User login
How to control migraines in patients with psychiatric disorders
Many of the 28 million people who suffer from migraine headaches each year1 need psychiatric care in addition to headache relief. Migraine headaches often coexist with depression,2 anxiety/panic disorders,2,3 bipolar disorder,4 and phobias,5 as well as with stroke6 and epilepsy.7 A study of 995 young adults found that anxiety disorders, phobias, major depression, panic disorder, and obsessive-compulsive disorder were two to five times more prevalent among migraine sufferers than among a control group (Table 1 ).2
Migraine sufferers know that at any time an attack could hamper their ability to work, care for their families, or engage in social activities. A nationwide study of migraineurs found that attacks often impaired their relationships with family and friends.8
Psychiatrists should screen patients for a history of migraine or other headaches and carefully consider the relationship between migraines and psychiatric disorders when prescribing treatment. In this article, we outline acute and preventive headache treatments and present two cases to help you treat these patients appropriately.
Table 1
PSYCHIATRIC COMORBIDITIES IN PATIENTS WITH VS. WITHOUT MIGRAINES*
| Migraineurs (%) (n = 128) | Controls (%) (n = 879) | |
|---|---|---|
| Any anxiety | 54 | 27 |
| Generalized anxiety disorder | 10 | 2 |
| Phobia | 40 | 21 |
| Major depression | 35 | 10 |
| Panic disorder | 11 | 2 |
| Obsessive-compulsive disorder | 9 | 2 |
| * Prevalence Source: Breslau N, Davis GC. Cephalalgia 1992;12(2):85-90. | ||
Table 2
THREE TYPES OF PRIMARY HEADACHE: DIAGNOSTIC CRITERIA
| Headache type | Age of onset (years) | Location | Duration | Frequency/timing | Severity | Quality | Features |
|---|---|---|---|---|---|---|---|
| Migraine | 10 to 40 | Hemicranial | 4 to 72 hr | Variable | Moderate to severe | Throbbing, steady ache | Nausea; vomiting; photo/phono/osmophobia; neurologic deficits; aura |
| Tension-type | 20 to 50 | Bilateral/generalized | 30 min to 7 days+ | Variable | Dull ache, may wax and wane | Tight, band-like pressure | Generally none |
| Cluster | 15 to 40 | Unilateral, periorbital or retro-orbital | 15 to 180 min | 1 to 8 times per day or night | Excruciating | Boring, piercing | Ipsilateral, conjunctival injection, nasal congestion, rhinorrhea, miosis, facial seating |
| Source: Classification and diagnostic criteria for headache disorders, cranial neuralgias and facial pain. Headache Classification Committee of the International Headache Society. Cephalalgia 1988;8(suppl 7):1-96. | |||||||
Headache definitions and diagnosis
Primary or secondary. Under the International Headache Society’s (IHS) 1988 headache classification and diagnostic criteria,9 headaches are primary or secondary:
- Primary headaches are benign recurrent headaches that commonly present in practice.
- Secondary headaches occur much less frequently and are caused by underlying pathology.
The possibility of secondary headache should be ruled out before a primary headache can be diagnosed. The following headache features should cause concern:
- Severe headache with abrupt onset
- Subacute or progressive headache over days or months
- Headache, nausea, vomiting, and fever not explained by systemic illness
- New-onset headache late in life
- Headache with neurologic signs or symptoms such as confusion, decreased level of consciousness, meningismus, or papilledema
- Headache following head trauma
- Patient history of sickle cell disease, malignancy, or HIV.
Headache types. The three major types of primary headache are migraine, tension-type, and cluster (Table 2 ). Tension-type is the most common, is often mild, and is either self-treated with over-the-counter medications or ignored. Migraine is the most troublesome headache in everyday practice. Cluster is the most severe and fortunately is rare.
Migraine with aura and migraine without aura are separate diagnoses. IHS criteria for diagnosing migraines without aura are listed in Table 3. According to the IHS, migraine with aura (or “classic migraine”) fulfills all the criteria for migraine without aura, with fully reversible neurologic symptoms indicating focal cerebral cortical and/or brain stem dysfunction.
Auras. About 15% of migraineurs experience auras. Symptoms develop within 5 to 20 minutes, usually last less than 1 hour, and fade before the headache’s onset. Gradual onset and history of previous attacks helps to distinguish aura from transient ischemic attacks. Auras may manifest as visual, sensory, motor, or brain-stem symptoms, or as combinations of these:
- Visual auras are most common, presenting as localized visual loss (scotoma), with flashing lights (scintillation) at margins or jagged edges (fortification).
- Sensory auras present as facial or limb paresthesias.
- Motor auras manifest as weakness or lack of coordination.
- Brain stem auras manifest as vertigo or double vision.
Migraine aura is considered part of the headache’s prodrome, which may occur days or hours before the headache’s onset. The aura may bring about:
- an altered mental state (e.g., depression, hyperactivity, euphoria, difficulty concentrating, dysphasia)
- neurologic symptoms (e.g., photophobia, phonophobia, hyperosmia, yawning)
- general bodily discomforts (e.g., anorexia, food craving, diarrhea, thirst, urination, fluid retention, cold feeling).
Despite their sometimes severe effects, migraines often remain undiagnosed.10 Migraine should be suspected in patients with recurrent moderate to severe disabling headaches (Box).11-15
Case 1: “Bad, sick headaches”
Ms. A, 23, a single parent with a 2-year-old child, has had trouble staying employed because of repeated illnesses. She made 17 visits to her primary care physician within 26 months. While her main complaint was headache, she also complained of other aches and pains, a lack of energy, and insomnia. Numerous examinations revealed no physical abnormalities.
She reported having “bad, sick headaches” that sometimes lasted 2 to 3 days. Bed rest helped but this was not always possible. The headache was throbbing and usually one-sided. She had no aura, and ibuprofen gave partial relief. She noted that her mother gets similar headaches.
Table 3
DIAGNOSTIC REQUIREMENTS FOR MIGRAINE WITHOUT AURA
Mandatory
|
At least 2 of the following:
|
| During headache At least one of the following:
|
| Additional features Migraine prodrome—A range of general, neurologic, and mental changes may occur hours or days before the headache’s onset General—Anorexia, food craving, diarrhea or constipation, thirst, urination, fluid retention, cold feeling Mental—Depression, hyperactivity, euphoria, difficulty concentrating, dysphasia Neurologic—Photophobia, phonophobia, hyperosmia, yawning |
| SOURCE: Classification and diagnostic criteria for headache disorders, cranial neuralgias and facial pain. Headache Classification Committee of the International Headache Society. Cephalalgia 1988;8(suppl 7):1-96. |
Ms. A was diagnosed with migraine without aura, and she was treated with sumatriptan, 100 mg (1 or 2 doses, as needed). Her headaches responded well to this treatment, but the frequency of attacks remained unchanged. She requested a change in her medicine.
The underlying mechanisms of migraine headaches are not completely understood.
Vascular causes. A recently described neurovascular mechanism11 suggests that perivascular neurogenic inflammation involving meningeal vessels causes migraine. The triptan drugs have been found to reverse this process and relieve the headache.12
Positron emission tomography has demonstrated increased blood flow during acute migraine in midline brain stem structures. This suggests the presence of a central migraine generator in that location.13
Heredity. A rare form of migraine, familial hemiplegic migraine, is associated with a genetic abnormality on chromosome 19.14
Nitric oxide. Nitroglycerine-induced migraine headache, caused by the release of nitric oxide in cerebral vessels, can be reversed by nitrous oxide synthase inhibitors, thus opening up intriguing possibilities of new therapeutic agents and increased understanding of underlying migraine mechanisms.15
Treating migraines
Acute treatment. Migraineurs whose attacks are infrequent and mild may find OTC analgesics or NSAIDs adequate. Most patients, however, require specific migraine treatment, usually with triptans. Acute oral treatment options include sumatriptan, 50 to 100 mg; rizatriptan, 10 mg; zolmitriptan, 2.5 to 5 mg; and eletriptan, 40 mg.
In case of vomiting or nausea, options include sumatriptan, 20 mg nasal spray or 6 mg SC; rizatriptan, 10 mg on a dissolving wafer; or dihydroergotamine, 2 mg nasal spray or 1 mg IM or SC. For severe nausea or vomiting, an anti-nauseant (e.g., prochlorperazine suppositories, 25 mg) may be of value.
Preventive treatment. Preventive treatment may be warranted, depending on attack frequency, severity, and the extent of disability caused. One prolonged, severe attack per month that responds poorly to acute treatment may indicate the need for preventive treatment. A range of preventative treatments is available (Table 4).
In Ms. A’s case, oral sumatriptan lessened the severity of the migraine attacks, and the addition of nortriptyline, 50 mg/d, reduced frequency by about 50%. She felt more energetic overall and was sleeping better.
Treating the psychiatric comorbidity
Behavioral therapy is used as an adjunct to pharmacologic headache treatment. This approach is usually considered after a poor or adverse response to treatment, or when pharmacologic treatment is contraindicated (e.g., during pregnancy).
Relaxation training, biofeedback, and cognitive-behavioral stress management are the most commonly used forms of behavioral therapy. Thirty-five to 55% improvement in migraine has been reported following such treatments.16
Cognitive-behavioral intervention has been shown to be effective in depression17 and anxiety disorders.18 When either psychiatric problem is comorbid with migraine, cognitive therapy can improve both the migraine and the psychiatric comorbidity.
Pharmacologic therapy. Depression is commonly associated with migraine and may be caused by living with chronic disabling headaches over time. In such cases, the depression will improve as the migraine responds to treatment. However, in cases where comorbid depression or anxiety trigger or exacerbate acute migraine attacks, neither the migraine nor the psychiatric problem responds until the underlying psychopathology is treated. In such cases, simultaneous psychiatric and migraine pharmacologic treatment is required.
We recommend that you treat the psychiatric comorbidity as it would be treated without a co-existing migraine. Be advised, however, that monoamine oxidase inhibitors are contraindicated in depression during the 2 weeks before treating the comorbid migraine with a triptan. If the patient does not respond or if there is concern regarding possible underlying pathology, consult with a clinician who specializes in headache treatment.
Precipitating and aggravating factors
Headache triggers. Helping patients to recognize headache triggers and aggravating factors is an important element in treating and preventing migraines. Identifying these factors in the patient history can help you establish a diagnosis and implement steps to avoid or reduce attack severity.
Table 4
TREATMENT OPTIONS FOR PREVENTING MIGRAINE ATTACKS
| Drug | Efficacy* | Side effects* | Indications | Contraindications |
|---|---|---|---|---|
| β blockers | 4+ | 2+ | Hypertension | Depression, asthma, diabetes, hypotension, congestive heart failure, peripheral vascular disease |
| Ca channel blockers | 2+ | 1+ | Hypertension, angina, asthma, migraine aura | Constipation, hypotension |
| Tricyclic antidepressants | 4+ | 2+ | Depression, anxiety disorders, insomnia | Heart block, urinary retention, mania |
| Selective serotonin reuptake inhibitors | 2+ | 1+ | Depression, obsessive-compulsive disorder | Mania |
| Monoamine oxidase inhibitors | 4+ | 4+ | Depression | Dietary restrictions |
| Divalproex/valproate | 4+ | 2+ | Epilepsy, anxiety disorders, mania | Liver disease, bleeding disorders, hair loss |
| Naproxen | 2+ | 2+ | Arthritis, other pain disorders | Gastritis, peptic ulcer |
| * Ratings on a scale from 1+ (lowest) to 4+ (highest). Table partially derived from data in: Silberstein SD, Lipton RB, Goadsby PJ, Smith, R (eds). Headache in primary care. Oxford, UK: Isis Medical Media, 1999. | ||||
Common migraine headache triggers include menstruation, stress, relaxation after stress, fatigue, too much or too little sleep, skipping meals, weather changes, high humidity, glare and flickering lights, loud or high-pitched noises, smoke or dust, strong perfumes or cooking aromas. Food triggers cause 10% of migraine cases. Chocolate, strong cheeses, red wine, beer, citrus fruits, and foods with monosodium glutamate and nitrate preservatives are common food triggers.
Tension-type headaches are triggered by stress or the end of a stress-filled day. Triggers for cluster-type headaches include alcohol, smoking during the cluster phase, and lying down during an attack.
Case 2: Flying the unfriendly skies
Ms. B, 38, is a mother of three who works as a flight attendant. She is separated from her husband and had filed for divorce because of repeated spousal abuse. She has visited her primary care physician multiple times for migraine, sinus problems, backache, and coccygodynia. Orthopedic and rectal examinations revealed no abnormalities.
Her headaches met the IHS diagnostic criteria for migraine with aura, and these responded well to zolmitriptan, 5 mg. The headaches usually occurred during days off from work, but her sinus problems also led to headaches and nasal stuffiness when she flew. Her headaches eventually occurred almost daily.
Her supervisor was unsympathetic. An otolaryngologist had prescribed decongestants and a course of desensitization, both of which brought only transient relief.
A counselor at work recommended that Ms. B go on sick leave and accept a transfer to a non-flying job. The patient was tearful and felt overwhelmed by her problems. She felt that life was no longer worth living. She agreed to see a psychiatrist, who diagnosed depression and anxiety disorder. The psychiatrist prescribed citalopram, 20 mg/d, and agreed to see her regularly to monitor progress.
Discussion. As a migraineur, Ms. B was at increased risk for depression and anxiety disorders.19 Migraine with aura is associated with an increased lifetime prevalence of suicidal ideation and suicide attempts.20
The exact mechanisms by which migraine and depression are related are unknown. Each disorder increases the risk for developing the other. The specificity of this relationship is strengthened by the fact that depression is not associated with a greater risk of severe nonmigrainous headache, even though a severe nonmigrainous headache may cause depression.21
The patient in case 1 responded well when an antidepressant was added to her treatment. In her case, the diagnosis of a depressive disorder remained an open question. Migraine attacks are known to be associated with mood change, lethargy, and cognitive changes. The picture may be further confounded because migraine without depression responds well to prophylaxis with antidepressants.
The patient in case 2, however, presented with a complex of interrelated headache and psychiatric problems of potentially dangerous proportions. Psychiatric problems in migraineurs may be deep-seated, and these patients may require urgent, specialized attention to avoid further serious disability and a possible tragic outcome.
Related resources
- Silberstein SD, Lipton RB, Goadsby PJ, Smith, R, eds. Headache in primary care. Oxford, UK: Isis Medical Media, 1999.
- Silberstein SD, Lipton RB, Dalessio DJ. Wolff’s headache and other head pain (7th ed). New York: Oxford University Press, 2001.
- Davidoff RA. Migraine. Manifestations, pathogenesis and management (2nd ed). New York: Oxford University Press, 2002.
- International Headache Society. http://www.i-h-s.org
Drug brand names
- Citalopram • Celexa
- Dihydroergotamine • Migranal
- Eletriptan • Relpax
- Rizatriptan • Maxalt
- Sumatriptan • Imitrex
- Valproate sodium • Depakote
- Zolmitriptan • Zomig
Disclosure
Dr. Smith reports that he serves as a consultant to and is on the speakers’ bureau of AstraZeneca Pharmaceuticals.
Dr. Hasse reports no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
1. Lipton RB, Stewart WF, Diamond S, Diamond M, Reed M. Prevalence and burden of migraine in the United States: data from the American Migraine Study II. Headache 2001;41(7):646-57.
2. Breslau N, Davis GC. Migraine, major depression and panic disorder: A prospective epidemiologic study of young adults. Cephalalgia 1992;12(2):85-90.
3. Stewart WF, Linet MS, Celentano DD. Migraine headaches and panic attacks. Psychosom Med 1989;51(5):559-69.
4. Mersky H, Peatfield RC. Headache in the psychiatrically ill. In: Olesen J, Tfelt-Hensen P, Welch KMA (eds). The headaches (2nd ed). Baltimore: Lippincott, Williams and Wilkins, 1999;962-3.
5. Davidoff RA. Comorbidity. In: Davidoff RA (ed). Migraine manifestations, pathogenesis, and management (2nd ed). Oxford, UK: Oxford University Press, 2002;21-2.
6. Chang CL, Donaghy M, Poulter N. Migraine and stroke in young women: case-control study. BMJ 1999;318(7175):13-8.
7. Migraine-epilepsy relationships: epidemiological and genetic aspects. In: Andermann FA, Lugaresi E (eds). Migraine and epilepsy. Boston: Butterworths, 1987.
8. Smith R. Impact of migraine on the family. Headache 1998;38(6):423-6.
9. Classification and diagnostic criteria for headache disorders, cranial neuralgias and facial pain. Headache Classification Committee of the International Headache Society. Cephalalgia 1988;8(suppl 7):1-96.
10. Smith R, Hasse LA, Ritchey PN, et al. Extent of migraine and migrainous headache in headache NOS patients in family practice. Cephalalgia 2001;21:291-2.
11. Olesen J, Friberg L, et al. Basic mechanisms in vascular headache. Neurol Clin 1990;8:801-15.
12. Sumatriptan—an oral dose-defining study. The Oral Sumatriptan Dose-Defining Study Group. Eur Neurol 1991;31(5):300-5.
13. Diener HC. Positron emission tomography studies in headache. Headache 1997;37(10):622-5.
14. Joutel A, Bousser MG, V Biousse, et al. A gene for familial hemiplegic migraine maps to chromosome 19. Nat Genet 1993;5(1):40-5.
15. Iadecola C, Pelligrino DA, Moskowitz MA, Lassen NA. Nitric oxide synthase inhibition and cerebrovascular regulation. J Cereb Blood Flow Metab 1994;14(2):175-92.
16. Holroyd KA, Penzien DB, Lipchik GL. Efficacy of Behavioral Treatments. In: Silberstein SD, Lipton RB, Dalessio DJ (eds). Wolf’s headache and other head pain (7th ed). New York: Oxford University Press, 2001;563-6.
17. Robinson LA, Berman JS, Neimeyer RA. Psychotherapy for the treatment of depression: A comprehensive review of controlled outcome research. Psychol Bull 1990;108:30-49.
18. Gould RA, Otto MW, et al. Cognitive behavioral and pharmacological treatment of generalized anxiety disorder. Behav Ther 1997;28:285-305.
19. Breslau N, Andreski P. Migraine, personality and psychiatric comorbidity. Headache 1995;35(7):382-6.
20. Breslau N. Migraine, suicidal ideation, and suicide attempts. Neurology 1992;42(2):392-5.
21. Breslau N, Schultz LR, Stewart WF, et al. Headache and major depression: is the association specific to migraine? Neurology 2000;54(2):308-13.
Many of the 28 million people who suffer from migraine headaches each year1 need psychiatric care in addition to headache relief. Migraine headaches often coexist with depression,2 anxiety/panic disorders,2,3 bipolar disorder,4 and phobias,5 as well as with stroke6 and epilepsy.7 A study of 995 young adults found that anxiety disorders, phobias, major depression, panic disorder, and obsessive-compulsive disorder were two to five times more prevalent among migraine sufferers than among a control group (Table 1 ).2
Migraine sufferers know that at any time an attack could hamper their ability to work, care for their families, or engage in social activities. A nationwide study of migraineurs found that attacks often impaired their relationships with family and friends.8
Psychiatrists should screen patients for a history of migraine or other headaches and carefully consider the relationship between migraines and psychiatric disorders when prescribing treatment. In this article, we outline acute and preventive headache treatments and present two cases to help you treat these patients appropriately.
Table 1
PSYCHIATRIC COMORBIDITIES IN PATIENTS WITH VS. WITHOUT MIGRAINES*
| Migraineurs (%) (n = 128) | Controls (%) (n = 879) | |
|---|---|---|
| Any anxiety | 54 | 27 |
| Generalized anxiety disorder | 10 | 2 |
| Phobia | 40 | 21 |
| Major depression | 35 | 10 |
| Panic disorder | 11 | 2 |
| Obsessive-compulsive disorder | 9 | 2 |
| * Prevalence Source: Breslau N, Davis GC. Cephalalgia 1992;12(2):85-90. | ||
Table 2
THREE TYPES OF PRIMARY HEADACHE: DIAGNOSTIC CRITERIA
| Headache type | Age of onset (years) | Location | Duration | Frequency/timing | Severity | Quality | Features |
|---|---|---|---|---|---|---|---|
| Migraine | 10 to 40 | Hemicranial | 4 to 72 hr | Variable | Moderate to severe | Throbbing, steady ache | Nausea; vomiting; photo/phono/osmophobia; neurologic deficits; aura |
| Tension-type | 20 to 50 | Bilateral/generalized | 30 min to 7 days+ | Variable | Dull ache, may wax and wane | Tight, band-like pressure | Generally none |
| Cluster | 15 to 40 | Unilateral, periorbital or retro-orbital | 15 to 180 min | 1 to 8 times per day or night | Excruciating | Boring, piercing | Ipsilateral, conjunctival injection, nasal congestion, rhinorrhea, miosis, facial seating |
| Source: Classification and diagnostic criteria for headache disorders, cranial neuralgias and facial pain. Headache Classification Committee of the International Headache Society. Cephalalgia 1988;8(suppl 7):1-96. | |||||||
Headache definitions and diagnosis
Primary or secondary. Under the International Headache Society’s (IHS) 1988 headache classification and diagnostic criteria,9 headaches are primary or secondary:
- Primary headaches are benign recurrent headaches that commonly present in practice.
- Secondary headaches occur much less frequently and are caused by underlying pathology.
The possibility of secondary headache should be ruled out before a primary headache can be diagnosed. The following headache features should cause concern:
- Severe headache with abrupt onset
- Subacute or progressive headache over days or months
- Headache, nausea, vomiting, and fever not explained by systemic illness
- New-onset headache late in life
- Headache with neurologic signs or symptoms such as confusion, decreased level of consciousness, meningismus, or papilledema
- Headache following head trauma
- Patient history of sickle cell disease, malignancy, or HIV.
Headache types. The three major types of primary headache are migraine, tension-type, and cluster (Table 2 ). Tension-type is the most common, is often mild, and is either self-treated with over-the-counter medications or ignored. Migraine is the most troublesome headache in everyday practice. Cluster is the most severe and fortunately is rare.
Migraine with aura and migraine without aura are separate diagnoses. IHS criteria for diagnosing migraines without aura are listed in Table 3. According to the IHS, migraine with aura (or “classic migraine”) fulfills all the criteria for migraine without aura, with fully reversible neurologic symptoms indicating focal cerebral cortical and/or brain stem dysfunction.
Auras. About 15% of migraineurs experience auras. Symptoms develop within 5 to 20 minutes, usually last less than 1 hour, and fade before the headache’s onset. Gradual onset and history of previous attacks helps to distinguish aura from transient ischemic attacks. Auras may manifest as visual, sensory, motor, or brain-stem symptoms, or as combinations of these:
- Visual auras are most common, presenting as localized visual loss (scotoma), with flashing lights (scintillation) at margins or jagged edges (fortification).
- Sensory auras present as facial or limb paresthesias.
- Motor auras manifest as weakness or lack of coordination.
- Brain stem auras manifest as vertigo or double vision.
Migraine aura is considered part of the headache’s prodrome, which may occur days or hours before the headache’s onset. The aura may bring about:
- an altered mental state (e.g., depression, hyperactivity, euphoria, difficulty concentrating, dysphasia)
- neurologic symptoms (e.g., photophobia, phonophobia, hyperosmia, yawning)
- general bodily discomforts (e.g., anorexia, food craving, diarrhea, thirst, urination, fluid retention, cold feeling).
Despite their sometimes severe effects, migraines often remain undiagnosed.10 Migraine should be suspected in patients with recurrent moderate to severe disabling headaches (Box).11-15
Case 1: “Bad, sick headaches”
Ms. A, 23, a single parent with a 2-year-old child, has had trouble staying employed because of repeated illnesses. She made 17 visits to her primary care physician within 26 months. While her main complaint was headache, she also complained of other aches and pains, a lack of energy, and insomnia. Numerous examinations revealed no physical abnormalities.
She reported having “bad, sick headaches” that sometimes lasted 2 to 3 days. Bed rest helped but this was not always possible. The headache was throbbing and usually one-sided. She had no aura, and ibuprofen gave partial relief. She noted that her mother gets similar headaches.
Table 3
DIAGNOSTIC REQUIREMENTS FOR MIGRAINE WITHOUT AURA
Mandatory
|
At least 2 of the following:
|
| During headache At least one of the following:
|
| Additional features Migraine prodrome—A range of general, neurologic, and mental changes may occur hours or days before the headache’s onset General—Anorexia, food craving, diarrhea or constipation, thirst, urination, fluid retention, cold feeling Mental—Depression, hyperactivity, euphoria, difficulty concentrating, dysphasia Neurologic—Photophobia, phonophobia, hyperosmia, yawning |
| SOURCE: Classification and diagnostic criteria for headache disorders, cranial neuralgias and facial pain. Headache Classification Committee of the International Headache Society. Cephalalgia 1988;8(suppl 7):1-96. |
Ms. A was diagnosed with migraine without aura, and she was treated with sumatriptan, 100 mg (1 or 2 doses, as needed). Her headaches responded well to this treatment, but the frequency of attacks remained unchanged. She requested a change in her medicine.
The underlying mechanisms of migraine headaches are not completely understood.
Vascular causes. A recently described neurovascular mechanism11 suggests that perivascular neurogenic inflammation involving meningeal vessels causes migraine. The triptan drugs have been found to reverse this process and relieve the headache.12
Positron emission tomography has demonstrated increased blood flow during acute migraine in midline brain stem structures. This suggests the presence of a central migraine generator in that location.13
Heredity. A rare form of migraine, familial hemiplegic migraine, is associated with a genetic abnormality on chromosome 19.14
Nitric oxide. Nitroglycerine-induced migraine headache, caused by the release of nitric oxide in cerebral vessels, can be reversed by nitrous oxide synthase inhibitors, thus opening up intriguing possibilities of new therapeutic agents and increased understanding of underlying migraine mechanisms.15
Treating migraines
Acute treatment. Migraineurs whose attacks are infrequent and mild may find OTC analgesics or NSAIDs adequate. Most patients, however, require specific migraine treatment, usually with triptans. Acute oral treatment options include sumatriptan, 50 to 100 mg; rizatriptan, 10 mg; zolmitriptan, 2.5 to 5 mg; and eletriptan, 40 mg.
In case of vomiting or nausea, options include sumatriptan, 20 mg nasal spray or 6 mg SC; rizatriptan, 10 mg on a dissolving wafer; or dihydroergotamine, 2 mg nasal spray or 1 mg IM or SC. For severe nausea or vomiting, an anti-nauseant (e.g., prochlorperazine suppositories, 25 mg) may be of value.
Preventive treatment. Preventive treatment may be warranted, depending on attack frequency, severity, and the extent of disability caused. One prolonged, severe attack per month that responds poorly to acute treatment may indicate the need for preventive treatment. A range of preventative treatments is available (Table 4).
In Ms. A’s case, oral sumatriptan lessened the severity of the migraine attacks, and the addition of nortriptyline, 50 mg/d, reduced frequency by about 50%. She felt more energetic overall and was sleeping better.
Treating the psychiatric comorbidity
Behavioral therapy is used as an adjunct to pharmacologic headache treatment. This approach is usually considered after a poor or adverse response to treatment, or when pharmacologic treatment is contraindicated (e.g., during pregnancy).
Relaxation training, biofeedback, and cognitive-behavioral stress management are the most commonly used forms of behavioral therapy. Thirty-five to 55% improvement in migraine has been reported following such treatments.16
Cognitive-behavioral intervention has been shown to be effective in depression17 and anxiety disorders.18 When either psychiatric problem is comorbid with migraine, cognitive therapy can improve both the migraine and the psychiatric comorbidity.
Pharmacologic therapy. Depression is commonly associated with migraine and may be caused by living with chronic disabling headaches over time. In such cases, the depression will improve as the migraine responds to treatment. However, in cases where comorbid depression or anxiety trigger or exacerbate acute migraine attacks, neither the migraine nor the psychiatric problem responds until the underlying psychopathology is treated. In such cases, simultaneous psychiatric and migraine pharmacologic treatment is required.
We recommend that you treat the psychiatric comorbidity as it would be treated without a co-existing migraine. Be advised, however, that monoamine oxidase inhibitors are contraindicated in depression during the 2 weeks before treating the comorbid migraine with a triptan. If the patient does not respond or if there is concern regarding possible underlying pathology, consult with a clinician who specializes in headache treatment.
Precipitating and aggravating factors
Headache triggers. Helping patients to recognize headache triggers and aggravating factors is an important element in treating and preventing migraines. Identifying these factors in the patient history can help you establish a diagnosis and implement steps to avoid or reduce attack severity.
Table 4
TREATMENT OPTIONS FOR PREVENTING MIGRAINE ATTACKS
| Drug | Efficacy* | Side effects* | Indications | Contraindications |
|---|---|---|---|---|
| β blockers | 4+ | 2+ | Hypertension | Depression, asthma, diabetes, hypotension, congestive heart failure, peripheral vascular disease |
| Ca channel blockers | 2+ | 1+ | Hypertension, angina, asthma, migraine aura | Constipation, hypotension |
| Tricyclic antidepressants | 4+ | 2+ | Depression, anxiety disorders, insomnia | Heart block, urinary retention, mania |
| Selective serotonin reuptake inhibitors | 2+ | 1+ | Depression, obsessive-compulsive disorder | Mania |
| Monoamine oxidase inhibitors | 4+ | 4+ | Depression | Dietary restrictions |
| Divalproex/valproate | 4+ | 2+ | Epilepsy, anxiety disorders, mania | Liver disease, bleeding disorders, hair loss |
| Naproxen | 2+ | 2+ | Arthritis, other pain disorders | Gastritis, peptic ulcer |
| * Ratings on a scale from 1+ (lowest) to 4+ (highest). Table partially derived from data in: Silberstein SD, Lipton RB, Goadsby PJ, Smith, R (eds). Headache in primary care. Oxford, UK: Isis Medical Media, 1999. | ||||
Common migraine headache triggers include menstruation, stress, relaxation after stress, fatigue, too much or too little sleep, skipping meals, weather changes, high humidity, glare and flickering lights, loud or high-pitched noises, smoke or dust, strong perfumes or cooking aromas. Food triggers cause 10% of migraine cases. Chocolate, strong cheeses, red wine, beer, citrus fruits, and foods with monosodium glutamate and nitrate preservatives are common food triggers.
Tension-type headaches are triggered by stress or the end of a stress-filled day. Triggers for cluster-type headaches include alcohol, smoking during the cluster phase, and lying down during an attack.
Case 2: Flying the unfriendly skies
Ms. B, 38, is a mother of three who works as a flight attendant. She is separated from her husband and had filed for divorce because of repeated spousal abuse. She has visited her primary care physician multiple times for migraine, sinus problems, backache, and coccygodynia. Orthopedic and rectal examinations revealed no abnormalities.
Her headaches met the IHS diagnostic criteria for migraine with aura, and these responded well to zolmitriptan, 5 mg. The headaches usually occurred during days off from work, but her sinus problems also led to headaches and nasal stuffiness when she flew. Her headaches eventually occurred almost daily.
Her supervisor was unsympathetic. An otolaryngologist had prescribed decongestants and a course of desensitization, both of which brought only transient relief.
A counselor at work recommended that Ms. B go on sick leave and accept a transfer to a non-flying job. The patient was tearful and felt overwhelmed by her problems. She felt that life was no longer worth living. She agreed to see a psychiatrist, who diagnosed depression and anxiety disorder. The psychiatrist prescribed citalopram, 20 mg/d, and agreed to see her regularly to monitor progress.
Discussion. As a migraineur, Ms. B was at increased risk for depression and anxiety disorders.19 Migraine with aura is associated with an increased lifetime prevalence of suicidal ideation and suicide attempts.20
The exact mechanisms by which migraine and depression are related are unknown. Each disorder increases the risk for developing the other. The specificity of this relationship is strengthened by the fact that depression is not associated with a greater risk of severe nonmigrainous headache, even though a severe nonmigrainous headache may cause depression.21
The patient in case 1 responded well when an antidepressant was added to her treatment. In her case, the diagnosis of a depressive disorder remained an open question. Migraine attacks are known to be associated with mood change, lethargy, and cognitive changes. The picture may be further confounded because migraine without depression responds well to prophylaxis with antidepressants.
The patient in case 2, however, presented with a complex of interrelated headache and psychiatric problems of potentially dangerous proportions. Psychiatric problems in migraineurs may be deep-seated, and these patients may require urgent, specialized attention to avoid further serious disability and a possible tragic outcome.
Related resources
- Silberstein SD, Lipton RB, Goadsby PJ, Smith, R, eds. Headache in primary care. Oxford, UK: Isis Medical Media, 1999.
- Silberstein SD, Lipton RB, Dalessio DJ. Wolff’s headache and other head pain (7th ed). New York: Oxford University Press, 2001.
- Davidoff RA. Migraine. Manifestations, pathogenesis and management (2nd ed). New York: Oxford University Press, 2002.
- International Headache Society. http://www.i-h-s.org
Drug brand names
- Citalopram • Celexa
- Dihydroergotamine • Migranal
- Eletriptan • Relpax
- Rizatriptan • Maxalt
- Sumatriptan • Imitrex
- Valproate sodium • Depakote
- Zolmitriptan • Zomig
Disclosure
Dr. Smith reports that he serves as a consultant to and is on the speakers’ bureau of AstraZeneca Pharmaceuticals.
Dr. Hasse reports no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
Many of the 28 million people who suffer from migraine headaches each year1 need psychiatric care in addition to headache relief. Migraine headaches often coexist with depression,2 anxiety/panic disorders,2,3 bipolar disorder,4 and phobias,5 as well as with stroke6 and epilepsy.7 A study of 995 young adults found that anxiety disorders, phobias, major depression, panic disorder, and obsessive-compulsive disorder were two to five times more prevalent among migraine sufferers than among a control group (Table 1 ).2
Migraine sufferers know that at any time an attack could hamper their ability to work, care for their families, or engage in social activities. A nationwide study of migraineurs found that attacks often impaired their relationships with family and friends.8
Psychiatrists should screen patients for a history of migraine or other headaches and carefully consider the relationship between migraines and psychiatric disorders when prescribing treatment. In this article, we outline acute and preventive headache treatments and present two cases to help you treat these patients appropriately.
Table 1
PSYCHIATRIC COMORBIDITIES IN PATIENTS WITH VS. WITHOUT MIGRAINES*
| Migraineurs (%) (n = 128) | Controls (%) (n = 879) | |
|---|---|---|
| Any anxiety | 54 | 27 |
| Generalized anxiety disorder | 10 | 2 |
| Phobia | 40 | 21 |
| Major depression | 35 | 10 |
| Panic disorder | 11 | 2 |
| Obsessive-compulsive disorder | 9 | 2 |
| * Prevalence Source: Breslau N, Davis GC. Cephalalgia 1992;12(2):85-90. | ||
Table 2
THREE TYPES OF PRIMARY HEADACHE: DIAGNOSTIC CRITERIA
| Headache type | Age of onset (years) | Location | Duration | Frequency/timing | Severity | Quality | Features |
|---|---|---|---|---|---|---|---|
| Migraine | 10 to 40 | Hemicranial | 4 to 72 hr | Variable | Moderate to severe | Throbbing, steady ache | Nausea; vomiting; photo/phono/osmophobia; neurologic deficits; aura |
| Tension-type | 20 to 50 | Bilateral/generalized | 30 min to 7 days+ | Variable | Dull ache, may wax and wane | Tight, band-like pressure | Generally none |
| Cluster | 15 to 40 | Unilateral, periorbital or retro-orbital | 15 to 180 min | 1 to 8 times per day or night | Excruciating | Boring, piercing | Ipsilateral, conjunctival injection, nasal congestion, rhinorrhea, miosis, facial seating |
| Source: Classification and diagnostic criteria for headache disorders, cranial neuralgias and facial pain. Headache Classification Committee of the International Headache Society. Cephalalgia 1988;8(suppl 7):1-96. | |||||||
Headache definitions and diagnosis
Primary or secondary. Under the International Headache Society’s (IHS) 1988 headache classification and diagnostic criteria,9 headaches are primary or secondary:
- Primary headaches are benign recurrent headaches that commonly present in practice.
- Secondary headaches occur much less frequently and are caused by underlying pathology.
The possibility of secondary headache should be ruled out before a primary headache can be diagnosed. The following headache features should cause concern:
- Severe headache with abrupt onset
- Subacute or progressive headache over days or months
- Headache, nausea, vomiting, and fever not explained by systemic illness
- New-onset headache late in life
- Headache with neurologic signs or symptoms such as confusion, decreased level of consciousness, meningismus, or papilledema
- Headache following head trauma
- Patient history of sickle cell disease, malignancy, or HIV.
Headache types. The three major types of primary headache are migraine, tension-type, and cluster (Table 2 ). Tension-type is the most common, is often mild, and is either self-treated with over-the-counter medications or ignored. Migraine is the most troublesome headache in everyday practice. Cluster is the most severe and fortunately is rare.
Migraine with aura and migraine without aura are separate diagnoses. IHS criteria for diagnosing migraines without aura are listed in Table 3. According to the IHS, migraine with aura (or “classic migraine”) fulfills all the criteria for migraine without aura, with fully reversible neurologic symptoms indicating focal cerebral cortical and/or brain stem dysfunction.
Auras. About 15% of migraineurs experience auras. Symptoms develop within 5 to 20 minutes, usually last less than 1 hour, and fade before the headache’s onset. Gradual onset and history of previous attacks helps to distinguish aura from transient ischemic attacks. Auras may manifest as visual, sensory, motor, or brain-stem symptoms, or as combinations of these:
- Visual auras are most common, presenting as localized visual loss (scotoma), with flashing lights (scintillation) at margins or jagged edges (fortification).
- Sensory auras present as facial or limb paresthesias.
- Motor auras manifest as weakness or lack of coordination.
- Brain stem auras manifest as vertigo or double vision.
Migraine aura is considered part of the headache’s prodrome, which may occur days or hours before the headache’s onset. The aura may bring about:
- an altered mental state (e.g., depression, hyperactivity, euphoria, difficulty concentrating, dysphasia)
- neurologic symptoms (e.g., photophobia, phonophobia, hyperosmia, yawning)
- general bodily discomforts (e.g., anorexia, food craving, diarrhea, thirst, urination, fluid retention, cold feeling).
Despite their sometimes severe effects, migraines often remain undiagnosed.10 Migraine should be suspected in patients with recurrent moderate to severe disabling headaches (Box).11-15
Case 1: “Bad, sick headaches”
Ms. A, 23, a single parent with a 2-year-old child, has had trouble staying employed because of repeated illnesses. She made 17 visits to her primary care physician within 26 months. While her main complaint was headache, she also complained of other aches and pains, a lack of energy, and insomnia. Numerous examinations revealed no physical abnormalities.
She reported having “bad, sick headaches” that sometimes lasted 2 to 3 days. Bed rest helped but this was not always possible. The headache was throbbing and usually one-sided. She had no aura, and ibuprofen gave partial relief. She noted that her mother gets similar headaches.
Table 3
DIAGNOSTIC REQUIREMENTS FOR MIGRAINE WITHOUT AURA
Mandatory
|
At least 2 of the following:
|
| During headache At least one of the following:
|
| Additional features Migraine prodrome—A range of general, neurologic, and mental changes may occur hours or days before the headache’s onset General—Anorexia, food craving, diarrhea or constipation, thirst, urination, fluid retention, cold feeling Mental—Depression, hyperactivity, euphoria, difficulty concentrating, dysphasia Neurologic—Photophobia, phonophobia, hyperosmia, yawning |
| SOURCE: Classification and diagnostic criteria for headache disorders, cranial neuralgias and facial pain. Headache Classification Committee of the International Headache Society. Cephalalgia 1988;8(suppl 7):1-96. |
Ms. A was diagnosed with migraine without aura, and she was treated with sumatriptan, 100 mg (1 or 2 doses, as needed). Her headaches responded well to this treatment, but the frequency of attacks remained unchanged. She requested a change in her medicine.
The underlying mechanisms of migraine headaches are not completely understood.
Vascular causes. A recently described neurovascular mechanism11 suggests that perivascular neurogenic inflammation involving meningeal vessels causes migraine. The triptan drugs have been found to reverse this process and relieve the headache.12
Positron emission tomography has demonstrated increased blood flow during acute migraine in midline brain stem structures. This suggests the presence of a central migraine generator in that location.13
Heredity. A rare form of migraine, familial hemiplegic migraine, is associated with a genetic abnormality on chromosome 19.14
Nitric oxide. Nitroglycerine-induced migraine headache, caused by the release of nitric oxide in cerebral vessels, can be reversed by nitrous oxide synthase inhibitors, thus opening up intriguing possibilities of new therapeutic agents and increased understanding of underlying migraine mechanisms.15
Treating migraines
Acute treatment. Migraineurs whose attacks are infrequent and mild may find OTC analgesics or NSAIDs adequate. Most patients, however, require specific migraine treatment, usually with triptans. Acute oral treatment options include sumatriptan, 50 to 100 mg; rizatriptan, 10 mg; zolmitriptan, 2.5 to 5 mg; and eletriptan, 40 mg.
In case of vomiting or nausea, options include sumatriptan, 20 mg nasal spray or 6 mg SC; rizatriptan, 10 mg on a dissolving wafer; or dihydroergotamine, 2 mg nasal spray or 1 mg IM or SC. For severe nausea or vomiting, an anti-nauseant (e.g., prochlorperazine suppositories, 25 mg) may be of value.
Preventive treatment. Preventive treatment may be warranted, depending on attack frequency, severity, and the extent of disability caused. One prolonged, severe attack per month that responds poorly to acute treatment may indicate the need for preventive treatment. A range of preventative treatments is available (Table 4).
In Ms. A’s case, oral sumatriptan lessened the severity of the migraine attacks, and the addition of nortriptyline, 50 mg/d, reduced frequency by about 50%. She felt more energetic overall and was sleeping better.
Treating the psychiatric comorbidity
Behavioral therapy is used as an adjunct to pharmacologic headache treatment. This approach is usually considered after a poor or adverse response to treatment, or when pharmacologic treatment is contraindicated (e.g., during pregnancy).
Relaxation training, biofeedback, and cognitive-behavioral stress management are the most commonly used forms of behavioral therapy. Thirty-five to 55% improvement in migraine has been reported following such treatments.16
Cognitive-behavioral intervention has been shown to be effective in depression17 and anxiety disorders.18 When either psychiatric problem is comorbid with migraine, cognitive therapy can improve both the migraine and the psychiatric comorbidity.
Pharmacologic therapy. Depression is commonly associated with migraine and may be caused by living with chronic disabling headaches over time. In such cases, the depression will improve as the migraine responds to treatment. However, in cases where comorbid depression or anxiety trigger or exacerbate acute migraine attacks, neither the migraine nor the psychiatric problem responds until the underlying psychopathology is treated. In such cases, simultaneous psychiatric and migraine pharmacologic treatment is required.
We recommend that you treat the psychiatric comorbidity as it would be treated without a co-existing migraine. Be advised, however, that monoamine oxidase inhibitors are contraindicated in depression during the 2 weeks before treating the comorbid migraine with a triptan. If the patient does not respond or if there is concern regarding possible underlying pathology, consult with a clinician who specializes in headache treatment.
Precipitating and aggravating factors
Headache triggers. Helping patients to recognize headache triggers and aggravating factors is an important element in treating and preventing migraines. Identifying these factors in the patient history can help you establish a diagnosis and implement steps to avoid or reduce attack severity.
Table 4
TREATMENT OPTIONS FOR PREVENTING MIGRAINE ATTACKS
| Drug | Efficacy* | Side effects* | Indications | Contraindications |
|---|---|---|---|---|
| β blockers | 4+ | 2+ | Hypertension | Depression, asthma, diabetes, hypotension, congestive heart failure, peripheral vascular disease |
| Ca channel blockers | 2+ | 1+ | Hypertension, angina, asthma, migraine aura | Constipation, hypotension |
| Tricyclic antidepressants | 4+ | 2+ | Depression, anxiety disorders, insomnia | Heart block, urinary retention, mania |
| Selective serotonin reuptake inhibitors | 2+ | 1+ | Depression, obsessive-compulsive disorder | Mania |
| Monoamine oxidase inhibitors | 4+ | 4+ | Depression | Dietary restrictions |
| Divalproex/valproate | 4+ | 2+ | Epilepsy, anxiety disorders, mania | Liver disease, bleeding disorders, hair loss |
| Naproxen | 2+ | 2+ | Arthritis, other pain disorders | Gastritis, peptic ulcer |
| * Ratings on a scale from 1+ (lowest) to 4+ (highest). Table partially derived from data in: Silberstein SD, Lipton RB, Goadsby PJ, Smith, R (eds). Headache in primary care. Oxford, UK: Isis Medical Media, 1999. | ||||
Common migraine headache triggers include menstruation, stress, relaxation after stress, fatigue, too much or too little sleep, skipping meals, weather changes, high humidity, glare and flickering lights, loud or high-pitched noises, smoke or dust, strong perfumes or cooking aromas. Food triggers cause 10% of migraine cases. Chocolate, strong cheeses, red wine, beer, citrus fruits, and foods with monosodium glutamate and nitrate preservatives are common food triggers.
Tension-type headaches are triggered by stress or the end of a stress-filled day. Triggers for cluster-type headaches include alcohol, smoking during the cluster phase, and lying down during an attack.
Case 2: Flying the unfriendly skies
Ms. B, 38, is a mother of three who works as a flight attendant. She is separated from her husband and had filed for divorce because of repeated spousal abuse. She has visited her primary care physician multiple times for migraine, sinus problems, backache, and coccygodynia. Orthopedic and rectal examinations revealed no abnormalities.
Her headaches met the IHS diagnostic criteria for migraine with aura, and these responded well to zolmitriptan, 5 mg. The headaches usually occurred during days off from work, but her sinus problems also led to headaches and nasal stuffiness when she flew. Her headaches eventually occurred almost daily.
Her supervisor was unsympathetic. An otolaryngologist had prescribed decongestants and a course of desensitization, both of which brought only transient relief.
A counselor at work recommended that Ms. B go on sick leave and accept a transfer to a non-flying job. The patient was tearful and felt overwhelmed by her problems. She felt that life was no longer worth living. She agreed to see a psychiatrist, who diagnosed depression and anxiety disorder. The psychiatrist prescribed citalopram, 20 mg/d, and agreed to see her regularly to monitor progress.
Discussion. As a migraineur, Ms. B was at increased risk for depression and anxiety disorders.19 Migraine with aura is associated with an increased lifetime prevalence of suicidal ideation and suicide attempts.20
The exact mechanisms by which migraine and depression are related are unknown. Each disorder increases the risk for developing the other. The specificity of this relationship is strengthened by the fact that depression is not associated with a greater risk of severe nonmigrainous headache, even though a severe nonmigrainous headache may cause depression.21
The patient in case 1 responded well when an antidepressant was added to her treatment. In her case, the diagnosis of a depressive disorder remained an open question. Migraine attacks are known to be associated with mood change, lethargy, and cognitive changes. The picture may be further confounded because migraine without depression responds well to prophylaxis with antidepressants.
The patient in case 2, however, presented with a complex of interrelated headache and psychiatric problems of potentially dangerous proportions. Psychiatric problems in migraineurs may be deep-seated, and these patients may require urgent, specialized attention to avoid further serious disability and a possible tragic outcome.
Related resources
- Silberstein SD, Lipton RB, Goadsby PJ, Smith, R, eds. Headache in primary care. Oxford, UK: Isis Medical Media, 1999.
- Silberstein SD, Lipton RB, Dalessio DJ. Wolff’s headache and other head pain (7th ed). New York: Oxford University Press, 2001.
- Davidoff RA. Migraine. Manifestations, pathogenesis and management (2nd ed). New York: Oxford University Press, 2002.
- International Headache Society. http://www.i-h-s.org
Drug brand names
- Citalopram • Celexa
- Dihydroergotamine • Migranal
- Eletriptan • Relpax
- Rizatriptan • Maxalt
- Sumatriptan • Imitrex
- Valproate sodium • Depakote
- Zolmitriptan • Zomig
Disclosure
Dr. Smith reports that he serves as a consultant to and is on the speakers’ bureau of AstraZeneca Pharmaceuticals.
Dr. Hasse reports no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
1. Lipton RB, Stewart WF, Diamond S, Diamond M, Reed M. Prevalence and burden of migraine in the United States: data from the American Migraine Study II. Headache 2001;41(7):646-57.
2. Breslau N, Davis GC. Migraine, major depression and panic disorder: A prospective epidemiologic study of young adults. Cephalalgia 1992;12(2):85-90.
3. Stewart WF, Linet MS, Celentano DD. Migraine headaches and panic attacks. Psychosom Med 1989;51(5):559-69.
4. Mersky H, Peatfield RC. Headache in the psychiatrically ill. In: Olesen J, Tfelt-Hensen P, Welch KMA (eds). The headaches (2nd ed). Baltimore: Lippincott, Williams and Wilkins, 1999;962-3.
5. Davidoff RA. Comorbidity. In: Davidoff RA (ed). Migraine manifestations, pathogenesis, and management (2nd ed). Oxford, UK: Oxford University Press, 2002;21-2.
6. Chang CL, Donaghy M, Poulter N. Migraine and stroke in young women: case-control study. BMJ 1999;318(7175):13-8.
7. Migraine-epilepsy relationships: epidemiological and genetic aspects. In: Andermann FA, Lugaresi E (eds). Migraine and epilepsy. Boston: Butterworths, 1987.
8. Smith R. Impact of migraine on the family. Headache 1998;38(6):423-6.
9. Classification and diagnostic criteria for headache disorders, cranial neuralgias and facial pain. Headache Classification Committee of the International Headache Society. Cephalalgia 1988;8(suppl 7):1-96.
10. Smith R, Hasse LA, Ritchey PN, et al. Extent of migraine and migrainous headache in headache NOS patients in family practice. Cephalalgia 2001;21:291-2.
11. Olesen J, Friberg L, et al. Basic mechanisms in vascular headache. Neurol Clin 1990;8:801-15.
12. Sumatriptan—an oral dose-defining study. The Oral Sumatriptan Dose-Defining Study Group. Eur Neurol 1991;31(5):300-5.
13. Diener HC. Positron emission tomography studies in headache. Headache 1997;37(10):622-5.
14. Joutel A, Bousser MG, V Biousse, et al. A gene for familial hemiplegic migraine maps to chromosome 19. Nat Genet 1993;5(1):40-5.
15. Iadecola C, Pelligrino DA, Moskowitz MA, Lassen NA. Nitric oxide synthase inhibition and cerebrovascular regulation. J Cereb Blood Flow Metab 1994;14(2):175-92.
16. Holroyd KA, Penzien DB, Lipchik GL. Efficacy of Behavioral Treatments. In: Silberstein SD, Lipton RB, Dalessio DJ (eds). Wolf’s headache and other head pain (7th ed). New York: Oxford University Press, 2001;563-6.
17. Robinson LA, Berman JS, Neimeyer RA. Psychotherapy for the treatment of depression: A comprehensive review of controlled outcome research. Psychol Bull 1990;108:30-49.
18. Gould RA, Otto MW, et al. Cognitive behavioral and pharmacological treatment of generalized anxiety disorder. Behav Ther 1997;28:285-305.
19. Breslau N, Andreski P. Migraine, personality and psychiatric comorbidity. Headache 1995;35(7):382-6.
20. Breslau N. Migraine, suicidal ideation, and suicide attempts. Neurology 1992;42(2):392-5.
21. Breslau N, Schultz LR, Stewart WF, et al. Headache and major depression: is the association specific to migraine? Neurology 2000;54(2):308-13.
1. Lipton RB, Stewart WF, Diamond S, Diamond M, Reed M. Prevalence and burden of migraine in the United States: data from the American Migraine Study II. Headache 2001;41(7):646-57.
2. Breslau N, Davis GC. Migraine, major depression and panic disorder: A prospective epidemiologic study of young adults. Cephalalgia 1992;12(2):85-90.
3. Stewart WF, Linet MS, Celentano DD. Migraine headaches and panic attacks. Psychosom Med 1989;51(5):559-69.
4. Mersky H, Peatfield RC. Headache in the psychiatrically ill. In: Olesen J, Tfelt-Hensen P, Welch KMA (eds). The headaches (2nd ed). Baltimore: Lippincott, Williams and Wilkins, 1999;962-3.
5. Davidoff RA. Comorbidity. In: Davidoff RA (ed). Migraine manifestations, pathogenesis, and management (2nd ed). Oxford, UK: Oxford University Press, 2002;21-2.
6. Chang CL, Donaghy M, Poulter N. Migraine and stroke in young women: case-control study. BMJ 1999;318(7175):13-8.
7. Migraine-epilepsy relationships: epidemiological and genetic aspects. In: Andermann FA, Lugaresi E (eds). Migraine and epilepsy. Boston: Butterworths, 1987.
8. Smith R. Impact of migraine on the family. Headache 1998;38(6):423-6.
9. Classification and diagnostic criteria for headache disorders, cranial neuralgias and facial pain. Headache Classification Committee of the International Headache Society. Cephalalgia 1988;8(suppl 7):1-96.
10. Smith R, Hasse LA, Ritchey PN, et al. Extent of migraine and migrainous headache in headache NOS patients in family practice. Cephalalgia 2001;21:291-2.
11. Olesen J, Friberg L, et al. Basic mechanisms in vascular headache. Neurol Clin 1990;8:801-15.
12. Sumatriptan—an oral dose-defining study. The Oral Sumatriptan Dose-Defining Study Group. Eur Neurol 1991;31(5):300-5.
13. Diener HC. Positron emission tomography studies in headache. Headache 1997;37(10):622-5.
14. Joutel A, Bousser MG, V Biousse, et al. A gene for familial hemiplegic migraine maps to chromosome 19. Nat Genet 1993;5(1):40-5.
15. Iadecola C, Pelligrino DA, Moskowitz MA, Lassen NA. Nitric oxide synthase inhibition and cerebrovascular regulation. J Cereb Blood Flow Metab 1994;14(2):175-92.
16. Holroyd KA, Penzien DB, Lipchik GL. Efficacy of Behavioral Treatments. In: Silberstein SD, Lipton RB, Dalessio DJ (eds). Wolf’s headache and other head pain (7th ed). New York: Oxford University Press, 2001;563-6.
17. Robinson LA, Berman JS, Neimeyer RA. Psychotherapy for the treatment of depression: A comprehensive review of controlled outcome research. Psychol Bull 1990;108:30-49.
18. Gould RA, Otto MW, et al. Cognitive behavioral and pharmacological treatment of generalized anxiety disorder. Behav Ther 1997;28:285-305.
19. Breslau N, Andreski P. Migraine, personality and psychiatric comorbidity. Headache 1995;35(7):382-6.
20. Breslau N. Migraine, suicidal ideation, and suicide attempts. Neurology 1992;42(2):392-5.
21. Breslau N, Schultz LR, Stewart WF, et al. Headache and major depression: is the association specific to migraine? Neurology 2000;54(2):308-13.
Borderline personality disorder: The lability of psychiatric diagnosis
Not everyone agrees that borderline personality disorder (BPD) should be a diagnostic category. BPD became “official” with DSM-III in 1980, although the term had been used for 40 years to describe various patient groups. Being listed in DSM-III legitimized BPD, which was thought to represent a specific—though not necessarily distinct—diagnostic category.
The history of the BPD diagnosis and opinions as to its usefulness can be viewed as a microcosm of psychiatric diagnosis in general. Before DSM-III, diagnoses were broadly defined and did not contain specific inclusion or exclusion criteria.1 For the 5 to 10 years prior to DSM-III, however, two assumptions developed:
- distinct diagnostic categories did, in fact, exist
- by rigorously defining and studying those categories we could develop more specific and effective treatments for our patients.2
The specificity and exclusivity that we assumed we could achieve by categorical diagnoses, however, remain a distant wish. Comorbidity appears more common in psychiatry than was originally thought and confounds both treatment and outcome.3 Also, many patients appear treatment-resistant, despite fitting neatly into diagnostic categories.4
Miss A, age 35, presents to the emergency room with a long history of intermittent depression and self-mutilation. She has never been hospitalized nor on psychotropic medication but has been in and out of psychotherapy for years. She has had intermittent depressive episodes for many years, though the episodes often lasted 2 to 3 weeks and appeared to correct themselves spontaneously.
Agitated and afraid. She is extremely agitated when she arrives at the emergency department. She has hardly slept or eaten but insists she is not hungry. She reports that she cannot concentrate or do her work as an accountant. She says she is hearing voices, knows they are in her head, but nonetheless is terrified that something horrible is about to happen—though she cannot say what it might be.
Voice ‘calling my name.’ When the psychiatric resident inquires further, Miss A says a male voice is calling her name and mumbling some short phrase she cannot understand. She says she has heard the voice the last few days, perhaps for 10 to 15 minutes every few hours, particularly when she ruminates about how she messed up a relationship with her now ex-boyfriend. The breakup occurred 1 week ago.
Feeling detached. She claims she has never heard voices before but describes periods when she has felt detached and unreal. Often these were short-term dissociative episodes that occurred in the wake of what she perceived as a personal failure or a distressful interpersonal encounter (often with a man). Relationships frequently were very difficult for her, and she felt she could easily go from infatuation to detesting someone.
Diagnosis? Talking appears to calm her down. After being in the emergency room for 2 hours, she says she no longer hears the voice. The resident tells the attending psychiatrist he believes the patient is in a major depressive episode, perhaps a psychotic depression, and proposes starting antidepressant treatment. The attending argues that the patient appears to have borderline personality disorder and suggests that she be sent home without medication and given an appointment to the outpatient clinic within the next few days.
As psychiatry considers DSM-V, questions linger as to whether BPD (and personality disorder in general) should remain as a categorical diagnosis or if dimensional measures may be more appropriate. Dimensions imply that no one ever fits into a given box because no specific box exists. Rather, patients are described as being closer to or more distant from a prototypic model of the diagnosis. In personality disorders, the dimensions most often mentioned are cognition, impulsivity, emotional lability, environmental hyperreactivity, and anxiety. The case report (above) illustrates the interplay of these dimensions in a typical patient with presumed BPD.
What’s in a name?
The symptom complex or syndrome that bears the name borderline personality disorder has probably existed for as long as people have thought about patients in psychopathologic terms.5 Before 1980, the term “borderline” applied primarily to two separate but overlapping concepts:
- Patients thought to reside on the “border” with psychosis, such as the patient in our case example. They seemed to have an underlying psychotic disorder, but the psychosis—if it surfaced—appeared briefly, was not exceptionally deep or firmly held, and was not regularly evident or immediately accessible to the clinician.
- Patients who appeared to occupy the space between neurosis and psychosis. This concept evolved into the idea of a character or personality disorder distinguished primarily by unstable interpersonal relationships, a confused or inconsistent sense of identity, and emotional instability.
How DSM is changing. Comparing the disorders listed in DSM-IV (1994)6 versus DSM-II (1968)1 suggests that psychiatry has become enamored of the naming process. For example, DSM-II lists anxiety neurosis (300.0), phobic neurosis (300.2), and obsessive-compulsive neurosis (300.3), whereas DSM-IV lists 11 different categories of anxiety disorders.
But beyond naming, subsequent DSMs have differed even more dramatically from DSM-II. We have seen a shift from describing a diagnostic category with a simple explanatory paragraph to lists of specific inclusion and exclusion criteria. These more-specific lists imply that they define categories closer to some reality or authenticity than did previous definitions.
Before DSM-III, the borderline concept was conceived in broad object relational and psychodynamic terms. In contrast, DSM-III produced a definitive set of criteria and required that a subset be met before the diagnosis could be made.7 An example of this criteria-based model is shown in Box 1, which lists the DSM-IV-TR criteria for BPD.
Some psychiatrists objected that BPD was solely a psychoanalytic construct and too theoretical for inclusion in DSM-III. Others argued that if BPD were not defined, it would be difficult to study the clinical usefulness of that definition or any other. Nonetheless, many have argued that BPD does not exist, though to what category BPD patients should belong has changed over the years:
- Is BPD nothing more than a milder or unusual presentation of an affective disorder8 or actually bipolar II disorder?9
- Is it a presentation of posttraumatic stress disorder (PTSD) called “complex PTSD,”10-11 or an adult presentation of attention-deficit/ hyperactivity or other brain disorder?12
- Is it a stigmatizing diagnosis that we apply to patients whom we do not like?13
In truth, the diagnosis of BPD reflects a particular clinical presentation no more or less accurately than many of the well-accepted axis I disorders. Despite recent advances in the neurosciences, the dilemma we face as psychiatrists is that we make a diagnosis based upon what we see in the clinical setting (i.e., a phenotype). Yet in labeling what we believe is a specific psychiatric disorder, we make assumptions—for better or for worse, consciously or unconsciously—about pathophysiology and indirectly about genotype.
A pervasive pattern of instability of interpersonal relationships, self-image, and affects and marked impulsivity beginning by early adulthood and present in a variety of contexts, as indicated by five (or more) of the following:
- Frantic efforts to avoid real or imagined abandonment
- A pattern of unstable and intense interpersonal relationships characterized by alternating between extremes of idealization and devaluation
- Identity disturbance: markedly and persistent unstable self-image or sense of self
- Impulsivity in at least two areas that are potentially self-damaging (spending, sex, substance abuse, binge eating, reckless driving)
- Recurrent suicidal behavior, gestures, or threats; self-mutilating behavior
- Affective instability due to a marked reactivity of mood
- Chronic feelings of emptiness
- Inappropriate, intense anger or difficulty controlling anger
- Transient, stress-related paranoid ideation or severe dissociative symptoms
Source: DSM-IV6
Defining the borderline personality
Stern first used the term “borderline” in 1938 to describe patients who appeared to occupy the border between neurosis and psychosis.14 In 1942, Deutsch described the “as if” personality in patients who seemed chameleon-like. They could adapt or play the role demanded of them in specific situations, yet elsewhere—as in the analyst’s office—they had little sense of themselves and were thought to be internally disorganized and probably psychotic.15
Border to psychosis. The idea that borderline-type patients were psychotic continued in Hoch and Polatin’s description of the “pseudoneurotic schizophrenic,”16 a patient who appeared severely neurotic but was thought to employ many defenses and interpersonal styles to ward off a fundamental inner psychosis. Knight used the label “borderline states”17 to describe severely ill patients who were not frankly psychotic but fell within the realm of psychosis without qualifying for a diagnosis of schizophrenia. Knight was the first person to use the term “borderline” as a diagnostic entity, though simultaneously he argued against its use as a label because the term lacked precision.
Psychotic character. About the same time, Schmideberg characterized a group of patients whose emotional lability or affective reactivity seemed to be a consistent aspect of their clinical presentation. She believed this appearance of “stable instability”18 represented the patient’s characterologic adaptation to the world.
Frosch coined the term “psychotic character”19 that aptly captured both the characterologic and the border-to-psychosis aspects of these patients’ clinical picture. According to Frosch, these patients appeared to regress readily into psychotic thinking, yet they did not lose their ability to test reality.
Affective and emotional instability. Thus until the 1960s, the term borderline was applied primarily to patients who appeared to occupy the border between neurosis and psychosis but were thought to be closer to psychotic than neurotic. And this sitting close to the edge of psychosis appeared to be a stable condition.
Most of the attention up until this point had been paid to how these patients thought—with little attention to their affective lability or emotional instability, save for Schmideberg’s comments. In the 1960s, however, the term borderline was applied somewhat differently—not completely divorced from previous concepts but with greater emphasis on borderline as a stable but psychopathologic functioning of the personality that included affective and emotional instability and an impaired sense of self.
- Intense affect, usually depressive or hostile
- History of impulsive, often self-destructive behavior
- Social adaptiveness that may mask a disturbed identity
- Brief psychotic episodes, often paranoid and evident in unstructured situations
- “Loose thinking” or primitive answers on unstructured psychological tests
- Relationships vacillate between transient superficiality and intense dependency
Impaired personality organization. In 1967, Kernberg published a seminal article in the history of BPD diagnosis. Although he did not discuss the diagnosis of BPD, Kernberg did develop a concept concerning a specific organization of the personality based upon impaired object relations. This impaired organization could apply across several personality disorders. The construct, named borderline personality organization (BPO),20 was defined by:
- an impaired sense of identity and lack of integration of one’s own identity
- use of primitive defenses, including splitting, rage, and regression
- ability to test reality.
Kernberg’s theory is too complex to summarize here, but he—along with Roy Grinker—is responsible for placing BPD on the diagnostic map. He was the first to describe BPO (and by extension BPD) in terms of a personality disorder.
Grinker’s ‘core’ group. Almost simultaneously (in 1968), Grinker published a careful study of 50 hospitalized patients. His work on the “borderline syndrome”21 revealed four subgroups to which the label of borderline had been applied:
- those occupying the border with psychosis
- those occupying the border with neurosis
- those similar to Deutsch’s “as if” group
- the “core” borderline group.
The core group—with its symptoms of anger and loneliness, a nonintegrated sense of self, and labile and oscillating interpersonal relationships— defined patients closest to our current definition.
Six criteria for BPD. In 1975, Gunderson and Singer published an article that greatly influenced our definition of BPD. They reviewed major descriptive accounts of BPD or BPD-like syndromes22 and proposed six diagnostic criteria (Box 2), though they did not identify a specific number or subset of the criteria as needing to be met for the diagnosis. (It is important to note that the term BPD did not become official for 5 more years.)
DSM-IV’s definition of BPD retains four of Gunderson and Singer‘s criteria among the nine it lists (five being necessary for a diagnosis of BPD). Missing are:
- social adaptiveness—though DSM-IV does say that social adaptiveness may be superficial (as in the “as if” personality) and may hide a disturbed identity6
- and the criterion relating to psychological test performance (this omission reflects a movement since 1980 away from listing “psychological” or psychodynamic criteria in the DSM).
DSM-III. BPD was included in DSM-III7 following an important study that tried to determine whether the term “borderline” refers to patients at the border of psychosis or to a stable group with mood instability and affective lability as part of a personality disorder. Spitzer et al23 asked 808 clinicians to describe patients they would label as borderline and to use 22 items gleaned from the literature to score two of their own patients:
- one patient who the clinician felt truly had borderline personality, borderline personality organization, or borderline schizophrenia
- and a control patient who was not diagnosed as psychotic and did not fall into any borderline category.
- The concept of abandonment, introduced in DSM-III-R, replaced the concept of aloneness in DSM-III.
- In DSM-III and DSM-III-R, a patient needed to meet 5 of 8 criteria for a diagnosis of BPD.
- DSM-IV introduced the ninth criterion, “transient, stress-related paranoid ideation or severe dissociative symptoms.” Since then, a patient has needed to meet 5 of 9 criteria for a diagnosis of BPD.
Their responses showed that BPD and schizotypal personality disorder (SPD) were separate, independent (though not mutually exclusive) disorders. Spitzer et al preserved the “schizotypal” label in DSM-III to describe the personality disorder that closely matched the border-to-psychosis subset. The other criteria set, which they labeled the “unstable personality item set,” was renamed “borderline” in DSM-III to describe the personality disorder that closely matched the emotional lability subset.
From one DSM edition to another, the concept of brief transient psychotic episodes has been included in and excluded from the diagnosis of borderline personality disorder (BPD).
In DSM-III. Because of work by Spitzer et al, these “experiences” were placed within schizotypal personality disorder (SPD) in DSM-III in 1980, though historically they had always been within the borderline concept and were one of Gunderson and Singer’s six criteria for diagnosing BPD (Box 2).22
Out of DSM-III-R. Research in the late 1980s suggested that when patients with BPD were depressed, they had a greater tendency to have psychotic–like episodes.24 Evidence indicated that attributing these psychotic and dissociative phenomena to SPD, rather than—perhaps more appropriately—to BPD, was one of the main reasons for the overlap between the definitions of BPD and SPD.25 Therefore, in DSM-III-R, the transient psychotic/dissociative criterion was removed from the SPD criteria set.
Back in DSM-IV. The criterion “transient stress-related paranoid ideation or severe dissociative symptoms” was placed into the BPD criteria set in DSM-IV. In DSM-IV, these symptoms were further characterized as usually not of “sufficient severity or duration to warrant an additional diagnosis.”
What is “sufficient” duration? The psychotic episodes of BPD last for minutes to hours and often appear when the patient imagines being (or actually is) abandoned by others. Not all agree that the criteria for BPD are met if these episodes last longer (e.g.,a day or two). In that case, they may exceed the transient time frame. More research is needed to better understand the quality and duration of these psychotic-like phenomena.
Not everyone agrees with renaming the unstable set “borderline” because the word:
- has always been ambiguous
- does not connote or denote any specific criteria or characteristic of patients who bear the label
- brands the patient as untreatable, defiant, or just “bad.”
Post-DSM-III: Where are we now?
