User login
Patient-centered primed communication and goals-of-care discussions
Clinical question: Can primed communication increase the frequency of goals-of-care conversations in the outpatient setting?
Background: Effective outpatient communication helps patients and families with serious illnesses with increased quality of life, improved quality of the dying process, and decreased resource utilization at the end of life.
Study design: Cluster-randomized trial.
Setting: Multicenter, primary care, and subspecialty clinics for adults in the Pacific Northwest.
Synopsis: Patients with advanced age and/or severe chronic medical conditions were selected to participate. The median survival for these patients was 2 years. Clinicians were eligible to participate if they had five or more of the selected patients in their panel.
In the intervention group (57 clinicians and 184 patients), all patients were surveyed to identify preferences, barriers, and facilitators for goals-of-care discussions. These data were compiled into “Jumpstart Tips” and distributed to providers before a visit with a study patient. The control group (57 clinicians and 211 patients) had patients complete these surveys but no information was provided to clinicians.
The “Jumpstart Tips” led to an increase in patient-reported (74% vs. 31%; P less than .001) and EHR-documented (62% vs. 17%; P less than .001) occurrences of goals-of-care discussions. Patients also reported increased quality of these conversations (4.6 vs. 2.1; P = .01).
However, no significant improvements were noted in goal-concordant care, depression, or anxiety scores, which may have been because of selection bias and overall difficulty in defining goal-concordant care.
Bottom line: Patient-centered primed communication can increase the frequency and quality of goals-of-care discussions in the outpatient setting.
Citation: Curtis JR et al. Effect of a patient and clinician communication-priming intervention on patient-reported goals-of-care discussions between patients with serious illness and clinicians: A randomized clinical trial. JAMA Intern Med. 2018 Jul 1;178(7):930-40.
Dr. Chowdury is an assistant professor in the division of hospital medicine, University of Colorado, Denver.
Clinical question: Can primed communication increase the frequency of goals-of-care conversations in the outpatient setting?
Background: Effective outpatient communication helps patients and families with serious illnesses with increased quality of life, improved quality of the dying process, and decreased resource utilization at the end of life.
Study design: Cluster-randomized trial.
Setting: Multicenter, primary care, and subspecialty clinics for adults in the Pacific Northwest.
Synopsis: Patients with advanced age and/or severe chronic medical conditions were selected to participate. The median survival for these patients was 2 years. Clinicians were eligible to participate if they had five or more of the selected patients in their panel.
In the intervention group (57 clinicians and 184 patients), all patients were surveyed to identify preferences, barriers, and facilitators for goals-of-care discussions. These data were compiled into “Jumpstart Tips” and distributed to providers before a visit with a study patient. The control group (57 clinicians and 211 patients) had patients complete these surveys but no information was provided to clinicians.
The “Jumpstart Tips” led to an increase in patient-reported (74% vs. 31%; P less than .001) and EHR-documented (62% vs. 17%; P less than .001) occurrences of goals-of-care discussions. Patients also reported increased quality of these conversations (4.6 vs. 2.1; P = .01).
However, no significant improvements were noted in goal-concordant care, depression, or anxiety scores, which may have been because of selection bias and overall difficulty in defining goal-concordant care.
Bottom line: Patient-centered primed communication can increase the frequency and quality of goals-of-care discussions in the outpatient setting.
Citation: Curtis JR et al. Effect of a patient and clinician communication-priming intervention on patient-reported goals-of-care discussions between patients with serious illness and clinicians: A randomized clinical trial. JAMA Intern Med. 2018 Jul 1;178(7):930-40.
Dr. Chowdury is an assistant professor in the division of hospital medicine, University of Colorado, Denver.
Clinical question: Can primed communication increase the frequency of goals-of-care conversations in the outpatient setting?
Background: Effective outpatient communication helps patients and families with serious illnesses with increased quality of life, improved quality of the dying process, and decreased resource utilization at the end of life.
Study design: Cluster-randomized trial.
Setting: Multicenter, primary care, and subspecialty clinics for adults in the Pacific Northwest.
Synopsis: Patients with advanced age and/or severe chronic medical conditions were selected to participate. The median survival for these patients was 2 years. Clinicians were eligible to participate if they had five or more of the selected patients in their panel.
In the intervention group (57 clinicians and 184 patients), all patients were surveyed to identify preferences, barriers, and facilitators for goals-of-care discussions. These data were compiled into “Jumpstart Tips” and distributed to providers before a visit with a study patient. The control group (57 clinicians and 211 patients) had patients complete these surveys but no information was provided to clinicians.
The “Jumpstart Tips” led to an increase in patient-reported (74% vs. 31%; P less than .001) and EHR-documented (62% vs. 17%; P less than .001) occurrences of goals-of-care discussions. Patients also reported increased quality of these conversations (4.6 vs. 2.1; P = .01).
However, no significant improvements were noted in goal-concordant care, depression, or anxiety scores, which may have been because of selection bias and overall difficulty in defining goal-concordant care.
Bottom line: Patient-centered primed communication can increase the frequency and quality of goals-of-care discussions in the outpatient setting.
Citation: Curtis JR et al. Effect of a patient and clinician communication-priming intervention on patient-reported goals-of-care discussions between patients with serious illness and clinicians: A randomized clinical trial. JAMA Intern Med. 2018 Jul 1;178(7):930-40.
Dr. Chowdury is an assistant professor in the division of hospital medicine, University of Colorado, Denver.
Hospitalist groups explore use of medical scribes
Can scribes reduce doctors’ job stress?
Physician stress and burnout remain major concerns for the U.S. health care system, with frustrations over the electronic health record (EHR) driving much of the dissatisfaction experienced by hospitalists and other physicians in the hospital.1 Underlying the EHR conundrum is a deeper question: Is entering clinical data on a computer the best use of a doctor’s time and professional skills? Or could a portion of that clerical function be delegated to nonphysicians?
Trained medical scribes, charting specialists who input EHR data for physicians on rounds, have been offered as a solution to potentially affect job stress for physicians and shorten their work days. But while scribes have been used and tested by different hospitalist groups around the country, the concept has not taken off in hospital medicine the way it has in certain other settings, such as emergency departments.
“The demand for scribes doesn’t seem to have materialized in a big way for hospital medicine,” said John Nelson, MD, MHM, a hospitalist and consultant in Bellevue, Wash., and a cofounder of the Society of Hospital Medicine. “I’m not convinced that scribes have had a big impact on hospitalist burnout.” It’s difficult to share scribes between doctors on a shift, and it’s a problem if the scribe and doctor get physically separated in the hospital. There’s also the question of who should pay the scribe’s salary, Dr. Nelson said.
Frustrations with the EHR can be a major factor in the experience of physician burnout, but Dr. Nelson said hospitalists can get proficient more quickly because they’re using the same computer system all day. “The bigger problem is that other doctors like surgeons don’t learn how to use the EHR and dump their routine tasks involving the EHR on the hospitalist, which means more work that is less satisfying.”
Could pairing a scribe with a hospitalist improve efficiency and decrease costs relative to the expense of employing the scribe? Are there specific settings, applications, and caseloads in hospital medicine where it makes more sense to use a scribe to support and assist doctors while they’re meeting with patients, with the doctor reviewing and editing the scribe’s work for accuracy? Could the scribe even help with physician staffing shortages by making doctors more productive?
TeamHealth, a national physician services company based in Knoxville, Tenn., has used scribes in emergency departments for years but had concluded that they made less sense for its hospitalist groups after a failure to document significant net increases in productivity, according to a 2015 report in The Hospitalist.2 Michael Corvini, MD, FACP, FACEP, TeamHealth’s new regional medical director for acute care services, said he brought extensive positive experience with scribes to his new job and is quite excited about their potential for hospital medicine. “When I came to TeamHealth in July, I began to suggest that there was unrealized potential for scribes,” he said.
Dr. Corvini noted that a potential benefit of scribes for patients is that their presence may allow for more face time with the doctor. Providers, relieved of worrying about completing the chart in its entirety would be more able to focus on the patient and critical thinking. There are even benefits for scribes themselves. Often scribes are medical students, and those who are interested in pursuing a future in the health professions gain invaluable experience in the workings of medicine. “They are making a real contribution to patient care. They are a member of the health care team,” he said.
Dr. Corvini sees two primary areas in which scribes can contribute to hospital medicine. The first is shadowing the physician who is admitting patients during a high-volume admissions shift. Regular tasks like capturing the patient’s medication list and populating the History and Physical document lend themselves well to data entry by scribes, in contrast to completing more routine daily progress notes, which does not.
“They can also be helpful when there is a major transition from paper charting to the EHR or from one EHR system to another, when there is a lot of stress on the physician and risk for lost billing revenue,” Dr. Corvini said. “If scribes are trained in a particular EHR, they could help teach the physician how to use it.” TeamHealth is now in the process of running a trial of scribes at one of its sites, and the organization plans to measure productivity, provider satisfaction, and HCAHPS patient satisfaction scores.
A workaround – or a problem solver?
In a 2015 Viewpoint article in JAMA,3 George Gellert, MD, MPH, MPA, former chief medical information officer for the CHRISTUS Santa Rosa health system in San Antonio, Texas, and his coauthors labeled the use of scribes as a “workaround” that could curtail efforts to make EHRs more functionally operational because their use allows physicians to be satisfied with inferior EHR products.
In an interview, Dr. Gellert stated that he hasn’t changed his views about the negative consequences of scribes on EHR improvement. “The work of clinicians in using and advancing EHR technology is presently the only method we have for massively distributing and ensuring the use of evidence-based medicine,” he said. “That in turn is a critical strategy for reducing high rates of medical errors through a variety of decision-support applications.”
For better or worse, EHRs are an essential part of the solution to the epidemic of preventable, medical error–caused patient deaths, Dr. Gellert said. He also believes that substantial progress has already been made in advancing EHR usability, as reflected in the most recent product releases by leading EHR companies. However, considerable evolution is still needed in both usability and optimization of clinical decision support.
“With respect to your readers, my recommendation is to not use medical scribes, or else delimit their use to only where absolutely required. Instead, develop systematic processes to regularly capture specific physician concerns with the EHR being used, and transmit that critical information to their EHR vendor with a clear expectation that the manufacturer will address the issue in the near term, or at least in their next major product iteration or generation,” Dr. Gellert said.
By contrast, at the Management of the Hospitalized Patient conference in San Francisco in October 2015, Christine Sinsky, MD, FACP, vice president for professional satisfaction at the American Medical Association, identified documentation assistance as a helpful intervention for physician stress and burnout.4 In a recent email, Dr. Sinsky called documentation assistance “the most powerful intervention to give patients the time, attention, and care they need from their physicians. The data entry and data retrieval work of health care has grown over the last decade. Sharing this work with nonphysicians allows society to get the most value for its investment in physicians’ training.”
Dr. Sinsky calls documentation assistance – such as that provided by medical scribes – “a logical and strategic delegation of work according to ability for greater value,” not a workaround. She said it makes patient care safer by allowing physicians to focus on medical decision making and relationship building – rather than record keeping.
Experience from the front lines
Eric Edwards, MD, FAAP, FHM, of the division of hospital medicine at the University of North Carolina’s Hillsborough Hospital campus, recently presented a poster on his group’s experience with medical scribes at a meeting of the North Carolina Triangle Chapter of SHM. Their research concluded that scribes can be successfully incorporated into an inpatient hospital medicine practice and thus increase provider satisfaction and decrease the time clinicians spend charting.
“We were able to get the support of the hospital administration to pilot the use of scribes 3 days per week, which we’ve now done for almost a year,” Dr. Edwards said. Scribes are employed through a local company, MedScribes, and they work alongside admitting hospitalists during their 10-hour shifts. The hospitalists have been overwhelmingly positive about their experience, he said. “We established that it saves the physician 15 minutes per patient encounter by helping with documentation.”
It’s important that the scribe gets to know an individual provider’s personal preferences, Dr. Edwards said. Some hospitalists create their own charting templates. There’s also a need to train the clinician in how to use the medical scribe. For example, physicians are instructed to call out physical findings during their exam, which simultaneously informs the patient while allowing the scribe to document the exam.
“We are working on getting more formal data about the scribe experience,” he added. “But we have found that our providers love it, and it improves their efficiency and productivity. The danger is if the physician becomes too reliant on the scribe and fails to exercise due diligence in reviewing the scribe’s notes to ensure that all relevant information is in the chart and irrelevant information is not. We need to make sure we are carefully reviewing and signing off on the scribe’s notes,” he explained.
“I think we’re years away from improving the EHR to the point that would allow us to call it doctor friendly,” Dr. Edwards said. “For now, the scribe is a great way to alleviate some of the physician’s burden. But for hospitalist groups to use scribes successfully, it can’t be done haphazardly. We are lucky to have an experienced local scribe company to partner with. They provide systematic training and orientation. It’s also important that scribes are trained in the specific EHR that they will be using.”
Christine Lum Lung, MD, SFHM, CEO and medical director of Northern Colorado Hospitalists, a hospital medicine group at the University of Colorado’s North Campus hospitals in Fort Collins, has been studying the use of scribes since 2014. “We had a gap in bringing on new doctors fast enough for our group’s needs, so I looked into the return on investment from scribes and pitched it to our group,” she said. “It’s difficult to say what has been the actual impact on caseload, but we all think it has reduced physician workdays by an hour or greater.”
The 32-member hospitalist group, which covers two facilities, has a designated director of scribes who periodically surveys the hospitalists’ satisfaction with the scribes. “Now we all embrace the use of scribes. Satisfaction is high, and quality of life has improved,” Dr. Lum Lung said. “It’s hard to quantify, but we feel like it helps with burnout for us to be able to leave work earlier, and it alleviates some of the other stresses in our workday.”
She said scribes are important to the medical team not just with managing the EHR but also with other burdens such as documenting compliance with code status, VTEs, and other quality requirements, and to help with other regulatory issues. Scribes can look up lab values and radiology reports. When there are downtimes, they can prepare discharge plans.
Typically, there are five scribes on duty for 18 hours a day at each hospital, Dr. Lum Lung said. But only those doctors primarily doing admissions are assured of having a scribe to round with them. “Most doctors in the group would say the greatest efficiency of scribes is with admitting,” she said. The company that provides scribes to the UC hospitals, ScribeAmerica, handles administration, training, and human resource issues, and the scribe team has a designated Lead Scribe and Quality Scribe at their facility.
Studying the benefits
Andrew Friedson, PhD, a health care economist at the University of Colorado in Denver, recently conducted a 9-month randomized experiment in three hospital emergency rooms in the Denver area to determine the effects of scribes on measures of emergency physician productivity.5 He found that scribes reduced patient wait times in the emergency department by about 13 minutes per patient, while greatly decreasing the amount of time physicians spent after a shift completing their charting, which thus lowered overtime costs for ED physicians.
“This is one of the first times medical scribes have been studied with a randomized, controlled trial,” Dr. Friedson said. “I tracked the amount of overtime, patient waiting, and charge capture for each encounter. These were hospitals where the emergency doctors weren’t allowed to go home until their charting was done.” He discovered that there was a large drop in the time between when patients arrived at the ED and when a decision was made regarding whether to admit them. Additionally, charge capture increased significantly, and physicians had more time to perform medical procedures. Dr. Friedson believes that his findings hold implications for other settings and medical groups, including hospital medicine. To the extent that scribes free up hospitalists to perform tasks other than charting, they should provide an efficiency benefit.
