User login
Poor sleep due to ADHD or ADHD due to poor sleep?
The day wouldn’t be so bad if he would just go to sleep at night! How many times have you heard this plea from parents of your patients with ADHD? Sleep is important for everyone, but getting enough is both more important and more difficult for children with ADHD. About three-quarters of children with ADHD have significant problems with sleep, most even before any medication treatment. And inadequate sleep can exacerbate or even cause ADHD symptoms!
Solving sleep problems for children with ADHD is not always simple. The kinds of sleep issues that are more common in children (and adults) with ADHD, compared with typical children, include behavioral bedtime resistance, circadian rhythm sleep disorder (CRSD), insomnia, morning sleepiness, night waking, periodic limb movement disorder (PLMD), restless leg syndrome (RLS), and sleep disordered breathing (SDB). Such a broad differential means a careful history and sometimes even lab studies may be needed.
Both initial and follow-up visits for ADHD should include a sleep history or, ideally, a tool such as BEARS sleep screening tool or Children’s Sleep Habits Questionnaire and a 2-week sleep diary (http://www.sleepfoundation.org/). These are good ways to collect signs of allergies or apnea (for SDB), limb movements or limb pain (for RLS or PLMD), mouth breathing, night waking, and snoring.
You also need to ask about alcohol, drugs, caffeine, and nicotine; asthma; comorbid conditions such as mental health disorders or their treatments; and enuresis (alone or part of nocturnal seizures).
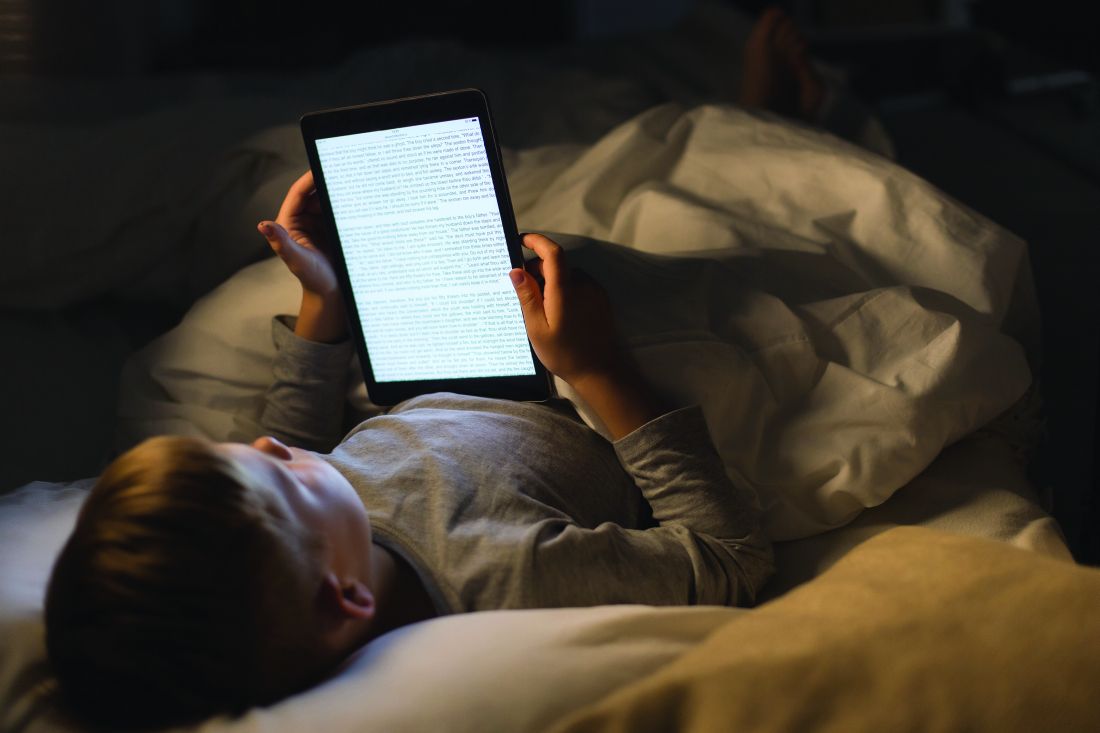
Do I need to remind you to find out about electronics activating the child before bedtime – hidden under the covers, or signaling messages from friends in the middle of the night – and to encourage limits on these? Some sleep disorders warrant polysomnography in a sleep lab or from MyZeo.com (for PLMD and some SDB) or ferritin less than 50 mg/L (for RLS) for diagnosis and to guide treatment. Nasal steroids, antihistamines, or montelukast may help SDB when there are enlarged tonsils or adenoids, but adenotonsillectomy is usually curative.
The first line and most effective treatment for sleep problems in children with or without ADHD is improving sleep hygiene. The key component is establishing habits for the entire sleep cycle: a steady pattern of reduced stimulation in the hour before bedtime (sans electronics); a friendly rather than irritated bedtime routine; and the same bedtime and wake up time, ideally 7 days per week. Bedtime stories read to the child can soothe at any age, not just toddlers! Of course, both children and families want fun and special occasions. For most, varying bedtime by up to 1 hour won’t mess up their biological clock, but for some even this should be avoided. Sleeping alone in a cool, dark, quiet room, nightly in the same bed (not used for other activities), is considered the ideal. Earplugs, white noise generators, and eye masks may be helpful. If sleeping with siblings is a necessity, bedtimes can be staggered to put the child to bed earlier or after others are asleep.
Struggles postponing bedtime may be part of a pattern of oppositionality common in ADHD, but the child may not be tired due to being off schedule (from CRSD), napping on the bus or after school, sleeping in mornings, or unrealistic parent expectations for sleep duration. Parents may want their hyperactive children to give them a break and go to bed at 8 p.m., but children aged 6-10 years need only 10-11 hours and those aged 10-17 years need 8.5-9.25 hours of sleep.
Not tired may instead be “wired” from lingering stimulant effects or even lack of such medication leaving the child overactive or rebounding from earlier medications. Lower afternoon doses or shorter-acting medication may solve lasting medication issues, but sometimes an additional low dose of stimulants actually will help a child with ADHD settle at bedtime. All stimulant medications can prolong sleep onset, often by 30 minutes, but this varies by individual and tends to resolve on its own a few weeks after a new or changed medicine. Switching medication category may allow a child to fall asleep faster. Atomoxetine and alpha agonists are less likely to delay sleep than methylphenidate (MPH).
What if sleep hygiene, behavioral methods, and adjusting ADHD medications is not enough? If sleep issues are causing significant problems, medication for sleep is worth a try. Controlled-release melatonin 1-2 hours before bedtime has data for effectiveness. There is no defined dose, so the lowest effective dose should be used, but 3-6 mg may be needed. Because many families with a child with ADHD are not organized enough to give medicine on this schedule, sublingual melatonin that acts in 15-20 minutes is a good alternative or even first choice. Clonidine 0.05-0.2 mg 1 hour before bedtime speeds sleep onset, lasts 3 hours, and does not carry over to sedation the next day. Stronger psychopharmaceuticals can assist sleep onset, including low dose mirtazapine or trazodone, but have the side effect of daytime sleepiness.
Management of waking in the middle of the night can be more difficult to treat as sleep drive has been dissipated. First, consider whether trips out of bed reflect a sleep association that has not been extinguished. Daytime atomoxetine or, better yet, MPH may improve night waking, and sometimes even a low-dose evening, long-acting medication, such as osmotic release oral system (OROS) extended release methylphenidate HCL (OROS MPH), helps. Short-acting clonidine or melatonin in the middle of the night or bedtime mirtazapine or trazodone also may be worth a try.
When dealing with sleep, keep in mind that 50% or more of children with ADHD have a coexisting mental health disorder. Anxiety, separation anxiety, depression, and dysthymia all often affect sleep onset, night waking, and sometimes early morning waking. The child or teen may need extra reassurance or company at bedtime (siblings or pets may suffice). Reading positive stories or playing soft music may be better at setting a positive mood and sense of safety for sleep, certainly more so than social media, which should be avoided.
Keep in mind that substance use is more common in ADHD as well as with those other mental health conditions and can interfere with restful sleep and make RLS worse. Bipolar disorder can be mistaken for ADHD as it often presents with hyperactivity but also can be comorbid. Sleep problems are increased sixfold when both are present. Prolonged periods awake at night and diminished need for sleep are signs that help differentiate bipolar from ADHD. Medication management for the bipolar disorder with atypicals can reduce sleep latency and reduce REM sleep, but also causes morning fatigue. Medications to treat other mental health problems can help sleep onset (for example, anticonvulsants, atypicals), or prolong it (SSRIs), change REM states (atypicals), and even exacerbate RLS (SSRIs). You can make changes or work with the child’s mental health specialist if medications are causing significant sleep problems.
When we help improve sleep for children with ADHD, it can lessen not only ADHD symptoms but also some symptoms of other mental health disorders, improve learning and behavior, and greatly improve family quality of life!
Dr. Howard is assistant professor of pediatrics at Johns Hopkins University, Baltimore, and creator of CHADIS (www.CHADIS.com). She had no other relevant disclosures. Dr. Howard’s contribution to this publication was as a paid expert to MDedge News. E-mail her at [email protected].
The day wouldn’t be so bad if he would just go to sleep at night! How many times have you heard this plea from parents of your patients with ADHD? Sleep is important for everyone, but getting enough is both more important and more difficult for children with ADHD. About three-quarters of children with ADHD have significant problems with sleep, most even before any medication treatment. And inadequate sleep can exacerbate or even cause ADHD symptoms!
Solving sleep problems for children with ADHD is not always simple. The kinds of sleep issues that are more common in children (and adults) with ADHD, compared with typical children, include behavioral bedtime resistance, circadian rhythm sleep disorder (CRSD), insomnia, morning sleepiness, night waking, periodic limb movement disorder (PLMD), restless leg syndrome (RLS), and sleep disordered breathing (SDB). Such a broad differential means a careful history and sometimes even lab studies may be needed.
Both initial and follow-up visits for ADHD should include a sleep history or, ideally, a tool such as BEARS sleep screening tool or Children’s Sleep Habits Questionnaire and a 2-week sleep diary (http://www.sleepfoundation.org/). These are good ways to collect signs of allergies or apnea (for SDB), limb movements or limb pain (for RLS or PLMD), mouth breathing, night waking, and snoring.
You also need to ask about alcohol, drugs, caffeine, and nicotine; asthma; comorbid conditions such as mental health disorders or their treatments; and enuresis (alone or part of nocturnal seizures).
Do I need to remind you to find out about electronics activating the child before bedtime – hidden under the covers, or signaling messages from friends in the middle of the night – and to encourage limits on these? Some sleep disorders warrant polysomnography in a sleep lab or from MyZeo.com (for PLMD and some SDB) or ferritin less than 50 mg/L (for RLS) for diagnosis and to guide treatment. Nasal steroids, antihistamines, or montelukast may help SDB when there are enlarged tonsils or adenoids, but adenotonsillectomy is usually curative.
The first line and most effective treatment for sleep problems in children with or without ADHD is improving sleep hygiene. The key component is establishing habits for the entire sleep cycle: a steady pattern of reduced stimulation in the hour before bedtime (sans electronics); a friendly rather than irritated bedtime routine; and the same bedtime and wake up time, ideally 7 days per week. Bedtime stories read to the child can soothe at any age, not just toddlers! Of course, both children and families want fun and special occasions. For most, varying bedtime by up to 1 hour won’t mess up their biological clock, but for some even this should be avoided. Sleeping alone in a cool, dark, quiet room, nightly in the same bed (not used for other activities), is considered the ideal. Earplugs, white noise generators, and eye masks may be helpful. If sleeping with siblings is a necessity, bedtimes can be staggered to put the child to bed earlier or after others are asleep.
Struggles postponing bedtime may be part of a pattern of oppositionality common in ADHD, but the child may not be tired due to being off schedule (from CRSD), napping on the bus or after school, sleeping in mornings, or unrealistic parent expectations for sleep duration. Parents may want their hyperactive children to give them a break and go to bed at 8 p.m., but children aged 6-10 years need only 10-11 hours and those aged 10-17 years need 8.5-9.25 hours of sleep.
Not tired may instead be “wired” from lingering stimulant effects or even lack of such medication leaving the child overactive or rebounding from earlier medications. Lower afternoon doses or shorter-acting medication may solve lasting medication issues, but sometimes an additional low dose of stimulants actually will help a child with ADHD settle at bedtime. All stimulant medications can prolong sleep onset, often by 30 minutes, but this varies by individual and tends to resolve on its own a few weeks after a new or changed medicine. Switching medication category may allow a child to fall asleep faster. Atomoxetine and alpha agonists are less likely to delay sleep than methylphenidate (MPH).
What if sleep hygiene, behavioral methods, and adjusting ADHD medications is not enough? If sleep issues are causing significant problems, medication for sleep is worth a try. Controlled-release melatonin 1-2 hours before bedtime has data for effectiveness. There is no defined dose, so the lowest effective dose should be used, but 3-6 mg may be needed. Because many families with a child with ADHD are not organized enough to give medicine on this schedule, sublingual melatonin that acts in 15-20 minutes is a good alternative or even first choice. Clonidine 0.05-0.2 mg 1 hour before bedtime speeds sleep onset, lasts 3 hours, and does not carry over to sedation the next day. Stronger psychopharmaceuticals can assist sleep onset, including low dose mirtazapine or trazodone, but have the side effect of daytime sleepiness.
Management of waking in the middle of the night can be more difficult to treat as sleep drive has been dissipated. First, consider whether trips out of bed reflect a sleep association that has not been extinguished. Daytime atomoxetine or, better yet, MPH may improve night waking, and sometimes even a low-dose evening, long-acting medication, such as osmotic release oral system (OROS) extended release methylphenidate HCL (OROS MPH), helps. Short-acting clonidine or melatonin in the middle of the night or bedtime mirtazapine or trazodone also may be worth a try.
When dealing with sleep, keep in mind that 50% or more of children with ADHD have a coexisting mental health disorder. Anxiety, separation anxiety, depression, and dysthymia all often affect sleep onset, night waking, and sometimes early morning waking. The child or teen may need extra reassurance or company at bedtime (siblings or pets may suffice). Reading positive stories or playing soft music may be better at setting a positive mood and sense of safety for sleep, certainly more so than social media, which should be avoided.
Keep in mind that substance use is more common in ADHD as well as with those other mental health conditions and can interfere with restful sleep and make RLS worse. Bipolar disorder can be mistaken for ADHD as it often presents with hyperactivity but also can be comorbid. Sleep problems are increased sixfold when both are present. Prolonged periods awake at night and diminished need for sleep are signs that help differentiate bipolar from ADHD. Medication management for the bipolar disorder with atypicals can reduce sleep latency and reduce REM sleep, but also causes morning fatigue. Medications to treat other mental health problems can help sleep onset (for example, anticonvulsants, atypicals), or prolong it (SSRIs), change REM states (atypicals), and even exacerbate RLS (SSRIs). You can make changes or work with the child’s mental health specialist if medications are causing significant sleep problems.
When we help improve sleep for children with ADHD, it can lessen not only ADHD symptoms but also some symptoms of other mental health disorders, improve learning and behavior, and greatly improve family quality of life!
Dr. Howard is assistant professor of pediatrics at Johns Hopkins University, Baltimore, and creator of CHADIS (www.CHADIS.com). She had no other relevant disclosures. Dr. Howard’s contribution to this publication was as a paid expert to MDedge News. E-mail her at [email protected].
The day wouldn’t be so bad if he would just go to sleep at night! How many times have you heard this plea from parents of your patients with ADHD? Sleep is important for everyone, but getting enough is both more important and more difficult for children with ADHD. About three-quarters of children with ADHD have significant problems with sleep, most even before any medication treatment. And inadequate sleep can exacerbate or even cause ADHD symptoms!
Solving sleep problems for children with ADHD is not always simple. The kinds of sleep issues that are more common in children (and adults) with ADHD, compared with typical children, include behavioral bedtime resistance, circadian rhythm sleep disorder (CRSD), insomnia, morning sleepiness, night waking, periodic limb movement disorder (PLMD), restless leg syndrome (RLS), and sleep disordered breathing (SDB). Such a broad differential means a careful history and sometimes even lab studies may be needed.
Both initial and follow-up visits for ADHD should include a sleep history or, ideally, a tool such as BEARS sleep screening tool or Children’s Sleep Habits Questionnaire and a 2-week sleep diary (http://www.sleepfoundation.org/). These are good ways to collect signs of allergies or apnea (for SDB), limb movements or limb pain (for RLS or PLMD), mouth breathing, night waking, and snoring.
You also need to ask about alcohol, drugs, caffeine, and nicotine; asthma; comorbid conditions such as mental health disorders or their treatments; and enuresis (alone or part of nocturnal seizures).
Do I need to remind you to find out about electronics activating the child before bedtime – hidden under the covers, or signaling messages from friends in the middle of the night – and to encourage limits on these? Some sleep disorders warrant polysomnography in a sleep lab or from MyZeo.com (for PLMD and some SDB) or ferritin less than 50 mg/L (for RLS) for diagnosis and to guide treatment. Nasal steroids, antihistamines, or montelukast may help SDB when there are enlarged tonsils or adenoids, but adenotonsillectomy is usually curative.
The first line and most effective treatment for sleep problems in children with or without ADHD is improving sleep hygiene. The key component is establishing habits for the entire sleep cycle: a steady pattern of reduced stimulation in the hour before bedtime (sans electronics); a friendly rather than irritated bedtime routine; and the same bedtime and wake up time, ideally 7 days per week. Bedtime stories read to the child can soothe at any age, not just toddlers! Of course, both children and families want fun and special occasions. For most, varying bedtime by up to 1 hour won’t mess up their biological clock, but for some even this should be avoided. Sleeping alone in a cool, dark, quiet room, nightly in the same bed (not used for other activities), is considered the ideal. Earplugs, white noise generators, and eye masks may be helpful. If sleeping with siblings is a necessity, bedtimes can be staggered to put the child to bed earlier or after others are asleep.
Struggles postponing bedtime may be part of a pattern of oppositionality common in ADHD, but the child may not be tired due to being off schedule (from CRSD), napping on the bus or after school, sleeping in mornings, or unrealistic parent expectations for sleep duration. Parents may want their hyperactive children to give them a break and go to bed at 8 p.m., but children aged 6-10 years need only 10-11 hours and those aged 10-17 years need 8.5-9.25 hours of sleep.
Not tired may instead be “wired” from lingering stimulant effects or even lack of such medication leaving the child overactive or rebounding from earlier medications. Lower afternoon doses or shorter-acting medication may solve lasting medication issues, but sometimes an additional low dose of stimulants actually will help a child with ADHD settle at bedtime. All stimulant medications can prolong sleep onset, often by 30 minutes, but this varies by individual and tends to resolve on its own a few weeks after a new or changed medicine. Switching medication category may allow a child to fall asleep faster. Atomoxetine and alpha agonists are less likely to delay sleep than methylphenidate (MPH).
What if sleep hygiene, behavioral methods, and adjusting ADHD medications is not enough? If sleep issues are causing significant problems, medication for sleep is worth a try. Controlled-release melatonin 1-2 hours before bedtime has data for effectiveness. There is no defined dose, so the lowest effective dose should be used, but 3-6 mg may be needed. Because many families with a child with ADHD are not organized enough to give medicine on this schedule, sublingual melatonin that acts in 15-20 minutes is a good alternative or even first choice. Clonidine 0.05-0.2 mg 1 hour before bedtime speeds sleep onset, lasts 3 hours, and does not carry over to sedation the next day. Stronger psychopharmaceuticals can assist sleep onset, including low dose mirtazapine or trazodone, but have the side effect of daytime sleepiness.
Management of waking in the middle of the night can be more difficult to treat as sleep drive has been dissipated. First, consider whether trips out of bed reflect a sleep association that has not been extinguished. Daytime atomoxetine or, better yet, MPH may improve night waking, and sometimes even a low-dose evening, long-acting medication, such as osmotic release oral system (OROS) extended release methylphenidate HCL (OROS MPH), helps. Short-acting clonidine or melatonin in the middle of the night or bedtime mirtazapine or trazodone also may be worth a try.
When dealing with sleep, keep in mind that 50% or more of children with ADHD have a coexisting mental health disorder. Anxiety, separation anxiety, depression, and dysthymia all often affect sleep onset, night waking, and sometimes early morning waking. The child or teen may need extra reassurance or company at bedtime (siblings or pets may suffice). Reading positive stories or playing soft music may be better at setting a positive mood and sense of safety for sleep, certainly more so than social media, which should be avoided.
Keep in mind that substance use is more common in ADHD as well as with those other mental health conditions and can interfere with restful sleep and make RLS worse. Bipolar disorder can be mistaken for ADHD as it often presents with hyperactivity but also can be comorbid. Sleep problems are increased sixfold when both are present. Prolonged periods awake at night and diminished need for sleep are signs that help differentiate bipolar from ADHD. Medication management for the bipolar disorder with atypicals can reduce sleep latency and reduce REM sleep, but also causes morning fatigue. Medications to treat other mental health problems can help sleep onset (for example, anticonvulsants, atypicals), or prolong it (SSRIs), change REM states (atypicals), and even exacerbate RLS (SSRIs). You can make changes or work with the child’s mental health specialist if medications are causing significant sleep problems.
When we help improve sleep for children with ADHD, it can lessen not only ADHD symptoms but also some symptoms of other mental health disorders, improve learning and behavior, and greatly improve family quality of life!
Dr. Howard is assistant professor of pediatrics at Johns Hopkins University, Baltimore, and creator of CHADIS (www.CHADIS.com). She had no other relevant disclosures. Dr. Howard’s contribution to this publication was as a paid expert to MDedge News. E-mail her at [email protected].
