User login
The estimated glomerular filtration rate as a test for chronic kidney disease: Problems and solutions
At the American Society of Nephrology Renal Week 2010, one of the authors (A.D.R.) presented the following question at an In-Depth Nephrology Course on Geriatric Nephrology:
A 65-year-old woman donated a kidney to her son. Before donation, her serum creatinine level was 1.0 mg/dL, her estimated glomerular filtration rate (GFR) was 56 mL/min/1.73 m2, and her measured GFR was 82 mL/min/1.73 m2, which was below the 2.5th percentile for 20-year-old potential kidney donors. The patient had no albuminuria or hypertension and was otherwise healthy. The kidney was biopsied during the transplant surgery. The biopsy revealed 2 of 20 glomeruli as globally sclerosed, a focus of tubular atrophy, and mild arteriosclerosis (findings present in less than 2.5% of 20-year-old donors).
Choose one. Prior to donation, this woman had:
- Chronic kidney disease (CKD), and she should not have donated her kidney
- CKD, but kidney donation was reasonable
- Age-related (senescent) changes in her kidneys, and should not have donated her kidney
- Age-related (senescent) changes in her kidneys, but kidney donation was reasonable
Using an electronic response system, 36 (82%) of 44 physicians in the audience chose the last option, even though this patient meets the current definition of CKD (an estimated GFR less than 60 mL/min/1.73 m2) and has chronic parenchymal damage documented by a kidney biopsy.
PROBLEMS WITH THE GFR AND CKD CLASSIFICATION
This question highlights several key problems with the GFR and CKD classification.
First, in low-risk populations such as potential kidney donors, serum-creatinine-based equations such as the Modification of Diet in Renal Disease (MDRD) equation and the Chronic Kidney Disease Epidemiology Study (CKD-EPI) equation substantially underestimate the GFR.1
Second, many healthy older adults with normal serum creatinine levels have an estimated GFR and a measured GFR below the normal range for young adults.2
Third, many healthy older adults have evidence of chronic parenchymal damage on renal biopsy, unlike healthy young adults.3
Finally, many health care providers did not previously recognize that people with a normal serum creatinine level could have a reduced GFR, and widespread use of the estimated GFR has addressed this problem. However, many physicians remain skeptical about efforts this past decade to classify age-related changes in kidney function as a “disease” in the absence of a clear benefit to older patients.4
TWO POINTS ABOUT THE ESTIMATED GFR
In this issue of the Cleveland Clinic Journal of Medicine, Simon and colleagues5 provide a balanced assessment of the benefits and pitfalls of using the estimated GFR in clinical practice. Two points they make deserve further discussion:
Bigger people make more creatinine. GFR can be reported in units of milliliters per minute, or in units normalized to body surface area (mL/min/1.73 m2). Contemporary equations for identifying and classifying CKD use the latter, because the GFR is considered inappropriately low when metabolic waste is not being adequately cleared. It is intuitive that smaller people require less absolute GFR than larger people, who generate more metabolic waste. Indexing GFR to 1.73 m2 assumes that body surface area is a good surrogate for metabolic waste generation. However, whether body surface area is the best surrogate for the rate of metabolic waste generation has long been a subject of debate.6
The relationship between GFR and serum creatinine is not linear. Due to the inverse relationship between serum creatinine and GFR, a small change in serum creatinine from 0.9 to 1.2 mg/dL will represent a relatively large change in GFR (eg, 85 to 65 mL/min/1.73 m2), whereas a large change in serum creatinine from 5 to 9 mg/dL will represent a smaller change in GFR (eg, 10 to 5 mL/min/1.73 m2). The latter may be of great concern since it represents a fall in GFR to levels at which dialysis is likely needed. With the former, subtle changes in serum creatinine represent large changes in GFR, but there is also much more day-to-day variability in GFR in the normal or near-normal range than in the advanced range of kidney disease. This is one of the reasons the MDRD and CKD-EPI equations were developed, using logarithmic models that emphasize percentage instead of absolute differences in GFR.
BEYOND CREATININE?
As Simon and colleagues point out,5 although serum creatinine is a flawed surrogate for GFR, there are many problems with determining GFR by other means.
Direct GFR measurement relies on the use of an exogenous marker such as inulin or iothalamate that is infused or injected, followed by timed urine and plasma measurements to calculate GFR by the urinary clearance method (UV/P, where U is the concentration of the marker in the urine, V is the urine volume, and P is the concentration of the marker in the plasma). Alternatively, timed plasma measurements of the marker alone can be used to determine GFR by the plasma clearance method. The problem is that direct GFR measurement is costly, invasive, imprecise, time-consuming, and impractical in most clinical settings.
Exogenous markers for determining GFR are chosen because they are metabolically inert, are cleared by glomerular filtration without tubular secretion or reabsorption, and have no extrarenal clearance via the liver or intestines. Endogenous markers such as serum creatinine do not fulfill all of these ideal criteria.
Simon and colleagues highlight the problem of using the estimated GFR to screen for CKD in populations of ostensibly healthy persons.5 The MDRD and CKD-EPI equations contain demographic variables to approximate the creatinine generation rate. The primary source of creatinine generation is muscle, and the coefficients in these equations reflect the higher muscle mass of younger individuals, males, and African Americans. However, any creatinine-based equation is fundamentally flawed because overall health also affects muscle mass: healthy people have greater muscle mass than people with chronic illness, including those with CKD. Therefore, at the same serum creatinine level, a healthy person has a higher GFR than a patient with CKD.1,7 This problem leads to circular reasoning, since you need to know whether the patient has CKD or is healthy in order to accurately estimate GFR, but estimated GFR is being used to determine whether the patient is healthy or has CKD.
Therefore, other endogenous markers that are also eliminated via glomerular filtration, such as cystatin C, have been used to construct equations that estimate GFR. Unfortunately, factors other than GFR, such as inflammation, can also influence blood cystatin C levels. This in turn impairs the accuracy of equations that use cystatin C to estimate GFR in the general population.8 No known endogenous marker of GFR can be used in all patients without any confounding factors.
To rectify this problem, recent studies have investigated the use of a confirmatory test to determine which patients with a creatinine-based estimated GFR less than 60 mL/min/1.73 m2 actually have kidney disease or have a false-positive result due to higher-than-average creatinine generation. Both albuminuria and elevated serum cystatin C are examples of useful confirmatory tests that substantially decrease the misdiagnosis of CKD in healthy adults with an estimated GFR less than 60 mL/min/1.73 m2.9,10
Imagine if we identified and staged systemic lupus erythematosus on the basis of antinuclear antibody levels alone: this would parallel the current approach that largely uses serum creatinine alone to classify CKD. Confirmatory tests and considering patient-specific risk factors could avoid potential harm to healthy individuals and yet retain gains that have been made to improve the interpretation of serum creatinine levels in CKD patients.
- Tent H, Rook M, Stevens LA, et a.l Renal function equations before and after living kidney donation: a within-individual comparison of performance at different levels of renal function. Clin J Am Soc Nephrol 2010; 5:1960–1968.
- Poggio ED, Rule AD, Tanchanco R, et al. Demographic and clinical characteristics associated with glomerular filtration rates in living kidney donors. Kidney Int 2009; 75:1079–1087.
- Rule AD, Amer H, Cornell LD, et al. The association between age and nephrosclerosis on renal biopsy among healthy adults. Ann Intern Med 2010; 152:561–567.
- Spence D. Bad medicine: chronic kidney disease. BMJ 2010; 340:c3188.
- Simon J, Amde M, Poggio E. Interpreting the estimated glomerular filtration rate in the primary care setting: benefits and pitfalls. Cleve Clin J Med 2011; 78:189–195.
- Daugirdas JT, Meyer K, Greene T, Butler RS, Poggio ED. Scaling of measured glomerular filtration rate in kidney donor candidates by anthropometric estimates of body surface area, body water, metabolic rate, or liver size. Clin J Am Soc Nephrol 2009; 4:1575–1583.
- Rule AD, Larson TS, Bergstralh EJ, Slezak JM, Jacobsen SJ, Cosio FG. Using serum creatinine to estimate glomerular filtration rate: accuracy in good health and in chronic kidney disease. Ann Intern Med 2004; 141:929–937.
- Eriksen BO, Mathisen UD, Melsom T, et al. Cystatin C is not a better estimator of GFR than plasma creatinine in the general population. Kidney Int 2010; 78:1305–1311.
- Tonelli M, Muntner P, Lloyd A, et al. Using proteinuria and estimated glomerular filtration rate to classify risk in patients with chronic kidney disease: a cohort study. Ann Intern Med 2011; 154:12–21.
- Peralta CA, Katz R, Sarnak MJ, et al. Cystatin C identifies chronic kidney disease patients at higher risk for complications. J Am Soc Nephrol 2011; 22:147–155.
At the American Society of Nephrology Renal Week 2010, one of the authors (A.D.R.) presented the following question at an In-Depth Nephrology Course on Geriatric Nephrology:
A 65-year-old woman donated a kidney to her son. Before donation, her serum creatinine level was 1.0 mg/dL, her estimated glomerular filtration rate (GFR) was 56 mL/min/1.73 m2, and her measured GFR was 82 mL/min/1.73 m2, which was below the 2.5th percentile for 20-year-old potential kidney donors. The patient had no albuminuria or hypertension and was otherwise healthy. The kidney was biopsied during the transplant surgery. The biopsy revealed 2 of 20 glomeruli as globally sclerosed, a focus of tubular atrophy, and mild arteriosclerosis (findings present in less than 2.5% of 20-year-old donors).
Choose one. Prior to donation, this woman had:
- Chronic kidney disease (CKD), and she should not have donated her kidney
- CKD, but kidney donation was reasonable
- Age-related (senescent) changes in her kidneys, and should not have donated her kidney
- Age-related (senescent) changes in her kidneys, but kidney donation was reasonable
Using an electronic response system, 36 (82%) of 44 physicians in the audience chose the last option, even though this patient meets the current definition of CKD (an estimated GFR less than 60 mL/min/1.73 m2) and has chronic parenchymal damage documented by a kidney biopsy.
PROBLEMS WITH THE GFR AND CKD CLASSIFICATION
This question highlights several key problems with the GFR and CKD classification.
First, in low-risk populations such as potential kidney donors, serum-creatinine-based equations such as the Modification of Diet in Renal Disease (MDRD) equation and the Chronic Kidney Disease Epidemiology Study (CKD-EPI) equation substantially underestimate the GFR.1
Second, many healthy older adults with normal serum creatinine levels have an estimated GFR and a measured GFR below the normal range for young adults.2
Third, many healthy older adults have evidence of chronic parenchymal damage on renal biopsy, unlike healthy young adults.3
Finally, many health care providers did not previously recognize that people with a normal serum creatinine level could have a reduced GFR, and widespread use of the estimated GFR has addressed this problem. However, many physicians remain skeptical about efforts this past decade to classify age-related changes in kidney function as a “disease” in the absence of a clear benefit to older patients.4
TWO POINTS ABOUT THE ESTIMATED GFR
In this issue of the Cleveland Clinic Journal of Medicine, Simon and colleagues5 provide a balanced assessment of the benefits and pitfalls of using the estimated GFR in clinical practice. Two points they make deserve further discussion:
Bigger people make more creatinine. GFR can be reported in units of milliliters per minute, or in units normalized to body surface area (mL/min/1.73 m2). Contemporary equations for identifying and classifying CKD use the latter, because the GFR is considered inappropriately low when metabolic waste is not being adequately cleared. It is intuitive that smaller people require less absolute GFR than larger people, who generate more metabolic waste. Indexing GFR to 1.73 m2 assumes that body surface area is a good surrogate for metabolic waste generation. However, whether body surface area is the best surrogate for the rate of metabolic waste generation has long been a subject of debate.6
The relationship between GFR and serum creatinine is not linear. Due to the inverse relationship between serum creatinine and GFR, a small change in serum creatinine from 0.9 to 1.2 mg/dL will represent a relatively large change in GFR (eg, 85 to 65 mL/min/1.73 m2), whereas a large change in serum creatinine from 5 to 9 mg/dL will represent a smaller change in GFR (eg, 10 to 5 mL/min/1.73 m2). The latter may be of great concern since it represents a fall in GFR to levels at which dialysis is likely needed. With the former, subtle changes in serum creatinine represent large changes in GFR, but there is also much more day-to-day variability in GFR in the normal or near-normal range than in the advanced range of kidney disease. This is one of the reasons the MDRD and CKD-EPI equations were developed, using logarithmic models that emphasize percentage instead of absolute differences in GFR.
BEYOND CREATININE?
As Simon and colleagues point out,5 although serum creatinine is a flawed surrogate for GFR, there are many problems with determining GFR by other means.
Direct GFR measurement relies on the use of an exogenous marker such as inulin or iothalamate that is infused or injected, followed by timed urine and plasma measurements to calculate GFR by the urinary clearance method (UV/P, where U is the concentration of the marker in the urine, V is the urine volume, and P is the concentration of the marker in the plasma). Alternatively, timed plasma measurements of the marker alone can be used to determine GFR by the plasma clearance method. The problem is that direct GFR measurement is costly, invasive, imprecise, time-consuming, and impractical in most clinical settings.
Exogenous markers for determining GFR are chosen because they are metabolically inert, are cleared by glomerular filtration without tubular secretion or reabsorption, and have no extrarenal clearance via the liver or intestines. Endogenous markers such as serum creatinine do not fulfill all of these ideal criteria.
Simon and colleagues highlight the problem of using the estimated GFR to screen for CKD in populations of ostensibly healthy persons.5 The MDRD and CKD-EPI equations contain demographic variables to approximate the creatinine generation rate. The primary source of creatinine generation is muscle, and the coefficients in these equations reflect the higher muscle mass of younger individuals, males, and African Americans. However, any creatinine-based equation is fundamentally flawed because overall health also affects muscle mass: healthy people have greater muscle mass than people with chronic illness, including those with CKD. Therefore, at the same serum creatinine level, a healthy person has a higher GFR than a patient with CKD.1,7 This problem leads to circular reasoning, since you need to know whether the patient has CKD or is healthy in order to accurately estimate GFR, but estimated GFR is being used to determine whether the patient is healthy or has CKD.
Therefore, other endogenous markers that are also eliminated via glomerular filtration, such as cystatin C, have been used to construct equations that estimate GFR. Unfortunately, factors other than GFR, such as inflammation, can also influence blood cystatin C levels. This in turn impairs the accuracy of equations that use cystatin C to estimate GFR in the general population.8 No known endogenous marker of GFR can be used in all patients without any confounding factors.
To rectify this problem, recent studies have investigated the use of a confirmatory test to determine which patients with a creatinine-based estimated GFR less than 60 mL/min/1.73 m2 actually have kidney disease or have a false-positive result due to higher-than-average creatinine generation. Both albuminuria and elevated serum cystatin C are examples of useful confirmatory tests that substantially decrease the misdiagnosis of CKD in healthy adults with an estimated GFR less than 60 mL/min/1.73 m2.9,10
Imagine if we identified and staged systemic lupus erythematosus on the basis of antinuclear antibody levels alone: this would parallel the current approach that largely uses serum creatinine alone to classify CKD. Confirmatory tests and considering patient-specific risk factors could avoid potential harm to healthy individuals and yet retain gains that have been made to improve the interpretation of serum creatinine levels in CKD patients.
At the American Society of Nephrology Renal Week 2010, one of the authors (A.D.R.) presented the following question at an In-Depth Nephrology Course on Geriatric Nephrology:
A 65-year-old woman donated a kidney to her son. Before donation, her serum creatinine level was 1.0 mg/dL, her estimated glomerular filtration rate (GFR) was 56 mL/min/1.73 m2, and her measured GFR was 82 mL/min/1.73 m2, which was below the 2.5th percentile for 20-year-old potential kidney donors. The patient had no albuminuria or hypertension and was otherwise healthy. The kidney was biopsied during the transplant surgery. The biopsy revealed 2 of 20 glomeruli as globally sclerosed, a focus of tubular atrophy, and mild arteriosclerosis (findings present in less than 2.5% of 20-year-old donors).
Choose one. Prior to donation, this woman had:
- Chronic kidney disease (CKD), and she should not have donated her kidney
- CKD, but kidney donation was reasonable
- Age-related (senescent) changes in her kidneys, and should not have donated her kidney
- Age-related (senescent) changes in her kidneys, but kidney donation was reasonable
Using an electronic response system, 36 (82%) of 44 physicians in the audience chose the last option, even though this patient meets the current definition of CKD (an estimated GFR less than 60 mL/min/1.73 m2) and has chronic parenchymal damage documented by a kidney biopsy.
PROBLEMS WITH THE GFR AND CKD CLASSIFICATION
This question highlights several key problems with the GFR and CKD classification.
First, in low-risk populations such as potential kidney donors, serum-creatinine-based equations such as the Modification of Diet in Renal Disease (MDRD) equation and the Chronic Kidney Disease Epidemiology Study (CKD-EPI) equation substantially underestimate the GFR.1
Second, many healthy older adults with normal serum creatinine levels have an estimated GFR and a measured GFR below the normal range for young adults.2
Third, many healthy older adults have evidence of chronic parenchymal damage on renal biopsy, unlike healthy young adults.3
Finally, many health care providers did not previously recognize that people with a normal serum creatinine level could have a reduced GFR, and widespread use of the estimated GFR has addressed this problem. However, many physicians remain skeptical about efforts this past decade to classify age-related changes in kidney function as a “disease” in the absence of a clear benefit to older patients.4
TWO POINTS ABOUT THE ESTIMATED GFR
In this issue of the Cleveland Clinic Journal of Medicine, Simon and colleagues5 provide a balanced assessment of the benefits and pitfalls of using the estimated GFR in clinical practice. Two points they make deserve further discussion:
Bigger people make more creatinine. GFR can be reported in units of milliliters per minute, or in units normalized to body surface area (mL/min/1.73 m2). Contemporary equations for identifying and classifying CKD use the latter, because the GFR is considered inappropriately low when metabolic waste is not being adequately cleared. It is intuitive that smaller people require less absolute GFR than larger people, who generate more metabolic waste. Indexing GFR to 1.73 m2 assumes that body surface area is a good surrogate for metabolic waste generation. However, whether body surface area is the best surrogate for the rate of metabolic waste generation has long been a subject of debate.6
The relationship between GFR and serum creatinine is not linear. Due to the inverse relationship between serum creatinine and GFR, a small change in serum creatinine from 0.9 to 1.2 mg/dL will represent a relatively large change in GFR (eg, 85 to 65 mL/min/1.73 m2), whereas a large change in serum creatinine from 5 to 9 mg/dL will represent a smaller change in GFR (eg, 10 to 5 mL/min/1.73 m2). The latter may be of great concern since it represents a fall in GFR to levels at which dialysis is likely needed. With the former, subtle changes in serum creatinine represent large changes in GFR, but there is also much more day-to-day variability in GFR in the normal or near-normal range than in the advanced range of kidney disease. This is one of the reasons the MDRD and CKD-EPI equations were developed, using logarithmic models that emphasize percentage instead of absolute differences in GFR.
BEYOND CREATININE?
As Simon and colleagues point out,5 although serum creatinine is a flawed surrogate for GFR, there are many problems with determining GFR by other means.
Direct GFR measurement relies on the use of an exogenous marker such as inulin or iothalamate that is infused or injected, followed by timed urine and plasma measurements to calculate GFR by the urinary clearance method (UV/P, where U is the concentration of the marker in the urine, V is the urine volume, and P is the concentration of the marker in the plasma). Alternatively, timed plasma measurements of the marker alone can be used to determine GFR by the plasma clearance method. The problem is that direct GFR measurement is costly, invasive, imprecise, time-consuming, and impractical in most clinical settings.
Exogenous markers for determining GFR are chosen because they are metabolically inert, are cleared by glomerular filtration without tubular secretion or reabsorption, and have no extrarenal clearance via the liver or intestines. Endogenous markers such as serum creatinine do not fulfill all of these ideal criteria.
Simon and colleagues highlight the problem of using the estimated GFR to screen for CKD in populations of ostensibly healthy persons.5 The MDRD and CKD-EPI equations contain demographic variables to approximate the creatinine generation rate. The primary source of creatinine generation is muscle, and the coefficients in these equations reflect the higher muscle mass of younger individuals, males, and African Americans. However, any creatinine-based equation is fundamentally flawed because overall health also affects muscle mass: healthy people have greater muscle mass than people with chronic illness, including those with CKD. Therefore, at the same serum creatinine level, a healthy person has a higher GFR than a patient with CKD.1,7 This problem leads to circular reasoning, since you need to know whether the patient has CKD or is healthy in order to accurately estimate GFR, but estimated GFR is being used to determine whether the patient is healthy or has CKD.
Therefore, other endogenous markers that are also eliminated via glomerular filtration, such as cystatin C, have been used to construct equations that estimate GFR. Unfortunately, factors other than GFR, such as inflammation, can also influence blood cystatin C levels. This in turn impairs the accuracy of equations that use cystatin C to estimate GFR in the general population.8 No known endogenous marker of GFR can be used in all patients without any confounding factors.
To rectify this problem, recent studies have investigated the use of a confirmatory test to determine which patients with a creatinine-based estimated GFR less than 60 mL/min/1.73 m2 actually have kidney disease or have a false-positive result due to higher-than-average creatinine generation. Both albuminuria and elevated serum cystatin C are examples of useful confirmatory tests that substantially decrease the misdiagnosis of CKD in healthy adults with an estimated GFR less than 60 mL/min/1.73 m2.9,10
Imagine if we identified and staged systemic lupus erythematosus on the basis of antinuclear antibody levels alone: this would parallel the current approach that largely uses serum creatinine alone to classify CKD. Confirmatory tests and considering patient-specific risk factors could avoid potential harm to healthy individuals and yet retain gains that have been made to improve the interpretation of serum creatinine levels in CKD patients.
- Tent H, Rook M, Stevens LA, et a.l Renal function equations before and after living kidney donation: a within-individual comparison of performance at different levels of renal function. Clin J Am Soc Nephrol 2010; 5:1960–1968.
- Poggio ED, Rule AD, Tanchanco R, et al. Demographic and clinical characteristics associated with glomerular filtration rates in living kidney donors. Kidney Int 2009; 75:1079–1087.
- Rule AD, Amer H, Cornell LD, et al. The association between age and nephrosclerosis on renal biopsy among healthy adults. Ann Intern Med 2010; 152:561–567.
- Spence D. Bad medicine: chronic kidney disease. BMJ 2010; 340:c3188.
- Simon J, Amde M, Poggio E. Interpreting the estimated glomerular filtration rate in the primary care setting: benefits and pitfalls. Cleve Clin J Med 2011; 78:189–195.
- Daugirdas JT, Meyer K, Greene T, Butler RS, Poggio ED. Scaling of measured glomerular filtration rate in kidney donor candidates by anthropometric estimates of body surface area, body water, metabolic rate, or liver size. Clin J Am Soc Nephrol 2009; 4:1575–1583.
- Rule AD, Larson TS, Bergstralh EJ, Slezak JM, Jacobsen SJ, Cosio FG. Using serum creatinine to estimate glomerular filtration rate: accuracy in good health and in chronic kidney disease. Ann Intern Med 2004; 141:929–937.
- Eriksen BO, Mathisen UD, Melsom T, et al. Cystatin C is not a better estimator of GFR than plasma creatinine in the general population. Kidney Int 2010; 78:1305–1311.
- Tonelli M, Muntner P, Lloyd A, et al. Using proteinuria and estimated glomerular filtration rate to classify risk in patients with chronic kidney disease: a cohort study. Ann Intern Med 2011; 154:12–21.
- Peralta CA, Katz R, Sarnak MJ, et al. Cystatin C identifies chronic kidney disease patients at higher risk for complications. J Am Soc Nephrol 2011; 22:147–155.
- Tent H, Rook M, Stevens LA, et a.l Renal function equations before and after living kidney donation: a within-individual comparison of performance at different levels of renal function. Clin J Am Soc Nephrol 2010; 5:1960–1968.
- Poggio ED, Rule AD, Tanchanco R, et al. Demographic and clinical characteristics associated with glomerular filtration rates in living kidney donors. Kidney Int 2009; 75:1079–1087.
- Rule AD, Amer H, Cornell LD, et al. The association between age and nephrosclerosis on renal biopsy among healthy adults. Ann Intern Med 2010; 152:561–567.
- Spence D. Bad medicine: chronic kidney disease. BMJ 2010; 340:c3188.
- Simon J, Amde M, Poggio E. Interpreting the estimated glomerular filtration rate in the primary care setting: benefits and pitfalls. Cleve Clin J Med 2011; 78:189–195.
- Daugirdas JT, Meyer K, Greene T, Butler RS, Poggio ED. Scaling of measured glomerular filtration rate in kidney donor candidates by anthropometric estimates of body surface area, body water, metabolic rate, or liver size. Clin J Am Soc Nephrol 2009; 4:1575–1583.
- Rule AD, Larson TS, Bergstralh EJ, Slezak JM, Jacobsen SJ, Cosio FG. Using serum creatinine to estimate glomerular filtration rate: accuracy in good health and in chronic kidney disease. Ann Intern Med 2004; 141:929–937.
- Eriksen BO, Mathisen UD, Melsom T, et al. Cystatin C is not a better estimator of GFR than plasma creatinine in the general population. Kidney Int 2010; 78:1305–1311.
- Tonelli M, Muntner P, Lloyd A, et al. Using proteinuria and estimated glomerular filtration rate to classify risk in patients with chronic kidney disease: a cohort study. Ann Intern Med 2011; 154:12–21.
- Peralta CA, Katz R, Sarnak MJ, et al. Cystatin C identifies chronic kidney disease patients at higher risk for complications. J Am Soc Nephrol 2011; 22:147–155.
Hospitalists in Disaster Response
In the last decade, natural disasters such as the Indonesian tsunami of 2004, Hurricane Katrina in 2004, and the Pakistani earthquake of 2005 have brought attention to the importance of diverse but complementary medical professional roles in humanitarian medical aid.14 Natural disasters that cause significant physical trauma to large populations often necessitate initial multidisciplinary responder teams comprised of surgeons, anesthesiologists, emergency medicine physicians, surgical technologists, nurses, psychiatrists, and public health specialists. Their roles are to manage life‐threatening injuries, provide immediate triage, help affected individuals deal with intense psychological shock, and address critical population‐based needs such as water, food, and sanitation. Meanwhile, general medical, pediatric, rehabilitative, and long‐term psychiatric services often constitute a secondary tier of disaster response, providing postsurgical care, managing acute medical illnesses, mitigating psychological trauma, rehabilitating injuries, and providing vaccinations to at‐risk individuals. Hospitalists can play an important role in postcatastrophe recovery services as experts in acute care, stewards of care transitions, and drivers of systems improvement.
The earthquake that occurred January 12, 2010 in Haiti is a dramatic illustration of the importance of a multidisciplinary approach to disaster relief. The 7.0‐magnitude earthquake near Port‐au‐Prince ravaged an already crippled health care system, severely damaging the country's primary academic medical center, and killed the entire class of second‐year nursing students. The death toll has been estimated to be nearly one‐quarter of a million people.5 Victims awaiting surgery, recovering from surgery, or in need of other immediate medical attention quickly inundated any existing health facilities. The following stories describe the authors' respective experiences in Haiti after the earthquake.
JC: I arrived 4 days after the earthquake to a hospital outside of Port‐au‐Prince, spared from destruction, but filled with hundreds of patients with crush injuries and severe fractures. On rounds with the surgical team, I observed that venous thromboembolism (VTE) prophylaxis had not yet been initiated, and I was concerned that patients might die from pulmonary embolism. In the overwhelming urgency of providing life‐saving surgery to as many patients as possible, this simple measure had been overlooked. After discussion with our team and our Haitian medical colleagues, we initiated subcutaneous heparin on all eligible patients and made arrangements to receive further shipments of heparin to accommodate the influx of patients.
A nearby school and church had been annexed into makeshift extensions of the hospital wards. The volume and pace of incoming injuries was such that as soon as a patient was taken to surgery, another patient would often take his or her place in the bed. The rapid movement of patients to and from x‐ray, surgery, and postsurgical care created challenges around effective and accurate communication among multiple care providers. We decided that nonsurgical personnel would triage newly arriving patients and round on patients daily. Each nonsurgical physician was responsible for staffing a particular location. This zone‐defense approach ensured that the surgeons maximized their time in the operating rooms. We also instituted a basic system of portable medical records kept with each patient at all times, allowing personnel to easily and quickly assess care given to date, and to write notes and orders.
Presurgical and postsurgical wound infections became a common event, with the risk of ensuing sepsis. Antibiotic use was dependent on the preferences of individual surgeons and also on the available supply. As a result, antimicrobial treatments were highly variable and sometimes inadequate. The internists on the team proposed standard antibiotic guidelines for open fractures, for contaminated wounds, and for postoperative wounds; these regimens were approved and implemented by Haitian staff and the rest of the team.
Internists recognized the first complications of rhabdomyolysis from crush injuries and delays in receiving medical attention. Malaise, oliguria, and volume overload were often the only clues we had for severe renal failure. We had a functional lab capable of checking complete blood counts, urinalysis and creatinine, but we had a limited supply of serum potassium assays. We only used the latter in confirmed cases of rhabdomyolysis, and on several occasions we diagnosed severe hyperkalemia. Using bedside automated electrical defibrillation devices for monitoring, we sustained these patients on calcium gluconate until they could be transferred to an external dialysis unit run by Mdecins Sans Frontires in Port‐au‐Prince.6 As the number of rhabdomyolysis cases increased, we instigated creatinine rounds on patients arriving with large crush injuries, and we evaluated urine output daily until patients were clinically stable from this threat. We also helped the Haitian staff treat the omnipresent problem of pain and advised renal dosing of medications in renal failure and elderly patients.
GH: The situation 3 months after the earthquake was medically less dire but highlights the evolving importance of generalists in the aftermath of the quake.710 For many Haitian patients, the earthquake had become a universal point of reference for their symptomatology. Anorexia, amenorrhea, headaches, epigastric pain, even fungating soft tissue masses, were all reported to be depi tranbleman t a (since the earthquake) and were often somatic manifestations of a psychologically devastating event. At a hospital in Carrefour, I cared for patients presenting with dramatic sequelae of chronic diseases that had been undertreated due to the destruction of the Haitian medical infrastructurehypertensive coma, diabetic ketoacidosis, cerebral malaria, decompensated liver disease, and severe chronic anemia (including a patient with a hemoglobin of 3 mg/dL). I encountered many patients with infections exacerbated by excessive crowding in tent communities, such as typhoid and tuberculosis. At this particular hospital, priorities appropriately placed on surgical and postsurgical care required the team to devise creative solutions for the care and placement of medical patients, such as restructuring the emergency department and creating a rehabilitation tent on the hospital grounds. While few Haitian internists were present, a number of Haitian obstetricians were on site and helped manage medical conditions within the scope of their experience, such as hypertension, abdominal pain, and genitourinary infections. The expatriate orthopedic surgeons on site sought the consultative skills of hospitalists for preoperative management, postoperative complications, and comorbid conditions.
This hospital was largely sustained by rotating teams of volunteers, which underscored the importance of establishing a flexible system that would accommodate the turnover of personnel and fluctuating levels of professional expertise. The team used a tiered model for acute care delivery designating responsibilities based on the number of nurses, physicians, and other providers available. We collaborated with Haitian physicians to establish a routine of handoff rounds. Finally, we created and centralized documentation such as clinical protocols, contact numbers, and helpful tips for our successors.
Hospitalists have valuable skills to offer in medical responses to natural catastrophes.5 Our fluency with acute care environments becomes a pluripotent asset in disaster relief. Our experiences in assessing acuity are vital in assisting with inpatient triage. Our familiarity with the comanagement model facilitates partnership with other disciplines to optimize the distribution of skill sets without neglecting the overall well‐being of patients. Our clinical expertise in treating the vulnerable elderly, VTE, renal failure, pain management, postoperative infections, sepsis, and many other conditions can bolster medical relief efforts, even when the foremost need is surgical. The hospitalist's core competencies in healthcare systems11 can support recovery initiatives in medical facilities, particularly in the domains of drug safety, resource allocation, information management, team‐based methods, and care transitions. Our respective experiences also suggest the potential value of hospitalists in domestic, in addition to international, disaster response initiatives. Since large‐scale calamities may result in the hospitalization of overwhelming numbers of victims,12 hospitalists may be well‐positioned to assist our emergency medicine and public health colleagues, who currently (and fittingly) lead domestic efforts in disaster relief.
Tragedies like the earthquake in Haiti serve as a sobering reminder that a comprehensive multidisciplinary approach is required as medical disaster relief shifts from a life‐saving focus to one of life‐preserving care.13, 14 Hospitalists can play a vital role in these restorative efforts.
Acknowledgements
The authors thank their hospitalist colleagues at Beth Israel Deaconess who generously covered our shifts and encouraged us to write about our experiences.
- ,.Health impact of the 2004 Andaman Nicobar earthquake and tsunami in Indonesia.Prehosp Disaster Med.2009;24(6):493–499.
- ,,,.Medical response to hurricanes Katrina and Rita: local public health preparedness in action.J Public Health Manag Pract.2007;13(5):441–446.
- .Nephrology in earthquakes: sharing experiences and information.Clin J Am Soc Nephrol.2007;2(4):803–808.
- The Hospitalist. November2005. Hurricane Katrina: tragedy and hope. Available at: http://www.the‐hospitalist.org/details/article/255673/Hurricane_Katrina_Tragedy_and_Hope.html. Accessed August 2010.
- Washington Post. February 10,2010. Haiti raises earthquake toll to 230,000. Available at: http://www.washingtonpost.com/wp‐dyn/content/article/2010/02/09/AR2010020904447.html. Accessed August 2010.
- Médecins sans Frontiéres. About us. Available at: http://www.msf.org/msfinternational/aboutmsf/. Accessed August 2010.
- ,,, et al.Practicing internal medicine onboard the USNS COMFORT in the aftermath of the Haitian earthquake.Ann Intern Med.2010;152(11):733–737.
- Minnesota Medicine. April2010. Help for Haiti. Available at: http://www.minnesotamedicine.com/PastIssues/April2010/CoverstoryApril2010/tabid/3370/Default.aspx. Accessed August 2010.
- The Hospitalist. April2010. Hospitalists in Haiti. Available at: http://www.the‐hospitalist.org/details/article/590287/Hospitalists_in_Haiti.html. Accessed August 2010.
- .Haiti earthquake relief, phase two–long‐term needs and local resources.N Engl J Med.2010;362(20):1858–1861.
- ,,,,.The core competencies in hospital medicine: a framework for curriculum development by the society of hospital medicine. J Hosp Med.2006;(1 Suppl 1):2–95.
- ,,, et al.The impact of the Tsunami on hospitalizations at the tertiary care hospital in the Southern Province of Sri Lanka.Am J Disaster Med.2008;3(3):147–155.
- ,,.Short communication: patterns of chronic and acute diseases after natural disasters ‐ a study from the International Committee of the Red Cross field hospital in Banda Aceh after the 2004 Indian Ocean tsunami.Trop Med Int Health.2007;12(11):1338–1341.
- ,,.Characterisation of patients treated at the Red Cross field hospital in Kashmir during the first three weeks of operation.Emerg Med J.2006;23(8):654–656.
In the last decade, natural disasters such as the Indonesian tsunami of 2004, Hurricane Katrina in 2004, and the Pakistani earthquake of 2005 have brought attention to the importance of diverse but complementary medical professional roles in humanitarian medical aid.14 Natural disasters that cause significant physical trauma to large populations often necessitate initial multidisciplinary responder teams comprised of surgeons, anesthesiologists, emergency medicine physicians, surgical technologists, nurses, psychiatrists, and public health specialists. Their roles are to manage life‐threatening injuries, provide immediate triage, help affected individuals deal with intense psychological shock, and address critical population‐based needs such as water, food, and sanitation. Meanwhile, general medical, pediatric, rehabilitative, and long‐term psychiatric services often constitute a secondary tier of disaster response, providing postsurgical care, managing acute medical illnesses, mitigating psychological trauma, rehabilitating injuries, and providing vaccinations to at‐risk individuals. Hospitalists can play an important role in postcatastrophe recovery services as experts in acute care, stewards of care transitions, and drivers of systems improvement.
The earthquake that occurred January 12, 2010 in Haiti is a dramatic illustration of the importance of a multidisciplinary approach to disaster relief. The 7.0‐magnitude earthquake near Port‐au‐Prince ravaged an already crippled health care system, severely damaging the country's primary academic medical center, and killed the entire class of second‐year nursing students. The death toll has been estimated to be nearly one‐quarter of a million people.5 Victims awaiting surgery, recovering from surgery, or in need of other immediate medical attention quickly inundated any existing health facilities. The following stories describe the authors' respective experiences in Haiti after the earthquake.
JC: I arrived 4 days after the earthquake to a hospital outside of Port‐au‐Prince, spared from destruction, but filled with hundreds of patients with crush injuries and severe fractures. On rounds with the surgical team, I observed that venous thromboembolism (VTE) prophylaxis had not yet been initiated, and I was concerned that patients might die from pulmonary embolism. In the overwhelming urgency of providing life‐saving surgery to as many patients as possible, this simple measure had been overlooked. After discussion with our team and our Haitian medical colleagues, we initiated subcutaneous heparin on all eligible patients and made arrangements to receive further shipments of heparin to accommodate the influx of patients.
A nearby school and church had been annexed into makeshift extensions of the hospital wards. The volume and pace of incoming injuries was such that as soon as a patient was taken to surgery, another patient would often take his or her place in the bed. The rapid movement of patients to and from x‐ray, surgery, and postsurgical care created challenges around effective and accurate communication among multiple care providers. We decided that nonsurgical personnel would triage newly arriving patients and round on patients daily. Each nonsurgical physician was responsible for staffing a particular location. This zone‐defense approach ensured that the surgeons maximized their time in the operating rooms. We also instituted a basic system of portable medical records kept with each patient at all times, allowing personnel to easily and quickly assess care given to date, and to write notes and orders.
