User login
Reducing alarm fatigue
Monitoring from a centralized location
Hospitalists hearing the constant noise from cardiac telemetry monitoring systems can experience alarm fatigue – a nationwide phenomenon that can lead to an increase in patient deaths.
The American Heart Association reports that fewer than one in four adults survived an in-hospital cardiac arrest in 2013; other studies showed that up to 44% of inpatient cardiac arrests were not detected appropriately, according to the Cleveland Clinic.
Clinicians at the Cleveland Clinic have tried centralized monitoring to address the problem. They’ve established a “mission control” center, where off-site personnel monitor sensors and high-definition cameras and vital signs such as blood pressure, heart rate, and respiration. On-site action is requested when appropriate; unimportant alarms are dismissed.
In August 2016, results from the first 13 months of the Cleveland Clinic program were published in JAMA. They revealed that the monitoring system could help reduce rates of unimportant alarms with no increase in cardiopulmonary arrest events. The centralized unit monitored 99,048 patient orders, and ultimately detected serious problems and accurately notified on-site staff for 79% of 3,243 events, which included a rhythm and/or rate change within 1 hour or less of the event. Accurate notification to on-site hospital staff was more than 84%.
Since then, improvements to the system have continued, according to Cleveland Clinic, and include doubling the number of monitored patients per technician and improved clinical outcomes.
Reference
Cleveland Clinic: Consult QD – An update on the centralized cardiac telemetry monitoring unit
Monitoring from a centralized location
Monitoring from a centralized location
Hospitalists hearing the constant noise from cardiac telemetry monitoring systems can experience alarm fatigue – a nationwide phenomenon that can lead to an increase in patient deaths.
The American Heart Association reports that fewer than one in four adults survived an in-hospital cardiac arrest in 2013; other studies showed that up to 44% of inpatient cardiac arrests were not detected appropriately, according to the Cleveland Clinic.
Clinicians at the Cleveland Clinic have tried centralized monitoring to address the problem. They’ve established a “mission control” center, where off-site personnel monitor sensors and high-definition cameras and vital signs such as blood pressure, heart rate, and respiration. On-site action is requested when appropriate; unimportant alarms are dismissed.
In August 2016, results from the first 13 months of the Cleveland Clinic program were published in JAMA. They revealed that the monitoring system could help reduce rates of unimportant alarms with no increase in cardiopulmonary arrest events. The centralized unit monitored 99,048 patient orders, and ultimately detected serious problems and accurately notified on-site staff for 79% of 3,243 events, which included a rhythm and/or rate change within 1 hour or less of the event. Accurate notification to on-site hospital staff was more than 84%.
Since then, improvements to the system have continued, according to Cleveland Clinic, and include doubling the number of monitored patients per technician and improved clinical outcomes.
Reference
Cleveland Clinic: Consult QD – An update on the centralized cardiac telemetry monitoring unit
Hospitalists hearing the constant noise from cardiac telemetry monitoring systems can experience alarm fatigue – a nationwide phenomenon that can lead to an increase in patient deaths.
The American Heart Association reports that fewer than one in four adults survived an in-hospital cardiac arrest in 2013; other studies showed that up to 44% of inpatient cardiac arrests were not detected appropriately, according to the Cleveland Clinic.
Clinicians at the Cleveland Clinic have tried centralized monitoring to address the problem. They’ve established a “mission control” center, where off-site personnel monitor sensors and high-definition cameras and vital signs such as blood pressure, heart rate, and respiration. On-site action is requested when appropriate; unimportant alarms are dismissed.
In August 2016, results from the first 13 months of the Cleveland Clinic program were published in JAMA. They revealed that the monitoring system could help reduce rates of unimportant alarms with no increase in cardiopulmonary arrest events. The centralized unit monitored 99,048 patient orders, and ultimately detected serious problems and accurately notified on-site staff for 79% of 3,243 events, which included a rhythm and/or rate change within 1 hour or less of the event. Accurate notification to on-site hospital staff was more than 84%.
Since then, improvements to the system have continued, according to Cleveland Clinic, and include doubling the number of monitored patients per technician and improved clinical outcomes.
Reference
Cleveland Clinic: Consult QD – An update on the centralized cardiac telemetry monitoring unit
“You have a pending query”
Specificity is essential in documentation and coding
Throughout medical training, you learn to write complete and detailed notes to communicate with other physicians. As a student and resident, you are praised when you succinctly analyze and address all patient problems while justifying your orders for the day. But notes do not exist just to document patient care; they are the template by which our actual quality of care is judged and our patients’ severity of illness is captured.
Like it or not, ICD-10 coding, documentation, denials, calls, and emails from administrators are integral parts of a hospitalist’s day-to-day job. Why? The specificity and comprehensiveness of diagnoses affect such metrics as hospital length of stay, mortality, and Case Mix Index documentation.
Good documentation can lead to better severity of illness (SOI) and risk of mortality (ROM) scores, better patient safety indicator (PSI) scores, better Healthgrades scores, better University Hospital Consortium (UHC) scores, and decreased Recovery Audit Contractor (RAC) denials as well as appropriate reimbursement. Good documentation can even lead to improved patient care and better perceived treatment outcomes.
It is no surprise that many hospital administrators invest time and money in staff to support the proper usage of language in your notes. Of course, sometimes these well-meaning “queries” can throw you into emotional turmoil as you try to understand what was not clear in your excellent note about your patient’s heart failure exacerbation. In this article, we will try to help you take your specificity and comprehensiveness of diagnoses to the next level.
Basics of billing
Physicians do not need to become coders but it is helpful to have some understanding of what happens behind the scenes. Not everyone realizes that physician billing is completely different from hospital billing. Physician billing pertains to the care provided by the clinician, whereas hospital billing pertains to the overall care the patient received.
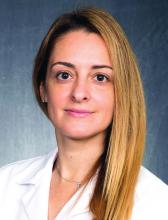
Below is an example of a case of pneumonia, (see Table 1) which shows the importance of specificity. Just by specifying ‘Aspiration’ for the type of pneumonia, we increased the SOI and the expected ROM appropriately. Also see a change in relative weight (RW): Each diagnosis-related group (DRG) is assigned a relative weight = estimated use of resources, and payment per case is based on estimated resource consumption = relative weight x “blended rate for each hospital.”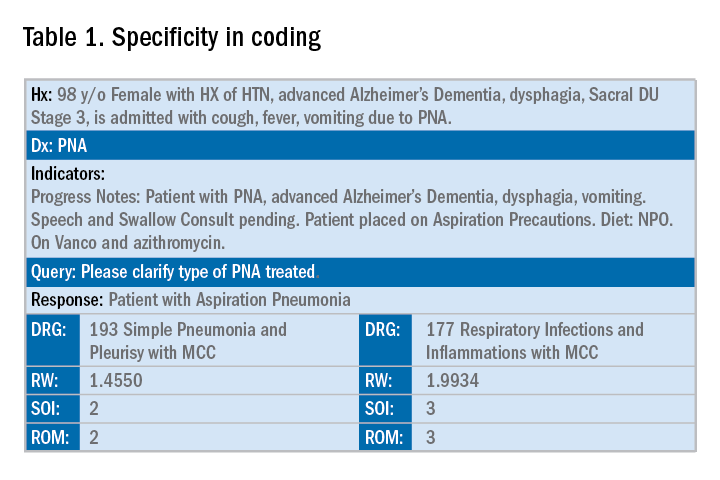
In addition to specificity, it is important to include all secondary diagnosis (know as cc/MCC – complication or comorbidity or a major complication or comorbidity – in the coding world). Table 2 is an example of using the correct terms and documenting secondary diagnosis. By documenting the type and severity of malnutrition we again increase the expected risk of mortality and the severity of illness.
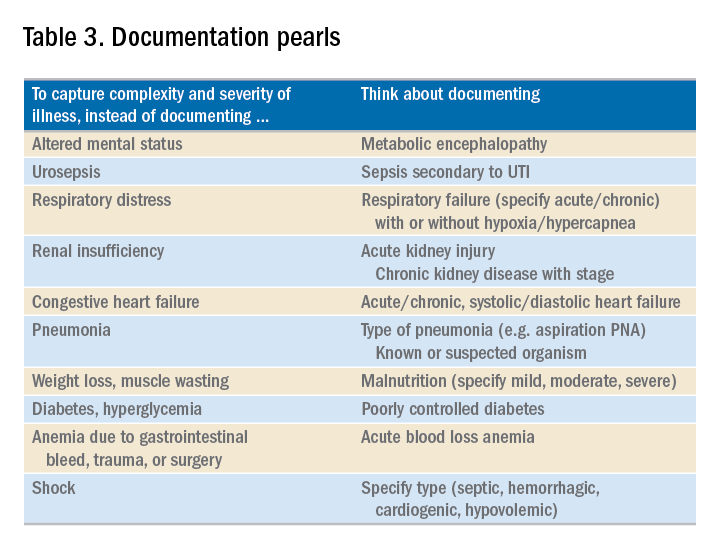
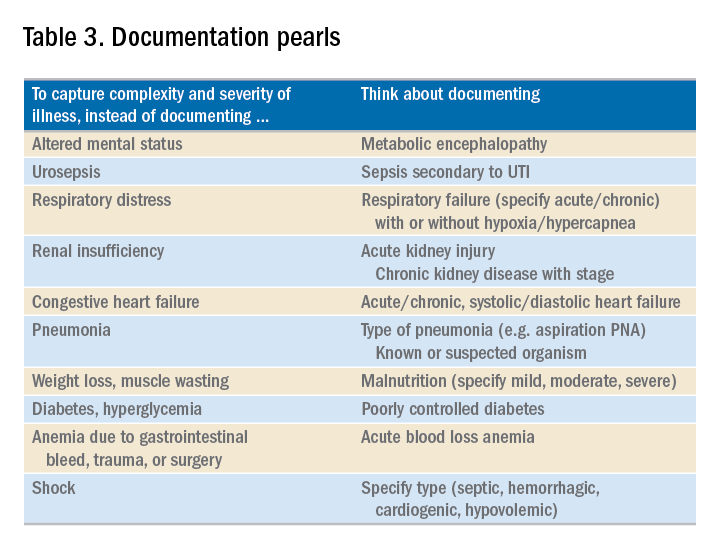
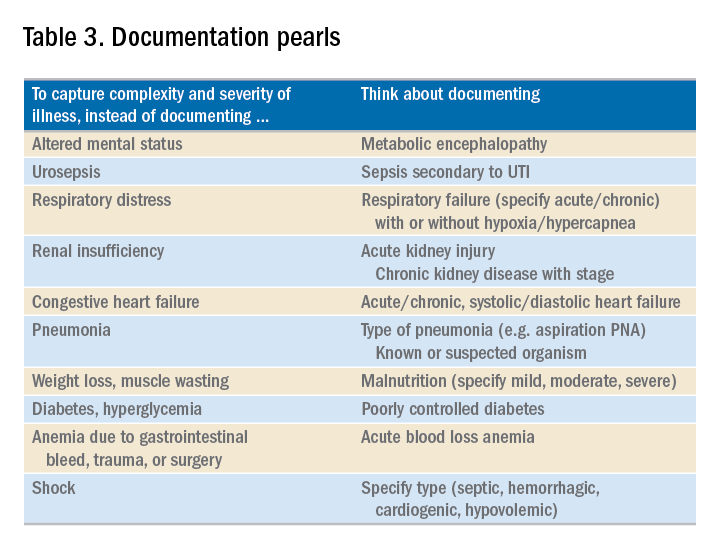
Physicians often do a lot more than what we record in the chart. Learning to document accurately to show the true clinical picture is an important skill set. Here are some tips to help understand and even avoid calls for better documentation.
- Use the terms “probable,” “possible,” “suspected,” or “likely” in documenting uncertain diagnoses (i.e., conditions for which physicians find clinical evidence that leads to a suspicion but not a definitive diagnosis). If conditions are ruled out or confirmed, clearly state so. If it remains uncertain, remember to carry this “possible” or “probable” diagnosis all the way through to the discharge summary or final progress note.
- Use linking of diagnoses when appropriate. For example, if the patient’s neuropathy, nephropathy, and retinopathy are related to their uncontrolled insulin dependent diabetes, state “uncontrolled insulin-dependent DMII with A1c of 11 complicated with nephropathy, neuropathy, and retinopathy.” The coders cannot link these diagnoses, and when you link them, you show a higher complexity of your patient. Remember to link the diagnoses only when they are truly related – this is where your medical knowledge and expertise come into play.
- Use the highest specificity of evidence that supports your medical decision making. You don’t need to be too verbose, all you need is evidence supporting your medical decision making and treatment plan. Think of it as demonstrating the logic of your diagnosis to another physician.
- Use Acuity (acute, chronic, acute on chronic, mild, moderate, severe, etc.) per diagnosis. For example, if you say heart failure exacerbation, it makes perfect sense to your medical colleagues, but in the coding world, it means nothing. Specify if it is acute, or acute on chronic, heart failure.
- Use status of each diagnosis. Is the condition improving, worsening, or resolved? Status does not have to be mentioned in all progress notes. Try to include this descriptor in the discharge summary and the day of the event.
- Always document the clinical significance of any abnormal laboratory, radiology reports, or pathology finding. Coders cannot use test results as a basis for coding unless a clinician has reviewed, interpreted, and documented the significance of the results in the progress note. Simply copying and pasting a report in the notes is not considered clinical acknowledgment. Shorthand notes like “Na=150, start hydration with 0.45% saline” is not acceptable. The actual diagnosis has to be written (i.e. “hypernatremia”). In addition, coders cannot code from nursing, dietitian, respiratory, and physical therapy notes. For example, if nursing documents that a patient has a pressure ulcer the clinician must still document the diagnosis of pressure ulcer, location, and stage. Although dietitian notes may state a body mass index greater than 40, coders cannot assume that patient is morbidly obese. Physician documentation is needed to support the obesity code assignment.
- Document all conditions that affect the patient’s stay, including complications and chronic conditions for which medications have been ordered. These secondary diagnoses paint the most accurate clinical picture and provide information needed to calculate important data, such as complexity and severity of patient illness and mortality risk. A patient with community-acquired pneumonia without other comorbidities requires fewer resources and has a greater chance of a good outcome than does the same patient with complications, such as acute heart failure.
- Downcoding brings losses, upcoding brings fines. Exaggerating the severity of patient conditions can lead to payer audits, reimbursement take backs, and charges of abuse and fraudulent billing. Never stretch the truth. Make sure you can support every diagnosis in the patient’s chart using clinical criteria.
You may be frustrated by the need to choose specific words about diagnoses that seem obvious to you without these descriptors. But accurate documentation can make a huge difference in your hospital’s bottom line and published metrics. Understanding the relative impact of changing your terminology can help you make these changes, until the language becomes second nature. Your hospital administrators will be grateful – and you just might cut down your queries!
