User login
Four pillars of a successful practice: 2. Attract new patients
Pillar 1: Keep your current patients happy (March 2013)
Dr. Baum describes his number one strategy to retain patients (Audiocast, March 2013)
Pillar 3: Obtain and maintain physician referrals (June 2013)
Pillar 4: Motivate your staff (August 2013)
External marketing is nothing more than making potential patients aware of your service and areas of expertise. The public truly does not mind marketing, as long as it believes you are communicating useful information and providing value. Nevertheless, such marketing—getting the word out to the public and potential referring physicians—takes some physicians out of their comfort zone. Some doctors think that marketing is synonymous with advertising.
The truth is, you can make the public aware of your services and expertise in an ethical and professional fashion without spending large amounts of money on advertising or hiring an expensive consultant.
How?
The essence of external marketing is writing, speaking, and making use of the Internet. In this article, I review simple, inexpensive techniques to increase your visibility among your peers and in your community. These techniques do not require additional staff or anything more than minimal assistance from your hospital’s public relations and marketing departments and the creation of a few PowerPoint slides that will hold the attention of your audience. A future article will describe Internet marketing strategies.
Try your hand at public speaking
Few of us are natural-born orators, but if you get started on the speaking circuit and acquire effective skills, you’ll be amazed at the demand for your presentations and the commensurate number of new patients filling your appointment book. When you take your message to the podium, audiences have an opportunity not only to learn more about your medical topic and how it applies to their health and wellness, but also to interact with you before and after the presentation.
Most of us have been asked to give a presentation to a lay audience at some time or another. How many of us have set off with a PowerPoint presentation from a pharmaceutical company that contains information far too technical for a nonmedical audience? Is it any wonder that so few talks motivate new patients to call our practices?
How to get invited to speak at local events
Even if you have a knack for public speaking, you still need to generate invitations for speaking engagements. I systematically contact meeting planners at various churches, service organizations like the Junior League, women’s book clubs, and patient advocacy groups, such as the American Cancer Society and American Diabetes Association. A list of these organizations and clubs can be obtained from the Chamber of Commerce in your community.
When I began public speaking, I created a public relations packet and sent it to meeting planners in the community. The packet contained a brief biography that outlined my credentials, listed organizations or groups to which I have given talks in the past, and provided a few testimonials from previous audience members. I also included a fact sheet (see the box on this page) and several articles on the topic to be covered. The articles were written by me for local outlets or written by others for publication in national magazines or other lay publications.
After I delivered a talk, I hung around to answer questions. I also made sure to have plenty of business cards to hand out, as well as my practice brochure and articles that pertained to the topic I had just presented.
Overactive bladder: You don’t have to depend on Depends!
Overactive bladder is a common disorder that affects millions of American women and men. Most people who have this condition suffer in silence and do not seek help from a health-care professional. The good news: Most sufferers can be helped.
Overactive bladder:
- affects 33 million American men and women
- can result in reclusive behavior
- can be a source of tremendous embarrassment
- can cause recurrent urinary tract infections
- hinders workplace interactions
- limits personal mobility
- can cause skin infections
- may lead to falls and fractures
- may lead to nursing home institutionalization
- is expensive—economic costs exceeded $35 billion in 2008.
Help is available. No one needs to depend on Depends!
If you would like additional information on this topic, or you are interested in having Dr. Neil Baum speak to your group about overactive bladder and other urologic problems, please call (504) 891-8454 or write to Dr. Baum at [email protected].
Don’t overlook support groups and group appointments
Conducting a support group is an excellent way to target a specific diagnosis or disease state. If you can identify women who have a chronic problem, such as pelvic pain, incontinence, or endometriosis, and invite them to a meeting, you’ll find that they appreciate your interest and expertise and often become patients in your practice. Women who attend these meetings get to know who you are, what you do, and where to find you.
Start by organizing your current patients. I have discovered that it is easiest to start with patients in your own practice when organizing these meetings. These women know others with similar problems and soon invite them to your group.
How to start a support group
Choose a date for your meeting. Keep the following in mind:
- Select a date 2 or 3 months in the future. Decide on several possible alternative dates as well. Don’t choose a date near a major holiday. Because I practice in New Orleans, for example, I would never pick a date a week before or after Mardi Gras.
- Tuesday and Wednesday evenings are the best nights of the week. Most people do not schedule social engagements during the middle of the week.
- If your target audience is senior citizens, they may not be able to attend or drive at night. A Saturday morning or weekday afternoon meeting might be better for them.
- At the meeting, provide a sign-in sheet to record the names and email addresses of all who attend. You can use this list to contact attendees later through an online newsletter.
Within 1 week after your support group presentation, send a follow-up email and appropriate additional information to attendees on your sign-in sheet. The letter should thank them for attending and let them know you are available to answer any questions. You can then add their names to your database and contact them periodically when new treatments or diagnostic techniques become available.
Ethnic communities require special attention
With so many different ethnicities in many US metropolitan areas, you may have an opportunity to attract new patients from these groups. If possible, try to learn to speak the language of the ethnic group you primarily serve—you will have an advantage in attracting foreign-born immigrants if you can speak their language. Alternatively, you can serve their needs by having someone on staff who can translate for you.
Be aware, however, that professional medical interpreters recommend employing a trained medical professional to manage the translation. Without specific training in the language and familiarity with the nuances of translating during a medical examination, diagnostic cues and treatment recommendations may be missed or misinterpreted.
Some translation services specialize in medical translation. You can contact the service and request a translator in nearly any language, including Vietnamese, Russian, Serbian, and Afrikaans, and they will arrange for a translator to arrive at a designated time. The fees are reasonable, and using such a service ensures that you can communicate with patients when neither you nor a staffer speaks the language.
It is still a good idea for you to learn some basic vocabulary, such as greetings, farewells, and the names of body parts. Not only will this make diagnoses more efficient, it will make your patients feel welcome.
Provide translations of your educational materials for patients who are more comfortable with a language besides English. If these materials are not already available from pharmaceutical or medical manufacturing companies, have the most frequently used information translated. The nearest university or college might be a good resource. The language departments at these institutions often can refer you to people who do translations on a freelance basis.
Be sure to add information to your Web site and other social media that makes it clear that you accept patients who speak other languages.
Consider writing articles for lay publications
How many referrals or new patients do you get from articles you have written for professional journals?
There is a good chance that your answer is the same as mine: “None.”
My CV lists nearly 175 articles that have been published in peer-reviewed professional journals, but I have not seen a single referral or new patient as a result. However, I have written several hundred articles for local newspapers and magazines that have generated hundreds of new patient visits to my practice.
Become a media resource: Write, be proactive, be responsive
By writing articles for the local press, you can easily become a media resource. Reporters and editors will notice your pieces. Often they will contact you for articles or ask you for quotations to be included in articles they are writing. If you are responsive, they will keep you in their database as an expert to call on whenever your specialty is in the news.
You can promote this transition yourself. When Whoopi Goldberg shared her experience with urinary incontinence on the television talk show The View, I contacted my local paper, the Times-Picayune, and offered to provide information about the problems of incontinence and overactive bladder and how an outpatient evaluation can often lead to cure of this disease.
What should you write about?
Topics of interest to lay readers in your community undoubtedly include wellness, menopause, cancer prevention, female sexual dysfunction, and vaginal rejuvenation. You can create an interesting article about new procedures, new treatments, a unique case with an excellent result, or the use of new technologies, such as new in-office procedures for permanent contraception.
Like medical skills, writing skills can be learned and polished. The more you do it, the better you get. The better you get, the more women you will attract to your practice.
Use your Web site to attract new patients
For most ObGyns, the majority of patients they serve come from within their community. A clinician’s service area usually encompasses no more than three to five zip codes or a 25- to 50-mile radius. All of us enjoy seeing a patient who has traveled more than 100 miles to see us for a gynecologic problem. Imagine the excitement when a patient from 1,000, 5,000, or even 10,000 miles away contacts your office for an appointment. This is exactly what a Web site can do for you and your practice. (Note: In a future article, I will focus on Internet marketing.)
Blogging offers an opportunity to engage potential patients
If you have a Web site, then you’ve already taken the most critical step toward marketing your practice in an increasingly Internet-savvy age. Today’s patients rely on the Internet for personal health information; they also expect a level of interaction and communication from their clinician on the Web. That’s because popular social media platforms, like Facebook and Twitter, are growing rapidly, enabling patients to use a variety of social media resources for support, education, and treatment decisions. A static Web site that consists only of your practice name, staff biographies, your office address and phone numbers, and a map to guide patients to your practice won’t cut it any longer in terms of patient expectations.
Health-care practitioners are just beginning to embrace social media—Facebook, Twitter, YouTube, and blogging—as an important component of their Internet marketing strategy. Blogging is easy, quick, and free. In many cases, a blog already is integrated with the rest of your professionally designed Web site. To get started, you just need to contribute content to the blog.
Although a blog won’t deliver an instant return on investment, it can, with time, build awareness of your practice and help promote your services to existing and potential patients. Blogs are driven by content, and a blog tied to your practice gives you the freedom to write and publish content that is unique to you and your practice. Written effectively, blogs present the perfect opportunity to interact with your patients while promoting your services.
Blogs also can improve your search engine ranking significantly. By adding new content to your blog on a regular basis, you ensure that search engines “crawl” your site more often. More important, blogs make it possible to dually publish content on other social media sites, functioning as the nucleus of your social media maintenance. Regular posts to your blog can be synced with your Facebook and Twitter accounts for seamless social networking.
Choose a snappy headline
Few patients will read a blog post with a headline that doesn’t entice them in some way. A compelling headline is essential to get your visitor to read the rest of the article and revisit your blog for new posts in the future.
Think of your blog title as a billboard. Consider that you are trying to attract the attention of drivers who have only a few seconds to look at your signage. The same is true for the title of your blog. Visitors often read the title and make a decision about whether to read the rest of the content. For example, an article entitled “Evaluation and treatment of urinary incontinence” probably would not get the eyeballs to stick, compared with a headline like “You don’t have to depend on Depends!” Doctors tend to think conservatively and may generate bland titles more suitable for a medical journal. I suggest that you think more like a tabloid journalist to attract readers to your blog.
Keep blog posts lay-friendly
Because patients will be reading your blog, remember to write for them and not for your colleagues. Be conversational and avoid overusing medical terminology that your readers won’t appreciate or understand. Try to target your writing to the 10th grade level so that you attract both educated and less educated readers. Some blog sites evaluate your writing to determine its grade level and will assist you in keeping your material understandable by most readers.
For example, Writing Sample Analyzer uses syllable counts and sentence length to determine the average grade level of your material (http://sarahktyler.com/code/sam ple.php). And the Readability Calculator at http://www.online-utility.org/english/readability_test_and_improve.jsp is also useful. In general, these tools penalize writers for polysyllabic words and long, complex sentences. Your writing will score higher when you use simpler diction and write short sentences.
Educate, rather than advertise.
Blogs should be used to support your online marketing efforts and provide patients with important information about your practice and services. A blog is not designed to be an advertising tool. Using it as such a tool will cause readers to lose interest fast. If you think education first, your material will be attractive to readers and they may call your office for an appointment.
Some organizational pointers:
- Avoid lengthy blog posts; they can lose reader interest. Pages with a lot of white space are easier to scan and more likely to keep patients reading. Say enough to get your point across, but don’t lose your readers’ attention with irrelevant information.
- Include subheadings and bullet points every few paragraphs so readers can quickly browse your post for the information they want.
Provide fresh, unique content that is new and interesting. Offer advice and tips for improved health, and inform patients about new technology and treatments that are specific to your practice. For example, if you offer a noninvasive approach to a medical problem using a procedure that is new in your community, write a post on this topic and include a testimonial from one of your treated patients. This strategy is very effective at generating new patients.
Don’t let your content get stale
Post to your blog regularly, providing new and updated content. Once you develop an audience, keep them coming back by adhering to a schedule. Every update you make to your blog counts as fresh content—a significant factor search engines use to rank Web sites. I suggest that you consider blogging at a minimum of once a week.
We are in the age of social media. The social media train is leaving the station, and you better get on board. The easiest way to start is by creating and posting regularly on your blog site.
External marketing to attract new patients to your ObGyn practice basically consists of writing and speaking. If you want to market outside your practice, you need to think about putting your writing and speaking skills into action. So, speak up and get your pen or computer working!
We want to hear from you! Tell us what you think.
CLICK HERE to access recent articles on managing your ObGyn practice.
Pillar 1: Keep your current patients happy (March 2013)
Dr. Baum describes his number one strategy to retain patients (Audiocast, March 2013)
Pillar 3: Obtain and maintain physician referrals (June 2013)
Pillar 4: Motivate your staff (August 2013)
External marketing is nothing more than making potential patients aware of your service and areas of expertise. The public truly does not mind marketing, as long as it believes you are communicating useful information and providing value. Nevertheless, such marketing—getting the word out to the public and potential referring physicians—takes some physicians out of their comfort zone. Some doctors think that marketing is synonymous with advertising.
The truth is, you can make the public aware of your services and expertise in an ethical and professional fashion without spending large amounts of money on advertising or hiring an expensive consultant.
How?
The essence of external marketing is writing, speaking, and making use of the Internet. In this article, I review simple, inexpensive techniques to increase your visibility among your peers and in your community. These techniques do not require additional staff or anything more than minimal assistance from your hospital’s public relations and marketing departments and the creation of a few PowerPoint slides that will hold the attention of your audience. A future article will describe Internet marketing strategies.
Try your hand at public speaking
Few of us are natural-born orators, but if you get started on the speaking circuit and acquire effective skills, you’ll be amazed at the demand for your presentations and the commensurate number of new patients filling your appointment book. When you take your message to the podium, audiences have an opportunity not only to learn more about your medical topic and how it applies to their health and wellness, but also to interact with you before and after the presentation.
Most of us have been asked to give a presentation to a lay audience at some time or another. How many of us have set off with a PowerPoint presentation from a pharmaceutical company that contains information far too technical for a nonmedical audience? Is it any wonder that so few talks motivate new patients to call our practices?
How to get invited to speak at local events
Even if you have a knack for public speaking, you still need to generate invitations for speaking engagements. I systematically contact meeting planners at various churches, service organizations like the Junior League, women’s book clubs, and patient advocacy groups, such as the American Cancer Society and American Diabetes Association. A list of these organizations and clubs can be obtained from the Chamber of Commerce in your community.
When I began public speaking, I created a public relations packet and sent it to meeting planners in the community. The packet contained a brief biography that outlined my credentials, listed organizations or groups to which I have given talks in the past, and provided a few testimonials from previous audience members. I also included a fact sheet (see the box on this page) and several articles on the topic to be covered. The articles were written by me for local outlets or written by others for publication in national magazines or other lay publications.
After I delivered a talk, I hung around to answer questions. I also made sure to have plenty of business cards to hand out, as well as my practice brochure and articles that pertained to the topic I had just presented.
Overactive bladder: You don’t have to depend on Depends!
Overactive bladder is a common disorder that affects millions of American women and men. Most people who have this condition suffer in silence and do not seek help from a health-care professional. The good news: Most sufferers can be helped.
Overactive bladder:
- affects 33 million American men and women
- can result in reclusive behavior
- can be a source of tremendous embarrassment
- can cause recurrent urinary tract infections
- hinders workplace interactions
- limits personal mobility
- can cause skin infections
- may lead to falls and fractures
- may lead to nursing home institutionalization
- is expensive—economic costs exceeded $35 billion in 2008.
Help is available. No one needs to depend on Depends!
If you would like additional information on this topic, or you are interested in having Dr. Neil Baum speak to your group about overactive bladder and other urologic problems, please call (504) 891-8454 or write to Dr. Baum at [email protected].
Don’t overlook support groups and group appointments
Conducting a support group is an excellent way to target a specific diagnosis or disease state. If you can identify women who have a chronic problem, such as pelvic pain, incontinence, or endometriosis, and invite them to a meeting, you’ll find that they appreciate your interest and expertise and often become patients in your practice. Women who attend these meetings get to know who you are, what you do, and where to find you.
Start by organizing your current patients. I have discovered that it is easiest to start with patients in your own practice when organizing these meetings. These women know others with similar problems and soon invite them to your group.
How to start a support group
Choose a date for your meeting. Keep the following in mind:
- Select a date 2 or 3 months in the future. Decide on several possible alternative dates as well. Don’t choose a date near a major holiday. Because I practice in New Orleans, for example, I would never pick a date a week before or after Mardi Gras.
- Tuesday and Wednesday evenings are the best nights of the week. Most people do not schedule social engagements during the middle of the week.
- If your target audience is senior citizens, they may not be able to attend or drive at night. A Saturday morning or weekday afternoon meeting might be better for them.
- At the meeting, provide a sign-in sheet to record the names and email addresses of all who attend. You can use this list to contact attendees later through an online newsletter.
Within 1 week after your support group presentation, send a follow-up email and appropriate additional information to attendees on your sign-in sheet. The letter should thank them for attending and let them know you are available to answer any questions. You can then add their names to your database and contact them periodically when new treatments or diagnostic techniques become available.
Ethnic communities require special attention
With so many different ethnicities in many US metropolitan areas, you may have an opportunity to attract new patients from these groups. If possible, try to learn to speak the language of the ethnic group you primarily serve—you will have an advantage in attracting foreign-born immigrants if you can speak their language. Alternatively, you can serve their needs by having someone on staff who can translate for you.
Be aware, however, that professional medical interpreters recommend employing a trained medical professional to manage the translation. Without specific training in the language and familiarity with the nuances of translating during a medical examination, diagnostic cues and treatment recommendations may be missed or misinterpreted.
Some translation services specialize in medical translation. You can contact the service and request a translator in nearly any language, including Vietnamese, Russian, Serbian, and Afrikaans, and they will arrange for a translator to arrive at a designated time. The fees are reasonable, and using such a service ensures that you can communicate with patients when neither you nor a staffer speaks the language.
It is still a good idea for you to learn some basic vocabulary, such as greetings, farewells, and the names of body parts. Not only will this make diagnoses more efficient, it will make your patients feel welcome.
Provide translations of your educational materials for patients who are more comfortable with a language besides English. If these materials are not already available from pharmaceutical or medical manufacturing companies, have the most frequently used information translated. The nearest university or college might be a good resource. The language departments at these institutions often can refer you to people who do translations on a freelance basis.
Be sure to add information to your Web site and other social media that makes it clear that you accept patients who speak other languages.
Consider writing articles for lay publications
How many referrals or new patients do you get from articles you have written for professional journals?
There is a good chance that your answer is the same as mine: “None.”
My CV lists nearly 175 articles that have been published in peer-reviewed professional journals, but I have not seen a single referral or new patient as a result. However, I have written several hundred articles for local newspapers and magazines that have generated hundreds of new patient visits to my practice.
