User login
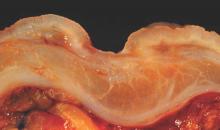
Four genes linked to phenotypic traits of Crohn’s disease
Four gene loci in patients with Crohn’s disease were significantly linked with phenotypic traits such as erythema nodosum or having a complicated or mild course of disease, researchers reported in the April issue of Gastroenterology (doi:10.1053/j.gastro.2014.12.030).
The work is the first genome-wide study to link specific genetic loci with clinically relevant traits in patients with Crohn’s disease (CD), said Dr. Arnald Alonso at the Vall d’Hebron Research Institute and the University of Catalonia in Barcelona and his associates. “Importantly, these new loci have not been previously described as risk factors for CD,” the researchers said. “Our results therefore demonstrate the existence of a genetic component for disease heterogeneity that is independent of the genetic variation associated with the susceptibility to Crohn’s disease.”
Crohn’s disease varies greatly in terms of severity, location of pathology, complications, and other factors. Genome-wide association studies have linked 140 genetic “risk loci” with susceptibility to CD, but past work has only found one gene locus (NOD2) that is definitively linked a single clinical trait of CD (ileal pathology), the investigators noted. For their genome-wide association study, they genotyped 576,818 single nucleotide polymorphisms in a discovery cohort of 1,090 CD patients of European ancestry who presented at university hospitals in Spain between 2007 and 2010, as well as 1,493 healthy controls. They examined associations between these genetic markers and 17 characteristics (or phenotypes) of CD related to disease location, disease behavior and course, age at onset, and extra-intestinal manifestations of CD. Next, the investigators studied a separate “replication” cohort of 1,296 CD patients in order to assess the 57 markers that had been most strongly associated (P < .0002) with CD phenotypes among the discovery cohort (Gastroenterology, http://www.gastrojournal.org/article/S0016-5085(14)01582-0/abstract).
These combined analyses showed that clinical phenotypes in CD were most significantly linked with four markers, including MAGI1, CLCA2, 2q24.1, and LY75, reported the investigators. The MAGI1 gene was found to predict complicated structuring disease course and stricturing behavior in CD, although it did not appear to speed its onset, they said. The gene encodes proteins that have been found to play an important role in the tight junctions between epithelial cells, and consequently in intestinal barrier function, they noted, adding that disruption of that mucosal integrity contributes to the pathogenesis of ulcerative colitis and CD. “Importantly, an increased intestinal permeability has been described in patients with active CD as well as in their first-degree relatives,” they added. “This evidence strongly suggests that increased intestinal permeability is not only a consequence of intestinal inflammation occurring in CD patients, but it is rather a risk factor for CD.”
The other three loci that were significantly associated with CD traits predicted ileal involvement (CLCA2), erythema nodosum (LY75), and having a mild disease course (2q24.1), the researchers reported. Taken together, the findings “indicate a genetic basis for the clinical heterogeneity observed for this inflammatory bowel disease,” concluded Dr. Alonso and his associates. “Further functional studies of these new loci will provide a better understanding of the biological mechanisms that are involved in the development of these relevant clinical phenotypes.”
The Spanish Ministry of Economy and Competitiveness funded the study. The investigators reported having no relevant financial disclosures.
Four gene loci in patients with Crohn’s disease were significantly linked with phenotypic traits such as erythema nodosum or having a complicated or mild course of disease, researchers reported in the April issue of Gastroenterology (doi:10.1053/j.gastro.2014.12.030).
The work is the first genome-wide study to link specific genetic loci with clinically relevant traits in patients with Crohn’s disease (CD), said Dr. Arnald Alonso at the Vall d’Hebron Research Institute and the University of Catalonia in Barcelona and his associates. “Importantly, these new loci have not been previously described as risk factors for CD,” the researchers said. “Our results therefore demonstrate the existence of a genetic component for disease heterogeneity that is independent of the genetic variation associated with the susceptibility to Crohn’s disease.”
Crohn’s disease varies greatly in terms of severity, location of pathology, complications, and other factors. Genome-wide association studies have linked 140 genetic “risk loci” with susceptibility to CD, but past work has only found one gene locus (NOD2) that is definitively linked a single clinical trait of CD (ileal pathology), the investigators noted. For their genome-wide association study, they genotyped 576,818 single nucleotide polymorphisms in a discovery cohort of 1,090 CD patients of European ancestry who presented at university hospitals in Spain between 2007 and 2010, as well as 1,493 healthy controls. They examined associations between these genetic markers and 17 characteristics (or phenotypes) of CD related to disease location, disease behavior and course, age at onset, and extra-intestinal manifestations of CD. Next, the investigators studied a separate “replication” cohort of 1,296 CD patients in order to assess the 57 markers that had been most strongly associated (P < .0002) with CD phenotypes among the discovery cohort (Gastroenterology, http://www.gastrojournal.org/article/S0016-5085(14)01582-0/abstract).
These combined analyses showed that clinical phenotypes in CD were most significantly linked with four markers, including MAGI1, CLCA2, 2q24.1, and LY75, reported the investigators. The MAGI1 gene was found to predict complicated structuring disease course and stricturing behavior in CD, although it did not appear to speed its onset, they said. The gene encodes proteins that have been found to play an important role in the tight junctions between epithelial cells, and consequently in intestinal barrier function, they noted, adding that disruption of that mucosal integrity contributes to the pathogenesis of ulcerative colitis and CD. “Importantly, an increased intestinal permeability has been described in patients with active CD as well as in their first-degree relatives,” they added. “This evidence strongly suggests that increased intestinal permeability is not only a consequence of intestinal inflammation occurring in CD patients, but it is rather a risk factor for CD.”
The other three loci that were significantly associated with CD traits predicted ileal involvement (CLCA2), erythema nodosum (LY75), and having a mild disease course (2q24.1), the researchers reported. Taken together, the findings “indicate a genetic basis for the clinical heterogeneity observed for this inflammatory bowel disease,” concluded Dr. Alonso and his associates. “Further functional studies of these new loci will provide a better understanding of the biological mechanisms that are involved in the development of these relevant clinical phenotypes.”
The Spanish Ministry of Economy and Competitiveness funded the study. The investigators reported having no relevant financial disclosures.
Four gene loci in patients with Crohn’s disease were significantly linked with phenotypic traits such as erythema nodosum or having a complicated or mild course of disease, researchers reported in the April issue of Gastroenterology (doi:10.1053/j.gastro.2014.12.030).
The work is the first genome-wide study to link specific genetic loci with clinically relevant traits in patients with Crohn’s disease (CD), said Dr. Arnald Alonso at the Vall d’Hebron Research Institute and the University of Catalonia in Barcelona and his associates. “Importantly, these new loci have not been previously described as risk factors for CD,” the researchers said. “Our results therefore demonstrate the existence of a genetic component for disease heterogeneity that is independent of the genetic variation associated with the susceptibility to Crohn’s disease.”
Crohn’s disease varies greatly in terms of severity, location of pathology, complications, and other factors. Genome-wide association studies have linked 140 genetic “risk loci” with susceptibility to CD, but past work has only found one gene locus (NOD2) that is definitively linked a single clinical trait of CD (ileal pathology), the investigators noted. For their genome-wide association study, they genotyped 576,818 single nucleotide polymorphisms in a discovery cohort of 1,090 CD patients of European ancestry who presented at university hospitals in Spain between 2007 and 2010, as well as 1,493 healthy controls. They examined associations between these genetic markers and 17 characteristics (or phenotypes) of CD related to disease location, disease behavior and course, age at onset, and extra-intestinal manifestations of CD. Next, the investigators studied a separate “replication” cohort of 1,296 CD patients in order to assess the 57 markers that had been most strongly associated (P < .0002) with CD phenotypes among the discovery cohort (Gastroenterology, http://www.gastrojournal.org/article/S0016-5085(14)01582-0/abstract).
These combined analyses showed that clinical phenotypes in CD were most significantly linked with four markers, including MAGI1, CLCA2, 2q24.1, and LY75, reported the investigators. The MAGI1 gene was found to predict complicated structuring disease course and stricturing behavior in CD, although it did not appear to speed its onset, they said. The gene encodes proteins that have been found to play an important role in the tight junctions between epithelial cells, and consequently in intestinal barrier function, they noted, adding that disruption of that mucosal integrity contributes to the pathogenesis of ulcerative colitis and CD. “Importantly, an increased intestinal permeability has been described in patients with active CD as well as in their first-degree relatives,” they added. “This evidence strongly suggests that increased intestinal permeability is not only a consequence of intestinal inflammation occurring in CD patients, but it is rather a risk factor for CD.”
The other three loci that were significantly associated with CD traits predicted ileal involvement (CLCA2), erythema nodosum (LY75), and having a mild disease course (2q24.1), the researchers reported. Taken together, the findings “indicate a genetic basis for the clinical heterogeneity observed for this inflammatory bowel disease,” concluded Dr. Alonso and his associates. “Further functional studies of these new loci will provide a better understanding of the biological mechanisms that are involved in the development of these relevant clinical phenotypes.”
The Spanish Ministry of Economy and Competitiveness funded the study. The investigators reported having no relevant financial disclosures.
FROM GASTROENTEROLOGY
Key clinical point: Four gene loci in patients with Crohn’s disease (CD) were significantly linked with phenotypic traits of the disease.
Major finding: The genes were associated with complicated structuring disease course and stricturing behavior (MAGI1), ileal involvement (CLCA2), erythema nodosum (LY75), and having a mild disease course (2q24.1).
Data source: Genome-wide association study of two cohorts of 1,090 and 1,296 CD patients, and 1,493 controls.
Disclosures: The Spanish Ministry of Economy and Competitiveness funded the study. The investigators reported having no relevant financial disclosures.
Two-thirds of endoscopists met colonic adenoma detection benchmarks
Two-thirds of endoscopists met national quality benchmarks for detecting colonic adenomas, but detection rates varied eightfold among male patients and 27-fold among female patients, according to a retrospective community-based cohort study.
These ranges narrowed somewhat when researchers controlled for patient-specific factors, such as age and sex, said Dr. Christopher Jensen and his associates at Kaiser Permanente Division of Research in Oakland, Calif. But researchers found that adjusting for those variables had little effect on how endoscopists ranked in terms of adenoma detection rates (ADRs) compared with their peers. Based on those findings, evaluators probably only need to account for patient demographics when comparing ADRs for endoscopists who tend to see very distinct types of patients, the investigators wrote in the April issue of Clinical Gastroenterology and Hepatology 2014 Oct 25. (doi:10.1016/j.cgh.2014.10.020).
Colorectal cancer remains the second leading cause of cancer mortality in the United States, and prevention hinges on detecting and removing precancerous adenomatous polyps of the colon. For this reason, organizations such as the U.S. Multi-Society Task Force on Colorectal Cancer and the U.S. Centers for Medicaid and Medicare Services have recommended benchmark ADRs of at least 25% for male patients and 15% for female patients. Although some studies have examined how characteristics of physicians and their practices affect ADRs, none have previously assessed effects of patient-specific variables, Dr. Jensen and his associates said (Clin. Gastroenterol. Hepatol. http://www.ncbi.nlm.nih.gov/pubmed/25445767.
The investigators retrospectively studied 108,662 colonoscopies and 20,792 screening colonoscopies carried out by 102 endoscopists at Kaiser Permanente Northern California between 2006 and 2008. They calculated ADRs for each physician before and after they adjusted for the patients’ age, sex, race/ethnicity, and family history of colorectal cancer.
Source: American Gastroenterological Association
In all, 67% of examiners met the gastrointestinal society guidelines for ADRs in male patients, and 68% met guidelines for female patients, the researchers found. But ADRs among the examiners ranged widely – from 7.7% to 61.5% for male patients and from 1.7% to 45.6% for females, the investigators said. Adjustments for patient demographics and family history of colorectal cancer cut the variation from 8-fold down to 3-fold for male patients, and from 27-fold to 5-fold for females. However, physicians’ absolute rankings among their peers remained similar before and after controlling for patient case mix. “Moderate differences in patient demographics between physicians are unlikely to substantially change rates of adenoma detection,” concluded Dr. Jensen and his associates. “The findings raise the question of whether adenoma detection rates should routinely be adjusted for case mix,” they added. “The need for adjustment will likely depend on the degree of variation between physicians in patient case mix, and how rates are used as a performance metric. Adjusted rates would likely only be needed in settings where physicians had very different patient demographics relative to sex and age.”
The study was funded by the Kaiser Permanente Community Benefits program, the National Cancer Institute, and the National Institute of Diabetes and Digestive and Kidney Diseases. The investigators reported having no relevant financial disclosures.
Two-thirds of endoscopists met national quality benchmarks for detecting colonic adenomas, but detection rates varied eightfold among male patients and 27-fold among female patients, according to a retrospective community-based cohort study.
These ranges narrowed somewhat when researchers controlled for patient-specific factors, such as age and sex, said Dr. Christopher Jensen and his associates at Kaiser Permanente Division of Research in Oakland, Calif. But researchers found that adjusting for those variables had little effect on how endoscopists ranked in terms of adenoma detection rates (ADRs) compared with their peers. Based on those findings, evaluators probably only need to account for patient demographics when comparing ADRs for endoscopists who tend to see very distinct types of patients, the investigators wrote in the April issue of Clinical Gastroenterology and Hepatology 2014 Oct 25. (doi:10.1016/j.cgh.2014.10.020).
Colorectal cancer remains the second leading cause of cancer mortality in the United States, and prevention hinges on detecting and removing precancerous adenomatous polyps of the colon. For this reason, organizations such as the U.S. Multi-Society Task Force on Colorectal Cancer and the U.S. Centers for Medicaid and Medicare Services have recommended benchmark ADRs of at least 25% for male patients and 15% for female patients. Although some studies have examined how characteristics of physicians and their practices affect ADRs, none have previously assessed effects of patient-specific variables, Dr. Jensen and his associates said (Clin. Gastroenterol. Hepatol. http://www.ncbi.nlm.nih.gov/pubmed/25445767.
The investigators retrospectively studied 108,662 colonoscopies and 20,792 screening colonoscopies carried out by 102 endoscopists at Kaiser Permanente Northern California between 2006 and 2008. They calculated ADRs for each physician before and after they adjusted for the patients’ age, sex, race/ethnicity, and family history of colorectal cancer.
Source: American Gastroenterological Association
In all, 67% of examiners met the gastrointestinal society guidelines for ADRs in male patients, and 68% met guidelines for female patients, the researchers found. But ADRs among the examiners ranged widely – from 7.7% to 61.5% for male patients and from 1.7% to 45.6% for females, the investigators said. Adjustments for patient demographics and family history of colorectal cancer cut the variation from 8-fold down to 3-fold for male patients, and from 27-fold to 5-fold for females. However, physicians’ absolute rankings among their peers remained similar before and after controlling for patient case mix. “Moderate differences in patient demographics between physicians are unlikely to substantially change rates of adenoma detection,” concluded Dr. Jensen and his associates. “The findings raise the question of whether adenoma detection rates should routinely be adjusted for case mix,” they added. “The need for adjustment will likely depend on the degree of variation between physicians in patient case mix, and how rates are used as a performance metric. Adjusted rates would likely only be needed in settings where physicians had very different patient demographics relative to sex and age.”
The study was funded by the Kaiser Permanente Community Benefits program, the National Cancer Institute, and the National Institute of Diabetes and Digestive and Kidney Diseases. The investigators reported having no relevant financial disclosures.
Two-thirds of endoscopists met national quality benchmarks for detecting colonic adenomas, but detection rates varied eightfold among male patients and 27-fold among female patients, according to a retrospective community-based cohort study.
