User login
Addressing the Needs of Patients With Chronic Pain
Chronic pain is a common health care problem that remains a significant burden for the VHA.1,2 Some reports indicate that nearly 50% of VA patients report chronic pain.3,4 Both within and outside the VHA, primary care providers (PCPs) generally manage patients with chronic pain.5,6 Historically, a biomedical approach to chronic pain also included the use of opioid medications, which may have contributed to increased opioid-related morbidity and mortality especially among the veteran patient population.7-9 The use of opioids also is controversial due to concerns about adverse effects (AEs), long-term efficacy, functional outcomes, and the potential for drug abuse and addiction.10 Consequently, alternative treatment options that incorporate an interdisciplinary approach have gained significant interest among pain care providers.11 Interdisciplinary programs have been shown to improve functional status and psychological well-being and to reduce pain severity and opioid use.12-14 These benefits may persist for a decade or longer.15
Background
The Stepped Care Model for Pain Management (SCM-PM) is a specific pain treatment approach promoted by the VA National Pain Management Directive.16 This systematically adjusted approach is associated with improved patient satisfaction and health outcomes for pain and depression.17,18 At its core, the model promotes engaging patients as active participants in their care along with a team of doctors who can offer an integrated, evidence-based, multimodal, interdisciplinary treatment plan.
To successfully implement this strategy at the VA, patient aligned care teams (PACT) assess and manage patients with common pain conditions through collaboration with mental health, complementary and integrative health services, physical therapy, and other programs, such as opioid renewal clinics and pain schools.19 This collaborative care approach, which the PCP initiates, is step 1 of the SCM-PM. If initial treatment is not successful and patients are not improving as expected, specialty care consultation and collaborative comanagement through interdisciplinary pain specialty teams are sought (step 2). Finally, step 3 involves tertiary, interdisciplinary care, including access to advanced diagnostic and pain rehabilitation programs accredited by the Commission for Accreditation of Rehabilitation Facilities (CARF).
Although the advantages of interdisciplinary pain programs are clear, resource limitations as well as challenges related to competencies of the PCPs, nurses, and associated health care professionals in pain assessment and management can make implementation of these programs, including the SCM-PM, difficult for many clinics and facilities. Thus, identifying effective chronic pain models and strategies, incorporating the philosophy and key elements of interdisciplinary programs, and accounting for facility resources and capacity are all important.
At the Ann Arbor VAMC, development of a comprehensive interdisciplinary team started with the implementation of joint sessions with a clinical pharmacist and health psychologist embedded in primary care to enhance access to behavioral pain management interventions.20 This program was subsequently expanded to include a pain physician, 2 pain-focused physical therapists (PTs) and a pain nurse.
This article describes a novel team approach for providing more comprehensive, interdisciplinary care for patients with chronic pain along with the initial results for the patients who were part of an outpatient pain group program (OPGP).
Methods
Developing a more interdisciplinary pain management program included integrating different services and creating a strategy for comprehensive evaluation and management of patients with chronic pain. After patients were referred to the interdisciplinary pain clinic by their PCP, they received a systematically structured multidimensional assessment. The primary focus of this assessment was to create an individually directed treatment approach based on the patient’s responses to previous treatments and information collected from several questionnaires administered prior to evaluation. This information helped guide individual patient decision making and actively engaged patients in their care, thus following one of the central tenants of the SCM-PM model. Moreover, functional restoration was at the core of each patient’s evaluation and management. The primary focus was on nonpharmacologic treatment options that included psychological, physical, and occupational therapy; self-management; education; and complementary and alternative therapies. These modalities were offered either individually or in a group setting.
The first step after referral was an evaluation that followed the main core principles for complex disease management described by Tauben and Theodore.21 All new patients were asked to complete a 2-question pain intensity and pain interference measure, the 4-question Patient Health Questionnaire (PHQ-4), 4-question Primary Care-PTSD screening tool (PC-PTSD), and the STOP-BANG questionnaire to assess the risk for obstructive sleep apnea.22-24 Each measure allowed the physician to identify specific problem areas and formulate a treatment plan that would incorporate PTs or occupational therapists, psychologists and/or clinical specialists, and pharmacists if needed.
Patients who were found to have or expressed significant disability because of pain and who wished to learn pain self-management strategies could participate in an 8-week OPGP. This program included the use of cognitive behavioral therapy (CBT) strategies along with group physical therapy classes. Some patients also received individual therapies concurrently with the 8-week OPGP. Patients were excluded from participating in the OPGP only if their current medical or psychiatric status precluded them from full engagement and maximum benefit as determined by the pain physician and psychologist.
Participants and Intervention
Program participants were patients with a chronic pain diagnosis who enrolled in the interdisciplinary pain team OPGP between April 2016 and April 2017. Most patients were referred by their PCPs due to chronic low back, neck, joint or neuropathic pain, although many presented with multiple pain areas. The onset of pain often was a result of a service-related injury or overuse, or the etiology was unknown.
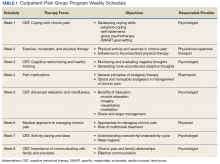
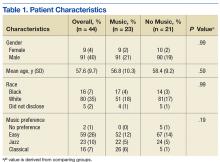
A board-certified pain physician, licensed clinical psychologist, 2 licensed PTs, and a clinical pharmacist led the OPGP sessions. The program was composed of 3-hour-long sessions held weekly for 8 consecutive weeks. Each week, a member of the team covered a specific topic (Table 1).
These sessions focused on the importance of exercise, movement, and physical therapy; appropriate use of medications for managing chronic pain; pacing activities and body mechanics; and the medical approach to managing chronic pain. In addition to didactic presentations, interaction and therapeutic dialogue was encouraged among patients. The education portion of each weekly session lasted about 90 minutes, including a short break. Then, following another short break, patients proceeded to the physical therapy area and engaged in an individualized, monitored exercise program, conducted by the team PTs. Patients also were issued pedometers and encouraged to track their steps each day. Education in improving posture and body mechanics was a key component of the exercise portion of the program so patients could resume their normal daily activities and regain enjoyment in their life. Pain outcomemeasures were collected at admission and immediately before discharge.
Medication management also was an important part of the program for some patients and included tapering off opioids and other drugs and implementing trials of adjuvant pain medications shown to help chronic pain. For some patients, this medication management continued after the patient completed the program.
Measures
The Pain Outcome Questionnaire (POQ) is a 19-item, self-report measure of pain treatment outcomes. Pain rating, mobility, activities of daily living, vitality, negative effect, and fear are the functioning domains evaluated, and the subscale scores are added to produce a total score. The POQ was developed from samples of veterans undergoing inpatient or outpatient pain treatment at VA facilities. For each of the subscales and the total score, higher values indicate poorer outcomes. In normative outpatient VA samples, a total score of 71 is at the 25th percentile, and 120 is at the 75th percentile. The POQ has been shown to have good reliability and validity among veterans in an outpatient setting.25
The Pain Catastrophizing Scale (PCS) is a 13-item scale designed to measure various levels of pain catastrophizing.26 Each item is rated on a 5-point Likert-type scale, from 0 (not at all) to 4 (all the time). The PCS consists of 3 subscale domains: rumination, 4 items; magnification, 3 items; and helplessness, 6 items. Responses to all items also can be added to produce a total score from 0 to 52, with higher scores indicating a higher level of catastrophic thinking related to pain. This project evaluated both the total score and the 3 subscale scores.
The Pain Self-Efficacy Questionnaire (PSEQ) is a 10-item questionnaire that assesses confidence in an individual’s ability to cope or to perform activities despite the pain.27 The PSEQ covers a range of functions, including household chores, socializing, work, as well as coping with pain without medications. Each question has a 7-point Likert scale response: 0 = not at all confident, and 7 = completely confident, to produce a total score from 0 to 60. Higher scores indicate stronger pain self-efficacy, which has been shown to be associated with return to work and maintenance of functional gains.
The Patient Health Questionnaire-4 (PHQ-4) is a 4-item instrument used to screen for depression and anxiety in outpatient medical settings.22 Patients indicate how often they have been bothered by certain problems on a 4-point Likert scale, from 0 (not at all) to 3 (nearly every day). The PHQ-4 provides a total score (0-12) with scores of 6 to 8 indicating moderate and 9 to 12 indicating severe psychological distress; 2 subscale scores, 1 for anxiety (2 questions) and 1 for depression (2 questions). For this analysis, the total PHQ-4 score has been dichotomized with 1 indicating a score in the moderate or severe range vs 0 for a score of mild or no psychological distress. Likewise, each of the subscale scores have been dichotomized with 1 indicating a score of 3 or greater, which is considered a positive screen.
The 6-minute walk test (6MWT) measures the distance (in feet) an individual can walk over a total of 6 minutes on a hard, flat surface.28 Even though the individual can walk at a self-selected pace and rest if needed during the test, the goal is for the patient to walk as far as possible over the course of 6 minutes. The 6MWT provides information regarding functional capacity, response to therapy, and prognosis across a range of chronic conditions, including pain.
Data Analysis
Data analysis included the use of both descriptive and comparative statistics. A descriptive analysis was conducted to examine the characteristics of patients who did and did not complete the OPGP. Specific outcomes for those individuals who completed the program, and thus had complete pre- and post-OPGP information, then were compared. Paired t tests were used to compare differences in continuous measures between baseline (pre-OPGP) and the 8-week follow-up (post-OPGP). Comparisons involving dichotomous measures were made using the Fisher exact test. A 2-sided α with a P value .05 was considered statistically significant. All statistical analyses were conducted using STATA version 14.1 (StataCorp, College Station, TX).
Results
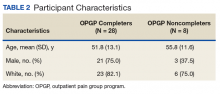
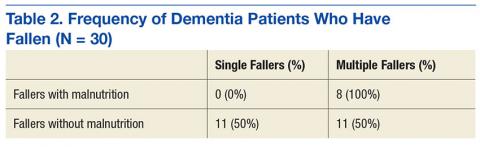
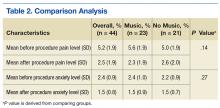
A total of 36 patients enrolled, and 28 (77%) completed the OPGP. Patients who did not complete the program (n = 8) either self-discharged due to lack of interest or had difficulty in consistently making their appointments and decided not to continue (Table 2).
Outcomes for OPGP Completers
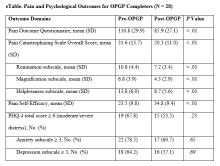
Improvements were observed for all outcome domains among patients who completed the program (eTable).
Discussion
This report describes the novel model for improving delivery of chronic pain management services implemented at the Ann Arbor VAMC through the development of a multidisciplinary pain PACT. The program included using a systematically structured multidimensional approach to identify appropriate treatments and delivery of interdisciplinary care for patients with chronic pain through an OPGP. The authors’ findings establish the feasibility and acceptability of the OPGP. More than 75% of those enrolled completed the program, indicating the promising potential of this approach with significant improvements observed for several pain-related outcomes among those who completed the 8-week program.
Stepped care is a well-established approach to managing complex chronic pain conditions. The approach adds increased levels of treatment intensity when there is no improvement after initial, simple measures are instituted (eg, over-the-counter pain medications, physical therapy, life style changes). Understanding the complexity of the pain experience while treating the patient and not simply the pain has the highest likelihood of helping patients with chronic pain. Given the prevalence of chronic pain among patients in primary care nationally, measurement-based pain care potentially could result in an earlier referral to appropriate care well before pain becomes intractable and chronic.
Growing evidence shows that multidisciplinary treatments reduce pain symptoms and intensity, medication, health care provider use, and improve quality of life.11-15,29,30 A systematic review by van Tulder and colleagues, for example, noted improvements in physical parameters, such as range of motion and flexibility and behavioral health parameters, including anxiety, depression, and cognition.29 Similarly, the cohort of patients who participated in the OPGP showed statistically significant improvements in several domains of pain-related distress and functioning following treatment, including pain catastrophizing, pain self-efficacy, and the multicomponent pain outcomes questionnaires. Functional improvement also was observed by comparing the distance walked in 6 minutes before and after program completion.
There is significant variation in duration of rehabilitation programs lasting from 2 weeks to 12 weeks or longer. These sessions consist of half days, daily sessions, weekly sessions, and monthly sessions. Inconsistencies also exist among programs that use 3 to 280 professional contact hours. Although it has been shown that programs with more than 100 hours of professional contact tended to have better outcomes than did those with less than 30 hours of contact, Stratton and colleagues reported that a 6-week group program was equivalent or better than a 12- and 10-week group program among veterans.11,31 These findings along with staffing and resource constraints led to the implementation of the 8-week OPGP with fewer than 30 hours of contact time per group. These results have important practical implications, as shorter treatments may offer comparable therapeutic impact than do longer, more time-intensive protocols.
Limitations
These findings were derived from a quality improvement project within one institution, and several limitations exist. Although the broader purpose of the article was to show how the fundamentals of creating a cohesive multidisciplinary chronic pain team can be implemented within the VA setting, the highlighted outcomes were primarily from participants in the OPGP Since this was not a controlled or experimental study and given potential sample size and selections issues as well as the lack of longer-term follow-up information, further study is needed to draw definitive conclusions about program effectiveness, despite promising preliminary results. In addition, medication use, such as opioids either before or after completion of the program, was not included as part of this evaluation. As previously discussed, medication management for some patients continued beyond the 8-week time frame of the OPGP. Nonetheless, understanding the impact of this team approach on opioid use also is an important topic for future research.
Despite these limitations, the described model could be a feasible option for improving pain management in outpatient practices not only within the VA but in community settings.
Conclusion
These results suggest that the use of short-term, structured therapeutic protocols could be a potentially effective strategy for the behavioral treatment of chronic pain conditions among veterans. The development and implementation of effective, innovative, evidence-based practice to address the needs of patients with chronic pain is an important priority for maximizing clinical service delivery and meeting the needs of the nation’s veterans.
Acknowledgments
The authors thank the previous Associate Chief of Staff, Ambulatory Care, Clinton Greenstone, MD, and Director of Primary Care Adam Tremblay, MD, for their vision, leadership, and support of the team and its efforts.
This work was supported in part through a Department of Veterans Affairs Health Services Research and Development Service Research Career Scientist Award (RCS 11-222) awarded to Sarah Krein, PhD.
1. Kerns RD, Otis J, Rosenberg R, Reid MC. Veterans’ reports of pain and associations with ratings of health, health-risk behaviors, affective distress, and use of the healthcare system. J Rehabil Res Dev. 2003;40(5):371-379.
2. Yu W, Ravelo A, Wagner TH, et al. Prevalence and cost of chronic conditions in the VA health care system. Med Care Res Rev. 2003;60(suppl 3):146S-167S.
3. Gironda RJ, Clark ME, Massengale JP, Walker RL. Pain among veterans of operations Enduring Freedom and Iraqi Freedom. Pain Med. 2006;7(4):339-343.
4. Cifu DX, Taylor BC, Carne WF, et al. Traumatic brain injury, posttraumatic stress disorder, and pain diagnoses in OIF/OEF/OND veterans. J Rehabil Res Dev. 2013;50(9):1169-1176.
5. Breuer B, Cruciani R, Portenoy RK. Pain management by primary care physicians, pain physicians, chiropractors, and acupuncturists: a national survey. South Med J. 2010;103(8):738-747.
6. Bergman AA, Matthias MS, Coffing JM, Krebs EE. Contrasting tensions between patients and PCPs in chronic pain management: a qualitative study. Pain Med. 2013;14(11):1689-1697.
7. Caudill-Slosberg MA, Schwartz LM, Woloshin S. Office visits and analgesic prescriptions for musculoskeletal pain in US: 1980 vs. 2000. Pain. 2004;109(3):514-519.
8. Zedler B, Xie L, Wang L, et al. Risk factors for serious prescription opioid-related toxicity or overdose among Veterans Health Administration patients. Pain Med. 2014;15(11):1911-1929.
9. Bohnert AS, Valenstein M, Bair MJ, et al. Association between opioid prescribing patterns and opioid overdose-related deaths. JAMA. 2011;305(13):1315-1321.
10. Chou R, Clark E, Helfand M. Comparative efficacy and safety of long-acting oral opioids for chronic non-cancer pain: a systematic review. J Pain Symptom Manage. 2003;26(5):1026-1048.
11. Guzmán J, Esmail R, Karjalainen K, Malmivaara A, Irvin E, Bombardier C. Multidisciplinary rehabilitation for chronic low back pain: systematic review. BMJ. 2001;322(7301):1511-1516.
12. Gatchel RJ, Okifuji A. Evidence-based scientific data documenting the treatment and cost-effectiveness of comprehensive pain programs for chronic nonmalignant pain. J Pain. 2006;7(11):779-793.
13. Flor H, Fydrich T, Turk DC. Efficacy of multidisciplinary pain treatment centers: a meta-analytic review. Pain. 1992;49(2):221-230.
14. Scascighini L, Toma V, Dober-Spielmann S, Sprott H. Multidisciplinary treatment for chronic pain: a systematic review of interventions and outcomes. Rheumatology (Oxford). 2008;47(5):670-678.
15. Patrick LE, Altmaier EM, Found EM. Long-term outcomes in multidisciplinary treatment of chronic low back pain: results of a 13-year follow-up. Spine (Phila Pa 1976). 2004;29(8):850-855.
16. Moore BA, Anderson D, Dorflinger L, et al. Stepped care model for pain management and quality of pain care in long-term opioid therapy. J Rehabil Res Dev. 2016;53(1):137-146.
17. Anderson DR, Zlateva I, Coman EN, Khatri K, Tian T, Kerns RD. Improving pain care through implementation of the stepped care model at a multisite community health center. J Pain Res. 2016;9:1021-1029.
18. Scott EL, Kroenke K, Wu J, Yu Z. Beneficial effects of improvement in depression, pain catastrophizing, and anxiety on pain outcomes: a 12-month longitudinal analysis. J Pain. 2016;17(2):215-222.
19. Kerns RD, Philip EJ, Lee AW, Rosenberger PH. Implementation of the Veterans Health Administration national pain management strategy. Transl Behav Med. 2011;1(4):635-643.
20. Bloor LE, Fisher C, Grix B, Zaleon CR, Wice S. Conjoint sessions with clinical pharmacy and health psychology for chronic pain. Fed Pract. 2017;34(4):35-41.
21. Tauben D, Theodore BR. Measurement-based stepped care approach to interdisciplinary chronic pain management. In: Benzon HT, Rathmell JP, Wu CL, et al, eds. Practical Management of Pain. 5th ed. Philadelphia, PA: Elsevier Mosby; 2013:37-46.
22. Kroenke K, Spitzer RL, Williams JB, Löwe B. An ultra-brief screening scale for anxiety and depression: the PHQ-4. Psychosomatics. 2009;50(6):613-621.
23. Ouimette P, Wade M, Prins A, Schohn M. Identifying PTSD in primary care: comparison of the primary care-PTSD screen (PC-PTSD) and the general health questionnaire-12 (GHQ). J Anxiety Disord. 2008;22(2):337-343.
24. Chung F, Yegneswaran B, Liao P, et al. STOP questionnaire: a tool to screen patients for obstructive sleep apnea. Anesthesiology. 2008;108(5):812-821.
25. Clark ME, Gironda RJ, Young RW. Development and validation of the pain outcomes questionnaire-VA. J Rehabil Res Dev. 2003;40(5):381-395.
26. Sullivan MJL, Bishop SR, Pivik J. The pain catastrophizing scale: development and validation. Psychol Assess. 1995;7(4):524-532.
27. Nicholas MK. The pain self-efficacy questionnaire: taking pain into account. Eur J Pain. 2007;11(2):153-163.
28. Peppin JF, Marcum S, Kirsh KL. The chronic pain patient and functional assessment: use of the 6-minute walk test in a multidisciplinary pain clinic. Curr Med Res Opin. 2014;30(3):361-365.
29. van Tulder MW, Ostelo R, Vlaeyen JW, Linton SJ, Morley SJ, Assendelft WJ. Behavioral treatment for chronic low back pain: a systematic review within the framework of the Cochrane back review group. Spine (Phila Pa 1976). 2000;25(20):2688-2699.
30. Sanders SH, Harden RN, Vicente PJ. Evidence-based clinical practice guidelines for interdisciplinary rehabilitation of chronic nonmalignant pain syndrome patients. Pain Pract. 2005;5(4):303-315.
31. Stratton KJ, Bender MC, Cameron JJ, Pickett TC. Development and evaluation of a behavioral pain management treatment program in a veterans affairs medical center. Mil Med. 2015;180(3):263-268.
Chronic pain is a common health care problem that remains a significant burden for the VHA.1,2 Some reports indicate that nearly 50% of VA patients report chronic pain.3,4 Both within and outside the VHA, primary care providers (PCPs) generally manage patients with chronic pain.5,6 Historically, a biomedical approach to chronic pain also included the use of opioid medications, which may have contributed to increased opioid-related morbidity and mortality especially among the veteran patient population.7-9 The use of opioids also is controversial due to concerns about adverse effects (AEs), long-term efficacy, functional outcomes, and the potential for drug abuse and addiction.10 Consequently, alternative treatment options that incorporate an interdisciplinary approach have gained significant interest among pain care providers.11 Interdisciplinary programs have been shown to improve functional status and psychological well-being and to reduce pain severity and opioid use.12-14 These benefits may persist for a decade or longer.15
Background
The Stepped Care Model for Pain Management (SCM-PM) is a specific pain treatment approach promoted by the VA National Pain Management Directive.16 This systematically adjusted approach is associated with improved patient satisfaction and health outcomes for pain and depression.17,18 At its core, the model promotes engaging patients as active participants in their care along with a team of doctors who can offer an integrated, evidence-based, multimodal, interdisciplinary treatment plan.
To successfully implement this strategy at the VA, patient aligned care teams (PACT) assess and manage patients with common pain conditions through collaboration with mental health, complementary and integrative health services, physical therapy, and other programs, such as opioid renewal clinics and pain schools.19 This collaborative care approach, which the PCP initiates, is step 1 of the SCM-PM. If initial treatment is not successful and patients are not improving as expected, specialty care consultation and collaborative comanagement through interdisciplinary pain specialty teams are sought (step 2). Finally, step 3 involves tertiary, interdisciplinary care, including access to advanced diagnostic and pain rehabilitation programs accredited by the Commission for Accreditation of Rehabilitation Facilities (CARF).
Although the advantages of interdisciplinary pain programs are clear, resource limitations as well as challenges related to competencies of the PCPs, nurses, and associated health care professionals in pain assessment and management can make implementation of these programs, including the SCM-PM, difficult for many clinics and facilities. Thus, identifying effective chronic pain models and strategies, incorporating the philosophy and key elements of interdisciplinary programs, and accounting for facility resources and capacity are all important.
At the Ann Arbor VAMC, development of a comprehensive interdisciplinary team started with the implementation of joint sessions with a clinical pharmacist and health psychologist embedded in primary care to enhance access to behavioral pain management interventions.20 This program was subsequently expanded to include a pain physician, 2 pain-focused physical therapists (PTs) and a pain nurse.
This article describes a novel team approach for providing more comprehensive, interdisciplinary care for patients with chronic pain along with the initial results for the patients who were part of an outpatient pain group program (OPGP).
Methods
Developing a more interdisciplinary pain management program included integrating different services and creating a strategy for comprehensive evaluation and management of patients with chronic pain. After patients were referred to the interdisciplinary pain clinic by their PCP, they received a systematically structured multidimensional assessment. The primary focus of this assessment was to create an individually directed treatment approach based on the patient’s responses to previous treatments and information collected from several questionnaires administered prior to evaluation. This information helped guide individual patient decision making and actively engaged patients in their care, thus following one of the central tenants of the SCM-PM model. Moreover, functional restoration was at the core of each patient’s evaluation and management. The primary focus was on nonpharmacologic treatment options that included psychological, physical, and occupational therapy; self-management; education; and complementary and alternative therapies. These modalities were offered either individually or in a group setting.
The first step after referral was an evaluation that followed the main core principles for complex disease management described by Tauben and Theodore.21 All new patients were asked to complete a 2-question pain intensity and pain interference measure, the 4-question Patient Health Questionnaire (PHQ-4), 4-question Primary Care-PTSD screening tool (PC-PTSD), and the STOP-BANG questionnaire to assess the risk for obstructive sleep apnea.22-24 Each measure allowed the physician to identify specific problem areas and formulate a treatment plan that would incorporate PTs or occupational therapists, psychologists and/or clinical specialists, and pharmacists if needed.
Patients who were found to have or expressed significant disability because of pain and who wished to learn pain self-management strategies could participate in an 8-week OPGP. This program included the use of cognitive behavioral therapy (CBT) strategies along with group physical therapy classes. Some patients also received individual therapies concurrently with the 8-week OPGP. Patients were excluded from participating in the OPGP only if their current medical or psychiatric status precluded them from full engagement and maximum benefit as determined by the pain physician and psychologist.
Participants and Intervention
Program participants were patients with a chronic pain diagnosis who enrolled in the interdisciplinary pain team OPGP between April 2016 and April 2017. Most patients were referred by their PCPs due to chronic low back, neck, joint or neuropathic pain, although many presented with multiple pain areas. The onset of pain often was a result of a service-related injury or overuse, or the etiology was unknown.
A board-certified pain physician, licensed clinical psychologist, 2 licensed PTs, and a clinical pharmacist led the OPGP sessions. The program was composed of 3-hour-long sessions held weekly for 8 consecutive weeks. Each week, a member of the team covered a specific topic (Table 1).
These sessions focused on the importance of exercise, movement, and physical therapy; appropriate use of medications for managing chronic pain; pacing activities and body mechanics; and the medical approach to managing chronic pain. In addition to didactic presentations, interaction and therapeutic dialogue was encouraged among patients. The education portion of each weekly session lasted about 90 minutes, including a short break. Then, following another short break, patients proceeded to the physical therapy area and engaged in an individualized, monitored exercise program, conducted by the team PTs. Patients also were issued pedometers and encouraged to track their steps each day. Education in improving posture and body mechanics was a key component of the exercise portion of the program so patients could resume their normal daily activities and regain enjoyment in their life. Pain outcomemeasures were collected at admission and immediately before discharge.
Medication management also was an important part of the program for some patients and included tapering off opioids and other drugs and implementing trials of adjuvant pain medications shown to help chronic pain. For some patients, this medication management continued after the patient completed the program.
Measures
The Pain Outcome Questionnaire (POQ) is a 19-item, self-report measure of pain treatment outcomes. Pain rating, mobility, activities of daily living, vitality, negative effect, and fear are the functioning domains evaluated, and the subscale scores are added to produce a total score. The POQ was developed from samples of veterans undergoing inpatient or outpatient pain treatment at VA facilities. For each of the subscales and the total score, higher values indicate poorer outcomes. In normative outpatient VA samples, a total score of 71 is at the 25th percentile, and 120 is at the 75th percentile. The POQ has been shown to have good reliability and validity among veterans in an outpatient setting.25
The Pain Catastrophizing Scale (PCS) is a 13-item scale designed to measure various levels of pain catastrophizing.26 Each item is rated on a 5-point Likert-type scale, from 0 (not at all) to 4 (all the time). The PCS consists of 3 subscale domains: rumination, 4 items; magnification, 3 items; and helplessness, 6 items. Responses to all items also can be added to produce a total score from 0 to 52, with higher scores indicating a higher level of catastrophic thinking related to pain. This project evaluated both the total score and the 3 subscale scores.
The Pain Self-Efficacy Questionnaire (PSEQ) is a 10-item questionnaire that assesses confidence in an individual’s ability to cope or to perform activities despite the pain.27 The PSEQ covers a range of functions, including household chores, socializing, work, as well as coping with pain without medications. Each question has a 7-point Likert scale response: 0 = not at all confident, and 7 = completely confident, to produce a total score from 0 to 60. Higher scores indicate stronger pain self-efficacy, which has been shown to be associated with return to work and maintenance of functional gains.
The Patient Health Questionnaire-4 (PHQ-4) is a 4-item instrument used to screen for depression and anxiety in outpatient medical settings.22 Patients indicate how often they have been bothered by certain problems on a 4-point Likert scale, from 0 (not at all) to 3 (nearly every day). The PHQ-4 provides a total score (0-12) with scores of 6 to 8 indicating moderate and 9 to 12 indicating severe psychological distress; 2 subscale scores, 1 for anxiety (2 questions) and 1 for depression (2 questions). For this analysis, the total PHQ-4 score has been dichotomized with 1 indicating a score in the moderate or severe range vs 0 for a score of mild or no psychological distress. Likewise, each of the subscale scores have been dichotomized with 1 indicating a score of 3 or greater, which is considered a positive screen.
The 6-minute walk test (6MWT) measures the distance (in feet) an individual can walk over a total of 6 minutes on a hard, flat surface.28 Even though the individual can walk at a self-selected pace and rest if needed during the test, the goal is for the patient to walk as far as possible over the course of 6 minutes. The 6MWT provides information regarding functional capacity, response to therapy, and prognosis across a range of chronic conditions, including pain.
Data Analysis
Data analysis included the use of both descriptive and comparative statistics. A descriptive analysis was conducted to examine the characteristics of patients who did and did not complete the OPGP. Specific outcomes for those individuals who completed the program, and thus had complete pre- and post-OPGP information, then were compared. Paired t tests were used to compare differences in continuous measures between baseline (pre-OPGP) and the 8-week follow-up (post-OPGP). Comparisons involving dichotomous measures were made using the Fisher exact test. A 2-sided α with a P value .05 was considered statistically significant. All statistical analyses were conducted using STATA version 14.1 (StataCorp, College Station, TX).
Results
A total of 36 patients enrolled, and 28 (77%) completed the OPGP. Patients who did not complete the program (n = 8) either self-discharged due to lack of interest or had difficulty in consistently making their appointments and decided not to continue (Table 2).
Outcomes for OPGP Completers
Improvements were observed for all outcome domains among patients who completed the program (eTable).
Discussion
This report describes the novel model for improving delivery of chronic pain management services implemented at the Ann Arbor VAMC through the development of a multidisciplinary pain PACT. The program included using a systematically structured multidimensional approach to identify appropriate treatments and delivery of interdisciplinary care for patients with chronic pain through an OPGP. The authors’ findings establish the feasibility and acceptability of the OPGP. More than 75% of those enrolled completed the program, indicating the promising potential of this approach with significant improvements observed for several pain-related outcomes among those who completed the 8-week program.
Stepped care is a well-established approach to managing complex chronic pain conditions. The approach adds increased levels of treatment intensity when there is no improvement after initial, simple measures are instituted (eg, over-the-counter pain medications, physical therapy, life style changes). Understanding the complexity of the pain experience while treating the patient and not simply the pain has the highest likelihood of helping patients with chronic pain. Given the prevalence of chronic pain among patients in primary care nationally, measurement-based pain care potentially could result in an earlier referral to appropriate care well before pain becomes intractable and chronic.
Growing evidence shows that multidisciplinary treatments reduce pain symptoms and intensity, medication, health care provider use, and improve quality of life.11-15,29,30 A systematic review by van Tulder and colleagues, for example, noted improvements in physical parameters, such as range of motion and flexibility and behavioral health parameters, including anxiety, depression, and cognition.29 Similarly, the cohort of patients who participated in the OPGP showed statistically significant improvements in several domains of pain-related distress and functioning following treatment, including pain catastrophizing, pain self-efficacy, and the multicomponent pain outcomes questionnaires. Functional improvement also was observed by comparing the distance walked in 6 minutes before and after program completion.
There is significant variation in duration of rehabilitation programs lasting from 2 weeks to 12 weeks or longer. These sessions consist of half days, daily sessions, weekly sessions, and monthly sessions. Inconsistencies also exist among programs that use 3 to 280 professional contact hours. Although it has been shown that programs with more than 100 hours of professional contact tended to have better outcomes than did those with less than 30 hours of contact, Stratton and colleagues reported that a 6-week group program was equivalent or better than a 12- and 10-week group program among veterans.11,31 These findings along with staffing and resource constraints led to the implementation of the 8-week OPGP with fewer than 30 hours of contact time per group. These results have important practical implications, as shorter treatments may offer comparable therapeutic impact than do longer, more time-intensive protocols.
Limitations
These findings were derived from a quality improvement project within one institution, and several limitations exist. Although the broader purpose of the article was to show how the fundamentals of creating a cohesive multidisciplinary chronic pain team can be implemented within the VA setting, the highlighted outcomes were primarily from participants in the OPGP Since this was not a controlled or experimental study and given potential sample size and selections issues as well as the lack of longer-term follow-up information, further study is needed to draw definitive conclusions about program effectiveness, despite promising preliminary results. In addition, medication use, such as opioids either before or after completion of the program, was not included as part of this evaluation. As previously discussed, medication management for some patients continued beyond the 8-week time frame of the OPGP. Nonetheless, understanding the impact of this team approach on opioid use also is an important topic for future research.
Despite these limitations, the described model could be a feasible option for improving pain management in outpatient practices not only within the VA but in community settings.
Conclusion
These results suggest that the use of short-term, structured therapeutic protocols could be a potentially effective strategy for the behavioral treatment of chronic pain conditions among veterans. The development and implementation of effective, innovative, evidence-based practice to address the needs of patients with chronic pain is an important priority for maximizing clinical service delivery and meeting the needs of the nation’s veterans.
Acknowledgments
The authors thank the previous Associate Chief of Staff, Ambulatory Care, Clinton Greenstone, MD, and Director of Primary Care Adam Tremblay, MD, for their vision, leadership, and support of the team and its efforts.
This work was supported in part through a Department of Veterans Affairs Health Services Research and Development Service Research Career Scientist Award (RCS 11-222) awarded to Sarah Krein, PhD.
Chronic pain is a common health care problem that remains a significant burden for the VHA.1,2 Some reports indicate that nearly 50% of VA patients report chronic pain.3,4 Both within and outside the VHA, primary care providers (PCPs) generally manage patients with chronic pain.5,6 Historically, a biomedical approach to chronic pain also included the use of opioid medications, which may have contributed to increased opioid-related morbidity and mortality especially among the veteran patient population.7-9 The use of opioids also is controversial due to concerns about adverse effects (AEs), long-term efficacy, functional outcomes, and the potential for drug abuse and addiction.10 Consequently, alternative treatment options that incorporate an interdisciplinary approach have gained significant interest among pain care providers.11 Interdisciplinary programs have been shown to improve functional status and psychological well-being and to reduce pain severity and opioid use.12-14 These benefits may persist for a decade or longer.15
Background
The Stepped Care Model for Pain Management (SCM-PM) is a specific pain treatment approach promoted by the VA National Pain Management Directive.16 This systematically adjusted approach is associated with improved patient satisfaction and health outcomes for pain and depression.17,18 At its core, the model promotes engaging patients as active participants in their care along with a team of doctors who can offer an integrated, evidence-based, multimodal, interdisciplinary treatment plan.
To successfully implement this strategy at the VA, patient aligned care teams (PACT) assess and manage patients with common pain conditions through collaboration with mental health, complementary and integrative health services, physical therapy, and other programs, such as opioid renewal clinics and pain schools.19 This collaborative care approach, which the PCP initiates, is step 1 of the SCM-PM. If initial treatment is not successful and patients are not improving as expected, specialty care consultation and collaborative comanagement through interdisciplinary pain specialty teams are sought (step 2). Finally, step 3 involves tertiary, interdisciplinary care, including access to advanced diagnostic and pain rehabilitation programs accredited by the Commission for Accreditation of Rehabilitation Facilities (CARF).
Although the advantages of interdisciplinary pain programs are clear, resource limitations as well as challenges related to competencies of the PCPs, nurses, and associated health care professionals in pain assessment and management can make implementation of these programs, including the SCM-PM, difficult for many clinics and facilities. Thus, identifying effective chronic pain models and strategies, incorporating the philosophy and key elements of interdisciplinary programs, and accounting for facility resources and capacity are all important.
At the Ann Arbor VAMC, development of a comprehensive interdisciplinary team started with the implementation of joint sessions with a clinical pharmacist and health psychologist embedded in primary care to enhance access to behavioral pain management interventions.20 This program was subsequently expanded to include a pain physician, 2 pain-focused physical therapists (PTs) and a pain nurse.
This article describes a novel team approach for providing more comprehensive, interdisciplinary care for patients with chronic pain along with the initial results for the patients who were part of an outpatient pain group program (OPGP).
Methods
Developing a more interdisciplinary pain management program included integrating different services and creating a strategy for comprehensive evaluation and management of patients with chronic pain. After patients were referred to the interdisciplinary pain clinic by their PCP, they received a systematically structured multidimensional assessment. The primary focus of this assessment was to create an individually directed treatment approach based on the patient’s responses to previous treatments and information collected from several questionnaires administered prior to evaluation. This information helped guide individual patient decision making and actively engaged patients in their care, thus following one of the central tenants of the SCM-PM model. Moreover, functional restoration was at the core of each patient’s evaluation and management. The primary focus was on nonpharmacologic treatment options that included psychological, physical, and occupational therapy; self-management; education; and complementary and alternative therapies. These modalities were offered either individually or in a group setting.
The first step after referral was an evaluation that followed the main core principles for complex disease management described by Tauben and Theodore.21 All new patients were asked to complete a 2-question pain intensity and pain interference measure, the 4-question Patient Health Questionnaire (PHQ-4), 4-question Primary Care-PTSD screening tool (PC-PTSD), and the STOP-BANG questionnaire to assess the risk for obstructive sleep apnea.22-24 Each measure allowed the physician to identify specific problem areas and formulate a treatment plan that would incorporate PTs or occupational therapists, psychologists and/or clinical specialists, and pharmacists if needed.
Patients who were found to have or expressed significant disability because of pain and who wished to learn pain self-management strategies could participate in an 8-week OPGP. This program included the use of cognitive behavioral therapy (CBT) strategies along with group physical therapy classes. Some patients also received individual therapies concurrently with the 8-week OPGP. Patients were excluded from participating in the OPGP only if their current medical or psychiatric status precluded them from full engagement and maximum benefit as determined by the pain physician and psychologist.
Participants and Intervention
Program participants were patients with a chronic pain diagnosis who enrolled in the interdisciplinary pain team OPGP between April 2016 and April 2017. Most patients were referred by their PCPs due to chronic low back, neck, joint or neuropathic pain, although many presented with multiple pain areas. The onset of pain often was a result of a service-related injury or overuse, or the etiology was unknown.
A board-certified pain physician, licensed clinical psychologist, 2 licensed PTs, and a clinical pharmacist led the OPGP sessions. The program was composed of 3-hour-long sessions held weekly for 8 consecutive weeks. Each week, a member of the team covered a specific topic (Table 1).
These sessions focused on the importance of exercise, movement, and physical therapy; appropriate use of medications for managing chronic pain; pacing activities and body mechanics; and the medical approach to managing chronic pain. In addition to didactic presentations, interaction and therapeutic dialogue was encouraged among patients. The education portion of each weekly session lasted about 90 minutes, including a short break. Then, following another short break, patients proceeded to the physical therapy area and engaged in an individualized, monitored exercise program, conducted by the team PTs. Patients also were issued pedometers and encouraged to track their steps each day. Education in improving posture and body mechanics was a key component of the exercise portion of the program so patients could resume their normal daily activities and regain enjoyment in their life. Pain outcomemeasures were collected at admission and immediately before discharge.
Medication management also was an important part of the program for some patients and included tapering off opioids and other drugs and implementing trials of adjuvant pain medications shown to help chronic pain. For some patients, this medication management continued after the patient completed the program.
Measures
The Pain Outcome Questionnaire (POQ) is a 19-item, self-report measure of pain treatment outcomes. Pain rating, mobility, activities of daily living, vitality, negative effect, and fear are the functioning domains evaluated, and the subscale scores are added to produce a total score. The POQ was developed from samples of veterans undergoing inpatient or outpatient pain treatment at VA facilities. For each of the subscales and the total score, higher values indicate poorer outcomes. In normative outpatient VA samples, a total score of 71 is at the 25th percentile, and 120 is at the 75th percentile. The POQ has been shown to have good reliability and validity among veterans in an outpatient setting.25
The Pain Catastrophizing Scale (PCS) is a 13-item scale designed to measure various levels of pain catastrophizing.26 Each item is rated on a 5-point Likert-type scale, from 0 (not at all) to 4 (all the time). The PCS consists of 3 subscale domains: rumination, 4 items; magnification, 3 items; and helplessness, 6 items. Responses to all items also can be added to produce a total score from 0 to 52, with higher scores indicating a higher level of catastrophic thinking related to pain. This project evaluated both the total score and the 3 subscale scores.
The Pain Self-Efficacy Questionnaire (PSEQ) is a 10-item questionnaire that assesses confidence in an individual’s ability to cope or to perform activities despite the pain.27 The PSEQ covers a range of functions, including household chores, socializing, work, as well as coping with pain without medications. Each question has a 7-point Likert scale response: 0 = not at all confident, and 7 = completely confident, to produce a total score from 0 to 60. Higher scores indicate stronger pain self-efficacy, which has been shown to be associated with return to work and maintenance of functional gains.
The Patient Health Questionnaire-4 (PHQ-4) is a 4-item instrument used to screen for depression and anxiety in outpatient medical settings.22 Patients indicate how often they have been bothered by certain problems on a 4-point Likert scale, from 0 (not at all) to 3 (nearly every day). The PHQ-4 provides a total score (0-12) with scores of 6 to 8 indicating moderate and 9 to 12 indicating severe psychological distress; 2 subscale scores, 1 for anxiety (2 questions) and 1 for depression (2 questions). For this analysis, the total PHQ-4 score has been dichotomized with 1 indicating a score in the moderate or severe range vs 0 for a score of mild or no psychological distress. Likewise, each of the subscale scores have been dichotomized with 1 indicating a score of 3 or greater, which is considered a positive screen.
The 6-minute walk test (6MWT) measures the distance (in feet) an individual can walk over a total of 6 minutes on a hard, flat surface.28 Even though the individual can walk at a self-selected pace and rest if needed during the test, the goal is for the patient to walk as far as possible over the course of 6 minutes. The 6MWT provides information regarding functional capacity, response to therapy, and prognosis across a range of chronic conditions, including pain.
Data Analysis
Data analysis included the use of both descriptive and comparative statistics. A descriptive analysis was conducted to examine the characteristics of patients who did and did not complete the OPGP. Specific outcomes for those individuals who completed the program, and thus had complete pre- and post-OPGP information, then were compared. Paired t tests were used to compare differences in continuous measures between baseline (pre-OPGP) and the 8-week follow-up (post-OPGP). Comparisons involving dichotomous measures were made using the Fisher exact test. A 2-sided α with a P value .05 was considered statistically significant. All statistical analyses were conducted using STATA version 14.1 (StataCorp, College Station, TX).
Results
A total of 36 patients enrolled, and 28 (77%) completed the OPGP. Patients who did not complete the program (n = 8) either self-discharged due to lack of interest or had difficulty in consistently making their appointments and decided not to continue (Table 2).
Outcomes for OPGP Completers
Improvements were observed for all outcome domains among patients who completed the program (eTable).
Discussion
This report describes the novel model for improving delivery of chronic pain management services implemented at the Ann Arbor VAMC through the development of a multidisciplinary pain PACT. The program included using a systematically structured multidimensional approach to identify appropriate treatments and delivery of interdisciplinary care for patients with chronic pain through an OPGP. The authors’ findings establish the feasibility and acceptability of the OPGP. More than 75% of those enrolled completed the program, indicating the promising potential of this approach with significant improvements observed for several pain-related outcomes among those who completed the 8-week program.
Stepped care is a well-established approach to managing complex chronic pain conditions. The approach adds increased levels of treatment intensity when there is no improvement after initial, simple measures are instituted (eg, over-the-counter pain medications, physical therapy, life style changes). Understanding the complexity of the pain experience while treating the patient and not simply the pain has the highest likelihood of helping patients with chronic pain. Given the prevalence of chronic pain among patients in primary care nationally, measurement-based pain care potentially could result in an earlier referral to appropriate care well before pain becomes intractable and chronic.
Growing evidence shows that multidisciplinary treatments reduce pain symptoms and intensity, medication, health care provider use, and improve quality of life.11-15,29,30 A systematic review by van Tulder and colleagues, for example, noted improvements in physical parameters, such as range of motion and flexibility and behavioral health parameters, including anxiety, depression, and cognition.29 Similarly, the cohort of patients who participated in the OPGP showed statistically significant improvements in several domains of pain-related distress and functioning following treatment, including pain catastrophizing, pain self-efficacy, and the multicomponent pain outcomes questionnaires. Functional improvement also was observed by comparing the distance walked in 6 minutes before and after program completion.
There is significant variation in duration of rehabilitation programs lasting from 2 weeks to 12 weeks or longer. These sessions consist of half days, daily sessions, weekly sessions, and monthly sessions. Inconsistencies also exist among programs that use 3 to 280 professional contact hours. Although it has been shown that programs with more than 100 hours of professional contact tended to have better outcomes than did those with less than 30 hours of contact, Stratton and colleagues reported that a 6-week group program was equivalent or better than a 12- and 10-week group program among veterans.11,31 These findings along with staffing and resource constraints led to the implementation of the 8-week OPGP with fewer than 30 hours of contact time per group. These results have important practical implications, as shorter treatments may offer comparable therapeutic impact than do longer, more time-intensive protocols.
Limitations
These findings were derived from a quality improvement project within one institution, and several limitations exist. Although the broader purpose of the article was to show how the fundamentals of creating a cohesive multidisciplinary chronic pain team can be implemented within the VA setting, the highlighted outcomes were primarily from participants in the OPGP Since this was not a controlled or experimental study and given potential sample size and selections issues as well as the lack of longer-term follow-up information, further study is needed to draw definitive conclusions about program effectiveness, despite promising preliminary results. In addition, medication use, such as opioids either before or after completion of the program, was not included as part of this evaluation. As previously discussed, medication management for some patients continued beyond the 8-week time frame of the OPGP. Nonetheless, understanding the impact of this team approach on opioid use also is an important topic for future research.
Despite these limitations, the described model could be a feasible option for improving pain management in outpatient practices not only within the VA but in community settings.
Conclusion
These results suggest that the use of short-term, structured therapeutic protocols could be a potentially effective strategy for the behavioral treatment of chronic pain conditions among veterans. The development and implementation of effective, innovative, evidence-based practice to address the needs of patients with chronic pain is an important priority for maximizing clinical service delivery and meeting the needs of the nation’s veterans.
Acknowledgments
The authors thank the previous Associate Chief of Staff, Ambulatory Care, Clinton Greenstone, MD, and Director of Primary Care Adam Tremblay, MD, for their vision, leadership, and support of the team and its efforts.
This work was supported in part through a Department of Veterans Affairs Health Services Research and Development Service Research Career Scientist Award (RCS 11-222) awarded to Sarah Krein, PhD.
1. Kerns RD, Otis J, Rosenberg R, Reid MC. Veterans’ reports of pain and associations with ratings of health, health-risk behaviors, affective distress, and use of the healthcare system. J Rehabil Res Dev. 2003;40(5):371-379.
2. Yu W, Ravelo A, Wagner TH, et al. Prevalence and cost of chronic conditions in the VA health care system. Med Care Res Rev. 2003;60(suppl 3):146S-167S.
3. Gironda RJ, Clark ME, Massengale JP, Walker RL. Pain among veterans of operations Enduring Freedom and Iraqi Freedom. Pain Med. 2006;7(4):339-343.
