User login
What's the best way to monitor low-risk patients with a history of differentiated thyroid cancer?
A recombinant human thyrotropin (rhTSH)-stimulated serum thyroglobulin (Tg) level alone is sufficient to monitor for recurrent disease in low-risk patients with a history of differentiated thyroid cancer (DTC) (strength of recommendation [SOR] A, meta-analysis). Low-risk patients are defined as patients who have undergone total thyroidectomy and radioactive iodine (I131) remnant ablation therapy and show no clinical evidence of recurrent disease.
Evidence summary
An estimated 37,340 new cases of thyroid cancer are diagnosed annually in the United States, typically in people between 20 and 55 years of age. The most common type of thyroid cancer is DTC, which includes papillary and follicular carcinoma. Papillary carcinoma accounts for 80% of all thyroid cancers, and follicular carcinoma accounts for 10%.
The 5-year survival rate for all cases of DTC is 97%. Although the disease has a favorable prognosis, an estimated 1630 patients were expected to die of it in 2009 because of its prevalence.1
The goal: Find recurrent disease early
The purpose of surveillance protocols in thyroid cancer is early detection of recurrent disease. Expert debate about DTC surveillance centers on the disease’s low incidence and prolonged clinical course, as well as a lack of prospective randomized clinical trials. Current guidelines were developed from large retrospective cohort studies of patients observed over several decades.
rhTSH-stimulated Tg is the new surveillance standard
All major professional organizations support the consensus that an rhTSH-stimulated serum Tg is adequate to follow-up low-risk patients. This test replaces the previous accepted standard of thyroid hormone withdrawal (THW)-stimulated measurements. Moreover, rhTSH-stimulated serum Tg is comparable to a THW-stimulated measurement for detecting recurrent disease, when a cutoff value of 2 mcg/L is used.2
rhTSH testing has similar sensitivity to THW
A 2004 meta-analysis examined 46 studies with a total of 9094 patients. THW-stimulated Tg measurements after thyroid remnant ablation had a sensitivity of 96% (95% confidence interval [CI], 93.5%-98.7%) and a specificity of 94% (95% CI, 93.3%-96.1%). For rhTSH-stimulated serum Tg measurements, sensitivity and specificity were 92% (95% CI, 88.9%-96.1%) and 88% (95% CI, 85.4%-90.6%), respectively.
Because the difference in sensitivity between THW-stimulated and rhTSH-stimulated serum Tg isn’t statistically significant, rhTSH can be used for Tg testing without significantly decreasing detection of DTC recurrence. The slightly lower specificity of rhTSH may lead to unnecessary additional testing because of a few more false-positive results. However, this risk should be weighed against the benefits of reducing morbidity by avoiding the need to withhold thyroid hormone replacement therapy before testing.3
Thyroglobulin measurements: How they compare to body scanning
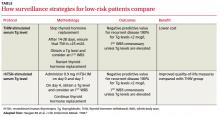
A 1999 prospective cohort study of 229 patients with DTC compared the accuracy of I131 whole body scanning with serum Tg measurement after both rhTSH and THW stimulation (TABLE). The results of the whole body scan were concordant with the rhTSH-stimulated and THW-stimulated Tg measurements in 89% of the patients (P=.108).
Using a cutoff value of ≥2 mcg/L for recurrent disease, an elevated Tg level was detected in 52% of patients with localized thyroid bed disease after rhTSH stimulation and in 56% of patients after THW stimulation. An elevated Tg level after rhTSH stimulation was found in 100% of patients with metastatic disease. Symptoms of hypothyroidism, including overall quality-of-life scores, were significantly better in the rhTSH group than the THW group (P<.01).4
rhTSH-stimulated Tg: Accuracy with a lower cost
A retrospective cohort study of 107 patients determined that rhTSH-stimulated serum Tg levels alone are sensitive enough to identify recurrent disease in low-risk patients. Levels greater than 2 mcg/L had a sensitivity and negative predictive value of 100% and a false-positive rate of 9%—a statistically and clinically significant improvement in accuracy over a whole body scan obtained after rhTSH stimulation, which had a sensitivity of only 27%, negative predictive value of 92%, and false-positive rate of 9% (P<.05). In low-risk patients, rhTSH-stimulated serum Tg measurement is the most accurate and least costly method of surveillance because of its high negative predictive value.5
Whole body scanning doesn’t enhance surveillance accuracy
This conclusion is supported by a cohort study that prospectively followed 99 patients with a history of DTC who underwent serum Tg measurement and an I131 whole body scan obtained after rhTSH stimulation and were followed by neck ultrasound 6 to 12 months after ablation treatment. The whole body scan was negative in 95% of the patients, with a sensitivity of 0%. Serum Tg was positive in 19 of these patients. Neck ultrasound confirmed positive lymph nodes in 7 patients, of whom 5 were Tg-positive. The I131 whole body scan added no benefit to the accuracy of surveillance.6
Recommendations
The British Thyroid Association and the American Thyroid Association recommend performing a physical examination with serum TSH, Tg, and antithyroglobulin antibodies at 6 and 12 months postablation, then annually if the patient is disease free.7,8
In low-risk patients, stimulated serum Tg measurement alone is an acceptable initial follow-up; a value of ≥2 mcg/L indicates a need for further evaluation. If serum Tg is undetectable under TSH stimulation, subsequent long-term follow-up by serum Tg levels alone while under TSH suppression is sufficient. TSH stimulation can be achieved by THW or rhTSH.7-9
A whole body scan rarely adds valuable additional information. Periodic neck ultrasound should be performed, however.7-9
Acknowledgement
The opinions and assertions contained herein are the private views of the authors and not to be construed as official or as reflecting the views of the US Air Force Medical Service or the US Air Force at large.
A recombinant human thyrotropin (rhTSH)-stimulated serum thyroglobulin (Tg) level alone is sufficient to monitor for recurrent disease in low-risk patients with a history of differentiated thyroid cancer (DTC) (strength of recommendation [SOR] A, meta-analysis). Low-risk patients are defined as patients who have undergone total thyroidectomy and radioactive iodine (I131) remnant ablation therapy and show no clinical evidence of recurrent disease.
Evidence summary
An estimated 37,340 new cases of thyroid cancer are diagnosed annually in the United States, typically in people between 20 and 55 years of age. The most common type of thyroid cancer is DTC, which includes papillary and follicular carcinoma. Papillary carcinoma accounts for 80% of all thyroid cancers, and follicular carcinoma accounts for 10%.
The 5-year survival rate for all cases of DTC is 97%. Although the disease has a favorable prognosis, an estimated 1630 patients were expected to die of it in 2009 because of its prevalence.1
The goal: Find recurrent disease early
The purpose of surveillance protocols in thyroid cancer is early detection of recurrent disease. Expert debate about DTC surveillance centers on the disease’s low incidence and prolonged clinical course, as well as a lack of prospective randomized clinical trials. Current guidelines were developed from large retrospective cohort studies of patients observed over several decades.
rhTSH-stimulated Tg is the new surveillance standard
All major professional organizations support the consensus that an rhTSH-stimulated serum Tg is adequate to follow-up low-risk patients. This test replaces the previous accepted standard of thyroid hormone withdrawal (THW)-stimulated measurements. Moreover, rhTSH-stimulated serum Tg is comparable to a THW-stimulated measurement for detecting recurrent disease, when a cutoff value of 2 mcg/L is used.2
rhTSH testing has similar sensitivity to THW
A 2004 meta-analysis examined 46 studies with a total of 9094 patients. THW-stimulated Tg measurements after thyroid remnant ablation had a sensitivity of 96% (95% confidence interval [CI], 93.5%-98.7%) and a specificity of 94% (95% CI, 93.3%-96.1%). For rhTSH-stimulated serum Tg measurements, sensitivity and specificity were 92% (95% CI, 88.9%-96.1%) and 88% (95% CI, 85.4%-90.6%), respectively.
Because the difference in sensitivity between THW-stimulated and rhTSH-stimulated serum Tg isn’t statistically significant, rhTSH can be used for Tg testing without significantly decreasing detection of DTC recurrence. The slightly lower specificity of rhTSH may lead to unnecessary additional testing because of a few more false-positive results. However, this risk should be weighed against the benefits of reducing morbidity by avoiding the need to withhold thyroid hormone replacement therapy before testing.3
Thyroglobulin measurements: How they compare to body scanning
A 1999 prospective cohort study of 229 patients with DTC compared the accuracy of I131 whole body scanning with serum Tg measurement after both rhTSH and THW stimulation (TABLE). The results of the whole body scan were concordant with the rhTSH-stimulated and THW-stimulated Tg measurements in 89% of the patients (P=.108).
Using a cutoff value of ≥2 mcg/L for recurrent disease, an elevated Tg level was detected in 52% of patients with localized thyroid bed disease after rhTSH stimulation and in 56% of patients after THW stimulation. An elevated Tg level after rhTSH stimulation was found in 100% of patients with metastatic disease. Symptoms of hypothyroidism, including overall quality-of-life scores, were significantly better in the rhTSH group than the THW group (P<.01).4
rhTSH-stimulated Tg: Accuracy with a lower cost
A retrospective cohort study of 107 patients determined that rhTSH-stimulated serum Tg levels alone are sensitive enough to identify recurrent disease in low-risk patients. Levels greater than 2 mcg/L had a sensitivity and negative predictive value of 100% and a false-positive rate of 9%—a statistically and clinically significant improvement in accuracy over a whole body scan obtained after rhTSH stimulation, which had a sensitivity of only 27%, negative predictive value of 92%, and false-positive rate of 9% (P<.05). In low-risk patients, rhTSH-stimulated serum Tg measurement is the most accurate and least costly method of surveillance because of its high negative predictive value.5
Whole body scanning doesn’t enhance surveillance accuracy
This conclusion is supported by a cohort study that prospectively followed 99 patients with a history of DTC who underwent serum Tg measurement and an I131 whole body scan obtained after rhTSH stimulation and were followed by neck ultrasound 6 to 12 months after ablation treatment. The whole body scan was negative in 95% of the patients, with a sensitivity of 0%. Serum Tg was positive in 19 of these patients. Neck ultrasound confirmed positive lymph nodes in 7 patients, of whom 5 were Tg-positive. The I131 whole body scan added no benefit to the accuracy of surveillance.6
Recommendations
The British Thyroid Association and the American Thyroid Association recommend performing a physical examination with serum TSH, Tg, and antithyroglobulin antibodies at 6 and 12 months postablation, then annually if the patient is disease free.7,8
In low-risk patients, stimulated serum Tg measurement alone is an acceptable initial follow-up; a value of ≥2 mcg/L indicates a need for further evaluation. If serum Tg is undetectable under TSH stimulation, subsequent long-term follow-up by serum Tg levels alone while under TSH suppression is sufficient. TSH stimulation can be achieved by THW or rhTSH.7-9
A whole body scan rarely adds valuable additional information. Periodic neck ultrasound should be performed, however.7-9
Acknowledgement
The opinions and assertions contained herein are the private views of the authors and not to be construed as official or as reflecting the views of the US Air Force Medical Service or the US Air Force at large.
A recombinant human thyrotropin (rhTSH)-stimulated serum thyroglobulin (Tg) level alone is sufficient to monitor for recurrent disease in low-risk patients with a history of differentiated thyroid cancer (DTC) (strength of recommendation [SOR] A, meta-analysis). Low-risk patients are defined as patients who have undergone total thyroidectomy and radioactive iodine (I131) remnant ablation therapy and show no clinical evidence of recurrent disease.
Evidence summary
An estimated 37,340 new cases of thyroid cancer are diagnosed annually in the United States, typically in people between 20 and 55 years of age. The most common type of thyroid cancer is DTC, which includes papillary and follicular carcinoma. Papillary carcinoma accounts for 80% of all thyroid cancers, and follicular carcinoma accounts for 10%.
The 5-year survival rate for all cases of DTC is 97%. Although the disease has a favorable prognosis, an estimated 1630 patients were expected to die of it in 2009 because of its prevalence.1
The goal: Find recurrent disease early
The purpose of surveillance protocols in thyroid cancer is early detection of recurrent disease. Expert debate about DTC surveillance centers on the disease’s low incidence and prolonged clinical course, as well as a lack of prospective randomized clinical trials. Current guidelines were developed from large retrospective cohort studies of patients observed over several decades.
rhTSH-stimulated Tg is the new surveillance standard
All major professional organizations support the consensus that an rhTSH-stimulated serum Tg is adequate to follow-up low-risk patients. This test replaces the previous accepted standard of thyroid hormone withdrawal (THW)-stimulated measurements. Moreover, rhTSH-stimulated serum Tg is comparable to a THW-stimulated measurement for detecting recurrent disease, when a cutoff value of 2 mcg/L is used.2
rhTSH testing has similar sensitivity to THW
A 2004 meta-analysis examined 46 studies with a total of 9094 patients. THW-stimulated Tg measurements after thyroid remnant ablation had a sensitivity of 96% (95% confidence interval [CI], 93.5%-98.7%) and a specificity of 94% (95% CI, 93.3%-96.1%). For rhTSH-stimulated serum Tg measurements, sensitivity and specificity were 92% (95% CI, 88.9%-96.1%) and 88% (95% CI, 85.4%-90.6%), respectively.
Because the difference in sensitivity between THW-stimulated and rhTSH-stimulated serum Tg isn’t statistically significant, rhTSH can be used for Tg testing without significantly decreasing detection of DTC recurrence. The slightly lower specificity of rhTSH may lead to unnecessary additional testing because of a few more false-positive results. However, this risk should be weighed against the benefits of reducing morbidity by avoiding the need to withhold thyroid hormone replacement therapy before testing.3
Thyroglobulin measurements: How they compare to body scanning
A 1999 prospective cohort study of 229 patients with DTC compared the accuracy of I131 whole body scanning with serum Tg measurement after both rhTSH and THW stimulation (TABLE). The results of the whole body scan were concordant with the rhTSH-stimulated and THW-stimulated Tg measurements in 89% of the patients (P=.108).
Using a cutoff value of ≥2 mcg/L for recurrent disease, an elevated Tg level was detected in 52% of patients with localized thyroid bed disease after rhTSH stimulation and in 56% of patients after THW stimulation. An elevated Tg level after rhTSH stimulation was found in 100% of patients with metastatic disease. Symptoms of hypothyroidism, including overall quality-of-life scores, were significantly better in the rhTSH group than the THW group (P<.01).4
rhTSH-stimulated Tg: Accuracy with a lower cost
A retrospective cohort study of 107 patients determined that rhTSH-stimulated serum Tg levels alone are sensitive enough to identify recurrent disease in low-risk patients. Levels greater than 2 mcg/L had a sensitivity and negative predictive value of 100% and a false-positive rate of 9%—a statistically and clinically significant improvement in accuracy over a whole body scan obtained after rhTSH stimulation, which had a sensitivity of only 27%, negative predictive value of 92%, and false-positive rate of 9% (P<.05). In low-risk patients, rhTSH-stimulated serum Tg measurement is the most accurate and least costly method of surveillance because of its high negative predictive value.5
Whole body scanning doesn’t enhance surveillance accuracy
This conclusion is supported by a cohort study that prospectively followed 99 patients with a history of DTC who underwent serum Tg measurement and an I131 whole body scan obtained after rhTSH stimulation and were followed by neck ultrasound 6 to 12 months after ablation treatment. The whole body scan was negative in 95% of the patients, with a sensitivity of 0%. Serum Tg was positive in 19 of these patients. Neck ultrasound confirmed positive lymph nodes in 7 patients, of whom 5 were Tg-positive. The I131 whole body scan added no benefit to the accuracy of surveillance.6
Recommendations
The British Thyroid Association and the American Thyroid Association recommend performing a physical examination with serum TSH, Tg, and antithyroglobulin antibodies at 6 and 12 months postablation, then annually if the patient is disease free.7,8
In low-risk patients, stimulated serum Tg measurement alone is an acceptable initial follow-up; a value of ≥2 mcg/L indicates a need for further evaluation. If serum Tg is undetectable under TSH stimulation, subsequent long-term follow-up by serum Tg levels alone while under TSH suppression is sufficient. TSH stimulation can be achieved by THW or rhTSH.7-9
A whole body scan rarely adds valuable additional information. Periodic neck ultrasound should be performed, however.7-9
Acknowledgement
The opinions and assertions contained herein are the private views of the authors and not to be construed as official or as reflecting the views of the US Air Force Medical Service or the US Air Force at large.
Evidence-based answers from the Family Physicians Inquiries Network
What does the evidence tell us about treating very-high-risk patients to an LDL
Not much. No studies directly compare low-density lipoprotein (LDL) levels <70 mg/dL to levels of 71 to 100 mg/dL in very-high-risk patients. However, no evidence suggests a "floor" for LDL cholesterol levels beyond which further reductions of heart disease risk can’t be achieved (strength of recommendation [SOR]: A, systematic reviews of randomized controlled trials [RCTs]). The target LDL cholesterol of <70 mg/dL is based on data extrapolated from RCTs (SOR: B).
Comparing larger (80 mg) with smaller doses of atorvastatin shows that larger doses reduce LDL and major cardiac events more than smaller doses. No studies report patient-oriented outcomes of treatments for patients who fail to reach target LDL levels <100 mg/dL.
Clinical Commentary
Treatment benefits—and potential barriers
As this review demonstrates, patients at very high risk of coronary artery disease may derive benefit from lowering LDL cholesterol to <70 mg/dL. Attempting to reach this goal for such patients seems to be a “no-brainer.” In reality, however, several possible barriers to treatment exist, including:
- The goal may be unachievable, even with the highest dose of statins, combination therapy, and lifestyle changes.
- The risk of myopathy (which is rare) or adverse side effects (less rare) is proportional to the statin dose and may prevent certain patients from achieving the goal.
- For most statins, cost increases with dosage.
- For patients with multiple comorbidities, the incremental health benefit of intensive LDL lowering may not be significant.
As with any medical intervention, you should explain all risks and benefits to the patient, who should participate actively in the decision to pursue the goal of intensively lowering LDL cholesterol.
Wail Malaty, MD
Mountain Area Health Education Center Family Practice
Rural Residency, University of North Carolina School of
Medicine, Hendersonville
Evidence summary
The National Cholesterol Education Program’s definition of “very high risk” for coronary heart disease (CHD) encompasses established CHD and CHD equivalents, including diabetes, peripheral arterial disease, abdominal aortic aneurysm, symptomatic carotid artery disease, and multiple cardiac risk factors that confer a 10-year calculated cardiac risk greater than 20%.1
Statin dosage: Bigger is better
The Treating to New Targets (TNT) study showed that in patients with stable CHD, intensive lipid lowering with atorvastatin 80 mg daily delivered significant clinical benefit beyond that provided by atorvastatin 10 mg daily.2 The mean LDL achieved in TNT was 77 mg/dL on 80 mg atorvastatin, compared with 101 mg/dL on 10 mg.
Patients with diabetes who took 80 mg had a 2.26% absolute risk reduction for major cardiovascular events (number needed to treat=43). Secondary outcomes—including all cardiovascular events, cerebrovascular events, and congestive heart failure with hospitalization—also improved on 80 mg atorvastatin.
Although this study enrolled a total of 10,001 patients with clinically evident CHD, it was not sufficiently powered to demonstrate differences in overall mortality between the 2 groups. While it is clear that patients in the 80-mg group had better outcomes than patients in the lower-dose group, the exact role of LDL lowering cannot be easily separated from other potentially beneficial effects of the higher dose of atorvastatin.
How low should LDL go? What the studies show
In the Heart Protection Study, patients with CHD, other occlusive arterial disease, or diabetes were randomized to 40 mg simvastatin or placebo.3 Simvastatin reduced relative risk of CHD—regardless of baseline LDL—even in patients with a baseline LDL <116 mg/dL.
Further analysis showed that among the many types of high-risk patients, 5 years of simvastatin at 40 mg daily would prevent about 70 to 100 people in 1000 from suffering at least 1 major vascular event (myocardial infarction, stroke, or the need for revascularization). Interestingly, patients with relatively smaller reductions in LDL (those in the lowest third) showed the same decrease in CHD events as patients in the highest third—although the overall difference in LDL wasn’t large.
A meta-analysis of these and other studies concluded that intensive lipid lowering with high-dose statin therapy confers a significant benefit over standard-dose therapy for preventing predominantly nonfatal cardiovascular events.4 The safety and tolerability of higher and standard statin doses are similar.2 Two additional meta-analyses supported the use of intensive statin regimens to reduce cardiovascular risk, but didn’t find evidence for lowering LDL to a particular target level.5,6
Meta-analysis: The lower the LDL, the lower the risk of CHD
The ENHANCE study, a double-blind, randomized trial conducted over a period of 24 months, compared the effects of 80 mg per day of simvastatin with either placebo or 10 mg per day of ezetimibe in 720 patients with familial hypercholesterolemia. The primary outcome measure was a change in intimamedia thickness of the walls of the carotid and femoral arteries. The results of the study have raised the question of whether it is appropriate to target LDL cholesterol primarily to reduce CHD risk, because ezetimibe did not affect carotid artery intima-media thickness, despite its effectiveness in reducing LDL cholesterol.7
However, an earlier 19-trial metaregression analysis (81,859 patients with stable CHD) demonstrated that each 1% reduction in LDL cholesterol corresponded to a 1% decrease in risk for CHD. This result held true regardless of different approaches to treatment, which included diet, bile-acid sequestrant, statins, or ileal bypass surgery.8
Recommendations
The Adult Treatment Panel (ATP) III guidelines recommend an LDL level <100 mg/dL for high-risk patients (CHD or a CHD risk equivalent).9 An update to the ATP III guidelines states that the LDL goal of <100 mg/dL was as low as could be supported by clinical trial evidence at the time of publication and was also the practical limit of LDL reduction that could be achieved with standard treatment in most high-risk patients.1 The ATP III update offers the option of treating high-risk patients to a target LDL <70 mg/dL and clarifies that recent trials have shown no significant side effects associated with very low LDL levels.
Recent American Diabetes Association guidelines state that the LDL target should be <100 mg/dL in patients with diabetes, with the option of treating patients with both overt CHD and diabetes to an LDL of <70 mg/dL.10
1. Grundy SM, Cleeman JI, Merz CNB, et al. Implications of recent clinical trials for the National Cholesterol Education Program Adult Treatment Panel III Guidelines. Circulation. 2004;110:227-239.
2. LaRosa JC, Grundy SM, Waters DD, et al. Intensive lipid lowering with atorvastatin in patients with stable coronary disease. N Engl J Med. 2005;352:1425-1435.
3. Heart Protection Study Collaborative Group. MRC/BHF Heart protection study of cholesterol lowering with simvastatin in 20,536 high-risk individuals: a randomised placebo-controlled trial. Lancet. 2002;360:7-22.
4. Cannon CP, Steinberg BA, Murphy SA, et al. Meta-analysis of cardiovascular outcomes trials comparing intensive versus moderate statin therapy. J Am Coll Cardiol. 2006;48:438-445.
5. Hayward RA, Hofer TP, Vijan, S. Narrative review: lack of evidence for recommended low-density lipoprotein treatment targets: a solvable problem. Ann Intern Med. 2006;145:520-530.
6. Kiranbir J, Majumdar SR, McAlister FA. The efficacy and safety of intensive statin therapy: a meta-analysis of randomized trials. CMAJ. 2008;178:576-584.
7. Kasselstein JJ, Akdim F, Stroes ES, et al. Simvastatin with or without ezetimibe in familial hypercholesterolemia. N Engl J Med. 2008;358:1431-1443.
8. Robinson JG, Smith B, Maheshwari N, et al. Pleiotropic effects of statins: benefit beyond cholesterol reduction? A meta-regression analysis. J Am Coll Cardiol. 2005;46:1855-1862.
9. National Cholesterol Education Program Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults. Third report of the National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III). Circulation. 2002;106:3143-3421.
10. American Diabetes Association. Executive summary: standards of medical care in diabetes care—2008. Diabetes Care. 2008;31(suppl 1):S5-S11.
Not much. No studies directly compare low-density lipoprotein (LDL) levels <70 mg/dL to levels of 71 to 100 mg/dL in very-high-risk patients. However, no evidence suggests a "floor" for LDL cholesterol levels beyond which further reductions of heart disease risk can’t be achieved (strength of recommendation [SOR]: A, systematic reviews of randomized controlled trials [RCTs]). The target LDL cholesterol of <70 mg/dL is based on data extrapolated from RCTs (SOR: B).
Comparing larger (80 mg) with smaller doses of atorvastatin shows that larger doses reduce LDL and major cardiac events more than smaller doses. No studies report patient-oriented outcomes of treatments for patients who fail to reach target LDL levels <100 mg/dL.
Clinical Commentary
Treatment benefits—and potential barriers
As this review demonstrates, patients at very high risk of coronary artery disease may derive benefit from lowering LDL cholesterol to <70 mg/dL. Attempting to reach this goal for such patients seems to be a “no-brainer.” In reality, however, several possible barriers to treatment exist, including:
- The goal may be unachievable, even with the highest dose of statins, combination therapy, and lifestyle changes.
- The risk of myopathy (which is rare) or adverse side effects (less rare) is proportional to the statin dose and may prevent certain patients from achieving the goal.
- For most statins, cost increases with dosage.
- For patients with multiple comorbidities, the incremental health benefit of intensive LDL lowering may not be significant.
