User login
Life is beautiful
A crimson November San Diego sunset over the Pacific Ocean. Seeing your parents dance on their 50th wedding anniversary. A stein of cold Oktoberfest beer. Your car, freshly detailed. Your name written in black ink on a Starbucks Pumpkin Latte. A nicely everted surgical wound.
The smile on your daughter’s face when descending the stairs after a huge trick-or-treat score. A perfectly arranged Mayo stand, oh, exactly as you like it. An empty EMR in basket. A flap close on the nose that closes just so.
A Red Sox World series win (again). Lollipop lamb chops sizzling on the grill on a chilly Saturday tailgating morning. The answer to 14 down that leads to all the other answers you’ve desperately been trying to solve. The “ting” sound that Mimosa glasses make toasting Sunday brunch with friends. The next episode of Black Mirror launching automatically. A brilliant orange maple tree against a brilliant blue sky. The fissures on the crust of a still-warm loaf of Italian bread.
An elderly woman, her husband, daughter, and son-in-law who waited weeks and traveled miles to see you because they know you care. And they insist on seeing only you. A man who comes to see you without his wife this time just because he wanted to tell you in person how much they appreciated your care for her in the end. Opening your mailbox to see the September issue of Vogue, waiting for you to tear off the plastic. An as-yet-untouched Sunday New York Times. The sound of wood popping in the fireplace. The string of melted marshmallow down your son’s arm still attached to a s’more at the other end. 7-7-7 on your dollar slot at the casino. Eight-year-old girls at the center of the field celebrating a Sunday morning soccer victory. Departures showing your flight, gate 8, on time.
The smell of incense. The smell of lightly roasting garlic and olive oil. The smell of your wife’s perfume. The smell of wet leaves. The smell of your favorite scented candle. The smell of burning firewood on an early-morning walk in the Rockies. Snow falling. Snow crunching under your feet. Snow melting.
Remembering the uproarious laughter after your belly flop into the pool back in July. Steph Curry shooting a 3 in slow motion. Snoopy floating over 5th Avenue on Thanksgiving morning. The sound of wrapping paper being stuffed into garbage bags when the opening is done. A prior auth letter of approval. The feeling when you turn that first page of a brand-new Stephen King book. The feel of the grip on your fairway wood. Seeing your favorite movie pop up on Amazon Prime. The head massage your stylist gives you when washing your hair. The near pain of a really good massage.
The warmth of a child on your lap. The bark your dog gives when he sees you for the first time today as if it has been a million years. The crack of your favorite beer can opening. The ding when your microwave popcorn is ready. That warm feeling when you realize that, no, you don’t need any filter for that picture, it is ready to post exactly the way it is. The smile on your medical assistant’s face when you hand her a gratitude card. The ping that an email makes when you’re dying to hear back. The pride you feel when you execute a downward-facing dog and the instructor tells everyone to do it just like you. The smell of balsam fir. A podcast episode so good, you sit in your driveway to finish listening. A patient with a delightful British accent. The feel of pasta dough in your hands after adding just the right amount of flour and water so it’s now ready to go. Watching the Red Sox win the World Series (Wait, did I say that already?). The sound of your laptop keyboard clicking away while you write this piece. The feeling that 2019 is going to be your best year ever.
I promise it will be a more beautiful place where you are when you’re done.
Dr. Benabio is director of Healthcare Transformation and chief of dermatology at Kaiser Permanente San Diego. The opinions expressed in this column are his own and do not represent those of Kaiser Permanente. Dr. Benabio is @Dermdoc on Twitter. Write to him at [email protected].
A crimson November San Diego sunset over the Pacific Ocean. Seeing your parents dance on their 50th wedding anniversary. A stein of cold Oktoberfest beer. Your car, freshly detailed. Your name written in black ink on a Starbucks Pumpkin Latte. A nicely everted surgical wound.
The smile on your daughter’s face when descending the stairs after a huge trick-or-treat score. A perfectly arranged Mayo stand, oh, exactly as you like it. An empty EMR in basket. A flap close on the nose that closes just so.
A Red Sox World series win (again). Lollipop lamb chops sizzling on the grill on a chilly Saturday tailgating morning. The answer to 14 down that leads to all the other answers you’ve desperately been trying to solve. The “ting” sound that Mimosa glasses make toasting Sunday brunch with friends. The next episode of Black Mirror launching automatically. A brilliant orange maple tree against a brilliant blue sky. The fissures on the crust of a still-warm loaf of Italian bread.
An elderly woman, her husband, daughter, and son-in-law who waited weeks and traveled miles to see you because they know you care. And they insist on seeing only you. A man who comes to see you without his wife this time just because he wanted to tell you in person how much they appreciated your care for her in the end. Opening your mailbox to see the September issue of Vogue, waiting for you to tear off the plastic. An as-yet-untouched Sunday New York Times. The sound of wood popping in the fireplace. The string of melted marshmallow down your son’s arm still attached to a s’more at the other end. 7-7-7 on your dollar slot at the casino. Eight-year-old girls at the center of the field celebrating a Sunday morning soccer victory. Departures showing your flight, gate 8, on time.
The smell of incense. The smell of lightly roasting garlic and olive oil. The smell of your wife’s perfume. The smell of wet leaves. The smell of your favorite scented candle. The smell of burning firewood on an early-morning walk in the Rockies. Snow falling. Snow crunching under your feet. Snow melting.
Remembering the uproarious laughter after your belly flop into the pool back in July. Steph Curry shooting a 3 in slow motion. Snoopy floating over 5th Avenue on Thanksgiving morning. The sound of wrapping paper being stuffed into garbage bags when the opening is done. A prior auth letter of approval. The feeling when you turn that first page of a brand-new Stephen King book. The feel of the grip on your fairway wood. Seeing your favorite movie pop up on Amazon Prime. The head massage your stylist gives you when washing your hair. The near pain of a really good massage.
The warmth of a child on your lap. The bark your dog gives when he sees you for the first time today as if it has been a million years. The crack of your favorite beer can opening. The ding when your microwave popcorn is ready. That warm feeling when you realize that, no, you don’t need any filter for that picture, it is ready to post exactly the way it is. The smile on your medical assistant’s face when you hand her a gratitude card. The ping that an email makes when you’re dying to hear back. The pride you feel when you execute a downward-facing dog and the instructor tells everyone to do it just like you. The smell of balsam fir. A podcast episode so good, you sit in your driveway to finish listening. A patient with a delightful British accent. The feel of pasta dough in your hands after adding just the right amount of flour and water so it’s now ready to go. Watching the Red Sox win the World Series (Wait, did I say that already?). The sound of your laptop keyboard clicking away while you write this piece. The feeling that 2019 is going to be your best year ever.
I promise it will be a more beautiful place where you are when you’re done.
Dr. Benabio is director of Healthcare Transformation and chief of dermatology at Kaiser Permanente San Diego. The opinions expressed in this column are his own and do not represent those of Kaiser Permanente. Dr. Benabio is @Dermdoc on Twitter. Write to him at [email protected].
A crimson November San Diego sunset over the Pacific Ocean. Seeing your parents dance on their 50th wedding anniversary. A stein of cold Oktoberfest beer. Your car, freshly detailed. Your name written in black ink on a Starbucks Pumpkin Latte. A nicely everted surgical wound.
The smile on your daughter’s face when descending the stairs after a huge trick-or-treat score. A perfectly arranged Mayo stand, oh, exactly as you like it. An empty EMR in basket. A flap close on the nose that closes just so.
A Red Sox World series win (again). Lollipop lamb chops sizzling on the grill on a chilly Saturday tailgating morning. The answer to 14 down that leads to all the other answers you’ve desperately been trying to solve. The “ting” sound that Mimosa glasses make toasting Sunday brunch with friends. The next episode of Black Mirror launching automatically. A brilliant orange maple tree against a brilliant blue sky. The fissures on the crust of a still-warm loaf of Italian bread.
An elderly woman, her husband, daughter, and son-in-law who waited weeks and traveled miles to see you because they know you care. And they insist on seeing only you. A man who comes to see you without his wife this time just because he wanted to tell you in person how much they appreciated your care for her in the end. Opening your mailbox to see the September issue of Vogue, waiting for you to tear off the plastic. An as-yet-untouched Sunday New York Times. The sound of wood popping in the fireplace. The string of melted marshmallow down your son’s arm still attached to a s’more at the other end. 7-7-7 on your dollar slot at the casino. Eight-year-old girls at the center of the field celebrating a Sunday morning soccer victory. Departures showing your flight, gate 8, on time.
The smell of incense. The smell of lightly roasting garlic and olive oil. The smell of your wife’s perfume. The smell of wet leaves. The smell of your favorite scented candle. The smell of burning firewood on an early-morning walk in the Rockies. Snow falling. Snow crunching under your feet. Snow melting.
Remembering the uproarious laughter after your belly flop into the pool back in July. Steph Curry shooting a 3 in slow motion. Snoopy floating over 5th Avenue on Thanksgiving morning. The sound of wrapping paper being stuffed into garbage bags when the opening is done. A prior auth letter of approval. The feeling when you turn that first page of a brand-new Stephen King book. The feel of the grip on your fairway wood. Seeing your favorite movie pop up on Amazon Prime. The head massage your stylist gives you when washing your hair. The near pain of a really good massage.
The warmth of a child on your lap. The bark your dog gives when he sees you for the first time today as if it has been a million years. The crack of your favorite beer can opening. The ding when your microwave popcorn is ready. That warm feeling when you realize that, no, you don’t need any filter for that picture, it is ready to post exactly the way it is. The smile on your medical assistant’s face when you hand her a gratitude card. The ping that an email makes when you’re dying to hear back. The pride you feel when you execute a downward-facing dog and the instructor tells everyone to do it just like you. The smell of balsam fir. A podcast episode so good, you sit in your driveway to finish listening. A patient with a delightful British accent. The feel of pasta dough in your hands after adding just the right amount of flour and water so it’s now ready to go. Watching the Red Sox win the World Series (Wait, did I say that already?). The sound of your laptop keyboard clicking away while you write this piece. The feeling that 2019 is going to be your best year ever.
I promise it will be a more beautiful place where you are when you’re done.
Dr. Benabio is director of Healthcare Transformation and chief of dermatology at Kaiser Permanente San Diego. The opinions expressed in this column are his own and do not represent those of Kaiser Permanente. Dr. Benabio is @Dermdoc on Twitter. Write to him at [email protected].
Superheroes
Who’s your favorite superhero? I realize this might be impossible to answer – Marvel and DC Comics alone have thousands of heroes from which to choose. I recently visited the Seattle Museum of Pop Culture, known as MoPOP, where they have an awesome exhibit on the history of Marvel. I left understanding why superheroes are perennially popular and why we need them. I also felt a little more powerful myself.
The Avengers might seem like just a marketing scheme created to take your movie money. They’re more than that. Superheroes like Thor and Black Widow appear in all cultures and throughout time. There are short and tall, black and white, young and old, gay and straight, Muslim and Jewish, European, Asian, and African superheroes. The characters in The Iliad were superheroes to the ancients. In India today, you can buy comics featuring Lord Shiva.
Superheroes change with time, often reflecting our struggles and values. Captain America was created in 1941 to allay our fear of the then-metastasizing Nazis. The most popular Marvel hero at the MoPOP right now is Black Panther. Next year Captain Marvel will be released. Also known as Carol Danvers, Captain Marvel is one of Marvel Comics’ strongest women, a female Air Force officer with superhuman strength and speed.
Heroes change with the times and are metaphors for the real-life challenges we face and our abilities to overcome them. Superhero stories are our own stories.
When I was a kid, Spider-Man was my favorite. I watched him every afternoon at 3 o’clock when I got home from school. Spidey is a nerdy, little kid who can perform amazing feats to keep people safe and to right societal wrongs. Being a little kid who similarly loved science, he seemed like a good role model at the time. Interestingly, Spidey might have helped me. A couple of studies have shown that kids who pretend to be superheroes, like Batman for example, perform better on tasks, compared with those who aren’t pretending. In some ways, this strategy of imagining to have superpowers is an antidote to the impostor syndrome, a common experience of feeling powerless and undeserving of your position or role. By imagining that they have superpowers, children behave commensurately with these beliefs, which can help them develop self-efficacy at a critical period of development.