Become a media resource: Write, be proactive, be responsive
By writing articles for the local press, you can easily become a media resource. Reporters and editors will notice your pieces. Often they will contact you for articles or ask you for quotations to be included in articles they are writing. If you are responsive, they will keep you in their database as an expert to call on whenever your specialty is in the news.
You can promote this transition yourself. When Whoopi Goldberg shared her experience with urinary incontinence on the television talk show The View, I contacted my local paper, the Times-Picayune, and offered to provide information about the problems of incontinence and overactive bladder and how an outpatient evaluation can often lead to cure of this disease.
What should you write about?
Topics of interest to lay readers in your community undoubtedly include wellness, menopause, cancer prevention, female sexual dysfunction, and vaginal rejuvenation. You can create an interesting article about new procedures, new treatments, a unique case with an excellent result, or the use of new technologies, such as new in-office procedures for permanent contraception.
Like medical skills, writing skills can be learned and polished. The more you do it, the better you get. The better you get, the more women you will attract to your practice.
Use your Web site to attract new patients
For most ObGyns, the majority of patients they serve come from within their community. A clinician’s service area usually encompasses no more than three to five zip codes or a 25- to 50-mile radius. All of us enjoy seeing a patient who has traveled more than 100 miles to see us for a gynecologic problem. Imagine the excitement when a patient from 1,000, 5,000, or even 10,000 miles away contacts your office for an appointment. This is exactly what a Web site can do for you and your practice. (Note: In a future article, I will focus on Internet marketing.)
Blogging offers an opportunity to engage potential patients
If you have a Web site, then you’ve already taken the most critical step toward marketing your practice in an increasingly Internet-savvy age. Today’s patients rely on the Internet for personal health information; they also expect a level of interaction and communication from their clinician on the Web. That’s because popular social media platforms, like Facebook and Twitter, are growing rapidly, enabling patients to use a variety of social media resources for support, education, and treatment decisions. A static Web site that consists only of your practice name, staff biographies, your office address and phone numbers, and a map to guide patients to your practice won’t cut it any longer in terms of patient expectations.
Health-care practitioners are just beginning to embrace social media—Facebook, Twitter, YouTube, and blogging—as an important component of their Internet marketing strategy. Blogging is easy, quick, and free. In many cases, a blog already is integrated with the rest of your professionally designed Web site. To get started, you just need to contribute content to the blog.
Although a blog won’t deliver an instant return on investment, it can, with time, build awareness of your practice and help promote your services to existing and potential patients. Blogs are driven by content, and a blog tied to your practice gives you the freedom to write and publish content that is unique to you and your practice. Written effectively, blogs present the perfect opportunity to interact with your patients while promoting your services.
Blogs also can improve your search engine ranking significantly. By adding new content to your blog on a regular basis, you ensure that search engines “crawl” your site more often. More important, blogs make it possible to dually publish content on other social media sites, functioning as the nucleus of your social media maintenance. Regular posts to your blog can be synced with your Facebook and Twitter accounts for seamless social networking.
Choose a snappy headline
Few patients will read a blog post with a headline that doesn’t entice them in some way. A compelling headline is essential to get your visitor to read the rest of the article and revisit your blog for new posts in the future.
Think of your blog title as a billboard. Consider that you are trying to attract the attention of drivers who have only a few seconds to look at your signage. The same is true for the title of your blog. Visitors often read the title and make a decision about whether to read the rest of the content. For example, an article entitled “Evaluation and treatment of urinary incontinence” probably would not get the eyeballs to stick, compared with a headline like “You don’t have to depend on Depends!” Doctors tend to think conservatively and may generate bland titles more suitable for a medical journal. I suggest that you think more like a tabloid journalist to attract readers to your blog.
Keep blog posts lay-friendly
Because patients will be reading your blog, remember to write for them and not for your colleagues. Be conversational and avoid overusing medical terminology that your readers won’t appreciate or understand. Try to target your writing to the 10th grade level so that you attract both educated and less educated readers. Some blog sites evaluate your writing to determine its grade level and will assist you in keeping your material understandable by most readers.
For example, Writing Sample Analyzer uses syllable counts and sentence length to determine the average grade level of your material (http://sarahktyler.com/code/sam ple.php). And the Readability Calculator at http://www.online-utility.org/english/readability_test_and_improve.jsp is also useful. In general, these tools penalize writers for polysyllabic words and long, complex sentences. Your writing will score higher when you use simpler diction and write short sentences.
Educate, rather than advertise.
Blogs should be used to support your online marketing efforts and provide patients with important information about your practice and services. A blog is not designed to be an advertising tool. Using it as such a tool will cause readers to lose interest fast. If you think education first, your material will be attractive to readers and they may call your office for an appointment.
Some organizational pointers:
- Avoid lengthy blog posts; they can lose reader interest. Pages with a lot of white space are easier to scan and more likely to keep patients reading. Say enough to get your point across, but don’t lose your readers’ attention with irrelevant information.
- Include subheadings and bullet points every few paragraphs so readers can quickly browse your post for the information they want.
Provide fresh, unique content that is new and interesting. Offer advice and tips for improved health, and inform patients about new technology and treatments that are specific to your practice. For example, if you offer a noninvasive approach to a medical problem using a procedure that is new in your community, write a post on this topic and include a testimonial from one of your treated patients. This strategy is very effective at generating new patients.
Don’t let your content get stale
Post to your blog regularly, providing new and updated content. Once you develop an audience, keep them coming back by adhering to a schedule. Every update you make to your blog counts as fresh content—a significant factor search engines use to rank Web sites. I suggest that you consider blogging at a minimum of once a week.
We are in the age of social media. The social media train is leaving the station, and you better get on board. The easiest way to start is by creating and posting regularly on your blog site.
External marketing to attract new patients to your ObGyn practice basically consists of writing and speaking. If you want to market outside your practice, you need to think about putting your writing and speaking skills into action. So, speak up and get your pen or computer working!
We want to hear from you! Tell us what you think.
CLICK HERE to access recent articles on managing your ObGyn practice.
Pillar 1: Keep your current patients happy (March 2013)
Dr. Baum describes his number one strategy to retain patients (Audiocast, March 2013)
Pillar 3: Obtain and maintain physician referrals (June 2013)
Pillar 4: Motivate your staff (August 2013)
External marketing is nothing more than making potential patients aware of your service and areas of expertise. The public truly does not mind marketing, as long as it believes you are communicating useful information and providing value. Nevertheless, such marketing—getting the word out to the public and potential referring physicians—takes some physicians out of their comfort zone. Some doctors think that marketing is synonymous with advertising.
The truth is, you can make the public aware of your services and expertise in an ethical and professional fashion without spending large amounts of money on advertising or hiring an expensive consultant.
How?
The essence of external marketing is writing, speaking, and making use of the Internet. In this article, I review simple, inexpensive techniques to increase your visibility among your peers and in your community. These techniques do not require additional staff or anything more than minimal assistance from your hospital’s public relations and marketing departments and the creation of a few PowerPoint slides that will hold the attention of your audience. A future article will describe Internet marketing strategies.
Try your hand at public speaking
Few of us are natural-born orators, but if you get started on the speaking circuit and acquire effective skills, you’ll be amazed at the demand for your presentations and the commensurate number of new patients filling your appointment book. When you take your message to the podium, audiences have an opportunity not only to learn more about your medical topic and how it applies to their health and wellness, but also to interact with you before and after the presentation.
Most of us have been asked to give a presentation to a lay audience at some time or another. How many of us have set off with a PowerPoint presentation from a pharmaceutical company that contains information far too technical for a nonmedical audience? Is it any wonder that so few talks motivate new patients to call our practices?
How to get invited to speak at local events
Even if you have a knack for public speaking, you still need to generate invitations for speaking engagements. I systematically contact meeting planners at various churches, service organizations like the Junior League, women’s book clubs, and patient advocacy groups, such as the American Cancer Society and American Diabetes Association. A list of these organizations and clubs can be obtained from the Chamber of Commerce in your community.
When I began public speaking, I created a public relations packet and sent it to meeting planners in the community. The packet contained a brief biography that outlined my credentials, listed organizations or groups to which I have given talks in the past, and provided a few testimonials from previous audience members. I also included a fact sheet (see the box on this page) and several articles on the topic to be covered. The articles were written by me for local outlets or written by others for publication in national magazines or other lay publications.
After I delivered a talk, I hung around to answer questions. I also made sure to have plenty of business cards to hand out, as well as my practice brochure and articles that pertained to the topic I had just presented.
Overactive bladder: You don’t have to depend on Depends!
Overactive bladder is a common disorder that affects millions of American women and men. Most people who have this condition suffer in silence and do not seek help from a health-care professional. The good news: Most sufferers can be helped.
Overactive bladder:
- affects 33 million American men and women
- can result in reclusive behavior
- can be a source of tremendous embarrassment
- can cause recurrent urinary tract infections
- hinders workplace interactions
- limits personal mobility
- can cause skin infections
- may lead to falls and fractures
- may lead to nursing home institutionalization
- is expensive—economic costs exceeded $35 billion in 2008.
Help is available. No one needs to depend on Depends!
If you would like additional information on this topic, or you are interested in having Dr. Neil Baum speak to your group about overactive bladder and other urologic problems, please call (504) 891-8454 or write to Dr. Baum at [email protected].
Don’t overlook support groups and group appointments
Conducting a support group is an excellent way to target a specific diagnosis or disease state. If you can identify women who have a chronic problem, such as pelvic pain, incontinence, or endometriosis, and invite them to a meeting, you’ll find that they appreciate your interest and expertise and often become patients in your practice. Women who attend these meetings get to know who you are, what you do, and where to find you.
Start by organizing your current patients. I have discovered that it is easiest to start with patients in your own practice when organizing these meetings. These women know others with similar problems and soon invite them to your group.
How to start a support group
Choose a date for your meeting. Keep the following in mind:
- Select a date 2 or 3 months in the future. Decide on several possible alternative dates as well. Don’t choose a date near a major holiday. Because I practice in New Orleans, for example, I would never pick a date a week before or after Mardi Gras.
- Tuesday and Wednesday evenings are the best nights of the week. Most people do not schedule social engagements during the middle of the week.
- If your target audience is senior citizens, they may not be able to attend or drive at night. A Saturday morning or weekday afternoon meeting might be better for them.
- At the meeting, provide a sign-in sheet to record the names and email addresses of all who attend. You can use this list to contact attendees later through an online newsletter.
Within 1 week after your support group presentation, send a follow-up email and appropriate additional information to attendees on your sign-in sheet. The letter should thank them for attending and let them know you are available to answer any questions. You can then add their names to your database and contact them periodically when new treatments or diagnostic techniques become available.
Ethnic communities require special attention
With so many different ethnicities in many US metropolitan areas, you may have an opportunity to attract new patients from these groups. If possible, try to learn to speak the language of the ethnic group you primarily serve—you will have an advantage in attracting foreign-born immigrants if you can speak their language. Alternatively, you can serve their needs by having someone on staff who can translate for you.
Be aware, however, that professional medical interpreters recommend employing a trained medical professional to manage the translation. Without specific training in the language and familiarity with the nuances of translating during a medical examination, diagnostic cues and treatment recommendations may be missed or misinterpreted.
Some translation services specialize in medical translation. You can contact the service and request a translator in nearly any language, including Vietnamese, Russian, Serbian, and Afrikaans, and they will arrange for a translator to arrive at a designated time. The fees are reasonable, and using such a service ensures that you can communicate with patients when neither you nor a staffer speaks the language.
It is still a good idea for you to learn some basic vocabulary, such as greetings, farewells, and the names of body parts. Not only will this make diagnoses more efficient, it will make your patients feel welcome.
Provide translations of your educational materials for patients who are more comfortable with a language besides English. If these materials are not already available from pharmaceutical or medical manufacturing companies, have the most frequently used information translated. The nearest university or college might be a good resource. The language departments at these institutions often can refer you to people who do translations on a freelance basis.
Be sure to add information to your Web site and other social media that makes it clear that you accept patients who speak other languages.
Consider writing articles for lay publications
How many referrals or new patients do you get from articles you have written for professional journals?
There is a good chance that your answer is the same as mine: “None.”
My CV lists nearly 175 articles that have been published in peer-reviewed professional journals, but I have not seen a single referral or new patient as a result. However, I have written several hundred articles for local newspapers and magazines that have generated hundreds of new patient visits to my practice.
Become a media resource: Write, be proactive, be responsive
By writing articles for the local press, you can easily become a media resource. Reporters and editors will notice your pieces. Often they will contact you for articles or ask you for quotations to be included in articles they are writing. If you are responsive, they will keep you in their database as an expert to call on whenever your specialty is in the news.
You can promote this transition yourself. When Whoopi Goldberg shared her experience with urinary incontinence on the television talk show The View, I contacted my local paper, the Times-Picayune, and offered to provide information about the problems of incontinence and overactive bladder and how an outpatient evaluation can often lead to cure of this disease.
What should you write about?
Topics of interest to lay readers in your community undoubtedly include wellness, menopause, cancer prevention, female sexual dysfunction, and vaginal rejuvenation. You can create an interesting article about new procedures, new treatments, a unique case with an excellent result, or the use of new technologies, such as new in-office procedures for permanent contraception.
Like medical skills, writing skills can be learned and polished. The more you do it, the better you get. The better you get, the more women you will attract to your practice.
Use your Web site to attract new patients
For most ObGyns, the majority of patients they serve come from within their community. A clinician’s service area usually encompasses no more than three to five zip codes or a 25- to 50-mile radius. All of us enjoy seeing a patient who has traveled more than 100 miles to see us for a gynecologic problem. Imagine the excitement when a patient from 1,000, 5,000, or even 10,000 miles away contacts your office for an appointment. This is exactly what a Web site can do for you and your practice. (Note: In a future article, I will focus on Internet marketing.)
Blogging offers an opportunity to engage potential patients
If you have a Web site, then you’ve already taken the most critical step toward marketing your practice in an increasingly Internet-savvy age. Today’s patients rely on the Internet for personal health information; they also expect a level of interaction and communication from their clinician on the Web. That’s because popular social media platforms, like Facebook and Twitter, are growing rapidly, enabling patients to use a variety of social media resources for support, education, and treatment decisions. A static Web site that consists only of your practice name, staff biographies, your office address and phone numbers, and a map to guide patients to your practice won’t cut it any longer in terms of patient expectations.
Health-care practitioners are just beginning to embrace social media—Facebook, Twitter, YouTube, and blogging—as an important component of their Internet marketing strategy. Blogging is easy, quick, and free. In many cases, a blog already is integrated with the rest of your professionally designed Web site. To get started, you just need to contribute content to the blog.
Although a blog won’t deliver an instant return on investment, it can, with time, build awareness of your practice and help promote your services to existing and potential patients. Blogs are driven by content, and a blog tied to your practice gives you the freedom to write and publish content that is unique to you and your practice. Written effectively, blogs present the perfect opportunity to interact with your patients while promoting your services.
Blogs also can improve your search engine ranking significantly. By adding new content to your blog on a regular basis, you ensure that search engines “crawl” your site more often. More important, blogs make it possible to dually publish content on other social media sites, functioning as the nucleus of your social media maintenance. Regular posts to your blog can be synced with your Facebook and Twitter accounts for seamless social networking.
Choose a snappy headline
Few patients will read a blog post with a headline that doesn’t entice them in some way. A compelling headline is essential to get your visitor to read the rest of the article and revisit your blog for new posts in the future.
Think of your blog title as a billboard. Consider that you are trying to attract the attention of drivers who have only a few seconds to look at your signage. The same is true for the title of your blog. Visitors often read the title and make a decision about whether to read the rest of the content. For example, an article entitled “Evaluation and treatment of urinary incontinence” probably would not get the eyeballs to stick, compared with a headline like “You don’t have to depend on Depends!” Doctors tend to think conservatively and may generate bland titles more suitable for a medical journal. I suggest that you think more like a tabloid journalist to attract readers to your blog.
Keep blog posts lay-friendly
Because patients will be reading your blog, remember to write for them and not for your colleagues. Be conversational and avoid overusing medical terminology that your readers won’t appreciate or understand. Try to target your writing to the 10th grade level so that you attract both educated and less educated readers. Some blog sites evaluate your writing to determine its grade level and will assist you in keeping your material understandable by most readers.
For example, Writing Sample Analyzer uses syllable counts and sentence length to determine the average grade level of your material (http://sarahktyler.com/code/sam ple.php). And the Readability Calculator at http://www.online-utility.org/english/readability_test_and_improve.jsp is also useful. In general, these tools penalize writers for polysyllabic words and long, complex sentences. Your writing will score higher when you use simpler diction and write short sentences.
Educate, rather than advertise.
Blogs should be used to support your online marketing efforts and provide patients with important information about your practice and services. A blog is not designed to be an advertising tool. Using it as such a tool will cause readers to lose interest fast. If you think education first, your material will be attractive to readers and they may call your office for an appointment.
Some organizational pointers:
- Avoid lengthy blog posts; they can lose reader interest. Pages with a lot of white space are easier to scan and more likely to keep patients reading. Say enough to get your point across, but don’t lose your readers’ attention with irrelevant information.
- Include subheadings and bullet points every few paragraphs so readers can quickly browse your post for the information they want.
Provide fresh, unique content that is new and interesting. Offer advice and tips for improved health, and inform patients about new technology and treatments that are specific to your practice. For example, if you offer a noninvasive approach to a medical problem using a procedure that is new in your community, write a post on this topic and include a testimonial from one of your treated patients. This strategy is very effective at generating new patients.
Don’t let your content get stale
Post to your blog regularly, providing new and updated content. Once you develop an audience, keep them coming back by adhering to a schedule. Every update you make to your blog counts as fresh content—a significant factor search engines use to rank Web sites. I suggest that you consider blogging at a minimum of once a week.
We are in the age of social media. The social media train is leaving the station, and you better get on board. The easiest way to start is by creating and posting regularly on your blog site.
External marketing to attract new patients to your ObGyn practice basically consists of writing and speaking. If you want to market outside your practice, you need to think about putting your writing and speaking skills into action. So, speak up and get your pen or computer working!
We want to hear from you! Tell us what you think.
CLICK HERE to access recent articles on managing your ObGyn practice.
Drive Change in an ACO
From informal polls I’ve recently conducted of hospitalists, many are not even aware they are part of an accountable-care organization (ACO). And if they are aware, they might not be engaging in meaningful dialogue with ACO leaders about their role in these organizations. But, in the long term, ACOs will need to bring hospitalists to the table in order to be successful.
Are You Part of an ACO?
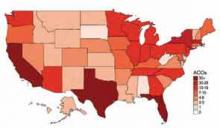
David Muhlestein, who blogs for Health Affairs, tracks the growth of ACOs around the country. He states that, as of Jan. 31, there were 428 ACOs in the U.S. (see Figure 1).1 In terms of numbers, Florida, Texas, and California lead the nation with 42, 33, and 46 ACOs, respectively. So it is likely that you are part of an ACO. If you are unsure, ask your chief medical officer or president of the medical staff.
