User login
2016 Medicare fee schedule: What should you know?
The comments are in and shaping of the final Medicare Physician Fee Schedule for 2016 rests now in the hands of officials at the Centers for Medicare & Medicaid Services. What are the key provisions doctors need to know about to practice successfully in 2016? Experts gave their opinions in a webinar sponsored by the American Health Lawyers Association (AHLA).
Physician Quality Reporting System (PQRS)
CMS proposes to audit not only physician participants, but also vendors who submit quality measure data on behalf of doctors, under the 2016 proposed fee schedule. The agency recommends that vendors make available contact information for each eligible practitioner on behalf of whom it submits data and retain data submitted to CMS for PQRS for 7 years.
Doctors who fail to report on nine quality measures for PQRS will not automatically face trouble, according to Daniel F. Shay, a health law attorney in Philadelphia. In general, individual physicians in PQRS must report on at least nine measures covering three National Quality Strategy (NQS) domains for at least 50% of their Medicare patient base. But if fewer than nine measures are reported, physicians have the chance to explain themselves.
“In some cases, a practice may not have at least nine measures that apply to it, Mr. Shay said. “The [eligible practitioner] would then be able to report on fewer than nine measures, but would be subject to the measure application validity process, which basically means CMS audits the provider to prove they couldn’t have reported on all of the required measures.”
Also, CMS proposes extending participation in PQRS to doctors who practice in critical access hospitals, according to the 2016 proposed fee schedule. PQRS is a voluntary quality reporting program that applies adjustments to payments based on benchmarks. CMS is suggesting that physicians who practice in certain critical access hospitals now have the option to participate in the program – such doctors were previously excluded.
Incident to service
When overseeing care that is “incident to” service, CMS proposes that billing physicians also act as supervising physicians. The proposal could significantly impact group practices who do not typically use that structure, said Washington health law attorney Julie E. Kass during the AHLA webinar.
Incident to is defined as services furnished incident to a physician’s professional services over the course of a patient’s diagnosis or treatment. Medicare pays for services rendered by employees of a physician only when all “incident to” criteria are met. Those criteria include that services rendered by nonphysicians are under the direct supervision of a physician physically in the same office suite. In the proposed 2016 rule, CMS seeks to clarify that the billing physician must be the same physician who supervises the ancillary personnel. Previously, group practices may have billed under the provider who ordered the treatment, according to Ms. Kass.
“It sounds simple, but then you put it into the context of what happens in a real life practice,” she said. “I think a lot of practices, in operationalizing this rule, have generally used the ordering physician as the physician who billed for the service without paying a lot of attention to who was the actual supervising physician.”
Group practices may want to rethink how they bill for incident to services, and ensure the billing physician is the one who supervises the treatment, she advised.
The Stark Law
Proposed changes to regulations implementing the Stark Law could make it easier for physicians to hire new nonphysician providers (NPP) to provide primary care. Under the fee schedule proposal, hospitals would be allowed to assist in the recruitment of health professionals for physician practices. Currently, hospitals may not because remuneration could be considered a compensation relationship between the hospital and physician practice. The proposed change aims to promote care team collaboration and help curb primary care shortages.
The exception would permit recruitment assistance and retention payment from a hospital, rural health clinic, or federally qualified health center to a physician practice to employ an NPP. However, the NPP would have to be a bona fide employee of the physician practice and provide primary care services. CMS defines an NPP as a physician assistant, nurse practitioner, clinical nurse specialist, or certified nurse-midwife. CMS is also recommending a cap on the total remuneration and duration of assistance provided.
The limits aim to “make sure the physicians have skin in the game in bringing in the NPP,” Ms. Kass said. “It’s not all going to be the burden of hospital to provide recruiting assistance, but rather the physician has to need and want the NPP enough to be willing to bring them in as well without total support and assistance.”
Value-Based Payment Modifier Program
CMS proposes a new way to determine the extent of payment cuts and bonuses in the Value-Based Payment Modifier program. The program evaluates the performance of solo practitioners and groups on the quality and cost of care they provide to fee-for-service Medicare patients.
In 2016, the agency proposes to adjust payments based on the size of the participating group and to determine that size by reviewing claims data and its Provider Enrollment, Chain, and Ownership System (PECOS)-generated list. CMS would apply whichever number is lower in PECOS or claims data.
Now is a good time for doctors to check their PECOS data to ensure the information is accurate and up to date, Mr. Shay recommended.
As many expected, the Value-Based Payment Modifier is slowly expanding to encompass more physicians. Beginning Jan. 1, 2015, the value modifier was applied to physician payments under the fee schedule for groups of 100 or more. In January 2016, it will be applied to physician payments for doctors in groups of 10 or more. In 2017, the modifier will apply to solo practitioners and physicians in groups of two or more. (All modifiers are based on performance periods 2 years prior.)
PQRS will continue to play a central role in the Value-Based Payment Modifier system, Mr. Shay added. CMS is proposing to use the PQRS reporting period for 2016 as the basis for the 2018 value modifier. The agency will draw from the group reporting option and individual EP reporting mechanisms proposed for 2016.
“We’re seeing just more interconnection between these two systems,” Mr. Shay said.
Physician Compare
Physicians should expect to have more information about their performance reported to the Physician Compare website under the proposed 2016 fee schedule. The site already continues information on physician education, location, group affiliations, and status in quality programs. CMS now wants to include performance rates on 2015 PQRS cardiovascular disease prevention measures for doctors who report them, in support of the Million Hearts program. Additionally, CMS proposes that groups receiving a pay increase under the Value-Based Payment Modifier Program report the data to the website. Doctors also would continue reporting information about patient experiences under the Consumer Assessment of Healthcare Providers & Systems (CAHPS) survey program. The surveys are designed to capture a patient’s experience receiving care from their physician.
