User login
Presidential Address: 'Changing Me to We in Vascular Care'
When R. Clement Darling III, MD, took to the podium at the Vascular Annual Meeting to present his presidential address, he highlighted the importance of teamwork and collaboration in training, in maintaining personal well-being, and most importantly, in patient care.
His talk, titled, “Looking Forward Through the Past: Changing Me to We in the Evolution of Team-based Vascular Care,” addressed these issues through a very personal lens. To make his point, Dr. Darling outlined four key take-home concepts that he had found useful “over five decades of working in an operating room as a technologist, a student and a surgeon,” and as chief of the division of vascular surgery at Albany Medical Center Hospital (N.Y.). These formed the basis of his entire address:
1. “None of us is as smart as all of us.” We learn from each other which is the foundation of team-based training.
2. The key to resilience, healing and health, whether for our patients or for ourselves, is caring and supporting each other more.
3. Failure is not an end result. It is the path to success through learning.
4. Remember the past but look to the future. The best predictor of future behavior is the past, but the future we are experiencing now, is like no other!”
Dr. Darling spoke from the heart about the importance of his colleagues and his parents, especially the role of his father as a pioneer in vascular surgery, and of the women in his life as role models.
He stressed how “one of the invaluable things I have learned is the value of failure, evaluating the past to avoid the same mistakes and the benefit of the TEAM in providing support and care.”
“Every day we’re asked to do the impossible and every day we get up, go to work. We do the best we can. We can make the best plans, treat the sickest patients and get a tremendous fulfillment for what we do in what we do. We do the right thing for the patient,” Dr. Darling explained, in summarizing the passion that he feels for vascular surgery.
“We are always willing to do and try the impossible. We’re always willing to be the last person to call when things look bleak. It brings me great glee whenever we get called to the operating room and people look around and go, ‘oh thank God, the vascular surgeon’s here.’ Our colleagues in other specialties are often afraid of blood vessels, afraid of death, afraid of complications. We thrust ourselves every day into situations where nobody else will go,” he added.
“As vascular surgeons we face failure and roadblocks daily yet still persist where others are scared to tread. Many of you have faced far worse barriers of discrimination and unreasonable arbitrary barriers, and I am constantly humbled by your ability to overcome them,” Dr. Darling said. He pointed out that: “This innate ability to focus on the problem is what makes vascular surgeons great. No problem is too complex, no detail is too small. We do the right thing despite the odds against us. We do right by the patient.”
After telling some of his own stories of “failure,” to illustrate its importance as a learning tool, Dr. Darling spoke of one person’s reception of his application to join the SVS: “When I applied for membership to the Society for Vascular Surgery, someone had written a note saying that ‘I should never be considered, nor was I deserving to be a member of the SVS, and never should I be admitted into this austere society.’”
Throughout his address, Dr. Darling re-emphasized the importance of teams and the collaborative nature of patient care. “The SVS has developed strong partnerships with the Society for Vascular Nursing, The American Venous Forum, The Society for Vascular Ultrasound, and is seeking to strengthen relationships with the regional vascular societies, VESS, the Society for Clinical Vascular Surgery, The Society for Vascular Medicine, the American Heart Association, and many others.
“The SVS is developing these relationships with the patient at the center, and with purpose, focusing on ‘shared vision,’ of specific advancements, programs, and initiatives that will advance quality of care. By tapping into this vast array of talent Vascular Surgery will become more agile, intelligent and thoughtful in our care of vascular patients,” Dr. Darling predicted.
But vascular surgeons must become comfortable with moving from the concept of “captain of the ship” to the role of team leadership, he emphasized, if they are to truly succeed in their careers and in providing optimal patient care.
“Currently, each patient coming to your service touches over 100 staff during their experience. This includes your office, vascular lab, angio suite, recovery room, hospital floor, ICU, CT scanner to name a few.” This is part of the need for the evolution from ‘captain’ to ‘leader,’ he added.
“If you have not had any formal training in leadership or team development, I strongly suggest you add this to your learning portfolio,” Dr. Darling counseled. “The SVS is addressing this through its Leadership and Diversity Committee, and you will see an expanding array of learning opportunities in the future.”
With regard to his own tenure as SVS President: “I am proud that during my year as president, the SVS has invested in several new Task Forces to address critical future issues including: Alternative Payment Models for vascular surgery; a national inpatient and outpatient vascular certification program; a focus on our own health, wellness, and potential ways to mitigate potential burnout; and Dr. Makaroun will be taking on the issues of vascular surgery valuation and workforce in the new Task Force on the Future of Vascular Surgery.”
He further discussed the role SVS is playing in helping to define the future of vascular surgery.
“As we work to strengthen our brand and identity, the SVS Executive Board has supported, and thanks, Amy Reed and Will Jordan for their leadership in the APDVS [Association of Program Directors of Vascular Surgery], and for taking the first step toward attaining a separate Vascular Residency Review Committee or RRC.” In addition, he described how “SVS is also working closely, and collaboratively, with the American Board of Surgery, and the Vascular Surgery Board, to complete the work that was begun a decade ago, and achieve an autonomous vascular surgery board that is an equal partner and stakeholder in the ABS.”
Dr. Darling then outlined one of his major concerns and interests: the exit path of senior vascular surgeons, and how this is often a tremendous waste of talent and expertise. “In the last decade of work when senior surgeons are trying to transition to non-clinical work, I think we throw away much of their intellectual skill and experience in dealing with vascular surgery problems,” he said. He urged that “as our senior surgeons leave clinical practice, we need to use their intellectual expertise and experience in a more productive way.”
The Society for Vascular Surgery is establishing pathways for leadership and pathways to train people in administration, he added.
Turning back to the extreme importance of teamwork, Dr. Darling addressed the future.
“We, physicians, nurses, PAs, technologists, staff, and administrators, need to work together, think together, to grow together, not only for our patients, but for our partners and our families. We are all part of the vascular team,” Dr. Darling said.
When R. Clement Darling III, MD, took to the podium at the Vascular Annual Meeting to present his presidential address, he highlighted the importance of teamwork and collaboration in training, in maintaining personal well-being, and most importantly, in patient care.
His talk, titled, “Looking Forward Through the Past: Changing Me to We in the Evolution of Team-based Vascular Care,” addressed these issues through a very personal lens. To make his point, Dr. Darling outlined four key take-home concepts that he had found useful “over five decades of working in an operating room as a technologist, a student and a surgeon,” and as chief of the division of vascular surgery at Albany Medical Center Hospital (N.Y.). These formed the basis of his entire address:
1. “None of us is as smart as all of us.” We learn from each other which is the foundation of team-based training.
2. The key to resilience, healing and health, whether for our patients or for ourselves, is caring and supporting each other more.
3. Failure is not an end result. It is the path to success through learning.
4. Remember the past but look to the future. The best predictor of future behavior is the past, but the future we are experiencing now, is like no other!”
Dr. Darling spoke from the heart about the importance of his colleagues and his parents, especially the role of his father as a pioneer in vascular surgery, and of the women in his life as role models.
He stressed how “one of the invaluable things I have learned is the value of failure, evaluating the past to avoid the same mistakes and the benefit of the TEAM in providing support and care.”
“Every day we’re asked to do the impossible and every day we get up, go to work. We do the best we can. We can make the best plans, treat the sickest patients and get a tremendous fulfillment for what we do in what we do. We do the right thing for the patient,” Dr. Darling explained, in summarizing the passion that he feels for vascular surgery.
“We are always willing to do and try the impossible. We’re always willing to be the last person to call when things look bleak. It brings me great glee whenever we get called to the operating room and people look around and go, ‘oh thank God, the vascular surgeon’s here.’ Our colleagues in other specialties are often afraid of blood vessels, afraid of death, afraid of complications. We thrust ourselves every day into situations where nobody else will go,” he added.
“As vascular surgeons we face failure and roadblocks daily yet still persist where others are scared to tread. Many of you have faced far worse barriers of discrimination and unreasonable arbitrary barriers, and I am constantly humbled by your ability to overcome them,” Dr. Darling said. He pointed out that: “This innate ability to focus on the problem is what makes vascular surgeons great. No problem is too complex, no detail is too small. We do the right thing despite the odds against us. We do right by the patient.”
After telling some of his own stories of “failure,” to illustrate its importance as a learning tool, Dr. Darling spoke of one person’s reception of his application to join the SVS: “When I applied for membership to the Society for Vascular Surgery, someone had written a note saying that ‘I should never be considered, nor was I deserving to be a member of the SVS, and never should I be admitted into this austere society.’”
Throughout his address, Dr. Darling re-emphasized the importance of teams and the collaborative nature of patient care. “The SVS has developed strong partnerships with the Society for Vascular Nursing, The American Venous Forum, The Society for Vascular Ultrasound, and is seeking to strengthen relationships with the regional vascular societies, VESS, the Society for Clinical Vascular Surgery, The Society for Vascular Medicine, the American Heart Association, and many others.
“The SVS is developing these relationships with the patient at the center, and with purpose, focusing on ‘shared vision,’ of specific advancements, programs, and initiatives that will advance quality of care. By tapping into this vast array of talent Vascular Surgery will become more agile, intelligent and thoughtful in our care of vascular patients,” Dr. Darling predicted.
But vascular surgeons must become comfortable with moving from the concept of “captain of the ship” to the role of team leadership, he emphasized, if they are to truly succeed in their careers and in providing optimal patient care.
“Currently, each patient coming to your service touches over 100 staff during their experience. This includes your office, vascular lab, angio suite, recovery room, hospital floor, ICU, CT scanner to name a few.” This is part of the need for the evolution from ‘captain’ to ‘leader,’ he added.
“If you have not had any formal training in leadership or team development, I strongly suggest you add this to your learning portfolio,” Dr. Darling counseled. “The SVS is addressing this through its Leadership and Diversity Committee, and you will see an expanding array of learning opportunities in the future.”
With regard to his own tenure as SVS President: “I am proud that during my year as president, the SVS has invested in several new Task Forces to address critical future issues including: Alternative Payment Models for vascular surgery; a national inpatient and outpatient vascular certification program; a focus on our own health, wellness, and potential ways to mitigate potential burnout; and Dr. Makaroun will be taking on the issues of vascular surgery valuation and workforce in the new Task Force on the Future of Vascular Surgery.”
He further discussed the role SVS is playing in helping to define the future of vascular surgery.
“As we work to strengthen our brand and identity, the SVS Executive Board has supported, and thanks, Amy Reed and Will Jordan for their leadership in the APDVS [Association of Program Directors of Vascular Surgery], and for taking the first step toward attaining a separate Vascular Residency Review Committee or RRC.” In addition, he described how “SVS is also working closely, and collaboratively, with the American Board of Surgery, and the Vascular Surgery Board, to complete the work that was begun a decade ago, and achieve an autonomous vascular surgery board that is an equal partner and stakeholder in the ABS.”
Dr. Darling then outlined one of his major concerns and interests: the exit path of senior vascular surgeons, and how this is often a tremendous waste of talent and expertise. “In the last decade of work when senior surgeons are trying to transition to non-clinical work, I think we throw away much of their intellectual skill and experience in dealing with vascular surgery problems,” he said. He urged that “as our senior surgeons leave clinical practice, we need to use their intellectual expertise and experience in a more productive way.”
The Society for Vascular Surgery is establishing pathways for leadership and pathways to train people in administration, he added.
Turning back to the extreme importance of teamwork, Dr. Darling addressed the future.
“We, physicians, nurses, PAs, technologists, staff, and administrators, need to work together, think together, to grow together, not only for our patients, but for our partners and our families. We are all part of the vascular team,” Dr. Darling said.
When R. Clement Darling III, MD, took to the podium at the Vascular Annual Meeting to present his presidential address, he highlighted the importance of teamwork and collaboration in training, in maintaining personal well-being, and most importantly, in patient care.
His talk, titled, “Looking Forward Through the Past: Changing Me to We in the Evolution of Team-based Vascular Care,” addressed these issues through a very personal lens. To make his point, Dr. Darling outlined four key take-home concepts that he had found useful “over five decades of working in an operating room as a technologist, a student and a surgeon,” and as chief of the division of vascular surgery at Albany Medical Center Hospital (N.Y.). These formed the basis of his entire address:
1. “None of us is as smart as all of us.” We learn from each other which is the foundation of team-based training.
2. The key to resilience, healing and health, whether for our patients or for ourselves, is caring and supporting each other more.
3. Failure is not an end result. It is the path to success through learning.
4. Remember the past but look to the future. The best predictor of future behavior is the past, but the future we are experiencing now, is like no other!”
Dr. Darling spoke from the heart about the importance of his colleagues and his parents, especially the role of his father as a pioneer in vascular surgery, and of the women in his life as role models.
He stressed how “one of the invaluable things I have learned is the value of failure, evaluating the past to avoid the same mistakes and the benefit of the TEAM in providing support and care.”
“Every day we’re asked to do the impossible and every day we get up, go to work. We do the best we can. We can make the best plans, treat the sickest patients and get a tremendous fulfillment for what we do in what we do. We do the right thing for the patient,” Dr. Darling explained, in summarizing the passion that he feels for vascular surgery.
“We are always willing to do and try the impossible. We’re always willing to be the last person to call when things look bleak. It brings me great glee whenever we get called to the operating room and people look around and go, ‘oh thank God, the vascular surgeon’s here.’ Our colleagues in other specialties are often afraid of blood vessels, afraid of death, afraid of complications. We thrust ourselves every day into situations where nobody else will go,” he added.
“As vascular surgeons we face failure and roadblocks daily yet still persist where others are scared to tread. Many of you have faced far worse barriers of discrimination and unreasonable arbitrary barriers, and I am constantly humbled by your ability to overcome them,” Dr. Darling said. He pointed out that: “This innate ability to focus on the problem is what makes vascular surgeons great. No problem is too complex, no detail is too small. We do the right thing despite the odds against us. We do right by the patient.”
After telling some of his own stories of “failure,” to illustrate its importance as a learning tool, Dr. Darling spoke of one person’s reception of his application to join the SVS: “When I applied for membership to the Society for Vascular Surgery, someone had written a note saying that ‘I should never be considered, nor was I deserving to be a member of the SVS, and never should I be admitted into this austere society.’”
Throughout his address, Dr. Darling re-emphasized the importance of teams and the collaborative nature of patient care. “The SVS has developed strong partnerships with the Society for Vascular Nursing, The American Venous Forum, The Society for Vascular Ultrasound, and is seeking to strengthen relationships with the regional vascular societies, VESS, the Society for Clinical Vascular Surgery, The Society for Vascular Medicine, the American Heart Association, and many others.
“The SVS is developing these relationships with the patient at the center, and with purpose, focusing on ‘shared vision,’ of specific advancements, programs, and initiatives that will advance quality of care. By tapping into this vast array of talent Vascular Surgery will become more agile, intelligent and thoughtful in our care of vascular patients,” Dr. Darling predicted.
But vascular surgeons must become comfortable with moving from the concept of “captain of the ship” to the role of team leadership, he emphasized, if they are to truly succeed in their careers and in providing optimal patient care.
“Currently, each patient coming to your service touches over 100 staff during their experience. This includes your office, vascular lab, angio suite, recovery room, hospital floor, ICU, CT scanner to name a few.” This is part of the need for the evolution from ‘captain’ to ‘leader,’ he added.
“If you have not had any formal training in leadership or team development, I strongly suggest you add this to your learning portfolio,” Dr. Darling counseled. “The SVS is addressing this through its Leadership and Diversity Committee, and you will see an expanding array of learning opportunities in the future.”
