User login
Termination of pregnancy for medical reasons: A mental health perspective
Termination of pregnancy for medical reasons (TFMR) occurs when a pregnancy is ended due to medical complications that threaten the health of a pregnant individual and/or fetus, or when a fetus has a poor prognosis or life-limiting diagnosis. It is distinct from the American College of Obstetricians and Gynecologists identification of all abortions as medically indicated. Common indications for TFMR include life-threatening pregnancy complications (eg, placental abruption, hyperemesis gravidarum, exacerbation of psychiatric illness), chromosomal abnormalities (eg, Trisomy 13, 18, and 21; Klinefelter syndrome), and fetal anomalies (eg, neural tube defects, cardiac defects, renal agenesis). In this article, we discuss the negative psychological outcomes of TFMR, and how to screen and intervene to best help women who experience TFMR.
Psychiatric sequelae of TFMR
Unlike abortions in general, negative psychological outcomes are common among women who experience TFMR.1 Nearly one-half of women develop symptoms of posttraumatic stress disorder (PTSD), and approximately one-fourth show signs of depression at 4 months after termination.2 Such symptoms usually improve with time but may return around trauma anniversaries (date of diagnosis or termination). Women with a history of trauma, a prior psychiatric diagnosis, and/or no living children are at greater risk. Self-blame, doubt, and high levels of distress are also risk factors.2-4 Protective factors include positive coping strategies (such as acceptance or reframing), higher perceived social support, and high self-efficacy.3,4
Screening: What to ask, and how
Use open-ended questions to ask about a patient’s obstetric history:
- Have you ever been pregnant?
- If you’re comfortable sharing, what were the outcomes of these pregnancies?
If a woman discloses that she has experienced a TFMR, screen for and normalize psychiatric outcomes by asking:
- Symptoms of grief, depression, and anxiety are common after TFMR. Have you experienced such symptoms?
- What impact has terminating your pregnancy for medical reasons had on your mental health?
Screening tools such as the General Self-Efficacy Scale can help assess predictive factors, while other scales can assess specific diagnoses (eg, Patient Health Questionaire-9 for depression, Impact of Event Scale-Revised and PTSD Checklist for DSM-5 for trauma-related symptoms, Traumatic Grief Inventory Self Report Version for pathological grief). The Edinburgh Postnatal Depression Scale can assess for depression, but if you use this instrument, exclude statements that reference a current pregnancy or recent delivery.
How to best help
Interventions should be specific and targeted. Thus, consider the individual nature of the experience and variation in attachment that can occur over time.5 OB-GYN and perinatal psychiatry clinicians can recommend local resources and support groups that specifically focus on TFMR, rather than on general pregnancy loss. Refer patients to therapists who specialize in pregnancy loss, reproductive trauma, and/or TFMR. Cognitive-behavioral therapy and acceptance and commitment therapy may be appropriate and effective.3 Online support groups (such as Termination of Pregnancy for Medical Reasons; www.facebook.com/groups/TFMRgroup/) can supplement or fill gaps in local resources. Suggest books that discuss TFMR, such
1. González-Ramos Z, Zuriguel-Pérez E, Albacar-Riobóo N, et al. The emotional responses of women when terminating a pregnancy for medical reasons: a scoping review. Midwifery. 2021;103:103095. doi:10.1016/j.midw.2021.103095
2. Korenromp MJ, Page-Christiaens GCML, van den Bout J, et al. Adjustment to termination of pregnancy for fetal anomaly: a longitudinal study in women at 4, 8, and 16 months. Am J Obstet Gynecol. 2009;201(2):160.e1-7.
3. Lafarge C, Mitchell K, Fox P. Perinatal grief following a termination of pregnancy for foetal abnormality: the impact of coping strategies. Prenat Diagn. 2013;33(12):1173-1182.
4. Korenromp MJ, Christiaens GC, van den Bout J, et al. Long-term psychological consequences of pregnancy termination for fetal abnormality: a cross-sectional study. Prenat Diagn. 2005;25(3):253-260.
5. Lou S, Hvidtjørn D, Jørgensen ML, Vogel I. “I had to think: this is not a child.” A qualitative exploration of how women/couples articulate their relation to the fetus/child following termination of a wanted pregnancy due to Down syndrome. Sex Reprod Healthc. 2021;28:100606. doi: 10.1016/j.srhc.2021.100606
6. Brooks C (ed.). Our Heartbreaking Choices: Forty-Six Women Share Their Stories of Interrupting a Much-Wanted Pregnancy. iUniverse; 2008.
Termination of pregnancy for medical reasons (TFMR) occurs when a pregnancy is ended due to medical complications that threaten the health of a pregnant individual and/or fetus, or when a fetus has a poor prognosis or life-limiting diagnosis. It is distinct from the American College of Obstetricians and Gynecologists identification of all abortions as medically indicated. Common indications for TFMR include life-threatening pregnancy complications (eg, placental abruption, hyperemesis gravidarum, exacerbation of psychiatric illness), chromosomal abnormalities (eg, Trisomy 13, 18, and 21; Klinefelter syndrome), and fetal anomalies (eg, neural tube defects, cardiac defects, renal agenesis). In this article, we discuss the negative psychological outcomes of TFMR, and how to screen and intervene to best help women who experience TFMR.
Psychiatric sequelae of TFMR
Unlike abortions in general, negative psychological outcomes are common among women who experience TFMR.1 Nearly one-half of women develop symptoms of posttraumatic stress disorder (PTSD), and approximately one-fourth show signs of depression at 4 months after termination.2 Such symptoms usually improve with time but may return around trauma anniversaries (date of diagnosis or termination). Women with a history of trauma, a prior psychiatric diagnosis, and/or no living children are at greater risk. Self-blame, doubt, and high levels of distress are also risk factors.2-4 Protective factors include positive coping strategies (such as acceptance or reframing), higher perceived social support, and high self-efficacy.3,4
Screening: What to ask, and how
Use open-ended questions to ask about a patient’s obstetric history:
- Have you ever been pregnant?
- If you’re comfortable sharing, what were the outcomes of these pregnancies?
If a woman discloses that she has experienced a TFMR, screen for and normalize psychiatric outcomes by asking:
- Symptoms of grief, depression, and anxiety are common after TFMR. Have you experienced such symptoms?
- What impact has terminating your pregnancy for medical reasons had on your mental health?
Screening tools such as the General Self-Efficacy Scale can help assess predictive factors, while other scales can assess specific diagnoses (eg, Patient Health Questionaire-9 for depression, Impact of Event Scale-Revised and PTSD Checklist for DSM-5 for trauma-related symptoms, Traumatic Grief Inventory Self Report Version for pathological grief). The Edinburgh Postnatal Depression Scale can assess for depression, but if you use this instrument, exclude statements that reference a current pregnancy or recent delivery.
How to best help
Interventions should be specific and targeted. Thus, consider the individual nature of the experience and variation in attachment that can occur over time.5 OB-GYN and perinatal psychiatry clinicians can recommend local resources and support groups that specifically focus on TFMR, rather than on general pregnancy loss. Refer patients to therapists who specialize in pregnancy loss, reproductive trauma, and/or TFMR. Cognitive-behavioral therapy and acceptance and commitment therapy may be appropriate and effective.3 Online support groups (such as Termination of Pregnancy for Medical Reasons; www.facebook.com/groups/TFMRgroup/) can supplement or fill gaps in local resources. Suggest books that discuss TFMR, such
Termination of pregnancy for medical reasons (TFMR) occurs when a pregnancy is ended due to medical complications that threaten the health of a pregnant individual and/or fetus, or when a fetus has a poor prognosis or life-limiting diagnosis. It is distinct from the American College of Obstetricians and Gynecologists identification of all abortions as medically indicated. Common indications for TFMR include life-threatening pregnancy complications (eg, placental abruption, hyperemesis gravidarum, exacerbation of psychiatric illness), chromosomal abnormalities (eg, Trisomy 13, 18, and 21; Klinefelter syndrome), and fetal anomalies (eg, neural tube defects, cardiac defects, renal agenesis). In this article, we discuss the negative psychological outcomes of TFMR, and how to screen and intervene to best help women who experience TFMR.
Psychiatric sequelae of TFMR
Unlike abortions in general, negative psychological outcomes are common among women who experience TFMR.1 Nearly one-half of women develop symptoms of posttraumatic stress disorder (PTSD), and approximately one-fourth show signs of depression at 4 months after termination.2 Such symptoms usually improve with time but may return around trauma anniversaries (date of diagnosis or termination). Women with a history of trauma, a prior psychiatric diagnosis, and/or no living children are at greater risk. Self-blame, doubt, and high levels of distress are also risk factors.2-4 Protective factors include positive coping strategies (such as acceptance or reframing), higher perceived social support, and high self-efficacy.3,4
Screening: What to ask, and how
Use open-ended questions to ask about a patient’s obstetric history:
- Have you ever been pregnant?
- If you’re comfortable sharing, what were the outcomes of these pregnancies?
If a woman discloses that she has experienced a TFMR, screen for and normalize psychiatric outcomes by asking:
- Symptoms of grief, depression, and anxiety are common after TFMR. Have you experienced such symptoms?
- What impact has terminating your pregnancy for medical reasons had on your mental health?
Screening tools such as the General Self-Efficacy Scale can help assess predictive factors, while other scales can assess specific diagnoses (eg, Patient Health Questionaire-9 for depression, Impact of Event Scale-Revised and PTSD Checklist for DSM-5 for trauma-related symptoms, Traumatic Grief Inventory Self Report Version for pathological grief). The Edinburgh Postnatal Depression Scale can assess for depression, but if you use this instrument, exclude statements that reference a current pregnancy or recent delivery.
How to best help
Interventions should be specific and targeted. Thus, consider the individual nature of the experience and variation in attachment that can occur over time.5 OB-GYN and perinatal psychiatry clinicians can recommend local resources and support groups that specifically focus on TFMR, rather than on general pregnancy loss. Refer patients to therapists who specialize in pregnancy loss, reproductive trauma, and/or TFMR. Cognitive-behavioral therapy and acceptance and commitment therapy may be appropriate and effective.3 Online support groups (such as Termination of Pregnancy for Medical Reasons; www.facebook.com/groups/TFMRgroup/) can supplement or fill gaps in local resources. Suggest books that discuss TFMR, such
1. González-Ramos Z, Zuriguel-Pérez E, Albacar-Riobóo N, et al. The emotional responses of women when terminating a pregnancy for medical reasons: a scoping review. Midwifery. 2021;103:103095. doi:10.1016/j.midw.2021.103095
2. Korenromp MJ, Page-Christiaens GCML, van den Bout J, et al. Adjustment to termination of pregnancy for fetal anomaly: a longitudinal study in women at 4, 8, and 16 months. Am J Obstet Gynecol. 2009;201(2):160.e1-7.
3. Lafarge C, Mitchell K, Fox P. Perinatal grief following a termination of pregnancy for foetal abnormality: the impact of coping strategies. Prenat Diagn. 2013;33(12):1173-1182.