Mr. Shay noted that one concern with the Physician Compare website is that doctors have little recourse to challenge information on the site. Physicians have only a 30-day window to review information about themselves and correct errors.
“There is no formal appeals mechanism for the website,” Mr. Shay.
CMS is currently reviewing feedback and comments submitted about the proposed physician fee schedule before issuing the final schedule, usually in November.
On Twitter @legal_med
The comments are in and shaping of the final Medicare Physician Fee Schedule for 2016 rests now in the hands of officials at the Centers for Medicare & Medicaid Services. What are the key provisions doctors need to know about to practice successfully in 2016? Experts gave their opinions in a webinar sponsored by the American Health Lawyers Association (AHLA).
Physician Quality Reporting System (PQRS)
CMS proposes to audit not only physician participants, but also vendors who submit quality measure data on behalf of doctors, under the 2016 proposed fee schedule. The agency recommends that vendors make available contact information for each eligible practitioner on behalf of whom it submits data and retain data submitted to CMS for PQRS for 7 years.
Doctors who fail to report on nine quality measures for PQRS will not automatically face trouble, according to Daniel F. Shay, a health law attorney in Philadelphia. In general, individual physicians in PQRS must report on at least nine measures covering three National Quality Strategy (NQS) domains for at least 50% of their Medicare patient base. But if fewer than nine measures are reported, physicians have the chance to explain themselves.
“In some cases, a practice may not have at least nine measures that apply to it, Mr. Shay said. “The [eligible practitioner] would then be able to report on fewer than nine measures, but would be subject to the measure application validity process, which basically means CMS audits the provider to prove they couldn’t have reported on all of the required measures.”
Also, CMS proposes extending participation in PQRS to doctors who practice in critical access hospitals, according to the 2016 proposed fee schedule. PQRS is a voluntary quality reporting program that applies adjustments to payments based on benchmarks. CMS is suggesting that physicians who practice in certain critical access hospitals now have the option to participate in the program – such doctors were previously excluded.
Incident to service
When overseeing care that is “incident to” service, CMS proposes that billing physicians also act as supervising physicians. The proposal could significantly impact group practices who do not typically use that structure, said Washington health law attorney Julie E. Kass during the AHLA webinar.
Incident to is defined as services furnished incident to a physician’s professional services over the course of a patient’s diagnosis or treatment. Medicare pays for services rendered by employees of a physician only when all “incident to” criteria are met. Those criteria include that services rendered by nonphysicians are under the direct supervision of a physician physically in the same office suite. In the proposed 2016 rule, CMS seeks to clarify that the billing physician must be the same physician who supervises the ancillary personnel. Previously, group practices may have billed under the provider who ordered the treatment, according to Ms. Kass.
“It sounds simple, but then you put it into the context of what happens in a real life practice,” she said. “I think a lot of practices, in operationalizing this rule, have generally used the ordering physician as the physician who billed for the service without paying a lot of attention to who was the actual supervising physician.”
Group practices may want to rethink how they bill for incident to services, and ensure the billing physician is the one who supervises the treatment, she advised.
The Stark Law
Proposed changes to regulations implementing the Stark Law could make it easier for physicians to hire new nonphysician providers (NPP) to provide primary care. Under the fee schedule proposal, hospitals would be allowed to assist in the recruitment of health professionals for physician practices. Currently, hospitals may not because remuneration could be considered a compensation relationship between the hospital and physician practice. The proposed change aims to promote care team collaboration and help curb primary care shortages.
The exception would permit recruitment assistance and retention payment from a hospital, rural health clinic, or federally qualified health center to a physician practice to employ an NPP. However, the NPP would have to be a bona fide employee of the physician practice and provide primary care services. CMS defines an NPP as a physician assistant, nurse practitioner, clinical nurse specialist, or certified nurse-midwife. CMS is also recommending a cap on the total remuneration and duration of assistance provided.
The limits aim to “make sure the physicians have skin in the game in bringing in the NPP,” Ms. Kass said. “It’s not all going to be the burden of hospital to provide recruiting assistance, but rather the physician has to need and want the NPP enough to be willing to bring them in as well without total support and assistance.”
Value-Based Payment Modifier Program
CMS proposes a new way to determine the extent of payment cuts and bonuses in the Value-Based Payment Modifier program. The program evaluates the performance of solo practitioners and groups on the quality and cost of care they provide to fee-for-service Medicare patients.
In 2016, the agency proposes to adjust payments based on the size of the participating group and to determine that size by reviewing claims data and its Provider Enrollment, Chain, and Ownership System (PECOS)-generated list. CMS would apply whichever number is lower in PECOS or claims data.
Now is a good time for doctors to check their PECOS data to ensure the information is accurate and up to date, Mr. Shay recommended.
As many expected, the Value-Based Payment Modifier is slowly expanding to encompass more physicians. Beginning Jan. 1, 2015, the value modifier was applied to physician payments under the fee schedule for groups of 100 or more. In January 2016, it will be applied to physician payments for doctors in groups of 10 or more. In 2017, the modifier will apply to solo practitioners and physicians in groups of two or more. (All modifiers are based on performance periods 2 years prior.)
PQRS will continue to play a central role in the Value-Based Payment Modifier system, Mr. Shay added. CMS is proposing to use the PQRS reporting period for 2016 as the basis for the 2018 value modifier. The agency will draw from the group reporting option and individual EP reporting mechanisms proposed for 2016.
“We’re seeing just more interconnection between these two systems,” Mr. Shay said.
Physician Compare
Physicians should expect to have more information about their performance reported to the Physician Compare website under the proposed 2016 fee schedule. The site already continues information on physician education, location, group affiliations, and status in quality programs. CMS now wants to include performance rates on 2015 PQRS cardiovascular disease prevention measures for doctors who report them, in support of the Million Hearts program. Additionally, CMS proposes that groups receiving a pay increase under the Value-Based Payment Modifier Program report the data to the website. Doctors also would continue reporting information about patient experiences under the Consumer Assessment of Healthcare Providers & Systems (CAHPS) survey program. The surveys are designed to capture a patient’s experience receiving care from their physician.