With regard to his own tenure as SVS President: “I am proud that during my year as president, the SVS has invested in several new Task Forces to address critical future issues including: Alternative Payment Models for vascular surgery; a national inpatient and outpatient vascular certification program; a focus on our own health, wellness, and potential ways to mitigate potential burnout; and Dr. Makaroun will be taking on the issues of vascular surgery valuation and workforce in the new Task Force on the Future of Vascular Surgery.”
He further discussed the role SVS is playing in helping to define the future of vascular surgery.
“As we work to strengthen our brand and identity, the SVS Executive Board has supported, and thanks, Amy Reed and Will Jordan for their leadership in the APDVS [Association of Program Directors of Vascular Surgery], and for taking the first step toward attaining a separate Vascular Residency Review Committee or RRC.” In addition, he described how “SVS is also working closely, and collaboratively, with the American Board of Surgery, and the Vascular Surgery Board, to complete the work that was begun a decade ago, and achieve an autonomous vascular surgery board that is an equal partner and stakeholder in the ABS.”
Dr. Darling then outlined one of his major concerns and interests: the exit path of senior vascular surgeons, and how this is often a tremendous waste of talent and expertise. “In the last decade of work when senior surgeons are trying to transition to non-clinical work, I think we throw away much of their intellectual skill and experience in dealing with vascular surgery problems,” he said. He urged that “as our senior surgeons leave clinical practice, we need to use their intellectual expertise and experience in a more productive way.”
The Society for Vascular Surgery is establishing pathways for leadership and pathways to train people in administration, he added.
Turning back to the extreme importance of teamwork, Dr. Darling addressed the future.
“We, physicians, nurses, PAs, technologists, staff, and administrators, need to work together, think together, to grow together, not only for our patients, but for our partners and our families. We are all part of the vascular team,” Dr. Darling said.
Resident debt burden may cloud professional future
Surgical trainees have a large, potentially unmanageable debt burden and are in need of long-term financial education to help better navigate the growing cost of medical education, according to new research.
“Surgical residents are highly leveraged financially and have minimal financial training,” Sarah E. Tevis, MD, of the University of Texas MD Anderson Cancer Center, Houston, and her colleagues wrote in a study in the Journal of the American College of Surgeons. “This places residents in a volatile financial situation as they complete their training and start accumulating debt liabilities, such as mortgages and child care, in the face of tremendous amounts of educational and other debt liabilities.”
Studies of resident debt load typically account for medical education debt, but not for other debts such as undergraduate loans, consumer debt, and mortgages. Residents’ actual debt burden may be considerably higher than has been reported.
The researchers sent surveys to all surgical residents at the University of Wisconsin, Madison, in 2015, with 105 responding (an 80% response rate). Of those responding, 38% reported having more than $200,000 in educational debt, and 82% had a moderate- or high-risk debt-to-asset ratio.
“We found that surgical residents are dangerously overleveraged, with 70% of residents found to have high debt-to-asset ratios,” Dr. Tevis and her colleagues wrote, with the addition of mortgages and vehicle debt on top of educational debt being the key factors of moving residents into the high-risk debt-to-asset category.
The debt-to-asset ratio was calculated as the sum of student loan debt + nonstudent loan debt + credit card balance + mortgage debt + vehicle debt divided by the value of home and other real estate + value of household vehicles + amount in savings + value of retirement investment. A debt-to-asset ratio of 0.5 to 0.9 was considered moderate risk, with a ratio greater than or equal to 0.9 considered high risk.
The debt-to-income ratio was calculated as the sum of student loan debt + nonstudent loan debt + credit card balance + mortgage debt + vehicle debt divided by total household income. A high-risk ratio defined as being greater than 0.4, the line at which surgical trainees might be restricted from obtaining a traditional mortgage.
Total household income included personal income, domestic partner income, military income, and any income from moonlighting, rental properties, and other sources of revenue. Assets included home and second home purchase prices when applicable, value of vehicles, amount in savings, value of retirement accounts, and value of investments. Contributors to debt included student loan, nonstudent loan, mortgage, vehicle financing, and credit card balances.
Salary data for U.S. residents, which strictly tracked U.S. inflation, was calculated over a 15-year period (2000-2015) using data from the Association of American Medical Colleges for comparison.
In examining debt-to-income, researchers found that “83% of residents have a high-risk debt-to-income ratio [greater than 0.4],” the authors wrote. “We found that the majority of residents were classified in the high financial risk exposure cohort when comprehensive total debt liabilities were considered. In this group of highly leveraged residents, over 80% of residents were dangerously unable to manage regular monthly liabilities with their current level of income.”
No statistically significant association between sex, residency year, residency program, or who manages finances and risk debt-to-asset ratios were found in this study.
The authors noted that, although this study did not look at the psychological impact of significant debt load and lack of training on how to manage finances, these factors have been shown in other studies to correlate with resident burnout and psychological stress.
Bruce A. Harms, MD, FACS, coauthor of the study said in an interview, “We are in an evolving era in surgery and in health care in general and financial resources are being stretched. We don’t know for sure that the rising educational debt and overall debt burden as residents enter their prime years will drive the next generation of physicians to certain career choices. It may even perhaps drive a given fully trained young surgeon away from a practice that is more exposed to an underserved population. Excessive financial debt induced stress may influence a resident’s decision on what they do with their skill set but to what degree is largely unknown.”
Dr. Harms added that residents may assume that when they eventually enter practice, they will have a pathway and the means to deal with educational debt. “They would be correct in that starting salaries are keeping pace with inflation. However, in many instances, they are also entering a time in their lives when they will be taking on additional debt in the form of home mortgage, family, and child care costs. I believe, in most instances, residents are focused almost totally on their residency training and many other financial considerations take a back seat and ‘we’ll deal with our debt problem in the future’ attitude. Residents for the most part don’t have the financial means and resources to deal with debt anyway during the course of their lengthy residency training. The exception would be having a secondary income from a spouse or partner that would allow for a more robust debt-attrition strategy. Also, residents are likely not focused on or considering a strategy for the best return on investment of their time, additional expense, and career delay from their prolonged pathway to becoming a fully trained surgeon.”
The bottom line is that basic financial educational is not included in core surgical training even though most surgical residents would like some degree of financial education. That is the basic problem and shortcoming of existing residency training programs, Dr. Tevis and her colleagues wrote.
Given the financial burdens that education and other factors are placing on surgical residents, Dr. Tevis and her colleagues proposed “that formal training in the business of medicine and personal finance for surgical residents be strongly considered at the training program level or in partnership with other organizations, such as the American College of Surgeons, in an effort to improve the financial status of residents and prepare them for their careers, both personally and professionally.”
Dr. Harms noted, “It is probable that in most cases, educational loan debt principal is not being paid down to any significant degree given the current residency salary structure. We can only hope that residents are given some degree of good information on strategies for managing educational loan debt, which may include federally sponsored loan repayment programs such as [those offered] through NIH-sponsored research or federal loan forgiveness programs that residents may qualify for. In most cases, federal loan forgiveness programs require a minimum monthly payment that is calculated based upon current income. As an absolute minimum, interest payments should be made as additional interest debt will add significantly to the overall debt burden as interest will continue to accrue.”
Getting that financial training early could have significant benefits on the back end. The study authors noted that salary data from the Association of American Medical Colleges showed assistant professor salaries mirrored inflation metrics, but even better, surgeon salaries continued to exceed inflation-indexed targets and continued upward trends even through recession periods.
“Therefore, the financial pathway, built on increases in surgeon starting salaries exceeding annual inflation, presently still exists for deleveraging of critical debt exposure if personal finances are optimally managed,” the authors stated.
The study did have its limitations. It did not include certain variable expenses such as utilities, food, and other shopping habits, although that may have been captured as the survey asked respondents to list other “major” sources of income and debt. It also was limited to surgical residents at a single institution and may not be applicable to other specialties or geographic locations. It did not assess whether residents with mortgage payments were able to make educational loan payments beyond the minimum.
The investigators reported no conflicts.
SOURCE: Tevis SE et al. J Am Coll Surg. 2018 May 31. doi: 10.1016/j.jamcollsurg.2018.05.002.
Surgical trainees have a large, potentially unmanageable debt burden and are in need of long-term financial education to help better navigate the growing cost of medical education, according to new research.
“Surgical residents are highly leveraged financially and have minimal financial training,” Sarah E. Tevis, MD, of the University of Texas MD Anderson Cancer Center, Houston, and her colleagues wrote in a study in the Journal of the American College of Surgeons. “This places residents in a volatile financial situation as they complete their training and start accumulating debt liabilities, such as mortgages and child care, in the face of tremendous amounts of educational and other debt liabilities.”
Studies of resident debt load typically account for medical education debt, but not for other debts such as undergraduate loans, consumer debt, and mortgages. Residents’ actual debt burden may be considerably higher than has been reported.
The researchers sent surveys to all surgical residents at the University of Wisconsin, Madison, in 2015, with 105 responding (an 80% response rate). Of those responding, 38% reported having more than $200,000 in educational debt, and 82% had a moderate- or high-risk debt-to-asset ratio.
“We found that surgical residents are dangerously overleveraged, with 70% of residents found to have high debt-to-asset ratios,” Dr. Tevis and her colleagues wrote, with the addition of mortgages and vehicle debt on top of educational debt being the key factors of moving residents into the high-risk debt-to-asset category.
The debt-to-asset ratio was calculated as the sum of student loan debt + nonstudent loan debt + credit card balance + mortgage debt + vehicle debt divided by the value of home and other real estate + value of household vehicles + amount in savings + value of retirement investment. A debt-to-asset ratio of 0.5 to 0.9 was considered moderate risk, with a ratio greater than or equal to 0.9 considered high risk.
The debt-to-income ratio was calculated as the sum of student loan debt + nonstudent loan debt + credit card balance + mortgage debt + vehicle debt divided by total household income. A high-risk ratio defined as being greater than 0.4, the line at which surgical trainees might be restricted from obtaining a traditional mortgage.
Total household income included personal income, domestic partner income, military income, and any income from moonlighting, rental properties, and other sources of revenue. Assets included home and second home purchase prices when applicable, value of vehicles, amount in savings, value of retirement accounts, and value of investments. Contributors to debt included student loan, nonstudent loan, mortgage, vehicle financing, and credit card balances.
Salary data for U.S. residents, which strictly tracked U.S. inflation, was calculated over a 15-year period (2000-2015) using data from the Association of American Medical Colleges for comparison.
In examining debt-to-income, researchers found that “83% of residents have a high-risk debt-to-income ratio [greater than 0.4],” the authors wrote. “We found that the majority of residents were classified in the high financial risk exposure cohort when comprehensive total debt liabilities were considered. In this group of highly leveraged residents, over 80% of residents were dangerously unable to manage regular monthly liabilities with their current level of income.”
No statistically significant association between sex, residency year, residency program, or who manages finances and risk debt-to-asset ratios were found in this study.
The authors noted that, although this study did not look at the psychological impact of significant debt load and lack of training on how to manage finances, these factors have been shown in other studies to correlate with resident burnout and psychological stress.
Bruce A. Harms, MD, FACS, coauthor of the study said in an interview, “We are in an evolving era in surgery and in health care in general and financial resources are being stretched. We don’t know for sure that the rising educational debt and overall debt burden as residents enter their prime years will drive the next generation of physicians to certain career choices. It may even perhaps drive a given fully trained young surgeon away from a practice that is more exposed to an underserved population. Excessive financial debt induced stress may influence a resident’s decision on what they do with their skill set but to what degree is largely unknown.”
Dr. Harms added that residents may assume that when they eventually enter practice, they will have a pathway and the means to deal with educational debt. “They would be correct in that starting salaries are keeping pace with inflation. However, in many instances, they are also entering a time in their lives when they will be taking on additional debt in the form of home mortgage, family, and child care costs. I believe, in most instances, residents are focused almost totally on their residency training and many other financial considerations take a back seat and ‘we’ll deal with our debt problem in the future’ attitude. Residents for the most part don’t have the financial means and resources to deal with debt anyway during the course of their lengthy residency training. The exception would be having a secondary income from a spouse or partner that would allow for a more robust debt-attrition strategy. Also, residents are likely not focused on or considering a strategy for the best return on investment of their time, additional expense, and career delay from their prolonged pathway to becoming a fully trained surgeon.”
The bottom line is that basic financial educational is not included in core surgical training even though most surgical residents would like some degree of financial education. That is the basic problem and shortcoming of existing residency training programs, Dr. Tevis and her colleagues wrote.
Given the financial burdens that education and other factors are placing on surgical residents, Dr. Tevis and her colleagues proposed “that formal training in the business of medicine and personal finance for surgical residents be strongly considered at the training program level or in partnership with other organizations, such as the American College of Surgeons, in an effort to improve the financial status of residents and prepare them for their careers, both personally and professionally.”
Dr. Harms noted, “It is probable that in most cases, educational loan debt principal is not being paid down to any significant degree given the current residency salary structure. We can only hope that residents are given some degree of good information on strategies for managing educational loan debt, which may include federally sponsored loan repayment programs such as [those offered] through NIH-sponsored research or federal loan forgiveness programs that residents may qualify for. In most cases, federal loan forgiveness programs require a minimum monthly payment that is calculated based upon current income. As an absolute minimum, interest payments should be made as additional interest debt will add significantly to the overall debt burden as interest will continue to accrue.”
Getting that financial training early could have significant benefits on the back end. The study authors noted that salary data from the Association of American Medical Colleges showed assistant professor salaries mirrored inflation metrics, but even better, surgeon salaries continued to exceed inflation-indexed targets and continued upward trends even through recession periods.
“Therefore, the financial pathway, built on increases in surgeon starting salaries exceeding annual inflation, presently still exists for deleveraging of critical debt exposure if personal finances are optimally managed,” the authors stated.
The study did have its limitations. It did not include certain variable expenses such as utilities, food, and other shopping habits, although that may have been captured as the survey asked respondents to list other “major” sources of income and debt. It also was limited to surgical residents at a single institution and may not be applicable to other specialties or geographic locations. It did not assess whether residents with mortgage payments were able to make educational loan payments beyond the minimum.
The investigators reported no conflicts.
SOURCE: Tevis SE et al. J Am Coll Surg. 2018 May 31. doi: 10.1016/j.jamcollsurg.2018.05.002.
Surgical trainees have a large, potentially unmanageable debt burden and are in need of long-term financial education to help better navigate the growing cost of medical education, according to new research.
“Surgical residents are highly leveraged financially and have minimal financial training,” Sarah E. Tevis, MD, of the University of Texas MD Anderson Cancer Center, Houston, and her colleagues wrote in a study in the Journal of the American College of Surgeons. “This places residents in a volatile financial situation as they complete their training and start accumulating debt liabilities, such as mortgages and child care, in the face of tremendous amounts of educational and other debt liabilities.”
Studies of resident debt load typically account for medical education debt, but not for other debts such as undergraduate loans, consumer debt, and mortgages. Residents’ actual debt burden may be considerably higher than has been reported.
The researchers sent surveys to all surgical residents at the University of Wisconsin, Madison, in 2015, with 105 responding (an 80% response rate). Of those responding, 38% reported having more than $200,000 in educational debt, and 82% had a moderate- or high-risk debt-to-asset ratio.
“We found that surgical residents are dangerously overleveraged, with 70% of residents found to have high debt-to-asset ratios,” Dr. Tevis and her colleagues wrote, with the addition of mortgages and vehicle debt on top of educational debt being the key factors of moving residents into the high-risk debt-to-asset category.
The debt-to-asset ratio was calculated as the sum of student loan debt + nonstudent loan debt + credit card balance + mortgage debt + vehicle debt divided by the value of home and other real estate + value of household vehicles + amount in savings + value of retirement investment. A debt-to-asset ratio of 0.5 to 0.9 was considered moderate risk, with a ratio greater than or equal to 0.9 considered high risk.
