User login
Pentoxifylline beat placebo in acute pancreatitis trial
Patients with acute pancreatitis who received pentoxifylline had fewer ICU admissions and shorter ICU and hospital stays than placebo-treated controls, according to a small, randomized double-blind trial reported in Gastroenterology.
“We showed that a single-institution drug trial for acute pancreatitis is feasible and that pentoxifylline is safe, cheap, and might have efficacy,” wrote Dr. Santhi Vege and his associates at the Mayo Clinic in Rochester, Minn. “This sets the stage for a larger trial of this drug in all patients with acute pancreatitis, to realize the goal of finding an effective drug that can be given within 24 hours of diagnosis in any setting.”
Tumor necrosis factor–alpha is a key culprit in severe acute pancreatitis, including pancreatic and peripancreatic necrosis, systemic inflammatory response syndrome, and persistent organ failure, the researchers noted. Pentoxifylline is a nonselective phosphodiesterase inhibitor that has been found safe and effective in other TNF-alpha–mediated diseases such as acute alcoholic hepatitis, but few studies in humans have evaluated the drug for acute pancreatitis, they said (Gastroenterology 2015 June 22 [doi:10.1053/j.gastro.2015.04.019]). For their study, the investigators randomized 28 patients with predicted severe acute pancreatitis to either placebo or 400 mg pentoxifylline given orally at enrollment and then three times a day for 72 hours. Both groups also received standard of care treatments such as antibiotics and fluid therapy, and had comparable baseline characteristics including age, sex, body mass index, Acute Physiology and Chronic Health Evaluation scores, systemic inflammatory response syndrome scores, and inflammatory marker levels, the researchers said.
Significantly fewer patients who received pentoxifylline needed to stay in the hospital for more than 4 days (14% vs. 57% for the placebo group; P = .046), and the maximum length of ICU stay was 0 days for the intervention group, compared with 13 days for the control group (P = .03), the investigators reported. Analyses of several other outcome measures also favored pentoxifylline over placebo, but did not reach statistical significance in the small study, including the need for ICU transfer (0% for pentoxifylline patients vs. 28% of the placebo group; P = .098) and the median length of hospitalization (for pentoxifylline: 3 days, range 1-5 days; for placebo: 5 days; range 1-30 days; P = .06).
The treatment and control groups did not significantly differ in terms of levels of inflammatory markers, including circulating TNF-alpha, said the investigators. Differences in levels of TNF-alpha, interleukin-6, IL-8, and C-reactive protein “may be significant if the sample size is larger,” they added.
The exact mechanism by which pentoxifylline affects acute pancreatitis is unclear, but the production of pancreatic TNF-alpha peaks about 24-36 hours into an episode of the disease, so patients might benefit from receiving pentoxifylline sooner than the 72-hour window dictated by the study protocol, said Dr. Vege and his associates. “Initiating drug therapy within a few hours is challenging, although a 24-hour cutoff time may be feasible in appropriate settings,” they wrote.
A scholarly opportunity award from the Mayo Clinic helped fund the work. The investigators reported having no relevant financial conflicts of interest.
The study of acute pancreatitis (AP) is economically and scientifically essential because acute pancreatitis is the most common reason for hospitalization among patients with GI diseases, consumes considerable resources, and is treated primarily with supportive measures. The pilot study by Dr. Vege and his colleagues reports that pentoxifylline treatment is safe for patients with severe acute pancreatitis and is associated with a promising reduction in ICU utilization and duration in patients requiring a hospital stay >4 days.

|
| Dr. Matthew J. DiMagno |
This study is not only provocative but also raises the hypothesis-generating question of how pentoxifylline might exert a salutary effect without reducing blood tumor necrosis factor–alpha levels (or IL-6, IL-8, or C-reactive protein levels). The authors ascribe this discordance to the timing of administering pentoxifylline and to potential TNF-alpha independent effects. Biologically, pancreatic TNF-alpha levels increase within the first 30-60 minutes of onset of acute pancreatitis (Am. J. Surg. 1998;175:76-83). In experimental AP, pentoxifylline ameliorates severity, but data are conflicting about whether prophylactic or delayed (Surgery 1996;120:515-21) antagonism of TNF-alpha signaling is more protective. Clinically relevant data suggest that prophylactic administration of pentoxifylline does not prevent postendoscopic retrograde cholangiopancreatography pancreatitis (Gastrointest. Endosc. 2007;66:513-8), but nonprophylactic administration of pentoxifylline improves short-term survival in alcoholic hepatitis without significantly reducing blood TNF-alpha levels (Gastroenterology 2000;119:1637-48). Hence, pentoxifylline appears to ameliorate AP and alcoholic hepatitis through TNF-alpha independent signaling, conceivably by targeting the microcirculation, as described for patients with claudication (Angiology 1994;45:339-45).
Future studies might test this hypothesis by determining whether pentoxifylline blunts increases in deleterious vascular factors (for example, angiopoietin-2) [Am. J. Gastroenterol. 2010;105:2287-92; J. Am. Coll. Surg. 2014;218:26-32; Am. J. Gastroenterol. 2011;106:1859-61]) and reduces vascular complications that correlate with the need for ICU care and more severe AP.
Dr. Matthew J. DiMagno is in the division of gastroenterology and hepatology, department of internal medicine, University of Michigan, Ann Arbor. He serves as chair of the American Gastroenterological Association Institute Council Section on Pancreatic Disorders. He declared no relevant financial conflicts of interest.
The study of acute pancreatitis (AP) is economically and scientifically essential because acute pancreatitis is the most common reason for hospitalization among patients with GI diseases, consumes considerable resources, and is treated primarily with supportive measures. The pilot study by Dr. Vege and his colleagues reports that pentoxifylline treatment is safe for patients with severe acute pancreatitis and is associated with a promising reduction in ICU utilization and duration in patients requiring a hospital stay >4 days.

|
| Dr. Matthew J. DiMagno |
This study is not only provocative but also raises the hypothesis-generating question of how pentoxifylline might exert a salutary effect without reducing blood tumor necrosis factor–alpha levels (or IL-6, IL-8, or C-reactive protein levels). The authors ascribe this discordance to the timing of administering pentoxifylline and to potential TNF-alpha independent effects. Biologically, pancreatic TNF-alpha levels increase within the first 30-60 minutes of onset of acute pancreatitis (Am. J. Surg. 1998;175:76-83). In experimental AP, pentoxifylline ameliorates severity, but data are conflicting about whether prophylactic or delayed (Surgery 1996;120:515-21) antagonism of TNF-alpha signaling is more protective. Clinically relevant data suggest that prophylactic administration of pentoxifylline does not prevent postendoscopic retrograde cholangiopancreatography pancreatitis (Gastrointest. Endosc. 2007;66:513-8), but nonprophylactic administration of pentoxifylline improves short-term survival in alcoholic hepatitis without significantly reducing blood TNF-alpha levels (Gastroenterology 2000;119:1637-48). Hence, pentoxifylline appears to ameliorate AP and alcoholic hepatitis through TNF-alpha independent signaling, conceivably by targeting the microcirculation, as described for patients with claudication (Angiology 1994;45:339-45).
Future studies might test this hypothesis by determining whether pentoxifylline blunts increases in deleterious vascular factors (for example, angiopoietin-2) [Am. J. Gastroenterol. 2010;105:2287-92; J. Am. Coll. Surg. 2014;218:26-32; Am. J. Gastroenterol. 2011;106:1859-61]) and reduces vascular complications that correlate with the need for ICU care and more severe AP.
Dr. Matthew J. DiMagno is in the division of gastroenterology and hepatology, department of internal medicine, University of Michigan, Ann Arbor. He serves as chair of the American Gastroenterological Association Institute Council Section on Pancreatic Disorders. He declared no relevant financial conflicts of interest.
The study of acute pancreatitis (AP) is economically and scientifically essential because acute pancreatitis is the most common reason for hospitalization among patients with GI diseases, consumes considerable resources, and is treated primarily with supportive measures. The pilot study by Dr. Vege and his colleagues reports that pentoxifylline treatment is safe for patients with severe acute pancreatitis and is associated with a promising reduction in ICU utilization and duration in patients requiring a hospital stay >4 days.

|
| Dr. Matthew J. DiMagno |
This study is not only provocative but also raises the hypothesis-generating question of how pentoxifylline might exert a salutary effect without reducing blood tumor necrosis factor–alpha levels (or IL-6, IL-8, or C-reactive protein levels). The authors ascribe this discordance to the timing of administering pentoxifylline and to potential TNF-alpha independent effects. Biologically, pancreatic TNF-alpha levels increase within the first 30-60 minutes of onset of acute pancreatitis (Am. J. Surg. 1998;175:76-83). In experimental AP, pentoxifylline ameliorates severity, but data are conflicting about whether prophylactic or delayed (Surgery 1996;120:515-21) antagonism of TNF-alpha signaling is more protective. Clinically relevant data suggest that prophylactic administration of pentoxifylline does not prevent postendoscopic retrograde cholangiopancreatography pancreatitis (Gastrointest. Endosc. 2007;66:513-8), but nonprophylactic administration of pentoxifylline improves short-term survival in alcoholic hepatitis without significantly reducing blood TNF-alpha levels (Gastroenterology 2000;119:1637-48). Hence, pentoxifylline appears to ameliorate AP and alcoholic hepatitis through TNF-alpha independent signaling, conceivably by targeting the microcirculation, as described for patients with claudication (Angiology 1994;45:339-45).
Future studies might test this hypothesis by determining whether pentoxifylline blunts increases in deleterious vascular factors (for example, angiopoietin-2) [Am. J. Gastroenterol. 2010;105:2287-92; J. Am. Coll. Surg. 2014;218:26-32; Am. J. Gastroenterol. 2011;106:1859-61]) and reduces vascular complications that correlate with the need for ICU care and more severe AP.
Dr. Matthew J. DiMagno is in the division of gastroenterology and hepatology, department of internal medicine, University of Michigan, Ann Arbor. He serves as chair of the American Gastroenterological Association Institute Council Section on Pancreatic Disorders. He declared no relevant financial conflicts of interest.
Patients with acute pancreatitis who received pentoxifylline had fewer ICU admissions and shorter ICU and hospital stays than placebo-treated controls, according to a small, randomized double-blind trial reported in Gastroenterology.
“We showed that a single-institution drug trial for acute pancreatitis is feasible and that pentoxifylline is safe, cheap, and might have efficacy,” wrote Dr. Santhi Vege and his associates at the Mayo Clinic in Rochester, Minn. “This sets the stage for a larger trial of this drug in all patients with acute pancreatitis, to realize the goal of finding an effective drug that can be given within 24 hours of diagnosis in any setting.”
Tumor necrosis factor–alpha is a key culprit in severe acute pancreatitis, including pancreatic and peripancreatic necrosis, systemic inflammatory response syndrome, and persistent organ failure, the researchers noted. Pentoxifylline is a nonselective phosphodiesterase inhibitor that has been found safe and effective in other TNF-alpha–mediated diseases such as acute alcoholic hepatitis, but few studies in humans have evaluated the drug for acute pancreatitis, they said (Gastroenterology 2015 June 22 [doi:10.1053/j.gastro.2015.04.019]). For their study, the investigators randomized 28 patients with predicted severe acute pancreatitis to either placebo or 400 mg pentoxifylline given orally at enrollment and then three times a day for 72 hours. Both groups also received standard of care treatments such as antibiotics and fluid therapy, and had comparable baseline characteristics including age, sex, body mass index, Acute Physiology and Chronic Health Evaluation scores, systemic inflammatory response syndrome scores, and inflammatory marker levels, the researchers said.
Significantly fewer patients who received pentoxifylline needed to stay in the hospital for more than 4 days (14% vs. 57% for the placebo group; P = .046), and the maximum length of ICU stay was 0 days for the intervention group, compared with 13 days for the control group (P = .03), the investigators reported. Analyses of several other outcome measures also favored pentoxifylline over placebo, but did not reach statistical significance in the small study, including the need for ICU transfer (0% for pentoxifylline patients vs. 28% of the placebo group; P = .098) and the median length of hospitalization (for pentoxifylline: 3 days, range 1-5 days; for placebo: 5 days; range 1-30 days; P = .06).
The treatment and control groups did not significantly differ in terms of levels of inflammatory markers, including circulating TNF-alpha, said the investigators. Differences in levels of TNF-alpha, interleukin-6, IL-8, and C-reactive protein “may be significant if the sample size is larger,” they added.
The exact mechanism by which pentoxifylline affects acute pancreatitis is unclear, but the production of pancreatic TNF-alpha peaks about 24-36 hours into an episode of the disease, so patients might benefit from receiving pentoxifylline sooner than the 72-hour window dictated by the study protocol, said Dr. Vege and his associates. “Initiating drug therapy within a few hours is challenging, although a 24-hour cutoff time may be feasible in appropriate settings,” they wrote.
A scholarly opportunity award from the Mayo Clinic helped fund the work. The investigators reported having no relevant financial conflicts of interest.
Patients with acute pancreatitis who received pentoxifylline had fewer ICU admissions and shorter ICU and hospital stays than placebo-treated controls, according to a small, randomized double-blind trial reported in Gastroenterology.
“We showed that a single-institution drug trial for acute pancreatitis is feasible and that pentoxifylline is safe, cheap, and might have efficacy,” wrote Dr. Santhi Vege and his associates at the Mayo Clinic in Rochester, Minn. “This sets the stage for a larger trial of this drug in all patients with acute pancreatitis, to realize the goal of finding an effective drug that can be given within 24 hours of diagnosis in any setting.”
Tumor necrosis factor–alpha is a key culprit in severe acute pancreatitis, including pancreatic and peripancreatic necrosis, systemic inflammatory response syndrome, and persistent organ failure, the researchers noted. Pentoxifylline is a nonselective phosphodiesterase inhibitor that has been found safe and effective in other TNF-alpha–mediated diseases such as acute alcoholic hepatitis, but few studies in humans have evaluated the drug for acute pancreatitis, they said (Gastroenterology 2015 June 22 [doi:10.1053/j.gastro.2015.04.019]). For their study, the investigators randomized 28 patients with predicted severe acute pancreatitis to either placebo or 400 mg pentoxifylline given orally at enrollment and then three times a day for 72 hours. Both groups also received standard of care treatments such as antibiotics and fluid therapy, and had comparable baseline characteristics including age, sex, body mass index, Acute Physiology and Chronic Health Evaluation scores, systemic inflammatory response syndrome scores, and inflammatory marker levels, the researchers said.
Significantly fewer patients who received pentoxifylline needed to stay in the hospital for more than 4 days (14% vs. 57% for the placebo group; P = .046), and the maximum length of ICU stay was 0 days for the intervention group, compared with 13 days for the control group (P = .03), the investigators reported. Analyses of several other outcome measures also favored pentoxifylline over placebo, but did not reach statistical significance in the small study, including the need for ICU transfer (0% for pentoxifylline patients vs. 28% of the placebo group; P = .098) and the median length of hospitalization (for pentoxifylline: 3 days, range 1-5 days; for placebo: 5 days; range 1-30 days; P = .06).
The treatment and control groups did not significantly differ in terms of levels of inflammatory markers, including circulating TNF-alpha, said the investigators. Differences in levels of TNF-alpha, interleukin-6, IL-8, and C-reactive protein “may be significant if the sample size is larger,” they added.
The exact mechanism by which pentoxifylline affects acute pancreatitis is unclear, but the production of pancreatic TNF-alpha peaks about 24-36 hours into an episode of the disease, so patients might benefit from receiving pentoxifylline sooner than the 72-hour window dictated by the study protocol, said Dr. Vege and his associates. “Initiating drug therapy within a few hours is challenging, although a 24-hour cutoff time may be feasible in appropriate settings,” they wrote.
A scholarly opportunity award from the Mayo Clinic helped fund the work. The investigators reported having no relevant financial conflicts of interest.
FROM GASTROENTEROLOGY
Key clinical point: Pentoxifylline topped placebo for several outcome measures among patients with severe acute pancreatitis.
Major finding: Significantly fewer patients who received pentoxifylline needed to stay in the hospital for more than 4 days (14% vs. 57% for the placebo group; P = .046).
Data source: A single-center, randomized placebo-controlled trial of 28 patients with predicted severe acute pancreatitis.
Disclosures: A scholarly opportunity award from the Mayo Clinic supported the work. The investigators reported having no relevant financial conflicts of interest.