Mr. Shay noted that one concern with the Physician Compare website is that doctors have little recourse to challenge information on the site. Physicians have only a 30-day window to review information about themselves and correct errors.
“There is no formal appeals mechanism for the website,” Mr. Shay.
CMS is currently reviewing feedback and comments submitted about the proposed physician fee schedule before issuing the final schedule, usually in November.
On Twitter @legal_med
The comments are in and shaping of the final Medicare Physician Fee Schedule for 2016 rests now in the hands of officials at the Centers for Medicare & Medicaid Services. What are the key provisions doctors need to know about to practice successfully in 2016? Experts gave their opinions in a webinar sponsored by the American Health Lawyers Association (AHLA).
Physician Quality Reporting System (PQRS)
CMS proposes to audit not only physician participants, but also vendors who submit quality measure data on behalf of doctors, under the 2016 proposed fee schedule. The agency recommends that vendors make available contact information for each eligible practitioner on behalf of whom it submits data and retain data submitted to CMS for PQRS for 7 years.
Doctors who fail to report on nine quality measures for PQRS will not automatically face trouble, according to Daniel F. Shay, a health law attorney in Philadelphia. In general, individual physicians in PQRS must report on at least nine measures covering three National Quality Strategy (NQS) domains for at least 50% of their Medicare patient base. But if fewer than nine measures are reported, physicians have the chance to explain themselves.
“In some cases, a practice may not have at least nine measures that apply to it, Mr. Shay said. “The [eligible practitioner] would then be able to report on fewer than nine measures, but would be subject to the measure application validity process, which basically means CMS audits the provider to prove they couldn’t have reported on all of the required measures.”
Also, CMS proposes extending participation in PQRS to doctors who practice in critical access hospitals, according to the 2016 proposed fee schedule. PQRS is a voluntary quality reporting program that applies adjustments to payments based on benchmarks. CMS is suggesting that physicians who practice in certain critical access hospitals now have the option to participate in the program – such doctors were previously excluded.
Incident to service
When overseeing care that is “incident to” service, CMS proposes that billing physicians also act as supervising physicians. The proposal could significantly impact group practices who do not typically use that structure, said Washington health law attorney Julie E. Kass during the AHLA webinar.
Incident to is defined as services furnished incident to a physician’s professional services over the course of a patient’s diagnosis or treatment. Medicare pays for services rendered by employees of a physician only when all “incident to” criteria are met. Those criteria include that services rendered by nonphysicians are under the direct supervision of a physician physically in the same office suite. In the proposed 2016 rule, CMS seeks to clarify that the billing physician must be the same physician who supervises the ancillary personnel. Previously, group practices may have billed under the provider who ordered the treatment, according to Ms. Kass.
“It sounds simple, but then you put it into the context of what happens in a real life practice,” she said. “I think a lot of practices, in operationalizing this rule, have generally used the ordering physician as the physician who billed for the service without paying a lot of attention to who was the actual supervising physician.”
Group practices may want to rethink how they bill for incident to services, and ensure the billing physician is the one who supervises the treatment, she advised.
The Stark Law
Proposed changes to regulations implementing the Stark Law could make it easier for physicians to hire new nonphysician providers (NPP) to provide primary care. Under the fee schedule proposal, hospitals would be allowed to assist in the recruitment of health professionals for physician practices. Currently, hospitals may not because remuneration could be considered a compensation relationship between the hospital and physician practice. The proposed change aims to promote care team collaboration and help curb primary care shortages.
The exception would permit recruitment assistance and retention payment from a hospital, rural health clinic, or federally qualified health center to a physician practice to employ an NPP. However, the NPP would have to be a bona fide employee of the physician practice and provide primary care services. CMS defines an NPP as a physician assistant, nurse practitioner, clinical nurse specialist, or certified nurse-midwife. CMS is also recommending a cap on the total remuneration and duration of assistance provided.
The limits aim to “make sure the physicians have skin in the game in bringing in the NPP,” Ms. Kass said. “It’s not all going to be the burden of hospital to provide recruiting assistance, but rather the physician has to need and want the NPP enough to be willing to bring them in as well without total support and assistance.”
Value-Based Payment Modifier Program
CMS proposes a new way to determine the extent of payment cuts and bonuses in the Value-Based Payment Modifier program. The program evaluates the performance of solo practitioners and groups on the quality and cost of care they provide to fee-for-service Medicare patients.
In 2016, the agency proposes to adjust payments based on the size of the participating group and to determine that size by reviewing claims data and its Provider Enrollment, Chain, and Ownership System (PECOS)-generated list. CMS would apply whichever number is lower in PECOS or claims data.
Now is a good time for doctors to check their PECOS data to ensure the information is accurate and up to date, Mr. Shay recommended.
As many expected, the Value-Based Payment Modifier is slowly expanding to encompass more physicians. Beginning Jan. 1, 2015, the value modifier was applied to physician payments under the fee schedule for groups of 100 or more. In January 2016, it will be applied to physician payments for doctors in groups of 10 or more. In 2017, the modifier will apply to solo practitioners and physicians in groups of two or more. (All modifiers are based on performance periods 2 years prior.)
PQRS will continue to play a central role in the Value-Based Payment Modifier system, Mr. Shay added. CMS is proposing to use the PQRS reporting period for 2016 as the basis for the 2018 value modifier. The agency will draw from the group reporting option and individual EP reporting mechanisms proposed for 2016.
“We’re seeing just more interconnection between these two systems,” Mr. Shay said.
