User login
Bob Wachter Puts Forward Spin on Patient Safety, Quality of Care at HM13
Most hospitalists have heard the adage “If you’ve seen one hospitalist group, you’ve seen one hospitalist group.” Another HM truism is “If you’ve seen one SHM annual meeting, then you’ve seen Bob Wachter, MD, MHM.”
Dr. Wachter, professor, chief of the division of hospital medicine, and chief of the medical service at the University of California at San Francisco Medical Center, is to HM conventions as warfarin is to anticoagulation. His keynote address is the finale to the yearly confab, and HM13’s version is scheduled for noon May 19 at the Gaylord National Harbor Resort & Convention Center in National Harbor, Md.
This year’s address is titled “Quality, Safety, and IT: A Decade of Successes, Failures, Surprises, and Epiphanies.” Dr. Wachter spoke recently with The Hospitalist about his annual tradition.
Question: With your interest in the intersection between healthcare and politics, to be back in D.C. has to be something enjoyable for you to write and talk about.
Answer: It’s a very interesting time in the life of healthcare, in that now that everybody knows that the [Affordable Care Act] is real and not going away, and we’re actually beginning to implement parts of it, you can kind of see what the future is going to look like, and everybody’s responding. And there are parts of that that are very exciting, because they’re forcing us to think about value in new ways. [And] there are parts of it that are somewhat frustrating.
Q: Does that give the hospitalist community the chance to ride herd on more global issues?
A: I think that’s the most optimistic interpretation—that we stick to our knitting, that we continue to be the leaders in improvement, and eventually all of the deals will be done, lawyers will be dismissed, and people will turn back to focusing on performance and say to us, “Thank goodness you’ve been doing this work, because now we realize that it’s not just about contracts; it’s about how we deliver care, and you’re the ones that have been leading the way.”
Q: What’s the most realistic interpretation?
A: This work gets less attention and less support than it needs. … I think we’re going to go through three to five years where we’re continuing to do the work. It’s really important—in many ways, it’s as important as growing—but as its importance is growing, the importance of other things that require more tending-to by the senior leadership is growing even faster. The risk is that there will be a disconnect.
Q: When you see the literature that suggests just how difficult the nuts and bolts implementation of reform is, what message do you want to get across to the people who are going to be listening, in terms of actually implementing all of this?
A: The message I don’t want to get across is “frustration, burnout, and it’s not worth it.” The endgame is worth it. The endgame is not even elective. We have to get to a place where we’re delivering higher-quality, safer, more satisfying care to patients at a lower cost. We’re in a unique position to deliver on that promise. … This is really tough stuff, and it takes time and it takes learning.
Check out our 6-minute feature video: "Five Reasons You Should Attend HM13"
Richard Quinn is a freelance writer in New Jersey.
Most hospitalists have heard the adage “If you’ve seen one hospitalist group, you’ve seen one hospitalist group.” Another HM truism is “If you’ve seen one SHM annual meeting, then you’ve seen Bob Wachter, MD, MHM.”
Dr. Wachter, professor, chief of the division of hospital medicine, and chief of the medical service at the University of California at San Francisco Medical Center, is to HM conventions as warfarin is to anticoagulation. His keynote address is the finale to the yearly confab, and HM13’s version is scheduled for noon May 19 at the Gaylord National Harbor Resort & Convention Center in National Harbor, Md.
This year’s address is titled “Quality, Safety, and IT: A Decade of Successes, Failures, Surprises, and Epiphanies.” Dr. Wachter spoke recently with The Hospitalist about his annual tradition.
Question: With your interest in the intersection between healthcare and politics, to be back in D.C. has to be something enjoyable for you to write and talk about.
Answer: It’s a very interesting time in the life of healthcare, in that now that everybody knows that the [Affordable Care Act] is real and not going away, and we’re actually beginning to implement parts of it, you can kind of see what the future is going to look like, and everybody’s responding. And there are parts of that that are very exciting, because they’re forcing us to think about value in new ways. [And] there are parts of it that are somewhat frustrating.
Q: Does that give the hospitalist community the chance to ride herd on more global issues?
A: I think that’s the most optimistic interpretation—that we stick to our knitting, that we continue to be the leaders in improvement, and eventually all of the deals will be done, lawyers will be dismissed, and people will turn back to focusing on performance and say to us, “Thank goodness you’ve been doing this work, because now we realize that it’s not just about contracts; it’s about how we deliver care, and you’re the ones that have been leading the way.”
Q: What’s the most realistic interpretation?
A: This work gets less attention and less support than it needs. … I think we’re going to go through three to five years where we’re continuing to do the work. It’s really important—in many ways, it’s as important as growing—but as its importance is growing, the importance of other things that require more tending-to by the senior leadership is growing even faster. The risk is that there will be a disconnect.
Q: When you see the literature that suggests just how difficult the nuts and bolts implementation of reform is, what message do you want to get across to the people who are going to be listening, in terms of actually implementing all of this?
A: The message I don’t want to get across is “frustration, burnout, and it’s not worth it.” The endgame is worth it. The endgame is not even elective. We have to get to a place where we’re delivering higher-quality, safer, more satisfying care to patients at a lower cost. We’re in a unique position to deliver on that promise. … This is really tough stuff, and it takes time and it takes learning.
Check out our 6-minute feature video: "Five Reasons You Should Attend HM13"
Richard Quinn is a freelance writer in New Jersey.
Most hospitalists have heard the adage “If you’ve seen one hospitalist group, you’ve seen one hospitalist group.” Another HM truism is “If you’ve seen one SHM annual meeting, then you’ve seen Bob Wachter, MD, MHM.”
Dr. Wachter, professor, chief of the division of hospital medicine, and chief of the medical service at the University of California at San Francisco Medical Center, is to HM conventions as warfarin is to anticoagulation. His keynote address is the finale to the yearly confab, and HM13’s version is scheduled for noon May 19 at the Gaylord National Harbor Resort & Convention Center in National Harbor, Md.
This year’s address is titled “Quality, Safety, and IT: A Decade of Successes, Failures, Surprises, and Epiphanies.” Dr. Wachter spoke recently with The Hospitalist about his annual tradition.
Question: With your interest in the intersection between healthcare and politics, to be back in D.C. has to be something enjoyable for you to write and talk about.
Answer: It’s a very interesting time in the life of healthcare, in that now that everybody knows that the [Affordable Care Act] is real and not going away, and we’re actually beginning to implement parts of it, you can kind of see what the future is going to look like, and everybody’s responding. And there are parts of that that are very exciting, because they’re forcing us to think about value in new ways. [And] there are parts of it that are somewhat frustrating.
Q: Does that give the hospitalist community the chance to ride herd on more global issues?
A: I think that’s the most optimistic interpretation—that we stick to our knitting, that we continue to be the leaders in improvement, and eventually all of the deals will be done, lawyers will be dismissed, and people will turn back to focusing on performance and say to us, “Thank goodness you’ve been doing this work, because now we realize that it’s not just about contracts; it’s about how we deliver care, and you’re the ones that have been leading the way.”
Q: What’s the most realistic interpretation?
A: This work gets less attention and less support than it needs. … I think we’re going to go through three to five years where we’re continuing to do the work. It’s really important—in many ways, it’s as important as growing—but as its importance is growing, the importance of other things that require more tending-to by the senior leadership is growing even faster. The risk is that there will be a disconnect.
Q: When you see the literature that suggests just how difficult the nuts and bolts implementation of reform is, what message do you want to get across to the people who are going to be listening, in terms of actually implementing all of this?
A: The message I don’t want to get across is “frustration, burnout, and it’s not worth it.” The endgame is worth it. The endgame is not even elective. We have to get to a place where we’re delivering higher-quality, safer, more satisfying care to patients at a lower cost. We’re in a unique position to deliver on that promise. … This is really tough stuff, and it takes time and it takes learning.
Check out our 6-minute feature video: "Five Reasons You Should Attend HM13"
Richard Quinn is a freelance writer in New Jersey.
UCLA Exec: Patient-Centered Approach Essential to Quality of Hospital Care

–David Feinberg, MD, MBA, president of UCLA Health System in Los Angeles
Patient satisfaction is a buzzword in HM circles, as compensation is increasingly tied to performance in keeping inpatients happy. David Feinberg, MD, MBA, president of UCLA Health System in Los Angeles, could be called a guru of patient satisfaction.
Just don’t tell him that.
“I hope I’m not seen as ‘patient satisfaction,’” he says. “I hope I’m seen as ‘patient centeredness.’ And patient satisfaction is a key piece of patient centeredness.”
Dr. Feinberg, who assumed his current role UCLA Health System in 2011, is a national voice for pushing a patient-centric model of care delivery. To wit, he will be one of the keynote speakers at HM13 next month at the Gaylord National Resort & Convention Center in National Harbor, Md. His address is fittingly titled “Healing Humankind One Patient at a Time.”
The Hospitalist spoke to Dr. Feinberg about his message to hospitalists.
Question: What do you think is the evolution of patient centeredness, as that becomes more of a focus for others?
Answer: Patient centeredness to me is the true north, and I think everything else that we’ve done that isn’t patient-centered has been a distraction. … It’s why we signed up to get into healthcare. It’s what we should be doing today and tonight, and it should guide our future tomorrow. It would be like me saying to the restaurateur, “How important is the food?”
Q: Is it something that hasn’t always been done?