From DSM-III evolved the hope that psychiatry could describe valid, well-defined diagnostic categories. Lost in the DSM-III enthusiasm was the fact that the categories were based upon theoretic constructs—theories no more or less valid than other theories that had preceded them. Because some of these categories were based upon empiric data— such as the Spitzer et al study—these diagnoses were perceived as more valid and more related to pathophysiology and perhaps genotype than prior constructs and definitions.
In the 1980s and early 1990s, a proliferation of studies attempted to examine the validity and reliability of DSM-III definitions, and BPD became the most studied of the personality disorders. The BPD concept took hold, even though several studies did not support it and despite refinements in subsequent DSM editions (Box 3).
One refinement in the BPD construct applied to transient psychotic or psychotic-like experiences, including dissociative phenomena. Yet questions remain about the duration of these transient episodes (Box 4).
Categorical versus dimensional
The categorical concept of BPD is facing new scrutiny,26,27 as recent studies have implied that biological disturbances may be spread across a number of personality disorders.28 If biological findings are found to be more closely allied with genotypic variations (alleles),29 then perhaps a dimensional classification system is needed for BPD and personality disorders in general.
On the other hand, categories provide a well-defined population that we can study and try to delineate from other populations, whereas dimensions—while perhaps closer to the reality of clinical presentation—may allow too much variability for research to proceed without confounding restraints.
BPD will continue to evolve, as will all psychiatric diagnostic categories, but the need to modify its definition does not negate its usefulness and clinical applicability. Most of our patients do not read the DSM before coming to us. They present with symptom complexes and problems that demand that we listen to what they say and understand who they are while we also try to fit them—as best we can—into categories or dimensions30 that help us choose the most appropriate interventions.
Related resources
- BPD Sanctuary (borderline personality disorder education, communities, support, books, and resources) http://www.mhsanctuary.com/borderline/ Borderline Central (resources for people who care about someone with borderline personality disorder) http://www.bpdcentral.com/
- Gunderson JG. Borderline personality disorder: a clinical guide. Washington, DC: American Psychiatric Publishing, Inc., 200l.
- Paris J (ed). Borderline personality disorder. Psych Clin N Am 2000;23:1 (entire volume devoted to BPD).
- Silk KR (ed). Biological and neurobehavioral studies of borderline personality disorder. Washington, DC: American Psychiatric Press, 1994.
1. Diagnostic and statistical manual of mental disorders (2nd ed). Washington, DC: American Psychiatric Association, 1968.
2. Feighner JP, Robins E, Guze SB, et al. Diagnostic criteria for use in psychiatric research. Arch Gen Psychiatry 1972;26:57-63.
3. Merikangas KR, Angst J, Eaton W, et al. Comorbidity and boundaries of affective disorders with anxiety disorders and substance misuse: results of an international task force. Br J Psychiatry 1996;30(suppl):58-67.
4. Nierenberg AA. DeCecco LM.Definitions of antidepressant treatment response, remission, nonresponse, partial response, and other relevant outcomes: a focus on treatment-resistant depression. J Clin Psychiatry 2001;62(suppl 16):5-9.
5. Stone MH (ed). Essential papers on borderline disorders: one hundred years at the border. New York: New York University Press, 1986.
6. Diagnostic and statistical manual of mental disorders (4th ed). Washington, DC: American Psychiatric Association, 1994.
7. Diagnostic and statistical manual of mental disorders (3rd ed). Washington, DC: American Psychiatric Association, 1980.
8. Akiskal HS. Subaffective disorders: dysthymic, cyclothymic and bipolar II disorders in the “borderline” realm. Psychiatric Clin N Am 1981;4:25-46.
9. Henry C, Mitropoulou V, New AS, et al. Affective instability and impulsivity in borderline personality and bipolar II disorders: similarities and differences. J Psychiatric Res 2001;35:307-12.
10. Herman JL, van der Kolk BA. Traumatic antecedents of borderline personality disorder. In: van der Kolk, BA. Psychological trauma. Washington, DC: American Psychiatric Press, 1987;111-26.
11. Silk KR, Lee S, Hill EM, Lohr NE. Borderline symptoms and severity of sexual abuse. Am J Psychiatry 1995;152:1059-64.
12. Streeter CC, Van Reekum R, Shorr RI, Bachman DL. Prior head injury in male veterans with borderline personality disorder. J Nerv Ment Dis 1995;183:577-81.
13. Maltsberger JT. Countertransference in borderline conditions: some further notes. Int J Psychoanal Psychother 1982-83;9:125-34.
14. Stern A. Psychoanalytic investigation and therapy in the borderline group of neuroses. Psychoanal Q 1938;7:467-89.
15. Deutsch H. Some forms of emotional disturbance and their relationship to schizophrenia. Psychoanal Q 1942;11:301-21.
16. Hoch P, Polatin P. Pseudoneurotic forms of schizophrenia. Psychiatric Q 1949;23:248-76.
17. Knight R. Borderline states. Bull Menn Clin 1953;17:1-12.
18. Schmideberg M. The treatment of psychopaths and borderline patients. Am J Psychotherapy 1947;1:45-70.
19. Frosch J. The psychotic character: clinical psychiatric considerations. Psychiatric Q 1964;38:81-96.
20. Kernberg O. Borderline personality organization. J Am Psychoanal Assoc 1967;15:641-85.
21. Grinker RR, Werble B, Drye R. The borderline syndrome: a behavioral study of ego functions. New York: Basic Books, 1968.
22. Gunderson JG, Singer MT. Defining borderline patients: an overview. Am J Psychiatry 1975;132:1-10.
23. Spitzer RL, Endicott J, Gibbon M. Crossing the border into borderline personality and borderline schizophrenia: the development of criteria. Arch Gen Psychiatry 1979;36:17-24.
24. Silk KR, Lohr NE, Westen D, Goodrich S. Psychosis in borderline patients with depression. J Personality Disord 1989;3:92-100.
25. Silk KR, Westen D, Lohr NE, et al. DSM-III and DSM-III-R schizotypal symptoms in borderline personality disorder. Comprehen Psychiatry 1990;31:103-10.
26. Livesley WJ, Jang KL, Vernon PA. Phenotypic and genetic structure of traits delineating personality disorder. Arch Gen Psychiatry 1998;55:941-8.
27. McCrae RR, Yang J, Costa PT, Jr, et al. Personality profiles and the prediction of categorical personality disorders. J Personality 2001;69:155-74.
28. Siever LJ, Davis KL. A psychobiological perspective on the personality disorders. Am J Psychiatry 1991;148:1647-58.
29. New AS, Gelernter J, Goodman M, et al. Suicide, impulsive aggression, and HTR1B genotype. Biolog Psychiatry 2001;50:62-5.
30. Oldham JM, Skodol AE. Charting the future of axis II. J Personality Disord 2000;14:17-29.
Not everyone agrees that borderline personality disorder (BPD) should be a diagnostic category. BPD became “official” with DSM-III in 1980, although the term had been used for 40 years to describe various patient groups. Being listed in DSM-III legitimized BPD, which was thought to represent a specific—though not necessarily distinct—diagnostic category.
The history of the BPD diagnosis and opinions as to its usefulness can be viewed as a microcosm of psychiatric diagnosis in general. Before DSM-III, diagnoses were broadly defined and did not contain specific inclusion or exclusion criteria.1 For the 5 to 10 years prior to DSM-III, however, two assumptions developed:
- distinct diagnostic categories did, in fact, exist
- by rigorously defining and studying those categories we could develop more specific and effective treatments for our patients.2
The specificity and exclusivity that we assumed we could achieve by categorical diagnoses, however, remain a distant wish. Comorbidity appears more common in psychiatry than was originally thought and confounds both treatment and outcome.3 Also, many patients appear treatment-resistant, despite fitting neatly into diagnostic categories.4
Miss A, age 35, presents to the emergency room with a long history of intermittent depression and self-mutilation. She has never been hospitalized nor on psychotropic medication but has been in and out of psychotherapy for years. She has had intermittent depressive episodes for many years, though the episodes often lasted 2 to 3 weeks and appeared to correct themselves spontaneously.
Agitated and afraid. She is extremely agitated when she arrives at the emergency department. She has hardly slept or eaten but insists she is not hungry. She reports that she cannot concentrate or do her work as an accountant. She says she is hearing voices, knows they are in her head, but nonetheless is terrified that something horrible is about to happen—though she cannot say what it might be.
Voice ‘calling my name.’ When the psychiatric resident inquires further, Miss A says a male voice is calling her name and mumbling some short phrase she cannot understand. She says she has heard the voice the last few days, perhaps for 10 to 15 minutes every few hours, particularly when she ruminates about how she messed up a relationship with her now ex-boyfriend. The breakup occurred 1 week ago.
Feeling detached. She claims she has never heard voices before but describes periods when she has felt detached and unreal. Often these were short-term dissociative episodes that occurred in the wake of what she perceived as a personal failure or a distressful interpersonal encounter (often with a man). Relationships frequently were very difficult for her, and she felt she could easily go from infatuation to detesting someone.
Diagnosis? Talking appears to calm her down. After being in the emergency room for 2 hours, she says she no longer hears the voice. The resident tells the attending psychiatrist he believes the patient is in a major depressive episode, perhaps a psychotic depression, and proposes starting antidepressant treatment. The attending argues that the patient appears to have borderline personality disorder and suggests that she be sent home without medication and given an appointment to the outpatient clinic within the next few days.
As psychiatry considers DSM-V, questions linger as to whether BPD (and personality disorder in general) should remain as a categorical diagnosis or if dimensional measures may be more appropriate. Dimensions imply that no one ever fits into a given box because no specific box exists. Rather, patients are described as being closer to or more distant from a prototypic model of the diagnosis. In personality disorders, the dimensions most often mentioned are cognition, impulsivity, emotional lability, environmental hyperreactivity, and anxiety. The case report (above) illustrates the interplay of these dimensions in a typical patient with presumed BPD.
What’s in a name?
The symptom complex or syndrome that bears the name borderline personality disorder has probably existed for as long as people have thought about patients in psychopathologic terms.5 Before 1980, the term “borderline” applied primarily to two separate but overlapping concepts:
- Patients thought to reside on the “border” with psychosis, such as the patient in our case example. They seemed to have an underlying psychotic disorder, but the psychosis—if it surfaced—appeared briefly, was not exceptionally deep or firmly held, and was not regularly evident or immediately accessible to the clinician.
- Patients who appeared to occupy the space between neurosis and psychosis. This concept evolved into the idea of a character or personality disorder distinguished primarily by unstable interpersonal relationships, a confused or inconsistent sense of identity, and emotional instability.
How DSM is changing. Comparing the disorders listed in DSM-IV (1994)6 versus DSM-II (1968)1 suggests that psychiatry has become enamored of the naming process. For example, DSM-II lists anxiety neurosis (300.0), phobic neurosis (300.2), and obsessive-compulsive neurosis (300.3), whereas DSM-IV lists 11 different categories of anxiety disorders.
But beyond naming, subsequent DSMs have differed even more dramatically from DSM-II. We have seen a shift from describing a diagnostic category with a simple explanatory paragraph to lists of specific inclusion and exclusion criteria. These more-specific lists imply that they define categories closer to some reality or authenticity than did previous definitions.
Before DSM-III, the borderline concept was conceived in broad object relational and psychodynamic terms. In contrast, DSM-III produced a definitive set of criteria and required that a subset be met before the diagnosis could be made.7 An example of this criteria-based model is shown in Box 1, which lists the DSM-IV-TR criteria for BPD.
Some psychiatrists objected that BPD was solely a psychoanalytic construct and too theoretical for inclusion in DSM-III. Others argued that if BPD were not defined, it would be difficult to study the clinical usefulness of that definition or any other. Nonetheless, many have argued that BPD does not exist, though to what category BPD patients should belong has changed over the years:
- Is BPD nothing more than a milder or unusual presentation of an affective disorder8 or actually bipolar II disorder?9
- Is it a presentation of posttraumatic stress disorder (PTSD) called “complex PTSD,”10-11 or an adult presentation of attention-deficit/ hyperactivity or other brain disorder?12
- Is it a stigmatizing diagnosis that we apply to patients whom we do not like?13
In truth, the diagnosis of BPD reflects a particular clinical presentation no more or less accurately than many of the well-accepted axis I disorders. Despite recent advances in the neurosciences, the dilemma we face as psychiatrists is that we make a diagnosis based upon what we see in the clinical setting (i.e., a phenotype). Yet in labeling what we believe is a specific psychiatric disorder, we make assumptions—for better or for worse, consciously or unconsciously—about pathophysiology and indirectly about genotype.
A pervasive pattern of instability of interpersonal relationships, self-image, and affects and marked impulsivity beginning by early adulthood and present in a variety of contexts, as indicated by five (or more) of the following:
- Frantic efforts to avoid real or imagined abandonment
- A pattern of unstable and intense interpersonal relationships characterized by alternating between extremes of idealization and devaluation
- Identity disturbance: markedly and persistent unstable self-image or sense of self
- Impulsivity in at least two areas that are potentially self-damaging (spending, sex, substance abuse, binge eating, reckless driving)
- Recurrent suicidal behavior, gestures, or threats; self-mutilating behavior
- Affective instability due to a marked reactivity of mood
- Chronic feelings of emptiness
- Inappropriate, intense anger or difficulty controlling anger
- Transient, stress-related paranoid ideation or severe dissociative symptoms
Source: DSM-IV6
Defining the borderline personality
Stern first used the term “borderline” in 1938 to describe patients who appeared to occupy the border between neurosis and psychosis.14 In 1942, Deutsch described the “as if” personality in patients who seemed chameleon-like. They could adapt or play the role demanded of them in specific situations, yet elsewhere—as in the analyst’s office—they had little sense of themselves and were thought to be internally disorganized and probably psychotic.15
Border to psychosis. The idea that borderline-type patients were psychotic continued in Hoch and Polatin’s description of the “pseudoneurotic schizophrenic,”16 a patient who appeared severely neurotic but was thought to employ many defenses and interpersonal styles to ward off a fundamental inner psychosis. Knight used the label “borderline states”17 to describe severely ill patients who were not frankly psychotic but fell within the realm of psychosis without qualifying for a diagnosis of schizophrenia. Knight was the first person to use the term “borderline” as a diagnostic entity, though simultaneously he argued against its use as a label because the term lacked precision.
Psychotic character. About the same time, Schmideberg characterized a group of patients whose emotional lability or affective reactivity seemed to be a consistent aspect of their clinical presentation. She believed this appearance of “stable instability”18 represented the patient’s characterologic adaptation to the world.
Frosch coined the term “psychotic character”19 that aptly captured both the characterologic and the border-to-psychosis aspects of these patients’ clinical picture. According to Frosch, these patients appeared to regress readily into psychotic thinking, yet they did not lose their ability to test reality.
Affective and emotional instability. Thus until the 1960s, the term borderline was applied primarily to patients who appeared to occupy the border between neurosis and psychosis but were thought to be closer to psychotic than neurotic. And this sitting close to the edge of psychosis appeared to be a stable condition.
Most of the attention up until this point had been paid to how these patients thought—with little attention to their affective lability or emotional instability, save for Schmideberg’s comments. In the 1960s, however, the term borderline was applied somewhat differently—not completely divorced from previous concepts but with greater emphasis on borderline as a stable but psychopathologic functioning of the personality that included affective and emotional instability and an impaired sense of self.
- Intense affect, usually depressive or hostile
- History of impulsive, often self-destructive behavior
- Social adaptiveness that may mask a disturbed identity
- Brief psychotic episodes, often paranoid and evident in unstructured situations
- “Loose thinking” or primitive answers on unstructured psychological tests
- Relationships vacillate between transient superficiality and intense dependency
Impaired personality organization. In 1967, Kernberg published a seminal article in the history of BPD diagnosis. Although he did not discuss the diagnosis of BPD, Kernberg did develop a concept concerning a specific organization of the personality based upon impaired object relations. This impaired organization could apply across several personality disorders. The construct, named borderline personality organization (BPO),20 was defined by:
- an impaired sense of identity and lack of integration of one’s own identity
- use of primitive defenses, including splitting, rage, and regression
- ability to test reality.
Kernberg’s theory is too complex to summarize here, but he—along with Roy Grinker—is responsible for placing BPD on the diagnostic map. He was the first to describe BPO (and by extension BPD) in terms of a personality disorder.
Grinker’s ‘core’ group. Almost simultaneously (in 1968), Grinker published a careful study of 50 hospitalized patients. His work on the “borderline syndrome”21 revealed four subgroups to which the label of borderline had been applied:
- those occupying the border with psychosis
- those occupying the border with neurosis
- those similar to Deutsch’s “as if” group
- the “core” borderline group.
The core group—with its symptoms of anger and loneliness, a nonintegrated sense of self, and labile and oscillating interpersonal relationships— defined patients closest to our current definition.
Six criteria for BPD. In 1975, Gunderson and Singer published an article that greatly influenced our definition of BPD. They reviewed major descriptive accounts of BPD or BPD-like syndromes22 and proposed six diagnostic criteria (Box 2), though they did not identify a specific number or subset of the criteria as needing to be met for the diagnosis. (It is important to note that the term BPD did not become official for 5 more years.)
DSM-IV’s definition of BPD retains four of Gunderson and Singer‘s criteria among the nine it lists (five being necessary for a diagnosis of BPD). Missing are:
- social adaptiveness—though DSM-IV does say that social adaptiveness may be superficial (as in the “as if” personality) and may hide a disturbed identity6
- and the criterion relating to psychological test performance (this omission reflects a movement since 1980 away from listing “psychological” or psychodynamic criteria in the DSM).
DSM-III. BPD was included in DSM-III7 following an important study that tried to determine whether the term “borderline” refers to patients at the border of psychosis or to a stable group with mood instability and affective lability as part of a personality disorder. Spitzer et al23 asked 808 clinicians to describe patients they would label as borderline and to use 22 items gleaned from the literature to score two of their own patients:
- one patient who the clinician felt truly had borderline personality, borderline personality organization, or borderline schizophrenia
- and a control patient who was not diagnosed as psychotic and did not fall into any borderline category.
- The concept of abandonment, introduced in DSM-III-R, replaced the concept of aloneness in DSM-III.
- In DSM-III and DSM-III-R, a patient needed to meet 5 of 8 criteria for a diagnosis of BPD.
- DSM-IV introduced the ninth criterion, “transient, stress-related paranoid ideation or severe dissociative symptoms.” Since then, a patient has needed to meet 5 of 9 criteria for a diagnosis of BPD.
Their responses showed that BPD and schizotypal personality disorder (SPD) were separate, independent (though not mutually exclusive) disorders. Spitzer et al preserved the “schizotypal” label in DSM-III to describe the personality disorder that closely matched the border-to-psychosis subset. The other criteria set, which they labeled the “unstable personality item set,” was renamed “borderline” in DSM-III to describe the personality disorder that closely matched the emotional lability subset.
From one DSM edition to another, the concept of brief transient psychotic episodes has been included in and excluded from the diagnosis of borderline personality disorder (BPD).
In DSM-III. Because of work by Spitzer et al, these “experiences” were placed within schizotypal personality disorder (SPD) in DSM-III in 1980, though historically they had always been within the borderline concept and were one of Gunderson and Singer’s six criteria for diagnosing BPD (Box 2).22
Out of DSM-III-R. Research in the late 1980s suggested that when patients with BPD were depressed, they had a greater tendency to have psychotic–like episodes.24 Evidence indicated that attributing these psychotic and dissociative phenomena to SPD, rather than—perhaps more appropriately—to BPD, was one of the main reasons for the overlap between the definitions of BPD and SPD.25 Therefore, in DSM-III-R, the transient psychotic/dissociative criterion was removed from the SPD criteria set.
Back in DSM-IV. The criterion “transient stress-related paranoid ideation or severe dissociative symptoms” was placed into the BPD criteria set in DSM-IV. In DSM-IV, these symptoms were further characterized as usually not of “sufficient severity or duration to warrant an additional diagnosis.”
What is “sufficient” duration? The psychotic episodes of BPD last for minutes to hours and often appear when the patient imagines being (or actually is) abandoned by others. Not all agree that the criteria for BPD are met if these episodes last longer (e.g.,a day or two). In that case, they may exceed the transient time frame. More research is needed to better understand the quality and duration of these psychotic-like phenomena.
Not everyone agrees with renaming the unstable set “borderline” because the word:
- has always been ambiguous
- does not connote or denote any specific criteria or characteristic of patients who bear the label
- brands the patient as untreatable, defiant, or just “bad.”
Post-DSM-III: Where are we now?
From DSM-III evolved the hope that psychiatry could describe valid, well-defined diagnostic categories. Lost in the DSM-III enthusiasm was the fact that the categories were based upon theoretic constructs—theories no more or less valid than other theories that had preceded them. Because some of these categories were based upon empiric data— such as the Spitzer et al study—these diagnoses were perceived as more valid and more related to pathophysiology and perhaps genotype than prior constructs and definitions.
In the 1980s and early 1990s, a proliferation of studies attempted to examine the validity and reliability of DSM-III definitions, and BPD became the most studied of the personality disorders. The BPD concept took hold, even though several studies did not support it and despite refinements in subsequent DSM editions (Box 3).
One refinement in the BPD construct applied to transient psychotic or psychotic-like experiences, including dissociative phenomena. Yet questions remain about the duration of these transient episodes (Box 4).
Categorical versus dimensional
The categorical concept of BPD is facing new scrutiny,26,27 as recent studies have implied that biological disturbances may be spread across a number of personality disorders.28 If biological findings are found to be more closely allied with genotypic variations (alleles),29 then perhaps a dimensional classification system is needed for BPD and personality disorders in general.
On the other hand, categories provide a well-defined population that we can study and try to delineate from other populations, whereas dimensions—while perhaps closer to the reality of clinical presentation—may allow too much variability for research to proceed without confounding restraints.
BPD will continue to evolve, as will all psychiatric diagnostic categories, but the need to modify its definition does not negate its usefulness and clinical applicability. Most of our patients do not read the DSM before coming to us. They present with symptom complexes and problems that demand that we listen to what they say and understand who they are while we also try to fit them—as best we can—into categories or dimensions30 that help us choose the most appropriate interventions.
Related resources
- BPD Sanctuary (borderline personality disorder education, communities, support, books, and resources) http://www.mhsanctuary.com/borderline/ Borderline Central (resources for people who care about someone with borderline personality disorder) http://www.bpdcentral.com/
- Gunderson JG. Borderline personality disorder: a clinical guide. Washington, DC: American Psychiatric Publishing, Inc., 200l.
- Paris J (ed). Borderline personality disorder. Psych Clin N Am 2000;23:1 (entire volume devoted to BPD).
- Silk KR (ed). Biological and neurobehavioral studies of borderline personality disorder. Washington, DC: American Psychiatric Press, 1994.
Not everyone agrees that borderline personality disorder (BPD) should be a diagnostic category. BPD became “official” with DSM-III in 1980, although the term had been used for 40 years to describe various patient groups. Being listed in DSM-III legitimized BPD, which was thought to represent a specific—though not necessarily distinct—diagnostic category.
The history of the BPD diagnosis and opinions as to its usefulness can be viewed as a microcosm of psychiatric diagnosis in general. Before DSM-III, diagnoses were broadly defined and did not contain specific inclusion or exclusion criteria.1 For the 5 to 10 years prior to DSM-III, however, two assumptions developed:
- distinct diagnostic categories did, in fact, exist
- by rigorously defining and studying those categories we could develop more specific and effective treatments for our patients.2
The specificity and exclusivity that we assumed we could achieve by categorical diagnoses, however, remain a distant wish. Comorbidity appears more common in psychiatry than was originally thought and confounds both treatment and outcome.3 Also, many patients appear treatment-resistant, despite fitting neatly into diagnostic categories.4
Miss A, age 35, presents to the emergency room with a long history of intermittent depression and self-mutilation. She has never been hospitalized nor on psychotropic medication but has been in and out of psychotherapy for years. She has had intermittent depressive episodes for many years, though the episodes often lasted 2 to 3 weeks and appeared to correct themselves spontaneously.
Agitated and afraid. She is extremely agitated when she arrives at the emergency department. She has hardly slept or eaten but insists she is not hungry. She reports that she cannot concentrate or do her work as an accountant. She says she is hearing voices, knows they are in her head, but nonetheless is terrified that something horrible is about to happen—though she cannot say what it might be.
Voice ‘calling my name.’ When the psychiatric resident inquires further, Miss A says a male voice is calling her name and mumbling some short phrase she cannot understand. She says she has heard the voice the last few days, perhaps for 10 to 15 minutes every few hours, particularly when she ruminates about how she messed up a relationship with her now ex-boyfriend. The breakup occurred 1 week ago.
Feeling detached. She claims she has never heard voices before but describes periods when she has felt detached and unreal. Often these were short-term dissociative episodes that occurred in the wake of what she perceived as a personal failure or a distressful interpersonal encounter (often with a man). Relationships frequently were very difficult for her, and she felt she could easily go from infatuation to detesting someone.
Diagnosis? Talking appears to calm her down. After being in the emergency room for 2 hours, she says she no longer hears the voice. The resident tells the attending psychiatrist he believes the patient is in a major depressive episode, perhaps a psychotic depression, and proposes starting antidepressant treatment. The attending argues that the patient appears to have borderline personality disorder and suggests that she be sent home without medication and given an appointment to the outpatient clinic within the next few days.
As psychiatry considers DSM-V, questions linger as to whether BPD (and personality disorder in general) should remain as a categorical diagnosis or if dimensional measures may be more appropriate. Dimensions imply that no one ever fits into a given box because no specific box exists. Rather, patients are described as being closer to or more distant from a prototypic model of the diagnosis. In personality disorders, the dimensions most often mentioned are cognition, impulsivity, emotional lability, environmental hyperreactivity, and anxiety. The case report (above) illustrates the interplay of these dimensions in a typical patient with presumed BPD.
What’s in a name?
The symptom complex or syndrome that bears the name borderline personality disorder has probably existed for as long as people have thought about patients in psychopathologic terms.5 Before 1980, the term “borderline” applied primarily to two separate but overlapping concepts:
- Patients thought to reside on the “border” with psychosis, such as the patient in our case example. They seemed to have an underlying psychotic disorder, but the psychosis—if it surfaced—appeared briefly, was not exceptionally deep or firmly held, and was not regularly evident or immediately accessible to the clinician.
- Patients who appeared to occupy the space between neurosis and psychosis. This concept evolved into the idea of a character or personality disorder distinguished primarily by unstable interpersonal relationships, a confused or inconsistent sense of identity, and emotional instability.
How DSM is changing. Comparing the disorders listed in DSM-IV (1994)6 versus DSM-II (1968)1 suggests that psychiatry has become enamored of the naming process. For example, DSM-II lists anxiety neurosis (300.0), phobic neurosis (300.2), and obsessive-compulsive neurosis (300.3), whereas DSM-IV lists 11 different categories of anxiety disorders.
But beyond naming, subsequent DSMs have differed even more dramatically from DSM-II. We have seen a shift from describing a diagnostic category with a simple explanatory paragraph to lists of specific inclusion and exclusion criteria. These more-specific lists imply that they define categories closer to some reality or authenticity than did previous definitions.
Before DSM-III, the borderline concept was conceived in broad object relational and psychodynamic terms. In contrast, DSM-III produced a definitive set of criteria and required that a subset be met before the diagnosis could be made.7 An example of this criteria-based model is shown in Box 1, which lists the DSM-IV-TR criteria for BPD.
Some psychiatrists objected that BPD was solely a psychoanalytic construct and too theoretical for inclusion in DSM-III. Others argued that if BPD were not defined, it would be difficult to study the clinical usefulness of that definition or any other. Nonetheless, many have argued that BPD does not exist, though to what category BPD patients should belong has changed over the years:
- Is BPD nothing more than a milder or unusual presentation of an affective disorder8 or actually bipolar II disorder?9
- Is it a presentation of posttraumatic stress disorder (PTSD) called “complex PTSD,”10-11 or an adult presentation of attention-deficit/ hyperactivity or other brain disorder?12
- Is it a stigmatizing diagnosis that we apply to patients whom we do not like?13
In truth, the diagnosis of BPD reflects a particular clinical presentation no more or less accurately than many of the well-accepted axis I disorders. Despite recent advances in the neurosciences, the dilemma we face as psychiatrists is that we make a diagnosis based upon what we see in the clinical setting (i.e., a phenotype). Yet in labeling what we believe is a specific psychiatric disorder, we make assumptions—for better or for worse, consciously or unconsciously—about pathophysiology and indirectly about genotype.
A pervasive pattern of instability of interpersonal relationships, self-image, and affects and marked impulsivity beginning by early adulthood and present in a variety of contexts, as indicated by five (or more) of the following:
- Frantic efforts to avoid real or imagined abandonment
- A pattern of unstable and intense interpersonal relationships characterized by alternating between extremes of idealization and devaluation
- Identity disturbance: markedly and persistent unstable self-image or sense of self
- Impulsivity in at least two areas that are potentially self-damaging (spending, sex, substance abuse, binge eating, reckless driving)
- Recurrent suicidal behavior, gestures, or threats; self-mutilating behavior
- Affective instability due to a marked reactivity of mood
- Chronic feelings of emptiness
- Inappropriate, intense anger or difficulty controlling anger
- Transient, stress-related paranoid ideation or severe dissociative symptoms
Source: DSM-IV6
Defining the borderline personality
Stern first used the term “borderline” in 1938 to describe patients who appeared to occupy the border between neurosis and psychosis.14 In 1942, Deutsch described the “as if” personality in patients who seemed chameleon-like. They could adapt or play the role demanded of them in specific situations, yet elsewhere—as in the analyst’s office—they had little sense of themselves and were thought to be internally disorganized and probably psychotic.15
Border to psychosis. The idea that borderline-type patients were psychotic continued in Hoch and Polatin’s description of the “pseudoneurotic schizophrenic,”16 a patient who appeared severely neurotic but was thought to employ many defenses and interpersonal styles to ward off a fundamental inner psychosis. Knight used the label “borderline states”17 to describe severely ill patients who were not frankly psychotic but fell within the realm of psychosis without qualifying for a diagnosis of schizophrenia. Knight was the first person to use the term “borderline” as a diagnostic entity, though simultaneously he argued against its use as a label because the term lacked precision.
Psychotic character. About the same time, Schmideberg characterized a group of patients whose emotional lability or affective reactivity seemed to be a consistent aspect of their clinical presentation. She believed this appearance of “stable instability”18 represented the patient’s characterologic adaptation to the world.
Frosch coined the term “psychotic character”19 that aptly captured both the characterologic and the border-to-psychosis aspects of these patients’ clinical picture. According to Frosch, these patients appeared to regress readily into psychotic thinking, yet they did not lose their ability to test reality.
Affective and emotional instability. Thus until the 1960s, the term borderline was applied primarily to patients who appeared to occupy the border between neurosis and psychosis but were thought to be closer to psychotic than neurotic. And this sitting close to the edge of psychosis appeared to be a stable condition.
Most of the attention up until this point had been paid to how these patients thought—with little attention to their affective lability or emotional instability, save for Schmideberg’s comments. In the 1960s, however, the term borderline was applied somewhat differently—not completely divorced from previous concepts but with greater emphasis on borderline as a stable but psychopathologic functioning of the personality that included affective and emotional instability and an impaired sense of self.
- Intense affect, usually depressive or hostile
- History of impulsive, often self-destructive behavior
- Social adaptiveness that may mask a disturbed identity
- Brief psychotic episodes, often paranoid and evident in unstructured situations
- “Loose thinking” or primitive answers on unstructured psychological tests
- Relationships vacillate between transient superficiality and intense dependency
Impaired personality organization. In 1967, Kernberg published a seminal article in the history of BPD diagnosis. Although he did not discuss the diagnosis of BPD, Kernberg did develop a concept concerning a specific organization of the personality based upon impaired object relations. This impaired organization could apply across several personality disorders. The construct, named borderline personality organization (BPO),20 was defined by:
- an impaired sense of identity and lack of integration of one’s own identity
- use of primitive defenses, including splitting, rage, and regression
- ability to test reality.
Kernberg’s theory is too complex to summarize here, but he—along with Roy Grinker—is responsible for placing BPD on the diagnostic map. He was the first to describe BPO (and by extension BPD) in terms of a personality disorder.
Grinker’s ‘core’ group. Almost simultaneously (in 1968), Grinker published a careful study of 50 hospitalized patients. His work on the “borderline syndrome”21 revealed four subgroups to which the label of borderline had been applied:
- those occupying the border with psychosis
- those occupying the border with neurosis
- those similar to Deutsch’s “as if” group
- the “core” borderline group.
The core group—with its symptoms of anger and loneliness, a nonintegrated sense of self, and labile and oscillating interpersonal relationships— defined patients closest to our current definition.
Six criteria for BPD. In 1975, Gunderson and Singer published an article that greatly influenced our definition of BPD. They reviewed major descriptive accounts of BPD or BPD-like syndromes22 and proposed six diagnostic criteria (Box 2), though they did not identify a specific number or subset of the criteria as needing to be met for the diagnosis. (It is important to note that the term BPD did not become official for 5 more years.)
DSM-IV’s definition of BPD retains four of Gunderson and Singer‘s criteria among the nine it lists (five being necessary for a diagnosis of BPD). Missing are:
- social adaptiveness—though DSM-IV does say that social adaptiveness may be superficial (as in the “as if” personality) and may hide a disturbed identity6
- and the criterion relating to psychological test performance (this omission reflects a movement since 1980 away from listing “psychological” or psychodynamic criteria in the DSM).
DSM-III. BPD was included in DSM-III7 following an important study that tried to determine whether the term “borderline” refers to patients at the border of psychosis or to a stable group with mood instability and affective lability as part of a personality disorder. Spitzer et al23 asked 808 clinicians to describe patients they would label as borderline and to use 22 items gleaned from the literature to score two of their own patients:
- one patient who the clinician felt truly had borderline personality, borderline personality organization, or borderline schizophrenia
- and a control patient who was not diagnosed as psychotic and did not fall into any borderline category.
- The concept of abandonment, introduced in DSM-III-R, replaced the concept of aloneness in DSM-III.
- In DSM-III and DSM-III-R, a patient needed to meet 5 of 8 criteria for a diagnosis of BPD.
- DSM-IV introduced the ninth criterion, “transient, stress-related paranoid ideation or severe dissociative symptoms.” Since then, a patient has needed to meet 5 of 9 criteria for a diagnosis of BPD.
Their responses showed that BPD and schizotypal personality disorder (SPD) were separate, independent (though not mutually exclusive) disorders. Spitzer et al preserved the “schizotypal” label in DSM-III to describe the personality disorder that closely matched the border-to-psychosis subset. The other criteria set, which they labeled the “unstable personality item set,” was renamed “borderline” in DSM-III to describe the personality disorder that closely matched the emotional lability subset.
From one DSM edition to another, the concept of brief transient psychotic episodes has been included in and excluded from the diagnosis of borderline personality disorder (BPD).
In DSM-III. Because of work by Spitzer et al, these “experiences” were placed within schizotypal personality disorder (SPD) in DSM-III in 1980, though historically they had always been within the borderline concept and were one of Gunderson and Singer’s six criteria for diagnosing BPD (Box 2).22
Out of DSM-III-R. Research in the late 1980s suggested that when patients with BPD were depressed, they had a greater tendency to have psychotic–like episodes.24 Evidence indicated that attributing these psychotic and dissociative phenomena to SPD, rather than—perhaps more appropriately—to BPD, was one of the main reasons for the overlap between the definitions of BPD and SPD.25 Therefore, in DSM-III-R, the transient psychotic/dissociative criterion was removed from the SPD criteria set.
Back in DSM-IV. The criterion “transient stress-related paranoid ideation or severe dissociative symptoms” was placed into the BPD criteria set in DSM-IV. In DSM-IV, these symptoms were further characterized as usually not of “sufficient severity or duration to warrant an additional diagnosis.”
What is “sufficient” duration? The psychotic episodes of BPD last for minutes to hours and often appear when the patient imagines being (or actually is) abandoned by others. Not all agree that the criteria for BPD are met if these episodes last longer (e.g.,a day or two). In that case, they may exceed the transient time frame. More research is needed to better understand the quality and duration of these psychotic-like phenomena.
Not everyone agrees with renaming the unstable set “borderline” because the word:
- has always been ambiguous
- does not connote or denote any specific criteria or characteristic of patients who bear the label
- brands the patient as untreatable, defiant, or just “bad.”
Post-DSM-III: Where are we now?
From DSM-III evolved the hope that psychiatry could describe valid, well-defined diagnostic categories. Lost in the DSM-III enthusiasm was the fact that the categories were based upon theoretic constructs—theories no more or less valid than other theories that had preceded them. Because some of these categories were based upon empiric data— such as the Spitzer et al study—these diagnoses were perceived as more valid and more related to pathophysiology and perhaps genotype than prior constructs and definitions.
In the 1980s and early 1990s, a proliferation of studies attempted to examine the validity and reliability of DSM-III definitions, and BPD became the most studied of the personality disorders. The BPD concept took hold, even though several studies did not support it and despite refinements in subsequent DSM editions (Box 3).
One refinement in the BPD construct applied to transient psychotic or psychotic-like experiences, including dissociative phenomena. Yet questions remain about the duration of these transient episodes (Box 4).
Categorical versus dimensional
The categorical concept of BPD is facing new scrutiny,26,27 as recent studies have implied that biological disturbances may be spread across a number of personality disorders.28 If biological findings are found to be more closely allied with genotypic variations (alleles),29 then perhaps a dimensional classification system is needed for BPD and personality disorders in general.
On the other hand, categories provide a well-defined population that we can study and try to delineate from other populations, whereas dimensions—while perhaps closer to the reality of clinical presentation—may allow too much variability for research to proceed without confounding restraints.
BPD will continue to evolve, as will all psychiatric diagnostic categories, but the need to modify its definition does not negate its usefulness and clinical applicability. Most of our patients do not read the DSM before coming to us. They present with symptom complexes and problems that demand that we listen to what they say and understand who they are while we also try to fit them—as best we can—into categories or dimensions30 that help us choose the most appropriate interventions.
Related resources
- BPD Sanctuary (borderline personality disorder education, communities, support, books, and resources) http://www.mhsanctuary.com/borderline/ Borderline Central (resources for people who care about someone with borderline personality disorder) http://www.bpdcentral.com/
- Gunderson JG. Borderline personality disorder: a clinical guide. Washington, DC: American Psychiatric Publishing, Inc., 200l.
- Paris J (ed). Borderline personality disorder. Psych Clin N Am 2000;23:1 (entire volume devoted to BPD).
- Silk KR (ed). Biological and neurobehavioral studies of borderline personality disorder. Washington, DC: American Psychiatric Press, 1994.
1. Diagnostic and statistical manual of mental disorders (2nd ed). Washington, DC: American Psychiatric Association, 1968.
2. Feighner JP, Robins E, Guze SB, et al. Diagnostic criteria for use in psychiatric research. Arch Gen Psychiatry 1972;26:57-63.
3. Merikangas KR, Angst J, Eaton W, et al. Comorbidity and boundaries of affective disorders with anxiety disorders and substance misuse: results of an international task force. Br J Psychiatry 1996;30(suppl):58-67.
4. Nierenberg AA. DeCecco LM.Definitions of antidepressant treatment response, remission, nonresponse, partial response, and other relevant outcomes: a focus on treatment-resistant depression. J Clin Psychiatry 2001;62(suppl 16):5-9.
5. Stone MH (ed). Essential papers on borderline disorders: one hundred years at the border. New York: New York University Press, 1986.
6. Diagnostic and statistical manual of mental disorders (4th ed). Washington, DC: American Psychiatric Association, 1994.
7. Diagnostic and statistical manual of mental disorders (3rd ed). Washington, DC: American Psychiatric Association, 1980.
8. Akiskal HS. Subaffective disorders: dysthymic, cyclothymic and bipolar II disorders in the “borderline” realm. Psychiatric Clin N Am 1981;4:25-46.
9. Henry C, Mitropoulou V, New AS, et al. Affective instability and impulsivity in borderline personality and bipolar II disorders: similarities and differences. J Psychiatric Res 2001;35:307-12.
10. Herman JL, van der Kolk BA. Traumatic antecedents of borderline personality disorder. In: van der Kolk, BA. Psychological trauma. Washington, DC: American Psychiatric Press, 1987;111-26.
11. Silk KR, Lee S, Hill EM, Lohr NE. Borderline symptoms and severity of sexual abuse. Am J Psychiatry 1995;152:1059-64.
12. Streeter CC, Van Reekum R, Shorr RI, Bachman DL. Prior head injury in male veterans with borderline personality disorder. J Nerv Ment Dis 1995;183:577-81.
13. Maltsberger JT. Countertransference in borderline conditions: some further notes. Int J Psychoanal Psychother 1982-83;9:125-34.
14. Stern A. Psychoanalytic investigation and therapy in the borderline group of neuroses. Psychoanal Q 1938;7:467-89.
15. Deutsch H. Some forms of emotional disturbance and their relationship to schizophrenia. Psychoanal Q 1942;11:301-21.
16. Hoch P, Polatin P. Pseudoneurotic forms of schizophrenia. Psychiatric Q 1949;23:248-76.
17. Knight R. Borderline states. Bull Menn Clin 1953;17:1-12.
18. Schmideberg M. The treatment of psychopaths and borderline patients. Am J Psychotherapy 1947;1:45-70.
19. Frosch J. The psychotic character: clinical psychiatric considerations. Psychiatric Q 1964;38:81-96.
20. Kernberg O. Borderline personality organization. J Am Psychoanal Assoc 1967;15:641-85.
21. Grinker RR, Werble B, Drye R. The borderline syndrome: a behavioral study of ego functions. New York: Basic Books, 1968.
22. Gunderson JG, Singer MT. Defining borderline patients: an overview. Am J Psychiatry 1975;132:1-10.
23. Spitzer RL, Endicott J, Gibbon M. Crossing the border into borderline personality and borderline schizophrenia: the development of criteria. Arch Gen Psychiatry 1979;36:17-24.
24. Silk KR, Lohr NE, Westen D, Goodrich S. Psychosis in borderline patients with depression. J Personality Disord 1989;3:92-100.
25. Silk KR, Westen D, Lohr NE, et al. DSM-III and DSM-III-R schizotypal symptoms in borderline personality disorder. Comprehen Psychiatry 1990;31:103-10.
26. Livesley WJ, Jang KL, Vernon PA. Phenotypic and genetic structure of traits delineating personality disorder. Arch Gen Psychiatry 1998;55:941-8.
27. McCrae RR, Yang J, Costa PT, Jr, et al. Personality profiles and the prediction of categorical personality disorders. J Personality 2001;69:155-74.
28. Siever LJ, Davis KL. A psychobiological perspective on the personality disorders. Am J Psychiatry 1991;148:1647-58.
29. New AS, Gelernter J, Goodman M, et al. Suicide, impulsive aggression, and HTR1B genotype. Biolog Psychiatry 2001;50:62-5.
30. Oldham JM, Skodol AE. Charting the future of axis II. J Personality Disord 2000;14:17-29.
1. Diagnostic and statistical manual of mental disorders (2nd ed). Washington, DC: American Psychiatric Association, 1968.
2. Feighner JP, Robins E, Guze SB, et al. Diagnostic criteria for use in psychiatric research. Arch Gen Psychiatry 1972;26:57-63.
3. Merikangas KR, Angst J, Eaton W, et al. Comorbidity and boundaries of affective disorders with anxiety disorders and substance misuse: results of an international task force. Br J Psychiatry 1996;30(suppl):58-67.
4. Nierenberg AA. DeCecco LM.Definitions of antidepressant treatment response, remission, nonresponse, partial response, and other relevant outcomes: a focus on treatment-resistant depression. J Clin Psychiatry 2001;62(suppl 16):5-9.
5. Stone MH (ed). Essential papers on borderline disorders: one hundred years at the border. New York: New York University Press, 1986.
6. Diagnostic and statistical manual of mental disorders (4th ed). Washington, DC: American Psychiatric Association, 1994.
7. Diagnostic and statistical manual of mental disorders (3rd ed). Washington, DC: American Psychiatric Association, 1980.
8. Akiskal HS. Subaffective disorders: dysthymic, cyclothymic and bipolar II disorders in the “borderline” realm. Psychiatric Clin N Am 1981;4:25-46.
9. Henry C, Mitropoulou V, New AS, et al. Affective instability and impulsivity in borderline personality and bipolar II disorders: similarities and differences. J Psychiatric Res 2001;35:307-12.
10. Herman JL, van der Kolk BA. Traumatic antecedents of borderline personality disorder. In: van der Kolk, BA. Psychological trauma. Washington, DC: American Psychiatric Press, 1987;111-26.
11. Silk KR, Lee S, Hill EM, Lohr NE. Borderline symptoms and severity of sexual abuse. Am J Psychiatry 1995;152:1059-64.
12. Streeter CC, Van Reekum R, Shorr RI, Bachman DL. Prior head injury in male veterans with borderline personality disorder. J Nerv Ment Dis 1995;183:577-81.
13. Maltsberger JT. Countertransference in borderline conditions: some further notes. Int J Psychoanal Psychother 1982-83;9:125-34.
14. Stern A. Psychoanalytic investigation and therapy in the borderline group of neuroses. Psychoanal Q 1938;7:467-89.
15. Deutsch H. Some forms of emotional disturbance and their relationship to schizophrenia. Psychoanal Q 1942;11:301-21.
16. Hoch P, Polatin P. Pseudoneurotic forms of schizophrenia. Psychiatric Q 1949;23:248-76.
17. Knight R. Borderline states. Bull Menn Clin 1953;17:1-12.
18. Schmideberg M. The treatment of psychopaths and borderline patients. Am J Psychotherapy 1947;1:45-70.
19. Frosch J. The psychotic character: clinical psychiatric considerations. Psychiatric Q 1964;38:81-96.
20. Kernberg O. Borderline personality organization. J Am Psychoanal Assoc 1967;15:641-85.
21. Grinker RR, Werble B, Drye R. The borderline syndrome: a behavioral study of ego functions. New York: Basic Books, 1968.
22. Gunderson JG, Singer MT. Defining borderline patients: an overview. Am J Psychiatry 1975;132:1-10.
23. Spitzer RL, Endicott J, Gibbon M. Crossing the border into borderline personality and borderline schizophrenia: the development of criteria. Arch Gen Psychiatry 1979;36:17-24.
24. Silk KR, Lohr NE, Westen D, Goodrich S. Psychosis in borderline patients with depression. J Personality Disord 1989;3:92-100.
25. Silk KR, Westen D, Lohr NE, et al. DSM-III and DSM-III-R schizotypal symptoms in borderline personality disorder. Comprehen Psychiatry 1990;31:103-10.
26. Livesley WJ, Jang KL, Vernon PA. Phenotypic and genetic structure of traits delineating personality disorder. Arch Gen Psychiatry 1998;55:941-8.
27. McCrae RR, Yang J, Costa PT, Jr, et al. Personality profiles and the prediction of categorical personality disorders. J Personality 2001;69:155-74.
28. Siever LJ, Davis KL. A psychobiological perspective on the personality disorders. Am J Psychiatry 1991;148:1647-58.
29. New AS, Gelernter J, Goodman M, et al. Suicide, impulsive aggression, and HTR1B genotype. Biolog Psychiatry 2001;50:62-5.
30. Oldham JM, Skodol AE. Charting the future of axis II. J Personality Disord 2000;14:17-29.
ADHD and substance abuse: 4 therapeutic options for patients with addictions
Should you prescribe a stimulant to treat attention and hyperactivity problems in teenagers and adults with a history of substance abuse? Evidence suggests that using a stimulant to treat attention-deficit/hyperactivity disorder (ADHD) may place such patients at risk for stimulant abuse or for relapse into abuse of other substances. But a stimulant may be the only option for patients whose ADHD symptoms do not respond to alternate medications, such as antidepressants.
Growing numbers of adults are being treated for ADHD. Because substance abuse problems are common in adults with ADHD (Box 1 ),1-3 prescribing an antidepressant instead of a stimulant in some cases may be prudent. Consider the following factors when choosing ADHD therapy for patients with a history of substance abuse.
Prevalence of stimulant use and abuse
In the United States, more than 95% of medications prescribed for children and adults with ADHD are stimulants—usually methylphenidate.4 Stimulant use has increased as more children and adults are diagnosed with ADHD. Methylphenidate prescriptions increased five-fold from 1990 to 1995.5 Visits to psychiatrists and physicians that included stimulant prescriptions grew from 570,000 to 2.86 million from 1985 to 1994, with most of that increase occurring during visits to primary care and other physicians.6
When used as prescribed, methylphenidate is safe and effective for treating most children and adults with ADHD. Methylphenidate’s pharmacologic properties, however, are similar to those of amphetamines and cocaine (Box 2, Figure 1),7,8 which is why methylphenidate is a schedule-II controlled substance.
Published data. Fifteen reports of methylphenidate abuse were published in the medical literature between 1960 and 1999,7 but little is known about the prevalence of stimulant abuse among patients with ADHD. Banov and colleagues recently published what may be the only data available, when they reported that 3 of 37 (8%) patients abused the stimulants they were prescribed for ADHD.9 The three patients who abused stimulants had histories of drug and alcohol abuse at study entry. In all three cases, stimulant abuse did not develop immediately but became apparent within 6 months after the study began.
In a study of 651 students ages 11 to 18 in Wisconsin and Minnesota, more than one-third of those taking stimulants reported being asked to sell or trade their medications. More than one-half of those not taking ADHD medications said they knew someone who sold or gave away his or her medication.10
Stimulant theft, recreational use. Methylphenidate has been identified as the third most abused prescribed substance in the United States.11 It was the 10th most frequently stolen controlled drug from pharmacies between 1990 and 1995, and 700,000 dosage units were reported stolen in 1996 and 1997.12
As many as 50% of adults with ADHD have substance abuse problems (including alcohol, cocaine, and marijuana), and as many as 30% have antisocial personality disorder (with increased potential for drug-seeking behaviors).1 Compared with the general population, persons with ADHD have an earlier onset of substance abuse that is less responsive to treatment and more likely to progress from alcohol to other drugs.2
The elevated risk of substance abuse in ADHD may be related to a subtle lack of response to normal positive and negative reinforcements. Hunt has outlined four neurobehavioral deficits that define ADHD.3 Besides inattention, hyperarousal, and impulsiveness, he proposes that persons with ADHD have a reward system deficit. They may gravitate toward substance abuse because drugs, alcohol, and nicotine provide stronger rewards than life’s more subtle social interactions.
The popular media have reported recreational use of methylphenidate—with street names such as “R-Ball” and “Vitamin R”—among teens and college students.13 Illegal stimulants are perceived to be easily accessible on college campuses, but no data have been reported.
The use of stimulant medication for ADHD patients with substance abuse problems remains controversial. For such patients, this author reserves stimulant medication for those:
- whose ADHD symptoms have not responded adequately to alternate treatments
- who have been reliable with prescription medications
- and whose functional level is seriously impaired by their ADHD.
Antidepressants vs. stimulants
Although few well-designed controlled studies have been published, four antidepressants appear to be reasonably equivalent in effectiveness for adults with ADHD and do not carry potential for stimulant abuse.14
Desipraime, bupropion, venlafaxine, and the experimental drug atomoxetine (Table 1) all increase norepinephrine at the synapse by inhibiting presynaptic reuptake. Though dopamine has traditionally been considered the neurotransmitter of choice for ADHD treatment, norepinephrine may be equally potent.
Impulse control center. Several lines of research have recently established a connection between the prefrontal cortex, norepinephrine, and ADHD.15 This evidence suggests that the prefrontal cortex plays a major role in inhibiting impulses and responses to distractions:
Figure 1
PET scans of the brain using carbon 11 (11C)-labeled cocaine and methylphenidate HCl show similar distributions in the striatium when the drugs are administered intravenously.
Source: Reproduced with permission from Volkow ND, Ding YS, Fowler JS, et al. Is methylphenidate like cocaine? Studies on their pharmacokinetics and distribution in the human brain. Arch Gen Psychiatry 1995;52:456-63.
Stimulants are classified as schedule-II drugs because they produce powerful reinforcing effects by increasing synaptic dopamine.7 Positron-emission tomography (PET) scans using carbon labeling have shown similar distributions of methylphenidate and cocaine in the brain (Figure 1).8 When administered intravenously, both drugs occupy the same receptors in the striatum and produce a “high” that parallels rapid neuronal uptake. Methylphenidate and cocaine similarly increase stimulation of the postsynaptic neuron by blocking the dopamine reuptake pump (dopamine transporter).
How a substance gets to the brain’s euphoric receptors greatly affects its addictive properties. Delivery systems with rapid onset—smoking, “snorting,” or IV injection—have much greater ability to produce a “high” than do oral or transdermal routes. The greater the “high,” the greater the potential for abuse.
Because methylphenidate is prescribed for oral use, the potential for abuse is minimal. However, we need to be extremely cautious when giving methylphenidate or similar stimulant medications to patients who have shown they are unable to control their abuse of other substances.
Stimulants can also re-ignite a dormant substance abuse problem. Though little has been written about this in the medical literature, Elizabeth Wurtzel, author of the controversial Prozac Nation, chronicles the resumption of her cocaine abuse in More, Now, Again: A Memoir of Addiction. She contends that after her doctor added methylphenidate to augment treatment of partially remitting depression, she began abusing it and eventually was using 40 tablets per day before slipping back into cocaine dependence.
- Patients with prefrontal cortex deficits can have problems with inattention and poor impulse control.
- Patients with ADHD have frontal lobe impairments, as neuropsychological testing and imaging studies have shown.
- Norepinephrine neurons, with cell bodies in the locus coeruleus, have projections that terminate in the prefrontal cortex.
- Agents with norepinephrine activity, but without mood-altering properties (e.g., clonidine), have been shown to improve ADHD symptoms.
Table 1
ADHD IN ADULTS: ANTIDEPRESSANT DOSAGES AND SIDE EFFECTS
| Medication | Class | Effective dosage | Side effects |
|---|---|---|---|
| Desipramine | Tricyclic | 100 to 200 mg/d | Sedation, weight gain, dry mouth, constipation, orthostatic hypotension, prolonged cardiac conduction time; may be lethal in overdose |
| Bupropion SR | Norepinephrine and dopamine reuptake inhibitor | 150 mg bid to 200 mg bid | Headaches, insomnia, agitation, increased risk of seizures |
| Venlafaxine XR | Serotonin and norepinephrine reuptake inhibitor | 75 to 225 mg/d | Nausea, sexual side effects, agitation, increased blood pressure at higher dosages |
| Atomoxetine* | Norepinephrine reuptake inhibitor | To be determined | To be determined |
| * Investigational agent; not FDA-approved | |||
Additional evidence suggests that the prefrontal cortex has projections back to the locus coeruleus, which may explain the relationship between the two areas. It may be that the brain’s higher-functioning areas, such as the prefrontal cortex, provide intelligent screening of impulses from the brain’s older areas, such as the locus coeruleus. Therefore, increased prefrontal cortex activity may modulate some impulses that ADHD patients cannot control otherwise.

No ‘high’ with antidepressants. Patients with ADHD who have experienced the powerful effects of street drugs such as cocaine, methamphetamine, or even alcohol may report that antidepressants do not provide the effect they desire. It is difficult to know if these patients are reporting a lack of benefit or simply the absence of a euphoric “high” they are used to experiencing with substances of abuse. The newer antidepressants do not activate the brain’s euphoric receptors to an appreciable degree.
Patients who take stimulants as prescribed also do not report a “high” but can detect the medication’s presence and absence. Most do not crave this feeling, but substance abusers tend to like it. A patient recently told me he didn’t think stimulants improved his ADHD, but said, “I just liked the way they made me feel.”
Desipramine
The tricyclic antidepressant desipramine is a potent norepinephrine reuptake inhibitor that is effective in treating ADHD in children and adults. In a double-blind, placebo-controlled study of adults with ADHD, subjects receiving desipramine showed robust improvement in symptom scores on the ADHD Rating Scale,16 compared with those receiving the placebo (Figure 2).17
During the 6-week trial, 41 adults with ADHD received desipramine, 200 mg/d, or a placebo. Those receiving desipramine showed significant improvement in 12 of 14 ADHD symptoms and less hyperactivity, impulsivity, and inattentiveness, whereas those receiving the placebo showed no improvement. According to the study criteria, 68% of those who received desipramine and none who received the placebo were considered positive responders.
Though no head-to-head studies have compared desipramine with methylphenidate, the same researchers conducted a similar placebo-controlled study with methylphenidate. The 6-week symptom score on the ADHD Rating Scale was 12.5 for methylphenidate, compared with a score of 12 for desipramine.18
Recommendation. Desipramine may be the most effective of the antidepressant treatments for patients with ADHD. Because of its side effects, however, it is not this author’s first choice and is usually reserved for patients whose symptoms fail to respond to other antidepressants. Desipramine can cause sedation, dry mouth, and constipation, which are related to blockade of adrenergic, histamine, and muscarinic cholinergic receptors. It also can be lethal in overdose.
Some substance abusers lose confidence in a medication that they cannot feel working. The side effects of desipramine, which can be intolerable for some patients, can reassure others with a history of substance abuse that they are being medicated.
Bupropion
Bupropion is a unique antidepressant that inhibits the presynaptic reuptake of dopamine and norepinephrine. Open-label studies demonstrate good responses to bupropion by adults with ADHD. One placebo-controlled, double-blind study found improved ADHD symptoms in 76% of patients receiving bupropion SR, compared with 37% of those receiving a placebo; the difference was statistically significant.19
Figure 2 IMPROVED ADHD SYMPTOMS WITH DESIPRAMINE
Adults with ADHD who received desipramine, 200 mg/d, in a double-blind trial showed significantly less hyperactivity, impulsivity, and inattentiveness after 6 weeks of therapy than a control group that received a placebo.
Source: Adapted with permission from Wilens TE, Biederman J, Prince J, et al. Six-week, double-blind, placebo-controlled study of desipramine for adult attention-deficit/hyperactivity disorder. Am J Psychiatry 1996;153:1147-53.Another study of adults with ADHD compared bupropion SR to methylphenidate and a placebo.20 Using a primary outcome of the Clinical Global Impression (CGI) scale, response rates were 64% for bupropion SR, 50% for methylphenidate, and 27% for the placebo. The difference in response rates between the two agents was not statistically significant (p = 0.14).
Recommendation. The risk of seizures with bupropion is about 1 in 1,000. Therefore, bupropion should not be given to patients with a seizure disorder or to those with conditions that alter the seizure threshold (e.g., eating disorders, recent head trauma, or benzodiazepine withdrawal).21
This author uses bupropion as first-line treatment for appropriate patients with ADHD and a substance abuse history. Bupropion’s mild benefit with smoking cessation may provide some crossover effect for other substances of abuse. The low incidence of sexual side effects is another benefit. Drawbacks include twice-daily dosing and lack of a robust effect on attention and concentration.
Venlafaxine
Venlafaxine is a potent inhibitor of serotonin reuptake, a moderate inhibitor of norepinephrine, and a mild inhibitor of dopamine. Venlafaxine has displayed response rates similar to those of desipramine and bupropion in open-label studies in adults with ADHD,14 but no placebo-controlled studies exist.
As noted above, these antidepressants are believed to improve ADHD symptoms by making norepinephrine more available at the synapse. Hypothetically, then, one would need to administer venlafaxine at dosages that adequately inhibit the norepinephrine reuptake receptor. Venlafaxine XR, 150 mg/d, provides significant norepinephrine activity, according to several lines of evidence.
Recently, Upadhyaya et al reported the use of venlafaxine in one of the few treatment studies of patients with ADHD and comorbid alcohol/cocaine abuse. In an open-label trial, 10 subjects received venlafaxine, up to 300 mg/d, along with psychotherapy and attendance at Alcoholics Anonymous meetings. The nine who completed 4 weeks of treatment showed significantly improved ADHD symptoms and decreased alcohol craving.22
Recommendation. Venlafaxine is this author’s second choice for patients with ADHD and substance abuse problems. Sexual side effects that some patients experience with venlafaxine can limit its use. Some clinicians are concerned about increases in blood pressure associated with venlafaxine, although significant changes do not seem to occur at dosages below 300 mg/d.23
Atomoxetine
Atomoxetine is an investigational antidepressant in phase-III trials as a treatment for ADHD. Evidence shows atomoxetine to be a potent inhibitor of the presynaptic norepinephrine transporter, with minimal affinity for other neurotransmitter receptors. Initial studies suggest that atomoxetine is effective for adults and children with ADHD:
- In a small, double-blind, placebo-controlled, crossover trial, 11 of 20 adults showed improvement in ADHD symptoms within 3 weeks of starting atomoxetine.24
- In 297 children and adolescents, atomoxetine at dosages averaging approximately 1.2 mg/kg/d was more effective than a placebo in reducing ADHD symptoms and improving social and family functioning. Treatment was well tolerated and without significant side effects.25
- In a randomized open-label trial, 228 children received atomoxetine or methylphenidate. Both treatments significantly reduced inattention and hyperactive/impulsive symptoms.26
Related resources
- Arnsten AF. Genetics of childhood disorders (XVIII). ADHD, Part 2: Norepinephrine has a critical modulatory influence on prefrontal cortical function. J Am Acad Child Adolesc Psychiatry. 2000;39:1201-3.
- Ward MF, Wender PH, Reimherr FW. The Wender Utah Rating Scale: An aid in the retrospective diagnosis of childhood attention-deficit/hyperactivity disorder. Am J Psychiatry. 1993;150:885-90.
- Research Report: Prescription Drugs—abuse and addiction. National Institute on Drug Abuse, Substance Abuse and Mental Health Services Administration.
Drug brand names
- Bupropion • Wellbutrin
- Desipramine • Norpramin
- Methylphenidate • Ritalin, Concerta
- Venlafaxine • Effexor
Disclosure
Dr. Higgins reports that he is on the speakers’ bureaus for Wyeth-Ayerst Pharmaceuticals and Eli Lilly and Co.
1. Mannuzza S, Klein RG, Bessler A, et al. Adult outcome of hyperactive boys. Educational achievement, occupational rank, and psychiatric status. Arch Gen Psychiatry 1993;50:565-76.
2. Sullivan MA, Rudnik-Levin F. Attention deficit/hyperactivity disorder and substance abuse. Diagnostic and therapeutic considerations. Ann NY Acad Sci 2001;931:251-70.
3. Hunt RD. Nosology, neurobiology, and clinical patterns of ADHD in adults. Psychiatric Ann 1997;27:572-81.
4. Taylor MA. Evaluation and management of attention-deficit hyperactivity disorder. Am Fam Phys 1997;55:887-904.
5. Diller LH. The run on Ritalin. Attention deficit disorder and stimulant treatment in the 1990s. Hasting Center Report 1996;26:12-18.
6. Pincus HA, Tanielian TL, Marcus SC, et al. Prescribing trends in psychotrophic medications: primary care, psychiatry, and other medical specialties. JAMA 1998;279:526-31.
7. Mortan WA, Stockton GG. Methylphenidate abuse and psychiatric side effects. J Clin Psychiatry (Primary Care) 2000;2:159-64.
8. Volkow ND, Ding YS, Fowler JS, et al. Is methylphenidate like cocaine? Studies on their pharmacokinetics and distribution in the human brain. Arch Gen Psychiatry 1995;52:456-63.
9. Banov MD, Palmer T, Brody E. Antidepressants are as effective as stimulants in the long-term treatment of ADHD in Adults. Primary Psychiatry 2001;8:54-7.
10. Moline S, Frankenberger W. Use of stimulant medication for treatment of attention-deficit/hyperactivity disorder. A survey of middle and high school students attitudes. Psychology in the Schools 2001;38:569-84.
11. Prescription drugs: abuse and addiction. National Institute on Drug Abuse Research Report Series. NIH publication number 01-4881, July 2001.
12. Mann A. Illicit methylphenidate trade appears widespread. Clinical Psychiatry News June 2000;28(6):5-
13. ABCNews.com. http://more/abcnews.go.com/sections/living/DailyNews/ritalin0505.html
14. Higgins ES. A comparative analysis of antidepressants and stimulants for the treatment of adults with attention-deficit hyperactivity disorder. J Fam Pract 1999;48:15-20.
15. Arnsten AF, Steere JC, Hunt RD. The contribution of alpha2-noradrenergic mechanisms to prefrontal cortical cognitive function. Arch Gen Psychiatry 1996;53:448-55.
16. DuPaul G. The ADHD Rating Scale: normative data, reliability, and validity. Worcester, MA: University of Massachusetts Medical School, 1990.
17. Wilens TE, Biederman J, Prince J, et al. Six-week, double-blind, placebo-controlled study of desipramine for adult attention-deficit/hyperactivity disorder. Am J Psychiatry 1996;153:1147-53.
18. Spencer T, Wilens T, Biederman J, Faraone SV, Ablon JS, Lapey K. A double-blind, crossover comparison of methylphenidate and placebo in adults with childhood-onset attention-deficit/hyperactivity disorder. Arch Gen Psychiatry 1995;52:434-43.
19. Wilens TE, Spencer TJ, Biederman J, et al. A controlled clinical trial of bupropion for attention-deficit/hyperactivity disorder in adults. Am J Psychiatry 2001;158:282-8.
20. Kuperman S, Perry PJ, Gaffney GR, et al. Bupropion SR vs. methylphenidate vs. placebo for attention-deficit/hyperactivity disorder in adults. Ann Clin Psychiatry 2001;13:129-34.
21. Wooltorton E. Bupropion (Zyban, Wellbutrin SR): reports of death, seizures, serum sickness. Can Med J 2002;166:68.-
22. Upadhyaya HP, Brady KT, Sethuraman G, et al. Venlafaxine treatment of patients with comorbid alcohol/cocaine abuse and attention-deficit/hyperactivity disorder: a pilot study. J Clin Psychopharmacol 2001;21:116-8.
23. Thase ME. Effects of venlafaxine on blood pressure: a meta-analysis of original data from 3744 depressed patients. J Clin Psychiatry 1998;59:502-8.
24. Spencer T, Biederman J, Wilens T, Prince J, Hatch M. Effectiveness and tolerability of tomoxetine in adults with attention-deficit/hyperactivity disorder. Am J Psychiatry 1998;155:693-5.
25. Michelson D, Faries D, Wernicke J, et al. Atomoxetine in the treatment of children and adolescents with attention-deficit/hyperactivity disorder: a randomized, placebo-controlled, dose-response study. Pediatrics 2001;108:E83.-
26. Kratochvil C, Heiligenstein JH, Dittmann R, et al. Atomoxetine and methylphenidate treatment in ADHD children: a randomized, open-label trial (presentation). Honolulu: American Academy of Child and Adolescent Psychiatry, October, 2001.
Should you prescribe a stimulant to treat attention and hyperactivity problems in teenagers and adults with a history of substance abuse? Evidence suggests that using a stimulant to treat attention-deficit/hyperactivity disorder (ADHD) may place such patients at risk for stimulant abuse or for relapse into abuse of other substances. But a stimulant may be the only option for patients whose ADHD symptoms do not respond to alternate medications, such as antidepressants.
Growing numbers of adults are being treated for ADHD. Because substance abuse problems are common in adults with ADHD (Box 1 ),1-3 prescribing an antidepressant instead of a stimulant in some cases may be prudent. Consider the following factors when choosing ADHD therapy for patients with a history of substance abuse.
Prevalence of stimulant use and abuse
In the United States, more than 95% of medications prescribed for children and adults with ADHD are stimulants—usually methylphenidate.4 Stimulant use has increased as more children and adults are diagnosed with ADHD. Methylphenidate prescriptions increased five-fold from 1990 to 1995.5 Visits to psychiatrists and physicians that included stimulant prescriptions grew from 570,000 to 2.86 million from 1985 to 1994, with most of that increase occurring during visits to primary care and other physicians.6
When used as prescribed, methylphenidate is safe and effective for treating most children and adults with ADHD. Methylphenidate’s pharmacologic properties, however, are similar to those of amphetamines and cocaine (Box 2, Figure 1),7,8 which is why methylphenidate is a schedule-II controlled substance.
Published data. Fifteen reports of methylphenidate abuse were published in the medical literature between 1960 and 1999,7 but little is known about the prevalence of stimulant abuse among patients with ADHD. Banov and colleagues recently published what may be the only data available, when they reported that 3 of 37 (8%) patients abused the stimulants they were prescribed for ADHD.9 The three patients who abused stimulants had histories of drug and alcohol abuse at study entry. In all three cases, stimulant abuse did not develop immediately but became apparent within 6 months after the study began.