Presurgical and postsurgical wound infections became a common event, with the risk of ensuing sepsis. Antibiotic use was dependent on the preferences of individual surgeons and also on the available supply. As a result, antimicrobial treatments were highly variable and sometimes inadequate. The internists on the team proposed standard antibiotic guidelines for open fractures, for contaminated wounds, and for postoperative wounds; these regimens were approved and implemented by Haitian staff and the rest of the team.
Internists recognized the first complications of rhabdomyolysis from crush injuries and delays in receiving medical attention. Malaise, oliguria, and volume overload were often the only clues we had for severe renal failure. We had a functional lab capable of checking complete blood counts, urinalysis and creatinine, but we had a limited supply of serum potassium assays. We only used the latter in confirmed cases of rhabdomyolysis, and on several occasions we diagnosed severe hyperkalemia. Using bedside automated electrical defibrillation devices for monitoring, we sustained these patients on calcium gluconate until they could be transferred to an external dialysis unit run by Mdecins Sans Frontires in Port‐au‐Prince.6 As the number of rhabdomyolysis cases increased, we instigated creatinine rounds on patients arriving with large crush injuries, and we evaluated urine output daily until patients were clinically stable from this threat. We also helped the Haitian staff treat the omnipresent problem of pain and advised renal dosing of medications in renal failure and elderly patients.
GH: The situation 3 months after the earthquake was medically less dire but highlights the evolving importance of generalists in the aftermath of the quake.710 For many Haitian patients, the earthquake had become a universal point of reference for their symptomatology. Anorexia, amenorrhea, headaches, epigastric pain, even fungating soft tissue masses, were all reported to be depi tranbleman t a (since the earthquake) and were often somatic manifestations of a psychologically devastating event. At a hospital in Carrefour, I cared for patients presenting with dramatic sequelae of chronic diseases that had been undertreated due to the destruction of the Haitian medical infrastructurehypertensive coma, diabetic ketoacidosis, cerebral malaria, decompensated liver disease, and severe chronic anemia (including a patient with a hemoglobin of 3 mg/dL). I encountered many patients with infections exacerbated by excessive crowding in tent communities, such as typhoid and tuberculosis. At this particular hospital, priorities appropriately placed on surgical and postsurgical care required the team to devise creative solutions for the care and placement of medical patients, such as restructuring the emergency department and creating a rehabilitation tent on the hospital grounds. While few Haitian internists were present, a number of Haitian obstetricians were on site and helped manage medical conditions within the scope of their experience, such as hypertension, abdominal pain, and genitourinary infections. The expatriate orthopedic surgeons on site sought the consultative skills of hospitalists for preoperative management, postoperative complications, and comorbid conditions.
This hospital was largely sustained by rotating teams of volunteers, which underscored the importance of establishing a flexible system that would accommodate the turnover of personnel and fluctuating levels of professional expertise. The team used a tiered model for acute care delivery designating responsibilities based on the number of nurses, physicians, and other providers available. We collaborated with Haitian physicians to establish a routine of handoff rounds. Finally, we created and centralized documentation such as clinical protocols, contact numbers, and helpful tips for our successors.
Hospitalists have valuable skills to offer in medical responses to natural catastrophes.5 Our fluency with acute care environments becomes a pluripotent asset in disaster relief. Our experiences in assessing acuity are vital in assisting with inpatient triage. Our familiarity with the comanagement model facilitates partnership with other disciplines to optimize the distribution of skill sets without neglecting the overall well‐being of patients. Our clinical expertise in treating the vulnerable elderly, VTE, renal failure, pain management, postoperative infections, sepsis, and many other conditions can bolster medical relief efforts, even when the foremost need is surgical. The hospitalist's core competencies in healthcare systems11 can support recovery initiatives in medical facilities, particularly in the domains of drug safety, resource allocation, information management, team‐based methods, and care transitions. Our respective experiences also suggest the potential value of hospitalists in domestic, in addition to international, disaster response initiatives. Since large‐scale calamities may result in the hospitalization of overwhelming numbers of victims,12 hospitalists may be well‐positioned to assist our emergency medicine and public health colleagues, who currently (and fittingly) lead domestic efforts in disaster relief.
Tragedies like the earthquake in Haiti serve as a sobering reminder that a comprehensive multidisciplinary approach is required as medical disaster relief shifts from a life‐saving focus to one of life‐preserving care.13, 14 Hospitalists can play a vital role in these restorative efforts.
Acknowledgements
The authors thank their hospitalist colleagues at Beth Israel Deaconess who generously covered our shifts and encouraged us to write about our experiences.
In the last decade, natural disasters such as the Indonesian tsunami of 2004, Hurricane Katrina in 2004, and the Pakistani earthquake of 2005 have brought attention to the importance of diverse but complementary medical professional roles in humanitarian medical aid.14 Natural disasters that cause significant physical trauma to large populations often necessitate initial multidisciplinary responder teams comprised of surgeons, anesthesiologists, emergency medicine physicians, surgical technologists, nurses, psychiatrists, and public health specialists. Their roles are to manage life‐threatening injuries, provide immediate triage, help affected individuals deal with intense psychological shock, and address critical population‐based needs such as water, food, and sanitation. Meanwhile, general medical, pediatric, rehabilitative, and long‐term psychiatric services often constitute a secondary tier of disaster response, providing postsurgical care, managing acute medical illnesses, mitigating psychological trauma, rehabilitating injuries, and providing vaccinations to at‐risk individuals. Hospitalists can play an important role in postcatastrophe recovery services as experts in acute care, stewards of care transitions, and drivers of systems improvement.
The earthquake that occurred January 12, 2010 in Haiti is a dramatic illustration of the importance of a multidisciplinary approach to disaster relief. The 7.0‐magnitude earthquake near Port‐au‐Prince ravaged an already crippled health care system, severely damaging the country's primary academic medical center, and killed the entire class of second‐year nursing students. The death toll has been estimated to be nearly one‐quarter of a million people.5 Victims awaiting surgery, recovering from surgery, or in need of other immediate medical attention quickly inundated any existing health facilities. The following stories describe the authors' respective experiences in Haiti after the earthquake.
JC: I arrived 4 days after the earthquake to a hospital outside of Port‐au‐Prince, spared from destruction, but filled with hundreds of patients with crush injuries and severe fractures. On rounds with the surgical team, I observed that venous thromboembolism (VTE) prophylaxis had not yet been initiated, and I was concerned that patients might die from pulmonary embolism. In the overwhelming urgency of providing life‐saving surgery to as many patients as possible, this simple measure had been overlooked. After discussion with our team and our Haitian medical colleagues, we initiated subcutaneous heparin on all eligible patients and made arrangements to receive further shipments of heparin to accommodate the influx of patients.
A nearby school and church had been annexed into makeshift extensions of the hospital wards. The volume and pace of incoming injuries was such that as soon as a patient was taken to surgery, another patient would often take his or her place in the bed. The rapid movement of patients to and from x‐ray, surgery, and postsurgical care created challenges around effective and accurate communication among multiple care providers. We decided that nonsurgical personnel would triage newly arriving patients and round on patients daily. Each nonsurgical physician was responsible for staffing a particular location. This zone‐defense approach ensured that the surgeons maximized their time in the operating rooms. We also instituted a basic system of portable medical records kept with each patient at all times, allowing personnel to easily and quickly assess care given to date, and to write notes and orders.
Presurgical and postsurgical wound infections became a common event, with the risk of ensuing sepsis. Antibiotic use was dependent on the preferences of individual surgeons and also on the available supply. As a result, antimicrobial treatments were highly variable and sometimes inadequate. The internists on the team proposed standard antibiotic guidelines for open fractures, for contaminated wounds, and for postoperative wounds; these regimens were approved and implemented by Haitian staff and the rest of the team.
Internists recognized the first complications of rhabdomyolysis from crush injuries and delays in receiving medical attention. Malaise, oliguria, and volume overload were often the only clues we had for severe renal failure. We had a functional lab capable of checking complete blood counts, urinalysis and creatinine, but we had a limited supply of serum potassium assays. We only used the latter in confirmed cases of rhabdomyolysis, and on several occasions we diagnosed severe hyperkalemia. Using bedside automated electrical defibrillation devices for monitoring, we sustained these patients on calcium gluconate until they could be transferred to an external dialysis unit run by Mdecins Sans Frontires in Port‐au‐Prince.6 As the number of rhabdomyolysis cases increased, we instigated creatinine rounds on patients arriving with large crush injuries, and we evaluated urine output daily until patients were clinically stable from this threat. We also helped the Haitian staff treat the omnipresent problem of pain and advised renal dosing of medications in renal failure and elderly patients.
GH: The situation 3 months after the earthquake was medically less dire but highlights the evolving importance of generalists in the aftermath of the quake.710 For many Haitian patients, the earthquake had become a universal point of reference for their symptomatology. Anorexia, amenorrhea, headaches, epigastric pain, even fungating soft tissue masses, were all reported to be depi tranbleman t a (since the earthquake) and were often somatic manifestations of a psychologically devastating event. At a hospital in Carrefour, I cared for patients presenting with dramatic sequelae of chronic diseases that had been undertreated due to the destruction of the Haitian medical infrastructurehypertensive coma, diabetic ketoacidosis, cerebral malaria, decompensated liver disease, and severe chronic anemia (including a patient with a hemoglobin of 3 mg/dL). I encountered many patients with infections exacerbated by excessive crowding in tent communities, such as typhoid and tuberculosis. At this particular hospital, priorities appropriately placed on surgical and postsurgical care required the team to devise creative solutions for the care and placement of medical patients, such as restructuring the emergency department and creating a rehabilitation tent on the hospital grounds. While few Haitian internists were present, a number of Haitian obstetricians were on site and helped manage medical conditions within the scope of their experience, such as hypertension, abdominal pain, and genitourinary infections. The expatriate orthopedic surgeons on site sought the consultative skills of hospitalists for preoperative management, postoperative complications, and comorbid conditions.
This hospital was largely sustained by rotating teams of volunteers, which underscored the importance of establishing a flexible system that would accommodate the turnover of personnel and fluctuating levels of professional expertise. The team used a tiered model for acute care delivery designating responsibilities based on the number of nurses, physicians, and other providers available. We collaborated with Haitian physicians to establish a routine of handoff rounds. Finally, we created and centralized documentation such as clinical protocols, contact numbers, and helpful tips for our successors.
Hospitalists have valuable skills to offer in medical responses to natural catastrophes.5 Our fluency with acute care environments becomes a pluripotent asset in disaster relief. Our experiences in assessing acuity are vital in assisting with inpatient triage. Our familiarity with the comanagement model facilitates partnership with other disciplines to optimize the distribution of skill sets without neglecting the overall well‐being of patients. Our clinical expertise in treating the vulnerable elderly, VTE, renal failure, pain management, postoperative infections, sepsis, and many other conditions can bolster medical relief efforts, even when the foremost need is surgical. The hospitalist's core competencies in healthcare systems11 can support recovery initiatives in medical facilities, particularly in the domains of drug safety, resource allocation, information management, team‐based methods, and care transitions. Our respective experiences also suggest the potential value of hospitalists in domestic, in addition to international, disaster response initiatives. Since large‐scale calamities may result in the hospitalization of overwhelming numbers of victims,12 hospitalists may be well‐positioned to assist our emergency medicine and public health colleagues, who currently (and fittingly) lead domestic efforts in disaster relief.
Tragedies like the earthquake in Haiti serve as a sobering reminder that a comprehensive multidisciplinary approach is required as medical disaster relief shifts from a life‐saving focus to one of life‐preserving care.13, 14 Hospitalists can play a vital role in these restorative efforts.
Acknowledgements
The authors thank their hospitalist colleagues at Beth Israel Deaconess who generously covered our shifts and encouraged us to write about our experiences.
- ,.Health impact of the 2004 Andaman Nicobar earthquake and tsunami in Indonesia.Prehosp Disaster Med.2009;24(6):493–499.
- ,,,.Medical response to hurricanes Katrina and Rita: local public health preparedness in action.J Public Health Manag Pract.2007;13(5):441–446.
- .Nephrology in earthquakes: sharing experiences and information.Clin J Am Soc Nephrol.2007;2(4):803–808.
- The Hospitalist. November2005. Hurricane Katrina: tragedy and hope. Available at: http://www.the‐hospitalist.org/details/article/255673/Hurricane_Katrina_Tragedy_and_Hope.html. Accessed August 2010.
- Washington Post. February 10,2010. Haiti raises earthquake toll to 230,000. Available at: http://www.washingtonpost.com/wp‐dyn/content/article/2010/02/09/AR2010020904447.html. Accessed August 2010.
- Médecins sans Frontiéres. About us. Available at: http://www.msf.org/msfinternational/aboutmsf/. Accessed August 2010.
- ,,, et al.Practicing internal medicine onboard the USNS COMFORT in the aftermath of the Haitian earthquake.Ann Intern Med.2010;152(11):733–737.
- Minnesota Medicine. April2010. Help for Haiti. Available at: http://www.minnesotamedicine.com/PastIssues/April2010/CoverstoryApril2010/tabid/3370/Default.aspx. Accessed August 2010.
- The Hospitalist. April2010. Hospitalists in Haiti. Available at: http://www.the‐hospitalist.org/details/article/590287/Hospitalists_in_Haiti.html. Accessed August 2010.
- .Haiti earthquake relief, phase two–long‐term needs and local resources.N Engl J Med.2010;362(20):1858–1861.
- ,,,,.The core competencies in hospital medicine: a framework for curriculum development by the society of hospital medicine. J Hosp Med.2006;(1 Suppl 1):2–95.
- ,,, et al.The impact of the Tsunami on hospitalizations at the tertiary care hospital in the Southern Province of Sri Lanka.Am J Disaster Med.2008;3(3):147–155.
- ,,.Short communication: patterns of chronic and acute diseases after natural disasters ‐ a study from the International Committee of the Red Cross field hospital in Banda Aceh after the 2004 Indian Ocean tsunami.Trop Med Int Health.2007;12(11):1338–1341.
- ,,.Characterisation of patients treated at the Red Cross field hospital in Kashmir during the first three weeks of operation.Emerg Med J.2006;23(8):654–656.
- ,.Health impact of the 2004 Andaman Nicobar earthquake and tsunami in Indonesia.Prehosp Disaster Med.2009;24(6):493–499.
- ,,,.Medical response to hurricanes Katrina and Rita: local public health preparedness in action.J Public Health Manag Pract.2007;13(5):441–446.
- .Nephrology in earthquakes: sharing experiences and information.Clin J Am Soc Nephrol.2007;2(4):803–808.
- The Hospitalist. November2005. Hurricane Katrina: tragedy and hope. Available at: http://www.the‐hospitalist.org/details/article/255673/Hurricane_Katrina_Tragedy_and_Hope.html. Accessed August 2010.
- Washington Post. February 10,2010. Haiti raises earthquake toll to 230,000. Available at: http://www.washingtonpost.com/wp‐dyn/content/article/2010/02/09/AR2010020904447.html. Accessed August 2010.
- Médecins sans Frontiéres. About us. Available at: http://www.msf.org/msfinternational/aboutmsf/. Accessed August 2010.
- ,,, et al.Practicing internal medicine onboard the USNS COMFORT in the aftermath of the Haitian earthquake.Ann Intern Med.2010;152(11):733–737.
- Minnesota Medicine. April2010. Help for Haiti. Available at: http://www.minnesotamedicine.com/PastIssues/April2010/CoverstoryApril2010/tabid/3370/Default.aspx. Accessed August 2010.
- The Hospitalist. April2010. Hospitalists in Haiti. Available at: http://www.the‐hospitalist.org/details/article/590287/Hospitalists_in_Haiti.html. Accessed August 2010.
- .Haiti earthquake relief, phase two–long‐term needs and local resources.N Engl J Med.2010;362(20):1858–1861.
- ,,,,.The core competencies in hospital medicine: a framework for curriculum development by the society of hospital medicine. J Hosp Med.2006;(1 Suppl 1):2–95.
- ,,, et al.The impact of the Tsunami on hospitalizations at the tertiary care hospital in the Southern Province of Sri Lanka.Am J Disaster Med.2008;3(3):147–155.
- ,,.Short communication: patterns of chronic and acute diseases after natural disasters ‐ a study from the International Committee of the Red Cross field hospital in Banda Aceh after the 2004 Indian Ocean tsunami.Trop Med Int Health.2007;12(11):1338–1341.
- ,,.Characterisation of patients treated at the Red Cross field hospital in Kashmir during the first three weeks of operation.Emerg Med J.2006;23(8):654–656.
Understanding Hospital Readmissions
Hospital readmissions pose a major problem both to the patient and the fiscal stability of our health care system.1 Many interventions have attempted to tackle this problem. Interventions exist that utilize transition coaches working intensively with hospitalized patients or nurses performing postdischarge home visits or phoning patients.2, 3 Although beneficial, these strategies are costly and require additional, highly trained personnel. Consequently, they have been difficult to sustain financially in a fee‐for‐service environment, and difficult to generalize at other locales. Recent policies to decrease hospital payments for readmissions will incentivize hospitals to implement discharge programs.4 However, all hospital systems will still want to do this in the most efficient manner possible.
One important way to maximize benefits and minimize costs is to target the most intensive, expensive interventions to the highest risk patients who are most likely to be rehospitalized. By targeting the highest risk patients, we could significantly reduce costs. However, models predicting rehospitalization have had limited accuracy, even for condition‐specific models such as heart failure. Two studies in this issue work to better identify high‐risk patients. Mudge and colleagues5 prospectively examined risk factors for recurrent readmissions in an Australian hospital and found that chronic disease, depression, and underweight were independent risk factors for repeat readmission. Allaudeen6 examined risk factors for readmission to their own institution among general medicine patients. In a retrospective analysis of administrative data, they found that several variables predicted hospital readmission, including black race, insurance coverage through Medicaid, prescription of steroids or narcotics, and diagnoses of heart failure, renal disease, cancer, anemia, and weight loss.
These studies raise two questions that are critical if we are to develop better predictive modeling of who will benefit most from intensive interventions to reduce readmissions. First, what are the risk factors for preventable hospitalizations? People with multiple readmissions seem an obvious target on which to focus. However, it may be that these individuals are just very sick with multiple comorbidities, and many of their readmissions may not be preventable. Rich and colleagues reported that a multidisciplinary discharge intervention reduced readmissions for heart failure by 56%.7 What is often forgotten is that in their pilot study they were not able to reduce admissions for the most severely ill, and their final study population excluded the sickest patients. By targeting moderate‐risk patients, they were able to reduce readmissions significantly.8 In the studies by Mudge et al.5 and Allaudeen,6 the fact that chronic diseases predicted rehospitalization is only moderately helpful. It is possible, perhaps likely, that many of the readmissions for heart failure were preventable while many of the readmissions for cancer were not. The challenge for researchers is to develop methods for classifying admissions/readmissions as preventable.9 Using a defined set of diagnostic categories to classify readmissions (eg, ambulatory care sensitive conditions) may misclassify many cases.10 Determining preventable hospitalizations through detailed chart review is expensive and may have limited interobserver reliability. Nevertheless, physician review and classification may be necessary for future research to advance the field.
Second, what predictor variables are causally related to preventable hospitalizations (and presumably actionable), and which are merely markers of true causal factors and therefore harder to interpret and more difficult to act upon? In addition to chronic disease, Mudge et al.5 found that depression and low body mass index were independent risk factors for readmission. These conditions often go hand in hand. Patients who are burdened with chronic disease may be depressed and not eat. Conversely, patients who are depressed may not eat and allow their chronic disease to worsen. But it seems that depression is the more likely of the two to be causal. Depression is an important predictor of medication nonadherence and worsening illness.11, 12 Screening hospitalized patients for depression could provide valuable information on which patients may need treatment or more rigorous postdischarge follow‐up. In contrast, being underweight may not truly cause readmissions, but could be a marker of frailty and difficulty in meeting activities of daily living.
Similarly, Allaudeen6 found that black race, Medicaid use, steroid use, and narcotic use were independently associated with hospital readmission (in addition to chronic diseases and weight loss). Can being on steroids or narcotics cause readmissions? Does enrollment in Medicaid or being of black race cause one to be readmitted? While these may be markers which are statistically significant, they are unlikely to be true causes of rehospitalization. It is more likely that these variables are markers for true causal factors, such as financial barriers to medications or access barriers to primary care. Many other studies have used administrative databases to examine variables linked to readmission. We need to drill deeper to determine what is actually causing readmissions. Did the patient misinterpret how to take their steroid taper or were they so sick that they needed to return to the hospital? Perhaps they decided to wait on taking the steroids until they spoke with their primary care physician. This deeper level of understanding cannot be ascertained through third party administrative data sets. Primary data collection is needed to correctly determine who to target and the specific foci of interventions.
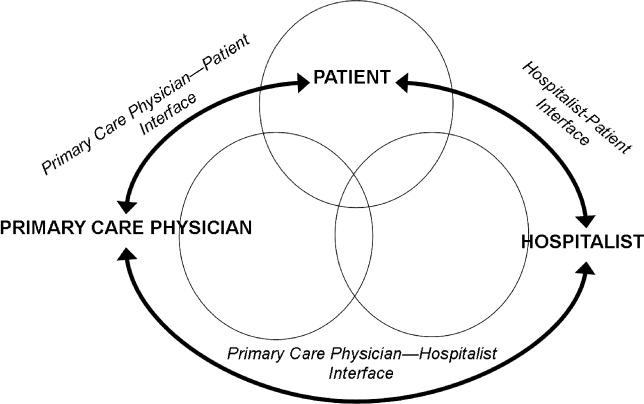
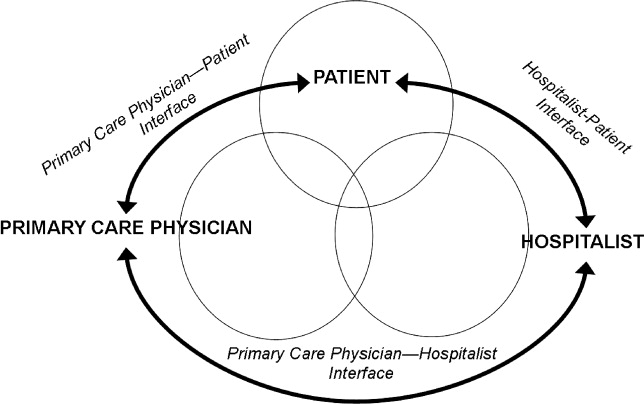
Future research on risk factors for readmissions (and interventions to decrease readmissions) should begin with a theoretical framework that addresses the patient, the hospital, and the receiving outpatient primary care physician or specialist, and the interfaces between each pair that could lead to preventable readmissions (see Figure 1).
With every potential variable affecting readmission, we need to systematically evaluate whether they are causal and preventable. When a variable is both causal and modifiable, we can then develop interventions to target these variables. We designed Table 1 as a framework to consider when moving forward in creating and implementing interventions.
| Factor | Potential Intervention |
|---|---|
| |
| Patient | |
| Cognition | Screening for cognition at discharge. Increase support at home. Inclusion of surrogate or caregiver in explaining discharge instructions. Additional use of a surrogate in explaining discharge instructions. |
| Depression | Screening for depression during the hospitalization and at discharge. Treatment of depression. Increased outpatient support to monitor depression. |
| Health literacy | Screening for health literacy. Involvement of hospital staff, social support network, and outpatient primary care physician to reinforce discharge instructions. |
| Support at home | Assess home support for patient. Increase phone call and home aid support following discharge for those with inadequate support. |
| Functional ability | Assess physical function throughout hospitalization and at discharge. Involve physical therapy early in the hospitalization and postdischarge. |
| Financial assets | Assess ability to pay for medications and transportation to follow‐up appointments. Work with social work on improving access. |
| Chronic disease (ie, congestive heart failure) | Improve patient education of disease and medications. Increase home support to monitor health status. Increase frequency of outpatient visits as needed. |
| Primary care physician | |
| PatientPCP interface | Via phone call to patient at discharge, reinforce so the patient understands disease process (eg, heart failure exacerbation triggers), will take medications started during hospitalization, and recognizes early precipitants of hospitalization. |
| PCPHospitalist interface | Encourage adequate communication about past medical problems and individualized issues pertinent to care plans. |
| Quality of outpatient primary care | Adhere to guidelines of care recommended by advisory standards. Ensure patients receive optimal outpatient care. |
| Medication reconciliation | Ensure that admission and discharge medication reconciliation is perfect. Update outpatient medication list with inpatient medication changes. |
| Follow‐up of pending tests | Create trigger system of pending tests for recently discharged patients. |
| Access to rapid follow‐up appointments | Incentivize physicians of recently discharged patients to offer follow‐up appointments in 1 week or less. |
| Hospitalist | |
| PatientHospitalist interface | Improve communication with patient on how to access physicians if residual postdischarge questions. |
| HospitalistPCP interface | Encourage adequate communication of hospital course and postdischarge plan. |
| Quality of inpatient hospital care | Ensure patients receive optimal inpatient care. Assess patient clinical stability and determine optimal time for discharge. |
| Written discharge instructions | Create easily understandable discharge instructions. Install checks to limit human errors. Ensure patient has copy on discharge. |
| Verbal discharge instructions | Learn to use teach‐back methodology to assess patient understanding of discharge instructions. Work to eliminate multiple sources (eg, consulting physicians, nurses, therapists) giving conflicting verbal discharge information. |
| Medication reconciliation | Utilize outpatient physician notes and pharmacy records to corroborate patient lists. Ensure that admission and discharge medication reconciliation is perfect. |
| Pending tests | Ensure discharge summary includes information and is communicated to PCP for follow‐up in timely manner. |
| Home services | Arrange for home support and nursing services to assist with patients needs postdischarge. Assess whether the patient knows of pending home services and means of contacting services if they do not occur. |
To advance this area, we need to be stringent about how we perform research and interpret findings. Studies that examine risk factors for readmission to a single hospital may be biased; for example, in the study by Allaudeen,6 it is possible that patients with Medicaid may have been equally likely to be readmitted to any hospital but more likely to be readmitted to the hospital that was the sole source of admission data. Even if findings from a single site are valid, they may not be generalizable. Ideally, studies of risk factors (and interventions to reduce readmissions) should be conducted in multiple sites that can track all hospitalizations and examine differences in risk factors for rehospitalization across hospitals. We have learned a tremendous amount over the last few years about risk markers for all‐cause readmission, and interventions to improve safety and quality of transitions in care. To advance further, multicenter studies are needed that focus on plausible causal variables of preventable readmissions and risk factors beyond the walls of the hospital (eg, access and quality of outpatient care for newly discharged patients). Only then will we better understand which patients can have their readmissions prevented and how to improve upon current strategies to improve outcomes.
- ,,. Nationwide Frequency and Costs of Potentially Preventable Hospitalizations,2006. April 2009. Available at: http://www.hcup‐us.ahrq.gov/reports/statbriefs/sb72.jsp. Accessed December 8, 2010.
- ,,,,,.Preparing patients and caregivers to participate in care delivered across settings: the care transitions intervention.J Am Geriatr Soc.2004;52(11):1817–1825.
- ,,, et al.A reengineered hospital discharge program to decrease rehospitalization: a randomized trial.Ann Int Med.2009;150(3):178–187.
- Sec. 3025.Hospital readmissions reduction program. The Patient Protection and Affordable Care Act. HR 3590. Acts of Congress, 111th second session. January 5,2010.
- ,,,,,,.Recurrent readmissions in medical patients: a prospective study.J Hosp Med.2011;6 (this issue).
- ,,,.Redefining identifiable readmission risk factors for general medicine patients.J Hosp Med.2011;6 (this issue).
- ,,,,,.A multidisciplinary intervention to prevent the readmission of elderly patients with congestive heart failure.N Engl J Med.1995;333(18):1190–1195.
- ,,, et al.Prevention of readmission in elderly patients with congestive heart failure: results of a prospective, randomized pilot study.J Gen Intern Med.1993;8(11):585–590.
- ,,,,,.Hospital readmissions and quality of care.Med Care.1999;37(5):490–501.
- ,,,.Ambulatory care sensitive conditions: terminology and disease coding need to be more specific to aid policy makers and clinicians.Public Health.2009;123(2):169–173.
- ,,,,.Depression is an important contributor to low medication adherence in hemodialyzed patients and transplant recipients.Kidney Int.2009;75(11):1223–1229.
- ,,, et al.Depression, medication adherence, and service utilization in systemic lupus erythematosus.Arthritis Rheum.2009;61(2):240–246.
Hospital readmissions pose a major problem both to the patient and the fiscal stability of our health care system.1 Many interventions have attempted to tackle this problem. Interventions exist that utilize transition coaches working intensively with hospitalized patients or nurses performing postdischarge home visits or phoning patients.2, 3 Although beneficial, these strategies are costly and require additional, highly trained personnel. Consequently, they have been difficult to sustain financially in a fee‐for‐service environment, and difficult to generalize at other locales. Recent policies to decrease hospital payments for readmissions will incentivize hospitals to implement discharge programs.4 However, all hospital systems will still want to do this in the most efficient manner possible.
One important way to maximize benefits and minimize costs is to target the most intensive, expensive interventions to the highest risk patients who are most likely to be rehospitalized. By targeting the highest risk patients, we could significantly reduce costs. However, models predicting rehospitalization have had limited accuracy, even for condition‐specific models such as heart failure. Two studies in this issue work to better identify high‐risk patients. Mudge and colleagues5 prospectively examined risk factors for recurrent readmissions in an Australian hospital and found that chronic disease, depression, and underweight were independent risk factors for repeat readmission. Allaudeen6 examined risk factors for readmission to their own institution among general medicine patients. In a retrospective analysis of administrative data, they found that several variables predicted hospital readmission, including black race, insurance coverage through Medicaid, prescription of steroids or narcotics, and diagnoses of heart failure, renal disease, cancer, anemia, and weight loss.
These studies raise two questions that are critical if we are to develop better predictive modeling of who will benefit most from intensive interventions to reduce readmissions. First, what are the risk factors for preventable hospitalizations? People with multiple readmissions seem an obvious target on which to focus. However, it may be that these individuals are just very sick with multiple comorbidities, and many of their readmissions may not be preventable. Rich and colleagues reported that a multidisciplinary discharge intervention reduced readmissions for heart failure by 56%.7 What is often forgotten is that in their pilot study they were not able to reduce admissions for the most severely ill, and their final study population excluded the sickest patients. By targeting moderate‐risk patients, they were able to reduce readmissions significantly.8 In the studies by Mudge et al.5 and Allaudeen,6 the fact that chronic diseases predicted rehospitalization is only moderately helpful. It is possible, perhaps likely, that many of the readmissions for heart failure were preventable while many of the readmissions for cancer were not. The challenge for researchers is to develop methods for classifying admissions/readmissions as preventable.9 Using a defined set of diagnostic categories to classify readmissions (eg, ambulatory care sensitive conditions) may misclassify many cases.10 Determining preventable hospitalizations through detailed chart review is expensive and may have limited interobserver reliability. Nevertheless, physician review and classification may be necessary for future research to advance the field.
Second, what predictor variables are causally related to preventable hospitalizations (and presumably actionable), and which are merely markers of true causal factors and therefore harder to interpret and more difficult to act upon? In addition to chronic disease, Mudge et al.5 found that depression and low body mass index were independent risk factors for readmission. These conditions often go hand in hand. Patients who are burdened with chronic disease may be depressed and not eat. Conversely, patients who are depressed may not eat and allow their chronic disease to worsen. But it seems that depression is the more likely of the two to be causal. Depression is an important predictor of medication nonadherence and worsening illness.11, 12 Screening hospitalized patients for depression could provide valuable information on which patients may need treatment or more rigorous postdischarge follow‐up. In contrast, being underweight may not truly cause readmissions, but could be a marker of frailty and difficulty in meeting activities of daily living.
Similarly, Allaudeen6 found that black race, Medicaid use, steroid use, and narcotic use were independently associated with hospital readmission (in addition to chronic diseases and weight loss). Can being on steroids or narcotics cause readmissions? Does enrollment in Medicaid or being of black race cause one to be readmitted? While these may be markers which are statistically significant, they are unlikely to be true causes of rehospitalization. It is more likely that these variables are markers for true causal factors, such as financial barriers to medications or access barriers to primary care. Many other studies have used administrative databases to examine variables linked to readmission. We need to drill deeper to determine what is actually causing readmissions. Did the patient misinterpret how to take their steroid taper or were they so sick that they needed to return to the hospital? Perhaps they decided to wait on taking the steroids until they spoke with their primary care physician. This deeper level of understanding cannot be ascertained through third party administrative data sets. Primary data collection is needed to correctly determine who to target and the specific foci of interventions.
Future research on risk factors for readmissions (and interventions to decrease readmissions) should begin with a theoretical framework that addresses the patient, the hospital, and the receiving outpatient primary care physician or specialist, and the interfaces between each pair that could lead to preventable readmissions (see Figure 1).
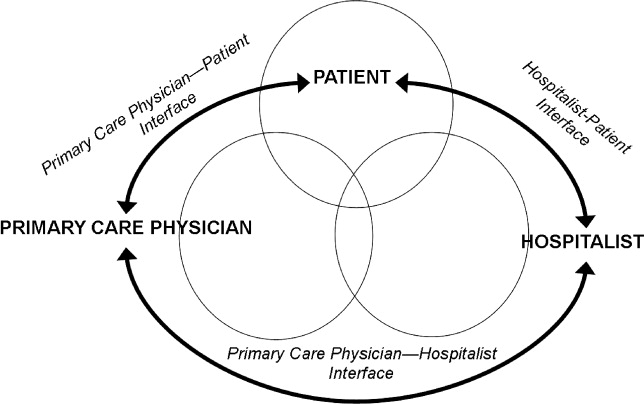
With every potential variable affecting readmission, we need to systematically evaluate whether they are causal and preventable. When a variable is both causal and modifiable, we can then develop interventions to target these variables. We designed Table 1 as a framework to consider when moving forward in creating and implementing interventions.
| Factor | Potential Intervention |
|---|---|
| |
| Patient | |
| Cognition | Screening for cognition at discharge. Increase support at home. Inclusion of surrogate or caregiver in explaining discharge instructions. Additional use of a surrogate in explaining discharge instructions. |
| Depression | Screening for depression during the hospitalization and at discharge. Treatment of depression. Increased outpatient support to monitor depression. |
| Health literacy | Screening for health literacy. Involvement of hospital staff, social support network, and outpatient primary care physician to reinforce discharge instructions. |
| Support at home | Assess home support for patient. Increase phone call and home aid support following discharge for those with inadequate support. |
| Functional ability | Assess physical function throughout hospitalization and at discharge. Involve physical therapy early in the hospitalization and postdischarge. |
| Financial assets | Assess ability to pay for medications and transportation to follow‐up appointments. Work with social work on improving access. |
| Chronic disease (ie, congestive heart failure) | Improve patient education of disease and medications. Increase home support to monitor health status. Increase frequency of outpatient visits as needed. |
| Primary care physician | |
| PatientPCP interface | Via phone call to patient at discharge, reinforce so the patient understands disease process (eg, heart failure exacerbation triggers), will take medications started during hospitalization, and recognizes early precipitants of hospitalization. |
| PCPHospitalist interface | Encourage adequate communication about past medical problems and individualized issues pertinent to care plans. |
| Quality of outpatient primary care | Adhere to guidelines of care recommended by advisory standards. Ensure patients receive optimal outpatient care. |
| Medication reconciliation | Ensure that admission and discharge medication reconciliation is perfect. Update outpatient medication list with inpatient medication changes. |
| Follow‐up of pending tests | Create trigger system of pending tests for recently discharged patients. |
| Access to rapid follow‐up appointments | Incentivize physicians of recently discharged patients to offer follow‐up appointments in 1 week or less. |
| Hospitalist | |
| PatientHospitalist interface | Improve communication with patient on how to access physicians if residual postdischarge questions. |
| HospitalistPCP interface | Encourage adequate communication of hospital course and postdischarge plan. |
| Quality of inpatient hospital care | Ensure patients receive optimal inpatient care. Assess patient clinical stability and determine optimal time for discharge. |
| Written discharge instructions | Create easily understandable discharge instructions. Install checks to limit human errors. Ensure patient has copy on discharge. |
| Verbal discharge instructions | Learn to use teach‐back methodology to assess patient understanding of discharge instructions. Work to eliminate multiple sources (eg, consulting physicians, nurses, therapists) giving conflicting verbal discharge information. |
| Medication reconciliation | Utilize outpatient physician notes and pharmacy records to corroborate patient lists. Ensure that admission and discharge medication reconciliation is perfect. |
| Pending tests | Ensure discharge summary includes information and is communicated to PCP for follow‐up in timely manner. |
| Home services | Arrange for home support and nursing services to assist with patients needs postdischarge. Assess whether the patient knows of pending home services and means of contacting services if they do not occur. |
To advance this area, we need to be stringent about how we perform research and interpret findings. Studies that examine risk factors for readmission to a single hospital may be biased; for example, in the study by Allaudeen,6 it is possible that patients with Medicaid may have been equally likely to be readmitted to any hospital but more likely to be readmitted to the hospital that was the sole source of admission data. Even if findings from a single site are valid, they may not be generalizable. Ideally, studies of risk factors (and interventions to reduce readmissions) should be conducted in multiple sites that can track all hospitalizations and examine differences in risk factors for rehospitalization across hospitals. We have learned a tremendous amount over the last few years about risk markers for all‐cause readmission, and interventions to improve safety and quality of transitions in care. To advance further, multicenter studies are needed that focus on plausible causal variables of preventable readmissions and risk factors beyond the walls of the hospital (eg, access and quality of outpatient care for newly discharged patients). Only then will we better understand which patients can have their readmissions prevented and how to improve upon current strategies to improve outcomes.
Hospital readmissions pose a major problem both to the patient and the fiscal stability of our health care system.1 Many interventions have attempted to tackle this problem. Interventions exist that utilize transition coaches working intensively with hospitalized patients or nurses performing postdischarge home visits or phoning patients.2, 3 Although beneficial, these strategies are costly and require additional, highly trained personnel. Consequently, they have been difficult to sustain financially in a fee‐for‐service environment, and difficult to generalize at other locales. Recent policies to decrease hospital payments for readmissions will incentivize hospitals to implement discharge programs.4 However, all hospital systems will still want to do this in the most efficient manner possible.