The debt-to-income ratio was calculated as the sum of student loan debt + nonstudent loan debt + credit card balance + mortgage debt + vehicle debt divided by total household income. A high-risk ratio defined as being greater than 0.4, the line at which surgical trainees might be restricted from obtaining a traditional mortgage.
Total household income included personal income, domestic partner income, military income, and any income from moonlighting, rental properties, and other sources of revenue. Assets included home and second home purchase prices when applicable, value of vehicles, amount in savings, value of retirement accounts, and value of investments. Contributors to debt included student loan, nonstudent loan, mortgage, vehicle financing, and credit card balances.
Salary data for U.S. residents, which strictly tracked U.S. inflation, was calculated over a 15-year period (2000-2015) using data from the Association of American Medical Colleges for comparison.
In examining debt-to-income, researchers found that “83% of residents have a high-risk debt-to-income ratio [greater than 0.4],” the authors wrote. “We found that the majority of residents were classified in the high financial risk exposure cohort when comprehensive total debt liabilities were considered. In this group of highly leveraged residents, over 80% of residents were dangerously unable to manage regular monthly liabilities with their current level of income.”
No statistically significant association between sex, residency year, residency program, or who manages finances and risk debt-to-asset ratios were found in this study.
The authors noted that, although this study did not look at the psychological impact of significant debt load and lack of training on how to manage finances, these factors have been shown in other studies to correlate with resident burnout and psychological stress.
Bruce A. Harms, MD, FACS, coauthor of the study said in an interview, “We are in an evolving era in surgery and in health care in general and financial resources are being stretched. We don’t know for sure that the rising educational debt and overall debt burden as residents enter their prime years will drive the next generation of physicians to certain career choices. It may even perhaps drive a given fully trained young surgeon away from a practice that is more exposed to an underserved population. Excessive financial debt induced stress may influence a resident’s decision on what they do with their skill set but to what degree is largely unknown.”
Dr. Harms added that residents may assume that when they eventually enter practice, they will have a pathway and the means to deal with educational debt. “They would be correct in that starting salaries are keeping pace with inflation. However, in many instances, they are also entering a time in their lives when they will be taking on additional debt in the form of home mortgage, family, and child care costs. I believe, in most instances, residents are focused almost totally on their residency training and many other financial considerations take a back seat and ‘we’ll deal with our debt problem in the future’ attitude. Residents for the most part don’t have the financial means and resources to deal with debt anyway during the course of their lengthy residency training. The exception would be having a secondary income from a spouse or partner that would allow for a more robust debt-attrition strategy. Also, residents are likely not focused on or considering a strategy for the best return on investment of their time, additional expense, and career delay from their prolonged pathway to becoming a fully trained surgeon.”
The bottom line is that basic financial educational is not included in core surgical training even though most surgical residents would like some degree of financial education. That is the basic problem and shortcoming of existing residency training programs, Dr. Tevis and her colleagues wrote.
Given the financial burdens that education and other factors are placing on surgical residents, Dr. Tevis and her colleagues proposed “that formal training in the business of medicine and personal finance for surgical residents be strongly considered at the training program level or in partnership with other organizations, such as the American College of Surgeons, in an effort to improve the financial status of residents and prepare them for their careers, both personally and professionally.”
Dr. Harms noted, “It is probable that in most cases, educational loan debt principal is not being paid down to any significant degree given the current residency salary structure. We can only hope that residents are given some degree of good information on strategies for managing educational loan debt, which may include federally sponsored loan repayment programs such as [those offered] through NIH-sponsored research or federal loan forgiveness programs that residents may qualify for. In most cases, federal loan forgiveness programs require a minimum monthly payment that is calculated based upon current income. As an absolute minimum, interest payments should be made as additional interest debt will add significantly to the overall debt burden as interest will continue to accrue.”
Getting that financial training early could have significant benefits on the back end. The study authors noted that salary data from the Association of American Medical Colleges showed assistant professor salaries mirrored inflation metrics, but even better, surgeon salaries continued to exceed inflation-indexed targets and continued upward trends even through recession periods.
“Therefore, the financial pathway, built on increases in surgeon starting salaries exceeding annual inflation, presently still exists for deleveraging of critical debt exposure if personal finances are optimally managed,” the authors stated.
The study did have its limitations. It did not include certain variable expenses such as utilities, food, and other shopping habits, although that may have been captured as the survey asked respondents to list other “major” sources of income and debt. It also was limited to surgical residents at a single institution and may not be applicable to other specialties or geographic locations. It did not assess whether residents with mortgage payments were able to make educational loan payments beyond the minimum.
The investigators reported no conflicts.
SOURCE: Tevis SE et al. J Am Coll Surg. 2018 May 31. doi: 10.1016/j.jamcollsurg.2018.05.002.
FROM THE JOURNAL OF THE AMERICAN COLLEGE OF SURGEONS
Key clinical point: Residents’ actual debt may be considerably higher than has been reported.
Major finding: More than one-third of surgical residents responding to a survey reported more than $200,000 in educational debt.
Study details: An analysis of responses to a survey from 105 surgical residents at the University of Wisconsin.
Disclosures: The study authors reported no disclosures.
Source: Tevis SE et al. J Am Coll Surg. 2018 May 31. doi: 10.1016/j.jamcollsurg.2018.05.002.
Peer mentorship, groups help combat burnout in female physicians
NEW YORK – Female physicians are at higher risk for burnout compared with their male counterparts, and the reasons and potential solutions for the problem were addressed at a symposium during the annual meeting of the American Psychiatric Association.
The work environment for women has improved over time, but lingering implicit and unconscious biases are part of the reason for the high burnout rate among women who are physicians, as are some inherent biological differences, according to Cynthia M. Stonnington, MD, of the Mayo Clinic, Phoenix.
In this video interview, Dr. Stonnington, symposium chair, discussed potential solutions, including facilitated peer mentorship and group support. She also reviewed recent data on how group support can be of benefit, and noted that “there is power in numbers.
“,” she said.
Dr. Stonnington reported having no disclosures.
NEW YORK – Female physicians are at higher risk for burnout compared with their male counterparts, and the reasons and potential solutions for the problem were addressed at a symposium during the annual meeting of the American Psychiatric Association.
The work environment for women has improved over time, but lingering implicit and unconscious biases are part of the reason for the high burnout rate among women who are physicians, as are some inherent biological differences, according to Cynthia M. Stonnington, MD, of the Mayo Clinic, Phoenix.
In this video interview, Dr. Stonnington, symposium chair, discussed potential solutions, including facilitated peer mentorship and group support. She also reviewed recent data on how group support can be of benefit, and noted that “there is power in numbers.
“,” she said.
Dr. Stonnington reported having no disclosures.
NEW YORK – Female physicians are at higher risk for burnout compared with their male counterparts, and the reasons and potential solutions for the problem were addressed at a symposium during the annual meeting of the American Psychiatric Association.
The work environment for women has improved over time, but lingering implicit and unconscious biases are part of the reason for the high burnout rate among women who are physicians, as are some inherent biological differences, according to Cynthia M. Stonnington, MD, of the Mayo Clinic, Phoenix.
In this video interview, Dr. Stonnington, symposium chair, discussed potential solutions, including facilitated peer mentorship and group support. She also reviewed recent data on how group support can be of benefit, and noted that “there is power in numbers.
“,” she said.
Dr. Stonnington reported having no disclosures.
REPORTING FROM APA
VIDEO: Fix physician burnout? You need more than yoga
NEW ORLEANS – Among a growing number of physicians, the words of a Righteous Brothers’ song ring true about their careers: They’ve lost that loving feeling.
For burned-out physicians, “they’ve lost that sense that they’re making a difference,” explained Susan Thompson Hingle, MD, of Southern Illinois University in Springfield. And the solutions aren’t simple. “You can’t yoga your way out of this,” Dr. Hingle cautioned.
At the annual meeting of the American College of Physicians, Dr. Hingle and Daisy Smith, MD, vice president of clinical programs at the ACP, talked about solutions to burnout, including how more traditional approaches can boost physician well-being, such as team-based care, physician champions, and increasing the pool of primary care providers.
But they also detailed ways that struggling physicians can find support from an unlikely source: their patients.
Dr. Smith’s video interview:
Dr. Hingle’s video interview:
NEW ORLEANS – Among a growing number of physicians, the words of a Righteous Brothers’ song ring true about their careers: They’ve lost that loving feeling.
For burned-out physicians, “they’ve lost that sense that they’re making a difference,” explained Susan Thompson Hingle, MD, of Southern Illinois University in Springfield. And the solutions aren’t simple. “You can’t yoga your way out of this,” Dr. Hingle cautioned.
At the annual meeting of the American College of Physicians, Dr. Hingle and Daisy Smith, MD, vice president of clinical programs at the ACP, talked about solutions to burnout, including how more traditional approaches can boost physician well-being, such as team-based care, physician champions, and increasing the pool of primary care providers.
But they also detailed ways that struggling physicians can find support from an unlikely source: their patients.
Dr. Smith’s video interview:
Dr. Hingle’s video interview:
NEW ORLEANS – Among a growing number of physicians, the words of a Righteous Brothers’ song ring true about their careers: They’ve lost that loving feeling.
For burned-out physicians, “they’ve lost that sense that they’re making a difference,” explained Susan Thompson Hingle, MD, of Southern Illinois University in Springfield. And the solutions aren’t simple. “You can’t yoga your way out of this,” Dr. Hingle cautioned.
At the annual meeting of the American College of Physicians, Dr. Hingle and Daisy Smith, MD, vice president of clinical programs at the ACP, talked about solutions to burnout, including how more traditional approaches can boost physician well-being, such as team-based care, physician champions, and increasing the pool of primary care providers.
But they also detailed ways that struggling physicians can find support from an unlikely source: their patients.
Dr. Smith’s video interview:
Dr. Hingle’s video interview:
REPORTING FROM ACP INTERNAL MEDICINE
I am not your burnout expert
Look, I am not a burnout expert. And neither are you (presumably). None of us know much, but that won’t stop the regulations from coming. Program directors are already being asked to provide “wellness plans.” Through the SVS, experts have been enlisted to help, but it is now clear that what works for others won’t necessarily work for vascular surgeons. The next step is up to us. We are the only ones with detailed knowledge of our lives. I believe we are moving closer to answers but still face a few significant hurdles. Don’t worry, there are solutions. Hear me out …
Previously, I shared three studies with you, which found that vascular surgeons had the highest rates of suicidal ideation and career dissatisfaction among surgeons while spending more hours in the hospital than any other specialty. So what has been done to address these horrific numbers? Very little. We need answers now, but most of the data are over 10 years old. Much has changed in our specialty. The endovascular revolution created an entirely new working paradigm. A busy vascular surgeon used to perform 300 cases annually; now this number approaches 1,000. More procedures means more clerical work. Lead aprons and radiation exposure have added new ergonomic and medical concerns. Reimbursement dynamics now favor shorter, more frequent patient interactions over longer, more complex cases. We are benchmarked against old work standards while CPT bundling continuously lowers current RVU designations. EMR was supposed to make our lives better; it has done the opposite. Patient-centered health care has become a mantra, but the measures taken often backfire. Practicing medicine where the desired outcome is a high score on patient satisfaction surveys will likely lead to unnecessary tests, poor cost allocation, and low physician fulfillment. Quality of care is now measured scrupulously while the quality of our lives remains undocumented.
In the absence of organized reform, burnout appears to be increasing. A recent Mayo Clinic–AMA study found the current prevalence to be 54% among physicians. All of this has not happened overnight. I believe practicing vascular surgeons are resilient by default. The majority of us trained prior to the enforcement of duty hour restrictions. Out of high school, I enrolled in a 6-year BA/MD program (skipping 2 years of college seemed like a great idea in high school, less so when I got there). Half of my class never finished. In my intern year, six of the eight categorical residents dropped out. My odds of reaching PGY 2 were 12.5%. Fuzzy math aside, all of your stories are similar. We have proved our resilience over and over again. What is happening here is different.
Burnout is described as emotional exhaustion, low self-esteem, and depersonalization/cynicism. It develops slowly, progressively as stressors increase. A common thread seems to be the feeling that you alone are not enough. Examine your daily life. What are your most common stressors? For me, they relate to time management, clinical documentation, and whatever fresh hell my kids’ teachers have cooked up for “school projects.”
*****Scene*****
Wife: Can you help Luke (kindergarten) finish his diorama? It needs to be a scale depiction of his 3 favorite scenes from Wagner’s Ring cycle.
Me: Sure, I just need to complete the wind tunnel testing on Jack’s (3rd grade) carbon-neutral peanut-free alternative fuel source rocket booster.
Off stage – 7th Grade Son: The genetically modified spiders got loose again!
*****End Scene*****
We want to do a good job, but more hurdles are placed in our way. A recent AMA/Dartmouth Hitchcock study found that 50% of physicians’ time is spent performing data entry and other administrative work. Only 27% of time was spent on patient care. Every hour of face-to-face patient time requires 2 hours of EMR/clerical work. We are trapped in a bureaucratic prison. For years, every quality initiative was solved with a new form. To enter a simple note today, we must first “establish our relationship” with the patient, then ably click through a minefield of “warning boxes” signifying impending DVT prophylaxis catastrophes and antibiotic crimes and misdemeanors, next we scroll through a pre-populated postapocalyptic hellscape of minute- by-minute vital sign entries and lab values dating back to inception. Then, and only then, finally, ON PAGE 11, we can meagerly type: Patient at wound care, will come back on evening rounds.
Another important component of the burnout syndrome is dehumanization. Recently I spoke with Donald Zimmerman, PhD, author of the textbook “Person-Focused Health Care Management.” His thoughts on health care were dramatically altered after spending 43 days in an ICU following abdominal aortic aneurysm repair. He describes the experience as “my worst nightmare that then got worse and then never ended.” While we can learn from his experience, how many of us were trained to face this horror? Dehumanization is a natural protective response, especially when we have so little time for patient interactions. Compassion fatigue sets in when we don’t have the time and resources to care for our patients.While poor outcomes have been cited as a result of burnout, this appears to be an end-stage result. The Minimizing Error, Maximizing Outcome (MEMO) study funded by the AHRQ found that physicians often served as a buffer between their patients and poor medical environments. The organizational flaws that led to burnout also independently resulted in substandard patient care. The burnout physicians experienced was a symptom of the defective health care system and not causative of the poor care. Doctors were literally sacrificing their well-being to care for their patients.
Not surprisingly, attitudes regarding burnout vary significantly between health care executives and physicians. A New England Journal of Medicine survey of their Insights Council found that 96% of respondents agreed that burnout is a moderate or serious problem, although physicians were significantly more likely than executives to rate the problem as “serious.” Opinions on solutions varied as well, with executives more likely to support redesign of EMR, while physicians favored reduction of documentation and clerical work. Obviously the physicians’ solution would be more costly to the corporation as the executives deflected the problem back to the EMR designers. Neither group favored the use of resilience/wellness programs as a primary solution.
Of all the remedies proposed, I find resilience training to be especially egregious. Studies consistently show a 40%-50% prevalence of burnout among physicians. How can this be an individual problem? Why train doctors to endure a broken system? This type of problem solving is why burnout continues to flourish. Doctors are not suffering from a disease but rather exhibiting a symptom.
