User login
No biopsy for 21% of adults with celiac disease
Patients with celiac disease often do not receive a biopsy or nutritional recommendations at diagnosis, according to the findings of a large survey study.
Strikingly, 21% of respondents did not have a confirmatory duodenal biopsy, reported Andrew M. Joelson, MD, of Columbia University Medical Center, New York, and his associates. Gastroenterologists diagnosed 66% of biopsied patients but only 31% of nonbiopsied patients (P less than .001). “Patients require more education about management of celiac disease and referral to gastroenterologists for duodenal biopsy confirmation,” the researchers wrote in the May issue of Clinical Gastroenterology and Hepatology.
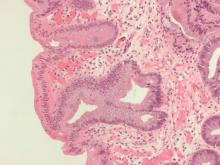
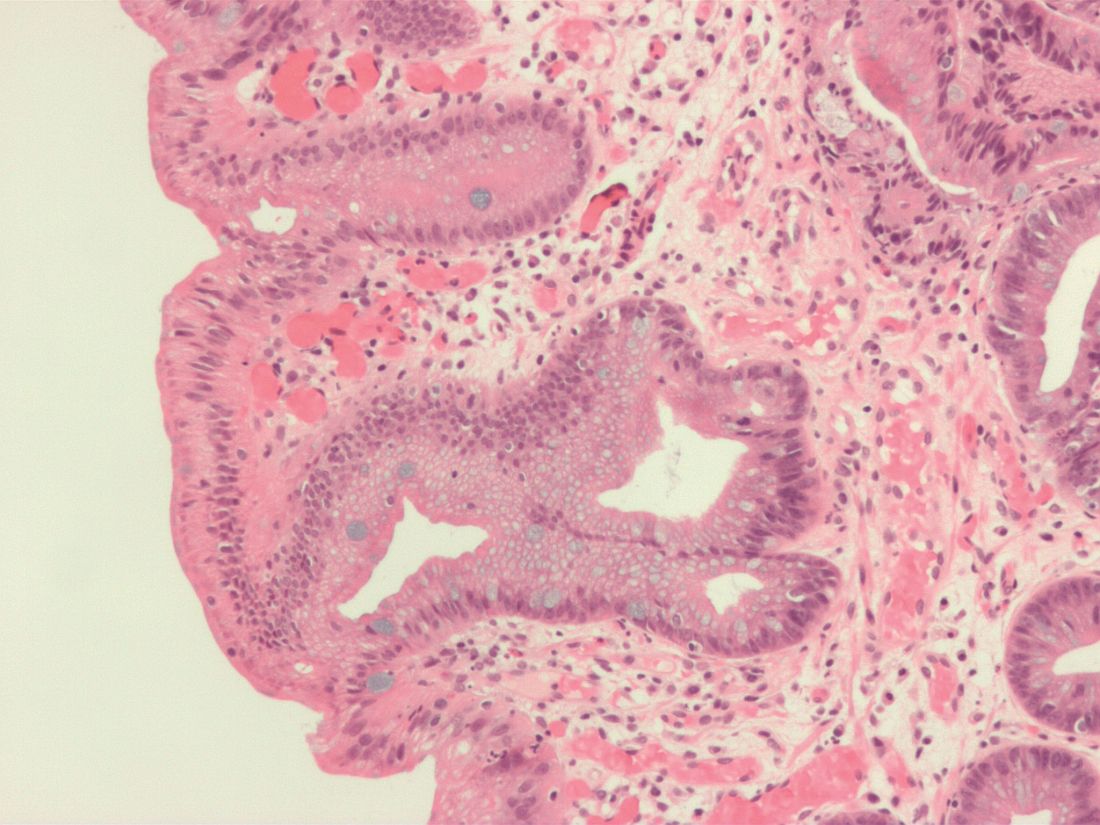
Classic small-bowel findings in celiac disease (intraepithelial lymphocytes, crypt hyperplasia, and villous atrophy) are not pathognomonic, making serology important for diagnosis. European guidelines discuss forgoing biopsy in children whose antitissue transglutaminase antibody titers are at least 10-fold above the upper limit of normal. However, the American College of Gastroenterology and the American Gastroenterological Association continue to recommend combining serology with confirmatory small bowel biopsy. The extent to which physicians follow this advice is unclear, the researchers noted.
Therefore, they analyzed data from a questionnaire posted on the Celiac Disease Foundation website during a 7-month period in 2016. Among 982 adults with self-reported celiac disease, 780 said their diagnosis included both serology and biopsy and 202 said they received serology only. Only 40% of these nonbiopsied respondents said they sought nutritional counseling at diagnosis, compared with 59% of biopsied patients (P less than .001). Patients diagnosed by serology alone also were more likely to report using dietary supplements to aid gluten digestion (20% vs. 9% of biopsied respondents; P less than .001).
These associations remained statistically significant after adjustment for age and sex, said the researchers. Nonbiopsied patients had a significantly lower odds of having been diagnosed by a gastroenterologist (odds ratio, 0.16; 95% confidence interval, 0.07-0.37) and seeking nutritional counseling (OR, 0.45; 95% CI, 0.33-0.63) and were significantly more likely to use digestive supplements (OR, 2.61; 95%, CI 1.62-4.19).
Fully 87% of respondents always followed a strict gluten-free diet, but symptoms persisted in 65% of those who were not biopsied, compared with only 51% of those who were biopsied. There were too few responses to this question for the difference between groups to reach statistical significance, but the finding might reflect the greater diagnostic accuracy of biopsy, the researchers said. However, they cautioned that none of the associations in this study were necessarily causal, diagnoses were not independently validated, and the reliability of self-reported celiac diagnosis remains unclear.
Survey respondents also were self-selected – for example, 91% self-identified as white and 60% reported having a bachelor’s degree, compared with only about 77% and one-third of adults captured by U.S. Census Bureau data from 2017.
“Although these characteristics may limit the generalizability of our findings, this study nevertheless reflects a population of celiac disease that is not typically studied, such as those not attending large academic celiac disease centers, and those diagnosed without the involvement of a gastroenterologist,” the researchers wrote. “Future studies are warranted to further characterize this population regarding the long-term consequences of forgoing the duodenal biopsy, and to develop educational interventions to promote evidence-based diagnosis and management of celiac disease.”
SOURCE: Joelson AM et al. Clin Gastroenterol Hepatol. 2018 Sep 10. doi: 10.1016/j.cgh.2018.09.006.
Self-reported celiac disease diagnosis is not validated and perhaps more inaccurate now with the rise of other gluten-related disorders. Although misdiagnosis is possible, the finding in this study by Joelson et al. that 21% of self-reported celiac adults said they never had a confirmatory biopsy is remarkable. Another important observation is the low-quality celiac care among nonbiopsed adults, with less formal nutritional counseling and high use of gluten digestive supplements and persistent symptoms.
Nowadays, biopsy confirmation may not be necessary for all. There is strong evidence for nonbiopsy diagnosis in selected symptomatic children with high titers of tissue transglutaminase antibodies (more than 10 times the upper limit of normal) and a positive endomysial antibody in a second sample. Whether the nonbiopsy approach could be applicable also in adults remains controversial. Current guidelines recommend biopsy confirmation in all adults. However, emerging evidence favors celiac disease diagnosis without use of biopsy in selected adults.
Although the debate regarding pros and cons of nonbiopsy diagnosis is far from an end, this approach is here to stay. In the future, regardless of the method selected to confirm celiac disease diagnosis, the overall quality of celiac care should be ensured.
Alberto Rubio-Tapia, MD, is an assistant professor of medicine at the Mayo Clinic, Rochester, Minn. He has no conflicts of interest.
Self-reported celiac disease diagnosis is not validated and perhaps more inaccurate now with the rise of other gluten-related disorders. Although misdiagnosis is possible, the finding in this study by Joelson et al. that 21% of self-reported celiac adults said they never had a confirmatory biopsy is remarkable. Another important observation is the low-quality celiac care among nonbiopsed adults, with less formal nutritional counseling and high use of gluten digestive supplements and persistent symptoms.
Nowadays, biopsy confirmation may not be necessary for all. There is strong evidence for nonbiopsy diagnosis in selected symptomatic children with high titers of tissue transglutaminase antibodies (more than 10 times the upper limit of normal) and a positive endomysial antibody in a second sample. Whether the nonbiopsy approach could be applicable also in adults remains controversial. Current guidelines recommend biopsy confirmation in all adults. However, emerging evidence favors celiac disease diagnosis without use of biopsy in selected adults.
Although the debate regarding pros and cons of nonbiopsy diagnosis is far from an end, this approach is here to stay. In the future, regardless of the method selected to confirm celiac disease diagnosis, the overall quality of celiac care should be ensured.
Alberto Rubio-Tapia, MD, is an assistant professor of medicine at the Mayo Clinic, Rochester, Minn. He has no conflicts of interest.
Self-reported celiac disease diagnosis is not validated and perhaps more inaccurate now with the rise of other gluten-related disorders. Although misdiagnosis is possible, the finding in this study by Joelson et al. that 21% of self-reported celiac adults said they never had a confirmatory biopsy is remarkable. Another important observation is the low-quality celiac care among nonbiopsed adults, with less formal nutritional counseling and high use of gluten digestive supplements and persistent symptoms.
Nowadays, biopsy confirmation may not be necessary for all. There is strong evidence for nonbiopsy diagnosis in selected symptomatic children with high titers of tissue transglutaminase antibodies (more than 10 times the upper limit of normal) and a positive endomysial antibody in a second sample. Whether the nonbiopsy approach could be applicable also in adults remains controversial. Current guidelines recommend biopsy confirmation in all adults. However, emerging evidence favors celiac disease diagnosis without use of biopsy in selected adults.
Although the debate regarding pros and cons of nonbiopsy diagnosis is far from an end, this approach is here to stay. In the future, regardless of the method selected to confirm celiac disease diagnosis, the overall quality of celiac care should be ensured.
Alberto Rubio-Tapia, MD, is an assistant professor of medicine at the Mayo Clinic, Rochester, Minn. He has no conflicts of interest.
Patients with celiac disease often do not receive a biopsy or nutritional recommendations at diagnosis, according to the findings of a large survey study.
Strikingly, 21% of respondents did not have a confirmatory duodenal biopsy, reported Andrew M. Joelson, MD, of Columbia University Medical Center, New York, and his associates. Gastroenterologists diagnosed 66% of biopsied patients but only 31% of nonbiopsied patients (P less than .001). “Patients require more education about management of celiac disease and referral to gastroenterologists for duodenal biopsy confirmation,” the researchers wrote in the May issue of Clinical Gastroenterology and Hepatology.
Classic small-bowel findings in celiac disease (intraepithelial lymphocytes, crypt hyperplasia, and villous atrophy) are not pathognomonic, making serology important for diagnosis. European guidelines discuss forgoing biopsy in children whose antitissue transglutaminase antibody titers are at least 10-fold above the upper limit of normal. However, the American College of Gastroenterology and the American Gastroenterological Association continue to recommend combining serology with confirmatory small bowel biopsy. The extent to which physicians follow this advice is unclear, the researchers noted.
Therefore, they analyzed data from a questionnaire posted on the Celiac Disease Foundation website during a 7-month period in 2016. Among 982 adults with self-reported celiac disease, 780 said their diagnosis included both serology and biopsy and 202 said they received serology only. Only 40% of these nonbiopsied respondents said they sought nutritional counseling at diagnosis, compared with 59% of biopsied patients (P less than .001). Patients diagnosed by serology alone also were more likely to report using dietary supplements to aid gluten digestion (20% vs. 9% of biopsied respondents; P less than .001).
These associations remained statistically significant after adjustment for age and sex, said the researchers. Nonbiopsied patients had a significantly lower odds of having been diagnosed by a gastroenterologist (odds ratio, 0.16; 95% confidence interval, 0.07-0.37) and seeking nutritional counseling (OR, 0.45; 95% CI, 0.33-0.63) and were significantly more likely to use digestive supplements (OR, 2.61; 95%, CI 1.62-4.19).
Fully 87% of respondents always followed a strict gluten-free diet, but symptoms persisted in 65% of those who were not biopsied, compared with only 51% of those who were biopsied. There were too few responses to this question for the difference between groups to reach statistical significance, but the finding might reflect the greater diagnostic accuracy of biopsy, the researchers said. However, they cautioned that none of the associations in this study were necessarily causal, diagnoses were not independently validated, and the reliability of self-reported celiac diagnosis remains unclear.
Survey respondents also were self-selected – for example, 91% self-identified as white and 60% reported having a bachelor’s degree, compared with only about 77% and one-third of adults captured by U.S. Census Bureau data from 2017.
“Although these characteristics may limit the generalizability of our findings, this study nevertheless reflects a population of celiac disease that is not typically studied, such as those not attending large academic celiac disease centers, and those diagnosed without the involvement of a gastroenterologist,” the researchers wrote. “Future studies are warranted to further characterize this population regarding the long-term consequences of forgoing the duodenal biopsy, and to develop educational interventions to promote evidence-based diagnosis and management of celiac disease.”
SOURCE: Joelson AM et al. Clin Gastroenterol Hepatol. 2018 Sep 10. doi: 10.1016/j.cgh.2018.09.006.
Patients with celiac disease often do not receive a biopsy or nutritional recommendations at diagnosis, according to the findings of a large survey study.
Strikingly, 21% of respondents did not have a confirmatory duodenal biopsy, reported Andrew M. Joelson, MD, of Columbia University Medical Center, New York, and his associates. Gastroenterologists diagnosed 66% of biopsied patients but only 31% of nonbiopsied patients (P less than .001). “Patients require more education about management of celiac disease and referral to gastroenterologists for duodenal biopsy confirmation,” the researchers wrote in the May issue of Clinical Gastroenterology and Hepatology.
Classic small-bowel findings in celiac disease (intraepithelial lymphocytes, crypt hyperplasia, and villous atrophy) are not pathognomonic, making serology important for diagnosis. European guidelines discuss forgoing biopsy in children whose antitissue transglutaminase antibody titers are at least 10-fold above the upper limit of normal. However, the American College of Gastroenterology and the American Gastroenterological Association continue to recommend combining serology with confirmatory small bowel biopsy. The extent to which physicians follow this advice is unclear, the researchers noted.
Therefore, they analyzed data from a questionnaire posted on the Celiac Disease Foundation website during a 7-month period in 2016. Among 982 adults with self-reported celiac disease, 780 said their diagnosis included both serology and biopsy and 202 said they received serology only. Only 40% of these nonbiopsied respondents said they sought nutritional counseling at diagnosis, compared with 59% of biopsied patients (P less than .001). Patients diagnosed by serology alone also were more likely to report using dietary supplements to aid gluten digestion (20% vs. 9% of biopsied respondents; P less than .001).
These associations remained statistically significant after adjustment for age and sex, said the researchers. Nonbiopsied patients had a significantly lower odds of having been diagnosed by a gastroenterologist (odds ratio, 0.16; 95% confidence interval, 0.07-0.37) and seeking nutritional counseling (OR, 0.45; 95% CI, 0.33-0.63) and were significantly more likely to use digestive supplements (OR, 2.61; 95%, CI 1.62-4.19).
Fully 87% of respondents always followed a strict gluten-free diet, but symptoms persisted in 65% of those who were not biopsied, compared with only 51% of those who were biopsied. There were too few responses to this question for the difference between groups to reach statistical significance, but the finding might reflect the greater diagnostic accuracy of biopsy, the researchers said. However, they cautioned that none of the associations in this study were necessarily causal, diagnoses were not independently validated, and the reliability of self-reported celiac diagnosis remains unclear.
Survey respondents also were self-selected – for example, 91% self-identified as white and 60% reported having a bachelor’s degree, compared with only about 77% and one-third of adults captured by U.S. Census Bureau data from 2017.