So why hasn’t the medical scribe caught on in a bigger way for hospitalists, compared with ED physicians? For Dr. Corvini, the ED is an obvious, high-pressure, high-volume setting where the cost of the scribe can be easily recouped. “That doesn’t exist in such an obvious fashion in hospital medicine, except where high-volume admissions are concentrated in a single physician’s caseload,” he said. Not all hospitalist groups will fit that model. Some may divide admissions between hospitalists on a shift, and others may not be large enough to experience significant caseload pressures.
“EDs are obviously time pressured, and once scribes demonstrate the ability to produce documentation in a high-quality fashion, they are quickly accepted. In hospital medicine, the time pressures are different – not necessarily less, but different,” Dr. Corvini said. There are also differences in physician responsibilities between the ED and hospital medicine, as well as in physicians’ willingness to let go of documentation responsibilities. “My prediction, if the scribe test is rolled out successfully in TeamHealth, with measurable benefits, it will be adopted in other settings where it fits.”
References
1. Shanafelt TD et al. Relationship between clerical burden and characteristics of the electronic environment with physician burnout and professional satisfaction. Mayo Clin Proc. 2016 Jul;91(7):836-48.
2. Collins TR. Use of medical scribes spurs debate about costs, difficulties of electronic health records. The Hospitalist; 2015 Oct.
3. Gellert GA et al. The rise of the medical scribe industry: Implications for the advancement of electronic health records. JAMA; 2015;313(13):1315-6.
4. Beresford L. Electronic Health Records Key Driver of Physician Burnout. The Hospitalist; 2015 Dec.
5. Friedson AI. Medical scribes as an input in healthcare production: Evidence from a randomized experiment. Am J Health Econ. 2017 Oct 2. doi: /10.1162/ajhe_a_00103.
Can scribes reduce doctors’ job stress?
Can scribes reduce doctors’ job stress?
Physician stress and burnout remain major concerns for the U.S. health care system, with frustrations over the electronic health record (EHR) driving much of the dissatisfaction experienced by hospitalists and other physicians in the hospital.1 Underlying the EHR conundrum is a deeper question: Is entering clinical data on a computer the best use of a doctor’s time and professional skills? Or could a portion of that clerical function be delegated to nonphysicians?
Trained medical scribes, charting specialists who input EHR data for physicians on rounds, have been offered as a solution to potentially affect job stress for physicians and shorten their work days. But while scribes have been used and tested by different hospitalist groups around the country, the concept has not taken off in hospital medicine the way it has in certain other settings, such as emergency departments.
“The demand for scribes doesn’t seem to have materialized in a big way for hospital medicine,” said John Nelson, MD, MHM, a hospitalist and consultant in Bellevue, Wash., and a cofounder of the Society of Hospital Medicine. “I’m not convinced that scribes have had a big impact on hospitalist burnout.” It’s difficult to share scribes between doctors on a shift, and it’s a problem if the scribe and doctor get physically separated in the hospital. There’s also the question of who should pay the scribe’s salary, Dr. Nelson said.
Frustrations with the EHR can be a major factor in the experience of physician burnout, but Dr. Nelson said hospitalists can get proficient more quickly because they’re using the same computer system all day. “The bigger problem is that other doctors like surgeons don’t learn how to use the EHR and dump their routine tasks involving the EHR on the hospitalist, which means more work that is less satisfying.”
Could pairing a scribe with a hospitalist improve efficiency and decrease costs relative to the expense of employing the scribe? Are there specific settings, applications, and caseloads in hospital medicine where it makes more sense to use a scribe to support and assist doctors while they’re meeting with patients, with the doctor reviewing and editing the scribe’s work for accuracy? Could the scribe even help with physician staffing shortages by making doctors more productive?
TeamHealth, a national physician services company based in Knoxville, Tenn., has used scribes in emergency departments for years but had concluded that they made less sense for its hospitalist groups after a failure to document significant net increases in productivity, according to a 2015 report in The Hospitalist.2 Michael Corvini, MD, FACP, FACEP, TeamHealth’s new regional medical director for acute care services, said he brought extensive positive experience with scribes to his new job and is quite excited about their potential for hospital medicine. “When I came to TeamHealth in July, I began to suggest that there was unrealized potential for scribes,” he said.
Dr. Corvini noted that a potential benefit of scribes for patients is that their presence may allow for more face time with the doctor. Providers, relieved of worrying about completing the chart in its entirety would be more able to focus on the patient and critical thinking. There are even benefits for scribes themselves. Often scribes are medical students, and those who are interested in pursuing a future in the health professions gain invaluable experience in the workings of medicine. “They are making a real contribution to patient care. They are a member of the health care team,” he said.
Dr. Corvini sees two primary areas in which scribes can contribute to hospital medicine. The first is shadowing the physician who is admitting patients during a high-volume admissions shift. Regular tasks like capturing the patient’s medication list and populating the History and Physical document lend themselves well to data entry by scribes, in contrast to completing more routine daily progress notes, which does not.
“They can also be helpful when there is a major transition from paper charting to the EHR or from one EHR system to another, when there is a lot of stress on the physician and risk for lost billing revenue,” Dr. Corvini said. “If scribes are trained in a particular EHR, they could help teach the physician how to use it.” TeamHealth is now in the process of running a trial of scribes at one of its sites, and the organization plans to measure productivity, provider satisfaction, and HCAHPS patient satisfaction scores.
A workaround – or a problem solver?
In a 2015 Viewpoint article in JAMA,3 George Gellert, MD, MPH, MPA, former chief medical information officer for the CHRISTUS Santa Rosa health system in San Antonio, Texas, and his coauthors labeled the use of scribes as a “workaround” that could curtail efforts to make EHRs more functionally operational because their use allows physicians to be satisfied with inferior EHR products.
In an interview, Dr. Gellert stated that he hasn’t changed his views about the negative consequences of scribes on EHR improvement. “The work of clinicians in using and advancing EHR technology is presently the only method we have for massively distributing and ensuring the use of evidence-based medicine,” he said. “That in turn is a critical strategy for reducing high rates of medical errors through a variety of decision-support applications.”
For better or worse, EHRs are an essential part of the solution to the epidemic of preventable, medical error–caused patient deaths, Dr. Gellert said. He also believes that substantial progress has already been made in advancing EHR usability, as reflected in the most recent product releases by leading EHR companies. However, considerable evolution is still needed in both usability and optimization of clinical decision support.
“With respect to your readers, my recommendation is to not use medical scribes, or else delimit their use to only where absolutely required. Instead, develop systematic processes to regularly capture specific physician concerns with the EHR being used, and transmit that critical information to their EHR vendor with a clear expectation that the manufacturer will address the issue in the near term, or at least in their next major product iteration or generation,” Dr. Gellert said.
By contrast, at the Management of the Hospitalized Patient conference in San Francisco in October 2015, Christine Sinsky, MD, FACP, vice president for professional satisfaction at the American Medical Association, identified documentation assistance as a helpful intervention for physician stress and burnout.4 In a recent email, Dr. Sinsky called documentation assistance “the most powerful intervention to give patients the time, attention, and care they need from their physicians. The data entry and data retrieval work of health care has grown over the last decade. Sharing this work with nonphysicians allows society to get the most value for its investment in physicians’ training.”
Dr. Sinsky calls documentation assistance – such as that provided by medical scribes – “a logical and strategic delegation of work according to ability for greater value,” not a workaround. She said it makes patient care safer by allowing physicians to focus on medical decision making and relationship building – rather than record keeping.
Experience from the front lines
Eric Edwards, MD, FAAP, FHM, of the division of hospital medicine at the University of North Carolina’s Hillsborough Hospital campus, recently presented a poster on his group’s experience with medical scribes at a meeting of the North Carolina Triangle Chapter of SHM. Their research concluded that scribes can be successfully incorporated into an inpatient hospital medicine practice and thus increase provider satisfaction and decrease the time clinicians spend charting.
“We were able to get the support of the hospital administration to pilot the use of scribes 3 days per week, which we’ve now done for almost a year,” Dr. Edwards said. Scribes are employed through a local company, MedScribes, and they work alongside admitting hospitalists during their 10-hour shifts. The hospitalists have been overwhelmingly positive about their experience, he said. “We established that it saves the physician 15 minutes per patient encounter by helping with documentation.”
It’s important that the scribe gets to know an individual provider’s personal preferences, Dr. Edwards said. Some hospitalists create their own charting templates. There’s also a need to train the clinician in how to use the medical scribe. For example, physicians are instructed to call out physical findings during their exam, which simultaneously informs the patient while allowing the scribe to document the exam.
“We are working on getting more formal data about the scribe experience,” he added. “But we have found that our providers love it, and it improves their efficiency and productivity. The danger is if the physician becomes too reliant on the scribe and fails to exercise due diligence in reviewing the scribe’s notes to ensure that all relevant information is in the chart and irrelevant information is not. We need to make sure we are carefully reviewing and signing off on the scribe’s notes,” he explained.
“I think we’re years away from improving the EHR to the point that would allow us to call it doctor friendly,” Dr. Edwards said. “For now, the scribe is a great way to alleviate some of the physician’s burden. But for hospitalist groups to use scribes successfully, it can’t be done haphazardly. We are lucky to have an experienced local scribe company to partner with. They provide systematic training and orientation. It’s also important that scribes are trained in the specific EHR that they will be using.”
Christine Lum Lung, MD, SFHM, CEO and medical director of Northern Colorado Hospitalists, a hospital medicine group at the University of Colorado’s North Campus hospitals in Fort Collins, has been studying the use of scribes since 2014. “We had a gap in bringing on new doctors fast enough for our group’s needs, so I looked into the return on investment from scribes and pitched it to our group,” she said. “It’s difficult to say what has been the actual impact on caseload, but we all think it has reduced physician workdays by an hour or greater.”
The 32-member hospitalist group, which covers two facilities, has a designated director of scribes who periodically surveys the hospitalists’ satisfaction with the scribes. “Now we all embrace the use of scribes. Satisfaction is high, and quality of life has improved,” Dr. Lum Lung said. “It’s hard to quantify, but we feel like it helps with burnout for us to be able to leave work earlier, and it alleviates some of the other stresses in our workday.”
She said scribes are important to the medical team not just with managing the EHR but also with other burdens such as documenting compliance with code status, VTEs, and other quality requirements, and to help with other regulatory issues. Scribes can look up lab values and radiology reports. When there are downtimes, they can prepare discharge plans.
Typically, there are five scribes on duty for 18 hours a day at each hospital, Dr. Lum Lung said. But only those doctors primarily doing admissions are assured of having a scribe to round with them. “Most doctors in the group would say the greatest efficiency of scribes is with admitting,” she said. The company that provides scribes to the UC hospitals, ScribeAmerica, handles administration, training, and human resource issues, and the scribe team has a designated Lead Scribe and Quality Scribe at their facility.
Studying the benefits
Andrew Friedson, PhD, a health care economist at the University of Colorado in Denver, recently conducted a 9-month randomized experiment in three hospital emergency rooms in the Denver area to determine the effects of scribes on measures of emergency physician productivity.5 He found that scribes reduced patient wait times in the emergency department by about 13 minutes per patient, while greatly decreasing the amount of time physicians spent after a shift completing their charting, which thus lowered overtime costs for ED physicians.
“This is one of the first times medical scribes have been studied with a randomized, controlled trial,” Dr. Friedson said. “I tracked the amount of overtime, patient waiting, and charge capture for each encounter. These were hospitals where the emergency doctors weren’t allowed to go home until their charting was done.” He discovered that there was a large drop in the time between when patients arrived at the ED and when a decision was made regarding whether to admit them. Additionally, charge capture increased significantly, and physicians had more time to perform medical procedures. Dr. Friedson believes that his findings hold implications for other settings and medical groups, including hospital medicine. To the extent that scribes free up hospitalists to perform tasks other than charting, they should provide an efficiency benefit.
So why hasn’t the medical scribe caught on in a bigger way for hospitalists, compared with ED physicians? For Dr. Corvini, the ED is an obvious, high-pressure, high-volume setting where the cost of the scribe can be easily recouped. “That doesn’t exist in such an obvious fashion in hospital medicine, except where high-volume admissions are concentrated in a single physician’s caseload,” he said. Not all hospitalist groups will fit that model. Some may divide admissions between hospitalists on a shift, and others may not be large enough to experience significant caseload pressures.
“EDs are obviously time pressured, and once scribes demonstrate the ability to produce documentation in a high-quality fashion, they are quickly accepted. In hospital medicine, the time pressures are different – not necessarily less, but different,” Dr. Corvini said. There are also differences in physician responsibilities between the ED and hospital medicine, as well as in physicians’ willingness to let go of documentation responsibilities. “My prediction, if the scribe test is rolled out successfully in TeamHealth, with measurable benefits, it will be adopted in other settings where it fits.”
References
1. Shanafelt TD et al. Relationship between clerical burden and characteristics of the electronic environment with physician burnout and professional satisfaction. Mayo Clin Proc. 2016 Jul;91(7):836-48.
2. Collins TR. Use of medical scribes spurs debate about costs, difficulties of electronic health records. The Hospitalist; 2015 Oct.
3. Gellert GA et al. The rise of the medical scribe industry: Implications for the advancement of electronic health records. JAMA; 2015;313(13):1315-6.
4. Beresford L. Electronic Health Records Key Driver of Physician Burnout. The Hospitalist; 2015 Dec.
5. Friedson AI. Medical scribes as an input in healthcare production: Evidence from a randomized experiment. Am J Health Econ. 2017 Oct 2. doi: /10.1162/ajhe_a_00103.
Physician stress and burnout remain major concerns for the U.S. health care system, with frustrations over the electronic health record (EHR) driving much of the dissatisfaction experienced by hospitalists and other physicians in the hospital.1 Underlying the EHR conundrum is a deeper question: Is entering clinical data on a computer the best use of a doctor’s time and professional skills? Or could a portion of that clerical function be delegated to nonphysicians?
Trained medical scribes, charting specialists who input EHR data for physicians on rounds, have been offered as a solution to potentially affect job stress for physicians and shorten their work days. But while scribes have been used and tested by different hospitalist groups around the country, the concept has not taken off in hospital medicine the way it has in certain other settings, such as emergency departments.
“The demand for scribes doesn’t seem to have materialized in a big way for hospital medicine,” said John Nelson, MD, MHM, a hospitalist and consultant in Bellevue, Wash., and a cofounder of the Society of Hospital Medicine. “I’m not convinced that scribes have had a big impact on hospitalist burnout.” It’s difficult to share scribes between doctors on a shift, and it’s a problem if the scribe and doctor get physically separated in the hospital. There’s also the question of who should pay the scribe’s salary, Dr. Nelson said.
Frustrations with the EHR can be a major factor in the experience of physician burnout, but Dr. Nelson said hospitalists can get proficient more quickly because they’re using the same computer system all day. “The bigger problem is that other doctors like surgeons don’t learn how to use the EHR and dump their routine tasks involving the EHR on the hospitalist, which means more work that is less satisfying.”