To arrive at possible solutions, let’s look at the elite athlete analogy. What are you trained to do? What are your exceptional skills? For me it is clearly EMR documentation (just checking to see if any of my residents have read this far). How many of us would describe ourselves as expert at billing? Paperwork? Medication reconciliation? Discharge summaries? Should LeBron James hawk 16-ounce Miller Lites in the nosebleeds during halftime? This may sound like I am expressing a cocky attitude that these tasks are beneath us, but we now have concrete evidence that forcing physicians to perform these duties hurts patient care and literally kills us. Full stop. Physician burnout can lead to suicide in the absence of clinical depression.
While hopelessness is part and parcel of the burnout syndrome, there are now potential solutions within our grasp. Clearly a reduction in clerical duties will be a key component of any realistic plan. Our time must be proportioned. Few of us are asking to work less. Reducing patient interactions while increasing the average time of these encounters has been shown to reduce burnout without decreasing work hours. We want to do a good job. It is time to remove these barriers.
Our next steps have already been taken, and for me it represents the best example of the potential of Vascular Specialist and the SVS. Under the leadership of SVS President Clem Darling, MD, and Executive Director Ken Slaw, PhD, a task force was created to address this issue. Ably chaired by Dawn Coleman, MD, and including Sam Money, MD, from the SVS Executive Council and Past SVS President Julie Freischlag, MD, the task force has collaborated with actual burnout experts Tait Shanafelt, MD, and Susan Hallbeck, PhD, to create a survey designed to identify the causes, prevalence, and potential solutions to the burnout problem in vascular surgery.
The first survey has been completed and will be issued to all SVS members this month to coincide with the SCVS annual symposium. The second, which will focus more on physical issues, will be released during the VAM in June.
Look, no one hates surveys more than I do. We simply have to get this information. Each survey is designed to only take 10 minutes. Things are going to change one way or another. Let’s lead, not wait to follow. With your help this will be the last time I write this ignorantly on this crisis. Vascular surgeons are few in number but this gives us the potential to deliver the most comprehensive self-assessment any specialty has ever performed. Lend your voice to the coming change.
Finally, there are now innovations in use which have proved beneficial in mitigating burnout. A Stanford University School of Medicine program allows physicians to “bank” time spent on committees, teaching, or other administrative duties and exchange these credits for home delivery meals, cleaning services, or even work tasks such as grant applications and paper writing. While the physicians could certainly afford to pay for these assistances, the success of the program demonstrates it is the time saved in arranging the services that the doctors truly valued. Our happiness seems to excel when we spend our time performing the tasks for which we are best suited.
It is time to change. When a system reaches this point, something breaks. Let’s stop being the thing that breaks. Fill out the survey. Get involved. There is time to act before we all burn out on burnout.
Dr. Sheahan is the Claude C. Craighead Jr. Professor and Chair, Division of Vascular and Endovascular Surgery, Louisiana State University Health Sciences Center, New Orleans.
Look, I am not a burnout expert. And neither are you (presumably). None of us know much, but that won’t stop the regulations from coming. Program directors are already being asked to provide “wellness plans.” Through the SVS, experts have been enlisted to help, but it is now clear that what works for others won’t necessarily work for vascular surgeons. The next step is up to us. We are the only ones with detailed knowledge of our lives. I believe we are moving closer to answers but still face a few significant hurdles. Don’t worry, there are solutions. Hear me out …
Previously, I shared three studies with you, which found that vascular surgeons had the highest rates of suicidal ideation and career dissatisfaction among surgeons while spending more hours in the hospital than any other specialty. So what has been done to address these horrific numbers? Very little. We need answers now, but most of the data are over 10 years old. Much has changed in our specialty. The endovascular revolution created an entirely new working paradigm. A busy vascular surgeon used to perform 300 cases annually; now this number approaches 1,000. More procedures means more clerical work. Lead aprons and radiation exposure have added new ergonomic and medical concerns. Reimbursement dynamics now favor shorter, more frequent patient interactions over longer, more complex cases. We are benchmarked against old work standards while CPT bundling continuously lowers current RVU designations. EMR was supposed to make our lives better; it has done the opposite. Patient-centered health care has become a mantra, but the measures taken often backfire. Practicing medicine where the desired outcome is a high score on patient satisfaction surveys will likely lead to unnecessary tests, poor cost allocation, and low physician fulfillment. Quality of care is now measured scrupulously while the quality of our lives remains undocumented.
In the absence of organized reform, burnout appears to be increasing. A recent Mayo Clinic–AMA study found the current prevalence to be 54% among physicians. All of this has not happened overnight. I believe practicing vascular surgeons are resilient by default. The majority of us trained prior to the enforcement of duty hour restrictions. Out of high school, I enrolled in a 6-year BA/MD program (skipping 2 years of college seemed like a great idea in high school, less so when I got there). Half of my class never finished. In my intern year, six of the eight categorical residents dropped out. My odds of reaching PGY 2 were 12.5%. Fuzzy math aside, all of your stories are similar. We have proved our resilience over and over again. What is happening here is different.
Burnout is described as emotional exhaustion, low self-esteem, and depersonalization/cynicism. It develops slowly, progressively as stressors increase. A common thread seems to be the feeling that you alone are not enough. Examine your daily life. What are your most common stressors? For me, they relate to time management, clinical documentation, and whatever fresh hell my kids’ teachers have cooked up for “school projects.”
*****Scene*****
Wife: Can you help Luke (kindergarten) finish his diorama? It needs to be a scale depiction of his 3 favorite scenes from Wagner’s Ring cycle.
Me: Sure, I just need to complete the wind tunnel testing on Jack’s (3rd grade) carbon-neutral peanut-free alternative fuel source rocket booster.
Off stage – 7th Grade Son: The genetically modified spiders got loose again!
*****End Scene*****
We want to do a good job, but more hurdles are placed in our way. A recent AMA/Dartmouth Hitchcock study found that 50% of physicians’ time is spent performing data entry and other administrative work. Only 27% of time was spent on patient care. Every hour of face-to-face patient time requires 2 hours of EMR/clerical work. We are trapped in a bureaucratic prison. For years, every quality initiative was solved with a new form. To enter a simple note today, we must first “establish our relationship” with the patient, then ably click through a minefield of “warning boxes” signifying impending DVT prophylaxis catastrophes and antibiotic crimes and misdemeanors, next we scroll through a pre-populated postapocalyptic hellscape of minute- by-minute vital sign entries and lab values dating back to inception. Then, and only then, finally, ON PAGE 11, we can meagerly type: Patient at wound care, will come back on evening rounds.
Another important component of the burnout syndrome is dehumanization. Recently I spoke with Donald Zimmerman, PhD, author of the textbook “Person-Focused Health Care Management.” His thoughts on health care were dramatically altered after spending 43 days in an ICU following abdominal aortic aneurysm repair. He describes the experience as “my worst nightmare that then got worse and then never ended.” While we can learn from his experience, how many of us were trained to face this horror? Dehumanization is a natural protective response, especially when we have so little time for patient interactions. Compassion fatigue sets in when we don’t have the time and resources to care for our patients.While poor outcomes have been cited as a result of burnout, this appears to be an end-stage result. The Minimizing Error, Maximizing Outcome (MEMO) study funded by the AHRQ found that physicians often served as a buffer between their patients and poor medical environments. The organizational flaws that led to burnout also independently resulted in substandard patient care. The burnout physicians experienced was a symptom of the defective health care system and not causative of the poor care. Doctors were literally sacrificing their well-being to care for their patients.
Not surprisingly, attitudes regarding burnout vary significantly between health care executives and physicians. A New England Journal of Medicine survey of their Insights Council found that 96% of respondents agreed that burnout is a moderate or serious problem, although physicians were significantly more likely than executives to rate the problem as “serious.” Opinions on solutions varied as well, with executives more likely to support redesign of EMR, while physicians favored reduction of documentation and clerical work. Obviously the physicians’ solution would be more costly to the corporation as the executives deflected the problem back to the EMR designers. Neither group favored the use of resilience/wellness programs as a primary solution.
Of all the remedies proposed, I find resilience training to be especially egregious. Studies consistently show a 40%-50% prevalence of burnout among physicians. How can this be an individual problem? Why train doctors to endure a broken system? This type of problem solving is why burnout continues to flourish. Doctors are not suffering from a disease but rather exhibiting a symptom.
To arrive at possible solutions, let’s look at the elite athlete analogy. What are you trained to do? What are your exceptional skills? For me it is clearly EMR documentation (just checking to see if any of my residents have read this far). How many of us would describe ourselves as expert at billing? Paperwork? Medication reconciliation? Discharge summaries? Should LeBron James hawk 16-ounce Miller Lites in the nosebleeds during halftime? This may sound like I am expressing a cocky attitude that these tasks are beneath us, but we now have concrete evidence that forcing physicians to perform these duties hurts patient care and literally kills us. Full stop. Physician burnout can lead to suicide in the absence of clinical depression.
While hopelessness is part and parcel of the burnout syndrome, there are now potential solutions within our grasp. Clearly a reduction in clerical duties will be a key component of any realistic plan. Our time must be proportioned. Few of us are asking to work less. Reducing patient interactions while increasing the average time of these encounters has been shown to reduce burnout without decreasing work hours. We want to do a good job. It is time to remove these barriers.
Our next steps have already been taken, and for me it represents the best example of the potential of Vascular Specialist and the SVS. Under the leadership of SVS President Clem Darling, MD, and Executive Director Ken Slaw, PhD, a task force was created to address this issue. Ably chaired by Dawn Coleman, MD, and including Sam Money, MD, from the SVS Executive Council and Past SVS President Julie Freischlag, MD, the task force has collaborated with actual burnout experts Tait Shanafelt, MD, and Susan Hallbeck, PhD, to create a survey designed to identify the causes, prevalence, and potential solutions to the burnout problem in vascular surgery.
The first survey has been completed and will be issued to all SVS members this month to coincide with the SCVS annual symposium. The second, which will focus more on physical issues, will be released during the VAM in June.
Look, no one hates surveys more than I do. We simply have to get this information. Each survey is designed to only take 10 minutes. Things are going to change one way or another. Let’s lead, not wait to follow. With your help this will be the last time I write this ignorantly on this crisis. Vascular surgeons are few in number but this gives us the potential to deliver the most comprehensive self-assessment any specialty has ever performed. Lend your voice to the coming change.
Finally, there are now innovations in use which have proved beneficial in mitigating burnout. A Stanford University School of Medicine program allows physicians to “bank” time spent on committees, teaching, or other administrative duties and exchange these credits for home delivery meals, cleaning services, or even work tasks such as grant applications and paper writing. While the physicians could certainly afford to pay for these assistances, the success of the program demonstrates it is the time saved in arranging the services that the doctors truly valued. Our happiness seems to excel when we spend our time performing the tasks for which we are best suited.
It is time to change. When a system reaches this point, something breaks. Let’s stop being the thing that breaks. Fill out the survey. Get involved. There is time to act before we all burn out on burnout.
Dr. Sheahan is the Claude C. Craighead Jr. Professor and Chair, Division of Vascular and Endovascular Surgery, Louisiana State University Health Sciences Center, New Orleans.
Look, I am not a burnout expert. And neither are you (presumably). None of us know much, but that won’t stop the regulations from coming. Program directors are already being asked to provide “wellness plans.” Through the SVS, experts have been enlisted to help, but it is now clear that what works for others won’t necessarily work for vascular surgeons. The next step is up to us. We are the only ones with detailed knowledge of our lives. I believe we are moving closer to answers but still face a few significant hurdles. Don’t worry, there are solutions. Hear me out …
Previously, I shared three studies with you, which found that vascular surgeons had the highest rates of suicidal ideation and career dissatisfaction among surgeons while spending more hours in the hospital than any other specialty. So what has been done to address these horrific numbers? Very little. We need answers now, but most of the data are over 10 years old. Much has changed in our specialty. The endovascular revolution created an entirely new working paradigm. A busy vascular surgeon used to perform 300 cases annually; now this number approaches 1,000. More procedures means more clerical work. Lead aprons and radiation exposure have added new ergonomic and medical concerns. Reimbursement dynamics now favor shorter, more frequent patient interactions over longer, more complex cases. We are benchmarked against old work standards while CPT bundling continuously lowers current RVU designations. EMR was supposed to make our lives better; it has done the opposite. Patient-centered health care has become a mantra, but the measures taken often backfire. Practicing medicine where the desired outcome is a high score on patient satisfaction surveys will likely lead to unnecessary tests, poor cost allocation, and low physician fulfillment. Quality of care is now measured scrupulously while the quality of our lives remains undocumented.
In the absence of organized reform, burnout appears to be increasing. A recent Mayo Clinic–AMA study found the current prevalence to be 54% among physicians. All of this has not happened overnight. I believe practicing vascular surgeons are resilient by default. The majority of us trained prior to the enforcement of duty hour restrictions. Out of high school, I enrolled in a 6-year BA/MD program (skipping 2 years of college seemed like a great idea in high school, less so when I got there). Half of my class never finished. In my intern year, six of the eight categorical residents dropped out. My odds of reaching PGY 2 were 12.5%. Fuzzy math aside, all of your stories are similar. We have proved our resilience over and over again. What is happening here is different.
Burnout is described as emotional exhaustion, low self-esteem, and depersonalization/cynicism. It develops slowly, progressively as stressors increase. A common thread seems to be the feeling that you alone are not enough. Examine your daily life. What are your most common stressors? For me, they relate to time management, clinical documentation, and whatever fresh hell my kids’ teachers have cooked up for “school projects.”
*****Scene*****
Wife: Can you help Luke (kindergarten) finish his diorama? It needs to be a scale depiction of his 3 favorite scenes from Wagner’s Ring cycle.
Me: Sure, I just need to complete the wind tunnel testing on Jack’s (3rd grade) carbon-neutral peanut-free alternative fuel source rocket booster.
Off stage – 7th Grade Son: The genetically modified spiders got loose again!
*****End Scene*****
We want to do a good job, but more hurdles are placed in our way. A recent AMA/Dartmouth Hitchcock study found that 50% of physicians’ time is spent performing data entry and other administrative work. Only 27% of time was spent on patient care. Every hour of face-to-face patient time requires 2 hours of EMR/clerical work. We are trapped in a bureaucratic prison. For years, every quality initiative was solved with a new form. To enter a simple note today, we must first “establish our relationship” with the patient, then ably click through a minefield of “warning boxes” signifying impending DVT prophylaxis catastrophes and antibiotic crimes and misdemeanors, next we scroll through a pre-populated postapocalyptic hellscape of minute- by-minute vital sign entries and lab values dating back to inception. Then, and only then, finally, ON PAGE 11, we can meagerly type: Patient at wound care, will come back on evening rounds.
Another important component of the burnout syndrome is dehumanization. Recently I spoke with Donald Zimmerman, PhD, author of the textbook “Person-Focused Health Care Management.” His thoughts on health care were dramatically altered after spending 43 days in an ICU following abdominal aortic aneurysm repair. He describes the experience as “my worst nightmare that then got worse and then never ended.” While we can learn from his experience, how many of us were trained to face this horror? Dehumanization is a natural protective response, especially when we have so little time for patient interactions. Compassion fatigue sets in when we don’t have the time and resources to care for our patients.While poor outcomes have been cited as a result of burnout, this appears to be an end-stage result. The Minimizing Error, Maximizing Outcome (MEMO) study funded by the AHRQ found that physicians often served as a buffer between their patients and poor medical environments. The organizational flaws that led to burnout also independently resulted in substandard patient care. The burnout physicians experienced was a symptom of the defective health care system and not causative of the poor care. Doctors were literally sacrificing their well-being to care for their patients.