“Although these characteristics may limit the generalizability of our findings, this study nevertheless reflects a population of celiac disease that is not typically studied, such as those not attending large academic celiac disease centers, and those diagnosed without the involvement of a gastroenterologist,” the researchers wrote. “Future studies are warranted to further characterize this population regarding the long-term consequences of forgoing the duodenal biopsy, and to develop educational interventions to promote evidence-based diagnosis and management of celiac disease.”
SOURCE: Joelson AM et al. Clin Gastroenterol Hepatol. 2018 Sep 10. doi: 10.1016/j.cgh.2018.09.006.
FROM CLINICAL GASTROENTEROLOGY AND HEPATOLOGY
AGA Clinical Practice Update: Switching between biologics and biosimilars in inflammatory bowel disease
Patients with inflammatory bowel disease (IBD) will soon have access to new biosimilars to infliximab, adalimumab, and other monoclonal antibodies, experts wrote in an American Gastroenterological Association clinical practice update.
“It is anticipated that biosimilars for IBD are here to stay,” wrote Laura E. Raffals, MD, of the Mayo Clinic in Rochester, Minn., and her associates in Clinical Gastroenterology and Hepatology. “Provided that the regulatory pathway remains rigorous and postmarketing surveillance is performed adequately, clinicians and patients can be reassured that these agents will provide the same well-described effectiveness for moderate to severe Crohn’s disease and ulcerative colitis, without new safety concerns.”
Evidence supports the use of biosimilars in IBD, but switching patients in stable remission on infliximab (Remicade) to a biosimilar, namely infliximab-dyyb (Inflectra), should remain a case-by-case choice, according to an AGA clinical practice update. Pending more safety data, the update’s authors recommended against nonmedical switches during pregnancy and urge special attention when considering whether to switch children.
Biologics have revolutionized IBD treatment, but at a steep price. As patents expire, companies have developed biosimilar agents that aim to conserve safety and efficacy at lower cost. Studies support this idea, although whether initiating or switching to biosimilars will save patients (versus hospitals or payers) money “remains to be seen,” the practice update states.
The FDA approval process for biosimilars is more rigorous than that for generics, but it skips the multiple phases of clinical trials required to approve reference biologics. Instead, the FDA requires robust evidence that the biosimilar has comparable structure, function, immunogenicity, animal toxicity, pharmacokinetics and pharmacodynamics, and clinical safety and efficacy in humans. Under U.S. law, a biosimilar cannot be FDA approved if its clinically active components differ from the reference product or it shows clinically meaningful differences in safety, potency, or purity.
So far, five biosimilars have been approved by the FDA for use in IBD, although not all are on the market yet: infliximab-dyyb (Inflectra), adalimumab-atta (Amjevita), infliximab-abda (Renflexis), adalimumab-adbm (Cyltezo), and infliximab-qbtx (Ixifi). Most postmarketing studies of their use involved patients on stable doses of Remicade who switched to biosimilar infliximab-dyyb (Inflectra).
The best known of these studies is the double-blind, randomized NOR-SWITCH trial, in which patients with Crohn’s disease, ulcerative colitis, spondyloarthritis, rheumatoid arthritis, psoriatic arthritis, or chronic plaque psoriasis on Remicade either continued it or switched to biosimilar infliximab-dyyb (Inflectra). At week 52, both safety and the likelihood of worsening disease activity were similar regardless of treatment randomization. The study was not powered to assess subgroup outcomes in Crohn’s disease or ulcerative colitis, the practice update notes.
More recently, the results of the 16-week SECURE trial also indicated that switching to infliximab-dyyb (Inflectra) was safe and well tolerated by patients with remitted IBD. However, the FDA has not yet designated any biosimilar as “interchangeable” with an approved biologic confirmed safe in multiple switches, the practice update notes. As a result, state laws prohibit patients from being switched to a biosimilar without notification. Both the NOR-SWITCH and SECURE trials were done in Europe.
Clinicians also must understand that antidrug antibodies to originator and biosimilar infliximab cross-react with each other, the experts emphasized. Switching patients with antibodies to Remicade or a biosimilar to the other product therefore risks an immediate hypersensitivity reaction, including life-threatening anaphylaxis.
The authors disclosed no external funding sources. One author disclosed ties to AbbVie, Janssen, Pfizer, Merck, Samsung Bioepis, and Amgen. The rest reported having no conflicts of interest.
SOURCE: Raffals LA et al. Clin Gastroenterol Hepatol. 2018 Sep 6. doi: 10.1016/j.cgh.2018.08.064.
Patients with inflammatory bowel disease (IBD) will soon have access to new biosimilars to infliximab, adalimumab, and other monoclonal antibodies, experts wrote in an American Gastroenterological Association clinical practice update.
“It is anticipated that biosimilars for IBD are here to stay,” wrote Laura E. Raffals, MD, of the Mayo Clinic in Rochester, Minn., and her associates in Clinical Gastroenterology and Hepatology. “Provided that the regulatory pathway remains rigorous and postmarketing surveillance is performed adequately, clinicians and patients can be reassured that these agents will provide the same well-described effectiveness for moderate to severe Crohn’s disease and ulcerative colitis, without new safety concerns.”
Evidence supports the use of biosimilars in IBD, but switching patients in stable remission on infliximab (Remicade) to a biosimilar, namely infliximab-dyyb (Inflectra), should remain a case-by-case choice, according to an AGA clinical practice update. Pending more safety data, the update’s authors recommended against nonmedical switches during pregnancy and urge special attention when considering whether to switch children.
Biologics have revolutionized IBD treatment, but at a steep price. As patents expire, companies have developed biosimilar agents that aim to conserve safety and efficacy at lower cost. Studies support this idea, although whether initiating or switching to biosimilars will save patients (versus hospitals or payers) money “remains to be seen,” the practice update states.
The FDA approval process for biosimilars is more rigorous than that for generics, but it skips the multiple phases of clinical trials required to approve reference biologics. Instead, the FDA requires robust evidence that the biosimilar has comparable structure, function, immunogenicity, animal toxicity, pharmacokinetics and pharmacodynamics, and clinical safety and efficacy in humans. Under U.S. law, a biosimilar cannot be FDA approved if its clinically active components differ from the reference product or it shows clinically meaningful differences in safety, potency, or purity.
So far, five biosimilars have been approved by the FDA for use in IBD, although not all are on the market yet: infliximab-dyyb (Inflectra), adalimumab-atta (Amjevita), infliximab-abda (Renflexis), adalimumab-adbm (Cyltezo), and infliximab-qbtx (Ixifi). Most postmarketing studies of their use involved patients on stable doses of Remicade who switched to biosimilar infliximab-dyyb (Inflectra).
The best known of these studies is the double-blind, randomized NOR-SWITCH trial, in which patients with Crohn’s disease, ulcerative colitis, spondyloarthritis, rheumatoid arthritis, psoriatic arthritis, or chronic plaque psoriasis on Remicade either continued it or switched to biosimilar infliximab-dyyb (Inflectra). At week 52, both safety and the likelihood of worsening disease activity were similar regardless of treatment randomization. The study was not powered to assess subgroup outcomes in Crohn’s disease or ulcerative colitis, the practice update notes.
More recently, the results of the 16-week SECURE trial also indicated that switching to infliximab-dyyb (Inflectra) was safe and well tolerated by patients with remitted IBD. However, the FDA has not yet designated any biosimilar as “interchangeable” with an approved biologic confirmed safe in multiple switches, the practice update notes. As a result, state laws prohibit patients from being switched to a biosimilar without notification. Both the NOR-SWITCH and SECURE trials were done in Europe.
Clinicians also must understand that antidrug antibodies to originator and biosimilar infliximab cross-react with each other, the experts emphasized. Switching patients with antibodies to Remicade or a biosimilar to the other product therefore risks an immediate hypersensitivity reaction, including life-threatening anaphylaxis.
The authors disclosed no external funding sources. One author disclosed ties to AbbVie, Janssen, Pfizer, Merck, Samsung Bioepis, and Amgen. The rest reported having no conflicts of interest.
SOURCE: Raffals LA et al. Clin Gastroenterol Hepatol. 2018 Sep 6. doi: 10.1016/j.cgh.2018.08.064.
Patients with inflammatory bowel disease (IBD) will soon have access to new biosimilars to infliximab, adalimumab, and other monoclonal antibodies, experts wrote in an American Gastroenterological Association clinical practice update.
“It is anticipated that biosimilars for IBD are here to stay,” wrote Laura E. Raffals, MD, of the Mayo Clinic in Rochester, Minn., and her associates in Clinical Gastroenterology and Hepatology. “Provided that the regulatory pathway remains rigorous and postmarketing surveillance is performed adequately, clinicians and patients can be reassured that these agents will provide the same well-described effectiveness for moderate to severe Crohn’s disease and ulcerative colitis, without new safety concerns.”
Evidence supports the use of biosimilars in IBD, but switching patients in stable remission on infliximab (Remicade) to a biosimilar, namely infliximab-dyyb (Inflectra), should remain a case-by-case choice, according to an AGA clinical practice update. Pending more safety data, the update’s authors recommended against nonmedical switches during pregnancy and urge special attention when considering whether to switch children.
Biologics have revolutionized IBD treatment, but at a steep price. As patents expire, companies have developed biosimilar agents that aim to conserve safety and efficacy at lower cost. Studies support this idea, although whether initiating or switching to biosimilars will save patients (versus hospitals or payers) money “remains to be seen,” the practice update states.
The FDA approval process for biosimilars is more rigorous than that for generics, but it skips the multiple phases of clinical trials required to approve reference biologics. Instead, the FDA requires robust evidence that the biosimilar has comparable structure, function, immunogenicity, animal toxicity, pharmacokinetics and pharmacodynamics, and clinical safety and efficacy in humans. Under U.S. law, a biosimilar cannot be FDA approved if its clinically active components differ from the reference product or it shows clinically meaningful differences in safety, potency, or purity.
So far, five biosimilars have been approved by the FDA for use in IBD, although not all are on the market yet: infliximab-dyyb (Inflectra), adalimumab-atta (Amjevita), infliximab-abda (Renflexis), adalimumab-adbm (Cyltezo), and infliximab-qbtx (Ixifi). Most postmarketing studies of their use involved patients on stable doses of Remicade who switched to biosimilar infliximab-dyyb (Inflectra).
The best known of these studies is the double-blind, randomized NOR-SWITCH trial, in which patients with Crohn’s disease, ulcerative colitis, spondyloarthritis, rheumatoid arthritis, psoriatic arthritis, or chronic plaque psoriasis on Remicade either continued it or switched to biosimilar infliximab-dyyb (Inflectra). At week 52, both safety and the likelihood of worsening disease activity were similar regardless of treatment randomization. The study was not powered to assess subgroup outcomes in Crohn’s disease or ulcerative colitis, the practice update notes.
More recently, the results of the 16-week SECURE trial also indicated that switching to infliximab-dyyb (Inflectra) was safe and well tolerated by patients with remitted IBD. However, the FDA has not yet designated any biosimilar as “interchangeable” with an approved biologic confirmed safe in multiple switches, the practice update notes. As a result, state laws prohibit patients from being switched to a biosimilar without notification. Both the NOR-SWITCH and SECURE trials were done in Europe.
Clinicians also must understand that antidrug antibodies to originator and biosimilar infliximab cross-react with each other, the experts emphasized. Switching patients with antibodies to Remicade or a biosimilar to the other product therefore risks an immediate hypersensitivity reaction, including life-threatening anaphylaxis.
The authors disclosed no external funding sources. One author disclosed ties to AbbVie, Janssen, Pfizer, Merck, Samsung Bioepis, and Amgen. The rest reported having no conflicts of interest.
SOURCE: Raffals LA et al. Clin Gastroenterol Hepatol. 2018 Sep 6. doi: 10.1016/j.cgh.2018.08.064.
FROM CLINICAL GASTROENTEROLOGY AND HEPATOLOGY
Study eyes biomarkers of regorafenib response in hepatocellular carcinoma
.
“In the absence of established or predefined biomarkers for regorafenib, we performed a broad exploratory biomarker analyses at the DNA, RNA, and protein level that represents a much more comprehensive approach than previous studies of regorafenib or sorafenib,” wrote Michael Teufel, PhD, of Bayer Healthcare Pharmaceuticals in Whippany, N.J., and his associates. The preplanned, retrospective analysis of data from the phase 3 RESOURCE trial was reported in Gastroenterology.
The randomized trial included 567 patients whose hepatocellular carcinoma had progressed on sorafenib. Regorafenib significantly outperformed placebo with regard to overall survival (OS). Dr. Teufel and his associates performed next-generation sequencing on 17 archived tumor samples containing sufficient tissue (all from regorafenib recipients). They also performed immune profiling on 46 tumor samples (32 from regorafenib recipients and 14 from placebo recipients), protein analysis on 499 plasma samples (332 from regorafenib recipients and 167 from placebo recipients), and microRNA analysis on 343 plasma samples (234 regorafenib recipients and 109 placebo recipients).
Among 266 proteins tested, decreased levels of 5 proteins correlated with significantly longer OS on regorafenib therapy. These proteins are involved in inflammation or hepatocellular carcinogenesis, the researchers noted. Importantly, none were associated with survival independent of treatment. These five proteins included angiopoietin 1 (hazard ratio for OS, 0.53; 95% confidence interval, 0.38-0.73), cystatin B (hazard ratio, 0.47; 95% CI, 0.34-0.64); the latency-associated peptide of transforming growth factor beta (HR, 0.46; 95% CI, 0.33-0.64), oxidized low-density lipoprotein receptor 1 (HR, 0.54; 95% CI, 0.41-0.72), and C-C motif chemokine ligand 3 (HR, 0.54; 95% CI, 0.39-0.74).
Additionally, baseline concentrations of 47 of the 266 proteins correlated with a time to progression (TPP) benefit on regorafenib therapy (adjusted P less than or equal to .05 for each). The 47 proteins included all 5 that predicted an OS benefit. All but two proteins (calbindin and gelsolin) showed the same directional effect as for OS (that is, low expression predicted response).
Nine plasma microRNA’s levels correlated with improved OS on regorafenib (adjusted P less than or equal to .05): MIR30A, MIR122, MIR125B, MIR200A, MIR374B, MIR15B, MIR107, MIR320, and MIR645. Notably, expression was linked to longer OS specifically among patients with the Hoshida S3 subtype of hepatocellular carcinoma. Next-generation sequencing of tumor samples also identified 49 variants in 27 oncogenes or tumor-suppressor genes. Mutations in CTNNB1 were found in 3 of 10 patients who progressed on regorafenib, and VEGFA amplification was found in 1 of 7 regorafenib responders.
“Thus far, rational biomarker selection has been unsuccessful in identifying predictive markers for regorafenib in colorectal cancer and gastrointestinal stromal tumors,” the researchers commented. “The broader approach used in this study is not only biologically warranted considering the heterogeneity of hepatocellular carcinoma tumors, but is also needed due to the multiple targets and pathways affected by MKIs such as regorafenib. Levels of these circulating biomarkers and genetic features of tumors might be used to identify patients with hepatocellular carcinoma most likely to respond to regorafenib.”
Bayer funded the study, provided the study drug, and was involved in all aspects of the study. Dr. Teufel and three coinvestigators are Bayer employees. Dr. Teufel and two coinvestigators own stock in Bayer. Three other coinvestigators disclosed ties to Bayer and other pharmaceutical companies.
SOURCE: Teufel M et al. Gastroenterology. 2019 Jan 30. doi: 10.1053/j.gastro.2019.01.261.
.
“In the absence of established or predefined biomarkers for regorafenib, we performed a broad exploratory biomarker analyses at the DNA, RNA, and protein level that represents a much more comprehensive approach than previous studies of regorafenib or sorafenib,” wrote Michael Teufel, PhD, of Bayer Healthcare Pharmaceuticals in Whippany, N.J., and his associates. The preplanned, retrospective analysis of data from the phase 3 RESOURCE trial was reported in Gastroenterology.