4. Cifu DX, Taylor BC, Carne WF, et al. Traumatic brain injury, posttraumatic stress disorder, and pain diagnoses in OIF/OEF/OND veterans. J Rehabil Res Dev. 2013;50(9):1169-1176.
5. Breuer B, Cruciani R, Portenoy RK. Pain management by primary care physicians, pain physicians, chiropractors, and acupuncturists: a national survey. South Med J. 2010;103(8):738-747.
6. Bergman AA, Matthias MS, Coffing JM, Krebs EE. Contrasting tensions between patients and PCPs in chronic pain management: a qualitative study. Pain Med. 2013;14(11):1689-1697.
7. Caudill-Slosberg MA, Schwartz LM, Woloshin S. Office visits and analgesic prescriptions for musculoskeletal pain in US: 1980 vs. 2000. Pain. 2004;109(3):514-519.
8. Zedler B, Xie L, Wang L, et al. Risk factors for serious prescription opioid-related toxicity or overdose among Veterans Health Administration patients. Pain Med. 2014;15(11):1911-1929.
9. Bohnert AS, Valenstein M, Bair MJ, et al. Association between opioid prescribing patterns and opioid overdose-related deaths. JAMA. 2011;305(13):1315-1321.
10. Chou R, Clark E, Helfand M. Comparative efficacy and safety of long-acting oral opioids for chronic non-cancer pain: a systematic review. J Pain Symptom Manage. 2003;26(5):1026-1048.
11. Guzmán J, Esmail R, Karjalainen K, Malmivaara A, Irvin E, Bombardier C. Multidisciplinary rehabilitation for chronic low back pain: systematic review. BMJ. 2001;322(7301):1511-1516.
12. Gatchel RJ, Okifuji A. Evidence-based scientific data documenting the treatment and cost-effectiveness of comprehensive pain programs for chronic nonmalignant pain. J Pain. 2006;7(11):779-793.
13. Flor H, Fydrich T, Turk DC. Efficacy of multidisciplinary pain treatment centers: a meta-analytic review. Pain. 1992;49(2):221-230.
14. Scascighini L, Toma V, Dober-Spielmann S, Sprott H. Multidisciplinary treatment for chronic pain: a systematic review of interventions and outcomes. Rheumatology (Oxford). 2008;47(5):670-678.
15. Patrick LE, Altmaier EM, Found EM. Long-term outcomes in multidisciplinary treatment of chronic low back pain: results of a 13-year follow-up. Spine (Phila Pa 1976). 2004;29(8):850-855.
16. Moore BA, Anderson D, Dorflinger L, et al. Stepped care model for pain management and quality of pain care in long-term opioid therapy. J Rehabil Res Dev. 2016;53(1):137-146.
17. Anderson DR, Zlateva I, Coman EN, Khatri K, Tian T, Kerns RD. Improving pain care through implementation of the stepped care model at a multisite community health center. J Pain Res. 2016;9:1021-1029.
18. Scott EL, Kroenke K, Wu J, Yu Z. Beneficial effects of improvement in depression, pain catastrophizing, and anxiety on pain outcomes: a 12-month longitudinal analysis. J Pain. 2016;17(2):215-222.
19. Kerns RD, Philip EJ, Lee AW, Rosenberger PH. Implementation of the Veterans Health Administration national pain management strategy. Transl Behav Med. 2011;1(4):635-643.
20. Bloor LE, Fisher C, Grix B, Zaleon CR, Wice S. Conjoint sessions with clinical pharmacy and health psychology for chronic pain. Fed Pract. 2017;34(4):35-41.
21. Tauben D, Theodore BR. Measurement-based stepped care approach to interdisciplinary chronic pain management. In: Benzon HT, Rathmell JP, Wu CL, et al, eds. Practical Management of Pain. 5th ed. Philadelphia, PA: Elsevier Mosby; 2013:37-46.
22. Kroenke K, Spitzer RL, Williams JB, Löwe B. An ultra-brief screening scale for anxiety and depression: the PHQ-4. Psychosomatics. 2009;50(6):613-621.
23. Ouimette P, Wade M, Prins A, Schohn M. Identifying PTSD in primary care: comparison of the primary care-PTSD screen (PC-PTSD) and the general health questionnaire-12 (GHQ). J Anxiety Disord. 2008;22(2):337-343.
24. Chung F, Yegneswaran B, Liao P, et al. STOP questionnaire: a tool to screen patients for obstructive sleep apnea. Anesthesiology. 2008;108(5):812-821.
25. Clark ME, Gironda RJ, Young RW. Development and validation of the pain outcomes questionnaire-VA. J Rehabil Res Dev. 2003;40(5):381-395.
26. Sullivan MJL, Bishop SR, Pivik J. The pain catastrophizing scale: development and validation. Psychol Assess. 1995;7(4):524-532.
27. Nicholas MK. The pain self-efficacy questionnaire: taking pain into account. Eur J Pain. 2007;11(2):153-163.
28. Peppin JF, Marcum S, Kirsh KL. The chronic pain patient and functional assessment: use of the 6-minute walk test in a multidisciplinary pain clinic. Curr Med Res Opin. 2014;30(3):361-365.
29. van Tulder MW, Ostelo R, Vlaeyen JW, Linton SJ, Morley SJ, Assendelft WJ. Behavioral treatment for chronic low back pain: a systematic review within the framework of the Cochrane back review group. Spine (Phila Pa 1976). 2000;25(20):2688-2699.
30. Sanders SH, Harden RN, Vicente PJ. Evidence-based clinical practice guidelines for interdisciplinary rehabilitation of chronic nonmalignant pain syndrome patients. Pain Pract. 2005;5(4):303-315.
31. Stratton KJ, Bender MC, Cameron JJ, Pickett TC. Development and evaluation of a behavioral pain management treatment program in a veterans affairs medical center. Mil Med. 2015;180(3):263-268.
1. Kerns RD, Otis J, Rosenberg R, Reid MC. Veterans’ reports of pain and associations with ratings of health, health-risk behaviors, affective distress, and use of the healthcare system. J Rehabil Res Dev. 2003;40(5):371-379.
2. Yu W, Ravelo A, Wagner TH, et al. Prevalence and cost of chronic conditions in the VA health care system. Med Care Res Rev. 2003;60(suppl 3):146S-167S.
3. Gironda RJ, Clark ME, Massengale JP, Walker RL. Pain among veterans of operations Enduring Freedom and Iraqi Freedom. Pain Med. 2006;7(4):339-343.
4. Cifu DX, Taylor BC, Carne WF, et al. Traumatic brain injury, posttraumatic stress disorder, and pain diagnoses in OIF/OEF/OND veterans. J Rehabil Res Dev. 2013;50(9):1169-1176.
5. Breuer B, Cruciani R, Portenoy RK. Pain management by primary care physicians, pain physicians, chiropractors, and acupuncturists: a national survey. South Med J. 2010;103(8):738-747.
6. Bergman AA, Matthias MS, Coffing JM, Krebs EE. Contrasting tensions between patients and PCPs in chronic pain management: a qualitative study. Pain Med. 2013;14(11):1689-1697.
7. Caudill-Slosberg MA, Schwartz LM, Woloshin S. Office visits and analgesic prescriptions for musculoskeletal pain in US: 1980 vs. 2000. Pain. 2004;109(3):514-519.
8. Zedler B, Xie L, Wang L, et al. Risk factors for serious prescription opioid-related toxicity or overdose among Veterans Health Administration patients. Pain Med. 2014;15(11):1911-1929.
9. Bohnert AS, Valenstein M, Bair MJ, et al. Association between opioid prescribing patterns and opioid overdose-related deaths. JAMA. 2011;305(13):1315-1321.
10. Chou R, Clark E, Helfand M. Comparative efficacy and safety of long-acting oral opioids for chronic non-cancer pain: a systematic review. J Pain Symptom Manage. 2003;26(5):1026-1048.
11. Guzmán J, Esmail R, Karjalainen K, Malmivaara A, Irvin E, Bombardier C. Multidisciplinary rehabilitation for chronic low back pain: systematic review. BMJ. 2001;322(7301):1511-1516.
12. Gatchel RJ, Okifuji A. Evidence-based scientific data documenting the treatment and cost-effectiveness of comprehensive pain programs for chronic nonmalignant pain. J Pain. 2006;7(11):779-793.
13. Flor H, Fydrich T, Turk DC. Efficacy of multidisciplinary pain treatment centers: a meta-analytic review. Pain. 1992;49(2):221-230.
14. Scascighini L, Toma V, Dober-Spielmann S, Sprott H. Multidisciplinary treatment for chronic pain: a systematic review of interventions and outcomes. Rheumatology (Oxford). 2008;47(5):670-678.
15. Patrick LE, Altmaier EM, Found EM. Long-term outcomes in multidisciplinary treatment of chronic low back pain: results of a 13-year follow-up. Spine (Phila Pa 1976). 2004;29(8):850-855.
16. Moore BA, Anderson D, Dorflinger L, et al. Stepped care model for pain management and quality of pain care in long-term opioid therapy. J Rehabil Res Dev. 2016;53(1):137-146.
17. Anderson DR, Zlateva I, Coman EN, Khatri K, Tian T, Kerns RD. Improving pain care through implementation of the stepped care model at a multisite community health center. J Pain Res. 2016;9:1021-1029.
18. Scott EL, Kroenke K, Wu J, Yu Z. Beneficial effects of improvement in depression, pain catastrophizing, and anxiety on pain outcomes: a 12-month longitudinal analysis. J Pain. 2016;17(2):215-222.
19. Kerns RD, Philip EJ, Lee AW, Rosenberger PH. Implementation of the Veterans Health Administration national pain management strategy. Transl Behav Med. 2011;1(4):635-643.
20. Bloor LE, Fisher C, Grix B, Zaleon CR, Wice S. Conjoint sessions with clinical pharmacy and health psychology for chronic pain. Fed Pract. 2017;34(4):35-41.
21. Tauben D, Theodore BR. Measurement-based stepped care approach to interdisciplinary chronic pain management. In: Benzon HT, Rathmell JP, Wu CL, et al, eds. Practical Management of Pain. 5th ed. Philadelphia, PA: Elsevier Mosby; 2013:37-46.
22. Kroenke K, Spitzer RL, Williams JB, Löwe B. An ultra-brief screening scale for anxiety and depression: the PHQ-4. Psychosomatics. 2009;50(6):613-621.
23. Ouimette P, Wade M, Prins A, Schohn M. Identifying PTSD in primary care: comparison of the primary care-PTSD screen (PC-PTSD) and the general health questionnaire-12 (GHQ). J Anxiety Disord. 2008;22(2):337-343.
24. Chung F, Yegneswaran B, Liao P, et al. STOP questionnaire: a tool to screen patients for obstructive sleep apnea. Anesthesiology. 2008;108(5):812-821.
25. Clark ME, Gironda RJ, Young RW. Development and validation of the pain outcomes questionnaire-VA. J Rehabil Res Dev. 2003;40(5):381-395.
26. Sullivan MJL, Bishop SR, Pivik J. The pain catastrophizing scale: development and validation. Psychol Assess. 1995;7(4):524-532.
27. Nicholas MK. The pain self-efficacy questionnaire: taking pain into account. Eur J Pain. 2007;11(2):153-163.
28. Peppin JF, Marcum S, Kirsh KL. The chronic pain patient and functional assessment: use of the 6-minute walk test in a multidisciplinary pain clinic. Curr Med Res Opin. 2014;30(3):361-365.
29. van Tulder MW, Ostelo R, Vlaeyen JW, Linton SJ, Morley SJ, Assendelft WJ. Behavioral treatment for chronic low back pain: a systematic review within the framework of the Cochrane back review group. Spine (Phila Pa 1976). 2000;25(20):2688-2699.
30. Sanders SH, Harden RN, Vicente PJ. Evidence-based clinical practice guidelines for interdisciplinary rehabilitation of chronic nonmalignant pain syndrome patients. Pain Pract. 2005;5(4):303-315.
31. Stratton KJ, Bender MC, Cameron JJ, Pickett TC. Development and evaluation of a behavioral pain management treatment program in a veterans affairs medical center. Mil Med. 2015;180(3):263-268.
Psychotherapy Telemental Health Center and Regional Pilot
Within VHA, telemental health (TMH) refers to behavioral health services that are provided remotely, using secure communication technologies, to veterans who are separated by distance from their mental health providers.1 Telemental health sometimes involves video teleconferencing (VTC) technology, where a veteran (or group of veterans) in one location and a provider in a different location are able to communicate in real time through a computer monitor or television screen.2 In the VHA, TMH visits are typically conducted from a central location (such as a medical center hospital) to a community-based outpatient clinic (CBOC), but pilot projects have also tested VTC in homes as well.1,3,4
In addition to providing timely access to behavioral health services in rural or underserved locations, TMH eliminates travel that may be disruptive or costly and allows mental health providers to consult with or provide supervision to one another. Telemental health can be used to make diagnoses, manage care, perform checkups, and provide long-term, follow-up care. Other uses for TMH include clinical assessment, individual and group psychotherapy, psycho-educational interventions, cognitive testing, and general psychiatric care.1,5,6 More recently, TMH has been used to provide evidence-based psychotherapies (EBPs) to individuals with posttraumatic stress disorder (PTSD) and other mental health diagnoses.6,7 Such care may be particularly advantageous for veterans with PTSD, because traveling can be a burden for them or a trigger for PTSD symptoms.
Although interactive video technology is becoming widely available, its use is limited in health care systems due to lack of knowledge, education, logistical guidance, and technical training. The authors have conducted EBPs using VTC across VISN 22 in both office-to-office and office-to-home modalities and are providing EBPs using VTC to CBOCs in other VISNs across the western U.S. This article addresses these issues, outlining the necessary steps required to establish a TMH clinic and to share the successes of the EBP TMH Center and Regional Pilot used at VISN 22.
Telemental Health
Telemental health is an effective alternative to in-person treatment and is well regarded by both mental health providers and veterans. Overall, mental health providers believe it can help reduce the stigma associated with traditional mental health care and ease transportation-related issues for veterans. Telemental health allows access to care for veterans living in rural or remote areas in addition to those who are incarcerated or are otherwise unable to attend visits at primary VA facilities.2,8-10 In an assessment of TMH services in 40 CBOCs across VISN 16, most CBOC mental health providers found it to be an acceptable alternative to face-to-face care, recognize the value of TMH, and endorse a willingness to use and expand TMH programs within their clinics.11
Veterans who participated in TMH via VTC have expressed satisfaction with the decreased travel time and expenses, fewer interactions with crowds, and fewer parking problems.12 Several studies suggested that veterans preferred TMH to in-person contact due to more rapid access to care and specialists who would otherwise be unavailable at remote locations.5,10 Similarly, veterans who avoid in-person mental health care were more open to remote therapy for many of the reasons listed earlier. Studies suggest that veterans from both rural and urban locations are generally receptive to receiving mental health services via TMH.5,10
Several studies have found that TMH services may have advantages over standard in-person care. These advantages include decreasing transportation costs, travel time, and time missed at work and increasing system coverage area.13 Overall, both veterans and providers reported similar satisfaction between VTC and in-person sessions and, in some cases, prefer VTC interactions due to a sense of “easing into” intense therapies or having a “therapeutic distance” as treatment begins.12
Utility
Previous studies have shown that TMH can be used successfully to provide psychopharmacologic treatment to veterans who have major depressive disorder or schizophrenia, among other psychiatric disorders.5,8,14 Recent studies have focused on the feasibility of providing EBPs via TMH, particularly for the treatment of PTSD.12,15 Studies have shown that TMH services via VTC can be used successfully to provide cognitive behavioral therapy (CBT), cognitive processing therapy (CPT), and prolonged exposure therapy (PE).16-21 In these studies, both PE and CPT delivered via TMH were found to be as efficacious as in-person formats. Furthermore, TMH services were successfully used in individual and group sessions.
Research has emphasized the benefits of TMH for veterans who are uncomfortable in crowds, waiting rooms, or hospital lobbies.7,12,18 For patients with PTSD who are initially limited by fears related to driving, TMH can facilitate access to care. Veterans with PTSD often avoid reminders of trauma (ie, uniforms, evidence of physical injury, artwork, photographs related to war), which can often be found at the larger VAMCs. These veterans may find mental health care services in their homes or at local CBOCs more appealing.7,12,18
Implementation
Prior to the implementation of telehealth services, many CBOC providers would refer veterans in need of specialty care to the nearest VAMC, which were sometimes many hours away.1 In response to travel and access concerns, the VA has implemented various telehealth modalities, including TMH.
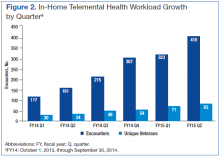
In 2008, about 230,000 veterans received mental health services via real-time clinical VTC at 300 VA CBOCs, and about 40,000 veterans enrolled in the In-Home Telehealth program.22 By 2011, > 380,000 veterans used clinic-based telehealth services and about 100,000 veterans used the in-home program.1 Between 2006 and 2008, the 98,000 veterans who used TMH modalities had fewer hospital admissions compared with those who did not; overall, the need for hospital services decreased by about 25% for those using TMH services.23
Although research suggests that TMH is an effective treatment modality, it does have limitations. A recent study noted several visual and audio difficulties that can emerge, including pixilation, “tracer” images with movement, low resolution, “frozen” or “choppy” images, delays in sound, echoes, or “mechanical sounding” voices.12 In some cases, physical details, such as crying, sniffling, or fidgeting, could not be clearly observed.12 Overall, these unforeseen issues can impact the ability to give and receive care through TMH modalities. Proper procedures need to be developed and implemented for each site.
Getting Started
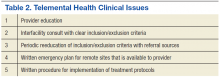
Using TMH to provide mental health care at other VHA facilities requires planning and preparation. Logistics, such as preparation of the room and equipment, should be considered. Similarly, veteran and provider convenience must be considered.2,11 Before starting TMH at any VA facility, professionals working with the audiovisual technology and providing TMH care must complete necessary VA Talent Management System courses and obtain copies of certificates to assure they have met the appropriate training criteria. Providers must be credentialed to provide TMH services, including the telehealth curriculum offered by VA Employee Educational Services.2,24 An appropriate memorandum of understanding (MOU) must be created, and credentialing and privileging must also be acquired.
In addition to provider training, an information technology representative who can administer technical support as needed must be selected for both the provider and remote locations. Technologic complications can make TMH implementation much more challenging.12 As such, it is important to assure that both the veteran and the provider have the necessary TMH equipment. The selected communication device must be compatible with the technology requirements at the provider and remote facilities.12
In addition to designated technical support, the VISN TMH coordinator needs to have point-of-contact information for those who can assist with each site’s telehealth services and address the demand for EBP for PTSD or other desired services. After this information has been obtained, relationships must be developed and maintained with local leadership at each site, associated telehealth coordinators, and evidence-based therapy coordinators.
After contact has been established with remote facilities and the demand for services has been determined, there are several agreements and procedures to put in place before starting TMH services. An initial step is to develop a MOU agreement between the VISN TMH center and remote
sites that allows providers’ credentials and privileges to be shared. Also, it is important to establish a service agreement that outlines the procedures for staff at the remote site. This agreement includes checking in veterans, setting up the TMH rooms, transferring homework to VISN TMH providers, and connecting with the VISN TMH provider. In addition to service agreements, emergency procedures must be in place to ensure the safety of the veterans and the staff.24
After these agreements have been completed, the VISN TMH providers will have to complete request forms to obtain access to the Computerized Patient Record System at the remote facilities, which then must be approved by the Information Security Officer at that site. This is separate from the request at the provider’s site.12 It is essential to have points of contact for questions regarding this process. In order to facilitate referrals for TMH, electronic interfacility consult requests must be developed. Local staff need to collaborate with VISN TMH staff to ensure that the consult addresses the referral facilities need to meet the appropriate requirements.
Before the initiation of TMH services, each TMH provider has to establish clinics for scheduling appointments and obtaining workload credit. Program support assistants at the provider and remote sites must work together to ensure clinics are established correctly. This collaboration is essential for coding of visits and clinic mapping. After the clinics are “built,” appointment times will be set up based on the availability of the provider, support staff, and rooms at the remote site for the TMH session.
Once a consult is initiated, the VISN TMH EBP coordinator will review the consult and the veteran’s chart to ensure initial inclusion/exclusion criteria are met before accepting or canceling the consult. If the consult is accepted, a VISN TMH provider is assigned to the case and contacts the veteran to discuss the referral and (if the veteran is appropriate and interested) initiate services at the closest CBOC or at home. The VISN TMH regional center staff enter the appointment time for the veteran at both facility sites. The VISN TMH provider also coordinates with the CBOC staff to ensure that the veteran is checked in to the appointment and is provided with any questionnaires and necessary homework.
During the first session, the provider obtains consent from the veteran to engage in TMH services, conducts an assessment, and establishes rapport. The provider works with the veteran to develop a treatment plan for PTSD or other mental health diagnosis that will include the type of EBP. At the end of the first session, the next appointment is scheduled, and treatment materials are either mailed to the veteran or given to him or her onsite. After completing EBP, the VISN TMH center works with the referring provider to find follow-up services for the veteran.
The various steps necessary to begin an interfacility TMH clinic are summarized in Table 1.
Provider Training
Despite strong evidence of success, many providers remained skeptical about the efficacy of TMH. One study indicated that several providers in VISN 16 rarely used the established TMH programs because they were not familiar with them and applied TMH only for medication checks and consults.11 This skepticism was present in providers preparing to offer TMH as well as in providers referring veterans for TMH services. However, once providers better understood the TMH programs and had more experience using them, they were significantly more likely to use TMH for initial evaluations and ongoing psychotherapy. For these reasons, proper training and educational opportunities for practicing providers are vital to TMH implementation.9,11
To be proficient, providers need to become familiar with various TMH applications.10 Health care networks implementing TMH must ensure that their providers are well trained and prepared to give and receive proper consultation and support. Providers must also acquire several skills and familiarize themselves with available tools.9 In educating providers on the process and use of TMH, the authors suggest the following steps for TMH application:
- Learn new ways to chart in multiple systems and know how to troubleshoot during connectivity issues.
- Have an established administrative support collaborator at outpatient clinics to fax and exchange veteran homework.12
- The TMH clinic culture must be embedded where the veteran is being served in order to allow for a more realistic therapeutic feel. This type of clinic setting will allow for referrals at the veteran site and the availability to coordinate emergency procedures in the remote clinic.
Clinical Issues
Ongoing clinical issues need to be addressed continuously. Initially, referrals may be plentiful but not always appropriate. It is important to have an understanding with referring providers and remote sites about what constitutes a “good referral” as well as alternate referral options. It is imperative to outline inclusion and exclusion criteria that are clear and concise for referring providers. It is often helpful to revisit these criteria with potential referral sources after initiating services.
With the ability to provide inhome services, it is important to identify specific inclusion/exclusion criteria. Recommendations are based on research and clinical applications for exclusions, which are available on the Office of Technology Services website. These include imminent suicidality or homicidality, serious personality disorder or problematic character traits, acute substance disorders, psychotic disorders, and bipolar disorder. It is important to use sound clinical judgment, because the usual safeguards present in a remote clinic are not available for inhome services. Emergency planning is one of the most important aspects of the in-home TMH health services that are provided. The information for the emergency plan is obtained prior to initiation of services.
Emergency Plans
Each remote clinic that provides services to veterans must have an emergency plan that details procedures, phone numbers, and resources in case of medical and psychological emergencies as well as natural disasters. The VISN TMH provider will need to have a copy of the emergency plan as well as a list of contacts in case of an emergency during a TMH session.
It is recommended that TMH providers have several ways to contact key staff who can assist during an emergency. Usually the clinical coordinator and telehealth technician are the first responders to be alerted by the TMH provider during an emergency. They will then institute the remote clinic’s emergency protocol. Discussing these procedures and reviewing them with staff regularly is advisable, as key contacts may change.
In a psychological emergency, the VISN TMH provider may assist in implementing emergency procedures until a clinical counterpart at the remote site can be alerted. In the authors’ experience, VISN TMH providers have successfully de-escalated and diffused potentially emergent situations by maintaining constant realtime communication with veterans and staff by using VTC as well as interoffice communication. By offering assistance to veterans and staff during challenging situations, the VISN TMH provider will not only decrease concerns of veterans, but oftentimes integrate themselves into the treatment team of the remote clinic. The role of a VISN TMH provider can be isolative, with minimal contact with remote clinic staff, so it is important to increase visibility among staff at a remote site by communication with them even when there is not an emergency.
Treatment protocols may be determined by either administrative or clinical factors. With certain TMH interventions, the rooms used for veterans may be available for only certain periods, which may or may not fit with treatment protocols. For example, if a room is available for only an hour but a treatment protocol session is for 90 minutes, then another time slot needs to be found or a different treatment considered and offered. Although it is not ideal to have treatment protocols determined by scheduling factors, the reality of shared space at remote sites requires flexibility.
Sharing Materials and Homework Another clinical issue that is often overlooked is how to implement specific treatment protocols that entail the exchange of materials between VISN TMH providers and veterans. If materials will need to be exchanged between provider and veteran, a plan will have to be in place to facilitate this. The service agreement addresses these details, but remote staff may not always be aware of the details.
If a TMH provider opts to use faxes to send materials between a veteran and a provider, a desktop faxing program is recommended so veteran privacy is not compromised. Often, providers will wait to begin sessions until after they have received materials, but this may result in a delayed
session. One solution TMH providers can implement is mailing the materials and questionnaires to veterans before the session with clear instructions to complete them beforehand. Once the veteran arrives for the TMH session, she or he will verbally respond to the questionnaire and treatment materials. This will add time to a session but minimizes potential delays. Many of the clinical VTC units have movable cameras, so veterans can tilt the camera to show providers the forms and questionnaires.
The various steps necessary to address TMH clinical issues are summarized in Table 2.
VISIN 22 Pilot Project
The VISN 22 EBP TMH Center and Regional Pilot, based at the VA San Diego Healthcare System, was tasked with developing and providing TMH EBP services for PTSD across VISN 22 and adjacent West Coast VISNs. In addition to creating standardized procedures, troubleshooting guides were established to assist other programs with implementation. The primary focus was to increase access to EBPs for veterans with PTSD in areas where there was either no available trained providers or delays for specific services. The program established 16 clinics as well as in-home
services in VISN 22, VISN 21, and VISN 20. In fiscal year (FY) 2013, the VISN 22 EBP TMH Center and Regional Pilot provided 1,657 EBP encounters via TMH to 234 unique veterans with PTSD (Table 3).
The pilot project collected data to evaluate program effectiveness. The data were de-identified before being sent to the VA Central Office (VACO) TMH program manager. The following items were collected for the pilot: (1) clinical information; (2) consent to engage in treatment and telehealth; (3) release of information to share de-identified data to VACO for program monitoring; (4) demographic form; (5) Beck Depression Inventory-II (every other week); (6) PTSD Checklist (every other week); (7) World Health Organization Quality of Life (sessions 1, 7, final); (8) Wechsler Adult Intelligence Scale-Revised (sessions 3, 7, final); (9) satisfaction survey (final); (10) mileage not driven by veterans who receive TMH services; (11) travel pay saved by VA; (12) no-show rates; and (13) veteran, TMH provider, and referral provider satisfaction.
The growth in number of encounters and number of unique veterans has increased steadily from the first quarter of FY14 through the second quarter of FY15 (Figure 1).
In January 2013, in-home TMH services were piloted. Although occasional technical difficulties occurred, 143 EBP encounters via TMH were provided to 42 unique veterans in 2013. The service has continued to expand, and in the first half of FY14, services were provided to 64 unique veterans for a total of 278 encounters, saving veterans 3,220 travel miles and saving the VA $1,336 in travel reimbursement. In-home TMH services will continue to expand as more providers in a variety of programs are being trained by the San Diego staff on how to provide these services to veterans in their homes. In addition to decreasing mileage and travel pay, the no-show rates are lower for TMH appointments in general (averaged 8%-10% vs facility no-show rate average of 13.5%) and with the use of inhome TMH, no-show rates were kept to 2%. The growth in the number of in-home encounters and the number of unique veterans has also increased steadily from the first quarter of FY14 thru the second quarter of FY15 (Figure 2).
In-Home TMH Services
The VISN 22 EBP TMH Center and Regional Pilot often requests to have an in-person meeting with a veteran before starting TMH services in order to complete a waiver to download the software used by the VA for real-time video in-home services, a Release of Information for a Primary Support Person form, and an emergency plan.
It is also recommended that information about the veteran’s Internet connection, type of computer, type of software, presence of a camera and speakers, e-mail address, and access to secure messaging are obtained. During the initial contact with a veteran, the provider will discuss the rules and requirements to ensure HIPAA compliance. The veteran will need to have a private area for the call (not a restaurant, car, or other place where Wi-Fi is offered). Even with these discussions, some veterans will initiate services from a public place or a room in their home where family members will enter and exit frequently.
Although not required, it is recommended to have the veteran identify a primary support person and complete a release form to allow the TMH provider to contact that person in an emergency. The support person may be a person in the home (adult family member or caregiver) or someone nearby (neighbor, friend, or family member) who can contact emergency services if needed. After the necessary information is gathered and the veteran agrees to the conditions of participation, a test call will be completed. The TMH provider is often the person to conduct this call, but if available, a telehealth technician or facility telehealth coordinator may assist. The TMH provider may help the veteran download the appropriate software that is sent from the VA Scheduler software. The veteran initiates the call with the provider. Once the connection is made, the session may begin. Sites that are currently conducting in-home services have provided guides to veterans and newer TMH providers to outline the necessary steps for initiating services.
It is recommended that any provider interested in providing in-home TMH services use the Office of Technological Services help desk to assist in troubleshooting difficulties with connectivity. Challenges have included the software used for in-home TMH, periodic Internet outages, and compatibility issues.
Veteran Satisfaction
Veteran satisfaction was measured through a self-report satisfaction survey. The survey included 12 questions assessing overall experience in using TMH services. Eleven of the 12 questions included a 5-point Likert scale (1 = strongly disagree, 5 = strongly agree); the last question was openended for additional comments.
A summary of the survey response of the initial 29 veterans who received TMH services suggested the following: (1) Veterans felt comfortable with using the TMH equipment and were able to see their clinician clearly; (2) Technical assistance was sufficient; (3) During the TMH session, they related to the provider as if it were a face-to-face meeting and that their needs were met; and (4) Veterans reported extremely high satisfaction with TMH and would refer TMH care to other veterans. Veterans found clinic locations very convenient and preferred the TMH modality of mental health services delivery to the alternative of travelling a long distance to see their provider (Table 4).
Written comments and recommendations from veterans supported the survey results. Most reported that they saved time and the convenience of the clinic allowed them to receive the treatment they need without interfering with their work schedule. However, some veterans still experienced trouble with travel to the remote clinic. Others felt their experience was different from the one they expected or they had a good experience via TMH but preferred face-to-face care.
Conclusion
The VISN 22 EBP TMH Center and Regional Pilot have established the infrastructure of interfacility clinics to use EBPs for the treatment of PTSD. Also, the center has provided consultation and guidance to facilities interested in developing their own TMH programs. The TMH Center now plans to expand mental health services and include medication management and EBP services for non-PTSD psychiatric diagnoses. The established infrastructure will allow providers from one facility to cover the mental health service needs of other facilities when there are absences or gaps due to leave or delays/challenges in hiring in rural locations. Finally, TMH offers the potential to offer after-hours services to veterans in other time zones during providers’ regular tours of duty.
Several other TMH programs are now expanding services into veterans’ homes. There are several sites within the VHA that have piloted this TMH modality and developed guidelines and recommendations for further expansion. Currently VACO is encouraging all VHA facilities to increase in-home telehealth services, and the Office of Telehealth Services provides details on implementation. Interested parties are encouraged to routinely visit the VACO website for updated information.
Developing and implementing a new TMH program can be an arduous task, but the program has great potential to provide veteran-centered care. As TMH sessions progress, the provider and veteran become less aware of the camera and software and more aware of the therapeutic process. Challenges and delays in implementation are to be expected—these can occur frequently during the development and implementation stages of a TMH program. Maintaining consistent communication with staff at remote sites is essential for the success of any program.
As the VHA focuses on veterancentered care, TMH services will improve access to providers with specific, needed expertise. The authors hope these experiences can facilitate the continued growth of TMH and assuage any concerns a facility or provider may have about this modality of care. Delivery of TMH care can be challenging, but the ability to provide these services to veterans at times and locations convenient to them makes these challenges worthwhile.
Acknowledgments
Dr. Hauser wishes to thank Cathy, Anika, Jirina, Katia, and Max Hauser, and Alba Pillwein for their continued support. In memory of Beverly Ostroski.
Author disclosures
The authors report no actual or potential conflicts of interest with regard to this article.
Disclaimer
The opinions expressed herein are those of the authors and do not necessarily reflect those of Federal Practitioner, Frontline Medical Communications Inc., the U.S. Government, or any of its agencies. This article may discuss unlabeled or investigational use of certain drugs. Please review the complete prescribing information for specific drugs or drug combinations—including indications, contraindications, warnings, and adverse effects—before administering pharmacologic therapy to patients.
1. U.S. Department of Veterans Affairs. What is telehealth? U.S. Department of Veterans Affairs Website. http://www.telehealth.va.gov. Update May 13, 2014. Accessed April 30, 2015.
2. Morland LA, Greene CJ, Rosen C, Mauldin PD, Frueh CB. Issues in the design of a randomized noninferiority clinical trial of telemental health psychotherapy for rural combat veterans with PTSD. Contemp Clin Trials. 2009;30(6):513-522.
3. Strachan M, Gros DF, Ruggiero KJ, Lejuez CW, Acierno R. An integrated approach to delivering exposure-based treatment for symptoms of PTSD and depression in OIF/OEF veterans: preliminary findings. Behav Ther. 2012;43(3):560-569.
4. Yuen EK, Gros DF, Price M, et al. Randomized controlled trial of home-based telehealth versus in-person prolonged exposure for combat-related PTSD in veterans: preliminary results. J Clin Psychol. 2015;71(6):500-512.
5. Ruskin PE, Reed S, Kumar R, et al. Reliability and acceptability of psychiatric diagnosis via telecommunication and audiovisual technology. Psychiatr Serv. 1998;49(8):1086-1088.
6. Gros DF, Morland LA, Greene CJ, et al. Delivery of evidence-based psychotherapy via video telehealth. J Psychopathol Behav Assess. 2013;35(4):506-521.
7. Backhaus A, Agha Z, Maglione ML, et al. Videoconferencing psychotherapy: a systematic review. Psychol Serv. 2012;9(2):111-131.
8. Egede LE, Frueh CB, Richardson LK, et al. Rationale and design: telepsychology service delivery for depressed elderly veterans. Trials. 2009;10:22.
9. Frueh BC, Deitsch SE, Santos AB, et al. Procedural and methodological issues in telepsychiatry research and program development. Psychiatr Serv. 2000;51(12):1522-1527.
10. Grubaugh AL, Cain GD, Elhai JD, Patrick SL, Frueh BC. Attitudes toward medical and mental health care delivered via telehealth applications among rural and urban primary care patients. J Nerv Ment Dis. 2008;196(2):166-170.
11. Jameson JP, Farmer MS, Head KJ, Fortney J, Teal CR. VA community mental health service providers’ utilization of and attitudes towards telemental health care: the gatekeeper’s perspective. J Rural Health. 2011;27(4):425-432.
12. Thorp SR, Fidler J, Moreno L, Floto E, Agha Z. Lessons learned from studies of psychotherapy for posttraumatic stress disorder via video teleconferencing. Psychol Serv. 2012;9(2):197-199.
13. Gros DF, Yoder M, Tuerk PW, Lozano BE, Acierno R. Exposure therapy for PTSD delivered to veterans via telehealth: predictors of treatment completion and outcome and comparison to treatment delivered in person. Behav Ther. 2011;42(2):276-283.
14. Zarate CA Jr, Weinstock L, Cukor P, et al. Applicability of telemedicine for assessing patients with schizophrenia: acceptance and reliability. J Clin Psychiatry. 1997;58(1):22-25.
15. Jones AM, Shealy KM, Reid-Quiñones K, et al. Guidelines for establishing a telemental health program to provide evidence-based therapy for trauma-exposed children and families. Psychol Serv. 2014;11(4):398-409.
16. Frueh BC, Monnier J, Grubaugh AL, Elhai JD, Yim E, Knapp R. Therapist adherence and competence with manualized cognitive-behavioral therapy for PTSD delivered via videoconferencing technology. Behav Modif. 2007;31(6):856-866.
17. Morland LA, Hynes AK, Mackintosh MA, Resick PA, Chard KM. Group cognitive processing therapy delivered to veterans via telehealth: a pilot cohort. J Trauma Stress. 2011;24(4):465-469.
18. Tuerk PW, Yoder M, Ruggiero KJ, Gros DF, Acierno R. A pilot study of prolonged exposure therapy for posttraumatic stress disorder delivered via telehealth technology. J Trauma Stress. 2010;23(1):116-123.
19. Fortney JC, Pyne JM, Kimbrell TA, et al. Telemedicine- based collaborative care for posttraumatic stress disorder: a randomized clinical trial. JAMA Psychiatry. 2015;72(1):58-67.
20. Germain V, Marchand A, Bouchard S, Drouin MS, Guay S. Effectiveness of cognitive behavioural therapy administered by videoconference for posttraumatic stress disorder. Cogn Behav Ther. 2009;38(1):42-53.
21. Morland LA, Mackintosh M, Greene CJ, et al. Cognitive processing therapy for posttraumatic stress disorder delivered to rural veterans via telemental health: a randomized noninferiority clinical trial. J Clin Psychiatry. 2014;75(5):470-476.
22. Tuerk PW, Fortney J, Bosworth HB, et al. Toward the development of national telehealth services: the role of Veterans Health Administration and future directions for research. Telemed J E Health. 2010;16(1):115-117.
23. Godleski L, Darkins A, Peters J. Outcomes of 98,609 U.S. Department of Veterans Affairs patients enrolled in telemental health services, 2006-2010. Psychiatr Serv. 2012;63(4):383-385.
24. Strachan M, Gros DF, Yuen E, Ruggiero KJ, Foa EB, Acierno R. Home-based telehealth to deliver evidence-based psychotherapy in veterans with PTSD. Contemp Clin Trials. 2012;33(2):402-409.
Within VHA, telemental health (TMH) refers to behavioral health services that are provided remotely, using secure communication technologies, to veterans who are separated by distance from their mental health providers.1 Telemental health sometimes involves video teleconferencing (VTC) technology, where a veteran (or group of veterans) in one location and a provider in a different location are able to communicate in real time through a computer monitor or television screen.2 In the VHA, TMH visits are typically conducted from a central location (such as a medical center hospital) to a community-based outpatient clinic (CBOC), but pilot projects have also tested VTC in homes as well.1,3,4
In addition to providing timely access to behavioral health services in rural or underserved locations, TMH eliminates travel that may be disruptive or costly and allows mental health providers to consult with or provide supervision to one another. Telemental health can be used to make diagnoses, manage care, perform checkups, and provide long-term, follow-up care. Other uses for TMH include clinical assessment, individual and group psychotherapy, psycho-educational interventions, cognitive testing, and general psychiatric care.1,5,6 More recently, TMH has been used to provide evidence-based psychotherapies (EBPs) to individuals with posttraumatic stress disorder (PTSD) and other mental health diagnoses.6,7 Such care may be particularly advantageous for veterans with PTSD, because traveling can be a burden for them or a trigger for PTSD symptoms.
Although interactive video technology is becoming widely available, its use is limited in health care systems due to lack of knowledge, education, logistical guidance, and technical training. The authors have conducted EBPs using VTC across VISN 22 in both office-to-office and office-to-home modalities and are providing EBPs using VTC to CBOCs in other VISNs across the western U.S. This article addresses these issues, outlining the necessary steps required to establish a TMH clinic and to share the successes of the EBP TMH Center and Regional Pilot used at VISN 22.
Telemental Health
Telemental health is an effective alternative to in-person treatment and is well regarded by both mental health providers and veterans. Overall, mental health providers believe it can help reduce the stigma associated with traditional mental health care and ease transportation-related issues for veterans. Telemental health allows access to care for veterans living in rural or remote areas in addition to those who are incarcerated or are otherwise unable to attend visits at primary VA facilities.2,8-10 In an assessment of TMH services in 40 CBOCs across VISN 16, most CBOC mental health providers found it to be an acceptable alternative to face-to-face care, recognize the value of TMH, and endorse a willingness to use and expand TMH programs within their clinics.11
Veterans who participated in TMH via VTC have expressed satisfaction with the decreased travel time and expenses, fewer interactions with crowds, and fewer parking problems.12 Several studies suggested that veterans preferred TMH to in-person contact due to more rapid access to care and specialists who would otherwise be unavailable at remote locations.5,10 Similarly, veterans who avoid in-person mental health care were more open to remote therapy for many of the reasons listed earlier. Studies suggest that veterans from both rural and urban locations are generally receptive to receiving mental health services via TMH.5,10
Several studies have found that TMH services may have advantages over standard in-person care. These advantages include decreasing transportation costs, travel time, and time missed at work and increasing system coverage area.13 Overall, both veterans and providers reported similar satisfaction between VTC and in-person sessions and, in some cases, prefer VTC interactions due to a sense of “easing into” intense therapies or having a “therapeutic distance” as treatment begins.12
Utility
Previous studies have shown that TMH can be used successfully to provide psychopharmacologic treatment to veterans who have major depressive disorder or schizophrenia, among other psychiatric disorders.5,8,14 Recent studies have focused on the feasibility of providing EBPs via TMH, particularly for the treatment of PTSD.12,15 Studies have shown that TMH services via VTC can be used successfully to provide cognitive behavioral therapy (CBT), cognitive processing therapy (CPT), and prolonged exposure therapy (PE).16-21 In these studies, both PE and CPT delivered via TMH were found to be as efficacious as in-person formats. Furthermore, TMH services were successfully used in individual and group sessions.
Research has emphasized the benefits of TMH for veterans who are uncomfortable in crowds, waiting rooms, or hospital lobbies.7,12,18 For patients with PTSD who are initially limited by fears related to driving, TMH can facilitate access to care. Veterans with PTSD often avoid reminders of trauma (ie, uniforms, evidence of physical injury, artwork, photographs related to war), which can often be found at the larger VAMCs. These veterans may find mental health care services in their homes or at local CBOCs more appealing.7,12,18
Implementation
Prior to the implementation of telehealth services, many CBOC providers would refer veterans in need of specialty care to the nearest VAMC, which were sometimes many hours away.1 In response to travel and access concerns, the VA has implemented various telehealth modalities, including TMH.
In 2008, about 230,000 veterans received mental health services via real-time clinical VTC at 300 VA CBOCs, and about 40,000 veterans enrolled in the In-Home Telehealth program.22 By 2011, > 380,000 veterans used clinic-based telehealth services and about 100,000 veterans used the in-home program.1 Between 2006 and 2008, the 98,000 veterans who used TMH modalities had fewer hospital admissions compared with those who did not; overall, the need for hospital services decreased by about 25% for those using TMH services.23
Although research suggests that TMH is an effective treatment modality, it does have limitations. A recent study noted several visual and audio difficulties that can emerge, including pixilation, “tracer” images with movement, low resolution, “frozen” or “choppy” images, delays in sound, echoes, or “mechanical sounding” voices.12 In some cases, physical details, such as crying, sniffling, or fidgeting, could not be clearly observed.12 Overall, these unforeseen issues can impact the ability to give and receive care through TMH modalities. Proper procedures need to be developed and implemented for each site.
Getting Started
Using TMH to provide mental health care at other VHA facilities requires planning and preparation. Logistics, such as preparation of the room and equipment, should be considered. Similarly, veteran and provider convenience must be considered.2,11 Before starting TMH at any VA facility, professionals working with the audiovisual technology and providing TMH care must complete necessary VA Talent Management System courses and obtain copies of certificates to assure they have met the appropriate training criteria. Providers must be credentialed to provide TMH services, including the telehealth curriculum offered by VA Employee Educational Services.2,24 An appropriate memorandum of understanding (MOU) must be created, and credentialing and privileging must also be acquired.
In addition to provider training, an information technology representative who can administer technical support as needed must be selected for both the provider and remote locations. Technologic complications can make TMH implementation much more challenging.12 As such, it is important to assure that both the veteran and the provider have the necessary TMH equipment. The selected communication device must be compatible with the technology requirements at the provider and remote facilities.12
In addition to designated technical support, the VISN TMH coordinator needs to have point-of-contact information for those who can assist with each site’s telehealth services and address the demand for EBP for PTSD or other desired services. After this information has been obtained, relationships must be developed and maintained with local leadership at each site, associated telehealth coordinators, and evidence-based therapy coordinators.
After contact has been established with remote facilities and the demand for services has been determined, there are several agreements and procedures to put in place before starting TMH services. An initial step is to develop a MOU agreement between the VISN TMH center and remote
sites that allows providers’ credentials and privileges to be shared. Also, it is important to establish a service agreement that outlines the procedures for staff at the remote site. This agreement includes checking in veterans, setting up the TMH rooms, transferring homework to VISN TMH providers, and connecting with the VISN TMH provider. In addition to service agreements, emergency procedures must be in place to ensure the safety of the veterans and the staff.24
After these agreements have been completed, the VISN TMH providers will have to complete request forms to obtain access to the Computerized Patient Record System at the remote facilities, which then must be approved by the Information Security Officer at that site. This is separate from the request at the provider’s site.12 It is essential to have points of contact for questions regarding this process. In order to facilitate referrals for TMH, electronic interfacility consult requests must be developed. Local staff need to collaborate with VISN TMH staff to ensure that the consult addresses the referral facilities need to meet the appropriate requirements.
Before the initiation of TMH services, each TMH provider has to establish clinics for scheduling appointments and obtaining workload credit. Program support assistants at the provider and remote sites must work together to ensure clinics are established correctly. This collaboration is essential for coding of visits and clinic mapping. After the clinics are “built,” appointment times will be set up based on the availability of the provider, support staff, and rooms at the remote site for the TMH session.
Once a consult is initiated, the VISN TMH EBP coordinator will review the consult and the veteran’s chart to ensure initial inclusion/exclusion criteria are met before accepting or canceling the consult. If the consult is accepted, a VISN TMH provider is assigned to the case and contacts the veteran to discuss the referral and (if the veteran is appropriate and interested) initiate services at the closest CBOC or at home. The VISN TMH regional center staff enter the appointment time for the veteran at both facility sites. The VISN TMH provider also coordinates with the CBOC staff to ensure that the veteran is checked in to the appointment and is provided with any questionnaires and necessary homework.
During the first session, the provider obtains consent from the veteran to engage in TMH services, conducts an assessment, and establishes rapport. The provider works with the veteran to develop a treatment plan for PTSD or other mental health diagnosis that will include the type of EBP. At the end of the first session, the next appointment is scheduled, and treatment materials are either mailed to the veteran or given to him or her onsite. After completing EBP, the VISN TMH center works with the referring provider to find follow-up services for the veteran.
The various steps necessary to begin an interfacility TMH clinic are summarized in Table 1.