As with any medical intervention, you should explain all risks and benefits to the patient, who should participate actively in the decision to pursue the goal of intensively lowering LDL cholesterol.
Wail Malaty, MD
Mountain Area Health Education Center Family Practice
Rural Residency, University of North Carolina School of
Medicine, Hendersonville
Evidence summary
The National Cholesterol Education Program’s definition of “very high risk” for coronary heart disease (CHD) encompasses established CHD and CHD equivalents, including diabetes, peripheral arterial disease, abdominal aortic aneurysm, symptomatic carotid artery disease, and multiple cardiac risk factors that confer a 10-year calculated cardiac risk greater than 20%.1
Statin dosage: Bigger is better
The Treating to New Targets (TNT) study showed that in patients with stable CHD, intensive lipid lowering with atorvastatin 80 mg daily delivered significant clinical benefit beyond that provided by atorvastatin 10 mg daily.2 The mean LDL achieved in TNT was 77 mg/dL on 80 mg atorvastatin, compared with 101 mg/dL on 10 mg.
Patients with diabetes who took 80 mg had a 2.26% absolute risk reduction for major cardiovascular events (number needed to treat=43). Secondary outcomes—including all cardiovascular events, cerebrovascular events, and congestive heart failure with hospitalization—also improved on 80 mg atorvastatin.
Although this study enrolled a total of 10,001 patients with clinically evident CHD, it was not sufficiently powered to demonstrate differences in overall mortality between the 2 groups. While it is clear that patients in the 80-mg group had better outcomes than patients in the lower-dose group, the exact role of LDL lowering cannot be easily separated from other potentially beneficial effects of the higher dose of atorvastatin.
How low should LDL go? What the studies show
In the Heart Protection Study, patients with CHD, other occlusive arterial disease, or diabetes were randomized to 40 mg simvastatin or placebo.3 Simvastatin reduced relative risk of CHD—regardless of baseline LDL—even in patients with a baseline LDL <116 mg/dL.
Further analysis showed that among the many types of high-risk patients, 5 years of simvastatin at 40 mg daily would prevent about 70 to 100 people in 1000 from suffering at least 1 major vascular event (myocardial infarction, stroke, or the need for revascularization). Interestingly, patients with relatively smaller reductions in LDL (those in the lowest third) showed the same decrease in CHD events as patients in the highest third—although the overall difference in LDL wasn’t large.
A meta-analysis of these and other studies concluded that intensive lipid lowering with high-dose statin therapy confers a significant benefit over standard-dose therapy for preventing predominantly nonfatal cardiovascular events.4 The safety and tolerability of higher and standard statin doses are similar.2 Two additional meta-analyses supported the use of intensive statin regimens to reduce cardiovascular risk, but didn’t find evidence for lowering LDL to a particular target level.5,6
Meta-analysis: The lower the LDL, the lower the risk of CHD
The ENHANCE study, a double-blind, randomized trial conducted over a period of 24 months, compared the effects of 80 mg per day of simvastatin with either placebo or 10 mg per day of ezetimibe in 720 patients with familial hypercholesterolemia. The primary outcome measure was a change in intimamedia thickness of the walls of the carotid and femoral arteries. The results of the study have raised the question of whether it is appropriate to target LDL cholesterol primarily to reduce CHD risk, because ezetimibe did not affect carotid artery intima-media thickness, despite its effectiveness in reducing LDL cholesterol.7
However, an earlier 19-trial metaregression analysis (81,859 patients with stable CHD) demonstrated that each 1% reduction in LDL cholesterol corresponded to a 1% decrease in risk for CHD. This result held true regardless of different approaches to treatment, which included diet, bile-acid sequestrant, statins, or ileal bypass surgery.8
Recommendations
The Adult Treatment Panel (ATP) III guidelines recommend an LDL level <100 mg/dL for high-risk patients (CHD or a CHD risk equivalent).9 An update to the ATP III guidelines states that the LDL goal of <100 mg/dL was as low as could be supported by clinical trial evidence at the time of publication and was also the practical limit of LDL reduction that could be achieved with standard treatment in most high-risk patients.1 The ATP III update offers the option of treating high-risk patients to a target LDL <70 mg/dL and clarifies that recent trials have shown no significant side effects associated with very low LDL levels.
Recent American Diabetes Association guidelines state that the LDL target should be <100 mg/dL in patients with diabetes, with the option of treating patients with both overt CHD and diabetes to an LDL of <70 mg/dL.10
Not much. No studies directly compare low-density lipoprotein (LDL) levels <70 mg/dL to levels of 71 to 100 mg/dL in very-high-risk patients. However, no evidence suggests a "floor" for LDL cholesterol levels beyond which further reductions of heart disease risk can’t be achieved (strength of recommendation [SOR]: A, systematic reviews of randomized controlled trials [RCTs]). The target LDL cholesterol of <70 mg/dL is based on data extrapolated from RCTs (SOR: B).
Comparing larger (80 mg) with smaller doses of atorvastatin shows that larger doses reduce LDL and major cardiac events more than smaller doses. No studies report patient-oriented outcomes of treatments for patients who fail to reach target LDL levels <100 mg/dL.
Clinical Commentary
Treatment benefits—and potential barriers
As this review demonstrates, patients at very high risk of coronary artery disease may derive benefit from lowering LDL cholesterol to <70 mg/dL. Attempting to reach this goal for such patients seems to be a “no-brainer.” In reality, however, several possible barriers to treatment exist, including:
- The goal may be unachievable, even with the highest dose of statins, combination therapy, and lifestyle changes.
- The risk of myopathy (which is rare) or adverse side effects (less rare) is proportional to the statin dose and may prevent certain patients from achieving the goal.
- For most statins, cost increases with dosage.
- For patients with multiple comorbidities, the incremental health benefit of intensive LDL lowering may not be significant.
As with any medical intervention, you should explain all risks and benefits to the patient, who should participate actively in the decision to pursue the goal of intensively lowering LDL cholesterol.
Wail Malaty, MD
Mountain Area Health Education Center Family Practice
Rural Residency, University of North Carolina School of
Medicine, Hendersonville
Evidence summary
The National Cholesterol Education Program’s definition of “very high risk” for coronary heart disease (CHD) encompasses established CHD and CHD equivalents, including diabetes, peripheral arterial disease, abdominal aortic aneurysm, symptomatic carotid artery disease, and multiple cardiac risk factors that confer a 10-year calculated cardiac risk greater than 20%.1
Statin dosage: Bigger is better
The Treating to New Targets (TNT) study showed that in patients with stable CHD, intensive lipid lowering with atorvastatin 80 mg daily delivered significant clinical benefit beyond that provided by atorvastatin 10 mg daily.2 The mean LDL achieved in TNT was 77 mg/dL on 80 mg atorvastatin, compared with 101 mg/dL on 10 mg.
Patients with diabetes who took 80 mg had a 2.26% absolute risk reduction for major cardiovascular events (number needed to treat=43). Secondary outcomes—including all cardiovascular events, cerebrovascular events, and congestive heart failure with hospitalization—also improved on 80 mg atorvastatin.
Although this study enrolled a total of 10,001 patients with clinically evident CHD, it was not sufficiently powered to demonstrate differences in overall mortality between the 2 groups. While it is clear that patients in the 80-mg group had better outcomes than patients in the lower-dose group, the exact role of LDL lowering cannot be easily separated from other potentially beneficial effects of the higher dose of atorvastatin.
How low should LDL go? What the studies show
In the Heart Protection Study, patients with CHD, other occlusive arterial disease, or diabetes were randomized to 40 mg simvastatin or placebo.3 Simvastatin reduced relative risk of CHD—regardless of baseline LDL—even in patients with a baseline LDL <116 mg/dL.
Further analysis showed that among the many types of high-risk patients, 5 years of simvastatin at 40 mg daily would prevent about 70 to 100 people in 1000 from suffering at least 1 major vascular event (myocardial infarction, stroke, or the need for revascularization). Interestingly, patients with relatively smaller reductions in LDL (those in the lowest third) showed the same decrease in CHD events as patients in the highest third—although the overall difference in LDL wasn’t large.
A meta-analysis of these and other studies concluded that intensive lipid lowering with high-dose statin therapy confers a significant benefit over standard-dose therapy for preventing predominantly nonfatal cardiovascular events.4 The safety and tolerability of higher and standard statin doses are similar.2 Two additional meta-analyses supported the use of intensive statin regimens to reduce cardiovascular risk, but didn’t find evidence for lowering LDL to a particular target level.5,6
Meta-analysis: The lower the LDL, the lower the risk of CHD
The ENHANCE study, a double-blind, randomized trial conducted over a period of 24 months, compared the effects of 80 mg per day of simvastatin with either placebo or 10 mg per day of ezetimibe in 720 patients with familial hypercholesterolemia. The primary outcome measure was a change in intimamedia thickness of the walls of the carotid and femoral arteries. The results of the study have raised the question of whether it is appropriate to target LDL cholesterol primarily to reduce CHD risk, because ezetimibe did not affect carotid artery intima-media thickness, despite its effectiveness in reducing LDL cholesterol.7
However, an earlier 19-trial metaregression analysis (81,859 patients with stable CHD) demonstrated that each 1% reduction in LDL cholesterol corresponded to a 1% decrease in risk for CHD. This result held true regardless of different approaches to treatment, which included diet, bile-acid sequestrant, statins, or ileal bypass surgery.8
Recommendations
The Adult Treatment Panel (ATP) III guidelines recommend an LDL level <100 mg/dL for high-risk patients (CHD or a CHD risk equivalent).9 An update to the ATP III guidelines states that the LDL goal of <100 mg/dL was as low as could be supported by clinical trial evidence at the time of publication and was also the practical limit of LDL reduction that could be achieved with standard treatment in most high-risk patients.1 The ATP III update offers the option of treating high-risk patients to a target LDL <70 mg/dL and clarifies that recent trials have shown no significant side effects associated with very low LDL levels.
Recent American Diabetes Association guidelines state that the LDL target should be <100 mg/dL in patients with diabetes, with the option of treating patients with both overt CHD and diabetes to an LDL of <70 mg/dL.10
1. Grundy SM, Cleeman JI, Merz CNB, et al. Implications of recent clinical trials for the National Cholesterol Education Program Adult Treatment Panel III Guidelines. Circulation. 2004;110:227-239.
2. LaRosa JC, Grundy SM, Waters DD, et al. Intensive lipid lowering with atorvastatin in patients with stable coronary disease. N Engl J Med. 2005;352:1425-1435.
3. Heart Protection Study Collaborative Group. MRC/BHF Heart protection study of cholesterol lowering with simvastatin in 20,536 high-risk individuals: a randomised placebo-controlled trial. Lancet. 2002;360:7-22.
4. Cannon CP, Steinberg BA, Murphy SA, et al. Meta-analysis of cardiovascular outcomes trials comparing intensive versus moderate statin therapy. J Am Coll Cardiol. 2006;48:438-445.
5. Hayward RA, Hofer TP, Vijan, S. Narrative review: lack of evidence for recommended low-density lipoprotein treatment targets: a solvable problem. Ann Intern Med. 2006;145:520-530.
6. Kiranbir J, Majumdar SR, McAlister FA. The efficacy and safety of intensive statin therapy: a meta-analysis of randomized trials. CMAJ. 2008;178:576-584.
7. Kasselstein JJ, Akdim F, Stroes ES, et al. Simvastatin with or without ezetimibe in familial hypercholesterolemia. N Engl J Med. 2008;358:1431-1443.
8. Robinson JG, Smith B, Maheshwari N, et al. Pleiotropic effects of statins: benefit beyond cholesterol reduction? A meta-regression analysis. J Am Coll Cardiol. 2005;46:1855-1862.
9. National Cholesterol Education Program Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults. Third report of the National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III). Circulation. 2002;106:3143-3421.
10. American Diabetes Association. Executive summary: standards of medical care in diabetes care—2008. Diabetes Care. 2008;31(suppl 1):S5-S11.
1. Grundy SM, Cleeman JI, Merz CNB, et al. Implications of recent clinical trials for the National Cholesterol Education Program Adult Treatment Panel III Guidelines. Circulation. 2004;110:227-239.
2. LaRosa JC, Grundy SM, Waters DD, et al. Intensive lipid lowering with atorvastatin in patients with stable coronary disease. N Engl J Med. 2005;352:1425-1435.
3. Heart Protection Study Collaborative Group. MRC/BHF Heart protection study of cholesterol lowering with simvastatin in 20,536 high-risk individuals: a randomised placebo-controlled trial. Lancet. 2002;360:7-22.
4. Cannon CP, Steinberg BA, Murphy SA, et al. Meta-analysis of cardiovascular outcomes trials comparing intensive versus moderate statin therapy. J Am Coll Cardiol. 2006;48:438-445.
5. Hayward RA, Hofer TP, Vijan, S. Narrative review: lack of evidence for recommended low-density lipoprotein treatment targets: a solvable problem. Ann Intern Med. 2006;145:520-530.
6. Kiranbir J, Majumdar SR, McAlister FA. The efficacy and safety of intensive statin therapy: a meta-analysis of randomized trials. CMAJ. 2008;178:576-584.
7. Kasselstein JJ, Akdim F, Stroes ES, et al. Simvastatin with or without ezetimibe in familial hypercholesterolemia. N Engl J Med. 2008;358:1431-1443.
8. Robinson JG, Smith B, Maheshwari N, et al. Pleiotropic effects of statins: benefit beyond cholesterol reduction? A meta-regression analysis. J Am Coll Cardiol. 2005;46:1855-1862.
9. National Cholesterol Education Program Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults. Third report of the National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III). Circulation. 2002;106:3143-3421.
10. American Diabetes Association. Executive summary: standards of medical care in diabetes care—2008. Diabetes Care. 2008;31(suppl 1):S5-S11.
Evidence-based answers from the Family Physicians Inquiries Network
Which strategies work best to prevent obesity in adults?
A/PHYSICAL ACTIVITY AND DIETARY MODIFICATION WORK BEST. Family involvement, regular weight monitoring, and behavior modification also can help.
Regular physical activity decreases long-term weight gain (strength of recommendation [SOR]: B, 2 high-quality, randomized controlled trials [RCTs]). Decreasing fat intake (SOR: B, 1 high-quality systematic review) and increasing fruit and vegetable consumption (SOR: B, 1 high-quality RCT) also may decrease weight gain. Combined dietary and physical activity interventions prevent weight gain (SOR: B, 1 high-quality systematic review).
Family involvement helps maintain weight (SOR:B, 2 small RCTs). Daily or weekly weight monitoring reduces long-term weight gain (SOR:B, 2 RCTs).
Clinic-based, direct-contact, and Web-based programs that include behavior modification may reduce weight gain in adults (SOR: C, 3 RCTs). Behavior modification delivered by personal contact is more effective than mail, Internet, or self-directed modification programs (SOR:B, 2 RCTs).
Evidence summary
A recent systematic review of obesity prevention studies found 9 RCTs demonstrating that dietary and physical activity interventions can prevent weight gain, but lacking sufficient evidence to recommend a specific type of program.1
A systematic review of the effects of physical activity on weight reduction and maintenance analyzed 46 studies, including 8 RCTs that investigated interventions to reduce weight and 3 that examined measures to maintain it.2 More than 80% of the studies showed a benefit from physical exercise. Prevention of weight gain appears to be dose-dependent. More exercise leads to less weight gain; a minimum of 1.5 hours per week of moderate exercise is needed to prevent weight gain.2
Less fat, more vegetables spur weight loss
The Women’s Health Initiative studied 46,808 postmenopausal women between 50 and 79 years of age who were randomly assigned to an intervention or control group.3 The intervention group received intensive group and individual counseling from dieticians aimed at reducing fat intake to 20%, increasing consumption of vegetables and fruits to 5 or more servings per day, and increasing consumption of grains to 6 or more servings per day. The control group received dietary education materials. Neither group had weight loss or calorie restriction goals or differences in physical activity.
The intervention group had a mean decrease in weight 1.9 kg greater than the controls at 1 year (P<.001) and 0.4 kg at 7.5 years (P<.01). Weight loss was greater in women who consumed more fruits and vegetables and greatest among women who decreased energy intake from fat.
A family-based intervention lowers BMI in females
A family-based trial of weight gain prevention randomized 82 families to a group that was encouraged to eat 2 servings of cereal a day and increase activity by 2000 steps a day, or to a control group.4 In the intervention group, body mass index (BMI) decreased by 0.4% in mothers (P=.027), and BMI percentage for age decreased by 2.6% in daughters (P<.01). Male family members showed no significant differences, however.
Family ties, self-weighing improve weight control
A systematic review of family-spouse involvement in weight control and weight loss found that involving spouses tended to improve the effectiveness of weight control.5
Two studies, 1 an RCT, found an association between self-weighing and preventing weight gain.6,7 Patients who weighed themselves daily or weekly were less likely to gain weight than patients who weighed themselves monthly, yearly, or never.
Getting personal helps modify behavior
Three RCTs compared clinic-based, Web-based, and self-directed advice and counseling to prevent weight gain (2 studies) and maintain weight loss (1 study). In the first study, 67 patients were assigned to 4 months of clinic-based or home-based counseling to increase exercise and reduce fat intake, or to a control group.8 Weight change was–1.9 kg in the clinic-based group,–1.3 kg in the home-based group, and +0.22 kg in the control group (P=.007).
In the second study, 1032 overweight or obese adults with hypertension and/or dyslipidemia who completed a weight-loss program were randomly assigned to receive monthly personal contact, unlimited access to a Web-based intervention, or a self-directed control group.9 At 30 months, participants in the personal contact group had regained less weight than the Web-based or control groups (4.0, 5.1, and 5.5 kg, respectively; P<.01).
A third RCT randomized 284 healthy 25- to 44-year-old women with BMI <30 kg/m2 to group meetings, lessons by mail, or a control group that received an information booklet. The study found no significant difference among the 3 groups in weight maintenance at a 3-year follow-up; 40% maintained weight, and 60% gained more than 2 pounds.10
Recommendations
Wide consensus supports screening by either BMI or height and weight. The US Preventive Services Task Force (USPSTF) recommends intensive counseling for everyone with a BMI ≥30 kg/m2 coupled with behavioral modification to promote sustained weight loss.11 The USPSTF found insufficient evidence to support less intensive counseling for obese patients or counseling of any intensity for overweight patients.
The Canadian Task Force on Preventive Health Care found insufficient evidence to recommend for or against BMI measurement during routine health evaluations of the general population.12
The American Diabetes Association13 and the American College of Preventive Medicine14 recommend counseling and behavior modification for all adults to prevent obesity.
1. Lemmens VE, Oenema A, Klepp KI, et al. A systematic review of the evidence regarding efficacy of obesity prevention interventions among adults. Obes Rev. 2008;9:446-455.
2. Fogelholm M, Kukkonen-Harjula K. Does physical activity prevent weight gain—a systematic review. Obes Rev. 2000;1:95-111.
3. Howard BV, Manson JE, Stefanick ML, et al. Low-fat dietary pattern and weight change over 7 years: the Women’s Health Initiative Dietary Modification Trial. JAMA. 2006;295:39-49.
4. Rodearmel SJ, Wyatt HR, Barry MJ, et al. A family-based approach to preventing excessive weight gain. Obesity (Silver Spring). 2006;14:1392-1401.
5. McLean N, Griffin S, Toney K, et al. Family involvement in weight control, weight maintenance and weight-loss interventions: a systematic review of randomised trials. Int J Obes Relat Metab Disord. 2003;27:987-1005.
6. Linde JA, Jeffery RW, French SA, et al. Self-weighing in weight gain prevention and weight loss trials. Ann Behav Med. 2005;30:210-216.
7. Levitsky DA, Garay J, Nausbaum M, et al. Monitoring weight daily blocks the freshman weight gain: a model for combating the epidemic of obesity. Int J Obes (London). 2006;30:1003-1010.
8. Leermarkers EA, Jakicic JM, Viteri J, et al. Clinic-based vs. home-based interventions for preventing weight gain in men. Obes Res. 1998;6:346-352.
9. Svetkey LP, Stevens VJ, Brantley PJ, et al. Comparison of strategies for sustaining weight loss: the weight loss maintenance randomized controlled trial. JAMA. 2008;299:1139-1148.
10. Levine MD, Klem ML, Kalarchian MA, et al. Weight gain prevention among women. Obesity (Silver Spring). 2007;15:1267-1277.
11. US Preventive Services Task Force. Screening for Obesity in Adults. Rockville, Md: AHRQ; December 2003. Available at: www.ahrq.gov/clinic/uspstf/uspsobes.htm. Accessed May 6, 2008.
12. Douketis JD, Feightner JW, Attia J, et al. Periodic health examination, 1999 update: 1. detection, prevention and treatment of obesity. Canadian Task Force on Preventive Health Care. CMAJ. 1999;160:513-525.
13. Franz MJ, Bantle JP, Beebe CA, et al. Evidence-based nutrition principles and recommendations for the treatment and prevention of diabetes and related complications. Diabetes Care. 2002;25:148-198.
14. Nawaz H, Katz D. American College of Preventive Medicine Medical Practice Policy Statement. Weight management counseling for overweight adults. Am J Prev Med. 2001;21:73-78.
A/PHYSICAL ACTIVITY AND DIETARY MODIFICATION WORK BEST. Family involvement, regular weight monitoring, and behavior modification also can help.
Regular physical activity decreases long-term weight gain (strength of recommendation [SOR]: B, 2 high-quality, randomized controlled trials [RCTs]). Decreasing fat intake (SOR: B, 1 high-quality systematic review) and increasing fruit and vegetable consumption (SOR: B, 1 high-quality RCT) also may decrease weight gain. Combined dietary and physical activity interventions prevent weight gain (SOR: B, 1 high-quality systematic review).
Family involvement helps maintain weight (SOR:B, 2 small RCTs). Daily or weekly weight monitoring reduces long-term weight gain (SOR:B, 2 RCTs).
Clinic-based, direct-contact, and Web-based programs that include behavior modification may reduce weight gain in adults (SOR: C, 3 RCTs). Behavior modification delivered by personal contact is more effective than mail, Internet, or self-directed modification programs (SOR:B, 2 RCTs).
Evidence summary
A recent systematic review of obesity prevention studies found 9 RCTs demonstrating that dietary and physical activity interventions can prevent weight gain, but lacking sufficient evidence to recommend a specific type of program.1
A systematic review of the effects of physical activity on weight reduction and maintenance analyzed 46 studies, including 8 RCTs that investigated interventions to reduce weight and 3 that examined measures to maintain it.2 More than 80% of the studies showed a benefit from physical exercise. Prevention of weight gain appears to be dose-dependent. More exercise leads to less weight gain; a minimum of 1.5 hours per week of moderate exercise is needed to prevent weight gain.2
Less fat, more vegetables spur weight loss
The Women’s Health Initiative studied 46,808 postmenopausal women between 50 and 79 years of age who were randomly assigned to an intervention or control group.3 The intervention group received intensive group and individual counseling from dieticians aimed at reducing fat intake to 20%, increasing consumption of vegetables and fruits to 5 or more servings per day, and increasing consumption of grains to 6 or more servings per day. The control group received dietary education materials. Neither group had weight loss or calorie restriction goals or differences in physical activity.
The intervention group had a mean decrease in weight 1.9 kg greater than the controls at 1 year (P<.001) and 0.4 kg at 7.5 years (P<.01). Weight loss was greater in women who consumed more fruits and vegetables and greatest among women who decreased energy intake from fat.
A family-based intervention lowers BMI in females
A family-based trial of weight gain prevention randomized 82 families to a group that was encouraged to eat 2 servings of cereal a day and increase activity by 2000 steps a day, or to a control group.4 In the intervention group, body mass index (BMI) decreased by 0.4% in mothers (P=.027), and BMI percentage for age decreased by 2.6% in daughters (P<.01). Male family members showed no significant differences, however.
Family ties, self-weighing improve weight control
A systematic review of family-spouse involvement in weight control and weight loss found that involving spouses tended to improve the effectiveness of weight control.5
Two studies, 1 an RCT, found an association between self-weighing and preventing weight gain.6,7 Patients who weighed themselves daily or weekly were less likely to gain weight than patients who weighed themselves monthly, yearly, or never.
Getting personal helps modify behavior
Three RCTs compared clinic-based, Web-based, and self-directed advice and counseling to prevent weight gain (2 studies) and maintain weight loss (1 study). In the first study, 67 patients were assigned to 4 months of clinic-based or home-based counseling to increase exercise and reduce fat intake, or to a control group.8 Weight change was–1.9 kg in the clinic-based group,–1.3 kg in the home-based group, and +0.22 kg in the control group (P=.007).
In the second study, 1032 overweight or obese adults with hypertension and/or dyslipidemia who completed a weight-loss program were randomly assigned to receive monthly personal contact, unlimited access to a Web-based intervention, or a self-directed control group.9 At 30 months, participants in the personal contact group had regained less weight than the Web-based or control groups (4.0, 5.1, and 5.5 kg, respectively; P<.01).