In a study of 651 students ages 11 to 18 in Wisconsin and Minnesota, more than one-third of those taking stimulants reported being asked to sell or trade their medications. More than one-half of those not taking ADHD medications said they knew someone who sold or gave away his or her medication.10
Stimulant theft, recreational use. Methylphenidate has been identified as the third most abused prescribed substance in the United States.11 It was the 10th most frequently stolen controlled drug from pharmacies between 1990 and 1995, and 700,000 dosage units were reported stolen in 1996 and 1997.12
As many as 50% of adults with ADHD have substance abuse problems (including alcohol, cocaine, and marijuana), and as many as 30% have antisocial personality disorder (with increased potential for drug-seeking behaviors).1 Compared with the general population, persons with ADHD have an earlier onset of substance abuse that is less responsive to treatment and more likely to progress from alcohol to other drugs.2
The elevated risk of substance abuse in ADHD may be related to a subtle lack of response to normal positive and negative reinforcements. Hunt has outlined four neurobehavioral deficits that define ADHD.3 Besides inattention, hyperarousal, and impulsiveness, he proposes that persons with ADHD have a reward system deficit. They may gravitate toward substance abuse because drugs, alcohol, and nicotine provide stronger rewards than life’s more subtle social interactions.
The popular media have reported recreational use of methylphenidate—with street names such as “R-Ball” and “Vitamin R”—among teens and college students.13 Illegal stimulants are perceived to be easily accessible on college campuses, but no data have been reported.
The use of stimulant medication for ADHD patients with substance abuse problems remains controversial. For such patients, this author reserves stimulant medication for those:
- whose ADHD symptoms have not responded adequately to alternate treatments
- who have been reliable with prescription medications
- and whose functional level is seriously impaired by their ADHD.
Antidepressants vs. stimulants
Although few well-designed controlled studies have been published, four antidepressants appear to be reasonably equivalent in effectiveness for adults with ADHD and do not carry potential for stimulant abuse.14
Desipraime, bupropion, venlafaxine, and the experimental drug atomoxetine (Table 1) all increase norepinephrine at the synapse by inhibiting presynaptic reuptake. Though dopamine has traditionally been considered the neurotransmitter of choice for ADHD treatment, norepinephrine may be equally potent.
Impulse control center. Several lines of research have recently established a connection between the prefrontal cortex, norepinephrine, and ADHD.15 This evidence suggests that the prefrontal cortex plays a major role in inhibiting impulses and responses to distractions:
Figure 1
PET scans of the brain using carbon 11 (11C)-labeled cocaine and methylphenidate HCl show similar distributions in the striatium when the drugs are administered intravenously.
Source: Reproduced with permission from Volkow ND, Ding YS, Fowler JS, et al. Is methylphenidate like cocaine? Studies on their pharmacokinetics and distribution in the human brain. Arch Gen Psychiatry 1995;52:456-63.
Stimulants are classified as schedule-II drugs because they produce powerful reinforcing effects by increasing synaptic dopamine.7 Positron-emission tomography (PET) scans using carbon labeling have shown similar distributions of methylphenidate and cocaine in the brain (Figure 1).8 When administered intravenously, both drugs occupy the same receptors in the striatum and produce a “high” that parallels rapid neuronal uptake. Methylphenidate and cocaine similarly increase stimulation of the postsynaptic neuron by blocking the dopamine reuptake pump (dopamine transporter).
How a substance gets to the brain’s euphoric receptors greatly affects its addictive properties. Delivery systems with rapid onset—smoking, “snorting,” or IV injection—have much greater ability to produce a “high” than do oral or transdermal routes. The greater the “high,” the greater the potential for abuse.
Because methylphenidate is prescribed for oral use, the potential for abuse is minimal. However, we need to be extremely cautious when giving methylphenidate or similar stimulant medications to patients who have shown they are unable to control their abuse of other substances.
Stimulants can also re-ignite a dormant substance abuse problem. Though little has been written about this in the medical literature, Elizabeth Wurtzel, author of the controversial Prozac Nation, chronicles the resumption of her cocaine abuse in More, Now, Again: A Memoir of Addiction. She contends that after her doctor added methylphenidate to augment treatment of partially remitting depression, she began abusing it and eventually was using 40 tablets per day before slipping back into cocaine dependence.
- Patients with prefrontal cortex deficits can have problems with inattention and poor impulse control.
- Patients with ADHD have frontal lobe impairments, as neuropsychological testing and imaging studies have shown.
- Norepinephrine neurons, with cell bodies in the locus coeruleus, have projections that terminate in the prefrontal cortex.
- Agents with norepinephrine activity, but without mood-altering properties (e.g., clonidine), have been shown to improve ADHD symptoms.
Table 1
ADHD IN ADULTS: ANTIDEPRESSANT DOSAGES AND SIDE EFFECTS
| Medication | Class | Effective dosage | Side effects |
|---|---|---|---|
| Desipramine | Tricyclic | 100 to 200 mg/d | Sedation, weight gain, dry mouth, constipation, orthostatic hypotension, prolonged cardiac conduction time; may be lethal in overdose |
| Bupropion SR | Norepinephrine and dopamine reuptake inhibitor | 150 mg bid to 200 mg bid | Headaches, insomnia, agitation, increased risk of seizures |
| Venlafaxine XR | Serotonin and norepinephrine reuptake inhibitor | 75 to 225 mg/d | Nausea, sexual side effects, agitation, increased blood pressure at higher dosages |
| Atomoxetine* | Norepinephrine reuptake inhibitor | To be determined | To be determined |
| * Investigational agent; not FDA-approved | |||
Additional evidence suggests that the prefrontal cortex has projections back to the locus coeruleus, which may explain the relationship between the two areas. It may be that the brain’s higher-functioning areas, such as the prefrontal cortex, provide intelligent screening of impulses from the brain’s older areas, such as the locus coeruleus. Therefore, increased prefrontal cortex activity may modulate some impulses that ADHD patients cannot control otherwise.

No ‘high’ with antidepressants. Patients with ADHD who have experienced the powerful effects of street drugs such as cocaine, methamphetamine, or even alcohol may report that antidepressants do not provide the effect they desire. It is difficult to know if these patients are reporting a lack of benefit or simply the absence of a euphoric “high” they are used to experiencing with substances of abuse. The newer antidepressants do not activate the brain’s euphoric receptors to an appreciable degree.
Patients who take stimulants as prescribed also do not report a “high” but can detect the medication’s presence and absence. Most do not crave this feeling, but substance abusers tend to like it. A patient recently told me he didn’t think stimulants improved his ADHD, but said, “I just liked the way they made me feel.”
Desipramine
The tricyclic antidepressant desipramine is a potent norepinephrine reuptake inhibitor that is effective in treating ADHD in children and adults. In a double-blind, placebo-controlled study of adults with ADHD, subjects receiving desipramine showed robust improvement in symptom scores on the ADHD Rating Scale,16 compared with those receiving the placebo (Figure 2).17
During the 6-week trial, 41 adults with ADHD received desipramine, 200 mg/d, or a placebo. Those receiving desipramine showed significant improvement in 12 of 14 ADHD symptoms and less hyperactivity, impulsivity, and inattentiveness, whereas those receiving the placebo showed no improvement. According to the study criteria, 68% of those who received desipramine and none who received the placebo were considered positive responders.
Though no head-to-head studies have compared desipramine with methylphenidate, the same researchers conducted a similar placebo-controlled study with methylphenidate. The 6-week symptom score on the ADHD Rating Scale was 12.5 for methylphenidate, compared with a score of 12 for desipramine.18
Recommendation. Desipramine may be the most effective of the antidepressant treatments for patients with ADHD. Because of its side effects, however, it is not this author’s first choice and is usually reserved for patients whose symptoms fail to respond to other antidepressants. Desipramine can cause sedation, dry mouth, and constipation, which are related to blockade of adrenergic, histamine, and muscarinic cholinergic receptors. It also can be lethal in overdose.
Some substance abusers lose confidence in a medication that they cannot feel working. The side effects of desipramine, which can be intolerable for some patients, can reassure others with a history of substance abuse that they are being medicated.
Bupropion
Bupropion is a unique antidepressant that inhibits the presynaptic reuptake of dopamine and norepinephrine. Open-label studies demonstrate good responses to bupropion by adults with ADHD. One placebo-controlled, double-blind study found improved ADHD symptoms in 76% of patients receiving bupropion SR, compared with 37% of those receiving a placebo; the difference was statistically significant.19
Figure 2 IMPROVED ADHD SYMPTOMS WITH DESIPRAMINE
Adults with ADHD who received desipramine, 200 mg/d, in a double-blind trial showed significantly less hyperactivity, impulsivity, and inattentiveness after 6 weeks of therapy than a control group that received a placebo.
Source: Adapted with permission from Wilens TE, Biederman J, Prince J, et al. Six-week, double-blind, placebo-controlled study of desipramine for adult attention-deficit/hyperactivity disorder. Am J Psychiatry 1996;153:1147-53.Another study of adults with ADHD compared bupropion SR to methylphenidate and a placebo.20 Using a primary outcome of the Clinical Global Impression (CGI) scale, response rates were 64% for bupropion SR, 50% for methylphenidate, and 27% for the placebo. The difference in response rates between the two agents was not statistically significant (p = 0.14).
Recommendation. The risk of seizures with bupropion is about 1 in 1,000. Therefore, bupropion should not be given to patients with a seizure disorder or to those with conditions that alter the seizure threshold (e.g., eating disorders, recent head trauma, or benzodiazepine withdrawal).21
This author uses bupropion as first-line treatment for appropriate patients with ADHD and a substance abuse history. Bupropion’s mild benefit with smoking cessation may provide some crossover effect for other substances of abuse. The low incidence of sexual side effects is another benefit. Drawbacks include twice-daily dosing and lack of a robust effect on attention and concentration.
Venlafaxine
Venlafaxine is a potent inhibitor of serotonin reuptake, a moderate inhibitor of norepinephrine, and a mild inhibitor of dopamine. Venlafaxine has displayed response rates similar to those of desipramine and bupropion in open-label studies in adults with ADHD,14 but no placebo-controlled studies exist.
As noted above, these antidepressants are believed to improve ADHD symptoms by making norepinephrine more available at the synapse. Hypothetically, then, one would need to administer venlafaxine at dosages that adequately inhibit the norepinephrine reuptake receptor. Venlafaxine XR, 150 mg/d, provides significant norepinephrine activity, according to several lines of evidence.
Recently, Upadhyaya et al reported the use of venlafaxine in one of the few treatment studies of patients with ADHD and comorbid alcohol/cocaine abuse. In an open-label trial, 10 subjects received venlafaxine, up to 300 mg/d, along with psychotherapy and attendance at Alcoholics Anonymous meetings. The nine who completed 4 weeks of treatment showed significantly improved ADHD symptoms and decreased alcohol craving.22
Recommendation. Venlafaxine is this author’s second choice for patients with ADHD and substance abuse problems. Sexual side effects that some patients experience with venlafaxine can limit its use. Some clinicians are concerned about increases in blood pressure associated with venlafaxine, although significant changes do not seem to occur at dosages below 300 mg/d.23
Atomoxetine
Atomoxetine is an investigational antidepressant in phase-III trials as a treatment for ADHD. Evidence shows atomoxetine to be a potent inhibitor of the presynaptic norepinephrine transporter, with minimal affinity for other neurotransmitter receptors. Initial studies suggest that atomoxetine is effective for adults and children with ADHD:
- In a small, double-blind, placebo-controlled, crossover trial, 11 of 20 adults showed improvement in ADHD symptoms within 3 weeks of starting atomoxetine.24
- In 297 children and adolescents, atomoxetine at dosages averaging approximately 1.2 mg/kg/d was more effective than a placebo in reducing ADHD symptoms and improving social and family functioning. Treatment was well tolerated and without significant side effects.25
- In a randomized open-label trial, 228 children received atomoxetine or methylphenidate. Both treatments significantly reduced inattention and hyperactive/impulsive symptoms.26
Related resources
- Arnsten AF. Genetics of childhood disorders (XVIII). ADHD, Part 2: Norepinephrine has a critical modulatory influence on prefrontal cortical function. J Am Acad Child Adolesc Psychiatry. 2000;39:1201-3.
- Ward MF, Wender PH, Reimherr FW. The Wender Utah Rating Scale: An aid in the retrospective diagnosis of childhood attention-deficit/hyperactivity disorder. Am J Psychiatry. 1993;150:885-90.
- Research Report: Prescription Drugs—abuse and addiction. National Institute on Drug Abuse, Substance Abuse and Mental Health Services Administration.
Drug brand names
- Bupropion • Wellbutrin
- Desipramine • Norpramin
- Methylphenidate • Ritalin, Concerta
- Venlafaxine • Effexor
Disclosure
Dr. Higgins reports that he is on the speakers’ bureaus for Wyeth-Ayerst Pharmaceuticals and Eli Lilly and Co.
Should you prescribe a stimulant to treat attention and hyperactivity problems in teenagers and adults with a history of substance abuse? Evidence suggests that using a stimulant to treat attention-deficit/hyperactivity disorder (ADHD) may place such patients at risk for stimulant abuse or for relapse into abuse of other substances. But a stimulant may be the only option for patients whose ADHD symptoms do not respond to alternate medications, such as antidepressants.
Growing numbers of adults are being treated for ADHD. Because substance abuse problems are common in adults with ADHD (Box 1 ),1-3 prescribing an antidepressant instead of a stimulant in some cases may be prudent. Consider the following factors when choosing ADHD therapy for patients with a history of substance abuse.
Prevalence of stimulant use and abuse
In the United States, more than 95% of medications prescribed for children and adults with ADHD are stimulants—usually methylphenidate.4 Stimulant use has increased as more children and adults are diagnosed with ADHD. Methylphenidate prescriptions increased five-fold from 1990 to 1995.5 Visits to psychiatrists and physicians that included stimulant prescriptions grew from 570,000 to 2.86 million from 1985 to 1994, with most of that increase occurring during visits to primary care and other physicians.6
When used as prescribed, methylphenidate is safe and effective for treating most children and adults with ADHD. Methylphenidate’s pharmacologic properties, however, are similar to those of amphetamines and cocaine (Box 2, Figure 1),7,8 which is why methylphenidate is a schedule-II controlled substance.
Published data. Fifteen reports of methylphenidate abuse were published in the medical literature between 1960 and 1999,7 but little is known about the prevalence of stimulant abuse among patients with ADHD. Banov and colleagues recently published what may be the only data available, when they reported that 3 of 37 (8%) patients abused the stimulants they were prescribed for ADHD.9 The three patients who abused stimulants had histories of drug and alcohol abuse at study entry. In all three cases, stimulant abuse did not develop immediately but became apparent within 6 months after the study began.
In a study of 651 students ages 11 to 18 in Wisconsin and Minnesota, more than one-third of those taking stimulants reported being asked to sell or trade their medications. More than one-half of those not taking ADHD medications said they knew someone who sold or gave away his or her medication.10
Stimulant theft, recreational use. Methylphenidate has been identified as the third most abused prescribed substance in the United States.11 It was the 10th most frequently stolen controlled drug from pharmacies between 1990 and 1995, and 700,000 dosage units were reported stolen in 1996 and 1997.12
As many as 50% of adults with ADHD have substance abuse problems (including alcohol, cocaine, and marijuana), and as many as 30% have antisocial personality disorder (with increased potential for drug-seeking behaviors).1 Compared with the general population, persons with ADHD have an earlier onset of substance abuse that is less responsive to treatment and more likely to progress from alcohol to other drugs.2
The elevated risk of substance abuse in ADHD may be related to a subtle lack of response to normal positive and negative reinforcements. Hunt has outlined four neurobehavioral deficits that define ADHD.3 Besides inattention, hyperarousal, and impulsiveness, he proposes that persons with ADHD have a reward system deficit. They may gravitate toward substance abuse because drugs, alcohol, and nicotine provide stronger rewards than life’s more subtle social interactions.
The popular media have reported recreational use of methylphenidate—with street names such as “R-Ball” and “Vitamin R”—among teens and college students.13 Illegal stimulants are perceived to be easily accessible on college campuses, but no data have been reported.
The use of stimulant medication for ADHD patients with substance abuse problems remains controversial. For such patients, this author reserves stimulant medication for those:
- whose ADHD symptoms have not responded adequately to alternate treatments
- who have been reliable with prescription medications
- and whose functional level is seriously impaired by their ADHD.
Antidepressants vs. stimulants
Although few well-designed controlled studies have been published, four antidepressants appear to be reasonably equivalent in effectiveness for adults with ADHD and do not carry potential for stimulant abuse.14
Desipraime, bupropion, venlafaxine, and the experimental drug atomoxetine (Table 1) all increase norepinephrine at the synapse by inhibiting presynaptic reuptake. Though dopamine has traditionally been considered the neurotransmitter of choice for ADHD treatment, norepinephrine may be equally potent.
Impulse control center. Several lines of research have recently established a connection between the prefrontal cortex, norepinephrine, and ADHD.15 This evidence suggests that the prefrontal cortex plays a major role in inhibiting impulses and responses to distractions:
Figure 1
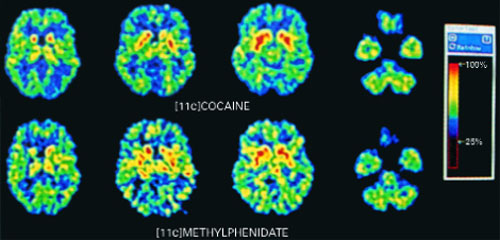
PET scans of the brain using carbon 11 (11C)-labeled cocaine and methylphenidate HCl show similar distributions in the striatium when the drugs are administered intravenously.
Source: Reproduced with permission from Volkow ND, Ding YS, Fowler JS, et al. Is methylphenidate like cocaine? Studies on their pharmacokinetics and distribution in the human brain. Arch Gen Psychiatry 1995;52:456-63.
Stimulants are classified as schedule-II drugs because they produce powerful reinforcing effects by increasing synaptic dopamine.7 Positron-emission tomography (PET) scans using carbon labeling have shown similar distributions of methylphenidate and cocaine in the brain (Figure 1).8 When administered intravenously, both drugs occupy the same receptors in the striatum and produce a “high” that parallels rapid neuronal uptake. Methylphenidate and cocaine similarly increase stimulation of the postsynaptic neuron by blocking the dopamine reuptake pump (dopamine transporter).
How a substance gets to the brain’s euphoric receptors greatly affects its addictive properties. Delivery systems with rapid onset—smoking, “snorting,” or IV injection—have much greater ability to produce a “high” than do oral or transdermal routes. The greater the “high,” the greater the potential for abuse.
Because methylphenidate is prescribed for oral use, the potential for abuse is minimal. However, we need to be extremely cautious when giving methylphenidate or similar stimulant medications to patients who have shown they are unable to control their abuse of other substances.
Stimulants can also re-ignite a dormant substance abuse problem. Though little has been written about this in the medical literature, Elizabeth Wurtzel, author of the controversial Prozac Nation, chronicles the resumption of her cocaine abuse in More, Now, Again: A Memoir of Addiction. She contends that after her doctor added methylphenidate to augment treatment of partially remitting depression, she began abusing it and eventually was using 40 tablets per day before slipping back into cocaine dependence.
- Patients with prefrontal cortex deficits can have problems with inattention and poor impulse control.
- Patients with ADHD have frontal lobe impairments, as neuropsychological testing and imaging studies have shown.
- Norepinephrine neurons, with cell bodies in the locus coeruleus, have projections that terminate in the prefrontal cortex.
- Agents with norepinephrine activity, but without mood-altering properties (e.g., clonidine), have been shown to improve ADHD symptoms.
Table 1
ADHD IN ADULTS: ANTIDEPRESSANT DOSAGES AND SIDE EFFECTS
| Medication | Class | Effective dosage | Side effects |
|---|---|---|---|
| Desipramine | Tricyclic | 100 to 200 mg/d | Sedation, weight gain, dry mouth, constipation, orthostatic hypotension, prolonged cardiac conduction time; may be lethal in overdose |
| Bupropion SR | Norepinephrine and dopamine reuptake inhibitor | 150 mg bid to 200 mg bid | Headaches, insomnia, agitation, increased risk of seizures |
| Venlafaxine XR | Serotonin and norepinephrine reuptake inhibitor | 75 to 225 mg/d | Nausea, sexual side effects, agitation, increased blood pressure at higher dosages |
| Atomoxetine* | Norepinephrine reuptake inhibitor | To be determined | To be determined |
| * Investigational agent; not FDA-approved | |||
Additional evidence suggests that the prefrontal cortex has projections back to the locus coeruleus, which may explain the relationship between the two areas. It may be that the brain’s higher-functioning areas, such as the prefrontal cortex, provide intelligent screening of impulses from the brain’s older areas, such as the locus coeruleus. Therefore, increased prefrontal cortex activity may modulate some impulses that ADHD patients cannot control otherwise.

No ‘high’ with antidepressants. Patients with ADHD who have experienced the powerful effects of street drugs such as cocaine, methamphetamine, or even alcohol may report that antidepressants do not provide the effect they desire. It is difficult to know if these patients are reporting a lack of benefit or simply the absence of a euphoric “high” they are used to experiencing with substances of abuse. The newer antidepressants do not activate the brain’s euphoric receptors to an appreciable degree.
Patients who take stimulants as prescribed also do not report a “high” but can detect the medication’s presence and absence. Most do not crave this feeling, but substance abusers tend to like it. A patient recently told me he didn’t think stimulants improved his ADHD, but said, “I just liked the way they made me feel.”
Desipramine
The tricyclic antidepressant desipramine is a potent norepinephrine reuptake inhibitor that is effective in treating ADHD in children and adults. In a double-blind, placebo-controlled study of adults with ADHD, subjects receiving desipramine showed robust improvement in symptom scores on the ADHD Rating Scale,16 compared with those receiving the placebo (Figure 2).17
During the 6-week trial, 41 adults with ADHD received desipramine, 200 mg/d, or a placebo. Those receiving desipramine showed significant improvement in 12 of 14 ADHD symptoms and less hyperactivity, impulsivity, and inattentiveness, whereas those receiving the placebo showed no improvement. According to the study criteria, 68% of those who received desipramine and none who received the placebo were considered positive responders.
Though no head-to-head studies have compared desipramine with methylphenidate, the same researchers conducted a similar placebo-controlled study with methylphenidate. The 6-week symptom score on the ADHD Rating Scale was 12.5 for methylphenidate, compared with a score of 12 for desipramine.18
Recommendation. Desipramine may be the most effective of the antidepressant treatments for patients with ADHD. Because of its side effects, however, it is not this author’s first choice and is usually reserved for patients whose symptoms fail to respond to other antidepressants. Desipramine can cause sedation, dry mouth, and constipation, which are related to blockade of adrenergic, histamine, and muscarinic cholinergic receptors. It also can be lethal in overdose.
Some substance abusers lose confidence in a medication that they cannot feel working. The side effects of desipramine, which can be intolerable for some patients, can reassure others with a history of substance abuse that they are being medicated.
Bupropion
Bupropion is a unique antidepressant that inhibits the presynaptic reuptake of dopamine and norepinephrine. Open-label studies demonstrate good responses to bupropion by adults with ADHD. One placebo-controlled, double-blind study found improved ADHD symptoms in 76% of patients receiving bupropion SR, compared with 37% of those receiving a placebo; the difference was statistically significant.19
Figure 2 IMPROVED ADHD SYMPTOMS WITH DESIPRAMINE
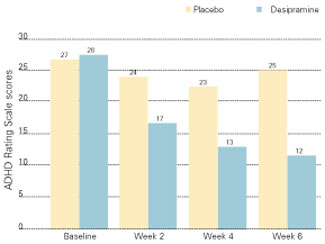
Adults with ADHD who received desipramine, 200 mg/d, in a double-blind trial showed significantly less hyperactivity, impulsivity, and inattentiveness after 6 weeks of therapy than a control group that received a placebo.
Source: Adapted with permission from Wilens TE, Biederman J, Prince J, et al. Six-week, double-blind, placebo-controlled study of desipramine for adult attention-deficit/hyperactivity disorder. Am J Psychiatry 1996;153:1147-53.Another study of adults with ADHD compared bupropion SR to methylphenidate and a placebo.20 Using a primary outcome of the Clinical Global Impression (CGI) scale, response rates were 64% for bupropion SR, 50% for methylphenidate, and 27% for the placebo. The difference in response rates between the two agents was not statistically significant (p = 0.14).
Recommendation. The risk of seizures with bupropion is about 1 in 1,000. Therefore, bupropion should not be given to patients with a seizure disorder or to those with conditions that alter the seizure threshold (e.g., eating disorders, recent head trauma, or benzodiazepine withdrawal).21
This author uses bupropion as first-line treatment for appropriate patients with ADHD and a substance abuse history. Bupropion’s mild benefit with smoking cessation may provide some crossover effect for other substances of abuse. The low incidence of sexual side effects is another benefit. Drawbacks include twice-daily dosing and lack of a robust effect on attention and concentration.
Venlafaxine
Venlafaxine is a potent inhibitor of serotonin reuptake, a moderate inhibitor of norepinephrine, and a mild inhibitor of dopamine. Venlafaxine has displayed response rates similar to those of desipramine and bupropion in open-label studies in adults with ADHD,14 but no placebo-controlled studies exist.
As noted above, these antidepressants are believed to improve ADHD symptoms by making norepinephrine more available at the synapse. Hypothetically, then, one would need to administer venlafaxine at dosages that adequately inhibit the norepinephrine reuptake receptor. Venlafaxine XR, 150 mg/d, provides significant norepinephrine activity, according to several lines of evidence.
Recently, Upadhyaya et al reported the use of venlafaxine in one of the few treatment studies of patients with ADHD and comorbid alcohol/cocaine abuse. In an open-label trial, 10 subjects received venlafaxine, up to 300 mg/d, along with psychotherapy and attendance at Alcoholics Anonymous meetings. The nine who completed 4 weeks of treatment showed significantly improved ADHD symptoms and decreased alcohol craving.22
Recommendation. Venlafaxine is this author’s second choice for patients with ADHD and substance abuse problems. Sexual side effects that some patients experience with venlafaxine can limit its use. Some clinicians are concerned about increases in blood pressure associated with venlafaxine, although significant changes do not seem to occur at dosages below 300 mg/d.23
Atomoxetine
Atomoxetine is an investigational antidepressant in phase-III trials as a treatment for ADHD. Evidence shows atomoxetine to be a potent inhibitor of the presynaptic norepinephrine transporter, with minimal affinity for other neurotransmitter receptors. Initial studies suggest that atomoxetine is effective for adults and children with ADHD:
- In a small, double-blind, placebo-controlled, crossover trial, 11 of 20 adults showed improvement in ADHD symptoms within 3 weeks of starting atomoxetine.24
- In 297 children and adolescents, atomoxetine at dosages averaging approximately 1.2 mg/kg/d was more effective than a placebo in reducing ADHD symptoms and improving social and family functioning. Treatment was well tolerated and without significant side effects.25
- In a randomized open-label trial, 228 children received atomoxetine or methylphenidate. Both treatments significantly reduced inattention and hyperactive/impulsive symptoms.26
Related resources
- Arnsten AF. Genetics of childhood disorders (XVIII). ADHD, Part 2: Norepinephrine has a critical modulatory influence on prefrontal cortical function. J Am Acad Child Adolesc Psychiatry. 2000;39:1201-3.
- Ward MF, Wender PH, Reimherr FW. The Wender Utah Rating Scale: An aid in the retrospective diagnosis of childhood attention-deficit/hyperactivity disorder. Am J Psychiatry. 1993;150:885-90.
- Research Report: Prescription Drugs—abuse and addiction. National Institute on Drug Abuse, Substance Abuse and Mental Health Services Administration.
Drug brand names
- Bupropion • Wellbutrin
- Desipramine • Norpramin
- Methylphenidate • Ritalin, Concerta
- Venlafaxine • Effexor
Disclosure
Dr. Higgins reports that he is on the speakers’ bureaus for Wyeth-Ayerst Pharmaceuticals and Eli Lilly and Co.
1. Mannuzza S, Klein RG, Bessler A, et al. Adult outcome of hyperactive boys. Educational achievement, occupational rank, and psychiatric status. Arch Gen Psychiatry 1993;50:565-76.
2. Sullivan MA, Rudnik-Levin F. Attention deficit/hyperactivity disorder and substance abuse. Diagnostic and therapeutic considerations. Ann NY Acad Sci 2001;931:251-70.
3. Hunt RD. Nosology, neurobiology, and clinical patterns of ADHD in adults. Psychiatric Ann 1997;27:572-81.
4. Taylor MA. Evaluation and management of attention-deficit hyperactivity disorder. Am Fam Phys 1997;55:887-904.
5. Diller LH. The run on Ritalin. Attention deficit disorder and stimulant treatment in the 1990s. Hasting Center Report 1996;26:12-18.
6. Pincus HA, Tanielian TL, Marcus SC, et al. Prescribing trends in psychotrophic medications: primary care, psychiatry, and other medical specialties. JAMA 1998;279:526-31.
7. Mortan WA, Stockton GG. Methylphenidate abuse and psychiatric side effects. J Clin Psychiatry (Primary Care) 2000;2:159-64.
8. Volkow ND, Ding YS, Fowler JS, et al. Is methylphenidate like cocaine? Studies on their pharmacokinetics and distribution in the human brain. Arch Gen Psychiatry 1995;52:456-63.
9. Banov MD, Palmer T, Brody E. Antidepressants are as effective as stimulants in the long-term treatment of ADHD in Adults. Primary Psychiatry 2001;8:54-7.
10. Moline S, Frankenberger W. Use of stimulant medication for treatment of attention-deficit/hyperactivity disorder. A survey of middle and high school students attitudes. Psychology in the Schools 2001;38:569-84.
11. Prescription drugs: abuse and addiction. National Institute on Drug Abuse Research Report Series. NIH publication number 01-4881, July 2001.
12. Mann A. Illicit methylphenidate trade appears widespread. Clinical Psychiatry News June 2000;28(6):5-
13. ABCNews.com. http://more/abcnews.go.com/sections/living/DailyNews/ritalin0505.html
14. Higgins ES. A comparative analysis of antidepressants and stimulants for the treatment of adults with attention-deficit hyperactivity disorder. J Fam Pract 1999;48:15-20.
15. Arnsten AF, Steere JC, Hunt RD. The contribution of alpha2-noradrenergic mechanisms to prefrontal cortical cognitive function. Arch Gen Psychiatry 1996;53:448-55.
16. DuPaul G. The ADHD Rating Scale: normative data, reliability, and validity. Worcester, MA: University of Massachusetts Medical School, 1990.
17. Wilens TE, Biederman J, Prince J, et al. Six-week, double-blind, placebo-controlled study of desipramine for adult attention-deficit/hyperactivity disorder. Am J Psychiatry 1996;153:1147-53.
18. Spencer T, Wilens T, Biederman J, Faraone SV, Ablon JS, Lapey K. A double-blind, crossover comparison of methylphenidate and placebo in adults with childhood-onset attention-deficit/hyperactivity disorder. Arch Gen Psychiatry 1995;52:434-43.
19. Wilens TE, Spencer TJ, Biederman J, et al. A controlled clinical trial of bupropion for attention-deficit/hyperactivity disorder in adults. Am J Psychiatry 2001;158:282-8.
20. Kuperman S, Perry PJ, Gaffney GR, et al. Bupropion SR vs. methylphenidate vs. placebo for attention-deficit/hyperactivity disorder in adults. Ann Clin Psychiatry 2001;13:129-34.
21. Wooltorton E. Bupropion (Zyban, Wellbutrin SR): reports of death, seizures, serum sickness. Can Med J 2002;166:68.-
22. Upadhyaya HP, Brady KT, Sethuraman G, et al. Venlafaxine treatment of patients with comorbid alcohol/cocaine abuse and attention-deficit/hyperactivity disorder: a pilot study. J Clin Psychopharmacol 2001;21:116-8.
23. Thase ME. Effects of venlafaxine on blood pressure: a meta-analysis of original data from 3744 depressed patients. J Clin Psychiatry 1998;59:502-8.
24. Spencer T, Biederman J, Wilens T, Prince J, Hatch M. Effectiveness and tolerability of tomoxetine in adults with attention-deficit/hyperactivity disorder. Am J Psychiatry 1998;155:693-5.
25. Michelson D, Faries D, Wernicke J, et al. Atomoxetine in the treatment of children and adolescents with attention-deficit/hyperactivity disorder: a randomized, placebo-controlled, dose-response study. Pediatrics 2001;108:E83.-
26. Kratochvil C, Heiligenstein JH, Dittmann R, et al. Atomoxetine and methylphenidate treatment in ADHD children: a randomized, open-label trial (presentation). Honolulu: American Academy of Child and Adolescent Psychiatry, October, 2001.
1. Mannuzza S, Klein RG, Bessler A, et al. Adult outcome of hyperactive boys. Educational achievement, occupational rank, and psychiatric status. Arch Gen Psychiatry 1993;50:565-76.
2. Sullivan MA, Rudnik-Levin F. Attention deficit/hyperactivity disorder and substance abuse. Diagnostic and therapeutic considerations. Ann NY Acad Sci 2001;931:251-70.
3. Hunt RD. Nosology, neurobiology, and clinical patterns of ADHD in adults. Psychiatric Ann 1997;27:572-81.
4. Taylor MA. Evaluation and management of attention-deficit hyperactivity disorder. Am Fam Phys 1997;55:887-904.
5. Diller LH. The run on Ritalin. Attention deficit disorder and stimulant treatment in the 1990s. Hasting Center Report 1996;26:12-18.
6. Pincus HA, Tanielian TL, Marcus SC, et al. Prescribing trends in psychotrophic medications: primary care, psychiatry, and other medical specialties. JAMA 1998;279:526-31.
7. Mortan WA, Stockton GG. Methylphenidate abuse and psychiatric side effects. J Clin Psychiatry (Primary Care) 2000;2:159-64.
8. Volkow ND, Ding YS, Fowler JS, et al. Is methylphenidate like cocaine? Studies on their pharmacokinetics and distribution in the human brain. Arch Gen Psychiatry 1995;52:456-63.
9. Banov MD, Palmer T, Brody E. Antidepressants are as effective as stimulants in the long-term treatment of ADHD in Adults. Primary Psychiatry 2001;8:54-7.
10. Moline S, Frankenberger W. Use of stimulant medication for treatment of attention-deficit/hyperactivity disorder. A survey of middle and high school students attitudes. Psychology in the Schools 2001;38:569-84.
11. Prescription drugs: abuse and addiction. National Institute on Drug Abuse Research Report Series. NIH publication number 01-4881, July 2001.
12. Mann A. Illicit methylphenidate trade appears widespread. Clinical Psychiatry News June 2000;28(6):5-
13. ABCNews.com. http://more/abcnews.go.com/sections/living/DailyNews/ritalin0505.html
14. Higgins ES. A comparative analysis of antidepressants and stimulants for the treatment of adults with attention-deficit hyperactivity disorder. J Fam Pract 1999;48:15-20.
15. Arnsten AF, Steere JC, Hunt RD. The contribution of alpha2-noradrenergic mechanisms to prefrontal cortical cognitive function. Arch Gen Psychiatry 1996;53:448-55.
16. DuPaul G. The ADHD Rating Scale: normative data, reliability, and validity. Worcester, MA: University of Massachusetts Medical School, 1990.
17. Wilens TE, Biederman J, Prince J, et al. Six-week, double-blind, placebo-controlled study of desipramine for adult attention-deficit/hyperactivity disorder. Am J Psychiatry 1996;153:1147-53.
18. Spencer T, Wilens T, Biederman J, Faraone SV, Ablon JS, Lapey K. A double-blind, crossover comparison of methylphenidate and placebo in adults with childhood-onset attention-deficit/hyperactivity disorder. Arch Gen Psychiatry 1995;52:434-43.
19. Wilens TE, Spencer TJ, Biederman J, et al. A controlled clinical trial of bupropion for attention-deficit/hyperactivity disorder in adults. Am J Psychiatry 2001;158:282-8.
20. Kuperman S, Perry PJ, Gaffney GR, et al. Bupropion SR vs. methylphenidate vs. placebo for attention-deficit/hyperactivity disorder in adults. Ann Clin Psychiatry 2001;13:129-34.
21. Wooltorton E. Bupropion (Zyban, Wellbutrin SR): reports of death, seizures, serum sickness. Can Med J 2002;166:68.-
22. Upadhyaya HP, Brady KT, Sethuraman G, et al. Venlafaxine treatment of patients with comorbid alcohol/cocaine abuse and attention-deficit/hyperactivity disorder: a pilot study. J Clin Psychopharmacol 2001;21:116-8.
23. Thase ME. Effects of venlafaxine on blood pressure: a meta-analysis of original data from 3744 depressed patients. J Clin Psychiatry 1998;59:502-8.
24. Spencer T, Biederman J, Wilens T, Prince J, Hatch M. Effectiveness and tolerability of tomoxetine in adults with attention-deficit/hyperactivity disorder. Am J Psychiatry 1998;155:693-5.
25. Michelson D, Faries D, Wernicke J, et al. Atomoxetine in the treatment of children and adolescents with attention-deficit/hyperactivity disorder: a randomized, placebo-controlled, dose-response study. Pediatrics 2001;108:E83.-
26. Kratochvil C, Heiligenstein JH, Dittmann R, et al. Atomoxetine and methylphenidate treatment in ADHD children: a randomized, open-label trial (presentation). Honolulu: American Academy of Child and Adolescent Psychiatry, October, 2001.
Using atypicals for patients without psychosis: The strength of evidence varies with the diagnosis
Antipsychotics—particularly the atypicals—have therapeutic properties that make them potential candidates for treating a variety of disorders in children and adolescents. As has occurred in adults, the use of atypical antipsychotics is expanding beyond schizophrenia to pediatric affective and nonpsychotic conditions.
In part 1 of this article, we examined the evidence for using atypical antipsychotics in childhood/adolescent-onset schizophrenia, bipolar disorder, and psychotic depression. Our search of the literature suggested two concerns to keep in mind when prescribing antipsychotics to children and adolescents:
- Side effects—weight gain, metabolic disturbances, hyperprolactinemia, and cardiac conduction abnormalities—are health concerns for all patients but particularly for children and adolescents, who may require years of exposure to atypical antipsychotics.
- Administering medications to children and adolescents requires special precautions because younger patients respond differently than do adults to psychotropic medications.
In part 2, we look at more limited evidence for using atypicals in children with anxiety disorders, autism and developmental disorders, Tourette’s and other tic disorders, disruptive behavior disorders, anorexia nervosa (Box 1)1-3, and stuttering (Box 2)4.
Anorexia nervosa was treated in the 1960s with chlorpromazine at dosages as high as 1,600 mg/d and often in combination with insulin. Weight increased and hospital stays decreased over the short term, but side effects—including seizures in 5 of 30 patients in one study—greatly complicated treatment. With longer follow-up, weight gain did not improve significantly, and (interestingly) purging behavior emerged.1 Treatment outcomes were unclear in double-blind, placebo-controlled, crossover studies of pimozide and sulpiride.2
Atypical antipsychotics are being investigated for adjunctive treatment of anorexia nervosa. Case reports have described olanzapine’s efficacy in weight gain and psychological improvement in patients with severe symptoms.3
Weight restoration is the most essential step in treating children and adolescents with anorexia nervosa. In this regard, the weight gain associated with using atypical antipsychotics may offer adjunctive benefit. Atypicals also may decrease relapse rates by treating comorbid personality traits (e.g., rigidity and obsessionality) and by restoring cognition in delusional patients. Such claims are speculative but worthy of investigation.
Anxiety disorders: Limited use for antipsychotics
Anxiety disorders are among the most prevalent psychopathologies in the pediatric population, and current treatment recommendations strongly focus on psychotherapeutic interventions. Pharmacologic interventions, however—including imipramine, selective serotonin reuptake inhibitors, and even benzodiazepines—can offer an important adjunct to behavioral and other nonpharmacologic therapies, particularly at the onset of illness and before behavioral techniques are learned.
The American Academy of Child and Adolescent Psychiatry’s 1997 practice parameters for anxiety disorders do not recommend using neuroleptics in the absence of comorbidity—such as Tourette’s syndrome or psychosis—because of concerns about impaired cognition and tardive dyskinesia.5 The clinician should also be aware that “neuroleptic separation anxiety syndrome” has been described in children who developed school phobia in response to haloperidol or pimozide while being treated for Tourette’s disorder.
Similar reports describe separation anxiety in two adolescent boys and one prepubertal boy treated with adjunctive low-dose risperidone for obsessive-compulsive disorder (OCD), attention-deficit/hyperactivity disorder (ADHD), and behavioral disruption. Two of the boys were subsequently treated with olanzapine without a recurrence of anxiety.
It seems unlikely that atypical antipsychotics will play a significant role in managing pediatric anxiety. Controlled studies for this indication are limited. Alternate pharmacologic options are considered safer and are themselves recommended only as adjuncts to other interventions.
Clinicians will no doubt be tempted to try atypicals in lieu of benzodiazepines for severe OCD (and perhaps even for severe anxiety) in this young population. If an antipsychotic trial is initiated, we recommend clear documentation of poor response to other interventions, notations of comorbidity, judicious dosing, and close monitoring. Psychotic symptoms associated with posttraumatic stress disorder may be a reasonable indication for antipsychotic use, but more research is needed.
Autism: Improving behavioral symptoms
Pharmacotherapy for children with autism and pervasive developmental disorders (PDD) generally targets aggression, irritability, stereotypic behavior, hyperactivity, self-abusive behavior, and self-stimulatory behavior. Almost all classes of psychotropics—including antipsychotics, selective serotonin reuptake inhibitors, tricyclic antidepressants, lithium, mood stabilizers, and anxiolytics—have been tested in clinical trials, with varying degrees of success.
Haloperidol has been shown to improve behavioral symptoms, including educational learning.6 Dyskinesias—including tardive dyskinesia—remain a concern, however, with long-term use of haloperidol in children.
Recently, attention has turned to atypical antipsychotics, with their lower risk of extrapyramidal symptoms (EPS). Double-blind, placebo-controlled studies have demonstrated the efficacy of these agents in treating autistic and developmental disorders; risperidone and olanzapine have been studied most extensively.
Risperidone. A 16-week open-label trial of 24 children ages 3 to 6 with autistic disorders demonstrated modest improvement with risperidone, 0.5 mg/d. At least 25% improvement was seen in:
- the Children’s Psychiatric Rating Scale (CPRS)
- hyperactivity, fidgetiness, rhythmic motions, mood lability, and angry affect, as measured by the Childhood Autism Rating Scale (CARS)
- functional impairment, as determined by the Children’s Global Assessment Scale (C-GAS).
Overall, risperidone was well-tolerated at this low dosage, although two children did not complete the study because of side effects. Three children gained more than 10% of their body weight.7
In a 12-month semi-naturalistic prospective study, 11 children and adolescents ages 7 to 17 (mean age 12.3) with autism (n=9) or PDD (n=2) were treated with risperidone. Starting dosage was 0.5 mg/d, mean dosage was 2.7 mg/d, and maximum dosage was 6 mg/d (0.1/mg/kg/d). Behavioral symptoms improved significantly with risperidone in 10 of the 11 subjects during the first 6 months of treatment. Autism’s core symptoms were also mildly improved, although more slowly and later in treatment. Risperidone continued to work in patients treated for 12 months, whereas behavioral symptoms reemerged in those who discontinued drug therapy after 6 months. Weight gain was the most common side effect.
After 6 months of therapy two patients developed facial dystonia, which resolved after the risperidone dosage was reduced or discontinued. Amenorrhea was observed in one patient, but no changes were reported in liver function, blood tests, or electrocardiogram (ECG) readings.8
Haloperidol and risperidone have shown efficacy in managing stuttering in double-blind studies. Olanzapine has improved stuttering symptoms in three case reports: a 10-year-old boy, a 16-year-old youth with developmental stuttering, and a 9-year-old boy with medication-induced stuttering.4 These studies, albeit very limited, suggest that antipsychotics may be an appropriate option for managing this impairing disorder.
Others have contributed greatly to our understanding of using atypicals in treating autism and PDD.9,10 Posey et al reported using risperidone to treat two boys, ages 23 months and 29 months. In both cases, aggression was reduced and social relatedness improved significantly. One patient’s treatment was complicated by dose-related presistent tachycardia and QTc prolongation.9
McDougle conducted an initial prospective, 12-week, open-label study examining risperidone treatment in 18 children and adolescents (15 boys and 3 girls, mean age 10) with PDD,10 followed by an 8-week, double-blind, placebo-controlled study of risperidone in 100 children with autistic disorders (excluding Asperger’s disorder).11 Mean dosage was 2.1 mg/d (0.75 mg to 3.5 mg/d) divided into two doses. The study examined the benefit in a relatively young cohort (Tanner stages I and II—children who have yet to complete sexual development).
After 2 to 4 weeks of treatment, irritability improved most significantly (>25% improvement on the Aberrant Behavior Checklist), and stereotypic behavior also improved. Inappropriate speech patterns did not change. Anecdotal reports suggested that social relatedness improved, although quantitative evaluation was inconclusive. EPS, as measured by the Simpson Angus EPS score, were mild and generally seen in early treatment. Side effects included increased appetite, weight gain, decreased energy, and sedation.11
Olanzapine. Most studies of olanzapine in children and adolescents with autistic disorders have been open-label:
Eight patients (four adults, ages 18 to 42, and four children, ages 5 to 17) were treated with olanzapine, mean dosage 7.8 mg/d for 12 weeks. Seven completed the study, and six were rated “much improved” or “very much improved” on the global improvement item of the Clinical Global Impression (CGI) scale. Hyperactivity, aggression, anger, and self-injurious behavior improved significantly, as did social relatedness, affectual reactions, sensory responses, and language use. The drug was well tolerated, with the most significant side effect being increased appetite and weight gain (mean increase 8.3 kg).12
In an open-label pilot study, 12 children with autism (mean age 8) were randomly assigned to 6 weeks of treatment with olanzapine (mean final dosage 7.9 mg/d) or haloperidol (mean final dosage 1.4 mg/d). Symptoms were reduced in both groups. Five of six children in the olanzapine group and three of six children in the haloperidol group were noted as responders, according to the CGI improvement item and the Children’s Psychiatric Rating Scale (CPRS) Autism Factor. Drowsiness and weight gain were seen with olanzapine.13
Similar results were obtained in another study, with significant improvements in irritability, hyperactivity, and excessive speech, as evaluated by the Aberrant Behavior Checklist.14,15
Summary. Atypical antipsychotics appear to be effective and well tolerated in children and adolescents with autistic and developmental disorders. Double-blind, placebo-controlled studies confirm the benefit of risperidone; open-label trials likewise suggest the benefit of olanzapine. Research is limited on quetiapine and ziprasidone in this population.
Weight gain appears to be the most problematic side effect and should be monitored. Early dietary education and discussion with the patient, parents, and family can help keep weight gain to a minimum.
Tourette’s disorder: Modest benefit
Tourette’s disorder and simple motor or vocal tics have traditionally been treated with the older neuroleptics, particularly haloperidol and pimozide. These agents have fallen out of favor in younger patients, however, because of the risk of short- and long-term side effects, including EPS, tardive dyskinesia, cognitive blunting, and school phobia.
Clinicians have turned to alternate agents, such as clonidine and guanfacine (alpha-2 agonists) to treat tic disorders, and now are trying atypical antipsychotics. In open and controlled studies, the atypicals have demonstrated moderate improvement in Tourette’s disorder. Even so, none of the newer agents has shown benefits comparable to haloperidol, which recently demonstrated 66% improvement in tic symptoms when compared with a placebo.16 For example:
- ziprasidone—35% improvement in tic symptoms when compared with a placebo17
- risperidone—44% improvement when compared with a placebo in 17 pediatric patients18
- clozapine—no effect on tic symptoms16 (clozapine causes little or no dopamine [D2] blockade, which most likely explains this result)
- olanzapine—modest to moderate benefit, but somewhat less effective than risperidone or ziprasidone (small sample size and inclusion of adult patients have confounded interpretation in the studies examining response to risperidone and olanzapine).16,17
Sedation was the most common side effect seen with use of risperidone, ziprasidone, or olanzapine, and weight gain was particularly problematic with olanzapine.16 No ECG abnormalities were noted in the 28 children treated with ziprasidone.17
Disruptive behavior: Improved conduct
The disruptive behavior disorders of childhood and adolescence include conduct disorder and oppositional defiant disorder. The only two antipsychotic medications approved to treat behavioral symptoms are chlorpromazine and thioridazine. These indications were approved in the 1980s, based on limited trials with poor statistical comparison and controlled study groups. Moreover, thioridazine has since been issued a black-box warning because of concerns about cardiac complications from QTc prolongation.
Among the typical antipsychotics, haloperidol has been studied the most extensively in disruptive behavior disorders, although it is not FDA-approved for this indication. Haloperidol has decreased destructive and aggressive behavior, oppositionality, and hostility, and has improved scores on children’s psychiatric and CGI scales.19
More recent studies have examined the role of atypical antipsychotics in disruptive behavior disorders, primarily risperidone.
Risperidone. In a double-blind, placebo-controlled study, use of risperidone (average dosage 0.75 to 1.50 mg/d) improved aggression and delinquent behavior in 20 children, ages 5 to 15, diagnosed with conduct disorder.20 In a larger 6-week, multisite, double-blind, placebo-controlled study, researchers examined the use of risperidone (mean dosage 1.11 mg/kg/d) in 118 children with conduct problems and borderline intellectual functioning (60% had oppositional defiant disorder, 40% had conduct disorder, and 60% had ADHD). Behaviors—anxious, hyperactive, self-injurious, isolative, and stereotypic—improved, as did adaptive skills. The most common side effects were sedation, GI distress, weight gain, hyperprolactinemia, rhinitis, and headaches.21 Replication of this study produced similar findings.22
In an extension study of conduct disorder, 34 children ages 5 to 14 with comorbid borderline intellectual functioning were treated for approximately 1 year with risperidone (mean dosage 1.48 mg/d). Clinical benefit, defined by statistically significant improvement in the conduct problem subscale of the Nisonger Child Behavior Rating Form, was noted throughout the study. Prolactin levels were elevated after 3 months of treatment but declined thereafter.23
No controlled studies have been published using olanzapine in children and adolescents with disruptive behavior disorders. As other medications—lithium, anticonvulsants, and psychostimulants—are available for symptomatic treatment of this population, questions remain. Are antipsychotics the best class of medication for this purpose, and should they be tried as first-line therapy? Few studies have compared the efficacy of antipsychotics and other pharmacologic options.
Summary
Pharmacotherapy of childhood psychiatric conditions is complex and an extremely underdeveloped area of research. Even so, clinicians are experimenting with the use of atypical antipsychotics on a trial-and-error basis or as adjuncts to other medications for childhood conditions beyond schizophrenia.24
Even more than in adult populations, judicious use of atypical antipsychotics is warranted in children and adolescents because of potential long-term consequences. The risk of interfering with normal development and the unique pharmacokinetics of childhood are important considerations. At the same time, atypical antipsychotics may offer the potential to improve behavior and function in children with intractable psychiatric conditions.
Related resources
- Pappadopulas E, Jensen PS, Schur SB, et al. Real world atypical antipsychotic prescribing practices in public child and adolescent inpatient settings. Schizophr Bull 2002;28(1):111-121.
- Malone RP, Sheikh R, Zito JM. Novel antipsychotic medications is the treatment of children and adolescents. Psychiatr Serv 1999; 50(2):171-174.
Drug brand names
- Chlorpromazine • Thorazine
- Clonidine • Catapres
- Clozapine • Clozaril
- Guanfacine • Tenex
- Haloperidol • Haldol
- Olanzapine • Zyprexa
- Pimozide • Orap
- Quetiapine • Seroquel
- Risperidone • Risperdal
- Thioridazine • Mellaril
- Ziprasidone • Geodon
Disclosure
Dr. Londino reports that she serves as a consultant to Eli Lilly and Co.
Ms. Wiggins reports no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
Dr. Buckley reports that he receives grant support from and serves as a consultant and speaker for AstraZeneca Pharmaceuticals, Eli Lilly and Co., Janssen Pharmaceutica, and Novartis Pharmaceuticals Corp.
1. Dally P, Sargant W. A new treatment of anorexia nervosa. BMJ 1960;1:1770-3.
2. Vandereycken W, Pierloot R. Pimozide combined with behavior therapy in the short-term treatment of anorexia nervosa. Acta Psychiatr Scand 1982;66:445-50.
3. Hanson L. Olanzapine in the treatment of anorexia nervosa. Br J Psychiatry 1999;175:592.-
4. Lavid N, Franklin DL, Maguire GA. Management of child and adolescent stuttering with olanzapine: three case reports. Ann Clin Psychiatry 1999;11(4):233-6.
5. American Academy of Child and Adolescent Psychiatry. AACAP official action: practice parameters for the assessment and treatment of children and adolescents with anxiety disorders. J Am Acad Child Adolesc Psychiatry 1997;36:69-84.
6. Anderson LT, Campbell M, Grega DM, et al. Haloperidol in the treatment of infantile autism: effects on learning and behavioral symptoms. Am J Psychiatry 1984;141(10):1195-1202.
7. Masi G, Cosenza A, Mucci M, Brovedani P. Open trial of risperidone in 24 young children with pervasive developmental disorders. J Am Acad Child Adolesc Psychiatry 2001;40(10):1206-14.
8. Zuddis A, Di Martino A, Muglia P, et al. Long-term risperidone for pervasive developmental disorder: efficacy, tolerability, and discontinuation. J Child Adolesc Psychopharmacol 2000;10(2):79-90.
9. Posey DJ, Walsh KH, Wilson GA, McDougle CJ. Risperidone in the treatment of two very young children with autism. J Child Adolesc Psychopharmacol 1999;9(4):273-6.
10. McDougle CJ, Homes JP, Bronson MR, et al. Risperidone treatment of children and adolescents with pervasive developmental disorders: a prospective open-label study. J Am Acad Child Adolesc Psychiatry 1997;36:685-93.
11. McCracken JT, McGough J, et al. Risperidone in children with autism and serious behavioral problems. Research Units on Pediatric Psychopharmacology Autism Network. N Eng J Med. 2002;347(5):314-21.
12. Potenza MN, Holmes JP, Kanes SJ, McDougle CJ. Olanzapine treatment of children, adolescents, and adults with pervasive developmental disorders: an open-label pilot study. J Clin Psychopharmacol 1999;19:37-44.
13. Malone RP, Cater J, Sheikh RM, et al. Olanzapine versus haloperidol in children with autistic disorder: an open pilot study. J Am Acad Child Adolesc Psychiatry 2001;40:887-94.
14. Kemner C, van Engeland H, Tuynman-Qua H. An open-label study of olanzapine in children with pervasive development disorder. Eur Neuropsychopharmacol 1999;9(suppl 5):S287-S288.
15. Kemner C, van Engeland H, Tuynman-Qua H. An open-label study of olanzapine in children with PDD. Schizophr Res 2000;41(1, suppl 1):194.-
16. Scahill L, Chappell PB, King RA, et al. Pharmacologic treatment of tic disorders. Child Adolesc Clin North Am 2000;9:99-117.
17. Sallee FR, Kurlan R, Goetz CG, et al. Ziprasidone treatment of children and adolescents with Tourette’s syndrome: a pilot study. J Am Acad Child Adolesc Psychiatry 2000;39:292-9.
18. Bruggeman R, van der Linden C, Buitelaar JK, et al. Risperidone versus pimozide in Tourette’s disorder: a comparative double-blind parallel-group study. J Clin Psychiatry 2001;50:912-24.
19. Campbell M, Small AM, Green WH, et al. Behavioral efficacy of haloperidol and lithium carbonate: a comparison of hospitalized aggressive children with conduct disorder. Arch Gen Psychiatry 1984;41:650-6.
20. Findling RL, McNamara NK, Branicky LA, et al. A double blind pilot study of risperidone in the treatment of conduct disorder. J Am Acad Child Adolesc Psychiatry 2000;39:509-16.
21. Aman MG, Findling RL, Derivan A, et al. Safety and efficacy of risperidone in children with significant conduct problems and borderline IQ or mental retardation. Brussels, Belgium: 22nd Collegium Internationale Neuro-psychopharmacologicum Congress, July 2000.
22. Turgay A, Snyder R, Fishman S, et al. and the Conduct Research Group. Risperidone versus placebo for conduct and other disruptive behavior disorders in children with subaverage IQ (poster presentation). Victoria, British Columbia, Canada: Canadian Psychiatric Association annual meeting, October 2000.
23. Holford LE, Peter E, Van der Walt A. Risperidone for behavior disorders in children with mental retardation (poster presentation). New York: American Academy of Child and Adolescent Psychiatry annual meeting, October 2000.
24. La Via MC, Gray N, Kaye WH. Case reports of olanzapine treatment of anorexia nervosa. Int J Eating Disord 2000;27:363-6.
Antipsychotics—particularly the atypicals—have therapeutic properties that make them potential candidates for treating a variety of disorders in children and adolescents. As has occurred in adults, the use of atypical antipsychotics is expanding beyond schizophrenia to pediatric affective and nonpsychotic conditions.
In part 1 of this article, we examined the evidence for using atypical antipsychotics in childhood/adolescent-onset schizophrenia, bipolar disorder, and psychotic depression. Our search of the literature suggested two concerns to keep in mind when prescribing antipsychotics to children and adolescents:
- Side effects—weight gain, metabolic disturbances, hyperprolactinemia, and cardiac conduction abnormalities—are health concerns for all patients but particularly for children and adolescents, who may require years of exposure to atypical antipsychotics.
- Administering medications to children and adolescents requires special precautions because younger patients respond differently than do adults to psychotropic medications.
In part 2, we look at more limited evidence for using atypicals in children with anxiety disorders, autism and developmental disorders, Tourette’s and other tic disorders, disruptive behavior disorders, anorexia nervosa (Box 1)1-3, and stuttering (Box 2)4.
Anorexia nervosa was treated in the 1960s with chlorpromazine at dosages as high as 1,600 mg/d and often in combination with insulin. Weight increased and hospital stays decreased over the short term, but side effects—including seizures in 5 of 30 patients in one study—greatly complicated treatment. With longer follow-up, weight gain did not improve significantly, and (interestingly) purging behavior emerged.1 Treatment outcomes were unclear in double-blind, placebo-controlled, crossover studies of pimozide and sulpiride.2
Atypical antipsychotics are being investigated for adjunctive treatment of anorexia nervosa. Case reports have described olanzapine’s efficacy in weight gain and psychological improvement in patients with severe symptoms.3
Weight restoration is the most essential step in treating children and adolescents with anorexia nervosa. In this regard, the weight gain associated with using atypical antipsychotics may offer adjunctive benefit. Atypicals also may decrease relapse rates by treating comorbid personality traits (e.g., rigidity and obsessionality) and by restoring cognition in delusional patients. Such claims are speculative but worthy of investigation.
Anxiety disorders: Limited use for antipsychotics
Anxiety disorders are among the most prevalent psychopathologies in the pediatric population, and current treatment recommendations strongly focus on psychotherapeutic interventions. Pharmacologic interventions, however—including imipramine, selective serotonin reuptake inhibitors, and even benzodiazepines—can offer an important adjunct to behavioral and other nonpharmacologic therapies, particularly at the onset of illness and before behavioral techniques are learned.
The American Academy of Child and Adolescent Psychiatry’s 1997 practice parameters for anxiety disorders do not recommend using neuroleptics in the absence of comorbidity—such as Tourette’s syndrome or psychosis—because of concerns about impaired cognition and tardive dyskinesia.5 The clinician should also be aware that “neuroleptic separation anxiety syndrome” has been described in children who developed school phobia in response to haloperidol or pimozide while being treated for Tourette’s disorder.
Similar reports describe separation anxiety in two adolescent boys and one prepubertal boy treated with adjunctive low-dose risperidone for obsessive-compulsive disorder (OCD), attention-deficit/hyperactivity disorder (ADHD), and behavioral disruption. Two of the boys were subsequently treated with olanzapine without a recurrence of anxiety.
It seems unlikely that atypical antipsychotics will play a significant role in managing pediatric anxiety. Controlled studies for this indication are limited. Alternate pharmacologic options are considered safer and are themselves recommended only as adjuncts to other interventions.
Clinicians will no doubt be tempted to try atypicals in lieu of benzodiazepines for severe OCD (and perhaps even for severe anxiety) in this young population. If an antipsychotic trial is initiated, we recommend clear documentation of poor response to other interventions, notations of comorbidity, judicious dosing, and close monitoring. Psychotic symptoms associated with posttraumatic stress disorder may be a reasonable indication for antipsychotic use, but more research is needed.
Autism: Improving behavioral symptoms
Pharmacotherapy for children with autism and pervasive developmental disorders (PDD) generally targets aggression, irritability, stereotypic behavior, hyperactivity, self-abusive behavior, and self-stimulatory behavior. Almost all classes of psychotropics—including antipsychotics, selective serotonin reuptake inhibitors, tricyclic antidepressants, lithium, mood stabilizers, and anxiolytics—have been tested in clinical trials, with varying degrees of success.
Haloperidol has been shown to improve behavioral symptoms, including educational learning.6 Dyskinesias—including tardive dyskinesia—remain a concern, however, with long-term use of haloperidol in children.
Recently, attention has turned to atypical antipsychotics, with their lower risk of extrapyramidal symptoms (EPS). Double-blind, placebo-controlled studies have demonstrated the efficacy of these agents in treating autistic and developmental disorders; risperidone and olanzapine have been studied most extensively.
Risperidone. A 16-week open-label trial of 24 children ages 3 to 6 with autistic disorders demonstrated modest improvement with risperidone, 0.5 mg/d. At least 25% improvement was seen in:
- the Children’s Psychiatric Rating Scale (CPRS)
- hyperactivity, fidgetiness, rhythmic motions, mood lability, and angry affect, as measured by the Childhood Autism Rating Scale (CARS)
- functional impairment, as determined by the Children’s Global Assessment Scale (C-GAS).
Overall, risperidone was well-tolerated at this low dosage, although two children did not complete the study because of side effects. Three children gained more than 10% of their body weight.7
In a 12-month semi-naturalistic prospective study, 11 children and adolescents ages 7 to 17 (mean age 12.3) with autism (n=9) or PDD (n=2) were treated with risperidone. Starting dosage was 0.5 mg/d, mean dosage was 2.7 mg/d, and maximum dosage was 6 mg/d (0.1/mg/kg/d). Behavioral symptoms improved significantly with risperidone in 10 of the 11 subjects during the first 6 months of treatment. Autism’s core symptoms were also mildly improved, although more slowly and later in treatment. Risperidone continued to work in patients treated for 12 months, whereas behavioral symptoms reemerged in those who discontinued drug therapy after 6 months. Weight gain was the most common side effect.
After 6 months of therapy two patients developed facial dystonia, which resolved after the risperidone dosage was reduced or discontinued. Amenorrhea was observed in one patient, but no changes were reported in liver function, blood tests, or electrocardiogram (ECG) readings.8
Haloperidol and risperidone have shown efficacy in managing stuttering in double-blind studies. Olanzapine has improved stuttering symptoms in three case reports: a 10-year-old boy, a 16-year-old youth with developmental stuttering, and a 9-year-old boy with medication-induced stuttering.4 These studies, albeit very limited, suggest that antipsychotics may be an appropriate option for managing this impairing disorder.
Others have contributed greatly to our understanding of using atypicals in treating autism and PDD.9,10 Posey et al reported using risperidone to treat two boys, ages 23 months and 29 months. In both cases, aggression was reduced and social relatedness improved significantly. One patient’s treatment was complicated by dose-related presistent tachycardia and QTc prolongation.9
McDougle conducted an initial prospective, 12-week, open-label study examining risperidone treatment in 18 children and adolescents (15 boys and 3 girls, mean age 10) with PDD,10 followed by an 8-week, double-blind, placebo-controlled study of risperidone in 100 children with autistic disorders (excluding Asperger’s disorder).11 Mean dosage was 2.1 mg/d (0.75 mg to 3.5 mg/d) divided into two doses. The study examined the benefit in a relatively young cohort (Tanner stages I and II—children who have yet to complete sexual development).
After 2 to 4 weeks of treatment, irritability improved most significantly (>25% improvement on the Aberrant Behavior Checklist), and stereotypic behavior also improved. Inappropriate speech patterns did not change. Anecdotal reports suggested that social relatedness improved, although quantitative evaluation was inconclusive. EPS, as measured by the Simpson Angus EPS score, were mild and generally seen in early treatment. Side effects included increased appetite, weight gain, decreased energy, and sedation.11
Olanzapine. Most studies of olanzapine in children and adolescents with autistic disorders have been open-label:
Eight patients (four adults, ages 18 to 42, and four children, ages 5 to 17) were treated with olanzapine, mean dosage 7.8 mg/d for 12 weeks. Seven completed the study, and six were rated “much improved” or “very much improved” on the global improvement item of the Clinical Global Impression (CGI) scale. Hyperactivity, aggression, anger, and self-injurious behavior improved significantly, as did social relatedness, affectual reactions, sensory responses, and language use. The drug was well tolerated, with the most significant side effect being increased appetite and weight gain (mean increase 8.3 kg).12
In an open-label pilot study, 12 children with autism (mean age 8) were randomly assigned to 6 weeks of treatment with olanzapine (mean final dosage 7.9 mg/d) or haloperidol (mean final dosage 1.4 mg/d). Symptoms were reduced in both groups. Five of six children in the olanzapine group and three of six children in the haloperidol group were noted as responders, according to the CGI improvement item and the Children’s Psychiatric Rating Scale (CPRS) Autism Factor. Drowsiness and weight gain were seen with olanzapine.13
Similar results were obtained in another study, with significant improvements in irritability, hyperactivity, and excessive speech, as evaluated by the Aberrant Behavior Checklist.14,15
Summary. Atypical antipsychotics appear to be effective and well tolerated in children and adolescents with autistic and developmental disorders. Double-blind, placebo-controlled studies confirm the benefit of risperidone; open-label trials likewise suggest the benefit of olanzapine. Research is limited on quetiapine and ziprasidone in this population.
Weight gain appears to be the most problematic side effect and should be monitored. Early dietary education and discussion with the patient, parents, and family can help keep weight gain to a minimum.
Tourette’s disorder: Modest benefit
Tourette’s disorder and simple motor or vocal tics have traditionally been treated with the older neuroleptics, particularly haloperidol and pimozide. These agents have fallen out of favor in younger patients, however, because of the risk of short- and long-term side effects, including EPS, tardive dyskinesia, cognitive blunting, and school phobia.
Clinicians have turned to alternate agents, such as clonidine and guanfacine (alpha-2 agonists) to treat tic disorders, and now are trying atypical antipsychotics. In open and controlled studies, the atypicals have demonstrated moderate improvement in Tourette’s disorder. Even so, none of the newer agents has shown benefits comparable to haloperidol, which recently demonstrated 66% improvement in tic symptoms when compared with a placebo.16 For example:
- ziprasidone—35% improvement in tic symptoms when compared with a placebo17
- risperidone—44% improvement when compared with a placebo in 17 pediatric patients18
- clozapine—no effect on tic symptoms16 (clozapine causes little or no dopamine [D2] blockade, which most likely explains this result)
- olanzapine—modest to moderate benefit, but somewhat less effective than risperidone or ziprasidone (small sample size and inclusion of adult patients have confounded interpretation in the studies examining response to risperidone and olanzapine).16,17
Sedation was the most common side effect seen with use of risperidone, ziprasidone, or olanzapine, and weight gain was particularly problematic with olanzapine.16 No ECG abnormalities were noted in the 28 children treated with ziprasidone.17
Disruptive behavior: Improved conduct
The disruptive behavior disorders of childhood and adolescence include conduct disorder and oppositional defiant disorder. The only two antipsychotic medications approved to treat behavioral symptoms are chlorpromazine and thioridazine. These indications were approved in the 1980s, based on limited trials with poor statistical comparison and controlled study groups. Moreover, thioridazine has since been issued a black-box warning because of concerns about cardiac complications from QTc prolongation.
Among the typical antipsychotics, haloperidol has been studied the most extensively in disruptive behavior disorders, although it is not FDA-approved for this indication. Haloperidol has decreased destructive and aggressive behavior, oppositionality, and hostility, and has improved scores on children’s psychiatric and CGI scales.19
More recent studies have examined the role of atypical antipsychotics in disruptive behavior disorders, primarily risperidone.
Risperidone. In a double-blind, placebo-controlled study, use of risperidone (average dosage 0.75 to 1.50 mg/d) improved aggression and delinquent behavior in 20 children, ages 5 to 15, diagnosed with conduct disorder.20 In a larger 6-week, multisite, double-blind, placebo-controlled study, researchers examined the use of risperidone (mean dosage 1.11 mg/kg/d) in 118 children with conduct problems and borderline intellectual functioning (60% had oppositional defiant disorder, 40% had conduct disorder, and 60% had ADHD). Behaviors—anxious, hyperactive, self-injurious, isolative, and stereotypic—improved, as did adaptive skills. The most common side effects were sedation, GI distress, weight gain, hyperprolactinemia, rhinitis, and headaches.21 Replication of this study produced similar findings.22
In an extension study of conduct disorder, 34 children ages 5 to 14 with comorbid borderline intellectual functioning were treated for approximately 1 year with risperidone (mean dosage 1.48 mg/d). Clinical benefit, defined by statistically significant improvement in the conduct problem subscale of the Nisonger Child Behavior Rating Form, was noted throughout the study. Prolactin levels were elevated after 3 months of treatment but declined thereafter.23
No controlled studies have been published using olanzapine in children and adolescents with disruptive behavior disorders. As other medications—lithium, anticonvulsants, and psychostimulants—are available for symptomatic treatment of this population, questions remain. Are antipsychotics the best class of medication for this purpose, and should they be tried as first-line therapy? Few studies have compared the efficacy of antipsychotics and other pharmacologic options.