Provider Training
Despite strong evidence of success, many providers remained skeptical about the efficacy of TMH. One study indicated that several providers in VISN 16 rarely used the established TMH programs because they were not familiar with them and applied TMH only for medication checks and consults.11 This skepticism was present in providers preparing to offer TMH as well as in providers referring veterans for TMH services. However, once providers better understood the TMH programs and had more experience using them, they were significantly more likely to use TMH for initial evaluations and ongoing psychotherapy. For these reasons, proper training and educational opportunities for practicing providers are vital to TMH implementation.9,11
To be proficient, providers need to become familiar with various TMH applications.10 Health care networks implementing TMH must ensure that their providers are well trained and prepared to give and receive proper consultation and support. Providers must also acquire several skills and familiarize themselves with available tools.9 In educating providers on the process and use of TMH, the authors suggest the following steps for TMH application:
- Learn new ways to chart in multiple systems and know how to troubleshoot during connectivity issues.
- Have an established administrative support collaborator at outpatient clinics to fax and exchange veteran homework.12
- The TMH clinic culture must be embedded where the veteran is being served in order to allow for a more realistic therapeutic feel. This type of clinic setting will allow for referrals at the veteran site and the availability to coordinate emergency procedures in the remote clinic.
Clinical Issues
Ongoing clinical issues need to be addressed continuously. Initially, referrals may be plentiful but not always appropriate. It is important to have an understanding with referring providers and remote sites about what constitutes a “good referral” as well as alternate referral options. It is imperative to outline inclusion and exclusion criteria that are clear and concise for referring providers. It is often helpful to revisit these criteria with potential referral sources after initiating services.
With the ability to provide inhome services, it is important to identify specific inclusion/exclusion criteria. Recommendations are based on research and clinical applications for exclusions, which are available on the Office of Technology Services website. These include imminent suicidality or homicidality, serious personality disorder or problematic character traits, acute substance disorders, psychotic disorders, and bipolar disorder. It is important to use sound clinical judgment, because the usual safeguards present in a remote clinic are not available for inhome services. Emergency planning is one of the most important aspects of the in-home TMH health services that are provided. The information for the emergency plan is obtained prior to initiation of services.
Emergency Plans
Each remote clinic that provides services to veterans must have an emergency plan that details procedures, phone numbers, and resources in case of medical and psychological emergencies as well as natural disasters. The VISN TMH provider will need to have a copy of the emergency plan as well as a list of contacts in case of an emergency during a TMH session.
It is recommended that TMH providers have several ways to contact key staff who can assist during an emergency. Usually the clinical coordinator and telehealth technician are the first responders to be alerted by the TMH provider during an emergency. They will then institute the remote clinic’s emergency protocol. Discussing these procedures and reviewing them with staff regularly is advisable, as key contacts may change.
In a psychological emergency, the VISN TMH provider may assist in implementing emergency procedures until a clinical counterpart at the remote site can be alerted. In the authors’ experience, VISN TMH providers have successfully de-escalated and diffused potentially emergent situations by maintaining constant realtime communication with veterans and staff by using VTC as well as interoffice communication. By offering assistance to veterans and staff during challenging situations, the VISN TMH provider will not only decrease concerns of veterans, but oftentimes integrate themselves into the treatment team of the remote clinic. The role of a VISN TMH provider can be isolative, with minimal contact with remote clinic staff, so it is important to increase visibility among staff at a remote site by communication with them even when there is not an emergency.
Treatment protocols may be determined by either administrative or clinical factors. With certain TMH interventions, the rooms used for veterans may be available for only certain periods, which may or may not fit with treatment protocols. For example, if a room is available for only an hour but a treatment protocol session is for 90 minutes, then another time slot needs to be found or a different treatment considered and offered. Although it is not ideal to have treatment protocols determined by scheduling factors, the reality of shared space at remote sites requires flexibility.
Sharing Materials and Homework Another clinical issue that is often overlooked is how to implement specific treatment protocols that entail the exchange of materials between VISN TMH providers and veterans. If materials will need to be exchanged between provider and veteran, a plan will have to be in place to facilitate this. The service agreement addresses these details, but remote staff may not always be aware of the details.
If a TMH provider opts to use faxes to send materials between a veteran and a provider, a desktop faxing program is recommended so veteran privacy is not compromised. Often, providers will wait to begin sessions until after they have received materials, but this may result in a delayed
session. One solution TMH providers can implement is mailing the materials and questionnaires to veterans before the session with clear instructions to complete them beforehand. Once the veteran arrives for the TMH session, she or he will verbally respond to the questionnaire and treatment materials. This will add time to a session but minimizes potential delays. Many of the clinical VTC units have movable cameras, so veterans can tilt the camera to show providers the forms and questionnaires.
The various steps necessary to address TMH clinical issues are summarized in Table 2.
VISIN 22 Pilot Project
The VISN 22 EBP TMH Center and Regional Pilot, based at the VA San Diego Healthcare System, was tasked with developing and providing TMH EBP services for PTSD across VISN 22 and adjacent West Coast VISNs. In addition to creating standardized procedures, troubleshooting guides were established to assist other programs with implementation. The primary focus was to increase access to EBPs for veterans with PTSD in areas where there was either no available trained providers or delays for specific services. The program established 16 clinics as well as in-home
services in VISN 22, VISN 21, and VISN 20. In fiscal year (FY) 2013, the VISN 22 EBP TMH Center and Regional Pilot provided 1,657 EBP encounters via TMH to 234 unique veterans with PTSD (Table 3).
The pilot project collected data to evaluate program effectiveness. The data were de-identified before being sent to the VA Central Office (VACO) TMH program manager. The following items were collected for the pilot: (1) clinical information; (2) consent to engage in treatment and telehealth; (3) release of information to share de-identified data to VACO for program monitoring; (4) demographic form; (5) Beck Depression Inventory-II (every other week); (6) PTSD Checklist (every other week); (7) World Health Organization Quality of Life (sessions 1, 7, final); (8) Wechsler Adult Intelligence Scale-Revised (sessions 3, 7, final); (9) satisfaction survey (final); (10) mileage not driven by veterans who receive TMH services; (11) travel pay saved by VA; (12) no-show rates; and (13) veteran, TMH provider, and referral provider satisfaction.
The growth in number of encounters and number of unique veterans has increased steadily from the first quarter of FY14 through the second quarter of FY15 (Figure 1).
In January 2013, in-home TMH services were piloted. Although occasional technical difficulties occurred, 143 EBP encounters via TMH were provided to 42 unique veterans in 2013. The service has continued to expand, and in the first half of FY14, services were provided to 64 unique veterans for a total of 278 encounters, saving veterans 3,220 travel miles and saving the VA $1,336 in travel reimbursement. In-home TMH services will continue to expand as more providers in a variety of programs are being trained by the San Diego staff on how to provide these services to veterans in their homes. In addition to decreasing mileage and travel pay, the no-show rates are lower for TMH appointments in general (averaged 8%-10% vs facility no-show rate average of 13.5%) and with the use of inhome TMH, no-show rates were kept to 2%. The growth in the number of in-home encounters and the number of unique veterans has also increased steadily from the first quarter of FY14 thru the second quarter of FY15 (Figure 2).
In-Home TMH Services
The VISN 22 EBP TMH Center and Regional Pilot often requests to have an in-person meeting with a veteran before starting TMH services in order to complete a waiver to download the software used by the VA for real-time video in-home services, a Release of Information for a Primary Support Person form, and an emergency plan.
It is also recommended that information about the veteran’s Internet connection, type of computer, type of software, presence of a camera and speakers, e-mail address, and access to secure messaging are obtained. During the initial contact with a veteran, the provider will discuss the rules and requirements to ensure HIPAA compliance. The veteran will need to have a private area for the call (not a restaurant, car, or other place where Wi-Fi is offered). Even with these discussions, some veterans will initiate services from a public place or a room in their home where family members will enter and exit frequently.
Although not required, it is recommended to have the veteran identify a primary support person and complete a release form to allow the TMH provider to contact that person in an emergency. The support person may be a person in the home (adult family member or caregiver) or someone nearby (neighbor, friend, or family member) who can contact emergency services if needed. After the necessary information is gathered and the veteran agrees to the conditions of participation, a test call will be completed. The TMH provider is often the person to conduct this call, but if available, a telehealth technician or facility telehealth coordinator may assist. The TMH provider may help the veteran download the appropriate software that is sent from the VA Scheduler software. The veteran initiates the call with the provider. Once the connection is made, the session may begin. Sites that are currently conducting in-home services have provided guides to veterans and newer TMH providers to outline the necessary steps for initiating services.
It is recommended that any provider interested in providing in-home TMH services use the Office of Technological Services help desk to assist in troubleshooting difficulties with connectivity. Challenges have included the software used for in-home TMH, periodic Internet outages, and compatibility issues.
Veteran Satisfaction
Veteran satisfaction was measured through a self-report satisfaction survey. The survey included 12 questions assessing overall experience in using TMH services. Eleven of the 12 questions included a 5-point Likert scale (1 = strongly disagree, 5 = strongly agree); the last question was openended for additional comments.
A summary of the survey response of the initial 29 veterans who received TMH services suggested the following: (1) Veterans felt comfortable with using the TMH equipment and were able to see their clinician clearly; (2) Technical assistance was sufficient; (3) During the TMH session, they related to the provider as if it were a face-to-face meeting and that their needs were met; and (4) Veterans reported extremely high satisfaction with TMH and would refer TMH care to other veterans. Veterans found clinic locations very convenient and preferred the TMH modality of mental health services delivery to the alternative of travelling a long distance to see their provider (Table 4).
Written comments and recommendations from veterans supported the survey results. Most reported that they saved time and the convenience of the clinic allowed them to receive the treatment they need without interfering with their work schedule. However, some veterans still experienced trouble with travel to the remote clinic. Others felt their experience was different from the one they expected or they had a good experience via TMH but preferred face-to-face care.
Conclusion
The VISN 22 EBP TMH Center and Regional Pilot have established the infrastructure of interfacility clinics to use EBPs for the treatment of PTSD. Also, the center has provided consultation and guidance to facilities interested in developing their own TMH programs. The TMH Center now plans to expand mental health services and include medication management and EBP services for non-PTSD psychiatric diagnoses. The established infrastructure will allow providers from one facility to cover the mental health service needs of other facilities when there are absences or gaps due to leave or delays/challenges in hiring in rural locations. Finally, TMH offers the potential to offer after-hours services to veterans in other time zones during providers’ regular tours of duty.
Several other TMH programs are now expanding services into veterans’ homes. There are several sites within the VHA that have piloted this TMH modality and developed guidelines and recommendations for further expansion. Currently VACO is encouraging all VHA facilities to increase in-home telehealth services, and the Office of Telehealth Services provides details on implementation. Interested parties are encouraged to routinely visit the VACO website for updated information.
Developing and implementing a new TMH program can be an arduous task, but the program has great potential to provide veteran-centered care. As TMH sessions progress, the provider and veteran become less aware of the camera and software and more aware of the therapeutic process. Challenges and delays in implementation are to be expected—these can occur frequently during the development and implementation stages of a TMH program. Maintaining consistent communication with staff at remote sites is essential for the success of any program.
As the VHA focuses on veterancentered care, TMH services will improve access to providers with specific, needed expertise. The authors hope these experiences can facilitate the continued growth of TMH and assuage any concerns a facility or provider may have about this modality of care. Delivery of TMH care can be challenging, but the ability to provide these services to veterans at times and locations convenient to them makes these challenges worthwhile.
Acknowledgments
Dr. Hauser wishes to thank Cathy, Anika, Jirina, Katia, and Max Hauser, and Alba Pillwein for their continued support. In memory of Beverly Ostroski.
Author disclosures
The authors report no actual or potential conflicts of interest with regard to this article.
Disclaimer
The opinions expressed herein are those of the authors and do not necessarily reflect those of Federal Practitioner, Frontline Medical Communications Inc., the U.S. Government, or any of its agencies. This article may discuss unlabeled or investigational use of certain drugs. Please review the complete prescribing information for specific drugs or drug combinations—including indications, contraindications, warnings, and adverse effects—before administering pharmacologic therapy to patients.
Within VHA, telemental health (TMH) refers to behavioral health services that are provided remotely, using secure communication technologies, to veterans who are separated by distance from their mental health providers.1 Telemental health sometimes involves video teleconferencing (VTC) technology, where a veteran (or group of veterans) in one location and a provider in a different location are able to communicate in real time through a computer monitor or television screen.2 In the VHA, TMH visits are typically conducted from a central location (such as a medical center hospital) to a community-based outpatient clinic (CBOC), but pilot projects have also tested VTC in homes as well.1,3,4
In addition to providing timely access to behavioral health services in rural or underserved locations, TMH eliminates travel that may be disruptive or costly and allows mental health providers to consult with or provide supervision to one another. Telemental health can be used to make diagnoses, manage care, perform checkups, and provide long-term, follow-up care. Other uses for TMH include clinical assessment, individual and group psychotherapy, psycho-educational interventions, cognitive testing, and general psychiatric care.1,5,6 More recently, TMH has been used to provide evidence-based psychotherapies (EBPs) to individuals with posttraumatic stress disorder (PTSD) and other mental health diagnoses.6,7 Such care may be particularly advantageous for veterans with PTSD, because traveling can be a burden for them or a trigger for PTSD symptoms.
Although interactive video technology is becoming widely available, its use is limited in health care systems due to lack of knowledge, education, logistical guidance, and technical training. The authors have conducted EBPs using VTC across VISN 22 in both office-to-office and office-to-home modalities and are providing EBPs using VTC to CBOCs in other VISNs across the western U.S. This article addresses these issues, outlining the necessary steps required to establish a TMH clinic and to share the successes of the EBP TMH Center and Regional Pilot used at VISN 22.
Telemental Health
Telemental health is an effective alternative to in-person treatment and is well regarded by both mental health providers and veterans. Overall, mental health providers believe it can help reduce the stigma associated with traditional mental health care and ease transportation-related issues for veterans. Telemental health allows access to care for veterans living in rural or remote areas in addition to those who are incarcerated or are otherwise unable to attend visits at primary VA facilities.2,8-10 In an assessment of TMH services in 40 CBOCs across VISN 16, most CBOC mental health providers found it to be an acceptable alternative to face-to-face care, recognize the value of TMH, and endorse a willingness to use and expand TMH programs within their clinics.11
Veterans who participated in TMH via VTC have expressed satisfaction with the decreased travel time and expenses, fewer interactions with crowds, and fewer parking problems.12 Several studies suggested that veterans preferred TMH to in-person contact due to more rapid access to care and specialists who would otherwise be unavailable at remote locations.5,10 Similarly, veterans who avoid in-person mental health care were more open to remote therapy for many of the reasons listed earlier. Studies suggest that veterans from both rural and urban locations are generally receptive to receiving mental health services via TMH.5,10
Several studies have found that TMH services may have advantages over standard in-person care. These advantages include decreasing transportation costs, travel time, and time missed at work and increasing system coverage area.13 Overall, both veterans and providers reported similar satisfaction between VTC and in-person sessions and, in some cases, prefer VTC interactions due to a sense of “easing into” intense therapies or having a “therapeutic distance” as treatment begins.12
Utility
Previous studies have shown that TMH can be used successfully to provide psychopharmacologic treatment to veterans who have major depressive disorder or schizophrenia, among other psychiatric disorders.5,8,14 Recent studies have focused on the feasibility of providing EBPs via TMH, particularly for the treatment of PTSD.12,15 Studies have shown that TMH services via VTC can be used successfully to provide cognitive behavioral therapy (CBT), cognitive processing therapy (CPT), and prolonged exposure therapy (PE).16-21 In these studies, both PE and CPT delivered via TMH were found to be as efficacious as in-person formats. Furthermore, TMH services were successfully used in individual and group sessions.
Research has emphasized the benefits of TMH for veterans who are uncomfortable in crowds, waiting rooms, or hospital lobbies.7,12,18 For patients with PTSD who are initially limited by fears related to driving, TMH can facilitate access to care. Veterans with PTSD often avoid reminders of trauma (ie, uniforms, evidence of physical injury, artwork, photographs related to war), which can often be found at the larger VAMCs. These veterans may find mental health care services in their homes or at local CBOCs more appealing.7,12,18
Implementation
Prior to the implementation of telehealth services, many CBOC providers would refer veterans in need of specialty care to the nearest VAMC, which were sometimes many hours away.1 In response to travel and access concerns, the VA has implemented various telehealth modalities, including TMH.
In 2008, about 230,000 veterans received mental health services via real-time clinical VTC at 300 VA CBOCs, and about 40,000 veterans enrolled in the In-Home Telehealth program.22 By 2011, > 380,000 veterans used clinic-based telehealth services and about 100,000 veterans used the in-home program.1 Between 2006 and 2008, the 98,000 veterans who used TMH modalities had fewer hospital admissions compared with those who did not; overall, the need for hospital services decreased by about 25% for those using TMH services.23
Although research suggests that TMH is an effective treatment modality, it does have limitations. A recent study noted several visual and audio difficulties that can emerge, including pixilation, “tracer” images with movement, low resolution, “frozen” or “choppy” images, delays in sound, echoes, or “mechanical sounding” voices.12 In some cases, physical details, such as crying, sniffling, or fidgeting, could not be clearly observed.12 Overall, these unforeseen issues can impact the ability to give and receive care through TMH modalities. Proper procedures need to be developed and implemented for each site.
Getting Started
Using TMH to provide mental health care at other VHA facilities requires planning and preparation. Logistics, such as preparation of the room and equipment, should be considered. Similarly, veteran and provider convenience must be considered.2,11 Before starting TMH at any VA facility, professionals working with the audiovisual technology and providing TMH care must complete necessary VA Talent Management System courses and obtain copies of certificates to assure they have met the appropriate training criteria. Providers must be credentialed to provide TMH services, including the telehealth curriculum offered by VA Employee Educational Services.2,24 An appropriate memorandum of understanding (MOU) must be created, and credentialing and privileging must also be acquired.
In addition to provider training, an information technology representative who can administer technical support as needed must be selected for both the provider and remote locations. Technologic complications can make TMH implementation much more challenging.12 As such, it is important to assure that both the veteran and the provider have the necessary TMH equipment. The selected communication device must be compatible with the technology requirements at the provider and remote facilities.12
In addition to designated technical support, the VISN TMH coordinator needs to have point-of-contact information for those who can assist with each site’s telehealth services and address the demand for EBP for PTSD or other desired services. After this information has been obtained, relationships must be developed and maintained with local leadership at each site, associated telehealth coordinators, and evidence-based therapy coordinators.
After contact has been established with remote facilities and the demand for services has been determined, there are several agreements and procedures to put in place before starting TMH services. An initial step is to develop a MOU agreement between the VISN TMH center and remote
sites that allows providers’ credentials and privileges to be shared. Also, it is important to establish a service agreement that outlines the procedures for staff at the remote site. This agreement includes checking in veterans, setting up the TMH rooms, transferring homework to VISN TMH providers, and connecting with the VISN TMH provider. In addition to service agreements, emergency procedures must be in place to ensure the safety of the veterans and the staff.24
After these agreements have been completed, the VISN TMH providers will have to complete request forms to obtain access to the Computerized Patient Record System at the remote facilities, which then must be approved by the Information Security Officer at that site. This is separate from the request at the provider’s site.12 It is essential to have points of contact for questions regarding this process. In order to facilitate referrals for TMH, electronic interfacility consult requests must be developed. Local staff need to collaborate with VISN TMH staff to ensure that the consult addresses the referral facilities need to meet the appropriate requirements.
Before the initiation of TMH services, each TMH provider has to establish clinics for scheduling appointments and obtaining workload credit. Program support assistants at the provider and remote sites must work together to ensure clinics are established correctly. This collaboration is essential for coding of visits and clinic mapping. After the clinics are “built,” appointment times will be set up based on the availability of the provider, support staff, and rooms at the remote site for the TMH session.
Once a consult is initiated, the VISN TMH EBP coordinator will review the consult and the veteran’s chart to ensure initial inclusion/exclusion criteria are met before accepting or canceling the consult. If the consult is accepted, a VISN TMH provider is assigned to the case and contacts the veteran to discuss the referral and (if the veteran is appropriate and interested) initiate services at the closest CBOC or at home. The VISN TMH regional center staff enter the appointment time for the veteran at both facility sites. The VISN TMH provider also coordinates with the CBOC staff to ensure that the veteran is checked in to the appointment and is provided with any questionnaires and necessary homework.
During the first session, the provider obtains consent from the veteran to engage in TMH services, conducts an assessment, and establishes rapport. The provider works with the veteran to develop a treatment plan for PTSD or other mental health diagnosis that will include the type of EBP. At the end of the first session, the next appointment is scheduled, and treatment materials are either mailed to the veteran or given to him or her onsite. After completing EBP, the VISN TMH center works with the referring provider to find follow-up services for the veteran.
The various steps necessary to begin an interfacility TMH clinic are summarized in Table 1.
Provider Training
Despite strong evidence of success, many providers remained skeptical about the efficacy of TMH. One study indicated that several providers in VISN 16 rarely used the established TMH programs because they were not familiar with them and applied TMH only for medication checks and consults.11 This skepticism was present in providers preparing to offer TMH as well as in providers referring veterans for TMH services. However, once providers better understood the TMH programs and had more experience using them, they were significantly more likely to use TMH for initial evaluations and ongoing psychotherapy. For these reasons, proper training and educational opportunities for practicing providers are vital to TMH implementation.9,11
To be proficient, providers need to become familiar with various TMH applications.10 Health care networks implementing TMH must ensure that their providers are well trained and prepared to give and receive proper consultation and support. Providers must also acquire several skills and familiarize themselves with available tools.9 In educating providers on the process and use of TMH, the authors suggest the following steps for TMH application:
- Learn new ways to chart in multiple systems and know how to troubleshoot during connectivity issues.
- Have an established administrative support collaborator at outpatient clinics to fax and exchange veteran homework.12
- The TMH clinic culture must be embedded where the veteran is being served in order to allow for a more realistic therapeutic feel. This type of clinic setting will allow for referrals at the veteran site and the availability to coordinate emergency procedures in the remote clinic.
Clinical Issues
Ongoing clinical issues need to be addressed continuously. Initially, referrals may be plentiful but not always appropriate. It is important to have an understanding with referring providers and remote sites about what constitutes a “good referral” as well as alternate referral options. It is imperative to outline inclusion and exclusion criteria that are clear and concise for referring providers. It is often helpful to revisit these criteria with potential referral sources after initiating services.
With the ability to provide inhome services, it is important to identify specific inclusion/exclusion criteria. Recommendations are based on research and clinical applications for exclusions, which are available on the Office of Technology Services website. These include imminent suicidality or homicidality, serious personality disorder or problematic character traits, acute substance disorders, psychotic disorders, and bipolar disorder. It is important to use sound clinical judgment, because the usual safeguards present in a remote clinic are not available for inhome services. Emergency planning is one of the most important aspects of the in-home TMH health services that are provided. The information for the emergency plan is obtained prior to initiation of services.
Emergency Plans
Each remote clinic that provides services to veterans must have an emergency plan that details procedures, phone numbers, and resources in case of medical and psychological emergencies as well as natural disasters. The VISN TMH provider will need to have a copy of the emergency plan as well as a list of contacts in case of an emergency during a TMH session.
It is recommended that TMH providers have several ways to contact key staff who can assist during an emergency. Usually the clinical coordinator and telehealth technician are the first responders to be alerted by the TMH provider during an emergency. They will then institute the remote clinic’s emergency protocol. Discussing these procedures and reviewing them with staff regularly is advisable, as key contacts may change.
In a psychological emergency, the VISN TMH provider may assist in implementing emergency procedures until a clinical counterpart at the remote site can be alerted. In the authors’ experience, VISN TMH providers have successfully de-escalated and diffused potentially emergent situations by maintaining constant realtime communication with veterans and staff by using VTC as well as interoffice communication. By offering assistance to veterans and staff during challenging situations, the VISN TMH provider will not only decrease concerns of veterans, but oftentimes integrate themselves into the treatment team of the remote clinic. The role of a VISN TMH provider can be isolative, with minimal contact with remote clinic staff, so it is important to increase visibility among staff at a remote site by communication with them even when there is not an emergency.
Treatment protocols may be determined by either administrative or clinical factors. With certain TMH interventions, the rooms used for veterans may be available for only certain periods, which may or may not fit with treatment protocols. For example, if a room is available for only an hour but a treatment protocol session is for 90 minutes, then another time slot needs to be found or a different treatment considered and offered. Although it is not ideal to have treatment protocols determined by scheduling factors, the reality of shared space at remote sites requires flexibility.
Sharing Materials and Homework Another clinical issue that is often overlooked is how to implement specific treatment protocols that entail the exchange of materials between VISN TMH providers and veterans. If materials will need to be exchanged between provider and veteran, a plan will have to be in place to facilitate this. The service agreement addresses these details, but remote staff may not always be aware of the details.
If a TMH provider opts to use faxes to send materials between a veteran and a provider, a desktop faxing program is recommended so veteran privacy is not compromised. Often, providers will wait to begin sessions until after they have received materials, but this may result in a delayed
session. One solution TMH providers can implement is mailing the materials and questionnaires to veterans before the session with clear instructions to complete them beforehand. Once the veteran arrives for the TMH session, she or he will verbally respond to the questionnaire and treatment materials. This will add time to a session but minimizes potential delays. Many of the clinical VTC units have movable cameras, so veterans can tilt the camera to show providers the forms and questionnaires.
The various steps necessary to address TMH clinical issues are summarized in Table 2.
VISIN 22 Pilot Project
The VISN 22 EBP TMH Center and Regional Pilot, based at the VA San Diego Healthcare System, was tasked with developing and providing TMH EBP services for PTSD across VISN 22 and adjacent West Coast VISNs. In addition to creating standardized procedures, troubleshooting guides were established to assist other programs with implementation. The primary focus was to increase access to EBPs for veterans with PTSD in areas where there was either no available trained providers or delays for specific services. The program established 16 clinics as well as in-home
services in VISN 22, VISN 21, and VISN 20. In fiscal year (FY) 2013, the VISN 22 EBP TMH Center and Regional Pilot provided 1,657 EBP encounters via TMH to 234 unique veterans with PTSD (Table 3).
The pilot project collected data to evaluate program effectiveness. The data were de-identified before being sent to the VA Central Office (VACO) TMH program manager. The following items were collected for the pilot: (1) clinical information; (2) consent to engage in treatment and telehealth; (3) release of information to share de-identified data to VACO for program monitoring; (4) demographic form; (5) Beck Depression Inventory-II (every other week); (6) PTSD Checklist (every other week); (7) World Health Organization Quality of Life (sessions 1, 7, final); (8) Wechsler Adult Intelligence Scale-Revised (sessions 3, 7, final); (9) satisfaction survey (final); (10) mileage not driven by veterans who receive TMH services; (11) travel pay saved by VA; (12) no-show rates; and (13) veteran, TMH provider, and referral provider satisfaction.
The growth in number of encounters and number of unique veterans has increased steadily from the first quarter of FY14 through the second quarter of FY15 (Figure 1).
In January 2013, in-home TMH services were piloted. Although occasional technical difficulties occurred, 143 EBP encounters via TMH were provided to 42 unique veterans in 2013. The service has continued to expand, and in the first half of FY14, services were provided to 64 unique veterans for a total of 278 encounters, saving veterans 3,220 travel miles and saving the VA $1,336 in travel reimbursement. In-home TMH services will continue to expand as more providers in a variety of programs are being trained by the San Diego staff on how to provide these services to veterans in their homes. In addition to decreasing mileage and travel pay, the no-show rates are lower for TMH appointments in general (averaged 8%-10% vs facility no-show rate average of 13.5%) and with the use of inhome TMH, no-show rates were kept to 2%. The growth in the number of in-home encounters and the number of unique veterans has also increased steadily from the first quarter of FY14 thru the second quarter of FY15 (Figure 2).
In-Home TMH Services
The VISN 22 EBP TMH Center and Regional Pilot often requests to have an in-person meeting with a veteran before starting TMH services in order to complete a waiver to download the software used by the VA for real-time video in-home services, a Release of Information for a Primary Support Person form, and an emergency plan.
It is also recommended that information about the veteran’s Internet connection, type of computer, type of software, presence of a camera and speakers, e-mail address, and access to secure messaging are obtained. During the initial contact with a veteran, the provider will discuss the rules and requirements to ensure HIPAA compliance. The veteran will need to have a private area for the call (not a restaurant, car, or other place where Wi-Fi is offered). Even with these discussions, some veterans will initiate services from a public place or a room in their home where family members will enter and exit frequently.
Although not required, it is recommended to have the veteran identify a primary support person and complete a release form to allow the TMH provider to contact that person in an emergency. The support person may be a person in the home (adult family member or caregiver) or someone nearby (neighbor, friend, or family member) who can contact emergency services if needed. After the necessary information is gathered and the veteran agrees to the conditions of participation, a test call will be completed. The TMH provider is often the person to conduct this call, but if available, a telehealth technician or facility telehealth coordinator may assist. The TMH provider may help the veteran download the appropriate software that is sent from the VA Scheduler software. The veteran initiates the call with the provider. Once the connection is made, the session may begin. Sites that are currently conducting in-home services have provided guides to veterans and newer TMH providers to outline the necessary steps for initiating services.
It is recommended that any provider interested in providing in-home TMH services use the Office of Technological Services help desk to assist in troubleshooting difficulties with connectivity. Challenges have included the software used for in-home TMH, periodic Internet outages, and compatibility issues.
Veteran Satisfaction
Veteran satisfaction was measured through a self-report satisfaction survey. The survey included 12 questions assessing overall experience in using TMH services. Eleven of the 12 questions included a 5-point Likert scale (1 = strongly disagree, 5 = strongly agree); the last question was openended for additional comments.
A summary of the survey response of the initial 29 veterans who received TMH services suggested the following: (1) Veterans felt comfortable with using the TMH equipment and were able to see their clinician clearly; (2) Technical assistance was sufficient; (3) During the TMH session, they related to the provider as if it were a face-to-face meeting and that their needs were met; and (4) Veterans reported extremely high satisfaction with TMH and would refer TMH care to other veterans. Veterans found clinic locations very convenient and preferred the TMH modality of mental health services delivery to the alternative of travelling a long distance to see their provider (Table 4).
Written comments and recommendations from veterans supported the survey results. Most reported that they saved time and the convenience of the clinic allowed them to receive the treatment they need without interfering with their work schedule. However, some veterans still experienced trouble with travel to the remote clinic. Others felt their experience was different from the one they expected or they had a good experience via TMH but preferred face-to-face care.
Conclusion
The VISN 22 EBP TMH Center and Regional Pilot have established the infrastructure of interfacility clinics to use EBPs for the treatment of PTSD. Also, the center has provided consultation and guidance to facilities interested in developing their own TMH programs. The TMH Center now plans to expand mental health services and include medication management and EBP services for non-PTSD psychiatric diagnoses. The established infrastructure will allow providers from one facility to cover the mental health service needs of other facilities when there are absences or gaps due to leave or delays/challenges in hiring in rural locations. Finally, TMH offers the potential to offer after-hours services to veterans in other time zones during providers’ regular tours of duty.
Several other TMH programs are now expanding services into veterans’ homes. There are several sites within the VHA that have piloted this TMH modality and developed guidelines and recommendations for further expansion. Currently VACO is encouraging all VHA facilities to increase in-home telehealth services, and the Office of Telehealth Services provides details on implementation. Interested parties are encouraged to routinely visit the VACO website for updated information.
Developing and implementing a new TMH program can be an arduous task, but the program has great potential to provide veteran-centered care. As TMH sessions progress, the provider and veteran become less aware of the camera and software and more aware of the therapeutic process. Challenges and delays in implementation are to be expected—these can occur frequently during the development and implementation stages of a TMH program. Maintaining consistent communication with staff at remote sites is essential for the success of any program.
As the VHA focuses on veterancentered care, TMH services will improve access to providers with specific, needed expertise. The authors hope these experiences can facilitate the continued growth of TMH and assuage any concerns a facility or provider may have about this modality of care. Delivery of TMH care can be challenging, but the ability to provide these services to veterans at times and locations convenient to them makes these challenges worthwhile.
Acknowledgments
Dr. Hauser wishes to thank Cathy, Anika, Jirina, Katia, and Max Hauser, and Alba Pillwein for their continued support. In memory of Beverly Ostroski.
Author disclosures
The authors report no actual or potential conflicts of interest with regard to this article.
Disclaimer
The opinions expressed herein are those of the authors and do not necessarily reflect those of Federal Practitioner, Frontline Medical Communications Inc., the U.S. Government, or any of its agencies. This article may discuss unlabeled or investigational use of certain drugs. Please review the complete prescribing information for specific drugs or drug combinations—including indications, contraindications, warnings, and adverse effects—before administering pharmacologic therapy to patients.
1. U.S. Department of Veterans Affairs. What is telehealth? U.S. Department of Veterans Affairs Website. http://www.telehealth.va.gov. Update May 13, 2014. Accessed April 30, 2015.
2. Morland LA, Greene CJ, Rosen C, Mauldin PD, Frueh CB. Issues in the design of a randomized noninferiority clinical trial of telemental health psychotherapy for rural combat veterans with PTSD. Contemp Clin Trials. 2009;30(6):513-522.
3. Strachan M, Gros DF, Ruggiero KJ, Lejuez CW, Acierno R. An integrated approach to delivering exposure-based treatment for symptoms of PTSD and depression in OIF/OEF veterans: preliminary findings. Behav Ther. 2012;43(3):560-569.
4. Yuen EK, Gros DF, Price M, et al. Randomized controlled trial of home-based telehealth versus in-person prolonged exposure for combat-related PTSD in veterans: preliminary results. J Clin Psychol. 2015;71(6):500-512.
5. Ruskin PE, Reed S, Kumar R, et al. Reliability and acceptability of psychiatric diagnosis via telecommunication and audiovisual technology. Psychiatr Serv. 1998;49(8):1086-1088.
6. Gros DF, Morland LA, Greene CJ, et al. Delivery of evidence-based psychotherapy via video telehealth. J Psychopathol Behav Assess. 2013;35(4):506-521.
7. Backhaus A, Agha Z, Maglione ML, et al. Videoconferencing psychotherapy: a systematic review. Psychol Serv. 2012;9(2):111-131.
8. Egede LE, Frueh CB, Richardson LK, et al. Rationale and design: telepsychology service delivery for depressed elderly veterans. Trials. 2009;10:22.
9. Frueh BC, Deitsch SE, Santos AB, et al. Procedural and methodological issues in telepsychiatry research and program development. Psychiatr Serv. 2000;51(12):1522-1527.
10. Grubaugh AL, Cain GD, Elhai JD, Patrick SL, Frueh BC. Attitudes toward medical and mental health care delivered via telehealth applications among rural and urban primary care patients. J Nerv Ment Dis. 2008;196(2):166-170.
11. Jameson JP, Farmer MS, Head KJ, Fortney J, Teal CR. VA community mental health service providers’ utilization of and attitudes towards telemental health care: the gatekeeper’s perspective. J Rural Health. 2011;27(4):425-432.
12. Thorp SR, Fidler J, Moreno L, Floto E, Agha Z. Lessons learned from studies of psychotherapy for posttraumatic stress disorder via video teleconferencing. Psychol Serv. 2012;9(2):197-199.
13. Gros DF, Yoder M, Tuerk PW, Lozano BE, Acierno R. Exposure therapy for PTSD delivered to veterans via telehealth: predictors of treatment completion and outcome and comparison to treatment delivered in person. Behav Ther. 2011;42(2):276-283.
14. Zarate CA Jr, Weinstock L, Cukor P, et al. Applicability of telemedicine for assessing patients with schizophrenia: acceptance and reliability. J Clin Psychiatry. 1997;58(1):22-25.
15. Jones AM, Shealy KM, Reid-Quiñones K, et al. Guidelines for establishing a telemental health program to provide evidence-based therapy for trauma-exposed children and families. Psychol Serv. 2014;11(4):398-409.
16. Frueh BC, Monnier J, Grubaugh AL, Elhai JD, Yim E, Knapp R. Therapist adherence and competence with manualized cognitive-behavioral therapy for PTSD delivered via videoconferencing technology. Behav Modif. 2007;31(6):856-866.
17. Morland LA, Hynes AK, Mackintosh MA, Resick PA, Chard KM. Group cognitive processing therapy delivered to veterans via telehealth: a pilot cohort. J Trauma Stress. 2011;24(4):465-469.
18. Tuerk PW, Yoder M, Ruggiero KJ, Gros DF, Acierno R. A pilot study of prolonged exposure therapy for posttraumatic stress disorder delivered via telehealth technology. J Trauma Stress. 2010;23(1):116-123.
19. Fortney JC, Pyne JM, Kimbrell TA, et al. Telemedicine- based collaborative care for posttraumatic stress disorder: a randomized clinical trial. JAMA Psychiatry. 2015;72(1):58-67.
20. Germain V, Marchand A, Bouchard S, Drouin MS, Guay S. Effectiveness of cognitive behavioural therapy administered by videoconference for posttraumatic stress disorder. Cogn Behav Ther. 2009;38(1):42-53.
21. Morland LA, Mackintosh M, Greene CJ, et al. Cognitive processing therapy for posttraumatic stress disorder delivered to rural veterans via telemental health: a randomized noninferiority clinical trial. J Clin Psychiatry. 2014;75(5):470-476.
22. Tuerk PW, Fortney J, Bosworth HB, et al. Toward the development of national telehealth services: the role of Veterans Health Administration and future directions for research. Telemed J E Health. 2010;16(1):115-117.
23. Godleski L, Darkins A, Peters J. Outcomes of 98,609 U.S. Department of Veterans Affairs patients enrolled in telemental health services, 2006-2010. Psychiatr Serv. 2012;63(4):383-385.
24. Strachan M, Gros DF, Yuen E, Ruggiero KJ, Foa EB, Acierno R. Home-based telehealth to deliver evidence-based psychotherapy in veterans with PTSD. Contemp Clin Trials. 2012;33(2):402-409.
1. U.S. Department of Veterans Affairs. What is telehealth? U.S. Department of Veterans Affairs Website. http://www.telehealth.va.gov. Update May 13, 2014. Accessed April 30, 2015.
2. Morland LA, Greene CJ, Rosen C, Mauldin PD, Frueh CB. Issues in the design of a randomized noninferiority clinical trial of telemental health psychotherapy for rural combat veterans with PTSD. Contemp Clin Trials. 2009;30(6):513-522.
3. Strachan M, Gros DF, Ruggiero KJ, Lejuez CW, Acierno R. An integrated approach to delivering exposure-based treatment for symptoms of PTSD and depression in OIF/OEF veterans: preliminary findings. Behav Ther. 2012;43(3):560-569.
4. Yuen EK, Gros DF, Price M, et al. Randomized controlled trial of home-based telehealth versus in-person prolonged exposure for combat-related PTSD in veterans: preliminary results. J Clin Psychol. 2015;71(6):500-512.
5. Ruskin PE, Reed S, Kumar R, et al. Reliability and acceptability of psychiatric diagnosis via telecommunication and audiovisual technology. Psychiatr Serv. 1998;49(8):1086-1088.
6. Gros DF, Morland LA, Greene CJ, et al. Delivery of evidence-based psychotherapy via video telehealth. J Psychopathol Behav Assess. 2013;35(4):506-521.
7. Backhaus A, Agha Z, Maglione ML, et al. Videoconferencing psychotherapy: a systematic review. Psychol Serv. 2012;9(2):111-131.
8. Egede LE, Frueh CB, Richardson LK, et al. Rationale and design: telepsychology service delivery for depressed elderly veterans. Trials. 2009;10:22.
9. Frueh BC, Deitsch SE, Santos AB, et al. Procedural and methodological issues in telepsychiatry research and program development. Psychiatr Serv. 2000;51(12):1522-1527.
10. Grubaugh AL, Cain GD, Elhai JD, Patrick SL, Frueh BC. Attitudes toward medical and mental health care delivered via telehealth applications among rural and urban primary care patients. J Nerv Ment Dis. 2008;196(2):166-170.
11. Jameson JP, Farmer MS, Head KJ, Fortney J, Teal CR. VA community mental health service providers’ utilization of and attitudes towards telemental health care: the gatekeeper’s perspective. J Rural Health. 2011;27(4):425-432.
12. Thorp SR, Fidler J, Moreno L, Floto E, Agha Z. Lessons learned from studies of psychotherapy for posttraumatic stress disorder via video teleconferencing. Psychol Serv. 2012;9(2):197-199.
13. Gros DF, Yoder M, Tuerk PW, Lozano BE, Acierno R. Exposure therapy for PTSD delivered to veterans via telehealth: predictors of treatment completion and outcome and comparison to treatment delivered in person. Behav Ther. 2011;42(2):276-283.
14. Zarate CA Jr, Weinstock L, Cukor P, et al. Applicability of telemedicine for assessing patients with schizophrenia: acceptance and reliability. J Clin Psychiatry. 1997;58(1):22-25.
15. Jones AM, Shealy KM, Reid-Quiñones K, et al. Guidelines for establishing a telemental health program to provide evidence-based therapy for trauma-exposed children and families. Psychol Serv. 2014;11(4):398-409.
16. Frueh BC, Monnier J, Grubaugh AL, Elhai JD, Yim E, Knapp R. Therapist adherence and competence with manualized cognitive-behavioral therapy for PTSD delivered via videoconferencing technology. Behav Modif. 2007;31(6):856-866.
17. Morland LA, Hynes AK, Mackintosh MA, Resick PA, Chard KM. Group cognitive processing therapy delivered to veterans via telehealth: a pilot cohort. J Trauma Stress. 2011;24(4):465-469.
18. Tuerk PW, Yoder M, Ruggiero KJ, Gros DF, Acierno R. A pilot study of prolonged exposure therapy for posttraumatic stress disorder delivered via telehealth technology. J Trauma Stress. 2010;23(1):116-123.
19. Fortney JC, Pyne JM, Kimbrell TA, et al. Telemedicine- based collaborative care for posttraumatic stress disorder: a randomized clinical trial. JAMA Psychiatry. 2015;72(1):58-67.
20. Germain V, Marchand A, Bouchard S, Drouin MS, Guay S. Effectiveness of cognitive behavioural therapy administered by videoconference for posttraumatic stress disorder. Cogn Behav Ther. 2009;38(1):42-53.
21. Morland LA, Mackintosh M, Greene CJ, et al. Cognitive processing therapy for posttraumatic stress disorder delivered to rural veterans via telemental health: a randomized noninferiority clinical trial. J Clin Psychiatry. 2014;75(5):470-476.
22. Tuerk PW, Fortney J, Bosworth HB, et al. Toward the development of national telehealth services: the role of Veterans Health Administration and future directions for research. Telemed J E Health. 2010;16(1):115-117.
23. Godleski L, Darkins A, Peters J. Outcomes of 98,609 U.S. Department of Veterans Affairs patients enrolled in telemental health services, 2006-2010. Psychiatr Serv. 2012;63(4):383-385.
24. Strachan M, Gros DF, Yuen E, Ruggiero KJ, Foa EB, Acierno R. Home-based telehealth to deliver evidence-based psychotherapy in veterans with PTSD. Contemp Clin Trials. 2012;33(2):402-409.
Conjoint Sessions With Clinical Pharmacy and Health Psychology for Chronic Pain
Providing comprehensive, integrated, behavioral intervention services to address the prevalent condition of chronic, noncancer pain is a growing concern. Although the biopsychosocial model (BPS) and stepped-care approaches have been understood and discussed for some time, clinician and patient understanding and investment in these approaches continue to face challenges. Moreover, even when resources (eg, staffing, referral options, space) are available, clinicians and patients must engage in meaningful communication to achieve this type of care.
Importantly, engagement means moving beyond diagnosis and assessment and offering interventions that provide psychoeducation related to the chronic pain cycle. These interventions address maladaptive cognitions and beliefs about movement and pain; promote paced, daily physical activity and engagement in life; and help increase coping skills to improve low mood or distress, all fundamental components of the BPS understanding of chronic pain.
Background
Chronic, noncancer pain is a prevalent presentation in primary care settings in the U.S. and even more so for veterans.1 Fifty percent of male veterans and 75% of female veterans report chronic pain as an important condition that impacts their health.2 An important aspect of this prevalence is the focus on opioid pain medication and medical procedures, both of which draw more narrowly on the biomedical model. Additional information on the longer term use of pain procedures and opioid medications is now available,and given some risks and limitations (eg, tolerance, decreasing efficacy, opioid-induced medical complications), the need to study and offer other options is gaining attention.3 Behavioral chronic pain management has a clear historic role that draws on the BPS modeland Gate Control Theory.3-6
More recently, the National Strategy of Chronic Pain collaborative and stepped-care models extended this literature, outlining collaboration and levels of care depending on the chronicity of the pain experience as well as co-occurring conditions and patient presentations.7,8 The Commission on Accreditation of Rehabilitation Facilities (CARF), the gold standard in interdisciplinary pain management programs, calls for further resources and coordination of these efforts, including a tertiary level of care representing the highest step in the stepped-care model.8
These interdisciplinary, integrative pain management programs, which include functional restoration and cognitive behavioral therapy (CBT) interventions, have been effective for the treatment of chronic pain.9-12However, the staffing, resources, clinical access, and coordination of this complex care may not be feasible in many health care settings. For example, a 2005 survey reported that there were only 200 multidisciplinary pain programs in the U.S., and only 84 of them were CARF accredited.13 By 2011 the number of CARF-accredited programs had decreased to 64 (the number of nonaccredited programs was not reported for 2011).13
Furthermore, engagement in behavioral pain management services is a challenge: Studies show that psychosocial interventions are underused, and a majority of studies may not report quantitatively or qualitatively on patient adherence or engagement in these services.14 These realities introduce the idea that coordinated appointments between 2 or 3 different disciplines available in primary care may be a feasible step toward implementing more comprehensive, optimal care models.
Behavioral pain management interventions that uphold the BPS also call on the idea of active self-management. Therefore, effective communication is fundamental at both the provider-patient and interprofessional levels to enhance engagement in health care, receptiveness to interventions, and to self-management of chronic pain.11,15 How clinicians conceptualize, hold assumptions about, and communicate with patients about chronic pain management has received more attention.15,16
Clinician Considerations for Pain Management
On theclinicians’ side, monitoring assumptions about patients and awareness of their beliefs as well as the care itself are foundational in patient interactions, impacting the success of patient engagement. Awareness of the language used in these interactions and how clinicians collaborate with other professionals become salient. Coupled with the reality of high attrition, this discussion lends itself in important ways to the motivational interviewing (MI) approach that aims to meet patients “where they are” by use of open-ended questions and reflective listening to guide the conversation in the direction of contemplating or actual behavior change.17 For example, “What do you think are the best ways to manage your pain?” and “It sounds like sometimes the medicine helps, but you also want more options to feel in control of your pain.”
Given the historic focus on the biomedical approach to chronic pain, including the use of opioid medications and medical procedures as well as traditional challenges to engagement in CBT, researchers have explored whether alternative methods may increase participation and improve outcomes for behavioral self-management.3 Drawing on a history of assessing readiness for change in pain management, Kerns and colleagues offered tailored cognitive strategies or behavioral skills training depending on patient preferences.18,19 These researchers also incorporated motivational enhancement strategies in the tailored interventions and compared engagement with standard CBT for chronic pain protocol. Although they did not find significant differences in engagement between the 2 groups, participation and treatment adherence were associated with posttreatment improvements in both groups.19 Taking a step back from enhancing intervention engagement, first assessing readiness to self-manage becomes another salient exploration and step in the process.