The randomized trial included 567 patients whose hepatocellular carcinoma had progressed on sorafenib. Regorafenib significantly outperformed placebo with regard to overall survival (OS). Dr. Teufel and his associates performed next-generation sequencing on 17 archived tumor samples containing sufficient tissue (all from regorafenib recipients). They also performed immune profiling on 46 tumor samples (32 from regorafenib recipients and 14 from placebo recipients), protein analysis on 499 plasma samples (332 from regorafenib recipients and 167 from placebo recipients), and microRNA analysis on 343 plasma samples (234 regorafenib recipients and 109 placebo recipients).
Among 266 proteins tested, decreased levels of 5 proteins correlated with significantly longer OS on regorafenib therapy. These proteins are involved in inflammation or hepatocellular carcinogenesis, the researchers noted. Importantly, none were associated with survival independent of treatment. These five proteins included angiopoietin 1 (hazard ratio for OS, 0.53; 95% confidence interval, 0.38-0.73), cystatin B (hazard ratio, 0.47; 95% CI, 0.34-0.64); the latency-associated peptide of transforming growth factor beta (HR, 0.46; 95% CI, 0.33-0.64), oxidized low-density lipoprotein receptor 1 (HR, 0.54; 95% CI, 0.41-0.72), and C-C motif chemokine ligand 3 (HR, 0.54; 95% CI, 0.39-0.74).
Additionally, baseline concentrations of 47 of the 266 proteins correlated with a time to progression (TPP) benefit on regorafenib therapy (adjusted P less than or equal to .05 for each). The 47 proteins included all 5 that predicted an OS benefit. All but two proteins (calbindin and gelsolin) showed the same directional effect as for OS (that is, low expression predicted response).
Nine plasma microRNA’s levels correlated with improved OS on regorafenib (adjusted P less than or equal to .05): MIR30A, MIR122, MIR125B, MIR200A, MIR374B, MIR15B, MIR107, MIR320, and MIR645. Notably, expression was linked to longer OS specifically among patients with the Hoshida S3 subtype of hepatocellular carcinoma. Next-generation sequencing of tumor samples also identified 49 variants in 27 oncogenes or tumor-suppressor genes. Mutations in CTNNB1 were found in 3 of 10 patients who progressed on regorafenib, and VEGFA amplification was found in 1 of 7 regorafenib responders.
“Thus far, rational biomarker selection has been unsuccessful in identifying predictive markers for regorafenib in colorectal cancer and gastrointestinal stromal tumors,” the researchers commented. “The broader approach used in this study is not only biologically warranted considering the heterogeneity of hepatocellular carcinoma tumors, but is also needed due to the multiple targets and pathways affected by MKIs such as regorafenib. Levels of these circulating biomarkers and genetic features of tumors might be used to identify patients with hepatocellular carcinoma most likely to respond to regorafenib.”
Bayer funded the study, provided the study drug, and was involved in all aspects of the study. Dr. Teufel and three coinvestigators are Bayer employees. Dr. Teufel and two coinvestigators own stock in Bayer. Three other coinvestigators disclosed ties to Bayer and other pharmaceutical companies.
SOURCE: Teufel M et al. Gastroenterology. 2019 Jan 30. doi: 10.1053/j.gastro.2019.01.261.
.
“In the absence of established or predefined biomarkers for regorafenib, we performed a broad exploratory biomarker analyses at the DNA, RNA, and protein level that represents a much more comprehensive approach than previous studies of regorafenib or sorafenib,” wrote Michael Teufel, PhD, of Bayer Healthcare Pharmaceuticals in Whippany, N.J., and his associates. The preplanned, retrospective analysis of data from the phase 3 RESOURCE trial was reported in Gastroenterology.
The randomized trial included 567 patients whose hepatocellular carcinoma had progressed on sorafenib. Regorafenib significantly outperformed placebo with regard to overall survival (OS). Dr. Teufel and his associates performed next-generation sequencing on 17 archived tumor samples containing sufficient tissue (all from regorafenib recipients). They also performed immune profiling on 46 tumor samples (32 from regorafenib recipients and 14 from placebo recipients), protein analysis on 499 plasma samples (332 from regorafenib recipients and 167 from placebo recipients), and microRNA analysis on 343 plasma samples (234 regorafenib recipients and 109 placebo recipients).
Among 266 proteins tested, decreased levels of 5 proteins correlated with significantly longer OS on regorafenib therapy. These proteins are involved in inflammation or hepatocellular carcinogenesis, the researchers noted. Importantly, none were associated with survival independent of treatment. These five proteins included angiopoietin 1 (hazard ratio for OS, 0.53; 95% confidence interval, 0.38-0.73), cystatin B (hazard ratio, 0.47; 95% CI, 0.34-0.64); the latency-associated peptide of transforming growth factor beta (HR, 0.46; 95% CI, 0.33-0.64), oxidized low-density lipoprotein receptor 1 (HR, 0.54; 95% CI, 0.41-0.72), and C-C motif chemokine ligand 3 (HR, 0.54; 95% CI, 0.39-0.74).
Additionally, baseline concentrations of 47 of the 266 proteins correlated with a time to progression (TPP) benefit on regorafenib therapy (adjusted P less than or equal to .05 for each). The 47 proteins included all 5 that predicted an OS benefit. All but two proteins (calbindin and gelsolin) showed the same directional effect as for OS (that is, low expression predicted response).
Nine plasma microRNA’s levels correlated with improved OS on regorafenib (adjusted P less than or equal to .05): MIR30A, MIR122, MIR125B, MIR200A, MIR374B, MIR15B, MIR107, MIR320, and MIR645. Notably, expression was linked to longer OS specifically among patients with the Hoshida S3 subtype of hepatocellular carcinoma. Next-generation sequencing of tumor samples also identified 49 variants in 27 oncogenes or tumor-suppressor genes. Mutations in CTNNB1 were found in 3 of 10 patients who progressed on regorafenib, and VEGFA amplification was found in 1 of 7 regorafenib responders.
“Thus far, rational biomarker selection has been unsuccessful in identifying predictive markers for regorafenib in colorectal cancer and gastrointestinal stromal tumors,” the researchers commented. “The broader approach used in this study is not only biologically warranted considering the heterogeneity of hepatocellular carcinoma tumors, but is also needed due to the multiple targets and pathways affected by MKIs such as regorafenib. Levels of these circulating biomarkers and genetic features of tumors might be used to identify patients with hepatocellular carcinoma most likely to respond to regorafenib.”
Bayer funded the study, provided the study drug, and was involved in all aspects of the study. Dr. Teufel and three coinvestigators are Bayer employees. Dr. Teufel and two coinvestigators own stock in Bayer. Three other coinvestigators disclosed ties to Bayer and other pharmaceutical companies.
SOURCE: Teufel M et al. Gastroenterology. 2019 Jan 30. doi: 10.1053/j.gastro.2019.01.261.
FROM GASTROENTEROLOGY
Mucosal impedance contour rapidly distinguished GERD, non-GERD, and eosinophilic esophagitis
.
Source: American Gastroenterological Association
Each group showed a significantly different (P less than .01) pattern of mucosal impedance (MI), or disruption of mucosal integrity, along the esophageal axis, wrote Dhyanesh A. Patel, MD, of Vanderbilt University Medical Center in Nashville, Tenn., and his associates. Patients without GERD had higher MI values along all esophageal segments, while GERD was characterized by below-normal values in the distal esophagus only, and eosinophilic esophagitis led to low values throughout the esophagus.
The findings were validated in a separate patient cohort, and the only reported adverse event was an episode of mild chest pain. “This contour heatmap could easily be employed to establish a diagnosis during endoscopy, independent of biopsy or pH monitoring,” the investigators wrote in Gastroenterology. They cautioned that the balloon catheter cannot be safely used in patients with severe fibrostenotic disease.
Current definitive diagnostics for GERD leave much to be desired. Transnasal probes are imprecise and uncomfortable, and they can be insensitive if discomfort causes patients to vary normal activity or skip meals. Wireless ambulatory pH monitoring is more tolerable but unreliable and measures only acidity of refluxed material at a single point along the esophagus. These tests also “fail to account for day-to-day variability of reflux, as they only provide a 24- to 48-hour snapshot of a disease process that is chronic in nature,” the researchers wrote. Eosinophilic esophagitis is becoming more common and usually requires proximal and distal biopsies for diagnosis.
Mucosal impedance contour pattern testing is based on the fact that both GERD and eosinophilic esophagitis involve increased distance between esophageal epithelial cells. The amount of intercellular dilatation correlates inversely with MI values. In proof-of-concept studies, individuals with GERD, non-GERD, eosinophilic esophagitis, and achalasia had distinct MI patterns. However, these studies tested a single-channel catheter system that took only point measurements and was subject to interoperator variability. To improve on this concept, Dr. Patel and his associates mounted radial and axial sensors on a balloon catheter to measure MI at 180-degree intervals along a 10-cm esophageal segment.
They tested the new device prospectively in 69 patients undergoing esophagogastroduodenoscopy with or without pH monitoring (which was used as the standard). In all, 24 patients had GERD, 21 had eosinophilic esophagitis, and 24 had normal findings. By using the intercept and slope of the balloon MI measurements, the researchers detected GERD with an area under the receiver operating characteristic curve (AUC) of 0.67, eosinophilic esophagitis with an AUC of 0.84, and non-GERD with an AUC of 0.83.
These findings held up in a separate validation cohort of 36 patients (28 with GERD and eight with eosinophilic esophagitis) from three tertiary care centers. The probability of eosinophilic esophagitis was highest in patients with low distal MI values (that is, a low intercept) and a low slope (showing that MI values remained low proximally). A low distal MI intercept with a steeper positive slope suggested GERD, while a higher distal MI intercept with a steep slope signified non-GERD.
The system “potentially obviates the need for 24- to 48-hour ambulatory wireless pH monitoring or esophageal biopsies for histopathology,” the researchers concluded. “This can help reduce diagnostic and treatment latency and might allow for monitoring disease activity over time.”
The National Institutes of Health funded the external validation analysis. Diversatek Healthcare, which patented the device together with Vanderbilt University, gave research funding to four coinvestigators, including the senior author. Dr. Patel and the other five coinvestigators reported having no conflicts of interest.
SOURCE: Patel DA et al. Gastroenterology. 2019 Jan 31. doi: 10.1053/j.gastro.2019.01.253.
Evaluating esophageal disorders such as GERD or eosinophilic esophagitis can be time consuming for patients in clinical practice and requires multiple visits to complete testing and obtain results. Other than visualizing complications of reflux such as erosive esophagitis or Barrett’s esophagus, there has been no immediate option to diagnose GERD in standard practice during routine endoscopy. Furthermore, the decision to pursue long-term medication or surgery for GERD relies on a brief pH assessment to be truly representative of a patient’s everyday symptoms. Follow-up of eosinophilic esophagitis requires repeated upper endoscopies with biopsies after every incremental change in medication or diet, which unsurprisingly, can reduce compliance with ongoing management for what is often a readily treatable condition.
Both GERD and eosinophilic esophagitis can be characterized by changes in esophageal mucosal impedance. Rather than directly measuring the pH or eosinophil counts, Dr. Patel and associates prospectively validated the diagnostic test performance of an add-on endoscopic mucosal impedance device that might enable the gastroenterologist to rule out GERD or rule in eosinophilic esophagitis during the index endoscopy with reasonable accuracy (AUC above 0.8 to rule out GERD or rule in eosinophilic esophagitis) while adding 2-3 minutes of procedure time. One patient was admitted for chest pain after use of the device but was discharged without complication, and the authors caution against use in severe fibrostenotic disease.
While work to refine a clinical prediction model with this technology is ongoing, the promise of diagnosing and following common esophageal conditions of GERD and eosinophilic esophagitis during endoscopy would have clear value in expediting care and enhancing compliance with treatment.
Eric D. Shah, MD, MBA, is assistant professor of medicine, director of gastrointestinal motility, esophageal, and swallowing disorders center, Geisel School of Medicine, Dartmouth College, Hanover, N.H. He has no disclosures.
Evaluating esophageal disorders such as GERD or eosinophilic esophagitis can be time consuming for patients in clinical practice and requires multiple visits to complete testing and obtain results. Other than visualizing complications of reflux such as erosive esophagitis or Barrett’s esophagus, there has been no immediate option to diagnose GERD in standard practice during routine endoscopy. Furthermore, the decision to pursue long-term medication or surgery for GERD relies on a brief pH assessment to be truly representative of a patient’s everyday symptoms. Follow-up of eosinophilic esophagitis requires repeated upper endoscopies with biopsies after every incremental change in medication or diet, which unsurprisingly, can reduce compliance with ongoing management for what is often a readily treatable condition.
Both GERD and eosinophilic esophagitis can be characterized by changes in esophageal mucosal impedance. Rather than directly measuring the pH or eosinophil counts, Dr. Patel and associates prospectively validated the diagnostic test performance of an add-on endoscopic mucosal impedance device that might enable the gastroenterologist to rule out GERD or rule in eosinophilic esophagitis during the index endoscopy with reasonable accuracy (AUC above 0.8 to rule out GERD or rule in eosinophilic esophagitis) while adding 2-3 minutes of procedure time. One patient was admitted for chest pain after use of the device but was discharged without complication, and the authors caution against use in severe fibrostenotic disease.
While work to refine a clinical prediction model with this technology is ongoing, the promise of diagnosing and following common esophageal conditions of GERD and eosinophilic esophagitis during endoscopy would have clear value in expediting care and enhancing compliance with treatment.
Eric D. Shah, MD, MBA, is assistant professor of medicine, director of gastrointestinal motility, esophageal, and swallowing disorders center, Geisel School of Medicine, Dartmouth College, Hanover, N.H. He has no disclosures.
Evaluating esophageal disorders such as GERD or eosinophilic esophagitis can be time consuming for patients in clinical practice and requires multiple visits to complete testing and obtain results. Other than visualizing complications of reflux such as erosive esophagitis or Barrett’s esophagus, there has been no immediate option to diagnose GERD in standard practice during routine endoscopy. Furthermore, the decision to pursue long-term medication or surgery for GERD relies on a brief pH assessment to be truly representative of a patient’s everyday symptoms. Follow-up of eosinophilic esophagitis requires repeated upper endoscopies with biopsies after every incremental change in medication or diet, which unsurprisingly, can reduce compliance with ongoing management for what is often a readily treatable condition.
Both GERD and eosinophilic esophagitis can be characterized by changes in esophageal mucosal impedance. Rather than directly measuring the pH or eosinophil counts, Dr. Patel and associates prospectively validated the diagnostic test performance of an add-on endoscopic mucosal impedance device that might enable the gastroenterologist to rule out GERD or rule in eosinophilic esophagitis during the index endoscopy with reasonable accuracy (AUC above 0.8 to rule out GERD or rule in eosinophilic esophagitis) while adding 2-3 minutes of procedure time. One patient was admitted for chest pain after use of the device but was discharged without complication, and the authors caution against use in severe fibrostenotic disease.
While work to refine a clinical prediction model with this technology is ongoing, the promise of diagnosing and following common esophageal conditions of GERD and eosinophilic esophagitis during endoscopy would have clear value in expediting care and enhancing compliance with treatment.
Eric D. Shah, MD, MBA, is assistant professor of medicine, director of gastrointestinal motility, esophageal, and swallowing disorders center, Geisel School of Medicine, Dartmouth College, Hanover, N.H. He has no disclosures.
.
Source: American Gastroenterological Association
Each group showed a significantly different (P less than .01) pattern of mucosal impedance (MI), or disruption of mucosal integrity, along the esophageal axis, wrote Dhyanesh A. Patel, MD, of Vanderbilt University Medical Center in Nashville, Tenn., and his associates. Patients without GERD had higher MI values along all esophageal segments, while GERD was characterized by below-normal values in the distal esophagus only, and eosinophilic esophagitis led to low values throughout the esophagus.