Managing psychosis in youth
Strong feelings – such as intense anxiety, irritability, or depressed mood – may affect every child for brief periods of time during their development. Parents and pediatricians are wise to not treat them as psychiatric disorders unless they persist for weeks, impair functioning, or are dramatically severe. Psychosis – marked by hallucinations, perceptual distortions, or profoundly disorganized thinking and behavior – typically looks dramatically severe. Even when psychotic symptoms are mild or brief, they can cause very serious distress for parents and clinicians. The worry is that they may represent a “first break,” a psychotic episode that requires much work for recovery, or the beginning of a lifelong struggle with schizophrenia or other chronic psychotic illness.
While it is important to recognize schizophrenia early – because early interventions are thought to improve the course of the disease – schizophrenia in childhood is rare. It is not commonly recognized that psychotic or psychoticlike symptoms are much more common than schizophrenia. While it is important to begin a thoughtful evaluation when a child or teenager presents with psychosis, it also is important to know that the majority of young people who experience psychotic symptoms do not have schizophrenia or other psychotic illness.
Psychosis describes symptoms in which there has been some “break with reality,” often in the form of hallucinations (seeing or hearing things which are not objectively present) or of distorted perceptions (such as paranoia or grandiosity). “Subsyndromal psychotic symptoms” occur when a person experiences these perceptual disturbances but has doubt about whether or not they are real. In frank psychosis, patients have a “fixed and firm” belief in the truth or accuracy of their perceptions, no matter the evidence against them. The voices they hear or hallucinations they see are “real” and there is a wholehearted belief that what the voice says or what they are seeing is as true as what you or I see and hear.
Schizophrenia is a diagnosis that requires the presence of both these “positive” psychotic symptoms and “negative” symptoms of flat affect; loss of motivation, social, or motor abilities; and cognitive impairment. These symptoms typically emerge in late adolescence (median age, 18 years) in males and early adulthood (median age, 25 years) in females, with another (smaller) peak in incidence in middle age. Importantly, the negative symptoms often emerge first so there often is a history of subtle cognitive decline and social withdrawal, one of the most common patterns in children, before psychosis emerges. Schizophrenia is quite rare, with a prevalence of slightly under 1% of the global population, an annual incidence of approximately 15 people per 100,000, and 1 in 40,000 in children under 13 years old, according to the National Institute of Mental Health. Psychotic symptoms are much more common than schizophrenia, affecting approximately 5% of the adult population at any point in time. They are even more common in children and adolescents. A meta-analysis of population-based studies of psychotic symptoms in youth demonstrated a median prevalence of 17% in children aged 9-12 years and 7.5% in adolescents aged 13-18 years.1 Of course, as with all statistics, much depends on the definitions used to identify this high prevalence rate.
Children and adolescents who report psychotic symptoms are at increased risk for developing schizophrenia, compared with the general population, but most youth with psychotic symptoms will not go on to develop schizophrenia. They are more likely to indicate other, nonpsychotic psychiatric illnesses, such as anxiety or mood disorders, including depression, obsessive compulsive disorder (OCD), and PTSD. In younger children, these symptoms may prove to be benign, but in adolescents they usually indicate the presence of a psychiatric illness. In one study, 57% of children aged 11-13 years with psychotic symptoms were found to have a nonpsychotic psychiatric illness, but the rate jumped to 80% for those aged 13-15 years with psychotic symptoms.2 So while psychosis in teenagers only rarely indicates schizophrenia, these symptoms usually indicate the presence of a psychiatric illness, and a psychiatric evaluation should be initiated.
If a child in your practice presents with psychotic symptoms, it is appropriate to assess their safety and then start a medical work-up. Find out from your patient or their parents if their behavior has been affected by their perceptual disturbances. Are they frightened and avoiding school? Are they withdrawing from social relationships? Is their sleep disrupted? Have they been more impulsive or unpredictable? If their behavior has been affected, you should refer to a child psychiatrist to perform a full diagnostic evaluation and help with management of these symptoms.
Your medical work-up should include a drug screen, blood count, metabolic panel, and thyroid function test. Medications, particularly stimulants, steroids, and anticholinergics can cause psychotic symptoms in high doses or vulnerable patients (such as those with a developmental disorder or traumatic brain injury). If the physical or neurologic exam are suggestive, further investigation of the many potential medical sources of psychotic symptoms in youth can be pursued to rule out autoimmune illnesses, endocrine disorders, metabolic illnesses, heavy metal poisoning, neurologic diseases, infectious diseases, and nutritional deficits. It is worth noting that childhood sleep disorders also can present with psychosis. Persistent psychotic symptoms in children are very hard to evaluate and may be the harbinger of a serious psychiatric disorder, so even if the medical work-up is negative and the persistent symptoms are mild and not causing a safety concern, a referral to a child psychiatrist for a full mental health evaluation is appropriate.
Psychotic symptoms in an adolescent sometimes are easier to assess, more worrisome for serious mental illness, and are a high-risk category for self-destructive behavior and substance use. Before you begin a medical work-up, you always should assess for safety, including suicide risk, if your adolescent patient presents with psychotic symptoms. Screening for symptoms of mood, anxiety, and substance use disorders also can help reveal the nature of their presenting problem. If your adolescent patient is using drugs, that does not rule out the possibility of an underlying mood, anxiety, or thought disorder. While intoxication with many drugs may precipitate psychotic symptoms (including stimulants, hallucinogens, and marijuana), others may precipitate psychosis in withdrawal states (alcohol, benzodiazepines, and other CNS depressants). It also is important to note that adolescents with emerging schizophrenia have very high rates of comorbid substance abuse (as high as 60%), so their drug use may not be the cause of their psychotic symptoms. There also is emerging evidence that use of certain drugs during sensitive developmental periods can significantly increase the likelihood of developing schizophrenia in vulnerable populations, such as with regular marijuana use in adolescents who have a family history of schizophrenia.
For those rare pediatric patients who present with both negative and positive symptoms of emerging schizophrenia, early diagnosis and treatment has shown promise in improving the course of the disease. Cognitive-behavioral therapy (CBT) for psychosis has shown promise in lowering the rates of conversion to schizophrenia in select patient populations. This therapy teaches strategies for improving reality testing, cognitive flexibility, and social skills. The social skills appear to be especially important for improving adaptive function, even in those patients who progress to schizophrenia. Family therapies, focused on improving family cohesion, communication, and adaptive functioning, appear to improve family well-being and the course of the patient’s illness (such as fewer and less severe psychotic episodes and improved mood and adaptive function). Early use of antipsychotic medications also appears to improve the course of the illness.
While schizophrenia is not curable, early detection (perhaps by a pediatrician), referral, and treatment can be powerfully protective for patients and their families.
Dr. Swick is physician in chief at Ohana, Center for Child and Adolescent Behavioral Health, Community Hospital of the Monterey (Calif.) Peninsula. Dr. Jellinek is professor emeritus of psychiatry and pediatrics, Harvard Medical School, Boston. Email them at [email protected].
References
1. Psychol Med. 2012 Sep;42(9):1857-63.
2. Br J Psychiatry. 2012 Jul;201(1):26-32.
Strong feelings – such as intense anxiety, irritability, or depressed mood – may affect every child for brief periods of time during their development. Parents and pediatricians are wise to not treat them as psychiatric disorders unless they persist for weeks, impair functioning, or are dramatically severe. Psychosis – marked by hallucinations, perceptual distortions, or profoundly disorganized thinking and behavior – typically looks dramatically severe. Even when psychotic symptoms are mild or brief, they can cause very serious distress for parents and clinicians. The worry is that they may represent a “first break,” a psychotic episode that requires much work for recovery, or the beginning of a lifelong struggle with schizophrenia or other chronic psychotic illness.
While it is important to recognize schizophrenia early – because early interventions are thought to improve the course of the disease – schizophrenia in childhood is rare. It is not commonly recognized that psychotic or psychoticlike symptoms are much more common than schizophrenia. While it is important to begin a thoughtful evaluation when a child or teenager presents with psychosis, it also is important to know that the majority of young people who experience psychotic symptoms do not have schizophrenia or other psychotic illness.
Psychosis describes symptoms in which there has been some “break with reality,” often in the form of hallucinations (seeing or hearing things which are not objectively present) or of distorted perceptions (such as paranoia or grandiosity). “Subsyndromal psychotic symptoms” occur when a person experiences these perceptual disturbances but has doubt about whether or not they are real. In frank psychosis, patients have a “fixed and firm” belief in the truth or accuracy of their perceptions, no matter the evidence against them. The voices they hear or hallucinations they see are “real” and there is a wholehearted belief that what the voice says or what they are seeing is as true as what you or I see and hear.
Schizophrenia is a diagnosis that requires the presence of both these “positive” psychotic symptoms and “negative” symptoms of flat affect; loss of motivation, social, or motor abilities; and cognitive impairment. These symptoms typically emerge in late adolescence (median age, 18 years) in males and early adulthood (median age, 25 years) in females, with another (smaller) peak in incidence in middle age. Importantly, the negative symptoms often emerge first so there often is a history of subtle cognitive decline and social withdrawal, one of the most common patterns in children, before psychosis emerges. Schizophrenia is quite rare, with a prevalence of slightly under 1% of the global population, an annual incidence of approximately 15 people per 100,000, and 1 in 40,000 in children under 13 years old, according to the National Institute of Mental Health. Psychotic symptoms are much more common than schizophrenia, affecting approximately 5% of the adult population at any point in time. They are even more common in children and adolescents. A meta-analysis of population-based studies of psychotic symptoms in youth demonstrated a median prevalence of 17% in children aged 9-12 years and 7.5% in adolescents aged 13-18 years.1 Of course, as with all statistics, much depends on the definitions used to identify this high prevalence rate.
Children and adolescents who report psychotic symptoms are at increased risk for developing schizophrenia, compared with the general population, but most youth with psychotic symptoms will not go on to develop schizophrenia. They are more likely to indicate other, nonpsychotic psychiatric illnesses, such as anxiety or mood disorders, including depression, obsessive compulsive disorder (OCD), and PTSD. In younger children, these symptoms may prove to be benign, but in adolescents they usually indicate the presence of a psychiatric illness. In one study, 57% of children aged 11-13 years with psychotic symptoms were found to have a nonpsychotic psychiatric illness, but the rate jumped to 80% for those aged 13-15 years with psychotic symptoms.2 So while psychosis in teenagers only rarely indicates schizophrenia, these symptoms usually indicate the presence of a psychiatric illness, and a psychiatric evaluation should be initiated.
If a child in your practice presents with psychotic symptoms, it is appropriate to assess their safety and then start a medical work-up. Find out from your patient or their parents if their behavior has been affected by their perceptual disturbances. Are they frightened and avoiding school? Are they withdrawing from social relationships? Is their sleep disrupted? Have they been more impulsive or unpredictable? If their behavior has been affected, you should refer to a child psychiatrist to perform a full diagnostic evaluation and help with management of these symptoms.
Your medical work-up should include a drug screen, blood count, metabolic panel, and thyroid function test. Medications, particularly stimulants, steroids, and anticholinergics can cause psychotic symptoms in high doses or vulnerable patients (such as those with a developmental disorder or traumatic brain injury). If the physical or neurologic exam are suggestive, further investigation of the many potential medical sources of psychotic symptoms in youth can be pursued to rule out autoimmune illnesses, endocrine disorders, metabolic illnesses, heavy metal poisoning, neurologic diseases, infectious diseases, and nutritional deficits. It is worth noting that childhood sleep disorders also can present with psychosis. Persistent psychotic symptoms in children are very hard to evaluate and may be the harbinger of a serious psychiatric disorder, so even if the medical work-up is negative and the persistent symptoms are mild and not causing a safety concern, a referral to a child psychiatrist for a full mental health evaluation is appropriate.
Psychotic symptoms in an adolescent sometimes are easier to assess, more worrisome for serious mental illness, and are a high-risk category for self-destructive behavior and substance use. Before you begin a medical work-up, you always should assess for safety, including suicide risk, if your adolescent patient presents with psychotic symptoms. Screening for symptoms of mood, anxiety, and substance use disorders also can help reveal the nature of their presenting problem. If your adolescent patient is using drugs, that does not rule out the possibility of an underlying mood, anxiety, or thought disorder. While intoxication with many drugs may precipitate psychotic symptoms (including stimulants, hallucinogens, and marijuana), others may precipitate psychosis in withdrawal states (alcohol, benzodiazepines, and other CNS depressants). It also is important to note that adolescents with emerging schizophrenia have very high rates of comorbid substance abuse (as high as 60%), so their drug use may not be the cause of their psychotic symptoms. There also is emerging evidence that use of certain drugs during sensitive developmental periods can significantly increase the likelihood of developing schizophrenia in vulnerable populations, such as with regular marijuana use in adolescents who have a family history of schizophrenia.
For those rare pediatric patients who present with both negative and positive symptoms of emerging schizophrenia, early diagnosis and treatment has shown promise in improving the course of the disease. Cognitive-behavioral therapy (CBT) for psychosis has shown promise in lowering the rates of conversion to schizophrenia in select patient populations. This therapy teaches strategies for improving reality testing, cognitive flexibility, and social skills. The social skills appear to be especially important for improving adaptive function, even in those patients who progress to schizophrenia. Family therapies, focused on improving family cohesion, communication, and adaptive functioning, appear to improve family well-being and the course of the patient’s illness (such as fewer and less severe psychotic episodes and improved mood and adaptive function). Early use of antipsychotic medications also appears to improve the course of the illness.
While schizophrenia is not curable, early detection (perhaps by a pediatrician), referral, and treatment can be powerfully protective for patients and their families.
Dr. Swick is physician in chief at Ohana, Center for Child and Adolescent Behavioral Health, Community Hospital of the Monterey (Calif.) Peninsula. Dr. Jellinek is professor emeritus of psychiatry and pediatrics, Harvard Medical School, Boston. Email them at [email protected].
References
1. Psychol Med. 2012 Sep;42(9):1857-63.
2. Br J Psychiatry. 2012 Jul;201(1):26-32.
Strong feelings – such as intense anxiety, irritability, or depressed mood – may affect every child for brief periods of time during their development. Parents and pediatricians are wise to not treat them as psychiatric disorders unless they persist for weeks, impair functioning, or are dramatically severe. Psychosis – marked by hallucinations, perceptual distortions, or profoundly disorganized thinking and behavior – typically looks dramatically severe. Even when psychotic symptoms are mild or brief, they can cause very serious distress for parents and clinicians. The worry is that they may represent a “first break,” a psychotic episode that requires much work for recovery, or the beginning of a lifelong struggle with schizophrenia or other chronic psychotic illness.
While it is important to recognize schizophrenia early – because early interventions are thought to improve the course of the disease – schizophrenia in childhood is rare. It is not commonly recognized that psychotic or psychoticlike symptoms are much more common than schizophrenia. While it is important to begin a thoughtful evaluation when a child or teenager presents with psychosis, it also is important to know that the majority of young people who experience psychotic symptoms do not have schizophrenia or other psychotic illness.
Psychosis describes symptoms in which there has been some “break with reality,” often in the form of hallucinations (seeing or hearing things which are not objectively present) or of distorted perceptions (such as paranoia or grandiosity). “Subsyndromal psychotic symptoms” occur when a person experiences these perceptual disturbances but has doubt about whether or not they are real. In frank psychosis, patients have a “fixed and firm” belief in the truth or accuracy of their perceptions, no matter the evidence against them. The voices they hear or hallucinations they see are “real” and there is a wholehearted belief that what the voice says or what they are seeing is as true as what you or I see and hear.
Schizophrenia is a diagnosis that requires the presence of both these “positive” psychotic symptoms and “negative” symptoms of flat affect; loss of motivation, social, or motor abilities; and cognitive impairment. These symptoms typically emerge in late adolescence (median age, 18 years) in males and early adulthood (median age, 25 years) in females, with another (smaller) peak in incidence in middle age. Importantly, the negative symptoms often emerge first so there often is a history of subtle cognitive decline and social withdrawal, one of the most common patterns in children, before psychosis emerges. Schizophrenia is quite rare, with a prevalence of slightly under 1% of the global population, an annual incidence of approximately 15 people per 100,000, and 1 in 40,000 in children under 13 years old, according to the National Institute of Mental Health. Psychotic symptoms are much more common than schizophrenia, affecting approximately 5% of the adult population at any point in time. They are even more common in children and adolescents. A meta-analysis of population-based studies of psychotic symptoms in youth demonstrated a median prevalence of 17% in children aged 9-12 years and 7.5% in adolescents aged 13-18 years.1 Of course, as with all statistics, much depends on the definitions used to identify this high prevalence rate.
Children and adolescents who report psychotic symptoms are at increased risk for developing schizophrenia, compared with the general population, but most youth with psychotic symptoms will not go on to develop schizophrenia. They are more likely to indicate other, nonpsychotic psychiatric illnesses, such as anxiety or mood disorders, including depression, obsessive compulsive disorder (OCD), and PTSD. In younger children, these symptoms may prove to be benign, but in adolescents they usually indicate the presence of a psychiatric illness. In one study, 57% of children aged 11-13 years with psychotic symptoms were found to have a nonpsychotic psychiatric illness, but the rate jumped to 80% for those aged 13-15 years with psychotic symptoms.2 So while psychosis in teenagers only rarely indicates schizophrenia, these symptoms usually indicate the presence of a psychiatric illness, and a psychiatric evaluation should be initiated.
If a child in your practice presents with psychotic symptoms, it is appropriate to assess their safety and then start a medical work-up. Find out from your patient or their parents if their behavior has been affected by their perceptual disturbances. Are they frightened and avoiding school? Are they withdrawing from social relationships? Is their sleep disrupted? Have they been more impulsive or unpredictable? If their behavior has been affected, you should refer to a child psychiatrist to perform a full diagnostic evaluation and help with management of these symptoms.
Your medical work-up should include a drug screen, blood count, metabolic panel, and thyroid function test. Medications, particularly stimulants, steroids, and anticholinergics can cause psychotic symptoms in high doses or vulnerable patients (such as those with a developmental disorder or traumatic brain injury). If the physical or neurologic exam are suggestive, further investigation of the many potential medical sources of psychotic symptoms in youth can be pursued to rule out autoimmune illnesses, endocrine disorders, metabolic illnesses, heavy metal poisoning, neurologic diseases, infectious diseases, and nutritional deficits. It is worth noting that childhood sleep disorders also can present with psychosis. Persistent psychotic symptoms in children are very hard to evaluate and may be the harbinger of a serious psychiatric disorder, so even if the medical work-up is negative and the persistent symptoms are mild and not causing a safety concern, a referral to a child psychiatrist for a full mental health evaluation is appropriate.
Psychotic symptoms in an adolescent sometimes are easier to assess, more worrisome for serious mental illness, and are a high-risk category for self-destructive behavior and substance use. Before you begin a medical work-up, you always should assess for safety, including suicide risk, if your adolescent patient presents with psychotic symptoms. Screening for symptoms of mood, anxiety, and substance use disorders also can help reveal the nature of their presenting problem. If your adolescent patient is using drugs, that does not rule out the possibility of an underlying mood, anxiety, or thought disorder. While intoxication with many drugs may precipitate psychotic symptoms (including stimulants, hallucinogens, and marijuana), others may precipitate psychosis in withdrawal states (alcohol, benzodiazepines, and other CNS depressants). It also is important to note that adolescents with emerging schizophrenia have very high rates of comorbid substance abuse (as high as 60%), so their drug use may not be the cause of their psychotic symptoms. There also is emerging evidence that use of certain drugs during sensitive developmental periods can significantly increase the likelihood of developing schizophrenia in vulnerable populations, such as with regular marijuana use in adolescents who have a family history of schizophrenia.
For those rare pediatric patients who present with both negative and positive symptoms of emerging schizophrenia, early diagnosis and treatment has shown promise in improving the course of the disease. Cognitive-behavioral therapy (CBT) for psychosis has shown promise in lowering the rates of conversion to schizophrenia in select patient populations. This therapy teaches strategies for improving reality testing, cognitive flexibility, and social skills. The social skills appear to be especially important for improving adaptive function, even in those patients who progress to schizophrenia. Family therapies, focused on improving family cohesion, communication, and adaptive functioning, appear to improve family well-being and the course of the patient’s illness (such as fewer and less severe psychotic episodes and improved mood and adaptive function). Early use of antipsychotic medications also appears to improve the course of the illness.
While schizophrenia is not curable, early detection (perhaps by a pediatrician), referral, and treatment can be powerfully protective for patients and their families.
Dr. Swick is physician in chief at Ohana, Center for Child and Adolescent Behavioral Health, Community Hospital of the Monterey (Calif.) Peninsula. Dr. Jellinek is professor emeritus of psychiatry and pediatrics, Harvard Medical School, Boston. Email them at [email protected].
References
1. Psychol Med. 2012 Sep;42(9):1857-63.
2. Br J Psychiatry. 2012 Jul;201(1):26-32.
It’s all in the timing
It is often fun and sometimes exhausting watching the speed with which children run around or switch from one game to another. A lot of us were attracted to pediatrics to share the quick joy of children and also the speed of their physical recovery. We get to see premature infants gain an ounce a day, and see wounds heal in less than a week. We give advice on sleep and see success in a month. We and the families get used to quick fixes.
Parents and children are forewarned and reassured by our knowledge about how long things typically take: Respiratory syncytial virus (RSV) peaks in 5 days, colic lessens in 3 months, changing sleep patterns takes 3 weeks, habit formation 6 weeks, menses come 2 years after breast development, and so on. But the timing of daily parenting is rarely as predictable. Sometimes a child’s clock is running fast, making waiting even seconds for a snack or a bathroom difficult; other times are slow, as when walking down the sidewalk noticing every leaf. The child’s clock is independent of the adult’s – and complicated by clocks of siblings.
