User login
Intramuscular midazolam superior in sedating acutely agitated adults
Clinical question: How effective are intramuscular midazolam, olanzapine, ziprasidone, and haloperidol at sedating acutely agitated adults in the emergency department?
Background: Acute agitation is commonly seen in the ED and sometimes requires parenteral medications to keep patients and staff safe. Although many medications, including benzodiazepines and antipsychotics, are used, there is no consensus regarding which medications are most effective and safe for acute agitation.
Study design: Prospective observational study.
Setting: Emergency department of an inner-city Level 1 adult and pediatric trauma center.
Synopsis: This study enrolled 737 adults in the ED who presented with acute agitation and treated them with either haloperidol 5 mg, ziprasidone 20 mg, olanzapine 10 mg, midazolam 5 mg, or haloperidol 10 mg intramuscularly, based on predetermined 3-week blocks. The main outcome was the proportion of patients adequately sedated at 15 minutes, based on Altered Mental Status Scale score less than 1. A total of 650 patients (88%) were agitated from alcohol intoxication.
Midazolam resulted in a statistically higher proportion of patients adequately sedated, compared with ziprasidone (difference, 18%; 95% confidence interval, 6%-29%), haloperidol 5 mg (difference, 30%; 95% CI, 19%-41%), and haloperidol 10 mg (difference, 28%; 95% CI,17%-39%). Midazolam resulted in a higher proportion of patients adequately sedated, compared with olanzapine (difference 9%), but this difference was not statistically significant because the confidence interval crossed 1 (95% CI, –1%-20%). Olanzapine resulted in a statistically higher proportion of patients adequately sedated, compared with haloperidol 5 mg (difference 20%; 95% CI, 10%-31%) and 10 mg (difference 18%; 95% CI, 7%-29%). Adverse effects were rare.
Bottom line: Intramuscular midazolam is safe and may be more effective for treating acute agitation in the emergency department than standard antipsychotics.
Citation: Klein LR et al. Intramuscular midazolam, olanzapine, ziprasidone, or haloperidol for treating acute agitation in the emergency department. Ann Emerg Med. 2018 Jun 6. doi: https://doi.org/10.1016/j.annemergmed.2018.04.027.
Dr. Jenkins is assistant professor of medicine and an academic hospitalist, University of Utah, Salt Lake City.
Clinical question: How effective are intramuscular midazolam, olanzapine, ziprasidone, and haloperidol at sedating acutely agitated adults in the emergency department?
Background: Acute agitation is commonly seen in the ED and sometimes requires parenteral medications to keep patients and staff safe. Although many medications, including benzodiazepines and antipsychotics, are used, there is no consensus regarding which medications are most effective and safe for acute agitation.
Study design: Prospective observational study.
Setting: Emergency department of an inner-city Level 1 adult and pediatric trauma center.
Synopsis: This study enrolled 737 adults in the ED who presented with acute agitation and treated them with either haloperidol 5 mg, ziprasidone 20 mg, olanzapine 10 mg, midazolam 5 mg, or haloperidol 10 mg intramuscularly, based on predetermined 3-week blocks. The main outcome was the proportion of patients adequately sedated at 15 minutes, based on Altered Mental Status Scale score less than 1. A total of 650 patients (88%) were agitated from alcohol intoxication.
Midazolam resulted in a statistically higher proportion of patients adequately sedated, compared with ziprasidone (difference, 18%; 95% confidence interval, 6%-29%), haloperidol 5 mg (difference, 30%; 95% CI, 19%-41%), and haloperidol 10 mg (difference, 28%; 95% CI,17%-39%). Midazolam resulted in a higher proportion of patients adequately sedated, compared with olanzapine (difference 9%), but this difference was not statistically significant because the confidence interval crossed 1 (95% CI, –1%-20%). Olanzapine resulted in a statistically higher proportion of patients adequately sedated, compared with haloperidol 5 mg (difference 20%; 95% CI, 10%-31%) and 10 mg (difference 18%; 95% CI, 7%-29%). Adverse effects were rare.
Bottom line: Intramuscular midazolam is safe and may be more effective for treating acute agitation in the emergency department than standard antipsychotics.
Citation: Klein LR et al. Intramuscular midazolam, olanzapine, ziprasidone, or haloperidol for treating acute agitation in the emergency department. Ann Emerg Med. 2018 Jun 6. doi: https://doi.org/10.1016/j.annemergmed.2018.04.027.
Dr. Jenkins is assistant professor of medicine and an academic hospitalist, University of Utah, Salt Lake City.
Clinical question: How effective are intramuscular midazolam, olanzapine, ziprasidone, and haloperidol at sedating acutely agitated adults in the emergency department?
Background: Acute agitation is commonly seen in the ED and sometimes requires parenteral medications to keep patients and staff safe. Although many medications, including benzodiazepines and antipsychotics, are used, there is no consensus regarding which medications are most effective and safe for acute agitation.
Study design: Prospective observational study.
Setting: Emergency department of an inner-city Level 1 adult and pediatric trauma center.
Synopsis: This study enrolled 737 adults in the ED who presented with acute agitation and treated them with either haloperidol 5 mg, ziprasidone 20 mg, olanzapine 10 mg, midazolam 5 mg, or haloperidol 10 mg intramuscularly, based on predetermined 3-week blocks. The main outcome was the proportion of patients adequately sedated at 15 minutes, based on Altered Mental Status Scale score less than 1. A total of 650 patients (88%) were agitated from alcohol intoxication.
Midazolam resulted in a statistically higher proportion of patients adequately sedated, compared with ziprasidone (difference, 18%; 95% confidence interval, 6%-29%), haloperidol 5 mg (difference, 30%; 95% CI, 19%-41%), and haloperidol 10 mg (difference, 28%; 95% CI,17%-39%). Midazolam resulted in a higher proportion of patients adequately sedated, compared with olanzapine (difference 9%), but this difference was not statistically significant because the confidence interval crossed 1 (95% CI, –1%-20%). Olanzapine resulted in a statistically higher proportion of patients adequately sedated, compared with haloperidol 5 mg (difference 20%; 95% CI, 10%-31%) and 10 mg (difference 18%; 95% CI, 7%-29%). Adverse effects were rare.
Bottom line: Intramuscular midazolam is safe and may be more effective for treating acute agitation in the emergency department than standard antipsychotics.
Citation: Klein LR et al. Intramuscular midazolam, olanzapine, ziprasidone, or haloperidol for treating acute agitation in the emergency department. Ann Emerg Med. 2018 Jun 6. doi: https://doi.org/10.1016/j.annemergmed.2018.04.027.
Dr. Jenkins is assistant professor of medicine and an academic hospitalist, University of Utah, Salt Lake City.
Metformin associated with acidosis only in patients with eGFR 30 mL/min per 1.73 m 2
Clinical question: Does metformin increase the risk of lactic acidosis in chronic kidney disease (CKD)?
Background: Metformin is first-line therapy for type 2 diabetes mellitus (DM) because of its low cost, safety, and potential cardiovascular benefit, but fear of lactic acidosis has limited its use in CKD. The risk of acidosis in CKD patients with varying levels of renal function has not been clearly defined.
Study design: Retrospective community-based cohort study.
Setting: Geisinger Health System in Pennsylvania.
Synopsis: A total of 75,413 patients were identified with diagnostic codes or medication prescriptions indicating DM. Forty-five percent of patients were taking metformin at enrollment, increasing by 18% over the 5.7 years of median follow-up. The primary outcome was inpatient acidosis, defined by an ICD-9-CM code capturing multiple forms of acidosis but excluding diabetic ketoacidosis.
When metformin users and nonusers were compared, risk of acidosis was similar for the entire cohort and for subgroups of patients with an estimated glomerular filtration rate (eGFR) greater than 90, 60-89, 45-59, and 30-44. Conversely, metformin use was associated with a higher risk of acidosis in patients with eGFR less than 30 (adjusted hazard ratio, 2.07; 95% confidence interval, 1.33-3.22). Metformin not increasing the risk of acidosis at eGFR greater than 30 also was noted in an additional analysis using sulfonylurea medications as an active comparator and was replicated in a separate database with 82,000 patients from 350 private health systems. As with all observational studies, this study is limited by the potential for residual confounding.
Bottom line: Metformin appears to be safe in CKD patients with eGFR above 30 mL/min per 1.73 m2.
Citation: Lazarus B et al. Association of metformin use with risk of lactic acidosis across the range of kidney function: A community- based cohort study. JAMA Int Med. 2018;178(7):903-10.
Dr. Wanner is director, hospital medicine section, and associate chief, division of general internal medicine, University of Utah, Salt Lake City.
Clinical question: Does metformin increase the risk of lactic acidosis in chronic kidney disease (CKD)?
Background: Metformin is first-line therapy for type 2 diabetes mellitus (DM) because of its low cost, safety, and potential cardiovascular benefit, but fear of lactic acidosis has limited its use in CKD. The risk of acidosis in CKD patients with varying levels of renal function has not been clearly defined.
Study design: Retrospective community-based cohort study.
Setting: Geisinger Health System in Pennsylvania.
Synopsis: A total of 75,413 patients were identified with diagnostic codes or medication prescriptions indicating DM. Forty-five percent of patients were taking metformin at enrollment, increasing by 18% over the 5.7 years of median follow-up. The primary outcome was inpatient acidosis, defined by an ICD-9-CM code capturing multiple forms of acidosis but excluding diabetic ketoacidosis.
When metformin users and nonusers were compared, risk of acidosis was similar for the entire cohort and for subgroups of patients with an estimated glomerular filtration rate (eGFR) greater than 90, 60-89, 45-59, and 30-44. Conversely, metformin use was associated with a higher risk of acidosis in patients with eGFR less than 30 (adjusted hazard ratio, 2.07; 95% confidence interval, 1.33-3.22). Metformin not increasing the risk of acidosis at eGFR greater than 30 also was noted in an additional analysis using sulfonylurea medications as an active comparator and was replicated in a separate database with 82,000 patients from 350 private health systems. As with all observational studies, this study is limited by the potential for residual confounding.
Bottom line: Metformin appears to be safe in CKD patients with eGFR above 30 mL/min per 1.73 m2.
Citation: Lazarus B et al. Association of metformin use with risk of lactic acidosis across the range of kidney function: A community- based cohort study. JAMA Int Med. 2018;178(7):903-10.
Dr. Wanner is director, hospital medicine section, and associate chief, division of general internal medicine, University of Utah, Salt Lake City.
Clinical question: Does metformin increase the risk of lactic acidosis in chronic kidney disease (CKD)?
Background: Metformin is first-line therapy for type 2 diabetes mellitus (DM) because of its low cost, safety, and potential cardiovascular benefit, but fear of lactic acidosis has limited its use in CKD. The risk of acidosis in CKD patients with varying levels of renal function has not been clearly defined.
Study design: Retrospective community-based cohort study.
Setting: Geisinger Health System in Pennsylvania.
Synopsis: A total of 75,413 patients were identified with diagnostic codes or medication prescriptions indicating DM. Forty-five percent of patients were taking metformin at enrollment, increasing by 18% over the 5.7 years of median follow-up. The primary outcome was inpatient acidosis, defined by an ICD-9-CM code capturing multiple forms of acidosis but excluding diabetic ketoacidosis.
When metformin users and nonusers were compared, risk of acidosis was similar for the entire cohort and for subgroups of patients with an estimated glomerular filtration rate (eGFR) greater than 90, 60-89, 45-59, and 30-44. Conversely, metformin use was associated with a higher risk of acidosis in patients with eGFR less than 30 (adjusted hazard ratio, 2.07; 95% confidence interval, 1.33-3.22). Metformin not increasing the risk of acidosis at eGFR greater than 30 also was noted in an additional analysis using sulfonylurea medications as an active comparator and was replicated in a separate database with 82,000 patients from 350 private health systems. As with all observational studies, this study is limited by the potential for residual confounding.
Bottom line: Metformin appears to be safe in CKD patients with eGFR above 30 mL/min per 1.73 m2.
Citation: Lazarus B et al. Association of metformin use with risk of lactic acidosis across the range of kidney function: A community- based cohort study. JAMA Int Med. 2018;178(7):903-10.
Dr. Wanner is director, hospital medicine section, and associate chief, division of general internal medicine, University of Utah, Salt Lake City.
Prioritize oral route for inpatient opioids with subcutaneous route as alternative
Clinical question: Can adoption of a local opioid standard of practice for hospitalized patients reduce intravenous and overall opioid exposure while providing effective pain control?
Background: Inpatient use of intravenous opioids may be excessive, considering that oral opioids may provide more consistent pain control with less risk of adverse effects. If oral treatment is not possible, subcutaneous administration of opioids is an effective and possibly less addictive alternative to the intravenous route.
Study design: Historical control pilot study.
Setting: Single adult general medicine unit in an urban academic medical center.
Synopsis: A 6-month historical period with 287 patients was compared with a 3-month intervention period with 127 patients. The intervention consisted of a clinical practice standard that was presented to medical and nursing staff via didactic sessions and email. The standard recommended the oral route for opioids in patients tolerating oral intake and endorsed subcutaneous over intravenous administration.
Intravenous doses decreased by 84% (0.06 vs. 0.39 doses/patient-day; P less than .001), the daily rate of patients receiving any parenteral opioid decreased by 57% (6% vs. 14%; P less than .001), and the mean daily overall morphine-milligram equivalents decreased by 31% (6.30 vs. 9.11). Pain scores were unchanged for hospital days 1 through 3 but were significantly improved on day 4 (P = .004) and day 5 (P = .009).
Limitations of this study include the small number of patients on one unit, in one institution, with one clinician group. Attractive features of the intervention include its scalability and potential for augmentation via additional processes such as EHR changes, prescribing restrictions, and pharmacy monitoring.
Bottom line: A standard of practice intervention with peer-to-peer education was associated with decreased intravenous opioid exposure, decreased total opioid exposure, and effective pain control.
Citation: Ackerman AL et al. Association of an opioid standard of practice intervention with intravenous opioid exposure in hospitalized patients. JAMA Int Med. 2018;178(6):759-63.
Dr. Wanner is director, hospital medicine section, and associate chief, division of general internal medicine, University of Utah, Salt Lake City.
Clinical question: Can adoption of a local opioid standard of practice for hospitalized patients reduce intravenous and overall opioid exposure while providing effective pain control?
Background: Inpatient use of intravenous opioids may be excessive, considering that oral opioids may provide more consistent pain control with less risk of adverse effects. If oral treatment is not possible, subcutaneous administration of opioids is an effective and possibly less addictive alternative to the intravenous route.
Study design: Historical control pilot study.
Setting: Single adult general medicine unit in an urban academic medical center.
Synopsis: A 6-month historical period with 287 patients was compared with a 3-month intervention period with 127 patients. The intervention consisted of a clinical practice standard that was presented to medical and nursing staff via didactic sessions and email. The standard recommended the oral route for opioids in patients tolerating oral intake and endorsed subcutaneous over intravenous administration.
Intravenous doses decreased by 84% (0.06 vs. 0.39 doses/patient-day; P less than .001), the daily rate of patients receiving any parenteral opioid decreased by 57% (6% vs. 14%; P less than .001), and the mean daily overall morphine-milligram equivalents decreased by 31% (6.30 vs. 9.11). Pain scores were unchanged for hospital days 1 through 3 but were significantly improved on day 4 (P = .004) and day 5 (P = .009).
Limitations of this study include the small number of patients on one unit, in one institution, with one clinician group. Attractive features of the intervention include its scalability and potential for augmentation via additional processes such as EHR changes, prescribing restrictions, and pharmacy monitoring.
Bottom line: A standard of practice intervention with peer-to-peer education was associated with decreased intravenous opioid exposure, decreased total opioid exposure, and effective pain control.
Citation: Ackerman AL et al. Association of an opioid standard of practice intervention with intravenous opioid exposure in hospitalized patients. JAMA Int Med. 2018;178(6):759-63.
Dr. Wanner is director, hospital medicine section, and associate chief, division of general internal medicine, University of Utah, Salt Lake City.
Clinical question: Can adoption of a local opioid standard of practice for hospitalized patients reduce intravenous and overall opioid exposure while providing effective pain control?
Background: Inpatient use of intravenous opioids may be excessive, considering that oral opioids may provide more consistent pain control with less risk of adverse effects. If oral treatment is not possible, subcutaneous administration of opioids is an effective and possibly less addictive alternative to the intravenous route.
