User login
15 Things Dermatologists Think Hospitalists Need to Know
- Maintain a broader range of differential diagnoses before ruling in or out something more concrete.
- Attend dermatology lectures as part of primary care’s continuing medical education courses.
- Review a good basic dermatology atlas from time to time.
- Learn to correctly describe lesions to a dermatologist by phone.
- Don’t assume that groin rashes are all fungal.
- Don’t mistakenly associate a drug-related reaction with a medication given one to two days before the onset of a rash.
- Consider involving a dermatologist to help manage open skin lesions, particularly if you’re unsure of the cause.
- Prescribe an adequate quantity of topical corticosteroids for the duration of treatment.
- Beware of painful or blistering rashes, especially if they involve the mucosa of the mouth, eyes, or genitals.
- Watch out for zoster, widespread herpes, pemphigus, and pemphigoid.
- Pay attention to itching in the wrists, genital region, and web spaces of fingers and toes.
- Be mindful of the rapid onset of purpuric lesions on the skin.
- Avoid consults for improving rashes and seborrheic keratosis, as well as nonurgent outpatient issues, such as psoriasis, rosacea, or a history of skin cancer.
- Don’t prescribe combined betamethasone/clotrimazole, also known as Lotrisone, for chronic scaly hands, feet, or groin.
- Encourage patients to follow up with a dermatologist on an outpatient basis.
Dermatologic diseases tend to receive little attention at most U.S. medical schools—typically only several days of lectures or a few weeks of clinical exposure.
“Not surprisingly, many general practitioners may feel unprepared to address hospitalized patients with challenging dermatologic findings,” says R. Samuel Hopkins, MD, assistant professor of dermatology and assistant residency program director at Oregon Health & Science University in Portland.
Few studies have examined the quality of inpatient dermatologic care. One study, a retrospective chart review at a Midwestern university hospital, found that the primary ward team submitted an accurate dermatologic diagnosis in only 23.9% of cases. Meanwhile, consultation with a dermatologist led to a change or addition to treatment in 77% of patients (Dermatol Online J. 2010;16(2):12).
“Given that medical schools may not be able to dedicate more time to managing dermatologic conditions, the burden of education may fall on post-graduate programs and continuing medical education to fill this gap,” Dr. Hopkins says. To further complicate matters, “it is difficult in many hospitals to obtain a dermatology consult on an inpatient, reflecting the limited access hospitalists often have to dermatologists.”
The most frequently encountered dermatologic conditions in the hospital setting are drug eruptions and skin infections. Dermatitis is the most misdiagnosed condition by nondermatologists in hospitals, says Russell Vinik, MD, co-director of the hospitalist group at the University of Utah Health Care in Salt Lake City.
The majority of skin issues don’t require a dermatologist’s input, but some do. “Clearly, there’s also the rash that we just don’t know what it is,” Dr. Vinik says. When in doubt, it’s best to err on the safe side and call the specialist.
Here’s how to assess whether to manage a dermatologic case yourself, or how to involve a dermatologist for appropriate diagnosis and treatment. In general, Dr. Hopkins says, “Whether one can handle a case on their own or not is a case-by-case decision by the hospitalist based on their comfort with their diagnosis and management.”
Maintain a broader range of differential diagnoses before ruling in or out something more concrete.
“Very often, patients with skin diseases are given a specific diagnosis without consideration of mimickers,” says Daniela Kroshinsky, MD, MPH, assistant professor of dermatology at Harvard Medical School in Boston.
“Cellulitis is a great example. People will come in with hot, red skin and be diagnosed with and treated for cellulitis but really have stasis dermatitis, Lyme [disease], gout, et cetera,” says Dr. Kroshinsky, who also is director of pediatric dermatology and director of inpatient dermatology, education, and research at Massachusetts General Hospital.
“The clinical picture of warm, red, tender skin can fit many conditions but is most often called cellulitis by nondermatologists,” she explains. “It’s not clear why, but I would suspect this is because cellulitis is one of the few dermatologic conditions taught in medical school, while the mimickers get less attention.”
Attend dermatology lectures as part of primary care’s continuing medical education courses.
This would increase your knowledge of skin conditions affecting hospitalized patients, Dr. Kroshinsky says. If there is a dermatologic consultant for your hospital, work closely with this specialist until you feel comfortable making diagnoses and incorporating treatment plans.
Similarly, if you are a resident who is interested in a career in hospital medicine, consider doing a rotation in dermatology.
Review a good basic dermatology atlas from time to time.
This keeps your mind open to differential diagnoses for a given situation that you may encounter in the hospital setting. A more comprehensive book or online reference can be helpful to peruse after seeing a patient with a particular rash, Dr. Kroshinsky says.
Learn to correctly describe lesions to a dermatologist by phone.
When a specialist isn’t available on site, the phone communication is vital to the specialist. This includes familiarizing yourself with some of the more life-threatening dermatologic problems, such as drug-induced hypersensitivity reactions. It will be easier to recognize when an urgent dermatologic consultation is required. Sometimes this is necessary when a patient doesn’t respond to treatment for a reasonable and presumed diagnosis—when one condition seems to mimic the symptoms of another, says Lindy Fox, MD, associate professor of clinical dermatology at the University of California at San Francisco and director of its hospital dermatology consultation service.
Don’t assume that groin rashes are all fungal.
In fact, there is a very large differential diagnosis for intertriginous eruptions, Dr. Fox says. Perform a KOH test (potassium hydroxide) and fungal cultures on intertriginous eruptions. If no fungus is identified or the patient is not responding appropriately to therapy, call for a dermatologic consultation.
Don’t mistakenly associate a drug-related reaction with a medication given one to two days before the onset of a rash.
It is typically seven to 10 days post-exposure that a drug eruption develops, Dr. Fox says. He suggests making a drug chart to highlight dates of medication administration. This helps pinpoint the most likely culprit based on timing and the probability that a certain drug may induce cutaneous eruptions. Correct identification of the type of drug eruption (e.g. simple drug eruption vs. hypersensitivity vs. potentially deadly Stevens-Johnson syndrome) is important.
Consider involving a dermatologist to help manage open skin lesions, particularly if you’re unsure of the cause.
There are many different causes of skin ulcers. Trauma, infections, and even malignancies can present as open wounds. Leg ulcers may be due to venous stasis, but they also can be caused by arterial insufficiency, vasculitis, and other conditions. A dermatologist might opt to perform a skin biopsy to help diagnose the lesion.
“Wound-care nurses can be very helpful in managing skin lesions, but they do not always have the experience needed to correctly diagnose the underlying problem,” says Kathryn Schwarzenberger, MD, professor of medicine at the University of Vermont College of Medicine in Burlington. “If you’re thinking of calling the wound-care nurse, think of calling the dermatologist first.”
Prescribe an adequate quantity of topical corticosteroids for the duration of treatment.
“It’s really important to provide enough medicine,” Dr. Schwarzenberger says. Typically, a patient will receive a small tube, apply the contents, and find that “it’s enough medicine to cover their body once. This doesn’t work if you intended to have the patient apply it all over for two weeks.”
It takes, on average, 30 g of a topical medication to cover the body once. With topical steroids, prescribing an insufficient quantity “dooms your therapy to failure.”
Allergic reactions from these medications are rare, and some insurance companies charge the same regardless of the size. Prescribing a small amount initially might incur an additional expense for the patient.
Beware of painful or blistering rashes, especially if they involve the mucosa of the mouth, eyes, or genitals.
“These symptoms can be associated with potentially deadly toxic epidermal necrolysis,” says Daniel Aires, MD, JD, director of the division of dermatology at the University of Kansas School of Medicine in Kansas City, Kan. “Consult dermatology immediately. The sooner treatment is begun, the better the odds of survival.”
If a rash involves the eye, call an ophthalmologist and a dermatologist. “Eyes are more likely than skin to develop chronic complications after resolution of an acute condition,” he says.
For a rash involving primarily the mouth, call an otolaryngologist, a dentist, or both, as well as a dermatologist. These specialists are more skilled in visualizing and treating oral conditions.
Watch out for zoster, widespread herpes, pemphigus, and pemphigoid.
These blistering conditions require urgent diagnosis and treatment, so a dermatologist’s expertise is needed quickly, Dr. Aires says. Even without the presence of blisters, a single region of the skin or “dermatome” gives pause for concern.
“This could be a sign of zoster, which is especially dangerous in immunosuppressed or otherwise debilitated patients,” he cautions. “Either perform a culture and begin treatment, or consult dermatology, or do both.”
Pay attention to itching in the wrists, genital region, and web spaces of fingers and toes.
This may be due to scabies infestation. “Scabies can spread rapidly throughout a hospital ward,” Dr. Aires says. What to do: Scrape for scabies, consider a trial of topical treatment, and consult a dermatologist if you’re unsure.
Be mindful of the rapid onset of purpuric lesionscon the skin.
They warrant suspicion of such conditions as vasculitis, hypercoaguable states, and disseminated angiotropic infections, says Dr. Hopkins of Oregon Health & Science University. “The shape and size of purpuric skin lesions help determine the etiology. A few characteristic examples include papular purpura and retiform purpura. Papular purpura [raised purpuric papules] may suggest vasculitis. Purpura that forms net-like patches is called retiform purpura and suggests a vaso-occlusive process, such as from a hypercoaguable state, embolic phenomena, or calciphylaxis.”
13 Avoid consults for improving rashes and seborrheic keratosis, as well as nonurgent outpatient issues, such as psoriasis, rosacea, or a history of skin cancer. These conditions “are more easily addressed in a clinic, as opposed to in a hospital, where the patient is lying in a bed feeling ill with IV tubes in place,” Dr. Aires says. “It also reflects respect for the dermatologist’s time. Inpatient dermatology can be pretty busy, so it’s preferable to consult primarily for urgent skin issues.” Consultations can be costly, too, and most patients would rather avoid additional medical bills.
Don’t prescribe combined betamethasone/clotrimazole, also known as Lotrisone, for chronic scaly hands, feet, or groin.
Although it is not harmful, “it is not usually a great choice for typical ‘dermatophyte’ fungal infections, such as athlete’s foot and ‘jock itch,’” Dr. Aires says. “Over-the-counter Lamisil is better, particularly following daily use of 10-minute soaks in 50-50 vinegar-water. Even for yeast infections, miconazole is better than clotrimazole.”
As for betamethasone, this “component is way too strong for the groin area and can cause atrophy or worse,” he says.

—Daniela Kroshinsky, MD, MPH, director of inpatient dermatology, education, and research, Massachusetts General Hospital, Boston
Encourage patients to follow up with a dermatologist on an outpatient basis.
By heeding this advice, patients are less likely to return to the ED for skin conditions that can be managed in an office, says Kirsten Flynn, MD, a dermatologist at Banner Health Center in Sun City West, Ariz. Inpatient admissions by dermatologists have been decreasing over the years. Most patients with skin diseases or cutaneous manifestations of systemic illnesses are admitted to hospitals by other physicians.
“Many dermatologists are happy to fit in urgent consults in their clinics. Drug eruptions are by far the most common consultation request,” says Dr. Flynn, who notes that high-dose IV steroids can cause complications, such as gastrointestinal bleeding, bowel perforation, opportunistic infections, and exacerbation of underlying diseases. “In most cases, removing the offending agent and providing supportive care is the best option.”
Susan Kreimer is a freelance writer in New York.
- Maintain a broader range of differential diagnoses before ruling in or out something more concrete.
- Attend dermatology lectures as part of primary care’s continuing medical education courses.
- Review a good basic dermatology atlas from time to time.
- Learn to correctly describe lesions to a dermatologist by phone.
- Don’t assume that groin rashes are all fungal.
- Don’t mistakenly associate a drug-related reaction with a medication given one to two days before the onset of a rash.
- Consider involving a dermatologist to help manage open skin lesions, particularly if you’re unsure of the cause.
- Prescribe an adequate quantity of topical corticosteroids for the duration of treatment.
- Beware of painful or blistering rashes, especially if they involve the mucosa of the mouth, eyes, or genitals.
- Watch out for zoster, widespread herpes, pemphigus, and pemphigoid.
- Pay attention to itching in the wrists, genital region, and web spaces of fingers and toes.
- Be mindful of the rapid onset of purpuric lesions on the skin.
- Avoid consults for improving rashes and seborrheic keratosis, as well as nonurgent outpatient issues, such as psoriasis, rosacea, or a history of skin cancer.
- Don’t prescribe combined betamethasone/clotrimazole, also known as Lotrisone, for chronic scaly hands, feet, or groin.
- Encourage patients to follow up with a dermatologist on an outpatient basis.
Dermatologic diseases tend to receive little attention at most U.S. medical schools—typically only several days of lectures or a few weeks of clinical exposure.
“Not surprisingly, many general practitioners may feel unprepared to address hospitalized patients with challenging dermatologic findings,” says R. Samuel Hopkins, MD, assistant professor of dermatology and assistant residency program director at Oregon Health & Science University in Portland.
Few studies have examined the quality of inpatient dermatologic care. One study, a retrospective chart review at a Midwestern university hospital, found that the primary ward team submitted an accurate dermatologic diagnosis in only 23.9% of cases. Meanwhile, consultation with a dermatologist led to a change or addition to treatment in 77% of patients (Dermatol Online J. 2010;16(2):12).
“Given that medical schools may not be able to dedicate more time to managing dermatologic conditions, the burden of education may fall on post-graduate programs and continuing medical education to fill this gap,” Dr. Hopkins says. To further complicate matters, “it is difficult in many hospitals to obtain a dermatology consult on an inpatient, reflecting the limited access hospitalists often have to dermatologists.”
The most frequently encountered dermatologic conditions in the hospital setting are drug eruptions and skin infections. Dermatitis is the most misdiagnosed condition by nondermatologists in hospitals, says Russell Vinik, MD, co-director of the hospitalist group at the University of Utah Health Care in Salt Lake City.
The majority of skin issues don’t require a dermatologist’s input, but some do. “Clearly, there’s also the rash that we just don’t know what it is,” Dr. Vinik says. When in doubt, it’s best to err on the safe side and call the specialist.
Here’s how to assess whether to manage a dermatologic case yourself, or how to involve a dermatologist for appropriate diagnosis and treatment. In general, Dr. Hopkins says, “Whether one can handle a case on their own or not is a case-by-case decision by the hospitalist based on their comfort with their diagnosis and management.”
Maintain a broader range of differential diagnoses before ruling in or out something more concrete.
“Very often, patients with skin diseases are given a specific diagnosis without consideration of mimickers,” says Daniela Kroshinsky, MD, MPH, assistant professor of dermatology at Harvard Medical School in Boston.
“Cellulitis is a great example. People will come in with hot, red skin and be diagnosed with and treated for cellulitis but really have stasis dermatitis, Lyme [disease], gout, et cetera,” says Dr. Kroshinsky, who also is director of pediatric dermatology and director of inpatient dermatology, education, and research at Massachusetts General Hospital.
“The clinical picture of warm, red, tender skin can fit many conditions but is most often called cellulitis by nondermatologists,” she explains. “It’s not clear why, but I would suspect this is because cellulitis is one of the few dermatologic conditions taught in medical school, while the mimickers get less attention.”
Attend dermatology lectures as part of primary care’s continuing medical education courses.
This would increase your knowledge of skin conditions affecting hospitalized patients, Dr. Kroshinsky says. If there is a dermatologic consultant for your hospital, work closely with this specialist until you feel comfortable making diagnoses and incorporating treatment plans.
Similarly, if you are a resident who is interested in a career in hospital medicine, consider doing a rotation in dermatology.
