User login
Culture-Conscious Lip Enhancement
Lip enhancement is a commonly performed aesthetic procedure in the United States. However, in the literature, anthropometric measurements defining the ideal lip proportions are computed and reported based on the white face. These proportions do not reflect the ethnic variations in Hispanic, Asian, and black lip dimensions.
In a study in the Journal of Plastic Reconstructive Aesthetic Surgery, Wong et al. evaluated three-dimensional models of male and female white, Chinese, and Korean subjects using surface-imaging technology (2010;63:2032-9). In both the Chinese and Korean patient groups, there were significant differences in lip parameters and lip-projection volumes, compared with whites, thus revealing measurable differences in the Asian lip morphology. Similarly, Hispanics and blacks do not exhibit the common 2/3 to 1/3 lip height proportions that are commonly used to define the "ideal" lip proportions in whites.
Skin of color patients often have full upper and lower lips, often with a 1/2 to 1/2 height ratio. In addition, photodamage and fine rhytids are not as common in these patients. Mandibular retraction in the lower face leads to perioral volume loss and ptosis of the lateral oral commissures, the development of the prejowl sulcus, and loss of lip volume.
Rejuvenation of the lip and perioral area in skin of color patients should involve the symmetry, shape, and projection of the lips in the context of their ethnicity and the structural differences in their faces. The extent and pattern of volume loss in the perioral region and the lower face should also be evaluated and treated. Revolumizing the lower face in conjunction with revolumizing the lips can produce perioral lifting and global lifting of the mouth and lower face.
Lip enhancement in skin of color patients should involve an understanding of both the inherent differences in the perception of beauty in skin of color patients and the differences in the mechanism of aging. Volumizing and recontouring of the perioral region is best approached in the context of what is thought to be aesthetically pleasing based on patient’s culture, ethnicity, and facial structure.
--Lily Talakoub, M.D.
Lip enhancement is a commonly performed aesthetic procedure in the United States. However, in the literature, anthropometric measurements defining the ideal lip proportions are computed and reported based on the white face. These proportions do not reflect the ethnic variations in Hispanic, Asian, and black lip dimensions.
In a study in the Journal of Plastic Reconstructive Aesthetic Surgery, Wong et al. evaluated three-dimensional models of male and female white, Chinese, and Korean subjects using surface-imaging technology (2010;63:2032-9). In both the Chinese and Korean patient groups, there were significant differences in lip parameters and lip-projection volumes, compared with whites, thus revealing measurable differences in the Asian lip morphology. Similarly, Hispanics and blacks do not exhibit the common 2/3 to 1/3 lip height proportions that are commonly used to define the "ideal" lip proportions in whites.
Skin of color patients often have full upper and lower lips, often with a 1/2 to 1/2 height ratio. In addition, photodamage and fine rhytids are not as common in these patients. Mandibular retraction in the lower face leads to perioral volume loss and ptosis of the lateral oral commissures, the development of the prejowl sulcus, and loss of lip volume.
Rejuvenation of the lip and perioral area in skin of color patients should involve the symmetry, shape, and projection of the lips in the context of their ethnicity and the structural differences in their faces. The extent and pattern of volume loss in the perioral region and the lower face should also be evaluated and treated. Revolumizing the lower face in conjunction with revolumizing the lips can produce perioral lifting and global lifting of the mouth and lower face.
Lip enhancement in skin of color patients should involve an understanding of both the inherent differences in the perception of beauty in skin of color patients and the differences in the mechanism of aging. Volumizing and recontouring of the perioral region is best approached in the context of what is thought to be aesthetically pleasing based on patient’s culture, ethnicity, and facial structure.
--Lily Talakoub, M.D.
Lip enhancement is a commonly performed aesthetic procedure in the United States. However, in the literature, anthropometric measurements defining the ideal lip proportions are computed and reported based on the white face. These proportions do not reflect the ethnic variations in Hispanic, Asian, and black lip dimensions.
In a study in the Journal of Plastic Reconstructive Aesthetic Surgery, Wong et al. evaluated three-dimensional models of male and female white, Chinese, and Korean subjects using surface-imaging technology (2010;63:2032-9). In both the Chinese and Korean patient groups, there were significant differences in lip parameters and lip-projection volumes, compared with whites, thus revealing measurable differences in the Asian lip morphology. Similarly, Hispanics and blacks do not exhibit the common 2/3 to 1/3 lip height proportions that are commonly used to define the "ideal" lip proportions in whites.
Skin of color patients often have full upper and lower lips, often with a 1/2 to 1/2 height ratio. In addition, photodamage and fine rhytids are not as common in these patients. Mandibular retraction in the lower face leads to perioral volume loss and ptosis of the lateral oral commissures, the development of the prejowl sulcus, and loss of lip volume.
Rejuvenation of the lip and perioral area in skin of color patients should involve the symmetry, shape, and projection of the lips in the context of their ethnicity and the structural differences in their faces. The extent and pattern of volume loss in the perioral region and the lower face should also be evaluated and treated. Revolumizing the lower face in conjunction with revolumizing the lips can produce perioral lifting and global lifting of the mouth and lower face.
Lip enhancement in skin of color patients should involve an understanding of both the inherent differences in the perception of beauty in skin of color patients and the differences in the mechanism of aging. Volumizing and recontouring of the perioral region is best approached in the context of what is thought to be aesthetically pleasing based on patient’s culture, ethnicity, and facial structure.
--Lily Talakoub, M.D.
Innovative Methods of UV Protection
One of the main reasons patients with darker skin don't apply sunscreen is because they believe they are at low or no risk for ultraviolet damage, according to the results of a survey that I conducted with Dr. Brooke Jackson and Dr. Chikoti Mibenge.
Our findings were presented in a poster at the American Academy of Dermatology's Summer Academy Meeting in Boston.
The study, conducted by surveying 105 patients in Chicago, revealed that 60% of black patients do not wear sunscreen regularly. Additionally, many darker skinned patients reported not liking the whitish or chalky appearance that sunscreens often leave.
However, sunscreen manufacturers are making more elegant formulations of both chemical and physical blockers that do not leave a whitish hue on darker skin.
Sun protective clothing, hats, parasols or umbrellas, avoiding peak hours of sun intensity, and avoiding tanning are all common methods we recommend to patients to protect themselves. Lesser known methods that we can also recommend to our patients include:
Heliocare
Heliocare tablets contain Polypodium leucotomos extract, a fern native to Central and South America rich in antioxidants which protect against formation of free radicals from UV exposure, particularly UVA. The science is based off of the fact that the fern, which was once aquatic, adapted to life on land and created its own protection from UV rays. The recommended dose is 1 tablet each morning or 2 tablets before intense sun exposure. The effect begins 30 minutes after consumption and is still active 2.5 hours after consumption. Total elimination is estimated to be about 8 hours, but pharmacokinetics for elimination have not been published. Numerous published studies have reported its benefits with regards to UV protection. A head-to-head study of UV protection from heliocare versus other powerful antioxidant supplements would be interesting.
Algae and Coral
At King's College in London, research is being done on the photoprotective effect of coral. In a press release last year, Dr. Paul Long reported that algae living within coral produces a sunscreen-like compound that not only protects the algae and coral from UV damage, but also the fish that feed on the coral. The part the algae play is thought to be part of the shikimate pathway found only in microbes and plants. A sunscreen tablet with this ingredient for human use is in the works.
Strawberries
Strawberries, as well as other darker colored berries, are known to contain polyphenols, which are antioxidants. Researchers in Italy and Spain tested a strawberry extract on cultured human fibroblasts to see if there was a photoprotective effect. They added strawberry extract in different concentrations to all but the control group. They then exposed the samples to a dose of UV light "equivalent to 90 minutes of midday summer sun in the French Riviera," said lead investigator Maurizio Battino. The results demonstrated that strawberry extract, especially at a concentration of 0.5 mg/ml, provided UVA protection. It not only boosted cell survival and viability, but also minimized DNA damage when compared with control cells.
Perhaps there will be topical sunscreens that contain strawberry extract in the future. Other foods high in antioxidants that may have sun protective benefits include:
Colored peppers and yellow squash (high in carotenoids).
Tomatoes and watermelon (high in lycopene).
Dark berries, such as blueberries, acai, blackberries, cranberries (rich in anthocyanin).
Turmeric root (curcumin).
Pomegranate (ellegic acid).
Green and black tea (catechins).
Dark cocoa (flavanols).
Green leafy vegetables, such as spinach and kale (xanthophylls, oxygenated carotenoids).
Fish, such as mackerel, salmon, trout, herring, and sardines (omega 3 fatty acids).
These are not a replacement for the more common methods of sun protection, but they may certainly provide an added benefit.
- Naissan Wesley, M.D.
Do you have questions about treating patients with darker skin? If so, send them to [email protected].
One of the main reasons patients with darker skin don't apply sunscreen is because they believe they are at low or no risk for ultraviolet damage, according to the results of a survey that I conducted with Dr. Brooke Jackson and Dr. Chikoti Mibenge.
Our findings were presented in a poster at the American Academy of Dermatology's Summer Academy Meeting in Boston.
The study, conducted by surveying 105 patients in Chicago, revealed that 60% of black patients do not wear sunscreen regularly. Additionally, many darker skinned patients reported not liking the whitish or chalky appearance that sunscreens often leave.
However, sunscreen manufacturers are making more elegant formulations of both chemical and physical blockers that do not leave a whitish hue on darker skin.
Sun protective clothing, hats, parasols or umbrellas, avoiding peak hours of sun intensity, and avoiding tanning are all common methods we recommend to patients to protect themselves. Lesser known methods that we can also recommend to our patients include:
Heliocare
Heliocare tablets contain Polypodium leucotomos extract, a fern native to Central and South America rich in antioxidants which protect against formation of free radicals from UV exposure, particularly UVA. The science is based off of the fact that the fern, which was once aquatic, adapted to life on land and created its own protection from UV rays. The recommended dose is 1 tablet each morning or 2 tablets before intense sun exposure. The effect begins 30 minutes after consumption and is still active 2.5 hours after consumption. Total elimination is estimated to be about 8 hours, but pharmacokinetics for elimination have not been published. Numerous published studies have reported its benefits with regards to UV protection. A head-to-head study of UV protection from heliocare versus other powerful antioxidant supplements would be interesting.
Algae and Coral
At King's College in London, research is being done on the photoprotective effect of coral. In a press release last year, Dr. Paul Long reported that algae living within coral produces a sunscreen-like compound that not only protects the algae and coral from UV damage, but also the fish that feed on the coral. The part the algae play is thought to be part of the shikimate pathway found only in microbes and plants. A sunscreen tablet with this ingredient for human use is in the works.
Strawberries
Strawberries, as well as other darker colored berries, are known to contain polyphenols, which are antioxidants. Researchers in Italy and Spain tested a strawberry extract on cultured human fibroblasts to see if there was a photoprotective effect. They added strawberry extract in different concentrations to all but the control group. They then exposed the samples to a dose of UV light "equivalent to 90 minutes of midday summer sun in the French Riviera," said lead investigator Maurizio Battino. The results demonstrated that strawberry extract, especially at a concentration of 0.5 mg/ml, provided UVA protection. It not only boosted cell survival and viability, but also minimized DNA damage when compared with control cells.
Perhaps there will be topical sunscreens that contain strawberry extract in the future. Other foods high in antioxidants that may have sun protective benefits include:
Colored peppers and yellow squash (high in carotenoids).
Tomatoes and watermelon (high in lycopene).
Dark berries, such as blueberries, acai, blackberries, cranberries (rich in anthocyanin).
Turmeric root (curcumin).
Pomegranate (ellegic acid).
Green and black tea (catechins).
Dark cocoa (flavanols).