This strategy can work for adults too. Military men and women will adopt heroes like Punisher for their battalions, surgeons will don Superman scrub caps, and athletes will take nicknames like Batman for their professional personas. It is a strategy our ancient ancestors deployed, imagining they had the power of Hercules going into battle. No doubt, the energizing, empowering emotion we feel when we think of superheroes is why they are still so popular today. It is why you walk with a bit more swagger when you exit the theater of a good hero flick.
So indulge in a little Wonder Woman and Daredevil and Jessica Jones, even after Halloween has passed. When you do, remember they are here because they are us. and one that we need.
Nowadays, I probably relate most to Captain America: Lead a team, help make each team member better. And, yet, looking at Chris Evans, the actor who plays Captain America, it’s clear I need a lot more time at the gym. Or maybe I could just try to get bitten by a spider.
“Can he swing from a thread? Take a look overhead. Hey, there, there goes the Spider-Man!”
Dr. Benabio is director of Healthcare Transformation and chief of dermatology at Kaiser Permanente San Diego. The opinions expressed in this column are his own and do not represent those of Kaiser Permanente. Dr. Benabio is @Dermdoc on Twitter. Write to him at [email protected].
Who’s your favorite superhero? I realize this might be impossible to answer – Marvel and DC Comics alone have thousands of heroes from which to choose. I recently visited the Seattle Museum of Pop Culture, known as MoPOP, where they have an awesome exhibit on the history of Marvel. I left understanding why superheroes are perennially popular and why we need them. I also felt a little more powerful myself.
The Avengers might seem like just a marketing scheme created to take your movie money. They’re more than that. Superheroes like Thor and Black Widow appear in all cultures and throughout time. There are short and tall, black and white, young and old, gay and straight, Muslim and Jewish, European, Asian, and African superheroes. The characters in The Iliad were superheroes to the ancients. In India today, you can buy comics featuring Lord Shiva.
Superheroes change with time, often reflecting our struggles and values. Captain America was created in 1941 to allay our fear of the then-metastasizing Nazis. The most popular Marvel hero at the MoPOP right now is Black Panther. Next year Captain Marvel will be released. Also known as Carol Danvers, Captain Marvel is one of Marvel Comics’ strongest women, a female Air Force officer with superhuman strength and speed.
Heroes change with the times and are metaphors for the real-life challenges we face and our abilities to overcome them. Superhero stories are our own stories.
When I was a kid, Spider-Man was my favorite. I watched him every afternoon at 3 o’clock when I got home from school. Spidey is a nerdy, little kid who can perform amazing feats to keep people safe and to right societal wrongs. Being a little kid who similarly loved science, he seemed like a good role model at the time. Interestingly, Spidey might have helped me. A couple of studies have shown that kids who pretend to be superheroes, like Batman for example, perform better on tasks, compared with those who aren’t pretending. In some ways, this strategy of imagining to have superpowers is an antidote to the impostor syndrome, a common experience of feeling powerless and undeserving of your position or role. By imagining that they have superpowers, children behave commensurately with these beliefs, which can help them develop self-efficacy at a critical period of development.
This strategy can work for adults too. Military men and women will adopt heroes like Punisher for their battalions, surgeons will don Superman scrub caps, and athletes will take nicknames like Batman for their professional personas. It is a strategy our ancient ancestors deployed, imagining they had the power of Hercules going into battle. No doubt, the energizing, empowering emotion we feel when we think of superheroes is why they are still so popular today. It is why you walk with a bit more swagger when you exit the theater of a good hero flick.
So indulge in a little Wonder Woman and Daredevil and Jessica Jones, even after Halloween has passed. When you do, remember they are here because they are us. and one that we need.
Nowadays, I probably relate most to Captain America: Lead a team, help make each team member better. And, yet, looking at Chris Evans, the actor who plays Captain America, it’s clear I need a lot more time at the gym. Or maybe I could just try to get bitten by a spider.
“Can he swing from a thread? Take a look overhead. Hey, there, there goes the Spider-Man!”
Dr. Benabio is director of Healthcare Transformation and chief of dermatology at Kaiser Permanente San Diego. The opinions expressed in this column are his own and do not represent those of Kaiser Permanente. Dr. Benabio is @Dermdoc on Twitter. Write to him at [email protected].
Who’s your favorite superhero? I realize this might be impossible to answer – Marvel and DC Comics alone have thousands of heroes from which to choose. I recently visited the Seattle Museum of Pop Culture, known as MoPOP, where they have an awesome exhibit on the history of Marvel. I left understanding why superheroes are perennially popular and why we need them. I also felt a little more powerful myself.
The Avengers might seem like just a marketing scheme created to take your movie money. They’re more than that. Superheroes like Thor and Black Widow appear in all cultures and throughout time. There are short and tall, black and white, young and old, gay and straight, Muslim and Jewish, European, Asian, and African superheroes. The characters in The Iliad were superheroes to the ancients. In India today, you can buy comics featuring Lord Shiva.
Superheroes change with time, often reflecting our struggles and values. Captain America was created in 1941 to allay our fear of the then-metastasizing Nazis. The most popular Marvel hero at the MoPOP right now is Black Panther. Next year Captain Marvel will be released. Also known as Carol Danvers, Captain Marvel is one of Marvel Comics’ strongest women, a female Air Force officer with superhuman strength and speed.
Heroes change with the times and are metaphors for the real-life challenges we face and our abilities to overcome them. Superhero stories are our own stories.
When I was a kid, Spider-Man was my favorite. I watched him every afternoon at 3 o’clock when I got home from school. Spidey is a nerdy, little kid who can perform amazing feats to keep people safe and to right societal wrongs. Being a little kid who similarly loved science, he seemed like a good role model at the time. Interestingly, Spidey might have helped me. A couple of studies have shown that kids who pretend to be superheroes, like Batman for example, perform better on tasks, compared with those who aren’t pretending. In some ways, this strategy of imagining to have superpowers is an antidote to the impostor syndrome, a common experience of feeling powerless and undeserving of your position or role. By imagining that they have superpowers, children behave commensurately with these beliefs, which can help them develop self-efficacy at a critical period of development.
This strategy can work for adults too. Military men and women will adopt heroes like Punisher for their battalions, surgeons will don Superman scrub caps, and athletes will take nicknames like Batman for their professional personas. It is a strategy our ancient ancestors deployed, imagining they had the power of Hercules going into battle. No doubt, the energizing, empowering emotion we feel when we think of superheroes is why they are still so popular today. It is why you walk with a bit more swagger when you exit the theater of a good hero flick.
So indulge in a little Wonder Woman and Daredevil and Jessica Jones, even after Halloween has passed. When you do, remember they are here because they are us. and one that we need.
Nowadays, I probably relate most to Captain America: Lead a team, help make each team member better. And, yet, looking at Chris Evans, the actor who plays Captain America, it’s clear I need a lot more time at the gym. Or maybe I could just try to get bitten by a spider.
“Can he swing from a thread? Take a look overhead. Hey, there, there goes the Spider-Man!”
Dr. Benabio is director of Healthcare Transformation and chief of dermatology at Kaiser Permanente San Diego. The opinions expressed in this column are his own and do not represent those of Kaiser Permanente. Dr. Benabio is @Dermdoc on Twitter. Write to him at [email protected].
Slowing down
This past Labor Day weekend, I did something radical. I slowed down. Way down. My wife slowed down with me, which helped. We spent the weekend close to home walking, talking, reading, contemplating, planning, assessing, doing puzzles and crosswords, and imbibing a craft beer or two, slowly, of course. Why? Because of Adam Grant, PhD, the organizational psychologist at the University of Pennsylvania’s Wharton School of Business, Philadelphia. I had recently reread his 2016 book I’m a big fan; he’s one of those professors who makes you fervently wish you were a student again, someone who will provoke you and challenge your way of thinking.
Dr. Grant’s basic premise, which he has proved through research, is that procrastination boosts productivity. Here’s how: Let’s say you’re facing a challenge or difficult task. He says to start working on it immediately, then take some time away for reflection. This “quick to start and slow to finish” method allows your brain to continually percolate on the problem. An incomplete task stays partially active in your brain. When you come back to it you often see it with fresh eyes. You will experience your highest productivity when you are toggling between these two modes.
This makes sense, and Dr. Grant cites numerous examples from Leonardo da Vinci to the founders of Warby-Parker, as examples of success. But how can it benefit physicians? Many of us are “precrastinators,” people who tend to complete or at least begin tasks as soon as possible, even when it’s unnecessary or not urgent. Unlike some jobs in which it’s easier to take a break from a project and return to it with more creative solutions, we often are racing against a clock to see more patients, read more slides, answer more emails, and make more phone calls. We are perpetually frenetic, which is not conducive to original thinking.
If this sounds like you, then you are likely to benefit from deliberate procrastination. Here are a few ways to slow down:
- Put it on your calendar. Yes, I see the irony, but it works. Start by scheduling one hour a week where you are to accomplish nothing. You can fill this time with whatever your mind wants to do at that moment.
- When faced with a diagnostic dilemma or treatment failure, resist the urge to solve that problem in that moment. Save that note for later, tell the patient you will call him back or bring him back for a visit later. Even if you’re not actively working on it, it will incubate somewhere in your brain, allowing more divergent thought processes to take over. It’s a little like trying to solve a crossword that seems impossible in the moment and then answers suddenly appear without effort.
- Take up a hobby: Play the guitar, learn to make pasta, climb a big rock. When you are fully engaged in such pursuits it requires complete mental focus. When you revisit the difficult problem you’re working on, you will likely see it from different perspectives.
- Meditate: Meditation requires our brains and bodies to slow down. It can help reduce self-doubt and criticism which stifle problem solving.
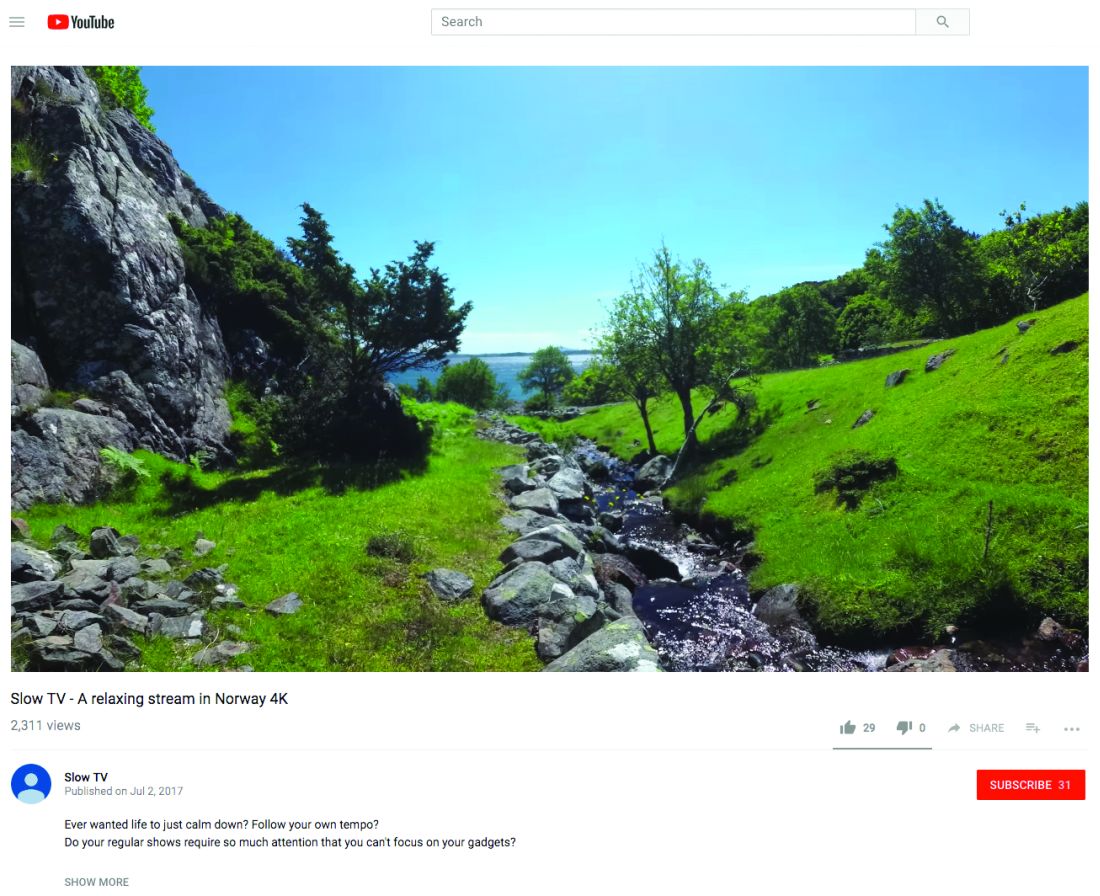
- Watch Slow TV. Slow TV is a Scandinavian phenomenon where you sit and watch meditative video such as a 7-hour train cam from Bergen, Norway, to Oslo. There’s no dialogue, no plot, no commercials. It’s just 7 hours of track and train and is weirdly comforting.