Review a good basic dermatology atlas from time to time.
This keeps your mind open to differential diagnoses for a given situation that you may encounter in the hospital setting. A more comprehensive book or online reference can be helpful to peruse after seeing a patient with a particular rash, Dr. Kroshinsky says.
Learn to correctly describe lesions to a dermatologist by phone.
When a specialist isn’t available on site, the phone communication is vital to the specialist. This includes familiarizing yourself with some of the more life-threatening dermatologic problems, such as drug-induced hypersensitivity reactions. It will be easier to recognize when an urgent dermatologic consultation is required. Sometimes this is necessary when a patient doesn’t respond to treatment for a reasonable and presumed diagnosis—when one condition seems to mimic the symptoms of another, says Lindy Fox, MD, associate professor of clinical dermatology at the University of California at San Francisco and director of its hospital dermatology consultation service.
Don’t assume that groin rashes are all fungal.
In fact, there is a very large differential diagnosis for intertriginous eruptions, Dr. Fox says. Perform a KOH test (potassium hydroxide) and fungal cultures on intertriginous eruptions. If no fungus is identified or the patient is not responding appropriately to therapy, call for a dermatologic consultation.
Don’t mistakenly associate a drug-related reaction with a medication given one to two days before the onset of a rash.
It is typically seven to 10 days post-exposure that a drug eruption develops, Dr. Fox says. He suggests making a drug chart to highlight dates of medication administration. This helps pinpoint the most likely culprit based on timing and the probability that a certain drug may induce cutaneous eruptions. Correct identification of the type of drug eruption (e.g. simple drug eruption vs. hypersensitivity vs. potentially deadly Stevens-Johnson syndrome) is important.
Consider involving a dermatologist to help manage open skin lesions, particularly if you’re unsure of the cause.
There are many different causes of skin ulcers. Trauma, infections, and even malignancies can present as open wounds. Leg ulcers may be due to venous stasis, but they also can be caused by arterial insufficiency, vasculitis, and other conditions. A dermatologist might opt to perform a skin biopsy to help diagnose the lesion.
“Wound-care nurses can be very helpful in managing skin lesions, but they do not always have the experience needed to correctly diagnose the underlying problem,” says Kathryn Schwarzenberger, MD, professor of medicine at the University of Vermont College of Medicine in Burlington. “If you’re thinking of calling the wound-care nurse, think of calling the dermatologist first.”
Prescribe an adequate quantity of topical corticosteroids for the duration of treatment.
“It’s really important to provide enough medicine,” Dr. Schwarzenberger says. Typically, a patient will receive a small tube, apply the contents, and find that “it’s enough medicine to cover their body once. This doesn’t work if you intended to have the patient apply it all over for two weeks.”
It takes, on average, 30 g of a topical medication to cover the body once. With topical steroids, prescribing an insufficient quantity “dooms your therapy to failure.”
Allergic reactions from these medications are rare, and some insurance companies charge the same regardless of the size. Prescribing a small amount initially might incur an additional expense for the patient.
Beware of painful or blistering rashes, especially if they involve the mucosa of the mouth, eyes, or genitals.
“These symptoms can be associated with potentially deadly toxic epidermal necrolysis,” says Daniel Aires, MD, JD, director of the division of dermatology at the University of Kansas School of Medicine in Kansas City, Kan. “Consult dermatology immediately. The sooner treatment is begun, the better the odds of survival.”
If a rash involves the eye, call an ophthalmologist and a dermatologist. “Eyes are more likely than skin to develop chronic complications after resolution of an acute condition,” he says.
For a rash involving primarily the mouth, call an otolaryngologist, a dentist, or both, as well as a dermatologist. These specialists are more skilled in visualizing and treating oral conditions.
Watch out for zoster, widespread herpes, pemphigus, and pemphigoid.
These blistering conditions require urgent diagnosis and treatment, so a dermatologist’s expertise is needed quickly, Dr. Aires says. Even without the presence of blisters, a single region of the skin or “dermatome” gives pause for concern.
“This could be a sign of zoster, which is especially dangerous in immunosuppressed or otherwise debilitated patients,” he cautions. “Either perform a culture and begin treatment, or consult dermatology, or do both.”
Pay attention to itching in the wrists, genital region, and web spaces of fingers and toes.
This may be due to scabies infestation. “Scabies can spread rapidly throughout a hospital ward,” Dr. Aires says. What to do: Scrape for scabies, consider a trial of topical treatment, and consult a dermatologist if you’re unsure.
Be mindful of the rapid onset of purpuric lesionscon the skin.
They warrant suspicion of such conditions as vasculitis, hypercoaguable states, and disseminated angiotropic infections, says Dr. Hopkins of Oregon Health & Science University. “The shape and size of purpuric skin lesions help determine the etiology. A few characteristic examples include papular purpura and retiform purpura. Papular purpura [raised purpuric papules] may suggest vasculitis. Purpura that forms net-like patches is called retiform purpura and suggests a vaso-occlusive process, such as from a hypercoaguable state, embolic phenomena, or calciphylaxis.”
13 Avoid consults for improving rashes and seborrheic keratosis, as well as nonurgent outpatient issues, such as psoriasis, rosacea, or a history of skin cancer. These conditions “are more easily addressed in a clinic, as opposed to in a hospital, where the patient is lying in a bed feeling ill with IV tubes in place,” Dr. Aires says. “It also reflects respect for the dermatologist’s time. Inpatient dermatology can be pretty busy, so it’s preferable to consult primarily for urgent skin issues.” Consultations can be costly, too, and most patients would rather avoid additional medical bills.
Don’t prescribe combined betamethasone/clotrimazole, also known as Lotrisone, for chronic scaly hands, feet, or groin.
Although it is not harmful, “it is not usually a great choice for typical ‘dermatophyte’ fungal infections, such as athlete’s foot and ‘jock itch,’” Dr. Aires says. “Over-the-counter Lamisil is better, particularly following daily use of 10-minute soaks in 50-50 vinegar-water. Even for yeast infections, miconazole is better than clotrimazole.”
As for betamethasone, this “component is way too strong for the groin area and can cause atrophy or worse,” he says.

—Daniela Kroshinsky, MD, MPH, director of inpatient dermatology, education, and research, Massachusetts General Hospital, Boston
Encourage patients to follow up with a dermatologist on an outpatient basis.
By heeding this advice, patients are less likely to return to the ED for skin conditions that can be managed in an office, says Kirsten Flynn, MD, a dermatologist at Banner Health Center in Sun City West, Ariz. Inpatient admissions by dermatologists have been decreasing over the years. Most patients with skin diseases or cutaneous manifestations of systemic illnesses are admitted to hospitals by other physicians.
“Many dermatologists are happy to fit in urgent consults in their clinics. Drug eruptions are by far the most common consultation request,” says Dr. Flynn, who notes that high-dose IV steroids can cause complications, such as gastrointestinal bleeding, bowel perforation, opportunistic infections, and exacerbation of underlying diseases. “In most cases, removing the offending agent and providing supportive care is the best option.”
Susan Kreimer is a freelance writer in New York.
- Maintain a broader range of differential diagnoses before ruling in or out something more concrete.
- Attend dermatology lectures as part of primary care’s continuing medical education courses.
- Review a good basic dermatology atlas from time to time.
- Learn to correctly describe lesions to a dermatologist by phone.
- Don’t assume that groin rashes are all fungal.
- Don’t mistakenly associate a drug-related reaction with a medication given one to two days before the onset of a rash.
- Consider involving a dermatologist to help manage open skin lesions, particularly if you’re unsure of the cause.
- Prescribe an adequate quantity of topical corticosteroids for the duration of treatment.
- Beware of painful or blistering rashes, especially if they involve the mucosa of the mouth, eyes, or genitals.
- Watch out for zoster, widespread herpes, pemphigus, and pemphigoid.
- Pay attention to itching in the wrists, genital region, and web spaces of fingers and toes.
- Be mindful of the rapid onset of purpuric lesions on the skin.
- Avoid consults for improving rashes and seborrheic keratosis, as well as nonurgent outpatient issues, such as psoriasis, rosacea, or a history of skin cancer.
- Don’t prescribe combined betamethasone/clotrimazole, also known as Lotrisone, for chronic scaly hands, feet, or groin.
- Encourage patients to follow up with a dermatologist on an outpatient basis.
Dermatologic diseases tend to receive little attention at most U.S. medical schools—typically only several days of lectures or a few weeks of clinical exposure.
“Not surprisingly, many general practitioners may feel unprepared to address hospitalized patients with challenging dermatologic findings,” says R. Samuel Hopkins, MD, assistant professor of dermatology and assistant residency program director at Oregon Health & Science University in Portland.
Few studies have examined the quality of inpatient dermatologic care. One study, a retrospective chart review at a Midwestern university hospital, found that the primary ward team submitted an accurate dermatologic diagnosis in only 23.9% of cases. Meanwhile, consultation with a dermatologist led to a change or addition to treatment in 77% of patients (Dermatol Online J. 2010;16(2):12).
“Given that medical schools may not be able to dedicate more time to managing dermatologic conditions, the burden of education may fall on post-graduate programs and continuing medical education to fill this gap,” Dr. Hopkins says. To further complicate matters, “it is difficult in many hospitals to obtain a dermatology consult on an inpatient, reflecting the limited access hospitalists often have to dermatologists.”
The most frequently encountered dermatologic conditions in the hospital setting are drug eruptions and skin infections. Dermatitis is the most misdiagnosed condition by nondermatologists in hospitals, says Russell Vinik, MD, co-director of the hospitalist group at the University of Utah Health Care in Salt Lake City.
The majority of skin issues don’t require a dermatologist’s input, but some do. “Clearly, there’s also the rash that we just don’t know what it is,” Dr. Vinik says. When in doubt, it’s best to err on the safe side and call the specialist.
Here’s how to assess whether to manage a dermatologic case yourself, or how to involve a dermatologist for appropriate diagnosis and treatment. In general, Dr. Hopkins says, “Whether one can handle a case on their own or not is a case-by-case decision by the hospitalist based on their comfort with their diagnosis and management.”
Maintain a broader range of differential diagnoses before ruling in or out something more concrete.
“Very often, patients with skin diseases are given a specific diagnosis without consideration of mimickers,” says Daniela Kroshinsky, MD, MPH, assistant professor of dermatology at Harvard Medical School in Boston.
“Cellulitis is a great example. People will come in with hot, red skin and be diagnosed with and treated for cellulitis but really have stasis dermatitis, Lyme [disease], gout, et cetera,” says Dr. Kroshinsky, who also is director of pediatric dermatology and director of inpatient dermatology, education, and research at Massachusetts General Hospital.
“The clinical picture of warm, red, tender skin can fit many conditions but is most often called cellulitis by nondermatologists,” she explains. “It’s not clear why, but I would suspect this is because cellulitis is one of the few dermatologic conditions taught in medical school, while the mimickers get less attention.”
Attend dermatology lectures as part of primary care’s continuing medical education courses.
This would increase your knowledge of skin conditions affecting hospitalized patients, Dr. Kroshinsky says. If there is a dermatologic consultant for your hospital, work closely with this specialist until you feel comfortable making diagnoses and incorporating treatment plans.
Similarly, if you are a resident who is interested in a career in hospital medicine, consider doing a rotation in dermatology.
Review a good basic dermatology atlas from time to time.
This keeps your mind open to differential diagnoses for a given situation that you may encounter in the hospital setting. A more comprehensive book or online reference can be helpful to peruse after seeing a patient with a particular rash, Dr. Kroshinsky says.
Learn to correctly describe lesions to a dermatologist by phone.
When a specialist isn’t available on site, the phone communication is vital to the specialist. This includes familiarizing yourself with some of the more life-threatening dermatologic problems, such as drug-induced hypersensitivity reactions. It will be easier to recognize when an urgent dermatologic consultation is required. Sometimes this is necessary when a patient doesn’t respond to treatment for a reasonable and presumed diagnosis—when one condition seems to mimic the symptoms of another, says Lindy Fox, MD, associate professor of clinical dermatology at the University of California at San Francisco and director of its hospital dermatology consultation service.
Don’t assume that groin rashes are all fungal.
In fact, there is a very large differential diagnosis for intertriginous eruptions, Dr. Fox says. Perform a KOH test (potassium hydroxide) and fungal cultures on intertriginous eruptions. If no fungus is identified or the patient is not responding appropriately to therapy, call for a dermatologic consultation.
Don’t mistakenly associate a drug-related reaction with a medication given one to two days before the onset of a rash.
It is typically seven to 10 days post-exposure that a drug eruption develops, Dr. Fox says. He suggests making a drug chart to highlight dates of medication administration. This helps pinpoint the most likely culprit based on timing and the probability that a certain drug may induce cutaneous eruptions. Correct identification of the type of drug eruption (e.g. simple drug eruption vs. hypersensitivity vs. potentially deadly Stevens-Johnson syndrome) is important.
Consider involving a dermatologist to help manage open skin lesions, particularly if you’re unsure of the cause.
There are many different causes of skin ulcers. Trauma, infections, and even malignancies can present as open wounds. Leg ulcers may be due to venous stasis, but they also can be caused by arterial insufficiency, vasculitis, and other conditions. A dermatologist might opt to perform a skin biopsy to help diagnose the lesion.
“Wound-care nurses can be very helpful in managing skin lesions, but they do not always have the experience needed to correctly diagnose the underlying problem,” says Kathryn Schwarzenberger, MD, professor of medicine at the University of Vermont College of Medicine in Burlington. “If you’re thinking of calling the wound-care nurse, think of calling the dermatologist first.”
Prescribe an adequate quantity of topical corticosteroids for the duration of treatment.
“It’s really important to provide enough medicine,” Dr. Schwarzenberger says. Typically, a patient will receive a small tube, apply the contents, and find that “it’s enough medicine to cover their body once. This doesn’t work if you intended to have the patient apply it all over for two weeks.”
It takes, on average, 30 g of a topical medication to cover the body once. With topical steroids, prescribing an insufficient quantity “dooms your therapy to failure.”
Allergic reactions from these medications are rare, and some insurance companies charge the same regardless of the size. Prescribing a small amount initially might incur an additional expense for the patient.
Beware of painful or blistering rashes, especially if they involve the mucosa of the mouth, eyes, or genitals.
“These symptoms can be associated with potentially deadly toxic epidermal necrolysis,” says Daniel Aires, MD, JD, director of the division of dermatology at the University of Kansas School of Medicine in Kansas City, Kan. “Consult dermatology immediately. The sooner treatment is begun, the better the odds of survival.”
If a rash involves the eye, call an ophthalmologist and a dermatologist. “Eyes are more likely than skin to develop chronic complications after resolution of an acute condition,” he says.
For a rash involving primarily the mouth, call an otolaryngologist, a dentist, or both, as well as a dermatologist. These specialists are more skilled in visualizing and treating oral conditions.
Watch out for zoster, widespread herpes, pemphigus, and pemphigoid.
These blistering conditions require urgent diagnosis and treatment, so a dermatologist’s expertise is needed quickly, Dr. Aires says. Even without the presence of blisters, a single region of the skin or “dermatome” gives pause for concern.
“This could be a sign of zoster, which is especially dangerous in immunosuppressed or otherwise debilitated patients,” he cautions. “Either perform a culture and begin treatment, or consult dermatology, or do both.”
Pay attention to itching in the wrists, genital region, and web spaces of fingers and toes.
This may be due to scabies infestation. “Scabies can spread rapidly throughout a hospital ward,” Dr. Aires says. What to do: Scrape for scabies, consider a trial of topical treatment, and consult a dermatologist if you’re unsure.