A: It’s pathetic. You’re totally right. We’ve lost our way.
Q: If it’s so common-sense, how did we lose our way?
A: It really became, to me, the coin of the realm in medicine was how much the doctor made, how great their reputation was. It even got to the point of: You were a good doctor if your waiting room was packed. … I keep saying the waiting room should be for the doctors. The patient shouldn’t have to wait. You should be back in the exam room and the doctor should be waiting to see you. So we’ve got to completely change the paradigm. … It’s really the patient who’s at the top of the pyramid. And I just think we’ve lost that completely.
Q: How does a hospitalist engage quickly to ensure that they’re trying to accomplish patient centeredness and manage outcomes properly?
A: Hospitalists have a unique opportunity there, because everybody remembers when they got put in the hospital. It is a big deal when you’re hospitalized. Your family is in a vulnerable state, everybody is in a heightened sense of alertness and focus. Think about how important those four days are around education, around myths and demystifying, around beliefs and disbelief.
Check out our 6-minute feature video: "Five Reasons You Should Attend HM13"
Q: So what is the one thing you want hospitalists to take away from your address?
A: That they should join with all of us who want to heal humankind; that they are healers, above all.
Q: How do you translate “I want to be a healer” to the grind of daily work?
A: Well, I don’t think this is a grind. I think that when you’re in this healing profession, that you come here with a purpose. I think if we asked them to look at their personal statements of why they went into med school, every single one of them has something to do with, “I was sick as a kid, my grandmother got sick, I had had this doctor who was a role model, I like to help people, I was a volunteer and I met this patient.” Everyone says that. So this is different than trying to inspire the workers at Costco. These are people that, by definition, have gone and chosen this. We know they’re all smart. They could have all become investment bankers, they could have all become schoolteachers, but what they chose was to go into this field that’s about healing others, and that’s what I think we need to and what I would want them to do, is to get back in touch with themselves because I know it’s there. By definition, it’s there.
Q: Then why don’t more people just make that connection? What is the hurdle?
A: There are a lot of distractions. There are a lot of things coming your way. Worrying about your own life; doctors have lives at home. Worrying about the pressures of making a living. Some of this stuff is really, really hard. There are a million things going on. I believe, and I hope at UCLA, that we believe the strategy to make all of that stuff work is to get it right with the patient. And if you get it right with the patient, then all of that other stuff seems to fall into place and starts to make sense. The finances work out. The market share works out. The healthcare reform works out. I think it is the answer.
Richard Quinn is a freelance writer in New Jersey.

–David Feinberg, MD, MBA, president of UCLA Health System in Los Angeles
Patient satisfaction is a buzzword in HM circles, as compensation is increasingly tied to performance in keeping inpatients happy. David Feinberg, MD, MBA, president of UCLA Health System in Los Angeles, could be called a guru of patient satisfaction.
Just don’t tell him that.
“I hope I’m not seen as ‘patient satisfaction,’” he says. “I hope I’m seen as ‘patient centeredness.’ And patient satisfaction is a key piece of patient centeredness.”
Dr. Feinberg, who assumed his current role UCLA Health System in 2011, is a national voice for pushing a patient-centric model of care delivery. To wit, he will be one of the keynote speakers at HM13 next month at the Gaylord National Resort & Convention Center in National Harbor, Md. His address is fittingly titled “Healing Humankind One Patient at a Time.”
The Hospitalist spoke to Dr. Feinberg about his message to hospitalists.
Question: What do you think is the evolution of patient centeredness, as that becomes more of a focus for others?
Answer: Patient centeredness to me is the true north, and I think everything else that we’ve done that isn’t patient-centered has been a distraction. … It’s why we signed up to get into healthcare. It’s what we should be doing today and tonight, and it should guide our future tomorrow. It would be like me saying to the restaurateur, “How important is the food?”
Q: Is it something that hasn’t always been done?
A: It’s pathetic. You’re totally right. We’ve lost our way.
Q: If it’s so common-sense, how did we lose our way?
A: It really became, to me, the coin of the realm in medicine was how much the doctor made, how great their reputation was. It even got to the point of: You were a good doctor if your waiting room was packed. … I keep saying the waiting room should be for the doctors. The patient shouldn’t have to wait. You should be back in the exam room and the doctor should be waiting to see you. So we’ve got to completely change the paradigm. … It’s really the patient who’s at the top of the pyramid. And I just think we’ve lost that completely.
Q: How does a hospitalist engage quickly to ensure that they’re trying to accomplish patient centeredness and manage outcomes properly?
A: Hospitalists have a unique opportunity there, because everybody remembers when they got put in the hospital. It is a big deal when you’re hospitalized. Your family is in a vulnerable state, everybody is in a heightened sense of alertness and focus. Think about how important those four days are around education, around myths and demystifying, around beliefs and disbelief.
Check out our 6-minute feature video: "Five Reasons You Should Attend HM13"
Q: So what is the one thing you want hospitalists to take away from your address?
A: That they should join with all of us who want to heal humankind; that they are healers, above all.
Q: How do you translate “I want to be a healer” to the grind of daily work?
A: Well, I don’t think this is a grind. I think that when you’re in this healing profession, that you come here with a purpose. I think if we asked them to look at their personal statements of why they went into med school, every single one of them has something to do with, “I was sick as a kid, my grandmother got sick, I had had this doctor who was a role model, I like to help people, I was a volunteer and I met this patient.” Everyone says that. So this is different than trying to inspire the workers at Costco. These are people that, by definition, have gone and chosen this. We know they’re all smart. They could have all become investment bankers, they could have all become schoolteachers, but what they chose was to go into this field that’s about healing others, and that’s what I think we need to and what I would want them to do, is to get back in touch with themselves because I know it’s there. By definition, it’s there.
Q: Then why don’t more people just make that connection? What is the hurdle?
A: There are a lot of distractions. There are a lot of things coming your way. Worrying about your own life; doctors have lives at home. Worrying about the pressures of making a living. Some of this stuff is really, really hard. There are a million things going on. I believe, and I hope at UCLA, that we believe the strategy to make all of that stuff work is to get it right with the patient. And if you get it right with the patient, then all of that other stuff seems to fall into place and starts to make sense. The finances work out. The market share works out. The healthcare reform works out. I think it is the answer.
Richard Quinn is a freelance writer in New Jersey.

–David Feinberg, MD, MBA, president of UCLA Health System in Los Angeles
Patient satisfaction is a buzzword in HM circles, as compensation is increasingly tied to performance in keeping inpatients happy. David Feinberg, MD, MBA, president of UCLA Health System in Los Angeles, could be called a guru of patient satisfaction.
Just don’t tell him that.
“I hope I’m not seen as ‘patient satisfaction,’” he says. “I hope I’m seen as ‘patient centeredness.’ And patient satisfaction is a key piece of patient centeredness.”
Dr. Feinberg, who assumed his current role UCLA Health System in 2011, is a national voice for pushing a patient-centric model of care delivery. To wit, he will be one of the keynote speakers at HM13 next month at the Gaylord National Resort & Convention Center in National Harbor, Md. His address is fittingly titled “Healing Humankind One Patient at a Time.”
The Hospitalist spoke to Dr. Feinberg about his message to hospitalists.
Question: What do you think is the evolution of patient centeredness, as that becomes more of a focus for others?
Answer: Patient centeredness to me is the true north, and I think everything else that we’ve done that isn’t patient-centered has been a distraction. … It’s why we signed up to get into healthcare. It’s what we should be doing today and tonight, and it should guide our future tomorrow. It would be like me saying to the restaurateur, “How important is the food?”
Q: Is it something that hasn’t always been done?
A: It’s pathetic. You’re totally right. We’ve lost our way.
Q: If it’s so common-sense, how did we lose our way?
A: It really became, to me, the coin of the realm in medicine was how much the doctor made, how great their reputation was. It even got to the point of: You were a good doctor if your waiting room was packed. … I keep saying the waiting room should be for the doctors. The patient shouldn’t have to wait. You should be back in the exam room and the doctor should be waiting to see you. So we’ve got to completely change the paradigm. … It’s really the patient who’s at the top of the pyramid. And I just think we’ve lost that completely.
Q: How does a hospitalist engage quickly to ensure that they’re trying to accomplish patient centeredness and manage outcomes properly?
A: Hospitalists have a unique opportunity there, because everybody remembers when they got put in the hospital. It is a big deal when you’re hospitalized. Your family is in a vulnerable state, everybody is in a heightened sense of alertness and focus. Think about how important those four days are around education, around myths and demystifying, around beliefs and disbelief.
Check out our 6-minute feature video: "Five Reasons You Should Attend HM13"
Q: So what is the one thing you want hospitalists to take away from your address?
A: That they should join with all of us who want to heal humankind; that they are healers, above all.
Q: How do you translate “I want to be a healer” to the grind of daily work?
A: Well, I don’t think this is a grind. I think that when you’re in this healing profession, that you come here with a purpose. I think if we asked them to look at their personal statements of why they went into med school, every single one of them has something to do with, “I was sick as a kid, my grandmother got sick, I had had this doctor who was a role model, I like to help people, I was a volunteer and I met this patient.” Everyone says that. So this is different than trying to inspire the workers at Costco. These are people that, by definition, have gone and chosen this. We know they’re all smart. They could have all become investment bankers, they could have all become schoolteachers, but what they chose was to go into this field that’s about healing others, and that’s what I think we need to and what I would want them to do, is to get back in touch with themselves because I know it’s there. By definition, it’s there.
