User login
The skill set of the ‘pluripotent’ hospitalist
Editor’s note: National Hospitalist Day occurs the first Thursday in March annually, and serves to celebrate the fastest growing specialty in modern medicine and hospitalists’ enduring contributions to the evolving health care landscape. On National Hospitalist Day in 2021, SHM convened a virtual roundtable with a diverse group of hospitalists to discuss skill set, wellness, and other key issues for hospitalists. To listen to the entire roundtable discussion, visit this Explore The Space podcast episode.
A hospitalist isn’t just a physician who happens to work in a hospital. They are medical professionals with a robust skill set that they use both inside and outside the hospital setting. But what skill sets do hospitalists need to become successful in their careers? And what skill sets does a “pluripotent” hospitalist need in their armamentarium?
These were the issues discussed by participants of a virtual roundtable discussion on National Hospitalist Day – March 4, 2021 – as part of a joint effort of the Society of Hospital Medicine and the Explore the Space podcast.
Maylyn S. Martinez, MD, clinician-researcher and clinical associate at the University of Chicago, sees her hospitalist and research skill sets as two “buckets” of skills she can sort through, with diagnostic, knowledge-based care coordination, and interpersonal skills as lanes where she can focus and improve. “I’m always trying to work in, and sharpen, and find ways to get better at something in each of those every day,” she said.
For Anika Kumar, MD, FHM, pediatric editor of the Hospitalist and clinical assistant professor of pediatrics at the Cleveland Clinic Lerner College of Medicine, much of her work is focused on problem solving. “I approach that as: ‘How do I come up with my differential diagnosis, and how do I diagnose the patient?’ I think that the lanes are a little bit different, but there is some overlap.”
Adaptability is another important part of the skill set for the hospitalist, Ndidi Unaka, MD, MEd, associate professor in the division of hospital medicine at Cincinnati Children’s Hospital Medical Center, said during the discussion. “I think we all really value teamwork, and we take on the role of being the coordinator and making sure things are getting done in a seamless and thoughtful manner. Communicating with families, communicating with our research team, communicating with primary care physicians. I think that is something we’re very used to doing, and I think we do it well. I think we don’t shy away from difficult conversations with consultants. And I think that’s what makes being a hospitalist so amazing.”
Achieving wellness as a hospitalist
Another topic discussed during the roundtable was “comprehensive care for the hospitalist” and how they can achieve a sense of wellness for themselves. Gurpreet Dhaliwal, MD, clinician-educator and professor of medicine at the University of California, San Francisco, said long-term satisfaction in one’s career is less about compensation and more about autonomy, mastery, and purpose.
“Autonomy is shrinking a little bit in health care. But if we connect to our purpose – ‘what are we doing here and how do we connect?’ – it’s either learning about patients and their stories, being with a team of people that you work with, that really builds that purpose,” he said.
Regarding mastery, there’s “tremendous joy if you’re in an environment where people value your mastery, whether it is working in a team or communicating or diagnosing or doing a procedure. If you think of setting up the work environment and those things are in place, I think a lot of wellness can actually happen at work, even though another component, of course, is balancing your life outside of work,” Dr. Dhaliwal said.
This may seem out of reach during COVID-19, but wellness is still achievable during the pandemic, Dr. Martinez said. Her time is spent 75% as a researcher and 25% as a clinician, which is her ideal balance. “I enjoy doing my research, doing my own statistics and writing grants and just learning about this problem that I’ve developed an interest in,” she said. “I just think that’s an important piece for people to focus on as far as health care for the hospitalist, is that there’s no no-one-size-fits-all, that’s for sure.”
Dr. Kumar noted that her clinical time gives her energy for nonclinical work. “I love my clinical time. It’s one of my favorite things that I do,” she said. Although she is tired at the end of the week, “I feel like I am not only giving back to my patients and my team, but I’m also giving back to myself and reminding myself why it is I do what I do every day,” she said.
Wellness for Dr. Unaka meant remembering what drew her to medicine. “It was definitely the opportunity to build strong relationships with patients and families,” she said. While these encounters can sometimes be heavy and stay with a hospitalist, “the fact that we’re in it with them is something that gives a lot of us purpose. I think that when I reflect on all of those things, I’m so happy that I’m in the role that I am.”
Unique skills during COVID-19
Mark Shapiro, MD, hospitalist and host of the roundtable and the Explore the Space podcast, also asked the panelists what skills they unexpectedly leveraged during the pandemic. Communication – with colleagues and with the community they serve – was a universal answer among the panelists.
“I learned – really from seeing some of our senior leaders here do it so well – the importance of being visible, particularly at a time when people were not together and more isolated,” Dr. Unaka said. “I think being able to be visible when you can, in order to deliver really complicated or tough news or communicate about uncertainty, for instance. Being here for our residents – many of our interns moved here sight unseen. I think they needed to feel like they had some sense of normalcy and a sense of community. I really learned how important it was to be visible, and available, and how important the little things mattered.”
Dr. Martinez said that worrying about her patients with COVID-19 in the hospital and the uncertainty around the disease kept her up at night. “I think we always have a hard time leaving work at work and getting a good night’s sleep. I just could not let go of worrying about these patients and having terrible insomnia, trying to leave work at work and I couldn’t – even after they were discharged.”
Dr. Shapiro said the skill he most needed to work on during the pandemic was his courage. “I remember the first time I took care of COVID patients. I was scared. I have no problems saying that out loud. That was a scary experience.”
The demeanor of the nurses on his unit, who had already seen patients with COVID-19, helped ground him during those moments and gave him the courage to move forward. “They’d already been doing it and they were the same. Same affect, same jokes, same everything,” he said. “That actually really helped, and I’ve leaned on that every time I’ve been back on our COVID service.”
Importance of mental health
The COVID-19 pandemic has also shined a light on the importance of mental health. “I think it is important to acknowledge that as hospitalists who have been out on the bleeding edge for a year, mental health is critically important, and we know that we face shortages in that space for the public at large and also for our profession,” Dr. Shapiro said.
When asked about what mental health and self-care looks like for her, Dr. Kumar referenced the need for exercise, meditation, and yoga. “My mental health was better knowing that the people closest to me – whether they be colleagues or friends or family – their mental health was also in a good place and they were also in a good place. And that helped to build me up,” she said.
Dr. Unaka called attention to the stigma around mental health, particularly among physicians, and the lack of resources to address the issue. “It’s a real problem,” she said. “I think it’s at a point where we as a profession need to advocate on behalf of each other and on behalf of our trainees. And honestly, I think we need to view mental health as just ‘health’ and stop separating it out in order for us to move to a place where people feel like they can access what they need without feeling shame about it.”
Editor’s note: National Hospitalist Day occurs the first Thursday in March annually, and serves to celebrate the fastest growing specialty in modern medicine and hospitalists’ enduring contributions to the evolving health care landscape. On National Hospitalist Day in 2021, SHM convened a virtual roundtable with a diverse group of hospitalists to discuss skill set, wellness, and other key issues for hospitalists. To listen to the entire roundtable discussion, visit this Explore The Space podcast episode.
A hospitalist isn’t just a physician who happens to work in a hospital. They are medical professionals with a robust skill set that they use both inside and outside the hospital setting. But what skill sets do hospitalists need to become successful in their careers? And what skill sets does a “pluripotent” hospitalist need in their armamentarium?
These were the issues discussed by participants of a virtual roundtable discussion on National Hospitalist Day – March 4, 2021 – as part of a joint effort of the Society of Hospital Medicine and the Explore the Space podcast.
Maylyn S. Martinez, MD, clinician-researcher and clinical associate at the University of Chicago, sees her hospitalist and research skill sets as two “buckets” of skills she can sort through, with diagnostic, knowledge-based care coordination, and interpersonal skills as lanes where she can focus and improve. “I’m always trying to work in, and sharpen, and find ways to get better at something in each of those every day,” she said.
For Anika Kumar, MD, FHM, pediatric editor of the Hospitalist and clinical assistant professor of pediatrics at the Cleveland Clinic Lerner College of Medicine, much of her work is focused on problem solving. “I approach that as: ‘How do I come up with my differential diagnosis, and how do I diagnose the patient?’ I think that the lanes are a little bit different, but there is some overlap.”
Adaptability is another important part of the skill set for the hospitalist, Ndidi Unaka, MD, MEd, associate professor in the division of hospital medicine at Cincinnati Children’s Hospital Medical Center, said during the discussion. “I think we all really value teamwork, and we take on the role of being the coordinator and making sure things are getting done in a seamless and thoughtful manner. Communicating with families, communicating with our research team, communicating with primary care physicians. I think that is something we’re very used to doing, and I think we do it well. I think we don’t shy away from difficult conversations with consultants. And I think that’s what makes being a hospitalist so amazing.”
Achieving wellness as a hospitalist
Another topic discussed during the roundtable was “comprehensive care for the hospitalist” and how they can achieve a sense of wellness for themselves. Gurpreet Dhaliwal, MD, clinician-educator and professor of medicine at the University of California, San Francisco, said long-term satisfaction in one’s career is less about compensation and more about autonomy, mastery, and purpose.
“Autonomy is shrinking a little bit in health care. But if we connect to our purpose – ‘what are we doing here and how do we connect?’ – it’s either learning about patients and their stories, being with a team of people that you work with, that really builds that purpose,” he said.
Regarding mastery, there’s “tremendous joy if you’re in an environment where people value your mastery, whether it is working in a team or communicating or diagnosing or doing a procedure. If you think of setting up the work environment and those things are in place, I think a lot of wellness can actually happen at work, even though another component, of course, is balancing your life outside of work,” Dr. Dhaliwal said.
This may seem out of reach during COVID-19, but wellness is still achievable during the pandemic, Dr. Martinez said. Her time is spent 75% as a researcher and 25% as a clinician, which is her ideal balance. “I enjoy doing my research, doing my own statistics and writing grants and just learning about this problem that I’ve developed an interest in,” she said. “I just think that’s an important piece for people to focus on as far as health care for the hospitalist, is that there’s no no-one-size-fits-all, that’s for sure.”
Dr. Kumar noted that her clinical time gives her energy for nonclinical work. “I love my clinical time. It’s one of my favorite things that I do,” she said. Although she is tired at the end of the week, “I feel like I am not only giving back to my patients and my team, but I’m also giving back to myself and reminding myself why it is I do what I do every day,” she said.
Wellness for Dr. Unaka meant remembering what drew her to medicine. “It was definitely the opportunity to build strong relationships with patients and families,” she said. While these encounters can sometimes be heavy and stay with a hospitalist, “the fact that we’re in it with them is something that gives a lot of us purpose. I think that when I reflect on all of those things, I’m so happy that I’m in the role that I am.”
Unique skills during COVID-19
Mark Shapiro, MD, hospitalist and host of the roundtable and the Explore the Space podcast, also asked the panelists what skills they unexpectedly leveraged during the pandemic. Communication – with colleagues and with the community they serve – was a universal answer among the panelists.
“I learned – really from seeing some of our senior leaders here do it so well – the importance of being visible, particularly at a time when people were not together and more isolated,” Dr. Unaka said. “I think being able to be visible when you can, in order to deliver really complicated or tough news or communicate about uncertainty, for instance. Being here for our residents – many of our interns moved here sight unseen. I think they needed to feel like they had some sense of normalcy and a sense of community. I really learned how important it was to be visible, and available, and how important the little things mattered.”
Dr. Martinez said that worrying about her patients with COVID-19 in the hospital and the uncertainty around the disease kept her up at night. “I think we always have a hard time leaving work at work and getting a good night’s sleep. I just could not let go of worrying about these patients and having terrible insomnia, trying to leave work at work and I couldn’t – even after they were discharged.”
Dr. Shapiro said the skill he most needed to work on during the pandemic was his courage. “I remember the first time I took care of COVID patients. I was scared. I have no problems saying that out loud. That was a scary experience.”
The demeanor of the nurses on his unit, who had already seen patients with COVID-19, helped ground him during those moments and gave him the courage to move forward. “They’d already been doing it and they were the same. Same affect, same jokes, same everything,” he said. “That actually really helped, and I’ve leaned on that every time I’ve been back on our COVID service.”
Importance of mental health
The COVID-19 pandemic has also shined a light on the importance of mental health. “I think it is important to acknowledge that as hospitalists who have been out on the bleeding edge for a year, mental health is critically important, and we know that we face shortages in that space for the public at large and also for our profession,” Dr. Shapiro said.
When asked about what mental health and self-care looks like for her, Dr. Kumar referenced the need for exercise, meditation, and yoga. “My mental health was better knowing that the people closest to me – whether they be colleagues or friends or family – their mental health was also in a good place and they were also in a good place. And that helped to build me up,” she said.
Dr. Unaka called attention to the stigma around mental health, particularly among physicians, and the lack of resources to address the issue. “It’s a real problem,” she said. “I think it’s at a point where we as a profession need to advocate on behalf of each other and on behalf of our trainees. And honestly, I think we need to view mental health as just ‘health’ and stop separating it out in order for us to move to a place where people feel like they can access what they need without feeling shame about it.”
Editor’s note: National Hospitalist Day occurs the first Thursday in March annually, and serves to celebrate the fastest growing specialty in modern medicine and hospitalists’ enduring contributions to the evolving health care landscape. On National Hospitalist Day in 2021, SHM convened a virtual roundtable with a diverse group of hospitalists to discuss skill set, wellness, and other key issues for hospitalists. To listen to the entire roundtable discussion, visit this Explore The Space podcast episode.
A hospitalist isn’t just a physician who happens to work in a hospital. They are medical professionals with a robust skill set that they use both inside and outside the hospital setting. But what skill sets do hospitalists need to become successful in their careers? And what skill sets does a “pluripotent” hospitalist need in their armamentarium?
These were the issues discussed by participants of a virtual roundtable discussion on National Hospitalist Day – March 4, 2021 – as part of a joint effort of the Society of Hospital Medicine and the Explore the Space podcast.
Maylyn S. Martinez, MD, clinician-researcher and clinical associate at the University of Chicago, sees her hospitalist and research skill sets as two “buckets” of skills she can sort through, with diagnostic, knowledge-based care coordination, and interpersonal skills as lanes where she can focus and improve. “I’m always trying to work in, and sharpen, and find ways to get better at something in each of those every day,” she said.
For Anika Kumar, MD, FHM, pediatric editor of the Hospitalist and clinical assistant professor of pediatrics at the Cleveland Clinic Lerner College of Medicine, much of her work is focused on problem solving. “I approach that as: ‘How do I come up with my differential diagnosis, and how do I diagnose the patient?’ I think that the lanes are a little bit different, but there is some overlap.”
Adaptability is another important part of the skill set for the hospitalist, Ndidi Unaka, MD, MEd, associate professor in the division of hospital medicine at Cincinnati Children’s Hospital Medical Center, said during the discussion. “I think we all really value teamwork, and we take on the role of being the coordinator and making sure things are getting done in a seamless and thoughtful manner. Communicating with families, communicating with our research team, communicating with primary care physicians. I think that is something we’re very used to doing, and I think we do it well. I think we don’t shy away from difficult conversations with consultants. And I think that’s what makes being a hospitalist so amazing.”
Achieving wellness as a hospitalist
Another topic discussed during the roundtable was “comprehensive care for the hospitalist” and how they can achieve a sense of wellness for themselves. Gurpreet Dhaliwal, MD, clinician-educator and professor of medicine at the University of California, San Francisco, said long-term satisfaction in one’s career is less about compensation and more about autonomy, mastery, and purpose.
“Autonomy is shrinking a little bit in health care. But if we connect to our purpose – ‘what are we doing here and how do we connect?’ – it’s either learning about patients and their stories, being with a team of people that you work with, that really builds that purpose,” he said.
Regarding mastery, there’s “tremendous joy if you’re in an environment where people value your mastery, whether it is working in a team or communicating or diagnosing or doing a procedure. If you think of setting up the work environment and those things are in place, I think a lot of wellness can actually happen at work, even though another component, of course, is balancing your life outside of work,” Dr. Dhaliwal said.
This may seem out of reach during COVID-19, but wellness is still achievable during the pandemic, Dr. Martinez said. Her time is spent 75% as a researcher and 25% as a clinician, which is her ideal balance. “I enjoy doing my research, doing my own statistics and writing grants and just learning about this problem that I’ve developed an interest in,” she said. “I just think that’s an important piece for people to focus on as far as health care for the hospitalist, is that there’s no no-one-size-fits-all, that’s for sure.”
Dr. Kumar noted that her clinical time gives her energy for nonclinical work. “I love my clinical time. It’s one of my favorite things that I do,” she said. Although she is tired at the end of the week, “I feel like I am not only giving back to my patients and my team, but I’m also giving back to myself and reminding myself why it is I do what I do every day,” she said.
Wellness for Dr. Unaka meant remembering what drew her to medicine. “It was definitely the opportunity to build strong relationships with patients and families,” she said. While these encounters can sometimes be heavy and stay with a hospitalist, “the fact that we’re in it with them is something that gives a lot of us purpose. I think that when I reflect on all of those things, I’m so happy that I’m in the role that I am.”
Unique skills during COVID-19
Mark Shapiro, MD, hospitalist and host of the roundtable and the Explore the Space podcast, also asked the panelists what skills they unexpectedly leveraged during the pandemic. Communication – with colleagues and with the community they serve – was a universal answer among the panelists.
“I learned – really from seeing some of our senior leaders here do it so well – the importance of being visible, particularly at a time when people were not together and more isolated,” Dr. Unaka said. “I think being able to be visible when you can, in order to deliver really complicated or tough news or communicate about uncertainty, for instance. Being here for our residents – many of our interns moved here sight unseen. I think they needed to feel like they had some sense of normalcy and a sense of community. I really learned how important it was to be visible, and available, and how important the little things mattered.”
Dr. Martinez said that worrying about her patients with COVID-19 in the hospital and the uncertainty around the disease kept her up at night. “I think we always have a hard time leaving work at work and getting a good night’s sleep. I just could not let go of worrying about these patients and having terrible insomnia, trying to leave work at work and I couldn’t – even after they were discharged.”
Dr. Shapiro said the skill he most needed to work on during the pandemic was his courage. “I remember the first time I took care of COVID patients. I was scared. I have no problems saying that out loud. That was a scary experience.”
The demeanor of the nurses on his unit, who had already seen patients with COVID-19, helped ground him during those moments and gave him the courage to move forward. “They’d already been doing it and they were the same. Same affect, same jokes, same everything,” he said. “That actually really helped, and I’ve leaned on that every time I’ve been back on our COVID service.”
Importance of mental health
The COVID-19 pandemic has also shined a light on the importance of mental health. “I think it is important to acknowledge that as hospitalists who have been out on the bleeding edge for a year, mental health is critically important, and we know that we face shortages in that space for the public at large and also for our profession,” Dr. Shapiro said.
When asked about what mental health and self-care looks like for her, Dr. Kumar referenced the need for exercise, meditation, and yoga. “My mental health was better knowing that the people closest to me – whether they be colleagues or friends or family – their mental health was also in a good place and they were also in a good place. And that helped to build me up,” she said.
Dr. Unaka called attention to the stigma around mental health, particularly among physicians, and the lack of resources to address the issue. “It’s a real problem,” she said. “I think it’s at a point where we as a profession need to advocate on behalf of each other and on behalf of our trainees. And honestly, I think we need to view mental health as just ‘health’ and stop separating it out in order for us to move to a place where people feel like they can access what they need without feeling shame about it.”
Virtual is the new real
Why did we fall short on maximizing telehealth’s value in the COVID-19 pandemic?
The COVID-19 pandemic catalyzed the transformation of Internet-based, remotely accessible innovative technologies. Internet-based customer service delivery technology was rapidly adopted and utilized by several services industries, but health care systems in most of the countries across the world faced unique challenges in adopting the technology for the delivery of health care services. The health care ecosystem of the United States was not immune to such challenges, and several significant barriers surfaced while the pandemic was underway.
Complexly structured, fragmented, unprepared, and overly burnt-out health systems in the United States arguably have fallen short of maximizing the value of telehealth in delivering safe, easily accessible, comprehensive, and cost-effective health care services. In this essay, we examine the reasons for such a suboptimal performance and discuss a few important strategies that may be useful in maximizing the value of telehealth value in several, appropriate health care services.
Hospitals and telehealth
Are hospitalists preparing ourselves “not to see” patients in a hospital-based health care delivery setting? If you have not yet started yet, now may be the right time! Yes, a certain percentage of doctor-patient encounters in hospital settings will remain virtual forever.
A well-established telehealth infrastructure is rarely found in most U.S. hospitals, although the COVID-19 pandemic has unexpectedly boosted the rapid growth of telehealth in the country.1 Public health emergency declarations in the United States in the face of the COVID-19 crisis have facilitated two important initiatives to restore health care delivery amidst formal and informal lockdowns that brought states to a grinding halt. These extend from expansion of virtual services, including telehealth, virtual check-ins, and e-visits, to the decision by the Department of Health & Human Services Office of Civil Rights to exercise enforcement discretion and waive penalties for the use of relatively inexpensive, non–public-facing mobile and other audiovisual technology tools.2
Hospital-based care in the United States taps nearly 33% of national health expenditure. An additional 30% of national health expenditure that is related to physicians, prescriptions, and other facilities is indirectly influenced by care delivered at health care facilities.3 Studies show that about 20% of ED visits could potentially be avoided via virtual urgent care offerings.4 A rapidly changing health care ecosystem is proving formidable for most hospital systems, and a test for their resilience and agility. Not just the implementation of telehealth is challenging, but getting it right is the key success factor.
Hospital-based telehealth
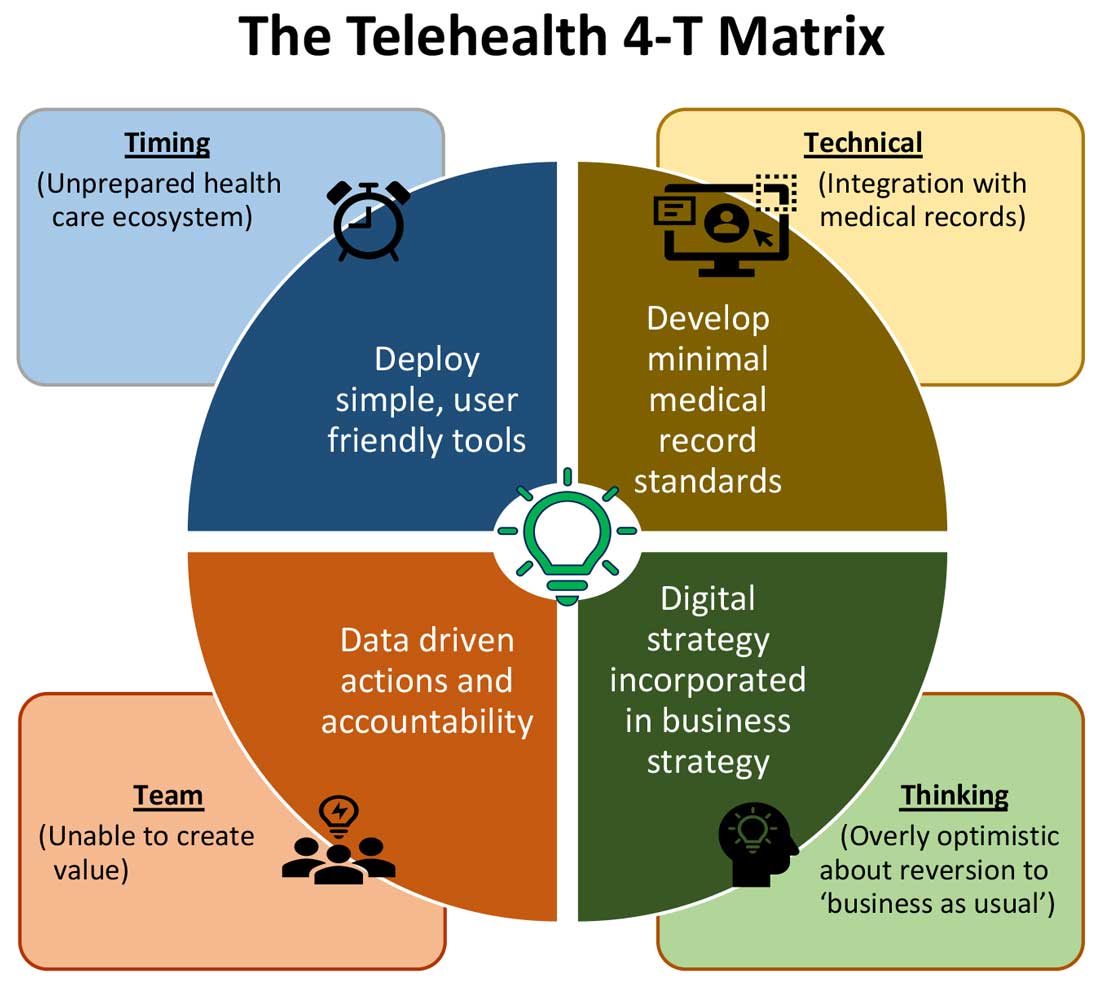
Expansion of telehealth coverage by the Centers for Medicare & Medicaid Services and most commercial payers did not quite ride the pandemic-induced momentum across the care continuum. Hospitals are lagging far behind ambulatory care in implementing telehealth. As illustrated in the “4-T Matrix” (see graphic) we would like to examine four key reasons for such a sluggish initial uptake and try to propose four important strategies that may help us to maximize the value created by telehealth technologies.