Be mindful of the rapid onset of purpuric lesionscon the skin.
They warrant suspicion of such conditions as vasculitis, hypercoaguable states, and disseminated angiotropic infections, says Dr. Hopkins of Oregon Health & Science University. “The shape and size of purpuric skin lesions help determine the etiology. A few characteristic examples include papular purpura and retiform purpura. Papular purpura [raised purpuric papules] may suggest vasculitis. Purpura that forms net-like patches is called retiform purpura and suggests a vaso-occlusive process, such as from a hypercoaguable state, embolic phenomena, or calciphylaxis.”
13 Avoid consults for improving rashes and seborrheic keratosis, as well as nonurgent outpatient issues, such as psoriasis, rosacea, or a history of skin cancer. These conditions “are more easily addressed in a clinic, as opposed to in a hospital, where the patient is lying in a bed feeling ill with IV tubes in place,” Dr. Aires says. “It also reflects respect for the dermatologist’s time. Inpatient dermatology can be pretty busy, so it’s preferable to consult primarily for urgent skin issues.” Consultations can be costly, too, and most patients would rather avoid additional medical bills.
Don’t prescribe combined betamethasone/clotrimazole, also known as Lotrisone, for chronic scaly hands, feet, or groin.
Although it is not harmful, “it is not usually a great choice for typical ‘dermatophyte’ fungal infections, such as athlete’s foot and ‘jock itch,’” Dr. Aires says. “Over-the-counter Lamisil is better, particularly following daily use of 10-minute soaks in 50-50 vinegar-water. Even for yeast infections, miconazole is better than clotrimazole.”
As for betamethasone, this “component is way too strong for the groin area and can cause atrophy or worse,” he says.

—Daniela Kroshinsky, MD, MPH, director of inpatient dermatology, education, and research, Massachusetts General Hospital, Boston
Encourage patients to follow up with a dermatologist on an outpatient basis.
By heeding this advice, patients are less likely to return to the ED for skin conditions that can be managed in an office, says Kirsten Flynn, MD, a dermatologist at Banner Health Center in Sun City West, Ariz. Inpatient admissions by dermatologists have been decreasing over the years. Most patients with skin diseases or cutaneous manifestations of systemic illnesses are admitted to hospitals by other physicians.
“Many dermatologists are happy to fit in urgent consults in their clinics. Drug eruptions are by far the most common consultation request,” says Dr. Flynn, who notes that high-dose IV steroids can cause complications, such as gastrointestinal bleeding, bowel perforation, opportunistic infections, and exacerbation of underlying diseases. “In most cases, removing the offending agent and providing supportive care is the best option.”
Susan Kreimer is a freelance writer in New York.
Rival Hospitalists Can Bring Havoc, or Healthy Competition to Hospitals
In November 2011, the board of directors of Lee Memorial Health System in Fort Myers, Fla., voted to close access at its four hospitals to any hospitalist who didn’t already practice there or wasn’t affiliated with private practices that contracted with the health system. According to a report in a local newspaper, the proliferation of competing hospitalist practices at Lee Memorial was contributing to high rates of patient and referring physician dissatisfaction and hospitalist turnover.1 As a result, the board limited new hospitalists from entering practice in their facilities until they could develop “rules of engagement” for the existing hospitalists through new contracts and standards of practice.
The Lee Memorial example of multiple, competing hospitalist groups—and individuals practicing hospital medicine, also known as “lone wolf” hospitalists—causing havoc is atypical of the fledgling medical specialty, which has seen rapid growth the past two decades. Even so, veteran hospitalists confirm that nowadays, with nearly 40,000 hospitalists practicing in a majority of U.S. hospitals, it’s not uncommon to have multiple groups or individuals working under the same hospital roof. What is concerning to some in the specialty is how the competition can turn ugly, especially considering SHM espouses such virtues as teamwork, leadership, and quality improvement (QI).
Even so, situations arise when multiple HM groups under one roof don’t get along. Sometimes those groups or individual practitioners compete, head to head, for new admissions. Some hospitals have patient populations carved out by capitated medical groups or staff/group model HMOs. Some specialty groups, cardiology or orthopedics, for example, choose to contract hospitalist groups for their patients, setting up potential conflicts with new admissions. Other hospitals have “lone wolf” hospitalists, basically a practice of one.
No matter the dynamic, hospital administrators are frustrated with their inability to control competitive situations, especially when competing groups or individuals do not act in conjunction with their strategic goals.
Depending on hospital bylaws and state regulations, it might be difficult to exclude hospitalists from practicing in the hospital or to cut off competition. Some hospitals even welcome competition—as a prime virtue in its own right, a way to advance quality, or to guard against staffing shortages. The challenge, hospitalists and administrators say, is to encourage multiple groups to work amicably alongside each other, cooperating on the hospital’s larger mission and working toward its quality targets—and to make sure clinicians focus less on competition and more on patients (see “The Magic Bullet: Communication,”).

—Lowell Palmer, MD, FHM, hospitalist, Southwest Washington Medical Center, Vancouver
Purposeful, Team-Based Medicine
Scott Nygaard, MD, Lee Memorial’s chief medical officer for physician services, announced on Aug. 29, 2012, that the health system was contracting with a newly formed medical group called Inpatient Specialists of Southwest Florida (ISSF), a partnership between Cape Coral, Fla.-based Hospitalist Group of Southwest Florida (HGSF) and national management company Cogent HMG based in Brentwood, Tenn. HGSF and Cogent HMG already had established practices in two of Lee’s four hospitals.
Other existing hospitalist groups are permitted to continue practicing in these hospitals, although only a contracted group will be able to recruit or add new physicians, Dr. Nygaard says.
“The bylaws did not allow us to formally close access for staff already in practice,” he said. Physicians have the option of joining ISSF, and eventually, he says, the other groups dwindled in numbers through attrition. As Lee Memorial’s sole provider of hospitalist care, ISSF’s long-term goal is to put HM on a similar footing with other hospital-based specialties, such as emergency medicine and anesthesiology.
As of late 2012, six hospitalist groups and more than 80 hospitalists practice at Lee Memorial hospitals; 40 of those hospitalists belong to ISSF. “The other groups were all offered an opportunity to discuss a contractual relationship with the system, but they declined,” Dr. Nygaard says.
The remaining groups had worked amicably alongside each other but in an atmosphere Dr. Nygaard likens to a flea market, with each group practicing its own separate business and business model.
A standardized approach conducive to achieving the hospital’s quality and performance targets was lacking, however. As a result, Lee Memorial implemented an HM standard of care within the system. It helped somewhat, Dr. Nygaard says, but it didn’t fix all of the competition problems.
“We have learned that variation is the enemy of quality, especially in the highly complex environment of an acute-care hospital, trying to generate the kinds of measurable results we are now being asked to provide,” he explains. “We need to be more organized, structured, and purposeful in an era of team-based medicine. You need committed, aligned partnerships offering appropriate incentives.”
The ISSF contract contains such performance incentives.
“The joint venture formalizes an informal, long-standing, collaborative relationship” between the two participating HM groups, says Joseph Daley, MD, co-founder and director of quality services for Hospitalist Group of Southwest Florida. “We bring substantial, local expertise to the table, and have been quality partners with both Lee Memorial and Cogent HMG.”
And, as of April, Lee Memorial spokesperson Mary Briggs reported patient satisfaction scores for hospitalists are improving. “We believe the changes put in place were the right ones,” she emailed The Hospitalist.

—Scott Nygaard, MD, chief medical officer for physician services, Lee Memorial Health System, Fort Myers, Fla.
Supply and Demand
Every local hospital environment is different, with HM group arrangements shaped to a large degree by supply and demand for physicians, says Brian Hazen, MD, chief of hospital medicine at Inova Fairfax Hospital in Falls Church, Va., one of five hospitals in the Inova system. Inova Fairfax employs the hospitalists in Dr. Hazen’s group but is also home to other groups, including a neurohospitalist service and about a half dozen solo practitioners. Dr. Hazen’s group receives administrative support from the hospital and primarily is assigned patients through the ED. Some of the private hospitalists don’t want to take ED call, he says, instead preferring to get referrals of insured patients from primary-care-physician groups.
“Here in the D.C. area, we’re reasonably well staffed by hospitalists, but we’re not fighting over patients. In fact, if it weren’t for the private physicians, we’d have trouble meeting current staffing needs,” Dr. Hazen says. “I have also seen competition in other hospital settings, but I haven’t been in a situation where the doctors were fighting over patients.”
The “lone wolf” hospitalists at Inova Fairfax work very hard, Dr. Hazen adds. “A lot of them have private practices, see patients in the hospital, and also take call. If one of them has to leave town on short notice, we can help them out. On the flip side, if we’re busy in the emergency department, we’ll call on them,” he says.
The ED receives instruction on which hospitalist group admits which patient, but sometimes referral mistakes are made.
“If we accidently admit a patient who should have gone to one of the private people, who depend on these admissions for their income, I let them choose whether we should continue to see that patient or do a transfer,” Dr. Hazen says. “For the most part, we all try to be nice people.”
In the current health-care environment, hospital administrators might be reluctant to erect barriers to multiple hospitalist practices under one roof for fear of restraining trade, just as they don’t stand in the way of primary-care physicians who want to follow their own patients into the hospital. It might be easier to enact equally enforced requirements for the credentialing and privileging of all hospitalists who want to practice at the hospital, spelling out expectations in such areas as following protocols. (In 2011, SHM issued a position paper on hospitalist credentialing that addressed the appropriate time to institute a credentialing category with privileging criteria for hospitalists, and how to preserve maximum flexibility within this process.)2
Hospitals can limit who they contract with, who gets administrative support—and how much—using financial and quality performance to shape contracting decisions. In many communities, that could serve as an excluder of multiple groups in the same building, but in other locales, the payor mix might be attractive enough for physicians to survive on billing alone, says Leslie Flores, MPH, of Nelson Flores Hospital Medicine Consultants. If the hospital isn’t providing financial support, it will have less influence over how that group does things.
Dr. Hazen says his employed hospitalist group at Inova Fairfax is represented on more than 20 hospital committees and quality initiatives in the hospital, and has demonstrated its alignment with the hospital’s goals. Recently, in response to the administration’s concerns about throughput, his group initiated geographic, multidisciplinary rounding.
“I can do this because I have elite physicians, and because I protect them from unreasonable expectations,” he says. “Everyone needs to understand that the hospital needs to survive, so the hospital has a right to expect certain things from its hospitalists, such as performance on length of stay, throughput, other core measures, and promptly answering pages. Everyone should understand that those are the rules. Being fair, honest, and transparent about expectations is not an unreasonable expectation.”
Competition among hospitalists should be on a professional basis, experts emphasize, and cooperation is in everyone’s best interests. But Lowell Palmer, MD, FHM, a hospitalist at Southwest Washington Medical Center in Vancouver, Wash., thinks competition can be a healthy thing for hospitalist groups.
“It forces us to make sure the services we provide are meeting the customer’s expectations,” says Dr. Palmer, who works with Cogent Physician Services, one of the three HM groups at Southwest Washington. “We can and do learn from each other.”
Impact of Health-Care Reform
Beware the transformation health-care reform is having on the dynamics of hospital-based practice and the competitive landscape facing more hospitalist groups, says Roger Heroux, MHA, PhD, CHE, consultant with Hospitalist Management Resources LLC. Reforms mean hospitalists are seeing an increased emphasis on coordinating with post-acute-care providers, improving care transitions, preventing readmissions, and meeting hospital targets for quality and patient safety.
Primary-care groups, accountable-care organizations (ACOs), and health plans could choose specific hospitalist practices they want to partner with to manage the care of their hospitalized members, but they will have clear performance expectations that those groups will need to meet, spelled out in benchmarks. Or, as some experts believe, they might opt to bring in their own hospitalist group.
“We’re spending our time working with existing hospitalist programs to help them be more efficient and effective, to manage risk, and to become aggressive about meeting the clinical benchmarks,” Heroux says. Hospitals, ACOs, and capitated groups can’t afford not to have a high-performing hospitalist program, so this will become a hallmark of survival for hospitalist programs as well. “In a highly managed environment, patients will be managed by a hospitalist group that is responsive to these expectations,” he says.
Larry Beresford is a freelance writer in Oakland, Calif.
References
- Gluck F. Lee Memorial Health Systems’ hospitalists under new controls. Fort Myers News Press. Dec. 1, 2011.
- Society of Hospital Medicine Position Statement on Hospitalist Credentialing and Medical Staff Privileges. SHM website. Available at: http://www.hospitalmedicine.org/AM/Template.cfm?Section=Where_We_Stand&Template=/CM/HTMLDisplay.cfm&ContentID=28262. Accessed April 1, 2013.
In November 2011, the board of directors of Lee Memorial Health System in Fort Myers, Fla., voted to close access at its four hospitals to any hospitalist who didn’t already practice there or wasn’t affiliated with private practices that contracted with the health system. According to a report in a local newspaper, the proliferation of competing hospitalist practices at Lee Memorial was contributing to high rates of patient and referring physician dissatisfaction and hospitalist turnover.1 As a result, the board limited new hospitalists from entering practice in their facilities until they could develop “rules of engagement” for the existing hospitalists through new contracts and standards of practice.
The Lee Memorial example of multiple, competing hospitalist groups—and individuals practicing hospital medicine, also known as “lone wolf” hospitalists—causing havoc is atypical of the fledgling medical specialty, which has seen rapid growth the past two decades. Even so, veteran hospitalists confirm that nowadays, with nearly 40,000 hospitalists practicing in a majority of U.S. hospitals, it’s not uncommon to have multiple groups or individuals working under the same hospital roof. What is concerning to some in the specialty is how the competition can turn ugly, especially considering SHM espouses such virtues as teamwork, leadership, and quality improvement (QI).
Even so, situations arise when multiple HM groups under one roof don’t get along. Sometimes those groups or individual practitioners compete, head to head, for new admissions. Some hospitals have patient populations carved out by capitated medical groups or staff/group model HMOs. Some specialty groups, cardiology or orthopedics, for example, choose to contract hospitalist groups for their patients, setting up potential conflicts with new admissions. Other hospitals have “lone wolf” hospitalists, basically a practice of one.
No matter the dynamic, hospital administrators are frustrated with their inability to control competitive situations, especially when competing groups or individuals do not act in conjunction with their strategic goals.
Depending on hospital bylaws and state regulations, it might be difficult to exclude hospitalists from practicing in the hospital or to cut off competition. Some hospitals even welcome competition—as a prime virtue in its own right, a way to advance quality, or to guard against staffing shortages. The challenge, hospitalists and administrators say, is to encourage multiple groups to work amicably alongside each other, cooperating on the hospital’s larger mission and working toward its quality targets—and to make sure clinicians focus less on competition and more on patients (see “The Magic Bullet: Communication,”).

—Lowell Palmer, MD, FHM, hospitalist, Southwest Washington Medical Center, Vancouver
Purposeful, Team-Based Medicine
Scott Nygaard, MD, Lee Memorial’s chief medical officer for physician services, announced on Aug. 29, 2012, that the health system was contracting with a newly formed medical group called Inpatient Specialists of Southwest Florida (ISSF), a partnership between Cape Coral, Fla.-based Hospitalist Group of Southwest Florida (HGSF) and national management company Cogent HMG based in Brentwood, Tenn. HGSF and Cogent HMG already had established practices in two of Lee’s four hospitals.
