User login
Hospital Readmissions Reduction Program may be doing more harm than good
A Medicare program aimed at lowering readmissions to hospitals could be having an adverse effect on mortality.
Results from a retrospective cohort study of hospitalizations for heart failure, acute myocardial infarction, and pneumonia among Medicare beneficiaries aged 65 years and older between April 1, 2005 and March 31, 2015 (covering the period before and after the Medicare Hospital Readmissions Reduction Program was announced in April 2010 and implemented in October 2012) found a significant increase in 30-day post discharge mortality among heart failure and pneumonia patients.
“Most concerning, however, is the possibility that the relationship between the HRRP and postdischarge mortality for heart failure and pneumonia is causal, indicating that the HRRP led to changes in quality of care that adversely affected patients,” Rishi Wadhera, MD, Harvard Medical School, Boston, and his colleagues wrote in a report published Dec. 25, 2018, in JAMA.
They looked at 8.3 million hospitalizations for heart failure, acute MI, and pneumonia, among whom 7.9 million were alive at the time of discharge. There were roughly 270,000 deaths within 30 days of discharge for heart failure; 128,000 for acute MI; and 246,000 for pneumonia.
To examine trends, the timing was divided into four periods: two prior to the announcement of the HRRP (April 2005–September 2007 and October 2007–March 2010); a third covering the time when the HRRP was announced (April 2010–September 2012); and the fourth when HRRP was implemented (October 2012–March 2015).
They found that among patients discharged with heart failure, 30-day mortality was rising even before the announcement of the HRRP, by 0.27% from the first period to the second period. That baseline trend continued when the HRRP was announced, by 0.49%, from second period to third. The difference in change between those periods was 0.22%. After implementation, 30-day mortality increased by 0.52%, with a difference in change from the third period of 0.25%. Both changes were statistically significant.
Among pneumonia patients, postdischarge mortality was stable before HRRP, but significantly increased after HRRP announcement, by 0.26%, with a difference in change from the second period to the third period of 0.22%. After implementation, the 30-day postdischarge mortality was 0.44%, with a significant difference in change of 0.40%.
Acute MI was a different story. Postdischarge mortality decreased significantly after the implementation of the HRRP, by 0.22%. The difference in change was –0.26%.
The authors suggested that “some hospitals may have focused more resources and efforts on reducing or avoiding readmissions than on prioritizing survival.” They add that the increases in heart failure morbidity could be related to patients with more severe heart conditions.
They noted that “although hospitals that reduce readmissions also appear to reduce mortality, this hospital-level concordance does not reflect the change in readmissions and mortality at the level of the patient population, which is arguably of greater importance to individual patients and to public health.”
Further research is needed to understand whether the increase in 30-day postdischarge mortality is a result of the HRRP, the authors concluded.
SOURCE: Wadhera R et al. JAMA. 2018 Dec 25. doi: 10.1001/jama.2018.19232.
Evidence in this study shows that while the Hospital Readmissions Reduction Program my be succeeding in reducing hospital admissions, little evidence is available to show that it is having a positive effect on patient outcomes.
The Centers for Medicare & Medicaid Services needs to reexamine the program and find alternative methods that are both effective at reducing hospital readmissions while at the same time protect patients from unintentional harm, including death.
Gregg C. Fonarow, MD , University of California Medical Center, Los Angeles, in an editorial published in JAMA, Dec. 25, 2018. doi:10.1001/jama.2018.19325 .
Evidence in this study shows that while the Hospital Readmissions Reduction Program my be succeeding in reducing hospital admissions, little evidence is available to show that it is having a positive effect on patient outcomes.
The Centers for Medicare & Medicaid Services needs to reexamine the program and find alternative methods that are both effective at reducing hospital readmissions while at the same time protect patients from unintentional harm, including death.
Gregg C. Fonarow, MD , University of California Medical Center, Los Angeles, in an editorial published in JAMA, Dec. 25, 2018. doi:10.1001/jama.2018.19325 .
Evidence in this study shows that while the Hospital Readmissions Reduction Program my be succeeding in reducing hospital admissions, little evidence is available to show that it is having a positive effect on patient outcomes.
The Centers for Medicare & Medicaid Services needs to reexamine the program and find alternative methods that are both effective at reducing hospital readmissions while at the same time protect patients from unintentional harm, including death.
Gregg C. Fonarow, MD , University of California Medical Center, Los Angeles, in an editorial published in JAMA, Dec. 25, 2018. doi:10.1001/jama.2018.19325 .
A Medicare program aimed at lowering readmissions to hospitals could be having an adverse effect on mortality.
Results from a retrospective cohort study of hospitalizations for heart failure, acute myocardial infarction, and pneumonia among Medicare beneficiaries aged 65 years and older between April 1, 2005 and March 31, 2015 (covering the period before and after the Medicare Hospital Readmissions Reduction Program was announced in April 2010 and implemented in October 2012) found a significant increase in 30-day post discharge mortality among heart failure and pneumonia patients.
“Most concerning, however, is the possibility that the relationship between the HRRP and postdischarge mortality for heart failure and pneumonia is causal, indicating that the HRRP led to changes in quality of care that adversely affected patients,” Rishi Wadhera, MD, Harvard Medical School, Boston, and his colleagues wrote in a report published Dec. 25, 2018, in JAMA.
They looked at 8.3 million hospitalizations for heart failure, acute MI, and pneumonia, among whom 7.9 million were alive at the time of discharge. There were roughly 270,000 deaths within 30 days of discharge for heart failure; 128,000 for acute MI; and 246,000 for pneumonia.
To examine trends, the timing was divided into four periods: two prior to the announcement of the HRRP (April 2005–September 2007 and October 2007–March 2010); a third covering the time when the HRRP was announced (April 2010–September 2012); and the fourth when HRRP was implemented (October 2012–March 2015).
They found that among patients discharged with heart failure, 30-day mortality was rising even before the announcement of the HRRP, by 0.27% from the first period to the second period. That baseline trend continued when the HRRP was announced, by 0.49%, from second period to third. The difference in change between those periods was 0.22%. After implementation, 30-day mortality increased by 0.52%, with a difference in change from the third period of 0.25%. Both changes were statistically significant.
Among pneumonia patients, postdischarge mortality was stable before HRRP, but significantly increased after HRRP announcement, by 0.26%, with a difference in change from the second period to the third period of 0.22%. After implementation, the 30-day postdischarge mortality was 0.44%, with a significant difference in change of 0.40%.
Acute MI was a different story. Postdischarge mortality decreased significantly after the implementation of the HRRP, by 0.22%. The difference in change was –0.26%.
The authors suggested that “some hospitals may have focused more resources and efforts on reducing or avoiding readmissions than on prioritizing survival.” They add that the increases in heart failure morbidity could be related to patients with more severe heart conditions.
They noted that “although hospitals that reduce readmissions also appear to reduce mortality, this hospital-level concordance does not reflect the change in readmissions and mortality at the level of the patient population, which is arguably of greater importance to individual patients and to public health.”
Further research is needed to understand whether the increase in 30-day postdischarge mortality is a result of the HRRP, the authors concluded.
SOURCE: Wadhera R et al. JAMA. 2018 Dec 25. doi: 10.1001/jama.2018.19232.
A Medicare program aimed at lowering readmissions to hospitals could be having an adverse effect on mortality.
Results from a retrospective cohort study of hospitalizations for heart failure, acute myocardial infarction, and pneumonia among Medicare beneficiaries aged 65 years and older between April 1, 2005 and March 31, 2015 (covering the period before and after the Medicare Hospital Readmissions Reduction Program was announced in April 2010 and implemented in October 2012) found a significant increase in 30-day post discharge mortality among heart failure and pneumonia patients.
“Most concerning, however, is the possibility that the relationship between the HRRP and postdischarge mortality for heart failure and pneumonia is causal, indicating that the HRRP led to changes in quality of care that adversely affected patients,” Rishi Wadhera, MD, Harvard Medical School, Boston, and his colleagues wrote in a report published Dec. 25, 2018, in JAMA.
They looked at 8.3 million hospitalizations for heart failure, acute MI, and pneumonia, among whom 7.9 million were alive at the time of discharge. There were roughly 270,000 deaths within 30 days of discharge for heart failure; 128,000 for acute MI; and 246,000 for pneumonia.
To examine trends, the timing was divided into four periods: two prior to the announcement of the HRRP (April 2005–September 2007 and October 2007–March 2010); a third covering the time when the HRRP was announced (April 2010–September 2012); and the fourth when HRRP was implemented (October 2012–March 2015).
They found that among patients discharged with heart failure, 30-day mortality was rising even before the announcement of the HRRP, by 0.27% from the first period to the second period. That baseline trend continued when the HRRP was announced, by 0.49%, from second period to third. The difference in change between those periods was 0.22%. After implementation, 30-day mortality increased by 0.52%, with a difference in change from the third period of 0.25%. Both changes were statistically significant.
Among pneumonia patients, postdischarge mortality was stable before HRRP, but significantly increased after HRRP announcement, by 0.26%, with a difference in change from the second period to the third period of 0.22%. After implementation, the 30-day postdischarge mortality was 0.44%, with a significant difference in change of 0.40%.
Acute MI was a different story. Postdischarge mortality decreased significantly after the implementation of the HRRP, by 0.22%. The difference in change was –0.26%.
The authors suggested that “some hospitals may have focused more resources and efforts on reducing or avoiding readmissions than on prioritizing survival.” They add that the increases in heart failure morbidity could be related to patients with more severe heart conditions.
They noted that “although hospitals that reduce readmissions also appear to reduce mortality, this hospital-level concordance does not reflect the change in readmissions and mortality at the level of the patient population, which is arguably of greater importance to individual patients and to public health.”
Further research is needed to understand whether the increase in 30-day postdischarge mortality is a result of the HRRP, the authors concluded.
SOURCE: Wadhera R et al. JAMA. 2018 Dec 25. doi: 10.1001/jama.2018.19232.
FROM JAMA
Key clinical point:
Major finding: Heart failure patients saw mortality increase 0.52% after HRRP launched.
Study details: A retrospective cohort study across 10 years, including time before and after the implementation of the HRRP.
Disclosures: The Richard A. and Susan F. Smith Center for Outcomes Research in Cardiology funded the study. No relevant conflicts of interest were disclosed.
Source: Wadhera R et al. JAMA 2018 Dec 25. doi: 10.1001/jama.2018.19232.
HIPAA compliance: Three cases to learn from
Data security experts say three HIPAA violations that resulted in significant fines by the Office for Civil Rights (OCR) in 2018 hold important lessons for health professionals about safeguarding records and training staff in HIPAA compliance.
Read on to learn how the cases unfolded and what knowledge practices can gain from the common HIPAA mistakes.
Who? Allergy Associates of Hartford, Conn.
What happened? A patient contacted a local television station to complain about a dispute between herself and a physician at Allergy Associates in Hartford, Conn. The disagreement stemmed from the office turning away the patient because she allegedly brought her service animal, according to a Nov. 26 announcement by the Department of Health & Human Services. The reporter contacted the doctor in question for a news story and, in responding, the physician disclosed protected patient information to the reporter.
What else? An OCR investigation determined that a privacy officer with Allergy Associates had instructed the physician not to respond to the media about the complaint or to respond with “no comment”; that advice was disregarded. The practice then failed to discipline the physician or take any corrective action following the disclosure, according to the OCR.
How much? The OCR imposed a $125,000 fine on the practice and a corrective action plan that includes 2 years of OCR monitoring.
Lessons learned: Had the practice disciplined the physician or taken corrective action after the disclosure, the OCR may not have penalized the group so severely, according to Jennifer Mitchell, a Cincinnati-based health law attorney and vice chair of the American Bar Association eHealth, Privacy, & Security Interest Group.
“In my opinion, the government levied these penalties because the provider did not sanction the doctor,” Ms. Mitchell said in an interview. “Health care entities need to take proper steps to remediate and, at a minimum, hold their workforce responsible for their behavior and ensure that it won’t happen again.”
The case emphasizes the need to train team members on media protocols and to ensure that protected health information is not mistakenly released. In addition to implementing policies and procedures, practices must also be willing to discipline health professionals when violations occur.
“A health care provider’s natural inclination is to defend themselves if they are being accused by a patient,” she said. “However, under the HIPAA rules, health care providers have to understand that they are prohibited from making such public statements about any patient.”
Who? Advanced Care Hospitalists of Lakeland, Fla.
What happened? Advanced Care Hospitalists (ACH) received billing services from an individual who represented himself to be affiliated with a Florida-based company named Doctor’s First Choice Billing. A local hospital later notified ACH that patient information, including names and Social Security numbers, were viewable on the First Choice website. ACH identified at least 400 patients affected by the breach and reported the breach to the OCR. However, ACH later determined that an additional 8,855 patients may have been affected and revised its OCR notification.
What else? During its investigation, the OCR found that the hospitalist group had never entered into a business associate agreement for billing services with First Choice, as required by HIPAA, and that the practice also failed to adopt any policies regarding business associate agreements until 2014, according to a Dec. 4 announcement from HHS.
How much? The OCR fined the practice $500,000 and also imposed a robust corrective action plan that includes an enterprise-wide risk analysis and the adoption of business associate agreements. Roger Severino, OCR director, called the case especially troubling because “the practice allowed the names and Social Security numbers of thousands of patients to be exposed on the Internet after it failed to follow basic security requirements under HIPAA.”
Lessons learned: The case illustrates the importance of having a business associate agreement in place for all third parties that may have access to protected health information, said Clinton Mikel, a Farmington Hills, Mich., health law attorney specializing in HIPAA compliance.
Under HIPAA, a business associate is defined as a person or entity, other than a member of the workforce of a covered entity, who “performs functions or activities on behalf of, or provides certain services to, a covered entity that involve access by the business associate to protected health information.”
HIPAA requires that covered entities enter into contracts with business associates to ensure appropriate safeguarding of protected health information.
“If your business associate has a breach, your practice must report the breach to OCR and your patients,” Mr. Mikel said in an interview. “The OCR will then investigate your practice and your relationship with the business associate. Just because the breach and fault clearly happened elsewhere, you will still be investigated, and could face a penalty if HIPAA requirements weren’t met.”
Who? Filefax of Northbrook, Ill.
What happened? The OCR opened an investigation after receiving an anonymous complaint that medical records obtained from Filefax, a company that provided storage, maintenance, and delivery of medical records for health professionals, were left unmonitored at a shredding and recycling facility. OCR’s investigation revealed that a person left the records of 2,150 patients at the recycling plant and that the records contained protected health information, according to an HHS announcement. It is unclear if the person worked for Filefax.
What else? The OCR discovered that, in a related incident, an individual who obtained medical records from Filefax left them unattended in an unlocked truck in the Filefax parking lot.
How much? The OCR imposed a $100,000 fine on Filefax. The company is no longer in business; however, a court-appointed liquidator has agreed to properly store and dispose of the remaining records.
Lessons learned: Although the case did not involve a health provider, the circumstances are applicable to physicians, particularly when practices move or close, Mr. Mikel said. In some cases, a former patient may contact a shuttered practice only to learn their record cannot be located, or worse, that a breach has occurred.
“[Such a case is] ripe for a patient to complain to OCR,” he said. “OCR doesn’t care if you’re closed or retired, they’re going to look.”
HIPAA requires thatcovered entities apply appropriate administrative, technical, and physical safeguards to protect the privacy of protected health information in any form when moving or closing. The safeguards must prevent prohibited uses and disclosures of protected health information in connection with the disposal of such information, according to the rule. The HHS provides guidance for the disposing of medical records; further, the American Academy of Family Physicians has created a checklist on closing a practice that addresses the transferring of medical records.
Without taking the correct measures, doctors may end up drawing scrutiny from OCR and face a potential fine if violations are found, experts said.
“Covered entities and business associates need to be aware that OCR is committed to enforcing HIPAA regardless of whether a covered entity is opening its doors or closing them,” Mr. Severino of the OCR said in a statement. “HIPAA still applies.”
Data security experts say three HIPAA violations that resulted in significant fines by the Office for Civil Rights (OCR) in 2018 hold important lessons for health professionals about safeguarding records and training staff in HIPAA compliance.