1. Timing
The health care system has always lagged far behind other service industries in terms of technology adaptation. Because of the unique nature of health care services, face-to-face interaction supersedes all other forms of communication. A rapidly evolving pandemic was not matched by simultaneous technology education for patients and providers. The enormous choice of hard-to-navigate telehealth tools; time and labor-intensive implementation; and uncertainty around payer, policy, and regulatory expectations might have precluded providers from the rapid adoption of telehealth in the hospital setting. Patients’ specific characteristics, such as the absence of technology-centered education, information, age, comorbidities, lack of technical literacy, and dependency on caregivers contributed to the suboptimal response from patients and families.
Deploying simple, ubiquitous, user-friendly, and technologically less challenging telehealth solutions may be a better approach to increase the adoption of such solutions by providers and patients. Hospitals need to develop and distribute telehealth user guides in all possible modes of communication. Provider-centric in-service sessions, workshops, and live support by “superuser teams” often work well in reducing end-user resistance.
2. Technical
Current electronic medical records vary widely in their features and offerings, and their ability to interact with third-party software and platforms. Dissatisfaction of end users with EMRs is well known, as is their likely relationship to burnout. Recent research continues to show a strong relationship between EMR usability and the odds of burnout among physicians.5 In the current climate, administrators and health informaticists have the responsibility to avoid adding increased burdens to end users.
Another issue is the limited connectivity in many remote/rural areas that would impact implementation of telehealth platforms. Studies indicate that 33% of rural Americans lack access to high-speed broadband Internet to support video visits.6 The recent successful implementation of telehealth across 530 providers in 75 ambulatory practices operated by Munson Healthcare, a rural health system in northern Michigan, sheds light on the technology’s enormous potential in providing safe access to rural populations.6,7
Privacy and safety of patient data is of paramount importance. According to a national poll on healthy aging by the University of Michigan in May 2019, targeting older adults, 47% of survey responders expressed difficulty using technology and 49% of survey responders were concerned about privacy.8 Use of certification and other tools offered by the Office of the National Coordinator for Health Information Technology would help reassure users, and the ability to capture and share images between providers would be of immense benefit in facilitating e-consults.
The need of the hour is redesigned work flow, to help providers adopt and use virtual care/telehealth efficiently. Work flow redesign must be coupled with technological advances to allow seamless integration of third-party telehealth platforms into existing EMR systems or built directly into EMRs. Use of quality metrics and analytical tools specific to telehealth would help measure the technology’s impact on patient care, outcomes, and end-user/provider experience.
3. Teams and training
Outcomes of health care interventions are often determined by the effectiveness of teams. Irrespective of how robust health care systems may have been initially, rapidly spreading infectious diseases like COVID-19 can quickly derail the system, bringing the workforce and patients to a breaking point.5 Decentralized, uncoordinated, and siloed efforts by individual teams across the care continuum were contributing factors for the partial success of telehealth care delivery pathways. The hospital systems with telehealth-ready teams at the start of the COVID-19 pandemic were so rare that the knowledge and technical training opportunities for innovators grew severalfold during the pandemic.
As per the American Medical Association, telehealth success is massively dependent on building the right team. Core, leadership, advisory, and implementation teams comprised of clinical representatives, end users, administrative personnel, executive members of the organization, technical experts, and payment/policy experts should be put together before implementing a telehealth strategy.9 Seamless integration of hospital-based care with ambulatory care via a telehealth platform is only complete when care managers are trained and deployed to fulfill the needs of a diverse group of patients. Deriving overall value from telehealth is only possible when there is a skill development, training and mentoring team put in place.
4. Thinking
In most U.S. hospitals, inpatient health care is equally distributed between nonprocedure and procedure-based services. Hospitals resorted to suspension of nonemergent procedures to mitigate the risk of spreading COVID-19. This was further compounded by many patients’ self-selection to defer care, an abrupt reduction in the influx of patients from the referral base because of suboptimally operating ambulatory care services, leading to low hospital occupancy.
Hospitals across the nation have gone through a massive short-term financial crunch and unfavorable cash-flow forecast, which prompted a paradoxical work-force reduction. While some argue that it may be akin to strategic myopia, the authors believed that such a response is strategically imperative to keep the hospital afloat. It is reasonable to attribute the paucity of innovation to constrained resources, and health systems are simply staying overly optimistic about “weathering the storm” and reverting soon to “business as usual.” The technological framework necessary for deploying a telehealth solution often comes with a price. Financially challenged hospital systems rarely exercise any capital-intensive activities. By contrast, telehealth adoption by ambulatory care can result in quicker resumption of patient care in community settings. A lack of operational and infrastructure synchrony between ambulatory and in-hospital systems has failed to capture telehealth-driven inpatient volume. For example, direct admissions from ambulatory telehealth referrals was a missed opportunity in several places. Referrals for labs, diagnostic tests, and other allied services could have helped hospitals offset their fixed costs. Similarly, work flows related to discharge and postdischarge follow up rarely embrace telehealth tools or telehealth care pathways. A brisk change in the health care ecosystem is partly responsible for this.
Digital strategy needs to be incorporated into business strategy. For the reasons already discussed, telehealth technology is not a “nice to have” anymore, but a “must have.” At present, providers are of the opinion that about 20% of their patient services can be delivered via a telehealth platform. Similar trends are observed among patients, as a new modality of access to care is increasingly beneficial to them. Telehealth must be incorporated in standardized hospital work flows. Use of telehealth for preoperative clearance will greatly minimize same-day surgery cancellations. Given the potential shortage in resources, telehealth adoption for inpatient consultations will help systems conserve personal protective equipment, minimize the risk of staff exposure to COVID-19, and improve efficiency.
Digital strategy also prompts the reengineering of care delivery.10 Excessive and unused physical capacity can be converted into digital care hubs. Health maintenance, prevention, health promotion, health education, and chronic disease management not only can serve a variety of patient groups but can also help address the “last-mile problem” in health care. A successful digital strategy usually has three important components – Commitment: Hospital leadership is committed to include digital transformation as a strategic objective; Cost: Digital strategy is added as a line item in the budget; and Control: Measurable metrics are put in place to monitor the performance, impact, and influence of the digital strategy.
Conclusion
For decades, most U.S. health systems occupied the periphery of technological transformation when compared to the rest of the service industry. While most health systems took a heroic approach to the adoption of telehealth during COVID-19, despite being unprepared, the need for a systematic telehealth deployment is far from being adequately fulfilled. The COVID-19 pandemic brought permanent changes to several business disciplines globally. Given the impact of the pandemic on the health and overall wellbeing of American society, the U.S. health care industry must leave no stone unturned in its quest for transformation.
Dr. Lingisetty is a hospitalist and physician executive at Baptist Health System, Little Rock, Ark, and is cofounder/president of SHM’s Arkansas chapter. Dr. Prasad is medical director of care management and a hospitalist at Advocate Aurora Health in Milwaukee. He is cochair of SHM’s IT Special Interest Group, sits on the HQPS committee, and is president of SHM’s Wisconsin chapter. Dr. Palabindala is the medical director, utilization management, and physician advisory services at the University of Mississippi Medical Center and an associate professor of medicine and academic hospitalist at the University of Mississippi, both in Jackson.
References
1. Finnegan M. “Telehealth booms amid COVID-19 crisis.” Computerworld. 2020 Apr 27. www.computerworld.com/article/3540315/telehealth-booms-amid-covid-19-crisis-virtual-care-is-here-to-stay.html. Accessed 2020 Sep 12.
2. Department of Health & Human Services. “OCR Announces Notification of Enforcement Discretion for Telehealth Remote Communications During the COVID-19 Nationwide Public Health Emergency.” 2020 Mar 17. www.hhs.gov/about/news/2020/03/17/ocr-announces-notification-of-enforcement-discretion-for-telehealth-remote-communications-during-the-covid-19.html. Accessed 2020 Sep 12.
3. National Center for Health Statistics. “Health Expenditures.” www.cdc.gov/nchs/fastats/health-expenditures.htm. Accessed 2020 Sep 12.
4. Bestsennyy O et al. “Telehealth: A post–COVID-19 reality?” McKinsey & Company. 2020 May 29. www.mckinsey.com/industries/healthcare-systems-and-services/our-insights/telehealth-a-quarter-trillion-dollar-post-covid-19-reality. Accessed 2020 Sep 12.
5. Melnick ER et al. The Association Between Perceived Electronic Health Record Usability and Professional Burnout Among U.S. Physicians. Mayo Clin Proc. 2020 March;95(3):476-87.
6. Hirko KA et al. Telehealth in response to the COVID-19 pandemic: Implications for rural health disparities. J Am Med Inform Assoc. 2020 Nov;27(11):1816-8. .
7. American Academy of Family Physicians. “Study Examines Telehealth, Rural Disparities in Pandemic.” 2020 July 30. www.aafp.org/news/practice-professional-issues/20200730ruraltelehealth.html. Accessed 2020 Dec 15.
8. Kurlander J et al. “Virtual Visits: Telehealth and Older Adults.” National Poll on Healthy Aging. 2019 Oct. hdl.handle.net/2027.42/151376.
9. American Medical Association. Telehealth Implementation Playbook. 2019. www.ama-assn.org/system/files/2020-04/ama-telehealth-implementation-playbook.pdf.
10. Smith AC et al. Telehealth for global emergencies: Implications for coronavirus disease 2019 (COVID-19). J Telemed Telecare. 2020 Jun;26(5):309-13.
Why did we fall short on maximizing telehealth’s value in the COVID-19 pandemic?
Why did we fall short on maximizing telehealth’s value in the COVID-19 pandemic?
The COVID-19 pandemic catalyzed the transformation of Internet-based, remotely accessible innovative technologies. Internet-based customer service delivery technology was rapidly adopted and utilized by several services industries, but health care systems in most of the countries across the world faced unique challenges in adopting the technology for the delivery of health care services. The health care ecosystem of the United States was not immune to such challenges, and several significant barriers surfaced while the pandemic was underway.
Complexly structured, fragmented, unprepared, and overly burnt-out health systems in the United States arguably have fallen short of maximizing the value of telehealth in delivering safe, easily accessible, comprehensive, and cost-effective health care services. In this essay, we examine the reasons for such a suboptimal performance and discuss a few important strategies that may be useful in maximizing the value of telehealth value in several, appropriate health care services.
Hospitals and telehealth
Are hospitalists preparing ourselves “not to see” patients in a hospital-based health care delivery setting? If you have not yet started yet, now may be the right time! Yes, a certain percentage of doctor-patient encounters in hospital settings will remain virtual forever.
A well-established telehealth infrastructure is rarely found in most U.S. hospitals, although the COVID-19 pandemic has unexpectedly boosted the rapid growth of telehealth in the country.1 Public health emergency declarations in the United States in the face of the COVID-19 crisis have facilitated two important initiatives to restore health care delivery amidst formal and informal lockdowns that brought states to a grinding halt. These extend from expansion of virtual services, including telehealth, virtual check-ins, and e-visits, to the decision by the Department of Health & Human Services Office of Civil Rights to exercise enforcement discretion and waive penalties for the use of relatively inexpensive, non–public-facing mobile and other audiovisual technology tools.2
Hospital-based care in the United States taps nearly 33% of national health expenditure. An additional 30% of national health expenditure that is related to physicians, prescriptions, and other facilities is indirectly influenced by care delivered at health care facilities.3 Studies show that about 20% of ED visits could potentially be avoided via virtual urgent care offerings.4 A rapidly changing health care ecosystem is proving formidable for most hospital systems, and a test for their resilience and agility. Not just the implementation of telehealth is challenging, but getting it right is the key success factor.
Hospital-based telehealth
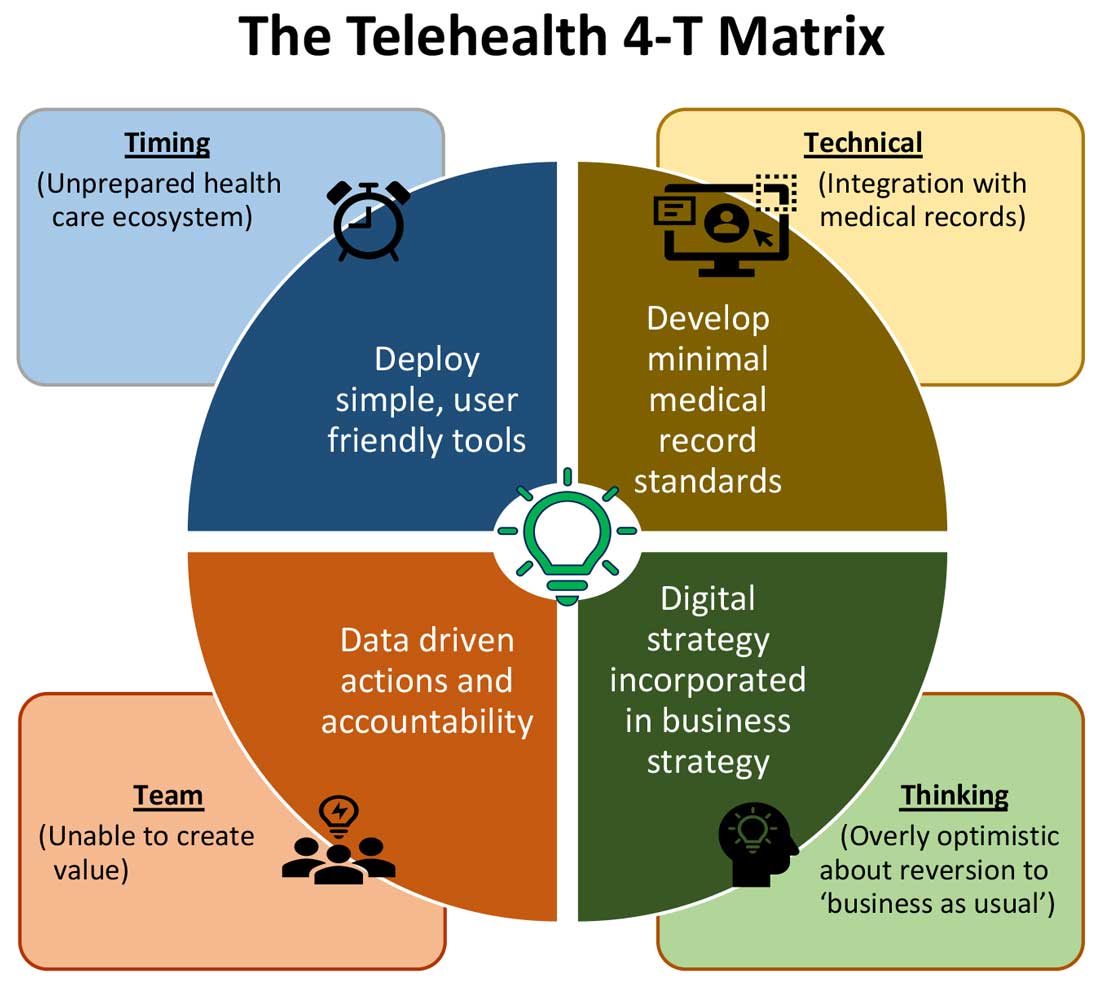
Expansion of telehealth coverage by the Centers for Medicare & Medicaid Services and most commercial payers did not quite ride the pandemic-induced momentum across the care continuum. Hospitals are lagging far behind ambulatory care in implementing telehealth. As illustrated in the “4-T Matrix” (see graphic) we would like to examine four key reasons for such a sluggish initial uptake and try to propose four important strategies that may help us to maximize the value created by telehealth technologies.
1. Timing
The health care system has always lagged far behind other service industries in terms of technology adaptation. Because of the unique nature of health care services, face-to-face interaction supersedes all other forms of communication. A rapidly evolving pandemic was not matched by simultaneous technology education for patients and providers. The enormous choice of hard-to-navigate telehealth tools; time and labor-intensive implementation; and uncertainty around payer, policy, and regulatory expectations might have precluded providers from the rapid adoption of telehealth in the hospital setting. Patients’ specific characteristics, such as the absence of technology-centered education, information, age, comorbidities, lack of technical literacy, and dependency on caregivers contributed to the suboptimal response from patients and families.
Deploying simple, ubiquitous, user-friendly, and technologically less challenging telehealth solutions may be a better approach to increase the adoption of such solutions by providers and patients. Hospitals need to develop and distribute telehealth user guides in all possible modes of communication. Provider-centric in-service sessions, workshops, and live support by “superuser teams” often work well in reducing end-user resistance.
2. Technical
Current electronic medical records vary widely in their features and offerings, and their ability to interact with third-party software and platforms. Dissatisfaction of end users with EMRs is well known, as is their likely relationship to burnout. Recent research continues to show a strong relationship between EMR usability and the odds of burnout among physicians.5 In the current climate, administrators and health informaticists have the responsibility to avoid adding increased burdens to end users.
Another issue is the limited connectivity in many remote/rural areas that would impact implementation of telehealth platforms. Studies indicate that 33% of rural Americans lack access to high-speed broadband Internet to support video visits.6 The recent successful implementation of telehealth across 530 providers in 75 ambulatory practices operated by Munson Healthcare, a rural health system in northern Michigan, sheds light on the technology’s enormous potential in providing safe access to rural populations.6,7
Privacy and safety of patient data is of paramount importance. According to a national poll on healthy aging by the University of Michigan in May 2019, targeting older adults, 47% of survey responders expressed difficulty using technology and 49% of survey responders were concerned about privacy.8 Use of certification and other tools offered by the Office of the National Coordinator for Health Information Technology would help reassure users, and the ability to capture and share images between providers would be of immense benefit in facilitating e-consults.
The need of the hour is redesigned work flow, to help providers adopt and use virtual care/telehealth efficiently. Work flow redesign must be coupled with technological advances to allow seamless integration of third-party telehealth platforms into existing EMR systems or built directly into EMRs. Use of quality metrics and analytical tools specific to telehealth would help measure the technology’s impact on patient care, outcomes, and end-user/provider experience.
3. Teams and training
Outcomes of health care interventions are often determined by the effectiveness of teams. Irrespective of how robust health care systems may have been initially, rapidly spreading infectious diseases like COVID-19 can quickly derail the system, bringing the workforce and patients to a breaking point.5 Decentralized, uncoordinated, and siloed efforts by individual teams across the care continuum were contributing factors for the partial success of telehealth care delivery pathways. The hospital systems with telehealth-ready teams at the start of the COVID-19 pandemic were so rare that the knowledge and technical training opportunities for innovators grew severalfold during the pandemic.
As per the American Medical Association, telehealth success is massively dependent on building the right team. Core, leadership, advisory, and implementation teams comprised of clinical representatives, end users, administrative personnel, executive members of the organization, technical experts, and payment/policy experts should be put together before implementing a telehealth strategy.9 Seamless integration of hospital-based care with ambulatory care via a telehealth platform is only complete when care managers are trained and deployed to fulfill the needs of a diverse group of patients. Deriving overall value from telehealth is only possible when there is a skill development, training and mentoring team put in place.
4. Thinking
In most U.S. hospitals, inpatient health care is equally distributed between nonprocedure and procedure-based services. Hospitals resorted to suspension of nonemergent procedures to mitigate the risk of spreading COVID-19. This was further compounded by many patients’ self-selection to defer care, an abrupt reduction in the influx of patients from the referral base because of suboptimally operating ambulatory care services, leading to low hospital occupancy.
Hospitals across the nation have gone through a massive short-term financial crunch and unfavorable cash-flow forecast, which prompted a paradoxical work-force reduction. While some argue that it may be akin to strategic myopia, the authors believed that such a response is strategically imperative to keep the hospital afloat. It is reasonable to attribute the paucity of innovation to constrained resources, and health systems are simply staying overly optimistic about “weathering the storm” and reverting soon to “business as usual.” The technological framework necessary for deploying a telehealth solution often comes with a price. Financially challenged hospital systems rarely exercise any capital-intensive activities. By contrast, telehealth adoption by ambulatory care can result in quicker resumption of patient care in community settings. A lack of operational and infrastructure synchrony between ambulatory and in-hospital systems has failed to capture telehealth-driven inpatient volume. For example, direct admissions from ambulatory telehealth referrals was a missed opportunity in several places. Referrals for labs, diagnostic tests, and other allied services could have helped hospitals offset their fixed costs. Similarly, work flows related to discharge and postdischarge follow up rarely embrace telehealth tools or telehealth care pathways. A brisk change in the health care ecosystem is partly responsible for this.
Digital strategy needs to be incorporated into business strategy. For the reasons already discussed, telehealth technology is not a “nice to have” anymore, but a “must have.” At present, providers are of the opinion that about 20% of their patient services can be delivered via a telehealth platform. Similar trends are observed among patients, as a new modality of access to care is increasingly beneficial to them. Telehealth must be incorporated in standardized hospital work flows. Use of telehealth for preoperative clearance will greatly minimize same-day surgery cancellations. Given the potential shortage in resources, telehealth adoption for inpatient consultations will help systems conserve personal protective equipment, minimize the risk of staff exposure to COVID-19, and improve efficiency.
Digital strategy also prompts the reengineering of care delivery.10 Excessive and unused physical capacity can be converted into digital care hubs. Health maintenance, prevention, health promotion, health education, and chronic disease management not only can serve a variety of patient groups but can also help address the “last-mile problem” in health care. A successful digital strategy usually has three important components – Commitment: Hospital leadership is committed to include digital transformation as a strategic objective; Cost: Digital strategy is added as a line item in the budget; and Control: Measurable metrics are put in place to monitor the performance, impact, and influence of the digital strategy.
Conclusion
For decades, most U.S. health systems occupied the periphery of technological transformation when compared to the rest of the service industry. While most health systems took a heroic approach to the adoption of telehealth during COVID-19, despite being unprepared, the need for a systematic telehealth deployment is far from being adequately fulfilled. The COVID-19 pandemic brought permanent changes to several business disciplines globally. Given the impact of the pandemic on the health and overall wellbeing of American society, the U.S. health care industry must leave no stone unturned in its quest for transformation.
Dr. Lingisetty is a hospitalist and physician executive at Baptist Health System, Little Rock, Ark, and is cofounder/president of SHM’s Arkansas chapter. Dr. Prasad is medical director of care management and a hospitalist at Advocate Aurora Health in Milwaukee. He is cochair of SHM’s IT Special Interest Group, sits on the HQPS committee, and is president of SHM’s Wisconsin chapter. Dr. Palabindala is the medical director, utilization management, and physician advisory services at the University of Mississippi Medical Center and an associate professor of medicine and academic hospitalist at the University of Mississippi, both in Jackson.
References
1. Finnegan M. “Telehealth booms amid COVID-19 crisis.” Computerworld. 2020 Apr 27. www.computerworld.com/article/3540315/telehealth-booms-amid-covid-19-crisis-virtual-care-is-here-to-stay.html. Accessed 2020 Sep 12.