Green leafy vegetables, such as spinach and kale (xanthophylls, oxygenated carotenoids).
Fish, such as mackerel, salmon, trout, herring, and sardines (omega 3 fatty acids).
These are not a replacement for the more common methods of sun protection, but they may certainly provide an added benefit.
- Naissan Wesley, M.D.
Do you have questions about treating patients with darker skin? If so, send them to [email protected].
One of the main reasons patients with darker skin don't apply sunscreen is because they believe they are at low or no risk for ultraviolet damage, according to the results of a survey that I conducted with Dr. Brooke Jackson and Dr. Chikoti Mibenge.
Our findings were presented in a poster at the American Academy of Dermatology's Summer Academy Meeting in Boston.
The study, conducted by surveying 105 patients in Chicago, revealed that 60% of black patients do not wear sunscreen regularly. Additionally, many darker skinned patients reported not liking the whitish or chalky appearance that sunscreens often leave.
However, sunscreen manufacturers are making more elegant formulations of both chemical and physical blockers that do not leave a whitish hue on darker skin.
Sun protective clothing, hats, parasols or umbrellas, avoiding peak hours of sun intensity, and avoiding tanning are all common methods we recommend to patients to protect themselves. Lesser known methods that we can also recommend to our patients include:
Heliocare
Heliocare tablets contain Polypodium leucotomos extract, a fern native to Central and South America rich in antioxidants which protect against formation of free radicals from UV exposure, particularly UVA. The science is based off of the fact that the fern, which was once aquatic, adapted to life on land and created its own protection from UV rays. The recommended dose is 1 tablet each morning or 2 tablets before intense sun exposure. The effect begins 30 minutes after consumption and is still active 2.5 hours after consumption. Total elimination is estimated to be about 8 hours, but pharmacokinetics for elimination have not been published. Numerous published studies have reported its benefits with regards to UV protection. A head-to-head study of UV protection from heliocare versus other powerful antioxidant supplements would be interesting.
Algae and Coral
At King's College in London, research is being done on the photoprotective effect of coral. In a press release last year, Dr. Paul Long reported that algae living within coral produces a sunscreen-like compound that not only protects the algae and coral from UV damage, but also the fish that feed on the coral. The part the algae play is thought to be part of the shikimate pathway found only in microbes and plants. A sunscreen tablet with this ingredient for human use is in the works.
Strawberries
Strawberries, as well as other darker colored berries, are known to contain polyphenols, which are antioxidants. Researchers in Italy and Spain tested a strawberry extract on cultured human fibroblasts to see if there was a photoprotective effect. They added strawberry extract in different concentrations to all but the control group. They then exposed the samples to a dose of UV light "equivalent to 90 minutes of midday summer sun in the French Riviera," said lead investigator Maurizio Battino. The results demonstrated that strawberry extract, especially at a concentration of 0.5 mg/ml, provided UVA protection. It not only boosted cell survival and viability, but also minimized DNA damage when compared with control cells.
Perhaps there will be topical sunscreens that contain strawberry extract in the future. Other foods high in antioxidants that may have sun protective benefits include:
Colored peppers and yellow squash (high in carotenoids).
Tomatoes and watermelon (high in lycopene).
Dark berries, such as blueberries, acai, blackberries, cranberries (rich in anthocyanin).
Turmeric root (curcumin).
Pomegranate (ellegic acid).
Green and black tea (catechins).
Dark cocoa (flavanols).
Green leafy vegetables, such as spinach and kale (xanthophylls, oxygenated carotenoids).
Fish, such as mackerel, salmon, trout, herring, and sardines (omega 3 fatty acids).
These are not a replacement for the more common methods of sun protection, but they may certainly provide an added benefit.
- Naissan Wesley, M.D.
Do you have questions about treating patients with darker skin? If so, send them to [email protected].
Optimized Pulsed Light Clears Vascular Lesions
PRAGUE – Optimized pulsed light therapy using Palomar Medical Technologies’ proprietary MaxG handpiece proved safe and efficient for the treatment of port wine stains and capillary malformations in an open study.
The MaxG is next-generation intense pulsed light therapy. The advance lies in a handpiece optimized so as to use a dual-band spectrum with two peaks: one at 500-670 nm and another at 870-1,200 nm. The peak in the visible light range targets small, superficial vessels, while the one in the near infrared addresses deeper vessels. Thus, optimized pulsed light (OPL) is able to achieve uniform heating and pulse width matched to a target vessel’s depth and size, Dr. Maurice A. Adatto explained at the annual congress of the European Academy of Dermatology and Venereology.
For years, pulsed dye laser therapy has been considered the gold standard in the treatment of vascular lesions. But recent published data demonstrate that while the laser can coagulate vessels quite nicely at the surface, the coagulation isn’t nearly as good for deeper vessels. In animal models, the OPL achieves greater increases in temperature compared with the pulsed dye laser at the purpuric threshold fluence in deeper and larger capillaries, said Dr. Adatto, who is medical director of the SkinPulse Dermatology & Laser Center in Geneva.
Dr. Adatto presented a two-center series of 16 OPL-treated adults and adolescents with vascular lesions on the face, neck, trunk, and lower limbs. The procedures were performed by him at the center in Geneva, and by his coinvestigator Dr. David Friedman in Jerusalem. The OPL handpiece was attached to Palomar’s Icon intense pulsed light device.
Outcomes were objectively assessed using the Antera 3D camera, made by Miravex, which provides high-definition clinical photographs along with quantitative measurement of hemoglobin and melanin clearance in treated areas. Assessments were done at 2-4 days and 1-2 months post-treatment.
The efficacy was impressive, and the side effects were far milder and more transitory than can occur with pulsed dye laser therapy, according to the dermatologist.
The majority of patients – 10 of 16 – achieved 50% or greater improvement in one to four OPL sessions. After the first treatment, four patients had roughly a 20% improvement, five were 25%-49% better, three showed 50%-74% clearance, and two patients showed 80% and 100% clearance.
Side effects consisted of 3-5 days of purpura and 1-3 days of local edema. To date, OPL for vascular lesions hasn’t resulted in any scars or in hypo- or hyperpigmentation.
As for the technical details, Dr. Adatto utilized one pass with 50 J/cm2 at 10 ms, while Dr. Friedman used a two-pass technique: the first at 34-36 J/cm2 at 10 ms, followed by a second at 22-28 J/cm2 at 5 ms. Treatment sessions were carried out at 4- to 6-week intervals.
In response to audience questions, Dr. Adatto said that his anecdotal experience has been that once a patient achieves greater than about 50% improvement, be it with a single OPL treatment session or after three, the therapeutic gain of additional sessions is smaller than with the initial ones.
"You can gain another 10% or so with another session for someone who has 70% improvement, but that’s it. You will reach a plateau," he said.
Dr. Adatto is now planning a similar study using OPL to treat vascular lesions in a pediatric population.
The study was funded by Palomar Medical Technologies. Dr. Adatto has received research funds from and is an adviser to Palomar and numerous other laser and intense pulsed light device manufacturers.
PRAGUE – Optimized pulsed light therapy using Palomar Medical Technologies’ proprietary MaxG handpiece proved safe and efficient for the treatment of port wine stains and capillary malformations in an open study.
The MaxG is next-generation intense pulsed light therapy. The advance lies in a handpiece optimized so as to use a dual-band spectrum with two peaks: one at 500-670 nm and another at 870-1,200 nm. The peak in the visible light range targets small, superficial vessels, while the one in the near infrared addresses deeper vessels. Thus, optimized pulsed light (OPL) is able to achieve uniform heating and pulse width matched to a target vessel’s depth and size, Dr. Maurice A. Adatto explained at the annual congress of the European Academy of Dermatology and Venereology.
For years, pulsed dye laser therapy has been considered the gold standard in the treatment of vascular lesions. But recent published data demonstrate that while the laser can coagulate vessels quite nicely at the surface, the coagulation isn’t nearly as good for deeper vessels. In animal models, the OPL achieves greater increases in temperature compared with the pulsed dye laser at the purpuric threshold fluence in deeper and larger capillaries, said Dr. Adatto, who is medical director of the SkinPulse Dermatology & Laser Center in Geneva.
Dr. Adatto presented a two-center series of 16 OPL-treated adults and adolescents with vascular lesions on the face, neck, trunk, and lower limbs. The procedures were performed by him at the center in Geneva, and by his coinvestigator Dr. David Friedman in Jerusalem. The OPL handpiece was attached to Palomar’s Icon intense pulsed light device.
Outcomes were objectively assessed using the Antera 3D camera, made by Miravex, which provides high-definition clinical photographs along with quantitative measurement of hemoglobin and melanin clearance in treated areas. Assessments were done at 2-4 days and 1-2 months post-treatment.
The efficacy was impressive, and the side effects were far milder and more transitory than can occur with pulsed dye laser therapy, according to the dermatologist.
The majority of patients – 10 of 16 – achieved 50% or greater improvement in one to four OPL sessions. After the first treatment, four patients had roughly a 20% improvement, five were 25%-49% better, three showed 50%-74% clearance, and two patients showed 80% and 100% clearance.
Side effects consisted of 3-5 days of purpura and 1-3 days of local edema. To date, OPL for vascular lesions hasn’t resulted in any scars or in hypo- or hyperpigmentation.
As for the technical details, Dr. Adatto utilized one pass with 50 J/cm2 at 10 ms, while Dr. Friedman used a two-pass technique: the first at 34-36 J/cm2 at 10 ms, followed by a second at 22-28 J/cm2 at 5 ms. Treatment sessions were carried out at 4- to 6-week intervals.
In response to audience questions, Dr. Adatto said that his anecdotal experience has been that once a patient achieves greater than about 50% improvement, be it with a single OPL treatment session or after three, the therapeutic gain of additional sessions is smaller than with the initial ones.
"You can gain another 10% or so with another session for someone who has 70% improvement, but that’s it. You will reach a plateau," he said.
Dr. Adatto is now planning a similar study using OPL to treat vascular lesions in a pediatric population.
The study was funded by Palomar Medical Technologies. Dr. Adatto has received research funds from and is an adviser to Palomar and numerous other laser and intense pulsed light device manufacturers.
PRAGUE – Optimized pulsed light therapy using Palomar Medical Technologies’ proprietary MaxG handpiece proved safe and efficient for the treatment of port wine stains and capillary malformations in an open study.
The MaxG is next-generation intense pulsed light therapy. The advance lies in a handpiece optimized so as to use a dual-band spectrum with two peaks: one at 500-670 nm and another at 870-1,200 nm. The peak in the visible light range targets small, superficial vessels, while the one in the near infrared addresses deeper vessels. Thus, optimized pulsed light (OPL) is able to achieve uniform heating and pulse width matched to a target vessel’s depth and size, Dr. Maurice A. Adatto explained at the annual congress of the European Academy of Dermatology and Venereology.
For years, pulsed dye laser therapy has been considered the gold standard in the treatment of vascular lesions. But recent published data demonstrate that while the laser can coagulate vessels quite nicely at the surface, the coagulation isn’t nearly as good for deeper vessels. In animal models, the OPL achieves greater increases in temperature compared with the pulsed dye laser at the purpuric threshold fluence in deeper and larger capillaries, said Dr. Adatto, who is medical director of the SkinPulse Dermatology & Laser Center in Geneva.
Dr. Adatto presented a two-center series of 16 OPL-treated adults and adolescents with vascular lesions on the face, neck, trunk, and lower limbs. The procedures were performed by him at the center in Geneva, and by his coinvestigator Dr. David Friedman in Jerusalem. The OPL handpiece was attached to Palomar’s Icon intense pulsed light device.