Study design: Historical control pilot study.
Setting: Single adult general medicine unit in an urban academic medical center.
Synopsis: A 6-month historical period with 287 patients was compared with a 3-month intervention period with 127 patients. The intervention consisted of a clinical practice standard that was presented to medical and nursing staff via didactic sessions and email. The standard recommended the oral route for opioids in patients tolerating oral intake and endorsed subcutaneous over intravenous administration.
Intravenous doses decreased by 84% (0.06 vs. 0.39 doses/patient-day; P less than .001), the daily rate of patients receiving any parenteral opioid decreased by 57% (6% vs. 14%; P less than .001), and the mean daily overall morphine-milligram equivalents decreased by 31% (6.30 vs. 9.11). Pain scores were unchanged for hospital days 1 through 3 but were significantly improved on day 4 (P = .004) and day 5 (P = .009).
Limitations of this study include the small number of patients on one unit, in one institution, with one clinician group. Attractive features of the intervention include its scalability and potential for augmentation via additional processes such as EHR changes, prescribing restrictions, and pharmacy monitoring.
Bottom line: A standard of practice intervention with peer-to-peer education was associated with decreased intravenous opioid exposure, decreased total opioid exposure, and effective pain control.
Citation: Ackerman AL et al. Association of an opioid standard of practice intervention with intravenous opioid exposure in hospitalized patients. JAMA Int Med. 2018;178(6):759-63.
Dr. Wanner is director, hospital medicine section, and associate chief, division of general internal medicine, University of Utah, Salt Lake City.
Lower grip strength associated with worse health outcomes
Background: Previous studies have shown that lower muscle function is associated with increased mortality; however, studies have not been able to fully examine associations with age and disease-specific mortality.
Study design: Prospective, population-based study.
Setting: Large population cohort in the United Kingdom (UK Biobank).
Synopsis: The UK Biobank population included 502,293 individuals, aged 40-69 years, recruited during April 2007–December 2010, with grip strength data available. Mean follow-up was 7.1 years for all-cause and disease-specific mortality. Cox proportional hazard models were used to report hazard ratios (HR) per 5-kg decrease in grip strength and were controlled for multiple sociodemographic and lifestyle factors. A lower grip strength was found to correlate with all-cause mortality (HR, 1.16 in women; HR, 1.20 in men) as well as incidence of and mortality from cardiovascular disease, respiratory disease, and cancer. Hazard ratios were higher among younger age groups with similar lower grip strength. The use of grip strength also improved the prediction of an office-based mortality risk score from cardiovascular disease.
Bottom line: Grip strength is a useful and easy-to-obtain measurement that is associated with all-cause and disease-specific morbidity and can be used to improve the prediction of an office-based risk score.
Citation: Celis-Morales CA et al. Associations of grip strength with cardiovascular, respiratory, and cancer outcomes and all-cause mortality: Prospective cohort study of half a million UK Biobank participants. BMJ. 2018;361:k1651.
Dr. Marr is assistant professor of medicine and an academic hospitalist, University of Utah, Salt Lake City.
Background: Previous studies have shown that lower muscle function is associated with increased mortality; however, studies have not been able to fully examine associations with age and disease-specific mortality.
Study design: Prospective, population-based study.
Setting: Large population cohort in the United Kingdom (UK Biobank).
Synopsis: The UK Biobank population included 502,293 individuals, aged 40-69 years, recruited during April 2007–December 2010, with grip strength data available. Mean follow-up was 7.1 years for all-cause and disease-specific mortality. Cox proportional hazard models were used to report hazard ratios (HR) per 5-kg decrease in grip strength and were controlled for multiple sociodemographic and lifestyle factors. A lower grip strength was found to correlate with all-cause mortality (HR, 1.16 in women; HR, 1.20 in men) as well as incidence of and mortality from cardiovascular disease, respiratory disease, and cancer. Hazard ratios were higher among younger age groups with similar lower grip strength. The use of grip strength also improved the prediction of an office-based mortality risk score from cardiovascular disease.
Bottom line: Grip strength is a useful and easy-to-obtain measurement that is associated with all-cause and disease-specific morbidity and can be used to improve the prediction of an office-based risk score.
Citation: Celis-Morales CA et al. Associations of grip strength with cardiovascular, respiratory, and cancer outcomes and all-cause mortality: Prospective cohort study of half a million UK Biobank participants. BMJ. 2018;361:k1651.
Dr. Marr is assistant professor of medicine and an academic hospitalist, University of Utah, Salt Lake City.
Background: Previous studies have shown that lower muscle function is associated with increased mortality; however, studies have not been able to fully examine associations with age and disease-specific mortality.
Study design: Prospective, population-based study.
Setting: Large population cohort in the United Kingdom (UK Biobank).
Synopsis: The UK Biobank population included 502,293 individuals, aged 40-69 years, recruited during April 2007–December 2010, with grip strength data available. Mean follow-up was 7.1 years for all-cause and disease-specific mortality. Cox proportional hazard models were used to report hazard ratios (HR) per 5-kg decrease in grip strength and were controlled for multiple sociodemographic and lifestyle factors. A lower grip strength was found to correlate with all-cause mortality (HR, 1.16 in women; HR, 1.20 in men) as well as incidence of and mortality from cardiovascular disease, respiratory disease, and cancer. Hazard ratios were higher among younger age groups with similar lower grip strength. The use of grip strength also improved the prediction of an office-based mortality risk score from cardiovascular disease.
Bottom line: Grip strength is a useful and easy-to-obtain measurement that is associated with all-cause and disease-specific morbidity and can be used to improve the prediction of an office-based risk score.
Citation: Celis-Morales CA et al. Associations of grip strength with cardiovascular, respiratory, and cancer outcomes and all-cause mortality: Prospective cohort study of half a million UK Biobank participants. BMJ. 2018;361:k1651.
Dr. Marr is assistant professor of medicine and an academic hospitalist, University of Utah, Salt Lake City.
VTE prophylaxis often overused in low-risk patients
Background: Per Chest guidelines, VTE prophylaxis is recommended for hospitalized patients at increased risk for VTE but is not recommended for low-risk patients. Risk stratification can be guided by the Padua Prediction Score to categorize patients.
Study design: Multicenter observational study.
Setting: A total of 52 U.S. hospitals (Michigan Hospital Medicine Safety Consortium database).
Synopsis: Patients admitted during Jan. 1, 2015–Dec. 21, 2016, to 52 non–intensive care medical units for 2 or more days were analyzed and stratified as high or low risk for VTE using the Padua Prediction Score. Excessive VTE prophylaxis was defined as low-risk patients prescribed pharmacologic or mechanical prophylaxis, high-risk patients receiving therapy despite a contraindication to prophylaxis, or any patient who received both mechanical and pharmacologic therapy. Underuse of VTE prophylaxis included high-risk patients who did not receive pharmacologic or mechanical prophylaxis. Of the 44,775 patients included in the study, 32,549 were low risk, and 77.9% (25,369 patients) received excessive VTE prophylaxis. Overtreatment also was present in high-risk patients with and without a contraindication to VTE prophylaxis (26.9% and 32.3%, respectively). Underuse of VTE prophylaxis occurred in 2,693 high-risk patients (22%).
Bottom line: Patients who are at low risk for VTE by Padua Prediction Score often are prescribed pharmacologic or mechanical prophylaxis that may be unnecessary. Overuse of VTE prophylaxis was more common than is underuse.
Citation: Grant PJ et al. Use of venous thromboembolism prophylaxis in hospitalized patients. JAMA Intern Med. 2018 Aug 1;178(8):1122-4. Published online May 21, 2018.
Dr. Marr is assistant professor of medicine and an academic hospitalist, University of Utah, Salt Lake City.
Background: Per Chest guidelines, VTE prophylaxis is recommended for hospitalized patients at increased risk for VTE but is not recommended for low-risk patients. Risk stratification can be guided by the Padua Prediction Score to categorize patients.
Study design: Multicenter observational study.
Setting: A total of 52 U.S. hospitals (Michigan Hospital Medicine Safety Consortium database).
Synopsis: Patients admitted during Jan. 1, 2015–Dec. 21, 2016, to 52 non–intensive care medical units for 2 or more days were analyzed and stratified as high or low risk for VTE using the Padua Prediction Score. Excessive VTE prophylaxis was defined as low-risk patients prescribed pharmacologic or mechanical prophylaxis, high-risk patients receiving therapy despite a contraindication to prophylaxis, or any patient who received both mechanical and pharmacologic therapy. Underuse of VTE prophylaxis included high-risk patients who did not receive pharmacologic or mechanical prophylaxis. Of the 44,775 patients included in the study, 32,549 were low risk, and 77.9% (25,369 patients) received excessive VTE prophylaxis. Overtreatment also was present in high-risk patients with and without a contraindication to VTE prophylaxis (26.9% and 32.3%, respectively). Underuse of VTE prophylaxis occurred in 2,693 high-risk patients (22%).
Bottom line: Patients who are at low risk for VTE by Padua Prediction Score often are prescribed pharmacologic or mechanical prophylaxis that may be unnecessary. Overuse of VTE prophylaxis was more common than is underuse.
Citation: Grant PJ et al. Use of venous thromboembolism prophylaxis in hospitalized patients. JAMA Intern Med. 2018 Aug 1;178(8):1122-4. Published online May 21, 2018.
Dr. Marr is assistant professor of medicine and an academic hospitalist, University of Utah, Salt Lake City.
Background: Per Chest guidelines, VTE prophylaxis is recommended for hospitalized patients at increased risk for VTE but is not recommended for low-risk patients. Risk stratification can be guided by the Padua Prediction Score to categorize patients.
Study design: Multicenter observational study.
Setting: A total of 52 U.S. hospitals (Michigan Hospital Medicine Safety Consortium database).
Synopsis: Patients admitted during Jan. 1, 2015–Dec. 21, 2016, to 52 non–intensive care medical units for 2 or more days were analyzed and stratified as high or low risk for VTE using the Padua Prediction Score. Excessive VTE prophylaxis was defined as low-risk patients prescribed pharmacologic or mechanical prophylaxis, high-risk patients receiving therapy despite a contraindication to prophylaxis, or any patient who received both mechanical and pharmacologic therapy. Underuse of VTE prophylaxis included high-risk patients who did not receive pharmacologic or mechanical prophylaxis. Of the 44,775 patients included in the study, 32,549 were low risk, and 77.9% (25,369 patients) received excessive VTE prophylaxis. Overtreatment also was present in high-risk patients with and without a contraindication to VTE prophylaxis (26.9% and 32.3%, respectively). Underuse of VTE prophylaxis occurred in 2,693 high-risk patients (22%).
Bottom line: Patients who are at low risk for VTE by Padua Prediction Score often are prescribed pharmacologic or mechanical prophylaxis that may be unnecessary. Overuse of VTE prophylaxis was more common than is underuse.
Citation: Grant PJ et al. Use of venous thromboembolism prophylaxis in hospitalized patients. JAMA Intern Med. 2018 Aug 1;178(8):1122-4. Published online May 21, 2018.
Dr. Marr is assistant professor of medicine and an academic hospitalist, University of Utah, Salt Lake City.
Looking into the future and making history
Emergence of population health management
For the first time ever, on March 7, 2019, tens of thousands of hospitalists across the United States and around the world will celebrate their day, National Hospitalist Day.
On this day, we will honor the hard work and dedication of hospitalists in the care of millions of hospitalized patients. With more than 62,000 hospitalists across the United States, hospital medicine has been the fastest growing medical specialty and among the largest of all specialties in medicine. Hospitalists now lead clinical care in over 75% of U.S. hospitals, caring for patients in their communities. We educate the future providers of health care by serving as teachers and mentors. We push the boundaries of science in hospital care through innovative research that defines the evidence-based practices for our field. Hospitalists, proudly celebrate all that we have accomplished together on March 7, and moving forward, every first Thursday in March annually.
The Society for Hospital Medicine’s celebration of National Hospitalist Day will include spotlights on hospitalists, a social medical campaign, downloadable customizable posters, and much more. Stay tuned for details!
Attend the only meeting designed just for you
Be among the thousands of hospitalists who will celebrate hospital medicine in person at Hospital Medicine 2019 (HM19), March 24-27 in National Harbor, Md.
While at HM19, check out more than 20 educational tracks, including clinical updates, diagnostic reasoning, and health policy. New this year are two mini tracks: “Between the Guidelines” and “Clinical Mastery”. Between the Guidelines explores how we can address some of the most challenging cases we encounter in hospital medicine, where clear guidelines don’t exist. Clinical Mastery is designed to enhance our bedside diagnostic skills, from ECGs to ultrasounds.
Get ready to vote in HM19’s “The Great Debate” – pairing two talented clinicians who will debate opposing sides of challenging clinical decisions that we encounter on the front lines of health care delivery. Attendees have the opportunity to hear the two sides and then vote on who they believe has the right approach. There are six precourses planned for HM19, with a new offering in Palliative Care and Pain Management. This year, the annual conference also features additional sessions for our NP/PA attendees. They include specific workshops as well as a track that includes 4 didactic sessions. Lastly, HM19 will offer CME, MOC, AOS, AAFP, and Pharmacology credits to address the needs of our attendees.
Looking into the future
While hospitalists are a vital part of U.S. health care, our delivery systems are in transition with greater focus on value-based care. To ensure hospital medicine continues to thrive in today’s dynamic scene, SHM’s Board of Directors held a strategic meeting in October 2018 to focus on the role of hospitalists and hospital medicine in population health management.
There are many hospitalists across the nation who are currently involved in population health management. These range from medical directors to vice presidents of accountable care organizations, population health management, or value-based care. Hospitalists are seeking communities focused on population health management to share best practices and learn from each other. To address this, SHM’s Advocacy and Public Policy HMX community has served as a meeting point to discuss issues related to value-based care. To join the discussion, visit the community by logging in at hospitalmedicine.org/hmx. Furthermore, at HM19, hospitalists will have the opportunity to meet face to face regarding these issues in the Advocacy Special Interest Forum.
Key points: Population health management
- Source of truth
SHM has served as the source of reliable and trusted information about hospital medicine. We will continue to develop content and resources specific to population health management on our website so hospitalists can easily access this information. To increase our awareness about population health management, presenters at HM19 will integrate a slide about the implications of population health management on their clinical topic. These slides will illustrate the clinical and nonclinical services that are necessary to enhance the patient’s quality of care and life. In addition to best practice care, these slides will highlight topics like the role of style modification and prevention, risk stratification, chronic disease management, and care coordination throughout the continuum of care.
- Advocating for us
In addition to providing a home for hospitalists to collaborate regarding population health management, SHM will advance this agenda from a regulatory perspective. The Public Policy and Performance Measurement & Reporting Committees are actively evaluating and leading the transition from value to volume. SHM is also working with potential key partners and organizations in the areas of primary care, skilled nursing facilities, and accountable care organizations that will help improve the effectiveness of delivering population health management.
- Creating expertise
SHM will lead best practice development for tools and skills that are necessary for hospitalists to lead population health management. Telemedicine is an increasingly critical tool as we help manage our patients in other facilities, inpatient or skilled nursing facilities, as well as at home. SHM has developed a white paper about telemedicine in hospital medicine that highlights modalities, offerings, implementation of programs, and work flows necessary for success. You can find it under “Resources” at hospitalmedicine.org/telemedicine.
SHM will continue to actively develop tools that appropriately address the challenges we’re facing. From National Hospitalist Day to population health management, this is an exciting time in hospital medicine – I hope to see you at HM19 to celebrate our specialty and our bright future.
Dr. Afsar is president of the Society of Hospital Medicine, and chief ambulatory officer and chief medical officer for accountable care organizations at UC Irvine Health.
Emergence of population health management
Emergence of population health management
For the first time ever, on March 7, 2019, tens of thousands of hospitalists across the United States and around the world will celebrate their day, National Hospitalist Day.
On this day, we will honor the hard work and dedication of hospitalists in the care of millions of hospitalized patients. With more than 62,000 hospitalists across the United States, hospital medicine has been the fastest growing medical specialty and among the largest of all specialties in medicine. Hospitalists now lead clinical care in over 75% of U.S. hospitals, caring for patients in their communities. We educate the future providers of health care by serving as teachers and mentors. We push the boundaries of science in hospital care through innovative research that defines the evidence-based practices for our field. Hospitalists, proudly celebrate all that we have accomplished together on March 7, and moving forward, every first Thursday in March annually.