Not surprisingly, attitudes regarding burnout vary significantly between health care executives and physicians. A New England Journal of Medicine survey of their Insights Council found that 96% of respondents agreed that burnout is a moderate or serious problem, although physicians were significantly more likely than executives to rate the problem as “serious.” Opinions on solutions varied as well, with executives more likely to support redesign of EMR, while physicians favored reduction of documentation and clerical work. Obviously the physicians’ solution would be more costly to the corporation as the executives deflected the problem back to the EMR designers. Neither group favored the use of resilience/wellness programs as a primary solution.
Of all the remedies proposed, I find resilience training to be especially egregious. Studies consistently show a 40%-50% prevalence of burnout among physicians. How can this be an individual problem? Why train doctors to endure a broken system? This type of problem solving is why burnout continues to flourish. Doctors are not suffering from a disease but rather exhibiting a symptom.
To arrive at possible solutions, let’s look at the elite athlete analogy. What are you trained to do? What are your exceptional skills? For me it is clearly EMR documentation (just checking to see if any of my residents have read this far). How many of us would describe ourselves as expert at billing? Paperwork? Medication reconciliation? Discharge summaries? Should LeBron James hawk 16-ounce Miller Lites in the nosebleeds during halftime? This may sound like I am expressing a cocky attitude that these tasks are beneath us, but we now have concrete evidence that forcing physicians to perform these duties hurts patient care and literally kills us. Full stop. Physician burnout can lead to suicide in the absence of clinical depression.
While hopelessness is part and parcel of the burnout syndrome, there are now potential solutions within our grasp. Clearly a reduction in clerical duties will be a key component of any realistic plan. Our time must be proportioned. Few of us are asking to work less. Reducing patient interactions while increasing the average time of these encounters has been shown to reduce burnout without decreasing work hours. We want to do a good job. It is time to remove these barriers.
Our next steps have already been taken, and for me it represents the best example of the potential of Vascular Specialist and the SVS. Under the leadership of SVS President Clem Darling, MD, and Executive Director Ken Slaw, PhD, a task force was created to address this issue. Ably chaired by Dawn Coleman, MD, and including Sam Money, MD, from the SVS Executive Council and Past SVS President Julie Freischlag, MD, the task force has collaborated with actual burnout experts Tait Shanafelt, MD, and Susan Hallbeck, PhD, to create a survey designed to identify the causes, prevalence, and potential solutions to the burnout problem in vascular surgery.
The first survey has been completed and will be issued to all SVS members this month to coincide with the SCVS annual symposium. The second, which will focus more on physical issues, will be released during the VAM in June.
Look, no one hates surveys more than I do. We simply have to get this information. Each survey is designed to only take 10 minutes. Things are going to change one way or another. Let’s lead, not wait to follow. With your help this will be the last time I write this ignorantly on this crisis. Vascular surgeons are few in number but this gives us the potential to deliver the most comprehensive self-assessment any specialty has ever performed. Lend your voice to the coming change.
Finally, there are now innovations in use which have proved beneficial in mitigating burnout. A Stanford University School of Medicine program allows physicians to “bank” time spent on committees, teaching, or other administrative duties and exchange these credits for home delivery meals, cleaning services, or even work tasks such as grant applications and paper writing. While the physicians could certainly afford to pay for these assistances, the success of the program demonstrates it is the time saved in arranging the services that the doctors truly valued. Our happiness seems to excel when we spend our time performing the tasks for which we are best suited.
It is time to change. When a system reaches this point, something breaks. Let’s stop being the thing that breaks. Fill out the survey. Get involved. There is time to act before we all burn out on burnout.
Dr. Sheahan is the Claude C. Craighead Jr. Professor and Chair, Division of Vascular and Endovascular Surgery, Louisiana State University Health Sciences Center, New Orleans.
How real is resident burnout?
JACKSONVILLE, FLA. – Burnout is commonly ascribed to surgical residents, but reliable estimates of the numbers involved and a clear, comparable definition of burnout remain elusive.
A large study of general surgery residents has found that almost one in four have at least one symptom of burnout daily and more than two in five report poor psychiatric well-being, according to results of a survey reported at the Association for Academic Surgery/Society of University Surgeons Academic Surgical Congress.
“Twenty-two percent of general surgery residents report at least one symptom of burnout daily,” said Daniel “Brock” Hewitt, MD, a research fellow in the Surgical Outcomes and Quality Improvement Center in the department of surgery, Feinberg School of Medicine, Northwestern University, Chicago. “Poor resident wellness is associated with more duty-hour violations, feeling unprepared for residency, and an increase in self-reported medical errors. However, burnout is not associated with worse surgical outcomes.”
The study, undertaken with grant support from The American Board of Surgery, Accreditation of Graduate Medical Education, American College of Surgeons and Agency for Healthcare Research and Quality, provided three significant insights into resident wellness, Dr. Hewitt said. “When measuring the level of burnout, careful consideration should be given to how burnout is defined,” he said. “Secondly, wellness interventions with attention to preparedness for residency and duty-hour restrictions may help alleviate burnout. And finally, with the significant impact it does have on the individual physician, we believe that burnout needs to be addressed regardless of its impact on patient outcomes.”
The study drew on a questionnaire given to residents immediately following the 2017 American Board of Surgery In-Training Examination (ABSITE), which 3,789 general surgery residents from 115 general surgery programs completed. The survey had a 99.3% response rate. The survey evaluated two factors associated with resident wellness: burnout and poor psychiatric well-being. “Poor wellness is prevalent among physicians and trainees and is associated with depression, suicidal ideation, attrition, and absenteeism,” Dr. Hewitt said.
But to measure burnout, the researchers had to first define it. The instrument Dr. Hewitt and coauthors used is the Maslach Burnout Inventory, named for University of California at Berkley psychology professor Christina Maslach, PhD. It quantifies three different factors for burnout: emotional exhaustion; depersonalization or cynicism; and a low sense of personal accomplishment. This study defined “burnout” as having feelings of both emotional exhaustion and depersonalization, and dismissed the third measure of burnout because physicians rarely posses a low sense of personal accomplishment.
Overall, 22.3% reported one sign or symptom of burnout daily, and 56.5% did so on a weekly basis, Dr. Hewitt said.
However, Dr. Hewitt noted, burnout measurement thresholds can vary “because burnout itself is not an actual diagnosis.” Studies have calculated the burnout rate among surgeons at 28% to 69% (J Am Coll Surg. 2016:222:1230-9). A recent systematic review found up to eight different cutoffs used to define “high burnout” (Cogent Med. 2016 7 Oct; doi.org/10.1080/2331205X.2016.1237605; J Am Coll Surg, 2016:223:440-51)
How studies of physician burnout establish cutoffs and which Maslach Burnout Inventory subscales they measure has an impact on the rates of burnout they report, Dr. Hewitt said. For this study, the researchers used the Maslach scores in the top quartile in both emotional exhaustion and depersonalization to define burnout. “Burnout is probably best defined as a continuum from engagement on the one end and burnout on the other, so there’s some combination of the [Maslach] subscales that lead to burnout,” he said.
Among survey respondents, 19.5% reported high Maslach scores for emotional exhaustion and 9% of depersonalization on a daily basis (6.2% reported both)--22.3% reported at least one daily. On a weekly basis, 54.2% reported high scores for emotional exhaustion and 25.6% high scores for depersonalization, with 56.5% reporting at least one and 22.4% reporting both.
To evaluate residents’ sense of psychiatric well-being, the study used the General Health Questionnaire (Psychol Med. 1998;28:915-21). Among survey respondents, 43% met criteria for poor psychiatric well-being.
Burnout rates among men and women were identical, but a significantly higher percentage of women had poor psychiatric well-being: 48.4% to 39.7% of men.
Burnout and psychiatric well-being scores also varied depending on post-graduate year. Second- and third-year residents were significantly more likely to report burnout, compared to first-year residents, Dr. Hewitt said. Rates of poor psychiatric well-being were lowest for fourth- and fifth-year residents.
Most pronounced was the impact of 80-hour duty week violations had on residents’ sense of burnout and poor psychiatric well-being. Burnout rates were 8.4% for those who reported no monthly duty-hour violations, but doubled and quadrupled with more frequent monthly duty-hour violations: 16.1% for those who reported one to four violations a month; and 35% for those who reported five or more. Dr. Hewitt also noted wellness rates for those in the standard and flexible policy groups in Flexibility In duty hour Requirements for Surgical Trainees Trial (FIRST Trial) programs were similar.
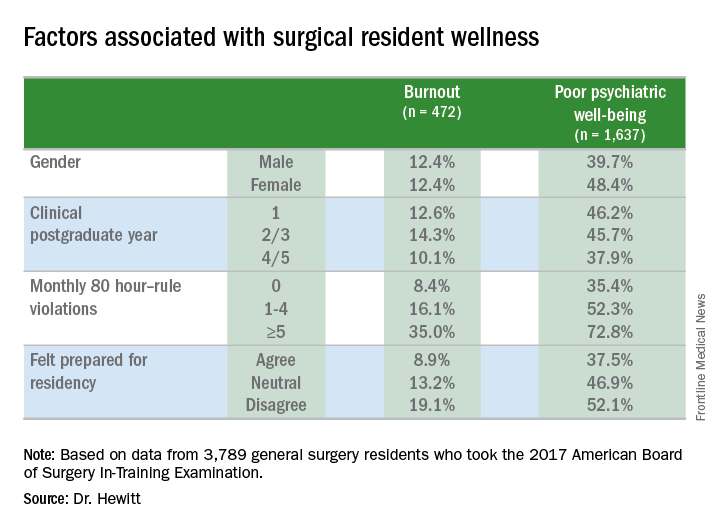
Another factor that contributed to burnout and poor psychiatric well-being was a sense of unpreparedness for residency, Dr. Hewitt said. Burnout rates for those who felt prepared were 8.9% vs. 19.1% for those who didn’t feel prepared. The disparity was less drastic, but nonetheless significant, for poor psychiatric well-being: 37.5% for those who felt prepared and 52.1% for those who didn’t.
With regard to outcomes, Dr. Hewitt said, “Residents in the highest quartile of burnout and the highest quartile of poor psychiatric well-being were significantly more likely to report a near miss or harmful medical error.” Among the burnout group, highest quartile rates were 39.3% for a near miss and 14.4% for a harmful medical error vs. 11.1% and 2.4%, respectively, for the lowest quartile. Among surgical residents who reported poor psychiatric well-being, highest quartile rates were 31.9% for a near miss and 13.2% for a harmful medical error vs. 12.5% and 2.1%, respectively, for those in the lowest quartile.
The study also analyzed outcomes for 134,877 surgical patients and found no association of overall morbidity and death or serious morbidity with resident wellness. “However,” Dr. Hewitt said, “when we look at mortality and failure to rescue, we can see an association with burnout, specifically in programs that have high levels of burnout; these patients have significantly lower odds of mortality and failure to rescue.” Each has an adjusted odds ratios of 0.81.
Among the study limitations Dr. Hewitt noted were its cross-sectional nature that led to inferences of association, not identification of causation; residents completing the survey after the ABSITE may have influenced their answers; and the fact it did not account for certain intermediate factors such as physician or nursing burnout or institutional quality measures.
The American Board of Surgery, Accreditation of Graduate Medical Education, American College of Surgeons and Agency for Healthcare Research and Quality provided grants to support the research.
SOURCE: Hewitt B et al. abstract 21.01
JACKSONVILLE, FLA. – Burnout is commonly ascribed to surgical residents, but reliable estimates of the numbers involved and a clear, comparable definition of burnout remain elusive.
A large study of general surgery residents has found that almost one in four have at least one symptom of burnout daily and more than two in five report poor psychiatric well-being, according to results of a survey reported at the Association for Academic Surgery/Society of University Surgeons Academic Surgical Congress.
“Twenty-two percent of general surgery residents report at least one symptom of burnout daily,” said Daniel “Brock” Hewitt, MD, a research fellow in the Surgical Outcomes and Quality Improvement Center in the department of surgery, Feinberg School of Medicine, Northwestern University, Chicago. “Poor resident wellness is associated with more duty-hour violations, feeling unprepared for residency, and an increase in self-reported medical errors. However, burnout is not associated with worse surgical outcomes.”
The study, undertaken with grant support from The American Board of Surgery, Accreditation of Graduate Medical Education, American College of Surgeons and Agency for Healthcare Research and Quality, provided three significant insights into resident wellness, Dr. Hewitt said. “When measuring the level of burnout, careful consideration should be given to how burnout is defined,” he said. “Secondly, wellness interventions with attention to preparedness for residency and duty-hour restrictions may help alleviate burnout. And finally, with the significant impact it does have on the individual physician, we believe that burnout needs to be addressed regardless of its impact on patient outcomes.”
The study drew on a questionnaire given to residents immediately following the 2017 American Board of Surgery In-Training Examination (ABSITE), which 3,789 general surgery residents from 115 general surgery programs completed. The survey had a 99.3% response rate. The survey evaluated two factors associated with resident wellness: burnout and poor psychiatric well-being. “Poor wellness is prevalent among physicians and trainees and is associated with depression, suicidal ideation, attrition, and absenteeism,” Dr. Hewitt said.
But to measure burnout, the researchers had to first define it. The instrument Dr. Hewitt and coauthors used is the Maslach Burnout Inventory, named for University of California at Berkley psychology professor Christina Maslach, PhD. It quantifies three different factors for burnout: emotional exhaustion; depersonalization or cynicism; and a low sense of personal accomplishment. This study defined “burnout” as having feelings of both emotional exhaustion and depersonalization, and dismissed the third measure of burnout because physicians rarely posses a low sense of personal accomplishment.
Overall, 22.3% reported one sign or symptom of burnout daily, and 56.5% did so on a weekly basis, Dr. Hewitt said.
However, Dr. Hewitt noted, burnout measurement thresholds can vary “because burnout itself is not an actual diagnosis.” Studies have calculated the burnout rate among surgeons at 28% to 69% (J Am Coll Surg. 2016:222:1230-9). A recent systematic review found up to eight different cutoffs used to define “high burnout” (Cogent Med. 2016 7 Oct; doi.org/10.1080/2331205X.2016.1237605; J Am Coll Surg, 2016:223:440-51)
How studies of physician burnout establish cutoffs and which Maslach Burnout Inventory subscales they measure has an impact on the rates of burnout they report, Dr. Hewitt said. For this study, the researchers used the Maslach scores in the top quartile in both emotional exhaustion and depersonalization to define burnout. “Burnout is probably best defined as a continuum from engagement on the one end and burnout on the other, so there’s some combination of the [Maslach] subscales that lead to burnout,” he said.
Among survey respondents, 19.5% reported high Maslach scores for emotional exhaustion and 9% of depersonalization on a daily basis (6.2% reported both)--22.3% reported at least one daily. On a weekly basis, 54.2% reported high scores for emotional exhaustion and 25.6% high scores for depersonalization, with 56.5% reporting at least one and 22.4% reporting both.
To evaluate residents’ sense of psychiatric well-being, the study used the General Health Questionnaire (Psychol Med. 1998;28:915-21). Among survey respondents, 43% met criteria for poor psychiatric well-being.
Burnout rates among men and women were identical, but a significantly higher percentage of women had poor psychiatric well-being: 48.4% to 39.7% of men.
Burnout and psychiatric well-being scores also varied depending on post-graduate year. Second- and third-year residents were significantly more likely to report burnout, compared to first-year residents, Dr. Hewitt said. Rates of poor psychiatric well-being were lowest for fourth- and fifth-year residents.