If you want to learn more, then when you get a chance, Google “slow living” and explore. Of course, some of you precrastinators probably have already started before finishing this column.
Dr. Benabio is director of Healthcare Transformation and chief of dermatology at Kaiser Permanente San Diego. The opinions expressed in this column are his own and do not represent those of Kaiser Permanente. Dr. Benabio is @Dermdoc on Twitter. Write to him at [email protected].
This past Labor Day weekend, I did something radical. I slowed down. Way down. My wife slowed down with me, which helped. We spent the weekend close to home walking, talking, reading, contemplating, planning, assessing, doing puzzles and crosswords, and imbibing a craft beer or two, slowly, of course. Why? Because of Adam Grant, PhD, the organizational psychologist at the University of Pennsylvania’s Wharton School of Business, Philadelphia. I had recently reread his 2016 book I’m a big fan; he’s one of those professors who makes you fervently wish you were a student again, someone who will provoke you and challenge your way of thinking.
Dr. Grant’s basic premise, which he has proved through research, is that procrastination boosts productivity. Here’s how: Let’s say you’re facing a challenge or difficult task. He says to start working on it immediately, then take some time away for reflection. This “quick to start and slow to finish” method allows your brain to continually percolate on the problem. An incomplete task stays partially active in your brain. When you come back to it you often see it with fresh eyes. You will experience your highest productivity when you are toggling between these two modes.
This makes sense, and Dr. Grant cites numerous examples from Leonardo da Vinci to the founders of Warby-Parker, as examples of success. But how can it benefit physicians? Many of us are “precrastinators,” people who tend to complete or at least begin tasks as soon as possible, even when it’s unnecessary or not urgent. Unlike some jobs in which it’s easier to take a break from a project and return to it with more creative solutions, we often are racing against a clock to see more patients, read more slides, answer more emails, and make more phone calls. We are perpetually frenetic, which is not conducive to original thinking.
If this sounds like you, then you are likely to benefit from deliberate procrastination. Here are a few ways to slow down:
- Put it on your calendar. Yes, I see the irony, but it works. Start by scheduling one hour a week where you are to accomplish nothing. You can fill this time with whatever your mind wants to do at that moment.
- When faced with a diagnostic dilemma or treatment failure, resist the urge to solve that problem in that moment. Save that note for later, tell the patient you will call him back or bring him back for a visit later. Even if you’re not actively working on it, it will incubate somewhere in your brain, allowing more divergent thought processes to take over. It’s a little like trying to solve a crossword that seems impossible in the moment and then answers suddenly appear without effort.
- Take up a hobby: Play the guitar, learn to make pasta, climb a big rock. When you are fully engaged in such pursuits it requires complete mental focus. When you revisit the difficult problem you’re working on, you will likely see it from different perspectives.
- Meditate: Meditation requires our brains and bodies to slow down. It can help reduce self-doubt and criticism which stifle problem solving.
- Watch Slow TV. Slow TV is a Scandinavian phenomenon where you sit and watch meditative video such as a 7-hour train cam from Bergen, Norway, to Oslo. There’s no dialogue, no plot, no commercials. It’s just 7 hours of track and train and is weirdly comforting.
If you want to learn more, then when you get a chance, Google “slow living” and explore. Of course, some of you precrastinators probably have already started before finishing this column.
Dr. Benabio is director of Healthcare Transformation and chief of dermatology at Kaiser Permanente San Diego. The opinions expressed in this column are his own and do not represent those of Kaiser Permanente. Dr. Benabio is @Dermdoc on Twitter. Write to him at [email protected].
This past Labor Day weekend, I did something radical. I slowed down. Way down. My wife slowed down with me, which helped. We spent the weekend close to home walking, talking, reading, contemplating, planning, assessing, doing puzzles and crosswords, and imbibing a craft beer or two, slowly, of course. Why? Because of Adam Grant, PhD, the organizational psychologist at the University of Pennsylvania’s Wharton School of Business, Philadelphia. I had recently reread his 2016 book I’m a big fan; he’s one of those professors who makes you fervently wish you were a student again, someone who will provoke you and challenge your way of thinking.
Dr. Grant’s basic premise, which he has proved through research, is that procrastination boosts productivity. Here’s how: Let’s say you’re facing a challenge or difficult task. He says to start working on it immediately, then take some time away for reflection. This “quick to start and slow to finish” method allows your brain to continually percolate on the problem. An incomplete task stays partially active in your brain. When you come back to it you often see it with fresh eyes. You will experience your highest productivity when you are toggling between these two modes.
This makes sense, and Dr. Grant cites numerous examples from Leonardo da Vinci to the founders of Warby-Parker, as examples of success. But how can it benefit physicians? Many of us are “precrastinators,” people who tend to complete or at least begin tasks as soon as possible, even when it’s unnecessary or not urgent. Unlike some jobs in which it’s easier to take a break from a project and return to it with more creative solutions, we often are racing against a clock to see more patients, read more slides, answer more emails, and make more phone calls. We are perpetually frenetic, which is not conducive to original thinking.
If this sounds like you, then you are likely to benefit from deliberate procrastination. Here are a few ways to slow down:
- Put it on your calendar. Yes, I see the irony, but it works. Start by scheduling one hour a week where you are to accomplish nothing. You can fill this time with whatever your mind wants to do at that moment.
- When faced with a diagnostic dilemma or treatment failure, resist the urge to solve that problem in that moment. Save that note for later, tell the patient you will call him back or bring him back for a visit later. Even if you’re not actively working on it, it will incubate somewhere in your brain, allowing more divergent thought processes to take over. It’s a little like trying to solve a crossword that seems impossible in the moment and then answers suddenly appear without effort.
- Take up a hobby: Play the guitar, learn to make pasta, climb a big rock. When you are fully engaged in such pursuits it requires complete mental focus. When you revisit the difficult problem you’re working on, you will likely see it from different perspectives.
- Meditate: Meditation requires our brains and bodies to slow down. It can help reduce self-doubt and criticism which stifle problem solving.
- Watch Slow TV. Slow TV is a Scandinavian phenomenon where you sit and watch meditative video such as a 7-hour train cam from Bergen, Norway, to Oslo. There’s no dialogue, no plot, no commercials. It’s just 7 hours of track and train and is weirdly comforting.
If you want to learn more, then when you get a chance, Google “slow living” and explore. Of course, some of you precrastinators probably have already started before finishing this column.
Dr. Benabio is director of Healthcare Transformation and chief of dermatology at Kaiser Permanente San Diego. The opinions expressed in this column are his own and do not represent those of Kaiser Permanente. Dr. Benabio is @Dermdoc on Twitter. Write to him at [email protected].
Creating positive patient experiences
Let’s start with an exercise, shall we? What was the last vacation you went on? How would you rate that vacation on a scale of 1-10?
How you came up with that score is likely not entirely reflective of your actual experience. Understanding how we remember experiences is critical for the work we do everyday.
My last vacation was in Alaska. I’d rate it a 9 out of 10. How did I come up with that score? It is not the mean score of the entire trip as you might expect. Rather, I took a shortcut and thought only about the highlights to come up with a number. We remember, and evaluate, our experiences as a series of discrete events. In considering these events, it is only the highs, the lows, and the transitions that matter. Think about the score you gave your vacation. What specific moments did you remember?
This phenomenon is not specific to vacations. It applies to all service experiences. When your patients evaluate you, they will ignore most of what occurred and focus on only a few moments. Fair or not, it is from these bits only that they will rate their entire experience. This information helps us devise strategies to achieve high satisfaction scores: Focus on the high points, address the low points, if any, and be sure the transitions are pleasant.
For example, a patient might come to see you for a procedure. It could be something positive, such as injection of cosmetic filler or something negative like a colonoscopy. Either way, being finished with the procedure will likely be the best part for them. Don’t rush this time; instead of quickly moving on, take a moment to acknowledge you’re done, how well the patient did, or how much better they will now look or feel. Engaging with your patient at this moment can improve the salience of their experience and increase the likelihood that she or he will remember the appointment favorably and rate you accordingly, if given the opportunity.
In the same way, if you are aware your patient has experienced something negative, try to respond to it right away. Acknowledge if she or he expressed frustration, such as a long wait or pain, then take a minute to address or reframe it. Blunting the severity of the service failure can blunt their recall of it. This will make it less likely that it becomes a memorable part of their experience.
Last, transitions matter. These are the moments when your patient shifts from one setting to another, such as arriving at your office, moving from the waiting room to the exam room, and wrapping up the visit with the receptionist. Many of these moments will be managed by your staff. Therefore, invest time reminding them of their importance and teaching them tips and techniques to help patients transition smoothly and to feel well cared for. There will likely be a wonderful return on investment for them, you and, most importantly, your patients.
Dr. Benabio is director of Healthcare Transformation and chief of dermatology at Kaiser Permanente San Diego. The opinions expressed in this column are his own and do not represent those of Kaiser Permanente. Dr. Benabio is @Dermdoc on Twitter. Write to him at [email protected].
Let’s start with an exercise, shall we? What was the last vacation you went on? How would you rate that vacation on a scale of 1-10?
How you came up with that score is likely not entirely reflective of your actual experience. Understanding how we remember experiences is critical for the work we do everyday.
My last vacation was in Alaska. I’d rate it a 9 out of 10. How did I come up with that score? It is not the mean score of the entire trip as you might expect. Rather, I took a shortcut and thought only about the highlights to come up with a number. We remember, and evaluate, our experiences as a series of discrete events. In considering these events, it is only the highs, the lows, and the transitions that matter. Think about the score you gave your vacation. What specific moments did you remember?
This phenomenon is not specific to vacations. It applies to all service experiences. When your patients evaluate you, they will ignore most of what occurred and focus on only a few moments. Fair or not, it is from these bits only that they will rate their entire experience. This information helps us devise strategies to achieve high satisfaction scores: Focus on the high points, address the low points, if any, and be sure the transitions are pleasant.
For example, a patient might come to see you for a procedure. It could be something positive, such as injection of cosmetic filler or something negative like a colonoscopy. Either way, being finished with the procedure will likely be the best part for them. Don’t rush this time; instead of quickly moving on, take a moment to acknowledge you’re done, how well the patient did, or how much better they will now look or feel. Engaging with your patient at this moment can improve the salience of their experience and increase the likelihood that she or he will remember the appointment favorably and rate you accordingly, if given the opportunity.
In the same way, if you are aware your patient has experienced something negative, try to respond to it right away. Acknowledge if she or he expressed frustration, such as a long wait or pain, then take a minute to address or reframe it. Blunting the severity of the service failure can blunt their recall of it. This will make it less likely that it becomes a memorable part of their experience.
Last, transitions matter. These are the moments when your patient shifts from one setting to another, such as arriving at your office, moving from the waiting room to the exam room, and wrapping up the visit with the receptionist. Many of these moments will be managed by your staff. Therefore, invest time reminding them of their importance and teaching them tips and techniques to help patients transition smoothly and to feel well cared for. There will likely be a wonderful return on investment for them, you and, most importantly, your patients.
Dr. Benabio is director of Healthcare Transformation and chief of dermatology at Kaiser Permanente San Diego. The opinions expressed in this column are his own and do not represent those of Kaiser Permanente. Dr. Benabio is @Dermdoc on Twitter. Write to him at [email protected].
Let’s start with an exercise, shall we? What was the last vacation you went on? How would you rate that vacation on a scale of 1-10?