Could pairing a scribe with a hospitalist improve efficiency and decrease costs relative to the expense of employing the scribe? Are there specific settings, applications, and caseloads in hospital medicine where it makes more sense to use a scribe to support and assist doctors while they’re meeting with patients, with the doctor reviewing and editing the scribe’s work for accuracy? Could the scribe even help with physician staffing shortages by making doctors more productive?
TeamHealth, a national physician services company based in Knoxville, Tenn., has used scribes in emergency departments for years but had concluded that they made less sense for its hospitalist groups after a failure to document significant net increases in productivity, according to a 2015 report in The Hospitalist.2 Michael Corvini, MD, FACP, FACEP, TeamHealth’s new regional medical director for acute care services, said he brought extensive positive experience with scribes to his new job and is quite excited about their potential for hospital medicine. “When I came to TeamHealth in July, I began to suggest that there was unrealized potential for scribes,” he said.
Dr. Corvini noted that a potential benefit of scribes for patients is that their presence may allow for more face time with the doctor. Providers, relieved of worrying about completing the chart in its entirety would be more able to focus on the patient and critical thinking. There are even benefits for scribes themselves. Often scribes are medical students, and those who are interested in pursuing a future in the health professions gain invaluable experience in the workings of medicine. “They are making a real contribution to patient care. They are a member of the health care team,” he said.
Dr. Corvini sees two primary areas in which scribes can contribute to hospital medicine. The first is shadowing the physician who is admitting patients during a high-volume admissions shift. Regular tasks like capturing the patient’s medication list and populating the History and Physical document lend themselves well to data entry by scribes, in contrast to completing more routine daily progress notes, which does not.
“They can also be helpful when there is a major transition from paper charting to the EHR or from one EHR system to another, when there is a lot of stress on the physician and risk for lost billing revenue,” Dr. Corvini said. “If scribes are trained in a particular EHR, they could help teach the physician how to use it.” TeamHealth is now in the process of running a trial of scribes at one of its sites, and the organization plans to measure productivity, provider satisfaction, and HCAHPS patient satisfaction scores.
A workaround – or a problem solver?
In a 2015 Viewpoint article in JAMA,3 George Gellert, MD, MPH, MPA, former chief medical information officer for the CHRISTUS Santa Rosa health system in San Antonio, Texas, and his coauthors labeled the use of scribes as a “workaround” that could curtail efforts to make EHRs more functionally operational because their use allows physicians to be satisfied with inferior EHR products.
In an interview, Dr. Gellert stated that he hasn’t changed his views about the negative consequences of scribes on EHR improvement. “The work of clinicians in using and advancing EHR technology is presently the only method we have for massively distributing and ensuring the use of evidence-based medicine,” he said. “That in turn is a critical strategy for reducing high rates of medical errors through a variety of decision-support applications.”
For better or worse, EHRs are an essential part of the solution to the epidemic of preventable, medical error–caused patient deaths, Dr. Gellert said. He also believes that substantial progress has already been made in advancing EHR usability, as reflected in the most recent product releases by leading EHR companies. However, considerable evolution is still needed in both usability and optimization of clinical decision support.
“With respect to your readers, my recommendation is to not use medical scribes, or else delimit their use to only where absolutely required. Instead, develop systematic processes to regularly capture specific physician concerns with the EHR being used, and transmit that critical information to their EHR vendor with a clear expectation that the manufacturer will address the issue in the near term, or at least in their next major product iteration or generation,” Dr. Gellert said.
By contrast, at the Management of the Hospitalized Patient conference in San Francisco in October 2015, Christine Sinsky, MD, FACP, vice president for professional satisfaction at the American Medical Association, identified documentation assistance as a helpful intervention for physician stress and burnout.4 In a recent email, Dr. Sinsky called documentation assistance “the most powerful intervention to give patients the time, attention, and care they need from their physicians. The data entry and data retrieval work of health care has grown over the last decade. Sharing this work with nonphysicians allows society to get the most value for its investment in physicians’ training.”
Dr. Sinsky calls documentation assistance – such as that provided by medical scribes – “a logical and strategic delegation of work according to ability for greater value,” not a workaround. She said it makes patient care safer by allowing physicians to focus on medical decision making and relationship building – rather than record keeping.
Experience from the front lines
Eric Edwards, MD, FAAP, FHM, of the division of hospital medicine at the University of North Carolina’s Hillsborough Hospital campus, recently presented a poster on his group’s experience with medical scribes at a meeting of the North Carolina Triangle Chapter of SHM. Their research concluded that scribes can be successfully incorporated into an inpatient hospital medicine practice and thus increase provider satisfaction and decrease the time clinicians spend charting.
“We were able to get the support of the hospital administration to pilot the use of scribes 3 days per week, which we’ve now done for almost a year,” Dr. Edwards said. Scribes are employed through a local company, MedScribes, and they work alongside admitting hospitalists during their 10-hour shifts. The hospitalists have been overwhelmingly positive about their experience, he said. “We established that it saves the physician 15 minutes per patient encounter by helping with documentation.”
It’s important that the scribe gets to know an individual provider’s personal preferences, Dr. Edwards said. Some hospitalists create their own charting templates. There’s also a need to train the clinician in how to use the medical scribe. For example, physicians are instructed to call out physical findings during their exam, which simultaneously informs the patient while allowing the scribe to document the exam.
“We are working on getting more formal data about the scribe experience,” he added. “But we have found that our providers love it, and it improves their efficiency and productivity. The danger is if the physician becomes too reliant on the scribe and fails to exercise due diligence in reviewing the scribe’s notes to ensure that all relevant information is in the chart and irrelevant information is not. We need to make sure we are carefully reviewing and signing off on the scribe’s notes,” he explained.
“I think we’re years away from improving the EHR to the point that would allow us to call it doctor friendly,” Dr. Edwards said. “For now, the scribe is a great way to alleviate some of the physician’s burden. But for hospitalist groups to use scribes successfully, it can’t be done haphazardly. We are lucky to have an experienced local scribe company to partner with. They provide systematic training and orientation. It’s also important that scribes are trained in the specific EHR that they will be using.”
Christine Lum Lung, MD, SFHM, CEO and medical director of Northern Colorado Hospitalists, a hospital medicine group at the University of Colorado’s North Campus hospitals in Fort Collins, has been studying the use of scribes since 2014. “We had a gap in bringing on new doctors fast enough for our group’s needs, so I looked into the return on investment from scribes and pitched it to our group,” she said. “It’s difficult to say what has been the actual impact on caseload, but we all think it has reduced physician workdays by an hour or greater.”
The 32-member hospitalist group, which covers two facilities, has a designated director of scribes who periodically surveys the hospitalists’ satisfaction with the scribes. “Now we all embrace the use of scribes. Satisfaction is high, and quality of life has improved,” Dr. Lum Lung said. “It’s hard to quantify, but we feel like it helps with burnout for us to be able to leave work earlier, and it alleviates some of the other stresses in our workday.”
She said scribes are important to the medical team not just with managing the EHR but also with other burdens such as documenting compliance with code status, VTEs, and other quality requirements, and to help with other regulatory issues. Scribes can look up lab values and radiology reports. When there are downtimes, they can prepare discharge plans.
Typically, there are five scribes on duty for 18 hours a day at each hospital, Dr. Lum Lung said. But only those doctors primarily doing admissions are assured of having a scribe to round with them. “Most doctors in the group would say the greatest efficiency of scribes is with admitting,” she said. The company that provides scribes to the UC hospitals, ScribeAmerica, handles administration, training, and human resource issues, and the scribe team has a designated Lead Scribe and Quality Scribe at their facility.
Studying the benefits
Andrew Friedson, PhD, a health care economist at the University of Colorado in Denver, recently conducted a 9-month randomized experiment in three hospital emergency rooms in the Denver area to determine the effects of scribes on measures of emergency physician productivity.5 He found that scribes reduced patient wait times in the emergency department by about 13 minutes per patient, while greatly decreasing the amount of time physicians spent after a shift completing their charting, which thus lowered overtime costs for ED physicians.
“This is one of the first times medical scribes have been studied with a randomized, controlled trial,” Dr. Friedson said. “I tracked the amount of overtime, patient waiting, and charge capture for each encounter. These were hospitals where the emergency doctors weren’t allowed to go home until their charting was done.” He discovered that there was a large drop in the time between when patients arrived at the ED and when a decision was made regarding whether to admit them. Additionally, charge capture increased significantly, and physicians had more time to perform medical procedures. Dr. Friedson believes that his findings hold implications for other settings and medical groups, including hospital medicine. To the extent that scribes free up hospitalists to perform tasks other than charting, they should provide an efficiency benefit.
So why hasn’t the medical scribe caught on in a bigger way for hospitalists, compared with ED physicians? For Dr. Corvini, the ED is an obvious, high-pressure, high-volume setting where the cost of the scribe can be easily recouped. “That doesn’t exist in such an obvious fashion in hospital medicine, except where high-volume admissions are concentrated in a single physician’s caseload,” he said. Not all hospitalist groups will fit that model. Some may divide admissions between hospitalists on a shift, and others may not be large enough to experience significant caseload pressures.
“EDs are obviously time pressured, and once scribes demonstrate the ability to produce documentation in a high-quality fashion, they are quickly accepted. In hospital medicine, the time pressures are different – not necessarily less, but different,” Dr. Corvini said. There are also differences in physician responsibilities between the ED and hospital medicine, as well as in physicians’ willingness to let go of documentation responsibilities. “My prediction, if the scribe test is rolled out successfully in TeamHealth, with measurable benefits, it will be adopted in other settings where it fits.”
References
1. Shanafelt TD et al. Relationship between clerical burden and characteristics of the electronic environment with physician burnout and professional satisfaction. Mayo Clin Proc. 2016 Jul;91(7):836-48.
2. Collins TR. Use of medical scribes spurs debate about costs, difficulties of electronic health records. The Hospitalist; 2015 Oct.
3. Gellert GA et al. The rise of the medical scribe industry: Implications for the advancement of electronic health records. JAMA; 2015;313(13):1315-6.
4. Beresford L. Electronic Health Records Key Driver of Physician Burnout. The Hospitalist; 2015 Dec.
5. Friedson AI. Medical scribes as an input in healthcare production: Evidence from a randomized experiment. Am J Health Econ. 2017 Oct 2. doi: /10.1162/ajhe_a_00103.
Opiate-prescribing standard decreases opiate use in hospitalized patients
Clinical question: Can an opiate-prescribing standard that favors oral and subcutaneous over intravenous administration reduce exposure to intravenous opiates for hospitalized adults?
Background: IV opiates, while effective for analgesia, may have a higher addictive potential because of the rapid and intermittent rises of peak concentrations. Subcutaneous and/or oral administration is a proven method of opioid delivery with similar bioavailability and efficacy of intravenous administration with more favorable pharmacokinetics.
Study design: Intervention-based quality improvement project.
Setting: Adult general medicine inpatient unit in an urban academic center.
Synopsis: Clinical leadership of the study unit collaborated to create an opiate-prescribing standard recommending oral over parenteral opioids and subcutaneous over IV if parental administration was required. The standard was promoted and reinforced with prescriber and nurse education, and prescribers were able to order intravenous opiates per usual protocol.
After a 6-month preintervention control period of 4,500 patient-days, the 3-month intervention period included 2,459 patient-days and led to a 84% decrease in IV opiate doses (0.06 vs. 0.39; P less than .001) and a 55% decrease in parenteral doses (0.18 vs. 0.39; P less than .001). Surprisingly there was a 23% decrease in overall doses of opiates (0.73 vs. 0.95; P = .02). Pain scores were similar between the two groups during hospital days 1-3 and improved in the intervention group between days 4 and 5.
This study was limited by a narrow focus, unblinded participants, and nursing-reported pain scores. While promising, more information is needed before establishing conclusions on a broader scale.
Bottom line: Establishing and promoting an opioid prescribing standard on a single unit led to a decrease in intravenous, parenteral, and overall opiates prescribed with similar or improved pain scores.
Citation: Ackerman AL et al. Association of an opioid standard of practice intervention with intravenous opioid exposure in hospitalized patients. JAMA Intern Med. 2018 Jun 1;178(6):759-63.
Dr. Chowdury is an assistant professor in the division of hospital medicine, University of Colorado, Denver.
Clinical question: Can an opiate-prescribing standard that favors oral and subcutaneous over intravenous administration reduce exposure to intravenous opiates for hospitalized adults?
Background: IV opiates, while effective for analgesia, may have a higher addictive potential because of the rapid and intermittent rises of peak concentrations. Subcutaneous and/or oral administration is a proven method of opioid delivery with similar bioavailability and efficacy of intravenous administration with more favorable pharmacokinetics.
Study design: Intervention-based quality improvement project.
Setting: Adult general medicine inpatient unit in an urban academic center.
Synopsis: Clinical leadership of the study unit collaborated to create an opiate-prescribing standard recommending oral over parenteral opioids and subcutaneous over IV if parental administration was required. The standard was promoted and reinforced with prescriber and nurse education, and prescribers were able to order intravenous opiates per usual protocol.
After a 6-month preintervention control period of 4,500 patient-days, the 3-month intervention period included 2,459 patient-days and led to a 84% decrease in IV opiate doses (0.06 vs. 0.39; P less than .001) and a 55% decrease in parenteral doses (0.18 vs. 0.39; P less than .001). Surprisingly there was a 23% decrease in overall doses of opiates (0.73 vs. 0.95; P = .02). Pain scores were similar between the two groups during hospital days 1-3 and improved in the intervention group between days 4 and 5.
This study was limited by a narrow focus, unblinded participants, and nursing-reported pain scores. While promising, more information is needed before establishing conclusions on a broader scale.
Bottom line: Establishing and promoting an opioid prescribing standard on a single unit led to a decrease in intravenous, parenteral, and overall opiates prescribed with similar or improved pain scores.
Citation: Ackerman AL et al. Association of an opioid standard of practice intervention with intravenous opioid exposure in hospitalized patients. JAMA Intern Med. 2018 Jun 1;178(6):759-63.
Dr. Chowdury is an assistant professor in the division of hospital medicine, University of Colorado, Denver.
Clinical question: Can an opiate-prescribing standard that favors oral and subcutaneous over intravenous administration reduce exposure to intravenous opiates for hospitalized adults?
Background: IV opiates, while effective for analgesia, may have a higher addictive potential because of the rapid and intermittent rises of peak concentrations. Subcutaneous and/or oral administration is a proven method of opioid delivery with similar bioavailability and efficacy of intravenous administration with more favorable pharmacokinetics.
Study design: Intervention-based quality improvement project.
Setting: Adult general medicine inpatient unit in an urban academic center.
Synopsis: Clinical leadership of the study unit collaborated to create an opiate-prescribing standard recommending oral over parenteral opioids and subcutaneous over IV if parental administration was required. The standard was promoted and reinforced with prescriber and nurse education, and prescribers were able to order intravenous opiates per usual protocol.
After a 6-month preintervention control period of 4,500 patient-days, the 3-month intervention period included 2,459 patient-days and led to a 84% decrease in IV opiate doses (0.06 vs. 0.39; P less than .001) and a 55% decrease in parenteral doses (0.18 vs. 0.39; P less than .001). Surprisingly there was a 23% decrease in overall doses of opiates (0.73 vs. 0.95; P = .02). Pain scores were similar between the two groups during hospital days 1-3 and improved in the intervention group between days 4 and 5.
This study was limited by a narrow focus, unblinded participants, and nursing-reported pain scores. While promising, more information is needed before establishing conclusions on a broader scale.