Parent pace also is determined by many factors unrelated to the child: work demands, deadlines, train schedules, something in the oven, needs of siblings, and so on. To those can be added intrinsic factors affecting parent’s tolerance to shifting pace to the child’s such as temperament, fatigue, illness, pain, or even adult ADHD. And don’t forget caffeine (or other drugs) affecting the internal metronome. When impatience with the child is a complaint, it is useful to ask, “What makes waiting for your child difficult for you?”
When discussing time, I find it important to discuss the poison “s-word” of parenting – “should.” This trickster often comes from time illusions in childrearing. After seeing so many behaviors change quickly, parents expect all change to be equally fast. She should be able to sleep through the night by now! He should be able to dress and get to the table in 5 minutes. And sometimes it is the parent’s s-word that creates pain – I should love pushing for as long as she wants to swing, if I am a good parent. The problem with thinking “should” is that it implies willful or moral behavior, and it may prompt a judgmental or punitive parental response.
Otherwise well intentioned, cooperative children who take longer to shift their attention from homework to shower can be seen as oppositional. Worse yet, if the example used is from playing video games (something fun) to getting to the bus stop (an undesirable shift), you may hear parents critically say, “He only wants to do what he wants to do.” When examining examples (always key to helping with behavior), pointing out that all kinds of transitions are difficult for this child may be educational and allow for a more reasoned response. And specifically being on electronics puts adults as well as children in a time warp which is hard to escape.
There are many kinds of thwarted expectations, but expectations about how long things take are pretty universal. Frustration generates anger and even can lead to violence, such as road rage. Children – who all step to the beat of a different drummer, especially those with different “clocks” such as in ADHD – may experience frustration most of the day. This can manifest as irritability for them and sometimes as an irritable response back from the parent.
The first step in adapting to differences in parent and child pace is to realize that time is the problem. Naming it, saying “we are on toddler time,” can be a “signal to self” to slow down. Generations of children loved Mr. Rogers because he always conveyed having all the time in the world for the person he was with. It actually does not take as long as it feels at first to do this. Listening while keeping eye contact, breathing deeply, and waiting until two breaths after the child goes silent before speaking or moving conveys your interest and respect. For some behaviors, such as tantrums, such quiet attention may be all that is needed to resolve the issue. We adults can practice this, but even infants can be helped to develop patience by reinforcement with brief attention from their caregivers for tiny increments of waiting.
I sometimes suggest that parents time behaviors to develop perspective, reset expectations, practice waiting, and perhaps even distract themselves from intervening and making things worse by lending attention to negative behaviors. Timing as observation can be helpful for tantrums, breath holding spells, whining, and sibling squabbles; maximum times for baths and video games; minimum times for meals, sitting to poop, and special time. Timers are not just for Time Out! “Visual timers” that show green then yellow then red and sometimes flashing lights as warnings of an upcoming stopping point are helpful for children preschool and older. These timers help them to develop a better sense of time and begin managing their own transitions. A game of guessing how long things take can build timing skills and patience. I think every child past preschool benefits from a wristwatch, first to build time sense, and second to avoid looking at a smartphone to see the hour, then being distracted by content! Diaries of behaviors over time are a staple of behavior change plans, with the added benefit of lending perspective on actually how often and how long a troublesome behavior occurs. Practicing mindfulness – nonjudgmental watching of our thoughts and feelings, often with deep breathing and relaxation – also can help both children and adults build time tolerance.
Children have little control over their daily schedule. Surrendering when you can for them to do things at their own pace can reduce their frustration, build the parent-child relationship, and promote positive behaviors. Plus family life is more enjoyable lived slower. You even can remind parents that “the days are long but the years are short” before their children will be grown and gone.
Dr. Howard is an assistant professor of pediatrics at Johns Hopkins University, Baltimore, and creator of CHADIS. She had no other relevant disclosures. Dr. Howard’s contribution to this publication was as a paid expert to MDedge News. Email her at [email protected].
It is often fun and sometimes exhausting watching the speed with which children run around or switch from one game to another. A lot of us were attracted to pediatrics to share the quick joy of children and also the speed of their physical recovery. We get to see premature infants gain an ounce a day, and see wounds heal in less than a week. We give advice on sleep and see success in a month. We and the families get used to quick fixes.
Parents and children are forewarned and reassured by our knowledge about how long things typically take: Respiratory syncytial virus (RSV) peaks in 5 days, colic lessens in 3 months, changing sleep patterns takes 3 weeks, habit formation 6 weeks, menses come 2 years after breast development, and so on. But the timing of daily parenting is rarely as predictable. Sometimes a child’s clock is running fast, making waiting even seconds for a snack or a bathroom difficult; other times are slow, as when walking down the sidewalk noticing every leaf. The child’s clock is independent of the adult’s – and complicated by clocks of siblings.
Parent pace also is determined by many factors unrelated to the child: work demands, deadlines, train schedules, something in the oven, needs of siblings, and so on. To those can be added intrinsic factors affecting parent’s tolerance to shifting pace to the child’s such as temperament, fatigue, illness, pain, or even adult ADHD. And don’t forget caffeine (or other drugs) affecting the internal metronome. When impatience with the child is a complaint, it is useful to ask, “What makes waiting for your child difficult for you?”
When discussing time, I find it important to discuss the poison “s-word” of parenting – “should.” This trickster often comes from time illusions in childrearing. After seeing so many behaviors change quickly, parents expect all change to be equally fast. She should be able to sleep through the night by now! He should be able to dress and get to the table in 5 minutes. And sometimes it is the parent’s s-word that creates pain – I should love pushing for as long as she wants to swing, if I am a good parent. The problem with thinking “should” is that it implies willful or moral behavior, and it may prompt a judgmental or punitive parental response.
Otherwise well intentioned, cooperative children who take longer to shift their attention from homework to shower can be seen as oppositional. Worse yet, if the example used is from playing video games (something fun) to getting to the bus stop (an undesirable shift), you may hear parents critically say, “He only wants to do what he wants to do.” When examining examples (always key to helping with behavior), pointing out that all kinds of transitions are difficult for this child may be educational and allow for a more reasoned response. And specifically being on electronics puts adults as well as children in a time warp which is hard to escape.
There are many kinds of thwarted expectations, but expectations about how long things take are pretty universal. Frustration generates anger and even can lead to violence, such as road rage. Children – who all step to the beat of a different drummer, especially those with different “clocks” such as in ADHD – may experience frustration most of the day. This can manifest as irritability for them and sometimes as an irritable response back from the parent.
The first step in adapting to differences in parent and child pace is to realize that time is the problem. Naming it, saying “we are on toddler time,” can be a “signal to self” to slow down. Generations of children loved Mr. Rogers because he always conveyed having all the time in the world for the person he was with. It actually does not take as long as it feels at first to do this. Listening while keeping eye contact, breathing deeply, and waiting until two breaths after the child goes silent before speaking or moving conveys your interest and respect. For some behaviors, such as tantrums, such quiet attention may be all that is needed to resolve the issue. We adults can practice this, but even infants can be helped to develop patience by reinforcement with brief attention from their caregivers for tiny increments of waiting.
I sometimes suggest that parents time behaviors to develop perspective, reset expectations, practice waiting, and perhaps even distract themselves from intervening and making things worse by lending attention to negative behaviors. Timing as observation can be helpful for tantrums, breath holding spells, whining, and sibling squabbles; maximum times for baths and video games; minimum times for meals, sitting to poop, and special time. Timers are not just for Time Out! “Visual timers” that show green then yellow then red and sometimes flashing lights as warnings of an upcoming stopping point are helpful for children preschool and older. These timers help them to develop a better sense of time and begin managing their own transitions. A game of guessing how long things take can build timing skills and patience. I think every child past preschool benefits from a wristwatch, first to build time sense, and second to avoid looking at a smartphone to see the hour, then being distracted by content! Diaries of behaviors over time are a staple of behavior change plans, with the added benefit of lending perspective on actually how often and how long a troublesome behavior occurs. Practicing mindfulness – nonjudgmental watching of our thoughts and feelings, often with deep breathing and relaxation – also can help both children and adults build time tolerance.
Children have little control over their daily schedule. Surrendering when you can for them to do things at their own pace can reduce their frustration, build the parent-child relationship, and promote positive behaviors. Plus family life is more enjoyable lived slower. You even can remind parents that “the days are long but the years are short” before their children will be grown and gone.
Dr. Howard is an assistant professor of pediatrics at Johns Hopkins University, Baltimore, and creator of CHADIS. She had no other relevant disclosures. Dr. Howard’s contribution to this publication was as a paid expert to MDedge News. Email her at [email protected].
It is often fun and sometimes exhausting watching the speed with which children run around or switch from one game to another. A lot of us were attracted to pediatrics to share the quick joy of children and also the speed of their physical recovery. We get to see premature infants gain an ounce a day, and see wounds heal in less than a week. We give advice on sleep and see success in a month. We and the families get used to quick fixes.
Parents and children are forewarned and reassured by our knowledge about how long things typically take: Respiratory syncytial virus (RSV) peaks in 5 days, colic lessens in 3 months, changing sleep patterns takes 3 weeks, habit formation 6 weeks, menses come 2 years after breast development, and so on. But the timing of daily parenting is rarely as predictable. Sometimes a child’s clock is running fast, making waiting even seconds for a snack or a bathroom difficult; other times are slow, as when walking down the sidewalk noticing every leaf. The child’s clock is independent of the adult’s – and complicated by clocks of siblings.
Parent pace also is determined by many factors unrelated to the child: work demands, deadlines, train schedules, something in the oven, needs of siblings, and so on. To those can be added intrinsic factors affecting parent’s tolerance to shifting pace to the child’s such as temperament, fatigue, illness, pain, or even adult ADHD. And don’t forget caffeine (or other drugs) affecting the internal metronome. When impatience with the child is a complaint, it is useful to ask, “What makes waiting for your child difficult for you?”
When discussing time, I find it important to discuss the poison “s-word” of parenting – “should.” This trickster often comes from time illusions in childrearing. After seeing so many behaviors change quickly, parents expect all change to be equally fast. She should be able to sleep through the night by now! He should be able to dress and get to the table in 5 minutes. And sometimes it is the parent’s s-word that creates pain – I should love pushing for as long as she wants to swing, if I am a good parent. The problem with thinking “should” is that it implies willful or moral behavior, and it may prompt a judgmental or punitive parental response.
Otherwise well intentioned, cooperative children who take longer to shift their attention from homework to shower can be seen as oppositional. Worse yet, if the example used is from playing video games (something fun) to getting to the bus stop (an undesirable shift), you may hear parents critically say, “He only wants to do what he wants to do.” When examining examples (always key to helping with behavior), pointing out that all kinds of transitions are difficult for this child may be educational and allow for a more reasoned response. And specifically being on electronics puts adults as well as children in a time warp which is hard to escape.
There are many kinds of thwarted expectations, but expectations about how long things take are pretty universal. Frustration generates anger and even can lead to violence, such as road rage. Children – who all step to the beat of a different drummer, especially those with different “clocks” such as in ADHD – may experience frustration most of the day. This can manifest as irritability for them and sometimes as an irritable response back from the parent.
The first step in adapting to differences in parent and child pace is to realize that time is the problem. Naming it, saying “we are on toddler time,” can be a “signal to self” to slow down. Generations of children loved Mr. Rogers because he always conveyed having all the time in the world for the person he was with. It actually does not take as long as it feels at first to do this. Listening while keeping eye contact, breathing deeply, and waiting until two breaths after the child goes silent before speaking or moving conveys your interest and respect. For some behaviors, such as tantrums, such quiet attention may be all that is needed to resolve the issue. We adults can practice this, but even infants can be helped to develop patience by reinforcement with brief attention from their caregivers for tiny increments of waiting.
I sometimes suggest that parents time behaviors to develop perspective, reset expectations, practice waiting, and perhaps even distract themselves from intervening and making things worse by lending attention to negative behaviors. Timing as observation can be helpful for tantrums, breath holding spells, whining, and sibling squabbles; maximum times for baths and video games; minimum times for meals, sitting to poop, and special time. Timers are not just for Time Out! “Visual timers” that show green then yellow then red and sometimes flashing lights as warnings of an upcoming stopping point are helpful for children preschool and older. These timers help them to develop a better sense of time and begin managing their own transitions. A game of guessing how long things take can build timing skills and patience. I think every child past preschool benefits from a wristwatch, first to build time sense, and second to avoid looking at a smartphone to see the hour, then being distracted by content! Diaries of behaviors over time are a staple of behavior change plans, with the added benefit of lending perspective on actually how often and how long a troublesome behavior occurs. Practicing mindfulness – nonjudgmental watching of our thoughts and feelings, often with deep breathing and relaxation – also can help both children and adults build time tolerance.
Children have little control over their daily schedule. Surrendering when you can for them to do things at their own pace can reduce their frustration, build the parent-child relationship, and promote positive behaviors. Plus family life is more enjoyable lived slower. You even can remind parents that “the days are long but the years are short” before their children will be grown and gone.
Dr. Howard is an assistant professor of pediatrics at Johns Hopkins University, Baltimore, and creator of CHADIS. She had no other relevant disclosures. Dr. Howard’s contribution to this publication was as a paid expert to MDedge News. Email her at [email protected].
Dr. Barbara J. Howard will receive the 2019 C. Anderson Aldrich Award
The award is given by the AAP Section on Developmental and Behavioral Pediatrics to “recognize physicians who have made outstanding contributions to the field of child development,” according to the AAP. Previous recipients of the award include pediatricians such as Benjamin M. Spock, MD, and T. Berry Brazelton, MD, as well as psychoanalyst Anna Freud and child psychologist Erik H. Erickson.
Dr. Howard is a developmental-behavioral pediatrician who is an assistant professor of pediatrics at Johns Hopkins University, Baltimore, where she codirected a fellowship program to train developmental and behavioral pediatricians. She is a creator of CHADIS, an innovative online system that provides previsit questionnaires that allows physicians “to collect patient-generated data that can be used to support clinical and shared decisions, track data, and create quality improvement reports,” according to the CHADIS website. She has given free monthly case conferences through a federal grant for 30 years, initially in person and more recently through a national webcast. Over the last 2 decades, Dr. Howard has written about practical approaches to developmental and behavioral problems children experience for this newspaper in her Behavioral Consult column.
Michael S. Jellinek, MD, professor emeritus of psychiatry and pediatrics at the Harvard Medical School, Boston, said in an interview, “Barbara’s dedication to the emotional health of children has made an enormous difference. In addition to her clinical care and writing, her development of CHADIS has helped pediatricians recognize and treat thousands upon thousands of children. She is most deserving of this high honor.”
The award is given by the AAP Section on Developmental and Behavioral Pediatrics to “recognize physicians who have made outstanding contributions to the field of child development,” according to the AAP. Previous recipients of the award include pediatricians such as Benjamin M. Spock, MD, and T. Berry Brazelton, MD, as well as psychoanalyst Anna Freud and child psychologist Erik H. Erickson.
Dr. Howard is a developmental-behavioral pediatrician who is an assistant professor of pediatrics at Johns Hopkins University, Baltimore, where she codirected a fellowship program to train developmental and behavioral pediatricians. She is a creator of CHADIS, an innovative online system that provides previsit questionnaires that allows physicians “to collect patient-generated data that can be used to support clinical and shared decisions, track data, and create quality improvement reports,” according to the CHADIS website. She has given free monthly case conferences through a federal grant for 30 years, initially in person and more recently through a national webcast. Over the last 2 decades, Dr. Howard has written about practical approaches to developmental and behavioral problems children experience for this newspaper in her Behavioral Consult column.
Michael S. Jellinek, MD, professor emeritus of psychiatry and pediatrics at the Harvard Medical School, Boston, said in an interview, “Barbara’s dedication to the emotional health of children has made an enormous difference. In addition to her clinical care and writing, her development of CHADIS has helped pediatricians recognize and treat thousands upon thousands of children. She is most deserving of this high honor.”
The award is given by the AAP Section on Developmental and Behavioral Pediatrics to “recognize physicians who have made outstanding contributions to the field of child development,” according to the AAP. Previous recipients of the award include pediatricians such as Benjamin M. Spock, MD, and T. Berry Brazelton, MD, as well as psychoanalyst Anna Freud and child psychologist Erik H. Erickson.
Dr. Howard is a developmental-behavioral pediatrician who is an assistant professor of pediatrics at Johns Hopkins University, Baltimore, where she codirected a fellowship program to train developmental and behavioral pediatricians. She is a creator of CHADIS, an innovative online system that provides previsit questionnaires that allows physicians “to collect patient-generated data that can be used to support clinical and shared decisions, track data, and create quality improvement reports,” according to the CHADIS website. She has given free monthly case conferences through a federal grant for 30 years, initially in person and more recently through a national webcast. Over the last 2 decades, Dr. Howard has written about practical approaches to developmental and behavioral problems children experience for this newspaper in her Behavioral Consult column.
Michael S. Jellinek, MD, professor emeritus of psychiatry and pediatrics at the Harvard Medical School, Boston, said in an interview, “Barbara’s dedication to the emotional health of children has made an enormous difference. In addition to her clinical care and writing, her development of CHADIS has helped pediatricians recognize and treat thousands upon thousands of children. She is most deserving of this high honor.”
Encourage participation in team sports
Participation in sports, competitive team sports in particular, is very good for the physical well-being and emotional development of children and adolescents. Specifically, there is growing evidence that sports promote healthy development socially and emotionally, protecting against drug use, poor body image, and against psychiatric illness in youth.
Sustaining academic productivity and team sports is demanding. By the middle of autumn, the amount of homework can begin to wear on teenagers, and the burden of getting them to practices and games can wear on parents. It can be very tempting for youth and their parents to drop team sports in high school, and turn their time and effort more completely to the serious work of school. But advocating for your patients and their parents to protect the time for team sports participation will pay dividends in the health and well-being of your patients and may even support rather than detract from academic performance.
The benefits of regular exercise for physical health are well established. Most teenagers do not get the recommended 60 minutes daily of moderate to vigorous physical activity. Participating in a team sport enforces this level of activity, in ways that parents typically don’t have to enforce. This level of physical activity typically promotes healthy eating and a healthy weight. Daily exercise promotes adequate, restful sleep, one of the most critical (and usually compromised) components of adolescent health. These exercise habits are easier to maintain into adulthood – when they protect against cardiovascular and inflammatory diseases – if they have been established early.
Beyond physical health, participation in team sports has been shown to promote good mental health and protect against psychiatric illnesses. They generally are less likely to use drugs and more likely to have a healthy body image than are their nonathlete peers. It is worth noting that the mental health benefits of team sports are even more robust than the benefits of solitary exercise in teenagers,1 possibly because of the social connections to peers and adults that grow out of them.
In the Monitoring the Future surveys (biannual national surveys of high school student health and behaviors funded by the National Institutes of Health) from 2010 to 2015, teenagers who participated in team sports were more likely to describe higher self-esteem and lower levels of loneliness. It is important to note that it has been difficult to establish the causal direction of the association between team sports and mental health in youth. We need more prospective randomized controlled trials to assert that the benefit is not simply an artifact of healthier youth choosing to participate in sports, but actually an active consequence of that choice. For now, though, we can say with confidence that physical activity promotes good mental health in youth and may protect against mental illness.
While student athletes benefit from the opportunity to develop deep social connections – ones forged in the intense setting of competition, collaboration, and sustained teamwork – they also benefit from strong mentorship connections with adults, including coaches, trainers, and even the parents of teammates who participate in all of the efforts that go into team sports in youth. While it might seem that all of the mental and physical benefits must be offset by lower academic performance, it turns out that is not the case. It is well established that regular exercise promotes healthy cognitive function, including processing speed, working memory, and even creativity. According to data from the Monitoring the Future survey, adolescents who participated in team sports were more likely to have As and to plan on attending a 4-year college than were their nonathlete peers.
Beyond the physiologic and social benefits of exercise, team sports provide adolescents with a powerful opportunity to get comfortable with failure. Even the best athletes cannot win all the time, and sports are unique in building failure into the work. Practice is almost entirely about failure, gradually getting better at something that is difficult. While everyone aims to win, they also prepare to struggle and lose. Athletes must learn how to persevere through a match that they are losing, and then pick themselves up and prepare again for the next match. When young people get comfortable with facing and managing challenges, managing setbacks and failure, they are ready to face the larger challenges, setbacks, and failures of adult life.
Team sports enable young people to learn what they are actually capable of managing – they build resilience. This promotion of resilience is illustrated in recent research that demonstrated that team sports may be especially protective for young people who have experienced trauma (adverse childhood experiences, or “ACEs”). Researchers at the University of California, Los Angeles, followed teenagers with and without high ACE scores into their mid 20s. They found that those with high ACE scores who participated in team sports as adolescents were 24% less likely to have depression and 30% less likely to have anxiety diagnoses as adults, compared with their peers who did not participate in team sports.2
Of course, the details matter in team sports. If your patients are participating and they or their parents are worried about spending so much time on something other than homework, talk to them about all of these exceptional benefits of team sports. But the culture of the team matters also. Some teams may be focused on winning at all costs, or have a practice culture that is humiliating or bullying. Some teams may have a culture of partying after games, with binge drinking and drug use. Ask your patients about whether they feel they are respected members of the team, and if effort and sportsmanship are valued as well as performance. Do they trust their coaches? Do they believe their coaches know and care about them? If your patients are not participating in a team sport, encourage them to find one (or more) that engage their interests. The benefits of track and field, crew, and tennis can be just as robust as the benefits of football or soccer. Speak with your patients and their parents about the payoff for their physical, mental, and developmental health the time and effort they are putting into a team sport can provide.