2. Department of Health & Human Services. “OCR Announces Notification of Enforcement Discretion for Telehealth Remote Communications During the COVID-19 Nationwide Public Health Emergency.” 2020 Mar 17. www.hhs.gov/about/news/2020/03/17/ocr-announces-notification-of-enforcement-discretion-for-telehealth-remote-communications-during-the-covid-19.html. Accessed 2020 Sep 12.
3. National Center for Health Statistics. “Health Expenditures.” www.cdc.gov/nchs/fastats/health-expenditures.htm. Accessed 2020 Sep 12.
4. Bestsennyy O et al. “Telehealth: A post–COVID-19 reality?” McKinsey & Company. 2020 May 29. www.mckinsey.com/industries/healthcare-systems-and-services/our-insights/telehealth-a-quarter-trillion-dollar-post-covid-19-reality. Accessed 2020 Sep 12.
5. Melnick ER et al. The Association Between Perceived Electronic Health Record Usability and Professional Burnout Among U.S. Physicians. Mayo Clin Proc. 2020 March;95(3):476-87.
6. Hirko KA et al. Telehealth in response to the COVID-19 pandemic: Implications for rural health disparities. J Am Med Inform Assoc. 2020 Nov;27(11):1816-8. .
7. American Academy of Family Physicians. “Study Examines Telehealth, Rural Disparities in Pandemic.” 2020 July 30. www.aafp.org/news/practice-professional-issues/20200730ruraltelehealth.html. Accessed 2020 Dec 15.
8. Kurlander J et al. “Virtual Visits: Telehealth and Older Adults.” National Poll on Healthy Aging. 2019 Oct. hdl.handle.net/2027.42/151376.
9. American Medical Association. Telehealth Implementation Playbook. 2019. www.ama-assn.org/system/files/2020-04/ama-telehealth-implementation-playbook.pdf.
10. Smith AC et al. Telehealth for global emergencies: Implications for coronavirus disease 2019 (COVID-19). J Telemed Telecare. 2020 Jun;26(5):309-13.
The COVID-19 pandemic catalyzed the transformation of Internet-based, remotely accessible innovative technologies. Internet-based customer service delivery technology was rapidly adopted and utilized by several services industries, but health care systems in most of the countries across the world faced unique challenges in adopting the technology for the delivery of health care services. The health care ecosystem of the United States was not immune to such challenges, and several significant barriers surfaced while the pandemic was underway.
Complexly structured, fragmented, unprepared, and overly burnt-out health systems in the United States arguably have fallen short of maximizing the value of telehealth in delivering safe, easily accessible, comprehensive, and cost-effective health care services. In this essay, we examine the reasons for such a suboptimal performance and discuss a few important strategies that may be useful in maximizing the value of telehealth value in several, appropriate health care services.
Hospitals and telehealth
Are hospitalists preparing ourselves “not to see” patients in a hospital-based health care delivery setting? If you have not yet started yet, now may be the right time! Yes, a certain percentage of doctor-patient encounters in hospital settings will remain virtual forever.
A well-established telehealth infrastructure is rarely found in most U.S. hospitals, although the COVID-19 pandemic has unexpectedly boosted the rapid growth of telehealth in the country.1 Public health emergency declarations in the United States in the face of the COVID-19 crisis have facilitated two important initiatives to restore health care delivery amidst formal and informal lockdowns that brought states to a grinding halt. These extend from expansion of virtual services, including telehealth, virtual check-ins, and e-visits, to the decision by the Department of Health & Human Services Office of Civil Rights to exercise enforcement discretion and waive penalties for the use of relatively inexpensive, non–public-facing mobile and other audiovisual technology tools.2
Hospital-based care in the United States taps nearly 33% of national health expenditure. An additional 30% of national health expenditure that is related to physicians, prescriptions, and other facilities is indirectly influenced by care delivered at health care facilities.3 Studies show that about 20% of ED visits could potentially be avoided via virtual urgent care offerings.4 A rapidly changing health care ecosystem is proving formidable for most hospital systems, and a test for their resilience and agility. Not just the implementation of telehealth is challenging, but getting it right is the key success factor.
Hospital-based telehealth
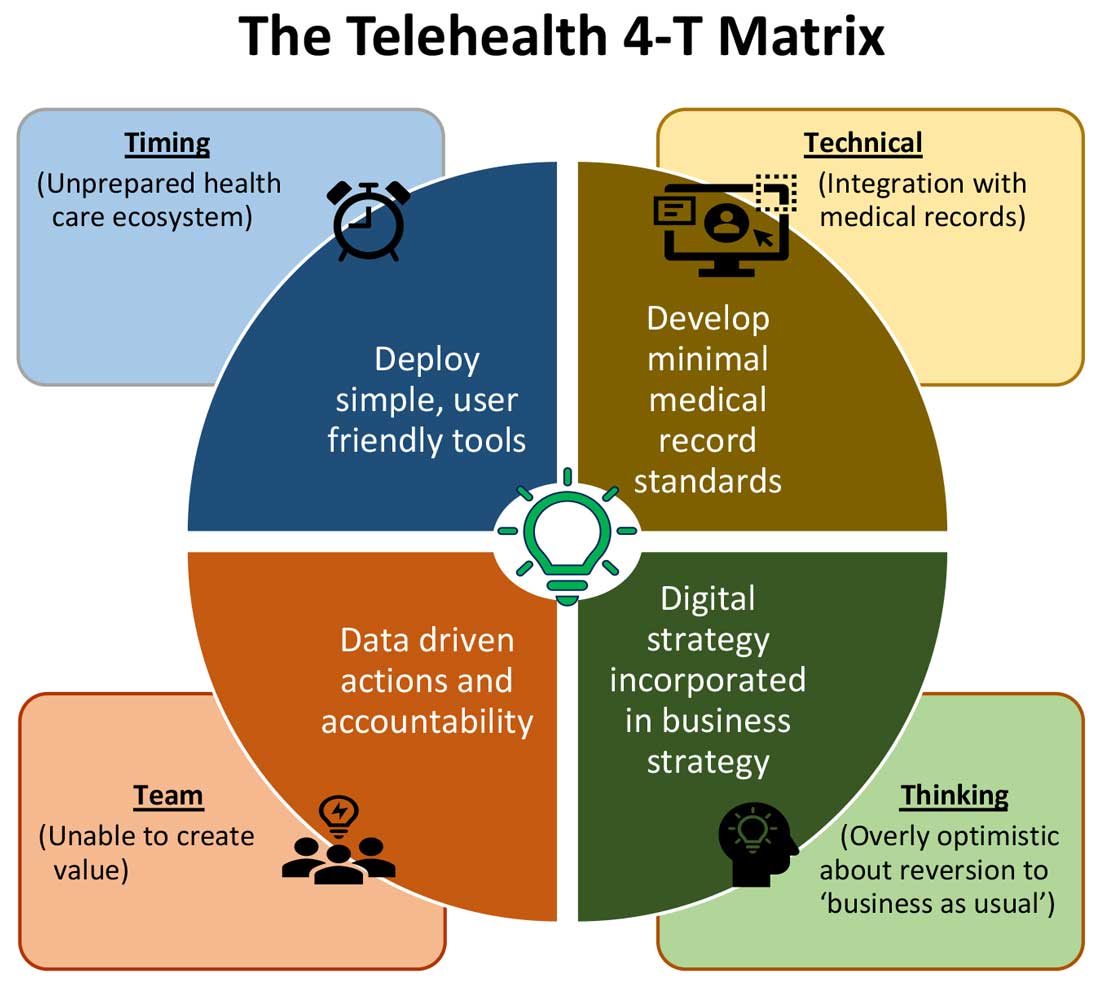
Expansion of telehealth coverage by the Centers for Medicare & Medicaid Services and most commercial payers did not quite ride the pandemic-induced momentum across the care continuum. Hospitals are lagging far behind ambulatory care in implementing telehealth. As illustrated in the “4-T Matrix” (see graphic) we would like to examine four key reasons for such a sluggish initial uptake and try to propose four important strategies that may help us to maximize the value created by telehealth technologies.
1. Timing
The health care system has always lagged far behind other service industries in terms of technology adaptation. Because of the unique nature of health care services, face-to-face interaction supersedes all other forms of communication. A rapidly evolving pandemic was not matched by simultaneous technology education for patients and providers. The enormous choice of hard-to-navigate telehealth tools; time and labor-intensive implementation; and uncertainty around payer, policy, and regulatory expectations might have precluded providers from the rapid adoption of telehealth in the hospital setting. Patients’ specific characteristics, such as the absence of technology-centered education, information, age, comorbidities, lack of technical literacy, and dependency on caregivers contributed to the suboptimal response from patients and families.
Deploying simple, ubiquitous, user-friendly, and technologically less challenging telehealth solutions may be a better approach to increase the adoption of such solutions by providers and patients. Hospitals need to develop and distribute telehealth user guides in all possible modes of communication. Provider-centric in-service sessions, workshops, and live support by “superuser teams” often work well in reducing end-user resistance.
2. Technical
Current electronic medical records vary widely in their features and offerings, and their ability to interact with third-party software and platforms. Dissatisfaction of end users with EMRs is well known, as is their likely relationship to burnout. Recent research continues to show a strong relationship between EMR usability and the odds of burnout among physicians.5 In the current climate, administrators and health informaticists have the responsibility to avoid adding increased burdens to end users.
Another issue is the limited connectivity in many remote/rural areas that would impact implementation of telehealth platforms. Studies indicate that 33% of rural Americans lack access to high-speed broadband Internet to support video visits.6 The recent successful implementation of telehealth across 530 providers in 75 ambulatory practices operated by Munson Healthcare, a rural health system in northern Michigan, sheds light on the technology’s enormous potential in providing safe access to rural populations.6,7
Privacy and safety of patient data is of paramount importance. According to a national poll on healthy aging by the University of Michigan in May 2019, targeting older adults, 47% of survey responders expressed difficulty using technology and 49% of survey responders were concerned about privacy.8 Use of certification and other tools offered by the Office of the National Coordinator for Health Information Technology would help reassure users, and the ability to capture and share images between providers would be of immense benefit in facilitating e-consults.
The need of the hour is redesigned work flow, to help providers adopt and use virtual care/telehealth efficiently. Work flow redesign must be coupled with technological advances to allow seamless integration of third-party telehealth platforms into existing EMR systems or built directly into EMRs. Use of quality metrics and analytical tools specific to telehealth would help measure the technology’s impact on patient care, outcomes, and end-user/provider experience.
3. Teams and training
Outcomes of health care interventions are often determined by the effectiveness of teams. Irrespective of how robust health care systems may have been initially, rapidly spreading infectious diseases like COVID-19 can quickly derail the system, bringing the workforce and patients to a breaking point.5 Decentralized, uncoordinated, and siloed efforts by individual teams across the care continuum were contributing factors for the partial success of telehealth care delivery pathways. The hospital systems with telehealth-ready teams at the start of the COVID-19 pandemic were so rare that the knowledge and technical training opportunities for innovators grew severalfold during the pandemic.
As per the American Medical Association, telehealth success is massively dependent on building the right team. Core, leadership, advisory, and implementation teams comprised of clinical representatives, end users, administrative personnel, executive members of the organization, technical experts, and payment/policy experts should be put together before implementing a telehealth strategy.9 Seamless integration of hospital-based care with ambulatory care via a telehealth platform is only complete when care managers are trained and deployed to fulfill the needs of a diverse group of patients. Deriving overall value from telehealth is only possible when there is a skill development, training and mentoring team put in place.
4. Thinking
In most U.S. hospitals, inpatient health care is equally distributed between nonprocedure and procedure-based services. Hospitals resorted to suspension of nonemergent procedures to mitigate the risk of spreading COVID-19. This was further compounded by many patients’ self-selection to defer care, an abrupt reduction in the influx of patients from the referral base because of suboptimally operating ambulatory care services, leading to low hospital occupancy.
Hospitals across the nation have gone through a massive short-term financial crunch and unfavorable cash-flow forecast, which prompted a paradoxical work-force reduction. While some argue that it may be akin to strategic myopia, the authors believed that such a response is strategically imperative to keep the hospital afloat. It is reasonable to attribute the paucity of innovation to constrained resources, and health systems are simply staying overly optimistic about “weathering the storm” and reverting soon to “business as usual.” The technological framework necessary for deploying a telehealth solution often comes with a price. Financially challenged hospital systems rarely exercise any capital-intensive activities. By contrast, telehealth adoption by ambulatory care can result in quicker resumption of patient care in community settings. A lack of operational and infrastructure synchrony between ambulatory and in-hospital systems has failed to capture telehealth-driven inpatient volume. For example, direct admissions from ambulatory telehealth referrals was a missed opportunity in several places. Referrals for labs, diagnostic tests, and other allied services could have helped hospitals offset their fixed costs. Similarly, work flows related to discharge and postdischarge follow up rarely embrace telehealth tools or telehealth care pathways. A brisk change in the health care ecosystem is partly responsible for this.
Digital strategy needs to be incorporated into business strategy. For the reasons already discussed, telehealth technology is not a “nice to have” anymore, but a “must have.” At present, providers are of the opinion that about 20% of their patient services can be delivered via a telehealth platform. Similar trends are observed among patients, as a new modality of access to care is increasingly beneficial to them. Telehealth must be incorporated in standardized hospital work flows. Use of telehealth for preoperative clearance will greatly minimize same-day surgery cancellations. Given the potential shortage in resources, telehealth adoption for inpatient consultations will help systems conserve personal protective equipment, minimize the risk of staff exposure to COVID-19, and improve efficiency.
Digital strategy also prompts the reengineering of care delivery.10 Excessive and unused physical capacity can be converted into digital care hubs. Health maintenance, prevention, health promotion, health education, and chronic disease management not only can serve a variety of patient groups but can also help address the “last-mile problem” in health care. A successful digital strategy usually has three important components – Commitment: Hospital leadership is committed to include digital transformation as a strategic objective; Cost: Digital strategy is added as a line item in the budget; and Control: Measurable metrics are put in place to monitor the performance, impact, and influence of the digital strategy.
Conclusion
For decades, most U.S. health systems occupied the periphery of technological transformation when compared to the rest of the service industry. While most health systems took a heroic approach to the adoption of telehealth during COVID-19, despite being unprepared, the need for a systematic telehealth deployment is far from being adequately fulfilled. The COVID-19 pandemic brought permanent changes to several business disciplines globally. Given the impact of the pandemic on the health and overall wellbeing of American society, the U.S. health care industry must leave no stone unturned in its quest for transformation.
Dr. Lingisetty is a hospitalist and physician executive at Baptist Health System, Little Rock, Ark, and is cofounder/president of SHM’s Arkansas chapter. Dr. Prasad is medical director of care management and a hospitalist at Advocate Aurora Health in Milwaukee. He is cochair of SHM’s IT Special Interest Group, sits on the HQPS committee, and is president of SHM’s Wisconsin chapter. Dr. Palabindala is the medical director, utilization management, and physician advisory services at the University of Mississippi Medical Center and an associate professor of medicine and academic hospitalist at the University of Mississippi, both in Jackson.
References
1. Finnegan M. “Telehealth booms amid COVID-19 crisis.” Computerworld. 2020 Apr 27. www.computerworld.com/article/3540315/telehealth-booms-amid-covid-19-crisis-virtual-care-is-here-to-stay.html. Accessed 2020 Sep 12.
2. Department of Health & Human Services. “OCR Announces Notification of Enforcement Discretion for Telehealth Remote Communications During the COVID-19 Nationwide Public Health Emergency.” 2020 Mar 17. www.hhs.gov/about/news/2020/03/17/ocr-announces-notification-of-enforcement-discretion-for-telehealth-remote-communications-during-the-covid-19.html. Accessed 2020 Sep 12.
3. National Center for Health Statistics. “Health Expenditures.” www.cdc.gov/nchs/fastats/health-expenditures.htm. Accessed 2020 Sep 12.
4. Bestsennyy O et al. “Telehealth: A post–COVID-19 reality?” McKinsey & Company. 2020 May 29. www.mckinsey.com/industries/healthcare-systems-and-services/our-insights/telehealth-a-quarter-trillion-dollar-post-covid-19-reality. Accessed 2020 Sep 12.
5. Melnick ER et al. The Association Between Perceived Electronic Health Record Usability and Professional Burnout Among U.S. Physicians. Mayo Clin Proc. 2020 March;95(3):476-87.
6. Hirko KA et al. Telehealth in response to the COVID-19 pandemic: Implications for rural health disparities. J Am Med Inform Assoc. 2020 Nov;27(11):1816-8. .
7. American Academy of Family Physicians. “Study Examines Telehealth, Rural Disparities in Pandemic.” 2020 July 30. www.aafp.org/news/practice-professional-issues/20200730ruraltelehealth.html. Accessed 2020 Dec 15.
8. Kurlander J et al. “Virtual Visits: Telehealth and Older Adults.” National Poll on Healthy Aging. 2019 Oct. hdl.handle.net/2027.42/151376.
9. American Medical Association. Telehealth Implementation Playbook. 2019. www.ama-assn.org/system/files/2020-04/ama-telehealth-implementation-playbook.pdf.
10. Smith AC et al. Telehealth for global emergencies: Implications for coronavirus disease 2019 (COVID-19). J Telemed Telecare. 2020 Jun;26(5):309-13.
Hospitalist movers and shakers – March 2021
Vivek H. Murthy, MD, was named by President Joe Biden as his selection for Surgeon General of the United States. Dr. Murthy filled the same role from 2014-17 during President Barack Obama’s administration.
Dr. Murthy was a hospitalist and an instructor at Brigham and Women’s Hospital at Harvard Medical School prior to becoming surgeon general the first time. He also is the founder of Doctors for America.
David Tupponce, MD, recently was named the new president of Allegheny Health Network’s Grove City (Pa.) Medical Center. He takes over for interim president Allan Klapper, MD, who filled the position since August 2020.
Dr. Tupponce comes to Grove City Medical Center after a successful tenure as president of Central Maine Medical Center (Lewiston, Maine), where he grew its physician group and fine-tuned the hospital quality program. Prior to that, he was chief executive officer at Tenet Healthcare’s Abrazo Scottsdale (Ariz.) Campus and CEO at Paradise Valley Hospital (Phoenix, Ariz.).
Dr. Tupponce is familiar with western Pennsylvania, having earned a master’s degree in medical management from Carnegie Mellon University in Pittsburgh. He also was chief resident at the University of Pittsburgh Medical Center.
Malcolm Mar Fan, MD, has been elevated to medical director of the Hospitalist Group at Evangelical Community Hospital (Lewisburg, Pa.). In the newly established position, Dr. Mar Fan will oversee all operations for the facility’s hospitalist program.
Dr. Mar Fan has been a hospitalist at Evangelical since 2014 after completing his internist residency at Albert Einstein Medical Center in Philadelphia. He has played a major role on Evangelical’s Peri-operative Glucose Management Committee and its Informatics Committee for Impatient and Outpatient Electronic Health Records.
Lyon County (Kansas) recently announced that Ladun Oyenuga, MD, has been appointed as public health officer for the county. She began her tenure on January 1.
Dr. Oyenuga is a hospitalist at Newman Regional Health (Emporia, Kan.). She is a native of Nigeria and did her residency at Harlem (N.Y.) Hospital Center. She has been with Newman since 2017.
Cherese Mari Laulhere BirthCare Center (Long Beach, Calif.) recently announced the addition of an OB hospitalist program at Miller Children’s & Women’s Hospital. OB hospitalists, or laborists, care for women with obstetrical issues while in the hospital.
At Cherese Mari Laulhere, OB hospitalists will be on hand 24 hours a day to assist patients’ OB/GYNs or to fill in if the personal physician cannot get to the hospital quickly.
Hospitalists at Nationwide Children’s (Columbus, Ohio) are now providing care for children who are hospitalized at Adena Regional Medical Center (Chillicothe, Ohio).
It is an expansion of an ongoing partnership between the two hospitals. Adena and Nationwide Children’s have been working together in helping to care for children in the south central and southern Ohio region since 2011. Nationwide Children’s hospitalists will round in special care and the well-baby nursery at Adena, as well as provide education programs for Adena providers and staff.
MultiCare Health System (Tacoma, Wash.) has announced that it will expand its hospitalist program partnership with Sound Physicians, also based in Tacoma, to create a region-wide, cohesive group of providers. The goal is to help ensure efficient management of inpatient populations as a region instead of at the individual hospital level, and will allow MultiCare to implement standard tools, processes and regionwide best practices.
The hospitalist programs at Tacoma General Hospital, Allenmore Hospital and Covington Medical Center will transition to Sound Physicians on April 5, 2021. Sound hospitalists are already working at three other MultiCare facilities – Tacoma General Hospital, Allenmore Hospital, and Covington Medical Center.
Vivek H. Murthy, MD, was named by President Joe Biden as his selection for Surgeon General of the United States. Dr. Murthy filled the same role from 2014-17 during President Barack Obama’s administration.
Dr. Murthy was a hospitalist and an instructor at Brigham and Women’s Hospital at Harvard Medical School prior to becoming surgeon general the first time. He also is the founder of Doctors for America.
David Tupponce, MD, recently was named the new president of Allegheny Health Network’s Grove City (Pa.) Medical Center. He takes over for interim president Allan Klapper, MD, who filled the position since August 2020.
Dr. Tupponce comes to Grove City Medical Center after a successful tenure as president of Central Maine Medical Center (Lewiston, Maine), where he grew its physician group and fine-tuned the hospital quality program. Prior to that, he was chief executive officer at Tenet Healthcare’s Abrazo Scottsdale (Ariz.) Campus and CEO at Paradise Valley Hospital (Phoenix, Ariz.).
Dr. Tupponce is familiar with western Pennsylvania, having earned a master’s degree in medical management from Carnegie Mellon University in Pittsburgh. He also was chief resident at the University of Pittsburgh Medical Center.
Malcolm Mar Fan, MD, has been elevated to medical director of the Hospitalist Group at Evangelical Community Hospital (Lewisburg, Pa.). In the newly established position, Dr. Mar Fan will oversee all operations for the facility’s hospitalist program.
Dr. Mar Fan has been a hospitalist at Evangelical since 2014 after completing his internist residency at Albert Einstein Medical Center in Philadelphia. He has played a major role on Evangelical’s Peri-operative Glucose Management Committee and its Informatics Committee for Impatient and Outpatient Electronic Health Records.
Lyon County (Kansas) recently announced that Ladun Oyenuga, MD, has been appointed as public health officer for the county. She began her tenure on January 1.
Dr. Oyenuga is a hospitalist at Newman Regional Health (Emporia, Kan.). She is a native of Nigeria and did her residency at Harlem (N.Y.) Hospital Center. She has been with Newman since 2017.
Cherese Mari Laulhere BirthCare Center (Long Beach, Calif.) recently announced the addition of an OB hospitalist program at Miller Children’s & Women’s Hospital. OB hospitalists, or laborists, care for women with obstetrical issues while in the hospital.
At Cherese Mari Laulhere, OB hospitalists will be on hand 24 hours a day to assist patients’ OB/GYNs or to fill in if the personal physician cannot get to the hospital quickly.
Hospitalists at Nationwide Children’s (Columbus, Ohio) are now providing care for children who are hospitalized at Adena Regional Medical Center (Chillicothe, Ohio).
It is an expansion of an ongoing partnership between the two hospitals. Adena and Nationwide Children’s have been working together in helping to care for children in the south central and southern Ohio region since 2011. Nationwide Children’s hospitalists will round in special care and the well-baby nursery at Adena, as well as provide education programs for Adena providers and staff.
MultiCare Health System (Tacoma, Wash.) has announced that it will expand its hospitalist program partnership with Sound Physicians, also based in Tacoma, to create a region-wide, cohesive group of providers. The goal is to help ensure efficient management of inpatient populations as a region instead of at the individual hospital level, and will allow MultiCare to implement standard tools, processes and regionwide best practices.
The hospitalist programs at Tacoma General Hospital, Allenmore Hospital and Covington Medical Center will transition to Sound Physicians on April 5, 2021. Sound hospitalists are already working at three other MultiCare facilities – Tacoma General Hospital, Allenmore Hospital, and Covington Medical Center.