Read on to learn how the cases unfolded and what knowledge practices can gain from the common HIPAA mistakes.
Who? Allergy Associates of Hartford, Conn.
What happened? A patient contacted a local television station to complain about a dispute between herself and a physician at Allergy Associates in Hartford, Conn. The disagreement stemmed from the office turning away the patient because she allegedly brought her service animal, according to a Nov. 26 announcement by the Department of Health & Human Services. The reporter contacted the doctor in question for a news story and, in responding, the physician disclosed protected patient information to the reporter.
What else? An OCR investigation determined that a privacy officer with Allergy Associates had instructed the physician not to respond to the media about the complaint or to respond with “no comment”; that advice was disregarded. The practice then failed to discipline the physician or take any corrective action following the disclosure, according to the OCR.
How much? The OCR imposed a $125,000 fine on the practice and a corrective action plan that includes 2 years of OCR monitoring.
Lessons learned: Had the practice disciplined the physician or taken corrective action after the disclosure, the OCR may not have penalized the group so severely, according to Jennifer Mitchell, a Cincinnati-based health law attorney and vice chair of the American Bar Association eHealth, Privacy, & Security Interest Group.
“In my opinion, the government levied these penalties because the provider did not sanction the doctor,” Ms. Mitchell said in an interview. “Health care entities need to take proper steps to remediate and, at a minimum, hold their workforce responsible for their behavior and ensure that it won’t happen again.”
The case emphasizes the need to train team members on media protocols and to ensure that protected health information is not mistakenly released. In addition to implementing policies and procedures, practices must also be willing to discipline health professionals when violations occur.
“A health care provider’s natural inclination is to defend themselves if they are being accused by a patient,” she said. “However, under the HIPAA rules, health care providers have to understand that they are prohibited from making such public statements about any patient.”
Who? Advanced Care Hospitalists of Lakeland, Fla.
What happened? Advanced Care Hospitalists (ACH) received billing services from an individual who represented himself to be affiliated with a Florida-based company named Doctor’s First Choice Billing. A local hospital later notified ACH that patient information, including names and Social Security numbers, were viewable on the First Choice website. ACH identified at least 400 patients affected by the breach and reported the breach to the OCR. However, ACH later determined that an additional 8,855 patients may have been affected and revised its OCR notification.
What else? During its investigation, the OCR found that the hospitalist group had never entered into a business associate agreement for billing services with First Choice, as required by HIPAA, and that the practice also failed to adopt any policies regarding business associate agreements until 2014, according to a Dec. 4 announcement from HHS.
How much? The OCR fined the practice $500,000 and also imposed a robust corrective action plan that includes an enterprise-wide risk analysis and the adoption of business associate agreements. Roger Severino, OCR director, called the case especially troubling because “the practice allowed the names and Social Security numbers of thousands of patients to be exposed on the Internet after it failed to follow basic security requirements under HIPAA.”
Lessons learned: The case illustrates the importance of having a business associate agreement in place for all third parties that may have access to protected health information, said Clinton Mikel, a Farmington Hills, Mich., health law attorney specializing in HIPAA compliance.
Under HIPAA, a business associate is defined as a person or entity, other than a member of the workforce of a covered entity, who “performs functions or activities on behalf of, or provides certain services to, a covered entity that involve access by the business associate to protected health information.”
HIPAA requires that covered entities enter into contracts with business associates to ensure appropriate safeguarding of protected health information.
“If your business associate has a breach, your practice must report the breach to OCR and your patients,” Mr. Mikel said in an interview. “The OCR will then investigate your practice and your relationship with the business associate. Just because the breach and fault clearly happened elsewhere, you will still be investigated, and could face a penalty if HIPAA requirements weren’t met.”
Who? Filefax of Northbrook, Ill.
What happened? The OCR opened an investigation after receiving an anonymous complaint that medical records obtained from Filefax, a company that provided storage, maintenance, and delivery of medical records for health professionals, were left unmonitored at a shredding and recycling facility. OCR’s investigation revealed that a person left the records of 2,150 patients at the recycling plant and that the records contained protected health information, according to an HHS announcement. It is unclear if the person worked for Filefax.
What else? The OCR discovered that, in a related incident, an individual who obtained medical records from Filefax left them unattended in an unlocked truck in the Filefax parking lot.
How much? The OCR imposed a $100,000 fine on Filefax. The company is no longer in business; however, a court-appointed liquidator has agreed to properly store and dispose of the remaining records.
Lessons learned: Although the case did not involve a health provider, the circumstances are applicable to physicians, particularly when practices move or close, Mr. Mikel said. In some cases, a former patient may contact a shuttered practice only to learn their record cannot be located, or worse, that a breach has occurred.
“[Such a case is] ripe for a patient to complain to OCR,” he said. “OCR doesn’t care if you’re closed or retired, they’re going to look.”
HIPAA requires thatcovered entities apply appropriate administrative, technical, and physical safeguards to protect the privacy of protected health information in any form when moving or closing. The safeguards must prevent prohibited uses and disclosures of protected health information in connection with the disposal of such information, according to the rule. The HHS provides guidance for the disposing of medical records; further, the American Academy of Family Physicians has created a checklist on closing a practice that addresses the transferring of medical records.
Without taking the correct measures, doctors may end up drawing scrutiny from OCR and face a potential fine if violations are found, experts said.
“Covered entities and business associates need to be aware that OCR is committed to enforcing HIPAA regardless of whether a covered entity is opening its doors or closing them,” Mr. Severino of the OCR said in a statement. “HIPAA still applies.”
Data security experts say three HIPAA violations that resulted in significant fines by the Office for Civil Rights (OCR) in 2018 hold important lessons for health professionals about safeguarding records and training staff in HIPAA compliance.
Read on to learn how the cases unfolded and what knowledge practices can gain from the common HIPAA mistakes.
Who? Allergy Associates of Hartford, Conn.
What happened? A patient contacted a local television station to complain about a dispute between herself and a physician at Allergy Associates in Hartford, Conn. The disagreement stemmed from the office turning away the patient because she allegedly brought her service animal, according to a Nov. 26 announcement by the Department of Health & Human Services. The reporter contacted the doctor in question for a news story and, in responding, the physician disclosed protected patient information to the reporter.
What else? An OCR investigation determined that a privacy officer with Allergy Associates had instructed the physician not to respond to the media about the complaint or to respond with “no comment”; that advice was disregarded. The practice then failed to discipline the physician or take any corrective action following the disclosure, according to the OCR.
How much? The OCR imposed a $125,000 fine on the practice and a corrective action plan that includes 2 years of OCR monitoring.
Lessons learned: Had the practice disciplined the physician or taken corrective action after the disclosure, the OCR may not have penalized the group so severely, according to Jennifer Mitchell, a Cincinnati-based health law attorney and vice chair of the American Bar Association eHealth, Privacy, & Security Interest Group.
“In my opinion, the government levied these penalties because the provider did not sanction the doctor,” Ms. Mitchell said in an interview. “Health care entities need to take proper steps to remediate and, at a minimum, hold their workforce responsible for their behavior and ensure that it won’t happen again.”
The case emphasizes the need to train team members on media protocols and to ensure that protected health information is not mistakenly released. In addition to implementing policies and procedures, practices must also be willing to discipline health professionals when violations occur.
“A health care provider’s natural inclination is to defend themselves if they are being accused by a patient,” she said. “However, under the HIPAA rules, health care providers have to understand that they are prohibited from making such public statements about any patient.”
Who? Advanced Care Hospitalists of Lakeland, Fla.
What happened? Advanced Care Hospitalists (ACH) received billing services from an individual who represented himself to be affiliated with a Florida-based company named Doctor’s First Choice Billing. A local hospital later notified ACH that patient information, including names and Social Security numbers, were viewable on the First Choice website. ACH identified at least 400 patients affected by the breach and reported the breach to the OCR. However, ACH later determined that an additional 8,855 patients may have been affected and revised its OCR notification.
What else? During its investigation, the OCR found that the hospitalist group had never entered into a business associate agreement for billing services with First Choice, as required by HIPAA, and that the practice also failed to adopt any policies regarding business associate agreements until 2014, according to a Dec. 4 announcement from HHS.
How much? The OCR fined the practice $500,000 and also imposed a robust corrective action plan that includes an enterprise-wide risk analysis and the adoption of business associate agreements. Roger Severino, OCR director, called the case especially troubling because “the practice allowed the names and Social Security numbers of thousands of patients to be exposed on the Internet after it failed to follow basic security requirements under HIPAA.”
Lessons learned: The case illustrates the importance of having a business associate agreement in place for all third parties that may have access to protected health information, said Clinton Mikel, a Farmington Hills, Mich., health law attorney specializing in HIPAA compliance.
Under HIPAA, a business associate is defined as a person or entity, other than a member of the workforce of a covered entity, who “performs functions or activities on behalf of, or provides certain services to, a covered entity that involve access by the business associate to protected health information.”
HIPAA requires that covered entities enter into contracts with business associates to ensure appropriate safeguarding of protected health information.
“If your business associate has a breach, your practice must report the breach to OCR and your patients,” Mr. Mikel said in an interview. “The OCR will then investigate your practice and your relationship with the business associate. Just because the breach and fault clearly happened elsewhere, you will still be investigated, and could face a penalty if HIPAA requirements weren’t met.”
Who? Filefax of Northbrook, Ill.
What happened? The OCR opened an investigation after receiving an anonymous complaint that medical records obtained from Filefax, a company that provided storage, maintenance, and delivery of medical records for health professionals, were left unmonitored at a shredding and recycling facility. OCR’s investigation revealed that a person left the records of 2,150 patients at the recycling plant and that the records contained protected health information, according to an HHS announcement. It is unclear if the person worked for Filefax.
What else? The OCR discovered that, in a related incident, an individual who obtained medical records from Filefax left them unattended in an unlocked truck in the Filefax parking lot.
How much? The OCR imposed a $100,000 fine on Filefax. The company is no longer in business; however, a court-appointed liquidator has agreed to properly store and dispose of the remaining records.
Lessons learned: Although the case did not involve a health provider, the circumstances are applicable to physicians, particularly when practices move or close, Mr. Mikel said. In some cases, a former patient may contact a shuttered practice only to learn their record cannot be located, or worse, that a breach has occurred.
“[Such a case is] ripe for a patient to complain to OCR,” he said. “OCR doesn’t care if you’re closed or retired, they’re going to look.”
HIPAA requires thatcovered entities apply appropriate administrative, technical, and physical safeguards to protect the privacy of protected health information in any form when moving or closing. The safeguards must prevent prohibited uses and disclosures of protected health information in connection with the disposal of such information, according to the rule. The HHS provides guidance for the disposing of medical records; further, the American Academy of Family Physicians has created a checklist on closing a practice that addresses the transferring of medical records.
Without taking the correct measures, doctors may end up drawing scrutiny from OCR and face a potential fine if violations are found, experts said.
“Covered entities and business associates need to be aware that OCR is committed to enforcing HIPAA regardless of whether a covered entity is opening its doors or closing them,” Mr. Severino of the OCR said in a statement. “HIPAA still applies.”
How can I improve opioid safety at my hospital?
Quality improvement is essential
Case
A 67-year-old opioid-naive male with a history of obstructive sleep apnea and chronic kidney disease became unresponsive 2 days after hip replacement. Physical exam revealed a respiratory rate of 6 breaths/minute and oxygen saturation of 82%. He had received 6 doses of 6-mg IV morphine within the past 7 hours. How can I improve opioid safety at my hospital?
Background
Opioids are the most commonly prescribed class of medication in the hospital and the second–most common class causing adverse drug events (ADEs), the most serious being respiratory depression and death.1
Opioid ADEs and side effects can cause prolonged length of stay and patient suffering. These vary from potentially life-threatening events such as serotonin syndrome and adrenal insufficiency to more manageable problems still requiring intervention such as constipation, urinary retention, cognitive impairment, nausea, and vomiting. Treatment of side effects can lead to complications, including side effects from antiemetics and urinary tract infections from catheters.
A 4-year review found 700 deaths in the United States attributed to patient-controlled analgesia (PCA) use.2 Another study revealed that one out of every 200 patients has postoperative respiratory depression attributable to opioids.3
It is estimated that 2 million patients a year become chronic opioid users. Inpatient opioid prescribing contributes to this problem;4 for instance, 5.9% of patients after minor surgery and 6.5% after major surgery become chronic opioid users if discharged with an opioid.5 Calcaterra et al. found 25% of opioid-naive medical patients received an opioid at discharge from a medical service.6 Those patients had an odds ratio of 4.90 for becoming a chronic opioid user that year.6
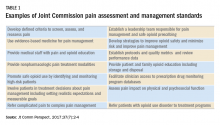
Most hospitals have incomplete or outdated policies and procedures for safe opioid prescribing and administration.7 The Joint Commission on Accreditation of Healthcare Organizations has specific pain standards for pain assessment, pain management, and safe opioid prescribing for hospitals. Additions and revisions were developed to go into effect Jan. 1, 2018. (Table 1)8
Quality improvement
Quality improvement (QI) is an effective way to improve opioid safety. The Society of Hospital Medicine has developed a QI guide, “Reducing adverse drug events related to opioids” or “RADEO,” to increase safety and decrease serious ADEs attributable to opioids.7
The steps in the RADEO program are as follows:
1. Assemble your team
It is critical to identify and include stakeholders from multiple disciplines on your project team. This team will be essential to develop a practical project, identify barriers, create solutions, and gain buy-in from medical staff and administrative leadership.
Front-line staff will have invaluable insight and need to be team members. The majority of interventions are performed by nurses; therefore, nursing leadership and input is essential. Representatives from pharmacy, information technology, and the quality department will be extremely valuable team members to guide you through the correct approach to a successful QI project.
A project champion can keep a high profile for the project and build and lead the team.
Identify an “executive sponsor” such as your CEO, CMO, or CNO. This leader will focus the team on issues critical to your organization, such as accreditation from governmental agencies, and help you obtain dedicated time and resources. Aligning with hospital goals will make your project a priority.
Coordinate with existing opioid initiative teams in the hospital to integrate efforts. This will keep the work of different departments aligned and allow you to learn from pitfalls and barriers the other groups experienced.
Patients/families contribute a unique and valuable perspective. Consider including a member of your hospital’s patient and family advisory council on your team.
2. Perform a needs assessment
Determine the current state of your hospital including: opioid prescribers; opioids prescribed; areas with increased ADEs or naloxone use; formulary restrictions, policies, or guidelines for monitoring, prescribing, and administering opioids; order sets; safety alerts; provider education; or patient education.
Your risk management or quality department may be able to a share root cause analysis of ADEs related to opioids. Joint Commission and CMS recommendations as well as other regulatory requirements may shape your QI interventions.8
Most importantly, review all of the concerns and priorities of your diverse team, which will identify areas of most pressing need and provide insight regarding needs you have not considered.
3. Develop SMART aims
Frame your QI project into a series of well-defined, clear SMART aims.9
Specific: Who will carry out the intervention? Who is your target population? What will be improved? In what way will it be improved?
Measurable: What will be measured? How it will be measured? Does it measure the outcome that needs to be improved?
Attainable/achievable: Ensure you have the resources and time to achieve the aim.
Relevant: Ensure each aim moves your team toward the project vision.
Timely: The aim should be achieved within a realistic time frame, long enough to meet goals but not so long that interest is lost.
An example of a poor aim is “Clinicians will improve knowledge of opioids.”
An example of a SMART aim is “75% of inpatient opioid prescribers including MDs, NPs, and PAs will complete and pass the opioid safety training module by July 1, 2018.”
4. Choose metrics
Outcome metrics measure if the intervention has improved patient safety, for example, measuring a decrease in opioid related ADEs. Structure metrics are the physical and organizational properties of the health care delivery setting, for example, the presence of EMR opioid safety. Processes are communication and practice patterns, for example, adherence to policy by examining nursing documentation of pain assessments.
5. Development and implementation 7,10
Use PDSA for development and implementation of the QI intervention.