How ACOs Work
All ACOs seek to manage a group, or population, of patients as efficiently as possible while maintaining or improving quality of care. For Medicare ACOs, the goal is to bring together hospitals and physicians in order to share savings derived from efficiencies in care. But before any savings can be shared, the Medicare ACO must demonstrate that it achieved high-quality care across four domains, totaling 33 individual quality measures. (see Table 1)
Main Flavors of ACOs
There are two types of ACOs: private ACOs and Medicare ACOs. Prior to Medicare ACOs, which were launched in January 2012, there were 150 private-sector ACOs, and this number continues to grow. Private ACOs represent a heterogeneous group in terms of reimbursement model. Some operate under shared savings programs; others use full or partial capitation, bundled payments, and/or other types of arrangements. But nearly all ACOs operate under the premise that the incentives used to make care more efficient and less costly can only be applied if measurable quality is maintained or improved. ACOs do not pay doctors or hospitals more unless high quality is demonstrated.
ACO Quality Measures and Hospitalists
Most of the 33 quality measures required by Medicare ACOs are based in ambulatory practice. These include measures related to blood pressure, immunizations, cancer, and fall-risk screening, and measures for diabetics, such as lipids and hemoglobin A1C. However, there are a few measures for which hospitalists should share in accountability, including:
- All-cause hospital readmission rate—risk-standardized;
- Ambulatory sensitive condition hospital admission rates (CHF, COPD); and
- Medication reconciliation after discharge from an inpatient facility.
Four Key Actions for Hospitalists
Hospitalists make a significant contribution to the quality and the financial performance of ACOs. In addition to the quality metrics cited above, hospitalists impact the inpatient portion of the overall population’s cost of care. Furthermore, hospitalists are vital partners in the care coordination required for an ACO to be successful.
Here are four actions I suggest taking in order for your hospitalist group to be effective as participants in an ACO:
- Have a representative from your group participate in ACO committees that address hospital utilization and related matters, such as care coordination impacting pre- and post-hospital care.
- Learn how to work with ACO case managers on care transitions, including post-discharge follow-up and information transfer.
- Understand an ACO’s approach to engagement of and coordination with post-acute-care facilities. The ability of a post-acute facility, such a skilled nursing facility, to accept patients who have complex care needs, to manage changes in condition in the facility when appropriate, and to send complete information upon transfer to the hospital are important strategies for an ACO’s success.
- Understand how an ACO reports quality and cost performance and how savings will be shared among participants.
Mindset Change
If hospitalists are part of the chain of ACO physicians and providers held accountable for the health of a population of patients, we must work more closely with the medical home/neighborhood, post-acute-care facilities, and home-care providers. The change in mindset will occur only if we have a set of tools to get the job done, such as case managers and information technology, and the appropriate incentives to support better care coordination. I encourage my fellow hospitalists to make things happen, instead of taking a passive role in this monumental transformation.
Reference
Dr. Whitcomb is medical director of healthcare quality at Baystate Medical Center in Springfield, Mass. He is a co-founder and past president of SHM. Email him at [email protected].
From informal polls I’ve recently conducted of hospitalists, many are not even aware they are part of an accountable-care organization (ACO). And if they are aware, they might not be engaging in meaningful dialogue with ACO leaders about their role in these organizations. But, in the long term, ACOs will need to bring hospitalists to the table in order to be successful.
Are You Part of an ACO?
David Muhlestein, who blogs for Health Affairs, tracks the growth of ACOs around the country. He states that, as of Jan. 31, there were 428 ACOs in the U.S. (see Figure 1).1 In terms of numbers, Florida, Texas, and California lead the nation with 42, 33, and 46 ACOs, respectively. So it is likely that you are part of an ACO. If you are unsure, ask your chief medical officer or president of the medical staff.
How ACOs Work
All ACOs seek to manage a group, or population, of patients as efficiently as possible while maintaining or improving quality of care. For Medicare ACOs, the goal is to bring together hospitals and physicians in order to share savings derived from efficiencies in care. But before any savings can be shared, the Medicare ACO must demonstrate that it achieved high-quality care across four domains, totaling 33 individual quality measures. (see Table 1)
Main Flavors of ACOs
There are two types of ACOs: private ACOs and Medicare ACOs. Prior to Medicare ACOs, which were launched in January 2012, there were 150 private-sector ACOs, and this number continues to grow. Private ACOs represent a heterogeneous group in terms of reimbursement model. Some operate under shared savings programs; others use full or partial capitation, bundled payments, and/or other types of arrangements. But nearly all ACOs operate under the premise that the incentives used to make care more efficient and less costly can only be applied if measurable quality is maintained or improved. ACOs do not pay doctors or hospitals more unless high quality is demonstrated.
ACO Quality Measures and Hospitalists
Most of the 33 quality measures required by Medicare ACOs are based in ambulatory practice. These include measures related to blood pressure, immunizations, cancer, and fall-risk screening, and measures for diabetics, such as lipids and hemoglobin A1C. However, there are a few measures for which hospitalists should share in accountability, including:
- All-cause hospital readmission rate—risk-standardized;
- Ambulatory sensitive condition hospital admission rates (CHF, COPD); and
- Medication reconciliation after discharge from an inpatient facility.
Four Key Actions for Hospitalists
Hospitalists make a significant contribution to the quality and the financial performance of ACOs. In addition to the quality metrics cited above, hospitalists impact the inpatient portion of the overall population’s cost of care. Furthermore, hospitalists are vital partners in the care coordination required for an ACO to be successful.
Here are four actions I suggest taking in order for your hospitalist group to be effective as participants in an ACO:
- Have a representative from your group participate in ACO committees that address hospital utilization and related matters, such as care coordination impacting pre- and post-hospital care.
- Learn how to work with ACO case managers on care transitions, including post-discharge follow-up and information transfer.
- Understand an ACO’s approach to engagement of and coordination with post-acute-care facilities. The ability of a post-acute facility, such a skilled nursing facility, to accept patients who have complex care needs, to manage changes in condition in the facility when appropriate, and to send complete information upon transfer to the hospital are important strategies for an ACO’s success.
- Understand how an ACO reports quality and cost performance and how savings will be shared among participants.
Mindset Change
If hospitalists are part of the chain of ACO physicians and providers held accountable for the health of a population of patients, we must work more closely with the medical home/neighborhood, post-acute-care facilities, and home-care providers. The change in mindset will occur only if we have a set of tools to get the job done, such as case managers and information technology, and the appropriate incentives to support better care coordination. I encourage my fellow hospitalists to make things happen, instead of taking a passive role in this monumental transformation.
Reference
Dr. Whitcomb is medical director of healthcare quality at Baystate Medical Center in Springfield, Mass. He is a co-founder and past president of SHM. Email him at [email protected].
From informal polls I’ve recently conducted of hospitalists, many are not even aware they are part of an accountable-care organization (ACO). And if they are aware, they might not be engaging in meaningful dialogue with ACO leaders about their role in these organizations. But, in the long term, ACOs will need to bring hospitalists to the table in order to be successful.
Are You Part of an ACO?
David Muhlestein, who blogs for Health Affairs, tracks the growth of ACOs around the country. He states that, as of Jan. 31, there were 428 ACOs in the U.S. (see Figure 1).1 In terms of numbers, Florida, Texas, and California lead the nation with 42, 33, and 46 ACOs, respectively. So it is likely that you are part of an ACO. If you are unsure, ask your chief medical officer or president of the medical staff.
How ACOs Work
All ACOs seek to manage a group, or population, of patients as efficiently as possible while maintaining or improving quality of care. For Medicare ACOs, the goal is to bring together hospitals and physicians in order to share savings derived from efficiencies in care. But before any savings can be shared, the Medicare ACO must demonstrate that it achieved high-quality care across four domains, totaling 33 individual quality measures. (see Table 1)
Main Flavors of ACOs
There are two types of ACOs: private ACOs and Medicare ACOs. Prior to Medicare ACOs, which were launched in January 2012, there were 150 private-sector ACOs, and this number continues to grow. Private ACOs represent a heterogeneous group in terms of reimbursement model. Some operate under shared savings programs; others use full or partial capitation, bundled payments, and/or other types of arrangements. But nearly all ACOs operate under the premise that the incentives used to make care more efficient and less costly can only be applied if measurable quality is maintained or improved. ACOs do not pay doctors or hospitals more unless high quality is demonstrated.
ACO Quality Measures and Hospitalists
Most of the 33 quality measures required by Medicare ACOs are based in ambulatory practice. These include measures related to blood pressure, immunizations, cancer, and fall-risk screening, and measures for diabetics, such as lipids and hemoglobin A1C. However, there are a few measures for which hospitalists should share in accountability, including:
- All-cause hospital readmission rate—risk-standardized;
- Ambulatory sensitive condition hospital admission rates (CHF, COPD); and
- Medication reconciliation after discharge from an inpatient facility.
Four Key Actions for Hospitalists
Hospitalists make a significant contribution to the quality and the financial performance of ACOs. In addition to the quality metrics cited above, hospitalists impact the inpatient portion of the overall population’s cost of care. Furthermore, hospitalists are vital partners in the care coordination required for an ACO to be successful.
Here are four actions I suggest taking in order for your hospitalist group to be effective as participants in an ACO:
- Have a representative from your group participate in ACO committees that address hospital utilization and related matters, such as care coordination impacting pre- and post-hospital care.
- Learn how to work with ACO case managers on care transitions, including post-discharge follow-up and information transfer.
- Understand an ACO’s approach to engagement of and coordination with post-acute-care facilities. The ability of a post-acute facility, such a skilled nursing facility, to accept patients who have complex care needs, to manage changes in condition in the facility when appropriate, and to send complete information upon transfer to the hospital are important strategies for an ACO’s success.
- Understand how an ACO reports quality and cost performance and how savings will be shared among participants.
Mindset Change
If hospitalists are part of the chain of ACO physicians and providers held accountable for the health of a population of patients, we must work more closely with the medical home/neighborhood, post-acute-care facilities, and home-care providers. The change in mindset will occur only if we have a set of tools to get the job done, such as case managers and information technology, and the appropriate incentives to support better care coordination. I encourage my fellow hospitalists to make things happen, instead of taking a passive role in this monumental transformation.
Reference
Dr. Whitcomb is medical director of healthcare quality at Baystate Medical Center in Springfield, Mass. He is a co-founder and past president of SHM. Email him at [email protected].
Should I retire early?
Much has been written of the widespread concern among America’s physicians over upcoming changes in our health care system. Dire predictions of impending doom have prompted many to consider early retirement.
I do not share such concerns, for what that is worth; but if you do, and you are serious about retiring sooner than planned, now would be a great time to take a close look at your financial situation.
Many doctors have a false sense of security about their money; most of us save too little. We either miscalculate or underestimate how much we’ll need to last through retirement.
We tend to live longer than we think we will, and as such we run the risk of outliving our savings. And we don’t face facts about long-term care. Not nearly enough of us have long-term care insurance, or the means to self-fund an extended long-term care situation.
Many people lack a clear idea of where their retirement income will come from, and even when they do, they don’t know how to manage their savings correctly. Doctors in particular are notorious for not understanding investments. Many attempt to manage their practice’s retirement plans with inadequate knowledge of how the investments within their plans work.
So how will you know if you can safely retire before Obamacare gets up to speed? Of course, as with everything else, it depends. But to arrive at any sort of reliable ballpark figure, you’ll need to know three things: (1) how much you realistically expect to spend annually after retirement; (2) how much principal you will need to generate that annual income; and (3) how far your present savings are from that target figure.
An oft-quoted rule of thumb is that in retirement you should plan to spend about 70% of what you are spending now. In my opinion, that’s nonsense. While a few significant expenses, such as disability and malpractice insurance premiums, will be eliminated, other expenses, such as travel, recreation, and medical care (including long-term care insurance, which no one should be without), will increase. My wife and I are assuming we will spend about the same in retirement as we spend now, and I suggest you do too.
Once you know how much money you will spend per year, you can calculate how much money – in interest- and dividend-producing assets – will be needed to generate that amount.
Ideally, you will want to spend only the interest and dividends; by leaving the principal untouched you will never run short, even if you retire at an unusually young age, or longevity runs in your family (or both). Most financial advisers use the 5% rule: You can safely assume a minimum average of 5% annual return on your nest egg. So if you want to spend $100,000 per year, you will need $2 million in assets; for $200,000, you’ll need $4 million.
This is where you may discover – if your present savings are a long way from your target figure – that early retirement is not a realistic option. Better, though, to make that unpleasant discovery now, rather than face the frightening prospect of running out of money at an advanced age. Don’t be tempted to close a wide gap in a hurry with high-return/high-risk investments, which often backfire, leaving you further than ever from retirement.
Of course, it goes without saying that debt can destroy the best-laid retirement plans. If you carry significant debt, pay it off as soon as possible, and certainly before you retire.
Even if you have no plans to retire in the immediate future, it is never too soon to think about retirement. Young physicians often defer contributing to their retirement plans because they want to save for a new house, or college for their children. But there are tangible tax benefits that you get now, because your contributions usually reduce your taxable income, and your investment grows tax-free until you take it out.
For long-term planning, the most foolproof strategy – seldom employed, because it’s boring – is to sock away a fixed amount per month (after your retirement plan has been funded) in a mutual fund. For example, $1,000 per month for 25 years with the market earning 10% overall comes to almost $2 million, with the power of compounded interest working for you.
Dr. Eastern practices dermatology and dermatologic surgery in Belleville, N.J.
Much has been written of the widespread concern among America’s physicians over upcoming changes in our health care system. Dire predictions of impending doom have prompted many to consider early retirement.
I do not share such concerns, for what that is worth; but if you do, and you are serious about retiring sooner than planned, now would be a great time to take a close look at your financial situation.
Many doctors have a false sense of security about their money; most of us save too little. We either miscalculate or underestimate how much we’ll need to last through retirement.
We tend to live longer than we think we will, and as such we run the risk of outliving our savings. And we don’t face facts about long-term care. Not nearly enough of us have long-term care insurance, or the means to self-fund an extended long-term care situation.
Many people lack a clear idea of where their retirement income will come from, and even when they do, they don’t know how to manage their savings correctly. Doctors in particular are notorious for not understanding investments. Many attempt to manage their practice’s retirement plans with inadequate knowledge of how the investments within their plans work.
So how will you know if you can safely retire before Obamacare gets up to speed? Of course, as with everything else, it depends. But to arrive at any sort of reliable ballpark figure, you’ll need to know three things: (1) how much you realistically expect to spend annually after retirement; (2) how much principal you will need to generate that annual income; and (3) how far your present savings are from that target figure.
An oft-quoted rule of thumb is that in retirement you should plan to spend about 70% of what you are spending now. In my opinion, that’s nonsense. While a few significant expenses, such as disability and malpractice insurance premiums, will be eliminated, other expenses, such as travel, recreation, and medical care (including long-term care insurance, which no one should be without), will increase. My wife and I are assuming we will spend about the same in retirement as we spend now, and I suggest you do too.
Once you know how much money you will spend per year, you can calculate how much money – in interest- and dividend-producing assets – will be needed to generate that amount.
Ideally, you will want to spend only the interest and dividends; by leaving the principal untouched you will never run short, even if you retire at an unusually young age, or longevity runs in your family (or both). Most financial advisers use the 5% rule: You can safely assume a minimum average of 5% annual return on your nest egg. So if you want to spend $100,000 per year, you will need $2 million in assets; for $200,000, you’ll need $4 million.
This is where you may discover – if your present savings are a long way from your target figure – that early retirement is not a realistic option. Better, though, to make that unpleasant discovery now, rather than face the frightening prospect of running out of money at an advanced age. Don’t be tempted to close a wide gap in a hurry with high-return/high-risk investments, which often backfire, leaving you further than ever from retirement.
Of course, it goes without saying that debt can destroy the best-laid retirement plans. If you carry significant debt, pay it off as soon as possible, and certainly before you retire.
Even if you have no plans to retire in the immediate future, it is never too soon to think about retirement. Young physicians often defer contributing to their retirement plans because they want to save for a new house, or college for their children. But there are tangible tax benefits that you get now, because your contributions usually reduce your taxable income, and your investment grows tax-free until you take it out.
For long-term planning, the most foolproof strategy – seldom employed, because it’s boring – is to sock away a fixed amount per month (after your retirement plan has been funded) in a mutual fund. For example, $1,000 per month for 25 years with the market earning 10% overall comes to almost $2 million, with the power of compounded interest working for you.
Dr. Eastern practices dermatology and dermatologic surgery in Belleville, N.J.
Much has been written of the widespread concern among America’s physicians over upcoming changes in our health care system. Dire predictions of impending doom have prompted many to consider early retirement.
I do not share such concerns, for what that is worth; but if you do, and you are serious about retiring sooner than planned, now would be a great time to take a close look at your financial situation.
Many doctors have a false sense of security about their money; most of us save too little. We either miscalculate or underestimate how much we’ll need to last through retirement.
We tend to live longer than we think we will, and as such we run the risk of outliving our savings. And we don’t face facts about long-term care. Not nearly enough of us have long-term care insurance, or the means to self-fund an extended long-term care situation.
Many people lack a clear idea of where their retirement income will come from, and even when they do, they don’t know how to manage their savings correctly. Doctors in particular are notorious for not understanding investments. Many attempt to manage their practice’s retirement plans with inadequate knowledge of how the investments within their plans work.
So how will you know if you can safely retire before Obamacare gets up to speed? Of course, as with everything else, it depends. But to arrive at any sort of reliable ballpark figure, you’ll need to know three things: (1) how much you realistically expect to spend annually after retirement; (2) how much principal you will need to generate that annual income; and (3) how far your present savings are from that target figure.
An oft-quoted rule of thumb is that in retirement you should plan to spend about 70% of what you are spending now. In my opinion, that’s nonsense. While a few significant expenses, such as disability and malpractice insurance premiums, will be eliminated, other expenses, such as travel, recreation, and medical care (including long-term care insurance, which no one should be without), will increase. My wife and I are assuming we will spend about the same in retirement as we spend now, and I suggest you do too.
Once you know how much money you will spend per year, you can calculate how much money – in interest- and dividend-producing assets – will be needed to generate that amount.
Ideally, you will want to spend only the interest and dividends; by leaving the principal untouched you will never run short, even if you retire at an unusually young age, or longevity runs in your family (or both). Most financial advisers use the 5% rule: You can safely assume a minimum average of 5% annual return on your nest egg. So if you want to spend $100,000 per year, you will need $2 million in assets; for $200,000, you’ll need $4 million.