The findings were validated in a separate patient cohort, and the only reported adverse event was an episode of mild chest pain. “This contour heatmap could easily be employed to establish a diagnosis during endoscopy, independent of biopsy or pH monitoring,” the investigators wrote in Gastroenterology. They cautioned that the balloon catheter cannot be safely used in patients with severe fibrostenotic disease.
Current definitive diagnostics for GERD leave much to be desired. Transnasal probes are imprecise and uncomfortable, and they can be insensitive if discomfort causes patients to vary normal activity or skip meals. Wireless ambulatory pH monitoring is more tolerable but unreliable and measures only acidity of refluxed material at a single point along the esophagus. These tests also “fail to account for day-to-day variability of reflux, as they only provide a 24- to 48-hour snapshot of a disease process that is chronic in nature,” the researchers wrote. Eosinophilic esophagitis is becoming more common and usually requires proximal and distal biopsies for diagnosis.
Mucosal impedance contour pattern testing is based on the fact that both GERD and eosinophilic esophagitis involve increased distance between esophageal epithelial cells. The amount of intercellular dilatation correlates inversely with MI values. In proof-of-concept studies, individuals with GERD, non-GERD, eosinophilic esophagitis, and achalasia had distinct MI patterns. However, these studies tested a single-channel catheter system that took only point measurements and was subject to interoperator variability. To improve on this concept, Dr. Patel and his associates mounted radial and axial sensors on a balloon catheter to measure MI at 180-degree intervals along a 10-cm esophageal segment.
They tested the new device prospectively in 69 patients undergoing esophagogastroduodenoscopy with or without pH monitoring (which was used as the standard). In all, 24 patients had GERD, 21 had eosinophilic esophagitis, and 24 had normal findings. By using the intercept and slope of the balloon MI measurements, the researchers detected GERD with an area under the receiver operating characteristic curve (AUC) of 0.67, eosinophilic esophagitis with an AUC of 0.84, and non-GERD with an AUC of 0.83.
These findings held up in a separate validation cohort of 36 patients (28 with GERD and eight with eosinophilic esophagitis) from three tertiary care centers. The probability of eosinophilic esophagitis was highest in patients with low distal MI values (that is, a low intercept) and a low slope (showing that MI values remained low proximally). A low distal MI intercept with a steeper positive slope suggested GERD, while a higher distal MI intercept with a steep slope signified non-GERD.
The system “potentially obviates the need for 24- to 48-hour ambulatory wireless pH monitoring or esophageal biopsies for histopathology,” the researchers concluded. “This can help reduce diagnostic and treatment latency and might allow for monitoring disease activity over time.”
The National Institutes of Health funded the external validation analysis. Diversatek Healthcare, which patented the device together with Vanderbilt University, gave research funding to four coinvestigators, including the senior author. Dr. Patel and the other five coinvestigators reported having no conflicts of interest.
SOURCE: Patel DA et al. Gastroenterology. 2019 Jan 31. doi: 10.1053/j.gastro.2019.01.253.
.
Source: American Gastroenterological Association
Each group showed a significantly different (P less than .01) pattern of mucosal impedance (MI), or disruption of mucosal integrity, along the esophageal axis, wrote Dhyanesh A. Patel, MD, of Vanderbilt University Medical Center in Nashville, Tenn., and his associates. Patients without GERD had higher MI values along all esophageal segments, while GERD was characterized by below-normal values in the distal esophagus only, and eosinophilic esophagitis led to low values throughout the esophagus.
The findings were validated in a separate patient cohort, and the only reported adverse event was an episode of mild chest pain. “This contour heatmap could easily be employed to establish a diagnosis during endoscopy, independent of biopsy or pH monitoring,” the investigators wrote in Gastroenterology. They cautioned that the balloon catheter cannot be safely used in patients with severe fibrostenotic disease.
Current definitive diagnostics for GERD leave much to be desired. Transnasal probes are imprecise and uncomfortable, and they can be insensitive if discomfort causes patients to vary normal activity or skip meals. Wireless ambulatory pH monitoring is more tolerable but unreliable and measures only acidity of refluxed material at a single point along the esophagus. These tests also “fail to account for day-to-day variability of reflux, as they only provide a 24- to 48-hour snapshot of a disease process that is chronic in nature,” the researchers wrote. Eosinophilic esophagitis is becoming more common and usually requires proximal and distal biopsies for diagnosis.
Mucosal impedance contour pattern testing is based on the fact that both GERD and eosinophilic esophagitis involve increased distance between esophageal epithelial cells. The amount of intercellular dilatation correlates inversely with MI values. In proof-of-concept studies, individuals with GERD, non-GERD, eosinophilic esophagitis, and achalasia had distinct MI patterns. However, these studies tested a single-channel catheter system that took only point measurements and was subject to interoperator variability. To improve on this concept, Dr. Patel and his associates mounted radial and axial sensors on a balloon catheter to measure MI at 180-degree intervals along a 10-cm esophageal segment.
They tested the new device prospectively in 69 patients undergoing esophagogastroduodenoscopy with or without pH monitoring (which was used as the standard). In all, 24 patients had GERD, 21 had eosinophilic esophagitis, and 24 had normal findings. By using the intercept and slope of the balloon MI measurements, the researchers detected GERD with an area under the receiver operating characteristic curve (AUC) of 0.67, eosinophilic esophagitis with an AUC of 0.84, and non-GERD with an AUC of 0.83.
These findings held up in a separate validation cohort of 36 patients (28 with GERD and eight with eosinophilic esophagitis) from three tertiary care centers. The probability of eosinophilic esophagitis was highest in patients with low distal MI values (that is, a low intercept) and a low slope (showing that MI values remained low proximally). A low distal MI intercept with a steeper positive slope suggested GERD, while a higher distal MI intercept with a steep slope signified non-GERD.
The system “potentially obviates the need for 24- to 48-hour ambulatory wireless pH monitoring or esophageal biopsies for histopathology,” the researchers concluded. “This can help reduce diagnostic and treatment latency and might allow for monitoring disease activity over time.”
The National Institutes of Health funded the external validation analysis. Diversatek Healthcare, which patented the device together with Vanderbilt University, gave research funding to four coinvestigators, including the senior author. Dr. Patel and the other five coinvestigators reported having no conflicts of interest.
SOURCE: Patel DA et al. Gastroenterology. 2019 Jan 31. doi: 10.1053/j.gastro.2019.01.253.
FROM GASTROENTEROLOGY
One-time, universal hepatitis C testing cost effective, researchers say
Universal one-time screening for hepatitis C virus infection is cost effective, compared with birth cohort screening alone, according to the results of a study published in Clinical Gastroenterology and Hepatology.
The Centers for Disease Control and Prevention and the U.S. Preventive Services Task Force recommend testing all individuals born between 1945 and 1965 in addition to injection drug users and other high-risk individuals. But so-called birth cohort screening does not reflect the recent spike in hepatitis C virus (HCV) cases among younger persons in the United States, nor the current recommendation to treat nearly all chronic HCV cases, wrote Mark H. Eckman, MD, of the University of Cincinnati, and his associates.
Using a computer program called Decision Maker, they modeled the cost-effectiveness of universal one-time testing, birth cohort screening, and no screening based on quality-adjusted life-years (QALYS) and 2017 U.S. dollars. They assumed that all HCV-infected patients were treatment naive, treatment eligible, and asymptomatic (for example, had no decompensated cirrhosis). They used efficacy data from the ASTRAL trials of sofosbuvir-velpatasvir as well as the ENDURANCE, SURVEYOR, and EXPEDITION trials of glecaprevir-pibrentasvir. In the model, patients who did not achieve a sustained viral response to treatment went on to complete a 12-week triple direct-acting antiviral (DAA) regimen (sofosbuvir, velpatasvir, and voxilaprevir).
Based on these assumptions, universal one-time screening and treatment of infected individuals cost less than $50,000 per QALY gained, making it highly cost effective, compared with no screening, the investigators wrote. Universal screening also was highly cost effective when compared with birth cohort screening, costing $11,378 for each QALY gained.
“Analyses performed during the era of first-generation DAAs and interferon-based treatment regimens found birth-cohort screening to be ‘cost effective,’ ” the researchers wrote. “However, the availability of a new generation of highly effective, non–interferon-based oral regimens, with fewer side effects and shorter treatment courses, has altered the dynamic around the question of screening.” They pointed to another recent study in which universal one-time HCV testing was more cost effective than birth cohort screening.
Such findings have spurred experts to revisit guidelines on HCV screening, but universal testing is controversial when some states, counties, and communities have a low HCV prevalence. In the model, universal one-time HCV screening was cost effective (less than $50,000 per QALY gained), compared with birth cohort screening as long as prevalence exceeded 0.07% among adults not born between 1945 and 1965. The current prevalence estimate in this group is 0.29%, which is probably low because it does not account for the rising incidence among younger adults, the researchers wrote. In an ideal world, all clinics and hospitals would implement an HCV testing program, but in the real world of scarce resources, “data regarding the cost-effectiveness threshold can guide local policy decisions by directing testing services to settings in which they generate sufficient benefit for the cost.”
Partial funding came from the National Foundation for the Centers for Disease Control and Prevention (CDC Foundation), with funding provided through multiple donors to the CDC Foundation’s Viral Hepatitis Action Coalition. Dr. Eckman reported grant support from Merck and one coinvestigator reported ties to AbbVie, Gilead, Merck, and several other pharmaceutical companies.
SOURCE: Eckman MH et al. Clin Gastroenterol Hepatol. 2018 Sep 7. doi: 10.1016/j.cgh.2018.08.080.
Universal one-time screening for hepatitis C virus infection is cost effective, compared with birth cohort screening alone, according to the results of a study published in Clinical Gastroenterology and Hepatology.
The Centers for Disease Control and Prevention and the U.S. Preventive Services Task Force recommend testing all individuals born between 1945 and 1965 in addition to injection drug users and other high-risk individuals. But so-called birth cohort screening does not reflect the recent spike in hepatitis C virus (HCV) cases among younger persons in the United States, nor the current recommendation to treat nearly all chronic HCV cases, wrote Mark H. Eckman, MD, of the University of Cincinnati, and his associates.
Using a computer program called Decision Maker, they modeled the cost-effectiveness of universal one-time testing, birth cohort screening, and no screening based on quality-adjusted life-years (QALYS) and 2017 U.S. dollars. They assumed that all HCV-infected patients were treatment naive, treatment eligible, and asymptomatic (for example, had no decompensated cirrhosis). They used efficacy data from the ASTRAL trials of sofosbuvir-velpatasvir as well as the ENDURANCE, SURVEYOR, and EXPEDITION trials of glecaprevir-pibrentasvir. In the model, patients who did not achieve a sustained viral response to treatment went on to complete a 12-week triple direct-acting antiviral (DAA) regimen (sofosbuvir, velpatasvir, and voxilaprevir).
Based on these assumptions, universal one-time screening and treatment of infected individuals cost less than $50,000 per QALY gained, making it highly cost effective, compared with no screening, the investigators wrote. Universal screening also was highly cost effective when compared with birth cohort screening, costing $11,378 for each QALY gained.
“Analyses performed during the era of first-generation DAAs and interferon-based treatment regimens found birth-cohort screening to be ‘cost effective,’ ” the researchers wrote. “However, the availability of a new generation of highly effective, non–interferon-based oral regimens, with fewer side effects and shorter treatment courses, has altered the dynamic around the question of screening.” They pointed to another recent study in which universal one-time HCV testing was more cost effective than birth cohort screening.
Such findings have spurred experts to revisit guidelines on HCV screening, but universal testing is controversial when some states, counties, and communities have a low HCV prevalence. In the model, universal one-time HCV screening was cost effective (less than $50,000 per QALY gained), compared with birth cohort screening as long as prevalence exceeded 0.07% among adults not born between 1945 and 1965. The current prevalence estimate in this group is 0.29%, which is probably low because it does not account for the rising incidence among younger adults, the researchers wrote. In an ideal world, all clinics and hospitals would implement an HCV testing program, but in the real world of scarce resources, “data regarding the cost-effectiveness threshold can guide local policy decisions by directing testing services to settings in which they generate sufficient benefit for the cost.”
Partial funding came from the National Foundation for the Centers for Disease Control and Prevention (CDC Foundation), with funding provided through multiple donors to the CDC Foundation’s Viral Hepatitis Action Coalition. Dr. Eckman reported grant support from Merck and one coinvestigator reported ties to AbbVie, Gilead, Merck, and several other pharmaceutical companies.
SOURCE: Eckman MH et al. Clin Gastroenterol Hepatol. 2018 Sep 7. doi: 10.1016/j.cgh.2018.08.080.
Universal one-time screening for hepatitis C virus infection is cost effective, compared with birth cohort screening alone, according to the results of a study published in Clinical Gastroenterology and Hepatology.
The Centers for Disease Control and Prevention and the U.S. Preventive Services Task Force recommend testing all individuals born between 1945 and 1965 in addition to injection drug users and other high-risk individuals. But so-called birth cohort screening does not reflect the recent spike in hepatitis C virus (HCV) cases among younger persons in the United States, nor the current recommendation to treat nearly all chronic HCV cases, wrote Mark H. Eckman, MD, of the University of Cincinnati, and his associates.
Using a computer program called Decision Maker, they modeled the cost-effectiveness of universal one-time testing, birth cohort screening, and no screening based on quality-adjusted life-years (QALYS) and 2017 U.S. dollars. They assumed that all HCV-infected patients were treatment naive, treatment eligible, and asymptomatic (for example, had no decompensated cirrhosis). They used efficacy data from the ASTRAL trials of sofosbuvir-velpatasvir as well as the ENDURANCE, SURVEYOR, and EXPEDITION trials of glecaprevir-pibrentasvir. In the model, patients who did not achieve a sustained viral response to treatment went on to complete a 12-week triple direct-acting antiviral (DAA) regimen (sofosbuvir, velpatasvir, and voxilaprevir).
Based on these assumptions, universal one-time screening and treatment of infected individuals cost less than $50,000 per QALY gained, making it highly cost effective, compared with no screening, the investigators wrote. Universal screening also was highly cost effective when compared with birth cohort screening, costing $11,378 for each QALY gained.
“Analyses performed during the era of first-generation DAAs and interferon-based treatment regimens found birth-cohort screening to be ‘cost effective,’ ” the researchers wrote. “However, the availability of a new generation of highly effective, non–interferon-based oral regimens, with fewer side effects and shorter treatment courses, has altered the dynamic around the question of screening.” They pointed to another recent study in which universal one-time HCV testing was more cost effective than birth cohort screening.
Such findings have spurred experts to revisit guidelines on HCV screening, but universal testing is controversial when some states, counties, and communities have a low HCV prevalence. In the model, universal one-time HCV screening was cost effective (less than $50,000 per QALY gained), compared with birth cohort screening as long as prevalence exceeded 0.07% among adults not born between 1945 and 1965. The current prevalence estimate in this group is 0.29%, which is probably low because it does not account for the rising incidence among younger adults, the researchers wrote. In an ideal world, all clinics and hospitals would implement an HCV testing program, but in the real world of scarce resources, “data regarding the cost-effectiveness threshold can guide local policy decisions by directing testing services to settings in which they generate sufficient benefit for the cost.”
Partial funding came from the National Foundation for the Centers for Disease Control and Prevention (CDC Foundation), with funding provided through multiple donors to the CDC Foundation’s Viral Hepatitis Action Coalition. Dr. Eckman reported grant support from Merck and one coinvestigator reported ties to AbbVie, Gilead, Merck, and several other pharmaceutical companies.
SOURCE: Eckman MH et al. Clin Gastroenterol Hepatol. 2018 Sep 7. doi: 10.1016/j.cgh.2018.08.080.
FROM CLINICAL GASTROENTEROLOGY AND HEPATOLOGY
High-calorie diet may worsen Wilson disease
A high-calorie diet may cause earlier onset of more severe Wilson disease, according to a rodent study.