4. Korenromp MJ, Christiaens GC, van den Bout J, et al. Long-term psychological consequences of pregnancy termination for fetal abnormality: a cross-sectional study. Prenat Diagn. 2005;25(3):253-260.
5. Lou S, Hvidtjørn D, Jørgensen ML, Vogel I. “I had to think: this is not a child.” A qualitative exploration of how women/couples articulate their relation to the fetus/child following termination of a wanted pregnancy due to Down syndrome. Sex Reprod Healthc. 2021;28:100606. doi: 10.1016/j.srhc.2021.100606
6. Brooks C (ed.). Our Heartbreaking Choices: Forty-Six Women Share Their Stories of Interrupting a Much-Wanted Pregnancy. iUniverse; 2008.
1. González-Ramos Z, Zuriguel-Pérez E, Albacar-Riobóo N, et al. The emotional responses of women when terminating a pregnancy for medical reasons: a scoping review. Midwifery. 2021;103:103095. doi:10.1016/j.midw.2021.103095
2. Korenromp MJ, Page-Christiaens GCML, van den Bout J, et al. Adjustment to termination of pregnancy for fetal anomaly: a longitudinal study in women at 4, 8, and 16 months. Am J Obstet Gynecol. 2009;201(2):160.e1-7.
3. Lafarge C, Mitchell K, Fox P. Perinatal grief following a termination of pregnancy for foetal abnormality: the impact of coping strategies. Prenat Diagn. 2013;33(12):1173-1182.
4. Korenromp MJ, Christiaens GC, van den Bout J, et al. Long-term psychological consequences of pregnancy termination for fetal abnormality: a cross-sectional study. Prenat Diagn. 2005;25(3):253-260.
5. Lou S, Hvidtjørn D, Jørgensen ML, Vogel I. “I had to think: this is not a child.” A qualitative exploration of how women/couples articulate their relation to the fetus/child following termination of a wanted pregnancy due to Down syndrome. Sex Reprod Healthc. 2021;28:100606. doi: 10.1016/j.srhc.2021.100606
6. Brooks C (ed.). Our Heartbreaking Choices: Forty-Six Women Share Their Stories of Interrupting a Much-Wanted Pregnancy. iUniverse; 2008.
BOARDING psychiatric patients in the ED: Key strategies
Boarding of psychiatric patients in the emergency department (ED) has been well documented.1 Numerous researchers have discussed ways to address this public health crisis. In this Pearl, I use the acronym BOARDING to provide key strategies for psychiatric clinicians managing psychiatric patients who are boarding in an ED.
Be vigilant. As a patient’s time waiting in the ED increases, watch for clinical blind spots. New medical problems,2 psychiatric issues, or medication errors3 may unexpectedly arise since the patient was originally stabilized by emergency medicine clinicians.
Orders. Since the patient could be waiting in the ED for 24 hours or longer, consider starting orders (eg, precautions, medications, diet, vital sign checks, labs, etc) as you would for a patient in an inpatient psychiatric unit or a dedicated psychiatric ED.
AWOL. Unlike inpatient psychiatric units, EDs generally are not locked. Extra resources (eg, sitter, safety alarm bracelet) may be needed to help prevent patients from leaving this setting unnoticed, especially those on involuntary psychiatric holds.
Re-evaluate. Ideally, re-evaluate the patient every shift. Does the patient still need an inpatient psychiatric setting? Can the involuntary psychiatric hold be discontinued?
Disposition. Is there a family member or reliable caregiver to whom the patient can be discharged? Can the patient go to a shelter or be stabilized in a short-term residential program, instead of an inpatient psychiatric unit?
Inpatient. If the patient waits 24 hours or longer, begin thinking like an inpatient psychiatric clinician. Are there any interventions you can reasonably begin in the ED that you would otherwise begin on an inpatient psychiatric unit?
Nursing. Work with ED nursing staff to familiarize them with the patient’s specific needs.
Guidelines. With the input of clinical and administrative leadership, establish local hospital-based guidelines for managing psychiatric patients who are boarding in the ED.
1. Nordstrom K, Berlin JS, Nash SS, et al. Boarding of mentally ill patients in emergency departments: American Psychiatric Association Resource Document. West J Emerg Med. 2019;20(5):690-695.
2. Garfinkel E, Rose D, Strouse K, et al. Psychiatric emergency department boarding: from catatonia to cardiac arrest. Am J Emerg Med. 2019;37(3):543-544.
3. Bakhsh HT, Perona SJ, Shields WA, et al. Medication errors in psychiatric patients boarded in the emergency department. Int J Risk Saf Med. 2014;26(4):191-198.
Boarding of psychiatric patients in the emergency department (ED) has been well documented.1 Numerous researchers have discussed ways to address this public health crisis. In this Pearl, I use the acronym BOARDING to provide key strategies for psychiatric clinicians managing psychiatric patients who are boarding in an ED.
Be vigilant. As a patient’s time waiting in the ED increases, watch for clinical blind spots. New medical problems,2 psychiatric issues, or medication errors3 may unexpectedly arise since the patient was originally stabilized by emergency medicine clinicians.
Orders. Since the patient could be waiting in the ED for 24 hours or longer, consider starting orders (eg, precautions, medications, diet, vital sign checks, labs, etc) as you would for a patient in an inpatient psychiatric unit or a dedicated psychiatric ED.
AWOL. Unlike inpatient psychiatric units, EDs generally are not locked. Extra resources (eg, sitter, safety alarm bracelet) may be needed to help prevent patients from leaving this setting unnoticed, especially those on involuntary psychiatric holds.
Re-evaluate. Ideally, re-evaluate the patient every shift. Does the patient still need an inpatient psychiatric setting? Can the involuntary psychiatric hold be discontinued?
Disposition. Is there a family member or reliable caregiver to whom the patient can be discharged? Can the patient go to a shelter or be stabilized in a short-term residential program, instead of an inpatient psychiatric unit?
Inpatient. If the patient waits 24 hours or longer, begin thinking like an inpatient psychiatric clinician. Are there any interventions you can reasonably begin in the ED that you would otherwise begin on an inpatient psychiatric unit?
Nursing. Work with ED nursing staff to familiarize them with the patient’s specific needs.
Guidelines. With the input of clinical and administrative leadership, establish local hospital-based guidelines for managing psychiatric patients who are boarding in the ED.
Boarding of psychiatric patients in the emergency department (ED) has been well documented.1 Numerous researchers have discussed ways to address this public health crisis. In this Pearl, I use the acronym BOARDING to provide key strategies for psychiatric clinicians managing psychiatric patients who are boarding in an ED.
Be vigilant. As a patient’s time waiting in the ED increases, watch for clinical blind spots. New medical problems,2 psychiatric issues, or medication errors3 may unexpectedly arise since the patient was originally stabilized by emergency medicine clinicians.
Orders. Since the patient could be waiting in the ED for 24 hours or longer, consider starting orders (eg, precautions, medications, diet, vital sign checks, labs, etc) as you would for a patient in an inpatient psychiatric unit or a dedicated psychiatric ED.
AWOL. Unlike inpatient psychiatric units, EDs generally are not locked. Extra resources (eg, sitter, safety alarm bracelet) may be needed to help prevent patients from leaving this setting unnoticed, especially those on involuntary psychiatric holds.
Re-evaluate. Ideally, re-evaluate the patient every shift. Does the patient still need an inpatient psychiatric setting? Can the involuntary psychiatric hold be discontinued?
Disposition. Is there a family member or reliable caregiver to whom the patient can be discharged? Can the patient go to a shelter or be stabilized in a short-term residential program, instead of an inpatient psychiatric unit?
Inpatient. If the patient waits 24 hours or longer, begin thinking like an inpatient psychiatric clinician. Are there any interventions you can reasonably begin in the ED that you would otherwise begin on an inpatient psychiatric unit?
Nursing. Work with ED nursing staff to familiarize them with the patient’s specific needs.
Guidelines. With the input of clinical and administrative leadership, establish local hospital-based guidelines for managing psychiatric patients who are boarding in the ED.
1. Nordstrom K, Berlin JS, Nash SS, et al. Boarding of mentally ill patients in emergency departments: American Psychiatric Association Resource Document. West J Emerg Med. 2019;20(5):690-695.
2. Garfinkel E, Rose D, Strouse K, et al. Psychiatric emergency department boarding: from catatonia to cardiac arrest. Am J Emerg Med. 2019;37(3):543-544.
3. Bakhsh HT, Perona SJ, Shields WA, et al. Medication errors in psychiatric patients boarded in the emergency department. Int J Risk Saf Med. 2014;26(4):191-198.
1. Nordstrom K, Berlin JS, Nash SS, et al. Boarding of mentally ill patients in emergency departments: American Psychiatric Association Resource Document. West J Emerg Med. 2019;20(5):690-695.
2. Garfinkel E, Rose D, Strouse K, et al. Psychiatric emergency department boarding: from catatonia to cardiac arrest. Am J Emerg Med. 2019;37(3):543-544.
3. Bakhsh HT, Perona SJ, Shields WA, et al. Medication errors in psychiatric patients boarded in the emergency department. Int J Risk Saf Med. 2014;26(4):191-198.
How to ‘cybersecure’ your practice
The health care sector is not immune from cybersecurity attacks (malicious attempts to access or damage a computer or network system). Between October 2019 and October 2021, 857 data breaches were reported to the United States Department of Health and Human Services.1 The 3 main types of breaches reported were theft, hacking/IT incident, or unauthorized access/disclosure.1 Health care has become a common target due to the availability of valuable patient information (health, personal, and financial), the industry’s financial stability and resource capacity, and network susceptibility.2 The top 2 cybersecurity threats facing physician practices are:
- ransomware attacks, in which an external party uses a type of malicious software (malware) that prevents you from accessing your computer files, systems, or networks, and demands you pay a ransom for their return.
- employee-related threats, such as the theft or destruction of sensitive information by a disgruntled employee.3
The financial implications of health care–related cybersecurity threats coupled with exposure to potential litigation associated with breaches of confidentiality result in a need to “cybersecure” your practice.2 In this article, I outline steps to take to protect your practice against such threats. Although the recommendations I provide will increase your practice’s cybersecurity fortification, they are not exhaustive, and you may need to consult with an IT specialist to help protect your data and network.
Improve your network protection. A broadband internet connection is always operating, which makes it continuously susceptible to cybersecurity attacks. Install a firewall (a network security system that monitors and controls network traffic and permits or blocks traffic based on a defined set of rules) between your practice’s internal computer network and the internet.4 For maximum protection, enable all available firewall settings in your operating software.2 Prevent unauthorized access by ensuring that all network passwords are strong (ie, they include a combination of uppercase and lowercase letters, numbers, and symbols). Consider using different networks for online communication and for storing sensitive information.2 Create separate Wi-Fi networks for your practice and for your patients, and use unique passwords for each that are not easily guessed.4 If you or your employees use a virtual private network (VPN) to remotely access your practice’s network, ensure that all devices used to do so (cell phones, tablets, etc) are encrypted and secured with strong passwords.