This is where you may discover – if your present savings are a long way from your target figure – that early retirement is not a realistic option. Better, though, to make that unpleasant discovery now, rather than face the frightening prospect of running out of money at an advanced age. Don’t be tempted to close a wide gap in a hurry with high-return/high-risk investments, which often backfire, leaving you further than ever from retirement.
Of course, it goes without saying that debt can destroy the best-laid retirement plans. If you carry significant debt, pay it off as soon as possible, and certainly before you retire.
Even if you have no plans to retire in the immediate future, it is never too soon to think about retirement. Young physicians often defer contributing to their retirement plans because they want to save for a new house, or college for their children. But there are tangible tax benefits that you get now, because your contributions usually reduce your taxable income, and your investment grows tax-free until you take it out.
For long-term planning, the most foolproof strategy – seldom employed, because it’s boring – is to sock away a fixed amount per month (after your retirement plan has been funded) in a mutual fund. For example, $1,000 per month for 25 years with the market earning 10% overall comes to almost $2 million, with the power of compounded interest working for you.
Dr. Eastern practices dermatology and dermatologic surgery in Belleville, N.J.
SHM Tallies Ratio of Hospital Respondents' Observation Admissions to Inpatient Admission Encounters
SHM added a new item to its 2012 State of Hospital Medicine report: the ratio of respondents’ observation admissions to inpatient admission encounters. This metric was added because observation encounters have been increasing, with financial effects on hospitals and patients. SHM survey respondents reported a 20% observation rate for both adult and pediatric practice groups (see Figure 1).
Under observation status, services that used to be billed as inpatient status (e.g. chest pain evaluation, treatment of asthma exacerbation) must be billed by the hospital at much lower outpatient rates. Some hospitals have responded to this financial pressure by creating observation units or making other operational adjustments. One recent analysis suggested that nationwide adoption of such efforts could save billions of dollars.1
Becoming lean enough to do short work in short time, though, does not address all of the observation-related issues facing hospitals. When the Centers for Medicare & Medicaid Services’ (CMS) Recovery Audit Contractors (RACs) determine retrospectively that an inpatient admission should have been an observation encounter, the hospital’s payment is not downgraded but forfeited.2 This development has prompted hospitals to preemptively opt for observation status for certain patients. Case managers and providers increasingly are spending time reviewing inpatient versus observation status throughout a patient’s stay. Many hospitals have turned to third-party contractors to help review observation status.
Observation status has financial implications for patients as well. In the past year, USA Today, The Wall Street Journal, and CNN Money all have reported on patients hit with unexpected out-of-pocket expenses related to observation care.3,4,5 A common theme: Medicare patient hospitalized with an acute fracture, managed nonoperatively but requiring rehabilitation prior to returning home. These patients found out too late that observation, a status they were often unaware of, did not qualify for CMS’ three-day inpatient requirement to cover rehabilitation costs. Some patients were charged exorbitant prices for noncovered “outpatient” services, such as providing their routine medications.
Advocacy groups have joined the fray on patients’ behalf, and legal challenges have ensued. AARP and others are educating patients about observation status—and their right to challenge it. The Center for Medicare Advocacy (www.kslaw.com/Library/publication/HH111411_Bagnall.pdf) has filed a lawsuit against the U.S. Department of Health and Human Services on behalf of patients hit with uncovered rehabilitation costs, and the American Hospital Association has teamed with several hospitals to sue over funds forfeited in RAC audits (www.aha.org/content/12/121101-aha-hhs-medicare-com.pdf). Both houses of Congress have legislation (H.R. 1543 and S. 818) seeking to count observation days toward the Medicare three-day rule. For its part, CMS has promised to review observation status and, hopefully, clarify the rules.
Hospitalists, meanwhile, are gearing up for more observation care. The 2012 State of Hospital Medicine report shows that 37% of adult groups and 28% of pediatric groups reported having primary responsibility for observation or short-stay units. My own hospital runs both a clinical decision unit in the ED and a short-stay unit staffed by our hospitalist group. As SHM tracks observation status in future surveys, HM groups will be able to follow this phenomenon among their colleagues and benchmark their own rates of observation encounters.
Dr. Creamer is medical director of the short-stay unit at MetroHealth Medical Center in Cleveland and a member of SHM’s Practice Analysis Committee.
References
- Feng Z, Wright DB, Mor V. Sharp rise in Medicare enrollees being held in hospitals for observation raises concerns about causes and consequences. Health Aff (Millwood). 2012;31(6):1251-1259.
- Baugh CW, Venkatesh AK, Hilton JA, Samuel PA, Schuur JD, Bohan JS. Making greater use of dedicated hospital observation units for many short-stay patients could save $3.1 billion a year. Health Aff (Millwood). 2012;31(10):2314-2323.
- Gengler A. The painful new trend in Medicare. CNN Money website. Available at: http://money.cnn.com/2012/08/07/pf/medicare-rehab-costs.moneymag/index.htm. Accessed March 6, 2013.
- Jaffe S. Patients held for observation can face steep drug bills. USA Today website. Available at: http://usatoday30.usatoday.com/money/industries/health/drugs/story/2012-04-30/drugs-can-be-expensive-in-observation-care/54646378/1. Accessed March 6, 2013.
- Landro L. Filling a gap between ERs and inpatient rooms. The Wall Street Journal website. Available at: http://online.wsj.com/article/SB10001424052970204349404578101060863887052.html. Accessed March 6, 2013.
SHM added a new item to its 2012 State of Hospital Medicine report: the ratio of respondents’ observation admissions to inpatient admission encounters. This metric was added because observation encounters have been increasing, with financial effects on hospitals and patients. SHM survey respondents reported a 20% observation rate for both adult and pediatric practice groups (see Figure 1).
Under observation status, services that used to be billed as inpatient status (e.g. chest pain evaluation, treatment of asthma exacerbation) must be billed by the hospital at much lower outpatient rates. Some hospitals have responded to this financial pressure by creating observation units or making other operational adjustments. One recent analysis suggested that nationwide adoption of such efforts could save billions of dollars.1
Becoming lean enough to do short work in short time, though, does not address all of the observation-related issues facing hospitals. When the Centers for Medicare & Medicaid Services’ (CMS) Recovery Audit Contractors (RACs) determine retrospectively that an inpatient admission should have been an observation encounter, the hospital’s payment is not downgraded but forfeited.2 This development has prompted hospitals to preemptively opt for observation status for certain patients. Case managers and providers increasingly are spending time reviewing inpatient versus observation status throughout a patient’s stay. Many hospitals have turned to third-party contractors to help review observation status.
Observation status has financial implications for patients as well. In the past year, USA Today, The Wall Street Journal, and CNN Money all have reported on patients hit with unexpected out-of-pocket expenses related to observation care.3,4,5 A common theme: Medicare patient hospitalized with an acute fracture, managed nonoperatively but requiring rehabilitation prior to returning home. These patients found out too late that observation, a status they were often unaware of, did not qualify for CMS’ three-day inpatient requirement to cover rehabilitation costs. Some patients were charged exorbitant prices for noncovered “outpatient” services, such as providing their routine medications.
Advocacy groups have joined the fray on patients’ behalf, and legal challenges have ensued. AARP and others are educating patients about observation status—and their right to challenge it. The Center for Medicare Advocacy (www.kslaw.com/Library/publication/HH111411_Bagnall.pdf) has filed a lawsuit against the U.S. Department of Health and Human Services on behalf of patients hit with uncovered rehabilitation costs, and the American Hospital Association has teamed with several hospitals to sue over funds forfeited in RAC audits (www.aha.org/content/12/121101-aha-hhs-medicare-com.pdf). Both houses of Congress have legislation (H.R. 1543 and S. 818) seeking to count observation days toward the Medicare three-day rule. For its part, CMS has promised to review observation status and, hopefully, clarify the rules.
Hospitalists, meanwhile, are gearing up for more observation care. The 2012 State of Hospital Medicine report shows that 37% of adult groups and 28% of pediatric groups reported having primary responsibility for observation or short-stay units. My own hospital runs both a clinical decision unit in the ED and a short-stay unit staffed by our hospitalist group. As SHM tracks observation status in future surveys, HM groups will be able to follow this phenomenon among their colleagues and benchmark their own rates of observation encounters.
Dr. Creamer is medical director of the short-stay unit at MetroHealth Medical Center in Cleveland and a member of SHM’s Practice Analysis Committee.
References
- Feng Z, Wright DB, Mor V. Sharp rise in Medicare enrollees being held in hospitals for observation raises concerns about causes and consequences. Health Aff (Millwood). 2012;31(6):1251-1259.
- Baugh CW, Venkatesh AK, Hilton JA, Samuel PA, Schuur JD, Bohan JS. Making greater use of dedicated hospital observation units for many short-stay patients could save $3.1 billion a year. Health Aff (Millwood). 2012;31(10):2314-2323.
- Gengler A. The painful new trend in Medicare. CNN Money website. Available at: http://money.cnn.com/2012/08/07/pf/medicare-rehab-costs.moneymag/index.htm. Accessed March 6, 2013.
- Jaffe S. Patients held for observation can face steep drug bills. USA Today website. Available at: http://usatoday30.usatoday.com/money/industries/health/drugs/story/2012-04-30/drugs-can-be-expensive-in-observation-care/54646378/1. Accessed March 6, 2013.
- Landro L. Filling a gap between ERs and inpatient rooms. The Wall Street Journal website. Available at: http://online.wsj.com/article/SB10001424052970204349404578101060863887052.html. Accessed March 6, 2013.
SHM added a new item to its 2012 State of Hospital Medicine report: the ratio of respondents’ observation admissions to inpatient admission encounters. This metric was added because observation encounters have been increasing, with financial effects on hospitals and patients. SHM survey respondents reported a 20% observation rate for both adult and pediatric practice groups (see Figure 1).
Under observation status, services that used to be billed as inpatient status (e.g. chest pain evaluation, treatment of asthma exacerbation) must be billed by the hospital at much lower outpatient rates. Some hospitals have responded to this financial pressure by creating observation units or making other operational adjustments. One recent analysis suggested that nationwide adoption of such efforts could save billions of dollars.1
Becoming lean enough to do short work in short time, though, does not address all of the observation-related issues facing hospitals. When the Centers for Medicare & Medicaid Services’ (CMS) Recovery Audit Contractors (RACs) determine retrospectively that an inpatient admission should have been an observation encounter, the hospital’s payment is not downgraded but forfeited.2 This development has prompted hospitals to preemptively opt for observation status for certain patients. Case managers and providers increasingly are spending time reviewing inpatient versus observation status throughout a patient’s stay. Many hospitals have turned to third-party contractors to help review observation status.
Observation status has financial implications for patients as well. In the past year, USA Today, The Wall Street Journal, and CNN Money all have reported on patients hit with unexpected out-of-pocket expenses related to observation care.3,4,5 A common theme: Medicare patient hospitalized with an acute fracture, managed nonoperatively but requiring rehabilitation prior to returning home. These patients found out too late that observation, a status they were often unaware of, did not qualify for CMS’ three-day inpatient requirement to cover rehabilitation costs. Some patients were charged exorbitant prices for noncovered “outpatient” services, such as providing their routine medications.
Advocacy groups have joined the fray on patients’ behalf, and legal challenges have ensued. AARP and others are educating patients about observation status—and their right to challenge it. The Center for Medicare Advocacy (www.kslaw.com/Library/publication/HH111411_Bagnall.pdf) has filed a lawsuit against the U.S. Department of Health and Human Services on behalf of patients hit with uncovered rehabilitation costs, and the American Hospital Association has teamed with several hospitals to sue over funds forfeited in RAC audits (www.aha.org/content/12/121101-aha-hhs-medicare-com.pdf). Both houses of Congress have legislation (H.R. 1543 and S. 818) seeking to count observation days toward the Medicare three-day rule. For its part, CMS has promised to review observation status and, hopefully, clarify the rules.
Hospitalists, meanwhile, are gearing up for more observation care. The 2012 State of Hospital Medicine report shows that 37% of adult groups and 28% of pediatric groups reported having primary responsibility for observation or short-stay units. My own hospital runs both a clinical decision unit in the ED and a short-stay unit staffed by our hospitalist group. As SHM tracks observation status in future surveys, HM groups will be able to follow this phenomenon among their colleagues and benchmark their own rates of observation encounters.
Dr. Creamer is medical director of the short-stay unit at MetroHealth Medical Center in Cleveland and a member of SHM’s Practice Analysis Committee.
References
- Feng Z, Wright DB, Mor V. Sharp rise in Medicare enrollees being held in hospitals for observation raises concerns about causes and consequences. Health Aff (Millwood). 2012;31(6):1251-1259.
- Baugh CW, Venkatesh AK, Hilton JA, Samuel PA, Schuur JD, Bohan JS. Making greater use of dedicated hospital observation units for many short-stay patients could save $3.1 billion a year. Health Aff (Millwood). 2012;31(10):2314-2323.
- Gengler A. The painful new trend in Medicare. CNN Money website. Available at: http://money.cnn.com/2012/08/07/pf/medicare-rehab-costs.moneymag/index.htm. Accessed March 6, 2013.
- Jaffe S. Patients held for observation can face steep drug bills. USA Today website. Available at: http://usatoday30.usatoday.com/money/industries/health/drugs/story/2012-04-30/drugs-can-be-expensive-in-observation-care/54646378/1. Accessed March 6, 2013.
- Landro L. Filling a gap between ERs and inpatient rooms. The Wall Street Journal website. Available at: http://online.wsj.com/article/SB10001424052970204349404578101060863887052.html. Accessed March 6, 2013.
Affordable Care Act (ACA) Provision Carries Pay Raise for Some Hospitalists
For those who remain unaware, hospitalists who care for Medicaid patients will be getting a raise in 2013 and 2014. The reason is that the Affordable Care Act (ACA) requires Medicaid rates for specified primary-care services to be equal to those of Medicare rates during those two years, with the federal government paying the difference. Hospitalists generally meet the requirements and, therefore, will see this pay increase for their applicable Medicaid billing. For some context of the scope of this change, on average, Medicaid pays physicians at 66% of the national Medicare rates, although there is significant variation among the states.
To qualify, a physician must have a specialty designation of family medicine, internal medicine, or pediatrics, then further attest to board certification in one of those specialties or related subspecialties. Alternatively, the physician must have a 60% claims history for the specified evaluation and management (E&M) codes.
Multiple parties who have heard reports about state plans for Medicaid parity recently have contacted SHM; the plans, they report, intentionally would exclude hospitalists from the promised increase. There are variations on the explanation for the exclusion and where the idea is coming from, but the inquiries follow this general theme: “Since the definition of eligible physicians remains a grey area, states are developing alternative plans with a more narrow interpretation of the qualifying factors for the increase. These plans are only including physicians who practice in the community setting (i.e. not the hospital setting).”
This is demonstrably wrong. Even if states are having these discussions, such a plan is not going to come to fruition. The final rule for Medicaid parity, which essentially has the effect of law, is very clear: It does not allow for differing eligibility or alternate state plans.
The Centers for Medicare & Medicaid Services (CMS) specifically stated in the final rule that the increase is not limited to office-based primary-care services, but it will also include hospital observation and consultation for inpatient services provided by nonadmitting physicians, ED services, and critical-care services. In other words, a hospitalist who attests eligibility for their respective state Medicaid agency and bills 99231-3, 99221-3, 99238-9, etc., will receive the increased payment for these codes.
In response to an SHM inquiry for further clarification, CMS officials have stated, “The regulation requires that qualified physicians billing eligible codes receive higher payment. States do not have the latitude to exclude physicians simply because they practice in hospitals.”
It is possible that some confusion might be arising due to the recent controversies around the upcoming Medicaid expansion, which would extend Medicaid eligibility to individuals who earn up to 138% of the federal poverty line. Some states have chosen to opt out of this expansion and have publicly fought its implementation. The Medicaid parity provision is parallel to, but independent of, Medicaid expansion. Even if a state opts out of the expansion, the Medicaid payment increase for primary-care services should remain unaffected.
This isn’t to say that the Medicaid parity provision is a certainty. With the eyes of Congress turned toward budget cuts and austerity, the funds allocated for this temporary increase could easily be targeted. Regardless, any change in eligibility would require a rule change at the federal level, which is unlikely.
Many states have already devoted much time and effort on plans to implement the provision, and the plans were due to be submitted to CMS on March 31. It is pretty late in the game to consider changes. Barring an unlikely rule change or total elimination of funding, it is clear that hospitalists are eligible for the payment bump and should remain so.
Josh Boswell is SHM’s senior manager of government relations.
For those who remain unaware, hospitalists who care for Medicaid patients will be getting a raise in 2013 and 2014. The reason is that the Affordable Care Act (ACA) requires Medicaid rates for specified primary-care services to be equal to those of Medicare rates during those two years, with the federal government paying the difference. Hospitalists generally meet the requirements and, therefore, will see this pay increase for their applicable Medicaid billing. For some context of the scope of this change, on average, Medicaid pays physicians at 66% of the national Medicare rates, although there is significant variation among the states.
To qualify, a physician must have a specialty designation of family medicine, internal medicine, or pediatrics, then further attest to board certification in one of those specialties or related subspecialties. Alternatively, the physician must have a 60% claims history for the specified evaluation and management (E&M) codes.
Multiple parties who have heard reports about state plans for Medicaid parity recently have contacted SHM; the plans, they report, intentionally would exclude hospitalists from the promised increase. There are variations on the explanation for the exclusion and where the idea is coming from, but the inquiries follow this general theme: “Since the definition of eligible physicians remains a grey area, states are developing alternative plans with a more narrow interpretation of the qualifying factors for the increase. These plans are only including physicians who practice in the community setting (i.e. not the hospital setting).”
This is demonstrably wrong. Even if states are having these discussions, such a plan is not going to come to fruition. The final rule for Medicaid parity, which essentially has the effect of law, is very clear: It does not allow for differing eligibility or alternate state plans.
The Centers for Medicare & Medicaid Services (CMS) specifically stated in the final rule that the increase is not limited to office-based primary-care services, but it will also include hospital observation and consultation for inpatient services provided by nonadmitting physicians, ED services, and critical-care services. In other words, a hospitalist who attests eligibility for their respective state Medicaid agency and bills 99231-3, 99221-3, 99238-9, etc., will receive the increased payment for these codes.
In response to an SHM inquiry for further clarification, CMS officials have stated, “The regulation requires that qualified physicians billing eligible codes receive higher payment. States do not have the latitude to exclude physicians simply because they practice in hospitals.”
It is possible that some confusion might be arising due to the recent controversies around the upcoming Medicaid expansion, which would extend Medicaid eligibility to individuals who earn up to 138% of the federal poverty line. Some states have chosen to opt out of this expansion and have publicly fought its implementation. The Medicaid parity provision is parallel to, but independent of, Medicaid expansion. Even if a state opts out of the expansion, the Medicaid payment increase for primary-care services should remain unaffected.