Other existing hospitalist groups are permitted to continue practicing in these hospitals, although only a contracted group will be able to recruit or add new physicians, Dr. Nygaard says.
“The bylaws did not allow us to formally close access for staff already in practice,” he said. Physicians have the option of joining ISSF, and eventually, he says, the other groups dwindled in numbers through attrition. As Lee Memorial’s sole provider of hospitalist care, ISSF’s long-term goal is to put HM on a similar footing with other hospital-based specialties, such as emergency medicine and anesthesiology.
As of late 2012, six hospitalist groups and more than 80 hospitalists practice at Lee Memorial hospitals; 40 of those hospitalists belong to ISSF. “The other groups were all offered an opportunity to discuss a contractual relationship with the system, but they declined,” Dr. Nygaard says.
The remaining groups had worked amicably alongside each other but in an atmosphere Dr. Nygaard likens to a flea market, with each group practicing its own separate business and business model.
A standardized approach conducive to achieving the hospital’s quality and performance targets was lacking, however. As a result, Lee Memorial implemented an HM standard of care within the system. It helped somewhat, Dr. Nygaard says, but it didn’t fix all of the competition problems.
“We have learned that variation is the enemy of quality, especially in the highly complex environment of an acute-care hospital, trying to generate the kinds of measurable results we are now being asked to provide,” he explains. “We need to be more organized, structured, and purposeful in an era of team-based medicine. You need committed, aligned partnerships offering appropriate incentives.”
The ISSF contract contains such performance incentives.
“The joint venture formalizes an informal, long-standing, collaborative relationship” between the two participating HM groups, says Joseph Daley, MD, co-founder and director of quality services for Hospitalist Group of Southwest Florida. “We bring substantial, local expertise to the table, and have been quality partners with both Lee Memorial and Cogent HMG.”
And, as of April, Lee Memorial spokesperson Mary Briggs reported patient satisfaction scores for hospitalists are improving. “We believe the changes put in place were the right ones,” she emailed The Hospitalist.

—Scott Nygaard, MD, chief medical officer for physician services, Lee Memorial Health System, Fort Myers, Fla.
Supply and Demand
Every local hospital environment is different, with HM group arrangements shaped to a large degree by supply and demand for physicians, says Brian Hazen, MD, chief of hospital medicine at Inova Fairfax Hospital in Falls Church, Va., one of five hospitals in the Inova system. Inova Fairfax employs the hospitalists in Dr. Hazen’s group but is also home to other groups, including a neurohospitalist service and about a half dozen solo practitioners. Dr. Hazen’s group receives administrative support from the hospital and primarily is assigned patients through the ED. Some of the private hospitalists don’t want to take ED call, he says, instead preferring to get referrals of insured patients from primary-care-physician groups.
“Here in the D.C. area, we’re reasonably well staffed by hospitalists, but we’re not fighting over patients. In fact, if it weren’t for the private physicians, we’d have trouble meeting current staffing needs,” Dr. Hazen says. “I have also seen competition in other hospital settings, but I haven’t been in a situation where the doctors were fighting over patients.”
The “lone wolf” hospitalists at Inova Fairfax work very hard, Dr. Hazen adds. “A lot of them have private practices, see patients in the hospital, and also take call. If one of them has to leave town on short notice, we can help them out. On the flip side, if we’re busy in the emergency department, we’ll call on them,” he says.
The ED receives instruction on which hospitalist group admits which patient, but sometimes referral mistakes are made.
“If we accidently admit a patient who should have gone to one of the private people, who depend on these admissions for their income, I let them choose whether we should continue to see that patient or do a transfer,” Dr. Hazen says. “For the most part, we all try to be nice people.”
In the current health-care environment, hospital administrators might be reluctant to erect barriers to multiple hospitalist practices under one roof for fear of restraining trade, just as they don’t stand in the way of primary-care physicians who want to follow their own patients into the hospital. It might be easier to enact equally enforced requirements for the credentialing and privileging of all hospitalists who want to practice at the hospital, spelling out expectations in such areas as following protocols. (In 2011, SHM issued a position paper on hospitalist credentialing that addressed the appropriate time to institute a credentialing category with privileging criteria for hospitalists, and how to preserve maximum flexibility within this process.)2
Hospitals can limit who they contract with, who gets administrative support—and how much—using financial and quality performance to shape contracting decisions. In many communities, that could serve as an excluder of multiple groups in the same building, but in other locales, the payor mix might be attractive enough for physicians to survive on billing alone, says Leslie Flores, MPH, of Nelson Flores Hospital Medicine Consultants. If the hospital isn’t providing financial support, it will have less influence over how that group does things.
Dr. Hazen says his employed hospitalist group at Inova Fairfax is represented on more than 20 hospital committees and quality initiatives in the hospital, and has demonstrated its alignment with the hospital’s goals. Recently, in response to the administration’s concerns about throughput, his group initiated geographic, multidisciplinary rounding.
“I can do this because I have elite physicians, and because I protect them from unreasonable expectations,” he says. “Everyone needs to understand that the hospital needs to survive, so the hospital has a right to expect certain things from its hospitalists, such as performance on length of stay, throughput, other core measures, and promptly answering pages. Everyone should understand that those are the rules. Being fair, honest, and transparent about expectations is not an unreasonable expectation.”
Competition among hospitalists should be on a professional basis, experts emphasize, and cooperation is in everyone’s best interests. But Lowell Palmer, MD, FHM, a hospitalist at Southwest Washington Medical Center in Vancouver, Wash., thinks competition can be a healthy thing for hospitalist groups.
“It forces us to make sure the services we provide are meeting the customer’s expectations,” says Dr. Palmer, who works with Cogent Physician Services, one of the three HM groups at Southwest Washington. “We can and do learn from each other.”
Impact of Health-Care Reform
Beware the transformation health-care reform is having on the dynamics of hospital-based practice and the competitive landscape facing more hospitalist groups, says Roger Heroux, MHA, PhD, CHE, consultant with Hospitalist Management Resources LLC. Reforms mean hospitalists are seeing an increased emphasis on coordinating with post-acute-care providers, improving care transitions, preventing readmissions, and meeting hospital targets for quality and patient safety.
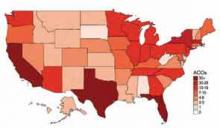
Primary-care groups, accountable-care organizations (ACOs), and health plans could choose specific hospitalist practices they want to partner with to manage the care of their hospitalized members, but they will have clear performance expectations that those groups will need to meet, spelled out in benchmarks. Or, as some experts believe, they might opt to bring in their own hospitalist group.
“We’re spending our time working with existing hospitalist programs to help them be more efficient and effective, to manage risk, and to become aggressive about meeting the clinical benchmarks,” Heroux says. Hospitals, ACOs, and capitated groups can’t afford not to have a high-performing hospitalist program, so this will become a hallmark of survival for hospitalist programs as well. “In a highly managed environment, patients will be managed by a hospitalist group that is responsive to these expectations,” he says.
Larry Beresford is a freelance writer in Oakland, Calif.
References
- Gluck F. Lee Memorial Health Systems’ hospitalists under new controls. Fort Myers News Press. Dec. 1, 2011.
- Society of Hospital Medicine Position Statement on Hospitalist Credentialing and Medical Staff Privileges. SHM website. Available at: http://www.hospitalmedicine.org/AM/Template.cfm?Section=Where_We_Stand&Template=/CM/HTMLDisplay.cfm&ContentID=28262. Accessed April 1, 2013.
In November 2011, the board of directors of Lee Memorial Health System in Fort Myers, Fla., voted to close access at its four hospitals to any hospitalist who didn’t already practice there or wasn’t affiliated with private practices that contracted with the health system. According to a report in a local newspaper, the proliferation of competing hospitalist practices at Lee Memorial was contributing to high rates of patient and referring physician dissatisfaction and hospitalist turnover.1 As a result, the board limited new hospitalists from entering practice in their facilities until they could develop “rules of engagement” for the existing hospitalists through new contracts and standards of practice.
The Lee Memorial example of multiple, competing hospitalist groups—and individuals practicing hospital medicine, also known as “lone wolf” hospitalists—causing havoc is atypical of the fledgling medical specialty, which has seen rapid growth the past two decades. Even so, veteran hospitalists confirm that nowadays, with nearly 40,000 hospitalists practicing in a majority of U.S. hospitals, it’s not uncommon to have multiple groups or individuals working under the same hospital roof. What is concerning to some in the specialty is how the competition can turn ugly, especially considering SHM espouses such virtues as teamwork, leadership, and quality improvement (QI).
Even so, situations arise when multiple HM groups under one roof don’t get along. Sometimes those groups or individual practitioners compete, head to head, for new admissions. Some hospitals have patient populations carved out by capitated medical groups or staff/group model HMOs. Some specialty groups, cardiology or orthopedics, for example, choose to contract hospitalist groups for their patients, setting up potential conflicts with new admissions. Other hospitals have “lone wolf” hospitalists, basically a practice of one.
No matter the dynamic, hospital administrators are frustrated with their inability to control competitive situations, especially when competing groups or individuals do not act in conjunction with their strategic goals.
Depending on hospital bylaws and state regulations, it might be difficult to exclude hospitalists from practicing in the hospital or to cut off competition. Some hospitals even welcome competition—as a prime virtue in its own right, a way to advance quality, or to guard against staffing shortages. The challenge, hospitalists and administrators say, is to encourage multiple groups to work amicably alongside each other, cooperating on the hospital’s larger mission and working toward its quality targets—and to make sure clinicians focus less on competition and more on patients (see “The Magic Bullet: Communication,”).

—Lowell Palmer, MD, FHM, hospitalist, Southwest Washington Medical Center, Vancouver
Purposeful, Team-Based Medicine
Scott Nygaard, MD, Lee Memorial’s chief medical officer for physician services, announced on Aug. 29, 2012, that the health system was contracting with a newly formed medical group called Inpatient Specialists of Southwest Florida (ISSF), a partnership between Cape Coral, Fla.-based Hospitalist Group of Southwest Florida (HGSF) and national management company Cogent HMG based in Brentwood, Tenn. HGSF and Cogent HMG already had established practices in two of Lee’s four hospitals.
Other existing hospitalist groups are permitted to continue practicing in these hospitals, although only a contracted group will be able to recruit or add new physicians, Dr. Nygaard says.
“The bylaws did not allow us to formally close access for staff already in practice,” he said. Physicians have the option of joining ISSF, and eventually, he says, the other groups dwindled in numbers through attrition. As Lee Memorial’s sole provider of hospitalist care, ISSF’s long-term goal is to put HM on a similar footing with other hospital-based specialties, such as emergency medicine and anesthesiology.
As of late 2012, six hospitalist groups and more than 80 hospitalists practice at Lee Memorial hospitals; 40 of those hospitalists belong to ISSF. “The other groups were all offered an opportunity to discuss a contractual relationship with the system, but they declined,” Dr. Nygaard says.
The remaining groups had worked amicably alongside each other but in an atmosphere Dr. Nygaard likens to a flea market, with each group practicing its own separate business and business model.
A standardized approach conducive to achieving the hospital’s quality and performance targets was lacking, however. As a result, Lee Memorial implemented an HM standard of care within the system. It helped somewhat, Dr. Nygaard says, but it didn’t fix all of the competition problems.
“We have learned that variation is the enemy of quality, especially in the highly complex environment of an acute-care hospital, trying to generate the kinds of measurable results we are now being asked to provide,” he explains. “We need to be more organized, structured, and purposeful in an era of team-based medicine. You need committed, aligned partnerships offering appropriate incentives.”
The ISSF contract contains such performance incentives.
“The joint venture formalizes an informal, long-standing, collaborative relationship” between the two participating HM groups, says Joseph Daley, MD, co-founder and director of quality services for Hospitalist Group of Southwest Florida. “We bring substantial, local expertise to the table, and have been quality partners with both Lee Memorial and Cogent HMG.”
And, as of April, Lee Memorial spokesperson Mary Briggs reported patient satisfaction scores for hospitalists are improving. “We believe the changes put in place were the right ones,” she emailed The Hospitalist.

—Scott Nygaard, MD, chief medical officer for physician services, Lee Memorial Health System, Fort Myers, Fla.
Supply and Demand
Every local hospital environment is different, with HM group arrangements shaped to a large degree by supply and demand for physicians, says Brian Hazen, MD, chief of hospital medicine at Inova Fairfax Hospital in Falls Church, Va., one of five hospitals in the Inova system. Inova Fairfax employs the hospitalists in Dr. Hazen’s group but is also home to other groups, including a neurohospitalist service and about a half dozen solo practitioners. Dr. Hazen’s group receives administrative support from the hospital and primarily is assigned patients through the ED. Some of the private hospitalists don’t want to take ED call, he says, instead preferring to get referrals of insured patients from primary-care-physician groups.
“Here in the D.C. area, we’re reasonably well staffed by hospitalists, but we’re not fighting over patients. In fact, if it weren’t for the private physicians, we’d have trouble meeting current staffing needs,” Dr. Hazen says. “I have also seen competition in other hospital settings, but I haven’t been in a situation where the doctors were fighting over patients.”
The “lone wolf” hospitalists at Inova Fairfax work very hard, Dr. Hazen adds. “A lot of them have private practices, see patients in the hospital, and also take call. If one of them has to leave town on short notice, we can help them out. On the flip side, if we’re busy in the emergency department, we’ll call on them,” he says.
The ED receives instruction on which hospitalist group admits which patient, but sometimes referral mistakes are made.
“If we accidently admit a patient who should have gone to one of the private people, who depend on these admissions for their income, I let them choose whether we should continue to see that patient or do a transfer,” Dr. Hazen says. “For the most part, we all try to be nice people.”
In the current health-care environment, hospital administrators might be reluctant to erect barriers to multiple hospitalist practices under one roof for fear of restraining trade, just as they don’t stand in the way of primary-care physicians who want to follow their own patients into the hospital. It might be easier to enact equally enforced requirements for the credentialing and privileging of all hospitalists who want to practice at the hospital, spelling out expectations in such areas as following protocols. (In 2011, SHM issued a position paper on hospitalist credentialing that addressed the appropriate time to institute a credentialing category with privileging criteria for hospitalists, and how to preserve maximum flexibility within this process.)2
Hospitals can limit who they contract with, who gets administrative support—and how much—using financial and quality performance to shape contracting decisions. In many communities, that could serve as an excluder of multiple groups in the same building, but in other locales, the payor mix might be attractive enough for physicians to survive on billing alone, says Leslie Flores, MPH, of Nelson Flores Hospital Medicine Consultants. If the hospital isn’t providing financial support, it will have less influence over how that group does things.
Dr. Hazen says his employed hospitalist group at Inova Fairfax is represented on more than 20 hospital committees and quality initiatives in the hospital, and has demonstrated its alignment with the hospital’s goals. Recently, in response to the administration’s concerns about throughput, his group initiated geographic, multidisciplinary rounding.
“I can do this because I have elite physicians, and because I protect them from unreasonable expectations,” he says. “Everyone needs to understand that the hospital needs to survive, so the hospital has a right to expect certain things from its hospitalists, such as performance on length of stay, throughput, other core measures, and promptly answering pages. Everyone should understand that those are the rules. Being fair, honest, and transparent about expectations is not an unreasonable expectation.”
Competition among hospitalists should be on a professional basis, experts emphasize, and cooperation is in everyone’s best interests. But Lowell Palmer, MD, FHM, a hospitalist at Southwest Washington Medical Center in Vancouver, Wash., thinks competition can be a healthy thing for hospitalist groups.