Bottom line: Establishing and promoting an opioid prescribing standard on a single unit led to a decrease in intravenous, parenteral, and overall opiates prescribed with similar or improved pain scores.
Citation: Ackerman AL et al. Association of an opioid standard of practice intervention with intravenous opioid exposure in hospitalized patients. JAMA Intern Med. 2018 Jun 1;178(6):759-63.
Dr. Chowdury is an assistant professor in the division of hospital medicine, University of Colorado, Denver.
Burden of atrial fibrillation associated with stroke risk
Background: Atrial fibrillation (AF) is a well-known risk factor for ischemic stroke; however, it is unclear if atrial fibrillation burden in patients with PAF is correlated with increased stroke risk.
Study design: Retrospective cohort chart review study during October 2011–October 2016.
Setting: Outpatients in two Kaiser Permanente California health systems.
Synopsis: Among 1,965 adult patients with PAF not on anticoagulation therapy, PAF burden was defined as the percentage time spent in AF during 14-day ECG monitoring. Outcomes included hospitalization for ischemic stroke or arterial thromboembolism while not taking anticoagulants.
Patients in the highest tertile of PAF burden (less than 11%) had 215% higher risk of thromboembolic events, compared with those with lower PAF burden (less than 11%), yielding a hazard ratio of 3.15 (95% confidence interval, 1.51-6.61), even after adjustment.
This study was limited by short ECG monitoring period (14 days), low total number of events (29 total events, 17 in the highest tertile), and no minimum follow-up time. Further, with all patients insured in a single health care system, and excluded on disenrollment from the health plan, selection bias could have affected the results.
Bottom line: In patients with PAF, a larger AF burden (greater than 11%) is associated with increased risk of ischemic stroke. Assessment of AF burden may help determine the need for anticoagulation for stroke prevention.
Citation: Go AS et al. Association of burden of atrial fibrillation with risk of ischemic stroke in adults with paroxysmal atrial fibrillation: the KP-RHYTHM study. JAMA Cardiol. 2018 Jul 1;3(7):601-8.
Dr. Hanna is an assistant professor in the division of hospital medicine, University of Colorado, Denver.
Background: Atrial fibrillation (AF) is a well-known risk factor for ischemic stroke; however, it is unclear if atrial fibrillation burden in patients with PAF is correlated with increased stroke risk.
Study design: Retrospective cohort chart review study during October 2011–October 2016.
Setting: Outpatients in two Kaiser Permanente California health systems.
Synopsis: Among 1,965 adult patients with PAF not on anticoagulation therapy, PAF burden was defined as the percentage time spent in AF during 14-day ECG monitoring. Outcomes included hospitalization for ischemic stroke or arterial thromboembolism while not taking anticoagulants.
Patients in the highest tertile of PAF burden (less than 11%) had 215% higher risk of thromboembolic events, compared with those with lower PAF burden (less than 11%), yielding a hazard ratio of 3.15 (95% confidence interval, 1.51-6.61), even after adjustment.
This study was limited by short ECG monitoring period (14 days), low total number of events (29 total events, 17 in the highest tertile), and no minimum follow-up time. Further, with all patients insured in a single health care system, and excluded on disenrollment from the health plan, selection bias could have affected the results.
Bottom line: In patients with PAF, a larger AF burden (greater than 11%) is associated with increased risk of ischemic stroke. Assessment of AF burden may help determine the need for anticoagulation for stroke prevention.
Citation: Go AS et al. Association of burden of atrial fibrillation with risk of ischemic stroke in adults with paroxysmal atrial fibrillation: the KP-RHYTHM study. JAMA Cardiol. 2018 Jul 1;3(7):601-8.
Dr. Hanna is an assistant professor in the division of hospital medicine, University of Colorado, Denver.
Background: Atrial fibrillation (AF) is a well-known risk factor for ischemic stroke; however, it is unclear if atrial fibrillation burden in patients with PAF is correlated with increased stroke risk.
Study design: Retrospective cohort chart review study during October 2011–October 2016.
Setting: Outpatients in two Kaiser Permanente California health systems.
Synopsis: Among 1,965 adult patients with PAF not on anticoagulation therapy, PAF burden was defined as the percentage time spent in AF during 14-day ECG monitoring. Outcomes included hospitalization for ischemic stroke or arterial thromboembolism while not taking anticoagulants.
Patients in the highest tertile of PAF burden (less than 11%) had 215% higher risk of thromboembolic events, compared with those with lower PAF burden (less than 11%), yielding a hazard ratio of 3.15 (95% confidence interval, 1.51-6.61), even after adjustment.
This study was limited by short ECG monitoring period (14 days), low total number of events (29 total events, 17 in the highest tertile), and no minimum follow-up time. Further, with all patients insured in a single health care system, and excluded on disenrollment from the health plan, selection bias could have affected the results.
Bottom line: In patients with PAF, a larger AF burden (greater than 11%) is associated with increased risk of ischemic stroke. Assessment of AF burden may help determine the need for anticoagulation for stroke prevention.
Citation: Go AS et al. Association of burden of atrial fibrillation with risk of ischemic stroke in adults with paroxysmal atrial fibrillation: the KP-RHYTHM study. JAMA Cardiol. 2018 Jul 1;3(7):601-8.
Dr. Hanna is an assistant professor in the division of hospital medicine, University of Colorado, Denver.
Liberal oxygen therapy associated with increased mortality
Background: An increasing body of literature suggests that hyperoxia may be harmful, yet liberal use of supplemental oxygen remains widespread.
Study design: Systematic review and meta-analysis.
Setting: Acutely ill hospitalized adults.
Synopsis: The authors performed a meta-analysis of 25 randomized controlled trials of oxygen therapy in acutely ill adults, encompassing 16,037 patients comparing liberal oxygen strategy (median fraction of inspired oxygen,, 0.52; interquartile range, 0.39-0.85) to conservative oxygen strategy (median FiO2, 0.21; IQR, 0.21-025). Results showed the liberal oxygen strategy was associated with higher in-hospital (risk ratio, 1.21; 95% confidence interval, 1.03-1.43) and 30-day (RR, 1.14, 95% CI, 1.01-1.28) mortality, without a difference in length of stay or disability.
Much like transfusion thresholds, more may not always be better when it comes to supplemental oxygen. Hospitalists should consider the harmful effects of hyperoxia when caring for patients on supplemental oxygen. Unfortunately, median blood oxygen saturation during therapy was not available for each group in this trial, so more research is needed to clearly define the upper limit of oxygen saturation at which harm outweighs benefit.
Bottom line: When compared to conservative oxygen administration, liberal oxygen therapy increases mortality in acutely ill adults.
Citation: Chu DK et al. Mortality and morbidity in acutely ill adults treated with liberal versus conservative oxygen therapy (IOTA): a systematic review and meta-analysis. Lancet. 2018;391:1693-705.
Dr. Metter is an assistant professor in the division of hospital medicine, University of Colorado, Denver.
Background: An increasing body of literature suggests that hyperoxia may be harmful, yet liberal use of supplemental oxygen remains widespread.
Study design: Systematic review and meta-analysis.
Setting: Acutely ill hospitalized adults.
Synopsis: The authors performed a meta-analysis of 25 randomized controlled trials of oxygen therapy in acutely ill adults, encompassing 16,037 patients comparing liberal oxygen strategy (median fraction of inspired oxygen,, 0.52; interquartile range, 0.39-0.85) to conservative oxygen strategy (median FiO2, 0.21; IQR, 0.21-025). Results showed the liberal oxygen strategy was associated with higher in-hospital (risk ratio, 1.21; 95% confidence interval, 1.03-1.43) and 30-day (RR, 1.14, 95% CI, 1.01-1.28) mortality, without a difference in length of stay or disability.
Much like transfusion thresholds, more may not always be better when it comes to supplemental oxygen. Hospitalists should consider the harmful effects of hyperoxia when caring for patients on supplemental oxygen. Unfortunately, median blood oxygen saturation during therapy was not available for each group in this trial, so more research is needed to clearly define the upper limit of oxygen saturation at which harm outweighs benefit.
Bottom line: When compared to conservative oxygen administration, liberal oxygen therapy increases mortality in acutely ill adults.
Citation: Chu DK et al. Mortality and morbidity in acutely ill adults treated with liberal versus conservative oxygen therapy (IOTA): a systematic review and meta-analysis. Lancet. 2018;391:1693-705.
Dr. Metter is an assistant professor in the division of hospital medicine, University of Colorado, Denver.
Background: An increasing body of literature suggests that hyperoxia may be harmful, yet liberal use of supplemental oxygen remains widespread.
Study design: Systematic review and meta-analysis.
Setting: Acutely ill hospitalized adults.
Synopsis: The authors performed a meta-analysis of 25 randomized controlled trials of oxygen therapy in acutely ill adults, encompassing 16,037 patients comparing liberal oxygen strategy (median fraction of inspired oxygen,, 0.52; interquartile range, 0.39-0.85) to conservative oxygen strategy (median FiO2, 0.21; IQR, 0.21-025). Results showed the liberal oxygen strategy was associated with higher in-hospital (risk ratio, 1.21; 95% confidence interval, 1.03-1.43) and 30-day (RR, 1.14, 95% CI, 1.01-1.28) mortality, without a difference in length of stay or disability.
Much like transfusion thresholds, more may not always be better when it comes to supplemental oxygen. Hospitalists should consider the harmful effects of hyperoxia when caring for patients on supplemental oxygen. Unfortunately, median blood oxygen saturation during therapy was not available for each group in this trial, so more research is needed to clearly define the upper limit of oxygen saturation at which harm outweighs benefit.
Bottom line: When compared to conservative oxygen administration, liberal oxygen therapy increases mortality in acutely ill adults.
Citation: Chu DK et al. Mortality and morbidity in acutely ill adults treated with liberal versus conservative oxygen therapy (IOTA): a systematic review and meta-analysis. Lancet. 2018;391:1693-705.
Dr. Metter is an assistant professor in the division of hospital medicine, University of Colorado, Denver.
Surgical repair of hip fractures in nursing home patients
Clinical question: Does surgical repair of hip fractures in nursing home residents with advanced dementia reduce adverse outcomes?
Background: Hip fractures are common in the advanced dementia nursing home population. The benefit of surgical repair is unclear in this population given significant baseline functional disability and limited life expectancy.
Study design: Retrospective cohort study.
Setting: Medicare claims data set.
Synopsis: Among 3,083 nursing home residents with advanced dementia and hip fracture, nearly 85% underwent surgical repair. The 30-day mortality rate in the nonsurgical group was 30.6%, compared with 11.5% in the surgical group. In an adjusted model, the surgical group had decreased risk of death, compared with the nonsurgical group (hazard ratio, 0.88; 95% confidence interval, 0.79-0.98). In additional adjusted models, surgical patients also had decreased risk of pressure ulcers (HR 0.64; 95% CI, 0.47-0.86) and less pain (HR, 0.78; 95% CI, 0.61-0.99). Limitations included the observational nature of the study. Although the models were adjusted, unmeasured confounding may have contributed to the findings.
Bottom line: Surgical repair of hip fractures in nursing home patients with advanced dementia reduces post-fracture mortality, pain, and pressure ulcer risk.
Citation: Berry SD et al. Association of clinical outcomes with surgical repair of hip fracture vs. nonsurgical management in nursing home residents with advanced dementia. JAMA Intern Med. 2018;178(6):774-80.
Dr. Abramowicz is an assistant professor in the division of hospital medicine, University of Colorado, Denver.
Clinical question: Does surgical repair of hip fractures in nursing home residents with advanced dementia reduce adverse outcomes?
Background: Hip fractures are common in the advanced dementia nursing home population. The benefit of surgical repair is unclear in this population given significant baseline functional disability and limited life expectancy.
Study design: Retrospective cohort study.
Setting: Medicare claims data set.
Synopsis: Among 3,083 nursing home residents with advanced dementia and hip fracture, nearly 85% underwent surgical repair. The 30-day mortality rate in the nonsurgical group was 30.6%, compared with 11.5% in the surgical group. In an adjusted model, the surgical group had decreased risk of death, compared with the nonsurgical group (hazard ratio, 0.88; 95% confidence interval, 0.79-0.98). In additional adjusted models, surgical patients also had decreased risk of pressure ulcers (HR 0.64; 95% CI, 0.47-0.86) and less pain (HR, 0.78; 95% CI, 0.61-0.99). Limitations included the observational nature of the study. Although the models were adjusted, unmeasured confounding may have contributed to the findings.
Bottom line: Surgical repair of hip fractures in nursing home patients with advanced dementia reduces post-fracture mortality, pain, and pressure ulcer risk.
Citation: Berry SD et al. Association of clinical outcomes with surgical repair of hip fracture vs. nonsurgical management in nursing home residents with advanced dementia. JAMA Intern Med. 2018;178(6):774-80.
Dr. Abramowicz is an assistant professor in the division of hospital medicine, University of Colorado, Denver.
Clinical question: Does surgical repair of hip fractures in nursing home residents with advanced dementia reduce adverse outcomes?
Background: Hip fractures are common in the advanced dementia nursing home population. The benefit of surgical repair is unclear in this population given significant baseline functional disability and limited life expectancy.
Study design: Retrospective cohort study.
Setting: Medicare claims data set.
Synopsis: Among 3,083 nursing home residents with advanced dementia and hip fracture, nearly 85% underwent surgical repair. The 30-day mortality rate in the nonsurgical group was 30.6%, compared with 11.5% in the surgical group. In an adjusted model, the surgical group had decreased risk of death, compared with the nonsurgical group (hazard ratio, 0.88; 95% confidence interval, 0.79-0.98). In additional adjusted models, surgical patients also had decreased risk of pressure ulcers (HR 0.64; 95% CI, 0.47-0.86) and less pain (HR, 0.78; 95% CI, 0.61-0.99). Limitations included the observational nature of the study. Although the models were adjusted, unmeasured confounding may have contributed to the findings.
Bottom line: Surgical repair of hip fractures in nursing home patients with advanced dementia reduces post-fracture mortality, pain, and pressure ulcer risk.
Citation: Berry SD et al. Association of clinical outcomes with surgical repair of hip fracture vs. nonsurgical management in nursing home residents with advanced dementia. JAMA Intern Med. 2018;178(6):774-80.
Dr. Abramowicz is an assistant professor in the division of hospital medicine, University of Colorado, Denver.
BNP levels and mortality in patients with and without heart failure
Clinical question: Does B-type natriuretic peptide (BNP) have prognostic value outside of heart failure (HF) patients?
Background: BNP levels are influenced by both cardiac and extracardiac stimuli and thus might have prognostic value outside of the traditional use to guide therapy for HF patients.
Study design: Retrospective cohort study of the Vanderbilt electronic health record.
Setting: Vanderbilt University Medical Center, Nashville, Tenn.
Synopsis: The study evaluated 30,487 patients with at least two BNP values for 2002-2015. Within this cohort, 62% of patients did not have a HF diagnosis. Risk of death was elevated in all patients regardless of HF status as BNP values rose. An increase from the 25th to 75th percentile in BNP value was associated with an increased risk of death in non-HF patients (hazard ratio, 2.08; 95% confidence interval, 1.99-2.2). Additionally, in a multivariate analysis BNP was the strongest predictor of death, compared with traditional risk factors in both HF and non-HF patients. The main limitation to this study was the use of ICD codes for diagnosis of HF.