This isn’t to say that the Medicaid parity provision is a certainty. With the eyes of Congress turned toward budget cuts and austerity, the funds allocated for this temporary increase could easily be targeted. Regardless, any change in eligibility would require a rule change at the federal level, which is unlikely.
Many states have already devoted much time and effort on plans to implement the provision, and the plans were due to be submitted to CMS on March 31. It is pretty late in the game to consider changes. Barring an unlikely rule change or total elimination of funding, it is clear that hospitalists are eligible for the payment bump and should remain so.
Josh Boswell is SHM’s senior manager of government relations.
For those who remain unaware, hospitalists who care for Medicaid patients will be getting a raise in 2013 and 2014. The reason is that the Affordable Care Act (ACA) requires Medicaid rates for specified primary-care services to be equal to those of Medicare rates during those two years, with the federal government paying the difference. Hospitalists generally meet the requirements and, therefore, will see this pay increase for their applicable Medicaid billing. For some context of the scope of this change, on average, Medicaid pays physicians at 66% of the national Medicare rates, although there is significant variation among the states.
To qualify, a physician must have a specialty designation of family medicine, internal medicine, or pediatrics, then further attest to board certification in one of those specialties or related subspecialties. Alternatively, the physician must have a 60% claims history for the specified evaluation and management (E&M) codes.
Multiple parties who have heard reports about state plans for Medicaid parity recently have contacted SHM; the plans, they report, intentionally would exclude hospitalists from the promised increase. There are variations on the explanation for the exclusion and where the idea is coming from, but the inquiries follow this general theme: “Since the definition of eligible physicians remains a grey area, states are developing alternative plans with a more narrow interpretation of the qualifying factors for the increase. These plans are only including physicians who practice in the community setting (i.e. not the hospital setting).”
This is demonstrably wrong. Even if states are having these discussions, such a plan is not going to come to fruition. The final rule for Medicaid parity, which essentially has the effect of law, is very clear: It does not allow for differing eligibility or alternate state plans.
The Centers for Medicare & Medicaid Services (CMS) specifically stated in the final rule that the increase is not limited to office-based primary-care services, but it will also include hospital observation and consultation for inpatient services provided by nonadmitting physicians, ED services, and critical-care services. In other words, a hospitalist who attests eligibility for their respective state Medicaid agency and bills 99231-3, 99221-3, 99238-9, etc., will receive the increased payment for these codes.
In response to an SHM inquiry for further clarification, CMS officials have stated, “The regulation requires that qualified physicians billing eligible codes receive higher payment. States do not have the latitude to exclude physicians simply because they practice in hospitals.”
It is possible that some confusion might be arising due to the recent controversies around the upcoming Medicaid expansion, which would extend Medicaid eligibility to individuals who earn up to 138% of the federal poverty line. Some states have chosen to opt out of this expansion and have publicly fought its implementation. The Medicaid parity provision is parallel to, but independent of, Medicaid expansion. Even if a state opts out of the expansion, the Medicaid payment increase for primary-care services should remain unaffected.
This isn’t to say that the Medicaid parity provision is a certainty. With the eyes of Congress turned toward budget cuts and austerity, the funds allocated for this temporary increase could easily be targeted. Regardless, any change in eligibility would require a rule change at the federal level, which is unlikely.
Many states have already devoted much time and effort on plans to implement the provision, and the plans were due to be submitted to CMS on March 31. It is pretty late in the game to consider changes. Barring an unlikely rule change or total elimination of funding, it is clear that hospitalists are eligible for the payment bump and should remain so.
Josh Boswell is SHM’s senior manager of government relations.
John Nelson: Excessive Workload a Concern for Many Hospitalists
“Forty percent of physicians reported that their typical inpatient census exceeded safe levels at least monthly.”1
This quote is taken from an article by Henry Michtalik and colleagues that appeared at the end of January this year in JAMA Internal Medicine. In 2010 the authors conducted an on-line survey asking hospitalists their perceptions of their workload. Respondents indicated that with concerning frequency a high workload prevented them from adequately discussing with patients treatment options or answering questions, delay admitting or discharging patients until the next day or shift, or in some other way risk patient safety or the overall quality of their work.
This alarming finding matches my anecdotal experience working with many different hospitalist groups around the country. I think few hospitalists were surprised by the survey’s findings. Excess hospitalist workloads are indeed a problem in some settings, and those who bear them are typically not shy about speaking out.
The demand for hospitalists has exceeded the supply of doctors available to do the work throughout the history of the field. Under the weight of stunningly rapid growth in referral volume, from about 1995 to 2002, it was reasonably common for the original doctors in a hospitalist practice to become overwhelmed and leave for other work after a year or two, sometimes resulting in the collapse of the practice. Most practices are no longer in such a rapid-growth phase, but for many of them, staffing has not yet caught up with workload. The result can be chronic excess work, and even if daily patient volume is not seen as being unsafe, the number of days or shifts worked might be excessive and lead to fatigue and poor performance.
Other Workload Data
The respondents to the Michtalik survey reported that regardless of any assistance, “they could safely see 15 patients per shift, if their effort was 100% clinical.” What we don’t know is how long their shifts were, whether they included things like ICU coverage, and how many shifts they work consecutively or in a year.
SHM’s 2012 State of Hospital Medicine report, which is based on 2011 data, provides additional context. It shows that hospitalists serving adult patients report a median 2,092 billed encounters annually (mean 2,245, standard deviation 1,161). They spread this work over a median 185 shifts (“work periods”) annually (mean 192). While there are lots of methodological problems in manipulating those numbers further, 2,092 encounters divided by 185 shifts yields 11.3 encounters per shift. These numbers exclude academicians who typically spend significant time in activities other than direct patient care, and I’m intentionally ignoring such issues as the night-shift doctor, who typically has low productivity, bringing down the average per full-time doctor in a practice.
The numbers from both surveys are sort of fuzzy because they aren’t audited or verified, but the 2012 State of Hospital Medicine data suggest that typical workloads aren’t too high in most practices, yet 40% of respondents in the Michtalik survey said they were high enough—unreasonably high—to risk quality and safety at least once a month.
One way to reconcile these findings is to take into account the standard deviation in daily volume in a single practice of about 30% to 40% on above or below the mean. If a hospitalist averages 14 encounters each day shift, then he should expect that the daily number might vary between about eight and 20. The Michtalik survey responses were likely reflecting the shifts on the high end.
Perspective
I wonder what a survey of physician workload opinions in other specialties would show, or what a survey of workers across all segments of the U.S. workforce in and out of healthcare would show. Of course, many or most jobs outside of healthcare don’t risk another’s health or well-being as significantly as ours do, but it would still be instructive to know how people in general think about the work they do.
I suspect a significant number of people across many different jobs feel like too much work is expected of them, and they can point to the ways their performance suffers as a result. It is difficult to know what portion of those who report too much work is just complaining versus a thoughtful self-reflection of the determinants of their performance. Lots of hospitalists do face worrisome high workloads, but some would probably still complain even with a much lower workload.
What Can Be Done?
For those practices facing remarkably high patient volumes, the solution is to make sure you’re recruiting additional doctors, and/or NPs/PAs, as fast as you can. But a portion of these practices must first convince their employers that more staff is needed. Some practices face a real uphill battle in getting the required additional funding, and the place to start is with a careful analysis of your current workload—based on hard numbers from your practice, not just anecdotes and estimates.
Don’t forget that some hospitalists put themselves in the position of having to manage high daily patient volumes by choosing a schedule of relatively few worked days annually. For example, a group working a seven-on/seven-off schedule that also has 14 shifts of time off means that each doctor will work only 168.5 shifts annually. Compressing a year’s worth of work into only 168 shifts means that each shift will be busy, and many will involve patient volumes that exceed what is seen as safe.
It could make more sense to titrate that same work volume over more annual shifts so that the average shift is less busy. I would love to see the Michtalik data segregated by those who work many shifts annually versus those who work few shifts. It is possible that those working more shifts have reported excessive workloads less often.
SHM has a role in influencing hospitalist workloads and promotes dissemination of data and opinions about it. At HM13 next month in Washington, D.C., I am leading a session titled “Hospitalist Workload: Is 15 the Right Number?” Although it won’t provide the “right” workload for all hospitalists, it will offer worthwhile data and food for thought.
It is much more difficult to do studies of how workload influences performance than something like effects of sleep deprivation on performance, so we may never get clear answers. You could take some consolation in the fact that successive surveys have shown little change or even modest decreases in annual patient encounters. But then again, maybe that hasn’t helped with excess work since providing hospital care gets harder and more complex every year.
Dr. Nelson has been a practicing hospitalist since 1988. He is co-founder and past president of SHM, and principal in Nelson Flores Hospital Medicine Consultants. He is co-director for SHM's "Best Practices in Managing a Hospital Medicine Program" course. Write to him at [email protected].
Reference
“Forty percent of physicians reported that their typical inpatient census exceeded safe levels at least monthly.”1
This quote is taken from an article by Henry Michtalik and colleagues that appeared at the end of January this year in JAMA Internal Medicine. In 2010 the authors conducted an on-line survey asking hospitalists their perceptions of their workload. Respondents indicated that with concerning frequency a high workload prevented them from adequately discussing with patients treatment options or answering questions, delay admitting or discharging patients until the next day or shift, or in some other way risk patient safety or the overall quality of their work.
This alarming finding matches my anecdotal experience working with many different hospitalist groups around the country. I think few hospitalists were surprised by the survey’s findings. Excess hospitalist workloads are indeed a problem in some settings, and those who bear them are typically not shy about speaking out.
The demand for hospitalists has exceeded the supply of doctors available to do the work throughout the history of the field. Under the weight of stunningly rapid growth in referral volume, from about 1995 to 2002, it was reasonably common for the original doctors in a hospitalist practice to become overwhelmed and leave for other work after a year or two, sometimes resulting in the collapse of the practice. Most practices are no longer in such a rapid-growth phase, but for many of them, staffing has not yet caught up with workload. The result can be chronic excess work, and even if daily patient volume is not seen as being unsafe, the number of days or shifts worked might be excessive and lead to fatigue and poor performance.
Other Workload Data
The respondents to the Michtalik survey reported that regardless of any assistance, “they could safely see 15 patients per shift, if their effort was 100% clinical.” What we don’t know is how long their shifts were, whether they included things like ICU coverage, and how many shifts they work consecutively or in a year.
SHM’s 2012 State of Hospital Medicine report, which is based on 2011 data, provides additional context. It shows that hospitalists serving adult patients report a median 2,092 billed encounters annually (mean 2,245, standard deviation 1,161). They spread this work over a median 185 shifts (“work periods”) annually (mean 192). While there are lots of methodological problems in manipulating those numbers further, 2,092 encounters divided by 185 shifts yields 11.3 encounters per shift. These numbers exclude academicians who typically spend significant time in activities other than direct patient care, and I’m intentionally ignoring such issues as the night-shift doctor, who typically has low productivity, bringing down the average per full-time doctor in a practice.
The numbers from both surveys are sort of fuzzy because they aren’t audited or verified, but the 2012 State of Hospital Medicine data suggest that typical workloads aren’t too high in most practices, yet 40% of respondents in the Michtalik survey said they were high enough—unreasonably high—to risk quality and safety at least once a month.
One way to reconcile these findings is to take into account the standard deviation in daily volume in a single practice of about 30% to 40% on above or below the mean. If a hospitalist averages 14 encounters each day shift, then he should expect that the daily number might vary between about eight and 20. The Michtalik survey responses were likely reflecting the shifts on the high end.
Perspective
I wonder what a survey of physician workload opinions in other specialties would show, or what a survey of workers across all segments of the U.S. workforce in and out of healthcare would show. Of course, many or most jobs outside of healthcare don’t risk another’s health or well-being as significantly as ours do, but it would still be instructive to know how people in general think about the work they do.
I suspect a significant number of people across many different jobs feel like too much work is expected of them, and they can point to the ways their performance suffers as a result. It is difficult to know what portion of those who report too much work is just complaining versus a thoughtful self-reflection of the determinants of their performance. Lots of hospitalists do face worrisome high workloads, but some would probably still complain even with a much lower workload.
What Can Be Done?
For those practices facing remarkably high patient volumes, the solution is to make sure you’re recruiting additional doctors, and/or NPs/PAs, as fast as you can. But a portion of these practices must first convince their employers that more staff is needed. Some practices face a real uphill battle in getting the required additional funding, and the place to start is with a careful analysis of your current workload—based on hard numbers from your practice, not just anecdotes and estimates.
Don’t forget that some hospitalists put themselves in the position of having to manage high daily patient volumes by choosing a schedule of relatively few worked days annually. For example, a group working a seven-on/seven-off schedule that also has 14 shifts of time off means that each doctor will work only 168.5 shifts annually. Compressing a year’s worth of work into only 168 shifts means that each shift will be busy, and many will involve patient volumes that exceed what is seen as safe.
It could make more sense to titrate that same work volume over more annual shifts so that the average shift is less busy. I would love to see the Michtalik data segregated by those who work many shifts annually versus those who work few shifts. It is possible that those working more shifts have reported excessive workloads less often.
SHM has a role in influencing hospitalist workloads and promotes dissemination of data and opinions about it. At HM13 next month in Washington, D.C., I am leading a session titled “Hospitalist Workload: Is 15 the Right Number?” Although it won’t provide the “right” workload for all hospitalists, it will offer worthwhile data and food for thought.
It is much more difficult to do studies of how workload influences performance than something like effects of sleep deprivation on performance, so we may never get clear answers. You could take some consolation in the fact that successive surveys have shown little change or even modest decreases in annual patient encounters. But then again, maybe that hasn’t helped with excess work since providing hospital care gets harder and more complex every year.
Dr. Nelson has been a practicing hospitalist since 1988. He is co-founder and past president of SHM, and principal in Nelson Flores Hospital Medicine Consultants. He is co-director for SHM's "Best Practices in Managing a Hospital Medicine Program" course. Write to him at [email protected].
Reference
“Forty percent of physicians reported that their typical inpatient census exceeded safe levels at least monthly.”1
This quote is taken from an article by Henry Michtalik and colleagues that appeared at the end of January this year in JAMA Internal Medicine. In 2010 the authors conducted an on-line survey asking hospitalists their perceptions of their workload. Respondents indicated that with concerning frequency a high workload prevented them from adequately discussing with patients treatment options or answering questions, delay admitting or discharging patients until the next day or shift, or in some other way risk patient safety or the overall quality of their work.
This alarming finding matches my anecdotal experience working with many different hospitalist groups around the country. I think few hospitalists were surprised by the survey’s findings. Excess hospitalist workloads are indeed a problem in some settings, and those who bear them are typically not shy about speaking out.
The demand for hospitalists has exceeded the supply of doctors available to do the work throughout the history of the field. Under the weight of stunningly rapid growth in referral volume, from about 1995 to 2002, it was reasonably common for the original doctors in a hospitalist practice to become overwhelmed and leave for other work after a year or two, sometimes resulting in the collapse of the practice. Most practices are no longer in such a rapid-growth phase, but for many of them, staffing has not yet caught up with workload. The result can be chronic excess work, and even if daily patient volume is not seen as being unsafe, the number of days or shifts worked might be excessive and lead to fatigue and poor performance.
Other Workload Data
The respondents to the Michtalik survey reported that regardless of any assistance, “they could safely see 15 patients per shift, if their effort was 100% clinical.” What we don’t know is how long their shifts were, whether they included things like ICU coverage, and how many shifts they work consecutively or in a year.
SHM’s 2012 State of Hospital Medicine report, which is based on 2011 data, provides additional context. It shows that hospitalists serving adult patients report a median 2,092 billed encounters annually (mean 2,245, standard deviation 1,161). They spread this work over a median 185 shifts (“work periods”) annually (mean 192). While there are lots of methodological problems in manipulating those numbers further, 2,092 encounters divided by 185 shifts yields 11.3 encounters per shift. These numbers exclude academicians who typically spend significant time in activities other than direct patient care, and I’m intentionally ignoring such issues as the night-shift doctor, who typically has low productivity, bringing down the average per full-time doctor in a practice.
The numbers from both surveys are sort of fuzzy because they aren’t audited or verified, but the 2012 State of Hospital Medicine data suggest that typical workloads aren’t too high in most practices, yet 40% of respondents in the Michtalik survey said they were high enough—unreasonably high—to risk quality and safety at least once a month.
One way to reconcile these findings is to take into account the standard deviation in daily volume in a single practice of about 30% to 40% on above or below the mean. If a hospitalist averages 14 encounters each day shift, then he should expect that the daily number might vary between about eight and 20. The Michtalik survey responses were likely reflecting the shifts on the high end.
Perspective
I wonder what a survey of physician workload opinions in other specialties would show, or what a survey of workers across all segments of the U.S. workforce in and out of healthcare would show. Of course, many or most jobs outside of healthcare don’t risk another’s health or well-being as significantly as ours do, but it would still be instructive to know how people in general think about the work they do.
I suspect a significant number of people across many different jobs feel like too much work is expected of them, and they can point to the ways their performance suffers as a result. It is difficult to know what portion of those who report too much work is just complaining versus a thoughtful self-reflection of the determinants of their performance. Lots of hospitalists do face worrisome high workloads, but some would probably still complain even with a much lower workload.
What Can Be Done?
For those practices facing remarkably high patient volumes, the solution is to make sure you’re recruiting additional doctors, and/or NPs/PAs, as fast as you can. But a portion of these practices must first convince their employers that more staff is needed. Some practices face a real uphill battle in getting the required additional funding, and the place to start is with a careful analysis of your current workload—based on hard numbers from your practice, not just anecdotes and estimates.
Don’t forget that some hospitalists put themselves in the position of having to manage high daily patient volumes by choosing a schedule of relatively few worked days annually. For example, a group working a seven-on/seven-off schedule that also has 14 shifts of time off means that each doctor will work only 168.5 shifts annually. Compressing a year’s worth of work into only 168 shifts means that each shift will be busy, and many will involve patient volumes that exceed what is seen as safe.
It could make more sense to titrate that same work volume over more annual shifts so that the average shift is less busy. I would love to see the Michtalik data segregated by those who work many shifts annually versus those who work few shifts. It is possible that those working more shifts have reported excessive workloads less often.
SHM has a role in influencing hospitalist workloads and promotes dissemination of data and opinions about it. At HM13 next month in Washington, D.C., I am leading a session titled “Hospitalist Workload: Is 15 the Right Number?” Although it won’t provide the “right” workload for all hospitalists, it will offer worthwhile data and food for thought.
It is much more difficult to do studies of how workload influences performance than something like effects of sleep deprivation on performance, so we may never get clear answers. You could take some consolation in the fact that successive surveys have shown little change or even modest decreases in annual patient encounters. But then again, maybe that hasn’t helped with excess work since providing hospital care gets harder and more complex every year.