Q: Then why don’t more people just make that connection? What is the hurdle?
A: There are a lot of distractions. There are a lot of things coming your way. Worrying about your own life; doctors have lives at home. Worrying about the pressures of making a living. Some of this stuff is really, really hard. There are a million things going on. I believe, and I hope at UCLA, that we believe the strategy to make all of that stuff work is to get it right with the patient. And if you get it right with the patient, then all of that other stuff seems to fall into place and starts to make sense. The finances work out. The market share works out. The healthcare reform works out. I think it is the answer.
Richard Quinn is a freelance writer in New Jersey.
Medicare CMO Encourages Hospitalists to Become Experts in Managing Quality Patient Care

–Patrick Conway, MD, MSc, FAAP, SFHM, chief medical officer, Centers for Medicaid & Medicare Service
Patrick Conway, MD, MSc, FAAP, SFHM, chief medical officer of the Centers for Medicaid & Medicare Services (CMS), often says that physicians need to come to the proverbial table to tell CMS what they think is best. So it’s fitting that at HM13 at the Gaylord National Resort & Convention Center in National Harbor, Md., Dr. Conway will be a keynote speaker who can deliver his message of quality through teamwork to more than 2,500 hospitalists.
A pediatric hospitalist who also serves as director of the Office of Clinical Standards and Quality at the U.S. Department of Health and Human Services in Washington, D.C., Dr. Conway will paint a picture of what hospitalists can do to become the quality-improvement (QI) leaders healthcare needs in the coming years in a presentation titled “The Ideal Hospitalist in 2014 and Beyond: Active Change Agent.”
“Are hospitalists going to accept that challenge?” he asks. “I hope they are.”
This is the second year in a row that Dr. Conway will be a plenary speaker. Last year in San Diego, he told a packed room that CMS had to move from a “passive payor to an active facilitator and catalyst for quality improvement,” says Danielle Scheurer, MD, MSCR, SFHM, physician editor of The Hospitalist. Or, in his own words: “better health, better care, and lower cost.”
But many of the issues in his 2012 commentary were in flux. The Affordable Care Act (ACA), now moving through the slow process of implementation, was then still a law very much in doubt. It wasn’t until last summer that the law was upheld by a bitterly divided U.S. Supreme Court and it became clear much of the proposed reforms would move forward.
This year, he will urge hospitalists to step up their focus on patient-centered outcomes and stop questioning whether that should be the way the HM and other physicians should be judged.
“Given the changing context of payment, hospitalists are going to have to become true experts in managing the quality of care,” Dr. Conway says. “The days of you just graduating residency, seeing as many patients as you can, and you go home at the end of the day—that’s gone for hospital medicine.”
Check out our 6-minute feature video: "Five Reasons You Should Attend HM13"
Hospitalists can take charge of quality initiatives via involvement with accountable-care organizations (ACOs), health exchanges, and CMS’ value-based purchasing modifier (VBPM). In part, HM is perfectly positioned to assume leadership roles over the next few years because hospitalists already work across multiple departments.
“Hospital medicine is already ahead of a lot of specialties,” Dr. Conway says. “Hospital medicine physicians are already taking on much larger roles in their systems. I think you’re going to see an increasing trend.”
Richard Quinn is a freelance writer in New Jersey.

–Patrick Conway, MD, MSc, FAAP, SFHM, chief medical officer, Centers for Medicaid & Medicare Service
Patrick Conway, MD, MSc, FAAP, SFHM, chief medical officer of the Centers for Medicaid & Medicare Services (CMS), often says that physicians need to come to the proverbial table to tell CMS what they think is best. So it’s fitting that at HM13 at the Gaylord National Resort & Convention Center in National Harbor, Md., Dr. Conway will be a keynote speaker who can deliver his message of quality through teamwork to more than 2,500 hospitalists.
A pediatric hospitalist who also serves as director of the Office of Clinical Standards and Quality at the U.S. Department of Health and Human Services in Washington, D.C., Dr. Conway will paint a picture of what hospitalists can do to become the quality-improvement (QI) leaders healthcare needs in the coming years in a presentation titled “The Ideal Hospitalist in 2014 and Beyond: Active Change Agent.”
“Are hospitalists going to accept that challenge?” he asks. “I hope they are.”
This is the second year in a row that Dr. Conway will be a plenary speaker. Last year in San Diego, he told a packed room that CMS had to move from a “passive payor to an active facilitator and catalyst for quality improvement,” says Danielle Scheurer, MD, MSCR, SFHM, physician editor of The Hospitalist. Or, in his own words: “better health, better care, and lower cost.”
But many of the issues in his 2012 commentary were in flux. The Affordable Care Act (ACA), now moving through the slow process of implementation, was then still a law very much in doubt. It wasn’t until last summer that the law was upheld by a bitterly divided U.S. Supreme Court and it became clear much of the proposed reforms would move forward.
This year, he will urge hospitalists to step up their focus on patient-centered outcomes and stop questioning whether that should be the way the HM and other physicians should be judged.
“Given the changing context of payment, hospitalists are going to have to become true experts in managing the quality of care,” Dr. Conway says. “The days of you just graduating residency, seeing as many patients as you can, and you go home at the end of the day—that’s gone for hospital medicine.”
Check out our 6-minute feature video: "Five Reasons You Should Attend HM13"
Hospitalists can take charge of quality initiatives via involvement with accountable-care organizations (ACOs), health exchanges, and CMS’ value-based purchasing modifier (VBPM). In part, HM is perfectly positioned to assume leadership roles over the next few years because hospitalists already work across multiple departments.
“Hospital medicine is already ahead of a lot of specialties,” Dr. Conway says. “Hospital medicine physicians are already taking on much larger roles in their systems. I think you’re going to see an increasing trend.”
Richard Quinn is a freelance writer in New Jersey.

–Patrick Conway, MD, MSc, FAAP, SFHM, chief medical officer, Centers for Medicaid & Medicare Service
Patrick Conway, MD, MSc, FAAP, SFHM, chief medical officer of the Centers for Medicaid & Medicare Services (CMS), often says that physicians need to come to the proverbial table to tell CMS what they think is best. So it’s fitting that at HM13 at the Gaylord National Resort & Convention Center in National Harbor, Md., Dr. Conway will be a keynote speaker who can deliver his message of quality through teamwork to more than 2,500 hospitalists.
A pediatric hospitalist who also serves as director of the Office of Clinical Standards and Quality at the U.S. Department of Health and Human Services in Washington, D.C., Dr. Conway will paint a picture of what hospitalists can do to become the quality-improvement (QI) leaders healthcare needs in the coming years in a presentation titled “The Ideal Hospitalist in 2014 and Beyond: Active Change Agent.”
“Are hospitalists going to accept that challenge?” he asks. “I hope they are.”
This is the second year in a row that Dr. Conway will be a plenary speaker. Last year in San Diego, he told a packed room that CMS had to move from a “passive payor to an active facilitator and catalyst for quality improvement,” says Danielle Scheurer, MD, MSCR, SFHM, physician editor of The Hospitalist. Or, in his own words: “better health, better care, and lower cost.”
But many of the issues in his 2012 commentary were in flux. The Affordable Care Act (ACA), now moving through the slow process of implementation, was then still a law very much in doubt. It wasn’t until last summer that the law was upheld by a bitterly divided U.S. Supreme Court and it became clear much of the proposed reforms would move forward.
This year, he will urge hospitalists to step up their focus on patient-centered outcomes and stop questioning whether that should be the way the HM and other physicians should be judged.
“Given the changing context of payment, hospitalists are going to have to become true experts in managing the quality of care,” Dr. Conway says. “The days of you just graduating residency, seeing as many patients as you can, and you go home at the end of the day—that’s gone for hospital medicine.”
Check out our 6-minute feature video: "Five Reasons You Should Attend HM13"
Hospitalists can take charge of quality initiatives via involvement with accountable-care organizations (ACOs), health exchanges, and CMS’ value-based purchasing modifier (VBPM). In part, HM is perfectly positioned to assume leadership roles over the next few years because hospitalists already work across multiple departments.
“Hospital medicine is already ahead of a lot of specialties,” Dr. Conway says. “Hospital medicine physicians are already taking on much larger roles in their systems. I think you’re going to see an increasing trend.”
Richard Quinn is a freelance writer in New Jersey.
Team Hospitalist Recommends Nine Don’t-Miss Sessions at HM13
Eight educational tracks, an equal number of credit bearing pre-courses, a score of small-group forums, three plenaries, and an SHM Town Hall meeting offers a lot of professional development in a four-day span. But that’s just a sampling of what HM13 has slated May 16-19 at the Gaylord National Resort & Convention Center in National Harbor, Md., just outside Washington, D.C.
So how does one get the most value out of the conference?
“The highest-yield content is going to depend on what your background is and how to spend that time in a way that augments your knowledge, your perspective, or your exposure to like-minded colleagues in a very individual way,” says HM13 course director Daniel Brotman, MD, FACP, SFHM, director of the hospitalist program at Johns Hopkins Hospital in Baltimore. “One of the things that’s so cool about hospital medicine is its diversity.”