Plan: Determine the intervention group such as a specific unit, number of units, and if there will be a control group. Determine who will collect the data, if baseline data will be collected, and who will analyze the data. Your information technology department will be essential to determine if the data can be collected via the EMR and how. Input from your multidisciplinary team is critical to anticipate unintended consequences, such as limiting opioid prescribing at discharge inadvertently increasing emergency department visits for pain control.
Do: Start as a small pilot study to make it as easy as possible to implement the project and begin data collection. A small-scale intervention will be more manageable and allow rapid responses to unanticipated problems.
Study: Analyze the data early to determine if the intervention is improving opioid safety and if alterations are needed. At this stage both process metrics (are processes being followed?) and outcome metrics (is the process leading to a desired outcome?) are important.
Act: Based on data analysis, refine the intervention as necessary. You may have to repeat cycles of PDSA to develop the final intervention. Then implement the final intervention to the entire hospital.
The Joint Commission recommendations for opioid QI
The Joint Commission recommends7 the following to reduce opioid-related respiratory depression:
- Effective processes which include processes such as tracking and analyzing ADEs related to opioids.
- Safe technology which includes using technology such as the EMR to monitor opioid prescribing of greater than 90 morphine milligram equivalents.
- Effective tools which include valid and reliable tools to improve opioid safety, such as the Pasero Opioid Induced Sedation Scale (POSS).
- Opioid education and training which includes provider and patient education such as patient discharge education.
Education
Develop educational interventions to ensure medical and hospital staff are aware of new processes, with an emphasis on “why.”7 If possible, use web-based programs that provide CME. Improve education interventions by using multiple live, interactive, and multimedia exposures.
Principles for successful interventions
- Keep it simple for the end user. This makes it more likely that the intervention is performed. Minimize complex tasks such as calculations and if possible design automated processes.
- Build your process into current work flow. If possible simplify or streamline work flow. A project that competes with staff’s other tasks and competing priorities is doomed to fail. It is critical to have input from those performing the intervention to develop a user-friendly and less disruptive intervention.
- Design reliability into the process. Make your intervention the default action. Build prompts into the work flow. Standardize the intervention into the work flow. And, consider having the intervention at scheduled intervals.7
Opioid safety QI interventions
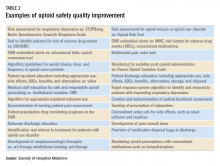
Interventions for improving opioid safety and reducing opioid -elated ADEs may be generalized into areas including risk screening and assessment, pain treatment, opioid administration, pain assessment, post opioid administration monitoring, and patient and provider education (Table 2).7
Back to the case
The patient received naloxone. His respiratory rate and oxygen saturation returned to normal. His dose of morphine was reduced and his interval increased. A multimodal approach was implemented including low-dose scheduled acetaminophen. There were no further ADEs while maintaining good pain control.
A multidisciplinary opioid task force was created and performed a hospital-wide review of opioid ADEs. Opportunities for improvement were identified and new procedures implemented. The Pasero opioid sedation scale (POSS) was added to the nursing work flow to monitor patients who received an opioid for sedation. An algorithm was developed for opioid-naive patients including guidance for opioid selection, dosing, and frequency. Multiple pain control modalities were added to pain control order sets. Annual training was developed for opioid prescribers, pharmacists, and nurses regarding safe and responsible use of opioids.
And, lastly, in-hospital and discharge patient education was developed for patients and families to be well-informed of opioid risk and benefit including how to identify and respond to ADEs.
Bottom line
Quality improvement is an effective method to improve patient safety and reduce serious adverse events related to opioids in the hospital setting.
Dr. Holmes-Maybank, is codirector, Fundamentals of Patient Care Year 1 and Internship 101, and chair, Clinical Competency Examination Committee, division of hospital medicine, Medical University of South Carolina. Dr. Frederickson is medical director, Hospital Medicine and Palliative Care at CHI Health, Omaha, Neb., and assistant professor at Creighton University School of Medicine, Omaha.
References
1. Davies EC et al. Adverse drug reactions in hospital inpatients: a prospective analysis of 3695 patient-episodes. PLoS One. 2009;4(2):e4439. doi: 10.1371/journal.pone.0004439. Epub 2009 Feb 11.
2. Association for the Advancement of Medical Instrumentation. Infusing patients safely: Priority issues from the AAMI/FDA Infusion Device Summit. 2010;1-39.
3. Dahan Aet al. Incidence, reversal, and prevention of opioid-induced respiratory depression. Anesthesiology. 2010;112:226-238. doi: 10.1097/ALN.0b013e3181c38c25.
4. Estimate about opioid users.
5. Brummett CM et al. New persistent opioid use after minor and major surgical procedures in U.S. adults. JAMA Surg. 2017;152(6):e170504. doi: 10.1001/jamasurg.2017.0504.
6. Calcaterra SL et al. Opioid prescribing at hospital discharge contributes to chronic opioid use. J Gen Intern Med. 2016;31(5):478-85. doi: 10.1007/s11606-015-3539-4.
7. Frederickson TW et al. Reducing adverse drug events related to opioids implementation guide. Philadelphia: Society of Hospital Medicine, 2015.
8. Joint Commission enhances pain assessment and management requirements for accredited hospitals. The Joint Commission Perspectives. 2017;37(7):2-4.
9. Minnesota Department of Health. SMART objectives.
10. Agency for Healthcare Research and Quality. Health Literacy Universal Precautions Toolkit, 2nd Edition.
Plan-Do-Study-Act (PDSA) Directions and Examples.
Recommended reading
Dowell D et al. CDC guideline for prescribing opioids for chronic pain – United States, 2016. Recommendations and Reports. 2016 Mar 18;65(1):1-49.
Frederickson TW et al. Using the 2018 guidelines from the Joint Commission to kickstart your hospital’s program to reduce opioid-induced ventilatory impairment. Anesthesia Patient Safety Foundation Newsletter. 2018;33(1):1-32.
Herzig SJ et al. Safe opioid prescribing for acute noncancer pain in hospitalized adults: a systematic review of existing guidelines. J Hosp Med. 2018 Apr;13(4):256-62. doi: 10.12788/jhm.2979.
Herzig SJ et al. Improving the safety of opioid use for acute noncancer pain in hospitalized adults: a consensus statement from the society of hospital medicine. J Hosp Med. 2018 Apr;13(4):263-71. doi: 10.12788/jhm.2980.
Joint Commission enhances pain assessment and management requirements for accredited hospitals. The Joint Commission Perspectives. 2017;37(7):2-4.
Key points
- Quality improvement is required by the Joint Commission and is an effective method to improve opioid safety in the hospital setting.
- It is critical to the success of a QI project to develop a multidisciplinary team.
- Input from frontline users of the intervention is essential to produce an effective intervention.
- Executive sponsorship and aligning the goals of your QI project with those of your institution will prioritize your project and increase resource availability.
Quiz
1. Based on a needs assessment at your hospital you assemble a multidisciplinary team to improve education for patients discharged on opioids. You recognize the importance of multidisciplinary input to develop a successful intervention for discharge education. Essential team members include all EXCEPT the following:
a. Executive sponsor
b. Patient representative
c. Nursing
d. Medical student representative ---- CORRECT
Explanation: The assembly of a multidisciplinary team is critical to the success of a QI intervention. An executive sponsor may assist you in aligning your goals with that of the hospital and provide resources for its development and implementation. Patient input would help determine how to best deliver the education. Lastly, the individuals carrying out the intervention are essential to develop an intervention that will easy for the end user and increase the likelihood of being used, in this case nursing.
2. You performed a review of naloxone use at your hospital and find that it is greater than similar hospitals. Prior to starting the QI project, you review SHM’s “Reducing adverse events related to opioids implementation guide” and learn that keys to success for QI implementation include:
a. A team of primarily hospitalists
b. Implementing the intervention hospital wide
c. Information technology input for data collection ---- CORRECT
d. No team – it is more effective to work alone
Explanation: Successful implementation of a QI project involves a multidisciplinary team. It is critical to involve information technology early in the development of the project to determine how and if the data can be collected from the EMR. It is best to pilot the intervention on one or two units to make alterations as needed rapidly and perfect the final intervention prior to rolling it out to the entire hospital.
3. You have assembled a multidisciplinary team to respond to the newly revised JCAHO pain standards. An example of a requirement from the new and revised JCAHO standards for pain assessment and management includes:
a. Programs for physician wellness
b. No opioids for chronic pain
c. No more than 5 days of opioids for acute pain
d. Nonpharmacologic pain management options ---- CORRECT
Explanation: JCAHO released new and revised requirements for pain assessment and management including offering nonpharmacologic pain management options. (See Table 1)
4. Your multidisciplinary QI team decides to develop a project to reduce respiratory depression in patients receiving opioids by monitoring for sedation with the Pasero Opioid Induced Sedation Scale. Principles for successful QI interventions include:
a. Complex tasks
b. Make the intervention a default action ---- CORRECT
c. Avoid EMR prompts
d. Competing with other hospital priorities
Explanation: Principles for successful QI interventions include keeping tasks simple, ensuring the intervention does not compete with other priorities, making the intervention the default action, installing prompts in the EMR, and standardizing the intervention into the work flow.
Quality improvement is essential
Quality improvement is essential
Case
A 67-year-old opioid-naive male with a history of obstructive sleep apnea and chronic kidney disease became unresponsive 2 days after hip replacement. Physical exam revealed a respiratory rate of 6 breaths/minute and oxygen saturation of 82%. He had received 6 doses of 6-mg IV morphine within the past 7 hours. How can I improve opioid safety at my hospital?
Background
Opioids are the most commonly prescribed class of medication in the hospital and the second–most common class causing adverse drug events (ADEs), the most serious being respiratory depression and death.1
Opioid ADEs and side effects can cause prolonged length of stay and patient suffering. These vary from potentially life-threatening events such as serotonin syndrome and adrenal insufficiency to more manageable problems still requiring intervention such as constipation, urinary retention, cognitive impairment, nausea, and vomiting. Treatment of side effects can lead to complications, including side effects from antiemetics and urinary tract infections from catheters.
A 4-year review found 700 deaths in the United States attributed to patient-controlled analgesia (PCA) use.2 Another study revealed that one out of every 200 patients has postoperative respiratory depression attributable to opioids.3
It is estimated that 2 million patients a year become chronic opioid users. Inpatient opioid prescribing contributes to this problem;4 for instance, 5.9% of patients after minor surgery and 6.5% after major surgery become chronic opioid users if discharged with an opioid.5 Calcaterra et al. found 25% of opioid-naive medical patients received an opioid at discharge from a medical service.6 Those patients had an odds ratio of 4.90 for becoming a chronic opioid user that year.6
Most hospitals have incomplete or outdated policies and procedures for safe opioid prescribing and administration.7 The Joint Commission on Accreditation of Healthcare Organizations has specific pain standards for pain assessment, pain management, and safe opioid prescribing for hospitals. Additions and revisions were developed to go into effect Jan. 1, 2018. (Table 1)8
Quality improvement
Quality improvement (QI) is an effective way to improve opioid safety. The Society of Hospital Medicine has developed a QI guide, “Reducing adverse drug events related to opioids” or “RADEO,” to increase safety and decrease serious ADEs attributable to opioids.7
The steps in the RADEO program are as follows:
1. Assemble your team
It is critical to identify and include stakeholders from multiple disciplines on your project team. This team will be essential to develop a practical project, identify barriers, create solutions, and gain buy-in from medical staff and administrative leadership.
Front-line staff will have invaluable insight and need to be team members. The majority of interventions are performed by nurses; therefore, nursing leadership and input is essential. Representatives from pharmacy, information technology, and the quality department will be extremely valuable team members to guide you through the correct approach to a successful QI project.
A project champion can keep a high profile for the project and build and lead the team.
Identify an “executive sponsor” such as your CEO, CMO, or CNO. This leader will focus the team on issues critical to your organization, such as accreditation from governmental agencies, and help you obtain dedicated time and resources. Aligning with hospital goals will make your project a priority.
Coordinate with existing opioid initiative teams in the hospital to integrate efforts. This will keep the work of different departments aligned and allow you to learn from pitfalls and barriers the other groups experienced.
Patients/families contribute a unique and valuable perspective. Consider including a member of your hospital’s patient and family advisory council on your team.
2. Perform a needs assessment
Determine the current state of your hospital including: opioid prescribers; opioids prescribed; areas with increased ADEs or naloxone use; formulary restrictions, policies, or guidelines for monitoring, prescribing, and administering opioids; order sets; safety alerts; provider education; or patient education.
Your risk management or quality department may be able to a share root cause analysis of ADEs related to opioids. Joint Commission and CMS recommendations as well as other regulatory requirements may shape your QI interventions.8
Most importantly, review all of the concerns and priorities of your diverse team, which will identify areas of most pressing need and provide insight regarding needs you have not considered.
3. Develop SMART aims
Frame your QI project into a series of well-defined, clear SMART aims.9
Specific: Who will carry out the intervention? Who is your target population? What will be improved? In what way will it be improved?
Measurable: What will be measured? How it will be measured? Does it measure the outcome that needs to be improved?
Attainable/achievable: Ensure you have the resources and time to achieve the aim.
Relevant: Ensure each aim moves your team toward the project vision.
Timely: The aim should be achieved within a realistic time frame, long enough to meet goals but not so long that interest is lost.
An example of a poor aim is “Clinicians will improve knowledge of opioids.”
An example of a SMART aim is “75% of inpatient opioid prescribers including MDs, NPs, and PAs will complete and pass the opioid safety training module by July 1, 2018.”
4. Choose metrics
Outcome metrics measure if the intervention has improved patient safety, for example, measuring a decrease in opioid related ADEs. Structure metrics are the physical and organizational properties of the health care delivery setting, for example, the presence of EMR opioid safety. Processes are communication and practice patterns, for example, adherence to policy by examining nursing documentation of pain assessments.
5. Development and implementation 7,10
Use PDSA for development and implementation of the QI intervention.
Plan: Determine the intervention group such as a specific unit, number of units, and if there will be a control group. Determine who will collect the data, if baseline data will be collected, and who will analyze the data. Your information technology department will be essential to determine if the data can be collected via the EMR and how. Input from your multidisciplinary team is critical to anticipate unintended consequences, such as limiting opioid prescribing at discharge inadvertently increasing emergency department visits for pain control.
Do: Start as a small pilot study to make it as easy as possible to implement the project and begin data collection. A small-scale intervention will be more manageable and allow rapid responses to unanticipated problems.
Study: Analyze the data early to determine if the intervention is improving opioid safety and if alterations are needed. At this stage both process metrics (are processes being followed?) and outcome metrics (is the process leading to a desired outcome?) are important.
Act: Based on data analysis, refine the intervention as necessary. You may have to repeat cycles of PDSA to develop the final intervention. Then implement the final intervention to the entire hospital.
The Joint Commission recommendations for opioid QI
The Joint Commission recommends7 the following to reduce opioid-related respiratory depression:
- Effective processes which include processes such as tracking and analyzing ADEs related to opioids.
- Safe technology which includes using technology such as the EMR to monitor opioid prescribing of greater than 90 morphine milligram equivalents.
- Effective tools which include valid and reliable tools to improve opioid safety, such as the Pasero Opioid Induced Sedation Scale (POSS).
- Opioid education and training which includes provider and patient education such as patient discharge education.
Education
Develop educational interventions to ensure medical and hospital staff are aware of new processes, with an emphasis on “why.”7 If possible, use web-based programs that provide CME. Improve education interventions by using multiple live, interactive, and multimedia exposures.
Principles for successful interventions
- Keep it simple for the end user. This makes it more likely that the intervention is performed. Minimize complex tasks such as calculations and if possible design automated processes.
- Build your process into current work flow. If possible simplify or streamline work flow. A project that competes with staff’s other tasks and competing priorities is doomed to fail. It is critical to have input from those performing the intervention to develop a user-friendly and less disruptive intervention.