The Society for Hospital Medicine’s celebration of National Hospitalist Day will include spotlights on hospitalists, a social medical campaign, downloadable customizable posters, and much more. Stay tuned for details!
Attend the only meeting designed just for you
Be among the thousands of hospitalists who will celebrate hospital medicine in person at Hospital Medicine 2019 (HM19), March 24-27 in National Harbor, Md.
While at HM19, check out more than 20 educational tracks, including clinical updates, diagnostic reasoning, and health policy. New this year are two mini tracks: “Between the Guidelines” and “Clinical Mastery”. Between the Guidelines explores how we can address some of the most challenging cases we encounter in hospital medicine, where clear guidelines don’t exist. Clinical Mastery is designed to enhance our bedside diagnostic skills, from ECGs to ultrasounds.
Get ready to vote in HM19’s “The Great Debate” – pairing two talented clinicians who will debate opposing sides of challenging clinical decisions that we encounter on the front lines of health care delivery. Attendees have the opportunity to hear the two sides and then vote on who they believe has the right approach. There are six precourses planned for HM19, with a new offering in Palliative Care and Pain Management. This year, the annual conference also features additional sessions for our NP/PA attendees. They include specific workshops as well as a track that includes 4 didactic sessions. Lastly, HM19 will offer CME, MOC, AOS, AAFP, and Pharmacology credits to address the needs of our attendees.
Looking into the future
While hospitalists are a vital part of U.S. health care, our delivery systems are in transition with greater focus on value-based care. To ensure hospital medicine continues to thrive in today’s dynamic scene, SHM’s Board of Directors held a strategic meeting in October 2018 to focus on the role of hospitalists and hospital medicine in population health management.
There are many hospitalists across the nation who are currently involved in population health management. These range from medical directors to vice presidents of accountable care organizations, population health management, or value-based care. Hospitalists are seeking communities focused on population health management to share best practices and learn from each other. To address this, SHM’s Advocacy and Public Policy HMX community has served as a meeting point to discuss issues related to value-based care. To join the discussion, visit the community by logging in at hospitalmedicine.org/hmx. Furthermore, at HM19, hospitalists will have the opportunity to meet face to face regarding these issues in the Advocacy Special Interest Forum.
Key points: Population health management
- Source of truth
SHM has served as the source of reliable and trusted information about hospital medicine. We will continue to develop content and resources specific to population health management on our website so hospitalists can easily access this information. To increase our awareness about population health management, presenters at HM19 will integrate a slide about the implications of population health management on their clinical topic. These slides will illustrate the clinical and nonclinical services that are necessary to enhance the patient’s quality of care and life. In addition to best practice care, these slides will highlight topics like the role of style modification and prevention, risk stratification, chronic disease management, and care coordination throughout the continuum of care.
- Advocating for us
In addition to providing a home for hospitalists to collaborate regarding population health management, SHM will advance this agenda from a regulatory perspective. The Public Policy and Performance Measurement & Reporting Committees are actively evaluating and leading the transition from value to volume. SHM is also working with potential key partners and organizations in the areas of primary care, skilled nursing facilities, and accountable care organizations that will help improve the effectiveness of delivering population health management.
- Creating expertise
SHM will lead best practice development for tools and skills that are necessary for hospitalists to lead population health management. Telemedicine is an increasingly critical tool as we help manage our patients in other facilities, inpatient or skilled nursing facilities, as well as at home. SHM has developed a white paper about telemedicine in hospital medicine that highlights modalities, offerings, implementation of programs, and work flows necessary for success. You can find it under “Resources” at hospitalmedicine.org/telemedicine.
SHM will continue to actively develop tools that appropriately address the challenges we’re facing. From National Hospitalist Day to population health management, this is an exciting time in hospital medicine – I hope to see you at HM19 to celebrate our specialty and our bright future.
Dr. Afsar is president of the Society of Hospital Medicine, and chief ambulatory officer and chief medical officer for accountable care organizations at UC Irvine Health.
For the first time ever, on March 7, 2019, tens of thousands of hospitalists across the United States and around the world will celebrate their day, National Hospitalist Day.
On this day, we will honor the hard work and dedication of hospitalists in the care of millions of hospitalized patients. With more than 62,000 hospitalists across the United States, hospital medicine has been the fastest growing medical specialty and among the largest of all specialties in medicine. Hospitalists now lead clinical care in over 75% of U.S. hospitals, caring for patients in their communities. We educate the future providers of health care by serving as teachers and mentors. We push the boundaries of science in hospital care through innovative research that defines the evidence-based practices for our field. Hospitalists, proudly celebrate all that we have accomplished together on March 7, and moving forward, every first Thursday in March annually.
The Society for Hospital Medicine’s celebration of National Hospitalist Day will include spotlights on hospitalists, a social medical campaign, downloadable customizable posters, and much more. Stay tuned for details!
Attend the only meeting designed just for you
Be among the thousands of hospitalists who will celebrate hospital medicine in person at Hospital Medicine 2019 (HM19), March 24-27 in National Harbor, Md.
While at HM19, check out more than 20 educational tracks, including clinical updates, diagnostic reasoning, and health policy. New this year are two mini tracks: “Between the Guidelines” and “Clinical Mastery”. Between the Guidelines explores how we can address some of the most challenging cases we encounter in hospital medicine, where clear guidelines don’t exist. Clinical Mastery is designed to enhance our bedside diagnostic skills, from ECGs to ultrasounds.
Get ready to vote in HM19’s “The Great Debate” – pairing two talented clinicians who will debate opposing sides of challenging clinical decisions that we encounter on the front lines of health care delivery. Attendees have the opportunity to hear the two sides and then vote on who they believe has the right approach. There are six precourses planned for HM19, with a new offering in Palliative Care and Pain Management. This year, the annual conference also features additional sessions for our NP/PA attendees. They include specific workshops as well as a track that includes 4 didactic sessions. Lastly, HM19 will offer CME, MOC, AOS, AAFP, and Pharmacology credits to address the needs of our attendees.
Looking into the future
While hospitalists are a vital part of U.S. health care, our delivery systems are in transition with greater focus on value-based care. To ensure hospital medicine continues to thrive in today’s dynamic scene, SHM’s Board of Directors held a strategic meeting in October 2018 to focus on the role of hospitalists and hospital medicine in population health management.
There are many hospitalists across the nation who are currently involved in population health management. These range from medical directors to vice presidents of accountable care organizations, population health management, or value-based care. Hospitalists are seeking communities focused on population health management to share best practices and learn from each other. To address this, SHM’s Advocacy and Public Policy HMX community has served as a meeting point to discuss issues related to value-based care. To join the discussion, visit the community by logging in at hospitalmedicine.org/hmx. Furthermore, at HM19, hospitalists will have the opportunity to meet face to face regarding these issues in the Advocacy Special Interest Forum.
Key points: Population health management
- Source of truth
SHM has served as the source of reliable and trusted information about hospital medicine. We will continue to develop content and resources specific to population health management on our website so hospitalists can easily access this information. To increase our awareness about population health management, presenters at HM19 will integrate a slide about the implications of population health management on their clinical topic. These slides will illustrate the clinical and nonclinical services that are necessary to enhance the patient’s quality of care and life. In addition to best practice care, these slides will highlight topics like the role of style modification and prevention, risk stratification, chronic disease management, and care coordination throughout the continuum of care.
- Advocating for us
In addition to providing a home for hospitalists to collaborate regarding population health management, SHM will advance this agenda from a regulatory perspective. The Public Policy and Performance Measurement & Reporting Committees are actively evaluating and leading the transition from value to volume. SHM is also working with potential key partners and organizations in the areas of primary care, skilled nursing facilities, and accountable care organizations that will help improve the effectiveness of delivering population health management.
- Creating expertise
SHM will lead best practice development for tools and skills that are necessary for hospitalists to lead population health management. Telemedicine is an increasingly critical tool as we help manage our patients in other facilities, inpatient or skilled nursing facilities, as well as at home. SHM has developed a white paper about telemedicine in hospital medicine that highlights modalities, offerings, implementation of programs, and work flows necessary for success. You can find it under “Resources” at hospitalmedicine.org/telemedicine.
SHM will continue to actively develop tools that appropriately address the challenges we’re facing. From National Hospitalist Day to population health management, this is an exciting time in hospital medicine – I hope to see you at HM19 to celebrate our specialty and our bright future.
Dr. Afsar is president of the Society of Hospital Medicine, and chief ambulatory officer and chief medical officer for accountable care organizations at UC Irvine Health.
Flu season showing signs of decline
The 2018-2019 flu season may have peaked as measures of influenza-like illness (ILI) activity dropped in the first week of the new year, according to the U.S. Centers for Disease Control and Prevention.

The proportion of outpatients visits for ILI dropped to 3.5% for the week ending Jan. 5, 2019, after reaching 4.0% the previous week. Outpatient ILI visits first topped the national baseline of 2.2% during the week ending Dec. 8, 2018, and have remained above that value for 5 consecutive weeks, the CDC’s influenza division said on Jan. 11.
Flu activity reported by the states reflects the national drop: 10 states came in at level 10 on the CDC’s 1-10 scale of activity for the week ending Jan. 5 – down from 12 the week before – and a total of 15 were in the high range from 8 to 10, compared with 19 the previous week, the CDC said. Two states, Mississippi and Texas, dropped from level 10 to level 7, which the CDC categorizes as moderate activity.
A total of 73 ILI-related deaths were reported during the week ending Dec. 29 (the latest with data available; reporting less than 68% complete), which already exceeds the 71 deaths reported for the week ending Dec. 22 (reporting 85% complete). Flu deaths totaled 437 through the first 13 weeks of the 2018-2019 season, compared with the 1,659 that occurred during weeks 1-13 of the very severe 2017-2018 season, CDC data show.
For the week ending Jan. 5, the CDC received reports of three flu-related pediatric deaths, all of which occurred the previous week. For the season so far, there have been 16 pediatric deaths, compared with 20 at this point in the 2017-2018 season.
Estimates released during the flu season for the first time show that between 6 and 7 million Americans have been infected since Oct. 1, 2018, and that 69,000-84,000 people have been hospitalized with the flu through Jan. 5, 2019. These cumulative totals have previously been available only at the end of the season, the CDC noted.
The 2018-2019 flu season may have peaked as measures of influenza-like illness (ILI) activity dropped in the first week of the new year, according to the U.S. Centers for Disease Control and Prevention.

The proportion of outpatients visits for ILI dropped to 3.5% for the week ending Jan. 5, 2019, after reaching 4.0% the previous week. Outpatient ILI visits first topped the national baseline of 2.2% during the week ending Dec. 8, 2018, and have remained above that value for 5 consecutive weeks, the CDC’s influenza division said on Jan. 11.
Flu activity reported by the states reflects the national drop: 10 states came in at level 10 on the CDC’s 1-10 scale of activity for the week ending Jan. 5 – down from 12 the week before – and a total of 15 were in the high range from 8 to 10, compared with 19 the previous week, the CDC said. Two states, Mississippi and Texas, dropped from level 10 to level 7, which the CDC categorizes as moderate activity.
A total of 73 ILI-related deaths were reported during the week ending Dec. 29 (the latest with data available; reporting less than 68% complete), which already exceeds the 71 deaths reported for the week ending Dec. 22 (reporting 85% complete). Flu deaths totaled 437 through the first 13 weeks of the 2018-2019 season, compared with the 1,659 that occurred during weeks 1-13 of the very severe 2017-2018 season, CDC data show.
For the week ending Jan. 5, the CDC received reports of three flu-related pediatric deaths, all of which occurred the previous week. For the season so far, there have been 16 pediatric deaths, compared with 20 at this point in the 2017-2018 season.
Estimates released during the flu season for the first time show that between 6 and 7 million Americans have been infected since Oct. 1, 2018, and that 69,000-84,000 people have been hospitalized with the flu through Jan. 5, 2019. These cumulative totals have previously been available only at the end of the season, the CDC noted.
The 2018-2019 flu season may have peaked as measures of influenza-like illness (ILI) activity dropped in the first week of the new year, according to the U.S. Centers for Disease Control and Prevention.

The proportion of outpatients visits for ILI dropped to 3.5% for the week ending Jan. 5, 2019, after reaching 4.0% the previous week. Outpatient ILI visits first topped the national baseline of 2.2% during the week ending Dec. 8, 2018, and have remained above that value for 5 consecutive weeks, the CDC’s influenza division said on Jan. 11.
Flu activity reported by the states reflects the national drop: 10 states came in at level 10 on the CDC’s 1-10 scale of activity for the week ending Jan. 5 – down from 12 the week before – and a total of 15 were in the high range from 8 to 10, compared with 19 the previous week, the CDC said. Two states, Mississippi and Texas, dropped from level 10 to level 7, which the CDC categorizes as moderate activity.
A total of 73 ILI-related deaths were reported during the week ending Dec. 29 (the latest with data available; reporting less than 68% complete), which already exceeds the 71 deaths reported for the week ending Dec. 22 (reporting 85% complete). Flu deaths totaled 437 through the first 13 weeks of the 2018-2019 season, compared with the 1,659 that occurred during weeks 1-13 of the very severe 2017-2018 season, CDC data show.
For the week ending Jan. 5, the CDC received reports of three flu-related pediatric deaths, all of which occurred the previous week. For the season so far, there have been 16 pediatric deaths, compared with 20 at this point in the 2017-2018 season.
Estimates released during the flu season for the first time show that between 6 and 7 million Americans have been infected since Oct. 1, 2018, and that 69,000-84,000 people have been hospitalized with the flu through Jan. 5, 2019. These cumulative totals have previously been available only at the end of the season, the CDC noted.
Hospitalist movers and shakers – January 2019
The Michigan chapter of the Society of Hospital Medicine has named Peter Watson, MD, SFHM, as state Hospitalist of the Year. Dr. Watson is the vice president of care management and outcomes for Health Alliance Plan (HAP) in Detroit. The Michigan chapter cited Dr. Watson’s leadership in hospital medicine and “generosity of spirit” as reasons for his selection.
Dr. Watson oversees nurses, social workers, and support staff while also serving as HAP Midwest Health Plan’s medical director. He’s a founding member of the Michigan SHM chapter, which he formerly represented as president.
Dr. Watson spent 11 years overseeing the Henry Ford Medical Group’s hospitalist program prior to joining HAP, and still works as an attending hospitalist for Henry Ford.
Hyung (Harry) Cho, MD, was named the inaugural chief value officer for NYC Health + Hospitals, which includes 11 hospitals in New York and is the largest public health system in the United States. He will oversee systemwide initiatives in value improvement and the reduction of unnecessary testing and treatment.
Prior to this appointment, Dr. Cho served as an academic hospitalist at Mount Sinai Hospital for 7 years, leading high-value care initiatives. Currently, he is a senior fellow with the Lown Institute in Brookline, Mass., and director of quality improvement implementation for the High Value Practice Academic Alliance.
Nick Fitterman, MD, SFHM, has been promoted to executive director at Huntington (N.Y.) Hospital. Dr. Fitterman has been a long-time physician and administrator at Huntington, serving previously as vice chair of medicine as well as head of hospitalists.
Dr. Fitterman has served as president of SHM’s Long Island chapter.
Previously, Dr. Fitterman was chief resident at the State University of New York at Stony Brook, and he remains an associate professor at Hofstra University, Hempstead, N.Y.
Allen Kachalia, MD, was named director of the Armstrong Institute for Patient Safety and Quality and senior vice president of patient safety and quality for Johns Hopkins Medicine in Baltimore. Dr. Kachalia is a general internist who has been an active academic hospitalist at Brigham and Women’s Hospital in Boston.
Dr. Kachalia will oversee patient safety and quality across all of Hopkins Medicine, with a focus on ending preventable harm, improving outcomes and patient experience, and reducing waste in the system’s delivery of care. He also will guide academic efforts for the Armstrong Institute, formed recently thanks to a $10 million gift.
In addition to his hospitalist work, Dr. Kachalia comes to Hopkins after serving as chief quality officer and vice president of quality and safety at Brigham Health.