But don’t take Dr. Brotman’s well-educated word for it. Here’s a list of recommendations from Team Hospitalist, the only reader-involvement group of its kind in HM, on events they would not miss this year.
The New Anticoagulants: When Should We Be Using Them?
2:45 p.m., May 17
Dr. Ma: “I’m very interested about the new anticoagulants talk. What I’m curious to see is what the speaker thinks about the survivability of these medications in our society, with so many lawyers. Pradaxa already has fallen out of favor. Let’s see what happens to Xarelto.”
How do CFOs Value Their Hospitalist Programs?
2:50 p.m., May 18
Dr. Ma: “The problem today is CFOs have to valuate their hospitalists in the setting of other specialists who also receive subsidies. There is less money to be spent on hospitalists, as other specialists vie for this allotment of savings from hospital-based value purchasing.”
Check out our 6-minute feature video: "Five Reasons You Should Attend HM13"
Mentoring/Coaching an Improvement Team: Lessons from SHM’s Mentored Implementation Programs
2:45 p.m., May 17
Dr. Perumalswami: “As a Project BOOST physician mentor in Illinois, I would highly recommend the session because the discussion will involve an inside look into valuable experience-based observations and analysis for the success of any process improvement team. The nature of teams and the culture of improvement at various sites will also be discussed. There will be a mentee side of the presentation, too, which will help other mentors of implementation programs better understand what the issues are ‘from the other side.’”
Strategies to Improve Communication with Patients and Families to Improve Care
2:45 p.m., May 17
Dr. Hale: “It is well known in pediatrics that you are treating two patients: both the child and the parents. If the family has a shared understanding of the child’s illness and there is collaboration for the care plan, there will be improved care.”
Neonatal HSV: When to Consider It, How to Evaluate for It, and How to Treat It
11 a.m., May 18
Dr. Hale: “Neonatal HSV is a devastating disease. It is essential to recognize high-risk patients to decrease morbidity and mortality for this illness. There have been recent updates in the understanding of epidemiology of this disease that can assist the provider in recognizing high-risk patients.”
Supporting Transition for Youth with Special Healthcare Needs: Coordinating Care and Preparing to Pass the Baton
4:15 p.m., May 18
Dr. Hale: “The transition of adolescents and young adults from pediatric-care teams to adult-medicine-care teams should be seamless for the sake of the patient, but often it is a blurry transition over the course of years. This session is high-yield for both pediatric and adult hospitalists.”
Getting Ready for Physician Value-Based Purchasing
9:50 a.m., May 19
Dr. Simone: “Dr. [Pat] Torcson’s presentation last year was one of the best at HM12, and I expect this year to be the same. He chairs SHM’s Performance Measurement and Reporting Committee and is well versed in these matters. He speaks in terms that will capture all audiences, whether they are experienced or new to the business aspects of medicine. Highly recommended.”
BOOSTing the Hospital Discharge Process: What Works and What Doesn’t
10:35 a.m., May 17
Dr. Simone: “Both panelists are excellent presenters as well as leading authorities when it comes to discharge processes. This presentation is very timely with the new CMS payment system, which penalizes unnecessary and unexpected readmissions.”
Success Stories: How to Integrate NPs and PAs into a Hospitalist Practice
4:15 p.m., May 18
Cardin: “This is an important session because, as every hard-working hospitalist knows, there simply aren’t enough physicians to fill the needs of our medically complex hospitalized patients. It is simply a reality that there will be an increased need in the future for mid-level providers, and it is valuable to maximize the success of a program by learning how to assimilate them into hospitalized practice.”
Diagnostic Errors and the Hospitalist: Why They Happen and How to Avoid Them
12:45 p.m., May 17
Cardin: “Half of practicing medicine is pattern recognition, and if there are patterns to making diagnostic errors, it would be so valuable to be aware of them. We have tremendous responsibility when caring for patients, and I think it is always beneficial to learn from mistakes.”
Richard Quinn is a freelance writer in New Jersey.
Eight educational tracks, an equal number of credit bearing pre-courses, a score of small-group forums, three plenaries, and an SHM Town Hall meeting offers a lot of professional development in a four-day span. But that’s just a sampling of what HM13 has slated May 16-19 at the Gaylord National Resort & Convention Center in National Harbor, Md., just outside Washington, D.C.
So how does one get the most value out of the conference?
“The highest-yield content is going to depend on what your background is and how to spend that time in a way that augments your knowledge, your perspective, or your exposure to like-minded colleagues in a very individual way,” says HM13 course director Daniel Brotman, MD, FACP, SFHM, director of the hospitalist program at Johns Hopkins Hospital in Baltimore. “One of the things that’s so cool about hospital medicine is its diversity.”
But don’t take Dr. Brotman’s well-educated word for it. Here’s a list of recommendations from Team Hospitalist, the only reader-involvement group of its kind in HM, on events they would not miss this year.
The New Anticoagulants: When Should We Be Using Them?
2:45 p.m., May 17
Dr. Ma: “I’m very interested about the new anticoagulants talk. What I’m curious to see is what the speaker thinks about the survivability of these medications in our society, with so many lawyers. Pradaxa already has fallen out of favor. Let’s see what happens to Xarelto.”
How do CFOs Value Their Hospitalist Programs?
2:50 p.m., May 18
Dr. Ma: “The problem today is CFOs have to valuate their hospitalists in the setting of other specialists who also receive subsidies. There is less money to be spent on hospitalists, as other specialists vie for this allotment of savings from hospital-based value purchasing.”
Check out our 6-minute feature video: "Five Reasons You Should Attend HM13"
Mentoring/Coaching an Improvement Team: Lessons from SHM’s Mentored Implementation Programs
2:45 p.m., May 17
Dr. Perumalswami: “As a Project BOOST physician mentor in Illinois, I would highly recommend the session because the discussion will involve an inside look into valuable experience-based observations and analysis for the success of any process improvement team. The nature of teams and the culture of improvement at various sites will also be discussed. There will be a mentee side of the presentation, too, which will help other mentors of implementation programs better understand what the issues are ‘from the other side.’”
Strategies to Improve Communication with Patients and Families to Improve Care
2:45 p.m., May 17
Dr. Hale: “It is well known in pediatrics that you are treating two patients: both the child and the parents. If the family has a shared understanding of the child’s illness and there is collaboration for the care plan, there will be improved care.”
Neonatal HSV: When to Consider It, How to Evaluate for It, and How to Treat It
11 a.m., May 18
Dr. Hale: “Neonatal HSV is a devastating disease. It is essential to recognize high-risk patients to decrease morbidity and mortality for this illness. There have been recent updates in the understanding of epidemiology of this disease that can assist the provider in recognizing high-risk patients.”
Supporting Transition for Youth with Special Healthcare Needs: Coordinating Care and Preparing to Pass the Baton
4:15 p.m., May 18
Dr. Hale: “The transition of adolescents and young adults from pediatric-care teams to adult-medicine-care teams should be seamless for the sake of the patient, but often it is a blurry transition over the course of years. This session is high-yield for both pediatric and adult hospitalists.”
Getting Ready for Physician Value-Based Purchasing
9:50 a.m., May 19
Dr. Simone: “Dr. [Pat] Torcson’s presentation last year was one of the best at HM12, and I expect this year to be the same. He chairs SHM’s Performance Measurement and Reporting Committee and is well versed in these matters. He speaks in terms that will capture all audiences, whether they are experienced or new to the business aspects of medicine. Highly recommended.”
BOOSTing the Hospital Discharge Process: What Works and What Doesn’t
10:35 a.m., May 17
Dr. Simone: “Both panelists are excellent presenters as well as leading authorities when it comes to discharge processes. This presentation is very timely with the new CMS payment system, which penalizes unnecessary and unexpected readmissions.”
Success Stories: How to Integrate NPs and PAs into a Hospitalist Practice
4:15 p.m., May 18
Cardin: “This is an important session because, as every hard-working hospitalist knows, there simply aren’t enough physicians to fill the needs of our medically complex hospitalized patients. It is simply a reality that there will be an increased need in the future for mid-level providers, and it is valuable to maximize the success of a program by learning how to assimilate them into hospitalized practice.”
Diagnostic Errors and the Hospitalist: Why They Happen and How to Avoid Them
12:45 p.m., May 17
Cardin: “Half of practicing medicine is pattern recognition, and if there are patterns to making diagnostic errors, it would be so valuable to be aware of them. We have tremendous responsibility when caring for patients, and I think it is always beneficial to learn from mistakes.”
Richard Quinn is a freelance writer in New Jersey.
Eight educational tracks, an equal number of credit bearing pre-courses, a score of small-group forums, three plenaries, and an SHM Town Hall meeting offers a lot of professional development in a four-day span. But that’s just a sampling of what HM13 has slated May 16-19 at the Gaylord National Resort & Convention Center in National Harbor, Md., just outside Washington, D.C.
So how does one get the most value out of the conference?
“The highest-yield content is going to depend on what your background is and how to spend that time in a way that augments your knowledge, your perspective, or your exposure to like-minded colleagues in a very individual way,” says HM13 course director Daniel Brotman, MD, FACP, SFHM, director of the hospitalist program at Johns Hopkins Hospital in Baltimore. “One of the things that’s so cool about hospital medicine is its diversity.”
But don’t take Dr. Brotman’s well-educated word for it. Here’s a list of recommendations from Team Hospitalist, the only reader-involvement group of its kind in HM, on events they would not miss this year.