- Design reliability into the process. Make your intervention the default action. Build prompts into the work flow. Standardize the intervention into the work flow. And, consider having the intervention at scheduled intervals.7
Opioid safety QI interventions
Interventions for improving opioid safety and reducing opioid -elated ADEs may be generalized into areas including risk screening and assessment, pain treatment, opioid administration, pain assessment, post opioid administration monitoring, and patient and provider education (Table 2).7
Back to the case
The patient received naloxone. His respiratory rate and oxygen saturation returned to normal. His dose of morphine was reduced and his interval increased. A multimodal approach was implemented including low-dose scheduled acetaminophen. There were no further ADEs while maintaining good pain control.
A multidisciplinary opioid task force was created and performed a hospital-wide review of opioid ADEs. Opportunities for improvement were identified and new procedures implemented. The Pasero opioid sedation scale (POSS) was added to the nursing work flow to monitor patients who received an opioid for sedation. An algorithm was developed for opioid-naive patients including guidance for opioid selection, dosing, and frequency. Multiple pain control modalities were added to pain control order sets. Annual training was developed for opioid prescribers, pharmacists, and nurses regarding safe and responsible use of opioids.
And, lastly, in-hospital and discharge patient education was developed for patients and families to be well-informed of opioid risk and benefit including how to identify and respond to ADEs.
Bottom line
Quality improvement is an effective method to improve patient safety and reduce serious adverse events related to opioids in the hospital setting.
Dr. Holmes-Maybank, is codirector, Fundamentals of Patient Care Year 1 and Internship 101, and chair, Clinical Competency Examination Committee, division of hospital medicine, Medical University of South Carolina. Dr. Frederickson is medical director, Hospital Medicine and Palliative Care at CHI Health, Omaha, Neb., and assistant professor at Creighton University School of Medicine, Omaha.
References
1. Davies EC et al. Adverse drug reactions in hospital inpatients: a prospective analysis of 3695 patient-episodes. PLoS One. 2009;4(2):e4439. doi: 10.1371/journal.pone.0004439. Epub 2009 Feb 11.
2. Association for the Advancement of Medical Instrumentation. Infusing patients safely: Priority issues from the AAMI/FDA Infusion Device Summit. 2010;1-39.
3. Dahan Aet al. Incidence, reversal, and prevention of opioid-induced respiratory depression. Anesthesiology. 2010;112:226-238. doi: 10.1097/ALN.0b013e3181c38c25.
4. Estimate about opioid users.
5. Brummett CM et al. New persistent opioid use after minor and major surgical procedures in U.S. adults. JAMA Surg. 2017;152(6):e170504. doi: 10.1001/jamasurg.2017.0504.
6. Calcaterra SL et al. Opioid prescribing at hospital discharge contributes to chronic opioid use. J Gen Intern Med. 2016;31(5):478-85. doi: 10.1007/s11606-015-3539-4.
7. Frederickson TW et al. Reducing adverse drug events related to opioids implementation guide. Philadelphia: Society of Hospital Medicine, 2015.
8. Joint Commission enhances pain assessment and management requirements for accredited hospitals. The Joint Commission Perspectives. 2017;37(7):2-4.
9. Minnesota Department of Health. SMART objectives.
10. Agency for Healthcare Research and Quality. Health Literacy Universal Precautions Toolkit, 2nd Edition.
Plan-Do-Study-Act (PDSA) Directions and Examples.
Recommended reading
Dowell D et al. CDC guideline for prescribing opioids for chronic pain – United States, 2016. Recommendations and Reports. 2016 Mar 18;65(1):1-49.
Frederickson TW et al. Using the 2018 guidelines from the Joint Commission to kickstart your hospital’s program to reduce opioid-induced ventilatory impairment. Anesthesia Patient Safety Foundation Newsletter. 2018;33(1):1-32.
Herzig SJ et al. Safe opioid prescribing for acute noncancer pain in hospitalized adults: a systematic review of existing guidelines. J Hosp Med. 2018 Apr;13(4):256-62. doi: 10.12788/jhm.2979.
Herzig SJ et al. Improving the safety of opioid use for acute noncancer pain in hospitalized adults: a consensus statement from the society of hospital medicine. J Hosp Med. 2018 Apr;13(4):263-71. doi: 10.12788/jhm.2980.
Joint Commission enhances pain assessment and management requirements for accredited hospitals. The Joint Commission Perspectives. 2017;37(7):2-4.
Key points
- Quality improvement is required by the Joint Commission and is an effective method to improve opioid safety in the hospital setting.
- It is critical to the success of a QI project to develop a multidisciplinary team.
- Input from frontline users of the intervention is essential to produce an effective intervention.
- Executive sponsorship and aligning the goals of your QI project with those of your institution will prioritize your project and increase resource availability.
Quiz
1. Based on a needs assessment at your hospital you assemble a multidisciplinary team to improve education for patients discharged on opioids. You recognize the importance of multidisciplinary input to develop a successful intervention for discharge education. Essential team members include all EXCEPT the following:
a. Executive sponsor
b. Patient representative
c. Nursing
d. Medical student representative ---- CORRECT
Explanation: The assembly of a multidisciplinary team is critical to the success of a QI intervention. An executive sponsor may assist you in aligning your goals with that of the hospital and provide resources for its development and implementation. Patient input would help determine how to best deliver the education. Lastly, the individuals carrying out the intervention are essential to develop an intervention that will easy for the end user and increase the likelihood of being used, in this case nursing.
2. You performed a review of naloxone use at your hospital and find that it is greater than similar hospitals. Prior to starting the QI project, you review SHM’s “Reducing adverse events related to opioids implementation guide” and learn that keys to success for QI implementation include:
a. A team of primarily hospitalists
b. Implementing the intervention hospital wide
c. Information technology input for data collection ---- CORRECT
d. No team – it is more effective to work alone
Explanation: Successful implementation of a QI project involves a multidisciplinary team. It is critical to involve information technology early in the development of the project to determine how and if the data can be collected from the EMR. It is best to pilot the intervention on one or two units to make alterations as needed rapidly and perfect the final intervention prior to rolling it out to the entire hospital.
3. You have assembled a multidisciplinary team to respond to the newly revised JCAHO pain standards. An example of a requirement from the new and revised JCAHO standards for pain assessment and management includes:
a. Programs for physician wellness
b. No opioids for chronic pain
c. No more than 5 days of opioids for acute pain
d. Nonpharmacologic pain management options ---- CORRECT
Explanation: JCAHO released new and revised requirements for pain assessment and management including offering nonpharmacologic pain management options. (See Table 1)
4. Your multidisciplinary QI team decides to develop a project to reduce respiratory depression in patients receiving opioids by monitoring for sedation with the Pasero Opioid Induced Sedation Scale. Principles for successful QI interventions include:
a. Complex tasks
b. Make the intervention a default action ---- CORRECT
c. Avoid EMR prompts
d. Competing with other hospital priorities
Explanation: Principles for successful QI interventions include keeping tasks simple, ensuring the intervention does not compete with other priorities, making the intervention the default action, installing prompts in the EMR, and standardizing the intervention into the work flow.
Case
A 67-year-old opioid-naive male with a history of obstructive sleep apnea and chronic kidney disease became unresponsive 2 days after hip replacement. Physical exam revealed a respiratory rate of 6 breaths/minute and oxygen saturation of 82%. He had received 6 doses of 6-mg IV morphine within the past 7 hours. How can I improve opioid safety at my hospital?
Background
Opioids are the most commonly prescribed class of medication in the hospital and the second–most common class causing adverse drug events (ADEs), the most serious being respiratory depression and death.1
Opioid ADEs and side effects can cause prolonged length of stay and patient suffering. These vary from potentially life-threatening events such as serotonin syndrome and adrenal insufficiency to more manageable problems still requiring intervention such as constipation, urinary retention, cognitive impairment, nausea, and vomiting. Treatment of side effects can lead to complications, including side effects from antiemetics and urinary tract infections from catheters.
A 4-year review found 700 deaths in the United States attributed to patient-controlled analgesia (PCA) use.2 Another study revealed that one out of every 200 patients has postoperative respiratory depression attributable to opioids.3
It is estimated that 2 million patients a year become chronic opioid users. Inpatient opioid prescribing contributes to this problem;4 for instance, 5.9% of patients after minor surgery and 6.5% after major surgery become chronic opioid users if discharged with an opioid.5 Calcaterra et al. found 25% of opioid-naive medical patients received an opioid at discharge from a medical service.6 Those patients had an odds ratio of 4.90 for becoming a chronic opioid user that year.6
Most hospitals have incomplete or outdated policies and procedures for safe opioid prescribing and administration.7 The Joint Commission on Accreditation of Healthcare Organizations has specific pain standards for pain assessment, pain management, and safe opioid prescribing for hospitals. Additions and revisions were developed to go into effect Jan. 1, 2018. (Table 1)8
Quality improvement
Quality improvement (QI) is an effective way to improve opioid safety. The Society of Hospital Medicine has developed a QI guide, “Reducing adverse drug events related to opioids” or “RADEO,” to increase safety and decrease serious ADEs attributable to opioids.7
The steps in the RADEO program are as follows:
1. Assemble your team
It is critical to identify and include stakeholders from multiple disciplines on your project team. This team will be essential to develop a practical project, identify barriers, create solutions, and gain buy-in from medical staff and administrative leadership.
Front-line staff will have invaluable insight and need to be team members. The majority of interventions are performed by nurses; therefore, nursing leadership and input is essential. Representatives from pharmacy, information technology, and the quality department will be extremely valuable team members to guide you through the correct approach to a successful QI project.
A project champion can keep a high profile for the project and build and lead the team.
Identify an “executive sponsor” such as your CEO, CMO, or CNO. This leader will focus the team on issues critical to your organization, such as accreditation from governmental agencies, and help you obtain dedicated time and resources. Aligning with hospital goals will make your project a priority.
Coordinate with existing opioid initiative teams in the hospital to integrate efforts. This will keep the work of different departments aligned and allow you to learn from pitfalls and barriers the other groups experienced.
Patients/families contribute a unique and valuable perspective. Consider including a member of your hospital’s patient and family advisory council on your team.
2. Perform a needs assessment
Determine the current state of your hospital including: opioid prescribers; opioids prescribed; areas with increased ADEs or naloxone use; formulary restrictions, policies, or guidelines for monitoring, prescribing, and administering opioids; order sets; safety alerts; provider education; or patient education.
Your risk management or quality department may be able to a share root cause analysis of ADEs related to opioids. Joint Commission and CMS recommendations as well as other regulatory requirements may shape your QI interventions.8
Most importantly, review all of the concerns and priorities of your diverse team, which will identify areas of most pressing need and provide insight regarding needs you have not considered.
3. Develop SMART aims
Frame your QI project into a series of well-defined, clear SMART aims.9
Specific: Who will carry out the intervention? Who is your target population? What will be improved? In what way will it be improved?
Measurable: What will be measured? How it will be measured? Does it measure the outcome that needs to be improved?
Attainable/achievable: Ensure you have the resources and time to achieve the aim.
Relevant: Ensure each aim moves your team toward the project vision.
Timely: The aim should be achieved within a realistic time frame, long enough to meet goals but not so long that interest is lost.
An example of a poor aim is “Clinicians will improve knowledge of opioids.”
An example of a SMART aim is “75% of inpatient opioid prescribers including MDs, NPs, and PAs will complete and pass the opioid safety training module by July 1, 2018.”
4. Choose metrics
Outcome metrics measure if the intervention has improved patient safety, for example, measuring a decrease in opioid related ADEs. Structure metrics are the physical and organizational properties of the health care delivery setting, for example, the presence of EMR opioid safety. Processes are communication and practice patterns, for example, adherence to policy by examining nursing documentation of pain assessments.
5. Development and implementation 7,10
Use PDSA for development and implementation of the QI intervention.
Plan: Determine the intervention group such as a specific unit, number of units, and if there will be a control group. Determine who will collect the data, if baseline data will be collected, and who will analyze the data. Your information technology department will be essential to determine if the data can be collected via the EMR and how. Input from your multidisciplinary team is critical to anticipate unintended consequences, such as limiting opioid prescribing at discharge inadvertently increasing emergency department visits for pain control.
Do: Start as a small pilot study to make it as easy as possible to implement the project and begin data collection. A small-scale intervention will be more manageable and allow rapid responses to unanticipated problems.
Study: Analyze the data early to determine if the intervention is improving opioid safety and if alterations are needed. At this stage both process metrics (are processes being followed?) and outcome metrics (is the process leading to a desired outcome?) are important.
Act: Based on data analysis, refine the intervention as necessary. You may have to repeat cycles of PDSA to develop the final intervention. Then implement the final intervention to the entire hospital.
The Joint Commission recommendations for opioid QI
The Joint Commission recommends7 the following to reduce opioid-related respiratory depression:
- Effective processes which include processes such as tracking and analyzing ADEs related to opioids.
- Safe technology which includes using technology such as the EMR to monitor opioid prescribing of greater than 90 morphine milligram equivalents.
- Effective tools which include valid and reliable tools to improve opioid safety, such as the Pasero Opioid Induced Sedation Scale (POSS).
- Opioid education and training which includes provider and patient education such as patient discharge education.
Education
Develop educational interventions to ensure medical and hospital staff are aware of new processes, with an emphasis on “why.”7 If possible, use web-based programs that provide CME. Improve education interventions by using multiple live, interactive, and multimedia exposures.
Principles for successful interventions
- Keep it simple for the end user. This makes it more likely that the intervention is performed. Minimize complex tasks such as calculations and if possible design automated processes.
- Build your process into current work flow. If possible simplify or streamline work flow. A project that competes with staff’s other tasks and competing priorities is doomed to fail. It is critical to have input from those performing the intervention to develop a user-friendly and less disruptive intervention.
- Design reliability into the process. Make your intervention the default action. Build prompts into the work flow. Standardize the intervention into the work flow. And, consider having the intervention at scheduled intervals.7
Opioid safety QI interventions
Interventions for improving opioid safety and reducing opioid -elated ADEs may be generalized into areas including risk screening and assessment, pain treatment, opioid administration, pain assessment, post opioid administration monitoring, and patient and provider education (Table 2).7
Back to the case
The patient received naloxone. His respiratory rate and oxygen saturation returned to normal. His dose of morphine was reduced and his interval increased. A multimodal approach was implemented including low-dose scheduled acetaminophen. There were no further ADEs while maintaining good pain control.
A multidisciplinary opioid task force was created and performed a hospital-wide review of opioid ADEs. Opportunities for improvement were identified and new procedures implemented. The Pasero opioid sedation scale (POSS) was added to the nursing work flow to monitor patients who received an opioid for sedation. An algorithm was developed for opioid-naive patients including guidance for opioid selection, dosing, and frequency. Multiple pain control modalities were added to pain control order sets. Annual training was developed for opioid prescribers, pharmacists, and nurses regarding safe and responsible use of opioids.
And, lastly, in-hospital and discharge patient education was developed for patients and families to be well-informed of opioid risk and benefit including how to identify and respond to ADEs.
Bottom line
Quality improvement is an effective method to improve patient safety and reduce serious adverse events related to opioids in the hospital setting.
Dr. Holmes-Maybank, is codirector, Fundamentals of Patient Care Year 1 and Internship 101, and chair, Clinical Competency Examination Committee, division of hospital medicine, Medical University of South Carolina. Dr. Frederickson is medical director, Hospital Medicine and Palliative Care at CHI Health, Omaha, Neb., and assistant professor at Creighton University School of Medicine, Omaha.
References
1. Davies EC et al. Adverse drug reactions in hospital inpatients: a prospective analysis of 3695 patient-episodes. PLoS One. 2009;4(2):e4439. doi: 10.1371/journal.pone.0004439. Epub 2009 Feb 11.
2. Association for the Advancement of Medical Instrumentation. Infusing patients safely: Priority issues from the AAMI/FDA Infusion Device Summit. 2010;1-39.
3. Dahan Aet al. Incidence, reversal, and prevention of opioid-induced respiratory depression. Anesthesiology. 2010;112:226-238. doi: 10.1097/ALN.0b013e3181c38c25.
4. Estimate about opioid users.
5. Brummett CM et al. New persistent opioid use after minor and major surgical procedures in U.S. adults. JAMA Surg. 2017;152(6):e170504. doi: 10.1001/jamasurg.2017.0504.