“It forces us to make sure the services we provide are meeting the customer’s expectations,” says Dr. Palmer, who works with Cogent Physician Services, one of the three HM groups at Southwest Washington. “We can and do learn from each other.”
Impact of Health-Care Reform
Beware the transformation health-care reform is having on the dynamics of hospital-based practice and the competitive landscape facing more hospitalist groups, says Roger Heroux, MHA, PhD, CHE, consultant with Hospitalist Management Resources LLC. Reforms mean hospitalists are seeing an increased emphasis on coordinating with post-acute-care providers, improving care transitions, preventing readmissions, and meeting hospital targets for quality and patient safety.
Primary-care groups, accountable-care organizations (ACOs), and health plans could choose specific hospitalist practices they want to partner with to manage the care of their hospitalized members, but they will have clear performance expectations that those groups will need to meet, spelled out in benchmarks. Or, as some experts believe, they might opt to bring in their own hospitalist group.
“We’re spending our time working with existing hospitalist programs to help them be more efficient and effective, to manage risk, and to become aggressive about meeting the clinical benchmarks,” Heroux says. Hospitals, ACOs, and capitated groups can’t afford not to have a high-performing hospitalist program, so this will become a hallmark of survival for hospitalist programs as well. “In a highly managed environment, patients will be managed by a hospitalist group that is responsive to these expectations,” he says.
Larry Beresford is a freelance writer in Oakland, Calif.
References
- Gluck F. Lee Memorial Health Systems’ hospitalists under new controls. Fort Myers News Press. Dec. 1, 2011.
- Society of Hospital Medicine Position Statement on Hospitalist Credentialing and Medical Staff Privileges. SHM website. Available at: http://www.hospitalmedicine.org/AM/Template.cfm?Section=Where_We_Stand&Template=/CM/HTMLDisplay.cfm&ContentID=28262. Accessed April 1, 2013.
UCSF Engages Hospitalists to Improve Patient Communication
In a poster presented at HM12, Kathryn Quinn, MPH, CPPS, FACHE, described how her quality team at the University of California at San Francisco (UCSF) developed a checklist to improve physician communication with patients, then taught it to the attending hospitalist faculty.1 The project began with a list of 29 best practices for patient-physician interaction, as identified in medical literature. Hospitalists then voted for the elements they felt were most important to their practice, as well as those best able to be measured, and a top-10 list was created.
Quinn, the program manager for quality and safety in the division of hospital medicine at UCSF, says the communication best practices were “chosen by the people whose practices we are trying to change.”
The quality team presented the best practices in one-hour training sessions that included small-group role plays, explains co-investigator and UCSF hospitalist Diane Sliwka, MD. The training extended to outpatient physicians, medical specialists, and chief residents. Participants also were provided a laminated pocket card listing the interventions. They also received feedback from structured observations with patients on service.
Quinn says UCSF hospitalists have improved at knocking and asking permission to enter patient rooms, introducing themselves by name and role, and encouraging questions at the end of the interaction. They have been less successful at inquiring about the patient’s concerns early in the interview and at discussing duration of treatment and next steps.
“We learned that it takes more than just talk,” Quinn says. “Just telling physicians how to improve communication doesn’t mean it’s easy to do.”
Still to be determined is the project’s impact on patient satisfaction scores, although the hospitalists reported that they found the training and feedback helpful.
References
- Quinn K, Neeman N, Mourad M, Sliwka D. Communication coaching: A multifaceted intervention to improve physician-patient communication [abstract]. J Hosp Med. 2012;7 Suppl 2:S108.
- Sokol PE, Wynia MK. There and Home Again, Safely: Five Responsibilities of Ambulatory Practices in High Quality Care Transitions. American Medical Association website. http://www.ama-assn.org/resources/doc/patient-safety/ambulatory-practices.pdf. Accessed February 12, 2013.
- Dharmarajan K, Hsieh AF, Lin Z, et al. Diagnoses and timing of 30-day readmissions after hospitalization for heart failure, acute myocardial infarction, or pneumonia. JAMA. 2013;309(4):355-363.
- JAMA Internal Medicine. Nearly one-third of physicians report missing electronic notification of test results. JAMA Internal Medicine website. Available at: http://media.jamanetwork.com/news-item/nearly-one-third-of-physicians-report-missing-electronic-notification-of-test-results/.Accessed April 8, 2013.
- Miliard M. VA enlists telehealth for disasters. Healthcare IT News website. http://www.healthcareitnews.com/news/va-enlists-telehealth-disasters. Published February 27, 2013. Accessed April 1, 2013.
In a poster presented at HM12, Kathryn Quinn, MPH, CPPS, FACHE, described how her quality team at the University of California at San Francisco (UCSF) developed a checklist to improve physician communication with patients, then taught it to the attending hospitalist faculty.1 The project began with a list of 29 best practices for patient-physician interaction, as identified in medical literature. Hospitalists then voted for the elements they felt were most important to their practice, as well as those best able to be measured, and a top-10 list was created.
Quinn, the program manager for quality and safety in the division of hospital medicine at UCSF, says the communication best practices were “chosen by the people whose practices we are trying to change.”
The quality team presented the best practices in one-hour training sessions that included small-group role plays, explains co-investigator and UCSF hospitalist Diane Sliwka, MD. The training extended to outpatient physicians, medical specialists, and chief residents. Participants also were provided a laminated pocket card listing the interventions. They also received feedback from structured observations with patients on service.
Quinn says UCSF hospitalists have improved at knocking and asking permission to enter patient rooms, introducing themselves by name and role, and encouraging questions at the end of the interaction. They have been less successful at inquiring about the patient’s concerns early in the interview and at discussing duration of treatment and next steps.
“We learned that it takes more than just talk,” Quinn says. “Just telling physicians how to improve communication doesn’t mean it’s easy to do.”
Still to be determined is the project’s impact on patient satisfaction scores, although the hospitalists reported that they found the training and feedback helpful.
References
- Quinn K, Neeman N, Mourad M, Sliwka D. Communication coaching: A multifaceted intervention to improve physician-patient communication [abstract]. J Hosp Med. 2012;7 Suppl 2:S108.
- Sokol PE, Wynia MK. There and Home Again, Safely: Five Responsibilities of Ambulatory Practices in High Quality Care Transitions. American Medical Association website. http://www.ama-assn.org/resources/doc/patient-safety/ambulatory-practices.pdf. Accessed February 12, 2013.
- Dharmarajan K, Hsieh AF, Lin Z, et al. Diagnoses and timing of 30-day readmissions after hospitalization for heart failure, acute myocardial infarction, or pneumonia. JAMA. 2013;309(4):355-363.
- JAMA Internal Medicine. Nearly one-third of physicians report missing electronic notification of test results. JAMA Internal Medicine website. Available at: http://media.jamanetwork.com/news-item/nearly-one-third-of-physicians-report-missing-electronic-notification-of-test-results/.Accessed April 8, 2013.
- Miliard M. VA enlists telehealth for disasters. Healthcare IT News website. http://www.healthcareitnews.com/news/va-enlists-telehealth-disasters. Published February 27, 2013. Accessed April 1, 2013.
In a poster presented at HM12, Kathryn Quinn, MPH, CPPS, FACHE, described how her quality team at the University of California at San Francisco (UCSF) developed a checklist to improve physician communication with patients, then taught it to the attending hospitalist faculty.1 The project began with a list of 29 best practices for patient-physician interaction, as identified in medical literature. Hospitalists then voted for the elements they felt were most important to their practice, as well as those best able to be measured, and a top-10 list was created.
Quinn, the program manager for quality and safety in the division of hospital medicine at UCSF, says the communication best practices were “chosen by the people whose practices we are trying to change.”
The quality team presented the best practices in one-hour training sessions that included small-group role plays, explains co-investigator and UCSF hospitalist Diane Sliwka, MD. The training extended to outpatient physicians, medical specialists, and chief residents. Participants also were provided a laminated pocket card listing the interventions. They also received feedback from structured observations with patients on service.
Quinn says UCSF hospitalists have improved at knocking and asking permission to enter patient rooms, introducing themselves by name and role, and encouraging questions at the end of the interaction. They have been less successful at inquiring about the patient’s concerns early in the interview and at discussing duration of treatment and next steps.
“We learned that it takes more than just talk,” Quinn says. “Just telling physicians how to improve communication doesn’t mean it’s easy to do.”
Still to be determined is the project’s impact on patient satisfaction scores, although the hospitalists reported that they found the training and feedback helpful.
References
- Quinn K, Neeman N, Mourad M, Sliwka D. Communication coaching: A multifaceted intervention to improve physician-patient communication [abstract]. J Hosp Med. 2012;7 Suppl 2:S108.
- Sokol PE, Wynia MK. There and Home Again, Safely: Five Responsibilities of Ambulatory Practices in High Quality Care Transitions. American Medical Association website. http://www.ama-assn.org/resources/doc/patient-safety/ambulatory-practices.pdf. Accessed February 12, 2013.
- Dharmarajan K, Hsieh AF, Lin Z, et al. Diagnoses and timing of 30-day readmissions after hospitalization for heart failure, acute myocardial infarction, or pneumonia. JAMA. 2013;309(4):355-363.
- JAMA Internal Medicine. Nearly one-third of physicians report missing electronic notification of test results. JAMA Internal Medicine website. Available at: http://media.jamanetwork.com/news-item/nearly-one-third-of-physicians-report-missing-electronic-notification-of-test-results/.Accessed April 8, 2013.
- Miliard M. VA enlists telehealth for disasters. Healthcare IT News website. http://www.healthcareitnews.com/news/va-enlists-telehealth-disasters. Published February 27, 2013. Accessed April 1, 2013.
Hospitalists Can Get Ahead Through Quality and Patient Safety Initiatives
Are you a hospitalist who, on daily rounds, often thinks, “There’s got to be a better way to do this”? You might be just the type of person who can carve a niche for yourself in hospital quality and patient safety—and advance your career in the process.
Successful navigation of the quality-improvement (QI) and patient-safety domains, according to three veteran hospitalists, requires an initial passion and an incremental approach. Now is an especially good time, they agree, for young hospitalists to engage in these types of initiatives.
Why Do It?
In her capacity as president of the Mid-Atlantic Business Unit for Brentwood, Tenn.-based CogentHMG, Julia Wright, MD, SFHM, FACP, often encourages young recruits to consider participation in QI and patient-safety initiatives. She admits that the transition from residency to a busy HM practice, with its higher patient volumes and a faster pace, can be daunting at first. Still, she tries to cultivate interest in initiatives and establish a realistic timeframe for involvement.
There are many reasons to consider this as a career step. Dr. Wright says that quality and patient safety dovetail with hospitalists’ initial reasons for choosing medicine: to improve patients’ lives.
Janet Nagamine, RN, MD, SFHM, former patient safety officer and assistant chief of quality at Kaiser Permanente in Santa Clara, Calif., describes the fit this way: “I might be a good doctor, but as a hospitalist, I rely on many others within the system to deliver, so my patients can’t get good care until the entire system is running well,” she says. “There are all kinds of opportunities to fix our [hospital] system, and I really believe that hospitalists cannot separate themselves from that engagement.”
Elizabeth Gundersen, MD, FHM, of Fort Lauderdale, Fla., agrees that it’s a natural step to think about the ways to make a difference on a larger level. At her former institution, the University of Massachusetts (UMass) Medical School in Worcester, she parlayed her interest in QI to work her way up from ground-level hospitalist to associate chief of her division and quality officer for the hospital. “Physicians get a lot of satisfaction from helping individual patients,” she says. “One thing I really liked about getting involved with quality improvement was being able to make a difference for patients on a systems level.”
An Incremental Path
The path to her current position began with a very specific issue for Dr. Nagamine, an SHM board member who also serves as a Project BOOST co-investigator. “Although I have been doing patient safety since before they had a name for it, I didn’t start out saying that I wanted a career in quality and safety,” she says. “I was trying to take better care of my patients with diabetes, but controlling their glucose was extremely challenging because all the related variables—timing and amount of their insulin dosage, when and how much they had eaten—were charted in different places. This made it hard to adjust their insulin appropriately.”
It quickly became clear to Dr. Nagamine that the solution had to be systemic. She realized that something as basic as taking care of her patients with diabetes required multiple departments (i.e. dietary, nursing, and pharmacy) to furnish information in an integrated manner. So she joined the diabetes committee and went to work on the issue. She helped devise a flow chart that could be used by all relevant departments. A further evolution on the path emanated from one of her patients receiving the wrong medication. She joined the medication safety committee, became chair, “and the next thing you know, I’m in charge of patient safety, and an assistant chief of quality.”
Training Is Necessary
QI and patient-safety methodologies have become sophisticated disciplines in the past two decades, Dr. Wright says. Access to training in QI basics now is readily available to early-career hospitalists. For example, CogentHMG offers program support for QI so that anyone interested “doesn’t have to start from scratch anymore; we can help show them the way and support them in doing it.”
This month, HM13 (www.hospital medicine2013.org)—just outside Washington, D.C.—will offer multiple sessions on quality, as well as the “Initiating Quality Improvement Projects with Built-In Sustainment” workshop, led by Center for Comprehensive Access and Delivery Research and Evaluation (CADRE) core investigator Peter Kaboli, MD, MS, who will address sustainability.
Beyond methodological tools, success in quality and patient safety requires the ability to motivate people, often across multiple disciplines, Dr. Nagamine says. “If you want things to work better, you must invite the right people to the table. For example, we often forget to include key nonclinical stakeholders,” she adds.
When working with hospitals across the country to implement rapid-response tTeams, Dr. Nagamine often reminds them to invite the operators, or “key people,” in the process.
“If you put patient safety at the core of your initiative and create the context for that, most people will agree that it’s the right thing to do and will get on board, even if it’s an extra step for them,” she says. “Know your audience, listen to their perspective, and learn what matters to them. And to most people, it matters that they give good patient care.”
Gretchen Henkel is a freelance writer in California.
Are you a hospitalist who, on daily rounds, often thinks, “There’s got to be a better way to do this”? You might be just the type of person who can carve a niche for yourself in hospital quality and patient safety—and advance your career in the process.
Successful navigation of the quality-improvement (QI) and patient-safety domains, according to three veteran hospitalists, requires an initial passion and an incremental approach. Now is an especially good time, they agree, for young hospitalists to engage in these types of initiatives.
Why Do It?
In her capacity as president of the Mid-Atlantic Business Unit for Brentwood, Tenn.-based CogentHMG, Julia Wright, MD, SFHM, FACP, often encourages young recruits to consider participation in QI and patient-safety initiatives. She admits that the transition from residency to a busy HM practice, with its higher patient volumes and a faster pace, can be daunting at first. Still, she tries to cultivate interest in initiatives and establish a realistic timeframe for involvement.
There are many reasons to consider this as a career step. Dr. Wright says that quality and patient safety dovetail with hospitalists’ initial reasons for choosing medicine: to improve patients’ lives.
Janet Nagamine, RN, MD, SFHM, former patient safety officer and assistant chief of quality at Kaiser Permanente in Santa Clara, Calif., describes the fit this way: “I might be a good doctor, but as a hospitalist, I rely on many others within the system to deliver, so my patients can’t get good care until the entire system is running well,” she says. “There are all kinds of opportunities to fix our [hospital] system, and I really believe that hospitalists cannot separate themselves from that engagement.”
Elizabeth Gundersen, MD, FHM, of Fort Lauderdale, Fla., agrees that it’s a natural step to think about the ways to make a difference on a larger level. At her former institution, the University of Massachusetts (UMass) Medical School in Worcester, she parlayed her interest in QI to work her way up from ground-level hospitalist to associate chief of her division and quality officer for the hospital. “Physicians get a lot of satisfaction from helping individual patients,” she says. “One thing I really liked about getting involved with quality improvement was being able to make a difference for patients on a systems level.”