The New Anticoagulants: When Should We Be Using Them?
2:45 p.m., May 17
Dr. Ma: “I’m very interested about the new anticoagulants talk. What I’m curious to see is what the speaker thinks about the survivability of these medications in our society, with so many lawyers. Pradaxa already has fallen out of favor. Let’s see what happens to Xarelto.”
How do CFOs Value Their Hospitalist Programs?
2:50 p.m., May 18
Dr. Ma: “The problem today is CFOs have to valuate their hospitalists in the setting of other specialists who also receive subsidies. There is less money to be spent on hospitalists, as other specialists vie for this allotment of savings from hospital-based value purchasing.”
Check out our 6-minute feature video: "Five Reasons You Should Attend HM13"
Mentoring/Coaching an Improvement Team: Lessons from SHM’s Mentored Implementation Programs
2:45 p.m., May 17
Dr. Perumalswami: “As a Project BOOST physician mentor in Illinois, I would highly recommend the session because the discussion will involve an inside look into valuable experience-based observations and analysis for the success of any process improvement team. The nature of teams and the culture of improvement at various sites will also be discussed. There will be a mentee side of the presentation, too, which will help other mentors of implementation programs better understand what the issues are ‘from the other side.’”
Strategies to Improve Communication with Patients and Families to Improve Care
2:45 p.m., May 17
Dr. Hale: “It is well known in pediatrics that you are treating two patients: both the child and the parents. If the family has a shared understanding of the child’s illness and there is collaboration for the care plan, there will be improved care.”
Neonatal HSV: When to Consider It, How to Evaluate for It, and How to Treat It
11 a.m., May 18
Dr. Hale: “Neonatal HSV is a devastating disease. It is essential to recognize high-risk patients to decrease morbidity and mortality for this illness. There have been recent updates in the understanding of epidemiology of this disease that can assist the provider in recognizing high-risk patients.”
Supporting Transition for Youth with Special Healthcare Needs: Coordinating Care and Preparing to Pass the Baton
4:15 p.m., May 18
Dr. Hale: “The transition of adolescents and young adults from pediatric-care teams to adult-medicine-care teams should be seamless for the sake of the patient, but often it is a blurry transition over the course of years. This session is high-yield for both pediatric and adult hospitalists.”
Getting Ready for Physician Value-Based Purchasing
9:50 a.m., May 19
Dr. Simone: “Dr. [Pat] Torcson’s presentation last year was one of the best at HM12, and I expect this year to be the same. He chairs SHM’s Performance Measurement and Reporting Committee and is well versed in these matters. He speaks in terms that will capture all audiences, whether they are experienced or new to the business aspects of medicine. Highly recommended.”
BOOSTing the Hospital Discharge Process: What Works and What Doesn’t
10:35 a.m., May 17
Dr. Simone: “Both panelists are excellent presenters as well as leading authorities when it comes to discharge processes. This presentation is very timely with the new CMS payment system, which penalizes unnecessary and unexpected readmissions.”
Success Stories: How to Integrate NPs and PAs into a Hospitalist Practice
4:15 p.m., May 18
Cardin: “This is an important session because, as every hard-working hospitalist knows, there simply aren’t enough physicians to fill the needs of our medically complex hospitalized patients. It is simply a reality that there will be an increased need in the future for mid-level providers, and it is valuable to maximize the success of a program by learning how to assimilate them into hospitalized practice.”
Diagnostic Errors and the Hospitalist: Why They Happen and How to Avoid Them
12:45 p.m., May 17
Cardin: “Half of practicing medicine is pattern recognition, and if there are patterns to making diagnostic errors, it would be so valuable to be aware of them. We have tremendous responsibility when caring for patients, and I think it is always beneficial to learn from mistakes.”
Richard Quinn is a freelance writer in New Jersey.
Danielle Scheurer: Thousands of Hospitalists Set Their Sights on HM13
SHM’s annual meeting—or annui conventus, for you Latin lovers—is right around the corner, so be sure to cement your intentions and prepare to go if you have not already.
Now a “longstanding” tradition, the annual meeting serves many purposes, one of which is to act as a reservoir of time for individual hospitalists and for hospitalist groups to reflect on where they have been, where they are now, and where they are (or would like to be) going. A brief history of the SHM annual meeting makes us quickly realize how far we have come, and how far we have to go.
Where We’ve Been
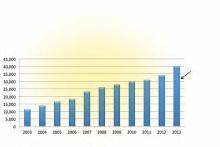
The annual meeting’s history dates back to 1998, when a rogue gathering of about 100 self-proclaimed hospitalists gathered at the National Association of Inpatient Physicians (NAIP) meeting in San Diego. From the year before the first annual meeting to the year after the first annual meeting, membership in NAIP had grown from about 20 hospitalists to about 800 hospitalists. That rapidity of growth had never been seen by another specialty in the history of modern medicine. By the 2003 annual meeting in San Diego, the name had officially changed to the Society of Hospital Medicine, and membership had grown to more than 3,000; less than 10 years later, when the meeting returned to San Diego, membership had grown to more than 10,000. These continued steady increases in both membership size and attendance at the meeting serves as a testimony to the strength of the field and the leadership of the society.
Check out our 6-minute feature video: "Five Reasons You Should Attend HM13"
Where We Are Now
Growth: SHM’s annual meeting now has a track record to be reckoned with. The number of attendees expected for 2013 is a staggering 3,000, which is only a portion of the more than 11,000 SHM members who can actually take time away from their busy practices to attend. The event has now expanded to more than three and a half days, including eight pre-courses and more than 100 workshops/breakout sessions to meet the needs of most any hospitalist. The number of submissions for the Research, Innovations, and Clinical Vignettes competition has steadily risen over the years, topping an all-time record of 800 submissions in 2013. This is a testimony to the curiosity and productivity of so many hospitalists and HM groups.
Advocacy: SHM has been a longstanding and considerable advocate for healthcare reform for more than a decade. With the annual meeting in Washington, D.C., this year, and in lieu of the pre-courses, more than 100 hospitalists and SHM staff will be making a field trip to Capitol Hill to advocate for changes in the structure and payment within the medical industry, to promote good patient care for those we serve, and to promote continued research for better ways of delivering care in the future. Over the course of 2012, SHM submitted more than 20 influential advocacy letters to a variety of stakeholders on topics ranging from sustainable growth rate (SGR) repeal to Agency for Healthcare Research and Quality (AHRQ) funding.
Impact: The annual meeting is not just bigger and longer; it is better. The quality and reputation of the plenary, breakout, and workshop speakers is tremendous, with this year’s plenary speakers including Patrick Conway, chief medical officer of CMS, and David Feinberg, president of UCLA Health System and CEO of UCLA Hospital System. The annual award ceremony will recognize a highly qualified repertoire of dedicated hospitalists and teams and reflect the number and quality of those involved in HM in the areas of clinical excellence, teaching, research, service, and teamwork. The annual Fellows in Hospital Medicine induction will include more than 300 additional fellows and senior fellows, which is a testimony to the level of involvement so many hospitalists have within our specialty.
Where We Are Going
Growth: I suspect the annual meeting will continue to grow in size, and it will expand to better serve the needs of other types of hospital-based physicians (neurologists, obstetricians, etc.), other types of practitioners (NPs, PAs, other specialty nurses), and other types of professionals (administrators and executives). It likely will attract an international community of hospitalists as other nations identify and execute better models of care for hospitalized patients.
Advocacy: SHM and the annual meeting will continue to serve as a nidus for directing the best pathways toward a better healthcare system. It will continue to serve as an avenue by which we partner with and/or influence impactful organizations, such as federal, state, and local governments, the Centers for Medicare & Medicaid Services (CMS), the Joint Commission, and the American Hospital Association, to name a few.
Impact: SHM and the annual meeting will expand its role as the focus for learning and sharing new research and innovations within the field. It will serve as a platform for initiating and spreading standardized evidence-based implementation of best practices through a repertoire of mentored implementation programs. And it will continue to serve as proof of the strength of our hospital medicine community as we spread into every U.S. hospital system and beyond.
Reputation: The future of our annual meeting and reputation will be dependent on how fast and how carefully we craft the pathway for HM. Currently, about half of all the nation’s hospitalists have been in practice for five years or less. We will need to carefully focus on how to be compassionate providers and system advocates—not just shift workers and billing specialists. We will have to be the mentors by which other countries define best practice for inpatient care, including what ideal training for a hospitalist should look like, and what their scope of practice should entail.
If you ask one of the attendees of the first annui conventus what it was like, they will say it was a small mom-and-pop gathering of disparate physicians, with a pie-in-the-sky idea of the future of hospitalist practice. And someday, when our current generation of hospitalists attends an international conference of hospitalists, in Prague, in 2033, we can say, “Remember when we met in that tiny hotel in D.C. in 2013?”
Dr. Scheurer is a hospitalist and chief quality officer at the Medical University of South Carolina in Charleston. She is physician editor of The Hospitalist. Email her at [email protected].
SHM’s annual meeting—or annui conventus, for you Latin lovers—is right around the corner, so be sure to cement your intentions and prepare to go if you have not already.
Now a “longstanding” tradition, the annual meeting serves many purposes, one of which is to act as a reservoir of time for individual hospitalists and for hospitalist groups to reflect on where they have been, where they are now, and where they are (or would like to be) going. A brief history of the SHM annual meeting makes us quickly realize how far we have come, and how far we have to go.