Most pronounced was the impact of 80-hour duty week violations had on residents’ sense of burnout and poor psychiatric well-being. Burnout rates were 8.4% for those who reported no monthly duty-hour violations, but doubled and quadrupled with more frequent monthly duty-hour violations: 16.1% for those who reported one to four violations a month; and 35% for those who reported five or more. Dr. Hewitt also noted wellness rates for those in the standard and flexible policy groups in Flexibility In duty hour Requirements for Surgical Trainees Trial (FIRST Trial) programs were similar.
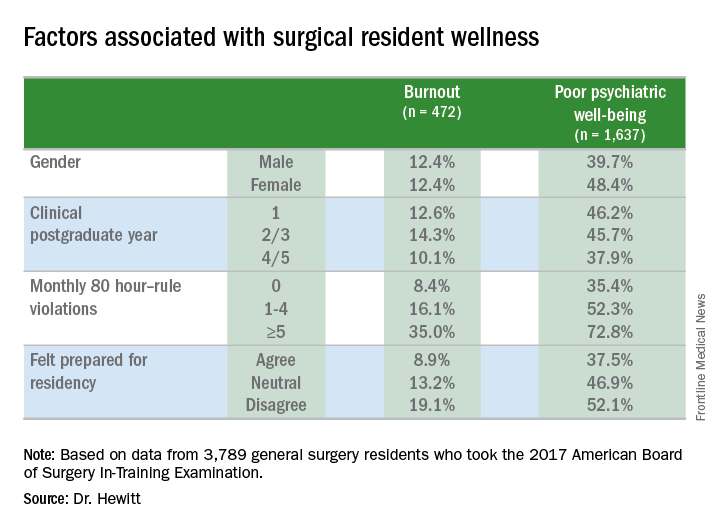
Another factor that contributed to burnout and poor psychiatric well-being was a sense of unpreparedness for residency, Dr. Hewitt said. Burnout rates for those who felt prepared were 8.9% vs. 19.1% for those who didn’t feel prepared. The disparity was less drastic, but nonetheless significant, for poor psychiatric well-being: 37.5% for those who felt prepared and 52.1% for those who didn’t.
With regard to outcomes, Dr. Hewitt said, “Residents in the highest quartile of burnout and the highest quartile of poor psychiatric well-being were significantly more likely to report a near miss or harmful medical error.” Among the burnout group, highest quartile rates were 39.3% for a near miss and 14.4% for a harmful medical error vs. 11.1% and 2.4%, respectively, for the lowest quartile. Among surgical residents who reported poor psychiatric well-being, highest quartile rates were 31.9% for a near miss and 13.2% for a harmful medical error vs. 12.5% and 2.1%, respectively, for those in the lowest quartile.
The study also analyzed outcomes for 134,877 surgical patients and found no association of overall morbidity and death or serious morbidity with resident wellness. “However,” Dr. Hewitt said, “when we look at mortality and failure to rescue, we can see an association with burnout, specifically in programs that have high levels of burnout; these patients have significantly lower odds of mortality and failure to rescue.” Each has an adjusted odds ratios of 0.81.
Among the study limitations Dr. Hewitt noted were its cross-sectional nature that led to inferences of association, not identification of causation; residents completing the survey after the ABSITE may have influenced their answers; and the fact it did not account for certain intermediate factors such as physician or nursing burnout or institutional quality measures.
The American Board of Surgery, Accreditation of Graduate Medical Education, American College of Surgeons and Agency for Healthcare Research and Quality provided grants to support the research.
SOURCE: Hewitt B et al. abstract 21.01
JACKSONVILLE, FLA. – Burnout is commonly ascribed to surgical residents, but reliable estimates of the numbers involved and a clear, comparable definition of burnout remain elusive.
A large study of general surgery residents has found that almost one in four have at least one symptom of burnout daily and more than two in five report poor psychiatric well-being, according to results of a survey reported at the Association for Academic Surgery/Society of University Surgeons Academic Surgical Congress.
“Twenty-two percent of general surgery residents report at least one symptom of burnout daily,” said Daniel “Brock” Hewitt, MD, a research fellow in the Surgical Outcomes and Quality Improvement Center in the department of surgery, Feinberg School of Medicine, Northwestern University, Chicago. “Poor resident wellness is associated with more duty-hour violations, feeling unprepared for residency, and an increase in self-reported medical errors. However, burnout is not associated with worse surgical outcomes.”
The study, undertaken with grant support from The American Board of Surgery, Accreditation of Graduate Medical Education, American College of Surgeons and Agency for Healthcare Research and Quality, provided three significant insights into resident wellness, Dr. Hewitt said. “When measuring the level of burnout, careful consideration should be given to how burnout is defined,” he said. “Secondly, wellness interventions with attention to preparedness for residency and duty-hour restrictions may help alleviate burnout. And finally, with the significant impact it does have on the individual physician, we believe that burnout needs to be addressed regardless of its impact on patient outcomes.”
The study drew on a questionnaire given to residents immediately following the 2017 American Board of Surgery In-Training Examination (ABSITE), which 3,789 general surgery residents from 115 general surgery programs completed. The survey had a 99.3% response rate. The survey evaluated two factors associated with resident wellness: burnout and poor psychiatric well-being. “Poor wellness is prevalent among physicians and trainees and is associated with depression, suicidal ideation, attrition, and absenteeism,” Dr. Hewitt said.
But to measure burnout, the researchers had to first define it. The instrument Dr. Hewitt and coauthors used is the Maslach Burnout Inventory, named for University of California at Berkley psychology professor Christina Maslach, PhD. It quantifies three different factors for burnout: emotional exhaustion; depersonalization or cynicism; and a low sense of personal accomplishment. This study defined “burnout” as having feelings of both emotional exhaustion and depersonalization, and dismissed the third measure of burnout because physicians rarely posses a low sense of personal accomplishment.
Overall, 22.3% reported one sign or symptom of burnout daily, and 56.5% did so on a weekly basis, Dr. Hewitt said.
However, Dr. Hewitt noted, burnout measurement thresholds can vary “because burnout itself is not an actual diagnosis.” Studies have calculated the burnout rate among surgeons at 28% to 69% (J Am Coll Surg. 2016:222:1230-9). A recent systematic review found up to eight different cutoffs used to define “high burnout” (Cogent Med. 2016 7 Oct; doi.org/10.1080/2331205X.2016.1237605; J Am Coll Surg, 2016:223:440-51)
How studies of physician burnout establish cutoffs and which Maslach Burnout Inventory subscales they measure has an impact on the rates of burnout they report, Dr. Hewitt said. For this study, the researchers used the Maslach scores in the top quartile in both emotional exhaustion and depersonalization to define burnout. “Burnout is probably best defined as a continuum from engagement on the one end and burnout on the other, so there’s some combination of the [Maslach] subscales that lead to burnout,” he said.
Among survey respondents, 19.5% reported high Maslach scores for emotional exhaustion and 9% of depersonalization on a daily basis (6.2% reported both)--22.3% reported at least one daily. On a weekly basis, 54.2% reported high scores for emotional exhaustion and 25.6% high scores for depersonalization, with 56.5% reporting at least one and 22.4% reporting both.
To evaluate residents’ sense of psychiatric well-being, the study used the General Health Questionnaire (Psychol Med. 1998;28:915-21). Among survey respondents, 43% met criteria for poor psychiatric well-being.
Burnout rates among men and women were identical, but a significantly higher percentage of women had poor psychiatric well-being: 48.4% to 39.7% of men.
Burnout and psychiatric well-being scores also varied depending on post-graduate year. Second- and third-year residents were significantly more likely to report burnout, compared to first-year residents, Dr. Hewitt said. Rates of poor psychiatric well-being were lowest for fourth- and fifth-year residents.
Most pronounced was the impact of 80-hour duty week violations had on residents’ sense of burnout and poor psychiatric well-being. Burnout rates were 8.4% for those who reported no monthly duty-hour violations, but doubled and quadrupled with more frequent monthly duty-hour violations: 16.1% for those who reported one to four violations a month; and 35% for those who reported five or more. Dr. Hewitt also noted wellness rates for those in the standard and flexible policy groups in Flexibility In duty hour Requirements for Surgical Trainees Trial (FIRST Trial) programs were similar.
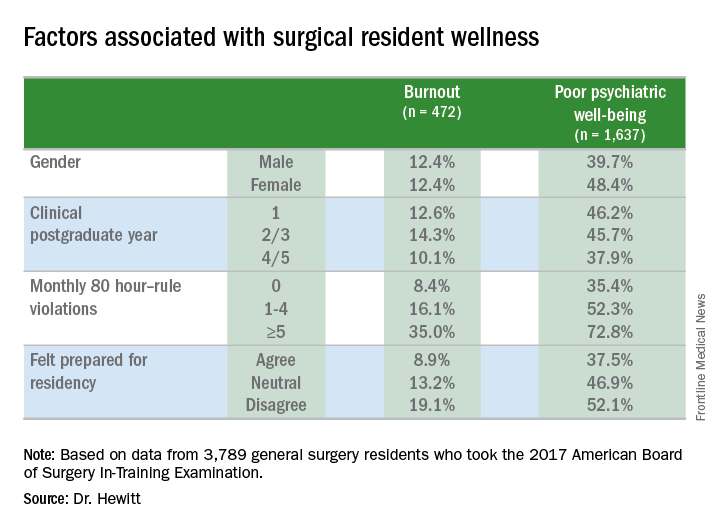
Another factor that contributed to burnout and poor psychiatric well-being was a sense of unpreparedness for residency, Dr. Hewitt said. Burnout rates for those who felt prepared were 8.9% vs. 19.1% for those who didn’t feel prepared. The disparity was less drastic, but nonetheless significant, for poor psychiatric well-being: 37.5% for those who felt prepared and 52.1% for those who didn’t.
With regard to outcomes, Dr. Hewitt said, “Residents in the highest quartile of burnout and the highest quartile of poor psychiatric well-being were significantly more likely to report a near miss or harmful medical error.” Among the burnout group, highest quartile rates were 39.3% for a near miss and 14.4% for a harmful medical error vs. 11.1% and 2.4%, respectively, for the lowest quartile. Among surgical residents who reported poor psychiatric well-being, highest quartile rates were 31.9% for a near miss and 13.2% for a harmful medical error vs. 12.5% and 2.1%, respectively, for those in the lowest quartile.
The study also analyzed outcomes for 134,877 surgical patients and found no association of overall morbidity and death or serious morbidity with resident wellness. “However,” Dr. Hewitt said, “when we look at mortality and failure to rescue, we can see an association with burnout, specifically in programs that have high levels of burnout; these patients have significantly lower odds of mortality and failure to rescue.” Each has an adjusted odds ratios of 0.81.
Among the study limitations Dr. Hewitt noted were its cross-sectional nature that led to inferences of association, not identification of causation; residents completing the survey after the ABSITE may have influenced their answers; and the fact it did not account for certain intermediate factors such as physician or nursing burnout or institutional quality measures.
The American Board of Surgery, Accreditation of Graduate Medical Education, American College of Surgeons and Agency for Healthcare Research and Quality provided grants to support the research.
SOURCE: Hewitt B et al. abstract 21.01
AT THE ANNUAL ACADEMIC SURGICAL CONGRESS
Key clinical point: Almost one in four surgical residents manifest a daily symptom of burnout.
Major finding: Overall 22.8% of daily and 44.3% had poor psychiatric well-being scores.
Study details: Surveys completed by 3,789 general surgery residents during the American Board of Surgery In-Training Examination in January 2017.
Disclosures: The American Board of Surgery, Accreditation of Graduate Medical Education, American College of Surgeons and Agency for Healthcare Research and Quality provided grants to support the research.
Source: Hewitt B et al. abstract 21.01
'This has to change': Surgeon pain, disability on the rise
The evidence has been accumulating for decades: Practicing surgery can exact a toll on surgeons’ physical well-being in ways that can shorten careers and contribute to professional dissatisfaction.
“Ergonomists have described the surgeon’s work environment and working conditions as equal to, if not at times harsher than, those of certain industrial workers,” wrote Sherise Epstein, MPH, and the coauthors of the systematic review and meta-analysis of studies addressing the issue. Ms. Epstein, currently a 4th-year medical student at the University of California, San Diego, and her team found a high prevalence of work-related musculoskeletal disorders and pain among surgeons and interventionalists, with pooled prevalence estimates for pain among these physicians ranging from 35% to 60% of all respondents. Cervical spine disease, rotator cuff pathology, and degenerative lumbar spine disease were each reported by nearly one in five respondents in the pooled analyses, with increasing prevalence over the duration of the study period (JAMA Surg. 2017 Dec 27. doi:10.1001/jamasurg.2017.49).
These findings, called “worrisome” by the study’s authors, come at a time when the demand for surgeons and interventionalists is expected soon to outstrip supply, and point to a major stressor for a profession already plagued by high rates of burnout and depression.
The results of the study are in line with previous work that finds a high – and increasing – rate of pain and disability among at-risk physicians, who endure long work hours, awkward positioning, and few opportunities for breaks.
The study also suggested a possible linkage between work-related pain and other factors, such as burnout and depression, that lead to attrition in the surgical profession.
Adrian Park, MD, FACS, a general surgeon who has long studied the issue of work-related musculoskeletal disorders (MSDs) among surgeons and interventionalists, was not surprised by the study’s findings. “This just goes to further the narrative, which is a consistent one: These aren’t just sporadic instances of individual surgeons having a tough time; this is an increasingly broadly recognized problem. ... These are the consequences of surgeons simply getting up and going to work each week,” Dr. Park said in an interview.
To take a long view of the published data on work-related injury and pain for at-risk physicians, Ms. Epstein and her collaborators identified 126 articles reporting physician work-related MSDs that met quality standards; the studies spanned 1974 to 2016, and 23 countries were represented.
A total of 21 articles were eventually included in the meta-analysis, which included responses from 5,828 physicians. Most of the respondents were male (78.5%), with a mean age of 46 years and a mean 12.8 years in practice. The mean number of hours spent in procedures per week was 14.4.
Sixteen cross-sectional studies included in the meta-analysis examined injury prevalence, with 14 studies eventually meeting eligibility criteria for quantitative synthesis. A total of 4,245 physicians were included in this portion of the analysis; 1,232 were orthopedic surgeons, 1,118 were interventional cardiologists, and 582 were general surgeons (a variety of other subspecialties made up the remainder).
The career prevalence of degenerative lumbar spine disease was estimated at 19%, with prevalence increasing over time in a series of surveys of interventional cardiologists, said Ms. Epstein and her colleagues. Among this group, the prevalence climbed from 6.5% in 1997 to 24.7% in 2015, an increase in prevalence of over 18%, they said. The investigators’ estimate of lumbar spine disease prevalence from their own data also showed an increase, to 21%, for studies published within the past decade.
Rotator cuff pathology during the study period was estimated at 18% overall, and carpal tunnel syndrome at 9% overall; carpal tunnel syndrome also appears to be increasing in prevalence, estimated at 12% within the last decade.
Musculoskeletal pain that was judged to be work related was common, as reported in 18 cross-sectional studies. Taken together, the studies used a total of five validated tools that measured both pain prevalence and related disability. Twelve of the studies met criteria for inclusion in the quantitative synthesis.
Neck, back, and shoulder pain were all common in this group of surgeons and interventionalists. Neck pain had a 60% estimated 12-month prevalence, and shoulder pain was almost as common, with a 52% prevalence; back pain was reported for about half (49%) of respondents.
Just 10 of the included studies addressed disability burden, said Ms. Epstein and her colleagues. Overall, 12% of physicians responding in this subset of studies reported that they required work modification, leave of absence, or early retirement because of work-related MSDs.