These ranges narrowed somewhat when researchers controlled for patient-specific factors, such as age and sex, said Dr. Christopher Jensen and his associates at Kaiser Permanente Division of Research in Oakland, Calif. But researchers found that adjusting for those variables had little effect on how endoscopists ranked in terms of adenoma detection rates (ADRs) compared with their peers. Based on those findings, evaluators probably only need to account for patient demographics when comparing ADRs for endoscopists who tend to see very distinct types of patients, the investigators wrote in the April issue of Clinical Gastroenterology and Hepatology 2014 Oct 25. (doi:10.1016/j.cgh.2014.10.020).
Colorectal cancer remains the second leading cause of cancer mortality in the United States, and prevention hinges on detecting and removing precancerous adenomatous polyps of the colon. For this reason, organizations such as the U.S. Multi-Society Task Force on Colorectal Cancer and the U.S. Centers for Medicaid and Medicare Services have recommended benchmark ADRs of at least 25% for male patients and 15% for female patients. Although some studies have examined how characteristics of physicians and their practices affect ADRs, none have previously assessed effects of patient-specific variables, Dr. Jensen and his associates said (Clin. Gastroenterol. Hepatol. http://www.ncbi.nlm.nih.gov/pubmed/25445767.
The investigators retrospectively studied 108,662 colonoscopies and 20,792 screening colonoscopies carried out by 102 endoscopists at Kaiser Permanente Northern California between 2006 and 2008. They calculated ADRs for each physician before and after they adjusted for the patients’ age, sex, race/ethnicity, and family history of colorectal cancer.
Source: American Gastroenterological Association
In all, 67% of examiners met the gastrointestinal society guidelines for ADRs in male patients, and 68% met guidelines for female patients, the researchers found. But ADRs among the examiners ranged widely – from 7.7% to 61.5% for male patients and from 1.7% to 45.6% for females, the investigators said. Adjustments for patient demographics and family history of colorectal cancer cut the variation from 8-fold down to 3-fold for male patients, and from 27-fold to 5-fold for females. However, physicians’ absolute rankings among their peers remained similar before and after controlling for patient case mix. “Moderate differences in patient demographics between physicians are unlikely to substantially change rates of adenoma detection,” concluded Dr. Jensen and his associates. “The findings raise the question of whether adenoma detection rates should routinely be adjusted for case mix,” they added. “The need for adjustment will likely depend on the degree of variation between physicians in patient case mix, and how rates are used as a performance metric. Adjusted rates would likely only be needed in settings where physicians had very different patient demographics relative to sex and age.”
The study was funded by the Kaiser Permanente Community Benefits program, the National Cancer Institute, and the National Institute of Diabetes and Digestive and Kidney Diseases. The investigators reported having no relevant financial disclosures.
FROM CLINICAL GASTROENTEROLOGY AND HEPATOLOGY
Key clinical point: About two-thirds of endoscopists met recommended benchmarks for detecting colonic adenomas.
Major finding: About two-thirds of endoscopists met specialist society guidelines for ADRs, and patient demographics had little effect on physician rankings.
Data source: Retrospective, community-based cohort study of 108,662 colonoscopies and 20,792 screening colonoscopies carried out by 102 endoscopists.
Disclosures: The study was funded by the Kaiser Permanente Community Benefits program, the National Cancer Institute, and the National Institute of Diabetes and Digestive and Kidney Diseases. The investigators reported having no relevant financial disclosures.
Study found two-way link between IBD and cervical cancer
Women with Crohn’s disease had about a 53% greater risk of developing cervical cancer compared with controls, and women with inflammatory bowel disease had a significantly greater risk of having had cervical neoplasia years earlier, according to a large population-based study reported in the April issue of Clinical Gastroenterology and Hepatology (http://dx.doi.org/10.1016/j.cgh.2014.07.036).
“We found a two-way association between inflammatory bowel disease, notably Crohn’s disease, and neoplastic lesions of the uterine cervix. This observation is not explained by differences in screening activity,” said Dr. Christine Rungoe at Statens Serum Institut in Copenhagen and her associates. “Patients with IBD should be encouraged to follow the screening program for cervical neoplasia, and clinicians should be aware of the slightly increased risk of HPV-related cervical lesions in IBD patients.”
Studies of IBD and cervical neoplasia have yielded mixed results as to a possible association. Some experts have postulated that underlying immunologic changes or the use of immunosuppressive drugs in IBD could thwart patients’ ability to clear HPV infections, thereby increasing their risk of developing cervical neoplasia. To explore that possibility, Dr. Rungoe and her associates compared rates of cervical dysplasia or cervical cancer among 27,408 women newly diagnosed with ulcerative colitis or Crohn’s disease and 1,508,334 controls without IBD. They identified cases and controls from a national patient registry of about 4 million women living in Denmark during 1979-2011. They also calculated the likelihood of a cervical neoplasia diagnosis preceding IBD.
Source: American Gastroenterological Association
Women with Crohn’s disease had a 26% higher rate of low-grade intraepithelial lesions of the cervix, a 28% greater incidence of high-grade lesions, and a 53% greater risk of cervical cancer compared with controls, the researchers reported (incidence rate ratios and 95% confidence intervals, respectively: 1.26, 1.07-1.48; 1.28, 1.13-1.45; and 1.53, 1.04-2.27). Women with ulcerative colitis also had about a 12%-15% increase in risk of developing cervical dysplasia, compared with controls (IRR for low-grade lesions, 1.15; 95% CI, 1.00-1.32; IRR for high-grade lesions, 1.12; 95% CI, 1.01-1.25), but no significant increase in cervical cancer risk.
Notably, women newly diagnosed with IBD had a “markedly elevated” odds of having been diagnosed with cervical neoplasia up to 10 years beforehand, the investigators reported. “This is a novel finding that may suggest a yet unexplored common susceptibility to IBD and cervical neoplasia, rather than an etiologic role of IBD or its treatment in development of cervical neoplasia,” they said.
Treatment with common IBD therapies such as azathioprine, mesalamine, and corticosteroids did not affect rates of cervical neoplasia, but women with Crohn’s disease who had used tumor necrosis factor–alpha antagonists had an 85% increase in high-grade intraepithelial cervical lesions. They also had a 2% increase in risk of these lesions for each filled prescription for hormonal contraceptives.
The frequency of cervical screening was slightly higher among women with ulcerative colitis, compared with controls, but was similar between controls and women with Crohn’s disease, the investigators noted.
The study was funded in part by the Danish Council of Independent Research. The investigators reported having no relevant financial disclosures.
The possibility that intraepithelial neoplasia or dysplasia of the uterine cervix might occur more frequently in women with inflammatory bowel disease (IBD) was raised almost 10 years ago. It stands to reason that some women with Crohn's disease or ulcerative colitis might be at increased risk of cervical dysplasia - after all, the primary driver of cervical neoplasia is infection with human papillomavirus, many patients with IBD are on drugs that suppress the immune system, and other immunosuppressive states (for example, HIV infection, post organ transplant) have been associated with higher rates of cervical dysplasia and cancer. However, the results of studies on this question have been conflicting.
These researchers from the Statens Serum Institut in Copenhagen have harnessed the power of the nationwide Danish medical informatics system to answer many epidemiologic questions about various aspects of IBD. The researchers identified a cohort of more than 18,000 women with ulcerative colitis, more than 8,000 women with Crohn's, and more than 1.5 million women with neither, and "followed" them through a pathology registry for cervical dysplasia and through a cancer registry for cervical cancer. Access to a prescription registry allowed stratification of risk based on medication use. Careful review of the methods section of the paper suggests that this study was well designed and executed.
Women with ulcerative colitis were about 15% more likely than controls to develop dysplasia, but the cancer risk was not increased. Women with Crohn's disease were about 25% more likely to develop dysplasia relative to controls and more than 50% more likely to develop cervical cancer. There were no significant differences in neoplasia risk when stratified by medication use, although there were trends toward increased risk of high-grade cervical dysplasia in women with Crohn's disease who were prescribed azathioprine or anti-tumor necrosis factor agents. Interestingly, the risk of cervical neoplasia was elevated in women well before the diagnosis of IBD.
The study confirms that there is an elevated risk of cervical dysplasia and cancer among women with IBD, and that the risk seems slightly higher in those with Crohn's disease. The finding of the increased risk of neoplasia well before the diagnosis of IBD suggests that perhaps a relative state of immunosuppression exists in patients who are ultimately diagnosed with IBD. In some respects, I found this to be the most intriguing aspect of the paper, and it needs to be explored further in both prospective and retrospective studies.
Dr. Edward V. Loftus Jr., AGAF is professor of medicine and director of the inflammatory bowel disease interest group, division of gastroenterology and hepatology, at the Mayo Clinic, Rochester, Minn. He has consulted for and received research support from UCB, AbbVie, and Janssen.
The possibility that intraepithelial neoplasia or dysplasia of the uterine cervix might occur more frequently in women with inflammatory bowel disease (IBD) was raised almost 10 years ago. It stands to reason that some women with Crohn's disease or ulcerative colitis might be at increased risk of cervical dysplasia - after all, the primary driver of cervical neoplasia is infection with human papillomavirus, many patients with IBD are on drugs that suppress the immune system, and other immunosuppressive states (for example, HIV infection, post organ transplant) have been associated with higher rates of cervical dysplasia and cancer. However, the results of studies on this question have been conflicting.
These researchers from the Statens Serum Institut in Copenhagen have harnessed the power of the nationwide Danish medical informatics system to answer many epidemiologic questions about various aspects of IBD. The researchers identified a cohort of more than 18,000 women with ulcerative colitis, more than 8,000 women with Crohn's, and more than 1.5 million women with neither, and "followed" them through a pathology registry for cervical dysplasia and through a cancer registry for cervical cancer. Access to a prescription registry allowed stratification of risk based on medication use. Careful review of the methods section of the paper suggests that this study was well designed and executed.
Women with ulcerative colitis were about 15% more likely than controls to develop dysplasia, but the cancer risk was not increased. Women with Crohn's disease were about 25% more likely to develop dysplasia relative to controls and more than 50% more likely to develop cervical cancer. There were no significant differences in neoplasia risk when stratified by medication use, although there were trends toward increased risk of high-grade cervical dysplasia in women with Crohn's disease who were prescribed azathioprine or anti-tumor necrosis factor agents. Interestingly, the risk of cervical neoplasia was elevated in women well before the diagnosis of IBD.
The study confirms that there is an elevated risk of cervical dysplasia and cancer among women with IBD, and that the risk seems slightly higher in those with Crohn's disease. The finding of the increased risk of neoplasia well before the diagnosis of IBD suggests that perhaps a relative state of immunosuppression exists in patients who are ultimately diagnosed with IBD. In some respects, I found this to be the most intriguing aspect of the paper, and it needs to be explored further in both prospective and retrospective studies.
Dr. Edward V. Loftus Jr., AGAF is professor of medicine and director of the inflammatory bowel disease interest group, division of gastroenterology and hepatology, at the Mayo Clinic, Rochester, Minn. He has consulted for and received research support from UCB, AbbVie, and Janssen.
The possibility that intraepithelial neoplasia or dysplasia of the uterine cervix might occur more frequently in women with inflammatory bowel disease (IBD) was raised almost 10 years ago. It stands to reason that some women with Crohn's disease or ulcerative colitis might be at increased risk of cervical dysplasia - after all, the primary driver of cervical neoplasia is infection with human papillomavirus, many patients with IBD are on drugs that suppress the immune system, and other immunosuppressive states (for example, HIV infection, post organ transplant) have been associated with higher rates of cervical dysplasia and cancer. However, the results of studies on this question have been conflicting.
These researchers from the Statens Serum Institut in Copenhagen have harnessed the power of the nationwide Danish medical informatics system to answer many epidemiologic questions about various aspects of IBD. The researchers identified a cohort of more than 18,000 women with ulcerative colitis, more than 8,000 women with Crohn's, and more than 1.5 million women with neither, and "followed" them through a pathology registry for cervical dysplasia and through a cancer registry for cervical cancer. Access to a prescription registry allowed stratification of risk based on medication use. Careful review of the methods section of the paper suggests that this study was well designed and executed.
Women with ulcerative colitis were about 15% more likely than controls to develop dysplasia, but the cancer risk was not increased. Women with Crohn's disease were about 25% more likely to develop dysplasia relative to controls and more than 50% more likely to develop cervical cancer. There were no significant differences in neoplasia risk when stratified by medication use, although there were trends toward increased risk of high-grade cervical dysplasia in women with Crohn's disease who were prescribed azathioprine or anti-tumor necrosis factor agents. Interestingly, the risk of cervical neoplasia was elevated in women well before the diagnosis of IBD.
The study confirms that there is an elevated risk of cervical dysplasia and cancer among women with IBD, and that the risk seems slightly higher in those with Crohn's disease. The finding of the increased risk of neoplasia well before the diagnosis of IBD suggests that perhaps a relative state of immunosuppression exists in patients who are ultimately diagnosed with IBD. In some respects, I found this to be the most intriguing aspect of the paper, and it needs to be explored further in both prospective and retrospective studies.
Dr. Edward V. Loftus Jr., AGAF is professor of medicine and director of the inflammatory bowel disease interest group, division of gastroenterology and hepatology, at the Mayo Clinic, Rochester, Minn. He has consulted for and received research support from UCB, AbbVie, and Janssen.
Women with Crohn’s disease had about a 53% greater risk of developing cervical cancer compared with controls, and women with inflammatory bowel disease had a significantly greater risk of having had cervical neoplasia years earlier, according to a large population-based study reported in the April issue of Clinical Gastroenterology and Hepatology (http://dx.doi.org/10.1016/j.cgh.2014.07.036).
“We found a two-way association between inflammatory bowel disease, notably Crohn’s disease, and neoplastic lesions of the uterine cervix. This observation is not explained by differences in screening activity,” said Dr. Christine Rungoe at Statens Serum Institut in Copenhagen and her associates. “Patients with IBD should be encouraged to follow the screening program for cervical neoplasia, and clinicians should be aware of the slightly increased risk of HPV-related cervical lesions in IBD patients.”
Studies of IBD and cervical neoplasia have yielded mixed results as to a possible association. Some experts have postulated that underlying immunologic changes or the use of immunosuppressive drugs in IBD could thwart patients’ ability to clear HPV infections, thereby increasing their risk of developing cervical neoplasia. To explore that possibility, Dr. Rungoe and her associates compared rates of cervical dysplasia or cervical cancer among 27,408 women newly diagnosed with ulcerative colitis or Crohn’s disease and 1,508,334 controls without IBD. They identified cases and controls from a national patient registry of about 4 million women living in Denmark during 1979-2011. They also calculated the likelihood of a cervical neoplasia diagnosis preceding IBD.
Source: American Gastroenterological Association
Women with Crohn’s disease had a 26% higher rate of low-grade intraepithelial lesions of the cervix, a 28% greater incidence of high-grade lesions, and a 53% greater risk of cervical cancer compared with controls, the researchers reported (incidence rate ratios and 95% confidence intervals, respectively: 1.26, 1.07-1.48; 1.28, 1.13-1.45; and 1.53, 1.04-2.27). Women with ulcerative colitis also had about a 12%-15% increase in risk of developing cervical dysplasia, compared with controls (IRR for low-grade lesions, 1.15; 95% CI, 1.00-1.32; IRR for high-grade lesions, 1.12; 95% CI, 1.01-1.25), but no significant increase in cervical cancer risk.
Notably, women newly diagnosed with IBD had a “markedly elevated” odds of having been diagnosed with cervical neoplasia up to 10 years beforehand, the investigators reported. “This is a novel finding that may suggest a yet unexplored common susceptibility to IBD and cervical neoplasia, rather than an etiologic role of IBD or its treatment in development of cervical neoplasia,” they said.
Treatment with common IBD therapies such as azathioprine, mesalamine, and corticosteroids did not affect rates of cervical neoplasia, but women with Crohn’s disease who had used tumor necrosis factor–alpha antagonists had an 85% increase in high-grade intraepithelial cervical lesions. They also had a 2% increase in risk of these lesions for each filled prescription for hormonal contraceptives.