Where We’ve Been
The annual meeting’s history dates back to 1998, when a rogue gathering of about 100 self-proclaimed hospitalists gathered at the National Association of Inpatient Physicians (NAIP) meeting in San Diego. From the year before the first annual meeting to the year after the first annual meeting, membership in NAIP had grown from about 20 hospitalists to about 800 hospitalists. That rapidity of growth had never been seen by another specialty in the history of modern medicine. By the 2003 annual meeting in San Diego, the name had officially changed to the Society of Hospital Medicine, and membership had grown to more than 3,000; less than 10 years later, when the meeting returned to San Diego, membership had grown to more than 10,000. These continued steady increases in both membership size and attendance at the meeting serves as a testimony to the strength of the field and the leadership of the society.
Check out our 6-minute feature video: "Five Reasons You Should Attend HM13"
Where We Are Now
Growth: SHM’s annual meeting now has a track record to be reckoned with. The number of attendees expected for 2013 is a staggering 3,000, which is only a portion of the more than 11,000 SHM members who can actually take time away from their busy practices to attend. The event has now expanded to more than three and a half days, including eight pre-courses and more than 100 workshops/breakout sessions to meet the needs of most any hospitalist. The number of submissions for the Research, Innovations, and Clinical Vignettes competition has steadily risen over the years, topping an all-time record of 800 submissions in 2013. This is a testimony to the curiosity and productivity of so many hospitalists and HM groups.
Advocacy: SHM has been a longstanding and considerable advocate for healthcare reform for more than a decade. With the annual meeting in Washington, D.C., this year, and in lieu of the pre-courses, more than 100 hospitalists and SHM staff will be making a field trip to Capitol Hill to advocate for changes in the structure and payment within the medical industry, to promote good patient care for those we serve, and to promote continued research for better ways of delivering care in the future. Over the course of 2012, SHM submitted more than 20 influential advocacy letters to a variety of stakeholders on topics ranging from sustainable growth rate (SGR) repeal to Agency for Healthcare Research and Quality (AHRQ) funding.
Impact: The annual meeting is not just bigger and longer; it is better. The quality and reputation of the plenary, breakout, and workshop speakers is tremendous, with this year’s plenary speakers including Patrick Conway, chief medical officer of CMS, and David Feinberg, president of UCLA Health System and CEO of UCLA Hospital System. The annual award ceremony will recognize a highly qualified repertoire of dedicated hospitalists and teams and reflect the number and quality of those involved in HM in the areas of clinical excellence, teaching, research, service, and teamwork. The annual Fellows in Hospital Medicine induction will include more than 300 additional fellows and senior fellows, which is a testimony to the level of involvement so many hospitalists have within our specialty.
Where We Are Going
Growth: I suspect the annual meeting will continue to grow in size, and it will expand to better serve the needs of other types of hospital-based physicians (neurologists, obstetricians, etc.), other types of practitioners (NPs, PAs, other specialty nurses), and other types of professionals (administrators and executives). It likely will attract an international community of hospitalists as other nations identify and execute better models of care for hospitalized patients.
Advocacy: SHM and the annual meeting will continue to serve as a nidus for directing the best pathways toward a better healthcare system. It will continue to serve as an avenue by which we partner with and/or influence impactful organizations, such as federal, state, and local governments, the Centers for Medicare & Medicaid Services (CMS), the Joint Commission, and the American Hospital Association, to name a few.
Impact: SHM and the annual meeting will expand its role as the focus for learning and sharing new research and innovations within the field. It will serve as a platform for initiating and spreading standardized evidence-based implementation of best practices through a repertoire of mentored implementation programs. And it will continue to serve as proof of the strength of our hospital medicine community as we spread into every U.S. hospital system and beyond.
Reputation: The future of our annual meeting and reputation will be dependent on how fast and how carefully we craft the pathway for HM. Currently, about half of all the nation’s hospitalists have been in practice for five years or less. We will need to carefully focus on how to be compassionate providers and system advocates—not just shift workers and billing specialists. We will have to be the mentors by which other countries define best practice for inpatient care, including what ideal training for a hospitalist should look like, and what their scope of practice should entail.
If you ask one of the attendees of the first annui conventus what it was like, they will say it was a small mom-and-pop gathering of disparate physicians, with a pie-in-the-sky idea of the future of hospitalist practice. And someday, when our current generation of hospitalists attends an international conference of hospitalists, in Prague, in 2033, we can say, “Remember when we met in that tiny hotel in D.C. in 2013?”
Dr. Scheurer is a hospitalist and chief quality officer at the Medical University of South Carolina in Charleston. She is physician editor of The Hospitalist. Email her at [email protected].
SHM’s annual meeting—or annui conventus, for you Latin lovers—is right around the corner, so be sure to cement your intentions and prepare to go if you have not already.
Now a “longstanding” tradition, the annual meeting serves many purposes, one of which is to act as a reservoir of time for individual hospitalists and for hospitalist groups to reflect on where they have been, where they are now, and where they are (or would like to be) going. A brief history of the SHM annual meeting makes us quickly realize how far we have come, and how far we have to go.
Where We’ve Been
The annual meeting’s history dates back to 1998, when a rogue gathering of about 100 self-proclaimed hospitalists gathered at the National Association of Inpatient Physicians (NAIP) meeting in San Diego. From the year before the first annual meeting to the year after the first annual meeting, membership in NAIP had grown from about 20 hospitalists to about 800 hospitalists. That rapidity of growth had never been seen by another specialty in the history of modern medicine. By the 2003 annual meeting in San Diego, the name had officially changed to the Society of Hospital Medicine, and membership had grown to more than 3,000; less than 10 years later, when the meeting returned to San Diego, membership had grown to more than 10,000. These continued steady increases in both membership size and attendance at the meeting serves as a testimony to the strength of the field and the leadership of the society.
Check out our 6-minute feature video: "Five Reasons You Should Attend HM13"
Where We Are Now
Growth: SHM’s annual meeting now has a track record to be reckoned with. The number of attendees expected for 2013 is a staggering 3,000, which is only a portion of the more than 11,000 SHM members who can actually take time away from their busy practices to attend. The event has now expanded to more than three and a half days, including eight pre-courses and more than 100 workshops/breakout sessions to meet the needs of most any hospitalist. The number of submissions for the Research, Innovations, and Clinical Vignettes competition has steadily risen over the years, topping an all-time record of 800 submissions in 2013. This is a testimony to the curiosity and productivity of so many hospitalists and HM groups.
Advocacy: SHM has been a longstanding and considerable advocate for healthcare reform for more than a decade. With the annual meeting in Washington, D.C., this year, and in lieu of the pre-courses, more than 100 hospitalists and SHM staff will be making a field trip to Capitol Hill to advocate for changes in the structure and payment within the medical industry, to promote good patient care for those we serve, and to promote continued research for better ways of delivering care in the future. Over the course of 2012, SHM submitted more than 20 influential advocacy letters to a variety of stakeholders on topics ranging from sustainable growth rate (SGR) repeal to Agency for Healthcare Research and Quality (AHRQ) funding.
Impact: The annual meeting is not just bigger and longer; it is better. The quality and reputation of the plenary, breakout, and workshop speakers is tremendous, with this year’s plenary speakers including Patrick Conway, chief medical officer of CMS, and David Feinberg, president of UCLA Health System and CEO of UCLA Hospital System. The annual award ceremony will recognize a highly qualified repertoire of dedicated hospitalists and teams and reflect the number and quality of those involved in HM in the areas of clinical excellence, teaching, research, service, and teamwork. The annual Fellows in Hospital Medicine induction will include more than 300 additional fellows and senior fellows, which is a testimony to the level of involvement so many hospitalists have within our specialty.
Where We Are Going
Growth: I suspect the annual meeting will continue to grow in size, and it will expand to better serve the needs of other types of hospital-based physicians (neurologists, obstetricians, etc.), other types of practitioners (NPs, PAs, other specialty nurses), and other types of professionals (administrators and executives). It likely will attract an international community of hospitalists as other nations identify and execute better models of care for hospitalized patients.
Advocacy: SHM and the annual meeting will continue to serve as a nidus for directing the best pathways toward a better healthcare system. It will continue to serve as an avenue by which we partner with and/or influence impactful organizations, such as federal, state, and local governments, the Centers for Medicare & Medicaid Services (CMS), the Joint Commission, and the American Hospital Association, to name a few.
Impact: SHM and the annual meeting will expand its role as the focus for learning and sharing new research and innovations within the field. It will serve as a platform for initiating and spreading standardized evidence-based implementation of best practices through a repertoire of mentored implementation programs. And it will continue to serve as proof of the strength of our hospital medicine community as we spread into every U.S. hospital system and beyond.
Reputation: The future of our annual meeting and reputation will be dependent on how fast and how carefully we craft the pathway for HM. Currently, about half of all the nation’s hospitalists have been in practice for five years or less. We will need to carefully focus on how to be compassionate providers and system advocates—not just shift workers and billing specialists. We will have to be the mentors by which other countries define best practice for inpatient care, including what ideal training for a hospitalist should look like, and what their scope of practice should entail.