A third RCT randomized 284 healthy 25- to 44-year-old women with BMI <30 kg/m2 to group meetings, lessons by mail, or a control group that received an information booklet. The study found no significant difference among the 3 groups in weight maintenance at a 3-year follow-up; 40% maintained weight, and 60% gained more than 2 pounds.10
Recommendations
Wide consensus supports screening by either BMI or height and weight. The US Preventive Services Task Force (USPSTF) recommends intensive counseling for everyone with a BMI ≥30 kg/m2 coupled with behavioral modification to promote sustained weight loss.11 The USPSTF found insufficient evidence to support less intensive counseling for obese patients or counseling of any intensity for overweight patients.
The Canadian Task Force on Preventive Health Care found insufficient evidence to recommend for or against BMI measurement during routine health evaluations of the general population.12
The American Diabetes Association13 and the American College of Preventive Medicine14 recommend counseling and behavior modification for all adults to prevent obesity.
A/PHYSICAL ACTIVITY AND DIETARY MODIFICATION WORK BEST. Family involvement, regular weight monitoring, and behavior modification also can help.
Regular physical activity decreases long-term weight gain (strength of recommendation [SOR]: B, 2 high-quality, randomized controlled trials [RCTs]). Decreasing fat intake (SOR: B, 1 high-quality systematic review) and increasing fruit and vegetable consumption (SOR: B, 1 high-quality RCT) also may decrease weight gain. Combined dietary and physical activity interventions prevent weight gain (SOR: B, 1 high-quality systematic review).
Family involvement helps maintain weight (SOR:B, 2 small RCTs). Daily or weekly weight monitoring reduces long-term weight gain (SOR:B, 2 RCTs).
Clinic-based, direct-contact, and Web-based programs that include behavior modification may reduce weight gain in adults (SOR: C, 3 RCTs). Behavior modification delivered by personal contact is more effective than mail, Internet, or self-directed modification programs (SOR:B, 2 RCTs).
Evidence summary
A recent systematic review of obesity prevention studies found 9 RCTs demonstrating that dietary and physical activity interventions can prevent weight gain, but lacking sufficient evidence to recommend a specific type of program.1
A systematic review of the effects of physical activity on weight reduction and maintenance analyzed 46 studies, including 8 RCTs that investigated interventions to reduce weight and 3 that examined measures to maintain it.2 More than 80% of the studies showed a benefit from physical exercise. Prevention of weight gain appears to be dose-dependent. More exercise leads to less weight gain; a minimum of 1.5 hours per week of moderate exercise is needed to prevent weight gain.2
Less fat, more vegetables spur weight loss
The Women’s Health Initiative studied 46,808 postmenopausal women between 50 and 79 years of age who were randomly assigned to an intervention or control group.3 The intervention group received intensive group and individual counseling from dieticians aimed at reducing fat intake to 20%, increasing consumption of vegetables and fruits to 5 or more servings per day, and increasing consumption of grains to 6 or more servings per day. The control group received dietary education materials. Neither group had weight loss or calorie restriction goals or differences in physical activity.
The intervention group had a mean decrease in weight 1.9 kg greater than the controls at 1 year (P<.001) and 0.4 kg at 7.5 years (P<.01). Weight loss was greater in women who consumed more fruits and vegetables and greatest among women who decreased energy intake from fat.
A family-based intervention lowers BMI in females
A family-based trial of weight gain prevention randomized 82 families to a group that was encouraged to eat 2 servings of cereal a day and increase activity by 2000 steps a day, or to a control group.4 In the intervention group, body mass index (BMI) decreased by 0.4% in mothers (P=.027), and BMI percentage for age decreased by 2.6% in daughters (P<.01). Male family members showed no significant differences, however.
Family ties, self-weighing improve weight control
A systematic review of family-spouse involvement in weight control and weight loss found that involving spouses tended to improve the effectiveness of weight control.5
Two studies, 1 an RCT, found an association between self-weighing and preventing weight gain.6,7 Patients who weighed themselves daily or weekly were less likely to gain weight than patients who weighed themselves monthly, yearly, or never.
Getting personal helps modify behavior
Three RCTs compared clinic-based, Web-based, and self-directed advice and counseling to prevent weight gain (2 studies) and maintain weight loss (1 study). In the first study, 67 patients were assigned to 4 months of clinic-based or home-based counseling to increase exercise and reduce fat intake, or to a control group.8 Weight change was–1.9 kg in the clinic-based group,–1.3 kg in the home-based group, and +0.22 kg in the control group (P=.007).
In the second study, 1032 overweight or obese adults with hypertension and/or dyslipidemia who completed a weight-loss program were randomly assigned to receive monthly personal contact, unlimited access to a Web-based intervention, or a self-directed control group.9 At 30 months, participants in the personal contact group had regained less weight than the Web-based or control groups (4.0, 5.1, and 5.5 kg, respectively; P<.01).
A third RCT randomized 284 healthy 25- to 44-year-old women with BMI <30 kg/m2 to group meetings, lessons by mail, or a control group that received an information booklet. The study found no significant difference among the 3 groups in weight maintenance at a 3-year follow-up; 40% maintained weight, and 60% gained more than 2 pounds.10
Recommendations
Wide consensus supports screening by either BMI or height and weight. The US Preventive Services Task Force (USPSTF) recommends intensive counseling for everyone with a BMI ≥30 kg/m2 coupled with behavioral modification to promote sustained weight loss.11 The USPSTF found insufficient evidence to support less intensive counseling for obese patients or counseling of any intensity for overweight patients.
The Canadian Task Force on Preventive Health Care found insufficient evidence to recommend for or against BMI measurement during routine health evaluations of the general population.12
The American Diabetes Association13 and the American College of Preventive Medicine14 recommend counseling and behavior modification for all adults to prevent obesity.
1. Lemmens VE, Oenema A, Klepp KI, et al. A systematic review of the evidence regarding efficacy of obesity prevention interventions among adults. Obes Rev. 2008;9:446-455.
2. Fogelholm M, Kukkonen-Harjula K. Does physical activity prevent weight gain—a systematic review. Obes Rev. 2000;1:95-111.
3. Howard BV, Manson JE, Stefanick ML, et al. Low-fat dietary pattern and weight change over 7 years: the Women’s Health Initiative Dietary Modification Trial. JAMA. 2006;295:39-49.
4. Rodearmel SJ, Wyatt HR, Barry MJ, et al. A family-based approach to preventing excessive weight gain. Obesity (Silver Spring). 2006;14:1392-1401.
5. McLean N, Griffin S, Toney K, et al. Family involvement in weight control, weight maintenance and weight-loss interventions: a systematic review of randomised trials. Int J Obes Relat Metab Disord. 2003;27:987-1005.
6. Linde JA, Jeffery RW, French SA, et al. Self-weighing in weight gain prevention and weight loss trials. Ann Behav Med. 2005;30:210-216.
7. Levitsky DA, Garay J, Nausbaum M, et al. Monitoring weight daily blocks the freshman weight gain: a model for combating the epidemic of obesity. Int J Obes (London). 2006;30:1003-1010.
8. Leermarkers EA, Jakicic JM, Viteri J, et al. Clinic-based vs. home-based interventions for preventing weight gain in men. Obes Res. 1998;6:346-352.
9. Svetkey LP, Stevens VJ, Brantley PJ, et al. Comparison of strategies for sustaining weight loss: the weight loss maintenance randomized controlled trial. JAMA. 2008;299:1139-1148.
10. Levine MD, Klem ML, Kalarchian MA, et al. Weight gain prevention among women. Obesity (Silver Spring). 2007;15:1267-1277.
11. US Preventive Services Task Force. Screening for Obesity in Adults. Rockville, Md: AHRQ; December 2003. Available at: www.ahrq.gov/clinic/uspstf/uspsobes.htm. Accessed May 6, 2008.
12. Douketis JD, Feightner JW, Attia J, et al. Periodic health examination, 1999 update: 1. detection, prevention and treatment of obesity. Canadian Task Force on Preventive Health Care. CMAJ. 1999;160:513-525.
13. Franz MJ, Bantle JP, Beebe CA, et al. Evidence-based nutrition principles and recommendations for the treatment and prevention of diabetes and related complications. Diabetes Care. 2002;25:148-198.
14. Nawaz H, Katz D. American College of Preventive Medicine Medical Practice Policy Statement. Weight management counseling for overweight adults. Am J Prev Med. 2001;21:73-78.
1. Lemmens VE, Oenema A, Klepp KI, et al. A systematic review of the evidence regarding efficacy of obesity prevention interventions among adults. Obes Rev. 2008;9:446-455.
2. Fogelholm M, Kukkonen-Harjula K. Does physical activity prevent weight gain—a systematic review. Obes Rev. 2000;1:95-111.
3. Howard BV, Manson JE, Stefanick ML, et al. Low-fat dietary pattern and weight change over 7 years: the Women’s Health Initiative Dietary Modification Trial. JAMA. 2006;295:39-49.
4. Rodearmel SJ, Wyatt HR, Barry MJ, et al. A family-based approach to preventing excessive weight gain. Obesity (Silver Spring). 2006;14:1392-1401.
5. McLean N, Griffin S, Toney K, et al. Family involvement in weight control, weight maintenance and weight-loss interventions: a systematic review of randomised trials. Int J Obes Relat Metab Disord. 2003;27:987-1005.
6. Linde JA, Jeffery RW, French SA, et al. Self-weighing in weight gain prevention and weight loss trials. Ann Behav Med. 2005;30:210-216.
7. Levitsky DA, Garay J, Nausbaum M, et al. Monitoring weight daily blocks the freshman weight gain: a model for combating the epidemic of obesity. Int J Obes (London). 2006;30:1003-1010.
8. Leermarkers EA, Jakicic JM, Viteri J, et al. Clinic-based vs. home-based interventions for preventing weight gain in men. Obes Res. 1998;6:346-352.
9. Svetkey LP, Stevens VJ, Brantley PJ, et al. Comparison of strategies for sustaining weight loss: the weight loss maintenance randomized controlled trial. JAMA. 2008;299:1139-1148.
10. Levine MD, Klem ML, Kalarchian MA, et al. Weight gain prevention among women. Obesity (Silver Spring). 2007;15:1267-1277.
11. US Preventive Services Task Force. Screening for Obesity in Adults. Rockville, Md: AHRQ; December 2003. Available at: www.ahrq.gov/clinic/uspstf/uspsobes.htm. Accessed May 6, 2008.
12. Douketis JD, Feightner JW, Attia J, et al. Periodic health examination, 1999 update: 1. detection, prevention and treatment of obesity. Canadian Task Force on Preventive Health Care. CMAJ. 1999;160:513-525.
13. Franz MJ, Bantle JP, Beebe CA, et al. Evidence-based nutrition principles and recommendations for the treatment and prevention of diabetes and related complications. Diabetes Care. 2002;25:148-198.
14. Nawaz H, Katz D. American College of Preventive Medicine Medical Practice Policy Statement. Weight management counseling for overweight adults. Am J Prev Med. 2001;21:73-78.
Evidence-based answers from the Family Physicians Inquiries Network
Do intercontraction intervals predict when a woman at term should seek evaluation of labor?
NO; HOWEVER, A REDUCTION IN the intercontraction interval is associated with active labor (strength of recommendation [SOR]: B, cohort study).
Most primigravidas who have had regular contractions for 2 hours and multigravidas who have had regular contractions for 1 hour haven’t transitioned into the active phase of labor (SOR: B, cohort study).
Evidence summary
Multiple cohort studies demonstrate that the expected events of normal labor form a bell-shaped curve. The range of labor experiences makes predicting when a particular woman will enter active labor difficult.
When does latent labor become active labor?
The first stage of labor includes latent and active phases. The latent phase is defined as the period between onset of labor and cervical dilatation of 3 to 4 cm or the time between onset of regular contractions and escalation in the rate of cervical dilation. Regular contractions must be intense, last 60 seconds, and occur in a predictable pattern. Escalating cervical dilation is marked by a change in the cervical examination over a short period of time (usually 2 hours).1
The World Health Organization defines active labor as cervical dilation between 4 and 9 cm, with dilation usually occurring at 1 cm per hour or faster and accompanied by the beginning of fetal descent.2
Latent labor was initially described in a large prospective cohort of 10,293 term gravidas (including 4175 nulliparas and 5599 multiparas) followed from presentation to delivery.1 Cervical dilation was assessed by examination every 30 to 120 minutes, almost always performed by the same examiner throughout labor. In primigravidas, latent labor averaged 6.4 hours, with 95% of women completing the latent phase in 20.6 hours. In multigravidas, the mean duration of latent labor was 4.8 hours, with 95% of women transitioning to active labor in 13.6 hours.
Shorter intercontraction interval linked to active labor
A recently published cohort study of women presenting to labor and delivery found that a relative decrease in the intercontraction interval was associated with a diagnosis of labor (odds ratio=1.42; 95% confidence interval, 1.06-1.90). The study failed to define either active labor or decrease in the intercontraction interval.3
Earlier admission leads to more interventions and poorer outcomes
Many studies have suggested that admitting women to the hospital during the latent phase of labor is associated with more interventions and poorer outcomes. Two large retrospective cohort studies (N=2697 and 3220) found increased rates of cesarean section in women admitted during the latent phase.4,5 They also reported increased use of oxytocin, epidural analgesia, intrauterine pressure catheters, and fetal scalp electrodes, and increased rates of chorioamnionitis, postpartum infection, and neonatal intubation.4,5 See the TABLE for a summary of the effects of latent-phase admission.
TABLE
Consequences of hospital admission during latent vs active labor
| Nulliparous | Parous | |||||
|---|---|---|---|---|---|---|
| Consequence | Latent (%) | Active (%) | NNH | Latent (%) | Active (%) | NNH |
| Oxytocin4 | 43 | 27 | 6* | 20 | 9 | 9* |
| Epidural4 | 82 | 61 | 5* | 58 | 40 | 6* |
| Assisted vaginal delivery4 | 27 | 25 | 50 | 8 | 6 | 50 |
| Cesarean4 | 10 | 4 | 17* | 8 | 6 | 50 |
| Cesarean5 † | 14 | 7 | 14* | 3 | 1 | 50* |
| pH <7.14 | 4 | 3 | 100 | 3 | 2 | 100 |
| Apgar <74 | 4 | 2 | 50 | 3 | 2 | 100 |
| NNH, number needed to harm. | ||||||
| *Indicates relationship significant at the level <.05. | ||||||
| †Study by Bailit5 also showed significant associations for oxytocin, scalp pH, intrauterine pressure catheter, fetal scalp electrode, epidural, neonatal intubation, amnionitis, and postpartum infection. Raw data are unavailable for abstraction | ||||||
Labor assessment program reduced time in the labor ward
Labor assessment programs attempt to delay admission during early active labor. One randomized clinical trial (N=209) among low-risk women with reassuring maternal and fetal assessments in early labor divided the women into 2 groups when they presented for labor and delivery. One group received advice, encouragement, and support along with instructions to walk or return home and come back when labor became more active (defined as regular, painful contractions and dilation of at least 3 cm). The other group was admitted directly to the labor and delivery ward. The study found that early labor assessment decreased use of analgesics and oxytocin and reduced time spent in the labor ward.6
Recommendations
The American College of Obstetricians and Gynecologists (ACOG) acknowledges in patient education literature that distinguishing true from false labor is difficult. ACOG lists characteristics of each and recommend that a woman monitor the frequency of contractions for an hour and call the doctor’s office or hospital if she thinks she’s in labor.7
Similarly, a patient handout from the American College of Nurse-Midwives recommends calling the health care provider if contractions are ≤5 minutes apart for more than 1 hour, several contractions are so painful that the woman cannot walk or talk, or her water breaks.8
A standard textbook describes normal uterine contractions during active labor as occurring every 2 to 5 minutes, and as often as every 2 to 3 minutes.9
1. Friedman EA, Kroll BH. Computer analysis of labor progression. 3. Pattern variations by parity. J Reprod Med. 1971;6:179-183.
2. World Health Organization. Managing Complications in Pregnancy and Childbirth: A Guide for Midwives and Doctors. Geneva, Switzerland: Department of Reproductive Health and Research, Family and Community Health, World Health Organization; 2003.
3. Ragusa A, Monsur M, Zanini A, et al. Diagnosis of labor: a prospective study. Med Gen Med. 2005;7:61.-
4. Holmes P, Oppenheimer LW, Wen SW. The relationship between cervical dilatation at initial presentation in labour and subsequent intervention. BJOG. 2001;108:1120-1124.
5. Bailit JL, Dierker LR, Blanchard MH, et al. Outcomes of women presenting in active versus latent phase of spontaneous labor. Obstet Gynecol. 2005;105:77-79.
6. McNiven PS, Williams JI, Hodnett E, et al. An early labor assessment program: a randomized, controlled trial. Birth. 1998;25:5-10.
7. How to Tell When Labor Begins. Washington, DC: American College of Obstetricians and Gynecologists; 1999. Available at: www.acog.org/publications/patient_education/bp004.cfm. Accessed November 8, 2008.
8. Am I in Labor? Silver Spring, Md: American College of Nurse-Midwives; 2003. Available at: www.midwife.org/siteFiles/news/sharewithwomen48_4.pdf. Accessed November 7, 2008.
9. Kilpatrick S, Garrison E. Normal labor and delivery. In: Gabbe SG, Niebyl JR, Simpson JL, eds. Obstetrics: Normal and Problem Pregnancies. 5th ed. Philadelphia: Churchill Livingstone/Elsevier; 2007:303–317.
NO; HOWEVER, A REDUCTION IN the intercontraction interval is associated with active labor (strength of recommendation [SOR]: B, cohort study).
Most primigravidas who have had regular contractions for 2 hours and multigravidas who have had regular contractions for 1 hour haven’t transitioned into the active phase of labor (SOR: B, cohort study).
Evidence summary
Multiple cohort studies demonstrate that the expected events of normal labor form a bell-shaped curve. The range of labor experiences makes predicting when a particular woman will enter active labor difficult.
When does latent labor become active labor?
The first stage of labor includes latent and active phases. The latent phase is defined as the period between onset of labor and cervical dilatation of 3 to 4 cm or the time between onset of regular contractions and escalation in the rate of cervical dilation. Regular contractions must be intense, last 60 seconds, and occur in a predictable pattern. Escalating cervical dilation is marked by a change in the cervical examination over a short period of time (usually 2 hours).1
The World Health Organization defines active labor as cervical dilation between 4 and 9 cm, with dilation usually occurring at 1 cm per hour or faster and accompanied by the beginning of fetal descent.2
Latent labor was initially described in a large prospective cohort of 10,293 term gravidas (including 4175 nulliparas and 5599 multiparas) followed from presentation to delivery.1 Cervical dilation was assessed by examination every 30 to 120 minutes, almost always performed by the same examiner throughout labor. In primigravidas, latent labor averaged 6.4 hours, with 95% of women completing the latent phase in 20.6 hours. In multigravidas, the mean duration of latent labor was 4.8 hours, with 95% of women transitioning to active labor in 13.6 hours.
Shorter intercontraction interval linked to active labor
A recently published cohort study of women presenting to labor and delivery found that a relative decrease in the intercontraction interval was associated with a diagnosis of labor (odds ratio=1.42; 95% confidence interval, 1.06-1.90). The study failed to define either active labor or decrease in the intercontraction interval.3
Earlier admission leads to more interventions and poorer outcomes
Many studies have suggested that admitting women to the hospital during the latent phase of labor is associated with more interventions and poorer outcomes. Two large retrospective cohort studies (N=2697 and 3220) found increased rates of cesarean section in women admitted during the latent phase.4,5 They also reported increased use of oxytocin, epidural analgesia, intrauterine pressure catheters, and fetal scalp electrodes, and increased rates of chorioamnionitis, postpartum infection, and neonatal intubation.4,5 See the TABLE for a summary of the effects of latent-phase admission.
TABLE
Consequences of hospital admission during latent vs active labor
| Nulliparous | Parous | |||||
|---|---|---|---|---|---|---|
| Consequence | Latent (%) | Active (%) | NNH | Latent (%) | Active (%) | NNH |
| Oxytocin4 | 43 | 27 | 6* | 20 | 9 | 9* |
| Epidural4 | 82 | 61 | 5* | 58 | 40 | 6* |
| Assisted vaginal delivery4 | 27 | 25 | 50 | 8 | 6 | 50 |
| Cesarean4 | 10 | 4 | 17* | 8 | 6 | 50 |
| Cesarean5 † | 14 | 7 | 14* | 3 | 1 | 50* |
| pH <7.14 | 4 | 3 | 100 | 3 | 2 | 100 |
| Apgar <74 | 4 | 2 | 50 | 3 | 2 | 100 |
| NNH, number needed to harm. | ||||||
| *Indicates relationship significant at the level <.05. | ||||||
| †Study by Bailit5 also showed significant associations for oxytocin, scalp pH, intrauterine pressure catheter, fetal scalp electrode, epidural, neonatal intubation, amnionitis, and postpartum infection. Raw data are unavailable for abstraction | ||||||
Labor assessment program reduced time in the labor ward
Labor assessment programs attempt to delay admission during early active labor. One randomized clinical trial (N=209) among low-risk women with reassuring maternal and fetal assessments in early labor divided the women into 2 groups when they presented for labor and delivery. One group received advice, encouragement, and support along with instructions to walk or return home and come back when labor became more active (defined as regular, painful contractions and dilation of at least 3 cm). The other group was admitted directly to the labor and delivery ward. The study found that early labor assessment decreased use of analgesics and oxytocin and reduced time spent in the labor ward.6
Recommendations
The American College of Obstetricians and Gynecologists (ACOG) acknowledges in patient education literature that distinguishing true from false labor is difficult. ACOG lists characteristics of each and recommend that a woman monitor the frequency of contractions for an hour and call the doctor’s office or hospital if she thinks she’s in labor.7
Similarly, a patient handout from the American College of Nurse-Midwives recommends calling the health care provider if contractions are ≤5 minutes apart for more than 1 hour, several contractions are so painful that the woman cannot walk or talk, or her water breaks.8
A standard textbook describes normal uterine contractions during active labor as occurring every 2 to 5 minutes, and as often as every 2 to 3 minutes.9
NO; HOWEVER, A REDUCTION IN the intercontraction interval is associated with active labor (strength of recommendation [SOR]: B, cohort study).
Most primigravidas who have had regular contractions for 2 hours and multigravidas who have had regular contractions for 1 hour haven’t transitioned into the active phase of labor (SOR: B, cohort study).
Evidence summary
Multiple cohort studies demonstrate that the expected events of normal labor form a bell-shaped curve. The range of labor experiences makes predicting when a particular woman will enter active labor difficult.
When does latent labor become active labor?
The first stage of labor includes latent and active phases. The latent phase is defined as the period between onset of labor and cervical dilatation of 3 to 4 cm or the time between onset of regular contractions and escalation in the rate of cervical dilation. Regular contractions must be intense, last 60 seconds, and occur in a predictable pattern. Escalating cervical dilation is marked by a change in the cervical examination over a short period of time (usually 2 hours).1
The World Health Organization defines active labor as cervical dilation between 4 and 9 cm, with dilation usually occurring at 1 cm per hour or faster and accompanied by the beginning of fetal descent.2
Latent labor was initially described in a large prospective cohort of 10,293 term gravidas (including 4175 nulliparas and 5599 multiparas) followed from presentation to delivery.1 Cervical dilation was assessed by examination every 30 to 120 minutes, almost always performed by the same examiner throughout labor. In primigravidas, latent labor averaged 6.4 hours, with 95% of women completing the latent phase in 20.6 hours. In multigravidas, the mean duration of latent labor was 4.8 hours, with 95% of women transitioning to active labor in 13.6 hours.
Shorter intercontraction interval linked to active labor
A recently published cohort study of women presenting to labor and delivery found that a relative decrease in the intercontraction interval was associated with a diagnosis of labor (odds ratio=1.42; 95% confidence interval, 1.06-1.90). The study failed to define either active labor or decrease in the intercontraction interval.3
Earlier admission leads to more interventions and poorer outcomes
Many studies have suggested that admitting women to the hospital during the latent phase of labor is associated with more interventions and poorer outcomes. Two large retrospective cohort studies (N=2697 and 3220) found increased rates of cesarean section in women admitted during the latent phase.4,5 They also reported increased use of oxytocin, epidural analgesia, intrauterine pressure catheters, and fetal scalp electrodes, and increased rates of chorioamnionitis, postpartum infection, and neonatal intubation.4,5 See the TABLE for a summary of the effects of latent-phase admission.
