User login
Individualizing Insulin Therapy
The Evolution of Insulin Therapy in Diabetes Mellitus
The modern management of diabetes mellitus (DM) began with the discovery of insulin by Banting and Best in 1921 (see The Evolution of Insulin Therapy in Diabetes Mellitus in this supplement). Since that time, numerous additional classes of glucose-lowering agents have been introduced for the treatment of type 2 DM (T2DM). These medications primarily act by addressing 2 of the key defects of T2DM, insulin resistance and pancreatic β-cell dysfunction. T2DM is a progressive disease process that requires continued adjustment of therapy to maintain treatment goals. Most patients with T2DM will require insulin therapy at some point in their lives.
Role of Insulin in Type 2 Diabetes Mellitus Management
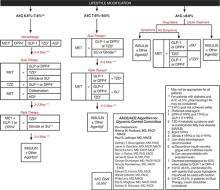
Consensus guidelines developed by the American Association of Clinical Endocrinologists/American College of Endocrinology (AACE/ACE) recommend initiating insulin when oral therapy fails to achieve glycemic control, A1C > 9.0% in treatment-naïve patients, or if the patient is symptomatic with glucose toxicity (polyuria, polydipsia, and weight loss) (FIGURE 1).1
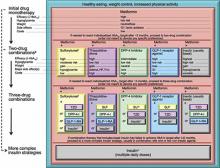
Similar consensus guidelines developed by the American Diabetes Association/European Association for the Study of Diabetes (ADA/EASD) advise the initiation of glucose-lowering therapy for most patients with T2DM with the combination of lifestyle modifications, diet, and metformin (FIGURE 2).2 For patients who do not achieve or maintain glycemic control over 3 months, or thereabouts, with metformin, a second oral agent should be added. Alternatives include a glucagon-like peptide-1 receptor (GLP-1R) agonist or basal insulin. Insulin should be strongly considered as initial therapy for a patient with significant symptoms of hyperglycemia and/or plasma glucose >300-350 mg/dL or A1C ≥10.0%.
The major role of insulin in the management of patients with T2DM stems from several important attributes. First, insulin is the only treatment that works in patients with advanced β-cell deficiency. It acts directly on tissues to regulate glucose homeostasis, unlike other glucose-lowering agents that require the presence of sufficient endogenous insulin to exert their effects as insulin sensitizers, secretagogues, incretin mimetics, amylin analogs, and other factors. This also means that the mechanism of action of insulin is complementary to those of other glucose-lowering agents. Second, there is less of a ceiling effect with insulin. That is, increasing the dose of insulin results in a progressive lowering of blood glucose in the majority of patients, with the major limitation being the risk for hypoglycemia. Third, the glucose-lowering efficacy of insulin is durable, unlike that of other glucose-lowering agents that depend on endogenous insulin secretion for continued effectiveness. Fourth, insulin improves the lipid profile, particularly triglyceride levels.2-5 Fifth, regarding the long-term safety and tolerability of insulin, it is well established that weight gain, likely mediated via reduction of glycosuria, and hypoglycemia are typically the most concerning adverse events encountered. Allergic reactions, which were a more common complication of animal-sourced insulins, are infrequent with the insulin analogs.6-17 Finally, the availability of insulin in different formulations allows for targeting fasting plasma glucose or postprandial glucose, and individualization of therapy (see The Evolution of Insulin Therapy in Diabetes Mellitus in this supplement.)
While both the AACE/ACE and ADA/EASD consensus guidelines provide treatment “algorithms,” both make it clear that these are suggested approaches suitable for the population with T2DM (FIGURE 1, FIGURE 2). The specific treatment approach must be individualized based on patient-specific factors such as age, comorbid conditions, and tolerance of hypoglycemia.
FIGURE 1
Role of insulin in the management of patients with type 2 diabetes mellitus according to the AACE/ACE1
AACE, American Association of Clinical Endocrinologists; ACE, American College of Endocrinology; AGI, α-glucosidase inhibitor; DPP4, dipeptidyl-peptidase-4 inhibitor; FPG, fasting plasma glucose; GLP-1, glucagon–like peptide-1 agonist; MET, metformin; PPG, postprandial glucose; SU, sulfonylurea; TZD, thiazolidinedione.
Reprinted from American Association of Clinical Endocrinologists. AACE/ACE Diabetes Algorithm for Glycemic Control. Available at https://www.aace.com/sites/default/files/GlycemicControlAlgorithmPPT.pdf. Accessed April 4, 2012, with permission from the American Association of Clinical Endocrinologists.
FIGURE 2
Role of insulin in the management of patients with type 2 diabetes mellitus according to the ADA/EASD2
Moving from the top to the bottom of the figure, potential sequences of antihyperglycemic therapy. In most patients, begin with lifestyle changes; metformin monotherapy is added at, or soon after, diagnosis (unless there are explicit contraindications). If the HbA1c target is not achieved after ~3 months, consider 1 of the 5 treatment options combined with metformin: an SU, TZD, DPP-4-i, GLP-1-RA, or basal insulin. (The order in the chart is determined by historical introduction and route of administration and is not meant to denote any specific preference.) Choice is based on patient and drug characteristics, with the over-riding goal of improving glycemic control while minimizing side effects. Shared decision making with the patient may help in the selection of therapeutic options. The figure displays drugs commonly used both in the United States and/or Europe. Rapid-acting secretagogues (meglitinides) may be used in place of SUs. Other drugs not shown (α-glucosidase inhibitors, colesevelam, dopamine agonists, pramlintide) may be used where available in selected patients but have modest efficacy and/or limiting side effects. In patients intolerant of, or with contraindications for, metformin, select initial drug from other classes depicted and proceed accordingly. In this circumstance, while published trials are generally lacking, it is reasonable to consider 3-drug combinations other than metformin. Insulin is likely to be more effective than most other agents as a third-line therapy, especially when HbA1c is very high (eg, ≥ 9.0%). The therapeutic regimen should include some basal insulin before moving to more complex insulin strategies. Dashed arrow line on the left-hand side of the figure denotes the option of a more rapid progression from a 2-drug combination directly to multiple daily insulin doses, in those patients with severe hyperglycemia (eg, HbA1c, ≥ 10.0–12.0%).
DPP-4, dipeptidyl peptidase-4; DPP-4-i, DPP-4 inhibitor; Fx’s, bone fractures; GI, gastrointestinal; GLP-1, glucagon-like peptide 1; GLP-1-RA, GLP-1 receptor agonist; HbA1c, hemoglobin A1c; HF, heart failure; NPH, neutral protamine Hagedorn; SU, sulfonylurea; TZD, thiazolidinedione.
aConsider beginning at this stage in patients with very high HbA1c (eg, ≥ 9%); bConsider rapid-acting, non-SU secretagogues (meglitinides) in patients with irregular meal schedules or who develop late postprandial hypoglycemia on SUs; cUsually a basal insulin (NPH, glargine, detemir) in combination with noninsulin agents; dCertain noninsulin agents may be continued with insulin. Consider beginning at this stage if patient presents with severe hyperglycemia (≥ 16.7–19.4 mmol/L [≥ 300–350 mg/dL]; HbA1c≥ 10.0–12.0%) with or without catabolic features (weight loss, ketosis, etc).
Diabetes Care by American Diabetes Association. Copyright 2012. Reproduced with permission of AMERICAN DIABETES ASSOCIATION in the format Journal via Copyright Clearance Center.
Individualizing Therapy
The importance of individualizing therapy in a way that allows patients with T2DM to effectively self-manage their disease cannot be overstated. A study involving 1381 patients with T2DM cared for by 42 primary care physicians was conducted to estimate the magnitude of effect that physicians have on glycemic control.18 Hierarchical linear modeling showed that physician-related factors were associated with a statistically significant but modest variability in A1C change (2%) for the entire patient group. On the face of it, this finding might be discouraging. Further analysis showed, however, that for patients whose A1C did improve, physician-related factors accounted for 5% of the overall change in A1C (P = .005). On the other hand, physician-related factors had no impact on patients whose A1C did not improve or worsened. These results support the role that physicians play in affecting patient outcomes. The results also make it clear that without a physician’s influence, a patient’s glycemic outcomes may be difficult to change. The question is: How best can a physician influence patient outcomes?
A 2011 survey of patients with DM, general practitioners, and DM specialists reported that clinicians tended to underestimate patients’ perceived seriousness of the disease, while overestimating patients’ level of distress. In addition, physicians had difficulty identifying which DM-related complications concerned patients most and the information and support patients needed to feel more at ease with DM. Patients placed greater importance on having easy access to their physicians rather than more time with them. But most importantly, the survey investigators concluded that patients generally wished for greater involvement in decision making and being provided more information.19 These findings suggest that patients understand that T2DM is a largely self-managed, chronic disease, and want a collaborative relationship with their physician.
Patient Barriers to Insulin Therapy
Numerous factors have been identified as impeding patients’ willingness to initiate insulin therapy (TABLE 1).20-24 Barriers often vary from patient to patient and, in fact, may change over time in an individual patient. It is crucial, therefore, to identify the root reasons for a patient’s apprehension with insulin when talking about options for intensifying treatment. Once insulin has been initiated, the patient should be asked about continuing or new concerns regarding insulin therapy (and DM management in general), including adherence.
TABLE 1
Barriers to insulin therapy identified by patients20-24
| Lack of understanding of serious nature of type 2 diabetes mellitus |
| Fear of addiction to insulin |
| Fear of hypoglycemia |
| Concern about weight gain |
| Repeated experiences of failing to achieve satisfactory glycemic control |
| Perception that quality of previous treatment was low |
| Needle phobia |
| Treatment complexity |
| Concern of social stigmatization |
| Perceived failure and low self-efficacy |
| Belief of becoming more ill |
| Out-of-pocket cost |
| Perceived negative impact on quality of life |
| Comorbidities such as poor eyesight, arthritis, forgetfulness |
A recent, international survey of 1400 patients with insulin-naïve T2DM reported that 3 negative beliefs about insulin were prominent: (1) feeling that the disease was worsening; (2) fear of injection; and (3) a feeling of personal failure.20 Certain patient comorbidities, such as poor eyesight, arthritis, and forgetfulness, might also serve as barriers to self-management of DM with insulin. Additional comorbidities may contribute as indirect barriers, such as the need for polypharmacy, which may make the initiation of additional treatments such as insulin logistically or financially difficult.
It is possible that the discussion about initiating insulin may uncover patient concerns about T2DM in general. The Diabetes Attitudes, Wishes, and Needs (DAWN) study reported that psychosocial issues were the major source of difficulty in patient self-management (TABLE 2).25 In fact, 85% of people who reported a high level of distress at the time of diagnosis of T2DM continued to experience psychological distress at a mean follow-up of 15 years.
TABLE 2
Patients experiencing various aspects of diabetes-related distress25
| Diabetes-related distress | Respondents who agree (%) |
|---|---|
| I feel stressed because of my diabetes. | 32.7 |
| I feel burned out because of my diabetes. | 18.1 |
| I feel that diabetes is preventing me from doing what I want to do. | 35.9 |
| I am constantly afraid of my diabetes getting worse. | 43.8 |
| I worry about not being able to carry out my family responsibilities in the future. | 30.1 |
| My diabetes causes me worries about my financial future. | 25.8 |
| My family and friends put too much pressure on me about my diabetes. | 14.7 |
| The community I live in is intolerant of diabetes. | 13.6 |
| Diabetes Care by American Diabetes Association. Copyright 2012. Reproduced with permission of AMERICAN DIABETES ASSOCIATION in the format Journal via Copyright Clearance Center. | |
Addressing psychosocial issues and other barriers is crucial in the discussion of self-management because those with more negative feelings about starting insulin are most unwilling to start insulin.20 One factor that may contribute to these negative feelings is repeated experiences of failing to achieve satisfactory glycemic control with oral glucose-lowering agents.23 Conversely, those who have experienced improved glycemic control with intensification of prior glucose-lowering therapy may be more accepting of initiating insulin therapy.23,26 These findings are a reminder of the importance of a treat-to-target approach to management, in which the target glycemic goal, generally A1C < 7.0%, is achieved within 2 to 3 months of diagnosis and maintained at that level through intensification of therapy as needed.
Addressing psychosocial issues can be a challenge in today’s busy primary care practice due to limited time and lack of training in the management of such issues. However, implementation of various strategies has been reported to facilitate and, in some cases, shorten a patient’s visit. For example, one small study reported that visits were shorter if the physician acknowledged and responded positively to a patient’s stated or implied concerns (17.6 minutes vs 20.1 minutes).27 Missing or ignoring the patient’s concerns often led the patient to bring up the same concern one or more additional times resulting in a longer office visit. These results underscore the importance of asking patients to identify their concerns or questions at the beginning of the office visit. The patient can fill out a questionnaire in the waiting room or be encouraged to write down and prioritize their questions and concerns specific to the visit. If the patient identifies more concerns or questions than can be reasonably addressed in one visit, there should be agreement to address the most pressing ones during the current visit and the remaining concerns and questions during the next visit. This “agenda-setting” approach has been reported to offer several advantages.28 From the patient’s perspective, the quality of the physician-patient interaction was much improved, in part because physicians took time to explain points in a way that was easy to understand. Advantages to the physician with an agenda-setting approach included “feeling more in control,” “less stressed by simply knowing what was on the patient’s mind,” “feeling less rushed,” and “enjoying patient encounters more.” Contrary to the study cited above, physicians found that patients’ visits often were longer, especially those of older patients. One physician, however, noted that the visit “takes more time now, but saves time later.” As noted in this study, additional time spent with the patient can lead to improved job satisfaction for the physician.29
The agenda-setting approach requires that the physician ask the patient to list his or her concerns and questions, and then actively listen to the patient. Once the agenda for the visit is established, employing the “ask, listen, empathize” communication style can lead to effective physician-patient communication and problem-solving. Using this approach, the physician asks questions to gain a clear understanding of the patient’s concerns and then uses active listening with little, if any, interruption.30,31 Since the goal is to solve problems with rather than for the patient, active listening without offering opinions, judgements, or advice while offering empathy is essential. Through reflection and discussion, the physician can help the patient to identify his or her issues and acceptable solutions.
The importance of good communication between physician and patient cannot be overstated. Additional communication skills to keep in mind are: (1) speak slowly using nonmedical language; (2) limit the amount of information and repeat it; (3) draw pictures and/or use visual aids; and (4) ask the patient to repeat instructions and key concepts. In addition to enhancing patients’ understanding, visual images may be particularly beneficial in keeping patients motivated to improve self-management, including adherence to therapy. For example, it may be helpful to graphically track the patient’s glycemic progress. This can be done by establishing an actionable A1C goal (generally < 7.0%) and a time frame to achieve the goal (eg, 2 to 3 months).32 A graph can be constructed beginning with the patient’s current, preinsulin A1C level, with updates at each visit. In addition to motivating the patient and reinforcing adherence, the graph can also be used to demonstrate when further treatment intensification is needed. Additional general strategies that can be employed when considering the initiation of insulin are shown in TABLE 3. Implementation of strategies such as these by family physicians provides patient outcomes comparable to those implemented by endocrinologists or diabetes specialists.33
TABLE 3
General strategies for initiating insulin therapy
| Invite the patient to take an active role in treatment decisions. |
| Remind the patient that type 2 diabetes is primarily self-managed. |
| Discuss the progressive nature of β-cell dysfunction in type 2 diabetes. |
| Emphasize the physiologic role of insulin to maintain glucose homeostasis. |
| Discuss that insulin will help to achieve glycemic control and minimize the risk for long-term complications. |
| Discuss that treatment will be modified as needed to maintain glycemic control and to best meet their needs, capabilities, and interest. |
| Utilize insulin pen devices whenever possible. |
| Emphasize the importance of lifestyle management. |
| Ask if hearing other patients talk of their experiences with insulin therapy would be helpful; consider a group office visit. |
| Discuss and provide the patient with an individualized, written action plan that includes insulin dosing, self-monitoring of blood glucose, and signs/symptoms of hypoglycemia and other adverse events with appropriate action(s) to take. |
| Simplify diabetes (and comorbidities) treatment whenever possible. |
The remainder of this article uses case studies to further explore various patient barriers to insulin therapy and strategies for addressing them with the patient. While other therapies may be appropriate in the case studies below as recommended by current guidelines, these case studies will focus on insulin. In addition, dosing strategies for initiating and intensifying insulin therapy are discussed. Changes to the treatment plan to adjust for comorbidities, such as hypertension and dyslipidemia, or for smoking cessation or aspirin therapy, are not addressed in these cases, but are crucial components of comprehensive management.
CASE STUDY 1
RF is a 49-year-old female insurance analyst diagnosed with T2DM 6 years ago. Initial therapy with lifestyle modifications and metformin has since been intensified. Glimepiride was added, then pioglitazone was added 1.5 years ago when the A1C had risen to 7.5%. There is no evidence of cardiovascular disease. She reports bothersome lower extremity edema and an 8-pound weight increase since starting pioglitazone treatment. RF states that she takes her medications every day, although she acknowledges that she sometimes forgets on Sundays.
Clinical Impression
After taking her history, performing a physical examination, and reviewing her laboratory and self-monitored blood glucose (SMBG) data, her physician concludes that her treatment plan needs to be changed (TABLE 4, TABLE 5).
TABLE 4
Case study 1: Chart notes
| Physical examination | Laboratory tests | Lifestyle habits | Current therapy | |
|---|---|---|---|---|
| Glucose-lowering | Other | |||
| BP: 126/80 mm Hg Weight: 176 lb (79.2 kg) BMI: 27 kg/m2 Eyes: no retinopathy Neurology: intact Skin: intact | SCr: 1.4 mg/dL Albuminuria: negative A1C: 8.2% Cholesterol: Total: 204 mg/dL LDL: 134 mg/dL HDL: 36 mg/dL | Exercise: Walks 2 miles 3-4 d/wk Nutrition: eats 3-4 meals/d | Metformin 1000 mg BID Glimepiride 8 mg QD Pioglitazone 45 mg QD | Lisinopril 30 mg QD Simvastatin 40 mg QD ASA 80 mg QD |
| ASA, acetylsalicylic acid; BMI, body mass index; BP, blood pressure; HDL, high-density lipoprotein; LDL, low-density lipoprotein; SCr, serum creatinine. | ||||
TABLE 5
Case study 1: Self-monitored blood glucose (mg/dL) over the previous 2 weeks
| Day | Fasting | 2 h Post-breakfast | 2 h Post-lunch | 2 h Post-dinner |
|---|---|---|---|---|
| Wednesday | 205 | |||
| Thursday | 158 | |||
| Friday | 179 | |||
| Saturday | 201 | 162 | ||
| Sunday | ||||
| Monday | 166 | |||
| Tuesday | 189 | |||
| Wednesday | ||||
| Thursday | 153 | 221 | ||
| Friday | 150 | |||
| Saturday | 199 | 186 | 213 | |
| Sunday | ||||
| Monday | 181 | |||
| Tuesday | 167 |
Treatment Plan
- Initiate basal insulin once daily in the evening.
- Continue glimepiride, but reduce pioglitazone to 15 mg once daily (or discontinue if cost is a concern).
- Ask RF to monitor fasting blood glucose and self-adjust insulin doses as appropriate.
Barriers
While discussing the need to change the treatment plan and the physician’s suggestion that RF begin basal insulin, RF asks her physician for another few months on her current regimen stating that she will try harder to take her medications on Sundays. She also voices concern that insulin treatment requires injections and that she is concerned about what her coworkers and friends might think. The physician confirms that these concerns are understandable; he also confirms that RF is fearful of needles. The following are possible responses that RF’s physician could use to address these concerns.
Patient’s concern: Perceived failure/low self-efficacy
Physician responses:
- We all forget to do things from time to time, but overall I think you have done a great job taking your medications.
- As we have talked about before, with T2DM there is a progressive loss of insulin production over time regardless of what you do. That is why we added glimepiride and then pioglita-zone and that is why we need to make a change now and put you back in control of your diabetes. It is likely that further changes will be needed and we can discuss and agree on them together.
Patient’s concern: Social stigmatization
Physician responses:
- We can begin by having you administer insulin once daily in the evening in the privacy of your home.
- The insulin can be administered with a device that looks like a pen. It is small and can be carried in your purse; it does not need to be refrigerated once opened. If the time comes that you will need to administer a dose of insulin during the day, you can easily administer the insulin discretely in a public restroom or your work area.
- The use of insulin is more common than it was even a few years ago. In fact, about 5 million people in the United States use insulin to replace what is missing, control blood sugars, and decrease the risk for diabetes complications.34
Patient’s concern: Fear of needles
Physician’s responses:
- Insulin can be injected using a pen device with short, ultrathin needles that makes most of the injections painless. I would like you to see how simple and painless the injection can be by using this sample pen here in the office.
- Many patients are concerned about giving themselves an injection at first, but they quickly become comfortable doing so.
Dosing
Treatment with basal insulin can be initiated using one of several approaches. Using the treat-to-target approach, basal insulin 10 U once daily is initiated.35 The starting dose should be reduced to 6 U if the initial pre-breakfast or pre-dinner blood glucose is < 126 mg/dL or the patient’s body mass index (BMI) is < 26 kg/m2.36 Alternatively, the ADA/EASD recommends starting with 0.2 U/kg, which may be more practical in very overweight or obese patients.2 Titration of the basal insulin dose can be accomplished using one of the following physician-directed or patient-driven treat-to-target titration algorithms (TABLE 6).35,37,38 The insulin dose should be titrated based on the pre-breakfast fasting blood glucose level.
TABLE 6
Physician-directed or patient-driven treat-to-target titration algorithms
| Riddle et al35 | Davies et al37 | Meneghini et al38 | ||||
|---|---|---|---|---|---|---|
| Start with 10 U/d bedtime basal insulin and adjust weekly | Start with 10* U/d bedtime basal insulin and adjust weekly (physician-directed) Or Start with a dose numerically equivalent to the highest FPG (in millimoles/L)† over the previous 7 days and adjust every 3 days (patient-managed) | Start with basal insulin once daily and adjust every 3 days | ||||
| Mean of self-monitored FPG values from preceding 2 days | Change in insulin dose (U/d)# | Mean of self-monitored FPG values from preceding 3 days | Change in insulin dose (U/d) (physician-directed) | Change in insulin dose (U/d) (patient-managed) | Mean of self-monitored FPG values from preceding 3 days | Change in insulin dose (U/d) |
| ≥180 mg/dL 140-180 mg/dL 120-140 mg/dL 100-120 mg/dL | +8 +6 +4 +2 | ≥180 mg/dL (≥10 mmol/L) 140-179 mg/dL (7.8-9.9 mmol/L) 120-139 mg/dL (6.7 – 7.7 mmol/L) 100-119 mg/dL (5.5-6.6 mmol/L) | +6 to +8 +4 +2 0 to +2 | +2 +2 +2 0 to +2 | >110 mg/dL 80-110 mg/dL <80 mg/dL | +3 0 -3 |
| FPG, fasting plasma glucose. *In insulin-naive patients. †For example, if the highest FPG over the previous 7 days was 7 mmol/L, start with 7 U.#Small insulin dose decreases (2-4 U/d per adjustment) were allowed if severe hypoglycemia (requiring assistance) or plasma-referenced glucose < 56 mg/dL was documented in the preceding week. Reproduced with permission. Meneghini LF, et al. J Fam Pract. 2011;60(9 Suppl 1):S21-S28. Quadrant HealthCom Inc. Copyright 2011. | ||||||
Follow-Up Visit
RF begins basal insulin 10 U in the evening and is given simple instructions for insulin dose titration based on fasting plasma glucose results. At her follow-up visit, RF reports that she has increased her basal insulin to 18 U administered once daily. Review of her SMBG results show that her blood glucose levels throughout the day have improved, but are still not at goal. RF’s physician commends her on the progress she has made. RF and her physician agree that she should continue to increase her basal insulin dose. Eight months after beginning basal insulin, RF is administering 28 U (0.35 U/kg) of basal insulin in the evening. Review of her SMBG results over the previous 2 weeks show that her blood glucose rises during the day and is highest after dinner; her current A1C is 7.2%.
Treatment Plan
- Discuss dietary and lifestyle complements to insulin therapy such as:
- Use SMBG to identify foods that raise her blood glucose.
CASE STUDY 2
LW is a 64-year-old male with longstanding hypertension diagnosed with T2DM 8 years ago for which he was treated initially with lifestyle management and metformin. He has since been treated with other oral agents as add-on therapy; glipizide was discontinued due to hypoglycemia when he skips meals (usually lunch); pioglitazone was discontinued after the patient expressed concerns about the risk for bladder cancer he heard on television. He has mild retinopathy and mild loss of vibration sensation in the feet; there is no evidence of cardiovascular disease. He was diagnosed with osteoarthritis 3 years ago.
Clinical Impression
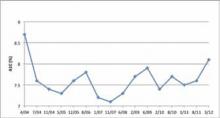
After taking his history, performing a physical examination, and reviewing his laboratory and SMBG data, his physician concludes that his treatment plan needs to be changed (FIGURE 3, TABLE 7, TABLE 8).
TABLE 7
Case study 2: Chart notes
| Physical examination | Laboratory tests | Lifestyle habits | Current therapy | |
|---|---|---|---|---|
| Glucose-lowering | Other | |||
| BP: 124/76 mm Hg Weight: 204 lb (92.7 kg) BMI: 31 kg/m2 Eyes: mild retinopathy Neurology: occasional tingling on bottom of right foot Skin: intact | SCr: 1.9 mg/dL eGFR: 51 mL/min Albuminuria: negative A1C: 8.1% Cholesterol: Total: 218 mg/dL LDL: 118 mg/dL HDL: 55 mg/dL Triglyceride: 204 mg/dL | Exercise: takes dog on occasional walk but otherwise sedentary Nutrition: eats 4 meals/d | Metformin 1000 mg BID Acarbose 50 mg TID Sitagliptin 100 mg QD | Lisinopril/HCTZ 20/25 mg QD Amlodipine 10 mg QD Acetaminophen extended-release 650 mg TID ASA 80 mg QD |
| ASA, acetylsalicylic acid; BMI, body mass index; BP, blood pressure; eGFR, estimated glomerular filtration rate; HCTZ, hydrochlorothiazide; HDL, high-density lipoprotein; LDL, low-density lipoprotein; SCr, serum creatinine. | ||||
TABLE 8
Case study 2: Self-monitored blood glucose (mg/dL) over the previous 2 weeks
| Day | Fasting | 2 h Post-breakfast | 2 h Post-lunch | 2 h Post-dinner |
|---|---|---|---|---|
| Tuesday | 135 | |||
| Wednesday | ||||
| Thursday | 196 | |||
| Friday | 152 | 174 | ||
| Saturday | ||||
| Sunday | 208 | |||
| Monday | 142 | 193 | ||
| Tuesday | ||||
| Wednesday | 130 | 156 | ||
| Thursday | ||||
| Friday | ||||
| Saturday | ||||
| Sunday | 151 | |||
| Monday |
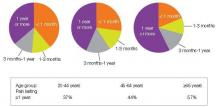
FIGURE 3
Case study 2: A1C levels for April 2004 to March 2012
Treatment Plan
- Discontinue metformin since LW’s serum creatinine is > 1.5 mg/dL.
- Initiate either basal insulin once daily in the evening or premix insulin at dinner.
- Ask LW to monitor his blood glucose and self-adjust insulin doses as appropriate.
- Stress the importance of exercise and proper nutrition; gain agreement on short-term goals for exercise and nutrition.
Barriers
LW’s physician recommends that his treatment plan be changed and insulin therapy initiated. LW quickly responds that previous changes to his treatment regimen have not resulted in his achieving an A1C < 7.0%. He also doubts that he can use a syringe to draw up the correct dose and then self-administer due to his arthritis. The following are possible responses his physician could use to address these concerns.
Patient concern: Repeated experience of failing to achieve glycemic control, ie, A1C < 7.0%
Physician responses:
- While achieving an A1C < 7.0% is a realistic goal that reduces the risks for vascular complications of diabetes, any reduction of A1C will be of benefit.
- I would like to work with you to implement a new plan that we both believe will enable you to improve your diabetes control and ideally achieve an A1C < 7.0%.
Patient concern: Self-administering due to arthritis
Physician responses:
- Instead of using a syringe and vial to draw up and administer insulin, I would like you to use an insulin pen device. As you can see, it is easy to handle and you can easily select the correct dose.
- If you choose to start on premix insulin, the pen device contains both types of insulin together in one dose.
Dosing
Treatment with basal insulin once daily in the evening can be initiated and titrated based on pre-breakfast blood glucose as in Case Study 1. Alternatively, treatment with premix insulin can be initiated at a dose of 12 U administered within 15 minutes of dinner initiation. The premix dose can be titrated using the algorithm employed in the 1-2-3 Study based on pre-breakfast blood glucose (TABLE 9).39 After 16 weeks, 41% of patients in the 1-2-3 Study achieved an A1C < 7.0% from a baseline A1C of 8.6%.
TABLE 9
1-2-3 Study algorithm39
| Pre-breakfast SMBG (mg/dL) | Adjustment of pre-dinner dose (U) |
|---|---|
| <80 | -3 |
| 80-110 | No change |
| 111-140 | +3 |
| 141-180 | +6 |
| > 180 | +9 |
| SMBG, self-monitored blood glucose. | |
Follow-Up Visit
LW began basal insulin 10 U in the evening. Over the next 5.5 months, he titrated his dose such that his current dose is 46 U (0.50 U/kg) in the evening. His current A1C is 7.3%. Review of his SMBG shows consistently high 2-hour post-lunch blood glucose levels. Although further increasing his basal insulin dose is an option, in most of the treat-to-target studies, the daily dose of basal insulin given once daily averaged between 0.4 and 0.6 U/kg.35,37,40,41 LW and his physician agree that adding rapid-acting insulin at lunch is the best option. The starting dose of rapid-acting bolus insulin is 4 to 6 U administered prior to the largest meal of the day or, as in this case, prior to the meal with the largest postprandial blood glucose excursion.42,43 Alternatively, the dose of rapid-acting insulin could be calculated as 10% of the total daily dose of basal insulin, which in this case is 5 U (10% x 46 U). The dose of basal insulin would be reduced by 5 U if the rapid-acting insulin is given at dinner in order to reduce the risk for nocturnal hypoglycemia. The dose of the bolus insulin can be titrated using the ExtraSTEP algorithm (TABLE 10).42 Alternatively, the SimpleSTEP algorithm can be used which does not require a 2-hour postprandial glucose measurement.42
TABLE 10
Algorithms for adjusting insulin aspart42
| ExtraSTEP algorithm | SimpleSTEP algorithm | |||
|---|---|---|---|---|
| 2-h Post-meal PG level (mg/dL) | Insulin aspart adjustment (U) | Pre-meal BG (mg/dL) | Bedtime BG (mg/dL) | Insulin aspart adjustment (U) |
| <72* | -2 | <72* | <72* | -2 |
| 72-144 | 0 | 72-108 | 72-144 | 0 |
| 145-180 | +2 | 109-162 | 145-180 | +2 |
| >180 | +4 | >162 | >180 | +4 |
| BG, blood glucose; PG, plasma glucose. *One or more PG values <72 mg/dL without obvious explanation. Reproduced with permission. Meneghini LF, et al. J Fam Pract. 2011;60(9 Suppl 1):S21-S28. Quadrant HealthCom Inc. Copyright 2011. | ||||
Plan
- Begin rapid-acting insulin 5 U at lunch.
- Continue basal insulin at 46 U in the evening.
- Ask LW to continue to titrate basal insulin based on the pre-breakfast blood glucose level and the lunch time bolus insulin dose based on the 2-hour post-lunch SMBG (ExtraSTEP); alternatively, adjust based on the pre-dinner blood glucose level (SimpleSTEP).
CASE STUDY 3
MB is a 46-year-old male who had not consulted a physician since having a physical examination 6 years ago. He presented 2 weeks ago with frequent urination (7-8 times/day) and feeling tired; he also noted losing 5 pounds (2.25 kg) over the preceding 3.5 months despite no changes in his diet. MB is a regional salesperson with an erratic schedule. During the week, he eats lunch and most dinners in a restaurant. On the weekend, he goes to a local bar with his friends. He does light yard work, but does not exercise regularly. He is a current smoker with a 36 pack-year history. Urinalysis shows ketonuria and microalbuminuria. His A1C reported back today is 10.8%, confirming a diagnosis of uncontrolled and symptomatic DM.
Clinical Impression
After taking his history, performing a physical examination, and reviewing his laboratory data, MB’s physician confirms a diagnosis of DM (TABLE 11). While it is likely that MB has T2DM, his physician wants to rule out type 1 DM and latent autoimmune diabetes of the adult (LADA), so he orders tests for antibodies (GAD, IA-2, ICA). The antibody testing is negative, making T2DM the most likely diagnosis.
TABLE 11
Case study 3: Chart notes
| Physical examination | Laboratory tests | Lifestyle habits | Current therapy | |
|---|---|---|---|---|
| Glucose-lowering | Other | |||
| BP: 142/88 mm Hg Weight: 176 lb (79.2 kg) BMI: 27 kg/m2 Eyes: no retinopathy Neurology: intact Skin: intact | SCr: 1.4 mg/dL Microalbumin:creatinine ratio: 140 mg/g creatinine Ketonuria: 1+ A1C: 10.8% Cholesterol: Total: 210 mg/dL LDL: 146 mg/dL HDL: 30 mg/dL | Exercise: light yard work, no regular exercise Nutrition: 3 meals/d, eats most meals in a restaurant (lunch M-F; dinner 3-4 nights/wk) | None | None |
| BMI, body mass index; BP, blood pressure; HDL, high-density lipoprotein; LDL, low-density lipoprotein; SCr, serum creatinine. | ||||
Treatment Plan
- Initiate basal-bolus therapy with fixed bolus doses of rapid-acting insulin at each meal (prandial insulin).
- Ask MB to monitor blood glucose before meals and at bedtime.
- Provide MB with a supplemental scale to correct hyperglycemia before meals.
- Stress the importance of exercise and proper nutrition; gain agreement for short-term goals for exercise and nutrition; refer for diabetes and nutrition education if available.
- Discuss the importance of smoking cessation; develop a plan.
- Consider metformin and other non-insulin therapies when A1C is under control.
Barriers
MB is surprised that he has T2DM and is clearly anxious at receiving the diagnosis. He expresses concern about starting insulin because his uncle died within a year of starting insulin. MB also recalls that his uncle was always giving himself shots and monitoring his blood glucose level. He wants to know whether there is a simpler treatment option if he agrees to start insulin treatment. He also wants to know whether he will have to remain on insulin for the rest of his life. The following are possible responses his physician could use to address these concerns.
Patient concern: Fear of death
Physician responses:
- Uncontrolled high blood sugars over a long period of time can cause serious complications, such as kidney and heart disease that can result in death. That is why it is important that we work together to gain control of your blood sugar levels over the next few months and then modify your treatment as needed to maintain control.
- Unfortunately for many patients in the past, treatment with insulin was not used until it was too late and people already had serious complications from DM. This is likely the case for your uncle.
Patient concern: Treatment complexity
Physician responses:
- Right now we have to control your blood glucose rapidly so your pancreas can regain some function and your body can better respond to insulin.
- I will also provide you with step-by-step written instructions you can follow that describe how to start insulin and how to monitor your blood glucose.
- We will communicate as often as you need to adjust your insulin doses over the next few weeks; when you feel comfortable, I can even show you how to adjust your insulin dose before a meal to correct a high blood sugar.
- We can try this treatment for 3 months and then reevaluate your response, how you feel, and whether you want to continue to modify your treatment plan to keep your blood sugars controlled.
Patient concern: Lack of understanding that T2DM is a serious disease
Physician responses:
- Please understand that T2DM is a serious disease that increases your risk for heart disease, stroke, blindness, and other diseases. Unfortunately, since diabetes does not cause bad symptoms until it is actually too late, many patients do not make the effort to properly control their diabetes. By working together, we can reduce the risk for these complications and do some screening tests to detect any complications before they become irreversible.
Dosing
There are several approaches to determining the initial doses of basal and prandial (bolus) insulin. One approach is to estimate the total daily dose (TDD) of insulin by multiplying the patient’s weight in kilograms by 0.5 U/kg/d.44 Half of the TDD is given as basal insulin replacement; the other half is divided into 3 fixed preprandial doses of rapid-acting insulin. When the patient is ready to take on more complex management, the supplemental dose for bolus insulin can be calculated using a correction factor. If the bolus insulin is a rapid-acting insulin analog, 1800 is divided by the TDD of insulin; 1500 is used for a short-acting human insulin. This correction factor is an estimate of the fall in blood glucose per unit of bolus insulin. In our patient, the TDD would be: 80 kg x 0.5 U/kg/d or 40 U/d of insulin. Thus, 1 U of insulin should lower the blood glucose by about 45 mg/dL (1800/40 U = 45 mg/dL). For every 45 mg/dL above the pre-meal target, the patient would add 1 U of rapid-acting insulin to correct the hyperglycemia over the next 4 to 5 hours. The basal and prandial insulin doses would be titrated on a periodic basis (perhaps every 1 to 2 weeks) until the daytime levels of blood glucose are on target. The fasting (pre-breakfast) blood glucose would be used to adjust the basal insulin dose, while the pre-lunch, pre-dinner, and bedtime blood glucose results would be used to adjust the pre-breakfast, pre-lunch, and pre-dinner prandial (rapid-acting) insulin doses, respectively.