Summary
Pharmacotherapy of childhood psychiatric conditions is complex and an extremely underdeveloped area of research. Even so, clinicians are experimenting with the use of atypical antipsychotics on a trial-and-error basis or as adjuncts to other medications for childhood conditions beyond schizophrenia.24
Even more than in adult populations, judicious use of atypical antipsychotics is warranted in children and adolescents because of potential long-term consequences. The risk of interfering with normal development and the unique pharmacokinetics of childhood are important considerations. At the same time, atypical antipsychotics may offer the potential to improve behavior and function in children with intractable psychiatric conditions.
Related resources
- Pappadopulas E, Jensen PS, Schur SB, et al. Real world atypical antipsychotic prescribing practices in public child and adolescent inpatient settings. Schizophr Bull 2002;28(1):111-121.
- Malone RP, Sheikh R, Zito JM. Novel antipsychotic medications is the treatment of children and adolescents. Psychiatr Serv 1999; 50(2):171-174.
Drug brand names
- Chlorpromazine • Thorazine
- Clonidine • Catapres
- Clozapine • Clozaril
- Guanfacine • Tenex
- Haloperidol • Haldol
- Olanzapine • Zyprexa
- Pimozide • Orap
- Quetiapine • Seroquel
- Risperidone • Risperdal
- Thioridazine • Mellaril
- Ziprasidone • Geodon
Disclosure
Dr. Londino reports that she serves as a consultant to Eli Lilly and Co.
Ms. Wiggins reports no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
Dr. Buckley reports that he receives grant support from and serves as a consultant and speaker for AstraZeneca Pharmaceuticals, Eli Lilly and Co., Janssen Pharmaceutica, and Novartis Pharmaceuticals Corp.
Antipsychotics—particularly the atypicals—have therapeutic properties that make them potential candidates for treating a variety of disorders in children and adolescents. As has occurred in adults, the use of atypical antipsychotics is expanding beyond schizophrenia to pediatric affective and nonpsychotic conditions.
In part 1 of this article, we examined the evidence for using atypical antipsychotics in childhood/adolescent-onset schizophrenia, bipolar disorder, and psychotic depression. Our search of the literature suggested two concerns to keep in mind when prescribing antipsychotics to children and adolescents:
- Side effects—weight gain, metabolic disturbances, hyperprolactinemia, and cardiac conduction abnormalities—are health concerns for all patients but particularly for children and adolescents, who may require years of exposure to atypical antipsychotics.
- Administering medications to children and adolescents requires special precautions because younger patients respond differently than do adults to psychotropic medications.
In part 2, we look at more limited evidence for using atypicals in children with anxiety disorders, autism and developmental disorders, Tourette’s and other tic disorders, disruptive behavior disorders, anorexia nervosa (Box 1)1-3, and stuttering (Box 2)4.
Anorexia nervosa was treated in the 1960s with chlorpromazine at dosages as high as 1,600 mg/d and often in combination with insulin. Weight increased and hospital stays decreased over the short term, but side effects—including seizures in 5 of 30 patients in one study—greatly complicated treatment. With longer follow-up, weight gain did not improve significantly, and (interestingly) purging behavior emerged.1 Treatment outcomes were unclear in double-blind, placebo-controlled, crossover studies of pimozide and sulpiride.2
Atypical antipsychotics are being investigated for adjunctive treatment of anorexia nervosa. Case reports have described olanzapine’s efficacy in weight gain and psychological improvement in patients with severe symptoms.3
Weight restoration is the most essential step in treating children and adolescents with anorexia nervosa. In this regard, the weight gain associated with using atypical antipsychotics may offer adjunctive benefit. Atypicals also may decrease relapse rates by treating comorbid personality traits (e.g., rigidity and obsessionality) and by restoring cognition in delusional patients. Such claims are speculative but worthy of investigation.
Anxiety disorders: Limited use for antipsychotics
Anxiety disorders are among the most prevalent psychopathologies in the pediatric population, and current treatment recommendations strongly focus on psychotherapeutic interventions. Pharmacologic interventions, however—including imipramine, selective serotonin reuptake inhibitors, and even benzodiazepines—can offer an important adjunct to behavioral and other nonpharmacologic therapies, particularly at the onset of illness and before behavioral techniques are learned.
The American Academy of Child and Adolescent Psychiatry’s 1997 practice parameters for anxiety disorders do not recommend using neuroleptics in the absence of comorbidity—such as Tourette’s syndrome or psychosis—because of concerns about impaired cognition and tardive dyskinesia.5 The clinician should also be aware that “neuroleptic separation anxiety syndrome” has been described in children who developed school phobia in response to haloperidol or pimozide while being treated for Tourette’s disorder.
Similar reports describe separation anxiety in two adolescent boys and one prepubertal boy treated with adjunctive low-dose risperidone for obsessive-compulsive disorder (OCD), attention-deficit/hyperactivity disorder (ADHD), and behavioral disruption. Two of the boys were subsequently treated with olanzapine without a recurrence of anxiety.
It seems unlikely that atypical antipsychotics will play a significant role in managing pediatric anxiety. Controlled studies for this indication are limited. Alternate pharmacologic options are considered safer and are themselves recommended only as adjuncts to other interventions.
Clinicians will no doubt be tempted to try atypicals in lieu of benzodiazepines for severe OCD (and perhaps even for severe anxiety) in this young population. If an antipsychotic trial is initiated, we recommend clear documentation of poor response to other interventions, notations of comorbidity, judicious dosing, and close monitoring. Psychotic symptoms associated with posttraumatic stress disorder may be a reasonable indication for antipsychotic use, but more research is needed.
Autism: Improving behavioral symptoms
Pharmacotherapy for children with autism and pervasive developmental disorders (PDD) generally targets aggression, irritability, stereotypic behavior, hyperactivity, self-abusive behavior, and self-stimulatory behavior. Almost all classes of psychotropics—including antipsychotics, selective serotonin reuptake inhibitors, tricyclic antidepressants, lithium, mood stabilizers, and anxiolytics—have been tested in clinical trials, with varying degrees of success.
Haloperidol has been shown to improve behavioral symptoms, including educational learning.6 Dyskinesias—including tardive dyskinesia—remain a concern, however, with long-term use of haloperidol in children.
Recently, attention has turned to atypical antipsychotics, with their lower risk of extrapyramidal symptoms (EPS). Double-blind, placebo-controlled studies have demonstrated the efficacy of these agents in treating autistic and developmental disorders; risperidone and olanzapine have been studied most extensively.
Risperidone. A 16-week open-label trial of 24 children ages 3 to 6 with autistic disorders demonstrated modest improvement with risperidone, 0.5 mg/d. At least 25% improvement was seen in:
- the Children’s Psychiatric Rating Scale (CPRS)
- hyperactivity, fidgetiness, rhythmic motions, mood lability, and angry affect, as measured by the Childhood Autism Rating Scale (CARS)
- functional impairment, as determined by the Children’s Global Assessment Scale (C-GAS).
Overall, risperidone was well-tolerated at this low dosage, although two children did not complete the study because of side effects. Three children gained more than 10% of their body weight.7
In a 12-month semi-naturalistic prospective study, 11 children and adolescents ages 7 to 17 (mean age 12.3) with autism (n=9) or PDD (n=2) were treated with risperidone. Starting dosage was 0.5 mg/d, mean dosage was 2.7 mg/d, and maximum dosage was 6 mg/d (0.1/mg/kg/d). Behavioral symptoms improved significantly with risperidone in 10 of the 11 subjects during the first 6 months of treatment. Autism’s core symptoms were also mildly improved, although more slowly and later in treatment. Risperidone continued to work in patients treated for 12 months, whereas behavioral symptoms reemerged in those who discontinued drug therapy after 6 months. Weight gain was the most common side effect.
After 6 months of therapy two patients developed facial dystonia, which resolved after the risperidone dosage was reduced or discontinued. Amenorrhea was observed in one patient, but no changes were reported in liver function, blood tests, or electrocardiogram (ECG) readings.8
Haloperidol and risperidone have shown efficacy in managing stuttering in double-blind studies. Olanzapine has improved stuttering symptoms in three case reports: a 10-year-old boy, a 16-year-old youth with developmental stuttering, and a 9-year-old boy with medication-induced stuttering.4 These studies, albeit very limited, suggest that antipsychotics may be an appropriate option for managing this impairing disorder.
Others have contributed greatly to our understanding of using atypicals in treating autism and PDD.9,10 Posey et al reported using risperidone to treat two boys, ages 23 months and 29 months. In both cases, aggression was reduced and social relatedness improved significantly. One patient’s treatment was complicated by dose-related presistent tachycardia and QTc prolongation.9
McDougle conducted an initial prospective, 12-week, open-label study examining risperidone treatment in 18 children and adolescents (15 boys and 3 girls, mean age 10) with PDD,10 followed by an 8-week, double-blind, placebo-controlled study of risperidone in 100 children with autistic disorders (excluding Asperger’s disorder).11 Mean dosage was 2.1 mg/d (0.75 mg to 3.5 mg/d) divided into two doses. The study examined the benefit in a relatively young cohort (Tanner stages I and II—children who have yet to complete sexual development).
After 2 to 4 weeks of treatment, irritability improved most significantly (>25% improvement on the Aberrant Behavior Checklist), and stereotypic behavior also improved. Inappropriate speech patterns did not change. Anecdotal reports suggested that social relatedness improved, although quantitative evaluation was inconclusive. EPS, as measured by the Simpson Angus EPS score, were mild and generally seen in early treatment. Side effects included increased appetite, weight gain, decreased energy, and sedation.11
Olanzapine. Most studies of olanzapine in children and adolescents with autistic disorders have been open-label:
Eight patients (four adults, ages 18 to 42, and four children, ages 5 to 17) were treated with olanzapine, mean dosage 7.8 mg/d for 12 weeks. Seven completed the study, and six were rated “much improved” or “very much improved” on the global improvement item of the Clinical Global Impression (CGI) scale. Hyperactivity, aggression, anger, and self-injurious behavior improved significantly, as did social relatedness, affectual reactions, sensory responses, and language use. The drug was well tolerated, with the most significant side effect being increased appetite and weight gain (mean increase 8.3 kg).12
In an open-label pilot study, 12 children with autism (mean age 8) were randomly assigned to 6 weeks of treatment with olanzapine (mean final dosage 7.9 mg/d) or haloperidol (mean final dosage 1.4 mg/d). Symptoms were reduced in both groups. Five of six children in the olanzapine group and three of six children in the haloperidol group were noted as responders, according to the CGI improvement item and the Children’s Psychiatric Rating Scale (CPRS) Autism Factor. Drowsiness and weight gain were seen with olanzapine.13
Similar results were obtained in another study, with significant improvements in irritability, hyperactivity, and excessive speech, as evaluated by the Aberrant Behavior Checklist.14,15
Summary. Atypical antipsychotics appear to be effective and well tolerated in children and adolescents with autistic and developmental disorders. Double-blind, placebo-controlled studies confirm the benefit of risperidone; open-label trials likewise suggest the benefit of olanzapine. Research is limited on quetiapine and ziprasidone in this population.
Weight gain appears to be the most problematic side effect and should be monitored. Early dietary education and discussion with the patient, parents, and family can help keep weight gain to a minimum.
Tourette’s disorder: Modest benefit
Tourette’s disorder and simple motor or vocal tics have traditionally been treated with the older neuroleptics, particularly haloperidol and pimozide. These agents have fallen out of favor in younger patients, however, because of the risk of short- and long-term side effects, including EPS, tardive dyskinesia, cognitive blunting, and school phobia.
Clinicians have turned to alternate agents, such as clonidine and guanfacine (alpha-2 agonists) to treat tic disorders, and now are trying atypical antipsychotics. In open and controlled studies, the atypicals have demonstrated moderate improvement in Tourette’s disorder. Even so, none of the newer agents has shown benefits comparable to haloperidol, which recently demonstrated 66% improvement in tic symptoms when compared with a placebo.16 For example:
- ziprasidone—35% improvement in tic symptoms when compared with a placebo17
- risperidone—44% improvement when compared with a placebo in 17 pediatric patients18
- clozapine—no effect on tic symptoms16 (clozapine causes little or no dopamine [D2] blockade, which most likely explains this result)
- olanzapine—modest to moderate benefit, but somewhat less effective than risperidone or ziprasidone (small sample size and inclusion of adult patients have confounded interpretation in the studies examining response to risperidone and olanzapine).16,17
Sedation was the most common side effect seen with use of risperidone, ziprasidone, or olanzapine, and weight gain was particularly problematic with olanzapine.16 No ECG abnormalities were noted in the 28 children treated with ziprasidone.17
Disruptive behavior: Improved conduct
The disruptive behavior disorders of childhood and adolescence include conduct disorder and oppositional defiant disorder. The only two antipsychotic medications approved to treat behavioral symptoms are chlorpromazine and thioridazine. These indications were approved in the 1980s, based on limited trials with poor statistical comparison and controlled study groups. Moreover, thioridazine has since been issued a black-box warning because of concerns about cardiac complications from QTc prolongation.
Among the typical antipsychotics, haloperidol has been studied the most extensively in disruptive behavior disorders, although it is not FDA-approved for this indication. Haloperidol has decreased destructive and aggressive behavior, oppositionality, and hostility, and has improved scores on children’s psychiatric and CGI scales.19
More recent studies have examined the role of atypical antipsychotics in disruptive behavior disorders, primarily risperidone.
Risperidone. In a double-blind, placebo-controlled study, use of risperidone (average dosage 0.75 to 1.50 mg/d) improved aggression and delinquent behavior in 20 children, ages 5 to 15, diagnosed with conduct disorder.20 In a larger 6-week, multisite, double-blind, placebo-controlled study, researchers examined the use of risperidone (mean dosage 1.11 mg/kg/d) in 118 children with conduct problems and borderline intellectual functioning (60% had oppositional defiant disorder, 40% had conduct disorder, and 60% had ADHD). Behaviors—anxious, hyperactive, self-injurious, isolative, and stereotypic—improved, as did adaptive skills. The most common side effects were sedation, GI distress, weight gain, hyperprolactinemia, rhinitis, and headaches.21 Replication of this study produced similar findings.22
In an extension study of conduct disorder, 34 children ages 5 to 14 with comorbid borderline intellectual functioning were treated for approximately 1 year with risperidone (mean dosage 1.48 mg/d). Clinical benefit, defined by statistically significant improvement in the conduct problem subscale of the Nisonger Child Behavior Rating Form, was noted throughout the study. Prolactin levels were elevated after 3 months of treatment but declined thereafter.23
No controlled studies have been published using olanzapine in children and adolescents with disruptive behavior disorders. As other medications—lithium, anticonvulsants, and psychostimulants—are available for symptomatic treatment of this population, questions remain. Are antipsychotics the best class of medication for this purpose, and should they be tried as first-line therapy? Few studies have compared the efficacy of antipsychotics and other pharmacologic options.
Summary
Pharmacotherapy of childhood psychiatric conditions is complex and an extremely underdeveloped area of research. Even so, clinicians are experimenting with the use of atypical antipsychotics on a trial-and-error basis or as adjuncts to other medications for childhood conditions beyond schizophrenia.24
Even more than in adult populations, judicious use of atypical antipsychotics is warranted in children and adolescents because of potential long-term consequences. The risk of interfering with normal development and the unique pharmacokinetics of childhood are important considerations. At the same time, atypical antipsychotics may offer the potential to improve behavior and function in children with intractable psychiatric conditions.
Related resources
- Pappadopulas E, Jensen PS, Schur SB, et al. Real world atypical antipsychotic prescribing practices in public child and adolescent inpatient settings. Schizophr Bull 2002;28(1):111-121.
- Malone RP, Sheikh R, Zito JM. Novel antipsychotic medications is the treatment of children and adolescents. Psychiatr Serv 1999; 50(2):171-174.
Drug brand names
- Chlorpromazine • Thorazine
- Clonidine • Catapres
- Clozapine • Clozaril
- Guanfacine • Tenex
- Haloperidol • Haldol
- Olanzapine • Zyprexa
- Pimozide • Orap
- Quetiapine • Seroquel
- Risperidone • Risperdal
- Thioridazine • Mellaril
- Ziprasidone • Geodon
Disclosure
Dr. Londino reports that she serves as a consultant to Eli Lilly and Co.
Ms. Wiggins reports no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
Dr. Buckley reports that he receives grant support from and serves as a consultant and speaker for AstraZeneca Pharmaceuticals, Eli Lilly and Co., Janssen Pharmaceutica, and Novartis Pharmaceuticals Corp.
1. Dally P, Sargant W. A new treatment of anorexia nervosa. BMJ 1960;1:1770-3.
2. Vandereycken W, Pierloot R. Pimozide combined with behavior therapy in the short-term treatment of anorexia nervosa. Acta Psychiatr Scand 1982;66:445-50.
3. Hanson L. Olanzapine in the treatment of anorexia nervosa. Br J Psychiatry 1999;175:592.-
4. Lavid N, Franklin DL, Maguire GA. Management of child and adolescent stuttering with olanzapine: three case reports. Ann Clin Psychiatry 1999;11(4):233-6.
5. American Academy of Child and Adolescent Psychiatry. AACAP official action: practice parameters for the assessment and treatment of children and adolescents with anxiety disorders. J Am Acad Child Adolesc Psychiatry 1997;36:69-84.
6. Anderson LT, Campbell M, Grega DM, et al. Haloperidol in the treatment of infantile autism: effects on learning and behavioral symptoms. Am J Psychiatry 1984;141(10):1195-1202.
7. Masi G, Cosenza A, Mucci M, Brovedani P. Open trial of risperidone in 24 young children with pervasive developmental disorders. J Am Acad Child Adolesc Psychiatry 2001;40(10):1206-14.
8. Zuddis A, Di Martino A, Muglia P, et al. Long-term risperidone for pervasive developmental disorder: efficacy, tolerability, and discontinuation. J Child Adolesc Psychopharmacol 2000;10(2):79-90.
9. Posey DJ, Walsh KH, Wilson GA, McDougle CJ. Risperidone in the treatment of two very young children with autism. J Child Adolesc Psychopharmacol 1999;9(4):273-6.
10. McDougle CJ, Homes JP, Bronson MR, et al. Risperidone treatment of children and adolescents with pervasive developmental disorders: a prospective open-label study. J Am Acad Child Adolesc Psychiatry 1997;36:685-93.
11. McCracken JT, McGough J, et al. Risperidone in children with autism and serious behavioral problems. Research Units on Pediatric Psychopharmacology Autism Network. N Eng J Med. 2002;347(5):314-21.
12. Potenza MN, Holmes JP, Kanes SJ, McDougle CJ. Olanzapine treatment of children, adolescents, and adults with pervasive developmental disorders: an open-label pilot study. J Clin Psychopharmacol 1999;19:37-44.
13. Malone RP, Cater J, Sheikh RM, et al. Olanzapine versus haloperidol in children with autistic disorder: an open pilot study. J Am Acad Child Adolesc Psychiatry 2001;40:887-94.
14. Kemner C, van Engeland H, Tuynman-Qua H. An open-label study of olanzapine in children with pervasive development disorder. Eur Neuropsychopharmacol 1999;9(suppl 5):S287-S288.
15. Kemner C, van Engeland H, Tuynman-Qua H. An open-label study of olanzapine in children with PDD. Schizophr Res 2000;41(1, suppl 1):194.-
16. Scahill L, Chappell PB, King RA, et al. Pharmacologic treatment of tic disorders. Child Adolesc Clin North Am 2000;9:99-117.
17. Sallee FR, Kurlan R, Goetz CG, et al. Ziprasidone treatment of children and adolescents with Tourette’s syndrome: a pilot study. J Am Acad Child Adolesc Psychiatry 2000;39:292-9.
18. Bruggeman R, van der Linden C, Buitelaar JK, et al. Risperidone versus pimozide in Tourette’s disorder: a comparative double-blind parallel-group study. J Clin Psychiatry 2001;50:912-24.
19. Campbell M, Small AM, Green WH, et al. Behavioral efficacy of haloperidol and lithium carbonate: a comparison of hospitalized aggressive children with conduct disorder. Arch Gen Psychiatry 1984;41:650-6.
20. Findling RL, McNamara NK, Branicky LA, et al. A double blind pilot study of risperidone in the treatment of conduct disorder. J Am Acad Child Adolesc Psychiatry 2000;39:509-16.
21. Aman MG, Findling RL, Derivan A, et al. Safety and efficacy of risperidone in children with significant conduct problems and borderline IQ or mental retardation. Brussels, Belgium: 22nd Collegium Internationale Neuro-psychopharmacologicum Congress, July 2000.
22. Turgay A, Snyder R, Fishman S, et al. and the Conduct Research Group. Risperidone versus placebo for conduct and other disruptive behavior disorders in children with subaverage IQ (poster presentation). Victoria, British Columbia, Canada: Canadian Psychiatric Association annual meeting, October 2000.
23. Holford LE, Peter E, Van der Walt A. Risperidone for behavior disorders in children with mental retardation (poster presentation). New York: American Academy of Child and Adolescent Psychiatry annual meeting, October 2000.
24. La Via MC, Gray N, Kaye WH. Case reports of olanzapine treatment of anorexia nervosa. Int J Eating Disord 2000;27:363-6.
1. Dally P, Sargant W. A new treatment of anorexia nervosa. BMJ 1960;1:1770-3.
2. Vandereycken W, Pierloot R. Pimozide combined with behavior therapy in the short-term treatment of anorexia nervosa. Acta Psychiatr Scand 1982;66:445-50.
3. Hanson L. Olanzapine in the treatment of anorexia nervosa. Br J Psychiatry 1999;175:592.-
4. Lavid N, Franklin DL, Maguire GA. Management of child and adolescent stuttering with olanzapine: three case reports. Ann Clin Psychiatry 1999;11(4):233-6.
5. American Academy of Child and Adolescent Psychiatry. AACAP official action: practice parameters for the assessment and treatment of children and adolescents with anxiety disorders. J Am Acad Child Adolesc Psychiatry 1997;36:69-84.
6. Anderson LT, Campbell M, Grega DM, et al. Haloperidol in the treatment of infantile autism: effects on learning and behavioral symptoms. Am J Psychiatry 1984;141(10):1195-1202.
7. Masi G, Cosenza A, Mucci M, Brovedani P. Open trial of risperidone in 24 young children with pervasive developmental disorders. J Am Acad Child Adolesc Psychiatry 2001;40(10):1206-14.
8. Zuddis A, Di Martino A, Muglia P, et al. Long-term risperidone for pervasive developmental disorder: efficacy, tolerability, and discontinuation. J Child Adolesc Psychopharmacol 2000;10(2):79-90.
9. Posey DJ, Walsh KH, Wilson GA, McDougle CJ. Risperidone in the treatment of two very young children with autism. J Child Adolesc Psychopharmacol 1999;9(4):273-6.
10. McDougle CJ, Homes JP, Bronson MR, et al. Risperidone treatment of children and adolescents with pervasive developmental disorders: a prospective open-label study. J Am Acad Child Adolesc Psychiatry 1997;36:685-93.
11. McCracken JT, McGough J, et al. Risperidone in children with autism and serious behavioral problems. Research Units on Pediatric Psychopharmacology Autism Network. N Eng J Med. 2002;347(5):314-21.
12. Potenza MN, Holmes JP, Kanes SJ, McDougle CJ. Olanzapine treatment of children, adolescents, and adults with pervasive developmental disorders: an open-label pilot study. J Clin Psychopharmacol 1999;19:37-44.
13. Malone RP, Cater J, Sheikh RM, et al. Olanzapine versus haloperidol in children with autistic disorder: an open pilot study. J Am Acad Child Adolesc Psychiatry 2001;40:887-94.
14. Kemner C, van Engeland H, Tuynman-Qua H. An open-label study of olanzapine in children with pervasive development disorder. Eur Neuropsychopharmacol 1999;9(suppl 5):S287-S288.
15. Kemner C, van Engeland H, Tuynman-Qua H. An open-label study of olanzapine in children with PDD. Schizophr Res 2000;41(1, suppl 1):194.-
16. Scahill L, Chappell PB, King RA, et al. Pharmacologic treatment of tic disorders. Child Adolesc Clin North Am 2000;9:99-117.
17. Sallee FR, Kurlan R, Goetz CG, et al. Ziprasidone treatment of children and adolescents with Tourette’s syndrome: a pilot study. J Am Acad Child Adolesc Psychiatry 2000;39:292-9.
18. Bruggeman R, van der Linden C, Buitelaar JK, et al. Risperidone versus pimozide in Tourette’s disorder: a comparative double-blind parallel-group study. J Clin Psychiatry 2001;50:912-24.
19. Campbell M, Small AM, Green WH, et al. Behavioral efficacy of haloperidol and lithium carbonate: a comparison of hospitalized aggressive children with conduct disorder. Arch Gen Psychiatry 1984;41:650-6.
20. Findling RL, McNamara NK, Branicky LA, et al. A double blind pilot study of risperidone in the treatment of conduct disorder. J Am Acad Child Adolesc Psychiatry 2000;39:509-16.
21. Aman MG, Findling RL, Derivan A, et al. Safety and efficacy of risperidone in children with significant conduct problems and borderline IQ or mental retardation. Brussels, Belgium: 22nd Collegium Internationale Neuro-psychopharmacologicum Congress, July 2000.
22. Turgay A, Snyder R, Fishman S, et al. and the Conduct Research Group. Risperidone versus placebo for conduct and other disruptive behavior disorders in children with subaverage IQ (poster presentation). Victoria, British Columbia, Canada: Canadian Psychiatric Association annual meeting, October 2000.
23. Holford LE, Peter E, Van der Walt A. Risperidone for behavior disorders in children with mental retardation (poster presentation). New York: American Academy of Child and Adolescent Psychiatry annual meeting, October 2000.
24. La Via MC, Gray N, Kaye WH. Case reports of olanzapine treatment of anorexia nervosa. Int J Eating Disord 2000;27:363-6.
From a trickle to a flood: Pipelines fill with psychotropics for children
Most psychotherapeutic drugs have been studied only in adults and are not approved for use in children and adolescents. Nevertheless, most drugs used in adult psychiatric treatment are widely prescribed to pediatric patients, and prescribing to this young population has increased dramatically (Box).1-3
Without the benefit of efficacy and safety data, one must rely on anecdotal reports and clinical judgment when choosing medications and determining dosages for children and adolescents. That may be changing soon, as more pediatric information is becoming available on psychotherapeutic drugs approved for adults and on agents under development.
Limited industry attention to pediatrics
The evidence gap between adult and pediatric practice4 can be attributed partly to child and adolescent psychiatry lagging behind adult psychiatry in embracing psychopharmacologic treatments. The primary reason, however, has been the pharmaceutical industry’s history of limited interest in studying pediatric populations.
An unprecedented step. In 1986 at Ciba-Geigy, I and colleagues Richard Katz, PhD, Phyllis Landau, MD, and Georges Moroz, MD, began developing clomipramine, the first drug approved in the United States to treat obsessive-compulsive disorder (OCD). Knowing that OCD onset is common in childhood or adolescence, we proposed doing a pediatric study concurrent with the adult studies that would provide the basis for regulatory approval.
Researchers have documented a dramatic increase in psychotropic prescriptions to children and adolescents in recent years.
Olfson et al1 reviewed national trends across 10 years. They found the overall annual rate of prescription of psychotherapeutic drugs to children increased from 1.4 per 100 children in 1987 to 3.9 per 100 in 1996. Stimulant and antidepressant drug prescriptions mostly accounted for this nearly threefold increase.
Rushton and Whitmire 2 reviewed a North Carolina Medicaid population and found the number of children prescribed stimulants increased from 6,407 in 1992 to 27,951 in 1998; the corresponding numbers for selective serotonin reuptake inhibitor (SSRI) prescriptions were 510 and 6,984. These represent a fourfold and greater than tenfold increase, respectively, across 7 years.
Zito et al 3 reported increases of 1.3- to 3.1-fold for stimulant and antidepressant prescriptions to preschool children (aged 2 to 4) between 1991 and 1995 in three healthcare settings.
Clinical development programs at other pharmaceutical companies followed suit when designing studies of selective serotonin reuptake inhibitors (SSRI) for OCD (SSRIs were just reaching the market as antidepressants). In some programs, pediatric studies were done after initial successful studies in adults with OCD. Even so, the industry continued to show little interest in including children and adolescents in routine clinical development of new drugs or in seeking regulatory approval for this population. This changed several years later, thanks to initiatives from the National Institute of Mental Health (NIMH) and the Food and Drug Administration (FDA).
RUPP and beyond
During the 1990s, NIMH convened meetings with the American Academy of Child and Adolescent Psychiatry (AACAP) and others that brought together representatives from academia, government, industry, and clinical practice, as well as patient advocates.7 Attendees discussed the need for new drug development to treat psychiatric disorders in children and adolescents and the obstacles to be overcome for progress to occur. As a result, NIMH in 1996 established Research Units in Pediatric Psychopharmacology (RUPP).
RUPP is a network of centers of excellence in child and adolescent psychopharmacology based in academic medical centers. Its purpose is to provide definitive studies of psychotropic drugs that are being used routinely in children and adolescents and to provide an infrastructure to support complicated multicenter trials. RUPP’s focus is practical, evaluating treatments used in clinical practice.
To date, RUPP has completed and reported the results of two significant studies:
Even so, RUPP has limitations. Its network cannot conduct studies on all psychotropic drugs that are in use today, and it is not positioned to evaluate investigational drugs (in development but not yet approved).
As a result, RUPP’s network can only partially satisfy psychiatrists’ need for information to guide the prescribing of psychotropics to children and adolescents.
FDA initiatives. Concurrent with the NIMH efforts, the FDA implemented the Pediatric Rule of 1994, which applied to all classes of drugs that might be used in younger patients. Under this rule, pharmaceutical manufacturers:
- were required to review existing data for using their drugs in a pediatric population
- could extrapolate efficacy data from adults to children, if the course of disease and effects of drug treatment were sufficiently similar in adult and pediatric patients and if appropriate pharmacokinetic and safety data were provided for younger patients.
FDAMA. The FDA’s next step was included in the FDA Modernization Act (FDAMA) of 1997, which allowed the agency to ask pharmaceutical manufacturers to generate safety and effectiveness data for drugs likely to be used in pediatrics. In exchange, manufacturers received 6 months’ marketing exclusivity (in addition to existing patent protection) for those drugs.
Many companies did sponsor additional safety and efficacy studies, although the incentive’s structure clearly favored drugs with high sales volume. For example, consider two products with annual sales of $200 million and $800 million, respectively. Six months of exclusive marketing rights would generate $400 million in additional revenue from the $800 million product—double the annual revenue of the $200 million product. The pharmaceutical company could obtain this benefit even if total pediatric use were quite small because the 6 months of exclusivity applied to all product sales, including pediatric and adult use.
The FDAMA had several other weaknesses:
- A manufacturer could obtain its benefit even if studies failed to demonstrate the product’s efficacy in the pediatric population.
- The regulation provided no incentive to develop pediatric data for drugs that had lost patent protection.
- It did not induce pharmaceutical companies to include pediatric studies early in drug development.
- for all new chemical entities (drugs in development and not yet approved)
- and for development programs seeking new indications, dosage forms, treatment regimens, or routes of administration for approved products.
- 32 drugs for cancer
- 24 vaccines
- 16 for cardiovascular disease
- 16 for cystic fibrosis
- 16 for infectious diseases
- 11 for psychiatric disorders
- 11 for respiratory disorders
- 10 for AIDS
- 10 for asthma
- 10 for genetic disorders
Source: Pharmaceutical Research and Manufacturers of America10
Drugs in development
As a result of these regulatory changes, the Pharmaceutical Research and Manufacturers of America (PhRMA) reports that nearly 200 drugs and vaccines are in development for children, (Box 2). In addition to the 11 drugs identified by PhRMA for treating psychiatric disorders in children and adolescents, at least another 10 were in the pipeline through the first 6 months of 2002 (Table).11 By the time you read this, some of the drugs may have been terminated from development, new drugs may have been added, and others will have emerged from the development process to receive FDA approval for pediatric use.
Indications. Among the 21 compounds listed in development for 10 different psychiatric indications, 16 are already approved for adult use. One—donepezil—is marketed for management of Alzheimer’s dementia symptoms, but for children and adolescents the agent is being developed for treatment of attention-deficit/hyperactivity disorder (ADHD).
Four other approved drugs appear to be in development for new indications, including mania (topiramate), autism (secretin), Tourette’s syndrome (mecamylamine), and ADHD (modafinil). Among the five new chemical entities (NCEs—investigational drugs not yet marketed with any indication), four appear to be in development for ADHD and one for a disorder of childhood listed only as behavioral disorders.
Table
PSYCHOTROPICS IN DEVELOPMENT FOR CHILDREN AND ADOLESCENTS, LISTED BY INDICATION
| Indication | Drugs in development | Company |
|---|---|---|
| Attention-deficit/hyperactivity disorder | ABT-089 | Abbott Laboratories |
| Atomoxetine | Eli Lilly and Co. | |
| Donepezil | Eisai | |
| Mecamylamine | Layton BioScience, Inc. | |
| Methylphenidate | ||
| Attenade | Celgene | |
| MethylPatch | Noven Pharmaceuticals | |
| Ritalin QD | Novartis Pharmaceuticals | |
| Modafinil | Cephalon | |
| SPD 420 | Cortex Pharmaceuticals | |
| SPD 503 | Shire Pharmaceuticals Group | |
| Depression | Fluoxetine | Eli Lilly and Co. |
| Mirtazepine | Organon | |
| Nefazodone | Brystol-Myers Squibb Co. | |
| Sertraline | Pfizer | |
| Venlafaxine | Wyeth | |
| Obsessive-compulsive disorder | Fluoxetine | Eli Lilly and Co. |
| Fluvoxamine | Solvay Pharmaceuticals | |
| Sertraline | Pfizer | |
| Anxiety | Busipirone | Bristol-Myers Squibb Co. |
| Tourette’s syndrome | Mecamylamine | Layton BioScience Inc. |
| Schizophrenia | Risperidone | Johnson & Johnson Pharmaceutical Research and Development |
| Mania | Topiramate | Johnson & Johnson Pharmaceutical Research and Development |
| Autism | Secretin | Repligen |
| Posttraumatic stress disorder | Sertraline | Pfizer |
The pharmaceutical companies’ decisions to conduct clinical trials in children and adolescents for this group of drugs may be attributable, to some extent, to incentives and the potential for financial gain. Whatever the reasons, the regulatory changes that stimulated this work will have accomplished their goal if they produce evidence of efficacy, safety, and tolerability of these marketed drugs in children and adolescents.
Noncommercial reserach. In addition to industry-sponsored drug development, much pediatric psychopharmacology research is also being conducted in academic and government settings. NIMH and the AACAP are sponsoring trials for a range of pediatric disorders, including ADHD, autism and other pervasive development disorders, bipolar disorder, body dysmorphic disorder, depression, OCD, PTSD, schizophrenia, social phobia, and Sydenham chorea.12,13
Unmet needs
The breadth of indications being investigated in pediatric psychopharmacology clinical trials shows that progress is being made. Missing are NCEs being developed for indications other than ADHD, but the FDA’s Final Pediatric Rule does create the expectation that pediatric studies will be included in all future new drug development programs.
Related resources
- Food and Drug Administration pediatric Web site. http://www.fda.gov/cder/pediatric
- American Academy of Child and Adolescent Psychiatry. Pediatric Psychopharmacology Initiative. http://www.aacap.org/research/ppi.htm
- Busipirone • BuSpar
- Clomipramine • Anafranil
- Donepezil • Aricept
- Fluoxetine • Prozac
- Fluvoxamine • Luvox
- Imipramine • Tofranil
- Mecamylamine • Inversine
- Methylphenidate • MethylPatch, Ritalin QD
- Mirtazapine • Remeron
- Modafinil • Provigil
- Nefazodone • Serzone
- R-methylphenidate • Attenade
- Risperidone • Risperdal
- Secretin • SecreFlo
- Sertraline • Zoloft
- Topiramate • Topamax
- Venlafaxine • Effexor XR
The author reports that he receives grant/research support from Synaptic Pharmaceutical Corp., is a consultant to GlaxoSmithKline, Elan Corp., and Cytospect, and owns stock in GlaxoSmithKline. No GlaxoSmithKline products are mentioned in this article.
1. Olfson M, Marcus SC, Weissman MM, Jensen PS. National trends in the use of psychotropic medications by children. J Am Acad Child Adolesc Psychiatry 2002;41(5):514-21.
2. Rushton JL, Whitmire JT. Pediatric stimulant and selective serotonin reuptake inhibitor prescription trends 1992 to 1998. Arch Pediatr Adolesc Med 2001;155:560-5.
3. Zito JM, Safer DJ, dosReis S, Gardner JF, Boles M, Lynch F. Trends in the prescribing of psychotropic medications to preschoolers. JAMA 2000;283:1025-30.
4. DeVeaugh-Geiss J. OCD: A model for closing the “gap” between adult and pediatric psychiatry. In: Maj M, Sartorius N, Okasha A, Zohar J (eds). World Psychiatric Association series, Evidence and experience in psychiatry (vol. 4). Obsessive-compulsive disorder. Chichester, UK: John Wiley & Sons, 2000:192-4.
5. DeVeaugh-Geiss J, Moroz G, Biederman J, et al. Clomipramine hydrochloride in childhood and adolescent obsessive compulsive disorder: a multicenter trial. J Am Acad Child Adolesc Psychiatry 1992;31(1):45-9.
6. Clomipramine Collaborative Study Group. Clomipramine in the treatment of obsessive compulsive disorder. Arch Gen Psychiatry 1991;48:730-8.
7. Vitiello B, Jensen P. Medication development and testing in children and adolescents: current problems, future directions. Arch Gen Psychiatry 1997;54:871-6.
8. Walkup J, Labellarte M, Riddle M, et al. Fluvoxamine for the treatment of anxiety disorders in children and adolescents. N Engl J Med 2001;344:1279-85.
9. RUPP Autism Network. A double-blind, placebo-controlled trial of risperidone in children with autism. N Engl J Med 2002;347:314-321.
10. Pharmaceutical Research and Manufacturers of America list of new medicines in development. Available at: http://www.phrma.org/searchcures/newmeds/. Accessed Aug. 26 2002.
11. R&D Directions, e-Knowledge Base online databases 2002 (a subscription database). Available at: www.pharmalive.com.
12. National Institute of Mental Health clinical trials. Available at: http://www.nimh.nih.gov/studies/index.cfm. Accessed July 2002.
13. American Academy of Child and Adolescent Psychiatry clinical trials and surveys. Available at: http://www.aacap.org/research/ctvn.htm. Accessed July 2002.
Most psychotherapeutic drugs have been studied only in adults and are not approved for use in children and adolescents. Nevertheless, most drugs used in adult psychiatric treatment are widely prescribed to pediatric patients, and prescribing to this young population has increased dramatically (Box).1-3
Without the benefit of efficacy and safety data, one must rely on anecdotal reports and clinical judgment when choosing medications and determining dosages for children and adolescents. That may be changing soon, as more pediatric information is becoming available on psychotherapeutic drugs approved for adults and on agents under development.
Limited industry attention to pediatrics
The evidence gap between adult and pediatric practice4 can be attributed partly to child and adolescent psychiatry lagging behind adult psychiatry in embracing psychopharmacologic treatments. The primary reason, however, has been the pharmaceutical industry’s history of limited interest in studying pediatric populations.
An unprecedented step. In 1986 at Ciba-Geigy, I and colleagues Richard Katz, PhD, Phyllis Landau, MD, and Georges Moroz, MD, began developing clomipramine, the first drug approved in the United States to treat obsessive-compulsive disorder (OCD). Knowing that OCD onset is common in childhood or adolescence, we proposed doing a pediatric study concurrent with the adult studies that would provide the basis for regulatory approval.
Researchers have documented a dramatic increase in psychotropic prescriptions to children and adolescents in recent years.
Olfson et al1 reviewed national trends across 10 years. They found the overall annual rate of prescription of psychotherapeutic drugs to children increased from 1.4 per 100 children in 1987 to 3.9 per 100 in 1996. Stimulant and antidepressant drug prescriptions mostly accounted for this nearly threefold increase.
Rushton and Whitmire 2 reviewed a North Carolina Medicaid population and found the number of children prescribed stimulants increased from 6,407 in 1992 to 27,951 in 1998; the corresponding numbers for selective serotonin reuptake inhibitor (SSRI) prescriptions were 510 and 6,984. These represent a fourfold and greater than tenfold increase, respectively, across 7 years.
Zito et al 3 reported increases of 1.3- to 3.1-fold for stimulant and antidepressant prescriptions to preschool children (aged 2 to 4) between 1991 and 1995 in three healthcare settings.
Clinical development programs at other pharmaceutical companies followed suit when designing studies of selective serotonin reuptake inhibitors (SSRI) for OCD (SSRIs were just reaching the market as antidepressants). In some programs, pediatric studies were done after initial successful studies in adults with OCD. Even so, the industry continued to show little interest in including children and adolescents in routine clinical development of new drugs or in seeking regulatory approval for this population. This changed several years later, thanks to initiatives from the National Institute of Mental Health (NIMH) and the Food and Drug Administration (FDA).
RUPP and beyond
During the 1990s, NIMH convened meetings with the American Academy of Child and Adolescent Psychiatry (AACAP) and others that brought together representatives from academia, government, industry, and clinical practice, as well as patient advocates.7 Attendees discussed the need for new drug development to treat psychiatric disorders in children and adolescents and the obstacles to be overcome for progress to occur. As a result, NIMH in 1996 established Research Units in Pediatric Psychopharmacology (RUPP).
RUPP is a network of centers of excellence in child and adolescent psychopharmacology based in academic medical centers. Its purpose is to provide definitive studies of psychotropic drugs that are being used routinely in children and adolescents and to provide an infrastructure to support complicated multicenter trials. RUPP’s focus is practical, evaluating treatments used in clinical practice.
To date, RUPP has completed and reported the results of two significant studies:
Even so, RUPP has limitations. Its network cannot conduct studies on all psychotropic drugs that are in use today, and it is not positioned to evaluate investigational drugs (in development but not yet approved).
As a result, RUPP’s network can only partially satisfy psychiatrists’ need for information to guide the prescribing of psychotropics to children and adolescents.
FDA initiatives. Concurrent with the NIMH efforts, the FDA implemented the Pediatric Rule of 1994, which applied to all classes of drugs that might be used in younger patients. Under this rule, pharmaceutical manufacturers:
- were required to review existing data for using their drugs in a pediatric population
- could extrapolate efficacy data from adults to children, if the course of disease and effects of drug treatment were sufficiently similar in adult and pediatric patients and if appropriate pharmacokinetic and safety data were provided for younger patients.
FDAMA. The FDA’s next step was included in the FDA Modernization Act (FDAMA) of 1997, which allowed the agency to ask pharmaceutical manufacturers to generate safety and effectiveness data for drugs likely to be used in pediatrics. In exchange, manufacturers received 6 months’ marketing exclusivity (in addition to existing patent protection) for those drugs.
Many companies did sponsor additional safety and efficacy studies, although the incentive’s structure clearly favored drugs with high sales volume. For example, consider two products with annual sales of $200 million and $800 million, respectively. Six months of exclusive marketing rights would generate $400 million in additional revenue from the $800 million product—double the annual revenue of the $200 million product. The pharmaceutical company could obtain this benefit even if total pediatric use were quite small because the 6 months of exclusivity applied to all product sales, including pediatric and adult use.
The FDAMA had several other weaknesses:
- A manufacturer could obtain its benefit even if studies failed to demonstrate the product’s efficacy in the pediatric population.
- The regulation provided no incentive to develop pediatric data for drugs that had lost patent protection.
- It did not induce pharmaceutical companies to include pediatric studies early in drug development.
- for all new chemical entities (drugs in development and not yet approved)
- and for development programs seeking new indications, dosage forms, treatment regimens, or routes of administration for approved products.
- 32 drugs for cancer
- 24 vaccines
- 16 for cardiovascular disease
- 16 for cystic fibrosis
- 16 for infectious diseases
- 11 for psychiatric disorders
- 11 for respiratory disorders
- 10 for AIDS
- 10 for asthma
- 10 for genetic disorders
Source: Pharmaceutical Research and Manufacturers of America10
Drugs in development
As a result of these regulatory changes, the Pharmaceutical Research and Manufacturers of America (PhRMA) reports that nearly 200 drugs and vaccines are in development for children, (Box 2). In addition to the 11 drugs identified by PhRMA for treating psychiatric disorders in children and adolescents, at least another 10 were in the pipeline through the first 6 months of 2002 (Table).11 By the time you read this, some of the drugs may have been terminated from development, new drugs may have been added, and others will have emerged from the development process to receive FDA approval for pediatric use.
Indications. Among the 21 compounds listed in development for 10 different psychiatric indications, 16 are already approved for adult use. One—donepezil—is marketed for management of Alzheimer’s dementia symptoms, but for children and adolescents the agent is being developed for treatment of attention-deficit/hyperactivity disorder (ADHD).
Four other approved drugs appear to be in development for new indications, including mania (topiramate), autism (secretin), Tourette’s syndrome (mecamylamine), and ADHD (modafinil). Among the five new chemical entities (NCEs—investigational drugs not yet marketed with any indication), four appear to be in development for ADHD and one for a disorder of childhood listed only as behavioral disorders.
Table
PSYCHOTROPICS IN DEVELOPMENT FOR CHILDREN AND ADOLESCENTS, LISTED BY INDICATION
| Indication | Drugs in development | Company |
|---|---|---|
| Attention-deficit/hyperactivity disorder | ABT-089 | Abbott Laboratories |
| Atomoxetine | Eli Lilly and Co. | |
| Donepezil | Eisai | |
| Mecamylamine | Layton BioScience, Inc. | |
| Methylphenidate | ||
| Attenade | Celgene | |
| MethylPatch | Noven Pharmaceuticals | |
| Ritalin QD | Novartis Pharmaceuticals | |
| Modafinil | Cephalon | |
| SPD 420 | Cortex Pharmaceuticals | |
| SPD 503 | Shire Pharmaceuticals Group | |
| Depression | Fluoxetine | Eli Lilly and Co. |
| Mirtazepine | Organon | |
| Nefazodone | Brystol-Myers Squibb Co. | |
| Sertraline | Pfizer | |
| Venlafaxine | Wyeth | |
| Obsessive-compulsive disorder | Fluoxetine | Eli Lilly and Co. |
| Fluvoxamine | Solvay Pharmaceuticals | |
| Sertraline | Pfizer | |
| Anxiety | Busipirone | Bristol-Myers Squibb Co. |
| Tourette’s syndrome | Mecamylamine | Layton BioScience Inc. |
| Schizophrenia | Risperidone | Johnson & Johnson Pharmaceutical Research and Development |
| Mania | Topiramate | Johnson & Johnson Pharmaceutical Research and Development |
| Autism | Secretin | Repligen |
| Posttraumatic stress disorder | Sertraline | Pfizer |
The pharmaceutical companies’ decisions to conduct clinical trials in children and adolescents for this group of drugs may be attributable, to some extent, to incentives and the potential for financial gain. Whatever the reasons, the regulatory changes that stimulated this work will have accomplished their goal if they produce evidence of efficacy, safety, and tolerability of these marketed drugs in children and adolescents.
Noncommercial reserach. In addition to industry-sponsored drug development, much pediatric psychopharmacology research is also being conducted in academic and government settings. NIMH and the AACAP are sponsoring trials for a range of pediatric disorders, including ADHD, autism and other pervasive development disorders, bipolar disorder, body dysmorphic disorder, depression, OCD, PTSD, schizophrenia, social phobia, and Sydenham chorea.12,13
Unmet needs
The breadth of indications being investigated in pediatric psychopharmacology clinical trials shows that progress is being made. Missing are NCEs being developed for indications other than ADHD, but the FDA’s Final Pediatric Rule does create the expectation that pediatric studies will be included in all future new drug development programs.
Related resources
- Food and Drug Administration pediatric Web site. http://www.fda.gov/cder/pediatric
- American Academy of Child and Adolescent Psychiatry. Pediatric Psychopharmacology Initiative. http://www.aacap.org/research/ppi.htm
- Busipirone • BuSpar
- Clomipramine • Anafranil
- Donepezil • Aricept
- Fluoxetine • Prozac
- Fluvoxamine • Luvox
- Imipramine • Tofranil
- Mecamylamine • Inversine
- Methylphenidate • MethylPatch, Ritalin QD
- Mirtazapine • Remeron
- Modafinil • Provigil
- Nefazodone • Serzone
- R-methylphenidate • Attenade
- Risperidone • Risperdal
- Secretin • SecreFlo
- Sertraline • Zoloft
- Topiramate • Topamax
- Venlafaxine • Effexor XR
The author reports that he receives grant/research support from Synaptic Pharmaceutical Corp., is a consultant to GlaxoSmithKline, Elan Corp., and Cytospect, and owns stock in GlaxoSmithKline. No GlaxoSmithKline products are mentioned in this article.
Most psychotherapeutic drugs have been studied only in adults and are not approved for use in children and adolescents. Nevertheless, most drugs used in adult psychiatric treatment are widely prescribed to pediatric patients, and prescribing to this young population has increased dramatically (Box).1-3
Without the benefit of efficacy and safety data, one must rely on anecdotal reports and clinical judgment when choosing medications and determining dosages for children and adolescents. That may be changing soon, as more pediatric information is becoming available on psychotherapeutic drugs approved for adults and on agents under development.
Limited industry attention to pediatrics
The evidence gap between adult and pediatric practice4 can be attributed partly to child and adolescent psychiatry lagging behind adult psychiatry in embracing psychopharmacologic treatments. The primary reason, however, has been the pharmaceutical industry’s history of limited interest in studying pediatric populations.
An unprecedented step. In 1986 at Ciba-Geigy, I and colleagues Richard Katz, PhD, Phyllis Landau, MD, and Georges Moroz, MD, began developing clomipramine, the first drug approved in the United States to treat obsessive-compulsive disorder (OCD). Knowing that OCD onset is common in childhood or adolescence, we proposed doing a pediatric study concurrent with the adult studies that would provide the basis for regulatory approval.
Researchers have documented a dramatic increase in psychotropic prescriptions to children and adolescents in recent years.
Olfson et al1 reviewed national trends across 10 years. They found the overall annual rate of prescription of psychotherapeutic drugs to children increased from 1.4 per 100 children in 1987 to 3.9 per 100 in 1996. Stimulant and antidepressant drug prescriptions mostly accounted for this nearly threefold increase.
Rushton and Whitmire 2 reviewed a North Carolina Medicaid population and found the number of children prescribed stimulants increased from 6,407 in 1992 to 27,951 in 1998; the corresponding numbers for selective serotonin reuptake inhibitor (SSRI) prescriptions were 510 and 6,984. These represent a fourfold and greater than tenfold increase, respectively, across 7 years.
Zito et al 3 reported increases of 1.3- to 3.1-fold for stimulant and antidepressant prescriptions to preschool children (aged 2 to 4) between 1991 and 1995 in three healthcare settings.
Clinical development programs at other pharmaceutical companies followed suit when designing studies of selective serotonin reuptake inhibitors (SSRI) for OCD (SSRIs were just reaching the market as antidepressants). In some programs, pediatric studies were done after initial successful studies in adults with OCD. Even so, the industry continued to show little interest in including children and adolescents in routine clinical development of new drugs or in seeking regulatory approval for this population. This changed several years later, thanks to initiatives from the National Institute of Mental Health (NIMH) and the Food and Drug Administration (FDA).
RUPP and beyond
During the 1990s, NIMH convened meetings with the American Academy of Child and Adolescent Psychiatry (AACAP) and others that brought together representatives from academia, government, industry, and clinical practice, as well as patient advocates.7 Attendees discussed the need for new drug development to treat psychiatric disorders in children and adolescents and the obstacles to be overcome for progress to occur. As a result, NIMH in 1996 established Research Units in Pediatric Psychopharmacology (RUPP).
RUPP is a network of centers of excellence in child and adolescent psychopharmacology based in academic medical centers. Its purpose is to provide definitive studies of psychotropic drugs that are being used routinely in children and adolescents and to provide an infrastructure to support complicated multicenter trials. RUPP’s focus is practical, evaluating treatments used in clinical practice.
To date, RUPP has completed and reported the results of two significant studies:
Even so, RUPP has limitations. Its network cannot conduct studies on all psychotropic drugs that are in use today, and it is not positioned to evaluate investigational drugs (in development but not yet approved).
As a result, RUPP’s network can only partially satisfy psychiatrists’ need for information to guide the prescribing of psychotropics to children and adolescents.
FDA initiatives. Concurrent with the NIMH efforts, the FDA implemented the Pediatric Rule of 1994, which applied to all classes of drugs that might be used in younger patients. Under this rule, pharmaceutical manufacturers:
- were required to review existing data for using their drugs in a pediatric population
- could extrapolate efficacy data from adults to children, if the course of disease and effects of drug treatment were sufficiently similar in adult and pediatric patients and if appropriate pharmacokinetic and safety data were provided for younger patients.
FDAMA. The FDA’s next step was included in the FDA Modernization Act (FDAMA) of 1997, which allowed the agency to ask pharmaceutical manufacturers to generate safety and effectiveness data for drugs likely to be used in pediatrics. In exchange, manufacturers received 6 months’ marketing exclusivity (in addition to existing patent protection) for those drugs.
Many companies did sponsor additional safety and efficacy studies, although the incentive’s structure clearly favored drugs with high sales volume. For example, consider two products with annual sales of $200 million and $800 million, respectively. Six months of exclusive marketing rights would generate $400 million in additional revenue from the $800 million product—double the annual revenue of the $200 million product. The pharmaceutical company could obtain this benefit even if total pediatric use were quite small because the 6 months of exclusivity applied to all product sales, including pediatric and adult use.
The FDAMA had several other weaknesses:
- A manufacturer could obtain its benefit even if studies failed to demonstrate the product’s efficacy in the pediatric population.
- The regulation provided no incentive to develop pediatric data for drugs that had lost patent protection.
- It did not induce pharmaceutical companies to include pediatric studies early in drug development.
- for all new chemical entities (drugs in development and not yet approved)
- and for development programs seeking new indications, dosage forms, treatment regimens, or routes of administration for approved products.
- 32 drugs for cancer
- 24 vaccines
- 16 for cardiovascular disease
- 16 for cystic fibrosis
- 16 for infectious diseases
- 11 for psychiatric disorders
- 11 for respiratory disorders
- 10 for AIDS
- 10 for asthma
- 10 for genetic disorders
Source: Pharmaceutical Research and Manufacturers of America10
Drugs in development
As a result of these regulatory changes, the Pharmaceutical Research and Manufacturers of America (PhRMA) reports that nearly 200 drugs and vaccines are in development for children, (Box 2). In addition to the 11 drugs identified by PhRMA for treating psychiatric disorders in children and adolescents, at least another 10 were in the pipeline through the first 6 months of 2002 (Table).11 By the time you read this, some of the drugs may have been terminated from development, new drugs may have been added, and others will have emerged from the development process to receive FDA approval for pediatric use.
Indications. Among the 21 compounds listed in development for 10 different psychiatric indications, 16 are already approved for adult use. One—donepezil—is marketed for management of Alzheimer’s dementia symptoms, but for children and adolescents the agent is being developed for treatment of attention-deficit/hyperactivity disorder (ADHD).
Four other approved drugs appear to be in development for new indications, including mania (topiramate), autism (secretin), Tourette’s syndrome (mecamylamine), and ADHD (modafinil). Among the five new chemical entities (NCEs—investigational drugs not yet marketed with any indication), four appear to be in development for ADHD and one for a disorder of childhood listed only as behavioral disorders.
Table
PSYCHOTROPICS IN DEVELOPMENT FOR CHILDREN AND ADOLESCENTS, LISTED BY INDICATION
| Indication | Drugs in development | Company |
|---|---|---|
| Attention-deficit/hyperactivity disorder | ABT-089 | Abbott Laboratories |
| Atomoxetine | Eli Lilly and Co. | |
| Donepezil | Eisai | |
| Mecamylamine | Layton BioScience, Inc. | |
| Methylphenidate | ||
| Attenade | Celgene | |
| MethylPatch | Noven Pharmaceuticals | |
| Ritalin QD | Novartis Pharmaceuticals | |
| Modafinil | Cephalon | |
| SPD 420 | Cortex Pharmaceuticals | |
| SPD 503 | Shire Pharmaceuticals Group | |
| Depression | Fluoxetine | Eli Lilly and Co. |
| Mirtazepine | Organon | |
| Nefazodone | Brystol-Myers Squibb Co. | |
| Sertraline | Pfizer | |
| Venlafaxine | Wyeth | |
| Obsessive-compulsive disorder | Fluoxetine | Eli Lilly and Co. |
| Fluvoxamine | Solvay Pharmaceuticals | |
| Sertraline | Pfizer | |
| Anxiety | Busipirone | Bristol-Myers Squibb Co. |
| Tourette’s syndrome | Mecamylamine | Layton BioScience Inc. |
| Schizophrenia | Risperidone | Johnson & Johnson Pharmaceutical Research and Development |
| Mania | Topiramate | Johnson & Johnson Pharmaceutical Research and Development |
| Autism | Secretin | Repligen |
| Posttraumatic stress disorder | Sertraline | Pfizer |
The pharmaceutical companies’ decisions to conduct clinical trials in children and adolescents for this group of drugs may be attributable, to some extent, to incentives and the potential for financial gain. Whatever the reasons, the regulatory changes that stimulated this work will have accomplished their goal if they produce evidence of efficacy, safety, and tolerability of these marketed drugs in children and adolescents.
Noncommercial reserach. In addition to industry-sponsored drug development, much pediatric psychopharmacology research is also being conducted in academic and government settings. NIMH and the AACAP are sponsoring trials for a range of pediatric disorders, including ADHD, autism and other pervasive development disorders, bipolar disorder, body dysmorphic disorder, depression, OCD, PTSD, schizophrenia, social phobia, and Sydenham chorea.12,13
Unmet needs
The breadth of indications being investigated in pediatric psychopharmacology clinical trials shows that progress is being made. Missing are NCEs being developed for indications other than ADHD, but the FDA’s Final Pediatric Rule does create the expectation that pediatric studies will be included in all future new drug development programs.
Related resources
- Food and Drug Administration pediatric Web site. http://www.fda.gov/cder/pediatric
- American Academy of Child and Adolescent Psychiatry. Pediatric Psychopharmacology Initiative. http://www.aacap.org/research/ppi.htm
- Busipirone • BuSpar
- Clomipramine • Anafranil
- Donepezil • Aricept
- Fluoxetine • Prozac
- Fluvoxamine • Luvox
- Imipramine • Tofranil
- Mecamylamine • Inversine
- Methylphenidate • MethylPatch, Ritalin QD
- Mirtazapine • Remeron
- Modafinil • Provigil
- Nefazodone • Serzone
- R-methylphenidate • Attenade
- Risperidone • Risperdal
- Secretin • SecreFlo
- Sertraline • Zoloft
- Topiramate • Topamax
- Venlafaxine • Effexor XR
The author reports that he receives grant/research support from Synaptic Pharmaceutical Corp., is a consultant to GlaxoSmithKline, Elan Corp., and Cytospect, and owns stock in GlaxoSmithKline. No GlaxoSmithKline products are mentioned in this article.
1. Olfson M, Marcus SC, Weissman MM, Jensen PS. National trends in the use of psychotropic medications by children. J Am Acad Child Adolesc Psychiatry 2002;41(5):514-21.
2. Rushton JL, Whitmire JT. Pediatric stimulant and selective serotonin reuptake inhibitor prescription trends 1992 to 1998. Arch Pediatr Adolesc Med 2001;155:560-5.
3. Zito JM, Safer DJ, dosReis S, Gardner JF, Boles M, Lynch F. Trends in the prescribing of psychotropic medications to preschoolers. JAMA 2000;283:1025-30.
4. DeVeaugh-Geiss J. OCD: A model for closing the “gap” between adult and pediatric psychiatry. In: Maj M, Sartorius N, Okasha A, Zohar J (eds). World Psychiatric Association series, Evidence and experience in psychiatry (vol. 4). Obsessive-compulsive disorder. Chichester, UK: John Wiley & Sons, 2000:192-4.
5. DeVeaugh-Geiss J, Moroz G, Biederman J, et al. Clomipramine hydrochloride in childhood and adolescent obsessive compulsive disorder: a multicenter trial. J Am Acad Child Adolesc Psychiatry 1992;31(1):45-9.
6. Clomipramine Collaborative Study Group. Clomipramine in the treatment of obsessive compulsive disorder. Arch Gen Psychiatry 1991;48:730-8.
7. Vitiello B, Jensen P. Medication development and testing in children and adolescents: current problems, future directions. Arch Gen Psychiatry 1997;54:871-6.
8. Walkup J, Labellarte M, Riddle M, et al. Fluvoxamine for the treatment of anxiety disorders in children and adolescents. N Engl J Med 2001;344:1279-85.
9. RUPP Autism Network. A double-blind, placebo-controlled trial of risperidone in children with autism. N Engl J Med 2002;347:314-321.
10. Pharmaceutical Research and Manufacturers of America list of new medicines in development. Available at: http://www.phrma.org/searchcures/newmeds/. Accessed Aug. 26 2002.
11. R&D Directions, e-Knowledge Base online databases 2002 (a subscription database). Available at: www.pharmalive.com.
12. National Institute of Mental Health clinical trials. Available at: http://www.nimh.nih.gov/studies/index.cfm. Accessed July 2002.
13. American Academy of Child and Adolescent Psychiatry clinical trials and surveys. Available at: http://www.aacap.org/research/ctvn.htm. Accessed July 2002.
1. Olfson M, Marcus SC, Weissman MM, Jensen PS. National trends in the use of psychotropic medications by children. J Am Acad Child Adolesc Psychiatry 2002;41(5):514-21.
2. Rushton JL, Whitmire JT. Pediatric stimulant and selective serotonin reuptake inhibitor prescription trends 1992 to 1998. Arch Pediatr Adolesc Med 2001;155:560-5.
3. Zito JM, Safer DJ, dosReis S, Gardner JF, Boles M, Lynch F. Trends in the prescribing of psychotropic medications to preschoolers. JAMA 2000;283:1025-30.
4. DeVeaugh-Geiss J. OCD: A model for closing the “gap” between adult and pediatric psychiatry. In: Maj M, Sartorius N, Okasha A, Zohar J (eds). World Psychiatric Association series, Evidence and experience in psychiatry (vol. 4). Obsessive-compulsive disorder. Chichester, UK: John Wiley & Sons, 2000:192-4.
5. DeVeaugh-Geiss J, Moroz G, Biederman J, et al. Clomipramine hydrochloride in childhood and adolescent obsessive compulsive disorder: a multicenter trial. J Am Acad Child Adolesc Psychiatry 1992;31(1):45-9.
6. Clomipramine Collaborative Study Group. Clomipramine in the treatment of obsessive compulsive disorder. Arch Gen Psychiatry 1991;48:730-8.
7. Vitiello B, Jensen P. Medication development and testing in children and adolescents: current problems, future directions. Arch Gen Psychiatry 1997;54:871-6.
8. Walkup J, Labellarte M, Riddle M, et al. Fluvoxamine for the treatment of anxiety disorders in children and adolescents. N Engl J Med 2001;344:1279-85.
9. RUPP Autism Network. A double-blind, placebo-controlled trial of risperidone in children with autism. N Engl J Med 2002;347:314-321.
10. Pharmaceutical Research and Manufacturers of America list of new medicines in development. Available at: http://www.phrma.org/searchcures/newmeds/. Accessed Aug. 26 2002.
11. R&D Directions, e-Knowledge Base online databases 2002 (a subscription database). Available at: www.pharmalive.com.
12. National Institute of Mental Health clinical trials. Available at: http://www.nimh.nih.gov/studies/index.cfm. Accessed July 2002.
13. American Academy of Child and Adolescent Psychiatry clinical trials and surveys. Available at: http://www.aacap.org/research/ctvn.htm. Accessed July 2002.
From a trickle to a flood: Pipelines fill with psychotropics for children
Most psychotherapeutic drugs have been studied only in adults and are not approved for use in children and adolescents. Nevertheless, most drugs used in adult psychiatric treatment are widely prescribed to pediatric patients, and prescribing to this young population has increased dramatically (Box).1-3
Without the benefit of efficacy and safety data, one must rely on anecdotal reports and clinical judgment when choosing medications and determining dosages for children and adolescents. That may be changing soon, as more pediatric information is becoming available on psychotherapeutic drugs approved for adults and on agents under development.
Limited industry attention to pediatrics
The evidence gap between adult and pediatric practice4 can be attributed partly to child and adolescent psychiatry lagging behind adult psychiatry in embracing psychopharmacologic treatments. The primary reason, however, has been the pharmaceutical industry’s history of limited interest in studying pediatric populations.
An unprecedented step. In 1986 at Ciba-Geigy, I and colleagues Richard Katz, PhD, Phyllis Landau, MD, and Georges Moroz, MD, began developing clomipramine, the first drug approved in the United States to treat obsessive-compulsive disorder (OCD). Knowing that OCD onset is common in childhood or adolescence, we proposed doing a pediatric study concurrent with the adult studies that would provide the basis for regulatory approval.
Researchers have documented a dramatic increase in psychotropic prescriptions to children and adolescents in recent years.
Olfson et al1 reviewed national trends across 10 years. They found the overall annual rate of prescription of psychotherapeutic drugs to children increased from 1.4 per 100 children in 1987 to 3.9 per 100 in 1996. Stimulant and antidepressant drug prescriptions mostly accounted for this nearly threefold increase.
Rushton and Whitmire 2 reviewed a North Carolina Medicaid population and found the number of children prescribed stimulants increased from 6,407 in 1992 to 27,951 in 1998; the corresponding numbers for selective serotonin reuptake inhibitor (SSRI) prescriptions were 510 and 6,984. These represent a fourfold and greater than tenfold increase, respectively, across 7 years.
Zito et al 3 reported increases of 1.3- to 3.1-fold for stimulant and antidepressant prescriptions to preschool children (aged 2 to 4) between 1991 and 1995 in three healthcare settings.
Clinical development programs at other pharmaceutical companies followed suit when designing studies of selective serotonin reuptake inhibitors (SSRI) for OCD (SSRIs were just reaching the market as antidepressants). In some programs, pediatric studies were done after initial successful studies in adults with OCD. Even so, the industry continued to show little interest in including children and adolescents in routine clinical development of new drugs or in seeking regulatory approval for this population. This changed several years later, thanks to initiatives from the National Institute of Mental Health (NIMH) and the Food and Drug Administration (FDA).
RUPP and beyond
During the 1990s, NIMH convened meetings with the American Academy of Child and Adolescent Psychiatry (AACAP) and others that brought together representatives from academia, government, industry, and clinical practice, as well as patient advocates.7 Attendees discussed the need for new drug development to treat psychiatric disorders in children and adolescents and the obstacles to be overcome for progress to occur. As a result, NIMH in 1996 established Research Units in Pediatric Psychopharmacology (RUPP).
RUPP is a network of centers of excellence in child and adolescent psychopharmacology based in academic medical centers. Its purpose is to provide definitive studies of psychotropic drugs that are being used routinely in children and adolescents and to provide an infrastructure to support complicated multicenter trials. RUPP’s focus is practical, evaluating treatments used in clinical practice.
To date, RUPP has completed and reported the results of two significant studies:
Even so, RUPP has limitations. Its network cannot conduct studies on all psychotropic drugs that are in use today, and it is not positioned to evaluate investigational drugs (in development but not yet approved).
As a result, RUPP’s network can only partially satisfy psychiatrists’ need for information to guide the prescribing of psychotropics to children and adolescents.
FDA initiatives. Concurrent with the NIMH efforts, the FDA implemented the Pediatric Rule of 1994, which applied to all classes of drugs that might be used in younger patients. Under this rule, pharmaceutical manufacturers:
- were required to review existing data for using their drugs in a pediatric population
- could extrapolate efficacy data from adults to children, if the course of disease and effects of drug treatment were sufficiently similar in adult and pediatric patients and if appropriate pharmacokinetic and safety data were provided for younger patients.