One important way to maximize benefits and minimize costs is to target the most intensive, expensive interventions to the highest risk patients who are most likely to be rehospitalized. By targeting the highest risk patients, we could significantly reduce costs. However, models predicting rehospitalization have had limited accuracy, even for condition‐specific models such as heart failure. Two studies in this issue work to better identify high‐risk patients. Mudge and colleagues5 prospectively examined risk factors for recurrent readmissions in an Australian hospital and found that chronic disease, depression, and underweight were independent risk factors for repeat readmission. Allaudeen6 examined risk factors for readmission to their own institution among general medicine patients. In a retrospective analysis of administrative data, they found that several variables predicted hospital readmission, including black race, insurance coverage through Medicaid, prescription of steroids or narcotics, and diagnoses of heart failure, renal disease, cancer, anemia, and weight loss.
These studies raise two questions that are critical if we are to develop better predictive modeling of who will benefit most from intensive interventions to reduce readmissions. First, what are the risk factors for preventable hospitalizations? People with multiple readmissions seem an obvious target on which to focus. However, it may be that these individuals are just very sick with multiple comorbidities, and many of their readmissions may not be preventable. Rich and colleagues reported that a multidisciplinary discharge intervention reduced readmissions for heart failure by 56%.7 What is often forgotten is that in their pilot study they were not able to reduce admissions for the most severely ill, and their final study population excluded the sickest patients. By targeting moderate‐risk patients, they were able to reduce readmissions significantly.8 In the studies by Mudge et al.5 and Allaudeen,6 the fact that chronic diseases predicted rehospitalization is only moderately helpful. It is possible, perhaps likely, that many of the readmissions for heart failure were preventable while many of the readmissions for cancer were not. The challenge for researchers is to develop methods for classifying admissions/readmissions as preventable.9 Using a defined set of diagnostic categories to classify readmissions (eg, ambulatory care sensitive conditions) may misclassify many cases.10 Determining preventable hospitalizations through detailed chart review is expensive and may have limited interobserver reliability. Nevertheless, physician review and classification may be necessary for future research to advance the field.
Second, what predictor variables are causally related to preventable hospitalizations (and presumably actionable), and which are merely markers of true causal factors and therefore harder to interpret and more difficult to act upon? In addition to chronic disease, Mudge et al.5 found that depression and low body mass index were independent risk factors for readmission. These conditions often go hand in hand. Patients who are burdened with chronic disease may be depressed and not eat. Conversely, patients who are depressed may not eat and allow their chronic disease to worsen. But it seems that depression is the more likely of the two to be causal. Depression is an important predictor of medication nonadherence and worsening illness.11, 12 Screening hospitalized patients for depression could provide valuable information on which patients may need treatment or more rigorous postdischarge follow‐up. In contrast, being underweight may not truly cause readmissions, but could be a marker of frailty and difficulty in meeting activities of daily living.
Similarly, Allaudeen6 found that black race, Medicaid use, steroid use, and narcotic use were independently associated with hospital readmission (in addition to chronic diseases and weight loss). Can being on steroids or narcotics cause readmissions? Does enrollment in Medicaid or being of black race cause one to be readmitted? While these may be markers which are statistically significant, they are unlikely to be true causes of rehospitalization. It is more likely that these variables are markers for true causal factors, such as financial barriers to medications or access barriers to primary care. Many other studies have used administrative databases to examine variables linked to readmission. We need to drill deeper to determine what is actually causing readmissions. Did the patient misinterpret how to take their steroid taper or were they so sick that they needed to return to the hospital? Perhaps they decided to wait on taking the steroids until they spoke with their primary care physician. This deeper level of understanding cannot be ascertained through third party administrative data sets. Primary data collection is needed to correctly determine who to target and the specific foci of interventions.
Future research on risk factors for readmissions (and interventions to decrease readmissions) should begin with a theoretical framework that addresses the patient, the hospital, and the receiving outpatient primary care physician or specialist, and the interfaces between each pair that could lead to preventable readmissions (see Figure 1).
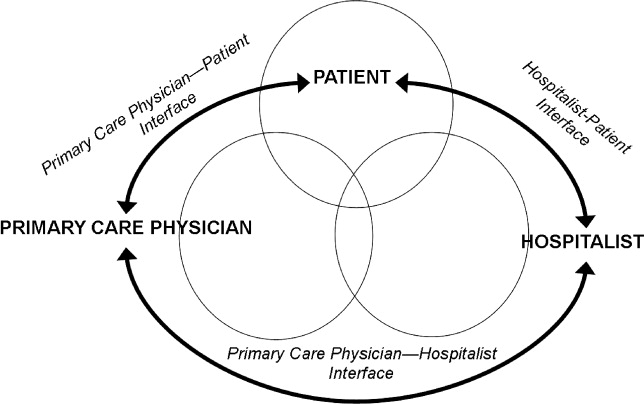
With every potential variable affecting readmission, we need to systematically evaluate whether they are causal and preventable. When a variable is both causal and modifiable, we can then develop interventions to target these variables. We designed Table 1 as a framework to consider when moving forward in creating and implementing interventions.
| Factor | Potential Intervention |
|---|---|
| |
| Patient | |
| Cognition | Screening for cognition at discharge. Increase support at home. Inclusion of surrogate or caregiver in explaining discharge instructions. Additional use of a surrogate in explaining discharge instructions. |
| Depression | Screening for depression during the hospitalization and at discharge. Treatment of depression. Increased outpatient support to monitor depression. |
| Health literacy | Screening for health literacy. Involvement of hospital staff, social support network, and outpatient primary care physician to reinforce discharge instructions. |
| Support at home | Assess home support for patient. Increase phone call and home aid support following discharge for those with inadequate support. |
| Functional ability | Assess physical function throughout hospitalization and at discharge. Involve physical therapy early in the hospitalization and postdischarge. |
| Financial assets | Assess ability to pay for medications and transportation to follow‐up appointments. Work with social work on improving access. |
| Chronic disease (ie, congestive heart failure) | Improve patient education of disease and medications. Increase home support to monitor health status. Increase frequency of outpatient visits as needed. |
| Primary care physician | |
| PatientPCP interface | Via phone call to patient at discharge, reinforce so the patient understands disease process (eg, heart failure exacerbation triggers), will take medications started during hospitalization, and recognizes early precipitants of hospitalization. |
| PCPHospitalist interface | Encourage adequate communication about past medical problems and individualized issues pertinent to care plans. |
| Quality of outpatient primary care | Adhere to guidelines of care recommended by advisory standards. Ensure patients receive optimal outpatient care. |
| Medication reconciliation | Ensure that admission and discharge medication reconciliation is perfect. Update outpatient medication list with inpatient medication changes. |
| Follow‐up of pending tests | Create trigger system of pending tests for recently discharged patients. |
| Access to rapid follow‐up appointments | Incentivize physicians of recently discharged patients to offer follow‐up appointments in 1 week or less. |
| Hospitalist | |
| PatientHospitalist interface | Improve communication with patient on how to access physicians if residual postdischarge questions. |
| HospitalistPCP interface | Encourage adequate communication of hospital course and postdischarge plan. |
| Quality of inpatient hospital care | Ensure patients receive optimal inpatient care. Assess patient clinical stability and determine optimal time for discharge. |
| Written discharge instructions | Create easily understandable discharge instructions. Install checks to limit human errors. Ensure patient has copy on discharge. |
| Verbal discharge instructions | Learn to use teach‐back methodology to assess patient understanding of discharge instructions. Work to eliminate multiple sources (eg, consulting physicians, nurses, therapists) giving conflicting verbal discharge information. |
| Medication reconciliation | Utilize outpatient physician notes and pharmacy records to corroborate patient lists. Ensure that admission and discharge medication reconciliation is perfect. |
| Pending tests | Ensure discharge summary includes information and is communicated to PCP for follow‐up in timely manner. |
| Home services | Arrange for home support and nursing services to assist with patients needs postdischarge. Assess whether the patient knows of pending home services and means of contacting services if they do not occur. |
To advance this area, we need to be stringent about how we perform research and interpret findings. Studies that examine risk factors for readmission to a single hospital may be biased; for example, in the study by Allaudeen,6 it is possible that patients with Medicaid may have been equally likely to be readmitted to any hospital but more likely to be readmitted to the hospital that was the sole source of admission data. Even if findings from a single site are valid, they may not be generalizable. Ideally, studies of risk factors (and interventions to reduce readmissions) should be conducted in multiple sites that can track all hospitalizations and examine differences in risk factors for rehospitalization across hospitals. We have learned a tremendous amount over the last few years about risk markers for all‐cause readmission, and interventions to improve safety and quality of transitions in care. To advance further, multicenter studies are needed that focus on plausible causal variables of preventable readmissions and risk factors beyond the walls of the hospital (eg, access and quality of outpatient care for newly discharged patients). Only then will we better understand which patients can have their readmissions prevented and how to improve upon current strategies to improve outcomes.
- ,,. Nationwide Frequency and Costs of Potentially Preventable Hospitalizations,2006. April 2009. Available at: http://www.hcup‐us.ahrq.gov/reports/statbriefs/sb72.jsp. Accessed December 8, 2010.
- ,,,,,.Preparing patients and caregivers to participate in care delivered across settings: the care transitions intervention.J Am Geriatr Soc.2004;52(11):1817–1825.
- ,,, et al.A reengineered hospital discharge program to decrease rehospitalization: a randomized trial.Ann Int Med.2009;150(3):178–187.
- Sec. 3025.Hospital readmissions reduction program. The Patient Protection and Affordable Care Act. HR 3590. Acts of Congress, 111th second session. January 5,2010.
- ,,,,,,.Recurrent readmissions in medical patients: a prospective study.J Hosp Med.2011;6 (this issue).
- ,,,.Redefining identifiable readmission risk factors for general medicine patients.J Hosp Med.2011;6 (this issue).
- ,,,,,.A multidisciplinary intervention to prevent the readmission of elderly patients with congestive heart failure.N Engl J Med.1995;333(18):1190–1195.
- ,,, et al.Prevention of readmission in elderly patients with congestive heart failure: results of a prospective, randomized pilot study.J Gen Intern Med.1993;8(11):585–590.
- ,,,,,.Hospital readmissions and quality of care.Med Care.1999;37(5):490–501.
- ,,,.Ambulatory care sensitive conditions: terminology and disease coding need to be more specific to aid policy makers and clinicians.Public Health.2009;123(2):169–173.
- ,,,,.Depression is an important contributor to low medication adherence in hemodialyzed patients and transplant recipients.Kidney Int.2009;75(11):1223–1229.
- ,,, et al.Depression, medication adherence, and service utilization in systemic lupus erythematosus.Arthritis Rheum.2009;61(2):240–246.
- ,,. Nationwide Frequency and Costs of Potentially Preventable Hospitalizations,2006. April 2009. Available at: http://www.hcup‐us.ahrq.gov/reports/statbriefs/sb72.jsp. Accessed December 8, 2010.
- ,,,,,.Preparing patients and caregivers to participate in care delivered across settings: the care transitions intervention.J Am Geriatr Soc.2004;52(11):1817–1825.
- ,,, et al.A reengineered hospital discharge program to decrease rehospitalization: a randomized trial.Ann Int Med.2009;150(3):178–187.
- Sec. 3025.Hospital readmissions reduction program. The Patient Protection and Affordable Care Act. HR 3590. Acts of Congress, 111th second session. January 5,2010.
- ,,,,,,.Recurrent readmissions in medical patients: a prospective study.J Hosp Med.2011;6 (this issue).
- ,,,.Redefining identifiable readmission risk factors for general medicine patients.J Hosp Med.2011;6 (this issue).
- ,,,,,.A multidisciplinary intervention to prevent the readmission of elderly patients with congestive heart failure.N Engl J Med.1995;333(18):1190–1195.
- ,,, et al.Prevention of readmission in elderly patients with congestive heart failure: results of a prospective, randomized pilot study.J Gen Intern Med.1993;8(11):585–590.
- ,,,,,.Hospital readmissions and quality of care.Med Care.1999;37(5):490–501.
- ,,,.Ambulatory care sensitive conditions: terminology and disease coding need to be more specific to aid policy makers and clinicians.Public Health.2009;123(2):169–173.
- ,,,,.Depression is an important contributor to low medication adherence in hemodialyzed patients and transplant recipients.Kidney Int.2009;75(11):1223–1229.
- ,,, et al.Depression, medication adherence, and service utilization in systemic lupus erythematosus.Arthritis Rheum.2009;61(2):240–246.
Off‐hours care: not so off
The word housestaff came from an era when you moved into the hospital (house) for your internship (staff). In those days, call every other night meant you missed half the learning opportunities. In those days, supervision was as remote as it could get. My, have things changed.
In 2003, the Accreditation Council for Graduate Medical Education (ACGME) implemented duty hour standards that called for restricting resident duty hours to no more than 80 hours per week, and no more than 24 continuous hours with an additional 6 hours for transfer of care.1 The expectation was that limiting work hours would have positive effects on outcomes, such as resident fatigue, the educational experience, and patient safety. A recent systematic review commissioned by the ACGME reviewed three decades worth of research on duty hours and patient safety. It reviewed laboratory studies of resident performance on clinical simulations, and tests of cognitive and fine motor skills under conditions of sleep deprivation. The results of these studies imply that limiting residents' duty hours should have positive effects on patient safety. However, that assumption has not been borne out. Paradoxically, examination of studies of alternative duty hour schedules, as well as the follow‐up studies on the impact of the New York duty hour rules and ACGME duty hour regulations have documented few measurable effects on patient safety.2 Thus, the simplistic view that fewer hours worked equals better patient care deserves a second‐look. In fact, a cause‐and‐effect relationship between resident fatigue and medical errors has yet to be proven.
The hospitalist movement was in full swing by 2003 and had already transformed the care of hospitalized patients. The early studies of hospitalists focused on cost and comparing outcomes with those of other providers. As many studies showed the economic benefit of hospitalists, residency programs began redesigning their inpatient services with hospitalists at the helm. Institutions sponsoring graduate medical education programs saw hospitalists as a necessary resource to enable and maintain compliance with duty hour reform. Some institutions created hospitalist‐only services with no housestaff (nonteaching services). Others created hospitalist teaching services that used indirect supervision at night from a hospitalist on‐call from home, while others had on‐site hospitalists at night that provided direct supervision of housestaff. It is clear that hospitalists are a versatile and valuable resource.
In this issue of the Journal of Hospital Medicine, Khanna and colleagues3 describe a retrospective medical record review at a large, urban academic hospital that evaluates the potential association between night admissions by night‐shiftbased hospitalists and a resident night float system, and hospitalization‐relevant outcomes. The outcomes included length of stay, hospital charges, Intensive Care Unit (ICU) transfers, Emergency Department visits within 30 days of discharge, 30‐day readmission rates, and poor outcomes within the first 24 hours of admission. Their results showed that night or weekend admission was not associated with worse hospitalization‐relevant outcomes. The extension of on‐site faculty supervision to nights, as well as awards for nursing excellence, likely had a strong positive impact on these outcomes. In some cases, night or weekend admission was associated with better outcomes, particularly in terms of ICU transfer during hospitalization and hospital charges. Maybe off‐hours care is not so off after all.
I am not sure where we are going, but the duty hour standards have been revised again. The new duty hour standards limit continuous duty hours for 1st‐year residents to 16, and all others to 24. Upper‐level residents can stay an additional 4 hours for transfer of care.4 Functionally, this proposed standard eliminates overnight call for 1st‐year residents. Although I would never advocate returning to the days of yore where autonomy and independence were the rule, I mourn the loss of extended shifts for 1st‐year residents. The loss of the extended shift will come at the expense of overnight call in many programs. I worry about the loss of some unique teaching moments for all residents, and the increased number of transitions in a patients' care. The hospital is a different place at night. It is less chaotic with fewer visitors, and there are less interruptions in patient care. There is time for teaching and learning because the work intensity is lower. The bedside teaching among senior and junior residents, during an acute patient episode in the middle of the night, is an experience that many of us would recount as an invaluable part of our training. It is also a time when on‐site faculty supervision and nurse staffing ratios are typically reduced. In other words, the entire system of care is different at night. This dichotomy in day versus night medicine has spurred research into whether patient outcomes differed between the two. Various investigators have looked at the differences in care, and there is some data to support that patient care outcomes are worse at night than during the day.58
The results from Khanna and colleagues3 are welcome news, since graduate medical education is undergoing a paradigm shift with further reductions in duty hours. Hospital‐based medicine is a 24‐hour operation, 7 days a week. We don't get to pick when patients are admitted or need care. In fact, this study demonstrates that 58% of the admissions came after 7 PM. It turns out that this pattern of admissions is not atypical.9 In light of the new standards, programs are left deciding where to deploy their 1st‐year resident resources. There are essentially two types of models to provide patient care off‐hours in the absence of an extended shift option: night float and night medicine. Night float implies that a trainee, usually a resident, comes from a different site or rotation to provide nocturnal care of a group of patients. That resident may do one isolated night of coverage or several nights in a row. The resident may perform cross‐cover functions, admit patients, or do both. Night medicine refers to having teams of housestaff at night along with an educational program as part of a rotation. The latter implies that trainees will get the full educational experience whether working days or nights. If one designs a model of care that puts 1st‐year residents where the volume is, they would come in late and leave early in the morning the next day. Both create more handoffs in patient care, which critics of these models have said lead to worse patient outcomes. This research challenges such earlier work and should make us all feel more comfortable that care at night does not need to be different if the proper systems are in place to manage it.
The graduate medical education community needs to take a step back and ask: Where are we going? As a long‐standing program director, I don't know anymore. As training has become competency‐based, and milestones are being developed for each level of training, we need to ask if reducing hours further is in the best interests of graduate medical education and, ultimately, the general public. I have long been interested in work intensity as a contributor to resident fatigue, burnout, and errors. A systematic review of resident workload and work activity looked at 21 studies examining resident time allocation and suggests that at least one‐third of resident time is spent on activities of limited educational value. Eight of the nine studies evaluating the impact of resident workload on patient care showed a negative impact on outcomes, including length of stay, mortality, patient satisfaction, medication errors, and lab utilization.10 If we are going to further restrict duty hours, then we need to transform the learning environment in a similar fashion. It does not seem logical to restrict duty hours further without a major redesign of the learning environment. I fear that all we have done is create more work compression because the system of care will be further strained in its weakest areas.
Hospitalists are uniquely poised to mitigate some of these concerns by being available for direct and indirect supervision, as well as being highly skilled at working in our complex systems. They are experts in systems‐based practice. The extension of direct faculty supervision to nights may be a major factor in eliminating the variances in care between nights and days. Not every program or institution will have the ability to employ night hospitalists, let alone have them in a supervisory and teaching role. Those that do can take great comfort in this research. Those that don't must challenge themselves to think about how to get there.
We all share the collective goal of producing the next generation of well‐trained physicians who will practice safe and effective care. As we begin to embrace competency‐based training, the prism through which we view patient safety must extend beyond duty hours and include learning environment reform. While the Khanna et al.3 study supports that off‐hours care is no longer off, we need to be careful that we don't drift too far towards shift work as the fundamental structure of medical training. In the beginning, residents lived in the hospital, thus the term. As we move through these stormy seas, we don't want to trade patient safety for transient trainees. There is a middle ground here that will be informed by future research. There is something to be said for living in your house.
- ACGME.Duty hour requirements. Available at: http://www.acgme.org/acWebsite/dutyHours/dh_ComProgrRequirmentsDutyHours0707.pdf. Accessed August 16,2010.
- ,,, et al.Systematic review of the literature on the impact of variation in residents' duty hour schedules on patient safety. Available at: http://acgme‐2010standards.org/pdf/Jefferson_Medical_College_Duty_Hours_Review.pdf. Accessed August 18,2010.
- ,,, et al.The association between night or weekend admission and hospitalization‐relevant patient outcomes.J Hosp Med2011;6:10–14.
- ACGME.Proposed duty hour standards. Available at: http://acgme‐2010standards.org/pdf/Proposed_Standards.pdf. Accessed August 16,2010.
- ,.Mortality among patients admitted to hospitals on weekends as compared with weekdays.N Engl J Med.2001;345(9):663–668.
- ,,, et al.Survival from in‐hospital cardiac arrest during nights and weekends.JAMA.2008;299(7):785–792.
- ,,,,.What effect does inpatient physician specialty and experience have on clinical outcomes and resource utilization on a general medicine service?J Gen Intern Med.2004;19:395–401.
- ,,,,,.Implementation of a voluntary hospitalist service at a community teaching hospital: improved clinical efficiency and patient outcomes.Ann Intern Med.2002;137:859–865.
- .Like night and day—shedding light on off‐hours care.N Engl J Med.2008;358(20):2091–2093.
- ,,.Systematic review of resident workload and work activity: impact on resident education and patient care. Available at: http://acgme‐2010standards.org/pdf/Resident_Duty_Hours_and_Related_Topics.pdf. Accessed on August 16,2010.
The word housestaff came from an era when you moved into the hospital (house) for your internship (staff). In those days, call every other night meant you missed half the learning opportunities. In those days, supervision was as remote as it could get. My, have things changed.
In 2003, the Accreditation Council for Graduate Medical Education (ACGME) implemented duty hour standards that called for restricting resident duty hours to no more than 80 hours per week, and no more than 24 continuous hours with an additional 6 hours for transfer of care.1 The expectation was that limiting work hours would have positive effects on outcomes, such as resident fatigue, the educational experience, and patient safety. A recent systematic review commissioned by the ACGME reviewed three decades worth of research on duty hours and patient safety. It reviewed laboratory studies of resident performance on clinical simulations, and tests of cognitive and fine motor skills under conditions of sleep deprivation. The results of these studies imply that limiting residents' duty hours should have positive effects on patient safety. However, that assumption has not been borne out. Paradoxically, examination of studies of alternative duty hour schedules, as well as the follow‐up studies on the impact of the New York duty hour rules and ACGME duty hour regulations have documented few measurable effects on patient safety.2 Thus, the simplistic view that fewer hours worked equals better patient care deserves a second‐look. In fact, a cause‐and‐effect relationship between resident fatigue and medical errors has yet to be proven.
The hospitalist movement was in full swing by 2003 and had already transformed the care of hospitalized patients. The early studies of hospitalists focused on cost and comparing outcomes with those of other providers. As many studies showed the economic benefit of hospitalists, residency programs began redesigning their inpatient services with hospitalists at the helm. Institutions sponsoring graduate medical education programs saw hospitalists as a necessary resource to enable and maintain compliance with duty hour reform. Some institutions created hospitalist‐only services with no housestaff (nonteaching services). Others created hospitalist teaching services that used indirect supervision at night from a hospitalist on‐call from home, while others had on‐site hospitalists at night that provided direct supervision of housestaff. It is clear that hospitalists are a versatile and valuable resource.
In this issue of the Journal of Hospital Medicine, Khanna and colleagues3 describe a retrospective medical record review at a large, urban academic hospital that evaluates the potential association between night admissions by night‐shiftbased hospitalists and a resident night float system, and hospitalization‐relevant outcomes. The outcomes included length of stay, hospital charges, Intensive Care Unit (ICU) transfers, Emergency Department visits within 30 days of discharge, 30‐day readmission rates, and poor outcomes within the first 24 hours of admission. Their results showed that night or weekend admission was not associated with worse hospitalization‐relevant outcomes. The extension of on‐site faculty supervision to nights, as well as awards for nursing excellence, likely had a strong positive impact on these outcomes. In some cases, night or weekend admission was associated with better outcomes, particularly in terms of ICU transfer during hospitalization and hospital charges. Maybe off‐hours care is not so off after all.
I am not sure where we are going, but the duty hour standards have been revised again. The new duty hour standards limit continuous duty hours for 1st‐year residents to 16, and all others to 24. Upper‐level residents can stay an additional 4 hours for transfer of care.4 Functionally, this proposed standard eliminates overnight call for 1st‐year residents. Although I would never advocate returning to the days of yore where autonomy and independence were the rule, I mourn the loss of extended shifts for 1st‐year residents. The loss of the extended shift will come at the expense of overnight call in many programs. I worry about the loss of some unique teaching moments for all residents, and the increased number of transitions in a patients' care. The hospital is a different place at night. It is less chaotic with fewer visitors, and there are less interruptions in patient care. There is time for teaching and learning because the work intensity is lower. The bedside teaching among senior and junior residents, during an acute patient episode in the middle of the night, is an experience that many of us would recount as an invaluable part of our training. It is also a time when on‐site faculty supervision and nurse staffing ratios are typically reduced. In other words, the entire system of care is different at night. This dichotomy in day versus night medicine has spurred research into whether patient outcomes differed between the two. Various investigators have looked at the differences in care, and there is some data to support that patient care outcomes are worse at night than during the day.58
The results from Khanna and colleagues3 are welcome news, since graduate medical education is undergoing a paradigm shift with further reductions in duty hours. Hospital‐based medicine is a 24‐hour operation, 7 days a week. We don't get to pick when patients are admitted or need care. In fact, this study demonstrates that 58% of the admissions came after 7 PM. It turns out that this pattern of admissions is not atypical.9 In light of the new standards, programs are left deciding where to deploy their 1st‐year resident resources. There are essentially two types of models to provide patient care off‐hours in the absence of an extended shift option: night float and night medicine. Night float implies that a trainee, usually a resident, comes from a different site or rotation to provide nocturnal care of a group of patients. That resident may do one isolated night of coverage or several nights in a row. The resident may perform cross‐cover functions, admit patients, or do both. Night medicine refers to having teams of housestaff at night along with an educational program as part of a rotation. The latter implies that trainees will get the full educational experience whether working days or nights. If one designs a model of care that puts 1st‐year residents where the volume is, they would come in late and leave early in the morning the next day. Both create more handoffs in patient care, which critics of these models have said lead to worse patient outcomes. This research challenges such earlier work and should make us all feel more comfortable that care at night does not need to be different if the proper systems are in place to manage it.
The graduate medical education community needs to take a step back and ask: Where are we going? As a long‐standing program director, I don't know anymore. As training has become competency‐based, and milestones are being developed for each level of training, we need to ask if reducing hours further is in the best interests of graduate medical education and, ultimately, the general public. I have long been interested in work intensity as a contributor to resident fatigue, burnout, and errors. A systematic review of resident workload and work activity looked at 21 studies examining resident time allocation and suggests that at least one‐third of resident time is spent on activities of limited educational value. Eight of the nine studies evaluating the impact of resident workload on patient care showed a negative impact on outcomes, including length of stay, mortality, patient satisfaction, medication errors, and lab utilization.10 If we are going to further restrict duty hours, then we need to transform the learning environment in a similar fashion. It does not seem logical to restrict duty hours further without a major redesign of the learning environment. I fear that all we have done is create more work compression because the system of care will be further strained in its weakest areas.
Hospitalists are uniquely poised to mitigate some of these concerns by being available for direct and indirect supervision, as well as being highly skilled at working in our complex systems. They are experts in systems‐based practice. The extension of direct faculty supervision to nights may be a major factor in eliminating the variances in care between nights and days. Not every program or institution will have the ability to employ night hospitalists, let alone have them in a supervisory and teaching role. Those that do can take great comfort in this research. Those that don't must challenge themselves to think about how to get there.
We all share the collective goal of producing the next generation of well‐trained physicians who will practice safe and effective care. As we begin to embrace competency‐based training, the prism through which we view patient safety must extend beyond duty hours and include learning environment reform. While the Khanna et al.3 study supports that off‐hours care is no longer off, we need to be careful that we don't drift too far towards shift work as the fundamental structure of medical training. In the beginning, residents lived in the hospital, thus the term. As we move through these stormy seas, we don't want to trade patient safety for transient trainees. There is a middle ground here that will be informed by future research. There is something to be said for living in your house.
The word housestaff came from an era when you moved into the hospital (house) for your internship (staff). In those days, call every other night meant you missed half the learning opportunities. In those days, supervision was as remote as it could get. My, have things changed.
In 2003, the Accreditation Council for Graduate Medical Education (ACGME) implemented duty hour standards that called for restricting resident duty hours to no more than 80 hours per week, and no more than 24 continuous hours with an additional 6 hours for transfer of care.1 The expectation was that limiting work hours would have positive effects on outcomes, such as resident fatigue, the educational experience, and patient safety. A recent systematic review commissioned by the ACGME reviewed three decades worth of research on duty hours and patient safety. It reviewed laboratory studies of resident performance on clinical simulations, and tests of cognitive and fine motor skills under conditions of sleep deprivation. The results of these studies imply that limiting residents' duty hours should have positive effects on patient safety. However, that assumption has not been borne out. Paradoxically, examination of studies of alternative duty hour schedules, as well as the follow‐up studies on the impact of the New York duty hour rules and ACGME duty hour regulations have documented few measurable effects on patient safety.2 Thus, the simplistic view that fewer hours worked equals better patient care deserves a second‐look. In fact, a cause‐and‐effect relationship between resident fatigue and medical errors has yet to be proven.
The hospitalist movement was in full swing by 2003 and had already transformed the care of hospitalized patients. The early studies of hospitalists focused on cost and comparing outcomes with those of other providers. As many studies showed the economic benefit of hospitalists, residency programs began redesigning their inpatient services with hospitalists at the helm. Institutions sponsoring graduate medical education programs saw hospitalists as a necessary resource to enable and maintain compliance with duty hour reform. Some institutions created hospitalist‐only services with no housestaff (nonteaching services). Others created hospitalist teaching services that used indirect supervision at night from a hospitalist on‐call from home, while others had on‐site hospitalists at night that provided direct supervision of housestaff. It is clear that hospitalists are a versatile and valuable resource.
In this issue of the Journal of Hospital Medicine, Khanna and colleagues3 describe a retrospective medical record review at a large, urban academic hospital that evaluates the potential association between night admissions by night‐shiftbased hospitalists and a resident night float system, and hospitalization‐relevant outcomes. The outcomes included length of stay, hospital charges, Intensive Care Unit (ICU) transfers, Emergency Department visits within 30 days of discharge, 30‐day readmission rates, and poor outcomes within the first 24 hours of admission. Their results showed that night or weekend admission was not associated with worse hospitalization‐relevant outcomes. The extension of on‐site faculty supervision to nights, as well as awards for nursing excellence, likely had a strong positive impact on these outcomes. In some cases, night or weekend admission was associated with better outcomes, particularly in terms of ICU transfer during hospitalization and hospital charges. Maybe off‐hours care is not so off after all.
I am not sure where we are going, but the duty hour standards have been revised again. The new duty hour standards limit continuous duty hours for 1st‐year residents to 16, and all others to 24. Upper‐level residents can stay an additional 4 hours for transfer of care.4 Functionally, this proposed standard eliminates overnight call for 1st‐year residents. Although I would never advocate returning to the days of yore where autonomy and independence were the rule, I mourn the loss of extended shifts for 1st‐year residents. The loss of the extended shift will come at the expense of overnight call in many programs. I worry about the loss of some unique teaching moments for all residents, and the increased number of transitions in a patients' care. The hospital is a different place at night. It is less chaotic with fewer visitors, and there are less interruptions in patient care. There is time for teaching and learning because the work intensity is lower. The bedside teaching among senior and junior residents, during an acute patient episode in the middle of the night, is an experience that many of us would recount as an invaluable part of our training. It is also a time when on‐site faculty supervision and nurse staffing ratios are typically reduced. In other words, the entire system of care is different at night. This dichotomy in day versus night medicine has spurred research into whether patient outcomes differed between the two. Various investigators have looked at the differences in care, and there is some data to support that patient care outcomes are worse at night than during the day.58
The results from Khanna and colleagues3 are welcome news, since graduate medical education is undergoing a paradigm shift with further reductions in duty hours. Hospital‐based medicine is a 24‐hour operation, 7 days a week. We don't get to pick when patients are admitted or need care. In fact, this study demonstrates that 58% of the admissions came after 7 PM. It turns out that this pattern of admissions is not atypical.9 In light of the new standards, programs are left deciding where to deploy their 1st‐year resident resources. There are essentially two types of models to provide patient care off‐hours in the absence of an extended shift option: night float and night medicine. Night float implies that a trainee, usually a resident, comes from a different site or rotation to provide nocturnal care of a group of patients. That resident may do one isolated night of coverage or several nights in a row. The resident may perform cross‐cover functions, admit patients, or do both. Night medicine refers to having teams of housestaff at night along with an educational program as part of a rotation. The latter implies that trainees will get the full educational experience whether working days or nights. If one designs a model of care that puts 1st‐year residents where the volume is, they would come in late and leave early in the morning the next day. Both create more handoffs in patient care, which critics of these models have said lead to worse patient outcomes. This research challenges such earlier work and should make us all feel more comfortable that care at night does not need to be different if the proper systems are in place to manage it.
The graduate medical education community needs to take a step back and ask: Where are we going? As a long‐standing program director, I don't know anymore. As training has become competency‐based, and milestones are being developed for each level of training, we need to ask if reducing hours further is in the best interests of graduate medical education and, ultimately, the general public. I have long been interested in work intensity as a contributor to resident fatigue, burnout, and errors. A systematic review of resident workload and work activity looked at 21 studies examining resident time allocation and suggests that at least one‐third of resident time is spent on activities of limited educational value. Eight of the nine studies evaluating the impact of resident workload on patient care showed a negative impact on outcomes, including length of stay, mortality, patient satisfaction, medication errors, and lab utilization.10 If we are going to further restrict duty hours, then we need to transform the learning environment in a similar fashion. It does not seem logical to restrict duty hours further without a major redesign of the learning environment. I fear that all we have done is create more work compression because the system of care will be further strained in its weakest areas.
Hospitalists are uniquely poised to mitigate some of these concerns by being available for direct and indirect supervision, as well as being highly skilled at working in our complex systems. They are experts in systems‐based practice. The extension of direct faculty supervision to nights may be a major factor in eliminating the variances in care between nights and days. Not every program or institution will have the ability to employ night hospitalists, let alone have them in a supervisory and teaching role. Those that do can take great comfort in this research. Those that don't must challenge themselves to think about how to get there.
We all share the collective goal of producing the next generation of well‐trained physicians who will practice safe and effective care. As we begin to embrace competency‐based training, the prism through which we view patient safety must extend beyond duty hours and include learning environment reform. While the Khanna et al.3 study supports that off‐hours care is no longer off, we need to be careful that we don't drift too far towards shift work as the fundamental structure of medical training. In the beginning, residents lived in the hospital, thus the term. As we move through these stormy seas, we don't want to trade patient safety for transient trainees. There is a middle ground here that will be informed by future research. There is something to be said for living in your house.
- ACGME.Duty hour requirements. Available at: http://www.acgme.org/acWebsite/dutyHours/dh_ComProgrRequirmentsDutyHours0707.pdf. Accessed August 16,2010.
- ,,, et al.Systematic review of the literature on the impact of variation in residents' duty hour schedules on patient safety. Available at: http://acgme‐2010standards.org/pdf/Jefferson_Medical_College_Duty_Hours_Review.pdf. Accessed August 18,2010.
- ,,, et al.The association between night or weekend admission and hospitalization‐relevant patient outcomes.J Hosp Med2011;6:10–14.
- ACGME.Proposed duty hour standards. Available at: http://acgme‐2010standards.org/pdf/Proposed_Standards.pdf. Accessed August 16,2010.
- ,.Mortality among patients admitted to hospitals on weekends as compared with weekdays.N Engl J Med.2001;345(9):663–668.
- ,,, et al.Survival from in‐hospital cardiac arrest during nights and weekends.JAMA.2008;299(7):785–792.
- ,,,,.What effect does inpatient physician specialty and experience have on clinical outcomes and resource utilization on a general medicine service?J Gen Intern Med.2004;19:395–401.
- ,,,,,.Implementation of a voluntary hospitalist service at a community teaching hospital: improved clinical efficiency and patient outcomes.Ann Intern Med.2002;137:859–865.
- .Like night and day—shedding light on off‐hours care.N Engl J Med.2008;358(20):2091–2093.
- ,,.Systematic review of resident workload and work activity: impact on resident education and patient care. Available at: http://acgme‐2010standards.org/pdf/Resident_Duty_Hours_and_Related_Topics.pdf. Accessed on August 16,2010.
- ACGME.Duty hour requirements. Available at: http://www.acgme.org/acWebsite/dutyHours/dh_ComProgrRequirmentsDutyHours0707.pdf. Accessed August 16,2010.
- ,,, et al.Systematic review of the literature on the impact of variation in residents' duty hour schedules on patient safety. Available at: http://acgme‐2010standards.org/pdf/Jefferson_Medical_College_Duty_Hours_Review.pdf. Accessed August 18,2010.
- ,,, et al.The association between night or weekend admission and hospitalization‐relevant patient outcomes.J Hosp Med2011;6:10–14.
- ACGME.Proposed duty hour standards. Available at: http://acgme‐2010standards.org/pdf/Proposed_Standards.pdf. Accessed August 16,2010.
- ,.Mortality among patients admitted to hospitals on weekends as compared with weekdays.N Engl J Med.2001;345(9):663–668.
- ,,, et al.Survival from in‐hospital cardiac arrest during nights and weekends.JAMA.2008;299(7):785–792.
- ,,,,.What effect does inpatient physician specialty and experience have on clinical outcomes and resource utilization on a general medicine service?J Gen Intern Med.2004;19:395–401.
- ,,,,,.Implementation of a voluntary hospitalist service at a community teaching hospital: improved clinical efficiency and patient outcomes.Ann Intern Med.2002;137:859–865.
- .Like night and day—shedding light on off‐hours care.N Engl J Med.2008;358(20):2091–2093.
- ,,.Systematic review of resident workload and work activity: impact on resident education and patient care. Available at: http://acgme‐2010standards.org/pdf/Resident_Duty_Hours_and_Related_Topics.pdf. Accessed on August 16,2010.