The frequency of cervical screening was slightly higher among women with ulcerative colitis, compared with controls, but was similar between controls and women with Crohn’s disease, the investigators noted.
The study was funded in part by the Danish Council of Independent Research. The investigators reported having no relevant financial disclosures.
Women with Crohn’s disease had about a 53% greater risk of developing cervical cancer compared with controls, and women with inflammatory bowel disease had a significantly greater risk of having had cervical neoplasia years earlier, according to a large population-based study reported in the April issue of Clinical Gastroenterology and Hepatology (http://dx.doi.org/10.1016/j.cgh.2014.07.036).
“We found a two-way association between inflammatory bowel disease, notably Crohn’s disease, and neoplastic lesions of the uterine cervix. This observation is not explained by differences in screening activity,” said Dr. Christine Rungoe at Statens Serum Institut in Copenhagen and her associates. “Patients with IBD should be encouraged to follow the screening program for cervical neoplasia, and clinicians should be aware of the slightly increased risk of HPV-related cervical lesions in IBD patients.”
Studies of IBD and cervical neoplasia have yielded mixed results as to a possible association. Some experts have postulated that underlying immunologic changes or the use of immunosuppressive drugs in IBD could thwart patients’ ability to clear HPV infections, thereby increasing their risk of developing cervical neoplasia. To explore that possibility, Dr. Rungoe and her associates compared rates of cervical dysplasia or cervical cancer among 27,408 women newly diagnosed with ulcerative colitis or Crohn’s disease and 1,508,334 controls without IBD. They identified cases and controls from a national patient registry of about 4 million women living in Denmark during 1979-2011. They also calculated the likelihood of a cervical neoplasia diagnosis preceding IBD.
Source: American Gastroenterological Association
Women with Crohn’s disease had a 26% higher rate of low-grade intraepithelial lesions of the cervix, a 28% greater incidence of high-grade lesions, and a 53% greater risk of cervical cancer compared with controls, the researchers reported (incidence rate ratios and 95% confidence intervals, respectively: 1.26, 1.07-1.48; 1.28, 1.13-1.45; and 1.53, 1.04-2.27). Women with ulcerative colitis also had about a 12%-15% increase in risk of developing cervical dysplasia, compared with controls (IRR for low-grade lesions, 1.15; 95% CI, 1.00-1.32; IRR for high-grade lesions, 1.12; 95% CI, 1.01-1.25), but no significant increase in cervical cancer risk.
Notably, women newly diagnosed with IBD had a “markedly elevated” odds of having been diagnosed with cervical neoplasia up to 10 years beforehand, the investigators reported. “This is a novel finding that may suggest a yet unexplored common susceptibility to IBD and cervical neoplasia, rather than an etiologic role of IBD or its treatment in development of cervical neoplasia,” they said.
Treatment with common IBD therapies such as azathioprine, mesalamine, and corticosteroids did not affect rates of cervical neoplasia, but women with Crohn’s disease who had used tumor necrosis factor–alpha antagonists had an 85% increase in high-grade intraepithelial cervical lesions. They also had a 2% increase in risk of these lesions for each filled prescription for hormonal contraceptives.
The frequency of cervical screening was slightly higher among women with ulcerative colitis, compared with controls, but was similar between controls and women with Crohn’s disease, the investigators noted.
The study was funded in part by the Danish Council of Independent Research. The investigators reported having no relevant financial disclosures.
FROM CLINICAL GASTROENTEROLOGY AND HEPATOLOGY
Key clinical point: Inflammatory bowel disease – particularly Crohn’s disease – might increase risk of cervical cancer.
Major finding: Women with Crohn’s disease had an estimated 53% increase in risk of developing cervical cancer, compared with controls.
Data source: Population-based cohort study of 27,408 women with inflammatory bowel disease and 1,508,334 controls.
Disclosures: The study was funded in part by the Danish Council of Independent Research. The investigators reported having no relevant financial disclosures.
Probiotics showed slight promise in post-resection Crohn’s prevention
A mixture of eight probiotic bacterial strains only somewhat outperformed placebo for preventing endoscopic recurrence after ileal resection in Crohn’s disease patients, according to a multicenter, randomized trial.
After 90 days of treatment, 9.3% of patients who received the probiotic mixture (VSL#3) had developed severe endoscopic recurrence, compared with 15.7% of the placebo group (P = .19), reported Dr. Richard Fedorak of the University of Alberta, Edmonton, and his associates.
The recurrence rate for the placebo group was about two-thirds lower than what the researchers had expected based on the sample size calculation, they noted. But the probiotic blend was linked to significantly significant decreases in colonic mucosal levels of proinflammatory cytokines, they reported (Clin. Gastroenterol. Hepatol. 2014 Nov. 6 [doi:10.1016/j.cgh.2014.10.031]).
Investigators have tested probiotics as a preventive therapy for Crohn’s disease because patients with active disease have less diverse intestinal microbiota, compared with those with quiescent disease or healthy controls. Past studies of single-strain probiotics have shown them to be no better than placebo for preventing endoscopic recurrence.
But in one small study, rifampin followed by VSL#3 outperformed mesalamine at 1 year (Gastroenterology 2000;118:A781), the researchers noted. “This mixture could confer protective effects where single-strain or lactobacillus-only formulations had failed,” they hypothesized.
To test that theory, the investigators randomized 120 patients with Crohn’s disease who had undergone ileal resection and ileocolonic anastomosis to twice-daily VSL#3 or placebo. Treatment began within 30 days after surgery and continued for 90 days, after which all patients received open-label VSL#3 for another 9 months.
Among patients who had nonsevere endoscopic lesions at day 90, 1-year rates of severe endoscopic recurrence were 10% for the early VSL#3 group, compared with 26.7% for the late VSL#3 group (P = .09), said the researchers. Likewise, combined rates of severe recurrence on days 90 and 365 were not statistically different, they reported. However, the early VSL#3 group had lower mucosal levels of 13 pro-inflammatory cytokines, compared with patients who received placebo until day 90 (P < .05). Measures of Crohn’s disease activity and disease-related quality of life scores were similar for both groups.
“Early treatment with VSL#3 had a larger effect than late treatment,” concluded the investigators. “Future larger studies will be needed to confirm the effect of VSL#3 in prevention of postoperative recurrence.”
The study was funded by VSL Pharmaceuticals, the Canadian Institutes of Health Research, and Crohn’s and Colitis Foundation of Canada. Dr. Fedorak reported having served on a speakers bureau for VSL Pharmaceuticals. The other authors declared no relevant conflicts of interest.
A mixture of eight probiotic bacterial strains only somewhat outperformed placebo for preventing endoscopic recurrence after ileal resection in Crohn’s disease patients, according to a multicenter, randomized trial.
After 90 days of treatment, 9.3% of patients who received the probiotic mixture (VSL#3) had developed severe endoscopic recurrence, compared with 15.7% of the placebo group (P = .19), reported Dr. Richard Fedorak of the University of Alberta, Edmonton, and his associates.
The recurrence rate for the placebo group was about two-thirds lower than what the researchers had expected based on the sample size calculation, they noted. But the probiotic blend was linked to significantly significant decreases in colonic mucosal levels of proinflammatory cytokines, they reported (Clin. Gastroenterol. Hepatol. 2014 Nov. 6 [doi:10.1016/j.cgh.2014.10.031]).
Investigators have tested probiotics as a preventive therapy for Crohn’s disease because patients with active disease have less diverse intestinal microbiota, compared with those with quiescent disease or healthy controls. Past studies of single-strain probiotics have shown them to be no better than placebo for preventing endoscopic recurrence.
But in one small study, rifampin followed by VSL#3 outperformed mesalamine at 1 year (Gastroenterology 2000;118:A781), the researchers noted. “This mixture could confer protective effects where single-strain or lactobacillus-only formulations had failed,” they hypothesized.
To test that theory, the investigators randomized 120 patients with Crohn’s disease who had undergone ileal resection and ileocolonic anastomosis to twice-daily VSL#3 or placebo. Treatment began within 30 days after surgery and continued for 90 days, after which all patients received open-label VSL#3 for another 9 months.
Among patients who had nonsevere endoscopic lesions at day 90, 1-year rates of severe endoscopic recurrence were 10% for the early VSL#3 group, compared with 26.7% for the late VSL#3 group (P = .09), said the researchers. Likewise, combined rates of severe recurrence on days 90 and 365 were not statistically different, they reported. However, the early VSL#3 group had lower mucosal levels of 13 pro-inflammatory cytokines, compared with patients who received placebo until day 90 (P < .05). Measures of Crohn’s disease activity and disease-related quality of life scores were similar for both groups.
“Early treatment with VSL#3 had a larger effect than late treatment,” concluded the investigators. “Future larger studies will be needed to confirm the effect of VSL#3 in prevention of postoperative recurrence.”
The study was funded by VSL Pharmaceuticals, the Canadian Institutes of Health Research, and Crohn’s and Colitis Foundation of Canada. Dr. Fedorak reported having served on a speakers bureau for VSL Pharmaceuticals. The other authors declared no relevant conflicts of interest.
A mixture of eight probiotic bacterial strains only somewhat outperformed placebo for preventing endoscopic recurrence after ileal resection in Crohn’s disease patients, according to a multicenter, randomized trial.
After 90 days of treatment, 9.3% of patients who received the probiotic mixture (VSL#3) had developed severe endoscopic recurrence, compared with 15.7% of the placebo group (P = .19), reported Dr. Richard Fedorak of the University of Alberta, Edmonton, and his associates.
The recurrence rate for the placebo group was about two-thirds lower than what the researchers had expected based on the sample size calculation, they noted. But the probiotic blend was linked to significantly significant decreases in colonic mucosal levels of proinflammatory cytokines, they reported (Clin. Gastroenterol. Hepatol. 2014 Nov. 6 [doi:10.1016/j.cgh.2014.10.031]).
Investigators have tested probiotics as a preventive therapy for Crohn’s disease because patients with active disease have less diverse intestinal microbiota, compared with those with quiescent disease or healthy controls. Past studies of single-strain probiotics have shown them to be no better than placebo for preventing endoscopic recurrence.
But in one small study, rifampin followed by VSL#3 outperformed mesalamine at 1 year (Gastroenterology 2000;118:A781), the researchers noted. “This mixture could confer protective effects where single-strain or lactobacillus-only formulations had failed,” they hypothesized.
To test that theory, the investigators randomized 120 patients with Crohn’s disease who had undergone ileal resection and ileocolonic anastomosis to twice-daily VSL#3 or placebo. Treatment began within 30 days after surgery and continued for 90 days, after which all patients received open-label VSL#3 for another 9 months.
Among patients who had nonsevere endoscopic lesions at day 90, 1-year rates of severe endoscopic recurrence were 10% for the early VSL#3 group, compared with 26.7% for the late VSL#3 group (P = .09), said the researchers. Likewise, combined rates of severe recurrence on days 90 and 365 were not statistically different, they reported. However, the early VSL#3 group had lower mucosal levels of 13 pro-inflammatory cytokines, compared with patients who received placebo until day 90 (P < .05). Measures of Crohn’s disease activity and disease-related quality of life scores were similar for both groups.
“Early treatment with VSL#3 had a larger effect than late treatment,” concluded the investigators. “Future larger studies will be needed to confirm the effect of VSL#3 in prevention of postoperative recurrence.”
The study was funded by VSL Pharmaceuticals, the Canadian Institutes of Health Research, and Crohn’s and Colitis Foundation of Canada. Dr. Fedorak reported having served on a speakers bureau for VSL Pharmaceuticals. The other authors declared no relevant conflicts of interest.
FROM CLINICAL GASTROENTEROLOGY AND HEPATOLOGY
Key clinical point: A mixture of eight bacterial probiotic strains somewhat outperformed placebo for preventing endoscopic recurrence in patients with Crohn’s disease.
Major finding: At day 90, severe endoscopic recurrence affected 9.3% of the treatment group and 15.7% of the placebo group (P =. 19)
Data source: Multicenter, randomized, double-blind study of 119 patients who had undergone ileal resection for Crohn’s disease.
Disclosures: The study was funded by VSL Pharmaceuticals, the Canadian Institutes of Health Research, and Crohn’s and Colitis Foundation of Canada. Dr. Fedorak reported having served on a speaker bureau for VSL Pharmaceuticals. The other authors declared no relevant conflicts of interest.
Infliximab most common cause of drug-induced liver injury
Infliximab caused liver injury in 8.3% of treated patients in a prospective study, exceeding rates for other tumor necrosis factor-alpha antagonists, investigators reported online in Clinical Gastroenterology and Hepatology.
The findings show that “liver injury associated with the use of TNF-alpha antagonists is more common than previously reported, occurring in 1 in 120 of those exposed to infliximab,” said Dr. Einar S. Björnsson at the University of Iceland in Reykjavik and his associates. Furthermore, neither anti-TNF treatment dose nor baseline antinuclear acid antibody (ANA) status predicted which patients would develop drug-induced liver injury (DILI), the researchers said.
Since emerging in the 1990s, anti-TNF agents have dramatically altered the treatment landscape for autoimmune diseases such as rheumatoid arthritis, psoriasis, and inflammatory bowel disease. Although they are known to cause liver damage in some patients, data on the topic mainly come from single case reports, the researchers said (Clin. Gastroenterol. Hepatol. 2014 [doi: http://dx.doi.org/10.1016/j.cgh.2014.07.062]) To better understand the association, the researchers prospectively studied patients who received anti-TNF agents between 2009 and 2013 at the University Hospital in Iceland. They defined liver injury as aspartate aminotransferase or alanine aminotransferase (ALT) levels that were at least triple the normal upper limit, or alkaline phosphatase levels of at least double the upper limit.
A total of 1,776 patients were treated with anti-TNF agents during the 5-year study period, the researchers reported. In all, 11 developed drug-induced liver injury (DILI), of which nine cases were caused by infliximab, they said. Liver injury developed in 8.3% of patients treated with infliximab, compared with only 3.7% of those who received adalimumab and 2.3% of those given etanercept, they added. In a past analysis, the researchers calculated that one in every 148 patients would develop DILI during 2 years of treatment with infliximab (Gastroenterology 2014;144:1419-25). Patients who developed DILI on one anti-TNF agent were able to switch therapies without DILI recurring, the investigators said. Seven patients were switched from infliximab to adalimumab, etanercept, or both, and one was switched to infliximab after developing DILI on adalimumab, they added.
The researchers also compared the 11 cases to 22 randomized controls matched by age, sex, underlying condition, and treatment. Notably, among the 11 patients diagnosed with DILI, just 1 (9%) was receiving methotrexate at the time of diagnosis, compared with 59% of the controls (P = .009), they reported. “The reason for this is not clear,” they added. “Methotrexate has been shown to lead to a decrease in circulating autoantibodies in cutaneous lupus erythematosus, but the influence of methotrexate could not be confirmed during infliximab treatment.”
Five of the 11 patients with DILI had liver biopsies, of which three showed severe acute hepatitis, two indicated mild unspecified chronic hepatitis, and one showed pure canalicular cholestasis, the researchers reported. About half the patients needed steroids acutely, but “the vast majority” did not need long-term steroid treatment, they said. Exactly how anti-TNF agents cause liver injury remains unclear, they added. Future studies might evaluate whether these drugs trigger CD4 T cells to react against liver cells, as is the case in classic autoimmune hepatitis, they said.
The researchers reported no funding sources and declared having no conflicts of interest.
Infliximab caused liver injury in 8.3% of treated patients in a prospective study, exceeding rates for other tumor necrosis factor-alpha antagonists, investigators reported online in Clinical Gastroenterology and Hepatology.