An alternative approach to initiating basal-bolus therapy is the PREFER algorithm.45 Here, the basal insulin dose is 10 U initially. The bolus doses are administered in a 3:1:2 ratio, so if the total of the 3 bolus doses is 12 U/d, the initial bolus doses would be 6 (breakfast), 2 (lunch), and 4 (dinner) U. The mean basal (once-daily) and bolus insulin doses observed in PREFER are shown in TABLE 12 and TABLE 13.
TABLE 12
Case study 3: Calculating initial basal-bolus insulin doses
| Algorithm | Calculations | Patient MB |
|---|---|---|
| Meneghini44 | TDD = (total body weight [kg]) (0.5 U/kg/d) Basal insulin dose* = (50%) (TDD) Bolus insulin dose† = (10%-20%) (TDD) | TDD = (0.5 U/kg/d)(80kg) = 40 U/d |
| Basal = (50%) (40 U/d) = 20 U/d | ||
| Bolus = (10%-20%) (40 U/d) = 4 to 8 U/meal | ||
| CF = 1800/40 U/d = 45 mg/dL per 1 unit | ||
| PREFER45 | Basal insulin dose* = 10 U (14 U if BMI > 32 kg/m2) Bolus insulin dose† = ratio of 3:1:2 (breakfast:lunch:dinner) Note: At week 26, the bolus insulin doses were divided into the 3 daily meals in approximately a 1:1:1 ratio | |
| BMI, body mass index; CF, correction factor; TDD, total daily dose of insulin. *Once daily; †Three meals per day. | ||
TABLE 13
Titrating the basal insulin dose using the PREFER algorithm45
| Pre-breakfast blood glucose (mg/dL) | Basal insulin dose adjustment (U) |
|---|---|
| < 56 | -4 |
| 56-72 | -2 |
| 73-125 | No change |
| 126-140 | +2 |
| 141-160 | +4 |
| 161-180 | +6 |
| 181-200 | +8 |
| > 200 | +10 |
Follow-up Visit
MB begins with basal insulin 20 U in the evening and bolus insulin at doses of 7 U before each meal. Over the next several months, MB has titrated his insulin doses; his current doses are: 32 U (basal), 11 U (bolus-breakfast), 7 U (bolus-lunch), and 10 U (bolus-dinner). He experienced 1 episode of mild hypoglycemia (SMBG, 50 mg/dL) one afternoon following a particularly active morning (TABLE 14). His current A1C is 7.4%. MB’s physician congratulates him on the progress he has made in dramatically lowering his blood glucose level—and his risk for diabetes-related complications. While MB appreciates his physician’s support and admits that he does not feel tired and generally feels better, which is likely due to resolution of glucotoxicity, he is not happy that he has gained 5.5 pounds (2.5 kg).46 He also finds the timing and administration of bolus insulin difficult.
TABLE 14
Case study 3: Self-monitored blood glucose (mg/dL) over the previous 2 weeks
| Day | Fasting | 2 h Post-breakfast | 2 h Post-lunch | 2 h Post-dinner |
|---|---|---|---|---|
| Wednesday | ||||
| Thursday | 168 | |||
| Friday | 106 | 166 | 174 | |
| Saturday | 88 | |||
| Sunday | 195 | |||
| Monday | 134 | |||
| Tuesday | 172 | |||
| Wednesday | 130 | 156 | ||
| Thursday | 112 | 168 | ||
| Friday | 92 | 164 | ||
| Saturday | 50 | 149 | 159 | 176 |
| Sunday | 94 | 174 | 210 | |
| Monday | 176 | 184 | ||
| Tuesday | 117 | 169 |
Plan
- Continue basal insulin once-daily in the evening.
- Add metformin 500 mg BID and increase to 1000 mg BID as tolerated.
- Consider weaning down the bolus insulin doses and substituting them with a GLP-1R agonist, dipeptidyl peptidase-4 inhibitor, or short-acting secretagogue. If so, continue rapid-acting insulin during transition. [Note: the following combinations are not currently approved by the US FDA: exenatide twice-daily and prandial insulin; exenatide once-weekly and insulin; liraglutide and prandial insulin; linagliptin and insulin.]
CASE STUDY 4
KW is a 62-year-old female diagnosed with T2DM 12 years ago. Treatment with lifestyle management and metformin initially provided glycemic control. Glimepiride was subsequently added and eventually the patient was started on basal insulin. The current dose of basal insulin is 60 U in the evening. Five months ago her A1C was found to be 7.9% and more recently 8.3%. She drinks alcohol occasionally and smokes. KW works as an executive secretary and has a consistent meal and activity schedule.
Clinical Impression
Following completion of the history, physical examination, and review of her laboratory data, KW’s physician concludes that her insulin regimen should be intensified (TABLE 15, TABLE 16).
TABLE 15
Case study 4: Chart notes
| Physical examination | Laboratory tests | Lifestyle habits | Current therapy | |
|---|---|---|---|---|
| Glucose-lowering | Other | |||
| BP: 126/78 mm Hg Weight: 176 lb (79.2 kg) BMI: 32 kg/m2 Eyes: no retinopathy Neurology: intact Skin: intact | SCr: 1.0 mg/dL Albuminuria: negative A1C: 8.3% Cholesterol Total: 172 mg/dL LDL: 96 mg/dL HDL: 46 mg/dL Triglycerides: 138 mg/dL | Exercise: sedentary Nutrition: 3 meals/d with large dinner | Metformin 1000 mg BID Basal insulin 60 U in the evening | ASA 80 mg QD Pravastatin 40 mg qHS |
| BMI, body mass index; BP, blood pressure; HDL, high-density lipoprotein; LDL, low-density lipoprotein; SCr, serum creatinine. | ||||
TABLE 16
Case study 4: Self-monitored blood glucose (mg/dL) over the previous 2 weeks
| Day | Fasting | 2 h Post-breakfast | 2 h Post-lunch | 2 h Post-dinner |
|---|---|---|---|---|
| Friday | ||||
| Saturday | 156 | 244 | ||
| Sunday | 253 | |||
| Monday | ||||
| Tuesday | ||||
| Wednesday | 148 | 227 | ||
| Thursday | ||||
| Friday | ||||
| Saturday | 179 | |||
| Sunday | 160 | |||
| Monday | ||||
| Tuesday | ||||
| Wednesday | ||||
| Thursday |
Plan
- Discontinue basal insulin.
- Begin premix insulin twice daily before breakfast and dinner.
- Ask KW to monitor blood glucose two times daily and, if appropriate, teach her how to self-adjust insulin doses.
- Stress the importance of exercise and proper nutrition; gain agreement on short-term goals for exercise and nutrition.
- Discuss the importance of smoking cessation; develop a plan.
Barriers
The physician discusses with KW that her consistent meal and activity schedule would make switching to premix insulin twice daily a good choice. KW is generally in agreement with the change, but wonders whether hypoglycemia might be more likely. She also asks if she might gain more weight in addition to the 3 pounds (1.35 kg) she has gained since starting basal insulin.
Patient concern: Hypoglycemia
Physician responses:
- Hypoglycemia remains a concern, and is more frequently seen with premix than with basal insulin; however, as long as you remain consistent with your meal and activity schedule, the risk for bad hypoglycemia is low.
- We should review your written action plan so that you are sure what signs or symptoms of a low blood sugar might occur and what you should do to treat them.
Patient concern: Weight gain
Physician responses:
- It is possible that you might gain a few additional pounds. You can avoid this by increasing your physical activity, and importantly, continue healthy eating. We should schedule a time for you to meet again with a dietician who can discuss options that might work for you.
Dosing
There are different approaches for converting from basal insulin to twice-daily premix insulin. One approach is to determine the TDD of basal insulin, and give half at breakfast and the other half at dinner as premix insulin.39 Since KW is taking 60 U of basal in the evening, she should take 30 U at breakfast and 30 U at dinner. Dose titration is according to the 1-2-3 Study algorithm shown in case study 2.
Another approach is to administer biphasic insulin aspart 70/30 0.2 U/kg before breakfast and 0.1 U/kg before dinner as was done in the PREFER study (TABLE 13).45 Subsequent dosing can be determined based on the PREFER algorithm below. Of note is that at study end, premix insulin doses were equally divided between breakfast and dinner. Breakfast and dinner doses are titrated based on blood glucose levels before dinner and breakfast, respectively. In the PREFER study, the use of premix insulin provided comparable A1C reduction as basal-bolus therapy (basal once daily + bolus TID) in insulin-naïve patients. However, patients previously treated with basal insulin such as KW experienced greater A1C reductions with basal-bolus insulin than with premix insulin.
1. Rodbard HW, Jellinger PS, Davidson JA, et al. Statement by an American Association of Clinical Endocrinologists/American College of Endocrinology consensus panel on type 2 diabetes mellitus: an algorithm for glycemic control [published correction appears in Endocr Pract. 2009;15(7):768-770]. Endocr Pract. 2009;15(6):540-559.
2. Inzucchi SE, Bergenstal RM, Buse JB, et al. Management of hyperglycemia in type 2 diabetes: a patient-centered approach: position statement of the American Diabetes Association (ADA) and the European Association for the Study of Diabetes (EASD) [published online ahead of print April 19, 2012]. Diabetes Care. doi:10.2337/dc12-0413.
3. Lalić NM, Micić D, Antić S, et al. Effect of biphasic insulin aspart on glucose and lipid control in patients with type 2 diabetes mellitus. Expert Opin Pharmacother. 2007;8(17):2895-2901.
4. Reynolds LR, Kingsley FJ, Karounos DG, Tannock LR. Differential effects of rosiglitazone and insulin glargine on inflammatory markers, glycemic control, and lipids in type 2 diabetes. Diabetes Res Clin Pract. 2007;77(2):180-187.
5. Rosak C, Jung R, Hofmann U. Insulin glargine maintains equivalent glycemic control and better lipometabolic control than NPH insulin in type 1 diabetes patients who missed a meal. Horm Metab Res. 2008;40(8):544-548.
6. Ampudia-Blasco FJ, Girbes J, Carmena R. A case of lipoatrophy with insulin glargine: long-acting insulin analogs are not exempt from this complication. Diabetes Care. 2005;28(12):2983.-
7. Griffin ME, Feder A, Tamborlane WV. Lipoatrophy associated with lispro insulin in insulin pump therapy: an old complication, a new cause? Diabetes Care. 2001;24(1):174.-
8. Fineberg SE, Huang J, Brunelle R, Gulliya KS, Anderson JH, Jr. Effect of long-term exposure to insulin lispro on the induction of antibody response in patients with type 1 or type 2 diabetes. Diabetes Care. 2003;26(1):89-96.
9. Moyes V, Driver R, Croom A, Mirakian R, Chowdhury TA. Insulin allergy in a patient with type 2 diabetes successfully treated with continuous subcutaneous insulin infusion. Diabet Med. 2006;23(2):204-206.
10. Ghosh S, McCann V, Bartle L, Collier A, Malik I. Allergy to insulin detemir. Diabet Med. 2007;24(11):1307.-
11. Blumer I. Severe, delayed insulin detemir injection site reaction. Diabet Med. 2008;25(8):1008.-
12. Pérez E, González R, Martínez J, Iglesias J, Matheu V. Detemir insulin-induced anaphylaxis. Ann Allergy Asthma Immunol. 2009;102(2):174-175.
13. Mollar-Puchades MA, Villanueva IL. Insulin glulisine in the treatment of allergy to rapid acting insulin and its rapid acting analogs. Diabetes Res Clin Pract. 2009;83(1):e21-e22.
14. Kawasaki F, Kamei S, Tatsumi F, et al. Gallbladder edema in type 1 diabetic patient due to delayed-type insulin allergy. Intern Med. 2009;48(17):1545-1549.
15. Wang C, Ding ZY, Shu SQ, et al. Severe insulin allergy after percutaneous transluminal coronary angioplasty. Clin Ther. 2009;31(3):569-574.
16. Ozaki N, Oiso Y. Immunologic tolerance to the insulin analogue glulisine. Diabetes Care. 2010;33(3):e39.-
17. Koroscil T, Kagzi Y, Zacharias D. Failure of multiple therapies in the treatment of a type 1 diabetic patient with insulin allergy: a case report. Endocr Pract. 2011;17(1):91-94.
18. Tuerk PW, Mueller M, Egede LE. Estimating physician effects on glycemic control in the treatment of diabetes: methods, effects sizes, and implications for treatment policy. Diabetes Care. 2008;31(5):869-873.
19. Hajos TR, Polonsky WH, Twisk JW, Dain MP, Snoek FJ. Do physicians understand type 2 diabetes patients’ perceptions of seriousness; the emotional impact and needs for care improvement? A cross-national survey. Patient Educ Couns. 2011;85(2):258-263.
20. Polonsky WH, Hajos TR, Dain MP, Snoek FJ. Are patients with type 2 diabetes reluctant to start insulin therapy? An examination of the scope and underpinnings of psychological insulin resistance in a large, international population. Curr Med Res Opin. 2011;27(6):1169-1174.
21. Nam S, Chesla C, Stotts NA, Kroon L, Janson SL. Factors associated with psychological insulin resistance in individuals with type 2 diabetes. Diabetes Care. 2010;33(8):1747-1749.
22. Nakar S, Yitzhaki G, Rosenberg R, Vinker S. Transition to insulin in type 2 diabetes: family physicians’ misconception of patients’ fears contributes to existing barriers. J Diabetes Complications. 2007;21(4):220-226.
23. Snoek FJ. Breaking the barriers to optimal glycaemic control—what physicians need to know from patients’ perspectives. Int J Clin Pract Suppl. 2002;(129):80-84.
24. Korytkowski M. When oral agents fail: practical barriers to starting insulin. Int J Obes Relat Metab Disord. 2002;26(Suppl 3):S18-S24.
25. Skovlund SE, Peyrot M. The Diabetes Attitudes, Wishes and Needs (DAWN) program: a new approach to improving outcomes of diabetes care. Diabetes Spectrum. 2005;18(3):136-142.
26. Jenkins N, Hallowell N, Farmer AJ, Holman RR, Lawton J. Initiating insulin as part of the Treating To Target in Type 2 Diabetes (4-T) trial: an interview study of patients’ and health professionals’ experiences. Diabetes Care. 2010;33(10):2178-2180.
27. Levinson W, Gorawara-Bhat R, Lamb J. A study of patient clues and physician responses in primary care and surgical settings. JAMA. 2000;284(8):1021-1027.
28. Rodriguez HP, Anastario MP, Frankel RM, et al. Can teaching agenda-setting skills to physicians improve clinical interaction quality? A controlled intervention. BMC Med Educ. 2008;8:3.-
29. Solomon J. How strategies for managing patient visit time affect physician job satisfaction: a qualitative analysis. J Gen Intern Med. 2008;23(6):775-780.
30. Funnell MM, Anderson RM. Empowerment and self-management of diabetes. Clin Diabetes. 2004;22(3):123-127.
31. Funnell MM, Anderson RM. Are patients or outcomes more important? Rev Endocrinol. 2008;2(8):49-51.
32. Shaefer CF. Clinical inertia: overcoming a major barrier to diabetes management. Insulin. 2006;1(2):61-64.
33. Harris S, Yale JF, Dempsey E, Gerstein H. Can family physicians help patients initiate basal insulin therapy successfully?: randomized trial of patient-titrated insulin glargine compared with standard oral therapy: lessons for family practice from the Canadian INSIGHT trial. Can Fam Physician. 2008;54(4):550-558.
34. Centers for Disease Control and Prevention. National diabetes fact sheet national estimates and general information on diabetes and prediabetes in the United States, 2011. Atlanta, GA: U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, 2011. http://www.cdc.gov/diabetes/pubs/pdf/ndfs_2011.pdf. Accessed February 10, 2011.
35. Riddle MC, Rosenstock J, Gerich J. Insulin Glargine 4002 Study Investigators. The treat-to-target trial: randomized addition of glargine or human NPH insulin to oral therapy of type 2 diabetic patients. Diabetes Care. 2003;26(11):3080-3086.
36. Hermansen K, Davies M, Derezinski T, Martinez Ravn G, Clauson P, Home P. A 26-week, randomized, parallel, treat-to-target trial comparing insulin detemir with NPH insulin as add-on therapy to oral glucose-lowering drugs in insulin-naive people with type 2 diabetes [published correction appears in Diabetes Care. 2007;30(4):1035]. Diabetes Care. 2006;29(6):1269-1274.
37. Davies M, Storms F, Shutler S, Bianchi-Biscay M, Gomis R. ATLANTUS Study Group. Improvement of glycemic control in subjects with poorly controlled type 2 diabetes: comparison of two treatment algorithms using insulin glargine. Diabetes Care. 2005;28(6):1282-1288.
38. Meneghini L, Koenen C, Weng W, Selam JL. The usage of a simplified self-titration dosing guideline (303 Algorithm) for insulin detemir in patients with type 2 diabetes—results of the randomized, controlled PREDICTIVE 303 study. Diabetes Obes Metab. 2007;9(6):902-913.
39. Garber AJ, Wahlen J, Wahl T, et al. Attainment of glycaemic goals in type 2 diabetes with once-, twice-, or thrice-daily dosing with biphasic insulin aspart 70/30 (The 1-2-3 study). Diabetes Obes Metab. 2006;8(1):58-66.
40. Philis-Tsimikas A, Charpentier G, Clauson P, Ravn GM, Roberts VL, Thorsteinsson B. Comparison of once-daily insulin detemir with NPH insulin added to a regimen of oral antidiabetic drugs in poorly controlled type 2 diabetes [published correction appears in Clin Ther. 2006;28(11):1967]. Clin Ther. 2006;28(10):1569-1581.
41. Blonde L, Merilainen M, Karwe V, Raskin P. TITRATE Study Group. Patient-directed titration for achieving glycaemic goals using a once-daily basal insulin analogue: an assessment of two different fasting plasma glucose targets—the TITRATE study. Diabetes Obes Metab. 2009;11(6):623-631.
42. Meneghini L, Mersebach H, Kumar S, Svendsen AL, Hermansen K. Comparison of 2 intensification regimens with rapid-acting insulin aspart in type 2 diabetes mellitus inadequately controlled by once-daily insulin detemir and oral antidiabetes drugs: the step-wise randomized study. Endocr Pract. 2011;17(5):727-736.
43. Lankisch MR, Ferlinz KC, Leahy JL, Scherbaum WA. Orals Plus Apidra and LANTUS (OPAL) study group. Introducing a simplified approach to insulin therapy in type 2 diabetes: a comparison of two single-dose regimens of insulin glulisine plus insulin glargine and oral antidiabetic drugs [published correction appears in Diabetes Obes Metab. 2010;12(5):461]. Diabetes Obes Metab 2008;10(12):1178-1185.
44. Meneghini L. Why and how to use insulin therapy earlier in the management of type 2 diabetes. South Med J. 2007;100(2):164-174.
45. Liebl A, Prager R, Binz K, Kaiser M, Bergenstal R, Gallwitz B. PREFER Study Group. Comparison of insulin analogue regimens in people with type 2 diabetes mellitus in the PREFER Study: a randomized controlled trial. Diabetes Obes Metab. 2009;11(1):45-52.
46. Braun A, Sämann A, Kubiak T, et al. Effects of metabolic control, patient education and initiation of insulin therapy on the quality of life of patients with type 2 diabetes mellitus. Patient Educ Couns. 2008;73(1):50-59.
The Evolution of Insulin Therapy in Diabetes Mellitus
The modern management of diabetes mellitus (DM) began with the discovery of insulin by Banting and Best in 1921 (see The Evolution of Insulin Therapy in Diabetes Mellitus in this supplement). Since that time, numerous additional classes of glucose-lowering agents have been introduced for the treatment of type 2 DM (T2DM). These medications primarily act by addressing 2 of the key defects of T2DM, insulin resistance and pancreatic β-cell dysfunction. T2DM is a progressive disease process that requires continued adjustment of therapy to maintain treatment goals. Most patients with T2DM will require insulin therapy at some point in their lives.
Role of Insulin in Type 2 Diabetes Mellitus Management
Consensus guidelines developed by the American Association of Clinical Endocrinologists/American College of Endocrinology (AACE/ACE) recommend initiating insulin when oral therapy fails to achieve glycemic control, A1C > 9.0% in treatment-naïve patients, or if the patient is symptomatic with glucose toxicity (polyuria, polydipsia, and weight loss) (FIGURE 1).1
Similar consensus guidelines developed by the American Diabetes Association/European Association for the Study of Diabetes (ADA/EASD) advise the initiation of glucose-lowering therapy for most patients with T2DM with the combination of lifestyle modifications, diet, and metformin (FIGURE 2).2 For patients who do not achieve or maintain glycemic control over 3 months, or thereabouts, with metformin, a second oral agent should be added. Alternatives include a glucagon-like peptide-1 receptor (GLP-1R) agonist or basal insulin. Insulin should be strongly considered as initial therapy for a patient with significant symptoms of hyperglycemia and/or plasma glucose >300-350 mg/dL or A1C ≥10.0%.
The major role of insulin in the management of patients with T2DM stems from several important attributes. First, insulin is the only treatment that works in patients with advanced β-cell deficiency. It acts directly on tissues to regulate glucose homeostasis, unlike other glucose-lowering agents that require the presence of sufficient endogenous insulin to exert their effects as insulin sensitizers, secretagogues, incretin mimetics, amylin analogs, and other factors. This also means that the mechanism of action of insulin is complementary to those of other glucose-lowering agents. Second, there is less of a ceiling effect with insulin. That is, increasing the dose of insulin results in a progressive lowering of blood glucose in the majority of patients, with the major limitation being the risk for hypoglycemia. Third, the glucose-lowering efficacy of insulin is durable, unlike that of other glucose-lowering agents that depend on endogenous insulin secretion for continued effectiveness. Fourth, insulin improves the lipid profile, particularly triglyceride levels.2-5 Fifth, regarding the long-term safety and tolerability of insulin, it is well established that weight gain, likely mediated via reduction of glycosuria, and hypoglycemia are typically the most concerning adverse events encountered. Allergic reactions, which were a more common complication of animal-sourced insulins, are infrequent with the insulin analogs.6-17 Finally, the availability of insulin in different formulations allows for targeting fasting plasma glucose or postprandial glucose, and individualization of therapy (see The Evolution of Insulin Therapy in Diabetes Mellitus in this supplement.)
While both the AACE/ACE and ADA/EASD consensus guidelines provide treatment “algorithms,” both make it clear that these are suggested approaches suitable for the population with T2DM (FIGURE 1, FIGURE 2). The specific treatment approach must be individualized based on patient-specific factors such as age, comorbid conditions, and tolerance of hypoglycemia.
FIGURE 1
Role of insulin in the management of patients with type 2 diabetes mellitus according to the AACE/ACE1
AACE, American Association of Clinical Endocrinologists; ACE, American College of Endocrinology; AGI, α-glucosidase inhibitor; DPP4, dipeptidyl-peptidase-4 inhibitor; FPG, fasting plasma glucose; GLP-1, glucagon–like peptide-1 agonist; MET, metformin; PPG, postprandial glucose; SU, sulfonylurea; TZD, thiazolidinedione.
Reprinted from American Association of Clinical Endocrinologists. AACE/ACE Diabetes Algorithm for Glycemic Control. Available at https://www.aace.com/sites/default/files/GlycemicControlAlgorithmPPT.pdf. Accessed April 4, 2012, with permission from the American Association of Clinical Endocrinologists.
FIGURE 2
Role of insulin in the management of patients with type 2 diabetes mellitus according to the ADA/EASD2
Moving from the top to the bottom of the figure, potential sequences of antihyperglycemic therapy. In most patients, begin with lifestyle changes; metformin monotherapy is added at, or soon after, diagnosis (unless there are explicit contraindications). If the HbA1c target is not achieved after ~3 months, consider 1 of the 5 treatment options combined with metformin: an SU, TZD, DPP-4-i, GLP-1-RA, or basal insulin. (The order in the chart is determined by historical introduction and route of administration and is not meant to denote any specific preference.) Choice is based on patient and drug characteristics, with the over-riding goal of improving glycemic control while minimizing side effects. Shared decision making with the patient may help in the selection of therapeutic options. The figure displays drugs commonly used both in the United States and/or Europe. Rapid-acting secretagogues (meglitinides) may be used in place of SUs. Other drugs not shown (α-glucosidase inhibitors, colesevelam, dopamine agonists, pramlintide) may be used where available in selected patients but have modest efficacy and/or limiting side effects. In patients intolerant of, or with contraindications for, metformin, select initial drug from other classes depicted and proceed accordingly. In this circumstance, while published trials are generally lacking, it is reasonable to consider 3-drug combinations other than metformin. Insulin is likely to be more effective than most other agents as a third-line therapy, especially when HbA1c is very high (eg, ≥ 9.0%). The therapeutic regimen should include some basal insulin before moving to more complex insulin strategies. Dashed arrow line on the left-hand side of the figure denotes the option of a more rapid progression from a 2-drug combination directly to multiple daily insulin doses, in those patients with severe hyperglycemia (eg, HbA1c, ≥ 10.0–12.0%).
DPP-4, dipeptidyl peptidase-4; DPP-4-i, DPP-4 inhibitor; Fx’s, bone fractures; GI, gastrointestinal; GLP-1, glucagon-like peptide 1; GLP-1-RA, GLP-1 receptor agonist; HbA1c, hemoglobin A1c; HF, heart failure; NPH, neutral protamine Hagedorn; SU, sulfonylurea; TZD, thiazolidinedione.
aConsider beginning at this stage in patients with very high HbA1c (eg, ≥ 9%); bConsider rapid-acting, non-SU secretagogues (meglitinides) in patients with irregular meal schedules or who develop late postprandial hypoglycemia on SUs; cUsually a basal insulin (NPH, glargine, detemir) in combination with noninsulin agents; dCertain noninsulin agents may be continued with insulin. Consider beginning at this stage if patient presents with severe hyperglycemia (≥ 16.7–19.4 mmol/L [≥ 300–350 mg/dL]; HbA1c≥ 10.0–12.0%) with or without catabolic features (weight loss, ketosis, etc).
Diabetes Care by American Diabetes Association. Copyright 2012. Reproduced with permission of AMERICAN DIABETES ASSOCIATION in the format Journal via Copyright Clearance Center.
Individualizing Therapy
The importance of individualizing therapy in a way that allows patients with T2DM to effectively self-manage their disease cannot be overstated. A study involving 1381 patients with T2DM cared for by 42 primary care physicians was conducted to estimate the magnitude of effect that physicians have on glycemic control.18 Hierarchical linear modeling showed that physician-related factors were associated with a statistically significant but modest variability in A1C change (2%) for the entire patient group. On the face of it, this finding might be discouraging. Further analysis showed, however, that for patients whose A1C did improve, physician-related factors accounted for 5% of the overall change in A1C (P = .005). On the other hand, physician-related factors had no impact on patients whose A1C did not improve or worsened. These results support the role that physicians play in affecting patient outcomes. The results also make it clear that without a physician’s influence, a patient’s glycemic outcomes may be difficult to change. The question is: How best can a physician influence patient outcomes?
A 2011 survey of patients with DM, general practitioners, and DM specialists reported that clinicians tended to underestimate patients’ perceived seriousness of the disease, while overestimating patients’ level of distress. In addition, physicians had difficulty identifying which DM-related complications concerned patients most and the information and support patients needed to feel more at ease with DM. Patients placed greater importance on having easy access to their physicians rather than more time with them. But most importantly, the survey investigators concluded that patients generally wished for greater involvement in decision making and being provided more information.19 These findings suggest that patients understand that T2DM is a largely self-managed, chronic disease, and want a collaborative relationship with their physician.
Patient Barriers to Insulin Therapy
Numerous factors have been identified as impeding patients’ willingness to initiate insulin therapy (TABLE 1).20-24 Barriers often vary from patient to patient and, in fact, may change over time in an individual patient. It is crucial, therefore, to identify the root reasons for a patient’s apprehension with insulin when talking about options for intensifying treatment. Once insulin has been initiated, the patient should be asked about continuing or new concerns regarding insulin therapy (and DM management in general), including adherence.
TABLE 1
Barriers to insulin therapy identified by patients20-24
| Lack of understanding of serious nature of type 2 diabetes mellitus |
| Fear of addiction to insulin |
| Fear of hypoglycemia |
| Concern about weight gain |
| Repeated experiences of failing to achieve satisfactory glycemic control |
| Perception that quality of previous treatment was low |
| Needle phobia |
| Treatment complexity |
| Concern of social stigmatization |
| Perceived failure and low self-efficacy |
| Belief of becoming more ill |
| Out-of-pocket cost |
| Perceived negative impact on quality of life |
| Comorbidities such as poor eyesight, arthritis, forgetfulness |
A recent, international survey of 1400 patients with insulin-naïve T2DM reported that 3 negative beliefs about insulin were prominent: (1) feeling that the disease was worsening; (2) fear of injection; and (3) a feeling of personal failure.20 Certain patient comorbidities, such as poor eyesight, arthritis, and forgetfulness, might also serve as barriers to self-management of DM with insulin. Additional comorbidities may contribute as indirect barriers, such as the need for polypharmacy, which may make the initiation of additional treatments such as insulin logistically or financially difficult.
It is possible that the discussion about initiating insulin may uncover patient concerns about T2DM in general. The Diabetes Attitudes, Wishes, and Needs (DAWN) study reported that psychosocial issues were the major source of difficulty in patient self-management (TABLE 2).25 In fact, 85% of people who reported a high level of distress at the time of diagnosis of T2DM continued to experience psychological distress at a mean follow-up of 15 years.
TABLE 2
Patients experiencing various aspects of diabetes-related distress25
| Diabetes-related distress | Respondents who agree (%) |
|---|---|
| I feel stressed because of my diabetes. | 32.7 |
| I feel burned out because of my diabetes. | 18.1 |
| I feel that diabetes is preventing me from doing what I want to do. | 35.9 |
| I am constantly afraid of my diabetes getting worse. | 43.8 |
| I worry about not being able to carry out my family responsibilities in the future. | 30.1 |
| My diabetes causes me worries about my financial future. | 25.8 |
| My family and friends put too much pressure on me about my diabetes. | 14.7 |
| The community I live in is intolerant of diabetes. | 13.6 |
| Diabetes Care by American Diabetes Association. Copyright 2012. Reproduced with permission of AMERICAN DIABETES ASSOCIATION in the format Journal via Copyright Clearance Center. | |
Addressing psychosocial issues and other barriers is crucial in the discussion of self-management because those with more negative feelings about starting insulin are most unwilling to start insulin.20 One factor that may contribute to these negative feelings is repeated experiences of failing to achieve satisfactory glycemic control with oral glucose-lowering agents.23 Conversely, those who have experienced improved glycemic control with intensification of prior glucose-lowering therapy may be more accepting of initiating insulin therapy.23,26 These findings are a reminder of the importance of a treat-to-target approach to management, in which the target glycemic goal, generally A1C < 7.0%, is achieved within 2 to 3 months of diagnosis and maintained at that level through intensification of therapy as needed.
Addressing psychosocial issues can be a challenge in today’s busy primary care practice due to limited time and lack of training in the management of such issues. However, implementation of various strategies has been reported to facilitate and, in some cases, shorten a patient’s visit. For example, one small study reported that visits were shorter if the physician acknowledged and responded positively to a patient’s stated or implied concerns (17.6 minutes vs 20.1 minutes).27 Missing or ignoring the patient’s concerns often led the patient to bring up the same concern one or more additional times resulting in a longer office visit. These results underscore the importance of asking patients to identify their concerns or questions at the beginning of the office visit. The patient can fill out a questionnaire in the waiting room or be encouraged to write down and prioritize their questions and concerns specific to the visit. If the patient identifies more concerns or questions than can be reasonably addressed in one visit, there should be agreement to address the most pressing ones during the current visit and the remaining concerns and questions during the next visit. This “agenda-setting” approach has been reported to offer several advantages.28 From the patient’s perspective, the quality of the physician-patient interaction was much improved, in part because physicians took time to explain points in a way that was easy to understand. Advantages to the physician with an agenda-setting approach included “feeling more in control,” “less stressed by simply knowing what was on the patient’s mind,” “feeling less rushed,” and “enjoying patient encounters more.” Contrary to the study cited above, physicians found that patients’ visits often were longer, especially those of older patients. One physician, however, noted that the visit “takes more time now, but saves time later.” As noted in this study, additional time spent with the patient can lead to improved job satisfaction for the physician.29
The agenda-setting approach requires that the physician ask the patient to list his or her concerns and questions, and then actively listen to the patient. Once the agenda for the visit is established, employing the “ask, listen, empathize” communication style can lead to effective physician-patient communication and problem-solving. Using this approach, the physician asks questions to gain a clear understanding of the patient’s concerns and then uses active listening with little, if any, interruption.30,31 Since the goal is to solve problems with rather than for the patient, active listening without offering opinions, judgements, or advice while offering empathy is essential. Through reflection and discussion, the physician can help the patient to identify his or her issues and acceptable solutions.
The importance of good communication between physician and patient cannot be overstated. Additional communication skills to keep in mind are: (1) speak slowly using nonmedical language; (2) limit the amount of information and repeat it; (3) draw pictures and/or use visual aids; and (4) ask the patient to repeat instructions and key concepts. In addition to enhancing patients’ understanding, visual images may be particularly beneficial in keeping patients motivated to improve self-management, including adherence to therapy. For example, it may be helpful to graphically track the patient’s glycemic progress. This can be done by establishing an actionable A1C goal (generally < 7.0%) and a time frame to achieve the goal (eg, 2 to 3 months).32 A graph can be constructed beginning with the patient’s current, preinsulin A1C level, with updates at each visit. In addition to motivating the patient and reinforcing adherence, the graph can also be used to demonstrate when further treatment intensification is needed. Additional general strategies that can be employed when considering the initiation of insulin are shown in TABLE 3. Implementation of strategies such as these by family physicians provides patient outcomes comparable to those implemented by endocrinologists or diabetes specialists.33
TABLE 3
General strategies for initiating insulin therapy
| Invite the patient to take an active role in treatment decisions. |
| Remind the patient that type 2 diabetes is primarily self-managed. |
| Discuss the progressive nature of β-cell dysfunction in type 2 diabetes. |
| Emphasize the physiologic role of insulin to maintain glucose homeostasis. |
| Discuss that insulin will help to achieve glycemic control and minimize the risk for long-term complications. |
| Discuss that treatment will be modified as needed to maintain glycemic control and to best meet their needs, capabilities, and interest. |
| Utilize insulin pen devices whenever possible. |
| Emphasize the importance of lifestyle management. |
| Ask if hearing other patients talk of their experiences with insulin therapy would be helpful; consider a group office visit. |
| Discuss and provide the patient with an individualized, written action plan that includes insulin dosing, self-monitoring of blood glucose, and signs/symptoms of hypoglycemia and other adverse events with appropriate action(s) to take. |
| Simplify diabetes (and comorbidities) treatment whenever possible. |
The remainder of this article uses case studies to further explore various patient barriers to insulin therapy and strategies for addressing them with the patient. While other therapies may be appropriate in the case studies below as recommended by current guidelines, these case studies will focus on insulin. In addition, dosing strategies for initiating and intensifying insulin therapy are discussed. Changes to the treatment plan to adjust for comorbidities, such as hypertension and dyslipidemia, or for smoking cessation or aspirin therapy, are not addressed in these cases, but are crucial components of comprehensive management.
CASE STUDY 1
RF is a 49-year-old female insurance analyst diagnosed with T2DM 6 years ago. Initial therapy with lifestyle modifications and metformin has since been intensified. Glimepiride was added, then pioglitazone was added 1.5 years ago when the A1C had risen to 7.5%. There is no evidence of cardiovascular disease. She reports bothersome lower extremity edema and an 8-pound weight increase since starting pioglitazone treatment. RF states that she takes her medications every day, although she acknowledges that she sometimes forgets on Sundays.
Clinical Impression
After taking her history, performing a physical examination, and reviewing her laboratory and self-monitored blood glucose (SMBG) data, her physician concludes that her treatment plan needs to be changed (TABLE 4, TABLE 5).