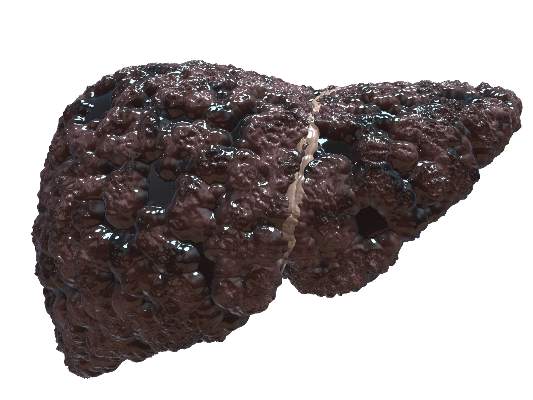
Lifestyle changes, surgical weight loss benefit NAFLD
Losing weight through lifestyle changes can significantly improve several measures of nonalcoholic fatty liver disease, particularly if patients lose at least 10% of their body weight, and bariatric surgery is a valid alternative if diet and exercise fail, according to two studies reported in the August issue of Gastroenterology (2015 Apr. 9 [doi:10.1053/j.gastro.2015.04.005]).
Global rates of nonalcoholic fatty liver disease (NAFLD) are up because of the “parallel epidemics” of obesity and type 2 diabetes mellitus, said Dr. Eduardo Vilar-Gomez of the National Institute of Hepatology in Havana, Cuba, who authored the study of lifestyle changes. There are no approved therapies for the more aggressive form of NAFLD, steatohepatitis, he and his associates said. In past studies, patients who lost about 7%-10% of their body weight substantially improved their NAFLD activity score and had reductions in steatosis, lobular inflammation, and ballooning, but the results did not extend to fibrosis, and prospective studies of the effect of lifestyle changes on histology are lacking, the researchers added .
To fill the gap, they followed 293 adults with histologically confirmed nonalcoholic steatohepatitis who completed a 52-week lifestyle intervention program that included keeping a food diary, restricting saturated fats to less than 10% of total intake, and walking at least 200 minutes a week. Patients had not received hypolipidemic treatment in the preceding 3 months and were not allowed to take insulin sensitizers or vitamin E, both of which are potentially beneficial for nonalcoholic steatohepatitis, the investigators said.
At the end of the yearlong program, steatohepatitis had resolved in 25% of patients, 47% had lower NAFLD activity scores, and 19% had regression of fibrosis, the researchers reported. Although only 30% of participants lost at least 5% of their body weight, weight loss correlated positively with resolution of steatohepatitis and with 2-point reductions in histologic activity scores (P <.001). Among patients who lost at least 10% of their body weight, 90% had resolution of steatohepatitis, 45% had regression of fibrosis, and all had improved histologic activity scores, even if they had negative risk factors such as female sex, a baseline body mass index of at least 35 kg/m2, and a baseline fasting glucose level of at least 5.5 mmol/L, the investigators added. “Our findings support the current recommendation for weight loss using lifestyle modification as the first step in the management of patients with nonalcoholic steatohepatitis,” they wrote.
But what if lifestyle changes fail? The impact of bariatric surgery on nonalcoholic steatohepatitis has not been well studied, said Dr. Guillaume Lassailly at CHRU Lille (France). He and his associates therefore followed 109 morbidly obese patients (BMI ≥40 kg/m2) with biopsy-confirmed nonalcoholic steatohepatitis who underwent bariatric surgery at a single tertiary hospital (Gastroenterology 2015 Apr. 25 [doi:10.1053/j.gastro.2015.04.014]) .
One year after surgery, 85% of patients had achieved disease resolution (95% confidence interval, 75.8%-92.2%), the investigators reported. Stratifying patients by baseline Brunt scores showed that those with milder presurgical disease were more likely to have complete resolution than were patients whose disease was severe (94% vs. 70%; P <.05), the researchers added. Histologic analyses supported the findings, revealing steatosis in 60% of presurgical tissue samples, compared with 10% of samples taken a year after surgery. In addition, average NAFLD disease scores dropped from 5 to 1 (P <.001), hepatocyte ballooning decreased in 84% of samples, lobular inflammation decreased in 67%, and Metavir fibrosis scores dropped in one-third of specimens.
Notably, BMI scores for patients with persistent postsurgical disease dropped by an average of only 9.1, compared with 12.3 for patients whose disease resolved (P = .005), said the researchers. Gastric bypass surgery achieved greater weight loss and improvements in disease status, compared with laparoscopic banding, they added. “The encouraging results of the present study suggest that bariatric surgery should be tested in multicenter, randomized controlled trials in morbidly or severely obese patients with nonalcoholic steatohepatitis who did not respond to lifestyle therapy,” they wrote.
The Cuban National Institute of Gastroenterology and Ministry of Health partially funded the study by Dr. Vilar-Gomez and his associates. The French Ministry of Health and the Conseil Regional Nord-Pas de Calais supported the work by Dr. Lassailly and his colleagues. All investigators declared having no relevant financial conflicts of interest.
Losing weight through lifestyle changes can significantly improve several measures of nonalcoholic fatty liver disease, particularly if patients lose at least 10% of their body weight, and bariatric surgery is a valid alternative if diet and exercise fail, according to two studies reported in the August issue of Gastroenterology (2015 Apr. 9 [doi:10.1053/j.gastro.2015.04.005]).
Global rates of nonalcoholic fatty liver disease (NAFLD) are up because of the “parallel epidemics” of obesity and type 2 diabetes mellitus, said Dr. Eduardo Vilar-Gomez of the National Institute of Hepatology in Havana, Cuba, who authored the study of lifestyle changes. There are no approved therapies for the more aggressive form of NAFLD, steatohepatitis, he and his associates said. In past studies, patients who lost about 7%-10% of their body weight substantially improved their NAFLD activity score and had reductions in steatosis, lobular inflammation, and ballooning, but the results did not extend to fibrosis, and prospective studies of the effect of lifestyle changes on histology are lacking, the researchers added .
To fill the gap, they followed 293 adults with histologically confirmed nonalcoholic steatohepatitis who completed a 52-week lifestyle intervention program that included keeping a food diary, restricting saturated fats to less than 10% of total intake, and walking at least 200 minutes a week. Patients had not received hypolipidemic treatment in the preceding 3 months and were not allowed to take insulin sensitizers or vitamin E, both of which are potentially beneficial for nonalcoholic steatohepatitis, the investigators said.
At the end of the yearlong program, steatohepatitis had resolved in 25% of patients, 47% had lower NAFLD activity scores, and 19% had regression of fibrosis, the researchers reported. Although only 30% of participants lost at least 5% of their body weight, weight loss correlated positively with resolution of steatohepatitis and with 2-point reductions in histologic activity scores (P <.001). Among patients who lost at least 10% of their body weight, 90% had resolution of steatohepatitis, 45% had regression of fibrosis, and all had improved histologic activity scores, even if they had negative risk factors such as female sex, a baseline body mass index of at least 35 kg/m2, and a baseline fasting glucose level of at least 5.5 mmol/L, the investigators added. “Our findings support the current recommendation for weight loss using lifestyle modification as the first step in the management of patients with nonalcoholic steatohepatitis,” they wrote.
But what if lifestyle changes fail? The impact of bariatric surgery on nonalcoholic steatohepatitis has not been well studied, said Dr. Guillaume Lassailly at CHRU Lille (France). He and his associates therefore followed 109 morbidly obese patients (BMI ≥40 kg/m2) with biopsy-confirmed nonalcoholic steatohepatitis who underwent bariatric surgery at a single tertiary hospital (Gastroenterology 2015 Apr. 25 [doi:10.1053/j.gastro.2015.04.014]) .
One year after surgery, 85% of patients had achieved disease resolution (95% confidence interval, 75.8%-92.2%), the investigators reported. Stratifying patients by baseline Brunt scores showed that those with milder presurgical disease were more likely to have complete resolution than were patients whose disease was severe (94% vs. 70%; P <.05), the researchers added. Histologic analyses supported the findings, revealing steatosis in 60% of presurgical tissue samples, compared with 10% of samples taken a year after surgery. In addition, average NAFLD disease scores dropped from 5 to 1 (P <.001), hepatocyte ballooning decreased in 84% of samples, lobular inflammation decreased in 67%, and Metavir fibrosis scores dropped in one-third of specimens.
Notably, BMI scores for patients with persistent postsurgical disease dropped by an average of only 9.1, compared with 12.3 for patients whose disease resolved (P = .005), said the researchers. Gastric bypass surgery achieved greater weight loss and improvements in disease status, compared with laparoscopic banding, they added. “The encouraging results of the present study suggest that bariatric surgery should be tested in multicenter, randomized controlled trials in morbidly or severely obese patients with nonalcoholic steatohepatitis who did not respond to lifestyle therapy,” they wrote.
The Cuban National Institute of Gastroenterology and Ministry of Health partially funded the study by Dr. Vilar-Gomez and his associates. The French Ministry of Health and the Conseil Regional Nord-Pas de Calais supported the work by Dr. Lassailly and his colleagues. All investigators declared having no relevant financial conflicts of interest.
Losing weight through lifestyle changes can significantly improve several measures of nonalcoholic fatty liver disease, particularly if patients lose at least 10% of their body weight, and bariatric surgery is a valid alternative if diet and exercise fail, according to two studies reported in the August issue of Gastroenterology (2015 Apr. 9 [doi:10.1053/j.gastro.2015.04.005]).
Global rates of nonalcoholic fatty liver disease (NAFLD) are up because of the “parallel epidemics” of obesity and type 2 diabetes mellitus, said Dr. Eduardo Vilar-Gomez of the National Institute of Hepatology in Havana, Cuba, who authored the study of lifestyle changes. There are no approved therapies for the more aggressive form of NAFLD, steatohepatitis, he and his associates said. In past studies, patients who lost about 7%-10% of their body weight substantially improved their NAFLD activity score and had reductions in steatosis, lobular inflammation, and ballooning, but the results did not extend to fibrosis, and prospective studies of the effect of lifestyle changes on histology are lacking, the researchers added .
To fill the gap, they followed 293 adults with histologically confirmed nonalcoholic steatohepatitis who completed a 52-week lifestyle intervention program that included keeping a food diary, restricting saturated fats to less than 10% of total intake, and walking at least 200 minutes a week. Patients had not received hypolipidemic treatment in the preceding 3 months and were not allowed to take insulin sensitizers or vitamin E, both of which are potentially beneficial for nonalcoholic steatohepatitis, the investigators said.
At the end of the yearlong program, steatohepatitis had resolved in 25% of patients, 47% had lower NAFLD activity scores, and 19% had regression of fibrosis, the researchers reported. Although only 30% of participants lost at least 5% of their body weight, weight loss correlated positively with resolution of steatohepatitis and with 2-point reductions in histologic activity scores (P <.001). Among patients who lost at least 10% of their body weight, 90% had resolution of steatohepatitis, 45% had regression of fibrosis, and all had improved histologic activity scores, even if they had negative risk factors such as female sex, a baseline body mass index of at least 35 kg/m2, and a baseline fasting glucose level of at least 5.5 mmol/L, the investigators added. “Our findings support the current recommendation for weight loss using lifestyle modification as the first step in the management of patients with nonalcoholic steatohepatitis,” they wrote.
But what if lifestyle changes fail? The impact of bariatric surgery on nonalcoholic steatohepatitis has not been well studied, said Dr. Guillaume Lassailly at CHRU Lille (France). He and his associates therefore followed 109 morbidly obese patients (BMI ≥40 kg/m2) with biopsy-confirmed nonalcoholic steatohepatitis who underwent bariatric surgery at a single tertiary hospital (Gastroenterology 2015 Apr. 25 [doi:10.1053/j.gastro.2015.04.014]) .
One year after surgery, 85% of patients had achieved disease resolution (95% confidence interval, 75.8%-92.2%), the investigators reported. Stratifying patients by baseline Brunt scores showed that those with milder presurgical disease were more likely to have complete resolution than were patients whose disease was severe (94% vs. 70%; P <.05), the researchers added. Histologic analyses supported the findings, revealing steatosis in 60% of presurgical tissue samples, compared with 10% of samples taken a year after surgery. In addition, average NAFLD disease scores dropped from 5 to 1 (P <.001), hepatocyte ballooning decreased in 84% of samples, lobular inflammation decreased in 67%, and Metavir fibrosis scores dropped in one-third of specimens.
Notably, BMI scores for patients with persistent postsurgical disease dropped by an average of only 9.1, compared with 12.3 for patients whose disease resolved (P = .005), said the researchers. Gastric bypass surgery achieved greater weight loss and improvements in disease status, compared with laparoscopic banding, they added. “The encouraging results of the present study suggest that bariatric surgery should be tested in multicenter, randomized controlled trials in morbidly or severely obese patients with nonalcoholic steatohepatitis who did not respond to lifestyle therapy,” they wrote.
The Cuban National Institute of Gastroenterology and Ministry of Health partially funded the study by Dr. Vilar-Gomez and his associates. The French Ministry of Health and the Conseil Regional Nord-Pas de Calais supported the work by Dr. Lassailly and his colleagues. All investigators declared having no relevant financial conflicts of interest.
FROM GASTROENTEROLOGY
Key clinical point: Losing weight through lifestyle changes or bariatric surgery can significantly improve several measures of nonalcoholic steatohepatitis.
Major finding: A yearlong diet and exercise program led to resolution of nonalcoholic steatohepatitis in 25% of patients, while bariatric surgery achieved that outcome for 85% of patients in a separate study.
Data source: Two prospective uncontrolled cohort studies of 402 total adults with nonalcoholic steatohepatitis (the more severe form of nonalcoholic fatty liver disease).
Disclosures: The Cuban National Institute of Gastroenterology and Ministry of Health partially funded the study by Dr. Vilar-Gomez and his associates. The French Ministry of Health and the Conseil Regional Nord-Pas de Calais supported the work by Dr. Lassailly and his colleagues. All investigators declared having no relevant financial conflicts of interest.
Adding enhanced MR to CT might improve diagnosis, outcomes in hepatocellular carcinoma
Among patients with single-nodule hepatocellular carcinomas diagnosed by computed tomography, further imaging with gadoxetic acid–enhanced magnetic resonance (MR) revealed more tumors and was tied to a 28% drop in cancer recurrence and a 35% drop in mortality, a retrospective cohort study reported in the June issue of Gastroenterology (doi.org/10.1053/j.gastro.2015.02.051) found.
“To the best of our knowledge, this is the first study to demonstrate that evaluation of hepatocellular carcinoma [HCC] with gadoxetic acid–enhanced MR imaging is associated with an improvement in the clinical outcome of patients, compared with that of a standard evaluation with dynamic CT,” said Dr. Hyung-Don Kim at the University of Ulsan in Seoul, South Korea and his associates. “This is clinically meaningful, given that the prognosis of patients with early-stage HCC is poor even after a curative treatment, mainly because of the high rate of early intrahepatic recurrence, and because there is no form of adjuvant therapy with a proven clinical benefit.” At least a third of early HCC recurrences might result from dissemination of primary tumor that went undetected at initial treatment, the researchers noted. To investigate the effects of gadoxetic acid–enhanced magnetic resonance imaging on HCC detection and subsequent survival, they retrospectively studied 700 patients in Seoul, South Korea, who had single-nodule HCCs diagnosed by dynamic four-phase CT. A total of 323 patients underwent additional imaging with gadoxetic acid–enhanced MR. These patients resembled CT-only patients in terms of baseline demographic characteristics, except that they were an average of 3 years younger (P < .001), had significantly higher median ALT levels (66 vs. 57 IU/mL; P < .006) and significantly higher platelet counts and lower alpha-fetoprotein levels, the investigators said.Gadoxetic acid–enhanced MR detected additional small HCC nodules in 16% of patients, and was tied to a 28% drop in likelihood of recurrence (hazard ratio, 0.72; 95% confidence interval, 0.54-0.96) and a 35% drop in risk of mortality (HR, 0.65; 95% CI, 0.44-0.96), the investigators reported. Rates of both recurrence-free and overall survival also were significantly higher for patients who underwent contrast-enhanced MR in addition to CT, compared with patients who underwent CT alone, and the differences held true in univariate, multivariate, inverse probability weighting analyses, and propensity score-matched analyses, they added.
“The major limitation of this study is that it was based on observational data,” commented the researchers. “Further studies that evaluate the effectiveness of gadoxetic acid–enhanced MR imaging for the evaluation of HCC in patients in other clinical settings are warranted.” The findings also need cautious interpretation because of the chance that selection bias led to more curable cases among patients who underwent MR in addition to CT, they said. The Korean Ministry of Health & Welfare and the Korean Association for the Study of Liver helped fund the research. One coauthor reported serving on the advisory boards of Bayer Healthcare, Bristol-Myers Squibb, and Gilead Science, and receiving research funding from Bayer, Gilead, and Novartis. The other investigators reported no conflicts of interest.