Reduce employee-related threats. Not every employee in your practice will need to access to your patients’ clinical or financial data. Limiting employee access to sensitive clinical or financial data can reduce the risks of employee-related cybersecurity threats.3 In addition, restrict an employee’s ability to install software on computers and other devices that belong to your practice.2
Frequently incorporate cybersecurity training, such as teaching your employees about the risks of clicking on links and attachments in emails and how to identify phishing attacks (in which an individual sends a fraudulent communication that appears to come from a reputable source in order to trick the recipient into revealing financial information, system credentials, or other sensitive data).2,3 Use multifactor authentication to verify an employee’s login identity, and change passwords often. Reinforce these policies at staff meetings and educate new employees about this process.3 If you need to fire an employee, consider deploying cybersurveillance software to monitor the behavior of all employees before the employee is terminated.3 Once the employee has been terminated, change all logins and passwords.
1. U.S. Department of Health and Human Services. Office for Civil Rights. Breach portal: Notice to the Secretary of HHS breach of unsecured protected health information. Accessed December 26, 2021. https://ocrportal.hhs.gov/ocr/breach/breach_report.jsf
2. Umali G. How to safeguard your practice from cybersecurity threats. Psychiatric News. 2021;56(12):23.
3. Cryts A. Top two cybersecurity threats facing physician practices. Physicians Practice. March 13, 2020. Accessed December 26, 2021. https://www.physicianspractice.com/view/top-two-cybersecurity-threats-facing-physician-practices
4. American Medical Association. Protect your practice and patients from cybersecurity threats. 2017. Accessed December 26, 2021. https://www.ama-assn.org/sites/ama-assn.org/files/corp/media-browser/public/government/advocacy/network-security.pdf
The health care sector is not immune from cybersecurity attacks (malicious attempts to access or damage a computer or network system). Between October 2019 and October 2021, 857 data breaches were reported to the United States Department of Health and Human Services.1 The 3 main types of breaches reported were theft, hacking/IT incident, or unauthorized access/disclosure.1 Health care has become a common target due to the availability of valuable patient information (health, personal, and financial), the industry’s financial stability and resource capacity, and network susceptibility.2 The top 2 cybersecurity threats facing physician practices are:
- ransomware attacks, in which an external party uses a type of malicious software (malware) that prevents you from accessing your computer files, systems, or networks, and demands you pay a ransom for their return.
- employee-related threats, such as the theft or destruction of sensitive information by a disgruntled employee.3
The financial implications of health care–related cybersecurity threats coupled with exposure to potential litigation associated with breaches of confidentiality result in a need to “cybersecure” your practice.2 In this article, I outline steps to take to protect your practice against such threats. Although the recommendations I provide will increase your practice’s cybersecurity fortification, they are not exhaustive, and you may need to consult with an IT specialist to help protect your data and network.
Improve your network protection. A broadband internet connection is always operating, which makes it continuously susceptible to cybersecurity attacks. Install a firewall (a network security system that monitors and controls network traffic and permits or blocks traffic based on a defined set of rules) between your practice’s internal computer network and the internet.4 For maximum protection, enable all available firewall settings in your operating software.2 Prevent unauthorized access by ensuring that all network passwords are strong (ie, they include a combination of uppercase and lowercase letters, numbers, and symbols). Consider using different networks for online communication and for storing sensitive information.2 Create separate Wi-Fi networks for your practice and for your patients, and use unique passwords for each that are not easily guessed.4 If you or your employees use a virtual private network (VPN) to remotely access your practice’s network, ensure that all devices used to do so (cell phones, tablets, etc) are encrypted and secured with strong passwords.
Reduce employee-related threats. Not every employee in your practice will need to access to your patients’ clinical or financial data. Limiting employee access to sensitive clinical or financial data can reduce the risks of employee-related cybersecurity threats.3 In addition, restrict an employee’s ability to install software on computers and other devices that belong to your practice.2
Frequently incorporate cybersecurity training, such as teaching your employees about the risks of clicking on links and attachments in emails and how to identify phishing attacks (in which an individual sends a fraudulent communication that appears to come from a reputable source in order to trick the recipient into revealing financial information, system credentials, or other sensitive data).2,3 Use multifactor authentication to verify an employee’s login identity, and change passwords often. Reinforce these policies at staff meetings and educate new employees about this process.3 If you need to fire an employee, consider deploying cybersurveillance software to monitor the behavior of all employees before the employee is terminated.3 Once the employee has been terminated, change all logins and passwords.
The health care sector is not immune from cybersecurity attacks (malicious attempts to access or damage a computer or network system). Between October 2019 and October 2021, 857 data breaches were reported to the United States Department of Health and Human Services.1 The 3 main types of breaches reported were theft, hacking/IT incident, or unauthorized access/disclosure.1 Health care has become a common target due to the availability of valuable patient information (health, personal, and financial), the industry’s financial stability and resource capacity, and network susceptibility.2 The top 2 cybersecurity threats facing physician practices are:
- ransomware attacks, in which an external party uses a type of malicious software (malware) that prevents you from accessing your computer files, systems, or networks, and demands you pay a ransom for their return.
- employee-related threats, such as the theft or destruction of sensitive information by a disgruntled employee.3
The financial implications of health care–related cybersecurity threats coupled with exposure to potential litigation associated with breaches of confidentiality result in a need to “cybersecure” your practice.2 In this article, I outline steps to take to protect your practice against such threats. Although the recommendations I provide will increase your practice’s cybersecurity fortification, they are not exhaustive, and you may need to consult with an IT specialist to help protect your data and network.
Improve your network protection. A broadband internet connection is always operating, which makes it continuously susceptible to cybersecurity attacks. Install a firewall (a network security system that monitors and controls network traffic and permits or blocks traffic based on a defined set of rules) between your practice’s internal computer network and the internet.4 For maximum protection, enable all available firewall settings in your operating software.2 Prevent unauthorized access by ensuring that all network passwords are strong (ie, they include a combination of uppercase and lowercase letters, numbers, and symbols). Consider using different networks for online communication and for storing sensitive information.2 Create separate Wi-Fi networks for your practice and for your patients, and use unique passwords for each that are not easily guessed.4 If you or your employees use a virtual private network (VPN) to remotely access your practice’s network, ensure that all devices used to do so (cell phones, tablets, etc) are encrypted and secured with strong passwords.
Reduce employee-related threats. Not every employee in your practice will need to access to your patients’ clinical or financial data. Limiting employee access to sensitive clinical or financial data can reduce the risks of employee-related cybersecurity threats.3 In addition, restrict an employee’s ability to install software on computers and other devices that belong to your practice.2
Frequently incorporate cybersecurity training, such as teaching your employees about the risks of clicking on links and attachments in emails and how to identify phishing attacks (in which an individual sends a fraudulent communication that appears to come from a reputable source in order to trick the recipient into revealing financial information, system credentials, or other sensitive data).2,3 Use multifactor authentication to verify an employee’s login identity, and change passwords often. Reinforce these policies at staff meetings and educate new employees about this process.3 If you need to fire an employee, consider deploying cybersurveillance software to monitor the behavior of all employees before the employee is terminated.3 Once the employee has been terminated, change all logins and passwords.
1. U.S. Department of Health and Human Services. Office for Civil Rights. Breach portal: Notice to the Secretary of HHS breach of unsecured protected health information. Accessed December 26, 2021. https://ocrportal.hhs.gov/ocr/breach/breach_report.jsf
2. Umali G. How to safeguard your practice from cybersecurity threats. Psychiatric News. 2021;56(12):23.
3. Cryts A. Top two cybersecurity threats facing physician practices. Physicians Practice. March 13, 2020. Accessed December 26, 2021. https://www.physicianspractice.com/view/top-two-cybersecurity-threats-facing-physician-practices
4. American Medical Association. Protect your practice and patients from cybersecurity threats. 2017. Accessed December 26, 2021. https://www.ama-assn.org/sites/ama-assn.org/files/corp/media-browser/public/government/advocacy/network-security.pdf
1. U.S. Department of Health and Human Services. Office for Civil Rights. Breach portal: Notice to the Secretary of HHS breach of unsecured protected health information. Accessed December 26, 2021. https://ocrportal.hhs.gov/ocr/breach/breach_report.jsf
2. Umali G. How to safeguard your practice from cybersecurity threats. Psychiatric News. 2021;56(12):23.
3. Cryts A. Top two cybersecurity threats facing physician practices. Physicians Practice. March 13, 2020. Accessed December 26, 2021. https://www.physicianspractice.com/view/top-two-cybersecurity-threats-facing-physician-practices
4. American Medical Association. Protect your practice and patients from cybersecurity threats. 2017. Accessed December 26, 2021. https://www.ama-assn.org/sites/ama-assn.org/files/corp/media-browser/public/government/advocacy/network-security.pdf
Managing bipolar disorder in women who are pregnant
Psychiatrists who treat women of childbearing age should consider that those women may become pregnant, and that women with psychiatric illness are more likely to have unplanned pregnancies.1 Thus, thoughtful perinatal medication choices should begin before pregnancy. Pregnancy is a time of vulnerability to psychiatric illness for many reasons, including physiologic changes that can affect mental status; changes in medication efficacy; and numerous stressors, such as new responsibilities and limited sleep.1,2 For the treatment of pregnant—or potentially pregnant—patients, we recommend the following.
Do not panic! Knee-jerk medication changes in response to learning a patient is pregnant can lead to an exacerbation of psychiatric symptoms, as well as decrease trust in clinicians.2 Switching to a medication with a purportedly “safer” reproductive profile may worsen psychiatric illness, while also exposing the fetus to a medication of unknown benefit. 2
Recognize the risk of untreated or undertreated psychiatric illness, either of which has the potential to harm both the woman and her fetus. For example, a pregnant woman in a manic state may be more likely to engage in risky behaviors, such as drug use or risky sexual activity, which can lead to adverse fetal outcomes. They may also present with a higher risk of suicide. Compared to nonpregnant women, pregnant women for whom lithium was discontinued were equally likely to experience illness recurrence and significantly more likely to experience postpartum illness recurrence.3 In addition, the risk of recurrence was greater after rapid discontinuation compared with gradual discontinuation.3
Accurately communicate research findings. Pregnancy risk categories are no longer used. A nuanced interpretation of the potential adverse effects of a medication, such as malformations, impaired fetal growth, birth outcomes (such as preterm birth), and neurodevelopmental sequelae is necessary. Physicians must accurately convey information about risks to their patients, including both the absolute risk of an adverse event and the possible range of severity. For example, lithium use during pregnancy confers a higher relative risk of Ebstein’s anomaly (a cardiac defect).4 However, the absolute incidence of this risk remains low: 0.6% of lithium-exposed infants vs 0.18% among unexposed infants.4 Ebstein’s anomaly also varies significantly in severity—serious cases may require surgery, but less serious cases need only monitoring. A reliable database that compiles the latest evidence may help in staying abreast of the latest data.