Dr. Swick is physician in chief at Ohana, Center for Child and Adolescent Behavioral Health, Community Hospital of the Monterey (Calif.) Peninsula. Dr. Jellinek is professor emeritus of psychiatry and pediatrics, Harvard Medical School, Boston. Email them at [email protected].
References
1. Int J Nutr Phys Act. 2013 Aug 15. doi: 10.1186/1479-5868-10-98.
2. JAMA Pediatr. 2019 Jul 1;173(7):681-8.
Participation in sports, competitive team sports in particular, is very good for the physical well-being and emotional development of children and adolescents. Specifically, there is growing evidence that sports promote healthy development socially and emotionally, protecting against drug use, poor body image, and against psychiatric illness in youth.
Sustaining academic productivity and team sports is demanding. By the middle of autumn, the amount of homework can begin to wear on teenagers, and the burden of getting them to practices and games can wear on parents. It can be very tempting for youth and their parents to drop team sports in high school, and turn their time and effort more completely to the serious work of school. But advocating for your patients and their parents to protect the time for team sports participation will pay dividends in the health and well-being of your patients and may even support rather than detract from academic performance.
The benefits of regular exercise for physical health are well established. Most teenagers do not get the recommended 60 minutes daily of moderate to vigorous physical activity. Participating in a team sport enforces this level of activity, in ways that parents typically don’t have to enforce. This level of physical activity typically promotes healthy eating and a healthy weight. Daily exercise promotes adequate, restful sleep, one of the most critical (and usually compromised) components of adolescent health. These exercise habits are easier to maintain into adulthood – when they protect against cardiovascular and inflammatory diseases – if they have been established early.
Beyond physical health, participation in team sports has been shown to promote good mental health and protect against psychiatric illnesses. They generally are less likely to use drugs and more likely to have a healthy body image than are their nonathlete peers. It is worth noting that the mental health benefits of team sports are even more robust than the benefits of solitary exercise in teenagers,1 possibly because of the social connections to peers and adults that grow out of them.
In the Monitoring the Future surveys (biannual national surveys of high school student health and behaviors funded by the National Institutes of Health) from 2010 to 2015, teenagers who participated in team sports were more likely to describe higher self-esteem and lower levels of loneliness. It is important to note that it has been difficult to establish the causal direction of the association between team sports and mental health in youth. We need more prospective randomized controlled trials to assert that the benefit is not simply an artifact of healthier youth choosing to participate in sports, but actually an active consequence of that choice. For now, though, we can say with confidence that physical activity promotes good mental health in youth and may protect against mental illness.
While student athletes benefit from the opportunity to develop deep social connections – ones forged in the intense setting of competition, collaboration, and sustained teamwork – they also benefit from strong mentorship connections with adults, including coaches, trainers, and even the parents of teammates who participate in all of the efforts that go into team sports in youth. While it might seem that all of the mental and physical benefits must be offset by lower academic performance, it turns out that is not the case. It is well established that regular exercise promotes healthy cognitive function, including processing speed, working memory, and even creativity. According to data from the Monitoring the Future survey, adolescents who participated in team sports were more likely to have As and to plan on attending a 4-year college than were their nonathlete peers.
Beyond the physiologic and social benefits of exercise, team sports provide adolescents with a powerful opportunity to get comfortable with failure. Even the best athletes cannot win all the time, and sports are unique in building failure into the work. Practice is almost entirely about failure, gradually getting better at something that is difficult. While everyone aims to win, they also prepare to struggle and lose. Athletes must learn how to persevere through a match that they are losing, and then pick themselves up and prepare again for the next match. When young people get comfortable with facing and managing challenges, managing setbacks and failure, they are ready to face the larger challenges, setbacks, and failures of adult life.
Team sports enable young people to learn what they are actually capable of managing – they build resilience. This promotion of resilience is illustrated in recent research that demonstrated that team sports may be especially protective for young people who have experienced trauma (adverse childhood experiences, or “ACEs”). Researchers at the University of California, Los Angeles, followed teenagers with and without high ACE scores into their mid 20s. They found that those with high ACE scores who participated in team sports as adolescents were 24% less likely to have depression and 30% less likely to have anxiety diagnoses as adults, compared with their peers who did not participate in team sports.2
Of course, the details matter in team sports. If your patients are participating and they or their parents are worried about spending so much time on something other than homework, talk to them about all of these exceptional benefits of team sports. But the culture of the team matters also. Some teams may be focused on winning at all costs, or have a practice culture that is humiliating or bullying. Some teams may have a culture of partying after games, with binge drinking and drug use. Ask your patients about whether they feel they are respected members of the team, and if effort and sportsmanship are valued as well as performance. Do they trust their coaches? Do they believe their coaches know and care about them? If your patients are not participating in a team sport, encourage them to find one (or more) that engage their interests. The benefits of track and field, crew, and tennis can be just as robust as the benefits of football or soccer. Speak with your patients and their parents about the payoff for their physical, mental, and developmental health the time and effort they are putting into a team sport can provide.
Dr. Swick is physician in chief at Ohana, Center for Child and Adolescent Behavioral Health, Community Hospital of the Monterey (Calif.) Peninsula. Dr. Jellinek is professor emeritus of psychiatry and pediatrics, Harvard Medical School, Boston. Email them at [email protected].
References
1. Int J Nutr Phys Act. 2013 Aug 15. doi: 10.1186/1479-5868-10-98.
2. JAMA Pediatr. 2019 Jul 1;173(7):681-8.
Participation in sports, competitive team sports in particular, is very good for the physical well-being and emotional development of children and adolescents. Specifically, there is growing evidence that sports promote healthy development socially and emotionally, protecting against drug use, poor body image, and against psychiatric illness in youth.
Sustaining academic productivity and team sports is demanding. By the middle of autumn, the amount of homework can begin to wear on teenagers, and the burden of getting them to practices and games can wear on parents. It can be very tempting for youth and their parents to drop team sports in high school, and turn their time and effort more completely to the serious work of school. But advocating for your patients and their parents to protect the time for team sports participation will pay dividends in the health and well-being of your patients and may even support rather than detract from academic performance.
The benefits of regular exercise for physical health are well established. Most teenagers do not get the recommended 60 minutes daily of moderate to vigorous physical activity. Participating in a team sport enforces this level of activity, in ways that parents typically don’t have to enforce. This level of physical activity typically promotes healthy eating and a healthy weight. Daily exercise promotes adequate, restful sleep, one of the most critical (and usually compromised) components of adolescent health. These exercise habits are easier to maintain into adulthood – when they protect against cardiovascular and inflammatory diseases – if they have been established early.
Beyond physical health, participation in team sports has been shown to promote good mental health and protect against psychiatric illnesses. They generally are less likely to use drugs and more likely to have a healthy body image than are their nonathlete peers. It is worth noting that the mental health benefits of team sports are even more robust than the benefits of solitary exercise in teenagers,1 possibly because of the social connections to peers and adults that grow out of them.
In the Monitoring the Future surveys (biannual national surveys of high school student health and behaviors funded by the National Institutes of Health) from 2010 to 2015, teenagers who participated in team sports were more likely to describe higher self-esteem and lower levels of loneliness. It is important to note that it has been difficult to establish the causal direction of the association between team sports and mental health in youth. We need more prospective randomized controlled trials to assert that the benefit is not simply an artifact of healthier youth choosing to participate in sports, but actually an active consequence of that choice. For now, though, we can say with confidence that physical activity promotes good mental health in youth and may protect against mental illness.
While student athletes benefit from the opportunity to develop deep social connections – ones forged in the intense setting of competition, collaboration, and sustained teamwork – they also benefit from strong mentorship connections with adults, including coaches, trainers, and even the parents of teammates who participate in all of the efforts that go into team sports in youth. While it might seem that all of the mental and physical benefits must be offset by lower academic performance, it turns out that is not the case. It is well established that regular exercise promotes healthy cognitive function, including processing speed, working memory, and even creativity. According to data from the Monitoring the Future survey, adolescents who participated in team sports were more likely to have As and to plan on attending a 4-year college than were their nonathlete peers.
Beyond the physiologic and social benefits of exercise, team sports provide adolescents with a powerful opportunity to get comfortable with failure. Even the best athletes cannot win all the time, and sports are unique in building failure into the work. Practice is almost entirely about failure, gradually getting better at something that is difficult. While everyone aims to win, they also prepare to struggle and lose. Athletes must learn how to persevere through a match that they are losing, and then pick themselves up and prepare again for the next match. When young people get comfortable with facing and managing challenges, managing setbacks and failure, they are ready to face the larger challenges, setbacks, and failures of adult life.
Team sports enable young people to learn what they are actually capable of managing – they build resilience. This promotion of resilience is illustrated in recent research that demonstrated that team sports may be especially protective for young people who have experienced trauma (adverse childhood experiences, or “ACEs”). Researchers at the University of California, Los Angeles, followed teenagers with and without high ACE scores into their mid 20s. They found that those with high ACE scores who participated in team sports as adolescents were 24% less likely to have depression and 30% less likely to have anxiety diagnoses as adults, compared with their peers who did not participate in team sports.2
Of course, the details matter in team sports. If your patients are participating and they or their parents are worried about spending so much time on something other than homework, talk to them about all of these exceptional benefits of team sports. But the culture of the team matters also. Some teams may be focused on winning at all costs, or have a practice culture that is humiliating or bullying. Some teams may have a culture of partying after games, with binge drinking and drug use. Ask your patients about whether they feel they are respected members of the team, and if effort and sportsmanship are valued as well as performance. Do they trust their coaches? Do they believe their coaches know and care about them? If your patients are not participating in a team sport, encourage them to find one (or more) that engage their interests. The benefits of track and field, crew, and tennis can be just as robust as the benefits of football or soccer. Speak with your patients and their parents about the payoff for their physical, mental, and developmental health the time and effort they are putting into a team sport can provide.
Dr. Swick is physician in chief at Ohana, Center for Child and Adolescent Behavioral Health, Community Hospital of the Monterey (Calif.) Peninsula. Dr. Jellinek is professor emeritus of psychiatry and pediatrics, Harvard Medical School, Boston. Email them at [email protected].
References
1. Int J Nutr Phys Act. 2013 Aug 15. doi: 10.1186/1479-5868-10-98.
2. JAMA Pediatr. 2019 Jul 1;173(7):681-8.
ALERT: Grandmother in the room!
One of the things that makes pediatrics challenging and potentially rewarding is that there are often multiple family members in the room for our visits.
With an expansion of our acknowledged role safeguarding and promoting a child’s current and future health to include asking about environmental and caregiving influences comes some tricky dynamics. The parent is in the room with a teen who has a secret love life. A father is in the room with the mother he threatens at home. The mother is in the room with the preschooler she has hit. There is risk but also opportunity for valuable discourse, discovery, and healing.
We now know that about 50% of the future morbidity of the child before us will be determined by the adverse childhood experiences (ACEs) they experience during the exact years (0-18) they are under our health supervision. Many of these risk factors come from home life and may be preventable or at least moderated. When we begin screening for ACEs we are asking the parents about bad things that happened when they were growing up.
The dilemma that came up recently was the grandmother in the room with the daughter she raised who is now caring for her own child. In this situation, you may be in the presence of the person whom the parent feels inflicted – or failed to prevent – the hurts being discussed.
“How are things at home?” you ask dutifully. Mother says “Fine,” but rolls her eyes. Grandma, sitting in the room looking at her phone, says something to the mother in a foreign language. You are in the dark, but sense friction.
Even in modern times, it is respectful to address the grandparent who is present first in a visit, introducing yourself, and finding out the relationship and living situation. Previsit questionnaires can help set visit priorities and alert you to what topics may be better discussed in private, perhaps including ACEs. It is important to ask the parent permission to discuss potentially sensitive topics when the grandparent is present or ask for the grandparent to step out of the room.
Why not just be sure the grandmother stays in the waiting room? If the hurts from the past still are affecting the mother now, moderating an open conversation about those experiences can be very valuable to reducing their impact on present parenting or dysfunctional coping strategies.
Some experts say that any enumeration of ACEs should include asking “Which of these are still bothering you now?” Saying, “Parenting often brings up memories of similar situations from when we were young that can tilt how we act toward our own children,” then asking, “Can we talk about those experiences you had?”
Eliciting the grandparent’s perspective with a question such as “What were those years of parenting like for you?” respects the significance of the grandparent’s role. The grandparents probably were young, stressed, and inexperienced when they were the mother’s primary caregivers. Or the grandparent may have gratefully erased memories of the tough moments but the parent clearly remembers the childhood pain, because hurts sear themselves into our brains more than positive or neutral experiences do. She or he may have been holding resentment against the grandparent and living it out for years and now in her/his parenting.
Suddenly, you and the parent may hear the grandparent reveal other factors that would never have been visible to the child then and may never have been brought up because the grandparent was working three jobs because the father was deployed; caring for a sick sibling; suffering from depression; being subject to an abusive alcoholic spouse; having to keep the children inside because of shooting in the neighborhood, etc. You may be able reframe what is said to point out that the grandparents “did the best they could at the time and with the resources and skills they possessed then.”
Mothers who had troubled relationships with their own mothers (e.g. insecure attachment) tend to pass these patterns down in their own parenting unless they have processed the experiences and come to a place of acceptance. People may process their past effectively on their own, some through mental health counseling or religion, but for others a brief “Ah ha!” moment may help settle the waters.
Ask the grandparent as well as the parent, “What are you hoping will go differently than when [parent] was growing up?” Some try to make up for what they see as their own mistakes by advocating coming down harder on their grandchildren than they did on their own. An example among my patients was the grandmother whose daughter had become a heroin user, who was very strict and critical in her determination that her granddaughter would not fall into the wrong crowd. Voicing this for her as a possible reason for her strident posture dramatically shifted her attitude.
Other times parents, maybe grateful for a place to live with the grandparents but also trapped there financially, are simmering with anger at the grandparents’ intrusions into their parenting choices. It can be useful to point out that grandparents, no longer caught up in careers, may feel the need to be useful and have a role by giving advice or bustling around cleaning and buying things for their grandchildren. Hey, any help can be welcome if you don’t take it as meaning you are not doing a good job! Although limits can be set.
Transitioning to regarding one’s grown child as an adult and letting them make their own choices and mistakes, waiting until asked for advice, can take a lot of tongue biting after years of active parenting. One essay I read about an adult’s fond memories of his father included the realization that some of the best parenting he recalled was when his father left things unsaid.
Cultural differences in parenting between grandparent and parent can be another source of stress. Assimilation happens fast in America. The newest generation is often trying very hard NOT to be like the “old country.” The parents’ turning away from the grandparents’ culture or religion can threaten their values and culture for which they may have sacrificed everything. Advising the parent to celebrate at least some traditions may reduce the tension at little cost.
As of 2016, 5% of U.S. children in two-parent families lived with a grandparent and 15% of single parents do. This is much higher in certain ethnic groups where living with your adult children is expected. Even if not living together, their influence may be great. Many parents report more stress than support from grandparents. Negative mother-in-law stories abound! That is why simply asking if the parent “has anyone to help them” as a way of assessing social support can be very misleading. You also may ask “Is that more a help or a problem?”
When grandparents undermine the parents’ rules, of course, a family meeting is in order. But grandparents, with the wisdom of years and reduced life pressure, tend to care for children more generously and less critically than when they were main caregivers, conveying unconditional love that can buffer stresses and be remembered by the beloved child forever.
Dr. Howard is assistant professor of pediatrics at Johns Hopkins University, Baltimore, and creator of CHADIS. She had no other relevant disclosures. Dr. Howard’s contribution to this publication was as a paid expert to MDedge News. E-mail her at [email protected].
One of the things that makes pediatrics challenging and potentially rewarding is that there are often multiple family members in the room for our visits.
With an expansion of our acknowledged role safeguarding and promoting a child’s current and future health to include asking about environmental and caregiving influences comes some tricky dynamics. The parent is in the room with a teen who has a secret love life. A father is in the room with the mother he threatens at home. The mother is in the room with the preschooler she has hit. There is risk but also opportunity for valuable discourse, discovery, and healing.
We now know that about 50% of the future morbidity of the child before us will be determined by the adverse childhood experiences (ACEs) they experience during the exact years (0-18) they are under our health supervision. Many of these risk factors come from home life and may be preventable or at least moderated. When we begin screening for ACEs we are asking the parents about bad things that happened when they were growing up.
The dilemma that came up recently was the grandmother in the room with the daughter she raised who is now caring for her own child. In this situation, you may be in the presence of the person whom the parent feels inflicted – or failed to prevent – the hurts being discussed.
“How are things at home?” you ask dutifully. Mother says “Fine,” but rolls her eyes. Grandma, sitting in the room looking at her phone, says something to the mother in a foreign language. You are in the dark, but sense friction.
Even in modern times, it is respectful to address the grandparent who is present first in a visit, introducing yourself, and finding out the relationship and living situation. Previsit questionnaires can help set visit priorities and alert you to what topics may be better discussed in private, perhaps including ACEs. It is important to ask the parent permission to discuss potentially sensitive topics when the grandparent is present or ask for the grandparent to step out of the room.
Why not just be sure the grandmother stays in the waiting room? If the hurts from the past still are affecting the mother now, moderating an open conversation about those experiences can be very valuable to reducing their impact on present parenting or dysfunctional coping strategies.
Some experts say that any enumeration of ACEs should include asking “Which of these are still bothering you now?” Saying, “Parenting often brings up memories of similar situations from when we were young that can tilt how we act toward our own children,” then asking, “Can we talk about those experiences you had?”
Eliciting the grandparent’s perspective with a question such as “What were those years of parenting like for you?” respects the significance of the grandparent’s role. The grandparents probably were young, stressed, and inexperienced when they were the mother’s primary caregivers. Or the grandparent may have gratefully erased memories of the tough moments but the parent clearly remembers the childhood pain, because hurts sear themselves into our brains more than positive or neutral experiences do. She or he may have been holding resentment against the grandparent and living it out for years and now in her/his parenting.
Suddenly, you and the parent may hear the grandparent reveal other factors that would never have been visible to the child then and may never have been brought up because the grandparent was working three jobs because the father was deployed; caring for a sick sibling; suffering from depression; being subject to an abusive alcoholic spouse; having to keep the children inside because of shooting in the neighborhood, etc. You may be able reframe what is said to point out that the grandparents “did the best they could at the time and with the resources and skills they possessed then.”
Mothers who had troubled relationships with their own mothers (e.g. insecure attachment) tend to pass these patterns down in their own parenting unless they have processed the experiences and come to a place of acceptance. People may process their past effectively on their own, some through mental health counseling or religion, but for others a brief “Ah ha!” moment may help settle the waters.
Ask the grandparent as well as the parent, “What are you hoping will go differently than when [parent] was growing up?” Some try to make up for what they see as their own mistakes by advocating coming down harder on their grandchildren than they did on their own. An example among my patients was the grandmother whose daughter had become a heroin user, who was very strict and critical in her determination that her granddaughter would not fall into the wrong crowd. Voicing this for her as a possible reason for her strident posture dramatically shifted her attitude.
Other times parents, maybe grateful for a place to live with the grandparents but also trapped there financially, are simmering with anger at the grandparents’ intrusions into their parenting choices. It can be useful to point out that grandparents, no longer caught up in careers, may feel the need to be useful and have a role by giving advice or bustling around cleaning and buying things for their grandchildren. Hey, any help can be welcome if you don’t take it as meaning you are not doing a good job! Although limits can be set.
Transitioning to regarding one’s grown child as an adult and letting them make their own choices and mistakes, waiting until asked for advice, can take a lot of tongue biting after years of active parenting. One essay I read about an adult’s fond memories of his father included the realization that some of the best parenting he recalled was when his father left things unsaid.
Cultural differences in parenting between grandparent and parent can be another source of stress. Assimilation happens fast in America. The newest generation is often trying very hard NOT to be like the “old country.” The parents’ turning away from the grandparents’ culture or religion can threaten their values and culture for which they may have sacrificed everything. Advising the parent to celebrate at least some traditions may reduce the tension at little cost.
As of 2016, 5% of U.S. children in two-parent families lived with a grandparent and 15% of single parents do. This is much higher in certain ethnic groups where living with your adult children is expected. Even if not living together, their influence may be great. Many parents report more stress than support from grandparents. Negative mother-in-law stories abound! That is why simply asking if the parent “has anyone to help them” as a way of assessing social support can be very misleading. You also may ask “Is that more a help or a problem?”
When grandparents undermine the parents’ rules, of course, a family meeting is in order. But grandparents, with the wisdom of years and reduced life pressure, tend to care for children more generously and less critically than when they were main caregivers, conveying unconditional love that can buffer stresses and be remembered by the beloved child forever.
Dr. Howard is assistant professor of pediatrics at Johns Hopkins University, Baltimore, and creator of CHADIS. She had no other relevant disclosures. Dr. Howard’s contribution to this publication was as a paid expert to MDedge News. E-mail her at [email protected].
One of the things that makes pediatrics challenging and potentially rewarding is that there are often multiple family members in the room for our visits.
With an expansion of our acknowledged role safeguarding and promoting a child’s current and future health to include asking about environmental and caregiving influences comes some tricky dynamics. The parent is in the room with a teen who has a secret love life. A father is in the room with the mother he threatens at home. The mother is in the room with the preschooler she has hit. There is risk but also opportunity for valuable discourse, discovery, and healing.
We now know that about 50% of the future morbidity of the child before us will be determined by the adverse childhood experiences (ACEs) they experience during the exact years (0-18) they are under our health supervision. Many of these risk factors come from home life and may be preventable or at least moderated. When we begin screening for ACEs we are asking the parents about bad things that happened when they were growing up.
The dilemma that came up recently was the grandmother in the room with the daughter she raised who is now caring for her own child. In this situation, you may be in the presence of the person whom the parent feels inflicted – or failed to prevent – the hurts being discussed.