Courtesy American Gastroenterological Association
Among patients with single-nodule hepatocellular carcinomas diagnosed by computed tomography, further imaging with gadoxetic acid–enhanced magnetic resonance (MR) revealed more tumors and was tied to a 28% drop in cancer recurrence and a 35% drop in mortality, a retrospective cohort study reported in the June issue of Gastroenterology (doi.org/10.1053/j.gastro.2015.02.051) found.
“To the best of our knowledge, this is the first study to demonstrate that evaluation of hepatocellular carcinoma [HCC] with gadoxetic acid–enhanced MR imaging is associated with an improvement in the clinical outcome of patients, compared with that of a standard evaluation with dynamic CT,” said Dr. Hyung-Don Kim at the University of Ulsan in Seoul, South Korea and his associates. “This is clinically meaningful, given that the prognosis of patients with early-stage HCC is poor even after a curative treatment, mainly because of the high rate of early intrahepatic recurrence, and because there is no form of adjuvant therapy with a proven clinical benefit.” At least a third of early HCC recurrences might result from dissemination of primary tumor that went undetected at initial treatment, the researchers noted. To investigate the effects of gadoxetic acid–enhanced magnetic resonance imaging on HCC detection and subsequent survival, they retrospectively studied 700 patients in Seoul, South Korea, who had single-nodule HCCs diagnosed by dynamic four-phase CT. A total of 323 patients underwent additional imaging with gadoxetic acid–enhanced MR. These patients resembled CT-only patients in terms of baseline demographic characteristics, except that they were an average of 3 years younger (P < .001), had significantly higher median ALT levels (66 vs. 57 IU/mL; P < .006) and significantly higher platelet counts and lower alpha-fetoprotein levels, the investigators said.Gadoxetic acid–enhanced MR detected additional small HCC nodules in 16% of patients, and was tied to a 28% drop in likelihood of recurrence (hazard ratio, 0.72; 95% confidence interval, 0.54-0.96) and a 35% drop in risk of mortality (HR, 0.65; 95% CI, 0.44-0.96), the investigators reported. Rates of both recurrence-free and overall survival also were significantly higher for patients who underwent contrast-enhanced MR in addition to CT, compared with patients who underwent CT alone, and the differences held true in univariate, multivariate, inverse probability weighting analyses, and propensity score-matched analyses, they added.
“The major limitation of this study is that it was based on observational data,” commented the researchers. “Further studies that evaluate the effectiveness of gadoxetic acid–enhanced MR imaging for the evaluation of HCC in patients in other clinical settings are warranted.” The findings also need cautious interpretation because of the chance that selection bias led to more curable cases among patients who underwent MR in addition to CT, they said. The Korean Ministry of Health & Welfare and the Korean Association for the Study of Liver helped fund the research. One coauthor reported serving on the advisory boards of Bayer Healthcare, Bristol-Myers Squibb, and Gilead Science, and receiving research funding from Bayer, Gilead, and Novartis. The other investigators reported no conflicts of interest.
Courtesy American Gastroenterological Association
Among patients with single-nodule hepatocellular carcinomas diagnosed by computed tomography, further imaging with gadoxetic acid–enhanced magnetic resonance (MR) revealed more tumors and was tied to a 28% drop in cancer recurrence and a 35% drop in mortality, a retrospective cohort study reported in the June issue of Gastroenterology (doi.org/10.1053/j.gastro.2015.02.051) found.
“To the best of our knowledge, this is the first study to demonstrate that evaluation of hepatocellular carcinoma [HCC] with gadoxetic acid–enhanced MR imaging is associated with an improvement in the clinical outcome of patients, compared with that of a standard evaluation with dynamic CT,” said Dr. Hyung-Don Kim at the University of Ulsan in Seoul, South Korea and his associates. “This is clinically meaningful, given that the prognosis of patients with early-stage HCC is poor even after a curative treatment, mainly because of the high rate of early intrahepatic recurrence, and because there is no form of adjuvant therapy with a proven clinical benefit.” At least a third of early HCC recurrences might result from dissemination of primary tumor that went undetected at initial treatment, the researchers noted. To investigate the effects of gadoxetic acid–enhanced magnetic resonance imaging on HCC detection and subsequent survival, they retrospectively studied 700 patients in Seoul, South Korea, who had single-nodule HCCs diagnosed by dynamic four-phase CT. A total of 323 patients underwent additional imaging with gadoxetic acid–enhanced MR. These patients resembled CT-only patients in terms of baseline demographic characteristics, except that they were an average of 3 years younger (P < .001), had significantly higher median ALT levels (66 vs. 57 IU/mL; P < .006) and significantly higher platelet counts and lower alpha-fetoprotein levels, the investigators said.Gadoxetic acid–enhanced MR detected additional small HCC nodules in 16% of patients, and was tied to a 28% drop in likelihood of recurrence (hazard ratio, 0.72; 95% confidence interval, 0.54-0.96) and a 35% drop in risk of mortality (HR, 0.65; 95% CI, 0.44-0.96), the investigators reported. Rates of both recurrence-free and overall survival also were significantly higher for patients who underwent contrast-enhanced MR in addition to CT, compared with patients who underwent CT alone, and the differences held true in univariate, multivariate, inverse probability weighting analyses, and propensity score-matched analyses, they added.
“The major limitation of this study is that it was based on observational data,” commented the researchers. “Further studies that evaluate the effectiveness of gadoxetic acid–enhanced MR imaging for the evaluation of HCC in patients in other clinical settings are warranted.” The findings also need cautious interpretation because of the chance that selection bias led to more curable cases among patients who underwent MR in addition to CT, they said. The Korean Ministry of Health & Welfare and the Korean Association for the Study of Liver helped fund the research. One coauthor reported serving on the advisory boards of Bayer Healthcare, Bristol-Myers Squibb, and Gilead Science, and receiving research funding from Bayer, Gilead, and Novartis. The other investigators reported no conflicts of interest.
Courtesy American Gastroenterological Association
Key clinical point: Gadoxetic acid–enhanced magnetic resonance (MR) imaging revealed smaller masses and was tied to better outcomes in patients with single-nodule hepatocellular carcinoma (HCC) diagnosed by computed tomography (CT).
Major finding: MR enhanced with gadoxetic acid detected additional HCC nodules in 16% of patients, and was tied to lower recurrence and mortality rates.
Data source: Retrospective study of 700 patients diagnosed with single-nodule HCC by dynamic four-phase CT.
Disclosures: The Korean Ministry of Health & Welfare and the Korean Association for the Study of Liver helped fund the research. One coauthor reported serving on the advisory boards of Bayer Healthcare, Bristol-Myers Squibb, and Gilead Science, and receiving research funding from Bayer, Gilead, and Novartis. The other investigators reported no conflicts of interest.
Referral centers varied significantly in IBD treatment approaches
Even high-volume referral centers varied significantly in their use of immunomodulators and some other therapies for patients with inflammatory bowel disease, particularly Crohn’s disease, a prospective cohort study found.
“The development and implementation of evidence-based standards of care may reduce variations and improve patient outcomes,” Dr. Ashwin Ananthakrishnan of Massachusetts General Hospital in Boston and his associates wrote in the June issue of Clinical Gastroenterology and Hepatology (2014 Nov. 21 [doi: 10.1016/j.cgh.2014.11.020]). “Because adherence to guidelines frequently is inadequate, a reduction of practice variation also requires continual improvement, including setting goals and repeated measurement of processes to identify how standardizing care impacts outcomes.”
New biologics have created increasingly diverse treatment options for patients with inflammatory bowel disease (IBD), but few studies have looked at how clinicians and patients choose treatment regimens in daily practice, the researchers noted. To explore the issue, they prospectively studied 1,659 adults with Crohn’s disease (CD) and 946 patients with ulcerative colitis who were treated at one of seven academic medical centers, all of which see a high volume of IBD patients.
Referral centers varied about threefold in their use of immunomodulators for CD (odds ratio for between-center differences, 3.34; 95% confidence interval, 2.09-5.32) in a model that controlled for age at diagnosis, sex, race, smoking status, and duration and extent or behavior of disease, the researchers reported. Use of immunomodulators for ulcerative colitis varied by more than twofold, they found (OR, 2.32; 95% CI, 1.05 to 5.13). Furthermore, they uncovered significant differences in use of oral mesalamine in both forms of IBD, and in the use of corticosteroids and immunomodulator-tumor necrosis factor antagonist combinations for CD, they said.
Treatment practices tended to vary more for CD than for ulcerative colitis, perhaps because CD spans a broader spectrum of pathologies or because clinicians have not yet reached consensus on early aggressive therapy or treatment strategies for CD, the researchers said. “Variations in treatment generally occur when there is uncertainty about the best practice,” they commented. “It is possible that the variations will diminish as evidence on effective IBD therapy grows and evidence-based guidelines become available and are implemented. The continued variation suggests that there is significant potential for standardization of care across referral and community practices.”
The study did not pinpoint reasons for discrepancies in practice, which could have reflected differences related to referring physicians’ or patients’ behaviors or expectations, the researchers said. But the findings did not reflect a single outlier center, and the cohort was not chosen to study variations between centers, which should have helped eliminate selection bias, they added.
The Leona M. and Harry B. Helmsley Charitable Trust funded the study. Dr. Ananthakrishnan reported advisory board payments from Cubist Pharmaceuticals and AbbVe. One coauthor reported financial conflicts of interest with numerous pharmaceutical companies. The other authors reported no conflicts of interest.
Jack Wennberg, a pioneer in quality improvement, was the first to recognize the association between significant variation in health care utilization and poor quality of care. The problem is that Wennberg published this in Science in 1973 (182:1102-8), and now, over 40 years later, we are just making progress for patients with Crohn’s disease and ulcerative colitis.
As a field, we now need to catch up and learn how to address this variation. It won’t be by solely measuring the differences between practices. As a proverb that was taught to me by experts at the Institute for Healthcare Improvement says, “You can’t fatten a cow by weighing it.” We could measure our practice patterns, quality metrics, and report them every day to claim our appropriate reimbursement from the Centers for Medicare & Medicaid Services, but this won’t improve patient outcomes or our understanding of what drives a better quality of life for our patients.
We need to take what Dr. Ananthakrishnan and his team have taught us to the next level. We need to learn from the Model for Improvement (Langley G.J., The improvement guide: A practical approach to enhancing organizational performance. San Francisco: Jossey-Bass, 2009), which teaches us that, to improve, we need to answer three questions: What are we trying to accomplish? How will we know that a change is an improvement? and What changes can we make that will result in an improvement? If we can apply these questions to changes that we want to make in our practices and systematically pursue answers, we will start to improve the quality of care delivered to our patients, as opposed to simply reporting that it is poor.
Dr. Corey A. Siegel, M.S., is director of the Dartmouth-Hitchcock Inflammatory Bowel Disease Center at Dartmouth-Hitchcock Medical Center, Lebanon, N.H. He is supported by AHRQ grant 1R01HS021747-01 and serves as consultant or on an advisory board for Abbvie, Amgen, Lilly, Janssen, Salix, Pfizer, Prometheus, Takeda, Theradiag, and UCB. He serves as a speaker for CME activities for AbbVie, Janssen, and Takeda, and has received grant support from Abbvie, Janssen, Salix, Takeda, and UCB. He is cochair of the Crohn’s and Colitis Foundation of America’s Quality of Care Program.
Jack Wennberg, a pioneer in quality improvement, was the first to recognize the association between significant variation in health care utilization and poor quality of care. The problem is that Wennberg published this in Science in 1973 (182:1102-8), and now, over 40 years later, we are just making progress for patients with Crohn’s disease and ulcerative colitis.
As a field, we now need to catch up and learn how to address this variation. It won’t be by solely measuring the differences between practices. As a proverb that was taught to me by experts at the Institute for Healthcare Improvement says, “You can’t fatten a cow by weighing it.” We could measure our practice patterns, quality metrics, and report them every day to claim our appropriate reimbursement from the Centers for Medicare & Medicaid Services, but this won’t improve patient outcomes or our understanding of what drives a better quality of life for our patients.
We need to take what Dr. Ananthakrishnan and his team have taught us to the next level. We need to learn from the Model for Improvement (Langley G.J., The improvement guide: A practical approach to enhancing organizational performance. San Francisco: Jossey-Bass, 2009), which teaches us that, to improve, we need to answer three questions: What are we trying to accomplish? How will we know that a change is an improvement? and What changes can we make that will result in an improvement? If we can apply these questions to changes that we want to make in our practices and systematically pursue answers, we will start to improve the quality of care delivered to our patients, as opposed to simply reporting that it is poor.
Dr. Corey A. Siegel, M.S., is director of the Dartmouth-Hitchcock Inflammatory Bowel Disease Center at Dartmouth-Hitchcock Medical Center, Lebanon, N.H. He is supported by AHRQ grant 1R01HS021747-01 and serves as consultant or on an advisory board for Abbvie, Amgen, Lilly, Janssen, Salix, Pfizer, Prometheus, Takeda, Theradiag, and UCB. He serves as a speaker for CME activities for AbbVie, Janssen, and Takeda, and has received grant support from Abbvie, Janssen, Salix, Takeda, and UCB. He is cochair of the Crohn’s and Colitis Foundation of America’s Quality of Care Program.
Jack Wennberg, a pioneer in quality improvement, was the first to recognize the association between significant variation in health care utilization and poor quality of care. The problem is that Wennberg published this in Science in 1973 (182:1102-8), and now, over 40 years later, we are just making progress for patients with Crohn’s disease and ulcerative colitis.
As a field, we now need to catch up and learn how to address this variation. It won’t be by solely measuring the differences between practices. As a proverb that was taught to me by experts at the Institute for Healthcare Improvement says, “You can’t fatten a cow by weighing it.” We could measure our practice patterns, quality metrics, and report them every day to claim our appropriate reimbursement from the Centers for Medicare & Medicaid Services, but this won’t improve patient outcomes or our understanding of what drives a better quality of life for our patients.
We need to take what Dr. Ananthakrishnan and his team have taught us to the next level. We need to learn from the Model for Improvement (Langley G.J., The improvement guide: A practical approach to enhancing organizational performance. San Francisco: Jossey-Bass, 2009), which teaches us that, to improve, we need to answer three questions: What are we trying to accomplish? How will we know that a change is an improvement? and What changes can we make that will result in an improvement? If we can apply these questions to changes that we want to make in our practices and systematically pursue answers, we will start to improve the quality of care delivered to our patients, as opposed to simply reporting that it is poor.
Dr. Corey A. Siegel, M.S., is director of the Dartmouth-Hitchcock Inflammatory Bowel Disease Center at Dartmouth-Hitchcock Medical Center, Lebanon, N.H. He is supported by AHRQ grant 1R01HS021747-01 and serves as consultant or on an advisory board for Abbvie, Amgen, Lilly, Janssen, Salix, Pfizer, Prometheus, Takeda, Theradiag, and UCB. He serves as a speaker for CME activities for AbbVie, Janssen, and Takeda, and has received grant support from Abbvie, Janssen, Salix, Takeda, and UCB. He is cochair of the Crohn’s and Colitis Foundation of America’s Quality of Care Program.
Even high-volume referral centers varied significantly in their use of immunomodulators and some other therapies for patients with inflammatory bowel disease, particularly Crohn’s disease, a prospective cohort study found.
“The development and implementation of evidence-based standards of care may reduce variations and improve patient outcomes,” Dr. Ashwin Ananthakrishnan of Massachusetts General Hospital in Boston and his associates wrote in the June issue of Clinical Gastroenterology and Hepatology (2014 Nov. 21 [doi: 10.1016/j.cgh.2014.11.020]). “Because adherence to guidelines frequently is inadequate, a reduction of practice variation also requires continual improvement, including setting goals and repeated measurement of processes to identify how standardizing care impacts outcomes.”
New biologics have created increasingly diverse treatment options for patients with inflammatory bowel disease (IBD), but few studies have looked at how clinicians and patients choose treatment regimens in daily practice, the researchers noted. To explore the issue, they prospectively studied 1,659 adults with Crohn’s disease (CD) and 946 patients with ulcerative colitis who were treated at one of seven academic medical centers, all of which see a high volume of IBD patients.