How you came up with that score is likely not entirely reflective of your actual experience. Understanding how we remember experiences is critical for the work we do everyday.
My last vacation was in Alaska. I’d rate it a 9 out of 10. How did I come up with that score? It is not the mean score of the entire trip as you might expect. Rather, I took a shortcut and thought only about the highlights to come up with a number. We remember, and evaluate, our experiences as a series of discrete events. In considering these events, it is only the highs, the lows, and the transitions that matter. Think about the score you gave your vacation. What specific moments did you remember?
This phenomenon is not specific to vacations. It applies to all service experiences. When your patients evaluate you, they will ignore most of what occurred and focus on only a few moments. Fair or not, it is from these bits only that they will rate their entire experience. This information helps us devise strategies to achieve high satisfaction scores: Focus on the high points, address the low points, if any, and be sure the transitions are pleasant.
For example, a patient might come to see you for a procedure. It could be something positive, such as injection of cosmetic filler or something negative like a colonoscopy. Either way, being finished with the procedure will likely be the best part for them. Don’t rush this time; instead of quickly moving on, take a moment to acknowledge you’re done, how well the patient did, or how much better they will now look or feel. Engaging with your patient at this moment can improve the salience of their experience and increase the likelihood that she or he will remember the appointment favorably and rate you accordingly, if given the opportunity.
In the same way, if you are aware your patient has experienced something negative, try to respond to it right away. Acknowledge if she or he expressed frustration, such as a long wait or pain, then take a minute to address or reframe it. Blunting the severity of the service failure can blunt their recall of it. This will make it less likely that it becomes a memorable part of their experience.
Last, transitions matter. These are the moments when your patient shifts from one setting to another, such as arriving at your office, moving from the waiting room to the exam room, and wrapping up the visit with the receptionist. Many of these moments will be managed by your staff. Therefore, invest time reminding them of their importance and teaching them tips and techniques to help patients transition smoothly and to feel well cared for. There will likely be a wonderful return on investment for them, you and, most importantly, your patients.
Dr. Benabio is director of Healthcare Transformation and chief of dermatology at Kaiser Permanente San Diego. The opinions expressed in this column are his own and do not represent those of Kaiser Permanente. Dr. Benabio is @Dermdoc on Twitter. Write to him at [email protected].
Tabata training
I’m in really good shape. Well, more like really not bad shape. I eat healthy food (see my previous column on diet) and work out nearly every day. I have done so for years. I’ve learned that working out doesn’t make much difference with my weight, but it makes a huge difference with my mood, even more so than meditating. That’s why I’ll never give it up.
My approach is to vary my routine, typically by month. I’ve done “BUD/S qualification” months where I do only push-ups, sit-ups, pull-ups, and runs to meet the minimum requirements for the Navy Seal Training. (It’s not as hard as you might think, although I’m pretty lenient on form.)
When I have an hour to exercise and I’m deep into a podcast, then I’ll just keep going. If I’m trying to work out a piece I’m writing, like this one, then I’ll go for a run along the harbor here in San Diego. If I have to catch an early flight or drive to LA for the day, then I might have only 15 minutes. In that instance, I do high-intensity sprints, also known as high-intensity interval training (HIIT). Although it’s hard to break a good sweat, these workouts are both challenging and rewarding.
Recently, I participated in a wonderful physician wellness program at Kaiser Permanente, San Diego, where, over several weeks, we learned about nutrition, practiced meditation, and did Tabatas. What’s a Tabata you ask? It’s a kick in the butt.
. Yup, it’s a 4-minute workout that consists of 20 seconds of all-out, maximum effort, followed by 10 seconds of rest. The specific move you do for Tabatas is up to you, but it’s recommended that it be the same move for all 4 minutes. I like burpees which work your entire body – you jump, you drop into a push-up position, you pull your feet back in, and jump again. (Check out a video on YouTube.)
When we started the class, I thought Tabatas would be too easy for a gym rat like me. Plus, there were pediatricians, and even radiologists there, so how hard could they be? Let’s just say I couldn’t sit for 2 days after my first session: That’s how hard.
Tabatas are also a quick way to torch calories. A study published in the Journal of Sports Science and Medicine in 2013 found subjects who performed a 20-minute Tabata session experienced improved cardiorespiratory endurance and increased calorie burn (J Sports Sci Med. 2013 Sep;12[3]: 612-3).
Sometimes on a Monday, which is typically my difficult day, I’ll break out a few burpees in my office between patients. The energy jolt is real, and unlike caffeine, doesn’t leave me shaky. Because Tabatas require physical and mental focus, they’re an effective way to clear your mind after a grueling patient visit or if you’re feeling distracted. You simply can’t be thinking about that late patient or angry email when you’re jumping and lunging at full speed.
All the physicians in our program liked the Tabatas; many were even better than me. (Turns out we have pediatricians and radiologists who do things like run the Boston marathon and win Spartan races).
And if you start doing Tabatas, feel free to email me if you need a recommendation for a standing desk – you might not be able to sit as much afterward.
Dr. Benabio is director of Healthcare Transformation and chief of dermatology at Kaiser Permanente San Diego. The opinions expressed in this column are his own and do not represent those of Kaiser Permanente. Dr. Benabio is @Dermdoc on Twitter. Write to him at [email protected].
I’m in really good shape. Well, more like really not bad shape. I eat healthy food (see my previous column on diet) and work out nearly every day. I have done so for years. I’ve learned that working out doesn’t make much difference with my weight, but it makes a huge difference with my mood, even more so than meditating. That’s why I’ll never give it up.
My approach is to vary my routine, typically by month. I’ve done “BUD/S qualification” months where I do only push-ups, sit-ups, pull-ups, and runs to meet the minimum requirements for the Navy Seal Training. (It’s not as hard as you might think, although I’m pretty lenient on form.)
When I have an hour to exercise and I’m deep into a podcast, then I’ll just keep going. If I’m trying to work out a piece I’m writing, like this one, then I’ll go for a run along the harbor here in San Diego. If I have to catch an early flight or drive to LA for the day, then I might have only 15 minutes. In that instance, I do high-intensity sprints, also known as high-intensity interval training (HIIT). Although it’s hard to break a good sweat, these workouts are both challenging and rewarding.
Recently, I participated in a wonderful physician wellness program at Kaiser Permanente, San Diego, where, over several weeks, we learned about nutrition, practiced meditation, and did Tabatas. What’s a Tabata you ask? It’s a kick in the butt.
. Yup, it’s a 4-minute workout that consists of 20 seconds of all-out, maximum effort, followed by 10 seconds of rest. The specific move you do for Tabatas is up to you, but it’s recommended that it be the same move for all 4 minutes. I like burpees which work your entire body – you jump, you drop into a push-up position, you pull your feet back in, and jump again. (Check out a video on YouTube.)
When we started the class, I thought Tabatas would be too easy for a gym rat like me. Plus, there were pediatricians, and even radiologists there, so how hard could they be? Let’s just say I couldn’t sit for 2 days after my first session: That’s how hard.
Tabatas are also a quick way to torch calories. A study published in the Journal of Sports Science and Medicine in 2013 found subjects who performed a 20-minute Tabata session experienced improved cardiorespiratory endurance and increased calorie burn (J Sports Sci Med. 2013 Sep;12[3]: 612-3).
Sometimes on a Monday, which is typically my difficult day, I’ll break out a few burpees in my office between patients. The energy jolt is real, and unlike caffeine, doesn’t leave me shaky. Because Tabatas require physical and mental focus, they’re an effective way to clear your mind after a grueling patient visit or if you’re feeling distracted. You simply can’t be thinking about that late patient or angry email when you’re jumping and lunging at full speed.
All the physicians in our program liked the Tabatas; many were even better than me. (Turns out we have pediatricians and radiologists who do things like run the Boston marathon and win Spartan races).
And if you start doing Tabatas, feel free to email me if you need a recommendation for a standing desk – you might not be able to sit as much afterward.
Dr. Benabio is director of Healthcare Transformation and chief of dermatology at Kaiser Permanente San Diego. The opinions expressed in this column are his own and do not represent those of Kaiser Permanente. Dr. Benabio is @Dermdoc on Twitter. Write to him at [email protected].
I’m in really good shape. Well, more like really not bad shape. I eat healthy food (see my previous column on diet) and work out nearly every day. I have done so for years. I’ve learned that working out doesn’t make much difference with my weight, but it makes a huge difference with my mood, even more so than meditating. That’s why I’ll never give it up.
My approach is to vary my routine, typically by month. I’ve done “BUD/S qualification” months where I do only push-ups, sit-ups, pull-ups, and runs to meet the minimum requirements for the Navy Seal Training. (It’s not as hard as you might think, although I’m pretty lenient on form.)
When I have an hour to exercise and I’m deep into a podcast, then I’ll just keep going. If I’m trying to work out a piece I’m writing, like this one, then I’ll go for a run along the harbor here in San Diego. If I have to catch an early flight or drive to LA for the day, then I might have only 15 minutes. In that instance, I do high-intensity sprints, also known as high-intensity interval training (HIIT). Although it’s hard to break a good sweat, these workouts are both challenging and rewarding.
Recently, I participated in a wonderful physician wellness program at Kaiser Permanente, San Diego, where, over several weeks, we learned about nutrition, practiced meditation, and did Tabatas. What’s a Tabata you ask? It’s a kick in the butt.
. Yup, it’s a 4-minute workout that consists of 20 seconds of all-out, maximum effort, followed by 10 seconds of rest. The specific move you do for Tabatas is up to you, but it’s recommended that it be the same move for all 4 minutes. I like burpees which work your entire body – you jump, you drop into a push-up position, you pull your feet back in, and jump again. (Check out a video on YouTube.)
When we started the class, I thought Tabatas would be too easy for a gym rat like me. Plus, there were pediatricians, and even radiologists there, so how hard could they be? Let’s just say I couldn’t sit for 2 days after my first session: That’s how hard.
Tabatas are also a quick way to torch calories. A study published in the Journal of Sports Science and Medicine in 2013 found subjects who performed a 20-minute Tabata session experienced improved cardiorespiratory endurance and increased calorie burn (J Sports Sci Med. 2013 Sep;12[3]: 612-3).
Sometimes on a Monday, which is typically my difficult day, I’ll break out a few burpees in my office between patients. The energy jolt is real, and unlike caffeine, doesn’t leave me shaky. Because Tabatas require physical and mental focus, they’re an effective way to clear your mind after a grueling patient visit or if you’re feeling distracted. You simply can’t be thinking about that late patient or angry email when you’re jumping and lunging at full speed.
All the physicians in our program liked the Tabatas; many were even better than me. (Turns out we have pediatricians and radiologists who do things like run the Boston marathon and win Spartan races).
And if you start doing Tabatas, feel free to email me if you need a recommendation for a standing desk – you might not be able to sit as much afterward.
Dr. Benabio is director of Healthcare Transformation and chief of dermatology at Kaiser Permanente San Diego. The opinions expressed in this column are his own and do not represent those of Kaiser Permanente. Dr. Benabio is @Dermdoc on Twitter. Write to him at [email protected].
What Alaska can teach us about burnout
Some people have nightmares of giant rats attacking from their basements, others encounter monsters from a Stephen King novel. My nightmares are of clinic where time is the beast pursuing me. In my nightmares, I’m running late and can’t get to my next patient, or I’m trapped somehow and unable to get to clinic at all.

Time demands that I provide patients access quickly, start clinic on time, double my speed to make up for add-ins, or worse, late patients. Time is a constant, relentless monster, one that has apparently infiltrated my subconscious. Yet, time is relative.
Over Memorial Day weekend, my wife and I flew from San Diego to Alaska. Somewhere between those places time transforms – early summer in San Diego becomes early spring in Alaska.
When we landed, daffodils were in bloom, buds on the alders were just arriving, and the sun struggled to warm the air to 50 degrees. The daytime defied gravity: it was daylight by 4 a.m. and still so after 11 p.m. We were the first visitors this season in our little cabin near Seward.