TABLE
Consequences of hospital admission during latent vs active labor
| Nulliparous | Parous | |||||
|---|---|---|---|---|---|---|
| Consequence | Latent (%) | Active (%) | NNH | Latent (%) | Active (%) | NNH |
| Oxytocin4 | 43 | 27 | 6* | 20 | 9 | 9* |
| Epidural4 | 82 | 61 | 5* | 58 | 40 | 6* |
| Assisted vaginal delivery4 | 27 | 25 | 50 | 8 | 6 | 50 |
| Cesarean4 | 10 | 4 | 17* | 8 | 6 | 50 |
| Cesarean5 † | 14 | 7 | 14* | 3 | 1 | 50* |
| pH <7.14 | 4 | 3 | 100 | 3 | 2 | 100 |
| Apgar <74 | 4 | 2 | 50 | 3 | 2 | 100 |
| NNH, number needed to harm. | ||||||
| *Indicates relationship significant at the level <.05. | ||||||
| †Study by Bailit5 also showed significant associations for oxytocin, scalp pH, intrauterine pressure catheter, fetal scalp electrode, epidural, neonatal intubation, amnionitis, and postpartum infection. Raw data are unavailable for abstraction | ||||||
Labor assessment program reduced time in the labor ward
Labor assessment programs attempt to delay admission during early active labor. One randomized clinical trial (N=209) among low-risk women with reassuring maternal and fetal assessments in early labor divided the women into 2 groups when they presented for labor and delivery. One group received advice, encouragement, and support along with instructions to walk or return home and come back when labor became more active (defined as regular, painful contractions and dilation of at least 3 cm). The other group was admitted directly to the labor and delivery ward. The study found that early labor assessment decreased use of analgesics and oxytocin and reduced time spent in the labor ward.6
Recommendations
The American College of Obstetricians and Gynecologists (ACOG) acknowledges in patient education literature that distinguishing true from false labor is difficult. ACOG lists characteristics of each and recommend that a woman monitor the frequency of contractions for an hour and call the doctor’s office or hospital if she thinks she’s in labor.7
Similarly, a patient handout from the American College of Nurse-Midwives recommends calling the health care provider if contractions are ≤5 minutes apart for more than 1 hour, several contractions are so painful that the woman cannot walk or talk, or her water breaks.8
A standard textbook describes normal uterine contractions during active labor as occurring every 2 to 5 minutes, and as often as every 2 to 3 minutes.9
1. Friedman EA, Kroll BH. Computer analysis of labor progression. 3. Pattern variations by parity. J Reprod Med. 1971;6:179-183.
2. World Health Organization. Managing Complications in Pregnancy and Childbirth: A Guide for Midwives and Doctors. Geneva, Switzerland: Department of Reproductive Health and Research, Family and Community Health, World Health Organization; 2003.
3. Ragusa A, Monsur M, Zanini A, et al. Diagnosis of labor: a prospective study. Med Gen Med. 2005;7:61.-
4. Holmes P, Oppenheimer LW, Wen SW. The relationship between cervical dilatation at initial presentation in labour and subsequent intervention. BJOG. 2001;108:1120-1124.
5. Bailit JL, Dierker LR, Blanchard MH, et al. Outcomes of women presenting in active versus latent phase of spontaneous labor. Obstet Gynecol. 2005;105:77-79.
6. McNiven PS, Williams JI, Hodnett E, et al. An early labor assessment program: a randomized, controlled trial. Birth. 1998;25:5-10.
7. How to Tell When Labor Begins. Washington, DC: American College of Obstetricians and Gynecologists; 1999. Available at: www.acog.org/publications/patient_education/bp004.cfm. Accessed November 8, 2008.
8. Am I in Labor? Silver Spring, Md: American College of Nurse-Midwives; 2003. Available at: www.midwife.org/siteFiles/news/sharewithwomen48_4.pdf. Accessed November 7, 2008.
9. Kilpatrick S, Garrison E. Normal labor and delivery. In: Gabbe SG, Niebyl JR, Simpson JL, eds. Obstetrics: Normal and Problem Pregnancies. 5th ed. Philadelphia: Churchill Livingstone/Elsevier; 2007:303–317.
1. Friedman EA, Kroll BH. Computer analysis of labor progression. 3. Pattern variations by parity. J Reprod Med. 1971;6:179-183.
2. World Health Organization. Managing Complications in Pregnancy and Childbirth: A Guide for Midwives and Doctors. Geneva, Switzerland: Department of Reproductive Health and Research, Family and Community Health, World Health Organization; 2003.
3. Ragusa A, Monsur M, Zanini A, et al. Diagnosis of labor: a prospective study. Med Gen Med. 2005;7:61.-
4. Holmes P, Oppenheimer LW, Wen SW. The relationship between cervical dilatation at initial presentation in labour and subsequent intervention. BJOG. 2001;108:1120-1124.
5. Bailit JL, Dierker LR, Blanchard MH, et al. Outcomes of women presenting in active versus latent phase of spontaneous labor. Obstet Gynecol. 2005;105:77-79.
6. McNiven PS, Williams JI, Hodnett E, et al. An early labor assessment program: a randomized, controlled trial. Birth. 1998;25:5-10.
7. How to Tell When Labor Begins. Washington, DC: American College of Obstetricians and Gynecologists; 1999. Available at: www.acog.org/publications/patient_education/bp004.cfm. Accessed November 8, 2008.
8. Am I in Labor? Silver Spring, Md: American College of Nurse-Midwives; 2003. Available at: www.midwife.org/siteFiles/news/sharewithwomen48_4.pdf. Accessed November 7, 2008.
9. Kilpatrick S, Garrison E. Normal labor and delivery. In: Gabbe SG, Niebyl JR, Simpson JL, eds. Obstetrics: Normal and Problem Pregnancies. 5th ed. Philadelphia: Churchill Livingstone/Elsevier; 2007:303–317.
Evidence-based answers from the Family Physicians Inquiries Network
Which asthma patients should get the pneumococcal vaccine?
ADULTS BETWEEN THE AGES OF 19 AND 64 YEARS who have chronic lung disease, including asthma, should get the vaccine, as should all patients 65 years and older (strength of recommendation [SOR]: C, consensus guidelines). Evidence doesn’t support routine vaccination of children with asthma or adults younger than 65 years who don’t have chronic lung disease to decrease asthma-related or pneumonia-related hospitalizations (SOR: B, 1 retrospective cohort study and 1 retrospective, case-controlled cohort study).
Evidence summary
A 5-year retrospective cohort study of 9170 patients evaluated the effect of pneumococcal vaccination on incidence and length of all-cause hospitalizations and hospitalizations related to respiratory and otorhinolaryngologic syndromes, including asthma and pneumonia.1 The vaccine was given to all patients older than 64 years (7834 patients [85%]) and any patient at risk for pneumococcal infection or complications, including patients with asthma, chronic obstructive pulmonary disease (COPD), bronchitis, chronic respiratory disease, cardiovascular disease, chronic renal failure, diabetes mellitus, immunodeficiency, and functional or anatomic asplenia (1336 patients [15%]).
The number of all-cause hospitalizations was reduced by 58% in patients who received the pneumococcal vaccine (relative risk [RR]=0.96; 95% confidence interval [CI], 0.94-0.98). In vaccinated patients with asthma (793 patients [8.7%]), asthma-related hospitalizations decreased by 78% (RR=1.82; 95% CI, 1.35-2.45; NNT=49) and average asthma-related length of hospital stay was shortened by about 2 days (P=.039). The study found no difference in pneumonia-related hospitalizations among all vaccinated patients.
Effect on younger patients is unclear
Because the investigators didn’t analyze asthma-related or pneumonia-related hospitalizations among asthmatic patients 64 years and younger, the effect of pneumococcal vaccination on this younger subgroup can’t be differentiated from the entire group of patients with asthma.1
What about pneumococcal hospitalization?
A retrospective, case-controlled cohort study examined the impact of pneumococcal vaccination on any pneumococcal-related hospitalization in patients with COPD or asthma.2 The study included 2746 adults with asthma (74.2% younger than 64 years) who were followed for about 2.1 years before and 2.6 years after vaccination.
Investigators found no significant differences in risk of pneumococcal-related hospitalization between asthma patients and controls throughout the study. They didn’t evaluate asthma-related hospital admissions.
Impact of vaccine on invasive disease in younger asthma patients?
A retrospective, nested, case-controlled study examined the relationship between asthma and invasive pneumococcal disease (IPD) in 6985 patients enrolled in Tennessee’s Medicaid program.3 Patients 2 to 49 years of age with any IPD diagnosis were identified using International Classification of Diseases (ICD-9-CM) codes and followed for 8 years.
Asthma patients without coexisting conditions that confer a high risk of IPD (such as diabetes, cardiac disease, and infection with human immunodeficiency virus) had a 14.7% risk of IPD compared with a risk of only 7.4% in age-matched controls (adjusted odds ratio=2.4; 95% CI, 1.7-3.4). The authors concluded that this Medicaid population with asthma had an increased incidence of IPD of 1 to 3 cases annually per 10,000 people. The effect of pneumococcal vaccination on the incidence of IPD in these younger asthma patients is unknown, however.3
Recommendations
The National Asthma Education and Prevention Program (NAEPP)4 and the Global Initiative for Asthma (GINA)5 make no recommendations regarding the administration of the pneumococcal vaccine.
The Advisory Committee on Immunization Practices (ACIP) recommends vaccination for all adults 65 years and older and adults 19 years and older with chronic lung disease, including asthma, or other chronic medical conditions such as cardiovascular diseases, diabetes, chronic liver diseases, chronic alcoholism, chronic renal failure, asplenia, and other immunocompromising conditions.6
The British Department of Health recommends vaccination with either the 7-valent conjugate or the 23-valent polysaccharide pneumococcal vaccine for all asthma patients taking systemic steroids longer than 1 month at a dose equivalent to prednisolone 20 mg daily and for children weighing less than 20 kg who take daily steroids at a dose of ≥1 mg/kg. Efficacy studies aren’t available to support this recommendation.7
1. Ansaldi F, Turello V, Lai P, et al. Effectiveness of a 23-valent polysaccharide vaccine in preventing pneumonia and non-invasive pneumococcal infection in elderly people: a large-scale retrospective cohort study. J Int Med Res. 2005;33:490-500.
2. Lee TA, Weaver FM, Weiss KB. Impact of pneumococcal vaccination on pneumonia rates in patients with COPD and asthma. J Gen Intern Med. 2007;22:62-67.
3. Talbot TR, Hartert TV, Mitchel E, et al. Asthma as a risk for invasive pneumococcal disease. N Engl J Med. 2005;352:2082-2090.
4. National Heart Lung and Blood Institute. Guidelines for the Diagnosis and Management of Asthma. Bethesda, Md: National Institutes of Health; 1991:11.
5. Global Initiative for Asthma (GINA). Global Strategy for Asthma Management and Prevention. Available at: www.ginasthma.org/Guidelineitem.asp?l1=2&l2=1&intId=60. Accessed December 10, 2007.
6. Centers for Disease Control and Prevention. Recommended adult immunization schedule—United States, 2009. MMWR Morb Mortal Wkly Rep. 2008;57(53):Q1-Q4.
7. Department of Health. Immunisation Against Infectious Disease 2006: The Green Book. London, England: Department of Health; 2007. Available at: www.dh.gov.uk/en/Policyandguidance/Healthandsocialcaretopics/Greenbook/DH_4097254. Accessed December 10, 2007.
ADULTS BETWEEN THE AGES OF 19 AND 64 YEARS who have chronic lung disease, including asthma, should get the vaccine, as should all patients 65 years and older (strength of recommendation [SOR]: C, consensus guidelines). Evidence doesn’t support routine vaccination of children with asthma or adults younger than 65 years who don’t have chronic lung disease to decrease asthma-related or pneumonia-related hospitalizations (SOR: B, 1 retrospective cohort study and 1 retrospective, case-controlled cohort study).
Evidence summary
A 5-year retrospective cohort study of 9170 patients evaluated the effect of pneumococcal vaccination on incidence and length of all-cause hospitalizations and hospitalizations related to respiratory and otorhinolaryngologic syndromes, including asthma and pneumonia.1 The vaccine was given to all patients older than 64 years (7834 patients [85%]) and any patient at risk for pneumococcal infection or complications, including patients with asthma, chronic obstructive pulmonary disease (COPD), bronchitis, chronic respiratory disease, cardiovascular disease, chronic renal failure, diabetes mellitus, immunodeficiency, and functional or anatomic asplenia (1336 patients [15%]).
The number of all-cause hospitalizations was reduced by 58% in patients who received the pneumococcal vaccine (relative risk [RR]=0.96; 95% confidence interval [CI], 0.94-0.98). In vaccinated patients with asthma (793 patients [8.7%]), asthma-related hospitalizations decreased by 78% (RR=1.82; 95% CI, 1.35-2.45; NNT=49) and average asthma-related length of hospital stay was shortened by about 2 days (P=.039). The study found no difference in pneumonia-related hospitalizations among all vaccinated patients.
Effect on younger patients is unclear
Because the investigators didn’t analyze asthma-related or pneumonia-related hospitalizations among asthmatic patients 64 years and younger, the effect of pneumococcal vaccination on this younger subgroup can’t be differentiated from the entire group of patients with asthma.1
What about pneumococcal hospitalization?
A retrospective, case-controlled cohort study examined the impact of pneumococcal vaccination on any pneumococcal-related hospitalization in patients with COPD or asthma.2 The study included 2746 adults with asthma (74.2% younger than 64 years) who were followed for about 2.1 years before and 2.6 years after vaccination.
Investigators found no significant differences in risk of pneumococcal-related hospitalization between asthma patients and controls throughout the study. They didn’t evaluate asthma-related hospital admissions.
Impact of vaccine on invasive disease in younger asthma patients?
A retrospective, nested, case-controlled study examined the relationship between asthma and invasive pneumococcal disease (IPD) in 6985 patients enrolled in Tennessee’s Medicaid program.3 Patients 2 to 49 years of age with any IPD diagnosis were identified using International Classification of Diseases (ICD-9-CM) codes and followed for 8 years.
Asthma patients without coexisting conditions that confer a high risk of IPD (such as diabetes, cardiac disease, and infection with human immunodeficiency virus) had a 14.7% risk of IPD compared with a risk of only 7.4% in age-matched controls (adjusted odds ratio=2.4; 95% CI, 1.7-3.4). The authors concluded that this Medicaid population with asthma had an increased incidence of IPD of 1 to 3 cases annually per 10,000 people. The effect of pneumococcal vaccination on the incidence of IPD in these younger asthma patients is unknown, however.3
Recommendations
The National Asthma Education and Prevention Program (NAEPP)4 and the Global Initiative for Asthma (GINA)5 make no recommendations regarding the administration of the pneumococcal vaccine.
The Advisory Committee on Immunization Practices (ACIP) recommends vaccination for all adults 65 years and older and adults 19 years and older with chronic lung disease, including asthma, or other chronic medical conditions such as cardiovascular diseases, diabetes, chronic liver diseases, chronic alcoholism, chronic renal failure, asplenia, and other immunocompromising conditions.6
The British Department of Health recommends vaccination with either the 7-valent conjugate or the 23-valent polysaccharide pneumococcal vaccine for all asthma patients taking systemic steroids longer than 1 month at a dose equivalent to prednisolone 20 mg daily and for children weighing less than 20 kg who take daily steroids at a dose of ≥1 mg/kg. Efficacy studies aren’t available to support this recommendation.7
ADULTS BETWEEN THE AGES OF 19 AND 64 YEARS who have chronic lung disease, including asthma, should get the vaccine, as should all patients 65 years and older (strength of recommendation [SOR]: C, consensus guidelines). Evidence doesn’t support routine vaccination of children with asthma or adults younger than 65 years who don’t have chronic lung disease to decrease asthma-related or pneumonia-related hospitalizations (SOR: B, 1 retrospective cohort study and 1 retrospective, case-controlled cohort study).
Evidence summary
A 5-year retrospective cohort study of 9170 patients evaluated the effect of pneumococcal vaccination on incidence and length of all-cause hospitalizations and hospitalizations related to respiratory and otorhinolaryngologic syndromes, including asthma and pneumonia.1 The vaccine was given to all patients older than 64 years (7834 patients [85%]) and any patient at risk for pneumococcal infection or complications, including patients with asthma, chronic obstructive pulmonary disease (COPD), bronchitis, chronic respiratory disease, cardiovascular disease, chronic renal failure, diabetes mellitus, immunodeficiency, and functional or anatomic asplenia (1336 patients [15%]).
The number of all-cause hospitalizations was reduced by 58% in patients who received the pneumococcal vaccine (relative risk [RR]=0.96; 95% confidence interval [CI], 0.94-0.98). In vaccinated patients with asthma (793 patients [8.7%]), asthma-related hospitalizations decreased by 78% (RR=1.82; 95% CI, 1.35-2.45; NNT=49) and average asthma-related length of hospital stay was shortened by about 2 days (P=.039). The study found no difference in pneumonia-related hospitalizations among all vaccinated patients.
Effect on younger patients is unclear
Because the investigators didn’t analyze asthma-related or pneumonia-related hospitalizations among asthmatic patients 64 years and younger, the effect of pneumococcal vaccination on this younger subgroup can’t be differentiated from the entire group of patients with asthma.1
What about pneumococcal hospitalization?
A retrospective, case-controlled cohort study examined the impact of pneumococcal vaccination on any pneumococcal-related hospitalization in patients with COPD or asthma.2 The study included 2746 adults with asthma (74.2% younger than 64 years) who were followed for about 2.1 years before and 2.6 years after vaccination.
Investigators found no significant differences in risk of pneumococcal-related hospitalization between asthma patients and controls throughout the study. They didn’t evaluate asthma-related hospital admissions.
Impact of vaccine on invasive disease in younger asthma patients?
A retrospective, nested, case-controlled study examined the relationship between asthma and invasive pneumococcal disease (IPD) in 6985 patients enrolled in Tennessee’s Medicaid program.3 Patients 2 to 49 years of age with any IPD diagnosis were identified using International Classification of Diseases (ICD-9-CM) codes and followed for 8 years.
Asthma patients without coexisting conditions that confer a high risk of IPD (such as diabetes, cardiac disease, and infection with human immunodeficiency virus) had a 14.7% risk of IPD compared with a risk of only 7.4% in age-matched controls (adjusted odds ratio=2.4; 95% CI, 1.7-3.4). The authors concluded that this Medicaid population with asthma had an increased incidence of IPD of 1 to 3 cases annually per 10,000 people. The effect of pneumococcal vaccination on the incidence of IPD in these younger asthma patients is unknown, however.3
Recommendations
The National Asthma Education and Prevention Program (NAEPP)4 and the Global Initiative for Asthma (GINA)5 make no recommendations regarding the administration of the pneumococcal vaccine.
The Advisory Committee on Immunization Practices (ACIP) recommends vaccination for all adults 65 years and older and adults 19 years and older with chronic lung disease, including asthma, or other chronic medical conditions such as cardiovascular diseases, diabetes, chronic liver diseases, chronic alcoholism, chronic renal failure, asplenia, and other immunocompromising conditions.6
The British Department of Health recommends vaccination with either the 7-valent conjugate or the 23-valent polysaccharide pneumococcal vaccine for all asthma patients taking systemic steroids longer than 1 month at a dose equivalent to prednisolone 20 mg daily and for children weighing less than 20 kg who take daily steroids at a dose of ≥1 mg/kg. Efficacy studies aren’t available to support this recommendation.7
1. Ansaldi F, Turello V, Lai P, et al. Effectiveness of a 23-valent polysaccharide vaccine in preventing pneumonia and non-invasive pneumococcal infection in elderly people: a large-scale retrospective cohort study. J Int Med Res. 2005;33:490-500.
2. Lee TA, Weaver FM, Weiss KB. Impact of pneumococcal vaccination on pneumonia rates in patients with COPD and asthma. J Gen Intern Med. 2007;22:62-67.
3. Talbot TR, Hartert TV, Mitchel E, et al. Asthma as a risk for invasive pneumococcal disease. N Engl J Med. 2005;352:2082-2090.
4. National Heart Lung and Blood Institute. Guidelines for the Diagnosis and Management of Asthma. Bethesda, Md: National Institutes of Health; 1991:11.
5. Global Initiative for Asthma (GINA). Global Strategy for Asthma Management and Prevention. Available at: www.ginasthma.org/Guidelineitem.asp?l1=2&l2=1&intId=60. Accessed December 10, 2007.
6. Centers for Disease Control and Prevention. Recommended adult immunization schedule—United States, 2009. MMWR Morb Mortal Wkly Rep. 2008;57(53):Q1-Q4.
7. Department of Health. Immunisation Against Infectious Disease 2006: The Green Book. London, England: Department of Health; 2007. Available at: www.dh.gov.uk/en/Policyandguidance/Healthandsocialcaretopics/Greenbook/DH_4097254. Accessed December 10, 2007.
1. Ansaldi F, Turello V, Lai P, et al. Effectiveness of a 23-valent polysaccharide vaccine in preventing pneumonia and non-invasive pneumococcal infection in elderly people: a large-scale retrospective cohort study. J Int Med Res. 2005;33:490-500.
2. Lee TA, Weaver FM, Weiss KB. Impact of pneumococcal vaccination on pneumonia rates in patients with COPD and asthma. J Gen Intern Med. 2007;22:62-67.
3. Talbot TR, Hartert TV, Mitchel E, et al. Asthma as a risk for invasive pneumococcal disease. N Engl J Med. 2005;352:2082-2090.
4. National Heart Lung and Blood Institute. Guidelines for the Diagnosis and Management of Asthma. Bethesda, Md: National Institutes of Health; 1991:11.
5. Global Initiative for Asthma (GINA). Global Strategy for Asthma Management and Prevention. Available at: www.ginasthma.org/Guidelineitem.asp?l1=2&l2=1&intId=60. Accessed December 10, 2007.
6. Centers for Disease Control and Prevention. Recommended adult immunization schedule—United States, 2009. MMWR Morb Mortal Wkly Rep. 2008;57(53):Q1-Q4.
7. Department of Health. Immunisation Against Infectious Disease 2006: The Green Book. London, England: Department of Health; 2007. Available at: www.dh.gov.uk/en/Policyandguidance/Healthandsocialcaretopics/Greenbook/DH_4097254. Accessed December 10, 2007.
Evidence-based answers from the Family Physicians Inquiries Network
What are the best prophylactic drugs for migraine?
BETA-BLOCKERS without intrinsic sympathomimetic activity, amitriptyline, divalproex sodium/sodium valproate, and topiramate are the most effective drugs for preventing episodic migraine (strength of recommendation: A, multiple, well-designed, randomized controlled trials [RCTs]).
Evidence summary
Many medications have been evaluated for migraine prophylaxis. However, very few head-to-head trials of more than 2 drugs have been published, and no recent meta-analyses of available drug classes have been performed. The most commonly evaluated outcome is a 50% reduction in headache frequency.
Propranolol and timolol offer consistent prevention
Propranolol and timolol have consistently demonstrated efficacy for preventing episodic migraine. In a 1991 meta-analysis, propranolol resulted in a 44% reduction in the headache index—a composite score that takes into account both intensity and duration—compared with a 14% reduction for placebo.1
Less evidence supports other beta-blockers
Atenolol, metoprolol, and nadolol have demonstrated a moderate effect, but less evidence exists to support their use.2 A recent trial comparing metoprolol and nebivolol demonstrated a positive response—defined as a 50% reduction in headache frequency—to each drug at 14 weeks (57% of metoprolol-treated and 50% of nebivolol-treated patients), but noted that nebivolol was better tolerated.3
Beta-blockers with intrinsic sympathomimetic activity (acebutolol, alprenolol, oxprenolol, pindolol) appear to be ineffective for migraine prevention.4
Amitriptyline works better than propranolol for some migraines
Amitriptyline is the most often studied antidepressant and the only one with consistent support for efficacy in preventing migraine. A 1981 trial found amitriptyline to be more effective than propranolol in mixed migraine-tension-type headache, whereas propranolol was more effective for migraine alone.5
Some support for fluoxetine, none for similar drugs
Limited evidence exists for the use of fluoxetine, 20 mg daily. A small 1999 study of patients with migraine without aura found a 57% reduction in total pain index—a value based on pain intensity and hours of headache per month—with fluoxetine compared with an insignificant 31% reduction with placebo.6
No evidence from controlled trials supports the use of fluvoxamine, paroxetine, sertraline, phenelzine, venlafaxine, mirtazapine, trazodone, or bupropion.4
Divalproex sodium, sodium valproate are effective
Divalproex sodium and sodium valproate show strong, consistent evidence of efficacy; they may be particularly useful for patients with prolonged or atypical migraine aura.4 Initial studies of delayed-release divalproex at doses ranging from 500 to 1500 mg daily found that 44% of divalproex-treated patients reported a 50% reduction in migraine frequency, compared with 21% in the placebo group (number needed to treat [NNT]=4).7
A more recent study of the extended-release form of divalproex sodium demonstrated a 4-week reduction in headache rate to 1.2 from a baseline of 4.4, compared with a decrease of 0.6 for placebo (95% confidence interval [CI] of treatment difference, 0.2-1.2).8
TABLE
Recommended drugs for migraine prophylaxis13
| Drug | Dose | Comments |
|---|---|---|
| Propranolol | 80-240 mg/d | May cause fatigue. When used in combination with rizatriptan, give a lower dose of rizatriptan. |
| Timolol | 20-30 mg/d | As with propranolol, may cause fatigue. Avoid β-blockers in patients with asthma or Raynaud’s disease. |
| Amitriptyline | 25-150 mg/d | Drowsiness, weight gain, and significant anticholinergic adverse events are common. |
| Divalproex sodium; Sodium valproate | 500-1500 mg/d; 800-1500 mg/d | Side effects include nausea, drowsiness, weight gain, hair loss, and tremor. Hepatotoxicity, pancreatitis, and hyperammonemia have been reported rarely. Pregnancy category D. |
| Topiramate | 100-200 mg/d | Paresthesia is the most common adverse event; fatigue, nausea, anorexia, and cognitive symptoms are less common. Carbonic anhydrase inhibition may cause metabolic acidosis. Acute myopia and angle closure glaucoma are rare events. |
Topiramate may decrease frequency as much as propranolol
Topiramate has significantly reduced the mean frequency of episodic migraine at doses of 100 to 200 mg daily and also improved secondary end points, including number of migraine days per month, use of acute medication, and daily activity.9 One study found that topiramate 100 mg daily had comparable efficacy to propranolol 160 mg daily; both drugs decreased monthly migraine frequency to 1.6 from a baseline of 4.9 with topiramate and 5.1 with propranolol (95% CI for the pair-wise difference of topiramate minus propranolol,-0.58 to 0.60).10
Anticonvulsants also reduce migraine frequency
A 2004 Cochrane review of anticonvulsant drugs for migraine prophylaxis found that anticonvulsants, as a class, reduce migraine frequency by about 1.3 attacks per 28 days when compared with placebo (based on 10 trials [N=902]). When analyzing data on relative frequency of migraines, data from 13 trials (N=1773) were combined and showed that anticonvulsants more than doubled the number of patients with a 50% or greater decrease in migraine frequency relative to placebo (relative risk=2.25; 95% CI, 1.79-2.84; NNT=3.9; 95% CI, 3.4-4.7).11
Other drugs to keep on your radar
Agents available in the United States that have at least limited evidence supporting their use to prevent episodic migraine include gabapentin, lisinopril, candesartan, memantine, riboflavin, magnesium, feverfew, coenzyme Q10, butterbur, and melatonin.