Referral centers varied about threefold in their use of immunomodulators for CD (odds ratio for between-center differences, 3.34; 95% confidence interval, 2.09-5.32) in a model that controlled for age at diagnosis, sex, race, smoking status, and duration and extent or behavior of disease, the researchers reported. Use of immunomodulators for ulcerative colitis varied by more than twofold, they found (OR, 2.32; 95% CI, 1.05 to 5.13). Furthermore, they uncovered significant differences in use of oral mesalamine in both forms of IBD, and in the use of corticosteroids and immunomodulator-tumor necrosis factor antagonist combinations for CD, they said.
Treatment practices tended to vary more for CD than for ulcerative colitis, perhaps because CD spans a broader spectrum of pathologies or because clinicians have not yet reached consensus on early aggressive therapy or treatment strategies for CD, the researchers said. “Variations in treatment generally occur when there is uncertainty about the best practice,” they commented. “It is possible that the variations will diminish as evidence on effective IBD therapy grows and evidence-based guidelines become available and are implemented. The continued variation suggests that there is significant potential for standardization of care across referral and community practices.”
The study did not pinpoint reasons for discrepancies in practice, which could have reflected differences related to referring physicians’ or patients’ behaviors or expectations, the researchers said. But the findings did not reflect a single outlier center, and the cohort was not chosen to study variations between centers, which should have helped eliminate selection bias, they added.
The Leona M. and Harry B. Helmsley Charitable Trust funded the study. Dr. Ananthakrishnan reported advisory board payments from Cubist Pharmaceuticals and AbbVe. One coauthor reported financial conflicts of interest with numerous pharmaceutical companies. The other authors reported no conflicts of interest.
Even high-volume referral centers varied significantly in their use of immunomodulators and some other therapies for patients with inflammatory bowel disease, particularly Crohn’s disease, a prospective cohort study found.
“The development and implementation of evidence-based standards of care may reduce variations and improve patient outcomes,” Dr. Ashwin Ananthakrishnan of Massachusetts General Hospital in Boston and his associates wrote in the June issue of Clinical Gastroenterology and Hepatology (2014 Nov. 21 [doi: 10.1016/j.cgh.2014.11.020]). “Because adherence to guidelines frequently is inadequate, a reduction of practice variation also requires continual improvement, including setting goals and repeated measurement of processes to identify how standardizing care impacts outcomes.”
New biologics have created increasingly diverse treatment options for patients with inflammatory bowel disease (IBD), but few studies have looked at how clinicians and patients choose treatment regimens in daily practice, the researchers noted. To explore the issue, they prospectively studied 1,659 adults with Crohn’s disease (CD) and 946 patients with ulcerative colitis who were treated at one of seven academic medical centers, all of which see a high volume of IBD patients.
Referral centers varied about threefold in their use of immunomodulators for CD (odds ratio for between-center differences, 3.34; 95% confidence interval, 2.09-5.32) in a model that controlled for age at diagnosis, sex, race, smoking status, and duration and extent or behavior of disease, the researchers reported. Use of immunomodulators for ulcerative colitis varied by more than twofold, they found (OR, 2.32; 95% CI, 1.05 to 5.13). Furthermore, they uncovered significant differences in use of oral mesalamine in both forms of IBD, and in the use of corticosteroids and immunomodulator-tumor necrosis factor antagonist combinations for CD, they said.
Treatment practices tended to vary more for CD than for ulcerative colitis, perhaps because CD spans a broader spectrum of pathologies or because clinicians have not yet reached consensus on early aggressive therapy or treatment strategies for CD, the researchers said. “Variations in treatment generally occur when there is uncertainty about the best practice,” they commented. “It is possible that the variations will diminish as evidence on effective IBD therapy grows and evidence-based guidelines become available and are implemented. The continued variation suggests that there is significant potential for standardization of care across referral and community practices.”
The study did not pinpoint reasons for discrepancies in practice, which could have reflected differences related to referring physicians’ or patients’ behaviors or expectations, the researchers said. But the findings did not reflect a single outlier center, and the cohort was not chosen to study variations between centers, which should have helped eliminate selection bias, they added.
The Leona M. and Harry B. Helmsley Charitable Trust funded the study. Dr. Ananthakrishnan reported advisory board payments from Cubist Pharmaceuticals and AbbVe. One coauthor reported financial conflicts of interest with numerous pharmaceutical companies. The other authors reported no conflicts of interest.
FROM CLINICAL GASTROENTEROLOGY AND HEPATOLOGY
Key clinical point: High-volume referral centers varied significantly in use of immunomodulators and other therapies for inflammatory bowel disease, especially Crohn’s disease.
Major finding: Centers varied as much as threefold in use of immunomodulators for CD (OR, 3.34; 95% CI, 2.09-4.32).
Data source: Prospective cohort study of 1,659 patients with Crohn’s disease and 946 patients with ulcerative colitis.
Disclosures: The Leona M. and Harry B. Helmsley Charitable Trust funded the study. Dr. Ananthakrishnan reported advisory board payments from Cubist Pharmaceuticals and AbbVie. One coauthor reported financial conflicts of interest with numerous pharmaceutical companies. The other authors reported no conflicts of interest.
Experts advocate ‘treat-to-target’ approach for Crohn’s disease
Patients with Crohn’s disease could benefit from a “treat-to-target” approach based on intervening early to reverse inflammation and gathering objective data to guide clinical decisions, according to a review article published in the June issue of Clinical Gastroenterology and Hepatology (2015 [doi:10.1016/j.cgh.2013.09.006]).
“In spite of available effective treatments, the development of complications such as stricture, fistula, and abscess that result in surgery and lead to a disabling course of Crohn’s disease remain common,” said Dr. Guillame Bouguen at the University of California, San Diego, and his associates. “This ‘natural history’ is not likely to improve unless the overall symptom-based therapeutic strategy for Crohn’s disease is changed,” they wrote.
Clinicians have historically managed Crohn’s disease (CD) by gradually intensifying treatments based on patients’ symptoms, but this approach has failed to achieve good long-term outcomes and puts patients at risk of bowel damage, the reviewers said. The advent of better drugs for other chronic inflammatory diseases, such as rheumatoid arthritis, “reinvigorated” treatment strategies to focus on intervening earlier and controlling inflammation as much as possible, including by augmenting the novel biologics with methotrexate or other older disease-modifying antirheumatic drugs, they said.A similar “treat-to-target” approach to CD would mean responding to objective evidence of inflammation before patients developed irreversible bowel damage, Dr. Bouguen and his associates said. The main treatment goal would be mucosal healing, but the target level would reflect individual comorbidities, demographic and behavioral factors, and risks of side effects. After refining the mucosal healing target, gastroenterologists would stick to it throughout treatment, and would adjust treatment based on imaging and other objective measures of bowel inflammation. Colonoscopies and related procedures would be performed every 6 months until ulcerations resolved, and every 1-2 years after that. To improve trust and adherence to treatment, gastroenterologists also would need to educate patients about the mucosal healing target and the plan for achieving that goal, the reviewers said.
Based on preliminary data, patients on azathioprine and tumor necrosis factor antagonists might be able to taper them after achieving sustained mucosal healing, although larger studies on the topic are lacking, said the reviewers. A treat-to-target approach also might help symptomatic CD patients who already have permanent bowel damage enhance their long-term quality of life and prevent worsening disability, the investigators said.The International Organization on Inflammatory Bowel Disease is leading a consensus effort to define the therapeutic target in the treatment of inflammatory bowel disease. “However, the principles of the treat-to-target strategy that uses both systematic follow-up of patients and therapy optimization focusing on inflammation and damage may persist,” they added. To better clarify whether a treat-to-target approach is useful in CD, researchers are enrolling patients in the REACT II trial, which will compare treatments that target mucosal healing with the conventional symptoms-based paradigm, they noted.The authors reported no funding sources. Dr. Bouguen reported receiving lecture fees from Abbott Laboratories, Ferring, and MSD Pharma. The other authors reported financial relationships with numerous pharmaceutical companies.
Patients with Crohn’s disease could benefit from a “treat-to-target” approach based on intervening early to reverse inflammation and gathering objective data to guide clinical decisions, according to a review article published in the June issue of Clinical Gastroenterology and Hepatology (2015 [doi:10.1016/j.cgh.2013.09.006]).
“In spite of available effective treatments, the development of complications such as stricture, fistula, and abscess that result in surgery and lead to a disabling course of Crohn’s disease remain common,” said Dr. Guillame Bouguen at the University of California, San Diego, and his associates. “This ‘natural history’ is not likely to improve unless the overall symptom-based therapeutic strategy for Crohn’s disease is changed,” they wrote.
Clinicians have historically managed Crohn’s disease (CD) by gradually intensifying treatments based on patients’ symptoms, but this approach has failed to achieve good long-term outcomes and puts patients at risk of bowel damage, the reviewers said. The advent of better drugs for other chronic inflammatory diseases, such as rheumatoid arthritis, “reinvigorated” treatment strategies to focus on intervening earlier and controlling inflammation as much as possible, including by augmenting the novel biologics with methotrexate or other older disease-modifying antirheumatic drugs, they said.A similar “treat-to-target” approach to CD would mean responding to objective evidence of inflammation before patients developed irreversible bowel damage, Dr. Bouguen and his associates said. The main treatment goal would be mucosal healing, but the target level would reflect individual comorbidities, demographic and behavioral factors, and risks of side effects. After refining the mucosal healing target, gastroenterologists would stick to it throughout treatment, and would adjust treatment based on imaging and other objective measures of bowel inflammation. Colonoscopies and related procedures would be performed every 6 months until ulcerations resolved, and every 1-2 years after that. To improve trust and adherence to treatment, gastroenterologists also would need to educate patients about the mucosal healing target and the plan for achieving that goal, the reviewers said.
Based on preliminary data, patients on azathioprine and tumor necrosis factor antagonists might be able to taper them after achieving sustained mucosal healing, although larger studies on the topic are lacking, said the reviewers. A treat-to-target approach also might help symptomatic CD patients who already have permanent bowel damage enhance their long-term quality of life and prevent worsening disability, the investigators said.The International Organization on Inflammatory Bowel Disease is leading a consensus effort to define the therapeutic target in the treatment of inflammatory bowel disease. “However, the principles of the treat-to-target strategy that uses both systematic follow-up of patients and therapy optimization focusing on inflammation and damage may persist,” they added. To better clarify whether a treat-to-target approach is useful in CD, researchers are enrolling patients in the REACT II trial, which will compare treatments that target mucosal healing with the conventional symptoms-based paradigm, they noted.The authors reported no funding sources. Dr. Bouguen reported receiving lecture fees from Abbott Laboratories, Ferring, and MSD Pharma. The other authors reported financial relationships with numerous pharmaceutical companies.
Patients with Crohn’s disease could benefit from a “treat-to-target” approach based on intervening early to reverse inflammation and gathering objective data to guide clinical decisions, according to a review article published in the June issue of Clinical Gastroenterology and Hepatology (2015 [doi:10.1016/j.cgh.2013.09.006]).
“In spite of available effective treatments, the development of complications such as stricture, fistula, and abscess that result in surgery and lead to a disabling course of Crohn’s disease remain common,” said Dr. Guillame Bouguen at the University of California, San Diego, and his associates. “This ‘natural history’ is not likely to improve unless the overall symptom-based therapeutic strategy for Crohn’s disease is changed,” they wrote.
Clinicians have historically managed Crohn’s disease (CD) by gradually intensifying treatments based on patients’ symptoms, but this approach has failed to achieve good long-term outcomes and puts patients at risk of bowel damage, the reviewers said. The advent of better drugs for other chronic inflammatory diseases, such as rheumatoid arthritis, “reinvigorated” treatment strategies to focus on intervening earlier and controlling inflammation as much as possible, including by augmenting the novel biologics with methotrexate or other older disease-modifying antirheumatic drugs, they said.A similar “treat-to-target” approach to CD would mean responding to objective evidence of inflammation before patients developed irreversible bowel damage, Dr. Bouguen and his associates said. The main treatment goal would be mucosal healing, but the target level would reflect individual comorbidities, demographic and behavioral factors, and risks of side effects. After refining the mucosal healing target, gastroenterologists would stick to it throughout treatment, and would adjust treatment based on imaging and other objective measures of bowel inflammation. Colonoscopies and related procedures would be performed every 6 months until ulcerations resolved, and every 1-2 years after that. To improve trust and adherence to treatment, gastroenterologists also would need to educate patients about the mucosal healing target and the plan for achieving that goal, the reviewers said.
Based on preliminary data, patients on azathioprine and tumor necrosis factor antagonists might be able to taper them after achieving sustained mucosal healing, although larger studies on the topic are lacking, said the reviewers. A treat-to-target approach also might help symptomatic CD patients who already have permanent bowel damage enhance their long-term quality of life and prevent worsening disability, the investigators said.The International Organization on Inflammatory Bowel Disease is leading a consensus effort to define the therapeutic target in the treatment of inflammatory bowel disease. “However, the principles of the treat-to-target strategy that uses both systematic follow-up of patients and therapy optimization focusing on inflammation and damage may persist,” they added. To better clarify whether a treat-to-target approach is useful in CD, researchers are enrolling patients in the REACT II trial, which will compare treatments that target mucosal healing with the conventional symptoms-based paradigm, they noted.The authors reported no funding sources. Dr. Bouguen reported receiving lecture fees from Abbott Laboratories, Ferring, and MSD Pharma. The other authors reported financial relationships with numerous pharmaceutical companies.
Key clinical point: A treat-to-target approach based on early control of inflammation and objective clinical data might benefit patients with Crohn’s disease.
Major finding: Using only symptoms to guide treatment decisions in Crohn’s disease has failed to achieve good long-term outcomes.
Data source: A review of 15 primary research and review articles.
Disclosures: The authors reported no funding sources. Dr. Bouguen reported receiving lecture fees from Abbott Laboratories, Ferring, and MSD Pharma. The other authors reported financial disclosures from numerous pharmaceutical companies.
Capsule colonoscopy improved, but limitations persist
When compared with conventional colonoscopy, capsule colonoscopy had a sensitivity of 88% and a specificity of 82% for detecting adenomas of at least 6 mm in asymptomatic subjects, a multicenter prospective study showed.
But the capsule detected only 29% of subjects who had sessile serrated polyps of at least 6 mm, and required more extensive bowel preparation than did conventional colonoscopy, Dr. Douglas K. Rex at Indiana University Hospital in Indianapolis and his associates reported in the May issue of Gastroenterology (2015 [doi:10.1053/j.gastro.2015.01.025]). “Given these considerations ... colonoscopy remains the gold standard for the detection of colorectal polyps,” said the researchers. “The capsule is a good test for the detection of patients with conventional adenomas 6 mm or larger in size and appears to be an appropriate imaging choice for patients who cannot undergo colonoscopy or had incomplete colonoscopy.”
Capsule endoscopy is useful for small-bowel imaging, but adapting the technology for colorectal studies has been difficult. A first-generation capsule detected only 74% of advanced adenomas in one prospective multicenter trial, the researchers noted. Since then, the PillCam COLON 2 capsule has been updated with motion detection, variable frame speed, and a wider angle view, they said. In smaller studies, it detected up to 89% of subjects with polyps of at least 6 mm, but its specificity was as low as 64%.
To further investigate the technology, researchers at 16 centers in the United States and Israel compared the second-generation capsule with conventional colonoscopy in an average-risk screening population of 884 asymptomatic subjects. Endoscopists were blinded as to technique, but performed unblinded follow-up colonoscopies in subjects who were positive on capsule but negative on conventional colonoscopy.
The capsule’s sensitivity was 81% (95% confidence interval, 77%-84%) and its specificity was 93% (91%-95%) for detecting subjects who had polyps of at least 6 mm, the researchers reported. Sensitivity was 80% (74%-86%) and specificity was 97% (96%-98%) for detecting subjects with polyps of at least 10 mm. For conventional adenomas of at least 6 mm, sensitivity was 88% (82%-93%) and specificity was 82% (80%-83%), and for adenomas of 10 mm or larger, sensitivity was 92% (82%-97%) and specificity was 95% (94%-95%).
“Lesions in the serrated class were not detected well by the capsule in this study, compared with conventional adenomas,” the researchers reported. Prior studies of the capsule did not look for serrated lesions, and in the current study sensitivities were only 29% and 33% for 6-mm and 10-mm lesions, respectively.