“Your hot water might take a bit to get hot,” our host, Jim, informed us. He wore a thick flannel shirt and Carhartt workman trousers. He leaned against the cabin’s door frame with one hand at the top and the other hanging from the weight of a DeWalt drill at his side. “I made these cabins myself,” he informed. I was anxious to move on, to unpack and start exploring, but every time I tried to break away from his conversation, he extended it. He shared how a cow and calf (that’s moose talk) had come through earlier that morning. Then he told us about working in the timber industry, starting by “pulling green chain” and working his way up to being the keeper of the saws. While he talked, I watched a raven drop down from the tall Sitka spruce to a branch just across from where we parked our car. Just behind Jim, the raven was not only watching, but also listening in on our conversation. Jim pointed, “That bit of snow over there was all that was left from the 12-foot-high snow earlier this year. It was an easy winter.” He then advised we should start our trip with a visit to Exit Glacier. It was reachable by road and an easy hike.
Staying upright on the steep trail to the glacier’s Harding Icefield concentrates the mind. Looking down and across the glacial outwash, I imagined how the ice once thousands of feet above my head carved a valley from rock. Ice compacted so completely and so deep that only blue light escapes. Indeed, a glacier is just a pile of unmelted snow, thousands of years in the making. The Kenai fjords, deep enough that humpback whales swim there, were carved from granite – at glacial speed. Some of the rocks there contain fossils all the way from the tropics. They were transported by the Pacific tectonic plate that has rotated counterclockwise from the equator to Alaska over millions of years – at tectonic speed. Life here has a way of sharpening your focus, allowing you to see perspective as exists in nature. Alaska is so old that an ob.gyn. could have seen his or her first patient here – a mother with a stillborn child – at the Upward Sun River, 11,500 years ago, where in 2013, the fossil remains of a late-term fetus dating back to that time was discovered. It is indeed relative.
After a long hike, a crispy, hot halibut sandwich, we made it back to our cabin. There was no WiFi or reliable cell service, no TV, no Netflix. We read in bed by daylight. I slept soundly, despite the bright light. No nightmares. No monsters.
The next morning, as I sipped my steaming coffee on our porch, the raven didn’t waste much time to stop by. He paused before coming nearly eye to eye on the roof of the firewood shed in front of me. He looked me up and down and cackled. Not a cawh, not warning me of my intrusion, but rather a vocalization. He just wanted to strike up a conversation with the first guest of the season. He had nothing but time.
On our last night, I lit a fire with wood Jim had cut for us (with help from lots of lighter fluid). Jim ambled over to say goodbye. When I mentioned we had a 2½ hour drive back to Anchorage, he said 3 hours wasn’t a long time for Alaskans. He’d made that drive many times when his kids were little just to take them to McDonald’s. I asked if he ever got burned out, living here. He gave a long pause, turning his chin up, letting the question sink in before constructing an answer. “Burned out? Huh. I don’t know. I guess like when I was pulling green chain in the saw mill. I was pretty tired by the end of the day. But that’s how we sleep so good in Alaska.”
He didn’t get it. In the lower 48, we rush, scramble, and hurry trying to outrun time. At the end, we’re burned out. In Alaska, they don’t know what burned out means. They do understand that time can’t be controlled or beaten. Rather, it is observed and appreciated. I hoped to bring a little of that perspective to clinic on Monday morning.
My recommendation to you if want to sleep better, with fewer nightmares, if you want to reduce your risk for burn out, then go to Alaska (or Montana, or Wyoming, or Idaho, or your backyard). .
Dr. Benabio is director of Healthcare Transformation and chief of dermatology at Kaiser Permanente San Diego. The opinions expressed in this column are his own and do not represent those of Kaiser Permanente. Dr. Benabio is @Dermdoc on Twitter. Write to him at [email protected].
Some people have nightmares of giant rats attacking from their basements, others encounter monsters from a Stephen King novel. My nightmares are of clinic where time is the beast pursuing me. In my nightmares, I’m running late and can’t get to my next patient, or I’m trapped somehow and unable to get to clinic at all.

Time demands that I provide patients access quickly, start clinic on time, double my speed to make up for add-ins, or worse, late patients. Time is a constant, relentless monster, one that has apparently infiltrated my subconscious. Yet, time is relative.
Over Memorial Day weekend, my wife and I flew from San Diego to Alaska. Somewhere between those places time transforms – early summer in San Diego becomes early spring in Alaska.
When we landed, daffodils were in bloom, buds on the alders were just arriving, and the sun struggled to warm the air to 50 degrees. The daytime defied gravity: it was daylight by 4 a.m. and still so after 11 p.m. We were the first visitors this season in our little cabin near Seward.
“Your hot water might take a bit to get hot,” our host, Jim, informed us. He wore a thick flannel shirt and Carhartt workman trousers. He leaned against the cabin’s door frame with one hand at the top and the other hanging from the weight of a DeWalt drill at his side. “I made these cabins myself,” he informed. I was anxious to move on, to unpack and start exploring, but every time I tried to break away from his conversation, he extended it. He shared how a cow and calf (that’s moose talk) had come through earlier that morning. Then he told us about working in the timber industry, starting by “pulling green chain” and working his way up to being the keeper of the saws. While he talked, I watched a raven drop down from the tall Sitka spruce to a branch just across from where we parked our car. Just behind Jim, the raven was not only watching, but also listening in on our conversation. Jim pointed, “That bit of snow over there was all that was left from the 12-foot-high snow earlier this year. It was an easy winter.” He then advised we should start our trip with a visit to Exit Glacier. It was reachable by road and an easy hike.
Staying upright on the steep trail to the glacier’s Harding Icefield concentrates the mind. Looking down and across the glacial outwash, I imagined how the ice once thousands of feet above my head carved a valley from rock. Ice compacted so completely and so deep that only blue light escapes. Indeed, a glacier is just a pile of unmelted snow, thousands of years in the making. The Kenai fjords, deep enough that humpback whales swim there, were carved from granite – at glacial speed. Some of the rocks there contain fossils all the way from the tropics. They were transported by the Pacific tectonic plate that has rotated counterclockwise from the equator to Alaska over millions of years – at tectonic speed. Life here has a way of sharpening your focus, allowing you to see perspective as exists in nature. Alaska is so old that an ob.gyn. could have seen his or her first patient here – a mother with a stillborn child – at the Upward Sun River, 11,500 years ago, where in 2013, the fossil remains of a late-term fetus dating back to that time was discovered. It is indeed relative.
After a long hike, a crispy, hot halibut sandwich, we made it back to our cabin. There was no WiFi or reliable cell service, no TV, no Netflix. We read in bed by daylight. I slept soundly, despite the bright light. No nightmares. No monsters.
The next morning, as I sipped my steaming coffee on our porch, the raven didn’t waste much time to stop by. He paused before coming nearly eye to eye on the roof of the firewood shed in front of me. He looked me up and down and cackled. Not a cawh, not warning me of my intrusion, but rather a vocalization. He just wanted to strike up a conversation with the first guest of the season. He had nothing but time.
On our last night, I lit a fire with wood Jim had cut for us (with help from lots of lighter fluid). Jim ambled over to say goodbye. When I mentioned we had a 2½ hour drive back to Anchorage, he said 3 hours wasn’t a long time for Alaskans. He’d made that drive many times when his kids were little just to take them to McDonald’s. I asked if he ever got burned out, living here. He gave a long pause, turning his chin up, letting the question sink in before constructing an answer. “Burned out? Huh. I don’t know. I guess like when I was pulling green chain in the saw mill. I was pretty tired by the end of the day. But that’s how we sleep so good in Alaska.”
He didn’t get it. In the lower 48, we rush, scramble, and hurry trying to outrun time. At the end, we’re burned out. In Alaska, they don’t know what burned out means. They do understand that time can’t be controlled or beaten. Rather, it is observed and appreciated. I hoped to bring a little of that perspective to clinic on Monday morning.
My recommendation to you if want to sleep better, with fewer nightmares, if you want to reduce your risk for burn out, then go to Alaska (or Montana, or Wyoming, or Idaho, or your backyard). .
Dr. Benabio is director of Healthcare Transformation and chief of dermatology at Kaiser Permanente San Diego. The opinions expressed in this column are his own and do not represent those of Kaiser Permanente. Dr. Benabio is @Dermdoc on Twitter. Write to him at [email protected].
Some people have nightmares of giant rats attacking from their basements, others encounter monsters from a Stephen King novel. My nightmares are of clinic where time is the beast pursuing me. In my nightmares, I’m running late and can’t get to my next patient, or I’m trapped somehow and unable to get to clinic at all.

Time demands that I provide patients access quickly, start clinic on time, double my speed to make up for add-ins, or worse, late patients. Time is a constant, relentless monster, one that has apparently infiltrated my subconscious. Yet, time is relative.
Over Memorial Day weekend, my wife and I flew from San Diego to Alaska. Somewhere between those places time transforms – early summer in San Diego becomes early spring in Alaska.
When we landed, daffodils were in bloom, buds on the alders were just arriving, and the sun struggled to warm the air to 50 degrees. The daytime defied gravity: it was daylight by 4 a.m. and still so after 11 p.m. We were the first visitors this season in our little cabin near Seward.
“Your hot water might take a bit to get hot,” our host, Jim, informed us. He wore a thick flannel shirt and Carhartt workman trousers. He leaned against the cabin’s door frame with one hand at the top and the other hanging from the weight of a DeWalt drill at his side. “I made these cabins myself,” he informed. I was anxious to move on, to unpack and start exploring, but every time I tried to break away from his conversation, he extended it. He shared how a cow and calf (that’s moose talk) had come through earlier that morning. Then he told us about working in the timber industry, starting by “pulling green chain” and working his way up to being the keeper of the saws. While he talked, I watched a raven drop down from the tall Sitka spruce to a branch just across from where we parked our car. Just behind Jim, the raven was not only watching, but also listening in on our conversation. Jim pointed, “That bit of snow over there was all that was left from the 12-foot-high snow earlier this year. It was an easy winter.” He then advised we should start our trip with a visit to Exit Glacier. It was reachable by road and an easy hike.
Staying upright on the steep trail to the glacier’s Harding Icefield concentrates the mind. Looking down and across the glacial outwash, I imagined how the ice once thousands of feet above my head carved a valley from rock. Ice compacted so completely and so deep that only blue light escapes. Indeed, a glacier is just a pile of unmelted snow, thousands of years in the making. The Kenai fjords, deep enough that humpback whales swim there, were carved from granite – at glacial speed. Some of the rocks there contain fossils all the way from the tropics. They were transported by the Pacific tectonic plate that has rotated counterclockwise from the equator to Alaska over millions of years – at tectonic speed. Life here has a way of sharpening your focus, allowing you to see perspective as exists in nature. Alaska is so old that an ob.gyn. could have seen his or her first patient here – a mother with a stillborn child – at the Upward Sun River, 11,500 years ago, where in 2013, the fossil remains of a late-term fetus dating back to that time was discovered. It is indeed relative.
After a long hike, a crispy, hot halibut sandwich, we made it back to our cabin. There was no WiFi or reliable cell service, no TV, no Netflix. We read in bed by daylight. I slept soundly, despite the bright light. No nightmares. No monsters.
The next morning, as I sipped my steaming coffee on our porch, the raven didn’t waste much time to stop by. He paused before coming nearly eye to eye on the roof of the firewood shed in front of me. He looked me up and down and cackled. Not a cawh, not warning me of my intrusion, but rather a vocalization. He just wanted to strike up a conversation with the first guest of the season. He had nothing but time.
On our last night, I lit a fire with wood Jim had cut for us (with help from lots of lighter fluid). Jim ambled over to say goodbye. When I mentioned we had a 2½ hour drive back to Anchorage, he said 3 hours wasn’t a long time for Alaskans. He’d made that drive many times when his kids were little just to take them to McDonald’s. I asked if he ever got burned out, living here. He gave a long pause, turning his chin up, letting the question sink in before constructing an answer. “Burned out? Huh. I don’t know. I guess like when I was pulling green chain in the saw mill. I was pretty tired by the end of the day. But that’s how we sleep so good in Alaska.”
He didn’t get it. In the lower 48, we rush, scramble, and hurry trying to outrun time. At the end, we’re burned out. In Alaska, they don’t know what burned out means. They do understand that time can’t be controlled or beaten. Rather, it is observed and appreciated. I hoped to bring a little of that perspective to clinic on Monday morning.