TABLE 4
Case study 1: Chart notes
| Physical examination | Laboratory tests | Lifestyle habits | Current therapy | |
|---|---|---|---|---|
| Glucose-lowering | Other | |||
| BP: 126/80 mm Hg Weight: 176 lb (79.2 kg) BMI: 27 kg/m2 Eyes: no retinopathy Neurology: intact Skin: intact | SCr: 1.4 mg/dL Albuminuria: negative A1C: 8.2% Cholesterol: Total: 204 mg/dL LDL: 134 mg/dL HDL: 36 mg/dL | Exercise: Walks 2 miles 3-4 d/wk Nutrition: eats 3-4 meals/d | Metformin 1000 mg BID Glimepiride 8 mg QD Pioglitazone 45 mg QD | Lisinopril 30 mg QD Simvastatin 40 mg QD ASA 80 mg QD |
| ASA, acetylsalicylic acid; BMI, body mass index; BP, blood pressure; HDL, high-density lipoprotein; LDL, low-density lipoprotein; SCr, serum creatinine. | ||||
TABLE 5
Case study 1: Self-monitored blood glucose (mg/dL) over the previous 2 weeks
| Day | Fasting | 2 h Post-breakfast | 2 h Post-lunch | 2 h Post-dinner |
|---|---|---|---|---|
| Wednesday | 205 | |||
| Thursday | 158 | |||
| Friday | 179 | |||
| Saturday | 201 | 162 | ||
| Sunday | ||||
| Monday | 166 | |||
| Tuesday | 189 | |||
| Wednesday | ||||
| Thursday | 153 | 221 | ||
| Friday | 150 | |||
| Saturday | 199 | 186 | 213 | |
| Sunday | ||||
| Monday | 181 | |||
| Tuesday | 167 |
Treatment Plan
- Initiate basal insulin once daily in the evening.
- Continue glimepiride, but reduce pioglitazone to 15 mg once daily (or discontinue if cost is a concern).
- Ask RF to monitor fasting blood glucose and self-adjust insulin doses as appropriate.
Barriers
While discussing the need to change the treatment plan and the physician’s suggestion that RF begin basal insulin, RF asks her physician for another few months on her current regimen stating that she will try harder to take her medications on Sundays. She also voices concern that insulin treatment requires injections and that she is concerned about what her coworkers and friends might think. The physician confirms that these concerns are understandable; he also confirms that RF is fearful of needles. The following are possible responses that RF’s physician could use to address these concerns.
Patient’s concern: Perceived failure/low self-efficacy
Physician responses:
- We all forget to do things from time to time, but overall I think you have done a great job taking your medications.
- As we have talked about before, with T2DM there is a progressive loss of insulin production over time regardless of what you do. That is why we added glimepiride and then pioglita-zone and that is why we need to make a change now and put you back in control of your diabetes. It is likely that further changes will be needed and we can discuss and agree on them together.
Patient’s concern: Social stigmatization
Physician responses:
- We can begin by having you administer insulin once daily in the evening in the privacy of your home.
- The insulin can be administered with a device that looks like a pen. It is small and can be carried in your purse; it does not need to be refrigerated once opened. If the time comes that you will need to administer a dose of insulin during the day, you can easily administer the insulin discretely in a public restroom or your work area.
- The use of insulin is more common than it was even a few years ago. In fact, about 5 million people in the United States use insulin to replace what is missing, control blood sugars, and decrease the risk for diabetes complications.34
Patient’s concern: Fear of needles
Physician’s responses:
- Insulin can be injected using a pen device with short, ultrathin needles that makes most of the injections painless. I would like you to see how simple and painless the injection can be by using this sample pen here in the office.
- Many patients are concerned about giving themselves an injection at first, but they quickly become comfortable doing so.
Dosing
Treatment with basal insulin can be initiated using one of several approaches. Using the treat-to-target approach, basal insulin 10 U once daily is initiated.35 The starting dose should be reduced to 6 U if the initial pre-breakfast or pre-dinner blood glucose is < 126 mg/dL or the patient’s body mass index (BMI) is < 26 kg/m2.36 Alternatively, the ADA/EASD recommends starting with 0.2 U/kg, which may be more practical in very overweight or obese patients.2 Titration of the basal insulin dose can be accomplished using one of the following physician-directed or patient-driven treat-to-target titration algorithms (TABLE 6).35,37,38 The insulin dose should be titrated based on the pre-breakfast fasting blood glucose level.
TABLE 6
Physician-directed or patient-driven treat-to-target titration algorithms
| Riddle et al35 | Davies et al37 | Meneghini et al38 | ||||
|---|---|---|---|---|---|---|
| Start with 10 U/d bedtime basal insulin and adjust weekly | Start with 10* U/d bedtime basal insulin and adjust weekly (physician-directed) Or Start with a dose numerically equivalent to the highest FPG (in millimoles/L)† over the previous 7 days and adjust every 3 days (patient-managed) | Start with basal insulin once daily and adjust every 3 days | ||||
| Mean of self-monitored FPG values from preceding 2 days | Change in insulin dose (U/d)# | Mean of self-monitored FPG values from preceding 3 days | Change in insulin dose (U/d) (physician-directed) | Change in insulin dose (U/d) (patient-managed) | Mean of self-monitored FPG values from preceding 3 days | Change in insulin dose (U/d) |
| ≥180 mg/dL 140-180 mg/dL 120-140 mg/dL 100-120 mg/dL | +8 +6 +4 +2 | ≥180 mg/dL (≥10 mmol/L) 140-179 mg/dL (7.8-9.9 mmol/L) 120-139 mg/dL (6.7 – 7.7 mmol/L) 100-119 mg/dL (5.5-6.6 mmol/L) | +6 to +8 +4 +2 0 to +2 | +2 +2 +2 0 to +2 | >110 mg/dL 80-110 mg/dL <80 mg/dL | +3 0 -3 |
| FPG, fasting plasma glucose. *In insulin-naive patients. †For example, if the highest FPG over the previous 7 days was 7 mmol/L, start with 7 U.#Small insulin dose decreases (2-4 U/d per adjustment) were allowed if severe hypoglycemia (requiring assistance) or plasma-referenced glucose < 56 mg/dL was documented in the preceding week. Reproduced with permission. Meneghini LF, et al. J Fam Pract. 2011;60(9 Suppl 1):S21-S28. Quadrant HealthCom Inc. Copyright 2011. | ||||||
Follow-Up Visit
RF begins basal insulin 10 U in the evening and is given simple instructions for insulin dose titration based on fasting plasma glucose results. At her follow-up visit, RF reports that she has increased her basal insulin to 18 U administered once daily. Review of her SMBG results show that her blood glucose levels throughout the day have improved, but are still not at goal. RF’s physician commends her on the progress she has made. RF and her physician agree that she should continue to increase her basal insulin dose. Eight months after beginning basal insulin, RF is administering 28 U (0.35 U/kg) of basal insulin in the evening. Review of her SMBG results over the previous 2 weeks show that her blood glucose rises during the day and is highest after dinner; her current A1C is 7.2%.
Treatment Plan
- Discuss dietary and lifestyle complements to insulin therapy such as:
- Use SMBG to identify foods that raise her blood glucose.
CASE STUDY 2
LW is a 64-year-old male with longstanding hypertension diagnosed with T2DM 8 years ago for which he was treated initially with lifestyle management and metformin. He has since been treated with other oral agents as add-on therapy; glipizide was discontinued due to hypoglycemia when he skips meals (usually lunch); pioglitazone was discontinued after the patient expressed concerns about the risk for bladder cancer he heard on television. He has mild retinopathy and mild loss of vibration sensation in the feet; there is no evidence of cardiovascular disease. He was diagnosed with osteoarthritis 3 years ago.
Clinical Impression
After taking his history, performing a physical examination, and reviewing his laboratory and SMBG data, his physician concludes that his treatment plan needs to be changed (FIGURE 3, TABLE 7, TABLE 8).
TABLE 7
Case study 2: Chart notes
| Physical examination | Laboratory tests | Lifestyle habits | Current therapy | |
|---|---|---|---|---|
| Glucose-lowering | Other | |||
| BP: 124/76 mm Hg Weight: 204 lb (92.7 kg) BMI: 31 kg/m2 Eyes: mild retinopathy Neurology: occasional tingling on bottom of right foot Skin: intact | SCr: 1.9 mg/dL eGFR: 51 mL/min Albuminuria: negative A1C: 8.1% Cholesterol: Total: 218 mg/dL LDL: 118 mg/dL HDL: 55 mg/dL Triglyceride: 204 mg/dL | Exercise: takes dog on occasional walk but otherwise sedentary Nutrition: eats 4 meals/d | Metformin 1000 mg BID Acarbose 50 mg TID Sitagliptin 100 mg QD | Lisinopril/HCTZ 20/25 mg QD Amlodipine 10 mg QD Acetaminophen extended-release 650 mg TID ASA 80 mg QD |
| ASA, acetylsalicylic acid; BMI, body mass index; BP, blood pressure; eGFR, estimated glomerular filtration rate; HCTZ, hydrochlorothiazide; HDL, high-density lipoprotein; LDL, low-density lipoprotein; SCr, serum creatinine. | ||||
TABLE 8
Case study 2: Self-monitored blood glucose (mg/dL) over the previous 2 weeks
| Day | Fasting | 2 h Post-breakfast | 2 h Post-lunch | 2 h Post-dinner |
|---|---|---|---|---|
| Tuesday | 135 | |||
| Wednesday | ||||
| Thursday | 196 | |||
| Friday | 152 | 174 | ||
| Saturday | ||||
| Sunday | 208 | |||
| Monday | 142 | 193 | ||
| Tuesday | ||||
| Wednesday | 130 | 156 | ||
| Thursday | ||||
| Friday | ||||
| Saturday | ||||
| Sunday | 151 | |||
| Monday |
FIGURE 3
Case study 2: A1C levels for April 2004 to March 2012
Treatment Plan
- Discontinue metformin since LW’s serum creatinine is > 1.5 mg/dL.
- Initiate either basal insulin once daily in the evening or premix insulin at dinner.
- Ask LW to monitor his blood glucose and self-adjust insulin doses as appropriate.
- Stress the importance of exercise and proper nutrition; gain agreement on short-term goals for exercise and nutrition.
Barriers
LW’s physician recommends that his treatment plan be changed and insulin therapy initiated. LW quickly responds that previous changes to his treatment regimen have not resulted in his achieving an A1C < 7.0%. He also doubts that he can use a syringe to draw up the correct dose and then self-administer due to his arthritis. The following are possible responses his physician could use to address these concerns.
Patient concern: Repeated experience of failing to achieve glycemic control, ie, A1C < 7.0%
Physician responses:
- While achieving an A1C < 7.0% is a realistic goal that reduces the risks for vascular complications of diabetes, any reduction of A1C will be of benefit.
- I would like to work with you to implement a new plan that we both believe will enable you to improve your diabetes control and ideally achieve an A1C < 7.0%.
Patient concern: Self-administering due to arthritis
Physician responses:
- Instead of using a syringe and vial to draw up and administer insulin, I would like you to use an insulin pen device. As you can see, it is easy to handle and you can easily select the correct dose.
- If you choose to start on premix insulin, the pen device contains both types of insulin together in one dose.
Dosing
Treatment with basal insulin once daily in the evening can be initiated and titrated based on pre-breakfast blood glucose as in Case Study 1. Alternatively, treatment with premix insulin can be initiated at a dose of 12 U administered within 15 minutes of dinner initiation. The premix dose can be titrated using the algorithm employed in the 1-2-3 Study based on pre-breakfast blood glucose (TABLE 9).39 After 16 weeks, 41% of patients in the 1-2-3 Study achieved an A1C < 7.0% from a baseline A1C of 8.6%.
TABLE 9
1-2-3 Study algorithm39
| Pre-breakfast SMBG (mg/dL) | Adjustment of pre-dinner dose (U) |
|---|---|
| <80 | -3 |
| 80-110 | No change |
| 111-140 | +3 |
| 141-180 | +6 |
| > 180 | +9 |
| SMBG, self-monitored blood glucose. | |
Follow-Up Visit
LW began basal insulin 10 U in the evening. Over the next 5.5 months, he titrated his dose such that his current dose is 46 U (0.50 U/kg) in the evening. His current A1C is 7.3%. Review of his SMBG shows consistently high 2-hour post-lunch blood glucose levels. Although further increasing his basal insulin dose is an option, in most of the treat-to-target studies, the daily dose of basal insulin given once daily averaged between 0.4 and 0.6 U/kg.35,37,40,41 LW and his physician agree that adding rapid-acting insulin at lunch is the best option. The starting dose of rapid-acting bolus insulin is 4 to 6 U administered prior to the largest meal of the day or, as in this case, prior to the meal with the largest postprandial blood glucose excursion.42,43 Alternatively, the dose of rapid-acting insulin could be calculated as 10% of the total daily dose of basal insulin, which in this case is 5 U (10% x 46 U). The dose of basal insulin would be reduced by 5 U if the rapid-acting insulin is given at dinner in order to reduce the risk for nocturnal hypoglycemia. The dose of the bolus insulin can be titrated using the ExtraSTEP algorithm (TABLE 10).42 Alternatively, the SimpleSTEP algorithm can be used which does not require a 2-hour postprandial glucose measurement.42
TABLE 10
Algorithms for adjusting insulin aspart42
| ExtraSTEP algorithm | SimpleSTEP algorithm | |||
|---|---|---|---|---|
| 2-h Post-meal PG level (mg/dL) | Insulin aspart adjustment (U) | Pre-meal BG (mg/dL) | Bedtime BG (mg/dL) | Insulin aspart adjustment (U) |
| <72* | -2 | <72* | <72* | -2 |
| 72-144 | 0 | 72-108 | 72-144 | 0 |
| 145-180 | +2 | 109-162 | 145-180 | +2 |
| >180 | +4 | >162 | >180 | +4 |
| BG, blood glucose; PG, plasma glucose. *One or more PG values <72 mg/dL without obvious explanation. Reproduced with permission. Meneghini LF, et al. J Fam Pract. 2011;60(9 Suppl 1):S21-S28. Quadrant HealthCom Inc. Copyright 2011. | ||||
Plan
- Begin rapid-acting insulin 5 U at lunch.
- Continue basal insulin at 46 U in the evening.
- Ask LW to continue to titrate basal insulin based on the pre-breakfast blood glucose level and the lunch time bolus insulin dose based on the 2-hour post-lunch SMBG (ExtraSTEP); alternatively, adjust based on the pre-dinner blood glucose level (SimpleSTEP).
CASE STUDY 3
MB is a 46-year-old male who had not consulted a physician since having a physical examination 6 years ago. He presented 2 weeks ago with frequent urination (7-8 times/day) and feeling tired; he also noted losing 5 pounds (2.25 kg) over the preceding 3.5 months despite no changes in his diet. MB is a regional salesperson with an erratic schedule. During the week, he eats lunch and most dinners in a restaurant. On the weekend, he goes to a local bar with his friends. He does light yard work, but does not exercise regularly. He is a current smoker with a 36 pack-year history. Urinalysis shows ketonuria and microalbuminuria. His A1C reported back today is 10.8%, confirming a diagnosis of uncontrolled and symptomatic DM.
Clinical Impression
After taking his history, performing a physical examination, and reviewing his laboratory data, MB’s physician confirms a diagnosis of DM (TABLE 11). While it is likely that MB has T2DM, his physician wants to rule out type 1 DM and latent autoimmune diabetes of the adult (LADA), so he orders tests for antibodies (GAD, IA-2, ICA). The antibody testing is negative, making T2DM the most likely diagnosis.
TABLE 11
Case study 3: Chart notes
| Physical examination | Laboratory tests | Lifestyle habits | Current therapy | |
|---|---|---|---|---|
| Glucose-lowering | Other | |||
| BP: 142/88 mm Hg Weight: 176 lb (79.2 kg) BMI: 27 kg/m2 Eyes: no retinopathy Neurology: intact Skin: intact | SCr: 1.4 mg/dL Microalbumin:creatinine ratio: 140 mg/g creatinine Ketonuria: 1+ A1C: 10.8% Cholesterol: Total: 210 mg/dL LDL: 146 mg/dL HDL: 30 mg/dL | Exercise: light yard work, no regular exercise Nutrition: 3 meals/d, eats most meals in a restaurant (lunch M-F; dinner 3-4 nights/wk) | None | None |
| BMI, body mass index; BP, blood pressure; HDL, high-density lipoprotein; LDL, low-density lipoprotein; SCr, serum creatinine. | ||||
Treatment Plan
- Initiate basal-bolus therapy with fixed bolus doses of rapid-acting insulin at each meal (prandial insulin).
- Ask MB to monitor blood glucose before meals and at bedtime.
- Provide MB with a supplemental scale to correct hyperglycemia before meals.
- Stress the importance of exercise and proper nutrition; gain agreement for short-term goals for exercise and nutrition; refer for diabetes and nutrition education if available.
- Discuss the importance of smoking cessation; develop a plan.
- Consider metformin and other non-insulin therapies when A1C is under control.
Barriers
MB is surprised that he has T2DM and is clearly anxious at receiving the diagnosis. He expresses concern about starting insulin because his uncle died within a year of starting insulin. MB also recalls that his uncle was always giving himself shots and monitoring his blood glucose level. He wants to know whether there is a simpler treatment option if he agrees to start insulin treatment. He also wants to know whether he will have to remain on insulin for the rest of his life. The following are possible responses his physician could use to address these concerns.
Patient concern: Fear of death
Physician responses:
- Uncontrolled high blood sugars over a long period of time can cause serious complications, such as kidney and heart disease that can result in death. That is why it is important that we work together to gain control of your blood sugar levels over the next few months and then modify your treatment as needed to maintain control.
- Unfortunately for many patients in the past, treatment with insulin was not used until it was too late and people already had serious complications from DM. This is likely the case for your uncle.
Patient concern: Treatment complexity
Physician responses:
- Right now we have to control your blood glucose rapidly so your pancreas can regain some function and your body can better respond to insulin.
- I will also provide you with step-by-step written instructions you can follow that describe how to start insulin and how to monitor your blood glucose.
- We will communicate as often as you need to adjust your insulin doses over the next few weeks; when you feel comfortable, I can even show you how to adjust your insulin dose before a meal to correct a high blood sugar.
- We can try this treatment for 3 months and then reevaluate your response, how you feel, and whether you want to continue to modify your treatment plan to keep your blood sugars controlled.
Patient concern: Lack of understanding that T2DM is a serious disease
Physician responses:
- Please understand that T2DM is a serious disease that increases your risk for heart disease, stroke, blindness, and other diseases. Unfortunately, since diabetes does not cause bad symptoms until it is actually too late, many patients do not make the effort to properly control their diabetes. By working together, we can reduce the risk for these complications and do some screening tests to detect any complications before they become irreversible.
Dosing
There are several approaches to determining the initial doses of basal and prandial (bolus) insulin. One approach is to estimate the total daily dose (TDD) of insulin by multiplying the patient’s weight in kilograms by 0.5 U/kg/d.44 Half of the TDD is given as basal insulin replacement; the other half is divided into 3 fixed preprandial doses of rapid-acting insulin. When the patient is ready to take on more complex management, the supplemental dose for bolus insulin can be calculated using a correction factor. If the bolus insulin is a rapid-acting insulin analog, 1800 is divided by the TDD of insulin; 1500 is used for a short-acting human insulin. This correction factor is an estimate of the fall in blood glucose per unit of bolus insulin. In our patient, the TDD would be: 80 kg x 0.5 U/kg/d or 40 U/d of insulin. Thus, 1 U of insulin should lower the blood glucose by about 45 mg/dL (1800/40 U = 45 mg/dL). For every 45 mg/dL above the pre-meal target, the patient would add 1 U of rapid-acting insulin to correct the hyperglycemia over the next 4 to 5 hours. The basal and prandial insulin doses would be titrated on a periodic basis (perhaps every 1 to 2 weeks) until the daytime levels of blood glucose are on target. The fasting (pre-breakfast) blood glucose would be used to adjust the basal insulin dose, while the pre-lunch, pre-dinner, and bedtime blood glucose results would be used to adjust the pre-breakfast, pre-lunch, and pre-dinner prandial (rapid-acting) insulin doses, respectively.
An alternative approach to initiating basal-bolus therapy is the PREFER algorithm.45 Here, the basal insulin dose is 10 U initially. The bolus doses are administered in a 3:1:2 ratio, so if the total of the 3 bolus doses is 12 U/d, the initial bolus doses would be 6 (breakfast), 2 (lunch), and 4 (dinner) U. The mean basal (once-daily) and bolus insulin doses observed in PREFER are shown in TABLE 12 and TABLE 13.
TABLE 12
Case study 3: Calculating initial basal-bolus insulin doses
| Algorithm | Calculations | Patient MB |
|---|---|---|
| Meneghini44 | TDD = (total body weight [kg]) (0.5 U/kg/d) Basal insulin dose* = (50%) (TDD) Bolus insulin dose† = (10%-20%) (TDD) | TDD = (0.5 U/kg/d)(80kg) = 40 U/d |
| Basal = (50%) (40 U/d) = 20 U/d | ||
| Bolus = (10%-20%) (40 U/d) = 4 to 8 U/meal | ||
| CF = 1800/40 U/d = 45 mg/dL per 1 unit | ||
| PREFER45 | Basal insulin dose* = 10 U (14 U if BMI > 32 kg/m2) Bolus insulin dose† = ratio of 3:1:2 (breakfast:lunch:dinner) Note: At week 26, the bolus insulin doses were divided into the 3 daily meals in approximately a 1:1:1 ratio | |
| BMI, body mass index; CF, correction factor; TDD, total daily dose of insulin. *Once daily; †Three meals per day. | ||
TABLE 13
Titrating the basal insulin dose using the PREFER algorithm45
| Pre-breakfast blood glucose (mg/dL) | Basal insulin dose adjustment (U) |
|---|---|
| < 56 | -4 |
| 56-72 | -2 |
| 73-125 | No change |
| 126-140 | +2 |
| 141-160 | +4 |
| 161-180 | +6 |
| 181-200 | +8 |
| > 200 | +10 |
Follow-up Visit
MB begins with basal insulin 20 U in the evening and bolus insulin at doses of 7 U before each meal. Over the next several months, MB has titrated his insulin doses; his current doses are: 32 U (basal), 11 U (bolus-breakfast), 7 U (bolus-lunch), and 10 U (bolus-dinner). He experienced 1 episode of mild hypoglycemia (SMBG, 50 mg/dL) one afternoon following a particularly active morning (TABLE 14). His current A1C is 7.4%. MB’s physician congratulates him on the progress he has made in dramatically lowering his blood glucose level—and his risk for diabetes-related complications. While MB appreciates his physician’s support and admits that he does not feel tired and generally feels better, which is likely due to resolution of glucotoxicity, he is not happy that he has gained 5.5 pounds (2.5 kg).46 He also finds the timing and administration of bolus insulin difficult.
TABLE 14
Case study 3: Self-monitored blood glucose (mg/dL) over the previous 2 weeks
| Day | Fasting | 2 h Post-breakfast | 2 h Post-lunch | 2 h Post-dinner |
|---|---|---|---|---|
| Wednesday | ||||
| Thursday | 168 | |||
| Friday | 106 | 166 | 174 | |
| Saturday | 88 | |||
| Sunday | 195 | |||
| Monday | 134 | |||
| Tuesday | 172 | |||
| Wednesday | 130 | 156 | ||
| Thursday | 112 | 168 | ||
| Friday | 92 | 164 | ||
| Saturday | 50 | 149 | 159 | 176 |
| Sunday | 94 | 174 | 210 | |
| Monday | 176 | 184 | ||
| Tuesday | 117 | 169 |
Plan
- Continue basal insulin once-daily in the evening.
- Add metformin 500 mg BID and increase to 1000 mg BID as tolerated.
- Consider weaning down the bolus insulin doses and substituting them with a GLP-1R agonist, dipeptidyl peptidase-4 inhibitor, or short-acting secretagogue. If so, continue rapid-acting insulin during transition. [Note: the following combinations are not currently approved by the US FDA: exenatide twice-daily and prandial insulin; exenatide once-weekly and insulin; liraglutide and prandial insulin; linagliptin and insulin.]
CASE STUDY 4
KW is a 62-year-old female diagnosed with T2DM 12 years ago. Treatment with lifestyle management and metformin initially provided glycemic control. Glimepiride was subsequently added and eventually the patient was started on basal insulin. The current dose of basal insulin is 60 U in the evening. Five months ago her A1C was found to be 7.9% and more recently 8.3%. She drinks alcohol occasionally and smokes. KW works as an executive secretary and has a consistent meal and activity schedule.
Clinical Impression
Following completion of the history, physical examination, and review of her laboratory data, KW’s physician concludes that her insulin regimen should be intensified (TABLE 15, TABLE 16).
TABLE 15
Case study 4: Chart notes
| Physical examination | Laboratory tests | Lifestyle habits | Current therapy | |
|---|---|---|---|---|
| Glucose-lowering | Other | |||
| BP: 126/78 mm Hg Weight: 176 lb (79.2 kg) BMI: 32 kg/m2 Eyes: no retinopathy Neurology: intact Skin: intact | SCr: 1.0 mg/dL Albuminuria: negative A1C: 8.3% Cholesterol Total: 172 mg/dL LDL: 96 mg/dL HDL: 46 mg/dL Triglycerides: 138 mg/dL | Exercise: sedentary Nutrition: 3 meals/d with large dinner | Metformin 1000 mg BID Basal insulin 60 U in the evening | ASA 80 mg QD Pravastatin 40 mg qHS |
| BMI, body mass index; BP, blood pressure; HDL, high-density lipoprotein; LDL, low-density lipoprotein; SCr, serum creatinine. | ||||
TABLE 16
Case study 4: Self-monitored blood glucose (mg/dL) over the previous 2 weeks
| Day | Fasting | 2 h Post-breakfast | 2 h Post-lunch | 2 h Post-dinner |
|---|---|---|---|---|
| Friday | ||||
| Saturday | 156 | 244 | ||
| Sunday | 253 | |||
| Monday | ||||
| Tuesday | ||||
| Wednesday | 148 | 227 | ||
| Thursday | ||||
| Friday | ||||
| Saturday | 179 | |||
| Sunday | 160 | |||
| Monday | ||||
| Tuesday | ||||
| Wednesday | ||||
| Thursday |
Plan
- Discontinue basal insulin.
- Begin premix insulin twice daily before breakfast and dinner.
- Ask KW to monitor blood glucose two times daily and, if appropriate, teach her how to self-adjust insulin doses.
- Stress the importance of exercise and proper nutrition; gain agreement on short-term goals for exercise and nutrition.
- Discuss the importance of smoking cessation; develop a plan.
Barriers
The physician discusses with KW that her consistent meal and activity schedule would make switching to premix insulin twice daily a good choice. KW is generally in agreement with the change, but wonders whether hypoglycemia might be more likely. She also asks if she might gain more weight in addition to the 3 pounds (1.35 kg) she has gained since starting basal insulin.
Patient concern: Hypoglycemia
Physician responses:
- Hypoglycemia remains a concern, and is more frequently seen with premix than with basal insulin; however, as long as you remain consistent with your meal and activity schedule, the risk for bad hypoglycemia is low.
- We should review your written action plan so that you are sure what signs or symptoms of a low blood sugar might occur and what you should do to treat them.
Patient concern: Weight gain
Physician responses:
- It is possible that you might gain a few additional pounds. You can avoid this by increasing your physical activity, and importantly, continue healthy eating. We should schedule a time for you to meet again with a dietician who can discuss options that might work for you.
Dosing
There are different approaches for converting from basal insulin to twice-daily premix insulin. One approach is to determine the TDD of basal insulin, and give half at breakfast and the other half at dinner as premix insulin.39 Since KW is taking 60 U of basal in the evening, she should take 30 U at breakfast and 30 U at dinner. Dose titration is according to the 1-2-3 Study algorithm shown in case study 2.
Another approach is to administer biphasic insulin aspart 70/30 0.2 U/kg before breakfast and 0.1 U/kg before dinner as was done in the PREFER study (TABLE 13).45 Subsequent dosing can be determined based on the PREFER algorithm below. Of note is that at study end, premix insulin doses were equally divided between breakfast and dinner. Breakfast and dinner doses are titrated based on blood glucose levels before dinner and breakfast, respectively. In the PREFER study, the use of premix insulin provided comparable A1C reduction as basal-bolus therapy (basal once daily + bolus TID) in insulin-naïve patients. However, patients previously treated with basal insulin such as KW experienced greater A1C reductions with basal-bolus insulin than with premix insulin.
The Evolution of Insulin Therapy in Diabetes Mellitus
The modern management of diabetes mellitus (DM) began with the discovery of insulin by Banting and Best in 1921 (see The Evolution of Insulin Therapy in Diabetes Mellitus in this supplement). Since that time, numerous additional classes of glucose-lowering agents have been introduced for the treatment of type 2 DM (T2DM). These medications primarily act by addressing 2 of the key defects of T2DM, insulin resistance and pancreatic β-cell dysfunction. T2DM is a progressive disease process that requires continued adjustment of therapy to maintain treatment goals. Most patients with T2DM will require insulin therapy at some point in their lives.
Role of Insulin in Type 2 Diabetes Mellitus Management
Consensus guidelines developed by the American Association of Clinical Endocrinologists/American College of Endocrinology (AACE/ACE) recommend initiating insulin when oral therapy fails to achieve glycemic control, A1C > 9.0% in treatment-naïve patients, or if the patient is symptomatic with glucose toxicity (polyuria, polydipsia, and weight loss) (FIGURE 1).1
Similar consensus guidelines developed by the American Diabetes Association/European Association for the Study of Diabetes (ADA/EASD) advise the initiation of glucose-lowering therapy for most patients with T2DM with the combination of lifestyle modifications, diet, and metformin (FIGURE 2).2 For patients who do not achieve or maintain glycemic control over 3 months, or thereabouts, with metformin, a second oral agent should be added. Alternatives include a glucagon-like peptide-1 receptor (GLP-1R) agonist or basal insulin. Insulin should be strongly considered as initial therapy for a patient with significant symptoms of hyperglycemia and/or plasma glucose >300-350 mg/dL or A1C ≥10.0%.
The major role of insulin in the management of patients with T2DM stems from several important attributes. First, insulin is the only treatment that works in patients with advanced β-cell deficiency. It acts directly on tissues to regulate glucose homeostasis, unlike other glucose-lowering agents that require the presence of sufficient endogenous insulin to exert their effects as insulin sensitizers, secretagogues, incretin mimetics, amylin analogs, and other factors. This also means that the mechanism of action of insulin is complementary to those of other glucose-lowering agents. Second, there is less of a ceiling effect with insulin. That is, increasing the dose of insulin results in a progressive lowering of blood glucose in the majority of patients, with the major limitation being the risk for hypoglycemia. Third, the glucose-lowering efficacy of insulin is durable, unlike that of other glucose-lowering agents that depend on endogenous insulin secretion for continued effectiveness. Fourth, insulin improves the lipid profile, particularly triglyceride levels.2-5 Fifth, regarding the long-term safety and tolerability of insulin, it is well established that weight gain, likely mediated via reduction of glycosuria, and hypoglycemia are typically the most concerning adverse events encountered. Allergic reactions, which were a more common complication of animal-sourced insulins, are infrequent with the insulin analogs.6-17 Finally, the availability of insulin in different formulations allows for targeting fasting plasma glucose or postprandial glucose, and individualization of therapy (see The Evolution of Insulin Therapy in Diabetes Mellitus in this supplement.)
While both the AACE/ACE and ADA/EASD consensus guidelines provide treatment “algorithms,” both make it clear that these are suggested approaches suitable for the population with T2DM (FIGURE 1, FIGURE 2). The specific treatment approach must be individualized based on patient-specific factors such as age, comorbid conditions, and tolerance of hypoglycemia.
FIGURE 1
Role of insulin in the management of patients with type 2 diabetes mellitus according to the AACE/ACE1
AACE, American Association of Clinical Endocrinologists; ACE, American College of Endocrinology; AGI, α-glucosidase inhibitor; DPP4, dipeptidyl-peptidase-4 inhibitor; FPG, fasting plasma glucose; GLP-1, glucagon–like peptide-1 agonist; MET, metformin; PPG, postprandial glucose; SU, sulfonylurea; TZD, thiazolidinedione.
Reprinted from American Association of Clinical Endocrinologists. AACE/ACE Diabetes Algorithm for Glycemic Control. Available at https://www.aace.com/sites/default/files/GlycemicControlAlgorithmPPT.pdf. Accessed April 4, 2012, with permission from the American Association of Clinical Endocrinologists.
FIGURE 2
Role of insulin in the management of patients with type 2 diabetes mellitus according to the ADA/EASD2
Moving from the top to the bottom of the figure, potential sequences of antihyperglycemic therapy. In most patients, begin with lifestyle changes; metformin monotherapy is added at, or soon after, diagnosis (unless there are explicit contraindications). If the HbA1c target is not achieved after ~3 months, consider 1 of the 5 treatment options combined with metformin: an SU, TZD, DPP-4-i, GLP-1-RA, or basal insulin. (The order in the chart is determined by historical introduction and route of administration and is not meant to denote any specific preference.) Choice is based on patient and drug characteristics, with the over-riding goal of improving glycemic control while minimizing side effects. Shared decision making with the patient may help in the selection of therapeutic options. The figure displays drugs commonly used both in the United States and/or Europe. Rapid-acting secretagogues (meglitinides) may be used in place of SUs. Other drugs not shown (α-glucosidase inhibitors, colesevelam, dopamine agonists, pramlintide) may be used where available in selected patients but have modest efficacy and/or limiting side effects. In patients intolerant of, or with contraindications for, metformin, select initial drug from other classes depicted and proceed accordingly. In this circumstance, while published trials are generally lacking, it is reasonable to consider 3-drug combinations other than metformin. Insulin is likely to be more effective than most other agents as a third-line therapy, especially when HbA1c is very high (eg, ≥ 9.0%). The therapeutic regimen should include some basal insulin before moving to more complex insulin strategies. Dashed arrow line on the left-hand side of the figure denotes the option of a more rapid progression from a 2-drug combination directly to multiple daily insulin doses, in those patients with severe hyperglycemia (eg, HbA1c, ≥ 10.0–12.0%).
DPP-4, dipeptidyl peptidase-4; DPP-4-i, DPP-4 inhibitor; Fx’s, bone fractures; GI, gastrointestinal; GLP-1, glucagon-like peptide 1; GLP-1-RA, GLP-1 receptor agonist; HbA1c, hemoglobin A1c; HF, heart failure; NPH, neutral protamine Hagedorn; SU, sulfonylurea; TZD, thiazolidinedione.
aConsider beginning at this stage in patients with very high HbA1c (eg, ≥ 9%); bConsider rapid-acting, non-SU secretagogues (meglitinides) in patients with irregular meal schedules or who develop late postprandial hypoglycemia on SUs; cUsually a basal insulin (NPH, glargine, detemir) in combination with noninsulin agents; dCertain noninsulin agents may be continued with insulin. Consider beginning at this stage if patient presents with severe hyperglycemia (≥ 16.7–19.4 mmol/L [≥ 300–350 mg/dL]; HbA1c≥ 10.0–12.0%) with or without catabolic features (weight loss, ketosis, etc).
Diabetes Care by American Diabetes Association. Copyright 2012. Reproduced with permission of AMERICAN DIABETES ASSOCIATION in the format Journal via Copyright Clearance Center.
Individualizing Therapy
The importance of individualizing therapy in a way that allows patients with T2DM to effectively self-manage their disease cannot be overstated. A study involving 1381 patients with T2DM cared for by 42 primary care physicians was conducted to estimate the magnitude of effect that physicians have on glycemic control.18 Hierarchical linear modeling showed that physician-related factors were associated with a statistically significant but modest variability in A1C change (2%) for the entire patient group. On the face of it, this finding might be discouraging. Further analysis showed, however, that for patients whose A1C did improve, physician-related factors accounted for 5% of the overall change in A1C (P = .005). On the other hand, physician-related factors had no impact on patients whose A1C did not improve or worsened. These results support the role that physicians play in affecting patient outcomes. The results also make it clear that without a physician’s influence, a patient’s glycemic outcomes may be difficult to change. The question is: How best can a physician influence patient outcomes?
A 2011 survey of patients with DM, general practitioners, and DM specialists reported that clinicians tended to underestimate patients’ perceived seriousness of the disease, while overestimating patients’ level of distress. In addition, physicians had difficulty identifying which DM-related complications concerned patients most and the information and support patients needed to feel more at ease with DM. Patients placed greater importance on having easy access to their physicians rather than more time with them. But most importantly, the survey investigators concluded that patients generally wished for greater involvement in decision making and being provided more information.19 These findings suggest that patients understand that T2DM is a largely self-managed, chronic disease, and want a collaborative relationship with their physician.
Patient Barriers to Insulin Therapy
Numerous factors have been identified as impeding patients’ willingness to initiate insulin therapy (TABLE 1).20-24 Barriers often vary from patient to patient and, in fact, may change over time in an individual patient. It is crucial, therefore, to identify the root reasons for a patient’s apprehension with insulin when talking about options for intensifying treatment. Once insulin has been initiated, the patient should be asked about continuing or new concerns regarding insulin therapy (and DM management in general), including adherence.
TABLE 1
Barriers to insulin therapy identified by patients20-24
| Lack of understanding of serious nature of type 2 diabetes mellitus |
| Fear of addiction to insulin |
| Fear of hypoglycemia |
| Concern about weight gain |
| Repeated experiences of failing to achieve satisfactory glycemic control |
| Perception that quality of previous treatment was low |
| Needle phobia |
| Treatment complexity |
| Concern of social stigmatization |
| Perceived failure and low self-efficacy |
| Belief of becoming more ill |
| Out-of-pocket cost |
| Perceived negative impact on quality of life |
| Comorbidities such as poor eyesight, arthritis, forgetfulness |
A recent, international survey of 1400 patients with insulin-naïve T2DM reported that 3 negative beliefs about insulin were prominent: (1) feeling that the disease was worsening; (2) fear of injection; and (3) a feeling of personal failure.20 Certain patient comorbidities, such as poor eyesight, arthritis, and forgetfulness, might also serve as barriers to self-management of DM with insulin. Additional comorbidities may contribute as indirect barriers, such as the need for polypharmacy, which may make the initiation of additional treatments such as insulin logistically or financially difficult.