An Incremental Path
The path to her current position began with a very specific issue for Dr. Nagamine, an SHM board member who also serves as a Project BOOST co-investigator. “Although I have been doing patient safety since before they had a name for it, I didn’t start out saying that I wanted a career in quality and safety,” she says. “I was trying to take better care of my patients with diabetes, but controlling their glucose was extremely challenging because all the related variables—timing and amount of their insulin dosage, when and how much they had eaten—were charted in different places. This made it hard to adjust their insulin appropriately.”
It quickly became clear to Dr. Nagamine that the solution had to be systemic. She realized that something as basic as taking care of her patients with diabetes required multiple departments (i.e. dietary, nursing, and pharmacy) to furnish information in an integrated manner. So she joined the diabetes committee and went to work on the issue. She helped devise a flow chart that could be used by all relevant departments. A further evolution on the path emanated from one of her patients receiving the wrong medication. She joined the medication safety committee, became chair, “and the next thing you know, I’m in charge of patient safety, and an assistant chief of quality.”
Training Is Necessary
QI and patient-safety methodologies have become sophisticated disciplines in the past two decades, Dr. Wright says. Access to training in QI basics now is readily available to early-career hospitalists. For example, CogentHMG offers program support for QI so that anyone interested “doesn’t have to start from scratch anymore; we can help show them the way and support them in doing it.”
This month, HM13 (www.hospital medicine2013.org)—just outside Washington, D.C.—will offer multiple sessions on quality, as well as the “Initiating Quality Improvement Projects with Built-In Sustainment” workshop, led by Center for Comprehensive Access and Delivery Research and Evaluation (CADRE) core investigator Peter Kaboli, MD, MS, who will address sustainability.
Beyond methodological tools, success in quality and patient safety requires the ability to motivate people, often across multiple disciplines, Dr. Nagamine says. “If you want things to work better, you must invite the right people to the table. For example, we often forget to include key nonclinical stakeholders,” she adds.
When working with hospitals across the country to implement rapid-response tTeams, Dr. Nagamine often reminds them to invite the operators, or “key people,” in the process.
“If you put patient safety at the core of your initiative and create the context for that, most people will agree that it’s the right thing to do and will get on board, even if it’s an extra step for them,” she says. “Know your audience, listen to their perspective, and learn what matters to them. And to most people, it matters that they give good patient care.”
Gretchen Henkel is a freelance writer in California.
Are you a hospitalist who, on daily rounds, often thinks, “There’s got to be a better way to do this”? You might be just the type of person who can carve a niche for yourself in hospital quality and patient safety—and advance your career in the process.
Successful navigation of the quality-improvement (QI) and patient-safety domains, according to three veteran hospitalists, requires an initial passion and an incremental approach. Now is an especially good time, they agree, for young hospitalists to engage in these types of initiatives.
Why Do It?
In her capacity as president of the Mid-Atlantic Business Unit for Brentwood, Tenn.-based CogentHMG, Julia Wright, MD, SFHM, FACP, often encourages young recruits to consider participation in QI and patient-safety initiatives. She admits that the transition from residency to a busy HM practice, with its higher patient volumes and a faster pace, can be daunting at first. Still, she tries to cultivate interest in initiatives and establish a realistic timeframe for involvement.
There are many reasons to consider this as a career step. Dr. Wright says that quality and patient safety dovetail with hospitalists’ initial reasons for choosing medicine: to improve patients’ lives.
Janet Nagamine, RN, MD, SFHM, former patient safety officer and assistant chief of quality at Kaiser Permanente in Santa Clara, Calif., describes the fit this way: “I might be a good doctor, but as a hospitalist, I rely on many others within the system to deliver, so my patients can’t get good care until the entire system is running well,” she says. “There are all kinds of opportunities to fix our [hospital] system, and I really believe that hospitalists cannot separate themselves from that engagement.”
Elizabeth Gundersen, MD, FHM, of Fort Lauderdale, Fla., agrees that it’s a natural step to think about the ways to make a difference on a larger level. At her former institution, the University of Massachusetts (UMass) Medical School in Worcester, she parlayed her interest in QI to work her way up from ground-level hospitalist to associate chief of her division and quality officer for the hospital. “Physicians get a lot of satisfaction from helping individual patients,” she says. “One thing I really liked about getting involved with quality improvement was being able to make a difference for patients on a systems level.”
An Incremental Path
The path to her current position began with a very specific issue for Dr. Nagamine, an SHM board member who also serves as a Project BOOST co-investigator. “Although I have been doing patient safety since before they had a name for it, I didn’t start out saying that I wanted a career in quality and safety,” she says. “I was trying to take better care of my patients with diabetes, but controlling their glucose was extremely challenging because all the related variables—timing and amount of their insulin dosage, when and how much they had eaten—were charted in different places. This made it hard to adjust their insulin appropriately.”
It quickly became clear to Dr. Nagamine that the solution had to be systemic. She realized that something as basic as taking care of her patients with diabetes required multiple departments (i.e. dietary, nursing, and pharmacy) to furnish information in an integrated manner. So she joined the diabetes committee and went to work on the issue. She helped devise a flow chart that could be used by all relevant departments. A further evolution on the path emanated from one of her patients receiving the wrong medication. She joined the medication safety committee, became chair, “and the next thing you know, I’m in charge of patient safety, and an assistant chief of quality.”
Training Is Necessary
QI and patient-safety methodologies have become sophisticated disciplines in the past two decades, Dr. Wright says. Access to training in QI basics now is readily available to early-career hospitalists. For example, CogentHMG offers program support for QI so that anyone interested “doesn’t have to start from scratch anymore; we can help show them the way and support them in doing it.”
This month, HM13 (www.hospital medicine2013.org)—just outside Washington, D.C.—will offer multiple sessions on quality, as well as the “Initiating Quality Improvement Projects with Built-In Sustainment” workshop, led by Center for Comprehensive Access and Delivery Research and Evaluation (CADRE) core investigator Peter Kaboli, MD, MS, who will address sustainability.
Beyond methodological tools, success in quality and patient safety requires the ability to motivate people, often across multiple disciplines, Dr. Nagamine says. “If you want things to work better, you must invite the right people to the table. For example, we often forget to include key nonclinical stakeholders,” she adds.
When working with hospitals across the country to implement rapid-response tTeams, Dr. Nagamine often reminds them to invite the operators, or “key people,” in the process.
“If you put patient safety at the core of your initiative and create the context for that, most people will agree that it’s the right thing to do and will get on board, even if it’s an extra step for them,” she says. “Know your audience, listen to their perspective, and learn what matters to them. And to most people, it matters that they give good patient care.”
Gretchen Henkel is a freelance writer in California.
Drive Change in an ACO
From informal polls I’ve recently conducted of hospitalists, many are not even aware they are part of an accountable-care organization (ACO). And if they are aware, they might not be engaging in meaningful dialogue with ACO leaders about their role in these organizations. But, in the long term, ACOs will need to bring hospitalists to the table in order to be successful.
Are You Part of an ACO?
David Muhlestein, who blogs for Health Affairs, tracks the growth of ACOs around the country. He states that, as of Jan. 31, there were 428 ACOs in the U.S. (see Figure 1).1 In terms of numbers, Florida, Texas, and California lead the nation with 42, 33, and 46 ACOs, respectively. So it is likely that you are part of an ACO. If you are unsure, ask your chief medical officer or president of the medical staff.
How ACOs Work
All ACOs seek to manage a group, or population, of patients as efficiently as possible while maintaining or improving quality of care. For Medicare ACOs, the goal is to bring together hospitals and physicians in order to share savings derived from efficiencies in care. But before any savings can be shared, the Medicare ACO must demonstrate that it achieved high-quality care across four domains, totaling 33 individual quality measures. (see Table 1)
Main Flavors of ACOs
There are two types of ACOs: private ACOs and Medicare ACOs. Prior to Medicare ACOs, which were launched in January 2012, there were 150 private-sector ACOs, and this number continues to grow. Private ACOs represent a heterogeneous group in terms of reimbursement model. Some operate under shared savings programs; others use full or partial capitation, bundled payments, and/or other types of arrangements. But nearly all ACOs operate under the premise that the incentives used to make care more efficient and less costly can only be applied if measurable quality is maintained or improved. ACOs do not pay doctors or hospitals more unless high quality is demonstrated.
ACO Quality Measures and Hospitalists
Most of the 33 quality measures required by Medicare ACOs are based in ambulatory practice. These include measures related to blood pressure, immunizations, cancer, and fall-risk screening, and measures for diabetics, such as lipids and hemoglobin A1C. However, there are a few measures for which hospitalists should share in accountability, including:
- All-cause hospital readmission rate—risk-standardized;
- Ambulatory sensitive condition hospital admission rates (CHF, COPD); and
- Medication reconciliation after discharge from an inpatient facility.
Four Key Actions for Hospitalists
Hospitalists make a significant contribution to the quality and the financial performance of ACOs. In addition to the quality metrics cited above, hospitalists impact the inpatient portion of the overall population’s cost of care. Furthermore, hospitalists are vital partners in the care coordination required for an ACO to be successful.
Here are four actions I suggest taking in order for your hospitalist group to be effective as participants in an ACO:
- Have a representative from your group participate in ACO committees that address hospital utilization and related matters, such as care coordination impacting pre- and post-hospital care.
- Learn how to work with ACO case managers on care transitions, including post-discharge follow-up and information transfer.
- Understand an ACO’s approach to engagement of and coordination with post-acute-care facilities. The ability of a post-acute facility, such a skilled nursing facility, to accept patients who have complex care needs, to manage changes in condition in the facility when appropriate, and to send complete information upon transfer to the hospital are important strategies for an ACO’s success.
- Understand how an ACO reports quality and cost performance and how savings will be shared among participants.
Mindset Change
If hospitalists are part of the chain of ACO physicians and providers held accountable for the health of a population of patients, we must work more closely with the medical home/neighborhood, post-acute-care facilities, and home-care providers. The change in mindset will occur only if we have a set of tools to get the job done, such as case managers and information technology, and the appropriate incentives to support better care coordination. I encourage my fellow hospitalists to make things happen, instead of taking a passive role in this monumental transformation.
Reference
Dr. Whitcomb is medical director of healthcare quality at Baystate Medical Center in Springfield, Mass. He is a co-founder and past president of SHM. Email him at [email protected].
From informal polls I’ve recently conducted of hospitalists, many are not even aware they are part of an accountable-care organization (ACO). And if they are aware, they might not be engaging in meaningful dialogue with ACO leaders about their role in these organizations. But, in the long term, ACOs will need to bring hospitalists to the table in order to be successful.
Are You Part of an ACO?
David Muhlestein, who blogs for Health Affairs, tracks the growth of ACOs around the country. He states that, as of Jan. 31, there were 428 ACOs in the U.S. (see Figure 1).1 In terms of numbers, Florida, Texas, and California lead the nation with 42, 33, and 46 ACOs, respectively. So it is likely that you are part of an ACO. If you are unsure, ask your chief medical officer or president of the medical staff.
How ACOs Work
All ACOs seek to manage a group, or population, of patients as efficiently as possible while maintaining or improving quality of care. For Medicare ACOs, the goal is to bring together hospitals and physicians in order to share savings derived from efficiencies in care. But before any savings can be shared, the Medicare ACO must demonstrate that it achieved high-quality care across four domains, totaling 33 individual quality measures. (see Table 1)
Main Flavors of ACOs
There are two types of ACOs: private ACOs and Medicare ACOs. Prior to Medicare ACOs, which were launched in January 2012, there were 150 private-sector ACOs, and this number continues to grow. Private ACOs represent a heterogeneous group in terms of reimbursement model. Some operate under shared savings programs; others use full or partial capitation, bundled payments, and/or other types of arrangements. But nearly all ACOs operate under the premise that the incentives used to make care more efficient and less costly can only be applied if measurable quality is maintained or improved. ACOs do not pay doctors or hospitals more unless high quality is demonstrated.
ACO Quality Measures and Hospitalists
Most of the 33 quality measures required by Medicare ACOs are based in ambulatory practice. These include measures related to blood pressure, immunizations, cancer, and fall-risk screening, and measures for diabetics, such as lipids and hemoglobin A1C. However, there are a few measures for which hospitalists should share in accountability, including:
- All-cause hospital readmission rate—risk-standardized;
- Ambulatory sensitive condition hospital admission rates (CHF, COPD); and
- Medication reconciliation after discharge from an inpatient facility.
Four Key Actions for Hospitalists
Hospitalists make a significant contribution to the quality and the financial performance of ACOs. In addition to the quality metrics cited above, hospitalists impact the inpatient portion of the overall population’s cost of care. Furthermore, hospitalists are vital partners in the care coordination required for an ACO to be successful.
Here are four actions I suggest taking in order for your hospitalist group to be effective as participants in an ACO:
- Have a representative from your group participate in ACO committees that address hospital utilization and related matters, such as care coordination impacting pre- and post-hospital care.
- Learn how to work with ACO case managers on care transitions, including post-discharge follow-up and information transfer.
- Understand an ACO’s approach to engagement of and coordination with post-acute-care facilities. The ability of a post-acute facility, such a skilled nursing facility, to accept patients who have complex care needs, to manage changes in condition in the facility when appropriate, and to send complete information upon transfer to the hospital are important strategies for an ACO’s success.
- Understand how an ACO reports quality and cost performance and how savings will be shared among participants.
Mindset Change
If hospitalists are part of the chain of ACO physicians and providers held accountable for the health of a population of patients, we must work more closely with the medical home/neighborhood, post-acute-care facilities, and home-care providers. The change in mindset will occur only if we have a set of tools to get the job done, such as case managers and information technology, and the appropriate incentives to support better care coordination. I encourage my fellow hospitalists to make things happen, instead of taking a passive role in this monumental transformation.
Reference
Dr. Whitcomb is medical director of healthcare quality at Baystate Medical Center in Springfield, Mass. He is a co-founder and past president of SHM. Email him at [email protected].
From informal polls I’ve recently conducted of hospitalists, many are not even aware they are part of an accountable-care organization (ACO). And if they are aware, they might not be engaging in meaningful dialogue with ACO leaders about their role in these organizations. But, in the long term, ACOs will need to bring hospitalists to the table in order to be successful.
Are You Part of an ACO?
David Muhlestein, who blogs for Health Affairs, tracks the growth of ACOs around the country. He states that, as of Jan. 31, there were 428 ACOs in the U.S. (see Figure 1).1 In terms of numbers, Florida, Texas, and California lead the nation with 42, 33, and 46 ACOs, respectively. So it is likely that you are part of an ACO. If you are unsure, ask your chief medical officer or president of the medical staff.
How ACOs Work
All ACOs seek to manage a group, or population, of patients as efficiently as possible while maintaining or improving quality of care. For Medicare ACOs, the goal is to bring together hospitals and physicians in order to share savings derived from efficiencies in care. But before any savings can be shared, the Medicare ACO must demonstrate that it achieved high-quality care across four domains, totaling 33 individual quality measures. (see Table 1)
Main Flavors of ACOs
There are two types of ACOs: private ACOs and Medicare ACOs. Prior to Medicare ACOs, which were launched in January 2012, there were 150 private-sector ACOs, and this number continues to grow. Private ACOs represent a heterogeneous group in terms of reimbursement model. Some operate under shared savings programs; others use full or partial capitation, bundled payments, and/or other types of arrangements. But nearly all ACOs operate under the premise that the incentives used to make care more efficient and less costly can only be applied if measurable quality is maintained or improved. ACOs do not pay doctors or hospitals more unless high quality is demonstrated.