Another element of engagement in services is referral to other clinicians. Dorflinger and colleagues made this point in a conceptual paper that broadly outlined interdisciplinary, integrative, and more comprehensive models of care for chronic pain.15 We know from integrated models that referral-based care may decrease the likelihood of participation in health care services. That is, if a patient needs to make a separate appointment and meet with a new clinician, they are more likely to decline, cancel, or not show, particularly if they are not “ready” for change. Co-located or embedded care and conjoint sessions that include a warm handoff or another clinician who joins the first appointment may reduce stigma and other relevant barriers for introducing a patient to new ideas.20
Using a conjoint session that involves a clinical pharmacy pain specialist and a health psychologist is one way in which veterans can be exposed to more chronic pain-related BPS concepts and behavioral health services than they might be exposed to otherwise. The purpose of this project was to bring awareness to a practical and clinically relevant integrated approach to the dissemination of BPS information for chronic pain management.
In providing this information through effective communication at the patient-provider and interprofessional levels, the clinicians’ intention was to increase patient engagement and use of BPS strategies in the self-management of chronic pain. This project also aimed to enhance engagement and improve the quality of services before acquiring additional positions and funding for a specialized pain management team. These sessions were offered at the VA Ann Arbor Healthcare System (VAAAHS) in Michigan. Quantitative and qualitative information was examined from the conjoint and subsequent sessions that occurred in this setting.
Methods
With the above concepts in mind, VAAAHS offered veterans conjoint sessions involving a health psychologist and clinical pharmacy specialist during a 3-month period while this resource was available. The conjoint sessions were part of a preexisting pharmacist-run pain medication clinic embedded in primary care. The conjoint session was presented to patients as part of general clinic flow to reduce stigma of engagement in psychological services and allow for the dissemination of BPS information.
Participants
The electronic health records (EHR) of 24 veteran patients with chronic pain, who participated in a conjoint health psychology/pain pharmacy session, were reviewed for the current study. Most of the patients were male (95.8%) and non-Hispanic white (91.7%); the remaining participants did not disclose their ethnicity. The mean age was 60.6 years (SD 7.1; range 50-80). A total of 75% had a mental health diagnosis, and 41.7% were in mental health treatment at the time of the conjoint appointment. Among the sample, 20.8% had a current diagnosis of a substance use disorder (SUD), and no individuals were in treatment for a SUD at the time of the conjoint appointment. Patients received an average of 1.5 conjoint sessions (SD 0.7; range 1-3).
Procedure
The veterans for this project were chosen from a panel of patients followed by the pain medication clinical pharmacy specialist in the primary care pain medication clinic. The selected veterans were offered a joint session with their clinical pharmacy provider and the health psychology resident during their scheduled visit in the pain medication clinic. Each veteran was informed that the goal of the joint visit was to enhance self-directed nonpharmacologic chronic pain management skills as an additional set of tools in the tool kit for particularly difficult pain days. Veterans were assured that their usual care would not be compromised if they declined the session.
During the encounter(s), the health psychologist contributed to the veteran’s care by using MI and CBT for chronic pain skills. The health psychologist further assessed concerns and needs and guided the discussion as appropriate. With veteran readiness, these discussions explored the degree of knowledge and cognitive and behavioral coping skills the patient used. These conjoint sessions also documented the types of discussions and degree of engagement in the encounter(s) as well additional referrals, complementary services, and/or offered follow-up services for either additional conjoint sessions or further health psychology-related services.
A total of 24 EHRs from these conjoint and subsequent encounters were reviewed for evidence of the procedures by a psychology intern involved in chronic pain management services. Of these 24 records, 6 also were reviewed by a board-certified health psychologist for consensus building and agreement on coding (Sidebar, Record Coding).
Using the coding system and SPSS Version 2.1 (IBM, Armonk NY), descriptive statistics were used to examine conjoint session content and new- or re-engagement in health psychology services following the conjoint sessions. For those patients who followed up with additional services, the content, type, and outcome of these services were explored. Next, linear regression was used to determine whether number of conjoint sessions was associated with a qualitative treatment outcome, and 2 logistic regressions were used to determine whether the number of sessions was associated with the likelihood of accepting services and follow-through with services after accepting them. An additional logistic regression examined whether having a mental health diagnosis (yes/no) was associated with whether the individual accepted additional health psychology services. Finally, independent sample t tests examined differences between those who accepted services vs those who declined follow-up services in substance use diagnosis, mental health diagnosis, and previous health psychology services engagement. Of note, given the small sample size, the Levene’s test for equality of variances was conducted and unequal variances were assumed.
Results
All 24 patients agreed to have the conjoint session with the clinical pharmacy specialist and health psychologist. Of the participants, 62.5% had no previous interaction with health psychology services. Among those who had previous encounters with health psychology services, 12.5% had participated in 1 or more group sessions, another 12.5% had participated in 1 or more individual sessions, and an additional 12.5% had been referred for health psychology services but had not followed through. A total of 10 participants represented a new- or re-engagement in health psychology services following the conjoint appointment. Two patients were referred for additional services as a result of their conjoint appointment (1 to specialty mental health and another to Primary Care-Mental Health Integration [PC-MHI]), and 1 of the participants followed through with the referral. Finally, with regard to the content of the initial session, 37.5% of the sessions contained some form of psychoeducation, 54.2% contained a functional assessment, and 41.7% contained an introduction of skills.
Half of the veterans participated in health psychology services beyond the initial conjoint session. Four of these veterans participated in additional conjoint sessions, and the remaining 8 engaged in health psychology services, which took the form of telephone sessions (3), in-person sessions (3), or a combination of both telephone and in-person sessions (2). Twelve veterans participated in an average of 3.4 (SD 3.7) follow-up sessions. In terms of the content of these follow-up sessions, across all formats and types, 3 included some introduction to coping skills, with no documented evidence of follow-through. For 2 of the veterans engaging in some type of follow-up, there was documented use of coping skills, and 2 used the coping skills with self-reported success and benefit. Finally, documentation revealed evidence that 3 of these veterans were not only using the coping skills with benefit, but also reported an improvement in pain management overall. One also was connected with a different service.
Regarding reasons for completion of services, 2 veterans were terminated due to completing treatment/meeting goals, 2 were terminated because they did not follow up after a session, 7 were terminated due to patient declining additional sessions, and 1 veteran was still receiving services at the time of the review. Linear regression indicated that the number of conjoint sessions was not associated with qualitative treatment outcome. Two logistic regressions indicated that number of conjoint sessions was not related to whether the veteran accepted follow-up services or whether the veteran followed through with services after accepting. Of note, logistic regression indicated that having a mental health diagnosiswas associated with a decreased likelihood of accepting health psychology services (P = .03). Regarding the independent samples t tests, veterans who did not accept follow-up services were more likely to have a mental health diagnosis (P = .03). The groups did not differ significantly with regard to substance use diagnosis or previous engagement in health psychology services.
Discussion
Results showed that all 24 veterans who were offered a conjoint session with a clinical pharmacy specialist and health psychologist engaged in at least 1 session. Half the veterans participated in further services as well. Both the initial conjoint and follow-up sessions offered a greater degree of communication related to the cognitive-behavioral and functional restoration components of behavioral pain management. Given that a majority of the sample had not participated in behavioral or mental health services previously, this may represent a greater penetration rate of exposure to mental health service for veterans than would have been available otherwise.
More specifically, qualitative results suggest that in these conjoint sessions, the veterans were exposed to behavioral psychotherapeutic approaches to chronic pain management (eg, health behavior change, motivational enhancement, health-related psychoeducation, and CBT for chronic pain) that again may not have been provided otherwise (ie, via referral and separately scheduled sessions). These findings are supported by theories consistent with the Transtheoretical Model, which indicates that individuals fall in varying degrees of readiness for behavioral change (ie, precontemplative, contemplative, planning, action, maintenance).21,22 Thus, behavioral intervention approaches must be adaptive and adjust format and communication, including the amount and type of psychoeducation offered. Moreover, the integrated theory of health behavior change in the context of chronic pain management calls for fostering awareness, knowledge, and beliefs through effective communication and education for a wide range of individuals who are at varying stages of change.23 In addition to the conjoint session and subsequent service(s) content that were reviewed and coded in this current project, future projects might draw on these theoretical models and code sessions for patients’ stages of change and assess whether a patient made progress across phases of change (eg, the patient shifted from contemplative to the planning stage of change).
Within this project’s conjoint sessions and consistent with MI principles, veterans were offered discussions related to the bidirectional and BPS aspects of their own chronic pain experience. That is, while discussing responses and adjustment to pain medication(s), veterans received reflections with MI and heard feedback related to their current coping strategies, methods to enhance coping, as well as potential psychosocial impacts of their chronic pain experience. With permission, veterans also were introduced to themes that comprised evidence-based CBT for chronic pain (CBT-CP) intervention. Understanding what change means in the context of chronic pain management is critical. That is, tipping the conversation toward consideration of alternative modalities (eg, relaxation, stress management, cognitions, and pain) in conjunction with or in place of the traditional modalities (eg, medication, pain procedures) is paramount.
Clinicians must listen for patient ambivalence related to procedures, interventions, medication changes, and/or the behavioral self-management of chronic pain. This type of active listening and exploration may be more likely when there is collaboration and effective team functioning among clinicians than when clinicians provide care independently. Future quality improvement (QI) or research projects could extend the EHR review and evaluate clinician-patient transcripts for fidelity to the CBT-CP and MI models. Such efforts could assess for associations between clinician MI consistent behaviors and change talk on the part of the patient. Furthermore, clinician communication and patient change talk from transcripts could be evaluated in relation to evidence from the EHR regarding patient use of coping skills and behavior change.
Consistent with behavioral health literature, having a mental health diagnosis was associated with declining additional behavioral health psychology services in this project. Research has shown that individuals with a mental health diagnosis tend to engage less in behavioral health self-management programs, such as chronic headache and weight management.24-26 This phenomenon lends support for the importance of health care professionals (HCPs) to increase access and exposure to mental and behavioral health services, such as the PC-MHI model.20 In fact, chronic pain management program development efforts within the VA system nationwide include collaboration with the PC-MHI services. One of the initial goals for PC-MHI services is to increase penetration rates into the general outpatient medical clinics and enhance engagement in mental health services.
Using conjoint sessions as was offered in the current project is one step in the development of more comprehensive interdisciplinary teams through interprofessional collaboration and the use of effective clinical communication. In turn, it will be important to directly explore the communication skills and attitudes of these HCPs with regard to interdisciplinary program development and collaboration as teams continue to integrate more broadly into the medical system and enhance chronic pain management services.11 Similarly, measuring the perceptions of clinical pharmacy specialists, physicians, health psychologists, or other clinical disciplines involved in chronic pain management could be another area to explore. More specific to MI, clinician confidence in the use of effective communication and MI skills represents still another area for future study.16
Limitations
Some limitations and suggested future directions found as part of this QI project have been outlined earlier. Other limitations include the used of a retrospective review of information available in patient medical charts. More developed measurement-based care or research could collect self-reports of patient satisfaction with care, functioning, knowledge, readiness for change, and mood in addition to what is noted and documented in clinical observations. Second, the sample was small and did not include any female and few younger veterans, even though these are important subpopulations when examining pain management services. When resources are available for a larger sample size, some exploratory analyses could be conducted for differences in engagement among subgroups. Third, this project may have further confounding variables as this was not an experimental or a controlled study, which could directly compare conjoint sessions with referral-based care and/or those not offered conjoint sessions.
Conclusion
The optimal method of behavioral pain management suggests the need for an interdisciplinary, coordinated team approach, in which the gold standard programs meet requirements set by CARF. However, on a practical level, optimal behavioral pain management may not be feasible at all health care facilities. Furthermore, in an effort to provide best practices to individuals with chronic pain, clinicians must be adaptive and skilled in using effective communication and specialized interventions, such as CBT and MI.
Approaching the more optimal behavioral self-management of chronic pain from a multimodal interdisciplinary perspective and further engaging veterans in this care is paramount. This project is merely one step in this effort that can shed light on the function and logistic outcomes of using a practical, integrated approach to chronic pain. It demonstrates that implementing best practices founded in sound theoretical models despite staffing and resource constraints is possible. Thus, continuing to explore the utility of alternate modalities may offer important applied and translational information to help disseminate and improve chronic pain management services.
Future research could focus on important subpopulations and enhance experimental design with pre- and postmeasures, controlling for possible confounding variables and if possible a controlled design.
Acknowledgments
This quality improvement project was unfunded, and approval was confirmed with the VA Ann Arbor Healthcare System Institutional Review Board and Research & Development committees. The authors also thank Associate Chief of Staff, Ambulatory Care, Clinton Greenstone, MD, and Chief of Primary Care Adam Tremblay, MD, for their leadership and support of these integrative services and quality improvement efforts. The authors especially recognize the veterans for whom they aim to provide the highest quality of services possible.
1. Brooks PM. The burden of musculoskeletal disease—a global perspective. Clin Rheumatol. 2006;25(6):778-781.
2. Haskell SG, Heapy A, Reid MC, Papas RK, Kerns RD. The prevalence and age-related characteristics of pain in a sample of women veterans receiving primary care. J Womens Health (Larchmt). 2006;15(7):862-869.
3. Roth RS, Geisser ME, Williams DA. Interventional pain medicine: retreat from the biopsychosocial model of pain. Transl Behav Med. 2012;2(1):106-116.
4. Engel GL. The need for a new medical model: a challenge for biomedicine. Science. 1977;196(4286):129-136.
5. Borrell-Carrió F, Suchman AL, Epstein RM. The biopsychosocial model 25 years later: principles, practice, and scientific inquiry. Ann Fam Med. 2004;2(6):576-582.
6. Wall PD. The gate control theory of pain mechanisms: a re-examination and re-statement. Brain. 1978;101(1):1-18.
7. Dobscha SK, Corson K, Perrin NA, et al. Collaborative care for chronic pain in primary care: a cluster randomized trial. JAMA. 2009;301(12):1242-1252.
8. Von Korff, Moore JC. Stepped care for back pain: activating approaches for primary care. Ann Intern Med. 2001;134(9, pt 2):911-917.
9. Oslund S, Robinson RC, Clark TC, et al. Long-term effectiveness of a comprehensive pain management program: strengthening the case for interdisciplinary care. Proc (Bayl Univ Med Cent). 2009;22(3):211-214.
10. Scascighini L, Toma V, Dober-Spielmann S, Sprott H. Multidisciplinary treatment for chronic pain: a systematic review of interventions and outcomes. Rheumatology (Oxford). 2008;47(5):670-678.
11. Gatchel RJ, McGeary DD, McGeary CA, Lippe B. Interdisciplinary chronic pain management: past, present, and future. Am Psychol. 2014;69(2):119-130.
12. McCracken LM, Turk DC. Behavioral and cognitive-behavioral treatment for chronic pain: outcome, predictors of outcome, and treatment process. Spine (Phila Pa 1976). 2002;27(22): 2564-2573.
13. Jeffery MM, Butler M, Stark A, Kane RL. Multidisciplinary Pain Programs for Chronic Noncancer Pain. Comparative Effectiveness Technical Briefs, No 8. Rockville, MD: Agency for Healthcare Research and Quality; 2011.
14. Ehde DM, Dilworth TM, Turner JA. Cognitive-behavioral therapy for individuals with chronic pain: efficacy, innovations, and directions for research. Am Psychol. 2014;69(2):153-166.
15. Dorflinger L, Kerns RD, Auerbach SM. Providers’ roles in enhancing patients’ adherence to pain self management. Transl Behav Med. 2013;3(1):39-46.
16. Pellico LH, Gilliam WP, Lee AW, Kerns RD. Hearing new voices: registered nurses and health technicians experience caring for chronic pain patients in primary care clinics. Open Nurs J. 2014;8:25-33.
17. Rollnick S, Miller WR, Butler CC, eds. Motivational Interviewing in Health Care: Helping Patients Change Behavior. New York, NY: The Guilford Press; 2008.
18. Kerns RD, Habib S. A critical review of the pain readiness to change model. J Pain. 2004;5(7):357-367.19. Kerns RD, Burns JW, Shulman M, et al. Can we improve cognitive-behavior therapy for chronic back pain treatment engagement and adherence? A controlled trial of tailored versus standard therapy. Health Psychol. 2014;33(9):938-947.
20. Kearney LK, Post EP, Zeiss A, Goldstein MG, Dundon M. The role of mental and behavioral health in the application of the patient-centered medical home in the Department of Veterans Affairs. Transl Behav Med. 2011;1(4):624-628.
21. Prochaska JO, DiClemente CC. Stages and processes of self-change of smoking: toward an integrative model of change. J Consult Clin Psychol. 1983;51(3):390-395.
22. Prochaska JO, DiClemente CC, Norcross JC. In search of how people change. Applications to addictive behaviors. Am Psychol. 1992;47(9):1102-1114.
23. Ryan P. Integrated theory of health behavior change: background and intervention development. Clin Nurse Spec. 2009;23(3):161-172.
24. Evans DD , Blanchard EB. Prediction of early termination from the self-regulatory treatment of chronic headache. Biofeedback Self Regul. 1988;13(3):245-256.
25. Maguen S, Hoerster KD, Littman AJ, et al. Iraq and Afghanistan veterans with PTSD participate less in VA’s weight loss program than those without PTSD. J Affect Disord. 2016;193:289-294.
26. Bloor LE. Improving weight management services for female veterans: design and participation factors with a women only program, and comparisons with gender neutral services. Med Res Arch. 2015;2.
Providing comprehensive, integrated, behavioral intervention services to address the prevalent condition of chronic, noncancer pain is a growing concern. Although the biopsychosocial model (BPS) and stepped-care approaches have been understood and discussed for some time, clinician and patient understanding and investment in these approaches continue to face challenges. Moreover, even when resources (eg, staffing, referral options, space) are available, clinicians and patients must engage in meaningful communication to achieve this type of care.
Importantly, engagement means moving beyond diagnosis and assessment and offering interventions that provide psychoeducation related to the chronic pain cycle. These interventions address maladaptive cognitions and beliefs about movement and pain; promote paced, daily physical activity and engagement in life; and help increase coping skills to improve low mood or distress, all fundamental components of the BPS understanding of chronic pain.
Background
Chronic, noncancer pain is a prevalent presentation in primary care settings in the U.S. and even more so for veterans.1 Fifty percent of male veterans and 75% of female veterans report chronic pain as an important condition that impacts their health.2 An important aspect of this prevalence is the focus on opioid pain medication and medical procedures, both of which draw more narrowly on the biomedical model. Additional information on the longer term use of pain procedures and opioid medications is now available,and given some risks and limitations (eg, tolerance, decreasing efficacy, opioid-induced medical complications), the need to study and offer other options is gaining attention.3 Behavioral chronic pain management has a clear historic role that draws on the BPS modeland Gate Control Theory.3-6
More recently, the National Strategy of Chronic Pain collaborative and stepped-care models extended this literature, outlining collaboration and levels of care depending on the chronicity of the pain experience as well as co-occurring conditions and patient presentations.7,8 The Commission on Accreditation of Rehabilitation Facilities (CARF), the gold standard in interdisciplinary pain management programs, calls for further resources and coordination of these efforts, including a tertiary level of care representing the highest step in the stepped-care model.8
These interdisciplinary, integrative pain management programs, which include functional restoration and cognitive behavioral therapy (CBT) interventions, have been effective for the treatment of chronic pain.9-12However, the staffing, resources, clinical access, and coordination of this complex care may not be feasible in many health care settings. For example, a 2005 survey reported that there were only 200 multidisciplinary pain programs in the U.S., and only 84 of them were CARF accredited.13 By 2011 the number of CARF-accredited programs had decreased to 64 (the number of nonaccredited programs was not reported for 2011).13
Furthermore, engagement in behavioral pain management services is a challenge: Studies show that psychosocial interventions are underused, and a majority of studies may not report quantitatively or qualitatively on patient adherence or engagement in these services.14 These realities introduce the idea that coordinated appointments between 2 or 3 different disciplines available in primary care may be a feasible step toward implementing more comprehensive, optimal care models.
Behavioral pain management interventions that uphold the BPS also call on the idea of active self-management. Therefore, effective communication is fundamental at both the provider-patient and interprofessional levels to enhance engagement in health care, receptiveness to interventions, and to self-management of chronic pain.11,15 How clinicians conceptualize, hold assumptions about, and communicate with patients about chronic pain management has received more attention.15,16
Clinician Considerations for Pain Management
On theclinicians’ side, monitoring assumptions about patients and awareness of their beliefs as well as the care itself are foundational in patient interactions, impacting the success of patient engagement. Awareness of the language used in these interactions and how clinicians collaborate with other professionals become salient. Coupled with the reality of high attrition, this discussion lends itself in important ways to the motivational interviewing (MI) approach that aims to meet patients “where they are” by use of open-ended questions and reflective listening to guide the conversation in the direction of contemplating or actual behavior change.17 For example, “What do you think are the best ways to manage your pain?” and “It sounds like sometimes the medicine helps, but you also want more options to feel in control of your pain.”
Given the historic focus on the biomedical approach to chronic pain, including the use of opioid medications and medical procedures as well as traditional challenges to engagement in CBT, researchers have explored whether alternative methods may increase participation and improve outcomes for behavioral self-management.3 Drawing on a history of assessing readiness for change in pain management, Kerns and colleagues offered tailored cognitive strategies or behavioral skills training depending on patient preferences.18,19 These researchers also incorporated motivational enhancement strategies in the tailored interventions and compared engagement with standard CBT for chronic pain protocol. Although they did not find significant differences in engagement between the 2 groups, participation and treatment adherence were associated with posttreatment improvements in both groups.19 Taking a step back from enhancing intervention engagement, first assessing readiness to self-manage becomes another salient exploration and step in the process.
Another element of engagement in services is referral to other clinicians. Dorflinger and colleagues made this point in a conceptual paper that broadly outlined interdisciplinary, integrative, and more comprehensive models of care for chronic pain.15 We know from integrated models that referral-based care may decrease the likelihood of participation in health care services. That is, if a patient needs to make a separate appointment and meet with a new clinician, they are more likely to decline, cancel, or not show, particularly if they are not “ready” for change. Co-located or embedded care and conjoint sessions that include a warm handoff or another clinician who joins the first appointment may reduce stigma and other relevant barriers for introducing a patient to new ideas.20
Using a conjoint session that involves a clinical pharmacy pain specialist and a health psychologist is one way in which veterans can be exposed to more chronic pain-related BPS concepts and behavioral health services than they might be exposed to otherwise. The purpose of this project was to bring awareness to a practical and clinically relevant integrated approach to the dissemination of BPS information for chronic pain management.
In providing this information through effective communication at the patient-provider and interprofessional levels, the clinicians’ intention was to increase patient engagement and use of BPS strategies in the self-management of chronic pain. This project also aimed to enhance engagement and improve the quality of services before acquiring additional positions and funding for a specialized pain management team. These sessions were offered at the VA Ann Arbor Healthcare System (VAAAHS) in Michigan. Quantitative and qualitative information was examined from the conjoint and subsequent sessions that occurred in this setting.
Methods
With the above concepts in mind, VAAAHS offered veterans conjoint sessions involving a health psychologist and clinical pharmacy specialist during a 3-month period while this resource was available. The conjoint sessions were part of a preexisting pharmacist-run pain medication clinic embedded in primary care. The conjoint session was presented to patients as part of general clinic flow to reduce stigma of engagement in psychological services and allow for the dissemination of BPS information.
Participants
The electronic health records (EHR) of 24 veteran patients with chronic pain, who participated in a conjoint health psychology/pain pharmacy session, were reviewed for the current study. Most of the patients were male (95.8%) and non-Hispanic white (91.7%); the remaining participants did not disclose their ethnicity. The mean age was 60.6 years (SD 7.1; range 50-80). A total of 75% had a mental health diagnosis, and 41.7% were in mental health treatment at the time of the conjoint appointment. Among the sample, 20.8% had a current diagnosis of a substance use disorder (SUD), and no individuals were in treatment for a SUD at the time of the conjoint appointment. Patients received an average of 1.5 conjoint sessions (SD 0.7; range 1-3).
Procedure
The veterans for this project were chosen from a panel of patients followed by the pain medication clinical pharmacy specialist in the primary care pain medication clinic. The selected veterans were offered a joint session with their clinical pharmacy provider and the health psychology resident during their scheduled visit in the pain medication clinic. Each veteran was informed that the goal of the joint visit was to enhance self-directed nonpharmacologic chronic pain management skills as an additional set of tools in the tool kit for particularly difficult pain days. Veterans were assured that their usual care would not be compromised if they declined the session.
During the encounter(s), the health psychologist contributed to the veteran’s care by using MI and CBT for chronic pain skills. The health psychologist further assessed concerns and needs and guided the discussion as appropriate. With veteran readiness, these discussions explored the degree of knowledge and cognitive and behavioral coping skills the patient used. These conjoint sessions also documented the types of discussions and degree of engagement in the encounter(s) as well additional referrals, complementary services, and/or offered follow-up services for either additional conjoint sessions or further health psychology-related services.
A total of 24 EHRs from these conjoint and subsequent encounters were reviewed for evidence of the procedures by a psychology intern involved in chronic pain management services. Of these 24 records, 6 also were reviewed by a board-certified health psychologist for consensus building and agreement on coding (Sidebar, Record Coding).
Using the coding system and SPSS Version 2.1 (IBM, Armonk NY), descriptive statistics were used to examine conjoint session content and new- or re-engagement in health psychology services following the conjoint sessions. For those patients who followed up with additional services, the content, type, and outcome of these services were explored. Next, linear regression was used to determine whether number of conjoint sessions was associated with a qualitative treatment outcome, and 2 logistic regressions were used to determine whether the number of sessions was associated with the likelihood of accepting services and follow-through with services after accepting them. An additional logistic regression examined whether having a mental health diagnosis (yes/no) was associated with whether the individual accepted additional health psychology services. Finally, independent sample t tests examined differences between those who accepted services vs those who declined follow-up services in substance use diagnosis, mental health diagnosis, and previous health psychology services engagement. Of note, given the small sample size, the Levene’s test for equality of variances was conducted and unequal variances were assumed.
Results
All 24 patients agreed to have the conjoint session with the clinical pharmacy specialist and health psychologist. Of the participants, 62.5% had no previous interaction with health psychology services. Among those who had previous encounters with health psychology services, 12.5% had participated in 1 or more group sessions, another 12.5% had participated in 1 or more individual sessions, and an additional 12.5% had been referred for health psychology services but had not followed through. A total of 10 participants represented a new- or re-engagement in health psychology services following the conjoint appointment. Two patients were referred for additional services as a result of their conjoint appointment (1 to specialty mental health and another to Primary Care-Mental Health Integration [PC-MHI]), and 1 of the participants followed through with the referral. Finally, with regard to the content of the initial session, 37.5% of the sessions contained some form of psychoeducation, 54.2% contained a functional assessment, and 41.7% contained an introduction of skills.
Half of the veterans participated in health psychology services beyond the initial conjoint session. Four of these veterans participated in additional conjoint sessions, and the remaining 8 engaged in health psychology services, which took the form of telephone sessions (3), in-person sessions (3), or a combination of both telephone and in-person sessions (2). Twelve veterans participated in an average of 3.4 (SD 3.7) follow-up sessions. In terms of the content of these follow-up sessions, across all formats and types, 3 included some introduction to coping skills, with no documented evidence of follow-through. For 2 of the veterans engaging in some type of follow-up, there was documented use of coping skills, and 2 used the coping skills with self-reported success and benefit. Finally, documentation revealed evidence that 3 of these veterans were not only using the coping skills with benefit, but also reported an improvement in pain management overall. One also was connected with a different service.
Regarding reasons for completion of services, 2 veterans were terminated due to completing treatment/meeting goals, 2 were terminated because they did not follow up after a session, 7 were terminated due to patient declining additional sessions, and 1 veteran was still receiving services at the time of the review. Linear regression indicated that the number of conjoint sessions was not associated with qualitative treatment outcome. Two logistic regressions indicated that number of conjoint sessions was not related to whether the veteran accepted follow-up services or whether the veteran followed through with services after accepting. Of note, logistic regression indicated that having a mental health diagnosiswas associated with a decreased likelihood of accepting health psychology services (P = .03). Regarding the independent samples t tests, veterans who did not accept follow-up services were more likely to have a mental health diagnosis (P = .03). The groups did not differ significantly with regard to substance use diagnosis or previous engagement in health psychology services.
Discussion
Results showed that all 24 veterans who were offered a conjoint session with a clinical pharmacy specialist and health psychologist engaged in at least 1 session. Half the veterans participated in further services as well. Both the initial conjoint and follow-up sessions offered a greater degree of communication related to the cognitive-behavioral and functional restoration components of behavioral pain management. Given that a majority of the sample had not participated in behavioral or mental health services previously, this may represent a greater penetration rate of exposure to mental health service for veterans than would have been available otherwise.
More specifically, qualitative results suggest that in these conjoint sessions, the veterans were exposed to behavioral psychotherapeutic approaches to chronic pain management (eg, health behavior change, motivational enhancement, health-related psychoeducation, and CBT for chronic pain) that again may not have been provided otherwise (ie, via referral and separately scheduled sessions). These findings are supported by theories consistent with the Transtheoretical Model, which indicates that individuals fall in varying degrees of readiness for behavioral change (ie, precontemplative, contemplative, planning, action, maintenance).21,22 Thus, behavioral intervention approaches must be adaptive and adjust format and communication, including the amount and type of psychoeducation offered. Moreover, the integrated theory of health behavior change in the context of chronic pain management calls for fostering awareness, knowledge, and beliefs through effective communication and education for a wide range of individuals who are at varying stages of change.23 In addition to the conjoint session and subsequent service(s) content that were reviewed and coded in this current project, future projects might draw on these theoretical models and code sessions for patients’ stages of change and assess whether a patient made progress across phases of change (eg, the patient shifted from contemplative to the planning stage of change).
Within this project’s conjoint sessions and consistent with MI principles, veterans were offered discussions related to the bidirectional and BPS aspects of their own chronic pain experience. That is, while discussing responses and adjustment to pain medication(s), veterans received reflections with MI and heard feedback related to their current coping strategies, methods to enhance coping, as well as potential psychosocial impacts of their chronic pain experience. With permission, veterans also were introduced to themes that comprised evidence-based CBT for chronic pain (CBT-CP) intervention. Understanding what change means in the context of chronic pain management is critical. That is, tipping the conversation toward consideration of alternative modalities (eg, relaxation, stress management, cognitions, and pain) in conjunction with or in place of the traditional modalities (eg, medication, pain procedures) is paramount.
Clinicians must listen for patient ambivalence related to procedures, interventions, medication changes, and/or the behavioral self-management of chronic pain. This type of active listening and exploration may be more likely when there is collaboration and effective team functioning among clinicians than when clinicians provide care independently. Future quality improvement (QI) or research projects could extend the EHR review and evaluate clinician-patient transcripts for fidelity to the CBT-CP and MI models. Such efforts could assess for associations between clinician MI consistent behaviors and change talk on the part of the patient. Furthermore, clinician communication and patient change talk from transcripts could be evaluated in relation to evidence from the EHR regarding patient use of coping skills and behavior change.
Consistent with behavioral health literature, having a mental health diagnosis was associated with declining additional behavioral health psychology services in this project. Research has shown that individuals with a mental health diagnosis tend to engage less in behavioral health self-management programs, such as chronic headache and weight management.24-26 This phenomenon lends support for the importance of health care professionals (HCPs) to increase access and exposure to mental and behavioral health services, such as the PC-MHI model.20 In fact, chronic pain management program development efforts within the VA system nationwide include collaboration with the PC-MHI services. One of the initial goals for PC-MHI services is to increase penetration rates into the general outpatient medical clinics and enhance engagement in mental health services.
Using conjoint sessions as was offered in the current project is one step in the development of more comprehensive interdisciplinary teams through interprofessional collaboration and the use of effective clinical communication. In turn, it will be important to directly explore the communication skills and attitudes of these HCPs with regard to interdisciplinary program development and collaboration as teams continue to integrate more broadly into the medical system and enhance chronic pain management services.11 Similarly, measuring the perceptions of clinical pharmacy specialists, physicians, health psychologists, or other clinical disciplines involved in chronic pain management could be another area to explore. More specific to MI, clinician confidence in the use of effective communication and MI skills represents still another area for future study.16
Limitations
Some limitations and suggested future directions found as part of this QI project have been outlined earlier. Other limitations include the used of a retrospective review of information available in patient medical charts. More developed measurement-based care or research could collect self-reports of patient satisfaction with care, functioning, knowledge, readiness for change, and mood in addition to what is noted and documented in clinical observations. Second, the sample was small and did not include any female and few younger veterans, even though these are important subpopulations when examining pain management services. When resources are available for a larger sample size, some exploratory analyses could be conducted for differences in engagement among subgroups. Third, this project may have further confounding variables as this was not an experimental or a controlled study, which could directly compare conjoint sessions with referral-based care and/or those not offered conjoint sessions.
Conclusion
The optimal method of behavioral pain management suggests the need for an interdisciplinary, coordinated team approach, in which the gold standard programs meet requirements set by CARF. However, on a practical level, optimal behavioral pain management may not be feasible at all health care facilities. Furthermore, in an effort to provide best practices to individuals with chronic pain, clinicians must be adaptive and skilled in using effective communication and specialized interventions, such as CBT and MI.
Approaching the more optimal behavioral self-management of chronic pain from a multimodal interdisciplinary perspective and further engaging veterans in this care is paramount. This project is merely one step in this effort that can shed light on the function and logistic outcomes of using a practical, integrated approach to chronic pain. It demonstrates that implementing best practices founded in sound theoretical models despite staffing and resource constraints is possible. Thus, continuing to explore the utility of alternate modalities may offer important applied and translational information to help disseminate and improve chronic pain management services.
Future research could focus on important subpopulations and enhance experimental design with pre- and postmeasures, controlling for possible confounding variables and if possible a controlled design.
Acknowledgments
This quality improvement project was unfunded, and approval was confirmed with the VA Ann Arbor Healthcare System Institutional Review Board and Research & Development committees. The authors also thank Associate Chief of Staff, Ambulatory Care, Clinton Greenstone, MD, and Chief of Primary Care Adam Tremblay, MD, for their leadership and support of these integrative services and quality improvement efforts. The authors especially recognize the veterans for whom they aim to provide the highest quality of services possible.
Providing comprehensive, integrated, behavioral intervention services to address the prevalent condition of chronic, noncancer pain is a growing concern. Although the biopsychosocial model (BPS) and stepped-care approaches have been understood and discussed for some time, clinician and patient understanding and investment in these approaches continue to face challenges. Moreover, even when resources (eg, staffing, referral options, space) are available, clinicians and patients must engage in meaningful communication to achieve this type of care.
Importantly, engagement means moving beyond diagnosis and assessment and offering interventions that provide psychoeducation related to the chronic pain cycle. These interventions address maladaptive cognitions and beliefs about movement and pain; promote paced, daily physical activity and engagement in life; and help increase coping skills to improve low mood or distress, all fundamental components of the BPS understanding of chronic pain.
Background
Chronic, noncancer pain is a prevalent presentation in primary care settings in the U.S. and even more so for veterans.1 Fifty percent of male veterans and 75% of female veterans report chronic pain as an important condition that impacts their health.2 An important aspect of this prevalence is the focus on opioid pain medication and medical procedures, both of which draw more narrowly on the biomedical model. Additional information on the longer term use of pain procedures and opioid medications is now available,and given some risks and limitations (eg, tolerance, decreasing efficacy, opioid-induced medical complications), the need to study and offer other options is gaining attention.3 Behavioral chronic pain management has a clear historic role that draws on the BPS modeland Gate Control Theory.3-6
More recently, the National Strategy of Chronic Pain collaborative and stepped-care models extended this literature, outlining collaboration and levels of care depending on the chronicity of the pain experience as well as co-occurring conditions and patient presentations.7,8 The Commission on Accreditation of Rehabilitation Facilities (CARF), the gold standard in interdisciplinary pain management programs, calls for further resources and coordination of these efforts, including a tertiary level of care representing the highest step in the stepped-care model.8
These interdisciplinary, integrative pain management programs, which include functional restoration and cognitive behavioral therapy (CBT) interventions, have been effective for the treatment of chronic pain.9-12However, the staffing, resources, clinical access, and coordination of this complex care may not be feasible in many health care settings. For example, a 2005 survey reported that there were only 200 multidisciplinary pain programs in the U.S., and only 84 of them were CARF accredited.13 By 2011 the number of CARF-accredited programs had decreased to 64 (the number of nonaccredited programs was not reported for 2011).13
Furthermore, engagement in behavioral pain management services is a challenge: Studies show that psychosocial interventions are underused, and a majority of studies may not report quantitatively or qualitatively on patient adherence or engagement in these services.14 These realities introduce the idea that coordinated appointments between 2 or 3 different disciplines available in primary care may be a feasible step toward implementing more comprehensive, optimal care models.
Behavioral pain management interventions that uphold the BPS also call on the idea of active self-management. Therefore, effective communication is fundamental at both the provider-patient and interprofessional levels to enhance engagement in health care, receptiveness to interventions, and to self-management of chronic pain.11,15 How clinicians conceptualize, hold assumptions about, and communicate with patients about chronic pain management has received more attention.15,16
Clinician Considerations for Pain Management
On theclinicians’ side, monitoring assumptions about patients and awareness of their beliefs as well as the care itself are foundational in patient interactions, impacting the success of patient engagement. Awareness of the language used in these interactions and how clinicians collaborate with other professionals become salient. Coupled with the reality of high attrition, this discussion lends itself in important ways to the motivational interviewing (MI) approach that aims to meet patients “where they are” by use of open-ended questions and reflective listening to guide the conversation in the direction of contemplating or actual behavior change.17 For example, “What do you think are the best ways to manage your pain?” and “It sounds like sometimes the medicine helps, but you also want more options to feel in control of your pain.”
Given the historic focus on the biomedical approach to chronic pain, including the use of opioid medications and medical procedures as well as traditional challenges to engagement in CBT, researchers have explored whether alternative methods may increase participation and improve outcomes for behavioral self-management.3 Drawing on a history of assessing readiness for change in pain management, Kerns and colleagues offered tailored cognitive strategies or behavioral skills training depending on patient preferences.18,19 These researchers also incorporated motivational enhancement strategies in the tailored interventions and compared engagement with standard CBT for chronic pain protocol. Although they did not find significant differences in engagement between the 2 groups, participation and treatment adherence were associated with posttreatment improvements in both groups.19 Taking a step back from enhancing intervention engagement, first assessing readiness to self-manage becomes another salient exploration and step in the process.
Another element of engagement in services is referral to other clinicians. Dorflinger and colleagues made this point in a conceptual paper that broadly outlined interdisciplinary, integrative, and more comprehensive models of care for chronic pain.15 We know from integrated models that referral-based care may decrease the likelihood of participation in health care services. That is, if a patient needs to make a separate appointment and meet with a new clinician, they are more likely to decline, cancel, or not show, particularly if they are not “ready” for change. Co-located or embedded care and conjoint sessions that include a warm handoff or another clinician who joins the first appointment may reduce stigma and other relevant barriers for introducing a patient to new ideas.20
Using a conjoint session that involves a clinical pharmacy pain specialist and a health psychologist is one way in which veterans can be exposed to more chronic pain-related BPS concepts and behavioral health services than they might be exposed to otherwise. The purpose of this project was to bring awareness to a practical and clinically relevant integrated approach to the dissemination of BPS information for chronic pain management.
In providing this information through effective communication at the patient-provider and interprofessional levels, the clinicians’ intention was to increase patient engagement and use of BPS strategies in the self-management of chronic pain. This project also aimed to enhance engagement and improve the quality of services before acquiring additional positions and funding for a specialized pain management team. These sessions were offered at the VA Ann Arbor Healthcare System (VAAAHS) in Michigan. Quantitative and qualitative information was examined from the conjoint and subsequent sessions that occurred in this setting.
Methods
With the above concepts in mind, VAAAHS offered veterans conjoint sessions involving a health psychologist and clinical pharmacy specialist during a 3-month period while this resource was available. The conjoint sessions were part of a preexisting pharmacist-run pain medication clinic embedded in primary care. The conjoint session was presented to patients as part of general clinic flow to reduce stigma of engagement in psychological services and allow for the dissemination of BPS information.
Participants
The electronic health records (EHR) of 24 veteran patients with chronic pain, who participated in a conjoint health psychology/pain pharmacy session, were reviewed for the current study. Most of the patients were male (95.8%) and non-Hispanic white (91.7%); the remaining participants did not disclose their ethnicity. The mean age was 60.6 years (SD 7.1; range 50-80). A total of 75% had a mental health diagnosis, and 41.7% were in mental health treatment at the time of the conjoint appointment. Among the sample, 20.8% had a current diagnosis of a substance use disorder (SUD), and no individuals were in treatment for a SUD at the time of the conjoint appointment. Patients received an average of 1.5 conjoint sessions (SD 0.7; range 1-3).
Procedure
The veterans for this project were chosen from a panel of patients followed by the pain medication clinical pharmacy specialist in the primary care pain medication clinic. The selected veterans were offered a joint session with their clinical pharmacy provider and the health psychology resident during their scheduled visit in the pain medication clinic. Each veteran was informed that the goal of the joint visit was to enhance self-directed nonpharmacologic chronic pain management skills as an additional set of tools in the tool kit for particularly difficult pain days. Veterans were assured that their usual care would not be compromised if they declined the session.
During the encounter(s), the health psychologist contributed to the veteran’s care by using MI and CBT for chronic pain skills. The health psychologist further assessed concerns and needs and guided the discussion as appropriate. With veteran readiness, these discussions explored the degree of knowledge and cognitive and behavioral coping skills the patient used. These conjoint sessions also documented the types of discussions and degree of engagement in the encounter(s) as well additional referrals, complementary services, and/or offered follow-up services for either additional conjoint sessions or further health psychology-related services.
A total of 24 EHRs from these conjoint and subsequent encounters were reviewed for evidence of the procedures by a psychology intern involved in chronic pain management services. Of these 24 records, 6 also were reviewed by a board-certified health psychologist for consensus building and agreement on coding (Sidebar, Record Coding).
Using the coding system and SPSS Version 2.1 (IBM, Armonk NY), descriptive statistics were used to examine conjoint session content and new- or re-engagement in health psychology services following the conjoint sessions. For those patients who followed up with additional services, the content, type, and outcome of these services were explored. Next, linear regression was used to determine whether number of conjoint sessions was associated with a qualitative treatment outcome, and 2 logistic regressions were used to determine whether the number of sessions was associated with the likelihood of accepting services and follow-through with services after accepting them. An additional logistic regression examined whether having a mental health diagnosis (yes/no) was associated with whether the individual accepted additional health psychology services. Finally, independent sample t tests examined differences between those who accepted services vs those who declined follow-up services in substance use diagnosis, mental health diagnosis, and previous health psychology services engagement. Of note, given the small sample size, the Levene’s test for equality of variances was conducted and unequal variances were assumed.
Results
All 24 patients agreed to have the conjoint session with the clinical pharmacy specialist and health psychologist. Of the participants, 62.5% had no previous interaction with health psychology services. Among those who had previous encounters with health psychology services, 12.5% had participated in 1 or more group sessions, another 12.5% had participated in 1 or more individual sessions, and an additional 12.5% had been referred for health psychology services but had not followed through. A total of 10 participants represented a new- or re-engagement in health psychology services following the conjoint appointment. Two patients were referred for additional services as a result of their conjoint appointment (1 to specialty mental health and another to Primary Care-Mental Health Integration [PC-MHI]), and 1 of the participants followed through with the referral. Finally, with regard to the content of the initial session, 37.5% of the sessions contained some form of psychoeducation, 54.2% contained a functional assessment, and 41.7% contained an introduction of skills.
Half of the veterans participated in health psychology services beyond the initial conjoint session. Four of these veterans participated in additional conjoint sessions, and the remaining 8 engaged in health psychology services, which took the form of telephone sessions (3), in-person sessions (3), or a combination of both telephone and in-person sessions (2). Twelve veterans participated in an average of 3.4 (SD 3.7) follow-up sessions. In terms of the content of these follow-up sessions, across all formats and types, 3 included some introduction to coping skills, with no documented evidence of follow-through. For 2 of the veterans engaging in some type of follow-up, there was documented use of coping skills, and 2 used the coping skills with self-reported success and benefit. Finally, documentation revealed evidence that 3 of these veterans were not only using the coping skills with benefit, but also reported an improvement in pain management overall. One also was connected with a different service.
Regarding reasons for completion of services, 2 veterans were terminated due to completing treatment/meeting goals, 2 were terminated because they did not follow up after a session, 7 were terminated due to patient declining additional sessions, and 1 veteran was still receiving services at the time of the review. Linear regression indicated that the number of conjoint sessions was not associated with qualitative treatment outcome. Two logistic regressions indicated that number of conjoint sessions was not related to whether the veteran accepted follow-up services or whether the veteran followed through with services after accepting. Of note, logistic regression indicated that having a mental health diagnosiswas associated with a decreased likelihood of accepting health psychology services (P = .03). Regarding the independent samples t tests, veterans who did not accept follow-up services were more likely to have a mental health diagnosis (P = .03). The groups did not differ significantly with regard to substance use diagnosis or previous engagement in health psychology services.
Discussion
Results showed that all 24 veterans who were offered a conjoint session with a clinical pharmacy specialist and health psychologist engaged in at least 1 session. Half the veterans participated in further services as well. Both the initial conjoint and follow-up sessions offered a greater degree of communication related to the cognitive-behavioral and functional restoration components of behavioral pain management. Given that a majority of the sample had not participated in behavioral or mental health services previously, this may represent a greater penetration rate of exposure to mental health service for veterans than would have been available otherwise.
More specifically, qualitative results suggest that in these conjoint sessions, the veterans were exposed to behavioral psychotherapeutic approaches to chronic pain management (eg, health behavior change, motivational enhancement, health-related psychoeducation, and CBT for chronic pain) that again may not have been provided otherwise (ie, via referral and separately scheduled sessions). These findings are supported by theories consistent with the Transtheoretical Model, which indicates that individuals fall in varying degrees of readiness for behavioral change (ie, precontemplative, contemplative, planning, action, maintenance).21,22 Thus, behavioral intervention approaches must be adaptive and adjust format and communication, including the amount and type of psychoeducation offered. Moreover, the integrated theory of health behavior change in the context of chronic pain management calls for fostering awareness, knowledge, and beliefs through effective communication and education for a wide range of individuals who are at varying stages of change.23 In addition to the conjoint session and subsequent service(s) content that were reviewed and coded in this current project, future projects might draw on these theoretical models and code sessions for patients’ stages of change and assess whether a patient made progress across phases of change (eg, the patient shifted from contemplative to the planning stage of change).
Within this project’s conjoint sessions and consistent with MI principles, veterans were offered discussions related to the bidirectional and BPS aspects of their own chronic pain experience. That is, while discussing responses and adjustment to pain medication(s), veterans received reflections with MI and heard feedback related to their current coping strategies, methods to enhance coping, as well as potential psychosocial impacts of their chronic pain experience. With permission, veterans also were introduced to themes that comprised evidence-based CBT for chronic pain (CBT-CP) intervention. Understanding what change means in the context of chronic pain management is critical. That is, tipping the conversation toward consideration of alternative modalities (eg, relaxation, stress management, cognitions, and pain) in conjunction with or in place of the traditional modalities (eg, medication, pain procedures) is paramount.