It is possible that the discussion about initiating insulin may uncover patient concerns about T2DM in general. The Diabetes Attitudes, Wishes, and Needs (DAWN) study reported that psychosocial issues were the major source of difficulty in patient self-management (TABLE 2).25 In fact, 85% of people who reported a high level of distress at the time of diagnosis of T2DM continued to experience psychological distress at a mean follow-up of 15 years.
TABLE 2
Patients experiencing various aspects of diabetes-related distress25
| Diabetes-related distress | Respondents who agree (%) |
|---|---|
| I feel stressed because of my diabetes. | 32.7 |
| I feel burned out because of my diabetes. | 18.1 |
| I feel that diabetes is preventing me from doing what I want to do. | 35.9 |
| I am constantly afraid of my diabetes getting worse. | 43.8 |
| I worry about not being able to carry out my family responsibilities in the future. | 30.1 |
| My diabetes causes me worries about my financial future. | 25.8 |
| My family and friends put too much pressure on me about my diabetes. | 14.7 |
| The community I live in is intolerant of diabetes. | 13.6 |
| Diabetes Care by American Diabetes Association. Copyright 2012. Reproduced with permission of AMERICAN DIABETES ASSOCIATION in the format Journal via Copyright Clearance Center. | |
Addressing psychosocial issues and other barriers is crucial in the discussion of self-management because those with more negative feelings about starting insulin are most unwilling to start insulin.20 One factor that may contribute to these negative feelings is repeated experiences of failing to achieve satisfactory glycemic control with oral glucose-lowering agents.23 Conversely, those who have experienced improved glycemic control with intensification of prior glucose-lowering therapy may be more accepting of initiating insulin therapy.23,26 These findings are a reminder of the importance of a treat-to-target approach to management, in which the target glycemic goal, generally A1C < 7.0%, is achieved within 2 to 3 months of diagnosis and maintained at that level through intensification of therapy as needed.
Addressing psychosocial issues can be a challenge in today’s busy primary care practice due to limited time and lack of training in the management of such issues. However, implementation of various strategies has been reported to facilitate and, in some cases, shorten a patient’s visit. For example, one small study reported that visits were shorter if the physician acknowledged and responded positively to a patient’s stated or implied concerns (17.6 minutes vs 20.1 minutes).27 Missing or ignoring the patient’s concerns often led the patient to bring up the same concern one or more additional times resulting in a longer office visit. These results underscore the importance of asking patients to identify their concerns or questions at the beginning of the office visit. The patient can fill out a questionnaire in the waiting room or be encouraged to write down and prioritize their questions and concerns specific to the visit. If the patient identifies more concerns or questions than can be reasonably addressed in one visit, there should be agreement to address the most pressing ones during the current visit and the remaining concerns and questions during the next visit. This “agenda-setting” approach has been reported to offer several advantages.28 From the patient’s perspective, the quality of the physician-patient interaction was much improved, in part because physicians took time to explain points in a way that was easy to understand. Advantages to the physician with an agenda-setting approach included “feeling more in control,” “less stressed by simply knowing what was on the patient’s mind,” “feeling less rushed,” and “enjoying patient encounters more.” Contrary to the study cited above, physicians found that patients’ visits often were longer, especially those of older patients. One physician, however, noted that the visit “takes more time now, but saves time later.” As noted in this study, additional time spent with the patient can lead to improved job satisfaction for the physician.29
The agenda-setting approach requires that the physician ask the patient to list his or her concerns and questions, and then actively listen to the patient. Once the agenda for the visit is established, employing the “ask, listen, empathize” communication style can lead to effective physician-patient communication and problem-solving. Using this approach, the physician asks questions to gain a clear understanding of the patient’s concerns and then uses active listening with little, if any, interruption.30,31 Since the goal is to solve problems with rather than for the patient, active listening without offering opinions, judgements, or advice while offering empathy is essential. Through reflection and discussion, the physician can help the patient to identify his or her issues and acceptable solutions.
The importance of good communication between physician and patient cannot be overstated. Additional communication skills to keep in mind are: (1) speak slowly using nonmedical language; (2) limit the amount of information and repeat it; (3) draw pictures and/or use visual aids; and (4) ask the patient to repeat instructions and key concepts. In addition to enhancing patients’ understanding, visual images may be particularly beneficial in keeping patients motivated to improve self-management, including adherence to therapy. For example, it may be helpful to graphically track the patient’s glycemic progress. This can be done by establishing an actionable A1C goal (generally < 7.0%) and a time frame to achieve the goal (eg, 2 to 3 months).32 A graph can be constructed beginning with the patient’s current, preinsulin A1C level, with updates at each visit. In addition to motivating the patient and reinforcing adherence, the graph can also be used to demonstrate when further treatment intensification is needed. Additional general strategies that can be employed when considering the initiation of insulin are shown in TABLE 3. Implementation of strategies such as these by family physicians provides patient outcomes comparable to those implemented by endocrinologists or diabetes specialists.33
TABLE 3
General strategies for initiating insulin therapy
| Invite the patient to take an active role in treatment decisions. |
| Remind the patient that type 2 diabetes is primarily self-managed. |
| Discuss the progressive nature of β-cell dysfunction in type 2 diabetes. |
| Emphasize the physiologic role of insulin to maintain glucose homeostasis. |
| Discuss that insulin will help to achieve glycemic control and minimize the risk for long-term complications. |
| Discuss that treatment will be modified as needed to maintain glycemic control and to best meet their needs, capabilities, and interest. |
| Utilize insulin pen devices whenever possible. |
| Emphasize the importance of lifestyle management. |
| Ask if hearing other patients talk of their experiences with insulin therapy would be helpful; consider a group office visit. |
| Discuss and provide the patient with an individualized, written action plan that includes insulin dosing, self-monitoring of blood glucose, and signs/symptoms of hypoglycemia and other adverse events with appropriate action(s) to take. |
| Simplify diabetes (and comorbidities) treatment whenever possible. |
The remainder of this article uses case studies to further explore various patient barriers to insulin therapy and strategies for addressing them with the patient. While other therapies may be appropriate in the case studies below as recommended by current guidelines, these case studies will focus on insulin. In addition, dosing strategies for initiating and intensifying insulin therapy are discussed. Changes to the treatment plan to adjust for comorbidities, such as hypertension and dyslipidemia, or for smoking cessation or aspirin therapy, are not addressed in these cases, but are crucial components of comprehensive management.
CASE STUDY 1
RF is a 49-year-old female insurance analyst diagnosed with T2DM 6 years ago. Initial therapy with lifestyle modifications and metformin has since been intensified. Glimepiride was added, then pioglitazone was added 1.5 years ago when the A1C had risen to 7.5%. There is no evidence of cardiovascular disease. She reports bothersome lower extremity edema and an 8-pound weight increase since starting pioglitazone treatment. RF states that she takes her medications every day, although she acknowledges that she sometimes forgets on Sundays.
Clinical Impression
After taking her history, performing a physical examination, and reviewing her laboratory and self-monitored blood glucose (SMBG) data, her physician concludes that her treatment plan needs to be changed (TABLE 4, TABLE 5).
TABLE 4
Case study 1: Chart notes
| Physical examination | Laboratory tests | Lifestyle habits | Current therapy | |
|---|---|---|---|---|
| Glucose-lowering | Other | |||
| BP: 126/80 mm Hg Weight: 176 lb (79.2 kg) BMI: 27 kg/m2 Eyes: no retinopathy Neurology: intact Skin: intact | SCr: 1.4 mg/dL Albuminuria: negative A1C: 8.2% Cholesterol: Total: 204 mg/dL LDL: 134 mg/dL HDL: 36 mg/dL | Exercise: Walks 2 miles 3-4 d/wk Nutrition: eats 3-4 meals/d | Metformin 1000 mg BID Glimepiride 8 mg QD Pioglitazone 45 mg QD | Lisinopril 30 mg QD Simvastatin 40 mg QD ASA 80 mg QD |
| ASA, acetylsalicylic acid; BMI, body mass index; BP, blood pressure; HDL, high-density lipoprotein; LDL, low-density lipoprotein; SCr, serum creatinine. | ||||
TABLE 5
Case study 1: Self-monitored blood glucose (mg/dL) over the previous 2 weeks
| Day | Fasting | 2 h Post-breakfast | 2 h Post-lunch | 2 h Post-dinner |
|---|---|---|---|---|
| Wednesday | 205 | |||
| Thursday | 158 | |||
| Friday | 179 | |||
| Saturday | 201 | 162 | ||
| Sunday | ||||
| Monday | 166 | |||
| Tuesday | 189 | |||
| Wednesday | ||||
| Thursday | 153 | 221 | ||
| Friday | 150 | |||
| Saturday | 199 | 186 | 213 | |
| Sunday | ||||
| Monday | 181 | |||
| Tuesday | 167 |
Treatment Plan
- Initiate basal insulin once daily in the evening.
- Continue glimepiride, but reduce pioglitazone to 15 mg once daily (or discontinue if cost is a concern).
- Ask RF to monitor fasting blood glucose and self-adjust insulin doses as appropriate.
Barriers
While discussing the need to change the treatment plan and the physician’s suggestion that RF begin basal insulin, RF asks her physician for another few months on her current regimen stating that she will try harder to take her medications on Sundays. She also voices concern that insulin treatment requires injections and that she is concerned about what her coworkers and friends might think. The physician confirms that these concerns are understandable; he also confirms that RF is fearful of needles. The following are possible responses that RF’s physician could use to address these concerns.
Patient’s concern: Perceived failure/low self-efficacy
Physician responses:
- We all forget to do things from time to time, but overall I think you have done a great job taking your medications.
- As we have talked about before, with T2DM there is a progressive loss of insulin production over time regardless of what you do. That is why we added glimepiride and then pioglita-zone and that is why we need to make a change now and put you back in control of your diabetes. It is likely that further changes will be needed and we can discuss and agree on them together.
Patient’s concern: Social stigmatization
Physician responses:
- We can begin by having you administer insulin once daily in the evening in the privacy of your home.
- The insulin can be administered with a device that looks like a pen. It is small and can be carried in your purse; it does not need to be refrigerated once opened. If the time comes that you will need to administer a dose of insulin during the day, you can easily administer the insulin discretely in a public restroom or your work area.
- The use of insulin is more common than it was even a few years ago. In fact, about 5 million people in the United States use insulin to replace what is missing, control blood sugars, and decrease the risk for diabetes complications.34
Patient’s concern: Fear of needles
Physician’s responses:
- Insulin can be injected using a pen device with short, ultrathin needles that makes most of the injections painless. I would like you to see how simple and painless the injection can be by using this sample pen here in the office.
- Many patients are concerned about giving themselves an injection at first, but they quickly become comfortable doing so.
Dosing
Treatment with basal insulin can be initiated using one of several approaches. Using the treat-to-target approach, basal insulin 10 U once daily is initiated.35 The starting dose should be reduced to 6 U if the initial pre-breakfast or pre-dinner blood glucose is < 126 mg/dL or the patient’s body mass index (BMI) is < 26 kg/m2.36 Alternatively, the ADA/EASD recommends starting with 0.2 U/kg, which may be more practical in very overweight or obese patients.2 Titration of the basal insulin dose can be accomplished using one of the following physician-directed or patient-driven treat-to-target titration algorithms (TABLE 6).35,37,38 The insulin dose should be titrated based on the pre-breakfast fasting blood glucose level.
TABLE 6
Physician-directed or patient-driven treat-to-target titration algorithms
| Riddle et al35 | Davies et al37 | Meneghini et al38 | ||||
|---|---|---|---|---|---|---|
| Start with 10 U/d bedtime basal insulin and adjust weekly | Start with 10* U/d bedtime basal insulin and adjust weekly (physician-directed) Or Start with a dose numerically equivalent to the highest FPG (in millimoles/L)† over the previous 7 days and adjust every 3 days (patient-managed) | Start with basal insulin once daily and adjust every 3 days | ||||
| Mean of self-monitored FPG values from preceding 2 days | Change in insulin dose (U/d)# | Mean of self-monitored FPG values from preceding 3 days | Change in insulin dose (U/d) (physician-directed) | Change in insulin dose (U/d) (patient-managed) | Mean of self-monitored FPG values from preceding 3 days | Change in insulin dose (U/d) |
| ≥180 mg/dL 140-180 mg/dL 120-140 mg/dL 100-120 mg/dL | +8 +6 +4 +2 | ≥180 mg/dL (≥10 mmol/L) 140-179 mg/dL (7.8-9.9 mmol/L) 120-139 mg/dL (6.7 – 7.7 mmol/L) 100-119 mg/dL (5.5-6.6 mmol/L) | +6 to +8 +4 +2 0 to +2 | +2 +2 +2 0 to +2 | >110 mg/dL 80-110 mg/dL <80 mg/dL | +3 0 -3 |
| FPG, fasting plasma glucose. *In insulin-naive patients. †For example, if the highest FPG over the previous 7 days was 7 mmol/L, start with 7 U.#Small insulin dose decreases (2-4 U/d per adjustment) were allowed if severe hypoglycemia (requiring assistance) or plasma-referenced glucose < 56 mg/dL was documented in the preceding week. Reproduced with permission. Meneghini LF, et al. J Fam Pract. 2011;60(9 Suppl 1):S21-S28. Quadrant HealthCom Inc. Copyright 2011. | ||||||
Follow-Up Visit
RF begins basal insulin 10 U in the evening and is given simple instructions for insulin dose titration based on fasting plasma glucose results. At her follow-up visit, RF reports that she has increased her basal insulin to 18 U administered once daily. Review of her SMBG results show that her blood glucose levels throughout the day have improved, but are still not at goal. RF’s physician commends her on the progress she has made. RF and her physician agree that she should continue to increase her basal insulin dose. Eight months after beginning basal insulin, RF is administering 28 U (0.35 U/kg) of basal insulin in the evening. Review of her SMBG results over the previous 2 weeks show that her blood glucose rises during the day and is highest after dinner; her current A1C is 7.2%.
Treatment Plan
- Discuss dietary and lifestyle complements to insulin therapy such as:
- Use SMBG to identify foods that raise her blood glucose.
CASE STUDY 2
LW is a 64-year-old male with longstanding hypertension diagnosed with T2DM 8 years ago for which he was treated initially with lifestyle management and metformin. He has since been treated with other oral agents as add-on therapy; glipizide was discontinued due to hypoglycemia when he skips meals (usually lunch); pioglitazone was discontinued after the patient expressed concerns about the risk for bladder cancer he heard on television. He has mild retinopathy and mild loss of vibration sensation in the feet; there is no evidence of cardiovascular disease. He was diagnosed with osteoarthritis 3 years ago.
Clinical Impression
After taking his history, performing a physical examination, and reviewing his laboratory and SMBG data, his physician concludes that his treatment plan needs to be changed (FIGURE 3, TABLE 7, TABLE 8).
TABLE 7
Case study 2: Chart notes
| Physical examination | Laboratory tests | Lifestyle habits | Current therapy | |
|---|---|---|---|---|
| Glucose-lowering | Other | |||
| BP: 124/76 mm Hg Weight: 204 lb (92.7 kg) BMI: 31 kg/m2 Eyes: mild retinopathy Neurology: occasional tingling on bottom of right foot Skin: intact | SCr: 1.9 mg/dL eGFR: 51 mL/min Albuminuria: negative A1C: 8.1% Cholesterol: Total: 218 mg/dL LDL: 118 mg/dL HDL: 55 mg/dL Triglyceride: 204 mg/dL | Exercise: takes dog on occasional walk but otherwise sedentary Nutrition: eats 4 meals/d | Metformin 1000 mg BID Acarbose 50 mg TID Sitagliptin 100 mg QD | Lisinopril/HCTZ 20/25 mg QD Amlodipine 10 mg QD Acetaminophen extended-release 650 mg TID ASA 80 mg QD |
| ASA, acetylsalicylic acid; BMI, body mass index; BP, blood pressure; eGFR, estimated glomerular filtration rate; HCTZ, hydrochlorothiazide; HDL, high-density lipoprotein; LDL, low-density lipoprotein; SCr, serum creatinine. | ||||
TABLE 8
Case study 2: Self-monitored blood glucose (mg/dL) over the previous 2 weeks
| Day | Fasting | 2 h Post-breakfast | 2 h Post-lunch | 2 h Post-dinner |
|---|---|---|---|---|
| Tuesday | 135 | |||
| Wednesday | ||||
| Thursday | 196 | |||
| Friday | 152 | 174 | ||
| Saturday | ||||
| Sunday | 208 | |||
| Monday | 142 | 193 | ||
| Tuesday | ||||
| Wednesday | 130 | 156 | ||
| Thursday | ||||
| Friday | ||||
| Saturday | ||||
| Sunday | 151 | |||
| Monday |
FIGURE 3
Case study 2: A1C levels for April 2004 to March 2012
Treatment Plan
- Discontinue metformin since LW’s serum creatinine is > 1.5 mg/dL.
- Initiate either basal insulin once daily in the evening or premix insulin at dinner.
- Ask LW to monitor his blood glucose and self-adjust insulin doses as appropriate.
- Stress the importance of exercise and proper nutrition; gain agreement on short-term goals for exercise and nutrition.
Barriers
LW’s physician recommends that his treatment plan be changed and insulin therapy initiated. LW quickly responds that previous changes to his treatment regimen have not resulted in his achieving an A1C < 7.0%. He also doubts that he can use a syringe to draw up the correct dose and then self-administer due to his arthritis. The following are possible responses his physician could use to address these concerns.
Patient concern: Repeated experience of failing to achieve glycemic control, ie, A1C < 7.0%
Physician responses:
- While achieving an A1C < 7.0% is a realistic goal that reduces the risks for vascular complications of diabetes, any reduction of A1C will be of benefit.
- I would like to work with you to implement a new plan that we both believe will enable you to improve your diabetes control and ideally achieve an A1C < 7.0%.
Patient concern: Self-administering due to arthritis
Physician responses:
- Instead of using a syringe and vial to draw up and administer insulin, I would like you to use an insulin pen device. As you can see, it is easy to handle and you can easily select the correct dose.
- If you choose to start on premix insulin, the pen device contains both types of insulin together in one dose.
Dosing
Treatment with basal insulin once daily in the evening can be initiated and titrated based on pre-breakfast blood glucose as in Case Study 1. Alternatively, treatment with premix insulin can be initiated at a dose of 12 U administered within 15 minutes of dinner initiation. The premix dose can be titrated using the algorithm employed in the 1-2-3 Study based on pre-breakfast blood glucose (TABLE 9).39 After 16 weeks, 41% of patients in the 1-2-3 Study achieved an A1C < 7.0% from a baseline A1C of 8.6%.
TABLE 9
1-2-3 Study algorithm39
| Pre-breakfast SMBG (mg/dL) | Adjustment of pre-dinner dose (U) |
|---|---|
| <80 | -3 |
| 80-110 | No change |
| 111-140 | +3 |
| 141-180 | +6 |
| > 180 | +9 |
| SMBG, self-monitored blood glucose. | |
Follow-Up Visit
LW began basal insulin 10 U in the evening. Over the next 5.5 months, he titrated his dose such that his current dose is 46 U (0.50 U/kg) in the evening. His current A1C is 7.3%. Review of his SMBG shows consistently high 2-hour post-lunch blood glucose levels. Although further increasing his basal insulin dose is an option, in most of the treat-to-target studies, the daily dose of basal insulin given once daily averaged between 0.4 and 0.6 U/kg.35,37,40,41 LW and his physician agree that adding rapid-acting insulin at lunch is the best option. The starting dose of rapid-acting bolus insulin is 4 to 6 U administered prior to the largest meal of the day or, as in this case, prior to the meal with the largest postprandial blood glucose excursion.42,43 Alternatively, the dose of rapid-acting insulin could be calculated as 10% of the total daily dose of basal insulin, which in this case is 5 U (10% x 46 U). The dose of basal insulin would be reduced by 5 U if the rapid-acting insulin is given at dinner in order to reduce the risk for nocturnal hypoglycemia. The dose of the bolus insulin can be titrated using the ExtraSTEP algorithm (TABLE 10).42 Alternatively, the SimpleSTEP algorithm can be used which does not require a 2-hour postprandial glucose measurement.42
TABLE 10
Algorithms for adjusting insulin aspart42
| ExtraSTEP algorithm | SimpleSTEP algorithm | |||
|---|---|---|---|---|
| 2-h Post-meal PG level (mg/dL) | Insulin aspart adjustment (U) | Pre-meal BG (mg/dL) | Bedtime BG (mg/dL) | Insulin aspart adjustment (U) |
| <72* | -2 | <72* | <72* | -2 |
| 72-144 | 0 | 72-108 | 72-144 | 0 |
| 145-180 | +2 | 109-162 | 145-180 | +2 |
| >180 | +4 | >162 | >180 | +4 |
| BG, blood glucose; PG, plasma glucose. *One or more PG values <72 mg/dL without obvious explanation. Reproduced with permission. Meneghini LF, et al. J Fam Pract. 2011;60(9 Suppl 1):S21-S28. Quadrant HealthCom Inc. Copyright 2011. | ||||
Plan
- Begin rapid-acting insulin 5 U at lunch.
- Continue basal insulin at 46 U in the evening.
- Ask LW to continue to titrate basal insulin based on the pre-breakfast blood glucose level and the lunch time bolus insulin dose based on the 2-hour post-lunch SMBG (ExtraSTEP); alternatively, adjust based on the pre-dinner blood glucose level (SimpleSTEP).
CASE STUDY 3
MB is a 46-year-old male who had not consulted a physician since having a physical examination 6 years ago. He presented 2 weeks ago with frequent urination (7-8 times/day) and feeling tired; he also noted losing 5 pounds (2.25 kg) over the preceding 3.5 months despite no changes in his diet. MB is a regional salesperson with an erratic schedule. During the week, he eats lunch and most dinners in a restaurant. On the weekend, he goes to a local bar with his friends. He does light yard work, but does not exercise regularly. He is a current smoker with a 36 pack-year history. Urinalysis shows ketonuria and microalbuminuria. His A1C reported back today is 10.8%, confirming a diagnosis of uncontrolled and symptomatic DM.
Clinical Impression
After taking his history, performing a physical examination, and reviewing his laboratory data, MB’s physician confirms a diagnosis of DM (TABLE 11). While it is likely that MB has T2DM, his physician wants to rule out type 1 DM and latent autoimmune diabetes of the adult (LADA), so he orders tests for antibodies (GAD, IA-2, ICA). The antibody testing is negative, making T2DM the most likely diagnosis.
TABLE 11
Case study 3: Chart notes
| Physical examination | Laboratory tests | Lifestyle habits | Current therapy | |
|---|---|---|---|---|
| Glucose-lowering | Other | |||
| BP: 142/88 mm Hg Weight: 176 lb (79.2 kg) BMI: 27 kg/m2 Eyes: no retinopathy Neurology: intact Skin: intact | SCr: 1.4 mg/dL Microalbumin:creatinine ratio: 140 mg/g creatinine Ketonuria: 1+ A1C: 10.8% Cholesterol: Total: 210 mg/dL LDL: 146 mg/dL HDL: 30 mg/dL | Exercise: light yard work, no regular exercise Nutrition: 3 meals/d, eats most meals in a restaurant (lunch M-F; dinner 3-4 nights/wk) | None | None |
| BMI, body mass index; BP, blood pressure; HDL, high-density lipoprotein; LDL, low-density lipoprotein; SCr, serum creatinine. | ||||
Treatment Plan
- Initiate basal-bolus therapy with fixed bolus doses of rapid-acting insulin at each meal (prandial insulin).
- Ask MB to monitor blood glucose before meals and at bedtime.
- Provide MB with a supplemental scale to correct hyperglycemia before meals.
- Stress the importance of exercise and proper nutrition; gain agreement for short-term goals for exercise and nutrition; refer for diabetes and nutrition education if available.
- Discuss the importance of smoking cessation; develop a plan.
- Consider metformin and other non-insulin therapies when A1C is under control.
Barriers
MB is surprised that he has T2DM and is clearly anxious at receiving the diagnosis. He expresses concern about starting insulin because his uncle died within a year of starting insulin. MB also recalls that his uncle was always giving himself shots and monitoring his blood glucose level. He wants to know whether there is a simpler treatment option if he agrees to start insulin treatment. He also wants to know whether he will have to remain on insulin for the rest of his life. The following are possible responses his physician could use to address these concerns.
Patient concern: Fear of death
Physician responses:
- Uncontrolled high blood sugars over a long period of time can cause serious complications, such as kidney and heart disease that can result in death. That is why it is important that we work together to gain control of your blood sugar levels over the next few months and then modify your treatment as needed to maintain control.
- Unfortunately for many patients in the past, treatment with insulin was not used until it was too late and people already had serious complications from DM. This is likely the case for your uncle.
Patient concern: Treatment complexity
Physician responses:
- Right now we have to control your blood glucose rapidly so your pancreas can regain some function and your body can better respond to insulin.
- I will also provide you with step-by-step written instructions you can follow that describe how to start insulin and how to monitor your blood glucose.
- We will communicate as often as you need to adjust your insulin doses over the next few weeks; when you feel comfortable, I can even show you how to adjust your insulin dose before a meal to correct a high blood sugar.
- We can try this treatment for 3 months and then reevaluate your response, how you feel, and whether you want to continue to modify your treatment plan to keep your blood sugars controlled.
Patient concern: Lack of understanding that T2DM is a serious disease
Physician responses:
- Please understand that T2DM is a serious disease that increases your risk for heart disease, stroke, blindness, and other diseases. Unfortunately, since diabetes does not cause bad symptoms until it is actually too late, many patients do not make the effort to properly control their diabetes. By working together, we can reduce the risk for these complications and do some screening tests to detect any complications before they become irreversible.
Dosing
There are several approaches to determining the initial doses of basal and prandial (bolus) insulin. One approach is to estimate the total daily dose (TDD) of insulin by multiplying the patient’s weight in kilograms by 0.5 U/kg/d.44 Half of the TDD is given as basal insulin replacement; the other half is divided into 3 fixed preprandial doses of rapid-acting insulin. When the patient is ready to take on more complex management, the supplemental dose for bolus insulin can be calculated using a correction factor. If the bolus insulin is a rapid-acting insulin analog, 1800 is divided by the TDD of insulin; 1500 is used for a short-acting human insulin. This correction factor is an estimate of the fall in blood glucose per unit of bolus insulin. In our patient, the TDD would be: 80 kg x 0.5 U/kg/d or 40 U/d of insulin. Thus, 1 U of insulin should lower the blood glucose by about 45 mg/dL (1800/40 U = 45 mg/dL). For every 45 mg/dL above the pre-meal target, the patient would add 1 U of rapid-acting insulin to correct the hyperglycemia over the next 4 to 5 hours. The basal and prandial insulin doses would be titrated on a periodic basis (perhaps every 1 to 2 weeks) until the daytime levels of blood glucose are on target. The fasting (pre-breakfast) blood glucose would be used to adjust the basal insulin dose, while the pre-lunch, pre-dinner, and bedtime blood glucose results would be used to adjust the pre-breakfast, pre-lunch, and pre-dinner prandial (rapid-acting) insulin doses, respectively.
An alternative approach to initiating basal-bolus therapy is the PREFER algorithm.45 Here, the basal insulin dose is 10 U initially. The bolus doses are administered in a 3:1:2 ratio, so if the total of the 3 bolus doses is 12 U/d, the initial bolus doses would be 6 (breakfast), 2 (lunch), and 4 (dinner) U. The mean basal (once-daily) and bolus insulin doses observed in PREFER are shown in TABLE 12 and TABLE 13.
TABLE 12
Case study 3: Calculating initial basal-bolus insulin doses
| Algorithm | Calculations | Patient MB |
|---|---|---|
| Meneghini44 | TDD = (total body weight [kg]) (0.5 U/kg/d) Basal insulin dose* = (50%) (TDD) Bolus insulin dose† = (10%-20%) (TDD) | TDD = (0.5 U/kg/d)(80kg) = 40 U/d |
| Basal = (50%) (40 U/d) = 20 U/d | ||
| Bolus = (10%-20%) (40 U/d) = 4 to 8 U/meal | ||
| CF = 1800/40 U/d = 45 mg/dL per 1 unit | ||
| PREFER45 | Basal insulin dose* = 10 U (14 U if BMI > 32 kg/m2) Bolus insulin dose† = ratio of 3:1:2 (breakfast:lunch:dinner) Note: At week 26, the bolus insulin doses were divided into the 3 daily meals in approximately a 1:1:1 ratio | |
| BMI, body mass index; CF, correction factor; TDD, total daily dose of insulin. *Once daily; †Three meals per day. | ||
TABLE 13
Titrating the basal insulin dose using the PREFER algorithm45
| Pre-breakfast blood glucose (mg/dL) | Basal insulin dose adjustment (U) |
|---|---|
| < 56 | -4 |
| 56-72 | -2 |
| 73-125 | No change |
| 126-140 | +2 |
| 141-160 | +4 |
| 161-180 | +6 |
| 181-200 | +8 |
| > 200 | +10 |
Follow-up Visit
MB begins with basal insulin 20 U in the evening and bolus insulin at doses of 7 U before each meal. Over the next several months, MB has titrated his insulin doses; his current doses are: 32 U (basal), 11 U (bolus-breakfast), 7 U (bolus-lunch), and 10 U (bolus-dinner). He experienced 1 episode of mild hypoglycemia (SMBG, 50 mg/dL) one afternoon following a particularly active morning (TABLE 14). His current A1C is 7.4%. MB’s physician congratulates him on the progress he has made in dramatically lowering his blood glucose level—and his risk for diabetes-related complications. While MB appreciates his physician’s support and admits that he does not feel tired and generally feels better, which is likely due to resolution of glucotoxicity, he is not happy that he has gained 5.5 pounds (2.5 kg).46 He also finds the timing and administration of bolus insulin difficult.
TABLE 14
Case study 3: Self-monitored blood glucose (mg/dL) over the previous 2 weeks
| Day | Fasting | 2 h Post-breakfast | 2 h Post-lunch | 2 h Post-dinner |
|---|---|---|---|---|
| Wednesday | ||||
| Thursday | 168 | |||
| Friday | 106 | 166 | 174 | |
| Saturday | 88 | |||
| Sunday | 195 | |||
| Monday | 134 | |||
| Tuesday | 172 | |||
| Wednesday | 130 | 156 | ||
| Thursday | 112 | 168 | ||
| Friday | 92 | 164 | ||
| Saturday | 50 | 149 | 159 | 176 |
| Sunday | 94 | 174 | 210 | |
| Monday | 176 | 184 | ||
| Tuesday | 117 | 169 |
Plan
- Continue basal insulin once-daily in the evening.
- Add metformin 500 mg BID and increase to 1000 mg BID as tolerated.
- Consider weaning down the bolus insulin doses and substituting them with a GLP-1R agonist, dipeptidyl peptidase-4 inhibitor, or short-acting secretagogue. If so, continue rapid-acting insulin during transition. [Note: the following combinations are not currently approved by the US FDA: exenatide twice-daily and prandial insulin; exenatide once-weekly and insulin; liraglutide and prandial insulin; linagliptin and insulin.]
CASE STUDY 4
KW is a 62-year-old female diagnosed with T2DM 12 years ago. Treatment with lifestyle management and metformin initially provided glycemic control. Glimepiride was subsequently added and eventually the patient was started on basal insulin. The current dose of basal insulin is 60 U in the evening. Five months ago her A1C was found to be 7.9% and more recently 8.3%. She drinks alcohol occasionally and smokes. KW works as an executive secretary and has a consistent meal and activity schedule.
Clinical Impression
Following completion of the history, physical examination, and review of her laboratory data, KW’s physician concludes that her insulin regimen should be intensified (TABLE 15, TABLE 16).
TABLE 15
Case study 4: Chart notes
| Physical examination | Laboratory tests | Lifestyle habits | Current therapy | |
|---|---|---|---|---|
| Glucose-lowering | Other | |||
| BP: 126/78 mm Hg Weight: 176 lb (79.2 kg) BMI: 32 kg/m2 Eyes: no retinopathy Neurology: intact Skin: intact | SCr: 1.0 mg/dL Albuminuria: negative A1C: 8.3% Cholesterol Total: 172 mg/dL LDL: 96 mg/dL HDL: 46 mg/dL Triglycerides: 138 mg/dL | Exercise: sedentary Nutrition: 3 meals/d with large dinner | Metformin 1000 mg BID Basal insulin 60 U in the evening | ASA 80 mg QD Pravastatin 40 mg qHS |
| BMI, body mass index; BP, blood pressure; HDL, high-density lipoprotein; LDL, low-density lipoprotein; SCr, serum creatinine. | ||||
TABLE 16
Case study 4: Self-monitored blood glucose (mg/dL) over the previous 2 weeks
| Day | Fasting | 2 h Post-breakfast | 2 h Post-lunch | 2 h Post-dinner |
|---|---|---|---|---|
| Friday | ||||
| Saturday | 156 | 244 | ||
| Sunday | 253 | |||
| Monday | ||||
| Tuesday | ||||
| Wednesday | 148 | 227 | ||
| Thursday | ||||
| Friday | ||||
| Saturday | 179 | |||
| Sunday | 160 | |||
| Monday | ||||
| Tuesday | ||||
| Wednesday | ||||
| Thursday |
Plan
- Discontinue basal insulin.
- Begin premix insulin twice daily before breakfast and dinner.
- Ask KW to monitor blood glucose two times daily and, if appropriate, teach her how to self-adjust insulin doses.
- Stress the importance of exercise and proper nutrition; gain agreement on short-term goals for exercise and nutrition.
- Discuss the importance of smoking cessation; develop a plan.
Barriers
The physician discusses with KW that her consistent meal and activity schedule would make switching to premix insulin twice daily a good choice. KW is generally in agreement with the change, but wonders whether hypoglycemia might be more likely. She also asks if she might gain more weight in addition to the 3 pounds (1.35 kg) she has gained since starting basal insulin.
Patient concern: Hypoglycemia
Physician responses:
- Hypoglycemia remains a concern, and is more frequently seen with premix than with basal insulin; however, as long as you remain consistent with your meal and activity schedule, the risk for bad hypoglycemia is low.
- We should review your written action plan so that you are sure what signs or symptoms of a low blood sugar might occur and what you should do to treat them.
Patient concern: Weight gain
Physician responses:
- It is possible that you might gain a few additional pounds. You can avoid this by increasing your physical activity, and importantly, continue healthy eating. We should schedule a time for you to meet again with a dietician who can discuss options that might work for you.
Dosing
There are different approaches for converting from basal insulin to twice-daily premix insulin. One approach is to determine the TDD of basal insulin, and give half at breakfast and the other half at dinner as premix insulin.39 Since KW is taking 60 U of basal in the evening, she should take 30 U at breakfast and 30 U at dinner. Dose titration is according to the 1-2-3 Study algorithm shown in case study 2.
Another approach is to administer biphasic insulin aspart 70/30 0.2 U/kg before breakfast and 0.1 U/kg before dinner as was done in the PREFER study (TABLE 13).45 Subsequent dosing can be determined based on the PREFER algorithm below. Of note is that at study end, premix insulin doses were equally divided between breakfast and dinner. Breakfast and dinner doses are titrated based on blood glucose levels before dinner and breakfast, respectively. In the PREFER study, the use of premix insulin provided comparable A1C reduction as basal-bolus therapy (basal once daily + bolus TID) in insulin-naïve patients. However, patients previously treated with basal insulin such as KW experienced greater A1C reductions with basal-bolus insulin than with premix insulin.
1. Rodbard HW, Jellinger PS, Davidson JA, et al. Statement by an American Association of Clinical Endocrinologists/American College of Endocrinology consensus panel on type 2 diabetes mellitus: an algorithm for glycemic control [published correction appears in Endocr Pract. 2009;15(7):768-770]. Endocr Pract. 2009;15(6):540-559.
2. Inzucchi SE, Bergenstal RM, Buse JB, et al. Management of hyperglycemia in type 2 diabetes: a patient-centered approach: position statement of the American Diabetes Association (ADA) and the European Association for the Study of Diabetes (EASD) [published online ahead of print April 19, 2012]. Diabetes Care. doi:10.2337/dc12-0413.
3. Lalić NM, Micić D, Antić S, et al. Effect of biphasic insulin aspart on glucose and lipid control in patients with type 2 diabetes mellitus. Expert Opin Pharmacother. 2007;8(17):2895-2901.
4. Reynolds LR, Kingsley FJ, Karounos DG, Tannock LR. Differential effects of rosiglitazone and insulin glargine on inflammatory markers, glycemic control, and lipids in type 2 diabetes. Diabetes Res Clin Pract. 2007;77(2):180-187.