ACO Quality Measures and Hospitalists
Most of the 33 quality measures required by Medicare ACOs are based in ambulatory practice. These include measures related to blood pressure, immunizations, cancer, and fall-risk screening, and measures for diabetics, such as lipids and hemoglobin A1C. However, there are a few measures for which hospitalists should share in accountability, including:
- All-cause hospital readmission rate—risk-standardized;
- Ambulatory sensitive condition hospital admission rates (CHF, COPD); and
- Medication reconciliation after discharge from an inpatient facility.
Four Key Actions for Hospitalists
Hospitalists make a significant contribution to the quality and the financial performance of ACOs. In addition to the quality metrics cited above, hospitalists impact the inpatient portion of the overall population’s cost of care. Furthermore, hospitalists are vital partners in the care coordination required for an ACO to be successful.
Here are four actions I suggest taking in order for your hospitalist group to be effective as participants in an ACO:
- Have a representative from your group participate in ACO committees that address hospital utilization and related matters, such as care coordination impacting pre- and post-hospital care.
- Learn how to work with ACO case managers on care transitions, including post-discharge follow-up and information transfer.
- Understand an ACO’s approach to engagement of and coordination with post-acute-care facilities. The ability of a post-acute facility, such a skilled nursing facility, to accept patients who have complex care needs, to manage changes in condition in the facility when appropriate, and to send complete information upon transfer to the hospital are important strategies for an ACO’s success.
- Understand how an ACO reports quality and cost performance and how savings will be shared among participants.
Mindset Change
If hospitalists are part of the chain of ACO physicians and providers held accountable for the health of a population of patients, we must work more closely with the medical home/neighborhood, post-acute-care facilities, and home-care providers. The change in mindset will occur only if we have a set of tools to get the job done, such as case managers and information technology, and the appropriate incentives to support better care coordination. I encourage my fellow hospitalists to make things happen, instead of taking a passive role in this monumental transformation.
Reference
Dr. Whitcomb is medical director of healthcare quality at Baystate Medical Center in Springfield, Mass. He is a co-founder and past president of SHM. Email him at [email protected].
Stricter Duty-Hour Regulations Tied to Diminished Patient Care
A new report has linked recent changes made to hospital residents’ duty-hour regulations with a reduction in some aspects of patient care.
The study compared the work model for duty-hour regulations implemented in 2011 by the Accreditation Council for Graduate Medical Education (ACGME), which mostly limits first-year residents to a maximum 16-hour shift and older residents to 24 hours, with less restrictive guidelines adopted in 2003. Previously, 30-hour shifts were permitted for all residents.
Researchers at Johns Hopkins University in Baltimore measured residents’ sleep duration, hospital admission volumes, residents’ educational opportunities, the number of handoffs, and patient satisfaction surveys during shifts worked by internal-medicine house staff trainees under both models. The researchers used a three-month crossover design.
Residents slept longer, as expected, but the data showed more handoffs, fewer chances to attend teaching conferences, and reduced intern presence during daytime shifts when trainees followed the more recent work model. The study authors associated the model adopted in 2011 with deterioration in continuity of patient care and perceived quality of care. One of the four house staff teams perceived such a reduced quality of patient care that it terminated the project early.
However, one resident program director says much more research needs to be done to determine the efficacy of the new work-hour rules, particularly on patient and resident satisfaction. “There are things that go along with duty-hours, such as access to information and really well-designed handoff systems, that I think would bring out the safety advantages of duty-hours,” says Ethan Fried, MD, MS, FACP, associate professor of clinical medicine, Columbia College of Physicians and Surgeons and vice chair for education, department of medicine, St. Luke’s-Roosevelt Hospital, both in New York, and a former president of the Association of Program Directors in Internal Medicine.
“One of the reasons you’re not seeing an inflection in safety is because you have duty-hours, but you haven’t got the other system that you need to make duty-hours work. What people have been focused on is pure safety, and that we haven’t been able to demonstrate actual improvement in morbidity, mortality or complications,” he adds. “It’s one of those cases where I don’t know if we’re necessarily asking the right questions.”
Visit our website for more information on duty-hours.
A new report has linked recent changes made to hospital residents’ duty-hour regulations with a reduction in some aspects of patient care.
The study compared the work model for duty-hour regulations implemented in 2011 by the Accreditation Council for Graduate Medical Education (ACGME), which mostly limits first-year residents to a maximum 16-hour shift and older residents to 24 hours, with less restrictive guidelines adopted in 2003. Previously, 30-hour shifts were permitted for all residents.
Researchers at Johns Hopkins University in Baltimore measured residents’ sleep duration, hospital admission volumes, residents’ educational opportunities, the number of handoffs, and patient satisfaction surveys during shifts worked by internal-medicine house staff trainees under both models. The researchers used a three-month crossover design.
Residents slept longer, as expected, but the data showed more handoffs, fewer chances to attend teaching conferences, and reduced intern presence during daytime shifts when trainees followed the more recent work model. The study authors associated the model adopted in 2011 with deterioration in continuity of patient care and perceived quality of care. One of the four house staff teams perceived such a reduced quality of patient care that it terminated the project early.
However, one resident program director says much more research needs to be done to determine the efficacy of the new work-hour rules, particularly on patient and resident satisfaction. “There are things that go along with duty-hours, such as access to information and really well-designed handoff systems, that I think would bring out the safety advantages of duty-hours,” says Ethan Fried, MD, MS, FACP, associate professor of clinical medicine, Columbia College of Physicians and Surgeons and vice chair for education, department of medicine, St. Luke’s-Roosevelt Hospital, both in New York, and a former president of the Association of Program Directors in Internal Medicine.
“One of the reasons you’re not seeing an inflection in safety is because you have duty-hours, but you haven’t got the other system that you need to make duty-hours work. What people have been focused on is pure safety, and that we haven’t been able to demonstrate actual improvement in morbidity, mortality or complications,” he adds. “It’s one of those cases where I don’t know if we’re necessarily asking the right questions.”
Visit our website for more information on duty-hours.
A new report has linked recent changes made to hospital residents’ duty-hour regulations with a reduction in some aspects of patient care.
The study compared the work model for duty-hour regulations implemented in 2011 by the Accreditation Council for Graduate Medical Education (ACGME), which mostly limits first-year residents to a maximum 16-hour shift and older residents to 24 hours, with less restrictive guidelines adopted in 2003. Previously, 30-hour shifts were permitted for all residents.
Researchers at Johns Hopkins University in Baltimore measured residents’ sleep duration, hospital admission volumes, residents’ educational opportunities, the number of handoffs, and patient satisfaction surveys during shifts worked by internal-medicine house staff trainees under both models. The researchers used a three-month crossover design.
Residents slept longer, as expected, but the data showed more handoffs, fewer chances to attend teaching conferences, and reduced intern presence during daytime shifts when trainees followed the more recent work model. The study authors associated the model adopted in 2011 with deterioration in continuity of patient care and perceived quality of care. One of the four house staff teams perceived such a reduced quality of patient care that it terminated the project early.
However, one resident program director says much more research needs to be done to determine the efficacy of the new work-hour rules, particularly on patient and resident satisfaction. “There are things that go along with duty-hours, such as access to information and really well-designed handoff systems, that I think would bring out the safety advantages of duty-hours,” says Ethan Fried, MD, MS, FACP, associate professor of clinical medicine, Columbia College of Physicians and Surgeons and vice chair for education, department of medicine, St. Luke’s-Roosevelt Hospital, both in New York, and a former president of the Association of Program Directors in Internal Medicine.
“One of the reasons you’re not seeing an inflection in safety is because you have duty-hours, but you haven’t got the other system that you need to make duty-hours work. What people have been focused on is pure safety, and that we haven’t been able to demonstrate actual improvement in morbidity, mortality or complications,” he adds. “It’s one of those cases where I don’t know if we’re necessarily asking the right questions.”
Visit our website for more information on duty-hours.
In the Literature: Hospital-Based Research You Need to Know
Clinical question: Is routine preoperative urine screening beneficial?
Background: The value of preoperative urine screening is unproven, except before urologic procedures. Furthermore, treatment of asymptomatic bacteriuria may lead to adverse events, including diarrhea, allergic reactions, and Clostridium difficile infection (CDI).
Study design: Retrospective chart review.
Setting: Patients who underwent cardiothoracic, orthopedic, and vascular surgeries at the Minneapolis Veterans Affairs Medical Center in 2010.
Synopsis: A total of 1,934 procedures were performed on 1,699 patients, most of which were orthopedics procedures (1,291 in 1,115 patients). A urine culture was obtained before 25% of procedures with significant variation by service (cardiothoracic, 85%; vascular, 48%; orthopedic, 4%). Bacteriuria was detected in 11% of urine cultures (54 of 489), but antimicrobial drugs were dispensed to just 16 patients.
To identify correlates of preoperative urine culture use, patients with and without urine cultures were compared. The rate of surgical-site infection was similar for both groups. Postoperative UTI was more frequent among patients with bacteriuria. Rates of diarrhea, allergy, and CDI did not differ. Paradoxically, patients treated for preoperative UTI were more likely to develop surgical-site infections (45% vs. 14%; P=0.03). Postoperative UTI was also more frequent among treated patients versus untreated patients (18% vs. 7%).
Bottom line: This is the largest study to assess outcomes for routine preoperative urine cultures. These findings demonstrate that preoperative screening for, and treatment of, asymptomatic bacteriuria should be avoided in patients undergoing nonurologic surgical procedures.
Citation: Drekonja DM, Zarmbinski B, Johnson JR. Preoperative urine culture at a veterans affairs medical center. JAMA Intern Med. 2013;173(1):71-72.
Visit our website for more physician reviews of recent HM-relevant literature.
Clinical question: Is routine preoperative urine screening beneficial?
Background: The value of preoperative urine screening is unproven, except before urologic procedures. Furthermore, treatment of asymptomatic bacteriuria may lead to adverse events, including diarrhea, allergic reactions, and Clostridium difficile infection (CDI).
Study design: Retrospective chart review.
Setting: Patients who underwent cardiothoracic, orthopedic, and vascular surgeries at the Minneapolis Veterans Affairs Medical Center in 2010.
Synopsis: A total of 1,934 procedures were performed on 1,699 patients, most of which were orthopedics procedures (1,291 in 1,115 patients). A urine culture was obtained before 25% of procedures with significant variation by service (cardiothoracic, 85%; vascular, 48%; orthopedic, 4%). Bacteriuria was detected in 11% of urine cultures (54 of 489), but antimicrobial drugs were dispensed to just 16 patients.
To identify correlates of preoperative urine culture use, patients with and without urine cultures were compared. The rate of surgical-site infection was similar for both groups. Postoperative UTI was more frequent among patients with bacteriuria. Rates of diarrhea, allergy, and CDI did not differ. Paradoxically, patients treated for preoperative UTI were more likely to develop surgical-site infections (45% vs. 14%; P=0.03). Postoperative UTI was also more frequent among treated patients versus untreated patients (18% vs. 7%).
Bottom line: This is the largest study to assess outcomes for routine preoperative urine cultures. These findings demonstrate that preoperative screening for, and treatment of, asymptomatic bacteriuria should be avoided in patients undergoing nonurologic surgical procedures.
Citation: Drekonja DM, Zarmbinski B, Johnson JR. Preoperative urine culture at a veterans affairs medical center. JAMA Intern Med. 2013;173(1):71-72.
Visit our website for more physician reviews of recent HM-relevant literature.
Clinical question: Is routine preoperative urine screening beneficial?
Background: The value of preoperative urine screening is unproven, except before urologic procedures. Furthermore, treatment of asymptomatic bacteriuria may lead to adverse events, including diarrhea, allergic reactions, and Clostridium difficile infection (CDI).
Study design: Retrospective chart review.
Setting: Patients who underwent cardiothoracic, orthopedic, and vascular surgeries at the Minneapolis Veterans Affairs Medical Center in 2010.
Synopsis: A total of 1,934 procedures were performed on 1,699 patients, most of which were orthopedics procedures (1,291 in 1,115 patients). A urine culture was obtained before 25% of procedures with significant variation by service (cardiothoracic, 85%; vascular, 48%; orthopedic, 4%). Bacteriuria was detected in 11% of urine cultures (54 of 489), but antimicrobial drugs were dispensed to just 16 patients.
To identify correlates of preoperative urine culture use, patients with and without urine cultures were compared. The rate of surgical-site infection was similar for both groups. Postoperative UTI was more frequent among patients with bacteriuria. Rates of diarrhea, allergy, and CDI did not differ. Paradoxically, patients treated for preoperative UTI were more likely to develop surgical-site infections (45% vs. 14%; P=0.03). Postoperative UTI was also more frequent among treated patients versus untreated patients (18% vs. 7%).
Bottom line: This is the largest study to assess outcomes for routine preoperative urine cultures. These findings demonstrate that preoperative screening for, and treatment of, asymptomatic bacteriuria should be avoided in patients undergoing nonurologic surgical procedures.
Citation: Drekonja DM, Zarmbinski B, Johnson JR. Preoperative urine culture at a veterans affairs medical center. JAMA Intern Med. 2013;173(1):71-72.
Visit our website for more physician reviews of recent HM-relevant literature.
Patient Prediction Model Trims Avoidable Hospital Readmissions
A new prediction model that uses a familiar phrase can help identify potentially avoidable hospital patient readmissions, according to a report in JAMA Internal Medicine.
The retrospective cohort study, "Potentially Avoidable 30-Day Hospital Readmissions in Medical Patients," used a model dubbed HOSPITAL to create a score that targets patients most likely to benefit from pre-discharge interventions. The model is based on seven factors: hemoglobin at discharge, discharge from an oncology service, sodium levels at discharge, procedure during the index admission, index type of admission, number of admissions in the prior 12 months, and length of stay. The HOSPITAL score had fair discriminatory power (C statistic 0.71) and good calibration, the authors noted.
"By definition, these [interventions] are expensive and you really want to reserve them for the patients that are most likely to benefit," says study co-author Jeffrey Schnipper, MD, MPH, FHM, director of clinical research and an associate physician in the general medicine division at Brigham and Women's Hospital in Boston.
The study identified 879 potentially avoidable discharges out of 10,731 eligible discharges, or 8.5%. The estimated potentially avoidable readmission risk was 18%. Dr. Schnipper says that in absolute reduction, the model could cut 2% to 3% of readmissions.
"This is an evolution of sophistication in how we think about this work," Dr. Schnipper adds. "Not all patients have a preventable readmission. Maybe some of those patients are more likely to benefit. The next step is to prove it. That's the gold standard and that’s our next study." TH
Visit our website for more information on 30-day readmissions.
A new prediction model that uses a familiar phrase can help identify potentially avoidable hospital patient readmissions, according to a report in JAMA Internal Medicine.
The retrospective cohort study, "Potentially Avoidable 30-Day Hospital Readmissions in Medical Patients," used a model dubbed HOSPITAL to create a score that targets patients most likely to benefit from pre-discharge interventions. The model is based on seven factors: hemoglobin at discharge, discharge from an oncology service, sodium levels at discharge, procedure during the index admission, index type of admission, number of admissions in the prior 12 months, and length of stay. The HOSPITAL score had fair discriminatory power (C statistic 0.71) and good calibration, the authors noted.