Dr. Nelson has been a practicing hospitalist since 1988. He is co-founder and past president of SHM, and principal in Nelson Flores Hospital Medicine Consultants. He is co-director for SHM's "Best Practices in Managing a Hospital Medicine Program" course. Write to him at [email protected].
Reference
Team Hospitalist Recommends Nine Don’t-Miss Sessions at HM13
Eight educational tracks, an equal number of credit bearing pre-courses, a score of small-group forums, three plenaries, and an SHM Town Hall meeting offers a lot of professional development in a four-day span. But that’s just a sampling of what HM13 has slated May 16-19 at the Gaylord National Resort & Convention Center in National Harbor, Md., just outside Washington, D.C.
So how does one get the most value out of the conference?
“The highest-yield content is going to depend on what your background is and how to spend that time in a way that augments your knowledge, your perspective, or your exposure to like-minded colleagues in a very individual way,” says HM13 course director Daniel Brotman, MD, FACP, SFHM, director of the hospitalist program at Johns Hopkins Hospital in Baltimore. “One of the things that’s so cool about hospital medicine is its diversity.”
But don’t take Dr. Brotman’s well-educated word for it. Here’s a list of recommendations from Team Hospitalist, the only reader-involvement group of its kind in HM, on events they would not miss this year.
The New Anticoagulants: When Should We Be Using Them?
2:45 p.m., May 17
Dr. Ma: “I’m very interested about the new anticoagulants talk. What I’m curious to see is what the speaker thinks about the survivability of these medications in our society, with so many lawyers. Pradaxa already has fallen out of favor. Let’s see what happens to Xarelto.”
How do CFOs Value Their Hospitalist Programs?
2:50 p.m., May 18
Dr. Ma: “The problem today is CFOs have to valuate their hospitalists in the setting of other specialists who also receive subsidies. There is less money to be spent on hospitalists, as other specialists vie for this allotment of savings from hospital-based value purchasing.”
Check out our 6-minute feature video: "Five Reasons You Should Attend HM13"
Mentoring/Coaching an Improvement Team: Lessons from SHM’s Mentored Implementation Programs
2:45 p.m., May 17
Dr. Perumalswami: “As a Project BOOST physician mentor in Illinois, I would highly recommend the session because the discussion will involve an inside look into valuable experience-based observations and analysis for the success of any process improvement team. The nature of teams and the culture of improvement at various sites will also be discussed. There will be a mentee side of the presentation, too, which will help other mentors of implementation programs better understand what the issues are ‘from the other side.’”
Strategies to Improve Communication with Patients and Families to Improve Care
2:45 p.m., May 17
Dr. Hale: “It is well known in pediatrics that you are treating two patients: both the child and the parents. If the family has a shared understanding of the child’s illness and there is collaboration for the care plan, there will be improved care.”
Neonatal HSV: When to Consider It, How to Evaluate for It, and How to Treat It
11 a.m., May 18
Dr. Hale: “Neonatal HSV is a devastating disease. It is essential to recognize high-risk patients to decrease morbidity and mortality for this illness. There have been recent updates in the understanding of epidemiology of this disease that can assist the provider in recognizing high-risk patients.”
Supporting Transition for Youth with Special Healthcare Needs: Coordinating Care and Preparing to Pass the Baton
4:15 p.m., May 18
Dr. Hale: “The transition of adolescents and young adults from pediatric-care teams to adult-medicine-care teams should be seamless for the sake of the patient, but often it is a blurry transition over the course of years. This session is high-yield for both pediatric and adult hospitalists.”
Getting Ready for Physician Value-Based Purchasing
9:50 a.m., May 19
Dr. Simone: “Dr. [Pat] Torcson’s presentation last year was one of the best at HM12, and I expect this year to be the same. He chairs SHM’s Performance Measurement and Reporting Committee and is well versed in these matters. He speaks in terms that will capture all audiences, whether they are experienced or new to the business aspects of medicine. Highly recommended.”
BOOSTing the Hospital Discharge Process: What Works and What Doesn’t
10:35 a.m., May 17
Dr. Simone: “Both panelists are excellent presenters as well as leading authorities when it comes to discharge processes. This presentation is very timely with the new CMS payment system, which penalizes unnecessary and unexpected readmissions.”
Success Stories: How to Integrate NPs and PAs into a Hospitalist Practice
4:15 p.m., May 18
Cardin: “This is an important session because, as every hard-working hospitalist knows, there simply aren’t enough physicians to fill the needs of our medically complex hospitalized patients. It is simply a reality that there will be an increased need in the future for mid-level providers, and it is valuable to maximize the success of a program by learning how to assimilate them into hospitalized practice.”
Diagnostic Errors and the Hospitalist: Why They Happen and How to Avoid Them
12:45 p.m., May 17
Cardin: “Half of practicing medicine is pattern recognition, and if there are patterns to making diagnostic errors, it would be so valuable to be aware of them. We have tremendous responsibility when caring for patients, and I think it is always beneficial to learn from mistakes.”
Richard Quinn is a freelance writer in New Jersey.
Eight educational tracks, an equal number of credit bearing pre-courses, a score of small-group forums, three plenaries, and an SHM Town Hall meeting offers a lot of professional development in a four-day span. But that’s just a sampling of what HM13 has slated May 16-19 at the Gaylord National Resort & Convention Center in National Harbor, Md., just outside Washington, D.C.
So how does one get the most value out of the conference?
“The highest-yield content is going to depend on what your background is and how to spend that time in a way that augments your knowledge, your perspective, or your exposure to like-minded colleagues in a very individual way,” says HM13 course director Daniel Brotman, MD, FACP, SFHM, director of the hospitalist program at Johns Hopkins Hospital in Baltimore. “One of the things that’s so cool about hospital medicine is its diversity.”
But don’t take Dr. Brotman’s well-educated word for it. Here’s a list of recommendations from Team Hospitalist, the only reader-involvement group of its kind in HM, on events they would not miss this year.
The New Anticoagulants: When Should We Be Using Them?
2:45 p.m., May 17
Dr. Ma: “I’m very interested about the new anticoagulants talk. What I’m curious to see is what the speaker thinks about the survivability of these medications in our society, with so many lawyers. Pradaxa already has fallen out of favor. Let’s see what happens to Xarelto.”
How do CFOs Value Their Hospitalist Programs?
2:50 p.m., May 18
Dr. Ma: “The problem today is CFOs have to valuate their hospitalists in the setting of other specialists who also receive subsidies. There is less money to be spent on hospitalists, as other specialists vie for this allotment of savings from hospital-based value purchasing.”
Check out our 6-minute feature video: "Five Reasons You Should Attend HM13"
Mentoring/Coaching an Improvement Team: Lessons from SHM’s Mentored Implementation Programs
2:45 p.m., May 17
Dr. Perumalswami: “As a Project BOOST physician mentor in Illinois, I would highly recommend the session because the discussion will involve an inside look into valuable experience-based observations and analysis for the success of any process improvement team. The nature of teams and the culture of improvement at various sites will also be discussed. There will be a mentee side of the presentation, too, which will help other mentors of implementation programs better understand what the issues are ‘from the other side.’”
Strategies to Improve Communication with Patients and Families to Improve Care
2:45 p.m., May 17
Dr. Hale: “It is well known in pediatrics that you are treating two patients: both the child and the parents. If the family has a shared understanding of the child’s illness and there is collaboration for the care plan, there will be improved care.”
Neonatal HSV: When to Consider It, How to Evaluate for It, and How to Treat It
11 a.m., May 18
Dr. Hale: “Neonatal HSV is a devastating disease. It is essential to recognize high-risk patients to decrease morbidity and mortality for this illness. There have been recent updates in the understanding of epidemiology of this disease that can assist the provider in recognizing high-risk patients.”
Supporting Transition for Youth with Special Healthcare Needs: Coordinating Care and Preparing to Pass the Baton
4:15 p.m., May 18
Dr. Hale: “The transition of adolescents and young adults from pediatric-care teams to adult-medicine-care teams should be seamless for the sake of the patient, but often it is a blurry transition over the course of years. This session is high-yield for both pediatric and adult hospitalists.”
Getting Ready for Physician Value-Based Purchasing
9:50 a.m., May 19
Dr. Simone: “Dr. [Pat] Torcson’s presentation last year was one of the best at HM12, and I expect this year to be the same. He chairs SHM’s Performance Measurement and Reporting Committee and is well versed in these matters. He speaks in terms that will capture all audiences, whether they are experienced or new to the business aspects of medicine. Highly recommended.”
BOOSTing the Hospital Discharge Process: What Works and What Doesn’t
10:35 a.m., May 17
Dr. Simone: “Both panelists are excellent presenters as well as leading authorities when it comes to discharge processes. This presentation is very timely with the new CMS payment system, which penalizes unnecessary and unexpected readmissions.”
Success Stories: How to Integrate NPs and PAs into a Hospitalist Practice
4:15 p.m., May 18
Cardin: “This is an important session because, as every hard-working hospitalist knows, there simply aren’t enough physicians to fill the needs of our medically complex hospitalized patients. It is simply a reality that there will be an increased need in the future for mid-level providers, and it is valuable to maximize the success of a program by learning how to assimilate them into hospitalized practice.”
Diagnostic Errors and the Hospitalist: Why They Happen and How to Avoid Them
12:45 p.m., May 17
Cardin: “Half of practicing medicine is pattern recognition, and if there are patterns to making diagnostic errors, it would be so valuable to be aware of them. We have tremendous responsibility when caring for patients, and I think it is always beneficial to learn from mistakes.”
Richard Quinn is a freelance writer in New Jersey.
Eight educational tracks, an equal number of credit bearing pre-courses, a score of small-group forums, three plenaries, and an SHM Town Hall meeting offers a lot of professional development in a four-day span. But that’s just a sampling of what HM13 has slated May 16-19 at the Gaylord National Resort & Convention Center in National Harbor, Md., just outside Washington, D.C.
So how does one get the most value out of the conference?
“The highest-yield content is going to depend on what your background is and how to spend that time in a way that augments your knowledge, your perspective, or your exposure to like-minded colleagues in a very individual way,” says HM13 course director Daniel Brotman, MD, FACP, SFHM, director of the hospitalist program at Johns Hopkins Hospital in Baltimore. “One of the things that’s so cool about hospital medicine is its diversity.”
But don’t take Dr. Brotman’s well-educated word for it. Here’s a list of recommendations from Team Hospitalist, the only reader-involvement group of its kind in HM, on events they would not miss this year.
The New Anticoagulants: When Should We Be Using Them?
2:45 p.m., May 17
Dr. Ma: “I’m very interested about the new anticoagulants talk. What I’m curious to see is what the speaker thinks about the survivability of these medications in our society, with so many lawyers. Pradaxa already has fallen out of favor. Let’s see what happens to Xarelto.”
How do CFOs Value Their Hospitalist Programs?
2:50 p.m., May 18
Dr. Ma: “The problem today is CFOs have to valuate their hospitalists in the setting of other specialists who also receive subsidies. There is less money to be spent on hospitalists, as other specialists vie for this allotment of savings from hospital-based value purchasing.”
Check out our 6-minute feature video: "Five Reasons You Should Attend HM13"
Mentoring/Coaching an Improvement Team: Lessons from SHM’s Mentored Implementation Programs
2:45 p.m., May 17
Dr. Perumalswami: “As a Project BOOST physician mentor in Illinois, I would highly recommend the session because the discussion will involve an inside look into valuable experience-based observations and analysis for the success of any process improvement team. The nature of teams and the culture of improvement at various sites will also be discussed. There will be a mentee side of the presentation, too, which will help other mentors of implementation programs better understand what the issues are ‘from the other side.’”
Strategies to Improve Communication with Patients and Families to Improve Care
2:45 p.m., May 17
Dr. Hale: “It is well known in pediatrics that you are treating two patients: both the child and the parents. If the family has a shared understanding of the child’s illness and there is collaboration for the care plan, there will be improved care.”
Neonatal HSV: When to Consider It, How to Evaluate for It, and How to Treat It
11 a.m., May 18
Dr. Hale: “Neonatal HSV is a devastating disease. It is essential to recognize high-risk patients to decrease morbidity and mortality for this illness. There have been recent updates in the understanding of epidemiology of this disease that can assist the provider in recognizing high-risk patients.”
Supporting Transition for Youth with Special Healthcare Needs: Coordinating Care and Preparing to Pass the Baton
4:15 p.m., May 18
Dr. Hale: “The transition of adolescents and young adults from pediatric-care teams to adult-medicine-care teams should be seamless for the sake of the patient, but often it is a blurry transition over the course of years. This session is high-yield for both pediatric and adult hospitalists.”
Getting Ready for Physician Value-Based Purchasing
9:50 a.m., May 19
Dr. Simone: “Dr. [Pat] Torcson’s presentation last year was one of the best at HM12, and I expect this year to be the same. He chairs SHM’s Performance Measurement and Reporting Committee and is well versed in these matters. He speaks in terms that will capture all audiences, whether they are experienced or new to the business aspects of medicine. Highly recommended.”
BOOSTing the Hospital Discharge Process: What Works and What Doesn’t
10:35 a.m., May 17
Dr. Simone: “Both panelists are excellent presenters as well as leading authorities when it comes to discharge processes. This presentation is very timely with the new CMS payment system, which penalizes unnecessary and unexpected readmissions.”
Success Stories: How to Integrate NPs and PAs into a Hospitalist Practice
4:15 p.m., May 18
Cardin: “This is an important session because, as every hard-working hospitalist knows, there simply aren’t enough physicians to fill the needs of our medically complex hospitalized patients. It is simply a reality that there will be an increased need in the future for mid-level providers, and it is valuable to maximize the success of a program by learning how to assimilate them into hospitalized practice.”
Diagnostic Errors and the Hospitalist: Why They Happen and How to Avoid Them
12:45 p.m., May 17
Cardin: “Half of practicing medicine is pattern recognition, and if there are patterns to making diagnostic errors, it would be so valuable to be aware of them. We have tremendous responsibility when caring for patients, and I think it is always beneficial to learn from mistakes.”
Richard Quinn is a freelance writer in New Jersey.
Two Accountable Care Organizations (ACOs) Share Their Strategies for Success
Success as an ACO likely won’t come from any one strategy, but from many. Christopher Kim, MD, MBA, SFHM, a hospitalist and associate professor of internal medicine at the University of Michigan, says the Michigan Pioneer ACO serving roughly 20,000 beneficiaries in the state’s southeastern region has benefited greatly from a variety of pre-existing relationships and initiatives. The university’s medical center, one of 10 participants in a Medicare ACO precursor called the Physician Group Practice demonstration project, was among the few sites to successfully meet the requirements and gain the full cost savings benefits in all five years.
The newer ACO, which officially launched in January 2012, pairs the university’s Faculty Group Practice with Integrated Health Associates Inc. (IHA), a large multispecialty private-practice group. Many IHA providers already had access to the university’s electronic health records so they could track admitted patients. One preliminary collaborative effort between the two entities hinted at a trend toward lower readmission rates among a small group of patients who were seen by a primary-care provider within seven days of a hospital discharge, underscoring the importance of a smooth transition.
Providers also have been able to tap into statewide initiatives aimed at improving quality and care coordination in key areas, such as cardiovascular disease, cancer, and hospital care transitions (sponsored by Blue Cross Blue Shield of Michigan).

—Christopher Kim, MD, MBA, SFHM, associate professor of internal medicine, University of Michigan Health System, Ann Arbor
“These programs helped physician organizations and hospitals throughout the state become familiar with best practices related to these kinds of conditions,” Dr. Kim says, “and I think partly because of that, we were very prepared to work on a quality-improvement initiative such as this while also improving efficiency.”
Listen to Dr. Kim discuss the added responsibility hospitalists in ACOs like the one formed between the university faculty and a large multi-specialty practice called Integrated Health Associates, Inc.
For stratifying beneficiaries by risk, the ACO has benefited from a separate initiative called the Michigan Primary Care Transformation Project, which uses the concept of a pyramid to classify increasingly complicated patients. A complex-case manager, typically an advanced practice nurse, acts as the point person for guiding patients in the upper half of the pyramid toward the best resources while preventing unnecessary duplication of tasks or consultation referrals. Optimal coordination means that hospitalists need to communicate effectively with these managers as well as with other providers.
From Medicare claims supplied by CMS, Beth Israel Deaconess Physician Organization (BIDPO) in the Boston metropolitan region has used software to identify its highest-risk patients, or those most likely to be admitted to the hospital within the next 12 months. As part of the process, BIDPO officials asked doctors to validate the results based on their own patient records and observations.
The ACO has hired nurse practitioners through a company called INSPIRIS Massachusetts to visit its sickest and frailest Medicare beneficiaries at home to prevent hospital admissions and to avoid post-discharge readmissions among the highest-risk patients. BIDPO also uses nurse care managers to do telephone-based care management for less acute patients, and is asking emergency department staff to recognize patients who could be sent home safely with appropriate care rather than be admitted. Patients with cellulitis, for example, could be treated via IV antibiotic therapy at home, a service made possible through a collaboration with a home infusion company.
Dr. Parker, BIDPO’s medical director, says hospitalists will be key to understanding the need for excellent inpatient care and thoughtful, comprehensive discharge planning that helps avoid adverse events post-discharge.
Success as an ACO likely won’t come from any one strategy, but from many. Christopher Kim, MD, MBA, SFHM, a hospitalist and associate professor of internal medicine at the University of Michigan, says the Michigan Pioneer ACO serving roughly 20,000 beneficiaries in the state’s southeastern region has benefited greatly from a variety of pre-existing relationships and initiatives. The university’s medical center, one of 10 participants in a Medicare ACO precursor called the Physician Group Practice demonstration project, was among the few sites to successfully meet the requirements and gain the full cost savings benefits in all five years.
The newer ACO, which officially launched in January 2012, pairs the university’s Faculty Group Practice with Integrated Health Associates Inc. (IHA), a large multispecialty private-practice group. Many IHA providers already had access to the university’s electronic health records so they could track admitted patients. One preliminary collaborative effort between the two entities hinted at a trend toward lower readmission rates among a small group of patients who were seen by a primary-care provider within seven days of a hospital discharge, underscoring the importance of a smooth transition.
Providers also have been able to tap into statewide initiatives aimed at improving quality and care coordination in key areas, such as cardiovascular disease, cancer, and hospital care transitions (sponsored by Blue Cross Blue Shield of Michigan).

—Christopher Kim, MD, MBA, SFHM, associate professor of internal medicine, University of Michigan Health System, Ann Arbor
“These programs helped physician organizations and hospitals throughout the state become familiar with best practices related to these kinds of conditions,” Dr. Kim says, “and I think partly because of that, we were very prepared to work on a quality-improvement initiative such as this while also improving efficiency.”
Listen to Dr. Kim discuss the added responsibility hospitalists in ACOs like the one formed between the university faculty and a large multi-specialty practice called Integrated Health Associates, Inc.