Physician Compare
Physicians should expect to have more information about their performance reported to the Physician Compare website under the proposed 2016 fee schedule. The site already continues information on physician education, location, group affiliations, and status in quality programs. CMS now wants to include performance rates on 2015 PQRS cardiovascular disease prevention measures for doctors who report them, in support of the Million Hearts program. Additionally, CMS proposes that groups receiving a pay increase under the Value-Based Payment Modifier Program report the data to the website. Doctors also would continue reporting information about patient experiences under the Consumer Assessment of Healthcare Providers & Systems (CAHPS) survey program. The surveys are designed to capture a patient’s experience receiving care from their physician.
Mr. Shay noted that one concern with the Physician Compare website is that doctors have little recourse to challenge information on the site. Physicians have only a 30-day window to review information about themselves and correct errors.
“There is no formal appeals mechanism for the website,” Mr. Shay.
CMS is currently reviewing feedback and comments submitted about the proposed physician fee schedule before issuing the final schedule, usually in November.
On Twitter @legal_med
ICD-10 testers recommend certified coders, lighter loads for October
The advice from those who have already tried coding with ICD-10? Hire a certified coder if you don’t have one on staff already.
“If a physician office doesn’t have a certified coder, it should,” according to Penny Osmon Bahr, director of Avastone Health Solutions, who took part in the final International Classification of Disease, tenth revision, “end-to-end” test conducted by the Centers for Medicare & Medicaid in July. “That’s just plain and simple.”
Ms. Osmon Bahr described coding as “the pulse point of how data are really consumed,” whether via ICD-10 or part of value-based contracting, research on patient outcomes, or incentives being driven by the CMS. “It takes coders to ensure that the data that is going out truly represents your patient population and the patients that you are treating.”
Some physician practices “haven’t invested in education for staff to become knowledgeable in coding or certified in coding. That could be a struggle as the world continues to evolve.”
Another bit of advice: Scale back on the number of patient visits you book in October. That will give extra time to learn and incorporate ICD-10 into work flows.
“One of the things that we’ve encouraged our physicians to do is they need to lighten their schedules in October to prepare for ICD-10 to make sure they are completing the documentation that’s needed and coding with the current codes,” Lori Albano, manager of EDI development and support with practice management and EHR software vendor Nextgen Healthcare of Atlanta. “So maybe the first 2 weeks they lighten [appointments] by 20%” and then set up a specific schedule to ramp back up to full capacity.
Ms. Albano also recommended a focused approach to learning new codes to help avoid being overwhelmed.
“Take the top 50-100 ICD-9 codes that you currently use and become familiar with those ICD-10 codes and the documentation required to support them,” she said. “Start documenting on that level now.”
Ms. Osmon Bahr also stressed thorough documentation.
“You always want to tell the most specific story about your patient that you can,” she said, based on the greater number and specificity of the ICD-10 code set.
Ms. Osmon Bahr and Ms. Albano both spoke positively of the experience of testing and said that CMS appears ready to make the transition. The agency announced on Aug. 28 that its final round of end-to-end testing found no new issues and that no CMS front-end issues led to claims rejections. Previous issues in prior test rounds have been resolved, the agency noted.
The advice from those who have already tried coding with ICD-10? Hire a certified coder if you don’t have one on staff already.
“If a physician office doesn’t have a certified coder, it should,” according to Penny Osmon Bahr, director of Avastone Health Solutions, who took part in the final International Classification of Disease, tenth revision, “end-to-end” test conducted by the Centers for Medicare & Medicaid in July. “That’s just plain and simple.”
Ms. Osmon Bahr described coding as “the pulse point of how data are really consumed,” whether via ICD-10 or part of value-based contracting, research on patient outcomes, or incentives being driven by the CMS. “It takes coders to ensure that the data that is going out truly represents your patient population and the patients that you are treating.”
Some physician practices “haven’t invested in education for staff to become knowledgeable in coding or certified in coding. That could be a struggle as the world continues to evolve.”
Another bit of advice: Scale back on the number of patient visits you book in October. That will give extra time to learn and incorporate ICD-10 into work flows.
“One of the things that we’ve encouraged our physicians to do is they need to lighten their schedules in October to prepare for ICD-10 to make sure they are completing the documentation that’s needed and coding with the current codes,” Lori Albano, manager of EDI development and support with practice management and EHR software vendor Nextgen Healthcare of Atlanta. “So maybe the first 2 weeks they lighten [appointments] by 20%” and then set up a specific schedule to ramp back up to full capacity.
Ms. Albano also recommended a focused approach to learning new codes to help avoid being overwhelmed.
“Take the top 50-100 ICD-9 codes that you currently use and become familiar with those ICD-10 codes and the documentation required to support them,” she said. “Start documenting on that level now.”
Ms. Osmon Bahr also stressed thorough documentation.
“You always want to tell the most specific story about your patient that you can,” she said, based on the greater number and specificity of the ICD-10 code set.
Ms. Osmon Bahr and Ms. Albano both spoke positively of the experience of testing and said that CMS appears ready to make the transition. The agency announced on Aug. 28 that its final round of end-to-end testing found no new issues and that no CMS front-end issues led to claims rejections. Previous issues in prior test rounds have been resolved, the agency noted.
The advice from those who have already tried coding with ICD-10? Hire a certified coder if you don’t have one on staff already.
“If a physician office doesn’t have a certified coder, it should,” according to Penny Osmon Bahr, director of Avastone Health Solutions, who took part in the final International Classification of Disease, tenth revision, “end-to-end” test conducted by the Centers for Medicare & Medicaid in July. “That’s just plain and simple.”
Ms. Osmon Bahr described coding as “the pulse point of how data are really consumed,” whether via ICD-10 or part of value-based contracting, research on patient outcomes, or incentives being driven by the CMS. “It takes coders to ensure that the data that is going out truly represents your patient population and the patients that you are treating.”
Some physician practices “haven’t invested in education for staff to become knowledgeable in coding or certified in coding. That could be a struggle as the world continues to evolve.”