In a separate arm of the analysis, Ms. Epstein and her collaborators looked at studies that discussed ergonomic assessments and interventions, using a qualitative approach. A total of 101 studies, 50 of them in the United States, were included. None of the studies, they said, “included long-term surveillance for work-related MSDs”; rather, they focused on short-term outcomes and, in some cases, on real-time electromyographic data.
Of the 101 studies looking at ergonomics, about a third (n = 38) looked primarily at ergonomically designed devices or technology, while another third (n = 37) focused on educational or behavioral interventions and modifications. These were the studies included in the investigators’ analysis.
A lack of awareness of ergonomic recommendations on the part of the surgeons themselves was identified in several studies. Several specialties, publishing in a total of eight countries, have put forward “at least one article describing a need for ergonomics education during medical training.” And, said the investigators, “A few studies have found that ergonomics education during medical training appears feasible, accepted, and effective at changing behaviors and reducing symptoms.”
In addition to the usual limitations inherent to the meta-analysis research design (selection bias, self-reported data, small samples of individual studies), the study was limited by the elusive nature of the topic. Work-related pain and disability among surgeons remains underreported and underestimated, according to both Dr. Park and the study investigators. Further research is needed, and the investigators wrote: “Ultimately, this work should be integrated with research on preventing surgeon burnout and attrition given shared risk factors.”
Micro breaks can help
What’s the solution? Dr. Park says that some fixes are low tech, and can be put in place immediately. He and his team implemented a series of brief breaks, taken every half hour during a procedure, that they dubbed “targeted stretching micro breaks.” These are 45- to 50-second breaks during which a series of exercise physiologist–designed brief stretches are undertaken that do not require breaking scrub.
In a study of 66 surgeons and operating room staff, Dr. Park, chair of the department of surgery at Anne Arundel Medical Center, Annapolis, Md., and his collaborators found that surgeons reported less pain and fatigue, and improved mental focus, when they took micro breaks during a procedure. When surgeons took micro breaks, operative time was no longer than when they didn’t take the breaks (Ann Surg. 2017 Feb;265[2]:340-6).
“We do this all the time in our operating room now,” said Dr. Park. “And it makes a difference in terms of pain, in terms of alertness, in terms of stamina. And it costs nothing.”
Major redesign of tools and workspace
Other targets for technological improvement include offering better-designed handles for laparoscopic instruments. “We’ve had one size fits all forever. Why has it taken us so long to recognize that there’s not one size of surgical hand?” asked Dr. Park. He made the point that the influx of women – whose hands are smaller on average than men’s – into the surgical professions makes this a particularly pressing issue.
“The high-tech piece is going to be a better understanding of the operative work flow,” said Dr. Park, calling for “a meaningful revisiting of the surgeon-device interface and the surgeon-patient interface.”
A fundamental redesign of the operating room will eventually be in order, he said, contrasting the surgeon’s environments with that of an airline pilot. In the cockpit, the pilot sees a “heads-up” display of a limited amount of data, with an eye to controlling the cognitive workload for the operator. By contrast, said Dr. Park, in the OR, there are “lights flashing, and things pinging,” and pieces of equipment don’t “talk” to each other, presenting sometimes overwhelming sensory input that just potentiates the stress of the environment. Operating room design, he said, should move toward an ergonomically improved and stimulus-controlled environment.
As the leader of the surgical team, and as a physician whose foremost concern is the patient on the table, the surgeon may inadvertently have fallen into a role where his or her well-being is neglected.
Dr. Park suggested that, in the surgical profession, “it has never felt safe or appropriate to talk about ourselves.” But for the good of the profession, and ultimately for patient care, “this has to change.”
Ms. Epstein and her coauthors reported no conflicts of interest. .
We rarely think of surgeons as athletes and certainly we sometimes don’t look like athletes, but surgery is a performance sport that includes strength and grace. Many surgeons are also very active outside the OR. So, not only OR activity but all the other activities are stacked upon our bodies. Posture, strength training, and ergonomics need to be part of our training just as it would for a pitcher for the Kansas City Royals. You wouldn’t expect the pitcher’s arm to last long without coaching and training physically. That player’s career would be shortened. Why would we expect surgeons to be different? Our game is 90% mental, but the other half is physical (with respect to Yogi Berra).
We rarely think of surgeons as athletes and certainly we sometimes don’t look like athletes, but surgery is a performance sport that includes strength and grace. Many surgeons are also very active outside the OR. So, not only OR activity but all the other activities are stacked upon our bodies. Posture, strength training, and ergonomics need to be part of our training just as it would for a pitcher for the Kansas City Royals. You wouldn’t expect the pitcher’s arm to last long without coaching and training physically. That player’s career would be shortened. Why would we expect surgeons to be different? Our game is 90% mental, but the other half is physical (with respect to Yogi Berra).
We rarely think of surgeons as athletes and certainly we sometimes don’t look like athletes, but surgery is a performance sport that includes strength and grace. Many surgeons are also very active outside the OR. So, not only OR activity but all the other activities are stacked upon our bodies. Posture, strength training, and ergonomics need to be part of our training just as it would for a pitcher for the Kansas City Royals. You wouldn’t expect the pitcher’s arm to last long without coaching and training physically. That player’s career would be shortened. Why would we expect surgeons to be different? Our game is 90% mental, but the other half is physical (with respect to Yogi Berra).
The evidence has been accumulating for decades: Practicing surgery can exact a toll on surgeons’ physical well-being in ways that can shorten careers and contribute to professional dissatisfaction.
“Ergonomists have described the surgeon’s work environment and working conditions as equal to, if not at times harsher than, those of certain industrial workers,” wrote Sherise Epstein, MPH, and the coauthors of the systematic review and meta-analysis of studies addressing the issue. Ms. Epstein, currently a 4th-year medical student at the University of California, San Diego, and her team found a high prevalence of work-related musculoskeletal disorders and pain among surgeons and interventionalists, with pooled prevalence estimates for pain among these physicians ranging from 35% to 60% of all respondents. Cervical spine disease, rotator cuff pathology, and degenerative lumbar spine disease were each reported by nearly one in five respondents in the pooled analyses, with increasing prevalence over the duration of the study period (JAMA Surg. 2017 Dec 27. doi:10.1001/jamasurg.2017.49).
These findings, called “worrisome” by the study’s authors, come at a time when the demand for surgeons and interventionalists is expected soon to outstrip supply, and point to a major stressor for a profession already plagued by high rates of burnout and depression.
The results of the study are in line with previous work that finds a high – and increasing – rate of pain and disability among at-risk physicians, who endure long work hours, awkward positioning, and few opportunities for breaks.
The study also suggested a possible linkage between work-related pain and other factors, such as burnout and depression, that lead to attrition in the surgical profession.
Adrian Park, MD, FACS, a general surgeon who has long studied the issue of work-related musculoskeletal disorders (MSDs) among surgeons and interventionalists, was not surprised by the study’s findings. “This just goes to further the narrative, which is a consistent one: These aren’t just sporadic instances of individual surgeons having a tough time; this is an increasingly broadly recognized problem. ... These are the consequences of surgeons simply getting up and going to work each week,” Dr. Park said in an interview.
To take a long view of the published data on work-related injury and pain for at-risk physicians, Ms. Epstein and her collaborators identified 126 articles reporting physician work-related MSDs that met quality standards; the studies spanned 1974 to 2016, and 23 countries were represented.
A total of 21 articles were eventually included in the meta-analysis, which included responses from 5,828 physicians. Most of the respondents were male (78.5%), with a mean age of 46 years and a mean 12.8 years in practice. The mean number of hours spent in procedures per week was 14.4.
Sixteen cross-sectional studies included in the meta-analysis examined injury prevalence, with 14 studies eventually meeting eligibility criteria for quantitative synthesis. A total of 4,245 physicians were included in this portion of the analysis; 1,232 were orthopedic surgeons, 1,118 were interventional cardiologists, and 582 were general surgeons (a variety of other subspecialties made up the remainder).
The career prevalence of degenerative lumbar spine disease was estimated at 19%, with prevalence increasing over time in a series of surveys of interventional cardiologists, said Ms. Epstein and her colleagues. Among this group, the prevalence climbed from 6.5% in 1997 to 24.7% in 2015, an increase in prevalence of over 18%, they said. The investigators’ estimate of lumbar spine disease prevalence from their own data also showed an increase, to 21%, for studies published within the past decade.
Rotator cuff pathology during the study period was estimated at 18% overall, and carpal tunnel syndrome at 9% overall; carpal tunnel syndrome also appears to be increasing in prevalence, estimated at 12% within the last decade.
Musculoskeletal pain that was judged to be work related was common, as reported in 18 cross-sectional studies. Taken together, the studies used a total of five validated tools that measured both pain prevalence and related disability. Twelve of the studies met criteria for inclusion in the quantitative synthesis.
Neck, back, and shoulder pain were all common in this group of surgeons and interventionalists. Neck pain had a 60% estimated 12-month prevalence, and shoulder pain was almost as common, with a 52% prevalence; back pain was reported for about half (49%) of respondents.
Just 10 of the included studies addressed disability burden, said Ms. Epstein and her colleagues. Overall, 12% of physicians responding in this subset of studies reported that they required work modification, leave of absence, or early retirement because of work-related MSDs.
In a separate arm of the analysis, Ms. Epstein and her collaborators looked at studies that discussed ergonomic assessments and interventions, using a qualitative approach. A total of 101 studies, 50 of them in the United States, were included. None of the studies, they said, “included long-term surveillance for work-related MSDs”; rather, they focused on short-term outcomes and, in some cases, on real-time electromyographic data.
Of the 101 studies looking at ergonomics, about a third (n = 38) looked primarily at ergonomically designed devices or technology, while another third (n = 37) focused on educational or behavioral interventions and modifications. These were the studies included in the investigators’ analysis.
A lack of awareness of ergonomic recommendations on the part of the surgeons themselves was identified in several studies. Several specialties, publishing in a total of eight countries, have put forward “at least one article describing a need for ergonomics education during medical training.” And, said the investigators, “A few studies have found that ergonomics education during medical training appears feasible, accepted, and effective at changing behaviors and reducing symptoms.”
In addition to the usual limitations inherent to the meta-analysis research design (selection bias, self-reported data, small samples of individual studies), the study was limited by the elusive nature of the topic. Work-related pain and disability among surgeons remains underreported and underestimated, according to both Dr. Park and the study investigators. Further research is needed, and the investigators wrote: “Ultimately, this work should be integrated with research on preventing surgeon burnout and attrition given shared risk factors.”
Micro breaks can help
What’s the solution? Dr. Park says that some fixes are low tech, and can be put in place immediately. He and his team implemented a series of brief breaks, taken every half hour during a procedure, that they dubbed “targeted stretching micro breaks.” These are 45- to 50-second breaks during which a series of exercise physiologist–designed brief stretches are undertaken that do not require breaking scrub.
In a study of 66 surgeons and operating room staff, Dr. Park, chair of the department of surgery at Anne Arundel Medical Center, Annapolis, Md., and his collaborators found that surgeons reported less pain and fatigue, and improved mental focus, when they took micro breaks during a procedure. When surgeons took micro breaks, operative time was no longer than when they didn’t take the breaks (Ann Surg. 2017 Feb;265[2]:340-6).
“We do this all the time in our operating room now,” said Dr. Park. “And it makes a difference in terms of pain, in terms of alertness, in terms of stamina. And it costs nothing.”
Major redesign of tools and workspace
Other targets for technological improvement include offering better-designed handles for laparoscopic instruments. “We’ve had one size fits all forever. Why has it taken us so long to recognize that there’s not one size of surgical hand?” asked Dr. Park. He made the point that the influx of women – whose hands are smaller on average than men’s – into the surgical professions makes this a particularly pressing issue.
“The high-tech piece is going to be a better understanding of the operative work flow,” said Dr. Park, calling for “a meaningful revisiting of the surgeon-device interface and the surgeon-patient interface.”
A fundamental redesign of the operating room will eventually be in order, he said, contrasting the surgeon’s environments with that of an airline pilot. In the cockpit, the pilot sees a “heads-up” display of a limited amount of data, with an eye to controlling the cognitive workload for the operator. By contrast, said Dr. Park, in the OR, there are “lights flashing, and things pinging,” and pieces of equipment don’t “talk” to each other, presenting sometimes overwhelming sensory input that just potentiates the stress of the environment. Operating room design, he said, should move toward an ergonomically improved and stimulus-controlled environment.
As the leader of the surgical team, and as a physician whose foremost concern is the patient on the table, the surgeon may inadvertently have fallen into a role where his or her well-being is neglected.
Dr. Park suggested that, in the surgical profession, “it has never felt safe or appropriate to talk about ourselves.” But for the good of the profession, and ultimately for patient care, “this has to change.”
Ms. Epstein and her coauthors reported no conflicts of interest. .
The evidence has been accumulating for decades: Practicing surgery can exact a toll on surgeons’ physical well-being in ways that can shorten careers and contribute to professional dissatisfaction.
“Ergonomists have described the surgeon’s work environment and working conditions as equal to, if not at times harsher than, those of certain industrial workers,” wrote Sherise Epstein, MPH, and the coauthors of the systematic review and meta-analysis of studies addressing the issue. Ms. Epstein, currently a 4th-year medical student at the University of California, San Diego, and her team found a high prevalence of work-related musculoskeletal disorders and pain among surgeons and interventionalists, with pooled prevalence estimates for pain among these physicians ranging from 35% to 60% of all respondents. Cervical spine disease, rotator cuff pathology, and degenerative lumbar spine disease were each reported by nearly one in five respondents in the pooled analyses, with increasing prevalence over the duration of the study period (JAMA Surg. 2017 Dec 27. doi:10.1001/jamasurg.2017.49).
These findings, called “worrisome” by the study’s authors, come at a time when the demand for surgeons and interventionalists is expected soon to outstrip supply, and point to a major stressor for a profession already plagued by high rates of burnout and depression.
The results of the study are in line with previous work that finds a high – and increasing – rate of pain and disability among at-risk physicians, who endure long work hours, awkward positioning, and few opportunities for breaks.
The study also suggested a possible linkage between work-related pain and other factors, such as burnout and depression, that lead to attrition in the surgical profession.
Adrian Park, MD, FACS, a general surgeon who has long studied the issue of work-related musculoskeletal disorders (MSDs) among surgeons and interventionalists, was not surprised by the study’s findings. “This just goes to further the narrative, which is a consistent one: These aren’t just sporadic instances of individual surgeons having a tough time; this is an increasingly broadly recognized problem. ... These are the consequences of surgeons simply getting up and going to work each week,” Dr. Park said in an interview.
To take a long view of the published data on work-related injury and pain for at-risk physicians, Ms. Epstein and her collaborators identified 126 articles reporting physician work-related MSDs that met quality standards; the studies spanned 1974 to 2016, and 23 countries were represented.
A total of 21 articles were eventually included in the meta-analysis, which included responses from 5,828 physicians. Most of the respondents were male (78.5%), with a mean age of 46 years and a mean 12.8 years in practice. The mean number of hours spent in procedures per week was 14.4.
Sixteen cross-sectional studies included in the meta-analysis examined injury prevalence, with 14 studies eventually meeting eligibility criteria for quantitative synthesis. A total of 4,245 physicians were included in this portion of the analysis; 1,232 were orthopedic surgeons, 1,118 were interventional cardiologists, and 582 were general surgeons (a variety of other subspecialties made up the remainder).
The career prevalence of degenerative lumbar spine disease was estimated at 19%, with prevalence increasing over time in a series of surveys of interventional cardiologists, said Ms. Epstein and her colleagues. Among this group, the prevalence climbed from 6.5% in 1997 to 24.7% in 2015, an increase in prevalence of over 18%, they said. The investigators’ estimate of lumbar spine disease prevalence from their own data also showed an increase, to 21%, for studies published within the past decade.