“How are things at home?” you ask dutifully. Mother says “Fine,” but rolls her eyes. Grandma, sitting in the room looking at her phone, says something to the mother in a foreign language. You are in the dark, but sense friction.
Even in modern times, it is respectful to address the grandparent who is present first in a visit, introducing yourself, and finding out the relationship and living situation. Previsit questionnaires can help set visit priorities and alert you to what topics may be better discussed in private, perhaps including ACEs. It is important to ask the parent permission to discuss potentially sensitive topics when the grandparent is present or ask for the grandparent to step out of the room.
Why not just be sure the grandmother stays in the waiting room? If the hurts from the past still are affecting the mother now, moderating an open conversation about those experiences can be very valuable to reducing their impact on present parenting or dysfunctional coping strategies.
Some experts say that any enumeration of ACEs should include asking “Which of these are still bothering you now?” Saying, “Parenting often brings up memories of similar situations from when we were young that can tilt how we act toward our own children,” then asking, “Can we talk about those experiences you had?”
Eliciting the grandparent’s perspective with a question such as “What were those years of parenting like for you?” respects the significance of the grandparent’s role. The grandparents probably were young, stressed, and inexperienced when they were the mother’s primary caregivers. Or the grandparent may have gratefully erased memories of the tough moments but the parent clearly remembers the childhood pain, because hurts sear themselves into our brains more than positive or neutral experiences do. She or he may have been holding resentment against the grandparent and living it out for years and now in her/his parenting.
Suddenly, you and the parent may hear the grandparent reveal other factors that would never have been visible to the child then and may never have been brought up because the grandparent was working three jobs because the father was deployed; caring for a sick sibling; suffering from depression; being subject to an abusive alcoholic spouse; having to keep the children inside because of shooting in the neighborhood, etc. You may be able reframe what is said to point out that the grandparents “did the best they could at the time and with the resources and skills they possessed then.”
Mothers who had troubled relationships with their own mothers (e.g. insecure attachment) tend to pass these patterns down in their own parenting unless they have processed the experiences and come to a place of acceptance. People may process their past effectively on their own, some through mental health counseling or religion, but for others a brief “Ah ha!” moment may help settle the waters.
Ask the grandparent as well as the parent, “What are you hoping will go differently than when [parent] was growing up?” Some try to make up for what they see as their own mistakes by advocating coming down harder on their grandchildren than they did on their own. An example among my patients was the grandmother whose daughter had become a heroin user, who was very strict and critical in her determination that her granddaughter would not fall into the wrong crowd. Voicing this for her as a possible reason for her strident posture dramatically shifted her attitude.
Other times parents, maybe grateful for a place to live with the grandparents but also trapped there financially, are simmering with anger at the grandparents’ intrusions into their parenting choices. It can be useful to point out that grandparents, no longer caught up in careers, may feel the need to be useful and have a role by giving advice or bustling around cleaning and buying things for their grandchildren. Hey, any help can be welcome if you don’t take it as meaning you are not doing a good job! Although limits can be set.
Transitioning to regarding one’s grown child as an adult and letting them make their own choices and mistakes, waiting until asked for advice, can take a lot of tongue biting after years of active parenting. One essay I read about an adult’s fond memories of his father included the realization that some of the best parenting he recalled was when his father left things unsaid.
Cultural differences in parenting between grandparent and parent can be another source of stress. Assimilation happens fast in America. The newest generation is often trying very hard NOT to be like the “old country.” The parents’ turning away from the grandparents’ culture or religion can threaten their values and culture for which they may have sacrificed everything. Advising the parent to celebrate at least some traditions may reduce the tension at little cost.
As of 2016, 5% of U.S. children in two-parent families lived with a grandparent and 15% of single parents do. This is much higher in certain ethnic groups where living with your adult children is expected. Even if not living together, their influence may be great. Many parents report more stress than support from grandparents. Negative mother-in-law stories abound! That is why simply asking if the parent “has anyone to help them” as a way of assessing social support can be very misleading. You also may ask “Is that more a help or a problem?”
When grandparents undermine the parents’ rules, of course, a family meeting is in order. But grandparents, with the wisdom of years and reduced life pressure, tend to care for children more generously and less critically than when they were main caregivers, conveying unconditional love that can buffer stresses and be remembered by the beloved child forever.
Dr. Howard is assistant professor of pediatrics at Johns Hopkins University, Baltimore, and creator of CHADIS. She had no other relevant disclosures. Dr. Howard’s contribution to this publication was as a paid expert to MDedge News. E-mail her at [email protected].
Family dinners are good medicine
Intuitively, we have come to believe that adding more to each family members’ schedule – a lesson, an activity, more homework time – is more enriching or meaningful than is a family dinner, which appears to have less direct impact. However, there is a growing body of evidence that, when an entire family eats dinner together 5 or more nights weekly, the emotional health and well-being of all family members is improved. Not only is their health improved, as there is a greater likelihood of eating nutritious food, but so are a child’s school performance and emotional well-being.
But less than 60% of children eat five or more meals with their parents each week (National Center on Addiction and Substance Abuse [CASA], 2012). Few people would suggest that encouraging families to eat dinner together is a bad idea, but time is the ultimate scarce resource. Preparing food and eating together takes time, and parents and children have many demands on that time that feel nonnegotiable, such as homework, exercise, team practice, or work obligations. When you meet with your patients and explain the tremendous health benefits of eating dinner together, you help your patients and their parents make informed decisions about how to rebalance time to prioritize family dinners that have real but fewer obvious impacts then do a piano lesson or dance class.
Of course, children who eat regular family dinners eat more fruits and vegetables and fewer fried foods and soft drinks than do their peers who eat dinner with their families less often. They are less likely to become obese in youth and more likely to eat healthily and maintain a healthy weight once they live on their own as adults.
Scientific evidence of the mental health benefits to children of eating meals with their families first emerged in the 1990s when the National Center on Addiction and Substance Abuse at Columbia University, New York, began surveying various family behaviors and correlating them with the risk of adolescent substance use and misuse. They found strong evidence that when families ate dinner together five or more times weekly (we’ll call this “frequent family dinners”), their adolescents were far less likely to initiate alcohol and cigarette use and less likely to regularly abuse alcohol and drugs. Subsequent studies have demonstrated that the protective effect may be greater for girls than boys and may be greater for alcohol, cigarettes, and marijuana than for other drugs. But earlier age of first use of substances substantially raises the risk of later addiction, so the health benefits of any delay in first use are significant.
Since CASA’s first studies in the 1990s, researchers began paying closer attention to family meals and a variety of psychiatric problems in youth. They demonstrated that frequent family dinners lowered the risk of other externalizing behaviors in youth, including risky sexual behaviors, threats of physical harm, aggression, fights leading to injury, and carrying or using a weapon.1,2 Frequent family dinners are associated with lower rates of disordered eating behaviors and disordered body image in adolescent girls.3,4 Multiple studies have found a powerful association between frequent family dinners and lower rates of depressive symptoms and suicide attempts in both male and female adolescents.1 Frequent family dinners even have been shown to mitigate against the risks of multiple poor health and academic outcomes in children with high adverse childhood experience (ACE) scores.5
Beyond protecting against problems, frequent family meals are associated with improved well-being and performance. Studies have demonstrated positive associations between frequent family meals and higher levels of self-esteem, self-efficacy, and well-being in adolescents, both male and female. They have consistently found significant associations between frequent family meals and higher grade point averages, commitment to learning, and rich vocabularies in children and adolescents, even after adjustment for demographic and other familial factors.6 And children are not the only ones who benefit. Frequent family meals even have been shown to be associated with higher self-reported levels of well-being and self-esteem, and lower levels of stress among parents.7,8 While investing the time in preparing meals and eating them together may sound stressful, it’s clear the benefits outweigh the risks for parents as well as for their children.
It is important to set the framework for what really matters in a family dinner so that your patients can enjoy all of these benefits. Parents may assume that the meal must be prepared from scratch with only fresh, local, or organic ingredients. But what matters most is that the food is delicious and nutritious, and that the time spent eating (and preparing it) is fun, and promotes conversation and connection. Homemade food usually is more nutritious and will bring more of the physical health benefits, but many store-bought ingredients or even take-out options can be healthy and can promote time for the family to sit together and connect. If parents enjoy preparing food, then it’s worthwhile! And they should not worry about having every member of the family together at every meal. Even if only one parent and child are present for a dinner, they each will enjoy the benefits.
Parents can use this time to help promote good habits in their children. Talking about why manners matter while practicing them at the table is powerful for young children. Let them know manners are how we show people that we care about them, whether by taking turns talking or chewing with our mouths closed! Older children and adolescents can learn about how effort is an essential ingredient in every important area in life, from school to meals. Tell them that sometimes the work or effort will be uncomfortable, and pitching in to share the effort lightens everyone’s load. When parents ask for help, they show their children how to do the same and that they have confidence in their child’s ability to be helpful.
Parents should share the joy of the effort, too! They can invite their young children to help with the meal preparation in age-appropriate ways: pulling herbs off of their stems, rinsing vegetables, sprinkling spices, or emptying a box of spaghetti into a pot of water. Older children feel honored to be given bigger responsibilities, such as carrying plates to the table or cutting vegetables (with supervision, when appropriate). And adolescents, exploring their interests and enjoying their independence, may enjoy building their own menus for the family, doing the shopping or leading the preparation of a dish or full meal themselves.
While there is a role for supporting good manners and helpful habits, help parents avoid getting into power struggles with their children over what they will eat or how they conduct themselves at the table. There should be reasonable rules and expectations around mealtime, and predictable, reasonable consequences. If children try a food and don’t like it, they can have a bowl of (nutritious) cereal and stay at the table with the family. Phones should not be allowed at the table, and televisions should be off during the meal (although music may enhance the sense of pleasure or celebration). Mealtime should be time for relaxing, listening, and connecting.
Offer some ideas about how to facilitate conversations. Asking about how a child’s day went may spark conversations sometimes, but usually people benefit from specific questions. What made you really laugh today? What did you have for lunch? Whom did you sit next to on the bus? If a parent starts by telling a story about his or her day, even better! This is especially potent if a parent talks about something embarrassing or challenging, or mentions a failure. Young children will have plenty of these stories, and adolescents build resilience by internalizing the idea that setbacks and difficulties are a normal, healthy part of every day. This is a great time to talk about current events, whether in the news, entertainment, or sports. And telling stories about when children were younger, when the parents were children, or even about grandparents or more distant ancestors is a wonderful way to engage children in the greater story of their family narrative, and is always engaging and memorable.
At a deeper level, the family dinner is a time that recognizes each person’s contribution to a discussion, and facilitates a calm discussion of the families’ history and values. There is connection, communication, and building of trust. Families that cannot schedule a minimum number of dinners or that have dinners filled with tension and conflict, are very likely to have children at risk. For those conflicted and often unhappy families, a pediatrician’s early recognition and intervention could make a meaningful difference.
Dr. Swick is physician in chief at Ohana, Center for Child and Adolescent Behavioral Health, Community Hospital of the Monterey (Calif.) Peninsula. Dr. Jellinek is professor emeritus of psychiatry and pediatrics, Harvard Medical School, Boston. Email them at [email protected].
References
1. J Adolesc Health. 2006;39(3):337-45.
2. J Adolesc. 2010;33(1):187-96.
3. J Adolesc Health. 2009;44(5):431-6.
4. Health Psychol. 2008;27(Suppl 2):s109-17.
5. J Adolesc Health. 2009;45(4):389-95.
6. Pediatrics. 2019 Jul 8. doi: 10.1542/peds.2018-945.
7. Arch Pediatr Adolesc Med. 2004;158(8):792-6.
8. Prev Med. 2018;113:7-12.
Intuitively, we have come to believe that adding more to each family members’ schedule – a lesson, an activity, more homework time – is more enriching or meaningful than is a family dinner, which appears to have less direct impact. However, there is a growing body of evidence that, when an entire family eats dinner together 5 or more nights weekly, the emotional health and well-being of all family members is improved. Not only is their health improved, as there is a greater likelihood of eating nutritious food, but so are a child’s school performance and emotional well-being.
But less than 60% of children eat five or more meals with their parents each week (National Center on Addiction and Substance Abuse [CASA], 2012). Few people would suggest that encouraging families to eat dinner together is a bad idea, but time is the ultimate scarce resource. Preparing food and eating together takes time, and parents and children have many demands on that time that feel nonnegotiable, such as homework, exercise, team practice, or work obligations. When you meet with your patients and explain the tremendous health benefits of eating dinner together, you help your patients and their parents make informed decisions about how to rebalance time to prioritize family dinners that have real but fewer obvious impacts then do a piano lesson or dance class.
Of course, children who eat regular family dinners eat more fruits and vegetables and fewer fried foods and soft drinks than do their peers who eat dinner with their families less often. They are less likely to become obese in youth and more likely to eat healthily and maintain a healthy weight once they live on their own as adults.
Scientific evidence of the mental health benefits to children of eating meals with their families first emerged in the 1990s when the National Center on Addiction and Substance Abuse at Columbia University, New York, began surveying various family behaviors and correlating them with the risk of adolescent substance use and misuse. They found strong evidence that when families ate dinner together five or more times weekly (we’ll call this “frequent family dinners”), their adolescents were far less likely to initiate alcohol and cigarette use and less likely to regularly abuse alcohol and drugs. Subsequent studies have demonstrated that the protective effect may be greater for girls than boys and may be greater for alcohol, cigarettes, and marijuana than for other drugs. But earlier age of first use of substances substantially raises the risk of later addiction, so the health benefits of any delay in first use are significant.
Since CASA’s first studies in the 1990s, researchers began paying closer attention to family meals and a variety of psychiatric problems in youth. They demonstrated that frequent family dinners lowered the risk of other externalizing behaviors in youth, including risky sexual behaviors, threats of physical harm, aggression, fights leading to injury, and carrying or using a weapon.1,2 Frequent family dinners are associated with lower rates of disordered eating behaviors and disordered body image in adolescent girls.3,4 Multiple studies have found a powerful association between frequent family dinners and lower rates of depressive symptoms and suicide attempts in both male and female adolescents.1 Frequent family dinners even have been shown to mitigate against the risks of multiple poor health and academic outcomes in children with high adverse childhood experience (ACE) scores.5
Beyond protecting against problems, frequent family meals are associated with improved well-being and performance. Studies have demonstrated positive associations between frequent family meals and higher levels of self-esteem, self-efficacy, and well-being in adolescents, both male and female. They have consistently found significant associations between frequent family meals and higher grade point averages, commitment to learning, and rich vocabularies in children and adolescents, even after adjustment for demographic and other familial factors.6 And children are not the only ones who benefit. Frequent family meals even have been shown to be associated with higher self-reported levels of well-being and self-esteem, and lower levels of stress among parents.7,8 While investing the time in preparing meals and eating them together may sound stressful, it’s clear the benefits outweigh the risks for parents as well as for their children.
It is important to set the framework for what really matters in a family dinner so that your patients can enjoy all of these benefits. Parents may assume that the meal must be prepared from scratch with only fresh, local, or organic ingredients. But what matters most is that the food is delicious and nutritious, and that the time spent eating (and preparing it) is fun, and promotes conversation and connection. Homemade food usually is more nutritious and will bring more of the physical health benefits, but many store-bought ingredients or even take-out options can be healthy and can promote time for the family to sit together and connect. If parents enjoy preparing food, then it’s worthwhile! And they should not worry about having every member of the family together at every meal. Even if only one parent and child are present for a dinner, they each will enjoy the benefits.
Parents can use this time to help promote good habits in their children. Talking about why manners matter while practicing them at the table is powerful for young children. Let them know manners are how we show people that we care about them, whether by taking turns talking or chewing with our mouths closed! Older children and adolescents can learn about how effort is an essential ingredient in every important area in life, from school to meals. Tell them that sometimes the work or effort will be uncomfortable, and pitching in to share the effort lightens everyone’s load. When parents ask for help, they show their children how to do the same and that they have confidence in their child’s ability to be helpful.
Parents should share the joy of the effort, too! They can invite their young children to help with the meal preparation in age-appropriate ways: pulling herbs off of their stems, rinsing vegetables, sprinkling spices, or emptying a box of spaghetti into a pot of water. Older children feel honored to be given bigger responsibilities, such as carrying plates to the table or cutting vegetables (with supervision, when appropriate). And adolescents, exploring their interests and enjoying their independence, may enjoy building their own menus for the family, doing the shopping or leading the preparation of a dish or full meal themselves.
While there is a role for supporting good manners and helpful habits, help parents avoid getting into power struggles with their children over what they will eat or how they conduct themselves at the table. There should be reasonable rules and expectations around mealtime, and predictable, reasonable consequences. If children try a food and don’t like it, they can have a bowl of (nutritious) cereal and stay at the table with the family. Phones should not be allowed at the table, and televisions should be off during the meal (although music may enhance the sense of pleasure or celebration). Mealtime should be time for relaxing, listening, and connecting.
Offer some ideas about how to facilitate conversations. Asking about how a child’s day went may spark conversations sometimes, but usually people benefit from specific questions. What made you really laugh today? What did you have for lunch? Whom did you sit next to on the bus? If a parent starts by telling a story about his or her day, even better! This is especially potent if a parent talks about something embarrassing or challenging, or mentions a failure. Young children will have plenty of these stories, and adolescents build resilience by internalizing the idea that setbacks and difficulties are a normal, healthy part of every day. This is a great time to talk about current events, whether in the news, entertainment, or sports. And telling stories about when children were younger, when the parents were children, or even about grandparents or more distant ancestors is a wonderful way to engage children in the greater story of their family narrative, and is always engaging and memorable.
At a deeper level, the family dinner is a time that recognizes each person’s contribution to a discussion, and facilitates a calm discussion of the families’ history and values. There is connection, communication, and building of trust. Families that cannot schedule a minimum number of dinners or that have dinners filled with tension and conflict, are very likely to have children at risk. For those conflicted and often unhappy families, a pediatrician’s early recognition and intervention could make a meaningful difference.
Dr. Swick is physician in chief at Ohana, Center for Child and Adolescent Behavioral Health, Community Hospital of the Monterey (Calif.) Peninsula. Dr. Jellinek is professor emeritus of psychiatry and pediatrics, Harvard Medical School, Boston. Email them at [email protected].
References
1. J Adolesc Health. 2006;39(3):337-45.
2. J Adolesc. 2010;33(1):187-96.
3. J Adolesc Health. 2009;44(5):431-6.
4. Health Psychol. 2008;27(Suppl 2):s109-17.
5. J Adolesc Health. 2009;45(4):389-95.
6. Pediatrics. 2019 Jul 8. doi: 10.1542/peds.2018-945.
7. Arch Pediatr Adolesc Med. 2004;158(8):792-6.
8. Prev Med. 2018;113:7-12.
Intuitively, we have come to believe that adding more to each family members’ schedule – a lesson, an activity, more homework time – is more enriching or meaningful than is a family dinner, which appears to have less direct impact. However, there is a growing body of evidence that, when an entire family eats dinner together 5 or more nights weekly, the emotional health and well-being of all family members is improved. Not only is their health improved, as there is a greater likelihood of eating nutritious food, but so are a child’s school performance and emotional well-being.
But less than 60% of children eat five or more meals with their parents each week (National Center on Addiction and Substance Abuse [CASA], 2012). Few people would suggest that encouraging families to eat dinner together is a bad idea, but time is the ultimate scarce resource. Preparing food and eating together takes time, and parents and children have many demands on that time that feel nonnegotiable, such as homework, exercise, team practice, or work obligations. When you meet with your patients and explain the tremendous health benefits of eating dinner together, you help your patients and their parents make informed decisions about how to rebalance time to prioritize family dinners that have real but fewer obvious impacts then do a piano lesson or dance class.
Of course, children who eat regular family dinners eat more fruits and vegetables and fewer fried foods and soft drinks than do their peers who eat dinner with their families less often. They are less likely to become obese in youth and more likely to eat healthily and maintain a healthy weight once they live on their own as adults.
Scientific evidence of the mental health benefits to children of eating meals with their families first emerged in the 1990s when the National Center on Addiction and Substance Abuse at Columbia University, New York, began surveying various family behaviors and correlating them with the risk of adolescent substance use and misuse. They found strong evidence that when families ate dinner together five or more times weekly (we’ll call this “frequent family dinners”), their adolescents were far less likely to initiate alcohol and cigarette use and less likely to regularly abuse alcohol and drugs. Subsequent studies have demonstrated that the protective effect may be greater for girls than boys and may be greater for alcohol, cigarettes, and marijuana than for other drugs. But earlier age of first use of substances substantially raises the risk of later addiction, so the health benefits of any delay in first use are significant.
Since CASA’s first studies in the 1990s, researchers began paying closer attention to family meals and a variety of psychiatric problems in youth. They demonstrated that frequent family dinners lowered the risk of other externalizing behaviors in youth, including risky sexual behaviors, threats of physical harm, aggression, fights leading to injury, and carrying or using a weapon.1,2 Frequent family dinners are associated with lower rates of disordered eating behaviors and disordered body image in adolescent girls.3,4 Multiple studies have found a powerful association between frequent family dinners and lower rates of depressive symptoms and suicide attempts in both male and female adolescents.1 Frequent family dinners even have been shown to mitigate against the risks of multiple poor health and academic outcomes in children with high adverse childhood experience (ACE) scores.5
Beyond protecting against problems, frequent family meals are associated with improved well-being and performance. Studies have demonstrated positive associations between frequent family meals and higher levels of self-esteem, self-efficacy, and well-being in adolescents, both male and female. They have consistently found significant associations between frequent family meals and higher grade point averages, commitment to learning, and rich vocabularies in children and adolescents, even after adjustment for demographic and other familial factors.6 And children are not the only ones who benefit. Frequent family meals even have been shown to be associated with higher self-reported levels of well-being and self-esteem, and lower levels of stress among parents.7,8 While investing the time in preparing meals and eating them together may sound stressful, it’s clear the benefits outweigh the risks for parents as well as for their children.