Vivek H. Murthy, MD, was named by President Joe Biden as his selection for Surgeon General of the United States. Dr. Murthy filled the same role from 2014-17 during President Barack Obama’s administration.
Dr. Murthy was a hospitalist and an instructor at Brigham and Women’s Hospital at Harvard Medical School prior to becoming surgeon general the first time. He also is the founder of Doctors for America.
David Tupponce, MD, recently was named the new president of Allegheny Health Network’s Grove City (Pa.) Medical Center. He takes over for interim president Allan Klapper, MD, who filled the position since August 2020.
Dr. Tupponce comes to Grove City Medical Center after a successful tenure as president of Central Maine Medical Center (Lewiston, Maine), where he grew its physician group and fine-tuned the hospital quality program. Prior to that, he was chief executive officer at Tenet Healthcare’s Abrazo Scottsdale (Ariz.) Campus and CEO at Paradise Valley Hospital (Phoenix, Ariz.).
Dr. Tupponce is familiar with western Pennsylvania, having earned a master’s degree in medical management from Carnegie Mellon University in Pittsburgh. He also was chief resident at the University of Pittsburgh Medical Center.
Malcolm Mar Fan, MD, has been elevated to medical director of the Hospitalist Group at Evangelical Community Hospital (Lewisburg, Pa.). In the newly established position, Dr. Mar Fan will oversee all operations for the facility’s hospitalist program.
Dr. Mar Fan has been a hospitalist at Evangelical since 2014 after completing his internist residency at Albert Einstein Medical Center in Philadelphia. He has played a major role on Evangelical’s Peri-operative Glucose Management Committee and its Informatics Committee for Impatient and Outpatient Electronic Health Records.
Lyon County (Kansas) recently announced that Ladun Oyenuga, MD, has been appointed as public health officer for the county. She began her tenure on January 1.
Dr. Oyenuga is a hospitalist at Newman Regional Health (Emporia, Kan.). She is a native of Nigeria and did her residency at Harlem (N.Y.) Hospital Center. She has been with Newman since 2017.
Cherese Mari Laulhere BirthCare Center (Long Beach, Calif.) recently announced the addition of an OB hospitalist program at Miller Children’s & Women’s Hospital. OB hospitalists, or laborists, care for women with obstetrical issues while in the hospital.
At Cherese Mari Laulhere, OB hospitalists will be on hand 24 hours a day to assist patients’ OB/GYNs or to fill in if the personal physician cannot get to the hospital quickly.
Hospitalists at Nationwide Children’s (Columbus, Ohio) are now providing care for children who are hospitalized at Adena Regional Medical Center (Chillicothe, Ohio).
It is an expansion of an ongoing partnership between the two hospitals. Adena and Nationwide Children’s have been working together in helping to care for children in the south central and southern Ohio region since 2011. Nationwide Children’s hospitalists will round in special care and the well-baby nursery at Adena, as well as provide education programs for Adena providers and staff.
MultiCare Health System (Tacoma, Wash.) has announced that it will expand its hospitalist program partnership with Sound Physicians, also based in Tacoma, to create a region-wide, cohesive group of providers. The goal is to help ensure efficient management of inpatient populations as a region instead of at the individual hospital level, and will allow MultiCare to implement standard tools, processes and regionwide best practices.
The hospitalist programs at Tacoma General Hospital, Allenmore Hospital and Covington Medical Center will transition to Sound Physicians on April 5, 2021. Sound hospitalists are already working at three other MultiCare facilities – Tacoma General Hospital, Allenmore Hospital, and Covington Medical Center.
SHM Fellowship Class of 2021
The Society of Hospital Medicine has announced its 2021 class of Master Fellows, Senior Fellows, and Fellows in Hospital Medicine.
All Fellowship classes are listed in alphabetical order.
Master Fellows Class of 2021
Nasim Afsar, MD, MBA, MHM
Shaun D. Frost, MD, MHM
Jeffrey L. Schnipper, MD, MPH, MHM
Senior Fellows Class of 2021
Akindele Adaramola, MD, MPH, SFHM
Ramesh Adhikari, MD, SFHM
Pankaj Agrawal, MD, SFHM
Robert L. Anderson, MD, SFHM
Glenda B. Atilano, MD, SFHM
Bi A. Awosika, MD, FACP, SFHM
David N. Aymond, MD, SFHM
Paula Bailey, MD, SFHM
Amit B. Bansal, MD, MBA, SFHM
Jamie K. Bartley, DO, FACP, SFHM
Stephen J. Behnke, MD, SFHM
Christina A. Beyer, MD, SFHM
Vinil K. Bhuma, MD, SFHM
John P. Biebelhausen, MD, MBA, SFHM
Matthew T. Calestino, MD, FACP, SFHM
Domingo Caparas Jr., MD, FAAFP, SFHM
Darren Caudill, DO, FACP, SFHM
Julie M. Cernanec, MD, FAAP, SFHM
Will Cushing, PA-C, SFHM
Douglas A. Dodds II, MD, FAAP, SFHM
Coley B. Duncan, MD, CPE, MMM, SFHM
Noah Finkel, MD, SFHM
Justin Glasgow, MD, PhD, SFHM
Taylor Goot, MD, SFHM
Craig G. Gunderson, MD, SFHM
Alan Hall, MD, SFHM
Vivian Hamlett, MD, SFHM
Kathrin Harrington, MD, SFHM
Hossan Hassan, MD, SFHM
Anand D. Hongalgi, MD, FACP, SFHM
Akshata Hopkins, MD, FAAP, SFHM
Neelima Kamineni, MD, SFHM
Sudheer R. Kantharajpur, MBBS, MD, MHA, SFHM
Prakash Karki, MD, SFHM
Susrutha Kotwal, MD, SFHM
Ethan Kuperman, MD, SFHM
Rumman A. Langah, MD, FACP, SFHM
Sean LaVine, MD, FACP, SFHM
Don S. Lee, MD, FACP, SFHM
Charmaine A. Lewis, MD, MPH, CLHM, SFHM
Rishi Likhi, MD, SFHM
Lenny Lopez, MD, MPH, SFHM
Anthony Macchiavelli, MD, SFHM
Brian McGillen, MD, FACP, SFHM
Parth H. Mehta, MBBS, MD, MPH, SFHM
Anuj Mehta, MBBS, MD, MBA, SFHM
Prem Nair, MD, FACP, SFHM
Don J. Neer, MD, FACP, SFHM
Shyam Odeti, MD, FAAFP, SFHM
Amy T. O’Linn, DO, SFHM
Mihir Patel, MD, FACP, MBA, MPH, SFHM
Kimberly S. Pedram, MD, FACP, SFHM
Thomas Pineo, DO, SFHM
Mauricio Pinto, MD, SFHM
Lakmali C. Ranathunga, MBBS, SFHM
Matthew Reuter, MD, SFHM
Erik P. Rufa, MD, SFHM
Dipali Ruby Sahoo, DO, MBA, SFHM
Chady Sarraf, MD, SFHM
Suchita S. Sata, MD, SFHM
Klint Schwenk, MD, FAAP, MBA, SFHM
Aaron M. Sebach, CRNP, DNP, MBA, PhD, SFHM
Kevin Sowti, MD, MBA, SFHM
Joseph G. Surber, DO, FAAFP, SFHM
Bright Thilagar, MD, SFHM
Thomas S. Trawick Jr., MD, SFHM
Rehman Usmani, MD, SFHM
Arash Velayati, MD, SFHM
Jose A. Ventura, MD, FAAFP, SFHM
Andre Wajner, MD, PhD, SFHM
Phillip D. Warr, MD, SFHM
Virginia E. Watson, MD, SFHM
Kristin R. Wise, MD, SFHM
Elham A. Yousef, MD, FACP, MBA, MSc, SFHM
Fellows Class of 2021
Elizabeth M. Aarons, MD, FHM
Suhail A. Abbasi, MD, FACP, FHM
Waqas Adeel, MD, FHM
Rajender K. Agarwal, MD, MBA, MPH, FHM
Khaalisha Ajala, MD, MBA, FHM
Faraz S. Alam, MD, FHM
Amee Amin, MD, FHM
Muhammad W. Amir, MD, FACP, FHM
Saba Asad, MD, FHM
Logan Atkins, MD, FHM
Navneet Attri, MD, FHM
Jennifer Barnett, PA, FHM
Karyn Baum, MD, FHM
Prabhjot Bedi, MD, FHM
Nicolle R. Benz, DO, FHM
Ricky Bhimani, MD, FHM
Elizabeth Blankenship, PA-C, FHM
Rahul Borsadia, MD, FHM
Kalpana Chalasani, MD, FHM
Rani Chikkanna, MD, FHM
Venu Chippa, MBBS, MD, FHM
Lisa M. Coontz, FNP, FHM
Christie Crawford, MD, FHM
Rene Daniel, MD, PhD, FHM
Elda Dede, FHM
Radha Denmark, CNP, FHM
Alvine N. Nwehla Desamours, PA-C, FHM
Satyendra Dhar, MD, FHM
Manuel Jose Diaz, MD, FHM
Tiffany Egbe, MD, FHM
Chinwe Egbo, MD, FHM
Mohammad A. Farkhondehpour, MD, FACP, FHM
Shaheen Faruque, MBBS, FHM
Chris W. Fellin, MD, FACP, FHM
Juan Carlos Fuentes-Rosales, MD, FACP, MPH, FHM
Evelyn W. Gathecha, MD, FHM
Benjamin P. Geisler, MD, FACP, MPH, FHM
Matthew George, MD, FHM
Sonia George, DO, FHM
Mirna Giordano, MD, FHM
Rebecca Gomez, MD, FHM
David Gonzales, MD, FHM
Maria A. Guevara Hernandez, MD, FACP, FHM
Shubhra Gupta, MBBS, FHM
Rohini Harvey, MD, FHM
Allison Heinen, DO, FHM
Hollie L. Hurner, PA-C, FHM
Doug Hutcheon, MD, FHM
Varalakshmi Janamanchi, MD, FHM
Brian Keegan, MD, FACP, FHM
Qasim Khalil, MD, FHM
Irfana Khan, MD, FHM
Muhammad O. Khan, MD, FAAFP, MBA, FHM
Smita Kohli, MD, FHM
Julie Kolinski, MD, FAAP, FHM
Ewa Kontny, MD, FHM
Sungmi Lian, MD, FHM
Brian Lichtenstein, MD, FHM
Fernando Madero Gorostieta, MD, FHM
Vipul Mahajan, MD, FACP, FHM
Neetu Mahendraker, MD, FHM
Victoria McCurry, MD, FHM
Bridget McGrath, PA-C, FHM
Evan Meadors, MD, FHM
Kapil Mehta, MD, FACP, MBA, FHM
Waseem Mohamed, MD, FHM
Ernest Murray, MD, FHM
Murali K. Nagubandi, MD, FHM
Jessica Nave Allen, MD, FHM
Peter Nwafor, MD, FACP, FHM
Ike Anthony Nwaobi, MBBS, MBA, FHM
Olugbenga B. Ojo, MD, FACP, MBA, FHM
Jacqueline Okere, MD, FHM
Ifedolapo S. Olanrewaju, MD, MBchB, FHM
Mobolaji Olulade, MD, FHM
Elizabeth H. Papetti, MBA, FHM
Love Patel, MBBS, FHM
Kamakshya P. Patra, MD, MMM, FHM
Charles Pizanis, MD, FHM
Rajat Prakash, MD, FHM
Chris Pribula, MD, FHM
Michael Puchaev, MD, FHM
Ryan Punsalan, MD, FHM
Bhavya Rajanna, MD, FHM
Miguel A. Ramirez, MD, FHM
Raymund Ramirez, MD, FHM
Sandeep Randhawa, MBBS, FHM
Rohit Rattan, MD, FHM
Denisha Powell Rawlings, MD, FHM
Praveen K. Reddy, MD, MPH, FHM
Michael Ree, DO, MPH, FHM
Patrick Rendon, MD, FHM
David J. Rizk, MD, FAAFP, MBA, FHM
Michael Roberts, MD, FHM
Edwin Rosas, MD, FHM
Devjit Roy, MD, FHM
Sabyasachi Roy, MD, FHM
Paul Sandroni, CMPE, MSM, FHM
Vijairam Selvaraj, MD, MPH, FHM
Megha Shah, MD, MMM, FHM
Edie Shen, MD, FHM
Gurpinder Singh, MD, FACP, FHM
Vishwas A. Singh, MD, FHM
Karen Slatkovsky, MD, FHM
Sean M. Snyder, MD, FHM
Jaclyn Spiegel, MD, FHM
Dale Stapler Jr., MD, FHM
Christina E. Stovall, MD, FHM
Daniel Suders, DO, FHM
Clayton Swalstad, CMPE, MSM, FHM
Harshil Swaminarayan, MD, FHM
Keniesha Thompson, MD, FHM
Tet Toe, MD, FACP, FHM
Christine Tsai, MD, FHM
Ajay Vaikuntam, MD, FHM
Valerie Vaughn, MD, FHM
Jane N. Wainaina, FACP, MBchB, FHM
Neshahthari Wijeyakuhan, MD, FACP, FHM
Chia-Shing Yang, MD, FHM
Jennifer Zagursky, MD, FHM
The Society of Hospital Medicine has announced its 2021 class of Master Fellows, Senior Fellows, and Fellows in Hospital Medicine.
All Fellowship classes are listed in alphabetical order.
Master Fellows Class of 2021
Nasim Afsar, MD, MBA, MHM
Shaun D. Frost, MD, MHM
Jeffrey L. Schnipper, MD, MPH, MHM
Senior Fellows Class of 2021
Akindele Adaramola, MD, MPH, SFHM
Ramesh Adhikari, MD, SFHM
Pankaj Agrawal, MD, SFHM
Robert L. Anderson, MD, SFHM
Glenda B. Atilano, MD, SFHM
Bi A. Awosika, MD, FACP, SFHM
David N. Aymond, MD, SFHM
Paula Bailey, MD, SFHM
Amit B. Bansal, MD, MBA, SFHM
Jamie K. Bartley, DO, FACP, SFHM
Stephen J. Behnke, MD, SFHM
Christina A. Beyer, MD, SFHM
Vinil K. Bhuma, MD, SFHM
John P. Biebelhausen, MD, MBA, SFHM
Matthew T. Calestino, MD, FACP, SFHM
Domingo Caparas Jr., MD, FAAFP, SFHM
Darren Caudill, DO, FACP, SFHM
Julie M. Cernanec, MD, FAAP, SFHM
Will Cushing, PA-C, SFHM
Douglas A. Dodds II, MD, FAAP, SFHM
Coley B. Duncan, MD, CPE, MMM, SFHM
Noah Finkel, MD, SFHM
Justin Glasgow, MD, PhD, SFHM
Taylor Goot, MD, SFHM
Craig G. Gunderson, MD, SFHM
Alan Hall, MD, SFHM
Vivian Hamlett, MD, SFHM
Kathrin Harrington, MD, SFHM
Hossan Hassan, MD, SFHM
Anand D. Hongalgi, MD, FACP, SFHM
Akshata Hopkins, MD, FAAP, SFHM
Neelima Kamineni, MD, SFHM
Sudheer R. Kantharajpur, MBBS, MD, MHA, SFHM
Prakash Karki, MD, SFHM
Susrutha Kotwal, MD, SFHM
Ethan Kuperman, MD, SFHM
Rumman A. Langah, MD, FACP, SFHM
Sean LaVine, MD, FACP, SFHM
Don S. Lee, MD, FACP, SFHM
Charmaine A. Lewis, MD, MPH, CLHM, SFHM
Rishi Likhi, MD, SFHM
Lenny Lopez, MD, MPH, SFHM
Anthony Macchiavelli, MD, SFHM
Brian McGillen, MD, FACP, SFHM
Parth H. Mehta, MBBS, MD, MPH, SFHM
Anuj Mehta, MBBS, MD, MBA, SFHM
Prem Nair, MD, FACP, SFHM
Don J. Neer, MD, FACP, SFHM
Shyam Odeti, MD, FAAFP, SFHM
Amy T. O’Linn, DO, SFHM
Mihir Patel, MD, FACP, MBA, MPH, SFHM
Kimberly S. Pedram, MD, FACP, SFHM
Thomas Pineo, DO, SFHM
Mauricio Pinto, MD, SFHM
Lakmali C. Ranathunga, MBBS, SFHM
Matthew Reuter, MD, SFHM
Erik P. Rufa, MD, SFHM
Dipali Ruby Sahoo, DO, MBA, SFHM
Chady Sarraf, MD, SFHM
Suchita S. Sata, MD, SFHM
Klint Schwenk, MD, FAAP, MBA, SFHM
Aaron M. Sebach, CRNP, DNP, MBA, PhD, SFHM
Kevin Sowti, MD, MBA, SFHM
Joseph G. Surber, DO, FAAFP, SFHM
Bright Thilagar, MD, SFHM
Thomas S. Trawick Jr., MD, SFHM
Rehman Usmani, MD, SFHM
Arash Velayati, MD, SFHM
Jose A. Ventura, MD, FAAFP, SFHM
Andre Wajner, MD, PhD, SFHM
Phillip D. Warr, MD, SFHM
Virginia E. Watson, MD, SFHM
Kristin R. Wise, MD, SFHM
Elham A. Yousef, MD, FACP, MBA, MSc, SFHM
Fellows Class of 2021
Elizabeth M. Aarons, MD, FHM
Suhail A. Abbasi, MD, FACP, FHM
Waqas Adeel, MD, FHM
Rajender K. Agarwal, MD, MBA, MPH, FHM
Khaalisha Ajala, MD, MBA, FHM
Faraz S. Alam, MD, FHM
Amee Amin, MD, FHM
Muhammad W. Amir, MD, FACP, FHM
Saba Asad, MD, FHM
Logan Atkins, MD, FHM
Navneet Attri, MD, FHM
Jennifer Barnett, PA, FHM
Karyn Baum, MD, FHM
Prabhjot Bedi, MD, FHM
Nicolle R. Benz, DO, FHM
Ricky Bhimani, MD, FHM
Elizabeth Blankenship, PA-C, FHM
Rahul Borsadia, MD, FHM
Kalpana Chalasani, MD, FHM
Rani Chikkanna, MD, FHM
Venu Chippa, MBBS, MD, FHM
Lisa M. Coontz, FNP, FHM
Christie Crawford, MD, FHM
Rene Daniel, MD, PhD, FHM
Elda Dede, FHM
Radha Denmark, CNP, FHM
Alvine N. Nwehla Desamours, PA-C, FHM
Satyendra Dhar, MD, FHM
Manuel Jose Diaz, MD, FHM
Tiffany Egbe, MD, FHM
Chinwe Egbo, MD, FHM
Mohammad A. Farkhondehpour, MD, FACP, FHM
Shaheen Faruque, MBBS, FHM
Chris W. Fellin, MD, FACP, FHM
Juan Carlos Fuentes-Rosales, MD, FACP, MPH, FHM
Evelyn W. Gathecha, MD, FHM
Benjamin P. Geisler, MD, FACP, MPH, FHM
Matthew George, MD, FHM
Sonia George, DO, FHM
Mirna Giordano, MD, FHM
Rebecca Gomez, MD, FHM
David Gonzales, MD, FHM
Maria A. Guevara Hernandez, MD, FACP, FHM
Shubhra Gupta, MBBS, FHM
Rohini Harvey, MD, FHM
Allison Heinen, DO, FHM
Hollie L. Hurner, PA-C, FHM
Doug Hutcheon, MD, FHM
Varalakshmi Janamanchi, MD, FHM
Brian Keegan, MD, FACP, FHM
Qasim Khalil, MD, FHM
Irfana Khan, MD, FHM
Muhammad O. Khan, MD, FAAFP, MBA, FHM
Smita Kohli, MD, FHM
Julie Kolinski, MD, FAAP, FHM
Ewa Kontny, MD, FHM
Sungmi Lian, MD, FHM
Brian Lichtenstein, MD, FHM
Fernando Madero Gorostieta, MD, FHM
Vipul Mahajan, MD, FACP, FHM
Neetu Mahendraker, MD, FHM
Victoria McCurry, MD, FHM
Bridget McGrath, PA-C, FHM
Evan Meadors, MD, FHM
Kapil Mehta, MD, FACP, MBA, FHM
Waseem Mohamed, MD, FHM
Ernest Murray, MD, FHM
Murali K. Nagubandi, MD, FHM
Jessica Nave Allen, MD, FHM
Peter Nwafor, MD, FACP, FHM
Ike Anthony Nwaobi, MBBS, MBA, FHM
Olugbenga B. Ojo, MD, FACP, MBA, FHM
Jacqueline Okere, MD, FHM
Ifedolapo S. Olanrewaju, MD, MBchB, FHM
Mobolaji Olulade, MD, FHM
Elizabeth H. Papetti, MBA, FHM
Love Patel, MBBS, FHM
Kamakshya P. Patra, MD, MMM, FHM
Charles Pizanis, MD, FHM
Rajat Prakash, MD, FHM
Chris Pribula, MD, FHM
Michael Puchaev, MD, FHM
Ryan Punsalan, MD, FHM
Bhavya Rajanna, MD, FHM
Miguel A. Ramirez, MD, FHM
Raymund Ramirez, MD, FHM
Sandeep Randhawa, MBBS, FHM
Rohit Rattan, MD, FHM
Denisha Powell Rawlings, MD, FHM
Praveen K. Reddy, MD, MPH, FHM
Michael Ree, DO, MPH, FHM
Patrick Rendon, MD, FHM
David J. Rizk, MD, FAAFP, MBA, FHM
Michael Roberts, MD, FHM
Edwin Rosas, MD, FHM
Devjit Roy, MD, FHM
Sabyasachi Roy, MD, FHM
Paul Sandroni, CMPE, MSM, FHM
Vijairam Selvaraj, MD, MPH, FHM
Megha Shah, MD, MMM, FHM
Edie Shen, MD, FHM
Gurpinder Singh, MD, FACP, FHM
Vishwas A. Singh, MD, FHM
Karen Slatkovsky, MD, FHM
Sean M. Snyder, MD, FHM
Jaclyn Spiegel, MD, FHM
Dale Stapler Jr., MD, FHM
Christina E. Stovall, MD, FHM
Daniel Suders, DO, FHM
Clayton Swalstad, CMPE, MSM, FHM
Harshil Swaminarayan, MD, FHM
Keniesha Thompson, MD, FHM
Tet Toe, MD, FACP, FHM
Christine Tsai, MD, FHM
Ajay Vaikuntam, MD, FHM
Valerie Vaughn, MD, FHM
Jane N. Wainaina, FACP, MBchB, FHM
Neshahthari Wijeyakuhan, MD, FACP, FHM
Chia-Shing Yang, MD, FHM
Jennifer Zagursky, MD, FHM
The Society of Hospital Medicine has announced its 2021 class of Master Fellows, Senior Fellows, and Fellows in Hospital Medicine.
All Fellowship classes are listed in alphabetical order.