The need for mentors in the odyssey of the academic hospitalist
This issue of the Journal of Hospital Medicine features an important contribution concerning the current state of academic hospital medicine. The survey of 57 hospitalists revealed what many of us already suspected: the state of mentorship in academic hospitalist groups is unsatisfactory.1
While the conclusion is alarming, it is also not surprising. Over the past decade academic medical centers enthusiastically hired hospitalists to improve efficiency for inpatient services and to lessen the effect of Accreditation Council for Graduate Medical Education (ACGME) regulations on duty hours and patient caps. Few departments of internal medicine, however, hired academic hospitalists with the intent of creating academic divisions. Thus many institutions appear to view hospitalists primarily as hospital employees ignoring their potential academic contributions, and as a result it should not be a surprise that many hospitalist groups lack the mentorship infrastructure of other divisions within a typical Department of Medicine. Compounding the hospital employee problem, the new field of academic hospital medicine has emerged only in the last decade, a time frame that has resulted in very few hospitalists qualified to serve as senior mentors.
We cannot easily remove these limitations: the past is the past, and over time, hospital medicine will mature and develop more senior mentors. But what should we do until that maturation occurs? We believe that the academic work of hospitalists, both in education and research (Quality and Patient Safety) are important endeavors too valuable to be left to chance. With 30,000 hospitalists delivering care, it is critical that research in the optimal delivery of this care be performed, targeting systems improvements to enact anticipated outcomes in quality and patient safety. The physicians who are regularly and intimately involved in this system of inpatient care delivery, the hospitalists, are best suited for identifying the unique features of the inpatient care system needing improvement. Mentorship is essential in ensuring the advancement of both areas, and the sustainability of hospital medicine in medical academe. The article by Harrison et al.1 both establishes the depth of these issues and provides important insights into potential solutions for closing this mentorship gap while the field matures.
Utilizing Other Mentors
No measure of systems change will make young hospitalists immediately experienced, such that they have the sophistication to be senior mentors for younger hospitalists. But we can compensate for this temporary gap in mentorship experience. First, in the next 5 to 10 years, young academic hospitalists need explicit direction from those within Departments of Medicine who do have this mentorship experience, even if these mentors do not work in hospital medicine. Mentors within General Internal Medicine or the subspecialties can still provide the guidance and support to ensure that academic hospitalists are engaging in the appropriate endeavors toward promotion and intellectual growth. Second, academic hospitalists have to seek out mentorship from afar through their participation in the organizations primarily devoted to the academic welfare of hospitalists: The Society of Hospital Medicine (SHM) and the Society of General Internal Medicine (SGIM). Both organizations sponsor mentorship programs, and regular attendance at regional and/or national meetings (followed by email correspondence) can greatly improve an academic hospitalist's career trajectory. Finally, midlevel and senior‐level hospitalists have to learn mentorship skills; mere experience in the field does not ensure acquisition of the necessary mentorship skills, anymore than experience in medicine ensures teaching skills. Mentorship is its own skill set, and receiving appropriate training via the SHM or SGIM national meetings or the Academic Hospitalist Academy (referenced below) is critical.
Defining Academic Expectations for Hospitalists
Harrison et al.1 note that academic hospitalists felt there was a lack of respect for the scholarly work that hospitalists do as part of their job, raising the proposition that the mentorship dearth for academic hospitalists might result from currently available mentors not knowing what to say. Even if mentors were plentiful today, we still must ask the question, What would the mentor advise the young hospitalist to do? The academic hospitalist offers extraordinary value to the Department, but in a way that is different from the standard R0RO‐1 Grant paradigm. Even if hospitalists acquire extramural funding, it will likely come from sources different from the National Institutes of Health (NIH): Agency for Healthcare Research and Quality (AHRQ), foundations (eg, The Robert Wood Johnson Foundation or The John A. Hartford Foundation), intramural hospital‐originating funding, etc. And while extramural funding may be a measure of a hospitalist's contribution to the Department, it should not be the only measure of the hospitalist's career development. There are 2 ways to get rich: acquire more money, or spend less money. Academic hospitalists, unlike other specialties in Medicine, are likely to fall into the latter category, by offering decreased hospital costs (ie, decreased length of stay, decreased never events, etc.). Further, hospitalists may save in opportunity costs: the hospitalist staffing a ward service is less costly than a subspecialist who could be performing procedures, or a basic science researcher who could be acquiring grants. The problem today is that there is no way to quantify this decreased loss, and having this sort of metric will greatly enable mentors to provide hospitalists with ways of showing value to the department outside of the standard NIH grant paradigm. The Quality Portfolio developed by the SGIM and the forthcoming Benchmarks for Academic Hospitalists Promotion white paper (as developed by the SHM's Academic Practice and Promotion Committee) will greatly improve the substance of mentorship for academic hospitalists.2 Leaders of academic hospital medicine must learn to educate chairs of medicine and medical school deans as to the value‐added services intrinsic in the integration of hospitalists into the academic environment.
Having an Academic Plan
Mentorship is a 2‐way relationship: the mentor has responsibilities, but so too, does the mentee. As we wait for the hospitalist field to further develop, new academic hospitalists must become proactive in seeking guidance in career development. The Academic Hospitalist Academy, cosponsored by SHM, SGIM, and ACLGIM, is an example of this type of training.3 As a part of this course, participants learn of the rules and the opportunities for success in academic hospital medicine. Success for academic hospitalist groups will likely follow from understanding what success looks like. The Academy provides an excellent program for distributing that knowledge.
Research Training in Hospital Medicine
Many traditionalists would insist that Hospital Medicine could evoke the same training paradigm as other subspecialties in medicine (ie, fellowships). Unfortunately there are not a sufficient number of GME‐funded positions to handle the number of hospitalists required to advance the mission of academic hospital medicine. Moreover, fellowship training for every academic hospitalist would be unlikely to produce the desired results of improving the delivery of inpatient care. The academic agenda for the hospitalist depends on understanding the hospital system, and then executing improvements that lead to safer, more efficient and effective care. In this way, the academic hospitalist academic training is much more akin to a Master of Business Administration (MBA) than it is to a Bachelor of Science (BS) degree: namely, via job immersion, the hospitalist develops a greater systems understanding that should inform his or her academic career. Thus, a fellowship right out of residency may not have the same urgency for the hospitalist as it does for the subspecialist. Nevertheless, those hospitalists seeking an academic scholarly career will experience major benefits from fellowship training. Academic hospitalists need not focus only on the few existing hospitalist fellowships; they can obtain the necessary training in research skills via a general medicine fellowship, of which there are many. For this cohort of hospitalists, we strongly encourage training in a general medicine, health services, or outcomes research fellowship, with an emphasis on research techniques as they apply to the measurement of quality, patient safety, and/or clinical education.
With respect to academic hospitalists, it is likely that nothing is as important as the question of mentorship. Even the hardest working hospitalist can lose their way without guidance and a roadmap; the mentor is central to both. But the lost opportunity is not borne by the individual physician alone; the academic department loses too. Because the hospitalist's value depends on sufficient familiarity with a specific system prior to leveraging improvements, the department accrues maximal benefits in efficiency and effectiveness only if it can maintain retention for at least 2 years.4 The turnover carries major costs; recruitment costs money, and every new hospitalist engenders major start‐up costs. Faculty members who become completely integrated into the department have higher retention rates than those who consider themselves outside the main stream. Mentorship will greatly increase the probability that hospitalists will progress and feel the importance to the department.
Academic hospital medicine must strive over the next 5 to 10 years to become totally integrated in the academic culture of every institution. This task will take great leadership both at the local level and at a national level. We agree with the authors that the SHM and the SGIM can both provide important assistance to young hospital medicine groups. We applaud the authors of this article for making explicit this next major challenge for the field.
- ,,,.Survey of US academic hospitalist leaders about mentorship and academic activities in hospitalist groups.J Hosp Med.2011;6:5–9.
- ,,,.Quality portfolio introduction – academic hospitalist taskforce quality portfolio rationale and development. Society of General Internal Medicine Website,2010. Available at:http://www.sgim.org/index.cfm?pageId=846. Accessed September 2010.
- The Academic Hospitalist Academy Website,2010. Available at:http://www.academichospitalist.org. Accessed September 2010.
- ,,, et al.Effects of physician experience on costs and outcomes on an academic general medicine service.Ann Intern Med.2002;137:866–874.
This issue of the Journal of Hospital Medicine features an important contribution concerning the current state of academic hospital medicine. The survey of 57 hospitalists revealed what many of us already suspected: the state of mentorship in academic hospitalist groups is unsatisfactory.1
While the conclusion is alarming, it is also not surprising. Over the past decade academic medical centers enthusiastically hired hospitalists to improve efficiency for inpatient services and to lessen the effect of Accreditation Council for Graduate Medical Education (ACGME) regulations on duty hours and patient caps. Few departments of internal medicine, however, hired academic hospitalists with the intent of creating academic divisions. Thus many institutions appear to view hospitalists primarily as hospital employees ignoring their potential academic contributions, and as a result it should not be a surprise that many hospitalist groups lack the mentorship infrastructure of other divisions within a typical Department of Medicine. Compounding the hospital employee problem, the new field of academic hospital medicine has emerged only in the last decade, a time frame that has resulted in very few hospitalists qualified to serve as senior mentors.
We cannot easily remove these limitations: the past is the past, and over time, hospital medicine will mature and develop more senior mentors. But what should we do until that maturation occurs? We believe that the academic work of hospitalists, both in education and research (Quality and Patient Safety) are important endeavors too valuable to be left to chance. With 30,000 hospitalists delivering care, it is critical that research in the optimal delivery of this care be performed, targeting systems improvements to enact anticipated outcomes in quality and patient safety. The physicians who are regularly and intimately involved in this system of inpatient care delivery, the hospitalists, are best suited for identifying the unique features of the inpatient care system needing improvement. Mentorship is essential in ensuring the advancement of both areas, and the sustainability of hospital medicine in medical academe. The article by Harrison et al.1 both establishes the depth of these issues and provides important insights into potential solutions for closing this mentorship gap while the field matures.
Utilizing Other Mentors
No measure of systems change will make young hospitalists immediately experienced, such that they have the sophistication to be senior mentors for younger hospitalists. But we can compensate for this temporary gap in mentorship experience. First, in the next 5 to 10 years, young academic hospitalists need explicit direction from those within Departments of Medicine who do have this mentorship experience, even if these mentors do not work in hospital medicine. Mentors within General Internal Medicine or the subspecialties can still provide the guidance and support to ensure that academic hospitalists are engaging in the appropriate endeavors toward promotion and intellectual growth. Second, academic hospitalists have to seek out mentorship from afar through their participation in the organizations primarily devoted to the academic welfare of hospitalists: The Society of Hospital Medicine (SHM) and the Society of General Internal Medicine (SGIM). Both organizations sponsor mentorship programs, and regular attendance at regional and/or national meetings (followed by email correspondence) can greatly improve an academic hospitalist's career trajectory. Finally, midlevel and senior‐level hospitalists have to learn mentorship skills; mere experience in the field does not ensure acquisition of the necessary mentorship skills, anymore than experience in medicine ensures teaching skills. Mentorship is its own skill set, and receiving appropriate training via the SHM or SGIM national meetings or the Academic Hospitalist Academy (referenced below) is critical.
Defining Academic Expectations for Hospitalists
Harrison et al.1 note that academic hospitalists felt there was a lack of respect for the scholarly work that hospitalists do as part of their job, raising the proposition that the mentorship dearth for academic hospitalists might result from currently available mentors not knowing what to say. Even if mentors were plentiful today, we still must ask the question, What would the mentor advise the young hospitalist to do? The academic hospitalist offers extraordinary value to the Department, but in a way that is different from the standard R0RO‐1 Grant paradigm. Even if hospitalists acquire extramural funding, it will likely come from sources different from the National Institutes of Health (NIH): Agency for Healthcare Research and Quality (AHRQ), foundations (eg, The Robert Wood Johnson Foundation or The John A. Hartford Foundation), intramural hospital‐originating funding, etc. And while extramural funding may be a measure of a hospitalist's contribution to the Department, it should not be the only measure of the hospitalist's career development. There are 2 ways to get rich: acquire more money, or spend less money. Academic hospitalists, unlike other specialties in Medicine, are likely to fall into the latter category, by offering decreased hospital costs (ie, decreased length of stay, decreased never events, etc.). Further, hospitalists may save in opportunity costs: the hospitalist staffing a ward service is less costly than a subspecialist who could be performing procedures, or a basic science researcher who could be acquiring grants. The problem today is that there is no way to quantify this decreased loss, and having this sort of metric will greatly enable mentors to provide hospitalists with ways of showing value to the department outside of the standard NIH grant paradigm. The Quality Portfolio developed by the SGIM and the forthcoming Benchmarks for Academic Hospitalists Promotion white paper (as developed by the SHM's Academic Practice and Promotion Committee) will greatly improve the substance of mentorship for academic hospitalists.2 Leaders of academic hospital medicine must learn to educate chairs of medicine and medical school deans as to the value‐added services intrinsic in the integration of hospitalists into the academic environment.
Having an Academic Plan
Mentorship is a 2‐way relationship: the mentor has responsibilities, but so too, does the mentee. As we wait for the hospitalist field to further develop, new academic hospitalists must become proactive in seeking guidance in career development. The Academic Hospitalist Academy, cosponsored by SHM, SGIM, and ACLGIM, is an example of this type of training.3 As a part of this course, participants learn of the rules and the opportunities for success in academic hospital medicine. Success for academic hospitalist groups will likely follow from understanding what success looks like. The Academy provides an excellent program for distributing that knowledge.
Research Training in Hospital Medicine
Many traditionalists would insist that Hospital Medicine could evoke the same training paradigm as other subspecialties in medicine (ie, fellowships). Unfortunately there are not a sufficient number of GME‐funded positions to handle the number of hospitalists required to advance the mission of academic hospital medicine. Moreover, fellowship training for every academic hospitalist would be unlikely to produce the desired results of improving the delivery of inpatient care. The academic agenda for the hospitalist depends on understanding the hospital system, and then executing improvements that lead to safer, more efficient and effective care. In this way, the academic hospitalist academic training is much more akin to a Master of Business Administration (MBA) than it is to a Bachelor of Science (BS) degree: namely, via job immersion, the hospitalist develops a greater systems understanding that should inform his or her academic career. Thus, a fellowship right out of residency may not have the same urgency for the hospitalist as it does for the subspecialist. Nevertheless, those hospitalists seeking an academic scholarly career will experience major benefits from fellowship training. Academic hospitalists need not focus only on the few existing hospitalist fellowships; they can obtain the necessary training in research skills via a general medicine fellowship, of which there are many. For this cohort of hospitalists, we strongly encourage training in a general medicine, health services, or outcomes research fellowship, with an emphasis on research techniques as they apply to the measurement of quality, patient safety, and/or clinical education.
With respect to academic hospitalists, it is likely that nothing is as important as the question of mentorship. Even the hardest working hospitalist can lose their way without guidance and a roadmap; the mentor is central to both. But the lost opportunity is not borne by the individual physician alone; the academic department loses too. Because the hospitalist's value depends on sufficient familiarity with a specific system prior to leveraging improvements, the department accrues maximal benefits in efficiency and effectiveness only if it can maintain retention for at least 2 years.4 The turnover carries major costs; recruitment costs money, and every new hospitalist engenders major start‐up costs. Faculty members who become completely integrated into the department have higher retention rates than those who consider themselves outside the main stream. Mentorship will greatly increase the probability that hospitalists will progress and feel the importance to the department.
Academic hospital medicine must strive over the next 5 to 10 years to become totally integrated in the academic culture of every institution. This task will take great leadership both at the local level and at a national level. We agree with the authors that the SHM and the SGIM can both provide important assistance to young hospital medicine groups. We applaud the authors of this article for making explicit this next major challenge for the field.
This issue of the Journal of Hospital Medicine features an important contribution concerning the current state of academic hospital medicine. The survey of 57 hospitalists revealed what many of us already suspected: the state of mentorship in academic hospitalist groups is unsatisfactory.1
While the conclusion is alarming, it is also not surprising. Over the past decade academic medical centers enthusiastically hired hospitalists to improve efficiency for inpatient services and to lessen the effect of Accreditation Council for Graduate Medical Education (ACGME) regulations on duty hours and patient caps. Few departments of internal medicine, however, hired academic hospitalists with the intent of creating academic divisions. Thus many institutions appear to view hospitalists primarily as hospital employees ignoring their potential academic contributions, and as a result it should not be a surprise that many hospitalist groups lack the mentorship infrastructure of other divisions within a typical Department of Medicine. Compounding the hospital employee problem, the new field of academic hospital medicine has emerged only in the last decade, a time frame that has resulted in very few hospitalists qualified to serve as senior mentors.
We cannot easily remove these limitations: the past is the past, and over time, hospital medicine will mature and develop more senior mentors. But what should we do until that maturation occurs? We believe that the academic work of hospitalists, both in education and research (Quality and Patient Safety) are important endeavors too valuable to be left to chance. With 30,000 hospitalists delivering care, it is critical that research in the optimal delivery of this care be performed, targeting systems improvements to enact anticipated outcomes in quality and patient safety. The physicians who are regularly and intimately involved in this system of inpatient care delivery, the hospitalists, are best suited for identifying the unique features of the inpatient care system needing improvement. Mentorship is essential in ensuring the advancement of both areas, and the sustainability of hospital medicine in medical academe. The article by Harrison et al.1 both establishes the depth of these issues and provides important insights into potential solutions for closing this mentorship gap while the field matures.
Utilizing Other Mentors
No measure of systems change will make young hospitalists immediately experienced, such that they have the sophistication to be senior mentors for younger hospitalists. But we can compensate for this temporary gap in mentorship experience. First, in the next 5 to 10 years, young academic hospitalists need explicit direction from those within Departments of Medicine who do have this mentorship experience, even if these mentors do not work in hospital medicine. Mentors within General Internal Medicine or the subspecialties can still provide the guidance and support to ensure that academic hospitalists are engaging in the appropriate endeavors toward promotion and intellectual growth. Second, academic hospitalists have to seek out mentorship from afar through their participation in the organizations primarily devoted to the academic welfare of hospitalists: The Society of Hospital Medicine (SHM) and the Society of General Internal Medicine (SGIM). Both organizations sponsor mentorship programs, and regular attendance at regional and/or national meetings (followed by email correspondence) can greatly improve an academic hospitalist's career trajectory. Finally, midlevel and senior‐level hospitalists have to learn mentorship skills; mere experience in the field does not ensure acquisition of the necessary mentorship skills, anymore than experience in medicine ensures teaching skills. Mentorship is its own skill set, and receiving appropriate training via the SHM or SGIM national meetings or the Academic Hospitalist Academy (referenced below) is critical.
Defining Academic Expectations for Hospitalists
Harrison et al.1 note that academic hospitalists felt there was a lack of respect for the scholarly work that hospitalists do as part of their job, raising the proposition that the mentorship dearth for academic hospitalists might result from currently available mentors not knowing what to say. Even if mentors were plentiful today, we still must ask the question, What would the mentor advise the young hospitalist to do? The academic hospitalist offers extraordinary value to the Department, but in a way that is different from the standard R0RO‐1 Grant paradigm. Even if hospitalists acquire extramural funding, it will likely come from sources different from the National Institutes of Health (NIH): Agency for Healthcare Research and Quality (AHRQ), foundations (eg, The Robert Wood Johnson Foundation or The John A. Hartford Foundation), intramural hospital‐originating funding, etc. And while extramural funding may be a measure of a hospitalist's contribution to the Department, it should not be the only measure of the hospitalist's career development. There are 2 ways to get rich: acquire more money, or spend less money. Academic hospitalists, unlike other specialties in Medicine, are likely to fall into the latter category, by offering decreased hospital costs (ie, decreased length of stay, decreased never events, etc.). Further, hospitalists may save in opportunity costs: the hospitalist staffing a ward service is less costly than a subspecialist who could be performing procedures, or a basic science researcher who could be acquiring grants. The problem today is that there is no way to quantify this decreased loss, and having this sort of metric will greatly enable mentors to provide hospitalists with ways of showing value to the department outside of the standard NIH grant paradigm. The Quality Portfolio developed by the SGIM and the forthcoming Benchmarks for Academic Hospitalists Promotion white paper (as developed by the SHM's Academic Practice and Promotion Committee) will greatly improve the substance of mentorship for academic hospitalists.2 Leaders of academic hospital medicine must learn to educate chairs of medicine and medical school deans as to the value‐added services intrinsic in the integration of hospitalists into the academic environment.
Having an Academic Plan
Mentorship is a 2‐way relationship: the mentor has responsibilities, but so too, does the mentee. As we wait for the hospitalist field to further develop, new academic hospitalists must become proactive in seeking guidance in career development. The Academic Hospitalist Academy, cosponsored by SHM, SGIM, and ACLGIM, is an example of this type of training.3 As a part of this course, participants learn of the rules and the opportunities for success in academic hospital medicine. Success for academic hospitalist groups will likely follow from understanding what success looks like. The Academy provides an excellent program for distributing that knowledge.
Research Training in Hospital Medicine
Many traditionalists would insist that Hospital Medicine could evoke the same training paradigm as other subspecialties in medicine (ie, fellowships). Unfortunately there are not a sufficient number of GME‐funded positions to handle the number of hospitalists required to advance the mission of academic hospital medicine. Moreover, fellowship training for every academic hospitalist would be unlikely to produce the desired results of improving the delivery of inpatient care. The academic agenda for the hospitalist depends on understanding the hospital system, and then executing improvements that lead to safer, more efficient and effective care. In this way, the academic hospitalist academic training is much more akin to a Master of Business Administration (MBA) than it is to a Bachelor of Science (BS) degree: namely, via job immersion, the hospitalist develops a greater systems understanding that should inform his or her academic career. Thus, a fellowship right out of residency may not have the same urgency for the hospitalist as it does for the subspecialist. Nevertheless, those hospitalists seeking an academic scholarly career will experience major benefits from fellowship training. Academic hospitalists need not focus only on the few existing hospitalist fellowships; they can obtain the necessary training in research skills via a general medicine fellowship, of which there are many. For this cohort of hospitalists, we strongly encourage training in a general medicine, health services, or outcomes research fellowship, with an emphasis on research techniques as they apply to the measurement of quality, patient safety, and/or clinical education.
With respect to academic hospitalists, it is likely that nothing is as important as the question of mentorship. Even the hardest working hospitalist can lose their way without guidance and a roadmap; the mentor is central to both. But the lost opportunity is not borne by the individual physician alone; the academic department loses too. Because the hospitalist's value depends on sufficient familiarity with a specific system prior to leveraging improvements, the department accrues maximal benefits in efficiency and effectiveness only if it can maintain retention for at least 2 years.4 The turnover carries major costs; recruitment costs money, and every new hospitalist engenders major start‐up costs. Faculty members who become completely integrated into the department have higher retention rates than those who consider themselves outside the main stream. Mentorship will greatly increase the probability that hospitalists will progress and feel the importance to the department.
Academic hospital medicine must strive over the next 5 to 10 years to become totally integrated in the academic culture of every institution. This task will take great leadership both at the local level and at a national level. We agree with the authors that the SHM and the SGIM can both provide important assistance to young hospital medicine groups. We applaud the authors of this article for making explicit this next major challenge for the field.
- ,,,.Survey of US academic hospitalist leaders about mentorship and academic activities in hospitalist groups.J Hosp Med.2011;6:5–9.
- ,,,.Quality portfolio introduction – academic hospitalist taskforce quality portfolio rationale and development. Society of General Internal Medicine Website,2010. Available at:http://www.sgim.org/index.cfm?pageId=846. Accessed September 2010.
- The Academic Hospitalist Academy Website,2010. Available at:http://www.academichospitalist.org. Accessed September 2010.
- ,,, et al.Effects of physician experience on costs and outcomes on an academic general medicine service.Ann Intern Med.2002;137:866–874.
- ,,,.Survey of US academic hospitalist leaders about mentorship and academic activities in hospitalist groups.J Hosp Med.2011;6:5–9.
- ,,,.Quality portfolio introduction – academic hospitalist taskforce quality portfolio rationale and development. Society of General Internal Medicine Website,2010. Available at:http://www.sgim.org/index.cfm?pageId=846. Accessed September 2010.
- The Academic Hospitalist Academy Website,2010. Available at:http://www.academichospitalist.org. Accessed September 2010.
- ,,, et al.Effects of physician experience on costs and outcomes on an academic general medicine service.Ann Intern Med.2002;137:866–874.
Intracerebral hemorrhage: Pick your poison
Anticoagulants have been helping patients at risk of thrombosis since the late 1930s.1,2 Although the indications for these agents are many, the development of anticoagulants beyond oral vitamin K antagonists and parenteral heparin has been slow. In the United States, the vitamin K antagonist warfarin (Coumadin) is still the only oral anticoagulant available.
The major complication of anticoagulant therapy is bleeding, and vitamin K antagonists have proven challenging to use in clinical practice.1,3 They have a narrow therapeutic window, they vary considerably in dose-response from patient to patient, and they are subject to significant interactions with other drugs and with foods. For these reasons, therapy must be monitored with laboratory testing, and good patient compliance and patient education are essential. Yet even with these measures, life-threatening hemorrhage still can occur.
In this issue of the Cleveland Clinic Journal of Medicine, Goldstein and Greenberg4 review warfarin-related intracerebral hemorrhage (ICH) and provide a framework for considering whether to resume anticoagulant therapy.
WHAT TO DO IN THE ACUTE PHASE
Goldstein and Greenberg divide the difficult clinical question of what to do after ICH into the acute phase and the chronic phase.
What to do in the acute phase appears straightforward, as the risk of hematoma expansion in the hours immediately after warfarin-related ICH outweighs the risk of arterial or venous thromboembolism. Anticoagulant reversal should be the primary consideration in the first 24 hours, and, assuming the patient does not have acute (< 4-week-old) deep vein thrombosis, intermittent pneumatic compression should be applied to the lower extremities to reduce the risk of venous thromboembolism associated with ICH.5
Prophylactic anticoagulation with subcutaneous fixed-dose heparin or low-molecular-weight heparin is recommended starting 72 hours after ICH is diagnosed, provided the patient is not underweight (< 50 kg), has relatively normal renal function (creatinine clearance > 30 mL/minute/1.73 m2) and normal platelet function, and does not have coagulopathy. 6 If any one of these criteria is not met, the risk of bleeding can be higher, even with only prophylactic doses of anticoagulant drugs. Prophylactic anticoagulation should be continued until hospital and rehabilitation discharge, typically 1 to 2 weeks after ICH, depending on the severity of the patient’s neurologic impairment.
If a patient with warfarin-related ICH has concomitant acute proximal deep vein thrombosis or pulmonary embolism (ie, < 4 weeks old), then caval interruption therapy would be indicated.7 Although retrievable inferior vena cava filters are increasingly preferred over permanent filters, it is important to recognize the relative lack of both longitudinal and prospective data on retrievable devices. Given that provoked venous thromboembolism requires a minimum of 3 months of anticoagulation, and retrievable filters generally need to be removed before 3 months, a retrievable filter should be chosen only if the clinician has already decided that oral anticoagulation will be restarted in the next 3 to 4 weeks after filter removal.
WHAT TO DO IN THE CHRONIC PHASE
A more difficult question in patients with warfarin-related ICH arises in the chronic phase: should oral anticoagulation be resumed at all?
Since the risk of ICH is related to the intensity of anticoagulation, a lower target international normalized ratio may be the best compromise, depending on the patient. Alternatively, antiplatelet therapy alone may offer some benefit with less risk of ICH.
THE NEWER ORAL ANTICOAGULANTS
As Goldstein and Greenberg mention, the ongoing development of new and potentially safer oral anticoagulants may affect how we approach these risk-benefit equations.
Three new oral anticoagulants—dabigatran (Pradaxa), apixaban, and rivaroxaban (Xarelto)—are being tested for various anticoagulant indications, and several phase III studies have recently closed or are nearing completion.
Dabigatran is an oral direct thrombin inhibitor currently available in Europe and Canada.
In the Randomized Evaluation of Long-term Anticoagulant Therapy (RE-LY) trial, the efficacy and safety of two different doses of dabigatran (110 mg twice daily or 150 mg twice daily) relative to warfarin were studied in more than 18,000 patients with atrial fibrillation. 9 The primary outcome measure was stroke or systemic embolism. Dabigatran 110 mg was not inferior to warfarin in terms of the primary outcome, while dabigatran 150 mg was superior. The rate of major bleeding was 3.36% per year in the warfarin group vs 2.71% in the 110-mg group (P = .003) and 3.11% in the 150-mg group (P not significant).
Additional safety data on this drug are available from the 2,500-patient RE-COVER trial.10 Dabigatran was not inferior to warfarin in the treatment of acute venous thromboembolism, with a similar rate of major bleeding and a lower rate of combined major plus nonmajor bleeding.
Apixaban, an oral direct factor Xa inhibitor, is in a phase III trial in patients with atrial fibrillation—Apixaban for Reduction in Stroke and Other Thromboembolic Events in Atrial Fibrillation (ARISTOTLE)11—comparing apixaban vs warfarin. Another phase III trial, AVERROES,12 was stopped early after a predefined interim analysis by the independent data-monitoring committee found clear evidence of benefit in the apixaban group.13 The AVERROES results were presented at the 2010 European Society of Cardiology Congress, August 28–September 1, Stockholm, Sweden.14
Rivaroxaban, another promising oral direct factor Xa inhibitor, is currently available in Europe and Canada for the prevention of thrombosis in orthopedic surgery patients. Rivaroxaban is also in large phase III trials for the treatment of acute venous thromboembolism15–17 and for the prevention of stroke in atrial fibrillation.18
Newer agents have drawbacks, too
These new agents need no laboratory monitoring, and they do not appear to be subject to the dose variability and the interactions with drugs and foods seen with vitamin K antagonists. As a result, they may pose less risk of anticoagulant-related ICH.
The decision to resume anticoagulation after anticoagulant-associated intracranial hemorrhage should be based on the risk of rebleeding vs the risk of thrombosis. Patients determined to be at high risk of thrombosis and low risk of rebleeding are the best candidates for resuming anticoagulation.
Still, for patients who suffer an anticoagulant- or warfarin-related ICH, these new anticoagulants are not likely to simplify the issue of restarting anticoagulant therapy. Unlike vitamin K antagonists, dabigatran and the direct factor Xa inhibitors have no known antidote for their anticoagulant effects. Animal data suggest that factor Xa concentrates may help,19 but for patients at risk of a second anticoagulant-related ICH, this does not provide much reassurance.
As with all clinical decisions in medicine, the potential benefits of any therapy should outweigh the risks. In the case of warfarin-related ICH, resuming anticoagulant therapy requires careful consideration of many factors, including patient preferences and tolerance of different levels of risk. As new and perhaps safer anticoagulants become available, clinicians may face such difficult questions less and less. But in the meantime, doctors and their patients are left to pick their poison.
- Ansell J, Hirsh J, Hylek E, Jacobson A, Crowther M, Palareti G; American College of Chest Physicians. Pharmacology and management of the vitamin K antagonists: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines (8th Edition). Chest 2008; 133(suppl 6):160S–198S.
- Hirsh J, Bauer KA, Donati MB, Gould M, Samama MM, Weitz JI; American College of Chest Physicians. Parenteral anticoagulants: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines (8th Edition). Chest 2008; 133(suppl 6):141S–159S.
- Schulman S, Beyth RJ, Kearon C, Levine MN; American College of Chest Physicians. Hemorrhagic complications of anticoagulant and thrombolytic treatment: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines (8th edition). Chest 2008; 133(suppl 6):257S–298S.
- Goldstein JN, Greenberg SM. Should anticoagulation be resumed after intracerebral hemorrhage? Cleve Clin J Med 2010; 77:791–799.
- Geerts WH, Bergqvist D, Pineo GF, et al; American College of Chest Physicians. Prevention of venous thromboembolism: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines (8th Edition). Chest 2008; 133(suppl 6):381S–453S.
- Michota F, Merli G. Anticoagulation in special patient populations: are special dosing considerations required? Cleve Clin J Med 2005; 72(suppl 1):S37–S42.
- Kearon C, Kahn SR, Agnelli G, Goldhaber S, Raskob GE, Comerota AJ; American College of Chest Physicians. Antithrombotic therapy for venous thromboembolic disease: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines (8th Edition). Chest 2008; 133(suppl 6):454S–545S.
- Douketis JD, Berger PB, Dunn AS, et al; American College of Chest Physicians. The perioperative management of antithrombotic therapy: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines (8th Edition). Chest 2008; 133(suppl 6):299S–339S.
- Connolly SJ, Ezekowitz MD, Yusuf S, et al; RE-LY Steering Committee and Investigators. Dabigatran versus warfarin in patients with atrial fibrillation. N Engl J Med 2009; 361:1139–1151.
- Schulman S, Kearon C, Kakkar AK, et al; RE-COVER Study Group. Dabigatran versus warfarin in the treatment of acute venous thromboembolism. N Engl J Med 2009; 361:2342–2352.
- Lopes RD, Alexander JH, Al-Khatib SM; ARISTOTLE Investigators. Apixaban for Reduction in Stroke and Other Thromboembolic Events in Atrial Fibrillation (ARISTOTLE) trial: design and rationale. Am Heart J 2010; 159:331–339.
- Eikelboom JW, O’Donnell M, Yusuf S, et al. Rationale and design of AVERROES: apixaban versus acetylsalicylic acid to prevent stroke in atrial fibrillation patients who have failed or are unsuitable for vitamin K antagonist treatment. Am Heart J 2010; 159:348–353.
- Pfizer/Bristol-Myers Squibb. AVERROES study of investigational agent apixaban closes early due to clear evidence of efficacy, June 9, 2010. www.theheart.org/article/1087291.do. Accessed September 26, 2010.
- Connolly SJ, Arnesen H. AVERROES: Apixaban versus acetylsalicylic acid. http://www.escardio.org/congresses/esc-2010/congress-reports/Pages/708-3-AVERROES.aspx. Accessed September 7, 2010.
- Once-daily oral direct factor Xa inhibitor rivaroxaban in the long-term prevention of recurrent symptomatic venous thromboembolism in patients with symptomatic deep-vein thrombosis or pulmonary embolism. The Einstein-Extension Study. http://clinicaltrials.gov/ct2/show/NCT00439725. Accessed September 26, 2010.
- Oral direct factor Xa inhibitor rivaroxaban in patients with acute symptomatic deep-vein thrombosis without symptomatic pulmonary embolism: Einstein-DVT Evaluation. http://clinicaltrials.gov/ct2/show/NCT00440193. Accessed September 26, 2010.
- Oral direct factor Xa inhibitor rivaroxaban in patients with acute symptomatic pulmonary embolism with or without symptomatic deep-vein thrombosis: Einstein-PE Evaluation. http://clinicaltrials.gov/ct2/show/NCT00439777. Accessed September 26, 2010.
- ROCKET AF Study Investigators. Rivaroxaban once-daily, oral, direct factor Xa inhibition compared with vitamin K antagonism for prevention of stroke and embolism trial in atrial fibrillation: rationale and design of the ROCKET AF study. Am Heart J 2010; 159:340–347.
- Weitz JI, Hirsh J, Samama MM; American College of Chest Physicians. New antithrombotic drugs: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines (8th Edition). Chest 2008; 133(suppl 6):234S–256S.
Anticoagulants have been helping patients at risk of thrombosis since the late 1930s.1,2 Although the indications for these agents are many, the development of anticoagulants beyond oral vitamin K antagonists and parenteral heparin has been slow. In the United States, the vitamin K antagonist warfarin (Coumadin) is still the only oral anticoagulant available.
The major complication of anticoagulant therapy is bleeding, and vitamin K antagonists have proven challenging to use in clinical practice.1,3 They have a narrow therapeutic window, they vary considerably in dose-response from patient to patient, and they are subject to significant interactions with other drugs and with foods. For these reasons, therapy must be monitored with laboratory testing, and good patient compliance and patient education are essential. Yet even with these measures, life-threatening hemorrhage still can occur.
In this issue of the Cleveland Clinic Journal of Medicine, Goldstein and Greenberg4 review warfarin-related intracerebral hemorrhage (ICH) and provide a framework for considering whether to resume anticoagulant therapy.
WHAT TO DO IN THE ACUTE PHASE
Goldstein and Greenberg divide the difficult clinical question of what to do after ICH into the acute phase and the chronic phase.
What to do in the acute phase appears straightforward, as the risk of hematoma expansion in the hours immediately after warfarin-related ICH outweighs the risk of arterial or venous thromboembolism. Anticoagulant reversal should be the primary consideration in the first 24 hours, and, assuming the patient does not have acute (< 4-week-old) deep vein thrombosis, intermittent pneumatic compression should be applied to the lower extremities to reduce the risk of venous thromboembolism associated with ICH.5
Prophylactic anticoagulation with subcutaneous fixed-dose heparin or low-molecular-weight heparin is recommended starting 72 hours after ICH is diagnosed, provided the patient is not underweight (< 50 kg), has relatively normal renal function (creatinine clearance > 30 mL/minute/1.73 m2) and normal platelet function, and does not have coagulopathy. 6 If any one of these criteria is not met, the risk of bleeding can be higher, even with only prophylactic doses of anticoagulant drugs. Prophylactic anticoagulation should be continued until hospital and rehabilitation discharge, typically 1 to 2 weeks after ICH, depending on the severity of the patient’s neurologic impairment.
If a patient with warfarin-related ICH has concomitant acute proximal deep vein thrombosis or pulmonary embolism (ie, < 4 weeks old), then caval interruption therapy would be indicated.7 Although retrievable inferior vena cava filters are increasingly preferred over permanent filters, it is important to recognize the relative lack of both longitudinal and prospective data on retrievable devices. Given that provoked venous thromboembolism requires a minimum of 3 months of anticoagulation, and retrievable filters generally need to be removed before 3 months, a retrievable filter should be chosen only if the clinician has already decided that oral anticoagulation will be restarted in the next 3 to 4 weeks after filter removal.
WHAT TO DO IN THE CHRONIC PHASE
A more difficult question in patients with warfarin-related ICH arises in the chronic phase: should oral anticoagulation be resumed at all?
Since the risk of ICH is related to the intensity of anticoagulation, a lower target international normalized ratio may be the best compromise, depending on the patient. Alternatively, antiplatelet therapy alone may offer some benefit with less risk of ICH.