Bottom line: BNP has predictive value for risk of death in non-HF patients; as BNP levels rise, regardless of HF status, so does risk of death.
Citation: York MK et al. B-type natriuretic peptide levels and mortality in patients with and without heart failure. J Am Coll Cardiol. 2018 May 15;71(19):2079-88.
Dr. Abramowicz is an assistant professor in the division of hospital medicine, University of Colorado, Denver.
Clinical question: Does B-type natriuretic peptide (BNP) have prognostic value outside of heart failure (HF) patients?
Background: BNP levels are influenced by both cardiac and extracardiac stimuli and thus might have prognostic value outside of the traditional use to guide therapy for HF patients.
Study design: Retrospective cohort study of the Vanderbilt electronic health record.
Setting: Vanderbilt University Medical Center, Nashville, Tenn.
Synopsis: The study evaluated 30,487 patients with at least two BNP values for 2002-2015. Within this cohort, 62% of patients did not have a HF diagnosis. Risk of death was elevated in all patients regardless of HF status as BNP values rose. An increase from the 25th to 75th percentile in BNP value was associated with an increased risk of death in non-HF patients (hazard ratio, 2.08; 95% confidence interval, 1.99-2.2). Additionally, in a multivariate analysis BNP was the strongest predictor of death, compared with traditional risk factors in both HF and non-HF patients. The main limitation to this study was the use of ICD codes for diagnosis of HF.
Bottom line: BNP has predictive value for risk of death in non-HF patients; as BNP levels rise, regardless of HF status, so does risk of death.
Citation: York MK et al. B-type natriuretic peptide levels and mortality in patients with and without heart failure. J Am Coll Cardiol. 2018 May 15;71(19):2079-88.
Dr. Abramowicz is an assistant professor in the division of hospital medicine, University of Colorado, Denver.
Clinical question: Does B-type natriuretic peptide (BNP) have prognostic value outside of heart failure (HF) patients?
Background: BNP levels are influenced by both cardiac and extracardiac stimuli and thus might have prognostic value outside of the traditional use to guide therapy for HF patients.
Study design: Retrospective cohort study of the Vanderbilt electronic health record.
Setting: Vanderbilt University Medical Center, Nashville, Tenn.
Synopsis: The study evaluated 30,487 patients with at least two BNP values for 2002-2015. Within this cohort, 62% of patients did not have a HF diagnosis. Risk of death was elevated in all patients regardless of HF status as BNP values rose. An increase from the 25th to 75th percentile in BNP value was associated with an increased risk of death in non-HF patients (hazard ratio, 2.08; 95% confidence interval, 1.99-2.2). Additionally, in a multivariate analysis BNP was the strongest predictor of death, compared with traditional risk factors in both HF and non-HF patients. The main limitation to this study was the use of ICD codes for diagnosis of HF.
Bottom line: BNP has predictive value for risk of death in non-HF patients; as BNP levels rise, regardless of HF status, so does risk of death.
Citation: York MK et al. B-type natriuretic peptide levels and mortality in patients with and without heart failure. J Am Coll Cardiol. 2018 May 15;71(19):2079-88.
Dr. Abramowicz is an assistant professor in the division of hospital medicine, University of Colorado, Denver.
Quick Byte: Palliative care
Rapid adoption of a key program
In 2015, 75% of U.S. hospitals with more than 50 beds had palliative care programs – a sharp increase from the 25% that had palliative care in 2000.
“The rapid adoption of this high-value program, which is voluntary and runs counter to the dominant culture in U.S. hospitals, was catalyzed by tens of millions of dollars in philanthropic support for innovation, dissemination, and professionalization in the palliative care field,” according to research published in Health Affairs.
Reference
Cassel JB et al. Palliative care leadership centers are key to the diffusion of palliative care innovation. Health Aff. 2018 Feb. doi: 10.1377/hlthaff.2017.1122.
Rapid adoption of a key program
Rapid adoption of a key program
In 2015, 75% of U.S. hospitals with more than 50 beds had palliative care programs – a sharp increase from the 25% that had palliative care in 2000.
“The rapid adoption of this high-value program, which is voluntary and runs counter to the dominant culture in U.S. hospitals, was catalyzed by tens of millions of dollars in philanthropic support for innovation, dissemination, and professionalization in the palliative care field,” according to research published in Health Affairs.
Reference
Cassel JB et al. Palliative care leadership centers are key to the diffusion of palliative care innovation. Health Aff. 2018 Feb. doi: 10.1377/hlthaff.2017.1122.
In 2015, 75% of U.S. hospitals with more than 50 beds had palliative care programs – a sharp increase from the 25% that had palliative care in 2000.
“The rapid adoption of this high-value program, which is voluntary and runs counter to the dominant culture in U.S. hospitals, was catalyzed by tens of millions of dollars in philanthropic support for innovation, dissemination, and professionalization in the palliative care field,” according to research published in Health Affairs.
Reference
Cassel JB et al. Palliative care leadership centers are key to the diffusion of palliative care innovation. Health Aff. 2018 Feb. doi: 10.1377/hlthaff.2017.1122.
Focus on patient experience to cut readmission rates
Incorporate patient-reported quality measures
Hospitalists have focused much attention on reducing 30-day readmission rates, at a time when 15-20% of health care dollars spent on those readmissions is considered potentially preventable.
But until very recently, no study has explored patient perceptions of the likelihood of readmission during index admission. Now, that’s changed.
“Our objective was to examine associations between patient perceptions of care during index hospital admission and 30-day readmission,” says Jocelyn Carter, MD, of Massachusetts General Hospital, Boston, and lead author of November 2017 study in BMJ Quality & Safety.
Enrolled in the study were 846 patients at two inpatient adult medicine units at Massachusetts General, Boston; 201 (23.8%) of these patients were readmitted within 30 days. In multivariable models adjusting for baseline differences, respondents who reported being “very satisfied” with the care received during the index hospitalization were less likely to be readmitted; participants reporting that doctors “always listened to them carefully” also were less likely to be readmitted.
“These findings are important since they suggest that engaging patients in an assessment of communication quality, unmet needs, concerns, and overall experience during admission may help to identify issues that might not be captured in standard postdischarge surveys when the appropriate time for quality improvement interventions has passed,” Dr. Carter said. “Incorporating patient-reported measures during index hospitalizations may improve readmission rates and help predict which patients are more likely to be readmitted.”
Reference
Carter J et al. The association between patient experience factors and likelihood of 30-day readmission: A prospective cohort study. BMJ Qual Saf. 16 Nov 2017. Accessed Feb 2, 2018.
Incorporate patient-reported quality measures
Incorporate patient-reported quality measures
Hospitalists have focused much attention on reducing 30-day readmission rates, at a time when 15-20% of health care dollars spent on those readmissions is considered potentially preventable.
But until very recently, no study has explored patient perceptions of the likelihood of readmission during index admission. Now, that’s changed.
“Our objective was to examine associations between patient perceptions of care during index hospital admission and 30-day readmission,” says Jocelyn Carter, MD, of Massachusetts General Hospital, Boston, and lead author of November 2017 study in BMJ Quality & Safety.
Enrolled in the study were 846 patients at two inpatient adult medicine units at Massachusetts General, Boston; 201 (23.8%) of these patients were readmitted within 30 days. In multivariable models adjusting for baseline differences, respondents who reported being “very satisfied” with the care received during the index hospitalization were less likely to be readmitted; participants reporting that doctors “always listened to them carefully” also were less likely to be readmitted.
“These findings are important since they suggest that engaging patients in an assessment of communication quality, unmet needs, concerns, and overall experience during admission may help to identify issues that might not be captured in standard postdischarge surveys when the appropriate time for quality improvement interventions has passed,” Dr. Carter said. “Incorporating patient-reported measures during index hospitalizations may improve readmission rates and help predict which patients are more likely to be readmitted.”
Reference
Carter J et al. The association between patient experience factors and likelihood of 30-day readmission: A prospective cohort study. BMJ Qual Saf. 16 Nov 2017. Accessed Feb 2, 2018.
Hospitalists have focused much attention on reducing 30-day readmission rates, at a time when 15-20% of health care dollars spent on those readmissions is considered potentially preventable.
But until very recently, no study has explored patient perceptions of the likelihood of readmission during index admission. Now, that’s changed.
“Our objective was to examine associations between patient perceptions of care during index hospital admission and 30-day readmission,” says Jocelyn Carter, MD, of Massachusetts General Hospital, Boston, and lead author of November 2017 study in BMJ Quality & Safety.
Enrolled in the study were 846 patients at two inpatient adult medicine units at Massachusetts General, Boston; 201 (23.8%) of these patients were readmitted within 30 days. In multivariable models adjusting for baseline differences, respondents who reported being “very satisfied” with the care received during the index hospitalization were less likely to be readmitted; participants reporting that doctors “always listened to them carefully” also were less likely to be readmitted.
“These findings are important since they suggest that engaging patients in an assessment of communication quality, unmet needs, concerns, and overall experience during admission may help to identify issues that might not be captured in standard postdischarge surveys when the appropriate time for quality improvement interventions has passed,” Dr. Carter said. “Incorporating patient-reported measures during index hospitalizations may improve readmission rates and help predict which patients are more likely to be readmitted.”
Reference
Carter J et al. The association between patient experience factors and likelihood of 30-day readmission: A prospective cohort study. BMJ Qual Saf. 16 Nov 2017. Accessed Feb 2, 2018.
How do you evaluate and treat a patient with C. difficile–associated disease?
Metronidazole is no longer recommended
Case
A 45-year-old woman on omeprazole for gastroesophageal reflux disease and recent treatment with ciprofloxacin for a urinary tract infection (UTI), who also has had several days of frequent watery stools, is admitted. She does not appear ill, and her abdominal exam is benign. She has normal renal function and white blood cell count. How should she be evaluated and treated for Clostridium difficile–associated disease (CDAD)?
Brief overview
C. difficile, a gram-positive anaerobic bacillus that exists in vegetative and spore forms, is a leading cause of hospital-associated diarrhea. C. difficile has a variety of presentations, ranging from asymptomatic colonization to CDAD, including severe diarrhea, ileus, and megacolon, and may be associated with a fatal outcome on rare occasions. The incidence of CDAD has been rising since the emergence of a hypervirulent strain (NAP1/BI/027) in the early 2000s and, not surprisingly, the number of deaths attributed to CDAD has also increased.1
CDAD requires acquisition of C. difficile as well as alteration in the colonic microbiota, often precipitated by antibiotics. The vegetative form of C. difficile can produce up to three toxins that are responsible for a cascade of reactions beginning with intestinal epithelial cell death followed by a significant inflammatory response and migration of neutrophils that eventually lead to the formation of the characteristic pseudomembranes.2
Until recently, the mainstay treatment for CDAD consisted of metronidazole and oral preparations of vancomycin. Recent results from randomized controlled trials and the increasing popularity of fecal microbiota transplant (FMT), however, have changed the therapeutic landscape of CDAD dramatically. Not surprisingly, the 2017 Infectious Diseases Society of America and the Society for Healthcare Epidemiology of America joint guidelines for CDAD represent a significant change to the treatment of CDAD, compared with previous guidelines.3
Overview of data
The hallmark of CDAD is a watery, nonbloody diarrhea. Given many other causes of diarrhea in hospitalized patients (e.g., direct effect of antibiotics, laxative use, tube feeding, etc.), hospitalists should focus on testing those patients who have three or more episodes of diarrhea in 24 hours and risk factors for CDAD (See Table 1).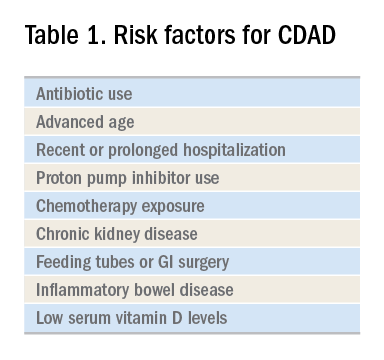
Exposure to antibiotics remains the greatest risk factor. It’s important to note that, while most patients develop CDAD within the first month after receiving systemic antibiotics, many patients remain at risk for up to 3 months.4 Although exposure to antibiotics, particularly in health care settings, is a significant risk factor for CDAD, up to 30%-40% of community-associated cases may not have a substantial antibiotic or health care facility exposure.5
Hospitalists should also not overlook the association between proton pump inhibitor (PPI) use and the development of CDAD.3 Although the IDSA/SHEA guidelines do not recommend discontinuation of PPIs solely for treatment or prevention of CDAD, at the minimum, the indication for their continued use in patients with CDAD should be revisited.
Testing for CDAD ranges from immunoassays that detect an enzyme common to all strains of C. difficile, glutamate dehydrogenase antigen (GDH), or toxins to nucleic acid amplification tests (NAATs), such as polymerase chain reaction [PCR]).1,6 GDH tests have high sensitivity but poor specificity, while testing for the toxin has high specificity but lower sensitivity (40%-80%) for CDAD.1 Although NAATs are highly sensitive and specific, they often have a poor positive predictive value in low-risk populations (e.g., those who do not have true diarrhea or whose diarrhea resolves before test results return). In these patients, a positive NAAT test may reflect colonization with toxigenic C. difficile, not necessarily CDAD. Except in rare instances, laboratories should only accept unformed stools for testing. Since the choice of testing for C. difficile varies by institution, hospitalists should understand the algorithm used by their respective hospitals and familiarize themselves with the sensitivity and specificity of each test.
Once a patient is diagnosed with CDAD, the hospitalist should assess the severity of the disease. The IDSA/SHEA guidelines still use leukocytosis and creatinine to separate mild from severe cases; the presence of fever and hypoalbuminemia also points to a more complicated course.3
The treatment of CDAD involves a strategy of withdrawing the putative culprit antibiotic(s) whenever possible and initiating of antibiotics effective against C. difficile. Following the publication of two randomized controlled trials demonstrating the inferiority of metronidazole to vancomycin in clinical cure of CDAD,2,7 the IDSA/SHEA guidelines no longer recommend metronidazole for the treatment of CDAD. Instead, a 10-day course of oral vancomycin or fidaxomicin has been recommended.2 Although fidaxomicin is associated with lower rates of recurrence of CDAD, it is also substantially more expensive than oral vancomycin, with a 10-day course often costing over $3,000.8 When choosing oral vancomycin for completion of therapy following discharge, hospitalists should also consider whether the dispensing outpatient pharmacy can provide the less-expensive liquid preparation of vancomycin. In resource-poor settings, consideration can still be given to metronidazole, an inexpensive drug, compared with both oral vancomycin and fidaxomicin. “Test of cure” with follow-up stool testing is not recommended.