Riane Dodge, PA, has been elevated to director of clinical education in physician assistant studies at Clarkson University, Potsdam, N.Y. The veteran physician assistant previously worked as a hospitalist in the Claxton Hepburn Medical Center in Ogdensburg, N.Y. There, she cared for patients in acute rehab, mental health, and on regular medical floors.
Dodge also has a background in urgent care and family medicine, and has experience as an emergency department technician.
BUSINESS MOVES
Surgical Affiliates of Sacramento, a surgical hospitalist provider with expertise in trauma, orthopedic, neurosurgery, and general surgery for hospital systems, has added partnerships with Christus Spohn Hospital South and Christus Spohn Hospital Shoreline in Corpus Christi, Texas.
Surgical Affiliates’ hospitalist system will provide round-the-clock emergency orthopedic surgery service to adult and pediatric patients in the two hospitals. With Surgical Affiliates’ help, Christus Spohn facilities will be able to cover its own patients, as well as those requiring transfer from regional hospitals.
Hospitalist surgeons will handle emergency surgeries and patient surgery consultations. Clinics will be provided at each facility to care for patients after they are discharged.
The Michigan chapter of the Society of Hospital Medicine has named Peter Watson, MD, SFHM, as state Hospitalist of the Year. Dr. Watson is the vice president of care management and outcomes for Health Alliance Plan (HAP) in Detroit. The Michigan chapter cited Dr. Watson’s leadership in hospital medicine and “generosity of spirit” as reasons for his selection.
Dr. Watson oversees nurses, social workers, and support staff while also serving as HAP Midwest Health Plan’s medical director. He’s a founding member of the Michigan SHM chapter, which he formerly represented as president.
Dr. Watson spent 11 years overseeing the Henry Ford Medical Group’s hospitalist program prior to joining HAP, and still works as an attending hospitalist for Henry Ford.
Hyung (Harry) Cho, MD, was named the inaugural chief value officer for NYC Health + Hospitals, which includes 11 hospitals in New York and is the largest public health system in the United States. He will oversee systemwide initiatives in value improvement and the reduction of unnecessary testing and treatment.
Prior to this appointment, Dr. Cho served as an academic hospitalist at Mount Sinai Hospital for 7 years, leading high-value care initiatives. Currently, he is a senior fellow with the Lown Institute in Brookline, Mass., and director of quality improvement implementation for the High Value Practice Academic Alliance.
Nick Fitterman, MD, SFHM, has been promoted to executive director at Huntington (N.Y.) Hospital. Dr. Fitterman has been a long-time physician and administrator at Huntington, serving previously as vice chair of medicine as well as head of hospitalists.
Dr. Fitterman has served as president of SHM’s Long Island chapter.
Previously, Dr. Fitterman was chief resident at the State University of New York at Stony Brook, and he remains an associate professor at Hofstra University, Hempstead, N.Y.
Allen Kachalia, MD, was named director of the Armstrong Institute for Patient Safety and Quality and senior vice president of patient safety and quality for Johns Hopkins Medicine in Baltimore. Dr. Kachalia is a general internist who has been an active academic hospitalist at Brigham and Women’s Hospital in Boston.
Dr. Kachalia will oversee patient safety and quality across all of Hopkins Medicine, with a focus on ending preventable harm, improving outcomes and patient experience, and reducing waste in the system’s delivery of care. He also will guide academic efforts for the Armstrong Institute, formed recently thanks to a $10 million gift.
In addition to his hospitalist work, Dr. Kachalia comes to Hopkins after serving as chief quality officer and vice president of quality and safety at Brigham Health.
Riane Dodge, PA, has been elevated to director of clinical education in physician assistant studies at Clarkson University, Potsdam, N.Y. The veteran physician assistant previously worked as a hospitalist in the Claxton Hepburn Medical Center in Ogdensburg, N.Y. There, she cared for patients in acute rehab, mental health, and on regular medical floors.
Dodge also has a background in urgent care and family medicine, and has experience as an emergency department technician.
BUSINESS MOVES
Surgical Affiliates of Sacramento, a surgical hospitalist provider with expertise in trauma, orthopedic, neurosurgery, and general surgery for hospital systems, has added partnerships with Christus Spohn Hospital South and Christus Spohn Hospital Shoreline in Corpus Christi, Texas.
Surgical Affiliates’ hospitalist system will provide round-the-clock emergency orthopedic surgery service to adult and pediatric patients in the two hospitals. With Surgical Affiliates’ help, Christus Spohn facilities will be able to cover its own patients, as well as those requiring transfer from regional hospitals.
Hospitalist surgeons will handle emergency surgeries and patient surgery consultations. Clinics will be provided at each facility to care for patients after they are discharged.
The Michigan chapter of the Society of Hospital Medicine has named Peter Watson, MD, SFHM, as state Hospitalist of the Year. Dr. Watson is the vice president of care management and outcomes for Health Alliance Plan (HAP) in Detroit. The Michigan chapter cited Dr. Watson’s leadership in hospital medicine and “generosity of spirit” as reasons for his selection.
Dr. Watson oversees nurses, social workers, and support staff while also serving as HAP Midwest Health Plan’s medical director. He’s a founding member of the Michigan SHM chapter, which he formerly represented as president.
Dr. Watson spent 11 years overseeing the Henry Ford Medical Group’s hospitalist program prior to joining HAP, and still works as an attending hospitalist for Henry Ford.
Hyung (Harry) Cho, MD, was named the inaugural chief value officer for NYC Health + Hospitals, which includes 11 hospitals in New York and is the largest public health system in the United States. He will oversee systemwide initiatives in value improvement and the reduction of unnecessary testing and treatment.
Prior to this appointment, Dr. Cho served as an academic hospitalist at Mount Sinai Hospital for 7 years, leading high-value care initiatives. Currently, he is a senior fellow with the Lown Institute in Brookline, Mass., and director of quality improvement implementation for the High Value Practice Academic Alliance.
Nick Fitterman, MD, SFHM, has been promoted to executive director at Huntington (N.Y.) Hospital. Dr. Fitterman has been a long-time physician and administrator at Huntington, serving previously as vice chair of medicine as well as head of hospitalists.
Dr. Fitterman has served as president of SHM’s Long Island chapter.
Previously, Dr. Fitterman was chief resident at the State University of New York at Stony Brook, and he remains an associate professor at Hofstra University, Hempstead, N.Y.
Allen Kachalia, MD, was named director of the Armstrong Institute for Patient Safety and Quality and senior vice president of patient safety and quality for Johns Hopkins Medicine in Baltimore. Dr. Kachalia is a general internist who has been an active academic hospitalist at Brigham and Women’s Hospital in Boston.
Dr. Kachalia will oversee patient safety and quality across all of Hopkins Medicine, with a focus on ending preventable harm, improving outcomes and patient experience, and reducing waste in the system’s delivery of care. He also will guide academic efforts for the Armstrong Institute, formed recently thanks to a $10 million gift.
In addition to his hospitalist work, Dr. Kachalia comes to Hopkins after serving as chief quality officer and vice president of quality and safety at Brigham Health.
Riane Dodge, PA, has been elevated to director of clinical education in physician assistant studies at Clarkson University, Potsdam, N.Y. The veteran physician assistant previously worked as a hospitalist in the Claxton Hepburn Medical Center in Ogdensburg, N.Y. There, she cared for patients in acute rehab, mental health, and on regular medical floors.
Dodge also has a background in urgent care and family medicine, and has experience as an emergency department technician.
BUSINESS MOVES
Surgical Affiliates of Sacramento, a surgical hospitalist provider with expertise in trauma, orthopedic, neurosurgery, and general surgery for hospital systems, has added partnerships with Christus Spohn Hospital South and Christus Spohn Hospital Shoreline in Corpus Christi, Texas.
Surgical Affiliates’ hospitalist system will provide round-the-clock emergency orthopedic surgery service to adult and pediatric patients in the two hospitals. With Surgical Affiliates’ help, Christus Spohn facilities will be able to cover its own patients, as well as those requiring transfer from regional hospitals.
Hospitalist surgeons will handle emergency surgeries and patient surgery consultations. Clinics will be provided at each facility to care for patients after they are discharged.
The state of hospital medicine in 2018
Productivity, pay, and roles remain center stage
In a national health care environment undergoing unprecedented transformation, the specialty of hospital medicine appears to be an island of relative stability, a conclusion that is supported by the principal findings from SHM’s 2018 State of Hospital Medicine (SoHM) report.
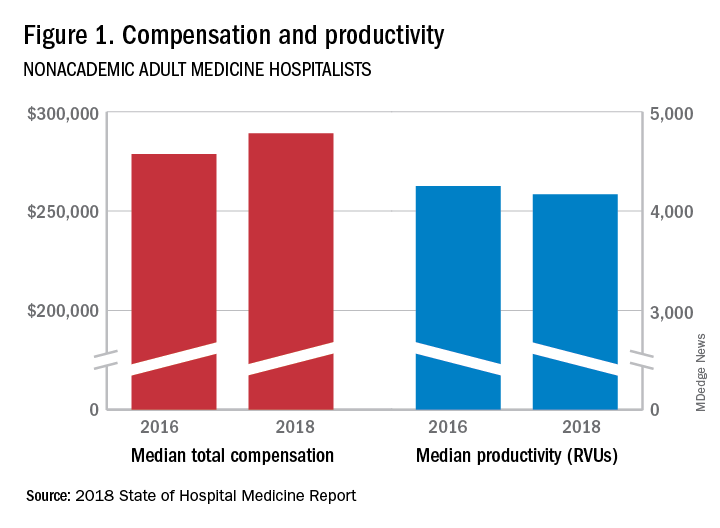
The report of hospitalist group practice characteristics, as well as other key data defining the field’s current status, that the Society of Hospital Medicine puts out every 2 years reveals that overall salaries for hospitalist physicians are up by 3.8% since 2016. Although productivity, as measured by work relative value units (RVUs), remained largely flat over the same period, financial support per full-time equivalent (FTE) physician position to hospitalist groups from their hospitals and health systems is up significantly.
Total support per FTE averaged $176,657 in 2018, 12% higher than in 2016, noted Leslie Flores, MHA, SFHM, of Nelson Flores Hospital Medicine Consultants, and a member of SHM’s Practice Analysis Committee, which oversees the biennial survey. Compensation and productivity data were collected by the Medical Group Management Association and licensed by SHM for inclusion in its report.
These findings – particularly the flat productivity – raise questions about long-term sustainability, Ms. Flores said. “What is going on? Do hospital administrators still recognize the value hospitalists bring to the operations and the quality of their hospitals? Or is paying the subsidy just a cost of doing business – a necessity for most hospitals in a setting where demand for hospitalist positions remains high?”
Andrew White, MD, FACP, SFHM, chair of SHM’s Practice Analysis Committee and director of the hospital medicine service at the University of Washington Medical Center, Seattle, said basic market forces dictate that it is “pretty much inconceivable” to run a modern hospital of any size without hospitalists.
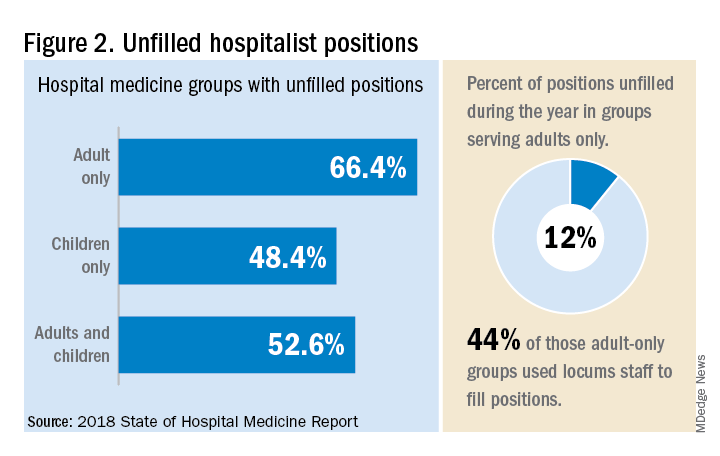
“Clearly, demand outstrips supply, which drives up salaries and support, whether CEOs feel that the hospitalist group is earning that support or not,” Dr. White said. “The unfilled hospitalist positions we identified speak to ongoing projected greater demand than supply. That said, hospitalists and group leaders can’t be complacent and must collaborate effectively with hospitals to provide highly valuable services.” Turnover of hospitalist positions was up slightly, he noted, at 7.4% in 2018, from 6.9% in 2016, reversing a trend of previous years.
But will these trends continue at a time when hospitals face continued pressure to cut costs, as the hospital medicine subsidy may represent one of their largest cost centers? Because the size of hospitalist groups continues to grow, hospitals’ total subsidy for hospital medicine is going up faster than the percentage increase in support per FTE.
How do hospitalists use the SoHM report?
Dr. White called the 2018 SoHM report the “most representative and balanced sample to date” of hospitalist group practices, with some of the highest quality data, thanks to more robust participation in the survey by pediatric groups and improved distribution among hospitalist management companies and academic programs.
“Not that past reports had major flaws, but this version is more authoritative, reflecting an intentional effort by our Practice Analysis Committee to bring in more participants from key groups,” he said.
The biennial report has been around long enough to achieve brand recognition in the field as the most authoritative source of information regarding hospitalist practice, he added. “We worked hard this year to balance the participants, with more of our responses than in the past coming from multi-hospital groups, whether 4 to 5 sites, or 20 to 30.”
Surveys were conducted online in January and February of 2018 in response to invitations mailed and emailed to targeted hospital medicine group leaders. A total of 569 groups completed the survey, representing 8,889 hospitalist FTEs, approximately 16% of the total hospitalist workforce. Responses were presented in several categories, including by size of program, region and employment model. Groups that care for adults only represented 87.9% of the surveys, while groups that care for children only were 6.7% and groups that care for both adults and children were 5.4%.
“This survey doesn’t tell us what should be best practice in hospital medicine,” Dr. White said, only what is actual current practice. He uses it in his own health system to not only contextualize and justify his group’s performance metrics for hospital administrators – relative to national and categorical averages – but also to see if the direction his group is following is consistent with what’s going on in the larger field.
“These data offer a very powerful resource regarding the trends in hospital medicine,” said Romil Chadha, MD, MPH, FACP, SFHM, associate division chief for operations in the division of hospital medicine at the University of Kentucky and UK Healthcare, Lexington. “It is my repository of data to go before my administrators for decisions that need to be made or to pilot new programs.”
Dr. Chadha also uses the data to help answer compensation, scheduling, and support questions from his group’s members.
Thomas McIlraith, MD, immediate past chairman of the hospital medicine department at Mercy Medical Group, Sacramento, Calif., said the report’s value is that it allows comparisons of salaries in different settings, and to see, for example, how night staffing is structured. “A lot of leaders I spoke to at SHM’s 2018 Leadership Academy in Vancouver were saying they didn’t feel up to parity with the national standards. You can use the report to look at the state of hospital medicine nationally and make comparisons,” he said.
Calls for more productivity
Roberta Himebaugh, MBA, SFHM, senior vice president of acute care services for the national hospitalist management company TeamHealth, and cochair of the SHM Practice Administrators Special Interest Group, said her company’s clients have traditionally asked for greater productivity from their hospitalist contracts as a way to decrease overall costs. Some markets are starting to see a change in that approach, she noted.
“Recently there’s been an increased focus on paying hospitalists to focus on quality rather than just productivity. Some of our clients are willing to pay for that, and we are trying to assign value to this non-billable time or adjust our productivity standards appropriately. I think hospitals definitely understand the value of non-billable services from hospitalists, but still will push us on the productivity targets,” Ms. Himebaugh said.
“I don’t believe hospital medicine can be sustainable long term on flat productivity or flat RVUs,” she added. “Yet the costs of burnout associated with pushing higher productivity are not sustainable, either.” So what are the answers? She said many inefficiencies are involved in responding to inquiries on the floor that could have been addressed another way, or waiting for the turnaround of diagnostic tests.
“Maybe we don’t need physicians to be in the hospital 24/7 if we have access to telehealth, or a partnership with the emergency department, or greater use of advanced care practice providers,” Ms. Himebaugh said. “Our hospitals are examining those options, and we have to look at how we can become more efficient and less costly. At TeamHealth, we are trying to staff for value – looking at patient flow patterns and adjusting our schedules accordingly. Is there a bolus of admissions tied to emergency department shift changes, or to certain days of the week? How can we move from the 12-hour shift that begins at 7 a.m. and ends at 7 p.m., and instead provide coverage for when the patients are there?”