Another bit of advice: Scale back on the number of patient visits you book in October. That will give extra time to learn and incorporate ICD-10 into work flows.
“One of the things that we’ve encouraged our physicians to do is they need to lighten their schedules in October to prepare for ICD-10 to make sure they are completing the documentation that’s needed and coding with the current codes,” Lori Albano, manager of EDI development and support with practice management and EHR software vendor Nextgen Healthcare of Atlanta. “So maybe the first 2 weeks they lighten [appointments] by 20%” and then set up a specific schedule to ramp back up to full capacity.
Ms. Albano also recommended a focused approach to learning new codes to help avoid being overwhelmed.
“Take the top 50-100 ICD-9 codes that you currently use and become familiar with those ICD-10 codes and the documentation required to support them,” she said. “Start documenting on that level now.”
Ms. Osmon Bahr also stressed thorough documentation.
“You always want to tell the most specific story about your patient that you can,” she said, based on the greater number and specificity of the ICD-10 code set.
Ms. Osmon Bahr and Ms. Albano both spoke positively of the experience of testing and said that CMS appears ready to make the transition. The agency announced on Aug. 28 that its final round of end-to-end testing found no new issues and that no CMS front-end issues led to claims rejections. Previous issues in prior test rounds have been resolved, the agency noted.
PQRS: Window is short to dispute the 2% pay cut
Assessments are complete, and the Centers for Medicare & Medicaid Services has determined which physician practices will face a pay cut – officially, a “downward payment adjustment” – for failing to comply with the Physician Quality Reporting System (PQRS). Doctors have just 2 months to challenge findings that they believe were made in error to spare themselves a cut in 2016.
The pay cut will apply to individual eligible practitioners and PQRS group practices that did not satisfactorily report data on quality measures in 2014. The 2% cut will be applied to all Part B covered services, according to a Sept. 9 CMS announcement.
To learn whether they are subject to the cut, physicians can review their 2014 PQRS feedback reports, which became available Sept. 8. The reports apply to doctors who submitted quality data in calendar year 2014. Feedback reports for 2015 will be available approximately this time next year.
To challenge PQRS determinations, physicians can submit an informal review between Sept. 9 and Nov. 9 and request that the CMS reevaluate incentive eligibility and adjustment determinations. Those requests can be made through the quality reporting portal. Physicians who request a review will be contacted via email of a final decision by the CMS within 90 days of their request. All decisions will be final and there will be no further review or appeal, according to the CMS.
It should not be surprising that physicians who did not satisfactorily comply with PQRS will see a 2% pay cut next year, said David Harlow, a health law and policy attorney based in Newton, Mass. What’s unusual, however, is that the informal review process does not include an avenue for an independent evaluation, Mr. Harlow said.
“It’s CMS reviewing a CMS decision,” he said in an interview. “From a provider perspective, there might be some skepticism about the independence of that review. CMS says this is not something that is subject to further administrative or judicial review. So there’s not an appeal.”
Mr. Harlow said that he would not be surprised if physician organizations advocate for further judicial relief in the process. CMS has previously provided avenues for administrative or judicial appeals of its decisions in other programs, he noted.
In its announcement, the agency outlined the ways in which physicians could have avoided the coming pay cut. This included reporting nine measures across three domains for 50% of Medicare patients, completing the GPRO Web Interface, or reporting at least one registry measures group for 20 patients, at least 11 of whom were Medicare Part B patients. Additionally, doctors could have reported three measures across one domain for 50% of Medicare patients, or satisfactorily participated in a qualified clinical data registry.
On Twitter @legal_med
Assessments are complete, and the Centers for Medicare & Medicaid Services has determined which physician practices will face a pay cut – officially, a “downward payment adjustment” – for failing to comply with the Physician Quality Reporting System (PQRS). Doctors have just 2 months to challenge findings that they believe were made in error to spare themselves a cut in 2016.
The pay cut will apply to individual eligible practitioners and PQRS group practices that did not satisfactorily report data on quality measures in 2014. The 2% cut will be applied to all Part B covered services, according to a Sept. 9 CMS announcement.
To learn whether they are subject to the cut, physicians can review their 2014 PQRS feedback reports, which became available Sept. 8. The reports apply to doctors who submitted quality data in calendar year 2014. Feedback reports for 2015 will be available approximately this time next year.
To challenge PQRS determinations, physicians can submit an informal review between Sept. 9 and Nov. 9 and request that the CMS reevaluate incentive eligibility and adjustment determinations. Those requests can be made through the quality reporting portal. Physicians who request a review will be contacted via email of a final decision by the CMS within 90 days of their request. All decisions will be final and there will be no further review or appeal, according to the CMS.
It should not be surprising that physicians who did not satisfactorily comply with PQRS will see a 2% pay cut next year, said David Harlow, a health law and policy attorney based in Newton, Mass. What’s unusual, however, is that the informal review process does not include an avenue for an independent evaluation, Mr. Harlow said.
“It’s CMS reviewing a CMS decision,” he said in an interview. “From a provider perspective, there might be some skepticism about the independence of that review. CMS says this is not something that is subject to further administrative or judicial review. So there’s not an appeal.”
Mr. Harlow said that he would not be surprised if physician organizations advocate for further judicial relief in the process. CMS has previously provided avenues for administrative or judicial appeals of its decisions in other programs, he noted.
In its announcement, the agency outlined the ways in which physicians could have avoided the coming pay cut. This included reporting nine measures across three domains for 50% of Medicare patients, completing the GPRO Web Interface, or reporting at least one registry measures group for 20 patients, at least 11 of whom were Medicare Part B patients. Additionally, doctors could have reported three measures across one domain for 50% of Medicare patients, or satisfactorily participated in a qualified clinical data registry.