It is important to set the framework for what really matters in a family dinner so that your patients can enjoy all of these benefits. Parents may assume that the meal must be prepared from scratch with only fresh, local, or organic ingredients. But what matters most is that the food is delicious and nutritious, and that the time spent eating (and preparing it) is fun, and promotes conversation and connection. Homemade food usually is more nutritious and will bring more of the physical health benefits, but many store-bought ingredients or even take-out options can be healthy and can promote time for the family to sit together and connect. If parents enjoy preparing food, then it’s worthwhile! And they should not worry about having every member of the family together at every meal. Even if only one parent and child are present for a dinner, they each will enjoy the benefits.
Parents can use this time to help promote good habits in their children. Talking about why manners matter while practicing them at the table is powerful for young children. Let them know manners are how we show people that we care about them, whether by taking turns talking or chewing with our mouths closed! Older children and adolescents can learn about how effort is an essential ingredient in every important area in life, from school to meals. Tell them that sometimes the work or effort will be uncomfortable, and pitching in to share the effort lightens everyone’s load. When parents ask for help, they show their children how to do the same and that they have confidence in their child’s ability to be helpful.
Parents should share the joy of the effort, too! They can invite their young children to help with the meal preparation in age-appropriate ways: pulling herbs off of their stems, rinsing vegetables, sprinkling spices, or emptying a box of spaghetti into a pot of water. Older children feel honored to be given bigger responsibilities, such as carrying plates to the table or cutting vegetables (with supervision, when appropriate). And adolescents, exploring their interests and enjoying their independence, may enjoy building their own menus for the family, doing the shopping or leading the preparation of a dish or full meal themselves.
While there is a role for supporting good manners and helpful habits, help parents avoid getting into power struggles with their children over what they will eat or how they conduct themselves at the table. There should be reasonable rules and expectations around mealtime, and predictable, reasonable consequences. If children try a food and don’t like it, they can have a bowl of (nutritious) cereal and stay at the table with the family. Phones should not be allowed at the table, and televisions should be off during the meal (although music may enhance the sense of pleasure or celebration). Mealtime should be time for relaxing, listening, and connecting.
Offer some ideas about how to facilitate conversations. Asking about how a child’s day went may spark conversations sometimes, but usually people benefit from specific questions. What made you really laugh today? What did you have for lunch? Whom did you sit next to on the bus? If a parent starts by telling a story about his or her day, even better! This is especially potent if a parent talks about something embarrassing or challenging, or mentions a failure. Young children will have plenty of these stories, and adolescents build resilience by internalizing the idea that setbacks and difficulties are a normal, healthy part of every day. This is a great time to talk about current events, whether in the news, entertainment, or sports. And telling stories about when children were younger, when the parents were children, or even about grandparents or more distant ancestors is a wonderful way to engage children in the greater story of their family narrative, and is always engaging and memorable.
At a deeper level, the family dinner is a time that recognizes each person’s contribution to a discussion, and facilitates a calm discussion of the families’ history and values. There is connection, communication, and building of trust. Families that cannot schedule a minimum number of dinners or that have dinners filled with tension and conflict, are very likely to have children at risk. For those conflicted and often unhappy families, a pediatrician’s early recognition and intervention could make a meaningful difference.
Dr. Swick is physician in chief at Ohana, Center for Child and Adolescent Behavioral Health, Community Hospital of the Monterey (Calif.) Peninsula. Dr. Jellinek is professor emeritus of psychiatry and pediatrics, Harvard Medical School, Boston. Email them at [email protected].
References
1. J Adolesc Health. 2006;39(3):337-45.
2. J Adolesc. 2010;33(1):187-96.
3. J Adolesc Health. 2009;44(5):431-6.
4. Health Psychol. 2008;27(Suppl 2):s109-17.
5. J Adolesc Health. 2009;45(4):389-95.
6. Pediatrics. 2019 Jul 8. doi: 10.1542/peds.2018-945.
7. Arch Pediatr Adolesc Med. 2004;158(8):792-6.
8. Prev Med. 2018;113:7-12.
Scoring below the cut but still depressed: What to do?
Depression is one of the most common mental health conditions in childhood, especially during socially turbulent adolescence when the brain is rapidly changing and parent-child relationships are strained by the teen’s striving for independence and identity. Often parents of teens call me worrying about possible depression, but in the next breath say “but maybe it is just puberty.” Because suicide is one of the most common causes of death among teens and is often associated with depression, we pediatricians have the scary job of sorting out symptoms and making a plan.
The Guidelines for Adolescent Depression in Primary Care (GLAD-PC)1,2 were revised in 2018 to help. This expert consensus document contains specific and practical guidance for all levels of depression. But for mild depression, GLAD-PC now advises pediatricians in Recommendation II to go beyond “watchful waiting.” It states, “After initial diagnosis,
Although a little vague, mild depression is diagnosed when there are “closer to 5” significant symptoms of depression, with “distressing but manageable” severity and only “mildly impaired” functioning. The most commonly used self-report adolescent depression screen, the Patient Health Questionnaire–Modified–9 (PHQ-9), has a recommended cut score of greater than 10, but 5-9 is considered mild depression symptoms. A clinical interview also is always required.
So what is this “active support” being recommended? After making an assessment of symptoms, severity, and impact – and ruling out significant suicide risk – the task is rather familiar to us from other medical conditions. We need to talk clearly and empathetically with the teen (and parents with consent) about depression and its neurological etiology, ask about contributing stress and genetic factors, and describe the typical course with optimism. This discussion is critical to pushing guilt or blame aside to rally family support. Substance use – (including alcohol) both a cause and attempted coping strategy for depression – must be addressed because it adds to risk for suicide or crashes and because it interacts with medicines.
Perhaps the biggest difference between active support for depression versus that for other conditions is that teens are likely reluctant, hopeless, and/or lacking energy to participate in the plan. The plan, therefore, needs to be approached in smaller steps and build on prior teen strengths, goals, or talents to motivate them and create reward to counteract general lethargy. You may know this teen used to play basketball, or sing at church, or love playing with a baby sister – all activities to try to reawaken. Parents can help recall these and are key to setting up opportunities.
GLAD-PC provides a “Self-Care Success!” worksheet of categories for goal setting for active support. These goals include:
- Stay physically active. Specified days/month, minutes/session, and dates and times.
- Engage spirituality and fun activities. Specify times/week, when, and with whom).
- Eat balanced meals. Specify number/day and names of foods.
- Spend time with people who can support you. Specify number/month, minutes/time, with whom, and doing what.
- Spend time relaxing. Specify days/week, minutes/time, and doing what.
- Determine small goals and simple steps. Establish these for a specified problem.
There is now evidence for these you can share with your teen patients and families.
Exercise
Exercise has a moderate effect size of 0.56 on depression, comparable to medications for mild to moderate depression and a useful adjunct to medications. The national Office of Disease Prevention and Health Promotion recommends that 6- to 17-year-olds get 60 minutes/day of moderate exercise or undertake vigorous “out of breath” exercise three times a week to maintain health. A meta-analysis of studies of yoga for people with depressive symptoms (not necessarily diagnosed depression) found reduced symptoms in 14 of 23 studies.
Pleasure
Advising fun has to include acknowledgment that a depressed teen is not motivated to do formerly fun things and may not get as much/any pleasure from it. You need to explain that “doing precedes feeling.” While what is fun is personal, new findings indicate that 2 hours/week “in nature” lowers stress, boosts mental health, and increases sense of well-being.
Nutrition
The MIND diet (Mediterranean-type diet high in leafy vegetables and berries but low in red meat) has evidence for lower odds of depression and psychological distress. Fatty acid supplements, specifically eicosapentaenoic acid at greater than 800 mg/day (930 mg), is better than placebo (P less than .001) for reducing mild depression within as little as 4 weeks. Natural S-Adenosyl-L-methionine (SAMe) has many studies showing benefit, according to National Center for Complementary and Alternative Medicine, a government-run website. NCCAM notes that St. John’s Wort has evidence for effectiveness equal to prescribed antidepressants for mild depression but with dangerous potential side effects, such as worsening of psychotic symptoms in bipolar disorder or schizophrenia, plus potentially life threatening drug interactions. While safe, valerian and probiotics have no evidence for reducing depression.
Social support
Family is usually the most important support for depressed teens even though they may be pushing family away, may refuse to come on outings, or may even refuse to come out of the bedroom. We should encourage parents and siblings to “hang out,” sitting quietly, available to listen rather than probing, cajoling, or nagging as they may have been doing. Parents also provide support by assuring adherence to visits, goals, and medications. Peer support helps a teen feel less alone and may increase social skills, but it can be difficult to sustain because friends may find depression threatening or give up when the teen avoids them and refuses activities. The National Association for Mental Illness has an online support group (www.strengthofus.org), as well as many excellent family resources. Sometimes medical efforts to be nonsectarian result in failure to recognize and remind teens and families of the value of religion, which is free and universally available, as a source of social support.
Relaxation
An evaluation of 15 studies concluded that relaxation techniques reduced depressive symptoms better than no treatment but not as much cognitive-behavior therapy (CBT). Yoga is another source of relaxation training. Mindfulness includes relaxation and specifies working to stay nonjudgmental about thoughts passing through one’s mind, recognizing and “arguing” with negative thinking, which is also part of CBT. Guided relaxation with a person, audiotape, or app (Calm or Headspace, among others) may be better for depressed teens because it inserts a voice to guide thoughts, which could potentially fend off ruminating on sad things.
Setting goals to address problems
In mild depression, compared with more endogenous moderate to severe major depressive disorder, a specific life stressor or relationship issue may be the precipitant. Identifying such factors (never forgetting possible trauma or abuse, which are harder to reveal), empathizing with the pain, and addressing them such as using Problem Solving Treatment for Primary Care (PST-PC) are within primary care skills. PST-PC involves four to six 30-minute sessions over 6-10 weeks during which you can provide perspective, help your patient set realistic goals and solutions to try out for situations that can be changed or coping strategies for emotion-focused unchangeable issues, iteratively check on progress via calls or televisits (the monitoring component), and renew problem-solving efforts as needed.
If mild depression fails to improve over several months or worsens, GLAD-PC describes evidence-based treatments. Even if it remits, your active support and monitoring should continue because depression tends to recur. You may not realize how valuable these seemingly simple active supports are to keeping mild depression in your teen patients at bay.
Dr. Howard is an assistant professor of pediatrics at Johns Hopkins University, Baltimore, and creator of CHADIS (www.CHADIS.com). She had no other relevant disclosures. Dr. Howard’s contribution to this publication was as a paid expert to MDedge News. E-mail her at [email protected].
References
1. Pediatrics. 2018 Mar 1. doi: 10.1542/peds.2017-4081.
2. Pediatrics. 2018 Mar 1. doi: 10.1542/peds.2017-4082.
Depression is one of the most common mental health conditions in childhood, especially during socially turbulent adolescence when the brain is rapidly changing and parent-child relationships are strained by the teen’s striving for independence and identity. Often parents of teens call me worrying about possible depression, but in the next breath say “but maybe it is just puberty.” Because suicide is one of the most common causes of death among teens and is often associated with depression, we pediatricians have the scary job of sorting out symptoms and making a plan.
The Guidelines for Adolescent Depression in Primary Care (GLAD-PC)1,2 were revised in 2018 to help. This expert consensus document contains specific and practical guidance for all levels of depression. But for mild depression, GLAD-PC now advises pediatricians in Recommendation II to go beyond “watchful waiting.” It states, “After initial diagnosis,
Although a little vague, mild depression is diagnosed when there are “closer to 5” significant symptoms of depression, with “distressing but manageable” severity and only “mildly impaired” functioning. The most commonly used self-report adolescent depression screen, the Patient Health Questionnaire–Modified–9 (PHQ-9), has a recommended cut score of greater than 10, but 5-9 is considered mild depression symptoms. A clinical interview also is always required.
So what is this “active support” being recommended? After making an assessment of symptoms, severity, and impact – and ruling out significant suicide risk – the task is rather familiar to us from other medical conditions. We need to talk clearly and empathetically with the teen (and parents with consent) about depression and its neurological etiology, ask about contributing stress and genetic factors, and describe the typical course with optimism. This discussion is critical to pushing guilt or blame aside to rally family support. Substance use – (including alcohol) both a cause and attempted coping strategy for depression – must be addressed because it adds to risk for suicide or crashes and because it interacts with medicines.
Perhaps the biggest difference between active support for depression versus that for other conditions is that teens are likely reluctant, hopeless, and/or lacking energy to participate in the plan. The plan, therefore, needs to be approached in smaller steps and build on prior teen strengths, goals, or talents to motivate them and create reward to counteract general lethargy. You may know this teen used to play basketball, or sing at church, or love playing with a baby sister – all activities to try to reawaken. Parents can help recall these and are key to setting up opportunities.
GLAD-PC provides a “Self-Care Success!” worksheet of categories for goal setting for active support. These goals include:
- Stay physically active. Specified days/month, minutes/session, and dates and times.
- Engage spirituality and fun activities. Specify times/week, when, and with whom).
- Eat balanced meals. Specify number/day and names of foods.
- Spend time with people who can support you. Specify number/month, minutes/time, with whom, and doing what.
- Spend time relaxing. Specify days/week, minutes/time, and doing what.
- Determine small goals and simple steps. Establish these for a specified problem.
There is now evidence for these you can share with your teen patients and families.
Exercise
Exercise has a moderate effect size of 0.56 on depression, comparable to medications for mild to moderate depression and a useful adjunct to medications. The national Office of Disease Prevention and Health Promotion recommends that 6- to 17-year-olds get 60 minutes/day of moderate exercise or undertake vigorous “out of breath” exercise three times a week to maintain health. A meta-analysis of studies of yoga for people with depressive symptoms (not necessarily diagnosed depression) found reduced symptoms in 14 of 23 studies.
Pleasure
Advising fun has to include acknowledgment that a depressed teen is not motivated to do formerly fun things and may not get as much/any pleasure from it. You need to explain that “doing precedes feeling.” While what is fun is personal, new findings indicate that 2 hours/week “in nature” lowers stress, boosts mental health, and increases sense of well-being.
Nutrition
The MIND diet (Mediterranean-type diet high in leafy vegetables and berries but low in red meat) has evidence for lower odds of depression and psychological distress. Fatty acid supplements, specifically eicosapentaenoic acid at greater than 800 mg/day (930 mg), is better than placebo (P less than .001) for reducing mild depression within as little as 4 weeks. Natural S-Adenosyl-L-methionine (SAMe) has many studies showing benefit, according to National Center for Complementary and Alternative Medicine, a government-run website. NCCAM notes that St. John’s Wort has evidence for effectiveness equal to prescribed antidepressants for mild depression but with dangerous potential side effects, such as worsening of psychotic symptoms in bipolar disorder or schizophrenia, plus potentially life threatening drug interactions. While safe, valerian and probiotics have no evidence for reducing depression.
Social support
Family is usually the most important support for depressed teens even though they may be pushing family away, may refuse to come on outings, or may even refuse to come out of the bedroom. We should encourage parents and siblings to “hang out,” sitting quietly, available to listen rather than probing, cajoling, or nagging as they may have been doing. Parents also provide support by assuring adherence to visits, goals, and medications. Peer support helps a teen feel less alone and may increase social skills, but it can be difficult to sustain because friends may find depression threatening or give up when the teen avoids them and refuses activities. The National Association for Mental Illness has an online support group (www.strengthofus.org), as well as many excellent family resources. Sometimes medical efforts to be nonsectarian result in failure to recognize and remind teens and families of the value of religion, which is free and universally available, as a source of social support.
Relaxation
An evaluation of 15 studies concluded that relaxation techniques reduced depressive symptoms better than no treatment but not as much cognitive-behavior therapy (CBT). Yoga is another source of relaxation training. Mindfulness includes relaxation and specifies working to stay nonjudgmental about thoughts passing through one’s mind, recognizing and “arguing” with negative thinking, which is also part of CBT. Guided relaxation with a person, audiotape, or app (Calm or Headspace, among others) may be better for depressed teens because it inserts a voice to guide thoughts, which could potentially fend off ruminating on sad things.
Setting goals to address problems
In mild depression, compared with more endogenous moderate to severe major depressive disorder, a specific life stressor or relationship issue may be the precipitant. Identifying such factors (never forgetting possible trauma or abuse, which are harder to reveal), empathizing with the pain, and addressing them such as using Problem Solving Treatment for Primary Care (PST-PC) are within primary care skills. PST-PC involves four to six 30-minute sessions over 6-10 weeks during which you can provide perspective, help your patient set realistic goals and solutions to try out for situations that can be changed or coping strategies for emotion-focused unchangeable issues, iteratively check on progress via calls or televisits (the monitoring component), and renew problem-solving efforts as needed.
If mild depression fails to improve over several months or worsens, GLAD-PC describes evidence-based treatments. Even if it remits, your active support and monitoring should continue because depression tends to recur. You may not realize how valuable these seemingly simple active supports are to keeping mild depression in your teen patients at bay.
Dr. Howard is an assistant professor of pediatrics at Johns Hopkins University, Baltimore, and creator of CHADIS (www.CHADIS.com). She had no other relevant disclosures. Dr. Howard’s contribution to this publication was as a paid expert to MDedge News. E-mail her at [email protected].
References
1. Pediatrics. 2018 Mar 1. doi: 10.1542/peds.2017-4081.
2. Pediatrics. 2018 Mar 1. doi: 10.1542/peds.2017-4082.
Depression is one of the most common mental health conditions in childhood, especially during socially turbulent adolescence when the brain is rapidly changing and parent-child relationships are strained by the teen’s striving for independence and identity. Often parents of teens call me worrying about possible depression, but in the next breath say “but maybe it is just puberty.” Because suicide is one of the most common causes of death among teens and is often associated with depression, we pediatricians have the scary job of sorting out symptoms and making a plan.
The Guidelines for Adolescent Depression in Primary Care (GLAD-PC)1,2 were revised in 2018 to help. This expert consensus document contains specific and practical guidance for all levels of depression. But for mild depression, GLAD-PC now advises pediatricians in Recommendation II to go beyond “watchful waiting.” It states, “After initial diagnosis,
Although a little vague, mild depression is diagnosed when there are “closer to 5” significant symptoms of depression, with “distressing but manageable” severity and only “mildly impaired” functioning. The most commonly used self-report adolescent depression screen, the Patient Health Questionnaire–Modified–9 (PHQ-9), has a recommended cut score of greater than 10, but 5-9 is considered mild depression symptoms. A clinical interview also is always required.
So what is this “active support” being recommended? After making an assessment of symptoms, severity, and impact – and ruling out significant suicide risk – the task is rather familiar to us from other medical conditions. We need to talk clearly and empathetically with the teen (and parents with consent) about depression and its neurological etiology, ask about contributing stress and genetic factors, and describe the typical course with optimism. This discussion is critical to pushing guilt or blame aside to rally family support. Substance use – (including alcohol) both a cause and attempted coping strategy for depression – must be addressed because it adds to risk for suicide or crashes and because it interacts with medicines.
Perhaps the biggest difference between active support for depression versus that for other conditions is that teens are likely reluctant, hopeless, and/or lacking energy to participate in the plan. The plan, therefore, needs to be approached in smaller steps and build on prior teen strengths, goals, or talents to motivate them and create reward to counteract general lethargy. You may know this teen used to play basketball, or sing at church, or love playing with a baby sister – all activities to try to reawaken. Parents can help recall these and are key to setting up opportunities.
GLAD-PC provides a “Self-Care Success!” worksheet of categories for goal setting for active support. These goals include:
- Stay physically active. Specified days/month, minutes/session, and dates and times.
- Engage spirituality and fun activities. Specify times/week, when, and with whom).
- Eat balanced meals. Specify number/day and names of foods.
- Spend time with people who can support you. Specify number/month, minutes/time, with whom, and doing what.
- Spend time relaxing. Specify days/week, minutes/time, and doing what.
- Determine small goals and simple steps. Establish these for a specified problem.
There is now evidence for these you can share with your teen patients and families.
Exercise
Exercise has a moderate effect size of 0.56 on depression, comparable to medications for mild to moderate depression and a useful adjunct to medications. The national Office of Disease Prevention and Health Promotion recommends that 6- to 17-year-olds get 60 minutes/day of moderate exercise or undertake vigorous “out of breath” exercise three times a week to maintain health. A meta-analysis of studies of yoga for people with depressive symptoms (not necessarily diagnosed depression) found reduced symptoms in 14 of 23 studies.
Pleasure
Advising fun has to include acknowledgment that a depressed teen is not motivated to do formerly fun things and may not get as much/any pleasure from it. You need to explain that “doing precedes feeling.” While what is fun is personal, new findings indicate that 2 hours/week “in nature” lowers stress, boosts mental health, and increases sense of well-being.
Nutrition
The MIND diet (Mediterranean-type diet high in leafy vegetables and berries but low in red meat) has evidence for lower odds of depression and psychological distress. Fatty acid supplements, specifically eicosapentaenoic acid at greater than 800 mg/day (930 mg), is better than placebo (P less than .001) for reducing mild depression within as little as 4 weeks. Natural S-Adenosyl-L-methionine (SAMe) has many studies showing benefit, according to National Center for Complementary and Alternative Medicine, a government-run website. NCCAM notes that St. John’s Wort has evidence for effectiveness equal to prescribed antidepressants for mild depression but with dangerous potential side effects, such as worsening of psychotic symptoms in bipolar disorder or schizophrenia, plus potentially life threatening drug interactions. While safe, valerian and probiotics have no evidence for reducing depression.