Dr. Rajda is medical director of clinical documentation and quality improvement for Mount Sinai Hospital in New York, and medical director for DRG appeals for the Mount Sinai Health System. She serves as assistant professor of medicine at Icahn School of Medicine at Mount Sinai. Dr. Fatemi is an assistant professor at the University of New Mexico, Albuquerque. She is director of documentation, coding, and billing for the division of hospital medicine at UNM. Dr. Reyna is assistant professor in the division of hospital medicine and medical director for clinical documentation and quality improvement at Mount Sinai Medical Center.
Specificity is essential in documentation and coding
Specificity is essential in documentation and coding
Throughout medical training, you learn to write complete and detailed notes to communicate with other physicians. As a student and resident, you are praised when you succinctly analyze and address all patient problems while justifying your orders for the day. But notes do not exist just to document patient care; they are the template by which our actual quality of care is judged and our patients’ severity of illness is captured.
Like it or not, ICD-10 coding, documentation, denials, calls, and emails from administrators are integral parts of a hospitalist’s day-to-day job. Why? The specificity and comprehensiveness of diagnoses affect such metrics as hospital length of stay, mortality, and Case Mix Index documentation.
Good documentation can lead to better severity of illness (SOI) and risk of mortality (ROM) scores, better patient safety indicator (PSI) scores, better Healthgrades scores, better University Hospital Consortium (UHC) scores, and decreased Recovery Audit Contractor (RAC) denials as well as appropriate reimbursement. Good documentation can even lead to improved patient care and better perceived treatment outcomes.
It is no surprise that many hospital administrators invest time and money in staff to support the proper usage of language in your notes. Of course, sometimes these well-meaning “queries” can throw you into emotional turmoil as you try to understand what was not clear in your excellent note about your patient’s heart failure exacerbation. In this article, we will try to help you take your specificity and comprehensiveness of diagnoses to the next level.
Basics of billing
Physicians do not need to become coders but it is helpful to have some understanding of what happens behind the scenes. Not everyone realizes that physician billing is completely different from hospital billing. Physician billing pertains to the care provided by the clinician, whereas hospital billing pertains to the overall care the patient received.
Below is an example of a case of pneumonia, (see Table 1) which shows the importance of specificity. Just by specifying ‘Aspiration’ for the type of pneumonia, we increased the SOI and the expected ROM appropriately. Also see a change in relative weight (RW): Each diagnosis-related group (DRG) is assigned a relative weight = estimated use of resources, and payment per case is based on estimated resource consumption = relative weight x “blended rate for each hospital.”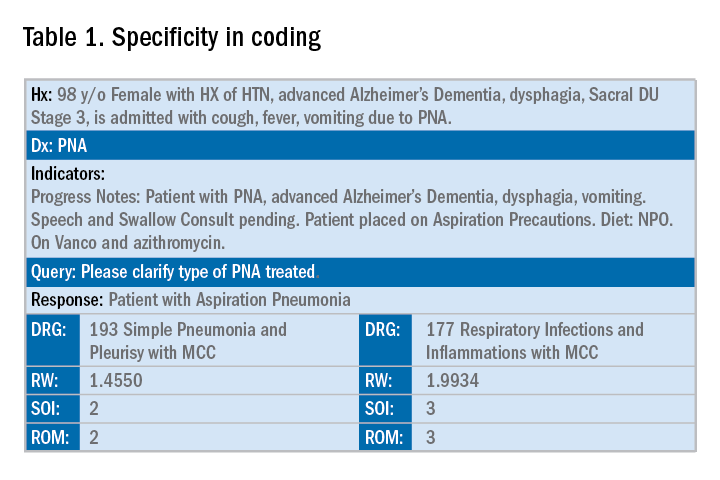
In addition to specificity, it is important to include all secondary diagnosis (know as cc/MCC – complication or comorbidity or a major complication or comorbidity – in the coding world). Table 2 is an example of using the correct terms and documenting secondary diagnosis. By documenting the type and severity of malnutrition we again increase the expected risk of mortality and the severity of illness.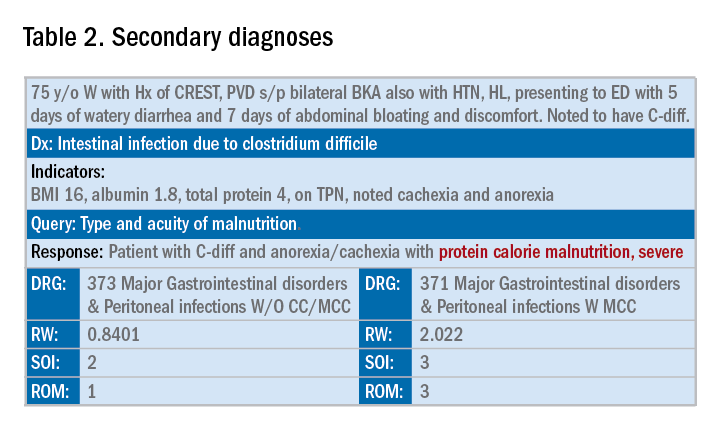
Physicians often do a lot more than what we record in the chart. Learning to document accurately to show the true clinical picture is an important skill set. Here are some tips to help understand and even avoid calls for better documentation.
- Use the terms “probable,” “possible,” “suspected,” or “likely” in documenting uncertain diagnoses (i.e., conditions for which physicians find clinical evidence that leads to a suspicion but not a definitive diagnosis). If conditions are ruled out or confirmed, clearly state so. If it remains uncertain, remember to carry this “possible” or “probable” diagnosis all the way through to the discharge summary or final progress note.
- Use linking of diagnoses when appropriate. For example, if the patient’s neuropathy, nephropathy, and retinopathy are related to their uncontrolled insulin dependent diabetes, state “uncontrolled insulin-dependent DMII with A1c of 11 complicated with nephropathy, neuropathy, and retinopathy.” The coders cannot link these diagnoses, and when you link them, you show a higher complexity of your patient. Remember to link the diagnoses only when they are truly related – this is where your medical knowledge and expertise come into play.
- Use the highest specificity of evidence that supports your medical decision making. You don’t need to be too verbose, all you need is evidence supporting your medical decision making and treatment plan. Think of it as demonstrating the logic of your diagnosis to another physician.
- Use Acuity (acute, chronic, acute on chronic, mild, moderate, severe, etc.) per diagnosis. For example, if you say heart failure exacerbation, it makes perfect sense to your medical colleagues, but in the coding world, it means nothing. Specify if it is acute, or acute on chronic, heart failure.
- Use status of each diagnosis. Is the condition improving, worsening, or resolved? Status does not have to be mentioned in all progress notes. Try to include this descriptor in the discharge summary and the day of the event.
- Always document the clinical significance of any abnormal laboratory, radiology reports, or pathology finding. Coders cannot use test results as a basis for coding unless a clinician has reviewed, interpreted, and documented the significance of the results in the progress note. Simply copying and pasting a report in the notes is not considered clinical acknowledgment. Shorthand notes like “Na=150, start hydration with 0.45% saline” is not acceptable. The actual diagnosis has to be written (i.e. “hypernatremia”). In addition, coders cannot code from nursing, dietitian, respiratory, and physical therapy notes. For example, if nursing documents that a patient has a pressure ulcer the clinician must still document the diagnosis of pressure ulcer, location, and stage. Although dietitian notes may state a body mass index greater than 40, coders cannot assume that patient is morbidly obese. Physician documentation is needed to support the obesity code assignment.
- Document all conditions that affect the patient’s stay, including complications and chronic conditions for which medications have been ordered. These secondary diagnoses paint the most accurate clinical picture and provide information needed to calculate important data, such as complexity and severity of patient illness and mortality risk. A patient with community-acquired pneumonia without other comorbidities requires fewer resources and has a greater chance of a good outcome than does the same patient with complications, such as acute heart failure.
- Downcoding brings losses, upcoding brings fines. Exaggerating the severity of patient conditions can lead to payer audits, reimbursement take backs, and charges of abuse and fraudulent billing. Never stretch the truth. Make sure you can support every diagnosis in the patient’s chart using clinical criteria.
You may be frustrated by the need to choose specific words about diagnoses that seem obvious to you without these descriptors. But accurate documentation can make a huge difference in your hospital’s bottom line and published metrics. Understanding the relative impact of changing your terminology can help you make these changes, until the language becomes second nature. Your hospital administrators will be grateful – and you just might cut down your queries!
Dr. Rajda is medical director of clinical documentation and quality improvement for Mount Sinai Hospital in New York, and medical director for DRG appeals for the Mount Sinai Health System. She serves as assistant professor of medicine at Icahn School of Medicine at Mount Sinai. Dr. Fatemi is an assistant professor at the University of New Mexico, Albuquerque. She is director of documentation, coding, and billing for the division of hospital medicine at UNM. Dr. Reyna is assistant professor in the division of hospital medicine and medical director for clinical documentation and quality improvement at Mount Sinai Medical Center.
Throughout medical training, you learn to write complete and detailed notes to communicate with other physicians. As a student and resident, you are praised when you succinctly analyze and address all patient problems while justifying your orders for the day. But notes do not exist just to document patient care; they are the template by which our actual quality of care is judged and our patients’ severity of illness is captured.
Like it or not, ICD-10 coding, documentation, denials, calls, and emails from administrators are integral parts of a hospitalist’s day-to-day job. Why? The specificity and comprehensiveness of diagnoses affect such metrics as hospital length of stay, mortality, and Case Mix Index documentation.
Good documentation can lead to better severity of illness (SOI) and risk of mortality (ROM) scores, better patient safety indicator (PSI) scores, better Healthgrades scores, better University Hospital Consortium (UHC) scores, and decreased Recovery Audit Contractor (RAC) denials as well as appropriate reimbursement. Good documentation can even lead to improved patient care and better perceived treatment outcomes.
It is no surprise that many hospital administrators invest time and money in staff to support the proper usage of language in your notes. Of course, sometimes these well-meaning “queries” can throw you into emotional turmoil as you try to understand what was not clear in your excellent note about your patient’s heart failure exacerbation. In this article, we will try to help you take your specificity and comprehensiveness of diagnoses to the next level.
Basics of billing
Physicians do not need to become coders but it is helpful to have some understanding of what happens behind the scenes. Not everyone realizes that physician billing is completely different from hospital billing. Physician billing pertains to the care provided by the clinician, whereas hospital billing pertains to the overall care the patient received.
Below is an example of a case of pneumonia, (see Table 1) which shows the importance of specificity. Just by specifying ‘Aspiration’ for the type of pneumonia, we increased the SOI and the expected ROM appropriately. Also see a change in relative weight (RW): Each diagnosis-related group (DRG) is assigned a relative weight = estimated use of resources, and payment per case is based on estimated resource consumption = relative weight x “blended rate for each hospital.”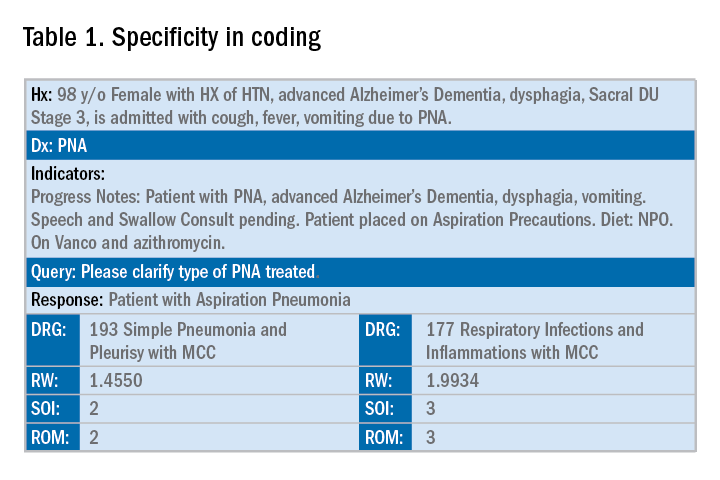
In addition to specificity, it is important to include all secondary diagnosis (know as cc/MCC – complication or comorbidity or a major complication or comorbidity – in the coding world). Table 2 is an example of using the correct terms and documenting secondary diagnosis. By documenting the type and severity of malnutrition we again increase the expected risk of mortality and the severity of illness.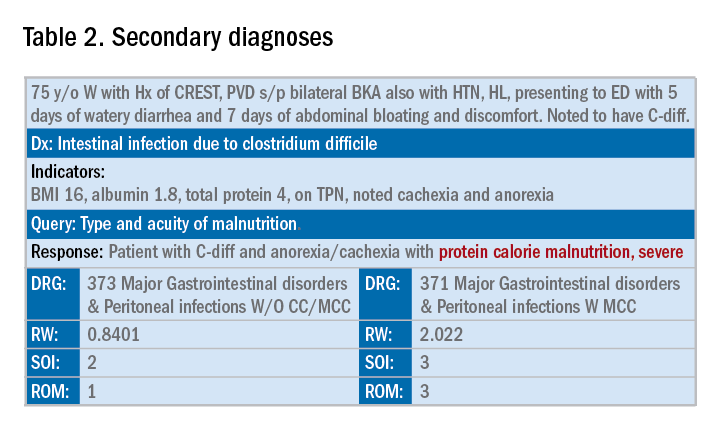
Physicians often do a lot more than what we record in the chart. Learning to document accurately to show the true clinical picture is an important skill set. Here are some tips to help understand and even avoid calls for better documentation.
- Use the terms “probable,” “possible,” “suspected,” or “likely” in documenting uncertain diagnoses (i.e., conditions for which physicians find clinical evidence that leads to a suspicion but not a definitive diagnosis). If conditions are ruled out or confirmed, clearly state so. If it remains uncertain, remember to carry this “possible” or “probable” diagnosis all the way through to the discharge summary or final progress note.
- Use linking of diagnoses when appropriate. For example, if the patient’s neuropathy, nephropathy, and retinopathy are related to their uncontrolled insulin dependent diabetes, state “uncontrolled insulin-dependent DMII with A1c of 11 complicated with nephropathy, neuropathy, and retinopathy.” The coders cannot link these diagnoses, and when you link them, you show a higher complexity of your patient. Remember to link the diagnoses only when they are truly related – this is where your medical knowledge and expertise come into play.
- Use the highest specificity of evidence that supports your medical decision making. You don’t need to be too verbose, all you need is evidence supporting your medical decision making and treatment plan. Think of it as demonstrating the logic of your diagnosis to another physician.
- Use Acuity (acute, chronic, acute on chronic, mild, moderate, severe, etc.) per diagnosis. For example, if you say heart failure exacerbation, it makes perfect sense to your medical colleagues, but in the coding world, it means nothing. Specify if it is acute, or acute on chronic, heart failure.
- Use status of each diagnosis. Is the condition improving, worsening, or resolved? Status does not have to be mentioned in all progress notes. Try to include this descriptor in the discharge summary and the day of the event.