Outcomes were objectively assessed using the Antera 3D camera, made by Miravex, which provides high-definition clinical photographs along with quantitative measurement of hemoglobin and melanin clearance in treated areas. Assessments were done at 2-4 days and 1-2 months post-treatment.
The efficacy was impressive, and the side effects were far milder and more transitory than can occur with pulsed dye laser therapy, according to the dermatologist.
The majority of patients – 10 of 16 – achieved 50% or greater improvement in one to four OPL sessions. After the first treatment, four patients had roughly a 20% improvement, five were 25%-49% better, three showed 50%-74% clearance, and two patients showed 80% and 100% clearance.
Side effects consisted of 3-5 days of purpura and 1-3 days of local edema. To date, OPL for vascular lesions hasn’t resulted in any scars or in hypo- or hyperpigmentation.
As for the technical details, Dr. Adatto utilized one pass with 50 J/cm2 at 10 ms, while Dr. Friedman used a two-pass technique: the first at 34-36 J/cm2 at 10 ms, followed by a second at 22-28 J/cm2 at 5 ms. Treatment sessions were carried out at 4- to 6-week intervals.
In response to audience questions, Dr. Adatto said that his anecdotal experience has been that once a patient achieves greater than about 50% improvement, be it with a single OPL treatment session or after three, the therapeutic gain of additional sessions is smaller than with the initial ones.
"You can gain another 10% or so with another session for someone who has 70% improvement, but that’s it. You will reach a plateau," he said.
Dr. Adatto is now planning a similar study using OPL to treat vascular lesions in a pediatric population.
The study was funded by Palomar Medical Technologies. Dr. Adatto has received research funds from and is an adviser to Palomar and numerous other laser and intense pulsed light device manufacturers.
AT THE ANNUAL CONGRESS OF THE EUROPEAN ACADEMY OF DERMATOLOGY AND VENEREOLOGY
Major Finding: Ten of 16 adults and adolescents who underwent dual-spectrum optimized pulsed light therapy for a variety of vascular lesions demonstrated 50% or greater improvement after one to four treatment sessions. Side effects were considerably milder than typically seen following pulsed dye laser therapy.
Data Source: This was an open study conducted at dermatology centers in Geneva and Jerusalem.
Disclosures: The study was funded by Palomar Medical Technologies, which markets the MaxG optimized pulsed light handpiece. The presenter is an advisor to Palomar and numerous other laser and intense pulsed light device manufacturers.
Botulinum Toxin Threading Yields More Uniform Result
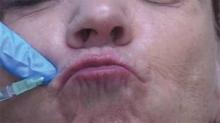
ATLANTA – The use of a threading technique, rather than the standard depot injection technique, when using botulinum toxin A to treat perioral and glabellar rhytides provides a more uniform and natural cosmetic result, according to Dr. H. William Higgins II.
Threading involves injecting the muscle along its normal anatomic course to paralyze the related muscle more evenly, he explained at the annual meeting of the American Society for Dermatologic Surgery.
For upper and lower lip treatment, for example, injections are made at a 20- to 30-degree angle, entering the skin at a location just lateral to the targeted rhytid. The toxin is dispensed while withdrawing, thereby threading the injection along the length of the orbicularis oris. This differs from the typical approach, which often involves a depot injection at an angle more perpendicular to the skin, said Dr. Higgins of Brown University in Providence, R.I.
For the glabellar lines, the threading technique involves four symmetrical injection points, with two points targeting each corrugator. Injections at the more medial points are made directly above the inner canthus, with intramuscular injections made perpendicularly to the skin in the traditional depot manner.
At the two lateral injection points, however, the needle is inserted in most cases just medial to the mid-pupillary lines, thereby targeting the "tail" of the corrugators, he explained.
"Similar to our approach at the orbicularis oris, rather than injecting at an angle more perpendicular to the skin, we inject at an angle of roughly 20-30 degrees, entering the skin at a location just medial to the glabellar rhytid we intend to treat. The needle is then directed laterally and slightly superiorly in order to follow the anatomy of the corrugator supercilii, and the injection is threaded along the muscle’s length while withdrawing," he explained.
This approach corrects for the inadequate responses sometimes seen when using the typical method of placing subepidermal blebs to produce localized microparesis of the targeted muscle, and could reduce the need for touch-up injections.
Cosmetic outcomes have been excellent and patient satisfaction high with the use of this technique, he said. In his experience, the technique has dramatically reduced the incidence of adverse effects.
"It has been documented that, even with conservative dosing, neuromodulator treatment of perioral rhytides can affect mouth function by weakening the lip sphincter, but this has not been the case in our patient population when using this technique," he said.
Similarly, when treating glabellar rhytides, the injection of the toxin at a more precise depth – and more evenly along the tail of the corrugators, has resulted in a reduced incidence of brow ptosis as well as more natural smoothing.
"This approach helps prevent the undesirable appearance of a 'forehead freeze,' " he said.
The threading technique also results in fewer needle sticks, which means less pain and bruising for the patients.
The use of a longer 1- or 1.5-inch needle could potentially allow for even fewer injections without compromising the result, Dr. Higgins noted.
"Furthermore, this technique could conceivably be applied on other areas of the face. Crow's feet, for example, could be treated with fewer threading injections rather than with multiple depot injections," he said.
Dr. Higgins reported having no relevant financial disclosures.
ATLANTA – The use of a threading technique, rather than the standard depot injection technique, when using botulinum toxin A to treat perioral and glabellar rhytides provides a more uniform and natural cosmetic result, according to Dr. H. William Higgins II.
Threading involves injecting the muscle along its normal anatomic course to paralyze the related muscle more evenly, he explained at the annual meeting of the American Society for Dermatologic Surgery.
For upper and lower lip treatment, for example, injections are made at a 20- to 30-degree angle, entering the skin at a location just lateral to the targeted rhytid. The toxin is dispensed while withdrawing, thereby threading the injection along the length of the orbicularis oris. This differs from the typical approach, which often involves a depot injection at an angle more perpendicular to the skin, said Dr. Higgins of Brown University in Providence, R.I.
For the glabellar lines, the threading technique involves four symmetrical injection points, with two points targeting each corrugator. Injections at the more medial points are made directly above the inner canthus, with intramuscular injections made perpendicularly to the skin in the traditional depot manner.
At the two lateral injection points, however, the needle is inserted in most cases just medial to the mid-pupillary lines, thereby targeting the "tail" of the corrugators, he explained.
"Similar to our approach at the orbicularis oris, rather than injecting at an angle more perpendicular to the skin, we inject at an angle of roughly 20-30 degrees, entering the skin at a location just medial to the glabellar rhytid we intend to treat. The needle is then directed laterally and slightly superiorly in order to follow the anatomy of the corrugator supercilii, and the injection is threaded along the muscle’s length while withdrawing," he explained.
This approach corrects for the inadequate responses sometimes seen when using the typical method of placing subepidermal blebs to produce localized microparesis of the targeted muscle, and could reduce the need for touch-up injections.
Cosmetic outcomes have been excellent and patient satisfaction high with the use of this technique, he said. In his experience, the technique has dramatically reduced the incidence of adverse effects.
"It has been documented that, even with conservative dosing, neuromodulator treatment of perioral rhytides can affect mouth function by weakening the lip sphincter, but this has not been the case in our patient population when using this technique," he said.
Similarly, when treating glabellar rhytides, the injection of the toxin at a more precise depth – and more evenly along the tail of the corrugators, has resulted in a reduced incidence of brow ptosis as well as more natural smoothing.
"This approach helps prevent the undesirable appearance of a 'forehead freeze,' " he said.
The threading technique also results in fewer needle sticks, which means less pain and bruising for the patients.
The use of a longer 1- or 1.5-inch needle could potentially allow for even fewer injections without compromising the result, Dr. Higgins noted.
"Furthermore, this technique could conceivably be applied on other areas of the face. Crow's feet, for example, could be treated with fewer threading injections rather than with multiple depot injections," he said.
Dr. Higgins reported having no relevant financial disclosures.
ATLANTA – The use of a threading technique, rather than the standard depot injection technique, when using botulinum toxin A to treat perioral and glabellar rhytides provides a more uniform and natural cosmetic result, according to Dr. H. William Higgins II.
Threading involves injecting the muscle along its normal anatomic course to paralyze the related muscle more evenly, he explained at the annual meeting of the American Society for Dermatologic Surgery.
For upper and lower lip treatment, for example, injections are made at a 20- to 30-degree angle, entering the skin at a location just lateral to the targeted rhytid. The toxin is dispensed while withdrawing, thereby threading the injection along the length of the orbicularis oris. This differs from the typical approach, which often involves a depot injection at an angle more perpendicular to the skin, said Dr. Higgins of Brown University in Providence, R.I.
For the glabellar lines, the threading technique involves four symmetrical injection points, with two points targeting each corrugator. Injections at the more medial points are made directly above the inner canthus, with intramuscular injections made perpendicularly to the skin in the traditional depot manner.
At the two lateral injection points, however, the needle is inserted in most cases just medial to the mid-pupillary lines, thereby targeting the "tail" of the corrugators, he explained.
"Similar to our approach at the orbicularis oris, rather than injecting at an angle more perpendicular to the skin, we inject at an angle of roughly 20-30 degrees, entering the skin at a location just medial to the glabellar rhytid we intend to treat. The needle is then directed laterally and slightly superiorly in order to follow the anatomy of the corrugator supercilii, and the injection is threaded along the muscle’s length while withdrawing," he explained.
This approach corrects for the inadequate responses sometimes seen when using the typical method of placing subepidermal blebs to produce localized microparesis of the targeted muscle, and could reduce the need for touch-up injections.
Cosmetic outcomes have been excellent and patient satisfaction high with the use of this technique, he said. In his experience, the technique has dramatically reduced the incidence of adverse effects.
"It has been documented that, even with conservative dosing, neuromodulator treatment of perioral rhytides can affect mouth function by weakening the lip sphincter, but this has not been the case in our patient population when using this technique," he said.
Similarly, when treating glabellar rhytides, the injection of the toxin at a more precise depth – and more evenly along the tail of the corrugators, has resulted in a reduced incidence of brow ptosis as well as more natural smoothing.
"This approach helps prevent the undesirable appearance of a 'forehead freeze,' " he said.
The threading technique also results in fewer needle sticks, which means less pain and bruising for the patients.
The use of a longer 1- or 1.5-inch needle could potentially allow for even fewer injections without compromising the result, Dr. Higgins noted.
"Furthermore, this technique could conceivably be applied on other areas of the face. Crow's feet, for example, could be treated with fewer threading injections rather than with multiple depot injections," he said.
Dr. Higgins reported having no relevant financial disclosures.
EXPERT ANALYSIS FROM THE ANNUAL MEETING OF THE AMERICAN SOCIETY FOR DERMATOLOGIC SURGERY
Pliaglis: Dermatologists Gain a Novel Topical Anesthetic
PRAGUE – A novel self-occlusive topical anesthetic cream newly approved by the Food and Drug Administration for local analgesia in superficial dermatologic procedures displayed persuasive evidence of efficacy in a phase III study highlighted at the annual congress of the European Academy of Dermatology and Venereology.
The topical anesthetic cream, called Pliaglis, incorporates lidocaine and tetracaine at 70 mg/g each. The FDA approved the product in October 2012 for use in conjunction with filler injections, laser-assisted tattoo removal, pulsed dye laser therapy, and other dermatologic procedures.
At the congress, Y. May Ma, Ph.D., presented the results of a multicenter phase III clinical trial involving 50 patients undergoing laser-assisted hair removal. Investigators applied Pliaglis to half of the skin surface scheduled for treatment and a placebo cream to the other half. Thirty minutes later dermatologists peeled off both materials and got to work.