The findings show that “liver injury associated with the use of TNF-alpha antagonists is more common than previously reported, occurring in 1 in 120 of those exposed to infliximab,” said Dr. Einar S. Björnsson at the University of Iceland in Reykjavik and his associates. Furthermore, neither anti-TNF treatment dose nor baseline antinuclear acid antibody (ANA) status predicted which patients would develop drug-induced liver injury (DILI), the researchers said.
Since emerging in the 1990s, anti-TNF agents have dramatically altered the treatment landscape for autoimmune diseases such as rheumatoid arthritis, psoriasis, and inflammatory bowel disease. Although they are known to cause liver damage in some patients, data on the topic mainly come from single case reports, the researchers said (Clin. Gastroenterol. Hepatol. 2014 [doi: http://dx.doi.org/10.1016/j.cgh.2014.07.062]) To better understand the association, the researchers prospectively studied patients who received anti-TNF agents between 2009 and 2013 at the University Hospital in Iceland. They defined liver injury as aspartate aminotransferase or alanine aminotransferase (ALT) levels that were at least triple the normal upper limit, or alkaline phosphatase levels of at least double the upper limit.
A total of 1,776 patients were treated with anti-TNF agents during the 5-year study period, the researchers reported. In all, 11 developed drug-induced liver injury (DILI), of which nine cases were caused by infliximab, they said. Liver injury developed in 8.3% of patients treated with infliximab, compared with only 3.7% of those who received adalimumab and 2.3% of those given etanercept, they added. In a past analysis, the researchers calculated that one in every 148 patients would develop DILI during 2 years of treatment with infliximab (Gastroenterology 2014;144:1419-25). Patients who developed DILI on one anti-TNF agent were able to switch therapies without DILI recurring, the investigators said. Seven patients were switched from infliximab to adalimumab, etanercept, or both, and one was switched to infliximab after developing DILI on adalimumab, they added.
The researchers also compared the 11 cases to 22 randomized controls matched by age, sex, underlying condition, and treatment. Notably, among the 11 patients diagnosed with DILI, just 1 (9%) was receiving methotrexate at the time of diagnosis, compared with 59% of the controls (P = .009), they reported. “The reason for this is not clear,” they added. “Methotrexate has been shown to lead to a decrease in circulating autoantibodies in cutaneous lupus erythematosus, but the influence of methotrexate could not be confirmed during infliximab treatment.”
Five of the 11 patients with DILI had liver biopsies, of which three showed severe acute hepatitis, two indicated mild unspecified chronic hepatitis, and one showed pure canalicular cholestasis, the researchers reported. About half the patients needed steroids acutely, but “the vast majority” did not need long-term steroid treatment, they said. Exactly how anti-TNF agents cause liver injury remains unclear, they added. Future studies might evaluate whether these drugs trigger CD4 T cells to react against liver cells, as is the case in classic autoimmune hepatitis, they said.
The researchers reported no funding sources and declared having no conflicts of interest.
Infliximab caused liver injury in 8.3% of treated patients in a prospective study, exceeding rates for other tumor necrosis factor-alpha antagonists, investigators reported online in Clinical Gastroenterology and Hepatology.
The findings show that “liver injury associated with the use of TNF-alpha antagonists is more common than previously reported, occurring in 1 in 120 of those exposed to infliximab,” said Dr. Einar S. Björnsson at the University of Iceland in Reykjavik and his associates. Furthermore, neither anti-TNF treatment dose nor baseline antinuclear acid antibody (ANA) status predicted which patients would develop drug-induced liver injury (DILI), the researchers said.
Since emerging in the 1990s, anti-TNF agents have dramatically altered the treatment landscape for autoimmune diseases such as rheumatoid arthritis, psoriasis, and inflammatory bowel disease. Although they are known to cause liver damage in some patients, data on the topic mainly come from single case reports, the researchers said (Clin. Gastroenterol. Hepatol. 2014 [doi: http://dx.doi.org/10.1016/j.cgh.2014.07.062]) To better understand the association, the researchers prospectively studied patients who received anti-TNF agents between 2009 and 2013 at the University Hospital in Iceland. They defined liver injury as aspartate aminotransferase or alanine aminotransferase (ALT) levels that were at least triple the normal upper limit, or alkaline phosphatase levels of at least double the upper limit.
A total of 1,776 patients were treated with anti-TNF agents during the 5-year study period, the researchers reported. In all, 11 developed drug-induced liver injury (DILI), of which nine cases were caused by infliximab, they said. Liver injury developed in 8.3% of patients treated with infliximab, compared with only 3.7% of those who received adalimumab and 2.3% of those given etanercept, they added. In a past analysis, the researchers calculated that one in every 148 patients would develop DILI during 2 years of treatment with infliximab (Gastroenterology 2014;144:1419-25). Patients who developed DILI on one anti-TNF agent were able to switch therapies without DILI recurring, the investigators said. Seven patients were switched from infliximab to adalimumab, etanercept, or both, and one was switched to infliximab after developing DILI on adalimumab, they added.
The researchers also compared the 11 cases to 22 randomized controls matched by age, sex, underlying condition, and treatment. Notably, among the 11 patients diagnosed with DILI, just 1 (9%) was receiving methotrexate at the time of diagnosis, compared with 59% of the controls (P = .009), they reported. “The reason for this is not clear,” they added. “Methotrexate has been shown to lead to a decrease in circulating autoantibodies in cutaneous lupus erythematosus, but the influence of methotrexate could not be confirmed during infliximab treatment.”
Five of the 11 patients with DILI had liver biopsies, of which three showed severe acute hepatitis, two indicated mild unspecified chronic hepatitis, and one showed pure canalicular cholestasis, the researchers reported. About half the patients needed steroids acutely, but “the vast majority” did not need long-term steroid treatment, they said. Exactly how anti-TNF agents cause liver injury remains unclear, they added. Future studies might evaluate whether these drugs trigger CD4 T cells to react against liver cells, as is the case in classic autoimmune hepatitis, they said.
The researchers reported no funding sources and declared having no conflicts of interest.
Key clinical point: Infliximab was the most common anti–tumor necrosis factor-alpha agent linked to liver injury.
Major finding: Rates of drug-induced liver injury were highest among patients treated with infliximab (8.3%), compared with 3.7% for adalimumab and 2.3% for etanercept.
Data source: Prospective study of 11 cases of drug-induced liver injury and 22 controls.
Disclosures: The researchers declared no funding sources or conflicts of interest.
H. pylori might help regulate gastric immunity
Chronic Helicobacter pylori infection suppresses interleukin-33 cytokine in the stomach, which inhibits the CD4+ T helper cell 2 (or Th2) response and may set the stage for gastric carcinoma, investigators reported online in Cellular and Molecular Gastroenterology and Hepatology.
But long-term rises in IL-33 also can trigger precancerous changes in the stomach by causing the immune system to skew excessively toward Th2 instead of Th1 immunity, said Jon Buzzelli and his associates at the University of Melbourne in Parkville, Australia.
“Despite the immune response being vastly different ... the outcome appears to be similar, as preneoplastic changes occur in both settings,” the researchers added. “In keeping with recent findings, these data suggest that H. pylori may be a beneficial organism that under certain circumstances may help to ensure that gastric immunity is tightly regulated.” (Cellular and Molecular Gastroenterology and Hepatology 2015 [http://dx.doi.org/10.1016/j.jcmgh.2014.12.003 5])
IL-33 is a member of a diverse group of cytokines called alarmins, which quickly trigger an immune response to injury or infection when released by dying cells. Fasted mice in the study that were given oral aspirin to induce gastric injury had elevated IL-33 expression, compared with controls 4 hours later, the investigators reported. “This demonstrates that IL-33 responds immediately to gastric insult through relocalization and transcriptional changes, and may be involved in gastric wound healing,” they added.
The researchers also found that gastric IL-33 levels in mice rose fourfold just 1 day after they were infected with H. pylori. But 2 months later, the mice’s IL-33 levels had fallen below those of controls, resembling the researchers’ comparison of H. pylori–positive and uninfected human stomach specimens, they said.
Furthermore, the drop in IL-33 caused a tilt away from Th2 toward Th1 immunity, which appeared to trigger precancerous changes to the gastric mucosa, the researchers added. “The inhibition of gastric IL-33 in response to chronic H. pylori infection may be a key event in gastric cancer progression,” they concluded.
But eliminating H. pylori might also cause problems in some cases, the findings suggested. The declining prevalence of helicobacteriosis in humans has accompanied a rise in Barrett’s esophagus, which precedes esophageal cancer, they noted. When the researchers administered extra IL-33 to mice – mimicking the absence of H. pylori – the cardia of their stomachs expanded and became markedly metaplastic, which precedes Barrett’s esophagus in humans, they noted. H. pylori might help prevent Barrett’s esophagus by suppressing IL-33 and thereby regulating Th2 immunity, they concluded.
The researchers also found that mice born and reared in a pathogen-free environment had lower IL-33 levels, compared with those in conventional housing, they said. Gastric IL-33 expression appeared to rise as bacterial load and diversity increased, supporting the idea that IL-33 functions in this setting as an alarmin, they added.
The investigators also examined whether the TFF2 gene – which helps regulate homeostasis in mucus cells – promoted IL-33 expression in the stomach, as it does in the lungs. Indeed, TFF2 knockout mice had about 40% less gastric IL-33, compared with wild-type mice, they said. Humans with chronic helicobacteriosis also have low TFF2 expression, which continues to fall as gastric cancer grows, they noted.
The study was funded by the Victorian Government’s Operational Infrastructure Support Program and National Health & Medical Research Council, Australia. The researchers reported no conflicts of interest.
Gastric adenocarcinoma is the second-leading cause of cancer-related death worldwide, and chronic infection with Helicobacter pylori is the strongest known risk factor for the development of this malignancy. H. pylori colonization rates hover around 80%-90% in developing countries, but only a fraction of infected individuals ever develop disease. It is increasingly apparent that gastric carcinogenesis is multifactorial, influenced by host responses, H. pylori virulence, and environmental cofactors.
Parasitic helminth infections among H. pylori-infected individuals have been associated with a lower risk for the development of gastric cancer, and experimental data from animal models of Helicobacter infection have demonstrated that concurrent helminth infection attenuates the host immune response and reduces gastric atrophy. Infection with H. pylori typically induces a Th1-polarized immune response, while helminths drive Th2 responses.
Concurrent infections with helminths is endemic in regions of some developing countries that have a high prevalence of H. pylori infection, but a lower than expected rate of gastric cancer. Buzzelli et al. provide fresh insights into the role that IL-33 plays in polarizing Th2 immune responses by demonstrating that chronic, but not acute, H. pylori infection suppresses IL-33, which ultimately leads to a predominant Th1 response. These findings may represent a novel mechanism (e.g., manipulation of IL-33) explaining why populations harboring concurrent helminth and H. pylori infection have a reduced risk of gastric cancer.
Jennifer M. Noto, Ph.D., and Richard M. Peek Jr., M.D., AGAF, of the department of medicine, division of gastroenterology, hepatology, and department of nutrition and cancer biology, Vanderbilt University, Nashville, Tenn. Dr. Noto and Dr. Peek declared that no conflict of interest exists. They acknowledge the following funding sources: NIH R01CA077955, R01DK058587, P01CA116087, and P30DK058404.
Gastric adenocarcinoma is the second-leading cause of cancer-related death worldwide, and chronic infection with Helicobacter pylori is the strongest known risk factor for the development of this malignancy. H. pylori colonization rates hover around 80%-90% in developing countries, but only a fraction of infected individuals ever develop disease. It is increasingly apparent that gastric carcinogenesis is multifactorial, influenced by host responses, H. pylori virulence, and environmental cofactors.
Parasitic helminth infections among H. pylori-infected individuals have been associated with a lower risk for the development of gastric cancer, and experimental data from animal models of Helicobacter infection have demonstrated that concurrent helminth infection attenuates the host immune response and reduces gastric atrophy. Infection with H. pylori typically induces a Th1-polarized immune response, while helminths drive Th2 responses.
Concurrent infections with helminths is endemic in regions of some developing countries that have a high prevalence of H. pylori infection, but a lower than expected rate of gastric cancer. Buzzelli et al. provide fresh insights into the role that IL-33 plays in polarizing Th2 immune responses by demonstrating that chronic, but not acute, H. pylori infection suppresses IL-33, which ultimately leads to a predominant Th1 response. These findings may represent a novel mechanism (e.g., manipulation of IL-33) explaining why populations harboring concurrent helminth and H. pylori infection have a reduced risk of gastric cancer.
Jennifer M. Noto, Ph.D., and Richard M. Peek Jr., M.D., AGAF, of the department of medicine, division of gastroenterology, hepatology, and department of nutrition and cancer biology, Vanderbilt University, Nashville, Tenn. Dr. Noto and Dr. Peek declared that no conflict of interest exists. They acknowledge the following funding sources: NIH R01CA077955, R01DK058587, P01CA116087, and P30DK058404.
Gastric adenocarcinoma is the second-leading cause of cancer-related death worldwide, and chronic infection with Helicobacter pylori is the strongest known risk factor for the development of this malignancy. H. pylori colonization rates hover around 80%-90% in developing countries, but only a fraction of infected individuals ever develop disease. It is increasingly apparent that gastric carcinogenesis is multifactorial, influenced by host responses, H. pylori virulence, and environmental cofactors.
Parasitic helminth infections among H. pylori-infected individuals have been associated with a lower risk for the development of gastric cancer, and experimental data from animal models of Helicobacter infection have demonstrated that concurrent helminth infection attenuates the host immune response and reduces gastric atrophy. Infection with H. pylori typically induces a Th1-polarized immune response, while helminths drive Th2 responses.
Concurrent infections with helminths is endemic in regions of some developing countries that have a high prevalence of H. pylori infection, but a lower than expected rate of gastric cancer. Buzzelli et al. provide fresh insights into the role that IL-33 plays in polarizing Th2 immune responses by demonstrating that chronic, but not acute, H. pylori infection suppresses IL-33, which ultimately leads to a predominant Th1 response. These findings may represent a novel mechanism (e.g., manipulation of IL-33) explaining why populations harboring concurrent helminth and H. pylori infection have a reduced risk of gastric cancer.
Jennifer M. Noto, Ph.D., and Richard M. Peek Jr., M.D., AGAF, of the department of medicine, division of gastroenterology, hepatology, and department of nutrition and cancer biology, Vanderbilt University, Nashville, Tenn. Dr. Noto and Dr. Peek declared that no conflict of interest exists. They acknowledge the following funding sources: NIH R01CA077955, R01DK058587, P01CA116087, and P30DK058404.
Chronic Helicobacter pylori infection suppresses interleukin-33 cytokine in the stomach, which inhibits the CD4+ T helper cell 2 (or Th2) response and may set the stage for gastric carcinoma, investigators reported online in Cellular and Molecular Gastroenterology and Hepatology.
But long-term rises in IL-33 also can trigger precancerous changes in the stomach by causing the immune system to skew excessively toward Th2 instead of Th1 immunity, said Jon Buzzelli and his associates at the University of Melbourne in Parkville, Australia.
“Despite the immune response being vastly different ... the outcome appears to be similar, as preneoplastic changes occur in both settings,” the researchers added. “In keeping with recent findings, these data suggest that H. pylori may be a beneficial organism that under certain circumstances may help to ensure that gastric immunity is tightly regulated.” (Cellular and Molecular Gastroenterology and Hepatology 2015 [http://dx.doi.org/10.1016/j.jcmgh.2014.12.003 5])
IL-33 is a member of a diverse group of cytokines called alarmins, which quickly trigger an immune response to injury or infection when released by dying cells. Fasted mice in the study that were given oral aspirin to induce gastric injury had elevated IL-33 expression, compared with controls 4 hours later, the investigators reported. “This demonstrates that IL-33 responds immediately to gastric insult through relocalization and transcriptional changes, and may be involved in gastric wound healing,” they added.