Master Fellows Class of 2021
Nasim Afsar, MD, MBA, MHM
Shaun D. Frost, MD, MHM
Jeffrey L. Schnipper, MD, MPH, MHM
Senior Fellows Class of 2021
Akindele Adaramola, MD, MPH, SFHM
Ramesh Adhikari, MD, SFHM
Pankaj Agrawal, MD, SFHM
Robert L. Anderson, MD, SFHM
Glenda B. Atilano, MD, SFHM
Bi A. Awosika, MD, FACP, SFHM
David N. Aymond, MD, SFHM
Paula Bailey, MD, SFHM
Amit B. Bansal, MD, MBA, SFHM
Jamie K. Bartley, DO, FACP, SFHM
Stephen J. Behnke, MD, SFHM
Christina A. Beyer, MD, SFHM
Vinil K. Bhuma, MD, SFHM
John P. Biebelhausen, MD, MBA, SFHM
Matthew T. Calestino, MD, FACP, SFHM
Domingo Caparas Jr., MD, FAAFP, SFHM
Darren Caudill, DO, FACP, SFHM
Julie M. Cernanec, MD, FAAP, SFHM
Will Cushing, PA-C, SFHM
Douglas A. Dodds II, MD, FAAP, SFHM
Coley B. Duncan, MD, CPE, MMM, SFHM
Noah Finkel, MD, SFHM
Justin Glasgow, MD, PhD, SFHM
Taylor Goot, MD, SFHM
Craig G. Gunderson, MD, SFHM
Alan Hall, MD, SFHM
Vivian Hamlett, MD, SFHM
Kathrin Harrington, MD, SFHM
Hossan Hassan, MD, SFHM
Anand D. Hongalgi, MD, FACP, SFHM
Akshata Hopkins, MD, FAAP, SFHM
Neelima Kamineni, MD, SFHM
Sudheer R. Kantharajpur, MBBS, MD, MHA, SFHM
Prakash Karki, MD, SFHM
Susrutha Kotwal, MD, SFHM
Ethan Kuperman, MD, SFHM
Rumman A. Langah, MD, FACP, SFHM
Sean LaVine, MD, FACP, SFHM
Don S. Lee, MD, FACP, SFHM
Charmaine A. Lewis, MD, MPH, CLHM, SFHM
Rishi Likhi, MD, SFHM
Lenny Lopez, MD, MPH, SFHM
Anthony Macchiavelli, MD, SFHM
Brian McGillen, MD, FACP, SFHM
Parth H. Mehta, MBBS, MD, MPH, SFHM
Anuj Mehta, MBBS, MD, MBA, SFHM
Prem Nair, MD, FACP, SFHM
Don J. Neer, MD, FACP, SFHM
Shyam Odeti, MD, FAAFP, SFHM
Amy T. O’Linn, DO, SFHM
Mihir Patel, MD, FACP, MBA, MPH, SFHM
Kimberly S. Pedram, MD, FACP, SFHM
Thomas Pineo, DO, SFHM
Mauricio Pinto, MD, SFHM
Lakmali C. Ranathunga, MBBS, SFHM
Matthew Reuter, MD, SFHM
Erik P. Rufa, MD, SFHM
Dipali Ruby Sahoo, DO, MBA, SFHM
Chady Sarraf, MD, SFHM
Suchita S. Sata, MD, SFHM
Klint Schwenk, MD, FAAP, MBA, SFHM
Aaron M. Sebach, CRNP, DNP, MBA, PhD, SFHM
Kevin Sowti, MD, MBA, SFHM
Joseph G. Surber, DO, FAAFP, SFHM
Bright Thilagar, MD, SFHM
Thomas S. Trawick Jr., MD, SFHM
Rehman Usmani, MD, SFHM
Arash Velayati, MD, SFHM
Jose A. Ventura, MD, FAAFP, SFHM
Andre Wajner, MD, PhD, SFHM
Phillip D. Warr, MD, SFHM
Virginia E. Watson, MD, SFHM
Kristin R. Wise, MD, SFHM
Elham A. Yousef, MD, FACP, MBA, MSc, SFHM
Fellows Class of 2021
Elizabeth M. Aarons, MD, FHM
Suhail A. Abbasi, MD, FACP, FHM
Waqas Adeel, MD, FHM
Rajender K. Agarwal, MD, MBA, MPH, FHM
Khaalisha Ajala, MD, MBA, FHM
Faraz S. Alam, MD, FHM
Amee Amin, MD, FHM
Muhammad W. Amir, MD, FACP, FHM
Saba Asad, MD, FHM
Logan Atkins, MD, FHM
Navneet Attri, MD, FHM
Jennifer Barnett, PA, FHM
Karyn Baum, MD, FHM
Prabhjot Bedi, MD, FHM
Nicolle R. Benz, DO, FHM
Ricky Bhimani, MD, FHM
Elizabeth Blankenship, PA-C, FHM
Rahul Borsadia, MD, FHM
Kalpana Chalasani, MD, FHM
Rani Chikkanna, MD, FHM
Venu Chippa, MBBS, MD, FHM
Lisa M. Coontz, FNP, FHM
Christie Crawford, MD, FHM
Rene Daniel, MD, PhD, FHM
Elda Dede, FHM
Radha Denmark, CNP, FHM
Alvine N. Nwehla Desamours, PA-C, FHM
Satyendra Dhar, MD, FHM
Manuel Jose Diaz, MD, FHM
Tiffany Egbe, MD, FHM
Chinwe Egbo, MD, FHM
Mohammad A. Farkhondehpour, MD, FACP, FHM
Shaheen Faruque, MBBS, FHM
Chris W. Fellin, MD, FACP, FHM
Juan Carlos Fuentes-Rosales, MD, FACP, MPH, FHM
Evelyn W. Gathecha, MD, FHM
Benjamin P. Geisler, MD, FACP, MPH, FHM
Matthew George, MD, FHM
Sonia George, DO, FHM
Mirna Giordano, MD, FHM
Rebecca Gomez, MD, FHM
David Gonzales, MD, FHM
Maria A. Guevara Hernandez, MD, FACP, FHM
Shubhra Gupta, MBBS, FHM
Rohini Harvey, MD, FHM
Allison Heinen, DO, FHM
Hollie L. Hurner, PA-C, FHM
Doug Hutcheon, MD, FHM
Varalakshmi Janamanchi, MD, FHM
Brian Keegan, MD, FACP, FHM
Qasim Khalil, MD, FHM
Irfana Khan, MD, FHM
Muhammad O. Khan, MD, FAAFP, MBA, FHM
Smita Kohli, MD, FHM
Julie Kolinski, MD, FAAP, FHM
Ewa Kontny, MD, FHM
Sungmi Lian, MD, FHM
Brian Lichtenstein, MD, FHM
Fernando Madero Gorostieta, MD, FHM
Vipul Mahajan, MD, FACP, FHM
Neetu Mahendraker, MD, FHM
Victoria McCurry, MD, FHM
Bridget McGrath, PA-C, FHM
Evan Meadors, MD, FHM
Kapil Mehta, MD, FACP, MBA, FHM
Waseem Mohamed, MD, FHM
Ernest Murray, MD, FHM
Murali K. Nagubandi, MD, FHM
Jessica Nave Allen, MD, FHM
Peter Nwafor, MD, FACP, FHM
Ike Anthony Nwaobi, MBBS, MBA, FHM
Olugbenga B. Ojo, MD, FACP, MBA, FHM
Jacqueline Okere, MD, FHM
Ifedolapo S. Olanrewaju, MD, MBchB, FHM
Mobolaji Olulade, MD, FHM
Elizabeth H. Papetti, MBA, FHM
Love Patel, MBBS, FHM
Kamakshya P. Patra, MD, MMM, FHM
Charles Pizanis, MD, FHM
Rajat Prakash, MD, FHM
Chris Pribula, MD, FHM
Michael Puchaev, MD, FHM
Ryan Punsalan, MD, FHM
Bhavya Rajanna, MD, FHM
Miguel A. Ramirez, MD, FHM
Raymund Ramirez, MD, FHM
Sandeep Randhawa, MBBS, FHM
Rohit Rattan, MD, FHM
Denisha Powell Rawlings, MD, FHM
Praveen K. Reddy, MD, MPH, FHM
Michael Ree, DO, MPH, FHM
Patrick Rendon, MD, FHM
David J. Rizk, MD, FAAFP, MBA, FHM
Michael Roberts, MD, FHM
Edwin Rosas, MD, FHM
Devjit Roy, MD, FHM
Sabyasachi Roy, MD, FHM
Paul Sandroni, CMPE, MSM, FHM
Vijairam Selvaraj, MD, MPH, FHM
Megha Shah, MD, MMM, FHM
Edie Shen, MD, FHM
Gurpinder Singh, MD, FACP, FHM
Vishwas A. Singh, MD, FHM
Karen Slatkovsky, MD, FHM
Sean M. Snyder, MD, FHM
Jaclyn Spiegel, MD, FHM
Dale Stapler Jr., MD, FHM
Christina E. Stovall, MD, FHM
Daniel Suders, DO, FHM
Clayton Swalstad, CMPE, MSM, FHM
Harshil Swaminarayan, MD, FHM
Keniesha Thompson, MD, FHM
Tet Toe, MD, FACP, FHM
Christine Tsai, MD, FHM
Ajay Vaikuntam, MD, FHM
Valerie Vaughn, MD, FHM
Jane N. Wainaina, FACP, MBchB, FHM
Neshahthari Wijeyakuhan, MD, FACP, FHM
Chia-Shing Yang, MD, FHM
Jennifer Zagursky, MD, FHM
Inclusivity needed in PHM fellowships
A year and a half ago, I found myself seated in a crowded hall at the national Pediatric Hospital Medicine (PHM) conference. Throughout the conference, trainees like me were warmly welcomed into small groups and lunch tables. I tried to keep my cool while PHM “celebrities” chatted with me in the elevator. Most sessions were prepared with plenty of chairs, and those that were not encouraged latecomers to grab a spot on the floor or the back wall – the more the merrier.
The intention of this “advice for applicants” meeting was to inspire and guide our next steps toward fellowship, but a discomforting reality loomed over us. It was the first year graduating pediatricians could not choose PHM board certification via the practice pathway – we needed an invitation in the form of a fellowship match.
The “hidden curriculum” was not subtle: People who scored a seat would keep their options open within the field of PHM, and those who did not had a murkier future. This message stood in stark contrast to the PHM inclusivity I had experienced all conference, and planted seeds of doubt: Was I welcome here? Did I “deserve” a seat?
I found the experience as a PHM fellowship applicant to be uncomfortable, and my all-too familiar friend “imposter syndrome” set up camp in my brain and made herself at home. I had no way of knowing how many programs to apply to, how many to interview at, or the chances of my matching at all. Once on the interview trail, I realized I was not alone in my discomfort – most applicants harbored some trepidation, and no one truly knew how the chips would fall on Match Day.
I am thrilled and relieved to have come out the other end in a great position. The team I work with and learn from is phenomenal. I am grateful that ACGME accreditation ensures structures are in place for fellows to be supported in their academic and educational efforts and have full confidence that the skills I gain in fellowship will help me contribute to progression of the field of PHM and improve my performance as a clinician-educator.
Sadly, each year PHM match day celebrations are dampened by the knowledge that a large portion of our colleagues are being left out in the cold with an “unmatched” notification in their inboxes. Approximately 200 graduating pediatricians become pediatric hospitalists each year,1 but only 68 fellowship positions were available in the United States for matriculation in 2020.2 In 2019, PHM fellowship candidates navigated the 6-month application journey with aspirations to further their training in the profession they love. Of the candidates who submitted a rank list committing to 2 or more years in PHM fellowship, 35% were denied.
Unfortunately, despite expansion of PHM fellowship programs and fifteen seats added from last year, we learned this December that there still are not enough positions to welcome qualified applicants with open arms: Thirty-three percent of candidates ranked PHM programs first in the NRMP but did not match – the highest unmatched percentage out of all pediatric subspecialties.3
The NRMP report shared a glimpse of our colleagues who received interview invitations and submitted a rank list, but this is likely an underestimation of pediatric graduates who wanted to obtain PHM board certification and wound up on a different path. Some residents anticipated the stiff competition and delayed their plans to apply for fellowship, while others matched into another subspecialty that was able to accommodate them. Many pediatric graduates joined the workforce directly as pediatric hospitalists knowing the practice pathway to certification is not available to them. Along with other physicians without board certification in PHM, they shoulder concerns of being withheld from professional advancement opportunities.
For the foreseeable future it is clear that pediatric hospitalists without board certification will be a large part of our community, and are crucial to providing high-quality care to hospitalized children nationally. In 2019, a national survey of pediatric hospital medicine groups revealed that 50% of pediatric hospitalist hires came directly out of residency, and only 8% of hires were fellowship trained.4 The same report revealed that 26% of physicians were board-certified.These percentages are likely to change over the next 5 years as the window of practice pathway certification closes and fellowship programs continue to expand. Only time will tell what the national prevalence of board-certified pediatric hospitalists settles out to be.
Historically, PHM fellowship graduates have assumed roles that include teaching and research responsibilities, and ACGME fellowship requirements have ensured that trainees graduate with skills in medical education and scholarship, and need only 4 weeks of training to be done in a community hospital.5 Pediatric hospitalists who do not pursue board certification are seeing the growing pool of PHM fellowship graduates prepared for positions in academic institutions. It is reasonable that they harbor concerns about being siloed toward primarily community hospital roles, and for community hospitalists to feel that this structure undervalues their role within the field of PHM.
At a time when inclusivity and community in medicine are receiving much-needed recognition, the current fellowship application climate has potential to create division within the PHM community. Newly graduating pediatric residents are among the populations disproportionately affected by the practice pathway cutoff. Like other subspecialties with ever-climbing steps up the “ivory tower” of academia and specialization within medicine, the inherent structure of the training pathway makes navigating it more difficult for pediatricians with professional, geographic, and economic diversity or constraints.
Med-Peds–trained colleagues have the added challenge of finding a fellowship position that is willing and able to support their concurrent internal medicine goals. International medical graduates make up about 20% of graduating residents each year, and just 11% of matched PHM fellows.3,6 Similarly, while DO medical graduates make up 20% of pediatric residents in the United States, only 10% of matched PHM fellows were DOs.3,6 New pediatricians with families or financial insecurity may be unable to invest in an expensive application process, move to a new city, and accept less than half of the average starting salary of a pediatric hospitalist for 2-3 years.7
The prevalence of implicit bias in medicine is well documented, and there is growing evidence that it negatively impacts candidate selection in medical education and contributes to minorities being underrepresented in the physician workforce.8 We must recognize the ways that adding a competitive costly hurdle may risk conflict with our mission to encourage diversity of representation within PHM leadership positions.
We have not yet successfully bridged the gap between qualified PHM fellowship candidates and available fellowship positions. I worry that this gap and the lack of transparency surrounding it is resulting in one portion of new pediatricians being welcomed by the subspecialty, and others feeling unsupported and alienated by the larger PHM community as early career physicians.
Right now, the only solution available is expansion of fellowship programs. We see progress with the new addition of fellowship positions every year, but finding funding for each position is often a lengthy endeavor, and the COVID-19 pandemic has tightened the purse strings of many children’s hospitals. It may be many years before the number of available fellowship positions more closely approximates the 200 pediatricians that become hospitalists each year.
The most equitable solution would be offering other avenues to board certification while this gap is being bridged, either by extending the practice pathway option, or making a third pathway that requires less institutional funding per fellow, but still incentivizes institutional investment in fellowship positions and resources (e.g., a pathway requiring some number of years in practice, plus 1 year in fellowship centered around a nonclinical academic curriculum).
In the absence of the solutions above, we collectively hold the responsibility of maintaining inclusivity and support of our PHM colleagues with and without board certification. One important strategy provided by Dr. Gregory Welsh9 is to incorporate community hospital medicine rotations into residency training. Sharing this side of PHM with residents may help some graduates avoid a training pathway they may not want or need. More importantly, it would raise trainee exposure and interest toward a service that is both expansive – approximately 70% of pediatric hospitalists practice in a community hospital – and crucial to children’s health nationally.
Pediatric hospitalists who are not eligible for board certification are vital and valued members of the PHM community, and as such need to maintain representation within PHM leadership. Professional development opportunities need to remain accessible outside of fellowship. The blossoming of virtual conferences and Zoom meet-ups in the face of the COVID-19 pandemic have shown us that with innovation (and a good Internet connection), networking and mentorship can be accomplished across thousands of miles.
While there’s great diversity within PHM, this subspecialty has a history of attracting pediatricians with some common core qualities: Grit, creativity, and the belief that a strong team is far greater than the sum of its parts. I have confidence that if we approach this PHM transition period with transparency about our goals and challenges, this community can emerge from it strong and united.
Dr. Ezzio is a first-year pediatric hospital medicine fellow at Helen DeVos Children’s Hospital in Grand Rapids, Mich. Her interests include medical education and advocacy. Dr. Ezzio would like to thank Dr. Jeri Kessenich and Dr. Rachel “Danielle” Fisher for their assistance in revising the article. To submit to, or for inquiries about, our PHM Fellows Column, please contact our Pediatrics Editor, Dr. Anika Kumar ([email protected]).
References
1. Leyenaar JK and Fritner MP. Graduating pediatric residents entering the hospital medicine workforce, 2006-2015. Acad Pediatr. 2018 Mar;18(2):200-7.
2. National Resident Matching Program. Results and data: Specialties matching service 2020 appointment year. Washington, DC 2020.
3. National Resident Matching Program. Results and data: Specialties matching service 2021 appointment year. Washington, DC 2021.
4. 2020 State of Hospital Medicine report. Society of Hospital Medicine. 2020.
5. Oshimura JM et al. Current roles and perceived needs of pediatric hospital medicine fellowship graduates. Hosp Pediatr. 2016;6(10):633-7.
6. National Resident Matching Program. Results and data: 2020 main residency match. Washington, DC 2020.
7. American Academy of Pediatrics Annual Survey of graduating residents 2003-2020.
8. Quinn Capers IV. How clinicians and educators can mitigate implicit bias in patient care and candidate selection in medical education. American Thoracic Society Scholar. 2020 Jun;1(3):211-17.
9. Welsh G. The importance of community pediatric hospital medicine. The Hospitalist. 2021 Jan;25(1):27.
A year and a half ago, I found myself seated in a crowded hall at the national Pediatric Hospital Medicine (PHM) conference. Throughout the conference, trainees like me were warmly welcomed into small groups and lunch tables. I tried to keep my cool while PHM “celebrities” chatted with me in the elevator. Most sessions were prepared with plenty of chairs, and those that were not encouraged latecomers to grab a spot on the floor or the back wall – the more the merrier.
The intention of this “advice for applicants” meeting was to inspire and guide our next steps toward fellowship, but a discomforting reality loomed over us. It was the first year graduating pediatricians could not choose PHM board certification via the practice pathway – we needed an invitation in the form of a fellowship match.
The “hidden curriculum” was not subtle: People who scored a seat would keep their options open within the field of PHM, and those who did not had a murkier future. This message stood in stark contrast to the PHM inclusivity I had experienced all conference, and planted seeds of doubt: Was I welcome here? Did I “deserve” a seat?
I found the experience as a PHM fellowship applicant to be uncomfortable, and my all-too familiar friend “imposter syndrome” set up camp in my brain and made herself at home. I had no way of knowing how many programs to apply to, how many to interview at, or the chances of my matching at all. Once on the interview trail, I realized I was not alone in my discomfort – most applicants harbored some trepidation, and no one truly knew how the chips would fall on Match Day.
I am thrilled and relieved to have come out the other end in a great position. The team I work with and learn from is phenomenal. I am grateful that ACGME accreditation ensures structures are in place for fellows to be supported in their academic and educational efforts and have full confidence that the skills I gain in fellowship will help me contribute to progression of the field of PHM and improve my performance as a clinician-educator.
Sadly, each year PHM match day celebrations are dampened by the knowledge that a large portion of our colleagues are being left out in the cold with an “unmatched” notification in their inboxes. Approximately 200 graduating pediatricians become pediatric hospitalists each year,1 but only 68 fellowship positions were available in the United States for matriculation in 2020.2 In 2019, PHM fellowship candidates navigated the 6-month application journey with aspirations to further their training in the profession they love. Of the candidates who submitted a rank list committing to 2 or more years in PHM fellowship, 35% were denied.
Unfortunately, despite expansion of PHM fellowship programs and fifteen seats added from last year, we learned this December that there still are not enough positions to welcome qualified applicants with open arms: Thirty-three percent of candidates ranked PHM programs first in the NRMP but did not match – the highest unmatched percentage out of all pediatric subspecialties.3
The NRMP report shared a glimpse of our colleagues who received interview invitations and submitted a rank list, but this is likely an underestimation of pediatric graduates who wanted to obtain PHM board certification and wound up on a different path. Some residents anticipated the stiff competition and delayed their plans to apply for fellowship, while others matched into another subspecialty that was able to accommodate them. Many pediatric graduates joined the workforce directly as pediatric hospitalists knowing the practice pathway to certification is not available to them. Along with other physicians without board certification in PHM, they shoulder concerns of being withheld from professional advancement opportunities.
For the foreseeable future it is clear that pediatric hospitalists without board certification will be a large part of our community, and are crucial to providing high-quality care to hospitalized children nationally. In 2019, a national survey of pediatric hospital medicine groups revealed that 50% of pediatric hospitalist hires came directly out of residency, and only 8% of hires were fellowship trained.4 The same report revealed that 26% of physicians were board-certified.These percentages are likely to change over the next 5 years as the window of practice pathway certification closes and fellowship programs continue to expand. Only time will tell what the national prevalence of board-certified pediatric hospitalists settles out to be.
Historically, PHM fellowship graduates have assumed roles that include teaching and research responsibilities, and ACGME fellowship requirements have ensured that trainees graduate with skills in medical education and scholarship, and need only 4 weeks of training to be done in a community hospital.5 Pediatric hospitalists who do not pursue board certification are seeing the growing pool of PHM fellowship graduates prepared for positions in academic institutions. It is reasonable that they harbor concerns about being siloed toward primarily community hospital roles, and for community hospitalists to feel that this structure undervalues their role within the field of PHM.
At a time when inclusivity and community in medicine are receiving much-needed recognition, the current fellowship application climate has potential to create division within the PHM community. Newly graduating pediatric residents are among the populations disproportionately affected by the practice pathway cutoff. Like other subspecialties with ever-climbing steps up the “ivory tower” of academia and specialization within medicine, the inherent structure of the training pathway makes navigating it more difficult for pediatricians with professional, geographic, and economic diversity or constraints.
Med-Peds–trained colleagues have the added challenge of finding a fellowship position that is willing and able to support their concurrent internal medicine goals. International medical graduates make up about 20% of graduating residents each year, and just 11% of matched PHM fellows.3,6 Similarly, while DO medical graduates make up 20% of pediatric residents in the United States, only 10% of matched PHM fellows were DOs.3,6 New pediatricians with families or financial insecurity may be unable to invest in an expensive application process, move to a new city, and accept less than half of the average starting salary of a pediatric hospitalist for 2-3 years.7
The prevalence of implicit bias in medicine is well documented, and there is growing evidence that it negatively impacts candidate selection in medical education and contributes to minorities being underrepresented in the physician workforce.8 We must recognize the ways that adding a competitive costly hurdle may risk conflict with our mission to encourage diversity of representation within PHM leadership positions.
We have not yet successfully bridged the gap between qualified PHM fellowship candidates and available fellowship positions. I worry that this gap and the lack of transparency surrounding it is resulting in one portion of new pediatricians being welcomed by the subspecialty, and others feeling unsupported and alienated by the larger PHM community as early career physicians.
Right now, the only solution available is expansion of fellowship programs. We see progress with the new addition of fellowship positions every year, but finding funding for each position is often a lengthy endeavor, and the COVID-19 pandemic has tightened the purse strings of many children’s hospitals. It may be many years before the number of available fellowship positions more closely approximates the 200 pediatricians that become hospitalists each year.
The most equitable solution would be offering other avenues to board certification while this gap is being bridged, either by extending the practice pathway option, or making a third pathway that requires less institutional funding per fellow, but still incentivizes institutional investment in fellowship positions and resources (e.g., a pathway requiring some number of years in practice, plus 1 year in fellowship centered around a nonclinical academic curriculum).
In the absence of the solutions above, we collectively hold the responsibility of maintaining inclusivity and support of our PHM colleagues with and without board certification. One important strategy provided by Dr. Gregory Welsh9 is to incorporate community hospital medicine rotations into residency training. Sharing this side of PHM with residents may help some graduates avoid a training pathway they may not want or need. More importantly, it would raise trainee exposure and interest toward a service that is both expansive – approximately 70% of pediatric hospitalists practice in a community hospital – and crucial to children’s health nationally.
Pediatric hospitalists who are not eligible for board certification are vital and valued members of the PHM community, and as such need to maintain representation within PHM leadership. Professional development opportunities need to remain accessible outside of fellowship. The blossoming of virtual conferences and Zoom meet-ups in the face of the COVID-19 pandemic have shown us that with innovation (and a good Internet connection), networking and mentorship can be accomplished across thousands of miles.