If translatable to humans, the results could explain “striking phenotype-genotype discrepancies” between patients with Wilson disease, and may give reason to monitor nutrition more closely, particularly dietary levels of fat and sugar, reported lead author Claudia Einer, a PhD candidate at the German Research Center for Environmental Health in Neuherberg, Germany, and her colleagues. Their findings clarify an association between impaired copper metabolism, which defines Wilson disease, and liver steatosis, a common finding in affected patients.
“Indeed, Wilson disease often may be misdiagnosed as nonalcoholic fatty liver disease (NAFLD),” the investigators wrote in Cellular and Molecular Gastroenterology and Hepatology. They noted that previous reports showed similar mitochondrial alterations in the livers of patients with NAFLD and those with Wilson disease. Furthermore, in a case report of two twins with Wilson disease, the twin with bulimia nervosa developed severe liver disease, whereas the other twin, who was undernourished, had mild liver disease. Considering these observations and other supportive evidence, the investigators tested this apparent relationship between a high-fat diet and liver damage in Wilson disease.
“The rationale of this study was that both enriched copper and fatty acids cause bioenergetic defects and therefore synergistically and detrimentally may coincide on hepatic mitochondria, which was found to be dramatically the case,” the investigators wrote.
The study involved homozygous Atp7b–/– rats, which mirror Wilson disease, and heterozygous Atp7b+/– rats, which served as control subjects because they lack copper accumulation. The high-calorie diet contained high fat and sugar levels to mirror “the eating habits in Western society, causing the ‘American-lifestyle-induced-obesity syndrome.’ ”
Within several weeks of starting the high-calorie diet, both control and Wilson disease rats showed higher liver triglyceride levels and visceral fat mass compared with rats on the normal diet, with liver histology also showing macrosteatosis and increased NAFLD Activity Score (NAS). Control rats maintained similar body and liver weights regardless of diet; in contrast, Wilson disease rats on the high-calorie diet showed increased liver weight, compared with Wilson disease rats on the normal diet. In addition, Wilson disease rats fed the high-calorie diet had clinical liver injury, supported by elevated aspartate aminotransferase (AST) levels and gross hepatic damage. Under the microscope, histology revealed widespread necrosis, apoptosis, inflammation, and fibrosis; findings were sufficient to constitute nonalcoholic steatohepatitis in all Wilson disease rats fed the high-calorie diet, compared with just one-third of the control rats receiving high calories. Additional testing showed that Wilson disease rats fed the high-calorie diet had disease onset 20 days sooner than did Wilson disease rats fed the normal diet.
“This is a remarkable disease acceleration,” the investigators noted, highlighting the median survival of 106 days in Wilson disease rats fed a normal diet.
Copper testing showed that Wilson disease rats fed the high-calorie diet had high serum levels of non–ceruloplasmin-bound copper, which is a sign of overt liver damage; based on histologic findings, the copper likely came from destroyed hepatocytes. Regardless of diet type, Wilson disease rats developed high levels of copper within the liver, suggesting comparable copper consumption via water sources. Regardless of genotype, the high-calorie diet led to higher mitochondrial copper levels than those of the normal diet, but Wilson disease rats showed the highest levels of copper sequestration in mitochondria, to an extreme degree.
“Importantly,” the investigators wrote, “such increased mitochondrial copper significantly correlated with a higher NAS and a progressive Histologic Activity Index score.”
Closer inspection showed that the mitochondria of Wilson disease rats were abnormal regardless of diet, but those fed the high-calorie diet had “a most severe mitochondrial phenotype,” including detached membranes and ballooned cristae.
“These structural impairments were paralleled by remarkable mitochondrial functional deficits,” the investigators reported, referring to a significant decrease in adenosine triphosphate production and an increase in mitochondrial H2O2. In response to these mitochondrial abnormalities, cholesterol-related enzymes quadrupled, most prominently for biliary excretion. The investigators summed up these hepatic events as a “toxic triad of adenosine triphosphate depletion, increased reactive oxygen species, and increased bile salts [that led] to an earlier onset of the disease and to enhanced disease progression.”
To complete the set of experiments, rats were given the copper chelator methanobactin. This treatment effectively mitigated structural and functional abnormalities in mitochondria, which drove serum levels of AST, copper, and bile salts toward normalcy. Although treatment halted overt liver damage, histology revealed that resolution was incomplete.
“We conclude that lipid accumulation in copper-burdened hepatocytes may represent a ‘second-hit’ in Wilson disease, inducing liver damage, and suggest that further research should establish whether dietary counseling of Wilson disease patients may be of therapeutic benefit,” the investigators concluded.
The study was funded by Deutsche Forschungsgemeinschaft and the WiFoMed Society. The investigators reported no conflicts of interest.
SOURCE: Einer et al. Cell Mol Gastroenterol Hepatol. 2019 Jan 11. doi: 10.1016/j.jcmgh.2018.12.005.
A high-calorie diet may cause earlier onset of more severe Wilson disease, according to a rodent study.
If translatable to humans, the results could explain “striking phenotype-genotype discrepancies” between patients with Wilson disease, and may give reason to monitor nutrition more closely, particularly dietary levels of fat and sugar, reported lead author Claudia Einer, a PhD candidate at the German Research Center for Environmental Health in Neuherberg, Germany, and her colleagues. Their findings clarify an association between impaired copper metabolism, which defines Wilson disease, and liver steatosis, a common finding in affected patients.
“Indeed, Wilson disease often may be misdiagnosed as nonalcoholic fatty liver disease (NAFLD),” the investigators wrote in Cellular and Molecular Gastroenterology and Hepatology. They noted that previous reports showed similar mitochondrial alterations in the livers of patients with NAFLD and those with Wilson disease. Furthermore, in a case report of two twins with Wilson disease, the twin with bulimia nervosa developed severe liver disease, whereas the other twin, who was undernourished, had mild liver disease. Considering these observations and other supportive evidence, the investigators tested this apparent relationship between a high-fat diet and liver damage in Wilson disease.
“The rationale of this study was that both enriched copper and fatty acids cause bioenergetic defects and therefore synergistically and detrimentally may coincide on hepatic mitochondria, which was found to be dramatically the case,” the investigators wrote.
The study involved homozygous Atp7b–/– rats, which mirror Wilson disease, and heterozygous Atp7b+/– rats, which served as control subjects because they lack copper accumulation. The high-calorie diet contained high fat and sugar levels to mirror “the eating habits in Western society, causing the ‘American-lifestyle-induced-obesity syndrome.’ ”
Within several weeks of starting the high-calorie diet, both control and Wilson disease rats showed higher liver triglyceride levels and visceral fat mass compared with rats on the normal diet, with liver histology also showing macrosteatosis and increased NAFLD Activity Score (NAS). Control rats maintained similar body and liver weights regardless of diet; in contrast, Wilson disease rats on the high-calorie diet showed increased liver weight, compared with Wilson disease rats on the normal diet. In addition, Wilson disease rats fed the high-calorie diet had clinical liver injury, supported by elevated aspartate aminotransferase (AST) levels and gross hepatic damage. Under the microscope, histology revealed widespread necrosis, apoptosis, inflammation, and fibrosis; findings were sufficient to constitute nonalcoholic steatohepatitis in all Wilson disease rats fed the high-calorie diet, compared with just one-third of the control rats receiving high calories. Additional testing showed that Wilson disease rats fed the high-calorie diet had disease onset 20 days sooner than did Wilson disease rats fed the normal diet.
“This is a remarkable disease acceleration,” the investigators noted, highlighting the median survival of 106 days in Wilson disease rats fed a normal diet.
Copper testing showed that Wilson disease rats fed the high-calorie diet had high serum levels of non–ceruloplasmin-bound copper, which is a sign of overt liver damage; based on histologic findings, the copper likely came from destroyed hepatocytes. Regardless of diet type, Wilson disease rats developed high levels of copper within the liver, suggesting comparable copper consumption via water sources. Regardless of genotype, the high-calorie diet led to higher mitochondrial copper levels than those of the normal diet, but Wilson disease rats showed the highest levels of copper sequestration in mitochondria, to an extreme degree.
“Importantly,” the investigators wrote, “such increased mitochondrial copper significantly correlated with a higher NAS and a progressive Histologic Activity Index score.”
Closer inspection showed that the mitochondria of Wilson disease rats were abnormal regardless of diet, but those fed the high-calorie diet had “a most severe mitochondrial phenotype,” including detached membranes and ballooned cristae.
“These structural impairments were paralleled by remarkable mitochondrial functional deficits,” the investigators reported, referring to a significant decrease in adenosine triphosphate production and an increase in mitochondrial H2O2. In response to these mitochondrial abnormalities, cholesterol-related enzymes quadrupled, most prominently for biliary excretion. The investigators summed up these hepatic events as a “toxic triad of adenosine triphosphate depletion, increased reactive oxygen species, and increased bile salts [that led] to an earlier onset of the disease and to enhanced disease progression.”
To complete the set of experiments, rats were given the copper chelator methanobactin. This treatment effectively mitigated structural and functional abnormalities in mitochondria, which drove serum levels of AST, copper, and bile salts toward normalcy. Although treatment halted overt liver damage, histology revealed that resolution was incomplete.
“We conclude that lipid accumulation in copper-burdened hepatocytes may represent a ‘second-hit’ in Wilson disease, inducing liver damage, and suggest that further research should establish whether dietary counseling of Wilson disease patients may be of therapeutic benefit,” the investigators concluded.
The study was funded by Deutsche Forschungsgemeinschaft and the WiFoMed Society. The investigators reported no conflicts of interest.
SOURCE: Einer et al. Cell Mol Gastroenterol Hepatol. 2019 Jan 11. doi: 10.1016/j.jcmgh.2018.12.005.
A high-calorie diet may cause earlier onset of more severe Wilson disease, according to a rodent study.
If translatable to humans, the results could explain “striking phenotype-genotype discrepancies” between patients with Wilson disease, and may give reason to monitor nutrition more closely, particularly dietary levels of fat and sugar, reported lead author Claudia Einer, a PhD candidate at the German Research Center for Environmental Health in Neuherberg, Germany, and her colleagues. Their findings clarify an association between impaired copper metabolism, which defines Wilson disease, and liver steatosis, a common finding in affected patients.
“Indeed, Wilson disease often may be misdiagnosed as nonalcoholic fatty liver disease (NAFLD),” the investigators wrote in Cellular and Molecular Gastroenterology and Hepatology. They noted that previous reports showed similar mitochondrial alterations in the livers of patients with NAFLD and those with Wilson disease. Furthermore, in a case report of two twins with Wilson disease, the twin with bulimia nervosa developed severe liver disease, whereas the other twin, who was undernourished, had mild liver disease. Considering these observations and other supportive evidence, the investigators tested this apparent relationship between a high-fat diet and liver damage in Wilson disease.
“The rationale of this study was that both enriched copper and fatty acids cause bioenergetic defects and therefore synergistically and detrimentally may coincide on hepatic mitochondria, which was found to be dramatically the case,” the investigators wrote.
The study involved homozygous Atp7b–/– rats, which mirror Wilson disease, and heterozygous Atp7b+/– rats, which served as control subjects because they lack copper accumulation. The high-calorie diet contained high fat and sugar levels to mirror “the eating habits in Western society, causing the ‘American-lifestyle-induced-obesity syndrome.’ ”
Within several weeks of starting the high-calorie diet, both control and Wilson disease rats showed higher liver triglyceride levels and visceral fat mass compared with rats on the normal diet, with liver histology also showing macrosteatosis and increased NAFLD Activity Score (NAS). Control rats maintained similar body and liver weights regardless of diet; in contrast, Wilson disease rats on the high-calorie diet showed increased liver weight, compared with Wilson disease rats on the normal diet. In addition, Wilson disease rats fed the high-calorie diet had clinical liver injury, supported by elevated aspartate aminotransferase (AST) levels and gross hepatic damage. Under the microscope, histology revealed widespread necrosis, apoptosis, inflammation, and fibrosis; findings were sufficient to constitute nonalcoholic steatohepatitis in all Wilson disease rats fed the high-calorie diet, compared with just one-third of the control rats receiving high calories. Additional testing showed that Wilson disease rats fed the high-calorie diet had disease onset 20 days sooner than did Wilson disease rats fed the normal diet.
“This is a remarkable disease acceleration,” the investigators noted, highlighting the median survival of 106 days in Wilson disease rats fed a normal diet.
Copper testing showed that Wilson disease rats fed the high-calorie diet had high serum levels of non–ceruloplasmin-bound copper, which is a sign of overt liver damage; based on histologic findings, the copper likely came from destroyed hepatocytes. Regardless of diet type, Wilson disease rats developed high levels of copper within the liver, suggesting comparable copper consumption via water sources. Regardless of genotype, the high-calorie diet led to higher mitochondrial copper levels than those of the normal diet, but Wilson disease rats showed the highest levels of copper sequestration in mitochondria, to an extreme degree.
“Importantly,” the investigators wrote, “such increased mitochondrial copper significantly correlated with a higher NAS and a progressive Histologic Activity Index score.”
Closer inspection showed that the mitochondria of Wilson disease rats were abnormal regardless of diet, but those fed the high-calorie diet had “a most severe mitochondrial phenotype,” including detached membranes and ballooned cristae.
“These structural impairments were paralleled by remarkable mitochondrial functional deficits,” the investigators reported, referring to a significant decrease in adenosine triphosphate production and an increase in mitochondrial H2O2. In response to these mitochondrial abnormalities, cholesterol-related enzymes quadrupled, most prominently for biliary excretion. The investigators summed up these hepatic events as a “toxic triad of adenosine triphosphate depletion, increased reactive oxygen species, and increased bile salts [that led] to an earlier onset of the disease and to enhanced disease progression.”
To complete the set of experiments, rats were given the copper chelator methanobactin. This treatment effectively mitigated structural and functional abnormalities in mitochondria, which drove serum levels of AST, copper, and bile salts toward normalcy. Although treatment halted overt liver damage, histology revealed that resolution was incomplete.
“We conclude that lipid accumulation in copper-burdened hepatocytes may represent a ‘second-hit’ in Wilson disease, inducing liver damage, and suggest that further research should establish whether dietary counseling of Wilson disease patients may be of therapeutic benefit,” the investigators concluded.
The study was funded by Deutsche Forschungsgemeinschaft and the WiFoMed Society. The investigators reported no conflicts of interest.
SOURCE: Einer et al. Cell Mol Gastroenterol Hepatol. 2019 Jan 11. doi: 10.1016/j.jcmgh.2018.12.005.
FROM CELLULAR AND MOLECULAR GASTROENTEROLOGY AND HEPATOLOGY
Novel capsid assembly modulator shows promise in HBV
For adults with chronic hepatitis B virus infection, treatment with a novel investigational capsid assembly modulator was well tolerated and showed antiviral activity against HBV, according to the results of a phase 1 study of 73 patients.
“Substantial and correlated reductions in serum HBV DNA and HBV RNA levels were observed consistently with the higher-dose cohorts and were notably greatest for combination treatment with NVR 3-778 and pegIFN [pegylated interferon],” Man Fung Yuen, MD, of the University of Hong Kong, and his associates wrote in a report published in Gastroenterology. Hence, this first-in-class capsid assembly modulator might help prolong treatment responses, “most likely as a component of new combination treatment regimens for HBV-infected patients.” However, one patient developed severe rash immediately after completing treatment that took 6 months of intensive outpatient treatment to resolve, they noted.
Chronic viral hepatitis due to HBV is a major cause of early death worldwide, and new therapies are needed to help prevent severe liver disease and liver death from this infection. Current treatments for HBV infection consist of nucleoside or nucleotide analogs or pegylated interferon. These suppress HBV replication in many patients, but most patients do not achieve durable responses. Consequently, most patients require long-term treatment with HBV nucleosides and nucleotide analogs, which they may find difficult to tolerate or adhere to and to which their infections can become resistant, the researchers said.