THE NEWER ORAL ANTICOAGULANTS
As Goldstein and Greenberg mention, the ongoing development of new and potentially safer oral anticoagulants may affect how we approach these risk-benefit equations.
Three new oral anticoagulants—dabigatran (Pradaxa), apixaban, and rivaroxaban (Xarelto)—are being tested for various anticoagulant indications, and several phase III studies have recently closed or are nearing completion.
Dabigatran is an oral direct thrombin inhibitor currently available in Europe and Canada.
In the Randomized Evaluation of Long-term Anticoagulant Therapy (RE-LY) trial, the efficacy and safety of two different doses of dabigatran (110 mg twice daily or 150 mg twice daily) relative to warfarin were studied in more than 18,000 patients with atrial fibrillation. 9 The primary outcome measure was stroke or systemic embolism. Dabigatran 110 mg was not inferior to warfarin in terms of the primary outcome, while dabigatran 150 mg was superior. The rate of major bleeding was 3.36% per year in the warfarin group vs 2.71% in the 110-mg group (P = .003) and 3.11% in the 150-mg group (P not significant).
Additional safety data on this drug are available from the 2,500-patient RE-COVER trial.10 Dabigatran was not inferior to warfarin in the treatment of acute venous thromboembolism, with a similar rate of major bleeding and a lower rate of combined major plus nonmajor bleeding.
Apixaban, an oral direct factor Xa inhibitor, is in a phase III trial in patients with atrial fibrillation—Apixaban for Reduction in Stroke and Other Thromboembolic Events in Atrial Fibrillation (ARISTOTLE)11—comparing apixaban vs warfarin. Another phase III trial, AVERROES,12 was stopped early after a predefined interim analysis by the independent data-monitoring committee found clear evidence of benefit in the apixaban group.13 The AVERROES results were presented at the 2010 European Society of Cardiology Congress, August 28–September 1, Stockholm, Sweden.14
Rivaroxaban, another promising oral direct factor Xa inhibitor, is currently available in Europe and Canada for the prevention of thrombosis in orthopedic surgery patients. Rivaroxaban is also in large phase III trials for the treatment of acute venous thromboembolism15–17 and for the prevention of stroke in atrial fibrillation.18
Newer agents have drawbacks, too
These new agents need no laboratory monitoring, and they do not appear to be subject to the dose variability and the interactions with drugs and foods seen with vitamin K antagonists. As a result, they may pose less risk of anticoagulant-related ICH.
The decision to resume anticoagulation after anticoagulant-associated intracranial hemorrhage should be based on the risk of rebleeding vs the risk of thrombosis. Patients determined to be at high risk of thrombosis and low risk of rebleeding are the best candidates for resuming anticoagulation.
Still, for patients who suffer an anticoagulant- or warfarin-related ICH, these new anticoagulants are not likely to simplify the issue of restarting anticoagulant therapy. Unlike vitamin K antagonists, dabigatran and the direct factor Xa inhibitors have no known antidote for their anticoagulant effects. Animal data suggest that factor Xa concentrates may help,19 but for patients at risk of a second anticoagulant-related ICH, this does not provide much reassurance.
As with all clinical decisions in medicine, the potential benefits of any therapy should outweigh the risks. In the case of warfarin-related ICH, resuming anticoagulant therapy requires careful consideration of many factors, including patient preferences and tolerance of different levels of risk. As new and perhaps safer anticoagulants become available, clinicians may face such difficult questions less and less. But in the meantime, doctors and their patients are left to pick their poison.
Anticoagulants have been helping patients at risk of thrombosis since the late 1930s.1,2 Although the indications for these agents are many, the development of anticoagulants beyond oral vitamin K antagonists and parenteral heparin has been slow. In the United States, the vitamin K antagonist warfarin (Coumadin) is still the only oral anticoagulant available.
The major complication of anticoagulant therapy is bleeding, and vitamin K antagonists have proven challenging to use in clinical practice.1,3 They have a narrow therapeutic window, they vary considerably in dose-response from patient to patient, and they are subject to significant interactions with other drugs and with foods. For these reasons, therapy must be monitored with laboratory testing, and good patient compliance and patient education are essential. Yet even with these measures, life-threatening hemorrhage still can occur.
In this issue of the Cleveland Clinic Journal of Medicine, Goldstein and Greenberg4 review warfarin-related intracerebral hemorrhage (ICH) and provide a framework for considering whether to resume anticoagulant therapy.
WHAT TO DO IN THE ACUTE PHASE
Goldstein and Greenberg divide the difficult clinical question of what to do after ICH into the acute phase and the chronic phase.
What to do in the acute phase appears straightforward, as the risk of hematoma expansion in the hours immediately after warfarin-related ICH outweighs the risk of arterial or venous thromboembolism. Anticoagulant reversal should be the primary consideration in the first 24 hours, and, assuming the patient does not have acute (< 4-week-old) deep vein thrombosis, intermittent pneumatic compression should be applied to the lower extremities to reduce the risk of venous thromboembolism associated with ICH.5
Prophylactic anticoagulation with subcutaneous fixed-dose heparin or low-molecular-weight heparin is recommended starting 72 hours after ICH is diagnosed, provided the patient is not underweight (< 50 kg), has relatively normal renal function (creatinine clearance > 30 mL/minute/1.73 m2) and normal platelet function, and does not have coagulopathy. 6 If any one of these criteria is not met, the risk of bleeding can be higher, even with only prophylactic doses of anticoagulant drugs. Prophylactic anticoagulation should be continued until hospital and rehabilitation discharge, typically 1 to 2 weeks after ICH, depending on the severity of the patient’s neurologic impairment.
If a patient with warfarin-related ICH has concomitant acute proximal deep vein thrombosis or pulmonary embolism (ie, < 4 weeks old), then caval interruption therapy would be indicated.7 Although retrievable inferior vena cava filters are increasingly preferred over permanent filters, it is important to recognize the relative lack of both longitudinal and prospective data on retrievable devices. Given that provoked venous thromboembolism requires a minimum of 3 months of anticoagulation, and retrievable filters generally need to be removed before 3 months, a retrievable filter should be chosen only if the clinician has already decided that oral anticoagulation will be restarted in the next 3 to 4 weeks after filter removal.
WHAT TO DO IN THE CHRONIC PHASE
A more difficult question in patients with warfarin-related ICH arises in the chronic phase: should oral anticoagulation be resumed at all?
Since the risk of ICH is related to the intensity of anticoagulation, a lower target international normalized ratio may be the best compromise, depending on the patient. Alternatively, antiplatelet therapy alone may offer some benefit with less risk of ICH.
THE NEWER ORAL ANTICOAGULANTS
As Goldstein and Greenberg mention, the ongoing development of new and potentially safer oral anticoagulants may affect how we approach these risk-benefit equations.
Three new oral anticoagulants—dabigatran (Pradaxa), apixaban, and rivaroxaban (Xarelto)—are being tested for various anticoagulant indications, and several phase III studies have recently closed or are nearing completion.
Dabigatran is an oral direct thrombin inhibitor currently available in Europe and Canada.
In the Randomized Evaluation of Long-term Anticoagulant Therapy (RE-LY) trial, the efficacy and safety of two different doses of dabigatran (110 mg twice daily or 150 mg twice daily) relative to warfarin were studied in more than 18,000 patients with atrial fibrillation. 9 The primary outcome measure was stroke or systemic embolism. Dabigatran 110 mg was not inferior to warfarin in terms of the primary outcome, while dabigatran 150 mg was superior. The rate of major bleeding was 3.36% per year in the warfarin group vs 2.71% in the 110-mg group (P = .003) and 3.11% in the 150-mg group (P not significant).
Additional safety data on this drug are available from the 2,500-patient RE-COVER trial.10 Dabigatran was not inferior to warfarin in the treatment of acute venous thromboembolism, with a similar rate of major bleeding and a lower rate of combined major plus nonmajor bleeding.
Apixaban, an oral direct factor Xa inhibitor, is in a phase III trial in patients with atrial fibrillation—Apixaban for Reduction in Stroke and Other Thromboembolic Events in Atrial Fibrillation (ARISTOTLE)11—comparing apixaban vs warfarin. Another phase III trial, AVERROES,12 was stopped early after a predefined interim analysis by the independent data-monitoring committee found clear evidence of benefit in the apixaban group.13 The AVERROES results were presented at the 2010 European Society of Cardiology Congress, August 28–September 1, Stockholm, Sweden.14
Rivaroxaban, another promising oral direct factor Xa inhibitor, is currently available in Europe and Canada for the prevention of thrombosis in orthopedic surgery patients. Rivaroxaban is also in large phase III trials for the treatment of acute venous thromboembolism15–17 and for the prevention of stroke in atrial fibrillation.18
Newer agents have drawbacks, too
These new agents need no laboratory monitoring, and they do not appear to be subject to the dose variability and the interactions with drugs and foods seen with vitamin K antagonists. As a result, they may pose less risk of anticoagulant-related ICH.
The decision to resume anticoagulation after anticoagulant-associated intracranial hemorrhage should be based on the risk of rebleeding vs the risk of thrombosis. Patients determined to be at high risk of thrombosis and low risk of rebleeding are the best candidates for resuming anticoagulation.
Still, for patients who suffer an anticoagulant- or warfarin-related ICH, these new anticoagulants are not likely to simplify the issue of restarting anticoagulant therapy. Unlike vitamin K antagonists, dabigatran and the direct factor Xa inhibitors have no known antidote for their anticoagulant effects. Animal data suggest that factor Xa concentrates may help,19 but for patients at risk of a second anticoagulant-related ICH, this does not provide much reassurance.
As with all clinical decisions in medicine, the potential benefits of any therapy should outweigh the risks. In the case of warfarin-related ICH, resuming anticoagulant therapy requires careful consideration of many factors, including patient preferences and tolerance of different levels of risk. As new and perhaps safer anticoagulants become available, clinicians may face such difficult questions less and less. But in the meantime, doctors and their patients are left to pick their poison.
- Ansell J, Hirsh J, Hylek E, Jacobson A, Crowther M, Palareti G; American College of Chest Physicians. Pharmacology and management of the vitamin K antagonists: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines (8th Edition). Chest 2008; 133(suppl 6):160S–198S.
- Hirsh J, Bauer KA, Donati MB, Gould M, Samama MM, Weitz JI; American College of Chest Physicians. Parenteral anticoagulants: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines (8th Edition). Chest 2008; 133(suppl 6):141S–159S.
- Schulman S, Beyth RJ, Kearon C, Levine MN; American College of Chest Physicians. Hemorrhagic complications of anticoagulant and thrombolytic treatment: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines (8th edition). Chest 2008; 133(suppl 6):257S–298S.
- Goldstein JN, Greenberg SM. Should anticoagulation be resumed after intracerebral hemorrhage? Cleve Clin J Med 2010; 77:791–799.
- Geerts WH, Bergqvist D, Pineo GF, et al; American College of Chest Physicians. Prevention of venous thromboembolism: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines (8th Edition). Chest 2008; 133(suppl 6):381S–453S.
- Michota F, Merli G. Anticoagulation in special patient populations: are special dosing considerations required? Cleve Clin J Med 2005; 72(suppl 1):S37–S42.
- Kearon C, Kahn SR, Agnelli G, Goldhaber S, Raskob GE, Comerota AJ; American College of Chest Physicians. Antithrombotic therapy for venous thromboembolic disease: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines (8th Edition). Chest 2008; 133(suppl 6):454S–545S.
- Douketis JD, Berger PB, Dunn AS, et al; American College of Chest Physicians. The perioperative management of antithrombotic therapy: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines (8th Edition). Chest 2008; 133(suppl 6):299S–339S.
- Connolly SJ, Ezekowitz MD, Yusuf S, et al; RE-LY Steering Committee and Investigators. Dabigatran versus warfarin in patients with atrial fibrillation. N Engl J Med 2009; 361:1139–1151.
- Schulman S, Kearon C, Kakkar AK, et al; RE-COVER Study Group. Dabigatran versus warfarin in the treatment of acute venous thromboembolism. N Engl J Med 2009; 361:2342–2352.
- Lopes RD, Alexander JH, Al-Khatib SM; ARISTOTLE Investigators. Apixaban for Reduction in Stroke and Other Thromboembolic Events in Atrial Fibrillation (ARISTOTLE) trial: design and rationale. Am Heart J 2010; 159:331–339.
- Eikelboom JW, O’Donnell M, Yusuf S, et al. Rationale and design of AVERROES: apixaban versus acetylsalicylic acid to prevent stroke in atrial fibrillation patients who have failed or are unsuitable for vitamin K antagonist treatment. Am Heart J 2010; 159:348–353.
- Pfizer/Bristol-Myers Squibb. AVERROES study of investigational agent apixaban closes early due to clear evidence of efficacy, June 9, 2010. www.theheart.org/article/1087291.do. Accessed September 26, 2010.
- Connolly SJ, Arnesen H. AVERROES: Apixaban versus acetylsalicylic acid. http://www.escardio.org/congresses/esc-2010/congress-reports/Pages/708-3-AVERROES.aspx. Accessed September 7, 2010.
- Once-daily oral direct factor Xa inhibitor rivaroxaban in the long-term prevention of recurrent symptomatic venous thromboembolism in patients with symptomatic deep-vein thrombosis or pulmonary embolism. The Einstein-Extension Study. http://clinicaltrials.gov/ct2/show/NCT00439725. Accessed September 26, 2010.
- Oral direct factor Xa inhibitor rivaroxaban in patients with acute symptomatic deep-vein thrombosis without symptomatic pulmonary embolism: Einstein-DVT Evaluation. http://clinicaltrials.gov/ct2/show/NCT00440193. Accessed September 26, 2010.
- Oral direct factor Xa inhibitor rivaroxaban in patients with acute symptomatic pulmonary embolism with or without symptomatic deep-vein thrombosis: Einstein-PE Evaluation. http://clinicaltrials.gov/ct2/show/NCT00439777. Accessed September 26, 2010.
- ROCKET AF Study Investigators. Rivaroxaban once-daily, oral, direct factor Xa inhibition compared with vitamin K antagonism for prevention of stroke and embolism trial in atrial fibrillation: rationale and design of the ROCKET AF study. Am Heart J 2010; 159:340–347.
- Weitz JI, Hirsh J, Samama MM; American College of Chest Physicians. New antithrombotic drugs: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines (8th Edition). Chest 2008; 133(suppl 6):234S–256S.
- Ansell J, Hirsh J, Hylek E, Jacobson A, Crowther M, Palareti G; American College of Chest Physicians. Pharmacology and management of the vitamin K antagonists: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines (8th Edition). Chest 2008; 133(suppl 6):160S–198S.
- Hirsh J, Bauer KA, Donati MB, Gould M, Samama MM, Weitz JI; American College of Chest Physicians. Parenteral anticoagulants: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines (8th Edition). Chest 2008; 133(suppl 6):141S–159S.
- Schulman S, Beyth RJ, Kearon C, Levine MN; American College of Chest Physicians. Hemorrhagic complications of anticoagulant and thrombolytic treatment: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines (8th edition). Chest 2008; 133(suppl 6):257S–298S.
- Goldstein JN, Greenberg SM. Should anticoagulation be resumed after intracerebral hemorrhage? Cleve Clin J Med 2010; 77:791–799.
- Geerts WH, Bergqvist D, Pineo GF, et al; American College of Chest Physicians. Prevention of venous thromboembolism: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines (8th Edition). Chest 2008; 133(suppl 6):381S–453S.
- Michota F, Merli G. Anticoagulation in special patient populations: are special dosing considerations required? Cleve Clin J Med 2005; 72(suppl 1):S37–S42.
- Kearon C, Kahn SR, Agnelli G, Goldhaber S, Raskob GE, Comerota AJ; American College of Chest Physicians. Antithrombotic therapy for venous thromboembolic disease: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines (8th Edition). Chest 2008; 133(suppl 6):454S–545S.
- Douketis JD, Berger PB, Dunn AS, et al; American College of Chest Physicians. The perioperative management of antithrombotic therapy: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines (8th Edition). Chest 2008; 133(suppl 6):299S–339S.
- Connolly SJ, Ezekowitz MD, Yusuf S, et al; RE-LY Steering Committee and Investigators. Dabigatran versus warfarin in patients with atrial fibrillation. N Engl J Med 2009; 361:1139–1151.
- Schulman S, Kearon C, Kakkar AK, et al; RE-COVER Study Group. Dabigatran versus warfarin in the treatment of acute venous thromboembolism. N Engl J Med 2009; 361:2342–2352.
- Lopes RD, Alexander JH, Al-Khatib SM; ARISTOTLE Investigators. Apixaban for Reduction in Stroke and Other Thromboembolic Events in Atrial Fibrillation (ARISTOTLE) trial: design and rationale. Am Heart J 2010; 159:331–339.
- Eikelboom JW, O’Donnell M, Yusuf S, et al. Rationale and design of AVERROES: apixaban versus acetylsalicylic acid to prevent stroke in atrial fibrillation patients who have failed or are unsuitable for vitamin K antagonist treatment. Am Heart J 2010; 159:348–353.
- Pfizer/Bristol-Myers Squibb. AVERROES study of investigational agent apixaban closes early due to clear evidence of efficacy, June 9, 2010. www.theheart.org/article/1087291.do. Accessed September 26, 2010.
- Connolly SJ, Arnesen H. AVERROES: Apixaban versus acetylsalicylic acid. http://www.escardio.org/congresses/esc-2010/congress-reports/Pages/708-3-AVERROES.aspx. Accessed September 7, 2010.
- Once-daily oral direct factor Xa inhibitor rivaroxaban in the long-term prevention of recurrent symptomatic venous thromboembolism in patients with symptomatic deep-vein thrombosis or pulmonary embolism. The Einstein-Extension Study. http://clinicaltrials.gov/ct2/show/NCT00439725. Accessed September 26, 2010.
- Oral direct factor Xa inhibitor rivaroxaban in patients with acute symptomatic deep-vein thrombosis without symptomatic pulmonary embolism: Einstein-DVT Evaluation. http://clinicaltrials.gov/ct2/show/NCT00440193. Accessed September 26, 2010.
- Oral direct factor Xa inhibitor rivaroxaban in patients with acute symptomatic pulmonary embolism with or without symptomatic deep-vein thrombosis: Einstein-PE Evaluation. http://clinicaltrials.gov/ct2/show/NCT00439777. Accessed September 26, 2010.
- ROCKET AF Study Investigators. Rivaroxaban once-daily, oral, direct factor Xa inhibition compared with vitamin K antagonism for prevention of stroke and embolism trial in atrial fibrillation: rationale and design of the ROCKET AF study. Am Heart J 2010; 159:340–347.
- Weitz JI, Hirsh J, Samama MM; American College of Chest Physicians. New antithrombotic drugs: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines (8th Edition). Chest 2008; 133(suppl 6):234S–256S.
Postcards from Our Students
During their junior medicine rotation, our students are asked to post to Blackboard (an online student forum) an anonymous essay about an issue of professionalism or ethics, either inspiring or troubling. In many ways, these vignettes are like postcards, written by visitors describing foreign cultures and norms. They represent a way for the students to debrief, but also provide an opportunity for us, as faculty, to reflect upon the way we practice and teach medicine. Many postingslike postcards from exotic or historic placesare inspiring stories of residents and faculty extending themselves for their patients. Unfortunately, unlike typical postcards, there are also essays that are troubling or provoking and challenge us to consider how we could improve the professional and ethical environment on our teams.
In order to begin a learning process with our faculty and housestaff, we have presented a number of these anonymous essays at both faculty and housestaff Department of Medicine conferences as well as our monthly hospital Ethics conference. The goal of these conferences was to gather as a moral community to reflect on our students' experience and consider ways in which our day to day practice as attendings could be informed by what they tell us. In addition, the junior medicine site directors have a session each quarter with their junior students to review some of the most significant issues brought up by their essays.
Practically, these vignettes and conferences serve three main purposes:
-
Raising Awareness: Many professional issues noted by our students occur under the radar. Attendings are often unaware of the issues of professionalism and/or ethics confronting our students and housestaff.
-
Exploring Attitudes: Some attending may underemphasize the importance of specific issues of professionalism and/or ethics. Open discussions at faculty or resident conferences create opportunities for individuals to reflect upon their own reactions and for the group to create a norm.
-
Sharing Skills: It is difficult to learn the practice of professionalism and ethics from a book. Skill in this area is gained primarily by experience. Conferences provide an excellent forum for seasoned physicians to share wisdom with less experienced physicians. In addition, important teaching points can be made: Students should not deliver bad news alone. Errors should be disclosed.
Following are 3 of the essays we presented, along with brief commentaries. At the end, we provide practical suggestions for individual attendings to improve the professional climate on their teams.
The Hospital Didn't Wait
Code. On 12, the surgical wards floor. Elise sprinted to the stairwell, dashed up to 12, and ran to the corner room as fast as she could. She could see the room before she got there. Instinctively, she started reviewing the steps she had memorized so many months ago. But when she finally arrived at the patient's bathroom, her thought process came to a jolting halt as she came upon the gruesome scene.
The 76‐year‐old patient had hanged himself with the cinching rope from his garment bag, and now dangled suspended from a high towel rack against the wall. Nurses from the floor started to file in, and without losing a beat Elise barked commands. Together they brought the man's body down to the floor, laid him on his back, and stripped off his hospital gown. Elise was in charge; deliberately but forcefully, she ordered a nurse to retrieve a defibrillator, and had another resident check for a pulse. There was none. Anesthesiology was here. Quickly and expertly, they shoved a plastic tube down his throat and began ventilation. The nurse placed on the electrodes between chest compressions then called to clear the body. Airway stepped back. The chest pumper stepped back. The body lurched forward as the defibrillator issued a long beep and discharged. Still no pulse. The cycle repeated.
Finally, Elise called a stop. Time of death, 19:37. By now there were about 20 people crammed in the patient room, all of whom had a separate role during the code. Some stayed behind, while the rest left to return to their interrupted work. The medical student didn't know what to think as he returned to the team room. His jaw was sorehad he been clenching it the whole time?and as he brought his hand up to rub his face, he saw that his knuckles were bloody. Somehow he had scraped them during the code. As he logged back into the computer to finish off his evening notes, he knew that he wouldn't have time to reflect until hours later when he returned home. Codes happened all the time. There was still work to be done in the hospital, and the hospital didn't wait.
The room had already been assigned to a patient waiting in the Emergency Department downstairs. That patient would be here in a few minutes. The hospital didn't wait.
When we presented this case in our conferences, there was universal agreement that such a traumatic event merits, even demands, team debriefing and processing. But in the real life aftermath of this traumatic event, the take‐home message for the medical student was that the hospital didn't wait for such discussions. We know this is not unique to our institution. In a study of 32 medical students who were asked to reflect on their most memorable patient death,1 debriefing sessions were rare and many students felt inadequately supported. While experienced clinicians may be accustomed to seeing patients die, students are new to the culture of the hospital, and have not had the chance to develop the defense mechanisms necessary to cope with this sort of experience. Angoff2 writes, As medical educators, we ought to ask our students how they are coping with long hours, fatigue, illness, suffering, and death. We ought to model and commend compassion and react to the deep feelings of our students in the same way we would teach them to react to the deep feelings of their patients.
I Told a Man Today That He Had Brain Cancer
The resident, intern, and I were huddled together in our team room when the report came back on the computer. New 3.5 2.3 1.7 cm contrast‐enhancing lesion seen anterior to genu of corpus callosum. Concerning for metastatic focus vs. lymphoma. Advise follow‐up. It wasn't unexpected but we had nevertheless been hoping for better.
The three of us went into his room and I was waiting to see how my resident would deliver the bad news, but she didn't. She simply said that we were continuing to do imaging studies and that a neurology team would be in touch. There were probably several reasons why she didn't tell him: not enough time, not her responsibility, or maybe she was just uncomfortable with it. Whatever the case, we left the room with my patient still oblivious to the awful mass now tangled in his head.
If my resident was taking a pass on this conversation, I knew it fell to me he needed to hear it from his primary team. I came back after rounds alone, sat down next to his bed, and told him that his MRI results had come back, and that I had unfortunate news.
I told him that the images showed that his lung cancer had spread to his brain.
I paused to give him a chance to let it sink in. He turned away and looked up at the ceiling.
Where is it? How big is it?
What now?
Reflecting on this case, our audiences were disturbed that a student would attempt this difficult conversation alone, while recognizing that the student clearly felt a sense of responsibility and desire to help his patient by sharing important information. We talked about how students may erroneously pick up a message that the team member who has spent the most time with a patient is the most obvious choice to have difficult conversations. We also noted that, unfortunately, sometimes students are directly asked by their team to shoulder this responsibility on their own. In this painful account, there is no mention of preparation, supervision, or support for the student before or after the encounter. The student perceived (rightly or wrongly) that the team leaders lacked comfort or skill to deliver the bad news, and stepped in. It is possible that the attending lacked the skill and ability to model an interaction, but more likely the deficit was in awareness and attitude. It is unlikely the attending knew that the student had this conversation alone. One of the major reasons we present these vignettes is to make attendings and housestaff more aware of issues that occur under their radar so that they can take preventative action. However, once the resident or attending found out that the student had this conversation alone, the student should be pulled aside for a 1:1 discussion. At the end of the day, the student should know that it was inappropriate to attempt this conversation alone
Rosenbaum3 reviewed a number of strategies to teach the skill of delivering bad news, from lecture and small group discussions to role play and standardized patients. When asked, students cited role‐modeling as the best way to learn how to deliver bad news.4 Observation of a veteran clinician provides a firm foundation for learning; but that is not enough. Unfortunately, we know from the literature (and our student vignettes suggest) that students and residents are unprepared to carry out these conversations properly, either because of misguided attitudes, lack of experience, or inadequate training.57 We conceptualize engaging in difficult conversations as a procedure, demanding a skill set. Mere observation of an expert executing this procedure is only a beginning. With any other skill, from successful completion of a lumbar puncture to initiating cardiopulmonary resuscitation (CPR), a student would never conclude that knowing the patient the best sufficiently credentials the student to undertake these procedures. We maintain that a difficult conversationbe it breaking bad news, discussing end‐of‐life care preferences, code status discussions, or prognosisis a clinical intervention, like any other procedure in medicine. If performed with skill and caution, it can bring about a stronger therapeutic relationship and increased support for the patient; if performed clumsily, it can lead to unintended adverse outcomes, including misunderstanding, mistrust, anxiety, and anger.
A Decimal Point Got Misplaced
On palliative care, I had a 90 year‐old man with end stage lung CA that presented to the ED with increasing SOB. The resident decided that giving him some morphine would be a good solution but was worried that too much would push him over the edge. He was thin; his O2 sats weren't that good After some discussion it was decided that 2.5 mg should be the starting amount. Unfortunately, when the note was written a decimal point got misplaced and he got 25 mg as a first dose. He ended up very sedated for most of the day but his breathing was ok.
The mistake was not discussed with the patient or the patient's family. While it did not cause any lasting harm, I wondered if telling the patient/patient's family that an error had been made would have been more ethically sound.
When we presented this case in our conferences, there was little controversy about whether the error should have been disclosed. The discussion did provide reinforcement for doing a simple but difficult task. Our analysis is that the nondiscussion of this error reflects a deficit in attitude and possibly skill. The team was aware of the error, but the resident and attending did not take the opportunity to disclose an error. They should have. We do not know whether the attending or resident felt unprepared to discuss this or were simply unimpressed with the adverse event. We do get the sense that the student did not feel comfortable raising the issue with the team. As such, it was a missed opportunity to seek help from any number of hospital resources and find encouragement to take on difficult encounters.
Much has been written about apologies.810 Disclosing errors and apologizing is the ethical standard, and many of our institutions have made it policy. Yet in the moment, it is embarrassing, anxiety provoking, and our concern about litigation looms large. Learning to do the right thing begins, perhaps with lectures and standardized patients, but only when students see it modeled by our housestaff and faculty, does it take root for good.
Our housestaff are quite good at managing medical issues, but they may still need help in creating the appropriate environment for professional learning and growth. This is 1 of the most important contributions an attending can make. We have emphasized that faculty have an important role to play in the area of professional development, reinforcing the rudimentary information preclinical students are presented with in the classroom and processing experiences residents are exposed to on a regular basis. If the hospital doesn't wait, then it is the attending physician's job to create the space and time for trainees to think about what is happening and ask if it could have been done better.
A number of seasoned clinical teachers have written about ways to improve teaching on the wards.11 Below, we will add to that discussion by considering practical ways to enhance learning about professionalism and ethics (see Table 1). Note should be made that while we focus on specific behaviors and activities, underlying all is the importance of availability, presence, and intention. Like all good teaching, these activities require planning and effort.
| Attending Activity | Examples |
|---|---|
| Creating an Open Climate | |
| Breaking Communication Barriers | Setting aside time for introductions and team building exercises at the beginning of a rotation, with attending participating equally with residents and students |
| Emphasizing attending availability to discuss or review problems of any kind | |
| Setting Clear Expectations | Emphasizing the importance of patient‐clinician or family‐clinician communication from the outset |
| Devoting some attending rounds to Difficult Conversations (e.g., breaking bad news or code status discussions) | |
| Explicitly stating that no ethical question is a stupid question and providing positive feedback for raising such questions for the team | |
| Regular Check‐ins | Establishing team communication rounds: 10 minutes every day to review a good, bad, or awkward interaction from the past day (e.g., family meeting, DNR discussion) |
| Setting aside time on rounds or during attending teaching sessions to explore the team's or an individual's emotional responses to a patient's death or deterioration | |
| Writing exercises that focus on our reactions to challenging situations that are shared with the group | |
| Supervision and Modeling | |
| Planning | Clarifying an agenda and practicing key phrases for a family meeting with the resident prior to meeting the family |
| Anticipating which patients may require a code status discussion and discussing a game plan on rounds | |
| Modeling | Students observe the attending facilitate a family meeting |
| Residents observe the attending apologizing for an error, no matter how small | |
| Attending thinks about an interpersonal conflict out loud and models asking patient‐relations for help | |
| Debriefing | Reviewing a family meeting with and giving feedback to the resident who facilitated |
| Reviewing a challenging code status discussion as a team |
Creating an Open Climate
The medical team, of which the attending, residents, and students are all a part, should not only be a unit that provides excellent medical care to its patients, but should also create a culture of continuous learning and improvement. As such, it is important to create a safe atmosphere where teachers are invested in the growth of their learners and learners feel free to question the prevailing logic and practice, including issues of professionalism and ethics. As Malcolm Gladwell12 describes in Outliers, Korean Air jets were crashing because subordinates were afraid to question their superiors. Once that culture changed, Korean Air safety improved dramatically. Similarly, breaking down some of the hierarchical barriers should improve the culture of a medical team. We typically make an effort to get to know our students and residents on a more personal basis: where they are from, who is in their family, what was their major, what are their interests outside of medicine, and what has been surprising to them in their training so far. Whether we set aside time when we first meet or e‐mail our questions before the first day, we aim for this to be 1 of the first team activities. We also share our own stories, making clear that the attending is part of the team, and not just an evaluating supervisor.
Vignette 1 describes the student's trauma of witnessing a code and the inability to process the event with anyone afterward. Failed resuscitation attempts are the most dramatic examples, but even expected deaths, nonfatal adverse events, and conflict between patients and providers may be traumatic for new trainees inexperienced with the reality of medicine. Attendings should be aware of these potentially traumatic events and make time to check in with the team members about how they are dealing with their emotions. Taking time on attending rounds, for example, allows the attending to not only model reflective practice and self‐care, but also elevates team support to a place traditionally reserved for discussions about diagnosis and treatment.
Supervision and Modeling
Vignettes 2 and 3 center around challenging communication tasks that require special training, including instruction, modeling, feedback, and practice. Unfortunately, as some of our student accounts document, many teaching opportunities are missed. As attendings, our duties include being aware of these opportunities, and being prepared to model competent patientor familydoctor interactions. Emphasizing the importance of the doctor‐patient relationship is in fact one of the key skills of an effective attending role model.13
When opportunities arise for any potentially difficult conversation, we make every effort to identify the issue, prebrief with the team about how to conduct the discussion, and either offer to model the conversation or be present to observe and provide feedback and debriefing afterwards. For example, by asking about all DNR discussions had with our patients, we gain insight into the skill level of our housestaff. As important, the housestaff understand that we believe that these conversations are vital to review during formal rounds, with the same attention we give to chest pain and electrocardiograms (ECGs).
Two key skills that develop with experience are the ability to know the limits of one's knowledge and to know when to ask for help. We try to be open about naming those limits and thinking about the other members of the larger healthcare team that may provide insight, skill, and expertise. We are used to doing this with medical questions (eg, asking the gastroenterology consult team to locate a source of bleeding). Asking our risk management, patient‐relations, or ethics services to assist with a difficult communication task or conflict with a family is no different, and often something the housestaff may not readily do.
We are grateful to our students and their postcards for the snapshots of our local medical culture. While we are gratified to read of excellent role modeling, we are also disappointed to read of situations which have left our students confused, demoralized and cynical. But if these exercises are to reach their full potential, they should tell us about where we would like to go, in addition to where we have been. We believe that our conferences have stimulated our faculty and housestaff to reflect on the professionalism lessons they are teaching. Reading the student postings has definitely affected our approach to teaching professionalism. They reinforce what every parent and educator knows: when it comes to teaching professionalism, communication and ethics, what matters most is the behavior of the teacher. Our words mean little if our actions do not live out what we espouse.
Acknowledgements
We are grateful for Michael Chan and his classmates from the NUFSM class of 2010 for their thoughtful essays. David Neely, Director of Undergraduate Education, Department of Medicine, Eytan Szmuilowicz, Palliative Medicine. Kathy Neely, Chairman of NMH Ethics Committee. Co‐director of Patient, Physician and Society. This article was previously published in this journal in Vol 5, Issue 5:E10E13 (2010) as online‐only.
- .This is just too awful; I just can't believe I experienced that.Acad Med.2005;80(7):634–640.
- .A piece of my mind.JAMA.2001;286(9):1017–1018.
- .Teaching medical students and residents skills for delivering bad news: a review of strategies.Acad Med.2004;79(2):107–117.
- .Third‐year medical students' experiences with dying patients during the internal medicine clerkship: a qualitative study of the informal curriculum.Acad Med.2005;80(7):641–647.
- ,,.How do medical residents discuss resuscitation with patients? Official journal of the Society for Research and Education in Primary Care Internal Medicine.J Gen Intern Med.1995;10(8):436–442.
- ,,.See one, do one, teach one? House staff experience discussing do‐not‐resuscitate orders.Arch Intern Med.1996;156(12):1285–1289.
- ,,,.Residents' end‐of‐life decision making with adult hospitalized patients: a review of the literature.Acad Med.2005:80(7)622–633.
- .Physician error and disclosure.Clin Obstet Gynecol.2008;51(4):700–708.
- .Revealing medical errors to your patients.Chest.2009;133:1064–1065.
- .Apology in medical practice.JAMA.2006;296:1401–1404.
- .What if Osler were one of us? Inpatient teaching today.J Gen Intern Med.1997;12(Suppl 2):S41–S48.
- Malcolm Gladwell.Outliers.New York:Little, Brown, Co.,2008: p.177–223.
- ,,,,.Attributes of excellent attending‐physician role models.N Engl J Med.1998;339(27):1986–1993.
During their junior medicine rotation, our students are asked to post to Blackboard (an online student forum) an anonymous essay about an issue of professionalism or ethics, either inspiring or troubling. In many ways, these vignettes are like postcards, written by visitors describing foreign cultures and norms. They represent a way for the students to debrief, but also provide an opportunity for us, as faculty, to reflect upon the way we practice and teach medicine. Many postingslike postcards from exotic or historic placesare inspiring stories of residents and faculty extending themselves for their patients. Unfortunately, unlike typical postcards, there are also essays that are troubling or provoking and challenge us to consider how we could improve the professional and ethical environment on our teams.
In order to begin a learning process with our faculty and housestaff, we have presented a number of these anonymous essays at both faculty and housestaff Department of Medicine conferences as well as our monthly hospital Ethics conference. The goal of these conferences was to gather as a moral community to reflect on our students' experience and consider ways in which our day to day practice as attendings could be informed by what they tell us. In addition, the junior medicine site directors have a session each quarter with their junior students to review some of the most significant issues brought up by their essays.
Practically, these vignettes and conferences serve three main purposes:
-
Raising Awareness: Many professional issues noted by our students occur under the radar. Attendings are often unaware of the issues of professionalism and/or ethics confronting our students and housestaff.
-
Exploring Attitudes: Some attending may underemphasize the importance of specific issues of professionalism and/or ethics. Open discussions at faculty or resident conferences create opportunities for individuals to reflect upon their own reactions and for the group to create a norm.
-
Sharing Skills: It is difficult to learn the practice of professionalism and ethics from a book. Skill in this area is gained primarily by experience. Conferences provide an excellent forum for seasoned physicians to share wisdom with less experienced physicians. In addition, important teaching points can be made: Students should not deliver bad news alone. Errors should be disclosed.
Following are 3 of the essays we presented, along with brief commentaries. At the end, we provide practical suggestions for individual attendings to improve the professional climate on their teams.
The Hospital Didn't Wait
Code. On 12, the surgical wards floor. Elise sprinted to the stairwell, dashed up to 12, and ran to the corner room as fast as she could. She could see the room before she got there. Instinctively, she started reviewing the steps she had memorized so many months ago. But when she finally arrived at the patient's bathroom, her thought process came to a jolting halt as she came upon the gruesome scene.
The 76‐year‐old patient had hanged himself with the cinching rope from his garment bag, and now dangled suspended from a high towel rack against the wall. Nurses from the floor started to file in, and without losing a beat Elise barked commands. Together they brought the man's body down to the floor, laid him on his back, and stripped off his hospital gown. Elise was in charge; deliberately but forcefully, she ordered a nurse to retrieve a defibrillator, and had another resident check for a pulse. There was none. Anesthesiology was here. Quickly and expertly, they shoved a plastic tube down his throat and began ventilation. The nurse placed on the electrodes between chest compressions then called to clear the body. Airway stepped back. The chest pumper stepped back. The body lurched forward as the defibrillator issued a long beep and discharged. Still no pulse. The cycle repeated.