Participants’ mean pain score for the laser procedure on a 0-100 visual analog scale was 23 for the Pliaglis-pretreated areas compared with 32 for hair removal on the control areas. Eighty percent of patients rated the analgesic effect as adequate on Pliaglis-pretreated skin areas, but only 52% did so for placebo-pretreated areas, reported Dr. Ma of Galderma Laboratories in Sophia Antipolis, France.
Blinded investigators rated 44% of patients as having no pain during laser therapy on areas that had been pretreated with Pliaglis, compared with an investigator-judged 22% pain-free procedure rate on placebo-pretreated areas.
Mild, transient stinging, redness, and erythema were fairly common on Pliaglis-treated skin, but quickly resolved without any intervention, Dr. Ma observed.
This study was funded by Galderma and presented by a full-time Galderma employee.
PRAGUE – A novel self-occlusive topical anesthetic cream newly approved by the Food and Drug Administration for local analgesia in superficial dermatologic procedures displayed persuasive evidence of efficacy in a phase III study highlighted at the annual congress of the European Academy of Dermatology and Venereology.
The topical anesthetic cream, called Pliaglis, incorporates lidocaine and tetracaine at 70 mg/g each. The FDA approved the product in October 2012 for use in conjunction with filler injections, laser-assisted tattoo removal, pulsed dye laser therapy, and other dermatologic procedures.
At the congress, Y. May Ma, Ph.D., presented the results of a multicenter phase III clinical trial involving 50 patients undergoing laser-assisted hair removal. Investigators applied Pliaglis to half of the skin surface scheduled for treatment and a placebo cream to the other half. Thirty minutes later dermatologists peeled off both materials and got to work.
Participants’ mean pain score for the laser procedure on a 0-100 visual analog scale was 23 for the Pliaglis-pretreated areas compared with 32 for hair removal on the control areas. Eighty percent of patients rated the analgesic effect as adequate on Pliaglis-pretreated skin areas, but only 52% did so for placebo-pretreated areas, reported Dr. Ma of Galderma Laboratories in Sophia Antipolis, France.
Blinded investigators rated 44% of patients as having no pain during laser therapy on areas that had been pretreated with Pliaglis, compared with an investigator-judged 22% pain-free procedure rate on placebo-pretreated areas.
Mild, transient stinging, redness, and erythema were fairly common on Pliaglis-treated skin, but quickly resolved without any intervention, Dr. Ma observed.
This study was funded by Galderma and presented by a full-time Galderma employee.
PRAGUE – A novel self-occlusive topical anesthetic cream newly approved by the Food and Drug Administration for local analgesia in superficial dermatologic procedures displayed persuasive evidence of efficacy in a phase III study highlighted at the annual congress of the European Academy of Dermatology and Venereology.
The topical anesthetic cream, called Pliaglis, incorporates lidocaine and tetracaine at 70 mg/g each. The FDA approved the product in October 2012 for use in conjunction with filler injections, laser-assisted tattoo removal, pulsed dye laser therapy, and other dermatologic procedures.
At the congress, Y. May Ma, Ph.D., presented the results of a multicenter phase III clinical trial involving 50 patients undergoing laser-assisted hair removal. Investigators applied Pliaglis to half of the skin surface scheduled for treatment and a placebo cream to the other half. Thirty minutes later dermatologists peeled off both materials and got to work.
Participants’ mean pain score for the laser procedure on a 0-100 visual analog scale was 23 for the Pliaglis-pretreated areas compared with 32 for hair removal on the control areas. Eighty percent of patients rated the analgesic effect as adequate on Pliaglis-pretreated skin areas, but only 52% did so for placebo-pretreated areas, reported Dr. Ma of Galderma Laboratories in Sophia Antipolis, France.
Blinded investigators rated 44% of patients as having no pain during laser therapy on areas that had been pretreated with Pliaglis, compared with an investigator-judged 22% pain-free procedure rate on placebo-pretreated areas.
Mild, transient stinging, redness, and erythema were fairly common on Pliaglis-treated skin, but quickly resolved without any intervention, Dr. Ma observed.
This study was funded by Galderma and presented by a full-time Galderma employee.
AT THE ANNUAL CONGRESS OF THE EUROPEAN ACADEMY OF DERMATOLOGY AND VENEREOLOGY
Major Finding: Eighty percent of patients who received a new self-occlusive topical anesthetic cream prior to laser-assisted hair removal indicated they experienced adequate analgesia.
Data Source: Data are from a phase III clinical trial involving 50 patients who received the novel anesthetic cream on half of the target skin area and a placebo cream on the other half.
Disclosures: This study was funded by Galderma and presented by a full-time Galderma employee.
New Treatment Option for Thick AKs Emerges
PRAGUE – Intensified photodynamic therapy assisted by ablative fractional laser resurfacing is a new and more effective way to treat thick actinic keratoses, according to Dr. Merete Haedersdal.
At 3 months’ follow-up, cure rates were significantly better with fractional CO2 laser-assisted photodynamic therapy (PDT) than with standard PDT in a randomized trial, she reported at the annual congress of the European Academy of Dermatology and Venereology.
"As a side benefit, the combined therapy gives a nice decrease in photoaging. There is photorejuvenation of the skin," noted Dr. Haedersdal of the University of Copenhagen.
Stand-alone PDT gets good results in thinner AKs, Bowen’s lesions, and basal cell carcinomas, both superficial and nodular. But effectiveness drops off considerably for thicker lesions.
That’s why Dr. Haedersdal and her Copenhagen colleagues, together with researchers at the Wellman Center for Photomedicine at Massachusetts General Hospital, Boston, where she has been a visiting scientist, are developing intensified PDT.
Basically, the dermatologists are using the fractional CO2 laser at 10,600 nm to drill tiny vertical channels surrounded by areas of unexposed skin. These channels facilitate uptake of the photosensitizing agent, rendering PDT more effective at greater depths. The enhanced uptake of photosensitizer is not merely a hypothesis; it has been documented via a marked increase in fluorescence intensity during illumination, she explained.
Dr. Haedersdal reported on 15 patients with a total of 212 AKs on severely photodamaged skin of the scalp and face. Two symmetrical randomly selected areas were chosen on each patient to receive one fractional CO2 laser-assisted PDT treatment and one standard PDT treatment. First, however, both treatment areas underwent curettage. Then one site was treated with the UltraPulse laser using the DeepFx handpiece set to 10 mJ per pulse and a single pulse density of 5%. The photosensitizing agent, methyl aminolevulinate cream, was then applied under occlusion for 3 hours at both sites. This was followed by illumination using a red light–emitting diode at 37 J/cm2.
At 3 months’ follow-up, the complete response rate of thicker grade II-III AKs was 88% with intensified PDT, compared with 59% with conventional PDT. For thinner grade I lesions, the complete response rates were 100% and 79%, respectively.
Only 3 new lesions arose at the intensified PDT-treated sites within 3 months, compared with 11 new lesions in areas that received standard PDT.
"So there might – in terms of avoiding future treatment procedures – be a benefit in combining the photothermal efficacy of the laser with the photochemical response from the PDT procedure," Dr. Haedersdal noted.
Pain scores were significantly higher during illumination in the intensified PDT areas, with a mean of 6.5 on a 1-10 scale compared with 5.4 on skin sites that got standard PDT. Erythema and crusting were also more intense at intensified PDT sites, and long-term pigmentary changes were more frequent at these sites as well.
"We have to be aware that the clinical reactions that we see from this new procedure are more intense than with conventional PDT. So for now we have to take care that we’re not using it for really large treatment areas because then the patients will have really intense phototoxic reactions," the dermatologist cautioned.
She and her coinvestigators are conducting an ongoing clinical trial combining mild daylight PDT and intensified PDT in organ transplant recipients, who are highly prone to the development of numerous skin cancers.
In pig models, the investigators are able to get the photosensitizing agent to a depth of 1.8 mm with the help of the fractional CO2 laser. This makes intensified PDT an attractive proposition for the treatment of basal cell carcinomas. Indeed, Dr. Haedersdal and her coinvestigators are now in the middle of a clinical trial of fractional CO2 laser-assisted PDT in patients with difficult-to-treat basal cell carcinomas.
"It seems very promising so far. We don’t have an evidence base yet, but I believe in it," she said.
The dermatologist reported serving on the advisory boards of Lumenis and Galderma, which are providing financial support for the development of intensified PDT.
European Academy of Dermatology and Venereology
PRAGUE – Intensified photodynamic therapy assisted by ablative fractional laser resurfacing is a new and more effective way to treat thick actinic keratoses, according to Dr. Merete Haedersdal.
At 3 months’ follow-up, cure rates were significantly better with fractional CO2 laser-assisted photodynamic therapy (PDT) than with standard PDT in a randomized trial, she reported at the annual congress of the European Academy of Dermatology and Venereology.
"As a side benefit, the combined therapy gives a nice decrease in photoaging. There is photorejuvenation of the skin," noted Dr. Haedersdal of the University of Copenhagen.
Stand-alone PDT gets good results in thinner AKs, Bowen’s lesions, and basal cell carcinomas, both superficial and nodular. But effectiveness drops off considerably for thicker lesions.
That’s why Dr. Haedersdal and her Copenhagen colleagues, together with researchers at the Wellman Center for Photomedicine at Massachusetts General Hospital, Boston, where she has been a visiting scientist, are developing intensified PDT.
Basically, the dermatologists are using the fractional CO2 laser at 10,600 nm to drill tiny vertical channels surrounded by areas of unexposed skin. These channels facilitate uptake of the photosensitizing agent, rendering PDT more effective at greater depths. The enhanced uptake of photosensitizer is not merely a hypothesis; it has been documented via a marked increase in fluorescence intensity during illumination, she explained.
Dr. Haedersdal reported on 15 patients with a total of 212 AKs on severely photodamaged skin of the scalp and face. Two symmetrical randomly selected areas were chosen on each patient to receive one fractional CO2 laser-assisted PDT treatment and one standard PDT treatment. First, however, both treatment areas underwent curettage. Then one site was treated with the UltraPulse laser using the DeepFx handpiece set to 10 mJ per pulse and a single pulse density of 5%. The photosensitizing agent, methyl aminolevulinate cream, was then applied under occlusion for 3 hours at both sites. This was followed by illumination using a red light–emitting diode at 37 J/cm2.
At 3 months’ follow-up, the complete response rate of thicker grade II-III AKs was 88% with intensified PDT, compared with 59% with conventional PDT. For thinner grade I lesions, the complete response rates were 100% and 79%, respectively.
Only 3 new lesions arose at the intensified PDT-treated sites within 3 months, compared with 11 new lesions in areas that received standard PDT.
"So there might – in terms of avoiding future treatment procedures – be a benefit in combining the photothermal efficacy of the laser with the photochemical response from the PDT procedure," Dr. Haedersdal noted.
Pain scores were significantly higher during illumination in the intensified PDT areas, with a mean of 6.5 on a 1-10 scale compared with 5.4 on skin sites that got standard PDT. Erythema and crusting were also more intense at intensified PDT sites, and long-term pigmentary changes were more frequent at these sites as well.
"We have to be aware that the clinical reactions that we see from this new procedure are more intense than with conventional PDT. So for now we have to take care that we’re not using it for really large treatment areas because then the patients will have really intense phototoxic reactions," the dermatologist cautioned.
She and her coinvestigators are conducting an ongoing clinical trial combining mild daylight PDT and intensified PDT in organ transplant recipients, who are highly prone to the development of numerous skin cancers.
In pig models, the investigators are able to get the photosensitizing agent to a depth of 1.8 mm with the help of the fractional CO2 laser. This makes intensified PDT an attractive proposition for the treatment of basal cell carcinomas. Indeed, Dr. Haedersdal and her coinvestigators are now in the middle of a clinical trial of fractional CO2 laser-assisted PDT in patients with difficult-to-treat basal cell carcinomas.