Clinicians must listen for patient ambivalence related to procedures, interventions, medication changes, and/or the behavioral self-management of chronic pain. This type of active listening and exploration may be more likely when there is collaboration and effective team functioning among clinicians than when clinicians provide care independently. Future quality improvement (QI) or research projects could extend the EHR review and evaluate clinician-patient transcripts for fidelity to the CBT-CP and MI models. Such efforts could assess for associations between clinician MI consistent behaviors and change talk on the part of the patient. Furthermore, clinician communication and patient change talk from transcripts could be evaluated in relation to evidence from the EHR regarding patient use of coping skills and behavior change.
Consistent with behavioral health literature, having a mental health diagnosis was associated with declining additional behavioral health psychology services in this project. Research has shown that individuals with a mental health diagnosis tend to engage less in behavioral health self-management programs, such as chronic headache and weight management.24-26 This phenomenon lends support for the importance of health care professionals (HCPs) to increase access and exposure to mental and behavioral health services, such as the PC-MHI model.20 In fact, chronic pain management program development efforts within the VA system nationwide include collaboration with the PC-MHI services. One of the initial goals for PC-MHI services is to increase penetration rates into the general outpatient medical clinics and enhance engagement in mental health services.
Using conjoint sessions as was offered in the current project is one step in the development of more comprehensive interdisciplinary teams through interprofessional collaboration and the use of effective clinical communication. In turn, it will be important to directly explore the communication skills and attitudes of these HCPs with regard to interdisciplinary program development and collaboration as teams continue to integrate more broadly into the medical system and enhance chronic pain management services.11 Similarly, measuring the perceptions of clinical pharmacy specialists, physicians, health psychologists, or other clinical disciplines involved in chronic pain management could be another area to explore. More specific to MI, clinician confidence in the use of effective communication and MI skills represents still another area for future study.16
Limitations
Some limitations and suggested future directions found as part of this QI project have been outlined earlier. Other limitations include the used of a retrospective review of information available in patient medical charts. More developed measurement-based care or research could collect self-reports of patient satisfaction with care, functioning, knowledge, readiness for change, and mood in addition to what is noted and documented in clinical observations. Second, the sample was small and did not include any female and few younger veterans, even though these are important subpopulations when examining pain management services. When resources are available for a larger sample size, some exploratory analyses could be conducted for differences in engagement among subgroups. Third, this project may have further confounding variables as this was not an experimental or a controlled study, which could directly compare conjoint sessions with referral-based care and/or those not offered conjoint sessions.
Conclusion
The optimal method of behavioral pain management suggests the need for an interdisciplinary, coordinated team approach, in which the gold standard programs meet requirements set by CARF. However, on a practical level, optimal behavioral pain management may not be feasible at all health care facilities. Furthermore, in an effort to provide best practices to individuals with chronic pain, clinicians must be adaptive and skilled in using effective communication and specialized interventions, such as CBT and MI.
Approaching the more optimal behavioral self-management of chronic pain from a multimodal interdisciplinary perspective and further engaging veterans in this care is paramount. This project is merely one step in this effort that can shed light on the function and logistic outcomes of using a practical, integrated approach to chronic pain. It demonstrates that implementing best practices founded in sound theoretical models despite staffing and resource constraints is possible. Thus, continuing to explore the utility of alternate modalities may offer important applied and translational information to help disseminate and improve chronic pain management services.
Future research could focus on important subpopulations and enhance experimental design with pre- and postmeasures, controlling for possible confounding variables and if possible a controlled design.
Acknowledgments
This quality improvement project was unfunded, and approval was confirmed with the VA Ann Arbor Healthcare System Institutional Review Board and Research & Development committees. The authors also thank Associate Chief of Staff, Ambulatory Care, Clinton Greenstone, MD, and Chief of Primary Care Adam Tremblay, MD, for their leadership and support of these integrative services and quality improvement efforts. The authors especially recognize the veterans for whom they aim to provide the highest quality of services possible.
1. Brooks PM. The burden of musculoskeletal disease—a global perspective. Clin Rheumatol. 2006;25(6):778-781.
2. Haskell SG, Heapy A, Reid MC, Papas RK, Kerns RD. The prevalence and age-related characteristics of pain in a sample of women veterans receiving primary care. J Womens Health (Larchmt). 2006;15(7):862-869.
3. Roth RS, Geisser ME, Williams DA. Interventional pain medicine: retreat from the biopsychosocial model of pain. Transl Behav Med. 2012;2(1):106-116.
4. Engel GL. The need for a new medical model: a challenge for biomedicine. Science. 1977;196(4286):129-136.
5. Borrell-Carrió F, Suchman AL, Epstein RM. The biopsychosocial model 25 years later: principles, practice, and scientific inquiry. Ann Fam Med. 2004;2(6):576-582.
6. Wall PD. The gate control theory of pain mechanisms: a re-examination and re-statement. Brain. 1978;101(1):1-18.
7. Dobscha SK, Corson K, Perrin NA, et al. Collaborative care for chronic pain in primary care: a cluster randomized trial. JAMA. 2009;301(12):1242-1252.
8. Von Korff, Moore JC. Stepped care for back pain: activating approaches for primary care. Ann Intern Med. 2001;134(9, pt 2):911-917.
9. Oslund S, Robinson RC, Clark TC, et al. Long-term effectiveness of a comprehensive pain management program: strengthening the case for interdisciplinary care. Proc (Bayl Univ Med Cent). 2009;22(3):211-214.
10. Scascighini L, Toma V, Dober-Spielmann S, Sprott H. Multidisciplinary treatment for chronic pain: a systematic review of interventions and outcomes. Rheumatology (Oxford). 2008;47(5):670-678.
11. Gatchel RJ, McGeary DD, McGeary CA, Lippe B. Interdisciplinary chronic pain management: past, present, and future. Am Psychol. 2014;69(2):119-130.
12. McCracken LM, Turk DC. Behavioral and cognitive-behavioral treatment for chronic pain: outcome, predictors of outcome, and treatment process. Spine (Phila Pa 1976). 2002;27(22): 2564-2573.
13. Jeffery MM, Butler M, Stark A, Kane RL. Multidisciplinary Pain Programs for Chronic Noncancer Pain. Comparative Effectiveness Technical Briefs, No 8. Rockville, MD: Agency for Healthcare Research and Quality; 2011.
14. Ehde DM, Dilworth TM, Turner JA. Cognitive-behavioral therapy for individuals with chronic pain: efficacy, innovations, and directions for research. Am Psychol. 2014;69(2):153-166.
15. Dorflinger L, Kerns RD, Auerbach SM. Providers’ roles in enhancing patients’ adherence to pain self management. Transl Behav Med. 2013;3(1):39-46.
16. Pellico LH, Gilliam WP, Lee AW, Kerns RD. Hearing new voices: registered nurses and health technicians experience caring for chronic pain patients in primary care clinics. Open Nurs J. 2014;8:25-33.
17. Rollnick S, Miller WR, Butler CC, eds. Motivational Interviewing in Health Care: Helping Patients Change Behavior. New York, NY: The Guilford Press; 2008.
18. Kerns RD, Habib S. A critical review of the pain readiness to change model. J Pain. 2004;5(7):357-367.19. Kerns RD, Burns JW, Shulman M, et al. Can we improve cognitive-behavior therapy for chronic back pain treatment engagement and adherence? A controlled trial of tailored versus standard therapy. Health Psychol. 2014;33(9):938-947.
20. Kearney LK, Post EP, Zeiss A, Goldstein MG, Dundon M. The role of mental and behavioral health in the application of the patient-centered medical home in the Department of Veterans Affairs. Transl Behav Med. 2011;1(4):624-628.
21. Prochaska JO, DiClemente CC. Stages and processes of self-change of smoking: toward an integrative model of change. J Consult Clin Psychol. 1983;51(3):390-395.
22. Prochaska JO, DiClemente CC, Norcross JC. In search of how people change. Applications to addictive behaviors. Am Psychol. 1992;47(9):1102-1114.
23. Ryan P. Integrated theory of health behavior change: background and intervention development. Clin Nurse Spec. 2009;23(3):161-172.
24. Evans DD , Blanchard EB. Prediction of early termination from the self-regulatory treatment of chronic headache. Biofeedback Self Regul. 1988;13(3):245-256.
25. Maguen S, Hoerster KD, Littman AJ, et al. Iraq and Afghanistan veterans with PTSD participate less in VA’s weight loss program than those without PTSD. J Affect Disord. 2016;193:289-294.
26. Bloor LE. Improving weight management services for female veterans: design and participation factors with a women only program, and comparisons with gender neutral services. Med Res Arch. 2015;2.
1. Brooks PM. The burden of musculoskeletal disease—a global perspective. Clin Rheumatol. 2006;25(6):778-781.
2. Haskell SG, Heapy A, Reid MC, Papas RK, Kerns RD. The prevalence and age-related characteristics of pain in a sample of women veterans receiving primary care. J Womens Health (Larchmt). 2006;15(7):862-869.
3. Roth RS, Geisser ME, Williams DA. Interventional pain medicine: retreat from the biopsychosocial model of pain. Transl Behav Med. 2012;2(1):106-116.
4. Engel GL. The need for a new medical model: a challenge for biomedicine. Science. 1977;196(4286):129-136.
5. Borrell-Carrió F, Suchman AL, Epstein RM. The biopsychosocial model 25 years later: principles, practice, and scientific inquiry. Ann Fam Med. 2004;2(6):576-582.
6. Wall PD. The gate control theory of pain mechanisms: a re-examination and re-statement. Brain. 1978;101(1):1-18.
7. Dobscha SK, Corson K, Perrin NA, et al. Collaborative care for chronic pain in primary care: a cluster randomized trial. JAMA. 2009;301(12):1242-1252.
8. Von Korff, Moore JC. Stepped care for back pain: activating approaches for primary care. Ann Intern Med. 2001;134(9, pt 2):911-917.
9. Oslund S, Robinson RC, Clark TC, et al. Long-term effectiveness of a comprehensive pain management program: strengthening the case for interdisciplinary care. Proc (Bayl Univ Med Cent). 2009;22(3):211-214.
10. Scascighini L, Toma V, Dober-Spielmann S, Sprott H. Multidisciplinary treatment for chronic pain: a systematic review of interventions and outcomes. Rheumatology (Oxford). 2008;47(5):670-678.
11. Gatchel RJ, McGeary DD, McGeary CA, Lippe B. Interdisciplinary chronic pain management: past, present, and future. Am Psychol. 2014;69(2):119-130.
12. McCracken LM, Turk DC. Behavioral and cognitive-behavioral treatment for chronic pain: outcome, predictors of outcome, and treatment process. Spine (Phila Pa 1976). 2002;27(22): 2564-2573.
13. Jeffery MM, Butler M, Stark A, Kane RL. Multidisciplinary Pain Programs for Chronic Noncancer Pain. Comparative Effectiveness Technical Briefs, No 8. Rockville, MD: Agency for Healthcare Research and Quality; 2011.
14. Ehde DM, Dilworth TM, Turner JA. Cognitive-behavioral therapy for individuals with chronic pain: efficacy, innovations, and directions for research. Am Psychol. 2014;69(2):153-166.
15. Dorflinger L, Kerns RD, Auerbach SM. Providers’ roles in enhancing patients’ adherence to pain self management. Transl Behav Med. 2013;3(1):39-46.
16. Pellico LH, Gilliam WP, Lee AW, Kerns RD. Hearing new voices: registered nurses and health technicians experience caring for chronic pain patients in primary care clinics. Open Nurs J. 2014;8:25-33.
17. Rollnick S, Miller WR, Butler CC, eds. Motivational Interviewing in Health Care: Helping Patients Change Behavior. New York, NY: The Guilford Press; 2008.
18. Kerns RD, Habib S. A critical review of the pain readiness to change model. J Pain. 2004;5(7):357-367.19. Kerns RD, Burns JW, Shulman M, et al. Can we improve cognitive-behavior therapy for chronic back pain treatment engagement and adherence? A controlled trial of tailored versus standard therapy. Health Psychol. 2014;33(9):938-947.
20. Kearney LK, Post EP, Zeiss A, Goldstein MG, Dundon M. The role of mental and behavioral health in the application of the patient-centered medical home in the Department of Veterans Affairs. Transl Behav Med. 2011;1(4):624-628.
21. Prochaska JO, DiClemente CC. Stages and processes of self-change of smoking: toward an integrative model of change. J Consult Clin Psychol. 1983;51(3):390-395.
22. Prochaska JO, DiClemente CC, Norcross JC. In search of how people change. Applications to addictive behaviors. Am Psychol. 1992;47(9):1102-1114.
23. Ryan P. Integrated theory of health behavior change: background and intervention development. Clin Nurse Spec. 2009;23(3):161-172.
24. Evans DD , Blanchard EB. Prediction of early termination from the self-regulatory treatment of chronic headache. Biofeedback Self Regul. 1988;13(3):245-256.
25. Maguen S, Hoerster KD, Littman AJ, et al. Iraq and Afghanistan veterans with PTSD participate less in VA’s weight loss program than those without PTSD. J Affect Disord. 2016;193:289-294.
26. Bloor LE. Improving weight management services for female veterans: design and participation factors with a women only program, and comparisons with gender neutral services. Med Res Arch. 2015;2.
Improving Caregiver Knowledge of Support Resources
In 2012, 1.3 million veterans who were wounded in action had a severe service-connected disability—nearly triple the number in 2001 (482,000).1 Given the increased number of wounded veterans, the need for caregivers also increased.
The act of caring for an individual with a chronic disability can be a daunting task for the caregiver. However, what is not so commonly recognized is the need for caregiver awareness of the available support resources. Caregivers who do not receive necessary support experience physical and emotional consequences that interfere with their ability to care for veterans with disabilities. Therefore, there is a significant need to provide adequate support for the caregiver to maintain optimum care of the veteran.2
Increased caregiver strain among family caregivers of veterans with long-term disabilities and their lack of knowledge of support resources is a clinical concern. A comprehensive review of the literature provided evidence that access and use of caregiver support resources improved caregiver quality of life.
The purpose of this project was to provide an educational intervention of caregiver resources that were available at the Durham VA Health Care System in North Carolina and in the surrounding community. The desired outcomes included (a) increasing the caregiver’s knowledge of resources available at the VA and within the community to decrease caregiver burden; and (b) assisting the caregiver in determining the best resources for the caregiver and patient. This project was deemed to be a quality improvement project and did not require institutional review board (IRB) approval.
Background
The term strain is used to describe the burden, trouble, or burnout that a caregiver encounters when caring for a person with a long-term illness or disability.3 Caregivers of veterans remain in their role longer and have a heavier burden of care than that of all other caregivers: 65% are in a high-burden caregiving situation compared with 31% nationally.4 The consequence of providing care without assistance has all the features of chronic stress.2 Moreover, the decline of the caregiver’s health can significantly compromise the ability to provide care.3
Empirical observations of the negative health effects of caregiving noted over the past 2 decades have helped convince policymakers that supporting caregivers is an important public health issue.2 To this end, Congress mandated legislation that required the VA to provide a support program for veteran caregivers. In May 2010, President Obama signed the Caregivers and Veterans Omnibus Health Services Act of 2010 into law.1
Supporting Literature
The VA caregiver resource program offers a variety of support resources.1 A better understanding of caregiver needs is necessary to provide the right support resources, improve the health and well-being of caregivers, and make decisions regarding individual caregiving situations.5 For example, respite care offers temporary or periodic relief from caregiving, allowing caregivers to attend to personal tasks, such as shopping, running errands, relaxing, and socializing. This service can increase the physical and mental well-being of the caregiver.6 Studies show that early use of support services is paramount in order for caregivers to receive the greatest positive impact.5
Chen and colleaguesconducted a study of 164 caregivers. The study showed that caregivers who received assistance with accessing the correct support resource exhibited considerably higher satisfaction with the services they received.7 Determining which support therapy was best for the caregiver and the patient for whom they were caring was seen as the initial step. Providing a tool that supplies all the information caregivers need as well as assisting them with accessing services more efficiently is beneficial.
The National Alliance for Caregiving conducted a study to evaluate the needs of caregivers of veterans of various conflicts.4 In the study, caregivers reported that a resource guide would be beneficial. Some of the services they wanted to include in the directory were VA disability benefits, respite care, home health care, hospice services, assisted living, rehabilitation therapies, caregiver support group information, and community resources.
Based on the literature, the author believed that better knowledge of support resources was needed for caregivers. The literature included detailed descriptions of how knowledge of support resources improved caregiver’s well-being by increasing his or her ability to cope with stress related to providing care. However, the literature could have provided a more elaborate discussion on this topic. That was the only weakness identified in each of the studies. Nonetheless, it was clearly noted that resource knowledge yielded a positive effect.
Methods
The project took place at the Durham VA Health Care System and was implemented from August 2015 to October 2015. The participants targeted were caregivers of veterans with disabilities who were considered the veteran’s primary caregiver. Participation was voluntary.
During the veteran’s clinic appointment, the caregiver was given an implied consent letter, pre- and postquestionnaire forms, and a caregiver resource manual. The manual included information on caregiver support resources at the Durham VA Health Care System and in the community (eg, adult day care centers; home-based primary care, hospice care, skilled care, and telehealth; homemaker and home health aide programs; respite care). Other information was provided, such as the Caregiver Support Program application process, contact names, numbers, and helpful websites. Before reading the manual, participants completed the prequestionnaire form and returned it the day of the veteran’s visit. After reading the manual, the caregiver was instructed to complete the postquestionnaire form.
The project coordinator (PC) collaborated with the Veteran Health Education coordinator in developing the caregiver resource manual and questionnaires to ensure that the material met the requirements set forth by the educational program within the Durham VA Health Care System. The PC also collaborated with the Caregiver Support Program subject experts, the chief and acting assistant chief of social work when formulating the contents of the manual and questionnaires. The questionnaires were used to assess the effectiveness of the manual.
The 3 questions on the prequestionnaire and 3 questions on the postquestionnaire were geared to measure the caregiver’s knowledge. There also were 4 questions on the postquestionnaire that were used to address manual revisions.
On the prequestionnaire form, the following questions were asked: (1) If you needed to find caregiver support resources, how much knowledge do you have finding the resources that fit your needs as well as the veteran’s needs? (2) Rate how aware you are with knowing what caregiver support resources are available at the VA and within the community; and (3) Would knowing which caregiver support resources to choose from at the VA and within the community decrease your stress level and give you “peace of mind?”
The same questions were asked postintervention, and the participants were asked to rate their knowledge after reviewing the manual. The participant’s responses on the questionnaires were measured using a 5-point Likert scale.
Participant Demographics
Demographic information was obtained from the cover letter distributed to each participant. The demographic information included age, gender, relationship to the veteran, and number of years to date in the current caregiving role. Participants eligible for inclusion in this project were primary caregivers of veterans with disabilities from all eras of conflict, aged ≥ 18 years.
Fifteen caregivers participated by returning the cover letter containing the implied consent, reading the manual, and completing the pre- and postquestionnaires. There was a wide age range of caregivers who participated, from 29 to 77 years. Of those who responded, there also was a wide range in time in their current caregiving role, ranging from 1 to 41 years. The mean number of years in the current caregiving role was 7 years.
Of the 15 participants, most were female spouses. There were no husbands who participated. The relative’s category included a cousin, a son, and a daughter. The “other” category included a son-in-law and a fiancé.
Data Analysis
Both outcomes were measured using the responses from questions 1 through 3 with the use of running a descriptive statistical analysis. In addition, a t test was used to determine statistical significance, set at α level < .05 of knowledge increase from pre- to postintervention data. Based on the facility, educational benchmarks were set at 80% with the 80% equal to 4 on the Likert scale. Therefore, 80% was the identified benchmark for this project. The goal was that > 70% of the participants would score 80% or better on the postquestionnaire.
Results
Both outcomes were met: (1) increasing the caregiver’s knowledge regarding resources available at the VA and within the community to decrease caregiver burden; and (2) assisting the caregiver in deciding which caregiver resources located in the manual were the right fit for the caregiver and the veteran for whom they were caring. The percentage of participants who scored 80% or better on the prequestionnaire was 54% (n = 8). The postquestionnaire outcomes were considered an improvement based on caregiver’s knowledge of support resources as well as whether the information in the manual decreased their stress level and gave them peace of mind. The intended outcome for the postquestionnaire was that > 70% of the participants would score ≥ 80% after the intervention. This goal was met as final results revealed 73% (n = 11) of the participants scored > 80% on the postquestionnaire.
The postresults supported that caregivers’ knowledge increased, they had peace of mind, and stress levels were decreased with the use of an educational intervention, a comprehensive Caregiver Resource Manual. The postquestionnaire revealed that all of the participants found the Caregiver Resource Manual easy to navigate, and 93% of participants found the Caregiver Resource Manual useful. Out of 15 participants, 8 provided comments. Seven provided positive comments, reporting that the information in the manual was interesting, the manual was simple/easy to read, and the outside resources listed were helpful.
The participant who provided a negative comment was one of the caregivers who did not meet the benchmark of 80% on the pre- or postquestionnaire. The participant was a 33-year-old wife of a veteran with disabilities who had been in the current caregiving role for 9 years. This participant reported that the Caregiver Resource Manual was not geared to younger caregivers, so she would not benefit from using the manual. This caregiver also was the only participant who reported that the Caregiver Resource Manual neither gave her peace of mind nor decreased her stress level.
Comments or suggestions would have been helpful from the other 8 individuals. Because it was not written in the IRB proposal to contact the participants other than to follow-up with telephone calls regarding unreturned questionnaires, no further contact was made with the participants.
Discussion
The preliminary success of this project suggests that there is a significant need for an educational conduit to ensure sufficient caregiver knowledge. Interprofessional collaborative efforts along with using information systems/technology to deliver the Caregiver Resource Manual electronically are important future consideration for improvement of the overall outcomes for a wide range of caregivers, veterans, and health care providers. Health care policy changes on the organizational level, systems level, and national level could further support caregivers of disabled veterans by enabling easy access to caregiver resources as a mandated practice.
Limitations
Limitations centered on the recruitment process. There were a total of 15 caregivers who participated. Although the participation did not meet the PC’s expectation, the final number of participants was adequate in obtaining data regarding evaluating the impact of this project.
Conclusion
The results of this project provided evidence that the Caregiver Resource Manual was effective. Caregivers gained a sense of knowledge and empowerment regarding available resources within the VA and the community. Providing the caregiver with peace of mind and improving the overall health and well-being of the caregiver and veteran were essential.
Moreover, just as the veterans who fought for freedom were equipped with full body armor to help protect them from the potential negative consequences of combat, caregivers who care for these brave soldiers are now equipped with a resource tool and a “full armor of knowledge” to care for their loved ones…our nation’s heroes…our veterans.
1. VA Health Care. Actions needed to address higher-than-expected demand for the family caregiver program. http://www.gao.gov/assets/670/665928.pdf. Published September 18, 2014. Accessed January 9, 2017.
2. Schulz R, Sherwood PR. Physical and mental health effects of family caregiving. Am J Nurs. 2008;108(suppl 9):23-27.
3. Centers for Disease Control; Kimberly-Clark Corporation. Assuring healthy caregivers, a public health approach to translating research into practice: the RE-AIM framework. https://www.cdc.gov /aging/pdf/caregiving_monograph.pdf. Published 2008. Accessed January 9, 2017.
4. National Alliance for Caregiving. Caregivers of veterans—serving on the home front report of study findings. http://www.caregiving.org/data/2010 _Caregivers_of_Veterans_FULLREPORT_WEB _FINAL.pdf. Published 2010. Accessed January 9, 2017.
5. Whittier S, Coon D, Aaker J. Caregiving support interventions. http://cssr.berkeley.edu/pdfs/famcare_04.pdf. Updated 2001. Accessed January 9, 2017.
6. Alzheimer’s Association. Respite care. http://www .alz.org/care/alzheimers-dementia-caregiver-respite.asp. Updated 2016. Accessed January 9, 2017.
7. Chen YM, Hedrick SC, Young HM. A pilot evaluation of the family caregiver support program. Eval Program Plann. 2010;33(2):113-119.
In 2012, 1.3 million veterans who were wounded in action had a severe service-connected disability—nearly triple the number in 2001 (482,000).1 Given the increased number of wounded veterans, the need for caregivers also increased.
The act of caring for an individual with a chronic disability can be a daunting task for the caregiver. However, what is not so commonly recognized is the need for caregiver awareness of the available support resources. Caregivers who do not receive necessary support experience physical and emotional consequences that interfere with their ability to care for veterans with disabilities. Therefore, there is a significant need to provide adequate support for the caregiver to maintain optimum care of the veteran.2
Increased caregiver strain among family caregivers of veterans with long-term disabilities and their lack of knowledge of support resources is a clinical concern. A comprehensive review of the literature provided evidence that access and use of caregiver support resources improved caregiver quality of life.
The purpose of this project was to provide an educational intervention of caregiver resources that were available at the Durham VA Health Care System in North Carolina and in the surrounding community. The desired outcomes included (a) increasing the caregiver’s knowledge of resources available at the VA and within the community to decrease caregiver burden; and (b) assisting the caregiver in determining the best resources for the caregiver and patient. This project was deemed to be a quality improvement project and did not require institutional review board (IRB) approval.
Background
The term strain is used to describe the burden, trouble, or burnout that a caregiver encounters when caring for a person with a long-term illness or disability.3 Caregivers of veterans remain in their role longer and have a heavier burden of care than that of all other caregivers: 65% are in a high-burden caregiving situation compared with 31% nationally.4 The consequence of providing care without assistance has all the features of chronic stress.2 Moreover, the decline of the caregiver’s health can significantly compromise the ability to provide care.3
Empirical observations of the negative health effects of caregiving noted over the past 2 decades have helped convince policymakers that supporting caregivers is an important public health issue.2 To this end, Congress mandated legislation that required the VA to provide a support program for veteran caregivers. In May 2010, President Obama signed the Caregivers and Veterans Omnibus Health Services Act of 2010 into law.1
Supporting Literature
The VA caregiver resource program offers a variety of support resources.1 A better understanding of caregiver needs is necessary to provide the right support resources, improve the health and well-being of caregivers, and make decisions regarding individual caregiving situations.5 For example, respite care offers temporary or periodic relief from caregiving, allowing caregivers to attend to personal tasks, such as shopping, running errands, relaxing, and socializing. This service can increase the physical and mental well-being of the caregiver.6 Studies show that early use of support services is paramount in order for caregivers to receive the greatest positive impact.5
Chen and colleaguesconducted a study of 164 caregivers. The study showed that caregivers who received assistance with accessing the correct support resource exhibited considerably higher satisfaction with the services they received.7 Determining which support therapy was best for the caregiver and the patient for whom they were caring was seen as the initial step. Providing a tool that supplies all the information caregivers need as well as assisting them with accessing services more efficiently is beneficial.
The National Alliance for Caregiving conducted a study to evaluate the needs of caregivers of veterans of various conflicts.4 In the study, caregivers reported that a resource guide would be beneficial. Some of the services they wanted to include in the directory were VA disability benefits, respite care, home health care, hospice services, assisted living, rehabilitation therapies, caregiver support group information, and community resources.
Based on the literature, the author believed that better knowledge of support resources was needed for caregivers. The literature included detailed descriptions of how knowledge of support resources improved caregiver’s well-being by increasing his or her ability to cope with stress related to providing care. However, the literature could have provided a more elaborate discussion on this topic. That was the only weakness identified in each of the studies. Nonetheless, it was clearly noted that resource knowledge yielded a positive effect.
Methods
The project took place at the Durham VA Health Care System and was implemented from August 2015 to October 2015. The participants targeted were caregivers of veterans with disabilities who were considered the veteran’s primary caregiver. Participation was voluntary.
During the veteran’s clinic appointment, the caregiver was given an implied consent letter, pre- and postquestionnaire forms, and a caregiver resource manual. The manual included information on caregiver support resources at the Durham VA Health Care System and in the community (eg, adult day care centers; home-based primary care, hospice care, skilled care, and telehealth; homemaker and home health aide programs; respite care). Other information was provided, such as the Caregiver Support Program application process, contact names, numbers, and helpful websites. Before reading the manual, participants completed the prequestionnaire form and returned it the day of the veteran’s visit. After reading the manual, the caregiver was instructed to complete the postquestionnaire form.
The project coordinator (PC) collaborated with the Veteran Health Education coordinator in developing the caregiver resource manual and questionnaires to ensure that the material met the requirements set forth by the educational program within the Durham VA Health Care System. The PC also collaborated with the Caregiver Support Program subject experts, the chief and acting assistant chief of social work when formulating the contents of the manual and questionnaires. The questionnaires were used to assess the effectiveness of the manual.
The 3 questions on the prequestionnaire and 3 questions on the postquestionnaire were geared to measure the caregiver’s knowledge. There also were 4 questions on the postquestionnaire that were used to address manual revisions.
On the prequestionnaire form, the following questions were asked: (1) If you needed to find caregiver support resources, how much knowledge do you have finding the resources that fit your needs as well as the veteran’s needs? (2) Rate how aware you are with knowing what caregiver support resources are available at the VA and within the community; and (3) Would knowing which caregiver support resources to choose from at the VA and within the community decrease your stress level and give you “peace of mind?”
The same questions were asked postintervention, and the participants were asked to rate their knowledge after reviewing the manual. The participant’s responses on the questionnaires were measured using a 5-point Likert scale.
Participant Demographics
Demographic information was obtained from the cover letter distributed to each participant. The demographic information included age, gender, relationship to the veteran, and number of years to date in the current caregiving role. Participants eligible for inclusion in this project were primary caregivers of veterans with disabilities from all eras of conflict, aged ≥ 18 years.
Fifteen caregivers participated by returning the cover letter containing the implied consent, reading the manual, and completing the pre- and postquestionnaires. There was a wide age range of caregivers who participated, from 29 to 77 years. Of those who responded, there also was a wide range in time in their current caregiving role, ranging from 1 to 41 years. The mean number of years in the current caregiving role was 7 years.
Of the 15 participants, most were female spouses. There were no husbands who participated. The relative’s category included a cousin, a son, and a daughter. The “other” category included a son-in-law and a fiancé.
Data Analysis
Both outcomes were measured using the responses from questions 1 through 3 with the use of running a descriptive statistical analysis. In addition, a t test was used to determine statistical significance, set at α level < .05 of knowledge increase from pre- to postintervention data. Based on the facility, educational benchmarks were set at 80% with the 80% equal to 4 on the Likert scale. Therefore, 80% was the identified benchmark for this project. The goal was that > 70% of the participants would score 80% or better on the postquestionnaire.
Results
Both outcomes were met: (1) increasing the caregiver’s knowledge regarding resources available at the VA and within the community to decrease caregiver burden; and (2) assisting the caregiver in deciding which caregiver resources located in the manual were the right fit for the caregiver and the veteran for whom they were caring. The percentage of participants who scored 80% or better on the prequestionnaire was 54% (n = 8). The postquestionnaire outcomes were considered an improvement based on caregiver’s knowledge of support resources as well as whether the information in the manual decreased their stress level and gave them peace of mind. The intended outcome for the postquestionnaire was that > 70% of the participants would score ≥ 80% after the intervention. This goal was met as final results revealed 73% (n = 11) of the participants scored > 80% on the postquestionnaire.
The postresults supported that caregivers’ knowledge increased, they had peace of mind, and stress levels were decreased with the use of an educational intervention, a comprehensive Caregiver Resource Manual. The postquestionnaire revealed that all of the participants found the Caregiver Resource Manual easy to navigate, and 93% of participants found the Caregiver Resource Manual useful. Out of 15 participants, 8 provided comments. Seven provided positive comments, reporting that the information in the manual was interesting, the manual was simple/easy to read, and the outside resources listed were helpful.
The participant who provided a negative comment was one of the caregivers who did not meet the benchmark of 80% on the pre- or postquestionnaire. The participant was a 33-year-old wife of a veteran with disabilities who had been in the current caregiving role for 9 years. This participant reported that the Caregiver Resource Manual was not geared to younger caregivers, so she would not benefit from using the manual. This caregiver also was the only participant who reported that the Caregiver Resource Manual neither gave her peace of mind nor decreased her stress level.
Comments or suggestions would have been helpful from the other 8 individuals. Because it was not written in the IRB proposal to contact the participants other than to follow-up with telephone calls regarding unreturned questionnaires, no further contact was made with the participants.
Discussion
The preliminary success of this project suggests that there is a significant need for an educational conduit to ensure sufficient caregiver knowledge. Interprofessional collaborative efforts along with using information systems/technology to deliver the Caregiver Resource Manual electronically are important future consideration for improvement of the overall outcomes for a wide range of caregivers, veterans, and health care providers. Health care policy changes on the organizational level, systems level, and national level could further support caregivers of disabled veterans by enabling easy access to caregiver resources as a mandated practice.
Limitations
Limitations centered on the recruitment process. There were a total of 15 caregivers who participated. Although the participation did not meet the PC’s expectation, the final number of participants was adequate in obtaining data regarding evaluating the impact of this project.
Conclusion
The results of this project provided evidence that the Caregiver Resource Manual was effective. Caregivers gained a sense of knowledge and empowerment regarding available resources within the VA and the community. Providing the caregiver with peace of mind and improving the overall health and well-being of the caregiver and veteran were essential.
Moreover, just as the veterans who fought for freedom were equipped with full body armor to help protect them from the potential negative consequences of combat, caregivers who care for these brave soldiers are now equipped with a resource tool and a “full armor of knowledge” to care for their loved ones…our nation’s heroes…our veterans.
In 2012, 1.3 million veterans who were wounded in action had a severe service-connected disability—nearly triple the number in 2001 (482,000).1 Given the increased number of wounded veterans, the need for caregivers also increased.
The act of caring for an individual with a chronic disability can be a daunting task for the caregiver. However, what is not so commonly recognized is the need for caregiver awareness of the available support resources. Caregivers who do not receive necessary support experience physical and emotional consequences that interfere with their ability to care for veterans with disabilities. Therefore, there is a significant need to provide adequate support for the caregiver to maintain optimum care of the veteran.2
Increased caregiver strain among family caregivers of veterans with long-term disabilities and their lack of knowledge of support resources is a clinical concern. A comprehensive review of the literature provided evidence that access and use of caregiver support resources improved caregiver quality of life.
The purpose of this project was to provide an educational intervention of caregiver resources that were available at the Durham VA Health Care System in North Carolina and in the surrounding community. The desired outcomes included (a) increasing the caregiver’s knowledge of resources available at the VA and within the community to decrease caregiver burden; and (b) assisting the caregiver in determining the best resources for the caregiver and patient. This project was deemed to be a quality improvement project and did not require institutional review board (IRB) approval.
Background
The term strain is used to describe the burden, trouble, or burnout that a caregiver encounters when caring for a person with a long-term illness or disability.3 Caregivers of veterans remain in their role longer and have a heavier burden of care than that of all other caregivers: 65% are in a high-burden caregiving situation compared with 31% nationally.4 The consequence of providing care without assistance has all the features of chronic stress.2 Moreover, the decline of the caregiver’s health can significantly compromise the ability to provide care.3
Empirical observations of the negative health effects of caregiving noted over the past 2 decades have helped convince policymakers that supporting caregivers is an important public health issue.2 To this end, Congress mandated legislation that required the VA to provide a support program for veteran caregivers. In May 2010, President Obama signed the Caregivers and Veterans Omnibus Health Services Act of 2010 into law.1
Supporting Literature
The VA caregiver resource program offers a variety of support resources.1 A better understanding of caregiver needs is necessary to provide the right support resources, improve the health and well-being of caregivers, and make decisions regarding individual caregiving situations.5 For example, respite care offers temporary or periodic relief from caregiving, allowing caregivers to attend to personal tasks, such as shopping, running errands, relaxing, and socializing. This service can increase the physical and mental well-being of the caregiver.6 Studies show that early use of support services is paramount in order for caregivers to receive the greatest positive impact.5
Chen and colleaguesconducted a study of 164 caregivers. The study showed that caregivers who received assistance with accessing the correct support resource exhibited considerably higher satisfaction with the services they received.7 Determining which support therapy was best for the caregiver and the patient for whom they were caring was seen as the initial step. Providing a tool that supplies all the information caregivers need as well as assisting them with accessing services more efficiently is beneficial.
The National Alliance for Caregiving conducted a study to evaluate the needs of caregivers of veterans of various conflicts.4 In the study, caregivers reported that a resource guide would be beneficial. Some of the services they wanted to include in the directory were VA disability benefits, respite care, home health care, hospice services, assisted living, rehabilitation therapies, caregiver support group information, and community resources.
Based on the literature, the author believed that better knowledge of support resources was needed for caregivers. The literature included detailed descriptions of how knowledge of support resources improved caregiver’s well-being by increasing his or her ability to cope with stress related to providing care. However, the literature could have provided a more elaborate discussion on this topic. That was the only weakness identified in each of the studies. Nonetheless, it was clearly noted that resource knowledge yielded a positive effect.
Methods
The project took place at the Durham VA Health Care System and was implemented from August 2015 to October 2015. The participants targeted were caregivers of veterans with disabilities who were considered the veteran’s primary caregiver. Participation was voluntary.
During the veteran’s clinic appointment, the caregiver was given an implied consent letter, pre- and postquestionnaire forms, and a caregiver resource manual. The manual included information on caregiver support resources at the Durham VA Health Care System and in the community (eg, adult day care centers; home-based primary care, hospice care, skilled care, and telehealth; homemaker and home health aide programs; respite care). Other information was provided, such as the Caregiver Support Program application process, contact names, numbers, and helpful websites. Before reading the manual, participants completed the prequestionnaire form and returned it the day of the veteran’s visit. After reading the manual, the caregiver was instructed to complete the postquestionnaire form.
The project coordinator (PC) collaborated with the Veteran Health Education coordinator in developing the caregiver resource manual and questionnaires to ensure that the material met the requirements set forth by the educational program within the Durham VA Health Care System. The PC also collaborated with the Caregiver Support Program subject experts, the chief and acting assistant chief of social work when formulating the contents of the manual and questionnaires. The questionnaires were used to assess the effectiveness of the manual.
The 3 questions on the prequestionnaire and 3 questions on the postquestionnaire were geared to measure the caregiver’s knowledge. There also were 4 questions on the postquestionnaire that were used to address manual revisions.
On the prequestionnaire form, the following questions were asked: (1) If you needed to find caregiver support resources, how much knowledge do you have finding the resources that fit your needs as well as the veteran’s needs? (2) Rate how aware you are with knowing what caregiver support resources are available at the VA and within the community; and (3) Would knowing which caregiver support resources to choose from at the VA and within the community decrease your stress level and give you “peace of mind?”
The same questions were asked postintervention, and the participants were asked to rate their knowledge after reviewing the manual. The participant’s responses on the questionnaires were measured using a 5-point Likert scale.
Participant Demographics
Demographic information was obtained from the cover letter distributed to each participant. The demographic information included age, gender, relationship to the veteran, and number of years to date in the current caregiving role. Participants eligible for inclusion in this project were primary caregivers of veterans with disabilities from all eras of conflict, aged ≥ 18 years.
Fifteen caregivers participated by returning the cover letter containing the implied consent, reading the manual, and completing the pre- and postquestionnaires. There was a wide age range of caregivers who participated, from 29 to 77 years. Of those who responded, there also was a wide range in time in their current caregiving role, ranging from 1 to 41 years. The mean number of years in the current caregiving role was 7 years.
Of the 15 participants, most were female spouses. There were no husbands who participated. The relative’s category included a cousin, a son, and a daughter. The “other” category included a son-in-law and a fiancé.
Data Analysis
Both outcomes were measured using the responses from questions 1 through 3 with the use of running a descriptive statistical analysis. In addition, a t test was used to determine statistical significance, set at α level < .05 of knowledge increase from pre- to postintervention data. Based on the facility, educational benchmarks were set at 80% with the 80% equal to 4 on the Likert scale. Therefore, 80% was the identified benchmark for this project. The goal was that > 70% of the participants would score 80% or better on the postquestionnaire.
Results
Both outcomes were met: (1) increasing the caregiver’s knowledge regarding resources available at the VA and within the community to decrease caregiver burden; and (2) assisting the caregiver in deciding which caregiver resources located in the manual were the right fit for the caregiver and the veteran for whom they were caring. The percentage of participants who scored 80% or better on the prequestionnaire was 54% (n = 8). The postquestionnaire outcomes were considered an improvement based on caregiver’s knowledge of support resources as well as whether the information in the manual decreased their stress level and gave them peace of mind. The intended outcome for the postquestionnaire was that > 70% of the participants would score ≥ 80% after the intervention. This goal was met as final results revealed 73% (n = 11) of the participants scored > 80% on the postquestionnaire.
The postresults supported that caregivers’ knowledge increased, they had peace of mind, and stress levels were decreased with the use of an educational intervention, a comprehensive Caregiver Resource Manual. The postquestionnaire revealed that all of the participants found the Caregiver Resource Manual easy to navigate, and 93% of participants found the Caregiver Resource Manual useful. Out of 15 participants, 8 provided comments. Seven provided positive comments, reporting that the information in the manual was interesting, the manual was simple/easy to read, and the outside resources listed were helpful.
The participant who provided a negative comment was one of the caregivers who did not meet the benchmark of 80% on the pre- or postquestionnaire. The participant was a 33-year-old wife of a veteran with disabilities who had been in the current caregiving role for 9 years. This participant reported that the Caregiver Resource Manual was not geared to younger caregivers, so she would not benefit from using the manual. This caregiver also was the only participant who reported that the Caregiver Resource Manual neither gave her peace of mind nor decreased her stress level.
Comments or suggestions would have been helpful from the other 8 individuals. Because it was not written in the IRB proposal to contact the participants other than to follow-up with telephone calls regarding unreturned questionnaires, no further contact was made with the participants.
Discussion
The preliminary success of this project suggests that there is a significant need for an educational conduit to ensure sufficient caregiver knowledge. Interprofessional collaborative efforts along with using information systems/technology to deliver the Caregiver Resource Manual electronically are important future consideration for improvement of the overall outcomes for a wide range of caregivers, veterans, and health care providers. Health care policy changes on the organizational level, systems level, and national level could further support caregivers of disabled veterans by enabling easy access to caregiver resources as a mandated practice.
Limitations
Limitations centered on the recruitment process. There were a total of 15 caregivers who participated. Although the participation did not meet the PC’s expectation, the final number of participants was adequate in obtaining data regarding evaluating the impact of this project.
Conclusion
The results of this project provided evidence that the Caregiver Resource Manual was effective. Caregivers gained a sense of knowledge and empowerment regarding available resources within the VA and the community. Providing the caregiver with peace of mind and improving the overall health and well-being of the caregiver and veteran were essential.
Moreover, just as the veterans who fought for freedom were equipped with full body armor to help protect them from the potential negative consequences of combat, caregivers who care for these brave soldiers are now equipped with a resource tool and a “full armor of knowledge” to care for their loved ones…our nation’s heroes…our veterans.
1. VA Health Care. Actions needed to address higher-than-expected demand for the family caregiver program. http://www.gao.gov/assets/670/665928.pdf. Published September 18, 2014. Accessed January 9, 2017.
2. Schulz R, Sherwood PR. Physical and mental health effects of family caregiving. Am J Nurs. 2008;108(suppl 9):23-27.
3. Centers for Disease Control; Kimberly-Clark Corporation. Assuring healthy caregivers, a public health approach to translating research into practice: the RE-AIM framework. https://www.cdc.gov /aging/pdf/caregiving_monograph.pdf. Published 2008. Accessed January 9, 2017.
4. National Alliance for Caregiving. Caregivers of veterans—serving on the home front report of study findings. http://www.caregiving.org/data/2010 _Caregivers_of_Veterans_FULLREPORT_WEB _FINAL.pdf. Published 2010. Accessed January 9, 2017.
5. Whittier S, Coon D, Aaker J. Caregiving support interventions. http://cssr.berkeley.edu/pdfs/famcare_04.pdf. Updated 2001. Accessed January 9, 2017.
6. Alzheimer’s Association. Respite care. http://www .alz.org/care/alzheimers-dementia-caregiver-respite.asp. Updated 2016. Accessed January 9, 2017.
7. Chen YM, Hedrick SC, Young HM. A pilot evaluation of the family caregiver support program. Eval Program Plann. 2010;33(2):113-119.
1. VA Health Care. Actions needed to address higher-than-expected demand for the family caregiver program. http://www.gao.gov/assets/670/665928.pdf. Published September 18, 2014. Accessed January 9, 2017.
2. Schulz R, Sherwood PR. Physical and mental health effects of family caregiving. Am J Nurs. 2008;108(suppl 9):23-27.
3. Centers for Disease Control; Kimberly-Clark Corporation. Assuring healthy caregivers, a public health approach to translating research into practice: the RE-AIM framework. https://www.cdc.gov /aging/pdf/caregiving_monograph.pdf. Published 2008. Accessed January 9, 2017.
4. National Alliance for Caregiving. Caregivers of veterans—serving on the home front report of study findings. http://www.caregiving.org/data/2010 _Caregivers_of_Veterans_FULLREPORT_WEB _FINAL.pdf. Published 2010. Accessed January 9, 2017.
5. Whittier S, Coon D, Aaker J. Caregiving support interventions. http://cssr.berkeley.edu/pdfs/famcare_04.pdf. Updated 2001. Accessed January 9, 2017.
6. Alzheimer’s Association. Respite care. http://www .alz.org/care/alzheimers-dementia-caregiver-respite.asp. Updated 2016. Accessed January 9, 2017.
7. Chen YM, Hedrick SC, Young HM. A pilot evaluation of the family caregiver support program. Eval Program Plann. 2010;33(2):113-119.
Malnutrition as a Fall Risk Factor
Falls often result in injuries with devastating outcomes. In the elderly, falls are the largest cause of injury, mortality, and functional decline, leading to 40% of nursing home admissions.1 Nationally, falls with injury are estimated to cost $19 billion in direct medical costs.2 According to the National Quality Forum (NQF), hospital falls resulting in injury are reportable events. Beginning in fiscal year 2015, reportable events labeled as hospital acquired conditions (HAC) are subject to nonpayment, creating increased regulatory and reimbursement pressure on hospitals.3
Due to the major impact of a fall, The Joint Commission (TJC) requires hospitals to assess a patient’s fall risk on admission and whenever the patient’s condition changes.4 Despite decades of research evaluating various predictive strategies to identify individuals at fall risk, nutritional issues as interactive risk factors have received little attention.
A comparative study on the validity of fall risk assessment scales revealed that tools claiming to predict risk factors do not work well.5 Falls are the result of multiple interactive, synergistic pathologies and risk factors. In a multivariate regression study conducted by Lichtenstein and colleagues in Canada, lower body weight was found to be a statistically significant risk factor for falling.6 In 2004, Oliver and colleagues conducted a systematic review of fall risk assessment tools that included validation testing with sufficient data to allow for calculation of sensitivity, specificity, negative and positive predictive values, odds ratios, and confidence intervals.5
Fourteen studies identified common fall risk factors. The majority of these studies identified impaired cognition as a risk factor.5 Of the 14 studies included in the systematic analysis of Oliver and colleagues,6-19 6 identified medications,6,8,11,12,17,18, and 8 noted weakness and unsteady gait as risk factors.6,9-11,14,16,18,19 Only 1 study noted anemia as a risk factor for falls among patients who were post cerebral vascular accident.11 Additionally, only 1 study noted an association between falls resulting in hip fracture and lower body weight.6
One in 4 adults admitted to a hospital is malnourished.20,21 Components of malnutrition, including but not limited to anemia, clinically significant weight loss, and vitamin D deficiency, may be unrecognized interactive risk factors that increase the risk of hospital falls. Malnutrition and dehydration symptoms include fatigue, dizziness, irritability, loss of muscle mass, impulsivity, and the potential for poor judgment. Therefore, it is likely that the severity of specific malnutrition parameters is associated with recurrent falls and possibly injurious falls.