If you ask one of the attendees of the first annui conventus what it was like, they will say it was a small mom-and-pop gathering of disparate physicians, with a pie-in-the-sky idea of the future of hospitalist practice. And someday, when our current generation of hospitalists attends an international conference of hospitalists, in Prague, in 2033, we can say, “Remember when we met in that tiny hotel in D.C. in 2013?”
Dr. Scheurer is a hospitalist and chief quality officer at the Medical University of South Carolina in Charleston. She is physician editor of The Hospitalist. Email her at [email protected].
Two Accountable Care Organizations (ACOs) Share Their Strategies for Success
Success as an ACO likely won’t come from any one strategy, but from many. Christopher Kim, MD, MBA, SFHM, a hospitalist and associate professor of internal medicine at the University of Michigan, says the Michigan Pioneer ACO serving roughly 20,000 beneficiaries in the state’s southeastern region has benefited greatly from a variety of pre-existing relationships and initiatives. The university’s medical center, one of 10 participants in a Medicare ACO precursor called the Physician Group Practice demonstration project, was among the few sites to successfully meet the requirements and gain the full cost savings benefits in all five years.
The newer ACO, which officially launched in January 2012, pairs the university’s Faculty Group Practice with Integrated Health Associates Inc. (IHA), a large multispecialty private-practice group. Many IHA providers already had access to the university’s electronic health records so they could track admitted patients. One preliminary collaborative effort between the two entities hinted at a trend toward lower readmission rates among a small group of patients who were seen by a primary-care provider within seven days of a hospital discharge, underscoring the importance of a smooth transition.
Providers also have been able to tap into statewide initiatives aimed at improving quality and care coordination in key areas, such as cardiovascular disease, cancer, and hospital care transitions (sponsored by Blue Cross Blue Shield of Michigan).

—Christopher Kim, MD, MBA, SFHM, associate professor of internal medicine, University of Michigan Health System, Ann Arbor
“These programs helped physician organizations and hospitals throughout the state become familiar with best practices related to these kinds of conditions,” Dr. Kim says, “and I think partly because of that, we were very prepared to work on a quality-improvement initiative such as this while also improving efficiency.”
Listen to Dr. Kim discuss the added responsibility hospitalists in ACOs like the one formed between the university faculty and a large multi-specialty practice called Integrated Health Associates, Inc.
For stratifying beneficiaries by risk, the ACO has benefited from a separate initiative called the Michigan Primary Care Transformation Project, which uses the concept of a pyramid to classify increasingly complicated patients. A complex-case manager, typically an advanced practice nurse, acts as the point person for guiding patients in the upper half of the pyramid toward the best resources while preventing unnecessary duplication of tasks or consultation referrals. Optimal coordination means that hospitalists need to communicate effectively with these managers as well as with other providers.
From Medicare claims supplied by CMS, Beth Israel Deaconess Physician Organization (BIDPO) in the Boston metropolitan region has used software to identify its highest-risk patients, or those most likely to be admitted to the hospital within the next 12 months. As part of the process, BIDPO officials asked doctors to validate the results based on their own patient records and observations.
The ACO has hired nurse practitioners through a company called INSPIRIS Massachusetts to visit its sickest and frailest Medicare beneficiaries at home to prevent hospital admissions and to avoid post-discharge readmissions among the highest-risk patients. BIDPO also uses nurse care managers to do telephone-based care management for less acute patients, and is asking emergency department staff to recognize patients who could be sent home safely with appropriate care rather than be admitted. Patients with cellulitis, for example, could be treated via IV antibiotic therapy at home, a service made possible through a collaboration with a home infusion company.
Dr. Parker, BIDPO’s medical director, says hospitalists will be key to understanding the need for excellent inpatient care and thoughtful, comprehensive discharge planning that helps avoid adverse events post-discharge.
Success as an ACO likely won’t come from any one strategy, but from many. Christopher Kim, MD, MBA, SFHM, a hospitalist and associate professor of internal medicine at the University of Michigan, says the Michigan Pioneer ACO serving roughly 20,000 beneficiaries in the state’s southeastern region has benefited greatly from a variety of pre-existing relationships and initiatives. The university’s medical center, one of 10 participants in a Medicare ACO precursor called the Physician Group Practice demonstration project, was among the few sites to successfully meet the requirements and gain the full cost savings benefits in all five years.
The newer ACO, which officially launched in January 2012, pairs the university’s Faculty Group Practice with Integrated Health Associates Inc. (IHA), a large multispecialty private-practice group. Many IHA providers already had access to the university’s electronic health records so they could track admitted patients. One preliminary collaborative effort between the two entities hinted at a trend toward lower readmission rates among a small group of patients who were seen by a primary-care provider within seven days of a hospital discharge, underscoring the importance of a smooth transition.
Providers also have been able to tap into statewide initiatives aimed at improving quality and care coordination in key areas, such as cardiovascular disease, cancer, and hospital care transitions (sponsored by Blue Cross Blue Shield of Michigan).

—Christopher Kim, MD, MBA, SFHM, associate professor of internal medicine, University of Michigan Health System, Ann Arbor
“These programs helped physician organizations and hospitals throughout the state become familiar with best practices related to these kinds of conditions,” Dr. Kim says, “and I think partly because of that, we were very prepared to work on a quality-improvement initiative such as this while also improving efficiency.”
Listen to Dr. Kim discuss the added responsibility hospitalists in ACOs like the one formed between the university faculty and a large multi-specialty practice called Integrated Health Associates, Inc.
For stratifying beneficiaries by risk, the ACO has benefited from a separate initiative called the Michigan Primary Care Transformation Project, which uses the concept of a pyramid to classify increasingly complicated patients. A complex-case manager, typically an advanced practice nurse, acts as the point person for guiding patients in the upper half of the pyramid toward the best resources while preventing unnecessary duplication of tasks or consultation referrals. Optimal coordination means that hospitalists need to communicate effectively with these managers as well as with other providers.
From Medicare claims supplied by CMS, Beth Israel Deaconess Physician Organization (BIDPO) in the Boston metropolitan region has used software to identify its highest-risk patients, or those most likely to be admitted to the hospital within the next 12 months. As part of the process, BIDPO officials asked doctors to validate the results based on their own patient records and observations.
The ACO has hired nurse practitioners through a company called INSPIRIS Massachusetts to visit its sickest and frailest Medicare beneficiaries at home to prevent hospital admissions and to avoid post-discharge readmissions among the highest-risk patients. BIDPO also uses nurse care managers to do telephone-based care management for less acute patients, and is asking emergency department staff to recognize patients who could be sent home safely with appropriate care rather than be admitted. Patients with cellulitis, for example, could be treated via IV antibiotic therapy at home, a service made possible through a collaboration with a home infusion company.
Dr. Parker, BIDPO’s medical director, says hospitalists will be key to understanding the need for excellent inpatient care and thoughtful, comprehensive discharge planning that helps avoid adverse events post-discharge.
Success as an ACO likely won’t come from any one strategy, but from many. Christopher Kim, MD, MBA, SFHM, a hospitalist and associate professor of internal medicine at the University of Michigan, says the Michigan Pioneer ACO serving roughly 20,000 beneficiaries in the state’s southeastern region has benefited greatly from a variety of pre-existing relationships and initiatives. The university’s medical center, one of 10 participants in a Medicare ACO precursor called the Physician Group Practice demonstration project, was among the few sites to successfully meet the requirements and gain the full cost savings benefits in all five years.
The newer ACO, which officially launched in January 2012, pairs the university’s Faculty Group Practice with Integrated Health Associates Inc. (IHA), a large multispecialty private-practice group. Many IHA providers already had access to the university’s electronic health records so they could track admitted patients. One preliminary collaborative effort between the two entities hinted at a trend toward lower readmission rates among a small group of patients who were seen by a primary-care provider within seven days of a hospital discharge, underscoring the importance of a smooth transition.
Providers also have been able to tap into statewide initiatives aimed at improving quality and care coordination in key areas, such as cardiovascular disease, cancer, and hospital care transitions (sponsored by Blue Cross Blue Shield of Michigan).

—Christopher Kim, MD, MBA, SFHM, associate professor of internal medicine, University of Michigan Health System, Ann Arbor
“These programs helped physician organizations and hospitals throughout the state become familiar with best practices related to these kinds of conditions,” Dr. Kim says, “and I think partly because of that, we were very prepared to work on a quality-improvement initiative such as this while also improving efficiency.”
Listen to Dr. Kim discuss the added responsibility hospitalists in ACOs like the one formed between the university faculty and a large multi-specialty practice called Integrated Health Associates, Inc.
For stratifying beneficiaries by risk, the ACO has benefited from a separate initiative called the Michigan Primary Care Transformation Project, which uses the concept of a pyramid to classify increasingly complicated patients. A complex-case manager, typically an advanced practice nurse, acts as the point person for guiding patients in the upper half of the pyramid toward the best resources while preventing unnecessary duplication of tasks or consultation referrals. Optimal coordination means that hospitalists need to communicate effectively with these managers as well as with other providers.
From Medicare claims supplied by CMS, Beth Israel Deaconess Physician Organization (BIDPO) in the Boston metropolitan region has used software to identify its highest-risk patients, or those most likely to be admitted to the hospital within the next 12 months. As part of the process, BIDPO officials asked doctors to validate the results based on their own patient records and observations.