My recommendation to you if want to sleep better, with fewer nightmares, if you want to reduce your risk for burn out, then go to Alaska (or Montana, or Wyoming, or Idaho, or your backyard). .
Dr. Benabio is director of Healthcare Transformation and chief of dermatology at Kaiser Permanente San Diego. The opinions expressed in this column are his own and do not represent those of Kaiser Permanente. Dr. Benabio is @Dermdoc on Twitter. Write to him at [email protected].
Diet
I’m about to embark on a controversial topic. Perhaps it’s safer to avoid, but I can’t put it off any longer. We need to talk about diet.
Discussing diet, like politics, religion, or salary, is best done just with oneself. Yet, I’m compelled to share what I’ve learned. First, I’m agnostic. I don’t believe you need to be vegan or paleo to be saved. I eat plant-based foods. I also eat things that eat plants. I’m sure you’d find a fine film of gluten in my kitchen. What I’ve learned is that for me, it doesn’t matter.
Specifically, I have little or nothing to eat from when I wake until dinner. As a busy dermatologist, that may seem draconian, but in fact it is easier than you might think. Patients are a constant all day, while hunger is fleeting. Got a craving at 10:15 a.m.? Easy. Walk in to see the next patient. Then repeat. Most days, this continues until 6:30 p.m. or so, when it’s time to head home. It’s not that hard, particularly when you don’t have anything in your office to eat except Dentyne Ice gum and green tea.
Now, this doesn’t always work. Why? Meetings. How do I manage fasting on those days? I don’t. If I know I have a lunch meeting scheduled, then I eat a healthy breakfast before I leave home, such as a protein smoothie or a bowl of hot oats with a dollop of Greek yogurt, sunflower seeds, walnuts, and berries. By eating a wholesome, well-balanced meal of fiber, carbs, lean protein, and good fats, I’m not starving before the meeting and am less likely to overeat. (That’s because I have also learned I’m not one of those enviable people who can simply say “no” to a crispy fish taco and guacamole if I’m hungry. I’m gonna eat it.) So, I avoid fasting and the inevitable frustration of breaking a fast on those days.
On days when I fast, I monitor how I feel. Fortunately, I have rarely felt hypoglycemic; except for that one Tuesday a couple of months ago. I had completed a long, hard early morning workout, and by mid-morning my hands were shaking and I felt nauseous. I quickly downed two RX bars and felt fine within minutes. Better for me, better for my patients.
Right now, intermittent fasting is working for me. Here’s my weekly plan:
I don’t fast on Fridays or weekends or when I travel. I eat out rarely. On weekends, my wife and I shop at the local farmers’ and fish markets to prepare ourselves for a week of healthy eating. And on Sundays, we continue our treasured family tradition of Sunday supper, which is basted with nostalgia and drizzled liberally with comfort. Often it requires long preparation, which is part of the appeal, and short attention is paid to its nutritional value. That’s not the point of Sunday dinner. A delicious dunk of fresh Italian bread in grassy-green olive oil or fresh pasta doused with homemade tomato basil sauce is the best possible meal I can have to prepare for a long, hard week ahead.
Dr. Benabio is director of Healthcare Transformation and chief of dermatology at Kaiser Permanente San Diego. The opinions expressed in this column are his own and do not represent those of Kaiser Permanente. Dr. Benabio is @Dermdoc on Twitter. Write to him at [email protected].
I’m about to embark on a controversial topic. Perhaps it’s safer to avoid, but I can’t put it off any longer. We need to talk about diet.
Discussing diet, like politics, religion, or salary, is best done just with oneself. Yet, I’m compelled to share what I’ve learned. First, I’m agnostic. I don’t believe you need to be vegan or paleo to be saved. I eat plant-based foods. I also eat things that eat plants. I’m sure you’d find a fine film of gluten in my kitchen. What I’ve learned is that for me, it doesn’t matter.
Specifically, I have little or nothing to eat from when I wake until dinner. As a busy dermatologist, that may seem draconian, but in fact it is easier than you might think. Patients are a constant all day, while hunger is fleeting. Got a craving at 10:15 a.m.? Easy. Walk in to see the next patient. Then repeat. Most days, this continues until 6:30 p.m. or so, when it’s time to head home. It’s not that hard, particularly when you don’t have anything in your office to eat except Dentyne Ice gum and green tea.
Now, this doesn’t always work. Why? Meetings. How do I manage fasting on those days? I don’t. If I know I have a lunch meeting scheduled, then I eat a healthy breakfast before I leave home, such as a protein smoothie or a bowl of hot oats with a dollop of Greek yogurt, sunflower seeds, walnuts, and berries. By eating a wholesome, well-balanced meal of fiber, carbs, lean protein, and good fats, I’m not starving before the meeting and am less likely to overeat. (That’s because I have also learned I’m not one of those enviable people who can simply say “no” to a crispy fish taco and guacamole if I’m hungry. I’m gonna eat it.) So, I avoid fasting and the inevitable frustration of breaking a fast on those days.
On days when I fast, I monitor how I feel. Fortunately, I have rarely felt hypoglycemic; except for that one Tuesday a couple of months ago. I had completed a long, hard early morning workout, and by mid-morning my hands were shaking and I felt nauseous. I quickly downed two RX bars and felt fine within minutes. Better for me, better for my patients.
Right now, intermittent fasting is working for me. Here’s my weekly plan:
I don’t fast on Fridays or weekends or when I travel. I eat out rarely. On weekends, my wife and I shop at the local farmers’ and fish markets to prepare ourselves for a week of healthy eating. And on Sundays, we continue our treasured family tradition of Sunday supper, which is basted with nostalgia and drizzled liberally with comfort. Often it requires long preparation, which is part of the appeal, and short attention is paid to its nutritional value. That’s not the point of Sunday dinner. A delicious dunk of fresh Italian bread in grassy-green olive oil or fresh pasta doused with homemade tomato basil sauce is the best possible meal I can have to prepare for a long, hard week ahead.
Dr. Benabio is director of Healthcare Transformation and chief of dermatology at Kaiser Permanente San Diego. The opinions expressed in this column are his own and do not represent those of Kaiser Permanente. Dr. Benabio is @Dermdoc on Twitter. Write to him at [email protected].
I’m about to embark on a controversial topic. Perhaps it’s safer to avoid, but I can’t put it off any longer. We need to talk about diet.
Discussing diet, like politics, religion, or salary, is best done just with oneself. Yet, I’m compelled to share what I’ve learned. First, I’m agnostic. I don’t believe you need to be vegan or paleo to be saved. I eat plant-based foods. I also eat things that eat plants. I’m sure you’d find a fine film of gluten in my kitchen. What I’ve learned is that for me, it doesn’t matter.
Specifically, I have little or nothing to eat from when I wake until dinner. As a busy dermatologist, that may seem draconian, but in fact it is easier than you might think. Patients are a constant all day, while hunger is fleeting. Got a craving at 10:15 a.m.? Easy. Walk in to see the next patient. Then repeat. Most days, this continues until 6:30 p.m. or so, when it’s time to head home. It’s not that hard, particularly when you don’t have anything in your office to eat except Dentyne Ice gum and green tea.
Now, this doesn’t always work. Why? Meetings. How do I manage fasting on those days? I don’t. If I know I have a lunch meeting scheduled, then I eat a healthy breakfast before I leave home, such as a protein smoothie or a bowl of hot oats with a dollop of Greek yogurt, sunflower seeds, walnuts, and berries. By eating a wholesome, well-balanced meal of fiber, carbs, lean protein, and good fats, I’m not starving before the meeting and am less likely to overeat. (That’s because I have also learned I’m not one of those enviable people who can simply say “no” to a crispy fish taco and guacamole if I’m hungry. I’m gonna eat it.) So, I avoid fasting and the inevitable frustration of breaking a fast on those days.
On days when I fast, I monitor how I feel. Fortunately, I have rarely felt hypoglycemic; except for that one Tuesday a couple of months ago. I had completed a long, hard early morning workout, and by mid-morning my hands were shaking and I felt nauseous. I quickly downed two RX bars and felt fine within minutes. Better for me, better for my patients.
Right now, intermittent fasting is working for me. Here’s my weekly plan:
I don’t fast on Fridays or weekends or when I travel. I eat out rarely. On weekends, my wife and I shop at the local farmers’ and fish markets to prepare ourselves for a week of healthy eating. And on Sundays, we continue our treasured family tradition of Sunday supper, which is basted with nostalgia and drizzled liberally with comfort. Often it requires long preparation, which is part of the appeal, and short attention is paid to its nutritional value. That’s not the point of Sunday dinner. A delicious dunk of fresh Italian bread in grassy-green olive oil or fresh pasta doused with homemade tomato basil sauce is the best possible meal I can have to prepare for a long, hard week ahead.
Dr. Benabio is director of Healthcare Transformation and chief of dermatology at Kaiser Permanente San Diego. The opinions expressed in this column are his own and do not represent those of Kaiser Permanente. Dr. Benabio is @Dermdoc on Twitter. Write to him at [email protected].
Grind it out
“And five more, four more, three more, two more, one more, and done!” Just when you thought you could not stand the searing pain any longer, it ends. Your spin instructor is not only helping you be fit, she is also teaching you an important lesson for life: Sometimes you just need to grind it out.
. College basketball teams need to simply grind it out to advance in the NCAA championship tournament. How might Tiger Woods recover from a disastrous few holes at the Masters? “He’ll just have to grind it out on the back nine.” How will you finally finish your PhD thesis? You’ll have to grind it out this month. It’s how I’m writing this column, how I got my taxes in on time, and, sometimes, how I get through clinic.
The phrase is used to describe something which needs to be done that is tedious, laborious, or joyless. Although the outcome of grinding it out is always pleasant, the task is often considered arduous.
In my dermatology practice, patient demand came in like a lion this March, and to meet our awesome access goals, we needed to add clinics on Saturdays, early mornings, and even a few nights. We met our goal, with supply to spare, and felt proud of our accomplishments. Physician wellness gurus (this author not included) say that, to avoid burnout from such excess work, you must find meaning in your work. Be grateful to help that 24-year-old with acne at 8:15 p.m. Think about how lucky you are to serve that lawyer with hand dermatitis at 8:45 p.m. Celebrate the mom’s cancer-free skin screening at 9:00 p.m. By finding meaning in our work, we’re told, we can achieve clinic nirvana. Except it doesn’t always work, and sometimes it serves us badly.
For the long days that ended in night clinic last month, I found myself counting down those last few patients – “four more, three more, two more, and last one.” I love my work and care about my patients, but sometimes I just have to grind it out. I’m proud of what I’ve accomplished.
Now it’s on to spin class.
Dr. Benabio is director of Healthcare Transformation and chief of dermatology at Kaiser Permanente San Diego. The opinions expressed in this column are his own and do not represent those of Kaiser Permanente. Dr. Benabio is @Dermdoc on Twitter. Write to him at [email protected].
“And five more, four more, three more, two more, one more, and done!” Just when you thought you could not stand the searing pain any longer, it ends. Your spin instructor is not only helping you be fit, she is also teaching you an important lesson for life: Sometimes you just need to grind it out.
. College basketball teams need to simply grind it out to advance in the NCAA championship tournament. How might Tiger Woods recover from a disastrous few holes at the Masters? “He’ll just have to grind it out on the back nine.” How will you finally finish your PhD thesis? You’ll have to grind it out this month. It’s how I’m writing this column, how I got my taxes in on time, and, sometimes, how I get through clinic.
The phrase is used to describe something which needs to be done that is tedious, laborious, or joyless. Although the outcome of grinding it out is always pleasant, the task is often considered arduous.
In my dermatology practice, patient demand came in like a lion this March, and to meet our awesome access goals, we needed to add clinics on Saturdays, early mornings, and even a few nights. We met our goal, with supply to spare, and felt proud of our accomplishments. Physician wellness gurus (this author not included) say that, to avoid burnout from such excess work, you must find meaning in your work. Be grateful to help that 24-year-old with acne at 8:15 p.m. Think about how lucky you are to serve that lawyer with hand dermatitis at 8:45 p.m. Celebrate the mom’s cancer-free skin screening at 9:00 p.m. By finding meaning in our work, we’re told, we can achieve clinic nirvana. Except it doesn’t always work, and sometimes it serves us badly.