Drugs so far proved ineffective in preventing episodic migraine include clonidine, carbamazepine, clonazepam, vigabatrin, oxcarbazepine, zonisamide, lamotrigine, nifedipine, and acetazolamide. Botulinum toxin type A given by intramuscular injection in the head and neck region has demonstrated limited efficacy in chronic headache disorders, but doesn’t prevent episodic migraine.12
Recommendations
The 2000 guidelines of the American Association of Neurology address Group 1 (first-line) drugs and Group 2 drugs:
Group 1 drugs (medium to high efficacy, good strength of evidence, and a range of severity [mild to moderate] and frequency [infrequent to frequent] of side effects) include amitriptyline, divalproex sodium, propranolol, and timolol.
Group 2 drugs (lower efficacy than Group 1, or limited strength of evidence, and mild to moderate side effects) include aspirin (but not combination products), atenolol, fenoprofen, feverfew, flurbiprofen, fluoxetine, gabapentin, guanfacine, ketoprofen, magnesium, mefenamic acid, metoprolol, nadolol, naproxen, nimodipine, verapamil, and vitamin B2.13
Topiramate was still under study when the guidelines were released and wasn’t approved by the US Food and Drug Administration for migraine prophylaxis until 2004. The 2000 guidelines are undergoing revision.
1. Holroyd KA, Penzien DB, Cordingley GE. Propranolol in the management of recurrent migraine: a meta-analytic review. Headache. 1991;31:333-340.
2. Silberstein SD, Goadsby PJ. Migraine: preventive treatment. Cephalalgia. 2002;22:491-512.
3. Schellenberg R, Lichtenthal A, Wöhling H, et al. Nebivolol and metoprolol for treating migraine: an advance on β-blocker treatment? Headache. 2008;48:118-125.
4. Snow V, Weiss K, Wall EM, et al. Pharmacologic management of acute attacks of migraine and prevention of migraine headache. Ann Intern Med. 2002;137:840-849.
5. Mathew NT. Prophylaxis of migraine and mixed headache: a randomized controlled study. Headache. 1981;21:105-109.
6. d’Amato CC, Pizza V, Marmolo T, et al. Fluoxetine for migraine prophylaxis: a double-blind trial. Headache. 1999;39:716-719.
7. Klapper J. Divalproex sodium in migraine prophylaxis: a dose-controlled study [published correction appears in Cephalalgia. 1997;17:798]. Cephalalgia. 1997;17:103-108.
8. Freitag FG, Collins SD, Carlson HA, et al. A randomized trial of divalproex sodium extended-release tablets in migraine prophylaxis. Neurology. 2002;58:1652-1659.
9. Kaniecki R. Neuromodulators for migraine prevention. Headache. 2008;48:586-600.
10. Diener HC, Tfelt-Hansen P, Dahlof C, et al. Topiramate in migraine prophylaxis—results from a placebo-controlled trial with propranolol as an active control. J Neurol. 2004;251:943-950.
11. Chronicle EP, Mulleners WM. Anticonvulsant drugs for migraine prophylaxis. Cochrane Database Syst Rev. 2004;(3):CD003226.
12. Blumenfeld AM, Schim JD, Chippendale TJ. Botulinum toxin type A and divalproex sodium for prophylactic treatment of episodic or chronic migraine. Headache. 2008;48:210-220.
13. Ramadan NM, Silberstein SD, Freitag FG, et al. Evidence-based guidelines for migraine headache in the primary care setting: pharmacological management for prevention of migraine. 2000. Available at: www.aan.com/professionals/practice/pdfs/gl0090.pdf. Accessed March 26, 2008.
BETA-BLOCKERS without intrinsic sympathomimetic activity, amitriptyline, divalproex sodium/sodium valproate, and topiramate are the most effective drugs for preventing episodic migraine (strength of recommendation: A, multiple, well-designed, randomized controlled trials [RCTs]).
Evidence summary
Many medications have been evaluated for migraine prophylaxis. However, very few head-to-head trials of more than 2 drugs have been published, and no recent meta-analyses of available drug classes have been performed. The most commonly evaluated outcome is a 50% reduction in headache frequency.
Propranolol and timolol offer consistent prevention
Propranolol and timolol have consistently demonstrated efficacy for preventing episodic migraine. In a 1991 meta-analysis, propranolol resulted in a 44% reduction in the headache index—a composite score that takes into account both intensity and duration—compared with a 14% reduction for placebo.1
Less evidence supports other beta-blockers
Atenolol, metoprolol, and nadolol have demonstrated a moderate effect, but less evidence exists to support their use.2 A recent trial comparing metoprolol and nebivolol demonstrated a positive response—defined as a 50% reduction in headache frequency—to each drug at 14 weeks (57% of metoprolol-treated and 50% of nebivolol-treated patients), but noted that nebivolol was better tolerated.3
Beta-blockers with intrinsic sympathomimetic activity (acebutolol, alprenolol, oxprenolol, pindolol) appear to be ineffective for migraine prevention.4
Amitriptyline works better than propranolol for some migraines
Amitriptyline is the most often studied antidepressant and the only one with consistent support for efficacy in preventing migraine. A 1981 trial found amitriptyline to be more effective than propranolol in mixed migraine-tension-type headache, whereas propranolol was more effective for migraine alone.5
Some support for fluoxetine, none for similar drugs
Limited evidence exists for the use of fluoxetine, 20 mg daily. A small 1999 study of patients with migraine without aura found a 57% reduction in total pain index—a value based on pain intensity and hours of headache per month—with fluoxetine compared with an insignificant 31% reduction with placebo.6
No evidence from controlled trials supports the use of fluvoxamine, paroxetine, sertraline, phenelzine, venlafaxine, mirtazapine, trazodone, or bupropion.4
Divalproex sodium, sodium valproate are effective
Divalproex sodium and sodium valproate show strong, consistent evidence of efficacy; they may be particularly useful for patients with prolonged or atypical migraine aura.4 Initial studies of delayed-release divalproex at doses ranging from 500 to 1500 mg daily found that 44% of divalproex-treated patients reported a 50% reduction in migraine frequency, compared with 21% in the placebo group (number needed to treat [NNT]=4).7
A more recent study of the extended-release form of divalproex sodium demonstrated a 4-week reduction in headache rate to 1.2 from a baseline of 4.4, compared with a decrease of 0.6 for placebo (95% confidence interval [CI] of treatment difference, 0.2-1.2).8
TABLE
Recommended drugs for migraine prophylaxis13
| Drug | Dose | Comments |
|---|---|---|
| Propranolol | 80-240 mg/d | May cause fatigue. When used in combination with rizatriptan, give a lower dose of rizatriptan. |
| Timolol | 20-30 mg/d | As with propranolol, may cause fatigue. Avoid β-blockers in patients with asthma or Raynaud’s disease. |
| Amitriptyline | 25-150 mg/d | Drowsiness, weight gain, and significant anticholinergic adverse events are common. |
| Divalproex sodium; Sodium valproate | 500-1500 mg/d; 800-1500 mg/d | Side effects include nausea, drowsiness, weight gain, hair loss, and tremor. Hepatotoxicity, pancreatitis, and hyperammonemia have been reported rarely. Pregnancy category D. |
| Topiramate | 100-200 mg/d | Paresthesia is the most common adverse event; fatigue, nausea, anorexia, and cognitive symptoms are less common. Carbonic anhydrase inhibition may cause metabolic acidosis. Acute myopia and angle closure glaucoma are rare events. |
Topiramate may decrease frequency as much as propranolol
Topiramate has significantly reduced the mean frequency of episodic migraine at doses of 100 to 200 mg daily and also improved secondary end points, including number of migraine days per month, use of acute medication, and daily activity.9 One study found that topiramate 100 mg daily had comparable efficacy to propranolol 160 mg daily; both drugs decreased monthly migraine frequency to 1.6 from a baseline of 4.9 with topiramate and 5.1 with propranolol (95% CI for the pair-wise difference of topiramate minus propranolol,-0.58 to 0.60).10
Anticonvulsants also reduce migraine frequency
A 2004 Cochrane review of anticonvulsant drugs for migraine prophylaxis found that anticonvulsants, as a class, reduce migraine frequency by about 1.3 attacks per 28 days when compared with placebo (based on 10 trials [N=902]). When analyzing data on relative frequency of migraines, data from 13 trials (N=1773) were combined and showed that anticonvulsants more than doubled the number of patients with a 50% or greater decrease in migraine frequency relative to placebo (relative risk=2.25; 95% CI, 1.79-2.84; NNT=3.9; 95% CI, 3.4-4.7).11
Other drugs to keep on your radar
Agents available in the United States that have at least limited evidence supporting their use to prevent episodic migraine include gabapentin, lisinopril, candesartan, memantine, riboflavin, magnesium, feverfew, coenzyme Q10, butterbur, and melatonin.
Drugs so far proved ineffective in preventing episodic migraine include clonidine, carbamazepine, clonazepam, vigabatrin, oxcarbazepine, zonisamide, lamotrigine, nifedipine, and acetazolamide. Botulinum toxin type A given by intramuscular injection in the head and neck region has demonstrated limited efficacy in chronic headache disorders, but doesn’t prevent episodic migraine.12
Recommendations
The 2000 guidelines of the American Association of Neurology address Group 1 (first-line) drugs and Group 2 drugs:
Group 1 drugs (medium to high efficacy, good strength of evidence, and a range of severity [mild to moderate] and frequency [infrequent to frequent] of side effects) include amitriptyline, divalproex sodium, propranolol, and timolol.
Group 2 drugs (lower efficacy than Group 1, or limited strength of evidence, and mild to moderate side effects) include aspirin (but not combination products), atenolol, fenoprofen, feverfew, flurbiprofen, fluoxetine, gabapentin, guanfacine, ketoprofen, magnesium, mefenamic acid, metoprolol, nadolol, naproxen, nimodipine, verapamil, and vitamin B2.13
Topiramate was still under study when the guidelines were released and wasn’t approved by the US Food and Drug Administration for migraine prophylaxis until 2004. The 2000 guidelines are undergoing revision.
BETA-BLOCKERS without intrinsic sympathomimetic activity, amitriptyline, divalproex sodium/sodium valproate, and topiramate are the most effective drugs for preventing episodic migraine (strength of recommendation: A, multiple, well-designed, randomized controlled trials [RCTs]).
Evidence summary
Many medications have been evaluated for migraine prophylaxis. However, very few head-to-head trials of more than 2 drugs have been published, and no recent meta-analyses of available drug classes have been performed. The most commonly evaluated outcome is a 50% reduction in headache frequency.
Propranolol and timolol offer consistent prevention
Propranolol and timolol have consistently demonstrated efficacy for preventing episodic migraine. In a 1991 meta-analysis, propranolol resulted in a 44% reduction in the headache index—a composite score that takes into account both intensity and duration—compared with a 14% reduction for placebo.1
Less evidence supports other beta-blockers
Atenolol, metoprolol, and nadolol have demonstrated a moderate effect, but less evidence exists to support their use.2 A recent trial comparing metoprolol and nebivolol demonstrated a positive response—defined as a 50% reduction in headache frequency—to each drug at 14 weeks (57% of metoprolol-treated and 50% of nebivolol-treated patients), but noted that nebivolol was better tolerated.3
Beta-blockers with intrinsic sympathomimetic activity (acebutolol, alprenolol, oxprenolol, pindolol) appear to be ineffective for migraine prevention.4
Amitriptyline works better than propranolol for some migraines
Amitriptyline is the most often studied antidepressant and the only one with consistent support for efficacy in preventing migraine. A 1981 trial found amitriptyline to be more effective than propranolol in mixed migraine-tension-type headache, whereas propranolol was more effective for migraine alone.5
Some support for fluoxetine, none for similar drugs
Limited evidence exists for the use of fluoxetine, 20 mg daily. A small 1999 study of patients with migraine without aura found a 57% reduction in total pain index—a value based on pain intensity and hours of headache per month—with fluoxetine compared with an insignificant 31% reduction with placebo.6
No evidence from controlled trials supports the use of fluvoxamine, paroxetine, sertraline, phenelzine, venlafaxine, mirtazapine, trazodone, or bupropion.4
Divalproex sodium, sodium valproate are effective
Divalproex sodium and sodium valproate show strong, consistent evidence of efficacy; they may be particularly useful for patients with prolonged or atypical migraine aura.4 Initial studies of delayed-release divalproex at doses ranging from 500 to 1500 mg daily found that 44% of divalproex-treated patients reported a 50% reduction in migraine frequency, compared with 21% in the placebo group (number needed to treat [NNT]=4).7
A more recent study of the extended-release form of divalproex sodium demonstrated a 4-week reduction in headache rate to 1.2 from a baseline of 4.4, compared with a decrease of 0.6 for placebo (95% confidence interval [CI] of treatment difference, 0.2-1.2).8
TABLE
Recommended drugs for migraine prophylaxis13
| Drug | Dose | Comments |
|---|---|---|
| Propranolol | 80-240 mg/d | May cause fatigue. When used in combination with rizatriptan, give a lower dose of rizatriptan. |
| Timolol | 20-30 mg/d | As with propranolol, may cause fatigue. Avoid β-blockers in patients with asthma or Raynaud’s disease. |
| Amitriptyline | 25-150 mg/d | Drowsiness, weight gain, and significant anticholinergic adverse events are common. |
| Divalproex sodium; Sodium valproate | 500-1500 mg/d; 800-1500 mg/d | Side effects include nausea, drowsiness, weight gain, hair loss, and tremor. Hepatotoxicity, pancreatitis, and hyperammonemia have been reported rarely. Pregnancy category D. |
| Topiramate | 100-200 mg/d | Paresthesia is the most common adverse event; fatigue, nausea, anorexia, and cognitive symptoms are less common. Carbonic anhydrase inhibition may cause metabolic acidosis. Acute myopia and angle closure glaucoma are rare events. |
Topiramate may decrease frequency as much as propranolol
Topiramate has significantly reduced the mean frequency of episodic migraine at doses of 100 to 200 mg daily and also improved secondary end points, including number of migraine days per month, use of acute medication, and daily activity.9 One study found that topiramate 100 mg daily had comparable efficacy to propranolol 160 mg daily; both drugs decreased monthly migraine frequency to 1.6 from a baseline of 4.9 with topiramate and 5.1 with propranolol (95% CI for the pair-wise difference of topiramate minus propranolol,-0.58 to 0.60).10
Anticonvulsants also reduce migraine frequency
A 2004 Cochrane review of anticonvulsant drugs for migraine prophylaxis found that anticonvulsants, as a class, reduce migraine frequency by about 1.3 attacks per 28 days when compared with placebo (based on 10 trials [N=902]). When analyzing data on relative frequency of migraines, data from 13 trials (N=1773) were combined and showed that anticonvulsants more than doubled the number of patients with a 50% or greater decrease in migraine frequency relative to placebo (relative risk=2.25; 95% CI, 1.79-2.84; NNT=3.9; 95% CI, 3.4-4.7).11
Other drugs to keep on your radar
Agents available in the United States that have at least limited evidence supporting their use to prevent episodic migraine include gabapentin, lisinopril, candesartan, memantine, riboflavin, magnesium, feverfew, coenzyme Q10, butterbur, and melatonin.
Drugs so far proved ineffective in preventing episodic migraine include clonidine, carbamazepine, clonazepam, vigabatrin, oxcarbazepine, zonisamide, lamotrigine, nifedipine, and acetazolamide. Botulinum toxin type A given by intramuscular injection in the head and neck region has demonstrated limited efficacy in chronic headache disorders, but doesn’t prevent episodic migraine.12
Recommendations
The 2000 guidelines of the American Association of Neurology address Group 1 (first-line) drugs and Group 2 drugs:
Group 1 drugs (medium to high efficacy, good strength of evidence, and a range of severity [mild to moderate] and frequency [infrequent to frequent] of side effects) include amitriptyline, divalproex sodium, propranolol, and timolol.
Group 2 drugs (lower efficacy than Group 1, or limited strength of evidence, and mild to moderate side effects) include aspirin (but not combination products), atenolol, fenoprofen, feverfew, flurbiprofen, fluoxetine, gabapentin, guanfacine, ketoprofen, magnesium, mefenamic acid, metoprolol, nadolol, naproxen, nimodipine, verapamil, and vitamin B2.13
Topiramate was still under study when the guidelines were released and wasn’t approved by the US Food and Drug Administration for migraine prophylaxis until 2004. The 2000 guidelines are undergoing revision.
1. Holroyd KA, Penzien DB, Cordingley GE. Propranolol in the management of recurrent migraine: a meta-analytic review. Headache. 1991;31:333-340.
2. Silberstein SD, Goadsby PJ. Migraine: preventive treatment. Cephalalgia. 2002;22:491-512.
3. Schellenberg R, Lichtenthal A, Wöhling H, et al. Nebivolol and metoprolol for treating migraine: an advance on β-blocker treatment? Headache. 2008;48:118-125.
4. Snow V, Weiss K, Wall EM, et al. Pharmacologic management of acute attacks of migraine and prevention of migraine headache. Ann Intern Med. 2002;137:840-849.
5. Mathew NT. Prophylaxis of migraine and mixed headache: a randomized controlled study. Headache. 1981;21:105-109.
6. d’Amato CC, Pizza V, Marmolo T, et al. Fluoxetine for migraine prophylaxis: a double-blind trial. Headache. 1999;39:716-719.
7. Klapper J. Divalproex sodium in migraine prophylaxis: a dose-controlled study [published correction appears in Cephalalgia. 1997;17:798]. Cephalalgia. 1997;17:103-108.
8. Freitag FG, Collins SD, Carlson HA, et al. A randomized trial of divalproex sodium extended-release tablets in migraine prophylaxis. Neurology. 2002;58:1652-1659.
9. Kaniecki R. Neuromodulators for migraine prevention. Headache. 2008;48:586-600.
10. Diener HC, Tfelt-Hansen P, Dahlof C, et al. Topiramate in migraine prophylaxis—results from a placebo-controlled trial with propranolol as an active control. J Neurol. 2004;251:943-950.
11. Chronicle EP, Mulleners WM. Anticonvulsant drugs for migraine prophylaxis. Cochrane Database Syst Rev. 2004;(3):CD003226.
12. Blumenfeld AM, Schim JD, Chippendale TJ. Botulinum toxin type A and divalproex sodium for prophylactic treatment of episodic or chronic migraine. Headache. 2008;48:210-220.
13. Ramadan NM, Silberstein SD, Freitag FG, et al. Evidence-based guidelines for migraine headache in the primary care setting: pharmacological management for prevention of migraine. 2000. Available at: www.aan.com/professionals/practice/pdfs/gl0090.pdf. Accessed March 26, 2008.
1. Holroyd KA, Penzien DB, Cordingley GE. Propranolol in the management of recurrent migraine: a meta-analytic review. Headache. 1991;31:333-340.
2. Silberstein SD, Goadsby PJ. Migraine: preventive treatment. Cephalalgia. 2002;22:491-512.
3. Schellenberg R, Lichtenthal A, Wöhling H, et al. Nebivolol and metoprolol for treating migraine: an advance on β-blocker treatment? Headache. 2008;48:118-125.
4. Snow V, Weiss K, Wall EM, et al. Pharmacologic management of acute attacks of migraine and prevention of migraine headache. Ann Intern Med. 2002;137:840-849.
5. Mathew NT. Prophylaxis of migraine and mixed headache: a randomized controlled study. Headache. 1981;21:105-109.
6. d’Amato CC, Pizza V, Marmolo T, et al. Fluoxetine for migraine prophylaxis: a double-blind trial. Headache. 1999;39:716-719.
7. Klapper J. Divalproex sodium in migraine prophylaxis: a dose-controlled study [published correction appears in Cephalalgia. 1997;17:798]. Cephalalgia. 1997;17:103-108.
8. Freitag FG, Collins SD, Carlson HA, et al. A randomized trial of divalproex sodium extended-release tablets in migraine prophylaxis. Neurology. 2002;58:1652-1659.
9. Kaniecki R. Neuromodulators for migraine prevention. Headache. 2008;48:586-600.
10. Diener HC, Tfelt-Hansen P, Dahlof C, et al. Topiramate in migraine prophylaxis—results from a placebo-controlled trial with propranolol as an active control. J Neurol. 2004;251:943-950.
11. Chronicle EP, Mulleners WM. Anticonvulsant drugs for migraine prophylaxis. Cochrane Database Syst Rev. 2004;(3):CD003226.
12. Blumenfeld AM, Schim JD, Chippendale TJ. Botulinum toxin type A and divalproex sodium for prophylactic treatment of episodic or chronic migraine. Headache. 2008;48:210-220.
13. Ramadan NM, Silberstein SD, Freitag FG, et al. Evidence-based guidelines for migraine headache in the primary care setting: pharmacological management for prevention of migraine. 2000. Available at: www.aan.com/professionals/practice/pdfs/gl0090.pdf. Accessed March 26, 2008.
Evidence-based answers from the Family Physicians Inquiries Network
When should you consider implanted nerve stimulators for lower back pain?
CONSIDER IT FOR PATIENTS WITH FAILED BACK SURGERY SYNDROME. These patients can gain more pain relief from spinal cord stimulation (SCS) than from reoperation (strength of recommendation [SOR]: A, 2 randomized controlled trials [RCTs]). SCS can also treat chronic low back pain effectively (SOR: B, cohort studies). It’s indicated when conservative measures have failed (SOR: C, expert opinion).
The side effects and failure rates of SCS are well documented and should be considered before recommending the therapy to patients (SOR: A, systematic review of RCTs and cohort studies).
Evidence summary
SCS systems comprise transcutaneously inserted leads that deliver low-voltage electronic stimulation to the spinal cord or targeted peripheral nerves. The resulting dermatomal parasthesia can be preferable to chronic painful stimuli. The voltage generator is located externally or implanted internally.
SCS can be used to treat patients with chronic and intractable pain, such as the pain caused by failed back surgery syndrome. The syndrome, defined as persistent or recurrent pain after lumbosacral spine surgery, occurs in 10% to 40% of patients who have undergone lumbosacral spine surgery.1
A 2005 prospective RCT enrolled 50 patients with failed back surgery syndrome who were considering reoperation.1 Twenty-four were randomized to SCS and 26 to reoperation. Success was defined as >50% pain relief measured by a validated visual analog pain scale. The average length of follow-up was 3 years. An intention-to-treat analysis demonstrated that 9 of 24 (38%) SCS insertions were successful, compared with 3 of 26 (12%) reoperations (P=.04; number needed to treat=3.8).
Low back pain shows significant response to stimulation
A 2004 systematic review of SCS for all indications included 51 studies and 2973 patients.2 Sixteen of the studies, with a total of 616 patients, focused on low back pain, specifically chronic back pain and failed back surgery syndrome. Two of the 16 studies were prospective controlled trials, 8 were prospective trials without controls, and 6 were retrospective studies.
Both prospective, controlled trials (total of 62 patients) demonstrated statistically significant (P<.05) results with SCS. One measured subjective pain and the other used crossover to the other treatment arm (SCS vs surgery) as a marker for treatment failure.
Consider the side effects
SCS isn’t without side effects. Cameron’s systematic review of 51 SCS studies reported rates for a number of complications ( TABLE ).2 The most common complication was lead migration—displacement of the spinal electrodes that can cause pain to recur.
TABLE
Major complications of SCS
| Complication | Rate |
|---|---|
| Lead migration | 13.2% |
| Lead breakage | 9.1% |
| Infection | 3.4% |
| Hardware malfunction | 2.9% |
| Unwanted stimulation | 2.4% |
| Battery failure | 1.6% |
| Pain over implant | 0.9% |
| SCS, spinal cord stimulation. | |
| Adapted from: Cameron T, et al. J Neurosurg.2 | |
Recommendations
Evidence-based guidelines for interventional techniques to control chronic pain, published in the January 2007 edition of Pain Physician, classify indications for SCS as follows:3
Strong indication: complex regional pain syndrome (CRPS)
Moderate indication: failed back surgery syndrome, chronic low back pain, and chronic lower extremity pain.