Hunger and inadequate food intake due to chronic disease or chronic food insecurity are real issues for the elderly. Insufficient caloric intake often leads to slow, progressive, and often unnoticed weight loss. The Academy of Nutrition and Dietetics (AND) and the American Association of Parenteral and Enteral Nutrition (ASPEN) have defined clinically significant weight loss categories to aid in the diagnosis of malnutrition. To aid in the diagnosis of various degrees of malnutrition, clinically significant weight loss is classified as ≥ 5% weight loss in 30 days; ≥ 7.5% weight loss in 90 days; > 10% in 180 days.21 The World Health Organization (WHO) identifies iron deficiency measured by hemoglobin (Hgb) value (for men < 13 g/dL) as the most common and widespread nutritional disorder in the world (Tables 1a, 1b, and 1c).22
Eat Well, Fall Less is a retrospective chart review approved by the Louis Stokes Cleveland VAMC (LSCVAMC) Internal Review Board. The review seeks to determine whether degree of weight loss and decline in Hgb and vitamin D deficiency, factors of malnutrition, are present in recurrent fallers vs single-event fallers. Researchers hypothesized that individuals who experienced recurrent falls during hospitalization would demonstrate a greater degree of clinically significant weight loss compared with those who had experienced a single fall. The second hypothesis was that recurrent fallers also would have lower Hgb values than that of single-event fallers. The tertiary hypothesis was that individuals with a greater degree of vitamin D deficiency were more likely to be recurrent fallers compared with single-event fallers.
In addition, dementia has been previously identified as an independent risk factor for falls and recurrent falls.23 During phase 2 of the study, the researchers hypothesized that in individuals with dementia, the concurrent diagnosis of malnutrition would be greatest in the recurrent fall population. A total of 30 subjects were included in the analysis.
Methods
Patient record search of note titles for falls was compiled daily. A random sample of 170 veterans who had experienced a fall was screened for study inclusion. Of the 170 charts, data from a total of 120 veterans who experienced a documented fall during a hospitalization between October 1, 2010 and October 31, 2012, were included in this analysis.
Eligibility Criteria and Baseline Characteristics
Chart reviews of veterans aged > 18 years experiencing a fall while hospitalized at the LSCVAMC between October 1, 2010 and October 31, 2012, were eligible to be included in this study. Each veteran needed to have 1 documented weight in a maximum of 24 months before the first fall and a minimum of 1 documented Hgb value prior to the first fall.
Patients were excluded if they had experienced a cerebrovascular accident or transient ischemic attack; a documented orthopedic fracture in the 12 months before the first fall; a documented amputation of a lower limb in the past 24 months; diagnosis of blindness; a lack of outpatient weight for greater than 24 months before the first fall; a history of volume overload, renal, cardiovascular, or other in nature during hospitalization; and alcoholism. Additionally, if any of the study investigators felt as though a patient had commorientes that made weight history inaccurate, those patients were excluded. Data were reviewed on 170 randomly selected subjects. A total of 50 subjects were excluded for not meeting the inclusion criteria; 120 individuals met eligible criteria. The patients who had experienced falls were divided into 2 groups: single-event fallers (1 fall documented during the study period) and recurrent fallers (2 or more falls documented during the study period). Fifty subjects were excluded from the final analysis because they met the following exclusion criteria: volume overload anytime in the 12 months before the documented fall (42); amputation of a lower limb before the fall (6); and prosthetic device alteration within the 12 months before the fall (3). One of the subjects was eliminated for both volume overload and amputation.
Data Collection
Data obtained from the Computerized Patient Record System review included age, gender, diagnosis, and body weight at the time of the first fall and 1 month, 3 months, 6 months, and 1 year before the first fall. Hemoglobin values at time of the first fall, 1 month, 3 months, 6 months, and 1 year before first documented fall also were collected. Vitamin D values and date of value also were collected. In year 2 of this multiphase retrospective review, charts again were reviewed and additional data collected, which included absence or presence of dementia along with type of dementia and the presence or absence of cancer. Year 2 data collection also included diagnosis of malnutrition by provider and registered dietitian assessment of degree of malnutrition.
Analysis
Data analysis comparing single-event fallers and frequent fallers was performed using IBM SPSS Statistic V22.0s. This pilot study has recognized weight loss and anemia as being associated with repeat falls. A 2-tailed t test was performed to evaluate differences in weight history, 25-hydroxyvitamin D, and Hgb characteristics between single fallers and frequent fallers. A repeated analysis of variance was performed to evaluate changes in weight and Hgb values over time for single and multiple falls. During phase 2 of this trial, a subanalysis comparing individuals with and without the diagnosis of dementia was conducted.
Results
The average age of the patients was 68 years. There was a significant decline in Hgb levels in both single-event fallers and frequent fallers at 12 and 6 months before the first fall event (95% confidence interval; P = .001). One year before the first fall, 28% of eventual fallers met WHO criteria for the diagnosis of mild anemia. One year before the first fall, none of the eventual fallers met WHO criteria for moderate or severe anemia. Using the lab data just before the first fall, 10% of fallers met WHO criteria for mild anemia, 48% met WHO criteria for moderate anemia, and 31% met WHO criteria for severe anemia. The degree of anemia in single-event fallers when compared with multiple-event fallers was insignificant. Interestingly, the degree of decline of Hgb value during the 6 months before the first fall event was notable for all fallers (Figure).
Only 60 of the 120 included patients had a documented vitamin D level. At the time of the fall, 46 patients had moderate vitamin D deficiency, and 23 patients had severe vitamin D deficiency, defined as < 32 mg/dL. The authors speculate that vitamin D status declines with malnutrition and increases fall risk.
Thirty participants were included in the dementia arm; 36.7% were single-event fallers, and 63.3% were multiple-event fallers (Table 2). The average age of the groups was 76.7 years and 73.9 years, respectively. Physician diagnosis of malnutrition was collected for both single- and multiple-event fallers. Of the single-event fallers with dementia, none had a diagnosis of malnutrition before the first hospital fall; and of the multiple-event fallers with dementia, all had a diagnosis of malnutrition before their first hospital fall. Individuals with a diagnosis of dementia and malnutrition fall frequently (P = .0028).
Discussion
In this study, falls occurred in a variety of patient populations. Both single-event fallers and recurrent fallers had a significant drop in Hgb values at 12, 6, and 3 months before the first fall. There was not a strong difference of the Hgb value between single-event falls and multiple fallers in the total population. Anemia was a significant risk factor for all fallers. The decline in the Hgb level before a fall is highly predictive of fall risk.
In individuals with dementia, those with the diagnosis of malnutrition are frequent fallers. A tool to assist in identification of this patient population along with a focused intervention strategy for this population is an area of needed research.
Further research is under way to determine which components of malnutrition diagnosis contribute to fall risk. If so, development of a fall assessment tool, including various components of malnutrition is warranted. Intervention strategies to reduce fall risk may soon include new nutrition and education techniques based on the faller constellation. Falls instruments that explore nutritional risk factors and falls should be investigated (ie, weight loss, vitamin D status, and anemia).
Falls occur in patients with a variety of risk factors (eg, mobility and cognition). The current screening instruments to assess fall risk factors do not sufficiently account for nutritional risk factors. In the Eat Well, Fall Less Study of hospitalized veterans, nutritional risk factors of anemia and weight loss also were associated with single- and multiple-event fallers. The AUTUMN falls instrument that includes critical elements of malnutrition, such as a decline in Hgb and weight loss, is currently being created and is in the process of being validated at LSCVAMC; this tool will incorporate components of malnutrition.
Acknowledgments
The authors acknowledge Michelle Pearson, Laura Guidotti, Adam Weier, Elizabeth Gable, and Shannon Corlett for their research contributions. In memory of Anne Raguso, RD, PhD, for her lifelong focus on nutrition research.
1. Centers for Disease Control and Prevention. Older adult falls: important facts about falls. http://www.cdc.gov/homeandrecreationalsafety/falls/adultfalls.html. Updated September 20, 2016. Accessed December 2, 2016.
2. Centers for Disease Control and Prevention. Older adult falls: cost of falls among older adults. http://www.cdc.gov/HomeandRecreationalSafety/Falls/fallcost.html. Updated August 19, 2016. Accessed December 2, 2016.
3. National Quality Forum. Serious reportable events in healthcare—2011 update: a consensus report https://www.qualityforum.org/Publications/2011/12/SRE_2011_Final_Report.aspx. Published 2011. Accessed December 2, 2016.
4. DuPree E. Taking a stand against falls. https://www.jointcommission.org/jc_physician_blog/taking_a_stand_against_falls. Published May1, 2014. Accessed December 2, 2016.
5. Oliver D, Daly F, Martin FC, McMurdo ME. Risk factors and risk assessment tools for falls in hospital in-patients: a systematic review. Age Ageing. 2004;33(2):122-130.
6. Lichtenstein MJ, Griffin MR, Cornell JE, Malcolm E, Ray WA. Risk factors for hip fractures occurring in the hospital. Am J Epidemiol. 1994;140(9):830-838.
7. Ballinger BR, Ramsay AC. Accidents and drug treatment in a psychiatric hospital. Br J Psychiatry. 1975;126:462-463.
8. Bates D, Pruess K, Souney P, Platt R. Serious falls in hospitalized patients correlates and resource utilization. Am J Med. 1995;99(2):137-143.
9. Byers V, Arrington ME, Finstuen K. Predictive risk factors associated with stroke patient falls in acute care settings. J Neurosci Nurs. 1990;22(3):147-154.
10. Chu LW, Pei CK, Chiu A, et al. Risk factors for falls in hospitalized older medical patients. J Gerontol A Biol Sci Med Sci. 1999;54(1):M38-M48.
11. Gales BJ, Menard SM. Relationship between administration of selected medications and falls in hospitalized elderly patients. Ann Pharmacother. 1995;29(4):354-358.
12. Gluck T, Wientjes HJ, Rai GS. An evaluation of risk factors for inpatient falls in acute care and rehabilitation elderly care wards. Gerontology. 1996:42(2):104-107.
13. Janken J, Reynolds B. Patient falls in the acute care setting: identifying risk factors. Nurs Res.1986;35(4):215-219.
14. Morse JM, Tylko SJ, Dixon HA. Characteristics of the fall-prone patient. Gerontologist. 1987;27(4):516-522.
15. Oliver D, Britton M, Seed P, Martin FC, Hopper AH. Development and evaluation of an evidenced based risk assessment tool (STRATIFY) to predict which elderly outpatients will fall: case-control and cohort studies. BMJ. 1997;315(7115):1049-1053.
16. Passaro A, Volpato S. Benzodiazepenes with different half-life and falling in a hospitalized population: the GIFA study. Gruppo Italiano di Farmacovigilanza nell’Anziano. J Clin Epidemol. 2000;53(12):1222-1229.
17. Salgado R, Lord SR, Packer J, Ehrlich F. Factors associated with falling in elderly hospitalized inpatients. Gerentology. 1994;40(6):325-331.
18. Schmidt NA. 1989 federal nursing service award winner. reducing patient falls: a research-based comprehensive fall prevention program. Mil Med. 1990;155(5):202-207.
19. Sutton JC, Standon PJ, Wallace WA. Patient accidents in hospital: incidence, documentation and significance. Br J Clin Pract. 1994;48(2):63-66.
20. White JV, Guenter P, Jensen G, Malone A, Schofield M; Academy of Nutrition and Dietetics Malnutrition Work Group; A.S.P.E.N. Malnutrition Task Force; A.S.P.E.N. Board of Directors. Consensus statement of the Academy of Nutrition and Dietetics/American Society for Parental and Enteral Nutrition: characteristics recommended for the identification and documentation of adult malnutrition (undernutrition). J Acad Nutr Diet. 2012;112(5):730-738.
21. Russell C, Elia M. Nutrition screening survey in the UK in 2008: hospitals, care homes and mental health units. http://www.bapen.org.uk/pdfs/nsw/nsw_report2008-09.pdf. Published 2009. Accessed December 2, 2016.
22. Cansado P, Ravasco P, Camilo M. A longitudinal study of hospital undernutrition in the elderly: comparison of four validated methods. J Nutr Health Aging. 2009;13(2):159-164.
23. World Health Organization. Nutrition: micronutrient deficiencies. http://www.who.int/nutrition/topics/ida/en. Accessed December 2, 2016.
Falls often result in injuries with devastating outcomes. In the elderly, falls are the largest cause of injury, mortality, and functional decline, leading to 40% of nursing home admissions.1 Nationally, falls with injury are estimated to cost $19 billion in direct medical costs.2 According to the National Quality Forum (NQF), hospital falls resulting in injury are reportable events. Beginning in fiscal year 2015, reportable events labeled as hospital acquired conditions (HAC) are subject to nonpayment, creating increased regulatory and reimbursement pressure on hospitals.3
Due to the major impact of a fall, The Joint Commission (TJC) requires hospitals to assess a patient’s fall risk on admission and whenever the patient’s condition changes.4 Despite decades of research evaluating various predictive strategies to identify individuals at fall risk, nutritional issues as interactive risk factors have received little attention.
A comparative study on the validity of fall risk assessment scales revealed that tools claiming to predict risk factors do not work well.5 Falls are the result of multiple interactive, synergistic pathologies and risk factors. In a multivariate regression study conducted by Lichtenstein and colleagues in Canada, lower body weight was found to be a statistically significant risk factor for falling.6 In 2004, Oliver and colleagues conducted a systematic review of fall risk assessment tools that included validation testing with sufficient data to allow for calculation of sensitivity, specificity, negative and positive predictive values, odds ratios, and confidence intervals.5
Fourteen studies identified common fall risk factors. The majority of these studies identified impaired cognition as a risk factor.5 Of the 14 studies included in the systematic analysis of Oliver and colleagues,6-19 6 identified medications,6,8,11,12,17,18, and 8 noted weakness and unsteady gait as risk factors.6,9-11,14,16,18,19 Only 1 study noted anemia as a risk factor for falls among patients who were post cerebral vascular accident.11 Additionally, only 1 study noted an association between falls resulting in hip fracture and lower body weight.6
One in 4 adults admitted to a hospital is malnourished.20,21 Components of malnutrition, including but not limited to anemia, clinically significant weight loss, and vitamin D deficiency, may be unrecognized interactive risk factors that increase the risk of hospital falls. Malnutrition and dehydration symptoms include fatigue, dizziness, irritability, loss of muscle mass, impulsivity, and the potential for poor judgment. Therefore, it is likely that the severity of specific malnutrition parameters is associated with recurrent falls and possibly injurious falls.
Hunger and inadequate food intake due to chronic disease or chronic food insecurity are real issues for the elderly. Insufficient caloric intake often leads to slow, progressive, and often unnoticed weight loss. The Academy of Nutrition and Dietetics (AND) and the American Association of Parenteral and Enteral Nutrition (ASPEN) have defined clinically significant weight loss categories to aid in the diagnosis of malnutrition. To aid in the diagnosis of various degrees of malnutrition, clinically significant weight loss is classified as ≥ 5% weight loss in 30 days; ≥ 7.5% weight loss in 90 days; > 10% in 180 days.21 The World Health Organization (WHO) identifies iron deficiency measured by hemoglobin (Hgb) value (for men < 13 g/dL) as the most common and widespread nutritional disorder in the world (Tables 1a, 1b, and 1c).22
Eat Well, Fall Less is a retrospective chart review approved by the Louis Stokes Cleveland VAMC (LSCVAMC) Internal Review Board. The review seeks to determine whether degree of weight loss and decline in Hgb and vitamin D deficiency, factors of malnutrition, are present in recurrent fallers vs single-event fallers. Researchers hypothesized that individuals who experienced recurrent falls during hospitalization would demonstrate a greater degree of clinically significant weight loss compared with those who had experienced a single fall. The second hypothesis was that recurrent fallers also would have lower Hgb values than that of single-event fallers. The tertiary hypothesis was that individuals with a greater degree of vitamin D deficiency were more likely to be recurrent fallers compared with single-event fallers.
In addition, dementia has been previously identified as an independent risk factor for falls and recurrent falls.23 During phase 2 of the study, the researchers hypothesized that in individuals with dementia, the concurrent diagnosis of malnutrition would be greatest in the recurrent fall population. A total of 30 subjects were included in the analysis.
Methods
Patient record search of note titles for falls was compiled daily. A random sample of 170 veterans who had experienced a fall was screened for study inclusion. Of the 170 charts, data from a total of 120 veterans who experienced a documented fall during a hospitalization between October 1, 2010 and October 31, 2012, were included in this analysis.
Eligibility Criteria and Baseline Characteristics
Chart reviews of veterans aged > 18 years experiencing a fall while hospitalized at the LSCVAMC between October 1, 2010 and October 31, 2012, were eligible to be included in this study. Each veteran needed to have 1 documented weight in a maximum of 24 months before the first fall and a minimum of 1 documented Hgb value prior to the first fall.
Patients were excluded if they had experienced a cerebrovascular accident or transient ischemic attack; a documented orthopedic fracture in the 12 months before the first fall; a documented amputation of a lower limb in the past 24 months; diagnosis of blindness; a lack of outpatient weight for greater than 24 months before the first fall; a history of volume overload, renal, cardiovascular, or other in nature during hospitalization; and alcoholism. Additionally, if any of the study investigators felt as though a patient had commorientes that made weight history inaccurate, those patients were excluded. Data were reviewed on 170 randomly selected subjects. A total of 50 subjects were excluded for not meeting the inclusion criteria; 120 individuals met eligible criteria. The patients who had experienced falls were divided into 2 groups: single-event fallers (1 fall documented during the study period) and recurrent fallers (2 or more falls documented during the study period). Fifty subjects were excluded from the final analysis because they met the following exclusion criteria: volume overload anytime in the 12 months before the documented fall (42); amputation of a lower limb before the fall (6); and prosthetic device alteration within the 12 months before the fall (3). One of the subjects was eliminated for both volume overload and amputation.
Data Collection
Data obtained from the Computerized Patient Record System review included age, gender, diagnosis, and body weight at the time of the first fall and 1 month, 3 months, 6 months, and 1 year before the first fall. Hemoglobin values at time of the first fall, 1 month, 3 months, 6 months, and 1 year before first documented fall also were collected. Vitamin D values and date of value also were collected. In year 2 of this multiphase retrospective review, charts again were reviewed and additional data collected, which included absence or presence of dementia along with type of dementia and the presence or absence of cancer. Year 2 data collection also included diagnosis of malnutrition by provider and registered dietitian assessment of degree of malnutrition.
Analysis
Data analysis comparing single-event fallers and frequent fallers was performed using IBM SPSS Statistic V22.0s. This pilot study has recognized weight loss and anemia as being associated with repeat falls. A 2-tailed t test was performed to evaluate differences in weight history, 25-hydroxyvitamin D, and Hgb characteristics between single fallers and frequent fallers. A repeated analysis of variance was performed to evaluate changes in weight and Hgb values over time for single and multiple falls. During phase 2 of this trial, a subanalysis comparing individuals with and without the diagnosis of dementia was conducted.
Results
The average age of the patients was 68 years. There was a significant decline in Hgb levels in both single-event fallers and frequent fallers at 12 and 6 months before the first fall event (95% confidence interval; P = .001). One year before the first fall, 28% of eventual fallers met WHO criteria for the diagnosis of mild anemia. One year before the first fall, none of the eventual fallers met WHO criteria for moderate or severe anemia. Using the lab data just before the first fall, 10% of fallers met WHO criteria for mild anemia, 48% met WHO criteria for moderate anemia, and 31% met WHO criteria for severe anemia. The degree of anemia in single-event fallers when compared with multiple-event fallers was insignificant. Interestingly, the degree of decline of Hgb value during the 6 months before the first fall event was notable for all fallers (Figure).
Only 60 of the 120 included patients had a documented vitamin D level. At the time of the fall, 46 patients had moderate vitamin D deficiency, and 23 patients had severe vitamin D deficiency, defined as < 32 mg/dL. The authors speculate that vitamin D status declines with malnutrition and increases fall risk.
Thirty participants were included in the dementia arm; 36.7% were single-event fallers, and 63.3% were multiple-event fallers (Table 2). The average age of the groups was 76.7 years and 73.9 years, respectively. Physician diagnosis of malnutrition was collected for both single- and multiple-event fallers. Of the single-event fallers with dementia, none had a diagnosis of malnutrition before the first hospital fall; and of the multiple-event fallers with dementia, all had a diagnosis of malnutrition before their first hospital fall. Individuals with a diagnosis of dementia and malnutrition fall frequently (P = .0028).
Discussion
In this study, falls occurred in a variety of patient populations. Both single-event fallers and recurrent fallers had a significant drop in Hgb values at 12, 6, and 3 months before the first fall. There was not a strong difference of the Hgb value between single-event falls and multiple fallers in the total population. Anemia was a significant risk factor for all fallers. The decline in the Hgb level before a fall is highly predictive of fall risk.
In individuals with dementia, those with the diagnosis of malnutrition are frequent fallers. A tool to assist in identification of this patient population along with a focused intervention strategy for this population is an area of needed research.
Further research is under way to determine which components of malnutrition diagnosis contribute to fall risk. If so, development of a fall assessment tool, including various components of malnutrition is warranted. Intervention strategies to reduce fall risk may soon include new nutrition and education techniques based on the faller constellation. Falls instruments that explore nutritional risk factors and falls should be investigated (ie, weight loss, vitamin D status, and anemia).
Falls occur in patients with a variety of risk factors (eg, mobility and cognition). The current screening instruments to assess fall risk factors do not sufficiently account for nutritional risk factors. In the Eat Well, Fall Less Study of hospitalized veterans, nutritional risk factors of anemia and weight loss also were associated with single- and multiple-event fallers. The AUTUMN falls instrument that includes critical elements of malnutrition, such as a decline in Hgb and weight loss, is currently being created and is in the process of being validated at LSCVAMC; this tool will incorporate components of malnutrition.
Acknowledgments
The authors acknowledge Michelle Pearson, Laura Guidotti, Adam Weier, Elizabeth Gable, and Shannon Corlett for their research contributions. In memory of Anne Raguso, RD, PhD, for her lifelong focus on nutrition research.
Falls often result in injuries with devastating outcomes. In the elderly, falls are the largest cause of injury, mortality, and functional decline, leading to 40% of nursing home admissions.1 Nationally, falls with injury are estimated to cost $19 billion in direct medical costs.2 According to the National Quality Forum (NQF), hospital falls resulting in injury are reportable events. Beginning in fiscal year 2015, reportable events labeled as hospital acquired conditions (HAC) are subject to nonpayment, creating increased regulatory and reimbursement pressure on hospitals.3
Due to the major impact of a fall, The Joint Commission (TJC) requires hospitals to assess a patient’s fall risk on admission and whenever the patient’s condition changes.4 Despite decades of research evaluating various predictive strategies to identify individuals at fall risk, nutritional issues as interactive risk factors have received little attention.
A comparative study on the validity of fall risk assessment scales revealed that tools claiming to predict risk factors do not work well.5 Falls are the result of multiple interactive, synergistic pathologies and risk factors. In a multivariate regression study conducted by Lichtenstein and colleagues in Canada, lower body weight was found to be a statistically significant risk factor for falling.6 In 2004, Oliver and colleagues conducted a systematic review of fall risk assessment tools that included validation testing with sufficient data to allow for calculation of sensitivity, specificity, negative and positive predictive values, odds ratios, and confidence intervals.5
Fourteen studies identified common fall risk factors. The majority of these studies identified impaired cognition as a risk factor.5 Of the 14 studies included in the systematic analysis of Oliver and colleagues,6-19 6 identified medications,6,8,11,12,17,18, and 8 noted weakness and unsteady gait as risk factors.6,9-11,14,16,18,19 Only 1 study noted anemia as a risk factor for falls among patients who were post cerebral vascular accident.11 Additionally, only 1 study noted an association between falls resulting in hip fracture and lower body weight.6
One in 4 adults admitted to a hospital is malnourished.20,21 Components of malnutrition, including but not limited to anemia, clinically significant weight loss, and vitamin D deficiency, may be unrecognized interactive risk factors that increase the risk of hospital falls. Malnutrition and dehydration symptoms include fatigue, dizziness, irritability, loss of muscle mass, impulsivity, and the potential for poor judgment. Therefore, it is likely that the severity of specific malnutrition parameters is associated with recurrent falls and possibly injurious falls.
Hunger and inadequate food intake due to chronic disease or chronic food insecurity are real issues for the elderly. Insufficient caloric intake often leads to slow, progressive, and often unnoticed weight loss. The Academy of Nutrition and Dietetics (AND) and the American Association of Parenteral and Enteral Nutrition (ASPEN) have defined clinically significant weight loss categories to aid in the diagnosis of malnutrition. To aid in the diagnosis of various degrees of malnutrition, clinically significant weight loss is classified as ≥ 5% weight loss in 30 days; ≥ 7.5% weight loss in 90 days; > 10% in 180 days.21 The World Health Organization (WHO) identifies iron deficiency measured by hemoglobin (Hgb) value (for men < 13 g/dL) as the most common and widespread nutritional disorder in the world (Tables 1a, 1b, and 1c).22
Eat Well, Fall Less is a retrospective chart review approved by the Louis Stokes Cleveland VAMC (LSCVAMC) Internal Review Board. The review seeks to determine whether degree of weight loss and decline in Hgb and vitamin D deficiency, factors of malnutrition, are present in recurrent fallers vs single-event fallers. Researchers hypothesized that individuals who experienced recurrent falls during hospitalization would demonstrate a greater degree of clinically significant weight loss compared with those who had experienced a single fall. The second hypothesis was that recurrent fallers also would have lower Hgb values than that of single-event fallers. The tertiary hypothesis was that individuals with a greater degree of vitamin D deficiency were more likely to be recurrent fallers compared with single-event fallers.
In addition, dementia has been previously identified as an independent risk factor for falls and recurrent falls.23 During phase 2 of the study, the researchers hypothesized that in individuals with dementia, the concurrent diagnosis of malnutrition would be greatest in the recurrent fall population. A total of 30 subjects were included in the analysis.
Methods
Patient record search of note titles for falls was compiled daily. A random sample of 170 veterans who had experienced a fall was screened for study inclusion. Of the 170 charts, data from a total of 120 veterans who experienced a documented fall during a hospitalization between October 1, 2010 and October 31, 2012, were included in this analysis.
Eligibility Criteria and Baseline Characteristics
Chart reviews of veterans aged > 18 years experiencing a fall while hospitalized at the LSCVAMC between October 1, 2010 and October 31, 2012, were eligible to be included in this study. Each veteran needed to have 1 documented weight in a maximum of 24 months before the first fall and a minimum of 1 documented Hgb value prior to the first fall.
Patients were excluded if they had experienced a cerebrovascular accident or transient ischemic attack; a documented orthopedic fracture in the 12 months before the first fall; a documented amputation of a lower limb in the past 24 months; diagnosis of blindness; a lack of outpatient weight for greater than 24 months before the first fall; a history of volume overload, renal, cardiovascular, or other in nature during hospitalization; and alcoholism. Additionally, if any of the study investigators felt as though a patient had commorientes that made weight history inaccurate, those patients were excluded. Data were reviewed on 170 randomly selected subjects. A total of 50 subjects were excluded for not meeting the inclusion criteria; 120 individuals met eligible criteria. The patients who had experienced falls were divided into 2 groups: single-event fallers (1 fall documented during the study period) and recurrent fallers (2 or more falls documented during the study period). Fifty subjects were excluded from the final analysis because they met the following exclusion criteria: volume overload anytime in the 12 months before the documented fall (42); amputation of a lower limb before the fall (6); and prosthetic device alteration within the 12 months before the fall (3). One of the subjects was eliminated for both volume overload and amputation.
Data Collection
Data obtained from the Computerized Patient Record System review included age, gender, diagnosis, and body weight at the time of the first fall and 1 month, 3 months, 6 months, and 1 year before the first fall. Hemoglobin values at time of the first fall, 1 month, 3 months, 6 months, and 1 year before first documented fall also were collected. Vitamin D values and date of value also were collected. In year 2 of this multiphase retrospective review, charts again were reviewed and additional data collected, which included absence or presence of dementia along with type of dementia and the presence or absence of cancer. Year 2 data collection also included diagnosis of malnutrition by provider and registered dietitian assessment of degree of malnutrition.
Analysis
Data analysis comparing single-event fallers and frequent fallers was performed using IBM SPSS Statistic V22.0s. This pilot study has recognized weight loss and anemia as being associated with repeat falls. A 2-tailed t test was performed to evaluate differences in weight history, 25-hydroxyvitamin D, and Hgb characteristics between single fallers and frequent fallers. A repeated analysis of variance was performed to evaluate changes in weight and Hgb values over time for single and multiple falls. During phase 2 of this trial, a subanalysis comparing individuals with and without the diagnosis of dementia was conducted.
Results
The average age of the patients was 68 years. There was a significant decline in Hgb levels in both single-event fallers and frequent fallers at 12 and 6 months before the first fall event (95% confidence interval; P = .001). One year before the first fall, 28% of eventual fallers met WHO criteria for the diagnosis of mild anemia. One year before the first fall, none of the eventual fallers met WHO criteria for moderate or severe anemia. Using the lab data just before the first fall, 10% of fallers met WHO criteria for mild anemia, 48% met WHO criteria for moderate anemia, and 31% met WHO criteria for severe anemia. The degree of anemia in single-event fallers when compared with multiple-event fallers was insignificant. Interestingly, the degree of decline of Hgb value during the 6 months before the first fall event was notable for all fallers (Figure).
Only 60 of the 120 included patients had a documented vitamin D level. At the time of the fall, 46 patients had moderate vitamin D deficiency, and 23 patients had severe vitamin D deficiency, defined as < 32 mg/dL. The authors speculate that vitamin D status declines with malnutrition and increases fall risk.
Thirty participants were included in the dementia arm; 36.7% were single-event fallers, and 63.3% were multiple-event fallers (Table 2). The average age of the groups was 76.7 years and 73.9 years, respectively. Physician diagnosis of malnutrition was collected for both single- and multiple-event fallers. Of the single-event fallers with dementia, none had a diagnosis of malnutrition before the first hospital fall; and of the multiple-event fallers with dementia, all had a diagnosis of malnutrition before their first hospital fall. Individuals with a diagnosis of dementia and malnutrition fall frequently (P = .0028).
Discussion
In this study, falls occurred in a variety of patient populations. Both single-event fallers and recurrent fallers had a significant drop in Hgb values at 12, 6, and 3 months before the first fall. There was not a strong difference of the Hgb value between single-event falls and multiple fallers in the total population. Anemia was a significant risk factor for all fallers. The decline in the Hgb level before a fall is highly predictive of fall risk.
In individuals with dementia, those with the diagnosis of malnutrition are frequent fallers. A tool to assist in identification of this patient population along with a focused intervention strategy for this population is an area of needed research.
Further research is under way to determine which components of malnutrition diagnosis contribute to fall risk. If so, development of a fall assessment tool, including various components of malnutrition is warranted. Intervention strategies to reduce fall risk may soon include new nutrition and education techniques based on the faller constellation. Falls instruments that explore nutritional risk factors and falls should be investigated (ie, weight loss, vitamin D status, and anemia).
Falls occur in patients with a variety of risk factors (eg, mobility and cognition). The current screening instruments to assess fall risk factors do not sufficiently account for nutritional risk factors. In the Eat Well, Fall Less Study of hospitalized veterans, nutritional risk factors of anemia and weight loss also were associated with single- and multiple-event fallers. The AUTUMN falls instrument that includes critical elements of malnutrition, such as a decline in Hgb and weight loss, is currently being created and is in the process of being validated at LSCVAMC; this tool will incorporate components of malnutrition.
Acknowledgments
The authors acknowledge Michelle Pearson, Laura Guidotti, Adam Weier, Elizabeth Gable, and Shannon Corlett for their research contributions. In memory of Anne Raguso, RD, PhD, for her lifelong focus on nutrition research.
1. Centers for Disease Control and Prevention. Older adult falls: important facts about falls. http://www.cdc.gov/homeandrecreationalsafety/falls/adultfalls.html. Updated September 20, 2016. Accessed December 2, 2016.
2. Centers for Disease Control and Prevention. Older adult falls: cost of falls among older adults. http://www.cdc.gov/HomeandRecreationalSafety/Falls/fallcost.html. Updated August 19, 2016. Accessed December 2, 2016.
3. National Quality Forum. Serious reportable events in healthcare—2011 update: a consensus report https://www.qualityforum.org/Publications/2011/12/SRE_2011_Final_Report.aspx. Published 2011. Accessed December 2, 2016.
4. DuPree E. Taking a stand against falls. https://www.jointcommission.org/jc_physician_blog/taking_a_stand_against_falls. Published May1, 2014. Accessed December 2, 2016.
5. Oliver D, Daly F, Martin FC, McMurdo ME. Risk factors and risk assessment tools for falls in hospital in-patients: a systematic review. Age Ageing. 2004;33(2):122-130.
6. Lichtenstein MJ, Griffin MR, Cornell JE, Malcolm E, Ray WA. Risk factors for hip fractures occurring in the hospital. Am J Epidemiol. 1994;140(9):830-838.
7. Ballinger BR, Ramsay AC. Accidents and drug treatment in a psychiatric hospital. Br J Psychiatry. 1975;126:462-463.
8. Bates D, Pruess K, Souney P, Platt R. Serious falls in hospitalized patients correlates and resource utilization. Am J Med. 1995;99(2):137-143.
9. Byers V, Arrington ME, Finstuen K. Predictive risk factors associated with stroke patient falls in acute care settings. J Neurosci Nurs. 1990;22(3):147-154.
10. Chu LW, Pei CK, Chiu A, et al. Risk factors for falls in hospitalized older medical patients. J Gerontol A Biol Sci Med Sci. 1999;54(1):M38-M48.
11. Gales BJ, Menard SM. Relationship between administration of selected medications and falls in hospitalized elderly patients. Ann Pharmacother. 1995;29(4):354-358.
12. Gluck T, Wientjes HJ, Rai GS. An evaluation of risk factors for inpatient falls in acute care and rehabilitation elderly care wards. Gerontology. 1996:42(2):104-107.
13. Janken J, Reynolds B. Patient falls in the acute care setting: identifying risk factors. Nurs Res.1986;35(4):215-219.
14. Morse JM, Tylko SJ, Dixon HA. Characteristics of the fall-prone patient. Gerontologist. 1987;27(4):516-522.
15. Oliver D, Britton M, Seed P, Martin FC, Hopper AH. Development and evaluation of an evidenced based risk assessment tool (STRATIFY) to predict which elderly outpatients will fall: case-control and cohort studies. BMJ. 1997;315(7115):1049-1053.
16. Passaro A, Volpato S. Benzodiazepenes with different half-life and falling in a hospitalized population: the GIFA study. Gruppo Italiano di Farmacovigilanza nell’Anziano. J Clin Epidemol. 2000;53(12):1222-1229.
17. Salgado R, Lord SR, Packer J, Ehrlich F. Factors associated with falling in elderly hospitalized inpatients. Gerentology. 1994;40(6):325-331.
18. Schmidt NA. 1989 federal nursing service award winner. reducing patient falls: a research-based comprehensive fall prevention program. Mil Med. 1990;155(5):202-207.
19. Sutton JC, Standon PJ, Wallace WA. Patient accidents in hospital: incidence, documentation and significance. Br J Clin Pract. 1994;48(2):63-66.
20. White JV, Guenter P, Jensen G, Malone A, Schofield M; Academy of Nutrition and Dietetics Malnutrition Work Group; A.S.P.E.N. Malnutrition Task Force; A.S.P.E.N. Board of Directors. Consensus statement of the Academy of Nutrition and Dietetics/American Society for Parental and Enteral Nutrition: characteristics recommended for the identification and documentation of adult malnutrition (undernutrition). J Acad Nutr Diet. 2012;112(5):730-738.
21. Russell C, Elia M. Nutrition screening survey in the UK in 2008: hospitals, care homes and mental health units. http://www.bapen.org.uk/pdfs/nsw/nsw_report2008-09.pdf. Published 2009. Accessed December 2, 2016.
22. Cansado P, Ravasco P, Camilo M. A longitudinal study of hospital undernutrition in the elderly: comparison of four validated methods. J Nutr Health Aging. 2009;13(2):159-164.
23. World Health Organization. Nutrition: micronutrient deficiencies. http://www.who.int/nutrition/topics/ida/en. Accessed December 2, 2016.
1. Centers for Disease Control and Prevention. Older adult falls: important facts about falls. http://www.cdc.gov/homeandrecreationalsafety/falls/adultfalls.html. Updated September 20, 2016. Accessed December 2, 2016.
2. Centers for Disease Control and Prevention. Older adult falls: cost of falls among older adults. http://www.cdc.gov/HomeandRecreationalSafety/Falls/fallcost.html. Updated August 19, 2016. Accessed December 2, 2016.
3. National Quality Forum. Serious reportable events in healthcare—2011 update: a consensus report https://www.qualityforum.org/Publications/2011/12/SRE_2011_Final_Report.aspx. Published 2011. Accessed December 2, 2016.
4. DuPree E. Taking a stand against falls. https://www.jointcommission.org/jc_physician_blog/taking_a_stand_against_falls. Published May1, 2014. Accessed December 2, 2016.
5. Oliver D, Daly F, Martin FC, McMurdo ME. Risk factors and risk assessment tools for falls in hospital in-patients: a systematic review. Age Ageing. 2004;33(2):122-130.
6. Lichtenstein MJ, Griffin MR, Cornell JE, Malcolm E, Ray WA. Risk factors for hip fractures occurring in the hospital. Am J Epidemiol. 1994;140(9):830-838.
7. Ballinger BR, Ramsay AC. Accidents and drug treatment in a psychiatric hospital. Br J Psychiatry. 1975;126:462-463.
8. Bates D, Pruess K, Souney P, Platt R. Serious falls in hospitalized patients correlates and resource utilization. Am J Med. 1995;99(2):137-143.
9. Byers V, Arrington ME, Finstuen K. Predictive risk factors associated with stroke patient falls in acute care settings. J Neurosci Nurs. 1990;22(3):147-154.
10. Chu LW, Pei CK, Chiu A, et al. Risk factors for falls in hospitalized older medical patients. J Gerontol A Biol Sci Med Sci. 1999;54(1):M38-M48.
11. Gales BJ, Menard SM. Relationship between administration of selected medications and falls in hospitalized elderly patients. Ann Pharmacother. 1995;29(4):354-358.
12. Gluck T, Wientjes HJ, Rai GS. An evaluation of risk factors for inpatient falls in acute care and rehabilitation elderly care wards. Gerontology. 1996:42(2):104-107.
13. Janken J, Reynolds B. Patient falls in the acute care setting: identifying risk factors. Nurs Res.1986;35(4):215-219.
14. Morse JM, Tylko SJ, Dixon HA. Characteristics of the fall-prone patient. Gerontologist. 1987;27(4):516-522.
15. Oliver D, Britton M, Seed P, Martin FC, Hopper AH. Development and evaluation of an evidenced based risk assessment tool (STRATIFY) to predict which elderly outpatients will fall: case-control and cohort studies. BMJ. 1997;315(7115):1049-1053.
16. Passaro A, Volpato S. Benzodiazepenes with different half-life and falling in a hospitalized population: the GIFA study. Gruppo Italiano di Farmacovigilanza nell’Anziano. J Clin Epidemol. 2000;53(12):1222-1229.
17. Salgado R, Lord SR, Packer J, Ehrlich F. Factors associated with falling in elderly hospitalized inpatients. Gerentology. 1994;40(6):325-331.
18. Schmidt NA. 1989 federal nursing service award winner. reducing patient falls: a research-based comprehensive fall prevention program. Mil Med. 1990;155(5):202-207.
19. Sutton JC, Standon PJ, Wallace WA. Patient accidents in hospital: incidence, documentation and significance. Br J Clin Pract. 1994;48(2):63-66.
20. White JV, Guenter P, Jensen G, Malone A, Schofield M; Academy of Nutrition and Dietetics Malnutrition Work Group; A.S.P.E.N. Malnutrition Task Force; A.S.P.E.N. Board of Directors. Consensus statement of the Academy of Nutrition and Dietetics/American Society for Parental and Enteral Nutrition: characteristics recommended for the identification and documentation of adult malnutrition (undernutrition). J Acad Nutr Diet. 2012;112(5):730-738.
21. Russell C, Elia M. Nutrition screening survey in the UK in 2008: hospitals, care homes and mental health units. http://www.bapen.org.uk/pdfs/nsw/nsw_report2008-09.pdf. Published 2009. Accessed December 2, 2016.
22. Cansado P, Ravasco P, Camilo M. A longitudinal study of hospital undernutrition in the elderly: comparison of four validated methods. J Nutr Health Aging. 2009;13(2):159-164.
23. World Health Organization. Nutrition: micronutrient deficiencies. http://www.who.int/nutrition/topics/ida/en. Accessed December 2, 2016.
Diabetes: Health Literacy Education Improves Veteran Outcomes
According to the National Academy of Medicine (NAM), health literacy is “the degree to which individuals have the capacity to obtain, process and understand basic health information and services needed to make appropriate health decisions.”1 Studies suggest that millions of patients have inadequate health literacy and cannot make fully informed decisions because of this lack of knowledge.2-4 A 2007 National Patient Safety Foundation report calculated that inadequate health literacy burdens the U.S. health care system with an additional $106 to $238 billion annually.5
In 2014, the American Diabetes Association reported that diabetes affects 29.1 million Americans (9.3%) and that by 2050 1 in 3 Americans will have diabetes.6 People with diabetes have health care costs 2.3 times higher than the cost for nondiabetic patients. The cost of taking care of patients with diabetes annually is about $245 billion.6 Without interventions that address health literacy and effective self-management to reduce the risks of complications and comorbidity, health care costs related to diabetes will continue to increase.
Literature Review
According to a U.S. Department of Education assessment on adult health literacy in 2003, 88% of adults in the U.S. have inadequate health literacy.2 About 90 million Americans lack health literacy skills, according to a 2004 NAM report.3 Heinrich, who conducted a review of U.S. studies on health literacy, concluded that about 25% of Americans have low health literacy.4
The Newest Vital Sign Tool
The Newest Vital Sign (NVS) tool is a free tool developed by Pfizer (New York, NY) for assessing health literacy. Participants are asked 6 questions about nutrition based on an ice cream nutrition label (Figure). The researcher records the participant’s responses, which accommodates participants who may have difficulty reading. The tool is scored from 0 to 6. A score of below 4 indicates the possibility of limited health literacy.7 This test can be completed in about 3 minutes, is widely accepted, and provides results comparable to more extensive literacy tests.8 A study conducted by Welch and colleagues suggested the NVS tool is both cost and time efficient.9 Ryan and colleagues found that 98% of patients in their study (n = 289) did not have objections to taking the NVS assessment.10
Escobedo and Weismuller’s study used the NVS health literacy tool to assess the health literacy of renal patients.3 In 2004, about 50,000 American patients with diabetes began treatment for kidney failure due to diabetes complications.6 Escobedo and Weismuller found that patients with diabetes with limited health literacy knowledge are more likely to be hospitalized, thus increasing health care costs.3 In addition, they discovered that these patients demonstrated poor adherence to prescribed treatment protocols. Welch, VanGeest, and Caskey conducted a case study on time, cost, and clinical utilization of the NVS health literacy tool and found that a patient’s lack of health literacy was linked to limited participation in personal medical decisions.7,9 Patient’s lack of knowledge was associated with delays in seeking treatment, poor self-management of the disease, and more hospital admissions.
Health Literacy and Diabetes
Studies specific to diabetes and inadequate health literacy support the premise that better health literacy leads to improved patient outcomes. Using the NVS tool, Heinrich conducted a study of the health literacy of 54 patients with diabetes in a primary care setting. The study showed that 65% had inadequate health literacy and that patients with diabetes with inadequate health literacy were more likely to have poor glycemic control compared with patients with diabetes and adequate health literacy levels.4 McCleary-Jones examined diet, foot care, and exercise of 50 African American participants with diabetes from a community health center, finding a positive relationship between health literacy and diabetes knowledge.11
Long and Gambling conducted a 2-year prospective, observational study that incorporated motivational interviewing and patient-centered care into a self-management program, examining the effectiveness of scheduled phone interventions to assist patients with diabetes in the management of their disease.12 The interventions used structured and consistent questions supported by a protocol and script that examined medication adherence and lifestyle choices. Long and Gambling concluded that “the findings demonstrate not only changes in the depth and detail of diabetes-related knowledge and confidence, but also enhanced competence in translating knowledge into every day self-care.”12 These researchers concluded that increased knowledge translated into better patient self-management of their disease. The Long and Gambling study included general self-management characteristics of monitoring HbA1c, diet, exercise, medication management, and general self-care. These researchers contend that diabetes self-management education must be a long-term endeavor to promote change.12
Mendoza and Rosenburg’s meta-analysis on self-management programs for diabetes and chronic conditions found a statistically significant 0.81% reduction in hemoglobin A1c (HbA1c). Characteristics of self-management programs that were linked to improved outcomes included nurse and provider education on medications, diet and/or exercise, and demonstrated use of motivational interviewing and biofeedback. Mendoza and Rosenburg suggested motivational interviewing focuses on the patient’s perspective and facilitates the process that the patient uses to assess their needs and to think about possible solutions.13 Mulimba and Bryo-Daniel found that motivational interviewing is a valuable tool for primary care nurses’ health promotion practice, and Thompson and colleagues found that it was effective in changing behavior.14,15
Nurse’s Role in Health Literacy
Nurses play a vital role in educating and securing adherence of patients in the management of their disease(s).13 In addition to educating patients, families, and friends of the family, nurses assist with helping them make informed decisions.16 The VHA uses the Specialty Care Access Network-Extension for Community Healthcare Outcomes (SCAN-ECHO) to teach health care staff about diabetes self-management education (DSME). Tisdel and colleagues found that DSME established through telemedicine or clinical mentoring improved patient outcomes.17 Mendoza and Rosenburgfound nurse-led DSME was linked to minimizing cardiovascular risk factors and improvements in HbA1c.13
Background
Staunton Community Based Outpatient Clinic (CBOC) in rural Virginia is a primary care clinic that serves veterans in the surrounding area. About one-fourth of the Staunton patients have diabetes. According to June 2014 data from the VHA Support Service Center, the physician at the Staunton CBOC was responsible for 946 patients (225 with diabetes) and the nurse practitioner was responsible for 707 (184 with diabetes). The VHA Support Service Center 2014 data indicated that veterans with poorly self-managed diabetes were at increased risk for poor outcomes, such as kidney failure, cardiovascular disease, and limb amputation. Veterans with diabetes use the emergency department more often and are admitted to the hospital more often than are veterans who do not have diabetes.18
Methods
The primary objective of this pilot study was to explore whether weekly structured nursing education sessions lasting 45 minutes and subsequent follow-up weekly conferences would improve their HbA1c for veterans identified as having ≥ 9 HbA1c and ≤ 3 health literacy score on the NVS 7 study assessment. Most recent HbA1c prior to beginning the study was used to identify potential participants. After completion of 12 weekly education interventions, an additional HbA1c was obtained.