For patients who require systemic antibiotics that precipitated their CDAD, it is common practice to extend CDAD treatment by providing a “tail” coverage with an agent effective against CDAD for 7-10 days following the completion of the inciting antibiotic. A common clinical question relates to the management of patients with prior history of CDAD but in need of a new round of systemic antibiotic therapy. In these patients, concurrent prophylactic doses of oral vancomycin have been found to be effective in preventing recurrence.9 The IDSA/SHEA guidelines conclude that “it may be prudent to administer low doses of vancomycin or fidaxomicin (e.g., 125 mg or 200 mg, respectively, once daily) while systemic antibiotics are administered.”3
For patients whose presentation extends beyond diarrhea, the IDSA/SHEA guidelines have changed the nomenclature for CDAD from “severe, complicated” to “fulminant.” Although there are no strict definitions, the IDSA/SHEA guidelines suggest that fulminant CDAD is characterized by “hypotension or shock, ileus, or megacolon.” In these patients, surgical intervention can be life saving, though mortality rates may remain over 50%.10 Hospitalists whose patients with CDAD are experiencing an acute abdomen or concern for colonic perforation, megacolon, shock, or organ system failure should obtain prompt surgical consultation. Antibiotic treatment should consist of a combination of higher doses of oral vancomycin and intravenous metronidazole (See Table 2).
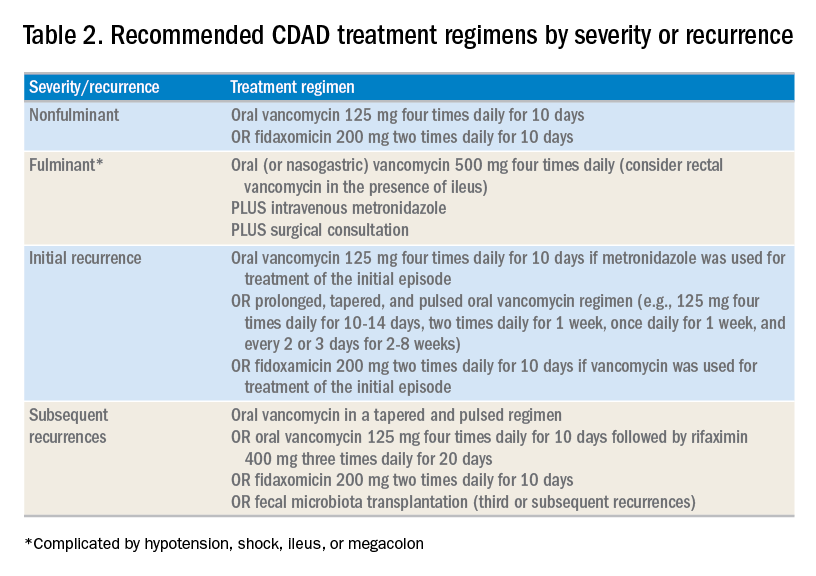
In addition to occasional treatment failures, a vexing characteristic of CDAD is its frequent recurrence rate, which may range from 15% to 30% or higher.11 The approach to recurrences is twofold: treatment of the C. difficile itself, and attempts to restore the colonic microbiome. The antibiotic treatment of the first recurrence of CDAD consists of either a 10-day course of fidaxomicin or a tapered, pulsed dose of vancomycin, which may be more effective than a repeat 10-day course of oral vancomycin.12 Although the treatment is unchanged for subsequent recurrences, the guidelines suggest consideration of rifaximin after a course of vancomycin (See Table 2).
Probiotics have been investigated as a means of restoring the colonic microbiome. Use of probiotics for both primary and secondary prevention of CDAD has resulted in conflicting data, with pooled analyses showing some benefit, while randomized controlled trials demonstrate less benefit.13 In addition, reports of bloodstream infections with Lactobacillus in frail patients and Saccharomyces in immunocompromised patients and those with central venous catheters raise doubts regarding their safety in certain patient populations.13 The IDSA/SHEA guidelines make no recommendations about the use of probiotics for the prevention of CDAD at this time.
Fecal microbiota transplant (FMT), however, does appear to be effective, especially in comparison to antibiotics alone in patients with multiple recurrences of CDAD.13 The IDSA/SHEA guidelines recommend consideration for FMT after the second recurrence of CDAD. The Fecal Microbiota Transplantation Workgroup has also proposed a set of guidelines for consideration of FMT when available (See Table 3).
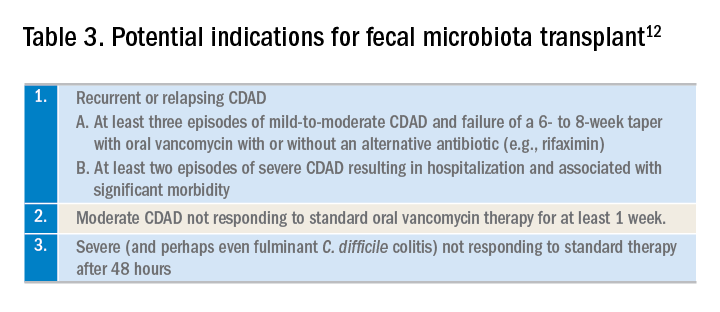
Application of data
The recent IDSA/SHEA guidelines have revised the treatment paradigm for CDAD. Most notably, metronidazole is no longer recommended for treatment of either initial or subsequent episodes of mild to severe CDAD, except when the cost of treatment may preclude the use of more effective therapies.
Initial episodes of mild to severe infection should be treated with either oral vancomycin or fidaxomicin. Recurrent episodes of CDAD should be treated with an agent different from that used for the initial episode, or with a pulsed, tapered regimen of oral vancomycin. FMT, where available, should be considered with multiple recurrences, or with moderate to severe infection not responding to standard therapy.
Fulminant CDAD, characterized by hypotension, shock, severe ileus, or megacolon, is a life-threatening medical emergency with a high mortality rate. Treatment should include high-dose oral vancomycin and intravenous metronidazole, with consideration of rectal vancomycin in patients with ileus. Immediate surgical consultation should be obtained to weigh the benefits of colectomy.
Back to our case
Our patient was treated with a 10-day course of vancomycin because this was uncomplicated CDAD and was her initial episode. Were she to develop a recurrence, she could be treated with a pulsed, tapered vancomycin regimen or fidaxomicin.
Bottom line
Vancomycin and fidaxomicin are recommended for the initial episode as well as recurrent CDAD. FMT should be considered for patients with multiple episodes of CDAD or treatment failures.
Dr. Roberts, Dr. Hillman, and Dr. Manian are hospitalists at Massachusetts General Hospital in Boston.
References
1. Louie TJ et al. Fidaxomicin versus vancomycin for Clostridium difficile infection. N Engl J Med. 2011 Feb 3;364:422-31. doi: 10.1056/NEJMoa0910812.
2. Burnham CA et al. Diagnosis of Clostridium difficile infection: an ongoing conundrum for clinicians and for clinical laboratories. Clin Microbiol Rev. 2013 Jul;26:604-30. doi: 10.1128/CMR.00016-13.
3. McDonald LC et al. Clinical Practice Guidelines for Clostridium difficile infection in adults and children: 2017 update by the Infectious Diseases Society of America (IDSA) and Society for Healthcare Epidemiology of America (SHEA). Clin Infect Dis. 2018 Mar 19;66:987-94. doi: 10.1093/cid/ciy149.
4. Hensgens MP et al. Time interval of increased risk for Clostridium difficile infection after exposure to antibiotics. J Antimicrob Chemother. 2012 Mar;67:742-8. doi: 10.1093/jac/dkr508. Epub 2011 Dec 6.
5. Chitnis AS et al. Epidemiology of community-associated Clostridium difficile infection, 2009 through 2011. JAMA Intern Med. 2013 Jul 22;173:1359-67. doi: 10.1001/jamainternmed.2013.7056.
6. Solomon DA et al. ID learning unit: Understanding and interpreting testing for Clostridium difficile. Open Forum Infectious Diseases. 2014 Mar;1(1);ofu007. doi: 10.1093/ofid/ofu007.
7. Johnson S et al. Vancomycin, metronidazole, or tolevamer for Clostridium difficile infection: results from two multinational, randomized, controlled trials. Clin Infect Dis. 2014 Aug 1;59(3):345-54. doi: 10.1093/cid/ciu313. Epub 2014 May 5.
8. https://m.goodrx.com/fidaxomicin, accessed June 24, 2018.
9. Van Hise NW et al. Efficacy of oral vancomycin in preventing recurrent Clostridium difficile infection in patients treated with systemic antimicrobial agents. Clin Infect Dis. 2016 Sep 1;63:651-3. doi: 10.1093/cid/ciw401. Epub 2016 Jun 17.
10. Sailhamer EA et al. Fulminant Clostridium difficile colitis: Patterns of care and predictors of mortality. Arch Surg. 2009;144:433-9. doi: 10.1001/archsurg.2009.51.
11. Zar FA et al. A comparison of vancomycin and metronidazole for the treatment of Clostridium difficile-associated diarrhea, stratified by disease severity. Clin Infect Dis. 2007;45:302-7. doi: 10.1086/519265. Epub 2007 Jun 19.
12. Bakken JS et al. Treating Clostridium difficile infection with fecal microbiota transplantation. Clin Gastroenterol Hepatol. 2011;9:1044-9. doi: 10.1016/j.cgh.2011.08.014. Epub 2011 Aug 24.
13. Crow JR et al. Probiotics and fecal microbiota transplant for primary and secondary prevention of Clostridium difficile infection. Pharmacotherapy. 2015 Nov;35:1016-25. doi: 10.1002/phar.1644. Epub 2015 Nov 2.
Additional reading
1. McDonald LC et al. Clinical practice guidelines for Clostridium difficile infection in adults and children: 2017 update by the Infectious Diseases Society of America (IDSA) and Society for Healthcare Epidemiology of America (SHEA). Clin Infect Dis. 2018 Mar 19;66:987-94. doi: 10.1093/cid/ciy149.
2. Burnham CA et al. Diagnosis of Clostridium difficile infection: an ongoing conundrum for clinicians and for clinical laboratories. Clin Microbiol Rev. 2013 Jul;26:604-30. doi: 10.1128/CMR.00016-13.
3. Crow JR, Davis SL, Chaykosky DM, Smith TT, Smith JM. Probiotics and fecal microbiota transplant for primary and secondary prevention of Clostridium difficile infection. Pharmacotherapy. 2015 Nov; 35:1016-25. doi: 10.1002/phar.1644. Epub 2015 Nov 2. Review.
Key points
1. Metronidazole is inferior to oral vancomycin and fidaxomicin for clinical cure of CDAD. The IDSA/SHEA guidelines now recommend a 10-day course of oral vancomycin or fidaxomicin for nonfulminant cases of CDAD.
2. For fulminant CDAD, the IDSA/SHEA guidelines suggest an increased dose of vancomycin and the addition of IV metronidazole. In such cases, surgical consultation should also be obtained.
3. After the second recurrence of Clostridium difficile infection, hospitalists should consider referral for FMT where available.
Quiz
The recent IDSA/SHEA guidelines no longer recommend metronidazole in the treatment of CDAD, except for which of the following scenarios (best answer)?
A. Treatment of a first episode of nonfulminant CDAD.
B. Treatment of recurrent CDAD following an initial course of oral vancomycin.
C. Treatment of fulminant infection with IV metronidazole in addition to oral or rectal vancomycin.
D. For prophylaxis following fecal microbiota transplant.
Answer: C. In fulminant infection, concurrent ileus may interfere with appropriate delivery of oral vancomycin to the colon. Adding intravenous metronidazole can allow this antibiotic to reach the bowel. Adding intravenous metronidazole to oral vancomycin is also recommended by IDSA/SHEA guidelines in cases of fulminant CDAD. Evidence from high-quality randomized controlled trials has shown that vancomycin is superior to oral metronidazole for treatment of initial and recurrent episodes of CDAD. There is no evidence to support the use of metronidazole for recurrent CDAD following an initial course of oral vancomycin or for prophylaxis following FMT.
Metronidazole is no longer recommended
Metronidazole is no longer recommended
Case
A 45-year-old woman on omeprazole for gastroesophageal reflux disease and recent treatment with ciprofloxacin for a urinary tract infection (UTI), who also has had several days of frequent watery stools, is admitted. She does not appear ill, and her abdominal exam is benign. She has normal renal function and white blood cell count. How should she be evaluated and treated for Clostridium difficile–associated disease (CDAD)?
Brief overview
C. difficile, a gram-positive anaerobic bacillus that exists in vegetative and spore forms, is a leading cause of hospital-associated diarrhea. C. difficile has a variety of presentations, ranging from asymptomatic colonization to CDAD, including severe diarrhea, ileus, and megacolon, and may be associated with a fatal outcome on rare occasions. The incidence of CDAD has been rising since the emergence of a hypervirulent strain (NAP1/BI/027) in the early 2000s and, not surprisingly, the number of deaths attributed to CDAD has also increased.1
CDAD requires acquisition of C. difficile as well as alteration in the colonic microbiota, often precipitated by antibiotics. The vegetative form of C. difficile can produce up to three toxins that are responsible for a cascade of reactions beginning with intestinal epithelial cell death followed by a significant inflammatory response and migration of neutrophils that eventually lead to the formation of the characteristic pseudomembranes.2
Until recently, the mainstay treatment for CDAD consisted of metronidazole and oral preparations of vancomycin. Recent results from randomized controlled trials and the increasing popularity of fecal microbiota transplant (FMT), however, have changed the therapeutic landscape of CDAD dramatically. Not surprisingly, the 2017 Infectious Diseases Society of America and the Society for Healthcare Epidemiology of America joint guidelines for CDAD represent a significant change to the treatment of CDAD, compared with previous guidelines.3
Overview of data
The hallmark of CDAD is a watery, nonbloody diarrhea. Given many other causes of diarrhea in hospitalized patients (e.g., direct effect of antibiotics, laxative use, tube feeding, etc.), hospitalists should focus on testing those patients who have three or more episodes of diarrhea in 24 hours and risk factors for CDAD (See Table 1).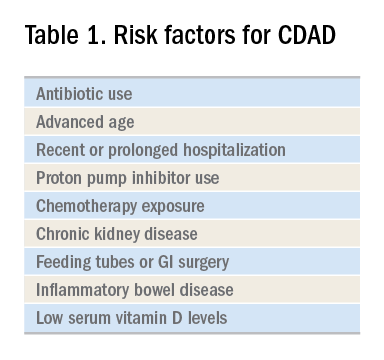
Exposure to antibiotics remains the greatest risk factor. It’s important to note that, while most patients develop CDAD within the first month after receiving systemic antibiotics, many patients remain at risk for up to 3 months.4 Although exposure to antibiotics, particularly in health care settings, is a significant risk factor for CDAD, up to 30%-40% of community-associated cases may not have a substantial antibiotic or health care facility exposure.5
Hospitalists should also not overlook the association between proton pump inhibitor (PPI) use and the development of CDAD.3 Although the IDSA/SHEA guidelines do not recommend discontinuation of PPIs solely for treatment or prevention of CDAD, at the minimum, the indication for their continued use in patients with CDAD should be revisited.
Testing for CDAD ranges from immunoassays that detect an enzyme common to all strains of C. difficile, glutamate dehydrogenase antigen (GDH), or toxins to nucleic acid amplification tests (NAATs), such as polymerase chain reaction [PCR]).1,6 GDH tests have high sensitivity but poor specificity, while testing for the toxin has high specificity but lower sensitivity (40%-80%) for CDAD.1 Although NAATs are highly sensitive and specific, they often have a poor positive predictive value in low-risk populations (e.g., those who do not have true diarrhea or whose diarrhea resolves before test results return). In these patients, a positive NAAT test may reflect colonization with toxigenic C. difficile, not necessarily CDAD. Except in rare instances, laboratories should only accept unformed stools for testing. Since the choice of testing for C. difficile varies by institution, hospitalists should understand the algorithm used by their respective hospitals and familiarize themselves with the sensitivity and specificity of each test.