The researchers also found that gastric IL-33 levels in mice rose fourfold just 1 day after they were infected with H. pylori. But 2 months later, the mice’s IL-33 levels had fallen below those of controls, resembling the researchers’ comparison of H. pylori–positive and uninfected human stomach specimens, they said.
Furthermore, the drop in IL-33 caused a tilt away from Th2 toward Th1 immunity, which appeared to trigger precancerous changes to the gastric mucosa, the researchers added. “The inhibition of gastric IL-33 in response to chronic H. pylori infection may be a key event in gastric cancer progression,” they concluded.
But eliminating H. pylori might also cause problems in some cases, the findings suggested. The declining prevalence of helicobacteriosis in humans has accompanied a rise in Barrett’s esophagus, which precedes esophageal cancer, they noted. When the researchers administered extra IL-33 to mice – mimicking the absence of H. pylori – the cardia of their stomachs expanded and became markedly metaplastic, which precedes Barrett’s esophagus in humans, they noted. H. pylori might help prevent Barrett’s esophagus by suppressing IL-33 and thereby regulating Th2 immunity, they concluded.
The researchers also found that mice born and reared in a pathogen-free environment had lower IL-33 levels, compared with those in conventional housing, they said. Gastric IL-33 expression appeared to rise as bacterial load and diversity increased, supporting the idea that IL-33 functions in this setting as an alarmin, they added.
The investigators also examined whether the TFF2 gene – which helps regulate homeostasis in mucus cells – promoted IL-33 expression in the stomach, as it does in the lungs. Indeed, TFF2 knockout mice had about 40% less gastric IL-33, compared with wild-type mice, they said. Humans with chronic helicobacteriosis also have low TFF2 expression, which continues to fall as gastric cancer grows, they noted.
The study was funded by the Victorian Government’s Operational Infrastructure Support Program and National Health & Medical Research Council, Australia. The researchers reported no conflicts of interest.
Chronic Helicobacter pylori infection suppresses interleukin-33 cytokine in the stomach, which inhibits the CD4+ T helper cell 2 (or Th2) response and may set the stage for gastric carcinoma, investigators reported online in Cellular and Molecular Gastroenterology and Hepatology.
But long-term rises in IL-33 also can trigger precancerous changes in the stomach by causing the immune system to skew excessively toward Th2 instead of Th1 immunity, said Jon Buzzelli and his associates at the University of Melbourne in Parkville, Australia.
“Despite the immune response being vastly different ... the outcome appears to be similar, as preneoplastic changes occur in both settings,” the researchers added. “In keeping with recent findings, these data suggest that H. pylori may be a beneficial organism that under certain circumstances may help to ensure that gastric immunity is tightly regulated.” (Cellular and Molecular Gastroenterology and Hepatology 2015 [http://dx.doi.org/10.1016/j.jcmgh.2014.12.003 5])
IL-33 is a member of a diverse group of cytokines called alarmins, which quickly trigger an immune response to injury or infection when released by dying cells. Fasted mice in the study that were given oral aspirin to induce gastric injury had elevated IL-33 expression, compared with controls 4 hours later, the investigators reported. “This demonstrates that IL-33 responds immediately to gastric insult through relocalization and transcriptional changes, and may be involved in gastric wound healing,” they added.
The researchers also found that gastric IL-33 levels in mice rose fourfold just 1 day after they were infected with H. pylori. But 2 months later, the mice’s IL-33 levels had fallen below those of controls, resembling the researchers’ comparison of H. pylori–positive and uninfected human stomach specimens, they said.
Furthermore, the drop in IL-33 caused a tilt away from Th2 toward Th1 immunity, which appeared to trigger precancerous changes to the gastric mucosa, the researchers added. “The inhibition of gastric IL-33 in response to chronic H. pylori infection may be a key event in gastric cancer progression,” they concluded.
But eliminating H. pylori might also cause problems in some cases, the findings suggested. The declining prevalence of helicobacteriosis in humans has accompanied a rise in Barrett’s esophagus, which precedes esophageal cancer, they noted. When the researchers administered extra IL-33 to mice – mimicking the absence of H. pylori – the cardia of their stomachs expanded and became markedly metaplastic, which precedes Barrett’s esophagus in humans, they noted. H. pylori might help prevent Barrett’s esophagus by suppressing IL-33 and thereby regulating Th2 immunity, they concluded.
The researchers also found that mice born and reared in a pathogen-free environment had lower IL-33 levels, compared with those in conventional housing, they said. Gastric IL-33 expression appeared to rise as bacterial load and diversity increased, supporting the idea that IL-33 functions in this setting as an alarmin, they added.
The investigators also examined whether the TFF2 gene – which helps regulate homeostasis in mucus cells – promoted IL-33 expression in the stomach, as it does in the lungs. Indeed, TFF2 knockout mice had about 40% less gastric IL-33, compared with wild-type mice, they said. Humans with chronic helicobacteriosis also have low TFF2 expression, which continues to fall as gastric cancer grows, they noted.
The study was funded by the Victorian Government’s Operational Infrastructure Support Program and National Health & Medical Research Council, Australia. The researchers reported no conflicts of interest.
FROM CELLULAR AND MOLECULAR GASTROENTEROLOGY AND HEPATOLOGY
Key clinical point: H. pylori may help regulate gastric immunity in some circumstances.
Major finding: Chronic gastric H. pylori infection lowered expression of IL-33, a cytokine that helps activate the CD4+ T helper cell 2 response.
Data source: Immunofluorescence, flow cytometry, and quantitative real-time polymerase chain reaction studies of tissue specimens from humans and mice.Disclosures: The study was funded by the Victorian Government’s Operational Infrastructure Support Program and NH&MRC Australia. The researchers reported no conflicts of interest.
Mutations found in almost 4% of pancreatic cancer patients
In a registry-based study, 3.8% of patients with pancreatic cancer had germline mutations in genes known to significantly increase cancer risk, researchers reported in the March issue of Gastroenterology.
“A small but clinically important proportion of pancreatic cancer is associated with mutations in known predisposition genes. The heterogeneity of mutations identified in this study shows the value of using a multiple-gene panel in pancreatic cancer,” said Robert Grant of the Ontario Institute for Cancer Research in Toronto and his associates.
Source: American Gastroenterological Association
Some patients had mutations in the BRCA and MMR genes, about which enough is known to help guide preventive measures and treatment decisions, the researchers noted. “Furthermore, all mutation carriers represent a high-risk subgroup of patients for pancreatic cancer researchers to consider for screening studies and for experimental targeted therapies,” the investigators wrote (Gastroenterology 2014 Dec. 2 [doi:10.1053/j.gastro.2014.11.042]).
For the study, the investigators carried out multigene next-generation sequencing of DNA from the blood and saliva of 290 patients with pancreatic cancer. The patients were randomly chosen from a population-based pancreatic cancer registry in Ontario. The researchers looked for mutations in 13 genes that have been previously linked to cancers: APC, ATM, BRCA1, BRCA2, CDKN2A, MLH1, MSH2, MSH6, PALB2, PMS2, PRSS1, STK11, and TP53. They found a total of 11 pathogenic germline mutations in seven of these genes, including 3 in the ATM gene, 1 in BRCA1,2 in BRCA2, 1 in MLH1, 2 in MSH2, 1 in MSH6, and 1 in TP53, they reported.
A total of 3.8% (95% confidence interval, 2.1%-5.6%) of the patients carried mutations, or about 1 in every 26 patients, said the researchers. Most mutations were linked to breast or colorectal cancer. Mutation carriers were significantly more likely to have been diagnosed with breast cancer or colorectal cancer themselves, or to have an affected first-degree relative (P < .01 for both), compared with other patients in the study.
Furthermore, the prevalence of mutations jumped to 10.7% (95% CI, 4.4%-11.1%) when the researchers looked only at patients with a personal or family history of breast cancer, and to 11.1% (95% CI, 3.0%-19.1%) in the subgroup of patients with a personal or family history of colorectal cancer, the investigators reported.
But mutation status was not linked with familial pancreatic cancer, nor with age at diagnosis, which “raises questions with important clinical implications,” said the researchers. “With decreasing sequencing costs, which patients should be referred for multiple-gene panel sequencing? What is the relevance of mutations in [patients] with atypical personal and family histories?”
Answering those questions would require studying many genes from large groups of patients with pancreatic cancer, they emphasized. For now, although multiple-gene panels cost about the same amount as single-gene tests, “the added value of simultaneously sequencing many genes remains uncertain, and likely depends on the clinical setting,” they said. Nonetheless, the analysis uncovered so many mutations in the cohort that the researchers would recommend multiple-gene testing of patients with pancreatic cancer, they said.
Patients were recruited into the registry based on pathology results, which would have excluded those with advanced pancreatic cancer who never had pathology testing, said the investigators. Also, study patients tended to be younger, to have been treated in academic centers, and to have resectable disease more often than other patients in Ontario with pancreatic cancer.
The work was funded by the Weston Garfield Foundation, Pancreatic Cancer Canada, National Cancer Institute, Mount Sinai Hospital Biospecimen Repository, and Teresa Bianco. The investigators declared having no conflicts of interest.
In a registry-based study, 3.8% of patients with pancreatic cancer had germline mutations in genes known to significantly increase cancer risk, researchers reported in the March issue of Gastroenterology.
“A small but clinically important proportion of pancreatic cancer is associated with mutations in known predisposition genes. The heterogeneity of mutations identified in this study shows the value of using a multiple-gene panel in pancreatic cancer,” said Robert Grant of the Ontario Institute for Cancer Research in Toronto and his associates.
Source: American Gastroenterological Association
Some patients had mutations in the BRCA and MMR genes, about which enough is known to help guide preventive measures and treatment decisions, the researchers noted. “Furthermore, all mutation carriers represent a high-risk subgroup of patients for pancreatic cancer researchers to consider for screening studies and for experimental targeted therapies,” the investigators wrote (Gastroenterology 2014 Dec. 2 [doi:10.1053/j.gastro.2014.11.042]).
For the study, the investigators carried out multigene next-generation sequencing of DNA from the blood and saliva of 290 patients with pancreatic cancer. The patients were randomly chosen from a population-based pancreatic cancer registry in Ontario. The researchers looked for mutations in 13 genes that have been previously linked to cancers: APC, ATM, BRCA1, BRCA2, CDKN2A, MLH1, MSH2, MSH6, PALB2, PMS2, PRSS1, STK11, and TP53. They found a total of 11 pathogenic germline mutations in seven of these genes, including 3 in the ATM gene, 1 in BRCA1,2 in BRCA2, 1 in MLH1, 2 in MSH2, 1 in MSH6, and 1 in TP53, they reported.
A total of 3.8% (95% confidence interval, 2.1%-5.6%) of the patients carried mutations, or about 1 in every 26 patients, said the researchers. Most mutations were linked to breast or colorectal cancer. Mutation carriers were significantly more likely to have been diagnosed with breast cancer or colorectal cancer themselves, or to have an affected first-degree relative (P < .01 for both), compared with other patients in the study.
Furthermore, the prevalence of mutations jumped to 10.7% (95% CI, 4.4%-11.1%) when the researchers looked only at patients with a personal or family history of breast cancer, and to 11.1% (95% CI, 3.0%-19.1%) in the subgroup of patients with a personal or family history of colorectal cancer, the investigators reported.
But mutation status was not linked with familial pancreatic cancer, nor with age at diagnosis, which “raises questions with important clinical implications,” said the researchers. “With decreasing sequencing costs, which patients should be referred for multiple-gene panel sequencing? What is the relevance of mutations in [patients] with atypical personal and family histories?”
Answering those questions would require studying many genes from large groups of patients with pancreatic cancer, they emphasized. For now, although multiple-gene panels cost about the same amount as single-gene tests, “the added value of simultaneously sequencing many genes remains uncertain, and likely depends on the clinical setting,” they said. Nonetheless, the analysis uncovered so many mutations in the cohort that the researchers would recommend multiple-gene testing of patients with pancreatic cancer, they said.
Patients were recruited into the registry based on pathology results, which would have excluded those with advanced pancreatic cancer who never had pathology testing, said the investigators. Also, study patients tended to be younger, to have been treated in academic centers, and to have resectable disease more often than other patients in Ontario with pancreatic cancer.
The work was funded by the Weston Garfield Foundation, Pancreatic Cancer Canada, National Cancer Institute, Mount Sinai Hospital Biospecimen Repository, and Teresa Bianco. The investigators declared having no conflicts of interest.
In a registry-based study, 3.8% of patients with pancreatic cancer had germline mutations in genes known to significantly increase cancer risk, researchers reported in the March issue of Gastroenterology.
“A small but clinically important proportion of pancreatic cancer is associated with mutations in known predisposition genes. The heterogeneity of mutations identified in this study shows the value of using a multiple-gene panel in pancreatic cancer,” said Robert Grant of the Ontario Institute for Cancer Research in Toronto and his associates.
Source: American Gastroenterological Association
Some patients had mutations in the BRCA and MMR genes, about which enough is known to help guide preventive measures and treatment decisions, the researchers noted. “Furthermore, all mutation carriers represent a high-risk subgroup of patients for pancreatic cancer researchers to consider for screening studies and for experimental targeted therapies,” the investigators wrote (Gastroenterology 2014 Dec. 2 [doi:10.1053/j.gastro.2014.11.042]).
For the study, the investigators carried out multigene next-generation sequencing of DNA from the blood and saliva of 290 patients with pancreatic cancer. The patients were randomly chosen from a population-based pancreatic cancer registry in Ontario. The researchers looked for mutations in 13 genes that have been previously linked to cancers: APC, ATM, BRCA1, BRCA2, CDKN2A, MLH1, MSH2, MSH6, PALB2, PMS2, PRSS1, STK11, and TP53. They found a total of 11 pathogenic germline mutations in seven of these genes, including 3 in the ATM gene, 1 in BRCA1,2 in BRCA2, 1 in MLH1, 2 in MSH2, 1 in MSH6, and 1 in TP53, they reported.
A total of 3.8% (95% confidence interval, 2.1%-5.6%) of the patients carried mutations, or about 1 in every 26 patients, said the researchers. Most mutations were linked to breast or colorectal cancer. Mutation carriers were significantly more likely to have been diagnosed with breast cancer or colorectal cancer themselves, or to have an affected first-degree relative (P < .01 for both), compared with other patients in the study.
Furthermore, the prevalence of mutations jumped to 10.7% (95% CI, 4.4%-11.1%) when the researchers looked only at patients with a personal or family history of breast cancer, and to 11.1% (95% CI, 3.0%-19.1%) in the subgroup of patients with a personal or family history of colorectal cancer, the investigators reported.
But mutation status was not linked with familial pancreatic cancer, nor with age at diagnosis, which “raises questions with important clinical implications,” said the researchers. “With decreasing sequencing costs, which patients should be referred for multiple-gene panel sequencing? What is the relevance of mutations in [patients] with atypical personal and family histories?”
Answering those questions would require studying many genes from large groups of patients with pancreatic cancer, they emphasized. For now, although multiple-gene panels cost about the same amount as single-gene tests, “the added value of simultaneously sequencing many genes remains uncertain, and likely depends on the clinical setting,” they said. Nonetheless, the analysis uncovered so many mutations in the cohort that the researchers would recommend multiple-gene testing of patients with pancreatic cancer, they said.
Patients were recruited into the registry based on pathology results, which would have excluded those with advanced pancreatic cancer who never had pathology testing, said the investigators. Also, study patients tended to be younger, to have been treated in academic centers, and to have resectable disease more often than other patients in Ontario with pancreatic cancer.
The work was funded by the Weston Garfield Foundation, Pancreatic Cancer Canada, National Cancer Institute, Mount Sinai Hospital Biospecimen Repository, and Teresa Bianco. The investigators declared having no conflicts of interest.
FROM GASTROENTEROLOGY
Key clinical point: In a registry-based study, 3.8% of patients with pancreatic cancer had mutations in seven genes known to substantially increase cancer risk.