FDAMA. The FDA’s next step was included in the FDA Modernization Act (FDAMA) of 1997, which allowed the agency to ask pharmaceutical manufacturers to generate safety and effectiveness data for drugs likely to be used in pediatrics. In exchange, manufacturers received 6 months’ marketing exclusivity (in addition to existing patent protection) for those drugs.
Many companies did sponsor additional safety and efficacy studies, although the incentive’s structure clearly favored drugs with high sales volume. For example, consider two products with annual sales of $200 million and $800 million, respectively. Six months of exclusive marketing rights would generate $400 million in additional revenue from the $800 million product—double the annual revenue of the $200 million product. The pharmaceutical company could obtain this benefit even if total pediatric use were quite small because the 6 months of exclusivity applied to all product sales, including pediatric and adult use.
The FDAMA had several other weaknesses:
- A manufacturer could obtain its benefit even if studies failed to demonstrate the product’s efficacy in the pediatric population.
- The regulation provided no incentive to develop pediatric data for drugs that had lost patent protection.
- It did not induce pharmaceutical companies to include pediatric studies early in drug development.
- for all new chemical entities (drugs in development and not yet approved)
- and for development programs seeking new indications, dosage forms, treatment regimens, or routes of administration for approved products.
- 32 drugs for cancer
- 24 vaccines
- 16 for cardiovascular disease
- 16 for cystic fibrosis
- 16 for infectious diseases
- 11 for psychiatric disorders
- 11 for respiratory disorders
- 10 for AIDS
- 10 for asthma
- 10 for genetic disorders
Source: Pharmaceutical Research and Manufacturers of America10
Drugs in development
As a result of these regulatory changes, the Pharmaceutical Research and Manufacturers of America (PhRMA) reports that nearly 200 drugs and vaccines are in development for children, (Box 2). In addition to the 11 drugs identified by PhRMA for treating psychiatric disorders in children and adolescents, at least another 10 were in the pipeline through the first 6 months of 2002 (Table).11 By the time you read this, some of the drugs may have been terminated from development, new drugs may have been added, and others will have emerged from the development process to receive FDA approval for pediatric use.
Indications. Among the 21 compounds listed in development for 10 different psychiatric indications, 16 are already approved for adult use. One—donepezil—is marketed for management of Alzheimer’s dementia symptoms, but for children and adolescents the agent is being developed for treatment of attention-deficit/hyperactivity disorder (ADHD).
Four other approved drugs appear to be in development for new indications, including mania (topiramate), autism (secretin), Tourette’s syndrome (mecamylamine), and ADHD (modafinil). Among the five new chemical entities (NCEs—investigational drugs not yet marketed with any indication), four appear to be in development for ADHD and one for a disorder of childhood listed only as behavioral disorders.
Table
PSYCHOTROPICS IN DEVELOPMENT FOR CHILDREN AND ADOLESCENTS, LISTED BY INDICATION
| Indication | Drugs in development | Company |
|---|---|---|
| Attention-deficit/hyperactivity disorder | ABT-089 | Abbott Laboratories |
| Atomoxetine | Eli Lilly and Co. | |
| Donepezil | Eisai | |
| Mecamylamine | Layton BioScience, Inc. | |
| Methylphenidate | ||
| Attenade | Celgene | |
| MethylPatch | Noven Pharmaceuticals | |
| Ritalin QD | Novartis Pharmaceuticals | |
| Modafinil | Cephalon | |
| SPD 420 | Cortex Pharmaceuticals | |
| SPD 503 | Shire Pharmaceuticals Group | |
| Depression | Fluoxetine | Eli Lilly and Co. |
| Mirtazepine | Organon | |
| Nefazodone | Brystol-Myers Squibb Co. | |
| Sertraline | Pfizer | |
| Venlafaxine | Wyeth | |
| Obsessive-compulsive disorder | Fluoxetine | Eli Lilly and Co. |
| Fluvoxamine | Solvay Pharmaceuticals | |
| Sertraline | Pfizer | |
| Anxiety | Busipirone | Bristol-Myers Squibb Co. |
| Tourette’s syndrome | Mecamylamine | Layton BioScience Inc. |
| Schizophrenia | Risperidone | Johnson & Johnson Pharmaceutical Research and Development |
| Mania | Topiramate | Johnson & Johnson Pharmaceutical Research and Development |
| Autism | Secretin | Repligen |
| Posttraumatic stress disorder | Sertraline | Pfizer |
The pharmaceutical companies’ decisions to conduct clinical trials in children and adolescents for this group of drugs may be attributable, to some extent, to incentives and the potential for financial gain. Whatever the reasons, the regulatory changes that stimulated this work will have accomplished their goal if they produce evidence of efficacy, safety, and tolerability of these marketed drugs in children and adolescents.
Noncommercial reserach. In addition to industry-sponsored drug development, much pediatric psychopharmacology research is also being conducted in academic and government settings. NIMH and the AACAP are sponsoring trials for a range of pediatric disorders, including ADHD, autism and other pervasive development disorders, bipolar disorder, body dysmorphic disorder, depression, OCD, PTSD, schizophrenia, social phobia, and Sydenham chorea.12,13
Unmet needs
The breadth of indications being investigated in pediatric psychopharmacology clinical trials shows that progress is being made. Missing are NCEs being developed for indications other than ADHD, but the FDA’s Final Pediatric Rule does create the expectation that pediatric studies will be included in all future new drug development programs.
Related resources
- Food and Drug Administration pediatric Web site. http://www.fda.gov/cder/pediatric
- American Academy of Child and Adolescent Psychiatry. Pediatric Psychopharmacology Initiative. http://www.aacap.org/research/ppi.htm
- Busipirone • BuSpar
- Clomipramine • Anafranil
- Donepezil • Aricept
- Fluoxetine • Prozac
- Fluvoxamine • Luvox
- Imipramine • Tofranil
- Mecamylamine • Inversine
- Methylphenidate • MethylPatch, Ritalin QD
- Mirtazapine • Remeron
- Modafinil • Provigil
- Nefazodone • Serzone
- R-methylphenidate • Attenade
- Risperidone • Risperdal
- Secretin • SecreFlo
- Sertraline • Zoloft
- Topiramate • Topamax
- Venlafaxine • Effexor XR
The author reports that he receives grant/research support from Synaptic Pharmaceutical Corp., is a consultant to GlaxoSmithKline, Elan Corp., and Cytospect, and owns stock in GlaxoSmithKline. No GlaxoSmithKline products are mentioned in this article.
1. Olfson M, Marcus SC, Weissman MM, Jensen PS. National trends in the use of psychotropic medications by children. J Am Acad Child Adolesc Psychiatry 2002;41(5):514-21.
2. Rushton JL, Whitmire JT. Pediatric stimulant and selective serotonin reuptake inhibitor prescription trends 1992 to 1998. Arch Pediatr Adolesc Med 2001;155:560-5.
3. Zito JM, Safer DJ, dosReis S, Gardner JF, Boles M, Lynch F. Trends in the prescribing of psychotropic medications to preschoolers. JAMA 2000;283:1025-30.
4. DeVeaugh-Geiss J. OCD: A model for closing the “gap” between adult and pediatric psychiatry. In: Maj M, Sartorius N, Okasha A, Zohar J (eds). World Psychiatric Association series, Evidence and experience in psychiatry (vol. 4). Obsessive-compulsive disorder. Chichester, UK: John Wiley & Sons, 2000:192-4.
5. DeVeaugh-Geiss J, Moroz G, Biederman J, et al. Clomipramine hydrochloride in childhood and adolescent obsessive compulsive disorder: a multicenter trial. J Am Acad Child Adolesc Psychiatry 1992;31(1):45-9.
6. Clomipramine Collaborative Study Group. Clomipramine in the treatment of obsessive compulsive disorder. Arch Gen Psychiatry 1991;48:730-8.
7. Vitiello B, Jensen P. Medication development and testing in children and adolescents: current problems, future directions. Arch Gen Psychiatry 1997;54:871-6.
8. Walkup J, Labellarte M, Riddle M, et al. Fluvoxamine for the treatment of anxiety disorders in children and adolescents. N Engl J Med 2001;344:1279-85.
9. RUPP Autism Network. A double-blind, placebo-controlled trial of risperidone in children with autism. N Engl J Med 2002;347:314-321.
10. Pharmaceutical Research and Manufacturers of America list of new medicines in development. Available at: http://www.phrma.org/searchcures/newmeds/. Accessed Aug. 26 2002.
11. R&D Directions, e-Knowledge Base online databases 2002 (a subscription database). Available at: www.pharmalive.com.
12. National Institute of Mental Health clinical trials. Available at: http://www.nimh.nih.gov/studies/index.cfm. Accessed July 2002.
13. American Academy of Child and Adolescent Psychiatry clinical trials and surveys. Available at: http://www.aacap.org/research/ctvn.htm. Accessed July 2002.
Most psychotherapeutic drugs have been studied only in adults and are not approved for use in children and adolescents. Nevertheless, most drugs used in adult psychiatric treatment are widely prescribed to pediatric patients, and prescribing to this young population has increased dramatically (Box).1-3
Without the benefit of efficacy and safety data, one must rely on anecdotal reports and clinical judgment when choosing medications and determining dosages for children and adolescents. That may be changing soon, as more pediatric information is becoming available on psychotherapeutic drugs approved for adults and on agents under development.
Limited industry attention to pediatrics
The evidence gap between adult and pediatric practice4 can be attributed partly to child and adolescent psychiatry lagging behind adult psychiatry in embracing psychopharmacologic treatments. The primary reason, however, has been the pharmaceutical industry’s history of limited interest in studying pediatric populations.
An unprecedented step. In 1986 at Ciba-Geigy, I and colleagues Richard Katz, PhD, Phyllis Landau, MD, and Georges Moroz, MD, began developing clomipramine, the first drug approved in the United States to treat obsessive-compulsive disorder (OCD). Knowing that OCD onset is common in childhood or adolescence, we proposed doing a pediatric study concurrent with the adult studies that would provide the basis for regulatory approval.
Researchers have documented a dramatic increase in psychotropic prescriptions to children and adolescents in recent years.
Olfson et al1 reviewed national trends across 10 years. They found the overall annual rate of prescription of psychotherapeutic drugs to children increased from 1.4 per 100 children in 1987 to 3.9 per 100 in 1996. Stimulant and antidepressant drug prescriptions mostly accounted for this nearly threefold increase.
Rushton and Whitmire 2 reviewed a North Carolina Medicaid population and found the number of children prescribed stimulants increased from 6,407 in 1992 to 27,951 in 1998; the corresponding numbers for selective serotonin reuptake inhibitor (SSRI) prescriptions were 510 and 6,984. These represent a fourfold and greater than tenfold increase, respectively, across 7 years.
Zito et al 3 reported increases of 1.3- to 3.1-fold for stimulant and antidepressant prescriptions to preschool children (aged 2 to 4) between 1991 and 1995 in three healthcare settings.
Clinical development programs at other pharmaceutical companies followed suit when designing studies of selective serotonin reuptake inhibitors (SSRI) for OCD (SSRIs were just reaching the market as antidepressants). In some programs, pediatric studies were done after initial successful studies in adults with OCD. Even so, the industry continued to show little interest in including children and adolescents in routine clinical development of new drugs or in seeking regulatory approval for this population. This changed several years later, thanks to initiatives from the National Institute of Mental Health (NIMH) and the Food and Drug Administration (FDA).
RUPP and beyond
During the 1990s, NIMH convened meetings with the American Academy of Child and Adolescent Psychiatry (AACAP) and others that brought together representatives from academia, government, industry, and clinical practice, as well as patient advocates.7 Attendees discussed the need for new drug development to treat psychiatric disorders in children and adolescents and the obstacles to be overcome for progress to occur. As a result, NIMH in 1996 established Research Units in Pediatric Psychopharmacology (RUPP).
RUPP is a network of centers of excellence in child and adolescent psychopharmacology based in academic medical centers. Its purpose is to provide definitive studies of psychotropic drugs that are being used routinely in children and adolescents and to provide an infrastructure to support complicated multicenter trials. RUPP’s focus is practical, evaluating treatments used in clinical practice.
To date, RUPP has completed and reported the results of two significant studies:
Even so, RUPP has limitations. Its network cannot conduct studies on all psychotropic drugs that are in use today, and it is not positioned to evaluate investigational drugs (in development but not yet approved).
As a result, RUPP’s network can only partially satisfy psychiatrists’ need for information to guide the prescribing of psychotropics to children and adolescents.
FDA initiatives. Concurrent with the NIMH efforts, the FDA implemented the Pediatric Rule of 1994, which applied to all classes of drugs that might be used in younger patients. Under this rule, pharmaceutical manufacturers:
- were required to review existing data for using their drugs in a pediatric population
- could extrapolate efficacy data from adults to children, if the course of disease and effects of drug treatment were sufficiently similar in adult and pediatric patients and if appropriate pharmacokinetic and safety data were provided for younger patients.
FDAMA. The FDA’s next step was included in the FDA Modernization Act (FDAMA) of 1997, which allowed the agency to ask pharmaceutical manufacturers to generate safety and effectiveness data for drugs likely to be used in pediatrics. In exchange, manufacturers received 6 months’ marketing exclusivity (in addition to existing patent protection) for those drugs.
Many companies did sponsor additional safety and efficacy studies, although the incentive’s structure clearly favored drugs with high sales volume. For example, consider two products with annual sales of $200 million and $800 million, respectively. Six months of exclusive marketing rights would generate $400 million in additional revenue from the $800 million product—double the annual revenue of the $200 million product. The pharmaceutical company could obtain this benefit even if total pediatric use were quite small because the 6 months of exclusivity applied to all product sales, including pediatric and adult use.
The FDAMA had several other weaknesses:
- A manufacturer could obtain its benefit even if studies failed to demonstrate the product’s efficacy in the pediatric population.
- The regulation provided no incentive to develop pediatric data for drugs that had lost patent protection.
- It did not induce pharmaceutical companies to include pediatric studies early in drug development.
- for all new chemical entities (drugs in development and not yet approved)
- and for development programs seeking new indications, dosage forms, treatment regimens, or routes of administration for approved products.
- 32 drugs for cancer
- 24 vaccines
- 16 for cardiovascular disease
- 16 for cystic fibrosis
- 16 for infectious diseases
- 11 for psychiatric disorders
- 11 for respiratory disorders
- 10 for AIDS
- 10 for asthma
- 10 for genetic disorders
Source: Pharmaceutical Research and Manufacturers of America10
Drugs in development
As a result of these regulatory changes, the Pharmaceutical Research and Manufacturers of America (PhRMA) reports that nearly 200 drugs and vaccines are in development for children, (Box 2). In addition to the 11 drugs identified by PhRMA for treating psychiatric disorders in children and adolescents, at least another 10 were in the pipeline through the first 6 months of 2002 (Table).11 By the time you read this, some of the drugs may have been terminated from development, new drugs may have been added, and others will have emerged from the development process to receive FDA approval for pediatric use.
Indications. Among the 21 compounds listed in development for 10 different psychiatric indications, 16 are already approved for adult use. One—donepezil—is marketed for management of Alzheimer’s dementia symptoms, but for children and adolescents the agent is being developed for treatment of attention-deficit/hyperactivity disorder (ADHD).
Four other approved drugs appear to be in development for new indications, including mania (topiramate), autism (secretin), Tourette’s syndrome (mecamylamine), and ADHD (modafinil). Among the five new chemical entities (NCEs—investigational drugs not yet marketed with any indication), four appear to be in development for ADHD and one for a disorder of childhood listed only as behavioral disorders.
Table
PSYCHOTROPICS IN DEVELOPMENT FOR CHILDREN AND ADOLESCENTS, LISTED BY INDICATION
| Indication | Drugs in development | Company |
|---|---|---|
| Attention-deficit/hyperactivity disorder | ABT-089 | Abbott Laboratories |
| Atomoxetine | Eli Lilly and Co. | |
| Donepezil | Eisai | |
| Mecamylamine | Layton BioScience, Inc. | |
| Methylphenidate | ||
| Attenade | Celgene | |
| MethylPatch | Noven Pharmaceuticals | |
| Ritalin QD | Novartis Pharmaceuticals | |
| Modafinil | Cephalon | |
| SPD 420 | Cortex Pharmaceuticals | |
| SPD 503 | Shire Pharmaceuticals Group | |
| Depression | Fluoxetine | Eli Lilly and Co. |
| Mirtazepine | Organon | |
| Nefazodone | Brystol-Myers Squibb Co. | |
| Sertraline | Pfizer | |
| Venlafaxine | Wyeth | |
| Obsessive-compulsive disorder | Fluoxetine | Eli Lilly and Co. |
| Fluvoxamine | Solvay Pharmaceuticals | |
| Sertraline | Pfizer | |
| Anxiety | Busipirone | Bristol-Myers Squibb Co. |
| Tourette’s syndrome | Mecamylamine | Layton BioScience Inc. |
| Schizophrenia | Risperidone | Johnson & Johnson Pharmaceutical Research and Development |
| Mania | Topiramate | Johnson & Johnson Pharmaceutical Research and Development |
| Autism | Secretin | Repligen |
| Posttraumatic stress disorder | Sertraline | Pfizer |
The pharmaceutical companies’ decisions to conduct clinical trials in children and adolescents for this group of drugs may be attributable, to some extent, to incentives and the potential for financial gain. Whatever the reasons, the regulatory changes that stimulated this work will have accomplished their goal if they produce evidence of efficacy, safety, and tolerability of these marketed drugs in children and adolescents.
Noncommercial reserach. In addition to industry-sponsored drug development, much pediatric psychopharmacology research is also being conducted in academic and government settings. NIMH and the AACAP are sponsoring trials for a range of pediatric disorders, including ADHD, autism and other pervasive development disorders, bipolar disorder, body dysmorphic disorder, depression, OCD, PTSD, schizophrenia, social phobia, and Sydenham chorea.12,13
Unmet needs
The breadth of indications being investigated in pediatric psychopharmacology clinical trials shows that progress is being made. Missing are NCEs being developed for indications other than ADHD, but the FDA’s Final Pediatric Rule does create the expectation that pediatric studies will be included in all future new drug development programs.
Related resources
- Food and Drug Administration pediatric Web site. http://www.fda.gov/cder/pediatric
- American Academy of Child and Adolescent Psychiatry. Pediatric Psychopharmacology Initiative. http://www.aacap.org/research/ppi.htm
- Busipirone • BuSpar
- Clomipramine • Anafranil
- Donepezil • Aricept
- Fluoxetine • Prozac
- Fluvoxamine • Luvox
- Imipramine • Tofranil
- Mecamylamine • Inversine
- Methylphenidate • MethylPatch, Ritalin QD
- Mirtazapine • Remeron
- Modafinil • Provigil
- Nefazodone • Serzone
- R-methylphenidate • Attenade
- Risperidone • Risperdal
- Secretin • SecreFlo
- Sertraline • Zoloft
- Topiramate • Topamax
- Venlafaxine • Effexor XR
The author reports that he receives grant/research support from Synaptic Pharmaceutical Corp., is a consultant to GlaxoSmithKline, Elan Corp., and Cytospect, and owns stock in GlaxoSmithKline. No GlaxoSmithKline products are mentioned in this article.
Most psychotherapeutic drugs have been studied only in adults and are not approved for use in children and adolescents. Nevertheless, most drugs used in adult psychiatric treatment are widely prescribed to pediatric patients, and prescribing to this young population has increased dramatically (Box).1-3
Without the benefit of efficacy and safety data, one must rely on anecdotal reports and clinical judgment when choosing medications and determining dosages for children and adolescents. That may be changing soon, as more pediatric information is becoming available on psychotherapeutic drugs approved for adults and on agents under development.
Limited industry attention to pediatrics
The evidence gap between adult and pediatric practice4 can be attributed partly to child and adolescent psychiatry lagging behind adult psychiatry in embracing psychopharmacologic treatments. The primary reason, however, has been the pharmaceutical industry’s history of limited interest in studying pediatric populations.
An unprecedented step. In 1986 at Ciba-Geigy, I and colleagues Richard Katz, PhD, Phyllis Landau, MD, and Georges Moroz, MD, began developing clomipramine, the first drug approved in the United States to treat obsessive-compulsive disorder (OCD). Knowing that OCD onset is common in childhood or adolescence, we proposed doing a pediatric study concurrent with the adult studies that would provide the basis for regulatory approval.
Researchers have documented a dramatic increase in psychotropic prescriptions to children and adolescents in recent years.
Olfson et al1 reviewed national trends across 10 years. They found the overall annual rate of prescription of psychotherapeutic drugs to children increased from 1.4 per 100 children in 1987 to 3.9 per 100 in 1996. Stimulant and antidepressant drug prescriptions mostly accounted for this nearly threefold increase.
Rushton and Whitmire 2 reviewed a North Carolina Medicaid population and found the number of children prescribed stimulants increased from 6,407 in 1992 to 27,951 in 1998; the corresponding numbers for selective serotonin reuptake inhibitor (SSRI) prescriptions were 510 and 6,984. These represent a fourfold and greater than tenfold increase, respectively, across 7 years.
Zito et al 3 reported increases of 1.3- to 3.1-fold for stimulant and antidepressant prescriptions to preschool children (aged 2 to 4) between 1991 and 1995 in three healthcare settings.
Clinical development programs at other pharmaceutical companies followed suit when designing studies of selective serotonin reuptake inhibitors (SSRI) for OCD (SSRIs were just reaching the market as antidepressants). In some programs, pediatric studies were done after initial successful studies in adults with OCD. Even so, the industry continued to show little interest in including children and adolescents in routine clinical development of new drugs or in seeking regulatory approval for this population. This changed several years later, thanks to initiatives from the National Institute of Mental Health (NIMH) and the Food and Drug Administration (FDA).
RUPP and beyond
During the 1990s, NIMH convened meetings with the American Academy of Child and Adolescent Psychiatry (AACAP) and others that brought together representatives from academia, government, industry, and clinical practice, as well as patient advocates.7 Attendees discussed the need for new drug development to treat psychiatric disorders in children and adolescents and the obstacles to be overcome for progress to occur. As a result, NIMH in 1996 established Research Units in Pediatric Psychopharmacology (RUPP).
RUPP is a network of centers of excellence in child and adolescent psychopharmacology based in academic medical centers. Its purpose is to provide definitive studies of psychotropic drugs that are being used routinely in children and adolescents and to provide an infrastructure to support complicated multicenter trials. RUPP’s focus is practical, evaluating treatments used in clinical practice.
To date, RUPP has completed and reported the results of two significant studies:
Even so, RUPP has limitations. Its network cannot conduct studies on all psychotropic drugs that are in use today, and it is not positioned to evaluate investigational drugs (in development but not yet approved).
As a result, RUPP’s network can only partially satisfy psychiatrists’ need for information to guide the prescribing of psychotropics to children and adolescents.
FDA initiatives. Concurrent with the NIMH efforts, the FDA implemented the Pediatric Rule of 1994, which applied to all classes of drugs that might be used in younger patients. Under this rule, pharmaceutical manufacturers:
- were required to review existing data for using their drugs in a pediatric population
- could extrapolate efficacy data from adults to children, if the course of disease and effects of drug treatment were sufficiently similar in adult and pediatric patients and if appropriate pharmacokinetic and safety data were provided for younger patients.
FDAMA. The FDA’s next step was included in the FDA Modernization Act (FDAMA) of 1997, which allowed the agency to ask pharmaceutical manufacturers to generate safety and effectiveness data for drugs likely to be used in pediatrics. In exchange, manufacturers received 6 months’ marketing exclusivity (in addition to existing patent protection) for those drugs.
Many companies did sponsor additional safety and efficacy studies, although the incentive’s structure clearly favored drugs with high sales volume. For example, consider two products with annual sales of $200 million and $800 million, respectively. Six months of exclusive marketing rights would generate $400 million in additional revenue from the $800 million product—double the annual revenue of the $200 million product. The pharmaceutical company could obtain this benefit even if total pediatric use were quite small because the 6 months of exclusivity applied to all product sales, including pediatric and adult use.
The FDAMA had several other weaknesses:
- A manufacturer could obtain its benefit even if studies failed to demonstrate the product’s efficacy in the pediatric population.
- The regulation provided no incentive to develop pediatric data for drugs that had lost patent protection.
- It did not induce pharmaceutical companies to include pediatric studies early in drug development.
- for all new chemical entities (drugs in development and not yet approved)
- and for development programs seeking new indications, dosage forms, treatment regimens, or routes of administration for approved products.
- 32 drugs for cancer
- 24 vaccines
- 16 for cardiovascular disease
- 16 for cystic fibrosis
- 16 for infectious diseases
- 11 for psychiatric disorders
- 11 for respiratory disorders
- 10 for AIDS
- 10 for asthma
- 10 for genetic disorders
Source: Pharmaceutical Research and Manufacturers of America10
Drugs in development
As a result of these regulatory changes, the Pharmaceutical Research and Manufacturers of America (PhRMA) reports that nearly 200 drugs and vaccines are in development for children, (Box 2). In addition to the 11 drugs identified by PhRMA for treating psychiatric disorders in children and adolescents, at least another 10 were in the pipeline through the first 6 months of 2002 (Table).11 By the time you read this, some of the drugs may have been terminated from development, new drugs may have been added, and others will have emerged from the development process to receive FDA approval for pediatric use.
Indications. Among the 21 compounds listed in development for 10 different psychiatric indications, 16 are already approved for adult use. One—donepezil—is marketed for management of Alzheimer’s dementia symptoms, but for children and adolescents the agent is being developed for treatment of attention-deficit/hyperactivity disorder (ADHD).
Four other approved drugs appear to be in development for new indications, including mania (topiramate), autism (secretin), Tourette’s syndrome (mecamylamine), and ADHD (modafinil). Among the five new chemical entities (NCEs—investigational drugs not yet marketed with any indication), four appear to be in development for ADHD and one for a disorder of childhood listed only as behavioral disorders.
Table
PSYCHOTROPICS IN DEVELOPMENT FOR CHILDREN AND ADOLESCENTS, LISTED BY INDICATION
| Indication | Drugs in development | Company |
|---|---|---|
| Attention-deficit/hyperactivity disorder | ABT-089 | Abbott Laboratories |
| Atomoxetine | Eli Lilly and Co. | |
| Donepezil | Eisai | |
| Mecamylamine | Layton BioScience, Inc. | |
| Methylphenidate | ||
| Attenade | Celgene | |
| MethylPatch | Noven Pharmaceuticals | |
| Ritalin QD | Novartis Pharmaceuticals | |
| Modafinil | Cephalon | |
| SPD 420 | Cortex Pharmaceuticals | |
| SPD 503 | Shire Pharmaceuticals Group | |
| Depression | Fluoxetine | Eli Lilly and Co. |
| Mirtazepine | Organon | |
| Nefazodone | Brystol-Myers Squibb Co. | |
| Sertraline | Pfizer | |
| Venlafaxine | Wyeth | |
| Obsessive-compulsive disorder | Fluoxetine | Eli Lilly and Co. |
| Fluvoxamine | Solvay Pharmaceuticals | |
| Sertraline | Pfizer | |
| Anxiety | Busipirone | Bristol-Myers Squibb Co. |
| Tourette’s syndrome | Mecamylamine | Layton BioScience Inc. |
| Schizophrenia | Risperidone | Johnson & Johnson Pharmaceutical Research and Development |
| Mania | Topiramate | Johnson & Johnson Pharmaceutical Research and Development |
| Autism | Secretin | Repligen |
| Posttraumatic stress disorder | Sertraline | Pfizer |
The pharmaceutical companies’ decisions to conduct clinical trials in children and adolescents for this group of drugs may be attributable, to some extent, to incentives and the potential for financial gain. Whatever the reasons, the regulatory changes that stimulated this work will have accomplished their goal if they produce evidence of efficacy, safety, and tolerability of these marketed drugs in children and adolescents.
Noncommercial reserach. In addition to industry-sponsored drug development, much pediatric psychopharmacology research is also being conducted in academic and government settings. NIMH and the AACAP are sponsoring trials for a range of pediatric disorders, including ADHD, autism and other pervasive development disorders, bipolar disorder, body dysmorphic disorder, depression, OCD, PTSD, schizophrenia, social phobia, and Sydenham chorea.12,13
Unmet needs
The breadth of indications being investigated in pediatric psychopharmacology clinical trials shows that progress is being made. Missing are NCEs being developed for indications other than ADHD, but the FDA’s Final Pediatric Rule does create the expectation that pediatric studies will be included in all future new drug development programs.
Related resources
- Food and Drug Administration pediatric Web site. http://www.fda.gov/cder/pediatric
- American Academy of Child and Adolescent Psychiatry. Pediatric Psychopharmacology Initiative. http://www.aacap.org/research/ppi.htm
- Busipirone • BuSpar
- Clomipramine • Anafranil
- Donepezil • Aricept
- Fluoxetine • Prozac
- Fluvoxamine • Luvox
- Imipramine • Tofranil
- Mecamylamine • Inversine
- Methylphenidate • MethylPatch, Ritalin QD
- Mirtazapine • Remeron
- Modafinil • Provigil
- Nefazodone • Serzone
- R-methylphenidate • Attenade
- Risperidone • Risperdal
- Secretin • SecreFlo
- Sertraline • Zoloft
- Topiramate • Topamax
- Venlafaxine • Effexor XR
The author reports that he receives grant/research support from Synaptic Pharmaceutical Corp., is a consultant to GlaxoSmithKline, Elan Corp., and Cytospect, and owns stock in GlaxoSmithKline. No GlaxoSmithKline products are mentioned in this article.
1. Olfson M, Marcus SC, Weissman MM, Jensen PS. National trends in the use of psychotropic medications by children. J Am Acad Child Adolesc Psychiatry 2002;41(5):514-21.
2. Rushton JL, Whitmire JT. Pediatric stimulant and selective serotonin reuptake inhibitor prescription trends 1992 to 1998. Arch Pediatr Adolesc Med 2001;155:560-5.
3. Zito JM, Safer DJ, dosReis S, Gardner JF, Boles M, Lynch F. Trends in the prescribing of psychotropic medications to preschoolers. JAMA 2000;283:1025-30.
4. DeVeaugh-Geiss J. OCD: A model for closing the “gap” between adult and pediatric psychiatry. In: Maj M, Sartorius N, Okasha A, Zohar J (eds). World Psychiatric Association series, Evidence and experience in psychiatry (vol. 4). Obsessive-compulsive disorder. Chichester, UK: John Wiley & Sons, 2000:192-4.
5. DeVeaugh-Geiss J, Moroz G, Biederman J, et al. Clomipramine hydrochloride in childhood and adolescent obsessive compulsive disorder: a multicenter trial. J Am Acad Child Adolesc Psychiatry 1992;31(1):45-9.
6. Clomipramine Collaborative Study Group. Clomipramine in the treatment of obsessive compulsive disorder. Arch Gen Psychiatry 1991;48:730-8.
7. Vitiello B, Jensen P. Medication development and testing in children and adolescents: current problems, future directions. Arch Gen Psychiatry 1997;54:871-6.
8. Walkup J, Labellarte M, Riddle M, et al. Fluvoxamine for the treatment of anxiety disorders in children and adolescents. N Engl J Med 2001;344:1279-85.
9. RUPP Autism Network. A double-blind, placebo-controlled trial of risperidone in children with autism. N Engl J Med 2002;347:314-321.
10. Pharmaceutical Research and Manufacturers of America list of new medicines in development. Available at: http://www.phrma.org/searchcures/newmeds/. Accessed Aug. 26 2002.
11. R&D Directions, e-Knowledge Base online databases 2002 (a subscription database). Available at: www.pharmalive.com.
12. National Institute of Mental Health clinical trials. Available at: http://www.nimh.nih.gov/studies/index.cfm. Accessed July 2002.
13. American Academy of Child and Adolescent Psychiatry clinical trials and surveys. Available at: http://www.aacap.org/research/ctvn.htm. Accessed July 2002.
1. Olfson M, Marcus SC, Weissman MM, Jensen PS. National trends in the use of psychotropic medications by children. J Am Acad Child Adolesc Psychiatry 2002;41(5):514-21.
2. Rushton JL, Whitmire JT. Pediatric stimulant and selective serotonin reuptake inhibitor prescription trends 1992 to 1998. Arch Pediatr Adolesc Med 2001;155:560-5.
3. Zito JM, Safer DJ, dosReis S, Gardner JF, Boles M, Lynch F. Trends in the prescribing of psychotropic medications to preschoolers. JAMA 2000;283:1025-30.
4. DeVeaugh-Geiss J. OCD: A model for closing the “gap” between adult and pediatric psychiatry. In: Maj M, Sartorius N, Okasha A, Zohar J (eds). World Psychiatric Association series, Evidence and experience in psychiatry (vol. 4). Obsessive-compulsive disorder. Chichester, UK: John Wiley & Sons, 2000:192-4.
5. DeVeaugh-Geiss J, Moroz G, Biederman J, et al. Clomipramine hydrochloride in childhood and adolescent obsessive compulsive disorder: a multicenter trial. J Am Acad Child Adolesc Psychiatry 1992;31(1):45-9.
6. Clomipramine Collaborative Study Group. Clomipramine in the treatment of obsessive compulsive disorder. Arch Gen Psychiatry 1991;48:730-8.
7. Vitiello B, Jensen P. Medication development and testing in children and adolescents: current problems, future directions. Arch Gen Psychiatry 1997;54:871-6.
8. Walkup J, Labellarte M, Riddle M, et al. Fluvoxamine for the treatment of anxiety disorders in children and adolescents. N Engl J Med 2001;344:1279-85.
9. RUPP Autism Network. A double-blind, placebo-controlled trial of risperidone in children with autism. N Engl J Med 2002;347:314-321.
10. Pharmaceutical Research and Manufacturers of America list of new medicines in development. Available at: http://www.phrma.org/searchcures/newmeds/. Accessed Aug. 26 2002.
11. R&D Directions, e-Knowledge Base online databases 2002 (a subscription database). Available at: www.pharmalive.com.
12. National Institute of Mental Health clinical trials. Available at: http://www.nimh.nih.gov/studies/index.cfm. Accessed July 2002.
13. American Academy of Child and Adolescent Psychiatry clinical trials and surveys. Available at: http://www.aacap.org/research/ctvn.htm. Accessed July 2002.
New uses for atypicals in pediatric patients: How to offer the benefits while minimizing side effects
Prescribing of atypical antipsychotics for children and adolescents is increasing, despite a lack of randomized controlled clinical trials. Like many psychiatrists, you may be treating pediatric patients with these medications for a variety of indications beyond psychosis.
Three factors are driving the use of atypical antipsychotics for broader indications:
- substantial evidence that these newer agents are safer and more effective than typical antipsychotics1
- inadequate response of childhood and adolescent psychiatric disorders to their primary treatments
- evidence that atypical antipsychotics have potential thymoleptic, antiaggressive, and anxiolytic properties.
These attributes already have expanded atypical antipsychotic use in adult patients. In fact, atypicals are being used more extensively in adults for affective and nonpsychotic conditions than for schizophrenia.2
In preparing the following two-part article for Current Psychiatry, we scoured the available literature—Medline, abstracts from scientific meetings, and American Academy of Child and Adolescent Psychiatry (AACAP) practice parameters—to examine the evolving role of atypical antipsychotics in children and adolescents. In part 1 of this article, we discuss using atypicals in childhood/adolescent-onset schizophrenia, bipolar disorder, and psychotic depression. In part 2, we look at evidence for using atypicals in children with autism and developmental disorders, Tourette’s and other tic disorders, disruptive behavior disorders, anorexia nervosa, anxiety disorders, and stuttering.
Before prescribing antipsychotic medications for children and adolescents, always conduct a comprehensive history and complete physical examination.
History. Include information about:
- seizures, head trauma, and cardiac or endocrine problems (often elicited with questions about fatigue, temperature intolerance, or weight concerns)
- perinatal history (apnea, Apgar scores, days in hospital)
- family history (e.g., significant medical problems).
Physical exam. Obtain baseline blood pressure, pulse, body weight and habitus, and laboratory tests—complete blood count, comprehensive metabolic profile with liver function tests, and cholesterol/triglyceride levels.
Educate the parent and child about possible side effects, whether they are likely to be transient or persistent, and ways to minimize them (e.g., bedtime dosing to prevent daytime sedation, dietary recommendations to lessen potential weight gain).
Monitor lab values and weight throughout treatment (compared with normal growth curves). Use words the child understands when asking about side effects (e.g., “Have you had leakage from your breasts?”). Continually weigh the benefits versus the risks of antipsychotics, and discuss this balance with the parent and child.
Shift in pharmacotherapy of schizophrenia.
One-quarter of patients with schizophrenia develop the disorder before age 15, and subtle psychotic manifestations are often observed in early childhood.3 In general, schizophrenia’s presenting symptoms are comparable in adults and children, but the childhood/adolescent-onset form is more severe.4,5
During the past 5 years, pharmacotherapy of adult schizophrenia has shifted dramatically away from typical antipsychotics. Atypical agents have shown greater efficacy and tolerability, especially with respect to extrapyramidal symptoms (EPS) and tardive dyskinesia (TD).1
In a recent survey, most general and specialist psychiatrists (86%) said they prefer using atypical antipsychotics as first-line treatment for new-onset schizophrenia and as maintenance therapy. They also reported using atypicals to treat patients with dementia (80%), personality disorders (69%), developmental delay/mental retardation (65%), and autism (40%).6
Translating adult findings to children. Most evidence of atypical antipsychotics’ efficacy and tolerability is derived from adult studies, which likely will continue to influence clinical practice more than the limited number of child and adolescent studies. In 1998, a thorough review of atypical antipsychotic use in child and adolescent psychiatry found only five blinded placebo-controlled clinical trials, 24 open-label trials, and 33 case series.7 A follow-up review in 1999 again found mainly case reports and case series, with a handful of controlled studies.8
Available atypical antipsychotics include clozapine, risperidone, olanzapine, quetiapine, and ziprasidone. An investigational agent—aripiprazole—is likely to be available soon for clinical use.
Issues in pediatric use of atypicals
When prescribing atypical antipsychotics, it is important to balance the benefit of treatment with the risk of exposing children to possible adverse effects. Side effects associated with atypicals include weight gain, secondary metabolic disturbances such as hyperglycemia, hyperprolactinemia, and cardiac conduction abnormalities. These side effects are health concerns for all patients but particularly for children and adolescents, who may require years of exposure to antipsychotics.
Weight gain. Younger patients may be particularly susceptible to weight gain with the use of the atypicals. In a state hospital adult population, Buckley et al found a strong inverse relationship between patient age and weight gain associated with atypical antipsychotic use.9 Key issues for pediatric populations are:
- Will children have difficulties losing weight over time?
- Will they stop their medications over time?
- Will they stop their medications because of this effect?
- Will they be further stigmatized at school because of obesity?
- Are they at increased risk to develop diabetes mellitus?
- What are the long-term consequences of antipsychotic-induced obesity and metabolic disturbances for this patient population?
Hyperprolactinemia in children and adolescents may lead to breast enlargement and galactorrhea, which are particularly distressing in this age group. Sustained elevation of prolactin may affect the regulation of other hormones, resulting in low estrogen and testosterone levels. The long-term impact of these changes on adolescent growth and development is unknown. Antipsychotic-induced hyperprolactinemia also may be associated with reduced bone density.10
Abnormal cardiac conduction. Thioridazine recently received a “black box” label warning from the FDA because of sudden deaths and a prolonged QTc interval seen on electrocardiogram (ECG) readings. Several other antipsychotics also show ECG evidence of QTc prolongation.11 However, the clinical significance of this finding is unclear.
Younger patients respond differently than do adults to antipsychotic medications because of developmental differences in pharmacokinetics: absorption, distribution, metabolism, and excretion.
Absorption. Stomach contents tend to be less acidic in younger persons than in adults, potentially slowing absorption of weakly acidic drugs. In theory, the absorption of antidepressants and psychostimulants is more likely to be altered than that of antipsychotics. Children may also have fewer and less diverse intestinal microflora, which may explain why phenothiazines (absorbed or metabolized in the intestinal wall) must be given at higher-than-adult oral dosages for clinical effect.12
Children may absorb certain psychotropic medications (e.g., imipramine) more rapidly than adults. This contributes to greater fluctuations in blood levels and possible cardiac toxicity—often a function of peak plasma concentrations.
Distribution. Drug distribution patterns in infants, children, and adolescents—especially those going through puberty—are not homogenous.13 Fat stores and the relative proportion of total body water to extracellular water affect distribution and change with development.
The proportion of fat to body weight is highest in the first year of life, declines steadily during childhood, increases prior to puberty, then declines thereafter. Thus, although individuals have variable degrees of fat stores, children in general have a lower proportion of body fat than adults and therefore a smaller volume of distribution. This becomes significant when prescribing antipsychotics, which are lipid-soluble.
If one considers only a drug’s distribution, one would expect to find a higher plasma concentration in a child if a child and an adult were given the same weight-adjusted dose of a lipophilic drug. Children, however, exhibit a lowerplasma concentration of lipophilic drugs than do adults because of differences in metabolism.13
Metabolism. Children’s increased metabolic rate is directly related to age-related changes in hepatic enzymes. In general, metabolic pathways for many drugs function at a low level during the perinatal period, mature by 6 months, peak between ages 1 and 5, and decline gradually to adult values by about age 15. Liver mass is also greater in children than in adults. Therefore, higher ratios of milligrams of drug to kilograms of body weight may be needed in children to achieve steady-state plasma levels comparable to those seen in adults.
Excretion. Infant and adult renal functioning are approximately the same. With the exception of lithium, developmental changes in renal function do not contribute substantially to age-related differences in psychotropic drug excretion.13
Summary. When compared with adults, children require a higher milligram-to-kilogram dosage of antipsychotics to achieve the same plasma concentration but clinically require a lower milligram-to-kilogram dosage—starting dosages usually less than one-half of an adult dose—to avoid unwanted side effects.
SUGGESTED DOSAGES OF ATYPICAL ANTIPSYCHOTICS
| Drug | FDA-approved dosages for psychosis in adults | For psychosis in children and adolescents | For bipolar disorder in children and adolescents |
|---|---|---|---|
| Clozapine | Initial: 25 mg bid; increase gradually to 300 to 800 mg/d in divided doses | Not recommended for children under age 16 Initial: 12.5 to 25 mg bid; increase gradually to 300 to 450 mg/d (divided) Increased risk of seizures; potential for agranulocytosis | Limited research |
| Olanzapine | Psychosis. Initial: 5 to 10 mg qd or 5 mg bid; increase to 20 mg qd or 10 mg bid Bipolar disorder. Similar initial; lower maintenance (10 to 20 mg qd or 10 mg bid can often be obtained) | Clinical benefit in children age 10 at 2.5 to 10 mg/d; For age >10, 5 to 20 mg qd or 10 mg bid may be used Sedation and weight gain are common side effects | Clinically beneficial at dosages comparable to those used in psychosis Maintenance dosage may be lower than that required in a primary psychotic disorder |
| Quetiapine | Initial: 25 mg bid; increase to 300 to 800 mg/d divided in two to three doses | Initial: 12.5 mg bid (50 kg) Maintenance: 50 mg bid (50 kg) Few controlled trials in children | Limited research |
| Risperidone | Initial: 2 mg/d; may be increased to 4 to 6 mg/d in divided doses | Clinical trials indicate benefit at 0.25 to 0.5 mg qd or bid May be increased as needed to 0.5 to 1.5 mg/d in single or divided doses | Clinically beneficial at dosages comparable to those used in psychosis |
| Ziprasidone | Initial: 20 to 40 mg bid; may be increased to 40 to 80 mg bid | Preliminary studies suggest benefit at 10 to 20 mg bid, increasing to 20 to 60 mg bid Not recommended as first-line therapy in this population | Limited research |
| * The FDA has not approved a specific indication for these agents for use in children and adolescents. In adult patients, atypical antipsychotics have been approved for psychosis, and olanzapine is FDA-approved for psychosis and mood disorders. | |||
Special care is required to decrease the risks associated with using antipsychotics in children and adolescents and to increase compliance with medication recommendations (Box 1).
Pharmacokinetics in children and adolescents
Administering medications to children and adolescents requires special precautions. Younger patients respond differently than adults to psychotropic medications because of differences in pharmacokinetics—how the body handles a drug—and pharmacodynamics—the drug’s effect on the body.
During a child’s growth and development, physiologic changes in absorption, distribution, metabolism, and excretion may affect drug delivery to target tissue (Box 2).12,13 Maturation of brain regions and neurotransmitter systems also may alter a medication’s effect at different ages.
Antipsychotic dosage recommendations and therapeutic ranges for children and adolescents have been published but are extrapolated from adult studies because studies in children are lacking. There is danger, however, in using body weight and proportionately reducing an adult dosage to obtain a pediatric dosage. The plasma concentration may ultimately be subtherapeutic or toxic.14
The liver metabolizes most antipsychotics. The higher rate of hepatic metabolism in children would suggest that on a milligram-to-kilogram basis a child or adolescent would need a higher dose. Children, however, require smaller weight-adjusted doses of antipsychotics than do adults to achieve the same therapeutic effect.15 Children have a greater density of dopamine D-1 and D-2 receptors than do adults, suggesting a greater sensitivity to the beneficial and adverse effects of antipsychotics. To date, dopamine receptor occupancy in children/adolescents with schizophrenia has not been studied with positron emission tomography.
Summary. Compared with adults, children require a reduced milligram-to-kilogram dosage of antipsychotics to achieve the same therapeutic effect and avoid unwanted side effects. Children younger than age 10 or weighing less than 50 kg typically should start with the lowest starting dose, given once or twice a day (Table). The dose should be slowly increased based on the presence of side effects and remission of symptoms.
Maximum daily dosages for children weighing less than 50 kg should rarely exceed one-half of an adult antipsychotic dosage, particularly when used for symptoms of disorders other than primary psychosis. However, dosages closer to those used in adults may be necessary when treating primary psychosis in early-onset schizophrenia, especially in an adolescent (Box 3).
An adolescent boy, age 13 and weighing 47 kg, presents with the chief complaint of paranoia, which is impairing his academic functioning. On examination, his interaction is guarded, and he exhibits severe emotional withdrawal and a paucity of thought content. His family history is significant for a maternal uncle with early-onset schizophrenia, which is chronic but under reasonable control with olanzapine, 10 mg bid.
The boy’s treatment is started with olanzapine, 2.5 mg once daily. After 2 weeks, the dosage is increased to 2.5 mg in the morning and 5 mg at bedtime, with good symptom resolution.
Childhood/adolescent-onset schizophrenia
Typical antipsychotics appear to have limited efficacy in childhood/adolescent-onset schizophrenia, based on a small number of available case series and relatively short open-label trials.16 In a single-arm, placebo-controlled trial, haloperidol was effective in 16 children ages 5 to 12, but its use was associated with substantial EPS. A similar intolerance was demonstrated in a comparative trial of thioridazine and thiothixene.
Less is known about the incidence of tardive dyskinesia, but there is no reason to believe that the rate is lower in children and adolescents than in adults with schizophrenia (estimated at 5% per year for the first 5 years of treatment).
Clozapine. Information is emerging on the efficacy and tolerability of atypical antipsychotics in childhood/adolescent-onset schizophrenia.16 Clozapine has been studied more than other atypicals, in part because of the severity of early-onset schizophrenia and because clozapine has been used in clinical practice longer than the other agents in that class.
Early case reports and small open-labeled trials confirmed that clozapine was effective for children and adolescents with schizophrenia who had failed prior antipsychotic treatments.17-19 A randomized, double-blind, controlled trial from the childhood schizophrenia division of the National Institute of Mental Health provided the most reliable information.17 In that 6-week treatment study, 21 severely ill adolescents (mean age 14) received clozapine, mean dosage 176 mg/d, or haloperidol, mean dosage 16 mg/d. Response to clozapine was greater for both positive and negative symptoms, and the difference was clinically and statistically significant. In addition, 62% of clozapine-treated patients were rated very much improved on the Clinical Global Impression (CGI) scale.
In the same trial, clozapine treatment was complicated by higher rates of adverse effects than are typically observed in adult studies:
- Sedation was reported in 90% of patients.
- 2 of 10 patients had a seizure during clozapine therapy.
- A 2% rate of agranulocytosis was disconcerting, given the lower adult rate (0.38%) and the brevity of the trial. As older age is a known risk factor for clozapine-induced agranulocytosis, it may be that children and the elderly are more susceptible to this side effect.
Olanzapine has been effective in this patient population at dosages up to 10 mg/d.7,16,21 In a pilot study, Kumra et al administered olanzapine to 23 children with schizophrenia who had not previously responded to neuroleptic treatment. After 8 weeks, the children improved on the Brief Psychiatric Rating Scale, the Scale for the Assessment for Negative Symptoms, and the Scale for the Assessment of Positive Symptoms.21
Similarities and differences in olanzapine’s side effects in adults and children/adolescents with schizophrenia were seen in a recent study. Children had more weight gain, sedation, and dystonia, whereas adults had significantly more cardiac arrhythmias.22
Quetiapine. McConville and colleagues examined the efficacy and tolerability of quetiapine in 10 adolescents with chronic psychosis (7 with schizoaffective disorder and 3 with bipolar disorder). In this 3-week study, quetiapine was well-tolerated; in several patients, dosages exceeded 750 mg/d. Psychotic symptoms were reduced, and there was global improvement in functioning.23
Other antipsychotics. There are no published data on the use of ziprasidone or aripiprazole in childhood/adolescent-onset schizophrenia.
Comparative data are very limited. One retrospective analysis compared the tolerability of risperidone, olanzapine, and quetiapine in 116 adolescent patients.24 Over 3 months, 75 patients received risperidone (mean 2.6 mg/d), 16 received olanzapine (mean 13.3 mg/d), and 25 were treated with quetiapine (mean 210.3 mg/d). Weight gain was the most common side effect; patients gained an average 8.6 lb with risperidone, 7.2 lb with quetiapine, and 14.1 lb with olanzapine. EPS were treated in seven (10%) patients taking risperidone, four (25%) taking olanzapine, and no patients taking quetiapine.
Bipolar disorder
As in the adult population, there has been substantial use of antipsychotics in children and adolescents with bipolar illness. Bipolar I disorder affects an estimated 0.6% of adolescents and is even being diagnosed in prepubertal patients.
Lithium, valproate, carbamazapine, and adjunctive treatment with benzodiazapines traditionally have been used to treat bipolar I disorders. Although practice guidelines recommend lithium and divalproex sodium as first-line treatments for bipolar illness, these recommendations are generally based on a preference for first-line agents that have potential use in maintenance treatment. The benefit of medications in bipolar disorder, however, is two-fold:
- Initial pharmacotherapy is usually instituted to target manic or mixed symptoms, and continued treatment is necessary to avoid relapse. The new antipsychotics—particularly risperidone, olanzapine, and quetiapine—are beneficial to treat agitated mania and disrupted sleep that may impair function and/or mandate inpatient stabilization. The highly sedative properties offer an acute benefit in restoring disrupted sleep.
- Psychotic symptoms seen in mania may need to be targeted independent of the mood symptoms and would thus suggest the use of an antipsychotic. In early-onset bipolar disorder, antipsychotics are used primarily as adjuncts to mood stabilizers.
- In the 1994 case report, an adolescent with bipolar disorder showed benefit when treated with clozapine.26
- In a retrospective chart review, 28 children ages 4 to 17 with bipolar disorder (25 mixed and 3 hypomanic) were treated with adjunctive risperidone for 6 months. Most (82%) showed significant improvement in mania and aggression on a mean dosage of 1.7 +/- 1.3 mg/d. Attention-deficit/hyperactivity disorder symptoms improved in 8% of the patients.27
- Affective symptoms (predominantly suggestive of bipolar disorder), aggression, and violent behavior in 11 children and adolescents ages 5 to 16 showed therapeutic response to an open trial of adjunctive low-dose (0.75 to 2.5 mg/d) risperidone.28
Olanzapine. Recent interest in olanzapine’s thymoleptic propertities has contributed to its clinical use in bipolar disorder, specifically in psychotic mania. Olanzapine has also been studied as long-term maintenance therapy in bipolar disorder. In a 47-week study, adult patients receiving olanzapine improved significantly more than those receiving valproate (47% vs. 34% by the Young Mania Rating Scale) after 3 weeks. Both medications were effective throughout the long-term, randomized, double-blind study.29
Two case series and one open trial have examined olanzapine as primary or adjunctive treatment for children and adolescents with bipolar disorder. In the open study, Frazier and colleagues gave olanzapine, 2.5 to 20 mg/d, to 23 children ages 5 to 14.30 After 8 weeks, the response rate was 61% (defined as 30% or greater improvement on the Young Mania Rating Scale). Weight gain was the predominant side effect (mean increase 5 kg).
Chang and colleagues demonstrated “marked improvement” in CGI scores when using olanzapine as adjunctive therapy for three youths with bipolar disorder.31 Similar findings were reported when treating seven youths with acute mania.32 Olanzapine’s broad affinity for dopaminergic and serotonergic receptors may explain these positive outcomes.
Other atypicals. No studies have been published on the use of quetiapine, ziprasidone, or aripiprazole in childhood mood disorders.
Psychotic depression
Psychosis can complicate depression in adults and adolescents. In a small study of adolescents with psychotic depression, Gellar et al demonstrated conventional neuroleptics’ benefit in combination with antidepressants.33 We have no data, however, on use of atypicals in childhood depression, and published accounts of depression in bipolar patients treated with atypicals are of some concern.
In one study,34 four of six patients with bipolar disorder developed dysphoric mood within 3 months of starting risperidone. Two met the criteria for major depression and required antidepressant therapy. This finding was somewhat surprising, given risperidone’s antidepressant benefit in some adults, most likely due to its 5-HT2 antagonistic effect. Frazier and colleagues similiarly noted that one patient discontinued treatment during an open-label trial examining the benefit of olanzapine in juvenile bipolar disorder.30
These findings in the adolescent bipolar population should not be ignored when you consider treating a primary depressive disorder with psychosis. Antipsychotics certainly can be useful for treating psychotic depression, especially acutely for stabilization and preventing harm to self. Atypical antipsychotics have consistently been proven to have less adverse side effects than typical antipsychotics and thus would be preferred in children and adolescents. Research is needed to examine possible worsening of dysphoria.
Related resources
- Hermann RC, Yang D, Ettner SL, et al. Prescription of antipsychotic drugs by office-based physicians in the United States, 1989-1997. Psychiatric Services 2002;53:425-30.
- Stigler KA, Potenza MN, McDougle CJ. Tolerability profile of atypical antipsychotics in children and adolescents (review). Paediatric Drugs 2001;3(12):927-94
- American Academy of Child and Adolescent Psychiatry http://www.aacap.org
- Clozapine • Clozaril
- Olanzapine • Zyprexa
- Quetiapine • Seroquel
- Risperidone • Risperdal
- Ziprasidone • Geodon
- Aripiprazole (investigational)
Dr. Londino reports that she serves as a consultant to Eli Lilly and Co.
Ms. Wiggins reports no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
Dr. Buckley reports that he receives grant support from and serves as a consultant and speaker for AstraZeneca Pharmaceuticals, Eli Lilly and Co., Janssen Pharmaceutica, and Novartis Pharmaceuticals Corp.
1. World Psychiatric Association. The usefulness and use of second-generation antipsychotic medications. Curr Opinion Psychiatry 2002;15(suppl):51-551.
2. Buckley PF. Broad therapeutic uses of atypical antipsychotic medications. Biol Psychiatry 2001;50:912-24.
3. Lieberman JA, Perkins D, Belger A, et al. The early stages of schizophrenia: speculations on pathogenesis, pathophysiology, and therapeutic approaches. Biol Psychiatry 2001;50:884-97.
4. Asarnow JR, Tompson MC, Goldstein MJ. Childhood-onset schizophrenia: a follow-up study. Schizophr Bull 1994;20:599-617.
5. Eggers C, Bunk D. The long-term course of childhood-onset schizophrenia: a 42-year follow-up study. Schizophr Bull 1997;23:105-17.
6. Buckley PF, Miller DD, Singer B, Donnenwirth K. The evolving clinical profile of atypical antipsychotic medications. Can J Psychiatry 2001;46:285.-
7. Toren P, Laor N, Weizman. Use of atypical neuroleptics in child and adolescent psychiatry. J Clin Psychiatry 1998;58:644-56.
8. Malone RP, Sheikh R, Zito JM. Novel antipsychotic medications in the treatment of children and adolescents. Psych Services 1999;50(2):171-4.
9. Singer B, Buckley PF, Friedman L, et al. Weight gain, diabetes mellitus, and the pharmacotherapy of schizophrenia. Schiophr Res 2001;49:276.-
10. Meaney AM. Elevated prolactin levels and the effect with atypical antipsychotics. Presentation at the Winter Workshop on Schizophrenia Research. Davos, Switzerland: February 2002.
11. Reilly JG, Ayis S, Ferrrier IN, et al. QTc interval abnormalities and psychotropic drug therapy in psychiatric patients. Lancet 2000;355:1048-52.
12. Lewis M (ed) Child and adolescent psychiatry Baltimore: Williams & Wilkins, 1996.
13. Jatlow PI. Psychotropic drug disposition during development. In: Popper C (ed). Psychiatric pharmacosciences of children and adolescents Washington, DC: American Psychiatric Press, 1987;29-44.
14. Janicak PG, Davis JM, Preskorn SH, et al (eds). Pharmacokinetics. In: Janicak PG, Davis JM, Preskorn SH, et al (eds). Principles and practice of psychopharmacotherapy Baltimore: Williams & Wilkins, 1993;59-79.
15. Verghese C, Kessel JB, Simpson GM. Pharmacokinetics of neuroleptics. Psychopharmacol Bull 1991;27(4):551-63.
16. Frangou S, Kumra S. Treatment of childhood-onset schizophrenia. In: Buckley PF, Waddington JL (eds). Schizophrenia and mood disorders: The new drug therapies in clinical practice Oxford, UK: Arnold, 2000;253:72.-
17. Kumra S, Frazier JA, Jacobsen LK, et al. Childhood-onset schizophrenia: A double-blind clozapine-haloperidol comparison. Arch Gen Psychiatr 1996;53:1090-7.
18. Remschmidt H, Schulz E, Martin M. An open trial of clozapine in thirty-six adolescents with schizophrenia. J Child Adolesc Psychiatry 1994;4:31-41.
19. Turetz M, Mozes T, Toren P, et al. An open trial of clozapine in neuroleptic-resistant childhood-onset schizophrenia. Br J Psychiatry 1997;170:507-10.
20. McGorry PD, et al. Risperidone for prodrome of schizophrenia. Arch Gen Psychiatry 2002 (in press).
21. Kumra S, Jacobsen LK, Lanane M, et al. Childhood-onset schizophrenia: An open-label study of olanzapine in adolescents. J Am Acad Adolesc Psychiatry 1998;37:377-85.
22. Woods SC, McGlashan TH. Adverse effects of olanzapine in adolescents and adults. Schizophr Res 2002;53:170.-
23. McConville B. Seroquel does not elevate prolactin levels in adolescents with selected psychotic disorders. Schizophr Res 2000;41:206.-
24. Grcevich S, Melamed L, Richards R. Comparative side effects of atypical antipsychotics in children and adolescents (poster presentation) Whistler, British Columbia: International Congress on Schizophrenia Research, April 2001.
25. American Academy of Child and Adolescent Psychiatry. AACAP official action: practice parameters for the assessment and treatment of children and adolescents with bipolar disorder. J Am Acad Child Adolesc Psychiatry 1997;36:138-57.
26. Fuchs DC. Clozapine treatment of bipolar disorder in a young adolescent. J Am Acad Child Adolesc Psych 1994;33:1299-1302.
27. Frazier JA, Meyer MC, Biederman J, et al. Risperidone treatment for juvenile bipolar disorder: a retrospective chart review. J Am Acad Child Adolesc Psych 1999;38:960-5.
28. Schreier HA. Risperidone for young children with mood disorders and aggressive behavior. J Child Adolesc Psychopharmacol 1998;8:49-59.
29. Tohen M, Baker RW, Altshuler L, et al. Olanzapine versus divalproex sodium for bipolar mania: a 47-week study. Eur Psychiatry 2002;17(suppl 1):109.-
30. Frazier JA, Biederman J, Jacobs TG, et al. Olanzapine in the treatment of bipolar disorder in juveniles. Schizophr Res 2000;41(1, suppl 1):194.-
31. Chang KD, Ketter TA. Mood stabilizer augmentation with olanzapine in acutely manic children. J Child Adolesc Psychopharmacol 2000;10:45-9.
32. Soutullo CA, Sorter MT, Foster KD, et al. Olanzapine in the treatment of adolescent acute mania: a report of seven cases. J Affect Dis 1999;53:279-83.
33. Gellar B, Cooper TB, Farooki ZQ, et al. Dose and plasma levels of nortriptyline and chlorpromazine in delusionally depressed adolescents and of nortriptyline in nondelusionally depressed adolescents. Am J Psych 1985;142:336-8.
34. Mandoki MW. Risperidone treatment of children and adolescents: increased risk of extrapyramidal side effects? J Clin Adolesc Psychopharmacol 1995;5:49-67.
Prescribing of atypical antipsychotics for children and adolescents is increasing, despite a lack of randomized controlled clinical trials. Like many psychiatrists, you may be treating pediatric patients with these medications for a variety of indications beyond psychosis.
Three factors are driving the use of atypical antipsychotics for broader indications:
- substantial evidence that these newer agents are safer and more effective than typical antipsychotics1
- inadequate response of childhood and adolescent psychiatric disorders to their primary treatments
- evidence that atypical antipsychotics have potential thymoleptic, antiaggressive, and anxiolytic properties.
These attributes already have expanded atypical antipsychotic use in adult patients. In fact, atypicals are being used more extensively in adults for affective and nonpsychotic conditions than for schizophrenia.2
In preparing the following two-part article for Current Psychiatry, we scoured the available literature—Medline, abstracts from scientific meetings, and American Academy of Child and Adolescent Psychiatry (AACAP) practice parameters—to examine the evolving role of atypical antipsychotics in children and adolescents. In part 1 of this article, we discuss using atypicals in childhood/adolescent-onset schizophrenia, bipolar disorder, and psychotic depression. In part 2, we look at evidence for using atypicals in children with autism and developmental disorders, Tourette’s and other tic disorders, disruptive behavior disorders, anorexia nervosa, anxiety disorders, and stuttering.
Before prescribing antipsychotic medications for children and adolescents, always conduct a comprehensive history and complete physical examination.
History. Include information about:
- seizures, head trauma, and cardiac or endocrine problems (often elicited with questions about fatigue, temperature intolerance, or weight concerns)
- perinatal history (apnea, Apgar scores, days in hospital)
- family history (e.g., significant medical problems).
Physical exam. Obtain baseline blood pressure, pulse, body weight and habitus, and laboratory tests—complete blood count, comprehensive metabolic profile with liver function tests, and cholesterol/triglyceride levels.
Educate the parent and child about possible side effects, whether they are likely to be transient or persistent, and ways to minimize them (e.g., bedtime dosing to prevent daytime sedation, dietary recommendations to lessen potential weight gain).
Monitor lab values and weight throughout treatment (compared with normal growth curves). Use words the child understands when asking about side effects (e.g., “Have you had leakage from your breasts?”). Continually weigh the benefits versus the risks of antipsychotics, and discuss this balance with the parent and child.
Shift in pharmacotherapy of schizophrenia.
One-quarter of patients with schizophrenia develop the disorder before age 15, and subtle psychotic manifestations are often observed in early childhood.3 In general, schizophrenia’s presenting symptoms are comparable in adults and children, but the childhood/adolescent-onset form is more severe.4,5
During the past 5 years, pharmacotherapy of adult schizophrenia has shifted dramatically away from typical antipsychotics. Atypical agents have shown greater efficacy and tolerability, especially with respect to extrapyramidal symptoms (EPS) and tardive dyskinesia (TD).1
In a recent survey, most general and specialist psychiatrists (86%) said they prefer using atypical antipsychotics as first-line treatment for new-onset schizophrenia and as maintenance therapy. They also reported using atypicals to treat patients with dementia (80%), personality disorders (69%), developmental delay/mental retardation (65%), and autism (40%).6
Translating adult findings to children. Most evidence of atypical antipsychotics’ efficacy and tolerability is derived from adult studies, which likely will continue to influence clinical practice more than the limited number of child and adolescent studies. In 1998, a thorough review of atypical antipsychotic use in child and adolescent psychiatry found only five blinded placebo-controlled clinical trials, 24 open-label trials, and 33 case series.7 A follow-up review in 1999 again found mainly case reports and case series, with a handful of controlled studies.8
Available atypical antipsychotics include clozapine, risperidone, olanzapine, quetiapine, and ziprasidone. An investigational agent—aripiprazole—is likely to be available soon for clinical use.
Issues in pediatric use of atypicals
When prescribing atypical antipsychotics, it is important to balance the benefit of treatment with the risk of exposing children to possible adverse effects. Side effects associated with atypicals include weight gain, secondary metabolic disturbances such as hyperglycemia, hyperprolactinemia, and cardiac conduction abnormalities. These side effects are health concerns for all patients but particularly for children and adolescents, who may require years of exposure to antipsychotics.
Weight gain. Younger patients may be particularly susceptible to weight gain with the use of the atypicals. In a state hospital adult population, Buckley et al found a strong inverse relationship between patient age and weight gain associated with atypical antipsychotic use.9 Key issues for pediatric populations are:
- Will children have difficulties losing weight over time?
- Will they stop their medications over time?
- Will they stop their medications because of this effect?
- Will they be further stigmatized at school because of obesity?
- Are they at increased risk to develop diabetes mellitus?
- What are the long-term consequences of antipsychotic-induced obesity and metabolic disturbances for this patient population?
Hyperprolactinemia in children and adolescents may lead to breast enlargement and galactorrhea, which are particularly distressing in this age group. Sustained elevation of prolactin may affect the regulation of other hormones, resulting in low estrogen and testosterone levels. The long-term impact of these changes on adolescent growth and development is unknown. Antipsychotic-induced hyperprolactinemia also may be associated with reduced bone density.10
Abnormal cardiac conduction. Thioridazine recently received a “black box” label warning from the FDA because of sudden deaths and a prolonged QTc interval seen on electrocardiogram (ECG) readings. Several other antipsychotics also show ECG evidence of QTc prolongation.11 However, the clinical significance of this finding is unclear.
Younger patients respond differently than do adults to antipsychotic medications because of developmental differences in pharmacokinetics: absorption, distribution, metabolism, and excretion.
Absorption. Stomach contents tend to be less acidic in younger persons than in adults, potentially slowing absorption of weakly acidic drugs. In theory, the absorption of antidepressants and psychostimulants is more likely to be altered than that of antipsychotics. Children may also have fewer and less diverse intestinal microflora, which may explain why phenothiazines (absorbed or metabolized in the intestinal wall) must be given at higher-than-adult oral dosages for clinical effect.12
Children may absorb certain psychotropic medications (e.g., imipramine) more rapidly than adults. This contributes to greater fluctuations in blood levels and possible cardiac toxicity—often a function of peak plasma concentrations.
Distribution. Drug distribution patterns in infants, children, and adolescents—especially those going through puberty—are not homogenous.13 Fat stores and the relative proportion of total body water to extracellular water affect distribution and change with development.
The proportion of fat to body weight is highest in the first year of life, declines steadily during childhood, increases prior to puberty, then declines thereafter. Thus, although individuals have variable degrees of fat stores, children in general have a lower proportion of body fat than adults and therefore a smaller volume of distribution. This becomes significant when prescribing antipsychotics, which are lipid-soluble.
If one considers only a drug’s distribution, one would expect to find a higher plasma concentration in a child if a child and an adult were given the same weight-adjusted dose of a lipophilic drug. Children, however, exhibit a lowerplasma concentration of lipophilic drugs than do adults because of differences in metabolism.13
Metabolism. Children’s increased metabolic rate is directly related to age-related changes in hepatic enzymes. In general, metabolic pathways for many drugs function at a low level during the perinatal period, mature by 6 months, peak between ages 1 and 5, and decline gradually to adult values by about age 15. Liver mass is also greater in children than in adults. Therefore, higher ratios of milligrams of drug to kilograms of body weight may be needed in children to achieve steady-state plasma levels comparable to those seen in adults.
Excretion. Infant and adult renal functioning are approximately the same. With the exception of lithium, developmental changes in renal function do not contribute substantially to age-related differences in psychotropic drug excretion.13
Summary. When compared with adults, children require a higher milligram-to-kilogram dosage of antipsychotics to achieve the same plasma concentration but clinically require a lower milligram-to-kilogram dosage—starting dosages usually less than one-half of an adult dose—to avoid unwanted side effects.