Mark Williams, MD, MHM, chief of the division of hospital medicine at the University of Kentucky, Lexington, said he appreciates the volume of data in the report but wishes for even more survey participants, which could make the breakouts for subgroups such as academic hospitalists more robust. Other current sources of hospitalist salary data include the Association of American Medical Colleges (AAMC), which produces compensation reports to help medical schools and teaching hospitals with benchmarking, and the Faculty Practice Solution Center developed jointly by AAMC and Vizient to provide faculty practice plans with analytic tools. The Medical Group Management Association (MGMA) is another valuable source of information, some of which was licensed for inclusion in the SoHM report.
“There is no source of absolute truth that hospitalists can point to,” Dr. Williams said. “I will present my data and my administrators will reply: ‘We have our own data.’ Our institution has consistently ranked first or second nationwide for the sickest patients. We take more Medicaid and dually eligible patients, who have a lot of social issues. They take a lot of time to manage medically and the RVUs don’t reflect that. And yet I’m still judged by my RVUs generated per hospitalist. Hospital administrators understandably want to get the most productivity, and they are looking for their own data for average productivity numbers.”
Ryan Brown, MD, specialty medical director for hospital medicine with Atrium Health in Charlotte, N.C., said that hospital medicine’s flat productivity trends would be difficult to sustain in the business world. But there aren’t easy or obvious ways to increase hospitalists’ productivity. The SoHM report also shows that as productivity increases, total compensation increases but at a lower rate, resulting in a gradual decrease in compensation per RVU.
Pressures to increase productivity can be a double-edged sword, Dr. Williams added. Demanding that doctors make more billable visits faster to generate more RVUs can be a recipe for burnout and turnover, with huge costs associated with recruiting replacements.
“If there was recent turnover of hospitalists at the hospital, with the need to find replacements, there may be institutional memory about that,” he said. “But where are hospitals spending their money? Bottom line, we still need to learn to cut our costs.”
How is hospitalist practice evolving?
In addition to payment and productivity data, the SoHM report provides a current picture of the evolving state of hospitalist group practices. A key thread is how the work hospitalists are doing, and the way they do it, is changing, with new information about comanagement roles, dedicated admitters, night coverage, geographic rounding, and the like.
Making greater use of nurse practitioners and physician assistants (NPs/PAs), may be one way to change the flat productivity trends, Dr. Brown said. With a cost per RVU that’s roughly half that of a doctor’s, NPs/PAs could contribute to the bottom line. But he sees surprisingly large variation in how hospitalist groups are using them. Typically, they are deployed at a ratio of four doctors to one NP/PA, but that ratio could be two to one or even one to one, he said.
Use of NPs/PAs by academic hospitalist groups is up, from 52.1% in 2016 to 75.7% in 2018. For adult-only groups, 76.8% had NPs/PAs, with higher rates in hospitals and health systems and lower rates in the West region. But a lot of groups are using these practitioners for nonproductive work, and some are failing to generate any billing income, Dr. Brown said.
“The rate at which NPs/PAs performed billable services was higher in physician-owned practices, resulting in a lower cost per RVU, suggesting that many practices may be underutilizing their NPs/PAs or not sharing the work.” Not every NP or PA wants to or is able to care for very complex patients, Dr. Brown said, “but you want a system where the NP and PA can work at the highest level permitted by state law.”
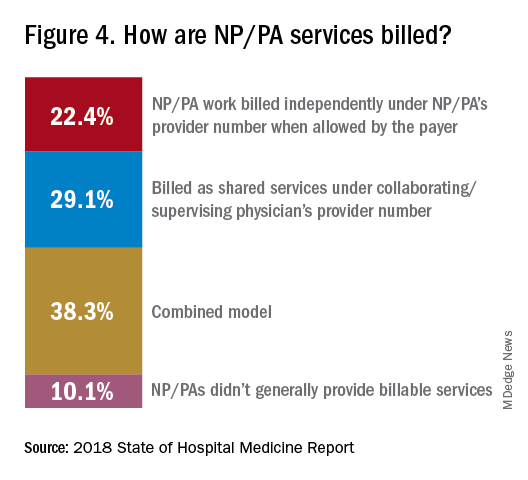
The predominant scheduling model of hospital medicine, 7 days on duty followed by 7 days off, has diminished somewhat in recent years. There appears to be some fluctuation and a gradual move away from 7 on/7 off toward some kind of variable approach, since the former may not be physically sustainable for the doctor over the long haul, Dr. Brown said. Some groups are experimenting with a combined approach.
“I think balancing workload with manpower has always been a challenge for our field. Maybe we should be working shorter shifts or fewer days and making sure our hospitalists aren’t ever sitting around idle,” he said. “And could we come in on nonclinical days to do administrative tasks? I think the solution is out there, but we haven’t created the algorithms to define that yet. If you could somehow use the data for volume, number of beds, nurse staffing, etc., by year and seasonally, you might be able to reliably predict census. This is about applying data hospitals already have in their electronic health records, but utilizing the data in ways that are more helpful.”
Dr. McIlraith added that a big driver of the future of hospital medicine will be the evolution of the EHR and the digitalization of health care, as hospitals learn how to leverage more of what’s in their EHRs. “The impact will grow for hospitalists through the creation and maturation of big data systems – and the learning that can be extracted from what’s contained in the electronic health record.”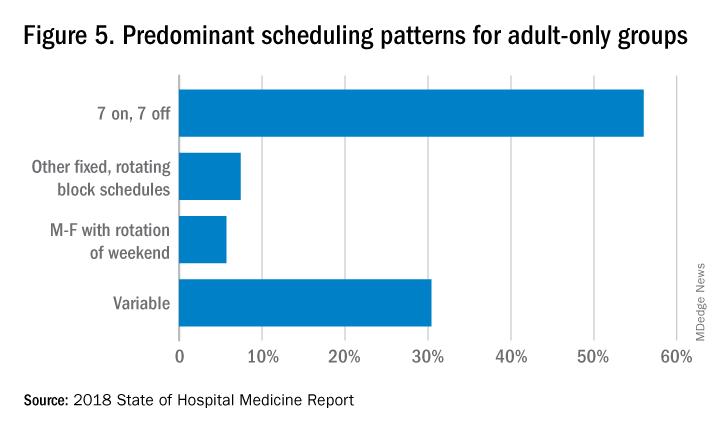
Another important question for hospitalist groups is their model of backup scheduling, to make sure there is a replacement available if a scheduled doctor calls in sick or if demand is unexpectedly high.
“In today’s world, this is how we have traditionally managed unpredictability,” Dr. Brown said. “You don’t know when you will need it, but if you need it, you want it immediately. So how do you pay for it – only when the doctor comes in, or also an amount just for being on call?” Some groups pay for both, he said, others for neither.
“We are a group of 70 hospitalists, and if someone is sick you can’t just shut down the service,” said Dr. Chadha. “We are one of the few to use incentives for both, which could include a 1-week decrease in clinical shifts in exchange for 2 weeks of backup. We have times with 25% usage of backup number 1, and 10% usage of backup number 2,” he noted. “But the goal is for our hospitalists to have assurances that there is a backup system and that it works.”
The presence of nocturnists in hospitals continues to rise, with 76.1% of adults-only groups having nocturnists, 27.6% of children-only groups, and 68.2% of adults and children groups. Geographic or unit-based hospital assignments have grown to 36.4% of adult-only groups.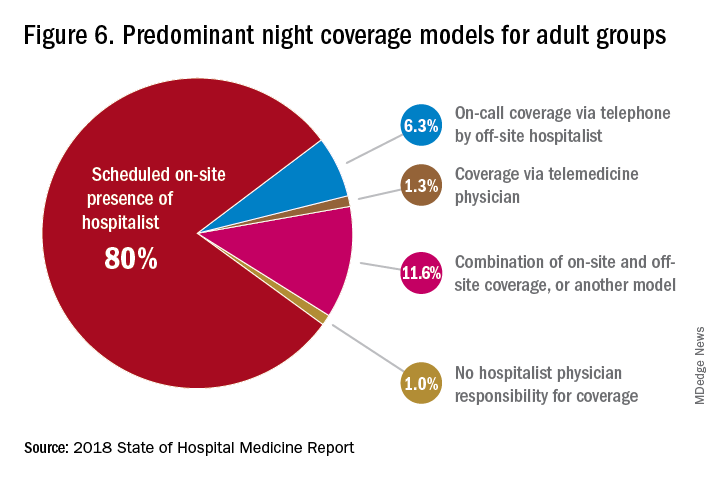
What are hospitalists’ other new roles?
“We have a large group of 50 doctors, with about 40 FTEs, and we are evolving from the traditional generalist role toward more subspecialty comanagement,” said Bryan Huang, MD, physician adviser and associate clinical professor in the division of hospital medicine at the University of California–San Diego. “Our hospitalists are asking what it means to be an academic hospitalist as our teaching roles have shrunk.”
Dr. Huang recently took on a new role as physician adviser for his hospital in such areas as utilization review, patient flow, and length of stay. “I’m spearheading a work group to address quality issues – all of which involve collaboration with other professionals. We also developed an admitting role here for a hospitalist whose sole role for the day is to admit patients.” Nationally up to 51.2% of hospitalist groups utilize a dedicated daytime admitter.
The report found that hospital services for which hospitalists are more likely to be attendings than consultants include GI/liver, 78.4%; palliative care, 77.3%; neurology/stroke, 73.6%; oncology, 67.8%; cardiology, 56.9%; and critical care, 50.7%. Conditions where hospitalists are more likely to consult rather than admit and attend include neurosurgery, orthopedics, general surgery, cardiovascular surgery, and other surgical subspecialties.
Other hospital services routinely provided by adult-only hospitalists include care of patients in an ICU setting (62.7%); primary responsibility for observation units (54.6%); primary clinical responsibility for rapid response teams (48.8%); primary responsibility for code blue or cardiac arrest teams (43.8%); nighttime admissions or tuck-in services (33.9%); and medical procedures (31.5%). For pediatric hospital medicine groups, care of healthy newborns and medical procedures were among the most common services provided, while for hospitalists serving adults and children, rapid response teams, ICUs, and specialty units were most common.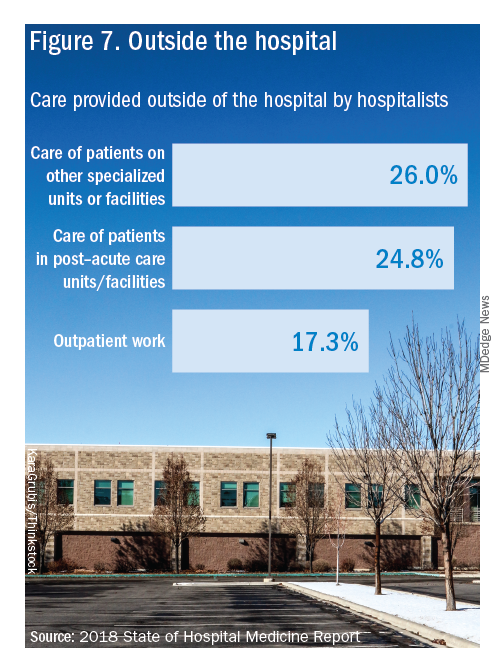
New models of payment for health care
As the larger health care system is being transformed by new payment models and benefit structures, including accountable care organizations (ACOs), value-based purchasing, bundled payments, and other forms of population-based coverage – which is described as a volume-to-value shift in health care – how are these new models affecting hospitalists?
Observers say penetration of these new models varies widely by locality but they haven’t had much direct impact on hospitalists’ practices – at least not yet. However, as hospitals and health systems find themselves needing to learn new ways to invest their resources differently in response to these trends, what matters to the hospital should be of great importance to the hospitalist group.
“I haven’t seen a lot of dramatic changes in how hospitalists engage with value-based purchasing,” Dr. White said. “If we know that someone is part of an ACO, the instinctual – and right – response is to treat them like any other patient. But we still need to be committed to not waste resources.”
Hospitalists are the best people to understand the intricacies of how the health care system works under value-based approaches, Dr. Huang said. “That’s why so many hospitalists have taken leadership positions in their hospitals. I think all of this translates to the practical, day-to-day work of hospitalists, reflected in our focus on readmissions and length of stay.”
Dr. Williams said the health care system still hasn’t turned the corner from fee-for-service to value-based purchasing. “It still represents a tiny fraction of the income of hospitalists. Hospitals still have to focus on the bottom line, as fee-for-service reimbursement for hospitalized patients continues to get squeezed, and ACOs aren’t exactly paying premium rates either. Ask almost any hospital CEO what drives their bottom line today and the answer is volume – along with optimizing productivity. Pretty much every place I look, the future does not look terribly rosy for hospitals.”
Ms. Himebaugh said she is bullish on hospital medicine, in the sense that it’s unlikely to go away anytime soon. “Hospitalists are needed and provide value. But I don’t think we have devised the right model yet. I’m not sure our current model is sustainable. We need to find new models we can afford that don’t require squeezing our providers.”
For more information about the 2018 State of Hospital Medicine Report, contact SHM’s Practice Management Department at: [email protected] or call 800-843-3360. See also: https://www.hospitalmedicine.org/practice-management/shms-state-of-hospital-medicine/.
Productivity, pay, and roles remain center stage
Productivity, pay, and roles remain center stage
In a national health care environment undergoing unprecedented transformation, the specialty of hospital medicine appears to be an island of relative stability, a conclusion that is supported by the principal findings from SHM’s 2018 State of Hospital Medicine (SoHM) report.
The report of hospitalist group practice characteristics, as well as other key data defining the field’s current status, that the Society of Hospital Medicine puts out every 2 years reveals that overall salaries for hospitalist physicians are up by 3.8% since 2016. Although productivity, as measured by work relative value units (RVUs), remained largely flat over the same period, financial support per full-time equivalent (FTE) physician position to hospitalist groups from their hospitals and health systems is up significantly.
Total support per FTE averaged $176,657 in 2018, 12% higher than in 2016, noted Leslie Flores, MHA, SFHM, of Nelson Flores Hospital Medicine Consultants, and a member of SHM’s Practice Analysis Committee, which oversees the biennial survey. Compensation and productivity data were collected by the Medical Group Management Association and licensed by SHM for inclusion in its report.
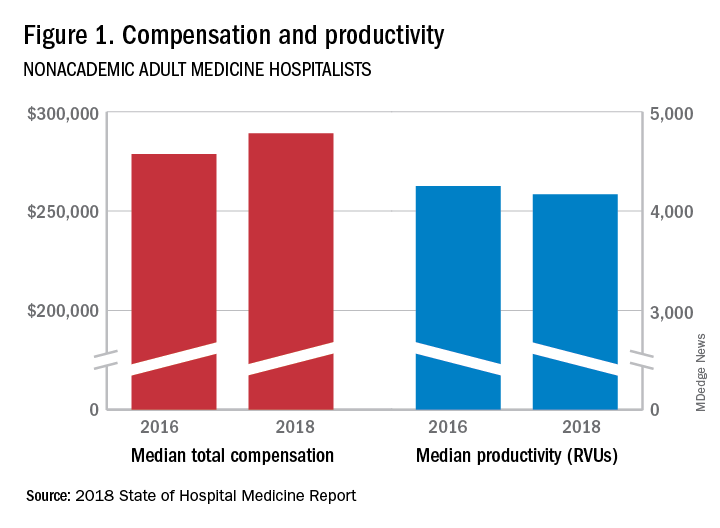
These findings – particularly the flat productivity – raise questions about long-term sustainability, Ms. Flores said. “What is going on? Do hospital administrators still recognize the value hospitalists bring to the operations and the quality of their hospitals? Or is paying the subsidy just a cost of doing business – a necessity for most hospitals in a setting where demand for hospitalist positions remains high?”
Andrew White, MD, FACP, SFHM, chair of SHM’s Practice Analysis Committee and director of the hospital medicine service at the University of Washington Medical Center, Seattle, said basic market forces dictate that it is “pretty much inconceivable” to run a modern hospital of any size without hospitalists.