For stratifying beneficiaries by risk, the ACO has benefited from a separate initiative called the Michigan Primary Care Transformation Project, which uses the concept of a pyramid to classify increasingly complicated patients. A complex-case manager, typically an advanced practice nurse, acts as the point person for guiding patients in the upper half of the pyramid toward the best resources while preventing unnecessary duplication of tasks or consultation referrals. Optimal coordination means that hospitalists need to communicate effectively with these managers as well as with other providers.
From Medicare claims supplied by CMS, Beth Israel Deaconess Physician Organization (BIDPO) in the Boston metropolitan region has used software to identify its highest-risk patients, or those most likely to be admitted to the hospital within the next 12 months. As part of the process, BIDPO officials asked doctors to validate the results based on their own patient records and observations.
The ACO has hired nurse practitioners through a company called INSPIRIS Massachusetts to visit its sickest and frailest Medicare beneficiaries at home to prevent hospital admissions and to avoid post-discharge readmissions among the highest-risk patients. BIDPO also uses nurse care managers to do telephone-based care management for less acute patients, and is asking emergency department staff to recognize patients who could be sent home safely with appropriate care rather than be admitted. Patients with cellulitis, for example, could be treated via IV antibiotic therapy at home, a service made possible through a collaboration with a home infusion company.
Dr. Parker, BIDPO’s medical director, says hospitalists will be key to understanding the need for excellent inpatient care and thoughtful, comprehensive discharge planning that helps avoid adverse events post-discharge.
Success as an ACO likely won’t come from any one strategy, but from many. Christopher Kim, MD, MBA, SFHM, a hospitalist and associate professor of internal medicine at the University of Michigan, says the Michigan Pioneer ACO serving roughly 20,000 beneficiaries in the state’s southeastern region has benefited greatly from a variety of pre-existing relationships and initiatives. The university’s medical center, one of 10 participants in a Medicare ACO precursor called the Physician Group Practice demonstration project, was among the few sites to successfully meet the requirements and gain the full cost savings benefits in all five years.
The newer ACO, which officially launched in January 2012, pairs the university’s Faculty Group Practice with Integrated Health Associates Inc. (IHA), a large multispecialty private-practice group. Many IHA providers already had access to the university’s electronic health records so they could track admitted patients. One preliminary collaborative effort between the two entities hinted at a trend toward lower readmission rates among a small group of patients who were seen by a primary-care provider within seven days of a hospital discharge, underscoring the importance of a smooth transition.
Providers also have been able to tap into statewide initiatives aimed at improving quality and care coordination in key areas, such as cardiovascular disease, cancer, and hospital care transitions (sponsored by Blue Cross Blue Shield of Michigan).

—Christopher Kim, MD, MBA, SFHM, associate professor of internal medicine, University of Michigan Health System, Ann Arbor
“These programs helped physician organizations and hospitals throughout the state become familiar with best practices related to these kinds of conditions,” Dr. Kim says, “and I think partly because of that, we were very prepared to work on a quality-improvement initiative such as this while also improving efficiency.”
Listen to Dr. Kim discuss the added responsibility hospitalists in ACOs like the one formed between the university faculty and a large multi-specialty practice called Integrated Health Associates, Inc.
For stratifying beneficiaries by risk, the ACO has benefited from a separate initiative called the Michigan Primary Care Transformation Project, which uses the concept of a pyramid to classify increasingly complicated patients. A complex-case manager, typically an advanced practice nurse, acts as the point person for guiding patients in the upper half of the pyramid toward the best resources while preventing unnecessary duplication of tasks or consultation referrals. Optimal coordination means that hospitalists need to communicate effectively with these managers as well as with other providers.
From Medicare claims supplied by CMS, Beth Israel Deaconess Physician Organization (BIDPO) in the Boston metropolitan region has used software to identify its highest-risk patients, or those most likely to be admitted to the hospital within the next 12 months. As part of the process, BIDPO officials asked doctors to validate the results based on their own patient records and observations.
The ACO has hired nurse practitioners through a company called INSPIRIS Massachusetts to visit its sickest and frailest Medicare beneficiaries at home to prevent hospital admissions and to avoid post-discharge readmissions among the highest-risk patients. BIDPO also uses nurse care managers to do telephone-based care management for less acute patients, and is asking emergency department staff to recognize patients who could be sent home safely with appropriate care rather than be admitted. Patients with cellulitis, for example, could be treated via IV antibiotic therapy at home, a service made possible through a collaboration with a home infusion company.
Dr. Parker, BIDPO’s medical director, says hospitalists will be key to understanding the need for excellent inpatient care and thoughtful, comprehensive discharge planning that helps avoid adverse events post-discharge.
Accountable Care Organizations (ACO) Gain Popularity with Physicians in Wake of Added Incentives, Revised Federal Rules
Throughout much of 2011, ambivalence plagued efforts by the Centers for Medicare & Medicaid Services (CMS) to expand the federal government’s reach into integrated care delivery to help improve patient outcomes while lowering costs. Critics panned the initial draft of regulations for a large accountable-care demonstration project called the Shared Savings Program, and prominent medical groups announced their intention to sit on the sidelines.
At the start of 2013, the atmosphere couldn’t be more different. CMS won over most of its critics with a well-received final version of the rules that provided more incentives for groups to form accountable-care organizations (ACOs), and the presidential election provided more clarity about the future of healthcare reform. Medical groups around the country are readily jumping on the ACO bandwagon, with its emphasis on shared responsibility among provider groups for a defined pool of patients.
Few medical groups have enough data to suggest whether their varied approaches to managing patient populations will lead to better-quality care that’s also more affordable; the first batch of Medicare ACO data isn’t expected until later this spring. And healthcare experts differ on which models and components are likely to make the biggest long-term impact; even the precise definition of an ACO remains a moving target. But industry observers say they’re surprised and encouraged not only by the speed with which the movement has taken off, but also by the breadth of models being investigated, the strong engagement of the private sector, and a spreading sense of cautious optimism.
“This is actually moving faster than I thought—faster than I think anybody thought,” says SHM Public Policy Committee chair Ron Greeno, MD, FCCP, MHM.
Although CMS still is in the beginning stages of its work and has focused most of its efforts on reviewing applications and providing feedback on organizations’ historical expenditure and utilization patterns, agency officials say the ACO initiative has not encountered any unexpected setbacks. “As with any new program, there are bumps along the way, but I don’t think we’ve experienced anything that is out of the ordinary,” says John Pilotte, director of Performance-Based Payment Policy in the Center for Medicare. “We’re pretty happy with where we are with the program.”
The Shared Savings Program, which Pilotte describes as “an easier on-ramp” to population management for providers and offers low financial risk in exchange for a modest level of shared cost savings, is proving especially popular. Combined, several hundred organizations submitted applications for the program’s second and third rounds, which began July 1, 2012, and Jan. 1, 2013, respectively.
“Two hundred twenty ACOs are currently up and running, and we expect to continue to add ACOs to the program annually,” Pilotte says.

—David Muhlestein, analyst, Leavitt Partners
Last January, another 32 groups joined Medicare’s Pioneer ACO program, designed for more experienced organizations with more resources. The groups assume more risk, and in return are more handsomely rewarded if they meet benchmarks.
All told, the tally of confirmed ACOs in the U.S. reached 428 by the end of January, according to Leavitt Partners, a Salt Lake City-based healthcare consulting firm that is tracking the growth of accountable care (see “A Sampling of Significant ACO Programs,” below). David Muhlestein, an analyst with Leavitt Partners, says private ACOs now account for roughly half of that total, a trend driven by their ability to experiment with different approaches and more easily track costs through clearly defined patient populations.
The central role for hospitalists within most ACOs is rooted in the reality that hospital care is the most expensive part of healthcare. Successfully implementing a plan to coordinate care and prevent hospital readmissions might not correlate directly with improved quality metrics, but it can lead to significant savings.
The diverse ACO models now being tested, however, could result in varying responsibilities for hospitalists, depending on the focal points of the sponsoring entities. After patients have been admitted to a hospital, for example, many hospitalists assume responsibility for managing inpatient care and the inpatient-outpatient handoff. A main goal of a physician-owned medical group, such as an independent practice association (IPA), by contrast, is to keep patients out of the hospital altogether, placing more of the focus on primary and specialty care. An IPA that forms an ACO, Muhlestein says, might hire its own hospitalists to monitor the care of patients in affiliated hospitals while using the association’s approach to limiting costs.
ACO participants also have varied widely in the effort expended to get up to speed. “Some people have said they haven’t had to make any major changes to their organization, while some people have had to drastically think how they provide care,” Muhlestein says. In general, many of the former have had the luxury of working within relatively integrated facilities and building upon existing frameworks, whereas many of the latter previously toiled away in silos and are now scrambling to establish more cohesive working relationships from scratch.
Optimism Abounds
Though many ACOs have only limited data so far, Muhlestein says most are generally optimistic that their early results will be positive. Even so, Dr. Greeno says, he fully expects the Pioneer ACOs to produce the best results among the Medicare demonstration projects. Those organizations already have successful track records in managing patient populations, and the Pioneer model’s incentives are stronger because the groups are assuming more risk. If the Pioneer ACO results are eclipsed by those of the Shared Savings Program, he says, “I’d fall out of my chair.”
The Beth Israel Deaconess Physician Organization (BIDPO) now has four global payment contracts, including its Pioneer ACO arrangement with CMS that serves 33,000 beneficiaries in the Boston metropolitan region. “The decision-making around joining was a recognition that the fee-for-service model is highly dysfunctional,” says Richard Parker, MD, BIDPO’s medical director. “Our organization and our leadership believed that most of the country, both private payor and governmental payor, would be moving toward global payment and that it would be to our advantage to get in early.”
Despite the complicated rollout and delays in receiving Medicare data on patients from CMS, Dr. Parker says, the feedback from both providers and patients has been mostly positive. “I would say, anecdotally, that the doctors seem appreciative that we’re trying to fix some of these gaps in care that we all know have existed for some time,” he says. “And, anecdotally from the patients, we get appreciation that we’re trying to take better care of them.”
Chris Coleman, chief financial officer for Phoenix-based Banner Health Network, another Pioneer ACO participant, says the project fits in well with his company’s decision “to transform itself into more of a value-based, performance-based provider.” Banner’s ACO, which serves about 50,000 beneficiaries, is still setting up needed systems, including a consistent platform for electronic medical records throughout the entire provider network. Even during the building phase, however, Coleman says company officials have been pleasantly surprised by the ACO’s positive effect on utilization, patient care, and apparent savings.
Although the company has only a partial year of Medicare claims to go by, Coleman says the data look “pretty good” so far and suggest the ACO is on track for modest savings of perhaps 3% or 4%. Like BIDPO, Banner has other shared-risk agreements in place, including one for a Medicare Advantage population and another with a private payor. So far, Coleman says, those arrangements also seem to be “performing positively.”
Dr. Greeno and other experts see the best ACO results coming from such rapidly growing private arrangements, and early published data have been generally encouraging.1 The ability to more narrowly define patient groups and assume more control over payments, he says, has allowed private ACOs to keep better track of costs and implement innovative population health interventions.

—Ron Greeno, MD, FCCP, MHM, SHM Public Policy Committee chair
Built to Last?
Whether public, private, or a hybrid between the two, some ACOs are trying to manage the care of their entire patient pool and look at everything that might help them accrue cost savings. Others are focusing only on the sickest patients to reach their quality improvement (QI) and savings goals, and targeting specific parameters, such as blood pressure or medication adherence, for patients with myocardial infarction.
Joane Goodroe, an Atlanta-based healthcare consultant, favors the latter approach, at least for new ACOs. Goodroe recommends adopting a streamlined strategy that will get an ACO up and running, then allow the group to gradually add to it, rather than waiting until all of the right pieces fall into place. Her own data analysis of Medicare patients, for example, suggests that a diabetic who’s been an inpatient can average $50,000 in yearly costs, compared with $2,400 for a diabetic who has never been admitted to a hospital.
Setting up a system to manage every diabetic patient from the start, she says, would require too much time and money. “If you try to build the perfect ACO structure, it’s going to be too expensive for the results you initially get back,” she says, making it seem like the ACO is an unsustainable failure. “You’ve got to figure out how to build a cost-effective infrastructure while you’re also improving the care of the patients, and the best place to go is to target your sickest patients first.”
CMS’ Advance Payment ACO Model is designed to help by providing upfront payments to smaller ACO organizations that might lack capital, giving them an advance on potential shared savings so they can install the infrastructure and support structures necessary to redesign care.
To maximize the overall chances of success, Dr. Parker says, ACO leadership should be fully engaged, and each organization should have enough resources to address its own care management and information technology needs. “My goal as medical director is to improve the quality of care of the patients and, hopefully, also improve the working life of the doctors and staff,” he says. “And my belief and expectation is that if we do that, the cost of care will ultimately go down.”
Bryn Nelson is a freelance medical writer in Seattle.
Reference
Throughout much of 2011, ambivalence plagued efforts by the Centers for Medicare & Medicaid Services (CMS) to expand the federal government’s reach into integrated care delivery to help improve patient outcomes while lowering costs. Critics panned the initial draft of regulations for a large accountable-care demonstration project called the Shared Savings Program, and prominent medical groups announced their intention to sit on the sidelines.
At the start of 2013, the atmosphere couldn’t be more different. CMS won over most of its critics with a well-received final version of the rules that provided more incentives for groups to form accountable-care organizations (ACOs), and the presidential election provided more clarity about the future of healthcare reform. Medical groups around the country are readily jumping on the ACO bandwagon, with its emphasis on shared responsibility among provider groups for a defined pool of patients.
Few medical groups have enough data to suggest whether their varied approaches to managing patient populations will lead to better-quality care that’s also more affordable; the first batch of Medicare ACO data isn’t expected until later this spring. And healthcare experts differ on which models and components are likely to make the biggest long-term impact; even the precise definition of an ACO remains a moving target. But industry observers say they’re surprised and encouraged not only by the speed with which the movement has taken off, but also by the breadth of models being investigated, the strong engagement of the private sector, and a spreading sense of cautious optimism.
“This is actually moving faster than I thought—faster than I think anybody thought,” says SHM Public Policy Committee chair Ron Greeno, MD, FCCP, MHM.
Although CMS still is in the beginning stages of its work and has focused most of its efforts on reviewing applications and providing feedback on organizations’ historical expenditure and utilization patterns, agency officials say the ACO initiative has not encountered any unexpected setbacks. “As with any new program, there are bumps along the way, but I don’t think we’ve experienced anything that is out of the ordinary,” says John Pilotte, director of Performance-Based Payment Policy in the Center for Medicare. “We’re pretty happy with where we are with the program.”
The Shared Savings Program, which Pilotte describes as “an easier on-ramp” to population management for providers and offers low financial risk in exchange for a modest level of shared cost savings, is proving especially popular. Combined, several hundred organizations submitted applications for the program’s second and third rounds, which began July 1, 2012, and Jan. 1, 2013, respectively.
“Two hundred twenty ACOs are currently up and running, and we expect to continue to add ACOs to the program annually,” Pilotte says.

—David Muhlestein, analyst, Leavitt Partners
Last January, another 32 groups joined Medicare’s Pioneer ACO program, designed for more experienced organizations with more resources. The groups assume more risk, and in return are more handsomely rewarded if they meet benchmarks.
All told, the tally of confirmed ACOs in the U.S. reached 428 by the end of January, according to Leavitt Partners, a Salt Lake City-based healthcare consulting firm that is tracking the growth of accountable care (see “A Sampling of Significant ACO Programs,” below). David Muhlestein, an analyst with Leavitt Partners, says private ACOs now account for roughly half of that total, a trend driven by their ability to experiment with different approaches and more easily track costs through clearly defined patient populations.
The central role for hospitalists within most ACOs is rooted in the reality that hospital care is the most expensive part of healthcare. Successfully implementing a plan to coordinate care and prevent hospital readmissions might not correlate directly with improved quality metrics, but it can lead to significant savings.
The diverse ACO models now being tested, however, could result in varying responsibilities for hospitalists, depending on the focal points of the sponsoring entities. After patients have been admitted to a hospital, for example, many hospitalists assume responsibility for managing inpatient care and the inpatient-outpatient handoff. A main goal of a physician-owned medical group, such as an independent practice association (IPA), by contrast, is to keep patients out of the hospital altogether, placing more of the focus on primary and specialty care. An IPA that forms an ACO, Muhlestein says, might hire its own hospitalists to monitor the care of patients in affiliated hospitals while using the association’s approach to limiting costs.
ACO participants also have varied widely in the effort expended to get up to speed. “Some people have said they haven’t had to make any major changes to their organization, while some people have had to drastically think how they provide care,” Muhlestein says. In general, many of the former have had the luxury of working within relatively integrated facilities and building upon existing frameworks, whereas many of the latter previously toiled away in silos and are now scrambling to establish more cohesive working relationships from scratch.
Optimism Abounds
Though many ACOs have only limited data so far, Muhlestein says most are generally optimistic that their early results will be positive. Even so, Dr. Greeno says, he fully expects the Pioneer ACOs to produce the best results among the Medicare demonstration projects. Those organizations already have successful track records in managing patient populations, and the Pioneer model’s incentives are stronger because the groups are assuming more risk. If the Pioneer ACO results are eclipsed by those of the Shared Savings Program, he says, “I’d fall out of my chair.”
The Beth Israel Deaconess Physician Organization (BIDPO) now has four global payment contracts, including its Pioneer ACO arrangement with CMS that serves 33,000 beneficiaries in the Boston metropolitan region. “The decision-making around joining was a recognition that the fee-for-service model is highly dysfunctional,” says Richard Parker, MD, BIDPO’s medical director. “Our organization and our leadership believed that most of the country, both private payor and governmental payor, would be moving toward global payment and that it would be to our advantage to get in early.”
Despite the complicated rollout and delays in receiving Medicare data on patients from CMS, Dr. Parker says, the feedback from both providers and patients has been mostly positive. “I would say, anecdotally, that the doctors seem appreciative that we’re trying to fix some of these gaps in care that we all know have existed for some time,” he says. “And, anecdotally from the patients, we get appreciation that we’re trying to take better care of them.”
Chris Coleman, chief financial officer for Phoenix-based Banner Health Network, another Pioneer ACO participant, says the project fits in well with his company’s decision “to transform itself into more of a value-based, performance-based provider.” Banner’s ACO, which serves about 50,000 beneficiaries, is still setting up needed systems, including a consistent platform for electronic medical records throughout the entire provider network. Even during the building phase, however, Coleman says company officials have been pleasantly surprised by the ACO’s positive effect on utilization, patient care, and apparent savings.
Although the company has only a partial year of Medicare claims to go by, Coleman says the data look “pretty good” so far and suggest the ACO is on track for modest savings of perhaps 3% or 4%. Like BIDPO, Banner has other shared-risk agreements in place, including one for a Medicare Advantage population and another with a private payor. So far, Coleman says, those arrangements also seem to be “performing positively.”