Major finding: Eleven pathogenic mutations were found in the ATM, BRCA1, BRCA2, MLH1, MSH2, MSH6, and TP53 genes.
Data source: Multiple-gene sequencing of 290 patients with pancreatic cancer.
Disclosures: The work was funded by the Weston Garfield Foundation, Pancreatic Cancer Canada, National Cancer Institute, Mount Sinai Hospital Biospecimen Repository, and Teresa Bianco. The investigators declared having no conflicts of interest.
Stress independently predicts peptic ulcers
High levels of psychological stress more than doubled the odds of peptic ulcers, and the link remained statistically significant even after controlling for factors such as Helicobacter pylori infection and cigarette smoking, according to a prospective study published in the March issue of Clinical Gastroenterology and Hepatology.
The findings contradict the widely accepted view that stress does not cause peptic ulcers, said Dr. Susan Levenstein of Aventino Medical Group in Rome and her associates. “Clinicians treating ulcer patients should investigate potential psychological stress among other risk factors,” they said.
Source: American Gastroenterological Association
Although “a vast literature links peptic ulcer to stress,” past studies suffered so many methodologic weaknesses that groups such as the U.S. National Institute of Diabetes and Digestive and Kidney Diseases rejected the evidence outright, Dr. Levenstein and her associates noted. Many studies were cross-sectional, for example, or did not control for confounders such as helicobacteriosis, they said.
To further study the effects of stress on ulcer risk, the researchers analyzed historical data from 76 patients who lacked a history of gastric and duodenal ulcers in 1982, but by 1994 had developed “distinct breach[es] in the mucosa” that were confirmed by endoscopy or contrast radiology. The researchers did not count erosions that lacked appreciable depth as ulcers, they noted (Clin. Gastroenterol. Hepatol. 2014 Aug. 8 [doi:10.1016/j.cgh.2014.07.052]).
Study subjects answered 12 questions about their stress levels, such as, “Do your hands easily shake?” “Do you often suffer from fits of dizziness?” “Do you constantly have thoughts that trouble and worry you?” and “Do you usually feel misunderstood by other people?” They answered these questions at baseline in 1982-1983, again in 1987-1988, and again in 1993-1994.
Respondents who scored in the top tertile for psychological stress had an ulcer incidence of 3.5%, compared with 1.6% for those in the lowest tertile (odds ratio, 2.2; 95% confidence interval, 1.2-3.9; P < .01), reported the investigators. And controlling for smoking, helicobacteriosis, use of nonsteroidal anti-inflammatory drugs, and low socioeconomic status only partially weakened the relationship between stress and ulcers, they said. After accounting for those risk factors, every one-point increase on the stress questionnaire still upped the odds of peptic ulcer by 12% (odds ratio, 1.12; 95% confidence interval, 1.01-1.23)they reported.
Helicobacteri pylori infection was the strongest independent predictor of ulcers (OR, 3.3; 95% CI, 2.02-5.69), while cigarette smoking came in a close second (OR, 2.91; 95% CI, 1.38-6.16), said the researchers. Notably, stress and helicobacteriosis did not seem to synergistically increase the chances of ulcers, they reported. “Stress affected H. pylori–related ulcers at least as much as those related to neither H. pylori nor nonsteroidal anti-inflammatory drugs,” they said.
Several factors might explain the stress-ulcer link, such as increased acid load, activation of the hypothalamic-pituitary-adrenal axis, shifts in blood flow, and cytokine activation that might impair gastrointestinal mucosal defenses, said the investigators. Although the baseline data in their study were more than 2 decades old, that meant that patients likely had not been treated to eradicate H. pylori and were less likely to have taken proton pump inhibitors than the current population that has over-the-counter access to PPIs, they added. They also noted that past studies found a particularly strong link between stress and bleeding or perforated ulcers, which have not declined as much as other types of ulcers. “These results support a multicausal model of peptic ulcer etiology, with intertwined biological and psychosocial components,” they concluded.
The Kirby Family Foundation funded the statistical analysis. The researchers reported no conflicts of interest.
Stress was the most frequently cited cause of ulcer disease before Helicobacter pylori was discovered. The harried executive who developed an ulcer was a widely accepted profile of an ulcer diathesis. When the role of H. pylori infection and NSAIDs became clear, the role of stress was downplayed and some articles and textbooks dismissed stress as a potential cause for ulcer disease.

|
Dr. Nimish Vakil |
Studies of New York City residents suggest a higher incidence of ulcer disease after the 9-11 attacks and studies from Japan have shown an increase in the incidence of ulcer disease after the nuclear reactor disaster. In this issue of Clinical Gastroenterology and Hepatology, Dr. Levenstein and her colleagues report the results of a study of stress and the incidence of ulcer disease in Danish subjects. In 1982-1983, a population-based study in Denmark collected sera and psychological data in over 3000 subjects and reinterviewed them in 1987-1988 and 1993-1994. An ad-hoc, unvalidated scale developed by the authors measured stress. It included a psychological scale used by the Danish military to identify recruits unsuitable for military service but also included tranquilizer use, working more than 40 hours a week, and unemployment. In multivariate analysis, they found that stress increased the risk for both gastric and duodenal ulcers, with an adjusted odds ratio of 1.19 per point increase in the stress scale for gastric ulcers (95% confidence interval, 1.03-1.37) and a odds ratio of 1.1 per point increase in the stress index for duodenal ulcers (95% CI, 0.98-1.27).
There are obvious limitations with this study: a historical cohort, an unvalidated stress scale, the inclusion of items that may not represent stress in some cultures (e.g., working more than 40 hours/week) and the lower bound of confidence intervals for risk which are very close to one. However, studies such as this tell us that we have been too quick to dismiss the role of stress in ulcer pathogenesis. With declining H. pylori prevalence and the development of safer NSAIDs, stress will undergo a renaissance in the pathogenesis of ulcer disease.
Dr. Nimish Vakil, AGAF, FASGE, FACP, is a physician specializing in gastroenterology at the Aurora Wilkinson Medical Clinic in Summit, Wisc. He is a consultant for Astra Zeneca, Ironwood, and Baxter Pharmaceuticals.
Stress was the most frequently cited cause of ulcer disease before Helicobacter pylori was discovered. The harried executive who developed an ulcer was a widely accepted profile of an ulcer diathesis. When the role of H. pylori infection and NSAIDs became clear, the role of stress was downplayed and some articles and textbooks dismissed stress as a potential cause for ulcer disease.

|
Dr. Nimish Vakil |
Studies of New York City residents suggest a higher incidence of ulcer disease after the 9-11 attacks and studies from Japan have shown an increase in the incidence of ulcer disease after the nuclear reactor disaster. In this issue of Clinical Gastroenterology and Hepatology, Dr. Levenstein and her colleagues report the results of a study of stress and the incidence of ulcer disease in Danish subjects. In 1982-1983, a population-based study in Denmark collected sera and psychological data in over 3000 subjects and reinterviewed them in 1987-1988 and 1993-1994. An ad-hoc, unvalidated scale developed by the authors measured stress. It included a psychological scale used by the Danish military to identify recruits unsuitable for military service but also included tranquilizer use, working more than 40 hours a week, and unemployment. In multivariate analysis, they found that stress increased the risk for both gastric and duodenal ulcers, with an adjusted odds ratio of 1.19 per point increase in the stress scale for gastric ulcers (95% confidence interval, 1.03-1.37) and a odds ratio of 1.1 per point increase in the stress index for duodenal ulcers (95% CI, 0.98-1.27).
There are obvious limitations with this study: a historical cohort, an unvalidated stress scale, the inclusion of items that may not represent stress in some cultures (e.g., working more than 40 hours/week) and the lower bound of confidence intervals for risk which are very close to one. However, studies such as this tell us that we have been too quick to dismiss the role of stress in ulcer pathogenesis. With declining H. pylori prevalence and the development of safer NSAIDs, stress will undergo a renaissance in the pathogenesis of ulcer disease.
Dr. Nimish Vakil, AGAF, FASGE, FACP, is a physician specializing in gastroenterology at the Aurora Wilkinson Medical Clinic in Summit, Wisc. He is a consultant for Astra Zeneca, Ironwood, and Baxter Pharmaceuticals.
Stress was the most frequently cited cause of ulcer disease before Helicobacter pylori was discovered. The harried executive who developed an ulcer was a widely accepted profile of an ulcer diathesis. When the role of H. pylori infection and NSAIDs became clear, the role of stress was downplayed and some articles and textbooks dismissed stress as a potential cause for ulcer disease.

|
Dr. Nimish Vakil |
Studies of New York City residents suggest a higher incidence of ulcer disease after the 9-11 attacks and studies from Japan have shown an increase in the incidence of ulcer disease after the nuclear reactor disaster. In this issue of Clinical Gastroenterology and Hepatology, Dr. Levenstein and her colleagues report the results of a study of stress and the incidence of ulcer disease in Danish subjects. In 1982-1983, a population-based study in Denmark collected sera and psychological data in over 3000 subjects and reinterviewed them in 1987-1988 and 1993-1994. An ad-hoc, unvalidated scale developed by the authors measured stress. It included a psychological scale used by the Danish military to identify recruits unsuitable for military service but also included tranquilizer use, working more than 40 hours a week, and unemployment. In multivariate analysis, they found that stress increased the risk for both gastric and duodenal ulcers, with an adjusted odds ratio of 1.19 per point increase in the stress scale for gastric ulcers (95% confidence interval, 1.03-1.37) and a odds ratio of 1.1 per point increase in the stress index for duodenal ulcers (95% CI, 0.98-1.27).
There are obvious limitations with this study: a historical cohort, an unvalidated stress scale, the inclusion of items that may not represent stress in some cultures (e.g., working more than 40 hours/week) and the lower bound of confidence intervals for risk which are very close to one. However, studies such as this tell us that we have been too quick to dismiss the role of stress in ulcer pathogenesis. With declining H. pylori prevalence and the development of safer NSAIDs, stress will undergo a renaissance in the pathogenesis of ulcer disease.
Dr. Nimish Vakil, AGAF, FASGE, FACP, is a physician specializing in gastroenterology at the Aurora Wilkinson Medical Clinic in Summit, Wisc. He is a consultant for Astra Zeneca, Ironwood, and Baxter Pharmaceuticals.
High levels of psychological stress more than doubled the odds of peptic ulcers, and the link remained statistically significant even after controlling for factors such as Helicobacter pylori infection and cigarette smoking, according to a prospective study published in the March issue of Clinical Gastroenterology and Hepatology.
The findings contradict the widely accepted view that stress does not cause peptic ulcers, said Dr. Susan Levenstein of Aventino Medical Group in Rome and her associates. “Clinicians treating ulcer patients should investigate potential psychological stress among other risk factors,” they said.
Source: American Gastroenterological Association
Although “a vast literature links peptic ulcer to stress,” past studies suffered so many methodologic weaknesses that groups such as the U.S. National Institute of Diabetes and Digestive and Kidney Diseases rejected the evidence outright, Dr. Levenstein and her associates noted. Many studies were cross-sectional, for example, or did not control for confounders such as helicobacteriosis, they said.
To further study the effects of stress on ulcer risk, the researchers analyzed historical data from 76 patients who lacked a history of gastric and duodenal ulcers in 1982, but by 1994 had developed “distinct breach[es] in the mucosa” that were confirmed by endoscopy or contrast radiology. The researchers did not count erosions that lacked appreciable depth as ulcers, they noted (Clin. Gastroenterol. Hepatol. 2014 Aug. 8 [doi:10.1016/j.cgh.2014.07.052]).
Study subjects answered 12 questions about their stress levels, such as, “Do your hands easily shake?” “Do you often suffer from fits of dizziness?” “Do you constantly have thoughts that trouble and worry you?” and “Do you usually feel misunderstood by other people?” They answered these questions at baseline in 1982-1983, again in 1987-1988, and again in 1993-1994.
Respondents who scored in the top tertile for psychological stress had an ulcer incidence of 3.5%, compared with 1.6% for those in the lowest tertile (odds ratio, 2.2; 95% confidence interval, 1.2-3.9; P < .01), reported the investigators. And controlling for smoking, helicobacteriosis, use of nonsteroidal anti-inflammatory drugs, and low socioeconomic status only partially weakened the relationship between stress and ulcers, they said. After accounting for those risk factors, every one-point increase on the stress questionnaire still upped the odds of peptic ulcer by 12% (odds ratio, 1.12; 95% confidence interval, 1.01-1.23)they reported.
Helicobacteri pylori infection was the strongest independent predictor of ulcers (OR, 3.3; 95% CI, 2.02-5.69), while cigarette smoking came in a close second (OR, 2.91; 95% CI, 1.38-6.16), said the researchers. Notably, stress and helicobacteriosis did not seem to synergistically increase the chances of ulcers, they reported. “Stress affected H. pylori–related ulcers at least as much as those related to neither H. pylori nor nonsteroidal anti-inflammatory drugs,” they said.
Several factors might explain the stress-ulcer link, such as increased acid load, activation of the hypothalamic-pituitary-adrenal axis, shifts in blood flow, and cytokine activation that might impair gastrointestinal mucosal defenses, said the investigators. Although the baseline data in their study were more than 2 decades old, that meant that patients likely had not been treated to eradicate H. pylori and were less likely to have taken proton pump inhibitors than the current population that has over-the-counter access to PPIs, they added. They also noted that past studies found a particularly strong link between stress and bleeding or perforated ulcers, which have not declined as much as other types of ulcers. “These results support a multicausal model of peptic ulcer etiology, with intertwined biological and psychosocial components,” they concluded.
The Kirby Family Foundation funded the statistical analysis. The researchers reported no conflicts of interest.
High levels of psychological stress more than doubled the odds of peptic ulcers, and the link remained statistically significant even after controlling for factors such as Helicobacter pylori infection and cigarette smoking, according to a prospective study published in the March issue of Clinical Gastroenterology and Hepatology.
The findings contradict the widely accepted view that stress does not cause peptic ulcers, said Dr. Susan Levenstein of Aventino Medical Group in Rome and her associates. “Clinicians treating ulcer patients should investigate potential psychological stress among other risk factors,” they said.
Source: American Gastroenterological Association
Although “a vast literature links peptic ulcer to stress,” past studies suffered so many methodologic weaknesses that groups such as the U.S. National Institute of Diabetes and Digestive and Kidney Diseases rejected the evidence outright, Dr. Levenstein and her associates noted. Many studies were cross-sectional, for example, or did not control for confounders such as helicobacteriosis, they said.
To further study the effects of stress on ulcer risk, the researchers analyzed historical data from 76 patients who lacked a history of gastric and duodenal ulcers in 1982, but by 1994 had developed “distinct breach[es] in the mucosa” that were confirmed by endoscopy or contrast radiology. The researchers did not count erosions that lacked appreciable depth as ulcers, they noted (Clin. Gastroenterol. Hepatol. 2014 Aug. 8 [doi:10.1016/j.cgh.2014.07.052]).
Study subjects answered 12 questions about their stress levels, such as, “Do your hands easily shake?” “Do you often suffer from fits of dizziness?” “Do you constantly have thoughts that trouble and worry you?” and “Do you usually feel misunderstood by other people?” They answered these questions at baseline in 1982-1983, again in 1987-1988, and again in 1993-1994.
Respondents who scored in the top tertile for psychological stress had an ulcer incidence of 3.5%, compared with 1.6% for those in the lowest tertile (odds ratio, 2.2; 95% confidence interval, 1.2-3.9; P < .01), reported the investigators. And controlling for smoking, helicobacteriosis, use of nonsteroidal anti-inflammatory drugs, and low socioeconomic status only partially weakened the relationship between stress and ulcers, they said. After accounting for those risk factors, every one-point increase on the stress questionnaire still upped the odds of peptic ulcer by 12% (odds ratio, 1.12; 95% confidence interval, 1.01-1.23)they reported.