5. Rosak C, Jung R, Hofmann U. Insulin glargine maintains equivalent glycemic control and better lipometabolic control than NPH insulin in type 1 diabetes patients who missed a meal. Horm Metab Res. 2008;40(8):544-548.
6. Ampudia-Blasco FJ, Girbes J, Carmena R. A case of lipoatrophy with insulin glargine: long-acting insulin analogs are not exempt from this complication. Diabetes Care. 2005;28(12):2983.-
7. Griffin ME, Feder A, Tamborlane WV. Lipoatrophy associated with lispro insulin in insulin pump therapy: an old complication, a new cause? Diabetes Care. 2001;24(1):174.-
8. Fineberg SE, Huang J, Brunelle R, Gulliya KS, Anderson JH, Jr. Effect of long-term exposure to insulin lispro on the induction of antibody response in patients with type 1 or type 2 diabetes. Diabetes Care. 2003;26(1):89-96.
9. Moyes V, Driver R, Croom A, Mirakian R, Chowdhury TA. Insulin allergy in a patient with type 2 diabetes successfully treated with continuous subcutaneous insulin infusion. Diabet Med. 2006;23(2):204-206.
10. Ghosh S, McCann V, Bartle L, Collier A, Malik I. Allergy to insulin detemir. Diabet Med. 2007;24(11):1307.-
11. Blumer I. Severe, delayed insulin detemir injection site reaction. Diabet Med. 2008;25(8):1008.-
12. Pérez E, González R, Martínez J, Iglesias J, Matheu V. Detemir insulin-induced anaphylaxis. Ann Allergy Asthma Immunol. 2009;102(2):174-175.
13. Mollar-Puchades MA, Villanueva IL. Insulin glulisine in the treatment of allergy to rapid acting insulin and its rapid acting analogs. Diabetes Res Clin Pract. 2009;83(1):e21-e22.
14. Kawasaki F, Kamei S, Tatsumi F, et al. Gallbladder edema in type 1 diabetic patient due to delayed-type insulin allergy. Intern Med. 2009;48(17):1545-1549.
15. Wang C, Ding ZY, Shu SQ, et al. Severe insulin allergy after percutaneous transluminal coronary angioplasty. Clin Ther. 2009;31(3):569-574.
16. Ozaki N, Oiso Y. Immunologic tolerance to the insulin analogue glulisine. Diabetes Care. 2010;33(3):e39.-
17. Koroscil T, Kagzi Y, Zacharias D. Failure of multiple therapies in the treatment of a type 1 diabetic patient with insulin allergy: a case report. Endocr Pract. 2011;17(1):91-94.
18. Tuerk PW, Mueller M, Egede LE. Estimating physician effects on glycemic control in the treatment of diabetes: methods, effects sizes, and implications for treatment policy. Diabetes Care. 2008;31(5):869-873.
19. Hajos TR, Polonsky WH, Twisk JW, Dain MP, Snoek FJ. Do physicians understand type 2 diabetes patients’ perceptions of seriousness; the emotional impact and needs for care improvement? A cross-national survey. Patient Educ Couns. 2011;85(2):258-263.
20. Polonsky WH, Hajos TR, Dain MP, Snoek FJ. Are patients with type 2 diabetes reluctant to start insulin therapy? An examination of the scope and underpinnings of psychological insulin resistance in a large, international population. Curr Med Res Opin. 2011;27(6):1169-1174.
21. Nam S, Chesla C, Stotts NA, Kroon L, Janson SL. Factors associated with psychological insulin resistance in individuals with type 2 diabetes. Diabetes Care. 2010;33(8):1747-1749.
22. Nakar S, Yitzhaki G, Rosenberg R, Vinker S. Transition to insulin in type 2 diabetes: family physicians’ misconception of patients’ fears contributes to existing barriers. J Diabetes Complications. 2007;21(4):220-226.
23. Snoek FJ. Breaking the barriers to optimal glycaemic control—what physicians need to know from patients’ perspectives. Int J Clin Pract Suppl. 2002;(129):80-84.
24. Korytkowski M. When oral agents fail: practical barriers to starting insulin. Int J Obes Relat Metab Disord. 2002;26(Suppl 3):S18-S24.
25. Skovlund SE, Peyrot M. The Diabetes Attitudes, Wishes and Needs (DAWN) program: a new approach to improving outcomes of diabetes care. Diabetes Spectrum. 2005;18(3):136-142.
26. Jenkins N, Hallowell N, Farmer AJ, Holman RR, Lawton J. Initiating insulin as part of the Treating To Target in Type 2 Diabetes (4-T) trial: an interview study of patients’ and health professionals’ experiences. Diabetes Care. 2010;33(10):2178-2180.
27. Levinson W, Gorawara-Bhat R, Lamb J. A study of patient clues and physician responses in primary care and surgical settings. JAMA. 2000;284(8):1021-1027.
28. Rodriguez HP, Anastario MP, Frankel RM, et al. Can teaching agenda-setting skills to physicians improve clinical interaction quality? A controlled intervention. BMC Med Educ. 2008;8:3.-
29. Solomon J. How strategies for managing patient visit time affect physician job satisfaction: a qualitative analysis. J Gen Intern Med. 2008;23(6):775-780.
30. Funnell MM, Anderson RM. Empowerment and self-management of diabetes. Clin Diabetes. 2004;22(3):123-127.
31. Funnell MM, Anderson RM. Are patients or outcomes more important? Rev Endocrinol. 2008;2(8):49-51.
32. Shaefer CF. Clinical inertia: overcoming a major barrier to diabetes management. Insulin. 2006;1(2):61-64.
33. Harris S, Yale JF, Dempsey E, Gerstein H. Can family physicians help patients initiate basal insulin therapy successfully?: randomized trial of patient-titrated insulin glargine compared with standard oral therapy: lessons for family practice from the Canadian INSIGHT trial. Can Fam Physician. 2008;54(4):550-558.
34. Centers for Disease Control and Prevention. National diabetes fact sheet national estimates and general information on diabetes and prediabetes in the United States, 2011. Atlanta, GA: U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, 2011. http://www.cdc.gov/diabetes/pubs/pdf/ndfs_2011.pdf. Accessed February 10, 2011.
35. Riddle MC, Rosenstock J, Gerich J. Insulin Glargine 4002 Study Investigators. The treat-to-target trial: randomized addition of glargine or human NPH insulin to oral therapy of type 2 diabetic patients. Diabetes Care. 2003;26(11):3080-3086.
36. Hermansen K, Davies M, Derezinski T, Martinez Ravn G, Clauson P, Home P. A 26-week, randomized, parallel, treat-to-target trial comparing insulin detemir with NPH insulin as add-on therapy to oral glucose-lowering drugs in insulin-naive people with type 2 diabetes [published correction appears in Diabetes Care. 2007;30(4):1035]. Diabetes Care. 2006;29(6):1269-1274.
37. Davies M, Storms F, Shutler S, Bianchi-Biscay M, Gomis R. ATLANTUS Study Group. Improvement of glycemic control in subjects with poorly controlled type 2 diabetes: comparison of two treatment algorithms using insulin glargine. Diabetes Care. 2005;28(6):1282-1288.
38. Meneghini L, Koenen C, Weng W, Selam JL. The usage of a simplified self-titration dosing guideline (303 Algorithm) for insulin detemir in patients with type 2 diabetes—results of the randomized, controlled PREDICTIVE 303 study. Diabetes Obes Metab. 2007;9(6):902-913.
39. Garber AJ, Wahlen J, Wahl T, et al. Attainment of glycaemic goals in type 2 diabetes with once-, twice-, or thrice-daily dosing with biphasic insulin aspart 70/30 (The 1-2-3 study). Diabetes Obes Metab. 2006;8(1):58-66.
40. Philis-Tsimikas A, Charpentier G, Clauson P, Ravn GM, Roberts VL, Thorsteinsson B. Comparison of once-daily insulin detemir with NPH insulin added to a regimen of oral antidiabetic drugs in poorly controlled type 2 diabetes [published correction appears in Clin Ther. 2006;28(11):1967]. Clin Ther. 2006;28(10):1569-1581.
41. Blonde L, Merilainen M, Karwe V, Raskin P. TITRATE Study Group. Patient-directed titration for achieving glycaemic goals using a once-daily basal insulin analogue: an assessment of two different fasting plasma glucose targets—the TITRATE study. Diabetes Obes Metab. 2009;11(6):623-631.
42. Meneghini L, Mersebach H, Kumar S, Svendsen AL, Hermansen K. Comparison of 2 intensification regimens with rapid-acting insulin aspart in type 2 diabetes mellitus inadequately controlled by once-daily insulin detemir and oral antidiabetes drugs: the step-wise randomized study. Endocr Pract. 2011;17(5):727-736.
43. Lankisch MR, Ferlinz KC, Leahy JL, Scherbaum WA. Orals Plus Apidra and LANTUS (OPAL) study group. Introducing a simplified approach to insulin therapy in type 2 diabetes: a comparison of two single-dose regimens of insulin glulisine plus insulin glargine and oral antidiabetic drugs [published correction appears in Diabetes Obes Metab. 2010;12(5):461]. Diabetes Obes Metab 2008;10(12):1178-1185.
44. Meneghini L. Why and how to use insulin therapy earlier in the management of type 2 diabetes. South Med J. 2007;100(2):164-174.
45. Liebl A, Prager R, Binz K, Kaiser M, Bergenstal R, Gallwitz B. PREFER Study Group. Comparison of insulin analogue regimens in people with type 2 diabetes mellitus in the PREFER Study: a randomized controlled trial. Diabetes Obes Metab. 2009;11(1):45-52.
46. Braun A, Sämann A, Kubiak T, et al. Effects of metabolic control, patient education and initiation of insulin therapy on the quality of life of patients with type 2 diabetes mellitus. Patient Educ Couns. 2008;73(1):50-59.
1. Rodbard HW, Jellinger PS, Davidson JA, et al. Statement by an American Association of Clinical Endocrinologists/American College of Endocrinology consensus panel on type 2 diabetes mellitus: an algorithm for glycemic control [published correction appears in Endocr Pract. 2009;15(7):768-770]. Endocr Pract. 2009;15(6):540-559.
2. Inzucchi SE, Bergenstal RM, Buse JB, et al. Management of hyperglycemia in type 2 diabetes: a patient-centered approach: position statement of the American Diabetes Association (ADA) and the European Association for the Study of Diabetes (EASD) [published online ahead of print April 19, 2012]. Diabetes Care. doi:10.2337/dc12-0413.
3. Lalić NM, Micić D, Antić S, et al. Effect of biphasic insulin aspart on glucose and lipid control in patients with type 2 diabetes mellitus. Expert Opin Pharmacother. 2007;8(17):2895-2901.
4. Reynolds LR, Kingsley FJ, Karounos DG, Tannock LR. Differential effects of rosiglitazone and insulin glargine on inflammatory markers, glycemic control, and lipids in type 2 diabetes. Diabetes Res Clin Pract. 2007;77(2):180-187.
5. Rosak C, Jung R, Hofmann U. Insulin glargine maintains equivalent glycemic control and better lipometabolic control than NPH insulin in type 1 diabetes patients who missed a meal. Horm Metab Res. 2008;40(8):544-548.
6. Ampudia-Blasco FJ, Girbes J, Carmena R. A case of lipoatrophy with insulin glargine: long-acting insulin analogs are not exempt from this complication. Diabetes Care. 2005;28(12):2983.-
7. Griffin ME, Feder A, Tamborlane WV. Lipoatrophy associated with lispro insulin in insulin pump therapy: an old complication, a new cause? Diabetes Care. 2001;24(1):174.-
8. Fineberg SE, Huang J, Brunelle R, Gulliya KS, Anderson JH, Jr. Effect of long-term exposure to insulin lispro on the induction of antibody response in patients with type 1 or type 2 diabetes. Diabetes Care. 2003;26(1):89-96.
9. Moyes V, Driver R, Croom A, Mirakian R, Chowdhury TA. Insulin allergy in a patient with type 2 diabetes successfully treated with continuous subcutaneous insulin infusion. Diabet Med. 2006;23(2):204-206.
10. Ghosh S, McCann V, Bartle L, Collier A, Malik I. Allergy to insulin detemir. Diabet Med. 2007;24(11):1307.-
11. Blumer I. Severe, delayed insulin detemir injection site reaction. Diabet Med. 2008;25(8):1008.-
12. Pérez E, González R, Martínez J, Iglesias J, Matheu V. Detemir insulin-induced anaphylaxis. Ann Allergy Asthma Immunol. 2009;102(2):174-175.
13. Mollar-Puchades MA, Villanueva IL. Insulin glulisine in the treatment of allergy to rapid acting insulin and its rapid acting analogs. Diabetes Res Clin Pract. 2009;83(1):e21-e22.
14. Kawasaki F, Kamei S, Tatsumi F, et al. Gallbladder edema in type 1 diabetic patient due to delayed-type insulin allergy. Intern Med. 2009;48(17):1545-1549.
15. Wang C, Ding ZY, Shu SQ, et al. Severe insulin allergy after percutaneous transluminal coronary angioplasty. Clin Ther. 2009;31(3):569-574.
16. Ozaki N, Oiso Y. Immunologic tolerance to the insulin analogue glulisine. Diabetes Care. 2010;33(3):e39.-
17. Koroscil T, Kagzi Y, Zacharias D. Failure of multiple therapies in the treatment of a type 1 diabetic patient with insulin allergy: a case report. Endocr Pract. 2011;17(1):91-94.
18. Tuerk PW, Mueller M, Egede LE. Estimating physician effects on glycemic control in the treatment of diabetes: methods, effects sizes, and implications for treatment policy. Diabetes Care. 2008;31(5):869-873.
19. Hajos TR, Polonsky WH, Twisk JW, Dain MP, Snoek FJ. Do physicians understand type 2 diabetes patients’ perceptions of seriousness; the emotional impact and needs for care improvement? A cross-national survey. Patient Educ Couns. 2011;85(2):258-263.
20. Polonsky WH, Hajos TR, Dain MP, Snoek FJ. Are patients with type 2 diabetes reluctant to start insulin therapy? An examination of the scope and underpinnings of psychological insulin resistance in a large, international population. Curr Med Res Opin. 2011;27(6):1169-1174.
21. Nam S, Chesla C, Stotts NA, Kroon L, Janson SL. Factors associated with psychological insulin resistance in individuals with type 2 diabetes. Diabetes Care. 2010;33(8):1747-1749.
22. Nakar S, Yitzhaki G, Rosenberg R, Vinker S. Transition to insulin in type 2 diabetes: family physicians’ misconception of patients’ fears contributes to existing barriers. J Diabetes Complications. 2007;21(4):220-226.
23. Snoek FJ. Breaking the barriers to optimal glycaemic control—what physicians need to know from patients’ perspectives. Int J Clin Pract Suppl. 2002;(129):80-84.
24. Korytkowski M. When oral agents fail: practical barriers to starting insulin. Int J Obes Relat Metab Disord. 2002;26(Suppl 3):S18-S24.
25. Skovlund SE, Peyrot M. The Diabetes Attitudes, Wishes and Needs (DAWN) program: a new approach to improving outcomes of diabetes care. Diabetes Spectrum. 2005;18(3):136-142.
26. Jenkins N, Hallowell N, Farmer AJ, Holman RR, Lawton J. Initiating insulin as part of the Treating To Target in Type 2 Diabetes (4-T) trial: an interview study of patients’ and health professionals’ experiences. Diabetes Care. 2010;33(10):2178-2180.
27. Levinson W, Gorawara-Bhat R, Lamb J. A study of patient clues and physician responses in primary care and surgical settings. JAMA. 2000;284(8):1021-1027.
28. Rodriguez HP, Anastario MP, Frankel RM, et al. Can teaching agenda-setting skills to physicians improve clinical interaction quality? A controlled intervention. BMC Med Educ. 2008;8:3.-
29. Solomon J. How strategies for managing patient visit time affect physician job satisfaction: a qualitative analysis. J Gen Intern Med. 2008;23(6):775-780.
30. Funnell MM, Anderson RM. Empowerment and self-management of diabetes. Clin Diabetes. 2004;22(3):123-127.
31. Funnell MM, Anderson RM. Are patients or outcomes more important? Rev Endocrinol. 2008;2(8):49-51.
32. Shaefer CF. Clinical inertia: overcoming a major barrier to diabetes management. Insulin. 2006;1(2):61-64.
33. Harris S, Yale JF, Dempsey E, Gerstein H. Can family physicians help patients initiate basal insulin therapy successfully?: randomized trial of patient-titrated insulin glargine compared with standard oral therapy: lessons for family practice from the Canadian INSIGHT trial. Can Fam Physician. 2008;54(4):550-558.
34. Centers for Disease Control and Prevention. National diabetes fact sheet national estimates and general information on diabetes and prediabetes in the United States, 2011. Atlanta, GA: U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, 2011. http://www.cdc.gov/diabetes/pubs/pdf/ndfs_2011.pdf. Accessed February 10, 2011.
35. Riddle MC, Rosenstock J, Gerich J. Insulin Glargine 4002 Study Investigators. The treat-to-target trial: randomized addition of glargine or human NPH insulin to oral therapy of type 2 diabetic patients. Diabetes Care. 2003;26(11):3080-3086.
36. Hermansen K, Davies M, Derezinski T, Martinez Ravn G, Clauson P, Home P. A 26-week, randomized, parallel, treat-to-target trial comparing insulin detemir with NPH insulin as add-on therapy to oral glucose-lowering drugs in insulin-naive people with type 2 diabetes [published correction appears in Diabetes Care. 2007;30(4):1035]. Diabetes Care. 2006;29(6):1269-1274.
37. Davies M, Storms F, Shutler S, Bianchi-Biscay M, Gomis R. ATLANTUS Study Group. Improvement of glycemic control in subjects with poorly controlled type 2 diabetes: comparison of two treatment algorithms using insulin glargine. Diabetes Care. 2005;28(6):1282-1288.
38. Meneghini L, Koenen C, Weng W, Selam JL. The usage of a simplified self-titration dosing guideline (303 Algorithm) for insulin detemir in patients with type 2 diabetes—results of the randomized, controlled PREDICTIVE 303 study. Diabetes Obes Metab. 2007;9(6):902-913.
39. Garber AJ, Wahlen J, Wahl T, et al. Attainment of glycaemic goals in type 2 diabetes with once-, twice-, or thrice-daily dosing with biphasic insulin aspart 70/30 (The 1-2-3 study). Diabetes Obes Metab. 2006;8(1):58-66.
40. Philis-Tsimikas A, Charpentier G, Clauson P, Ravn GM, Roberts VL, Thorsteinsson B. Comparison of once-daily insulin detemir with NPH insulin added to a regimen of oral antidiabetic drugs in poorly controlled type 2 diabetes [published correction appears in Clin Ther. 2006;28(11):1967]. Clin Ther. 2006;28(10):1569-1581.
41. Blonde L, Merilainen M, Karwe V, Raskin P. TITRATE Study Group. Patient-directed titration for achieving glycaemic goals using a once-daily basal insulin analogue: an assessment of two different fasting plasma glucose targets—the TITRATE study. Diabetes Obes Metab. 2009;11(6):623-631.
42. Meneghini L, Mersebach H, Kumar S, Svendsen AL, Hermansen K. Comparison of 2 intensification regimens with rapid-acting insulin aspart in type 2 diabetes mellitus inadequately controlled by once-daily insulin detemir and oral antidiabetes drugs: the step-wise randomized study. Endocr Pract. 2011;17(5):727-736.
43. Lankisch MR, Ferlinz KC, Leahy JL, Scherbaum WA. Orals Plus Apidra and LANTUS (OPAL) study group. Introducing a simplified approach to insulin therapy in type 2 diabetes: a comparison of two single-dose regimens of insulin glulisine plus insulin glargine and oral antidiabetic drugs [published correction appears in Diabetes Obes Metab. 2010;12(5):461]. Diabetes Obes Metab 2008;10(12):1178-1185.
44. Meneghini L. Why and how to use insulin therapy earlier in the management of type 2 diabetes. South Med J. 2007;100(2):164-174.
45. Liebl A, Prager R, Binz K, Kaiser M, Bergenstal R, Gallwitz B. PREFER Study Group. Comparison of insulin analogue regimens in people with type 2 diabetes mellitus in the PREFER Study: a randomized controlled trial. Diabetes Obes Metab. 2009;11(1):45-52.
46. Braun A, Sämann A, Kubiak T, et al. Effects of metabolic control, patient education and initiation of insulin therapy on the quality of life of patients with type 2 diabetes mellitus. Patient Educ Couns. 2008;73(1):50-59.
Update On Insulin Management in Type 2 Diabetes
JOURNAL SCANSummary of Key ArticlesIdentifying Challenges With Insulin Therapy and Assessing Treatment Strategies With Pramlintide
Summary of Key Articles
Identifying Challenges With Insulin Therapy and Assessing Treatment Strategies With Pramlintide
A supplement to Clinical Endocrinology News.
This supplement was sponsored by Amylin.
• Introduction
• Should Minimal Blood Glucose Variability Become the Gold Standard of Glycemic Control?
• Contributions of Fasting and Postprandial Plasma Glucose Increments to the Overall Diurnal Hyperglycemia of Type 2 Diabetic Patients
• Addition of Biphasic, Prandial, or Basal Insulin to Oral Therapy in Type 2 Diabetes
• Effects of Intensive Glucose Lowering in Type 2 Diabetes
• Pramlintide as an Adjunct to Insulin in Patients With Type 2 Diabetes in a Clinical Practice Setting Reduced A1C, Postprandial Glucose Excursions, and Weight
• Pramlintide as an Adjunct to Insulin Therapy Improves Long-Term Glycemic and Weight Control in Patients With Type 2 Diabetes: A 1-Year Randomized Controlled Trial
• Amylin Replacement with Primlintide as an Adjunct to Insulin Therapy Improves Long-Term Glycemic and Weight Control in Type 1 Diabetes Mellitus: A 1-Year, Randomized Controlled Trial
• Important Safety Information and SYMLIN Prescribing Information
Faculty/Faculty Disclosure
Steven V. Edelman, MD
Professor of Medicine, University of California, San Diego
Veterans Affairs Medical Center, San Diego, California
Founder and Director, Taking Control of Your Diabetes, 501(3)
Del Mar, California
Associate Clinical Professor of Medicine
Dr. Edelman is a consultant to and speaker for Amylin Pharmaceuticals, Inc., Eli Lilly and Company, Novo Nordisk A/S, and sanofi-aventis U.S., LLC.
Copyright © 2009 Elsevier Inc.
A supplement to Clinical Endocrinology News.
This supplement was sponsored by Amylin.
• Introduction
• Should Minimal Blood Glucose Variability Become the Gold Standard of Glycemic Control?
• Contributions of Fasting and Postprandial Plasma Glucose Increments to the Overall Diurnal Hyperglycemia of Type 2 Diabetic Patients
• Addition of Biphasic, Prandial, or Basal Insulin to Oral Therapy in Type 2 Diabetes
• Effects of Intensive Glucose Lowering in Type 2 Diabetes
• Pramlintide as an Adjunct to Insulin in Patients With Type 2 Diabetes in a Clinical Practice Setting Reduced A1C, Postprandial Glucose Excursions, and Weight
• Pramlintide as an Adjunct to Insulin Therapy Improves Long-Term Glycemic and Weight Control in Patients With Type 2 Diabetes: A 1-Year Randomized Controlled Trial
• Amylin Replacement with Primlintide as an Adjunct to Insulin Therapy Improves Long-Term Glycemic and Weight Control in Type 1 Diabetes Mellitus: A 1-Year, Randomized Controlled Trial
• Important Safety Information and SYMLIN Prescribing Information
Faculty/Faculty Disclosure
Steven V. Edelman, MD
Professor of Medicine, University of California, San Diego
Veterans Affairs Medical Center, San Diego, California
Founder and Director, Taking Control of Your Diabetes, 501(3)
Del Mar, California
Associate Clinical Professor of Medicine
Dr. Edelman is a consultant to and speaker for Amylin Pharmaceuticals, Inc., Eli Lilly and Company, Novo Nordisk A/S, and sanofi-aventis U.S., LLC.
Copyright © 2009 Elsevier Inc.
A supplement to Clinical Endocrinology News.
This supplement was sponsored by Amylin.
• Introduction
• Should Minimal Blood Glucose Variability Become the Gold Standard of Glycemic Control?
• Contributions of Fasting and Postprandial Plasma Glucose Increments to the Overall Diurnal Hyperglycemia of Type 2 Diabetic Patients
• Addition of Biphasic, Prandial, or Basal Insulin to Oral Therapy in Type 2 Diabetes
• Effects of Intensive Glucose Lowering in Type 2 Diabetes
• Pramlintide as an Adjunct to Insulin in Patients With Type 2 Diabetes in a Clinical Practice Setting Reduced A1C, Postprandial Glucose Excursions, and Weight
• Pramlintide as an Adjunct to Insulin Therapy Improves Long-Term Glycemic and Weight Control in Patients With Type 2 Diabetes: A 1-Year Randomized Controlled Trial
• Amylin Replacement with Primlintide as an Adjunct to Insulin Therapy Improves Long-Term Glycemic and Weight Control in Type 1 Diabetes Mellitus: A 1-Year, Randomized Controlled Trial
• Important Safety Information and SYMLIN Prescribing Information
Faculty/Faculty Disclosure
Steven V. Edelman, MD
Professor of Medicine, University of California, San Diego
Veterans Affairs Medical Center, San Diego, California
Founder and Director, Taking Control of Your Diabetes, 501(3)
Del Mar, California
Associate Clinical Professor of Medicine
Dr. Edelman is a consultant to and speaker for Amylin Pharmaceuticals, Inc., Eli Lilly and Company, Novo Nordisk A/S, and sanofi-aventis U.S., LLC.
Copyright © 2009 Elsevier Inc.
Summary of Key Articles
Identifying Challenges With Insulin Therapy and Assessing Treatment Strategies With Pramlintide
Summary of Key Articles
Identifying Challenges With Insulin Therapy and Assessing Treatment Strategies With Pramlintide
Case 1: Management Decisions in an Adult Comorbid Patient With Type 2 Diabetes Having Primary HyperlipidemiaCase 2: Colesevelam Hydrochloride for Management of a Patient With Type 2 Diabetes Mellitus and Hyperlipidemia
Case 2: Colesevelam Hydrochloride for Management of a Patient With Type 2 Diabetes Mellitus and Hyperlipidemia
A Case Studies Compendium supplement to Clinical Endocrinology News. This supplement was sponsored by Daiichi Sankyo, Inc.
• Background
• Current Visit
• Laboratory Results
• Clinical Discussion
• Endocrinologist Consultation
• New Treatment Regimen With Add-On Therapy
• Conclusions
Case 2 Topics
• Background
• Current Visit: Exam Findings
• Current Treatment Regimen
• Health History
• Laboratory Results
• Clinical Discussion
• Cardiologist Visit
• Three Months After Visiting the Cardiologist
• Add-On Therapy With Welchol for Patients With T2DM and CHD
• Treatment Goals for Alice
• Conclusions
Faculty/Faculty Disclosures
Yehuda Handelsman, MD, FACP, FACE
Medical Director
Metabolic Institute of America
Chair and Program Director
7th World Congress on InsulinResistance
Chair, International Committeefor Insulin Resistance
18372 Clark Street, Suite 212
Tarzana, CA 91356
E-mail:[email protected]
Web Site:www.TheMetabolicCenter.com
Dr Handelsman is a consultant for Bristol-Myers Squibb
Company, Daiichi Sankyo, Inc., GlaxoSmithKline, Medtronic, Merck, Tethys,
and Xoma; he has received clinical research grant funding from Daiichi Sankyo, Inc., GlaxoSmithKline, Novo Nordisk, and Takeda; and he ison the speakers bureau for AstraZeneca, Bristol-Myers Squibb, Daiichi Sankyo, Inc., GlaxoSmithKline, Merck, and Novartis. He also serves on the advisory board for CLINICAL ENDOCRINOLOGY NEWS.
Peter H. Jones, MD, FACP
Co-Director, Lipid Metabolism
and Atherosclerosis Clinic
Medical Director, Weight
Management Center
The Methodist Hospital
Associate Professor of Medicine
Section of Atherosclerosis andLipid Research
Baylor College of Medicine
Houston, TX 77030
E-mail: [email protected]
Dr Jones has disclosed that he has received support in the form of consulting agreements from Abbott Laboratories, AstraZeneca Pharmaceuticals LP, Daiichi Sankyo, Inc., and Merck.
Copyright © 2010 Elsevier Inc.
A Case Studies Compendium supplement to Clinical Endocrinology News. This supplement was sponsored by Daiichi Sankyo, Inc.
• Background
• Current Visit
• Laboratory Results
• Clinical Discussion
• Endocrinologist Consultation
• New Treatment Regimen With Add-On Therapy
• Conclusions
Case 2 Topics
• Background
• Current Visit: Exam Findings
• Current Treatment Regimen
• Health History
• Laboratory Results
• Clinical Discussion
• Cardiologist Visit
• Three Months After Visiting the Cardiologist
• Add-On Therapy With Welchol for Patients With T2DM and CHD
• Treatment Goals for Alice
• Conclusions
Faculty/Faculty Disclosures
Yehuda Handelsman, MD, FACP, FACE
Medical Director
Metabolic Institute of America
Chair and Program Director
7th World Congress on InsulinResistance
Chair, International Committeefor Insulin Resistance
18372 Clark Street, Suite 212
Tarzana, CA 91356
E-mail:[email protected]
Web Site:www.TheMetabolicCenter.com
Dr Handelsman is a consultant for Bristol-Myers Squibb
Company, Daiichi Sankyo, Inc., GlaxoSmithKline, Medtronic, Merck, Tethys,
and Xoma; he has received clinical research grant funding from Daiichi Sankyo, Inc., GlaxoSmithKline, Novo Nordisk, and Takeda; and he ison the speakers bureau for AstraZeneca, Bristol-Myers Squibb, Daiichi Sankyo, Inc., GlaxoSmithKline, Merck, and Novartis. He also serves on the advisory board for CLINICAL ENDOCRINOLOGY NEWS.
Peter H. Jones, MD, FACP
Co-Director, Lipid Metabolism
and Atherosclerosis Clinic
Medical Director, Weight
Management Center
The Methodist Hospital
Associate Professor of Medicine
Section of Atherosclerosis andLipid Research
Baylor College of Medicine
Houston, TX 77030
E-mail: [email protected]
Dr Jones has disclosed that he has received support in the form of consulting agreements from Abbott Laboratories, AstraZeneca Pharmaceuticals LP, Daiichi Sankyo, Inc., and Merck.
Copyright © 2010 Elsevier Inc.
A Case Studies Compendium supplement to Clinical Endocrinology News. This supplement was sponsored by Daiichi Sankyo, Inc.
• Background
• Current Visit
• Laboratory Results
• Clinical Discussion
• Endocrinologist Consultation
• New Treatment Regimen With Add-On Therapy
• Conclusions
Case 2 Topics
• Background
• Current Visit: Exam Findings
• Current Treatment Regimen
• Health History
• Laboratory Results
• Clinical Discussion
• Cardiologist Visit
• Three Months After Visiting the Cardiologist
• Add-On Therapy With Welchol for Patients With T2DM and CHD
• Treatment Goals for Alice
• Conclusions
Faculty/Faculty Disclosures
Yehuda Handelsman, MD, FACP, FACE
Medical Director
Metabolic Institute of America
Chair and Program Director
7th World Congress on InsulinResistance
Chair, International Committeefor Insulin Resistance
18372 Clark Street, Suite 212
Tarzana, CA 91356
E-mail:[email protected]
Web Site:www.TheMetabolicCenter.com
Dr Handelsman is a consultant for Bristol-Myers Squibb
Company, Daiichi Sankyo, Inc., GlaxoSmithKline, Medtronic, Merck, Tethys,
and Xoma; he has received clinical research grant funding from Daiichi Sankyo, Inc., GlaxoSmithKline, Novo Nordisk, and Takeda; and he ison the speakers bureau for AstraZeneca, Bristol-Myers Squibb, Daiichi Sankyo, Inc., GlaxoSmithKline, Merck, and Novartis. He also serves on the advisory board for CLINICAL ENDOCRINOLOGY NEWS.
Peter H. Jones, MD, FACP
Co-Director, Lipid Metabolism
and Atherosclerosis Clinic
Medical Director, Weight
Management Center
The Methodist Hospital
Associate Professor of Medicine
Section of Atherosclerosis andLipid Research
Baylor College of Medicine
Houston, TX 77030
E-mail: [email protected]
Dr Jones has disclosed that he has received support in the form of consulting agreements from Abbott Laboratories, AstraZeneca Pharmaceuticals LP, Daiichi Sankyo, Inc., and Merck.
Copyright © 2010 Elsevier Inc.
Case 2: Colesevelam Hydrochloride for Management of a Patient With Type 2 Diabetes Mellitus and Hyperlipidemia
Case 2: Colesevelam Hydrochloride for Management of a Patient With Type 2 Diabetes Mellitus and Hyperlipidemia
An Approach to the Management of Type 2 Diabetes Mellitus in Patients Receiving Add-On Therapy With Colesevelam HCl
A Journal Scan supplement to Clinical Endocrinology News. This supplement was sponsored by Daiichi Sankyo, Inc.
• Introduction
• Results of the Glucose-Lowering Effect of WelChol Study (GLOWS): A Randomized, Double-Blind, Placebo-Controlled Pilot Study Evaluating the Effect of Colesevelam Hydrochloride on Glycemic Control in Subjects with Type 2 Diabetes
• Efficacy and Safety of Colesevelam in Patients With Type 2 Diabetes Mellitus and Inadequate Glycemic Control Receiving Insulin-Based Therapy
• Colesevelam HCl Improves Glycemic Control and Reduces LDL Cholesterol in Patients With Inadequately Controlled Type 2 Diabetes on Sulfonylurea-Based Therapy
• Colesevelam Hydrochloride Therapy in Patients With Type 2 Diabetes Mellitus Treated With Metformin: Glucose and Lipid Effects
Faculty/Faculty Disclosures
Endocrinologist:
Harold E. Bays, MD, FACP, FACE
Medical Director/President
Louisville Metabolic and
Atherosclerosis Research Center
Louisville, Kentucky
Dr Bays has research grants, consultant fees, and speaker fees with Abbott Laboratories, Aegerion Pharmaceuticals, Akros Pharma Inc, Amarin, Amgen Inc., Amylin Pharmaceuticals, Inc., Arena Pharmaceuticals, Inc., Arete Therapeutics Inc., AstraZeneca, Bristol-Myers Squibb, Boehringer Ingelheim Corporation, Cargill, Inc., Daiichi Sankyo, Inc., Eli Lilly and Company, Essentialis, Inc., GlaxoSmithKline plc, Hoffmann-La Roche Inc., Home Access Health Corporation, InteKrin Therapeutics Inc., Isis Pharmaceuticals, Inc., Johnson & Johnson Services, Inc., Merck & Co., Inc.,Merck/Schering-Plough Pharmaceuticals, Metabolex, Inc., Neuromed Pharmaceuticals Ltd., NicOx, Novo Nordisk A/S, Orexigen Therapeutics, Inc., Pfizer Inc., Purdue Pharma L.P., sanofi-aventis US LLC, Sciele Pharma, Inc., Surface Logix, Inc., Takeda Pharmaceutical Company Limited, and VIVUS Inc.
Cardiologist:
Peter H. Jones, MD
Associate Professor of Medicine
Baylor College of Medicine
Houston, Texas
Dr Jones has consulting agreements with Abbott Laboratories, AstraZeneca, Daiichi Sankyo, Inc., and Merck/Schering-Plough Pharmaceuticals.
Copyright © 2010 Elsevier Inc.
A Journal Scan supplement to Clinical Endocrinology News. This supplement was sponsored by Daiichi Sankyo, Inc.
• Introduction
• Results of the Glucose-Lowering Effect of WelChol Study (GLOWS): A Randomized, Double-Blind, Placebo-Controlled Pilot Study Evaluating the Effect of Colesevelam Hydrochloride on Glycemic Control in Subjects with Type 2 Diabetes
• Efficacy and Safety of Colesevelam in Patients With Type 2 Diabetes Mellitus and Inadequate Glycemic Control Receiving Insulin-Based Therapy
• Colesevelam HCl Improves Glycemic Control and Reduces LDL Cholesterol in Patients With Inadequately Controlled Type 2 Diabetes on Sulfonylurea-Based Therapy
• Colesevelam Hydrochloride Therapy in Patients With Type 2 Diabetes Mellitus Treated With Metformin: Glucose and Lipid Effects
Faculty/Faculty Disclosures
Endocrinologist:
Harold E. Bays, MD, FACP, FACE
Medical Director/President
Louisville Metabolic and
Atherosclerosis Research Center
Louisville, Kentucky
Dr Bays has research grants, consultant fees, and speaker fees with Abbott Laboratories, Aegerion Pharmaceuticals, Akros Pharma Inc, Amarin, Amgen Inc., Amylin Pharmaceuticals, Inc., Arena Pharmaceuticals, Inc., Arete Therapeutics Inc., AstraZeneca, Bristol-Myers Squibb, Boehringer Ingelheim Corporation, Cargill, Inc., Daiichi Sankyo, Inc., Eli Lilly and Company, Essentialis, Inc., GlaxoSmithKline plc, Hoffmann-La Roche Inc., Home Access Health Corporation, InteKrin Therapeutics Inc., Isis Pharmaceuticals, Inc., Johnson & Johnson Services, Inc., Merck & Co., Inc.,Merck/Schering-Plough Pharmaceuticals, Metabolex, Inc., Neuromed Pharmaceuticals Ltd., NicOx, Novo Nordisk A/S, Orexigen Therapeutics, Inc., Pfizer Inc., Purdue Pharma L.P., sanofi-aventis US LLC, Sciele Pharma, Inc., Surface Logix, Inc., Takeda Pharmaceutical Company Limited, and VIVUS Inc.