- Always document the clinical significance of any abnormal laboratory, radiology reports, or pathology finding. Coders cannot use test results as a basis for coding unless a clinician has reviewed, interpreted, and documented the significance of the results in the progress note. Simply copying and pasting a report in the notes is not considered clinical acknowledgment. Shorthand notes like “Na=150, start hydration with 0.45% saline” is not acceptable. The actual diagnosis has to be written (i.e. “hypernatremia”). In addition, coders cannot code from nursing, dietitian, respiratory, and physical therapy notes. For example, if nursing documents that a patient has a pressure ulcer the clinician must still document the diagnosis of pressure ulcer, location, and stage. Although dietitian notes may state a body mass index greater than 40, coders cannot assume that patient is morbidly obese. Physician documentation is needed to support the obesity code assignment.
- Document all conditions that affect the patient’s stay, including complications and chronic conditions for which medications have been ordered. These secondary diagnoses paint the most accurate clinical picture and provide information needed to calculate important data, such as complexity and severity of patient illness and mortality risk. A patient with community-acquired pneumonia without other comorbidities requires fewer resources and has a greater chance of a good outcome than does the same patient with complications, such as acute heart failure.
- Downcoding brings losses, upcoding brings fines. Exaggerating the severity of patient conditions can lead to payer audits, reimbursement take backs, and charges of abuse and fraudulent billing. Never stretch the truth. Make sure you can support every diagnosis in the patient’s chart using clinical criteria.
You may be frustrated by the need to choose specific words about diagnoses that seem obvious to you without these descriptors. But accurate documentation can make a huge difference in your hospital’s bottom line and published metrics. Understanding the relative impact of changing your terminology can help you make these changes, until the language becomes second nature. Your hospital administrators will be grateful – and you just might cut down your queries!
Dr. Rajda is medical director of clinical documentation and quality improvement for Mount Sinai Hospital in New York, and medical director for DRG appeals for the Mount Sinai Health System. She serves as assistant professor of medicine at Icahn School of Medicine at Mount Sinai. Dr. Fatemi is an assistant professor at the University of New Mexico, Albuquerque. She is director of documentation, coding, and billing for the division of hospital medicine at UNM. Dr. Reyna is assistant professor in the division of hospital medicine and medical director for clinical documentation and quality improvement at Mount Sinai Medical Center.
NAIP to SHM: The importance of a name
Defining the hospitalist ‘brand’
The National Association of Inpatient Physicians (NAIP) “opened its doors” in the spring of 1998, welcoming the first 300 hospitalists. The term “hospitalist” was first coined in Bob Wachter’s 1996 New England Journal of Medicine article,1 although hospitalists were relatively few at that time, and the term not infrequently evoked controversy.
Having full-time hospital-based physicians was highly disruptive to the traditional culture of medicine, where hospital rounds were an integral part of a primary care physicians’ practice, professional identity, and referral patterns. Additionally, many hospital-based specialists were beginning to fill the hospitalist role.
The decision to include “inpatient physician” rather than “hospitalist” in the name was carefully considered and was intended to be inclusive, without alienating potential allies. Virtually any doctor working in a hospital could identify themselves as an inpatient physician, and all who wanted to participate were welcomed. It also was evident early on that this young specialty was going to comprise many different disciplines, including internal medicine, family practice, and pediatrics to name a few, and reaching out to all potential stakeholders was an urgent priority.
During its’ first 5 years, the field of hospital medicine grew rapidly, with NAIP membership nearing 2,000 members. The bimonthly newsletter The Hospitalist provided a vehicle to reach out to members and other stakeholders, and the annual meeting gave hospitalists a forum to gather, learn from each other, and enjoy camaraderie. Early research efforts focused on patient safety and, just as importantly, in 2002, the publication of the first Productivity and Compensation Survey (which is now known as SHM’s State of Hospital Medicine Report) and the initial development of The Hospitalist Core Competencies (first published in 2006, and now in its’ 2017 revision) all helped define the young specialty and gain acceptance.2,3
The term hospitalist became mainstream and accepted, and the name of our field, hospital medicine, has now become widely recognized.
Though the term “inpatient physician” had focused on physicians as a primary constituency, the successful growth of hospital medicine now increasingly depended upon other important constituencies and their understanding of the hospital medicine specialty and the role of hospitalists. These stakeholders included virtually all health care professionals and administrators, government officials at the federal, state, and local levels, patients, and the American public.
As NAIP leadership, it was our belief and intent that having a name that accurately portrayed hospitalists and hospital medicine would define our “brand” in an understandable way. This was especially important given the breadth and depth of the responsibilities that NAIP and its’ members were increasingly taking on in a rapidly changing health care system. Additionally, it was a top priority to find a name that would inspire confidence and passion among our members, stir a sense of loyalty and pride, and continue to be inclusive.
With this in mind, the NAIP board undertook a process to search for a new name in the spring of 2002. As NAIP President-Elect, stewarding the name change process was my responsibility.
In approaching this challenge, we initially evaluated the components of other professional organizations’ names, including academy, college, and society among others, and whether the specialist name or professional field was included. We then held focus groups among regional hospitalists, invited feedback from all NAIP members, and solicited leadership feedback from other professional organizations. All of these data were taken into our fall 2002 board meeting in St. Louis.
Prior to the meeting, it was agreed that making a name change would require a supermajority of two-thirds of the 11 voting board members (though only 10 ultimately attended the meeting). Also participating in the discussion were the nonvoting four ex-officio board members and the NAIP CEO. The initial discussion included presentations arguing for Hospital Medicine versus Hospitalist as part of the name. We then discussed and voted on the primary professional component of the name, with “Society” finally being chosen. After further discussion and a series of ballots, we arrived at the name “Society of Hospital Medicine.” In the final ballot, 7 out of 10 cast their votes in favor of this finalist, and our organization became The Society of Hospital Medicine. Our abbreviation SHM was to become our logo, which was developed in advance of our 2003 annual meeting.
In the 15 years since, the Society of Hospital Medicine has become well known to our constituents and stakeholders. SHM is recognized for its staunch advocacy, particularly at the federal level, with recent establishment of a Medicare specialty code designation for hospitalists, and support for endeavors such as Project Boost, which focused on patient transitions from hospital discharge to home.4,5,6 Hospitalists throughout the United States routinely manage hospitalized patients, and now have their specialty expertise recognized via Focused Practice in Hospital Medicine (Internal Medicine and Family Practice), and future specialty training and certification for pediatric hospitalists.7,8,9
The Journal of Hospital Medicine now highlights accomplishments in hospital medicine research and knowledge.10 Hospitalist leaders frequently are developed through the SHM Leadership Academy,11 and hospitalists increasingly fill diverse health care responsibilities in education, research, informatics, palliative care, performance improvement, administration, among many others. Of note, SHM membership currently exceeds 17,000 members, and now offers membership that includes nurse practitioners, physician assistants, fellows, residents, students, and practice administrators, among others.12
These achievements and many more have been driven by the efforts of past and present Society of Hospital Medicine members and staff, and like-minded, invested professionals and organizations. The name Society of Hospital Medicine (SHM) is highly familiar and well regarded by virtually all our stakeholders and is recognized for its proven leadership in continuing to define our brand, hospital medicine.
Dr. Dichter is an intensivist and associate professor of medicine at the University of Minnesota Medical Center, Minneapolis.
References
1. Wachter RM et al. The emerging role of “hospitalists” in the American health care system. N Eng J Med. 1996 Aug 15;335(7):514-7.
2. SHM’s State of Hospital Medicine Report 2018. Fall 2018.
3. Satyen N et al. Core competencies in hospital medicine 2017 Revision. J Hosp Med. 2017 Apr;12:S1.
4. Society of Hospital Medicine website, Policy & Advocacy homepage (accessed July 26, 2018).
5. CMS manual system, Oct. 28, 2016 (accessed July 26, 2018).
6. Society of Hospital Medicine website, Clinical Topics: Advancing successful care transitions to improve outcomes (accessed July 26, 2018).
7. American Board of Internal Medicine website, MOC requirements: Focused practice in hospital medicine (accessed July 26, 2018).
8. American Board of Family Medicine website, Designation of practice in hospital medicine (accessed July 26, 2018).
9. The American Board of Pediatrics website, Pediatric hospital medicine certification (accessed July 26, 2018).
10. Journal of Hospital Medicine official website (accessed July 26, 2018).
11. SHM Leadership Academy website (accessed July 26, 2018).
12. Society of Hospital Medicine website, About SHM membership (accessed July 26, 2018).
Defining the hospitalist ‘brand’
Defining the hospitalist ‘brand’
The National Association of Inpatient Physicians (NAIP) “opened its doors” in the spring of 1998, welcoming the first 300 hospitalists. The term “hospitalist” was first coined in Bob Wachter’s 1996 New England Journal of Medicine article,1 although hospitalists were relatively few at that time, and the term not infrequently evoked controversy.
Having full-time hospital-based physicians was highly disruptive to the traditional culture of medicine, where hospital rounds were an integral part of a primary care physicians’ practice, professional identity, and referral patterns. Additionally, many hospital-based specialists were beginning to fill the hospitalist role.
The decision to include “inpatient physician” rather than “hospitalist” in the name was carefully considered and was intended to be inclusive, without alienating potential allies. Virtually any doctor working in a hospital could identify themselves as an inpatient physician, and all who wanted to participate were welcomed. It also was evident early on that this young specialty was going to comprise many different disciplines, including internal medicine, family practice, and pediatrics to name a few, and reaching out to all potential stakeholders was an urgent priority.
During its’ first 5 years, the field of hospital medicine grew rapidly, with NAIP membership nearing 2,000 members. The bimonthly newsletter The Hospitalist provided a vehicle to reach out to members and other stakeholders, and the annual meeting gave hospitalists a forum to gather, learn from each other, and enjoy camaraderie. Early research efforts focused on patient safety and, just as importantly, in 2002, the publication of the first Productivity and Compensation Survey (which is now known as SHM’s State of Hospital Medicine Report) and the initial development of The Hospitalist Core Competencies (first published in 2006, and now in its’ 2017 revision) all helped define the young specialty and gain acceptance.2,3
The term hospitalist became mainstream and accepted, and the name of our field, hospital medicine, has now become widely recognized.
Though the term “inpatient physician” had focused on physicians as a primary constituency, the successful growth of hospital medicine now increasingly depended upon other important constituencies and their understanding of the hospital medicine specialty and the role of hospitalists. These stakeholders included virtually all health care professionals and administrators, government officials at the federal, state, and local levels, patients, and the American public.
As NAIP leadership, it was our belief and intent that having a name that accurately portrayed hospitalists and hospital medicine would define our “brand” in an understandable way. This was especially important given the breadth and depth of the responsibilities that NAIP and its’ members were increasingly taking on in a rapidly changing health care system. Additionally, it was a top priority to find a name that would inspire confidence and passion among our members, stir a sense of loyalty and pride, and continue to be inclusive.
With this in mind, the NAIP board undertook a process to search for a new name in the spring of 2002. As NAIP President-Elect, stewarding the name change process was my responsibility.
In approaching this challenge, we initially evaluated the components of other professional organizations’ names, including academy, college, and society among others, and whether the specialist name or professional field was included. We then held focus groups among regional hospitalists, invited feedback from all NAIP members, and solicited leadership feedback from other professional organizations. All of these data were taken into our fall 2002 board meeting in St. Louis.
Prior to the meeting, it was agreed that making a name change would require a supermajority of two-thirds of the 11 voting board members (though only 10 ultimately attended the meeting). Also participating in the discussion were the nonvoting four ex-officio board members and the NAIP CEO. The initial discussion included presentations arguing for Hospital Medicine versus Hospitalist as part of the name. We then discussed and voted on the primary professional component of the name, with “Society” finally being chosen. After further discussion and a series of ballots, we arrived at the name “Society of Hospital Medicine.” In the final ballot, 7 out of 10 cast their votes in favor of this finalist, and our organization became The Society of Hospital Medicine. Our abbreviation SHM was to become our logo, which was developed in advance of our 2003 annual meeting.
In the 15 years since, the Society of Hospital Medicine has become well known to our constituents and stakeholders. SHM is recognized for its staunch advocacy, particularly at the federal level, with recent establishment of a Medicare specialty code designation for hospitalists, and support for endeavors such as Project Boost, which focused on patient transitions from hospital discharge to home.4,5,6 Hospitalists throughout the United States routinely manage hospitalized patients, and now have their specialty expertise recognized via Focused Practice in Hospital Medicine (Internal Medicine and Family Practice), and future specialty training and certification for pediatric hospitalists.7,8,9
The Journal of Hospital Medicine now highlights accomplishments in hospital medicine research and knowledge.10 Hospitalist leaders frequently are developed through the SHM Leadership Academy,11 and hospitalists increasingly fill diverse health care responsibilities in education, research, informatics, palliative care, performance improvement, administration, among many others. Of note, SHM membership currently exceeds 17,000 members, and now offers membership that includes nurse practitioners, physician assistants, fellows, residents, students, and practice administrators, among others.12
These achievements and many more have been driven by the efforts of past and present Society of Hospital Medicine members and staff, and like-minded, invested professionals and organizations. The name Society of Hospital Medicine (SHM) is highly familiar and well regarded by virtually all our stakeholders and is recognized for its proven leadership in continuing to define our brand, hospital medicine.
Dr. Dichter is an intensivist and associate professor of medicine at the University of Minnesota Medical Center, Minneapolis.
References
1. Wachter RM et al. The emerging role of “hospitalists” in the American health care system. N Eng J Med. 1996 Aug 15;335(7):514-7.
2. SHM’s State of Hospital Medicine Report 2018. Fall 2018.
3. Satyen N et al. Core competencies in hospital medicine 2017 Revision. J Hosp Med. 2017 Apr;12:S1.
4. Society of Hospital Medicine website, Policy & Advocacy homepage (accessed July 26, 2018).
5. CMS manual system, Oct. 28, 2016 (accessed July 26, 2018).
6. Society of Hospital Medicine website, Clinical Topics: Advancing successful care transitions to improve outcomes (accessed July 26, 2018).
7. American Board of Internal Medicine website, MOC requirements: Focused practice in hospital medicine (accessed July 26, 2018).
8. American Board of Family Medicine website, Designation of practice in hospital medicine (accessed July 26, 2018).
9. The American Board of Pediatrics website, Pediatric hospital medicine certification (accessed July 26, 2018).
10. Journal of Hospital Medicine official website (accessed July 26, 2018).
11. SHM Leadership Academy website (accessed July 26, 2018).
12. Society of Hospital Medicine website, About SHM membership (accessed July 26, 2018).
The National Association of Inpatient Physicians (NAIP) “opened its doors” in the spring of 1998, welcoming the first 300 hospitalists. The term “hospitalist” was first coined in Bob Wachter’s 1996 New England Journal of Medicine article,1 although hospitalists were relatively few at that time, and the term not infrequently evoked controversy.
Having full-time hospital-based physicians was highly disruptive to the traditional culture of medicine, where hospital rounds were an integral part of a primary care physicians’ practice, professional identity, and referral patterns. Additionally, many hospital-based specialists were beginning to fill the hospitalist role.