Finally, Elise called a stop. Time of death, 19:37. By now there were about 20 people crammed in the patient room, all of whom had a separate role during the code. Some stayed behind, while the rest left to return to their interrupted work. The medical student didn't know what to think as he returned to the team room. His jaw was sorehad he been clenching it the whole time?and as he brought his hand up to rub his face, he saw that his knuckles were bloody. Somehow he had scraped them during the code. As he logged back into the computer to finish off his evening notes, he knew that he wouldn't have time to reflect until hours later when he returned home. Codes happened all the time. There was still work to be done in the hospital, and the hospital didn't wait.
The room had already been assigned to a patient waiting in the Emergency Department downstairs. That patient would be here in a few minutes. The hospital didn't wait.
When we presented this case in our conferences, there was universal agreement that such a traumatic event merits, even demands, team debriefing and processing. But in the real life aftermath of this traumatic event, the take‐home message for the medical student was that the hospital didn't wait for such discussions. We know this is not unique to our institution. In a study of 32 medical students who were asked to reflect on their most memorable patient death,1 debriefing sessions were rare and many students felt inadequately supported. While experienced clinicians may be accustomed to seeing patients die, students are new to the culture of the hospital, and have not had the chance to develop the defense mechanisms necessary to cope with this sort of experience. Angoff2 writes, As medical educators, we ought to ask our students how they are coping with long hours, fatigue, illness, suffering, and death. We ought to model and commend compassion and react to the deep feelings of our students in the same way we would teach them to react to the deep feelings of their patients.
I Told a Man Today That He Had Brain Cancer
The resident, intern, and I were huddled together in our team room when the report came back on the computer. New 3.5 2.3 1.7 cm contrast‐enhancing lesion seen anterior to genu of corpus callosum. Concerning for metastatic focus vs. lymphoma. Advise follow‐up. It wasn't unexpected but we had nevertheless been hoping for better.
The three of us went into his room and I was waiting to see how my resident would deliver the bad news, but she didn't. She simply said that we were continuing to do imaging studies and that a neurology team would be in touch. There were probably several reasons why she didn't tell him: not enough time, not her responsibility, or maybe she was just uncomfortable with it. Whatever the case, we left the room with my patient still oblivious to the awful mass now tangled in his head.
If my resident was taking a pass on this conversation, I knew it fell to me he needed to hear it from his primary team. I came back after rounds alone, sat down next to his bed, and told him that his MRI results had come back, and that I had unfortunate news.
I told him that the images showed that his lung cancer had spread to his brain.
I paused to give him a chance to let it sink in. He turned away and looked up at the ceiling.
Where is it? How big is it?
What now?
Reflecting on this case, our audiences were disturbed that a student would attempt this difficult conversation alone, while recognizing that the student clearly felt a sense of responsibility and desire to help his patient by sharing important information. We talked about how students may erroneously pick up a message that the team member who has spent the most time with a patient is the most obvious choice to have difficult conversations. We also noted that, unfortunately, sometimes students are directly asked by their team to shoulder this responsibility on their own. In this painful account, there is no mention of preparation, supervision, or support for the student before or after the encounter. The student perceived (rightly or wrongly) that the team leaders lacked comfort or skill to deliver the bad news, and stepped in. It is possible that the attending lacked the skill and ability to model an interaction, but more likely the deficit was in awareness and attitude. It is unlikely the attending knew that the student had this conversation alone. One of the major reasons we present these vignettes is to make attendings and housestaff more aware of issues that occur under their radar so that they can take preventative action. However, once the resident or attending found out that the student had this conversation alone, the student should be pulled aside for a 1:1 discussion. At the end of the day, the student should know that it was inappropriate to attempt this conversation alone
Rosenbaum3 reviewed a number of strategies to teach the skill of delivering bad news, from lecture and small group discussions to role play and standardized patients. When asked, students cited role‐modeling as the best way to learn how to deliver bad news.4 Observation of a veteran clinician provides a firm foundation for learning; but that is not enough. Unfortunately, we know from the literature (and our student vignettes suggest) that students and residents are unprepared to carry out these conversations properly, either because of misguided attitudes, lack of experience, or inadequate training.57 We conceptualize engaging in difficult conversations as a procedure, demanding a skill set. Mere observation of an expert executing this procedure is only a beginning. With any other skill, from successful completion of a lumbar puncture to initiating cardiopulmonary resuscitation (CPR), a student would never conclude that knowing the patient the best sufficiently credentials the student to undertake these procedures. We maintain that a difficult conversationbe it breaking bad news, discussing end‐of‐life care preferences, code status discussions, or prognosisis a clinical intervention, like any other procedure in medicine. If performed with skill and caution, it can bring about a stronger therapeutic relationship and increased support for the patient; if performed clumsily, it can lead to unintended adverse outcomes, including misunderstanding, mistrust, anxiety, and anger.
A Decimal Point Got Misplaced
On palliative care, I had a 90 year‐old man with end stage lung CA that presented to the ED with increasing SOB. The resident decided that giving him some morphine would be a good solution but was worried that too much would push him over the edge. He was thin; his O2 sats weren't that good After some discussion it was decided that 2.5 mg should be the starting amount. Unfortunately, when the note was written a decimal point got misplaced and he got 25 mg as a first dose. He ended up very sedated for most of the day but his breathing was ok.
The mistake was not discussed with the patient or the patient's family. While it did not cause any lasting harm, I wondered if telling the patient/patient's family that an error had been made would have been more ethically sound.
When we presented this case in our conferences, there was little controversy about whether the error should have been disclosed. The discussion did provide reinforcement for doing a simple but difficult task. Our analysis is that the nondiscussion of this error reflects a deficit in attitude and possibly skill. The team was aware of the error, but the resident and attending did not take the opportunity to disclose an error. They should have. We do not know whether the attending or resident felt unprepared to discuss this or were simply unimpressed with the adverse event. We do get the sense that the student did not feel comfortable raising the issue with the team. As such, it was a missed opportunity to seek help from any number of hospital resources and find encouragement to take on difficult encounters.
Much has been written about apologies.810 Disclosing errors and apologizing is the ethical standard, and many of our institutions have made it policy. Yet in the moment, it is embarrassing, anxiety provoking, and our concern about litigation looms large. Learning to do the right thing begins, perhaps with lectures and standardized patients, but only when students see it modeled by our housestaff and faculty, does it take root for good.
Our housestaff are quite good at managing medical issues, but they may still need help in creating the appropriate environment for professional learning and growth. This is 1 of the most important contributions an attending can make. We have emphasized that faculty have an important role to play in the area of professional development, reinforcing the rudimentary information preclinical students are presented with in the classroom and processing experiences residents are exposed to on a regular basis. If the hospital doesn't wait, then it is the attending physician's job to create the space and time for trainees to think about what is happening and ask if it could have been done better.
A number of seasoned clinical teachers have written about ways to improve teaching on the wards.11 Below, we will add to that discussion by considering practical ways to enhance learning about professionalism and ethics (see Table 1). Note should be made that while we focus on specific behaviors and activities, underlying all is the importance of availability, presence, and intention. Like all good teaching, these activities require planning and effort.
| Attending Activity | Examples |
|---|---|
| Creating an Open Climate | |
| Breaking Communication Barriers | Setting aside time for introductions and team building exercises at the beginning of a rotation, with attending participating equally with residents and students |
| Emphasizing attending availability to discuss or review problems of any kind | |
| Setting Clear Expectations | Emphasizing the importance of patient‐clinician or family‐clinician communication from the outset |
| Devoting some attending rounds to Difficult Conversations (e.g., breaking bad news or code status discussions) | |
| Explicitly stating that no ethical question is a stupid question and providing positive feedback for raising such questions for the team | |
| Regular Check‐ins | Establishing team communication rounds: 10 minutes every day to review a good, bad, or awkward interaction from the past day (e.g., family meeting, DNR discussion) |
| Setting aside time on rounds or during attending teaching sessions to explore the team's or an individual's emotional responses to a patient's death or deterioration | |
| Writing exercises that focus on our reactions to challenging situations that are shared with the group | |
| Supervision and Modeling | |
| Planning | Clarifying an agenda and practicing key phrases for a family meeting with the resident prior to meeting the family |
| Anticipating which patients may require a code status discussion and discussing a game plan on rounds | |
| Modeling | Students observe the attending facilitate a family meeting |
| Residents observe the attending apologizing for an error, no matter how small | |
| Attending thinks about an interpersonal conflict out loud and models asking patient‐relations for help | |
| Debriefing | Reviewing a family meeting with and giving feedback to the resident who facilitated |
| Reviewing a challenging code status discussion as a team |
Creating an Open Climate
The medical team, of which the attending, residents, and students are all a part, should not only be a unit that provides excellent medical care to its patients, but should also create a culture of continuous learning and improvement. As such, it is important to create a safe atmosphere where teachers are invested in the growth of their learners and learners feel free to question the prevailing logic and practice, including issues of professionalism and ethics. As Malcolm Gladwell12 describes in Outliers, Korean Air jets were crashing because subordinates were afraid to question their superiors. Once that culture changed, Korean Air safety improved dramatically. Similarly, breaking down some of the hierarchical barriers should improve the culture of a medical team. We typically make an effort to get to know our students and residents on a more personal basis: where they are from, who is in their family, what was their major, what are their interests outside of medicine, and what has been surprising to them in their training so far. Whether we set aside time when we first meet or e‐mail our questions before the first day, we aim for this to be 1 of the first team activities. We also share our own stories, making clear that the attending is part of the team, and not just an evaluating supervisor.
Vignette 1 describes the student's trauma of witnessing a code and the inability to process the event with anyone afterward. Failed resuscitation attempts are the most dramatic examples, but even expected deaths, nonfatal adverse events, and conflict between patients and providers may be traumatic for new trainees inexperienced with the reality of medicine. Attendings should be aware of these potentially traumatic events and make time to check in with the team members about how they are dealing with their emotions. Taking time on attending rounds, for example, allows the attending to not only model reflective practice and self‐care, but also elevates team support to a place traditionally reserved for discussions about diagnosis and treatment.
Supervision and Modeling
Vignettes 2 and 3 center around challenging communication tasks that require special training, including instruction, modeling, feedback, and practice. Unfortunately, as some of our student accounts document, many teaching opportunities are missed. As attendings, our duties include being aware of these opportunities, and being prepared to model competent patientor familydoctor interactions. Emphasizing the importance of the doctor‐patient relationship is in fact one of the key skills of an effective attending role model.13
When opportunities arise for any potentially difficult conversation, we make every effort to identify the issue, prebrief with the team about how to conduct the discussion, and either offer to model the conversation or be present to observe and provide feedback and debriefing afterwards. For example, by asking about all DNR discussions had with our patients, we gain insight into the skill level of our housestaff. As important, the housestaff understand that we believe that these conversations are vital to review during formal rounds, with the same attention we give to chest pain and electrocardiograms (ECGs).
Two key skills that develop with experience are the ability to know the limits of one's knowledge and to know when to ask for help. We try to be open about naming those limits and thinking about the other members of the larger healthcare team that may provide insight, skill, and expertise. We are used to doing this with medical questions (eg, asking the gastroenterology consult team to locate a source of bleeding). Asking our risk management, patient‐relations, or ethics services to assist with a difficult communication task or conflict with a family is no different, and often something the housestaff may not readily do.
We are grateful to our students and their postcards for the snapshots of our local medical culture. While we are gratified to read of excellent role modeling, we are also disappointed to read of situations which have left our students confused, demoralized and cynical. But if these exercises are to reach their full potential, they should tell us about where we would like to go, in addition to where we have been. We believe that our conferences have stimulated our faculty and housestaff to reflect on the professionalism lessons they are teaching. Reading the student postings has definitely affected our approach to teaching professionalism. They reinforce what every parent and educator knows: when it comes to teaching professionalism, communication and ethics, what matters most is the behavior of the teacher. Our words mean little if our actions do not live out what we espouse.
Acknowledgements
We are grateful for Michael Chan and his classmates from the NUFSM class of 2010 for their thoughtful essays. David Neely, Director of Undergraduate Education, Department of Medicine, Eytan Szmuilowicz, Palliative Medicine. Kathy Neely, Chairman of NMH Ethics Committee. Co‐director of Patient, Physician and Society. This article was previously published in this journal in Vol 5, Issue 5:E10E13 (2010) as online‐only.
During their junior medicine rotation, our students are asked to post to Blackboard (an online student forum) an anonymous essay about an issue of professionalism or ethics, either inspiring or troubling. In many ways, these vignettes are like postcards, written by visitors describing foreign cultures and norms. They represent a way for the students to debrief, but also provide an opportunity for us, as faculty, to reflect upon the way we practice and teach medicine. Many postingslike postcards from exotic or historic placesare inspiring stories of residents and faculty extending themselves for their patients. Unfortunately, unlike typical postcards, there are also essays that are troubling or provoking and challenge us to consider how we could improve the professional and ethical environment on our teams.
In order to begin a learning process with our faculty and housestaff, we have presented a number of these anonymous essays at both faculty and housestaff Department of Medicine conferences as well as our monthly hospital Ethics conference. The goal of these conferences was to gather as a moral community to reflect on our students' experience and consider ways in which our day to day practice as attendings could be informed by what they tell us. In addition, the junior medicine site directors have a session each quarter with their junior students to review some of the most significant issues brought up by their essays.
Practically, these vignettes and conferences serve three main purposes:
-
Raising Awareness: Many professional issues noted by our students occur under the radar. Attendings are often unaware of the issues of professionalism and/or ethics confronting our students and housestaff.
-
Exploring Attitudes: Some attending may underemphasize the importance of specific issues of professionalism and/or ethics. Open discussions at faculty or resident conferences create opportunities for individuals to reflect upon their own reactions and for the group to create a norm.
-
Sharing Skills: It is difficult to learn the practice of professionalism and ethics from a book. Skill in this area is gained primarily by experience. Conferences provide an excellent forum for seasoned physicians to share wisdom with less experienced physicians. In addition, important teaching points can be made: Students should not deliver bad news alone. Errors should be disclosed.
Following are 3 of the essays we presented, along with brief commentaries. At the end, we provide practical suggestions for individual attendings to improve the professional climate on their teams.
The Hospital Didn't Wait
Code. On 12, the surgical wards floor. Elise sprinted to the stairwell, dashed up to 12, and ran to the corner room as fast as she could. She could see the room before she got there. Instinctively, she started reviewing the steps she had memorized so many months ago. But when she finally arrived at the patient's bathroom, her thought process came to a jolting halt as she came upon the gruesome scene.
The 76‐year‐old patient had hanged himself with the cinching rope from his garment bag, and now dangled suspended from a high towel rack against the wall. Nurses from the floor started to file in, and without losing a beat Elise barked commands. Together they brought the man's body down to the floor, laid him on his back, and stripped off his hospital gown. Elise was in charge; deliberately but forcefully, she ordered a nurse to retrieve a defibrillator, and had another resident check for a pulse. There was none. Anesthesiology was here. Quickly and expertly, they shoved a plastic tube down his throat and began ventilation. The nurse placed on the electrodes between chest compressions then called to clear the body. Airway stepped back. The chest pumper stepped back. The body lurched forward as the defibrillator issued a long beep and discharged. Still no pulse. The cycle repeated.
Finally, Elise called a stop. Time of death, 19:37. By now there were about 20 people crammed in the patient room, all of whom had a separate role during the code. Some stayed behind, while the rest left to return to their interrupted work. The medical student didn't know what to think as he returned to the team room. His jaw was sorehad he been clenching it the whole time?and as he brought his hand up to rub his face, he saw that his knuckles were bloody. Somehow he had scraped them during the code. As he logged back into the computer to finish off his evening notes, he knew that he wouldn't have time to reflect until hours later when he returned home. Codes happened all the time. There was still work to be done in the hospital, and the hospital didn't wait.
The room had already been assigned to a patient waiting in the Emergency Department downstairs. That patient would be here in a few minutes. The hospital didn't wait.
When we presented this case in our conferences, there was universal agreement that such a traumatic event merits, even demands, team debriefing and processing. But in the real life aftermath of this traumatic event, the take‐home message for the medical student was that the hospital didn't wait for such discussions. We know this is not unique to our institution. In a study of 32 medical students who were asked to reflect on their most memorable patient death,1 debriefing sessions were rare and many students felt inadequately supported. While experienced clinicians may be accustomed to seeing patients die, students are new to the culture of the hospital, and have not had the chance to develop the defense mechanisms necessary to cope with this sort of experience. Angoff2 writes, As medical educators, we ought to ask our students how they are coping with long hours, fatigue, illness, suffering, and death. We ought to model and commend compassion and react to the deep feelings of our students in the same way we would teach them to react to the deep feelings of their patients.
I Told a Man Today That He Had Brain Cancer
The resident, intern, and I were huddled together in our team room when the report came back on the computer. New 3.5 2.3 1.7 cm contrast‐enhancing lesion seen anterior to genu of corpus callosum. Concerning for metastatic focus vs. lymphoma. Advise follow‐up. It wasn't unexpected but we had nevertheless been hoping for better.
The three of us went into his room and I was waiting to see how my resident would deliver the bad news, but she didn't. She simply said that we were continuing to do imaging studies and that a neurology team would be in touch. There were probably several reasons why she didn't tell him: not enough time, not her responsibility, or maybe she was just uncomfortable with it. Whatever the case, we left the room with my patient still oblivious to the awful mass now tangled in his head.
If my resident was taking a pass on this conversation, I knew it fell to me he needed to hear it from his primary team. I came back after rounds alone, sat down next to his bed, and told him that his MRI results had come back, and that I had unfortunate news.
I told him that the images showed that his lung cancer had spread to his brain.
I paused to give him a chance to let it sink in. He turned away and looked up at the ceiling.
Where is it? How big is it?
What now?
Reflecting on this case, our audiences were disturbed that a student would attempt this difficult conversation alone, while recognizing that the student clearly felt a sense of responsibility and desire to help his patient by sharing important information. We talked about how students may erroneously pick up a message that the team member who has spent the most time with a patient is the most obvious choice to have difficult conversations. We also noted that, unfortunately, sometimes students are directly asked by their team to shoulder this responsibility on their own. In this painful account, there is no mention of preparation, supervision, or support for the student before or after the encounter. The student perceived (rightly or wrongly) that the team leaders lacked comfort or skill to deliver the bad news, and stepped in. It is possible that the attending lacked the skill and ability to model an interaction, but more likely the deficit was in awareness and attitude. It is unlikely the attending knew that the student had this conversation alone. One of the major reasons we present these vignettes is to make attendings and housestaff more aware of issues that occur under their radar so that they can take preventative action. However, once the resident or attending found out that the student had this conversation alone, the student should be pulled aside for a 1:1 discussion. At the end of the day, the student should know that it was inappropriate to attempt this conversation alone
Rosenbaum3 reviewed a number of strategies to teach the skill of delivering bad news, from lecture and small group discussions to role play and standardized patients. When asked, students cited role‐modeling as the best way to learn how to deliver bad news.4 Observation of a veteran clinician provides a firm foundation for learning; but that is not enough. Unfortunately, we know from the literature (and our student vignettes suggest) that students and residents are unprepared to carry out these conversations properly, either because of misguided attitudes, lack of experience, or inadequate training.57 We conceptualize engaging in difficult conversations as a procedure, demanding a skill set. Mere observation of an expert executing this procedure is only a beginning. With any other skill, from successful completion of a lumbar puncture to initiating cardiopulmonary resuscitation (CPR), a student would never conclude that knowing the patient the best sufficiently credentials the student to undertake these procedures. We maintain that a difficult conversationbe it breaking bad news, discussing end‐of‐life care preferences, code status discussions, or prognosisis a clinical intervention, like any other procedure in medicine. If performed with skill and caution, it can bring about a stronger therapeutic relationship and increased support for the patient; if performed clumsily, it can lead to unintended adverse outcomes, including misunderstanding, mistrust, anxiety, and anger.
A Decimal Point Got Misplaced
On palliative care, I had a 90 year‐old man with end stage lung CA that presented to the ED with increasing SOB. The resident decided that giving him some morphine would be a good solution but was worried that too much would push him over the edge. He was thin; his O2 sats weren't that good After some discussion it was decided that 2.5 mg should be the starting amount. Unfortunately, when the note was written a decimal point got misplaced and he got 25 mg as a first dose. He ended up very sedated for most of the day but his breathing was ok.
The mistake was not discussed with the patient or the patient's family. While it did not cause any lasting harm, I wondered if telling the patient/patient's family that an error had been made would have been more ethically sound.
When we presented this case in our conferences, there was little controversy about whether the error should have been disclosed. The discussion did provide reinforcement for doing a simple but difficult task. Our analysis is that the nondiscussion of this error reflects a deficit in attitude and possibly skill. The team was aware of the error, but the resident and attending did not take the opportunity to disclose an error. They should have. We do not know whether the attending or resident felt unprepared to discuss this or were simply unimpressed with the adverse event. We do get the sense that the student did not feel comfortable raising the issue with the team. As such, it was a missed opportunity to seek help from any number of hospital resources and find encouragement to take on difficult encounters.
Much has been written about apologies.810 Disclosing errors and apologizing is the ethical standard, and many of our institutions have made it policy. Yet in the moment, it is embarrassing, anxiety provoking, and our concern about litigation looms large. Learning to do the right thing begins, perhaps with lectures and standardized patients, but only when students see it modeled by our housestaff and faculty, does it take root for good.
Our housestaff are quite good at managing medical issues, but they may still need help in creating the appropriate environment for professional learning and growth. This is 1 of the most important contributions an attending can make. We have emphasized that faculty have an important role to play in the area of professional development, reinforcing the rudimentary information preclinical students are presented with in the classroom and processing experiences residents are exposed to on a regular basis. If the hospital doesn't wait, then it is the attending physician's job to create the space and time for trainees to think about what is happening and ask if it could have been done better.
A number of seasoned clinical teachers have written about ways to improve teaching on the wards.11 Below, we will add to that discussion by considering practical ways to enhance learning about professionalism and ethics (see Table 1). Note should be made that while we focus on specific behaviors and activities, underlying all is the importance of availability, presence, and intention. Like all good teaching, these activities require planning and effort.
| Attending Activity | Examples |
|---|---|
| Creating an Open Climate | |
| Breaking Communication Barriers | Setting aside time for introductions and team building exercises at the beginning of a rotation, with attending participating equally with residents and students |
| Emphasizing attending availability to discuss or review problems of any kind | |
| Setting Clear Expectations | Emphasizing the importance of patient‐clinician or family‐clinician communication from the outset |
| Devoting some attending rounds to Difficult Conversations (e.g., breaking bad news or code status discussions) | |
| Explicitly stating that no ethical question is a stupid question and providing positive feedback for raising such questions for the team | |
| Regular Check‐ins | Establishing team communication rounds: 10 minutes every day to review a good, bad, or awkward interaction from the past day (e.g., family meeting, DNR discussion) |
| Setting aside time on rounds or during attending teaching sessions to explore the team's or an individual's emotional responses to a patient's death or deterioration | |
| Writing exercises that focus on our reactions to challenging situations that are shared with the group | |
| Supervision and Modeling | |
| Planning | Clarifying an agenda and practicing key phrases for a family meeting with the resident prior to meeting the family |
| Anticipating which patients may require a code status discussion and discussing a game plan on rounds | |
| Modeling | Students observe the attending facilitate a family meeting |
| Residents observe the attending apologizing for an error, no matter how small | |
| Attending thinks about an interpersonal conflict out loud and models asking patient‐relations for help | |
| Debriefing | Reviewing a family meeting with and giving feedback to the resident who facilitated |
| Reviewing a challenging code status discussion as a team |
Creating an Open Climate
The medical team, of which the attending, residents, and students are all a part, should not only be a unit that provides excellent medical care to its patients, but should also create a culture of continuous learning and improvement. As such, it is important to create a safe atmosphere where teachers are invested in the growth of their learners and learners feel free to question the prevailing logic and practice, including issues of professionalism and ethics. As Malcolm Gladwell12 describes in Outliers, Korean Air jets were crashing because subordinates were afraid to question their superiors. Once that culture changed, Korean Air safety improved dramatically. Similarly, breaking down some of the hierarchical barriers should improve the culture of a medical team. We typically make an effort to get to know our students and residents on a more personal basis: where they are from, who is in their family, what was their major, what are their interests outside of medicine, and what has been surprising to them in their training so far. Whether we set aside time when we first meet or e‐mail our questions before the first day, we aim for this to be 1 of the first team activities. We also share our own stories, making clear that the attending is part of the team, and not just an evaluating supervisor.
Vignette 1 describes the student's trauma of witnessing a code and the inability to process the event with anyone afterward. Failed resuscitation attempts are the most dramatic examples, but even expected deaths, nonfatal adverse events, and conflict between patients and providers may be traumatic for new trainees inexperienced with the reality of medicine. Attendings should be aware of these potentially traumatic events and make time to check in with the team members about how they are dealing with their emotions. Taking time on attending rounds, for example, allows the attending to not only model reflective practice and self‐care, but also elevates team support to a place traditionally reserved for discussions about diagnosis and treatment.
Supervision and Modeling
Vignettes 2 and 3 center around challenging communication tasks that require special training, including instruction, modeling, feedback, and practice. Unfortunately, as some of our student accounts document, many teaching opportunities are missed. As attendings, our duties include being aware of these opportunities, and being prepared to model competent patientor familydoctor interactions. Emphasizing the importance of the doctor‐patient relationship is in fact one of the key skills of an effective attending role model.13
When opportunities arise for any potentially difficult conversation, we make every effort to identify the issue, prebrief with the team about how to conduct the discussion, and either offer to model the conversation or be present to observe and provide feedback and debriefing afterwards. For example, by asking about all DNR discussions had with our patients, we gain insight into the skill level of our housestaff. As important, the housestaff understand that we believe that these conversations are vital to review during formal rounds, with the same attention we give to chest pain and electrocardiograms (ECGs).
Two key skills that develop with experience are the ability to know the limits of one's knowledge and to know when to ask for help. We try to be open about naming those limits and thinking about the other members of the larger healthcare team that may provide insight, skill, and expertise. We are used to doing this with medical questions (eg, asking the gastroenterology consult team to locate a source of bleeding). Asking our risk management, patient‐relations, or ethics services to assist with a difficult communication task or conflict with a family is no different, and often something the housestaff may not readily do.
We are grateful to our students and their postcards for the snapshots of our local medical culture. While we are gratified to read of excellent role modeling, we are also disappointed to read of situations which have left our students confused, demoralized and cynical. But if these exercises are to reach their full potential, they should tell us about where we would like to go, in addition to where we have been. We believe that our conferences have stimulated our faculty and housestaff to reflect on the professionalism lessons they are teaching. Reading the student postings has definitely affected our approach to teaching professionalism. They reinforce what every parent and educator knows: when it comes to teaching professionalism, communication and ethics, what matters most is the behavior of the teacher. Our words mean little if our actions do not live out what we espouse.
Acknowledgements
We are grateful for Michael Chan and his classmates from the NUFSM class of 2010 for their thoughtful essays. David Neely, Director of Undergraduate Education, Department of Medicine, Eytan Szmuilowicz, Palliative Medicine. Kathy Neely, Chairman of NMH Ethics Committee. Co‐director of Patient, Physician and Society. This article was previously published in this journal in Vol 5, Issue 5:E10E13 (2010) as online‐only.
- .This is just too awful; I just can't believe I experienced that.Acad Med.2005;80(7):634–640.
- .A piece of my mind.JAMA.2001;286(9):1017–1018.
- .Teaching medical students and residents skills for delivering bad news: a review of strategies.Acad Med.2004;79(2):107–117.
- .Third‐year medical students' experiences with dying patients during the internal medicine clerkship: a qualitative study of the informal curriculum.Acad Med.2005;80(7):641–647.
- ,,.How do medical residents discuss resuscitation with patients? Official journal of the Society for Research and Education in Primary Care Internal Medicine.J Gen Intern Med.1995;10(8):436–442.
- ,,.See one, do one, teach one? House staff experience discussing do‐not‐resuscitate orders.Arch Intern Med.1996;156(12):1285–1289.
- ,,,.Residents' end‐of‐life decision making with adult hospitalized patients: a review of the literature.Acad Med.2005:80(7)622–633.
- .Physician error and disclosure.Clin Obstet Gynecol.2008;51(4):700–708.
- .Revealing medical errors to your patients.Chest.2009;133:1064–1065.
- .Apology in medical practice.JAMA.2006;296:1401–1404.
- .What if Osler were one of us? Inpatient teaching today.J Gen Intern Med.1997;12(Suppl 2):S41–S48.
- Malcolm Gladwell.Outliers.New York:Little, Brown, Co.,2008: p.177–223.
- ,,,,.Attributes of excellent attending‐physician role models.N Engl J Med.1998;339(27):1986–1993.
- .This is just too awful; I just can't believe I experienced that.Acad Med.2005;80(7):634–640.
- .A piece of my mind.JAMA.2001;286(9):1017–1018.
- .Teaching medical students and residents skills for delivering bad news: a review of strategies.Acad Med.2004;79(2):107–117.
- .Third‐year medical students' experiences with dying patients during the internal medicine clerkship: a qualitative study of the informal curriculum.Acad Med.2005;80(7):641–647.
- ,,.How do medical residents discuss resuscitation with patients? Official journal of the Society for Research and Education in Primary Care Internal Medicine.J Gen Intern Med.1995;10(8):436–442.
- ,,.See one, do one, teach one? House staff experience discussing do‐not‐resuscitate orders.Arch Intern Med.1996;156(12):1285–1289.
- ,,,.Residents' end‐of‐life decision making with adult hospitalized patients: a review of the literature.Acad Med.2005:80(7)622–633.
- .Physician error and disclosure.Clin Obstet Gynecol.2008;51(4):700–708.
- .Revealing medical errors to your patients.Chest.2009;133:1064–1065.
- .Apology in medical practice.JAMA.2006;296:1401–1404.
- .What if Osler were one of us? Inpatient teaching today.J Gen Intern Med.1997;12(Suppl 2):S41–S48.
- Malcolm Gladwell.Outliers.New York:Little, Brown, Co.,2008: p.177–223.
- ,,,,.Attributes of excellent attending‐physician role models.N Engl J Med.1998;339(27):1986–1993.
Management of Inpatient Hyperglycemia
Hyperglycemia that develops acutely due to illness is associated with poor patient outcomes in hospitalized inpatients, especially those critically ill in the intensive care unit (ICU).18 In fact, those without a prior diagnosis of diabetes and therefore newly found to have hyperglycemia have worse outcomes than those who have a prior diagnosis of diabetes.1, 2, 4, 68 Many mechanisms have been put forward to explain the adverse outcomes related to hyperglycemia, including the release of counter‐regulatory hormones, increased lipolysis with free fatty acid release, the release of inflammatory cytokines and growth factors, increased reactive oxygen species with oxidative stress and altered immunoglobulin, and neutrophil phagocytic function.911
The practical importance of this was brought home by Furnary et al.12, 13 who showed that glycemic control using 3 days of intensive intravenous (IV) insulin therapy of diabetic patients undergoing cardiac surgical procedures was able to reduce significantly the risk of deep sternal wound infections and mortality and to bring these adverse outcomes to the same levels as those of nondiabetic patients. However, the benefits of intensive insulin therapy are not limited to those with diabetes and extend to those with critical illness‐induced hyperglycemia. In a landmark, randomized, prospective study from Belgium, van den Berghe et al.14 showed that the use of an intensive IV insulin protocol designed to maintain serum blood glucose 80 mg/dL to 110 mg/dL significantly decreased morbidity and mortality following admission to the surgical ICU (SICU). Of note, only 13% of the individuals in the study had a previously known diagnosis of diabetes, showing that hyperglycemia was common following SICU admission and glycemic control was beneficial regardless of diabetes status.14
These impressive benefits1214 led to the call for improved glycemic control in the hospital with glucose targets similar to those used in the Belgian study.15 The development of protocols for such treatment proceeded rapidly.16, 17 A meta‐analysis that reviewed 14 trials through May 1, 2006 of patients in SICUs showed a 31% reduction in mortality with intensive therapy, albeit at the expense of a substantially increased risk of hypoglycemia.18 Our own studies19 using 1 day of continuous insulin infusion followed by subcutaneous basal/bolus insulin for all hyperglycemic patients following coronary artery bypass surgery showed results similar to those of Furnary et al.12, 13
Subsequently, 3 large, multicenter studies of patients in medical ICU (MICU) and SICUs, the VISEP, NICE‐SUGAR, and GLUCONTROL studies, failed to show the benefit of intensive insulin therapy on mortality and all had very high rates of hypoglycemia.2022 The VISEP20 study was stopped prematurely because of excessive hypoglycemia in the intensive treatment arm and the GLUCONTROL study was stopped prematurely because of multiple protocol violations.22 The NICE‐SUGAR study actually showed an increased mortality in the intensively treated group21 but the target range for their control group was 140 mg/dL to 180 mg/dL rather than 180 mg/dL to 215 mg/dL and this likely accounted for the better mortality in their control group compared to other studies. Van den Berghe et al.,23 in a design similar to their earlier one in the SICU, found that intensive insulin therapy in the MICU resulted in significant reductions in new onset renal injury, MICU and hospital length of stay, and an improved ability to wean off mechanical ventilation; however, no improvement in mortality was found except for those whose MICU stay was >3 days duration. In a post hoc analysis of their combined SICU and MICU studies, van den Berghe et al.23 found that a glucose target of 110 mg/dL to 150 mg/dL accounted for about 75% of the mortality benefit with a low risk of hypoglycemia.24 A recent meta‐analysis that included data on 13,567 patients from 26 trials, including the NICE‐SUGAR study, concluded that although overall there was no mortality benefit from intensive insulin therapy there was benefit in the SICU but not in the MICU or mixed ICU units.25
As a result of these later studies, new recommendations from the American Association of Clinical Endocrinologists and the American Diabetes Association state that for optimal risk/benefit, the overall goal of inpatient treatment for most patients should be 140 mg/dL to 180 mg/dL, although a range of 110 mg/dL to 140 mg/dL may be appropriate for some patients.26 Stressed in this Consensus Statement is the need for experienced practitioners and systems to provide optimal implementation of protocols so as to provide adequate glycemic control without an undue amount of hypoglycemia. We have found that active individual patient management by experienced nurse practitioners who can modify existing protocols as needed provides better glycemic control with less hypoglycemia than nursing personnel adhering to a protocol without taking into account the myriad of factors affecting patients daily.16
Although hypoglycemia is certainly to be avoided and has been associated with increased mortality,6, 27 Kosiborod et al.7 showed that mortality in hyperglycemic patients following an acute myocardial infarction was not related to insulin‐induced hypoglycemia but to hypoglycemia unassociated with insulin use. In the latter case, the hypoglycemia is generally attributable to shock, sepsis, malnutrition, liver failure, renal failure, or multiorgan failure.
One of the potential hurdles to achievement of glycemic control in the critically ill is the labor‐intensive changes in patient care policies necessary to attain these goals. Particular concern lies in the ability of inpatient care providers to develop and implement successful insulin protocols. Intravenous insulin administration is effective and appropriate in the ICU and some non‐ICU settings, but administration of insulin subcutaneously is less nursing intensive and a more familiar hyperglycemia treatment option. However, glycemic control with subcutaneous insulin is only achieved using basal/bolus regimens and not with simple sliding‐scale regimens that omit basal insulin and attempt to treat rather than prevent hyperglycemia.28
In this issue of the Journal of Hospital Medicine, 3 articles deal with some of the practical aspects of inpatient hyperglycemia management. In ICU patients on continuous IV insulin infusions, Newton et al.29 demonstrated improved glycemic control without an increase in hypoglycemia when using a computer‐guided insulin algorithm using a hand‐held device (Glucommander) compared to a paper algorithm. A previous publication in JHM showed that when continuous insulin infusions were used on the regular hospital floors outside of the ICU, Smiley et al.30 found that 67% of patients achieved the targeted goal of 150 mg/dL by day 2. Wesorick et al.31 found that simply educating floor nurses as well as physicians and using standardized insulin protocols resulted in improved glycemic control and less hypoglycemia on inpatient services outside of the ICU. In the third paper, Ramos et al. found that those with glycosylated hemoglobin (HbA1c) levels >6.0%, a prior history of diabetes, or chronic steroid use did better with basal insulin than with no basal insulin when converting from insulin infusions.32 In contrast to their using only 40% of the stable insulin infusion rate for their basal dose, we found that 80% worked better.33 We also learned the hard way that overlap of the infusion by 2 hours to 4 hours after giving the basal insulin subcutaneous dose is just not carried out by the treating team because of timing and practical considerations. We now just give a dose of rapid acting insulin equal to 10% of the basal insulin dose at the time of the injection of the basal dose; this allows for the immediate cessation of the infusion without loss of glycemic control (Table 1).
|
| Measure HbA1c on admission to aid in discharge planning |
| Start insulin infusions in postoperative and other unstable patients if blood glucose >180 mg/dL on 2 or more occasions |
| Begin IV continuous insulin infusion using validated protocols |
| Glucose target: 140‐180 mg/dL* |
| When converting from IV to subcutaneous insulin |
| Give 80% of stable IV dose as glargine insulin |
| Give 10% of glargine dose as rapid acting insulin |
| Then stop insulin infusion |
| If starting with subcutaneous insulin without prior insulin infusion |
| Give 50% as long‐acting insulin (glargine or detemir) |
| Give 50% as rapid‐acting insulin, divided into 3 for the 3 meals |
Intensive insulin treatment in the ICU clearly results in better outcomes when compared to letting glucose levels remain greater than 200 mg/dL. A glucose target range of 140 mg/dL to 180 mg/dL provides improved mortality and morbidity with a low risk of hypoglycemia and is suitable for most hospitals. A more aggressive target range of 110 mg/dL to 140 mg/dL provides further improvement but increases the risk of hypoglycemia and would only be appropriate for those institutions with considerable experience with such therapy and demonstrated low rates of hypoglycemia. Work is still needed on devising the ideal treatment algorithm, regimens for conversion from IV to subcutaneous insulin, and discharge planning. However, the most important part of patient care we have found is the insertion of an intelligent and experienced brain between the patient and the insulin protocol.