Treat the psychiatric illness. Consider the optimal treatment for the psychiatric illness. Lithium remains the gold standard treatment for bipolar I disorder, regardless of reproductive status. Olanzapine and quetiapine are also commonly used and effective during pregnancy. This is an opportunity to conduct a detailed review of the patient’s previous medication regimens, including a review of medication trials and efficacy. Keep in mind that untreated bipolar disorder also carries an increased risk of adverse pregnancy outcomes.5
Consider pregnancy timing. Most organs form between weeks 3 to 8 of pregnancy. For example, if a medication potentially affects heart formation, but the patient is in the third trimester, explain to her that the heart has already been formed. Consider that medication may be required long-term and affect future pregnancies. Pregnant women require more frequent monitoring, because blood volume changes in pregnancy and postpartum can affect medication levels and efficacy. In addition, note whether a woman plans to breastfeed and be mindful of a medication’s profile in breastfeeding.
Ensure the patient can provide informed consent. Communicate your diagnostic formulation and treatment options. Consider involving the patient’s partner and/or support system in the discussion, if the patient consents. If a patient cannot provide informed consent, a surrogate decision-maker should be identified.6
Continue to: Collaborate with other clinicians
Collaborate with other clinicians, such as the patient’s OB/GYN and family medicine physician when possible. This will ensure that all clinicians are on the same page.
Plan for future pregnancies. Psychiatric medications can be long-term. Even patients who say they do not wish to become pregnant may someday become pregnant. Having discussions about medication choices, and their reproductive implications, prior to pregnancy allows patients to take an active role in their health.1,2
Consult a reproductive psychiatrist when indicated, and as early in the pregnancy as possible.
1. Friedman SH. The ethics of treating depression in pregnancy. J Prim Health Care. 2015;7(1):81-83.
2. Friedman SH, Reed E. Treating psychosis in pregnant women: a measured approach. Current Psychiatry. 2021; 20(7):34-35.
3. Viguera AC, Nonacs R, Cohen LS, et al. Risk of recurrence of bipolar disorder in pregnant and nonpregnant women after discontinuing lithium maintenance. Am J Psychiatry. 2000;157(2):179-184.
4. Patorno E, Huybrechts KF, Bateman BT, et al. Lithium use in pregnancy and the risk of cardiac malformations. N Engl J Med. 2017;376(23):2245-2254.
5. Bodén R, Lundgren M, Brandt L, et al. Risks of adverse pregnancy and birth outcomes in women treated or not treated with mood stabilisers for bipolar disorder: population based cohort study. BMJ. 2012;345:e7085. doi:10.1136/bmj.e7085
6. Ross NE, Webster TG, Tastenhoye CA, et al. Reproductive decision-making capacity in women with psychiatric illness: a systematic review. J Acad Consult Liaison Psychiatry. 2022:63(1);61-70.
Psychiatrists who treat women of childbearing age should consider that those women may become pregnant, and that women with psychiatric illness are more likely to have unplanned pregnancies.1 Thus, thoughtful perinatal medication choices should begin before pregnancy. Pregnancy is a time of vulnerability to psychiatric illness for many reasons, including physiologic changes that can affect mental status; changes in medication efficacy; and numerous stressors, such as new responsibilities and limited sleep.1,2 For the treatment of pregnant—or potentially pregnant—patients, we recommend the following.
Do not panic! Knee-jerk medication changes in response to learning a patient is pregnant can lead to an exacerbation of psychiatric symptoms, as well as decrease trust in clinicians.2 Switching to a medication with a purportedly “safer” reproductive profile may worsen psychiatric illness, while also exposing the fetus to a medication of unknown benefit. 2
Recognize the risk of untreated or undertreated psychiatric illness, either of which has the potential to harm both the woman and her fetus. For example, a pregnant woman in a manic state may be more likely to engage in risky behaviors, such as drug use or risky sexual activity, which can lead to adverse fetal outcomes. They may also present with a higher risk of suicide. Compared to nonpregnant women, pregnant women for whom lithium was discontinued were equally likely to experience illness recurrence and significantly more likely to experience postpartum illness recurrence.3 In addition, the risk of recurrence was greater after rapid discontinuation compared with gradual discontinuation.3
Accurately communicate research findings. Pregnancy risk categories are no longer used. A nuanced interpretation of the potential adverse effects of a medication, such as malformations, impaired fetal growth, birth outcomes (such as preterm birth), and neurodevelopmental sequelae is necessary. Physicians must accurately convey information about risks to their patients, including both the absolute risk of an adverse event and the possible range of severity. For example, lithium use during pregnancy confers a higher relative risk of Ebstein’s anomaly (a cardiac defect).4 However, the absolute incidence of this risk remains low: 0.6% of lithium-exposed infants vs 0.18% among unexposed infants.4 Ebstein’s anomaly also varies significantly in severity—serious cases may require surgery, but less serious cases need only monitoring. A reliable database that compiles the latest evidence may help in staying abreast of the latest data.
Treat the psychiatric illness. Consider the optimal treatment for the psychiatric illness. Lithium remains the gold standard treatment for bipolar I disorder, regardless of reproductive status. Olanzapine and quetiapine are also commonly used and effective during pregnancy. This is an opportunity to conduct a detailed review of the patient’s previous medication regimens, including a review of medication trials and efficacy. Keep in mind that untreated bipolar disorder also carries an increased risk of adverse pregnancy outcomes.5
Consider pregnancy timing. Most organs form between weeks 3 to 8 of pregnancy. For example, if a medication potentially affects heart formation, but the patient is in the third trimester, explain to her that the heart has already been formed. Consider that medication may be required long-term and affect future pregnancies. Pregnant women require more frequent monitoring, because blood volume changes in pregnancy and postpartum can affect medication levels and efficacy. In addition, note whether a woman plans to breastfeed and be mindful of a medication’s profile in breastfeeding.
Ensure the patient can provide informed consent. Communicate your diagnostic formulation and treatment options. Consider involving the patient’s partner and/or support system in the discussion, if the patient consents. If a patient cannot provide informed consent, a surrogate decision-maker should be identified.6
Continue to: Collaborate with other clinicians
Collaborate with other clinicians, such as the patient’s OB/GYN and family medicine physician when possible. This will ensure that all clinicians are on the same page.
Plan for future pregnancies. Psychiatric medications can be long-term. Even patients who say they do not wish to become pregnant may someday become pregnant. Having discussions about medication choices, and their reproductive implications, prior to pregnancy allows patients to take an active role in their health.1,2
Consult a reproductive psychiatrist when indicated, and as early in the pregnancy as possible.
Psychiatrists who treat women of childbearing age should consider that those women may become pregnant, and that women with psychiatric illness are more likely to have unplanned pregnancies.1 Thus, thoughtful perinatal medication choices should begin before pregnancy. Pregnancy is a time of vulnerability to psychiatric illness for many reasons, including physiologic changes that can affect mental status; changes in medication efficacy; and numerous stressors, such as new responsibilities and limited sleep.1,2 For the treatment of pregnant—or potentially pregnant—patients, we recommend the following.
Do not panic! Knee-jerk medication changes in response to learning a patient is pregnant can lead to an exacerbation of psychiatric symptoms, as well as decrease trust in clinicians.2 Switching to a medication with a purportedly “safer” reproductive profile may worsen psychiatric illness, while also exposing the fetus to a medication of unknown benefit. 2
Recognize the risk of untreated or undertreated psychiatric illness, either of which has the potential to harm both the woman and her fetus. For example, a pregnant woman in a manic state may be more likely to engage in risky behaviors, such as drug use or risky sexual activity, which can lead to adverse fetal outcomes. They may also present with a higher risk of suicide. Compared to nonpregnant women, pregnant women for whom lithium was discontinued were equally likely to experience illness recurrence and significantly more likely to experience postpartum illness recurrence.3 In addition, the risk of recurrence was greater after rapid discontinuation compared with gradual discontinuation.3
Accurately communicate research findings. Pregnancy risk categories are no longer used. A nuanced interpretation of the potential adverse effects of a medication, such as malformations, impaired fetal growth, birth outcomes (such as preterm birth), and neurodevelopmental sequelae is necessary. Physicians must accurately convey information about risks to their patients, including both the absolute risk of an adverse event and the possible range of severity. For example, lithium use during pregnancy confers a higher relative risk of Ebstein’s anomaly (a cardiac defect).4 However, the absolute incidence of this risk remains low: 0.6% of lithium-exposed infants vs 0.18% among unexposed infants.4 Ebstein’s anomaly also varies significantly in severity—serious cases may require surgery, but less serious cases need only monitoring. A reliable database that compiles the latest evidence may help in staying abreast of the latest data.
Treat the psychiatric illness. Consider the optimal treatment for the psychiatric illness. Lithium remains the gold standard treatment for bipolar I disorder, regardless of reproductive status. Olanzapine and quetiapine are also commonly used and effective during pregnancy. This is an opportunity to conduct a detailed review of the patient’s previous medication regimens, including a review of medication trials and efficacy. Keep in mind that untreated bipolar disorder also carries an increased risk of adverse pregnancy outcomes.5
Consider pregnancy timing. Most organs form between weeks 3 to 8 of pregnancy. For example, if a medication potentially affects heart formation, but the patient is in the third trimester, explain to her that the heart has already been formed. Consider that medication may be required long-term and affect future pregnancies. Pregnant women require more frequent monitoring, because blood volume changes in pregnancy and postpartum can affect medication levels and efficacy. In addition, note whether a woman plans to breastfeed and be mindful of a medication’s profile in breastfeeding.
Ensure the patient can provide informed consent. Communicate your diagnostic formulation and treatment options. Consider involving the patient’s partner and/or support system in the discussion, if the patient consents. If a patient cannot provide informed consent, a surrogate decision-maker should be identified.6
Continue to: Collaborate with other clinicians
Collaborate with other clinicians, such as the patient’s OB/GYN and family medicine physician when possible. This will ensure that all clinicians are on the same page.
Plan for future pregnancies. Psychiatric medications can be long-term. Even patients who say they do not wish to become pregnant may someday become pregnant. Having discussions about medication choices, and their reproductive implications, prior to pregnancy allows patients to take an active role in their health.1,2
Consult a reproductive psychiatrist when indicated, and as early in the pregnancy as possible.
1. Friedman SH. The ethics of treating depression in pregnancy. J Prim Health Care. 2015;7(1):81-83.
2. Friedman SH, Reed E. Treating psychosis in pregnant women: a measured approach. Current Psychiatry. 2021; 20(7):34-35.
3. Viguera AC, Nonacs R, Cohen LS, et al. Risk of recurrence of bipolar disorder in pregnant and nonpregnant women after discontinuing lithium maintenance. Am J Psychiatry. 2000;157(2):179-184.
4. Patorno E, Huybrechts KF, Bateman BT, et al. Lithium use in pregnancy and the risk of cardiac malformations. N Engl J Med. 2017;376(23):2245-2254.