"By definition, these [interventions] are expensive and you really want to reserve them for the patients that are most likely to benefit," says study co-author Jeffrey Schnipper, MD, MPH, FHM, director of clinical research and an associate physician in the general medicine division at Brigham and Women's Hospital in Boston.
The study identified 879 potentially avoidable discharges out of 10,731 eligible discharges, or 8.5%. The estimated potentially avoidable readmission risk was 18%. Dr. Schnipper says that in absolute reduction, the model could cut 2% to 3% of readmissions.
"This is an evolution of sophistication in how we think about this work," Dr. Schnipper adds. "Not all patients have a preventable readmission. Maybe some of those patients are more likely to benefit. The next step is to prove it. That's the gold standard and that’s our next study." TH
Visit our website for more information on 30-day readmissions.
A new prediction model that uses a familiar phrase can help identify potentially avoidable hospital patient readmissions, according to a report in JAMA Internal Medicine.
The retrospective cohort study, "Potentially Avoidable 30-Day Hospital Readmissions in Medical Patients," used a model dubbed HOSPITAL to create a score that targets patients most likely to benefit from pre-discharge interventions. The model is based on seven factors: hemoglobin at discharge, discharge from an oncology service, sodium levels at discharge, procedure during the index admission, index type of admission, number of admissions in the prior 12 months, and length of stay. The HOSPITAL score had fair discriminatory power (C statistic 0.71) and good calibration, the authors noted.
"By definition, these [interventions] are expensive and you really want to reserve them for the patients that are most likely to benefit," says study co-author Jeffrey Schnipper, MD, MPH, FHM, director of clinical research and an associate physician in the general medicine division at Brigham and Women's Hospital in Boston.
The study identified 879 potentially avoidable discharges out of 10,731 eligible discharges, or 8.5%. The estimated potentially avoidable readmission risk was 18%. Dr. Schnipper says that in absolute reduction, the model could cut 2% to 3% of readmissions.
"This is an evolution of sophistication in how we think about this work," Dr. Schnipper adds. "Not all patients have a preventable readmission. Maybe some of those patients are more likely to benefit. The next step is to prove it. That's the gold standard and that’s our next study." TH
Visit our website for more information on 30-day readmissions.
Hospitals Seek Ways to Defuse Angry Doctors
Everyone is prone to an angry outburst from time to time, and doctors are no exception. With well-documented, negative effects on morale, nurse retention, and patient safety, it's safe to say anger issues crop up from time to time among the nearly 40,000 practicing hospitalists throughout the U.S.
A recent article in Kaiser Health News describes efforts by hospitals to deal with physicians' tirades, such as a three-day counseling program developed at Vanderbilt University in Nashville, Tenn.
"All physicians need to be aware that there should be a 'zero tolerance' attitude for disruptive behavior, hospitalists included, and that disruptive behavior undermines a culture of safety, and therefore can put patients in danger," says Danielle Scheurer, MD, MSCR, SFHM, hospitalist and chief quality officer at Medical University of South Carolina in Charleston and physician editor of The Hospitalist.
In 2009, The Joint Commission issued a sentinel alert about intimidating and disruptive behaviors by physicians and the ways in which hospitals can address the issue.
The problem is not unique to any physician specialty, including hospitalists, says Alan Rosenstein, MD, an internist and disruptive behavior researcher based in San Francisco. A physician's training or personality might contribute to angry outbursts, but excessive workloads will cause pressure, stress, and burnout, which can lead to poor behavior.
"Hospitals can no longer afford to look the other way," Dr. Rosenstein says. "I look at physicians as a precious resource. The organizations they're affiliated with need to be more proactive and empathetic, intervening before the problem reaches the stage of requiring discipline through techniques such as coaching and stress management." TH
Visit our website for more information about the impact of workloads on hospitalists.
Everyone is prone to an angry outburst from time to time, and doctors are no exception. With well-documented, negative effects on morale, nurse retention, and patient safety, it's safe to say anger issues crop up from time to time among the nearly 40,000 practicing hospitalists throughout the U.S.
A recent article in Kaiser Health News describes efforts by hospitals to deal with physicians' tirades, such as a three-day counseling program developed at Vanderbilt University in Nashville, Tenn.
"All physicians need to be aware that there should be a 'zero tolerance' attitude for disruptive behavior, hospitalists included, and that disruptive behavior undermines a culture of safety, and therefore can put patients in danger," says Danielle Scheurer, MD, MSCR, SFHM, hospitalist and chief quality officer at Medical University of South Carolina in Charleston and physician editor of The Hospitalist.
In 2009, The Joint Commission issued a sentinel alert about intimidating and disruptive behaviors by physicians and the ways in which hospitals can address the issue.
The problem is not unique to any physician specialty, including hospitalists, says Alan Rosenstein, MD, an internist and disruptive behavior researcher based in San Francisco. A physician's training or personality might contribute to angry outbursts, but excessive workloads will cause pressure, stress, and burnout, which can lead to poor behavior.
"Hospitals can no longer afford to look the other way," Dr. Rosenstein says. "I look at physicians as a precious resource. The organizations they're affiliated with need to be more proactive and empathetic, intervening before the problem reaches the stage of requiring discipline through techniques such as coaching and stress management." TH
Visit our website for more information about the impact of workloads on hospitalists.
Everyone is prone to an angry outburst from time to time, and doctors are no exception. With well-documented, negative effects on morale, nurse retention, and patient safety, it's safe to say anger issues crop up from time to time among the nearly 40,000 practicing hospitalists throughout the U.S.
A recent article in Kaiser Health News describes efforts by hospitals to deal with physicians' tirades, such as a three-day counseling program developed at Vanderbilt University in Nashville, Tenn.
"All physicians need to be aware that there should be a 'zero tolerance' attitude for disruptive behavior, hospitalists included, and that disruptive behavior undermines a culture of safety, and therefore can put patients in danger," says Danielle Scheurer, MD, MSCR, SFHM, hospitalist and chief quality officer at Medical University of South Carolina in Charleston and physician editor of The Hospitalist.
In 2009, The Joint Commission issued a sentinel alert about intimidating and disruptive behaviors by physicians and the ways in which hospitals can address the issue.
The problem is not unique to any physician specialty, including hospitalists, says Alan Rosenstein, MD, an internist and disruptive behavior researcher based in San Francisco. A physician's training or personality might contribute to angry outbursts, but excessive workloads will cause pressure, stress, and burnout, which can lead to poor behavior.
"Hospitals can no longer afford to look the other way," Dr. Rosenstein says. "I look at physicians as a precious resource. The organizations they're affiliated with need to be more proactive and empathetic, intervening before the problem reaches the stage of requiring discipline through techniques such as coaching and stress management." TH
Visit our website for more information about the impact of workloads on hospitalists.
Affordable Care Act (ACA) Provision Carries Pay Raise for Some Hospitalists
For those who remain unaware, hospitalists who care for Medicaid patients will be getting a raise in 2013 and 2014. The reason is that the Affordable Care Act (ACA) requires Medicaid rates for specified primary-care services to be equal to those of Medicare rates during those two years, with the federal government paying the difference. Hospitalists generally meet the requirements and, therefore, will see this pay increase for their applicable Medicaid billing. For some context of the scope of this change, on average, Medicaid pays physicians at 66% of the national Medicare rates, although there is significant variation among the states.
To qualify, a physician must have a specialty designation of family medicine, internal medicine, or pediatrics, then further attest to board certification in one of those specialties or related subspecialties. Alternatively, the physician must have a 60% claims history for the specified evaluation and management (E&M) codes.
Multiple parties who have heard reports about state plans for Medicaid parity recently have contacted SHM; the plans, they report, intentionally would exclude hospitalists from the promised increase. There are variations on the explanation for the exclusion and where the idea is coming from, but the inquiries follow this general theme: “Since the definition of eligible physicians remains a grey area, states are developing alternative plans with a more narrow interpretation of the qualifying factors for the increase. These plans are only including physicians who practice in the community setting (i.e. not the hospital setting).”
This is demonstrably wrong. Even if states are having these discussions, such a plan is not going to come to fruition. The final rule for Medicaid parity, which essentially has the effect of law, is very clear: It does not allow for differing eligibility or alternate state plans.
The Centers for Medicare & Medicaid Services (CMS) specifically stated in the final rule that the increase is not limited to office-based primary-care services, but it will also include hospital observation and consultation for inpatient services provided by nonadmitting physicians, ED services, and critical-care services. In other words, a hospitalist who attests eligibility for their respective state Medicaid agency and bills 99231-3, 99221-3, 99238-9, etc., will receive the increased payment for these codes.
In response to an SHM inquiry for further clarification, CMS officials have stated, “The regulation requires that qualified physicians billing eligible codes receive higher payment. States do not have the latitude to exclude physicians simply because they practice in hospitals.”
It is possible that some confusion might be arising due to the recent controversies around the upcoming Medicaid expansion, which would extend Medicaid eligibility to individuals who earn up to 138% of the federal poverty line. Some states have chosen to opt out of this expansion and have publicly fought its implementation. The Medicaid parity provision is parallel to, but independent of, Medicaid expansion. Even if a state opts out of the expansion, the Medicaid payment increase for primary-care services should remain unaffected.
This isn’t to say that the Medicaid parity provision is a certainty. With the eyes of Congress turned toward budget cuts and austerity, the funds allocated for this temporary increase could easily be targeted. Regardless, any change in eligibility would require a rule change at the federal level, which is unlikely.
Many states have already devoted much time and effort on plans to implement the provision, and the plans were due to be submitted to CMS on March 31. It is pretty late in the game to consider changes. Barring an unlikely rule change or total elimination of funding, it is clear that hospitalists are eligible for the payment bump and should remain so.
Josh Boswell is SHM’s senior manager of government relations.
For those who remain unaware, hospitalists who care for Medicaid patients will be getting a raise in 2013 and 2014. The reason is that the Affordable Care Act (ACA) requires Medicaid rates for specified primary-care services to be equal to those of Medicare rates during those two years, with the federal government paying the difference. Hospitalists generally meet the requirements and, therefore, will see this pay increase for their applicable Medicaid billing. For some context of the scope of this change, on average, Medicaid pays physicians at 66% of the national Medicare rates, although there is significant variation among the states.
To qualify, a physician must have a specialty designation of family medicine, internal medicine, or pediatrics, then further attest to board certification in one of those specialties or related subspecialties. Alternatively, the physician must have a 60% claims history for the specified evaluation and management (E&M) codes.
Multiple parties who have heard reports about state plans for Medicaid parity recently have contacted SHM; the plans, they report, intentionally would exclude hospitalists from the promised increase. There are variations on the explanation for the exclusion and where the idea is coming from, but the inquiries follow this general theme: “Since the definition of eligible physicians remains a grey area, states are developing alternative plans with a more narrow interpretation of the qualifying factors for the increase. These plans are only including physicians who practice in the community setting (i.e. not the hospital setting).”
This is demonstrably wrong. Even if states are having these discussions, such a plan is not going to come to fruition. The final rule for Medicaid parity, which essentially has the effect of law, is very clear: It does not allow for differing eligibility or alternate state plans.
The Centers for Medicare & Medicaid Services (CMS) specifically stated in the final rule that the increase is not limited to office-based primary-care services, but it will also include hospital observation and consultation for inpatient services provided by nonadmitting physicians, ED services, and critical-care services. In other words, a hospitalist who attests eligibility for their respective state Medicaid agency and bills 99231-3, 99221-3, 99238-9, etc., will receive the increased payment for these codes.
In response to an SHM inquiry for further clarification, CMS officials have stated, “The regulation requires that qualified physicians billing eligible codes receive higher payment. States do not have the latitude to exclude physicians simply because they practice in hospitals.”
It is possible that some confusion might be arising due to the recent controversies around the upcoming Medicaid expansion, which would extend Medicaid eligibility to individuals who earn up to 138% of the federal poverty line. Some states have chosen to opt out of this expansion and have publicly fought its implementation. The Medicaid parity provision is parallel to, but independent of, Medicaid expansion. Even if a state opts out of the expansion, the Medicaid payment increase for primary-care services should remain unaffected.
This isn’t to say that the Medicaid parity provision is a certainty. With the eyes of Congress turned toward budget cuts and austerity, the funds allocated for this temporary increase could easily be targeted. Regardless, any change in eligibility would require a rule change at the federal level, which is unlikely.
Many states have already devoted much time and effort on plans to implement the provision, and the plans were due to be submitted to CMS on March 31. It is pretty late in the game to consider changes. Barring an unlikely rule change or total elimination of funding, it is clear that hospitalists are eligible for the payment bump and should remain so.
Josh Boswell is SHM’s senior manager of government relations.
For those who remain unaware, hospitalists who care for Medicaid patients will be getting a raise in 2013 and 2014. The reason is that the Affordable Care Act (ACA) requires Medicaid rates for specified primary-care services to be equal to those of Medicare rates during those two years, with the federal government paying the difference. Hospitalists generally meet the requirements and, therefore, will see this pay increase for their applicable Medicaid billing. For some context of the scope of this change, on average, Medicaid pays physicians at 66% of the national Medicare rates, although there is significant variation among the states.
To qualify, a physician must have a specialty designation of family medicine, internal medicine, or pediatrics, then further attest to board certification in one of those specialties or related subspecialties. Alternatively, the physician must have a 60% claims history for the specified evaluation and management (E&M) codes.
Multiple parties who have heard reports about state plans for Medicaid parity recently have contacted SHM; the plans, they report, intentionally would exclude hospitalists from the promised increase. There are variations on the explanation for the exclusion and where the idea is coming from, but the inquiries follow this general theme: “Since the definition of eligible physicians remains a grey area, states are developing alternative plans with a more narrow interpretation of the qualifying factors for the increase. These plans are only including physicians who practice in the community setting (i.e. not the hospital setting).”
This is demonstrably wrong. Even if states are having these discussions, such a plan is not going to come to fruition. The final rule for Medicaid parity, which essentially has the effect of law, is very clear: It does not allow for differing eligibility or alternate state plans.
The Centers for Medicare & Medicaid Services (CMS) specifically stated in the final rule that the increase is not limited to office-based primary-care services, but it will also include hospital observation and consultation for inpatient services provided by nonadmitting physicians, ED services, and critical-care services. In other words, a hospitalist who attests eligibility for their respective state Medicaid agency and bills 99231-3, 99221-3, 99238-9, etc., will receive the increased payment for these codes.
In response to an SHM inquiry for further clarification, CMS officials have stated, “The regulation requires that qualified physicians billing eligible codes receive higher payment. States do not have the latitude to exclude physicians simply because they practice in hospitals.”
It is possible that some confusion might be arising due to the recent controversies around the upcoming Medicaid expansion, which would extend Medicaid eligibility to individuals who earn up to 138% of the federal poverty line. Some states have chosen to opt out of this expansion and have publicly fought its implementation. The Medicaid parity provision is parallel to, but independent of, Medicaid expansion. Even if a state opts out of the expansion, the Medicaid payment increase for primary-care services should remain unaffected.
This isn’t to say that the Medicaid parity provision is a certainty. With the eyes of Congress turned toward budget cuts and austerity, the funds allocated for this temporary increase could easily be targeted. Regardless, any change in eligibility would require a rule change at the federal level, which is unlikely.
Many states have already devoted much time and effort on plans to implement the provision, and the plans were due to be submitted to CMS on March 31. It is pretty late in the game to consider changes. Barring an unlikely rule change or total elimination of funding, it is clear that hospitalists are eligible for the payment bump and should remain so.
Josh Boswell is SHM’s senior manager of government relations.