The Society of British Neurological Surgeons lists the following conditions as “good indications” for SCS: failed back surgery syndrome, CRPS, neuropathic pain from peripheral nerve damage, pain secondary to peripheral vascular disease, refractory angina, and brachial plexopathy.4
1. North RB, Kidd DH, Farrokhi F, et al. Spinal cord stimulation versus repeated lumbosacral spine surgery for chronic pain: a randomized, controlled trial. Neurosurgery. 2005;56:98-106.
2. Cameron T. Safety and efficacy of spinal cord stimulation for the treatment of chronic pain: a 20-year literature review. J Neurosurg. 2004;100(suppl 3 Spine):254-267.
3. Boswell MV, Trescot AM, Datta S, et al. American Society of Interventional Pain Physicians Interventional techniques: evidence-based practice guidelines in the management of chronic spinal pain. Pain Physician. 2007;10:7-111.
4. Society of British Neurological Surgeons/British Pain Society Spinal Cord Stimulation for the Management of Pain: Recommendations for Best Clinical Practice. London: British Pain Society; 2009. Available at: www.britishpainsociety.org/book_scs_main.pdf. Accessed October 3, 2009.
CONSIDER IT FOR PATIENTS WITH FAILED BACK SURGERY SYNDROME. These patients can gain more pain relief from spinal cord stimulation (SCS) than from reoperation (strength of recommendation [SOR]: A, 2 randomized controlled trials [RCTs]). SCS can also treat chronic low back pain effectively (SOR: B, cohort studies). It’s indicated when conservative measures have failed (SOR: C, expert opinion).
The side effects and failure rates of SCS are well documented and should be considered before recommending the therapy to patients (SOR: A, systematic review of RCTs and cohort studies).
Evidence summary
SCS systems comprise transcutaneously inserted leads that deliver low-voltage electronic stimulation to the spinal cord or targeted peripheral nerves. The resulting dermatomal parasthesia can be preferable to chronic painful stimuli. The voltage generator is located externally or implanted internally.
SCS can be used to treat patients with chronic and intractable pain, such as the pain caused by failed back surgery syndrome. The syndrome, defined as persistent or recurrent pain after lumbosacral spine surgery, occurs in 10% to 40% of patients who have undergone lumbosacral spine surgery.1
A 2005 prospective RCT enrolled 50 patients with failed back surgery syndrome who were considering reoperation.1 Twenty-four were randomized to SCS and 26 to reoperation. Success was defined as >50% pain relief measured by a validated visual analog pain scale. The average length of follow-up was 3 years. An intention-to-treat analysis demonstrated that 9 of 24 (38%) SCS insertions were successful, compared with 3 of 26 (12%) reoperations (P=.04; number needed to treat=3.8).
Low back pain shows significant response to stimulation
A 2004 systematic review of SCS for all indications included 51 studies and 2973 patients.2 Sixteen of the studies, with a total of 616 patients, focused on low back pain, specifically chronic back pain and failed back surgery syndrome. Two of the 16 studies were prospective controlled trials, 8 were prospective trials without controls, and 6 were retrospective studies.
Both prospective, controlled trials (total of 62 patients) demonstrated statistically significant (P<.05) results with SCS. One measured subjective pain and the other used crossover to the other treatment arm (SCS vs surgery) as a marker for treatment failure.
Consider the side effects
SCS isn’t without side effects. Cameron’s systematic review of 51 SCS studies reported rates for a number of complications ( TABLE ).2 The most common complication was lead migration—displacement of the spinal electrodes that can cause pain to recur.
TABLE
Major complications of SCS
| Complication | Rate |
|---|---|
| Lead migration | 13.2% |
| Lead breakage | 9.1% |
| Infection | 3.4% |
| Hardware malfunction | 2.9% |
| Unwanted stimulation | 2.4% |
| Battery failure | 1.6% |
| Pain over implant | 0.9% |
| SCS, spinal cord stimulation. | |
| Adapted from: Cameron T, et al. J Neurosurg.2 | |
Recommendations
Evidence-based guidelines for interventional techniques to control chronic pain, published in the January 2007 edition of Pain Physician, classify indications for SCS as follows:3
Strong indication: complex regional pain syndrome (CRPS)
Moderate indication: failed back surgery syndrome, chronic low back pain, and chronic lower extremity pain.
The Society of British Neurological Surgeons lists the following conditions as “good indications” for SCS: failed back surgery syndrome, CRPS, neuropathic pain from peripheral nerve damage, pain secondary to peripheral vascular disease, refractory angina, and brachial plexopathy.4
CONSIDER IT FOR PATIENTS WITH FAILED BACK SURGERY SYNDROME. These patients can gain more pain relief from spinal cord stimulation (SCS) than from reoperation (strength of recommendation [SOR]: A, 2 randomized controlled trials [RCTs]). SCS can also treat chronic low back pain effectively (SOR: B, cohort studies). It’s indicated when conservative measures have failed (SOR: C, expert opinion).
The side effects and failure rates of SCS are well documented and should be considered before recommending the therapy to patients (SOR: A, systematic review of RCTs and cohort studies).
Evidence summary
SCS systems comprise transcutaneously inserted leads that deliver low-voltage electronic stimulation to the spinal cord or targeted peripheral nerves. The resulting dermatomal parasthesia can be preferable to chronic painful stimuli. The voltage generator is located externally or implanted internally.
SCS can be used to treat patients with chronic and intractable pain, such as the pain caused by failed back surgery syndrome. The syndrome, defined as persistent or recurrent pain after lumbosacral spine surgery, occurs in 10% to 40% of patients who have undergone lumbosacral spine surgery.1
A 2005 prospective RCT enrolled 50 patients with failed back surgery syndrome who were considering reoperation.1 Twenty-four were randomized to SCS and 26 to reoperation. Success was defined as >50% pain relief measured by a validated visual analog pain scale. The average length of follow-up was 3 years. An intention-to-treat analysis demonstrated that 9 of 24 (38%) SCS insertions were successful, compared with 3 of 26 (12%) reoperations (P=.04; number needed to treat=3.8).
Low back pain shows significant response to stimulation
A 2004 systematic review of SCS for all indications included 51 studies and 2973 patients.2 Sixteen of the studies, with a total of 616 patients, focused on low back pain, specifically chronic back pain and failed back surgery syndrome. Two of the 16 studies were prospective controlled trials, 8 were prospective trials without controls, and 6 were retrospective studies.
Both prospective, controlled trials (total of 62 patients) demonstrated statistically significant (P<.05) results with SCS. One measured subjective pain and the other used crossover to the other treatment arm (SCS vs surgery) as a marker for treatment failure.
Consider the side effects
SCS isn’t without side effects. Cameron’s systematic review of 51 SCS studies reported rates for a number of complications ( TABLE ).2 The most common complication was lead migration—displacement of the spinal electrodes that can cause pain to recur.
TABLE
Major complications of SCS
| Complication | Rate |
|---|---|
| Lead migration | 13.2% |
| Lead breakage | 9.1% |
| Infection | 3.4% |
| Hardware malfunction | 2.9% |
| Unwanted stimulation | 2.4% |
| Battery failure | 1.6% |
| Pain over implant | 0.9% |
| SCS, spinal cord stimulation. | |
| Adapted from: Cameron T, et al. J Neurosurg.2 | |
Recommendations
Evidence-based guidelines for interventional techniques to control chronic pain, published in the January 2007 edition of Pain Physician, classify indications for SCS as follows:3
Strong indication: complex regional pain syndrome (CRPS)
Moderate indication: failed back surgery syndrome, chronic low back pain, and chronic lower extremity pain.
The Society of British Neurological Surgeons lists the following conditions as “good indications” for SCS: failed back surgery syndrome, CRPS, neuropathic pain from peripheral nerve damage, pain secondary to peripheral vascular disease, refractory angina, and brachial plexopathy.4
1. North RB, Kidd DH, Farrokhi F, et al. Spinal cord stimulation versus repeated lumbosacral spine surgery for chronic pain: a randomized, controlled trial. Neurosurgery. 2005;56:98-106.
2. Cameron T. Safety and efficacy of spinal cord stimulation for the treatment of chronic pain: a 20-year literature review. J Neurosurg. 2004;100(suppl 3 Spine):254-267.
3. Boswell MV, Trescot AM, Datta S, et al. American Society of Interventional Pain Physicians Interventional techniques: evidence-based practice guidelines in the management of chronic spinal pain. Pain Physician. 2007;10:7-111.
4. Society of British Neurological Surgeons/British Pain Society Spinal Cord Stimulation for the Management of Pain: Recommendations for Best Clinical Practice. London: British Pain Society; 2009. Available at: www.britishpainsociety.org/book_scs_main.pdf. Accessed October 3, 2009.
1. North RB, Kidd DH, Farrokhi F, et al. Spinal cord stimulation versus repeated lumbosacral spine surgery for chronic pain: a randomized, controlled trial. Neurosurgery. 2005;56:98-106.
2. Cameron T. Safety and efficacy of spinal cord stimulation for the treatment of chronic pain: a 20-year literature review. J Neurosurg. 2004;100(suppl 3 Spine):254-267.
3. Boswell MV, Trescot AM, Datta S, et al. American Society of Interventional Pain Physicians Interventional techniques: evidence-based practice guidelines in the management of chronic spinal pain. Pain Physician. 2007;10:7-111.
4. Society of British Neurological Surgeons/British Pain Society Spinal Cord Stimulation for the Management of Pain: Recommendations for Best Clinical Practice. London: British Pain Society; 2009. Available at: www.britishpainsociety.org/book_scs_main.pdf. Accessed October 3, 2009.
Evidence-based answers from the Family Physicians Inquiries Network
Should you use antibiotics to treat acute otitis media in children?
IN MOST CASES, NO. Antibiotics are not necessary to treat uncomplicated acute otitis media (AOM) in an otherwise healthy child (strength of recommendation [SOR]: A, systematic review). Children younger than 2 years and children with bilateral infection, high fever, or vomiting may experience modest symptom relief from antibiotics (SOR: B, cohort studies).
No evidence supports any of the commonly used antibiotic regimens over another (SOR: A, meta-analysis). Amoxicillin (80-90 mg/kg per day in 2 divided doses) is the recommended first-line regimen (SOR: C, expert consensus). In otherwise healthy children, 5 days of therapy should be sufficient (SOR: A; systematic review).
Discourage the use of antihistamines and decongestants because of their lack of efficacy and safety concerns, especially in children younger than 2 years.2 Pain control with acetaminophen and ibuprofen and topical analgesic ear drops should always be part of the treatment plan. Finally, counsel parents carefully, when indicated, about the significant harms of passive smoke.
Vincent Lo, MD
San Joaquin Family Medicine, French Camp, Calif
Evidence summary
Otitis media is the most common outpatient diagnosis in children.3 Although these infections usually resolve without treatment, it is common practice in the United States to prescribe antibiotics.4
Antibiotic benefits are small in uncomplicated disease
A Cochrane review of 8 randomized controlled trials (RCTs)—6 double-blinded, 2287 children total—compared antibiotics with placebo for uncomplicated AOM in otherwise healthy children.5 The review showed that children treated with antibiotics were no less likely to have pain at 24 hours after starting therapy than untreated children. However, 7% fewer children who received antibiotics had pain at 2 to 7 days than unmedicated children (number needed to treat [NNT]=15; 95% confidence interval [CI], 11-24).
Children treated with antibiotics had no significant decrease in recurrence of AOM (mean 0.70 vs 0.63; 95% CI, -0.22 to 0.34; odds ratio [OR]=0.99) or hearing loss (reported by a combination of tympanometry and audiometry). They did have an increase in nausea, diarrhea, and rash, however. Only 1 case of mastoiditis was reported in the included studies.5
Of note, 2 of the studies showed a modest increase in failure rates of placebo treatment for children younger than 2 years and children with bilateral disease. Antibiotics may benefit these groups. Overall, both the potential benefits and harms of antibiotics for AOM are small.5
More on which children may benefit from antibiotics
A secondary analysis of cohorts from 6 RCTs (a total of 824 children untreated for AOM) identified age younger than 2 years (OR=2.07; 95% CI, 1.47-2.91; P<.0001) and bilateral disease (OR=1.70; 95% CI, 1.19-2.41; P=.003) as independent risk factors for pain and fever at 3 to 7 days of illness. However, the study did not address whether antibiotics would actually mitigate the risk factors.6
In another secondary analysis of cohorts from a single RCT (315 patients), children with high temperature or vomiting who were treated immediately with antibiotics were less likely to be in distress by day 3 of illness (32% immediate vs 53% delayed; P=.045; NNT=5) or have night disturbance (26% immediate vs 59% delayed; P=.002; NNT=3). The greatest benefit occurred among children younger than 2 years and children with bilateral infection (NNT=4). The outcomes were reported by parents, who were not blinded.7
One regimen is as effective as another
In meta-analyses of subsets of a systematic review that included 74 RCTs and 6 cohort studies, the 1- to 7-day clinical failure rate among children not given antibiotics for AOM was 19% (95% CI, 0.10-0.28). Patients treated with ampicillin or amoxicillin had a 2- to 7-dayclinical failure rate of 7% (NNT=8; 95% CI, 0.04-0.20). Pooled analyses did not show any difference in efficacy between comparisons of penicillin, ampicillin, amoxicillin (2 or 3 times daily; standard or high dose), amoxicillin-clavulanate, cefaclor, cefixime, ceftriaxone, azithromycin, and trimethoprim-sulfamethoxazole.
An 8% higher incidence of diarrhea was noted for cefixime compared with amoxicillin (number needed to harm=12; 95% CI, 0.04-0.13). Azithromycin had a 19% lower adverse event rate than amoxicillin-clavulanate (NNT=5; 95% CI, 0.09-0.29).8
Five days of treatment are as good as 10
A 2000 Cochrane review found that 5 days of antibiotic therapy was as effective as a 10-day course of treatment in otherwise healthy children with uncomplicated AOM. A slight increase in signs, symptoms, relapse, or reinfection among children receiving 5 days of antibiotics was noted at 8 to 18 days after treatment (OR=1.52; 95% CI, 1.17-1.98), but the finding was no longer statistically significant at 30 days (OR=1.22; 95% CI, 0.98-1.54).9
Recommendations
The American Academy of Pediatrics recommends amoxicillin 80 to 90 mg/kg per day in 2 divided doses for:
- all children younger than 6 months with AOM
- children 6 to 24 months old with a certain diagnosis of AOM (rapid onset, signs of middle-ear effusion, and signs and symptoms of middle-ear inflammation) or severe illness (moderate to severe otalgia or fever ≥102.2°F [39°C])
- children older than 24 months with severe illness.
All other children may be observed if the caregiver consents and is able to monitor the child and if systems are in place for follow-up communication, reevaluation, or access to medication.
Children with a non-type-I penicillin allergy can be given a second- or third-generation cephalosporin, such as cefdinir (14 mg/kg per day in 1 or 2 doses), cefpodoxime (10 mg/kg per day in 1 dose), or cefuroxime (30 mg/kg per day in 2 divided doses). If the child is at high risk of anaphylaxis, 2 acceptable options are azithromycin (10 mg/kg on day 1 followed by 5 mg/kg per day for 4 days as a single daily dose) or clarithromycin (15 mg/kg per day in 2 divided doses).
Amoxicillin should not be given to children at risk for highly amoxicillin-resistant organisms (eg, children who have had antibiotics in the previous 30 days, concomitant purulent conjunctivitis, chronic prophylactic amoxicillin). The recommended alternative is high-dose amoxicillin-clavulanate (90 mg/kg per day of amoxicillin and 6.4 mg/kg per day of clavulanate in 2 divided doses).4
1. Siegel RM, Kiely M, Bien JP, et al. Treatment of otitis media with observation and a safety-net antibiotic prescription. Pediatrics. 2003;112(3 pt 1):527-531.
2. Griffin GH, Flynn C, Bailey RE, et al. Antihistamines and/or decongestants for otitis media with effusion (OME) in children. Cochrane Database Syst Rev. 2006;(4):CD003423.-
3. Bondy J, Berman S, Glazner J, et al. Direct expenditures related to otitis media diagnoses: extrapolations from a pediatric medicaid cohort. Pediatrics. 2000;105:e72.-
4. American Academy of Pediatrics Subcommittee on Management of Acute Otitis Media. Diagnosis and management of acute otitis media. Pediatrics. 2004;113:1451-1465.
5. Glasziou PP, Del Mar CB, Sanders SL, et al. Antibiotics for acute otitis media in children. Cochrane Database Syst Rev. 2004;(1):CD000219.-
6. Rovers MM, Glasziou P, Appelman CL, et al. Predictors of pain and/or fever at 3 to 7 days for children with acute otitis media not treated initially with antibiotics: a meta-analysis of individual patient data. Pediatrics. 2007;119:579-585.
7. Little P, Gould C, Moore M, et al. Predictors of poor outcomes and benefits from antibiotics in children with acute otitis media: pragmatic randomised trial. BMJ. 2002;325:22-27.
8. Takata Gl, Chan LS, Shekelle P, et al. Evidence assessment of management of acute otitis media: I. The role of antibiotics in treatment of uncomplicated acute otitis media. Pediatrics. 2001;108:239-247.
9. Kozyrskyj AL, Hildes-Ripstein GE, Longstaffe SE, et al. Short-course antibiotics for acute otitis media. Cochrane Database Syst Rev. 2000;(2):CD001095.-
IN MOST CASES, NO. Antibiotics are not necessary to treat uncomplicated acute otitis media (AOM) in an otherwise healthy child (strength of recommendation [SOR]: A, systematic review). Children younger than 2 years and children with bilateral infection, high fever, or vomiting may experience modest symptom relief from antibiotics (SOR: B, cohort studies).
No evidence supports any of the commonly used antibiotic regimens over another (SOR: A, meta-analysis). Amoxicillin (80-90 mg/kg per day in 2 divided doses) is the recommended first-line regimen (SOR: C, expert consensus). In otherwise healthy children, 5 days of therapy should be sufficient (SOR: A; systematic review).
Discourage the use of antihistamines and decongestants because of their lack of efficacy and safety concerns, especially in children younger than 2 years.2 Pain control with acetaminophen and ibuprofen and topical analgesic ear drops should always be part of the treatment plan. Finally, counsel parents carefully, when indicated, about the significant harms of passive smoke.
Vincent Lo, MD
San Joaquin Family Medicine, French Camp, Calif
Evidence summary
Otitis media is the most common outpatient diagnosis in children.3 Although these infections usually resolve without treatment, it is common practice in the United States to prescribe antibiotics.4
Antibiotic benefits are small in uncomplicated disease
A Cochrane review of 8 randomized controlled trials (RCTs)—6 double-blinded, 2287 children total—compared antibiotics with placebo for uncomplicated AOM in otherwise healthy children.5 The review showed that children treated with antibiotics were no less likely to have pain at 24 hours after starting therapy than untreated children. However, 7% fewer children who received antibiotics had pain at 2 to 7 days than unmedicated children (number needed to treat [NNT]=15; 95% confidence interval [CI], 11-24).
Children treated with antibiotics had no significant decrease in recurrence of AOM (mean 0.70 vs 0.63; 95% CI, -0.22 to 0.34; odds ratio [OR]=0.99) or hearing loss (reported by a combination of tympanometry and audiometry). They did have an increase in nausea, diarrhea, and rash, however. Only 1 case of mastoiditis was reported in the included studies.5
Of note, 2 of the studies showed a modest increase in failure rates of placebo treatment for children younger than 2 years and children with bilateral disease. Antibiotics may benefit these groups. Overall, both the potential benefits and harms of antibiotics for AOM are small.5
More on which children may benefit from antibiotics
A secondary analysis of cohorts from 6 RCTs (a total of 824 children untreated for AOM) identified age younger than 2 years (OR=2.07; 95% CI, 1.47-2.91; P<.0001) and bilateral disease (OR=1.70; 95% CI, 1.19-2.41; P=.003) as independent risk factors for pain and fever at 3 to 7 days of illness. However, the study did not address whether antibiotics would actually mitigate the risk factors.6
In another secondary analysis of cohorts from a single RCT (315 patients), children with high temperature or vomiting who were treated immediately with antibiotics were less likely to be in distress by day 3 of illness (32% immediate vs 53% delayed; P=.045; NNT=5) or have night disturbance (26% immediate vs 59% delayed; P=.002; NNT=3). The greatest benefit occurred among children younger than 2 years and children with bilateral infection (NNT=4). The outcomes were reported by parents, who were not blinded.7
One regimen is as effective as another
In meta-analyses of subsets of a systematic review that included 74 RCTs and 6 cohort studies, the 1- to 7-day clinical failure rate among children not given antibiotics for AOM was 19% (95% CI, 0.10-0.28). Patients treated with ampicillin or amoxicillin had a 2- to 7-dayclinical failure rate of 7% (NNT=8; 95% CI, 0.04-0.20). Pooled analyses did not show any difference in efficacy between comparisons of penicillin, ampicillin, amoxicillin (2 or 3 times daily; standard or high dose), amoxicillin-clavulanate, cefaclor, cefixime, ceftriaxone, azithromycin, and trimethoprim-sulfamethoxazole.
An 8% higher incidence of diarrhea was noted for cefixime compared with amoxicillin (number needed to harm=12; 95% CI, 0.04-0.13). Azithromycin had a 19% lower adverse event rate than amoxicillin-clavulanate (NNT=5; 95% CI, 0.09-0.29).8
Five days of treatment are as good as 10
A 2000 Cochrane review found that 5 days of antibiotic therapy was as effective as a 10-day course of treatment in otherwise healthy children with uncomplicated AOM. A slight increase in signs, symptoms, relapse, or reinfection among children receiving 5 days of antibiotics was noted at 8 to 18 days after treatment (OR=1.52; 95% CI, 1.17-1.98), but the finding was no longer statistically significant at 30 days (OR=1.22; 95% CI, 0.98-1.54).9
Recommendations
The American Academy of Pediatrics recommends amoxicillin 80 to 90 mg/kg per day in 2 divided doses for:
- all children younger than 6 months with AOM
- children 6 to 24 months old with a certain diagnosis of AOM (rapid onset, signs of middle-ear effusion, and signs and symptoms of middle-ear inflammation) or severe illness (moderate to severe otalgia or fever ≥102.2°F [39°C])
- children older than 24 months with severe illness.
All other children may be observed if the caregiver consents and is able to monitor the child and if systems are in place for follow-up communication, reevaluation, or access to medication.
Children with a non-type-I penicillin allergy can be given a second- or third-generation cephalosporin, such as cefdinir (14 mg/kg per day in 1 or 2 doses), cefpodoxime (10 mg/kg per day in 1 dose), or cefuroxime (30 mg/kg per day in 2 divided doses). If the child is at high risk of anaphylaxis, 2 acceptable options are azithromycin (10 mg/kg on day 1 followed by 5 mg/kg per day for 4 days as a single daily dose) or clarithromycin (15 mg/kg per day in 2 divided doses).
Amoxicillin should not be given to children at risk for highly amoxicillin-resistant organisms (eg, children who have had antibiotics in the previous 30 days, concomitant purulent conjunctivitis, chronic prophylactic amoxicillin). The recommended alternative is high-dose amoxicillin-clavulanate (90 mg/kg per day of amoxicillin and 6.4 mg/kg per day of clavulanate in 2 divided doses).4
IN MOST CASES, NO. Antibiotics are not necessary to treat uncomplicated acute otitis media (AOM) in an otherwise healthy child (strength of recommendation [SOR]: A, systematic review). Children younger than 2 years and children with bilateral infection, high fever, or vomiting may experience modest symptom relief from antibiotics (SOR: B, cohort studies).
No evidence supports any of the commonly used antibiotic regimens over another (SOR: A, meta-analysis). Amoxicillin (80-90 mg/kg per day in 2 divided doses) is the recommended first-line regimen (SOR: C, expert consensus). In otherwise healthy children, 5 days of therapy should be sufficient (SOR: A; systematic review).
Discourage the use of antihistamines and decongestants because of their lack of efficacy and safety concerns, especially in children younger than 2 years.2 Pain control with acetaminophen and ibuprofen and topical analgesic ear drops should always be part of the treatment plan. Finally, counsel parents carefully, when indicated, about the significant harms of passive smoke.
Vincent Lo, MD
San Joaquin Family Medicine, French Camp, Calif
Evidence summary
Otitis media is the most common outpatient diagnosis in children.3 Although these infections usually resolve without treatment, it is common practice in the United States to prescribe antibiotics.4
Antibiotic benefits are small in uncomplicated disease
A Cochrane review of 8 randomized controlled trials (RCTs)—6 double-blinded, 2287 children total—compared antibiotics with placebo for uncomplicated AOM in otherwise healthy children.5 The review showed that children treated with antibiotics were no less likely to have pain at 24 hours after starting therapy than untreated children. However, 7% fewer children who received antibiotics had pain at 2 to 7 days than unmedicated children (number needed to treat [NNT]=15; 95% confidence interval [CI], 11-24).