The software used to measure polyps during capsule colonoscopy had a 40% error range when tested on balls of known size, the researchers said. Therefore, there is a strict location-matching rule within the colon, but a liberal size rule that only required measurements to fall within 50% of one another to be considered a match. “Any set of matching rules for polyps detected by the capsule and colonoscopy might operate to increase or decrease the calculated sensitivity of the capsule incorrectly,” they added. Also, the adenoma detection rate for conventional colonoscopy was only 39%, and some polyps that were clearly seen on capsule were not visualized on regular colonoscopy. “In these cases, a polyp that should be a true positive for the capsule was counted as false,” they added. “Both colonoscopy and capsule are inferior for localization, compared with CT colonography. Inaccurate localization by one or both tests in this study could have reduced the sensitivity of the capsule.”
The investigators also had to exclude 77 patients because of inadequate cleansing and short transit times related to using sodium phosphate as a boost, they noted. The Food and Drug Administration label for the capsule is expected to reflect those limitations, they added.
Given Imaging funded the study and paid consulting or other fees to Dr. Rex and six coauthors. The other authors reported having no relevant conflicts of interest.
In the United States, colonoscopy is the primary screening test for colorectal cancer. However, because of issues with colonoscopy uptake, costs, and the small but finite risk of complications, the concept of a relatively noninvasive structural examination of the colon that can detect colorectal neoplasia is appealing to both patients and physicians.
Although capsule colonoscopy has emerged as a potential noninvasive tool for examining the entire colon, there are limited data on its accuracy for detecting conventional adenomas or sessile serrated polyps, particularly in an average-risk screening population.
In the May issue of Gastroenterology, Dr. Rex and colleagues report their results from a large, multicenter, prospective study evaluating the new second-generation capsule colonoscopy (PillCam COLON 2, Given Imaging) for detecting colorectal neoplasia in an average-risk screening population. Using optical colonoscopy as the reference standard, the capsule colonoscopy performed well for detecting conventional adenomas 6 mm or larger with a sensitivity and specificity of 88% and 82%, respectively.
In addition, the sensitivity and specificity of capsule colonoscopy for conventional adenomas 10 mm or larger were 92% and 95%, respectively. However, despite the high performance characteristics for detection of conventional adenomas, the capsule colonoscopy had limited accuracy for detecting sessile serrated polyps 10 mm or larger, with a sensitivity of 33%. Furthermore, nearly 10% of the enrolled subjects were excluded from the analysis due to poor bowel preparation and rapid transit time.
These issues aside, the Rex study provides important information about alternative screening modalities for detection of colorectal neoplasia, particularly for gastroenterologists who may be hesitant or unwilling to perform an optical colonoscopy in high-risk patients with significant co-morbidities or in patients who had an incomplete colonoscopy.
Dr. Jeffrey Lee, MAS is assistant clinical professor of medicine, division of gastroenterology, University of California, San Francisco. He has no conflicts of interest.
In the United States, colonoscopy is the primary screening test for colorectal cancer. However, because of issues with colonoscopy uptake, costs, and the small but finite risk of complications, the concept of a relatively noninvasive structural examination of the colon that can detect colorectal neoplasia is appealing to both patients and physicians.
Although capsule colonoscopy has emerged as a potential noninvasive tool for examining the entire colon, there are limited data on its accuracy for detecting conventional adenomas or sessile serrated polyps, particularly in an average-risk screening population.
In the May issue of Gastroenterology, Dr. Rex and colleagues report their results from a large, multicenter, prospective study evaluating the new second-generation capsule colonoscopy (PillCam COLON 2, Given Imaging) for detecting colorectal neoplasia in an average-risk screening population. Using optical colonoscopy as the reference standard, the capsule colonoscopy performed well for detecting conventional adenomas 6 mm or larger with a sensitivity and specificity of 88% and 82%, respectively.
In addition, the sensitivity and specificity of capsule colonoscopy for conventional adenomas 10 mm or larger were 92% and 95%, respectively. However, despite the high performance characteristics for detection of conventional adenomas, the capsule colonoscopy had limited accuracy for detecting sessile serrated polyps 10 mm or larger, with a sensitivity of 33%. Furthermore, nearly 10% of the enrolled subjects were excluded from the analysis due to poor bowel preparation and rapid transit time.
These issues aside, the Rex study provides important information about alternative screening modalities for detection of colorectal neoplasia, particularly for gastroenterologists who may be hesitant or unwilling to perform an optical colonoscopy in high-risk patients with significant co-morbidities or in patients who had an incomplete colonoscopy.
Dr. Jeffrey Lee, MAS is assistant clinical professor of medicine, division of gastroenterology, University of California, San Francisco. He has no conflicts of interest.
In the United States, colonoscopy is the primary screening test for colorectal cancer. However, because of issues with colonoscopy uptake, costs, and the small but finite risk of complications, the concept of a relatively noninvasive structural examination of the colon that can detect colorectal neoplasia is appealing to both patients and physicians.
Although capsule colonoscopy has emerged as a potential noninvasive tool for examining the entire colon, there are limited data on its accuracy for detecting conventional adenomas or sessile serrated polyps, particularly in an average-risk screening population.
In the May issue of Gastroenterology, Dr. Rex and colleagues report their results from a large, multicenter, prospective study evaluating the new second-generation capsule colonoscopy (PillCam COLON 2, Given Imaging) for detecting colorectal neoplasia in an average-risk screening population. Using optical colonoscopy as the reference standard, the capsule colonoscopy performed well for detecting conventional adenomas 6 mm or larger with a sensitivity and specificity of 88% and 82%, respectively.
In addition, the sensitivity and specificity of capsule colonoscopy for conventional adenomas 10 mm or larger were 92% and 95%, respectively. However, despite the high performance characteristics for detection of conventional adenomas, the capsule colonoscopy had limited accuracy for detecting sessile serrated polyps 10 mm or larger, with a sensitivity of 33%. Furthermore, nearly 10% of the enrolled subjects were excluded from the analysis due to poor bowel preparation and rapid transit time.
These issues aside, the Rex study provides important information about alternative screening modalities for detection of colorectal neoplasia, particularly for gastroenterologists who may be hesitant or unwilling to perform an optical colonoscopy in high-risk patients with significant co-morbidities or in patients who had an incomplete colonoscopy.
Dr. Jeffrey Lee, MAS is assistant clinical professor of medicine, division of gastroenterology, University of California, San Francisco. He has no conflicts of interest.
When compared with conventional colonoscopy, capsule colonoscopy had a sensitivity of 88% and a specificity of 82% for detecting adenomas of at least 6 mm in asymptomatic subjects, a multicenter prospective study showed.
But the capsule detected only 29% of subjects who had sessile serrated polyps of at least 6 mm, and required more extensive bowel preparation than did conventional colonoscopy, Dr. Douglas K. Rex at Indiana University Hospital in Indianapolis and his associates reported in the May issue of Gastroenterology (2015 [doi:10.1053/j.gastro.2015.01.025]). “Given these considerations ... colonoscopy remains the gold standard for the detection of colorectal polyps,” said the researchers. “The capsule is a good test for the detection of patients with conventional adenomas 6 mm or larger in size and appears to be an appropriate imaging choice for patients who cannot undergo colonoscopy or had incomplete colonoscopy.”
Capsule endoscopy is useful for small-bowel imaging, but adapting the technology for colorectal studies has been difficult. A first-generation capsule detected only 74% of advanced adenomas in one prospective multicenter trial, the researchers noted. Since then, the PillCam COLON 2 capsule has been updated with motion detection, variable frame speed, and a wider angle view, they said. In smaller studies, it detected up to 89% of subjects with polyps of at least 6 mm, but its specificity was as low as 64%.
To further investigate the technology, researchers at 16 centers in the United States and Israel compared the second-generation capsule with conventional colonoscopy in an average-risk screening population of 884 asymptomatic subjects. Endoscopists were blinded as to technique, but performed unblinded follow-up colonoscopies in subjects who were positive on capsule but negative on conventional colonoscopy.
The capsule’s sensitivity was 81% (95% confidence interval, 77%-84%) and its specificity was 93% (91%-95%) for detecting subjects who had polyps of at least 6 mm, the researchers reported. Sensitivity was 80% (74%-86%) and specificity was 97% (96%-98%) for detecting subjects with polyps of at least 10 mm. For conventional adenomas of at least 6 mm, sensitivity was 88% (82%-93%) and specificity was 82% (80%-83%), and for adenomas of 10 mm or larger, sensitivity was 92% (82%-97%) and specificity was 95% (94%-95%).
“Lesions in the serrated class were not detected well by the capsule in this study, compared with conventional adenomas,” the researchers reported. Prior studies of the capsule did not look for serrated lesions, and in the current study sensitivities were only 29% and 33% for 6-mm and 10-mm lesions, respectively.
The software used to measure polyps during capsule colonoscopy had a 40% error range when tested on balls of known size, the researchers said. Therefore, there is a strict location-matching rule within the colon, but a liberal size rule that only required measurements to fall within 50% of one another to be considered a match. “Any set of matching rules for polyps detected by the capsule and colonoscopy might operate to increase or decrease the calculated sensitivity of the capsule incorrectly,” they added. Also, the adenoma detection rate for conventional colonoscopy was only 39%, and some polyps that were clearly seen on capsule were not visualized on regular colonoscopy. “In these cases, a polyp that should be a true positive for the capsule was counted as false,” they added. “Both colonoscopy and capsule are inferior for localization, compared with CT colonography. Inaccurate localization by one or both tests in this study could have reduced the sensitivity of the capsule.”
The investigators also had to exclude 77 patients because of inadequate cleansing and short transit times related to using sodium phosphate as a boost, they noted. The Food and Drug Administration label for the capsule is expected to reflect those limitations, they added.
Given Imaging funded the study and paid consulting or other fees to Dr. Rex and six coauthors. The other authors reported having no relevant conflicts of interest.
When compared with conventional colonoscopy, capsule colonoscopy had a sensitivity of 88% and a specificity of 82% for detecting adenomas of at least 6 mm in asymptomatic subjects, a multicenter prospective study showed.
But the capsule detected only 29% of subjects who had sessile serrated polyps of at least 6 mm, and required more extensive bowel preparation than did conventional colonoscopy, Dr. Douglas K. Rex at Indiana University Hospital in Indianapolis and his associates reported in the May issue of Gastroenterology (2015 [doi:10.1053/j.gastro.2015.01.025]). “Given these considerations ... colonoscopy remains the gold standard for the detection of colorectal polyps,” said the researchers. “The capsule is a good test for the detection of patients with conventional adenomas 6 mm or larger in size and appears to be an appropriate imaging choice for patients who cannot undergo colonoscopy or had incomplete colonoscopy.”
Capsule endoscopy is useful for small-bowel imaging, but adapting the technology for colorectal studies has been difficult. A first-generation capsule detected only 74% of advanced adenomas in one prospective multicenter trial, the researchers noted. Since then, the PillCam COLON 2 capsule has been updated with motion detection, variable frame speed, and a wider angle view, they said. In smaller studies, it detected up to 89% of subjects with polyps of at least 6 mm, but its specificity was as low as 64%.
To further investigate the technology, researchers at 16 centers in the United States and Israel compared the second-generation capsule with conventional colonoscopy in an average-risk screening population of 884 asymptomatic subjects. Endoscopists were blinded as to technique, but performed unblinded follow-up colonoscopies in subjects who were positive on capsule but negative on conventional colonoscopy.
The capsule’s sensitivity was 81% (95% confidence interval, 77%-84%) and its specificity was 93% (91%-95%) for detecting subjects who had polyps of at least 6 mm, the researchers reported. Sensitivity was 80% (74%-86%) and specificity was 97% (96%-98%) for detecting subjects with polyps of at least 10 mm. For conventional adenomas of at least 6 mm, sensitivity was 88% (82%-93%) and specificity was 82% (80%-83%), and for adenomas of 10 mm or larger, sensitivity was 92% (82%-97%) and specificity was 95% (94%-95%).
“Lesions in the serrated class were not detected well by the capsule in this study, compared with conventional adenomas,” the researchers reported. Prior studies of the capsule did not look for serrated lesions, and in the current study sensitivities were only 29% and 33% for 6-mm and 10-mm lesions, respectively.
The software used to measure polyps during capsule colonoscopy had a 40% error range when tested on balls of known size, the researchers said. Therefore, there is a strict location-matching rule within the colon, but a liberal size rule that only required measurements to fall within 50% of one another to be considered a match. “Any set of matching rules for polyps detected by the capsule and colonoscopy might operate to increase or decrease the calculated sensitivity of the capsule incorrectly,” they added. Also, the adenoma detection rate for conventional colonoscopy was only 39%, and some polyps that were clearly seen on capsule were not visualized on regular colonoscopy. “In these cases, a polyp that should be a true positive for the capsule was counted as false,” they added. “Both colonoscopy and capsule are inferior for localization, compared with CT colonography. Inaccurate localization by one or both tests in this study could have reduced the sensitivity of the capsule.”
The investigators also had to exclude 77 patients because of inadequate cleansing and short transit times related to using sodium phosphate as a boost, they noted. The Food and Drug Administration label for the capsule is expected to reflect those limitations, they added.
Given Imaging funded the study and paid consulting or other fees to Dr. Rex and six coauthors. The other authors reported having no relevant conflicts of interest.
FROM GASTROENTEROLOGY
Key clinical point: Despite improvements in second-generation capsules, colonoscopy remains the gold standard for colorectal adenoma detection.
Major finding: Compared with conventional colonoscopy, the capsule showed 88% sensitivity and 82% specificity for detecting subjects who had adenomas of at least 6 mm.
Data source: Prospective, multicenter, single-blinded comparison of capsule and conventional colonoscopy in 884 asymptomatic subjects.
Disclosures: Given Imaging makes the capsule technology, funded the study, and paid consulting or other fees to Dr. Rex and six coauthors. The other authors reported no relevant conflicts of interest.
Acid exposure time found most useful in pH-impedance testing
pH-impedance testing best predicted response to reflux treatment when patients were off proton pump inhibitors, and abnormal acid exposure time was the single most useful testing parameter, a prospective study has found.
“Impedance-based reflux parameters complement but do not replace acid-based parameters in predicting symptom outcome from both medical and surgical antireflux therapy,” wrote Dr. Amit Patel and his associates at the Washington School of Medicine, St. Louis. The study appears in the May issue of Clinical Gastroenterology and Hepatology (doi:10.1016/j.cgh.2014.08.02).
“Because abnormal acid reflux time and symptom-reflux correlation parameters are detected more often when testing is performed off therapy, pH-impedance testing off antisecretory therapy maximizes prediction of symptomatic outcome from GERD [gastroesophageal reflux disease] therapy,” the researchers wrote.
Clinicians continue to debate the role of pH-impedance testing in management of GERD, whether testing should be performed on or off antisecretory therapy, and which testing parameters are most useful for predicting treatment response, the investigators noted. Therefore, they followed 187 adults with persistent GERD symptoms who underwent pH-impedance testing at their center during a 5-year period. Average age of patients was 54 years, almost 71% were female, and none had histopathologic evidence of esophageal motor disorders. Almost half had been off proton pump inhibitors for 7 days when tested, and 68% were managed medically as opposed to surgically.
Global symptom assessment (GSS) and dominant symptom intensity (DSI) scores both improved significantly during an average of 40 months of follow-up, the researchers said. After the researchers controlled for demographics, symptoms at presentation, use of proton pump inhibitors (PPI), and parameters that predicted treatment response in the univariate analyses, only abnormal acid exposure time (AET) predicted linear improvement in DSI scores (P =.027), while abnormal AET (P =.002) and symptom association probability (P =.026) predicted significant improvements in linear and dichotomous GSS, they reported. Abnormal AET and being off PPIs during testing also more than doubled the odds of at least a 50% improvement in GSS.
In contrast, dichotomous reflux exposure time did not predict response in any of the analyses, said the investigators. “Established thresholds for the total number of reflux events did not predict linear or dichotomous global symptom severity improvement,” they added. “Our data therefore suggest that performing pH-impedance testing off PPI therapy increases the yield of abnormal AET and symptom-reflux association with reflux events, facilitating predicting value for symptom improvement with both medical and surgical antireflux therapy.”
The researchers could not corroborate patients’ compliance with antisecretory therapy, assess the reasons physicians chose medical or surgical management, or evaluate the impact of the placebo effect or other factors unrelated to reflux, they said.
The study was partly funded by the National Institute for Diabetes and Digestive and Kidney Diseases, the National Institutes of Health, and the Washington University Department of Medicine Mentors in Medicine and Clinical Science Training and Research programs. The authors declared no relevant conflicts of interest.
pH-impedance testing best predicted response to reflux treatment when patients were off proton pump inhibitors, and abnormal acid exposure time was the single most useful testing parameter, a prospective study has found.