While there’s great diversity within PHM, this subspecialty has a history of attracting pediatricians with some common core qualities: Grit, creativity, and the belief that a strong team is far greater than the sum of its parts. I have confidence that if we approach this PHM transition period with transparency about our goals and challenges, this community can emerge from it strong and united.
Dr. Ezzio is a first-year pediatric hospital medicine fellow at Helen DeVos Children’s Hospital in Grand Rapids, Mich. Her interests include medical education and advocacy. Dr. Ezzio would like to thank Dr. Jeri Kessenich and Dr. Rachel “Danielle” Fisher for their assistance in revising the article. To submit to, or for inquiries about, our PHM Fellows Column, please contact our Pediatrics Editor, Dr. Anika Kumar ([email protected]).
References
1. Leyenaar JK and Fritner MP. Graduating pediatric residents entering the hospital medicine workforce, 2006-2015. Acad Pediatr. 2018 Mar;18(2):200-7.
2. National Resident Matching Program. Results and data: Specialties matching service 2020 appointment year. Washington, DC 2020.
3. National Resident Matching Program. Results and data: Specialties matching service 2021 appointment year. Washington, DC 2021.
4. 2020 State of Hospital Medicine report. Society of Hospital Medicine. 2020.
5. Oshimura JM et al. Current roles and perceived needs of pediatric hospital medicine fellowship graduates. Hosp Pediatr. 2016;6(10):633-7.
6. National Resident Matching Program. Results and data: 2020 main residency match. Washington, DC 2020.
7. American Academy of Pediatrics Annual Survey of graduating residents 2003-2020.
8. Quinn Capers IV. How clinicians and educators can mitigate implicit bias in patient care and candidate selection in medical education. American Thoracic Society Scholar. 2020 Jun;1(3):211-17.
9. Welsh G. The importance of community pediatric hospital medicine. The Hospitalist. 2021 Jan;25(1):27.
A year and a half ago, I found myself seated in a crowded hall at the national Pediatric Hospital Medicine (PHM) conference. Throughout the conference, trainees like me were warmly welcomed into small groups and lunch tables. I tried to keep my cool while PHM “celebrities” chatted with me in the elevator. Most sessions were prepared with plenty of chairs, and those that were not encouraged latecomers to grab a spot on the floor or the back wall – the more the merrier.
The intention of this “advice for applicants” meeting was to inspire and guide our next steps toward fellowship, but a discomforting reality loomed over us. It was the first year graduating pediatricians could not choose PHM board certification via the practice pathway – we needed an invitation in the form of a fellowship match.
The “hidden curriculum” was not subtle: People who scored a seat would keep their options open within the field of PHM, and those who did not had a murkier future. This message stood in stark contrast to the PHM inclusivity I had experienced all conference, and planted seeds of doubt: Was I welcome here? Did I “deserve” a seat?
I found the experience as a PHM fellowship applicant to be uncomfortable, and my all-too familiar friend “imposter syndrome” set up camp in my brain and made herself at home. I had no way of knowing how many programs to apply to, how many to interview at, or the chances of my matching at all. Once on the interview trail, I realized I was not alone in my discomfort – most applicants harbored some trepidation, and no one truly knew how the chips would fall on Match Day.
I am thrilled and relieved to have come out the other end in a great position. The team I work with and learn from is phenomenal. I am grateful that ACGME accreditation ensures structures are in place for fellows to be supported in their academic and educational efforts and have full confidence that the skills I gain in fellowship will help me contribute to progression of the field of PHM and improve my performance as a clinician-educator.
Sadly, each year PHM match day celebrations are dampened by the knowledge that a large portion of our colleagues are being left out in the cold with an “unmatched” notification in their inboxes. Approximately 200 graduating pediatricians become pediatric hospitalists each year,1 but only 68 fellowship positions were available in the United States for matriculation in 2020.2 In 2019, PHM fellowship candidates navigated the 6-month application journey with aspirations to further their training in the profession they love. Of the candidates who submitted a rank list committing to 2 or more years in PHM fellowship, 35% were denied.
Unfortunately, despite expansion of PHM fellowship programs and fifteen seats added from last year, we learned this December that there still are not enough positions to welcome qualified applicants with open arms: Thirty-three percent of candidates ranked PHM programs first in the NRMP but did not match – the highest unmatched percentage out of all pediatric subspecialties.3
The NRMP report shared a glimpse of our colleagues who received interview invitations and submitted a rank list, but this is likely an underestimation of pediatric graduates who wanted to obtain PHM board certification and wound up on a different path. Some residents anticipated the stiff competition and delayed their plans to apply for fellowship, while others matched into another subspecialty that was able to accommodate them. Many pediatric graduates joined the workforce directly as pediatric hospitalists knowing the practice pathway to certification is not available to them. Along with other physicians without board certification in PHM, they shoulder concerns of being withheld from professional advancement opportunities.
For the foreseeable future it is clear that pediatric hospitalists without board certification will be a large part of our community, and are crucial to providing high-quality care to hospitalized children nationally. In 2019, a national survey of pediatric hospital medicine groups revealed that 50% of pediatric hospitalist hires came directly out of residency, and only 8% of hires were fellowship trained.4 The same report revealed that 26% of physicians were board-certified.These percentages are likely to change over the next 5 years as the window of practice pathway certification closes and fellowship programs continue to expand. Only time will tell what the national prevalence of board-certified pediatric hospitalists settles out to be.
Historically, PHM fellowship graduates have assumed roles that include teaching and research responsibilities, and ACGME fellowship requirements have ensured that trainees graduate with skills in medical education and scholarship, and need only 4 weeks of training to be done in a community hospital.5 Pediatric hospitalists who do not pursue board certification are seeing the growing pool of PHM fellowship graduates prepared for positions in academic institutions. It is reasonable that they harbor concerns about being siloed toward primarily community hospital roles, and for community hospitalists to feel that this structure undervalues their role within the field of PHM.
At a time when inclusivity and community in medicine are receiving much-needed recognition, the current fellowship application climate has potential to create division within the PHM community. Newly graduating pediatric residents are among the populations disproportionately affected by the practice pathway cutoff. Like other subspecialties with ever-climbing steps up the “ivory tower” of academia and specialization within medicine, the inherent structure of the training pathway makes navigating it more difficult for pediatricians with professional, geographic, and economic diversity or constraints.
Med-Peds–trained colleagues have the added challenge of finding a fellowship position that is willing and able to support their concurrent internal medicine goals. International medical graduates make up about 20% of graduating residents each year, and just 11% of matched PHM fellows.3,6 Similarly, while DO medical graduates make up 20% of pediatric residents in the United States, only 10% of matched PHM fellows were DOs.3,6 New pediatricians with families or financial insecurity may be unable to invest in an expensive application process, move to a new city, and accept less than half of the average starting salary of a pediatric hospitalist for 2-3 years.7
The prevalence of implicit bias in medicine is well documented, and there is growing evidence that it negatively impacts candidate selection in medical education and contributes to minorities being underrepresented in the physician workforce.8 We must recognize the ways that adding a competitive costly hurdle may risk conflict with our mission to encourage diversity of representation within PHM leadership positions.
We have not yet successfully bridged the gap between qualified PHM fellowship candidates and available fellowship positions. I worry that this gap and the lack of transparency surrounding it is resulting in one portion of new pediatricians being welcomed by the subspecialty, and others feeling unsupported and alienated by the larger PHM community as early career physicians.
Right now, the only solution available is expansion of fellowship programs. We see progress with the new addition of fellowship positions every year, but finding funding for each position is often a lengthy endeavor, and the COVID-19 pandemic has tightened the purse strings of many children’s hospitals. It may be many years before the number of available fellowship positions more closely approximates the 200 pediatricians that become hospitalists each year.
The most equitable solution would be offering other avenues to board certification while this gap is being bridged, either by extending the practice pathway option, or making a third pathway that requires less institutional funding per fellow, but still incentivizes institutional investment in fellowship positions and resources (e.g., a pathway requiring some number of years in practice, plus 1 year in fellowship centered around a nonclinical academic curriculum).
In the absence of the solutions above, we collectively hold the responsibility of maintaining inclusivity and support of our PHM colleagues with and without board certification. One important strategy provided by Dr. Gregory Welsh9 is to incorporate community hospital medicine rotations into residency training. Sharing this side of PHM with residents may help some graduates avoid a training pathway they may not want or need. More importantly, it would raise trainee exposure and interest toward a service that is both expansive – approximately 70% of pediatric hospitalists practice in a community hospital – and crucial to children’s health nationally.
Pediatric hospitalists who are not eligible for board certification are vital and valued members of the PHM community, and as such need to maintain representation within PHM leadership. Professional development opportunities need to remain accessible outside of fellowship. The blossoming of virtual conferences and Zoom meet-ups in the face of the COVID-19 pandemic have shown us that with innovation (and a good Internet connection), networking and mentorship can be accomplished across thousands of miles.
While there’s great diversity within PHM, this subspecialty has a history of attracting pediatricians with some common core qualities: Grit, creativity, and the belief that a strong team is far greater than the sum of its parts. I have confidence that if we approach this PHM transition period with transparency about our goals and challenges, this community can emerge from it strong and united.
Dr. Ezzio is a first-year pediatric hospital medicine fellow at Helen DeVos Children’s Hospital in Grand Rapids, Mich. Her interests include medical education and advocacy. Dr. Ezzio would like to thank Dr. Jeri Kessenich and Dr. Rachel “Danielle” Fisher for their assistance in revising the article. To submit to, or for inquiries about, our PHM Fellows Column, please contact our Pediatrics Editor, Dr. Anika Kumar ([email protected]).
References
1. Leyenaar JK and Fritner MP. Graduating pediatric residents entering the hospital medicine workforce, 2006-2015. Acad Pediatr. 2018 Mar;18(2):200-7.
2. National Resident Matching Program. Results and data: Specialties matching service 2020 appointment year. Washington, DC 2020.
3. National Resident Matching Program. Results and data: Specialties matching service 2021 appointment year. Washington, DC 2021.
4. 2020 State of Hospital Medicine report. Society of Hospital Medicine. 2020.
5. Oshimura JM et al. Current roles and perceived needs of pediatric hospital medicine fellowship graduates. Hosp Pediatr. 2016;6(10):633-7.
6. National Resident Matching Program. Results and data: 2020 main residency match. Washington, DC 2020.
7. American Academy of Pediatrics Annual Survey of graduating residents 2003-2020.
8. Quinn Capers IV. How clinicians and educators can mitigate implicit bias in patient care and candidate selection in medical education. American Thoracic Society Scholar. 2020 Jun;1(3):211-17.
9. Welsh G. The importance of community pediatric hospital medicine. The Hospitalist. 2021 Jan;25(1):27.
Palliative care and hospital medicine partnerships in the pandemic
Patients dying without their loved ones, families forced to remotely decide goals of care without the physical presence or human connection of the care team, overworked staff physically isolated from their critically ill patients, and at-risk community members with uncertain and undocumented goals for care are among the universal challenges confronted by hospitals and hospitalists during this COVID-19 pandemic. Partnerships among hospital medicine (HM) and palliative care (PC) teams at Dell Medical School/Dell Seton Medical Center thrive on mutually shared core values of patient centered care – compassion, empathy, and humanity.
A key PC-HM collaboration was adapting our multidisciplinary huddle to focus on communication effectiveness and efficiency in the medical intensive care unit (MICU). Expanded interprofessional and cross-specialty collaboration promoted streamlined, succinct, and standardized communication with patients’ families while their loved ones were critically ill with COVID-19. The PC team attended daily MICU multidisciplinary huddles, attentive to both the medical and psychosocial updates for each patient. During huddles, residents or HM providers were asked to end their presentation with a clinical status “headline” and solicited feedback from the multidisciplinary team before messaging to the family. The PC team then communicated with families a succinct and cohesive medical update and continuously explored goals of care. This allowed the HM team, often overwhelmed with admissions, co-managing intensive care patients, and facilitating safe discharges, to focus on urgent issues while PC provided continuity and personalized support for patients and families. PC’s ability to synthesize and summarize clinical information from multiple teams and then provide cohesive updates in patient-friendly language modeled important communication skills for learners and simultaneously benefited HM providers.
Our chaplains, too, were central to facilitating timely, proactive conversations and documentation of Medical Power of Attorney (MPOA) for patients with COVID-19 admitted to our hospital. HM prioritized early admission conversations with patients to counsel them on severity of illness, prognosis based on risk factors, to elucidate wishes for intubation or resuscitation, and to capture their desired medical decision maker. HM was notified of all COVID and PUI admissions, allowing us to speak with even critically ill patients in the ER or ICU prior to intubation in order to quickly and accurately capture patients’ wishes for treatment and delegate decision makers. Our chaplains supported and supplemented these efforts by diligently and dutifully soliciting, hearing, and documenting patient MPOA delegates, with over 50% MPOA completion by 24 hours of hospitalization.
Another early PC-HM project, “Meet My Loved One,” was adapted from the University of Alabama at Birmingham Palliative and Comfort Unit. The absence of families visiting the ICU and sharing pictures, stories, anecdotes of our patients left a deeply felt, dehumanizing void in the halls and rooms of our hospital. To fill this space with life and humanity, furloughed medical students on their “transition of care” electives contacted family members of their “continuity” patients focusing primarily on those patients expected to have prolonged ICU or hospital stays and solicited personal, humanizing information about our patients. Questions included: “What is your loved one’s preferred name or nickname?” and “What are three things we should know to take better care of your loved one?” With family permission, we posted this information on the door outside the patient’s room. Nursing staff, in particular, appreciated getting to know their patients more personally and families appreciated the staff’s desire to know their loved one as an individual.
It is also important to acknowledge setbacks. Early efforts to engage technology proved more foe than friend. We continue to struggle with using our iPads for video visits. Most of our families prefer “WhatsApp” for video communication, which is not compatible with operating systems on early versions of the iPad, which were generously and widely donated by local school systems. Desperate to allow families to connect, many providers resorted to using personal devices to facilitate video visits and family meetings. And we discovered that many video visits caused more not less family angst, especially for critically ill patients. Families often required preparation and coaching on what to expect and how to interact with intubated, sedated, proned, and paralyzed loved ones.
Our hospital medicine and palliative care teams have an established strong partnership. The COVID-19 pandemic created novel communication challenges but our shared mission toward patient-centered care allowed us to effectively collaborate to bring the patients goals of care to the forefront aligning patients, families, physicians, nurses, and staff during the COVID-19 surge.
Dr. Johnston is associate professor at Dell Medical School at The University of Texas in Austin. She practices hospital medicine and inpatient palliative care at Dell Seton Medical Center. Dr. Cooremans is a resident physician at Dell Medical School. Dr. Salib is the internal medicine clerkship director and an associate professor at Dell Medical School. Dr. Nieto is an assistant professor and associate chief of the Division of Hospital Medicine at Dell Medical School. Dr. Patel is an assistant professor at Dell Medical School. This article is part of a series written by members of the Division of Hospital Medicine at Dell Medical School, exploring lessons learned from the coronavirus pandemic and outlining an approach for creating COVID-19 Centers of Excellence. The article first appeared in The Hospital Leader, the official blog of SHM.
Patients dying without their loved ones, families forced to remotely decide goals of care without the physical presence or human connection of the care team, overworked staff physically isolated from their critically ill patients, and at-risk community members with uncertain and undocumented goals for care are among the universal challenges confronted by hospitals and hospitalists during this COVID-19 pandemic. Partnerships among hospital medicine (HM) and palliative care (PC) teams at Dell Medical School/Dell Seton Medical Center thrive on mutually shared core values of patient centered care – compassion, empathy, and humanity.
A key PC-HM collaboration was adapting our multidisciplinary huddle to focus on communication effectiveness and efficiency in the medical intensive care unit (MICU). Expanded interprofessional and cross-specialty collaboration promoted streamlined, succinct, and standardized communication with patients’ families while their loved ones were critically ill with COVID-19. The PC team attended daily MICU multidisciplinary huddles, attentive to both the medical and psychosocial updates for each patient. During huddles, residents or HM providers were asked to end their presentation with a clinical status “headline” and solicited feedback from the multidisciplinary team before messaging to the family. The PC team then communicated with families a succinct and cohesive medical update and continuously explored goals of care. This allowed the HM team, often overwhelmed with admissions, co-managing intensive care patients, and facilitating safe discharges, to focus on urgent issues while PC provided continuity and personalized support for patients and families. PC’s ability to synthesize and summarize clinical information from multiple teams and then provide cohesive updates in patient-friendly language modeled important communication skills for learners and simultaneously benefited HM providers.
Our chaplains, too, were central to facilitating timely, proactive conversations and documentation of Medical Power of Attorney (MPOA) for patients with COVID-19 admitted to our hospital. HM prioritized early admission conversations with patients to counsel them on severity of illness, prognosis based on risk factors, to elucidate wishes for intubation or resuscitation, and to capture their desired medical decision maker. HM was notified of all COVID and PUI admissions, allowing us to speak with even critically ill patients in the ER or ICU prior to intubation in order to quickly and accurately capture patients’ wishes for treatment and delegate decision makers. Our chaplains supported and supplemented these efforts by diligently and dutifully soliciting, hearing, and documenting patient MPOA delegates, with over 50% MPOA completion by 24 hours of hospitalization.
Another early PC-HM project, “Meet My Loved One,” was adapted from the University of Alabama at Birmingham Palliative and Comfort Unit. The absence of families visiting the ICU and sharing pictures, stories, anecdotes of our patients left a deeply felt, dehumanizing void in the halls and rooms of our hospital. To fill this space with life and humanity, furloughed medical students on their “transition of care” electives contacted family members of their “continuity” patients focusing primarily on those patients expected to have prolonged ICU or hospital stays and solicited personal, humanizing information about our patients. Questions included: “What is your loved one’s preferred name or nickname?” and “What are three things we should know to take better care of your loved one?” With family permission, we posted this information on the door outside the patient’s room. Nursing staff, in particular, appreciated getting to know their patients more personally and families appreciated the staff’s desire to know their loved one as an individual.
It is also important to acknowledge setbacks. Early efforts to engage technology proved more foe than friend. We continue to struggle with using our iPads for video visits. Most of our families prefer “WhatsApp” for video communication, which is not compatible with operating systems on early versions of the iPad, which were generously and widely donated by local school systems. Desperate to allow families to connect, many providers resorted to using personal devices to facilitate video visits and family meetings. And we discovered that many video visits caused more not less family angst, especially for critically ill patients. Families often required preparation and coaching on what to expect and how to interact with intubated, sedated, proned, and paralyzed loved ones.
Our hospital medicine and palliative care teams have an established strong partnership. The COVID-19 pandemic created novel communication challenges but our shared mission toward patient-centered care allowed us to effectively collaborate to bring the patients goals of care to the forefront aligning patients, families, physicians, nurses, and staff during the COVID-19 surge.
Dr. Johnston is associate professor at Dell Medical School at The University of Texas in Austin. She practices hospital medicine and inpatient palliative care at Dell Seton Medical Center. Dr. Cooremans is a resident physician at Dell Medical School. Dr. Salib is the internal medicine clerkship director and an associate professor at Dell Medical School. Dr. Nieto is an assistant professor and associate chief of the Division of Hospital Medicine at Dell Medical School. Dr. Patel is an assistant professor at Dell Medical School. This article is part of a series written by members of the Division of Hospital Medicine at Dell Medical School, exploring lessons learned from the coronavirus pandemic and outlining an approach for creating COVID-19 Centers of Excellence. The article first appeared in The Hospital Leader, the official blog of SHM.
Patients dying without their loved ones, families forced to remotely decide goals of care without the physical presence or human connection of the care team, overworked staff physically isolated from their critically ill patients, and at-risk community members with uncertain and undocumented goals for care are among the universal challenges confronted by hospitals and hospitalists during this COVID-19 pandemic. Partnerships among hospital medicine (HM) and palliative care (PC) teams at Dell Medical School/Dell Seton Medical Center thrive on mutually shared core values of patient centered care – compassion, empathy, and humanity.
A key PC-HM collaboration was adapting our multidisciplinary huddle to focus on communication effectiveness and efficiency in the medical intensive care unit (MICU). Expanded interprofessional and cross-specialty collaboration promoted streamlined, succinct, and standardized communication with patients’ families while their loved ones were critically ill with COVID-19. The PC team attended daily MICU multidisciplinary huddles, attentive to both the medical and psychosocial updates for each patient. During huddles, residents or HM providers were asked to end their presentation with a clinical status “headline” and solicited feedback from the multidisciplinary team before messaging to the family. The PC team then communicated with families a succinct and cohesive medical update and continuously explored goals of care. This allowed the HM team, often overwhelmed with admissions, co-managing intensive care patients, and facilitating safe discharges, to focus on urgent issues while PC provided continuity and personalized support for patients and families. PC’s ability to synthesize and summarize clinical information from multiple teams and then provide cohesive updates in patient-friendly language modeled important communication skills for learners and simultaneously benefited HM providers.
Our chaplains, too, were central to facilitating timely, proactive conversations and documentation of Medical Power of Attorney (MPOA) for patients with COVID-19 admitted to our hospital. HM prioritized early admission conversations with patients to counsel them on severity of illness, prognosis based on risk factors, to elucidate wishes for intubation or resuscitation, and to capture their desired medical decision maker. HM was notified of all COVID and PUI admissions, allowing us to speak with even critically ill patients in the ER or ICU prior to intubation in order to quickly and accurately capture patients’ wishes for treatment and delegate decision makers. Our chaplains supported and supplemented these efforts by diligently and dutifully soliciting, hearing, and documenting patient MPOA delegates, with over 50% MPOA completion by 24 hours of hospitalization.
Another early PC-HM project, “Meet My Loved One,” was adapted from the University of Alabama at Birmingham Palliative and Comfort Unit. The absence of families visiting the ICU and sharing pictures, stories, anecdotes of our patients left a deeply felt, dehumanizing void in the halls and rooms of our hospital. To fill this space with life and humanity, furloughed medical students on their “transition of care” electives contacted family members of their “continuity” patients focusing primarily on those patients expected to have prolonged ICU or hospital stays and solicited personal, humanizing information about our patients. Questions included: “What is your loved one’s preferred name or nickname?” and “What are three things we should know to take better care of your loved one?” With family permission, we posted this information on the door outside the patient’s room. Nursing staff, in particular, appreciated getting to know their patients more personally and families appreciated the staff’s desire to know their loved one as an individual.
It is also important to acknowledge setbacks. Early efforts to engage technology proved more foe than friend. We continue to struggle with using our iPads for video visits. Most of our families prefer “WhatsApp” for video communication, which is not compatible with operating systems on early versions of the iPad, which were generously and widely donated by local school systems. Desperate to allow families to connect, many providers resorted to using personal devices to facilitate video visits and family meetings. And we discovered that many video visits caused more not less family angst, especially for critically ill patients. Families often required preparation and coaching on what to expect and how to interact with intubated, sedated, proned, and paralyzed loved ones.
Our hospital medicine and palliative care teams have an established strong partnership. The COVID-19 pandemic created novel communication challenges but our shared mission toward patient-centered care allowed us to effectively collaborate to bring the patients goals of care to the forefront aligning patients, families, physicians, nurses, and staff during the COVID-19 surge.
Dr. Johnston is associate professor at Dell Medical School at The University of Texas in Austin. She practices hospital medicine and inpatient palliative care at Dell Seton Medical Center. Dr. Cooremans is a resident physician at Dell Medical School. Dr. Salib is the internal medicine clerkship director and an associate professor at Dell Medical School. Dr. Nieto is an assistant professor and associate chief of the Division of Hospital Medicine at Dell Medical School. Dr. Patel is an assistant professor at Dell Medical School. This article is part of a series written by members of the Division of Hospital Medicine at Dell Medical School, exploring lessons learned from the coronavirus pandemic and outlining an approach for creating COVID-19 Centers of Excellence. The article first appeared in The Hospital Leader, the official blog of SHM.
Who do you call in those late, quiet hours, when all seems lost?