Rotator cuff pathology during the study period was estimated at 18% overall, and carpal tunnel syndrome at 9% overall; carpal tunnel syndrome also appears to be increasing in prevalence, estimated at 12% within the last decade.
Musculoskeletal pain that was judged to be work related was common, as reported in 18 cross-sectional studies. Taken together, the studies used a total of five validated tools that measured both pain prevalence and related disability. Twelve of the studies met criteria for inclusion in the quantitative synthesis.
Neck, back, and shoulder pain were all common in this group of surgeons and interventionalists. Neck pain had a 60% estimated 12-month prevalence, and shoulder pain was almost as common, with a 52% prevalence; back pain was reported for about half (49%) of respondents.
Just 10 of the included studies addressed disability burden, said Ms. Epstein and her colleagues. Overall, 12% of physicians responding in this subset of studies reported that they required work modification, leave of absence, or early retirement because of work-related MSDs.
In a separate arm of the analysis, Ms. Epstein and her collaborators looked at studies that discussed ergonomic assessments and interventions, using a qualitative approach. A total of 101 studies, 50 of them in the United States, were included. None of the studies, they said, “included long-term surveillance for work-related MSDs”; rather, they focused on short-term outcomes and, in some cases, on real-time electromyographic data.
Of the 101 studies looking at ergonomics, about a third (n = 38) looked primarily at ergonomically designed devices or technology, while another third (n = 37) focused on educational or behavioral interventions and modifications. These were the studies included in the investigators’ analysis.
A lack of awareness of ergonomic recommendations on the part of the surgeons themselves was identified in several studies. Several specialties, publishing in a total of eight countries, have put forward “at least one article describing a need for ergonomics education during medical training.” And, said the investigators, “A few studies have found that ergonomics education during medical training appears feasible, accepted, and effective at changing behaviors and reducing symptoms.”
In addition to the usual limitations inherent to the meta-analysis research design (selection bias, self-reported data, small samples of individual studies), the study was limited by the elusive nature of the topic. Work-related pain and disability among surgeons remains underreported and underestimated, according to both Dr. Park and the study investigators. Further research is needed, and the investigators wrote: “Ultimately, this work should be integrated with research on preventing surgeon burnout and attrition given shared risk factors.”
Micro breaks can help
What’s the solution? Dr. Park says that some fixes are low tech, and can be put in place immediately. He and his team implemented a series of brief breaks, taken every half hour during a procedure, that they dubbed “targeted stretching micro breaks.” These are 45- to 50-second breaks during which a series of exercise physiologist–designed brief stretches are undertaken that do not require breaking scrub.
In a study of 66 surgeons and operating room staff, Dr. Park, chair of the department of surgery at Anne Arundel Medical Center, Annapolis, Md., and his collaborators found that surgeons reported less pain and fatigue, and improved mental focus, when they took micro breaks during a procedure. When surgeons took micro breaks, operative time was no longer than when they didn’t take the breaks (Ann Surg. 2017 Feb;265[2]:340-6).
“We do this all the time in our operating room now,” said Dr. Park. “And it makes a difference in terms of pain, in terms of alertness, in terms of stamina. And it costs nothing.”
Major redesign of tools and workspace
Other targets for technological improvement include offering better-designed handles for laparoscopic instruments. “We’ve had one size fits all forever. Why has it taken us so long to recognize that there’s not one size of surgical hand?” asked Dr. Park. He made the point that the influx of women – whose hands are smaller on average than men’s – into the surgical professions makes this a particularly pressing issue.
“The high-tech piece is going to be a better understanding of the operative work flow,” said Dr. Park, calling for “a meaningful revisiting of the surgeon-device interface and the surgeon-patient interface.”
A fundamental redesign of the operating room will eventually be in order, he said, contrasting the surgeon’s environments with that of an airline pilot. In the cockpit, the pilot sees a “heads-up” display of a limited amount of data, with an eye to controlling the cognitive workload for the operator. By contrast, said Dr. Park, in the OR, there are “lights flashing, and things pinging,” and pieces of equipment don’t “talk” to each other, presenting sometimes overwhelming sensory input that just potentiates the stress of the environment. Operating room design, he said, should move toward an ergonomically improved and stimulus-controlled environment.
As the leader of the surgical team, and as a physician whose foremost concern is the patient on the table, the surgeon may inadvertently have fallen into a role where his or her well-being is neglected.
Dr. Park suggested that, in the surgical profession, “it has never felt safe or appropriate to talk about ourselves.” But for the good of the profession, and ultimately for patient care, “this has to change.”
Ms. Epstein and her coauthors reported no conflicts of interest. .
Vascular surgeons are top tier for burnout risk
CHICAGO – Vascular surgeons are solidly within the top tier of surgical subspecialists in terms of risk for burnout, Joan M. Anzia, MD, observed at a symposium on vascular surgery sponsored by Northwestern University.
Joining them in this unwelcome company with an elevated rate of lower quality of life are trauma surgeons, urologists, and otolaryngologists, according to the results of a 9-year-old national study of burnout and career satisfaction among American surgeons that has served as a wakeup call for the profession (Ann Surg. 2009 Sep;250[3]:463-71).
“This is where the biggest impact on burnout is going to be: institutional interventions to target the known drivers of burnout. Looking at nights on call, work compression, looking at the amount of time you guys spend in front of a computer documenting your EHR and your billing. Do you really need to do those things? You need help from midlevel professionals and others who can free you to practice at the top of your life, doing the work you love, which for most surgeons is being in the OR,” said Dr. Anzia, professor of psychiatry and behavioral sciences and the departmental vice chair of education at Northwestern University in Chicago.
The Society for Vascular Surgery is one of many professional specialty organizations that are focusing on the burnout problem. They are joined by the Association of American Medical Colleges, the Accreditation Council for Graduate Medical Education, the National Academy of Medicine, the Liaison Committee on Medical Education, the American Medical Association, and other interested groups.
“Since 2008, burnout rates in every specialty have increased by an average of an absolute 10%. That’s just remarkable, and it’s why people are very, very concerned,” noted the psychiatrist, who serves as the physician health liaison at Northwestern Memorial Hospital. In that capacity, she is frequently called upon to help physicians with the classic manifestations of burnout, including substance use disorders that arose as the practitioners tried to self-treat their burnout rather than seeking help.
“He reports only to the dean,” according to Dr. Anzia.
Why are vascular surgeons at such high risk for burnout? According to the Maslach Burnout Inventory, the leading psychological assessment tool for burnout, the syndrome has three main components: emotional exhaustion, a sense of loss of meaning in work, and feeling ineffective in one’s work. Studies show vascular surgeons often score high in all three domains.
Vascular surgeons’ work is extremely stressful. They average 20 hours per week in the OR, and almost 3 nights on call per week. They care for acutely ill patients and perform high-intensity, high-risk procedures in which unpredictable events are common.
“Work compression – not just workload, but facing multiple demands at once that you’re trying to balance – that’s one of the key drivers of burnout, and work compression is really common in vascular surgery,” Dr. Anzia noted.
In the national surgeon burnout study, younger surgeons and those with children still living at home were at increased risk for burnout. So were surgeons whose compensation was entirely based upon the Relative Value Unit system. The number of nights on call per week was another independent risk factor.
Dr. Shanafelt and his coinvestigators found that roughly 30% of respondent surgeons screened positive for depression, and 6.4% of the study population reported having suicidal thoughts within the past 12 months.
“We lose the equivalent of two to three medical school classes worth of physicians every year to suicide. And let me tell you: 98% of those folks, at the time they suicided, had major depression, which is eminently treatable. And the reason they weren’t treated was they, like most physicians, avoided treatment. They had difficulty accessing care. They were worried about stigma, life insurance, things like that. This is a huge problem which is mostly preventable, but we are not addressing it effectively,” Dr. Anzia said.
While institutional interventions aimed at the prevention of physician burnout such as spending less time on the electronic health record will have a major impact on the problem, thought leaders in medical education have come to realize that it also will be necessary to address the broader culture of medicine.
“There are so many implicit beliefs that every one of us grew up with, like ‘I work when I’m sick,’ or ‘I can work without sleep.’ All those things that we believe make us good physicians actually may not be entirely true,” the psychiatrist said.
She reported having no financial conflicts of interest regarding her presentation.
CHICAGO – Vascular surgeons are solidly within the top tier of surgical subspecialists in terms of risk for burnout, Joan M. Anzia, MD, observed at a symposium on vascular surgery sponsored by Northwestern University.
Joining them in this unwelcome company with an elevated rate of lower quality of life are trauma surgeons, urologists, and otolaryngologists, according to the results of a 9-year-old national study of burnout and career satisfaction among American surgeons that has served as a wakeup call for the profession (Ann Surg. 2009 Sep;250[3]:463-71).
“This is where the biggest impact on burnout is going to be: institutional interventions to target the known drivers of burnout. Looking at nights on call, work compression, looking at the amount of time you guys spend in front of a computer documenting your EHR and your billing. Do you really need to do those things? You need help from midlevel professionals and others who can free you to practice at the top of your life, doing the work you love, which for most surgeons is being in the OR,” said Dr. Anzia, professor of psychiatry and behavioral sciences and the departmental vice chair of education at Northwestern University in Chicago.
The Society for Vascular Surgery is one of many professional specialty organizations that are focusing on the burnout problem. They are joined by the Association of American Medical Colleges, the Accreditation Council for Graduate Medical Education, the National Academy of Medicine, the Liaison Committee on Medical Education, the American Medical Association, and other interested groups.
“Since 2008, burnout rates in every specialty have increased by an average of an absolute 10%. That’s just remarkable, and it’s why people are very, very concerned,” noted the psychiatrist, who serves as the physician health liaison at Northwestern Memorial Hospital. In that capacity, she is frequently called upon to help physicians with the classic manifestations of burnout, including substance use disorders that arose as the practitioners tried to self-treat their burnout rather than seeking help.
“He reports only to the dean,” according to Dr. Anzia.
Why are vascular surgeons at such high risk for burnout? According to the Maslach Burnout Inventory, the leading psychological assessment tool for burnout, the syndrome has three main components: emotional exhaustion, a sense of loss of meaning in work, and feeling ineffective in one’s work. Studies show vascular surgeons often score high in all three domains.
Vascular surgeons’ work is extremely stressful. They average 20 hours per week in the OR, and almost 3 nights on call per week. They care for acutely ill patients and perform high-intensity, high-risk procedures in which unpredictable events are common.
“Work compression – not just workload, but facing multiple demands at once that you’re trying to balance – that’s one of the key drivers of burnout, and work compression is really common in vascular surgery,” Dr. Anzia noted.
In the national surgeon burnout study, younger surgeons and those with children still living at home were at increased risk for burnout. So were surgeons whose compensation was entirely based upon the Relative Value Unit system. The number of nights on call per week was another independent risk factor.
Dr. Shanafelt and his coinvestigators found that roughly 30% of respondent surgeons screened positive for depression, and 6.4% of the study population reported having suicidal thoughts within the past 12 months.
“We lose the equivalent of two to three medical school classes worth of physicians every year to suicide. And let me tell you: 98% of those folks, at the time they suicided, had major depression, which is eminently treatable. And the reason they weren’t treated was they, like most physicians, avoided treatment. They had difficulty accessing care. They were worried about stigma, life insurance, things like that. This is a huge problem which is mostly preventable, but we are not addressing it effectively,” Dr. Anzia said.
While institutional interventions aimed at the prevention of physician burnout such as spending less time on the electronic health record will have a major impact on the problem, thought leaders in medical education have come to realize that it also will be necessary to address the broader culture of medicine.
“There are so many implicit beliefs that every one of us grew up with, like ‘I work when I’m sick,’ or ‘I can work without sleep.’ All those things that we believe make us good physicians actually may not be entirely true,” the psychiatrist said.
She reported having no financial conflicts of interest regarding her presentation.
CHICAGO – Vascular surgeons are solidly within the top tier of surgical subspecialists in terms of risk for burnout, Joan M. Anzia, MD, observed at a symposium on vascular surgery sponsored by Northwestern University.
Joining them in this unwelcome company with an elevated rate of lower quality of life are trauma surgeons, urologists, and otolaryngologists, according to the results of a 9-year-old national study of burnout and career satisfaction among American surgeons that has served as a wakeup call for the profession (Ann Surg. 2009 Sep;250[3]:463-71).
“This is where the biggest impact on burnout is going to be: institutional interventions to target the known drivers of burnout. Looking at nights on call, work compression, looking at the amount of time you guys spend in front of a computer documenting your EHR and your billing. Do you really need to do those things? You need help from midlevel professionals and others who can free you to practice at the top of your life, doing the work you love, which for most surgeons is being in the OR,” said Dr. Anzia, professor of psychiatry and behavioral sciences and the departmental vice chair of education at Northwestern University in Chicago.
The Society for Vascular Surgery is one of many professional specialty organizations that are focusing on the burnout problem. They are joined by the Association of American Medical Colleges, the Accreditation Council for Graduate Medical Education, the National Academy of Medicine, the Liaison Committee on Medical Education, the American Medical Association, and other interested groups.
“Since 2008, burnout rates in every specialty have increased by an average of an absolute 10%. That’s just remarkable, and it’s why people are very, very concerned,” noted the psychiatrist, who serves as the physician health liaison at Northwestern Memorial Hospital. In that capacity, she is frequently called upon to help physicians with the classic manifestations of burnout, including substance use disorders that arose as the practitioners tried to self-treat their burnout rather than seeking help.
“He reports only to the dean,” according to Dr. Anzia.
Why are vascular surgeons at such high risk for burnout? According to the Maslach Burnout Inventory, the leading psychological assessment tool for burnout, the syndrome has three main components: emotional exhaustion, a sense of loss of meaning in work, and feeling ineffective in one’s work. Studies show vascular surgeons often score high in all three domains.
Vascular surgeons’ work is extremely stressful. They average 20 hours per week in the OR, and almost 3 nights on call per week. They care for acutely ill patients and perform high-intensity, high-risk procedures in which unpredictable events are common.
“Work compression – not just workload, but facing multiple demands at once that you’re trying to balance – that’s one of the key drivers of burnout, and work compression is really common in vascular surgery,” Dr. Anzia noted.
In the national surgeon burnout study, younger surgeons and those with children still living at home were at increased risk for burnout. So were surgeons whose compensation was entirely based upon the Relative Value Unit system. The number of nights on call per week was another independent risk factor.
Dr. Shanafelt and his coinvestigators found that roughly 30% of respondent surgeons screened positive for depression, and 6.4% of the study population reported having suicidal thoughts within the past 12 months.
“We lose the equivalent of two to three medical school classes worth of physicians every year to suicide. And let me tell you: 98% of those folks, at the time they suicided, had major depression, which is eminently treatable. And the reason they weren’t treated was they, like most physicians, avoided treatment. They had difficulty accessing care. They were worried about stigma, life insurance, things like that. This is a huge problem which is mostly preventable, but we are not addressing it effectively,” Dr. Anzia said.
While institutional interventions aimed at the prevention of physician burnout such as spending less time on the electronic health record will have a major impact on the problem, thought leaders in medical education have come to realize that it also will be necessary to address the broader culture of medicine.
“There are so many implicit beliefs that every one of us grew up with, like ‘I work when I’m sick,’ or ‘I can work without sleep.’ All those things that we believe make us good physicians actually may not be entirely true,” the psychiatrist said.
She reported having no financial conflicts of interest regarding her presentation.
EXPERT ANALYSIS FROM THE NORTHWESTERN VASCULAR SYMPOSIUM