Cardiologist:
Peter H. Jones, MD
Associate Professor of Medicine
Baylor College of Medicine
Houston, Texas
Dr Jones has consulting agreements with Abbott Laboratories, AstraZeneca, Daiichi Sankyo, Inc., and Merck/Schering-Plough Pharmaceuticals.
Copyright © 2010 Elsevier Inc.
A Journal Scan supplement to Clinical Endocrinology News. This supplement was sponsored by Daiichi Sankyo, Inc.
• Introduction
• Results of the Glucose-Lowering Effect of WelChol Study (GLOWS): A Randomized, Double-Blind, Placebo-Controlled Pilot Study Evaluating the Effect of Colesevelam Hydrochloride on Glycemic Control in Subjects with Type 2 Diabetes
• Efficacy and Safety of Colesevelam in Patients With Type 2 Diabetes Mellitus and Inadequate Glycemic Control Receiving Insulin-Based Therapy
• Colesevelam HCl Improves Glycemic Control and Reduces LDL Cholesterol in Patients With Inadequately Controlled Type 2 Diabetes on Sulfonylurea-Based Therapy
• Colesevelam Hydrochloride Therapy in Patients With Type 2 Diabetes Mellitus Treated With Metformin: Glucose and Lipid Effects
Faculty/Faculty Disclosures
Endocrinologist:
Harold E. Bays, MD, FACP, FACE
Medical Director/President
Louisville Metabolic and
Atherosclerosis Research Center
Louisville, Kentucky
Dr Bays has research grants, consultant fees, and speaker fees with Abbott Laboratories, Aegerion Pharmaceuticals, Akros Pharma Inc, Amarin, Amgen Inc., Amylin Pharmaceuticals, Inc., Arena Pharmaceuticals, Inc., Arete Therapeutics Inc., AstraZeneca, Bristol-Myers Squibb, Boehringer Ingelheim Corporation, Cargill, Inc., Daiichi Sankyo, Inc., Eli Lilly and Company, Essentialis, Inc., GlaxoSmithKline plc, Hoffmann-La Roche Inc., Home Access Health Corporation, InteKrin Therapeutics Inc., Isis Pharmaceuticals, Inc., Johnson & Johnson Services, Inc., Merck & Co., Inc.,Merck/Schering-Plough Pharmaceuticals, Metabolex, Inc., Neuromed Pharmaceuticals Ltd., NicOx, Novo Nordisk A/S, Orexigen Therapeutics, Inc., Pfizer Inc., Purdue Pharma L.P., sanofi-aventis US LLC, Sciele Pharma, Inc., Surface Logix, Inc., Takeda Pharmaceutical Company Limited, and VIVUS Inc.
Cardiologist:
Peter H. Jones, MD
Associate Professor of Medicine
Baylor College of Medicine
Houston, Texas
Dr Jones has consulting agreements with Abbott Laboratories, AstraZeneca, Daiichi Sankyo, Inc., and Merck/Schering-Plough Pharmaceuticals.
Copyright © 2010 Elsevier Inc.
CASE STUDY: Management Decisions in a Comorbid Patient With Type 2 Diabetes Having Primary Hyperlipidemia
A supplement to Clinical Endocrinology News. This supplement was sponsored by Daiichi Sankyo, Inc.
• Background
• Current Visit
• Laboratory Results
• Clinical Discussion
• Endocrinologist Consultation
• New Treatment Regimen With Add-On Therapy
• Conclusions
Faculty
Yehuda Handelsman, MD, FACP, FACE
Medical Director, Metabolic Institute of America
Chair and Program Director, 7th World Congress on Insulin Resistance Chair, International Committee for Insulin Resistance
18372 Clark Street, Suite 212
Tarzana, CA 91356
E-mail:[email protected]
Web site:www.TheMetabolicCenter.com
Dr Handelsman is a consultant for Bristol-Myers Squibb Company, Daiichi Sankyo, Inc., GlaxoSmithKline, Medtronic, Merck, Xoma, and Tethys;he has received clinical research grant funding from Takeda, Daiichi Sankyo Inc., GlaxoSmithKline, and Novo Nordisk; and he is on the speakers bureau for AstraZeneca, Bristol-Myers Squibb, Daiichi Sankyo Inc., GlaxoSmithKline, Merck, and Novartis. He also serves on the advisory board for CLINICAL ENDOCRINOLOGY NEWS.
Copyright © 2010 Elsevier Inc.
A supplement to Clinical Endocrinology News. This supplement was sponsored by Daiichi Sankyo, Inc.
• Background
• Current Visit
• Laboratory Results
• Clinical Discussion
• Endocrinologist Consultation
• New Treatment Regimen With Add-On Therapy
• Conclusions
Faculty
Yehuda Handelsman, MD, FACP, FACE
Medical Director, Metabolic Institute of America
Chair and Program Director, 7th World Congress on Insulin Resistance Chair, International Committee for Insulin Resistance
18372 Clark Street, Suite 212
Tarzana, CA 91356
E-mail:[email protected]
Web site:www.TheMetabolicCenter.com
Dr Handelsman is a consultant for Bristol-Myers Squibb Company, Daiichi Sankyo, Inc., GlaxoSmithKline, Medtronic, Merck, Xoma, and Tethys;he has received clinical research grant funding from Takeda, Daiichi Sankyo Inc., GlaxoSmithKline, and Novo Nordisk; and he is on the speakers bureau for AstraZeneca, Bristol-Myers Squibb, Daiichi Sankyo Inc., GlaxoSmithKline, Merck, and Novartis. He also serves on the advisory board for CLINICAL ENDOCRINOLOGY NEWS.
Copyright © 2010 Elsevier Inc.
A supplement to Clinical Endocrinology News. This supplement was sponsored by Daiichi Sankyo, Inc.
• Background
• Current Visit
• Laboratory Results
• Clinical Discussion
• Endocrinologist Consultation
• New Treatment Regimen With Add-On Therapy
• Conclusions
Faculty
Yehuda Handelsman, MD, FACP, FACE
Medical Director, Metabolic Institute of America
Chair and Program Director, 7th World Congress on Insulin Resistance Chair, International Committee for Insulin Resistance
18372 Clark Street, Suite 212
Tarzana, CA 91356
E-mail:[email protected]
Web site:www.TheMetabolicCenter.com
Dr Handelsman is a consultant for Bristol-Myers Squibb Company, Daiichi Sankyo, Inc., GlaxoSmithKline, Medtronic, Merck, Xoma, and Tethys;he has received clinical research grant funding from Takeda, Daiichi Sankyo Inc., GlaxoSmithKline, and Novo Nordisk; and he is on the speakers bureau for AstraZeneca, Bristol-Myers Squibb, Daiichi Sankyo Inc., GlaxoSmithKline, Merck, and Novartis. He also serves on the advisory board for CLINICAL ENDOCRINOLOGY NEWS.
Copyright © 2010 Elsevier Inc.
Central pain states: a shift in thinking about chronic pain
What do we mean when we talk about pain? Traditionally pain is defined as an unpleasant sensory and emotional experience associated with actual or potential tissue damage.1 Pain can result when intense or noxious stimuli activate peripheral nociceptors. It serves as a warning against impending tissue damage and acts reflectively to protect against or minimize that damage.
We have known since the time of Descartes about the existence of an ascending sensory pain pathway that sends “distress” signals from the source of tissue damage to the brain. We also know of the Gate Control theory described by Melzack and Wall in 1965, in which stimulation of the skin evokes responses that transmit signal injury to transmission cells (the “gate”) in the dorsal horn of the spinal cord that continues to the brain, triggering response signals that modulate the activity of inhibitory cells (which close the “gate”), thereby decreasing the intensity of pain.2 But how do we explain pain in the absence of tissue damage, pain that is not triggered in the periphery, that often appears long after the noxious stimulus has stopped exerting its unpleasant effect?
Types of chronic pain
An estimated 116 million American adults suffer from chronic pain, defined as pain that lasts more than 3 months after onset and well into the phase of healing.1,3 According to a 2006 report from the Centers for Disease Control and Prevention with a special focus on pain, almost 57% of adults age 65 or older and 37% of younger adults ages 20–44 reported pain that lasted one year or more [Figure 1].4 Chronic pain exacts a cost of between $560 billion and $635 billion annually in medical treatment and lost productivity.5 There is a tremendous need to understand the molecular and cellular mechanisms of chronic pain in an effort to develop new, more effective treatments for these patients. This understanding may come as a result of our recent advances in visualizing the peripheral and central processes involved in pain. The emerging data suggest that for some individuals central factors play a key role in the maintenance and establishment of certain chronic pain conditions. That is, for some, the problem is really not inthe periphery.
| FIGURE 1: Pain duration by age group, 1999-2002 |
| Source: Centers for Disease Control and Prevention, National Center for Health Statistics, Health, United States, 2006. Data from theNational Health and Nutrition Examination Survey. |
Knee and hip pain. When peripheral tissue damage is unavoidable, the inflamed tissues and those nearby become hypersensitive, a protective response to guard the area during the period of healing. Conditions like chronic low-back pain and knee or hip osteoarthritis classically have been thought to be due to inflammation or damage to tissues in the back, knee, or hip. However, recent studies show that these conditions may have complex factors entailing both the peripheral and central nervous systems.
Analysis of data from the National Health and Nutrition Examination Survey (NHANES I) of patients with radiographic evidence of structural damage to the knee due to osteoarthritis found discordance between the amount of damage visible on x-ray and patients’ self-report of the degree of pain. In 319 patients with radiographic stage 2–4 knee osteoarthritis, only 47% reported knee pain, suggesting that something more than the degree of tissue injury was involved in the perception of pain.6,7 One explanation of these findings is that pain is a complex system incorporating structural changes, peripheral and central pain mechanisms, and subjective factors, including the patient’s history, psychological experience, genetics, and culture.
Diabetic neuropathy and postherpetic neuralgia. Chronic neuropathic pain results when there is actual damage to the nervous system—the peripheral nerve, dorsal root, or central nervous system. Peripheral neuropathic pain occurs after damage or alterations to sensory neurons. Some neuropathic pain disorders, such as diabetic neuropathy and postherpetic neuralgia, are well-defined disorders in which symptoms are unrelated to a stimulus and pain is related to peripheral as well as central processing.8
Stroke. Central poststroke pain, in which pain and hypersensitivity occurs in a body part due to injury to the corresponding part of the brain affected by the cerebrovascular lesion, is also considered a neuropathic pain syndrome. The onset of central poststroke pain typically occurs more than one month after the stroke, and exists with somatosensory abnormalities.9-11 For these types of neuropathies, altered function due to loss or damage of neuronal tissue is likely the cause of the pain condition.
Many of the people suffering from these central chronic pain conditions find it difficult to obtain relief, and probably will not benefit from surgeries or manipulations in the periphery. Instead, they may benefit from a targeted approach that addresses the central nervous system.
Recent studies on fibromyalgia and pain
Fibromyalgia (FM) may be considered the prototypical central pain disorder, in which the pain originates or is maintained in part in the central nervous system. Although new diagnostic criteria are being validated for this disorder, FM classically has been diagnosed by the detection of 11 of 18 tender points and the presence of chronic widespread pain for 3 months or longer.12
FM is a common disorder found to affect between 2% and 4% of the US population.13 It was one of the first disorders shown to have central factors predominant in the pathology, and as a result it has been the focus of numerous studies. Irritable bowel syndrome and chronic fatigue syndrome, often comorbid with FM, are also commonly studied. Until recently, these disorders have largely been considered “wastebasket” terms to categorize the complaints of patients with unexplained symptoms, because there were no objective signs to support their complaints. However with the advent of new imaging techniques to look into the brain and the central nervous system, researchers are finding very real physiological differences. For example, one study using sensory testing with thermal, mechanical, and electrical stimuli showed a correlation between FM patients’ subjective reports of pain and significantly altered cold and heat thresholds when compared with controls.14 Based on such studies it appears that patients with FM perceive stimuli as noxious at lower levels than healthy, pain-free controls.
Recent studies of FM have incorporated the use of functional magnetic resonance imaging (fMRI) to look at brain activations in response to painful stimuli. A study that included patients with FM and others with chronic low-back pain used fMRI to visualize the participants’ response to equal amounts of thumbnail pressure. In the FM and groups, 5 areas of neuronal activation within the cortex related to pain were detected, compared with only one activation in controls.15 Another study to evaluate the pattern of cerebral activation in FM patients found that in response to similar thumbnail pressures there were 13 regions of greater activation in the FM group compared with one region in the healthy control group.16 Additionally, mild pressure resulted in subjective pain reports and cerebral responses in the FM group that were similar to responses produced by twice the pressure applied in controls.
Another important area of research in pain processing looks at gray matter in the brain using voxel-based morphometry. A study of patients with FM found significantly less volume of gray matter and an age-associated decrease in gray matter that was 3.3 times greater than healthy controls.17
Using MRI to look at gray matter volume in patients with chronic musculoskeletal pain, significant differences in gray matter volume were found in osteoarthritis patients prior to hip arthroplasty compared with healthy controls. Specifically, areas of the thalamus, understood to play a role in central pain processing, showed decreased gray matter volume in the osteoarthritis group. Significantly, a comparison of gray matter volume 9 months after surgery showed that the levels of reduced thalamic gray matter volume in osteoarthritis patients “reversed” to levels similar to the those of the healthy control group.18
Although the mechanism that drives the loss or degradation of brain tissue in patients with chronic pain remains to be determined, one theory is that pain is associated with certain areas of the brain becoming hyperactive. Imaging studies using fMRI show that a constellation of regions typically are activated in pain processing, including the insula,
cingulate, primary somatosensory and secondary somatosensory cortices, amygdala, and thalamus [Figure 2].19 These regions have been shown to be more active in chronic pain states when patients respond to stimuli such as painful pressure or heat. Indeed, these regions have shown overamplification or augmentation of neural activity.
| FIGURE 2: Neuroanatomy of pain processing. Main brain regions that activate during a painful experience are highlighted as bilaterally active but with more dominant activation on the contralateral hemisphere (red). |
| Source: Tracey I. Br J Anaesth. 2008;101:32-39. |
Since overstimulation of nerve cells can trigger a toxic release of glutamate into surrounding tissues of the brain, this may cause nerve cells to die, ultimately reducing the amount of gray matter visualized in the brains of patients with chronic pain. In addition, some studies of FM have shown elevated levels of glutamate, an excitatory neurotransmitter that is known to cause excitotoxicity.20
Another significant consequence of long-term pain appears to be alterations in the normal connectivity of the brain, including the “default mode network” (DMN) which is noted to be important during the resting state. Recent studies of chronic pain suggest alterations in key DMN regions that may be related to the chronic pain state and existing comorbidities.21
The role of stress and depression in pain
The association among physical and psychosocial stressors, depression, and chronic pain syndromes has been the subject of numerous studies.
Posttraumatic stress disorder (PTSD) has been closely correlated with chronic pain. An example of one such stressor may be deployment to a military conflict. Soldiers and military personnel throughout history have reported a cluster of symptoms such as pain, fatigue, and cognitive impairment that are very similar to FM. From US military conflicts, these syndromes include Gulf War illness, the condition known as “shell shock” in World War I, and “soldier’s heart” during the Civil War.
A review of the literature addressing the association between chronic pain and PTSD by the Department of Veterans Affairs found such a high degree of correlation that the authors suggested clinicians who conduct diagnostic assessments for one disorder should also assess for the other.22 In a study that evaluated patients for FM, chronic fatigue, and psychiatric symptoms, patients with FM who had both tender points and diffuse pain were significantly more likely to have an increased prevalence of lifetime PTSD.23
The relationship between depression and chronic pain has been well documented. Kaiser Permanente surveyed patients seen in primary care and found that a significantly higher proportion of patients with major depressive disorder (MDD) reported chronic pain than did patients without MDD (66% vs 43%, respectively).24 These conditions share common physiologic features and a high degree of comorbidity.
A study of patients with FM and depressive symptoms or MDD looked at neural responses to painful pressure and found no association between the extent of depressive symptoms or MDD and neural activation in the primary and secondary cortices, areas associated with the sensation of pain. However, activation was seen in the amygdala and contralateral anterior insula, areas associated with affective pain processing.25
These findings were supported in a more recent study in which patients who met the criteria for FM were given a series of questionnaires to assess depressive symptoms, anxiety, and catastrophizing, and were tested for painful pressure responses using fMRI. The results established a correlation between this cluster of affective symptoms, but there was no correlation with clinical pain symptoms or responses to painful pressure.26 Rather than suggesting that there is no alignment between the mental and physical aspects of pain, results from both of these studies suggest that 2 independent pain networks exist to process the sensory and affective dimensions of pain, and that these pathways may operate simultaneously.
Pain in the clinical setting
The evidence is strong that many patients experience chronic pain that is not site-specific and arises not merely from the periphery but from intricate neural systems. With a new appreciation for the complexity of pain processing, the clinician is compelled to probe beyond, “Where does it hurt?” [Table].
| TABLE: Clinical diagnosis of central pain
|
When patients complain of widespread or chronic pain, the clinician is well advised to take the time to examine further by inquiring about depression, anxiety, fatigue, sleep disturbances, and cognitive difficulties in order to understand what is driving the patient’s symptoms.13 The results may be revealing. In a study of primary care patients, participants who complained of muscle pain, headache, and stomach pain were found to be 2.5 to 10 times more likely to screen positively for panic disorder, generalized anxiety, or MDD.27
An article in a following issue will discuss practical tools that can be used to assess comorbidities such as anxiety and depression, and interventions that might be helpful for central pain and neurorehabilitation. An approach that acknowledges the patient’s account of pain, recognizes the cluster of symptoms and conditions that can accompany pain, and utilizes a multidisciplinary approach for diagnosis and treatment will have the best chance of yielding positive outcomes.
Acknowledgement—The author wishes to thank Kristen Georgi for her assistance in the research and writing of this article.
REFERENCES
1. International Association for the Study of Pain. IASP taxonomy: pain terms. Pain. Available at: http://www.iasp-pain.org/AM/Template.cfm?Section=Pain_Defi...isplay.cfm&ContentID=1728#Pain.
2. Melzack R, Wall PD. Pain mechanisms. A new theory. Science. 1965;150:971-979.
3. Carr DB. How prevalent is chronic pain? Pain Clinical Updates. 2003;11:1-4. Available at: http://www.iasp-pain.org/AM/AMTemplate.cfm?Section=Home&CONTENTID=7594&TEMPLATE=/CM/ContentDisplay.cfm&SECTION=Home.
4. Washington, DC: US Department of Health and Human Services, Centers for Disease Control and Prevention; 2006. Bernstein AB, Makuc DM, Bilheimer LT. Health, United States, 2006. Available at: http: //www.cdc.gov/nchs/data/hus/hus06.pdf.
5. Institute of Medicine. Relieving pain in America: a blueprint for transforming prevention, care, education, and research. Washington, DC: National Academies Press; 2011.
6. Hannan MT, Felson DT, Pincus T. Analysis of the discordance between radiographic changes and knee pain in osteoarthritis of the knee. J Rheumatol. 2000;27:1513-1517.
7. Creamer P, Hochberg MC. Why does osteoarthritis of the knee hurt—sometimes? Br J Rheumatol. 1997;36:726-728.
8. Woolf CJ, Mannion RJ. Neuropathic pain: aetiology, symptoms, mechanisms, and management. Lancet. 1999;353:1959-1964.
9. Andersen G, Vestergaard K, Ingeman-Nielsen M, et al. Incidence of central post-stroke pain. Pain. 1995;61:187-193.
10. Bowsher D. Central pain: clinical and physiological characteristics. J Neurol Neurosurg Psychiatry. 1996;61:62-69.
11. Klit H, Finnerup NB, Jensen TS. Central post-stroke pain: clinical characteristics, pathophysiology, and management. Lancet. 2009;8:857-868.
12. Wolfe F, Smythe HA, Yunus MB, et al. The American College of Rheumatology 1990 criteria for the classification of fibromyalgia: report of the multicenter criteria committee. Arthritis Rheum. 1990;33:160-172.
13. Wolfe F, Ross K, Anderson J, et al. Aspects of fibromyalgia in the general population: sex, pain threshold, and fibromyalgia symptoms. J Rheumatol. 1995;22:151-156.
14. Desmeules JA, Cedraschi C, Rapiti E, et al. Neurolopshysiologic evidence for a central sensitization in patients with fibromyalgia. Arthritis Rheum. 2003;48:1420-1429.
15. Giesecke T, Gracely RH, Grant MAB, et al. Evidence of augmented central pain processing in idiopathic chronic low back pain. Arthritis Rheum. 2004;50:613-623.
16. Gracely RH, Petzke F, Wolf JM, et al. Functional magnetic resonance imaging evidence of augmented pain processing in fibromyalgia. Arthritis Rheum. 2002;46:1333-1343.
17. Kuchinad A, Schweinhardt P, Seminowicz DA, et al. Accelerated brain gray matter loss in fibromyalgia patients: premature aging of the brain? J Neurosci. 2007;27:4004-4007.
18. Gwilym SE, Fillipini N, Douaud G, et al. Thalamic atrophy associated with painful osteoarthritis of the hip is reversible after arthroplasty. Arthritis Rheum. 2010;62:2930-2940.
19. Tracey I. Imaging pain. Br J Anaesth. 2008;101:32-39.
20. Harris RE, Sundgren PC, Craig AD, et al. Elevated insular glutamate in fibromyalgia is associated with experimental pain. Arthritis Rheum. 2009;60:3146-3152.
21. Baliki MN, Geha PY, Apkarian AV, et al. Beyond feeling: chronic pain hurts the brain, disrupting the default-mode network dynamics. J Neurosci. 2008;28:
1398-1403.
22. Otis JD, Keane TM, Kerns RD. An examination of the relationship between chronic pain and posttraumatic stress disorder. J Rehabil Res Dev. 2003;40:397-406.
23. Roy-Byrne P, Smith WR, Goldberg N, et al. Posttraumatic stress disorder among patients with chronic pain and chronic fatigue. Psychol Med. 2004;34:
363-368.
24. Arnow BA, Hunkeler EM, Blasey CM, et al. Comorbid depression, chronic pain, and disability in primary care. Psychosom Med. 2006;68:262-268.
25. Giesecke T, Gracely RH, Williams DA, et al. The relationship between depression, clinical pain, and experimental pain in a chronic pain cohort. Arthritis Rheum. 2005;52:1577-1584.
26. Jensen KB, Petzke F, Carville S, et al. Anxiety and depressive symptoms in fibromyalgia are related to poor perception of health but not to pain sensitivity or cerebral processing of pain. Arthritis Rheum. 2010;62:3488-3495.
27. Means-Christensen AJ, Roy-Byrne PR, Sherbourne CD, et al. Relationships among pain, anxiety, and depression in primary care. Depress Anxiety. 2008;25:
593-600.
What do we mean when we talk about pain? Traditionally pain is defined as an unpleasant sensory and emotional experience associated with actual or potential tissue damage.1 Pain can result when intense or noxious stimuli activate peripheral nociceptors. It serves as a warning against impending tissue damage and acts reflectively to protect against or minimize that damage.
We have known since the time of Descartes about the existence of an ascending sensory pain pathway that sends “distress” signals from the source of tissue damage to the brain. We also know of the Gate Control theory described by Melzack and Wall in 1965, in which stimulation of the skin evokes responses that transmit signal injury to transmission cells (the “gate”) in the dorsal horn of the spinal cord that continues to the brain, triggering response signals that modulate the activity of inhibitory cells (which close the “gate”), thereby decreasing the intensity of pain.2 But how do we explain pain in the absence of tissue damage, pain that is not triggered in the periphery, that often appears long after the noxious stimulus has stopped exerting its unpleasant effect?
Types of chronic pain
An estimated 116 million American adults suffer from chronic pain, defined as pain that lasts more than 3 months after onset and well into the phase of healing.1,3 According to a 2006 report from the Centers for Disease Control and Prevention with a special focus on pain, almost 57% of adults age 65 or older and 37% of younger adults ages 20–44 reported pain that lasted one year or more [Figure 1].4 Chronic pain exacts a cost of between $560 billion and $635 billion annually in medical treatment and lost productivity.5 There is a tremendous need to understand the molecular and cellular mechanisms of chronic pain in an effort to develop new, more effective treatments for these patients. This understanding may come as a result of our recent advances in visualizing the peripheral and central processes involved in pain. The emerging data suggest that for some individuals central factors play a key role in the maintenance and establishment of certain chronic pain conditions. That is, for some, the problem is really not inthe periphery.
| FIGURE 1: Pain duration by age group, 1999-2002 |
| Source: Centers for Disease Control and Prevention, National Center for Health Statistics, Health, United States, 2006. Data from theNational Health and Nutrition Examination Survey. |
Knee and hip pain. When peripheral tissue damage is unavoidable, the inflamed tissues and those nearby become hypersensitive, a protective response to guard the area during the period of healing. Conditions like chronic low-back pain and knee or hip osteoarthritis classically have been thought to be due to inflammation or damage to tissues in the back, knee, or hip. However, recent studies show that these conditions may have complex factors entailing both the peripheral and central nervous systems.
Analysis of data from the National Health and Nutrition Examination Survey (NHANES I) of patients with radiographic evidence of structural damage to the knee due to osteoarthritis found discordance between the amount of damage visible on x-ray and patients’ self-report of the degree of pain. In 319 patients with radiographic stage 2–4 knee osteoarthritis, only 47% reported knee pain, suggesting that something more than the degree of tissue injury was involved in the perception of pain.6,7 One explanation of these findings is that pain is a complex system incorporating structural changes, peripheral and central pain mechanisms, and subjective factors, including the patient’s history, psychological experience, genetics, and culture.
Diabetic neuropathy and postherpetic neuralgia. Chronic neuropathic pain results when there is actual damage to the nervous system—the peripheral nerve, dorsal root, or central nervous system. Peripheral neuropathic pain occurs after damage or alterations to sensory neurons. Some neuropathic pain disorders, such as diabetic neuropathy and postherpetic neuralgia, are well-defined disorders in which symptoms are unrelated to a stimulus and pain is related to peripheral as well as central processing.8
Stroke. Central poststroke pain, in which pain and hypersensitivity occurs in a body part due to injury to the corresponding part of the brain affected by the cerebrovascular lesion, is also considered a neuropathic pain syndrome. The onset of central poststroke pain typically occurs more than one month after the stroke, and exists with somatosensory abnormalities.9-11 For these types of neuropathies, altered function due to loss or damage of neuronal tissue is likely the cause of the pain condition.
Many of the people suffering from these central chronic pain conditions find it difficult to obtain relief, and probably will not benefit from surgeries or manipulations in the periphery. Instead, they may benefit from a targeted approach that addresses the central nervous system.
Recent studies on fibromyalgia and pain
Fibromyalgia (FM) may be considered the prototypical central pain disorder, in which the pain originates or is maintained in part in the central nervous system. Although new diagnostic criteria are being validated for this disorder, FM classically has been diagnosed by the detection of 11 of 18 tender points and the presence of chronic widespread pain for 3 months or longer.12
FM is a common disorder found to affect between 2% and 4% of the US population.13 It was one of the first disorders shown to have central factors predominant in the pathology, and as a result it has been the focus of numerous studies. Irritable bowel syndrome and chronic fatigue syndrome, often comorbid with FM, are also commonly studied. Until recently, these disorders have largely been considered “wastebasket” terms to categorize the complaints of patients with unexplained symptoms, because there were no objective signs to support their complaints. However with the advent of new imaging techniques to look into the brain and the central nervous system, researchers are finding very real physiological differences. For example, one study using sensory testing with thermal, mechanical, and electrical stimuli showed a correlation between FM patients’ subjective reports of pain and significantly altered cold and heat thresholds when compared with controls.14 Based on such studies it appears that patients with FM perceive stimuli as noxious at lower levels than healthy, pain-free controls.
Recent studies of FM have incorporated the use of functional magnetic resonance imaging (fMRI) to look at brain activations in response to painful stimuli. A study that included patients with FM and others with chronic low-back pain used fMRI to visualize the participants’ response to equal amounts of thumbnail pressure. In the FM and groups, 5 areas of neuronal activation within the cortex related to pain were detected, compared with only one activation in controls.15 Another study to evaluate the pattern of cerebral activation in FM patients found that in response to similar thumbnail pressures there were 13 regions of greater activation in the FM group compared with one region in the healthy control group.16 Additionally, mild pressure resulted in subjective pain reports and cerebral responses in the FM group that were similar to responses produced by twice the pressure applied in controls.
Another important area of research in pain processing looks at gray matter in the brain using voxel-based morphometry. A study of patients with FM found significantly less volume of gray matter and an age-associated decrease in gray matter that was 3.3 times greater than healthy controls.17
Using MRI to look at gray matter volume in patients with chronic musculoskeletal pain, significant differences in gray matter volume were found in osteoarthritis patients prior to hip arthroplasty compared with healthy controls. Specifically, areas of the thalamus, understood to play a role in central pain processing, showed decreased gray matter volume in the osteoarthritis group. Significantly, a comparison of gray matter volume 9 months after surgery showed that the levels of reduced thalamic gray matter volume in osteoarthritis patients “reversed” to levels similar to the those of the healthy control group.18
Although the mechanism that drives the loss or degradation of brain tissue in patients with chronic pain remains to be determined, one theory is that pain is associated with certain areas of the brain becoming hyperactive. Imaging studies using fMRI show that a constellation of regions typically are activated in pain processing, including the insula,
cingulate, primary somatosensory and secondary somatosensory cortices, amygdala, and thalamus [Figure 2].19 These regions have been shown to be more active in chronic pain states when patients respond to stimuli such as painful pressure or heat. Indeed, these regions have shown overamplification or augmentation of neural activity.
| FIGURE 2: Neuroanatomy of pain processing. Main brain regions that activate during a painful experience are highlighted as bilaterally active but with more dominant activation on the contralateral hemisphere (red). |
| Source: Tracey I. Br J Anaesth. 2008;101:32-39. |
Since overstimulation of nerve cells can trigger a toxic release of glutamate into surrounding tissues of the brain, this may cause nerve cells to die, ultimately reducing the amount of gray matter visualized in the brains of patients with chronic pain. In addition, some studies of FM have shown elevated levels of glutamate, an excitatory neurotransmitter that is known to cause excitotoxicity.20
Another significant consequence of long-term pain appears to be alterations in the normal connectivity of the brain, including the “default mode network” (DMN) which is noted to be important during the resting state. Recent studies of chronic pain suggest alterations in key DMN regions that may be related to the chronic pain state and existing comorbidities.21
The role of stress and depression in pain
The association among physical and psychosocial stressors, depression, and chronic pain syndromes has been the subject of numerous studies.
Posttraumatic stress disorder (PTSD) has been closely correlated with chronic pain. An example of one such stressor may be deployment to a military conflict. Soldiers and military personnel throughout history have reported a cluster of symptoms such as pain, fatigue, and cognitive impairment that are very similar to FM. From US military conflicts, these syndromes include Gulf War illness, the condition known as “shell shock” in World War I, and “soldier’s heart” during the Civil War.
A review of the literature addressing the association between chronic pain and PTSD by the Department of Veterans Affairs found such a high degree of correlation that the authors suggested clinicians who conduct diagnostic assessments for one disorder should also assess for the other.22 In a study that evaluated patients for FM, chronic fatigue, and psychiatric symptoms, patients with FM who had both tender points and diffuse pain were significantly more likely to have an increased prevalence of lifetime PTSD.23
The relationship between depression and chronic pain has been well documented. Kaiser Permanente surveyed patients seen in primary care and found that a significantly higher proportion of patients with major depressive disorder (MDD) reported chronic pain than did patients without MDD (66% vs 43%, respectively).24 These conditions share common physiologic features and a high degree of comorbidity.
A study of patients with FM and depressive symptoms or MDD looked at neural responses to painful pressure and found no association between the extent of depressive symptoms or MDD and neural activation in the primary and secondary cortices, areas associated with the sensation of pain. However, activation was seen in the amygdala and contralateral anterior insula, areas associated with affective pain processing.25
These findings were supported in a more recent study in which patients who met the criteria for FM were given a series of questionnaires to assess depressive symptoms, anxiety, and catastrophizing, and were tested for painful pressure responses using fMRI. The results established a correlation between this cluster of affective symptoms, but there was no correlation with clinical pain symptoms or responses to painful pressure.26 Rather than suggesting that there is no alignment between the mental and physical aspects of pain, results from both of these studies suggest that 2 independent pain networks exist to process the sensory and affective dimensions of pain, and that these pathways may operate simultaneously.
Pain in the clinical setting
The evidence is strong that many patients experience chronic pain that is not site-specific and arises not merely from the periphery but from intricate neural systems. With a new appreciation for the complexity of pain processing, the clinician is compelled to probe beyond, “Where does it hurt?” [Table].
| TABLE: Clinical diagnosis of central pain
|
When patients complain of widespread or chronic pain, the clinician is well advised to take the time to examine further by inquiring about depression, anxiety, fatigue, sleep disturbances, and cognitive difficulties in order to understand what is driving the patient’s symptoms.13 The results may be revealing. In a study of primary care patients, participants who complained of muscle pain, headache, and stomach pain were found to be 2.5 to 10 times more likely to screen positively for panic disorder, generalized anxiety, or MDD.27
An article in a following issue will discuss practical tools that can be used to assess comorbidities such as anxiety and depression, and interventions that might be helpful for central pain and neurorehabilitation. An approach that acknowledges the patient’s account of pain, recognizes the cluster of symptoms and conditions that can accompany pain, and utilizes a multidisciplinary approach for diagnosis and treatment will have the best chance of yielding positive outcomes.
Acknowledgement—The author wishes to thank Kristen Georgi for her assistance in the research and writing of this article.
REFERENCES
1. International Association for the Study of Pain. IASP taxonomy: pain terms. Pain. Available at: http://www.iasp-pain.org/AM/Template.cfm?Section=Pain_Defi...isplay.cfm&ContentID=1728#Pain.
2. Melzack R, Wall PD. Pain mechanisms. A new theory. Science. 1965;150:971-979.
3. Carr DB. How prevalent is chronic pain? Pain Clinical Updates. 2003;11:1-4. Available at: http://www.iasp-pain.org/AM/AMTemplate.cfm?Section=Home&CONTENTID=7594&TEMPLATE=/CM/ContentDisplay.cfm&SECTION=Home.
4. Washington, DC: US Department of Health and Human Services, Centers for Disease Control and Prevention; 2006. Bernstein AB, Makuc DM, Bilheimer LT. Health, United States, 2006. Available at: http: //www.cdc.gov/nchs/data/hus/hus06.pdf.
5. Institute of Medicine. Relieving pain in America: a blueprint for transforming prevention, care, education, and research. Washington, DC: National Academies Press; 2011.
6. Hannan MT, Felson DT, Pincus T. Analysis of the discordance between radiographic changes and knee pain in osteoarthritis of the knee. J Rheumatol. 2000;27:1513-1517.
7. Creamer P, Hochberg MC. Why does osteoarthritis of the knee hurt—sometimes? Br J Rheumatol. 1997;36:726-728.
8. Woolf CJ, Mannion RJ. Neuropathic pain: aetiology, symptoms, mechanisms, and management. Lancet. 1999;353:1959-1964.
9. Andersen G, Vestergaard K, Ingeman-Nielsen M, et al. Incidence of central post-stroke pain. Pain. 1995;61:187-193.
10. Bowsher D. Central pain: clinical and physiological characteristics. J Neurol Neurosurg Psychiatry. 1996;61:62-69.
11. Klit H, Finnerup NB, Jensen TS. Central post-stroke pain: clinical characteristics, pathophysiology, and management. Lancet. 2009;8:857-868.
12. Wolfe F, Smythe HA, Yunus MB, et al. The American College of Rheumatology 1990 criteria for the classification of fibromyalgia: report of the multicenter criteria committee. Arthritis Rheum. 1990;33:160-172.
13. Wolfe F, Ross K, Anderson J, et al. Aspects of fibromyalgia in the general population: sex, pain threshold, and fibromyalgia symptoms. J Rheumatol. 1995;22:151-156.
14. Desmeules JA, Cedraschi C, Rapiti E, et al. Neurolopshysiologic evidence for a central sensitization in patients with fibromyalgia. Arthritis Rheum. 2003;48:1420-1429.