“Clearly, demand outstrips supply, which drives up salaries and support, whether CEOs feel that the hospitalist group is earning that support or not,” Dr. White said. “The unfilled hospitalist positions we identified speak to ongoing projected greater demand than supply. That said, hospitalists and group leaders can’t be complacent and must collaborate effectively with hospitals to provide highly valuable services.” Turnover of hospitalist positions was up slightly, he noted, at 7.4% in 2018, from 6.9% in 2016, reversing a trend of previous years.
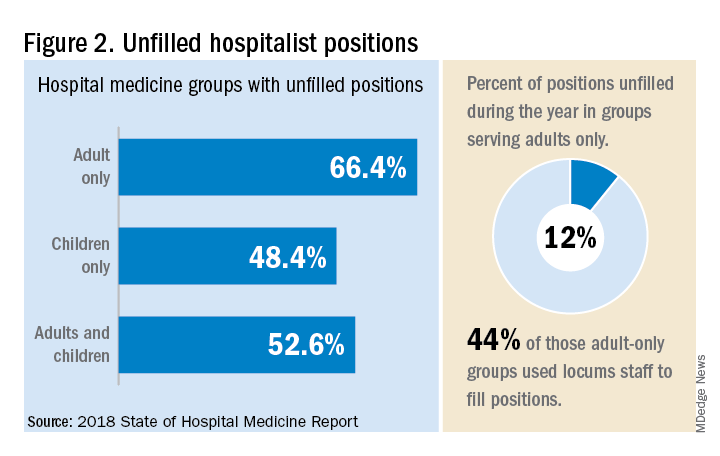
But will these trends continue at a time when hospitals face continued pressure to cut costs, as the hospital medicine subsidy may represent one of their largest cost centers? Because the size of hospitalist groups continues to grow, hospitals’ total subsidy for hospital medicine is going up faster than the percentage increase in support per FTE.
How do hospitalists use the SoHM report?
Dr. White called the 2018 SoHM report the “most representative and balanced sample to date” of hospitalist group practices, with some of the highest quality data, thanks to more robust participation in the survey by pediatric groups and improved distribution among hospitalist management companies and academic programs.
“Not that past reports had major flaws, but this version is more authoritative, reflecting an intentional effort by our Practice Analysis Committee to bring in more participants from key groups,” he said.
The biennial report has been around long enough to achieve brand recognition in the field as the most authoritative source of information regarding hospitalist practice, he added. “We worked hard this year to balance the participants, with more of our responses than in the past coming from multi-hospital groups, whether 4 to 5 sites, or 20 to 30.”
Surveys were conducted online in January and February of 2018 in response to invitations mailed and emailed to targeted hospital medicine group leaders. A total of 569 groups completed the survey, representing 8,889 hospitalist FTEs, approximately 16% of the total hospitalist workforce. Responses were presented in several categories, including by size of program, region and employment model. Groups that care for adults only represented 87.9% of the surveys, while groups that care for children only were 6.7% and groups that care for both adults and children were 5.4%.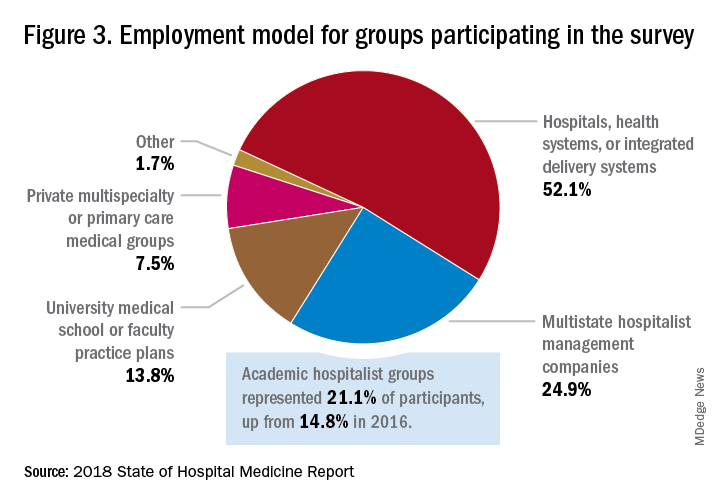
“This survey doesn’t tell us what should be best practice in hospital medicine,” Dr. White said, only what is actual current practice. He uses it in his own health system to not only contextualize and justify his group’s performance metrics for hospital administrators – relative to national and categorical averages – but also to see if the direction his group is following is consistent with what’s going on in the larger field.
“These data offer a very powerful resource regarding the trends in hospital medicine,” said Romil Chadha, MD, MPH, FACP, SFHM, associate division chief for operations in the division of hospital medicine at the University of Kentucky and UK Healthcare, Lexington. “It is my repository of data to go before my administrators for decisions that need to be made or to pilot new programs.”
Dr. Chadha also uses the data to help answer compensation, scheduling, and support questions from his group’s members.
Thomas McIlraith, MD, immediate past chairman of the hospital medicine department at Mercy Medical Group, Sacramento, Calif., said the report’s value is that it allows comparisons of salaries in different settings, and to see, for example, how night staffing is structured. “A lot of leaders I spoke to at SHM’s 2018 Leadership Academy in Vancouver were saying they didn’t feel up to parity with the national standards. You can use the report to look at the state of hospital medicine nationally and make comparisons,” he said.
Calls for more productivity
Roberta Himebaugh, MBA, SFHM, senior vice president of acute care services for the national hospitalist management company TeamHealth, and cochair of the SHM Practice Administrators Special Interest Group, said her company’s clients have traditionally asked for greater productivity from their hospitalist contracts as a way to decrease overall costs. Some markets are starting to see a change in that approach, she noted.
“Recently there’s been an increased focus on paying hospitalists to focus on quality rather than just productivity. Some of our clients are willing to pay for that, and we are trying to assign value to this non-billable time or adjust our productivity standards appropriately. I think hospitals definitely understand the value of non-billable services from hospitalists, but still will push us on the productivity targets,” Ms. Himebaugh said.
“I don’t believe hospital medicine can be sustainable long term on flat productivity or flat RVUs,” she added. “Yet the costs of burnout associated with pushing higher productivity are not sustainable, either.” So what are the answers? She said many inefficiencies are involved in responding to inquiries on the floor that could have been addressed another way, or waiting for the turnaround of diagnostic tests.
“Maybe we don’t need physicians to be in the hospital 24/7 if we have access to telehealth, or a partnership with the emergency department, or greater use of advanced care practice providers,” Ms. Himebaugh said. “Our hospitals are examining those options, and we have to look at how we can become more efficient and less costly. At TeamHealth, we are trying to staff for value – looking at patient flow patterns and adjusting our schedules accordingly. Is there a bolus of admissions tied to emergency department shift changes, or to certain days of the week? How can we move from the 12-hour shift that begins at 7 a.m. and ends at 7 p.m., and instead provide coverage for when the patients are there?”
Mark Williams, MD, MHM, chief of the division of hospital medicine at the University of Kentucky, Lexington, said he appreciates the volume of data in the report but wishes for even more survey participants, which could make the breakouts for subgroups such as academic hospitalists more robust. Other current sources of hospitalist salary data include the Association of American Medical Colleges (AAMC), which produces compensation reports to help medical schools and teaching hospitals with benchmarking, and the Faculty Practice Solution Center developed jointly by AAMC and Vizient to provide faculty practice plans with analytic tools. The Medical Group Management Association (MGMA) is another valuable source of information, some of which was licensed for inclusion in the SoHM report.
“There is no source of absolute truth that hospitalists can point to,” Dr. Williams said. “I will present my data and my administrators will reply: ‘We have our own data.’ Our institution has consistently ranked first or second nationwide for the sickest patients. We take more Medicaid and dually eligible patients, who have a lot of social issues. They take a lot of time to manage medically and the RVUs don’t reflect that. And yet I’m still judged by my RVUs generated per hospitalist. Hospital administrators understandably want to get the most productivity, and they are looking for their own data for average productivity numbers.”
Ryan Brown, MD, specialty medical director for hospital medicine with Atrium Health in Charlotte, N.C., said that hospital medicine’s flat productivity trends would be difficult to sustain in the business world. But there aren’t easy or obvious ways to increase hospitalists’ productivity. The SoHM report also shows that as productivity increases, total compensation increases but at a lower rate, resulting in a gradual decrease in compensation per RVU.
Pressures to increase productivity can be a double-edged sword, Dr. Williams added. Demanding that doctors make more billable visits faster to generate more RVUs can be a recipe for burnout and turnover, with huge costs associated with recruiting replacements.
“If there was recent turnover of hospitalists at the hospital, with the need to find replacements, there may be institutional memory about that,” he said. “But where are hospitals spending their money? Bottom line, we still need to learn to cut our costs.”
How is hospitalist practice evolving?
In addition to payment and productivity data, the SoHM report provides a current picture of the evolving state of hospitalist group practices. A key thread is how the work hospitalists are doing, and the way they do it, is changing, with new information about comanagement roles, dedicated admitters, night coverage, geographic rounding, and the like.
Making greater use of nurse practitioners and physician assistants (NPs/PAs), may be one way to change the flat productivity trends, Dr. Brown said. With a cost per RVU that’s roughly half that of a doctor’s, NPs/PAs could contribute to the bottom line. But he sees surprisingly large variation in how hospitalist groups are using them. Typically, they are deployed at a ratio of four doctors to one NP/PA, but that ratio could be two to one or even one to one, he said.
Use of NPs/PAs by academic hospitalist groups is up, from 52.1% in 2016 to 75.7% in 2018. For adult-only groups, 76.8% had NPs/PAs, with higher rates in hospitals and health systems and lower rates in the West region. But a lot of groups are using these practitioners for nonproductive work, and some are failing to generate any billing income, Dr. Brown said.
“The rate at which NPs/PAs performed billable services was higher in physician-owned practices, resulting in a lower cost per RVU, suggesting that many practices may be underutilizing their NPs/PAs or not sharing the work.” Not every NP or PA wants to or is able to care for very complex patients, Dr. Brown said, “but you want a system where the NP and PA can work at the highest level permitted by state law.”
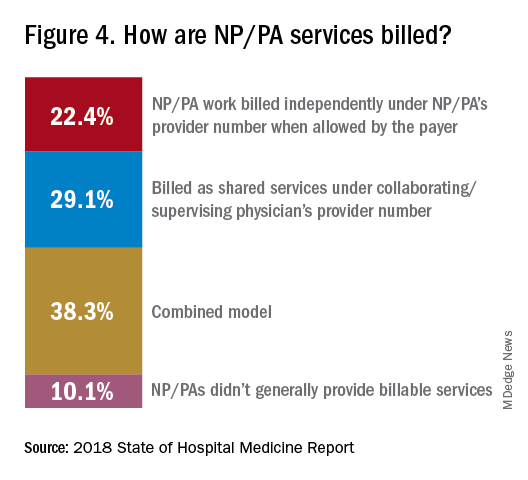
The predominant scheduling model of hospital medicine, 7 days on duty followed by 7 days off, has diminished somewhat in recent years. There appears to be some fluctuation and a gradual move away from 7 on/7 off toward some kind of variable approach, since the former may not be physically sustainable for the doctor over the long haul, Dr. Brown said. Some groups are experimenting with a combined approach.
“I think balancing workload with manpower has always been a challenge for our field. Maybe we should be working shorter shifts or fewer days and making sure our hospitalists aren’t ever sitting around idle,” he said. “And could we come in on nonclinical days to do administrative tasks? I think the solution is out there, but we haven’t created the algorithms to define that yet. If you could somehow use the data for volume, number of beds, nurse staffing, etc., by year and seasonally, you might be able to reliably predict census. This is about applying data hospitals already have in their electronic health records, but utilizing the data in ways that are more helpful.”
Dr. McIlraith added that a big driver of the future of hospital medicine will be the evolution of the EHR and the digitalization of health care, as hospitals learn how to leverage more of what’s in their EHRs. “The impact will grow for hospitalists through the creation and maturation of big data systems – and the learning that can be extracted from what’s contained in the electronic health record.”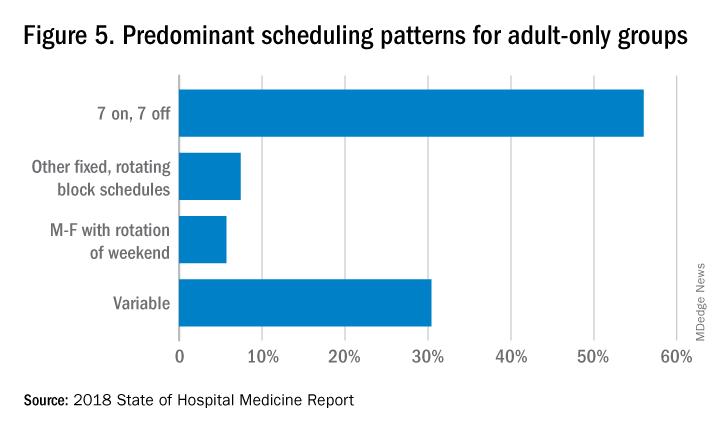
Another important question for hospitalist groups is their model of backup scheduling, to make sure there is a replacement available if a scheduled doctor calls in sick or if demand is unexpectedly high.
“In today’s world, this is how we have traditionally managed unpredictability,” Dr. Brown said. “You don’t know when you will need it, but if you need it, you want it immediately. So how do you pay for it – only when the doctor comes in, or also an amount just for being on call?” Some groups pay for both, he said, others for neither.
“We are a group of 70 hospitalists, and if someone is sick you can’t just shut down the service,” said Dr. Chadha. “We are one of the few to use incentives for both, which could include a 1-week decrease in clinical shifts in exchange for 2 weeks of backup. We have times with 25% usage of backup number 1, and 10% usage of backup number 2,” he noted. “But the goal is for our hospitalists to have assurances that there is a backup system and that it works.”
The presence of nocturnists in hospitals continues to rise, with 76.1% of adults-only groups having nocturnists, 27.6% of children-only groups, and 68.2% of adults and children groups. Geographic or unit-based hospital assignments have grown to 36.4% of adult-only groups.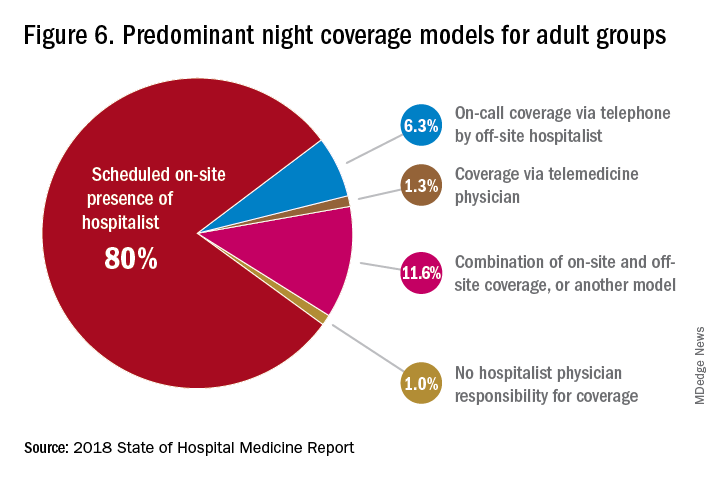
What are hospitalists’ other new roles?
“We have a large group of 50 doctors, with about 40 FTEs, and we are evolving from the traditional generalist role toward more subspecialty comanagement,” said Bryan Huang, MD, physician adviser and associate clinical professor in the division of hospital medicine at the University of California–San Diego. “Our hospitalists are asking what it means to be an academic hospitalist as our teaching roles have shrunk.”
Dr. Huang recently took on a new role as physician adviser for his hospital in such areas as utilization review, patient flow, and length of stay. “I’m spearheading a work group to address quality issues – all of which involve collaboration with other professionals. We also developed an admitting role here for a hospitalist whose sole role for the day is to admit patients.” Nationally up to 51.2% of hospitalist groups utilize a dedicated daytime admitter.
The report found that hospital services for which hospitalists are more likely to be attendings than consultants include GI/liver, 78.4%; palliative care, 77.3%; neurology/stroke, 73.6%; oncology, 67.8%; cardiology, 56.9%; and critical care, 50.7%. Conditions where hospitalists are more likely to consult rather than admit and attend include neurosurgery, orthopedics, general surgery, cardiovascular surgery, and other surgical subspecialties.