Children treated with antibiotics had no significant decrease in recurrence of AOM (mean 0.70 vs 0.63; 95% CI, -0.22 to 0.34; odds ratio [OR]=0.99) or hearing loss (reported by a combination of tympanometry and audiometry). They did have an increase in nausea, diarrhea, and rash, however. Only 1 case of mastoiditis was reported in the included studies.5
Of note, 2 of the studies showed a modest increase in failure rates of placebo treatment for children younger than 2 years and children with bilateral disease. Antibiotics may benefit these groups. Overall, both the potential benefits and harms of antibiotics for AOM are small.5
More on which children may benefit from antibiotics
A secondary analysis of cohorts from 6 RCTs (a total of 824 children untreated for AOM) identified age younger than 2 years (OR=2.07; 95% CI, 1.47-2.91; P<.0001) and bilateral disease (OR=1.70; 95% CI, 1.19-2.41; P=.003) as independent risk factors for pain and fever at 3 to 7 days of illness. However, the study did not address whether antibiotics would actually mitigate the risk factors.6
In another secondary analysis of cohorts from a single RCT (315 patients), children with high temperature or vomiting who were treated immediately with antibiotics were less likely to be in distress by day 3 of illness (32% immediate vs 53% delayed; P=.045; NNT=5) or have night disturbance (26% immediate vs 59% delayed; P=.002; NNT=3). The greatest benefit occurred among children younger than 2 years and children with bilateral infection (NNT=4). The outcomes were reported by parents, who were not blinded.7
One regimen is as effective as another
In meta-analyses of subsets of a systematic review that included 74 RCTs and 6 cohort studies, the 1- to 7-day clinical failure rate among children not given antibiotics for AOM was 19% (95% CI, 0.10-0.28). Patients treated with ampicillin or amoxicillin had a 2- to 7-dayclinical failure rate of 7% (NNT=8; 95% CI, 0.04-0.20). Pooled analyses did not show any difference in efficacy between comparisons of penicillin, ampicillin, amoxicillin (2 or 3 times daily; standard or high dose), amoxicillin-clavulanate, cefaclor, cefixime, ceftriaxone, azithromycin, and trimethoprim-sulfamethoxazole.
An 8% higher incidence of diarrhea was noted for cefixime compared with amoxicillin (number needed to harm=12; 95% CI, 0.04-0.13). Azithromycin had a 19% lower adverse event rate than amoxicillin-clavulanate (NNT=5; 95% CI, 0.09-0.29).8
Five days of treatment are as good as 10
A 2000 Cochrane review found that 5 days of antibiotic therapy was as effective as a 10-day course of treatment in otherwise healthy children with uncomplicated AOM. A slight increase in signs, symptoms, relapse, or reinfection among children receiving 5 days of antibiotics was noted at 8 to 18 days after treatment (OR=1.52; 95% CI, 1.17-1.98), but the finding was no longer statistically significant at 30 days (OR=1.22; 95% CI, 0.98-1.54).9
Recommendations
The American Academy of Pediatrics recommends amoxicillin 80 to 90 mg/kg per day in 2 divided doses for:
- all children younger than 6 months with AOM
- children 6 to 24 months old with a certain diagnosis of AOM (rapid onset, signs of middle-ear effusion, and signs and symptoms of middle-ear inflammation) or severe illness (moderate to severe otalgia or fever ≥102.2°F [39°C])
- children older than 24 months with severe illness.
All other children may be observed if the caregiver consents and is able to monitor the child and if systems are in place for follow-up communication, reevaluation, or access to medication.
Children with a non-type-I penicillin allergy can be given a second- or third-generation cephalosporin, such as cefdinir (14 mg/kg per day in 1 or 2 doses), cefpodoxime (10 mg/kg per day in 1 dose), or cefuroxime (30 mg/kg per day in 2 divided doses). If the child is at high risk of anaphylaxis, 2 acceptable options are azithromycin (10 mg/kg on day 1 followed by 5 mg/kg per day for 4 days as a single daily dose) or clarithromycin (15 mg/kg per day in 2 divided doses).
Amoxicillin should not be given to children at risk for highly amoxicillin-resistant organisms (eg, children who have had antibiotics in the previous 30 days, concomitant purulent conjunctivitis, chronic prophylactic amoxicillin). The recommended alternative is high-dose amoxicillin-clavulanate (90 mg/kg per day of amoxicillin and 6.4 mg/kg per day of clavulanate in 2 divided doses).4
1. Siegel RM, Kiely M, Bien JP, et al. Treatment of otitis media with observation and a safety-net antibiotic prescription. Pediatrics. 2003;112(3 pt 1):527-531.
2. Griffin GH, Flynn C, Bailey RE, et al. Antihistamines and/or decongestants for otitis media with effusion (OME) in children. Cochrane Database Syst Rev. 2006;(4):CD003423.-
3. Bondy J, Berman S, Glazner J, et al. Direct expenditures related to otitis media diagnoses: extrapolations from a pediatric medicaid cohort. Pediatrics. 2000;105:e72.-
4. American Academy of Pediatrics Subcommittee on Management of Acute Otitis Media. Diagnosis and management of acute otitis media. Pediatrics. 2004;113:1451-1465.
5. Glasziou PP, Del Mar CB, Sanders SL, et al. Antibiotics for acute otitis media in children. Cochrane Database Syst Rev. 2004;(1):CD000219.-
6. Rovers MM, Glasziou P, Appelman CL, et al. Predictors of pain and/or fever at 3 to 7 days for children with acute otitis media not treated initially with antibiotics: a meta-analysis of individual patient data. Pediatrics. 2007;119:579-585.
7. Little P, Gould C, Moore M, et al. Predictors of poor outcomes and benefits from antibiotics in children with acute otitis media: pragmatic randomised trial. BMJ. 2002;325:22-27.
8. Takata Gl, Chan LS, Shekelle P, et al. Evidence assessment of management of acute otitis media: I. The role of antibiotics in treatment of uncomplicated acute otitis media. Pediatrics. 2001;108:239-247.
9. Kozyrskyj AL, Hildes-Ripstein GE, Longstaffe SE, et al. Short-course antibiotics for acute otitis media. Cochrane Database Syst Rev. 2000;(2):CD001095.-
1. Siegel RM, Kiely M, Bien JP, et al. Treatment of otitis media with observation and a safety-net antibiotic prescription. Pediatrics. 2003;112(3 pt 1):527-531.
2. Griffin GH, Flynn C, Bailey RE, et al. Antihistamines and/or decongestants for otitis media with effusion (OME) in children. Cochrane Database Syst Rev. 2006;(4):CD003423.-
3. Bondy J, Berman S, Glazner J, et al. Direct expenditures related to otitis media diagnoses: extrapolations from a pediatric medicaid cohort. Pediatrics. 2000;105:e72.-
4. American Academy of Pediatrics Subcommittee on Management of Acute Otitis Media. Diagnosis and management of acute otitis media. Pediatrics. 2004;113:1451-1465.
5. Glasziou PP, Del Mar CB, Sanders SL, et al. Antibiotics for acute otitis media in children. Cochrane Database Syst Rev. 2004;(1):CD000219.-
6. Rovers MM, Glasziou P, Appelman CL, et al. Predictors of pain and/or fever at 3 to 7 days for children with acute otitis media not treated initially with antibiotics: a meta-analysis of individual patient data. Pediatrics. 2007;119:579-585.
7. Little P, Gould C, Moore M, et al. Predictors of poor outcomes and benefits from antibiotics in children with acute otitis media: pragmatic randomised trial. BMJ. 2002;325:22-27.
8. Takata Gl, Chan LS, Shekelle P, et al. Evidence assessment of management of acute otitis media: I. The role of antibiotics in treatment of uncomplicated acute otitis media. Pediatrics. 2001;108:239-247.
9. Kozyrskyj AL, Hildes-Ripstein GE, Longstaffe SE, et al. Short-course antibiotics for acute otitis media. Cochrane Database Syst Rev. 2000;(2):CD001095.-
Evidence-based answers from the Family Physicians Inquiries Network
Which interventions are best for alleviating nipple pain in nursing mothers?
THE BEST INTERVENTION IS EDUCATION on proper positioning and attachment of the infant (strength of recommendation [SOR]: A, a systematic review of randomized controlled trials [RCTs]). No single topical preparation has been consistently demonstrated to be superior to others for relieving nipple pain (SOR: B, inconsistent RCTs).
Topical agents that show some evidence of benefit include expressed breast milk, lanolin, warm water compresses, tea bag compresses, hydrogel dressings, a chlorhexidinealcohol spray, and a polyethylene film dressing (SOR: B, inconsistent RCTs). Several studies found these interventions to be equivalent to basic breast care, including keeping the nipple clean and dry (SOR: B, RCTs).
One type of glycerin-based hydrogel dressing was associated with an increased incidence of breast infections (SOR: B, inconsistent RCTs).
Evidence summary
Nipple pain during the first week of breastfeeding is common. Some studies report a prevalence as high as 96%.1 Because nipple pain has been identified as an important factor in a woman’s decision to discontinue breastfeeding, preventing or treating it is important not only to increase individual women’s comfort but also to promote breastfeeding generally.
We identified 2 systematic reviews and 3 additional RCTs of interventions to treat or prevent nipple pain. Most studies included women serving as their own control, randomizing 1 breast to intervention and the other to control treatment. The remainder of the studies randomized women to either the intervention or control group. Major limitations of the studies included their generally small size and lack of blinding of participants to their treatment group. In only 1 study were the participants blinded.1,2
Women who receive education have less pain
Two studies of educational sessions, 1 antenatal (N=75) and 1 immediately postnatal (N=160), reported less nipple pain in the intervention groups (number needed to treat [NNT]=1.6 and 5.6, respectively). The antenatal education study demonstrated higher continuation of breastfeeding at 6 weeks postpartum in the intervention group (NNT=4.5), whereas the postnatal study showed no significant difference in continuation of breastfeeding in the intervention group at 6 weeks, 3 months, and 6 months.1
No one topical agent is superior
No single topical agent emerged as clearly superior to others for preventing or treating nipple pain. Warm water compresses have the most data to support their use: 2 trials showed superiority to other agents or no treatment, 3 trials demonstrated equivalence to other agents or no treatment, and no trial showed inferiority to other agents.
Chlorhexidine spray was superior to a distilled water spray in 1 small RCT, the only double-blind study identified. A polyethylene film dressing decreased nipple pain in a single trial, but most women found it uncomfortable to remove.
Hydrogel dressing associated with infection
The only topical agent found to have any detrimental effect was a glycerin-based hydrogel dressing that was associated with an increased incidence of breast infections.1 The TABLE summarizes results of trials of topical agents for the treatment or prevention of nipple pain.1,3,4
Breast shields were ineffective in 1 RCT.1 In another RCT performed in Sweden, women who received peripartum care in a birthing center had more nipple pain than women who delivered in a traditional hospital setting (NNT=16).5
TABLE
How topical agents compare for treating or preventing nipple pain
| Agent* | Positive results | Equivalent results | Negative results |
|---|---|---|---|
| Expressed mother’s milk (EMM) | Superior to lanolin3 | Equivalent to warm water compresses and keeping nipples dry and clean1 Equivalent to tea bag compress1 Equivalent to lanolin1 Equivalent to lanolin, warm water compress, and no treatment1 Equivalent to no treatment3 | Inferior to warm water compress1 |
| Lanolin | Superior to hydrogel dressing1 | Equivalent to Emm1 Equivalent to warm water compress, Emm, and no treatment1 Equivalent to tea bag compress and no treatment1 Equivalent to no treatment1 Equivalent to hydrogel dressing and no treatment4 | Inferior to hydrogel dressing1 Inferior to Emm and no treatment3 |
| Hydrogel dressing | Superior to lanolin1 | Equivalent to lanolin and no treatment4 | Inferior to lanolin, associated with an increased rate of breast infections1 |
| Tea bag compress | Superior to no treatment1 | Equivalent to Emm1 Equivalent to warm water compress1 Equivalent to lanolin and no treatment1 | Inferior to warm water compress1 |
| Warm water compress | Superior to tea bag compress and Emm1 Superior to no treatment1 | Equivalent to Emm and keeping nipples dry and clean1 Equivalent to tea bag compress1 Equivalent to lanolin, Emm, and no treatment1 | |
| Chlorhexidine spray | Superior to distilled water spray1 | ||
| Polyethylene film dressing | Superior to no treatment1 | ||
| *Comparison treatments may appear more than once, based on results of studies found in the systematic review | |||
Recommendations
The International Lactation Consultant Association states that nipple pain is often the result of ineffective positioning and latch.6 The group recommends anticipatory guidance to prevent nipple pain. Additionally, a thorough clinical assessment of the nipple is indicated to rule out other causes, such as bacterial or fungal infection.
1. Morland-Schultz K, Hill PD. Prevention of and therapies for nipple pain: a systematic review. J Obstet Gynecol Neonatal Nurs. 2005;34:428-437.
2. Page T, Lockwood C, Guest K. Management of nipple pain and/or trauma associated with breastfeeding: a systematic review. JBI Rep. 2003;1:127-147.
3. Mohammadzadeh A, Farhat A, Esmaeily H. The effect of breast milk and lanolin on sore nipples. Saudi Med J. 2005;26:1231-1234.
4. Cadwell K, Turner-Maffei C, Blair A, et al. Pain reduction and treatment of sore nipples in nursing mothers. J Perinat Educ. 2004;13:29-35.
5. Waldenstrom U, Nilsson CA. No effect of birth centre care on either duration or experience of breastfeeding, but more complications: findings from a randomised controlled trial. Midwifery. 1994;10:8-17.
6. International Lactation Consultant Association. Clinical Guidelines for the Establishment of Exclusive Breastfeeding. Raleigh, NC: International Lactation Consultant Association; 2005. Available at: www.guideline.gov/summary/summary.aspx?doc_id=7662. Accessed July 5, 2009.
THE BEST INTERVENTION IS EDUCATION on proper positioning and attachment of the infant (strength of recommendation [SOR]: A, a systematic review of randomized controlled trials [RCTs]). No single topical preparation has been consistently demonstrated to be superior to others for relieving nipple pain (SOR: B, inconsistent RCTs).
Topical agents that show some evidence of benefit include expressed breast milk, lanolin, warm water compresses, tea bag compresses, hydrogel dressings, a chlorhexidinealcohol spray, and a polyethylene film dressing (SOR: B, inconsistent RCTs). Several studies found these interventions to be equivalent to basic breast care, including keeping the nipple clean and dry (SOR: B, RCTs).
One type of glycerin-based hydrogel dressing was associated with an increased incidence of breast infections (SOR: B, inconsistent RCTs).
Evidence summary
Nipple pain during the first week of breastfeeding is common. Some studies report a prevalence as high as 96%.1 Because nipple pain has been identified as an important factor in a woman’s decision to discontinue breastfeeding, preventing or treating it is important not only to increase individual women’s comfort but also to promote breastfeeding generally.
We identified 2 systematic reviews and 3 additional RCTs of interventions to treat or prevent nipple pain. Most studies included women serving as their own control, randomizing 1 breast to intervention and the other to control treatment. The remainder of the studies randomized women to either the intervention or control group. Major limitations of the studies included their generally small size and lack of blinding of participants to their treatment group. In only 1 study were the participants blinded.1,2
Women who receive education have less pain
Two studies of educational sessions, 1 antenatal (N=75) and 1 immediately postnatal (N=160), reported less nipple pain in the intervention groups (number needed to treat [NNT]=1.6 and 5.6, respectively). The antenatal education study demonstrated higher continuation of breastfeeding at 6 weeks postpartum in the intervention group (NNT=4.5), whereas the postnatal study showed no significant difference in continuation of breastfeeding in the intervention group at 6 weeks, 3 months, and 6 months.1
No one topical agent is superior
No single topical agent emerged as clearly superior to others for preventing or treating nipple pain. Warm water compresses have the most data to support their use: 2 trials showed superiority to other agents or no treatment, 3 trials demonstrated equivalence to other agents or no treatment, and no trial showed inferiority to other agents.
Chlorhexidine spray was superior to a distilled water spray in 1 small RCT, the only double-blind study identified. A polyethylene film dressing decreased nipple pain in a single trial, but most women found it uncomfortable to remove.
Hydrogel dressing associated with infection
The only topical agent found to have any detrimental effect was a glycerin-based hydrogel dressing that was associated with an increased incidence of breast infections.1 The TABLE summarizes results of trials of topical agents for the treatment or prevention of nipple pain.1,3,4
Breast shields were ineffective in 1 RCT.1 In another RCT performed in Sweden, women who received peripartum care in a birthing center had more nipple pain than women who delivered in a traditional hospital setting (NNT=16).5
TABLE
How topical agents compare for treating or preventing nipple pain
| Agent* | Positive results | Equivalent results | Negative results |
|---|---|---|---|
| Expressed mother’s milk (EMM) | Superior to lanolin3 | Equivalent to warm water compresses and keeping nipples dry and clean1 Equivalent to tea bag compress1 Equivalent to lanolin1 Equivalent to lanolin, warm water compress, and no treatment1 Equivalent to no treatment3 | Inferior to warm water compress1 |
| Lanolin | Superior to hydrogel dressing1 | Equivalent to Emm1 Equivalent to warm water compress, Emm, and no treatment1 Equivalent to tea bag compress and no treatment1 Equivalent to no treatment1 Equivalent to hydrogel dressing and no treatment4 | Inferior to hydrogel dressing1 Inferior to Emm and no treatment3 |
| Hydrogel dressing | Superior to lanolin1 | Equivalent to lanolin and no treatment4 | Inferior to lanolin, associated with an increased rate of breast infections1 |
| Tea bag compress | Superior to no treatment1 | Equivalent to Emm1 Equivalent to warm water compress1 Equivalent to lanolin and no treatment1 | Inferior to warm water compress1 |
| Warm water compress | Superior to tea bag compress and Emm1 Superior to no treatment1 | Equivalent to Emm and keeping nipples dry and clean1 Equivalent to tea bag compress1 Equivalent to lanolin, Emm, and no treatment1 | |
| Chlorhexidine spray | Superior to distilled water spray1 | ||
| Polyethylene film dressing | Superior to no treatment1 | ||
| *Comparison treatments may appear more than once, based on results of studies found in the systematic review | |||
Recommendations
The International Lactation Consultant Association states that nipple pain is often the result of ineffective positioning and latch.6 The group recommends anticipatory guidance to prevent nipple pain. Additionally, a thorough clinical assessment of the nipple is indicated to rule out other causes, such as bacterial or fungal infection.
THE BEST INTERVENTION IS EDUCATION on proper positioning and attachment of the infant (strength of recommendation [SOR]: A, a systematic review of randomized controlled trials [RCTs]). No single topical preparation has been consistently demonstrated to be superior to others for relieving nipple pain (SOR: B, inconsistent RCTs).
Topical agents that show some evidence of benefit include expressed breast milk, lanolin, warm water compresses, tea bag compresses, hydrogel dressings, a chlorhexidinealcohol spray, and a polyethylene film dressing (SOR: B, inconsistent RCTs). Several studies found these interventions to be equivalent to basic breast care, including keeping the nipple clean and dry (SOR: B, RCTs).
One type of glycerin-based hydrogel dressing was associated with an increased incidence of breast infections (SOR: B, inconsistent RCTs).
Evidence summary
Nipple pain during the first week of breastfeeding is common. Some studies report a prevalence as high as 96%.1 Because nipple pain has been identified as an important factor in a woman’s decision to discontinue breastfeeding, preventing or treating it is important not only to increase individual women’s comfort but also to promote breastfeeding generally.
We identified 2 systematic reviews and 3 additional RCTs of interventions to treat or prevent nipple pain. Most studies included women serving as their own control, randomizing 1 breast to intervention and the other to control treatment. The remainder of the studies randomized women to either the intervention or control group. Major limitations of the studies included their generally small size and lack of blinding of participants to their treatment group. In only 1 study were the participants blinded.1,2
Women who receive education have less pain
Two studies of educational sessions, 1 antenatal (N=75) and 1 immediately postnatal (N=160), reported less nipple pain in the intervention groups (number needed to treat [NNT]=1.6 and 5.6, respectively). The antenatal education study demonstrated higher continuation of breastfeeding at 6 weeks postpartum in the intervention group (NNT=4.5), whereas the postnatal study showed no significant difference in continuation of breastfeeding in the intervention group at 6 weeks, 3 months, and 6 months.1
No one topical agent is superior
No single topical agent emerged as clearly superior to others for preventing or treating nipple pain. Warm water compresses have the most data to support their use: 2 trials showed superiority to other agents or no treatment, 3 trials demonstrated equivalence to other agents or no treatment, and no trial showed inferiority to other agents.
Chlorhexidine spray was superior to a distilled water spray in 1 small RCT, the only double-blind study identified. A polyethylene film dressing decreased nipple pain in a single trial, but most women found it uncomfortable to remove.
Hydrogel dressing associated with infection
The only topical agent found to have any detrimental effect was a glycerin-based hydrogel dressing that was associated with an increased incidence of breast infections.1 The TABLE summarizes results of trials of topical agents for the treatment or prevention of nipple pain.1,3,4
Breast shields were ineffective in 1 RCT.1 In another RCT performed in Sweden, women who received peripartum care in a birthing center had more nipple pain than women who delivered in a traditional hospital setting (NNT=16).5
TABLE
How topical agents compare for treating or preventing nipple pain
| Agent* | Positive results | Equivalent results | Negative results |
|---|---|---|---|
| Expressed mother’s milk (EMM) | Superior to lanolin3 | Equivalent to warm water compresses and keeping nipples dry and clean1 Equivalent to tea bag compress1 Equivalent to lanolin1 Equivalent to lanolin, warm water compress, and no treatment1 Equivalent to no treatment3 | Inferior to warm water compress1 |
| Lanolin | Superior to hydrogel dressing1 | Equivalent to Emm1 Equivalent to warm water compress, Emm, and no treatment1 Equivalent to tea bag compress and no treatment1 Equivalent to no treatment1 Equivalent to hydrogel dressing and no treatment4 | Inferior to hydrogel dressing1 Inferior to Emm and no treatment3 |
| Hydrogel dressing | Superior to lanolin1 | Equivalent to lanolin and no treatment4 | Inferior to lanolin, associated with an increased rate of breast infections1 |
| Tea bag compress | Superior to no treatment1 | Equivalent to Emm1 Equivalent to warm water compress1 Equivalent to lanolin and no treatment1 | Inferior to warm water compress1 |
| Warm water compress | Superior to tea bag compress and Emm1 Superior to no treatment1 | Equivalent to Emm and keeping nipples dry and clean1 Equivalent to tea bag compress1 Equivalent to lanolin, Emm, and no treatment1 | |
| Chlorhexidine spray | Superior to distilled water spray1 | ||
| Polyethylene film dressing | Superior to no treatment1 | ||
| *Comparison treatments may appear more than once, based on results of studies found in the systematic review | |||
Recommendations
The International Lactation Consultant Association states that nipple pain is often the result of ineffective positioning and latch.6 The group recommends anticipatory guidance to prevent nipple pain. Additionally, a thorough clinical assessment of the nipple is indicated to rule out other causes, such as bacterial or fungal infection.
1. Morland-Schultz K, Hill PD. Prevention of and therapies for nipple pain: a systematic review. J Obstet Gynecol Neonatal Nurs. 2005;34:428-437.
2. Page T, Lockwood C, Guest K. Management of nipple pain and/or trauma associated with breastfeeding: a systematic review. JBI Rep. 2003;1:127-147.
3. Mohammadzadeh A, Farhat A, Esmaeily H. The effect of breast milk and lanolin on sore nipples. Saudi Med J. 2005;26:1231-1234.
4. Cadwell K, Turner-Maffei C, Blair A, et al. Pain reduction and treatment of sore nipples in nursing mothers. J Perinat Educ. 2004;13:29-35.
5. Waldenstrom U, Nilsson CA. No effect of birth centre care on either duration or experience of breastfeeding, but more complications: findings from a randomised controlled trial. Midwifery. 1994;10:8-17.
6. International Lactation Consultant Association. Clinical Guidelines for the Establishment of Exclusive Breastfeeding. Raleigh, NC: International Lactation Consultant Association; 2005. Available at: www.guideline.gov/summary/summary.aspx?doc_id=7662. Accessed July 5, 2009.
1. Morland-Schultz K, Hill PD. Prevention of and therapies for nipple pain: a systematic review. J Obstet Gynecol Neonatal Nurs. 2005;34:428-437.
2. Page T, Lockwood C, Guest K. Management of nipple pain and/or trauma associated with breastfeeding: a systematic review. JBI Rep. 2003;1:127-147.
3. Mohammadzadeh A, Farhat A, Esmaeily H. The effect of breast milk and lanolin on sore nipples. Saudi Med J. 2005;26:1231-1234.
4. Cadwell K, Turner-Maffei C, Blair A, et al. Pain reduction and treatment of sore nipples in nursing mothers. J Perinat Educ. 2004;13:29-35.
5. Waldenstrom U, Nilsson CA. No effect of birth centre care on either duration or experience of breastfeeding, but more complications: findings from a randomised controlled trial. Midwifery. 1994;10:8-17.
6. International Lactation Consultant Association. Clinical Guidelines for the Establishment of Exclusive Breastfeeding. Raleigh, NC: International Lactation Consultant Association; 2005. Available at: www.guideline.gov/summary/summary.aspx?doc_id=7662. Accessed July 5, 2009.
Evidence-based answers from the Family Physicians Inquiries Network
Do OTC remedies relieve cough in acute URIs?