The decision to include “inpatient physician” rather than “hospitalist” in the name was carefully considered and was intended to be inclusive, without alienating potential allies. Virtually any doctor working in a hospital could identify themselves as an inpatient physician, and all who wanted to participate were welcomed. It also was evident early on that this young specialty was going to comprise many different disciplines, including internal medicine, family practice, and pediatrics to name a few, and reaching out to all potential stakeholders was an urgent priority.
During its’ first 5 years, the field of hospital medicine grew rapidly, with NAIP membership nearing 2,000 members. The bimonthly newsletter The Hospitalist provided a vehicle to reach out to members and other stakeholders, and the annual meeting gave hospitalists a forum to gather, learn from each other, and enjoy camaraderie. Early research efforts focused on patient safety and, just as importantly, in 2002, the publication of the first Productivity and Compensation Survey (which is now known as SHM’s State of Hospital Medicine Report) and the initial development of The Hospitalist Core Competencies (first published in 2006, and now in its’ 2017 revision) all helped define the young specialty and gain acceptance.2,3
The term hospitalist became mainstream and accepted, and the name of our field, hospital medicine, has now become widely recognized.
Though the term “inpatient physician” had focused on physicians as a primary constituency, the successful growth of hospital medicine now increasingly depended upon other important constituencies and their understanding of the hospital medicine specialty and the role of hospitalists. These stakeholders included virtually all health care professionals and administrators, government officials at the federal, state, and local levels, patients, and the American public.
As NAIP leadership, it was our belief and intent that having a name that accurately portrayed hospitalists and hospital medicine would define our “brand” in an understandable way. This was especially important given the breadth and depth of the responsibilities that NAIP and its’ members were increasingly taking on in a rapidly changing health care system. Additionally, it was a top priority to find a name that would inspire confidence and passion among our members, stir a sense of loyalty and pride, and continue to be inclusive.
With this in mind, the NAIP board undertook a process to search for a new name in the spring of 2002. As NAIP President-Elect, stewarding the name change process was my responsibility.
In approaching this challenge, we initially evaluated the components of other professional organizations’ names, including academy, college, and society among others, and whether the specialist name or professional field was included. We then held focus groups among regional hospitalists, invited feedback from all NAIP members, and solicited leadership feedback from other professional organizations. All of these data were taken into our fall 2002 board meeting in St. Louis.
Prior to the meeting, it was agreed that making a name change would require a supermajority of two-thirds of the 11 voting board members (though only 10 ultimately attended the meeting). Also participating in the discussion were the nonvoting four ex-officio board members and the NAIP CEO. The initial discussion included presentations arguing for Hospital Medicine versus Hospitalist as part of the name. We then discussed and voted on the primary professional component of the name, with “Society” finally being chosen. After further discussion and a series of ballots, we arrived at the name “Society of Hospital Medicine.” In the final ballot, 7 out of 10 cast their votes in favor of this finalist, and our organization became The Society of Hospital Medicine. Our abbreviation SHM was to become our logo, which was developed in advance of our 2003 annual meeting.
In the 15 years since, the Society of Hospital Medicine has become well known to our constituents and stakeholders. SHM is recognized for its staunch advocacy, particularly at the federal level, with recent establishment of a Medicare specialty code designation for hospitalists, and support for endeavors such as Project Boost, which focused on patient transitions from hospital discharge to home.4,5,6 Hospitalists throughout the United States routinely manage hospitalized patients, and now have their specialty expertise recognized via Focused Practice in Hospital Medicine (Internal Medicine and Family Practice), and future specialty training and certification for pediatric hospitalists.7,8,9
The Journal of Hospital Medicine now highlights accomplishments in hospital medicine research and knowledge.10 Hospitalist leaders frequently are developed through the SHM Leadership Academy,11 and hospitalists increasingly fill diverse health care responsibilities in education, research, informatics, palliative care, performance improvement, administration, among many others. Of note, SHM membership currently exceeds 17,000 members, and now offers membership that includes nurse practitioners, physician assistants, fellows, residents, students, and practice administrators, among others.12
These achievements and many more have been driven by the efforts of past and present Society of Hospital Medicine members and staff, and like-minded, invested professionals and organizations. The name Society of Hospital Medicine (SHM) is highly familiar and well regarded by virtually all our stakeholders and is recognized for its proven leadership in continuing to define our brand, hospital medicine.
Dr. Dichter is an intensivist and associate professor of medicine at the University of Minnesota Medical Center, Minneapolis.
References
1. Wachter RM et al. The emerging role of “hospitalists” in the American health care system. N Eng J Med. 1996 Aug 15;335(7):514-7.
2. SHM’s State of Hospital Medicine Report 2018. Fall 2018.
3. Satyen N et al. Core competencies in hospital medicine 2017 Revision. J Hosp Med. 2017 Apr;12:S1.
4. Society of Hospital Medicine website, Policy & Advocacy homepage (accessed July 26, 2018).
5. CMS manual system, Oct. 28, 2016 (accessed July 26, 2018).
6. Society of Hospital Medicine website, Clinical Topics: Advancing successful care transitions to improve outcomes (accessed July 26, 2018).
7. American Board of Internal Medicine website, MOC requirements: Focused practice in hospital medicine (accessed July 26, 2018).
8. American Board of Family Medicine website, Designation of practice in hospital medicine (accessed July 26, 2018).
9. The American Board of Pediatrics website, Pediatric hospital medicine certification (accessed July 26, 2018).
10. Journal of Hospital Medicine official website (accessed July 26, 2018).
11. SHM Leadership Academy website (accessed July 26, 2018).
12. Society of Hospital Medicine website, About SHM membership (accessed July 26, 2018).
Paradigm shifts in palliative care
Better engagement with patients essential
A 57-year-old man is admitted to the hospital with new back pain, which has been getting worse over the past 6 days. He had been diagnosed with stage 4 lung cancer in mid-2017 and underwent treatment with a platinum-based double therapy.
The man also has a history of heroin use – as recently as two years earlier – and he was divorced not long ago. He has been using an old prescription for Vicodin to treat himself, taking as many as 10-12 tablets a day.
This man is an example of the kind of complicated patient hospitalists are called on to treat – complex pain in an era when opioid abuse is considered a public scourge. How is a hospitalist to handle a case like this?
Pain cases are far from the only types of increasingly complex, often palliative cases in which hospitalists are being asked to provide help. Care for the elderly is also becoming increasingly difficult as the U.S. population ages and as hospitalists step in to provide care in the absence of geriatricians. .
Pain management in the opioid era and the need for new approaches in elderly care were highlighted at the Hospital Medicine 2018 annual conference, with experts drawing attention to subtleties that are often overlooked in these sometimes desperate cases.
James Risser, MD, medical director of palliative care at Regions Hospital in Minneapolis, said the complex problems of the 57-year-old man with back pain amounted to an example of “pain’s greatest hits.”
That particular case underscores the need to identify individual types of pain, he said, because they all need to be handled differently. If hospitalists don’t consider all the different aspects of pain, a patient might endure more suffering than necessary.
“All of this pain is swirling around in a very complicated patient,” Dr. Risser said, noting that it is important to “tease out the individual parts” of a complex patient’s history.
“Pain is a very complicated construct, from the physical to the neurological to the emotional,” Dr. Risser said. “Pain is a subjective experience, and the way people interact with their pain really depends not just on physical pain but also their psychological state, their social state, and even their spiritual state.”
Understanding this array of causes has led Dr. Risser to approach the problem of pain from different angles – including perspectives that might not be traditional, he said.
“One of the things that I’ve gotten better at is taking a spiritual history,” he said. “I don’t know if that’s part of everybody’s armamentarium. But if you’re dealing with people who are very, very sick, sometimes that’s the fundamental fabric of how they live and how they die. If there are unresolved issues along those lines, it’s possible they could be experiencing their pain in a different or more severe way.”
Varieties of pain
Treatment depends on the pain type, Dr. Risser said. Somatic pain often responds to nonsteroidal anti-inflammatories or steroids.
Neuropathic pain usually responds poorly to anti-inflammatories and to opioids. There is some research suggesting methadone could be helpful, but the data are not very strong. The most common medications prescribed are antiseizure medications and antidepressants, such as gabapentin and serotonin, and norepinephrine reuptake inhibitors.
The question of cancer pain versus noncancer pain can be tricky, Dr. Risser said. If a person’s life expectancy is limited, there can be a reason, or even a requirement, to use higher-risk medications. But, he said, that doesn’t mean the patient still won’t have problems with overuse of pain medication.
“We have a lot of patients now living post cancer who have been put on methadone or have been put on Oxycontin, and now we’re trying to figure out what to do with them,” he said. “I don’t think it’s that clear anymore that there’s a massive difference between cancer and noncancer pain, especially for those survivors.”
Clinicians, he said, should “fix what can be fixed” – and with the right tools. “If you have a patient who’s got severe lower abdominal pain because they have a bladder full or urine, really the treatment would probably not be … opioids. It probably would be a Foley catheter,” he said.
Hospitalists should treat patients based on sound principles of pain management, Dr. Risser said, but “while you try to create a diagnostic framework, know that people continually defy the boxes we put them in.”
Indeed, in an era of pain-medication addiction, it might be a good idea to worry about prescribing opioids, but clinicians have to remember that their goal is to help patients get relief – and that they themselves bring biases to the table, said Amy Davis, DO, MS, of Drexel University, Philadelphia.
In a presentation at HM18, Dr. Davis displayed images of a variety of patients on a large screen – different races and genders, some in business attire, some rougher around the edges.
“Would pain decisions change based on what people look like?” she asked. “Can you really spot who the drug traffickers are? We need to remember that our biases play a huge role not only in the treatment of our patients but in their outcomes. I’m challenging everybody to start thinking about these folks not as drug-seekers but as comfort-seekers.”
When it comes right down to it, she said, patients want a better life, not their drug of choice.
“That is the nature of the disease. [The illegal drug] is not what they’re looking for in reality because that does not provide a good quality of life,” Dr. Davis said. “The [practice of medicine] is supposed to be about helping people live their lives, not just checking off boxes.”
People with an opioid use disorder are physically different, she said. The processing of pain stimuli by their brain and spinal cord is physically altered – they have an increased perception of pain and lower pain tolerance.
“This is not a character flaw,” Dr. Davis affirmed. The increased sensitivity to pain does not resolve with opioid cessation; it can last for decades. Clinicians may need to spend more time interacting with certain patients to get a sense of the physical and nonphysical pain from which they suffer.
“Consistent, open, nonjudgmental communication improves not only the information we gather from patients and families, but it actually changes the adherence,” Dr. Davis said. “Ultimately the treatment outcomes are what all of this is about.”
Paradigm shift
Another palliative care role that hospitalists often find themselves in is “comforter” of elderly patients.

Ryan Greysen, MD, MHS, chief of hospital medicine at the University of Pennsylvania, Philadelphia, said hospitals must respond to a shift in the paradigm of elderly care. To explain the nature of this change, he referenced the “paradigm shift” model devised by the philosopher of science Thomas Kuhn, PhD. According to Kuhn, science proceeds in a settled pattern for many years, but on the rare occasions, when there is a fundamental drift in thinking, new problems present themselves and put the old model in a crisis mode, which prompts an intellectual revolution and a shift in the paradigm itself.
“This is a way of thinking about changes in scientific paradigms, but I think it works in clinical practice as well,” Dr. Greysen said.
The need for a paradigm shift in the care of elderly inpatients has largely to do with demographics. By 2050, the number of people aged 65 years and older is expected to be about 80 million, roughly double what it was in 2000. The number of people aged 85 years and up is expected to be about 20 million, or about four times the total in 2000.
In 2010, 40% of the hospitalized population was over 65 years. In 2030, that will flip: Only 40% of inpatients will be under 65 years. This will mean that hospitalists must care for more patients who are older, and the patients themselves will have more complicated medical issues.
“To be ready for the aging century, we must be better able to adapt and address those things that affect seniors,” Dr. Greysen said. With the number of geriatricians falling, much more of this care will fall to hospitalists, he said.
More attention must be paid to the potential harms of hospital-based care to older patients: decreased muscle strength and aerobic capacity, vasomotor instability, lower bone density, poor ventilation, altered thirst and nutrition, and fragile skin, among others, Dr. Greysen said.
In a study published in 2015, Dr. Greysen assessed outcomes for elderly patients who were assessed before hospitalization for functional impairment. The more impaired they were, the more likely they were to be readmitted within 30 days of discharge – from a 13.5% readmission rate for those with no impairment up to 18.2% for those considered to have “dependency” in three or more activities of daily living.1
In another analysis, severe functional impairment – dependency in at least two activities of daily living – was associated with more post-acute care Medicare costs than neurological disorders or renal failure.2
Acute care for the elderly (ACE) programs, which have care specifically tailored to the needs of older patients, have been found to be associated with less functional decline, shorter lengths of stay, fewer adverse events, and lower costs and readmission rates, Dr. Greysen said.
These programs are becoming more common, but they are not spreading as quickly as perhaps they should, he said. In part, this is because of the “know-do” gap, in which practical steps that have been shown to work are not actually implemented because of assumptions that they are already in place or the mistaken belief that simple steps could not possibly make a difference.
Part of the paradigm shift that’s needed, Dr. Greysen said, is an appreciation of the concept of “posthospitalization syndrome,” which is composed of several domains: sleep, function, nutrition, symptom burden such as pain and discomfort, cognition, level of engagement, psychosocial status including emotional stress, and treatment burden including the adverse effects of medications.
Better patient engagement in discharge planning – including asking patients about whether they’ve had help reading hospital discharge–related documents, their level of education, and how often they are getting out of bed – is one necessary step toward change. Surveys of satisfaction using tablets and patient portals is another option, Dr. Greysen said.
The patients of the future will likely prompt their own change, he said, quoting from a 2013 publication.
“Possibly the most promising predictor for change in delivery of care is change in the patients themselves,” the authors wrote. “Baby boomers have redefined the norms at every stage of their lives. ... They will expect providers to engage them in shared decision making, elicit their health care goals and treatment preferences, communicate with providers across sites, and provide needed social supports.”3
References
1. Greysen SR et al. Functional impairment and hospital readmission in medicare seniors. JAMA Intern Med. 2015 Apr;175(4):559-65.
2. Greysen SR et al. Functional impairment: An unmeasured marker of medicare costs for postacute care of older adults. J Am Geriatr Soc. 2017 Sep;65(9):1996-2002.
3. Laura A. Levit, Erin P. Balogh, Sharyl J. Nass, and Patricia A. Ganz, eds. Delivering High-Quality Cancer Care: Charting a New Course for a System in Crisis. (Washington (DC): National Academies Press (US), 2013 Dec 27).
Better engagement with patients essential
Better engagement with patients essential
A 57-year-old man is admitted to the hospital with new back pain, which has been getting worse over the past 6 days. He had been diagnosed with stage 4 lung cancer in mid-2017 and underwent treatment with a platinum-based double therapy.