- ,,, et al.Stress hyperglycemia and prognosis of stroke in nondiabetic and diabetic patients: A systematic overview.Stroke.2001;32;2426–2432.
- ,,, et al.Hyperglycemia: an independent marker of in‐hospital mortality in patients with undiagnosed diabetes.J Clin Endocrinol Metab.2002;87;978–982.
- .Association between hyperglycemia and increased hospital mortality in a heterogeneous population of critically ill patients.Mayo Clin Proc.2003;78:1471–1478.
- ,,, et al.Influence of individual characteristics on outcome of glycemic control in intensive care unit patients with or without diabetes mellitus.Mayo Clin Proc.2005;80:1558–1567.
- ,,, et al.The relation between hyperglycemia and outcomes in 2,471 patients admitted to the hospital with community acquired pneumonia.Diabetes Care.2005;28:810–815.
- ,,, et al.Admission glucose and mortality in elderly patients hospitalized with acute myocardial infarction. Implications for patients with and without recognized diabetes.Circulation.2005;111:3078–3086.
- ,,, et al.Glucometrics in patients hospitalized with acute myocardial infarction. Defining the optimal outcomes‐based measure of risk.Circulation.2008;117:1018–1027.
- ,,, et al.Hyperglycemia‐related mortality in critically ill patients varies with admission diagnosis.Crit Care Med.2009;37:3001–3009.
- .Effect of insulin therapy on nonglycemic variables during acute illness.Endocr Pract.2004;10(Suppl 2):63–70.
- ,, et al.Therapy insight: the effect of tight glycemic control in acute illness.Nature Clin Pract Endocrinol Metab.2007;3:270–278.
- ,,.Stress hyperglycemia.Lancet.2009;373:1798–1807.
- ,,, et al.Continuous intravenous insulin infusion reduces the incidence of deep sternal wound infection in diabetic patients after cardiac surgical procedures.Ann Thorac Surg.1999;67:352–362.
- ,,, et al.Insulin infusion reduces mortality in patients undergoing coronary artery bypass grafting.J Thorac Cardiovasc Surg.2003;125:1007–1021.
- ,,, et al.Intensive insulin therapy in critically ill patients.N Engl J Med.2001;345:1359–1367.
- ,,, et al.American College of Endocrinology Position Statement on inpatient diabetes and metabolic control.Endocr Pract.2004;10:77–82.
- ,,, et al.Inpatient management of hyperglycemia: The Northwestern Experience.Endocr Pract.2006:12;491–505.
- ,,.Insulin infusion protocols for critically ill patients: a highlight of differences and similarities.Endocr Pract.2007;13:137–146.
- ,,, et al.Effect of perioperative insulin infusion on surgical morbidity and mortality: systematic review and meta‐analysis of randomized trials.Mayo Clin Proc.2008;83:418–430.
- ,,, et al.Reduction in surgical mortality and morbidity in diabetic patients undergoing cardiac surgery with a combined intravenous and subcutaneous insulin glucose management.Diabetes Care.2007;30:823–828.
- ,,, et al.Intensive insulin therapy and pentastarch resuscitation in severe sepsis.N Engl J Med.2008;358:125–139.
- ,,Su SY for the NICE‐SUGAR Study Investigators. Intensive versus conventional glucose control in critically ill patients.N Engl J Med.2009;360:1283–1297.
- ,,, et al.A prospective randomised multi‐centre controlled trial on tight glucose control by intensive insulin therapy in adult intensive care units: the Glucontrol Study.Intensive Care Med.2009;35:1738–1748.
- ,,, et al.Intensive insulin therapy in the medical ICU.N Engl J Med.2006;354:449–461.
- ,,, et al.Intensive insulin therapy in mixed medical/surgical intensive care units: benefit versus harm.Diabetes.2006;55:3151–3159.
- ,,, et al.Intensive insulin therapy and mortality among critically ill patients: a meta‐analysis including NIC‐SUGAR study data.CMAJ.2009;180:821–827.
- ,,, et al.American Association of Clinical Endocrinologists and American Diabetes Association consensus statement on inpatient glycemic control.Diabetes Care.2009;32:1119–1131.
- ,.Severe hypoglycemia in critically ill patients: risk factors and outcomes.Crit Care Med.2007;35:2262–2267.
- ,,, et al.Randomized study of basal‐bolus insulin therapy in the inpatient management of patients with type 2 diabetes (RABBIT 2 trial).Diabetes Care.2007;30:2181–2186.
- ,,, et al.A comparison study of continuous insulin infusion protocols in the Medical Intensive Care Unit: computer‐guided versus standard column‐based algorithms.J Hosp Med. 2010;5:432–437.
- ,,, et al.Safety and efficacy of continuous insulin infusion in noncritical care settings.J Hosp Med.2010;5(4):212–217.
- ,,, et al.Effects of an educational program and a standardized insulin order form on glycemic outcomes in non‐critically ill hospitalized patients.J Hosp Med. 2010;5:438–445.
- ,,, et al.Maintaining glycemic control when transitioning from infusion insulin: a protocol driven, multidisciplinary approach.J Hosp Med. 2010;5:446–451.
- ,,, et al.Conversion of intravenous insulin infusions to subcutaneously administered insulin glargine in patients with hyperglycemia.Endocr Pract.2006;12:641–650.
Hyperglycemia that develops acutely due to illness is associated with poor patient outcomes in hospitalized inpatients, especially those critically ill in the intensive care unit (ICU).18 In fact, those without a prior diagnosis of diabetes and therefore newly found to have hyperglycemia have worse outcomes than those who have a prior diagnosis of diabetes.1, 2, 4, 68 Many mechanisms have been put forward to explain the adverse outcomes related to hyperglycemia, including the release of counter‐regulatory hormones, increased lipolysis with free fatty acid release, the release of inflammatory cytokines and growth factors, increased reactive oxygen species with oxidative stress and altered immunoglobulin, and neutrophil phagocytic function.911
The practical importance of this was brought home by Furnary et al.12, 13 who showed that glycemic control using 3 days of intensive intravenous (IV) insulin therapy of diabetic patients undergoing cardiac surgical procedures was able to reduce significantly the risk of deep sternal wound infections and mortality and to bring these adverse outcomes to the same levels as those of nondiabetic patients. However, the benefits of intensive insulin therapy are not limited to those with diabetes and extend to those with critical illness‐induced hyperglycemia. In a landmark, randomized, prospective study from Belgium, van den Berghe et al.14 showed that the use of an intensive IV insulin protocol designed to maintain serum blood glucose 80 mg/dL to 110 mg/dL significantly decreased morbidity and mortality following admission to the surgical ICU (SICU). Of note, only 13% of the individuals in the study had a previously known diagnosis of diabetes, showing that hyperglycemia was common following SICU admission and glycemic control was beneficial regardless of diabetes status.14
These impressive benefits1214 led to the call for improved glycemic control in the hospital with glucose targets similar to those used in the Belgian study.15 The development of protocols for such treatment proceeded rapidly.16, 17 A meta‐analysis that reviewed 14 trials through May 1, 2006 of patients in SICUs showed a 31% reduction in mortality with intensive therapy, albeit at the expense of a substantially increased risk of hypoglycemia.18 Our own studies19 using 1 day of continuous insulin infusion followed by subcutaneous basal/bolus insulin for all hyperglycemic patients following coronary artery bypass surgery showed results similar to those of Furnary et al.12, 13
Subsequently, 3 large, multicenter studies of patients in medical ICU (MICU) and SICUs, the VISEP, NICE‐SUGAR, and GLUCONTROL studies, failed to show the benefit of intensive insulin therapy on mortality and all had very high rates of hypoglycemia.2022 The VISEP20 study was stopped prematurely because of excessive hypoglycemia in the intensive treatment arm and the GLUCONTROL study was stopped prematurely because of multiple protocol violations.22 The NICE‐SUGAR study actually showed an increased mortality in the intensively treated group21 but the target range for their control group was 140 mg/dL to 180 mg/dL rather than 180 mg/dL to 215 mg/dL and this likely accounted for the better mortality in their control group compared to other studies. Van den Berghe et al.,23 in a design similar to their earlier one in the SICU, found that intensive insulin therapy in the MICU resulted in significant reductions in new onset renal injury, MICU and hospital length of stay, and an improved ability to wean off mechanical ventilation; however, no improvement in mortality was found except for those whose MICU stay was >3 days duration. In a post hoc analysis of their combined SICU and MICU studies, van den Berghe et al.23 found that a glucose target of 110 mg/dL to 150 mg/dL accounted for about 75% of the mortality benefit with a low risk of hypoglycemia.24 A recent meta‐analysis that included data on 13,567 patients from 26 trials, including the NICE‐SUGAR study, concluded that although overall there was no mortality benefit from intensive insulin therapy there was benefit in the SICU but not in the MICU or mixed ICU units.25
As a result of these later studies, new recommendations from the American Association of Clinical Endocrinologists and the American Diabetes Association state that for optimal risk/benefit, the overall goal of inpatient treatment for most patients should be 140 mg/dL to 180 mg/dL, although a range of 110 mg/dL to 140 mg/dL may be appropriate for some patients.26 Stressed in this Consensus Statement is the need for experienced practitioners and systems to provide optimal implementation of protocols so as to provide adequate glycemic control without an undue amount of hypoglycemia. We have found that active individual patient management by experienced nurse practitioners who can modify existing protocols as needed provides better glycemic control with less hypoglycemia than nursing personnel adhering to a protocol without taking into account the myriad of factors affecting patients daily.16
Although hypoglycemia is certainly to be avoided and has been associated with increased mortality,6, 27 Kosiborod et al.7 showed that mortality in hyperglycemic patients following an acute myocardial infarction was not related to insulin‐induced hypoglycemia but to hypoglycemia unassociated with insulin use. In the latter case, the hypoglycemia is generally attributable to shock, sepsis, malnutrition, liver failure, renal failure, or multiorgan failure.
One of the potential hurdles to achievement of glycemic control in the critically ill is the labor‐intensive changes in patient care policies necessary to attain these goals. Particular concern lies in the ability of inpatient care providers to develop and implement successful insulin protocols. Intravenous insulin administration is effective and appropriate in the ICU and some non‐ICU settings, but administration of insulin subcutaneously is less nursing intensive and a more familiar hyperglycemia treatment option. However, glycemic control with subcutaneous insulin is only achieved using basal/bolus regimens and not with simple sliding‐scale regimens that omit basal insulin and attempt to treat rather than prevent hyperglycemia.28
In this issue of the Journal of Hospital Medicine, 3 articles deal with some of the practical aspects of inpatient hyperglycemia management. In ICU patients on continuous IV insulin infusions, Newton et al.29 demonstrated improved glycemic control without an increase in hypoglycemia when using a computer‐guided insulin algorithm using a hand‐held device (Glucommander) compared to a paper algorithm. A previous publication in JHM showed that when continuous insulin infusions were used on the regular hospital floors outside of the ICU, Smiley et al.30 found that 67% of patients achieved the targeted goal of 150 mg/dL by day 2. Wesorick et al.31 found that simply educating floor nurses as well as physicians and using standardized insulin protocols resulted in improved glycemic control and less hypoglycemia on inpatient services outside of the ICU. In the third paper, Ramos et al. found that those with glycosylated hemoglobin (HbA1c) levels >6.0%, a prior history of diabetes, or chronic steroid use did better with basal insulin than with no basal insulin when converting from insulin infusions.32 In contrast to their using only 40% of the stable insulin infusion rate for their basal dose, we found that 80% worked better.33 We also learned the hard way that overlap of the infusion by 2 hours to 4 hours after giving the basal insulin subcutaneous dose is just not carried out by the treating team because of timing and practical considerations. We now just give a dose of rapid acting insulin equal to 10% of the basal insulin dose at the time of the injection of the basal dose; this allows for the immediate cessation of the infusion without loss of glycemic control (Table 1).
|
| Measure HbA1c on admission to aid in discharge planning |
| Start insulin infusions in postoperative and other unstable patients if blood glucose >180 mg/dL on 2 or more occasions |
| Begin IV continuous insulin infusion using validated protocols |
| Glucose target: 140‐180 mg/dL* |
| When converting from IV to subcutaneous insulin |
| Give 80% of stable IV dose as glargine insulin |
| Give 10% of glargine dose as rapid acting insulin |
| Then stop insulin infusion |
| If starting with subcutaneous insulin without prior insulin infusion |
| Give 50% as long‐acting insulin (glargine or detemir) |
| Give 50% as rapid‐acting insulin, divided into 3 for the 3 meals |
Intensive insulin treatment in the ICU clearly results in better outcomes when compared to letting glucose levels remain greater than 200 mg/dL. A glucose target range of 140 mg/dL to 180 mg/dL provides improved mortality and morbidity with a low risk of hypoglycemia and is suitable for most hospitals. A more aggressive target range of 110 mg/dL to 140 mg/dL provides further improvement but increases the risk of hypoglycemia and would only be appropriate for those institutions with considerable experience with such therapy and demonstrated low rates of hypoglycemia. Work is still needed on devising the ideal treatment algorithm, regimens for conversion from IV to subcutaneous insulin, and discharge planning. However, the most important part of patient care we have found is the insertion of an intelligent and experienced brain between the patient and the insulin protocol.
Hyperglycemia that develops acutely due to illness is associated with poor patient outcomes in hospitalized inpatients, especially those critically ill in the intensive care unit (ICU).18 In fact, those without a prior diagnosis of diabetes and therefore newly found to have hyperglycemia have worse outcomes than those who have a prior diagnosis of diabetes.1, 2, 4, 68 Many mechanisms have been put forward to explain the adverse outcomes related to hyperglycemia, including the release of counter‐regulatory hormones, increased lipolysis with free fatty acid release, the release of inflammatory cytokines and growth factors, increased reactive oxygen species with oxidative stress and altered immunoglobulin, and neutrophil phagocytic function.911
The practical importance of this was brought home by Furnary et al.12, 13 who showed that glycemic control using 3 days of intensive intravenous (IV) insulin therapy of diabetic patients undergoing cardiac surgical procedures was able to reduce significantly the risk of deep sternal wound infections and mortality and to bring these adverse outcomes to the same levels as those of nondiabetic patients. However, the benefits of intensive insulin therapy are not limited to those with diabetes and extend to those with critical illness‐induced hyperglycemia. In a landmark, randomized, prospective study from Belgium, van den Berghe et al.14 showed that the use of an intensive IV insulin protocol designed to maintain serum blood glucose 80 mg/dL to 110 mg/dL significantly decreased morbidity and mortality following admission to the surgical ICU (SICU). Of note, only 13% of the individuals in the study had a previously known diagnosis of diabetes, showing that hyperglycemia was common following SICU admission and glycemic control was beneficial regardless of diabetes status.14
These impressive benefits1214 led to the call for improved glycemic control in the hospital with glucose targets similar to those used in the Belgian study.15 The development of protocols for such treatment proceeded rapidly.16, 17 A meta‐analysis that reviewed 14 trials through May 1, 2006 of patients in SICUs showed a 31% reduction in mortality with intensive therapy, albeit at the expense of a substantially increased risk of hypoglycemia.18 Our own studies19 using 1 day of continuous insulin infusion followed by subcutaneous basal/bolus insulin for all hyperglycemic patients following coronary artery bypass surgery showed results similar to those of Furnary et al.12, 13
Subsequently, 3 large, multicenter studies of patients in medical ICU (MICU) and SICUs, the VISEP, NICE‐SUGAR, and GLUCONTROL studies, failed to show the benefit of intensive insulin therapy on mortality and all had very high rates of hypoglycemia.2022 The VISEP20 study was stopped prematurely because of excessive hypoglycemia in the intensive treatment arm and the GLUCONTROL study was stopped prematurely because of multiple protocol violations.22 The NICE‐SUGAR study actually showed an increased mortality in the intensively treated group21 but the target range for their control group was 140 mg/dL to 180 mg/dL rather than 180 mg/dL to 215 mg/dL and this likely accounted for the better mortality in their control group compared to other studies. Van den Berghe et al.,23 in a design similar to their earlier one in the SICU, found that intensive insulin therapy in the MICU resulted in significant reductions in new onset renal injury, MICU and hospital length of stay, and an improved ability to wean off mechanical ventilation; however, no improvement in mortality was found except for those whose MICU stay was >3 days duration. In a post hoc analysis of their combined SICU and MICU studies, van den Berghe et al.23 found that a glucose target of 110 mg/dL to 150 mg/dL accounted for about 75% of the mortality benefit with a low risk of hypoglycemia.24 A recent meta‐analysis that included data on 13,567 patients from 26 trials, including the NICE‐SUGAR study, concluded that although overall there was no mortality benefit from intensive insulin therapy there was benefit in the SICU but not in the MICU or mixed ICU units.25
As a result of these later studies, new recommendations from the American Association of Clinical Endocrinologists and the American Diabetes Association state that for optimal risk/benefit, the overall goal of inpatient treatment for most patients should be 140 mg/dL to 180 mg/dL, although a range of 110 mg/dL to 140 mg/dL may be appropriate for some patients.26 Stressed in this Consensus Statement is the need for experienced practitioners and systems to provide optimal implementation of protocols so as to provide adequate glycemic control without an undue amount of hypoglycemia. We have found that active individual patient management by experienced nurse practitioners who can modify existing protocols as needed provides better glycemic control with less hypoglycemia than nursing personnel adhering to a protocol without taking into account the myriad of factors affecting patients daily.16
Although hypoglycemia is certainly to be avoided and has been associated with increased mortality,6, 27 Kosiborod et al.7 showed that mortality in hyperglycemic patients following an acute myocardial infarction was not related to insulin‐induced hypoglycemia but to hypoglycemia unassociated with insulin use. In the latter case, the hypoglycemia is generally attributable to shock, sepsis, malnutrition, liver failure, renal failure, or multiorgan failure.
One of the potential hurdles to achievement of glycemic control in the critically ill is the labor‐intensive changes in patient care policies necessary to attain these goals. Particular concern lies in the ability of inpatient care providers to develop and implement successful insulin protocols. Intravenous insulin administration is effective and appropriate in the ICU and some non‐ICU settings, but administration of insulin subcutaneously is less nursing intensive and a more familiar hyperglycemia treatment option. However, glycemic control with subcutaneous insulin is only achieved using basal/bolus regimens and not with simple sliding‐scale regimens that omit basal insulin and attempt to treat rather than prevent hyperglycemia.28
In this issue of the Journal of Hospital Medicine, 3 articles deal with some of the practical aspects of inpatient hyperglycemia management. In ICU patients on continuous IV insulin infusions, Newton et al.29 demonstrated improved glycemic control without an increase in hypoglycemia when using a computer‐guided insulin algorithm using a hand‐held device (Glucommander) compared to a paper algorithm. A previous publication in JHM showed that when continuous insulin infusions were used on the regular hospital floors outside of the ICU, Smiley et al.30 found that 67% of patients achieved the targeted goal of 150 mg/dL by day 2. Wesorick et al.31 found that simply educating floor nurses as well as physicians and using standardized insulin protocols resulted in improved glycemic control and less hypoglycemia on inpatient services outside of the ICU. In the third paper, Ramos et al. found that those with glycosylated hemoglobin (HbA1c) levels >6.0%, a prior history of diabetes, or chronic steroid use did better with basal insulin than with no basal insulin when converting from insulin infusions.32 In contrast to their using only 40% of the stable insulin infusion rate for their basal dose, we found that 80% worked better.33 We also learned the hard way that overlap of the infusion by 2 hours to 4 hours after giving the basal insulin subcutaneous dose is just not carried out by the treating team because of timing and practical considerations. We now just give a dose of rapid acting insulin equal to 10% of the basal insulin dose at the time of the injection of the basal dose; this allows for the immediate cessation of the infusion without loss of glycemic control (Table 1).
|
| Measure HbA1c on admission to aid in discharge planning |
| Start insulin infusions in postoperative and other unstable patients if blood glucose >180 mg/dL on 2 or more occasions |
| Begin IV continuous insulin infusion using validated protocols |
| Glucose target: 140‐180 mg/dL* |
| When converting from IV to subcutaneous insulin |
| Give 80% of stable IV dose as glargine insulin |
| Give 10% of glargine dose as rapid acting insulin |
| Then stop insulin infusion |
| If starting with subcutaneous insulin without prior insulin infusion |
| Give 50% as long‐acting insulin (glargine or detemir) |
| Give 50% as rapid‐acting insulin, divided into 3 for the 3 meals |
Intensive insulin treatment in the ICU clearly results in better outcomes when compared to letting glucose levels remain greater than 200 mg/dL. A glucose target range of 140 mg/dL to 180 mg/dL provides improved mortality and morbidity with a low risk of hypoglycemia and is suitable for most hospitals. A more aggressive target range of 110 mg/dL to 140 mg/dL provides further improvement but increases the risk of hypoglycemia and would only be appropriate for those institutions with considerable experience with such therapy and demonstrated low rates of hypoglycemia. Work is still needed on devising the ideal treatment algorithm, regimens for conversion from IV to subcutaneous insulin, and discharge planning. However, the most important part of patient care we have found is the insertion of an intelligent and experienced brain between the patient and the insulin protocol.
- ,,, et al.Stress hyperglycemia and prognosis of stroke in nondiabetic and diabetic patients: A systematic overview.Stroke.2001;32;2426–2432.
- ,,, et al.Hyperglycemia: an independent marker of in‐hospital mortality in patients with undiagnosed diabetes.J Clin Endocrinol Metab.2002;87;978–982.
- .Association between hyperglycemia and increased hospital mortality in a heterogeneous population of critically ill patients.Mayo Clin Proc.2003;78:1471–1478.
- ,,, et al.Influence of individual characteristics on outcome of glycemic control in intensive care unit patients with or without diabetes mellitus.Mayo Clin Proc.2005;80:1558–1567.
- ,,, et al.The relation between hyperglycemia and outcomes in 2,471 patients admitted to the hospital with community acquired pneumonia.Diabetes Care.2005;28:810–815.
- ,,, et al.Admission glucose and mortality in elderly patients hospitalized with acute myocardial infarction. Implications for patients with and without recognized diabetes.Circulation.2005;111:3078–3086.
- ,,, et al.Glucometrics in patients hospitalized with acute myocardial infarction. Defining the optimal outcomes‐based measure of risk.Circulation.2008;117:1018–1027.
- ,,, et al.Hyperglycemia‐related mortality in critically ill patients varies with admission diagnosis.Crit Care Med.2009;37:3001–3009.
- .Effect of insulin therapy on nonglycemic variables during acute illness.Endocr Pract.2004;10(Suppl 2):63–70.
- ,, et al.Therapy insight: the effect of tight glycemic control in acute illness.Nature Clin Pract Endocrinol Metab.2007;3:270–278.
- ,,.Stress hyperglycemia.Lancet.2009;373:1798–1807.
- ,,, et al.Continuous intravenous insulin infusion reduces the incidence of deep sternal wound infection in diabetic patients after cardiac surgical procedures.Ann Thorac Surg.1999;67:352–362.
- ,,, et al.Insulin infusion reduces mortality in patients undergoing coronary artery bypass grafting.J Thorac Cardiovasc Surg.2003;125:1007–1021.
- ,,, et al.Intensive insulin therapy in critically ill patients.N Engl J Med.2001;345:1359–1367.
- ,,, et al.American College of Endocrinology Position Statement on inpatient diabetes and metabolic control.Endocr Pract.2004;10:77–82.
- ,,, et al.Inpatient management of hyperglycemia: The Northwestern Experience.Endocr Pract.2006:12;491–505.
- ,,.Insulin infusion protocols for critically ill patients: a highlight of differences and similarities.Endocr Pract.2007;13:137–146.
- ,,, et al.Effect of perioperative insulin infusion on surgical morbidity and mortality: systematic review and meta‐analysis of randomized trials.Mayo Clin Proc.2008;83:418–430.
- ,,, et al.Reduction in surgical mortality and morbidity in diabetic patients undergoing cardiac surgery with a combined intravenous and subcutaneous insulin glucose management.Diabetes Care.2007;30:823–828.
- ,,, et al.Intensive insulin therapy and pentastarch resuscitation in severe sepsis.N Engl J Med.2008;358:125–139.
- ,,Su SY for the NICE‐SUGAR Study Investigators. Intensive versus conventional glucose control in critically ill patients.N Engl J Med.2009;360:1283–1297.
- ,,, et al.A prospective randomised multi‐centre controlled trial on tight glucose control by intensive insulin therapy in adult intensive care units: the Glucontrol Study.Intensive Care Med.2009;35:1738–1748.
- ,,, et al.Intensive insulin therapy in the medical ICU.N Engl J Med.2006;354:449–461.
- ,,, et al.Intensive insulin therapy in mixed medical/surgical intensive care units: benefit versus harm.Diabetes.2006;55:3151–3159.
- ,,, et al.Intensive insulin therapy and mortality among critically ill patients: a meta‐analysis including NIC‐SUGAR study data.CMAJ.2009;180:821–827.
- ,,, et al.American Association of Clinical Endocrinologists and American Diabetes Association consensus statement on inpatient glycemic control.Diabetes Care.2009;32:1119–1131.
- ,.Severe hypoglycemia in critically ill patients: risk factors and outcomes.Crit Care Med.2007;35:2262–2267.
- ,,, et al.Randomized study of basal‐bolus insulin therapy in the inpatient management of patients with type 2 diabetes (RABBIT 2 trial).Diabetes Care.2007;30:2181–2186.
- ,,, et al.A comparison study of continuous insulin infusion protocols in the Medical Intensive Care Unit: computer‐guided versus standard column‐based algorithms.J Hosp Med. 2010;5:432–437.
- ,,, et al.Safety and efficacy of continuous insulin infusion in noncritical care settings.J Hosp Med.2010;5(4):212–217.
- ,,, et al.Effects of an educational program and a standardized insulin order form on glycemic outcomes in non‐critically ill hospitalized patients.J Hosp Med. 2010;5:438–445.
- ,,, et al.Maintaining glycemic control when transitioning from infusion insulin: a protocol driven, multidisciplinary approach.J Hosp Med. 2010;5:446–451.
- ,,, et al.Conversion of intravenous insulin infusions to subcutaneously administered insulin glargine in patients with hyperglycemia.Endocr Pract.2006;12:641–650.
- ,,, et al.Stress hyperglycemia and prognosis of stroke in nondiabetic and diabetic patients: A systematic overview.Stroke.2001;32;2426–2432.
- ,,, et al.Hyperglycemia: an independent marker of in‐hospital mortality in patients with undiagnosed diabetes.J Clin Endocrinol Metab.2002;87;978–982.
- .Association between hyperglycemia and increased hospital mortality in a heterogeneous population of critically ill patients.Mayo Clin Proc.2003;78:1471–1478.
- ,,, et al.Influence of individual characteristics on outcome of glycemic control in intensive care unit patients with or without diabetes mellitus.Mayo Clin Proc.2005;80:1558–1567.
- ,,, et al.The relation between hyperglycemia and outcomes in 2,471 patients admitted to the hospital with community acquired pneumonia.Diabetes Care.2005;28:810–815.
- ,,, et al.Admission glucose and mortality in elderly patients hospitalized with acute myocardial infarction. Implications for patients with and without recognized diabetes.Circulation.2005;111:3078–3086.
- ,,, et al.Glucometrics in patients hospitalized with acute myocardial infarction. Defining the optimal outcomes‐based measure of risk.Circulation.2008;117:1018–1027.
- ,,, et al.Hyperglycemia‐related mortality in critically ill patients varies with admission diagnosis.Crit Care Med.2009;37:3001–3009.
- .Effect of insulin therapy on nonglycemic variables during acute illness.Endocr Pract.2004;10(Suppl 2):63–70.
- ,, et al.Therapy insight: the effect of tight glycemic control in acute illness.Nature Clin Pract Endocrinol Metab.2007;3:270–278.
- ,,.Stress hyperglycemia.Lancet.2009;373:1798–1807.
- ,,, et al.Continuous intravenous insulin infusion reduces the incidence of deep sternal wound infection in diabetic patients after cardiac surgical procedures.Ann Thorac Surg.1999;67:352–362.
- ,,, et al.Insulin infusion reduces mortality in patients undergoing coronary artery bypass grafting.J Thorac Cardiovasc Surg.2003;125:1007–1021.
- ,,, et al.Intensive insulin therapy in critically ill patients.N Engl J Med.2001;345:1359–1367.
- ,,, et al.American College of Endocrinology Position Statement on inpatient diabetes and metabolic control.Endocr Pract.2004;10:77–82.
- ,,, et al.Inpatient management of hyperglycemia: The Northwestern Experience.Endocr Pract.2006:12;491–505.
- ,,.Insulin infusion protocols for critically ill patients: a highlight of differences and similarities.Endocr Pract.2007;13:137–146.
- ,,, et al.Effect of perioperative insulin infusion on surgical morbidity and mortality: systematic review and meta‐analysis of randomized trials.Mayo Clin Proc.2008;83:418–430.
- ,,, et al.Reduction in surgical mortality and morbidity in diabetic patients undergoing cardiac surgery with a combined intravenous and subcutaneous insulin glucose management.Diabetes Care.2007;30:823–828.
- ,,, et al.Intensive insulin therapy and pentastarch resuscitation in severe sepsis.N Engl J Med.2008;358:125–139.
- ,,Su SY for the NICE‐SUGAR Study Investigators. Intensive versus conventional glucose control in critically ill patients.N Engl J Med.2009;360:1283–1297.
- ,,, et al.A prospective randomised multi‐centre controlled trial on tight glucose control by intensive insulin therapy in adult intensive care units: the Glucontrol Study.Intensive Care Med.2009;35:1738–1748.
- ,,, et al.Intensive insulin therapy in the medical ICU.N Engl J Med.2006;354:449–461.
- ,,, et al.Intensive insulin therapy in mixed medical/surgical intensive care units: benefit versus harm.Diabetes.2006;55:3151–3159.
- ,,, et al.Intensive insulin therapy and mortality among critically ill patients: a meta‐analysis including NIC‐SUGAR study data.CMAJ.2009;180:821–827.
- ,,, et al.American Association of Clinical Endocrinologists and American Diabetes Association consensus statement on inpatient glycemic control.Diabetes Care.2009;32:1119–1131.
- ,.Severe hypoglycemia in critically ill patients: risk factors and outcomes.Crit Care Med.2007;35:2262–2267.
- ,,, et al.Randomized study of basal‐bolus insulin therapy in the inpatient management of patients with type 2 diabetes (RABBIT 2 trial).Diabetes Care.2007;30:2181–2186.
- ,,, et al.A comparison study of continuous insulin infusion protocols in the Medical Intensive Care Unit: computer‐guided versus standard column‐based algorithms.J Hosp Med. 2010;5:432–437.
- ,,, et al.Safety and efficacy of continuous insulin infusion in noncritical care settings.J Hosp Med.2010;5(4):212–217.
- ,,, et al.Effects of an educational program and a standardized insulin order form on glycemic outcomes in non‐critically ill hospitalized patients.J Hosp Med. 2010;5:438–445.
- ,,, et al.Maintaining glycemic control when transitioning from infusion insulin: a protocol driven, multidisciplinary approach.J Hosp Med. 2010;5:446–451.
- ,,, et al.Conversion of intravenous insulin infusions to subcutaneously administered insulin glargine in patients with hyperglycemia.Endocr Pract.2006;12:641–650.
Is there a doctor in your house? Home health care of the future
Medical care at home is emerging as a “disruptive innovation” on the US health care scene. New models of home care offer the promise of better service, higher quality, and a better experience at a lower cost compared with nursing home and hospital care. A tall order, indeed! Pioneers like Dr. Bruce Leff, however, have already shown quite convincingly that “hospital at home” programs can be implemented and can deliver on these promises for patients who are eligible for hospital admission.1,2
In their essay “Bringing home the ‘medical home’ for older adults” in this issue of the Cleveland Clinic Journal of Medicine, Landers and colleagues discuss the opportunity of extending the medical home model to home health care as an integral part of the medical neighborhood to improve care coordination, reduce expensive hospitalizations, and improve the patient experience by caring for patients in their own homes. As a part of health care reform, the Center for Medicare and Medicaid Services intends to fund demonstration projects to determine to what extent home care can achieve these lofty goals.
A modernized, efficient, and effective home health care system would be a welcome improvement on the patchwork system we have had in the United States for the past 30 years. From my perspective as a family physician, this new legislation may provide the opportunity to get home health care right.
It did not start off on the right foot in the United States. Many home health agencies were established as independent, for-profit businesses detached from the primary care doctors who were ultimately responsible for patients’ care. Signing orders once a month on long forms that conveyed little useful information about my patients never seemed like adequate care oversight on my part. Communicating well with a dozen nurses I did not know or see on a regular basis was a daunting if not impossible task.
IT TAKES TWO TO PASS THE BATON
If home health care got off on the wrong foot in the United States in the 1970s, what then is the right foot?
To me, the key is a tight linkage of home health care to hospitals, physician offices, and nursing homes. Most elderly and frail people do not live out their lives in one venue. They move from home to hospital to nursing home and back again, often several times during their lives. These care transitions are fraught with the dangers of medication errors and forgotten test results. Home health care agencies can become experts in managing these dangerous care transitions.
Home health nurses and physicians can be experts at passing the baton without dropping it. Parenthetically, all physicians must become experts at passing the baton. It takes two to pass the baton successfully, whether it is from hospitalist to primary care physician, from home care nurse to primary care physician, or from primary care physician to hospitalist.
CHALLENGES: REIMBURSEMENT, COSTLY TECHNOLOGY, COMMUNICATION
What are the challenges Dr. Landers and his forward-thinking colleagues face in implementing modern medical care in the home?
Reimbursement is the obvious first issue. Current restrictions make it difficult to care for homebound and semi-homebound patients on more than an episodic basis. The proposed demonstration projects in home health must overcome this barrier.
Appropriate use of home health technology will be a second challenge, just as it is an opportunity. How much minute-by-minute information is really necessary for home monitoring? How expensive will the technology be? Will home health technology simply be another opportunity to make money, or will it really deliver economic value by preventing hospitalizations? Is fancy monitoring equipment more effective than low-tech daily phone calls and a scale in managing patients with congestive heart failure? How much monitoring and intervention is enough to achieve excellent outcomes? For congestive heart failure, there is good evidence from randomized clinical trials that telemonitoring reduces rates of all-cause mortality (relative risk 0.66, 95% confidence interval 0.54–0.81) and heart-failure-related hospitalizations (relative risk 0.79, 95% confidence interval 0.67–0.94).3
On the cost side of the value equation, what is the right “dose” of home health care for a given patient? At what point on the cost-quality curve does cost outweigh value? Integrating home health care into accountable health care organizations may be the only way to maximize quality and efficiency.
Communication challenges will be the toughest. If home health care becomes a well-developed island of care, I suspect we will not be much better off than we are now. Key to improving quality and lowering cost is effective communication across the spectrum of care. Can teams of doctors and other health care professionals who each claim a different venue as their territory—home, hospital, office, nursing home—provide the coordinated, evidence-based, and personalized medical care to which Dr. Landers and his colleagues aspire? I believe it is possible, but the jury is still out.
A seamless, shared electronic medical record is essential for communication, but current platforms are not designed to integrate home care, hospital, and office records. Several innovative home care companies are attempting to do so, however. Recently, Cleveland Clinic made home visit notes from its home care arm available to other providers on its electronic medical record platform.
Locating visiting nurses and home care physicians in proximity to primary care physician offices would greatly improve the chances of good communication. In a randomized trial of outpatient care of frail elderly patients living at home, having nurse care coordinators located in primary care physician offices resulted in fewer hospitalizations and nursing home placements and greater patient, family, and physician satisfaction compared with traditional outpatient care.4.5
NO MORE ‘BUSINESS AS USUAL’
In this time of economic uncertainty, at least one thing is certain: “business as usual” does not apply to US health care delivery. I am hopeful that innovative models of home care will find their proper niche as we seek to provide the right care for the right patient at the right time in the right venue and at the right price.
- Leff B, Burton L, Mader SL, et al. Comparison of functional outcomes associated with hospital at home care and traditional acute hospital care. J Am Geriatr Soc 2009; 57:273–278.
- Frick KD, Burton LC, Clark R, et al. Substitutive Hospital at Home for older persons: effects on costs. Am J Manag Care 2009; 15:49–56.
- Inglis SC, Clark RA, McAlister FA, et al. Structured telephone support or telemonitoring programmes for patients with chronic heart failure. Cochrane Database Syst Rev 2010; 8:CD007228.
- Boyd CM, Reider L, Frey K, et al. The effects of guided care on the perceived quality of health care for multi-morbid older persons: 18-month outcomes from a cluster-randomized controlled trial. J Gen Intern Med 2010; 25:235–242.
- Leff B, Reider L, Frick KD, et al. Guided care and the cost of complex healthcare: a preliminary report. Am J Manag Care 2009; 15:555–559.
Medical care at home is emerging as a “disruptive innovation” on the US health care scene. New models of home care offer the promise of better service, higher quality, and a better experience at a lower cost compared with nursing home and hospital care. A tall order, indeed! Pioneers like Dr. Bruce Leff, however, have already shown quite convincingly that “hospital at home” programs can be implemented and can deliver on these promises for patients who are eligible for hospital admission.1,2
In their essay “Bringing home the ‘medical home’ for older adults” in this issue of the Cleveland Clinic Journal of Medicine, Landers and colleagues discuss the opportunity of extending the medical home model to home health care as an integral part of the medical neighborhood to improve care coordination, reduce expensive hospitalizations, and improve the patient experience by caring for patients in their own homes. As a part of health care reform, the Center for Medicare and Medicaid Services intends to fund demonstration projects to determine to what extent home care can achieve these lofty goals.
A modernized, efficient, and effective home health care system would be a welcome improvement on the patchwork system we have had in the United States for the past 30 years. From my perspective as a family physician, this new legislation may provide the opportunity to get home health care right.