SUGGESTED DOSAGES OF ATYPICAL ANTIPSYCHOTICS
| Drug | FDA-approved dosages for psychosis in adults | For psychosis in children and adolescents | For bipolar disorder in children and adolescents |
|---|---|---|---|
| Clozapine | Initial: 25 mg bid; increase gradually to 300 to 800 mg/d in divided doses | Not recommended for children under age 16 Initial: 12.5 to 25 mg bid; increase gradually to 300 to 450 mg/d (divided) Increased risk of seizures; potential for agranulocytosis | Limited research |
| Olanzapine | Psychosis. Initial: 5 to 10 mg qd or 5 mg bid; increase to 20 mg qd or 10 mg bid Bipolar disorder. Similar initial; lower maintenance (10 to 20 mg qd or 10 mg bid can often be obtained) | Clinical benefit in children age 10 at 2.5 to 10 mg/d; For age >10, 5 to 20 mg qd or 10 mg bid may be used Sedation and weight gain are common side effects | Clinically beneficial at dosages comparable to those used in psychosis Maintenance dosage may be lower than that required in a primary psychotic disorder |
| Quetiapine | Initial: 25 mg bid; increase to 300 to 800 mg/d divided in two to three doses | Initial: 12.5 mg bid (50 kg) Maintenance: 50 mg bid (50 kg) Few controlled trials in children | Limited research |
| Risperidone | Initial: 2 mg/d; may be increased to 4 to 6 mg/d in divided doses | Clinical trials indicate benefit at 0.25 to 0.5 mg qd or bid May be increased as needed to 0.5 to 1.5 mg/d in single or divided doses | Clinically beneficial at dosages comparable to those used in psychosis |
| Ziprasidone | Initial: 20 to 40 mg bid; may be increased to 40 to 80 mg bid | Preliminary studies suggest benefit at 10 to 20 mg bid, increasing to 20 to 60 mg bid Not recommended as first-line therapy in this population | Limited research |
| * The FDA has not approved a specific indication for these agents for use in children and adolescents. In adult patients, atypical antipsychotics have been approved for psychosis, and olanzapine is FDA-approved for psychosis and mood disorders. | |||
Special care is required to decrease the risks associated with using antipsychotics in children and adolescents and to increase compliance with medication recommendations (Box 1).
Pharmacokinetics in children and adolescents
Administering medications to children and adolescents requires special precautions. Younger patients respond differently than adults to psychotropic medications because of differences in pharmacokinetics—how the body handles a drug—and pharmacodynamics—the drug’s effect on the body.
During a child’s growth and development, physiologic changes in absorption, distribution, metabolism, and excretion may affect drug delivery to target tissue (Box 2).12,13 Maturation of brain regions and neurotransmitter systems also may alter a medication’s effect at different ages.
Antipsychotic dosage recommendations and therapeutic ranges for children and adolescents have been published but are extrapolated from adult studies because studies in children are lacking. There is danger, however, in using body weight and proportionately reducing an adult dosage to obtain a pediatric dosage. The plasma concentration may ultimately be subtherapeutic or toxic.14
The liver metabolizes most antipsychotics. The higher rate of hepatic metabolism in children would suggest that on a milligram-to-kilogram basis a child or adolescent would need a higher dose. Children, however, require smaller weight-adjusted doses of antipsychotics than do adults to achieve the same therapeutic effect.15 Children have a greater density of dopamine D-1 and D-2 receptors than do adults, suggesting a greater sensitivity to the beneficial and adverse effects of antipsychotics. To date, dopamine receptor occupancy in children/adolescents with schizophrenia has not been studied with positron emission tomography.
Summary. Compared with adults, children require a reduced milligram-to-kilogram dosage of antipsychotics to achieve the same therapeutic effect and avoid unwanted side effects. Children younger than age 10 or weighing less than 50 kg typically should start with the lowest starting dose, given once or twice a day (Table). The dose should be slowly increased based on the presence of side effects and remission of symptoms.
Maximum daily dosages for children weighing less than 50 kg should rarely exceed one-half of an adult antipsychotic dosage, particularly when used for symptoms of disorders other than primary psychosis. However, dosages closer to those used in adults may be necessary when treating primary psychosis in early-onset schizophrenia, especially in an adolescent (Box 3).
An adolescent boy, age 13 and weighing 47 kg, presents with the chief complaint of paranoia, which is impairing his academic functioning. On examination, his interaction is guarded, and he exhibits severe emotional withdrawal and a paucity of thought content. His family history is significant for a maternal uncle with early-onset schizophrenia, which is chronic but under reasonable control with olanzapine, 10 mg bid.
The boy’s treatment is started with olanzapine, 2.5 mg once daily. After 2 weeks, the dosage is increased to 2.5 mg in the morning and 5 mg at bedtime, with good symptom resolution.
Childhood/adolescent-onset schizophrenia
Typical antipsychotics appear to have limited efficacy in childhood/adolescent-onset schizophrenia, based on a small number of available case series and relatively short open-label trials.16 In a single-arm, placebo-controlled trial, haloperidol was effective in 16 children ages 5 to 12, but its use was associated with substantial EPS. A similar intolerance was demonstrated in a comparative trial of thioridazine and thiothixene.
Less is known about the incidence of tardive dyskinesia, but there is no reason to believe that the rate is lower in children and adolescents than in adults with schizophrenia (estimated at 5% per year for the first 5 years of treatment).
Clozapine. Information is emerging on the efficacy and tolerability of atypical antipsychotics in childhood/adolescent-onset schizophrenia.16 Clozapine has been studied more than other atypicals, in part because of the severity of early-onset schizophrenia and because clozapine has been used in clinical practice longer than the other agents in that class.
Early case reports and small open-labeled trials confirmed that clozapine was effective for children and adolescents with schizophrenia who had failed prior antipsychotic treatments.17-19 A randomized, double-blind, controlled trial from the childhood schizophrenia division of the National Institute of Mental Health provided the most reliable information.17 In that 6-week treatment study, 21 severely ill adolescents (mean age 14) received clozapine, mean dosage 176 mg/d, or haloperidol, mean dosage 16 mg/d. Response to clozapine was greater for both positive and negative symptoms, and the difference was clinically and statistically significant. In addition, 62% of clozapine-treated patients were rated very much improved on the Clinical Global Impression (CGI) scale.
In the same trial, clozapine treatment was complicated by higher rates of adverse effects than are typically observed in adult studies:
- Sedation was reported in 90% of patients.
- 2 of 10 patients had a seizure during clozapine therapy.
- A 2% rate of agranulocytosis was disconcerting, given the lower adult rate (0.38%) and the brevity of the trial. As older age is a known risk factor for clozapine-induced agranulocytosis, it may be that children and the elderly are more susceptible to this side effect.
Olanzapine has been effective in this patient population at dosages up to 10 mg/d.7,16,21 In a pilot study, Kumra et al administered olanzapine to 23 children with schizophrenia who had not previously responded to neuroleptic treatment. After 8 weeks, the children improved on the Brief Psychiatric Rating Scale, the Scale for the Assessment for Negative Symptoms, and the Scale for the Assessment of Positive Symptoms.21
Similarities and differences in olanzapine’s side effects in adults and children/adolescents with schizophrenia were seen in a recent study. Children had more weight gain, sedation, and dystonia, whereas adults had significantly more cardiac arrhythmias.22
Quetiapine. McConville and colleagues examined the efficacy and tolerability of quetiapine in 10 adolescents with chronic psychosis (7 with schizoaffective disorder and 3 with bipolar disorder). In this 3-week study, quetiapine was well-tolerated; in several patients, dosages exceeded 750 mg/d. Psychotic symptoms were reduced, and there was global improvement in functioning.23
Other antipsychotics. There are no published data on the use of ziprasidone or aripiprazole in childhood/adolescent-onset schizophrenia.
Comparative data are very limited. One retrospective analysis compared the tolerability of risperidone, olanzapine, and quetiapine in 116 adolescent patients.24 Over 3 months, 75 patients received risperidone (mean 2.6 mg/d), 16 received olanzapine (mean 13.3 mg/d), and 25 were treated with quetiapine (mean 210.3 mg/d). Weight gain was the most common side effect; patients gained an average 8.6 lb with risperidone, 7.2 lb with quetiapine, and 14.1 lb with olanzapine. EPS were treated in seven (10%) patients taking risperidone, four (25%) taking olanzapine, and no patients taking quetiapine.
Bipolar disorder
As in the adult population, there has been substantial use of antipsychotics in children and adolescents with bipolar illness. Bipolar I disorder affects an estimated 0.6% of adolescents and is even being diagnosed in prepubertal patients.
Lithium, valproate, carbamazapine, and adjunctive treatment with benzodiazapines traditionally have been used to treat bipolar I disorders. Although practice guidelines recommend lithium and divalproex sodium as first-line treatments for bipolar illness, these recommendations are generally based on a preference for first-line agents that have potential use in maintenance treatment. The benefit of medications in bipolar disorder, however, is two-fold:
- Initial pharmacotherapy is usually instituted to target manic or mixed symptoms, and continued treatment is necessary to avoid relapse. The new antipsychotics—particularly risperidone, olanzapine, and quetiapine—are beneficial to treat agitated mania and disrupted sleep that may impair function and/or mandate inpatient stabilization. The highly sedative properties offer an acute benefit in restoring disrupted sleep.
- Psychotic symptoms seen in mania may need to be targeted independent of the mood symptoms and would thus suggest the use of an antipsychotic. In early-onset bipolar disorder, antipsychotics are used primarily as adjuncts to mood stabilizers.
- In the 1994 case report, an adolescent with bipolar disorder showed benefit when treated with clozapine.26
- In a retrospective chart review, 28 children ages 4 to 17 with bipolar disorder (25 mixed and 3 hypomanic) were treated with adjunctive risperidone for 6 months. Most (82%) showed significant improvement in mania and aggression on a mean dosage of 1.7 +/- 1.3 mg/d. Attention-deficit/hyperactivity disorder symptoms improved in 8% of the patients.27
- Affective symptoms (predominantly suggestive of bipolar disorder), aggression, and violent behavior in 11 children and adolescents ages 5 to 16 showed therapeutic response to an open trial of adjunctive low-dose (0.75 to 2.5 mg/d) risperidone.28
Olanzapine. Recent interest in olanzapine’s thymoleptic propertities has contributed to its clinical use in bipolar disorder, specifically in psychotic mania. Olanzapine has also been studied as long-term maintenance therapy in bipolar disorder. In a 47-week study, adult patients receiving olanzapine improved significantly more than those receiving valproate (47% vs. 34% by the Young Mania Rating Scale) after 3 weeks. Both medications were effective throughout the long-term, randomized, double-blind study.29
Two case series and one open trial have examined olanzapine as primary or adjunctive treatment for children and adolescents with bipolar disorder. In the open study, Frazier and colleagues gave olanzapine, 2.5 to 20 mg/d, to 23 children ages 5 to 14.30 After 8 weeks, the response rate was 61% (defined as 30% or greater improvement on the Young Mania Rating Scale). Weight gain was the predominant side effect (mean increase 5 kg).
Chang and colleagues demonstrated “marked improvement” in CGI scores when using olanzapine as adjunctive therapy for three youths with bipolar disorder.31 Similar findings were reported when treating seven youths with acute mania.32 Olanzapine’s broad affinity for dopaminergic and serotonergic receptors may explain these positive outcomes.
Other atypicals. No studies have been published on the use of quetiapine, ziprasidone, or aripiprazole in childhood mood disorders.
Psychotic depression
Psychosis can complicate depression in adults and adolescents. In a small study of adolescents with psychotic depression, Gellar et al demonstrated conventional neuroleptics’ benefit in combination with antidepressants.33 We have no data, however, on use of atypicals in childhood depression, and published accounts of depression in bipolar patients treated with atypicals are of some concern.
In one study,34 four of six patients with bipolar disorder developed dysphoric mood within 3 months of starting risperidone. Two met the criteria for major depression and required antidepressant therapy. This finding was somewhat surprising, given risperidone’s antidepressant benefit in some adults, most likely due to its 5-HT2 antagonistic effect. Frazier and colleagues similiarly noted that one patient discontinued treatment during an open-label trial examining the benefit of olanzapine in juvenile bipolar disorder.30
These findings in the adolescent bipolar population should not be ignored when you consider treating a primary depressive disorder with psychosis. Antipsychotics certainly can be useful for treating psychotic depression, especially acutely for stabilization and preventing harm to self. Atypical antipsychotics have consistently been proven to have less adverse side effects than typical antipsychotics and thus would be preferred in children and adolescents. Research is needed to examine possible worsening of dysphoria.
Related resources
- Hermann RC, Yang D, Ettner SL, et al. Prescription of antipsychotic drugs by office-based physicians in the United States, 1989-1997. Psychiatric Services 2002;53:425-30.
- Stigler KA, Potenza MN, McDougle CJ. Tolerability profile of atypical antipsychotics in children and adolescents (review). Paediatric Drugs 2001;3(12):927-94
- American Academy of Child and Adolescent Psychiatry http://www.aacap.org
- Clozapine • Clozaril
- Olanzapine • Zyprexa
- Quetiapine • Seroquel
- Risperidone • Risperdal
- Ziprasidone • Geodon
- Aripiprazole (investigational)
Dr. Londino reports that she serves as a consultant to Eli Lilly and Co.
Ms. Wiggins reports no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
Dr. Buckley reports that he receives grant support from and serves as a consultant and speaker for AstraZeneca Pharmaceuticals, Eli Lilly and Co., Janssen Pharmaceutica, and Novartis Pharmaceuticals Corp.
Prescribing of atypical antipsychotics for children and adolescents is increasing, despite a lack of randomized controlled clinical trials. Like many psychiatrists, you may be treating pediatric patients with these medications for a variety of indications beyond psychosis.
Three factors are driving the use of atypical antipsychotics for broader indications:
- substantial evidence that these newer agents are safer and more effective than typical antipsychotics1
- inadequate response of childhood and adolescent psychiatric disorders to their primary treatments
- evidence that atypical antipsychotics have potential thymoleptic, antiaggressive, and anxiolytic properties.
These attributes already have expanded atypical antipsychotic use in adult patients. In fact, atypicals are being used more extensively in adults for affective and nonpsychotic conditions than for schizophrenia.2
In preparing the following two-part article for Current Psychiatry, we scoured the available literature—Medline, abstracts from scientific meetings, and American Academy of Child and Adolescent Psychiatry (AACAP) practice parameters—to examine the evolving role of atypical antipsychotics in children and adolescents. In part 1 of this article, we discuss using atypicals in childhood/adolescent-onset schizophrenia, bipolar disorder, and psychotic depression. In part 2, we look at evidence for using atypicals in children with autism and developmental disorders, Tourette’s and other tic disorders, disruptive behavior disorders, anorexia nervosa, anxiety disorders, and stuttering.
Before prescribing antipsychotic medications for children and adolescents, always conduct a comprehensive history and complete physical examination.
History. Include information about:
- seizures, head trauma, and cardiac or endocrine problems (often elicited with questions about fatigue, temperature intolerance, or weight concerns)
- perinatal history (apnea, Apgar scores, days in hospital)
- family history (e.g., significant medical problems).
Physical exam. Obtain baseline blood pressure, pulse, body weight and habitus, and laboratory tests—complete blood count, comprehensive metabolic profile with liver function tests, and cholesterol/triglyceride levels.
Educate the parent and child about possible side effects, whether they are likely to be transient or persistent, and ways to minimize them (e.g., bedtime dosing to prevent daytime sedation, dietary recommendations to lessen potential weight gain).
Monitor lab values and weight throughout treatment (compared with normal growth curves). Use words the child understands when asking about side effects (e.g., “Have you had leakage from your breasts?”). Continually weigh the benefits versus the risks of antipsychotics, and discuss this balance with the parent and child.
Shift in pharmacotherapy of schizophrenia.
One-quarter of patients with schizophrenia develop the disorder before age 15, and subtle psychotic manifestations are often observed in early childhood.3 In general, schizophrenia’s presenting symptoms are comparable in adults and children, but the childhood/adolescent-onset form is more severe.4,5
During the past 5 years, pharmacotherapy of adult schizophrenia has shifted dramatically away from typical antipsychotics. Atypical agents have shown greater efficacy and tolerability, especially with respect to extrapyramidal symptoms (EPS) and tardive dyskinesia (TD).1
In a recent survey, most general and specialist psychiatrists (86%) said they prefer using atypical antipsychotics as first-line treatment for new-onset schizophrenia and as maintenance therapy. They also reported using atypicals to treat patients with dementia (80%), personality disorders (69%), developmental delay/mental retardation (65%), and autism (40%).6
Translating adult findings to children. Most evidence of atypical antipsychotics’ efficacy and tolerability is derived from adult studies, which likely will continue to influence clinical practice more than the limited number of child and adolescent studies. In 1998, a thorough review of atypical antipsychotic use in child and adolescent psychiatry found only five blinded placebo-controlled clinical trials, 24 open-label trials, and 33 case series.7 A follow-up review in 1999 again found mainly case reports and case series, with a handful of controlled studies.8
Available atypical antipsychotics include clozapine, risperidone, olanzapine, quetiapine, and ziprasidone. An investigational agent—aripiprazole—is likely to be available soon for clinical use.
Issues in pediatric use of atypicals
When prescribing atypical antipsychotics, it is important to balance the benefit of treatment with the risk of exposing children to possible adverse effects. Side effects associated with atypicals include weight gain, secondary metabolic disturbances such as hyperglycemia, hyperprolactinemia, and cardiac conduction abnormalities. These side effects are health concerns for all patients but particularly for children and adolescents, who may require years of exposure to antipsychotics.
Weight gain. Younger patients may be particularly susceptible to weight gain with the use of the atypicals. In a state hospital adult population, Buckley et al found a strong inverse relationship between patient age and weight gain associated with atypical antipsychotic use.9 Key issues for pediatric populations are:
- Will children have difficulties losing weight over time?
- Will they stop their medications over time?
- Will they stop their medications because of this effect?
- Will they be further stigmatized at school because of obesity?
- Are they at increased risk to develop diabetes mellitus?
- What are the long-term consequences of antipsychotic-induced obesity and metabolic disturbances for this patient population?
Hyperprolactinemia in children and adolescents may lead to breast enlargement and galactorrhea, which are particularly distressing in this age group. Sustained elevation of prolactin may affect the regulation of other hormones, resulting in low estrogen and testosterone levels. The long-term impact of these changes on adolescent growth and development is unknown. Antipsychotic-induced hyperprolactinemia also may be associated with reduced bone density.10
Abnormal cardiac conduction. Thioridazine recently received a “black box” label warning from the FDA because of sudden deaths and a prolonged QTc interval seen on electrocardiogram (ECG) readings. Several other antipsychotics also show ECG evidence of QTc prolongation.11 However, the clinical significance of this finding is unclear.
Younger patients respond differently than do adults to antipsychotic medications because of developmental differences in pharmacokinetics: absorption, distribution, metabolism, and excretion.
Absorption. Stomach contents tend to be less acidic in younger persons than in adults, potentially slowing absorption of weakly acidic drugs. In theory, the absorption of antidepressants and psychostimulants is more likely to be altered than that of antipsychotics. Children may also have fewer and less diverse intestinal microflora, which may explain why phenothiazines (absorbed or metabolized in the intestinal wall) must be given at higher-than-adult oral dosages for clinical effect.12
Children may absorb certain psychotropic medications (e.g., imipramine) more rapidly than adults. This contributes to greater fluctuations in blood levels and possible cardiac toxicity—often a function of peak plasma concentrations.
Distribution. Drug distribution patterns in infants, children, and adolescents—especially those going through puberty—are not homogenous.13 Fat stores and the relative proportion of total body water to extracellular water affect distribution and change with development.
The proportion of fat to body weight is highest in the first year of life, declines steadily during childhood, increases prior to puberty, then declines thereafter. Thus, although individuals have variable degrees of fat stores, children in general have a lower proportion of body fat than adults and therefore a smaller volume of distribution. This becomes significant when prescribing antipsychotics, which are lipid-soluble.
If one considers only a drug’s distribution, one would expect to find a higher plasma concentration in a child if a child and an adult were given the same weight-adjusted dose of a lipophilic drug. Children, however, exhibit a lowerplasma concentration of lipophilic drugs than do adults because of differences in metabolism.13
Metabolism. Children’s increased metabolic rate is directly related to age-related changes in hepatic enzymes. In general, metabolic pathways for many drugs function at a low level during the perinatal period, mature by 6 months, peak between ages 1 and 5, and decline gradually to adult values by about age 15. Liver mass is also greater in children than in adults. Therefore, higher ratios of milligrams of drug to kilograms of body weight may be needed in children to achieve steady-state plasma levels comparable to those seen in adults.
Excretion. Infant and adult renal functioning are approximately the same. With the exception of lithium, developmental changes in renal function do not contribute substantially to age-related differences in psychotropic drug excretion.13
Summary. When compared with adults, children require a higher milligram-to-kilogram dosage of antipsychotics to achieve the same plasma concentration but clinically require a lower milligram-to-kilogram dosage—starting dosages usually less than one-half of an adult dose—to avoid unwanted side effects.
SUGGESTED DOSAGES OF ATYPICAL ANTIPSYCHOTICS
| Drug | FDA-approved dosages for psychosis in adults | For psychosis in children and adolescents | For bipolar disorder in children and adolescents |
|---|---|---|---|
| Clozapine | Initial: 25 mg bid; increase gradually to 300 to 800 mg/d in divided doses | Not recommended for children under age 16 Initial: 12.5 to 25 mg bid; increase gradually to 300 to 450 mg/d (divided) Increased risk of seizures; potential for agranulocytosis | Limited research |
| Olanzapine | Psychosis. Initial: 5 to 10 mg qd or 5 mg bid; increase to 20 mg qd or 10 mg bid Bipolar disorder. Similar initial; lower maintenance (10 to 20 mg qd or 10 mg bid can often be obtained) | Clinical benefit in children age 10 at 2.5 to 10 mg/d; For age >10, 5 to 20 mg qd or 10 mg bid may be used Sedation and weight gain are common side effects | Clinically beneficial at dosages comparable to those used in psychosis Maintenance dosage may be lower than that required in a primary psychotic disorder |
| Quetiapine | Initial: 25 mg bid; increase to 300 to 800 mg/d divided in two to three doses | Initial: 12.5 mg bid (50 kg) Maintenance: 50 mg bid (50 kg) Few controlled trials in children | Limited research |
| Risperidone | Initial: 2 mg/d; may be increased to 4 to 6 mg/d in divided doses | Clinical trials indicate benefit at 0.25 to 0.5 mg qd or bid May be increased as needed to 0.5 to 1.5 mg/d in single or divided doses | Clinically beneficial at dosages comparable to those used in psychosis |
| Ziprasidone | Initial: 20 to 40 mg bid; may be increased to 40 to 80 mg bid | Preliminary studies suggest benefit at 10 to 20 mg bid, increasing to 20 to 60 mg bid Not recommended as first-line therapy in this population | Limited research |
| * The FDA has not approved a specific indication for these agents for use in children and adolescents. In adult patients, atypical antipsychotics have been approved for psychosis, and olanzapine is FDA-approved for psychosis and mood disorders. | |||
Special care is required to decrease the risks associated with using antipsychotics in children and adolescents and to increase compliance with medication recommendations (Box 1).
Pharmacokinetics in children and adolescents
Administering medications to children and adolescents requires special precautions. Younger patients respond differently than adults to psychotropic medications because of differences in pharmacokinetics—how the body handles a drug—and pharmacodynamics—the drug’s effect on the body.
During a child’s growth and development, physiologic changes in absorption, distribution, metabolism, and excretion may affect drug delivery to target tissue (Box 2).12,13 Maturation of brain regions and neurotransmitter systems also may alter a medication’s effect at different ages.
Antipsychotic dosage recommendations and therapeutic ranges for children and adolescents have been published but are extrapolated from adult studies because studies in children are lacking. There is danger, however, in using body weight and proportionately reducing an adult dosage to obtain a pediatric dosage. The plasma concentration may ultimately be subtherapeutic or toxic.14
The liver metabolizes most antipsychotics. The higher rate of hepatic metabolism in children would suggest that on a milligram-to-kilogram basis a child or adolescent would need a higher dose. Children, however, require smaller weight-adjusted doses of antipsychotics than do adults to achieve the same therapeutic effect.15 Children have a greater density of dopamine D-1 and D-2 receptors than do adults, suggesting a greater sensitivity to the beneficial and adverse effects of antipsychotics. To date, dopamine receptor occupancy in children/adolescents with schizophrenia has not been studied with positron emission tomography.
Summary. Compared with adults, children require a reduced milligram-to-kilogram dosage of antipsychotics to achieve the same therapeutic effect and avoid unwanted side effects. Children younger than age 10 or weighing less than 50 kg typically should start with the lowest starting dose, given once or twice a day (Table). The dose should be slowly increased based on the presence of side effects and remission of symptoms.
Maximum daily dosages for children weighing less than 50 kg should rarely exceed one-half of an adult antipsychotic dosage, particularly when used for symptoms of disorders other than primary psychosis. However, dosages closer to those used in adults may be necessary when treating primary psychosis in early-onset schizophrenia, especially in an adolescent (Box 3).
An adolescent boy, age 13 and weighing 47 kg, presents with the chief complaint of paranoia, which is impairing his academic functioning. On examination, his interaction is guarded, and he exhibits severe emotional withdrawal and a paucity of thought content. His family history is significant for a maternal uncle with early-onset schizophrenia, which is chronic but under reasonable control with olanzapine, 10 mg bid.
The boy’s treatment is started with olanzapine, 2.5 mg once daily. After 2 weeks, the dosage is increased to 2.5 mg in the morning and 5 mg at bedtime, with good symptom resolution.
Childhood/adolescent-onset schizophrenia
Typical antipsychotics appear to have limited efficacy in childhood/adolescent-onset schizophrenia, based on a small number of available case series and relatively short open-label trials.16 In a single-arm, placebo-controlled trial, haloperidol was effective in 16 children ages 5 to 12, but its use was associated with substantial EPS. A similar intolerance was demonstrated in a comparative trial of thioridazine and thiothixene.
Less is known about the incidence of tardive dyskinesia, but there is no reason to believe that the rate is lower in children and adolescents than in adults with schizophrenia (estimated at 5% per year for the first 5 years of treatment).
Clozapine. Information is emerging on the efficacy and tolerability of atypical antipsychotics in childhood/adolescent-onset schizophrenia.16 Clozapine has been studied more than other atypicals, in part because of the severity of early-onset schizophrenia and because clozapine has been used in clinical practice longer than the other agents in that class.
Early case reports and small open-labeled trials confirmed that clozapine was effective for children and adolescents with schizophrenia who had failed prior antipsychotic treatments.17-19 A randomized, double-blind, controlled trial from the childhood schizophrenia division of the National Institute of Mental Health provided the most reliable information.17 In that 6-week treatment study, 21 severely ill adolescents (mean age 14) received clozapine, mean dosage 176 mg/d, or haloperidol, mean dosage 16 mg/d. Response to clozapine was greater for both positive and negative symptoms, and the difference was clinically and statistically significant. In addition, 62% of clozapine-treated patients were rated very much improved on the Clinical Global Impression (CGI) scale.
In the same trial, clozapine treatment was complicated by higher rates of adverse effects than are typically observed in adult studies:
- Sedation was reported in 90% of patients.
- 2 of 10 patients had a seizure during clozapine therapy.
- A 2% rate of agranulocytosis was disconcerting, given the lower adult rate (0.38%) and the brevity of the trial. As older age is a known risk factor for clozapine-induced agranulocytosis, it may be that children and the elderly are more susceptible to this side effect.
Olanzapine has been effective in this patient population at dosages up to 10 mg/d.7,16,21 In a pilot study, Kumra et al administered olanzapine to 23 children with schizophrenia who had not previously responded to neuroleptic treatment. After 8 weeks, the children improved on the Brief Psychiatric Rating Scale, the Scale for the Assessment for Negative Symptoms, and the Scale for the Assessment of Positive Symptoms.21
Similarities and differences in olanzapine’s side effects in adults and children/adolescents with schizophrenia were seen in a recent study. Children had more weight gain, sedation, and dystonia, whereas adults had significantly more cardiac arrhythmias.22
Quetiapine. McConville and colleagues examined the efficacy and tolerability of quetiapine in 10 adolescents with chronic psychosis (7 with schizoaffective disorder and 3 with bipolar disorder). In this 3-week study, quetiapine was well-tolerated; in several patients, dosages exceeded 750 mg/d. Psychotic symptoms were reduced, and there was global improvement in functioning.23
Other antipsychotics. There are no published data on the use of ziprasidone or aripiprazole in childhood/adolescent-onset schizophrenia.
Comparative data are very limited. One retrospective analysis compared the tolerability of risperidone, olanzapine, and quetiapine in 116 adolescent patients.24 Over 3 months, 75 patients received risperidone (mean 2.6 mg/d), 16 received olanzapine (mean 13.3 mg/d), and 25 were treated with quetiapine (mean 210.3 mg/d). Weight gain was the most common side effect; patients gained an average 8.6 lb with risperidone, 7.2 lb with quetiapine, and 14.1 lb with olanzapine. EPS were treated in seven (10%) patients taking risperidone, four (25%) taking olanzapine, and no patients taking quetiapine.
Bipolar disorder
As in the adult population, there has been substantial use of antipsychotics in children and adolescents with bipolar illness. Bipolar I disorder affects an estimated 0.6% of adolescents and is even being diagnosed in prepubertal patients.
Lithium, valproate, carbamazapine, and adjunctive treatment with benzodiazapines traditionally have been used to treat bipolar I disorders. Although practice guidelines recommend lithium and divalproex sodium as first-line treatments for bipolar illness, these recommendations are generally based on a preference for first-line agents that have potential use in maintenance treatment. The benefit of medications in bipolar disorder, however, is two-fold:
- Initial pharmacotherapy is usually instituted to target manic or mixed symptoms, and continued treatment is necessary to avoid relapse. The new antipsychotics—particularly risperidone, olanzapine, and quetiapine—are beneficial to treat agitated mania and disrupted sleep that may impair function and/or mandate inpatient stabilization. The highly sedative properties offer an acute benefit in restoring disrupted sleep.
- Psychotic symptoms seen in mania may need to be targeted independent of the mood symptoms and would thus suggest the use of an antipsychotic. In early-onset bipolar disorder, antipsychotics are used primarily as adjuncts to mood stabilizers.
- In the 1994 case report, an adolescent with bipolar disorder showed benefit when treated with clozapine.26
- In a retrospective chart review, 28 children ages 4 to 17 with bipolar disorder (25 mixed and 3 hypomanic) were treated with adjunctive risperidone for 6 months. Most (82%) showed significant improvement in mania and aggression on a mean dosage of 1.7 +/- 1.3 mg/d. Attention-deficit/hyperactivity disorder symptoms improved in 8% of the patients.27
- Affective symptoms (predominantly suggestive of bipolar disorder), aggression, and violent behavior in 11 children and adolescents ages 5 to 16 showed therapeutic response to an open trial of adjunctive low-dose (0.75 to 2.5 mg/d) risperidone.28
Olanzapine. Recent interest in olanzapine’s thymoleptic propertities has contributed to its clinical use in bipolar disorder, specifically in psychotic mania. Olanzapine has also been studied as long-term maintenance therapy in bipolar disorder. In a 47-week study, adult patients receiving olanzapine improved significantly more than those receiving valproate (47% vs. 34% by the Young Mania Rating Scale) after 3 weeks. Both medications were effective throughout the long-term, randomized, double-blind study.29
Two case series and one open trial have examined olanzapine as primary or adjunctive treatment for children and adolescents with bipolar disorder. In the open study, Frazier and colleagues gave olanzapine, 2.5 to 20 mg/d, to 23 children ages 5 to 14.30 After 8 weeks, the response rate was 61% (defined as 30% or greater improvement on the Young Mania Rating Scale). Weight gain was the predominant side effect (mean increase 5 kg).
Chang and colleagues demonstrated “marked improvement” in CGI scores when using olanzapine as adjunctive therapy for three youths with bipolar disorder.31 Similar findings were reported when treating seven youths with acute mania.32 Olanzapine’s broad affinity for dopaminergic and serotonergic receptors may explain these positive outcomes.
Other atypicals. No studies have been published on the use of quetiapine, ziprasidone, or aripiprazole in childhood mood disorders.
Psychotic depression
Psychosis can complicate depression in adults and adolescents. In a small study of adolescents with psychotic depression, Gellar et al demonstrated conventional neuroleptics’ benefit in combination with antidepressants.33 We have no data, however, on use of atypicals in childhood depression, and published accounts of depression in bipolar patients treated with atypicals are of some concern.
In one study,34 four of six patients with bipolar disorder developed dysphoric mood within 3 months of starting risperidone. Two met the criteria for major depression and required antidepressant therapy. This finding was somewhat surprising, given risperidone’s antidepressant benefit in some adults, most likely due to its 5-HT2 antagonistic effect. Frazier and colleagues similiarly noted that one patient discontinued treatment during an open-label trial examining the benefit of olanzapine in juvenile bipolar disorder.30
These findings in the adolescent bipolar population should not be ignored when you consider treating a primary depressive disorder with psychosis. Antipsychotics certainly can be useful for treating psychotic depression, especially acutely for stabilization and preventing harm to self. Atypical antipsychotics have consistently been proven to have less adverse side effects than typical antipsychotics and thus would be preferred in children and adolescents. Research is needed to examine possible worsening of dysphoria.
Related resources
- Hermann RC, Yang D, Ettner SL, et al. Prescription of antipsychotic drugs by office-based physicians in the United States, 1989-1997. Psychiatric Services 2002;53:425-30.
- Stigler KA, Potenza MN, McDougle CJ. Tolerability profile of atypical antipsychotics in children and adolescents (review). Paediatric Drugs 2001;3(12):927-94
- American Academy of Child and Adolescent Psychiatry http://www.aacap.org
- Clozapine • Clozaril
- Olanzapine • Zyprexa
- Quetiapine • Seroquel
- Risperidone • Risperdal
- Ziprasidone • Geodon
- Aripiprazole (investigational)
Dr. Londino reports that she serves as a consultant to Eli Lilly and Co.
Ms. Wiggins reports no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
Dr. Buckley reports that he receives grant support from and serves as a consultant and speaker for AstraZeneca Pharmaceuticals, Eli Lilly and Co., Janssen Pharmaceutica, and Novartis Pharmaceuticals Corp.
1. World Psychiatric Association. The usefulness and use of second-generation antipsychotic medications. Curr Opinion Psychiatry 2002;15(suppl):51-551.
2. Buckley PF. Broad therapeutic uses of atypical antipsychotic medications. Biol Psychiatry 2001;50:912-24.
3. Lieberman JA, Perkins D, Belger A, et al. The early stages of schizophrenia: speculations on pathogenesis, pathophysiology, and therapeutic approaches. Biol Psychiatry 2001;50:884-97.
4. Asarnow JR, Tompson MC, Goldstein MJ. Childhood-onset schizophrenia: a follow-up study. Schizophr Bull 1994;20:599-617.
5. Eggers C, Bunk D. The long-term course of childhood-onset schizophrenia: a 42-year follow-up study. Schizophr Bull 1997;23:105-17.
6. Buckley PF, Miller DD, Singer B, Donnenwirth K. The evolving clinical profile of atypical antipsychotic medications. Can J Psychiatry 2001;46:285.-
7. Toren P, Laor N, Weizman. Use of atypical neuroleptics in child and adolescent psychiatry. J Clin Psychiatry 1998;58:644-56.
8. Malone RP, Sheikh R, Zito JM. Novel antipsychotic medications in the treatment of children and adolescents. Psych Services 1999;50(2):171-4.
9. Singer B, Buckley PF, Friedman L, et al. Weight gain, diabetes mellitus, and the pharmacotherapy of schizophrenia. Schiophr Res 2001;49:276.-
10. Meaney AM. Elevated prolactin levels and the effect with atypical antipsychotics. Presentation at the Winter Workshop on Schizophrenia Research. Davos, Switzerland: February 2002.
11. Reilly JG, Ayis S, Ferrrier IN, et al. QTc interval abnormalities and psychotropic drug therapy in psychiatric patients. Lancet 2000;355:1048-52.
12. Lewis M (ed) Child and adolescent psychiatry Baltimore: Williams & Wilkins, 1996.
13. Jatlow PI. Psychotropic drug disposition during development. In: Popper C (ed). Psychiatric pharmacosciences of children and adolescents Washington, DC: American Psychiatric Press, 1987;29-44.
14. Janicak PG, Davis JM, Preskorn SH, et al (eds). Pharmacokinetics. In: Janicak PG, Davis JM, Preskorn SH, et al (eds). Principles and practice of psychopharmacotherapy Baltimore: Williams & Wilkins, 1993;59-79.
15. Verghese C, Kessel JB, Simpson GM. Pharmacokinetics of neuroleptics. Psychopharmacol Bull 1991;27(4):551-63.
16. Frangou S, Kumra S. Treatment of childhood-onset schizophrenia. In: Buckley PF, Waddington JL (eds). Schizophrenia and mood disorders: The new drug therapies in clinical practice Oxford, UK: Arnold, 2000;253:72.-
17. Kumra S, Frazier JA, Jacobsen LK, et al. Childhood-onset schizophrenia: A double-blind clozapine-haloperidol comparison. Arch Gen Psychiatr 1996;53:1090-7.
18. Remschmidt H, Schulz E, Martin M. An open trial of clozapine in thirty-six adolescents with schizophrenia. J Child Adolesc Psychiatry 1994;4:31-41.
19. Turetz M, Mozes T, Toren P, et al. An open trial of clozapine in neuroleptic-resistant childhood-onset schizophrenia. Br J Psychiatry 1997;170:507-10.
20. McGorry PD, et al. Risperidone for prodrome of schizophrenia. Arch Gen Psychiatry 2002 (in press).
21. Kumra S, Jacobsen LK, Lanane M, et al. Childhood-onset schizophrenia: An open-label study of olanzapine in adolescents. J Am Acad Adolesc Psychiatry 1998;37:377-85.
22. Woods SC, McGlashan TH. Adverse effects of olanzapine in adolescents and adults. Schizophr Res 2002;53:170.-
23. McConville B. Seroquel does not elevate prolactin levels in adolescents with selected psychotic disorders. Schizophr Res 2000;41:206.-
24. Grcevich S, Melamed L, Richards R. Comparative side effects of atypical antipsychotics in children and adolescents (poster presentation) Whistler, British Columbia: International Congress on Schizophrenia Research, April 2001.
25. American Academy of Child and Adolescent Psychiatry. AACAP official action: practice parameters for the assessment and treatment of children and adolescents with bipolar disorder. J Am Acad Child Adolesc Psychiatry 1997;36:138-57.
26. Fuchs DC. Clozapine treatment of bipolar disorder in a young adolescent. J Am Acad Child Adolesc Psych 1994;33:1299-1302.
27. Frazier JA, Meyer MC, Biederman J, et al. Risperidone treatment for juvenile bipolar disorder: a retrospective chart review. J Am Acad Child Adolesc Psych 1999;38:960-5.
28. Schreier HA. Risperidone for young children with mood disorders and aggressive behavior. J Child Adolesc Psychopharmacol 1998;8:49-59.
29. Tohen M, Baker RW, Altshuler L, et al. Olanzapine versus divalproex sodium for bipolar mania: a 47-week study. Eur Psychiatry 2002;17(suppl 1):109.-
30. Frazier JA, Biederman J, Jacobs TG, et al. Olanzapine in the treatment of bipolar disorder in juveniles. Schizophr Res 2000;41(1, suppl 1):194.-
31. Chang KD, Ketter TA. Mood stabilizer augmentation with olanzapine in acutely manic children. J Child Adolesc Psychopharmacol 2000;10:45-9.
32. Soutullo CA, Sorter MT, Foster KD, et al. Olanzapine in the treatment of adolescent acute mania: a report of seven cases. J Affect Dis 1999;53:279-83.
33. Gellar B, Cooper TB, Farooki ZQ, et al. Dose and plasma levels of nortriptyline and chlorpromazine in delusionally depressed adolescents and of nortriptyline in nondelusionally depressed adolescents. Am J Psych 1985;142:336-8.
34. Mandoki MW. Risperidone treatment of children and adolescents: increased risk of extrapyramidal side effects? J Clin Adolesc Psychopharmacol 1995;5:49-67.
1. World Psychiatric Association. The usefulness and use of second-generation antipsychotic medications. Curr Opinion Psychiatry 2002;15(suppl):51-551.
2. Buckley PF. Broad therapeutic uses of atypical antipsychotic medications. Biol Psychiatry 2001;50:912-24.
3. Lieberman JA, Perkins D, Belger A, et al. The early stages of schizophrenia: speculations on pathogenesis, pathophysiology, and therapeutic approaches. Biol Psychiatry 2001;50:884-97.
4. Asarnow JR, Tompson MC, Goldstein MJ. Childhood-onset schizophrenia: a follow-up study. Schizophr Bull 1994;20:599-617.
5. Eggers C, Bunk D. The long-term course of childhood-onset schizophrenia: a 42-year follow-up study. Schizophr Bull 1997;23:105-17.
6. Buckley PF, Miller DD, Singer B, Donnenwirth K. The evolving clinical profile of atypical antipsychotic medications. Can J Psychiatry 2001;46:285.-
7. Toren P, Laor N, Weizman. Use of atypical neuroleptics in child and adolescent psychiatry. J Clin Psychiatry 1998;58:644-56.
8. Malone RP, Sheikh R, Zito JM. Novel antipsychotic medications in the treatment of children and adolescents. Psych Services 1999;50(2):171-4.
9. Singer B, Buckley PF, Friedman L, et al. Weight gain, diabetes mellitus, and the pharmacotherapy of schizophrenia. Schiophr Res 2001;49:276.-
10. Meaney AM. Elevated prolactin levels and the effect with atypical antipsychotics. Presentation at the Winter Workshop on Schizophrenia Research. Davos, Switzerland: February 2002.
11. Reilly JG, Ayis S, Ferrrier IN, et al. QTc interval abnormalities and psychotropic drug therapy in psychiatric patients. Lancet 2000;355:1048-52.
12. Lewis M (ed) Child and adolescent psychiatry Baltimore: Williams & Wilkins, 1996.
13. Jatlow PI. Psychotropic drug disposition during development. In: Popper C (ed). Psychiatric pharmacosciences of children and adolescents Washington, DC: American Psychiatric Press, 1987;29-44.
14. Janicak PG, Davis JM, Preskorn SH, et al (eds). Pharmacokinetics. In: Janicak PG, Davis JM, Preskorn SH, et al (eds). Principles and practice of psychopharmacotherapy Baltimore: Williams & Wilkins, 1993;59-79.
15. Verghese C, Kessel JB, Simpson GM. Pharmacokinetics of neuroleptics. Psychopharmacol Bull 1991;27(4):551-63.
16. Frangou S, Kumra S. Treatment of childhood-onset schizophrenia. In: Buckley PF, Waddington JL (eds). Schizophrenia and mood disorders: The new drug therapies in clinical practice Oxford, UK: Arnold, 2000;253:72.-
17. Kumra S, Frazier JA, Jacobsen LK, et al. Childhood-onset schizophrenia: A double-blind clozapine-haloperidol comparison. Arch Gen Psychiatr 1996;53:1090-7.
18. Remschmidt H, Schulz E, Martin M. An open trial of clozapine in thirty-six adolescents with schizophrenia. J Child Adolesc Psychiatry 1994;4:31-41.
19. Turetz M, Mozes T, Toren P, et al. An open trial of clozapine in neuroleptic-resistant childhood-onset schizophrenia. Br J Psychiatry 1997;170:507-10.
20. McGorry PD, et al. Risperidone for prodrome of schizophrenia. Arch Gen Psychiatry 2002 (in press).
21. Kumra S, Jacobsen LK, Lanane M, et al. Childhood-onset schizophrenia: An open-label study of olanzapine in adolescents. J Am Acad Adolesc Psychiatry 1998;37:377-85.
22. Woods SC, McGlashan TH. Adverse effects of olanzapine in adolescents and adults. Schizophr Res 2002;53:170.-
23. McConville B. Seroquel does not elevate prolactin levels in adolescents with selected psychotic disorders. Schizophr Res 2000;41:206.-
24. Grcevich S, Melamed L, Richards R. Comparative side effects of atypical antipsychotics in children and adolescents (poster presentation) Whistler, British Columbia: International Congress on Schizophrenia Research, April 2001.
25. American Academy of Child and Adolescent Psychiatry. AACAP official action: practice parameters for the assessment and treatment of children and adolescents with bipolar disorder. J Am Acad Child Adolesc Psychiatry 1997;36:138-57.
26. Fuchs DC. Clozapine treatment of bipolar disorder in a young adolescent. J Am Acad Child Adolesc Psych 1994;33:1299-1302.
27. Frazier JA, Meyer MC, Biederman J, et al. Risperidone treatment for juvenile bipolar disorder: a retrospective chart review. J Am Acad Child Adolesc Psych 1999;38:960-5.
28. Schreier HA. Risperidone for young children with mood disorders and aggressive behavior. J Child Adolesc Psychopharmacol 1998;8:49-59.
29. Tohen M, Baker RW, Altshuler L, et al. Olanzapine versus divalproex sodium for bipolar mania: a 47-week study. Eur Psychiatry 2002;17(suppl 1):109.-
30. Frazier JA, Biederman J, Jacobs TG, et al. Olanzapine in the treatment of bipolar disorder in juveniles. Schizophr Res 2000;41(1, suppl 1):194.-
31. Chang KD, Ketter TA. Mood stabilizer augmentation with olanzapine in acutely manic children. J Child Adolesc Psychopharmacol 2000;10:45-9.
32. Soutullo CA, Sorter MT, Foster KD, et al. Olanzapine in the treatment of adolescent acute mania: a report of seven cases. J Affect Dis 1999;53:279-83.
33. Gellar B, Cooper TB, Farooki ZQ, et al. Dose and plasma levels of nortriptyline and chlorpromazine in delusionally depressed adolescents and of nortriptyline in nondelusionally depressed adolescents. Am J Psych 1985;142:336-8.
34. Mandoki MW. Risperidone treatment of children and adolescents: increased risk of extrapyramidal side effects? J Clin Adolesc Psychopharmacol 1995;5:49-67.
Adult ADHD: Less hyperactivity, but lingering inattention and distress
Attention-deficit/hyperactivity disorder (ADHD) may be the only mental disorder that was discovered in children and later acknowledged in adults. Although controlled studies of adults with ADHD are few, we know that ADHD is common in adults, it can be diagnosed reliably, and 75% of those treated respond to treatment.1
The hallmark symptom of ADHD in children—hyperactivity—is usually attenuated in adults. In fact, some adults prefer the term ADD to ADHD because they are not hyperactive. This may be especially true of women, as their attention problems during childhood often were not recognized as ADHD (Box 1).
In childhood, girls with ADHD typically present with attention problems and over-talkativeness, rather than hyperactivity. Talking too much does not disrupt the classroom as much as the larger-scale misbehavior of boys with ADHD, so the diagnosis is often missed in these girls. Overtalkativeness was added to the DSM-III-R criteria for ADHD in 1987, after it was recognized as a symptom of overactivity.
Now in midlife, many women with undiagnosed ADHD have children with ADHD. As they bring their children to treatment, these women are recognizing similar attention deficit symptoms from their own childhoods and are getting the help they need. As adults, many have low self-esteem, low energy, and weight problems. Among adults with ADHD, these women may be the most underdiagnosed.
Characteristics of adult ADHD
Adults with ADHD visit a psychiatrist for a variety of reasons. Often they are parents of children diagnosed with ADHD, and the possibility that they are similarly affected has arisen during their children’s evaluation and treatment. Sometimes they have recognized themselves in consumer articles about ADHD, or others have seen them in this light.
Adults with ADHD continue to experience their childhood difficulties in sustaining attention, listening, following instructions, and organizing tasks; inattention to details; lack of sustained mental effort; losing things; distractibility, and forgetfulness. Typical complaints include underachievement and poor adjustment at work or home. Comorbid ADHD may also be identified in patients who present with depression, anxiety, substance misuse, and mood swings.
The cognitive impairment of ADHD continues into adulthood, even in adults without hyperactive symptoms. It may be that adults are not hyperactive because the basal ganglia, which control motor activity in the brain, have over the years accommodated the problem through behavior modification or neurodevelopmental changes in late adolescence.2
Children with ADHD have abnormal cerebrospinal fluid (CSF) and blood levels of the dopaminergic metabolite homovanillic acid (HVA), but adults with ADHD may not. The primary origin for CSF HVA is the nigrostriatum, which suggests that subcortical dopaminergic nuclei are more often affected in children than adults.2 This may mean that compensatory changes occur as persons with ADHD mature, or perhaps the forms of ADHD that persist into adulthood have a different pathology or pathophysiology.
Comorbidities with ADHD
Rarely does one see pure ADHD; comorbidity is the rule. ADHD can be diagnosed quickly if you know what to look for. But a facile diagnosis may overlook a comorbidity that must be treated first—especially if you plan to use stimulants. Many patients with ADHD also have bipolar disorder, and a smaller proportion of patients with bipolar disorder have undetected ADHD. Placing a patient with undetected bipolar disorder on a stimulant could precipitate mania.
Table 1
COMMON COMORBIDITIES WITH ADHD
| Bipolar disorder |
| Anxiety disorder |
| Depression |
| Drug dependence |
| Personality disorders |
| Somatoform disorders |
| Tourette’s disorder |
| Obsessive-compulsive disorder |
| Intermittent explosive disorder |
| Impulse control problems |
| Addictive behaviors |
| Sexual problems |
| Compulsive gambling |
| Learning disabilities |
| Asperger’s syndrome |
From the initial assessment, your treatment plan must address comorbid conditions (Table 1). This means taking a good history that includes corroborating information from relatives and data from the past, if possible. The case will then be much easier to manage, and quality of care greatly enhanced.
Stimulants: Usual first-choice therapy
In most cases, adult ADHD responds well to stimulant medications, although most available evidence is limited to studies in children. Several nonstimulant medications are also available, and the FDA is considering a new-drug application for a medication indicated for adult ADHD. Stimulants produce significant improvement in 30% of patients and mixed results in another 40%. Comorbidities may account for the 10 to 30% of patients who do not respond to stimulant therapy.
Methylphenidate, taken multiple times daily, is the most common treatment for ADHD. Dextroamphetamine and mixed salts of amphetamine also are used (Table 2).3 Patients usually respond to either methylphenidate or an amphetamine, and typically 25% of those who do not respond to one will respond to the other. When the clinical efficacy of amphetamines diminishes over time, many psychiatrists rotate medications. Replacing one amphetamine with another often eliminates the need to slowly increase the dosage and allows the clinician to maintain a relatively stable regimen.
When administering stimulants to adults, consider the individual’s total dosage requirement and daily schedule. Will he or she fare better with multiple daily dosing or a sustained-release form? How long is his or her average day? Does the patient have to be alert for 12 hours—or longer?
Some patients cannot sleep unless they take their last stimulant dose at bedtime. Others will have insomnia if a last dose is taken too late in the afternoon, especially with a sustained-release formulation.
When starting a patient on stimulants, begin with a 12-hour day and titrate the dosage—usually up, sometimes down—depending on response and side effects. Educating patients about their medications enables them to participate in decision-making.
Common side effects of stimulants include insomnia, decreased appetite, upset stomach, headache, anxiety, agitation, and increased pulse rate and blood pressure. The increase in blood pressure is usually less than 10%, but patients with poorly controlled hypertension should not be treated with stimulants until their blood pressure is well controlled. Until more is known about long-term effects, periodic assessment of blood pressure may be warranted.
Table 2
STIMULANT THERAPY FOR ADULTS WITH ADHD
| Stimulants | Starting dosage | Titration rate | Usual dosing interval | Maximum dosage in adults | |
|---|---|---|---|---|---|
| Methylphenidate | |||||
| Short-acting | |||||
| d, l-methylphenidate (Ritalin, Methylin) | 5 mg qd or 5 mg bid | 5 to 10 mg every 3 to 5 days | Every 3 to 4 hours Usually bid-tid | Average oral dosage 0.92 mg/kg/d; best response to 1.0 mg/kg/d16 | |
| Intermediate-acting | |||||
| d, l-methylphenidate (Ritalin SR, Metadate ER, Methylin ER) | 20 mg Ritalin SR; 10 mg Methylin ER or Metadate ER | 10 to 20 mg per week | qd to bid | ||
| d-methylphenidate (Focalin) | 2.5 mg bid | 2.5 to 5 mg per week | bid, at least 4 hours apart | ||
| Long-acting | |||||
| d, l-methylphenidate (Concerta) | 18 mg qd | 18 mg every 3 to 5 days | 12+ hours, usually qd | ||
| d, l-methylphenidate (Metadate CD) | 20 mg qd | 20 mg per week | qd | ||
| Amphetamine | |||||
| Short-acting | |||||
| (Dexedrine, Dextrostat) | 2.5 to 5 mg qd | 2.5 to 5 mg every 3 to 5 days | Every 4 to 6 hours Usually bid-tid | ||
| Intermediate-acting | |||||
| Mixed salts (Adderall) | 5 mg qd or 5 mg bid | 5 to 10 mg every 3 to 5 days | Every 4 to 6 hours Usually qd to bid | Average dosage 54 mg/d divided in two doses; maximum 30 mg bid | |
| (Dexedrine Spansule) | 5 or 10 mg qd | 5 mg per week | qd | ||
| Long-acting | |||||
| (Adderall XR) | 10 mg qd | 10 mg per week | qd | ||
| Stimulant | |||||
| Pemoline (Cylert) | 37.5 mg qd | 18.75 mg per week | qd; typical range 56.25 to 75 mg qd | Maximum dosage 112.5 mg/d | |
- Organized and orderly home and working environment
- Designated work/study space at home
- Designated coach to supervise work/study
- Healthy meals at regularly scheduled times
- Regular exercise
Adults with ADHD have been treated with mixed amphetamine salts with positive results. In a 7-week controlled, crossover study, 27 adults with ADHD received an average of 54 mg/d administered in two doses. Symptoms improved significantly—a 42% decrease on the ADHD Rating Scale. The medication was well-tolerated, and 70% of those receiving mixed amphetamine salts improved, compared with 7% of those who received a placebo.4
Duration of action of mixed salts of amphetamine has been measured at 3.5 hours with a 5-mg dose and 6.4 hours with a 20-mg dose.5 With methylphenidate, a dose of 12.5 mg worked for 4 hours. The maximum recommended dosage of mixed salts of amphetamine is 40 mg/d in divided doses.
Stimulant medications are well-tolerated. Addiction and the need for increased dosages can occur over long-term use (months to years). Reducing the dosage or switching from methylphenidate to an amphetamine variant can usually prevent these problems.
The FDA recently approved a single-enantiomer form of methylphenidate. It contains only the active “d” enantiomer, whereas the racemic mixture contains both the “d” and “l” enantiomers. Because the “l” enantiomer is inert, the resulting medication is more potent and may be prescribed at half the dosage of the racemic mixture.
Pemoline, a once-daily stimulant, is considered a second-line treatment because of reports of hepatic failure in some patients. Its use requires written informed consent and liver function tests at baseline and every 2 weeks. In a controlled trial, pemoline at high dosages (120 to 160 mg/d) was found moderately effective in adults with ADHD.6
Newer options: Longer-acting stimulants
Newer forms of slow-release methylphenidate and mixed amphetamine salts with sophisticated delivery systems are available.
Metadate CD is delivered in capsules containing beads with polymer coatings that dissolve and release their contents at different times. The capsules contain a 30:70 ratio of immediate- and extended-release beads.
Metadate CD has not been tested for adults in controlled clinical trials. In children ages 6 to 15, a single morning dose has been shown to be clinically effective in the morning and afternoon. A supplemental immediate-release capsule can be given in the morning if a patient’s medication levels need to be increased quickly. Dosage supplementation may also be required later in the day.
Concerta is delivered in 18-mg and 36-mg tablets. The immediate-release coating on the tablets delivers medication within the first hour. The drug inside then dissolves in the GI tract and is released at a controlled rate by osmotic pressure. The indigestible tablet is passed in the stool.
Concerta was investigated in children ages 6 to 12 and provides 10 to 12 hours of sustained medication. From child studies, we know that when a patient takes a 36-mg tablet at 6 AM, blood levels decline in late afternoon. An 18-mg dose at noon covers the 4 to 6 hours needed for evening chores.
Adderall XR is an extended-release, once-daily form of mixed amphetamine salts. No controlled trials of this formulation are available in adults with ADHD. Its efficacy was established after two clinical trials of children aged 6 to 12 who met DSM-IV criteria for ADHD.
Individualized and flexible dosing improves symptom control and compliance when treating adults with ADHD. For some patients, once-daily dosing is more convenient than multiple doses, while others prefer the immediate-release form because they like its midday “pause” and bid dosing. The immediate-release tablet allows the flexibility of bid or tid dosing, depending on the day’s requirements.
Antidepressants: Another choice
Antidepressants are usually considered second-line treatment for ADHD because of concerns about efficacy and side effects. The few available studies show antidepressants work as well as stimulants but more slowly. It is good practice, therefore, to advise patients that—unlike feeling the effect of a stimulant in 60 minutes—they will not feel an effect from an antidepressant for days or weeks, and that achieving an optimal effect may take 4 to 6 weeks.
Antidepressants have several advantages over stimulants. They are not classified as narcotics, work without the on-off effects of stimulants, and can treat comorbid depression and anxiety. For adult ADHD, the most effective agents work on the catecholamine systems—norepinephrine and/or dopamine. This includes the tricyclic antidepressants, MAO inhibitors, bupropion, and venlafaxine. The serotonin reuptake inhibitors have not shown promise in ADHD, nor have mirtazapine or nefazodone demonstrated much effect.
Desipramine, a tricyclic antidepressant, is a strong inhibitor of norepinephrine reuptake. In a double-blind, controlled study in 41 adults with ADHD, 68% of patients receiving desipramine, 200 mg/d, responded positively, compared with no patients who took a placebo.7
When venlafaxine was given in standard dosages to 10 adults with ADHD in an open, 8-week clinical trial, an effect was seen by week two. Of the nine patients who completed the study, seven were considered responders. Symptoms were reduced significantly with venlafaxine treatment, and most side effects were mild.8
In an open study, bupropion treatment resulted in moderate to marked response in 74% of 19 patients. Ten of those patients who responded chose to continue bupropion rather than their previous medication.9 In a 6-week controlled study of 40 patients, bupropion use was associated with a 42% reduction in ADHD symptoms in the 38 patients who completed the study. Patients who received a placebo showed only a 24% reduction in symptoms. According to the CGI, 52% of patients who received bupropion reported being “much improved” or “very improved” compared with 11% of those receiving a placebo.10
Other treatment options that have shown mixed results include modafinil, alpha-2a agonists, acetylcholinesterase inhibitors, and the histaminergic agents.
Managing adverse effects
Substance abuse Stimulant abuse has been a concern, but it has not become the problem many feared. In fact, some studies have found that methylphenidate may help stanch the craving for cocaine in adults with ADHD.11,12 Treating ADHD with pharmacotherapy also has been shown to reduce the risk for substance abuse in adolescence by 85%.13
With careful screening, you can usually identify drug-seeking behavior in adult patients. For patients with substance abuse problems, you can prescribe the nonstimulants.
Tics that can occur with stimulant medications usually can be suppressed by reducing the dosage, being vigilant, and waiting it out. Tics may ameliorate over weeks to months.
Cardiac and cognitive effects Long-term use of stimulant medications at high dosages has been associated with cardiac and cognitive toxicity, as noted in the 1998 NIH consensus statement on diagnosis and treatment of ADHD. It is important to provide patients with this information as part of their informed-consent briefing. (See “Related resources,” to view the consensus statement.)
Nonpharmacologic management
Nonpharmacologic treatments such as EEG biofeedback; psychoeducational approaches; and individual, family, and group psychotherapy are widely used to treat adults with ADHD. Clinicians and patients often perceive these interventions as beneficial, although none have been tested in randomized, placebo-controlled studies.
Patients often function better when their home and work environments are thoughtfully organized, with a designated work/study space and regularly scheduled times for meals, sleep, and exercise. An ADHD coach may facilitate such structure and discipline (Box 2).
New agents in the pipeline
Efforts are being made to increase awareness of adult ADHD and to improve its treatment. For example, the National Institute of Mental Health is funding research on adult ADHD and displays on its Web site a PET scan of an adult brain with ADHD (see “Related resources”).14 Several medications also are being developed to treat ADHD.
Atomoxetine, a nonstimulant medication awaiting FDA approval for adult ADHD, is a selective norepinephrine reuptake inhibitor. In a double-blind, placebo-controlled, crossover study of adults with well-characterized ADHD, 11 of 21 patients improved with use of atomoxetine, compared with 2 of 21 who improved with use of a placebo. The average dosage of 76 mg/d was well-tolerated.15 The 52% response rate is similar to the 54% average improvement rate reported for methylphenidate in previous studies of adult ADHD.
In clinical trials, atomoxetine was given bid. Insomnia was not a side effect, so bid dosing does not interfere with sleep. Approximately 10 to 15% of patients experienced weight loss as a side effect.
Other treatment options under development include:
- a transdermal system for delivery of methylphenidate16
- a novel nicotinic analogue
- glutamate AMPA receptor modulation
- omega-3 fatty acids.
- Hallowell EM, Ratey JJ. Driven to distraction: Recognizing and coping with attention deficit disorder from childhood through adulthood. New York: Simon and Schuster; Reprint edition 1995.
- Solanto MV, Arnstein AFT, Castellanos FX, eds. Stimulant drugs and ADHD: Basic and clinical neuroscience. New York: Oxford University Press; 2001.
- Weiss M, Trokenberg-Hechtman L, Weiss G. ADHD in adulthood: A guide to current theory, diagnosis, and treatment. Baltimore: Johns Hopkins University Press; 1999.
- National Institute of Mental Health. http://www.nimh.nih.gov
Drug brand names
- Atomoxetine • (investigational)
- Bupropion • Wellbutrin
- Desipramine • Norpramin
- Dextroamphetamine • Dexedrine, Dextrostat
- Methamphetamine • Desoxyn
- Methylphenidate • Focalin, Ritalin
- Methylphenidate SR • Concerta, Metadate CD, Metadate ER, Methylin ER, Ritalin SR
- Mixed salts of amphetamine • Adderall, Adderall XR
- Modafinil • Provigil
- Pemoline • Cylert
- Venlafaxine • Effexor
Disclosure
The author reports that he serves as a consultant to Eli Lilly and Company and is on the speaker’s bureaus of Wyeth Pharmaceuticals and AstraZeneca.
1. Gadrow KD, Weiss M. Attention-deficit/hyperactivity disorder in adults: beyond controversy. Arch Gen Psychiatry 2001;58(8):784-5.
2. Ernst M, Zametkin AJ, Matochik JA, Jons PH, Cohen RM. DOPA decarboxylase activity in attention deficit hyperactivity disorder adults. A [fluorine-18]fluorodopa positron emission tomographic study. J Neurosci 1998;18(15):5901-7.
3. Spencer T, Wilens T, Biederman J, Faraone SV, Ablon JS, Lapey K. A double-blind, crossover comparison of methylphenidate and placebo in adults with childhood-onset attention-deficit hyperactivity disorder. Arch Gen Psychiatry 1995;52:434-43.
4. Spencer T, Biederman J, Wilens T, et al. Efficacy of a mixed amphetamine salts compound in adults with attention-deficit/hyperactivity disorder. Arch Gen Psychiatry 2001;58(8):775-82.
5. Swanson J, Wigal S, Greenhill L, et al. Objective and subjective measures of the pharmacodynamic effects of Adderall in the treatment of children with ADHD in a controlled laboratory classroom setting. Psychopharmacol Bull 1998;34(1):55-60.
6. Wilens TE, Biederman J, Spencer TJ, et al. Controlled trial of high doses of pemoline for adults with attention-deficit/hyperactivity disorder. J Clin Psychopharmacol 1999;19(3):257-64.
7. Wilens TE, Biederman J, Mick E, Spencer TJ. A systematic assessment of tricyclic antidepressants in the treatment of adult attention-deficit hyperactivity disorder. J Nerv Ment Dis 1995;183(1):48-50.
8. Findling RL, Schwartz MA, Flannery DJ, Manos MJ. Venlafaxine in adults with attention-deficit/hyperactivity disorder: an open clinical trial. J Clin Psychiatry 1996;57(5):184-9.
9. Wender PH, Reimherr FW. Bupropion treatment of attention-deficit hyperactivity disorder in adults. Am J Psychiatry 1990;147(8):1018-20.
10. Wilens TE, Spencer TJ, et al. A controlled clinical trial of bupropion for attention deficit hyperactivity disorder in adults. Am J Psychiatry 2001;158(2):282-8.
11. Grabowski J, Roache JD, Schmitz JM, Rhoades H, et al. Replacement medication for cocaine dependence: methylphenidate. J Clin Psychopharmacol 1997;17(6):485-8.
12. Levin FR, Evans SM, McDowell DM, Kleber HD. Methylphenidate treatment for cocaine abusers with adult attention-deficit/hyperactivity disorder: a pilot study. J Clin Psychiatry 1998;59(6):300-5.
13. Biederman J, Wilens T, Mick E, Spencer T, Faraone SV. Pharmacotherapy of attention-deficit/hyperactivity disorder reduces risk for substance use disorder. Pediatrics 1999;104(2):e20.-
14. Zametkin AJ, Nordahl TE, Gross M, et al. Cerebral glucose metabolism in adults with hyperactivity of childhood onset. N Engl J Med 1990;323(20):1361-6.
15. Spencer T, Biederman J, Wilens T. Effectiveness and tolerability of atomoxetine in adults with attention deficit hyperactivity disorder. Am J Psychiatry 1998;155(5):693-5.
16. Noven Pharmaceuticals. The Science of Noven. Research and development. Transdermal technology. Available at: http://www.noven.com/research.htm.
Attention-deficit/hyperactivity disorder (ADHD) may be the only mental disorder that was discovered in children and later acknowledged in adults. Although controlled studies of adults with ADHD are few, we know that ADHD is common in adults, it can be diagnosed reliably, and 75% of those treated respond to treatment.1
The hallmark symptom of ADHD in children—hyperactivity—is usually attenuated in adults. In fact, some adults prefer the term ADD to ADHD because they are not hyperactive. This may be especially true of women, as their attention problems during childhood often were not recognized as ADHD (Box 1).
In childhood, girls with ADHD typically present with attention problems and over-talkativeness, rather than hyperactivity. Talking too much does not disrupt the classroom as much as the larger-scale misbehavior of boys with ADHD, so the diagnosis is often missed in these girls. Overtalkativeness was added to the DSM-III-R criteria for ADHD in 1987, after it was recognized as a symptom of overactivity.
Now in midlife, many women with undiagnosed ADHD have children with ADHD. As they bring their children to treatment, these women are recognizing similar attention deficit symptoms from their own childhoods and are getting the help they need. As adults, many have low self-esteem, low energy, and weight problems. Among adults with ADHD, these women may be the most underdiagnosed.
Characteristics of adult ADHD
Adults with ADHD visit a psychiatrist for a variety of reasons. Often they are parents of children diagnosed with ADHD, and the possibility that they are similarly affected has arisen during their children’s evaluation and treatment. Sometimes they have recognized themselves in consumer articles about ADHD, or others have seen them in this light.
Adults with ADHD continue to experience their childhood difficulties in sustaining attention, listening, following instructions, and organizing tasks; inattention to details; lack of sustained mental effort; losing things; distractibility, and forgetfulness. Typical complaints include underachievement and poor adjustment at work or home. Comorbid ADHD may also be identified in patients who present with depression, anxiety, substance misuse, and mood swings.
The cognitive impairment of ADHD continues into adulthood, even in adults without hyperactive symptoms. It may be that adults are not hyperactive because the basal ganglia, which control motor activity in the brain, have over the years accommodated the problem through behavior modification or neurodevelopmental changes in late adolescence.2
Children with ADHD have abnormal cerebrospinal fluid (CSF) and blood levels of the dopaminergic metabolite homovanillic acid (HVA), but adults with ADHD may not. The primary origin for CSF HVA is the nigrostriatum, which suggests that subcortical dopaminergic nuclei are more often affected in children than adults.2 This may mean that compensatory changes occur as persons with ADHD mature, or perhaps the forms of ADHD that persist into adulthood have a different pathology or pathophysiology.
Comorbidities with ADHD
Rarely does one see pure ADHD; comorbidity is the rule. ADHD can be diagnosed quickly if you know what to look for. But a facile diagnosis may overlook a comorbidity that must be treated first—especially if you plan to use stimulants. Many patients with ADHD also have bipolar disorder, and a smaller proportion of patients with bipolar disorder have undetected ADHD. Placing a patient with undetected bipolar disorder on a stimulant could precipitate mania.