Once a patient is diagnosed with CDAD, the hospitalist should assess the severity of the disease. The IDSA/SHEA guidelines still use leukocytosis and creatinine to separate mild from severe cases; the presence of fever and hypoalbuminemia also points to a more complicated course.3
The treatment of CDAD involves a strategy of withdrawing the putative culprit antibiotic(s) whenever possible and initiating of antibiotics effective against C. difficile. Following the publication of two randomized controlled trials demonstrating the inferiority of metronidazole to vancomycin in clinical cure of CDAD,2,7 the IDSA/SHEA guidelines no longer recommend metronidazole for the treatment of CDAD. Instead, a 10-day course of oral vancomycin or fidaxomicin has been recommended.2 Although fidaxomicin is associated with lower rates of recurrence of CDAD, it is also substantially more expensive than oral vancomycin, with a 10-day course often costing over $3,000.8 When choosing oral vancomycin for completion of therapy following discharge, hospitalists should also consider whether the dispensing outpatient pharmacy can provide the less-expensive liquid preparation of vancomycin. In resource-poor settings, consideration can still be given to metronidazole, an inexpensive drug, compared with both oral vancomycin and fidaxomicin. “Test of cure” with follow-up stool testing is not recommended.
For patients who require systemic antibiotics that precipitated their CDAD, it is common practice to extend CDAD treatment by providing a “tail” coverage with an agent effective against CDAD for 7-10 days following the completion of the inciting antibiotic. A common clinical question relates to the management of patients with prior history of CDAD but in need of a new round of systemic antibiotic therapy. In these patients, concurrent prophylactic doses of oral vancomycin have been found to be effective in preventing recurrence.9 The IDSA/SHEA guidelines conclude that “it may be prudent to administer low doses of vancomycin or fidaxomicin (e.g., 125 mg or 200 mg, respectively, once daily) while systemic antibiotics are administered.”3
For patients whose presentation extends beyond diarrhea, the IDSA/SHEA guidelines have changed the nomenclature for CDAD from “severe, complicated” to “fulminant.” Although there are no strict definitions, the IDSA/SHEA guidelines suggest that fulminant CDAD is characterized by “hypotension or shock, ileus, or megacolon.” In these patients, surgical intervention can be life saving, though mortality rates may remain over 50%.10 Hospitalists whose patients with CDAD are experiencing an acute abdomen or concern for colonic perforation, megacolon, shock, or organ system failure should obtain prompt surgical consultation. Antibiotic treatment should consist of a combination of higher doses of oral vancomycin and intravenous metronidazole (See Table 2).
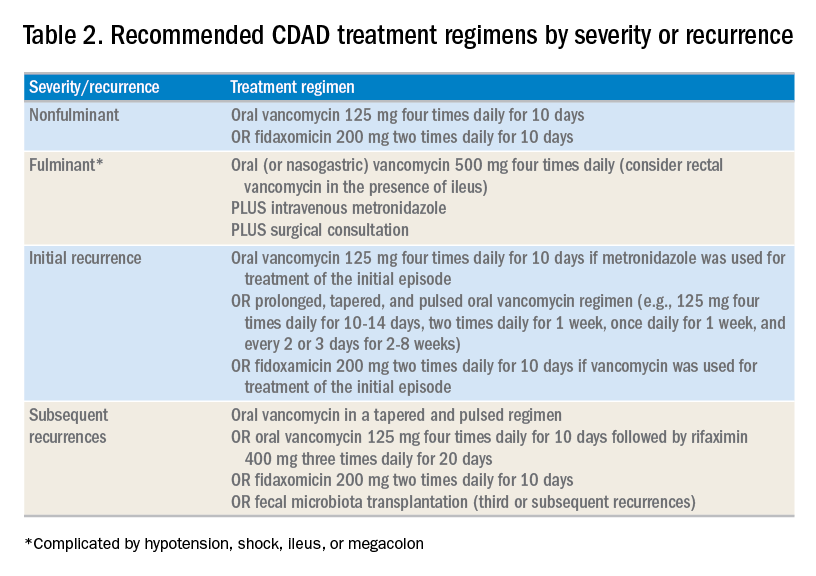
In addition to occasional treatment failures, a vexing characteristic of CDAD is its frequent recurrence rate, which may range from 15% to 30% or higher.11 The approach to recurrences is twofold: treatment of the C. difficile itself, and attempts to restore the colonic microbiome. The antibiotic treatment of the first recurrence of CDAD consists of either a 10-day course of fidaxomicin or a tapered, pulsed dose of vancomycin, which may be more effective than a repeat 10-day course of oral vancomycin.12 Although the treatment is unchanged for subsequent recurrences, the guidelines suggest consideration of rifaximin after a course of vancomycin (See Table 2).
Probiotics have been investigated as a means of restoring the colonic microbiome. Use of probiotics for both primary and secondary prevention of CDAD has resulted in conflicting data, with pooled analyses showing some benefit, while randomized controlled trials demonstrate less benefit.13 In addition, reports of bloodstream infections with Lactobacillus in frail patients and Saccharomyces in immunocompromised patients and those with central venous catheters raise doubts regarding their safety in certain patient populations.13 The IDSA/SHEA guidelines make no recommendations about the use of probiotics for the prevention of CDAD at this time.
Fecal microbiota transplant (FMT), however, does appear to be effective, especially in comparison to antibiotics alone in patients with multiple recurrences of CDAD.13 The IDSA/SHEA guidelines recommend consideration for FMT after the second recurrence of CDAD. The Fecal Microbiota Transplantation Workgroup has also proposed a set of guidelines for consideration of FMT when available (See Table 3).
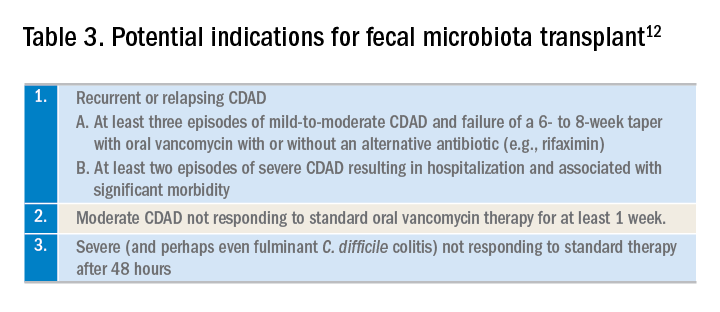
Application of data
The recent IDSA/SHEA guidelines have revised the treatment paradigm for CDAD. Most notably, metronidazole is no longer recommended for treatment of either initial or subsequent episodes of mild to severe CDAD, except when the cost of treatment may preclude the use of more effective therapies.
Initial episodes of mild to severe infection should be treated with either oral vancomycin or fidaxomicin. Recurrent episodes of CDAD should be treated with an agent different from that used for the initial episode, or with a pulsed, tapered regimen of oral vancomycin. FMT, where available, should be considered with multiple recurrences, or with moderate to severe infection not responding to standard therapy.
Fulminant CDAD, characterized by hypotension, shock, severe ileus, or megacolon, is a life-threatening medical emergency with a high mortality rate. Treatment should include high-dose oral vancomycin and intravenous metronidazole, with consideration of rectal vancomycin in patients with ileus. Immediate surgical consultation should be obtained to weigh the benefits of colectomy.
Back to our case
Our patient was treated with a 10-day course of vancomycin because this was uncomplicated CDAD and was her initial episode. Were she to develop a recurrence, she could be treated with a pulsed, tapered vancomycin regimen or fidaxomicin.
Bottom line
Vancomycin and fidaxomicin are recommended for the initial episode as well as recurrent CDAD. FMT should be considered for patients with multiple episodes of CDAD or treatment failures.
Dr. Roberts, Dr. Hillman, and Dr. Manian are hospitalists at Massachusetts General Hospital in Boston.
References
1. Louie TJ et al. Fidaxomicin versus vancomycin for Clostridium difficile infection. N Engl J Med. 2011 Feb 3;364:422-31. doi: 10.1056/NEJMoa0910812.
2. Burnham CA et al. Diagnosis of Clostridium difficile infection: an ongoing conundrum for clinicians and for clinical laboratories. Clin Microbiol Rev. 2013 Jul;26:604-30. doi: 10.1128/CMR.00016-13.
3. McDonald LC et al. Clinical Practice Guidelines for Clostridium difficile infection in adults and children: 2017 update by the Infectious Diseases Society of America (IDSA) and Society for Healthcare Epidemiology of America (SHEA). Clin Infect Dis. 2018 Mar 19;66:987-94. doi: 10.1093/cid/ciy149.
4. Hensgens MP et al. Time interval of increased risk for Clostridium difficile infection after exposure to antibiotics. J Antimicrob Chemother. 2012 Mar;67:742-8. doi: 10.1093/jac/dkr508. Epub 2011 Dec 6.
5. Chitnis AS et al. Epidemiology of community-associated Clostridium difficile infection, 2009 through 2011. JAMA Intern Med. 2013 Jul 22;173:1359-67. doi: 10.1001/jamainternmed.2013.7056.
6. Solomon DA et al. ID learning unit: Understanding and interpreting testing for Clostridium difficile. Open Forum Infectious Diseases. 2014 Mar;1(1);ofu007. doi: 10.1093/ofid/ofu007.
7. Johnson S et al. Vancomycin, metronidazole, or tolevamer for Clostridium difficile infection: results from two multinational, randomized, controlled trials. Clin Infect Dis. 2014 Aug 1;59(3):345-54. doi: 10.1093/cid/ciu313. Epub 2014 May 5.
8. https://m.goodrx.com/fidaxomicin, accessed June 24, 2018.
9. Van Hise NW et al. Efficacy of oral vancomycin in preventing recurrent Clostridium difficile infection in patients treated with systemic antimicrobial agents. Clin Infect Dis. 2016 Sep 1;63:651-3. doi: 10.1093/cid/ciw401. Epub 2016 Jun 17.
10. Sailhamer EA et al. Fulminant Clostridium difficile colitis: Patterns of care and predictors of mortality. Arch Surg. 2009;144:433-9. doi: 10.1001/archsurg.2009.51.
11. Zar FA et al. A comparison of vancomycin and metronidazole for the treatment of Clostridium difficile-associated diarrhea, stratified by disease severity. Clin Infect Dis. 2007;45:302-7. doi: 10.1086/519265. Epub 2007 Jun 19.
12. Bakken JS et al. Treating Clostridium difficile infection with fecal microbiota transplantation. Clin Gastroenterol Hepatol. 2011;9:1044-9. doi: 10.1016/j.cgh.2011.08.014. Epub 2011 Aug 24.
13. Crow JR et al. Probiotics and fecal microbiota transplant for primary and secondary prevention of Clostridium difficile infection. Pharmacotherapy. 2015 Nov;35:1016-25. doi: 10.1002/phar.1644. Epub 2015 Nov 2.
Additional reading
1. McDonald LC et al. Clinical practice guidelines for Clostridium difficile infection in adults and children: 2017 update by the Infectious Diseases Society of America (IDSA) and Society for Healthcare Epidemiology of America (SHEA). Clin Infect Dis. 2018 Mar 19;66:987-94. doi: 10.1093/cid/ciy149.
2. Burnham CA et al. Diagnosis of Clostridium difficile infection: an ongoing conundrum for clinicians and for clinical laboratories. Clin Microbiol Rev. 2013 Jul;26:604-30. doi: 10.1128/CMR.00016-13.
3. Crow JR, Davis SL, Chaykosky DM, Smith TT, Smith JM. Probiotics and fecal microbiota transplant for primary and secondary prevention of Clostridium difficile infection. Pharmacotherapy. 2015 Nov; 35:1016-25. doi: 10.1002/phar.1644. Epub 2015 Nov 2. Review.
Key points
1. Metronidazole is inferior to oral vancomycin and fidaxomicin for clinical cure of CDAD. The IDSA/SHEA guidelines now recommend a 10-day course of oral vancomycin or fidaxomicin for nonfulminant cases of CDAD.
2. For fulminant CDAD, the IDSA/SHEA guidelines suggest an increased dose of vancomycin and the addition of IV metronidazole. In such cases, surgical consultation should also be obtained.
3. After the second recurrence of Clostridium difficile infection, hospitalists should consider referral for FMT where available.
Quiz
The recent IDSA/SHEA guidelines no longer recommend metronidazole in the treatment of CDAD, except for which of the following scenarios (best answer)?
A. Treatment of a first episode of nonfulminant CDAD.
B. Treatment of recurrent CDAD following an initial course of oral vancomycin.
C. Treatment of fulminant infection with IV metronidazole in addition to oral or rectal vancomycin.
D. For prophylaxis following fecal microbiota transplant.
Answer: C. In fulminant infection, concurrent ileus may interfere with appropriate delivery of oral vancomycin to the colon. Adding intravenous metronidazole can allow this antibiotic to reach the bowel. Adding intravenous metronidazole to oral vancomycin is also recommended by IDSA/SHEA guidelines in cases of fulminant CDAD. Evidence from high-quality randomized controlled trials has shown that vancomycin is superior to oral metronidazole for treatment of initial and recurrent episodes of CDAD. There is no evidence to support the use of metronidazole for recurrent CDAD following an initial course of oral vancomycin or for prophylaxis following FMT.
Case
A 45-year-old woman on omeprazole for gastroesophageal reflux disease and recent treatment with ciprofloxacin for a urinary tract infection (UTI), who also has had several days of frequent watery stools, is admitted. She does not appear ill, and her abdominal exam is benign. She has normal renal function and white blood cell count. How should she be evaluated and treated for Clostridium difficile–associated disease (CDAD)?
Brief overview
C. difficile, a gram-positive anaerobic bacillus that exists in vegetative and spore forms, is a leading cause of hospital-associated diarrhea. C. difficile has a variety of presentations, ranging from asymptomatic colonization to CDAD, including severe diarrhea, ileus, and megacolon, and may be associated with a fatal outcome on rare occasions. The incidence of CDAD has been rising since the emergence of a hypervirulent strain (NAP1/BI/027) in the early 2000s and, not surprisingly, the number of deaths attributed to CDAD has also increased.1
CDAD requires acquisition of C. difficile as well as alteration in the colonic microbiota, often precipitated by antibiotics. The vegetative form of C. difficile can produce up to three toxins that are responsible for a cascade of reactions beginning with intestinal epithelial cell death followed by a significant inflammatory response and migration of neutrophils that eventually lead to the formation of the characteristic pseudomembranes.2
Until recently, the mainstay treatment for CDAD consisted of metronidazole and oral preparations of vancomycin. Recent results from randomized controlled trials and the increasing popularity of fecal microbiota transplant (FMT), however, have changed the therapeutic landscape of CDAD dramatically. Not surprisingly, the 2017 Infectious Diseases Society of America and the Society for Healthcare Epidemiology of America joint guidelines for CDAD represent a significant change to the treatment of CDAD, compared with previous guidelines.3
Overview of data
The hallmark of CDAD is a watery, nonbloody diarrhea. Given many other causes of diarrhea in hospitalized patients (e.g., direct effect of antibiotics, laxative use, tube feeding, etc.), hospitalists should focus on testing those patients who have three or more episodes of diarrhea in 24 hours and risk factors for CDAD (See Table 1).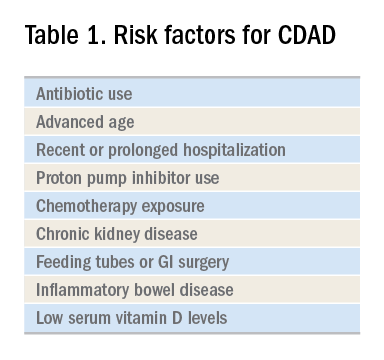
Exposure to antibiotics remains the greatest risk factor. It’s important to note that, while most patients develop CDAD within the first month after receiving systemic antibiotics, many patients remain at risk for up to 3 months.4 Although exposure to antibiotics, particularly in health care settings, is a significant risk factor for CDAD, up to 30%-40% of community-associated cases may not have a substantial antibiotic or health care facility exposure.5
Hospitalists should also not overlook the association between proton pump inhibitor (PPI) use and the development of CDAD.3 Although the IDSA/SHEA guidelines do not recommend discontinuation of PPIs solely for treatment or prevention of CDAD, at the minimum, the indication for their continued use in patients with CDAD should be revisited.