“Impedance-based reflux parameters complement but do not replace acid-based parameters in predicting symptom outcome from both medical and surgical antireflux therapy,” wrote Dr. Amit Patel and his associates at the Washington School of Medicine, St. Louis. The study appears in the May issue of Clinical Gastroenterology and Hepatology (doi:10.1016/j.cgh.2014.08.02).
“Because abnormal acid reflux time and symptom-reflux correlation parameters are detected more often when testing is performed off therapy, pH-impedance testing off antisecretory therapy maximizes prediction of symptomatic outcome from GERD [gastroesophageal reflux disease] therapy,” the researchers wrote.
Clinicians continue to debate the role of pH-impedance testing in management of GERD, whether testing should be performed on or off antisecretory therapy, and which testing parameters are most useful for predicting treatment response, the investigators noted. Therefore, they followed 187 adults with persistent GERD symptoms who underwent pH-impedance testing at their center during a 5-year period. Average age of patients was 54 years, almost 71% were female, and none had histopathologic evidence of esophageal motor disorders. Almost half had been off proton pump inhibitors for 7 days when tested, and 68% were managed medically as opposed to surgically.
Global symptom assessment (GSS) and dominant symptom intensity (DSI) scores both improved significantly during an average of 40 months of follow-up, the researchers said. After the researchers controlled for demographics, symptoms at presentation, use of proton pump inhibitors (PPI), and parameters that predicted treatment response in the univariate analyses, only abnormal acid exposure time (AET) predicted linear improvement in DSI scores (P =.027), while abnormal AET (P =.002) and symptom association probability (P =.026) predicted significant improvements in linear and dichotomous GSS, they reported. Abnormal AET and being off PPIs during testing also more than doubled the odds of at least a 50% improvement in GSS.
In contrast, dichotomous reflux exposure time did not predict response in any of the analyses, said the investigators. “Established thresholds for the total number of reflux events did not predict linear or dichotomous global symptom severity improvement,” they added. “Our data therefore suggest that performing pH-impedance testing off PPI therapy increases the yield of abnormal AET and symptom-reflux association with reflux events, facilitating predicting value for symptom improvement with both medical and surgical antireflux therapy.”
The researchers could not corroborate patients’ compliance with antisecretory therapy, assess the reasons physicians chose medical or surgical management, or evaluate the impact of the placebo effect or other factors unrelated to reflux, they said.
The study was partly funded by the National Institute for Diabetes and Digestive and Kidney Diseases, the National Institutes of Health, and the Washington University Department of Medicine Mentors in Medicine and Clinical Science Training and Research programs. The authors declared no relevant conflicts of interest.
pH-impedance testing best predicted response to reflux treatment when patients were off proton pump inhibitors, and abnormal acid exposure time was the single most useful testing parameter, a prospective study has found.
“Impedance-based reflux parameters complement but do not replace acid-based parameters in predicting symptom outcome from both medical and surgical antireflux therapy,” wrote Dr. Amit Patel and his associates at the Washington School of Medicine, St. Louis. The study appears in the May issue of Clinical Gastroenterology and Hepatology (doi:10.1016/j.cgh.2014.08.02).
“Because abnormal acid reflux time and symptom-reflux correlation parameters are detected more often when testing is performed off therapy, pH-impedance testing off antisecretory therapy maximizes prediction of symptomatic outcome from GERD [gastroesophageal reflux disease] therapy,” the researchers wrote.
Clinicians continue to debate the role of pH-impedance testing in management of GERD, whether testing should be performed on or off antisecretory therapy, and which testing parameters are most useful for predicting treatment response, the investigators noted. Therefore, they followed 187 adults with persistent GERD symptoms who underwent pH-impedance testing at their center during a 5-year period. Average age of patients was 54 years, almost 71% were female, and none had histopathologic evidence of esophageal motor disorders. Almost half had been off proton pump inhibitors for 7 days when tested, and 68% were managed medically as opposed to surgically.
Global symptom assessment (GSS) and dominant symptom intensity (DSI) scores both improved significantly during an average of 40 months of follow-up, the researchers said. After the researchers controlled for demographics, symptoms at presentation, use of proton pump inhibitors (PPI), and parameters that predicted treatment response in the univariate analyses, only abnormal acid exposure time (AET) predicted linear improvement in DSI scores (P =.027), while abnormal AET (P =.002) and symptom association probability (P =.026) predicted significant improvements in linear and dichotomous GSS, they reported. Abnormal AET and being off PPIs during testing also more than doubled the odds of at least a 50% improvement in GSS.
In contrast, dichotomous reflux exposure time did not predict response in any of the analyses, said the investigators. “Established thresholds for the total number of reflux events did not predict linear or dichotomous global symptom severity improvement,” they added. “Our data therefore suggest that performing pH-impedance testing off PPI therapy increases the yield of abnormal AET and symptom-reflux association with reflux events, facilitating predicting value for symptom improvement with both medical and surgical antireflux therapy.”
The researchers could not corroborate patients’ compliance with antisecretory therapy, assess the reasons physicians chose medical or surgical management, or evaluate the impact of the placebo effect or other factors unrelated to reflux, they said.
The study was partly funded by the National Institute for Diabetes and Digestive and Kidney Diseases, the National Institutes of Health, and the Washington University Department of Medicine Mentors in Medicine and Clinical Science Training and Research programs. The authors declared no relevant conflicts of interest.
Key clinical point: pH-impedance testing best predicted response to reflux treatment when patients were off proton pump inhibitors, and abnormal acid exposure time was the single most useful parameter.
Major finding: Acid exposure time consistently predicted response to antireflux therapy in univariate and multivariable analyses, while reflux exposure time did not.
Data source: Prospective, single-center study of 187 patients who underwent pH-impedance testing.
Disclosures: This study was partly funded by the National Institute for Diabetes and Digestive and Kidney Diseases, the National Institutes of Health, and the Washington University Department of Medicine Mentors in Medicine and Clinical Science Training and Research programs. The authors declared no relevant conflicts of interest.
Oxidized low-density lipoprotein predicted chronic HCV interferon response
Oxidized low-density lipoprotein prevented hepatitis C virus from entering liver cells and predicted interferon response among patients with chronic HCV infection, researchers reported online in the May issue of Cellular and Molecular Gastroenterology and Hepatology (2015 March 14 [doi:10.1016/j.jcmgh.2015.03.002]).
“Even as all-oral regimens begin to reach the market, interferon-based treatment will continue to be used in cost-restrained settings. Thus, there is a need for predictors of who is likely to respond to interferon and who will require a more expensive direct-acting antiviral combination regimen,” said Dr. Philipp Solbach of Medizinische Hochschule Hannover and the German Center for Infection Research and his associates. Combinations of interferon and viral entry inhibitors might benefit patients with chronic HCV infection (CHC), the investigators added.
Hepatitis C virus spreads between hepatocytes with the help of several cell surface receptors, including scavenger receptor class B type 1 (SR-BI). Research has shown that oxidized low-density lipoprotein (oxLDL) noncompetitively inhibits the interaction between SR-B1 and HCV. To further study the role of oxLDL in CHC pathology, the investigators used a commercial enzyme-linked immunosorbent assay test to measure serum levels in 379 patients with genotype 1 CHC from the INDIV-2 study. Patients in that study received a pegylated interferon-ribavirin combination for 24-72 weeks, depending on baseline viral load. Dr. Solbach and his associates also studied the effects of oxLDL on HCV replication in hepatoma cells.
Average serum oxLDL levels were significantly higher among patients who achieved SVR on peg-IFN/RBV than in those who did not (7.1 mU/L [standard deviation, 3.2] vs. 5.9 mU/L [SD, 2.6]; P < .001), the researchers reported. In the multivariate analysis, oxLDL levels independently predicted SVR, but were not associated with increased ALT or ferritin levels, both of which point to liver inflammation. Increased serum oxLDL also was linked to decreased infected cell loss rate, further supporting the idea that oxLDL helps inhibit cell-to-cell spread of HCV in chronically infected patients, they said.
Area under the receiver operative curve (AUROC) values were similar for LDL and oxLDL, indicating that one value was a good clinical indicator of the other, the investigators said. The optimal cutoff points to predict SVR in their model were 8.85 mU/L for oxLDL and 3.6 mmol/L for LDL.
In the in vitro study, oxLDL did not affect the sensitivity of HCV replication to interferon, but strongly inhibited the spread of HCV between adjacent hepatocytes, the investigators reported. “We found that oxLDL but not LDL potently inhibits cell-to-cell spread between neighboring cells,” they noted. “Cell-to-cell spread is thought to be the dominant route of new cell infection within the chronically infected liver.”
Taken together, the findings suggest that HCV needs to interact with SR-BI in order to spread between hepatocytes, that oxLDL can impede that interaction and thereby limit infection of naive cells, and that oxLDL is neither an inflammatory marker nor a modulator of interferon response, Dr. Solback and his associates said. “The slower second-phase decline of viral load during interferon-based therapy is thought to reflect a declining pool of infected hepatocytes, and the slope of second-phase decline and even more the estimated viral kinetic parameter describing the infected cell loss rate is predictive of eventual SVR,” they added. “The presence of an agent reducing the rate at which naive cells get infected might thus be beneficial.”
The Germany Center for Infection Research partially funded the study. Five coauthors reported having served as clinical researchers, consultants, or speakers for MSD/Merck and Roche. The other authors declared no conflicts of interest.
Despite the fact that significant advances in the treatment of hepatitis C have been made, it is still a major global health burden. In order to follow up on their previous observation that oxLDL acts as a hepatitis C virus (HCV) entry inhibitor by disrupting the interaction between HCV and one of its entry factors, scavenger receptor type B class I (SR-BI), Dr. Solbach and his associates analyzed the oxLDL levels of 379 patients from the INDIV-2 study chronically infected with HCV genotype 1. The authors demonstrated that baseline oxLDL serum levels were an independent predictor of a sustained virologic response in interferon-based treatment regimens and that LDL is a sufficient surrogate marker.
Clinicians, especially in resource-limited environments, may take oxLDL or LDL serum levels into consideration for treatment decisions, although these predictors are unlikely to broadly affect treatment decisions in real-world settings. The significance of this study lies more in adding to our understanding of the pathophysiology of HCV. The data presented here indicate that the observed effect of oxLDL is possibly due to an oxLDL-mediated inhibition of HCV cell-to-cell spread. Taken together with their previous observation that oxLDL interferes with the interaction of HCV and its entry factor SR-BI, the authors provide additional evidence that SR-BI may be needed for cell-to-cell spread of HCV and might thereby have implications for the further development of HCV entry inhibitors.
Dr. Markus von Schaewen and Dr. Alexander Ploss are in the department of molecular biology, Princeton University, Princeton, N.J. They had no conflicts of interest.
Despite the fact that significant advances in the treatment of hepatitis C have been made, it is still a major global health burden. In order to follow up on their previous observation that oxLDL acts as a hepatitis C virus (HCV) entry inhibitor by disrupting the interaction between HCV and one of its entry factors, scavenger receptor type B class I (SR-BI), Dr. Solbach and his associates analyzed the oxLDL levels of 379 patients from the INDIV-2 study chronically infected with HCV genotype 1. The authors demonstrated that baseline oxLDL serum levels were an independent predictor of a sustained virologic response in interferon-based treatment regimens and that LDL is a sufficient surrogate marker.
Clinicians, especially in resource-limited environments, may take oxLDL or LDL serum levels into consideration for treatment decisions, although these predictors are unlikely to broadly affect treatment decisions in real-world settings. The significance of this study lies more in adding to our understanding of the pathophysiology of HCV. The data presented here indicate that the observed effect of oxLDL is possibly due to an oxLDL-mediated inhibition of HCV cell-to-cell spread. Taken together with their previous observation that oxLDL interferes with the interaction of HCV and its entry factor SR-BI, the authors provide additional evidence that SR-BI may be needed for cell-to-cell spread of HCV and might thereby have implications for the further development of HCV entry inhibitors.
Dr. Markus von Schaewen and Dr. Alexander Ploss are in the department of molecular biology, Princeton University, Princeton, N.J. They had no conflicts of interest.
Despite the fact that significant advances in the treatment of hepatitis C have been made, it is still a major global health burden. In order to follow up on their previous observation that oxLDL acts as a hepatitis C virus (HCV) entry inhibitor by disrupting the interaction between HCV and one of its entry factors, scavenger receptor type B class I (SR-BI), Dr. Solbach and his associates analyzed the oxLDL levels of 379 patients from the INDIV-2 study chronically infected with HCV genotype 1. The authors demonstrated that baseline oxLDL serum levels were an independent predictor of a sustained virologic response in interferon-based treatment regimens and that LDL is a sufficient surrogate marker.
Clinicians, especially in resource-limited environments, may take oxLDL or LDL serum levels into consideration for treatment decisions, although these predictors are unlikely to broadly affect treatment decisions in real-world settings. The significance of this study lies more in adding to our understanding of the pathophysiology of HCV. The data presented here indicate that the observed effect of oxLDL is possibly due to an oxLDL-mediated inhibition of HCV cell-to-cell spread. Taken together with their previous observation that oxLDL interferes with the interaction of HCV and its entry factor SR-BI, the authors provide additional evidence that SR-BI may be needed for cell-to-cell spread of HCV and might thereby have implications for the further development of HCV entry inhibitors.
Dr. Markus von Schaewen and Dr. Alexander Ploss are in the department of molecular biology, Princeton University, Princeton, N.J. They had no conflicts of interest.
Oxidized low-density lipoprotein prevented hepatitis C virus from entering liver cells and predicted interferon response among patients with chronic HCV infection, researchers reported online in the May issue of Cellular and Molecular Gastroenterology and Hepatology (2015 March 14 [doi:10.1016/j.jcmgh.2015.03.002]).
“Even as all-oral regimens begin to reach the market, interferon-based treatment will continue to be used in cost-restrained settings. Thus, there is a need for predictors of who is likely to respond to interferon and who will require a more expensive direct-acting antiviral combination regimen,” said Dr. Philipp Solbach of Medizinische Hochschule Hannover and the German Center for Infection Research and his associates. Combinations of interferon and viral entry inhibitors might benefit patients with chronic HCV infection (CHC), the investigators added.
Hepatitis C virus spreads between hepatocytes with the help of several cell surface receptors, including scavenger receptor class B type 1 (SR-BI). Research has shown that oxidized low-density lipoprotein (oxLDL) noncompetitively inhibits the interaction between SR-B1 and HCV. To further study the role of oxLDL in CHC pathology, the investigators used a commercial enzyme-linked immunosorbent assay test to measure serum levels in 379 patients with genotype 1 CHC from the INDIV-2 study. Patients in that study received a pegylated interferon-ribavirin combination for 24-72 weeks, depending on baseline viral load. Dr. Solbach and his associates also studied the effects of oxLDL on HCV replication in hepatoma cells.
Average serum oxLDL levels were significantly higher among patients who achieved SVR on peg-IFN/RBV than in those who did not (7.1 mU/L [standard deviation, 3.2] vs. 5.9 mU/L [SD, 2.6]; P < .001), the researchers reported. In the multivariate analysis, oxLDL levels independently predicted SVR, but were not associated with increased ALT or ferritin levels, both of which point to liver inflammation. Increased serum oxLDL also was linked to decreased infected cell loss rate, further supporting the idea that oxLDL helps inhibit cell-to-cell spread of HCV in chronically infected patients, they said.
Area under the receiver operative curve (AUROC) values were similar for LDL and oxLDL, indicating that one value was a good clinical indicator of the other, the investigators said. The optimal cutoff points to predict SVR in their model were 8.85 mU/L for oxLDL and 3.6 mmol/L for LDL.
In the in vitro study, oxLDL did not affect the sensitivity of HCV replication to interferon, but strongly inhibited the spread of HCV between adjacent hepatocytes, the investigators reported. “We found that oxLDL but not LDL potently inhibits cell-to-cell spread between neighboring cells,” they noted. “Cell-to-cell spread is thought to be the dominant route of new cell infection within the chronically infected liver.”
Taken together, the findings suggest that HCV needs to interact with SR-BI in order to spread between hepatocytes, that oxLDL can impede that interaction and thereby limit infection of naive cells, and that oxLDL is neither an inflammatory marker nor a modulator of interferon response, Dr. Solback and his associates said. “The slower second-phase decline of viral load during interferon-based therapy is thought to reflect a declining pool of infected hepatocytes, and the slope of second-phase decline and even more the estimated viral kinetic parameter describing the infected cell loss rate is predictive of eventual SVR,” they added. “The presence of an agent reducing the rate at which naive cells get infected might thus be beneficial.”