Table 1
COMMON COMORBIDITIES WITH ADHD
| Bipolar disorder |
| Anxiety disorder |
| Depression |
| Drug dependence |
| Personality disorders |
| Somatoform disorders |
| Tourette’s disorder |
| Obsessive-compulsive disorder |
| Intermittent explosive disorder |
| Impulse control problems |
| Addictive behaviors |
| Sexual problems |
| Compulsive gambling |
| Learning disabilities |
| Asperger’s syndrome |
From the initial assessment, your treatment plan must address comorbid conditions (Table 1). This means taking a good history that includes corroborating information from relatives and data from the past, if possible. The case will then be much easier to manage, and quality of care greatly enhanced.
Stimulants: Usual first-choice therapy
In most cases, adult ADHD responds well to stimulant medications, although most available evidence is limited to studies in children. Several nonstimulant medications are also available, and the FDA is considering a new-drug application for a medication indicated for adult ADHD. Stimulants produce significant improvement in 30% of patients and mixed results in another 40%. Comorbidities may account for the 10 to 30% of patients who do not respond to stimulant therapy.
Methylphenidate, taken multiple times daily, is the most common treatment for ADHD. Dextroamphetamine and mixed salts of amphetamine also are used (Table 2).3 Patients usually respond to either methylphenidate or an amphetamine, and typically 25% of those who do not respond to one will respond to the other. When the clinical efficacy of amphetamines diminishes over time, many psychiatrists rotate medications. Replacing one amphetamine with another often eliminates the need to slowly increase the dosage and allows the clinician to maintain a relatively stable regimen.
When administering stimulants to adults, consider the individual’s total dosage requirement and daily schedule. Will he or she fare better with multiple daily dosing or a sustained-release form? How long is his or her average day? Does the patient have to be alert for 12 hours—or longer?
Some patients cannot sleep unless they take their last stimulant dose at bedtime. Others will have insomnia if a last dose is taken too late in the afternoon, especially with a sustained-release formulation.
When starting a patient on stimulants, begin with a 12-hour day and titrate the dosage—usually up, sometimes down—depending on response and side effects. Educating patients about their medications enables them to participate in decision-making.
Common side effects of stimulants include insomnia, decreased appetite, upset stomach, headache, anxiety, agitation, and increased pulse rate and blood pressure. The increase in blood pressure is usually less than 10%, but patients with poorly controlled hypertension should not be treated with stimulants until their blood pressure is well controlled. Until more is known about long-term effects, periodic assessment of blood pressure may be warranted.
Table 2
STIMULANT THERAPY FOR ADULTS WITH ADHD
| Stimulants | Starting dosage | Titration rate | Usual dosing interval | Maximum dosage in adults | |
|---|---|---|---|---|---|
| Methylphenidate | |||||
| Short-acting | |||||
| d, l-methylphenidate (Ritalin, Methylin) | 5 mg qd or 5 mg bid | 5 to 10 mg every 3 to 5 days | Every 3 to 4 hours Usually bid-tid | Average oral dosage 0.92 mg/kg/d; best response to 1.0 mg/kg/d16 | |
| Intermediate-acting | |||||
| d, l-methylphenidate (Ritalin SR, Metadate ER, Methylin ER) | 20 mg Ritalin SR; 10 mg Methylin ER or Metadate ER | 10 to 20 mg per week | qd to bid | ||
| d-methylphenidate (Focalin) | 2.5 mg bid | 2.5 to 5 mg per week | bid, at least 4 hours apart | ||
| Long-acting | |||||
| d, l-methylphenidate (Concerta) | 18 mg qd | 18 mg every 3 to 5 days | 12+ hours, usually qd | ||
| d, l-methylphenidate (Metadate CD) | 20 mg qd | 20 mg per week | qd | ||
| Amphetamine | |||||
| Short-acting | |||||
| (Dexedrine, Dextrostat) | 2.5 to 5 mg qd | 2.5 to 5 mg every 3 to 5 days | Every 4 to 6 hours Usually bid-tid | ||
| Intermediate-acting | |||||
| Mixed salts (Adderall) | 5 mg qd or 5 mg bid | 5 to 10 mg every 3 to 5 days | Every 4 to 6 hours Usually qd to bid | Average dosage 54 mg/d divided in two doses; maximum 30 mg bid | |
| (Dexedrine Spansule) | 5 or 10 mg qd | 5 mg per week | qd | ||
| Long-acting | |||||
| (Adderall XR) | 10 mg qd | 10 mg per week | qd | ||
| Stimulant | |||||
| Pemoline (Cylert) | 37.5 mg qd | 18.75 mg per week | qd; typical range 56.25 to 75 mg qd | Maximum dosage 112.5 mg/d | |
- Organized and orderly home and working environment
- Designated work/study space at home
- Designated coach to supervise work/study
- Healthy meals at regularly scheduled times
- Regular exercise
Adults with ADHD have been treated with mixed amphetamine salts with positive results. In a 7-week controlled, crossover study, 27 adults with ADHD received an average of 54 mg/d administered in two doses. Symptoms improved significantly—a 42% decrease on the ADHD Rating Scale. The medication was well-tolerated, and 70% of those receiving mixed amphetamine salts improved, compared with 7% of those who received a placebo.4
Duration of action of mixed salts of amphetamine has been measured at 3.5 hours with a 5-mg dose and 6.4 hours with a 20-mg dose.5 With methylphenidate, a dose of 12.5 mg worked for 4 hours. The maximum recommended dosage of mixed salts of amphetamine is 40 mg/d in divided doses.
Stimulant medications are well-tolerated. Addiction and the need for increased dosages can occur over long-term use (months to years). Reducing the dosage or switching from methylphenidate to an amphetamine variant can usually prevent these problems.
The FDA recently approved a single-enantiomer form of methylphenidate. It contains only the active “d” enantiomer, whereas the racemic mixture contains both the “d” and “l” enantiomers. Because the “l” enantiomer is inert, the resulting medication is more potent and may be prescribed at half the dosage of the racemic mixture.
Pemoline, a once-daily stimulant, is considered a second-line treatment because of reports of hepatic failure in some patients. Its use requires written informed consent and liver function tests at baseline and every 2 weeks. In a controlled trial, pemoline at high dosages (120 to 160 mg/d) was found moderately effective in adults with ADHD.6
Newer options: Longer-acting stimulants
Newer forms of slow-release methylphenidate and mixed amphetamine salts with sophisticated delivery systems are available.
Metadate CD is delivered in capsules containing beads with polymer coatings that dissolve and release their contents at different times. The capsules contain a 30:70 ratio of immediate- and extended-release beads.
Metadate CD has not been tested for adults in controlled clinical trials. In children ages 6 to 15, a single morning dose has been shown to be clinically effective in the morning and afternoon. A supplemental immediate-release capsule can be given in the morning if a patient’s medication levels need to be increased quickly. Dosage supplementation may also be required later in the day.
Concerta is delivered in 18-mg and 36-mg tablets. The immediate-release coating on the tablets delivers medication within the first hour. The drug inside then dissolves in the GI tract and is released at a controlled rate by osmotic pressure. The indigestible tablet is passed in the stool.
Concerta was investigated in children ages 6 to 12 and provides 10 to 12 hours of sustained medication. From child studies, we know that when a patient takes a 36-mg tablet at 6 AM, blood levels decline in late afternoon. An 18-mg dose at noon covers the 4 to 6 hours needed for evening chores.
Adderall XR is an extended-release, once-daily form of mixed amphetamine salts. No controlled trials of this formulation are available in adults with ADHD. Its efficacy was established after two clinical trials of children aged 6 to 12 who met DSM-IV criteria for ADHD.
Individualized and flexible dosing improves symptom control and compliance when treating adults with ADHD. For some patients, once-daily dosing is more convenient than multiple doses, while others prefer the immediate-release form because they like its midday “pause” and bid dosing. The immediate-release tablet allows the flexibility of bid or tid dosing, depending on the day’s requirements.
Antidepressants: Another choice
Antidepressants are usually considered second-line treatment for ADHD because of concerns about efficacy and side effects. The few available studies show antidepressants work as well as stimulants but more slowly. It is good practice, therefore, to advise patients that—unlike feeling the effect of a stimulant in 60 minutes—they will not feel an effect from an antidepressant for days or weeks, and that achieving an optimal effect may take 4 to 6 weeks.
Antidepressants have several advantages over stimulants. They are not classified as narcotics, work without the on-off effects of stimulants, and can treat comorbid depression and anxiety. For adult ADHD, the most effective agents work on the catecholamine systems—norepinephrine and/or dopamine. This includes the tricyclic antidepressants, MAO inhibitors, bupropion, and venlafaxine. The serotonin reuptake inhibitors have not shown promise in ADHD, nor have mirtazapine or nefazodone demonstrated much effect.
Desipramine, a tricyclic antidepressant, is a strong inhibitor of norepinephrine reuptake. In a double-blind, controlled study in 41 adults with ADHD, 68% of patients receiving desipramine, 200 mg/d, responded positively, compared with no patients who took a placebo.7
When venlafaxine was given in standard dosages to 10 adults with ADHD in an open, 8-week clinical trial, an effect was seen by week two. Of the nine patients who completed the study, seven were considered responders. Symptoms were reduced significantly with venlafaxine treatment, and most side effects were mild.8
In an open study, bupropion treatment resulted in moderate to marked response in 74% of 19 patients. Ten of those patients who responded chose to continue bupropion rather than their previous medication.9 In a 6-week controlled study of 40 patients, bupropion use was associated with a 42% reduction in ADHD symptoms in the 38 patients who completed the study. Patients who received a placebo showed only a 24% reduction in symptoms. According to the CGI, 52% of patients who received bupropion reported being “much improved” or “very improved” compared with 11% of those receiving a placebo.10
Other treatment options that have shown mixed results include modafinil, alpha-2a agonists, acetylcholinesterase inhibitors, and the histaminergic agents.
Managing adverse effects
Substance abuse Stimulant abuse has been a concern, but it has not become the problem many feared. In fact, some studies have found that methylphenidate may help stanch the craving for cocaine in adults with ADHD.11,12 Treating ADHD with pharmacotherapy also has been shown to reduce the risk for substance abuse in adolescence by 85%.13
With careful screening, you can usually identify drug-seeking behavior in adult patients. For patients with substance abuse problems, you can prescribe the nonstimulants.
Tics that can occur with stimulant medications usually can be suppressed by reducing the dosage, being vigilant, and waiting it out. Tics may ameliorate over weeks to months.
Cardiac and cognitive effects Long-term use of stimulant medications at high dosages has been associated with cardiac and cognitive toxicity, as noted in the 1998 NIH consensus statement on diagnosis and treatment of ADHD. It is important to provide patients with this information as part of their informed-consent briefing. (See “Related resources,” to view the consensus statement.)
Nonpharmacologic management
Nonpharmacologic treatments such as EEG biofeedback; psychoeducational approaches; and individual, family, and group psychotherapy are widely used to treat adults with ADHD. Clinicians and patients often perceive these interventions as beneficial, although none have been tested in randomized, placebo-controlled studies.
Patients often function better when their home and work environments are thoughtfully organized, with a designated work/study space and regularly scheduled times for meals, sleep, and exercise. An ADHD coach may facilitate such structure and discipline (Box 2).
New agents in the pipeline
Efforts are being made to increase awareness of adult ADHD and to improve its treatment. For example, the National Institute of Mental Health is funding research on adult ADHD and displays on its Web site a PET scan of an adult brain with ADHD (see “Related resources”).14 Several medications also are being developed to treat ADHD.
Atomoxetine, a nonstimulant medication awaiting FDA approval for adult ADHD, is a selective norepinephrine reuptake inhibitor. In a double-blind, placebo-controlled, crossover study of adults with well-characterized ADHD, 11 of 21 patients improved with use of atomoxetine, compared with 2 of 21 who improved with use of a placebo. The average dosage of 76 mg/d was well-tolerated.15 The 52% response rate is similar to the 54% average improvement rate reported for methylphenidate in previous studies of adult ADHD.
In clinical trials, atomoxetine was given bid. Insomnia was not a side effect, so bid dosing does not interfere with sleep. Approximately 10 to 15% of patients experienced weight loss as a side effect.
Other treatment options under development include:
- a transdermal system for delivery of methylphenidate16
- a novel nicotinic analogue
- glutamate AMPA receptor modulation
- omega-3 fatty acids.
- Hallowell EM, Ratey JJ. Driven to distraction: Recognizing and coping with attention deficit disorder from childhood through adulthood. New York: Simon and Schuster; Reprint edition 1995.
- Solanto MV, Arnstein AFT, Castellanos FX, eds. Stimulant drugs and ADHD: Basic and clinical neuroscience. New York: Oxford University Press; 2001.
- Weiss M, Trokenberg-Hechtman L, Weiss G. ADHD in adulthood: A guide to current theory, diagnosis, and treatment. Baltimore: Johns Hopkins University Press; 1999.
- National Institute of Mental Health. http://www.nimh.nih.gov
Drug brand names
- Atomoxetine • (investigational)
- Bupropion • Wellbutrin
- Desipramine • Norpramin
- Dextroamphetamine • Dexedrine, Dextrostat
- Methamphetamine • Desoxyn
- Methylphenidate • Focalin, Ritalin
- Methylphenidate SR • Concerta, Metadate CD, Metadate ER, Methylin ER, Ritalin SR
- Mixed salts of amphetamine • Adderall, Adderall XR
- Modafinil • Provigil
- Pemoline • Cylert
- Venlafaxine • Effexor
Disclosure
The author reports that he serves as a consultant to Eli Lilly and Company and is on the speaker’s bureaus of Wyeth Pharmaceuticals and AstraZeneca.
Attention-deficit/hyperactivity disorder (ADHD) may be the only mental disorder that was discovered in children and later acknowledged in adults. Although controlled studies of adults with ADHD are few, we know that ADHD is common in adults, it can be diagnosed reliably, and 75% of those treated respond to treatment.1
The hallmark symptom of ADHD in children—hyperactivity—is usually attenuated in adults. In fact, some adults prefer the term ADD to ADHD because they are not hyperactive. This may be especially true of women, as their attention problems during childhood often were not recognized as ADHD (Box 1).
In childhood, girls with ADHD typically present with attention problems and over-talkativeness, rather than hyperactivity. Talking too much does not disrupt the classroom as much as the larger-scale misbehavior of boys with ADHD, so the diagnosis is often missed in these girls. Overtalkativeness was added to the DSM-III-R criteria for ADHD in 1987, after it was recognized as a symptom of overactivity.
Now in midlife, many women with undiagnosed ADHD have children with ADHD. As they bring their children to treatment, these women are recognizing similar attention deficit symptoms from their own childhoods and are getting the help they need. As adults, many have low self-esteem, low energy, and weight problems. Among adults with ADHD, these women may be the most underdiagnosed.
Characteristics of adult ADHD
Adults with ADHD visit a psychiatrist for a variety of reasons. Often they are parents of children diagnosed with ADHD, and the possibility that they are similarly affected has arisen during their children’s evaluation and treatment. Sometimes they have recognized themselves in consumer articles about ADHD, or others have seen them in this light.
Adults with ADHD continue to experience their childhood difficulties in sustaining attention, listening, following instructions, and organizing tasks; inattention to details; lack of sustained mental effort; losing things; distractibility, and forgetfulness. Typical complaints include underachievement and poor adjustment at work or home. Comorbid ADHD may also be identified in patients who present with depression, anxiety, substance misuse, and mood swings.
The cognitive impairment of ADHD continues into adulthood, even in adults without hyperactive symptoms. It may be that adults are not hyperactive because the basal ganglia, which control motor activity in the brain, have over the years accommodated the problem through behavior modification or neurodevelopmental changes in late adolescence.2
Children with ADHD have abnormal cerebrospinal fluid (CSF) and blood levels of the dopaminergic metabolite homovanillic acid (HVA), but adults with ADHD may not. The primary origin for CSF HVA is the nigrostriatum, which suggests that subcortical dopaminergic nuclei are more often affected in children than adults.2 This may mean that compensatory changes occur as persons with ADHD mature, or perhaps the forms of ADHD that persist into adulthood have a different pathology or pathophysiology.
Comorbidities with ADHD
Rarely does one see pure ADHD; comorbidity is the rule. ADHD can be diagnosed quickly if you know what to look for. But a facile diagnosis may overlook a comorbidity that must be treated first—especially if you plan to use stimulants. Many patients with ADHD also have bipolar disorder, and a smaller proportion of patients with bipolar disorder have undetected ADHD. Placing a patient with undetected bipolar disorder on a stimulant could precipitate mania.
Table 1
COMMON COMORBIDITIES WITH ADHD
| Bipolar disorder |
| Anxiety disorder |
| Depression |
| Drug dependence |
| Personality disorders |
| Somatoform disorders |
| Tourette’s disorder |
| Obsessive-compulsive disorder |
| Intermittent explosive disorder |
| Impulse control problems |
| Addictive behaviors |
| Sexual problems |
| Compulsive gambling |
| Learning disabilities |
| Asperger’s syndrome |
From the initial assessment, your treatment plan must address comorbid conditions (Table 1). This means taking a good history that includes corroborating information from relatives and data from the past, if possible. The case will then be much easier to manage, and quality of care greatly enhanced.
Stimulants: Usual first-choice therapy
In most cases, adult ADHD responds well to stimulant medications, although most available evidence is limited to studies in children. Several nonstimulant medications are also available, and the FDA is considering a new-drug application for a medication indicated for adult ADHD. Stimulants produce significant improvement in 30% of patients and mixed results in another 40%. Comorbidities may account for the 10 to 30% of patients who do not respond to stimulant therapy.
Methylphenidate, taken multiple times daily, is the most common treatment for ADHD. Dextroamphetamine and mixed salts of amphetamine also are used (Table 2).3 Patients usually respond to either methylphenidate or an amphetamine, and typically 25% of those who do not respond to one will respond to the other. When the clinical efficacy of amphetamines diminishes over time, many psychiatrists rotate medications. Replacing one amphetamine with another often eliminates the need to slowly increase the dosage and allows the clinician to maintain a relatively stable regimen.
When administering stimulants to adults, consider the individual’s total dosage requirement and daily schedule. Will he or she fare better with multiple daily dosing or a sustained-release form? How long is his or her average day? Does the patient have to be alert for 12 hours—or longer?
Some patients cannot sleep unless they take their last stimulant dose at bedtime. Others will have insomnia if a last dose is taken too late in the afternoon, especially with a sustained-release formulation.
When starting a patient on stimulants, begin with a 12-hour day and titrate the dosage—usually up, sometimes down—depending on response and side effects. Educating patients about their medications enables them to participate in decision-making.
Common side effects of stimulants include insomnia, decreased appetite, upset stomach, headache, anxiety, agitation, and increased pulse rate and blood pressure. The increase in blood pressure is usually less than 10%, but patients with poorly controlled hypertension should not be treated with stimulants until their blood pressure is well controlled. Until more is known about long-term effects, periodic assessment of blood pressure may be warranted.
Table 2
STIMULANT THERAPY FOR ADULTS WITH ADHD
| Stimulants | Starting dosage | Titration rate | Usual dosing interval | Maximum dosage in adults | |
|---|---|---|---|---|---|
| Methylphenidate | |||||
| Short-acting | |||||
| d, l-methylphenidate (Ritalin, Methylin) | 5 mg qd or 5 mg bid | 5 to 10 mg every 3 to 5 days | Every 3 to 4 hours Usually bid-tid | Average oral dosage 0.92 mg/kg/d; best response to 1.0 mg/kg/d16 | |
| Intermediate-acting | |||||
| d, l-methylphenidate (Ritalin SR, Metadate ER, Methylin ER) | 20 mg Ritalin SR; 10 mg Methylin ER or Metadate ER | 10 to 20 mg per week | qd to bid | ||
| d-methylphenidate (Focalin) | 2.5 mg bid | 2.5 to 5 mg per week | bid, at least 4 hours apart | ||
| Long-acting | |||||
| d, l-methylphenidate (Concerta) | 18 mg qd | 18 mg every 3 to 5 days | 12+ hours, usually qd | ||
| d, l-methylphenidate (Metadate CD) | 20 mg qd | 20 mg per week | qd | ||
| Amphetamine | |||||
| Short-acting | |||||
| (Dexedrine, Dextrostat) | 2.5 to 5 mg qd | 2.5 to 5 mg every 3 to 5 days | Every 4 to 6 hours Usually bid-tid | ||
| Intermediate-acting | |||||
| Mixed salts (Adderall) | 5 mg qd or 5 mg bid | 5 to 10 mg every 3 to 5 days | Every 4 to 6 hours Usually qd to bid | Average dosage 54 mg/d divided in two doses; maximum 30 mg bid | |
| (Dexedrine Spansule) | 5 or 10 mg qd | 5 mg per week | qd | ||
| Long-acting | |||||
| (Adderall XR) | 10 mg qd | 10 mg per week | qd | ||
| Stimulant | |||||
| Pemoline (Cylert) | 37.5 mg qd | 18.75 mg per week | qd; typical range 56.25 to 75 mg qd | Maximum dosage 112.5 mg/d | |
- Organized and orderly home and working environment
- Designated work/study space at home
- Designated coach to supervise work/study
- Healthy meals at regularly scheduled times
- Regular exercise
Adults with ADHD have been treated with mixed amphetamine salts with positive results. In a 7-week controlled, crossover study, 27 adults with ADHD received an average of 54 mg/d administered in two doses. Symptoms improved significantly—a 42% decrease on the ADHD Rating Scale. The medication was well-tolerated, and 70% of those receiving mixed amphetamine salts improved, compared with 7% of those who received a placebo.4
Duration of action of mixed salts of amphetamine has been measured at 3.5 hours with a 5-mg dose and 6.4 hours with a 20-mg dose.5 With methylphenidate, a dose of 12.5 mg worked for 4 hours. The maximum recommended dosage of mixed salts of amphetamine is 40 mg/d in divided doses.
Stimulant medications are well-tolerated. Addiction and the need for increased dosages can occur over long-term use (months to years). Reducing the dosage or switching from methylphenidate to an amphetamine variant can usually prevent these problems.
The FDA recently approved a single-enantiomer form of methylphenidate. It contains only the active “d” enantiomer, whereas the racemic mixture contains both the “d” and “l” enantiomers. Because the “l” enantiomer is inert, the resulting medication is more potent and may be prescribed at half the dosage of the racemic mixture.
Pemoline, a once-daily stimulant, is considered a second-line treatment because of reports of hepatic failure in some patients. Its use requires written informed consent and liver function tests at baseline and every 2 weeks. In a controlled trial, pemoline at high dosages (120 to 160 mg/d) was found moderately effective in adults with ADHD.6
Newer options: Longer-acting stimulants
Newer forms of slow-release methylphenidate and mixed amphetamine salts with sophisticated delivery systems are available.
Metadate CD is delivered in capsules containing beads with polymer coatings that dissolve and release their contents at different times. The capsules contain a 30:70 ratio of immediate- and extended-release beads.
Metadate CD has not been tested for adults in controlled clinical trials. In children ages 6 to 15, a single morning dose has been shown to be clinically effective in the morning and afternoon. A supplemental immediate-release capsule can be given in the morning if a patient’s medication levels need to be increased quickly. Dosage supplementation may also be required later in the day.
Concerta is delivered in 18-mg and 36-mg tablets. The immediate-release coating on the tablets delivers medication within the first hour. The drug inside then dissolves in the GI tract and is released at a controlled rate by osmotic pressure. The indigestible tablet is passed in the stool.
Concerta was investigated in children ages 6 to 12 and provides 10 to 12 hours of sustained medication. From child studies, we know that when a patient takes a 36-mg tablet at 6 AM, blood levels decline in late afternoon. An 18-mg dose at noon covers the 4 to 6 hours needed for evening chores.
Adderall XR is an extended-release, once-daily form of mixed amphetamine salts. No controlled trials of this formulation are available in adults with ADHD. Its efficacy was established after two clinical trials of children aged 6 to 12 who met DSM-IV criteria for ADHD.
Individualized and flexible dosing improves symptom control and compliance when treating adults with ADHD. For some patients, once-daily dosing is more convenient than multiple doses, while others prefer the immediate-release form because they like its midday “pause” and bid dosing. The immediate-release tablet allows the flexibility of bid or tid dosing, depending on the day’s requirements.
Antidepressants: Another choice
Antidepressants are usually considered second-line treatment for ADHD because of concerns about efficacy and side effects. The few available studies show antidepressants work as well as stimulants but more slowly. It is good practice, therefore, to advise patients that—unlike feeling the effect of a stimulant in 60 minutes—they will not feel an effect from an antidepressant for days or weeks, and that achieving an optimal effect may take 4 to 6 weeks.
Antidepressants have several advantages over stimulants. They are not classified as narcotics, work without the on-off effects of stimulants, and can treat comorbid depression and anxiety. For adult ADHD, the most effective agents work on the catecholamine systems—norepinephrine and/or dopamine. This includes the tricyclic antidepressants, MAO inhibitors, bupropion, and venlafaxine. The serotonin reuptake inhibitors have not shown promise in ADHD, nor have mirtazapine or nefazodone demonstrated much effect.
Desipramine, a tricyclic antidepressant, is a strong inhibitor of norepinephrine reuptake. In a double-blind, controlled study in 41 adults with ADHD, 68% of patients receiving desipramine, 200 mg/d, responded positively, compared with no patients who took a placebo.7
When venlafaxine was given in standard dosages to 10 adults with ADHD in an open, 8-week clinical trial, an effect was seen by week two. Of the nine patients who completed the study, seven were considered responders. Symptoms were reduced significantly with venlafaxine treatment, and most side effects were mild.8
In an open study, bupropion treatment resulted in moderate to marked response in 74% of 19 patients. Ten of those patients who responded chose to continue bupropion rather than their previous medication.9 In a 6-week controlled study of 40 patients, bupropion use was associated with a 42% reduction in ADHD symptoms in the 38 patients who completed the study. Patients who received a placebo showed only a 24% reduction in symptoms. According to the CGI, 52% of patients who received bupropion reported being “much improved” or “very improved” compared with 11% of those receiving a placebo.10
Other treatment options that have shown mixed results include modafinil, alpha-2a agonists, acetylcholinesterase inhibitors, and the histaminergic agents.
Managing adverse effects
Substance abuse Stimulant abuse has been a concern, but it has not become the problem many feared. In fact, some studies have found that methylphenidate may help stanch the craving for cocaine in adults with ADHD.11,12 Treating ADHD with pharmacotherapy also has been shown to reduce the risk for substance abuse in adolescence by 85%.13
With careful screening, you can usually identify drug-seeking behavior in adult patients. For patients with substance abuse problems, you can prescribe the nonstimulants.
Tics that can occur with stimulant medications usually can be suppressed by reducing the dosage, being vigilant, and waiting it out. Tics may ameliorate over weeks to months.
Cardiac and cognitive effects Long-term use of stimulant medications at high dosages has been associated with cardiac and cognitive toxicity, as noted in the 1998 NIH consensus statement on diagnosis and treatment of ADHD. It is important to provide patients with this information as part of their informed-consent briefing. (See “Related resources,” to view the consensus statement.)
Nonpharmacologic management
Nonpharmacologic treatments such as EEG biofeedback; psychoeducational approaches; and individual, family, and group psychotherapy are widely used to treat adults with ADHD. Clinicians and patients often perceive these interventions as beneficial, although none have been tested in randomized, placebo-controlled studies.
Patients often function better when their home and work environments are thoughtfully organized, with a designated work/study space and regularly scheduled times for meals, sleep, and exercise. An ADHD coach may facilitate such structure and discipline (Box 2).
New agents in the pipeline
Efforts are being made to increase awareness of adult ADHD and to improve its treatment. For example, the National Institute of Mental Health is funding research on adult ADHD and displays on its Web site a PET scan of an adult brain with ADHD (see “Related resources”).14 Several medications also are being developed to treat ADHD.
Atomoxetine, a nonstimulant medication awaiting FDA approval for adult ADHD, is a selective norepinephrine reuptake inhibitor. In a double-blind, placebo-controlled, crossover study of adults with well-characterized ADHD, 11 of 21 patients improved with use of atomoxetine, compared with 2 of 21 who improved with use of a placebo. The average dosage of 76 mg/d was well-tolerated.15 The 52% response rate is similar to the 54% average improvement rate reported for methylphenidate in previous studies of adult ADHD.
In clinical trials, atomoxetine was given bid. Insomnia was not a side effect, so bid dosing does not interfere with sleep. Approximately 10 to 15% of patients experienced weight loss as a side effect.
Other treatment options under development include:
- a transdermal system for delivery of methylphenidate16
- a novel nicotinic analogue
- glutamate AMPA receptor modulation
- omega-3 fatty acids.
- Hallowell EM, Ratey JJ. Driven to distraction: Recognizing and coping with attention deficit disorder from childhood through adulthood. New York: Simon and Schuster; Reprint edition 1995.
- Solanto MV, Arnstein AFT, Castellanos FX, eds. Stimulant drugs and ADHD: Basic and clinical neuroscience. New York: Oxford University Press; 2001.
- Weiss M, Trokenberg-Hechtman L, Weiss G. ADHD in adulthood: A guide to current theory, diagnosis, and treatment. Baltimore: Johns Hopkins University Press; 1999.
- National Institute of Mental Health. http://www.nimh.nih.gov
Drug brand names
- Atomoxetine • (investigational)
- Bupropion • Wellbutrin
- Desipramine • Norpramin
- Dextroamphetamine • Dexedrine, Dextrostat
- Methamphetamine • Desoxyn
- Methylphenidate • Focalin, Ritalin
- Methylphenidate SR • Concerta, Metadate CD, Metadate ER, Methylin ER, Ritalin SR
- Mixed salts of amphetamine • Adderall, Adderall XR
- Modafinil • Provigil
- Pemoline • Cylert
- Venlafaxine • Effexor
Disclosure
The author reports that he serves as a consultant to Eli Lilly and Company and is on the speaker’s bureaus of Wyeth Pharmaceuticals and AstraZeneca.
1. Gadrow KD, Weiss M. Attention-deficit/hyperactivity disorder in adults: beyond controversy. Arch Gen Psychiatry 2001;58(8):784-5.
2. Ernst M, Zametkin AJ, Matochik JA, Jons PH, Cohen RM. DOPA decarboxylase activity in attention deficit hyperactivity disorder adults. A [fluorine-18]fluorodopa positron emission tomographic study. J Neurosci 1998;18(15):5901-7.
3. Spencer T, Wilens T, Biederman J, Faraone SV, Ablon JS, Lapey K. A double-blind, crossover comparison of methylphenidate and placebo in adults with childhood-onset attention-deficit hyperactivity disorder. Arch Gen Psychiatry 1995;52:434-43.
4. Spencer T, Biederman J, Wilens T, et al. Efficacy of a mixed amphetamine salts compound in adults with attention-deficit/hyperactivity disorder. Arch Gen Psychiatry 2001;58(8):775-82.
5. Swanson J, Wigal S, Greenhill L, et al. Objective and subjective measures of the pharmacodynamic effects of Adderall in the treatment of children with ADHD in a controlled laboratory classroom setting. Psychopharmacol Bull 1998;34(1):55-60.
6. Wilens TE, Biederman J, Spencer TJ, et al. Controlled trial of high doses of pemoline for adults with attention-deficit/hyperactivity disorder. J Clin Psychopharmacol 1999;19(3):257-64.
7. Wilens TE, Biederman J, Mick E, Spencer TJ. A systematic assessment of tricyclic antidepressants in the treatment of adult attention-deficit hyperactivity disorder. J Nerv Ment Dis 1995;183(1):48-50.
8. Findling RL, Schwartz MA, Flannery DJ, Manos MJ. Venlafaxine in adults with attention-deficit/hyperactivity disorder: an open clinical trial. J Clin Psychiatry 1996;57(5):184-9.
9. Wender PH, Reimherr FW. Bupropion treatment of attention-deficit hyperactivity disorder in adults. Am J Psychiatry 1990;147(8):1018-20.
10. Wilens TE, Spencer TJ, et al. A controlled clinical trial of bupropion for attention deficit hyperactivity disorder in adults. Am J Psychiatry 2001;158(2):282-8.
11. Grabowski J, Roache JD, Schmitz JM, Rhoades H, et al. Replacement medication for cocaine dependence: methylphenidate. J Clin Psychopharmacol 1997;17(6):485-8.
12. Levin FR, Evans SM, McDowell DM, Kleber HD. Methylphenidate treatment for cocaine abusers with adult attention-deficit/hyperactivity disorder: a pilot study. J Clin Psychiatry 1998;59(6):300-5.
13. Biederman J, Wilens T, Mick E, Spencer T, Faraone SV. Pharmacotherapy of attention-deficit/hyperactivity disorder reduces risk for substance use disorder. Pediatrics 1999;104(2):e20.-
14. Zametkin AJ, Nordahl TE, Gross M, et al. Cerebral glucose metabolism in adults with hyperactivity of childhood onset. N Engl J Med 1990;323(20):1361-6.
15. Spencer T, Biederman J, Wilens T. Effectiveness and tolerability of atomoxetine in adults with attention deficit hyperactivity disorder. Am J Psychiatry 1998;155(5):693-5.
16. Noven Pharmaceuticals. The Science of Noven. Research and development. Transdermal technology. Available at: http://www.noven.com/research.htm.
1. Gadrow KD, Weiss M. Attention-deficit/hyperactivity disorder in adults: beyond controversy. Arch Gen Psychiatry 2001;58(8):784-5.
2. Ernst M, Zametkin AJ, Matochik JA, Jons PH, Cohen RM. DOPA decarboxylase activity in attention deficit hyperactivity disorder adults. A [fluorine-18]fluorodopa positron emission tomographic study. J Neurosci 1998;18(15):5901-7.
3. Spencer T, Wilens T, Biederman J, Faraone SV, Ablon JS, Lapey K. A double-blind, crossover comparison of methylphenidate and placebo in adults with childhood-onset attention-deficit hyperactivity disorder. Arch Gen Psychiatry 1995;52:434-43.
4. Spencer T, Biederman J, Wilens T, et al. Efficacy of a mixed amphetamine salts compound in adults with attention-deficit/hyperactivity disorder. Arch Gen Psychiatry 2001;58(8):775-82.
5. Swanson J, Wigal S, Greenhill L, et al. Objective and subjective measures of the pharmacodynamic effects of Adderall in the treatment of children with ADHD in a controlled laboratory classroom setting. Psychopharmacol Bull 1998;34(1):55-60.
6. Wilens TE, Biederman J, Spencer TJ, et al. Controlled trial of high doses of pemoline for adults with attention-deficit/hyperactivity disorder. J Clin Psychopharmacol 1999;19(3):257-64.
7. Wilens TE, Biederman J, Mick E, Spencer TJ. A systematic assessment of tricyclic antidepressants in the treatment of adult attention-deficit hyperactivity disorder. J Nerv Ment Dis 1995;183(1):48-50.
8. Findling RL, Schwartz MA, Flannery DJ, Manos MJ. Venlafaxine in adults with attention-deficit/hyperactivity disorder: an open clinical trial. J Clin Psychiatry 1996;57(5):184-9.
9. Wender PH, Reimherr FW. Bupropion treatment of attention-deficit hyperactivity disorder in adults. Am J Psychiatry 1990;147(8):1018-20.
10. Wilens TE, Spencer TJ, et al. A controlled clinical trial of bupropion for attention deficit hyperactivity disorder in adults. Am J Psychiatry 2001;158(2):282-8.
11. Grabowski J, Roache JD, Schmitz JM, Rhoades H, et al. Replacement medication for cocaine dependence: methylphenidate. J Clin Psychopharmacol 1997;17(6):485-8.
12. Levin FR, Evans SM, McDowell DM, Kleber HD. Methylphenidate treatment for cocaine abusers with adult attention-deficit/hyperactivity disorder: a pilot study. J Clin Psychiatry 1998;59(6):300-5.
13. Biederman J, Wilens T, Mick E, Spencer T, Faraone SV. Pharmacotherapy of attention-deficit/hyperactivity disorder reduces risk for substance use disorder. Pediatrics 1999;104(2):e20.-
14. Zametkin AJ, Nordahl TE, Gross M, et al. Cerebral glucose metabolism in adults with hyperactivity of childhood onset. N Engl J Med 1990;323(20):1361-6.
15. Spencer T, Biederman J, Wilens T. Effectiveness and tolerability of atomoxetine in adults with attention deficit hyperactivity disorder. Am J Psychiatry 1998;155(5):693-5.
16. Noven Pharmaceuticals. The Science of Noven. Research and development. Transdermal technology. Available at: http://www.noven.com/research.htm.
Adult ADHD: Less hyperactivity, but lingering inattention and distress
Attention-deficit/hyperactivity disorder (ADHD) may be the only mental disorder that was discovered in children and later acknowledged in adults. Although controlled studies of adults with ADHD are few, we know that ADHD is common in adults, it can be diagnosed reliably, and 75% of those treated respond to treatment.1
The hallmark symptom of ADHD in children—hyperactivity—is usually attenuated in adults. In fact, some adults prefer the term ADD to ADHD because they are not hyperactive. This may be especially true of women, as their attention problems during childhood often were not recognized as ADHD (Box 1).
In childhood, girls with ADHD typically present with attention problems and over-talkativeness, rather than hyperactivity. Talking too much does not disrupt the classroom as much as the larger-scale misbehavior of boys with ADHD, so the diagnosis is often missed in these girls. Overtalkativeness was added to the DSM-III-R criteria for ADHD in 1987, after it was recognized as a symptom of overactivity.
Now in midlife, many women with undiagnosed ADHD have children with ADHD. As they bring their children to treatment, these women are recognizing similar attention deficit symptoms from their own childhoods and are getting the help they need. As adults, many have low self-esteem, low energy, and weight problems. Among adults with ADHD, these women may be the most underdiagnosed.
Characteristics of adult ADHD
Adults with ADHD visit a psychiatrist for a variety of reasons. Often they are parents of children diagnosed with ADHD, and the possibility that they are similarly affected has arisen during their children’s evaluation and treatment. Sometimes they have recognized themselves in consumer articles about ADHD, or others have seen them in this light.
Adults with ADHD continue to experience their childhood difficulties in sustaining attention, listening, following instructions, and organizing tasks; inattention to details; lack of sustained mental effort; losing things; distractibility, and forgetfulness. Typical complaints include underachievement and poor adjustment at work or home. Comorbid ADHD may also be identified in patients who present with depression, anxiety, substance misuse, and mood swings.
The cognitive impairment of ADHD continues into adulthood, even in adults without hyperactive symptoms. It may be that adults are not hyperactive because the basal ganglia, which control motor activity in the brain, have over the years accommodated the problem through behavior modification or neurodevelopmental changes in late adolescence.2
Children with ADHD have abnormal cerebrospinal fluid (CSF) and blood levels of the dopaminergic metabolite homovanillic acid (HVA), but adults with ADHD may not. The primary origin for CSF HVA is the nigrostriatum, which suggests that subcortical dopaminergic nuclei are more often affected in children than adults.2 This may mean that compensatory changes occur as persons with ADHD mature, or perhaps the forms of ADHD that persist into adulthood have a different pathology or pathophysiology.
Comorbidities with ADHD
Rarely does one see pure ADHD; comorbidity is the rule. ADHD can be diagnosed quickly if you know what to look for. But a facile diagnosis may overlook a comorbidity that must be treated first—especially if you plan to use stimulants. Many patients with ADHD also have bipolar disorder, and a smaller proportion of patients with bipolar disorder have undetected ADHD. Placing a patient with undetected bipolar disorder on a stimulant could precipitate mania.
Table 1
COMMON COMORBIDITIES WITH ADHD
| Bipolar disorder |
| Anxiety disorder |
| Depression |
| Drug dependence |
| Personality disorders |
| Somatoform disorders |
| Tourette’s disorder |
| Obsessive-compulsive disorder |
| Intermittent explosive disorder |
| Impulse control problems |
| Addictive behaviors |
| Sexual problems |
| Compulsive gambling |
| Learning disabilities |
| Asperger’s syndrome |
From the initial assessment, your treatment plan must address comorbid conditions (Table 1). This means taking a good history that includes corroborating information from relatives and data from the past, if possible. The case will then be much easier to manage, and quality of care greatly enhanced.
Stimulants: Usual first-choice therapy
In most cases, adult ADHD responds well to stimulant medications, although most available evidence is limited to studies in children. Several nonstimulant medications are also available, and the FDA is considering a new-drug application for a medication indicated for adult ADHD. Stimulants produce significant improvement in 30% of patients and mixed results in another 40%. Comorbidities may account for the 10 to 30% of patients who do not respond to stimulant therapy.
Methylphenidate, taken multiple times daily, is the most common treatment for ADHD. Dextroamphetamine and mixed salts of amphetamine also are used (Table 2).3 Patients usually respond to either methylphenidate or an amphetamine, and typically 25% of those who do not respond to one will respond to the other. When the clinical efficacy of amphetamines diminishes over time, many psychiatrists rotate medications. Replacing one amphetamine with another often eliminates the need to slowly increase the dosage and allows the clinician to maintain a relatively stable regimen.
When administering stimulants to adults, consider the individual’s total dosage requirement and daily schedule. Will he or she fare better with multiple daily dosing or a sustained-release form? How long is his or her average day? Does the patient have to be alert for 12 hours—or longer?
Some patients cannot sleep unless they take their last stimulant dose at bedtime. Others will have insomnia if a last dose is taken too late in the afternoon, especially with a sustained-release formulation.
When starting a patient on stimulants, begin with a 12-hour day and titrate the dosage—usually up, sometimes down—depending on response and side effects. Educating patients about their medications enables them to participate in decision-making.
Common side effects of stimulants include insomnia, decreased appetite, upset stomach, headache, anxiety, agitation, and increased pulse rate and blood pressure. The increase in blood pressure is usually less than 10%, but patients with poorly controlled hypertension should not be treated with stimulants until their blood pressure is well controlled. Until more is known about long-term effects, periodic assessment of blood pressure may be warranted.
Table 2
STIMULANT THERAPY FOR ADULTS WITH ADHD
| Stimulants | Starting dosage | Titration rate | Usual dosing interval | Maximum dosage in adults | |
|---|---|---|---|---|---|
| Methylphenidate | |||||
| Short-acting | |||||
| d, l-methylphenidate (Ritalin, Methylin) | 5 mg qd or 5 mg bid | 5 to 10 mg every 3 to 5 days | Every 3 to 4 hours Usually bid-tid | Average oral dosage 0.92 mg/kg/d; best response to 1.0 mg/kg/d16 | |
| Intermediate-acting | |||||
| d, l-methylphenidate (Ritalin SR, Metadate ER, Methylin ER) | 20 mg Ritalin SR; 10 mg Methylin ER or Metadate ER | 10 to 20 mg per week | qd to bid | ||
| d-methylphenidate (Focalin) | 2.5 mg bid | 2.5 to 5 mg per week | bid, at least 4 hours apart | ||
| Long-acting | |||||
| d, l-methylphenidate (Concerta) | 18 mg qd | 18 mg every 3 to 5 days | 12+ hours, usually qd | ||
| d, l-methylphenidate (Metadate CD) | 20 mg qd | 20 mg per week | qd | ||
| Amphetamine | |||||
| Short-acting | |||||
| (Dexedrine, Dextrostat) | 2.5 to 5 mg qd | 2.5 to 5 mg every 3 to 5 days | Every 4 to 6 hours Usually bid-tid | ||
| Intermediate-acting | |||||
| Mixed salts (Adderall) | 5 mg qd or 5 mg bid | 5 to 10 mg every 3 to 5 days | Every 4 to 6 hours Usually qd to bid | Average dosage 54 mg/d divided in two doses; maximum 30 mg bid | |
| (Dexedrine Spansule) | 5 or 10 mg qd | 5 mg per week | qd | ||
| Long-acting | |||||
| (Adderall XR) | 10 mg qd | 10 mg per week | qd | ||
| Stimulant | |||||
| Pemoline (Cylert) | 37.5 mg qd | 18.75 mg per week | qd; typical range 56.25 to 75 mg qd | Maximum dosage 112.5 mg/d | |
- Organized and orderly home and working environment
- Designated work/study space at home
- Designated coach to supervise work/study
- Healthy meals at regularly scheduled times
- Regular exercise
Adults with ADHD have been treated with mixed amphetamine salts with positive results. In a 7-week controlled, crossover study, 27 adults with ADHD received an average of 54 mg/d administered in two doses. Symptoms improved significantly—a 42% decrease on the ADHD Rating Scale. The medication was well-tolerated, and 70% of those receiving mixed amphetamine salts improved, compared with 7% of those who received a placebo.4
Duration of action of mixed salts of amphetamine has been measured at 3.5 hours with a 5-mg dose and 6.4 hours with a 20-mg dose.5 With methylphenidate, a dose of 12.5 mg worked for 4 hours. The maximum recommended dosage of mixed salts of amphetamine is 40 mg/d in divided doses.
Stimulant medications are well-tolerated. Addiction and the need for increased dosages can occur over long-term use (months to years). Reducing the dosage or switching from methylphenidate to an amphetamine variant can usually prevent these problems.
The FDA recently approved a single-enantiomer form of methylphenidate. It contains only the active “d” enantiomer, whereas the racemic mixture contains both the “d” and “l” enantiomers. Because the “l” enantiomer is inert, the resulting medication is more potent and may be prescribed at half the dosage of the racemic mixture.
Pemoline, a once-daily stimulant, is considered a second-line treatment because of reports of hepatic failure in some patients. Its use requires written informed consent and liver function tests at baseline and every 2 weeks. In a controlled trial, pemoline at high dosages (120 to 160 mg/d) was found moderately effective in adults with ADHD.6
Newer options: Longer-acting stimulants
Newer forms of slow-release methylphenidate and mixed amphetamine salts with sophisticated delivery systems are available.
Metadate CD is delivered in capsules containing beads with polymer coatings that dissolve and release their contents at different times. The capsules contain a 30:70 ratio of immediate- and extended-release beads.
Metadate CD has not been tested for adults in controlled clinical trials. In children ages 6 to 15, a single morning dose has been shown to be clinically effective in the morning and afternoon. A supplemental immediate-release capsule can be given in the morning if a patient’s medication levels need to be increased quickly. Dosage supplementation may also be required later in the day.
Concerta is delivered in 18-mg and 36-mg tablets. The immediate-release coating on the tablets delivers medication within the first hour. The drug inside then dissolves in the GI tract and is released at a controlled rate by osmotic pressure. The indigestible tablet is passed in the stool.
Concerta was investigated in children ages 6 to 12 and provides 10 to 12 hours of sustained medication. From child studies, we know that when a patient takes a 36-mg tablet at 6 AM, blood levels decline in late afternoon. An 18-mg dose at noon covers the 4 to 6 hours needed for evening chores.
Adderall XR is an extended-release, once-daily form of mixed amphetamine salts. No controlled trials of this formulation are available in adults with ADHD. Its efficacy was established after two clinical trials of children aged 6 to 12 who met DSM-IV criteria for ADHD.
Individualized and flexible dosing improves symptom control and compliance when treating adults with ADHD. For some patients, once-daily dosing is more convenient than multiple doses, while others prefer the immediate-release form because they like its midday “pause” and bid dosing. The immediate-release tablet allows the flexibility of bid or tid dosing, depending on the day’s requirements.
Antidepressants: Another choice
Antidepressants are usually considered second-line treatment for ADHD because of concerns about efficacy and side effects. The few available studies show antidepressants work as well as stimulants but more slowly. It is good practice, therefore, to advise patients that—unlike feeling the effect of a stimulant in 60 minutes—they will not feel an effect from an antidepressant for days or weeks, and that achieving an optimal effect may take 4 to 6 weeks.
Antidepressants have several advantages over stimulants. They are not classified as narcotics, work without the on-off effects of stimulants, and can treat comorbid depression and anxiety. For adult ADHD, the most effective agents work on the catecholamine systems—norepinephrine and/or dopamine. This includes the tricyclic antidepressants, MAO inhibitors, bupropion, and venlafaxine. The serotonin reuptake inhibitors have not shown promise in ADHD, nor have mirtazapine or nefazodone demonstrated much effect.
Desipramine, a tricyclic antidepressant, is a strong inhibitor of norepinephrine reuptake. In a double-blind, controlled study in 41 adults with ADHD, 68% of patients receiving desipramine, 200 mg/d, responded positively, compared with no patients who took a placebo.7
When venlafaxine was given in standard dosages to 10 adults with ADHD in an open, 8-week clinical trial, an effect was seen by week two. Of the nine patients who completed the study, seven were considered responders. Symptoms were reduced significantly with venlafaxine treatment, and most side effects were mild.8
In an open study, bupropion treatment resulted in moderate to marked response in 74% of 19 patients. Ten of those patients who responded chose to continue bupropion rather than their previous medication.9 In a 6-week controlled study of 40 patients, bupropion use was associated with a 42% reduction in ADHD symptoms in the 38 patients who completed the study. Patients who received a placebo showed only a 24% reduction in symptoms. According to the CGI, 52% of patients who received bupropion reported being “much improved” or “very improved” compared with 11% of those receiving a placebo.10
Other treatment options that have shown mixed results include modafinil, alpha-2a agonists, acetylcholinesterase inhibitors, and the histaminergic agents.
Managing adverse effects
Substance abuse Stimulant abuse has been a concern, but it has not become the problem many feared. In fact, some studies have found that methylphenidate may help stanch the craving for cocaine in adults with ADHD.11,12 Treating ADHD with pharmacotherapy also has been shown to reduce the risk for substance abuse in adolescence by 85%.13
With careful screening, you can usually identify drug-seeking behavior in adult patients. For patients with substance abuse problems, you can prescribe the nonstimulants.
Tics that can occur with stimulant medications usually can be suppressed by reducing the dosage, being vigilant, and waiting it out. Tics may ameliorate over weeks to months.
Cardiac and cognitive effects Long-term use of stimulant medications at high dosages has been associated with cardiac and cognitive toxicity, as noted in the 1998 NIH consensus statement on diagnosis and treatment of ADHD. It is important to provide patients with this information as part of their informed-consent briefing. (See “Related resources,” to view the consensus statement.)
Nonpharmacologic management
Nonpharmacologic treatments such as EEG biofeedback; psychoeducational approaches; and individual, family, and group psychotherapy are widely used to treat adults with ADHD. Clinicians and patients often perceive these interventions as beneficial, although none have been tested in randomized, placebo-controlled studies.
Patients often function better when their home and work environments are thoughtfully organized, with a designated work/study space and regularly scheduled times for meals, sleep, and exercise. An ADHD coach may facilitate such structure and discipline (Box 2).
New agents in the pipeline
Efforts are being made to increase awareness of adult ADHD and to improve its treatment. For example, the National Institute of Mental Health is funding research on adult ADHD and displays on its Web site a PET scan of an adult brain with ADHD (see “Related resources”).14 Several medications also are being developed to treat ADHD.
Atomoxetine, a nonstimulant medication awaiting FDA approval for adult ADHD, is a selective norepinephrine reuptake inhibitor. In a double-blind, placebo-controlled, crossover study of adults with well-characterized ADHD, 11 of 21 patients improved with use of atomoxetine, compared with 2 of 21 who improved with use of a placebo. The average dosage of 76 mg/d was well-tolerated.15 The 52% response rate is similar to the 54% average improvement rate reported for methylphenidate in previous studies of adult ADHD.
In clinical trials, atomoxetine was given bid. Insomnia was not a side effect, so bid dosing does not interfere with sleep. Approximately 10 to 15% of patients experienced weight loss as a side effect.
Other treatment options under development include:
- a transdermal system for delivery of methylphenidate16
- a novel nicotinic analogue
- glutamate AMPA receptor modulation
- omega-3 fatty acids.
- Hallowell EM, Ratey JJ. Driven to distraction: Recognizing and coping with attention deficit disorder from childhood through adulthood. New York: Simon and Schuster; Reprint edition 1995.
- Solanto MV, Arnstein AFT, Castellanos FX, eds. Stimulant drugs and ADHD: Basic and clinical neuroscience. New York: Oxford University Press; 2001.
- Weiss M, Trokenberg-Hechtman L, Weiss G. ADHD in adulthood: A guide to current theory, diagnosis, and treatment. Baltimore: Johns Hopkins University Press; 1999.
- National Institute of Mental Health. http://www.nimh.nih.gov
Drug brand names
- Atomoxetine • (investigational)
- Bupropion • Wellbutrin
- Desipramine • Norpramin
- Dextroamphetamine • Dexedrine, Dextrostat
- Methamphetamine • Desoxyn
- Methylphenidate • Focalin, Ritalin
- Methylphenidate SR • Concerta, Metadate CD, Metadate ER, Methylin ER, Ritalin SR
- Mixed salts of amphetamine • Adderall, Adderall XR
- Modafinil • Provigil
- Pemoline • Cylert
- Venlafaxine • Effexor
Disclosure
The author reports that he serves as a consultant to Eli Lilly and Company and is on the speaker’s bureaus of Wyeth Pharmaceuticals and AstraZeneca.
1. Gadrow KD, Weiss M. Attention-deficit/hyperactivity disorder in adults: beyond controversy. Arch Gen Psychiatry 2001;58(8):784-5.
2. Ernst M, Zametkin AJ, Matochik JA, Jons PH, Cohen RM. DOPA decarboxylase activity in attention deficit hyperactivity disorder adults. A [fluorine-18]fluorodopa positron emission tomographic study. J Neurosci 1998;18(15):5901-7.
3. Spencer T, Wilens T, Biederman J, Faraone SV, Ablon JS, Lapey K. A double-blind, crossover comparison of methylphenidate and placebo in adults with childhood-onset attention-deficit hyperactivity disorder. Arch Gen Psychiatry 1995;52:434-43.
4. Spencer T, Biederman J, Wilens T, et al. Efficacy of a mixed amphetamine salts compound in adults with attention-deficit/hyperactivity disorder. Arch Gen Psychiatry 2001;58(8):775-82.
5. Swanson J, Wigal S, Greenhill L, et al. Objective and subjective measures of the pharmacodynamic effects of Adderall in the treatment of children with ADHD in a controlled laboratory classroom setting. Psychopharmacol Bull 1998;34(1):55-60.
6. Wilens TE, Biederman J, Spencer TJ, et al. Controlled trial of high doses of pemoline for adults with attention-deficit/hyperactivity disorder. J Clin Psychopharmacol 1999;19(3):257-64.
7. Wilens TE, Biederman J, Mick E, Spencer TJ. A systematic assessment of tricyclic antidepressants in the treatment of adult attention-deficit hyperactivity disorder. J Nerv Ment Dis 1995;183(1):48-50.
8. Findling RL, Schwartz MA, Flannery DJ, Manos MJ. Venlafaxine in adults with attention-deficit/hyperactivity disorder: an open clinical trial. J Clin Psychiatry 1996;57(5):184-9.
9. Wender PH, Reimherr FW. Bupropion treatment of attention-deficit hyperactivity disorder in adults. Am J Psychiatry 1990;147(8):1018-20.
10. Wilens TE, Spencer TJ, et al. A controlled clinical trial of bupropion for attention deficit hyperactivity disorder in adults. Am J Psychiatry 2001;158(2):282-8.
11. Grabowski J, Roache JD, Schmitz JM, Rhoades H, et al. Replacement medication for cocaine dependence: methylphenidate. J Clin Psychopharmacol 1997;17(6):485-8.
12. Levin FR, Evans SM, McDowell DM, Kleber HD. Methylphenidate treatment for cocaine abusers with adult attention-deficit/hyperactivity disorder: a pilot study. J Clin Psychiatry 1998;59(6):300-5.
13. Biederman J, Wilens T, Mick E, Spencer T, Faraone SV. Pharmacotherapy of attention-deficit/hyperactivity disorder reduces risk for substance use disorder. Pediatrics 1999;104(2):e20.-
14. Zametkin AJ, Nordahl TE, Gross M, et al. Cerebral glucose metabolism in adults with hyperactivity of childhood onset. N Engl J Med 1990;323(20):1361-6.
15. Spencer T, Biederman J, Wilens T. Effectiveness and tolerability of atomoxetine in adults with attention deficit hyperactivity disorder. Am J Psychiatry 1998;155(5):693-5.
16. Noven Pharmaceuticals. The Science of Noven. Research and development. Transdermal technology. Available at: http://www.noven.com/research.htm.
Attention-deficit/hyperactivity disorder (ADHD) may be the only mental disorder that was discovered in children and later acknowledged in adults. Although controlled studies of adults with ADHD are few, we know that ADHD is common in adults, it can be diagnosed reliably, and 75% of those treated respond to treatment.1
The hallmark symptom of ADHD in children—hyperactivity—is usually attenuated in adults. In fact, some adults prefer the term ADD to ADHD because they are not hyperactive. This may be especially true of women, as their attention problems during childhood often were not recognized as ADHD (Box 1).
In childhood, girls with ADHD typically present with attention problems and over-talkativeness, rather than hyperactivity. Talking too much does not disrupt the classroom as much as the larger-scale misbehavior of boys with ADHD, so the diagnosis is often missed in these girls. Overtalkativeness was added to the DSM-III-R criteria for ADHD in 1987, after it was recognized as a symptom of overactivity.
Now in midlife, many women with undiagnosed ADHD have children with ADHD. As they bring their children to treatment, these women are recognizing similar attention deficit symptoms from their own childhoods and are getting the help they need. As adults, many have low self-esteem, low energy, and weight problems. Among adults with ADHD, these women may be the most underdiagnosed.
Characteristics of adult ADHD
Adults with ADHD visit a psychiatrist for a variety of reasons. Often they are parents of children diagnosed with ADHD, and the possibility that they are similarly affected has arisen during their children’s evaluation and treatment. Sometimes they have recognized themselves in consumer articles about ADHD, or others have seen them in this light.
Adults with ADHD continue to experience their childhood difficulties in sustaining attention, listening, following instructions, and organizing tasks; inattention to details; lack of sustained mental effort; losing things; distractibility, and forgetfulness. Typical complaints include underachievement and poor adjustment at work or home. Comorbid ADHD may also be identified in patients who present with depression, anxiety, substance misuse, and mood swings.
The cognitive impairment of ADHD continues into adulthood, even in adults without hyperactive symptoms. It may be that adults are not hyperactive because the basal ganglia, which control motor activity in the brain, have over the years accommodated the problem through behavior modification or neurodevelopmental changes in late adolescence.2
Children with ADHD have abnormal cerebrospinal fluid (CSF) and blood levels of the dopaminergic metabolite homovanillic acid (HVA), but adults with ADHD may not. The primary origin for CSF HVA is the nigrostriatum, which suggests that subcortical dopaminergic nuclei are more often affected in children than adults.2 This may mean that compensatory changes occur as persons with ADHD mature, or perhaps the forms of ADHD that persist into adulthood have a different pathology or pathophysiology.
Comorbidities with ADHD
Rarely does one see pure ADHD; comorbidity is the rule. ADHD can be diagnosed quickly if you know what to look for. But a facile diagnosis may overlook a comorbidity that must be treated first—especially if you plan to use stimulants. Many patients with ADHD also have bipolar disorder, and a smaller proportion of patients with bipolar disorder have undetected ADHD. Placing a patient with undetected bipolar disorder on a stimulant could precipitate mania.
Table 1
COMMON COMORBIDITIES WITH ADHD
| Bipolar disorder |
| Anxiety disorder |
| Depression |
| Drug dependence |
| Personality disorders |
| Somatoform disorders |
| Tourette’s disorder |
| Obsessive-compulsive disorder |
| Intermittent explosive disorder |
| Impulse control problems |
| Addictive behaviors |
| Sexual problems |
| Compulsive gambling |
| Learning disabilities |
| Asperger’s syndrome |
From the initial assessment, your treatment plan must address comorbid conditions (Table 1). This means taking a good history that includes corroborating information from relatives and data from the past, if possible. The case will then be much easier to manage, and quality of care greatly enhanced.
Stimulants: Usual first-choice therapy
In most cases, adult ADHD responds well to stimulant medications, although most available evidence is limited to studies in children. Several nonstimulant medications are also available, and the FDA is considering a new-drug application for a medication indicated for adult ADHD. Stimulants produce significant improvement in 30% of patients and mixed results in another 40%. Comorbidities may account for the 10 to 30% of patients who do not respond to stimulant therapy.
Methylphenidate, taken multiple times daily, is the most common treatment for ADHD. Dextroamphetamine and mixed salts of amphetamine also are used (Table 2).3 Patients usually respond to either methylphenidate or an amphetamine, and typically 25% of those who do not respond to one will respond to the other. When the clinical efficacy of amphetamines diminishes over time, many psychiatrists rotate medications. Replacing one amphetamine with another often eliminates the need to slowly increase the dosage and allows the clinician to maintain a relatively stable regimen.
When administering stimulants to adults, consider the individual’s total dosage requirement and daily schedule. Will he or she fare better with multiple daily dosing or a sustained-release form? How long is his or her average day? Does the patient have to be alert for 12 hours—or longer?
Some patients cannot sleep unless they take their last stimulant dose at bedtime. Others will have insomnia if a last dose is taken too late in the afternoon, especially with a sustained-release formulation.
When starting a patient on stimulants, begin with a 12-hour day and titrate the dosage—usually up, sometimes down—depending on response and side effects. Educating patients about their medications enables them to participate in decision-making.
Common side effects of stimulants include insomnia, decreased appetite, upset stomach, headache, anxiety, agitation, and increased pulse rate and blood pressure. The increase in blood pressure is usually less than 10%, but patients with poorly controlled hypertension should not be treated with stimulants until their blood pressure is well controlled. Until more is known about long-term effects, periodic assessment of blood pressure may be warranted.
Table 2
STIMULANT THERAPY FOR ADULTS WITH ADHD
| Stimulants | Starting dosage | Titration rate | Usual dosing interval | Maximum dosage in adults | |
|---|---|---|---|---|---|
| Methylphenidate | |||||
| Short-acting | |||||
| d, l-methylphenidate (Ritalin, Methylin) | 5 mg qd or 5 mg bid | 5 to 10 mg every 3 to 5 days | Every 3 to 4 hours Usually bid-tid | Average oral dosage 0.92 mg/kg/d; best response to 1.0 mg/kg/d16 | |
| Intermediate-acting | |||||
| d, l-methylphenidate (Ritalin SR, Metadate ER, Methylin ER) | 20 mg Ritalin SR; 10 mg Methylin ER or Metadate ER | 10 to 20 mg per week | qd to bid | ||
| d-methylphenidate (Focalin) | 2.5 mg bid | 2.5 to 5 mg per week | bid, at least 4 hours apart | ||
| Long-acting | |||||
| d, l-methylphenidate (Concerta) | 18 mg qd | 18 mg every 3 to 5 days | 12+ hours, usually qd | ||
| d, l-methylphenidate (Metadate CD) | 20 mg qd | 20 mg per week | qd | ||
| Amphetamine | |||||
| Short-acting | |||||
| (Dexedrine, Dextrostat) | 2.5 to 5 mg qd | 2.5 to 5 mg every 3 to 5 days | Every 4 to 6 hours Usually bid-tid | ||
| Intermediate-acting | |||||
| Mixed salts (Adderall) | 5 mg qd or 5 mg bid | 5 to 10 mg every 3 to 5 days | Every 4 to 6 hours Usually qd to bid | Average dosage 54 mg/d divided in two doses; maximum 30 mg bid | |
| (Dexedrine Spansule) | 5 or 10 mg qd | 5 mg per week | qd | ||
| Long-acting | |||||
| (Adderall XR) | 10 mg qd | 10 mg per week | qd | ||
| Stimulant | |||||
| Pemoline (Cylert) | 37.5 mg qd | 18.75 mg per week | qd; typical range 56.25 to 75 mg qd | Maximum dosage 112.5 mg/d | |
- Organized and orderly home and working environment
- Designated work/study space at home
- Designated coach to supervise work/study
- Healthy meals at regularly scheduled times
- Regular exercise
Adults with ADHD have been treated with mixed amphetamine salts with positive results. In a 7-week controlled, crossover study, 27 adults with ADHD received an average of 54 mg/d administered in two doses. Symptoms improved significantly—a 42% decrease on the ADHD Rating Scale. The medication was well-tolerated, and 70% of those receiving mixed amphetamine salts improved, compared with 7% of those who received a placebo.4
Duration of action of mixed salts of amphetamine has been measured at 3.5 hours with a 5-mg dose and 6.4 hours with a 20-mg dose.5 With methylphenidate, a dose of 12.5 mg worked for 4 hours. The maximum recommended dosage of mixed salts of amphetamine is 40 mg/d in divided doses.
Stimulant medications are well-tolerated. Addiction and the need for increased dosages can occur over long-term use (months to years). Reducing the dosage or switching from methylphenidate to an amphetamine variant can usually prevent these problems.
The FDA recently approved a single-enantiomer form of methylphenidate. It contains only the active “d” enantiomer, whereas the racemic mixture contains both the “d” and “l” enantiomers. Because the “l” enantiomer is inert, the resulting medication is more potent and may be prescribed at half the dosage of the racemic mixture.
Pemoline, a once-daily stimulant, is considered a second-line treatment because of reports of hepatic failure in some patients. Its use requires written informed consent and liver function tests at baseline and every 2 weeks. In a controlled trial, pemoline at high dosages (120 to 160 mg/d) was found moderately effective in adults with ADHD.6
Newer options: Longer-acting stimulants
Newer forms of slow-release methylphenidate and mixed amphetamine salts with sophisticated delivery systems are available.
Metadate CD is delivered in capsules containing beads with polymer coatings that dissolve and release their contents at different times. The capsules contain a 30:70 ratio of immediate- and extended-release beads.
Metadate CD has not been tested for adults in controlled clinical trials. In children ages 6 to 15, a single morning dose has been shown to be clinically effective in the morning and afternoon. A supplemental immediate-release capsule can be given in the morning if a patient’s medication levels need to be increased quickly. Dosage supplementation may also be required later in the day.
Concerta is delivered in 18-mg and 36-mg tablets. The immediate-release coating on the tablets delivers medication within the first hour. The drug inside then dissolves in the GI tract and is released at a controlled rate by osmotic pressure. The indigestible tablet is passed in the stool.
Concerta was investigated in children ages 6 to 12 and provides 10 to 12 hours of sustained medication. From child studies, we know that when a patient takes a 36-mg tablet at 6 AM, blood levels decline in late afternoon. An 18-mg dose at noon covers the 4 to 6 hours needed for evening chores.
Adderall XR is an extended-release, once-daily form of mixed amphetamine salts. No controlled trials of this formulation are available in adults with ADHD. Its efficacy was established after two clinical trials of children aged 6 to 12 who met DSM-IV criteria for ADHD.
Individualized and flexible dosing improves symptom control and compliance when treating adults with ADHD. For some patients, once-daily dosing is more convenient than multiple doses, while others prefer the immediate-release form because they like its midday “pause” and bid dosing. The immediate-release tablet allows the flexibility of bid or tid dosing, depending on the day’s requirements.
Antidepressants: Another choice
Antidepressants are usually considered second-line treatment for ADHD because of concerns about efficacy and side effects. The few available studies show antidepressants work as well as stimulants but more slowly. It is good practice, therefore, to advise patients that—unlike feeling the effect of a stimulant in 60 minutes—they will not feel an effect from an antidepressant for days or weeks, and that achieving an optimal effect may take 4 to 6 weeks.
Antidepressants have several advantages over stimulants. They are not classified as narcotics, work without the on-off effects of stimulants, and can treat comorbid depression and anxiety. For adult ADHD, the most effective agents work on the catecholamine systems—norepinephrine and/or dopamine. This includes the tricyclic antidepressants, MAO inhibitors, bupropion, and venlafaxine. The serotonin reuptake inhibitors have not shown promise in ADHD, nor have mirtazapine or nefazodone demonstrated much effect.
Desipramine, a tricyclic antidepressant, is a strong inhibitor of norepinephrine reuptake. In a double-blind, controlled study in 41 adults with ADHD, 68% of patients receiving desipramine, 200 mg/d, responded positively, compared with no patients who took a placebo.7
When venlafaxine was given in standard dosages to 10 adults with ADHD in an open, 8-week clinical trial, an effect was seen by week two. Of the nine patients who completed the study, seven were considered responders. Symptoms were reduced significantly with venlafaxine treatment, and most side effects were mild.8
In an open study, bupropion treatment resulted in moderate to marked response in 74% of 19 patients. Ten of those patients who responded chose to continue bupropion rather than their previous medication.9 In a 6-week controlled study of 40 patients, bupropion use was associated with a 42% reduction in ADHD symptoms in the 38 patients who completed the study. Patients who received a placebo showed only a 24% reduction in symptoms. According to the CGI, 52% of patients who received bupropion reported being “much improved” or “very improved” compared with 11% of those receiving a placebo.10
Other treatment options that have shown mixed results include modafinil, alpha-2a agonists, acetylcholinesterase inhibitors, and the histaminergic agents.