SOME DO. DEXTROMETHORPHAN (DM) for adults and honey for children provide some relief. DM may modestly decrease cough in adults compared with placebo (strength of recommendation [SOR]: B, systematic review of inconsistent or limited evidence). The data supporting zinc for the common cold are mixed (SOR: B, meta-analysis with inconsistent results). Antihistamines, antihistamine-decongestant combinations, and guaifenesin don’t provide greater relief than placebo in adults (SOR: B, systematic review of inconsistent or limited evidence).
In children, antihistamines, decongestants, DM, or combinations of them don’t relieve cough better than placebo (SOR: A, systematic review). Honey may modestly decrease frequency and severity of cough compared with DM or no treatment (SOR: B, small, randomized controlled trial [RCT]).
Clinical commentary
It appears that all of the common, troublesome symptoms of an upper respiratory infection can be managed just as well with over-the-counter (OTC) medications as with prescriptions: DM for cough; acetaminophen or naproxen sodium for fever and aches; decongestants or vapor rubs for nasal congestion. Spread the word!
It would be wonderful if the office visit for upper respiratory infection became a rarity—the health care system would save a lot of money. Presumably, patients would still come in wondering if they had something worse than a cold, but education during the first visit would help prevent repeat trips.
Jon O. Neher, MD
Valley Medical Center
Family Practice Residency,
University of Washington, Renton
Evidence summary
A Cochrane review found DM to be modestly effective in 2 of 3 studies.1 In the first study—a meta-analysis of 6 industry-sponsored RCTs of 710 adults—a single 30-mg dose of DM decreased coughing bouts by 12% (P=.004) and increased the time between bouts by 17 % (P=.002) in the 3 hours after treatment.
A second study of 3 successive industry-sponsored, blinded RCTs enrolling a total of 451 adults found that 30 mg of DM decreased cough counts between 19% and 36% (P<.05) over a 3-hour follow-up period. Neither of the 2 studies specified whether the outcome assessors were blinded to treatment groups.
A third double-blinded RCT evaluating a single 30-mg dose of DM in 43 adults during a 3-hour follow-up period showed no statistically significant improvement in cough outcomes compared with placebo.
A split decision on guaifenesin
The same Cochrane review also evaluated other medications for cough related to upper respiratory infection in adults.1 The results of 2 guaifenesin trials were split. In a double-blinded RCT of 239 adults, more patients taking guaifenesin reported decreased cough frequency and intensity (75% vs 31%; P<.01). However, another double-blinded RCT of 65 patients found guaifenesin to be no more effective than placebo in reducing subjective cough frequency.
Antihistamines don’t help, adding a decongestant isn’t much better
Three trials of antihistamines in a total of 1900 adults found that the drugs didn’t relieve cough symptoms more effectively than placebo. Antihistamine-decongestant combination trials produced split results. In 1 double-blinded RCT of 283 adults, loratadine-pseudoephedrine (5 and 120 mg, respectively) twice daily for 4 days didn’t decrease subjective cough scores more than placebo and was associated with more dry mouth, dizziness, headache, and insomnia (30% vs 21%; P value not reported).
Another partially double-blinded RCT of 73 adults reported that dexbrompheniramine-pseudoephedrine (6 and 120 mg, respectively) twice daily for 1 week decreased subjective cough severity (1.4 vs 2.0; P<.05) on a scale of 0 to 4 during days 3 to 5 of treatment. The combination was associated with increased dizziness and dry mouth, however (exact data not reported; P≤.01).
Codeine works no better than placebo
Two partially double-blinded RCTs of 163 adults found codeine (sold OTC in Canada) to be no more effective than placebo in relieving cough caused by the common cold.1
Zinc lozenges show mixed results
Zinc lozenges containing 13.3 mg of zinc acetate taken every 2 to 3 hours decreased the duration of cough from 5.35 to 2.14 days (P<.001) in a double-blinded placebo-controlled RCT of 50 adults.2 The most recent systematic review showed mixed results: Half the studies found no benefit for zinc in treating upper respiratory infection.3
In children, forget DM, antihistamines, decongestants
The previously mentioned Cochrane review1 also summarized studies in children. DM was no more effective than placebo for decreasing cough in 2 RCTs enrolling a total of 107 children. Another single-blinded RCT of 100 children showed that neither DM nor diphenhydramine relieved cough better than placebo.
Two RCTs involving a total of 237 children compared antihistamines with placebo. One double-blinded trial reported that clemastine and chlorpheniramine were no more effective than placebo. The other partially double-blinded trial found that diphenhydramine didn’t decrease cough frequency more than placebo.
Two double-blinded RCTs (total of 155 children) showed that antihistamine-decongestant combinations (brompheniramine-phenylpropanolamine and brompheniramine-phenylephrine-propanolamine) didn’t reduce cough more than placebo. No studies have evaluated guai-fenesin in children.1
Honey appears to help
In a partially double-blinded RCT (the “no treatment” group was not blinded) of 105 children, a single dose of buckwheat honey decreased cough frequency, as assessed by parents, by 1.89 points on the 7-point Likert scale compared with DM (1.39) and no treatment (0.92; P<.001). Overall improvement in symptom score averaged 10.71 out of a total 30 points for honey compared with 6.41 for no treatment (P=.04). Cough frequency and overall symptom scores for DM didn’t differ significantly from no treatment. Hyperactivity, nervousness, and insomnia were reported more often with honey (5 patients) than DM (2 patients) or no treatment (0 patients); (P=.04).4
Placebos work, but why?
In a review of 8 RCTs, the average reduction in cough in the placebo group (both capsules and syrups) was approximately 85% of that seen in the active medication group (range 56%-105%).5 Several factors may account for the efficacy of placebo, including lubrication of the pharynx by increased salivation caused by sweet or bitter vehicles. Sweet vehicles also may stimulate endogenous opioids that may suppress cough. In an unblinded RCT of 54 patients, a capsule placebo significantly decreased the number of coughs during a 15-minute follow-up compared with no treatment (18 vs 3; P=.0003).6
Recommendations
The American College of Chest Physicians recommends a first-generation antihistamine-decongestant combination or naproxen for acute cough in the common cold (SOR: A). Newer-generation, nonsedating antihistamines are not recommended (SOR: D).7
The US Food and Drug Administration (FDA) advises against using OTC cough and cold medicines in children younger than 2 years because of the risk of “serious and potentially life-threatening side effects.” The FDA also recommends taking significant precautions if these products are used in children older than 2 years, pending a complete FDA review of the medications for children 2 to 11 years. Manufacturers of children’s cough and cold remedies have changed the labels on the medications voluntarily to recommend that they not be given to children younger than 4 years.8
The American Academy of Pediatrics recommends that physicians clearly educate parents about the potential risks and lack of benefits of DM- and codeine-containing cough remedies.9
1. Smith SM, Schroeder K, Fahey T. Over-the-counter medications for acute cough in children and adults in ambulatory settings. Cochrane Database Syst Rev. 2008;(1):CD001831.-
2. Prasad AS, Beck FW, Bao B, et al. Duration and severity of symptoms and levels of plasma interleukin-1 receptor antagonist, soluble tumor necrosis factor receptor, and adhesion molecules in patients with common cold treated with zinc acetate. J Infect Dis. 2008;197:795-802.
3. Caruso TJ, Prober CG, Gwaltney JM. Treatment of naturally acquired common colds with zinc: a structured review. Clin Infect Dis. 2007;45:569-574.
4. Paul IM, Beiler J, McMonagle A, et al. Effect of honey, dextromethorphan, and no treatment on nocturnal cough and sleep quality for coughing children and their parents. Arch Pediatr Adolesc Med. 2007;161:1140-1146.
5. Eccles R. The powerful placebo in cough studies? Pulm Pharmacol Ther. 2002;15:303-308.
6. Lee PC, Jawad MS, Hull JD, et al. The antitussive effect of placebo treatment on cough associated with acute upper respiratory infection. Psychosom Med. 2005;67:314-317.
7. Pratter MR. Cough and the common cold: ACCP evidence-based clinical practice guidelines. Chest. 2006;129(suppl 1):72S-74S.
8. FDA Public Health Advisory. FDA Recommends that over-the-counter (OTC) cough and cold products not be used for infants and children under 2 years of age. Available at: www.fda.gov/drugs/drugsafety/publichealthadvisories/ucm051137.html. Page updated April 30, 2009. Accessed July 12, 2009.
9. American Academy of Pediatrics Committee on Drugs. Use of codeine- and dextromethorphan-containing cough remedies in children. Pediatrics. 1997;99:918-920.(Reaffirmed 2006).
SOME DO. DEXTROMETHORPHAN (DM) for adults and honey for children provide some relief. DM may modestly decrease cough in adults compared with placebo (strength of recommendation [SOR]: B, systematic review of inconsistent or limited evidence). The data supporting zinc for the common cold are mixed (SOR: B, meta-analysis with inconsistent results). Antihistamines, antihistamine-decongestant combinations, and guaifenesin don’t provide greater relief than placebo in adults (SOR: B, systematic review of inconsistent or limited evidence).
In children, antihistamines, decongestants, DM, or combinations of them don’t relieve cough better than placebo (SOR: A, systematic review). Honey may modestly decrease frequency and severity of cough compared with DM or no treatment (SOR: B, small, randomized controlled trial [RCT]).
Clinical commentary
It appears that all of the common, troublesome symptoms of an upper respiratory infection can be managed just as well with over-the-counter (OTC) medications as with prescriptions: DM for cough; acetaminophen or naproxen sodium for fever and aches; decongestants or vapor rubs for nasal congestion. Spread the word!
It would be wonderful if the office visit for upper respiratory infection became a rarity—the health care system would save a lot of money. Presumably, patients would still come in wondering if they had something worse than a cold, but education during the first visit would help prevent repeat trips.
Jon O. Neher, MD
Valley Medical Center
Family Practice Residency,
University of Washington, Renton
Evidence summary
A Cochrane review found DM to be modestly effective in 2 of 3 studies.1 In the first study—a meta-analysis of 6 industry-sponsored RCTs of 710 adults—a single 30-mg dose of DM decreased coughing bouts by 12% (P=.004) and increased the time between bouts by 17 % (P=.002) in the 3 hours after treatment.
A second study of 3 successive industry-sponsored, blinded RCTs enrolling a total of 451 adults found that 30 mg of DM decreased cough counts between 19% and 36% (P<.05) over a 3-hour follow-up period. Neither of the 2 studies specified whether the outcome assessors were blinded to treatment groups.
A third double-blinded RCT evaluating a single 30-mg dose of DM in 43 adults during a 3-hour follow-up period showed no statistically significant improvement in cough outcomes compared with placebo.
A split decision on guaifenesin
The same Cochrane review also evaluated other medications for cough related to upper respiratory infection in adults.1 The results of 2 guaifenesin trials were split. In a double-blinded RCT of 239 adults, more patients taking guaifenesin reported decreased cough frequency and intensity (75% vs 31%; P<.01). However, another double-blinded RCT of 65 patients found guaifenesin to be no more effective than placebo in reducing subjective cough frequency.
Antihistamines don’t help, adding a decongestant isn’t much better
Three trials of antihistamines in a total of 1900 adults found that the drugs didn’t relieve cough symptoms more effectively than placebo. Antihistamine-decongestant combination trials produced split results. In 1 double-blinded RCT of 283 adults, loratadine-pseudoephedrine (5 and 120 mg, respectively) twice daily for 4 days didn’t decrease subjective cough scores more than placebo and was associated with more dry mouth, dizziness, headache, and insomnia (30% vs 21%; P value not reported).
Another partially double-blinded RCT of 73 adults reported that dexbrompheniramine-pseudoephedrine (6 and 120 mg, respectively) twice daily for 1 week decreased subjective cough severity (1.4 vs 2.0; P<.05) on a scale of 0 to 4 during days 3 to 5 of treatment. The combination was associated with increased dizziness and dry mouth, however (exact data not reported; P≤.01).
Codeine works no better than placebo
Two partially double-blinded RCTs of 163 adults found codeine (sold OTC in Canada) to be no more effective than placebo in relieving cough caused by the common cold.1
Zinc lozenges show mixed results
Zinc lozenges containing 13.3 mg of zinc acetate taken every 2 to 3 hours decreased the duration of cough from 5.35 to 2.14 days (P<.001) in a double-blinded placebo-controlled RCT of 50 adults.2 The most recent systematic review showed mixed results: Half the studies found no benefit for zinc in treating upper respiratory infection.3
In children, forget DM, antihistamines, decongestants
The previously mentioned Cochrane review1 also summarized studies in children. DM was no more effective than placebo for decreasing cough in 2 RCTs enrolling a total of 107 children. Another single-blinded RCT of 100 children showed that neither DM nor diphenhydramine relieved cough better than placebo.
Two RCTs involving a total of 237 children compared antihistamines with placebo. One double-blinded trial reported that clemastine and chlorpheniramine were no more effective than placebo. The other partially double-blinded trial found that diphenhydramine didn’t decrease cough frequency more than placebo.
Two double-blinded RCTs (total of 155 children) showed that antihistamine-decongestant combinations (brompheniramine-phenylpropanolamine and brompheniramine-phenylephrine-propanolamine) didn’t reduce cough more than placebo. No studies have evaluated guai-fenesin in children.1
Honey appears to help
In a partially double-blinded RCT (the “no treatment” group was not blinded) of 105 children, a single dose of buckwheat honey decreased cough frequency, as assessed by parents, by 1.89 points on the 7-point Likert scale compared with DM (1.39) and no treatment (0.92; P<.001). Overall improvement in symptom score averaged 10.71 out of a total 30 points for honey compared with 6.41 for no treatment (P=.04). Cough frequency and overall symptom scores for DM didn’t differ significantly from no treatment. Hyperactivity, nervousness, and insomnia were reported more often with honey (5 patients) than DM (2 patients) or no treatment (0 patients); (P=.04).4
Placebos work, but why?
In a review of 8 RCTs, the average reduction in cough in the placebo group (both capsules and syrups) was approximately 85% of that seen in the active medication group (range 56%-105%).5 Several factors may account for the efficacy of placebo, including lubrication of the pharynx by increased salivation caused by sweet or bitter vehicles. Sweet vehicles also may stimulate endogenous opioids that may suppress cough. In an unblinded RCT of 54 patients, a capsule placebo significantly decreased the number of coughs during a 15-minute follow-up compared with no treatment (18 vs 3; P=.0003).6
Recommendations
The American College of Chest Physicians recommends a first-generation antihistamine-decongestant combination or naproxen for acute cough in the common cold (SOR: A). Newer-generation, nonsedating antihistamines are not recommended (SOR: D).7
The US Food and Drug Administration (FDA) advises against using OTC cough and cold medicines in children younger than 2 years because of the risk of “serious and potentially life-threatening side effects.” The FDA also recommends taking significant precautions if these products are used in children older than 2 years, pending a complete FDA review of the medications for children 2 to 11 years. Manufacturers of children’s cough and cold remedies have changed the labels on the medications voluntarily to recommend that they not be given to children younger than 4 years.8
The American Academy of Pediatrics recommends that physicians clearly educate parents about the potential risks and lack of benefits of DM- and codeine-containing cough remedies.9
SOME DO. DEXTROMETHORPHAN (DM) for adults and honey for children provide some relief. DM may modestly decrease cough in adults compared with placebo (strength of recommendation [SOR]: B, systematic review of inconsistent or limited evidence). The data supporting zinc for the common cold are mixed (SOR: B, meta-analysis with inconsistent results). Antihistamines, antihistamine-decongestant combinations, and guaifenesin don’t provide greater relief than placebo in adults (SOR: B, systematic review of inconsistent or limited evidence).
In children, antihistamines, decongestants, DM, or combinations of them don’t relieve cough better than placebo (SOR: A, systematic review). Honey may modestly decrease frequency and severity of cough compared with DM or no treatment (SOR: B, small, randomized controlled trial [RCT]).
Clinical commentary
It appears that all of the common, troublesome symptoms of an upper respiratory infection can be managed just as well with over-the-counter (OTC) medications as with prescriptions: DM for cough; acetaminophen or naproxen sodium for fever and aches; decongestants or vapor rubs for nasal congestion. Spread the word!
It would be wonderful if the office visit for upper respiratory infection became a rarity—the health care system would save a lot of money. Presumably, patients would still come in wondering if they had something worse than a cold, but education during the first visit would help prevent repeat trips.
Jon O. Neher, MD
Valley Medical Center
Family Practice Residency,
University of Washington, Renton
Evidence summary
A Cochrane review found DM to be modestly effective in 2 of 3 studies.1 In the first study—a meta-analysis of 6 industry-sponsored RCTs of 710 adults—a single 30-mg dose of DM decreased coughing bouts by 12% (P=.004) and increased the time between bouts by 17 % (P=.002) in the 3 hours after treatment.
A second study of 3 successive industry-sponsored, blinded RCTs enrolling a total of 451 adults found that 30 mg of DM decreased cough counts between 19% and 36% (P<.05) over a 3-hour follow-up period. Neither of the 2 studies specified whether the outcome assessors were blinded to treatment groups.
A third double-blinded RCT evaluating a single 30-mg dose of DM in 43 adults during a 3-hour follow-up period showed no statistically significant improvement in cough outcomes compared with placebo.
A split decision on guaifenesin
The same Cochrane review also evaluated other medications for cough related to upper respiratory infection in adults.1 The results of 2 guaifenesin trials were split. In a double-blinded RCT of 239 adults, more patients taking guaifenesin reported decreased cough frequency and intensity (75% vs 31%; P<.01). However, another double-blinded RCT of 65 patients found guaifenesin to be no more effective than placebo in reducing subjective cough frequency.
Antihistamines don’t help, adding a decongestant isn’t much better
Three trials of antihistamines in a total of 1900 adults found that the drugs didn’t relieve cough symptoms more effectively than placebo. Antihistamine-decongestant combination trials produced split results. In 1 double-blinded RCT of 283 adults, loratadine-pseudoephedrine (5 and 120 mg, respectively) twice daily for 4 days didn’t decrease subjective cough scores more than placebo and was associated with more dry mouth, dizziness, headache, and insomnia (30% vs 21%; P value not reported).
Another partially double-blinded RCT of 73 adults reported that dexbrompheniramine-pseudoephedrine (6 and 120 mg, respectively) twice daily for 1 week decreased subjective cough severity (1.4 vs 2.0; P<.05) on a scale of 0 to 4 during days 3 to 5 of treatment. The combination was associated with increased dizziness and dry mouth, however (exact data not reported; P≤.01).
Codeine works no better than placebo
Two partially double-blinded RCTs of 163 adults found codeine (sold OTC in Canada) to be no more effective than placebo in relieving cough caused by the common cold.1
Zinc lozenges show mixed results
Zinc lozenges containing 13.3 mg of zinc acetate taken every 2 to 3 hours decreased the duration of cough from 5.35 to 2.14 days (P<.001) in a double-blinded placebo-controlled RCT of 50 adults.2 The most recent systematic review showed mixed results: Half the studies found no benefit for zinc in treating upper respiratory infection.3
In children, forget DM, antihistamines, decongestants
The previously mentioned Cochrane review1 also summarized studies in children. DM was no more effective than placebo for decreasing cough in 2 RCTs enrolling a total of 107 children. Another single-blinded RCT of 100 children showed that neither DM nor diphenhydramine relieved cough better than placebo.
Two RCTs involving a total of 237 children compared antihistamines with placebo. One double-blinded trial reported that clemastine and chlorpheniramine were no more effective than placebo. The other partially double-blinded trial found that diphenhydramine didn’t decrease cough frequency more than placebo.
Two double-blinded RCTs (total of 155 children) showed that antihistamine-decongestant combinations (brompheniramine-phenylpropanolamine and brompheniramine-phenylephrine-propanolamine) didn’t reduce cough more than placebo. No studies have evaluated guai-fenesin in children.1
Honey appears to help
In a partially double-blinded RCT (the “no treatment” group was not blinded) of 105 children, a single dose of buckwheat honey decreased cough frequency, as assessed by parents, by 1.89 points on the 7-point Likert scale compared with DM (1.39) and no treatment (0.92; P<.001). Overall improvement in symptom score averaged 10.71 out of a total 30 points for honey compared with 6.41 for no treatment (P=.04). Cough frequency and overall symptom scores for DM didn’t differ significantly from no treatment. Hyperactivity, nervousness, and insomnia were reported more often with honey (5 patients) than DM (2 patients) or no treatment (0 patients); (P=.04).4
Placebos work, but why?
In a review of 8 RCTs, the average reduction in cough in the placebo group (both capsules and syrups) was approximately 85% of that seen in the active medication group (range 56%-105%).5 Several factors may account for the efficacy of placebo, including lubrication of the pharynx by increased salivation caused by sweet or bitter vehicles. Sweet vehicles also may stimulate endogenous opioids that may suppress cough. In an unblinded RCT of 54 patients, a capsule placebo significantly decreased the number of coughs during a 15-minute follow-up compared with no treatment (18 vs 3; P=.0003).6
Recommendations
The American College of Chest Physicians recommends a first-generation antihistamine-decongestant combination or naproxen for acute cough in the common cold (SOR: A). Newer-generation, nonsedating antihistamines are not recommended (SOR: D).7
The US Food and Drug Administration (FDA) advises against using OTC cough and cold medicines in children younger than 2 years because of the risk of “serious and potentially life-threatening side effects.” The FDA also recommends taking significant precautions if these products are used in children older than 2 years, pending a complete FDA review of the medications for children 2 to 11 years. Manufacturers of children’s cough and cold remedies have changed the labels on the medications voluntarily to recommend that they not be given to children younger than 4 years.8
The American Academy of Pediatrics recommends that physicians clearly educate parents about the potential risks and lack of benefits of DM- and codeine-containing cough remedies.9
1. Smith SM, Schroeder K, Fahey T. Over-the-counter medications for acute cough in children and adults in ambulatory settings. Cochrane Database Syst Rev. 2008;(1):CD001831.-
2. Prasad AS, Beck FW, Bao B, et al. Duration and severity of symptoms and levels of plasma interleukin-1 receptor antagonist, soluble tumor necrosis factor receptor, and adhesion molecules in patients with common cold treated with zinc acetate. J Infect Dis. 2008;197:795-802.
3. Caruso TJ, Prober CG, Gwaltney JM. Treatment of naturally acquired common colds with zinc: a structured review. Clin Infect Dis. 2007;45:569-574.
4. Paul IM, Beiler J, McMonagle A, et al. Effect of honey, dextromethorphan, and no treatment on nocturnal cough and sleep quality for coughing children and their parents. Arch Pediatr Adolesc Med. 2007;161:1140-1146.
5. Eccles R. The powerful placebo in cough studies? Pulm Pharmacol Ther. 2002;15:303-308.
6. Lee PC, Jawad MS, Hull JD, et al. The antitussive effect of placebo treatment on cough associated with acute upper respiratory infection. Psychosom Med. 2005;67:314-317.
7. Pratter MR. Cough and the common cold: ACCP evidence-based clinical practice guidelines. Chest. 2006;129(suppl 1):72S-74S.
8. FDA Public Health Advisory. FDA Recommends that over-the-counter (OTC) cough and cold products not be used for infants and children under 2 years of age. Available at: www.fda.gov/drugs/drugsafety/publichealthadvisories/ucm051137.html. Page updated April 30, 2009. Accessed July 12, 2009.
9. American Academy of Pediatrics Committee on Drugs. Use of codeine- and dextromethorphan-containing cough remedies in children. Pediatrics. 1997;99:918-920.(Reaffirmed 2006).
1. Smith SM, Schroeder K, Fahey T. Over-the-counter medications for acute cough in children and adults in ambulatory settings. Cochrane Database Syst Rev. 2008;(1):CD001831.-
2. Prasad AS, Beck FW, Bao B, et al. Duration and severity of symptoms and levels of plasma interleukin-1 receptor antagonist, soluble tumor necrosis factor receptor, and adhesion molecules in patients with common cold treated with zinc acetate. J Infect Dis. 2008;197:795-802.
3. Caruso TJ, Prober CG, Gwaltney JM. Treatment of naturally acquired common colds with zinc: a structured review. Clin Infect Dis. 2007;45:569-574.
4. Paul IM, Beiler J, McMonagle A, et al. Effect of honey, dextromethorphan, and no treatment on nocturnal cough and sleep quality for coughing children and their parents. Arch Pediatr Adolesc Med. 2007;161:1140-1146.
5. Eccles R. The powerful placebo in cough studies? Pulm Pharmacol Ther. 2002;15:303-308.
6. Lee PC, Jawad MS, Hull JD, et al. The antitussive effect of placebo treatment on cough associated with acute upper respiratory infection. Psychosom Med. 2005;67:314-317.
7. Pratter MR. Cough and the common cold: ACCP evidence-based clinical practice guidelines. Chest. 2006;129(suppl 1):72S-74S.
8. FDA Public Health Advisory. FDA Recommends that over-the-counter (OTC) cough and cold products not be used for infants and children under 2 years of age. Available at: www.fda.gov/drugs/drugsafety/publichealthadvisories/ucm051137.html. Page updated April 30, 2009. Accessed July 12, 2009.
9. American Academy of Pediatrics Committee on Drugs. Use of codeine- and dextromethorphan-containing cough remedies in children. Pediatrics. 1997;99:918-920.(Reaffirmed 2006).
Evidence-based answers from the Family Physicians Inquiries Network