On Twitter @legal_med
Assessments are complete, and the Centers for Medicare & Medicaid Services has determined which physician practices will face a pay cut – officially, a “downward payment adjustment” – for failing to comply with the Physician Quality Reporting System (PQRS). Doctors have just 2 months to challenge findings that they believe were made in error to spare themselves a cut in 2016.
The pay cut will apply to individual eligible practitioners and PQRS group practices that did not satisfactorily report data on quality measures in 2014. The 2% cut will be applied to all Part B covered services, according to a Sept. 9 CMS announcement.
To learn whether they are subject to the cut, physicians can review their 2014 PQRS feedback reports, which became available Sept. 8. The reports apply to doctors who submitted quality data in calendar year 2014. Feedback reports for 2015 will be available approximately this time next year.
To challenge PQRS determinations, physicians can submit an informal review between Sept. 9 and Nov. 9 and request that the CMS reevaluate incentive eligibility and adjustment determinations. Those requests can be made through the quality reporting portal. Physicians who request a review will be contacted via email of a final decision by the CMS within 90 days of their request. All decisions will be final and there will be no further review or appeal, according to the CMS.
It should not be surprising that physicians who did not satisfactorily comply with PQRS will see a 2% pay cut next year, said David Harlow, a health law and policy attorney based in Newton, Mass. What’s unusual, however, is that the informal review process does not include an avenue for an independent evaluation, Mr. Harlow said.
“It’s CMS reviewing a CMS decision,” he said in an interview. “From a provider perspective, there might be some skepticism about the independence of that review. CMS says this is not something that is subject to further administrative or judicial review. So there’s not an appeal.”
Mr. Harlow said that he would not be surprised if physician organizations advocate for further judicial relief in the process. CMS has previously provided avenues for administrative or judicial appeals of its decisions in other programs, he noted.
In its announcement, the agency outlined the ways in which physicians could have avoided the coming pay cut. This included reporting nine measures across three domains for 50% of Medicare patients, completing the GPRO Web Interface, or reporting at least one registry measures group for 20 patients, at least 11 of whom were Medicare Part B patients. Additionally, doctors could have reported three measures across one domain for 50% of Medicare patients, or satisfactorily participated in a qualified clinical data registry.
On Twitter @legal_med
Hospitalists' Role in Improving Patient Experience: A Baldridge Winner's Perspective
Understanding and improving the patient care experience has become a vital component of delivering high quality care. According to a new survey of American Society for Quality (ASQ) healthcare quality experts, more than 80% of respondents said improving communications between caregivers and patients and easing access to treatment across the entire continuum of care should be top priorities for improving patient experience. For Hill Country Memorial (HCM) in Fredericksburg, Texas, winner of the Malcolm Baldrige National Quality Award, accomplishing this kind of top-level patient experience performance involved engaging physicians—particularly hospitalists—using voice of the customer (VOC) input.
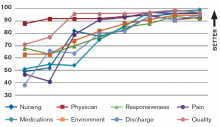
HCM did not achieve overnight success, however; instead, the facility achieved year-over-year improvement in finance and growth, patient experience, quality of care, and workforce environment and engagement (see Figure 1).
HCM developed a systematic VOC input-to-action process in which listening and learning methods during annual planning led them to institute a hospitalist program. Results included:
- Improved access to primary care, achieved by increasing the physicians’ hours of availability in their clinics, and improved work-life balance, enhancing engagement and alignment of the medical staff and HCM;
- Reductions in delays in admissions, discharges, and length of stay; and
- Real-time review and management of clinical data, not just during the daily rounding as had been done previously.
One of the major hurdles in the way of achieving patient satisfaction, according to the ASQ patient experience survey, is care that is fragmented and uncoordinated because of communication issues. HCM has overcome those hurdles using strategies such as a daily afternoon huddle in which hospitalists meet with a multidisciplinary team so that everyone understands patient action plans and current concerns. The process of discharge planning begins in these huddles so that more complex issues are initiated on day one of the hospital stay.
A new rounding communication process, called GIFT for greet, inform, find out, and time, has dramatically improved patient satisfaction and engagement. GIFT enables hospitalists to greet a patient with a personal introduction and an explanation of their position and responsibilities. Hospitalists always sit while engaging the patient, and they make it a point to acknowledge not only the patient but everyone present in the room. Personalized “baseball cards” featuring the hospitalist’s background, including personal interests and hobbies, are handed out to patients or family members. Hospitalists take time to inform the patient and appropriate family members and caregivers of all diagnostic test results and the clinical response of treatment to date. Treatment plans and further diagnostic tests or procedures are discussed. A report of all consultants who have joined or will be joining in the care, along with their roles in the treatment planned, is fully vetted.
One key to a successful patient experience is discovering the concerns of the patient, family members, friends, and caregivers. Emotional issues become as important as the physical needs of the patient; these are openly addressed. Ask not “What’s the matter?” but instead “What matters to you?”
Timing the hospitalist’s return to see the patient and the anticipated date of transition of care is the last item in the rounding interaction. The date should be as accurate as possible to reduce patient anxiety and help the patient understand that the hospitalist really cares.
The hospitalist program has also strengthened the relationship between nurses and physicians. Nurses know the hospitalists’ practice patterns well, which allows them to help manage patient interactions and minimize patient anxiety and frustration. The physician-patient relationship is reinforced when nurse leaders include hospitalist satisfaction questions during daily rounding to identify concerns that can be clarified or resolved in real time.
The systematic VOC approach has enabled HCM to design, manage, and improve its key work process at multiple levels of the organization. These processes are reviewed and refined periodically to respond to the changing healthcare environment and stay focused on creating value for customers.
Chip Caldwell is chairman of Caldwell Butler, a firm specializing in coaching organizations to achieve world class performance in margin improvement, patient experience, physician/clinical enterprise, and capacity optimization. Jayne Pope, MBA, RN, is CEO of Hill Country Memorial Hospital in Fredericksburg, Texas. James Partin, MD, is CMO at Hill Country Memorial.