"It seems very promising so far. We don’t have an evidence base yet, but I believe in it," she said.
The dermatologist reported serving on the advisory boards of Lumenis and Galderma, which are providing financial support for the development of intensified PDT.
PRAGUE – Intensified photodynamic therapy assisted by ablative fractional laser resurfacing is a new and more effective way to treat thick actinic keratoses, according to Dr. Merete Haedersdal.
At 3 months’ follow-up, cure rates were significantly better with fractional CO2 laser-assisted photodynamic therapy (PDT) than with standard PDT in a randomized trial, she reported at the annual congress of the European Academy of Dermatology and Venereology.
"As a side benefit, the combined therapy gives a nice decrease in photoaging. There is photorejuvenation of the skin," noted Dr. Haedersdal of the University of Copenhagen.
Stand-alone PDT gets good results in thinner AKs, Bowen’s lesions, and basal cell carcinomas, both superficial and nodular. But effectiveness drops off considerably for thicker lesions.
That’s why Dr. Haedersdal and her Copenhagen colleagues, together with researchers at the Wellman Center for Photomedicine at Massachusetts General Hospital, Boston, where she has been a visiting scientist, are developing intensified PDT.
Basically, the dermatologists are using the fractional CO2 laser at 10,600 nm to drill tiny vertical channels surrounded by areas of unexposed skin. These channels facilitate uptake of the photosensitizing agent, rendering PDT more effective at greater depths. The enhanced uptake of photosensitizer is not merely a hypothesis; it has been documented via a marked increase in fluorescence intensity during illumination, she explained.
Dr. Haedersdal reported on 15 patients with a total of 212 AKs on severely photodamaged skin of the scalp and face. Two symmetrical randomly selected areas were chosen on each patient to receive one fractional CO2 laser-assisted PDT treatment and one standard PDT treatment. First, however, both treatment areas underwent curettage. Then one site was treated with the UltraPulse laser using the DeepFx handpiece set to 10 mJ per pulse and a single pulse density of 5%. The photosensitizing agent, methyl aminolevulinate cream, was then applied under occlusion for 3 hours at both sites. This was followed by illumination using a red light–emitting diode at 37 J/cm2.
At 3 months’ follow-up, the complete response rate of thicker grade II-III AKs was 88% with intensified PDT, compared with 59% with conventional PDT. For thinner grade I lesions, the complete response rates were 100% and 79%, respectively.
Only 3 new lesions arose at the intensified PDT-treated sites within 3 months, compared with 11 new lesions in areas that received standard PDT.
"So there might – in terms of avoiding future treatment procedures – be a benefit in combining the photothermal efficacy of the laser with the photochemical response from the PDT procedure," Dr. Haedersdal noted.
Pain scores were significantly higher during illumination in the intensified PDT areas, with a mean of 6.5 on a 1-10 scale compared with 5.4 on skin sites that got standard PDT. Erythema and crusting were also more intense at intensified PDT sites, and long-term pigmentary changes were more frequent at these sites as well.
"We have to be aware that the clinical reactions that we see from this new procedure are more intense than with conventional PDT. So for now we have to take care that we’re not using it for really large treatment areas because then the patients will have really intense phototoxic reactions," the dermatologist cautioned.
She and her coinvestigators are conducting an ongoing clinical trial combining mild daylight PDT and intensified PDT in organ transplant recipients, who are highly prone to the development of numerous skin cancers.
In pig models, the investigators are able to get the photosensitizing agent to a depth of 1.8 mm with the help of the fractional CO2 laser. This makes intensified PDT an attractive proposition for the treatment of basal cell carcinomas. Indeed, Dr. Haedersdal and her coinvestigators are now in the middle of a clinical trial of fractional CO2 laser-assisted PDT in patients with difficult-to-treat basal cell carcinomas.
"It seems very promising so far. We don’t have an evidence base yet, but I believe in it," she said.
The dermatologist reported serving on the advisory boards of Lumenis and Galderma, which are providing financial support for the development of intensified PDT.
European Academy of Dermatology and Venereology
European Academy of Dermatology and Venereology
AT THE ANNUAL CONGRESS OF THE EUROPEAN ACADEMY OF DERMATOLOGY AND VENEREOLOGY
Major Finding: The complete cure rate was 88% for thick grade II-III actinic keratoses at 3 months after ablative fractional laser resurfacing that was followed immediately by photodynamic therapy. The cure rate was 59% with photodynamic therapy alone.
Data Source: This randomized trial included 15 patients with a total of 212 actinic keratoses on severely photodamaged skin on the scalp and face. Each patient underwent treatment using standard PDT on one affected area and intensified PDT with fractional CO2 laser therapy on another.
Disclosures: Dr. Haedersdal has received research grants from, and is an adviser to, Lumenis and Galderma, which are involved in the development of this novel therapy.
Dermatologic Laser Therapy Advances on Many Fronts
PRAGUE – It has been a big year for dermatologic laser therapy.
Among the major advances in the field seen during 2012 has been introduction of novel techniques for remodeling mature burn scars and removing tattoos, as well as welcome, albeit preliminary, data supporting laser therapy of onychomycosis, and – finally – some long-overdue first persuasive evidence of the effectiveness of a home-use, light-based device for unwanted hair removal, Dr. Merete Haedersdal said in a keynote year-in-review laser lecture at the annual congress of the European Academy of Dermatology and Venereology.
• Tattoos. Based upon the concept of selective photothermolysis coupled with recognition that tattoo pigment particles are really tiny – a mere 40-300 nm in size – dermatologists at SkinCare Physicians in Chestnut Hill (Mass.) treated 12 patients using a novel picosecond 755-nm alexandrite laser.
After an average of 4.2 treatment sessions spaced roughly 6 weeks apart, all 12 patients showed greater than 75% clearance upon blinded physician assessment. All 12 declared themselves either satisfied or extremely satisfied with their results (Arch. Dermatol. 2012;17:1-4).
This picosecond alexandrite laser delivers pulses 100 times shorter than the familiar nanosecond lasers. It’s not yet commercially available, but is expected to be quite soon, according to Dr. Haedersdal of the University of Copenhagen.
Meanwhile, Greek dermatologists have pioneered a laser technique for tattoo removal that entails four treatment passes separated by 20-minute intervals, all delivered in a single lengthy session. The underlying concept is that the downtime between passes allows the treated skin to relax and shed treatment-induced air bubbles. In an 18-patient study, the clinical results were demonstrably better with the four-pass technique than with conventional single-treatment sessions (J. Am. Acad. Dermatol. 2012;66:271-7).
Dr. Haedersdal said that she’s heard some colleagues who’ve tried the four-pass-in-a-session technique say they’re not convinced it really does work better than the standard approach. She has tweaked the technique somewhat to good effect in her own practice: She starts out removing a tattoo using the standard single-treatment-per-session method and sticks with it until there is no further improvement. Then she switches to the four-pass-per-session technique.
"I would say it works very nicely when we add it on," the dermatologist commented.
• Home-use hair-removal device effectiveness. The home-device market has been on fire in the United States for more than 5 years and in Europe for the last couple. It is a field that’s been long on claims and short on evidence of meaningful efficacy and safety – until 2012. Just in September, Dr. Ronald G. Wheeland, professor of dermatology and chief of dermatologic surgery at the University of Missouri, Columbia, published a case-controlled study that Dr. Haedersdal considers most welcome.
Thirteen patients underwent eight hair removal treatment sessions at monthly intervals using an 810-nm home-use diode laser marketed as the Tria Hair Removal Laser. Untreated areas of unwanted hair growth served as controls. At 1 year of follow-up after completing the eighth and final treatment, the mean hair count reduction was 44%, 49%, and 65%, respectively, in areas treated at fluences of 7, 12, and 20 J/cm2 compared with controls (Lasers Surg. Med. 2012;44:550-7).
In addition, Dr. Haedersdal coauthored a systematic literature review of the two approved diode laser devices and nine intense pulsed light devices marketed for home use for hair removal. The cumulative supporting evidence isn’t super strong: six prospective uncontrolled studies and one controlled study (J. Eur. Acad. Dermatol. Venereol. 2012;26:545-53).
"Clearly, there is something to this home therapy based on the Wheeland study and our systematic review. We really need some randomized comparative trials, though," she said.
• Home-device safety. This is an area of such great concern that she and her colleagues in the European Society for Laser Dermatology recently published hair-removal home-device safety guidelines (J. Eur. Acad. Dermatol. Venereol. 2012;26: 799-811).
"People just aren’t being trained in the safe use of these devices," she cautioned.
The risks associated with improper use include ocular injury, skin burns, and paradoxical hair growth, as is the case with devices used in physicians’ offices.
The paradoxical hair growth risk in untreated areas close by treated skin is an issue that has been largely beneath dermatologists’ radar prior to the European guidelines. The reported risk with professional devices used by dermatologists is 0.6%-10%. With home devices, who knows?
"It’s a real matter of concern these days. When you lower the fluences, the incidence of paradoxical hair growth may be even higher. There’s nothing in the literature yet, but I’m sure there will be in the next few years," Dr. Haedersdal said.
Patients at increased risk for paradoxical hair regrowth are women with darker skin types, typically with polycystic ovarian syndrome, who are undergoing facial treatment. The mechanism of paradoxical hair regrowth is unknown. Two leading possibilities are light-driven triggering of inflammatory mediators or stimulation of the hair cycle secondary to subtherapeutic thermal injury, she continued.
• Burn scars. A solid body of evidence has accrued regarding the efficacy and safety of both ablative and nonablative fractional lasers to remodel mature burn scars.
Particularly noteworthy was a recent prospective, single-arm, blinded-evaluator study in which a 1,550-nm nonablative fractional erbium laser was employed to treat burn scars in 10 patients. Ninety percent of patients showed improved skin texture and 80% demonstrated improvement in dyschromia, something that hasn’t previously been reported with laser therapy (Lasers Surg. Med. 2012;44:441-6).
The 13 published studies of nonablative fractional laser therapy for burn scars show 26%-50% improvement. That’s slightly less than the 26%-83% improvement reported in the 13 studies of ablative fractional lasers. On the other hand, nonablative fractional laser therapy entails fewer side effects: 1-3 days of erythema and a postinflammatory hyperpigmentation rate of up to 13%, compared with 3-14 days of erythema with ablative fractional laser therapy and a postinflammatory hyperpigmentation rate of up to 92%. As yet, though, there have been no head-to-head comparative studies of the two types of devices.
• Onychomycosis. This is a brand-new area for laser therapy. A recent review noted that, while the Food and Drug Administration has approved four YAG lasers for treatment of onychomycosis, the regulatory standards for device approval don’t require persuasive evidence of efficacy, unlike for drugs (J. Am. Podiatr. Med. Assoc. 2012;102:428-30). Although it’s a promising technology, the authors stated that there are as yet no data showing how laser therapy stacks up against existing standard treatments for onychomycosis in terms of efficacy.
Nevertheless, Dr. Haedersdal noted, attention-getting cure rates were seen in a recent Chinese study involving 154 laser-treated nails in 33 patients. The week-24 complete cure rate, both mycologic and clinical, was 51% after eight weekly treatments and 53% after four weekly treatments (Chin. Med. J. 2012;125:3288-91).
Dr. Haedersdal reported serving on the scientific advisory boards for Galderma, LEO Pharma, and Procter & Gamble.
PRAGUE – It has been a big year for dermatologic laser therapy.