The Salem VAMC and Eastern Mennonite University Institutional Review Board approved the study. Veterans’ questions were answered prior to signing consent forms. All data collected were kept confidential.
Veterans with ≥ 9 HbA1c were evaluated for possible participation. Forty-nine veterans met the criteria to participate in this pilot study. Exclusion criteria included diagnosis of any cognitive disorder, such as dementia, Alzheimer disease, or memory impairment. In addition, veterans unwilling or unable to commit to weekly follow-up sessions were excluded. The veterans eligible for participation were contacted by telephone, and 9 agreed to participate in the pilot study. Inclusion criteria included those aged ≥ 18 years and a diagnosis of diabetes with most recent HbA1c of ≥ 9 and a score of < 4 on the NVS health literacy assessment. After taking the NVS health literacy assessment, 6 of the 9 participants qualified to continue in the study.
Education interventions included assessing medication adherence, discussing diet, reviewing physical activity for the previous week (based on diet and activity logs), and reviewing home blood glucose monitoring. Weekly education sessions were either face-to-face or by telephone. This choice was given to accommodate veterans who may have had transportation issues. A total of 12 weekly appointments were scheduled for each participant, and education was directed at the specific needs and goals of each participant. Interventions for education were based on those found in previous studies.13,14,18,19
Data Collection and Analysis
All 6 participants were white male veterans who were diagnosed with diabetes for at least 3 years. Their ages ranged from 59 to 72. Three participants were service connected for diabetes and 3 were not. One participant dropped from the study after completing 4 appointments, stating he was just too busy to be available for a weekly appointment. Another participant completed 6 appointments and removed himself from the study due to time constraints. The 4 participants who completed the pilot study were followed for 12 weeks by a registered nurse (RN), and all had reductions in their HbA1c.
Participants were assessed at weekly appointments using a predetermined template for medication adherence, diet, activity, and blood glucose monitoring. Responses of the participants guided the education interventions to meet the individual veteran’s learning needs. For example, one veteran was given specific education on carbohydrate counting and another was educated on how to read food labels. Participants were also encouraged to express satisfaction, frustration, anger, or other emotions in managing their chronic illness. The premise for spending additional time with the veteran was to promote positive self-management behaviors as recommended by Radhakrishnan.19
Veterans who completed the study stated that the education interventions positively impacted their health status. One veteran was able to delay dialysis due to self-directed improvement in his lifestyle (exercising and watching his diet), which improved his HbA1c. This veteran attributed his health improvement to the individualized education sessions with the RN and knowing he had to be accountable to someone. Additionally, it was found there was a strong familial-social component to diabetes self-management. Several veterans were knowledgeable about diabetes self-management as evidenced by their responses to weekly questions. However, disease management for these veterans was strongly impacted by family and life events.
One veteran did not manage his disease for an entire week due to “being busy with a death in the family and planning for a wedding.” This veteran took his medication but did not check his blood glucose or monitor his diet. Another veteran spoke of eating ice cream and other concentrated sweets because his young grandson was with him for the week. A third veteran was able to manage his diet better when his wife packed snacks for him but when left to his own accord did not do well with his food selection. Even though these veterans understood how to effectively manage their diabetes, they may have chosen to inconsistently translate that knowledge into practice if they perceive those familial-social forces to be more important or more powerful.
Discussion
The findings from this small pilot study from a single clinic cannot be generalized. However, this pilot study adds to the literature of the positive impact of individualized, structured, tailored nursing interventions delivered with careful consideration of the participants’ personal goals and health care needs for diabetes self-management.
Participants monitored home blood glucose levels, diet, and activity and maintained adherence with prescribed diabetes medications. The HbA1c level for participants decreased by the end of the program. During the course of the pilot study a pharmacist managed the veterans’ medications. Participant 1 began a new medication regimen the first day of the study. Previously, the patient was self-regulating his medication. However, during the 12-week study, he had no medication adjustments. Participant 4 had several increases to his insulin dose (insulin aspart protamine and insulin aspart rdna origin) during the course of the study. Participants 5 and 6 had no medication adjustments during the study.
Even though participants had medication adjustments, which contributed to the HbA1c decrease, they became more aware of the medical need to control their blood sugar through the one-on-one education provided. Although there was variation in the depth and detail that participants maintained their food/activity log and home blood glucose monitoring, all participants agreed that they were more likely to be adherent with prescribed self-monitoring “knowing they were going to have to report self-monitoring information” to the RN.
Health care professionals may not realize the impact of familial-social events on blood glucose control. Veterans in this study found that having weekly sessions with the RN helped them through such events, even though they did not adhere strictly to their regimen. One suggestion is having veterans anticipate future familial-social events that may trigger nonadherence to their diabetes health plan and then discuss those events with the health care professional.
Future Research
This small exploratory pilot study has implications for future research. Increasing the study’s sample size and using a control group is recommended to compare veterans who have an educational intervention with those that do not and the impact it has on blood glucose control. The study was limited to 1 CBOC. Incorporating additional CBOCs could increase the sample size. Additionally, although this study was only 3 months in duration, a longer study could reveal significant patterns of change over time as well as the long-term benefit of a tailored educational intervention. In addition, adjusting the study inclusion criteria of > 9 HbA1c to include those with > 8 HbA1c also may increase the sample size.
Limited financial resources for the study could have negatively impacted the sample size. Incorporating recruitment or advertising strategy may increase the number of participants. Research also is needed on education interventions with a diverse group of male and female veterans that extends beyond 3 months. Exploring the value of including the veteran’s family in the education sessions is needed. Finally, this study examined only diabetes education. Researchers need to consider other diseases and the value of individualized education.
Limitations
Limitations included a small sample size and no control group. Due to the study’s small sample size, extrapolating data from it becomes difficult. However, this pilot study sets the groundwork for other researchers to expand the importance of education interventions and health literacy. Recruitment was challenging since an eligibility criterion was the NVS score, and patients were sometimes difficult to contact.7 The pilot study started with 6 white male participants but only 4 finished. During the course of the pilot study, 1 veteran had medication adjustments as part of routine care and 1 veteran had medication adjustments prior to the study, which could have altered the HbA1c results.
In hindsight, using the NVS to assess both prestudy with poststudy health literacy scores would have provided additional information about the education intervention. There is possible bias because the researcher was a VAMC employee, and the RN that implemented the interventions had previously worked with the patients.
Conclusion
Although this is a small descriptive pilot study, it adds to the body of research on the value of nurse-driven interventions to help veterans manage diabetes by enhancing their health literacy. It also raises questions and opportunities for further research into the power of familial-social influences on a veteran’s willingness to manage their diabetes. The majority of veterans who declined to participate in this study, even though they qualified, stated that they would “not follow any recommendations.” Further investigation is needed about why some veterans elect not to obtain help that could positively impact their health and possibly extend their life. Additionally, scientific quantitative and qualitative research is needed to evaluate the statistical significance between health care literacy and educational intervention on patient adherence among individuals diagnosed with diabetes.
1. Stiles E. Promoting health literacy in patients with diabetes. Nurs Stand. 2011;26(8):35-40.
2. Baum NH, Dowling RA. Health literacy: how do your patients rate? http://urologytimes.modernmedicine.com/urology-times/news/modernmedicine/modern-medicine-now/health-literacy-how-do-your-patients-rate. Published August 1, 2011. Accessed December 2, 2016.
3. Escobedo W, Weismuller P. Assessing health literacy in renal failure and kidney transplant patients. Prog Transplant. 2013;23(1):47-54.
4. Heinrich C. Health literacy: the sixth vital sign. J Am Acad Nurse Pract. 2012;24(4):218-223.
5. Roett MA, Wessel L. Help your patient “get” what you just said: health literacy guide. J Fam Pract. 2012;61(4):190-196.
6. American Diabetes Association. Statistics about diabetes. http://www.diabetes.org/diabetes-basics/statistics/?loc=feat1.Updated December 12, 2016. Accessed December 14, 2016.
7. Pfizer. The newest vital sign. http://www.pfizer.com/files/health/nvs_flipbook_english_final.pdf. Published February 2011. Accessed December 2, 2016.
8. Shah LC, West P, Bremmeyr K, Savoy-Moore RT. Health literacy instrument in family medicine: the “newest vital sign” ease of use and correlates. J Am Board Fam Med. 2010;23(2):195-203.
9. Welch VL, VanGeest JB, Caskey R. Time, costs, and clinical utilization of screening for health literacy: a case study using the Newest Vital Sign (NVS) instrument. J Am Board Fam Med. 2011;24(3):281-289.
10. Ryan JG, Leguen F, Weiss BD, et al. Will patients agree to have their literacy skills assessed in clinical practice? Health Educ Res. 2008;23(4):603-611.
11. McCleary-Jones V. Health literacy and its association with diabetes knowledge, self-efficacy and disease self-management among African Americans with diabetes mellitus. ABNF J. 2011;22(2):25-32.
12. Long AF, Gambling T. Enhancing health literacy and behavioral change within a tele-care education and support intervention for people with type 2 diabetes. Health Expect. 2012;15(3):267-282.
13. Mendoza M, Rosenberg T. Self-management of type 2 diabetes: A good idea-or not? J Fam Pract. 2013;62(5):244-248.
14. A Clifford Mulimba A, Byron-Daniel J. Motivational interviewing-based interventions and diabetes mellitus. Br J Nurs. 2014;23(1):8-14.
15. Thompson DR, Chair SY, Chan SW, Astin F, Davidson PM, Ski CF. Motivational interviewing: a useful approach to improving cardiovascular health? J Clin Nurs. 2011;20;(9-10):1236-1244.
16. Protheroe J, Rowlands G. Matching clinical information with levels of patient health literacy. Nurs Manag (Harrow). 2013;20(3):20-21.
17. Tisdel KA, Bedwell M, Tarkington PE, Mundy A, Fredrickson SK. Diabetes specialists share experience remotely with RN care managers. Fed Pract. 2013;30(suppl 7):15S-20S.
18. U.S. Department of Veterans Affairs, Veterans Health Administration Support Service Center. http://vssc.med.va.gov/AlphaIndex.asp?Ltr=D.
19. Radhakrishnan K. The efficacy of tailored interventions for self-management outcomes of type 2 diabetes, hypertension, or heart disease: a systemic review. J Adv Nurs. 2012;68(3):496-510.
According to the National Academy of Medicine (NAM), health literacy is “the degree to which individuals have the capacity to obtain, process and understand basic health information and services needed to make appropriate health decisions.”1 Studies suggest that millions of patients have inadequate health literacy and cannot make fully informed decisions because of this lack of knowledge.2-4 A 2007 National Patient Safety Foundation report calculated that inadequate health literacy burdens the U.S. health care system with an additional $106 to $238 billion annually.5
In 2014, the American Diabetes Association reported that diabetes affects 29.1 million Americans (9.3%) and that by 2050 1 in 3 Americans will have diabetes.6 People with diabetes have health care costs 2.3 times higher than the cost for nondiabetic patients. The cost of taking care of patients with diabetes annually is about $245 billion.6 Without interventions that address health literacy and effective self-management to reduce the risks of complications and comorbidity, health care costs related to diabetes will continue to increase.
Literature Review
According to a U.S. Department of Education assessment on adult health literacy in 2003, 88% of adults in the U.S. have inadequate health literacy.2 About 90 million Americans lack health literacy skills, according to a 2004 NAM report.3 Heinrich, who conducted a review of U.S. studies on health literacy, concluded that about 25% of Americans have low health literacy.4
The Newest Vital Sign Tool
The Newest Vital Sign (NVS) tool is a free tool developed by Pfizer (New York, NY) for assessing health literacy. Participants are asked 6 questions about nutrition based on an ice cream nutrition label (Figure). The researcher records the participant’s responses, which accommodates participants who may have difficulty reading. The tool is scored from 0 to 6. A score of below 4 indicates the possibility of limited health literacy.7 This test can be completed in about 3 minutes, is widely accepted, and provides results comparable to more extensive literacy tests.8 A study conducted by Welch and colleagues suggested the NVS tool is both cost and time efficient.9 Ryan and colleagues found that 98% of patients in their study (n = 289) did not have objections to taking the NVS assessment.10
Escobedo and Weismuller’s study used the NVS health literacy tool to assess the health literacy of renal patients.3 In 2004, about 50,000 American patients with diabetes began treatment for kidney failure due to diabetes complications.6 Escobedo and Weismuller found that patients with diabetes with limited health literacy knowledge are more likely to be hospitalized, thus increasing health care costs.3 In addition, they discovered that these patients demonstrated poor adherence to prescribed treatment protocols. Welch, VanGeest, and Caskey conducted a case study on time, cost, and clinical utilization of the NVS health literacy tool and found that a patient’s lack of health literacy was linked to limited participation in personal medical decisions.7,9 Patient’s lack of knowledge was associated with delays in seeking treatment, poor self-management of the disease, and more hospital admissions.
Health Literacy and Diabetes
Studies specific to diabetes and inadequate health literacy support the premise that better health literacy leads to improved patient outcomes. Using the NVS tool, Heinrich conducted a study of the health literacy of 54 patients with diabetes in a primary care setting. The study showed that 65% had inadequate health literacy and that patients with diabetes with inadequate health literacy were more likely to have poor glycemic control compared with patients with diabetes and adequate health literacy levels.4 McCleary-Jones examined diet, foot care, and exercise of 50 African American participants with diabetes from a community health center, finding a positive relationship between health literacy and diabetes knowledge.11
Long and Gambling conducted a 2-year prospective, observational study that incorporated motivational interviewing and patient-centered care into a self-management program, examining the effectiveness of scheduled phone interventions to assist patients with diabetes in the management of their disease.12 The interventions used structured and consistent questions supported by a protocol and script that examined medication adherence and lifestyle choices. Long and Gambling concluded that “the findings demonstrate not only changes in the depth and detail of diabetes-related knowledge and confidence, but also enhanced competence in translating knowledge into every day self-care.”12 These researchers concluded that increased knowledge translated into better patient self-management of their disease. The Long and Gambling study included general self-management characteristics of monitoring HbA1c, diet, exercise, medication management, and general self-care. These researchers contend that diabetes self-management education must be a long-term endeavor to promote change.12
Mendoza and Rosenburg’s meta-analysis on self-management programs for diabetes and chronic conditions found a statistically significant 0.81% reduction in hemoglobin A1c (HbA1c). Characteristics of self-management programs that were linked to improved outcomes included nurse and provider education on medications, diet and/or exercise, and demonstrated use of motivational interviewing and biofeedback. Mendoza and Rosenburg suggested motivational interviewing focuses on the patient’s perspective and facilitates the process that the patient uses to assess their needs and to think about possible solutions.13 Mulimba and Bryo-Daniel found that motivational interviewing is a valuable tool for primary care nurses’ health promotion practice, and Thompson and colleagues found that it was effective in changing behavior.14,15
Nurse’s Role in Health Literacy
Nurses play a vital role in educating and securing adherence of patients in the management of their disease(s).13 In addition to educating patients, families, and friends of the family, nurses assist with helping them make informed decisions.16 The VHA uses the Specialty Care Access Network-Extension for Community Healthcare Outcomes (SCAN-ECHO) to teach health care staff about diabetes self-management education (DSME). Tisdel and colleagues found that DSME established through telemedicine or clinical mentoring improved patient outcomes.17 Mendoza and Rosenburgfound nurse-led DSME was linked to minimizing cardiovascular risk factors and improvements in HbA1c.13
Background
Staunton Community Based Outpatient Clinic (CBOC) in rural Virginia is a primary care clinic that serves veterans in the surrounding area. About one-fourth of the Staunton patients have diabetes. According to June 2014 data from the VHA Support Service Center, the physician at the Staunton CBOC was responsible for 946 patients (225 with diabetes) and the nurse practitioner was responsible for 707 (184 with diabetes). The VHA Support Service Center 2014 data indicated that veterans with poorly self-managed diabetes were at increased risk for poor outcomes, such as kidney failure, cardiovascular disease, and limb amputation. Veterans with diabetes use the emergency department more often and are admitted to the hospital more often than are veterans who do not have diabetes.18
Methods
The primary objective of this pilot study was to explore whether weekly structured nursing education sessions lasting 45 minutes and subsequent follow-up weekly conferences would improve their HbA1c for veterans identified as having ≥ 9 HbA1c and ≤ 3 health literacy score on the NVS 7 study assessment. Most recent HbA1c prior to beginning the study was used to identify potential participants. After completion of 12 weekly education interventions, an additional HbA1c was obtained.
The Salem VAMC and Eastern Mennonite University Institutional Review Board approved the study. Veterans’ questions were answered prior to signing consent forms. All data collected were kept confidential.
Veterans with ≥ 9 HbA1c were evaluated for possible participation. Forty-nine veterans met the criteria to participate in this pilot study. Exclusion criteria included diagnosis of any cognitive disorder, such as dementia, Alzheimer disease, or memory impairment. In addition, veterans unwilling or unable to commit to weekly follow-up sessions were excluded. The veterans eligible for participation were contacted by telephone, and 9 agreed to participate in the pilot study. Inclusion criteria included those aged ≥ 18 years and a diagnosis of diabetes with most recent HbA1c of ≥ 9 and a score of < 4 on the NVS health literacy assessment. After taking the NVS health literacy assessment, 6 of the 9 participants qualified to continue in the study.
Education interventions included assessing medication adherence, discussing diet, reviewing physical activity for the previous week (based on diet and activity logs), and reviewing home blood glucose monitoring. Weekly education sessions were either face-to-face or by telephone. This choice was given to accommodate veterans who may have had transportation issues. A total of 12 weekly appointments were scheduled for each participant, and education was directed at the specific needs and goals of each participant. Interventions for education were based on those found in previous studies.13,14,18,19
Data Collection and Analysis
All 6 participants were white male veterans who were diagnosed with diabetes for at least 3 years. Their ages ranged from 59 to 72. Three participants were service connected for diabetes and 3 were not. One participant dropped from the study after completing 4 appointments, stating he was just too busy to be available for a weekly appointment. Another participant completed 6 appointments and removed himself from the study due to time constraints. The 4 participants who completed the pilot study were followed for 12 weeks by a registered nurse (RN), and all had reductions in their HbA1c.
Participants were assessed at weekly appointments using a predetermined template for medication adherence, diet, activity, and blood glucose monitoring. Responses of the participants guided the education interventions to meet the individual veteran’s learning needs. For example, one veteran was given specific education on carbohydrate counting and another was educated on how to read food labels. Participants were also encouraged to express satisfaction, frustration, anger, or other emotions in managing their chronic illness. The premise for spending additional time with the veteran was to promote positive self-management behaviors as recommended by Radhakrishnan.19
Veterans who completed the study stated that the education interventions positively impacted their health status. One veteran was able to delay dialysis due to self-directed improvement in his lifestyle (exercising and watching his diet), which improved his HbA1c. This veteran attributed his health improvement to the individualized education sessions with the RN and knowing he had to be accountable to someone. Additionally, it was found there was a strong familial-social component to diabetes self-management. Several veterans were knowledgeable about diabetes self-management as evidenced by their responses to weekly questions. However, disease management for these veterans was strongly impacted by family and life events.
One veteran did not manage his disease for an entire week due to “being busy with a death in the family and planning for a wedding.” This veteran took his medication but did not check his blood glucose or monitor his diet. Another veteran spoke of eating ice cream and other concentrated sweets because his young grandson was with him for the week. A third veteran was able to manage his diet better when his wife packed snacks for him but when left to his own accord did not do well with his food selection. Even though these veterans understood how to effectively manage their diabetes, they may have chosen to inconsistently translate that knowledge into practice if they perceive those familial-social forces to be more important or more powerful.
Discussion
The findings from this small pilot study from a single clinic cannot be generalized. However, this pilot study adds to the literature of the positive impact of individualized, structured, tailored nursing interventions delivered with careful consideration of the participants’ personal goals and health care needs for diabetes self-management.
Participants monitored home blood glucose levels, diet, and activity and maintained adherence with prescribed diabetes medications. The HbA1c level for participants decreased by the end of the program. During the course of the pilot study a pharmacist managed the veterans’ medications. Participant 1 began a new medication regimen the first day of the study. Previously, the patient was self-regulating his medication. However, during the 12-week study, he had no medication adjustments. Participant 4 had several increases to his insulin dose (insulin aspart protamine and insulin aspart rdna origin) during the course of the study. Participants 5 and 6 had no medication adjustments during the study.
Even though participants had medication adjustments, which contributed to the HbA1c decrease, they became more aware of the medical need to control their blood sugar through the one-on-one education provided. Although there was variation in the depth and detail that participants maintained their food/activity log and home blood glucose monitoring, all participants agreed that they were more likely to be adherent with prescribed self-monitoring “knowing they were going to have to report self-monitoring information” to the RN.
Health care professionals may not realize the impact of familial-social events on blood glucose control. Veterans in this study found that having weekly sessions with the RN helped them through such events, even though they did not adhere strictly to their regimen. One suggestion is having veterans anticipate future familial-social events that may trigger nonadherence to their diabetes health plan and then discuss those events with the health care professional.
Future Research
This small exploratory pilot study has implications for future research. Increasing the study’s sample size and using a control group is recommended to compare veterans who have an educational intervention with those that do not and the impact it has on blood glucose control. The study was limited to 1 CBOC. Incorporating additional CBOCs could increase the sample size. Additionally, although this study was only 3 months in duration, a longer study could reveal significant patterns of change over time as well as the long-term benefit of a tailored educational intervention. In addition, adjusting the study inclusion criteria of > 9 HbA1c to include those with > 8 HbA1c also may increase the sample size.
Limited financial resources for the study could have negatively impacted the sample size. Incorporating recruitment or advertising strategy may increase the number of participants. Research also is needed on education interventions with a diverse group of male and female veterans that extends beyond 3 months. Exploring the value of including the veteran’s family in the education sessions is needed. Finally, this study examined only diabetes education. Researchers need to consider other diseases and the value of individualized education.
Limitations
Limitations included a small sample size and no control group. Due to the study’s small sample size, extrapolating data from it becomes difficult. However, this pilot study sets the groundwork for other researchers to expand the importance of education interventions and health literacy. Recruitment was challenging since an eligibility criterion was the NVS score, and patients were sometimes difficult to contact.7 The pilot study started with 6 white male participants but only 4 finished. During the course of the pilot study, 1 veteran had medication adjustments as part of routine care and 1 veteran had medication adjustments prior to the study, which could have altered the HbA1c results.
In hindsight, using the NVS to assess both prestudy with poststudy health literacy scores would have provided additional information about the education intervention. There is possible bias because the researcher was a VAMC employee, and the RN that implemented the interventions had previously worked with the patients.
Conclusion
Although this is a small descriptive pilot study, it adds to the body of research on the value of nurse-driven interventions to help veterans manage diabetes by enhancing their health literacy. It also raises questions and opportunities for further research into the power of familial-social influences on a veteran’s willingness to manage their diabetes. The majority of veterans who declined to participate in this study, even though they qualified, stated that they would “not follow any recommendations.” Further investigation is needed about why some veterans elect not to obtain help that could positively impact their health and possibly extend their life. Additionally, scientific quantitative and qualitative research is needed to evaluate the statistical significance between health care literacy and educational intervention on patient adherence among individuals diagnosed with diabetes.
According to the National Academy of Medicine (NAM), health literacy is “the degree to which individuals have the capacity to obtain, process and understand basic health information and services needed to make appropriate health decisions.”1 Studies suggest that millions of patients have inadequate health literacy and cannot make fully informed decisions because of this lack of knowledge.2-4 A 2007 National Patient Safety Foundation report calculated that inadequate health literacy burdens the U.S. health care system with an additional $106 to $238 billion annually.5
In 2014, the American Diabetes Association reported that diabetes affects 29.1 million Americans (9.3%) and that by 2050 1 in 3 Americans will have diabetes.6 People with diabetes have health care costs 2.3 times higher than the cost for nondiabetic patients. The cost of taking care of patients with diabetes annually is about $245 billion.6 Without interventions that address health literacy and effective self-management to reduce the risks of complications and comorbidity, health care costs related to diabetes will continue to increase.
Literature Review
According to a U.S. Department of Education assessment on adult health literacy in 2003, 88% of adults in the U.S. have inadequate health literacy.2 About 90 million Americans lack health literacy skills, according to a 2004 NAM report.3 Heinrich, who conducted a review of U.S. studies on health literacy, concluded that about 25% of Americans have low health literacy.4
The Newest Vital Sign Tool
The Newest Vital Sign (NVS) tool is a free tool developed by Pfizer (New York, NY) for assessing health literacy. Participants are asked 6 questions about nutrition based on an ice cream nutrition label (Figure). The researcher records the participant’s responses, which accommodates participants who may have difficulty reading. The tool is scored from 0 to 6. A score of below 4 indicates the possibility of limited health literacy.7 This test can be completed in about 3 minutes, is widely accepted, and provides results comparable to more extensive literacy tests.8 A study conducted by Welch and colleagues suggested the NVS tool is both cost and time efficient.9 Ryan and colleagues found that 98% of patients in their study (n = 289) did not have objections to taking the NVS assessment.10
Escobedo and Weismuller’s study used the NVS health literacy tool to assess the health literacy of renal patients.3 In 2004, about 50,000 American patients with diabetes began treatment for kidney failure due to diabetes complications.6 Escobedo and Weismuller found that patients with diabetes with limited health literacy knowledge are more likely to be hospitalized, thus increasing health care costs.3 In addition, they discovered that these patients demonstrated poor adherence to prescribed treatment protocols. Welch, VanGeest, and Caskey conducted a case study on time, cost, and clinical utilization of the NVS health literacy tool and found that a patient’s lack of health literacy was linked to limited participation in personal medical decisions.7,9 Patient’s lack of knowledge was associated with delays in seeking treatment, poor self-management of the disease, and more hospital admissions.
Health Literacy and Diabetes
Studies specific to diabetes and inadequate health literacy support the premise that better health literacy leads to improved patient outcomes. Using the NVS tool, Heinrich conducted a study of the health literacy of 54 patients with diabetes in a primary care setting. The study showed that 65% had inadequate health literacy and that patients with diabetes with inadequate health literacy were more likely to have poor glycemic control compared with patients with diabetes and adequate health literacy levels.4 McCleary-Jones examined diet, foot care, and exercise of 50 African American participants with diabetes from a community health center, finding a positive relationship between health literacy and diabetes knowledge.11
Long and Gambling conducted a 2-year prospective, observational study that incorporated motivational interviewing and patient-centered care into a self-management program, examining the effectiveness of scheduled phone interventions to assist patients with diabetes in the management of their disease.12 The interventions used structured and consistent questions supported by a protocol and script that examined medication adherence and lifestyle choices. Long and Gambling concluded that “the findings demonstrate not only changes in the depth and detail of diabetes-related knowledge and confidence, but also enhanced competence in translating knowledge into every day self-care.”12 These researchers concluded that increased knowledge translated into better patient self-management of their disease. The Long and Gambling study included general self-management characteristics of monitoring HbA1c, diet, exercise, medication management, and general self-care. These researchers contend that diabetes self-management education must be a long-term endeavor to promote change.12
Mendoza and Rosenburg’s meta-analysis on self-management programs for diabetes and chronic conditions found a statistically significant 0.81% reduction in hemoglobin A1c (HbA1c). Characteristics of self-management programs that were linked to improved outcomes included nurse and provider education on medications, diet and/or exercise, and demonstrated use of motivational interviewing and biofeedback. Mendoza and Rosenburg suggested motivational interviewing focuses on the patient’s perspective and facilitates the process that the patient uses to assess their needs and to think about possible solutions.13 Mulimba and Bryo-Daniel found that motivational interviewing is a valuable tool for primary care nurses’ health promotion practice, and Thompson and colleagues found that it was effective in changing behavior.14,15
Nurse’s Role in Health Literacy
Nurses play a vital role in educating and securing adherence of patients in the management of their disease(s).13 In addition to educating patients, families, and friends of the family, nurses assist with helping them make informed decisions.16 The VHA uses the Specialty Care Access Network-Extension for Community Healthcare Outcomes (SCAN-ECHO) to teach health care staff about diabetes self-management education (DSME). Tisdel and colleagues found that DSME established through telemedicine or clinical mentoring improved patient outcomes.17 Mendoza and Rosenburgfound nurse-led DSME was linked to minimizing cardiovascular risk factors and improvements in HbA1c.13
Background
Staunton Community Based Outpatient Clinic (CBOC) in rural Virginia is a primary care clinic that serves veterans in the surrounding area. About one-fourth of the Staunton patients have diabetes. According to June 2014 data from the VHA Support Service Center, the physician at the Staunton CBOC was responsible for 946 patients (225 with diabetes) and the nurse practitioner was responsible for 707 (184 with diabetes). The VHA Support Service Center 2014 data indicated that veterans with poorly self-managed diabetes were at increased risk for poor outcomes, such as kidney failure, cardiovascular disease, and limb amputation. Veterans with diabetes use the emergency department more often and are admitted to the hospital more often than are veterans who do not have diabetes.18
Methods
The primary objective of this pilot study was to explore whether weekly structured nursing education sessions lasting 45 minutes and subsequent follow-up weekly conferences would improve their HbA1c for veterans identified as having ≥ 9 HbA1c and ≤ 3 health literacy score on the NVS 7 study assessment. Most recent HbA1c prior to beginning the study was used to identify potential participants. After completion of 12 weekly education interventions, an additional HbA1c was obtained.
The Salem VAMC and Eastern Mennonite University Institutional Review Board approved the study. Veterans’ questions were answered prior to signing consent forms. All data collected were kept confidential.
Veterans with ≥ 9 HbA1c were evaluated for possible participation. Forty-nine veterans met the criteria to participate in this pilot study. Exclusion criteria included diagnosis of any cognitive disorder, such as dementia, Alzheimer disease, or memory impairment. In addition, veterans unwilling or unable to commit to weekly follow-up sessions were excluded. The veterans eligible for participation were contacted by telephone, and 9 agreed to participate in the pilot study. Inclusion criteria included those aged ≥ 18 years and a diagnosis of diabetes with most recent HbA1c of ≥ 9 and a score of < 4 on the NVS health literacy assessment. After taking the NVS health literacy assessment, 6 of the 9 participants qualified to continue in the study.
Education interventions included assessing medication adherence, discussing diet, reviewing physical activity for the previous week (based on diet and activity logs), and reviewing home blood glucose monitoring. Weekly education sessions were either face-to-face or by telephone. This choice was given to accommodate veterans who may have had transportation issues. A total of 12 weekly appointments were scheduled for each participant, and education was directed at the specific needs and goals of each participant. Interventions for education were based on those found in previous studies.13,14,18,19
Data Collection and Analysis
All 6 participants were white male veterans who were diagnosed with diabetes for at least 3 years. Their ages ranged from 59 to 72. Three participants were service connected for diabetes and 3 were not. One participant dropped from the study after completing 4 appointments, stating he was just too busy to be available for a weekly appointment. Another participant completed 6 appointments and removed himself from the study due to time constraints. The 4 participants who completed the pilot study were followed for 12 weeks by a registered nurse (RN), and all had reductions in their HbA1c.
Participants were assessed at weekly appointments using a predetermined template for medication adherence, diet, activity, and blood glucose monitoring. Responses of the participants guided the education interventions to meet the individual veteran’s learning needs. For example, one veteran was given specific education on carbohydrate counting and another was educated on how to read food labels. Participants were also encouraged to express satisfaction, frustration, anger, or other emotions in managing their chronic illness. The premise for spending additional time with the veteran was to promote positive self-management behaviors as recommended by Radhakrishnan.19
Veterans who completed the study stated that the education interventions positively impacted their health status. One veteran was able to delay dialysis due to self-directed improvement in his lifestyle (exercising and watching his diet), which improved his HbA1c. This veteran attributed his health improvement to the individualized education sessions with the RN and knowing he had to be accountable to someone. Additionally, it was found there was a strong familial-social component to diabetes self-management. Several veterans were knowledgeable about diabetes self-management as evidenced by their responses to weekly questions. However, disease management for these veterans was strongly impacted by family and life events.
One veteran did not manage his disease for an entire week due to “being busy with a death in the family and planning for a wedding.” This veteran took his medication but did not check his blood glucose or monitor his diet. Another veteran spoke of eating ice cream and other concentrated sweets because his young grandson was with him for the week. A third veteran was able to manage his diet better when his wife packed snacks for him but when left to his own accord did not do well with his food selection. Even though these veterans understood how to effectively manage their diabetes, they may have chosen to inconsistently translate that knowledge into practice if they perceive those familial-social forces to be more important or more powerful.
Discussion
The findings from this small pilot study from a single clinic cannot be generalized. However, this pilot study adds to the literature of the positive impact of individualized, structured, tailored nursing interventions delivered with careful consideration of the participants’ personal goals and health care needs for diabetes self-management.
Participants monitored home blood glucose levels, diet, and activity and maintained adherence with prescribed diabetes medications. The HbA1c level for participants decreased by the end of the program. During the course of the pilot study a pharmacist managed the veterans’ medications. Participant 1 began a new medication regimen the first day of the study. Previously, the patient was self-regulating his medication. However, during the 12-week study, he had no medication adjustments. Participant 4 had several increases to his insulin dose (insulin aspart protamine and insulin aspart rdna origin) during the course of the study. Participants 5 and 6 had no medication adjustments during the study.
Even though participants had medication adjustments, which contributed to the HbA1c decrease, they became more aware of the medical need to control their blood sugar through the one-on-one education provided. Although there was variation in the depth and detail that participants maintained their food/activity log and home blood glucose monitoring, all participants agreed that they were more likely to be adherent with prescribed self-monitoring “knowing they were going to have to report self-monitoring information” to the RN.
Health care professionals may not realize the impact of familial-social events on blood glucose control. Veterans in this study found that having weekly sessions with the RN helped them through such events, even though they did not adhere strictly to their regimen. One suggestion is having veterans anticipate future familial-social events that may trigger nonadherence to their diabetes health plan and then discuss those events with the health care professional.
Future Research
This small exploratory pilot study has implications for future research. Increasing the study’s sample size and using a control group is recommended to compare veterans who have an educational intervention with those that do not and the impact it has on blood glucose control. The study was limited to 1 CBOC. Incorporating additional CBOCs could increase the sample size. Additionally, although this study was only 3 months in duration, a longer study could reveal significant patterns of change over time as well as the long-term benefit of a tailored educational intervention. In addition, adjusting the study inclusion criteria of > 9 HbA1c to include those with > 8 HbA1c also may increase the sample size.
Limited financial resources for the study could have negatively impacted the sample size. Incorporating recruitment or advertising strategy may increase the number of participants. Research also is needed on education interventions with a diverse group of male and female veterans that extends beyond 3 months. Exploring the value of including the veteran’s family in the education sessions is needed. Finally, this study examined only diabetes education. Researchers need to consider other diseases and the value of individualized education.
Limitations
Limitations included a small sample size and no control group. Due to the study’s small sample size, extrapolating data from it becomes difficult. However, this pilot study sets the groundwork for other researchers to expand the importance of education interventions and health literacy. Recruitment was challenging since an eligibility criterion was the NVS score, and patients were sometimes difficult to contact.7 The pilot study started with 6 white male participants but only 4 finished. During the course of the pilot study, 1 veteran had medication adjustments as part of routine care and 1 veteran had medication adjustments prior to the study, which could have altered the HbA1c results.
In hindsight, using the NVS to assess both prestudy with poststudy health literacy scores would have provided additional information about the education intervention. There is possible bias because the researcher was a VAMC employee, and the RN that implemented the interventions had previously worked with the patients.
Conclusion
Although this is a small descriptive pilot study, it adds to the body of research on the value of nurse-driven interventions to help veterans manage diabetes by enhancing their health literacy. It also raises questions and opportunities for further research into the power of familial-social influences on a veteran’s willingness to manage their diabetes. The majority of veterans who declined to participate in this study, even though they qualified, stated that they would “not follow any recommendations.” Further investigation is needed about why some veterans elect not to obtain help that could positively impact their health and possibly extend their life. Additionally, scientific quantitative and qualitative research is needed to evaluate the statistical significance between health care literacy and educational intervention on patient adherence among individuals diagnosed with diabetes.
1. Stiles E. Promoting health literacy in patients with diabetes. Nurs Stand. 2011;26(8):35-40.
2. Baum NH, Dowling RA. Health literacy: how do your patients rate? http://urologytimes.modernmedicine.com/urology-times/news/modernmedicine/modern-medicine-now/health-literacy-how-do-your-patients-rate. Published August 1, 2011. Accessed December 2, 2016.
3. Escobedo W, Weismuller P. Assessing health literacy in renal failure and kidney transplant patients. Prog Transplant. 2013;23(1):47-54.
4. Heinrich C. Health literacy: the sixth vital sign. J Am Acad Nurse Pract. 2012;24(4):218-223.
5. Roett MA, Wessel L. Help your patient “get” what you just said: health literacy guide. J Fam Pract. 2012;61(4):190-196.
6. American Diabetes Association. Statistics about diabetes. http://www.diabetes.org/diabetes-basics/statistics/?loc=feat1.Updated December 12, 2016. Accessed December 14, 2016.
7. Pfizer. The newest vital sign. http://www.pfizer.com/files/health/nvs_flipbook_english_final.pdf. Published February 2011. Accessed December 2, 2016.
8. Shah LC, West P, Bremmeyr K, Savoy-Moore RT. Health literacy instrument in family medicine: the “newest vital sign” ease of use and correlates. J Am Board Fam Med. 2010;23(2):195-203.
9. Welch VL, VanGeest JB, Caskey R. Time, costs, and clinical utilization of screening for health literacy: a case study using the Newest Vital Sign (NVS) instrument. J Am Board Fam Med. 2011;24(3):281-289.
10. Ryan JG, Leguen F, Weiss BD, et al. Will patients agree to have their literacy skills assessed in clinical practice? Health Educ Res. 2008;23(4):603-611.
11. McCleary-Jones V. Health literacy and its association with diabetes knowledge, self-efficacy and disease self-management among African Americans with diabetes mellitus. ABNF J. 2011;22(2):25-32.
12. Long AF, Gambling T. Enhancing health literacy and behavioral change within a tele-care education and support intervention for people with type 2 diabetes. Health Expect. 2012;15(3):267-282.
13. Mendoza M, Rosenberg T. Self-management of type 2 diabetes: A good idea-or not? J Fam Pract. 2013;62(5):244-248.
14. A Clifford Mulimba A, Byron-Daniel J. Motivational interviewing-based interventions and diabetes mellitus. Br J Nurs. 2014;23(1):8-14.
15. Thompson DR, Chair SY, Chan SW, Astin F, Davidson PM, Ski CF. Motivational interviewing: a useful approach to improving cardiovascular health? J Clin Nurs. 2011;20;(9-10):1236-1244.
16. Protheroe J, Rowlands G. Matching clinical information with levels of patient health literacy. Nurs Manag (Harrow). 2013;20(3):20-21.
17. Tisdel KA, Bedwell M, Tarkington PE, Mundy A, Fredrickson SK. Diabetes specialists share experience remotely with RN care managers. Fed Pract. 2013;30(suppl 7):15S-20S.
18. U.S. Department of Veterans Affairs, Veterans Health Administration Support Service Center. http://vssc.med.va.gov/AlphaIndex.asp?Ltr=D.
19. Radhakrishnan K. The efficacy of tailored interventions for self-management outcomes of type 2 diabetes, hypertension, or heart disease: a systemic review. J Adv Nurs. 2012;68(3):496-510.
1. Stiles E. Promoting health literacy in patients with diabetes. Nurs Stand. 2011;26(8):35-40.
2. Baum NH, Dowling RA. Health literacy: how do your patients rate? http://urologytimes.modernmedicine.com/urology-times/news/modernmedicine/modern-medicine-now/health-literacy-how-do-your-patients-rate. Published August 1, 2011. Accessed December 2, 2016.
3. Escobedo W, Weismuller P. Assessing health literacy in renal failure and kidney transplant patients. Prog Transplant. 2013;23(1):47-54.
4. Heinrich C. Health literacy: the sixth vital sign. J Am Acad Nurse Pract. 2012;24(4):218-223.
5. Roett MA, Wessel L. Help your patient “get” what you just said: health literacy guide. J Fam Pract. 2012;61(4):190-196.
6. American Diabetes Association. Statistics about diabetes. http://www.diabetes.org/diabetes-basics/statistics/?loc=feat1.Updated December 12, 2016. Accessed December 14, 2016.
7. Pfizer. The newest vital sign. http://www.pfizer.com/files/health/nvs_flipbook_english_final.pdf. Published February 2011. Accessed December 2, 2016.
8. Shah LC, West P, Bremmeyr K, Savoy-Moore RT. Health literacy instrument in family medicine: the “newest vital sign” ease of use and correlates. J Am Board Fam Med. 2010;23(2):195-203.
9. Welch VL, VanGeest JB, Caskey R. Time, costs, and clinical utilization of screening for health literacy: a case study using the Newest Vital Sign (NVS) instrument. J Am Board Fam Med. 2011;24(3):281-289.
10. Ryan JG, Leguen F, Weiss BD, et al. Will patients agree to have their literacy skills assessed in clinical practice? Health Educ Res. 2008;23(4):603-611.
11. McCleary-Jones V. Health literacy and its association with diabetes knowledge, self-efficacy and disease self-management among African Americans with diabetes mellitus. ABNF J. 2011;22(2):25-32.
12. Long AF, Gambling T. Enhancing health literacy and behavioral change within a tele-care education and support intervention for people with type 2 diabetes. Health Expect. 2012;15(3):267-282.
13. Mendoza M, Rosenberg T. Self-management of type 2 diabetes: A good idea-or not? J Fam Pract. 2013;62(5):244-248.
14. A Clifford Mulimba A, Byron-Daniel J. Motivational interviewing-based interventions and diabetes mellitus. Br J Nurs. 2014;23(1):8-14.
15. Thompson DR, Chair SY, Chan SW, Astin F, Davidson PM, Ski CF. Motivational interviewing: a useful approach to improving cardiovascular health? J Clin Nurs. 2011;20;(9-10):1236-1244.
16. Protheroe J, Rowlands G. Matching clinical information with levels of patient health literacy. Nurs Manag (Harrow). 2013;20(3):20-21.
17. Tisdel KA, Bedwell M, Tarkington PE, Mundy A, Fredrickson SK. Diabetes specialists share experience remotely with RN care managers. Fed Pract. 2013;30(suppl 7):15S-20S.
18. U.S. Department of Veterans Affairs, Veterans Health Administration Support Service Center. http://vssc.med.va.gov/AlphaIndex.asp?Ltr=D.
19. Radhakrishnan K. The efficacy of tailored interventions for self-management outcomes of type 2 diabetes, hypertension, or heart disease: a systemic review. J Adv Nurs. 2012;68(3):496-510.
“Where’s the Music?” Using Music Therapy for Pain Management
Staff at the Malcolm Randall VAMC (MRVAMC) outpatient pain clinic in Gainesville, Florida, found that procedures to reduce a patient’s pain could initially cause pain and anxiety. Typical nursing care plans involved measures to reduce anxiety in patients undergoing interventional procedures expected to produce pain, including identifying and reinforcing coping strategies, providing reassurance and comfort, and giving patients clear explanations slowly and calmly. The MRVAMC nursing staff therefore also advocated to add music therapy to the existing plan.
Background
As part of a quality improvement (QI) project, the authors conducted a literature search to find scientific evidence for the use of music therapy. Multiple medical databases were analyzed to find studies that included total time, dose of sedative medications, pain scores, patient experience, and willingness to repeat the same procedure in the future with use of music vs no music.1 The literature review revealed that music therapy demonstrated effectiveness in decreasing anxiety and pain, supporting relaxation, reducing sedation medication during procedures, and improving patient satisfaction.
As a result of the literature search the authors conducted a prospective, randomized controlled study to investigate music therapy as an adjunct intervention during painful procedures.
Radiofrequency Lesioning
One of the more common (and most painful) procedures performed at MRVAMC is radiofrequency lesioning (RFL).The procedure uses electrical pulses to block nerves for pain relief. Using fluoroscopy, the physician inserts a needle adjacent to the nerve that innervates the facet joint. The sensory and motor nerves are stimulated, causing a tingling or buzzing sensation and tapping. Once the tip of the needle is placed in the correct location, electrical pulses (small radiofrequency currents) are passed through the needle. A lesion is formed that temporarily interrupts the pain messages that the nerve sends to the brain. The procedure can take between30 and 60 minutes, which is longer than most pain clinic procedures.
Radiofrequency lesioning controls pain caused by degenerative disc disease, facet arthropathy, sacroiliac joints, stellate ganglions, and other nerve conditions. Due to the length of the RFL procedure, patients may experience pain and anxiety (as well as other complications, such as vasovagal responses).
The clinic staff anticipated that there would be 20 RFL procedures scheduled per week and selected it as the study procedure for 3 reasons: procedure length, high level of pain, and frequency performed.
After receiving approval from the University of Florida Institutional Review Board and VA Research and Development, the MRVAMC pain clinic initiated the study from September 2013 to April 2014. The purpose of the study was to measure the effects of music on patient’s self-reported anxiety and pain levels before and after nonsedating lumbar RFL.
Methods
Study Design
Veterans aged between 21 and 88 years who were scheduled to return for lumbar RFL and who did not require sedation were invited to participate. Sixty participants consented. The music group had 21 men and 2 women. The no-music group had 19 men and 2 women. Table 1 summarizes descriptive data. Table 2 describes the results of the comparison analysis. Patients were randomly assigned to either the music intervention group or no-music g
The study tools included the global anxiety VAS (GA-VAS) for pain and anxiety and a yes/no self-reported question, “Did music help?” for participants in the music group. Evaluation of the GA-VAS demonstrated reliability and validity and were patient friendly.2,3 Pain was recorded using a Likert scale of 0 for no pain and 10 for severe pain. Anxiety was recorded using a Likert scale of 0 for no anxiety and 4 for extreme anxiety.
Study subjects were recruited from patients who were on a maintenance lumbar RFL schedule, did not require sedation, and were willing to participate. If sedation was required, the patient was excluded from the study. Returning patients scheduled for RFL were informed about the music study and asked whether they were interested in participating. If they agreed, the study was explained in full, and informed consent was obtained prior to the day of their scheduled procedure. After obtaining informed consent, participants were asked to choose a music genre from 3 options: easy listening, jazz, or classical. Participants received a sealed envelope identifying their group (30 envelopes were created for each group) to be opened by the procedure nurse on the day of the procedure.4,5
Sixty participants consented to participate in the study. Of these 60 patients, 44 were studied. The 16 patients who did not participate had either a change in procedure or did not show for the appointment.
Data Collection
On procedure day, all participants completed the anxiety scale as well as a VAS pain scale (which is the MRVAMC standard of care), preoperatively and postprocedure. Envelopes were opened prior to going into the procedure room to prevent prior knowledge of who was assigned to the music group. Participants in the music intervention group listened to their preselected music on a portable CD player in the procedure room. The music was played softly so the patient could still hear and respond to the physicians instructions during the procedure. The no-music group received everything that the music intervention group received except for music (standard care throughout procedure, which consisted of nurse monitoring, measures to reduce fear and anxiety, and comfort measures). Procedures were performed with local anesthesia; neither group received moderate sedation.