The man also has a history of heroin use – as recently as two years earlier – and he was divorced not long ago. He has been using an old prescription for Vicodin to treat himself, taking as many as 10-12 tablets a day.
This man is an example of the kind of complicated patient hospitalists are called on to treat – complex pain in an era when opioid abuse is considered a public scourge. How is a hospitalist to handle a case like this?
Pain cases are far from the only types of increasingly complex, often palliative cases in which hospitalists are being asked to provide help. Care for the elderly is also becoming increasingly difficult as the U.S. population ages and as hospitalists step in to provide care in the absence of geriatricians. .
Pain management in the opioid era and the need for new approaches in elderly care were highlighted at the Hospital Medicine 2018 annual conference, with experts drawing attention to subtleties that are often overlooked in these sometimes desperate cases.
James Risser, MD, medical director of palliative care at Regions Hospital in Minneapolis, said the complex problems of the 57-year-old man with back pain amounted to an example of “pain’s greatest hits.”
That particular case underscores the need to identify individual types of pain, he said, because they all need to be handled differently. If hospitalists don’t consider all the different aspects of pain, a patient might endure more suffering than necessary.
“All of this pain is swirling around in a very complicated patient,” Dr. Risser said, noting that it is important to “tease out the individual parts” of a complex patient’s history.
“Pain is a very complicated construct, from the physical to the neurological to the emotional,” Dr. Risser said. “Pain is a subjective experience, and the way people interact with their pain really depends not just on physical pain but also their psychological state, their social state, and even their spiritual state.”
Understanding this array of causes has led Dr. Risser to approach the problem of pain from different angles – including perspectives that might not be traditional, he said.
“One of the things that I’ve gotten better at is taking a spiritual history,” he said. “I don’t know if that’s part of everybody’s armamentarium. But if you’re dealing with people who are very, very sick, sometimes that’s the fundamental fabric of how they live and how they die. If there are unresolved issues along those lines, it’s possible they could be experiencing their pain in a different or more severe way.”
Varieties of pain
Treatment depends on the pain type, Dr. Risser said. Somatic pain often responds to nonsteroidal anti-inflammatories or steroids.
Neuropathic pain usually responds poorly to anti-inflammatories and to opioids. There is some research suggesting methadone could be helpful, but the data are not very strong. The most common medications prescribed are antiseizure medications and antidepressants, such as gabapentin and serotonin, and norepinephrine reuptake inhibitors.
The question of cancer pain versus noncancer pain can be tricky, Dr. Risser said. If a person’s life expectancy is limited, there can be a reason, or even a requirement, to use higher-risk medications. But, he said, that doesn’t mean the patient still won’t have problems with overuse of pain medication.
“We have a lot of patients now living post cancer who have been put on methadone or have been put on Oxycontin, and now we’re trying to figure out what to do with them,” he said. “I don’t think it’s that clear anymore that there’s a massive difference between cancer and noncancer pain, especially for those survivors.”
Clinicians, he said, should “fix what can be fixed” – and with the right tools. “If you have a patient who’s got severe lower abdominal pain because they have a bladder full or urine, really the treatment would probably not be … opioids. It probably would be a Foley catheter,” he said.
Hospitalists should treat patients based on sound principles of pain management, Dr. Risser said, but “while you try to create a diagnostic framework, know that people continually defy the boxes we put them in.”
Indeed, in an era of pain-medication addiction, it might be a good idea to worry about prescribing opioids, but clinicians have to remember that their goal is to help patients get relief – and that they themselves bring biases to the table, said Amy Davis, DO, MS, of Drexel University, Philadelphia.
In a presentation at HM18, Dr. Davis displayed images of a variety of patients on a large screen – different races and genders, some in business attire, some rougher around the edges.
“Would pain decisions change based on what people look like?” she asked. “Can you really spot who the drug traffickers are? We need to remember that our biases play a huge role not only in the treatment of our patients but in their outcomes. I’m challenging everybody to start thinking about these folks not as drug-seekers but as comfort-seekers.”
When it comes right down to it, she said, patients want a better life, not their drug of choice.
“That is the nature of the disease. [The illegal drug] is not what they’re looking for in reality because that does not provide a good quality of life,” Dr. Davis said. “The [practice of medicine] is supposed to be about helping people live their lives, not just checking off boxes.”
People with an opioid use disorder are physically different, she said. The processing of pain stimuli by their brain and spinal cord is physically altered – they have an increased perception of pain and lower pain tolerance.
“This is not a character flaw,” Dr. Davis affirmed. The increased sensitivity to pain does not resolve with opioid cessation; it can last for decades. Clinicians may need to spend more time interacting with certain patients to get a sense of the physical and nonphysical pain from which they suffer.
“Consistent, open, nonjudgmental communication improves not only the information we gather from patients and families, but it actually changes the adherence,” Dr. Davis said. “Ultimately the treatment outcomes are what all of this is about.”
Paradigm shift
Another palliative care role that hospitalists often find themselves in is “comforter” of elderly patients.

Ryan Greysen, MD, MHS, chief of hospital medicine at the University of Pennsylvania, Philadelphia, said hospitals must respond to a shift in the paradigm of elderly care. To explain the nature of this change, he referenced the “paradigm shift” model devised by the philosopher of science Thomas Kuhn, PhD. According to Kuhn, science proceeds in a settled pattern for many years, but on the rare occasions, when there is a fundamental drift in thinking, new problems present themselves and put the old model in a crisis mode, which prompts an intellectual revolution and a shift in the paradigm itself.
“This is a way of thinking about changes in scientific paradigms, but I think it works in clinical practice as well,” Dr. Greysen said.
The need for a paradigm shift in the care of elderly inpatients has largely to do with demographics. By 2050, the number of people aged 65 years and older is expected to be about 80 million, roughly double what it was in 2000. The number of people aged 85 years and up is expected to be about 20 million, or about four times the total in 2000.
In 2010, 40% of the hospitalized population was over 65 years. In 2030, that will flip: Only 40% of inpatients will be under 65 years. This will mean that hospitalists must care for more patients who are older, and the patients themselves will have more complicated medical issues.
“To be ready for the aging century, we must be better able to adapt and address those things that affect seniors,” Dr. Greysen said. With the number of geriatricians falling, much more of this care will fall to hospitalists, he said.
More attention must be paid to the potential harms of hospital-based care to older patients: decreased muscle strength and aerobic capacity, vasomotor instability, lower bone density, poor ventilation, altered thirst and nutrition, and fragile skin, among others, Dr. Greysen said.
In a study published in 2015, Dr. Greysen assessed outcomes for elderly patients who were assessed before hospitalization for functional impairment. The more impaired they were, the more likely they were to be readmitted within 30 days of discharge – from a 13.5% readmission rate for those with no impairment up to 18.2% for those considered to have “dependency” in three or more activities of daily living.1
In another analysis, severe functional impairment – dependency in at least two activities of daily living – was associated with more post-acute care Medicare costs than neurological disorders or renal failure.2
Acute care for the elderly (ACE) programs, which have care specifically tailored to the needs of older patients, have been found to be associated with less functional decline, shorter lengths of stay, fewer adverse events, and lower costs and readmission rates, Dr. Greysen said.
These programs are becoming more common, but they are not spreading as quickly as perhaps they should, he said. In part, this is because of the “know-do” gap, in which practical steps that have been shown to work are not actually implemented because of assumptions that they are already in place or the mistaken belief that simple steps could not possibly make a difference.
Part of the paradigm shift that’s needed, Dr. Greysen said, is an appreciation of the concept of “posthospitalization syndrome,” which is composed of several domains: sleep, function, nutrition, symptom burden such as pain and discomfort, cognition, level of engagement, psychosocial status including emotional stress, and treatment burden including the adverse effects of medications.
Better patient engagement in discharge planning – including asking patients about whether they’ve had help reading hospital discharge–related documents, their level of education, and how often they are getting out of bed – is one necessary step toward change. Surveys of satisfaction using tablets and patient portals is another option, Dr. Greysen said.
The patients of the future will likely prompt their own change, he said, quoting from a 2013 publication.
“Possibly the most promising predictor for change in delivery of care is change in the patients themselves,” the authors wrote. “Baby boomers have redefined the norms at every stage of their lives. ... They will expect providers to engage them in shared decision making, elicit their health care goals and treatment preferences, communicate with providers across sites, and provide needed social supports.”3
References
1. Greysen SR et al. Functional impairment and hospital readmission in medicare seniors. JAMA Intern Med. 2015 Apr;175(4):559-65.
2. Greysen SR et al. Functional impairment: An unmeasured marker of medicare costs for postacute care of older adults. J Am Geriatr Soc. 2017 Sep;65(9):1996-2002.
3. Laura A. Levit, Erin P. Balogh, Sharyl J. Nass, and Patricia A. Ganz, eds. Delivering High-Quality Cancer Care: Charting a New Course for a System in Crisis. (Washington (DC): National Academies Press (US), 2013 Dec 27).
A 57-year-old man is admitted to the hospital with new back pain, which has been getting worse over the past 6 days. He had been diagnosed with stage 4 lung cancer in mid-2017 and underwent treatment with a platinum-based double therapy.
The man also has a history of heroin use – as recently as two years earlier – and he was divorced not long ago. He has been using an old prescription for Vicodin to treat himself, taking as many as 10-12 tablets a day.
This man is an example of the kind of complicated patient hospitalists are called on to treat – complex pain in an era when opioid abuse is considered a public scourge. How is a hospitalist to handle a case like this?
Pain cases are far from the only types of increasingly complex, often palliative cases in which hospitalists are being asked to provide help. Care for the elderly is also becoming increasingly difficult as the U.S. population ages and as hospitalists step in to provide care in the absence of geriatricians. .
Pain management in the opioid era and the need for new approaches in elderly care were highlighted at the Hospital Medicine 2018 annual conference, with experts drawing attention to subtleties that are often overlooked in these sometimes desperate cases.
James Risser, MD, medical director of palliative care at Regions Hospital in Minneapolis, said the complex problems of the 57-year-old man with back pain amounted to an example of “pain’s greatest hits.”
That particular case underscores the need to identify individual types of pain, he said, because they all need to be handled differently. If hospitalists don’t consider all the different aspects of pain, a patient might endure more suffering than necessary.
“All of this pain is swirling around in a very complicated patient,” Dr. Risser said, noting that it is important to “tease out the individual parts” of a complex patient’s history.
“Pain is a very complicated construct, from the physical to the neurological to the emotional,” Dr. Risser said. “Pain is a subjective experience, and the way people interact with their pain really depends not just on physical pain but also their psychological state, their social state, and even their spiritual state.”
Understanding this array of causes has led Dr. Risser to approach the problem of pain from different angles – including perspectives that might not be traditional, he said.
“One of the things that I’ve gotten better at is taking a spiritual history,” he said. “I don’t know if that’s part of everybody’s armamentarium. But if you’re dealing with people who are very, very sick, sometimes that’s the fundamental fabric of how they live and how they die. If there are unresolved issues along those lines, it’s possible they could be experiencing their pain in a different or more severe way.”
Varieties of pain
Treatment depends on the pain type, Dr. Risser said. Somatic pain often responds to nonsteroidal anti-inflammatories or steroids.
Neuropathic pain usually responds poorly to anti-inflammatories and to opioids. There is some research suggesting methadone could be helpful, but the data are not very strong. The most common medications prescribed are antiseizure medications and antidepressants, such as gabapentin and serotonin, and norepinephrine reuptake inhibitors.
The question of cancer pain versus noncancer pain can be tricky, Dr. Risser said. If a person’s life expectancy is limited, there can be a reason, or even a requirement, to use higher-risk medications. But, he said, that doesn’t mean the patient still won’t have problems with overuse of pain medication.
“We have a lot of patients now living post cancer who have been put on methadone or have been put on Oxycontin, and now we’re trying to figure out what to do with them,” he said. “I don’t think it’s that clear anymore that there’s a massive difference between cancer and noncancer pain, especially for those survivors.”
Clinicians, he said, should “fix what can be fixed” – and with the right tools. “If you have a patient who’s got severe lower abdominal pain because they have a bladder full or urine, really the treatment would probably not be … opioids. It probably would be a Foley catheter,” he said.
Hospitalists should treat patients based on sound principles of pain management, Dr. Risser said, but “while you try to create a diagnostic framework, know that people continually defy the boxes we put them in.”
Indeed, in an era of pain-medication addiction, it might be a good idea to worry about prescribing opioids, but clinicians have to remember that their goal is to help patients get relief – and that they themselves bring biases to the table, said Amy Davis, DO, MS, of Drexel University, Philadelphia.
In a presentation at HM18, Dr. Davis displayed images of a variety of patients on a large screen – different races and genders, some in business attire, some rougher around the edges.
“Would pain decisions change based on what people look like?” she asked. “Can you really spot who the drug traffickers are? We need to remember that our biases play a huge role not only in the treatment of our patients but in their outcomes. I’m challenging everybody to start thinking about these folks not as drug-seekers but as comfort-seekers.”
When it comes right down to it, she said, patients want a better life, not their drug of choice.
“That is the nature of the disease. [The illegal drug] is not what they’re looking for in reality because that does not provide a good quality of life,” Dr. Davis said. “The [practice of medicine] is supposed to be about helping people live their lives, not just checking off boxes.”
People with an opioid use disorder are physically different, she said. The processing of pain stimuli by their brain and spinal cord is physically altered – they have an increased perception of pain and lower pain tolerance.
“This is not a character flaw,” Dr. Davis affirmed. The increased sensitivity to pain does not resolve with opioid cessation; it can last for decades. Clinicians may need to spend more time interacting with certain patients to get a sense of the physical and nonphysical pain from which they suffer.
“Consistent, open, nonjudgmental communication improves not only the information we gather from patients and families, but it actually changes the adherence,” Dr. Davis said. “Ultimately the treatment outcomes are what all of this is about.”
Paradigm shift
Another palliative care role that hospitalists often find themselves in is “comforter” of elderly patients.

Ryan Greysen, MD, MHS, chief of hospital medicine at the University of Pennsylvania, Philadelphia, said hospitals must respond to a shift in the paradigm of elderly care. To explain the nature of this change, he referenced the “paradigm shift” model devised by the philosopher of science Thomas Kuhn, PhD. According to Kuhn, science proceeds in a settled pattern for many years, but on the rare occasions, when there is a fundamental drift in thinking, new problems present themselves and put the old model in a crisis mode, which prompts an intellectual revolution and a shift in the paradigm itself.
“This is a way of thinking about changes in scientific paradigms, but I think it works in clinical practice as well,” Dr. Greysen said.
The need for a paradigm shift in the care of elderly inpatients has largely to do with demographics. By 2050, the number of people aged 65 years and older is expected to be about 80 million, roughly double what it was in 2000. The number of people aged 85 years and up is expected to be about 20 million, or about four times the total in 2000.
In 2010, 40% of the hospitalized population was over 65 years. In 2030, that will flip: Only 40% of inpatients will be under 65 years. This will mean that hospitalists must care for more patients who are older, and the patients themselves will have more complicated medical issues.