15. Giesecke T, Gracely RH, Grant MAB, et al. Evidence of augmented central pain processing in idiopathic chronic low back pain. Arthritis Rheum. 2004;50:613-623.
16. Gracely RH, Petzke F, Wolf JM, et al. Functional magnetic resonance imaging evidence of augmented pain processing in fibromyalgia. Arthritis Rheum. 2002;46:1333-1343.
17. Kuchinad A, Schweinhardt P, Seminowicz DA, et al. Accelerated brain gray matter loss in fibromyalgia patients: premature aging of the brain? J Neurosci. 2007;27:4004-4007.
18. Gwilym SE, Fillipini N, Douaud G, et al. Thalamic atrophy associated with painful osteoarthritis of the hip is reversible after arthroplasty. Arthritis Rheum. 2010;62:2930-2940.
19. Tracey I. Imaging pain. Br J Anaesth. 2008;101:32-39.
20. Harris RE, Sundgren PC, Craig AD, et al. Elevated insular glutamate in fibromyalgia is associated with experimental pain. Arthritis Rheum. 2009;60:3146-3152.
21. Baliki MN, Geha PY, Apkarian AV, et al. Beyond feeling: chronic pain hurts the brain, disrupting the default-mode network dynamics. J Neurosci. 2008;28:
1398-1403.
22. Otis JD, Keane TM, Kerns RD. An examination of the relationship between chronic pain and posttraumatic stress disorder. J Rehabil Res Dev. 2003;40:397-406.
23. Roy-Byrne P, Smith WR, Goldberg N, et al. Posttraumatic stress disorder among patients with chronic pain and chronic fatigue. Psychol Med. 2004;34:
363-368.
24. Arnow BA, Hunkeler EM, Blasey CM, et al. Comorbid depression, chronic pain, and disability in primary care. Psychosom Med. 2006;68:262-268.
25. Giesecke T, Gracely RH, Williams DA, et al. The relationship between depression, clinical pain, and experimental pain in a chronic pain cohort. Arthritis Rheum. 2005;52:1577-1584.
26. Jensen KB, Petzke F, Carville S, et al. Anxiety and depressive symptoms in fibromyalgia are related to poor perception of health but not to pain sensitivity or cerebral processing of pain. Arthritis Rheum. 2010;62:3488-3495.
27. Means-Christensen AJ, Roy-Byrne PR, Sherbourne CD, et al. Relationships among pain, anxiety, and depression in primary care. Depress Anxiety. 2008;25:
593-600.
What do we mean when we talk about pain? Traditionally pain is defined as an unpleasant sensory and emotional experience associated with actual or potential tissue damage.1 Pain can result when intense or noxious stimuli activate peripheral nociceptors. It serves as a warning against impending tissue damage and acts reflectively to protect against or minimize that damage.
We have known since the time of Descartes about the existence of an ascending sensory pain pathway that sends “distress” signals from the source of tissue damage to the brain. We also know of the Gate Control theory described by Melzack and Wall in 1965, in which stimulation of the skin evokes responses that transmit signal injury to transmission cells (the “gate”) in the dorsal horn of the spinal cord that continues to the brain, triggering response signals that modulate the activity of inhibitory cells (which close the “gate”), thereby decreasing the intensity of pain.2 But how do we explain pain in the absence of tissue damage, pain that is not triggered in the periphery, that often appears long after the noxious stimulus has stopped exerting its unpleasant effect?
Types of chronic pain
An estimated 116 million American adults suffer from chronic pain, defined as pain that lasts more than 3 months after onset and well into the phase of healing.1,3 According to a 2006 report from the Centers for Disease Control and Prevention with a special focus on pain, almost 57% of adults age 65 or older and 37% of younger adults ages 20–44 reported pain that lasted one year or more [Figure 1].4 Chronic pain exacts a cost of between $560 billion and $635 billion annually in medical treatment and lost productivity.5 There is a tremendous need to understand the molecular and cellular mechanisms of chronic pain in an effort to develop new, more effective treatments for these patients. This understanding may come as a result of our recent advances in visualizing the peripheral and central processes involved in pain. The emerging data suggest that for some individuals central factors play a key role in the maintenance and establishment of certain chronic pain conditions. That is, for some, the problem is really not inthe periphery.
| FIGURE 1: Pain duration by age group, 1999-2002 |
| Source: Centers for Disease Control and Prevention, National Center for Health Statistics, Health, United States, 2006. Data from theNational Health and Nutrition Examination Survey. |
Knee and hip pain. When peripheral tissue damage is unavoidable, the inflamed tissues and those nearby become hypersensitive, a protective response to guard the area during the period of healing. Conditions like chronic low-back pain and knee or hip osteoarthritis classically have been thought to be due to inflammation or damage to tissues in the back, knee, or hip. However, recent studies show that these conditions may have complex factors entailing both the peripheral and central nervous systems.
Analysis of data from the National Health and Nutrition Examination Survey (NHANES I) of patients with radiographic evidence of structural damage to the knee due to osteoarthritis found discordance between the amount of damage visible on x-ray and patients’ self-report of the degree of pain. In 319 patients with radiographic stage 2–4 knee osteoarthritis, only 47% reported knee pain, suggesting that something more than the degree of tissue injury was involved in the perception of pain.6,7 One explanation of these findings is that pain is a complex system incorporating structural changes, peripheral and central pain mechanisms, and subjective factors, including the patient’s history, psychological experience, genetics, and culture.
Diabetic neuropathy and postherpetic neuralgia. Chronic neuropathic pain results when there is actual damage to the nervous system—the peripheral nerve, dorsal root, or central nervous system. Peripheral neuropathic pain occurs after damage or alterations to sensory neurons. Some neuropathic pain disorders, such as diabetic neuropathy and postherpetic neuralgia, are well-defined disorders in which symptoms are unrelated to a stimulus and pain is related to peripheral as well as central processing.8
Stroke. Central poststroke pain, in which pain and hypersensitivity occurs in a body part due to injury to the corresponding part of the brain affected by the cerebrovascular lesion, is also considered a neuropathic pain syndrome. The onset of central poststroke pain typically occurs more than one month after the stroke, and exists with somatosensory abnormalities.9-11 For these types of neuropathies, altered function due to loss or damage of neuronal tissue is likely the cause of the pain condition.
Many of the people suffering from these central chronic pain conditions find it difficult to obtain relief, and probably will not benefit from surgeries or manipulations in the periphery. Instead, they may benefit from a targeted approach that addresses the central nervous system.
Recent studies on fibromyalgia and pain
Fibromyalgia (FM) may be considered the prototypical central pain disorder, in which the pain originates or is maintained in part in the central nervous system. Although new diagnostic criteria are being validated for this disorder, FM classically has been diagnosed by the detection of 11 of 18 tender points and the presence of chronic widespread pain for 3 months or longer.12
FM is a common disorder found to affect between 2% and 4% of the US population.13 It was one of the first disorders shown to have central factors predominant in the pathology, and as a result it has been the focus of numerous studies. Irritable bowel syndrome and chronic fatigue syndrome, often comorbid with FM, are also commonly studied. Until recently, these disorders have largely been considered “wastebasket” terms to categorize the complaints of patients with unexplained symptoms, because there were no objective signs to support their complaints. However with the advent of new imaging techniques to look into the brain and the central nervous system, researchers are finding very real physiological differences. For example, one study using sensory testing with thermal, mechanical, and electrical stimuli showed a correlation between FM patients’ subjective reports of pain and significantly altered cold and heat thresholds when compared with controls.14 Based on such studies it appears that patients with FM perceive stimuli as noxious at lower levels than healthy, pain-free controls.
Recent studies of FM have incorporated the use of functional magnetic resonance imaging (fMRI) to look at brain activations in response to painful stimuli. A study that included patients with FM and others with chronic low-back pain used fMRI to visualize the participants’ response to equal amounts of thumbnail pressure. In the FM and groups, 5 areas of neuronal activation within the cortex related to pain were detected, compared with only one activation in controls.15 Another study to evaluate the pattern of cerebral activation in FM patients found that in response to similar thumbnail pressures there were 13 regions of greater activation in the FM group compared with one region in the healthy control group.16 Additionally, mild pressure resulted in subjective pain reports and cerebral responses in the FM group that were similar to responses produced by twice the pressure applied in controls.
Another important area of research in pain processing looks at gray matter in the brain using voxel-based morphometry. A study of patients with FM found significantly less volume of gray matter and an age-associated decrease in gray matter that was 3.3 times greater than healthy controls.17
Using MRI to look at gray matter volume in patients with chronic musculoskeletal pain, significant differences in gray matter volume were found in osteoarthritis patients prior to hip arthroplasty compared with healthy controls. Specifically, areas of the thalamus, understood to play a role in central pain processing, showed decreased gray matter volume in the osteoarthritis group. Significantly, a comparison of gray matter volume 9 months after surgery showed that the levels of reduced thalamic gray matter volume in osteoarthritis patients “reversed” to levels similar to the those of the healthy control group.18
Although the mechanism that drives the loss or degradation of brain tissue in patients with chronic pain remains to be determined, one theory is that pain is associated with certain areas of the brain becoming hyperactive. Imaging studies using fMRI show that a constellation of regions typically are activated in pain processing, including the insula,
cingulate, primary somatosensory and secondary somatosensory cortices, amygdala, and thalamus [Figure 2].19 These regions have been shown to be more active in chronic pain states when patients respond to stimuli such as painful pressure or heat. Indeed, these regions have shown overamplification or augmentation of neural activity.
| FIGURE 2: Neuroanatomy of pain processing. Main brain regions that activate during a painful experience are highlighted as bilaterally active but with more dominant activation on the contralateral hemisphere (red). |
| Source: Tracey I. Br J Anaesth. 2008;101:32-39. |
Since overstimulation of nerve cells can trigger a toxic release of glutamate into surrounding tissues of the brain, this may cause nerve cells to die, ultimately reducing the amount of gray matter visualized in the brains of patients with chronic pain. In addition, some studies of FM have shown elevated levels of glutamate, an excitatory neurotransmitter that is known to cause excitotoxicity.20
Another significant consequence of long-term pain appears to be alterations in the normal connectivity of the brain, including the “default mode network” (DMN) which is noted to be important during the resting state. Recent studies of chronic pain suggest alterations in key DMN regions that may be related to the chronic pain state and existing comorbidities.21
The role of stress and depression in pain
The association among physical and psychosocial stressors, depression, and chronic pain syndromes has been the subject of numerous studies.
Posttraumatic stress disorder (PTSD) has been closely correlated with chronic pain. An example of one such stressor may be deployment to a military conflict. Soldiers and military personnel throughout history have reported a cluster of symptoms such as pain, fatigue, and cognitive impairment that are very similar to FM. From US military conflicts, these syndromes include Gulf War illness, the condition known as “shell shock” in World War I, and “soldier’s heart” during the Civil War.
A review of the literature addressing the association between chronic pain and PTSD by the Department of Veterans Affairs found such a high degree of correlation that the authors suggested clinicians who conduct diagnostic assessments for one disorder should also assess for the other.22 In a study that evaluated patients for FM, chronic fatigue, and psychiatric symptoms, patients with FM who had both tender points and diffuse pain were significantly more likely to have an increased prevalence of lifetime PTSD.23
The relationship between depression and chronic pain has been well documented. Kaiser Permanente surveyed patients seen in primary care and found that a significantly higher proportion of patients with major depressive disorder (MDD) reported chronic pain than did patients without MDD (66% vs 43%, respectively).24 These conditions share common physiologic features and a high degree of comorbidity.
A study of patients with FM and depressive symptoms or MDD looked at neural responses to painful pressure and found no association between the extent of depressive symptoms or MDD and neural activation in the primary and secondary cortices, areas associated with the sensation of pain. However, activation was seen in the amygdala and contralateral anterior insula, areas associated with affective pain processing.25
These findings were supported in a more recent study in which patients who met the criteria for FM were given a series of questionnaires to assess depressive symptoms, anxiety, and catastrophizing, and were tested for painful pressure responses using fMRI. The results established a correlation between this cluster of affective symptoms, but there was no correlation with clinical pain symptoms or responses to painful pressure.26 Rather than suggesting that there is no alignment between the mental and physical aspects of pain, results from both of these studies suggest that 2 independent pain networks exist to process the sensory and affective dimensions of pain, and that these pathways may operate simultaneously.
Pain in the clinical setting
The evidence is strong that many patients experience chronic pain that is not site-specific and arises not merely from the periphery but from intricate neural systems. With a new appreciation for the complexity of pain processing, the clinician is compelled to probe beyond, “Where does it hurt?” [Table].
| TABLE: Clinical diagnosis of central pain
|
When patients complain of widespread or chronic pain, the clinician is well advised to take the time to examine further by inquiring about depression, anxiety, fatigue, sleep disturbances, and cognitive difficulties in order to understand what is driving the patient’s symptoms.13 The results may be revealing. In a study of primary care patients, participants who complained of muscle pain, headache, and stomach pain were found to be 2.5 to 10 times more likely to screen positively for panic disorder, generalized anxiety, or MDD.27
An article in a following issue will discuss practical tools that can be used to assess comorbidities such as anxiety and depression, and interventions that might be helpful for central pain and neurorehabilitation. An approach that acknowledges the patient’s account of pain, recognizes the cluster of symptoms and conditions that can accompany pain, and utilizes a multidisciplinary approach for diagnosis and treatment will have the best chance of yielding positive outcomes.
Acknowledgement—The author wishes to thank Kristen Georgi for her assistance in the research and writing of this article.
REFERENCES
1. International Association for the Study of Pain. IASP taxonomy: pain terms. Pain. Available at: http://www.iasp-pain.org/AM/Template.cfm?Section=Pain_Defi...isplay.cfm&ContentID=1728#Pain.
2. Melzack R, Wall PD. Pain mechanisms. A new theory. Science. 1965;150:971-979.
3. Carr DB. How prevalent is chronic pain? Pain Clinical Updates. 2003;11:1-4. Available at: http://www.iasp-pain.org/AM/AMTemplate.cfm?Section=Home&CONTENTID=7594&TEMPLATE=/CM/ContentDisplay.cfm&SECTION=Home.
4. Washington, DC: US Department of Health and Human Services, Centers for Disease Control and Prevention; 2006. Bernstein AB, Makuc DM, Bilheimer LT. Health, United States, 2006. Available at: http: //www.cdc.gov/nchs/data/hus/hus06.pdf.
5. Institute of Medicine. Relieving pain in America: a blueprint for transforming prevention, care, education, and research. Washington, DC: National Academies Press; 2011.
6. Hannan MT, Felson DT, Pincus T. Analysis of the discordance between radiographic changes and knee pain in osteoarthritis of the knee. J Rheumatol. 2000;27:1513-1517.
7. Creamer P, Hochberg MC. Why does osteoarthritis of the knee hurt—sometimes? Br J Rheumatol. 1997;36:726-728.
8. Woolf CJ, Mannion RJ. Neuropathic pain: aetiology, symptoms, mechanisms, and management. Lancet. 1999;353:1959-1964.
9. Andersen G, Vestergaard K, Ingeman-Nielsen M, et al. Incidence of central post-stroke pain. Pain. 1995;61:187-193.
10. Bowsher D. Central pain: clinical and physiological characteristics. J Neurol Neurosurg Psychiatry. 1996;61:62-69.
11. Klit H, Finnerup NB, Jensen TS. Central post-stroke pain: clinical characteristics, pathophysiology, and management. Lancet. 2009;8:857-868.
12. Wolfe F, Smythe HA, Yunus MB, et al. The American College of Rheumatology 1990 criteria for the classification of fibromyalgia: report of the multicenter criteria committee. Arthritis Rheum. 1990;33:160-172.
13. Wolfe F, Ross K, Anderson J, et al. Aspects of fibromyalgia in the general population: sex, pain threshold, and fibromyalgia symptoms. J Rheumatol. 1995;22:151-156.
14. Desmeules JA, Cedraschi C, Rapiti E, et al. Neurolopshysiologic evidence for a central sensitization in patients with fibromyalgia. Arthritis Rheum. 2003;48:1420-1429.
15. Giesecke T, Gracely RH, Grant MAB, et al. Evidence of augmented central pain processing in idiopathic chronic low back pain. Arthritis Rheum. 2004;50:613-623.
16. Gracely RH, Petzke F, Wolf JM, et al. Functional magnetic resonance imaging evidence of augmented pain processing in fibromyalgia. Arthritis Rheum. 2002;46:1333-1343.
17. Kuchinad A, Schweinhardt P, Seminowicz DA, et al. Accelerated brain gray matter loss in fibromyalgia patients: premature aging of the brain? J Neurosci. 2007;27:4004-4007.
18. Gwilym SE, Fillipini N, Douaud G, et al. Thalamic atrophy associated with painful osteoarthritis of the hip is reversible after arthroplasty. Arthritis Rheum. 2010;62:2930-2940.
19. Tracey I. Imaging pain. Br J Anaesth. 2008;101:32-39.
20. Harris RE, Sundgren PC, Craig AD, et al. Elevated insular glutamate in fibromyalgia is associated with experimental pain. Arthritis Rheum. 2009;60:3146-3152.
21. Baliki MN, Geha PY, Apkarian AV, et al. Beyond feeling: chronic pain hurts the brain, disrupting the default-mode network dynamics. J Neurosci. 2008;28:
1398-1403.
22. Otis JD, Keane TM, Kerns RD. An examination of the relationship between chronic pain and posttraumatic stress disorder. J Rehabil Res Dev. 2003;40:397-406.
23. Roy-Byrne P, Smith WR, Goldberg N, et al. Posttraumatic stress disorder among patients with chronic pain and chronic fatigue. Psychol Med. 2004;34:
363-368.
24. Arnow BA, Hunkeler EM, Blasey CM, et al. Comorbid depression, chronic pain, and disability in primary care. Psychosom Med. 2006;68:262-268.
25. Giesecke T, Gracely RH, Williams DA, et al. The relationship between depression, clinical pain, and experimental pain in a chronic pain cohort. Arthritis Rheum. 2005;52:1577-1584.
26. Jensen KB, Petzke F, Carville S, et al. Anxiety and depressive symptoms in fibromyalgia are related to poor perception of health but not to pain sensitivity or cerebral processing of pain. Arthritis Rheum. 2010;62:3488-3495.
27. Means-Christensen AJ, Roy-Byrne PR, Sherbourne CD, et al. Relationships among pain, anxiety, and depression in primary care. Depress Anxiety. 2008;25:
593-600.
Exploring the Role of Modified-Release Doxycycline in Rosacea

Topics
- Introduction - Exploring the Role of Modified-Release
- Doxycycline in Rosacea
- Comparing Antimicrobial and Anti-Inflammatory Doses of Oral Doxycycline in the Treatment of Rosacea
- Impact of Antibiotic Resistance on Dermatologic Practice
- The Effects of Modified-Release Doxycycline on Quality of Life
- Combining Anti-Inflammatory–Dose Doxycycline With Topical Metronidazole
To view the supplement, click the image above.
Faculty/Faculty Disclosure
Brian Berman, MD, PhD
Voluntary Professor of Dermatology and Cutaneous Surgery
University of Miami, Miller School of Medicine
Co-Director
Center for Clinical and Cosmetic Research, Skin & Cancer Associates, LLP,
Aventura, FL
Dr Berman has received funding for clinical grants from, is an investigator for, and is a consultant to, Galderma Laboratories, L.P.
Copyright © 2012 by Elsevier Inc.

Topics
- Introduction - Exploring the Role of Modified-Release
- Doxycycline in Rosacea
- Comparing Antimicrobial and Anti-Inflammatory Doses of Oral Doxycycline in the Treatment of Rosacea
- Impact of Antibiotic Resistance on Dermatologic Practice
- The Effects of Modified-Release Doxycycline on Quality of Life
- Combining Anti-Inflammatory–Dose Doxycycline With Topical Metronidazole
To view the supplement, click the image above.
Faculty/Faculty Disclosure
Brian Berman, MD, PhD
Voluntary Professor of Dermatology and Cutaneous Surgery
University of Miami, Miller School of Medicine
Co-Director
Center for Clinical and Cosmetic Research, Skin & Cancer Associates, LLP,
Aventura, FL
Dr Berman has received funding for clinical grants from, is an investigator for, and is a consultant to, Galderma Laboratories, L.P.
Copyright © 2012 by Elsevier Inc.

Topics
- Introduction - Exploring the Role of Modified-Release
- Doxycycline in Rosacea
- Comparing Antimicrobial and Anti-Inflammatory Doses of Oral Doxycycline in the Treatment of Rosacea
- Impact of Antibiotic Resistance on Dermatologic Practice
- The Effects of Modified-Release Doxycycline on Quality of Life
- Combining Anti-Inflammatory–Dose Doxycycline With Topical Metronidazole
To view the supplement, click the image above.
Faculty/Faculty Disclosure
Brian Berman, MD, PhD
Voluntary Professor of Dermatology and Cutaneous Surgery
University of Miami, Miller School of Medicine
Co-Director
Center for Clinical and Cosmetic Research, Skin & Cancer Associates, LLP,
Aventura, FL
Dr Berman has received funding for clinical grants from, is an investigator for, and is a consultant to, Galderma Laboratories, L.P.
Copyright © 2012 by Elsevier Inc.
Exploring the Role of Modified-Release Doxycycline in Rosacea
- Introduction - Exploring the Role of Modified-Release
- Doxycycline in Rosacea
- Comparing Antimicrobial and Anti-Inflammatory Doses of Oral Doxycycline in the Treatment of Rosacea
- Impact of Antibiotic Resistance on Dermatologic Practice
- The Effects of Modified-Release Doxycycline on Quality of Life
- Combining Anti-Inflammatory–Dose Doxycycline With Topical Metronidazole
To view the supplement, click the image above.
Faculty/Faculty Disclosure
Brian Berman, MD, PhD
Voluntary Professor of Dermatology and Cutaneous Surgery
University of Miami, Miller School of Medicine Co-Director
Center for Clinical and Cosmetic Research, Skin & Cancer Associates, LLP, Aventura, FL
Copyright (c) 2012 by Elsevier Inc.
- Introduction - Exploring the Role of Modified-Release
- Doxycycline in Rosacea
- Comparing Antimicrobial and Anti-Inflammatory Doses of Oral Doxycycline in the Treatment of Rosacea
- Impact of Antibiotic Resistance on Dermatologic Practice
- The Effects of Modified-Release Doxycycline on Quality of Life
- Combining Anti-Inflammatory–Dose Doxycycline With Topical Metronidazole
To view the supplement, click the image above.
Faculty/Faculty Disclosure
Brian Berman, MD, PhD
Voluntary Professor of Dermatology and Cutaneous Surgery
University of Miami, Miller School of Medicine Co-Director
Center for Clinical and Cosmetic Research, Skin & Cancer Associates, LLP, Aventura, FL
Copyright (c) 2012 by Elsevier Inc.
- Introduction - Exploring the Role of Modified-Release
- Doxycycline in Rosacea
- Comparing Antimicrobial and Anti-Inflammatory Doses of Oral Doxycycline in the Treatment of Rosacea
- Impact of Antibiotic Resistance on Dermatologic Practice
- The Effects of Modified-Release Doxycycline on Quality of Life
- Combining Anti-Inflammatory–Dose Doxycycline With Topical Metronidazole
To view the supplement, click the image above.
Faculty/Faculty Disclosure
Brian Berman, MD, PhD
Voluntary Professor of Dermatology and Cutaneous Surgery
University of Miami, Miller School of Medicine Co-Director
Center for Clinical and Cosmetic Research, Skin & Cancer Associates, LLP, Aventura, FL
Copyright (c) 2012 by Elsevier Inc.
Men, women, and migraine: The role of sex, hormones, obesity, and PTSD
Migraine is a common neurologic disorder that occurs in approximately 3 times as many females as males in the United States. Among 30,000 respondents, the American Migraine Study II found that the prevalence of migraine was 18.2% among females and 6.5% among males, and was much higher in females from age 12 across the lifespan.1 In comparison, for tension-type headache the female to male ratio of occurrence is 5:4, occurring only slightly more in females.2 The reasons for this disparity in migraine prevalence are not well understood. The disproportionate number of women of reproductive age with migraine suggests that hormonal factors may play a role, but the complex pathophysiology of migraine indicates additional factors are involved.3
Recent research on menstrual-related migraine and two significant comorbidities of migraine—obesity and posttraumatic stress disorder (PTSD)—shed new light on the differences in how men and women present with and experience this often disabling disorder.
Epidemiologic differences
The incidence of migraine, defined here as age of first onset, is different in boys and girls. For migraine without aura, age of first onset is approximately 10 to 11 years in boys versus 14 to 17 years in girls. For migraine with aura, age of first onset is approximately 5 years in boys and 12 to 13 years in girls.4
The picture of migraine differs by sex before and after puberty. Before age 12, boys have a higher incidence and prevalence of migraine. After age 12, prevalence increases for both sexes, peaking between age 35 to 45, with an increase in the female-to-male ratio from 2:1 at age 20 to 3.3:1 at age 40.5,6
Disparities in migraine symptoms
Common symptoms associated with severe or unilateral migraine pain include photophobia, phonophobia, and nausea. In the American Migraine Study II, the most frequently reported symptoms were pulsatile pain (85%of migraineurs), light sensitivity (80%), sound sensitivity (76%), nausea (73%), unilateral pain (59%), blurred vision (44%), aura (36%), and vomiting (29%).1 Females were more likely than males to report light sensitivity, sound sensitivity, and nausea. More females experienced 1 to 2 days of migraine-associated activity restriction than males (30.5% vs 22.9%).1 Separate studies have shown neck pain to be second after menstruation in its predictive value for onset of migraine, and to be more prevalent than nausea at the time of treatment.7,8
Migraine comorbidities
Migraine is known to be comorbid with a variety of disorders including psychiatric conditions such as depression and anxiety,9,10 and medical comorbidities such as stroke, epilepsy, and hypothyroidism.11-13 In women, migraine is also comorbid with endometriosis.14
Hormonal factors: Menstrual-related migraine
With migraine disproportionately affecting women of reproductive age, as many as 70% of female migraineurs are aware of a menstrual association with their headaches.15 A menstrual migraine is defined as migraine without aura that occurs during the 5-day window that begins 2 days before the onset of bleeding and extends through the third day of active bleeding—and that occurs in at least two-thirds of menstrual cycles.16 Approximately 14% of women experience what is termed pure menstrual migraine, meaning the only time they experience migraine is during menstruation. For women who also have migraines triggered by other mechanisms, the menstrual migraine is typically their most severe migraine of the month.
For many women, menstrual migraines are more painful, longer lasting, and more resistant to acute therapy than migraines occurring at other times.17,18 It is specifically the reduction in estradiol in the late luteal phase that appears to be the greatest trigger for menstrual migraine.
About two-thirds of women with migraine improve in menopause, particularly those for whom migraine attacks were associated with menstruation.19,20 As disabling as menstrual related migraine can be, clinically it is often found to coexist with chronic migraine and medication overuse headache.21
In a study that looked at the impact of eliminating menstrual migraine, investigators treated women with hormonal preventives based on the hypothesis that, because these agents confer no known benefit for migraines that are not hormonally triggered, use of these agents might allow them to separate out menstrual-related migraine and its effect on the overall clinical picture.21 Among 229 consecutive women seen in follow-up, 81% of those patients who were taking the hormonal preventive as prescribed had a complete resolution of menstrual-related migraine. Among those in whom menstrual migraine was eliminated, 58.9% reverted back to episodic migraine, compared with only 11% of patients whose menstrual-migraine was not eliminated.21 Resolution of menstrual-related migraine also was associated with resolution of medication overuse. Patients in whom menstrual-related migraine resolved were >2 times as likely to stop medication overuse as those in whom the migraines were not eliminated. The results offer preliminary evidence that hormonal regimens may be of benefit in preventing menstrual-related migraine.
Migraine and obesity
Obesity, which results from excessive adipose tissue in relation to fat free mass, has been shown in clinical and population-based studies to be associated with migraine.22-25 Both migraine and the distribution of adipose tissue change substantially based on age and sex.25 Following puberty, girls have an increase in the subcutaneous to visceral adipose tissue ratio as compared with boys, a pattern that continues through the reproductive years for women. Postmenopausal women see an increase in visceral
adipose tissue volume and a decrease in the subcutaneous to visceral adipose tissue volume compared with premenopausal women. Similarly, migraine prevalence increases in women of reproductive age as compared with those of postreproductive age and it is greater in women of reproductive age as compared with men.25
To evaluate the prevalence of migraine and severe headaches in men and women with and without total body obesity (TBO), as measured by body mass index (BMI) and abdominal obesity (Abd-O), Peterlin and colleagues analyzed data from 21,783 participants in the National Health and Nutrition Examination Survey.26 The investigators found that the relationship between migraine and obesity varies by age, sex, and the distribution of adipose tissue. For men and women of reproductive age, migraine prevalence increased in those with either TBO or Abd-O compared with those without. For postreproductive aged men and women (>55 years), migraine prevalence was not increased in those with either Abd-O or TBO. [Figure 1]
FIGURE 1: Migraine prevalence in men and women in relation to TBO and Abd-O
Total body obesity (TBO) was estimated based on BMI. Abdominal obesity (Abd-O) was estimated
based on waist circumference.
*P ≤ .001; † P ≤ .01; ‡ P ≤ .05
Source: Adapted with permission from Peterlin BL, et al. Migraine and obesity: Epidemiology,
mechanisms, and implications. Headache. 2010;50:631-636.
Vo et al observed similar findings for women of reproductive age in analyses of data from the Omega study. In a cohort of 3,733 women during early pregnancy, researchers found that obesity was associated with increased odds for migraine and that the risk of migraine increased with increasing obesity.27 Specifically, while the overall odds of migraine in women with obesity of any level was 48% greater than in women without obesity (OR 1.48; 95%CI: 1.12-1.96), those women with severe or class II obesity (BMI 35 to 39.9) had a >200% increased risk (OR 2.07; 95%CI: 1.27-3.39), and those with morbid or class III obesity (BMI ≥40) had a 275% increased risk of migraine, (OR 2.75; 95%CI: 1.60-4.70).27 Furthermore, Vo et al demonstrated that women with a history of pediatric migraine had 67% increased odds of gaining ≥22 pounds above their weight at the age of 18 (OR 1.67; 95% CI:1.13-2.47).27
An association between obesity and migraine was also found in two small studies that assessed the effects of bariatric surgery on headache frequency in morbidly obese, episodic migraineurs.28,29 In these studies, at 6 months after surgery the monthly headache frequency declined from approximately 4 headache days per month at baseline to just 1 to 2 headache days per month. Researchers also noted that following bariatric surgery, the migraine-associated symptoms were reduced and headache related disability improved significantly. Larger, controlled studies will be needed to substantiate these findings and determine the true effect size before bariatric surgery could be considered as a component of migraine therapy.30 However, these results highlight the observation that clinicians should give consideration to obesity as a potentially modifiable risk factor for episodic migraine.
Migraine and PTSD
Posttraumatic stress disorder (PTSD), the result of traumatic life stressors, has a lifetime prevalence of approximately 7%—3.6% among men and 9.7% among women—according to the National Comorbidity Survey Replication (NCS-R), a cross-sectional, general population survey of mental disorders.31 Interpersonal trauma (such as physical or sexual abuse) is the most common cause of PTSD, but it can also result from life-threatening situations such as natural and man-made disasters or military combat.32,33 In a secondary analysis of a the NCS-R, Peterlin and colleagues and found that 21.5% of episodic migraineurs and 19.2% of chronic daily headache sufferers fulfilled PTSD criteria.34
Although both migraine and PTSD are up to 3 times more common in women than men, recent data suggest that the association between migraine and PTSD is stronger in men.34,35 Using the NCS-R data, Peterlin and colleagues found a more than 3-4 fold increase in the odds ratio of PTSD in men with migraine versus women with migraine—a result that renders PTSD, to the knowledge of the investigators, the first mental disorder to be reported as having a greater prevalence in men with migraine than women with migraine.34[Figure 2]
FIGURE 2: Sex-specific odds ratio of PTSD in episodic migraine
Source: Adapted with permission from Peterlin BL, et al. Post-traumatic distress disorder and migraine:
Epidemiology, sex differences, and potential mechanisms. Headache. 2011;51(6)860-868.
The neurobiological mechanism linking PTSD to migraine is not known. Although a variety of theories exist—including low serotonin levels, dysfunctions of the autonomic system and hypothalamic-pituitary-adrenal axis (HPA) in both migraine and PTSD, and elevated baseline cortisol levels in migraineurs—it remains unclear why the association is stronger in men than in women.34 Some studies suggest that sex-related differences of the HPA axis may play a role.36,37 Others consider fMRI findings of sex differences in cerebral blood flow to pain centers in response to psychological distress.37 Further research into the sex-related differences of migraineurs with PTSD will likely reveal insights into new therapeutic directions for men and women with these disorders.
Implications for clinicians
The preceding data add to the understanding that numerous comorbidities exist in individuals with migraine. If a patient is a migraineur, screen for PTSD as well as depression and anxiety. Treatment with cognitive behavioral therapy—alone or in combination with pharmacological therapy—should be considered, since treatment of PTSD alone has been shown to have a beneficial effect on both pain and disability in chronic pain patients.38
Given that obesity is a modifiable risk factor, educate all migraine patients about the association with obesity in general, the increasing risk of migraine associated with increasing obesity, and the potential effect of weight gain/loss on headache frequency.26,27 Also inform patients about the potential effects migraine medications may have on their weight, and encourage them to eat a healthy diet, exercise, and avoid gaining excessive weight. If other comorbidities are involved, tailor the therapeutic regimen based on that combination. If a migraine patient is obese and has high blood pressure, look for an antihypertensive agent that is relatively weight-neutral.
Eliminating menstrual migraine should be an important treatment goal for patients in whom it is the most disabling migraine of the month. Hormonal preventives may be the best approach for women whose menstrual attacks are resistant to acute treatment.21
Disclosures
B. Lee Peterlin, DO, has received grant/research support from GlaxoSmithKline, has served as a consultant to Nautilus, and has served on the speaker’s bureau of Zogenix. She holds a provisional patent for use of adiponectin-modulating drugs for migraine.
Anne H. Calhoun, MD, has no conflicts of interest to report.
Fred Balzac has no conflicts of interest to report.
1. Lipton RB, Stewart WF, Diamond S, et al. Prevalence and burden of migraine in the United States: data from the American Migraine Study II. Headache. 2001;41:646-657.
2. Rasmussen BK, Jensen R, Schroll M, et al. Epidemiology of headache in a general population—a prevalence study. J Clin Epidemiol. 1991;44(11)1147-1157.
3. Peterlin BL, Katsnelson MJ, Calhoun AH. The associations between migraine, unipolar psychiatric comorbidities, and stress-related disorders and the role of estrogen. Curr Pain Headache Rep. 2009;13:404-412.
4. Stewart WF, Linet MS, Celentano DD, et al. Age- and sex-specific incidence rates of migraine with and without visual aura. Am J Epidemiol. 1991;134(10):1111-1120.
5. Stewart WF, Lipton RB, Celentano DD, et al. Prevalence of migraine headache in the United States: relation to age, income, race, and other sociodemographic factors. JAMA. 1992;267:64- 69.
6. Lipton RB, Stewart WF. Migraine in the United States: a review of epidemiology and health care use. Neurology. 1993;43(suppl 3):S6-10.
7. Wober C, Brannath W, Schmidt K, et al. Prospective analysis of factors related to migraine attacks: The PAMINA study. Cephalalgia. 2007;27:304-314.
8. Calhoun AH, Ford S, Millen C, et al. The prevalence of neck pain in migraine. Headache. 2010;50:1273-1277.
9. Breslau N, Lipton RB, Stewart WF, et al. Comorbidity of migraine and depression: Investigating potential etiology and prognosis. Neurology. 2003;60:1308-1312.
10. Stewart W, Breslau N, Keck PE Jr. Comorbidity of migraine and panic disorder. Neurology. 1994;44:S23-S27.
11. Scher AI, Terwindt GM, Picavet HS, et al. Cardiovascular risk factors and migraine: The GEM population based study. Neurology. 2005;64:614-620.
12. Ottman R, Lipton RB. Comorbidity of migraine and epilepsy. Neurology. 1994;44:2105-2110.
13. Moreau T, Manceau E, Giroud-Baleydier F, et al. Headache in hypothyroidism. Prevalence and outcome under thyroid hormone therapy. Cephalalgia. 1998;18:687-689.
14. Ferrero S, Pretta S, Bertoldi S, et al. Increased frequency of migraine among women with endometriosis. Hum Reprod. 2004;19:2927-2932.
15. MacGregor EA. “Menstrual” migraine: Towards a definition. Cephalalgia. 1996;16:11-21.
16. Calhoun AH, Hutchinson S. Hormonal therapies for menstrual migraine. Curr Pain Headache Rep.2009;13:381-385.
17. Granella F, Sances G, Allais G, et al. Characteristics of menstrual and nonmenstrual attacks in women with menstrually related migraine referred to headache centres. Cephalalgia. 2004;24:707-716.
18. MacGregor EA, Hackshaw A. Prevalence of migraine on each day of the natural menstrual cycle. Neurology. 2004;63:351-353.