Helicobacteri pylori infection was the strongest independent predictor of ulcers (OR, 3.3; 95% CI, 2.02-5.69), while cigarette smoking came in a close second (OR, 2.91; 95% CI, 1.38-6.16), said the researchers. Notably, stress and helicobacteriosis did not seem to synergistically increase the chances of ulcers, they reported. “Stress affected H. pylori–related ulcers at least as much as those related to neither H. pylori nor nonsteroidal anti-inflammatory drugs,” they said.
Several factors might explain the stress-ulcer link, such as increased acid load, activation of the hypothalamic-pituitary-adrenal axis, shifts in blood flow, and cytokine activation that might impair gastrointestinal mucosal defenses, said the investigators. Although the baseline data in their study were more than 2 decades old, that meant that patients likely had not been treated to eradicate H. pylori and were less likely to have taken proton pump inhibitors than the current population that has over-the-counter access to PPIs, they added. They also noted that past studies found a particularly strong link between stress and bleeding or perforated ulcers, which have not declined as much as other types of ulcers. “These results support a multicausal model of peptic ulcer etiology, with intertwined biological and psychosocial components,” they concluded.
The Kirby Family Foundation funded the statistical analysis. The researchers reported no conflicts of interest.
FROM CLINICAL GASTROENTEROLOGY AND HEPATOLOGY
Key clinical point: High stress levels independently predicted peptic ulcers.
Major finding: After adjustment for other risk factors, every one-point increase on a 12-item stress questionnaire increased the odds of peptic ulcers by 12% (OR, 1.12; 95% CI, 1.01-1.23).
Data source: Prospective, population-based study of 76 patients with peptic ulcers.
Disclosures: The Kirby Family Foundation funded the statistical analysis. The researchers reported no conflicts of interest.
Study linked gastric phenotypes, hormone levels to obesity
A prospective study linked obesity to faster gastric emptying time, higher fasted stomach volume, lower postprandial levels of the appetite-modifying hormone peptide tyrosine tyrosine, and higher postprandial levels of glucagonlike peptide–1, researchers reported in the March issue of Gastroenterology.
By understanding how patients’ obesity relates to these types of specific, quantifiable measures, clinicians might better tailor treatments based on their mechanisms of action, said Dr. Andres Acosta and his associates at Mayo Medical School, Rochester, Minn. “This observation has public health relevance, as it would usher in a new era of matching patients based on quantitative traits to pharmacotherapy, potentially enhancing drug efficacy in treatment of obesity, and reducing expenditures for both validating the efficacy of such medications and prescribing them to obese individuals in clinical practice,” the researchers said.
Source: American Gastroenterological Association
Extended-release phentermine-topiramate and other prescription weight-loss therapies vary from patient to patient in terms of efficacy, the researchers noted. For example, only about half of patients treated with phentermine-topiramate ER have been found to lose more than 10% of their body weight, while 30% lose less than 5% of body weight on the drug, they said. Furthermore, past studies have yielded conflicting data on whether gastric functions, such as emptying time and volume, predict body mass index (BMI), they noted (Gastroenterology 2014 Dec. 2 [doi:10.1053/j.gastro.2014.11.020]).
To explore these relationships, the investigators prospectively studied 328 adults and found that obese individuals had higher stomach volume when fasting (P = .03), faster gastric emptying (P < .001 for solids and P < .011 for liquids), lower levels of peptide tyrosine tyrosine (PYY) after eating (P = .003), and higher postprandial levels of glucagonlike peptide–1 (GLP-1) (P < .001), compared with normal-weight individuals.
Next, they carried out an expanded analysis that added retrospective data from another 181 adults. Among the 509 total subjects in that analysis, 85 were of normal weight (BMI, 18-24.9 kg/m2), 158 were overweight (BMI, 25-29.9 kg/m2), 135 fell within the obesity class I definition (BMI, 30-34.9 kg/m2), and 131 met the criteria for obesity class II (BMI greater than 35 kg/m2), the researchers reported. This study found that obese subjects ate more before feeling full (P = .038), compared with normal-weight individuals, as did patients whose waist circumference was abnormally high (P = .016), compared with subjects of normal girth, they added. In fact, for every 5 kg per m2 increase in BMI, individuals consumed about 50 calories more, and those with abnormal waist circumference consumed about 100 calories more at a buffet meal, compared with individuals whose waist circumference was normal (P = 0.016), they added.
The researchers also studied the effects of phentermine-topiramate ER on weight loss in 24 of the obese individuals, of whom half were randomized to the drug and half to placebo. The treatment group lost an average of 1.4 kg (standard deviation, 0.4 kg), compared with a 0.23-kg average loss for the placebo group (SD, 0.4 kg; P = 0.03), the investigators said. The treatment group also consumed fewer calories and had slower gastric emptying than the placebo group, they added. Furthermore, the amount of calories that individuals had previously consumed at a buffet meal was significantly linked with their response to phentermine-topiramate ER, they reported. Based on those results, obese individuals who tend to consume more than 1,000 calories at buffets could be expected to lose more than 1 kg per week on phentermine-topiramate ER, at least in the short term, they added.
Finally, factors related to satiety were found to explain 21% of differences among overweight and obese individuals, while gastric capacity explained 14% and psychological factors such as anxiety and depression explained 13%, the investigators said. Such measures “can serve as biomarkers to enrich selection of patients for treatment, based on the pharmacological effects of the medication,” they added. Just as satiety predicted response to phentermine-topiramate ER, other biomarkers might predict response to amylin agonists or GLP-1 agonists, they said.
The National Institutes of Health supported the study, and Vivus provided medication. The researchers reported having no conflicts of interest.
The last 2 decades have witnessed a dramatic rise in surgical as well as less invasive procedures to combat obesity and insulin resistance. However, it is clear that bariatric medicine/surgery has a long way to go. We have little or no knowledge about predictors of outcome and optimal selection for response to medical, surgical, or endoscopic interventions, leading to a "one-size-fits-all" approach, which may not be the most appropriate for treating obesity.
Perhaps an even more important problem is that therapies (such as drugs or balloons) may be ignored or even dismissed on the basis of overall disappointing results in large cohort studies, even though they may have the potential to produce much more significant weight loss in yet to be identified subgroups of patients.

|
| Dr. Pankaj Jay Pasricha |
With the expected proliferation of less invasive procedures with better patient acceptance, it becomes even more imperative, therefore, to start phenotyping patients across several dimensions including, but not limited, to the individual's gastrointestinal physiology and pathophysiology. In this article, Acosta et al. have taken a preliminary step in that direction, with a focus on gastric physiology and associated parameters of eating and satiety in a large group of obese patients. Their initial classification of "gastric phenotypes" needs to be validated further but provides a valuable framework to start building a more nuanced and tailored approach to interventions, particularly those that act predominantly on the stomach such as balloons, a dazzling variety of which are expected to appear on the market in the near future.
Dr. Pankaj Jay Pasricha, AGAF, is director of the Johns Hopkins Center for Neurogastroenterology; director of the Food Body and Mind Center at Johns Hopkins; professor of medicine and neurosciences, Johns Hopkins School of Medicine; and professor of innovation management, Johns Hopkins Carey School of Business, Baltimore. He has no conflicts of interest.
The last 2 decades have witnessed a dramatic rise in surgical as well as less invasive procedures to combat obesity and insulin resistance. However, it is clear that bariatric medicine/surgery has a long way to go. We have little or no knowledge about predictors of outcome and optimal selection for response to medical, surgical, or endoscopic interventions, leading to a "one-size-fits-all" approach, which may not be the most appropriate for treating obesity.
Perhaps an even more important problem is that therapies (such as drugs or balloons) may be ignored or even dismissed on the basis of overall disappointing results in large cohort studies, even though they may have the potential to produce much more significant weight loss in yet to be identified subgroups of patients.

|
| Dr. Pankaj Jay Pasricha |
With the expected proliferation of less invasive procedures with better patient acceptance, it becomes even more imperative, therefore, to start phenotyping patients across several dimensions including, but not limited, to the individual's gastrointestinal physiology and pathophysiology. In this article, Acosta et al. have taken a preliminary step in that direction, with a focus on gastric physiology and associated parameters of eating and satiety in a large group of obese patients. Their initial classification of "gastric phenotypes" needs to be validated further but provides a valuable framework to start building a more nuanced and tailored approach to interventions, particularly those that act predominantly on the stomach such as balloons, a dazzling variety of which are expected to appear on the market in the near future.
Dr. Pankaj Jay Pasricha, AGAF, is director of the Johns Hopkins Center for Neurogastroenterology; director of the Food Body and Mind Center at Johns Hopkins; professor of medicine and neurosciences, Johns Hopkins School of Medicine; and professor of innovation management, Johns Hopkins Carey School of Business, Baltimore. He has no conflicts of interest.
The last 2 decades have witnessed a dramatic rise in surgical as well as less invasive procedures to combat obesity and insulin resistance. However, it is clear that bariatric medicine/surgery has a long way to go. We have little or no knowledge about predictors of outcome and optimal selection for response to medical, surgical, or endoscopic interventions, leading to a "one-size-fits-all" approach, which may not be the most appropriate for treating obesity.
Perhaps an even more important problem is that therapies (such as drugs or balloons) may be ignored or even dismissed on the basis of overall disappointing results in large cohort studies, even though they may have the potential to produce much more significant weight loss in yet to be identified subgroups of patients.

|
| Dr. Pankaj Jay Pasricha |
With the expected proliferation of less invasive procedures with better patient acceptance, it becomes even more imperative, therefore, to start phenotyping patients across several dimensions including, but not limited, to the individual's gastrointestinal physiology and pathophysiology. In this article, Acosta et al. have taken a preliminary step in that direction, with a focus on gastric physiology and associated parameters of eating and satiety in a large group of obese patients. Their initial classification of "gastric phenotypes" needs to be validated further but provides a valuable framework to start building a more nuanced and tailored approach to interventions, particularly those that act predominantly on the stomach such as balloons, a dazzling variety of which are expected to appear on the market in the near future.
Dr. Pankaj Jay Pasricha, AGAF, is director of the Johns Hopkins Center for Neurogastroenterology; director of the Food Body and Mind Center at Johns Hopkins; professor of medicine and neurosciences, Johns Hopkins School of Medicine; and professor of innovation management, Johns Hopkins Carey School of Business, Baltimore. He has no conflicts of interest.
A prospective study linked obesity to faster gastric emptying time, higher fasted stomach volume, lower postprandial levels of the appetite-modifying hormone peptide tyrosine tyrosine, and higher postprandial levels of glucagonlike peptide–1, researchers reported in the March issue of Gastroenterology.
By understanding how patients’ obesity relates to these types of specific, quantifiable measures, clinicians might better tailor treatments based on their mechanisms of action, said Dr. Andres Acosta and his associates at Mayo Medical School, Rochester, Minn. “This observation has public health relevance, as it would usher in a new era of matching patients based on quantitative traits to pharmacotherapy, potentially enhancing drug efficacy in treatment of obesity, and reducing expenditures for both validating the efficacy of such medications and prescribing them to obese individuals in clinical practice,” the researchers said.
Source: American Gastroenterological Association
Extended-release phentermine-topiramate and other prescription weight-loss therapies vary from patient to patient in terms of efficacy, the researchers noted. For example, only about half of patients treated with phentermine-topiramate ER have been found to lose more than 10% of their body weight, while 30% lose less than 5% of body weight on the drug, they said. Furthermore, past studies have yielded conflicting data on whether gastric functions, such as emptying time and volume, predict body mass index (BMI), they noted (Gastroenterology 2014 Dec. 2 [doi:10.1053/j.gastro.2014.11.020]).
To explore these relationships, the investigators prospectively studied 328 adults and found that obese individuals had higher stomach volume when fasting (P = .03), faster gastric emptying (P < .001 for solids and P < .011 for liquids), lower levels of peptide tyrosine tyrosine (PYY) after eating (P = .003), and higher postprandial levels of glucagonlike peptide–1 (GLP-1) (P < .001), compared with normal-weight individuals.
Next, they carried out an expanded analysis that added retrospective data from another 181 adults. Among the 509 total subjects in that analysis, 85 were of normal weight (BMI, 18-24.9 kg/m2), 158 were overweight (BMI, 25-29.9 kg/m2), 135 fell within the obesity class I definition (BMI, 30-34.9 kg/m2), and 131 met the criteria for obesity class II (BMI greater than 35 kg/m2), the researchers reported. This study found that obese subjects ate more before feeling full (P = .038), compared with normal-weight individuals, as did patients whose waist circumference was abnormally high (P = .016), compared with subjects of normal girth, they added. In fact, for every 5 kg per m2 increase in BMI, individuals consumed about 50 calories more, and those with abnormal waist circumference consumed about 100 calories more at a buffet meal, compared with individuals whose waist circumference was normal (P = 0.016), they added.
The researchers also studied the effects of phentermine-topiramate ER on weight loss in 24 of the obese individuals, of whom half were randomized to the drug and half to placebo. The treatment group lost an average of 1.4 kg (standard deviation, 0.4 kg), compared with a 0.23-kg average loss for the placebo group (SD, 0.4 kg; P = 0.03), the investigators said. The treatment group also consumed fewer calories and had slower gastric emptying than the placebo group, they added. Furthermore, the amount of calories that individuals had previously consumed at a buffet meal was significantly linked with their response to phentermine-topiramate ER, they reported. Based on those results, obese individuals who tend to consume more than 1,000 calories at buffets could be expected to lose more than 1 kg per week on phentermine-topiramate ER, at least in the short term, they added.
Finally, factors related to satiety were found to explain 21% of differences among overweight and obese individuals, while gastric capacity explained 14% and psychological factors such as anxiety and depression explained 13%, the investigators said. Such measures “can serve as biomarkers to enrich selection of patients for treatment, based on the pharmacological effects of the medication,” they added. Just as satiety predicted response to phentermine-topiramate ER, other biomarkers might predict response to amylin agonists or GLP-1 agonists, they said.
The National Institutes of Health supported the study, and Vivus provided medication. The researchers reported having no conflicts of interest.
A prospective study linked obesity to faster gastric emptying time, higher fasted stomach volume, lower postprandial levels of the appetite-modifying hormone peptide tyrosine tyrosine, and higher postprandial levels of glucagonlike peptide–1, researchers reported in the March issue of Gastroenterology.
By understanding how patients’ obesity relates to these types of specific, quantifiable measures, clinicians might better tailor treatments based on their mechanisms of action, said Dr. Andres Acosta and his associates at Mayo Medical School, Rochester, Minn. “This observation has public health relevance, as it would usher in a new era of matching patients based on quantitative traits to pharmacotherapy, potentially enhancing drug efficacy in treatment of obesity, and reducing expenditures for both validating the efficacy of such medications and prescribing them to obese individuals in clinical practice,” the researchers said.
Source: American Gastroenterological Association
Extended-release phentermine-topiramate and other prescription weight-loss therapies vary from patient to patient in terms of efficacy, the researchers noted. For example, only about half of patients treated with phentermine-topiramate ER have been found to lose more than 10% of their body weight, while 30% lose less than 5% of body weight on the drug, they said. Furthermore, past studies have yielded conflicting data on whether gastric functions, such as emptying time and volume, predict body mass index (BMI), they noted (Gastroenterology 2014 Dec. 2 [doi:10.1053/j.gastro.2014.11.020]).
To explore these relationships, the investigators prospectively studied 328 adults and found that obese individuals had higher stomach volume when fasting (P = .03), faster gastric emptying (P < .001 for solids and P < .011 for liquids), lower levels of peptide tyrosine tyrosine (PYY) after eating (P = .003), and higher postprandial levels of glucagonlike peptide–1 (GLP-1) (P < .001), compared with normal-weight individuals.