The Germany Center for Infection Research partially funded the study. Five coauthors reported having served as clinical researchers, consultants, or speakers for MSD/Merck and Roche. The other authors declared no conflicts of interest.
Oxidized low-density lipoprotein prevented hepatitis C virus from entering liver cells and predicted interferon response among patients with chronic HCV infection, researchers reported online in the May issue of Cellular and Molecular Gastroenterology and Hepatology (2015 March 14 [doi:10.1016/j.jcmgh.2015.03.002]).
“Even as all-oral regimens begin to reach the market, interferon-based treatment will continue to be used in cost-restrained settings. Thus, there is a need for predictors of who is likely to respond to interferon and who will require a more expensive direct-acting antiviral combination regimen,” said Dr. Philipp Solbach of Medizinische Hochschule Hannover and the German Center for Infection Research and his associates. Combinations of interferon and viral entry inhibitors might benefit patients with chronic HCV infection (CHC), the investigators added.
Hepatitis C virus spreads between hepatocytes with the help of several cell surface receptors, including scavenger receptor class B type 1 (SR-BI). Research has shown that oxidized low-density lipoprotein (oxLDL) noncompetitively inhibits the interaction between SR-B1 and HCV. To further study the role of oxLDL in CHC pathology, the investigators used a commercial enzyme-linked immunosorbent assay test to measure serum levels in 379 patients with genotype 1 CHC from the INDIV-2 study. Patients in that study received a pegylated interferon-ribavirin combination for 24-72 weeks, depending on baseline viral load. Dr. Solbach and his associates also studied the effects of oxLDL on HCV replication in hepatoma cells.
Average serum oxLDL levels were significantly higher among patients who achieved SVR on peg-IFN/RBV than in those who did not (7.1 mU/L [standard deviation, 3.2] vs. 5.9 mU/L [SD, 2.6]; P < .001), the researchers reported. In the multivariate analysis, oxLDL levels independently predicted SVR, but were not associated with increased ALT or ferritin levels, both of which point to liver inflammation. Increased serum oxLDL also was linked to decreased infected cell loss rate, further supporting the idea that oxLDL helps inhibit cell-to-cell spread of HCV in chronically infected patients, they said.
Area under the receiver operative curve (AUROC) values were similar for LDL and oxLDL, indicating that one value was a good clinical indicator of the other, the investigators said. The optimal cutoff points to predict SVR in their model were 8.85 mU/L for oxLDL and 3.6 mmol/L for LDL.
In the in vitro study, oxLDL did not affect the sensitivity of HCV replication to interferon, but strongly inhibited the spread of HCV between adjacent hepatocytes, the investigators reported. “We found that oxLDL but not LDL potently inhibits cell-to-cell spread between neighboring cells,” they noted. “Cell-to-cell spread is thought to be the dominant route of new cell infection within the chronically infected liver.”
Taken together, the findings suggest that HCV needs to interact with SR-BI in order to spread between hepatocytes, that oxLDL can impede that interaction and thereby limit infection of naive cells, and that oxLDL is neither an inflammatory marker nor a modulator of interferon response, Dr. Solback and his associates said. “The slower second-phase decline of viral load during interferon-based therapy is thought to reflect a declining pool of infected hepatocytes, and the slope of second-phase decline and even more the estimated viral kinetic parameter describing the infected cell loss rate is predictive of eventual SVR,” they added. “The presence of an agent reducing the rate at which naive cells get infected might thus be beneficial.”
The Germany Center for Infection Research partially funded the study. Five coauthors reported having served as clinical researchers, consultants, or speakers for MSD/Merck and Roche. The other authors declared no conflicts of interest.
FROM CELLULAR AND MOLECULAR GASTROENTEROLOGY AND HEPATOLOGY
Key clinical point: Oxidized low-density lipoprotein prevented hepatitis C virus from entering hepatocytes and predicted interferon-based treatment response among patients with chronic HCV infection.
Major finding: Serum oxLDL levels independently predicted SVR after treatment with pegylated interferon/ribavirin (P < .001).
Data source: In vivo study of 379 patients with chronic genotype 1 HCV infection, and in vitro study of HCV replication in hepatoma cells.
Disclosures: The Germany Center for Infection Research partially funded the study. Five coauthors reported having served as clinical researchers, consultants, or speakers for MSD/Merck and Roche. The other authors reported no relevant conflicts of interest.
Inpatient cirrhosis mortality has dropped, except when patients had sepsis
Hospital mortality among patients with cirrhosis fell by 41% in the United States between 2002 and 2010, far outpacing improvements in survival among inpatients who did not have cirrhosis, researchers reported in the May issue of Gastroenterology (2015 [doi:10.1053/j.gastro.2015.01.032]).
The drop occurred even though cirrhosis inpatients were older and had more comorbidities by the end, compared with the beginning of the study, said Monica Schmidtat the University of North Carolina Liver Center and the Gillings School of Global Public Health in Chapel Hill, N.C., and her associates. The finding was “remarkably consistent across several cirrhosis complications, and [suggested] improving cirrhosis care that may extend beyond general improvements in inpatient care,” the researchers added. “On the other hand, sepsis had an increasing mortality risk, suggesting that cirrhotic patients may need a more tailored approach to sepsis,” they said.
Source: American Gastroenterological Association
New treatments have emerged in the past 10-15 years for several complications of cirrhosis, including hepatorenal syndrome, variceal bleeding, spontaneous bacterial peritonitis, ascites, and hepatocellular carcinoma, Ms. Schmidt and her associates noted. To study the extent to which these advances and updated guidelines have entered hospital practice, they examined 781,515 hospitalizations with a diagnosis of cirrhosis, and equal numbers of hospitalizations without cirrhosis or with congestive heart failure. Data were from the National Inpatient Sample of the Healthcare Cost and Utilization Project, which includes 46 states and is the single largest all-payer inpatient database in the country. Cohorts were matched by age, sex, and year of hospital discharge from 2002 through 2010.
Hospital mortality among cirrhosis patients dropped by 41% (from 9.1% to 5.4%) during the 8 years of the study, compared with declines of 44% for inpatients with congestive heart failure and 19% for inpatients without cirrhosis, the investigators said. Furthermore, the independent risk of dying in the hospital among cirrhosis patients declined steadily to 0.50 by the end of the study (95% confidence interval, 0.48-0.52), despite the population’s increasing age and medical complexity. Hospital mortality rates were higher for subgroups of cirrhosis patients with hepatorenal syndrome, hepatocellular carcinoma, variceal bleeding, and spontaneous bacterial peritonitis, but independent mortality risks for each of these conditions fell progressively over time, the investigators noted.
In contrast, cirrhosis inpatients with sepsis were 22% more likely to die in the hospital in 2010 than in 2002 (relative risk in 2002, 3.6; 95% CI, 3.3-3.95; RR in 2010, 4.6; 95% CI, 4.4-4.8), the researchers found. The increase was so marked that the mortality risk related to sepsis in 2010 exceeded even that for hepatorenal syndrome, they said. The unexpected finding contradicted a report of declining overall sepsis-related mortality, which was based on the same data source and a similar time period, the investigators noted.
“Cirrhosis patients have particularly poor hemodynamic reserve, with wider perturbations in immune inflammatory and compensatory responses that could hinder survival,” they commented. “Therefore, it is possible that cirrhosis patients are doing much worse with sepsis, compared with other patients. The surviving sepsis campaign may need guidelines that specifically target cirrhosis patients.”
The National Institutes of Health partly funded the study. The authors reported having no relevant conflicts of interest.
Hospital mortality among patients with cirrhosis fell by 41% in the United States between 2002 and 2010, far outpacing improvements in survival among inpatients who did not have cirrhosis, researchers reported in the May issue of Gastroenterology (2015 [doi:10.1053/j.gastro.2015.01.032]).
The drop occurred even though cirrhosis inpatients were older and had more comorbidities by the end, compared with the beginning of the study, said Monica Schmidtat the University of North Carolina Liver Center and the Gillings School of Global Public Health in Chapel Hill, N.C., and her associates. The finding was “remarkably consistent across several cirrhosis complications, and [suggested] improving cirrhosis care that may extend beyond general improvements in inpatient care,” the researchers added. “On the other hand, sepsis had an increasing mortality risk, suggesting that cirrhotic patients may need a more tailored approach to sepsis,” they said.
Source: American Gastroenterological Association
New treatments have emerged in the past 10-15 years for several complications of cirrhosis, including hepatorenal syndrome, variceal bleeding, spontaneous bacterial peritonitis, ascites, and hepatocellular carcinoma, Ms. Schmidt and her associates noted. To study the extent to which these advances and updated guidelines have entered hospital practice, they examined 781,515 hospitalizations with a diagnosis of cirrhosis, and equal numbers of hospitalizations without cirrhosis or with congestive heart failure. Data were from the National Inpatient Sample of the Healthcare Cost and Utilization Project, which includes 46 states and is the single largest all-payer inpatient database in the country. Cohorts were matched by age, sex, and year of hospital discharge from 2002 through 2010.
Hospital mortality among cirrhosis patients dropped by 41% (from 9.1% to 5.4%) during the 8 years of the study, compared with declines of 44% for inpatients with congestive heart failure and 19% for inpatients without cirrhosis, the investigators said. Furthermore, the independent risk of dying in the hospital among cirrhosis patients declined steadily to 0.50 by the end of the study (95% confidence interval, 0.48-0.52), despite the population’s increasing age and medical complexity. Hospital mortality rates were higher for subgroups of cirrhosis patients with hepatorenal syndrome, hepatocellular carcinoma, variceal bleeding, and spontaneous bacterial peritonitis, but independent mortality risks for each of these conditions fell progressively over time, the investigators noted.
In contrast, cirrhosis inpatients with sepsis were 22% more likely to die in the hospital in 2010 than in 2002 (relative risk in 2002, 3.6; 95% CI, 3.3-3.95; RR in 2010, 4.6; 95% CI, 4.4-4.8), the researchers found. The increase was so marked that the mortality risk related to sepsis in 2010 exceeded even that for hepatorenal syndrome, they said. The unexpected finding contradicted a report of declining overall sepsis-related mortality, which was based on the same data source and a similar time period, the investigators noted.
“Cirrhosis patients have particularly poor hemodynamic reserve, with wider perturbations in immune inflammatory and compensatory responses that could hinder survival,” they commented. “Therefore, it is possible that cirrhosis patients are doing much worse with sepsis, compared with other patients. The surviving sepsis campaign may need guidelines that specifically target cirrhosis patients.”
The National Institutes of Health partly funded the study. The authors reported having no relevant conflicts of interest.
Hospital mortality among patients with cirrhosis fell by 41% in the United States between 2002 and 2010, far outpacing improvements in survival among inpatients who did not have cirrhosis, researchers reported in the May issue of Gastroenterology (2015 [doi:10.1053/j.gastro.2015.01.032]).
The drop occurred even though cirrhosis inpatients were older and had more comorbidities by the end, compared with the beginning of the study, said Monica Schmidtat the University of North Carolina Liver Center and the Gillings School of Global Public Health in Chapel Hill, N.C., and her associates. The finding was “remarkably consistent across several cirrhosis complications, and [suggested] improving cirrhosis care that may extend beyond general improvements in inpatient care,” the researchers added. “On the other hand, sepsis had an increasing mortality risk, suggesting that cirrhotic patients may need a more tailored approach to sepsis,” they said.
Source: American Gastroenterological Association
New treatments have emerged in the past 10-15 years for several complications of cirrhosis, including hepatorenal syndrome, variceal bleeding, spontaneous bacterial peritonitis, ascites, and hepatocellular carcinoma, Ms. Schmidt and her associates noted. To study the extent to which these advances and updated guidelines have entered hospital practice, they examined 781,515 hospitalizations with a diagnosis of cirrhosis, and equal numbers of hospitalizations without cirrhosis or with congestive heart failure. Data were from the National Inpatient Sample of the Healthcare Cost and Utilization Project, which includes 46 states and is the single largest all-payer inpatient database in the country. Cohorts were matched by age, sex, and year of hospital discharge from 2002 through 2010.
Hospital mortality among cirrhosis patients dropped by 41% (from 9.1% to 5.4%) during the 8 years of the study, compared with declines of 44% for inpatients with congestive heart failure and 19% for inpatients without cirrhosis, the investigators said. Furthermore, the independent risk of dying in the hospital among cirrhosis patients declined steadily to 0.50 by the end of the study (95% confidence interval, 0.48-0.52), despite the population’s increasing age and medical complexity. Hospital mortality rates were higher for subgroups of cirrhosis patients with hepatorenal syndrome, hepatocellular carcinoma, variceal bleeding, and spontaneous bacterial peritonitis, but independent mortality risks for each of these conditions fell progressively over time, the investigators noted.
In contrast, cirrhosis inpatients with sepsis were 22% more likely to die in the hospital in 2010 than in 2002 (relative risk in 2002, 3.6; 95% CI, 3.3-3.95; RR in 2010, 4.6; 95% CI, 4.4-4.8), the researchers found. The increase was so marked that the mortality risk related to sepsis in 2010 exceeded even that for hepatorenal syndrome, they said. The unexpected finding contradicted a report of declining overall sepsis-related mortality, which was based on the same data source and a similar time period, the investigators noted.
“Cirrhosis patients have particularly poor hemodynamic reserve, with wider perturbations in immune inflammatory and compensatory responses that could hinder survival,” they commented. “Therefore, it is possible that cirrhosis patients are doing much worse with sepsis, compared with other patients. The surviving sepsis campaign may need guidelines that specifically target cirrhosis patients.”
The National Institutes of Health partly funded the study. The authors reported having no relevant conflicts of interest.
Key clinical point: Hospital mortality among cirrhosis patients has fallen markedly, but not when they also had sepsis.
Major finding: Inpatient mortality fell by 41%, but risk of death among cirrhosis patients who had sepsis rose by 22%.
Data source: Analysis of 781,515 hospitalizations of patients with cirrhosis and equal numbers of hospitalizations without cirrhosis or with congestive heart failure.
Disclosures: The National Institutes of Health partly funded the study. The authors reported having no relevant conflicts of interest.
All-oral simeprevir-sofosbuvir beat interferon-based regimen for HCV with compensated cirrhosis
Patients with compensated cirrhosis and chronic genotype 1 hepatitis C virus infections were significantly more likely to clear their infections and had fewer adverse effects when treated with simeprevir and sofosbuvir instead of peginterferon, ribavirin, and sofosbuvir, investigators reported in the April issue of Gastroenterology. “Patients given the interferon-containing regimen had a significantly greater rate of virologic relapse than patients given simeprevir and sofosbuvir ... and reported worse outcomes and more side effects,” said Dr. Brian L. Pearlman and his associates of Atlanta Medical Center and Emory University, Atlanta.
Liver disease associated with chronic hepatitis C virus (HCV) infection causes at least 350,000 deaths per year worldwide. Genotype 1 (GT-1) HCV is the most common HCV strain and the hardest to treat, especially when patients have cirrhosis. Treatments for chronic GT-1 HCV infections historically included interferon, but achieved only moderate rates of sustained virologic response (SVR) and caused adverse somatic and psychiatric effects. All-oral, interferon-free regimens are now in widespread use, but many of the pivotal trials were industry sponsored and had strict enrollment criteria, potentially limiting their generalizability in community settings, the researchers reported (Gastroenterology 2015 April [doi:10.1053/j.gastro.2014.12.027]).Their open-label trial included 82 patients with HCV GT-1a infection and Child’s grade A cirrhosis recruited from two clinical practices in Atlanta. Thirty-two of the patients were treatment naive, while 50 had previously not responded to peginterferon and ribavirin treatment. Patients were randomized to either 12 weeks of all-oral simeprevir (150 mg/day) and sofosbuvir (400 mg/day), or peginterferon alfa 2b (1.5 mcg/kg per week), ribavirin (1000-1200 mg/day), and sofosbuvir (400 mg/day).Fully 54 of 58 (93%) patients given the simeprevir-sofosbuvir regimen had undetectable levels of HCV RNA at 12 weeks (SVR12), compared with 18 of 24 (75%) patients who received the interferon-containing regimen (P = .02), the researchers reported. Rates of SVR12 among prior nonresponders were 92% and 64%, and were 95% and 80% for treatment-naive patients, although P-values did not reach statistical significance. The interferon group also had a higher rate of virologic relapse than did patients given simeprevir and sofosbuvir (P = .009), and had worse self-reported outcomes and more side effects, the researchers said. Patients in both groups who achieved SVR12 had higher quality-of-life scores than those who did not. Notably, almost half of patients were African American, a group that has historically had lower cure rates compared with other racial groups, said the investigators.