Other hospital services routinely provided by adult-only hospitalists include care of patients in an ICU setting (62.7%); primary responsibility for observation units (54.6%); primary clinical responsibility for rapid response teams (48.8%); primary responsibility for code blue or cardiac arrest teams (43.8%); nighttime admissions or tuck-in services (33.9%); and medical procedures (31.5%). For pediatric hospital medicine groups, care of healthy newborns and medical procedures were among the most common services provided, while for hospitalists serving adults and children, rapid response teams, ICUs, and specialty units were most common.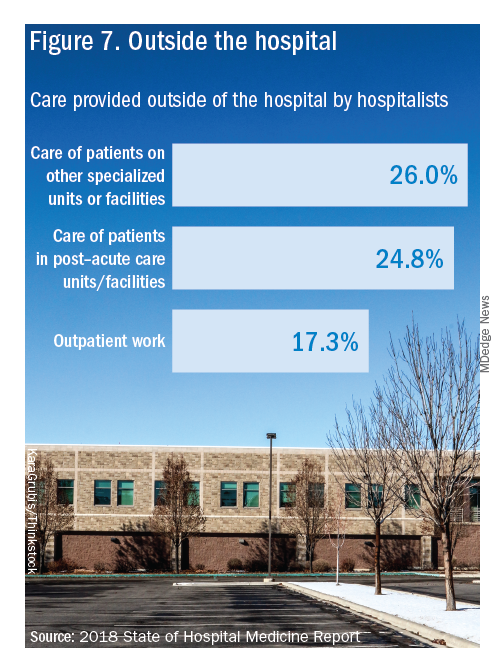
New models of payment for health care
As the larger health care system is being transformed by new payment models and benefit structures, including accountable care organizations (ACOs), value-based purchasing, bundled payments, and other forms of population-based coverage – which is described as a volume-to-value shift in health care – how are these new models affecting hospitalists?
Observers say penetration of these new models varies widely by locality but they haven’t had much direct impact on hospitalists’ practices – at least not yet. However, as hospitals and health systems find themselves needing to learn new ways to invest their resources differently in response to these trends, what matters to the hospital should be of great importance to the hospitalist group.
“I haven’t seen a lot of dramatic changes in how hospitalists engage with value-based purchasing,” Dr. White said. “If we know that someone is part of an ACO, the instinctual – and right – response is to treat them like any other patient. But we still need to be committed to not waste resources.”
Hospitalists are the best people to understand the intricacies of how the health care system works under value-based approaches, Dr. Huang said. “That’s why so many hospitalists have taken leadership positions in their hospitals. I think all of this translates to the practical, day-to-day work of hospitalists, reflected in our focus on readmissions and length of stay.”
Dr. Williams said the health care system still hasn’t turned the corner from fee-for-service to value-based purchasing. “It still represents a tiny fraction of the income of hospitalists. Hospitals still have to focus on the bottom line, as fee-for-service reimbursement for hospitalized patients continues to get squeezed, and ACOs aren’t exactly paying premium rates either. Ask almost any hospital CEO what drives their bottom line today and the answer is volume – along with optimizing productivity. Pretty much every place I look, the future does not look terribly rosy for hospitals.”
Ms. Himebaugh said she is bullish on hospital medicine, in the sense that it’s unlikely to go away anytime soon. “Hospitalists are needed and provide value. But I don’t think we have devised the right model yet. I’m not sure our current model is sustainable. We need to find new models we can afford that don’t require squeezing our providers.”
For more information about the 2018 State of Hospital Medicine Report, contact SHM’s Practice Management Department at: [email protected] or call 800-843-3360. See also: https://www.hospitalmedicine.org/practice-management/shms-state-of-hospital-medicine/.
In a national health care environment undergoing unprecedented transformation, the specialty of hospital medicine appears to be an island of relative stability, a conclusion that is supported by the principal findings from SHM’s 2018 State of Hospital Medicine (SoHM) report.
The report of hospitalist group practice characteristics, as well as other key data defining the field’s current status, that the Society of Hospital Medicine puts out every 2 years reveals that overall salaries for hospitalist physicians are up by 3.8% since 2016. Although productivity, as measured by work relative value units (RVUs), remained largely flat over the same period, financial support per full-time equivalent (FTE) physician position to hospitalist groups from their hospitals and health systems is up significantly.
Total support per FTE averaged $176,657 in 2018, 12% higher than in 2016, noted Leslie Flores, MHA, SFHM, of Nelson Flores Hospital Medicine Consultants, and a member of SHM’s Practice Analysis Committee, which oversees the biennial survey. Compensation and productivity data were collected by the Medical Group Management Association and licensed by SHM for inclusion in its report.
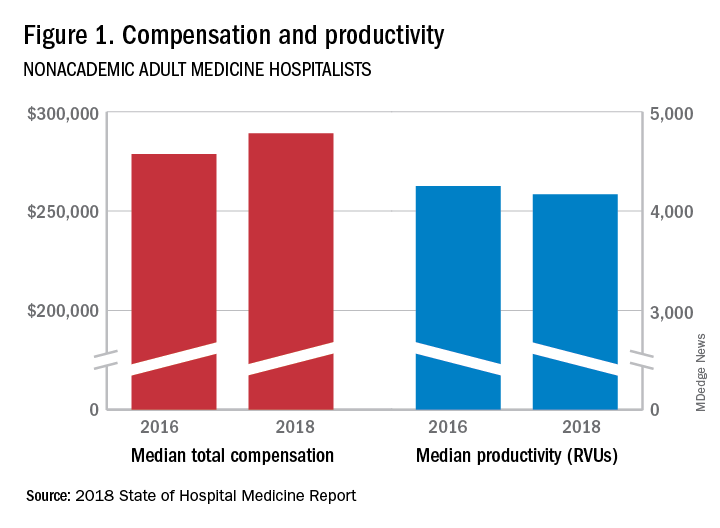
These findings – particularly the flat productivity – raise questions about long-term sustainability, Ms. Flores said. “What is going on? Do hospital administrators still recognize the value hospitalists bring to the operations and the quality of their hospitals? Or is paying the subsidy just a cost of doing business – a necessity for most hospitals in a setting where demand for hospitalist positions remains high?”
Andrew White, MD, FACP, SFHM, chair of SHM’s Practice Analysis Committee and director of the hospital medicine service at the University of Washington Medical Center, Seattle, said basic market forces dictate that it is “pretty much inconceivable” to run a modern hospital of any size without hospitalists.
“Clearly, demand outstrips supply, which drives up salaries and support, whether CEOs feel that the hospitalist group is earning that support or not,” Dr. White said. “The unfilled hospitalist positions we identified speak to ongoing projected greater demand than supply. That said, hospitalists and group leaders can’t be complacent and must collaborate effectively with hospitals to provide highly valuable services.” Turnover of hospitalist positions was up slightly, he noted, at 7.4% in 2018, from 6.9% in 2016, reversing a trend of previous years.
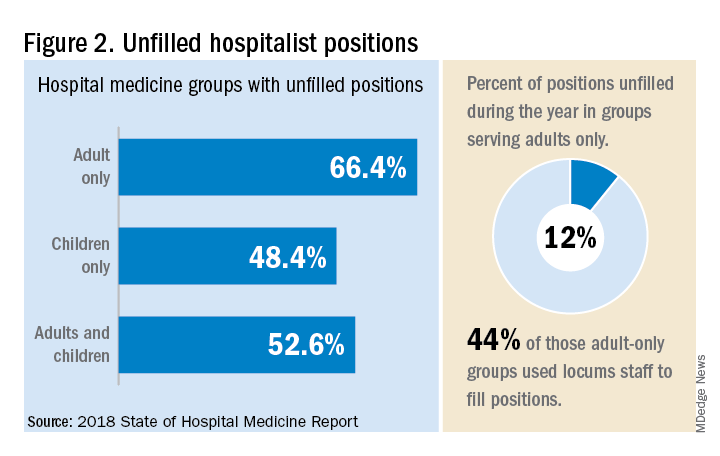
But will these trends continue at a time when hospitals face continued pressure to cut costs, as the hospital medicine subsidy may represent one of their largest cost centers? Because the size of hospitalist groups continues to grow, hospitals’ total subsidy for hospital medicine is going up faster than the percentage increase in support per FTE.
How do hospitalists use the SoHM report?
Dr. White called the 2018 SoHM report the “most representative and balanced sample to date” of hospitalist group practices, with some of the highest quality data, thanks to more robust participation in the survey by pediatric groups and improved distribution among hospitalist management companies and academic programs.
“Not that past reports had major flaws, but this version is more authoritative, reflecting an intentional effort by our Practice Analysis Committee to bring in more participants from key groups,” he said.
The biennial report has been around long enough to achieve brand recognition in the field as the most authoritative source of information regarding hospitalist practice, he added. “We worked hard this year to balance the participants, with more of our responses than in the past coming from multi-hospital groups, whether 4 to 5 sites, or 20 to 30.”
Surveys were conducted online in January and February of 2018 in response to invitations mailed and emailed to targeted hospital medicine group leaders. A total of 569 groups completed the survey, representing 8,889 hospitalist FTEs, approximately 16% of the total hospitalist workforce. Responses were presented in several categories, including by size of program, region and employment model. Groups that care for adults only represented 87.9% of the surveys, while groups that care for children only were 6.7% and groups that care for both adults and children were 5.4%.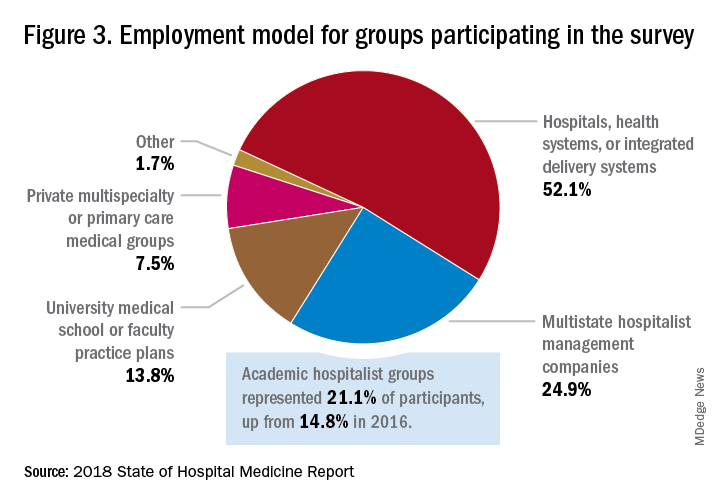
“This survey doesn’t tell us what should be best practice in hospital medicine,” Dr. White said, only what is actual current practice. He uses it in his own health system to not only contextualize and justify his group’s performance metrics for hospital administrators – relative to national and categorical averages – but also to see if the direction his group is following is consistent with what’s going on in the larger field.
“These data offer a very powerful resource regarding the trends in hospital medicine,” said Romil Chadha, MD, MPH, FACP, SFHM, associate division chief for operations in the division of hospital medicine at the University of Kentucky and UK Healthcare, Lexington. “It is my repository of data to go before my administrators for decisions that need to be made or to pilot new programs.”
Dr. Chadha also uses the data to help answer compensation, scheduling, and support questions from his group’s members.
Thomas McIlraith, MD, immediate past chairman of the hospital medicine department at Mercy Medical Group, Sacramento, Calif., said the report’s value is that it allows comparisons of salaries in different settings, and to see, for example, how night staffing is structured. “A lot of leaders I spoke to at SHM’s 2018 Leadership Academy in Vancouver were saying they didn’t feel up to parity with the national standards. You can use the report to look at the state of hospital medicine nationally and make comparisons,” he said.
Calls for more productivity
Roberta Himebaugh, MBA, SFHM, senior vice president of acute care services for the national hospitalist management company TeamHealth, and cochair of the SHM Practice Administrators Special Interest Group, said her company’s clients have traditionally asked for greater productivity from their hospitalist contracts as a way to decrease overall costs. Some markets are starting to see a change in that approach, she noted.
“Recently there’s been an increased focus on paying hospitalists to focus on quality rather than just productivity. Some of our clients are willing to pay for that, and we are trying to assign value to this non-billable time or adjust our productivity standards appropriately. I think hospitals definitely understand the value of non-billable services from hospitalists, but still will push us on the productivity targets,” Ms. Himebaugh said.
“I don’t believe hospital medicine can be sustainable long term on flat productivity or flat RVUs,” she added. “Yet the costs of burnout associated with pushing higher productivity are not sustainable, either.” So what are the answers? She said many inefficiencies are involved in responding to inquiries on the floor that could have been addressed another way, or waiting for the turnaround of diagnostic tests.
“Maybe we don’t need physicians to be in the hospital 24/7 if we have access to telehealth, or a partnership with the emergency department, or greater use of advanced care practice providers,” Ms. Himebaugh said. “Our hospitals are examining those options, and we have to look at how we can become more efficient and less costly. At TeamHealth, we are trying to staff for value – looking at patient flow patterns and adjusting our schedules accordingly. Is there a bolus of admissions tied to emergency department shift changes, or to certain days of the week? How can we move from the 12-hour shift that begins at 7 a.m. and ends at 7 p.m., and instead provide coverage for when the patients are there?”
Mark Williams, MD, MHM, chief of the division of hospital medicine at the University of Kentucky, Lexington, said he appreciates the volume of data in the report but wishes for even more survey participants, which could make the breakouts for subgroups such as academic hospitalists more robust. Other current sources of hospitalist salary data include the Association of American Medical Colleges (AAMC), which produces compensation reports to help medical schools and teaching hospitals with benchmarking, and the Faculty Practice Solution Center developed jointly by AAMC and Vizient to provide faculty practice plans with analytic tools. The Medical Group Management Association (MGMA) is another valuable source of information, some of which was licensed for inclusion in the SoHM report.
“There is no source of absolute truth that hospitalists can point to,” Dr. Williams said. “I will present my data and my administrators will reply: ‘We have our own data.’ Our institution has consistently ranked first or second nationwide for the sickest patients. We take more Medicaid and dually eligible patients, who have a lot of social issues. They take a lot of time to manage medically and the RVUs don’t reflect that. And yet I’m still judged by my RVUs generated per hospitalist. Hospital administrators understandably want to get the most productivity, and they are looking for their own data for average productivity numbers.”
Ryan Brown, MD, specialty medical director for hospital medicine with Atrium Health in Charlotte, N.C., said that hospital medicine’s flat productivity trends would be difficult to sustain in the business world. But there aren’t easy or obvious ways to increase hospitalists’ productivity. The SoHM report also shows that as productivity increases, total compensation increases but at a lower rate, resulting in a gradual decrease in compensation per RVU.
Pressures to increase productivity can be a double-edged sword, Dr. Williams added. Demanding that doctors make more billable visits faster to generate more RVUs can be a recipe for burnout and turnover, with huge costs associated with recruiting replacements.
“If there was recent turnover of hospitalists at the hospital, with the need to find replacements, there may be institutional memory about that,” he said. “But where are hospitals spending their money? Bottom line, we still need to learn to cut our costs.”
How is hospitalist practice evolving?
In addition to payment and productivity data, the SoHM report provides a current picture of the evolving state of hospitalist group practices. A key thread is how the work hospitalists are doing, and the way they do it, is changing, with new information about comanagement roles, dedicated admitters, night coverage, geographic rounding, and the like.
Making greater use of nurse practitioners and physician assistants (NPs/PAs), may be one way to change the flat productivity trends, Dr. Brown said. With a cost per RVU that’s roughly half that of a doctor’s, NPs/PAs could contribute to the bottom line. But he sees surprisingly large variation in how hospitalist groups are using them. Typically, they are deployed at a ratio of four doctors to one NP/PA, but that ratio could be two to one or even one to one, he said.
Use of NPs/PAs by academic hospitalist groups is up, from 52.1% in 2016 to 75.7% in 2018. For adult-only groups, 76.8% had NPs/PAs, with higher rates in hospitals and health systems and lower rates in the West region. But a lot of groups are using these practitioners for nonproductive work, and some are failing to generate any billing income, Dr. Brown said.
“The rate at which NPs/PAs performed billable services was higher in physician-owned practices, resulting in a lower cost per RVU, suggesting that many practices may be underutilizing their NPs/PAs or not sharing the work.” Not every NP or PA wants to or is able to care for very complex patients, Dr. Brown said, “but you want a system where the NP and PA can work at the highest level permitted by state law.”