19. Neri I, Granella F, Nappi R, et al. Characteristics of headache at menopause: a clinico-epidemiologic study. Maturitas.1993;17:31-37.
20. Brandes JL. The influence of estrogen on migraine: a systematic review. JAMA. 2006;295(15):1824-1830.
21. Calhoun A, Ford S. Elimination of menstrual-related migraine beneficially impacts chronification and medication overuse. Headache. 2008;48:1186-1193.
22. Scher AI, Stewart WF, Ricci JA, et al. Factors associated with the onset and remission of chronic daily headache in a population-based study. Pain. 2003;106:81-89.
23. Horev A, Wirguin I, Lantsberg L, et al. A high incidence of migraine with aura among morbidly obese women. Headache. 2005;45:936-938.
24. Ford ES, Li C, Pearson WS, et al. Body mass index and headaches: Findings from a national sample of US adults. Cephalalgia. 2008;28(12):1270-1276.
25. Peterlin BL, Rapoport AM, Kurth T. Migraine and obesity: Epidemiology, mechanisms, and implications. Headache. 2012;50:631-648.
26. Peterlin BL, Rosso AL, Rapoport AM, et al. Obesity and migraine: the effect of age, gender and adipose tissue distribution. Headache. 2010;50:52-62.
27. Vo M, Ainalem A, Qiu C, et al. Body mass index and adult weight gain among reproductive age women with migraine. Headache. 2011;51:559-569.
28. Novack V, Fuchs L, Lantsberg L, et al. Changes in headache frequency in premenopausal obese women with migraine after bariatric surgery: A case series. Cephalalgia. 2011;31(13):1336-1342.
29. Bond DS, Vithiananthan S, Nash JM, et al. Improvement of migraine headaches in severely obese patients after bariatric surgery. Neurology. 2011;76(13)1135-1138.
30. Peterlin BL. Bariatric surgery in obese migraineurs: Mounting evidence but important questions remain. Cephalalgia. 2011;31(13):1333-1335.
31. Kessler RC, Berglund P, Delmer O, et al. Lifetime prevalence and age-of-onset distributions of DSM-IV disorders in the National Comorbidity Survey Replication. Arch Gen Psychiatry. 2005;62(6):593-602.
32. Butterfield MI, Becker M, Marx CE. Posttraumatic stress disorder in women: Current concepts and treatments. Curr Psychiatry Rep. 2002;4:474-486.
33. Breslau N. The epidemiology of trauma, PTSD, and other posttrauma disorders. Trauma Violence Abuse. 2009;10(3):198-210.
34. Peterlin BL, Rosso AL, Sheftell FD, et al. Post-traumatic stress disorder, drug abuse and migraine: new findings from the National Comorbidity Survey Replication (NCS-R). Cephalalgia. 2011;31:235-244.
35. Peterlin BL, Nijjar SS, Tietjen GE. Post-traumatic stress disorder and migraine: epidemiology, sex differences, and potential mechanisms. Headache. 2011;51:860-868.
36. Rainero I, Ferrero M, Rubino E, et al. Endocrine function is altered in chronic migraine patient with medication-overuse. Headache. 2006;46:597-603.
37. Wang J, Korczykowski, Rao H, et al. Gender difference in neural response to psychological stress. Soc Cog Affect Neurosci. 2007;2:227-239.
38. Peterlin BL, Tietjen GE, Brandes JL, et al. Posttraumatic stress disorder in migraine. Headache. 2009;49:541-551.
Migraine is a common neurologic disorder that occurs in approximately 3 times as many females as males in the United States. Among 30,000 respondents, the American Migraine Study II found that the prevalence of migraine was 18.2% among females and 6.5% among males, and was much higher in females from age 12 across the lifespan.1 In comparison, for tension-type headache the female to male ratio of occurrence is 5:4, occurring only slightly more in females.2 The reasons for this disparity in migraine prevalence are not well understood. The disproportionate number of women of reproductive age with migraine suggests that hormonal factors may play a role, but the complex pathophysiology of migraine indicates additional factors are involved.3
Recent research on menstrual-related migraine and two significant comorbidities of migraine—obesity and posttraumatic stress disorder (PTSD)—shed new light on the differences in how men and women present with and experience this often disabling disorder.
Epidemiologic differences
The incidence of migraine, defined here as age of first onset, is different in boys and girls. For migraine without aura, age of first onset is approximately 10 to 11 years in boys versus 14 to 17 years in girls. For migraine with aura, age of first onset is approximately 5 years in boys and 12 to 13 years in girls.4
The picture of migraine differs by sex before and after puberty. Before age 12, boys have a higher incidence and prevalence of migraine. After age 12, prevalence increases for both sexes, peaking between age 35 to 45, with an increase in the female-to-male ratio from 2:1 at age 20 to 3.3:1 at age 40.5,6
Disparities in migraine symptoms
Common symptoms associated with severe or unilateral migraine pain include photophobia, phonophobia, and nausea. In the American Migraine Study II, the most frequently reported symptoms were pulsatile pain (85%of migraineurs), light sensitivity (80%), sound sensitivity (76%), nausea (73%), unilateral pain (59%), blurred vision (44%), aura (36%), and vomiting (29%).1 Females were more likely than males to report light sensitivity, sound sensitivity, and nausea. More females experienced 1 to 2 days of migraine-associated activity restriction than males (30.5% vs 22.9%).1 Separate studies have shown neck pain to be second after menstruation in its predictive value for onset of migraine, and to be more prevalent than nausea at the time of treatment.7,8
Migraine comorbidities
Migraine is known to be comorbid with a variety of disorders including psychiatric conditions such as depression and anxiety,9,10 and medical comorbidities such as stroke, epilepsy, and hypothyroidism.11-13 In women, migraine is also comorbid with endometriosis.14
Hormonal factors: Menstrual-related migraine
With migraine disproportionately affecting women of reproductive age, as many as 70% of female migraineurs are aware of a menstrual association with their headaches.15 A menstrual migraine is defined as migraine without aura that occurs during the 5-day window that begins 2 days before the onset of bleeding and extends through the third day of active bleeding—and that occurs in at least two-thirds of menstrual cycles.16 Approximately 14% of women experience what is termed pure menstrual migraine, meaning the only time they experience migraine is during menstruation. For women who also have migraines triggered by other mechanisms, the menstrual migraine is typically their most severe migraine of the month.
For many women, menstrual migraines are more painful, longer lasting, and more resistant to acute therapy than migraines occurring at other times.17,18 It is specifically the reduction in estradiol in the late luteal phase that appears to be the greatest trigger for menstrual migraine.
About two-thirds of women with migraine improve in menopause, particularly those for whom migraine attacks were associated with menstruation.19,20 As disabling as menstrual related migraine can be, clinically it is often found to coexist with chronic migraine and medication overuse headache.21
In a study that looked at the impact of eliminating menstrual migraine, investigators treated women with hormonal preventives based on the hypothesis that, because these agents confer no known benefit for migraines that are not hormonally triggered, use of these agents might allow them to separate out menstrual-related migraine and its effect on the overall clinical picture.21 Among 229 consecutive women seen in follow-up, 81% of those patients who were taking the hormonal preventive as prescribed had a complete resolution of menstrual-related migraine. Among those in whom menstrual migraine was eliminated, 58.9% reverted back to episodic migraine, compared with only 11% of patients whose menstrual-migraine was not eliminated.21 Resolution of menstrual-related migraine also was associated with resolution of medication overuse. Patients in whom menstrual-related migraine resolved were >2 times as likely to stop medication overuse as those in whom the migraines were not eliminated. The results offer preliminary evidence that hormonal regimens may be of benefit in preventing menstrual-related migraine.
Migraine and obesity
Obesity, which results from excessive adipose tissue in relation to fat free mass, has been shown in clinical and population-based studies to be associated with migraine.22-25 Both migraine and the distribution of adipose tissue change substantially based on age and sex.25 Following puberty, girls have an increase in the subcutaneous to visceral adipose tissue ratio as compared with boys, a pattern that continues through the reproductive years for women. Postmenopausal women see an increase in visceral
adipose tissue volume and a decrease in the subcutaneous to visceral adipose tissue volume compared with premenopausal women. Similarly, migraine prevalence increases in women of reproductive age as compared with those of postreproductive age and it is greater in women of reproductive age as compared with men.25
To evaluate the prevalence of migraine and severe headaches in men and women with and without total body obesity (TBO), as measured by body mass index (BMI) and abdominal obesity (Abd-O), Peterlin and colleagues analyzed data from 21,783 participants in the National Health and Nutrition Examination Survey.26 The investigators found that the relationship between migraine and obesity varies by age, sex, and the distribution of adipose tissue. For men and women of reproductive age, migraine prevalence increased in those with either TBO or Abd-O compared with those without. For postreproductive aged men and women (>55 years), migraine prevalence was not increased in those with either Abd-O or TBO. [Figure 1]
FIGURE 1: Migraine prevalence in men and women in relation to TBO and Abd-O
Total body obesity (TBO) was estimated based on BMI. Abdominal obesity (Abd-O) was estimated
based on waist circumference.
*P ≤ .001; † P ≤ .01; ‡ P ≤ .05
Source: Adapted with permission from Peterlin BL, et al. Migraine and obesity: Epidemiology,
mechanisms, and implications. Headache. 2010;50:631-636.
Vo et al observed similar findings for women of reproductive age in analyses of data from the Omega study. In a cohort of 3,733 women during early pregnancy, researchers found that obesity was associated with increased odds for migraine and that the risk of migraine increased with increasing obesity.27 Specifically, while the overall odds of migraine in women with obesity of any level was 48% greater than in women without obesity (OR 1.48; 95%CI: 1.12-1.96), those women with severe or class II obesity (BMI 35 to 39.9) had a >200% increased risk (OR 2.07; 95%CI: 1.27-3.39), and those with morbid or class III obesity (BMI ≥40) had a 275% increased risk of migraine, (OR 2.75; 95%CI: 1.60-4.70).27 Furthermore, Vo et al demonstrated that women with a history of pediatric migraine had 67% increased odds of gaining ≥22 pounds above their weight at the age of 18 (OR 1.67; 95% CI:1.13-2.47).27
An association between obesity and migraine was also found in two small studies that assessed the effects of bariatric surgery on headache frequency in morbidly obese, episodic migraineurs.28,29 In these studies, at 6 months after surgery the monthly headache frequency declined from approximately 4 headache days per month at baseline to just 1 to 2 headache days per month. Researchers also noted that following bariatric surgery, the migraine-associated symptoms were reduced and headache related disability improved significantly. Larger, controlled studies will be needed to substantiate these findings and determine the true effect size before bariatric surgery could be considered as a component of migraine therapy.30 However, these results highlight the observation that clinicians should give consideration to obesity as a potentially modifiable risk factor for episodic migraine.
Migraine and PTSD
Posttraumatic stress disorder (PTSD), the result of traumatic life stressors, has a lifetime prevalence of approximately 7%—3.6% among men and 9.7% among women—according to the National Comorbidity Survey Replication (NCS-R), a cross-sectional, general population survey of mental disorders.31 Interpersonal trauma (such as physical or sexual abuse) is the most common cause of PTSD, but it can also result from life-threatening situations such as natural and man-made disasters or military combat.32,33 In a secondary analysis of a the NCS-R, Peterlin and colleagues and found that 21.5% of episodic migraineurs and 19.2% of chronic daily headache sufferers fulfilled PTSD criteria.34
Although both migraine and PTSD are up to 3 times more common in women than men, recent data suggest that the association between migraine and PTSD is stronger in men.34,35 Using the NCS-R data, Peterlin and colleagues found a more than 3-4 fold increase in the odds ratio of PTSD in men with migraine versus women with migraine—a result that renders PTSD, to the knowledge of the investigators, the first mental disorder to be reported as having a greater prevalence in men with migraine than women with migraine.34[Figure 2]
FIGURE 2: Sex-specific odds ratio of PTSD in episodic migraine
Source: Adapted with permission from Peterlin BL, et al. Post-traumatic distress disorder and migraine:
Epidemiology, sex differences, and potential mechanisms. Headache. 2011;51(6)860-868.
The neurobiological mechanism linking PTSD to migraine is not known. Although a variety of theories exist—including low serotonin levels, dysfunctions of the autonomic system and hypothalamic-pituitary-adrenal axis (HPA) in both migraine and PTSD, and elevated baseline cortisol levels in migraineurs—it remains unclear why the association is stronger in men than in women.34 Some studies suggest that sex-related differences of the HPA axis may play a role.36,37 Others consider fMRI findings of sex differences in cerebral blood flow to pain centers in response to psychological distress.37 Further research into the sex-related differences of migraineurs with PTSD will likely reveal insights into new therapeutic directions for men and women with these disorders.
Implications for clinicians
The preceding data add to the understanding that numerous comorbidities exist in individuals with migraine. If a patient is a migraineur, screen for PTSD as well as depression and anxiety. Treatment with cognitive behavioral therapy—alone or in combination with pharmacological therapy—should be considered, since treatment of PTSD alone has been shown to have a beneficial effect on both pain and disability in chronic pain patients.38
Given that obesity is a modifiable risk factor, educate all migraine patients about the association with obesity in general, the increasing risk of migraine associated with increasing obesity, and the potential effect of weight gain/loss on headache frequency.26,27 Also inform patients about the potential effects migraine medications may have on their weight, and encourage them to eat a healthy diet, exercise, and avoid gaining excessive weight. If other comorbidities are involved, tailor the therapeutic regimen based on that combination. If a migraine patient is obese and has high blood pressure, look for an antihypertensive agent that is relatively weight-neutral.
Eliminating menstrual migraine should be an important treatment goal for patients in whom it is the most disabling migraine of the month. Hormonal preventives may be the best approach for women whose menstrual attacks are resistant to acute treatment.21
Disclosures
B. Lee Peterlin, DO, has received grant/research support from GlaxoSmithKline, has served as a consultant to Nautilus, and has served on the speaker’s bureau of Zogenix. She holds a provisional patent for use of adiponectin-modulating drugs for migraine.
Anne H. Calhoun, MD, has no conflicts of interest to report.
Fred Balzac has no conflicts of interest to report.
Migraine is a common neurologic disorder that occurs in approximately 3 times as many females as males in the United States. Among 30,000 respondents, the American Migraine Study II found that the prevalence of migraine was 18.2% among females and 6.5% among males, and was much higher in females from age 12 across the lifespan.1 In comparison, for tension-type headache the female to male ratio of occurrence is 5:4, occurring only slightly more in females.2 The reasons for this disparity in migraine prevalence are not well understood. The disproportionate number of women of reproductive age with migraine suggests that hormonal factors may play a role, but the complex pathophysiology of migraine indicates additional factors are involved.3
Recent research on menstrual-related migraine and two significant comorbidities of migraine—obesity and posttraumatic stress disorder (PTSD)—shed new light on the differences in how men and women present with and experience this often disabling disorder.
Epidemiologic differences
The incidence of migraine, defined here as age of first onset, is different in boys and girls. For migraine without aura, age of first onset is approximately 10 to 11 years in boys versus 14 to 17 years in girls. For migraine with aura, age of first onset is approximately 5 years in boys and 12 to 13 years in girls.4
The picture of migraine differs by sex before and after puberty. Before age 12, boys have a higher incidence and prevalence of migraine. After age 12, prevalence increases for both sexes, peaking between age 35 to 45, with an increase in the female-to-male ratio from 2:1 at age 20 to 3.3:1 at age 40.5,6
Disparities in migraine symptoms
Common symptoms associated with severe or unilateral migraine pain include photophobia, phonophobia, and nausea. In the American Migraine Study II, the most frequently reported symptoms were pulsatile pain (85%of migraineurs), light sensitivity (80%), sound sensitivity (76%), nausea (73%), unilateral pain (59%), blurred vision (44%), aura (36%), and vomiting (29%).1 Females were more likely than males to report light sensitivity, sound sensitivity, and nausea. More females experienced 1 to 2 days of migraine-associated activity restriction than males (30.5% vs 22.9%).1 Separate studies have shown neck pain to be second after menstruation in its predictive value for onset of migraine, and to be more prevalent than nausea at the time of treatment.7,8
Migraine comorbidities
Migraine is known to be comorbid with a variety of disorders including psychiatric conditions such as depression and anxiety,9,10 and medical comorbidities such as stroke, epilepsy, and hypothyroidism.11-13 In women, migraine is also comorbid with endometriosis.14
Hormonal factors: Menstrual-related migraine
With migraine disproportionately affecting women of reproductive age, as many as 70% of female migraineurs are aware of a menstrual association with their headaches.15 A menstrual migraine is defined as migraine without aura that occurs during the 5-day window that begins 2 days before the onset of bleeding and extends through the third day of active bleeding—and that occurs in at least two-thirds of menstrual cycles.16 Approximately 14% of women experience what is termed pure menstrual migraine, meaning the only time they experience migraine is during menstruation. For women who also have migraines triggered by other mechanisms, the menstrual migraine is typically their most severe migraine of the month.
For many women, menstrual migraines are more painful, longer lasting, and more resistant to acute therapy than migraines occurring at other times.17,18 It is specifically the reduction in estradiol in the late luteal phase that appears to be the greatest trigger for menstrual migraine.
About two-thirds of women with migraine improve in menopause, particularly those for whom migraine attacks were associated with menstruation.19,20 As disabling as menstrual related migraine can be, clinically it is often found to coexist with chronic migraine and medication overuse headache.21
In a study that looked at the impact of eliminating menstrual migraine, investigators treated women with hormonal preventives based on the hypothesis that, because these agents confer no known benefit for migraines that are not hormonally triggered, use of these agents might allow them to separate out menstrual-related migraine and its effect on the overall clinical picture.21 Among 229 consecutive women seen in follow-up, 81% of those patients who were taking the hormonal preventive as prescribed had a complete resolution of menstrual-related migraine. Among those in whom menstrual migraine was eliminated, 58.9% reverted back to episodic migraine, compared with only 11% of patients whose menstrual-migraine was not eliminated.21 Resolution of menstrual-related migraine also was associated with resolution of medication overuse. Patients in whom menstrual-related migraine resolved were >2 times as likely to stop medication overuse as those in whom the migraines were not eliminated. The results offer preliminary evidence that hormonal regimens may be of benefit in preventing menstrual-related migraine.
Migraine and obesity
Obesity, which results from excessive adipose tissue in relation to fat free mass, has been shown in clinical and population-based studies to be associated with migraine.22-25 Both migraine and the distribution of adipose tissue change substantially based on age and sex.25 Following puberty, girls have an increase in the subcutaneous to visceral adipose tissue ratio as compared with boys, a pattern that continues through the reproductive years for women. Postmenopausal women see an increase in visceral
adipose tissue volume and a decrease in the subcutaneous to visceral adipose tissue volume compared with premenopausal women. Similarly, migraine prevalence increases in women of reproductive age as compared with those of postreproductive age and it is greater in women of reproductive age as compared with men.25
To evaluate the prevalence of migraine and severe headaches in men and women with and without total body obesity (TBO), as measured by body mass index (BMI) and abdominal obesity (Abd-O), Peterlin and colleagues analyzed data from 21,783 participants in the National Health and Nutrition Examination Survey.26 The investigators found that the relationship between migraine and obesity varies by age, sex, and the distribution of adipose tissue. For men and women of reproductive age, migraine prevalence increased in those with either TBO or Abd-O compared with those without. For postreproductive aged men and women (>55 years), migraine prevalence was not increased in those with either Abd-O or TBO. [Figure 1]
FIGURE 1: Migraine prevalence in men and women in relation to TBO and Abd-O
Total body obesity (TBO) was estimated based on BMI. Abdominal obesity (Abd-O) was estimated
based on waist circumference.
*P ≤ .001; † P ≤ .01; ‡ P ≤ .05
Source: Adapted with permission from Peterlin BL, et al. Migraine and obesity: Epidemiology,
mechanisms, and implications. Headache. 2010;50:631-636.
Vo et al observed similar findings for women of reproductive age in analyses of data from the Omega study. In a cohort of 3,733 women during early pregnancy, researchers found that obesity was associated with increased odds for migraine and that the risk of migraine increased with increasing obesity.27 Specifically, while the overall odds of migraine in women with obesity of any level was 48% greater than in women without obesity (OR 1.48; 95%CI: 1.12-1.96), those women with severe or class II obesity (BMI 35 to 39.9) had a >200% increased risk (OR 2.07; 95%CI: 1.27-3.39), and those with morbid or class III obesity (BMI ≥40) had a 275% increased risk of migraine, (OR 2.75; 95%CI: 1.60-4.70).27 Furthermore, Vo et al demonstrated that women with a history of pediatric migraine had 67% increased odds of gaining ≥22 pounds above their weight at the age of 18 (OR 1.67; 95% CI:1.13-2.47).27
An association between obesity and migraine was also found in two small studies that assessed the effects of bariatric surgery on headache frequency in morbidly obese, episodic migraineurs.28,29 In these studies, at 6 months after surgery the monthly headache frequency declined from approximately 4 headache days per month at baseline to just 1 to 2 headache days per month. Researchers also noted that following bariatric surgery, the migraine-associated symptoms were reduced and headache related disability improved significantly. Larger, controlled studies will be needed to substantiate these findings and determine the true effect size before bariatric surgery could be considered as a component of migraine therapy.30 However, these results highlight the observation that clinicians should give consideration to obesity as a potentially modifiable risk factor for episodic migraine.
Migraine and PTSD
Posttraumatic stress disorder (PTSD), the result of traumatic life stressors, has a lifetime prevalence of approximately 7%—3.6% among men and 9.7% among women—according to the National Comorbidity Survey Replication (NCS-R), a cross-sectional, general population survey of mental disorders.31 Interpersonal trauma (such as physical or sexual abuse) is the most common cause of PTSD, but it can also result from life-threatening situations such as natural and man-made disasters or military combat.32,33 In a secondary analysis of a the NCS-R, Peterlin and colleagues and found that 21.5% of episodic migraineurs and 19.2% of chronic daily headache sufferers fulfilled PTSD criteria.34
Although both migraine and PTSD are up to 3 times more common in women than men, recent data suggest that the association between migraine and PTSD is stronger in men.34,35 Using the NCS-R data, Peterlin and colleagues found a more than 3-4 fold increase in the odds ratio of PTSD in men with migraine versus women with migraine—a result that renders PTSD, to the knowledge of the investigators, the first mental disorder to be reported as having a greater prevalence in men with migraine than women with migraine.34[Figure 2]
FIGURE 2: Sex-specific odds ratio of PTSD in episodic migraine
Source: Adapted with permission from Peterlin BL, et al. Post-traumatic distress disorder and migraine:
Epidemiology, sex differences, and potential mechanisms. Headache. 2011;51(6)860-868.
The neurobiological mechanism linking PTSD to migraine is not known. Although a variety of theories exist—including low serotonin levels, dysfunctions of the autonomic system and hypothalamic-pituitary-adrenal axis (HPA) in both migraine and PTSD, and elevated baseline cortisol levels in migraineurs—it remains unclear why the association is stronger in men than in women.34 Some studies suggest that sex-related differences of the HPA axis may play a role.36,37 Others consider fMRI findings of sex differences in cerebral blood flow to pain centers in response to psychological distress.37 Further research into the sex-related differences of migraineurs with PTSD will likely reveal insights into new therapeutic directions for men and women with these disorders.
Implications for clinicians
The preceding data add to the understanding that numerous comorbidities exist in individuals with migraine. If a patient is a migraineur, screen for PTSD as well as depression and anxiety. Treatment with cognitive behavioral therapy—alone or in combination with pharmacological therapy—should be considered, since treatment of PTSD alone has been shown to have a beneficial effect on both pain and disability in chronic pain patients.38
Given that obesity is a modifiable risk factor, educate all migraine patients about the association with obesity in general, the increasing risk of migraine associated with increasing obesity, and the potential effect of weight gain/loss on headache frequency.26,27 Also inform patients about the potential effects migraine medications may have on their weight, and encourage them to eat a healthy diet, exercise, and avoid gaining excessive weight. If other comorbidities are involved, tailor the therapeutic regimen based on that combination. If a migraine patient is obese and has high blood pressure, look for an antihypertensive agent that is relatively weight-neutral.
Eliminating menstrual migraine should be an important treatment goal for patients in whom it is the most disabling migraine of the month. Hormonal preventives may be the best approach for women whose menstrual attacks are resistant to acute treatment.21
Disclosures
B. Lee Peterlin, DO, has received grant/research support from GlaxoSmithKline, has served as a consultant to Nautilus, and has served on the speaker’s bureau of Zogenix. She holds a provisional patent for use of adiponectin-modulating drugs for migraine.
Anne H. Calhoun, MD, has no conflicts of interest to report.
Fred Balzac has no conflicts of interest to report.
1. Lipton RB, Stewart WF, Diamond S, et al. Prevalence and burden of migraine in the United States: data from the American Migraine Study II. Headache. 2001;41:646-657.
2. Rasmussen BK, Jensen R, Schroll M, et al. Epidemiology of headache in a general population—a prevalence study. J Clin Epidemiol. 1991;44(11)1147-1157.
3. Peterlin BL, Katsnelson MJ, Calhoun AH. The associations between migraine, unipolar psychiatric comorbidities, and stress-related disorders and the role of estrogen. Curr Pain Headache Rep. 2009;13:404-412.
4. Stewart WF, Linet MS, Celentano DD, et al. Age- and sex-specific incidence rates of migraine with and without visual aura. Am J Epidemiol. 1991;134(10):1111-1120.
5. Stewart WF, Lipton RB, Celentano DD, et al. Prevalence of migraine headache in the United States: relation to age, income, race, and other sociodemographic factors. JAMA. 1992;267:64- 69.
6. Lipton RB, Stewart WF. Migraine in the United States: a review of epidemiology and health care use. Neurology. 1993;43(suppl 3):S6-10.
7. Wober C, Brannath W, Schmidt K, et al. Prospective analysis of factors related to migraine attacks: The PAMINA study. Cephalalgia. 2007;27:304-314.
8. Calhoun AH, Ford S, Millen C, et al. The prevalence of neck pain in migraine. Headache. 2010;50:1273-1277.
9. Breslau N, Lipton RB, Stewart WF, et al. Comorbidity of migraine and depression: Investigating potential etiology and prognosis. Neurology. 2003;60:1308-1312.
10. Stewart W, Breslau N, Keck PE Jr. Comorbidity of migraine and panic disorder. Neurology. 1994;44:S23-S27.
11. Scher AI, Terwindt GM, Picavet HS, et al. Cardiovascular risk factors and migraine: The GEM population based study. Neurology. 2005;64:614-620.
12. Ottman R, Lipton RB. Comorbidity of migraine and epilepsy. Neurology. 1994;44:2105-2110.
13. Moreau T, Manceau E, Giroud-Baleydier F, et al. Headache in hypothyroidism. Prevalence and outcome under thyroid hormone therapy. Cephalalgia. 1998;18:687-689.
14. Ferrero S, Pretta S, Bertoldi S, et al. Increased frequency of migraine among women with endometriosis. Hum Reprod. 2004;19:2927-2932.
15. MacGregor EA. “Menstrual” migraine: Towards a definition. Cephalalgia. 1996;16:11-21.
16. Calhoun AH, Hutchinson S. Hormonal therapies for menstrual migraine. Curr Pain Headache Rep.2009;13:381-385.
17. Granella F, Sances G, Allais G, et al. Characteristics of menstrual and nonmenstrual attacks in women with menstrually related migraine referred to headache centres. Cephalalgia. 2004;24:707-716.
18. MacGregor EA, Hackshaw A. Prevalence of migraine on each day of the natural menstrual cycle. Neurology. 2004;63:351-353.
19. Neri I, Granella F, Nappi R, et al. Characteristics of headache at menopause: a clinico-epidemiologic study. Maturitas.1993;17:31-37.
20. Brandes JL. The influence of estrogen on migraine: a systematic review. JAMA. 2006;295(15):1824-1830.
21. Calhoun A, Ford S. Elimination of menstrual-related migraine beneficially impacts chronification and medication overuse. Headache. 2008;48:1186-1193.
22. Scher AI, Stewart WF, Ricci JA, et al. Factors associated with the onset and remission of chronic daily headache in a population-based study. Pain. 2003;106:81-89.
23. Horev A, Wirguin I, Lantsberg L, et al. A high incidence of migraine with aura among morbidly obese women. Headache. 2005;45:936-938.
24. Ford ES, Li C, Pearson WS, et al. Body mass index and headaches: Findings from a national sample of US adults. Cephalalgia. 2008;28(12):1270-1276.
25. Peterlin BL, Rapoport AM, Kurth T. Migraine and obesity: Epidemiology, mechanisms, and implications. Headache. 2012;50:631-648.
26. Peterlin BL, Rosso AL, Rapoport AM, et al. Obesity and migraine: the effect of age, gender and adipose tissue distribution. Headache. 2010;50:52-62.
27. Vo M, Ainalem A, Qiu C, et al. Body mass index and adult weight gain among reproductive age women with migraine. Headache. 2011;51:559-569.
28. Novack V, Fuchs L, Lantsberg L, et al. Changes in headache frequency in premenopausal obese women with migraine after bariatric surgery: A case series. Cephalalgia. 2011;31(13):1336-1342.
29. Bond DS, Vithiananthan S, Nash JM, et al. Improvement of migraine headaches in severely obese patients after bariatric surgery. Neurology. 2011;76(13)1135-1138.
30. Peterlin BL. Bariatric surgery in obese migraineurs: Mounting evidence but important questions remain. Cephalalgia. 2011;31(13):1333-1335.
31. Kessler RC, Berglund P, Delmer O, et al. Lifetime prevalence and age-of-onset distributions of DSM-IV disorders in the National Comorbidity Survey Replication. Arch Gen Psychiatry. 2005;62(6):593-602.
32. Butterfield MI, Becker M, Marx CE. Posttraumatic stress disorder in women: Current concepts and treatments. Curr Psychiatry Rep. 2002;4:474-486.
33. Breslau N. The epidemiology of trauma, PTSD, and other posttrauma disorders. Trauma Violence Abuse. 2009;10(3):198-210.
34. Peterlin BL, Rosso AL, Sheftell FD, et al. Post-traumatic stress disorder, drug abuse and migraine: new findings from the National Comorbidity Survey Replication (NCS-R). Cephalalgia. 2011;31:235-244.
35. Peterlin BL, Nijjar SS, Tietjen GE. Post-traumatic stress disorder and migraine: epidemiology, sex differences, and potential mechanisms. Headache. 2011;51:860-868.
36. Rainero I, Ferrero M, Rubino E, et al. Endocrine function is altered in chronic migraine patient with medication-overuse. Headache. 2006;46:597-603.
37. Wang J, Korczykowski, Rao H, et al. Gender difference in neural response to psychological stress. Soc Cog Affect Neurosci. 2007;2:227-239.
38. Peterlin BL, Tietjen GE, Brandes JL, et al. Posttraumatic stress disorder in migraine. Headache. 2009;49:541-551.
1. Lipton RB, Stewart WF, Diamond S, et al. Prevalence and burden of migraine in the United States: data from the American Migraine Study II. Headache. 2001;41:646-657.
2. Rasmussen BK, Jensen R, Schroll M, et al. Epidemiology of headache in a general population—a prevalence study. J Clin Epidemiol. 1991;44(11)1147-1157.
3. Peterlin BL, Katsnelson MJ, Calhoun AH. The associations between migraine, unipolar psychiatric comorbidities, and stress-related disorders and the role of estrogen. Curr Pain Headache Rep. 2009;13:404-412.
4. Stewart WF, Linet MS, Celentano DD, et al. Age- and sex-specific incidence rates of migraine with and without visual aura. Am J Epidemiol. 1991;134(10):1111-1120.
5. Stewart WF, Lipton RB, Celentano DD, et al. Prevalence of migraine headache in the United States: relation to age, income, race, and other sociodemographic factors. JAMA. 1992;267:64- 69.
6. Lipton RB, Stewart WF. Migraine in the United States: a review of epidemiology and health care use. Neurology. 1993;43(suppl 3):S6-10.
7. Wober C, Brannath W, Schmidt K, et al. Prospective analysis of factors related to migraine attacks: The PAMINA study. Cephalalgia. 2007;27:304-314.
8. Calhoun AH, Ford S, Millen C, et al. The prevalence of neck pain in migraine. Headache. 2010;50:1273-1277.
9. Breslau N, Lipton RB, Stewart WF, et al. Comorbidity of migraine and depression: Investigating potential etiology and prognosis. Neurology. 2003;60:1308-1312.
10. Stewart W, Breslau N, Keck PE Jr. Comorbidity of migraine and panic disorder. Neurology. 1994;44:S23-S27.
11. Scher AI, Terwindt GM, Picavet HS, et al. Cardiovascular risk factors and migraine: The GEM population based study. Neurology. 2005;64:614-620.
12. Ottman R, Lipton RB. Comorbidity of migraine and epilepsy. Neurology. 1994;44:2105-2110.
13. Moreau T, Manceau E, Giroud-Baleydier F, et al. Headache in hypothyroidism. Prevalence and outcome under thyroid hormone therapy. Cephalalgia. 1998;18:687-689.
14. Ferrero S, Pretta S, Bertoldi S, et al. Increased frequency of migraine among women with endometriosis. Hum Reprod. 2004;19:2927-2932.
15. MacGregor EA. “Menstrual” migraine: Towards a definition. Cephalalgia. 1996;16:11-21.
16. Calhoun AH, Hutchinson S. Hormonal therapies for menstrual migraine. Curr Pain Headache Rep.2009;13:381-385.
17. Granella F, Sances G, Allais G, et al. Characteristics of menstrual and nonmenstrual attacks in women with menstrually related migraine referred to headache centres. Cephalalgia. 2004;24:707-716.
18. MacGregor EA, Hackshaw A. Prevalence of migraine on each day of the natural menstrual cycle. Neurology. 2004;63:351-353.
19. Neri I, Granella F, Nappi R, et al. Characteristics of headache at menopause: a clinico-epidemiologic study. Maturitas.1993;17:31-37.
20. Brandes JL. The influence of estrogen on migraine: a systematic review. JAMA. 2006;295(15):1824-1830.
21. Calhoun A, Ford S. Elimination of menstrual-related migraine beneficially impacts chronification and medication overuse. Headache. 2008;48:1186-1193.
22. Scher AI, Stewart WF, Ricci JA, et al. Factors associated with the onset and remission of chronic daily headache in a population-based study. Pain. 2003;106:81-89.
23. Horev A, Wirguin I, Lantsberg L, et al. A high incidence of migraine with aura among morbidly obese women. Headache. 2005;45:936-938.
24. Ford ES, Li C, Pearson WS, et al. Body mass index and headaches: Findings from a national sample of US adults. Cephalalgia. 2008;28(12):1270-1276.
25. Peterlin BL, Rapoport AM, Kurth T. Migraine and obesity: Epidemiology, mechanisms, and implications. Headache. 2012;50:631-648.
26. Peterlin BL, Rosso AL, Rapoport AM, et al. Obesity and migraine: the effect of age, gender and adipose tissue distribution. Headache. 2010;50:52-62.
27. Vo M, Ainalem A, Qiu C, et al. Body mass index and adult weight gain among reproductive age women with migraine. Headache. 2011;51:559-569.
28. Novack V, Fuchs L, Lantsberg L, et al. Changes in headache frequency in premenopausal obese women with migraine after bariatric surgery: A case series. Cephalalgia. 2011;31(13):1336-1342.
29. Bond DS, Vithiananthan S, Nash JM, et al. Improvement of migraine headaches in severely obese patients after bariatric surgery. Neurology. 2011;76(13)1135-1138.
30. Peterlin BL. Bariatric surgery in obese migraineurs: Mounting evidence but important questions remain. Cephalalgia. 2011;31(13):1333-1335.
31. Kessler RC, Berglund P, Delmer O, et al. Lifetime prevalence and age-of-onset distributions of DSM-IV disorders in the National Comorbidity Survey Replication. Arch Gen Psychiatry. 2005;62(6):593-602.
32. Butterfield MI, Becker M, Marx CE. Posttraumatic stress disorder in women: Current concepts and treatments. Curr Psychiatry Rep. 2002;4:474-486.
33. Breslau N. The epidemiology of trauma, PTSD, and other posttrauma disorders. Trauma Violence Abuse. 2009;10(3):198-210.
34. Peterlin BL, Rosso AL, Sheftell FD, et al. Post-traumatic stress disorder, drug abuse and migraine: new findings from the National Comorbidity Survey Replication (NCS-R). Cephalalgia. 2011;31:235-244.
35. Peterlin BL, Nijjar SS, Tietjen GE. Post-traumatic stress disorder and migraine: epidemiology, sex differences, and potential mechanisms. Headache. 2011;51:860-868.
36. Rainero I, Ferrero M, Rubino E, et al. Endocrine function is altered in chronic migraine patient with medication-overuse. Headache. 2006;46:597-603.
37. Wang J, Korczykowski, Rao H, et al. Gender difference in neural response to psychological stress. Soc Cog Affect Neurosci. 2007;2:227-239.
38. Peterlin BL, Tietjen GE, Brandes JL, et al. Posttraumatic stress disorder in migraine. Headache. 2009;49:541-551.