6. Calcaterra SL et al. Opioid prescribing at hospital discharge contributes to chronic opioid use. J Gen Intern Med. 2016;31(5):478-85. doi: 10.1007/s11606-015-3539-4.
7. Frederickson TW et al. Reducing adverse drug events related to opioids implementation guide. Philadelphia: Society of Hospital Medicine, 2015.
8. Joint Commission enhances pain assessment and management requirements for accredited hospitals. The Joint Commission Perspectives. 2017;37(7):2-4.
9. Minnesota Department of Health. SMART objectives.
10. Agency for Healthcare Research and Quality. Health Literacy Universal Precautions Toolkit, 2nd Edition.
Plan-Do-Study-Act (PDSA) Directions and Examples.
Recommended reading
Dowell D et al. CDC guideline for prescribing opioids for chronic pain – United States, 2016. Recommendations and Reports. 2016 Mar 18;65(1):1-49.
Frederickson TW et al. Using the 2018 guidelines from the Joint Commission to kickstart your hospital’s program to reduce opioid-induced ventilatory impairment. Anesthesia Patient Safety Foundation Newsletter. 2018;33(1):1-32.
Herzig SJ et al. Safe opioid prescribing for acute noncancer pain in hospitalized adults: a systematic review of existing guidelines. J Hosp Med. 2018 Apr;13(4):256-62. doi: 10.12788/jhm.2979.
Herzig SJ et al. Improving the safety of opioid use for acute noncancer pain in hospitalized adults: a consensus statement from the society of hospital medicine. J Hosp Med. 2018 Apr;13(4):263-71. doi: 10.12788/jhm.2980.
Joint Commission enhances pain assessment and management requirements for accredited hospitals. The Joint Commission Perspectives. 2017;37(7):2-4.
Key points
- Quality improvement is required by the Joint Commission and is an effective method to improve opioid safety in the hospital setting.
- It is critical to the success of a QI project to develop a multidisciplinary team.
- Input from frontline users of the intervention is essential to produce an effective intervention.
- Executive sponsorship and aligning the goals of your QI project with those of your institution will prioritize your project and increase resource availability.
Quiz
1. Based on a needs assessment at your hospital you assemble a multidisciplinary team to improve education for patients discharged on opioids. You recognize the importance of multidisciplinary input to develop a successful intervention for discharge education. Essential team members include all EXCEPT the following:
a. Executive sponsor
b. Patient representative
c. Nursing
d. Medical student representative ---- CORRECT
Explanation: The assembly of a multidisciplinary team is critical to the success of a QI intervention. An executive sponsor may assist you in aligning your goals with that of the hospital and provide resources for its development and implementation. Patient input would help determine how to best deliver the education. Lastly, the individuals carrying out the intervention are essential to develop an intervention that will easy for the end user and increase the likelihood of being used, in this case nursing.
2. You performed a review of naloxone use at your hospital and find that it is greater than similar hospitals. Prior to starting the QI project, you review SHM’s “Reducing adverse events related to opioids implementation guide” and learn that keys to success for QI implementation include:
a. A team of primarily hospitalists
b. Implementing the intervention hospital wide
c. Information technology input for data collection ---- CORRECT
d. No team – it is more effective to work alone
Explanation: Successful implementation of a QI project involves a multidisciplinary team. It is critical to involve information technology early in the development of the project to determine how and if the data can be collected from the EMR. It is best to pilot the intervention on one or two units to make alterations as needed rapidly and perfect the final intervention prior to rolling it out to the entire hospital.
3. You have assembled a multidisciplinary team to respond to the newly revised JCAHO pain standards. An example of a requirement from the new and revised JCAHO standards for pain assessment and management includes:
a. Programs for physician wellness
b. No opioids for chronic pain
c. No more than 5 days of opioids for acute pain
d. Nonpharmacologic pain management options ---- CORRECT
Explanation: JCAHO released new and revised requirements for pain assessment and management including offering nonpharmacologic pain management options. (See Table 1)
4. Your multidisciplinary QI team decides to develop a project to reduce respiratory depression in patients receiving opioids by monitoring for sedation with the Pasero Opioid Induced Sedation Scale. Principles for successful QI interventions include:
a. Complex tasks
b. Make the intervention a default action ---- CORRECT
c. Avoid EMR prompts
d. Competing with other hospital priorities
Explanation: Principles for successful QI interventions include keeping tasks simple, ensuring the intervention does not compete with other priorities, making the intervention the default action, installing prompts in the EMR, and standardizing the intervention into the work flow.
Meal programs for dual eligibles
Do food delivery programs reduce the use of costly health services and decrease medical spending in a population of patients dually eligible for Medicare and Medicaid?
Researchers in Massachusetts wanted to determine whether home meal delivery of either medically tailored food or nontailored food reduces the use of selected health care services and medical spending in a sample of adult “dual eligibles.”
“Compared with matched nonparticipants, participants had fewer emergency department visits in both the medically tailored meal program and the nontailored food program,” the investigators found. “Participants in the medically tailored meal program also had fewer inpatient admissions and lower medical spending. Participation in the nontailored food program was not associated with fewer inpatient admissions but was associated with lower medical spending.”
Reference
Berkowitz SA et al. Meal delivery programs reduce the use of costly health care in dually eligible Medicare and Medicaid beneficiaries. Health Aff (Millwood). 2018 Apr;37(4):535-42.
Do food delivery programs reduce the use of costly health services and decrease medical spending in a population of patients dually eligible for Medicare and Medicaid?
Researchers in Massachusetts wanted to determine whether home meal delivery of either medically tailored food or nontailored food reduces the use of selected health care services and medical spending in a sample of adult “dual eligibles.”
“Compared with matched nonparticipants, participants had fewer emergency department visits in both the medically tailored meal program and the nontailored food program,” the investigators found. “Participants in the medically tailored meal program also had fewer inpatient admissions and lower medical spending. Participation in the nontailored food program was not associated with fewer inpatient admissions but was associated with lower medical spending.”
Reference
Berkowitz SA et al. Meal delivery programs reduce the use of costly health care in dually eligible Medicare and Medicaid beneficiaries. Health Aff (Millwood). 2018 Apr;37(4):535-42.
Do food delivery programs reduce the use of costly health services and decrease medical spending in a population of patients dually eligible for Medicare and Medicaid?
Researchers in Massachusetts wanted to determine whether home meal delivery of either medically tailored food or nontailored food reduces the use of selected health care services and medical spending in a sample of adult “dual eligibles.”
“Compared with matched nonparticipants, participants had fewer emergency department visits in both the medically tailored meal program and the nontailored food program,” the investigators found. “Participants in the medically tailored meal program also had fewer inpatient admissions and lower medical spending. Participation in the nontailored food program was not associated with fewer inpatient admissions but was associated with lower medical spending.”
Reference
Berkowitz SA et al. Meal delivery programs reduce the use of costly health care in dually eligible Medicare and Medicaid beneficiaries. Health Aff (Millwood). 2018 Apr;37(4):535-42.
How to assess an Antimicrobial Stewardship Program
A study compares the merits of DOT and DOTA
The currently recommended method for hospital antimicrobial stewardship programs (ASPs) to measure antibiotic use is Days of Therapy/1,000 patient-days, but there are a few disadvantages of using the DOT, said Maryrose Laguio-Vila, MD, coauthor of a recent study on stewardship.
“For accurate measurement, it requires information technology (IT) support to assist an ASP in generating reports of antibiotic prescriptions and administrations to patients, often from an electronic medical record (EMR). In hospitals where there is no EMR, DOT is probably not easily done and would have to be manually extracted (a herculean task),” she said. “Second, DOT tends to be an aggregate measurement of antibiotics used at an institution or hospital location; if an ASP does a specific intervention targeting a group of antibiotics or infectious indication, changes in the hospital-wide DOT or drug-class DOT may not accurately reflect the exact impact of an ASP’s intervention.”
The paper offers an alternative/supplemental method for ASPs to quantify their impact on antibiotic use without using an EMR or needing IT support: Days of Therapy Avoided. “DOTA can be tracked prospectively (or retrospectively) with each intervention an ASP makes, and calculates an exact amount of antibiotic use avoided,” Dr. Laguio-Vila said. “If the ASP also tracks the types of antibiotic recommendations made according to infectious indication, comparison of DOTA between indications – such as pneumonia versus UTI [urinary tract infection] – can lead to ideas of which type of indication needs clinical guidelines development, or order set revision, or which type of infection the ASP should target to reduce high-risk antibiotics.”
Also, she added, because most ASPs have several types of interventions at once (such as education on pneumonia guidelines, as well as penicillin-allergy assessment), aggregate assessments of institutional antibiotic use like the DOT cannot quantify how much impact a specific intervention has accomplished. DOTA may offer a fairer assessment of the direct changes in antibiotic use resulting from specific ASP activities, because tracking DOTA is extracted from each specific patient intervention.
“Now that the Joint Commission has a requirement that all hospitals seeking JC accreditation have some form of an ASP in place and measure antibiotic use in some way at their institution, there may be numerous hospitals facing the same challenges with calculating a DOT. DOTA would meet these requirements, but in a ‘low tech’ way,” Dr. Laguio-Vila said. “For hospitalists with interests in being the antibiotic steward or champion for their institution, DOTA is an option for measuring antibiotic use.”
Reference
Datta S et al. Days of therapy avoided: A novel method for measuring the impact of an antimicrobial stewardship program to stop antibiotics. J Hosp Med. 2018 Feb 8. doi: 10.12788/jhm.2927.
A study compares the merits of DOT and DOTA
A study compares the merits of DOT and DOTA
The currently recommended method for hospital antimicrobial stewardship programs (ASPs) to measure antibiotic use is Days of Therapy/1,000 patient-days, but there are a few disadvantages of using the DOT, said Maryrose Laguio-Vila, MD, coauthor of a recent study on stewardship.
“For accurate measurement, it requires information technology (IT) support to assist an ASP in generating reports of antibiotic prescriptions and administrations to patients, often from an electronic medical record (EMR). In hospitals where there is no EMR, DOT is probably not easily done and would have to be manually extracted (a herculean task),” she said. “Second, DOT tends to be an aggregate measurement of antibiotics used at an institution or hospital location; if an ASP does a specific intervention targeting a group of antibiotics or infectious indication, changes in the hospital-wide DOT or drug-class DOT may not accurately reflect the exact impact of an ASP’s intervention.”
The paper offers an alternative/supplemental method for ASPs to quantify their impact on antibiotic use without using an EMR or needing IT support: Days of Therapy Avoided. “DOTA can be tracked prospectively (or retrospectively) with each intervention an ASP makes, and calculates an exact amount of antibiotic use avoided,” Dr. Laguio-Vila said. “If the ASP also tracks the types of antibiotic recommendations made according to infectious indication, comparison of DOTA between indications – such as pneumonia versus UTI [urinary tract infection] – can lead to ideas of which type of indication needs clinical guidelines development, or order set revision, or which type of infection the ASP should target to reduce high-risk antibiotics.”
Also, she added, because most ASPs have several types of interventions at once (such as education on pneumonia guidelines, as well as penicillin-allergy assessment), aggregate assessments of institutional antibiotic use like the DOT cannot quantify how much impact a specific intervention has accomplished. DOTA may offer a fairer assessment of the direct changes in antibiotic use resulting from specific ASP activities, because tracking DOTA is extracted from each specific patient intervention.
“Now that the Joint Commission has a requirement that all hospitals seeking JC accreditation have some form of an ASP in place and measure antibiotic use in some way at their institution, there may be numerous hospitals facing the same challenges with calculating a DOT. DOTA would meet these requirements, but in a ‘low tech’ way,” Dr. Laguio-Vila said. “For hospitalists with interests in being the antibiotic steward or champion for their institution, DOTA is an option for measuring antibiotic use.”
Reference
Datta S et al. Days of therapy avoided: A novel method for measuring the impact of an antimicrobial stewardship program to stop antibiotics. J Hosp Med. 2018 Feb 8. doi: 10.12788/jhm.2927.
The currently recommended method for hospital antimicrobial stewardship programs (ASPs) to measure antibiotic use is Days of Therapy/1,000 patient-days, but there are a few disadvantages of using the DOT, said Maryrose Laguio-Vila, MD, coauthor of a recent study on stewardship.
“For accurate measurement, it requires information technology (IT) support to assist an ASP in generating reports of antibiotic prescriptions and administrations to patients, often from an electronic medical record (EMR). In hospitals where there is no EMR, DOT is probably not easily done and would have to be manually extracted (a herculean task),” she said. “Second, DOT tends to be an aggregate measurement of antibiotics used at an institution or hospital location; if an ASP does a specific intervention targeting a group of antibiotics or infectious indication, changes in the hospital-wide DOT or drug-class DOT may not accurately reflect the exact impact of an ASP’s intervention.”
The paper offers an alternative/supplemental method for ASPs to quantify their impact on antibiotic use without using an EMR or needing IT support: Days of Therapy Avoided. “DOTA can be tracked prospectively (or retrospectively) with each intervention an ASP makes, and calculates an exact amount of antibiotic use avoided,” Dr. Laguio-Vila said. “If the ASP also tracks the types of antibiotic recommendations made according to infectious indication, comparison of DOTA between indications – such as pneumonia versus UTI [urinary tract infection] – can lead to ideas of which type of indication needs clinical guidelines development, or order set revision, or which type of infection the ASP should target to reduce high-risk antibiotics.”
Also, she added, because most ASPs have several types of interventions at once (such as education on pneumonia guidelines, as well as penicillin-allergy assessment), aggregate assessments of institutional antibiotic use like the DOT cannot quantify how much impact a specific intervention has accomplished. DOTA may offer a fairer assessment of the direct changes in antibiotic use resulting from specific ASP activities, because tracking DOTA is extracted from each specific patient intervention.
“Now that the Joint Commission has a requirement that all hospitals seeking JC accreditation have some form of an ASP in place and measure antibiotic use in some way at their institution, there may be numerous hospitals facing the same challenges with calculating a DOT. DOTA would meet these requirements, but in a ‘low tech’ way,” Dr. Laguio-Vila said. “For hospitalists with interests in being the antibiotic steward or champion for their institution, DOTA is an option for measuring antibiotic use.”
Reference
Datta S et al. Days of therapy avoided: A novel method for measuring the impact of an antimicrobial stewardship program to stop antibiotics. J Hosp Med. 2018 Feb 8. doi: 10.12788/jhm.2927.
2018-2019 flu season starts in earnest
National flu activity moved solidly into above-average territory during the week ending Dec. 15, as Colorado and Georgia took the lead with the highest activity levels in the country, according to the Centers for Disease Control and Prevention.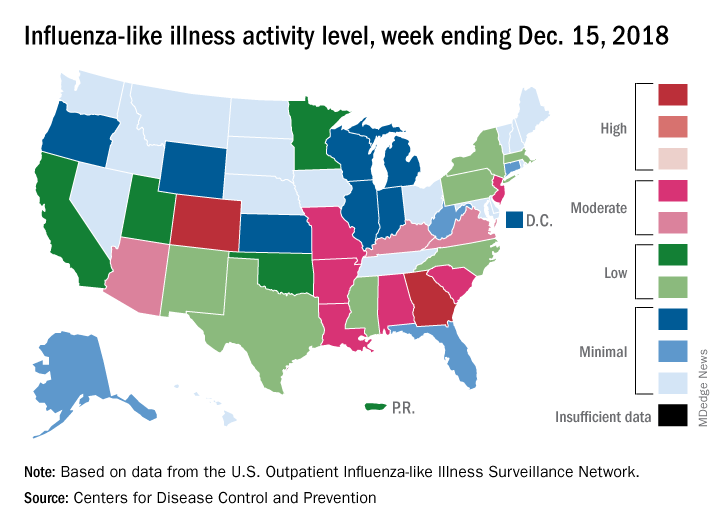
The proportion of outpatient visits for influenza-like illness (ILI) was 2.7% for the week, which was up from 2.3% the previous week and above the national baseline of 2.2%, the CDC reported. ILI is defined “as fever (temperature of 100°F [37.8°C] or greater) and cough and/or sore throat.”