Dr. Greeno and other experts see the best ACO results coming from such rapidly growing private arrangements, and early published data have been generally encouraging.1 The ability to more narrowly define patient groups and assume more control over payments, he says, has allowed private ACOs to keep better track of costs and implement innovative population health interventions.

—Ron Greeno, MD, FCCP, MHM, SHM Public Policy Committee chair
Built to Last?
Whether public, private, or a hybrid between the two, some ACOs are trying to manage the care of their entire patient pool and look at everything that might help them accrue cost savings. Others are focusing only on the sickest patients to reach their quality improvement (QI) and savings goals, and targeting specific parameters, such as blood pressure or medication adherence, for patients with myocardial infarction.
Joane Goodroe, an Atlanta-based healthcare consultant, favors the latter approach, at least for new ACOs. Goodroe recommends adopting a streamlined strategy that will get an ACO up and running, then allow the group to gradually add to it, rather than waiting until all of the right pieces fall into place. Her own data analysis of Medicare patients, for example, suggests that a diabetic who’s been an inpatient can average $50,000 in yearly costs, compared with $2,400 for a diabetic who has never been admitted to a hospital.
Setting up a system to manage every diabetic patient from the start, she says, would require too much time and money. “If you try to build the perfect ACO structure, it’s going to be too expensive for the results you initially get back,” she says, making it seem like the ACO is an unsustainable failure. “You’ve got to figure out how to build a cost-effective infrastructure while you’re also improving the care of the patients, and the best place to go is to target your sickest patients first.”
CMS’ Advance Payment ACO Model is designed to help by providing upfront payments to smaller ACO organizations that might lack capital, giving them an advance on potential shared savings so they can install the infrastructure and support structures necessary to redesign care.
To maximize the overall chances of success, Dr. Parker says, ACO leadership should be fully engaged, and each organization should have enough resources to address its own care management and information technology needs. “My goal as medical director is to improve the quality of care of the patients and, hopefully, also improve the working life of the doctors and staff,” he says. “And my belief and expectation is that if we do that, the cost of care will ultimately go down.”
Bryn Nelson is a freelance medical writer in Seattle.
Reference
Throughout much of 2011, ambivalence plagued efforts by the Centers for Medicare & Medicaid Services (CMS) to expand the federal government’s reach into integrated care delivery to help improve patient outcomes while lowering costs. Critics panned the initial draft of regulations for a large accountable-care demonstration project called the Shared Savings Program, and prominent medical groups announced their intention to sit on the sidelines.
At the start of 2013, the atmosphere couldn’t be more different. CMS won over most of its critics with a well-received final version of the rules that provided more incentives for groups to form accountable-care organizations (ACOs), and the presidential election provided more clarity about the future of healthcare reform. Medical groups around the country are readily jumping on the ACO bandwagon, with its emphasis on shared responsibility among provider groups for a defined pool of patients.
Few medical groups have enough data to suggest whether their varied approaches to managing patient populations will lead to better-quality care that’s also more affordable; the first batch of Medicare ACO data isn’t expected until later this spring. And healthcare experts differ on which models and components are likely to make the biggest long-term impact; even the precise definition of an ACO remains a moving target. But industry observers say they’re surprised and encouraged not only by the speed with which the movement has taken off, but also by the breadth of models being investigated, the strong engagement of the private sector, and a spreading sense of cautious optimism.
“This is actually moving faster than I thought—faster than I think anybody thought,” says SHM Public Policy Committee chair Ron Greeno, MD, FCCP, MHM.
Although CMS still is in the beginning stages of its work and has focused most of its efforts on reviewing applications and providing feedback on organizations’ historical expenditure and utilization patterns, agency officials say the ACO initiative has not encountered any unexpected setbacks. “As with any new program, there are bumps along the way, but I don’t think we’ve experienced anything that is out of the ordinary,” says John Pilotte, director of Performance-Based Payment Policy in the Center for Medicare. “We’re pretty happy with where we are with the program.”
The Shared Savings Program, which Pilotte describes as “an easier on-ramp” to population management for providers and offers low financial risk in exchange for a modest level of shared cost savings, is proving especially popular. Combined, several hundred organizations submitted applications for the program’s second and third rounds, which began July 1, 2012, and Jan. 1, 2013, respectively.
“Two hundred twenty ACOs are currently up and running, and we expect to continue to add ACOs to the program annually,” Pilotte says.

—David Muhlestein, analyst, Leavitt Partners
Last January, another 32 groups joined Medicare’s Pioneer ACO program, designed for more experienced organizations with more resources. The groups assume more risk, and in return are more handsomely rewarded if they meet benchmarks.
All told, the tally of confirmed ACOs in the U.S. reached 428 by the end of January, according to Leavitt Partners, a Salt Lake City-based healthcare consulting firm that is tracking the growth of accountable care (see “A Sampling of Significant ACO Programs,” below). David Muhlestein, an analyst with Leavitt Partners, says private ACOs now account for roughly half of that total, a trend driven by their ability to experiment with different approaches and more easily track costs through clearly defined patient populations.
The central role for hospitalists within most ACOs is rooted in the reality that hospital care is the most expensive part of healthcare. Successfully implementing a plan to coordinate care and prevent hospital readmissions might not correlate directly with improved quality metrics, but it can lead to significant savings.
The diverse ACO models now being tested, however, could result in varying responsibilities for hospitalists, depending on the focal points of the sponsoring entities. After patients have been admitted to a hospital, for example, many hospitalists assume responsibility for managing inpatient care and the inpatient-outpatient handoff. A main goal of a physician-owned medical group, such as an independent practice association (IPA), by contrast, is to keep patients out of the hospital altogether, placing more of the focus on primary and specialty care. An IPA that forms an ACO, Muhlestein says, might hire its own hospitalists to monitor the care of patients in affiliated hospitals while using the association’s approach to limiting costs.
ACO participants also have varied widely in the effort expended to get up to speed. “Some people have said they haven’t had to make any major changes to their organization, while some people have had to drastically think how they provide care,” Muhlestein says. In general, many of the former have had the luxury of working within relatively integrated facilities and building upon existing frameworks, whereas many of the latter previously toiled away in silos and are now scrambling to establish more cohesive working relationships from scratch.
Optimism Abounds
Though many ACOs have only limited data so far, Muhlestein says most are generally optimistic that their early results will be positive. Even so, Dr. Greeno says, he fully expects the Pioneer ACOs to produce the best results among the Medicare demonstration projects. Those organizations already have successful track records in managing patient populations, and the Pioneer model’s incentives are stronger because the groups are assuming more risk. If the Pioneer ACO results are eclipsed by those of the Shared Savings Program, he says, “I’d fall out of my chair.”
The Beth Israel Deaconess Physician Organization (BIDPO) now has four global payment contracts, including its Pioneer ACO arrangement with CMS that serves 33,000 beneficiaries in the Boston metropolitan region. “The decision-making around joining was a recognition that the fee-for-service model is highly dysfunctional,” says Richard Parker, MD, BIDPO’s medical director. “Our organization and our leadership believed that most of the country, both private payor and governmental payor, would be moving toward global payment and that it would be to our advantage to get in early.”
Despite the complicated rollout and delays in receiving Medicare data on patients from CMS, Dr. Parker says, the feedback from both providers and patients has been mostly positive. “I would say, anecdotally, that the doctors seem appreciative that we’re trying to fix some of these gaps in care that we all know have existed for some time,” he says. “And, anecdotally from the patients, we get appreciation that we’re trying to take better care of them.”
Chris Coleman, chief financial officer for Phoenix-based Banner Health Network, another Pioneer ACO participant, says the project fits in well with his company’s decision “to transform itself into more of a value-based, performance-based provider.” Banner’s ACO, which serves about 50,000 beneficiaries, is still setting up needed systems, including a consistent platform for electronic medical records throughout the entire provider network. Even during the building phase, however, Coleman says company officials have been pleasantly surprised by the ACO’s positive effect on utilization, patient care, and apparent savings.
Although the company has only a partial year of Medicare claims to go by, Coleman says the data look “pretty good” so far and suggest the ACO is on track for modest savings of perhaps 3% or 4%. Like BIDPO, Banner has other shared-risk agreements in place, including one for a Medicare Advantage population and another with a private payor. So far, Coleman says, those arrangements also seem to be “performing positively.”
Dr. Greeno and other experts see the best ACO results coming from such rapidly growing private arrangements, and early published data have been generally encouraging.1 The ability to more narrowly define patient groups and assume more control over payments, he says, has allowed private ACOs to keep better track of costs and implement innovative population health interventions.

—Ron Greeno, MD, FCCP, MHM, SHM Public Policy Committee chair
Built to Last?
Whether public, private, or a hybrid between the two, some ACOs are trying to manage the care of their entire patient pool and look at everything that might help them accrue cost savings. Others are focusing only on the sickest patients to reach their quality improvement (QI) and savings goals, and targeting specific parameters, such as blood pressure or medication adherence, for patients with myocardial infarction.
Joane Goodroe, an Atlanta-based healthcare consultant, favors the latter approach, at least for new ACOs. Goodroe recommends adopting a streamlined strategy that will get an ACO up and running, then allow the group to gradually add to it, rather than waiting until all of the right pieces fall into place. Her own data analysis of Medicare patients, for example, suggests that a diabetic who’s been an inpatient can average $50,000 in yearly costs, compared with $2,400 for a diabetic who has never been admitted to a hospital.
Setting up a system to manage every diabetic patient from the start, she says, would require too much time and money. “If you try to build the perfect ACO structure, it’s going to be too expensive for the results you initially get back,” she says, making it seem like the ACO is an unsustainable failure. “You’ve got to figure out how to build a cost-effective infrastructure while you’re also improving the care of the patients, and the best place to go is to target your sickest patients first.”
CMS’ Advance Payment ACO Model is designed to help by providing upfront payments to smaller ACO organizations that might lack capital, giving them an advance on potential shared savings so they can install the infrastructure and support structures necessary to redesign care.
To maximize the overall chances of success, Dr. Parker says, ACO leadership should be fully engaged, and each organization should have enough resources to address its own care management and information technology needs. “My goal as medical director is to improve the quality of care of the patients and, hopefully, also improve the working life of the doctors and staff,” he says. “And my belief and expectation is that if we do that, the cost of care will ultimately go down.”
Bryn Nelson is a freelance medical writer in Seattle.
Reference
The Future of ACOs Remains Cloudy
Experts disagree on what a sustainable accountable-care organization (ACO) will look like in the future. The shared savings model currently dominates the ACO landscape, but David Muhlestein, an analyst with Washington, D.C.-based healthcare consulting firm Leavitt Partners, says his firm’s interviews with participants suggest that very few see the approach as the best long-term answer. Some believe those capitated models of the 1990s—the much-despised HMOs with their narrowly defined networks and global payments to provider groups—could make a comeback in a slightly altered form. Others feel strongly that a bundled payment model, which provides more flexibility in where patients can go for care, will instead dominate. A few providers have even suggested that the shared savings experiment will eventually revert back to a fee-for-service approach.

—David Muhlestein, analyst, Leavitt Partners, Washington, D.C.
SHM Public Policy Committee chair Ron Greeno, MD, FCCP, MHM, says bundled payments and shared savings alone are unlikely to deliver optimal value within the integrated care structure.
“There’s just not enough incentive, and the organization that’s taking risk doesn’t have enough flexibility in terms of how they use resources,” says Dr. Greeno, chief medical officer of Cogent HMG. The real improvements, Dr. Greeno says, might not come until ACOs assume a more capitated structure in which they accept global risk and are given unfettered freedom in how they allocate payments. In the meantime, he says, Medicare could be simply trying to encourage organizations “to start dipping their toe in the water of integrated care.”
John Pilotte, director of performance-based payment policy in the Center for Medicare at CMS, agreed that one major aim of its Shared Savings Program is to provide a “new avenue for providers to work together to better coordinate care for Medicare fee-for-service beneficiaries, and to move away from volume-based incentives and to recognize and reward them for improving the quality and efficiency and effectiveness of the care they deliver.”
Muhlestein says his firm has spoken with many organizations that are carefully monitoring how the current ACOs are faring. “Right now, the ACOs that have formed are people who want to forge their own trail,” he says. “There are many more providers that want to follow some path, and they want to follow a path that has some evidence that it has been successful.”
The more paths that are taken, he says, the greater the likelihood that one or more will achieve success. And although healthcare analysts often talk about success in terms of controlling costs, Muhlestein says, quality improvement (QI) and better outcomes alone could prove alluring to would-be ACOs.
“Even if we don’t see a moderation in cost growth, but we do see an improvement in quality, there is the chance that the model could still stick around, because that’s enough,” he says. “Even if we’re paying the same amount, we’re getting better results, so our value has improved.”
Regardless of how the ACO experiment plays out, Dr. Greeno says, it represents a fundamental shift toward a more integrated, pay-for-performance healthcare system that will not be optional for providers in the near future.
“Everyone is going to be asked to perform at a higher level, and there’s going to be tremendous pressure on hospitalists to lead that performance,” he says. “My advice would be to embrace it—it’s a great opportunity to bring value to the healthcare system.” TH
Bryn Nelson is a freelance medical writer in Seattle.
Experts disagree on what a sustainable accountable-care organization (ACO) will look like in the future. The shared savings model currently dominates the ACO landscape, but David Muhlestein, an analyst with Washington, D.C.-based healthcare consulting firm Leavitt Partners, says his firm’s interviews with participants suggest that very few see the approach as the best long-term answer. Some believe those capitated models of the 1990s—the much-despised HMOs with their narrowly defined networks and global payments to provider groups—could make a comeback in a slightly altered form. Others feel strongly that a bundled payment model, which provides more flexibility in where patients can go for care, will instead dominate. A few providers have even suggested that the shared savings experiment will eventually revert back to a fee-for-service approach.

—David Muhlestein, analyst, Leavitt Partners, Washington, D.C.
SHM Public Policy Committee chair Ron Greeno, MD, FCCP, MHM, says bundled payments and shared savings alone are unlikely to deliver optimal value within the integrated care structure.
“There’s just not enough incentive, and the organization that’s taking risk doesn’t have enough flexibility in terms of how they use resources,” says Dr. Greeno, chief medical officer of Cogent HMG. The real improvements, Dr. Greeno says, might not come until ACOs assume a more capitated structure in which they accept global risk and are given unfettered freedom in how they allocate payments. In the meantime, he says, Medicare could be simply trying to encourage organizations “to start dipping their toe in the water of integrated care.”
John Pilotte, director of performance-based payment policy in the Center for Medicare at CMS, agreed that one major aim of its Shared Savings Program is to provide a “new avenue for providers to work together to better coordinate care for Medicare fee-for-service beneficiaries, and to move away from volume-based incentives and to recognize and reward them for improving the quality and efficiency and effectiveness of the care they deliver.”
Muhlestein says his firm has spoken with many organizations that are carefully monitoring how the current ACOs are faring. “Right now, the ACOs that have formed are people who want to forge their own trail,” he says. “There are many more providers that want to follow some path, and they want to follow a path that has some evidence that it has been successful.”
The more paths that are taken, he says, the greater the likelihood that one or more will achieve success. And although healthcare analysts often talk about success in terms of controlling costs, Muhlestein says, quality improvement (QI) and better outcomes alone could prove alluring to would-be ACOs.
“Even if we don’t see a moderation in cost growth, but we do see an improvement in quality, there is the chance that the model could still stick around, because that’s enough,” he says. “Even if we’re paying the same amount, we’re getting better results, so our value has improved.”
Regardless of how the ACO experiment plays out, Dr. Greeno says, it represents a fundamental shift toward a more integrated, pay-for-performance healthcare system that will not be optional for providers in the near future.
“Everyone is going to be asked to perform at a higher level, and there’s going to be tremendous pressure on hospitalists to lead that performance,” he says. “My advice would be to embrace it—it’s a great opportunity to bring value to the healthcare system.” TH
Bryn Nelson is a freelance medical writer in Seattle.
Experts disagree on what a sustainable accountable-care organization (ACO) will look like in the future. The shared savings model currently dominates the ACO landscape, but David Muhlestein, an analyst with Washington, D.C.-based healthcare consulting firm Leavitt Partners, says his firm’s interviews with participants suggest that very few see the approach as the best long-term answer. Some believe those capitated models of the 1990s—the much-despised HMOs with their narrowly defined networks and global payments to provider groups—could make a comeback in a slightly altered form. Others feel strongly that a bundled payment model, which provides more flexibility in where patients can go for care, will instead dominate. A few providers have even suggested that the shared savings experiment will eventually revert back to a fee-for-service approach.

—David Muhlestein, analyst, Leavitt Partners, Washington, D.C.
SHM Public Policy Committee chair Ron Greeno, MD, FCCP, MHM, says bundled payments and shared savings alone are unlikely to deliver optimal value within the integrated care structure.
“There’s just not enough incentive, and the organization that’s taking risk doesn’t have enough flexibility in terms of how they use resources,” says Dr. Greeno, chief medical officer of Cogent HMG. The real improvements, Dr. Greeno says, might not come until ACOs assume a more capitated structure in which they accept global risk and are given unfettered freedom in how they allocate payments. In the meantime, he says, Medicare could be simply trying to encourage organizations “to start dipping their toe in the water of integrated care.”
John Pilotte, director of performance-based payment policy in the Center for Medicare at CMS, agreed that one major aim of its Shared Savings Program is to provide a “new avenue for providers to work together to better coordinate care for Medicare fee-for-service beneficiaries, and to move away from volume-based incentives and to recognize and reward them for improving the quality and efficiency and effectiveness of the care they deliver.”
Muhlestein says his firm has spoken with many organizations that are carefully monitoring how the current ACOs are faring. “Right now, the ACOs that have formed are people who want to forge their own trail,” he says. “There are many more providers that want to follow some path, and they want to follow a path that has some evidence that it has been successful.”
The more paths that are taken, he says, the greater the likelihood that one or more will achieve success. And although healthcare analysts often talk about success in terms of controlling costs, Muhlestein says, quality improvement (QI) and better outcomes alone could prove alluring to would-be ACOs.
“Even if we don’t see a moderation in cost growth, but we do see an improvement in quality, there is the chance that the model could still stick around, because that’s enough,” he says. “Even if we’re paying the same amount, we’re getting better results, so our value has improved.”
Regardless of how the ACO experiment plays out, Dr. Greeno says, it represents a fundamental shift toward a more integrated, pay-for-performance healthcare system that will not be optional for providers in the near future.
“Everyone is going to be asked to perform at a higher level, and there’s going to be tremendous pressure on hospitalists to lead that performance,” he says. “My advice would be to embrace it—it’s a great opportunity to bring value to the healthcare system.” TH
Bryn Nelson is a freelance medical writer in Seattle.