Testing for CDAD ranges from immunoassays that detect an enzyme common to all strains of C. difficile, glutamate dehydrogenase antigen (GDH), or toxins to nucleic acid amplification tests (NAATs), such as polymerase chain reaction [PCR]).1,6 GDH tests have high sensitivity but poor specificity, while testing for the toxin has high specificity but lower sensitivity (40%-80%) for CDAD.1 Although NAATs are highly sensitive and specific, they often have a poor positive predictive value in low-risk populations (e.g., those who do not have true diarrhea or whose diarrhea resolves before test results return). In these patients, a positive NAAT test may reflect colonization with toxigenic C. difficile, not necessarily CDAD. Except in rare instances, laboratories should only accept unformed stools for testing. Since the choice of testing for C. difficile varies by institution, hospitalists should understand the algorithm used by their respective hospitals and familiarize themselves with the sensitivity and specificity of each test.
Once a patient is diagnosed with CDAD, the hospitalist should assess the severity of the disease. The IDSA/SHEA guidelines still use leukocytosis and creatinine to separate mild from severe cases; the presence of fever and hypoalbuminemia also points to a more complicated course.3
The treatment of CDAD involves a strategy of withdrawing the putative culprit antibiotic(s) whenever possible and initiating of antibiotics effective against C. difficile. Following the publication of two randomized controlled trials demonstrating the inferiority of metronidazole to vancomycin in clinical cure of CDAD,2,7 the IDSA/SHEA guidelines no longer recommend metronidazole for the treatment of CDAD. Instead, a 10-day course of oral vancomycin or fidaxomicin has been recommended.2 Although fidaxomicin is associated with lower rates of recurrence of CDAD, it is also substantially more expensive than oral vancomycin, with a 10-day course often costing over $3,000.8 When choosing oral vancomycin for completion of therapy following discharge, hospitalists should also consider whether the dispensing outpatient pharmacy can provide the less-expensive liquid preparation of vancomycin. In resource-poor settings, consideration can still be given to metronidazole, an inexpensive drug, compared with both oral vancomycin and fidaxomicin. “Test of cure” with follow-up stool testing is not recommended.
For patients who require systemic antibiotics that precipitated their CDAD, it is common practice to extend CDAD treatment by providing a “tail” coverage with an agent effective against CDAD for 7-10 days following the completion of the inciting antibiotic. A common clinical question relates to the management of patients with prior history of CDAD but in need of a new round of systemic antibiotic therapy. In these patients, concurrent prophylactic doses of oral vancomycin have been found to be effective in preventing recurrence.9 The IDSA/SHEA guidelines conclude that “it may be prudent to administer low doses of vancomycin or fidaxomicin (e.g., 125 mg or 200 mg, respectively, once daily) while systemic antibiotics are administered.”3
For patients whose presentation extends beyond diarrhea, the IDSA/SHEA guidelines have changed the nomenclature for CDAD from “severe, complicated” to “fulminant.” Although there are no strict definitions, the IDSA/SHEA guidelines suggest that fulminant CDAD is characterized by “hypotension or shock, ileus, or megacolon.” In these patients, surgical intervention can be life saving, though mortality rates may remain over 50%.10 Hospitalists whose patients with CDAD are experiencing an acute abdomen or concern for colonic perforation, megacolon, shock, or organ system failure should obtain prompt surgical consultation. Antibiotic treatment should consist of a combination of higher doses of oral vancomycin and intravenous metronidazole (See Table 2).
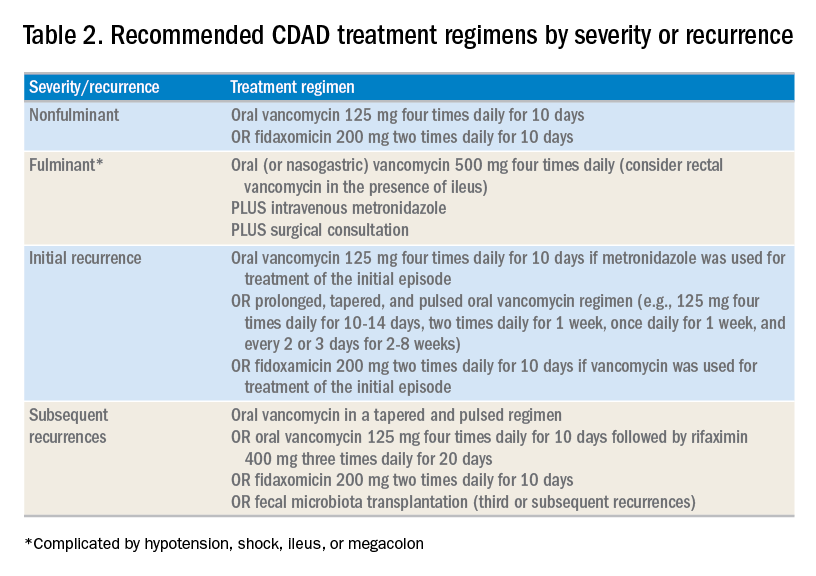
In addition to occasional treatment failures, a vexing characteristic of CDAD is its frequent recurrence rate, which may range from 15% to 30% or higher.11 The approach to recurrences is twofold: treatment of the C. difficile itself, and attempts to restore the colonic microbiome. The antibiotic treatment of the first recurrence of CDAD consists of either a 10-day course of fidaxomicin or a tapered, pulsed dose of vancomycin, which may be more effective than a repeat 10-day course of oral vancomycin.12 Although the treatment is unchanged for subsequent recurrences, the guidelines suggest consideration of rifaximin after a course of vancomycin (See Table 2).
Probiotics have been investigated as a means of restoring the colonic microbiome. Use of probiotics for both primary and secondary prevention of CDAD has resulted in conflicting data, with pooled analyses showing some benefit, while randomized controlled trials demonstrate less benefit.13 In addition, reports of bloodstream infections with Lactobacillus in frail patients and Saccharomyces in immunocompromised patients and those with central venous catheters raise doubts regarding their safety in certain patient populations.13 The IDSA/SHEA guidelines make no recommendations about the use of probiotics for the prevention of CDAD at this time.
Fecal microbiota transplant (FMT), however, does appear to be effective, especially in comparison to antibiotics alone in patients with multiple recurrences of CDAD.13 The IDSA/SHEA guidelines recommend consideration for FMT after the second recurrence of CDAD. The Fecal Microbiota Transplantation Workgroup has also proposed a set of guidelines for consideration of FMT when available (See Table 3).
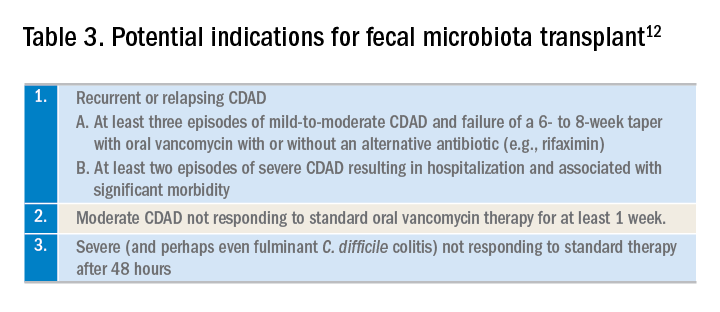
Application of data
The recent IDSA/SHEA guidelines have revised the treatment paradigm for CDAD. Most notably, metronidazole is no longer recommended for treatment of either initial or subsequent episodes of mild to severe CDAD, except when the cost of treatment may preclude the use of more effective therapies.
Initial episodes of mild to severe infection should be treated with either oral vancomycin or fidaxomicin. Recurrent episodes of CDAD should be treated with an agent different from that used for the initial episode, or with a pulsed, tapered regimen of oral vancomycin. FMT, where available, should be considered with multiple recurrences, or with moderate to severe infection not responding to standard therapy.
Fulminant CDAD, characterized by hypotension, shock, severe ileus, or megacolon, is a life-threatening medical emergency with a high mortality rate. Treatment should include high-dose oral vancomycin and intravenous metronidazole, with consideration of rectal vancomycin in patients with ileus. Immediate surgical consultation should be obtained to weigh the benefits of colectomy.
Back to our case
Our patient was treated with a 10-day course of vancomycin because this was uncomplicated CDAD and was her initial episode. Were she to develop a recurrence, she could be treated with a pulsed, tapered vancomycin regimen or fidaxomicin.
Bottom line
Vancomycin and fidaxomicin are recommended for the initial episode as well as recurrent CDAD. FMT should be considered for patients with multiple episodes of CDAD or treatment failures.
Dr. Roberts, Dr. Hillman, and Dr. Manian are hospitalists at Massachusetts General Hospital in Boston.
References
1. Louie TJ et al. Fidaxomicin versus vancomycin for Clostridium difficile infection. N Engl J Med. 2011 Feb 3;364:422-31. doi: 10.1056/NEJMoa0910812.
2. Burnham CA et al. Diagnosis of Clostridium difficile infection: an ongoing conundrum for clinicians and for clinical laboratories. Clin Microbiol Rev. 2013 Jul;26:604-30. doi: 10.1128/CMR.00016-13.
3. McDonald LC et al. Clinical Practice Guidelines for Clostridium difficile infection in adults and children: 2017 update by the Infectious Diseases Society of America (IDSA) and Society for Healthcare Epidemiology of America (SHEA). Clin Infect Dis. 2018 Mar 19;66:987-94. doi: 10.1093/cid/ciy149.
4. Hensgens MP et al. Time interval of increased risk for Clostridium difficile infection after exposure to antibiotics. J Antimicrob Chemother. 2012 Mar;67:742-8. doi: 10.1093/jac/dkr508. Epub 2011 Dec 6.
5. Chitnis AS et al. Epidemiology of community-associated Clostridium difficile infection, 2009 through 2011. JAMA Intern Med. 2013 Jul 22;173:1359-67. doi: 10.1001/jamainternmed.2013.7056.
6. Solomon DA et al. ID learning unit: Understanding and interpreting testing for Clostridium difficile. Open Forum Infectious Diseases. 2014 Mar;1(1);ofu007. doi: 10.1093/ofid/ofu007.
7. Johnson S et al. Vancomycin, metronidazole, or tolevamer for Clostridium difficile infection: results from two multinational, randomized, controlled trials. Clin Infect Dis. 2014 Aug 1;59(3):345-54. doi: 10.1093/cid/ciu313. Epub 2014 May 5.
8. https://m.goodrx.com/fidaxomicin, accessed June 24, 2018.
9. Van Hise NW et al. Efficacy of oral vancomycin in preventing recurrent Clostridium difficile infection in patients treated with systemic antimicrobial agents. Clin Infect Dis. 2016 Sep 1;63:651-3. doi: 10.1093/cid/ciw401. Epub 2016 Jun 17.
10. Sailhamer EA et al. Fulminant Clostridium difficile colitis: Patterns of care and predictors of mortality. Arch Surg. 2009;144:433-9. doi: 10.1001/archsurg.2009.51.
11. Zar FA et al. A comparison of vancomycin and metronidazole for the treatment of Clostridium difficile-associated diarrhea, stratified by disease severity. Clin Infect Dis. 2007;45:302-7. doi: 10.1086/519265. Epub 2007 Jun 19.
12. Bakken JS et al. Treating Clostridium difficile infection with fecal microbiota transplantation. Clin Gastroenterol Hepatol. 2011;9:1044-9. doi: 10.1016/j.cgh.2011.08.014. Epub 2011 Aug 24.
13. Crow JR et al. Probiotics and fecal microbiota transplant for primary and secondary prevention of Clostridium difficile infection. Pharmacotherapy. 2015 Nov;35:1016-25. doi: 10.1002/phar.1644. Epub 2015 Nov 2.
Additional reading
1. McDonald LC et al. Clinical practice guidelines for Clostridium difficile infection in adults and children: 2017 update by the Infectious Diseases Society of America (IDSA) and Society for Healthcare Epidemiology of America (SHEA). Clin Infect Dis. 2018 Mar 19;66:987-94. doi: 10.1093/cid/ciy149.
2. Burnham CA et al. Diagnosis of Clostridium difficile infection: an ongoing conundrum for clinicians and for clinical laboratories. Clin Microbiol Rev. 2013 Jul;26:604-30. doi: 10.1128/CMR.00016-13.
3. Crow JR, Davis SL, Chaykosky DM, Smith TT, Smith JM. Probiotics and fecal microbiota transplant for primary and secondary prevention of Clostridium difficile infection. Pharmacotherapy. 2015 Nov; 35:1016-25. doi: 10.1002/phar.1644. Epub 2015 Nov 2. Review.
Key points
1. Metronidazole is inferior to oral vancomycin and fidaxomicin for clinical cure of CDAD. The IDSA/SHEA guidelines now recommend a 10-day course of oral vancomycin or fidaxomicin for nonfulminant cases of CDAD.
2. For fulminant CDAD, the IDSA/SHEA guidelines suggest an increased dose of vancomycin and the addition of IV metronidazole. In such cases, surgical consultation should also be obtained.
3. After the second recurrence of Clostridium difficile infection, hospitalists should consider referral for FMT where available.
Quiz
The recent IDSA/SHEA guidelines no longer recommend metronidazole in the treatment of CDAD, except for which of the following scenarios (best answer)?
A. Treatment of a first episode of nonfulminant CDAD.
B. Treatment of recurrent CDAD following an initial course of oral vancomycin.
C. Treatment of fulminant infection with IV metronidazole in addition to oral or rectal vancomycin.
D. For prophylaxis following fecal microbiota transplant.
Answer: C. In fulminant infection, concurrent ileus may interfere with appropriate delivery of oral vancomycin to the colon. Adding intravenous metronidazole can allow this antibiotic to reach the bowel. Adding intravenous metronidazole to oral vancomycin is also recommended by IDSA/SHEA guidelines in cases of fulminant CDAD. Evidence from high-quality randomized controlled trials has shown that vancomycin is superior to oral metronidazole for treatment of initial and recurrent episodes of CDAD. There is no evidence to support the use of metronidazole for recurrent CDAD following an initial course of oral vancomycin or for prophylaxis following FMT.



