Colorado and Georgia both reported ILI activity of 10 on the CDC’s 1-10 scale, making them the only states in the “high” range (8-10). Nine states and New York City had activity levels in the “moderate” range (6-7), Puerto Rico and 11 states were in the “low” range (4-5), and 28 states and the District of Columbia were in the “minimal” range (1-3), the CDC said.
During the comparable period of last year’s high-severity flu season, which ultimately resulted in 900,000 flu-related hospitalizations and 80,000 deaths (185 pediatric), nine states were already at level 10. For the 2018-2019 season so far, there have been seven ILI-related pediatric deaths, CDC data show.
National flu activity moved solidly into above-average territory during the week ending Dec. 15, as Colorado and Georgia took the lead with the highest activity levels in the country, according to the Centers for Disease Control and Prevention.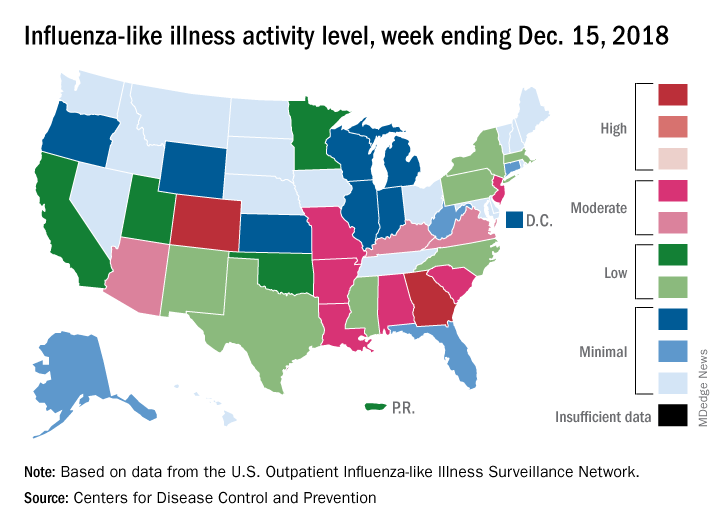
The proportion of outpatient visits for influenza-like illness (ILI) was 2.7% for the week, which was up from 2.3% the previous week and above the national baseline of 2.2%, the CDC reported. ILI is defined “as fever (temperature of 100°F [37.8°C] or greater) and cough and/or sore throat.”
Colorado and Georgia both reported ILI activity of 10 on the CDC’s 1-10 scale, making them the only states in the “high” range (8-10). Nine states and New York City had activity levels in the “moderate” range (6-7), Puerto Rico and 11 states were in the “low” range (4-5), and 28 states and the District of Columbia were in the “minimal” range (1-3), the CDC said.
During the comparable period of last year’s high-severity flu season, which ultimately resulted in 900,000 flu-related hospitalizations and 80,000 deaths (185 pediatric), nine states were already at level 10. For the 2018-2019 season so far, there have been seven ILI-related pediatric deaths, CDC data show.
National flu activity moved solidly into above-average territory during the week ending Dec. 15, as Colorado and Georgia took the lead with the highest activity levels in the country, according to the Centers for Disease Control and Prevention.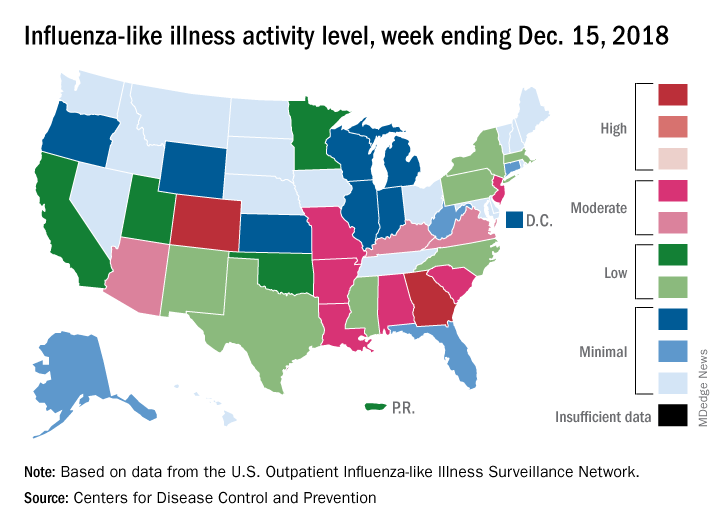
The proportion of outpatient visits for influenza-like illness (ILI) was 2.7% for the week, which was up from 2.3% the previous week and above the national baseline of 2.2%, the CDC reported. ILI is defined “as fever (temperature of 100°F [37.8°C] or greater) and cough and/or sore throat.”
Colorado and Georgia both reported ILI activity of 10 on the CDC’s 1-10 scale, making them the only states in the “high” range (8-10). Nine states and New York City had activity levels in the “moderate” range (6-7), Puerto Rico and 11 states were in the “low” range (4-5), and 28 states and the District of Columbia were in the “minimal” range (1-3), the CDC said.
During the comparable period of last year’s high-severity flu season, which ultimately resulted in 900,000 flu-related hospitalizations and 80,000 deaths (185 pediatric), nine states were already at level 10. For the 2018-2019 season so far, there have been seven ILI-related pediatric deaths, CDC data show.
Hospital medicine fellowships
Is it the right choice for me?
As Dr. Melanie Schaffer neared the end of her family medicine residency in the spring of 2015, she found herself considering a hospital medicine fellowship. Unsure if she could get a hospitalist job in an urban market given the outpatient focus of her training, Dr. Schaffer began searching for fellowships on the Society of Hospital Medicine website.1
Likewise, in 2014 Dr. Micah Prochaska was seriously contemplating a hospital medicine fellowship. He was about to graduate from internal medicine residency at the University of Chicago and was eager to gain skills and experience in clinical research.
In 2006, there were a total of 16 HM fellowship programs in the United States, catering to graduates of internal medicine, family medicine, and pediatric residencies.2 Since that time, the number of hospital medicine fellowships has grown considerably, paralleling the explosive growth of hospital medicine as a specialty. For example, at one point in the summer of 2018, the SHM website listed 13 clinical family practice fellowships, 29 internal medicine fellowships, and 26 pediatric fellowships. Each fellowship emphasized different aspects of hospital medicine including clinical practice, research, quality improvement, and leadership.
Now more than ever, residents interested in hospital medicine may get overwhelmed by the multitude of options for fellowship training. And the question remains: why pursue fellowship training in the first place?
“I learned that as a family physician it is harder to get a job as a hospitalist outside of smaller communities, and I wanted to have extra training and credentials,” Dr. Schaffer said. “I pursued a fellowship in hospital medicine to hone my inpatient skills, obtain more ICU exposure, and work on procedures.”
Dr. Schaffer’s online search eventually led her to the Advanced Hospital Medicine Fellowship at Swedish Medical Center in Seattle. This 1-year hospital medicine fellowship started in 2008 with an intentional clinical focus, aiming to provide additional training opportunities in hospital medicine primarily to family medicine residency graduates.
“The goal of our program is to bridge the gap between the training of family medicine and internal medicine so our trainees can refine and develop their inpatient skills,” said Dr. David Wilson, program director of the Swedish Hospitalist Fellowship.
During her fellowship year, Dr. Schaffer was caring for hospitalized adult patients on a general medical ward, with supervision from a dedicated group of teaching hospitalists. She also completed rotations in the ICU, on subspecialty services, and received advanced training in point-of-care ultrasound.
Now in her second year of practice as a full time adult hospitalist at Swedish Medical Center, Dr. Schaffer believes her year of hospital medicine fellowship prepared her well for her current position.
“I am constantly using the tools and knowledge I acquired during my fellowship year,” she said. “I would encourage anyone who has an interest in working on procedural skills and gaining more ICU exposure to pursue a similar fellowship.”
In contrast to Dr. Schaffer, Dr. Prochaska was satisfied with his clinical training but chose to pursue a hospital medicine fellowship to develop research skills. Prior to starting the 2-year Hospitalist Scholars Training Program at the University of Chicago in 2014, Dr. Prochaska had a clear vision of becoming a hospital medicine health outcomes investigator, and believed this career would not be possible without the additional training offered by a research-focused fellowship program.
The Hospitalist Scholars Program at the University of Chicago, one of the first programs of its kind, offers a built-in master’s degree to all participants. At the conclusion of his fellowship training in 2016, Dr. Prochaska completed his Master’s in Health Sciences, which gives considerable attention to biostatistics and epidemiology. According to Dr. Prochaska, the key to becoming a successful academic researcher lies in one’s ability to write grants and receive funding, a skill he honed during this fellowship.
Now on faculty at the University of Chicago in the Section of Hospital Medicine, Dr. Prochaska devotes approximately 75% of his time to research and 25% to patient care.
Beyond the research training and experience he gained during his hospital medicine fellowship, Dr. Prochaska said he values the mentorship afforded to him. He noted that one of the most meaningful experiences during his 2 years of fellowship was having the opportunity to sit down with his program directors, Dr. Vineet Arora and Dr. David Meltzer, to discuss the trajectory of his career in academic medicine.
“It is hard to find senior mentors in hospital medicine,” Dr. Prochaska said. “You could get a master’s degree on your own, but with the fellowship program, your mentors can help you think about the next steps in your career.”
For Dr. Schaffer and Dr. Prochaska, fellowship provided training and experience well-matched to their individual goals and helped foster their careers in hospital medicine. For some, however, a fellowship may not be a necessary step on the path to becoming a hospitalist. Many leaders in the field of hospital medicine have advanced in their careers without further training. In addition, receiving little more than a resident’s salary for an additional year or more during fellowship may not be financially tenable for some. Given the ongoing demand for hospitalists across the country, the lack of a fellowship on your resume may not significantly diminish your chances of securing a position, especially in the community setting.
In the end, the decision of whether to pursue a hospital medicine fellowship is a personal one, and the programs available are as varied as the individuals completing them. “Any hospitalist interested in more than simply patient care – potentially QI, medical education, policy, or administration – should consider a fellowship,” Dr. Prochaska said. “Hospitalists have a unique opportunity to be involved in all these areas, but there are absolutely critical skills you need to develop beyond your clinical skills to succeed.” Fellowships are one way to enhance these nonclinical skills.
The best advice to those considering a hospital medicine fellowship? Dedicate some time to engage in self-assessment and goal setting, before jumping to SHM’s online list of programs.
Ask yourself: “Where do I see myself in 10 years? What do I wish to accomplish in my career as a hospitalist? What additional training (clinical, research, quality improvement, leadership) might I need to achieve these goals? Will completion of a hospital medicine fellowship help me make this vision a reality?”
For Dr. Schaffer, a clinical practice–focused hospital medicine fellowship served as a necessary bridge between her family medicine residency and her current position as an adult hospitalist. While for Dr. Prochaska, a research-intensive hospital medicine fellowship was a key step in launching his academic career.
Of course, for many trainees at the end of residency, your self-assessment may lead you in the opposite direction. In that case it is time to find your first “real job” as an attending physician. But if you feel you need more training to meet your personal goals you should rest assured – whether now or in the future, there is almost certainly a hospital medicine fellowship that is right for you.
Dr. Schouten is a hospitalist at Mayo Clinic in Rochester, Minn., and serves on the Society of Hospital Medicine Physicians in Training Committee. Dr. Sundar is a hospitalist at Emory Saint Joseph’s Hospital in Sandy Springs, Ga., and serves as the Site Assistant Director for Education.
References
1. www.hospitalmedicine.org/membership/hospitalist-fellowships/
2. Ranji et al. “Hospital medicine fellowships: Works in progress.” American J Med. 2006 Jan;119(1):72.e1-7. doi: 10.1016/j.amjmed.2005.07.061.
Is it the right choice for me?
Is it the right choice for me?
As Dr. Melanie Schaffer neared the end of her family medicine residency in the spring of 2015, she found herself considering a hospital medicine fellowship. Unsure if she could get a hospitalist job in an urban market given the outpatient focus of her training, Dr. Schaffer began searching for fellowships on the Society of Hospital Medicine website.1
Likewise, in 2014 Dr. Micah Prochaska was seriously contemplating a hospital medicine fellowship. He was about to graduate from internal medicine residency at the University of Chicago and was eager to gain skills and experience in clinical research.
In 2006, there were a total of 16 HM fellowship programs in the United States, catering to graduates of internal medicine, family medicine, and pediatric residencies.2 Since that time, the number of hospital medicine fellowships has grown considerably, paralleling the explosive growth of hospital medicine as a specialty. For example, at one point in the summer of 2018, the SHM website listed 13 clinical family practice fellowships, 29 internal medicine fellowships, and 26 pediatric fellowships. Each fellowship emphasized different aspects of hospital medicine including clinical practice, research, quality improvement, and leadership.
Now more than ever, residents interested in hospital medicine may get overwhelmed by the multitude of options for fellowship training. And the question remains: why pursue fellowship training in the first place?
“I learned that as a family physician it is harder to get a job as a hospitalist outside of smaller communities, and I wanted to have extra training and credentials,” Dr. Schaffer said. “I pursued a fellowship in hospital medicine to hone my inpatient skills, obtain more ICU exposure, and work on procedures.”
Dr. Schaffer’s online search eventually led her to the Advanced Hospital Medicine Fellowship at Swedish Medical Center in Seattle. This 1-year hospital medicine fellowship started in 2008 with an intentional clinical focus, aiming to provide additional training opportunities in hospital medicine primarily to family medicine residency graduates.
“The goal of our program is to bridge the gap between the training of family medicine and internal medicine so our trainees can refine and develop their inpatient skills,” said Dr. David Wilson, program director of the Swedish Hospitalist Fellowship.
During her fellowship year, Dr. Schaffer was caring for hospitalized adult patients on a general medical ward, with supervision from a dedicated group of teaching hospitalists. She also completed rotations in the ICU, on subspecialty services, and received advanced training in point-of-care ultrasound.
Now in her second year of practice as a full time adult hospitalist at Swedish Medical Center, Dr. Schaffer believes her year of hospital medicine fellowship prepared her well for her current position.
“I am constantly using the tools and knowledge I acquired during my fellowship year,” she said. “I would encourage anyone who has an interest in working on procedural skills and gaining more ICU exposure to pursue a similar fellowship.”
In contrast to Dr. Schaffer, Dr. Prochaska was satisfied with his clinical training but chose to pursue a hospital medicine fellowship to develop research skills. Prior to starting the 2-year Hospitalist Scholars Training Program at the University of Chicago in 2014, Dr. Prochaska had a clear vision of becoming a hospital medicine health outcomes investigator, and believed this career would not be possible without the additional training offered by a research-focused fellowship program.
The Hospitalist Scholars Program at the University of Chicago, one of the first programs of its kind, offers a built-in master’s degree to all participants. At the conclusion of his fellowship training in 2016, Dr. Prochaska completed his Master’s in Health Sciences, which gives considerable attention to biostatistics and epidemiology. According to Dr. Prochaska, the key to becoming a successful academic researcher lies in one’s ability to write grants and receive funding, a skill he honed during this fellowship.
Now on faculty at the University of Chicago in the Section of Hospital Medicine, Dr. Prochaska devotes approximately 75% of his time to research and 25% to patient care.
Beyond the research training and experience he gained during his hospital medicine fellowship, Dr. Prochaska said he values the mentorship afforded to him. He noted that one of the most meaningful experiences during his 2 years of fellowship was having the opportunity to sit down with his program directors, Dr. Vineet Arora and Dr. David Meltzer, to discuss the trajectory of his career in academic medicine.
“It is hard to find senior mentors in hospital medicine,” Dr. Prochaska said. “You could get a master’s degree on your own, but with the fellowship program, your mentors can help you think about the next steps in your career.”
For Dr. Schaffer and Dr. Prochaska, fellowship provided training and experience well-matched to their individual goals and helped foster their careers in hospital medicine. For some, however, a fellowship may not be a necessary step on the path to becoming a hospitalist. Many leaders in the field of hospital medicine have advanced in their careers without further training. In addition, receiving little more than a resident’s salary for an additional year or more during fellowship may not be financially tenable for some. Given the ongoing demand for hospitalists across the country, the lack of a fellowship on your resume may not significantly diminish your chances of securing a position, especially in the community setting.