I swear by Apollo Physician and Asclepius and Hygeia and Panacea and all the gods and goddesses, making them my witnesses, that I will fulfill according to my ability and judgment this oath and this covenant.
On my desk sits a bust of Hygeia, a mask from Venice, next to a small sculpture and a figurine of the plague doctor. Nearby, there is a Klimt closeup of Hygeia, a postcard portraying Asclepius, St. Sebastian paintings, and quotes from Maimonides. They whisper secrets and nod to the challenges of the past. These medical specters, ancient voices of the past, keep me grounded. They speak, listen, and elevate me, too. They bring life into my otherwise quiet room.
We all began our careers swearing to Apollo, Asclepius, Hygeia, and Panacea when we recited the Hippocratic Oath. I call upon them, and other gods and totems, and saints and ancient healers, now more than ever. As an atheist, I don’t appeal to them as prayers, but as Hippocrates intended. I look to their supernatural healing powers as a source of strength and as revealers of the natural and observable phenomena.
Apollo was one of the Twelve Olympians, a God of medicine, father of Asclepius. He was a healer, though his arrows also bore the plagues of the Gods.
For centuries, Apollo was found floating above the marble dissection table in the Bologna anatomical theater, guiding students who dove into the secrets of the human body.
Asclepius, son of Apollo, was hailed as a god of medicine. He healed many from plagues at his temples throughout the Ancient Greek and Roman empires. He was mentored in the healing arts by the centaur, Chiron. His many daughters and sons represent various aspects of medicine including cures, healing, recovery, sanitation, and beauty. To Asclepius, temples were places of healing, an ancient ancestor to modern hospitals.
Two of his daughters, Panacea and Hygeia, gave us the healing words of panacea and hygiene. Today, these acts of hygiene, handwashing, mask-wearing, and sanitation are discussed across the world louder than ever. While we’re all wishing for a panacea, we know it will take all the attributes of medicine to get us through this pandemic.
Hospitalists are part of the frontline teams facing this pandemic head-on. Gowning up for MRSA isolation seems quaint nowadays.
My attendings spoke of their fears, up against the unknown while on service in the 1980s, when HIV appeared. 2014 brought the Ebola biocontainment units. Now, this generation works daily against a modern plague, where every day is a risk of exposure. When every patient is in isolation, the garb begins to reflect the PPE that emerged during a 17th-century plague epidemics, the plague doctor outfit.
Godfather II fans recall the famous portrayal of the August 16th festival to San Rocco play out in the streets of New York. For those stricken with COVID-19 and recovered, you emulate San Rocco, in your continued return to service.
The Scuola Grande di San Rocco, in Venice, is the epitome of healing and greatness in one building. Tintoretto, the great Venetian painter, assembled the story of healing through art and portraits of San Rocco. The scuola, a confraternity, was a community of healers, gathered in one place to look after the less fortunate.
Hospitalists march into the hospital risking their lives. We always wear PPE for MRSA, ESBL, or C. diff. And enter reverse isolation rooms wearing N95s for possible TB cases. But those don’t elevate to the volume, to the same fear, as gowning up for COVID-19.
Hospitalists, frontline health care workers, embody the story of San Sebastian, another plague saint who absorbed the arrows, the symbolic plagues, onto his own shoulders so no one else had to bear them. San Sebastian was a Christian persecuted by a Roman emperor once his beliefs were discovered. He is often laden with arrows in spots where buboes would have appeared: the armpits and the groin. His sacrifice for others’ recovery became a symbol of absorbing the plague, the wounds, and the impact of the arrows.
This sacrifice epitomizes the daily work the frontline nurses, ER docs, intensivists, hospitalists, and the entire hospital staff perform daily, bearing the slung arrows of coronavirus.
One of the images I think of frequently during this time lies atop Castel San Angelo in Rome. Built in 161 AD, it has served as a mausoleum, prison, papal residence, and is currently a museum. Atop San’Angelo stands St. Michael, the destroyer of the dragon. He is sheathing his sword in representation of the end of the plague in 590.
The arrows flow, yet the sword will be sheathed. Evil will be halted. The stories of these ancient totems and strength can give us strength as they remind us of the work that was done for centuries: pestilence, famine, war. The great killers never go away completely.
Fast forward to today
These medical specters serve as reminders of what makes the field of medicine so inspiring: the selfless acts, the fortitude of spirit, the healers, the long history, and the shoulders of giants we stand upon. From these stories, we spring the healing waters we bathe in to give us the courage to wake up and care for our patients each day. These specters encourage us to defeat any and all of the scourges that come our way.
I hear and read stories about the frontline heroes, the vaccine makers, the PPE creators, the health care workers, grocery store clerks, and teachers. I’m honored to hear of these stories and your sacrifices. I’m inspired to continue upholding your essence, your fight, and your stories. In keeping with ancient empire metaphors, you are taking the slings of the diseased arrows flying to our brethren as you try to keep yourself and others safe.
The sheathing of this sword will come. These arrows will be silenced. But until then, I lean on these pictures, these stories, and these saints, to give us all the strength to wake up each morning and continue healing.
They serve as reminders of what makes the field of medicine so great: the selfless acts, the fortitude of spirit, the healers, the long history, and the shoulders of giants we stand upon. From these stories spring the healing waters we bathe in to give us the courage to wake up and care for our patients each day and defeat any and all scourges that come our way.
So, who do you call in those late, quiet hours, when all seems lost?
Dr. Messler is the executive director, quality initiatives at Glytec and works as a hospitalist at Morton Plant Hospitalist group in Clearwater, Fla. This essay appeared initially on The Hospital Leader, the official blog of SHM.
I swear by Apollo Physician and Asclepius and Hygeia and Panacea and all the gods and goddesses, making them my witnesses, that I will fulfill according to my ability and judgment this oath and this covenant.
On my desk sits a bust of Hygeia, a mask from Venice, next to a small sculpture and a figurine of the plague doctor. Nearby, there is a Klimt closeup of Hygeia, a postcard portraying Asclepius, St. Sebastian paintings, and quotes from Maimonides. They whisper secrets and nod to the challenges of the past. These medical specters, ancient voices of the past, keep me grounded. They speak, listen, and elevate me, too. They bring life into my otherwise quiet room.
We all began our careers swearing to Apollo, Asclepius, Hygeia, and Panacea when we recited the Hippocratic Oath. I call upon them, and other gods and totems, and saints and ancient healers, now more than ever. As an atheist, I don’t appeal to them as prayers, but as Hippocrates intended. I look to their supernatural healing powers as a source of strength and as revealers of the natural and observable phenomena.
Apollo was one of the Twelve Olympians, a God of medicine, father of Asclepius. He was a healer, though his arrows also bore the plagues of the Gods.
For centuries, Apollo was found floating above the marble dissection table in the Bologna anatomical theater, guiding students who dove into the secrets of the human body.
Asclepius, son of Apollo, was hailed as a god of medicine. He healed many from plagues at his temples throughout the Ancient Greek and Roman empires. He was mentored in the healing arts by the centaur, Chiron. His many daughters and sons represent various aspects of medicine including cures, healing, recovery, sanitation, and beauty. To Asclepius, temples were places of healing, an ancient ancestor to modern hospitals.
Two of his daughters, Panacea and Hygeia, gave us the healing words of panacea and hygiene. Today, these acts of hygiene, handwashing, mask-wearing, and sanitation are discussed across the world louder than ever. While we’re all wishing for a panacea, we know it will take all the attributes of medicine to get us through this pandemic.
Hospitalists are part of the frontline teams facing this pandemic head-on. Gowning up for MRSA isolation seems quaint nowadays.
My attendings spoke of their fears, up against the unknown while on service in the 1980s, when HIV appeared. 2014 brought the Ebola biocontainment units. Now, this generation works daily against a modern plague, where every day is a risk of exposure. When every patient is in isolation, the garb begins to reflect the PPE that emerged during a 17th-century plague epidemics, the plague doctor outfit.
Godfather II fans recall the famous portrayal of the August 16th festival to San Rocco play out in the streets of New York. For those stricken with COVID-19 and recovered, you emulate San Rocco, in your continued return to service.
The Scuola Grande di San Rocco, in Venice, is the epitome of healing and greatness in one building. Tintoretto, the great Venetian painter, assembled the story of healing through art and portraits of San Rocco. The scuola, a confraternity, was a community of healers, gathered in one place to look after the less fortunate.
Hospitalists march into the hospital risking their lives. We always wear PPE for MRSA, ESBL, or C. diff. And enter reverse isolation rooms wearing N95s for possible TB cases. But those don’t elevate to the volume, to the same fear, as gowning up for COVID-19.
Hospitalists, frontline health care workers, embody the story of San Sebastian, another plague saint who absorbed the arrows, the symbolic plagues, onto his own shoulders so no one else had to bear them. San Sebastian was a Christian persecuted by a Roman emperor once his beliefs were discovered. He is often laden with arrows in spots where buboes would have appeared: the armpits and the groin. His sacrifice for others’ recovery became a symbol of absorbing the plague, the wounds, and the impact of the arrows.
This sacrifice epitomizes the daily work the frontline nurses, ER docs, intensivists, hospitalists, and the entire hospital staff perform daily, bearing the slung arrows of coronavirus.
One of the images I think of frequently during this time lies atop Castel San Angelo in Rome. Built in 161 AD, it has served as a mausoleum, prison, papal residence, and is currently a museum. Atop San’Angelo stands St. Michael, the destroyer of the dragon. He is sheathing his sword in representation of the end of the plague in 590.
The arrows flow, yet the sword will be sheathed. Evil will be halted. The stories of these ancient totems and strength can give us strength as they remind us of the work that was done for centuries: pestilence, famine, war. The great killers never go away completely.
Fast forward to today
These medical specters serve as reminders of what makes the field of medicine so inspiring: the selfless acts, the fortitude of spirit, the healers, the long history, and the shoulders of giants we stand upon. From these stories, we spring the healing waters we bathe in to give us the courage to wake up and care for our patients each day. These specters encourage us to defeat any and all of the scourges that come our way.
I hear and read stories about the frontline heroes, the vaccine makers, the PPE creators, the health care workers, grocery store clerks, and teachers. I’m honored to hear of these stories and your sacrifices. I’m inspired to continue upholding your essence, your fight, and your stories. In keeping with ancient empire metaphors, you are taking the slings of the diseased arrows flying to our brethren as you try to keep yourself and others safe.
The sheathing of this sword will come. These arrows will be silenced. But until then, I lean on these pictures, these stories, and these saints, to give us all the strength to wake up each morning and continue healing.
They serve as reminders of what makes the field of medicine so great: the selfless acts, the fortitude of spirit, the healers, the long history, and the shoulders of giants we stand upon. From these stories spring the healing waters we bathe in to give us the courage to wake up and care for our patients each day and defeat any and all scourges that come our way.
So, who do you call in those late, quiet hours, when all seems lost?
Dr. Messler is the executive director, quality initiatives at Glytec and works as a hospitalist at Morton Plant Hospitalist group in Clearwater, Fla. This essay appeared initially on The Hospital Leader, the official blog of SHM.
I swear by Apollo Physician and Asclepius and Hygeia and Panacea and all the gods and goddesses, making them my witnesses, that I will fulfill according to my ability and judgment this oath and this covenant.
On my desk sits a bust of Hygeia, a mask from Venice, next to a small sculpture and a figurine of the plague doctor. Nearby, there is a Klimt closeup of Hygeia, a postcard portraying Asclepius, St. Sebastian paintings, and quotes from Maimonides. They whisper secrets and nod to the challenges of the past. These medical specters, ancient voices of the past, keep me grounded. They speak, listen, and elevate me, too. They bring life into my otherwise quiet room.
We all began our careers swearing to Apollo, Asclepius, Hygeia, and Panacea when we recited the Hippocratic Oath. I call upon them, and other gods and totems, and saints and ancient healers, now more than ever. As an atheist, I don’t appeal to them as prayers, but as Hippocrates intended. I look to their supernatural healing powers as a source of strength and as revealers of the natural and observable phenomena.
Apollo was one of the Twelve Olympians, a God of medicine, father of Asclepius. He was a healer, though his arrows also bore the plagues of the Gods.
For centuries, Apollo was found floating above the marble dissection table in the Bologna anatomical theater, guiding students who dove into the secrets of the human body.
Asclepius, son of Apollo, was hailed as a god of medicine. He healed many from plagues at his temples throughout the Ancient Greek and Roman empires. He was mentored in the healing arts by the centaur, Chiron. His many daughters and sons represent various aspects of medicine including cures, healing, recovery, sanitation, and beauty. To Asclepius, temples were places of healing, an ancient ancestor to modern hospitals.
Two of his daughters, Panacea and Hygeia, gave us the healing words of panacea and hygiene. Today, these acts of hygiene, handwashing, mask-wearing, and sanitation are discussed across the world louder than ever. While we’re all wishing for a panacea, we know it will take all the attributes of medicine to get us through this pandemic.
Hospitalists are part of the frontline teams facing this pandemic head-on. Gowning up for MRSA isolation seems quaint nowadays.
My attendings spoke of their fears, up against the unknown while on service in the 1980s, when HIV appeared. 2014 brought the Ebola biocontainment units. Now, this generation works daily against a modern plague, where every day is a risk of exposure. When every patient is in isolation, the garb begins to reflect the PPE that emerged during a 17th-century plague epidemics, the plague doctor outfit.
Godfather II fans recall the famous portrayal of the August 16th festival to San Rocco play out in the streets of New York. For those stricken with COVID-19 and recovered, you emulate San Rocco, in your continued return to service.
The Scuola Grande di San Rocco, in Venice, is the epitome of healing and greatness in one building. Tintoretto, the great Venetian painter, assembled the story of healing through art and portraits of San Rocco. The scuola, a confraternity, was a community of healers, gathered in one place to look after the less fortunate.
Hospitalists march into the hospital risking their lives. We always wear PPE for MRSA, ESBL, or C. diff. And enter reverse isolation rooms wearing N95s for possible TB cases. But those don’t elevate to the volume, to the same fear, as gowning up for COVID-19.
Hospitalists, frontline health care workers, embody the story of San Sebastian, another plague saint who absorbed the arrows, the symbolic plagues, onto his own shoulders so no one else had to bear them. San Sebastian was a Christian persecuted by a Roman emperor once his beliefs were discovered. He is often laden with arrows in spots where buboes would have appeared: the armpits and the groin. His sacrifice for others’ recovery became a symbol of absorbing the plague, the wounds, and the impact of the arrows.
This sacrifice epitomizes the daily work the frontline nurses, ER docs, intensivists, hospitalists, and the entire hospital staff perform daily, bearing the slung arrows of coronavirus.
One of the images I think of frequently during this time lies atop Castel San Angelo in Rome. Built in 161 AD, it has served as a mausoleum, prison, papal residence, and is currently a museum. Atop San’Angelo stands St. Michael, the destroyer of the dragon. He is sheathing his sword in representation of the end of the plague in 590.
The arrows flow, yet the sword will be sheathed. Evil will be halted. The stories of these ancient totems and strength can give us strength as they remind us of the work that was done for centuries: pestilence, famine, war. The great killers never go away completely.
Fast forward to today
These medical specters serve as reminders of what makes the field of medicine so inspiring: the selfless acts, the fortitude of spirit, the healers, the long history, and the shoulders of giants we stand upon. From these stories, we spring the healing waters we bathe in to give us the courage to wake up and care for our patients each day. These specters encourage us to defeat any and all of the scourges that come our way.
I hear and read stories about the frontline heroes, the vaccine makers, the PPE creators, the health care workers, grocery store clerks, and teachers. I’m honored to hear of these stories and your sacrifices. I’m inspired to continue upholding your essence, your fight, and your stories. In keeping with ancient empire metaphors, you are taking the slings of the diseased arrows flying to our brethren as you try to keep yourself and others safe.
The sheathing of this sword will come. These arrows will be silenced. But until then, I lean on these pictures, these stories, and these saints, to give us all the strength to wake up each morning and continue healing.
They serve as reminders of what makes the field of medicine so great: the selfless acts, the fortitude of spirit, the healers, the long history, and the shoulders of giants we stand upon. From these stories spring the healing waters we bathe in to give us the courage to wake up and care for our patients each day and defeat any and all scourges that come our way.
So, who do you call in those late, quiet hours, when all seems lost?
Dr. Messler is the executive director, quality initiatives at Glytec and works as a hospitalist at Morton Plant Hospitalist group in Clearwater, Fla. This essay appeared initially on The Hospital Leader, the official blog of SHM.
Hospital medicine groups are getting larger
What are the implications for your workplace?
Although readers will be forgiven for missing the subtle change, the tables in the 2020 State of Hospital Medicine (SoHM) Report underwent a landmark structural change that echoes the growth of our field. In the latest SoHM Report, the hospital medicine group (HMG) size categories all increased significantly to reflect the fact that hospitalist groups have grown from a median of 9 physician full time equivalents (FTE) in 2016 to a median of 15.2 employed/contracted FTE (excluding FTE provided by locum tenens providers) in 2020.
For many years, the Report considered “large” adult HMGs to be those with 30 or more FTE of physicians, and smaller groups were organized by FTE categories of <5, 5-9, 10-19, and 20-29. Now the SoHM Report describes a large HMG as 50 employed/contracted FTE or greater, a category that represents 12.7% of HMGs serving adults. The other categories expanded to <5, 5-14, 15-29, and 30-49, respectively. Overall, HMGs are growing in size, and the SoHM displays new data slices that help leaders to compare their group to modern peers.
There are some caveats to consider. First, these figures only represent physician FTE, and essentially all these large groups employ NP/PA hospitalists as well. Second, these HMGs typically employ some part-time and contracted PRN physicians in this FTE count. In combination, these two factors mean that large HMGs often employ many more than 50 individual clinicians. In fact, the average number of physicians in this cohort was 72.3 before counting NP/PAs and locums. Third, do not interpret the portion of large groups in the survey (12.7%) as insignificant. Because each one employs so many total hospitalists, large HMGs collectively represent a common work environment for many hospitalists in the US. Lastly, although pediatric HMGs have grown, far fewer (3.1%) have over 50 FTE, so this column focuses on HMGs serving adults.
Why does it matter that groups are growing in size? The SoHM Report offers extensive data to answer this question. Here are a couple of highlights but consider buying the report to dig deeper. First, large groups are far more likely to offer variable scheduling. Although the 7-on, 7-off scheduling pattern is still the norm in all group sizes, large HMGs are most likely to offer something flexible that might enhance career sustainability for hospitalists. Second, large groups are the most likely to employ a few hospitalists with extra training, whether that be geriatrics, palliative care, pediatrics, or a medicine subspecialty. Working in a large group means you can ask for curbside consults from a diverse and well-trained bunch of colleagues. Third, large groups were most likely to employ nocturnists, meaning fewer night shifts are allocated to the hospitalists who want to focus on daytime work. From an individual perspective, there is a lot to like about working in a large HMG.
There are some drawbacks to larger groups, of course. Large groups can be less socially cohesive and the costs of managing 70-100 hospitalists typically grow well past the capacity of a single group leader. My personal belief is that these downsides can be solved through economies of scale and skilled management teams. In addition, a large group can afford to dedicate leadership FTE to niche hospitalist needs, such as career development and coaching, which are difficult to fund in small practices. This also provides more opportunities for staff hospitalists to begin taking on some leadership or administrative duties or branch out into related areas such as quality improvement, case management physician advisor roles, or IT expertise.
Ultimately, large groups typically represent the maturation of an HMG within a large hospital – it signifies that the hospital relies on that group to deliver great patient outcomes in every corner of the hospital. Where you practice remains a personal choice, but the emergence of large groups hints at the clout and sophistication hospitalists can build by banding together. Learn more about the full 2020 SoHM Report at hospitalmedicine.org/sohm.
Dr. White is associate professor of medicine at the University of Washington, Seattle. He is the chair of SHM’s Practice Analysis Committee.
What are the implications for your workplace?
What are the implications for your workplace?
Although readers will be forgiven for missing the subtle change, the tables in the 2020 State of Hospital Medicine (SoHM) Report underwent a landmark structural change that echoes the growth of our field. In the latest SoHM Report, the hospital medicine group (HMG) size categories all increased significantly to reflect the fact that hospitalist groups have grown from a median of 9 physician full time equivalents (FTE) in 2016 to a median of 15.2 employed/contracted FTE (excluding FTE provided by locum tenens providers) in 2020.
For many years, the Report considered “large” adult HMGs to be those with 30 or more FTE of physicians, and smaller groups were organized by FTE categories of <5, 5-9, 10-19, and 20-29. Now the SoHM Report describes a large HMG as 50 employed/contracted FTE or greater, a category that represents 12.7% of HMGs serving adults. The other categories expanded to <5, 5-14, 15-29, and 30-49, respectively. Overall, HMGs are growing in size, and the SoHM displays new data slices that help leaders to compare their group to modern peers.
There are some caveats to consider. First, these figures only represent physician FTE, and essentially all these large groups employ NP/PA hospitalists as well. Second, these HMGs typically employ some part-time and contracted PRN physicians in this FTE count. In combination, these two factors mean that large HMGs often employ many more than 50 individual clinicians. In fact, the average number of physicians in this cohort was 72.3 before counting NP/PAs and locums. Third, do not interpret the portion of large groups in the survey (12.7%) as insignificant. Because each one employs so many total hospitalists, large HMGs collectively represent a common work environment for many hospitalists in the US. Lastly, although pediatric HMGs have grown, far fewer (3.1%) have over 50 FTE, so this column focuses on HMGs serving adults.
Why does it matter that groups are growing in size? The SoHM Report offers extensive data to answer this question. Here are a couple of highlights but consider buying the report to dig deeper. First, large groups are far more likely to offer variable scheduling. Although the 7-on, 7-off scheduling pattern is still the norm in all group sizes, large HMGs are most likely to offer something flexible that might enhance career sustainability for hospitalists. Second, large groups are the most likely to employ a few hospitalists with extra training, whether that be geriatrics, palliative care, pediatrics, or a medicine subspecialty. Working in a large group means you can ask for curbside consults from a diverse and well-trained bunch of colleagues. Third, large groups were most likely to employ nocturnists, meaning fewer night shifts are allocated to the hospitalists who want to focus on daytime work. From an individual perspective, there is a lot to like about working in a large HMG.
There are some drawbacks to larger groups, of course. Large groups can be less socially cohesive and the costs of managing 70-100 hospitalists typically grow well past the capacity of a single group leader. My personal belief is that these downsides can be solved through economies of scale and skilled management teams. In addition, a large group can afford to dedicate leadership FTE to niche hospitalist needs, such as career development and coaching, which are difficult to fund in small practices. This also provides more opportunities for staff hospitalists to begin taking on some leadership or administrative duties or branch out into related areas such as quality improvement, case management physician advisor roles, or IT expertise.
Ultimately, large groups typically represent the maturation of an HMG within a large hospital – it signifies that the hospital relies on that group to deliver great patient outcomes in every corner of the hospital. Where you practice remains a personal choice, but the emergence of large groups hints at the clout and sophistication hospitalists can build by banding together. Learn more about the full 2020 SoHM Report at hospitalmedicine.org/sohm.
Dr. White is associate professor of medicine at the University of Washington, Seattle. He is the chair of SHM’s Practice Analysis Committee.
Although readers will be forgiven for missing the subtle change, the tables in the 2020 State of Hospital Medicine (SoHM) Report underwent a landmark structural change that echoes the growth of our field. In the latest SoHM Report, the hospital medicine group (HMG) size categories all increased significantly to reflect the fact that hospitalist groups have grown from a median of 9 physician full time equivalents (FTE) in 2016 to a median of 15.2 employed/contracted FTE (excluding FTE provided by locum tenens providers) in 2020.
For many years, the Report considered “large” adult HMGs to be those with 30 or more FTE of physicians, and smaller groups were organized by FTE categories of <5, 5-9, 10-19, and 20-29. Now the SoHM Report describes a large HMG as 50 employed/contracted FTE or greater, a category that represents 12.7% of HMGs serving adults. The other categories expanded to <5, 5-14, 15-29, and 30-49, respectively. Overall, HMGs are growing in size, and the SoHM displays new data slices that help leaders to compare their group to modern peers.