Among the major advances in the field seen during 2012 has been introduction of novel techniques for remodeling mature burn scars and removing tattoos, as well as welcome, albeit preliminary, data supporting laser therapy of onychomycosis, and – finally – some long-overdue first persuasive evidence of the effectiveness of a home-use, light-based device for unwanted hair removal, Dr. Merete Haedersdal said in a keynote year-in-review laser lecture at the annual congress of the European Academy of Dermatology and Venereology.
• Tattoos. Based upon the concept of selective photothermolysis coupled with recognition that tattoo pigment particles are really tiny – a mere 40-300 nm in size – dermatologists at SkinCare Physicians in Chestnut Hill (Mass.) treated 12 patients using a novel picosecond 755-nm alexandrite laser.
After an average of 4.2 treatment sessions spaced roughly 6 weeks apart, all 12 patients showed greater than 75% clearance upon blinded physician assessment. All 12 declared themselves either satisfied or extremely satisfied with their results (Arch. Dermatol. 2012;17:1-4).
This picosecond alexandrite laser delivers pulses 100 times shorter than the familiar nanosecond lasers. It’s not yet commercially available, but is expected to be quite soon, according to Dr. Haedersdal of the University of Copenhagen.
Meanwhile, Greek dermatologists have pioneered a laser technique for tattoo removal that entails four treatment passes separated by 20-minute intervals, all delivered in a single lengthy session. The underlying concept is that the downtime between passes allows the treated skin to relax and shed treatment-induced air bubbles. In an 18-patient study, the clinical results were demonstrably better with the four-pass technique than with conventional single-treatment sessions (J. Am. Acad. Dermatol. 2012;66:271-7).
Dr. Haedersdal said that she’s heard some colleagues who’ve tried the four-pass-in-a-session technique say they’re not convinced it really does work better than the standard approach. She has tweaked the technique somewhat to good effect in her own practice: She starts out removing a tattoo using the standard single-treatment-per-session method and sticks with it until there is no further improvement. Then she switches to the four-pass-per-session technique.
"I would say it works very nicely when we add it on," the dermatologist commented.
• Home-use hair-removal device effectiveness. The home-device market has been on fire in the United States for more than 5 years and in Europe for the last couple. It is a field that’s been long on claims and short on evidence of meaningful efficacy and safety – until 2012. Just in September, Dr. Ronald G. Wheeland, professor of dermatology and chief of dermatologic surgery at the University of Missouri, Columbia, published a case-controlled study that Dr. Haedersdal considers most welcome.
Thirteen patients underwent eight hair removal treatment sessions at monthly intervals using an 810-nm home-use diode laser marketed as the Tria Hair Removal Laser. Untreated areas of unwanted hair growth served as controls. At 1 year of follow-up after completing the eighth and final treatment, the mean hair count reduction was 44%, 49%, and 65%, respectively, in areas treated at fluences of 7, 12, and 20 J/cm2 compared with controls (Lasers Surg. Med. 2012;44:550-7).
In addition, Dr. Haedersdal coauthored a systematic literature review of the two approved diode laser devices and nine intense pulsed light devices marketed for home use for hair removal. The cumulative supporting evidence isn’t super strong: six prospective uncontrolled studies and one controlled study (J. Eur. Acad. Dermatol. Venereol. 2012;26:545-53).
"Clearly, there is something to this home therapy based on the Wheeland study and our systematic review. We really need some randomized comparative trials, though," she said.
• Home-device safety. This is an area of such great concern that she and her colleagues in the European Society for Laser Dermatology recently published hair-removal home-device safety guidelines (J. Eur. Acad. Dermatol. Venereol. 2012;26: 799-811).
"People just aren’t being trained in the safe use of these devices," she cautioned.
The risks associated with improper use include ocular injury, skin burns, and paradoxical hair growth, as is the case with devices used in physicians’ offices.
The paradoxical hair growth risk in untreated areas close by treated skin is an issue that has been largely beneath dermatologists’ radar prior to the European guidelines. The reported risk with professional devices used by dermatologists is 0.6%-10%. With home devices, who knows?
"It’s a real matter of concern these days. When you lower the fluences, the incidence of paradoxical hair growth may be even higher. There’s nothing in the literature yet, but I’m sure there will be in the next few years," Dr. Haedersdal said.
Patients at increased risk for paradoxical hair regrowth are women with darker skin types, typically with polycystic ovarian syndrome, who are undergoing facial treatment. The mechanism of paradoxical hair regrowth is unknown. Two leading possibilities are light-driven triggering of inflammatory mediators or stimulation of the hair cycle secondary to subtherapeutic thermal injury, she continued.
• Burn scars. A solid body of evidence has accrued regarding the efficacy and safety of both ablative and nonablative fractional lasers to remodel mature burn scars.
Particularly noteworthy was a recent prospective, single-arm, blinded-evaluator study in which a 1,550-nm nonablative fractional erbium laser was employed to treat burn scars in 10 patients. Ninety percent of patients showed improved skin texture and 80% demonstrated improvement in dyschromia, something that hasn’t previously been reported with laser therapy (Lasers Surg. Med. 2012;44:441-6).
The 13 published studies of nonablative fractional laser therapy for burn scars show 26%-50% improvement. That’s slightly less than the 26%-83% improvement reported in the 13 studies of ablative fractional lasers. On the other hand, nonablative fractional laser therapy entails fewer side effects: 1-3 days of erythema and a postinflammatory hyperpigmentation rate of up to 13%, compared with 3-14 days of erythema with ablative fractional laser therapy and a postinflammatory hyperpigmentation rate of up to 92%. As yet, though, there have been no head-to-head comparative studies of the two types of devices.
• Onychomycosis. This is a brand-new area for laser therapy. A recent review noted that, while the Food and Drug Administration has approved four YAG lasers for treatment of onychomycosis, the regulatory standards for device approval don’t require persuasive evidence of efficacy, unlike for drugs (J. Am. Podiatr. Med. Assoc. 2012;102:428-30). Although it’s a promising technology, the authors stated that there are as yet no data showing how laser therapy stacks up against existing standard treatments for onychomycosis in terms of efficacy.
Nevertheless, Dr. Haedersdal noted, attention-getting cure rates were seen in a recent Chinese study involving 154 laser-treated nails in 33 patients. The week-24 complete cure rate, both mycologic and clinical, was 51% after eight weekly treatments and 53% after four weekly treatments (Chin. Med. J. 2012;125:3288-91).
Dr. Haedersdal reported serving on the scientific advisory boards for Galderma, LEO Pharma, and Procter & Gamble.
PRAGUE – It has been a big year for dermatologic laser therapy.
Among the major advances in the field seen during 2012 has been introduction of novel techniques for remodeling mature burn scars and removing tattoos, as well as welcome, albeit preliminary, data supporting laser therapy of onychomycosis, and – finally – some long-overdue first persuasive evidence of the effectiveness of a home-use, light-based device for unwanted hair removal, Dr. Merete Haedersdal said in a keynote year-in-review laser lecture at the annual congress of the European Academy of Dermatology and Venereology.
• Tattoos. Based upon the concept of selective photothermolysis coupled with recognition that tattoo pigment particles are really tiny – a mere 40-300 nm in size – dermatologists at SkinCare Physicians in Chestnut Hill (Mass.) treated 12 patients using a novel picosecond 755-nm alexandrite laser.
After an average of 4.2 treatment sessions spaced roughly 6 weeks apart, all 12 patients showed greater than 75% clearance upon blinded physician assessment. All 12 declared themselves either satisfied or extremely satisfied with their results (Arch. Dermatol. 2012;17:1-4).
This picosecond alexandrite laser delivers pulses 100 times shorter than the familiar nanosecond lasers. It’s not yet commercially available, but is expected to be quite soon, according to Dr. Haedersdal of the University of Copenhagen.
Meanwhile, Greek dermatologists have pioneered a laser technique for tattoo removal that entails four treatment passes separated by 20-minute intervals, all delivered in a single lengthy session. The underlying concept is that the downtime between passes allows the treated skin to relax and shed treatment-induced air bubbles. In an 18-patient study, the clinical results were demonstrably better with the four-pass technique than with conventional single-treatment sessions (J. Am. Acad. Dermatol. 2012;66:271-7).
Dr. Haedersdal said that she’s heard some colleagues who’ve tried the four-pass-in-a-session technique say they’re not convinced it really does work better than the standard approach. She has tweaked the technique somewhat to good effect in her own practice: She starts out removing a tattoo using the standard single-treatment-per-session method and sticks with it until there is no further improvement. Then she switches to the four-pass-per-session technique.
"I would say it works very nicely when we add it on," the dermatologist commented.
• Home-use hair-removal device effectiveness. The home-device market has been on fire in the United States for more than 5 years and in Europe for the last couple. It is a field that’s been long on claims and short on evidence of meaningful efficacy and safety – until 2012. Just in September, Dr. Ronald G. Wheeland, professor of dermatology and chief of dermatologic surgery at the University of Missouri, Columbia, published a case-controlled study that Dr. Haedersdal considers most welcome.
Thirteen patients underwent eight hair removal treatment sessions at monthly intervals using an 810-nm home-use diode laser marketed as the Tria Hair Removal Laser. Untreated areas of unwanted hair growth served as controls. At 1 year of follow-up after completing the eighth and final treatment, the mean hair count reduction was 44%, 49%, and 65%, respectively, in areas treated at fluences of 7, 12, and 20 J/cm2 compared with controls (Lasers Surg. Med. 2012;44:550-7).
In addition, Dr. Haedersdal coauthored a systematic literature review of the two approved diode laser devices and nine intense pulsed light devices marketed for home use for hair removal. The cumulative supporting evidence isn’t super strong: six prospective uncontrolled studies and one controlled study (J. Eur. Acad. Dermatol. Venereol. 2012;26:545-53).
"Clearly, there is something to this home therapy based on the Wheeland study and our systematic review. We really need some randomized comparative trials, though," she said.
• Home-device safety. This is an area of such great concern that she and her colleagues in the European Society for Laser Dermatology recently published hair-removal home-device safety guidelines (J. Eur. Acad. Dermatol. Venereol. 2012;26: 799-811).
"People just aren’t being trained in the safe use of these devices," she cautioned.
The risks associated with improper use include ocular injury, skin burns, and paradoxical hair growth, as is the case with devices used in physicians’ offices.
The paradoxical hair growth risk in untreated areas close by treated skin is an issue that has been largely beneath dermatologists’ radar prior to the European guidelines. The reported risk with professional devices used by dermatologists is 0.6%-10%. With home devices, who knows?
"It’s a real matter of concern these days. When you lower the fluences, the incidence of paradoxical hair growth may be even higher. There’s nothing in the literature yet, but I’m sure there will be in the next few years," Dr. Haedersdal said.
Patients at increased risk for paradoxical hair regrowth are women with darker skin types, typically with polycystic ovarian syndrome, who are undergoing facial treatment. The mechanism of paradoxical hair regrowth is unknown. Two leading possibilities are light-driven triggering of inflammatory mediators or stimulation of the hair cycle secondary to subtherapeutic thermal injury, she continued.
• Burn scars. A solid body of evidence has accrued regarding the efficacy and safety of both ablative and nonablative fractional lasers to remodel mature burn scars.
Particularly noteworthy was a recent prospective, single-arm, blinded-evaluator study in which a 1,550-nm nonablative fractional erbium laser was employed to treat burn scars in 10 patients. Ninety percent of patients showed improved skin texture and 80% demonstrated improvement in dyschromia, something that hasn’t previously been reported with laser therapy (Lasers Surg. Med. 2012;44:441-6).