The HBV virion contains a viral core protein (HBc) that is required to encapsidate viral polymerase and pregenomic HBV RNA into a nucleocapsid. To target this process, researchers developed NVR 3-778, a first-in-class, orally bioavailable small molecule that binds HBc so that HBc forms a defective capsid that lacks nuclear material. Hence, NVR 3-778 is intended to stop the production of HBV nucleocapsids and keep infected cells from releasing the enveloped infectious viral particles that perpetuate HBV infection.
To assess the safety, pharmacokinetics, and antiviral activity of NVR 3-778, the researchers conducted a phase 1 study of 73 patients with chronic HBV infection who tested positive for hepatitis B e-antigen (HBeAg) and had no detectable cirrhosis. Patients were randomly assigned to receive oral NVR 3-778 (100 mg, 200 mg, or 400 mg daily or 600 mg or 1,000 mg twice daily ) or placebo for 28 days. Some patients received combination therapy with pegylated interferon plus either NVR 3-778 (600 mg twice daily) or placebo. Treatment was generally well tolerated, and adverse events were usually mild and deemed unrelated to therapy. No patient stopped treatment for adverse effects.
The only serious adverse event in the study consisted of grade 3 rash that developed in a 42-year-old male after 22 days of treatment at the lowest dose of NVR 3-778 (100 mg per day). This patient completed treatment and ultimately developed a severe papulovesicular rash with a predominantly acral distribution over the hands, arm, side of neck, and one leg (palmar plantar erythrodysesthesia), the researchers said. “There were no perioral or mucosal lesions, no ecchymotic skin involvement, no bullae, and no systemic manifestations or hematological abnormalities,” they wrote. “The rash was subsequently managed with a psoriasis-like treatment regimen of psoralen, ultraviolet light, and topical steroid ointment during outpatient follow-up and resolved after approximately 6 months.”
Another three cases of “minor” skin rash were considered probably related to treatment in the cohort that received 600 mg NVR 3-778 b.i.d. plus pegylated interferon, the investigators said. Two additional cases of mild rash were deemed unrelated to treatment.
“The observed reductions in HBV RNA confirmed the novel mechanism of NVR 3-778,” the researchers concluded. “This class of compounds can also inhibit replenishment of intranuclear covalently closed circular DNA over time and may have immunomodulatory properties.” Longer treatment periods would be needed to study these mechanisms and to quantify reductions in serum HBsAg and HBeAG, they noted.
Novira Therapeutics developed NVR 3-778 and is a Janssen Pharmaceutical Company. Janssen provided funding for editorial support. Dr. Yuen disclosed relationships with AbbVie, Biocartis, Bristol-Myers Squibb, Gilead Sciences, GlaxoSmithKline, Ionis, Roche, Vir Biotechnology, and several other pharmaceutical companies. Other coinvestigators disclosed ties to pharmaceutical companies; eight reported employment by Novira or a Janssen company.
SOURCE: Yuen MF et al. Gastroenterology. 2019 Jan 5. doi: 10.1053/j.gastro.2018.12.023.
For adults with chronic hepatitis B virus infection, treatment with a novel investigational capsid assembly modulator was well tolerated and showed antiviral activity against HBV, according to the results of a phase 1 study of 73 patients.
“Substantial and correlated reductions in serum HBV DNA and HBV RNA levels were observed consistently with the higher-dose cohorts and were notably greatest for combination treatment with NVR 3-778 and pegIFN [pegylated interferon],” Man Fung Yuen, MD, of the University of Hong Kong, and his associates wrote in a report published in Gastroenterology. Hence, this first-in-class capsid assembly modulator might help prolong treatment responses, “most likely as a component of new combination treatment regimens for HBV-infected patients.” However, one patient developed severe rash immediately after completing treatment that took 6 months of intensive outpatient treatment to resolve, they noted.
Chronic viral hepatitis due to HBV is a major cause of early death worldwide, and new therapies are needed to help prevent severe liver disease and liver death from this infection. Current treatments for HBV infection consist of nucleoside or nucleotide analogs or pegylated interferon. These suppress HBV replication in many patients, but most patients do not achieve durable responses. Consequently, most patients require long-term treatment with HBV nucleosides and nucleotide analogs, which they may find difficult to tolerate or adhere to and to which their infections can become resistant, the researchers said.
The HBV virion contains a viral core protein (HBc) that is required to encapsidate viral polymerase and pregenomic HBV RNA into a nucleocapsid. To target this process, researchers developed NVR 3-778, a first-in-class, orally bioavailable small molecule that binds HBc so that HBc forms a defective capsid that lacks nuclear material. Hence, NVR 3-778 is intended to stop the production of HBV nucleocapsids and keep infected cells from releasing the enveloped infectious viral particles that perpetuate HBV infection.
To assess the safety, pharmacokinetics, and antiviral activity of NVR 3-778, the researchers conducted a phase 1 study of 73 patients with chronic HBV infection who tested positive for hepatitis B e-antigen (HBeAg) and had no detectable cirrhosis. Patients were randomly assigned to receive oral NVR 3-778 (100 mg, 200 mg, or 400 mg daily or 600 mg or 1,000 mg twice daily ) or placebo for 28 days. Some patients received combination therapy with pegylated interferon plus either NVR 3-778 (600 mg twice daily) or placebo. Treatment was generally well tolerated, and adverse events were usually mild and deemed unrelated to therapy. No patient stopped treatment for adverse effects.
The only serious adverse event in the study consisted of grade 3 rash that developed in a 42-year-old male after 22 days of treatment at the lowest dose of NVR 3-778 (100 mg per day). This patient completed treatment and ultimately developed a severe papulovesicular rash with a predominantly acral distribution over the hands, arm, side of neck, and one leg (palmar plantar erythrodysesthesia), the researchers said. “There were no perioral or mucosal lesions, no ecchymotic skin involvement, no bullae, and no systemic manifestations or hematological abnormalities,” they wrote. “The rash was subsequently managed with a psoriasis-like treatment regimen of psoralen, ultraviolet light, and topical steroid ointment during outpatient follow-up and resolved after approximately 6 months.”
Another three cases of “minor” skin rash were considered probably related to treatment in the cohort that received 600 mg NVR 3-778 b.i.d. plus pegylated interferon, the investigators said. Two additional cases of mild rash were deemed unrelated to treatment.
“The observed reductions in HBV RNA confirmed the novel mechanism of NVR 3-778,” the researchers concluded. “This class of compounds can also inhibit replenishment of intranuclear covalently closed circular DNA over time and may have immunomodulatory properties.” Longer treatment periods would be needed to study these mechanisms and to quantify reductions in serum HBsAg and HBeAG, they noted.
Novira Therapeutics developed NVR 3-778 and is a Janssen Pharmaceutical Company. Janssen provided funding for editorial support. Dr. Yuen disclosed relationships with AbbVie, Biocartis, Bristol-Myers Squibb, Gilead Sciences, GlaxoSmithKline, Ionis, Roche, Vir Biotechnology, and several other pharmaceutical companies. Other coinvestigators disclosed ties to pharmaceutical companies; eight reported employment by Novira or a Janssen company.
SOURCE: Yuen MF et al. Gastroenterology. 2019 Jan 5. doi: 10.1053/j.gastro.2018.12.023.
For adults with chronic hepatitis B virus infection, treatment with a novel investigational capsid assembly modulator was well tolerated and showed antiviral activity against HBV, according to the results of a phase 1 study of 73 patients.
“Substantial and correlated reductions in serum HBV DNA and HBV RNA levels were observed consistently with the higher-dose cohorts and were notably greatest for combination treatment with NVR 3-778 and pegIFN [pegylated interferon],” Man Fung Yuen, MD, of the University of Hong Kong, and his associates wrote in a report published in Gastroenterology. Hence, this first-in-class capsid assembly modulator might help prolong treatment responses, “most likely as a component of new combination treatment regimens for HBV-infected patients.” However, one patient developed severe rash immediately after completing treatment that took 6 months of intensive outpatient treatment to resolve, they noted.
Chronic viral hepatitis due to HBV is a major cause of early death worldwide, and new therapies are needed to help prevent severe liver disease and liver death from this infection. Current treatments for HBV infection consist of nucleoside or nucleotide analogs or pegylated interferon. These suppress HBV replication in many patients, but most patients do not achieve durable responses. Consequently, most patients require long-term treatment with HBV nucleosides and nucleotide analogs, which they may find difficult to tolerate or adhere to and to which their infections can become resistant, the researchers said.
The HBV virion contains a viral core protein (HBc) that is required to encapsidate viral polymerase and pregenomic HBV RNA into a nucleocapsid. To target this process, researchers developed NVR 3-778, a first-in-class, orally bioavailable small molecule that binds HBc so that HBc forms a defective capsid that lacks nuclear material. Hence, NVR 3-778 is intended to stop the production of HBV nucleocapsids and keep infected cells from releasing the enveloped infectious viral particles that perpetuate HBV infection.
To assess the safety, pharmacokinetics, and antiviral activity of NVR 3-778, the researchers conducted a phase 1 study of 73 patients with chronic HBV infection who tested positive for hepatitis B e-antigen (HBeAg) and had no detectable cirrhosis. Patients were randomly assigned to receive oral NVR 3-778 (100 mg, 200 mg, or 400 mg daily or 600 mg or 1,000 mg twice daily ) or placebo for 28 days. Some patients received combination therapy with pegylated interferon plus either NVR 3-778 (600 mg twice daily) or placebo. Treatment was generally well tolerated, and adverse events were usually mild and deemed unrelated to therapy. No patient stopped treatment for adverse effects.
The only serious adverse event in the study consisted of grade 3 rash that developed in a 42-year-old male after 22 days of treatment at the lowest dose of NVR 3-778 (100 mg per day). This patient completed treatment and ultimately developed a severe papulovesicular rash with a predominantly acral distribution over the hands, arm, side of neck, and one leg (palmar plantar erythrodysesthesia), the researchers said. “There were no perioral or mucosal lesions, no ecchymotic skin involvement, no bullae, and no systemic manifestations or hematological abnormalities,” they wrote. “The rash was subsequently managed with a psoriasis-like treatment regimen of psoralen, ultraviolet light, and topical steroid ointment during outpatient follow-up and resolved after approximately 6 months.”
Another three cases of “minor” skin rash were considered probably related to treatment in the cohort that received 600 mg NVR 3-778 b.i.d. plus pegylated interferon, the investigators said. Two additional cases of mild rash were deemed unrelated to treatment.
“The observed reductions in HBV RNA confirmed the novel mechanism of NVR 3-778,” the researchers concluded. “This class of compounds can also inhibit replenishment of intranuclear covalently closed circular DNA over time and may have immunomodulatory properties.” Longer treatment periods would be needed to study these mechanisms and to quantify reductions in serum HBsAg and HBeAG, they noted.
Novira Therapeutics developed NVR 3-778 and is a Janssen Pharmaceutical Company. Janssen provided funding for editorial support. Dr. Yuen disclosed relationships with AbbVie, Biocartis, Bristol-Myers Squibb, Gilead Sciences, GlaxoSmithKline, Ionis, Roche, Vir Biotechnology, and several other pharmaceutical companies. Other coinvestigators disclosed ties to pharmaceutical companies; eight reported employment by Novira or a Janssen company.
SOURCE: Yuen MF et al. Gastroenterology. 2019 Jan 5. doi: 10.1053/j.gastro.2018.12.023.
FROM GASTROENTEROLOGY
AGA Clinical Practice Update: Surgical risk assessment and perioperative management in cirrhosis
Patients with cirrhosis should be risk stratified and counseled accordingly before all but the most urgent surgeries, cautions a clinical practice update from the American Gastroenterological Association.
These risks, which include mortality and reflect “the profound effects of hepatic synthetic dysfunction and portal hypertension,” require presurgical evaluation based on CTP score (Child-Pugh class), Model for End-Stage Liver Disease (MELD) score, Mayo Postoperative Mortality Risk Score, or another proven risk-stratification system, writes Patrick G. Northup, MD, of the University of Virginia, Charlottesville, together with his associates. “There is no single definitive risk-stratification system to determine operative risk in all patients with cirrhosis, and we recommend using multiple methods,” they elaborated in Clinical Gastroenterology and Hepatology.
The prevalence of cirrhosis is rising, affected patients are living longer, and liver disease is more advanced and may involve comorbidities that merit consideration of surgery, noted Dr. Northup and his associates. However, cirrhosis increases the risk for serious postoperative complications, including hepatic decompensation, worsening of liver synthetic function, exacerbated portal hypertension, wound dehiscence, pleural effusions, pneumonia, bacterial peritonitis, bleeding, and multiple organ failure. Because clinical trials of surgery in cirrhotic patients are lacking, the experts stress the need for case-by-case management.
There is no definite threshold that precludes all surgeries in cases of cirrhosis, but a Child-Pugh class C (CTP score over 10) or MELD score over 20 greatly increases the risk of postoperative decompensation and death. For these patients, “all but the most urgent and life-saving procedures” should be canceled or postponed until after liver transplantation, the experts wrote. For less severe cirrhosis, it is key to consider the type and anatomic site of the proposed surgery. Hepatobiliary surgeries, other intra-abdominal surgeries, cardiovascular surgeries, and thoracic procedures are most likely to lead to serious complications.
Preoperative care should emphasize control of ascites, variceal bleeding risk, and hepatic encephalopathy. Bleeding and clotting safety thresholds in cirrhosis are unknown, and individualized management, ideally with viscoelastic testing–directed therapy, is warranted instead of protocol transfusions to a target international normalized ratio (INR). Bleeding events are more common in critically ill patients with plasma fibrinogen ratios under 100 mg/dL.
Segmental hepatic resection (usually for malignancy), the most studied procedure in cirrhosis, is generally safe in the absence of clinically significant portal hypertension. For patients who do have portal hypertension, transjugular intrahepatic portosystemic shunt (TIPS) has not clearly been shown to outperform conservative management, although small case series have found that TIPS during deep pelvic or colonic resection decompresses abdominal collaterals.
Because of the risk of poor outcomes, patients with cirrhosis and incompletely controlled ascites should not undergo abdominal hernia repair unless they have an incarceration that is not manually reducible or suspected strangulation. Bariatric surgery is contraindicated in cases of clinically significant portal hypertension but otherwise can be performed at a center with cirrhosis expertise. Sleeve gastrectomy at the same time as liver transplantation is also an option for select patients with obesity.
Elective cholecystectomy should be avoided, and required cases should be performed in experienced centers. “The gallbladder wall may appear thickened on imaging, which may lead to the erroneous diagnosis of acute cholecystitis,” the experts noted. Hence, the diagnosis “should be made only in the appropriate clinical setting, usually in the presence of biliary pain.”
Hepatic decompensation after surgery can be severe enough to merit liver transplantation. There is no agreed-on MELD score that mandates liver transplant evaluation before elective surgery, but the experts recommend doing so if the MELD score is 15 or greater or if risk of mortality within 3 months after surgery exceeds 15%.
Postoperative management of patients with cirrhosis should include aggressive measures to prevent portal hypertension. Monitor renal function closely and avoid volume depletion or overload, the experts advised. Patients should receive only short-acting benzodiazepines and lower opiate doses, administered less often, than in the general population. Avoiding constipation is vital to minimize hepatic encephalopathy, which makes oral rifaximin a better choice than lactulose. Patients should not receive NSAIDs, which can impair renal blood flow. To prevent liver toxicity, they should not be discharged on opiate/acetaminophen combinations, which they might unknowingly take along with another drug that contains acetaminophen.
The experts disclosed no external funding sources and reported having no conflicts of interest.
SOURCE: Northup PG et al. Clin Gastroenterol Hepatol. 2018 Sep 28. doi: 10.1016/j.cgh.2018.09.043.