In the end, the decision of whether to pursue a hospital medicine fellowship is a personal one, and the programs available are as varied as the individuals completing them. “Any hospitalist interested in more than simply patient care – potentially QI, medical education, policy, or administration – should consider a fellowship,” Dr. Prochaska said. “Hospitalists have a unique opportunity to be involved in all these areas, but there are absolutely critical skills you need to develop beyond your clinical skills to succeed.” Fellowships are one way to enhance these nonclinical skills.
The best advice to those considering a hospital medicine fellowship? Dedicate some time to engage in self-assessment and goal setting, before jumping to SHM’s online list of programs.
Ask yourself: “Where do I see myself in 10 years? What do I wish to accomplish in my career as a hospitalist? What additional training (clinical, research, quality improvement, leadership) might I need to achieve these goals? Will completion of a hospital medicine fellowship help me make this vision a reality?”
For Dr. Schaffer, a clinical practice–focused hospital medicine fellowship served as a necessary bridge between her family medicine residency and her current position as an adult hospitalist. While for Dr. Prochaska, a research-intensive hospital medicine fellowship was a key step in launching his academic career.
Of course, for many trainees at the end of residency, your self-assessment may lead you in the opposite direction. In that case it is time to find your first “real job” as an attending physician. But if you feel you need more training to meet your personal goals you should rest assured – whether now or in the future, there is almost certainly a hospital medicine fellowship that is right for you.
Dr. Schouten is a hospitalist at Mayo Clinic in Rochester, Minn., and serves on the Society of Hospital Medicine Physicians in Training Committee. Dr. Sundar is a hospitalist at Emory Saint Joseph’s Hospital in Sandy Springs, Ga., and serves as the Site Assistant Director for Education.
References
1. www.hospitalmedicine.org/membership/hospitalist-fellowships/
2. Ranji et al. “Hospital medicine fellowships: Works in progress.” American J Med. 2006 Jan;119(1):72.e1-7. doi: 10.1016/j.amjmed.2005.07.061.
As Dr. Melanie Schaffer neared the end of her family medicine residency in the spring of 2015, she found herself considering a hospital medicine fellowship. Unsure if she could get a hospitalist job in an urban market given the outpatient focus of her training, Dr. Schaffer began searching for fellowships on the Society of Hospital Medicine website.1
Likewise, in 2014 Dr. Micah Prochaska was seriously contemplating a hospital medicine fellowship. He was about to graduate from internal medicine residency at the University of Chicago and was eager to gain skills and experience in clinical research.
In 2006, there were a total of 16 HM fellowship programs in the United States, catering to graduates of internal medicine, family medicine, and pediatric residencies.2 Since that time, the number of hospital medicine fellowships has grown considerably, paralleling the explosive growth of hospital medicine as a specialty. For example, at one point in the summer of 2018, the SHM website listed 13 clinical family practice fellowships, 29 internal medicine fellowships, and 26 pediatric fellowships. Each fellowship emphasized different aspects of hospital medicine including clinical practice, research, quality improvement, and leadership.
Now more than ever, residents interested in hospital medicine may get overwhelmed by the multitude of options for fellowship training. And the question remains: why pursue fellowship training in the first place?
“I learned that as a family physician it is harder to get a job as a hospitalist outside of smaller communities, and I wanted to have extra training and credentials,” Dr. Schaffer said. “I pursued a fellowship in hospital medicine to hone my inpatient skills, obtain more ICU exposure, and work on procedures.”
Dr. Schaffer’s online search eventually led her to the Advanced Hospital Medicine Fellowship at Swedish Medical Center in Seattle. This 1-year hospital medicine fellowship started in 2008 with an intentional clinical focus, aiming to provide additional training opportunities in hospital medicine primarily to family medicine residency graduates.
“The goal of our program is to bridge the gap between the training of family medicine and internal medicine so our trainees can refine and develop their inpatient skills,” said Dr. David Wilson, program director of the Swedish Hospitalist Fellowship.
During her fellowship year, Dr. Schaffer was caring for hospitalized adult patients on a general medical ward, with supervision from a dedicated group of teaching hospitalists. She also completed rotations in the ICU, on subspecialty services, and received advanced training in point-of-care ultrasound.
Now in her second year of practice as a full time adult hospitalist at Swedish Medical Center, Dr. Schaffer believes her year of hospital medicine fellowship prepared her well for her current position.
“I am constantly using the tools and knowledge I acquired during my fellowship year,” she said. “I would encourage anyone who has an interest in working on procedural skills and gaining more ICU exposure to pursue a similar fellowship.”
In contrast to Dr. Schaffer, Dr. Prochaska was satisfied with his clinical training but chose to pursue a hospital medicine fellowship to develop research skills. Prior to starting the 2-year Hospitalist Scholars Training Program at the University of Chicago in 2014, Dr. Prochaska had a clear vision of becoming a hospital medicine health outcomes investigator, and believed this career would not be possible without the additional training offered by a research-focused fellowship program.
The Hospitalist Scholars Program at the University of Chicago, one of the first programs of its kind, offers a built-in master’s degree to all participants. At the conclusion of his fellowship training in 2016, Dr. Prochaska completed his Master’s in Health Sciences, which gives considerable attention to biostatistics and epidemiology. According to Dr. Prochaska, the key to becoming a successful academic researcher lies in one’s ability to write grants and receive funding, a skill he honed during this fellowship.
Now on faculty at the University of Chicago in the Section of Hospital Medicine, Dr. Prochaska devotes approximately 75% of his time to research and 25% to patient care.
Beyond the research training and experience he gained during his hospital medicine fellowship, Dr. Prochaska said he values the mentorship afforded to him. He noted that one of the most meaningful experiences during his 2 years of fellowship was having the opportunity to sit down with his program directors, Dr. Vineet Arora and Dr. David Meltzer, to discuss the trajectory of his career in academic medicine.
“It is hard to find senior mentors in hospital medicine,” Dr. Prochaska said. “You could get a master’s degree on your own, but with the fellowship program, your mentors can help you think about the next steps in your career.”
For Dr. Schaffer and Dr. Prochaska, fellowship provided training and experience well-matched to their individual goals and helped foster their careers in hospital medicine. For some, however, a fellowship may not be a necessary step on the path to becoming a hospitalist. Many leaders in the field of hospital medicine have advanced in their careers without further training. In addition, receiving little more than a resident’s salary for an additional year or more during fellowship may not be financially tenable for some. Given the ongoing demand for hospitalists across the country, the lack of a fellowship on your resume may not significantly diminish your chances of securing a position, especially in the community setting.
In the end, the decision of whether to pursue a hospital medicine fellowship is a personal one, and the programs available are as varied as the individuals completing them. “Any hospitalist interested in more than simply patient care – potentially QI, medical education, policy, or administration – should consider a fellowship,” Dr. Prochaska said. “Hospitalists have a unique opportunity to be involved in all these areas, but there are absolutely critical skills you need to develop beyond your clinical skills to succeed.” Fellowships are one way to enhance these nonclinical skills.
The best advice to those considering a hospital medicine fellowship? Dedicate some time to engage in self-assessment and goal setting, before jumping to SHM’s online list of programs.
Ask yourself: “Where do I see myself in 10 years? What do I wish to accomplish in my career as a hospitalist? What additional training (clinical, research, quality improvement, leadership) might I need to achieve these goals? Will completion of a hospital medicine fellowship help me make this vision a reality?”
For Dr. Schaffer, a clinical practice–focused hospital medicine fellowship served as a necessary bridge between her family medicine residency and her current position as an adult hospitalist. While for Dr. Prochaska, a research-intensive hospital medicine fellowship was a key step in launching his academic career.
Of course, for many trainees at the end of residency, your self-assessment may lead you in the opposite direction. In that case it is time to find your first “real job” as an attending physician. But if you feel you need more training to meet your personal goals you should rest assured – whether now or in the future, there is almost certainly a hospital medicine fellowship that is right for you.
Dr. Schouten is a hospitalist at Mayo Clinic in Rochester, Minn., and serves on the Society of Hospital Medicine Physicians in Training Committee. Dr. Sundar is a hospitalist at Emory Saint Joseph’s Hospital in Sandy Springs, Ga., and serves as the Site Assistant Director for Education.
References
1. www.hospitalmedicine.org/membership/hospitalist-fellowships/
2. Ranji et al. “Hospital medicine fellowships: Works in progress.” American J Med. 2006 Jan;119(1):72.e1-7. doi: 10.1016/j.amjmed.2005.07.061.
Ingredients for effective team-based care
Changing times for U.S. health care
The current health care environment is undergoing a rapid transformation. In evolutionary biology, a theory exists called punctuated equilibrium. This theory suggests there are long periods of little or no morphological change amongst species and then, geologically speaking, short periods of rapid change in response to pressures within the environment. This rapid period of change adds significant diversity to the landscape of existing species. In health care, we are undergoing a period of “punctuation.”
A testament to the degree of change is a scan of the various consolidation activities occurring across the health care space. Some are more traditional, such as mergers of health systems with different or competing geographical footprints or hospitalist management companies that provide similar services and desire to increase their market share. Others that are more interesting are those that include mergers of seemingly different business lines or offerings, like CVS Health and Aetna; Humana and Kindred; or even organizations such as Amazon, Berkshire Hathaway, and JP Morgan hiring Atul Gawande as the CEO of their newly formed health care venture. The latter examples serve as an illustration of the reorganization that is occurring within health care delivery. This represents, at the very least, a blurring of the lines – if not a deconstruction and complete rebuild – of traditional lines of separation between payers, providers, employers, and retailers.
In other words, the silos are coming down, significant diversity in the landscape of existing species. A common theme across these changes is that most – if not all – participants will share some portion of the financial risk associated with these evolving models. High-deductible health plans, alternative payment models (APMs), and advanced APMs are examples of tactics and models that distribute the financial risk. The consolidations referenced above will likely continue to encourage distribution of the financial risk across patients, providers, employers, and payers.
A key theme coming into focus is that the evolving care delivery system will not be defined by bricks and mortar. Rather, it will follow the patient and go wherever he or she goes to meet his or her specific needs. This is why we’re seeing mergers comprised of a variety of assets, including personnel, technology, critical supplies (such as pharmaceuticals), and funding resources. This very purposeful and deliberate melting pot phenomenon will restructure and reformat the care delivery model.
To be successful within this new landscape, there will need to be a renewed focus on working within a collaborative model. The days of a single entity or provider being able to serve as the “be all” or “do all” is over, and the days of practicing medicine as the Lone Ranger are anachronistic. Instead, there is a need for health care providers to embrace and lead a team-based care model. Team-based care should have the patient at the center of the care delivery model and leverage the expertise of the various team members to practice at the “top of their expertise.”
In hospital medicine, this includes a variety of team members – from physicians, nurse practitioners, physician assistants, and clinical pharmacists to case managers, physical therapists, subject matter experts in quality improvement, and analysts – who identify operational priorities from the data rather than reporting predefined goals on dashboards. Although possibly a good start, this is by no means an exhaustive list of team members. The team will be defined by the goals the health care team aspires to achieve. These goals may include closer alignment with payers, employers, and post-acute partners; the goals will influence the composition of the team. Once the team is defined, the challenge will be to effectively integrate team members, so they are contributing their expertise to the patient care being delivered.
Some ingredients for effective team-based care include the following:
- Developing an effective process for engagement and providing a voice for all team members. Interdisciplinary team rounds where there is an established time for team members to plan and operationalize their plans around patient care can serve as an example of this type of structured process.
- Creating well-defined roles and responsibilities with key performance indicators to promote accountability. The team will have outcomes they are measuring and striving to impact, and each team member will have a role in achieving those goals. Being able to parse out and measure how each team member contributes to the overall outcome can be beneficial. This provides an opportunity for each team member to play a meaningful role in accomplishing the overall goal and allows for a measurement process to track success. For example, an overall team goal may be to have a specific percentage of eligible discharges completed by 11:00 a.m. To accomplish this goal, there may be specific objectives for the clinicians to have discharge orders in the chart by 9:30 a.m. and for case management to have communicated with any post-acute services the day before discharge. These specific accountability measures facilitate accomplishing the larger team goal.
- Developing a culture of safety and transparency. Effective teams promote an environment where all members are empowered and encouraged to speak and share their perspective and knowledge. Communication is based on the value it provides to accomplishing the team’s goals rather than based on a hierarchy which determines who contributes and when.
- Defining and then redefining the competencies required of the team to promote continued development and growth. In this time of dynamic change, the skill sets that helped us get where we are today may be different then the skill sets that are needed for success in the future. There will continue to be a need for functional and knowledge-based competencies in addition to the need to focus on competencies that engender a culture of team-based care. For example, hospitalist leaders will need to understand evidence-based medicine to support appropriate management of a septic patient and simultaneously understand evidence-based management/leadership to affect sepsis care across his or her health care system.
With this change in the health care environment come new and exciting opportunities. Hospital medicine has always elected to assume a leadership role in these times of change, these periods of “punctuation.” Development of effective team-based care is a great place for those of us working in hospital medicine to demonstrate our leadership as we care for our patients.
Dr. Frost is national medical director, hospital-based services, at LifePoint Health, Brentwood, Tenn. He is president-elect of the Society of Hospital Medicine.
Changing times for U.S. health care
Changing times for U.S. health care
The current health care environment is undergoing a rapid transformation. In evolutionary biology, a theory exists called punctuated equilibrium. This theory suggests there are long periods of little or no morphological change amongst species and then, geologically speaking, short periods of rapid change in response to pressures within the environment. This rapid period of change adds significant diversity to the landscape of existing species. In health care, we are undergoing a period of “punctuation.”
A testament to the degree of change is a scan of the various consolidation activities occurring across the health care space. Some are more traditional, such as mergers of health systems with different or competing geographical footprints or hospitalist management companies that provide similar services and desire to increase their market share. Others that are more interesting are those that include mergers of seemingly different business lines or offerings, like CVS Health and Aetna; Humana and Kindred; or even organizations such as Amazon, Berkshire Hathaway, and JP Morgan hiring Atul Gawande as the CEO of their newly formed health care venture. The latter examples serve as an illustration of the reorganization that is occurring within health care delivery. This represents, at the very least, a blurring of the lines – if not a deconstruction and complete rebuild – of traditional lines of separation between payers, providers, employers, and retailers.
In other words, the silos are coming down, significant diversity in the landscape of existing species. A common theme across these changes is that most – if not all – participants will share some portion of the financial risk associated with these evolving models. High-deductible health plans, alternative payment models (APMs), and advanced APMs are examples of tactics and models that distribute the financial risk. The consolidations referenced above will likely continue to encourage distribution of the financial risk across patients, providers, employers, and payers.
A key theme coming into focus is that the evolving care delivery system will not be defined by bricks and mortar. Rather, it will follow the patient and go wherever he or she goes to meet his or her specific needs. This is why we’re seeing mergers comprised of a variety of assets, including personnel, technology, critical supplies (such as pharmaceuticals), and funding resources. This very purposeful and deliberate melting pot phenomenon will restructure and reformat the care delivery model.
To be successful within this new landscape, there will need to be a renewed focus on working within a collaborative model. The days of a single entity or provider being able to serve as the “be all” or “do all” is over, and the days of practicing medicine as the Lone Ranger are anachronistic. Instead, there is a need for health care providers to embrace and lead a team-based care model. Team-based care should have the patient at the center of the care delivery model and leverage the expertise of the various team members to practice at the “top of their expertise.”
In hospital medicine, this includes a variety of team members – from physicians, nurse practitioners, physician assistants, and clinical pharmacists to case managers, physical therapists, subject matter experts in quality improvement, and analysts – who identify operational priorities from the data rather than reporting predefined goals on dashboards. Although possibly a good start, this is by no means an exhaustive list of team members. The team will be defined by the goals the health care team aspires to achieve. These goals may include closer alignment with payers, employers, and post-acute partners; the goals will influence the composition of the team. Once the team is defined, the challenge will be to effectively integrate team members, so they are contributing their expertise to the patient care being delivered.