5. Bodén R, Lundgren M, Brandt L, et al. Risks of adverse pregnancy and birth outcomes in women treated or not treated with mood stabilisers for bipolar disorder: population based cohort study. BMJ. 2012;345:e7085. doi:10.1136/bmj.e7085
6. Ross NE, Webster TG, Tastenhoye CA, et al. Reproductive decision-making capacity in women with psychiatric illness: a systematic review. J Acad Consult Liaison Psychiatry. 2022:63(1);61-70.
1. Friedman SH. The ethics of treating depression in pregnancy. J Prim Health Care. 2015;7(1):81-83.
2. Friedman SH, Reed E. Treating psychosis in pregnant women: a measured approach. Current Psychiatry. 2021; 20(7):34-35.
3. Viguera AC, Nonacs R, Cohen LS, et al. Risk of recurrence of bipolar disorder in pregnant and nonpregnant women after discontinuing lithium maintenance. Am J Psychiatry. 2000;157(2):179-184.
4. Patorno E, Huybrechts KF, Bateman BT, et al. Lithium use in pregnancy and the risk of cardiac malformations. N Engl J Med. 2017;376(23):2245-2254.
5. Bodén R, Lundgren M, Brandt L, et al. Risks of adverse pregnancy and birth outcomes in women treated or not treated with mood stabilisers for bipolar disorder: population based cohort study. BMJ. 2012;345:e7085. doi:10.1136/bmj.e7085
6. Ross NE, Webster TG, Tastenhoye CA, et al. Reproductive decision-making capacity in women with psychiatric illness: a systematic review. J Acad Consult Liaison Psychiatry. 2022:63(1);61-70.
Loneliness: How psychiatry can help
Loneliness is distress that occurs when the quality or quantity of social relationships are less than desired.1 It is a symptom of many psychiatric disorders, and can lead to multiple negative health consequences, including depression, sleep deprivation, executive dysfunction, accelerated cognitive decline, and hypertension. Loneliness can increase the likelihood of immunocompromising conditions, including (but not limited to) stroke, anxiety, and depression, resulting in frequent emergency department visits and costly health expenses.2 Up to 80% of individuals younger than age 18 and 40% of adults older than age 65 report being lonely at least sometimes, with levels of loneliness gradually diminishing during middle age and then increasing in older adults.1 Loneliness is such a common and pervasive problem that in 2017, the government of the United Kingdom created a commission on loneliness and developed a Minister of Loneliness to find solutions to reduce it.3 In this article, I discuss the detrimental impact loneliness can have on our patients, and steps we can take to address it.
What contributes to loneliness?
Most people prefer the company of others, but some psychiatric disorders can cause individuals to become antisocial. For example, patients with schizoid personality disorder avoid social activities and interaction with others. Other patients may want to form bonds with others but their psychiatric disorder hinders this. For example, those with paranoia and social anxiety may avoid interacting with people due to their mistrust of others or their actions. Patients with substance use disorders can drive away those closest to them and lose familial bonds as a result of their behaviors. Patients with depression might not have the energy to pursue relationships and often have faulty cognitive patterns that lead them to believe they are unloved and unwanted.
Situational factors play a significant role in feelings of loneliness. Loss of a job or friends, ending a relationship, death of a loved one, or social isolation as experienced by COVID-19 or other illnesses can lead to loneliness. Social factors such as lack of income or transportation can make it difficult to attend or take part in social activities and events.
Some patients with dementia express feeling lonely, even after a visit from loved ones, because they forget the visit occurred. Nursing home residents often experience loneliness. Children may feel lonely after being subjected to bullying. College students, especially freshmen who are away from home for the first time, report significant levels of loneliness. Members of the LGBTQ+ community are often lonely due to familial rejection, prejudice, and religious beliefs. Anyone can experience loneliness, even married individuals if the marriage is unsatisfying.
What can psychiatry do to help?
Fortunately, psychiatric clinicians can play a large role in helping patients with loneliness.
Assessment. Ask the patient about the status of their present relationships and if they are feeling lonely. If yes, ask additional questions to identify possible causes. Are there conflicts that can be resolved? Is there abuse? What do they believe is the cause of their loneliness, and what might be the solution? How would their life be different if they weren’t lonely?
Treatment. When indicated, pharmacologic interventions might relieve symptoms that interfere with relationships and social interactions. For example, several types of antidepressants can improve mood and reduce anxiety, and selective serotonin reuptake inhibitors may relieve panic symptoms. Benzodiazepines and beta-blockers can reduce symptoms of social anxiety. Antipsychotics can reduce paranoia. Stimulants can aid patients with attention-deficit/hyperactivity disorder by improving their ability to interact with others.
Continue to: Psychotherapy and counseling...
Psychotherapy and counseling can specifically target loneliness. Solution-focused therapy, for example, involves solving the problem by deciding which actions the patient needs to take to relieve symptoms of loneliness. Dialectal behavior therapy can help patients with borderline and other personality disorders regulate their emotions and accept their feelings. Cognitive therapy and rational emotive therapy use various techniques to assist patients in changing their negative thought patterns. For example, a therapist might assign a patient to introduce themselves to a stranger or attend an event with others. The assignment is then discussed at the next session. Client-centered, psychodynamic, and behavior therapies also may be appropriate for a patient experiencing loneliness. Positive psychology can aid patients by helping them appreciate and not discount others in their lives. Meditation and mindfulness can motivate individuals to live in the present and enjoy those around them.
Referral and psychosocial support can be offered to direct patients to social services for help in improving their living circumstances. For example, a patient with an alcohol use disorder may benefit from a referral to a self-help organization such as Alcoholics Anonymous, where they can receive additional support and develop friendships. Other resources might offer patients the ability to discuss solutions, such as the benefits of owning a pet, attending a class, or volunteering opportunities, to combat loneliness.
Living a purposeful life is essential to engaging with others and avoiding isolation. Many people have turned to online support rooms, chat rooms, gaming, and social media to maintain relationships and meet others. Excessive computer use can be detrimental, however, if used in a manner that doesn’t involve interaction with others.
Regardless of the specific intervention, psychiatrists and other psychiatric clinicians can play a major role in reducing a patient’s loneliness. Simply by being present, you are showing the patient that at least one person in their life listens and cares.
1. Hawkley LC, Cacioppo JT. Loneliness matters: a theoretical and empirical review of consequences and mechanisms. Ann Behav Med. 2010;40(2):218-227.
2. Pimlott N. The ministry of loneliness. Can Fam Physician. 2018;64(3):166.
3. Leach N. The health consequences of loneliness. Causes and health consequences of being lonely. 2020. Accessed March 24, 2022. https://www.awpnow.com/main/2020/02/04/the-health-consequences-of-loneliness/
Loneliness is distress that occurs when the quality or quantity of social relationships are less than desired.1 It is a symptom of many psychiatric disorders, and can lead to multiple negative health consequences, including depression, sleep deprivation, executive dysfunction, accelerated cognitive decline, and hypertension. Loneliness can increase the likelihood of immunocompromising conditions, including (but not limited to) stroke, anxiety, and depression, resulting in frequent emergency department visits and costly health expenses.2 Up to 80% of individuals younger than age 18 and 40% of adults older than age 65 report being lonely at least sometimes, with levels of loneliness gradually diminishing during middle age and then increasing in older adults.1 Loneliness is such a common and pervasive problem that in 2017, the government of the United Kingdom created a commission on loneliness and developed a Minister of Loneliness to find solutions to reduce it.3 In this article, I discuss the detrimental impact loneliness can have on our patients, and steps we can take to address it.
What contributes to loneliness?
Most people prefer the company of others, but some psychiatric disorders can cause individuals to become antisocial. For example, patients with schizoid personality disorder avoid social activities and interaction with others. Other patients may want to form bonds with others but their psychiatric disorder hinders this. For example, those with paranoia and social anxiety may avoid interacting with people due to their mistrust of others or their actions. Patients with substance use disorders can drive away those closest to them and lose familial bonds as a result of their behaviors. Patients with depression might not have the energy to pursue relationships and often have faulty cognitive patterns that lead them to believe they are unloved and unwanted.
Situational factors play a significant role in feelings of loneliness. Loss of a job or friends, ending a relationship, death of a loved one, or social isolation as experienced by COVID-19 or other illnesses can lead to loneliness. Social factors such as lack of income or transportation can make it difficult to attend or take part in social activities and events.
Some patients with dementia express feeling lonely, even after a visit from loved ones, because they forget the visit occurred. Nursing home residents often experience loneliness. Children may feel lonely after being subjected to bullying. College students, especially freshmen who are away from home for the first time, report significant levels of loneliness. Members of the LGBTQ+ community are often lonely due to familial rejection, prejudice, and religious beliefs. Anyone can experience loneliness, even married individuals if the marriage is unsatisfying.
What can psychiatry do to help?
Fortunately, psychiatric clinicians can play a large role in helping patients with loneliness.
Assessment. Ask the patient about the status of their present relationships and if they are feeling lonely. If yes, ask additional questions to identify possible causes. Are there conflicts that can be resolved? Is there abuse? What do they believe is the cause of their loneliness, and what might be the solution? How would their life be different if they weren’t lonely?
Treatment. When indicated, pharmacologic interventions might relieve symptoms that interfere with relationships and social interactions. For example, several types of antidepressants can improve mood and reduce anxiety, and selective serotonin reuptake inhibitors may relieve panic symptoms. Benzodiazepines and beta-blockers can reduce symptoms of social anxiety. Antipsychotics can reduce paranoia. Stimulants can aid patients with attention-deficit/hyperactivity disorder by improving their ability to interact with others.
Continue to: Psychotherapy and counseling...
Psychotherapy and counseling can specifically target loneliness. Solution-focused therapy, for example, involves solving the problem by deciding which actions the patient needs to take to relieve symptoms of loneliness. Dialectal behavior therapy can help patients with borderline and other personality disorders regulate their emotions and accept their feelings. Cognitive therapy and rational emotive therapy use various techniques to assist patients in changing their negative thought patterns. For example, a therapist might assign a patient to introduce themselves to a stranger or attend an event with others. The assignment is then discussed at the next session. Client-centered, psychodynamic, and behavior therapies also may be appropriate for a patient experiencing loneliness. Positive psychology can aid patients by helping them appreciate and not discount others in their lives. Meditation and mindfulness can motivate individuals to live in the present and enjoy those around them.
Referral and psychosocial support can be offered to direct patients to social services for help in improving their living circumstances. For example, a patient with an alcohol use disorder may benefit from a referral to a self-help organization such as Alcoholics Anonymous, where they can receive additional support and develop friendships. Other resources might offer patients the ability to discuss solutions, such as the benefits of owning a pet, attending a class, or volunteering opportunities, to combat loneliness.
Living a purposeful life is essential to engaging with others and avoiding isolation. Many people have turned to online support rooms, chat rooms, gaming, and social media to maintain relationships and meet others. Excessive computer use can be detrimental, however, if used in a manner that doesn’t involve interaction with others.