The ACO has hired nurse practitioners through a company called INSPIRIS Massachusetts to visit its sickest and frailest Medicare beneficiaries at home to prevent hospital admissions and to avoid post-discharge readmissions among the highest-risk patients. BIDPO also uses nurse care managers to do telephone-based care management for less acute patients, and is asking emergency department staff to recognize patients who could be sent home safely with appropriate care rather than be admitted. Patients with cellulitis, for example, could be treated via IV antibiotic therapy at home, a service made possible through a collaboration with a home infusion company.
Dr. Parker, BIDPO’s medical director, says hospitalists will be key to understanding the need for excellent inpatient care and thoughtful, comprehensive discharge planning that helps avoid adverse events post-discharge.
ONLINE EXCLUSIVE: Why Hospitalists Should Spread the Good Word on Capitol Hill
ONLINE EXCLUSIVE: The Medical Director of the National Alliance on Mental Illness Spotlights Hospitalist Communication, Attention to Discharge Details
Click here to listen to Dr. Duckworth
Click here to listen to Dr. Duckworth
Click here to listen to Dr. Duckworth
ONLINE EXCLUSIVE: Listen to SHM Annual Meeting Course Director and Keynote Speaker
Click here to listen to Dr. Brotman
Click here to listen to Dr. Feinberg
Check out our 6-minute feature video: "Five Reasons You Should Attend HM13"
Click here to listen to Dr. Brotman
Click here to listen to Dr. Feinberg
Check out our 6-minute feature video: "Five Reasons You Should Attend HM13"
Click here to listen to Dr. Brotman
Click here to listen to Dr. Feinberg
Check out our 6-minute feature video: "Five Reasons You Should Attend HM13"
Clarifying the Role of Hospitalists Focused on Family Medicine in the ICU
Clarifying Family-Practice Hospitalists’ Value, Focused-Practice Opportunities
I am writing regarding the letter and your response in the January 2013 issue of The Hospitalist regarding hospitalists trained in family medicine and practice in critical-care units. I am the chair of the Family Medicine Committee for SHM, a practicing hospitalist, and an SHM member for over 10 years. There is an error in your reply, in that physicians who are board-certified through the American Board of Family Medicine (ABFM) are indeed eligible to take the examination for Recognition of Focused Practice in Hospital Medicine (RFPHM). This examination is administered by the American Board of Internal Medicine (ABIM), and is the same examination for all physicians, regardless of whether their residency was completed in family or internal medicine.
I am proud to be among the six family physicians who took and passed the first examination in October 2010. Through 2012, there have been 28 family physicians who have passed this exam, and attained RFPHM (verbal communication from ABFM). According to the ABIM website, there have been 267 total physicians who have taken the examination through 2011, which includes family-medicine-trained physicians. There are a number of Maintenance of Certification (MOC) modules offered through the ABIM that are available to hospitalists trained in family medicine.
A prior study showed that 66% of hospitalists trained in family medicine practice in critical-care units (McElrath et al). You are correct that there is no current pathway for HTFM to pursue a critical-care fellowship or attain board certification by the SCCM, as diplomats of the ABFM are excluded. However, there are many hospitalists trained in family medicine providing excellent care to patients in critical-care units. There are clearly not enough board certified intensivists to provide the care.
—Kevin Ahern, MD, SFHM, chief hospitalist, Sound Physicians, Urbana, Ohio
Dr. Hospitalist responds:
You are absolutely correct in your point of clarification regarding the Recognition of Focused Practice in Hospital Medicine from the ABFM. I was aware of this at the time of the article; however, in my efforts to outline the proposed path from RFPHM to ICU certification, I focused solely on the ABIM pathway without mentioning the additional recognition available to family-practice physicians. In no way was this meant to denigrate the efforts or contributions of family-practice physicians to HM and SHM, but I could have been much more clear on this point. Having hired and worked alongside family-practice hospitalists, I know just how valuable you are.
The overall picture is consistent with what you described in that there are “clearly not enough board-certified intensivists” to fully staff ICUs. However, it is evident that it will be an uphill battle to sanction an alternate pathway that lets any hospitalist gain certification as an ICU physician. Truth be told, there are fundamental differences in the amount of ICU exposure between internal-medicine and family-practice training programs. As a result, in the current proposal there is no overt discussion of the role for family-practice hospitalists in the ICU. I think that this will continue to remain a conscious omission for both political and practical reasons.
Clarifying Family-Practice Hospitalists’ Value, Focused-Practice Opportunities
I am writing regarding the letter and your response in the January 2013 issue of The Hospitalist regarding hospitalists trained in family medicine and practice in critical-care units. I am the chair of the Family Medicine Committee for SHM, a practicing hospitalist, and an SHM member for over 10 years. There is an error in your reply, in that physicians who are board-certified through the American Board of Family Medicine (ABFM) are indeed eligible to take the examination for Recognition of Focused Practice in Hospital Medicine (RFPHM). This examination is administered by the American Board of Internal Medicine (ABIM), and is the same examination for all physicians, regardless of whether their residency was completed in family or internal medicine.
I am proud to be among the six family physicians who took and passed the first examination in October 2010. Through 2012, there have been 28 family physicians who have passed this exam, and attained RFPHM (verbal communication from ABFM). According to the ABIM website, there have been 267 total physicians who have taken the examination through 2011, which includes family-medicine-trained physicians. There are a number of Maintenance of Certification (MOC) modules offered through the ABIM that are available to hospitalists trained in family medicine.
A prior study showed that 66% of hospitalists trained in family medicine practice in critical-care units (McElrath et al). You are correct that there is no current pathway for HTFM to pursue a critical-care fellowship or attain board certification by the SCCM, as diplomats of the ABFM are excluded. However, there are many hospitalists trained in family medicine providing excellent care to patients in critical-care units. There are clearly not enough board certified intensivists to provide the care.
—Kevin Ahern, MD, SFHM, chief hospitalist, Sound Physicians, Urbana, Ohio
Dr. Hospitalist responds:
You are absolutely correct in your point of clarification regarding the Recognition of Focused Practice in Hospital Medicine from the ABFM. I was aware of this at the time of the article; however, in my efforts to outline the proposed path from RFPHM to ICU certification, I focused solely on the ABIM pathway without mentioning the additional recognition available to family-practice physicians. In no way was this meant to denigrate the efforts or contributions of family-practice physicians to HM and SHM, but I could have been much more clear on this point. Having hired and worked alongside family-practice hospitalists, I know just how valuable you are.
The overall picture is consistent with what you described in that there are “clearly not enough board-certified intensivists” to fully staff ICUs. However, it is evident that it will be an uphill battle to sanction an alternate pathway that lets any hospitalist gain certification as an ICU physician. Truth be told, there are fundamental differences in the amount of ICU exposure between internal-medicine and family-practice training programs. As a result, in the current proposal there is no overt discussion of the role for family-practice hospitalists in the ICU. I think that this will continue to remain a conscious omission for both political and practical reasons.
Clarifying Family-Practice Hospitalists’ Value, Focused-Practice Opportunities
I am writing regarding the letter and your response in the January 2013 issue of The Hospitalist regarding hospitalists trained in family medicine and practice in critical-care units. I am the chair of the Family Medicine Committee for SHM, a practicing hospitalist, and an SHM member for over 10 years. There is an error in your reply, in that physicians who are board-certified through the American Board of Family Medicine (ABFM) are indeed eligible to take the examination for Recognition of Focused Practice in Hospital Medicine (RFPHM). This examination is administered by the American Board of Internal Medicine (ABIM), and is the same examination for all physicians, regardless of whether their residency was completed in family or internal medicine.
I am proud to be among the six family physicians who took and passed the first examination in October 2010. Through 2012, there have been 28 family physicians who have passed this exam, and attained RFPHM (verbal communication from ABFM). According to the ABIM website, there have been 267 total physicians who have taken the examination through 2011, which includes family-medicine-trained physicians. There are a number of Maintenance of Certification (MOC) modules offered through the ABIM that are available to hospitalists trained in family medicine.
A prior study showed that 66% of hospitalists trained in family medicine practice in critical-care units (McElrath et al). You are correct that there is no current pathway for HTFM to pursue a critical-care fellowship or attain board certification by the SCCM, as diplomats of the ABFM are excluded. However, there are many hospitalists trained in family medicine providing excellent care to patients in critical-care units. There are clearly not enough board certified intensivists to provide the care.
—Kevin Ahern, MD, SFHM, chief hospitalist, Sound Physicians, Urbana, Ohio
Dr. Hospitalist responds:
You are absolutely correct in your point of clarification regarding the Recognition of Focused Practice in Hospital Medicine from the ABFM. I was aware of this at the time of the article; however, in my efforts to outline the proposed path from RFPHM to ICU certification, I focused solely on the ABIM pathway without mentioning the additional recognition available to family-practice physicians. In no way was this meant to denigrate the efforts or contributions of family-practice physicians to HM and SHM, but I could have been much more clear on this point. Having hired and worked alongside family-practice hospitalists, I know just how valuable you are.
The overall picture is consistent with what you described in that there are “clearly not enough board-certified intensivists” to fully staff ICUs. However, it is evident that it will be an uphill battle to sanction an alternate pathway that lets any hospitalist gain certification as an ICU physician. Truth be told, there are fundamental differences in the amount of ICU exposure between internal-medicine and family-practice training programs. As a result, in the current proposal there is no overt discussion of the role for family-practice hospitalists in the ICU. I think that this will continue to remain a conscious omission for both political and practical reasons.