Some ingredients for effective team-based care include the following:
- Developing an effective process for engagement and providing a voice for all team members. Interdisciplinary team rounds where there is an established time for team members to plan and operationalize their plans around patient care can serve as an example of this type of structured process.
- Creating well-defined roles and responsibilities with key performance indicators to promote accountability. The team will have outcomes they are measuring and striving to impact, and each team member will have a role in achieving those goals. Being able to parse out and measure how each team member contributes to the overall outcome can be beneficial. This provides an opportunity for each team member to play a meaningful role in accomplishing the overall goal and allows for a measurement process to track success. For example, an overall team goal may be to have a specific percentage of eligible discharges completed by 11:00 a.m. To accomplish this goal, there may be specific objectives for the clinicians to have discharge orders in the chart by 9:30 a.m. and for case management to have communicated with any post-acute services the day before discharge. These specific accountability measures facilitate accomplishing the larger team goal.
- Developing a culture of safety and transparency. Effective teams promote an environment where all members are empowered and encouraged to speak and share their perspective and knowledge. Communication is based on the value it provides to accomplishing the team’s goals rather than based on a hierarchy which determines who contributes and when.
- Defining and then redefining the competencies required of the team to promote continued development and growth. In this time of dynamic change, the skill sets that helped us get where we are today may be different then the skill sets that are needed for success in the future. There will continue to be a need for functional and knowledge-based competencies in addition to the need to focus on competencies that engender a culture of team-based care. For example, hospitalist leaders will need to understand evidence-based medicine to support appropriate management of a septic patient and simultaneously understand evidence-based management/leadership to affect sepsis care across his or her health care system.
With this change in the health care environment come new and exciting opportunities. Hospital medicine has always elected to assume a leadership role in these times of change, these periods of “punctuation.” Development of effective team-based care is a great place for those of us working in hospital medicine to demonstrate our leadership as we care for our patients.
Dr. Frost is national medical director, hospital-based services, at LifePoint Health, Brentwood, Tenn. He is president-elect of the Society of Hospital Medicine.
The current health care environment is undergoing a rapid transformation. In evolutionary biology, a theory exists called punctuated equilibrium. This theory suggests there are long periods of little or no morphological change amongst species and then, geologically speaking, short periods of rapid change in response to pressures within the environment. This rapid period of change adds significant diversity to the landscape of existing species. In health care, we are undergoing a period of “punctuation.”
A testament to the degree of change is a scan of the various consolidation activities occurring across the health care space. Some are more traditional, such as mergers of health systems with different or competing geographical footprints or hospitalist management companies that provide similar services and desire to increase their market share. Others that are more interesting are those that include mergers of seemingly different business lines or offerings, like CVS Health and Aetna; Humana and Kindred; or even organizations such as Amazon, Berkshire Hathaway, and JP Morgan hiring Atul Gawande as the CEO of their newly formed health care venture. The latter examples serve as an illustration of the reorganization that is occurring within health care delivery. This represents, at the very least, a blurring of the lines – if not a deconstruction and complete rebuild – of traditional lines of separation between payers, providers, employers, and retailers.
In other words, the silos are coming down, significant diversity in the landscape of existing species. A common theme across these changes is that most – if not all – participants will share some portion of the financial risk associated with these evolving models. High-deductible health plans, alternative payment models (APMs), and advanced APMs are examples of tactics and models that distribute the financial risk. The consolidations referenced above will likely continue to encourage distribution of the financial risk across patients, providers, employers, and payers.
A key theme coming into focus is that the evolving care delivery system will not be defined by bricks and mortar. Rather, it will follow the patient and go wherever he or she goes to meet his or her specific needs. This is why we’re seeing mergers comprised of a variety of assets, including personnel, technology, critical supplies (such as pharmaceuticals), and funding resources. This very purposeful and deliberate melting pot phenomenon will restructure and reformat the care delivery model.
To be successful within this new landscape, there will need to be a renewed focus on working within a collaborative model. The days of a single entity or provider being able to serve as the “be all” or “do all” is over, and the days of practicing medicine as the Lone Ranger are anachronistic. Instead, there is a need for health care providers to embrace and lead a team-based care model. Team-based care should have the patient at the center of the care delivery model and leverage the expertise of the various team members to practice at the “top of their expertise.”
In hospital medicine, this includes a variety of team members – from physicians, nurse practitioners, physician assistants, and clinical pharmacists to case managers, physical therapists, subject matter experts in quality improvement, and analysts – who identify operational priorities from the data rather than reporting predefined goals on dashboards. Although possibly a good start, this is by no means an exhaustive list of team members. The team will be defined by the goals the health care team aspires to achieve. These goals may include closer alignment with payers, employers, and post-acute partners; the goals will influence the composition of the team. Once the team is defined, the challenge will be to effectively integrate team members, so they are contributing their expertise to the patient care being delivered.
Some ingredients for effective team-based care include the following:
- Developing an effective process for engagement and providing a voice for all team members. Interdisciplinary team rounds where there is an established time for team members to plan and operationalize their plans around patient care can serve as an example of this type of structured process.
- Creating well-defined roles and responsibilities with key performance indicators to promote accountability. The team will have outcomes they are measuring and striving to impact, and each team member will have a role in achieving those goals. Being able to parse out and measure how each team member contributes to the overall outcome can be beneficial. This provides an opportunity for each team member to play a meaningful role in accomplishing the overall goal and allows for a measurement process to track success. For example, an overall team goal may be to have a specific percentage of eligible discharges completed by 11:00 a.m. To accomplish this goal, there may be specific objectives for the clinicians to have discharge orders in the chart by 9:30 a.m. and for case management to have communicated with any post-acute services the day before discharge. These specific accountability measures facilitate accomplishing the larger team goal.
- Developing a culture of safety and transparency. Effective teams promote an environment where all members are empowered and encouraged to speak and share their perspective and knowledge. Communication is based on the value it provides to accomplishing the team’s goals rather than based on a hierarchy which determines who contributes and when.
- Defining and then redefining the competencies required of the team to promote continued development and growth. In this time of dynamic change, the skill sets that helped us get where we are today may be different then the skill sets that are needed for success in the future. There will continue to be a need for functional and knowledge-based competencies in addition to the need to focus on competencies that engender a culture of team-based care. For example, hospitalist leaders will need to understand evidence-based medicine to support appropriate management of a septic patient and simultaneously understand evidence-based management/leadership to affect sepsis care across his or her health care system.
With this change in the health care environment come new and exciting opportunities. Hospital medicine has always elected to assume a leadership role in these times of change, these periods of “punctuation.” Development of effective team-based care is a great place for those of us working in hospital medicine to demonstrate our leadership as we care for our patients.
Dr. Frost is national medical director, hospital-based services, at LifePoint Health, Brentwood, Tenn. He is president-elect of the Society of Hospital Medicine.
Launching an HIV testing reminder
Trying a new tool to reduce infection rates
The world’s largest gay dating app, Grindr, changed its software earlier this year to create reminders for users to get regular HIV tests.
According to Grindr, 3.3 million users around the world visit the site daily; it sends those who opt into the service a reminder every 3-6 months to get a test. The message also directs them to the nearest testing site. Grindr also plans to give clinics, gay community centers, and other testing sites free advertising.
Among health care providers, the decision has been widely applauded. “This will ‘demedicalize’ testing and destigmatize it,” Perry N. Halkitis, PhD, dean of the Rutgers School of Public Health, in Newark, N.J., told the New York Times. “The more you make it normal, the more people are going to access it.”
Studies have shown that reminders by text or phone can triple or quadruple the chance that the recipient will get tested.
Reference
McNeil Jr. DG. Grindr App to Offer H.I.V. Test Reminders. The New York Times. March 26, 2018. Accessed April 5, 2018.
Trying a new tool to reduce infection rates
Trying a new tool to reduce infection rates
The world’s largest gay dating app, Grindr, changed its software earlier this year to create reminders for users to get regular HIV tests.
According to Grindr, 3.3 million users around the world visit the site daily; it sends those who opt into the service a reminder every 3-6 months to get a test. The message also directs them to the nearest testing site. Grindr also plans to give clinics, gay community centers, and other testing sites free advertising.
Among health care providers, the decision has been widely applauded. “This will ‘demedicalize’ testing and destigmatize it,” Perry N. Halkitis, PhD, dean of the Rutgers School of Public Health, in Newark, N.J., told the New York Times. “The more you make it normal, the more people are going to access it.”
Studies have shown that reminders by text or phone can triple or quadruple the chance that the recipient will get tested.
Reference
McNeil Jr. DG. Grindr App to Offer H.I.V. Test Reminders. The New York Times. March 26, 2018. Accessed April 5, 2018.
The world’s largest gay dating app, Grindr, changed its software earlier this year to create reminders for users to get regular HIV tests.
According to Grindr, 3.3 million users around the world visit the site daily; it sends those who opt into the service a reminder every 3-6 months to get a test. The message also directs them to the nearest testing site. Grindr also plans to give clinics, gay community centers, and other testing sites free advertising.
Among health care providers, the decision has been widely applauded. “This will ‘demedicalize’ testing and destigmatize it,” Perry N. Halkitis, PhD, dean of the Rutgers School of Public Health, in Newark, N.J., told the New York Times. “The more you make it normal, the more people are going to access it.”
Studies have shown that reminders by text or phone can triple or quadruple the chance that the recipient will get tested.
Reference
McNeil Jr. DG. Grindr App to Offer H.I.V. Test Reminders. The New York Times. March 26, 2018. Accessed April 5, 2018.
Designing a better EHR
Hospitals can create a more effective system
It’s well known that overuse is an enormous problem in medicine, and when it comes to antibiotics, the problem is even more striking.
“Half of all inpatient antibiotic use is inappropriate,” says Valerie Vaughn, MD, MSc, a hospitalist at the University of Michigan, Ann Arbor, and coauthor of a BMJ editorial about EHRs and antibiotic overuse.
“This has led to an increase in antibiotic-related adverse events (~20% of all hospitalized patients on antibiotics), Clostridium difficile infections (half a million infections and 29,000 deaths in U.S. annually), and resistant bacteria (which now account for nearly 12% of all bacterial infections, costing $2.2 billion annually).”
EHRs can be a tool to combat that trend – if they are well designed. Clinicians are influenced by the design of their electronic health record, Dr. Vaughn said. “Rather than leave its influence to chance, we should capitalize on what is known about design to promote appropriate testing and treatment through the EHR.” Hospitalists – integral to quality improvement – can have a role in making these changes.
“These improvements will be the most effective if behavioral economics and nudging are considered while designing,” Dr. Vaughn said. “For example, when creating order sets, list recommended options first and when possible make them the default,” she said. “This little change will greatly improve appropriate use.”
For every hour physicians spend on direct patient care, they spend another two with the EHR, Dr. Vaughn wrote. “Given this degree of attention, it is not surprising that the EHR influences physician behavior, especially the overuse of low-value medical care. … Displaying brand-name instead of generic options leads to more expensive prescribing. Allowing labs to be ordered recurrently increases unnecessary phlebotomy. Even individually listing inappropriate antibiotics (rather than grouping them) can make them more noticeable, resulting in more broad-spectrum use.”
“All hospitalists – and humans – are affected by knee-jerk responses. One of the most common in medicine is the urge to treat a positive culture or any positive test. Recognize this urge and resist!” she said. “Antibiotics may be the correct response, but clinicians should first think about whether treatment is necessary based on that patient’s symptoms and comorbidities. Resist the knee-jerk urge to give antibiotics for every positive culture.”
Reference
Vaughn VM et al. Thoughtless design of the electronic health record drives overuse, but purposeful design can nudge improved patient care. BMJ Qual Saf. 24 Mar 2018. doi: 10.1136/bmjqs-2017-007578.
Hospitals can create a more effective system
Hospitals can create a more effective system
It’s well known that overuse is an enormous problem in medicine, and when it comes to antibiotics, the problem is even more striking.
“Half of all inpatient antibiotic use is inappropriate,” says Valerie Vaughn, MD, MSc, a hospitalist at the University of Michigan, Ann Arbor, and coauthor of a BMJ editorial about EHRs and antibiotic overuse.
“This has led to an increase in antibiotic-related adverse events (~20% of all hospitalized patients on antibiotics), Clostridium difficile infections (half a million infections and 29,000 deaths in U.S. annually), and resistant bacteria (which now account for nearly 12% of all bacterial infections, costing $2.2 billion annually).”
EHRs can be a tool to combat that trend – if they are well designed. Clinicians are influenced by the design of their electronic health record, Dr. Vaughn said. “Rather than leave its influence to chance, we should capitalize on what is known about design to promote appropriate testing and treatment through the EHR.” Hospitalists – integral to quality improvement – can have a role in making these changes.
“These improvements will be the most effective if behavioral economics and nudging are considered while designing,” Dr. Vaughn said. “For example, when creating order sets, list recommended options first and when possible make them the default,” she said. “This little change will greatly improve appropriate use.”
For every hour physicians spend on direct patient care, they spend another two with the EHR, Dr. Vaughn wrote. “Given this degree of attention, it is not surprising that the EHR influences physician behavior, especially the overuse of low-value medical care. … Displaying brand-name instead of generic options leads to more expensive prescribing. Allowing labs to be ordered recurrently increases unnecessary phlebotomy. Even individually listing inappropriate antibiotics (rather than grouping them) can make them more noticeable, resulting in more broad-spectrum use.”
“All hospitalists – and humans – are affected by knee-jerk responses. One of the most common in medicine is the urge to treat a positive culture or any positive test. Recognize this urge and resist!” she said. “Antibiotics may be the correct response, but clinicians should first think about whether treatment is necessary based on that patient’s symptoms and comorbidities. Resist the knee-jerk urge to give antibiotics for every positive culture.”
Reference
Vaughn VM et al. Thoughtless design of the electronic health record drives overuse, but purposeful design can nudge improved patient care. BMJ Qual Saf. 24 Mar 2018. doi: 10.1136/bmjqs-2017-007578.
It’s well known that overuse is an enormous problem in medicine, and when it comes to antibiotics, the problem is even more striking.
“Half of all inpatient antibiotic use is inappropriate,” says Valerie Vaughn, MD, MSc, a hospitalist at the University of Michigan, Ann Arbor, and coauthor of a BMJ editorial about EHRs and antibiotic overuse.
“This has led to an increase in antibiotic-related adverse events (~20% of all hospitalized patients on antibiotics), Clostridium difficile infections (half a million infections and 29,000 deaths in U.S. annually), and resistant bacteria (which now account for nearly 12% of all bacterial infections, costing $2.2 billion annually).”
EHRs can be a tool to combat that trend – if they are well designed. Clinicians are influenced by the design of their electronic health record, Dr. Vaughn said. “Rather than leave its influence to chance, we should capitalize on what is known about design to promote appropriate testing and treatment through the EHR.” Hospitalists – integral to quality improvement – can have a role in making these changes.
“These improvements will be the most effective if behavioral economics and nudging are considered while designing,” Dr. Vaughn said. “For example, when creating order sets, list recommended options first and when possible make them the default,” she said. “This little change will greatly improve appropriate use.”
For every hour physicians spend on direct patient care, they spend another two with the EHR, Dr. Vaughn wrote. “Given this degree of attention, it is not surprising that the EHR influences physician behavior, especially the overuse of low-value medical care. … Displaying brand-name instead of generic options leads to more expensive prescribing. Allowing labs to be ordered recurrently increases unnecessary phlebotomy. Even individually listing inappropriate antibiotics (rather than grouping them) can make them more noticeable, resulting in more broad-spectrum use.”
“All hospitalists – and humans – are affected by knee-jerk responses. One of the most common in medicine is the urge to treat a positive culture or any positive test. Recognize this urge and resist!” she said. “Antibiotics may be the correct response, but clinicians should first think about whether treatment is necessary based on that patient’s symptoms and comorbidities. Resist the knee-jerk urge to give antibiotics for every positive culture.”
Reference
Vaughn VM et al. Thoughtless design of the electronic health record drives overuse, but purposeful design can nudge improved patient care. BMJ Qual Saf. 24 Mar 2018. doi: 10.1136/bmjqs-2017-007578.