“To be ready for the aging century, we must be better able to adapt and address those things that affect seniors,” Dr. Greysen said. With the number of geriatricians falling, much more of this care will fall to hospitalists, he said.
More attention must be paid to the potential harms of hospital-based care to older patients: decreased muscle strength and aerobic capacity, vasomotor instability, lower bone density, poor ventilation, altered thirst and nutrition, and fragile skin, among others, Dr. Greysen said.
In a study published in 2015, Dr. Greysen assessed outcomes for elderly patients who were assessed before hospitalization for functional impairment. The more impaired they were, the more likely they were to be readmitted within 30 days of discharge – from a 13.5% readmission rate for those with no impairment up to 18.2% for those considered to have “dependency” in three or more activities of daily living.1
In another analysis, severe functional impairment – dependency in at least two activities of daily living – was associated with more post-acute care Medicare costs than neurological disorders or renal failure.2
Acute care for the elderly (ACE) programs, which have care specifically tailored to the needs of older patients, have been found to be associated with less functional decline, shorter lengths of stay, fewer adverse events, and lower costs and readmission rates, Dr. Greysen said.
These programs are becoming more common, but they are not spreading as quickly as perhaps they should, he said. In part, this is because of the “know-do” gap, in which practical steps that have been shown to work are not actually implemented because of assumptions that they are already in place or the mistaken belief that simple steps could not possibly make a difference.
Part of the paradigm shift that’s needed, Dr. Greysen said, is an appreciation of the concept of “posthospitalization syndrome,” which is composed of several domains: sleep, function, nutrition, symptom burden such as pain and discomfort, cognition, level of engagement, psychosocial status including emotional stress, and treatment burden including the adverse effects of medications.
Better patient engagement in discharge planning – including asking patients about whether they’ve had help reading hospital discharge–related documents, their level of education, and how often they are getting out of bed – is one necessary step toward change. Surveys of satisfaction using tablets and patient portals is another option, Dr. Greysen said.
The patients of the future will likely prompt their own change, he said, quoting from a 2013 publication.
“Possibly the most promising predictor for change in delivery of care is change in the patients themselves,” the authors wrote. “Baby boomers have redefined the norms at every stage of their lives. ... They will expect providers to engage them in shared decision making, elicit their health care goals and treatment preferences, communicate with providers across sites, and provide needed social supports.”3
References
1. Greysen SR et al. Functional impairment and hospital readmission in medicare seniors. JAMA Intern Med. 2015 Apr;175(4):559-65.
2. Greysen SR et al. Functional impairment: An unmeasured marker of medicare costs for postacute care of older adults. J Am Geriatr Soc. 2017 Sep;65(9):1996-2002.
3. Laura A. Levit, Erin P. Balogh, Sharyl J. Nass, and Patricia A. Ganz, eds. Delivering High-Quality Cancer Care: Charting a New Course for a System in Crisis. (Washington (DC): National Academies Press (US), 2013 Dec 27).
Be proactive with prophylaxis to tame VTE
Venous thromboembolism (VTE) is the No. 1 cause of preventable deaths in hospitals, and 60% of all VTE cases occur during or following hospitalization, according to Jeffrey I. Weitz, MD, of McMaster University in Hamilton, Ont.
, he said in a webinar to promote World Thrombosis Day.
“To prevent VTE, people need to be aware of the problem,” he said. Hospitalization for any reason increases the risk of VTE, but thromboprophylaxis may be underused in medical patients, compared with surgical patients, because most surgical patients are automatically considered at risk.
Prevention of VTE involves understanding the risk factors, Dr. Weitz said. He pointed to a triad of conditions that promote clotting: slow blood flow, injury to the vessel wall, and increased clotability of the blood.
In a study of VTE risk factors, recent surgery with hospitalization and trauma topped the list, but hospitalization without recent surgery was associated with a nearly 8-fold increase in risk (Arch Intern Med. 2000;160[6]:809-15).
Evidence supports the value of anticoagulant prophylaxis, Dr. Weitz said. In a 2007 meta-analysis, use of anticoagulants reduced the risk of VTE by approximately 60% (Ann Intern Med. 2007 Feb 20;146[4]:278-88), and a 2011 update showed a reduction in risk of approximately 30% (Ann Intern Med. 2011 Nov 1;155[9]:602-15).
While risk assessment remains a challenge, several models can help, said Dr. Weitz.
Current guidelines from the American College of Chest Physicians suggest a shift toward individualized assessment of VTE risk, and the Centers for Medicare & Medicaid Services mandates VTE risk assessment, Dr. Weitz said.
He offered seven steps to improve prophylaxis in the hospital:
1. Obtain commitment from hospital leadership, including formation of a committee.
2. Have a written hospital policy on thromboprophylaxis.
3. Keep the policy simple and standard in terms of who gets prophylaxis and when.
4. Use order sets, computer order entry, and decision support.
5. Make the prophylaxis decision mandatory.
6. Involve of all the members of the care team and patients.
7. Use audits to measure improvement.
Several risk assessment models for VTE in hospitalized medical patients have been studied, including the Padua and IMPROVE models, Dr. Weitz said. For any model, factoring in the D-dimer can provide more information. “If D-dimer is increased more than twice the upper limit of normal, it is a risk factor for VTE,” he said.
Another consideration in thromboprophylaxis involves extending the duration of prophylaxis beyond the hospital stay, which is becoming a larger issue because of the pressure to move patients out of the hospital as quickly as possible, Dr. Weitz said. However, trials of extended thromboprophylaxis have yielded mixed results. Extended doses of medications, including rivaroxaban, enoxaparin, apixaban, and betrixaban can reduce the risk of VTE, but can also increase the risk of major bleeding.
“I think at this point we are not yet there at identifying patients who should have thromboprophylaxis beyond the hospital stay,” Dr. Weitz said.
But VTE risk should be assessed in all hospitalized patients, and “appropriate thromboprophylaxis is essential for reducing the burden of hospital-associated VTE,” he said.
Dr. Weitz encouraged clinicians to explore more resources for managing VTE risk at worldthrombosisday.org.
Dr. Weitz reported relationships with companies including Bayer, Boehringer-Ingelheim, Bristol-Myers Squibb, Daiichi-Sankyo, Pfizer, Portola, Ionis Pharmaceuticals, Janssen, Merck, Novartis, and Servier. He also reported research support from the Canadian Institutes of Health Research, Heart and Stroke Foundation of Canada, and the Canadian Fund for Innovation.
Venous thromboembolism (VTE) is the No. 1 cause of preventable deaths in hospitals, and 60% of all VTE cases occur during or following hospitalization, according to Jeffrey I. Weitz, MD, of McMaster University in Hamilton, Ont.
, he said in a webinar to promote World Thrombosis Day.
“To prevent VTE, people need to be aware of the problem,” he said. Hospitalization for any reason increases the risk of VTE, but thromboprophylaxis may be underused in medical patients, compared with surgical patients, because most surgical patients are automatically considered at risk.
Prevention of VTE involves understanding the risk factors, Dr. Weitz said. He pointed to a triad of conditions that promote clotting: slow blood flow, injury to the vessel wall, and increased clotability of the blood.
In a study of VTE risk factors, recent surgery with hospitalization and trauma topped the list, but hospitalization without recent surgery was associated with a nearly 8-fold increase in risk (Arch Intern Med. 2000;160[6]:809-15).
Evidence supports the value of anticoagulant prophylaxis, Dr. Weitz said. In a 2007 meta-analysis, use of anticoagulants reduced the risk of VTE by approximately 60% (Ann Intern Med. 2007 Feb 20;146[4]:278-88), and a 2011 update showed a reduction in risk of approximately 30% (Ann Intern Med. 2011 Nov 1;155[9]:602-15).
While risk assessment remains a challenge, several models can help, said Dr. Weitz.
Current guidelines from the American College of Chest Physicians suggest a shift toward individualized assessment of VTE risk, and the Centers for Medicare & Medicaid Services mandates VTE risk assessment, Dr. Weitz said.
He offered seven steps to improve prophylaxis in the hospital:
1. Obtain commitment from hospital leadership, including formation of a committee.
2. Have a written hospital policy on thromboprophylaxis.
3. Keep the policy simple and standard in terms of who gets prophylaxis and when.
4. Use order sets, computer order entry, and decision support.
5. Make the prophylaxis decision mandatory.
6. Involve of all the members of the care team and patients.
7. Use audits to measure improvement.
Several risk assessment models for VTE in hospitalized medical patients have been studied, including the Padua and IMPROVE models, Dr. Weitz said. For any model, factoring in the D-dimer can provide more information. “If D-dimer is increased more than twice the upper limit of normal, it is a risk factor for VTE,” he said.
Another consideration in thromboprophylaxis involves extending the duration of prophylaxis beyond the hospital stay, which is becoming a larger issue because of the pressure to move patients out of the hospital as quickly as possible, Dr. Weitz said. However, trials of extended thromboprophylaxis have yielded mixed results. Extended doses of medications, including rivaroxaban, enoxaparin, apixaban, and betrixaban can reduce the risk of VTE, but can also increase the risk of major bleeding.
“I think at this point we are not yet there at identifying patients who should have thromboprophylaxis beyond the hospital stay,” Dr. Weitz said.
But VTE risk should be assessed in all hospitalized patients, and “appropriate thromboprophylaxis is essential for reducing the burden of hospital-associated VTE,” he said.
Dr. Weitz encouraged clinicians to explore more resources for managing VTE risk at worldthrombosisday.org.
Dr. Weitz reported relationships with companies including Bayer, Boehringer-Ingelheim, Bristol-Myers Squibb, Daiichi-Sankyo, Pfizer, Portola, Ionis Pharmaceuticals, Janssen, Merck, Novartis, and Servier. He also reported research support from the Canadian Institutes of Health Research, Heart and Stroke Foundation of Canada, and the Canadian Fund for Innovation.
Venous thromboembolism (VTE) is the No. 1 cause of preventable deaths in hospitals, and 60% of all VTE cases occur during or following hospitalization, according to Jeffrey I. Weitz, MD, of McMaster University in Hamilton, Ont.
, he said in a webinar to promote World Thrombosis Day.
“To prevent VTE, people need to be aware of the problem,” he said. Hospitalization for any reason increases the risk of VTE, but thromboprophylaxis may be underused in medical patients, compared with surgical patients, because most surgical patients are automatically considered at risk.
Prevention of VTE involves understanding the risk factors, Dr. Weitz said. He pointed to a triad of conditions that promote clotting: slow blood flow, injury to the vessel wall, and increased clotability of the blood.
In a study of VTE risk factors, recent surgery with hospitalization and trauma topped the list, but hospitalization without recent surgery was associated with a nearly 8-fold increase in risk (Arch Intern Med. 2000;160[6]:809-15).
Evidence supports the value of anticoagulant prophylaxis, Dr. Weitz said. In a 2007 meta-analysis, use of anticoagulants reduced the risk of VTE by approximately 60% (Ann Intern Med. 2007 Feb 20;146[4]:278-88), and a 2011 update showed a reduction in risk of approximately 30% (Ann Intern Med. 2011 Nov 1;155[9]:602-15).
While risk assessment remains a challenge, several models can help, said Dr. Weitz.
Current guidelines from the American College of Chest Physicians suggest a shift toward individualized assessment of VTE risk, and the Centers for Medicare & Medicaid Services mandates VTE risk assessment, Dr. Weitz said.
He offered seven steps to improve prophylaxis in the hospital:
1. Obtain commitment from hospital leadership, including formation of a committee.
2. Have a written hospital policy on thromboprophylaxis.
3. Keep the policy simple and standard in terms of who gets prophylaxis and when.
4. Use order sets, computer order entry, and decision support.
5. Make the prophylaxis decision mandatory.
6. Involve of all the members of the care team and patients.
7. Use audits to measure improvement.
Several risk assessment models for VTE in hospitalized medical patients have been studied, including the Padua and IMPROVE models, Dr. Weitz said. For any model, factoring in the D-dimer can provide more information. “If D-dimer is increased more than twice the upper limit of normal, it is a risk factor for VTE,” he said.
Another consideration in thromboprophylaxis involves extending the duration of prophylaxis beyond the hospital stay, which is becoming a larger issue because of the pressure to move patients out of the hospital as quickly as possible, Dr. Weitz said. However, trials of extended thromboprophylaxis have yielded mixed results. Extended doses of medications, including rivaroxaban, enoxaparin, apixaban, and betrixaban can reduce the risk of VTE, but can also increase the risk of major bleeding.
“I think at this point we are not yet there at identifying patients who should have thromboprophylaxis beyond the hospital stay,” Dr. Weitz said.
But VTE risk should be assessed in all hospitalized patients, and “appropriate thromboprophylaxis is essential for reducing the burden of hospital-associated VTE,” he said.
Dr. Weitz encouraged clinicians to explore more resources for managing VTE risk at worldthrombosisday.org.
Dr. Weitz reported relationships with companies including Bayer, Boehringer-Ingelheim, Bristol-Myers Squibb, Daiichi-Sankyo, Pfizer, Portola, Ionis Pharmaceuticals, Janssen, Merck, Novartis, and Servier. He also reported research support from the Canadian Institutes of Health Research, Heart and Stroke Foundation of Canada, and the Canadian Fund for Innovation.
FROM WORLD THROMBOSIS DAY 2018 WEBINAR
Readmissions after GI bleeds
Clinical question: What is the rate of hospital readmission within 30 days of nonvariceal upper GI hemorrhage, and what are its effects on mortality, morbidity, and health care use in the United States?
Background: Nonvariceal upper GI hemorrhage is the most common GI emergency that leads to hospital admission (approximately 300,000 admissions/year in the United States). Because of the advances in endoscopic therapy and overall medical care, associated in-hospital mortality has been steadily decreasing. As a result of Medicare and Medicaid shifts toward an alternative payment model, quantifying hospital readmission rate after an episode of nonvariceal upper GI hemorrhage and measuring its effects on patient outcomes and resource use have become a key step in both improving treatment outcomes and health care reimbursement.
Study design: Retrospective study.
Setting: The Agency for Healthcare Research and Quality’s Healthcare Cost and Utilization Project Nationwide Readmission Database for the year 2014.
Synopsis: The study collected data on hospital readmissions for 203,220 adults who were hospitalized for urgent nonvariceal upper gastrointestinal hemorrhage and discharged. The primary outcome was rate of all-cause readmission within 30 days of discharge. Secondary outcomes were reasons for readmission, readmission mortality rate, morbidity (shock and prolonged mechanical ventilation), and resource use (length of stay and total hospitalization costs and charges).
The rate of readmission was determined to be 13%, with only 18% caused by recurrent nonvariceal upper gastrointestinal bleeding. The rate of death among readmissions was higher than that among index admissions, and a higher proportion of readmitted patients had morbidities requiring prolonged mechanical ventilation. The total economic in-hospital burden was $30.3 million in costs and $108 million in charges over the span of readmission-associated 133,368 hospital days. Independent predictors of readmission were having Medicaid insurance, having a higher comorbidity score, having a lower income, residence in a metropolitan area, hemorrhagic shock, and longer stays in the hospital.