Patients with cirrhosis should be risk stratified and counseled accordingly before all but the most urgent surgeries, cautions a clinical practice update from the American Gastroenterological Association.
These risks, which include mortality and reflect “the profound effects of hepatic synthetic dysfunction and portal hypertension,” require presurgical evaluation based on CTP score (Child-Pugh class), Model for End-Stage Liver Disease (MELD) score, Mayo Postoperative Mortality Risk Score, or another proven risk-stratification system, writes Patrick G. Northup, MD, of the University of Virginia, Charlottesville, together with his associates. “There is no single definitive risk-stratification system to determine operative risk in all patients with cirrhosis, and we recommend using multiple methods,” they elaborated in Clinical Gastroenterology and Hepatology.
The prevalence of cirrhosis is rising, affected patients are living longer, and liver disease is more advanced and may involve comorbidities that merit consideration of surgery, noted Dr. Northup and his associates. However, cirrhosis increases the risk for serious postoperative complications, including hepatic decompensation, worsening of liver synthetic function, exacerbated portal hypertension, wound dehiscence, pleural effusions, pneumonia, bacterial peritonitis, bleeding, and multiple organ failure. Because clinical trials of surgery in cirrhotic patients are lacking, the experts stress the need for case-by-case management.
There is no definite threshold that precludes all surgeries in cases of cirrhosis, but a Child-Pugh class C (CTP score over 10) or MELD score over 20 greatly increases the risk of postoperative decompensation and death. For these patients, “all but the most urgent and life-saving procedures” should be canceled or postponed until after liver transplantation, the experts wrote. For less severe cirrhosis, it is key to consider the type and anatomic site of the proposed surgery. Hepatobiliary surgeries, other intra-abdominal surgeries, cardiovascular surgeries, and thoracic procedures are most likely to lead to serious complications.
Preoperative care should emphasize control of ascites, variceal bleeding risk, and hepatic encephalopathy. Bleeding and clotting safety thresholds in cirrhosis are unknown, and individualized management, ideally with viscoelastic testing–directed therapy, is warranted instead of protocol transfusions to a target international normalized ratio (INR). Bleeding events are more common in critically ill patients with plasma fibrinogen ratios under 100 mg/dL.
Segmental hepatic resection (usually for malignancy), the most studied procedure in cirrhosis, is generally safe in the absence of clinically significant portal hypertension. For patients who do have portal hypertension, transjugular intrahepatic portosystemic shunt (TIPS) has not clearly been shown to outperform conservative management, although small case series have found that TIPS during deep pelvic or colonic resection decompresses abdominal collaterals.
Because of the risk of poor outcomes, patients with cirrhosis and incompletely controlled ascites should not undergo abdominal hernia repair unless they have an incarceration that is not manually reducible or suspected strangulation. Bariatric surgery is contraindicated in cases of clinically significant portal hypertension but otherwise can be performed at a center with cirrhosis expertise. Sleeve gastrectomy at the same time as liver transplantation is also an option for select patients with obesity.
Elective cholecystectomy should be avoided, and required cases should be performed in experienced centers. “The gallbladder wall may appear thickened on imaging, which may lead to the erroneous diagnosis of acute cholecystitis,” the experts noted. Hence, the diagnosis “should be made only in the appropriate clinical setting, usually in the presence of biliary pain.”
Hepatic decompensation after surgery can be severe enough to merit liver transplantation. There is no agreed-on MELD score that mandates liver transplant evaluation before elective surgery, but the experts recommend doing so if the MELD score is 15 or greater or if risk of mortality within 3 months after surgery exceeds 15%.
Postoperative management of patients with cirrhosis should include aggressive measures to prevent portal hypertension. Monitor renal function closely and avoid volume depletion or overload, the experts advised. Patients should receive only short-acting benzodiazepines and lower opiate doses, administered less often, than in the general population. Avoiding constipation is vital to minimize hepatic encephalopathy, which makes oral rifaximin a better choice than lactulose. Patients should not receive NSAIDs, which can impair renal blood flow. To prevent liver toxicity, they should not be discharged on opiate/acetaminophen combinations, which they might unknowingly take along with another drug that contains acetaminophen.
The experts disclosed no external funding sources and reported having no conflicts of interest.
SOURCE: Northup PG et al. Clin Gastroenterol Hepatol. 2018 Sep 28. doi: 10.1016/j.cgh.2018.09.043.
Patients with cirrhosis should be risk stratified and counseled accordingly before all but the most urgent surgeries, cautions a clinical practice update from the American Gastroenterological Association.
These risks, which include mortality and reflect “the profound effects of hepatic synthetic dysfunction and portal hypertension,” require presurgical evaluation based on CTP score (Child-Pugh class), Model for End-Stage Liver Disease (MELD) score, Mayo Postoperative Mortality Risk Score, or another proven risk-stratification system, writes Patrick G. Northup, MD, of the University of Virginia, Charlottesville, together with his associates. “There is no single definitive risk-stratification system to determine operative risk in all patients with cirrhosis, and we recommend using multiple methods,” they elaborated in Clinical Gastroenterology and Hepatology.
The prevalence of cirrhosis is rising, affected patients are living longer, and liver disease is more advanced and may involve comorbidities that merit consideration of surgery, noted Dr. Northup and his associates. However, cirrhosis increases the risk for serious postoperative complications, including hepatic decompensation, worsening of liver synthetic function, exacerbated portal hypertension, wound dehiscence, pleural effusions, pneumonia, bacterial peritonitis, bleeding, and multiple organ failure. Because clinical trials of surgery in cirrhotic patients are lacking, the experts stress the need for case-by-case management.
There is no definite threshold that precludes all surgeries in cases of cirrhosis, but a Child-Pugh class C (CTP score over 10) or MELD score over 20 greatly increases the risk of postoperative decompensation and death. For these patients, “all but the most urgent and life-saving procedures” should be canceled or postponed until after liver transplantation, the experts wrote. For less severe cirrhosis, it is key to consider the type and anatomic site of the proposed surgery. Hepatobiliary surgeries, other intra-abdominal surgeries, cardiovascular surgeries, and thoracic procedures are most likely to lead to serious complications.
Preoperative care should emphasize control of ascites, variceal bleeding risk, and hepatic encephalopathy. Bleeding and clotting safety thresholds in cirrhosis are unknown, and individualized management, ideally with viscoelastic testing–directed therapy, is warranted instead of protocol transfusions to a target international normalized ratio (INR). Bleeding events are more common in critically ill patients with plasma fibrinogen ratios under 100 mg/dL.
Segmental hepatic resection (usually for malignancy), the most studied procedure in cirrhosis, is generally safe in the absence of clinically significant portal hypertension. For patients who do have portal hypertension, transjugular intrahepatic portosystemic shunt (TIPS) has not clearly been shown to outperform conservative management, although small case series have found that TIPS during deep pelvic or colonic resection decompresses abdominal collaterals.
Because of the risk of poor outcomes, patients with cirrhosis and incompletely controlled ascites should not undergo abdominal hernia repair unless they have an incarceration that is not manually reducible or suspected strangulation. Bariatric surgery is contraindicated in cases of clinically significant portal hypertension but otherwise can be performed at a center with cirrhosis expertise. Sleeve gastrectomy at the same time as liver transplantation is also an option for select patients with obesity.
Elective cholecystectomy should be avoided, and required cases should be performed in experienced centers. “The gallbladder wall may appear thickened on imaging, which may lead to the erroneous diagnosis of acute cholecystitis,” the experts noted. Hence, the diagnosis “should be made only in the appropriate clinical setting, usually in the presence of biliary pain.”
Hepatic decompensation after surgery can be severe enough to merit liver transplantation. There is no agreed-on MELD score that mandates liver transplant evaluation before elective surgery, but the experts recommend doing so if the MELD score is 15 or greater or if risk of mortality within 3 months after surgery exceeds 15%.
Postoperative management of patients with cirrhosis should include aggressive measures to prevent portal hypertension. Monitor renal function closely and avoid volume depletion or overload, the experts advised. Patients should receive only short-acting benzodiazepines and lower opiate doses, administered less often, than in the general population. Avoiding constipation is vital to minimize hepatic encephalopathy, which makes oral rifaximin a better choice than lactulose. Patients should not receive NSAIDs, which can impair renal blood flow. To prevent liver toxicity, they should not be discharged on opiate/acetaminophen combinations, which they might unknowingly take along with another drug that contains acetaminophen.
The experts disclosed no external funding sources and reported having no conflicts of interest.
SOURCE: Northup PG et al. Clin Gastroenterol Hepatol. 2018 Sep 28. doi: 10.1016/j.cgh.2018.09.043.
FROM CLINICAL GASTROENTEROLOGY AND HEPATOLOGY
AGA Clinical Practice Update: Changing utility of serology and histologic measures in celiac disease
For children and adolescents with strong clinical suspicion for celiac disease, repeated transglutaminase-2-IgA (TG2-IgA) levels that are more than 10 times higher than the upper limit of normal often suffices for diagnosis, according to an American Gastroenterological Association clinical practice update and expert review.
This approach precludes the need for esophagogastroduodenoscopy (EGD) in about 30%-50% of cases, wrote Steffen Husby, MD, PhD, of Odense University Hospital (Denmark), together with his associates in Gastroenterology. “When such a strongly positive TG2-IgA is combined with a positive endomysial antibody in a second blood sample, the positive predictive value for celiac disease is virtually 100%.” But for adults, they recommend confirmatory histologic analysis of duodenal biopsies with Marsh classification, counting of lymphocytes per high-power field, and morphometry.
Transglutaminase-2 is the major autoantigen present in celiac disease and can now be assessed with accurate, convenient, high-throughput tests, such as enzyme-linked immunosorbent assays. To maximize test TG2-IgA accuracy, Dr. Husby and his associates recommend testing patients who have compatible signs and symptoms of celiac disease or are asymptomatic but have other risk factors, such as confirmed autoimmune diseases (type 1 diabetes, autoimmune thyroid or liver diseases), chromosome abnormalities (Down or Turner syndrome), or first-degree relatives with celiac disease.
Several other serologic tests are available but have a more limited role in diagnosing celiac disease, according to the practice update. Perhaps most useful is the endomysial antibody (EMA) test, which evaluates tissue-bound TG2-IgA. This test is highly specific but labor-intensive and user-sensitive and thus is best used to confirm a positive TG2-IgA result. Deamidated gliadin peptide antibody assays are less accurate than TG2-IgA, while HLA-DQ2/DQ8 testing is best reserved for cases where the diagnosis is complicated by a prior gluten-free diet or inconclusive antibody titers or histology.
For adults from populations with less than a 5% prevalence of celiac disease, all guidelines recommend following serology with confirmatory biopsy, and the experts concur. If biopsy was part of the initial work-up, they recommend performing confirmatory serology before starting a gluten-free diet. If the biopsy was negative but celiac disease is strongly suspected, they recommend TG2-IgA testing followed by repeat biopsies, when possible, either at the same time or in the future.
For children with suspected celiac disease, the North American Society for Pediatric Gastroenterology Hepatology and Nutrition recommends starting with biopsy, while the European Society for Paediatric Gastroenterology Hepatology and Nutrition suggests starting with quantitative TG2-IgA testing, followed by TG2-IgA, EMA, or HLA-DQ2/DQ8 assays if TG2-IgA is 10 times higher than the upper limit of normal. However, EGD with biopsies and even a gluten challenge may be needed if serology results are unclear, the experts state. They recommend against gluten-free or low-gluten diets prior to diagnosis, since these can lower the sensitivity of both histology and serology. If a patient has unclear test results and is already on a gluten-free diet, they suggest resuming eating three slices of wheat bread daily for 1-3 months, followed by TG2-IgA testing.
A small but important subgroup of patients have strong suspicion for celiac disease but are negative on IgA isotype tests because of IgA deficiency. In such suspected cases, the experts recommend measuring total IgA, IgG deamidated gliadin antibodies, and TG2-IgG levels. They note that IgG isotype testing for TG2 antibodies is not celiac specific outside the setting of IgA deficiency.
Serology has a useful but more limited role in managing celiac disease, according to the practice update. Negative TG2-IgA and other serology does not guarantee that the intestinal mucosa has healed, so patients with ongoing or relapsing symptoms without another obvious cause should have repeat biopsies. However, serology that stays positive over time usually indicates ongoing mucosal damage and gluten exposure, so these follow-up tests are appropriate 6 and 12 months after diagnosing celiac disease and yearly thereafter.
Dr. Husby reported receiving grant support from the University of Southern Denmark, the Region of Southern Denmark, and the Novo Nordisk Research Fund. He also reported receiving payments from Thermo Fisher Scientific and an advisory relationship with Inova. Two coauthors reported ties to Alba Therapeutics, Celimmune, Intrexon, GlaxoSmithKline, and several other pharmaceutical companies.
SOURCE: Husby S et al. Gastroenterology. 2018 Dec 19. doi: 10.1053/j.gastro.2018.12.010.
For children and adolescents with strong clinical suspicion for celiac disease, repeated transglutaminase-2-IgA (TG2-IgA) levels that are more than 10 times higher than the upper limit of normal often suffices for diagnosis, according to an American Gastroenterological Association clinical practice update and expert review.
This approach precludes the need for esophagogastroduodenoscopy (EGD) in about 30%-50% of cases, wrote Steffen Husby, MD, PhD, of Odense University Hospital (Denmark), together with his associates in Gastroenterology. “When such a strongly positive TG2-IgA is combined with a positive endomysial antibody in a second blood sample, the positive predictive value for celiac disease is virtually 100%.” But for adults, they recommend confirmatory histologic analysis of duodenal biopsies with Marsh classification, counting of lymphocytes per high-power field, and morphometry.
Transglutaminase-2 is the major autoantigen present in celiac disease and can now be assessed with accurate, convenient, high-throughput tests, such as enzyme-linked immunosorbent assays. To maximize test TG2-IgA accuracy, Dr. Husby and his associates recommend testing patients who have compatible signs and symptoms of celiac disease or are asymptomatic but have other risk factors, such as confirmed autoimmune diseases (type 1 diabetes, autoimmune thyroid or liver diseases), chromosome abnormalities (Down or Turner syndrome), or first-degree relatives with celiac disease.
Several other serologic tests are available but have a more limited role in diagnosing celiac disease, according to the practice update. Perhaps most useful is the endomysial antibody (EMA) test, which evaluates tissue-bound TG2-IgA. This test is highly specific but labor-intensive and user-sensitive and thus is best used to confirm a positive TG2-IgA result. Deamidated gliadin peptide antibody assays are less accurate than TG2-IgA, while HLA-DQ2/DQ8 testing is best reserved for cases where the diagnosis is complicated by a prior gluten-free diet or inconclusive antibody titers or histology.
For adults from populations with less than a 5% prevalence of celiac disease, all guidelines recommend following serology with confirmatory biopsy, and the experts concur. If biopsy was part of the initial work-up, they recommend performing confirmatory serology before starting a gluten-free diet. If the biopsy was negative but celiac disease is strongly suspected, they recommend TG2-IgA testing followed by repeat biopsies, when possible, either at the same time or in the future.
For children with suspected celiac disease, the North American Society for Pediatric Gastroenterology Hepatology and Nutrition recommends starting with biopsy, while the European Society for Paediatric Gastroenterology Hepatology and Nutrition suggests starting with quantitative TG2-IgA testing, followed by TG2-IgA, EMA, or HLA-DQ2/DQ8 assays if TG2-IgA is 10 times higher than the upper limit of normal. However, EGD with biopsies and even a gluten challenge may be needed if serology results are unclear, the experts state. They recommend against gluten-free or low-gluten diets prior to diagnosis, since these can lower the sensitivity of both histology and serology. If a patient has unclear test results and is already on a gluten-free diet, they suggest resuming eating three slices of wheat bread daily for 1-3 months, followed by TG2-IgA testing.