Managing adverse effects
Substance abuse Stimulant abuse has been a concern, but it has not become the problem many feared. In fact, some studies have found that methylphenidate may help stanch the craving for cocaine in adults with ADHD.11,12 Treating ADHD with pharmacotherapy also has been shown to reduce the risk for substance abuse in adolescence by 85%.13
With careful screening, you can usually identify drug-seeking behavior in adult patients. For patients with substance abuse problems, you can prescribe the nonstimulants.
Tics that can occur with stimulant medications usually can be suppressed by reducing the dosage, being vigilant, and waiting it out. Tics may ameliorate over weeks to months.
Cardiac and cognitive effects Long-term use of stimulant medications at high dosages has been associated with cardiac and cognitive toxicity, as noted in the 1998 NIH consensus statement on diagnosis and treatment of ADHD. It is important to provide patients with this information as part of their informed-consent briefing. (See “Related resources,” to view the consensus statement.)
Nonpharmacologic management
Nonpharmacologic treatments such as EEG biofeedback; psychoeducational approaches; and individual, family, and group psychotherapy are widely used to treat adults with ADHD. Clinicians and patients often perceive these interventions as beneficial, although none have been tested in randomized, placebo-controlled studies.
Patients often function better when their home and work environments are thoughtfully organized, with a designated work/study space and regularly scheduled times for meals, sleep, and exercise. An ADHD coach may facilitate such structure and discipline (Box 2).
New agents in the pipeline
Efforts are being made to increase awareness of adult ADHD and to improve its treatment. For example, the National Institute of Mental Health is funding research on adult ADHD and displays on its Web site a PET scan of an adult brain with ADHD (see “Related resources”).14 Several medications also are being developed to treat ADHD.
Atomoxetine, a nonstimulant medication awaiting FDA approval for adult ADHD, is a selective norepinephrine reuptake inhibitor. In a double-blind, placebo-controlled, crossover study of adults with well-characterized ADHD, 11 of 21 patients improved with use of atomoxetine, compared with 2 of 21 who improved with use of a placebo. The average dosage of 76 mg/d was well-tolerated.15 The 52% response rate is similar to the 54% average improvement rate reported for methylphenidate in previous studies of adult ADHD.
In clinical trials, atomoxetine was given bid. Insomnia was not a side effect, so bid dosing does not interfere with sleep. Approximately 10 to 15% of patients experienced weight loss as a side effect.
Other treatment options under development include:
- a transdermal system for delivery of methylphenidate16
- a novel nicotinic analogue
- glutamate AMPA receptor modulation
- omega-3 fatty acids.
- Hallowell EM, Ratey JJ. Driven to distraction: Recognizing and coping with attention deficit disorder from childhood through adulthood. New York: Simon and Schuster; Reprint edition 1995.
- Solanto MV, Arnstein AFT, Castellanos FX, eds. Stimulant drugs and ADHD: Basic and clinical neuroscience. New York: Oxford University Press; 2001.
- Weiss M, Trokenberg-Hechtman L, Weiss G. ADHD in adulthood: A guide to current theory, diagnosis, and treatment. Baltimore: Johns Hopkins University Press; 1999.
- National Institute of Mental Health. http://www.nimh.nih.gov
Drug brand names
- Atomoxetine • (investigational)
- Bupropion • Wellbutrin
- Desipramine • Norpramin
- Dextroamphetamine • Dexedrine, Dextrostat
- Methamphetamine • Desoxyn
- Methylphenidate • Focalin, Ritalin
- Methylphenidate SR • Concerta, Metadate CD, Metadate ER, Methylin ER, Ritalin SR
- Mixed salts of amphetamine • Adderall, Adderall XR
- Modafinil • Provigil
- Pemoline • Cylert
- Venlafaxine • Effexor
Disclosure
The author reports that he serves as a consultant to Eli Lilly and Company and is on the speaker’s bureaus of Wyeth Pharmaceuticals and AstraZeneca.
Attention-deficit/hyperactivity disorder (ADHD) may be the only mental disorder that was discovered in children and later acknowledged in adults. Although controlled studies of adults with ADHD are few, we know that ADHD is common in adults, it can be diagnosed reliably, and 75% of those treated respond to treatment.1
The hallmark symptom of ADHD in children—hyperactivity—is usually attenuated in adults. In fact, some adults prefer the term ADD to ADHD because they are not hyperactive. This may be especially true of women, as their attention problems during childhood often were not recognized as ADHD (Box 1).
In childhood, girls with ADHD typically present with attention problems and over-talkativeness, rather than hyperactivity. Talking too much does not disrupt the classroom as much as the larger-scale misbehavior of boys with ADHD, so the diagnosis is often missed in these girls. Overtalkativeness was added to the DSM-III-R criteria for ADHD in 1987, after it was recognized as a symptom of overactivity.
Now in midlife, many women with undiagnosed ADHD have children with ADHD. As they bring their children to treatment, these women are recognizing similar attention deficit symptoms from their own childhoods and are getting the help they need. As adults, many have low self-esteem, low energy, and weight problems. Among adults with ADHD, these women may be the most underdiagnosed.
Characteristics of adult ADHD
Adults with ADHD visit a psychiatrist for a variety of reasons. Often they are parents of children diagnosed with ADHD, and the possibility that they are similarly affected has arisen during their children’s evaluation and treatment. Sometimes they have recognized themselves in consumer articles about ADHD, or others have seen them in this light.
Adults with ADHD continue to experience their childhood difficulties in sustaining attention, listening, following instructions, and organizing tasks; inattention to details; lack of sustained mental effort; losing things; distractibility, and forgetfulness. Typical complaints include underachievement and poor adjustment at work or home. Comorbid ADHD may also be identified in patients who present with depression, anxiety, substance misuse, and mood swings.
The cognitive impairment of ADHD continues into adulthood, even in adults without hyperactive symptoms. It may be that adults are not hyperactive because the basal ganglia, which control motor activity in the brain, have over the years accommodated the problem through behavior modification or neurodevelopmental changes in late adolescence.2
Children with ADHD have abnormal cerebrospinal fluid (CSF) and blood levels of the dopaminergic metabolite homovanillic acid (HVA), but adults with ADHD may not. The primary origin for CSF HVA is the nigrostriatum, which suggests that subcortical dopaminergic nuclei are more often affected in children than adults.2 This may mean that compensatory changes occur as persons with ADHD mature, or perhaps the forms of ADHD that persist into adulthood have a different pathology or pathophysiology.
Comorbidities with ADHD
Rarely does one see pure ADHD; comorbidity is the rule. ADHD can be diagnosed quickly if you know what to look for. But a facile diagnosis may overlook a comorbidity that must be treated first—especially if you plan to use stimulants. Many patients with ADHD also have bipolar disorder, and a smaller proportion of patients with bipolar disorder have undetected ADHD. Placing a patient with undetected bipolar disorder on a stimulant could precipitate mania.
Table 1
COMMON COMORBIDITIES WITH ADHD
| Bipolar disorder |
| Anxiety disorder |
| Depression |
| Drug dependence |
| Personality disorders |
| Somatoform disorders |
| Tourette’s disorder |
| Obsessive-compulsive disorder |
| Intermittent explosive disorder |
| Impulse control problems |
| Addictive behaviors |
| Sexual problems |
| Compulsive gambling |
| Learning disabilities |
| Asperger’s syndrome |
From the initial assessment, your treatment plan must address comorbid conditions (Table 1). This means taking a good history that includes corroborating information from relatives and data from the past, if possible. The case will then be much easier to manage, and quality of care greatly enhanced.
Stimulants: Usual first-choice therapy
In most cases, adult ADHD responds well to stimulant medications, although most available evidence is limited to studies in children. Several nonstimulant medications are also available, and the FDA is considering a new-drug application for a medication indicated for adult ADHD. Stimulants produce significant improvement in 30% of patients and mixed results in another 40%. Comorbidities may account for the 10 to 30% of patients who do not respond to stimulant therapy.
Methylphenidate, taken multiple times daily, is the most common treatment for ADHD. Dextroamphetamine and mixed salts of amphetamine also are used (Table 2).3 Patients usually respond to either methylphenidate or an amphetamine, and typically 25% of those who do not respond to one will respond to the other. When the clinical efficacy of amphetamines diminishes over time, many psychiatrists rotate medications. Replacing one amphetamine with another often eliminates the need to slowly increase the dosage and allows the clinician to maintain a relatively stable regimen.
When administering stimulants to adults, consider the individual’s total dosage requirement and daily schedule. Will he or she fare better with multiple daily dosing or a sustained-release form? How long is his or her average day? Does the patient have to be alert for 12 hours—or longer?
Some patients cannot sleep unless they take their last stimulant dose at bedtime. Others will have insomnia if a last dose is taken too late in the afternoon, especially with a sustained-release formulation.
When starting a patient on stimulants, begin with a 12-hour day and titrate the dosage—usually up, sometimes down—depending on response and side effects. Educating patients about their medications enables them to participate in decision-making.
Common side effects of stimulants include insomnia, decreased appetite, upset stomach, headache, anxiety, agitation, and increased pulse rate and blood pressure. The increase in blood pressure is usually less than 10%, but patients with poorly controlled hypertension should not be treated with stimulants until their blood pressure is well controlled. Until more is known about long-term effects, periodic assessment of blood pressure may be warranted.
Table 2
STIMULANT THERAPY FOR ADULTS WITH ADHD
| Stimulants | Starting dosage | Titration rate | Usual dosing interval | Maximum dosage in adults | |
|---|---|---|---|---|---|
| Methylphenidate | |||||
| Short-acting | |||||
| d, l-methylphenidate (Ritalin, Methylin) | 5 mg qd or 5 mg bid | 5 to 10 mg every 3 to 5 days | Every 3 to 4 hours Usually bid-tid | Average oral dosage 0.92 mg/kg/d; best response to 1.0 mg/kg/d16 | |
| Intermediate-acting | |||||
| d, l-methylphenidate (Ritalin SR, Metadate ER, Methylin ER) | 20 mg Ritalin SR; 10 mg Methylin ER or Metadate ER | 10 to 20 mg per week | qd to bid | ||
| d-methylphenidate (Focalin) | 2.5 mg bid | 2.5 to 5 mg per week | bid, at least 4 hours apart | ||
| Long-acting | |||||
| d, l-methylphenidate (Concerta) | 18 mg qd | 18 mg every 3 to 5 days | 12+ hours, usually qd | ||
| d, l-methylphenidate (Metadate CD) | 20 mg qd | 20 mg per week | qd | ||
| Amphetamine | |||||
| Short-acting | |||||
| (Dexedrine, Dextrostat) | 2.5 to 5 mg qd | 2.5 to 5 mg every 3 to 5 days | Every 4 to 6 hours Usually bid-tid | ||
| Intermediate-acting | |||||
| Mixed salts (Adderall) | 5 mg qd or 5 mg bid | 5 to 10 mg every 3 to 5 days | Every 4 to 6 hours Usually qd to bid | Average dosage 54 mg/d divided in two doses; maximum 30 mg bid | |
| (Dexedrine Spansule) | 5 or 10 mg qd | 5 mg per week | qd | ||
| Long-acting | |||||
| (Adderall XR) | 10 mg qd | 10 mg per week | qd | ||
| Stimulant | |||||
| Pemoline (Cylert) | 37.5 mg qd | 18.75 mg per week | qd; typical range 56.25 to 75 mg qd | Maximum dosage 112.5 mg/d | |
- Organized and orderly home and working environment
- Designated work/study space at home
- Designated coach to supervise work/study
- Healthy meals at regularly scheduled times
- Regular exercise
Adults with ADHD have been treated with mixed amphetamine salts with positive results. In a 7-week controlled, crossover study, 27 adults with ADHD received an average of 54 mg/d administered in two doses. Symptoms improved significantly—a 42% decrease on the ADHD Rating Scale. The medication was well-tolerated, and 70% of those receiving mixed amphetamine salts improved, compared with 7% of those who received a placebo.4
Duration of action of mixed salts of amphetamine has been measured at 3.5 hours with a 5-mg dose and 6.4 hours with a 20-mg dose.5 With methylphenidate, a dose of 12.5 mg worked for 4 hours. The maximum recommended dosage of mixed salts of amphetamine is 40 mg/d in divided doses.
Stimulant medications are well-tolerated. Addiction and the need for increased dosages can occur over long-term use (months to years). Reducing the dosage or switching from methylphenidate to an amphetamine variant can usually prevent these problems.
The FDA recently approved a single-enantiomer form of methylphenidate. It contains only the active “d” enantiomer, whereas the racemic mixture contains both the “d” and “l” enantiomers. Because the “l” enantiomer is inert, the resulting medication is more potent and may be prescribed at half the dosage of the racemic mixture.
Pemoline, a once-daily stimulant, is considered a second-line treatment because of reports of hepatic failure in some patients. Its use requires written informed consent and liver function tests at baseline and every 2 weeks. In a controlled trial, pemoline at high dosages (120 to 160 mg/d) was found moderately effective in adults with ADHD.6
Newer options: Longer-acting stimulants
Newer forms of slow-release methylphenidate and mixed amphetamine salts with sophisticated delivery systems are available.
Metadate CD is delivered in capsules containing beads with polymer coatings that dissolve and release their contents at different times. The capsules contain a 30:70 ratio of immediate- and extended-release beads.
Metadate CD has not been tested for adults in controlled clinical trials. In children ages 6 to 15, a single morning dose has been shown to be clinically effective in the morning and afternoon. A supplemental immediate-release capsule can be given in the morning if a patient’s medication levels need to be increased quickly. Dosage supplementation may also be required later in the day.
Concerta is delivered in 18-mg and 36-mg tablets. The immediate-release coating on the tablets delivers medication within the first hour. The drug inside then dissolves in the GI tract and is released at a controlled rate by osmotic pressure. The indigestible tablet is passed in the stool.
Concerta was investigated in children ages 6 to 12 and provides 10 to 12 hours of sustained medication. From child studies, we know that when a patient takes a 36-mg tablet at 6 AM, blood levels decline in late afternoon. An 18-mg dose at noon covers the 4 to 6 hours needed for evening chores.
Adderall XR is an extended-release, once-daily form of mixed amphetamine salts. No controlled trials of this formulation are available in adults with ADHD. Its efficacy was established after two clinical trials of children aged 6 to 12 who met DSM-IV criteria for ADHD.
Individualized and flexible dosing improves symptom control and compliance when treating adults with ADHD. For some patients, once-daily dosing is more convenient than multiple doses, while others prefer the immediate-release form because they like its midday “pause” and bid dosing. The immediate-release tablet allows the flexibility of bid or tid dosing, depending on the day’s requirements.
Antidepressants: Another choice
Antidepressants are usually considered second-line treatment for ADHD because of concerns about efficacy and side effects. The few available studies show antidepressants work as well as stimulants but more slowly. It is good practice, therefore, to advise patients that—unlike feeling the effect of a stimulant in 60 minutes—they will not feel an effect from an antidepressant for days or weeks, and that achieving an optimal effect may take 4 to 6 weeks.
Antidepressants have several advantages over stimulants. They are not classified as narcotics, work without the on-off effects of stimulants, and can treat comorbid depression and anxiety. For adult ADHD, the most effective agents work on the catecholamine systems—norepinephrine and/or dopamine. This includes the tricyclic antidepressants, MAO inhibitors, bupropion, and venlafaxine. The serotonin reuptake inhibitors have not shown promise in ADHD, nor have mirtazapine or nefazodone demonstrated much effect.
Desipramine, a tricyclic antidepressant, is a strong inhibitor of norepinephrine reuptake. In a double-blind, controlled study in 41 adults with ADHD, 68% of patients receiving desipramine, 200 mg/d, responded positively, compared with no patients who took a placebo.7
When venlafaxine was given in standard dosages to 10 adults with ADHD in an open, 8-week clinical trial, an effect was seen by week two. Of the nine patients who completed the study, seven were considered responders. Symptoms were reduced significantly with venlafaxine treatment, and most side effects were mild.8
In an open study, bupropion treatment resulted in moderate to marked response in 74% of 19 patients. Ten of those patients who responded chose to continue bupropion rather than their previous medication.9 In a 6-week controlled study of 40 patients, bupropion use was associated with a 42% reduction in ADHD symptoms in the 38 patients who completed the study. Patients who received a placebo showed only a 24% reduction in symptoms. According to the CGI, 52% of patients who received bupropion reported being “much improved” or “very improved” compared with 11% of those receiving a placebo.10
Other treatment options that have shown mixed results include modafinil, alpha-2a agonists, acetylcholinesterase inhibitors, and the histaminergic agents.
Managing adverse effects
Substance abuse Stimulant abuse has been a concern, but it has not become the problem many feared. In fact, some studies have found that methylphenidate may help stanch the craving for cocaine in adults with ADHD.11,12 Treating ADHD with pharmacotherapy also has been shown to reduce the risk for substance abuse in adolescence by 85%.13
With careful screening, you can usually identify drug-seeking behavior in adult patients. For patients with substance abuse problems, you can prescribe the nonstimulants.
Tics that can occur with stimulant medications usually can be suppressed by reducing the dosage, being vigilant, and waiting it out. Tics may ameliorate over weeks to months.
Cardiac and cognitive effects Long-term use of stimulant medications at high dosages has been associated with cardiac and cognitive toxicity, as noted in the 1998 NIH consensus statement on diagnosis and treatment of ADHD. It is important to provide patients with this information as part of their informed-consent briefing. (See “Related resources,” to view the consensus statement.)
Nonpharmacologic management
Nonpharmacologic treatments such as EEG biofeedback; psychoeducational approaches; and individual, family, and group psychotherapy are widely used to treat adults with ADHD. Clinicians and patients often perceive these interventions as beneficial, although none have been tested in randomized, placebo-controlled studies.
Patients often function better when their home and work environments are thoughtfully organized, with a designated work/study space and regularly scheduled times for meals, sleep, and exercise. An ADHD coach may facilitate such structure and discipline (Box 2).
New agents in the pipeline
Efforts are being made to increase awareness of adult ADHD and to improve its treatment. For example, the National Institute of Mental Health is funding research on adult ADHD and displays on its Web site a PET scan of an adult brain with ADHD (see “Related resources”).14 Several medications also are being developed to treat ADHD.
Atomoxetine, a nonstimulant medication awaiting FDA approval for adult ADHD, is a selective norepinephrine reuptake inhibitor. In a double-blind, placebo-controlled, crossover study of adults with well-characterized ADHD, 11 of 21 patients improved with use of atomoxetine, compared with 2 of 21 who improved with use of a placebo. The average dosage of 76 mg/d was well-tolerated.15 The 52% response rate is similar to the 54% average improvement rate reported for methylphenidate in previous studies of adult ADHD.
In clinical trials, atomoxetine was given bid. Insomnia was not a side effect, so bid dosing does not interfere with sleep. Approximately 10 to 15% of patients experienced weight loss as a side effect.
Other treatment options under development include:
- a transdermal system for delivery of methylphenidate16
- a novel nicotinic analogue
- glutamate AMPA receptor modulation
- omega-3 fatty acids.
- Hallowell EM, Ratey JJ. Driven to distraction: Recognizing and coping with attention deficit disorder from childhood through adulthood. New York: Simon and Schuster; Reprint edition 1995.
- Solanto MV, Arnstein AFT, Castellanos FX, eds. Stimulant drugs and ADHD: Basic and clinical neuroscience. New York: Oxford University Press; 2001.
- Weiss M, Trokenberg-Hechtman L, Weiss G. ADHD in adulthood: A guide to current theory, diagnosis, and treatment. Baltimore: Johns Hopkins University Press; 1999.
- National Institute of Mental Health. http://www.nimh.nih.gov
Drug brand names
- Atomoxetine • (investigational)
- Bupropion • Wellbutrin
- Desipramine • Norpramin
- Dextroamphetamine • Dexedrine, Dextrostat
- Methamphetamine • Desoxyn
- Methylphenidate • Focalin, Ritalin
- Methylphenidate SR • Concerta, Metadate CD, Metadate ER, Methylin ER, Ritalin SR
- Mixed salts of amphetamine • Adderall, Adderall XR
- Modafinil • Provigil
- Pemoline • Cylert
- Venlafaxine • Effexor
Disclosure
The author reports that he serves as a consultant to Eli Lilly and Company and is on the speaker’s bureaus of Wyeth Pharmaceuticals and AstraZeneca.
1. Gadrow KD, Weiss M. Attention-deficit/hyperactivity disorder in adults: beyond controversy. Arch Gen Psychiatry 2001;58(8):784-5.
2. Ernst M, Zametkin AJ, Matochik JA, Jons PH, Cohen RM. DOPA decarboxylase activity in attention deficit hyperactivity disorder adults. A [fluorine-18]fluorodopa positron emission tomographic study. J Neurosci 1998;18(15):5901-7.
3. Spencer T, Wilens T, Biederman J, Faraone SV, Ablon JS, Lapey K. A double-blind, crossover comparison of methylphenidate and placebo in adults with childhood-onset attention-deficit hyperactivity disorder. Arch Gen Psychiatry 1995;52:434-43.
4. Spencer T, Biederman J, Wilens T, et al. Efficacy of a mixed amphetamine salts compound in adults with attention-deficit/hyperactivity disorder. Arch Gen Psychiatry 2001;58(8):775-82.
5. Swanson J, Wigal S, Greenhill L, et al. Objective and subjective measures of the pharmacodynamic effects of Adderall in the treatment of children with ADHD in a controlled laboratory classroom setting. Psychopharmacol Bull 1998;34(1):55-60.
6. Wilens TE, Biederman J, Spencer TJ, et al. Controlled trial of high doses of pemoline for adults with attention-deficit/hyperactivity disorder. J Clin Psychopharmacol 1999;19(3):257-64.
7. Wilens TE, Biederman J, Mick E, Spencer TJ. A systematic assessment of tricyclic antidepressants in the treatment of adult attention-deficit hyperactivity disorder. J Nerv Ment Dis 1995;183(1):48-50.
8. Findling RL, Schwartz MA, Flannery DJ, Manos MJ. Venlafaxine in adults with attention-deficit/hyperactivity disorder: an open clinical trial. J Clin Psychiatry 1996;57(5):184-9.
9. Wender PH, Reimherr FW. Bupropion treatment of attention-deficit hyperactivity disorder in adults. Am J Psychiatry 1990;147(8):1018-20.
10. Wilens TE, Spencer TJ, et al. A controlled clinical trial of bupropion for attention deficit hyperactivity disorder in adults. Am J Psychiatry 2001;158(2):282-8.
11. Grabowski J, Roache JD, Schmitz JM, Rhoades H, et al. Replacement medication for cocaine dependence: methylphenidate. J Clin Psychopharmacol 1997;17(6):485-8.
12. Levin FR, Evans SM, McDowell DM, Kleber HD. Methylphenidate treatment for cocaine abusers with adult attention-deficit/hyperactivity disorder: a pilot study. J Clin Psychiatry 1998;59(6):300-5.
13. Biederman J, Wilens T, Mick E, Spencer T, Faraone SV. Pharmacotherapy of attention-deficit/hyperactivity disorder reduces risk for substance use disorder. Pediatrics 1999;104(2):e20.-
14. Zametkin AJ, Nordahl TE, Gross M, et al. Cerebral glucose metabolism in adults with hyperactivity of childhood onset. N Engl J Med 1990;323(20):1361-6.
15. Spencer T, Biederman J, Wilens T. Effectiveness and tolerability of atomoxetine in adults with attention deficit hyperactivity disorder. Am J Psychiatry 1998;155(5):693-5.
16. Noven Pharmaceuticals. The Science of Noven. Research and development. Transdermal technology. Available at: http://www.noven.com/research.htm.
1. Gadrow KD, Weiss M. Attention-deficit/hyperactivity disorder in adults: beyond controversy. Arch Gen Psychiatry 2001;58(8):784-5.
2. Ernst M, Zametkin AJ, Matochik JA, Jons PH, Cohen RM. DOPA decarboxylase activity in attention deficit hyperactivity disorder adults. A [fluorine-18]fluorodopa positron emission tomographic study. J Neurosci 1998;18(15):5901-7.
3. Spencer T, Wilens T, Biederman J, Faraone SV, Ablon JS, Lapey K. A double-blind, crossover comparison of methylphenidate and placebo in adults with childhood-onset attention-deficit hyperactivity disorder. Arch Gen Psychiatry 1995;52:434-43.
4. Spencer T, Biederman J, Wilens T, et al. Efficacy of a mixed amphetamine salts compound in adults with attention-deficit/hyperactivity disorder. Arch Gen Psychiatry 2001;58(8):775-82.
5. Swanson J, Wigal S, Greenhill L, et al. Objective and subjective measures of the pharmacodynamic effects of Adderall in the treatment of children with ADHD in a controlled laboratory classroom setting. Psychopharmacol Bull 1998;34(1):55-60.
6. Wilens TE, Biederman J, Spencer TJ, et al. Controlled trial of high doses of pemoline for adults with attention-deficit/hyperactivity disorder. J Clin Psychopharmacol 1999;19(3):257-64.
7. Wilens TE, Biederman J, Mick E, Spencer TJ. A systematic assessment of tricyclic antidepressants in the treatment of adult attention-deficit hyperactivity disorder. J Nerv Ment Dis 1995;183(1):48-50.
8. Findling RL, Schwartz MA, Flannery DJ, Manos MJ. Venlafaxine in adults with attention-deficit/hyperactivity disorder: an open clinical trial. J Clin Psychiatry 1996;57(5):184-9.
9. Wender PH, Reimherr FW. Bupropion treatment of attention-deficit hyperactivity disorder in adults. Am J Psychiatry 1990;147(8):1018-20.
10. Wilens TE, Spencer TJ, et al. A controlled clinical trial of bupropion for attention deficit hyperactivity disorder in adults. Am J Psychiatry 2001;158(2):282-8.
11. Grabowski J, Roache JD, Schmitz JM, Rhoades H, et al. Replacement medication for cocaine dependence: methylphenidate. J Clin Psychopharmacol 1997;17(6):485-8.
12. Levin FR, Evans SM, McDowell DM, Kleber HD. Methylphenidate treatment for cocaine abusers with adult attention-deficit/hyperactivity disorder: a pilot study. J Clin Psychiatry 1998;59(6):300-5.
13. Biederman J, Wilens T, Mick E, Spencer T, Faraone SV. Pharmacotherapy of attention-deficit/hyperactivity disorder reduces risk for substance use disorder. Pediatrics 1999;104(2):e20.-
14. Zametkin AJ, Nordahl TE, Gross M, et al. Cerebral glucose metabolism in adults with hyperactivity of childhood onset. N Engl J Med 1990;323(20):1361-6.
15. Spencer T, Biederman J, Wilens T. Effectiveness and tolerability of atomoxetine in adults with attention deficit hyperactivity disorder. Am J Psychiatry 1998;155(5):693-5.
16. Noven Pharmaceuticals. The Science of Noven. Research and development. Transdermal technology. Available at: http://www.noven.com/research.htm.
One AA meeting doesn’t fit all: 6 keys to prescribing 12-step programs
“The meeting was like sitting in a chimney – I practically choked to death.”
“I was the only person there without a tattoo.”
Attending the wrong 12-step meeting can turn off some patients, despite the substance abuse treatment support offered by Alcoholics Anonymous (AA) and similar programs. Because of the stigma associated with alcohol or drug addiction, most patients are ambivalent at best about attending their first 12-step meetings. Feeling “out of place”—the most common turn-off—can transform this ambivalence into adamant resistance.
Simply advising an addicted patient to “call AA” is tantamount to giving a depressed patient a copy of the Physicians’ Desk Reference and telling him or her to pick an antidepressant. Not all 12-step meetings are alike; 50,000 AA meetings are held every week in the United States (Box 1).1-7 Recognizing the differences between the groups in your area will help you guide your patients to the best match.
In prescribing a 12-step program, consider these six patient factors: socioeconomic status, gender, age, attitude towards spirituality, smoking status, and drug of choice.
More than 50,000 AA meetings, 20,000 NA meetings, and at least 15,000 Alanon/Alateen meetings are held every week in the United States. Other 12-step fellowships that model the AA approach include Gamblers Anonymous, Sex and Love Addicts Anonymous, Overeaters Anonymous, Cocaine Anonymous, Smokers Anonymous, Debtors Anonymous, Dual Recovery Anonymous, and Co-dependence Anonymous.
The combined membership of AA, NA, and Alanon/Alateen is approximately 2 million. To put this in perspective, if the 12-step approach was a religion—as some have proposed1 —it would have more U.S. congregants than Buddhism and Hinduism combined.
Although 12-step therapy has been a central tenet of community-based substance abuse treatment for more than 50 years,2 only recently has it become a focus of clinical research. Two major national multicenter clinical trials3,4 and several important but smaller clinical studies5-7 have found that 12-step-oriented therapies achieve modestly better abstinence rates than the psychotherapies with which they were compared.
Socioeconomic status
Matching patients with meetings according to socioeconomic status is not elitist—it’s pragmatic. Patients generally feel most comfortable and relate most readily at meetings where they feel they have something in common with the other members. For example, when a newly recovering middle-class alcoholic visits an AA group that is frequented by homeless and unemployed alcoholics, chances are that he will become more ambivalent about attending meetings. After all, he was never “that bad.”
A good practice is to give your patients an up-to-date 12-step meeting directory (Box 2). Suggest that they identify the meetings where they think they will feel most comfortable, based on the neighborhoods in which they are held.
Patients in early recovery often are terrified of encountering someone they know at a 12-step meeting. One strategy for patients concerned about protecting their anonymity—as many are—is to attend meetings outside their own neighborhoods but still in areas that match their socioeconomic status. Similarly, referring patients to meetings that are “closed to members only” might reduce their concerns about exposure.
Once a patient has connected with a 12-step program, matching by socioeconomic status becomes less important. Many begin to see similarities between themselves and other addicted individuals from all walks of life. In the beginning, however, similarities attract.
Your patient’s gender
Though women were once a small minority in AA and Narcotics Anonymous (NA), today they make up about one-third of AA’s membership and more than 40% of NA.8 One factor that may have boosted the number of women attending 12-step programs is the increased availability of women-only meetings.
Most cities have women-only meetings, and they generally will be a good place for your female patients to begin. Evidence indicates that gender-specific treatment enhances treatment outcomes.9,10 Women-only meetings tend to be smaller than mixed groups, and the senior members are often particularly willing to welcome newcomers.
Although it is severely frowned upon, the phenomenon of AA or NA members attempting to become romantically or sexually involved with a newcomer is common enough that 12-step members have coined a term for it: “13-stepping.” Newly recovering patients are often emotionally vulnerable and at risk of becoming enmeshed in a potentially destructive relationship. Beginning recovery in gender-specific meetings helps to reduce this risk.
Your patient’s age
A 12-step meeting dominated by people with gray, blue, or no hair can quickly put off teens and young adults in early recovery. Though these meetings with older members are likely to include persons who have achieved long-term and healthy recovery (making such meetings ideal territory for finding a sponsor), finding peers of a similar age is also important.
Meetings intended for young people are identified in 12-step meeting directories, but many of these “young peoples’ ” meetings have a preponderance of members older than 30—quite ancient by a 16-year-old’s standards. Conversely, some generic 12-step meetings might have a cadre of teenagers that attend regularly—at least for a while.
In AA and NA, teens and young adults tend to travel in nomadic packs, linger for a few months, then move on. For this reason, having contacts familiar with the characteristics of local meetings can be invaluable as you try to match a younger patient with a 12-step meeting.
Attitude toward spirituality
One of patients’ most common complaints about 12-step meetings is their surprise at how “religious” the programs are. Insiders are quick to point out that 12-step programs are “spiritual” and not “religious,” but the distinction is moot to patients who are uneasy with this aspect of meetings. The talk about “God as I understand Him,” the opening and closing of meetings with prayers, and the generous adoption of Judeo-Christian practices can rub agnostic, atheistic, and otherwise spiritually indifferent patients the wrong way.
To protect your patients from being blind-sided, review with them some of the spiritual practices employed in 12-step programs before they attend their first meeting:
- Meetings begin with reading the Twelve Steps (Box 3) and other 12-step literature; all readings are peppered with spiritually-loaded words such as “God,” “Higher Power,” “prayer,” and “meditation.”
- Meetings end with a prayer in which the group stands and holds hands (in AA) or links their arms in a huddle (NA). [I advise patients who might find this activity intolerable to duck out to the rest room 5 minutes before the meeting ends.]
- Group leaders typically collect donations by passing the basket.
Certain meetings have a particularly heavy spiritual focus and might be appropriately prescribed for patients hungering for spiritual growth. But for patients who have had toxic encounters with religion or otherwise are ill-at-ease with spirituality or religious matters, starting out at one of the more spiritually hardcore 12-step meetings could be overwhelming. While your 12-step contact person is your best guide in these matters, the following points also apply:
- Meetings listed as “11th Step” or “God as I understand Him” meetings will have a strong spiritual focus.
- Meetings held on Sunday mornings often have the express purpose of focusing on spirituality.
- “Step” meetings generally have a more spiritual focus, as 11 of the 12 steps are aimed at eliciting a “spiritual awakening.”
- “Speaker” or “topic discussion” meetings tend to have a less spiritual focus, though this will vary with the meeting chairperson’s preferences.
- “Beginners” meetings, when available, are intended for new members and devote more time to helping the newcomer understand the 12-step approach to spirituality.
Unless you regularly attend 12-step meetings, it is impossible to know which groups would be the best match for your patients. Here are suggestions for matching your patient’s needs with local 12-step meetings:
- Use fellowship directories. All 12-step fellowships maintain directories of where and when meetings are held and whether meetings are nonsmoking or have other restrictions (e.g., gay-only, women-only). For directories, call local AA and NA fellowships (in the phone book’s white pages).
- Develop a 12-step contact list. Rehabilitation centers often have counselors on staff who are familiar with local 12-step meetings and can recommend those that match your patients’ characteristics. Counselors who are active AA or NA members can be a valuable resource in identifying subtle differences in meetings.
- Locate 12-step meetings for impaired professionals. Special 12-step meetings for nurses, physicians, and pharmacists are held in many cities. For technical reasons, these are not “official”12-step meetings and are not listed in 12-step directories. Times and locations can generally be obtained from local medical societies, impaired-professional programs, or treatment centers.
- We admitted we were powerless over alcohol—that our lives had become unmanageable.
- Cameto believe that a Power greater than ourselves could restore us to sanity.
- Made a decision to turn our will and our lives over to the care of God as we understood Him.
- Made a searching and fearless moral inventory of ourselves.
- Admitted to God, to ourselves, and to another human being the exact nature of our wrongs.
- Were entirely ready to have God remove all these defects of character.
- Humbly asked Him to remove our shortcomings.
- Made a list of all persons we had harmed, and became willing to make amends to them all.
- Made direct amends to such people wherever possible, except when to do so would injure them or others.
- Continued to take personal inventory and when we were wrong promptly admitted it.
- Sought through prayer and meditation to improve our conscious contact with God as we understood Him, praying only for knowledge of His will for us and the power to carry that out.
- Having had a spiritual awakening as the result of these steps, we tried to carry this message to alcoholics and to practice these principles in all our affairs.
Source: Alcoholics Anonymous
AA’s main text, the so-called “Big Book” (its real title is: Alcoholics Anonymous7) has a chapter titled, “We Agnostics.” AA has many long-time members who have found support in the fellowship but never “found God” or a belief in a higher power other than the fellowship itself. These secular 12-step members demonstrate one of the many ironies of AA and NA—that spiritual fellowships can work even for individuals who reject spirituality.
Patients who resist spirituality are advised to “take what you can use” from the fellowship and “leave the rest.” While 12-step members will propose that the newcomer keep an open mind about spirituality, patients should also be assured that a seat is always waiting for them, regardless.
Whether your patient smokes
Most 12-step meetings today are smoke-free, not because of enlightenment within the fellowships but because meetings are usually held in churches, synagogues, and health care facilities where smoking is banned. The perception that attending 12-step meetings can be harmful to your health is out-of-date. Nonetheless, because most meetings have banned smoking, the few in which smoking is allowed are thick with smoke.
In general, 12-step clubhouses are among the holdouts where smoking is allowed during and after meetings. A clubhouse is typically a storefront rented or acquired by AA/NA members where meetings are held around the clock. Given the evidence that quitting smoking may improve overall health,10,11 patients should be encouraged to begin their involvement in smoke-free fellowships, which are identified in 12-step directories.
Your patient’s drug of choice
As its name implies, AA is intended for persons who desire to stop drinking. In practice, however, much of AA’s membership is addicted to more than one substance, and—in some cases—the drug of choice might not be alcohol.
Narcotics Anonymous—contrary to what its name implies—is for individuals addicted to any drug, not just narcotics. Patients generally should be advised to join the fellowship (AA or NA) that best matches their substance use history. There is, however, at least one exception that might best be illustrated with an example:
After I recommended NA meetings to a middle-class nurse addicted to analgesics, she returned for her next appointment quite angry. She attended three different NA meetings, and “all of the members were either heroin or crack cocaine addicts.” It seemed to her that all of them were on probation or parole. She was very uncomfortable throughout the meetings and upset with my recommendation.
In matching patients with meetings, socioeconomic and cultural factors take precedence over biochemistry. At the neuronal level, a nurse addicted to analgesics has a lot in common with a heroin addict, but her ability to relate to another recovering person—particularly in early recovery—may be limited. Arguing with my patient or countering that other nurses were probably at the meetings she attended would not have eased her reluctance to return to NA or helped our therapeutic alliance.
NA meetings are generally attended by individuals addicted to illicit drugs: amphetamines, crack cocaine, cannabis, and heroin. In larger cities, other 12-step fellowships may focus on specific drugs, such as cocaine, but these are rare. Just as individuals addicted to prescription narcotics are a minority in the treatment population, they are also a minority in NA.
For this reason, our prior recommendation—to match patients to meetings based on socioeconomic status—applies. It’s good policy to recommend that patients addicted to prescription medications try both AA and NA meetings and decide where they feel most comfortable.
The third tradition of AA states, “the only requirement for AA membership is a desire to stop drinking.” Though a purist might suggest that our analgesics-dependent nurse should join NA, her need to connect culturally with similar persons in recovery argues strongly for her to blend in at open AA meetings. A social drinker who never fulfilled the diagnostic criteria for alcohol dependence, she will have a better chance of abstaining from analgesics if she abstains from alcohol as well. For this reason, she should qualify for AA membership because she does, in fact, have “a desire to stop drinking.”
Some professionals addicted to prescription drugs will feel at home in NA meetings, whereas others will react as my patient did. Having access to a 12-step contact person who knows about the demographics of local NA meetings can help you make the best patient/meeting match.
Related resources
- Alcoholics Anonymous. www.alcoholics-anonymous.org
- Narcotics Anonymous. www.na.org
- Alanon-Alateen. www.al-anon.org
1. The Church of God Anonymous (religion of the 12-step movement) http://www.churchofgodanonymous.org/index2.html
2. White W. Slaying the Dragon Bloomington, IL: Chestnut Health Systems, 1998.
3. Crits-Christoph P, Siqueland L, Blaine J, et al. Psychosocial treatments for cocaine dependence: National Institute on Drug Abuse Collaborative Cocaine Treatment Study. Arch Gen Psychiatry 1999;57(6):493-502.
4. Project Match. Matching alcoholism treatments to client heterogeneity: Project MATCH posttreatment drinking outcomes. J Studies Alcohol 1997;58(1):7-29.
5. Ouimette PC, Finney JW, Moos RH. Twelve-step and cognitive-behavioral treatment for substance abuse: A comparison of treatment effectiveness. J Consult Clin Psychology 1997;65:230-40.
6. Morgenstern J, Blanchard KA, Morgan TJ, Labouvie E, Hayaki J. Testing the effectiveness of cognitive-behavioral treatment for substance abuse in a community setting: Within treatment and post-treatment findings. J Consult Clin Psychology 2001;69:1007-17.
7. Alcoholics Anonymous (3rd ed). New York: Alcoholics Anonymous World Service, 1976.
8. Emrick CD, Tonigan SJ, Montgomery H, Little L. Alcoholics Anonymous: what is currently known. In: McCrady BS, Miller WR (eds). Research on Alcoholics Anonymous New Brunswick, NJ: Rutgers Center on Alcohol Studies Publications, 1993:45.
9. Blume S. Addiction in women. In: Galanter M, Kleber HD (eds). Textbook of substance abuse treatment (2nd ed). Washington, DC: American Psychiatric Press, 1999;485-91.
10. Jarvis TJ. Implications of gender for alcohol treatment research: a quantitative and qualitative review. Br J Addiction 1992;87:1249-61.
11. Bobo JK, McIlvain HE, Lando HA, Walker RD, Leed-Kelly A. Effect of smoking cessation counseling on recovery from alcoholism: findings from a randomized community intervention trial. Addiction 1998;93:877-87.
12. Burling TA, Marshall GD, Seidner AL. Smoking cessation for substance abuse inpatients. J Subs Abuse 1991;3(3):269-76.
“The meeting was like sitting in a chimney – I practically choked to death.”
“I was the only person there without a tattoo.”
Attending the wrong 12-step meeting can turn off some patients, despite the substance abuse treatment support offered by Alcoholics Anonymous (AA) and similar programs. Because of the stigma associated with alcohol or drug addiction, most patients are ambivalent at best about attending their first 12-step meetings. Feeling “out of place”—the most common turn-off—can transform this ambivalence into adamant resistance.
Simply advising an addicted patient to “call AA” is tantamount to giving a depressed patient a copy of the Physicians’ Desk Reference and telling him or her to pick an antidepressant. Not all 12-step meetings are alike; 50,000 AA meetings are held every week in the United States (Box 1).1-7 Recognizing the differences between the groups in your area will help you guide your patients to the best match.
In prescribing a 12-step program, consider these six patient factors: socioeconomic status, gender, age, attitude towards spirituality, smoking status, and drug of choice.
More than 50,000 AA meetings, 20,000 NA meetings, and at least 15,000 Alanon/Alateen meetings are held every week in the United States. Other 12-step fellowships that model the AA approach include Gamblers Anonymous, Sex and Love Addicts Anonymous, Overeaters Anonymous, Cocaine Anonymous, Smokers Anonymous, Debtors Anonymous, Dual Recovery Anonymous, and Co-dependence Anonymous.
The combined membership of AA, NA, and Alanon/Alateen is approximately 2 million. To put this in perspective, if the 12-step approach was a religion—as some have proposed1 —it would have more U.S. congregants than Buddhism and Hinduism combined.
Although 12-step therapy has been a central tenet of community-based substance abuse treatment for more than 50 years,2 only recently has it become a focus of clinical research. Two major national multicenter clinical trials3,4 and several important but smaller clinical studies5-7 have found that 12-step-oriented therapies achieve modestly better abstinence rates than the psychotherapies with which they were compared.
Socioeconomic status
Matching patients with meetings according to socioeconomic status is not elitist—it’s pragmatic. Patients generally feel most comfortable and relate most readily at meetings where they feel they have something in common with the other members. For example, when a newly recovering middle-class alcoholic visits an AA group that is frequented by homeless and unemployed alcoholics, chances are that he will become more ambivalent about attending meetings. After all, he was never “that bad.”
A good practice is to give your patients an up-to-date 12-step meeting directory (Box 2). Suggest that they identify the meetings where they think they will feel most comfortable, based on the neighborhoods in which they are held.
Patients in early recovery often are terrified of encountering someone they know at a 12-step meeting. One strategy for patients concerned about protecting their anonymity—as many are—is to attend meetings outside their own neighborhoods but still in areas that match their socioeconomic status. Similarly, referring patients to meetings that are “closed to members only” might reduce their concerns about exposure.
Once a patient has connected with a 12-step program, matching by socioeconomic status becomes less important. Many begin to see similarities between themselves and other addicted individuals from all walks of life. In the beginning, however, similarities attract.
Your patient’s gender
Though women were once a small minority in AA and Narcotics Anonymous (NA), today they make up about one-third of AA’s membership and more than 40% of NA.8 One factor that may have boosted the number of women attending 12-step programs is the increased availability of women-only meetings.
Most cities have women-only meetings, and they generally will be a good place for your female patients to begin. Evidence indicates that gender-specific treatment enhances treatment outcomes.9,10 Women-only meetings tend to be smaller than mixed groups, and the senior members are often particularly willing to welcome newcomers.
Although it is severely frowned upon, the phenomenon of AA or NA members attempting to become romantically or sexually involved with a newcomer is common enough that 12-step members have coined a term for it: “13-stepping.” Newly recovering patients are often emotionally vulnerable and at risk of becoming enmeshed in a potentially destructive relationship. Beginning recovery in gender-specific meetings helps to reduce this risk.
Your patient’s age
A 12-step meeting dominated by people with gray, blue, or no hair can quickly put off teens and young adults in early recovery. Though these meetings with older members are likely to include persons who have achieved long-term and healthy recovery (making such meetings ideal territory for finding a sponsor), finding peers of a similar age is also important.
Meetings intended for young people are identified in 12-step meeting directories, but many of these “young peoples’ ” meetings have a preponderance of members older than 30—quite ancient by a 16-year-old’s standards. Conversely, some generic 12-step meetings might have a cadre of teenagers that attend regularly—at least for a while.
In AA and NA, teens and young adults tend to travel in nomadic packs, linger for a few months, then move on. For this reason, having contacts familiar with the characteristics of local meetings can be invaluable as you try to match a younger patient with a 12-step meeting.
Attitude toward spirituality
One of patients’ most common complaints about 12-step meetings is their surprise at how “religious” the programs are. Insiders are quick to point out that 12-step programs are “spiritual” and not “religious,” but the distinction is moot to patients who are uneasy with this aspect of meetings. The talk about “God as I understand Him,” the opening and closing of meetings with prayers, and the generous adoption of Judeo-Christian practices can rub agnostic, atheistic, and otherwise spiritually indifferent patients the wrong way.
To protect your patients from being blind-sided, review with them some of the spiritual practices employed in 12-step programs before they attend their first meeting:
- Meetings begin with reading the Twelve Steps (Box 3) and other 12-step literature; all readings are peppered with spiritually-loaded words such as “God,” “Higher Power,” “prayer,” and “meditation.”
- Meetings end with a prayer in which the group stands and holds hands (in AA) or links their arms in a huddle (NA). [I advise patients who might find this activity intolerable to duck out to the rest room 5 minutes before the meeting ends.]
- Group leaders typically collect donations by passing the basket.
Certain meetings have a particularly heavy spiritual focus and might be appropriately prescribed for patients hungering for spiritual growth. But for patients who have had toxic encounters with religion or otherwise are ill-at-ease with spirituality or religious matters, starting out at one of the more spiritually hardcore 12-step meetings could be overwhelming. While your 12-step contact person is your best guide in these matters, the following points also apply:
- Meetings listed as “11th Step” or “God as I understand Him” meetings will have a strong spiritual focus.
- Meetings held on Sunday mornings often have the express purpose of focusing on spirituality.
- “Step” meetings generally have a more spiritual focus, as 11 of the 12 steps are aimed at eliciting a “spiritual awakening.”
- “Speaker” or “topic discussion” meetings tend to have a less spiritual focus, though this will vary with the meeting chairperson’s preferences.
- “Beginners” meetings, when available, are intended for new members and devote more time to helping the newcomer understand the 12-step approach to spirituality.
Unless you regularly attend 12-step meetings, it is impossible to know which groups would be the best match for your patients. Here are suggestions for matching your patient’s needs with local 12-step meetings:
- Use fellowship directories. All 12-step fellowships maintain directories of where and when meetings are held and whether meetings are nonsmoking or have other restrictions (e.g., gay-only, women-only). For directories, call local AA and NA fellowships (in the phone book’s white pages).
- Develop a 12-step contact list. Rehabilitation centers often have counselors on staff who are familiar with local 12-step meetings and can recommend those that match your patients’ characteristics. Counselors who are active AA or NA members can be a valuable resource in identifying subtle differences in meetings.
- Locate 12-step meetings for impaired professionals. Special 12-step meetings for nurses, physicians, and pharmacists are held in many cities. For technical reasons, these are not “official”12-step meetings and are not listed in 12-step directories. Times and locations can generally be obtained from local medical societies, impaired-professional programs, or treatment centers.
- We admitted we were powerless over alcohol—that our lives had become unmanageable.
- Cameto believe that a Power greater than ourselves could restore us to sanity.
- Made a decision to turn our will and our lives over to the care of God as we understood Him.
- Made a searching and fearless moral inventory of ourselves.
- Admitted to God, to ourselves, and to another human being the exact nature of our wrongs.
- Were entirely ready to have God remove all these defects of character.
- Humbly asked Him to remove our shortcomings.
- Made a list of all persons we had harmed, and became willing to make amends to them all.
- Made direct amends to such people wherever possible, except when to do so would injure them or others.
- Continued to take personal inventory and when we were wrong promptly admitted it.
- Sought through prayer and meditation to improve our conscious contact with God as we understood Him, praying only for knowledge of His will for us and the power to carry that out.
- Having had a spiritual awakening as the result of these steps, we tried to carry this message to alcoholics and to practice these principles in all our affairs.
Source: Alcoholics Anonymous
AA’s main text, the so-called “Big Book” (its real title is: Alcoholics Anonymous7) has a chapter titled, “We Agnostics.” AA has many long-time members who have found support in the fellowship but never “found God” or a belief in a higher power other than the fellowship itself. These secular 12-step members demonstrate one of the many ironies of AA and NA—that spiritual fellowships can work even for individuals who reject spirituality.
Patients who resist spirituality are advised to “take what you can use” from the fellowship and “leave the rest.” While 12-step members will propose that the newcomer keep an open mind about spirituality, patients should also be assured that a seat is always waiting for them, regardless.
Whether your patient smokes
Most 12-step meetings today are smoke-free, not because of enlightenment within the fellowships but because meetings are usually held in churches, synagogues, and health care facilities where smoking is banned. The perception that attending 12-step meetings can be harmful to your health is out-of-date. Nonetheless, because most meetings have banned smoking, the few in which smoking is allowed are thick with smoke.
In general, 12-step clubhouses are among the holdouts where smoking is allowed during and after meetings. A clubhouse is typically a storefront rented or acquired by AA/NA members where meetings are held around the clock. Given the evidence that quitting smoking may improve overall health,10,11 patients should be encouraged to begin their involvement in smoke-free fellowships, which are identified in 12-step directories.
Your patient’s drug of choice
As its name implies, AA is intended for persons who desire to stop drinking. In practice, however, much of AA’s membership is addicted to more than one substance, and—in some cases—the drug of choice might not be alcohol.
Narcotics Anonymous—contrary to what its name implies—is for individuals addicted to any drug, not just narcotics. Patients generally should be advised to join the fellowship (AA or NA) that best matches their substance use history. There is, however, at least one exception that might best be illustrated with an example:
After I recommended NA meetings to a middle-class nurse addicted to analgesics, she returned for her next appointment quite angry. She attended three different NA meetings, and “all of the members were either heroin or crack cocaine addicts.” It seemed to her that all of them were on probation or parole. She was very uncomfortable throughout the meetings and upset with my recommendation.
In matching patients with meetings, socioeconomic and cultural factors take precedence over biochemistry. At the neuronal level, a nurse addicted to analgesics has a lot in common with a heroin addict, but her ability to relate to another recovering person—particularly in early recovery—may be limited. Arguing with my patient or countering that other nurses were probably at the meetings she attended would not have eased her reluctance to return to NA or helped our therapeutic alliance.
NA meetings are generally attended by individuals addicted to illicit drugs: amphetamines, crack cocaine, cannabis, and heroin. In larger cities, other 12-step fellowships may focus on specific drugs, such as cocaine, but these are rare. Just as individuals addicted to prescription narcotics are a minority in the treatment population, they are also a minority in NA.
For this reason, our prior recommendation—to match patients to meetings based on socioeconomic status—applies. It’s good policy to recommend that patients addicted to prescription medications try both AA and NA meetings and decide where they feel most comfortable.
The third tradition of AA states, “the only requirement for AA membership is a desire to stop drinking.” Though a purist might suggest that our analgesics-dependent nurse should join NA, her need to connect culturally with similar persons in recovery argues strongly for her to blend in at open AA meetings. A social drinker who never fulfilled the diagnostic criteria for alcohol dependence, she will have a better chance of abstaining from analgesics if she abstains from alcohol as well. For this reason, she should qualify for AA membership because she does, in fact, have “a desire to stop drinking.”
Some professionals addicted to prescription drugs will feel at home in NA meetings, whereas others will react as my patient did. Having access to a 12-step contact person who knows about the demographics of local NA meetings can help you make the best patient/meeting match.
Related resources
- Alcoholics Anonymous. www.alcoholics-anonymous.org
- Narcotics Anonymous. www.na.org
- Alanon-Alateen. www.al-anon.org
“The meeting was like sitting in a chimney – I practically choked to death.”
“I was the only person there without a tattoo.”
Attending the wrong 12-step meeting can turn off some patients, despite the substance abuse treatment support offered by Alcoholics Anonymous (AA) and similar programs. Because of the stigma associated with alcohol or drug addiction, most patients are ambivalent at best about attending their first 12-step meetings. Feeling “out of place”—the most common turn-off—can transform this ambivalence into adamant resistance.
Simply advising an addicted patient to “call AA” is tantamount to giving a depressed patient a copy of the Physicians’ Desk Reference and telling him or her to pick an antidepressant. Not all 12-step meetings are alike; 50,000 AA meetings are held every week in the United States (Box 1).1-7 Recognizing the differences between the groups in your area will help you guide your patients to the best match.
In prescribing a 12-step program, consider these six patient factors: socioeconomic status, gender, age, attitude towards spirituality, smoking status, and drug of choice.
More than 50,000 AA meetings, 20,000 NA meetings, and at least 15,000 Alanon/Alateen meetings are held every week in the United States. Other 12-step fellowships that model the AA approach include Gamblers Anonymous, Sex and Love Addicts Anonymous, Overeaters Anonymous, Cocaine Anonymous, Smokers Anonymous, Debtors Anonymous, Dual Recovery Anonymous, and Co-dependence Anonymous.
The combined membership of AA, NA, and Alanon/Alateen is approximately 2 million. To put this in perspective, if the 12-step approach was a religion—as some have proposed1 —it would have more U.S. congregants than Buddhism and Hinduism combined.
Although 12-step therapy has been a central tenet of community-based substance abuse treatment for more than 50 years,2 only recently has it become a focus of clinical research. Two major national multicenter clinical trials3,4 and several important but smaller clinical studies5-7 have found that 12-step-oriented therapies achieve modestly better abstinence rates than the psychotherapies with which they were compared.
Socioeconomic status
Matching patients with meetings according to socioeconomic status is not elitist—it’s pragmatic. Patients generally feel most comfortable and relate most readily at meetings where they feel they have something in common with the other members. For example, when a newly recovering middle-class alcoholic visits an AA group that is frequented by homeless and unemployed alcoholics, chances are that he will become more ambivalent about attending meetings. After all, he was never “that bad.”
A good practice is to give your patients an up-to-date 12-step meeting directory (Box 2). Suggest that they identify the meetings where they think they will feel most comfortable, based on the neighborhoods in which they are held.
Patients in early recovery often are terrified of encountering someone they know at a 12-step meeting. One strategy for patients concerned about protecting their anonymity—as many are—is to attend meetings outside their own neighborhoods but still in areas that match their socioeconomic status. Similarly, referring patients to meetings that are “closed to members only” might reduce their concerns about exposure.
Once a patient has connected with a 12-step program, matching by socioeconomic status becomes less important. Many begin to see similarities between themselves and other addicted individuals from all walks of life. In the beginning, however, similarities attract.
Your patient’s gender
Though women were once a small minority in AA and Narcotics Anonymous (NA), today they make up about one-third of AA’s membership and more than 40% of NA.8 One factor that may have boosted the number of women attending 12-step programs is the increased availability of women-only meetings.
Most cities have women-only meetings, and they generally will be a good place for your female patients to begin. Evidence indicates that gender-specific treatment enhances treatment outcomes.9,10 Women-only meetings tend to be smaller than mixed groups, and the senior members are often particularly willing to welcome newcomers.
Although it is severely frowned upon, the phenomenon of AA or NA members attempting to become romantically or sexually involved with a newcomer is common enough that 12-step members have coined a term for it: “13-stepping.” Newly recovering patients are often emotionally vulnerable and at risk of becoming enmeshed in a potentially destructive relationship. Beginning recovery in gender-specific meetings helps to reduce this risk.
Your patient’s age
A 12-step meeting dominated by people with gray, blue, or no hair can quickly put off teens and young adults in early recovery. Though these meetings with older members are likely to include persons who have achieved long-term and healthy recovery (making such meetings ideal territory for finding a sponsor), finding peers of a similar age is also important.
Meetings intended for young people are identified in 12-step meeting directories, but many of these “young peoples’ ” meetings have a preponderance of members older than 30—quite ancient by a 16-year-old’s standards. Conversely, some generic 12-step meetings might have a cadre of teenagers that attend regularly—at least for a while.
In AA and NA, teens and young adults tend to travel in nomadic packs, linger for a few months, then move on. For this reason, having contacts familiar with the characteristics of local meetings can be invaluable as you try to match a younger patient with a 12-step meeting.
Attitude toward spirituality
One of patients’ most common complaints about 12-step meetings is their surprise at how “religious” the programs are. Insiders are quick to point out that 12-step programs are “spiritual” and not “religious,” but the distinction is moot to patients who are uneasy with this aspect of meetings. The talk about “God as I understand Him,” the opening and closing of meetings with prayers, and the generous adoption of Judeo-Christian practices can rub agnostic, atheistic, and otherwise spiritually indifferent patients the wrong way.
To protect your patients from being blind-sided, review with them some of the spiritual practices employed in 12-step programs before they attend their first meeting:
- Meetings begin with reading the Twelve Steps (Box 3) and other 12-step literature; all readings are peppered with spiritually-loaded words such as “God,” “Higher Power,” “prayer,” and “meditation.”
- Meetings end with a prayer in which the group stands and holds hands (in AA) or links their arms in a huddle (NA). [I advise patients who might find this activity intolerable to duck out to the rest room 5 minutes before the meeting ends.]
- Group leaders typically collect donations by passing the basket.
Certain meetings have a particularly heavy spiritual focus and might be appropriately prescribed for patients hungering for spiritual growth. But for patients who have had toxic encounters with religion or otherwise are ill-at-ease with spirituality or religious matters, starting out at one of the more spiritually hardcore 12-step meetings could be overwhelming. While your 12-step contact person is your best guide in these matters, the following points also apply:
- Meetings listed as “11th Step” or “God as I understand Him” meetings will have a strong spiritual focus.
- Meetings held on Sunday mornings often have the express purpose of focusing on spirituality.
- “Step” meetings generally have a more spiritual focus, as 11 of the 12 steps are aimed at eliciting a “spiritual awakening.”
- “Speaker” or “topic discussion” meetings tend to have a less spiritual focus, though this will vary with the meeting chairperson’s preferences.
- “Beginners” meetings, when available, are intended for new members and devote more time to helping the newcomer understand the 12-step approach to spirituality.
Unless you regularly attend 12-step meetings, it is impossible to know which groups would be the best match for your patients. Here are suggestions for matching your patient’s needs with local 12-step meetings:
- Use fellowship directories. All 12-step fellowships maintain directories of where and when meetings are held and whether meetings are nonsmoking or have other restrictions (e.g., gay-only, women-only). For directories, call local AA and NA fellowships (in the phone book’s white pages).
- Develop a 12-step contact list. Rehabilitation centers often have counselors on staff who are familiar with local 12-step meetings and can recommend those that match your patients’ characteristics. Counselors who are active AA or NA members can be a valuable resource in identifying subtle differences in meetings.
- Locate 12-step meetings for impaired professionals. Special 12-step meetings for nurses, physicians, and pharmacists are held in many cities. For technical reasons, these are not “official”12-step meetings and are not listed in 12-step directories. Times and locations can generally be obtained from local medical societies, impaired-professional programs, or treatment centers.
- We admitted we were powerless over alcohol—that our lives had become unmanageable.
- Cameto believe that a Power greater than ourselves could restore us to sanity.
- Made a decision to turn our will and our lives over to the care of God as we understood Him.
- Made a searching and fearless moral inventory of ourselves.
- Admitted to God, to ourselves, and to another human being the exact nature of our wrongs.
- Were entirely ready to have God remove all these defects of character.
- Humbly asked Him to remove our shortcomings.
- Made a list of all persons we had harmed, and became willing to make amends to them all.
- Made direct amends to such people wherever possible, except when to do so would injure them or others.
- Continued to take personal inventory and when we were wrong promptly admitted it.
- Sought through prayer and meditation to improve our conscious contact with God as we understood Him, praying only for knowledge of His will for us and the power to carry that out.
- Having had a spiritual awakening as the result of these steps, we tried to carry this message to alcoholics and to practice these principles in all our affairs.
Source: Alcoholics Anonymous
AA’s main text, the so-called “Big Book” (its real title is: Alcoholics Anonymous7) has a chapter titled, “We Agnostics.” AA has many long-time members who have found support in the fellowship but never “found God” or a belief in a higher power other than the fellowship itself. These secular 12-step members demonstrate one of the many ironies of AA and NA—that spiritual fellowships can work even for individuals who reject spirituality.
Patients who resist spirituality are advised to “take what you can use” from the fellowship and “leave the rest.” While 12-step members will propose that the newcomer keep an open mind about spirituality, patients should also be assured that a seat is always waiting for them, regardless.
Whether your patient smokes
Most 12-step meetings today are smoke-free, not because of enlightenment within the fellowships but because meetings are usually held in churches, synagogues, and health care facilities where smoking is banned. The perception that attending 12-step meetings can be harmful to your health is out-of-date. Nonetheless, because most meetings have banned smoking, the few in which smoking is allowed are thick with smoke.
In general, 12-step clubhouses are among the holdouts where smoking is allowed during and after meetings. A clubhouse is typically a storefront rented or acquired by AA/NA members where meetings are held around the clock. Given the evidence that quitting smoking may improve overall health,10,11 patients should be encouraged to begin their involvement in smoke-free fellowships, which are identified in 12-step directories.
Your patient’s drug of choice
As its name implies, AA is intended for persons who desire to stop drinking. In practice, however, much of AA’s membership is addicted to more than one substance, and—in some cases—the drug of choice might not be alcohol.
Narcotics Anonymous—contrary to what its name implies—is for individuals addicted to any drug, not just narcotics. Patients generally should be advised to join the fellowship (AA or NA) that best matches their substance use history. There is, however, at least one exception that might best be illustrated with an example:
After I recommended NA meetings to a middle-class nurse addicted to analgesics, she returned for her next appointment quite angry. She attended three different NA meetings, and “all of the members were either heroin or crack cocaine addicts.” It seemed to her that all of them were on probation or parole. She was very uncomfortable throughout the meetings and upset with my recommendation.
In matching patients with meetings, socioeconomic and cultural factors take precedence over biochemistry. At the neuronal level, a nurse addicted to analgesics has a lot in common with a heroin addict, but her ability to relate to another recovering person—particularly in early recovery—may be limited. Arguing with my patient or countering that other nurses were probably at the meetings she attended would not have eased her reluctance to return to NA or helped our therapeutic alliance.
NA meetings are generally attended by individuals addicted to illicit drugs: amphetamines, crack cocaine, cannabis, and heroin. In larger cities, other 12-step fellowships may focus on specific drugs, such as cocaine, but these are rare. Just as individuals addicted to prescription narcotics are a minority in the treatment population, they are also a minority in NA.
For this reason, our prior recommendation—to match patients to meetings based on socioeconomic status—applies. It’s good policy to recommend that patients addicted to prescription medications try both AA and NA meetings and decide where they feel most comfortable.
The third tradition of AA states, “the only requirement for AA membership is a desire to stop drinking.” Though a purist might suggest that our analgesics-dependent nurse should join NA, her need to connect culturally with similar persons in recovery argues strongly for her to blend in at open AA meetings. A social drinker who never fulfilled the diagnostic criteria for alcohol dependence, she will have a better chance of abstaining from analgesics if she abstains from alcohol as well. For this reason, she should qualify for AA membership because she does, in fact, have “a desire to stop drinking.”
Some professionals addicted to prescription drugs will feel at home in NA meetings, whereas others will react as my patient did. Having access to a 12-step contact person who knows about the demographics of local NA meetings can help you make the best patient/meeting match.
Related resources
- Alcoholics Anonymous. www.alcoholics-anonymous.org
- Narcotics Anonymous. www.na.org
- Alanon-Alateen. www.al-anon.org
1. The Church of God Anonymous (religion of the 12-step movement) http://www.churchofgodanonymous.org/index2.html
2. White W. Slaying the Dragon Bloomington, IL: Chestnut Health Systems, 1998.
3. Crits-Christoph P, Siqueland L, Blaine J, et al. Psychosocial treatments for cocaine dependence: National Institute on Drug Abuse Collaborative Cocaine Treatment Study. Arch Gen Psychiatry 1999;57(6):493-502.
4. Project Match. Matching alcoholism treatments to client heterogeneity: Project MATCH posttreatment drinking outcomes. J Studies Alcohol 1997;58(1):7-29.
5. Ouimette PC, Finney JW, Moos RH. Twelve-step and cognitive-behavioral treatment for substance abuse: A comparison of treatment effectiveness. J Consult Clin Psychology 1997;65:230-40.
6. Morgenstern J, Blanchard KA, Morgan TJ, Labouvie E, Hayaki J. Testing the effectiveness of cognitive-behavioral treatment for substance abuse in a community setting: Within treatment and post-treatment findings. J Consult Clin Psychology 2001;69:1007-17.
7. Alcoholics Anonymous (3rd ed). New York: Alcoholics Anonymous World Service, 1976.
8. Emrick CD, Tonigan SJ, Montgomery H, Little L. Alcoholics Anonymous: what is currently known. In: McCrady BS, Miller WR (eds). Research on Alcoholics Anonymous New Brunswick, NJ: Rutgers Center on Alcohol Studies Publications, 1993:45.
9. Blume S. Addiction in women. In: Galanter M, Kleber HD (eds). Textbook of substance abuse treatment (2nd ed). Washington, DC: American Psychiatric Press, 1999;485-91.
10. Jarvis TJ. Implications of gender for alcohol treatment research: a quantitative and qualitative review. Br J Addiction 1992;87:1249-61.
11. Bobo JK, McIlvain HE, Lando HA, Walker RD, Leed-Kelly A. Effect of smoking cessation counseling on recovery from alcoholism: findings from a randomized community intervention trial. Addiction 1998;93:877-87.
12. Burling TA, Marshall GD, Seidner AL. Smoking cessation for substance abuse inpatients. J Subs Abuse 1991;3(3):269-76.
1. The Church of God Anonymous (religion of the 12-step movement) http://www.churchofgodanonymous.org/index2.html
2. White W. Slaying the Dragon Bloomington, IL: Chestnut Health Systems, 1998.
3. Crits-Christoph P, Siqueland L, Blaine J, et al. Psychosocial treatments for cocaine dependence: National Institute on Drug Abuse Collaborative Cocaine Treatment Study. Arch Gen Psychiatry 1999;57(6):493-502.
4. Project Match. Matching alcoholism treatments to client heterogeneity: Project MATCH posttreatment drinking outcomes. J Studies Alcohol 1997;58(1):7-29.
5. Ouimette PC, Finney JW, Moos RH. Twelve-step and cognitive-behavioral treatment for substance abuse: A comparison of treatment effectiveness. J Consult Clin Psychology 1997;65:230-40.
6. Morgenstern J, Blanchard KA, Morgan TJ, Labouvie E, Hayaki J. Testing the effectiveness of cognitive-behavioral treatment for substance abuse in a community setting: Within treatment and post-treatment findings. J Consult Clin Psychology 2001;69:1007-17.
7. Alcoholics Anonymous (3rd ed). New York: Alcoholics Anonymous World Service, 1976.
8. Emrick CD, Tonigan SJ, Montgomery H, Little L. Alcoholics Anonymous: what is currently known. In: McCrady BS, Miller WR (eds). Research on Alcoholics Anonymous New Brunswick, NJ: Rutgers Center on Alcohol Studies Publications, 1993:45.
9. Blume S. Addiction in women. In: Galanter M, Kleber HD (eds). Textbook of substance abuse treatment (2nd ed). Washington, DC: American Psychiatric Press, 1999;485-91.
10. Jarvis TJ. Implications of gender for alcohol treatment research: a quantitative and qualitative review. Br J Addiction 1992;87:1249-61.
11. Bobo JK, McIlvain HE, Lando HA, Walker RD, Leed-Kelly A. Effect of smoking cessation counseling on recovery from alcoholism: findings from a randomized community intervention trial. Addiction 1998;93:877-87.
12. Burling TA, Marshall GD, Seidner AL. Smoking cessation for substance abuse inpatients. J Subs Abuse 1991;3(3):269-76.