The 13 published studies of nonablative fractional laser therapy for burn scars show 26%-50% improvement. That’s slightly less than the 26%-83% improvement reported in the 13 studies of ablative fractional lasers. On the other hand, nonablative fractional laser therapy entails fewer side effects: 1-3 days of erythema and a postinflammatory hyperpigmentation rate of up to 13%, compared with 3-14 days of erythema with ablative fractional laser therapy and a postinflammatory hyperpigmentation rate of up to 92%. As yet, though, there have been no head-to-head comparative studies of the two types of devices.
• Onychomycosis. This is a brand-new area for laser therapy. A recent review noted that, while the Food and Drug Administration has approved four YAG lasers for treatment of onychomycosis, the regulatory standards for device approval don’t require persuasive evidence of efficacy, unlike for drugs (J. Am. Podiatr. Med. Assoc. 2012;102:428-30). Although it’s a promising technology, the authors stated that there are as yet no data showing how laser therapy stacks up against existing standard treatments for onychomycosis in terms of efficacy.
Nevertheless, Dr. Haedersdal noted, attention-getting cure rates were seen in a recent Chinese study involving 154 laser-treated nails in 33 patients. The week-24 complete cure rate, both mycologic and clinical, was 51% after eight weekly treatments and 53% after four weekly treatments (Chin. Med. J. 2012;125:3288-91).
Dr. Haedersdal reported serving on the scientific advisory boards for Galderma, LEO Pharma, and Procter & Gamble.
EXPERT ANALYSIS FROM THE ANNUAL CONGRESS OF THE EUROPEAN ACADEMY OF DERMATOLOGY AND VENEREOLOGY
Cryolipolysis Appears Safe for All Skin Types
ATLANTA – Cryolipolysis appears as safe and effective in dark skin types as in lighter skin types, according to a review of outcomes in 396 patients.
The primary goal of the study was to assess whether this technology is safe in patients with dark skin types, given their increased risk for developing postinflammatory hyperpigmentation with cold exposure and other treatments such as laser treatments, Dr. Ava Shamban said at the annual meeting of the American Society for Dermatologic Surgery.
However, no differences were seen in efficacy or safety based on skin type or ethnicity in the patients who participated in the multicenter study, she said.
"Cryolipolysis is, indeed, a color-blind technology."
In fact, patients with darker skin types had slightly higher satisfaction with the procedure, raising the question of whether the treatment might even be more effective in these patients, said Dr. Shamban, a dermatologist in private practice in Santa Monica, Calif.
The patients were treated on the back, flank, and/or abdomen, with most having multiple areas treated. Fitzpatrick skin types II-VI were represented: 85 had type II, 185 had type III, 104 had type IV, 18 had type V, and 4 had type VI.
Numerous ethnicities also were represented: 7 patients were African American, 38 were Asian, 295 were white, 37 were Latino, 5 were Mediterranean, and 14 were of Middle Eastern descent.
Women comprised 84% of the study population, and patients ranged in age from 24 to 74 years, with most in their late 40s to early 50s, Dr. Shamban noted.
No major adverse events occurred. Some patients did, however, experience minor effects, including bruising in 16%, swelling in 20%, and both bruising and swelling in 4%, she said, adding that the incidence of these effects did not differ between those with Fitzpatrick skin types II-III and those with type IV-VI.
Satisfaction with the procedure and outcomes also did not differ between those groups in 201 patients who completed a patient-satisfaction assessment. Only 7% of 122 patients with skin types II-III and 4% of 79 patients with skin types IV-VI were unsatisfied with the results, Dr. Shamban said.
"Cryolipolysis is, indeed, a color-blind technology, and it is a safe and effective method to reduce fat and thickening in patients of all skin types and ethnicities," she concluded.
Dr. Shamban had no disclosures to report. Her coauthor, Dr. Vic Narurkar, reported serving as a consultant for Zeltiq, the maker of the CoolSculpting cryolipolysis system used in this study.
ATLANTA – Cryolipolysis appears as safe and effective in dark skin types as in lighter skin types, according to a review of outcomes in 396 patients.
The primary goal of the study was to assess whether this technology is safe in patients with dark skin types, given their increased risk for developing postinflammatory hyperpigmentation with cold exposure and other treatments such as laser treatments, Dr. Ava Shamban said at the annual meeting of the American Society for Dermatologic Surgery.
However, no differences were seen in efficacy or safety based on skin type or ethnicity in the patients who participated in the multicenter study, she said.
"Cryolipolysis is, indeed, a color-blind technology."
In fact, patients with darker skin types had slightly higher satisfaction with the procedure, raising the question of whether the treatment might even be more effective in these patients, said Dr. Shamban, a dermatologist in private practice in Santa Monica, Calif.
The patients were treated on the back, flank, and/or abdomen, with most having multiple areas treated. Fitzpatrick skin types II-VI were represented: 85 had type II, 185 had type III, 104 had type IV, 18 had type V, and 4 had type VI.
Numerous ethnicities also were represented: 7 patients were African American, 38 were Asian, 295 were white, 37 were Latino, 5 were Mediterranean, and 14 were of Middle Eastern descent.
Women comprised 84% of the study population, and patients ranged in age from 24 to 74 years, with most in their late 40s to early 50s, Dr. Shamban noted.
No major adverse events occurred. Some patients did, however, experience minor effects, including bruising in 16%, swelling in 20%, and both bruising and swelling in 4%, she said, adding that the incidence of these effects did not differ between those with Fitzpatrick skin types II-III and those with type IV-VI.
Satisfaction with the procedure and outcomes also did not differ between those groups in 201 patients who completed a patient-satisfaction assessment. Only 7% of 122 patients with skin types II-III and 4% of 79 patients with skin types IV-VI were unsatisfied with the results, Dr. Shamban said.
"Cryolipolysis is, indeed, a color-blind technology, and it is a safe and effective method to reduce fat and thickening in patients of all skin types and ethnicities," she concluded.
Dr. Shamban had no disclosures to report. Her coauthor, Dr. Vic Narurkar, reported serving as a consultant for Zeltiq, the maker of the CoolSculpting cryolipolysis system used in this study.
ATLANTA – Cryolipolysis appears as safe and effective in dark skin types as in lighter skin types, according to a review of outcomes in 396 patients.
The primary goal of the study was to assess whether this technology is safe in patients with dark skin types, given their increased risk for developing postinflammatory hyperpigmentation with cold exposure and other treatments such as laser treatments, Dr. Ava Shamban said at the annual meeting of the American Society for Dermatologic Surgery.
However, no differences were seen in efficacy or safety based on skin type or ethnicity in the patients who participated in the multicenter study, she said.
"Cryolipolysis is, indeed, a color-blind technology."
In fact, patients with darker skin types had slightly higher satisfaction with the procedure, raising the question of whether the treatment might even be more effective in these patients, said Dr. Shamban, a dermatologist in private practice in Santa Monica, Calif.
The patients were treated on the back, flank, and/or abdomen, with most having multiple areas treated. Fitzpatrick skin types II-VI were represented: 85 had type II, 185 had type III, 104 had type IV, 18 had type V, and 4 had type VI.
Numerous ethnicities also were represented: 7 patients were African American, 38 were Asian, 295 were white, 37 were Latino, 5 were Mediterranean, and 14 were of Middle Eastern descent.
Women comprised 84% of the study population, and patients ranged in age from 24 to 74 years, with most in their late 40s to early 50s, Dr. Shamban noted.
No major adverse events occurred. Some patients did, however, experience minor effects, including bruising in 16%, swelling in 20%, and both bruising and swelling in 4%, she said, adding that the incidence of these effects did not differ between those with Fitzpatrick skin types II-III and those with type IV-VI.
Satisfaction with the procedure and outcomes also did not differ between those groups in 201 patients who completed a patient-satisfaction assessment. Only 7% of 122 patients with skin types II-III and 4% of 79 patients with skin types IV-VI were unsatisfied with the results, Dr. Shamban said.
"Cryolipolysis is, indeed, a color-blind technology, and it is a safe and effective method to reduce fat and thickening in patients of all skin types and ethnicities," she concluded.
Dr. Shamban had no disclosures to report. Her coauthor, Dr. Vic Narurkar, reported serving as a consultant for Zeltiq, the maker of the CoolSculpting cryolipolysis system used in this study.
AT THE ANNUAL MEETING OF THE AMERICAN SOCIETY FOR DERMATOLOGIC SURGERY
Major Finding: No differences were seen in efficacy or safety based on skin type or ethnicity.
Data Source: This review of outcomes involved 396 patients.
Disclosures: Dr. Shamban had no disclosures to report. Her coauthor, Dr. Vic Narurkar, reported serving as a consultant for Zeltiq, the maker of the CoolSculpting cryolipolysis system used in this study.
Topical Fluorocarbon Speeds Tattoo Removal Process
ATLANTA – Applying the topical fluorocarbon perfluorodecalin prior to Q-switched laser treatment for tattoo removal allows for immediate retreatment of the tattoo, thereby improving results while decreasing overall treatment time, according to Dr. Roy Geronemus.
The findings have important implications for improving outcomes and patient satisfaction, given that tattoo removal can require 10-20 sessions, depending on factors such as the age and colors of the tattoo, and that tattoos – and thus tattoo removal – continue to increase in popularity, he said. "For a busy practice or impatient patients like we have in New York, this has been a nice advance," Dr. Geronemus said at the annual meeting of the American Society for Dermatologic Surgery.
The approach builds on the "R20 technique" described earlier this year in a study published in the Journal of the American Academy of Dermatology. R20 involves the use of multiple treatment passes that are made at 20-minute intervals.
Typically, after an initial pass, tiny white bubbles form in the superficial papillary dermis, appearing as a whitening of the skin. Retreatment while these bubbles are present elicits a limited reaction.
The R20 technique was developed when investigators found that the bubbles disappear after 20 minutes, and, thus, tested the technique in a study of 12 adults. The patients were randomized to a single treatment pass with a Q-switched alexandrite laser (5.5 J/cm2, 755 nm, 100-nanosecond pulse duration, 3-mm spot size) or to four passes at 20 minute intervals.
The first treatment caused an immediate whitening reaction, but little or no whitening occurred after subsequent passes at 20-minute intervals. However, at 90-day follow-up, significant improvement was seen in the R20 group, compared with the single-treatment group, and light microscopy demonstrated greater dispersion of tattoo ink with the R20 approach. (J. Am. Acad. Dermatol. 2012;66:271-7).
Despite the increased efficacy using this approach, the time required to complete four passes at 20-minute intervals makes it impractical in the clinical setting, said Dr. Geronemus, a dermatologist in private practice in New York.
"So with this idea in mind, we began to look at a concept that would allow us to re-treat tattoos immediately without waiting 20 minutes," he said, explaining that topical perfluorodecalin helps dissolve the gas seen after the application of the Q-switched laser and speeds the resolution of the whitening.
"Rather than waiting 20 minutes, the gas dissolves almost immediately, allowing you to re-treat, and we’re now re-treating three or four times in a matter of minutes rather than waiting the 80 minutes that the R20 technique would take for a four-time treatment session," he said.
In his experience, results with perfluorodecalin are comparable to those seen with the R20 technique – but with greater convenience for the patient.
His observations were confirmed on optical coherence tomography scanning, which demonstrated that cavitation levels are indeed reduced by the use of perfluorodecalin.
Dr. Geronemus is an investigator for Cutera, Cynosure, Palomar, Solta Medical, and Syneron. He is also on the medical advisory board for Cynosure, Lumenis, Photomedex, Syneron, and Zeltiq. He reported that he is a Zeltiq shareholder.
ATLANTA – Applying the topical fluorocarbon perfluorodecalin prior to Q-switched laser treatment for tattoo removal allows for immediate retreatment of the tattoo, thereby improving results while decreasing overall treatment time, according to Dr. Roy Geronemus.