Regardless of the specific intervention, psychiatrists and other psychiatric clinicians can play a major role in reducing a patient’s loneliness. Simply by being present, you are showing the patient that at least one person in their life listens and cares.
Loneliness is distress that occurs when the quality or quantity of social relationships are less than desired.1 It is a symptom of many psychiatric disorders, and can lead to multiple negative health consequences, including depression, sleep deprivation, executive dysfunction, accelerated cognitive decline, and hypertension. Loneliness can increase the likelihood of immunocompromising conditions, including (but not limited to) stroke, anxiety, and depression, resulting in frequent emergency department visits and costly health expenses.2 Up to 80% of individuals younger than age 18 and 40% of adults older than age 65 report being lonely at least sometimes, with levels of loneliness gradually diminishing during middle age and then increasing in older adults.1 Loneliness is such a common and pervasive problem that in 2017, the government of the United Kingdom created a commission on loneliness and developed a Minister of Loneliness to find solutions to reduce it.3 In this article, I discuss the detrimental impact loneliness can have on our patients, and steps we can take to address it.
What contributes to loneliness?
Most people prefer the company of others, but some psychiatric disorders can cause individuals to become antisocial. For example, patients with schizoid personality disorder avoid social activities and interaction with others. Other patients may want to form bonds with others but their psychiatric disorder hinders this. For example, those with paranoia and social anxiety may avoid interacting with people due to their mistrust of others or their actions. Patients with substance use disorders can drive away those closest to them and lose familial bonds as a result of their behaviors. Patients with depression might not have the energy to pursue relationships and often have faulty cognitive patterns that lead them to believe they are unloved and unwanted.
Situational factors play a significant role in feelings of loneliness. Loss of a job or friends, ending a relationship, death of a loved one, or social isolation as experienced by COVID-19 or other illnesses can lead to loneliness. Social factors such as lack of income or transportation can make it difficult to attend or take part in social activities and events.
Some patients with dementia express feeling lonely, even after a visit from loved ones, because they forget the visit occurred. Nursing home residents often experience loneliness. Children may feel lonely after being subjected to bullying. College students, especially freshmen who are away from home for the first time, report significant levels of loneliness. Members of the LGBTQ+ community are often lonely due to familial rejection, prejudice, and religious beliefs. Anyone can experience loneliness, even married individuals if the marriage is unsatisfying.
What can psychiatry do to help?
Fortunately, psychiatric clinicians can play a large role in helping patients with loneliness.
Assessment. Ask the patient about the status of their present relationships and if they are feeling lonely. If yes, ask additional questions to identify possible causes. Are there conflicts that can be resolved? Is there abuse? What do they believe is the cause of their loneliness, and what might be the solution? How would their life be different if they weren’t lonely?
Treatment. When indicated, pharmacologic interventions might relieve symptoms that interfere with relationships and social interactions. For example, several types of antidepressants can improve mood and reduce anxiety, and selective serotonin reuptake inhibitors may relieve panic symptoms. Benzodiazepines and beta-blockers can reduce symptoms of social anxiety. Antipsychotics can reduce paranoia. Stimulants can aid patients with attention-deficit/hyperactivity disorder by improving their ability to interact with others.
Continue to: Psychotherapy and counseling...
Psychotherapy and counseling can specifically target loneliness. Solution-focused therapy, for example, involves solving the problem by deciding which actions the patient needs to take to relieve symptoms of loneliness. Dialectal behavior therapy can help patients with borderline and other personality disorders regulate their emotions and accept their feelings. Cognitive therapy and rational emotive therapy use various techniques to assist patients in changing their negative thought patterns. For example, a therapist might assign a patient to introduce themselves to a stranger or attend an event with others. The assignment is then discussed at the next session. Client-centered, psychodynamic, and behavior therapies also may be appropriate for a patient experiencing loneliness. Positive psychology can aid patients by helping them appreciate and not discount others in their lives. Meditation and mindfulness can motivate individuals to live in the present and enjoy those around them.
Referral and psychosocial support can be offered to direct patients to social services for help in improving their living circumstances. For example, a patient with an alcohol use disorder may benefit from a referral to a self-help organization such as Alcoholics Anonymous, where they can receive additional support and develop friendships. Other resources might offer patients the ability to discuss solutions, such as the benefits of owning a pet, attending a class, or volunteering opportunities, to combat loneliness.
Living a purposeful life is essential to engaging with others and avoiding isolation. Many people have turned to online support rooms, chat rooms, gaming, and social media to maintain relationships and meet others. Excessive computer use can be detrimental, however, if used in a manner that doesn’t involve interaction with others.
Regardless of the specific intervention, psychiatrists and other psychiatric clinicians can play a major role in reducing a patient’s loneliness. Simply by being present, you are showing the patient that at least one person in their life listens and cares.
1. Hawkley LC, Cacioppo JT. Loneliness matters: a theoretical and empirical review of consequences and mechanisms. Ann Behav Med. 2010;40(2):218-227.
2. Pimlott N. The ministry of loneliness. Can Fam Physician. 2018;64(3):166.
3. Leach N. The health consequences of loneliness. Causes and health consequences of being lonely. 2020. Accessed March 24, 2022. https://www.awpnow.com/main/2020/02/04/the-health-consequences-of-loneliness/
1. Hawkley LC, Cacioppo JT. Loneliness matters: a theoretical and empirical review of consequences and mechanisms. Ann Behav Med. 2010;40(2):218-227.
2. Pimlott N. The ministry of loneliness. Can Fam Physician. 2018;64(3):166.
3. Leach N. The health consequences of loneliness. Causes and health consequences of being lonely. 2020. Accessed March 24, 2022. https://www.awpnow.com/main/2020/02/04/the-health-consequences-of-loneliness/
I STEP: Recognizing cognitive distortions in posttraumatic stress disorder
Evidence-based cognitive-behavioral therapies for posttraumatic stress disorder (PTSD) may employ cognitive restructuring. This psychotherapeutic technique entails recognizing and correcting maladaptive, inaccurate thoughts that perpetuate illness.1 For example, a clinician helps a patient recognize that the negative thought “Nobody loves me” following a romantic breakup is an overgeneralization. The patient is taught to self-correct this to “While my ex-girlfriend doesn’t love me, others do. It only feels like nobody loves me.”2
We introduce the acronym I STEP to help clinicians recognize several common distorted thoughts in PTSD. These tend to occur within stereotyped themes in PTSD,3 as outlined and illustrated below. Recognizing distorted thoughts in these patients will help clinicians understand and address psychological distress following trauma.
Intimacy/In-touch. Intimacy involves comfort in relationships, including but not limited to sexual intimacy. This requires being in touch emotionally with self and others. In trauma involving loss, fear of further loss may impair intimacy with others. Difficulty with self-intimacy impairs commitment to life’s goals and prompts unhelpful avoidance behaviors, such as difficulty being alone or self-injurious use of drugs or alcohol. Comfort in spending some portion of time alone with one’s thoughts and emotions is a life skill necessary to attain optimum function. Patients who are unable to tolerate their own emotions without constant company might have excessive anxiety when social supports are otherwise occupied. Such patients might seek excessive and repeated reassurance rather than learning to tolerate their own emotions and thoughts. They would then find it difficult to engage successfully in solo activities.
Safety. After trauma, patients may view themselves and others as unsafe, and may overestimate risk. For example, a pedestrian who is struck by a vehicle may believe that crossing a street will again result in getting hit by a car without appreciating that people frequently cross streets without injury or that crossing cautiously is an essential life skill. Parents who have suffered from trauma may unduly believe that their children are in danger when engaging in an activity generally considered to be safe. This may create challenges in parenting and impede their children’s ability to develop a sense of independence.
Trust. Trauma victims may unfairly blame themselves, leading them to mistrust their own judgment. Such patients may have difficulty making decisions confidently and independently, such as choosing a job or a romantic partner. When traumatized by another person or people, it can be difficult to maintain positive views of others or to accept others’ positive behaviors as genuine. For example, a common reaction following rape may be a generalized mistrust of all men.
Esteem. Patients’ self-esteem may suffer following trauma due to irrational self-blame or believing the “just world hypothesis”—the idea that bad things only happen to bad people. For example, a patient who suffers an assault by an acquaintance might think “I must be stupid if I couldn’t figure out that my friend was dangerous.”
Power. Traumatic events usually occur outside of one’s control. Survivors of trauma may lose confidence in their ability to control any aspect of their lives. Conversely, they may attempt to gain control of all of life’s circumstances, including those that are beyond anyone’s control. Control can be applied to emotions, behaviors, or events. A driver struck by a vehicle may think “I can’t control other drivers, so I have no power to control my safety while driving,” and hence give up driving. While there are things that are beyond our control, this extreme thought ignores things that we can control, such as wearing seatbelts or having the vehicle’s brakes regularly serviced.
1. Wenzel A. Basic strategies of cognitive behavioral therapy. Psychiatr Clin North Am. 2017;40(4):597-609.
2. Beck J. Cognitive behavioral therapy: basics and beyond. 2nd ed. The Guilford Press; 2011.
3. Resick PA, Monson CM, Chard KM. Cognitive processing therapy for PTSD. A comprehensive manual. The Guilford Press; 2017.
Evidence-based cognitive-behavioral therapies for posttraumatic stress disorder (PTSD) may employ cognitive restructuring. This psychotherapeutic technique entails recognizing and correcting maladaptive, inaccurate thoughts that perpetuate illness.1 For example, a clinician helps a patient recognize that the negative thought “Nobody loves me” following a romantic breakup is an overgeneralization. The patient is taught to self-correct this to “While my ex-girlfriend doesn’t love me, others do. It only feels like nobody loves me.”2
We introduce the acronym I STEP to help clinicians recognize several common distorted thoughts in PTSD. These tend to occur within stereotyped themes in PTSD,3 as outlined and illustrated below. Recognizing distorted thoughts in these patients will help clinicians understand and address psychological distress following trauma.
Intimacy/In-touch. Intimacy involves comfort in relationships, including but not limited to sexual intimacy. This requires being in touch emotionally with self and others. In trauma involving loss, fear of further loss may impair intimacy with others. Difficulty with self-intimacy impairs commitment to life’s goals and prompts unhelpful avoidance behaviors, such as difficulty being alone or self-injurious use of drugs or alcohol. Comfort in spending some portion of time alone with one’s thoughts and emotions is a life skill necessary to attain optimum function. Patients who are unable to tolerate their own emotions without constant company might have excessive anxiety when social supports are otherwise occupied. Such patients might seek excessive and repeated reassurance rather than learning to tolerate their own emotions and thoughts. They would then find it difficult to engage successfully in solo activities.
Safety. After trauma, patients may view themselves and others as unsafe, and may overestimate risk. For example, a pedestrian who is struck by a vehicle may believe that crossing a street will again result in getting hit by a car without appreciating that people frequently cross streets without injury or that crossing cautiously is an essential life skill. Parents who have suffered from trauma may unduly believe that their children are in danger when engaging in an activity generally considered to be safe. This may create challenges in parenting and impede their children’s ability to develop a sense of independence.