It did not start off on the right foot in the United States. Many home health agencies were established as independent, for-profit businesses detached from the primary care doctors who were ultimately responsible for patients’ care. Signing orders once a month on long forms that conveyed little useful information about my patients never seemed like adequate care oversight on my part. Communicating well with a dozen nurses I did not know or see on a regular basis was a daunting if not impossible task.
IT TAKES TWO TO PASS THE BATON
If home health care got off on the wrong foot in the United States in the 1970s, what then is the right foot?
To me, the key is a tight linkage of home health care to hospitals, physician offices, and nursing homes. Most elderly and frail people do not live out their lives in one venue. They move from home to hospital to nursing home and back again, often several times during their lives. These care transitions are fraught with the dangers of medication errors and forgotten test results. Home health care agencies can become experts in managing these dangerous care transitions.
Home health nurses and physicians can be experts at passing the baton without dropping it. Parenthetically, all physicians must become experts at passing the baton. It takes two to pass the baton successfully, whether it is from hospitalist to primary care physician, from home care nurse to primary care physician, or from primary care physician to hospitalist.
CHALLENGES: REIMBURSEMENT, COSTLY TECHNOLOGY, COMMUNICATION
What are the challenges Dr. Landers and his forward-thinking colleagues face in implementing modern medical care in the home?
Reimbursement is the obvious first issue. Current restrictions make it difficult to care for homebound and semi-homebound patients on more than an episodic basis. The proposed demonstration projects in home health must overcome this barrier.
Appropriate use of home health technology will be a second challenge, just as it is an opportunity. How much minute-by-minute information is really necessary for home monitoring? How expensive will the technology be? Will home health technology simply be another opportunity to make money, or will it really deliver economic value by preventing hospitalizations? Is fancy monitoring equipment more effective than low-tech daily phone calls and a scale in managing patients with congestive heart failure? How much monitoring and intervention is enough to achieve excellent outcomes? For congestive heart failure, there is good evidence from randomized clinical trials that telemonitoring reduces rates of all-cause mortality (relative risk 0.66, 95% confidence interval 0.54–0.81) and heart-failure-related hospitalizations (relative risk 0.79, 95% confidence interval 0.67–0.94).3
On the cost side of the value equation, what is the right “dose” of home health care for a given patient? At what point on the cost-quality curve does cost outweigh value? Integrating home health care into accountable health care organizations may be the only way to maximize quality and efficiency.
Communication challenges will be the toughest. If home health care becomes a well-developed island of care, I suspect we will not be much better off than we are now. Key to improving quality and lowering cost is effective communication across the spectrum of care. Can teams of doctors and other health care professionals who each claim a different venue as their territory—home, hospital, office, nursing home—provide the coordinated, evidence-based, and personalized medical care to which Dr. Landers and his colleagues aspire? I believe it is possible, but the jury is still out.
A seamless, shared electronic medical record is essential for communication, but current platforms are not designed to integrate home care, hospital, and office records. Several innovative home care companies are attempting to do so, however. Recently, Cleveland Clinic made home visit notes from its home care arm available to other providers on its electronic medical record platform.
Locating visiting nurses and home care physicians in proximity to primary care physician offices would greatly improve the chances of good communication. In a randomized trial of outpatient care of frail elderly patients living at home, having nurse care coordinators located in primary care physician offices resulted in fewer hospitalizations and nursing home placements and greater patient, family, and physician satisfaction compared with traditional outpatient care.4.5
NO MORE ‘BUSINESS AS USUAL’
In this time of economic uncertainty, at least one thing is certain: “business as usual” does not apply to US health care delivery. I am hopeful that innovative models of home care will find their proper niche as we seek to provide the right care for the right patient at the right time in the right venue and at the right price.
Medical care at home is emerging as a “disruptive innovation” on the US health care scene. New models of home care offer the promise of better service, higher quality, and a better experience at a lower cost compared with nursing home and hospital care. A tall order, indeed! Pioneers like Dr. Bruce Leff, however, have already shown quite convincingly that “hospital at home” programs can be implemented and can deliver on these promises for patients who are eligible for hospital admission.1,2
In their essay “Bringing home the ‘medical home’ for older adults” in this issue of the Cleveland Clinic Journal of Medicine, Landers and colleagues discuss the opportunity of extending the medical home model to home health care as an integral part of the medical neighborhood to improve care coordination, reduce expensive hospitalizations, and improve the patient experience by caring for patients in their own homes. As a part of health care reform, the Center for Medicare and Medicaid Services intends to fund demonstration projects to determine to what extent home care can achieve these lofty goals.
A modernized, efficient, and effective home health care system would be a welcome improvement on the patchwork system we have had in the United States for the past 30 years. From my perspective as a family physician, this new legislation may provide the opportunity to get home health care right.
It did not start off on the right foot in the United States. Many home health agencies were established as independent, for-profit businesses detached from the primary care doctors who were ultimately responsible for patients’ care. Signing orders once a month on long forms that conveyed little useful information about my patients never seemed like adequate care oversight on my part. Communicating well with a dozen nurses I did not know or see on a regular basis was a daunting if not impossible task.
IT TAKES TWO TO PASS THE BATON
If home health care got off on the wrong foot in the United States in the 1970s, what then is the right foot?
To me, the key is a tight linkage of home health care to hospitals, physician offices, and nursing homes. Most elderly and frail people do not live out their lives in one venue. They move from home to hospital to nursing home and back again, often several times during their lives. These care transitions are fraught with the dangers of medication errors and forgotten test results. Home health care agencies can become experts in managing these dangerous care transitions.
Home health nurses and physicians can be experts at passing the baton without dropping it. Parenthetically, all physicians must become experts at passing the baton. It takes two to pass the baton successfully, whether it is from hospitalist to primary care physician, from home care nurse to primary care physician, or from primary care physician to hospitalist.
CHALLENGES: REIMBURSEMENT, COSTLY TECHNOLOGY, COMMUNICATION
What are the challenges Dr. Landers and his forward-thinking colleagues face in implementing modern medical care in the home?
Reimbursement is the obvious first issue. Current restrictions make it difficult to care for homebound and semi-homebound patients on more than an episodic basis. The proposed demonstration projects in home health must overcome this barrier.
Appropriate use of home health technology will be a second challenge, just as it is an opportunity. How much minute-by-minute information is really necessary for home monitoring? How expensive will the technology be? Will home health technology simply be another opportunity to make money, or will it really deliver economic value by preventing hospitalizations? Is fancy monitoring equipment more effective than low-tech daily phone calls and a scale in managing patients with congestive heart failure? How much monitoring and intervention is enough to achieve excellent outcomes? For congestive heart failure, there is good evidence from randomized clinical trials that telemonitoring reduces rates of all-cause mortality (relative risk 0.66, 95% confidence interval 0.54–0.81) and heart-failure-related hospitalizations (relative risk 0.79, 95% confidence interval 0.67–0.94).3
On the cost side of the value equation, what is the right “dose” of home health care for a given patient? At what point on the cost-quality curve does cost outweigh value? Integrating home health care into accountable health care organizations may be the only way to maximize quality and efficiency.
Communication challenges will be the toughest. If home health care becomes a well-developed island of care, I suspect we will not be much better off than we are now. Key to improving quality and lowering cost is effective communication across the spectrum of care. Can teams of doctors and other health care professionals who each claim a different venue as their territory—home, hospital, office, nursing home—provide the coordinated, evidence-based, and personalized medical care to which Dr. Landers and his colleagues aspire? I believe it is possible, but the jury is still out.
A seamless, shared electronic medical record is essential for communication, but current platforms are not designed to integrate home care, hospital, and office records. Several innovative home care companies are attempting to do so, however. Recently, Cleveland Clinic made home visit notes from its home care arm available to other providers on its electronic medical record platform.
Locating visiting nurses and home care physicians in proximity to primary care physician offices would greatly improve the chances of good communication. In a randomized trial of outpatient care of frail elderly patients living at home, having nurse care coordinators located in primary care physician offices resulted in fewer hospitalizations and nursing home placements and greater patient, family, and physician satisfaction compared with traditional outpatient care.4.5
NO MORE ‘BUSINESS AS USUAL’
In this time of economic uncertainty, at least one thing is certain: “business as usual” does not apply to US health care delivery. I am hopeful that innovative models of home care will find their proper niche as we seek to provide the right care for the right patient at the right time in the right venue and at the right price.
- Leff B, Burton L, Mader SL, et al. Comparison of functional outcomes associated with hospital at home care and traditional acute hospital care. J Am Geriatr Soc 2009; 57:273–278.
- Frick KD, Burton LC, Clark R, et al. Substitutive Hospital at Home for older persons: effects on costs. Am J Manag Care 2009; 15:49–56.
- Inglis SC, Clark RA, McAlister FA, et al. Structured telephone support or telemonitoring programmes for patients with chronic heart failure. Cochrane Database Syst Rev 2010; 8:CD007228.
- Boyd CM, Reider L, Frey K, et al. The effects of guided care on the perceived quality of health care for multi-morbid older persons: 18-month outcomes from a cluster-randomized controlled trial. J Gen Intern Med 2010; 25:235–242.
- Leff B, Reider L, Frick KD, et al. Guided care and the cost of complex healthcare: a preliminary report. Am J Manag Care 2009; 15:555–559.
- Leff B, Burton L, Mader SL, et al. Comparison of functional outcomes associated with hospital at home care and traditional acute hospital care. J Am Geriatr Soc 2009; 57:273–278.
- Frick KD, Burton LC, Clark R, et al. Substitutive Hospital at Home for older persons: effects on costs. Am J Manag Care 2009; 15:49–56.
- Inglis SC, Clark RA, McAlister FA, et al. Structured telephone support or telemonitoring programmes for patients with chronic heart failure. Cochrane Database Syst Rev 2010; 8:CD007228.
- Boyd CM, Reider L, Frey K, et al. The effects of guided care on the perceived quality of health care for multi-morbid older persons: 18-month outcomes from a cluster-randomized controlled trial. J Gen Intern Med 2010; 25:235–242.
- Leff B, Reider L, Frick KD, et al. Guided care and the cost of complex healthcare: a preliminary report. Am J Manag Care 2009; 15:555–559.
Partnering to Improve Care Transitions
Hospital readmissions are common, costly in both economic and human terms, and often preventable. This perfect storm of attributes has placed hospital readmissions at the center of discourse among payers, providers, and policy makers, which is leading to innovations in care delivery. Evolving efforts to enhance discharge communication, to improve care coordination and accountability, and to meaningfully involve primary care, show promise of reducing readmissions.14 These pockets of success demonstrate that improving care transitions can increase quality of care while decreasing costs.
Within the hospital, it is now clear that the discharge process typically requires the same intensity of effort as admission. The hospitalist guides an interdisciplinary team, including nurses, pharmacists, case managers, and social workers, through a checklist of discharge tasks. Some tasks require substantial hospitalist involvement and expertise, such as medication reconciliationa detail‐oriented, time‐consuming process. Other tasks can be accomplished by team members, overseen by the hospitalist, such as scheduling timely follow‐up appointments, coordinating outpatient services, and assembling educational materials. Taken as a whole, significant time and effort must be devoted by the inpatient team to address the complex landscape of a patient's medical and psychosocial needs.
That of course, is only half of the equation, as patient care must be transferred to an equally invested outpatient team led by a primary care provider (PCP). Several influential medical societies have endorsed the medical home (a multidisciplinary care team led by a PCP) as the primary agent to coordinate patient care across settings.5 Indeed, promptly reconnecting with their PCP and primary care team after discharge can have profound meaning for patients, who may otherwise be unsupported with their postdischarge clinical needs. In this issue of the Journal of Hospital Medicine, 4 important articles provide evidence in support of an outpatient partner to actively assume patient care responsibility after hospital discharge.
van Walraven et al.6 conducted an elegant study to evaluate the impact of postdischarge PCP visits on readmissions. Following more than 5000 patients for nearly 6 months, they demonstrated that increased PCP follow‐up was significantly and independently associated with a decreased risk of hospital readmission. This confirms the positive impact that a primary care connection can have on postdischarge care. This study also highlights some challenges: 18% of the original cohort were excluded from the final analyses because they had only 1 or no PCP visit in the 6 months following discharge, indicating inadequate postdischarge follow‐up for a substantial sub‐group. Misky et al.7 similarly established that patients with timely PCP follow‐up (within one month of discharge) were 10 times less likely to be readmitted for the same condition as their index admission. These are also encouraging findings for those patients with PCP follow‐up. Yet among patients in their study, PCP follow‐up was even less common, with only 49% of patients having appointments within one month. Future studies should consider how more intensive outreach strategies might engage difficult‐to‐reach patients and communities.
PCP follow‐up may be beneficial because discharged patients often have ongoing issues that need to be addressed. Arora et al.8 surveyed inner city patients and their PCPs 2 weeks after hospital discharge to assess whether patients experienced any problems in the postdischarge period, and whether PCPs were aware of their patients' hospitalization. Nearly half of all patients recounted 1 or more postdischarge problems. The likelihood of reporting such a problem was twice as common among those patients whose PCP was unaware of their hospitalization. Again, this is strong validation of the importance of PCP involvement in posthospital care, but equally concerning is their finding that fully 3 in 10 PCPs were unaware of their patient's hospitalization.
Finally, Mitchell et al.9 further refine our understanding of risk factors for readmission. In an ethnically diverse inner city population, they screened 738 inpatients for depression. Among the 238 (32%) patients who screened positive, there was a marked 73% increase in hospital utilization (emergency department [ED] visits and readmissions) within 30 days of discharge.9 This confirms previous research that depression is a risk factor for rehospitalization.10 Depression, however, is amenable to treatment and receiving care through one's primary care practice can potentially mitigate how depression negatively affects patients' medication adherence, self‐care behavior, and ultimately readmission rates.
Collectively, these 4 articles give us reason to experience both despair and hope. It is discouraging that large numbers of patients do not have timely encounters with their PCP after discharge, confirming previous findings,11 and that too often PCPs are unaware of their patients' hospitalizations. In any other industry this sort of inefficiency and poor customer service would put a company out of business; that it persists in medicine is embarrassing. Because our medical system is not sufficiently incentivized by quality outcomes, such poor practices continue to be tolerated, and our patients suffer the consequences.
But we are also shown a way forward, with accumulating evidence complimenting existing studies that a primary care connection can improve the quality of postdischarge care and decrease readmissions.1214 Recognizing this central role of primary care, however, forces us to acknowledge the diminishing availability of primary care nationwide; in many inner city and rural locations, accessible primary care is largely nonexistent. This shortage must be corrected to attain needed access and to advance health care reform.
Postdischarge PCP involvement is particularly essential with shorter hospital stays, as patients will predictably have complex postdischarge needs as they complete their recuperation at home. Indeed, Arora et al.8 indicate that posthospitalization problems may be more the rule than the exception, and that specific types of problems can be foreseen. Most commonly reported were challenges obtaining follow‐up appointments, difficulties managing or obtaining medications, feeling unprepared for discharge, having unanswered questions, or needing an urgent reevaluation. While well organized predischarge efforts help to prepare patients, even the most perfect discharge process cannot anticipate all possible pitfalls. Fortunately, most postdischarge problems can be effectively handled by those who often know the patient best, the patient's primary care team. The outpatient team is ideally situated to assist patients with the logistics of accessing the care system, to provide ongoing education, and to help with such basic needs as transportation and social support. It makes sense that such personalized outreach can prevent small problems from blossoming into more serious issues that might ultimately require rehospitalization.
Upon discharge, patients and families are also often expected to assume new self‐care responsibilities, to implement new dietary restrictions, to use new medications, and to monitor and respond to new and evolving symptoms. Gaining the knowledge, the confidence, and the experience to adopt new behaviors is critical to successful postdischarge self‐care. Adult learning theory informs us that education is an ongoing process. Mastering new material occurs with repetition, over time, and under different circumstances. An ancient Chinese proverb encapsulates the key aspects of learning:
-
I hear and I forget;
-
I see and I remember;
-
I do and I understand.
Thus, a single didactic discharge session in the hospital is unlikely to provide patients with sufficient depth of understanding that one attains through experiential learning. Hospital‐based discharge teaching is further compromised in the setting of patient fatigue, anxiety and illness: it is not surprising that patients comprehend and retain only 50% of the medical information discussed with their physicians.15
While teach back has been effectively used to ensure that information is registered when initially presented, it does not ensure that information has been internalized in such a way that it can be utilized hours or days later. Instead, it is the active engagement with the primary care team that provides opportunities for ongoing learning, personalized to the educational needs of each patient. With nurses, dieticians, pharmacists, and medical educators playing a central guiding role, patients can receive appropriately tailored instruction, as well as opportunities to practically apply their new knowledge.
The evolving partnership among hospitals, hospitalists, and primary care holds great promise to reduce avoidable readmissions, and the Patient Protection and Affordable Care Act of 2010 will provide financial incentives to support this partnership. Health care reform aims to adjust hospital payments based on rates of preventable Medicare readmissions; bundling payments (paying for episodes of illness based on outcomes) and accountable care organizations (ACOs) will ideally foster seamless care coordination.16 Nurturing and developing this collaboration between the inpatient and outpatient care teams will be essential as we seek to provide patients the safest transition possible from the hospital to home.
- ,,, et al.A reengineered hospital discharge program to decrease rehospitalization: a randomized trial.Ann Intern Med.2009;150(3):178–187.
- ,,,.The care transitions intervention: results of a randomized controlled trial.Arch Intern Med.2006;166(17):1822–1828.
- ,,,.Redefining and redesigning hospital discharge to enhance patient care: a randomized controlled study.J Gen Intern Med.2008;23(8):1228–1233.
- ,,, et al.Reduction of 30‐day postdischarge hospital readmission or emergency department (ED) visit rates in high‐risk elderly medical patients through delivery of a targeted care bundle.J Hosp Med.2009;4(4):211–218.
- ,,, et al.Transitions of Care Consensus policy statement: American College of Physicians, Society of General Internal Medicine, Society of Hospital Medicine, American Geriatrics Society, American College Of Emergency Physicians, and Society for Academic Emergency Medicine.J Hosp Med.2009;4(6):364–370.
- et al.Independent association of provider and information continuity on outcomes after hospital discharge: implications for hospitalists.J Hosp Med.2010;5(7):398–405.
- et al.Post‐hospitalization transitions: examining the effects of timing of primary care follow‐up.J Hosp Med.2010;5(7):392–397.
- et al.Problems after discharge and understanding of communication with their PCPs among hospitalized seniors: a mixed methods study.J Hosp Med.2010;5(7):385–391.
- et al.Post‐discharge hospital utilization among adult medical inpatients with depressive symptoms.J Hosp Med.2010;5(7):378–384.
- ,,, et al.Depression Is a risk factor for rehospitalization in medical inpatients.Prim Care Companion J Clin Psychiatry.2007;9(4):256–262.
- ,,.Rehospitalizations among patients in the Medicare fee‐for‐service program.N Engl J Med. 22009;360(14):1418–1428.
- ,,,,.The effect of technology‐supported, multidisease care management on the mortality and hospitalization of seniors.J Am Geriatr Soc.2008;56(12):2195–2202.
- ,,, et al.Guided care and the cost of complex healthcare: a preliminary report.Am J Manag Care.2009;15(8):555–559.
- ,,, et al.Geriatric care management for low‐income seniors: a randomized controlled trial.JAMA.2007;298(22):2623–2633.
- .Patients' memory for medical information.J R Soc Med.2003;96(5):219–222.
- .Understanding the new vocabulary of healthcare reform.J Hosp Med.2010;5(4):197–199.
Hospital readmissions are common, costly in both economic and human terms, and often preventable. This perfect storm of attributes has placed hospital readmissions at the center of discourse among payers, providers, and policy makers, which is leading to innovations in care delivery. Evolving efforts to enhance discharge communication, to improve care coordination and accountability, and to meaningfully involve primary care, show promise of reducing readmissions.14 These pockets of success demonstrate that improving care transitions can increase quality of care while decreasing costs.
Within the hospital, it is now clear that the discharge process typically requires the same intensity of effort as admission. The hospitalist guides an interdisciplinary team, including nurses, pharmacists, case managers, and social workers, through a checklist of discharge tasks. Some tasks require substantial hospitalist involvement and expertise, such as medication reconciliationa detail‐oriented, time‐consuming process. Other tasks can be accomplished by team members, overseen by the hospitalist, such as scheduling timely follow‐up appointments, coordinating outpatient services, and assembling educational materials. Taken as a whole, significant time and effort must be devoted by the inpatient team to address the complex landscape of a patient's medical and psychosocial needs.
That of course, is only half of the equation, as patient care must be transferred to an equally invested outpatient team led by a primary care provider (PCP). Several influential medical societies have endorsed the medical home (a multidisciplinary care team led by a PCP) as the primary agent to coordinate patient care across settings.5 Indeed, promptly reconnecting with their PCP and primary care team after discharge can have profound meaning for patients, who may otherwise be unsupported with their postdischarge clinical needs. In this issue of the Journal of Hospital Medicine, 4 important articles provide evidence in support of an outpatient partner to actively assume patient care responsibility after hospital discharge.
van Walraven et al.6 conducted an elegant study to evaluate the impact of postdischarge PCP visits on readmissions. Following more than 5000 patients for nearly 6 months, they demonstrated that increased PCP follow‐up was significantly and independently associated with a decreased risk of hospital readmission. This confirms the positive impact that a primary care connection can have on postdischarge care. This study also highlights some challenges: 18% of the original cohort were excluded from the final analyses because they had only 1 or no PCP visit in the 6 months following discharge, indicating inadequate postdischarge follow‐up for a substantial sub‐group. Misky et al.7 similarly established that patients with timely PCP follow‐up (within one month of discharge) were 10 times less likely to be readmitted for the same condition as their index admission. These are also encouraging findings for those patients with PCP follow‐up. Yet among patients in their study, PCP follow‐up was even less common, with only 49% of patients having appointments within one month. Future studies should consider how more intensive outreach strategies might engage difficult‐to‐reach patients and communities.
PCP follow‐up may be beneficial because discharged patients often have ongoing issues that need to be addressed. Arora et al.8 surveyed inner city patients and their PCPs 2 weeks after hospital discharge to assess whether patients experienced any problems in the postdischarge period, and whether PCPs were aware of their patients' hospitalization. Nearly half of all patients recounted 1 or more postdischarge problems. The likelihood of reporting such a problem was twice as common among those patients whose PCP was unaware of their hospitalization. Again, this is strong validation of the importance of PCP involvement in posthospital care, but equally concerning is their finding that fully 3 in 10 PCPs were unaware of their patient's hospitalization.
Finally, Mitchell et al.9 further refine our understanding of risk factors for readmission. In an ethnically diverse inner city population, they screened 738 inpatients for depression. Among the 238 (32%) patients who screened positive, there was a marked 73% increase in hospital utilization (emergency department [ED] visits and readmissions) within 30 days of discharge.9 This confirms previous research that depression is a risk factor for rehospitalization.10 Depression, however, is amenable to treatment and receiving care through one's primary care practice can potentially mitigate how depression negatively affects patients' medication adherence, self‐care behavior, and ultimately readmission rates.
Collectively, these 4 articles give us reason to experience both despair and hope. It is discouraging that large numbers of patients do not have timely encounters with their PCP after discharge, confirming previous findings,11 and that too often PCPs are unaware of their patients' hospitalizations. In any other industry this sort of inefficiency and poor customer service would put a company out of business; that it persists in medicine is embarrassing. Because our medical system is not sufficiently incentivized by quality outcomes, such poor practices continue to be tolerated, and our patients suffer the consequences.
But we are also shown a way forward, with accumulating evidence complimenting existing studies that a primary care connection can improve the quality of postdischarge care and decrease readmissions.1214 Recognizing this central role of primary care, however, forces us to acknowledge the diminishing availability of primary care nationwide; in many inner city and rural locations, accessible primary care is largely nonexistent. This shortage must be corrected to attain needed access and to advance health care reform.
Postdischarge PCP involvement is particularly essential with shorter hospital stays, as patients will predictably have complex postdischarge needs as they complete their recuperation at home. Indeed, Arora et al.8 indicate that posthospitalization problems may be more the rule than the exception, and that specific types of problems can be foreseen. Most commonly reported were challenges obtaining follow‐up appointments, difficulties managing or obtaining medications, feeling unprepared for discharge, having unanswered questions, or needing an urgent reevaluation. While well organized predischarge efforts help to prepare patients, even the most perfect discharge process cannot anticipate all possible pitfalls. Fortunately, most postdischarge problems can be effectively handled by those who often know the patient best, the patient's primary care team. The outpatient team is ideally situated to assist patients with the logistics of accessing the care system, to provide ongoing education, and to help with such basic needs as transportation and social support. It makes sense that such personalized outreach can prevent small problems from blossoming into more serious issues that might ultimately require rehospitalization.
Upon discharge, patients and families are also often expected to assume new self‐care responsibilities, to implement new dietary restrictions, to use new medications, and to monitor and respond to new and evolving symptoms. Gaining the knowledge, the confidence, and the experience to adopt new behaviors is critical to successful postdischarge self‐care. Adult learning theory informs us that education is an ongoing process. Mastering new material occurs with repetition, over time, and under different circumstances. An ancient Chinese proverb encapsulates the key aspects of learning:
-
I hear and I forget;
-
I see and I remember;
-
I do and I understand.
Thus, a single didactic discharge session in the hospital is unlikely to provide patients with sufficient depth of understanding that one attains through experiential learning. Hospital‐based discharge teaching is further compromised in the setting of patient fatigue, anxiety and illness: it is not surprising that patients comprehend and retain only 50% of the medical information discussed with their physicians.15
While teach back has been effectively used to ensure that information is registered when initially presented, it does not ensure that information has been internalized in such a way that it can be utilized hours or days later. Instead, it is the active engagement with the primary care team that provides opportunities for ongoing learning, personalized to the educational needs of each patient. With nurses, dieticians, pharmacists, and medical educators playing a central guiding role, patients can receive appropriately tailored instruction, as well as opportunities to practically apply their new knowledge.
The evolving partnership among hospitals, hospitalists, and primary care holds great promise to reduce avoidable readmissions, and the Patient Protection and Affordable Care Act of 2010 will provide financial incentives to support this partnership. Health care reform aims to adjust hospital payments based on rates of preventable Medicare readmissions; bundling payments (paying for episodes of illness based on outcomes) and accountable care organizations (ACOs) will ideally foster seamless care coordination.16 Nurturing and developing this collaboration between the inpatient and outpatient care teams will be essential as we seek to provide patients the safest transition possible from the hospital to home.
Hospital readmissions are common, costly in both economic and human terms, and often preventable. This perfect storm of attributes has placed hospital readmissions at the center of discourse among payers, providers, and policy makers, which is leading to innovations in care delivery. Evolving efforts to enhance discharge communication, to improve care coordination and accountability, and to meaningfully involve primary care, show promise of reducing readmissions.14 These pockets of success demonstrate that improving care transitions can increase quality of care while decreasing costs.
Within the hospital, it is now clear that the discharge process typically requires the same intensity of effort as admission. The hospitalist guides an interdisciplinary team, including nurses, pharmacists, case managers, and social workers, through a checklist of discharge tasks. Some tasks require substantial hospitalist involvement and expertise, such as medication reconciliationa detail‐oriented, time‐consuming process. Other tasks can be accomplished by team members, overseen by the hospitalist, such as scheduling timely follow‐up appointments, coordinating outpatient services, and assembling educational materials. Taken as a whole, significant time and effort must be devoted by the inpatient team to address the complex landscape of a patient's medical and psychosocial needs.
That of course, is only half of the equation, as patient care must be transferred to an equally invested outpatient team led by a primary care provider (PCP). Several influential medical societies have endorsed the medical home (a multidisciplinary care team led by a PCP) as the primary agent to coordinate patient care across settings.5 Indeed, promptly reconnecting with their PCP and primary care team after discharge can have profound meaning for patients, who may otherwise be unsupported with their postdischarge clinical needs. In this issue of the Journal of Hospital Medicine, 4 important articles provide evidence in support of an outpatient partner to actively assume patient care responsibility after hospital discharge.
van Walraven et al.6 conducted an elegant study to evaluate the impact of postdischarge PCP visits on readmissions. Following more than 5000 patients for nearly 6 months, they demonstrated that increased PCP follow‐up was significantly and independently associated with a decreased risk of hospital readmission. This confirms the positive impact that a primary care connection can have on postdischarge care. This study also highlights some challenges: 18% of the original cohort were excluded from the final analyses because they had only 1 or no PCP visit in the 6 months following discharge, indicating inadequate postdischarge follow‐up for a substantial sub‐group. Misky et al.7 similarly established that patients with timely PCP follow‐up (within one month of discharge) were 10 times less likely to be readmitted for the same condition as their index admission. These are also encouraging findings for those patients with PCP follow‐up. Yet among patients in their study, PCP follow‐up was even less common, with only 49% of patients having appointments within one month. Future studies should consider how more intensive outreach strategies might engage difficult‐to‐reach patients and communities.
PCP follow‐up may be beneficial because discharged patients often have ongoing issues that need to be addressed. Arora et al.8 surveyed inner city patients and their PCPs 2 weeks after hospital discharge to assess whether patients experienced any problems in the postdischarge period, and whether PCPs were aware of their patients' hospitalization. Nearly half of all patients recounted 1 or more postdischarge problems. The likelihood of reporting such a problem was twice as common among those patients whose PCP was unaware of their hospitalization. Again, this is strong validation of the importance of PCP involvement in posthospital care, but equally concerning is their finding that fully 3 in 10 PCPs were unaware of their patient's hospitalization.
Finally, Mitchell et al.9 further refine our understanding of risk factors for readmission. In an ethnically diverse inner city population, they screened 738 inpatients for depression. Among the 238 (32%) patients who screened positive, there was a marked 73% increase in hospital utilization (emergency department [ED] visits and readmissions) within 30 days of discharge.9 This confirms previous research that depression is a risk factor for rehospitalization.10 Depression, however, is amenable to treatment and receiving care through one's primary care practice can potentially mitigate how depression negatively affects patients' medication adherence, self‐care behavior, and ultimately readmission rates.
Collectively, these 4 articles give us reason to experience both despair and hope. It is discouraging that large numbers of patients do not have timely encounters with their PCP after discharge, confirming previous findings,11 and that too often PCPs are unaware of their patients' hospitalizations. In any other industry this sort of inefficiency and poor customer service would put a company out of business; that it persists in medicine is embarrassing. Because our medical system is not sufficiently incentivized by quality outcomes, such poor practices continue to be tolerated, and our patients suffer the consequences.
But we are also shown a way forward, with accumulating evidence complimenting existing studies that a primary care connection can improve the quality of postdischarge care and decrease readmissions.1214 Recognizing this central role of primary care, however, forces us to acknowledge the diminishing availability of primary care nationwide; in many inner city and rural locations, accessible primary care is largely nonexistent. This shortage must be corrected to attain needed access and to advance health care reform.
Postdischarge PCP involvement is particularly essential with shorter hospital stays, as patients will predictably have complex postdischarge needs as they complete their recuperation at home. Indeed, Arora et al.8 indicate that posthospitalization problems may be more the rule than the exception, and that specific types of problems can be foreseen. Most commonly reported were challenges obtaining follow‐up appointments, difficulties managing or obtaining medications, feeling unprepared for discharge, having unanswered questions, or needing an urgent reevaluation. While well organized predischarge efforts help to prepare patients, even the most perfect discharge process cannot anticipate all possible pitfalls. Fortunately, most postdischarge problems can be effectively handled by those who often know the patient best, the patient's primary care team. The outpatient team is ideally situated to assist patients with the logistics of accessing the care system, to provide ongoing education, and to help with such basic needs as transportation and social support. It makes sense that such personalized outreach can prevent small problems from blossoming into more serious issues that might ultimately require rehospitalization.
Upon discharge, patients and families are also often expected to assume new self‐care responsibilities, to implement new dietary restrictions, to use new medications, and to monitor and respond to new and evolving symptoms. Gaining the knowledge, the confidence, and the experience to adopt new behaviors is critical to successful postdischarge self‐care. Adult learning theory informs us that education is an ongoing process. Mastering new material occurs with repetition, over time, and under different circumstances. An ancient Chinese proverb encapsulates the key aspects of learning:
-
I hear and I forget;
-
I see and I remember;
-
I do and I understand.
Thus, a single didactic discharge session in the hospital is unlikely to provide patients with sufficient depth of understanding that one attains through experiential learning. Hospital‐based discharge teaching is further compromised in the setting of patient fatigue, anxiety and illness: it is not surprising that patients comprehend and retain only 50% of the medical information discussed with their physicians.15
While teach back has been effectively used to ensure that information is registered when initially presented, it does not ensure that information has been internalized in such a way that it can be utilized hours or days later. Instead, it is the active engagement with the primary care team that provides opportunities for ongoing learning, personalized to the educational needs of each patient. With nurses, dieticians, pharmacists, and medical educators playing a central guiding role, patients can receive appropriately tailored instruction, as well as opportunities to practically apply their new knowledge.
The evolving partnership among hospitals, hospitalists, and primary care holds great promise to reduce avoidable readmissions, and the Patient Protection and Affordable Care Act of 2010 will provide financial incentives to support this partnership. Health care reform aims to adjust hospital payments based on rates of preventable Medicare readmissions; bundling payments (paying for episodes of illness based on outcomes) and accountable care organizations (ACOs) will ideally foster seamless care coordination.16 Nurturing and developing this collaboration between the inpatient and outpatient care teams will be essential as we seek to provide patients the safest transition possible from the hospital to home.
- ,,, et al.A reengineered hospital discharge program to decrease rehospitalization: a randomized trial.Ann Intern Med.2009;150(3):178–187.
- ,,,.The care transitions intervention: results of a randomized controlled trial.Arch Intern Med.2006;166(17):1822–1828.
- ,,,.Redefining and redesigning hospital discharge to enhance patient care: a randomized controlled study.J Gen Intern Med.2008;23(8):1228–1233.
- ,,, et al.Reduction of 30‐day postdischarge hospital readmission or emergency department (ED) visit rates in high‐risk elderly medical patients through delivery of a targeted care bundle.J Hosp Med.2009;4(4):211–218.
- ,,, et al.Transitions of Care Consensus policy statement: American College of Physicians, Society of General Internal Medicine, Society of Hospital Medicine, American Geriatrics Society, American College Of Emergency Physicians, and Society for Academic Emergency Medicine.J Hosp Med.2009;4(6):364–370.
- et al.Independent association of provider and information continuity on outcomes after hospital discharge: implications for hospitalists.J Hosp Med.2010;5(7):398–405.
- et al.Post‐hospitalization transitions: examining the effects of timing of primary care follow‐up.J Hosp Med.2010;5(7):392–397.
- et al.Problems after discharge and understanding of communication with their PCPs among hospitalized seniors: a mixed methods study.J Hosp Med.2010;5(7):385–391.
- et al.Post‐discharge hospital utilization among adult medical inpatients with depressive symptoms.J Hosp Med.2010;5(7):378–384.
- ,,, et al.Depression Is a risk factor for rehospitalization in medical inpatients.Prim Care Companion J Clin Psychiatry.2007;9(4):256–262.
- ,,.Rehospitalizations among patients in the Medicare fee‐for‐service program.N Engl J Med. 22009;360(14):1418–1428.
- ,,,,.The effect of technology‐supported, multidisease care management on the mortality and hospitalization of seniors.J Am Geriatr Soc.2008;56(12):2195–2202.
- ,,, et al.Guided care and the cost of complex healthcare: a preliminary report.Am J Manag Care.2009;15(8):555–559.
- ,,, et al.Geriatric care management for low‐income seniors: a randomized controlled trial.JAMA.2007;298(22):2623–2633.
- .Patients' memory for medical information.J R Soc Med.2003;96(5):219–222.
- .Understanding the new vocabulary of healthcare reform.J Hosp Med.2010;5(4):197–199.
- ,,, et al.A reengineered hospital discharge program to decrease rehospitalization: a randomized trial.Ann Intern Med.2009;150(3):178–187.
- ,,,.The care transitions intervention: results of a randomized controlled trial.Arch Intern Med.2006;166(17):1822–1828.
- ,,,.Redefining and redesigning hospital discharge to enhance patient care: a randomized controlled study.J Gen Intern Med.2008;23(8):1228–1233.
- ,,, et al.Reduction of 30‐day postdischarge hospital readmission or emergency department (ED) visit rates in high‐risk elderly medical patients through delivery of a targeted care bundle.J Hosp Med.2009;4(4):211–218.
- ,,, et al.Transitions of Care Consensus policy statement: American College of Physicians, Society of General Internal Medicine, Society of Hospital Medicine, American Geriatrics Society, American College Of Emergency Physicians, and Society for Academic Emergency Medicine.J Hosp Med.2009;4(6):364–370.
- et al.Independent association of provider and information continuity on outcomes after hospital discharge: implications for hospitalists.J Hosp Med.2010;5(7):398–405.
- et al.Post‐hospitalization transitions: examining the effects of timing of primary care follow‐up.J Hosp Med.2010;5(7):392–397.
- et al.Problems after discharge and understanding of communication with their PCPs among hospitalized seniors: a mixed methods study.J Hosp Med.2010;5(7):385–391.
- et al.Post‐discharge hospital utilization among adult medical inpatients with depressive symptoms.J Hosp Med.2010;5(7):378–384.
- ,,, et al.Depression Is a risk factor for rehospitalization in medical inpatients.Prim Care Companion J Clin Psychiatry.2007;9(4):256–262.
- ,,.Rehospitalizations among patients in the Medicare fee‐for‐service program.N Engl J Med. 22009;360(14):1418–1428.
- ,,,,.The effect of technology‐supported, multidisease care management on the mortality and hospitalization of seniors.J Am Geriatr Soc.2008;56(12):2195–2202.
- ,,, et al.Guided care and the cost of complex healthcare: a preliminary report.Am J Manag Care.2009;15(8):555–559.
- ,,, et al.Geriatric care management for low‐income seniors: a randomized controlled trial.JAMA.2007;298(22):2623–2633.
- .Patients' memory for medical information.J R Soc Med.2003;96(5):219–222.
- .Understanding the new vocabulary of healthcare reform.J Hosp Med.2010;5(4):197–199.