Social support
Family is usually the most important support for depressed teens even though they may be pushing family away, may refuse to come on outings, or may even refuse to come out of the bedroom. We should encourage parents and siblings to “hang out,” sitting quietly, available to listen rather than probing, cajoling, or nagging as they may have been doing. Parents also provide support by assuring adherence to visits, goals, and medications. Peer support helps a teen feel less alone and may increase social skills, but it can be difficult to sustain because friends may find depression threatening or give up when the teen avoids them and refuses activities. The National Association for Mental Illness has an online support group (www.strengthofus.org), as well as many excellent family resources. Sometimes medical efforts to be nonsectarian result in failure to recognize and remind teens and families of the value of religion, which is free and universally available, as a source of social support.
Relaxation
An evaluation of 15 studies concluded that relaxation techniques reduced depressive symptoms better than no treatment but not as much cognitive-behavior therapy (CBT). Yoga is another source of relaxation training. Mindfulness includes relaxation and specifies working to stay nonjudgmental about thoughts passing through one’s mind, recognizing and “arguing” with negative thinking, which is also part of CBT. Guided relaxation with a person, audiotape, or app (Calm or Headspace, among others) may be better for depressed teens because it inserts a voice to guide thoughts, which could potentially fend off ruminating on sad things.
Setting goals to address problems
In mild depression, compared with more endogenous moderate to severe major depressive disorder, a specific life stressor or relationship issue may be the precipitant. Identifying such factors (never forgetting possible trauma or abuse, which are harder to reveal), empathizing with the pain, and addressing them such as using Problem Solving Treatment for Primary Care (PST-PC) are within primary care skills. PST-PC involves four to six 30-minute sessions over 6-10 weeks during which you can provide perspective, help your patient set realistic goals and solutions to try out for situations that can be changed or coping strategies for emotion-focused unchangeable issues, iteratively check on progress via calls or televisits (the monitoring component), and renew problem-solving efforts as needed.
If mild depression fails to improve over several months or worsens, GLAD-PC describes evidence-based treatments. Even if it remits, your active support and monitoring should continue because depression tends to recur. You may not realize how valuable these seemingly simple active supports are to keeping mild depression in your teen patients at bay.
Dr. Howard is an assistant professor of pediatrics at Johns Hopkins University, Baltimore, and creator of CHADIS (www.CHADIS.com). She had no other relevant disclosures. Dr. Howard’s contribution to this publication was as a paid expert to MDedge News. E-mail her at [email protected].
References
1. Pediatrics. 2018 Mar 1. doi: 10.1542/peds.2017-4081.
2. Pediatrics. 2018 Mar 1. doi: 10.1542/peds.2017-4082.
Is there an epidemic of anxiety and depression among today’s adolescents?
It seems that every week there are fresh headlines about a mental health crisis in children and adolescents, reporting exploding rates of severe anxiety and depression in youth. These reports raise the question of whether or not there has been a significant change in their incidence: Are more children developing depressive and anxiety disorders? Are they having greater difficulty accessing care? Are the disorders more severe than they were in the past? Or are young people failing to develop appropriate skills to manage anxiety, sadness, and other forms of distress that are a normal (if unpleasant) part of life? These are important questions, as they will help us to advocate for the proper services to address the public health challenge that underlies this “epidemic.”
What do the data show?
It is important to start by noting that epidemiologic data on child psychiatry in the United States are not as robust as we might like. It was only in 1999 that the Surgeon General’s Report on Mental Health articulated that there was a need for a more systematic approach to collecting epidemiologic data on psychiatric illness in children and adolescents. At that time, the consensus was that approximately one in five children would develop a psychiatric illness by the age of 18 and that approximately 5% of all children would experience a severe or persistent mental illness.1 In the 2 decades since then there have been expanded efforts to collect data, including the addition of an adolescent supplement to the National Comorbidity Survey sponsored by the National Institute of Mental Health, although our current estimates still are based on representative surveys of thousands of U.S. children and teenagers, often with questionnaires filled out by their parents. Thus, we may have overestimates of some behavioral disorders that are obvious and of concern to parents or underestimates of certain internalizing disorders such as depression that can remain unstated and contained in the mind of the adolescent. And even with accurate current estimates, our ability to make statements about trends or changes in rates of disease is limited by the very short period of time in which we have been studying these disease rates in U.S. youth, some changes in definitions, and the unknown impact of increasing recognition rather than true change in incidence.
What is unequivocally clear is that psychiatric illnesses usually present in youth and that these illnesses are among the most common illnesses of youth. Current estimates are that nearly one in four young people will have a psychiatric illness (by The Diagnostic and Statistical Manual of Mental Disorders [DSM], Fifth Edition criteria) by the time they turn 18,2 although only 10% of youth will experience an illness that meets the Substance Abuse and Mental Health Services Administration criteria for a serious emotional disturbance, or one that has a substantial impact on a child’s ability to function socially, emotionally, and academically.3
While it once was believed that children did not experience psychiatric illness, we now know that the majority of psychiatric illnesses present during childhood, adolescence, and young adulthood. The Centers for Disease Control and Prevention estimates that 50% of lifetime psychiatric illness has presented by the age of 15 years and 75% by the age of 24. Only one-quarter of all lifetime psychiatric illnesses emerge in full adulthood, or after the age of 24. Early diagnosis and treatment can make a significant difference in the overall impact of serious illnesses such as schizophrenia and bipolar disorder. We also can state with confidence that anxiety disorders are the most common psychiatric illnesses of youth, making up over 30% of all diagnoses, followed by disorders of behavior (19%), mood (14%), and then substance use (11%).4 Even compared with asthma (with a prevalence of approximately 11%), widely considered to be among the most common disease of childhood, psychiatric illnesses are the most common in youth.
The question then is whether these numbers are changing. The National Comorbidity Survey conducted in 2014 found that the incidence of major depressive episodes in adolescents had increased significantly between 2005 and 2014, from 9% to 11%.5 This is a survey of nearly 200,000 youth across the United States, interviewed by phone with a structured questionnaire assessing their (self-reported) DSM criteria for a major depressive episode, along with other illnesses. During this time frame, access to specialty mental health providers increased among adolescents, alongside their rate of use of psychiatric medications and inpatient hospitalization.
In Europe, where they have more robust epidemiological data, there also has been a public perception of an increase in depression in adolescents. Studies there have suggested that prevalence rates have not changed significantly, and that the problem actually may be a function of a growing population, greater public awareness, and higher rates of psychological distress.6
In the United States, it is difficult to place the prevalence rates in a meaningful context, given the shorter time frame during which we have been following these rates in young people. It is worth highlighting that although the rates at which young people are gaining access to mental health clinicians, being prescribed medications, and being admitted to psychiatric hospitals all have increased, there has not been an associated decrease in the rate of illness or in the severity of symptoms. It certainly is possible that the increase in use of services by youth is being driven by the increased prevalence of this diagnosis, or it may be that other factors, such as those detailed in international studies, are driving this increase in the incidence of depression.
What about the suicide rate?
Another statistic that addressed the question of whether there may be an epidemic of anxiety and depression in adolescents is the recent increase in the suicide rate. While the rate of completed suicide in 15- to 24-year-olds has been trending upward over the last decade, it is worth noting that this phenomenon appears to be occurring across age groups and is not isolated to adolescents. While adolescents may have a unique underlying set of issues driving the increase, it also may be that factors affecting the entire population (access to firearms, the epidemic of opioid addiction) may be at the core of this worrisome trend.
What about the role of stress?
It is worth noting that there is evidence of an increased rate of psychological distress in adolescents and young adults separate from any increase in the rate of psychiatric illness. Surveys of adolescents in high school and entering college demonstrate higher self-reported rates of severe stress and anxiety. One survey from the American Psychological Association from August 2018 found teenagers reporting higher levels of stress and related sadness and anxiety than the levels among the adults who were surveyed. So more young people are struggling with feelings of anxiety and sadness, without necessarily meeting criteria for a psychiatric illness. This suggests that levels of external stressors may have increased, or that the establishment of healthy coping skills has somehow been compromised in young people, or both.
What can you do as a clinician?
While the broader question of whether actual incidence rates of depression are on the rise will not be settled any time soon, when a patient of yours complains of high levels of stress, anxiety, or feelings of depression, it is very possible that the individual has a psychiatric diagnosis. A quick screening evaluation, using a questionnaire such as the Pediatric Symptom Checklist and/or a brief interview, can indicate if the patient may benefit from a referral.
In addition, all children, including those who have a psychiatric diagnosis, will benefit from a calm, patient, supportive adult who is interested in their distress. It would be very helpful if you are ready to talk about healthy coping skills, and how they are developed over time and only in the setting of actually struggling with some adversity. Help them frame their source of stress as a challenge rather than a threat. Help them identify their meaningful supports, particularly adults who know them well, and offer concrete and practical advice and motivation. And remind them about how self-care is essential to managing the normal stress of adolescence. Have handouts (or virtual ones) ready on good sleep hygiene, the value of exercise, and fact-based nutritional guidance. Offer strategies to manage screen time so that it is a recharging break and not a time sink. Support their identification of other strategies to decompress and manage stress: Are they recharged by time with friends? Exercise? Playing music? Listening to music? Playing video games? They should be building their personalized list, and it should include more active as well as passive strategies. Educate them about the risks of using drugs and alcohol “to relax,” or only having one way of unwinding. Educate your patients and parents about the special value of a mindfulness practice, whether meditation, yoga, or any activity in which they practice a nonjudgmental observation and acceptance of strong emotions.
Accurate prevalence rates can help us consider the statistical probability of a psychiatric diagnosis. By talking with your patients about stressful feelings, you can consider the individual need for a fuller psychiatric evaluation while also helping them reframe their approach to stress to one that is more empowering, adaptive, and healthy.
Dr. Swick is physician in chief at Ohana, Center for Child and Adolescent Behavioral Health, Community Hospital of the Monterey (Calif.) Peninsula. Dr. Jellinek is professor emeritus of psychiatry and pediatrics, Harvard Medical School, Boston. Email them at [email protected].
References
1. Mental Health: A Report of the Surgeon General, National Institutes of Mental Health (1999).
2. Prevalence of psychiatric disorders in childhood and adolescence, in “Mental Health Services: A Public Health Perspective,” 2nd ed. (Oxford, UK: Oxford University Press; 2004, pp. 111-28).
3. Public Health Rep. 2006 May-Jun;121(3):303-10.
4. J Am Acad Child Adolesc Psychiatry. 2010 Oct;49(10):980-9.
5. Pediatrics. 2016 Dec;138(6):e20161878.
6. Depress Anxiety. 2014 Jun;31(6):506-16.
It seems that every week there are fresh headlines about a mental health crisis in children and adolescents, reporting exploding rates of severe anxiety and depression in youth. These reports raise the question of whether or not there has been a significant change in their incidence: Are more children developing depressive and anxiety disorders? Are they having greater difficulty accessing care? Are the disorders more severe than they were in the past? Or are young people failing to develop appropriate skills to manage anxiety, sadness, and other forms of distress that are a normal (if unpleasant) part of life? These are important questions, as they will help us to advocate for the proper services to address the public health challenge that underlies this “epidemic.”
What do the data show?
It is important to start by noting that epidemiologic data on child psychiatry in the United States are not as robust as we might like. It was only in 1999 that the Surgeon General’s Report on Mental Health articulated that there was a need for a more systematic approach to collecting epidemiologic data on psychiatric illness in children and adolescents. At that time, the consensus was that approximately one in five children would develop a psychiatric illness by the age of 18 and that approximately 5% of all children would experience a severe or persistent mental illness.1 In the 2 decades since then there have been expanded efforts to collect data, including the addition of an adolescent supplement to the National Comorbidity Survey sponsored by the National Institute of Mental Health, although our current estimates still are based on representative surveys of thousands of U.S. children and teenagers, often with questionnaires filled out by their parents. Thus, we may have overestimates of some behavioral disorders that are obvious and of concern to parents or underestimates of certain internalizing disorders such as depression that can remain unstated and contained in the mind of the adolescent. And even with accurate current estimates, our ability to make statements about trends or changes in rates of disease is limited by the very short period of time in which we have been studying these disease rates in U.S. youth, some changes in definitions, and the unknown impact of increasing recognition rather than true change in incidence.
What is unequivocally clear is that psychiatric illnesses usually present in youth and that these illnesses are among the most common illnesses of youth. Current estimates are that nearly one in four young people will have a psychiatric illness (by The Diagnostic and Statistical Manual of Mental Disorders [DSM], Fifth Edition criteria) by the time they turn 18,2 although only 10% of youth will experience an illness that meets the Substance Abuse and Mental Health Services Administration criteria for a serious emotional disturbance, or one that has a substantial impact on a child’s ability to function socially, emotionally, and academically.3
While it once was believed that children did not experience psychiatric illness, we now know that the majority of psychiatric illnesses present during childhood, adolescence, and young adulthood. The Centers for Disease Control and Prevention estimates that 50% of lifetime psychiatric illness has presented by the age of 15 years and 75% by the age of 24. Only one-quarter of all lifetime psychiatric illnesses emerge in full adulthood, or after the age of 24. Early diagnosis and treatment can make a significant difference in the overall impact of serious illnesses such as schizophrenia and bipolar disorder. We also can state with confidence that anxiety disorders are the most common psychiatric illnesses of youth, making up over 30% of all diagnoses, followed by disorders of behavior (19%), mood (14%), and then substance use (11%).4 Even compared with asthma (with a prevalence of approximately 11%), widely considered to be among the most common disease of childhood, psychiatric illnesses are the most common in youth.
The question then is whether these numbers are changing. The National Comorbidity Survey conducted in 2014 found that the incidence of major depressive episodes in adolescents had increased significantly between 2005 and 2014, from 9% to 11%.5 This is a survey of nearly 200,000 youth across the United States, interviewed by phone with a structured questionnaire assessing their (self-reported) DSM criteria for a major depressive episode, along with other illnesses. During this time frame, access to specialty mental health providers increased among adolescents, alongside their rate of use of psychiatric medications and inpatient hospitalization.
In Europe, where they have more robust epidemiological data, there also has been a public perception of an increase in depression in adolescents. Studies there have suggested that prevalence rates have not changed significantly, and that the problem actually may be a function of a growing population, greater public awareness, and higher rates of psychological distress.6
In the United States, it is difficult to place the prevalence rates in a meaningful context, given the shorter time frame during which we have been following these rates in young people. It is worth highlighting that although the rates at which young people are gaining access to mental health clinicians, being prescribed medications, and being admitted to psychiatric hospitals all have increased, there has not been an associated decrease in the rate of illness or in the severity of symptoms. It certainly is possible that the increase in use of services by youth is being driven by the increased prevalence of this diagnosis, or it may be that other factors, such as those detailed in international studies, are driving this increase in the incidence of depression.
What about the suicide rate?
Another statistic that addressed the question of whether there may be an epidemic of anxiety and depression in adolescents is the recent increase in the suicide rate. While the rate of completed suicide in 15- to 24-year-olds has been trending upward over the last decade, it is worth noting that this phenomenon appears to be occurring across age groups and is not isolated to adolescents. While adolescents may have a unique underlying set of issues driving the increase, it also may be that factors affecting the entire population (access to firearms, the epidemic of opioid addiction) may be at the core of this worrisome trend.
What about the role of stress?
It is worth noting that there is evidence of an increased rate of psychological distress in adolescents and young adults separate from any increase in the rate of psychiatric illness. Surveys of adolescents in high school and entering college demonstrate higher self-reported rates of severe stress and anxiety. One survey from the American Psychological Association from August 2018 found teenagers reporting higher levels of stress and related sadness and anxiety than the levels among the adults who were surveyed. So more young people are struggling with feelings of anxiety and sadness, without necessarily meeting criteria for a psychiatric illness. This suggests that levels of external stressors may have increased, or that the establishment of healthy coping skills has somehow been compromised in young people, or both.
What can you do as a clinician?
While the broader question of whether actual incidence rates of depression are on the rise will not be settled any time soon, when a patient of yours complains of high levels of stress, anxiety, or feelings of depression, it is very possible that the individual has a psychiatric diagnosis. A quick screening evaluation, using a questionnaire such as the Pediatric Symptom Checklist and/or a brief interview, can indicate if the patient may benefit from a referral.
In addition, all children, including those who have a psychiatric diagnosis, will benefit from a calm, patient, supportive adult who is interested in their distress. It would be very helpful if you are ready to talk about healthy coping skills, and how they are developed over time and only in the setting of actually struggling with some adversity. Help them frame their source of stress as a challenge rather than a threat. Help them identify their meaningful supports, particularly adults who know them well, and offer concrete and practical advice and motivation. And remind them about how self-care is essential to managing the normal stress of adolescence. Have handouts (or virtual ones) ready on good sleep hygiene, the value of exercise, and fact-based nutritional guidance. Offer strategies to manage screen time so that it is a recharging break and not a time sink. Support their identification of other strategies to decompress and manage stress: Are they recharged by time with friends? Exercise? Playing music? Listening to music? Playing video games? They should be building their personalized list, and it should include more active as well as passive strategies. Educate them about the risks of using drugs and alcohol “to relax,” or only having one way of unwinding. Educate your patients and parents about the special value of a mindfulness practice, whether meditation, yoga, or any activity in which they practice a nonjudgmental observation and acceptance of strong emotions.
Accurate prevalence rates can help us consider the statistical probability of a psychiatric diagnosis. By talking with your patients about stressful feelings, you can consider the individual need for a fuller psychiatric evaluation while also helping them reframe their approach to stress to one that is more empowering, adaptive, and healthy.
Dr. Swick is physician in chief at Ohana, Center for Child and Adolescent Behavioral Health, Community Hospital of the Monterey (Calif.) Peninsula. Dr. Jellinek is professor emeritus of psychiatry and pediatrics, Harvard Medical School, Boston. Email them at [email protected].
References
1. Mental Health: A Report of the Surgeon General, National Institutes of Mental Health (1999).
2. Prevalence of psychiatric disorders in childhood and adolescence, in “Mental Health Services: A Public Health Perspective,” 2nd ed. (Oxford, UK: Oxford University Press; 2004, pp. 111-28).
3. Public Health Rep. 2006 May-Jun;121(3):303-10.
4. J Am Acad Child Adolesc Psychiatry. 2010 Oct;49(10):980-9.
5. Pediatrics. 2016 Dec;138(6):e20161878.
6. Depress Anxiety. 2014 Jun;31(6):506-16.
It seems that every week there are fresh headlines about a mental health crisis in children and adolescents, reporting exploding rates of severe anxiety and depression in youth. These reports raise the question of whether or not there has been a significant change in their incidence: Are more children developing depressive and anxiety disorders? Are they having greater difficulty accessing care? Are the disorders more severe than they were in the past? Or are young people failing to develop appropriate skills to manage anxiety, sadness, and other forms of distress that are a normal (if unpleasant) part of life? These are important questions, as they will help us to advocate for the proper services to address the public health challenge that underlies this “epidemic.”
What do the data show?
It is important to start by noting that epidemiologic data on child psychiatry in the United States are not as robust as we might like. It was only in 1999 that the Surgeon General’s Report on Mental Health articulated that there was a need for a more systematic approach to collecting epidemiologic data on psychiatric illness in children and adolescents. At that time, the consensus was that approximately one in five children would develop a psychiatric illness by the age of 18 and that approximately 5% of all children would experience a severe or persistent mental illness.1 In the 2 decades since then there have been expanded efforts to collect data, including the addition of an adolescent supplement to the National Comorbidity Survey sponsored by the National Institute of Mental Health, although our current estimates still are based on representative surveys of thousands of U.S. children and teenagers, often with questionnaires filled out by their parents. Thus, we may have overestimates of some behavioral disorders that are obvious and of concern to parents or underestimates of certain internalizing disorders such as depression that can remain unstated and contained in the mind of the adolescent. And even with accurate current estimates, our ability to make statements about trends or changes in rates of disease is limited by the very short period of time in which we have been studying these disease rates in U.S. youth, some changes in definitions, and the unknown impact of increasing recognition rather than true change in incidence.
What is unequivocally clear is that psychiatric illnesses usually present in youth and that these illnesses are among the most common illnesses of youth. Current estimates are that nearly one in four young people will have a psychiatric illness (by The Diagnostic and Statistical Manual of Mental Disorders [DSM], Fifth Edition criteria) by the time they turn 18,2 although only 10% of youth will experience an illness that meets the Substance Abuse and Mental Health Services Administration criteria for a serious emotional disturbance, or one that has a substantial impact on a child’s ability to function socially, emotionally, and academically.3
While it once was believed that children did not experience psychiatric illness, we now know that the majority of psychiatric illnesses present during childhood, adolescence, and young adulthood. The Centers for Disease Control and Prevention estimates that 50% of lifetime psychiatric illness has presented by the age of 15 years and 75% by the age of 24. Only one-quarter of all lifetime psychiatric illnesses emerge in full adulthood, or after the age of 24. Early diagnosis and treatment can make a significant difference in the overall impact of serious illnesses such as schizophrenia and bipolar disorder. We also can state with confidence that anxiety disorders are the most common psychiatric illnesses of youth, making up over 30% of all diagnoses, followed by disorders of behavior (19%), mood (14%), and then substance use (11%).4 Even compared with asthma (with a prevalence of approximately 11%), widely considered to be among the most common disease of childhood, psychiatric illnesses are the most common in youth.
The question then is whether these numbers are changing. The National Comorbidity Survey conducted in 2014 found that the incidence of major depressive episodes in adolescents had increased significantly between 2005 and 2014, from 9% to 11%.5 This is a survey of nearly 200,000 youth across the United States, interviewed by phone with a structured questionnaire assessing their (self-reported) DSM criteria for a major depressive episode, along with other illnesses. During this time frame, access to specialty mental health providers increased among adolescents, alongside their rate of use of psychiatric medications and inpatient hospitalization.