Gender, age, and self-reported pain scores (before and after the lumber RFL procedure) were recorded in the patient’s chart and entered into the study database. Patients in both groups were queried before and after the procedure using the VAS to measure their pain and anxiety levels. Participants in the music intervention group were asked whether they felt that the music helped. They also were asked to provide feedback about their experience. Data were stored in locked filing cabinets, and all forms were de-identified.
Statistical Analysis
SAS version 9.2 (Cary, NC) was used for all analyses. Data were inspected for out-of-range values. The Fisher exact test was used to compare groups on categorical measures. An independent sample t test was used to compare groups on the age variable. Difference scores (formed by subtracting the after score from the before score) were analyzed using paired t tests. Analysis of covariance was used to test for significant group differences on the outcome variables of pain and anxiety with group as the independent variable and the preprocedure measure as the covariate. The level of significance was set at .05, and all testing was 2 sided.
Results
Of the 60 consenting patients, 44 participated in the study.Twenty-three were randomized to the music intervention and 21 to the no-music control group. Both pain and anxiety were significantly reduced (P < .0001) in the total sample (n = 44). The mean (SD) decrease in pain for all participants was 2.80 points (2.31) on a VAS of 0 to 10 and 0.86 points (0.93) decrease in anxiety. In the music intervention group, the mean decrease in pain and anxiety was 3.22 (2.66) and 1.00 (0.85), respectively. In the no-music group, the mean decrease in pain and anxiety was 2.33 (1.80) and 0.69 (1.00), respectively. The magnitude of pain decrease was larger in the music intervention group; however, the difference did not reach statistical significance.
Discussion
Although there was not a statistically significant difference in pain or anxiety reduction due to group assignment, a 2-point reduction in self-reported pain or anxiety may be considered clinically important and has been supported in older studies.6 Importantly, 87% of participants in the music intervention group reported that listening to music was helpful during the procedure (Figure 1).
Anxiety levels were not as high as expected when measured before and after the procedure, perhaps due to improvements in patient education and continuity of care (Figure 2). Since all participants were returning patients, they already were familiar with the procedure and the staff. Staff turnover rate is very low at this clinic, which may have contributed to the low anxiety rates among participants at baseline. Other contributing factors included good communication, expert technique, and teamwork.
During the study, few negative comments were noted. One participant did not hear the music due to faulty equipment setup. Another participant commented that the physician doing the procedure made negative remarks about the music the patient selected. A third participant commented that the music was too loud, and he was unable to hear the doctor’s instructions, indicating a need for guidelines.
There were many positive comments by participants in the music intervention group. Nurses reported comments such as “The music really helps”; “The music was great, but rock ‘n’ roll would be better”; and “Can I bring my own [music] next time?” Many patients returning for procedures frequently asked, “Where is the music?”
Limitations
Of the 60 consenting patients, only 44 participated, possibly lowering the power of the study to detect significant findings. During the study, the physician staff was reduced, resulting in fewer RFLs performed and causing the study to take longer to conduct and with fewer opportunities to recruit participants.
The CD players used for the study were old, and because earbuds could not be used, volume was difficult to modulate consistently. Earbuds were not used because patient participation was required during the procedure. Also, having only 3 music genres to choose from limited the participant’s choice.
Conclusion
Research supporting the use of music therapy to increase patient comfort is widely accepted and practiced.7 Music therapy is readily available, low risk, inexpensive, and does not require intense training by staff. It may reduce the need for moderate sedation and improve the overall patient experience. During the study, the MRVAMC nursing staff gained a greater appreciation of evidence-based practice; staff are more engaged in QI, based on their personal involvement in research.
Because 87% of the music therapy participants reported that music was helpful, the MRVAMC pain clinic plans to implement music therapy as a standard of care during RFL procedures and all procedure appointments. Music therapy may help reduce pain and anxiety during painful procedures. The goal is to continually increase patient satisfaction and overall procedure experience through integration of evidence-based practice.
Acknowledgments
The authors thank the study team who helped consent participants, perform the experiment, and gather and analyze data. They also acknowledge the pain clinic physicians, Dr. Egle Bavry and Dr. Heidi Goldstein, for their support throughout the study. Special thanks goes to Daniel Prince for his technical support.
1. Bechtold ML, Perez RA, Puli SR, Marshall JB. Effect of music on patients undergoing outpatient colonoscopy. World J Gastroenterol. 2006;12(45):7309-7312.
2. Miller SD, Duncan BL, Brown J, Sparks JA, Claud DA. The outcome rating scale: a preliminary study of the reliability, validity, and feasibility of a brief visual analog measure. J Brief Ther. 2003;2(2):91-100.
3. Williams VS, Morlock RJ, Feltner D. Psychometric evaluation of a visual analog scale for the assessment of anxiety. Health Qual Life Outcomes. 2010;8:57.
4. Dettori J. The random allocation process: two things you need to know. Evid Based Spine Care J. 2010;1(3):7-9.
5. Farrokhyar F, Bajammal S, Kahnamoui K, Bhandari M. Ensuring balanced groups in surgical trials. Can J Surg. 2010;53(6):418-423.
6. Hägg O, Fritzell P, Nordwall A; Swedish Lumbar Spine Study Group. The clinical importance of changes in outcome scores after treatment for chronic low back pain. Eur Spine J. 2003;12(1):12-20.
7. Sonke J. Music and the arts in health: a perspective from the United States. Music Arts Action. 2011;3(2):5-14
Staff at the Malcolm Randall VAMC (MRVAMC) outpatient pain clinic in Gainesville, Florida, found that procedures to reduce a patient’s pain could initially cause pain and anxiety. Typical nursing care plans involved measures to reduce anxiety in patients undergoing interventional procedures expected to produce pain, including identifying and reinforcing coping strategies, providing reassurance and comfort, and giving patients clear explanations slowly and calmly. The MRVAMC nursing staff therefore also advocated to add music therapy to the existing plan.
Background
As part of a quality improvement (QI) project, the authors conducted a literature search to find scientific evidence for the use of music therapy. Multiple medical databases were analyzed to find studies that included total time, dose of sedative medications, pain scores, patient experience, and willingness to repeat the same procedure in the future with use of music vs no music.1 The literature review revealed that music therapy demonstrated effectiveness in decreasing anxiety and pain, supporting relaxation, reducing sedation medication during procedures, and improving patient satisfaction.
As a result of the literature search the authors conducted a prospective, randomized controlled study to investigate music therapy as an adjunct intervention during painful procedures.
Radiofrequency Lesioning
One of the more common (and most painful) procedures performed at MRVAMC is radiofrequency lesioning (RFL).The procedure uses electrical pulses to block nerves for pain relief. Using fluoroscopy, the physician inserts a needle adjacent to the nerve that innervates the facet joint. The sensory and motor nerves are stimulated, causing a tingling or buzzing sensation and tapping. Once the tip of the needle is placed in the correct location, electrical pulses (small radiofrequency currents) are passed through the needle. A lesion is formed that temporarily interrupts the pain messages that the nerve sends to the brain. The procedure can take between30 and 60 minutes, which is longer than most pain clinic procedures.
Radiofrequency lesioning controls pain caused by degenerative disc disease, facet arthropathy, sacroiliac joints, stellate ganglions, and other nerve conditions. Due to the length of the RFL procedure, patients may experience pain and anxiety (as well as other complications, such as vasovagal responses).
The clinic staff anticipated that there would be 20 RFL procedures scheduled per week and selected it as the study procedure for 3 reasons: procedure length, high level of pain, and frequency performed.
After receiving approval from the University of Florida Institutional Review Board and VA Research and Development, the MRVAMC pain clinic initiated the study from September 2013 to April 2014. The purpose of the study was to measure the effects of music on patient’s self-reported anxiety and pain levels before and after nonsedating lumbar RFL.
Methods
Study Design
Veterans aged between 21 and 88 years who were scheduled to return for lumbar RFL and who did not require sedation were invited to participate. Sixty participants consented. The music group had 21 men and 2 women. The no-music group had 19 men and 2 women. Table 1 summarizes descriptive data. Table 2 describes the results of the comparison analysis. Patients were randomly assigned to either the music intervention group or no-music g
The study tools included the global anxiety VAS (GA-VAS) for pain and anxiety and a yes/no self-reported question, “Did music help?” for participants in the music group. Evaluation of the GA-VAS demonstrated reliability and validity and were patient friendly.2,3 Pain was recorded using a Likert scale of 0 for no pain and 10 for severe pain. Anxiety was recorded using a Likert scale of 0 for no anxiety and 4 for extreme anxiety.
Study subjects were recruited from patients who were on a maintenance lumbar RFL schedule, did not require sedation, and were willing to participate. If sedation was required, the patient was excluded from the study. Returning patients scheduled for RFL were informed about the music study and asked whether they were interested in participating. If they agreed, the study was explained in full, and informed consent was obtained prior to the day of their scheduled procedure. After obtaining informed consent, participants were asked to choose a music genre from 3 options: easy listening, jazz, or classical. Participants received a sealed envelope identifying their group (30 envelopes were created for each group) to be opened by the procedure nurse on the day of the procedure.4,5
Sixty participants consented to participate in the study. Of these 60 patients, 44 were studied. The 16 patients who did not participate had either a change in procedure or did not show for the appointment.
Data Collection
On procedure day, all participants completed the anxiety scale as well as a VAS pain scale (which is the MRVAMC standard of care), preoperatively and postprocedure. Envelopes were opened prior to going into the procedure room to prevent prior knowledge of who was assigned to the music group. Participants in the music intervention group listened to their preselected music on a portable CD player in the procedure room. The music was played softly so the patient could still hear and respond to the physicians instructions during the procedure. The no-music group received everything that the music intervention group received except for music (standard care throughout procedure, which consisted of nurse monitoring, measures to reduce fear and anxiety, and comfort measures). Procedures were performed with local anesthesia; neither group received moderate sedation.
Gender, age, and self-reported pain scores (before and after the lumber RFL procedure) were recorded in the patient’s chart and entered into the study database. Patients in both groups were queried before and after the procedure using the VAS to measure their pain and anxiety levels. Participants in the music intervention group were asked whether they felt that the music helped. They also were asked to provide feedback about their experience. Data were stored in locked filing cabinets, and all forms were de-identified.
Statistical Analysis
SAS version 9.2 (Cary, NC) was used for all analyses. Data were inspected for out-of-range values. The Fisher exact test was used to compare groups on categorical measures. An independent sample t test was used to compare groups on the age variable. Difference scores (formed by subtracting the after score from the before score) were analyzed using paired t tests. Analysis of covariance was used to test for significant group differences on the outcome variables of pain and anxiety with group as the independent variable and the preprocedure measure as the covariate. The level of significance was set at .05, and all testing was 2 sided.
Results
Of the 60 consenting patients, 44 participated in the study.Twenty-three were randomized to the music intervention and 21 to the no-music control group. Both pain and anxiety were significantly reduced (P < .0001) in the total sample (n = 44). The mean (SD) decrease in pain for all participants was 2.80 points (2.31) on a VAS of 0 to 10 and 0.86 points (0.93) decrease in anxiety. In the music intervention group, the mean decrease in pain and anxiety was 3.22 (2.66) and 1.00 (0.85), respectively. In the no-music group, the mean decrease in pain and anxiety was 2.33 (1.80) and 0.69 (1.00), respectively. The magnitude of pain decrease was larger in the music intervention group; however, the difference did not reach statistical significance.
Discussion
Although there was not a statistically significant difference in pain or anxiety reduction due to group assignment, a 2-point reduction in self-reported pain or anxiety may be considered clinically important and has been supported in older studies.6 Importantly, 87% of participants in the music intervention group reported that listening to music was helpful during the procedure (Figure 1).
Anxiety levels were not as high as expected when measured before and after the procedure, perhaps due to improvements in patient education and continuity of care (Figure 2). Since all participants were returning patients, they already were familiar with the procedure and the staff. Staff turnover rate is very low at this clinic, which may have contributed to the low anxiety rates among participants at baseline. Other contributing factors included good communication, expert technique, and teamwork.
During the study, few negative comments were noted. One participant did not hear the music due to faulty equipment setup. Another participant commented that the physician doing the procedure made negative remarks about the music the patient selected. A third participant commented that the music was too loud, and he was unable to hear the doctor’s instructions, indicating a need for guidelines.
There were many positive comments by participants in the music intervention group. Nurses reported comments such as “The music really helps”; “The music was great, but rock ‘n’ roll would be better”; and “Can I bring my own [music] next time?” Many patients returning for procedures frequently asked, “Where is the music?”
Limitations
Of the 60 consenting patients, only 44 participated, possibly lowering the power of the study to detect significant findings. During the study, the physician staff was reduced, resulting in fewer RFLs performed and causing the study to take longer to conduct and with fewer opportunities to recruit participants.
The CD players used for the study were old, and because earbuds could not be used, volume was difficult to modulate consistently. Earbuds were not used because patient participation was required during the procedure. Also, having only 3 music genres to choose from limited the participant’s choice.
Conclusion
Research supporting the use of music therapy to increase patient comfort is widely accepted and practiced.7 Music therapy is readily available, low risk, inexpensive, and does not require intense training by staff. It may reduce the need for moderate sedation and improve the overall patient experience. During the study, the MRVAMC nursing staff gained a greater appreciation of evidence-based practice; staff are more engaged in QI, based on their personal involvement in research.
Because 87% of the music therapy participants reported that music was helpful, the MRVAMC pain clinic plans to implement music therapy as a standard of care during RFL procedures and all procedure appointments. Music therapy may help reduce pain and anxiety during painful procedures. The goal is to continually increase patient satisfaction and overall procedure experience through integration of evidence-based practice.
Acknowledgments
The authors thank the study team who helped consent participants, perform the experiment, and gather and analyze data. They also acknowledge the pain clinic physicians, Dr. Egle Bavry and Dr. Heidi Goldstein, for their support throughout the study. Special thanks goes to Daniel Prince for his technical support.
Staff at the Malcolm Randall VAMC (MRVAMC) outpatient pain clinic in Gainesville, Florida, found that procedures to reduce a patient’s pain could initially cause pain and anxiety. Typical nursing care plans involved measures to reduce anxiety in patients undergoing interventional procedures expected to produce pain, including identifying and reinforcing coping strategies, providing reassurance and comfort, and giving patients clear explanations slowly and calmly. The MRVAMC nursing staff therefore also advocated to add music therapy to the existing plan.
Background
As part of a quality improvement (QI) project, the authors conducted a literature search to find scientific evidence for the use of music therapy. Multiple medical databases were analyzed to find studies that included total time, dose of sedative medications, pain scores, patient experience, and willingness to repeat the same procedure in the future with use of music vs no music.1 The literature review revealed that music therapy demonstrated effectiveness in decreasing anxiety and pain, supporting relaxation, reducing sedation medication during procedures, and improving patient satisfaction.
As a result of the literature search the authors conducted a prospective, randomized controlled study to investigate music therapy as an adjunct intervention during painful procedures.
Radiofrequency Lesioning
One of the more common (and most painful) procedures performed at MRVAMC is radiofrequency lesioning (RFL).The procedure uses electrical pulses to block nerves for pain relief. Using fluoroscopy, the physician inserts a needle adjacent to the nerve that innervates the facet joint. The sensory and motor nerves are stimulated, causing a tingling or buzzing sensation and tapping. Once the tip of the needle is placed in the correct location, electrical pulses (small radiofrequency currents) are passed through the needle. A lesion is formed that temporarily interrupts the pain messages that the nerve sends to the brain. The procedure can take between30 and 60 minutes, which is longer than most pain clinic procedures.
Radiofrequency lesioning controls pain caused by degenerative disc disease, facet arthropathy, sacroiliac joints, stellate ganglions, and other nerve conditions. Due to the length of the RFL procedure, patients may experience pain and anxiety (as well as other complications, such as vasovagal responses).
The clinic staff anticipated that there would be 20 RFL procedures scheduled per week and selected it as the study procedure for 3 reasons: procedure length, high level of pain, and frequency performed.
After receiving approval from the University of Florida Institutional Review Board and VA Research and Development, the MRVAMC pain clinic initiated the study from September 2013 to April 2014. The purpose of the study was to measure the effects of music on patient’s self-reported anxiety and pain levels before and after nonsedating lumbar RFL.
Methods
Study Design
Veterans aged between 21 and 88 years who were scheduled to return for lumbar RFL and who did not require sedation were invited to participate. Sixty participants consented. The music group had 21 men and 2 women. The no-music group had 19 men and 2 women. Table 1 summarizes descriptive data. Table 2 describes the results of the comparison analysis. Patients were randomly assigned to either the music intervention group or no-music g
The study tools included the global anxiety VAS (GA-VAS) for pain and anxiety and a yes/no self-reported question, “Did music help?” for participants in the music group. Evaluation of the GA-VAS demonstrated reliability and validity and were patient friendly.2,3 Pain was recorded using a Likert scale of 0 for no pain and 10 for severe pain. Anxiety was recorded using a Likert scale of 0 for no anxiety and 4 for extreme anxiety.
Study subjects were recruited from patients who were on a maintenance lumbar RFL schedule, did not require sedation, and were willing to participate. If sedation was required, the patient was excluded from the study. Returning patients scheduled for RFL were informed about the music study and asked whether they were interested in participating. If they agreed, the study was explained in full, and informed consent was obtained prior to the day of their scheduled procedure. After obtaining informed consent, participants were asked to choose a music genre from 3 options: easy listening, jazz, or classical. Participants received a sealed envelope identifying their group (30 envelopes were created for each group) to be opened by the procedure nurse on the day of the procedure.4,5
Sixty participants consented to participate in the study. Of these 60 patients, 44 were studied. The 16 patients who did not participate had either a change in procedure or did not show for the appointment.
Data Collection
On procedure day, all participants completed the anxiety scale as well as a VAS pain scale (which is the MRVAMC standard of care), preoperatively and postprocedure. Envelopes were opened prior to going into the procedure room to prevent prior knowledge of who was assigned to the music group. Participants in the music intervention group listened to their preselected music on a portable CD player in the procedure room. The music was played softly so the patient could still hear and respond to the physicians instructions during the procedure. The no-music group received everything that the music intervention group received except for music (standard care throughout procedure, which consisted of nurse monitoring, measures to reduce fear and anxiety, and comfort measures). Procedures were performed with local anesthesia; neither group received moderate sedation.
Gender, age, and self-reported pain scores (before and after the lumber RFL procedure) were recorded in the patient’s chart and entered into the study database. Patients in both groups were queried before and after the procedure using the VAS to measure their pain and anxiety levels. Participants in the music intervention group were asked whether they felt that the music helped. They also were asked to provide feedback about their experience. Data were stored in locked filing cabinets, and all forms were de-identified.
Statistical Analysis
SAS version 9.2 (Cary, NC) was used for all analyses. Data were inspected for out-of-range values. The Fisher exact test was used to compare groups on categorical measures. An independent sample t test was used to compare groups on the age variable. Difference scores (formed by subtracting the after score from the before score) were analyzed using paired t tests. Analysis of covariance was used to test for significant group differences on the outcome variables of pain and anxiety with group as the independent variable and the preprocedure measure as the covariate. The level of significance was set at .05, and all testing was 2 sided.
Results
Of the 60 consenting patients, 44 participated in the study.Twenty-three were randomized to the music intervention and 21 to the no-music control group. Both pain and anxiety were significantly reduced (P < .0001) in the total sample (n = 44). The mean (SD) decrease in pain for all participants was 2.80 points (2.31) on a VAS of 0 to 10 and 0.86 points (0.93) decrease in anxiety. In the music intervention group, the mean decrease in pain and anxiety was 3.22 (2.66) and 1.00 (0.85), respectively. In the no-music group, the mean decrease in pain and anxiety was 2.33 (1.80) and 0.69 (1.00), respectively. The magnitude of pain decrease was larger in the music intervention group; however, the difference did not reach statistical significance.
Discussion
Although there was not a statistically significant difference in pain or anxiety reduction due to group assignment, a 2-point reduction in self-reported pain or anxiety may be considered clinically important and has been supported in older studies.6 Importantly, 87% of participants in the music intervention group reported that listening to music was helpful during the procedure (Figure 1).
Anxiety levels were not as high as expected when measured before and after the procedure, perhaps due to improvements in patient education and continuity of care (Figure 2). Since all participants were returning patients, they already were familiar with the procedure and the staff. Staff turnover rate is very low at this clinic, which may have contributed to the low anxiety rates among participants at baseline. Other contributing factors included good communication, expert technique, and teamwork.
During the study, few negative comments were noted. One participant did not hear the music due to faulty equipment setup. Another participant commented that the physician doing the procedure made negative remarks about the music the patient selected. A third participant commented that the music was too loud, and he was unable to hear the doctor’s instructions, indicating a need for guidelines.
There were many positive comments by participants in the music intervention group. Nurses reported comments such as “The music really helps”; “The music was great, but rock ‘n’ roll would be better”; and “Can I bring my own [music] next time?” Many patients returning for procedures frequently asked, “Where is the music?”
Limitations
Of the 60 consenting patients, only 44 participated, possibly lowering the power of the study to detect significant findings. During the study, the physician staff was reduced, resulting in fewer RFLs performed and causing the study to take longer to conduct and with fewer opportunities to recruit participants.
The CD players used for the study were old, and because earbuds could not be used, volume was difficult to modulate consistently. Earbuds were not used because patient participation was required during the procedure. Also, having only 3 music genres to choose from limited the participant’s choice.
Conclusion
Research supporting the use of music therapy to increase patient comfort is widely accepted and practiced.7 Music therapy is readily available, low risk, inexpensive, and does not require intense training by staff. It may reduce the need for moderate sedation and improve the overall patient experience. During the study, the MRVAMC nursing staff gained a greater appreciation of evidence-based practice; staff are more engaged in QI, based on their personal involvement in research.
Because 87% of the music therapy participants reported that music was helpful, the MRVAMC pain clinic plans to implement music therapy as a standard of care during RFL procedures and all procedure appointments. Music therapy may help reduce pain and anxiety during painful procedures. The goal is to continually increase patient satisfaction and overall procedure experience through integration of evidence-based practice.
Acknowledgments
The authors thank the study team who helped consent participants, perform the experiment, and gather and analyze data. They also acknowledge the pain clinic physicians, Dr. Egle Bavry and Dr. Heidi Goldstein, for their support throughout the study. Special thanks goes to Daniel Prince for his technical support.
1. Bechtold ML, Perez RA, Puli SR, Marshall JB. Effect of music on patients undergoing outpatient colonoscopy. World J Gastroenterol. 2006;12(45):7309-7312.
2. Miller SD, Duncan BL, Brown J, Sparks JA, Claud DA. The outcome rating scale: a preliminary study of the reliability, validity, and feasibility of a brief visual analog measure. J Brief Ther. 2003;2(2):91-100.
3. Williams VS, Morlock RJ, Feltner D. Psychometric evaluation of a visual analog scale for the assessment of anxiety. Health Qual Life Outcomes. 2010;8:57.
4. Dettori J. The random allocation process: two things you need to know. Evid Based Spine Care J. 2010;1(3):7-9.
5. Farrokhyar F, Bajammal S, Kahnamoui K, Bhandari M. Ensuring balanced groups in surgical trials. Can J Surg. 2010;53(6):418-423.
6. Hägg O, Fritzell P, Nordwall A; Swedish Lumbar Spine Study Group. The clinical importance of changes in outcome scores after treatment for chronic low back pain. Eur Spine J. 2003;12(1):12-20.
7. Sonke J. Music and the arts in health: a perspective from the United States. Music Arts Action. 2011;3(2):5-14
1. Bechtold ML, Perez RA, Puli SR, Marshall JB. Effect of music on patients undergoing outpatient colonoscopy. World J Gastroenterol. 2006;12(45):7309-7312.
2. Miller SD, Duncan BL, Brown J, Sparks JA, Claud DA. The outcome rating scale: a preliminary study of the reliability, validity, and feasibility of a brief visual analog measure. J Brief Ther. 2003;2(2):91-100.
3. Williams VS, Morlock RJ, Feltner D. Psychometric evaluation of a visual analog scale for the assessment of anxiety. Health Qual Life Outcomes. 2010;8:57.
4. Dettori J. The random allocation process: two things you need to know. Evid Based Spine Care J. 2010;1(3):7-9.
5. Farrokhyar F, Bajammal S, Kahnamoui K, Bhandari M. Ensuring balanced groups in surgical trials. Can J Surg. 2010;53(6):418-423.
6. Hägg O, Fritzell P, Nordwall A; Swedish Lumbar Spine Study Group. The clinical importance of changes in outcome scores after treatment for chronic low back pain. Eur Spine J. 2003;12(1):12-20.
7. Sonke J. Music and the arts in health: a perspective from the United States. Music Arts Action. 2011;3(2):5-14
Baseball Reminiscence Therapy for Cognitively Impaired Veterans
The number of older veterans with dementia and depression has posed a growing health care concern. Before its 2012 closure, the Geriatric Research Education and Clinical Center (GRECC) at the VA St. Louis Health Care System (VASLHCS) in Missouri addressed this concern by creating a baseball reminiscence group pilot study to provide social support for veterans with dementia and depression.
Related: Development and Evaluation of a Geriatric Mood Management Program
Reminiscence therapy improves self-esteem, enhances mood, and promotes communication skills. Reminiscence therapy stimulates participants to share memories, which is helpful in relieving depressive symptoms and has shown positive effects on cognition.1,2
Dementia Management
In 2010, 563,758 veterans were diagnosed with dementia, including Alzheimer disease (AD).3 Although pharmacologic management of AD may slow its progression, AD cannot be prevented or reversed, and the treatments may cause adverse effects.4 Therefore, participation in support groups and supportive services should also be explored.
Currently, 70% of individuals with AD live at home, and most would like to remain there. Family caregivers provide 80% of the care in the home. Depending on the value placed on informal home care, the annual cost per patient for dementia care can be estimated between $41,689 and $56,290.5 The financial burden on family caregivers as well as on the veterans with dementia is increasing and needs to be addressed to improve the quality of care. Support groups may improve the quality of life (QOL) and care for both veterans and their caregivers.
Group Characteristics
Hoping to expand treatment options that would positively impact veterans, the VASLHCS GRECC created a reminiscence support group with the goal of improving the QOL for veterans with a diagnosis of dementia and depression. The group was modeled after the football reminiscence project of Scotland.6
Men and women with an interest in baseball and a diagnosis of either depression or dementia were invited. The presence of a family caregiver improved the probability of the veteran joining the group.
Related: Home-Based Video Telehealth for Veterans With Dementia
Ten of the original 14 recruits finished the first year with the group; 2 dropped out, 1 died, and 1 could not find transportation to the meetings. Of the 10 participating veterans, 3 had a depression diagnosis (Geriatric Depression Scale [GDS] scores between 8 and 12) and 7 had a mild-to-moderate dementia diagnosis (Saint Louis University Mental Status Examination [SLUMS] exam scores between 12 and 19). Four participants served in World War II, 4 served in Korea, and 2 served in Vietnam. Nine of the recruits were male; 1 was female. During the first year, 1 veteran entered the on-campus community living center following a hospitalization. This veteran continued to meet with the group during rehabilitation and on discharge went to an assisted living facility that provided transportation to VASLHCS. He participated until he died in year 2.
Cardinals Reminiscence League
The group gathered every 2 weeks for facilitated discussions. Meetings included guest speakers and sessions in which participants shared baseball memories. Field trips to the St. Louis Cardinals stadium for a tour, the St. Louis Cardinals Hall of Fame and Museum, a Cardinals game, or a local radio station kept veterans engaged.
After each meeting, participants were given a Scorecard (Figure). The Scorecard included the group logo, which reflected both military and baseball themes; contained information about the time, location, and subject of the next meeting; and provided a brief description of the story the veteran had shared at the meeting.
Caregivers reported that the Scorecard allowed them to continue the discussion at home. One caregiver reported that the card often contained old baseball stories he had heard as a child. He expressed gratitude for hearing a “voice” that the family feared had been silenced by dementia.
At the end of the first year of the program, caregivers for the veterans with dementia expressed gratitude and reported an improved mood for the veterans when they discussed baseball at home. The SLUMS scores for these 7 patients had not changed significantly. The veterans with depression did not have caregivers, so no caregiver data were collected, but their self-reported statements indicated they felt more energetic and hopeful than they had felt before joining the group. However, all 3 veterans with a prior depression diagnosis declined requests to retake the GDS at the end of the first year.
Related: Delirium in the Cardiac ICU
The VASLHCS baseball reminiscence group had 3 important partners. The St. Louis chapter of the Alzheimer’s Association provided expertise in facilitator and volunteer training. Voluntary Services at VASLHCS actively recruited volunteers. The third partner was the St. Louis Cardinals. The St. Louis Cardinals Hall of Fame and Museum produced books with laminated iconic baseball pictures from their archives for the reminiscence group. Meetings began with a review of the books.
Holding meetings at VASLHCS had many benefits. Participants could schedule medical appointments on the days the group met, thereby reducing transportation demands. Other veterans often contributed to the program, which increased the festive, social nature of the meetings. For example, one veteran, who practiced piano as part of his regular therapy, played Take Me Out to the Ballgame at the beginning and end of the meetings. Veterans who were on site for appointments or social events helped greet the participants in the parking lot and escorted them to the meeting room. The VASLHCS provided a safe, familiar environment in which the veterans and their caregivers could congregate and conduct other business as needed. Also, holding the meetings at VASLHCS reinforced that group members had 2 things in common: They were baseball fans, and they were veterans.
Conclusions
The baseball reminiscence support group helped promote camaraderie among veterans. This pilot project helped determine the feasibility and interest of the participants and volunteers and provided the following insights:
- Baseball reminiscence may appeal to men who do not feel comfortable in other types of support groups
- Properly trained facilitators were critical to the program
- Volunteers kept veterans engaged and promoted input from everyone
- Meeting reminders and follow-up calls kept caregivers apprised of activities
- Baseball is just one sport that can be used by a reminiscence group. Any sport that has a local fan base will provide volunteers and a core of interested veterans
- Memories of sporting events are traditionally exaggerated and rewritten as part of the social process, so there is no shame in forgetting facts or mixing up games
Support programs are often used with the hope of providing an improved QOL for participants. To document such outcomes, large, controlled, longitudinal studies are needed. Many patients with dementia and depression are unable to participate in these studies because of failing physical health, failing cognition, and caregiver fatigue. Pilot studies such as this one provide examples of social interventions that are not scientifically proven to be effective but are perceived to be of value by all involved: the veterans, their families, the volunteers, and the facilitators. This type of therapy provides a low-cost, social intervention and an opportunity for improved QOL and fun for veterans.
Author disclosures
The author reports no actual or potential conflicts of interest with regard to this article.
Disclaimer
The opinions expressed herein are those of the author and do not necessarily reflect those of Federal Practitioner, Frontline Medical Communications Inc., the U.S. Government, or any of its agencies. This article may discuss unlabeled or investigational use of certain drugs. Please review the complete prescribing information for specific drugs or drug combinations—including indications, contraindications, warnings, and adverse effects—before administering pharmacologic therapy to patients.
1. Wu L-F, Chuo LJ, Wu ST. The effect of group instrumental reminiscence therapy in older single veterans who live in a veterans home in Taiwan. Int J Geriatr Psychiatry. 2012;27(1):107-108.
2. Van Bogaert P, Van Grinsven R, Tolson D, Wouters K, Engelborghs S, Van der Mussele S. Effects of SolCos model-based individual reminiscence on older adults with mild to moderate dementia due to Alzheimer disease: a pilot study. J Am Med Dir Assoc. 2013;14(7):528.e9-e13.
3. U.S. Department of Veterans Affairs, Veterans Health Administration, Health Services Research & Development Service. A systematic evidence review of non-pharmacological interventions for behavioral symptoms of dementia. U.S. Department of Veterans Affairs Website. http://www.hsrd.research.va.gov/publications/esp/Dementia-Nonpharm.pdf. Published March 2011. Accessed August 30, 2015.
4. Alzheimer's Association. 2013 Alzheimer's disease facts and figures. Alzheimers Dement. 2013;9(2):208-245.
5. Hurd MD, Martorell P, Delavande A, Mullen KJ, Langa KM. Monetary costs of dementia in the United States. N Engl J Med. 2013;368(14):1326-1334.
6. Tolson D, Schofield I. Football reminiscence for men with dementia: lessons from a realistic evaluation. Nurs Inq. 2012;19(1):63-70.
The number of older veterans with dementia and depression has posed a growing health care concern. Before its 2012 closure, the Geriatric Research Education and Clinical Center (GRECC) at the VA St. Louis Health Care System (VASLHCS) in Missouri addressed this concern by creating a baseball reminiscence group pilot study to provide social support for veterans with dementia and depression.
Related: Development and Evaluation of a Geriatric Mood Management Program
Reminiscence therapy improves self-esteem, enhances mood, and promotes communication skills. Reminiscence therapy stimulates participants to share memories, which is helpful in relieving depressive symptoms and has shown positive effects on cognition.1,2
Dementia Management
In 2010, 563,758 veterans were diagnosed with dementia, including Alzheimer disease (AD).3 Although pharmacologic management of AD may slow its progression, AD cannot be prevented or reversed, and the treatments may cause adverse effects.4 Therefore, participation in support groups and supportive services should also be explored.
Currently, 70% of individuals with AD live at home, and most would like to remain there. Family caregivers provide 80% of the care in the home. Depending on the value placed on informal home care, the annual cost per patient for dementia care can be estimated between $41,689 and $56,290.5 The financial burden on family caregivers as well as on the veterans with dementia is increasing and needs to be addressed to improve the quality of care. Support groups may improve the quality of life (QOL) and care for both veterans and their caregivers.
Group Characteristics
Hoping to expand treatment options that would positively impact veterans, the VASLHCS GRECC created a reminiscence support group with the goal of improving the QOL for veterans with a diagnosis of dementia and depression. The group was modeled after the football reminiscence project of Scotland.6
Men and women with an interest in baseball and a diagnosis of either depression or dementia were invited. The presence of a family caregiver improved the probability of the veteran joining the group.
Related: Home-Based Video Telehealth for Veterans With Dementia
Ten of the original 14 recruits finished the first year with the group; 2 dropped out, 1 died, and 1 could not find transportation to the meetings. Of the 10 participating veterans, 3 had a depression diagnosis (Geriatric Depression Scale [GDS] scores between 8 and 12) and 7 had a mild-to-moderate dementia diagnosis (Saint Louis University Mental Status Examination [SLUMS] exam scores between 12 and 19). Four participants served in World War II, 4 served in Korea, and 2 served in Vietnam. Nine of the recruits were male; 1 was female. During the first year, 1 veteran entered the on-campus community living center following a hospitalization. This veteran continued to meet with the group during rehabilitation and on discharge went to an assisted living facility that provided transportation to VASLHCS. He participated until he died in year 2.
Cardinals Reminiscence League
The group gathered every 2 weeks for facilitated discussions. Meetings included guest speakers and sessions in which participants shared baseball memories. Field trips to the St. Louis Cardinals stadium for a tour, the St. Louis Cardinals Hall of Fame and Museum, a Cardinals game, or a local radio station kept veterans engaged.
After each meeting, participants were given a Scorecard (Figure). The Scorecard included the group logo, which reflected both military and baseball themes; contained information about the time, location, and subject of the next meeting; and provided a brief description of the story the veteran had shared at the meeting.
Caregivers reported that the Scorecard allowed them to continue the discussion at home. One caregiver reported that the card often contained old baseball stories he had heard as a child. He expressed gratitude for hearing a “voice” that the family feared had been silenced by dementia.
At the end of the first year of the program, caregivers for the veterans with dementia expressed gratitude and reported an improved mood for the veterans when they discussed baseball at home. The SLUMS scores for these 7 patients had not changed significantly. The veterans with depression did not have caregivers, so no caregiver data were collected, but their self-reported statements indicated they felt more energetic and hopeful than they had felt before joining the group. However, all 3 veterans with a prior depression diagnosis declined requests to retake the GDS at the end of the first year.
Related: Delirium in the Cardiac ICU
The VASLHCS baseball reminiscence group had 3 important partners. The St. Louis chapter of the Alzheimer’s Association provided expertise in facilitator and volunteer training. Voluntary Services at VASLHCS actively recruited volunteers. The third partner was the St. Louis Cardinals. The St. Louis Cardinals Hall of Fame and Museum produced books with laminated iconic baseball pictures from their archives for the reminiscence group. Meetings began with a review of the books.
Holding meetings at VASLHCS had many benefits. Participants could schedule medical appointments on the days the group met, thereby reducing transportation demands. Other veterans often contributed to the program, which increased the festive, social nature of the meetings. For example, one veteran, who practiced piano as part of his regular therapy, played Take Me Out to the Ballgame at the beginning and end of the meetings. Veterans who were on site for appointments or social events helped greet the participants in the parking lot and escorted them to the meeting room. The VASLHCS provided a safe, familiar environment in which the veterans and their caregivers could congregate and conduct other business as needed. Also, holding the meetings at VASLHCS reinforced that group members had 2 things in common: They were baseball fans, and they were veterans.
Conclusions
The baseball reminiscence support group helped promote camaraderie among veterans. This pilot project helped determine the feasibility and interest of the participants and volunteers and provided the following insights:
- Baseball reminiscence may appeal to men who do not feel comfortable in other types of support groups
- Properly trained facilitators were critical to the program
- Volunteers kept veterans engaged and promoted input from everyone
- Meeting reminders and follow-up calls kept caregivers apprised of activities
- Baseball is just one sport that can be used by a reminiscence group. Any sport that has a local fan base will provide volunteers and a core of interested veterans
- Memories of sporting events are traditionally exaggerated and rewritten as part of the social process, so there is no shame in forgetting facts or mixing up games
Support programs are often used with the hope of providing an improved QOL for participants. To document such outcomes, large, controlled, longitudinal studies are needed. Many patients with dementia and depression are unable to participate in these studies because of failing physical health, failing cognition, and caregiver fatigue. Pilot studies such as this one provide examples of social interventions that are not scientifically proven to be effective but are perceived to be of value by all involved: the veterans, their families, the volunteers, and the facilitators. This type of therapy provides a low-cost, social intervention and an opportunity for improved QOL and fun for veterans.
Author disclosures
The author reports no actual or potential conflicts of interest with regard to this article.
Disclaimer
The opinions expressed herein are those of the author and do not necessarily reflect those of Federal Practitioner, Frontline Medical Communications Inc., the U.S. Government, or any of its agencies. This article may discuss unlabeled or investigational use of certain drugs. Please review the complete prescribing information for specific drugs or drug combinations—including indications, contraindications, warnings, and adverse effects—before administering pharmacologic therapy to patients.
The number of older veterans with dementia and depression has posed a growing health care concern. Before its 2012 closure, the Geriatric Research Education and Clinical Center (GRECC) at the VA St. Louis Health Care System (VASLHCS) in Missouri addressed this concern by creating a baseball reminiscence group pilot study to provide social support for veterans with dementia and depression.
Related: Development and Evaluation of a Geriatric Mood Management Program
Reminiscence therapy improves self-esteem, enhances mood, and promotes communication skills. Reminiscence therapy stimulates participants to share memories, which is helpful in relieving depressive symptoms and has shown positive effects on cognition.1,2
Dementia Management
In 2010, 563,758 veterans were diagnosed with dementia, including Alzheimer disease (AD).3 Although pharmacologic management of AD may slow its progression, AD cannot be prevented or reversed, and the treatments may cause adverse effects.4 Therefore, participation in support groups and supportive services should also be explored.
Currently, 70% of individuals with AD live at home, and most would like to remain there. Family caregivers provide 80% of the care in the home. Depending on the value placed on informal home care, the annual cost per patient for dementia care can be estimated between $41,689 and $56,290.5 The financial burden on family caregivers as well as on the veterans with dementia is increasing and needs to be addressed to improve the quality of care. Support groups may improve the quality of life (QOL) and care for both veterans and their caregivers.
Group Characteristics
Hoping to expand treatment options that would positively impact veterans, the VASLHCS GRECC created a reminiscence support group with the goal of improving the QOL for veterans with a diagnosis of dementia and depression. The group was modeled after the football reminiscence project of Scotland.6
Men and women with an interest in baseball and a diagnosis of either depression or dementia were invited. The presence of a family caregiver improved the probability of the veteran joining the group.
Related: Home-Based Video Telehealth for Veterans With Dementia
Ten of the original 14 recruits finished the first year with the group; 2 dropped out, 1 died, and 1 could not find transportation to the meetings. Of the 10 participating veterans, 3 had a depression diagnosis (Geriatric Depression Scale [GDS] scores between 8 and 12) and 7 had a mild-to-moderate dementia diagnosis (Saint Louis University Mental Status Examination [SLUMS] exam scores between 12 and 19). Four participants served in World War II, 4 served in Korea, and 2 served in Vietnam. Nine of the recruits were male; 1 was female. During the first year, 1 veteran entered the on-campus community living center following a hospitalization. This veteran continued to meet with the group during rehabilitation and on discharge went to an assisted living facility that provided transportation to VASLHCS. He participated until he died in year 2.
Cardinals Reminiscence League
The group gathered every 2 weeks for facilitated discussions. Meetings included guest speakers and sessions in which participants shared baseball memories. Field trips to the St. Louis Cardinals stadium for a tour, the St. Louis Cardinals Hall of Fame and Museum, a Cardinals game, or a local radio station kept veterans engaged.
After each meeting, participants were given a Scorecard (Figure). The Scorecard included the group logo, which reflected both military and baseball themes; contained information about the time, location, and subject of the next meeting; and provided a brief description of the story the veteran had shared at the meeting.
Caregivers reported that the Scorecard allowed them to continue the discussion at home. One caregiver reported that the card often contained old baseball stories he had heard as a child. He expressed gratitude for hearing a “voice” that the family feared had been silenced by dementia.
At the end of the first year of the program, caregivers for the veterans with dementia expressed gratitude and reported an improved mood for the veterans when they discussed baseball at home. The SLUMS scores for these 7 patients had not changed significantly. The veterans with depression did not have caregivers, so no caregiver data were collected, but their self-reported statements indicated they felt more energetic and hopeful than they had felt before joining the group. However, all 3 veterans with a prior depression diagnosis declined requests to retake the GDS at the end of the first year.
Related: Delirium in the Cardiac ICU
The VASLHCS baseball reminiscence group had 3 important partners. The St. Louis chapter of the Alzheimer’s Association provided expertise in facilitator and volunteer training. Voluntary Services at VASLHCS actively recruited volunteers. The third partner was the St. Louis Cardinals. The St. Louis Cardinals Hall of Fame and Museum produced books with laminated iconic baseball pictures from their archives for the reminiscence group. Meetings began with a review of the books.
Holding meetings at VASLHCS had many benefits. Participants could schedule medical appointments on the days the group met, thereby reducing transportation demands. Other veterans often contributed to the program, which increased the festive, social nature of the meetings. For example, one veteran, who practiced piano as part of his regular therapy, played Take Me Out to the Ballgame at the beginning and end of the meetings. Veterans who were on site for appointments or social events helped greet the participants in the parking lot and escorted them to the meeting room. The VASLHCS provided a safe, familiar environment in which the veterans and their caregivers could congregate and conduct other business as needed. Also, holding the meetings at VASLHCS reinforced that group members had 2 things in common: They were baseball fans, and they were veterans.
Conclusions
The baseball reminiscence support group helped promote camaraderie among veterans. This pilot project helped determine the feasibility and interest of the participants and volunteers and provided the following insights:
- Baseball reminiscence may appeal to men who do not feel comfortable in other types of support groups
- Properly trained facilitators were critical to the program
- Volunteers kept veterans engaged and promoted input from everyone
- Meeting reminders and follow-up calls kept caregivers apprised of activities
- Baseball is just one sport that can be used by a reminiscence group. Any sport that has a local fan base will provide volunteers and a core of interested veterans
- Memories of sporting events are traditionally exaggerated and rewritten as part of the social process, so there is no shame in forgetting facts or mixing up games
Support programs are often used with the hope of providing an improved QOL for participants. To document such outcomes, large, controlled, longitudinal studies are needed. Many patients with dementia and depression are unable to participate in these studies because of failing physical health, failing cognition, and caregiver fatigue. Pilot studies such as this one provide examples of social interventions that are not scientifically proven to be effective but are perceived to be of value by all involved: the veterans, their families, the volunteers, and the facilitators. This type of therapy provides a low-cost, social intervention and an opportunity for improved QOL and fun for veterans.
Author disclosures
The author reports no actual or potential conflicts of interest with regard to this article.
Disclaimer
The opinions expressed herein are those of the author and do not necessarily reflect those of Federal Practitioner, Frontline Medical Communications Inc., the U.S. Government, or any of its agencies. This article may discuss unlabeled or investigational use of certain drugs. Please review the complete prescribing information for specific drugs or drug combinations—including indications, contraindications, warnings, and adverse effects—before administering pharmacologic therapy to patients.
1. Wu L-F, Chuo LJ, Wu ST. The effect of group instrumental reminiscence therapy in older single veterans who live in a veterans home in Taiwan. Int J Geriatr Psychiatry. 2012;27(1):107-108.
2. Van Bogaert P, Van Grinsven R, Tolson D, Wouters K, Engelborghs S, Van der Mussele S. Effects of SolCos model-based individual reminiscence on older adults with mild to moderate dementia due to Alzheimer disease: a pilot study. J Am Med Dir Assoc. 2013;14(7):528.e9-e13.
3. U.S. Department of Veterans Affairs, Veterans Health Administration, Health Services Research & Development Service. A systematic evidence review of non-pharmacological interventions for behavioral symptoms of dementia. U.S. Department of Veterans Affairs Website. http://www.hsrd.research.va.gov/publications/esp/Dementia-Nonpharm.pdf. Published March 2011. Accessed August 30, 2015.
4. Alzheimer's Association. 2013 Alzheimer's disease facts and figures. Alzheimers Dement. 2013;9(2):208-245.
5. Hurd MD, Martorell P, Delavande A, Mullen KJ, Langa KM. Monetary costs of dementia in the United States. N Engl J Med. 2013;368(14):1326-1334.
6. Tolson D, Schofield I. Football reminiscence for men with dementia: lessons from a realistic evaluation. Nurs Inq. 2012;19(1):63-70.
1. Wu L-F, Chuo LJ, Wu ST. The effect of group instrumental reminiscence therapy in older single veterans who live in a veterans home in Taiwan. Int J Geriatr Psychiatry. 2012;27(1):107-108.
2. Van Bogaert P, Van Grinsven R, Tolson D, Wouters K, Engelborghs S, Van der Mussele S. Effects of SolCos model-based individual reminiscence on older adults with mild to moderate dementia due to Alzheimer disease: a pilot study. J Am Med Dir Assoc. 2013;14(7):528.e9-e13.
3. U.S. Department of Veterans Affairs, Veterans Health Administration, Health Services Research & Development Service. A systematic evidence review of non-pharmacological interventions for behavioral symptoms of dementia. U.S. Department of Veterans Affairs Website. http://www.hsrd.research.va.gov/publications/esp/Dementia-Nonpharm.pdf. Published March 2011. Accessed August 30, 2015.
4. Alzheimer's Association. 2013 Alzheimer's disease facts and figures. Alzheimers Dement. 2013;9(2):208-245.
5. Hurd MD, Martorell P, Delavande A, Mullen KJ, Langa KM. Monetary costs of dementia in the United States. N Engl J Med. 2013;368(14):1326-1334.
6. Tolson D, Schofield I. Football reminiscence for men with dementia: lessons from a realistic evaluation. Nurs Inq. 2012;19(1):63-70.