For the long days that ended in night clinic last month, I found myself counting down those last few patients – “four more, three more, two more, and last one.” I love my work and care about my patients, but sometimes I just have to grind it out. I’m proud of what I’ve accomplished.
Now it’s on to spin class.
Dr. Benabio is director of Healthcare Transformation and chief of dermatology at Kaiser Permanente San Diego. The opinions expressed in this column are his own and do not represent those of Kaiser Permanente. Dr. Benabio is @Dermdoc on Twitter. Write to him at [email protected].
“And five more, four more, three more, two more, one more, and done!” Just when you thought you could not stand the searing pain any longer, it ends. Your spin instructor is not only helping you be fit, she is also teaching you an important lesson for life: Sometimes you just need to grind it out.
. College basketball teams need to simply grind it out to advance in the NCAA championship tournament. How might Tiger Woods recover from a disastrous few holes at the Masters? “He’ll just have to grind it out on the back nine.” How will you finally finish your PhD thesis? You’ll have to grind it out this month. It’s how I’m writing this column, how I got my taxes in on time, and, sometimes, how I get through clinic.
The phrase is used to describe something which needs to be done that is tedious, laborious, or joyless. Although the outcome of grinding it out is always pleasant, the task is often considered arduous.
In my dermatology practice, patient demand came in like a lion this March, and to meet our awesome access goals, we needed to add clinics on Saturdays, early mornings, and even a few nights. We met our goal, with supply to spare, and felt proud of our accomplishments. Physician wellness gurus (this author not included) say that, to avoid burnout from such excess work, you must find meaning in your work. Be grateful to help that 24-year-old with acne at 8:15 p.m. Think about how lucky you are to serve that lawyer with hand dermatitis at 8:45 p.m. Celebrate the mom’s cancer-free skin screening at 9:00 p.m. By finding meaning in our work, we’re told, we can achieve clinic nirvana. Except it doesn’t always work, and sometimes it serves us badly.
For the long days that ended in night clinic last month, I found myself counting down those last few patients – “four more, three more, two more, and last one.” I love my work and care about my patients, but sometimes I just have to grind it out. I’m proud of what I’ve accomplished.
Now it’s on to spin class.
Dr. Benabio is director of Healthcare Transformation and chief of dermatology at Kaiser Permanente San Diego. The opinions expressed in this column are his own and do not represent those of Kaiser Permanente. Dr. Benabio is @Dermdoc on Twitter. Write to him at [email protected].
Podcasts
you need no effort to enjoy them. Indeed, you can be actively engaged elsewhere: running, cycling, commuting, or simply loafing. The detail and richness of the sound also creates an intimate connection with the host in a way other mediums cannot. It feels like they are talking only to you.
Yet, there is a problem with podcasts: There are too many of them. If I listened continuously to the episodes in my queue it would take 6 months. I suppose I could see patients and listen at the same time. (Yes, I have a problem.) I also own far more books than I’ll ever read. Aspirational, I call it.
If, like me, you’re unable to dedicate your life to consuming podcasts, you might appreciate a few recommendations. Here’s a charcuterie board of tasty bits, carefully curated to avoid political allergies and Dunning-Kruger references.
1. Physicians Practice. It’s one of the oldest podcasts running and addresses a wide range of issues affecting health care professionals and the industry at large. Episodes are short (typically under 10 minutes) and address a range of issues relevant to both young and seasoned physicians With scores of podcasts from which to choose, I suggest just selecting one and jumping in. With episode titles such as “The Patient Empathy Problem Physicians Must Face” and “EHRs Not Designed with Real People in Mind, Expert Opines,” it’s easy to do.
2. UpToDate. If you’re looking for straight clinical talk buttressed with scientific evidence, then download UpToDate. Episodes typically feature interviews with one or two respected physician leaders who share their clinical findings. You can select episode topics based upon clinical specialty or simply start listening. Here is a sampling of topics: sentinel lymph node metastasis in melanoma; dexamethasone and acute pharyngitis pain in adults; management of anticoagulation for patients with nonvalvular atrial fibrillation. UpToDate states that it is entirely funded by user subscriptions and does not accept advertising or funding unrelated to subscriptions.
3. Bedside Rounds. The tagline for the podcast Bedside Rounds is “Because medicine is awesome.” This is not meant to be ironic. Creator and host, Adam Rodman, MD, a global health hospitalist who divides his time between Boston (at the Beth Israel Deaconess Medical Center) and Botswana, is that eager kid in the classroom who sits in the front row just because he’s so excited to be there. Unlike UpToDate, which focuses on current advances in clinical medicine, Bedside Rounds explores both the science and art of medicine through captivating stories heavily rooted in the history of medicine. Instead of brushing the dust off of your old medical books, tune in to Bedside Rounds to hear stories such as “Bone Portraits,” which explores the history of radiation, and “Curse of the Ninth,” which explores whether or not composer Gustav Mahler, worked his heart murmur into his famous Ninth Symphony.
4. The Adventures of Memento Mori. Creator and host, D.S. Moss, has created a podcast about death, or, to be more upbeat, the quest for the meaning of life. A screenwriter/producer, Mr. Moss deep dives into all things death. But it’s not as depressing as it sounds. “Memento mori,” he explains, is Latin for being mindful that you will die. As a result, Mr. Moss has created his podcast with the goal of encouraging listeners to live a more engaged, mindful, and meaningful life. We can apply many of these lessons to our own professional and personal lives and perhaps learn some ways to help our patients cope with terminal illness and mortality. Topics range from the emotional (“Thoughts in Passing,” which features several hospice patients) to the technological (“Digital Afterlife,” which explores what our digital legacies say about us), to the scientific (“The Science of Immortality,” which explores venture capital’s movement in the science of living forever).
5. Invisibilia. Invisibilia – Latin for invisible things – is an exploration of the “unseeable forces” that shape human behavior – our beliefs, thoughts, and assumptions. Hosts Alix Spiegel and Hanna Rosin, both of National Public Radio, seamlessly weave storytelling, interviewing, and scientific data to tackle a wide range of topics such as prejudice and implicit bias in “The Culture Inside” to people’s desire for radical change in “Bubble Hopping.” Part behavioral economics, part neuroscience, part sociology, part pop culture, fully fascinating.
6. Jocko Podcast. Jocko Willink, a retired Navy SEAL and motivational author and speaker, along with Echo Charles, conduct compelling interviews with leaders from various fields including the military, sports, medicine, and the arts. Mr. Willink’s style of motivation is refreshingly honest and direct. I have taken tips from his podcasts that have helped me become a more efficient and energetic physician and leader. Two fundamental themes that run through his podcast are the value of treating people well and of living your life with discipline. It gets you a long way as a Navy SEAL, as well as a doctor. One of my personal favorites is Episode 69: “The Real Top Gun. Battlefield, Work, and Life are Identical” with Elite Marine Fighter Pilot, David Berke. If that doesn’t pique your interest, no worries; there are over 100 episodes from which to choose.
There are many, many more podcasts I’d like to recommend, but I’ll show some discipline (thanks, Jocko) and save them for next time.
Dr. Benabio is director of Healthcare Transformation and chief of dermatology at Kaiser Permanente San Diego. The opinions expressed in this column are his own and do not represent those of Kaiser Permanente. Dr. Benabio is @Dermdoc on Twitter. Write to him at [email protected].
you need no effort to enjoy them. Indeed, you can be actively engaged elsewhere: running, cycling, commuting, or simply loafing. The detail and richness of the sound also creates an intimate connection with the host in a way other mediums cannot. It feels like they are talking only to you.
Yet, there is a problem with podcasts: There are too many of them. If I listened continuously to the episodes in my queue it would take 6 months. I suppose I could see patients and listen at the same time. (Yes, I have a problem.) I also own far more books than I’ll ever read. Aspirational, I call it.
If, like me, you’re unable to dedicate your life to consuming podcasts, you might appreciate a few recommendations. Here’s a charcuterie board of tasty bits, carefully curated to avoid political allergies and Dunning-Kruger references.
1. Physicians Practice. It’s one of the oldest podcasts running and addresses a wide range of issues affecting health care professionals and the industry at large. Episodes are short (typically under 10 minutes) and address a range of issues relevant to both young and seasoned physicians With scores of podcasts from which to choose, I suggest just selecting one and jumping in. With episode titles such as “The Patient Empathy Problem Physicians Must Face” and “EHRs Not Designed with Real People in Mind, Expert Opines,” it’s easy to do.
2. UpToDate. If you’re looking for straight clinical talk buttressed with scientific evidence, then download UpToDate. Episodes typically feature interviews with one or two respected physician leaders who share their clinical findings. You can select episode topics based upon clinical specialty or simply start listening. Here is a sampling of topics: sentinel lymph node metastasis in melanoma; dexamethasone and acute pharyngitis pain in adults; management of anticoagulation for patients with nonvalvular atrial fibrillation. UpToDate states that it is entirely funded by user subscriptions and does not accept advertising or funding unrelated to subscriptions.
3. Bedside Rounds. The tagline for the podcast Bedside Rounds is “Because medicine is awesome.” This is not meant to be ironic. Creator and host, Adam Rodman, MD, a global health hospitalist who divides his time between Boston (at the Beth Israel Deaconess Medical Center) and Botswana, is that eager kid in the classroom who sits in the front row just because he’s so excited to be there. Unlike UpToDate, which focuses on current advances in clinical medicine, Bedside Rounds explores both the science and art of medicine through captivating stories heavily rooted in the history of medicine. Instead of brushing the dust off of your old medical books, tune in to Bedside Rounds to hear stories such as “Bone Portraits,” which explores the history of radiation, and “Curse of the Ninth,” which explores whether or not composer Gustav Mahler, worked his heart murmur into his famous Ninth Symphony.
4. The Adventures of Memento Mori. Creator and host, D.S. Moss, has created a podcast about death, or, to be more upbeat, the quest for the meaning of life. A screenwriter/producer, Mr. Moss deep dives into all things death. But it’s not as depressing as it sounds. “Memento mori,” he explains, is Latin for being mindful that you will die. As a result, Mr. Moss has created his podcast with the goal of encouraging listeners to live a more engaged, mindful, and meaningful life. We can apply many of these lessons to our own professional and personal lives and perhaps learn some ways to help our patients cope with terminal illness and mortality. Topics range from the emotional (“Thoughts in Passing,” which features several hospice patients) to the technological (“Digital Afterlife,” which explores what our digital legacies say about us), to the scientific (“The Science of Immortality,” which explores venture capital’s movement in the science of living forever).
5. Invisibilia. Invisibilia – Latin for invisible things – is an exploration of the “unseeable forces” that shape human behavior – our beliefs, thoughts, and assumptions. Hosts Alix Spiegel and Hanna Rosin, both of National Public Radio, seamlessly weave storytelling, interviewing, and scientific data to tackle a wide range of topics such as prejudice and implicit bias in “The Culture Inside” to people’s desire for radical change in “Bubble Hopping.” Part behavioral economics, part neuroscience, part sociology, part pop culture, fully fascinating.
6. Jocko Podcast. Jocko Willink, a retired Navy SEAL and motivational author and speaker, along with Echo Charles, conduct compelling interviews with leaders from various fields including the military, sports, medicine, and the arts. Mr. Willink’s style of motivation is refreshingly honest and direct. I have taken tips from his podcasts that have helped me become a more efficient and energetic physician and leader. Two fundamental themes that run through his podcast are the value of treating people well and of living your life with discipline. It gets you a long way as a Navy SEAL, as well as a doctor. One of my personal favorites is Episode 69: “The Real Top Gun. Battlefield, Work, and Life are Identical” with Elite Marine Fighter Pilot, David Berke. If that doesn’t pique your interest, no worries; there are over 100 episodes from which to choose.
There are many, many more podcasts I’d like to recommend, but I’ll show some discipline (thanks, Jocko) and save them for next time.
Dr. Benabio is director of Healthcare Transformation and chief of dermatology at Kaiser Permanente San Diego. The opinions expressed in this column are his own and do not represent those of Kaiser Permanente. Dr. Benabio is @Dermdoc on Twitter. Write to him at [email protected].
you need no effort to enjoy them. Indeed, you can be actively engaged elsewhere: running, cycling, commuting, or simply loafing. The detail and richness of the sound also creates an intimate connection with the host in a way other mediums cannot. It feels like they are talking only to you.