Trust. Trauma victims may unfairly blame themselves, leading them to mistrust their own judgment. Such patients may have difficulty making decisions confidently and independently, such as choosing a job or a romantic partner. When traumatized by another person or people, it can be difficult to maintain positive views of others or to accept others’ positive behaviors as genuine. For example, a common reaction following rape may be a generalized mistrust of all men.
Esteem. Patients’ self-esteem may suffer following trauma due to irrational self-blame or believing the “just world hypothesis”—the idea that bad things only happen to bad people. For example, a patient who suffers an assault by an acquaintance might think “I must be stupid if I couldn’t figure out that my friend was dangerous.”
Power. Traumatic events usually occur outside of one’s control. Survivors of trauma may lose confidence in their ability to control any aspect of their lives. Conversely, they may attempt to gain control of all of life’s circumstances, including those that are beyond anyone’s control. Control can be applied to emotions, behaviors, or events. A driver struck by a vehicle may think “I can’t control other drivers, so I have no power to control my safety while driving,” and hence give up driving. While there are things that are beyond our control, this extreme thought ignores things that we can control, such as wearing seatbelts or having the vehicle’s brakes regularly serviced.
Evidence-based cognitive-behavioral therapies for posttraumatic stress disorder (PTSD) may employ cognitive restructuring. This psychotherapeutic technique entails recognizing and correcting maladaptive, inaccurate thoughts that perpetuate illness.1 For example, a clinician helps a patient recognize that the negative thought “Nobody loves me” following a romantic breakup is an overgeneralization. The patient is taught to self-correct this to “While my ex-girlfriend doesn’t love me, others do. It only feels like nobody loves me.”2
We introduce the acronym I STEP to help clinicians recognize several common distorted thoughts in PTSD. These tend to occur within stereotyped themes in PTSD,3 as outlined and illustrated below. Recognizing distorted thoughts in these patients will help clinicians understand and address psychological distress following trauma.
Intimacy/In-touch. Intimacy involves comfort in relationships, including but not limited to sexual intimacy. This requires being in touch emotionally with self and others. In trauma involving loss, fear of further loss may impair intimacy with others. Difficulty with self-intimacy impairs commitment to life’s goals and prompts unhelpful avoidance behaviors, such as difficulty being alone or self-injurious use of drugs or alcohol. Comfort in spending some portion of time alone with one’s thoughts and emotions is a life skill necessary to attain optimum function. Patients who are unable to tolerate their own emotions without constant company might have excessive anxiety when social supports are otherwise occupied. Such patients might seek excessive and repeated reassurance rather than learning to tolerate their own emotions and thoughts. They would then find it difficult to engage successfully in solo activities.
Safety. After trauma, patients may view themselves and others as unsafe, and may overestimate risk. For example, a pedestrian who is struck by a vehicle may believe that crossing a street will again result in getting hit by a car without appreciating that people frequently cross streets without injury or that crossing cautiously is an essential life skill. Parents who have suffered from trauma may unduly believe that their children are in danger when engaging in an activity generally considered to be safe. This may create challenges in parenting and impede their children’s ability to develop a sense of independence.
Trust. Trauma victims may unfairly blame themselves, leading them to mistrust their own judgment. Such patients may have difficulty making decisions confidently and independently, such as choosing a job or a romantic partner. When traumatized by another person or people, it can be difficult to maintain positive views of others or to accept others’ positive behaviors as genuine. For example, a common reaction following rape may be a generalized mistrust of all men.
Esteem. Patients’ self-esteem may suffer following trauma due to irrational self-blame or believing the “just world hypothesis”—the idea that bad things only happen to bad people. For example, a patient who suffers an assault by an acquaintance might think “I must be stupid if I couldn’t figure out that my friend was dangerous.”
Power. Traumatic events usually occur outside of one’s control. Survivors of trauma may lose confidence in their ability to control any aspect of their lives. Conversely, they may attempt to gain control of all of life’s circumstances, including those that are beyond anyone’s control. Control can be applied to emotions, behaviors, or events. A driver struck by a vehicle may think “I can’t control other drivers, so I have no power to control my safety while driving,” and hence give up driving. While there are things that are beyond our control, this extreme thought ignores things that we can control, such as wearing seatbelts or having the vehicle’s brakes regularly serviced.
1. Wenzel A. Basic strategies of cognitive behavioral therapy. Psychiatr Clin North Am. 2017;40(4):597-609.
2. Beck J. Cognitive behavioral therapy: basics and beyond. 2nd ed. The Guilford Press; 2011.
3. Resick PA, Monson CM, Chard KM. Cognitive processing therapy for PTSD. A comprehensive manual. The Guilford Press; 2017.
1. Wenzel A. Basic strategies of cognitive behavioral therapy. Psychiatr Clin North Am. 2017;40(4):597-609.
2. Beck J. Cognitive behavioral therapy: basics and beyond. 2nd ed. The Guilford Press; 2011.
3. Resick PA, Monson CM, Chard KM. Cognitive processing therapy for PTSD. A comprehensive manual. The Guilford Press; 2017.
Differentiating pediatric schizotypal disorder from schizophrenia and autism
Schizotypal disorder is a complex condition that is characterized by cognitive-perceptual impairments, oddness, disorganization, and interpersonal difficulties. It often is unrecognized or underdiagnosed. In DSM-5, schizotypal disorder is categorized a personality disorder, but it is also considered part of the schizophrenia spectrum disorders.1 The diagnostic criteria for schizotypal disorder are outlined in the Table.1,2
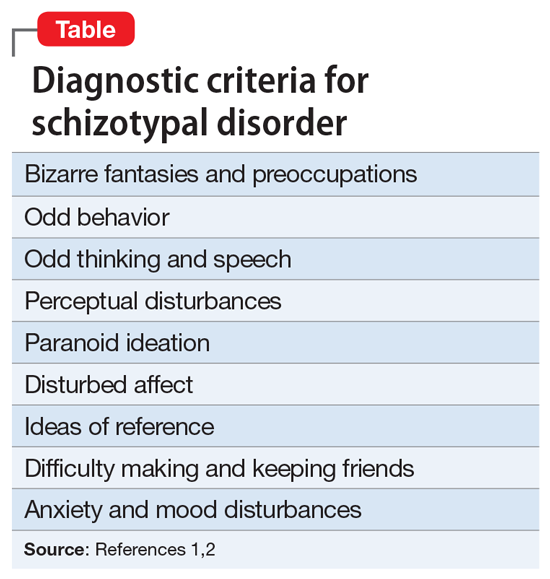
Although schizotypal disorder has a lifetime prevalence of approximately 4% in the general population of the United States,2 it can present during childhood or adolescence and may be overlooked in the differential diagnosis for psychotic symptoms in pediatric patients.3 Schizotypal disorder of childhood (SDC) can present with significant overlap with several pediatric diagnoses, including schizophrenia spectrum disorders and autism spectrum disorder (ASD), all of which may include psychotic symptoms and difficulties in interpersonal relationships. This overlap, combined with the lack of awareness of schizotypal disorder, can pose a diagnostic challenge. Better recognition of SDC could result in earlier and more effective treatment. In this article, we provide tips for differentiating SDC from childhood-onset schizophrenia and from ASD.
Differentiating SDC from schizophrenia
SDC may be mistaken for childhood-onset schizophrenia due to its perceptual disturbances (which may be interpreted as visual or auditory hallucinations), bizarre fantasies (which may be mistaken for overt delusions), paranoia, and odd behavior. Two ways to distinguish SDC from childhood schizophrenia are by clinical course and by severity of negative psychotic symptoms.
SDC tends to have an overall stable clinical course,4 with patients experiencing periods of time when they exhibit a more normal mental status complemented by fluctuations in symptom severity, which are exacerbated by stressors and followed by a return to baseline.3 SDC psychotic symptoms are predominantly positive, and patients typically do not demonstrate negative features beyond social difficulties. Childhood-onset schizophrenia is typically progressive and disabling, with worsening severity over time, and is much more likely to incorporate prominent negative symptoms.3
Differentiating SDC from ASD
SDC also demonstrates considerable diagnostic overlap with ASD, especially with regards to inappropriate affect; odd thinking, behavior, and speech; and social difficulties. Further complicating the diagnosis, ASD and SDC are comorbid in approximately 40% of ASD cases.3,5 The Melbourne Assessment of Schizotypy in Kids demonstrates validity in diagnosing schizotypal disorder in patients with comorbid ASD.5,6 For clinicians without easy access to advanced testing, 2 ways to distinguish SDC from ASD are the content of the odd behavior and thoughts, and the patient’s reaction to social deficits.
In SDC, odd behavior and thoughts most often revolve around daydreaming and a focus on “elaborate inner fantasies.”3,6 Unlike in ASD, in patients with SDC, behaviors don’t typically involve stereotyped mannerisms, the patient is unlikely to have rigid interests (apart from their fantasies), and there is not a particular focus on detail in the external world.3,6 Notably, imaginary companions are common in SDC; children with ASD are less likely to have an imaginary companion compared with children with SDC or those with no psychiatric diagnosis.6 Patients with SDC have social difficulties (often due to social anxiety stemming from their paranoia) but usually seek out interaction and are bothered by alienation, while patients with ASD may have less interest in social engagement.6
1. Diagnostic and Statistical Manual of Mental Disorders: DSM-5. 5th ed. American Psychiatric Association; 2013.
2. Pulay AJ, Stinson FS, Dawson DA, et al. Prevalence, correlates, disability, and comorbidity of DSM-IV schizotypal personality disorder: results from the wave 2 national epidemiologic survey on alcohol and related conditions. Prim Care Companion J Clin Psychiatry. 2009;11(2):53-67. doi:10.4088/pcc.08m00679
3. Tonge BJ, Testa R, Díaz-Arteche C, et al. Schizotypal disorder in children—a neglected diagnosis. Schizophrenia Bulletin Open. 2020;1(1):sgaa048. doi:10.1093/schizbullopen/sgaa048
4. Asarnow JR. Childhood-onset schizotypal disorder: a follow-up study and comparison with childhood-onset schizophrenia. J Child Adolesc Psychopharmacol. 2005;15(3):395-402.