Bottom line: Readmissions within 30 days of discharge for upper GI hemorrhage are associated with higher morbidity and mortality and lead to higher resource use.
Citation: Abougergi M et al. Thirty-day readmission among patients with nonvariceal upper gastrointestinal hemorrhage and effects on outcomes. Gastroenterology. 2018 Jul;155(1):38-46.
Dr. White is a hospitalist in the division of hospital medicine in the department of medicine at Loyola University Chicago, Maywood, Ill.
Clinical question: What is the rate of hospital readmission within 30 days of nonvariceal upper GI hemorrhage, and what are its effects on mortality, morbidity, and health care use in the United States?
Background: Nonvariceal upper GI hemorrhage is the most common GI emergency that leads to hospital admission (approximately 300,000 admissions/year in the United States). Because of the advances in endoscopic therapy and overall medical care, associated in-hospital mortality has been steadily decreasing. As a result of Medicare and Medicaid shifts toward an alternative payment model, quantifying hospital readmission rate after an episode of nonvariceal upper GI hemorrhage and measuring its effects on patient outcomes and resource use have become a key step in both improving treatment outcomes and health care reimbursement.
Study design: Retrospective study.
Setting: The Agency for Healthcare Research and Quality’s Healthcare Cost and Utilization Project Nationwide Readmission Database for the year 2014.
Synopsis: The study collected data on hospital readmissions for 203,220 adults who were hospitalized for urgent nonvariceal upper gastrointestinal hemorrhage and discharged. The primary outcome was rate of all-cause readmission within 30 days of discharge. Secondary outcomes were reasons for readmission, readmission mortality rate, morbidity (shock and prolonged mechanical ventilation), and resource use (length of stay and total hospitalization costs and charges).
The rate of readmission was determined to be 13%, with only 18% caused by recurrent nonvariceal upper gastrointestinal bleeding. The rate of death among readmissions was higher than that among index admissions, and a higher proportion of readmitted patients had morbidities requiring prolonged mechanical ventilation. The total economic in-hospital burden was $30.3 million in costs and $108 million in charges over the span of readmission-associated 133,368 hospital days. Independent predictors of readmission were having Medicaid insurance, having a higher comorbidity score, having a lower income, residence in a metropolitan area, hemorrhagic shock, and longer stays in the hospital.
Bottom line: Readmissions within 30 days of discharge for upper GI hemorrhage are associated with higher morbidity and mortality and lead to higher resource use.
Citation: Abougergi M et al. Thirty-day readmission among patients with nonvariceal upper gastrointestinal hemorrhage and effects on outcomes. Gastroenterology. 2018 Jul;155(1):38-46.
Dr. White is a hospitalist in the division of hospital medicine in the department of medicine at Loyola University Chicago, Maywood, Ill.
Clinical question: What is the rate of hospital readmission within 30 days of nonvariceal upper GI hemorrhage, and what are its effects on mortality, morbidity, and health care use in the United States?
Background: Nonvariceal upper GI hemorrhage is the most common GI emergency that leads to hospital admission (approximately 300,000 admissions/year in the United States). Because of the advances in endoscopic therapy and overall medical care, associated in-hospital mortality has been steadily decreasing. As a result of Medicare and Medicaid shifts toward an alternative payment model, quantifying hospital readmission rate after an episode of nonvariceal upper GI hemorrhage and measuring its effects on patient outcomes and resource use have become a key step in both improving treatment outcomes and health care reimbursement.
Study design: Retrospective study.
Setting: The Agency for Healthcare Research and Quality’s Healthcare Cost and Utilization Project Nationwide Readmission Database for the year 2014.
Synopsis: The study collected data on hospital readmissions for 203,220 adults who were hospitalized for urgent nonvariceal upper gastrointestinal hemorrhage and discharged. The primary outcome was rate of all-cause readmission within 30 days of discharge. Secondary outcomes were reasons for readmission, readmission mortality rate, morbidity (shock and prolonged mechanical ventilation), and resource use (length of stay and total hospitalization costs and charges).
The rate of readmission was determined to be 13%, with only 18% caused by recurrent nonvariceal upper gastrointestinal bleeding. The rate of death among readmissions was higher than that among index admissions, and a higher proportion of readmitted patients had morbidities requiring prolonged mechanical ventilation. The total economic in-hospital burden was $30.3 million in costs and $108 million in charges over the span of readmission-associated 133,368 hospital days. Independent predictors of readmission were having Medicaid insurance, having a higher comorbidity score, having a lower income, residence in a metropolitan area, hemorrhagic shock, and longer stays in the hospital.
Bottom line: Readmissions within 30 days of discharge for upper GI hemorrhage are associated with higher morbidity and mortality and lead to higher resource use.
Citation: Abougergi M et al. Thirty-day readmission among patients with nonvariceal upper gastrointestinal hemorrhage and effects on outcomes. Gastroenterology. 2018 Jul;155(1):38-46.
Dr. White is a hospitalist in the division of hospital medicine in the department of medicine at Loyola University Chicago, Maywood, Ill.
Smoking cessation drugs do not increase CV risk
Clinical question: Do pharmacotherapies used in tobacco cessation treatment significantly increase the risk of cardiovascular events?
Background: Although it is known that smoking cessation is the most beneficial enhancement of cardiovascular health, many clinicians may be hesitant to prescribe pharmacotherapies because of concerns regarding adverse events. This study reports the cardiovascular safety findings from EAGLES (Evaluating Adverse Events in a Global Smoking Cessation Study) and its nontreatment extension trial.
Study design: Double-blind, randomized, triple-dummy, placebo- and active-controlled trial and its nontreatment extension trial.
Setting: Conducted by 140 multinational centers, EAGLES was a trial in cohorts of smokers with and without psychiatric disease that assessed the safety and efficacy of pharmacotherapies used for smoking cessation.
The EAGLES extension trial is a nontreatment extension of EAGLES. It began with the first dose of medication and included those who completed an additional 28 weeks of observation.
Synopsis: The study included approximately 8,000 participants aged 18-75 years who smoked 10 or more cigarettes per day and were interested in quitting. The study monitored the development of a major adverse cardiovascular event (MACE), such as cardiovascular death, nonfatal myocardial infarction, or nonfatal stroke, during treatment with varenicline, bupropion hydrochloride, nicotine replacement therapy, and placebo therapy. Other end points included determining the occurrence of MACE along with other peripheral vascular disease that required either intervention, coronary revascularization, or hospitalization for unstable angina (MACE+).
There were no significant differences in time to MACE or MACE+ overall across all observation periods.
Possible limitations of the study were its exclusion criteria and baseline characteristics of participants. The study excluded participants with unstable psychiatric illness, active substance abuse, clinically significant cardiovascular disease in the 2 months prior to the study entry (MI or coronary artery bypass graft), clinically significant cerebrovascular disease in the 2 months prior to study entry (stroke or documented transient ischemic attack), or inadequate control of hypertension as judged by investigators at screening and baseline. Of the included participants, greater than 66% of the participants were in the low risk (less than 10%) cardiovascular risk category, less than 10% had diabetes, less than 5% had coronary heart disease, and less than 1% had carotid artery disease.
Bottom line: The findings provide evidence that, in a general population of smokers, smoking cessation medications do not increase the risk of serious cardiovascular events.
Citation: Benowitz N et al. Cardiovascular safety of varenicline, bupropion, and nicotine patch in smoker. JAMA Intern Med. 2018 May;178(5):622-31.
Dr. White is a hospitalist in the division of hospital medicine in the department of medicine at Loyola University Chicago, Maywood, Ill.
Clinical question: Do pharmacotherapies used in tobacco cessation treatment significantly increase the risk of cardiovascular events?
Background: Although it is known that smoking cessation is the most beneficial enhancement of cardiovascular health, many clinicians may be hesitant to prescribe pharmacotherapies because of concerns regarding adverse events. This study reports the cardiovascular safety findings from EAGLES (Evaluating Adverse Events in a Global Smoking Cessation Study) and its nontreatment extension trial.
Study design: Double-blind, randomized, triple-dummy, placebo- and active-controlled trial and its nontreatment extension trial.
Setting: Conducted by 140 multinational centers, EAGLES was a trial in cohorts of smokers with and without psychiatric disease that assessed the safety and efficacy of pharmacotherapies used for smoking cessation.
The EAGLES extension trial is a nontreatment extension of EAGLES. It began with the first dose of medication and included those who completed an additional 28 weeks of observation.
Synopsis: The study included approximately 8,000 participants aged 18-75 years who smoked 10 or more cigarettes per day and were interested in quitting. The study monitored the development of a major adverse cardiovascular event (MACE), such as cardiovascular death, nonfatal myocardial infarction, or nonfatal stroke, during treatment with varenicline, bupropion hydrochloride, nicotine replacement therapy, and placebo therapy. Other end points included determining the occurrence of MACE along with other peripheral vascular disease that required either intervention, coronary revascularization, or hospitalization for unstable angina (MACE+).
There were no significant differences in time to MACE or MACE+ overall across all observation periods.
Possible limitations of the study were its exclusion criteria and baseline characteristics of participants. The study excluded participants with unstable psychiatric illness, active substance abuse, clinically significant cardiovascular disease in the 2 months prior to the study entry (MI or coronary artery bypass graft), clinically significant cerebrovascular disease in the 2 months prior to study entry (stroke or documented transient ischemic attack), or inadequate control of hypertension as judged by investigators at screening and baseline. Of the included participants, greater than 66% of the participants were in the low risk (less than 10%) cardiovascular risk category, less than 10% had diabetes, less than 5% had coronary heart disease, and less than 1% had carotid artery disease.
Bottom line: The findings provide evidence that, in a general population of smokers, smoking cessation medications do not increase the risk of serious cardiovascular events.
Citation: Benowitz N et al. Cardiovascular safety of varenicline, bupropion, and nicotine patch in smoker. JAMA Intern Med. 2018 May;178(5):622-31.
Dr. White is a hospitalist in the division of hospital medicine in the department of medicine at Loyola University Chicago, Maywood, Ill.
Clinical question: Do pharmacotherapies used in tobacco cessation treatment significantly increase the risk of cardiovascular events?
Background: Although it is known that smoking cessation is the most beneficial enhancement of cardiovascular health, many clinicians may be hesitant to prescribe pharmacotherapies because of concerns regarding adverse events. This study reports the cardiovascular safety findings from EAGLES (Evaluating Adverse Events in a Global Smoking Cessation Study) and its nontreatment extension trial.
Study design: Double-blind, randomized, triple-dummy, placebo- and active-controlled trial and its nontreatment extension trial.
Setting: Conducted by 140 multinational centers, EAGLES was a trial in cohorts of smokers with and without psychiatric disease that assessed the safety and efficacy of pharmacotherapies used for smoking cessation.
The EAGLES extension trial is a nontreatment extension of EAGLES. It began with the first dose of medication and included those who completed an additional 28 weeks of observation.
Synopsis: The study included approximately 8,000 participants aged 18-75 years who smoked 10 or more cigarettes per day and were interested in quitting. The study monitored the development of a major adverse cardiovascular event (MACE), such as cardiovascular death, nonfatal myocardial infarction, or nonfatal stroke, during treatment with varenicline, bupropion hydrochloride, nicotine replacement therapy, and placebo therapy. Other end points included determining the occurrence of MACE along with other peripheral vascular disease that required either intervention, coronary revascularization, or hospitalization for unstable angina (MACE+).
There were no significant differences in time to MACE or MACE+ overall across all observation periods.
Possible limitations of the study were its exclusion criteria and baseline characteristics of participants. The study excluded participants with unstable psychiatric illness, active substance abuse, clinically significant cardiovascular disease in the 2 months prior to the study entry (MI or coronary artery bypass graft), clinically significant cerebrovascular disease in the 2 months prior to study entry (stroke or documented transient ischemic attack), or inadequate control of hypertension as judged by investigators at screening and baseline. Of the included participants, greater than 66% of the participants were in the low risk (less than 10%) cardiovascular risk category, less than 10% had diabetes, less than 5% had coronary heart disease, and less than 1% had carotid artery disease.
Bottom line: The findings provide evidence that, in a general population of smokers, smoking cessation medications do not increase the risk of serious cardiovascular events.
Citation: Benowitz N et al. Cardiovascular safety of varenicline, bupropion, and nicotine patch in smoker. JAMA Intern Med. 2018 May;178(5):622-31.
Dr. White is a hospitalist in the division of hospital medicine in the department of medicine at Loyola University Chicago, Maywood, Ill.
Association between hospice length of stay and health care costs
Background: Early hospice referral among Medicare patients is associated with lower rates of hospital admission, intensive care unit admission, and in-hospital death. However, it is not known whether there is association between early hospice referral and health care costs among patients with maintenance hemodialysis.
Study design: Cross-sectional observational study.
Setting: Using the United States Renal Data System registry.
Synopsis: With the use of data from the United States Renal Data System from 2000-2014, the study examined the relationship between health care utilization during the last month and that of the last week of life among patients with maintenance hemodialysis. The investigators used patients who had renal failure as a primary hospice diagnosis regardless of the decision to discontinue hemodialysis before death. Hospital admission, ICU admission, death in the hospital, and one or more inpatient intensive procedures were used as measures for health care utilization.
Among 154,186 (20%) patients receiving hospice service at the time of death, 41.5% enrolled in hospice within 3 days of death. Because more patients were referred to hospice very close to the time of death, the Medicare cost for hospice patients was similar to those patients not referred to hospice ($10,756 vs. $10,871; P = .08). Longer lengths of stay in hospice beyond 3 days were associated with lower rates of health care utilization and costs. Late hospice referral was also associated with inadequate pain control and emotional needs.
The study was not able to capture patients who had end-stage renal disease but were on hemodialysis. Patients with private insurance or those covered by Veterans Affairs were not included.
Bottom line: Half of hospice referrals among patients with maintenance hemodialysis occur within the last 3 day of life, which has no significant effect on end-of-life costs and health care utilization.
Citation: Wachterman MW et al. Association between hospice length of stay, health care utilization, and Medicare costs at the end of life among patients who received maintenance hemodialysis. Jama Intern Med. 2018;178(6):792-9.
Dr. Katsouli is a hospitalist in the division of hospital medicine in the department of medicine at Loyola University Chicago, Maywood, Ill.
Background: Early hospice referral among Medicare patients is associated with lower rates of hospital admission, intensive care unit admission, and in-hospital death. However, it is not known whether there is association between early hospice referral and health care costs among patients with maintenance hemodialysis.
Study design: Cross-sectional observational study.
Setting: Using the United States Renal Data System registry.