A small but important subgroup of patients have strong suspicion for celiac disease but are negative on IgA isotype tests because of IgA deficiency. In such suspected cases, the experts recommend measuring total IgA, IgG deamidated gliadin antibodies, and TG2-IgG levels. They note that IgG isotype testing for TG2 antibodies is not celiac specific outside the setting of IgA deficiency.
Serology has a useful but more limited role in managing celiac disease, according to the practice update. Negative TG2-IgA and other serology does not guarantee that the intestinal mucosa has healed, so patients with ongoing or relapsing symptoms without another obvious cause should have repeat biopsies. However, serology that stays positive over time usually indicates ongoing mucosal damage and gluten exposure, so these follow-up tests are appropriate 6 and 12 months after diagnosing celiac disease and yearly thereafter.
Dr. Husby reported receiving grant support from the University of Southern Denmark, the Region of Southern Denmark, and the Novo Nordisk Research Fund. He also reported receiving payments from Thermo Fisher Scientific and an advisory relationship with Inova. Two coauthors reported ties to Alba Therapeutics, Celimmune, Intrexon, GlaxoSmithKline, and several other pharmaceutical companies.
SOURCE: Husby S et al. Gastroenterology. 2018 Dec 19. doi: 10.1053/j.gastro.2018.12.010.
For children and adolescents with strong clinical suspicion for celiac disease, repeated transglutaminase-2-IgA (TG2-IgA) levels that are more than 10 times higher than the upper limit of normal often suffices for diagnosis, according to an American Gastroenterological Association clinical practice update and expert review.
This approach precludes the need for esophagogastroduodenoscopy (EGD) in about 30%-50% of cases, wrote Steffen Husby, MD, PhD, of Odense University Hospital (Denmark), together with his associates in Gastroenterology. “When such a strongly positive TG2-IgA is combined with a positive endomysial antibody in a second blood sample, the positive predictive value for celiac disease is virtually 100%.” But for adults, they recommend confirmatory histologic analysis of duodenal biopsies with Marsh classification, counting of lymphocytes per high-power field, and morphometry.
Transglutaminase-2 is the major autoantigen present in celiac disease and can now be assessed with accurate, convenient, high-throughput tests, such as enzyme-linked immunosorbent assays. To maximize test TG2-IgA accuracy, Dr. Husby and his associates recommend testing patients who have compatible signs and symptoms of celiac disease or are asymptomatic but have other risk factors, such as confirmed autoimmune diseases (type 1 diabetes, autoimmune thyroid or liver diseases), chromosome abnormalities (Down or Turner syndrome), or first-degree relatives with celiac disease.
Several other serologic tests are available but have a more limited role in diagnosing celiac disease, according to the practice update. Perhaps most useful is the endomysial antibody (EMA) test, which evaluates tissue-bound TG2-IgA. This test is highly specific but labor-intensive and user-sensitive and thus is best used to confirm a positive TG2-IgA result. Deamidated gliadin peptide antibody assays are less accurate than TG2-IgA, while HLA-DQ2/DQ8 testing is best reserved for cases where the diagnosis is complicated by a prior gluten-free diet or inconclusive antibody titers or histology.
For adults from populations with less than a 5% prevalence of celiac disease, all guidelines recommend following serology with confirmatory biopsy, and the experts concur. If biopsy was part of the initial work-up, they recommend performing confirmatory serology before starting a gluten-free diet. If the biopsy was negative but celiac disease is strongly suspected, they recommend TG2-IgA testing followed by repeat biopsies, when possible, either at the same time or in the future.
For children with suspected celiac disease, the North American Society for Pediatric Gastroenterology Hepatology and Nutrition recommends starting with biopsy, while the European Society for Paediatric Gastroenterology Hepatology and Nutrition suggests starting with quantitative TG2-IgA testing, followed by TG2-IgA, EMA, or HLA-DQ2/DQ8 assays if TG2-IgA is 10 times higher than the upper limit of normal. However, EGD with biopsies and even a gluten challenge may be needed if serology results are unclear, the experts state. They recommend against gluten-free or low-gluten diets prior to diagnosis, since these can lower the sensitivity of both histology and serology. If a patient has unclear test results and is already on a gluten-free diet, they suggest resuming eating three slices of wheat bread daily for 1-3 months, followed by TG2-IgA testing.
A small but important subgroup of patients have strong suspicion for celiac disease but are negative on IgA isotype tests because of IgA deficiency. In such suspected cases, the experts recommend measuring total IgA, IgG deamidated gliadin antibodies, and TG2-IgG levels. They note that IgG isotype testing for TG2 antibodies is not celiac specific outside the setting of IgA deficiency.
Serology has a useful but more limited role in managing celiac disease, according to the practice update. Negative TG2-IgA and other serology does not guarantee that the intestinal mucosa has healed, so patients with ongoing or relapsing symptoms without another obvious cause should have repeat biopsies. However, serology that stays positive over time usually indicates ongoing mucosal damage and gluten exposure, so these follow-up tests are appropriate 6 and 12 months after diagnosing celiac disease and yearly thereafter.
Dr. Husby reported receiving grant support from the University of Southern Denmark, the Region of Southern Denmark, and the Novo Nordisk Research Fund. He also reported receiving payments from Thermo Fisher Scientific and an advisory relationship with Inova. Two coauthors reported ties to Alba Therapeutics, Celimmune, Intrexon, GlaxoSmithKline, and several other pharmaceutical companies.
SOURCE: Husby S et al. Gastroenterology. 2018 Dec 19. doi: 10.1053/j.gastro.2018.12.010.
FROM GASTROENTEROLOGY
Interactive online module improved detection of Barrett’s esophagus neoplasia
An online educational tool for endoscopists helped improve their detection of Barrett’s esophagus–related neoplasia (BORN), researchers reported in the April issue of Gastroenterology.
In tests administered before and after training, endoscopists increased their rates of BORN detection by a median of 30% (P less than .001), reported J.J. Bergman, MD, PhD, of the University of Amsterdam, together with his associates. “To our knowledge, this is the first validated online, interactive endoscopic training program in our field,” they wrote. “Widespread use of this tool might improve management of Barrett’s esophagus by general endoscopists.”
To develop the program, the investigators recorded high-definition videos of upper endoscopies of patients with either BORN or nondysplastic Barrett’s esophagus. They sent these videos to three experts, who used special tools to superimpose their delineations of lesions.
Next, 68 general endoscopists (fellows, early-career general gastroenterologists, and senior general gastroenterologists) watched four batches of 20 videos each. The researchers compared the assessors’ interpretations with the experts’ to identify the 25 videos with the most educational impact. These were then shown in four batches of five to 121 new assessors (five videos were reserved for pre- and post testing).
From the first to the fourth batch of training videos, assessors sequentially improved their scores for detection, delineation, agreement delineation, and relative delineation of BORN, the researchers said. Among the 121 assessors in the second phase of development, median rates of detection of BORN rose by 30% after training. Furthermore, from baseline to the end of the study, scores rose by 46% for detection, 129% for delineation, 105% for agreement delineation, and 106% for relative delineation (all P less than .001). These improvements did not depend on the country of origin of the assessors or their level of endoscopic experience.
This module requires the use of high-definition videos whose resolution is not lost during replay or when viewed on the web, the researchers emphasized. They noted that the module is active, not passive – learners select the video frame to position a biopsy mark and delineate the lesion, and the software then gives them tailored feedback on their choice. Learners also can add and remove the experts’ delineations as well as their own during feedback sessions at the end of each batch of videos. This enables them to “fully appreciate the subtle appearance of the lesion on the selected time frame,” the investigators wrote.
By completing the training module, “general endoscopists with a wide range of experience and from different countries of origin can substantially and conveniently increase their skills for detection and delineation of early BORN lesions,” they concluded. “Therefore, the module could provide training in an essential upper gastrointestinal endoscopic skill that is not otherwise readily available.”
The investigators disclosed no external funding sources. They reported having no conflicts of interest.
SOURCE: Bergman JJ et al. Gastroenterology. 2019 Jan 2. doi: 10.1053/j.gastro.2018.12.021.
Endoscopic mucosal resection and ablation strategies offer the potential for minimally invasive, curative treatment for patients with Barrett’s esophagus–associated intramucosal neoplasia. For the gastroenterologist interested in endoscopic prevention and management of esophageal cancer, however, achieving proficiency in performance of these endoscopic techniques represents only part of the requisite preparatory experience. Acquisition of cognitive skills in lesion recognition is a fundamental and underappreciated component to a successful endoscopic treatment paradigm.
General endoscopist assessors were grouped into three groups based on level of experience. Following completion of the training module, scores in lesion detection and delineation increased irrespective of level of endoscopist experience.
The module is free, CME-accredited, and available for online use. Any endoscopist who performs Barrett’s screening, surveillance, and therapy should be motivated and incentivized to engage with this important educational tool.
Patrick Yachimski, MD, MPH, AGAF, is associate professor of medicine, director of pancreatobiliary endoscopy, division of gastroenterology, hepatology & nutrition, Vanderbilt University Medical Center, Nashville, Tenn. He has no conflicts.
Endoscopic mucosal resection and ablation strategies offer the potential for minimally invasive, curative treatment for patients with Barrett’s esophagus–associated intramucosal neoplasia. For the gastroenterologist interested in endoscopic prevention and management of esophageal cancer, however, achieving proficiency in performance of these endoscopic techniques represents only part of the requisite preparatory experience. Acquisition of cognitive skills in lesion recognition is a fundamental and underappreciated component to a successful endoscopic treatment paradigm.
General endoscopist assessors were grouped into three groups based on level of experience. Following completion of the training module, scores in lesion detection and delineation increased irrespective of level of endoscopist experience.
The module is free, CME-accredited, and available for online use. Any endoscopist who performs Barrett’s screening, surveillance, and therapy should be motivated and incentivized to engage with this important educational tool.
Patrick Yachimski, MD, MPH, AGAF, is associate professor of medicine, director of pancreatobiliary endoscopy, division of gastroenterology, hepatology & nutrition, Vanderbilt University Medical Center, Nashville, Tenn. He has no conflicts.
Endoscopic mucosal resection and ablation strategies offer the potential for minimally invasive, curative treatment for patients with Barrett’s esophagus–associated intramucosal neoplasia. For the gastroenterologist interested in endoscopic prevention and management of esophageal cancer, however, achieving proficiency in performance of these endoscopic techniques represents only part of the requisite preparatory experience. Acquisition of cognitive skills in lesion recognition is a fundamental and underappreciated component to a successful endoscopic treatment paradigm.
General endoscopist assessors were grouped into three groups based on level of experience. Following completion of the training module, scores in lesion detection and delineation increased irrespective of level of endoscopist experience.
The module is free, CME-accredited, and available for online use. Any endoscopist who performs Barrett’s screening, surveillance, and therapy should be motivated and incentivized to engage with this important educational tool.
Patrick Yachimski, MD, MPH, AGAF, is associate professor of medicine, director of pancreatobiliary endoscopy, division of gastroenterology, hepatology & nutrition, Vanderbilt University Medical Center, Nashville, Tenn. He has no conflicts.
An online educational tool for endoscopists helped improve their detection of Barrett’s esophagus–related neoplasia (BORN), researchers reported in the April issue of Gastroenterology.
In tests administered before and after training, endoscopists increased their rates of BORN detection by a median of 30% (P less than .001), reported J.J. Bergman, MD, PhD, of the University of Amsterdam, together with his associates. “To our knowledge, this is the first validated online, interactive endoscopic training program in our field,” they wrote. “Widespread use of this tool might improve management of Barrett’s esophagus by general endoscopists.”
To develop the program, the investigators recorded high-definition videos of upper endoscopies of patients with either BORN or nondysplastic Barrett’s esophagus. They sent these videos to three experts, who used special tools to superimpose their delineations of lesions.
Next, 68 general endoscopists (fellows, early-career general gastroenterologists, and senior general gastroenterologists) watched four batches of 20 videos each. The researchers compared the assessors’ interpretations with the experts’ to identify the 25 videos with the most educational impact. These were then shown in four batches of five to 121 new assessors (five videos were reserved for pre- and post testing).
From the first to the fourth batch of training videos, assessors sequentially improved their scores for detection, delineation, agreement delineation, and relative delineation of BORN, the researchers said. Among the 121 assessors in the second phase of development, median rates of detection of BORN rose by 30% after training. Furthermore, from baseline to the end of the study, scores rose by 46% for detection, 129% for delineation, 105% for agreement delineation, and 106% for relative delineation (all P less than .001). These improvements did not depend on the country of origin of the assessors or their level of endoscopic experience.
This module requires the use of high-definition videos whose resolution is not lost during replay or when viewed on the web, the researchers emphasized. They noted that the module is active, not passive – learners select the video frame to position a biopsy mark and delineate the lesion, and the software then gives them tailored feedback on their choice. Learners also can add and remove the experts’ delineations as well as their own during feedback sessions at the end of each batch of videos. This enables them to “fully appreciate the subtle appearance of the lesion on the selected time frame,” the investigators wrote.
By completing the training module, “general endoscopists with a wide range of experience and from different countries of origin can substantially and conveniently increase their skills for detection and delineation of early BORN lesions,” they concluded. “Therefore, the module could provide training in an essential upper gastrointestinal endoscopic skill that is not otherwise readily available.”
The investigators disclosed no external funding sources. They reported having no conflicts of interest.
SOURCE: Bergman JJ et al. Gastroenterology. 2019 Jan 2. doi: 10.1053/j.gastro.2018.12.021.
An online educational tool for endoscopists helped improve their detection of Barrett’s esophagus–related neoplasia (BORN), researchers reported in the April issue of Gastroenterology.
In tests administered before and after training, endoscopists increased their rates of BORN detection by a median of 30% (P less than .001), reported J.J. Bergman, MD, PhD, of the University of Amsterdam, together with his associates. “To our knowledge, this is the first validated online, interactive endoscopic training program in our field,” they wrote. “Widespread use of this tool might improve management of Barrett’s esophagus by general endoscopists.”
To develop the program, the investigators recorded high-definition videos of upper endoscopies of patients with either BORN or nondysplastic Barrett’s esophagus. They sent these videos to three experts, who used special tools to superimpose their delineations of lesions.
Next, 68 general endoscopists (fellows, early-career general gastroenterologists, and senior general gastroenterologists) watched four batches of 20 videos each. The researchers compared the assessors’ interpretations with the experts’ to identify the 25 videos with the most educational impact. These were then shown in four batches of five to 121 new assessors (five videos were reserved for pre- and post testing).
From the first to the fourth batch of training videos, assessors sequentially improved their scores for detection, delineation, agreement delineation, and relative delineation of BORN, the researchers said. Among the 121 assessors in the second phase of development, median rates of detection of BORN rose by 30% after training. Furthermore, from baseline to the end of the study, scores rose by 46% for detection, 129% for delineation, 105% for agreement delineation, and 106% for relative delineation (all P less than .001). These improvements did not depend on the country of origin of the assessors or their level of endoscopic experience.
This module requires the use of high-definition videos whose resolution is not lost during replay or when viewed on the web, the researchers emphasized. They noted that the module is active, not passive – learners select the video frame to position a biopsy mark and delineate the lesion, and the software then gives them tailored feedback on their choice. Learners also can add and remove the experts’ delineations as well as their own during feedback sessions at the end of each batch of videos. This enables them to “fully appreciate the subtle appearance of the lesion on the selected time frame,” the investigators wrote.
By completing the training module, “general endoscopists with a wide range of experience and from different countries of origin can substantially and conveniently increase their skills for detection and delineation of early BORN lesions,” they concluded. “Therefore, the module could provide training in an essential upper gastrointestinal endoscopic skill that is not otherwise readily available.”
The investigators disclosed no external funding sources. They reported having no conflicts of interest.
SOURCE: Bergman JJ et al. Gastroenterology. 2019 Jan 2. doi: 10.1053/j.gastro.2018.12.021.
FROM GASTROENTEROLOGY