5. Jones HP, Testa RR, Ross N, et al. The Melbourne Assessment of Schizotypy in Kids: a useful measure of childhood schizotypal personality disorder. Biomed Res Int. 2015;2015:635732. doi:10.1155/2015/635732
6. Poletti M, Raballo A. Childhood schizotypal features vs. high-functioning autism spectrum disorder: developmental overlaps and phenomenological differences. Schizophr Res. 2020;223:53-58. doi:10.1016/j.schres.2020.09.027
Schizotypal disorder is a complex condition that is characterized by cognitive-perceptual impairments, oddness, disorganization, and interpersonal difficulties. It often is unrecognized or underdiagnosed. In DSM-5, schizotypal disorder is categorized a personality disorder, but it is also considered part of the schizophrenia spectrum disorders.1 The diagnostic criteria for schizotypal disorder are outlined in the Table.1,2
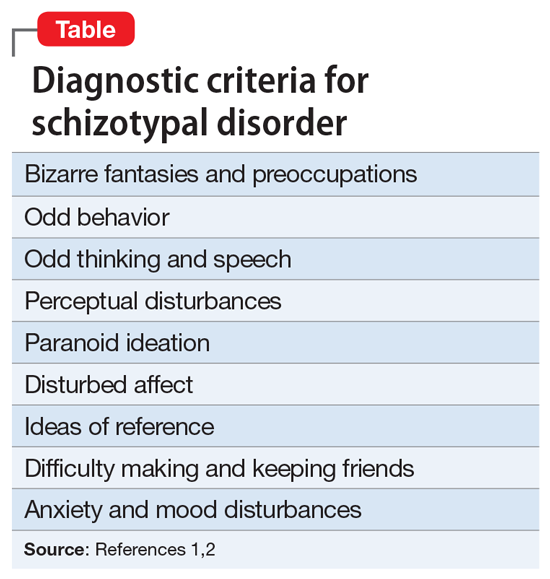
Although schizotypal disorder has a lifetime prevalence of approximately 4% in the general population of the United States,2 it can present during childhood or adolescence and may be overlooked in the differential diagnosis for psychotic symptoms in pediatric patients.3 Schizotypal disorder of childhood (SDC) can present with significant overlap with several pediatric diagnoses, including schizophrenia spectrum disorders and autism spectrum disorder (ASD), all of which may include psychotic symptoms and difficulties in interpersonal relationships. This overlap, combined with the lack of awareness of schizotypal disorder, can pose a diagnostic challenge. Better recognition of SDC could result in earlier and more effective treatment. In this article, we provide tips for differentiating SDC from childhood-onset schizophrenia and from ASD.
Differentiating SDC from schizophrenia
SDC may be mistaken for childhood-onset schizophrenia due to its perceptual disturbances (which may be interpreted as visual or auditory hallucinations), bizarre fantasies (which may be mistaken for overt delusions), paranoia, and odd behavior. Two ways to distinguish SDC from childhood schizophrenia are by clinical course and by severity of negative psychotic symptoms.
SDC tends to have an overall stable clinical course,4 with patients experiencing periods of time when they exhibit a more normal mental status complemented by fluctuations in symptom severity, which are exacerbated by stressors and followed by a return to baseline.3 SDC psychotic symptoms are predominantly positive, and patients typically do not demonstrate negative features beyond social difficulties. Childhood-onset schizophrenia is typically progressive and disabling, with worsening severity over time, and is much more likely to incorporate prominent negative symptoms.3
Differentiating SDC from ASD
SDC also demonstrates considerable diagnostic overlap with ASD, especially with regards to inappropriate affect; odd thinking, behavior, and speech; and social difficulties. Further complicating the diagnosis, ASD and SDC are comorbid in approximately 40% of ASD cases.3,5 The Melbourne Assessment of Schizotypy in Kids demonstrates validity in diagnosing schizotypal disorder in patients with comorbid ASD.5,6 For clinicians without easy access to advanced testing, 2 ways to distinguish SDC from ASD are the content of the odd behavior and thoughts, and the patient’s reaction to social deficits.
In SDC, odd behavior and thoughts most often revolve around daydreaming and a focus on “elaborate inner fantasies.”3,6 Unlike in ASD, in patients with SDC, behaviors don’t typically involve stereotyped mannerisms, the patient is unlikely to have rigid interests (apart from their fantasies), and there is not a particular focus on detail in the external world.3,6 Notably, imaginary companions are common in SDC; children with ASD are less likely to have an imaginary companion compared with children with SDC or those with no psychiatric diagnosis.6 Patients with SDC have social difficulties (often due to social anxiety stemming from their paranoia) but usually seek out interaction and are bothered by alienation, while patients with ASD may have less interest in social engagement.6
Schizotypal disorder is a complex condition that is characterized by cognitive-perceptual impairments, oddness, disorganization, and interpersonal difficulties. It often is unrecognized or underdiagnosed. In DSM-5, schizotypal disorder is categorized a personality disorder, but it is also considered part of the schizophrenia spectrum disorders.1 The diagnostic criteria for schizotypal disorder are outlined in the Table.1,2
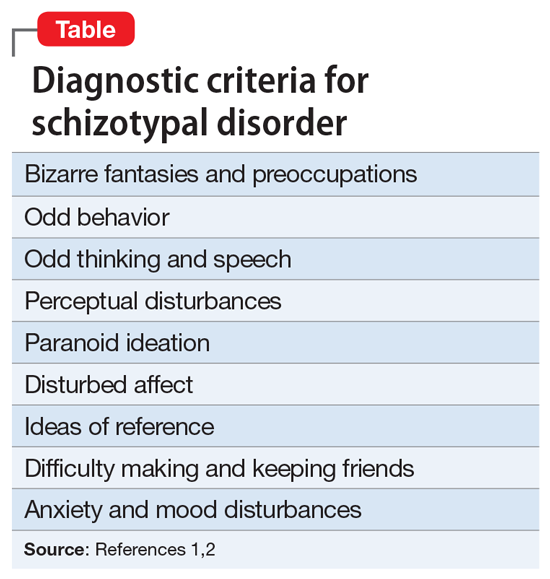
Although schizotypal disorder has a lifetime prevalence of approximately 4% in the general population of the United States,2 it can present during childhood or adolescence and may be overlooked in the differential diagnosis for psychotic symptoms in pediatric patients.3 Schizotypal disorder of childhood (SDC) can present with significant overlap with several pediatric diagnoses, including schizophrenia spectrum disorders and autism spectrum disorder (ASD), all of which may include psychotic symptoms and difficulties in interpersonal relationships. This overlap, combined with the lack of awareness of schizotypal disorder, can pose a diagnostic challenge. Better recognition of SDC could result in earlier and more effective treatment. In this article, we provide tips for differentiating SDC from childhood-onset schizophrenia and from ASD.
Differentiating SDC from schizophrenia
SDC may be mistaken for childhood-onset schizophrenia due to its perceptual disturbances (which may be interpreted as visual or auditory hallucinations), bizarre fantasies (which may be mistaken for overt delusions), paranoia, and odd behavior. Two ways to distinguish SDC from childhood schizophrenia are by clinical course and by severity of negative psychotic symptoms.
SDC tends to have an overall stable clinical course,4 with patients experiencing periods of time when they exhibit a more normal mental status complemented by fluctuations in symptom severity, which are exacerbated by stressors and followed by a return to baseline.3 SDC psychotic symptoms are predominantly positive, and patients typically do not demonstrate negative features beyond social difficulties. Childhood-onset schizophrenia is typically progressive and disabling, with worsening severity over time, and is much more likely to incorporate prominent negative symptoms.3
Differentiating SDC from ASD
SDC also demonstrates considerable diagnostic overlap with ASD, especially with regards to inappropriate affect; odd thinking, behavior, and speech; and social difficulties. Further complicating the diagnosis, ASD and SDC are comorbid in approximately 40% of ASD cases.3,5 The Melbourne Assessment of Schizotypy in Kids demonstrates validity in diagnosing schizotypal disorder in patients with comorbid ASD.5,6 For clinicians without easy access to advanced testing, 2 ways to distinguish SDC from ASD are the content of the odd behavior and thoughts, and the patient’s reaction to social deficits.
In SDC, odd behavior and thoughts most often revolve around daydreaming and a focus on “elaborate inner fantasies.”3,6 Unlike in ASD, in patients with SDC, behaviors don’t typically involve stereotyped mannerisms, the patient is unlikely to have rigid interests (apart from their fantasies), and there is not a particular focus on detail in the external world.3,6 Notably, imaginary companions are common in SDC; children with ASD are less likely to have an imaginary companion compared with children with SDC or those with no psychiatric diagnosis.6 Patients with SDC have social difficulties (often due to social anxiety stemming from their paranoia) but usually seek out interaction and are bothered by alienation, while patients with ASD may have less interest in social engagement.6
1. Diagnostic and Statistical Manual of Mental Disorders: DSM-5. 5th ed. American Psychiatric Association; 2013.
2. Pulay AJ, Stinson FS, Dawson DA, et al. Prevalence, correlates, disability, and comorbidity of DSM-IV schizotypal personality disorder: results from the wave 2 national epidemiologic survey on alcohol and related conditions. Prim Care Companion J Clin Psychiatry. 2009;11(2):53-67. doi:10.4088/pcc.08m00679
3. Tonge BJ, Testa R, Díaz-Arteche C, et al. Schizotypal disorder in children—a neglected diagnosis. Schizophrenia Bulletin Open. 2020;1(1):sgaa048. doi:10.1093/schizbullopen/sgaa048
4. Asarnow JR. Childhood-onset schizotypal disorder: a follow-up study and comparison with childhood-onset schizophrenia. J Child Adolesc Psychopharmacol. 2005;15(3):395-402.
5. Jones HP, Testa RR, Ross N, et al. The Melbourne Assessment of Schizotypy in Kids: a useful measure of childhood schizotypal personality disorder. Biomed Res Int. 2015;2015:635732. doi:10.1155/2015/635732
6. Poletti M, Raballo A. Childhood schizotypal features vs. high-functioning autism spectrum disorder: developmental overlaps and phenomenological differences. Schizophr Res. 2020;223:53-58. doi:10.1016/j.schres.2020.09.027
1. Diagnostic and Statistical Manual of Mental Disorders: DSM-5. 5th ed. American Psychiatric Association; 2013.
2. Pulay AJ, Stinson FS, Dawson DA, et al. Prevalence, correlates, disability, and comorbidity of DSM-IV schizotypal personality disorder: results from the wave 2 national epidemiologic survey on alcohol and related conditions. Prim Care Companion J Clin Psychiatry. 2009;11(2):53-67. doi:10.4088/pcc.08m00679
3. Tonge BJ, Testa R, Díaz-Arteche C, et al. Schizotypal disorder in children—a neglected diagnosis. Schizophrenia Bulletin Open. 2020;1(1):sgaa048. doi:10.1093/schizbullopen/sgaa048
4. Asarnow JR. Childhood-onset schizotypal disorder: a follow-up study and comparison with childhood-onset schizophrenia. J Child Adolesc Psychopharmacol. 2005;15(3):395-402.
5. Jones HP, Testa RR, Ross N, et al. The Melbourne Assessment of Schizotypy in Kids: a useful measure of childhood schizotypal personality disorder. Biomed Res Int. 2015;2015:635732. doi:10.1155/2015/635732
6. Poletti M, Raballo A. Childhood schizotypal features vs. high-functioning autism spectrum disorder: developmental overlaps and phenomenological differences. Schizophr Res. 2020;223:53-58. doi:10.1016/j.schres.2020.09.027