In Europe, where they have more robust epidemiological data, there also has been a public perception of an increase in depression in adolescents. Studies there have suggested that prevalence rates have not changed significantly, and that the problem actually may be a function of a growing population, greater public awareness, and higher rates of psychological distress.6
In the United States, it is difficult to place the prevalence rates in a meaningful context, given the shorter time frame during which we have been following these rates in young people. It is worth highlighting that although the rates at which young people are gaining access to mental health clinicians, being prescribed medications, and being admitted to psychiatric hospitals all have increased, there has not been an associated decrease in the rate of illness or in the severity of symptoms. It certainly is possible that the increase in use of services by youth is being driven by the increased prevalence of this diagnosis, or it may be that other factors, such as those detailed in international studies, are driving this increase in the incidence of depression.
What about the suicide rate?
Another statistic that addressed the question of whether there may be an epidemic of anxiety and depression in adolescents is the recent increase in the suicide rate. While the rate of completed suicide in 15- to 24-year-olds has been trending upward over the last decade, it is worth noting that this phenomenon appears to be occurring across age groups and is not isolated to adolescents. While adolescents may have a unique underlying set of issues driving the increase, it also may be that factors affecting the entire population (access to firearms, the epidemic of opioid addiction) may be at the core of this worrisome trend.
What about the role of stress?
It is worth noting that there is evidence of an increased rate of psychological distress in adolescents and young adults separate from any increase in the rate of psychiatric illness. Surveys of adolescents in high school and entering college demonstrate higher self-reported rates of severe stress and anxiety. One survey from the American Psychological Association from August 2018 found teenagers reporting higher levels of stress and related sadness and anxiety than the levels among the adults who were surveyed. So more young people are struggling with feelings of anxiety and sadness, without necessarily meeting criteria for a psychiatric illness. This suggests that levels of external stressors may have increased, or that the establishment of healthy coping skills has somehow been compromised in young people, or both.
What can you do as a clinician?
While the broader question of whether actual incidence rates of depression are on the rise will not be settled any time soon, when a patient of yours complains of high levels of stress, anxiety, or feelings of depression, it is very possible that the individual has a psychiatric diagnosis. A quick screening evaluation, using a questionnaire such as the Pediatric Symptom Checklist and/or a brief interview, can indicate if the patient may benefit from a referral.
In addition, all children, including those who have a psychiatric diagnosis, will benefit from a calm, patient, supportive adult who is interested in their distress. It would be very helpful if you are ready to talk about healthy coping skills, and how they are developed over time and only in the setting of actually struggling with some adversity. Help them frame their source of stress as a challenge rather than a threat. Help them identify their meaningful supports, particularly adults who know them well, and offer concrete and practical advice and motivation. And remind them about how self-care is essential to managing the normal stress of adolescence. Have handouts (or virtual ones) ready on good sleep hygiene, the value of exercise, and fact-based nutritional guidance. Offer strategies to manage screen time so that it is a recharging break and not a time sink. Support their identification of other strategies to decompress and manage stress: Are they recharged by time with friends? Exercise? Playing music? Listening to music? Playing video games? They should be building their personalized list, and it should include more active as well as passive strategies. Educate them about the risks of using drugs and alcohol “to relax,” or only having one way of unwinding. Educate your patients and parents about the special value of a mindfulness practice, whether meditation, yoga, or any activity in which they practice a nonjudgmental observation and acceptance of strong emotions.
Accurate prevalence rates can help us consider the statistical probability of a psychiatric diagnosis. By talking with your patients about stressful feelings, you can consider the individual need for a fuller psychiatric evaluation while also helping them reframe their approach to stress to one that is more empowering, adaptive, and healthy.
Dr. Swick is physician in chief at Ohana, Center for Child and Adolescent Behavioral Health, Community Hospital of the Monterey (Calif.) Peninsula. Dr. Jellinek is professor emeritus of psychiatry and pediatrics, Harvard Medical School, Boston. Email them at [email protected].
References
1. Mental Health: A Report of the Surgeon General, National Institutes of Mental Health (1999).
2. Prevalence of psychiatric disorders in childhood and adolescence, in “Mental Health Services: A Public Health Perspective,” 2nd ed. (Oxford, UK: Oxford University Press; 2004, pp. 111-28).
3. Public Health Rep. 2006 May-Jun;121(3):303-10.
4. J Am Acad Child Adolesc Psychiatry. 2010 Oct;49(10):980-9.
5. Pediatrics. 2016 Dec;138(6):e20161878.
6. Depress Anxiety. 2014 Jun;31(6):506-16.
Making an effective referral is surprisingly complex
Referrals actually are a complex procedure that can result in crucial health, developmental, and mental health benefits, yet patients attend referred services at wildly variable rates of 11%-81%, and for mental health and early intervention (EI) less than half the time.1 When surveyed, primary care providers (PCP) say that they want to share in the care of 75% of patients they refer, especially for mental health concerns. Yet after decades of practice, I can count on one hand the number of children I have referred to mental health or EI services for whom I received feedback from the specialist (here meaning agencies or providers outside the office). Lately, if the specialist is using the same EHR, I sometimes discover their note when reviewing the document list, but I was not cc’d. In fact, the most common outcome is that the patient never sees the specialist and we don’t find out until the next visit, often months later when precious time for intervention has passed. Less than 50% of children with a mental health issue that qualifies as a disorder are detected by PCPs, and less than half of those children complete a referral. But there are lots of reasons for that, you say, such as a lack of specialists. But less than half of referrals for toddlers with developmental delays are completed to EI services even when such services are available and free of cost.
What makes referrals so complicated? Lack of referral completion can come from structural factors and interpersonal factors. We and our patients both are frustrated by lack of specialty resources, specialists who do not accept our patient’s insurance (or any insurance), distance, transportation, hours of operation issues, overall life burdens or priorities of families, and of course, cost. We can help with a few of these, either with our own list or ideally with the help of a care coordinator or social worker keeping a list identifying local specialists, payment methods accepted, and perhaps reduced-cost care options or financial assistance. However, the interpersonal issues that can make or break a referral definitely are within our reach.
Some of the reasons patients report for not following through on a referral include not feeling that their PCP evaluated the situation adequately through history or that the PCP failed to perform tests, such as screens. Because 27% of referrals are made based on the first phone contact about an issue (a dump?), and most are made at the first visit an issue is considered (two-thirds for mental health referrals), this feeling is unsurprising and likely true.2 Families often do not know what kind of expertise we have to size up a need, especially if discussion about development or mental health have not been a regular part of care before a problem is detected. Parents of children with developmental delays who declined referral felt they were more expert on their child’s development than the PCP. Another reason given for not attending a referral is that the condition being referred for and what to expect from the referral, including logistics, was not clear to the parents of the patient. Low-literacy parents (30% of low-income samples) did not find written materials helpful. Parents referred to EI services, for example, sometimes thought they were being sent to Child Protective Services or feared notification of immigration. PCPs who have more time for visits and/or had a care navigator available to explain the process have more successful referrals (80%), especially if the manager makes the phone contact, which takes a parent on average seven calls to EI. In some cases, the parent does not agree that a consultation is needed. If this had been part of the referral discussion, a shared understanding might have been attained or an intermediate step chosen.
In many practices, language, literacy, and cultural differences are major barriers. Other barriers come from the parent or another family member denying there is an issue, not believing that the intervention being suggested is effective, concern over stigma for diagnoses such as mental illness or autism, not prioritizing therapies we recommend over other potential solutions such as home efforts or herbal medicine, or simple fear. The key here is for us to both give information and nonjudgmentally listen to the parent’s (or child’s) point of view and barriers, showing empathy by echoing their feelings, then using a motivational interviewing approach to weighing pros and cons of taking steps towards a referral. Requesting a “Talk Back” from the parent of what you tried to convey can assure understanding. The “warm hand off” to a smiling colocated professional that is so helpful at overcoming fear has recently been simulated by onsite tele-intake visits, resulting in 80% of patients keeping a visit for mental health care.3
For collaborative and cost-efficient care, we need to provide the specialist with data we have gathered, what questions we want answered, how best to communicate back, and what role we want in subsequent care. Referral completion is three times higher when PCPs schedule the appointment and communicate with the specialist. We need back a timely note or call about their impression, any tests or treatments initiated, and their ideas about sharing care going forward. A structured referral template makes for more satisfactory communication, but the key is actually sending and receiving it! Most PCPs surveyed count on the family to convey information back from a specialist. This respects their ownership of the issue, but what they tell us may be inaccurate, incomplete, and/or miss concerns the specialist may not have wanted to tell the patient, such as rare but serious possibilities being considered or delicate social issues uncovered.
Great discrepancies have been found between the frequency PCPs report providing information to specialists (69%) and what specialists report about frequency of receipt (38%). PCPs report hearing back about 21% of mental health referrals.4 Both may be true if referral information is lost in the system somewhere. Simply faxing the referral form to EI programs (that routinely contact families) rather than just giving families a phone number (33%) increased referral success to 58%! Text reminders also hold promise. Finally, with such low completion rates, tracking referrals made and information back is crucial, yet only 6 of 17 practices in one study did so.5 Apart from intra-EHR referral, newer software-as-a-service systems can transmit consent forms that include permission and information for the specialist to contact the patient and report on kept appointments (such as CHADIS) as well as exchanging results (such as Salesforce) that hold promise for closing the loop.
New interest by health care systems in better referrals is not just caused by care considerations, but for financial reasons. Specialty care costs more than primary care management, and missed specialist appointments are not only missed opportunities but also costly! And one-half of all outpatient visits are for referrals! This may become the best motivator for your practice or system to undertake a quality improvement project to improve this crucial primary care procedure.
Dr. Howard is assistant professor of pediatrics at Johns Hopkins University, Baltimore, and creator of CHADIS (www.CHADIS.com). She reported no other relevant disclosures. Dr. Howard’s contribution to this publication was as a paid expert to MDedge News. Email her at [email protected]
References
1. Acad Pediatr. 2014 May-Jun;14(3):315-23.
2. Hosp Community Psychiatry. 1992 May;43(5):489-93.
3. Pediatrics. 2019 Mar 1;143(3): e20182738.
4. Arch Pediatr Adolesc Med. 2000 May;154(5):499-506.
5. Pediatrics. 2010 Feb 1. doi: 10.1542/peds.2009-0388.
Referrals actually are a complex procedure that can result in crucial health, developmental, and mental health benefits, yet patients attend referred services at wildly variable rates of 11%-81%, and for mental health and early intervention (EI) less than half the time.1 When surveyed, primary care providers (PCP) say that they want to share in the care of 75% of patients they refer, especially for mental health concerns. Yet after decades of practice, I can count on one hand the number of children I have referred to mental health or EI services for whom I received feedback from the specialist (here meaning agencies or providers outside the office). Lately, if the specialist is using the same EHR, I sometimes discover their note when reviewing the document list, but I was not cc’d. In fact, the most common outcome is that the patient never sees the specialist and we don’t find out until the next visit, often months later when precious time for intervention has passed. Less than 50% of children with a mental health issue that qualifies as a disorder are detected by PCPs, and less than half of those children complete a referral. But there are lots of reasons for that, you say, such as a lack of specialists. But less than half of referrals for toddlers with developmental delays are completed to EI services even when such services are available and free of cost.
What makes referrals so complicated? Lack of referral completion can come from structural factors and interpersonal factors. We and our patients both are frustrated by lack of specialty resources, specialists who do not accept our patient’s insurance (or any insurance), distance, transportation, hours of operation issues, overall life burdens or priorities of families, and of course, cost. We can help with a few of these, either with our own list or ideally with the help of a care coordinator or social worker keeping a list identifying local specialists, payment methods accepted, and perhaps reduced-cost care options or financial assistance. However, the interpersonal issues that can make or break a referral definitely are within our reach.
Some of the reasons patients report for not following through on a referral include not feeling that their PCP evaluated the situation adequately through history or that the PCP failed to perform tests, such as screens. Because 27% of referrals are made based on the first phone contact about an issue (a dump?), and most are made at the first visit an issue is considered (two-thirds for mental health referrals), this feeling is unsurprising and likely true.2 Families often do not know what kind of expertise we have to size up a need, especially if discussion about development or mental health have not been a regular part of care before a problem is detected. Parents of children with developmental delays who declined referral felt they were more expert on their child’s development than the PCP. Another reason given for not attending a referral is that the condition being referred for and what to expect from the referral, including logistics, was not clear to the parents of the patient. Low-literacy parents (30% of low-income samples) did not find written materials helpful. Parents referred to EI services, for example, sometimes thought they were being sent to Child Protective Services or feared notification of immigration. PCPs who have more time for visits and/or had a care navigator available to explain the process have more successful referrals (80%), especially if the manager makes the phone contact, which takes a parent on average seven calls to EI. In some cases, the parent does not agree that a consultation is needed. If this had been part of the referral discussion, a shared understanding might have been attained or an intermediate step chosen.
In many practices, language, literacy, and cultural differences are major barriers. Other barriers come from the parent or another family member denying there is an issue, not believing that the intervention being suggested is effective, concern over stigma for diagnoses such as mental illness or autism, not prioritizing therapies we recommend over other potential solutions such as home efforts or herbal medicine, or simple fear. The key here is for us to both give information and nonjudgmentally listen to the parent’s (or child’s) point of view and barriers, showing empathy by echoing their feelings, then using a motivational interviewing approach to weighing pros and cons of taking steps towards a referral. Requesting a “Talk Back” from the parent of what you tried to convey can assure understanding. The “warm hand off” to a smiling colocated professional that is so helpful at overcoming fear has recently been simulated by onsite tele-intake visits, resulting in 80% of patients keeping a visit for mental health care.3
For collaborative and cost-efficient care, we need to provide the specialist with data we have gathered, what questions we want answered, how best to communicate back, and what role we want in subsequent care. Referral completion is three times higher when PCPs schedule the appointment and communicate with the specialist. We need back a timely note or call about their impression, any tests or treatments initiated, and their ideas about sharing care going forward. A structured referral template makes for more satisfactory communication, but the key is actually sending and receiving it! Most PCPs surveyed count on the family to convey information back from a specialist. This respects their ownership of the issue, but what they tell us may be inaccurate, incomplete, and/or miss concerns the specialist may not have wanted to tell the patient, such as rare but serious possibilities being considered or delicate social issues uncovered.
Great discrepancies have been found between the frequency PCPs report providing information to specialists (69%) and what specialists report about frequency of receipt (38%). PCPs report hearing back about 21% of mental health referrals.4 Both may be true if referral information is lost in the system somewhere. Simply faxing the referral form to EI programs (that routinely contact families) rather than just giving families a phone number (33%) increased referral success to 58%! Text reminders also hold promise. Finally, with such low completion rates, tracking referrals made and information back is crucial, yet only 6 of 17 practices in one study did so.5 Apart from intra-EHR referral, newer software-as-a-service systems can transmit consent forms that include permission and information for the specialist to contact the patient and report on kept appointments (such as CHADIS) as well as exchanging results (such as Salesforce) that hold promise for closing the loop.
New interest by health care systems in better referrals is not just caused by care considerations, but for financial reasons. Specialty care costs more than primary care management, and missed specialist appointments are not only missed opportunities but also costly! And one-half of all outpatient visits are for referrals! This may become the best motivator for your practice or system to undertake a quality improvement project to improve this crucial primary care procedure.
Dr. Howard is assistant professor of pediatrics at Johns Hopkins University, Baltimore, and creator of CHADIS (www.CHADIS.com). She reported no other relevant disclosures. Dr. Howard’s contribution to this publication was as a paid expert to MDedge News. Email her at [email protected]
References
1. Acad Pediatr. 2014 May-Jun;14(3):315-23.
2. Hosp Community Psychiatry. 1992 May;43(5):489-93.
3. Pediatrics. 2019 Mar 1;143(3): e20182738.
4. Arch Pediatr Adolesc Med. 2000 May;154(5):499-506.
5. Pediatrics. 2010 Feb 1. doi: 10.1542/peds.2009-0388.
Referrals actually are a complex procedure that can result in crucial health, developmental, and mental health benefits, yet patients attend referred services at wildly variable rates of 11%-81%, and for mental health and early intervention (EI) less than half the time.1 When surveyed, primary care providers (PCP) say that they want to share in the care of 75% of patients they refer, especially for mental health concerns. Yet after decades of practice, I can count on one hand the number of children I have referred to mental health or EI services for whom I received feedback from the specialist (here meaning agencies or providers outside the office). Lately, if the specialist is using the same EHR, I sometimes discover their note when reviewing the document list, but I was not cc’d. In fact, the most common outcome is that the patient never sees the specialist and we don’t find out until the next visit, often months later when precious time for intervention has passed. Less than 50% of children with a mental health issue that qualifies as a disorder are detected by PCPs, and less than half of those children complete a referral. But there are lots of reasons for that, you say, such as a lack of specialists. But less than half of referrals for toddlers with developmental delays are completed to EI services even when such services are available and free of cost.
What makes referrals so complicated? Lack of referral completion can come from structural factors and interpersonal factors. We and our patients both are frustrated by lack of specialty resources, specialists who do not accept our patient’s insurance (or any insurance), distance, transportation, hours of operation issues, overall life burdens or priorities of families, and of course, cost. We can help with a few of these, either with our own list or ideally with the help of a care coordinator or social worker keeping a list identifying local specialists, payment methods accepted, and perhaps reduced-cost care options or financial assistance. However, the interpersonal issues that can make or break a referral definitely are within our reach.
Some of the reasons patients report for not following through on a referral include not feeling that their PCP evaluated the situation adequately through history or that the PCP failed to perform tests, such as screens. Because 27% of referrals are made based on the first phone contact about an issue (a dump?), and most are made at the first visit an issue is considered (two-thirds for mental health referrals), this feeling is unsurprising and likely true.2 Families often do not know what kind of expertise we have to size up a need, especially if discussion about development or mental health have not been a regular part of care before a problem is detected. Parents of children with developmental delays who declined referral felt they were more expert on their child’s development than the PCP. Another reason given for not attending a referral is that the condition being referred for and what to expect from the referral, including logistics, was not clear to the parents of the patient. Low-literacy parents (30% of low-income samples) did not find written materials helpful. Parents referred to EI services, for example, sometimes thought they were being sent to Child Protective Services or feared notification of immigration. PCPs who have more time for visits and/or had a care navigator available to explain the process have more successful referrals (80%), especially if the manager makes the phone contact, which takes a parent on average seven calls to EI. In some cases, the parent does not agree that a consultation is needed. If this had been part of the referral discussion, a shared understanding might have been attained or an intermediate step chosen.
In many practices, language, literacy, and cultural differences are major barriers. Other barriers come from the parent or another family member denying there is an issue, not believing that the intervention being suggested is effective, concern over stigma for diagnoses such as mental illness or autism, not prioritizing therapies we recommend over other potential solutions such as home efforts or herbal medicine, or simple fear. The key here is for us to both give information and nonjudgmentally listen to the parent’s (or child’s) point of view and barriers, showing empathy by echoing their feelings, then using a motivational interviewing approach to weighing pros and cons of taking steps towards a referral. Requesting a “Talk Back” from the parent of what you tried to convey can assure understanding. The “warm hand off” to a smiling colocated professional that is so helpful at overcoming fear has recently been simulated by onsite tele-intake visits, resulting in 80% of patients keeping a visit for mental health care.3
For collaborative and cost-efficient care, we need to provide the specialist with data we have gathered, what questions we want answered, how best to communicate back, and what role we want in subsequent care. Referral completion is three times higher when PCPs schedule the appointment and communicate with the specialist. We need back a timely note or call about their impression, any tests or treatments initiated, and their ideas about sharing care going forward. A structured referral template makes for more satisfactory communication, but the key is actually sending and receiving it! Most PCPs surveyed count on the family to convey information back from a specialist. This respects their ownership of the issue, but what they tell us may be inaccurate, incomplete, and/or miss concerns the specialist may not have wanted to tell the patient, such as rare but serious possibilities being considered or delicate social issues uncovered.
Great discrepancies have been found between the frequency PCPs report providing information to specialists (69%) and what specialists report about frequency of receipt (38%). PCPs report hearing back about 21% of mental health referrals.4 Both may be true if referral information is lost in the system somewhere. Simply faxing the referral form to EI programs (that routinely contact families) rather than just giving families a phone number (33%) increased referral success to 58%! Text reminders also hold promise. Finally, with such low completion rates, tracking referrals made and information back is crucial, yet only 6 of 17 practices in one study did so.5 Apart from intra-EHR referral, newer software-as-a-service systems can transmit consent forms that include permission and information for the specialist to contact the patient and report on kept appointments (such as CHADIS) as well as exchanging results (such as Salesforce) that hold promise for closing the loop.
New interest by health care systems in better referrals is not just caused by care considerations, but for financial reasons. Specialty care costs more than primary care management, and missed specialist appointments are not only missed opportunities but also costly! And one-half of all outpatient visits are for referrals! This may become the best motivator for your practice or system to undertake a quality improvement project to improve this crucial primary care procedure.
Dr. Howard is assistant professor of pediatrics at Johns Hopkins University, Baltimore, and creator of CHADIS (www.CHADIS.com). She reported no other relevant disclosures. Dr. Howard’s contribution to this publication was as a paid expert to MDedge News. Email her at [email protected]
References
1. Acad Pediatr. 2014 May-Jun;14(3):315-23.
2. Hosp Community Psychiatry. 1992 May;43(5):489-93.
3. Pediatrics. 2019 Mar 1;143(3): e20182738.
4. Arch Pediatr Adolesc Med. 2000 May;154(5):499-506.
5. Pediatrics. 2010 Feb 1. doi: 10.1542/peds.2009-0388.