“Given that several new regimens for genotype 1 infection, including the sofosbuvir-ledipasvir combination pill, already have been approved, we believe that this study is very timely,” Dr. Pearlman and his associates said. “Although these are not head-to-head comparisons, the 12-week simeprevir and sofosbuvir regimen in this trial may compare favorably with the SVR rates for 12 weeks of sofosbuvir/ledipasvir and 12 weeks of the regimen, paritaprevir/ritonavir, ombitasvir and dasabuvir plus ribavirin for patients with cirrhosis, particularly for prior nonresponders to older therapies, with the caveat that many more patients were studied in the registration trials.”While industry-sponsored trials have had psychiatric exclusion criteria, several patients in the open-label trial had serious psychiatric conditions, said the researchers. A patient with stable bipolar disorder received the interferon-containing regimen, and two patients with stable schizophrenia received the all-oral regimen. None reported worsening psychiatric symptoms on treatment.
Dr. Pearlman reported having contracted research for Johnson & Johnson, Gilead, Abbvie, Bristol-Myers Squibb, Boehringer Ingelheim, and Merck; and having served on speaker and advisory boards for Johnson & Johnson, Gilead, and Abbvie. He also was an investigator and author in the COSMOS trial of simeprevir and sofosbuvir in patients with HCV/HIV coinfection. The other authors reported no conflicts of interest.
At the time of sofosbuvir (SOF) and simeprevir (SMV) approval, efficacy results of the combinations assessed in this study were still limited, especially in patients with cirrhosis, GT-1a, and/or previous nonresponse. The recent study by Dr. Pearlman and his associates aims to give light to some of the questions

|
| Dr. Xavier Forns |
raised. In this open-label trial, 82 patients with GT-1a cirrhosis (61% null responders) were recruited. Patients were randomized 2:1 to either 12 weeks of all-oral SMV/SOF or to peginterferon (PEG)/ribavirin (RBV)/SOF. Fully 93% of patients given the all-oral regimen achieved SVR12, compared with 75% who received the interferon-containing regimen. SVR12 rates were higher in the SMV/SOF arm than in the PEG/RBV/SOF arm, independent of previous response (92% vs. 64% in null responders and 95% vs. 80% in naive patients). Moreover, virologic relapse was lower in the all-oral arm (12.5% vs. 8%; P = .009). These results, however, are based on a limited number of patients, particularly in the interferon-containing arm. In addition, the PEG used in this study was alfa-2b, which has not been studied in combination with SOF in clinical trials (its potential impact is thus unknown). One important point of the study is the lack of prognostic value of early viral kinetics: Rapid virologic response was not related to SVR12, which has been a hallmark in previous interferon-based regimens.
Regarding safety and tolerance, there were poorer self-reported outcomes and more side effects in the interferon group. The latter seems obvious because of

|
| Dr. Sabela Lens |
the well-known interferon profile, but RBV has been associated with higher rates of anemia in patients with cirrhosis undergoing interferon-free regimens. The use of SMV/SOF without RBV is certainly a crucial point of the study.
With the inherent limitations of the small number of patients, the study by Dr. Pearlman and his associates supports a greater efficacy and a better tolerance for a regimen combining SMV/SOF as compared to PEG/RBV/SOF in patients with GT-1a cirrhosis.
Dr. Sabela Lens and Dr. Xavier Forns are in the Liver Unit, Hospital Clínic Barcelona, IDIBAPS and CIBERehd, University of Barcelona. Dr. Lens has acted as an adviser for Janssen, MSD, and Gilead, and Dr. Forns has acted as an adviser for Janssen, Abbvie, and Gilead and has received unrestricted grant support from Janssen and MSD.
At the time of sofosbuvir (SOF) and simeprevir (SMV) approval, efficacy results of the combinations assessed in this study were still limited, especially in patients with cirrhosis, GT-1a, and/or previous nonresponse. The recent study by Dr. Pearlman and his associates aims to give light to some of the questions

|
| Dr. Xavier Forns |
raised. In this open-label trial, 82 patients with GT-1a cirrhosis (61% null responders) were recruited. Patients were randomized 2:1 to either 12 weeks of all-oral SMV/SOF or to peginterferon (PEG)/ribavirin (RBV)/SOF. Fully 93% of patients given the all-oral regimen achieved SVR12, compared with 75% who received the interferon-containing regimen. SVR12 rates were higher in the SMV/SOF arm than in the PEG/RBV/SOF arm, independent of previous response (92% vs. 64% in null responders and 95% vs. 80% in naive patients). Moreover, virologic relapse was lower in the all-oral arm (12.5% vs. 8%; P = .009). These results, however, are based on a limited number of patients, particularly in the interferon-containing arm. In addition, the PEG used in this study was alfa-2b, which has not been studied in combination with SOF in clinical trials (its potential impact is thus unknown). One important point of the study is the lack of prognostic value of early viral kinetics: Rapid virologic response was not related to SVR12, which has been a hallmark in previous interferon-based regimens.
Regarding safety and tolerance, there were poorer self-reported outcomes and more side effects in the interferon group. The latter seems obvious because of

|
| Dr. Sabela Lens |
the well-known interferon profile, but RBV has been associated with higher rates of anemia in patients with cirrhosis undergoing interferon-free regimens. The use of SMV/SOF without RBV is certainly a crucial point of the study.
With the inherent limitations of the small number of patients, the study by Dr. Pearlman and his associates supports a greater efficacy and a better tolerance for a regimen combining SMV/SOF as compared to PEG/RBV/SOF in patients with GT-1a cirrhosis.
Dr. Sabela Lens and Dr. Xavier Forns are in the Liver Unit, Hospital Clínic Barcelona, IDIBAPS and CIBERehd, University of Barcelona. Dr. Lens has acted as an adviser for Janssen, MSD, and Gilead, and Dr. Forns has acted as an adviser for Janssen, Abbvie, and Gilead and has received unrestricted grant support from Janssen and MSD.
At the time of sofosbuvir (SOF) and simeprevir (SMV) approval, efficacy results of the combinations assessed in this study were still limited, especially in patients with cirrhosis, GT-1a, and/or previous nonresponse. The recent study by Dr. Pearlman and his associates aims to give light to some of the questions

|
| Dr. Xavier Forns |
raised. In this open-label trial, 82 patients with GT-1a cirrhosis (61% null responders) were recruited. Patients were randomized 2:1 to either 12 weeks of all-oral SMV/SOF or to peginterferon (PEG)/ribavirin (RBV)/SOF. Fully 93% of patients given the all-oral regimen achieved SVR12, compared with 75% who received the interferon-containing regimen. SVR12 rates were higher in the SMV/SOF arm than in the PEG/RBV/SOF arm, independent of previous response (92% vs. 64% in null responders and 95% vs. 80% in naive patients). Moreover, virologic relapse was lower in the all-oral arm (12.5% vs. 8%; P = .009). These results, however, are based on a limited number of patients, particularly in the interferon-containing arm. In addition, the PEG used in this study was alfa-2b, which has not been studied in combination with SOF in clinical trials (its potential impact is thus unknown). One important point of the study is the lack of prognostic value of early viral kinetics: Rapid virologic response was not related to SVR12, which has been a hallmark in previous interferon-based regimens.
Regarding safety and tolerance, there were poorer self-reported outcomes and more side effects in the interferon group. The latter seems obvious because of

|
| Dr. Sabela Lens |
the well-known interferon profile, but RBV has been associated with higher rates of anemia in patients with cirrhosis undergoing interferon-free regimens. The use of SMV/SOF without RBV is certainly a crucial point of the study.
With the inherent limitations of the small number of patients, the study by Dr. Pearlman and his associates supports a greater efficacy and a better tolerance for a regimen combining SMV/SOF as compared to PEG/RBV/SOF in patients with GT-1a cirrhosis.
Dr. Sabela Lens and Dr. Xavier Forns are in the Liver Unit, Hospital Clínic Barcelona, IDIBAPS and CIBERehd, University of Barcelona. Dr. Lens has acted as an adviser for Janssen, MSD, and Gilead, and Dr. Forns has acted as an adviser for Janssen, Abbvie, and Gilead and has received unrestricted grant support from Janssen and MSD.
Patients with compensated cirrhosis and chronic genotype 1 hepatitis C virus infections were significantly more likely to clear their infections and had fewer adverse effects when treated with simeprevir and sofosbuvir instead of peginterferon, ribavirin, and sofosbuvir, investigators reported in the April issue of Gastroenterology. “Patients given the interferon-containing regimen had a significantly greater rate of virologic relapse than patients given simeprevir and sofosbuvir ... and reported worse outcomes and more side effects,” said Dr. Brian L. Pearlman and his associates of Atlanta Medical Center and Emory University, Atlanta.
Liver disease associated with chronic hepatitis C virus (HCV) infection causes at least 350,000 deaths per year worldwide. Genotype 1 (GT-1) HCV is the most common HCV strain and the hardest to treat, especially when patients have cirrhosis. Treatments for chronic GT-1 HCV infections historically included interferon, but achieved only moderate rates of sustained virologic response (SVR) and caused adverse somatic and psychiatric effects. All-oral, interferon-free regimens are now in widespread use, but many of the pivotal trials were industry sponsored and had strict enrollment criteria, potentially limiting their generalizability in community settings, the researchers reported (Gastroenterology 2015 April [doi:10.1053/j.gastro.2014.12.027]).Their open-label trial included 82 patients with HCV GT-1a infection and Child’s grade A cirrhosis recruited from two clinical practices in Atlanta. Thirty-two of the patients were treatment naive, while 50 had previously not responded to peginterferon and ribavirin treatment. Patients were randomized to either 12 weeks of all-oral simeprevir (150 mg/day) and sofosbuvir (400 mg/day), or peginterferon alfa 2b (1.5 mcg/kg per week), ribavirin (1000-1200 mg/day), and sofosbuvir (400 mg/day).Fully 54 of 58 (93%) patients given the simeprevir-sofosbuvir regimen had undetectable levels of HCV RNA at 12 weeks (SVR12), compared with 18 of 24 (75%) patients who received the interferon-containing regimen (P = .02), the researchers reported. Rates of SVR12 among prior nonresponders were 92% and 64%, and were 95% and 80% for treatment-naive patients, although P-values did not reach statistical significance. The interferon group also had a higher rate of virologic relapse than did patients given simeprevir and sofosbuvir (P = .009), and had worse self-reported outcomes and more side effects, the researchers said. Patients in both groups who achieved SVR12 had higher quality-of-life scores than those who did not. Notably, almost half of patients were African American, a group that has historically had lower cure rates compared with other racial groups, said the investigators.
“Given that several new regimens for genotype 1 infection, including the sofosbuvir-ledipasvir combination pill, already have been approved, we believe that this study is very timely,” Dr. Pearlman and his associates said. “Although these are not head-to-head comparisons, the 12-week simeprevir and sofosbuvir regimen in this trial may compare favorably with the SVR rates for 12 weeks of sofosbuvir/ledipasvir and 12 weeks of the regimen, paritaprevir/ritonavir, ombitasvir and dasabuvir plus ribavirin for patients with cirrhosis, particularly for prior nonresponders to older therapies, with the caveat that many more patients were studied in the registration trials.”While industry-sponsored trials have had psychiatric exclusion criteria, several patients in the open-label trial had serious psychiatric conditions, said the researchers. A patient with stable bipolar disorder received the interferon-containing regimen, and two patients with stable schizophrenia received the all-oral regimen. None reported worsening psychiatric symptoms on treatment.
Dr. Pearlman reported having contracted research for Johnson & Johnson, Gilead, Abbvie, Bristol-Myers Squibb, Boehringer Ingelheim, and Merck; and having served on speaker and advisory boards for Johnson & Johnson, Gilead, and Abbvie. He also was an investigator and author in the COSMOS trial of simeprevir and sofosbuvir in patients with HCV/HIV coinfection. The other authors reported no conflicts of interest.
Patients with compensated cirrhosis and chronic genotype 1 hepatitis C virus infections were significantly more likely to clear their infections and had fewer adverse effects when treated with simeprevir and sofosbuvir instead of peginterferon, ribavirin, and sofosbuvir, investigators reported in the April issue of Gastroenterology. “Patients given the interferon-containing regimen had a significantly greater rate of virologic relapse than patients given simeprevir and sofosbuvir ... and reported worse outcomes and more side effects,” said Dr. Brian L. Pearlman and his associates of Atlanta Medical Center and Emory University, Atlanta.
Liver disease associated with chronic hepatitis C virus (HCV) infection causes at least 350,000 deaths per year worldwide. Genotype 1 (GT-1) HCV is the most common HCV strain and the hardest to treat, especially when patients have cirrhosis. Treatments for chronic GT-1 HCV infections historically included interferon, but achieved only moderate rates of sustained virologic response (SVR) and caused adverse somatic and psychiatric effects. All-oral, interferon-free regimens are now in widespread use, but many of the pivotal trials were industry sponsored and had strict enrollment criteria, potentially limiting their generalizability in community settings, the researchers reported (Gastroenterology 2015 April [doi:10.1053/j.gastro.2014.12.027]).Their open-label trial included 82 patients with HCV GT-1a infection and Child’s grade A cirrhosis recruited from two clinical practices in Atlanta. Thirty-two of the patients were treatment naive, while 50 had previously not responded to peginterferon and ribavirin treatment. Patients were randomized to either 12 weeks of all-oral simeprevir (150 mg/day) and sofosbuvir (400 mg/day), or peginterferon alfa 2b (1.5 mcg/kg per week), ribavirin (1000-1200 mg/day), and sofosbuvir (400 mg/day).Fully 54 of 58 (93%) patients given the simeprevir-sofosbuvir regimen had undetectable levels of HCV RNA at 12 weeks (SVR12), compared with 18 of 24 (75%) patients who received the interferon-containing regimen (P = .02), the researchers reported. Rates of SVR12 among prior nonresponders were 92% and 64%, and were 95% and 80% for treatment-naive patients, although P-values did not reach statistical significance. The interferon group also had a higher rate of virologic relapse than did patients given simeprevir and sofosbuvir (P = .009), and had worse self-reported outcomes and more side effects, the researchers said. Patients in both groups who achieved SVR12 had higher quality-of-life scores than those who did not. Notably, almost half of patients were African American, a group that has historically had lower cure rates compared with other racial groups, said the investigators.
“Given that several new regimens for genotype 1 infection, including the sofosbuvir-ledipasvir combination pill, already have been approved, we believe that this study is very timely,” Dr. Pearlman and his associates said. “Although these are not head-to-head comparisons, the 12-week simeprevir and sofosbuvir regimen in this trial may compare favorably with the SVR rates for 12 weeks of sofosbuvir/ledipasvir and 12 weeks of the regimen, paritaprevir/ritonavir, ombitasvir and dasabuvir plus ribavirin for patients with cirrhosis, particularly for prior nonresponders to older therapies, with the caveat that many more patients were studied in the registration trials.”While industry-sponsored trials have had psychiatric exclusion criteria, several patients in the open-label trial had serious psychiatric conditions, said the researchers. A patient with stable bipolar disorder received the interferon-containing regimen, and two patients with stable schizophrenia received the all-oral regimen. None reported worsening psychiatric symptoms on treatment.
Dr. Pearlman reported having contracted research for Johnson & Johnson, Gilead, Abbvie, Bristol-Myers Squibb, Boehringer Ingelheim, and Merck; and having served on speaker and advisory boards for Johnson & Johnson, Gilead, and Abbvie. He also was an investigator and author in the COSMOS trial of simeprevir and sofosbuvir in patients with HCV/HIV coinfection. The other authors reported no conflicts of interest.
Key clinical point: An all-oral simeprevir-sofosbuvir combination outperformed peginterferon/ribavirin/sofosbuvir in patients with genotype 1a HCV infection and compensated cirrhosis.
Major finding: Rates of sustained virologic response at 12 weeks were 93% for the simeprevir-sofosbuvir regimen and 75% for the interferon-containing regimen (P = .02).
Data source: Prospective open-label study of 82 treatment-naive and treatment-experienced patients with HCV infection and Child’s grade A cirrhosis.
Disclosures: Dr. Pearlman reported having contracted research for Johnson & Johnson, Gilead, Abbvie, Bristol-Myers Squibb, Boehringer Ingelheim, and Merck; and having served on speaker and advisory boards for Johnson & Johnson, Gilead, and Abbvie. Dr. Pearlman also reported having been an investigator and author in the COSMOS trial of sofosbuvir and simeprevir. The other authors reported no conflicts of interest.