Next, they carried out an expanded analysis that added retrospective data from another 181 adults. Among the 509 total subjects in that analysis, 85 were of normal weight (BMI, 18-24.9 kg/m2), 158 were overweight (BMI, 25-29.9 kg/m2), 135 fell within the obesity class I definition (BMI, 30-34.9 kg/m2), and 131 met the criteria for obesity class II (BMI greater than 35 kg/m2), the researchers reported. This study found that obese subjects ate more before feeling full (P = .038), compared with normal-weight individuals, as did patients whose waist circumference was abnormally high (P = .016), compared with subjects of normal girth, they added. In fact, for every 5 kg per m2 increase in BMI, individuals consumed about 50 calories more, and those with abnormal waist circumference consumed about 100 calories more at a buffet meal, compared with individuals whose waist circumference was normal (P = 0.016), they added.
The researchers also studied the effects of phentermine-topiramate ER on weight loss in 24 of the obese individuals, of whom half were randomized to the drug and half to placebo. The treatment group lost an average of 1.4 kg (standard deviation, 0.4 kg), compared with a 0.23-kg average loss for the placebo group (SD, 0.4 kg; P = 0.03), the investigators said. The treatment group also consumed fewer calories and had slower gastric emptying than the placebo group, they added. Furthermore, the amount of calories that individuals had previously consumed at a buffet meal was significantly linked with their response to phentermine-topiramate ER, they reported. Based on those results, obese individuals who tend to consume more than 1,000 calories at buffets could be expected to lose more than 1 kg per week on phentermine-topiramate ER, at least in the short term, they added.
Finally, factors related to satiety were found to explain 21% of differences among overweight and obese individuals, while gastric capacity explained 14% and psychological factors such as anxiety and depression explained 13%, the investigators said. Such measures “can serve as biomarkers to enrich selection of patients for treatment, based on the pharmacological effects of the medication,” they added. Just as satiety predicted response to phentermine-topiramate ER, other biomarkers might predict response to amylin agonists or GLP-1 agonists, they said.
The National Institutes of Health supported the study, and Vivus provided medication. The researchers reported having no conflicts of interest.
Key clinical point: Obesity was linked to lower satiety levels, faster gastric emptying, greater fasted gastric volume, and lower levels of PYY.
Major finding: Obese individuals had larger stomach volume when fasting (P = .03), faster gastric emptying (P < .001 for solids and P < .011 for liquids), lower levels of PYY after eating (P = .003), and higher postprandial levels of GLP-1 (P < .001), compared with normal-weight individuals.
Data source: Prospective study of 328 adults, expanded study of 509 adults, and nested randomized, controlled clinical trial of 24 obese adults.
Disclosures: The National Institutes of Health supported the study, and Vivus provided medication. The researchers reported having no conflicts of interest.
Human liver cells can induce antiviral reaction against hepatitis C
Immunity against the hepatitis C virus can be induced by cultured primary human liver sinusoidal endothelial cells, according to a study published in the February issue of Gastroenterology (doi:10.1053/j.gastro.2014.10.040).
“We found HLSECs [primary human LSECs] express many of the receptors implicated in HCV [hepatitis C virus] attachment and entry and HLSEC-to-hepatocyte contact was dispensable for uptake,” wrote lead author Dr. Silvia M. Giugliano of the University of Colorado, Denver, and her associates.
In a cohort study, investigators exposed HLSECs and immortalized liver endothelial cells (TMNK-1) to several variants of HCV: full-length transmitted/founder virus, sucrose-purified Japanese fulminant hepatitis–1 (JFH-1), a virus encoding a luciferase reporter, and the HCV-specific pathogen-associated molecular pattern molecules (PAMP, substrate for RIG-I). Cells were analyzed by using polymerase chain reaction (PCR), immunofluorescence, and immunohistochemical assays.
Results showed that HLSECs, regardless of contact between cells, were able to internalize HCV when exposed to it and replicate, though not translate HCV RNA. The HCV RNA “induced consistent and broad transcription of multiple interferons (IFNs) [via] pattern recognition receptors (TLR7 and retinoic acid-inducible gene 1).” Furthermore, supernatants from primary HLSECs transfected with HCV-specific PAMP molecules had larger inductions of IFNs and IFN-stimulated genes in HLSECs.
“Conditioned media from IFN-stimulated HLSECs induced expression of antiviral genes by uninfected primary human hepatocytes,” wrote Dr. Giugliano and her coauthors. “Exosomes, derived from HLSECs following stimulation with either type I or type III IFNs, controlled HCV replication in a dose-dependent manner.”
However, the investigators say that more study is required to understand why HCV is able to present so persistently if the means to combat the virus are so apparent in the immune system.
“These results raise a number of intriguing questions, for example, how the use of exogenous IFN to treat viral hepatitis could be expected to induce additional, previously unrecognized antiviral mechanisms involving HLSECs,” says the study. “Further work is warranted to understand why despite these innate immune responses, HCV is able to establish persistence and fail eradication with IFN-based antiviral therapy.”
The study supported by grants R21-AI103361 and U19 AI 1066328; Dr. Rosen received a Merit Review grant and Dr. Shaw received grant R21-AI 106000. The authors reported no financial conflicts of interest.
Liver sinusoidal endothelial cells (LSECs) are a large component of the liver immune system but are not very well characterized for their role in diseases like chronic hepatitis C virus (HCV) infection. Dr. Giugliano and her associates tested the antiviral activity of primary human LSECs and an immortalized LSEC cell line (TMNK-1), following exposure to several viral variants. These included naturally

|
| Dr. Arash Grakoui |
occurring founder genotype 1a virus, a JFH-1 infectious clone (cloned originally from a patient with fulminant hepatitis), a modified cell culture of adaptive JFH-1 virus expressing luciferase reporter, and HCV-specific pathogen-associated molecular pattern poly UC RNA that is a substrate for RIG-I. They found LSECs were able to acquire HCV in an LSEC-to-hepatocyte–contact independent manner but that these cells were not permissive for productive infection (replication). Importantly, viral RNA through HCV uptake induced robust transcription of type I and III interferon (IFN) by LSECs via TLR7 and RIG-I pathways. LSEC-derived IFN had antiviral effects on HCV-infected human hepatoma cell line, Huh7.5 cells in vitro, and this effect was mediated through the production of exosomes. The authors concluded that LSECs likely have an important antiviral role in HCV infection through bystander induction of an antiviral state. This study highlights the idea that these cells can function similarly to other innate/phagocytic cells like monocytes/macrophages and furthers the idea that innate activation of LSECs may have protective effects on the antiviral state of hepatocytes. Mechanisms of antiviral immunity by LSECs, whether it occurs through exosomes or IFN, will have a significant impact in the field as the answers will have relevance to numerous facets of liver immunology, including gene transfer, organ transplant, and response to other hepatotropic infections.
Dr. Arash Grakoui is an associate professor jointly appointed in the departments of medicine, division of infectious diseases and Yerkes National Primate Research Center, department of microbiology and immunology at Emory University, Atlanta. He has no conflicts of interest.
Liver sinusoidal endothelial cells (LSECs) are a large component of the liver immune system but are not very well characterized for their role in diseases like chronic hepatitis C virus (HCV) infection. Dr. Giugliano and her associates tested the antiviral activity of primary human LSECs and an immortalized LSEC cell line (TMNK-1), following exposure to several viral variants. These included naturally

|
| Dr. Arash Grakoui |
occurring founder genotype 1a virus, a JFH-1 infectious clone (cloned originally from a patient with fulminant hepatitis), a modified cell culture of adaptive JFH-1 virus expressing luciferase reporter, and HCV-specific pathogen-associated molecular pattern poly UC RNA that is a substrate for RIG-I. They found LSECs were able to acquire HCV in an LSEC-to-hepatocyte–contact independent manner but that these cells were not permissive for productive infection (replication). Importantly, viral RNA through HCV uptake induced robust transcription of type I and III interferon (IFN) by LSECs via TLR7 and RIG-I pathways. LSEC-derived IFN had antiviral effects on HCV-infected human hepatoma cell line, Huh7.5 cells in vitro, and this effect was mediated through the production of exosomes. The authors concluded that LSECs likely have an important antiviral role in HCV infection through bystander induction of an antiviral state. This study highlights the idea that these cells can function similarly to other innate/phagocytic cells like monocytes/macrophages and furthers the idea that innate activation of LSECs may have protective effects on the antiviral state of hepatocytes. Mechanisms of antiviral immunity by LSECs, whether it occurs through exosomes or IFN, will have a significant impact in the field as the answers will have relevance to numerous facets of liver immunology, including gene transfer, organ transplant, and response to other hepatotropic infections.
Dr. Arash Grakoui is an associate professor jointly appointed in the departments of medicine, division of infectious diseases and Yerkes National Primate Research Center, department of microbiology and immunology at Emory University, Atlanta. He has no conflicts of interest.
Liver sinusoidal endothelial cells (LSECs) are a large component of the liver immune system but are not very well characterized for their role in diseases like chronic hepatitis C virus (HCV) infection. Dr. Giugliano and her associates tested the antiviral activity of primary human LSECs and an immortalized LSEC cell line (TMNK-1), following exposure to several viral variants. These included naturally

|
| Dr. Arash Grakoui |
occurring founder genotype 1a virus, a JFH-1 infectious clone (cloned originally from a patient with fulminant hepatitis), a modified cell culture of adaptive JFH-1 virus expressing luciferase reporter, and HCV-specific pathogen-associated molecular pattern poly UC RNA that is a substrate for RIG-I. They found LSECs were able to acquire HCV in an LSEC-to-hepatocyte–contact independent manner but that these cells were not permissive for productive infection (replication). Importantly, viral RNA through HCV uptake induced robust transcription of type I and III interferon (IFN) by LSECs via TLR7 and RIG-I pathways. LSEC-derived IFN had antiviral effects on HCV-infected human hepatoma cell line, Huh7.5 cells in vitro, and this effect was mediated through the production of exosomes. The authors concluded that LSECs likely have an important antiviral role in HCV infection through bystander induction of an antiviral state. This study highlights the idea that these cells can function similarly to other innate/phagocytic cells like monocytes/macrophages and furthers the idea that innate activation of LSECs may have protective effects on the antiviral state of hepatocytes. Mechanisms of antiviral immunity by LSECs, whether it occurs through exosomes or IFN, will have a significant impact in the field as the answers will have relevance to numerous facets of liver immunology, including gene transfer, organ transplant, and response to other hepatotropic infections.
Dr. Arash Grakoui is an associate professor jointly appointed in the departments of medicine, division of infectious diseases and Yerkes National Primate Research Center, department of microbiology and immunology at Emory University, Atlanta. He has no conflicts of interest.
Immunity against the hepatitis C virus can be induced by cultured primary human liver sinusoidal endothelial cells, according to a study published in the February issue of Gastroenterology (doi:10.1053/j.gastro.2014.10.040).
“We found HLSECs [primary human LSECs] express many of the receptors implicated in HCV [hepatitis C virus] attachment and entry and HLSEC-to-hepatocyte contact was dispensable for uptake,” wrote lead author Dr. Silvia M. Giugliano of the University of Colorado, Denver, and her associates.
In a cohort study, investigators exposed HLSECs and immortalized liver endothelial cells (TMNK-1) to several variants of HCV: full-length transmitted/founder virus, sucrose-purified Japanese fulminant hepatitis–1 (JFH-1), a virus encoding a luciferase reporter, and the HCV-specific pathogen-associated molecular pattern molecules (PAMP, substrate for RIG-I). Cells were analyzed by using polymerase chain reaction (PCR), immunofluorescence, and immunohistochemical assays.
Results showed that HLSECs, regardless of contact between cells, were able to internalize HCV when exposed to it and replicate, though not translate HCV RNA. The HCV RNA “induced consistent and broad transcription of multiple interferons (IFNs) [via] pattern recognition receptors (TLR7 and retinoic acid-inducible gene 1).” Furthermore, supernatants from primary HLSECs transfected with HCV-specific PAMP molecules had larger inductions of IFNs and IFN-stimulated genes in HLSECs.
“Conditioned media from IFN-stimulated HLSECs induced expression of antiviral genes by uninfected primary human hepatocytes,” wrote Dr. Giugliano and her coauthors. “Exosomes, derived from HLSECs following stimulation with either type I or type III IFNs, controlled HCV replication in a dose-dependent manner.”
However, the investigators say that more study is required to understand why HCV is able to present so persistently if the means to combat the virus are so apparent in the immune system.
“These results raise a number of intriguing questions, for example, how the use of exogenous IFN to treat viral hepatitis could be expected to induce additional, previously unrecognized antiviral mechanisms involving HLSECs,” says the study. “Further work is warranted to understand why despite these innate immune responses, HCV is able to establish persistence and fail eradication with IFN-based antiviral therapy.”
The study supported by grants R21-AI103361 and U19 AI 1066328; Dr. Rosen received a Merit Review grant and Dr. Shaw received grant R21-AI 106000. The authors reported no financial conflicts of interest.
Immunity against the hepatitis C virus can be induced by cultured primary human liver sinusoidal endothelial cells, according to a study published in the February issue of Gastroenterology (doi:10.1053/j.gastro.2014.10.040).
“We found HLSECs [primary human LSECs] express many of the receptors implicated in HCV [hepatitis C virus] attachment and entry and HLSEC-to-hepatocyte contact was dispensable for uptake,” wrote lead author Dr. Silvia M. Giugliano of the University of Colorado, Denver, and her associates.
In a cohort study, investigators exposed HLSECs and immortalized liver endothelial cells (TMNK-1) to several variants of HCV: full-length transmitted/founder virus, sucrose-purified Japanese fulminant hepatitis–1 (JFH-1), a virus encoding a luciferase reporter, and the HCV-specific pathogen-associated molecular pattern molecules (PAMP, substrate for RIG-I). Cells were analyzed by using polymerase chain reaction (PCR), immunofluorescence, and immunohistochemical assays.
Results showed that HLSECs, regardless of contact between cells, were able to internalize HCV when exposed to it and replicate, though not translate HCV RNA. The HCV RNA “induced consistent and broad transcription of multiple interferons (IFNs) [via] pattern recognition receptors (TLR7 and retinoic acid-inducible gene 1).” Furthermore, supernatants from primary HLSECs transfected with HCV-specific PAMP molecules had larger inductions of IFNs and IFN-stimulated genes in HLSECs.
“Conditioned media from IFN-stimulated HLSECs induced expression of antiviral genes by uninfected primary human hepatocytes,” wrote Dr. Giugliano and her coauthors. “Exosomes, derived from HLSECs following stimulation with either type I or type III IFNs, controlled HCV replication in a dose-dependent manner.”
However, the investigators say that more study is required to understand why HCV is able to present so persistently if the means to combat the virus are so apparent in the immune system.
“These results raise a number of intriguing questions, for example, how the use of exogenous IFN to treat viral hepatitis could be expected to induce additional, previously unrecognized antiviral mechanisms involving HLSECs,” says the study. “Further work is warranted to understand why despite these innate immune responses, HCV is able to establish persistence and fail eradication with IFN-based antiviral therapy.”
The study supported by grants R21-AI103361 and U19 AI 1066328; Dr. Rosen received a Merit Review grant and Dr. Shaw received grant R21-AI 106000. The authors reported no financial conflicts of interest.
FROM GASTROENTEROLOGY
Key clinical point: Cultured primary human liver sinusoidal endothelial cells (HLSECs) induce self-amplifying interferon-mediated responses and release of exosomes with antiviral activity, thus allowing it to mediate immunity against the hepatitis C virus (HCV).
Major finding: HLSECs and CV-specific PAMP molecules induced IFNs and replicated HCV RNA when exposed to various forms of HCV.
Data source: Cohort study
Disclosures: Study supported by grants R21-AI103361 and U19 AI 1066328; Dr. Rosen received a Merit Review grant and Dr. Shaw received grant R21-AI 106000. The authors reported no financial conflicts of interest.