There are some caveats to consider. First, these figures only represent physician FTE, and essentially all these large groups employ NP/PA hospitalists as well. Second, these HMGs typically employ some part-time and contracted PRN physicians in this FTE count. In combination, these two factors mean that large HMGs often employ many more than 50 individual clinicians. In fact, the average number of physicians in this cohort was 72.3 before counting NP/PAs and locums. Third, do not interpret the portion of large groups in the survey (12.7%) as insignificant. Because each one employs so many total hospitalists, large HMGs collectively represent a common work environment for many hospitalists in the US. Lastly, although pediatric HMGs have grown, far fewer (3.1%) have over 50 FTE, so this column focuses on HMGs serving adults.
Why does it matter that groups are growing in size? The SoHM Report offers extensive data to answer this question. Here are a couple of highlights but consider buying the report to dig deeper. First, large groups are far more likely to offer variable scheduling. Although the 7-on, 7-off scheduling pattern is still the norm in all group sizes, large HMGs are most likely to offer something flexible that might enhance career sustainability for hospitalists. Second, large groups are the most likely to employ a few hospitalists with extra training, whether that be geriatrics, palliative care, pediatrics, or a medicine subspecialty. Working in a large group means you can ask for curbside consults from a diverse and well-trained bunch of colleagues. Third, large groups were most likely to employ nocturnists, meaning fewer night shifts are allocated to the hospitalists who want to focus on daytime work. From an individual perspective, there is a lot to like about working in a large HMG.
There are some drawbacks to larger groups, of course. Large groups can be less socially cohesive and the costs of managing 70-100 hospitalists typically grow well past the capacity of a single group leader. My personal belief is that these downsides can be solved through economies of scale and skilled management teams. In addition, a large group can afford to dedicate leadership FTE to niche hospitalist needs, such as career development and coaching, which are difficult to fund in small practices. This also provides more opportunities for staff hospitalists to begin taking on some leadership or administrative duties or branch out into related areas such as quality improvement, case management physician advisor roles, or IT expertise.
Ultimately, large groups typically represent the maturation of an HMG within a large hospital – it signifies that the hospital relies on that group to deliver great patient outcomes in every corner of the hospital. Where you practice remains a personal choice, but the emergence of large groups hints at the clout and sophistication hospitalists can build by banding together. Learn more about the full 2020 SoHM Report at hospitalmedicine.org/sohm.
Dr. White is associate professor of medicine at the University of Washington, Seattle. He is the chair of SHM’s Practice Analysis Committee.
Happy National Hospitalist Day!
Hospitalists across the United States have been and continue to be a critical part of our nation’s response to COVID-19. On National Hospitalist Day, Thursday, March 4, 2021, the Society of Hospital Medicine invites you to celebrate the individuals and teams that make up the hospital medicine community.

On this special day, SHM encourages you to share your story, showcase your team’s efforts to improve patient care, express your pride for the specialty, or share how you are making a difference in your hospital and in the lives of patients.
Here are just a few of the ways you can celebrate:
- Register for our live roundtable, featuring Mark Shapiro, MD, hospitalist and host of the Explore the Space podcast, and four hospitalist panelists, on March 4 at 7 p.m. ET/4 p.m. PT.
- Download shareable graphics, posters, Zoom backgrounds, and coloring book pages
- Enter our social media photo contest and follow the #HowWeHospitalist hashtag across all platforms
- Read special hospitalist profiles in the Hospitalist, including: Eric E. Howell, MD, MHM; Grace Huang, MD; Bridget McGrath, PA-C, FHM; and Harry Cho, MD, SFHM
Thank you for all you do and continue to do for hospital medicine. We hope you take some time today to celebrate you and your colleagues, as well as your commendable contributions to health care and the future of the specialty.
To learn more about National Hospitalist Day, visit hospitalmedicine.org/hospitalistday.
Hospitalists across the United States have been and continue to be a critical part of our nation’s response to COVID-19. On National Hospitalist Day, Thursday, March 4, 2021, the Society of Hospital Medicine invites you to celebrate the individuals and teams that make up the hospital medicine community.

On this special day, SHM encourages you to share your story, showcase your team’s efforts to improve patient care, express your pride for the specialty, or share how you are making a difference in your hospital and in the lives of patients.
Here are just a few of the ways you can celebrate:
- Register for our live roundtable, featuring Mark Shapiro, MD, hospitalist and host of the Explore the Space podcast, and four hospitalist panelists, on March 4 at 7 p.m. ET/4 p.m. PT.
- Download shareable graphics, posters, Zoom backgrounds, and coloring book pages
- Enter our social media photo contest and follow the #HowWeHospitalist hashtag across all platforms
- Read special hospitalist profiles in the Hospitalist, including: Eric E. Howell, MD, MHM; Grace Huang, MD; Bridget McGrath, PA-C, FHM; and Harry Cho, MD, SFHM
Thank you for all you do and continue to do for hospital medicine. We hope you take some time today to celebrate you and your colleagues, as well as your commendable contributions to health care and the future of the specialty.
To learn more about National Hospitalist Day, visit hospitalmedicine.org/hospitalistday.
Hospitalists across the United States have been and continue to be a critical part of our nation’s response to COVID-19. On National Hospitalist Day, Thursday, March 4, 2021, the Society of Hospital Medicine invites you to celebrate the individuals and teams that make up the hospital medicine community.

On this special day, SHM encourages you to share your story, showcase your team’s efforts to improve patient care, express your pride for the specialty, or share how you are making a difference in your hospital and in the lives of patients.
Here are just a few of the ways you can celebrate:
- Register for our live roundtable, featuring Mark Shapiro, MD, hospitalist and host of the Explore the Space podcast, and four hospitalist panelists, on March 4 at 7 p.m. ET/4 p.m. PT.
- Download shareable graphics, posters, Zoom backgrounds, and coloring book pages
- Enter our social media photo contest and follow the #HowWeHospitalist hashtag across all platforms
- Read special hospitalist profiles in the Hospitalist, including: Eric E. Howell, MD, MHM; Grace Huang, MD; Bridget McGrath, PA-C, FHM; and Harry Cho, MD, SFHM
Thank you for all you do and continue to do for hospital medicine. We hope you take some time today to celebrate you and your colleagues, as well as your commendable contributions to health care and the future of the specialty.
To learn more about National Hospitalist Day, visit hospitalmedicine.org/hospitalistday.
Owning all aspects of patient care: Bridget McGrath, PA-C, FHM
Editor’s note: This profile is part of the Society of Hospital Medicine’s celebration of National Hospitalist Day on March 4. National Hospitalist Day occurs the first Thursday in March annually and celebrates the fastest growing specialty in modern medicine and hospitalists’ enduring contributions to the evolving health care landscape.
Bridget McGrath, PA-C, FHM, is a physician assistant and director of the nurse practitioner/physician assistant service line for the section of hospital medicine at the University of Chicago. She is a cochair of SHM’s NP/PA Special Interest Group.
Where did you receive your PA education/training? Was your intention always to be a PA?
I graduated from the PA program at Butler University, Indianapolis, in 2014. In college, whenever I shadowed a PA, I was always impressed that each one loved their job and said they would never change it. That universal passion for the PA profession really made an impression on me.
At what point in your PA education/training did you decide to practice hospital medicine? What about it appealed to you?
That occurred during my clinical rotation year at Butler. I had always thought I wanted to practice neonatology, but during my clinical rotation I really fell in love with adult medicine. I recall that during my clinical rotation, the preceptor said to me that the goal was not to have me understand every aspect of medicine, but to learn how to exist in a hospital setting. I was exposed to the breadth of hospital medicine practice and I fell in love with the complexity, the variety, and the environment itself.
I initially accepted a job as a med-peds hospitalist PA – which brought both of my passions together at that time – at Schneck Medical Center in Seymour, Ind. During that time, Schneck was a 100-bed rural community hospital which had recently been the recipient of the Malcolm Baldrige National Quality Award. It was there that I was able to practice with a phenomenal group of physicians, nurses, and social workers who really took me under their wing and taught me how to be a hospitalist PA. I practiced at Schneck for 3 years, and then moved to the University of Chicago in 2017.
I am now the director of NP/PA services for the section of hospital medicine, overseeing a group of seven on our NP/PA team, within a larger group of about 60 physicians.
What are your favorite areas of clinical practice?
Like many hospitalists, I enjoy the variety of medicine that hospitalists practice. One area that I find especially rewarding is my time in our transplant comanagement services. To be able to walk with patients on their transplant journey is very rewarding, and I am very appreciative of the mentoring I have received from some of my colleagues with a deeper understanding of transplant medicine.
In my administrative role, I have the privilege of helping to expand the professional education and training of my colleagues. I have a passion for medical education, and we have been working to develop interprofessional educational opportunities within our section. I have had time to think about the imprint of NPs and PAs in academic medicine, and how we can continue to meet the professional educational needs of our section while improving the care of our patients.
What are the most challenging aspects of practicing hospital medicine?
The volume of diagnoses that we are expected to manage on a daily basis can be challenging. This challenges you to continue learning. The complexity of discharge planning, particularly for patients in underserved communities, can also be challenging. You have to make sure your patients are ready mentally, physically and emotionally for discharge. As a hospitalist, you are continuously thinking about how to optimize patients to leave your care. For example, patients have different insurance situations, different access to care at home – you are always managing the medical needs of your patient in the context of these other issues.
How does a hospitalist PA work differently from a PA in other care settings?
We are meant to be generalists. We serve as the main provider in owning our patients’ care. A hospitalist PA serves as a cog in the wheel, with connections to specialists, consultants, nurses, social workers, pharmacists, etc., and we are tasked with synthesizing all aspects of patient care to ensure the best outcome.
What has your experience taught you about how NPs and PAs can best fit into hospital medicine groups?
Each hospital medicine group will know how to best integrate their NPs and PAs based on the skillsets of their NPs and PAs, and the needs of the section and the hospital. I personally feel that the best way to utilize NPs and PAs is to allow them to own all aspects of patient care and work at the highest scope of practice. By doing this you empower the NP or PA to continue to develop their skill set and set a precedent of collaboration and respect for interprofessional care models within your section’s culture.
Scope of practice for an NP or PA is going to be based on a conglomeration of roles and bylaws. We are certified nationally, and our scope of practice is determined at the state level and the hospital by level. For the individual NP and PA, it really depends on the hospital medicine group, and how well a practice incorporates a sense of collegiality.
What kind of resources do hospitalist PAs need to succeed, either from SHM or from their own institutions?
There are a few key things that need to happen in order for hospital medicine groups to set up their NPs and PAs for success. The first is for PAs to have exposure to inpatient rotations during clinical rotations. A hospital medicine group also should have a very intentional onboarding process for NPs and PAs. They should also establish a culture of acceptance. To do this, they should utilize resources like SHM’s NP/PA Hospital Medicine Onboarding Toolkit and the SHM/American Academy of Physician Assistants Hospitalist Bootcamp On Demand.
Mentoring is also remarkably important. I have been incredibly blessed to have mentors that helped make me into the PA that I am. I could not have done what I did in the field without people taking a chance on me, and it is important to pass that on to the next generation of PAs.
How has COVID-19 changed the practice of hospital medicine, specifically for advanced practice providers?
The pandemic has demonstrated opportunities for teamwork and utilization of NPs and PAs. The COVID pandemic forced everyone to reflect on why they originally got into medicine – to help patients. I think there will be many doors opening for NPs and PAs, and many pathways for leadership.
The hospitalist leadership at the University of Chicago truly identified that we needed to make wellness a main priority during the beginning of the pandemic. We developed a wellness work group that I have been coleading.
What’s on the horizon for NPs and PAs in hospital medicine?
We are seeing significant increases in hospitalist program utilization, so this is a time where NPs and PAs can be advocates for our profession and articulate how we can use our backgrounds and training to build better care models in order to meet the needs of our patients.
I hope we will see more NPs and PAs assuming leadership roles to ensure that our voices are heard. We should also be advocating for more collaboration and teamwork with our MD and DO colleagues.
Do you have any advice for PA students interested in hospital medicine?
I always tell my students that they should be sponges – you are not expected to know everything as a hospitalist PA, but you are expected to continue learning in order to develop into the best PA you can be. Always be open to where your career path can take you. Hospital medicine is a relatively young field within medicine, and the diversity of our field is very exciting looking forward.
Editor’s note: This profile is part of the Society of Hospital Medicine’s celebration of National Hospitalist Day on March 4. National Hospitalist Day occurs the first Thursday in March annually and celebrates the fastest growing specialty in modern medicine and hospitalists’ enduring contributions to the evolving health care landscape.
Bridget McGrath, PA-C, FHM, is a physician assistant and director of the nurse practitioner/physician assistant service line for the section of hospital medicine at the University of Chicago. She is a cochair of SHM’s NP/PA Special Interest Group.
Where did you receive your PA education/training? Was your intention always to be a PA?
I graduated from the PA program at Butler University, Indianapolis, in 2014. In college, whenever I shadowed a PA, I was always impressed that each one loved their job and said they would never change it. That universal passion for the PA profession really made an impression on me.
At what point in your PA education/training did you decide to practice hospital medicine? What about it appealed to you?
That occurred during my clinical rotation year at Butler. I had always thought I wanted to practice neonatology, but during my clinical rotation I really fell in love with adult medicine. I recall that during my clinical rotation, the preceptor said to me that the goal was not to have me understand every aspect of medicine, but to learn how to exist in a hospital setting. I was exposed to the breadth of hospital medicine practice and I fell in love with the complexity, the variety, and the environment itself.
I initially accepted a job as a med-peds hospitalist PA – which brought both of my passions together at that time – at Schneck Medical Center in Seymour, Ind. During that time, Schneck was a 100-bed rural community hospital which had recently been the recipient of the Malcolm Baldrige National Quality Award. It was there that I was able to practice with a phenomenal group of physicians, nurses, and social workers who really took me under their wing and taught me how to be a hospitalist PA. I practiced at Schneck for 3 years, and then moved to the University of Chicago in 2017.
I am now the director of NP/PA services for the section of hospital medicine, overseeing a group of seven on our NP/PA team, within a larger group of about 60 physicians.
What are your favorite areas of clinical practice?
Like many hospitalists, I enjoy the variety of medicine that hospitalists practice. One area that I find especially rewarding is my time in our transplant comanagement services. To be able to walk with patients on their transplant journey is very rewarding, and I am very appreciative of the mentoring I have received from some of my colleagues with a deeper understanding of transplant medicine.
In my administrative role, I have the privilege of helping to expand the professional education and training of my colleagues. I have a passion for medical education, and we have been working to develop interprofessional educational opportunities within our section. I have had time to think about the imprint of NPs and PAs in academic medicine, and how we can continue to meet the professional educational needs of our section while improving the care of our patients.
What are the most challenging aspects of practicing hospital medicine?
The volume of diagnoses that we are expected to manage on a daily basis can be challenging. This challenges you to continue learning. The complexity of discharge planning, particularly for patients in underserved communities, can also be challenging. You have to make sure your patients are ready mentally, physically and emotionally for discharge. As a hospitalist, you are continuously thinking about how to optimize patients to leave your care. For example, patients have different insurance situations, different access to care at home – you are always managing the medical needs of your patient in the context of these other issues.
How does a hospitalist PA work differently from a PA in other care settings?
We are meant to be generalists. We serve as the main provider in owning our patients’ care. A hospitalist PA serves as a cog in the wheel, with connections to specialists, consultants, nurses, social workers, pharmacists, etc., and we are tasked with synthesizing all aspects of patient care to ensure the best outcome.
What has your experience taught you about how NPs and PAs can best fit into hospital medicine groups?
Each hospital medicine group will know how to best integrate their NPs and PAs based on the skillsets of their NPs and PAs, and the needs of the section and the hospital. I personally feel that the best way to utilize NPs and PAs is to allow them to own all aspects of patient care and work at the highest scope of practice. By doing this you empower the NP or PA to continue to develop their skill set and set a precedent of collaboration and respect for interprofessional care models within your section’s culture.
Scope of practice for an NP or PA is going to be based on a conglomeration of roles and bylaws. We are certified nationally, and our scope of practice is determined at the state level and the hospital by level. For the individual NP and PA, it really depends on the hospital medicine group, and how well a practice incorporates a sense of collegiality.
What kind of resources do hospitalist PAs need to succeed, either from SHM or from their own institutions?
There are a few key things that need to happen in order for hospital medicine groups to set up their NPs and PAs for success. The first is for PAs to have exposure to inpatient rotations during clinical rotations. A hospital medicine group also should have a very intentional onboarding process for NPs and PAs. They should also establish a culture of acceptance. To do this, they should utilize resources like SHM’s NP/PA Hospital Medicine Onboarding Toolkit and the SHM/American Academy of Physician Assistants Hospitalist Bootcamp On Demand.
Mentoring is also remarkably important. I have been incredibly blessed to have mentors that helped make me into the PA that I am. I could not have done what I did in the field without people taking a chance on me, and it is important to pass that on to the next generation of PAs.
How has COVID-19 changed the practice of hospital medicine, specifically for advanced practice providers?
The pandemic has demonstrated opportunities for teamwork and utilization of NPs and PAs. The COVID pandemic forced everyone to reflect on why they originally got into medicine – to help patients. I think there will be many doors opening for NPs and PAs, and many pathways for leadership.
The hospitalist leadership at the University of Chicago truly identified that we needed to make wellness a main priority during the beginning of the pandemic. We developed a wellness work group that I have been coleading.
What’s on the horizon for NPs and PAs in hospital medicine?
We are seeing significant increases in hospitalist program utilization, so this is a time where NPs and PAs can be advocates for our profession and articulate how we can use our backgrounds and training to build better care models in order to meet the needs of our patients.
I hope we will see more NPs and PAs assuming leadership roles to ensure that our voices are heard. We should also be advocating for more collaboration and teamwork with our MD and DO colleagues.
Do you have any advice for PA students interested in hospital medicine?
I always tell my students that they should be sponges – you are not expected to know everything as a hospitalist PA, but you are expected to continue learning in order to develop into the best PA you can be. Always be open to where your career path can take you. Hospital medicine is a relatively young field within medicine, and the diversity of our field is very exciting looking forward.
Editor’s note: This profile is part of the Society of Hospital Medicine’s celebration of National Hospitalist Day on March 4. National Hospitalist Day occurs the first Thursday in March annually and celebrates the fastest growing specialty in modern medicine and hospitalists’ enduring contributions to the evolving health care landscape.
Bridget McGrath, PA-C, FHM, is a physician assistant and director of the nurse practitioner/physician assistant service line for the section of hospital medicine at the University of Chicago. She is a cochair of SHM’s NP/PA Special Interest Group.
Where did you receive your PA education/training? Was your intention always to be a PA?
I graduated from the PA program at Butler University, Indianapolis, in 2014. In college, whenever I shadowed a PA, I was always impressed that each one loved their job and said they would never change it. That universal passion for the PA profession really made an impression on me.
At what point in your PA education/training did you decide to practice hospital medicine? What about it appealed to you?
That occurred during my clinical rotation year at Butler. I had always thought I wanted to practice neonatology, but during my clinical rotation I really fell in love with adult medicine. I recall that during my clinical rotation, the preceptor said to me that the goal was not to have me understand every aspect of medicine, but to learn how to exist in a hospital setting. I was exposed to the breadth of hospital medicine practice and I fell in love with the complexity, the variety, and the environment itself.
I initially accepted a job as a med-peds hospitalist PA – which brought both of my passions together at that time – at Schneck Medical Center in Seymour, Ind. During that time, Schneck was a 100-bed rural community hospital which had recently been the recipient of the Malcolm Baldrige National Quality Award. It was there that I was able to practice with a phenomenal group of physicians, nurses, and social workers who really took me under their wing and taught me how to be a hospitalist PA. I practiced at Schneck for 3 years, and then moved to the University of Chicago in 2017.
I am now the director of NP/PA services for the section of hospital medicine, overseeing a group of seven on our NP/PA team, within a larger group of about 60 physicians.
What are your favorite areas of clinical practice?
Like many hospitalists, I enjoy the variety of medicine that hospitalists practice. One area that I find especially rewarding is my time in our transplant comanagement services. To be able to walk with patients on their transplant journey is very rewarding, and I am very appreciative of the mentoring I have received from some of my colleagues with a deeper understanding of transplant medicine.
In my administrative role, I have the privilege of helping to expand the professional education and training of my colleagues. I have a passion for medical education, and we have been working to develop interprofessional educational opportunities within our section. I have had time to think about the imprint of NPs and PAs in academic medicine, and how we can continue to meet the professional educational needs of our section while improving the care of our patients.
What are the most challenging aspects of practicing hospital medicine?
The volume of diagnoses that we are expected to manage on a daily basis can be challenging. This challenges you to continue learning. The complexity of discharge planning, particularly for patients in underserved communities, can also be challenging. You have to make sure your patients are ready mentally, physically and emotionally for discharge. As a hospitalist, you are continuously thinking about how to optimize patients to leave your care. For example, patients have different insurance situations, different access to care at home – you are always managing the medical needs of your patient in the context of these other issues.
How does a hospitalist PA work differently from a PA in other care settings?
We are meant to be generalists. We serve as the main provider in owning our patients’ care. A hospitalist PA serves as a cog in the wheel, with connections to specialists, consultants, nurses, social workers, pharmacists, etc., and we are tasked with synthesizing all aspects of patient care to ensure the best outcome.
What has your experience taught you about how NPs and PAs can best fit into hospital medicine groups?
Each hospital medicine group will know how to best integrate their NPs and PAs based on the skillsets of their NPs and PAs, and the needs of the section and the hospital. I personally feel that the best way to utilize NPs and PAs is to allow them to own all aspects of patient care and work at the highest scope of practice. By doing this you empower the NP or PA to continue to develop their skill set and set a precedent of collaboration and respect for interprofessional care models within your section’s culture.
Scope of practice for an NP or PA is going to be based on a conglomeration of roles and bylaws. We are certified nationally, and our scope of practice is determined at the state level and the hospital by level. For the individual NP and PA, it really depends on the hospital medicine group, and how well a practice incorporates a sense of collegiality.
What kind of resources do hospitalist PAs need to succeed, either from SHM or from their own institutions?
There are a few key things that need to happen in order for hospital medicine groups to set up their NPs and PAs for success. The first is for PAs to have exposure to inpatient rotations during clinical rotations. A hospital medicine group also should have a very intentional onboarding process for NPs and PAs. They should also establish a culture of acceptance. To do this, they should utilize resources like SHM’s NP/PA Hospital Medicine Onboarding Toolkit and the SHM/American Academy of Physician Assistants Hospitalist Bootcamp On Demand.
Mentoring is also remarkably important. I have been incredibly blessed to have mentors that helped make me into the PA that I am. I could not have done what I did in the field without people taking a chance on me, and it is important to pass that on to the next generation of PAs.
How has COVID-19 changed the practice of hospital medicine, specifically for advanced practice providers?
The pandemic has demonstrated opportunities for teamwork and utilization of NPs and PAs. The COVID pandemic forced everyone to reflect on why they originally got into medicine – to help patients. I think there will be many doors opening for NPs and PAs, and many pathways for leadership.
The hospitalist leadership at the University of Chicago truly identified that we needed to make wellness a main priority during the beginning of the pandemic. We developed a wellness work group that I have been coleading.
What’s on the horizon for NPs and PAs in hospital medicine?
We are seeing significant increases in hospitalist program utilization, so this is a time where NPs and PAs can be advocates for our profession and articulate how we can use our backgrounds and training to build better care models in order to meet the needs of our patients.
I hope we will see more NPs and PAs assuming leadership roles to ensure that our voices are heard. We should also be advocating for more collaboration and teamwork with our MD and DO colleagues.
Do you have any advice for PA students interested in hospital medicine?
I always tell my students that they should be sponges – you are not expected to know everything as a hospitalist PA, but you are expected to continue learning in order to develop into the best PA you can be. Always be open to where your career path can take you. Hospital medicine is a relatively young field within medicine, and the diversity of our field is very exciting looking forward.