The findings have important implications for improving outcomes and patient satisfaction, given that tattoo removal can require 10-20 sessions, depending on factors such as the age and colors of the tattoo, and that tattoos – and thus tattoo removal – continue to increase in popularity, he said. "For a busy practice or impatient patients like we have in New York, this has been a nice advance," Dr. Geronemus said at the annual meeting of the American Society for Dermatologic Surgery.
The approach builds on the "R20 technique" described earlier this year in a study published in the Journal of the American Academy of Dermatology. R20 involves the use of multiple treatment passes that are made at 20-minute intervals.
Typically, after an initial pass, tiny white bubbles form in the superficial papillary dermis, appearing as a whitening of the skin. Retreatment while these bubbles are present elicits a limited reaction.
The R20 technique was developed when investigators found that the bubbles disappear after 20 minutes, and, thus, tested the technique in a study of 12 adults. The patients were randomized to a single treatment pass with a Q-switched alexandrite laser (5.5 J/cm2, 755 nm, 100-nanosecond pulse duration, 3-mm spot size) or to four passes at 20 minute intervals.
The first treatment caused an immediate whitening reaction, but little or no whitening occurred after subsequent passes at 20-minute intervals. However, at 90-day follow-up, significant improvement was seen in the R20 group, compared with the single-treatment group, and light microscopy demonstrated greater dispersion of tattoo ink with the R20 approach. (J. Am. Acad. Dermatol. 2012;66:271-7).
Despite the increased efficacy using this approach, the time required to complete four passes at 20-minute intervals makes it impractical in the clinical setting, said Dr. Geronemus, a dermatologist in private practice in New York.
"So with this idea in mind, we began to look at a concept that would allow us to re-treat tattoos immediately without waiting 20 minutes," he said, explaining that topical perfluorodecalin helps dissolve the gas seen after the application of the Q-switched laser and speeds the resolution of the whitening.
"Rather than waiting 20 minutes, the gas dissolves almost immediately, allowing you to re-treat, and we’re now re-treating three or four times in a matter of minutes rather than waiting the 80 minutes that the R20 technique would take for a four-time treatment session," he said.
In his experience, results with perfluorodecalin are comparable to those seen with the R20 technique – but with greater convenience for the patient.
His observations were confirmed on optical coherence tomography scanning, which demonstrated that cavitation levels are indeed reduced by the use of perfluorodecalin.
Dr. Geronemus is an investigator for Cutera, Cynosure, Palomar, Solta Medical, and Syneron. He is also on the medical advisory board for Cynosure, Lumenis, Photomedex, Syneron, and Zeltiq. He reported that he is a Zeltiq shareholder.
ATLANTA – Applying the topical fluorocarbon perfluorodecalin prior to Q-switched laser treatment for tattoo removal allows for immediate retreatment of the tattoo, thereby improving results while decreasing overall treatment time, according to Dr. Roy Geronemus.
The findings have important implications for improving outcomes and patient satisfaction, given that tattoo removal can require 10-20 sessions, depending on factors such as the age and colors of the tattoo, and that tattoos – and thus tattoo removal – continue to increase in popularity, he said. "For a busy practice or impatient patients like we have in New York, this has been a nice advance," Dr. Geronemus said at the annual meeting of the American Society for Dermatologic Surgery.
The approach builds on the "R20 technique" described earlier this year in a study published in the Journal of the American Academy of Dermatology. R20 involves the use of multiple treatment passes that are made at 20-minute intervals.
Typically, after an initial pass, tiny white bubbles form in the superficial papillary dermis, appearing as a whitening of the skin. Retreatment while these bubbles are present elicits a limited reaction.
The R20 technique was developed when investigators found that the bubbles disappear after 20 minutes, and, thus, tested the technique in a study of 12 adults. The patients were randomized to a single treatment pass with a Q-switched alexandrite laser (5.5 J/cm2, 755 nm, 100-nanosecond pulse duration, 3-mm spot size) or to four passes at 20 minute intervals.
The first treatment caused an immediate whitening reaction, but little or no whitening occurred after subsequent passes at 20-minute intervals. However, at 90-day follow-up, significant improvement was seen in the R20 group, compared with the single-treatment group, and light microscopy demonstrated greater dispersion of tattoo ink with the R20 approach. (J. Am. Acad. Dermatol. 2012;66:271-7).
Despite the increased efficacy using this approach, the time required to complete four passes at 20-minute intervals makes it impractical in the clinical setting, said Dr. Geronemus, a dermatologist in private practice in New York.
"So with this idea in mind, we began to look at a concept that would allow us to re-treat tattoos immediately without waiting 20 minutes," he said, explaining that topical perfluorodecalin helps dissolve the gas seen after the application of the Q-switched laser and speeds the resolution of the whitening.
"Rather than waiting 20 minutes, the gas dissolves almost immediately, allowing you to re-treat, and we’re now re-treating three or four times in a matter of minutes rather than waiting the 80 minutes that the R20 technique would take for a four-time treatment session," he said.
In his experience, results with perfluorodecalin are comparable to those seen with the R20 technique – but with greater convenience for the patient.
His observations were confirmed on optical coherence tomography scanning, which demonstrated that cavitation levels are indeed reduced by the use of perfluorodecalin.
Dr. Geronemus is an investigator for Cutera, Cynosure, Palomar, Solta Medical, and Syneron. He is also on the medical advisory board for Cynosure, Lumenis, Photomedex, Syneron, and Zeltiq. He reported that he is a Zeltiq shareholder.
EXPERT ANALYSIS FROM THE ANNUAL MEETING OF THE AMERICAN SOCIETY FOR DERMATOLOGIC SURGERY
Differences in the Stratum Corneum Barrier
Despite a growing worldwide population, there is still limited data on the physiology and structural differences in ethnic skin. Although the increased presence of melanin in skin of color confers a photo-protective effect, there are various differences in the stratum corneum that will influence skin physiology in different racial groups.
Barrier function of the skin depends on the structure of the corneocytes, lipid content, and transepidermal water loss.
Compared to white skin, black skin has more corneocyte layers and a more compact stratum corneum with greater intercellular cohesiveness (Semin. Cutan. Med. Surg. 2009;28:115-29). The epidermal barrier in darker skin has been shown to be stronger when exposed to mechanical or chemical challenge. Although the size of the individual corneocytes is the same in black and white skin, the desquamation rate in certain locations is higher in black skin. This is likely because of increased desquamatory enzyme levels, such as cathepsin L2 in the lamellar granules of darker pigmented individuals, leading to an "ashy" manifestation.
Black skin has the highest sebum content of all ethnicities but also the lowest ceramide level, and is, therefore, the most susceptible to transepidermal water loss and xerosis of the skin, when compared with other ethnic groups.
Asian skin has similar corneocyte architecture and transepidermal water loss when compared to white skin, but has decreased corneocyte cohesion, and, thus, a weaker barrier function when exposed to mechanical and chemical stimuli. Compared to white and black patients, Asian patients have the highest amount of ceramides and the least amount of transepidermal water loss.
Although no large, multiethnic group studies have been performed looking at all of the skin barrier physiologic properties and their relation to clinical signs of disease, several small studies do shed light on some of the ethnic variations in skin barrier function. In clinical practice, these small variations should play a role in ethnic-specific treatment regimens for common conditions, such as acne and atopic dermatitis.
In my practice, black patients with acne often have a high sebum content but cannot tolerate drying medications such as benzoyl peroxide. These patients often present with ashy, dry skin in certain areas and oily acne-prone skin in other areas, leading to more complex skin care regimens. Understanding these concepts can help tailor skin treatments for ethnic patients.
- Lily Talakoub, M.D.
Do you have questions about treating patients with darker skin? If so, send them to [email protected].
Despite a growing worldwide population, there is still limited data on the physiology and structural differences in ethnic skin. Although the increased presence of melanin in skin of color confers a photo-protective effect, there are various differences in the stratum corneum that will influence skin physiology in different racial groups.
Barrier function of the skin depends on the structure of the corneocytes, lipid content, and transepidermal water loss.
Compared to white skin, black skin has more corneocyte layers and a more compact stratum corneum with greater intercellular cohesiveness (Semin. Cutan. Med. Surg. 2009;28:115-29). The epidermal barrier in darker skin has been shown to be stronger when exposed to mechanical or chemical challenge. Although the size of the individual corneocytes is the same in black and white skin, the desquamation rate in certain locations is higher in black skin. This is likely because of increased desquamatory enzyme levels, such as cathepsin L2 in the lamellar granules of darker pigmented individuals, leading to an "ashy" manifestation.
Black skin has the highest sebum content of all ethnicities but also the lowest ceramide level, and is, therefore, the most susceptible to transepidermal water loss and xerosis of the skin, when compared with other ethnic groups.
Asian skin has similar corneocyte architecture and transepidermal water loss when compared to white skin, but has decreased corneocyte cohesion, and, thus, a weaker barrier function when exposed to mechanical and chemical stimuli. Compared to white and black patients, Asian patients have the highest amount of ceramides and the least amount of transepidermal water loss.
Although no large, multiethnic group studies have been performed looking at all of the skin barrier physiologic properties and their relation to clinical signs of disease, several small studies do shed light on some of the ethnic variations in skin barrier function. In clinical practice, these small variations should play a role in ethnic-specific treatment regimens for common conditions, such as acne and atopic dermatitis.
In my practice, black patients with acne often have a high sebum content but cannot tolerate drying medications such as benzoyl peroxide. These patients often present with ashy, dry skin in certain areas and oily acne-prone skin in other areas, leading to more complex skin care regimens. Understanding these concepts can help tailor skin treatments for ethnic patients.
- Lily Talakoub, M.D.
Do you have questions about treating patients with darker skin? If so, send them to [email protected].
Despite a growing worldwide population, there is still limited data on the physiology and structural differences in ethnic skin. Although the increased presence of melanin in skin of color confers a photo-protective effect, there are various differences in the stratum corneum that will influence skin physiology in different racial groups.
Barrier function of the skin depends on the structure of the corneocytes, lipid content, and transepidermal water loss.
Compared to white skin, black skin has more corneocyte layers and a more compact stratum corneum with greater intercellular cohesiveness (Semin. Cutan. Med. Surg. 2009;28:115-29). The epidermal barrier in darker skin has been shown to be stronger when exposed to mechanical or chemical challenge. Although the size of the individual corneocytes is the same in black and white skin, the desquamation rate in certain locations is higher in black skin. This is likely because of increased desquamatory enzyme levels, such as cathepsin L2 in the lamellar granules of darker pigmented individuals, leading to an "ashy" manifestation.
Black skin has the highest sebum content of all ethnicities but also the lowest ceramide level, and is, therefore, the most susceptible to transepidermal water loss and xerosis of the skin, when compared with other ethnic groups.
Asian skin has similar corneocyte architecture and transepidermal water loss when compared to white skin, but has decreased corneocyte cohesion, and, thus, a weaker barrier function when exposed to mechanical and chemical stimuli. Compared to white and black patients, Asian patients have the highest amount of ceramides and the least amount of transepidermal water loss.
Although no large, multiethnic group studies have been performed looking at all of the skin barrier physiologic properties and their relation to clinical signs of disease, several small studies do shed light on some of the ethnic variations in skin barrier function. In clinical practice, these small variations should play a role in ethnic-specific treatment regimens for common conditions, such as acne and atopic dermatitis.
In my practice, black patients with acne often have a high sebum content but cannot tolerate drying medications such as benzoyl peroxide. These patients often present with ashy, dry skin in certain areas and oily acne-prone skin in other areas, leading to more complex skin care regimens. Understanding these concepts can help tailor skin treatments for ethnic patients.
- Lily Talakoub, M.D.
Do you have questions about treating patients with darker skin? If so, send them to [email protected].