Understanding and improving the patient care experience has become a vital component of delivering high quality care. According to a new survey of American Society for Quality (ASQ) healthcare quality experts, more than 80% of respondents said improving communications between caregivers and patients and easing access to treatment across the entire continuum of care should be top priorities for improving patient experience. For Hill Country Memorial (HCM) in Fredericksburg, Texas, winner of the Malcolm Baldrige National Quality Award, accomplishing this kind of top-level patient experience performance involved engaging physicians—particularly hospitalists—using voice of the customer (VOC) input.
HCM did not achieve overnight success, however; instead, the facility achieved year-over-year improvement in finance and growth, patient experience, quality of care, and workforce environment and engagement (see Figure 1).
HCM developed a systematic VOC input-to-action process in which listening and learning methods during annual planning led them to institute a hospitalist program. Results included:
- Improved access to primary care, achieved by increasing the physicians’ hours of availability in their clinics, and improved work-life balance, enhancing engagement and alignment of the medical staff and HCM;
- Reductions in delays in admissions, discharges, and length of stay; and
- Real-time review and management of clinical data, not just during the daily rounding as had been done previously.
One of the major hurdles in the way of achieving patient satisfaction, according to the ASQ patient experience survey, is care that is fragmented and uncoordinated because of communication issues. HCM has overcome those hurdles using strategies such as a daily afternoon huddle in which hospitalists meet with a multidisciplinary team so that everyone understands patient action plans and current concerns. The process of discharge planning begins in these huddles so that more complex issues are initiated on day one of the hospital stay.
A new rounding communication process, called GIFT for greet, inform, find out, and time, has dramatically improved patient satisfaction and engagement. GIFT enables hospitalists to greet a patient with a personal introduction and an explanation of their position and responsibilities. Hospitalists always sit while engaging the patient, and they make it a point to acknowledge not only the patient but everyone present in the room. Personalized “baseball cards” featuring the hospitalist’s background, including personal interests and hobbies, are handed out to patients or family members. Hospitalists take time to inform the patient and appropriate family members and caregivers of all diagnostic test results and the clinical response of treatment to date. Treatment plans and further diagnostic tests or procedures are discussed. A report of all consultants who have joined or will be joining in the care, along with their roles in the treatment planned, is fully vetted.
One key to a successful patient experience is discovering the concerns of the patient, family members, friends, and caregivers. Emotional issues become as important as the physical needs of the patient; these are openly addressed. Ask not “What’s the matter?” but instead “What matters to you?”
Timing the hospitalist’s return to see the patient and the anticipated date of transition of care is the last item in the rounding interaction. The date should be as accurate as possible to reduce patient anxiety and help the patient understand that the hospitalist really cares.
The hospitalist program has also strengthened the relationship between nurses and physicians. Nurses know the hospitalists’ practice patterns well, which allows them to help manage patient interactions and minimize patient anxiety and frustration. The physician-patient relationship is reinforced when nurse leaders include hospitalist satisfaction questions during daily rounding to identify concerns that can be clarified or resolved in real time.
The systematic VOC approach has enabled HCM to design, manage, and improve its key work process at multiple levels of the organization. These processes are reviewed and refined periodically to respond to the changing healthcare environment and stay focused on creating value for customers.
Chip Caldwell is chairman of Caldwell Butler, a firm specializing in coaching organizations to achieve world class performance in margin improvement, patient experience, physician/clinical enterprise, and capacity optimization. Jayne Pope, MBA, RN, is CEO of Hill Country Memorial Hospital in Fredericksburg, Texas. James Partin, MD, is CMO at Hill Country Memorial.
Understanding and improving the patient care experience has become a vital component of delivering high quality care. According to a new survey of American Society for Quality (ASQ) healthcare quality experts, more than 80% of respondents said improving communications between caregivers and patients and easing access to treatment across the entire continuum of care should be top priorities for improving patient experience. For Hill Country Memorial (HCM) in Fredericksburg, Texas, winner of the Malcolm Baldrige National Quality Award, accomplishing this kind of top-level patient experience performance involved engaging physicians—particularly hospitalists—using voice of the customer (VOC) input.
HCM did not achieve overnight success, however; instead, the facility achieved year-over-year improvement in finance and growth, patient experience, quality of care, and workforce environment and engagement (see Figure 1).
HCM developed a systematic VOC input-to-action process in which listening and learning methods during annual planning led them to institute a hospitalist program. Results included:
- Improved access to primary care, achieved by increasing the physicians’ hours of availability in their clinics, and improved work-life balance, enhancing engagement and alignment of the medical staff and HCM;
- Reductions in delays in admissions, discharges, and length of stay; and
- Real-time review and management of clinical data, not just during the daily rounding as had been done previously.
One of the major hurdles in the way of achieving patient satisfaction, according to the ASQ patient experience survey, is care that is fragmented and uncoordinated because of communication issues. HCM has overcome those hurdles using strategies such as a daily afternoon huddle in which hospitalists meet with a multidisciplinary team so that everyone understands patient action plans and current concerns. The process of discharge planning begins in these huddles so that more complex issues are initiated on day one of the hospital stay.
A new rounding communication process, called GIFT for greet, inform, find out, and time, has dramatically improved patient satisfaction and engagement. GIFT enables hospitalists to greet a patient with a personal introduction and an explanation of their position and responsibilities. Hospitalists always sit while engaging the patient, and they make it a point to acknowledge not only the patient but everyone present in the room. Personalized “baseball cards” featuring the hospitalist’s background, including personal interests and hobbies, are handed out to patients or family members. Hospitalists take time to inform the patient and appropriate family members and caregivers of all diagnostic test results and the clinical response of treatment to date. Treatment plans and further diagnostic tests or procedures are discussed. A report of all consultants who have joined or will be joining in the care, along with their roles in the treatment planned, is fully vetted.