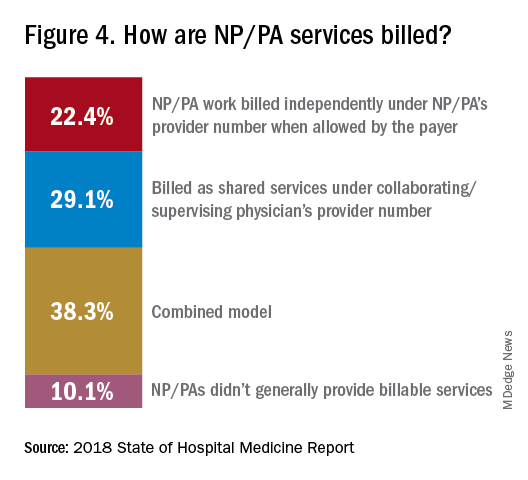
The predominant scheduling model of hospital medicine, 7 days on duty followed by 7 days off, has diminished somewhat in recent years. There appears to be some fluctuation and a gradual move away from 7 on/7 off toward some kind of variable approach, since the former may not be physically sustainable for the doctor over the long haul, Dr. Brown said. Some groups are experimenting with a combined approach.
“I think balancing workload with manpower has always been a challenge for our field. Maybe we should be working shorter shifts or fewer days and making sure our hospitalists aren’t ever sitting around idle,” he said. “And could we come in on nonclinical days to do administrative tasks? I think the solution is out there, but we haven’t created the algorithms to define that yet. If you could somehow use the data for volume, number of beds, nurse staffing, etc., by year and seasonally, you might be able to reliably predict census. This is about applying data hospitals already have in their electronic health records, but utilizing the data in ways that are more helpful.”
Dr. McIlraith added that a big driver of the future of hospital medicine will be the evolution of the EHR and the digitalization of health care, as hospitals learn how to leverage more of what’s in their EHRs. “The impact will grow for hospitalists through the creation and maturation of big data systems – and the learning that can be extracted from what’s contained in the electronic health record.”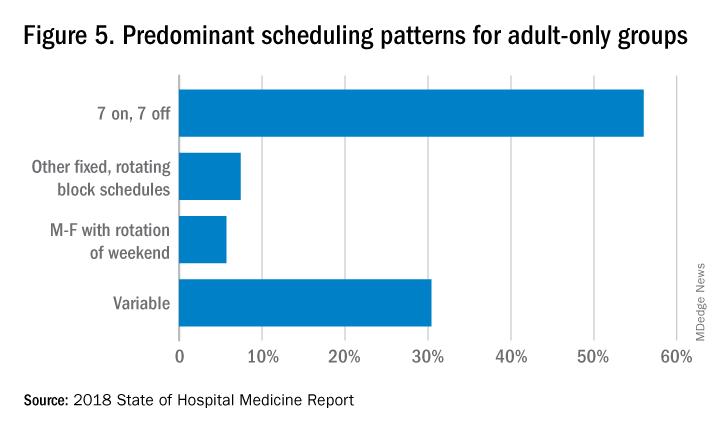
Another important question for hospitalist groups is their model of backup scheduling, to make sure there is a replacement available if a scheduled doctor calls in sick or if demand is unexpectedly high.
“In today’s world, this is how we have traditionally managed unpredictability,” Dr. Brown said. “You don’t know when you will need it, but if you need it, you want it immediately. So how do you pay for it – only when the doctor comes in, or also an amount just for being on call?” Some groups pay for both, he said, others for neither.
“We are a group of 70 hospitalists, and if someone is sick you can’t just shut down the service,” said Dr. Chadha. “We are one of the few to use incentives for both, which could include a 1-week decrease in clinical shifts in exchange for 2 weeks of backup. We have times with 25% usage of backup number 1, and 10% usage of backup number 2,” he noted. “But the goal is for our hospitalists to have assurances that there is a backup system and that it works.”
The presence of nocturnists in hospitals continues to rise, with 76.1% of adults-only groups having nocturnists, 27.6% of children-only groups, and 68.2% of adults and children groups. Geographic or unit-based hospital assignments have grown to 36.4% of adult-only groups.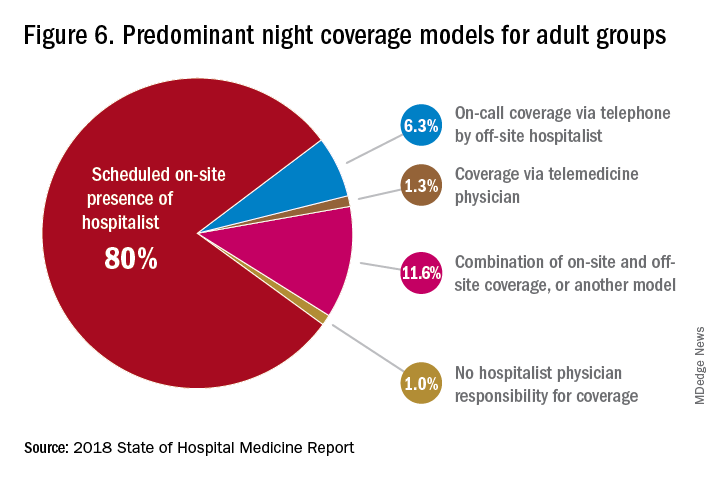
What are hospitalists’ other new roles?
“We have a large group of 50 doctors, with about 40 FTEs, and we are evolving from the traditional generalist role toward more subspecialty comanagement,” said Bryan Huang, MD, physician adviser and associate clinical professor in the division of hospital medicine at the University of California–San Diego. “Our hospitalists are asking what it means to be an academic hospitalist as our teaching roles have shrunk.”
Dr. Huang recently took on a new role as physician adviser for his hospital in such areas as utilization review, patient flow, and length of stay. “I’m spearheading a work group to address quality issues – all of which involve collaboration with other professionals. We also developed an admitting role here for a hospitalist whose sole role for the day is to admit patients.” Nationally up to 51.2% of hospitalist groups utilize a dedicated daytime admitter.
The report found that hospital services for which hospitalists are more likely to be attendings than consultants include GI/liver, 78.4%; palliative care, 77.3%; neurology/stroke, 73.6%; oncology, 67.8%; cardiology, 56.9%; and critical care, 50.7%. Conditions where hospitalists are more likely to consult rather than admit and attend include neurosurgery, orthopedics, general surgery, cardiovascular surgery, and other surgical subspecialties.
Other hospital services routinely provided by adult-only hospitalists include care of patients in an ICU setting (62.7%); primary responsibility for observation units (54.6%); primary clinical responsibility for rapid response teams (48.8%); primary responsibility for code blue or cardiac arrest teams (43.8%); nighttime admissions or tuck-in services (33.9%); and medical procedures (31.5%). For pediatric hospital medicine groups, care of healthy newborns and medical procedures were among the most common services provided, while for hospitalists serving adults and children, rapid response teams, ICUs, and specialty units were most common.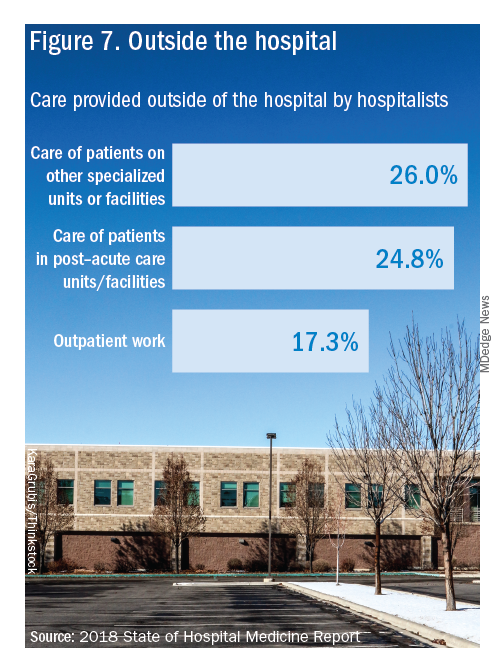
New models of payment for health care
As the larger health care system is being transformed by new payment models and benefit structures, including accountable care organizations (ACOs), value-based purchasing, bundled payments, and other forms of population-based coverage – which is described as a volume-to-value shift in health care – how are these new models affecting hospitalists?
Observers say penetration of these new models varies widely by locality but they haven’t had much direct impact on hospitalists’ practices – at least not yet. However, as hospitals and health systems find themselves needing to learn new ways to invest their resources differently in response to these trends, what matters to the hospital should be of great importance to the hospitalist group.
“I haven’t seen a lot of dramatic changes in how hospitalists engage with value-based purchasing,” Dr. White said. “If we know that someone is part of an ACO, the instinctual – and right – response is to treat them like any other patient. But we still need to be committed to not waste resources.”
Hospitalists are the best people to understand the intricacies of how the health care system works under value-based approaches, Dr. Huang said. “That’s why so many hospitalists have taken leadership positions in their hospitals. I think all of this translates to the practical, day-to-day work of hospitalists, reflected in our focus on readmissions and length of stay.”
Dr. Williams said the health care system still hasn’t turned the corner from fee-for-service to value-based purchasing. “It still represents a tiny fraction of the income of hospitalists. Hospitals still have to focus on the bottom line, as fee-for-service reimbursement for hospitalized patients continues to get squeezed, and ACOs aren’t exactly paying premium rates either. Ask almost any hospital CEO what drives their bottom line today and the answer is volume – along with optimizing productivity. Pretty much every place I look, the future does not look terribly rosy for hospitals.”
Ms. Himebaugh said she is bullish on hospital medicine, in the sense that it’s unlikely to go away anytime soon. “Hospitalists are needed and provide value. But I don’t think we have devised the right model yet. I’m not sure our current model is sustainable. We need to find new models we can afford that don’t require squeezing our providers.”
For more information about the 2018 State of Hospital Medicine Report, contact SHM’s Practice Management Department at: [email protected] or call 800-843-3360. See also: https://www.hospitalmedicine.org/practice-management/shms-state-of-hospital-medicine/.
SHM announces National Hospitalist Day
Inaugural day of recognition to honor hospital medicine care team
The Society of Hospital Medicine is proud to announce the inaugural National Hospitalist Day, to be held on Thursday, March 7, 2019. Occurring the first Thursday in March annually, National Hospitalist Day will serve to celebrate the fastest-growing specialty in modern medicine and hospitalists’ enduring contributions to the evolving health care landscape.
National Hospitalist Day was recently approved by the National Day Calendar and was one of approximately 30 national days to be approved for the year out of an applicant pool of more than 18,000.
“As the only society dedicated to the specialty of hospital medicine, it is appropriate that SHM spearhead a national day to recognize the countless contributions of hospitalists to health care, from clinical, academic, and leadership perspectives and more,” said Larry Wellikson, MD, MHM, chief executive officer of SHM. “We look forward to hospitalists across the nation contributing to the festivities and making this a tradition for years to come.”
In addition to celebrating hospitalists’ contributions to patient care, SHM will also be highlighting the diverse career paths of hospital medicine professionals, from frontline hospitalist physicians, nurse practitioners, and physician assistants to practice administrators, C-suite executives, and academic hospitalists.
Highlights of SHM’s campaign include the following:
- Downloadable customizable posters and assets for hospitals and individuals’ offices to celebrate their hospital medicine team, available on SHM’s website, hospitalmedicine.org.
- A series of spotlights of hospitalists at all stages of their careers in The Hospitalist, SHM’s monthly newsmagazine.
- A social media campaign inviting hospitalists and their employers to share their success stories using the hashtag #HowWeHospitalist, including banner graphics, profile photo overlays, and more.
- A social media contest to determine the most creative ways of celebrating use of the hashtag.
- A Twitter chat for hospitalists to celebrate virtually with their colleagues and peers from around the world.
“Hospitalists innovate, lead, and push the boundaries of clinical care and deserve to be recognized for their transformative contributions to health care,” said Eric E. Howell, MD, MHM, chief operating officer of SHM. “We hope this is the beginning of a long-standing tradition in honoring hospitalists and the noteworthy work they do.”
For more information, visit www.hospitalmedicine.org/hospitalistday.
Mr. Radler is marketing communications manager at the Society of Hospital Medicine.
Inaugural day of recognition to honor hospital medicine care team
Inaugural day of recognition to honor hospital medicine care team
The Society of Hospital Medicine is proud to announce the inaugural National Hospitalist Day, to be held on Thursday, March 7, 2019. Occurring the first Thursday in March annually, National Hospitalist Day will serve to celebrate the fastest-growing specialty in modern medicine and hospitalists’ enduring contributions to the evolving health care landscape.
National Hospitalist Day was recently approved by the National Day Calendar and was one of approximately 30 national days to be approved for the year out of an applicant pool of more than 18,000.
“As the only society dedicated to the specialty of hospital medicine, it is appropriate that SHM spearhead a national day to recognize the countless contributions of hospitalists to health care, from clinical, academic, and leadership perspectives and more,” said Larry Wellikson, MD, MHM, chief executive officer of SHM. “We look forward to hospitalists across the nation contributing to the festivities and making this a tradition for years to come.”
In addition to celebrating hospitalists’ contributions to patient care, SHM will also be highlighting the diverse career paths of hospital medicine professionals, from frontline hospitalist physicians, nurse practitioners, and physician assistants to practice administrators, C-suite executives, and academic hospitalists.
Highlights of SHM’s campaign include the following:
- Downloadable customizable posters and assets for hospitals and individuals’ offices to celebrate their hospital medicine team, available on SHM’s website, hospitalmedicine.org.
- A series of spotlights of hospitalists at all stages of their careers in The Hospitalist, SHM’s monthly newsmagazine.
- A social media campaign inviting hospitalists and their employers to share their success stories using the hashtag #HowWeHospitalist, including banner graphics, profile photo overlays, and more.
- A social media contest to determine the most creative ways of celebrating use of the hashtag.
- A Twitter chat for hospitalists to celebrate virtually with their colleagues and peers from around the world.
“Hospitalists innovate, lead, and push the boundaries of clinical care and deserve to be recognized for their transformative contributions to health care,” said Eric E. Howell, MD, MHM, chief operating officer of SHM. “We hope this is the beginning of a long-standing tradition in honoring hospitalists and the noteworthy work they do.”
For more information, visit www.hospitalmedicine.org/hospitalistday.
Mr. Radler is marketing communications manager at the Society of Hospital Medicine.
The Society of Hospital Medicine is proud to announce the inaugural National Hospitalist Day, to be held on Thursday, March 7, 2019. Occurring the first Thursday in March annually, National Hospitalist Day will serve to celebrate the fastest-growing specialty in modern medicine and hospitalists’ enduring contributions to the evolving health care landscape.
National Hospitalist Day was recently approved by the National Day Calendar and was one of approximately 30 national days to be approved for the year out of an applicant pool of more than 18,000.
“As the only society dedicated to the specialty of hospital medicine, it is appropriate that SHM spearhead a national day to recognize the countless contributions of hospitalists to health care, from clinical, academic, and leadership perspectives and more,” said Larry Wellikson, MD, MHM, chief executive officer of SHM. “We look forward to hospitalists across the nation contributing to the festivities and making this a tradition for years to come.”
In addition to celebrating hospitalists’ contributions to patient care, SHM will also be highlighting the diverse career paths of hospital medicine professionals, from frontline hospitalist physicians, nurse practitioners, and physician assistants to practice administrators, C-suite executives, and academic hospitalists.
Highlights of SHM’s campaign include the following:
- Downloadable customizable posters and assets for hospitals and individuals’ offices to celebrate their hospital medicine team, available on SHM’s website, hospitalmedicine.org.
- A series of spotlights of hospitalists at all stages of their careers in The Hospitalist, SHM’s monthly newsmagazine.
- A social media campaign inviting hospitalists and their employers to share their success stories using the hashtag #HowWeHospitalist, including banner graphics, profile photo overlays, and more.
- A social media contest to determine the most creative ways of celebrating use of the hashtag.
- A Twitter chat for hospitalists to celebrate virtually with their colleagues and peers from around the world.
“Hospitalists innovate, lead, and push the boundaries of clinical care and deserve to be recognized for their transformative contributions to health care,” said Eric E. Howell, MD, MHM, chief operating officer of SHM. “We hope this is the beginning of a long-standing tradition in honoring hospitalists and the noteworthy work they do.”
For more information, visit www.hospitalmedicine.org/hospitalistday.
Mr. Radler is marketing communications manager at the Society of Hospital Medicine.