Yet, there is a problem with podcasts: There are too many of them. If I listened continuously to the episodes in my queue it would take 6 months. I suppose I could see patients and listen at the same time. (Yes, I have a problem.) I also own far more books than I’ll ever read. Aspirational, I call it.
If, like me, you’re unable to dedicate your life to consuming podcasts, you might appreciate a few recommendations. Here’s a charcuterie board of tasty bits, carefully curated to avoid political allergies and Dunning-Kruger references.
1. Physicians Practice. It’s one of the oldest podcasts running and addresses a wide range of issues affecting health care professionals and the industry at large. Episodes are short (typically under 10 minutes) and address a range of issues relevant to both young and seasoned physicians With scores of podcasts from which to choose, I suggest just selecting one and jumping in. With episode titles such as “The Patient Empathy Problem Physicians Must Face” and “EHRs Not Designed with Real People in Mind, Expert Opines,” it’s easy to do.
2. UpToDate. If you’re looking for straight clinical talk buttressed with scientific evidence, then download UpToDate. Episodes typically feature interviews with one or two respected physician leaders who share their clinical findings. You can select episode topics based upon clinical specialty or simply start listening. Here is a sampling of topics: sentinel lymph node metastasis in melanoma; dexamethasone and acute pharyngitis pain in adults; management of anticoagulation for patients with nonvalvular atrial fibrillation. UpToDate states that it is entirely funded by user subscriptions and does not accept advertising or funding unrelated to subscriptions.
3. Bedside Rounds. The tagline for the podcast Bedside Rounds is “Because medicine is awesome.” This is not meant to be ironic. Creator and host, Adam Rodman, MD, a global health hospitalist who divides his time between Boston (at the Beth Israel Deaconess Medical Center) and Botswana, is that eager kid in the classroom who sits in the front row just because he’s so excited to be there. Unlike UpToDate, which focuses on current advances in clinical medicine, Bedside Rounds explores both the science and art of medicine through captivating stories heavily rooted in the history of medicine. Instead of brushing the dust off of your old medical books, tune in to Bedside Rounds to hear stories such as “Bone Portraits,” which explores the history of radiation, and “Curse of the Ninth,” which explores whether or not composer Gustav Mahler, worked his heart murmur into his famous Ninth Symphony.
4. The Adventures of Memento Mori. Creator and host, D.S. Moss, has created a podcast about death, or, to be more upbeat, the quest for the meaning of life. A screenwriter/producer, Mr. Moss deep dives into all things death. But it’s not as depressing as it sounds. “Memento mori,” he explains, is Latin for being mindful that you will die. As a result, Mr. Moss has created his podcast with the goal of encouraging listeners to live a more engaged, mindful, and meaningful life. We can apply many of these lessons to our own professional and personal lives and perhaps learn some ways to help our patients cope with terminal illness and mortality. Topics range from the emotional (“Thoughts in Passing,” which features several hospice patients) to the technological (“Digital Afterlife,” which explores what our digital legacies say about us), to the scientific (“The Science of Immortality,” which explores venture capital’s movement in the science of living forever).
5. Invisibilia. Invisibilia – Latin for invisible things – is an exploration of the “unseeable forces” that shape human behavior – our beliefs, thoughts, and assumptions. Hosts Alix Spiegel and Hanna Rosin, both of National Public Radio, seamlessly weave storytelling, interviewing, and scientific data to tackle a wide range of topics such as prejudice and implicit bias in “The Culture Inside” to people’s desire for radical change in “Bubble Hopping.” Part behavioral economics, part neuroscience, part sociology, part pop culture, fully fascinating.
6. Jocko Podcast. Jocko Willink, a retired Navy SEAL and motivational author and speaker, along with Echo Charles, conduct compelling interviews with leaders from various fields including the military, sports, medicine, and the arts. Mr. Willink’s style of motivation is refreshingly honest and direct. I have taken tips from his podcasts that have helped me become a more efficient and energetic physician and leader. Two fundamental themes that run through his podcast are the value of treating people well and of living your life with discipline. It gets you a long way as a Navy SEAL, as well as a doctor. One of my personal favorites is Episode 69: “The Real Top Gun. Battlefield, Work, and Life are Identical” with Elite Marine Fighter Pilot, David Berke. If that doesn’t pique your interest, no worries; there are over 100 episodes from which to choose.
There are many, many more podcasts I’d like to recommend, but I’ll show some discipline (thanks, Jocko) and save them for next time.
Dr. Benabio is director of Healthcare Transformation and chief of dermatology at Kaiser Permanente San Diego. The opinions expressed in this column are his own and do not represent those of Kaiser Permanente. Dr. Benabio is @Dermdoc on Twitter. Write to him at [email protected].
Impostor syndrome
Why are you bothering to read this? What could I offer that could possibly be useful to you? In fact, I was invited to write this column simply because I happened to be at the right conference at the right time. Soon, if not already, you’ll discover I’m actually not that clever. I’m an impostor.
I’ve thought this while staring at the blank page that is to be my article for the month. Reflecting on it, I realize you’ve probably had the same feelings of fraud at one time or another. It often occurs at moments of transition, such as when you were accepted into medical school or matched into a competitive specialty. Looking at your peers, watching how your colleagues perform, you feel you just aren’t smart enough to be there; either someone made a mistake or you just got lucky.
There are potentially positive aspects of impostor syndrome: Humility can make us more effective over time and more tolerable to be around. It also, however, can be destructive. When we feel undeserving, we grow anxious and focus ever more tightly on ourselves. It can be paralyzing. When you think about how you are perceived, you fail to be present and attentive to others around you. Believing you lack innate ability, you can slip into a fixed mindset and fail to grow. Trying to keep your insecurities a secret from others, the foundation of impostor syndrome, is stressful and will stoke the fire of burnout which threatens us all. Fortunately, there is a cure.
The first step in escaping this maladaptive experience is to do what I’ve just done: Share it with others. Find colleagues or partners who care about you and who can speak frankly. By sharing how you feel with others, you banish any power that impostor syndrome might have over you. You can’t worry about being a fraud once you’ve just announced that you are a fraud; the gig is up! Choose your confidantes carefully, as not everyone is suitable to help. Avoid sharing such feelings with your patients; it can erode their confidence in you.
Reframe how you interpret situations when you feel like an impostor. Committing an error doesn’t mean you’re incompetent; moreover, you needn’t be supremely confident to be competent. Marveling at others’ abilities doesn’t mean you could not perform as well. Remember, you don’t know how much effort and time they’ve invested, and chances are you’re underestimating the work they’ve put forth.
Last, take the time to write about your success. Journaling can be a powerful tool to make your successes more salient and remind you that you are truly accomplished. Try writing in the third person, telling the story of your journey and the obstacles you’ve overcome to reach your current prestigious destination. If you still feel like a fake sometimes, there is good news. Having some self-doubt correlates with success, probably because it keeps you motivated to work hard.
Did this article resonate with you? It should. It took me lots of drafts before I got it right.
Dr. Benabio is director of Healthcare Transformation and chief of dermatology at Kaiser Permanente San Diego. The opinions expressed in this column are his own and do not represent those of Kaiser Permanente. Dr. Benabio is @Dermdoc on Twitter. Write to him at [email protected].
Why are you bothering to read this? What could I offer that could possibly be useful to you? In fact, I was invited to write this column simply because I happened to be at the right conference at the right time. Soon, if not already, you’ll discover I’m actually not that clever. I’m an impostor.
I’ve thought this while staring at the blank page that is to be my article for the month. Reflecting on it, I realize you’ve probably had the same feelings of fraud at one time or another. It often occurs at moments of transition, such as when you were accepted into medical school or matched into a competitive specialty. Looking at your peers, watching how your colleagues perform, you feel you just aren’t smart enough to be there; either someone made a mistake or you just got lucky.
There are potentially positive aspects of impostor syndrome: Humility can make us more effective over time and more tolerable to be around. It also, however, can be destructive. When we feel undeserving, we grow anxious and focus ever more tightly on ourselves. It can be paralyzing. When you think about how you are perceived, you fail to be present and attentive to others around you. Believing you lack innate ability, you can slip into a fixed mindset and fail to grow. Trying to keep your insecurities a secret from others, the foundation of impostor syndrome, is stressful and will stoke the fire of burnout which threatens us all. Fortunately, there is a cure.
The first step in escaping this maladaptive experience is to do what I’ve just done: Share it with others. Find colleagues or partners who care about you and who can speak frankly. By sharing how you feel with others, you banish any power that impostor syndrome might have over you. You can’t worry about being a fraud once you’ve just announced that you are a fraud; the gig is up! Choose your confidantes carefully, as not everyone is suitable to help. Avoid sharing such feelings with your patients; it can erode their confidence in you.
Reframe how you interpret situations when you feel like an impostor. Committing an error doesn’t mean you’re incompetent; moreover, you needn’t be supremely confident to be competent. Marveling at others’ abilities doesn’t mean you could not perform as well. Remember, you don’t know how much effort and time they’ve invested, and chances are you’re underestimating the work they’ve put forth.
Last, take the time to write about your success. Journaling can be a powerful tool to make your successes more salient and remind you that you are truly accomplished. Try writing in the third person, telling the story of your journey and the obstacles you’ve overcome to reach your current prestigious destination. If you still feel like a fake sometimes, there is good news. Having some self-doubt correlates with success, probably because it keeps you motivated to work hard.
Did this article resonate with you? It should. It took me lots of drafts before I got it right.
Dr. Benabio is director of Healthcare Transformation and chief of dermatology at Kaiser Permanente San Diego. The opinions expressed in this column are his own and do not represent those of Kaiser Permanente. Dr. Benabio is @Dermdoc on Twitter. Write to him at [email protected].
Why are you bothering to read this? What could I offer that could possibly be useful to you? In fact, I was invited to write this column simply because I happened to be at the right conference at the right time. Soon, if not already, you’ll discover I’m actually not that clever. I’m an impostor.
I’ve thought this while staring at the blank page that is to be my article for the month. Reflecting on it, I realize you’ve probably had the same feelings of fraud at one time or another. It often occurs at moments of transition, such as when you were accepted into medical school or matched into a competitive specialty. Looking at your peers, watching how your colleagues perform, you feel you just aren’t smart enough to be there; either someone made a mistake or you just got lucky.
There are potentially positive aspects of impostor syndrome: Humility can make us more effective over time and more tolerable to be around. It also, however, can be destructive. When we feel undeserving, we grow anxious and focus ever more tightly on ourselves. It can be paralyzing. When you think about how you are perceived, you fail to be present and attentive to others around you. Believing you lack innate ability, you can slip into a fixed mindset and fail to grow. Trying to keep your insecurities a secret from others, the foundation of impostor syndrome, is stressful and will stoke the fire of burnout which threatens us all. Fortunately, there is a cure.
The first step in escaping this maladaptive experience is to do what I’ve just done: Share it with others. Find colleagues or partners who care about you and who can speak frankly. By sharing how you feel with others, you banish any power that impostor syndrome might have over you. You can’t worry about being a fraud once you’ve just announced that you are a fraud; the gig is up! Choose your confidantes carefully, as not everyone is suitable to help. Avoid sharing such feelings with your patients; it can erode their confidence in you.
Reframe how you interpret situations when you feel like an impostor. Committing an error doesn’t mean you’re incompetent; moreover, you needn’t be supremely confident to be competent. Marveling at others’ abilities doesn’t mean you could not perform as well. Remember, you don’t know how much effort and time they’ve invested, and chances are you’re underestimating the work they’ve put forth.
Last, take the time to write about your success. Journaling can be a powerful tool to make your successes more salient and remind you that you are truly accomplished. Try writing in the third person, telling the story of your journey and the obstacles you’ve overcome to reach your current prestigious destination. If you still feel like a fake sometimes, there is good news. Having some self-doubt correlates with success, probably because it keeps you motivated to work hard.
Did this article resonate with you? It should. It took me lots of drafts before I got it right.
Dr. Benabio is director of Healthcare Transformation and chief of dermatology at Kaiser Permanente San Diego. The opinions expressed in this column are his own and do not represent those of Kaiser Permanente. Dr. Benabio is @Dermdoc on Twitter. Write to him at [email protected].