Synopsis: With the use of data from the United States Renal Data System from 2000-2014, the study examined the relationship between health care utilization during the last month and that of the last week of life among patients with maintenance hemodialysis. The investigators used patients who had renal failure as a primary hospice diagnosis regardless of the decision to discontinue hemodialysis before death. Hospital admission, ICU admission, death in the hospital, and one or more inpatient intensive procedures were used as measures for health care utilization.
Among 154,186 (20%) patients receiving hospice service at the time of death, 41.5% enrolled in hospice within 3 days of death. Because more patients were referred to hospice very close to the time of death, the Medicare cost for hospice patients was similar to those patients not referred to hospice ($10,756 vs. $10,871; P = .08). Longer lengths of stay in hospice beyond 3 days were associated with lower rates of health care utilization and costs. Late hospice referral was also associated with inadequate pain control and emotional needs.
The study was not able to capture patients who had end-stage renal disease but were on hemodialysis. Patients with private insurance or those covered by Veterans Affairs were not included.
Bottom line: Half of hospice referrals among patients with maintenance hemodialysis occur within the last 3 day of life, which has no significant effect on end-of-life costs and health care utilization.
Citation: Wachterman MW et al. Association between hospice length of stay, health care utilization, and Medicare costs at the end of life among patients who received maintenance hemodialysis. Jama Intern Med. 2018;178(6):792-9.
Dr. Katsouli is a hospitalist in the division of hospital medicine in the department of medicine at Loyola University Chicago, Maywood, Ill.
Background: Early hospice referral among Medicare patients is associated with lower rates of hospital admission, intensive care unit admission, and in-hospital death. However, it is not known whether there is association between early hospice referral and health care costs among patients with maintenance hemodialysis.
Study design: Cross-sectional observational study.
Setting: Using the United States Renal Data System registry.
Synopsis: With the use of data from the United States Renal Data System from 2000-2014, the study examined the relationship between health care utilization during the last month and that of the last week of life among patients with maintenance hemodialysis. The investigators used patients who had renal failure as a primary hospice diagnosis regardless of the decision to discontinue hemodialysis before death. Hospital admission, ICU admission, death in the hospital, and one or more inpatient intensive procedures were used as measures for health care utilization.
Among 154,186 (20%) patients receiving hospice service at the time of death, 41.5% enrolled in hospice within 3 days of death. Because more patients were referred to hospice very close to the time of death, the Medicare cost for hospice patients was similar to those patients not referred to hospice ($10,756 vs. $10,871; P = .08). Longer lengths of stay in hospice beyond 3 days were associated with lower rates of health care utilization and costs. Late hospice referral was also associated with inadequate pain control and emotional needs.
The study was not able to capture patients who had end-stage renal disease but were on hemodialysis. Patients with private insurance or those covered by Veterans Affairs were not included.
Bottom line: Half of hospice referrals among patients with maintenance hemodialysis occur within the last 3 day of life, which has no significant effect on end-of-life costs and health care utilization.
Citation: Wachterman MW et al. Association between hospice length of stay, health care utilization, and Medicare costs at the end of life among patients who received maintenance hemodialysis. Jama Intern Med. 2018;178(6):792-9.
Dr. Katsouli is a hospitalist in the division of hospital medicine in the department of medicine at Loyola University Chicago, Maywood, Ill.
Discharge trends for septic shock survivors remain steady
SAN ANTONIO – While septic shock mortality has decreased since the Surviving Sepsis Campaign guidelines were introduced, discharge trends for survivors have not changed significantly over time, a recent analysis suggests.
The percentage of survivors discharged to subacute rehab or long-term facilities did not change appreciably over time, according to the 10-year retrospective analysis, presented at the annual meeting of the American College of Chest Physicians.
However, average length of stay did significantly trend downward over the decade analyzed, while total charge per septic shock admission significantly increased, according to investigator Di Pan, DO, Icahn School of Medicine at Mount Sinai, New York, and his colleagues.
This is one of few studies looking at outcomes in survivors of septic shock, as most analyses have primarily focused on mortality outcomes, the investigators said.
Their analysis was based on the 2004 to 2014 National (Nationwide) Inpatient Sample databases and included patients with a primary diagnosis of septic shock at discharge.
Out of nearly 1.8 million patients with septic shock in that cohort, about 1 million survived, according to data Dr. Pan and colleagues provided in an abstract of the presentation.
In-hospital mortality decreased from 51.7% in 2004 to 39.3% in 2014 (P less than .001), the investigators reported.
The proportion of survivors discharged to subacute rehab or long-term acute care facilities was 61.9% in 2004, and similarly, 62.4% in 2014 (P = .1), while the percentage discharged home was 17.1% in 2004 and 15.1% in 2014 (P = 0.55).
However, there was a small but statistically significant downtick in mean length of stay, from 12.6 days in 2004 to 11.05 days in 2014, the investigators said. Meanwhile, total hospitalization charges surged from $105,776 in 2004 to $134,394 over the same time period.
The first edition of the Surviving Sepsis Campaign guidelines for management of severe sepsis and septic shock was published in March 2004 in Critical Care Medicine.
Future studies and clinical trials should look beyond mortality outcomes to additionally evaluate morbidity outcomes in septic shock survivors, Dr. Pan and coauthors said in their report.
The researchers had no relationships to disclose relevant to the presented study.
SOURCE: Pan D et al. CHEST 2018. doi: 10.1016/j.chest.2018.08.339.
SAN ANTONIO – While septic shock mortality has decreased since the Surviving Sepsis Campaign guidelines were introduced, discharge trends for survivors have not changed significantly over time, a recent analysis suggests.
The percentage of survivors discharged to subacute rehab or long-term facilities did not change appreciably over time, according to the 10-year retrospective analysis, presented at the annual meeting of the American College of Chest Physicians.
However, average length of stay did significantly trend downward over the decade analyzed, while total charge per septic shock admission significantly increased, according to investigator Di Pan, DO, Icahn School of Medicine at Mount Sinai, New York, and his colleagues.
This is one of few studies looking at outcomes in survivors of septic shock, as most analyses have primarily focused on mortality outcomes, the investigators said.
Their analysis was based on the 2004 to 2014 National (Nationwide) Inpatient Sample databases and included patients with a primary diagnosis of septic shock at discharge.
Out of nearly 1.8 million patients with septic shock in that cohort, about 1 million survived, according to data Dr. Pan and colleagues provided in an abstract of the presentation.
In-hospital mortality decreased from 51.7% in 2004 to 39.3% in 2014 (P less than .001), the investigators reported.
The proportion of survivors discharged to subacute rehab or long-term acute care facilities was 61.9% in 2004, and similarly, 62.4% in 2014 (P = .1), while the percentage discharged home was 17.1% in 2004 and 15.1% in 2014 (P = 0.55).
However, there was a small but statistically significant downtick in mean length of stay, from 12.6 days in 2004 to 11.05 days in 2014, the investigators said. Meanwhile, total hospitalization charges surged from $105,776 in 2004 to $134,394 over the same time period.
The first edition of the Surviving Sepsis Campaign guidelines for management of severe sepsis and septic shock was published in March 2004 in Critical Care Medicine.
Future studies and clinical trials should look beyond mortality outcomes to additionally evaluate morbidity outcomes in septic shock survivors, Dr. Pan and coauthors said in their report.
The researchers had no relationships to disclose relevant to the presented study.
SOURCE: Pan D et al. CHEST 2018. doi: 10.1016/j.chest.2018.08.339.
SAN ANTONIO – While septic shock mortality has decreased since the Surviving Sepsis Campaign guidelines were introduced, discharge trends for survivors have not changed significantly over time, a recent analysis suggests.
The percentage of survivors discharged to subacute rehab or long-term facilities did not change appreciably over time, according to the 10-year retrospective analysis, presented at the annual meeting of the American College of Chest Physicians.
However, average length of stay did significantly trend downward over the decade analyzed, while total charge per septic shock admission significantly increased, according to investigator Di Pan, DO, Icahn School of Medicine at Mount Sinai, New York, and his colleagues.
This is one of few studies looking at outcomes in survivors of septic shock, as most analyses have primarily focused on mortality outcomes, the investigators said.
Their analysis was based on the 2004 to 2014 National (Nationwide) Inpatient Sample databases and included patients with a primary diagnosis of septic shock at discharge.
Out of nearly 1.8 million patients with septic shock in that cohort, about 1 million survived, according to data Dr. Pan and colleagues provided in an abstract of the presentation.
In-hospital mortality decreased from 51.7% in 2004 to 39.3% in 2014 (P less than .001), the investigators reported.
The proportion of survivors discharged to subacute rehab or long-term acute care facilities was 61.9% in 2004, and similarly, 62.4% in 2014 (P = .1), while the percentage discharged home was 17.1% in 2004 and 15.1% in 2014 (P = 0.55).
However, there was a small but statistically significant downtick in mean length of stay, from 12.6 days in 2004 to 11.05 days in 2014, the investigators said. Meanwhile, total hospitalization charges surged from $105,776 in 2004 to $134,394 over the same time period.
The first edition of the Surviving Sepsis Campaign guidelines for management of severe sepsis and septic shock was published in March 2004 in Critical Care Medicine.
Future studies and clinical trials should look beyond mortality outcomes to additionally evaluate morbidity outcomes in septic shock survivors, Dr. Pan and coauthors said in their report.
The researchers had no relationships to disclose relevant to the presented study.
SOURCE: Pan D et al. CHEST 2018. doi: 10.1016/j.chest.2018.08.339.
REPORTING FROM CHEST 2018
Key clinical point: While septic shock mortality has decreased over time, discharge trends for survivors have remained steady.
Major finding: In-hospital mortality dropped from about 52% to 39% over the 2004-2014 period, while discharges to subacute rehab or long-term facilities stayed around 62%.
Study details: Retrospective analysis of nearly 1.8 million patients with septic shock, of whom about 1 million survived.
Disclosures: The authors had no relationships to disclose relevant to the presented study.
Source: Pan D et al. CHEST 2018.
Perioperative gabapentin’s effect on postoperative opioid use
Background: Previous studies have shown that perioperative gabapentin has no effect on remote pain cessation but have not linked it with effects on remote opioid cessation. Also, most trials were limited to immediate postoperative use during hospital admission; limited data were available with extensive postoperative longitudinal follow-up.
Study design: Randomized, double-blind, placebo-controlled study.
Setting: Tertiary referral teaching hospital.
Synopsis: A randomized, double-blind trial including a total of 1,805 patients aged 18-75 years who were scheduled for eligible surgery was conducted at a single-center, tertiary referral teaching hospital. The treatment group received 1,200 mg of gabapentin preoperatively followed by 600 mg 3 times a day postoperatively. Meanwhile, the placebo group received lorazepam 0.5 mg preoperatively followed by inactive placebo postoperatively for 72 hours. With use of intention to treat analysis, this study showed that perioperative gabapentin did not affect time to postoperative pain resolution. However, a modest increase in the rate of opioid cessation was uncovered. Specifically, there was a 24% increase in the rate (hazard ratio, 1.24; 95% confidence interval, 1.00-1.54; P = .05) of opioid cessation after hospital discharge, with a median time of 25 days in the gabapentin group versus 32 days in the placebo group.
One caveat to the outcomes is that use of a gabapentin regimen may have increased after discharge date, which could have biased the outcome.
Bottom line: Perioperative gabapentin may promote opioid cessation and prevent the development of chronic opioid use after surgery.
Citation: Hah J et al. Effect of perioperative gabapentin on postoperative pain resolution and opioid cessation in a mixed surgical cohort. JAMA Surg. 2018;153(4):303-11.
Dr. Katsouli is a hospitalist in the division of hospital medicine in the department of medicine at Loyola University Chicago, Maywood, Ill.
Background: Previous studies have shown that perioperative gabapentin has no effect on remote pain cessation but have not linked it with effects on remote opioid cessation. Also, most trials were limited to immediate postoperative use during hospital admission; limited data were available with extensive postoperative longitudinal follow-up.
Study design: Randomized, double-blind, placebo-controlled study.
Setting: Tertiary referral teaching hospital.
Synopsis: A randomized, double-blind trial including a total of 1,805 patients aged 18-75 years who were scheduled for eligible surgery was conducted at a single-center, tertiary referral teaching hospital. The treatment group received 1,200 mg of gabapentin preoperatively followed by 600 mg 3 times a day postoperatively. Meanwhile, the placebo group received lorazepam 0.5 mg preoperatively followed by inactive placebo postoperatively for 72 hours. With use of intention to treat analysis, this study showed that perioperative gabapentin did not affect time to postoperative pain resolution. However, a modest increase in the rate of opioid cessation was uncovered. Specifically, there was a 24% increase in the rate (hazard ratio, 1.24; 95% confidence interval, 1.00-1.54; P = .05) of opioid cessation after hospital discharge, with a median time of 25 days in the gabapentin group versus 32 days in the placebo group.
One caveat to the outcomes is that use of a gabapentin regimen may have increased after discharge date, which could have biased the outcome.
Bottom line: Perioperative gabapentin may promote opioid cessation and prevent the development of chronic opioid use after surgery.
Citation: Hah J et al. Effect of perioperative gabapentin on postoperative pain resolution and opioid cessation in a mixed surgical cohort. JAMA Surg. 2018;153(4):303-11.
Dr. Katsouli is a hospitalist in the division of hospital medicine in the department of medicine at Loyola University Chicago, Maywood, Ill.
Background: Previous studies have shown that perioperative gabapentin has no effect on remote pain cessation but have not linked it with effects on remote opioid cessation. Also, most trials were limited to immediate postoperative use during hospital admission; limited data were available with extensive postoperative longitudinal follow-up.
Study design: Randomized, double-blind, placebo-controlled study.
Setting: Tertiary referral teaching hospital.
Synopsis: A randomized, double-blind trial including a total of 1,805 patients aged 18-75 years who were scheduled for eligible surgery was conducted at a single-center, tertiary referral teaching hospital. The treatment group received 1,200 mg of gabapentin preoperatively followed by 600 mg 3 times a day postoperatively. Meanwhile, the placebo group received lorazepam 0.5 mg preoperatively followed by inactive placebo postoperatively for 72 hours. With use of intention to treat analysis, this study showed that perioperative gabapentin did not affect time to postoperative pain resolution. However, a modest increase in the rate of opioid cessation was uncovered. Specifically, there was a 24% increase in the rate (hazard ratio, 1.24; 95% confidence interval, 1.00-1.54; P = .05) of opioid cessation after hospital discharge, with a median time of 25 days in the gabapentin group versus 32 days in the placebo group.
One caveat to the outcomes is that use of a gabapentin regimen may have increased after discharge date, which could have biased the outcome.
Bottom line: Perioperative gabapentin may promote opioid cessation and prevent the development of chronic opioid use after surgery.
Citation: Hah J et al. Effect of perioperative gabapentin on postoperative pain resolution and opioid cessation in a mixed surgical cohort. JAMA Surg. 2018;153(4):303-11.
Dr. Katsouli is a hospitalist in the division of hospital medicine in the department of medicine at Loyola University Chicago, Maywood, Ill.