One key to a successful patient experience is discovering the concerns of the patient, family members, friends, and caregivers. Emotional issues become as important as the physical needs of the patient; these are openly addressed. Ask not “What’s the matter?” but instead “What matters to you?”
Timing the hospitalist’s return to see the patient and the anticipated date of transition of care is the last item in the rounding interaction. The date should be as accurate as possible to reduce patient anxiety and help the patient understand that the hospitalist really cares.
The hospitalist program has also strengthened the relationship between nurses and physicians. Nurses know the hospitalists’ practice patterns well, which allows them to help manage patient interactions and minimize patient anxiety and frustration. The physician-patient relationship is reinforced when nurse leaders include hospitalist satisfaction questions during daily rounding to identify concerns that can be clarified or resolved in real time.
The systematic VOC approach has enabled HCM to design, manage, and improve its key work process at multiple levels of the organization. These processes are reviewed and refined periodically to respond to the changing healthcare environment and stay focused on creating value for customers.
Chip Caldwell is chairman of Caldwell Butler, a firm specializing in coaching organizations to achieve world class performance in margin improvement, patient experience, physician/clinical enterprise, and capacity optimization. Jayne Pope, MBA, RN, is CEO of Hill Country Memorial Hospital in Fredericksburg, Texas. James Partin, MD, is CMO at Hill Country Memorial.
Clinical Care Conundrums Provide Learning Potential for Hospitalists
At A Glance
Series: Hospital Medicine: Current Concepts
Title: Clinical Care Conundrums: Challenging Diagnoses in Hospital Medicine
Edited by: James C. Pile, Thomas E. Baudendistel, Brian Harte
Series Editors: Scott Flanders, Sanjay Saint
Pages: 208
Clinical Care Conundrums is written in 22 chapters, each discussing a clinical case presentation in a format similar to the series by the same name, published frequently in the Journal of Hospital Medicine.
An expert clinician’s approach to the “clinical conundrums” is disclosed using the presentation of an actual patient case in a prototypical “morning report” style. As in a patient care situation, sequential pieces of information are provided to the expert clinician, who is unfamiliar with the case. The focus of each case is the thought processes of both the clinical team caring for the patient and the commentator.
Excerpt
“Clinicians rely heavily on diagnostic test information, yet diagnostic tests are also susceptible to error. About 18% of critical laboratory results are judged nonrepresentative of the patient’s clinical condition after a chart review. …CT scans have 1.7% misinterpretation rate. Pathologic discrepancies occur in 11%-19% of cancer biopsy specimens. These data should remind clinicians to question…”
Each case provides great learning potential, not only in the unusual presentation of common diseases or more typical presentations of unusual diseases, but also in discussions of the possibilities in differential diagnoses. The range of information is wide. Readers are taken through discussions of conditions infrequently encountered but potentially fatal in the event of missed or delayed diagnosis, such as strongyloides hyperinfection, a condition that we are reminded is not always accompanied by eosinophilia. Some discussions of the more common conditions include:
- Evaluation of confusion;
- Etiologies of cirrhosis;
- Malignancies associated with hypercalcemia; and
- Work-up for new-onset seizures.
My interest remained high throughout the book, because I never knew what to expect. For example, a patient presenting with acute chest pain caused by esophageal perforation resulting in delayed diagnosis might follow the index case presentation of Whipple’s disease. We are also reminded that, despite the insistence of Gregory House, MD, (Dr. House is the titular character from the television series “House”) that “it’s never lupus,” it sometimes is actually lupus. A couple of interesting lupus cases are presented in a realistically perplexing manner, followed by beneficial discussion.
Analysis
The real value in this book lies in continued reminders of how and why clinicians make diagnostic errors. In fact, an early chapter in the book deals explicitly with improving diagnostic safety.
Robert Wachter, MD, MHM, reminds us in the introductory chapter that diagnostic errors comprise nearly one in five preventable adverse events. Until recently, diagnostic errors have been given relatively little attention, most likely because they are difficult to measure and harder to fix.
As hospital-based providers, the more awareness we have about the “anatomy and physiology” of both good and faulty decision making, the more likely we are to make better decisions. This book can be a crucial resource for any hospital-based care provider.
Dr. Lindsey is medical director of hospital-based physician services at Hospital Corporation of America (HCA).
At A Glance
Series: Hospital Medicine: Current Concepts
Title: Clinical Care Conundrums: Challenging Diagnoses in Hospital Medicine
Edited by: James C. Pile, Thomas E. Baudendistel, Brian Harte
Series Editors: Scott Flanders, Sanjay Saint
Pages: 208
Clinical Care Conundrums is written in 22 chapters, each discussing a clinical case presentation in a format similar to the series by the same name, published frequently in the Journal of Hospital Medicine.
An expert clinician’s approach to the “clinical conundrums” is disclosed using the presentation of an actual patient case in a prototypical “morning report” style. As in a patient care situation, sequential pieces of information are provided to the expert clinician, who is unfamiliar with the case. The focus of each case is the thought processes of both the clinical team caring for the patient and the commentator.
Excerpt
“Clinicians rely heavily on diagnostic test information, yet diagnostic tests are also susceptible to error. About 18% of critical laboratory results are judged nonrepresentative of the patient’s clinical condition after a chart review. …CT scans have 1.7% misinterpretation rate. Pathologic discrepancies occur in 11%-19% of cancer biopsy specimens. These data should remind clinicians to question…”
Each case provides great learning potential, not only in the unusual presentation of common diseases or more typical presentations of unusual diseases, but also in discussions of the possibilities in differential diagnoses. The range of information is wide. Readers are taken through discussions of conditions infrequently encountered but potentially fatal in the event of missed or delayed diagnosis, such as strongyloides hyperinfection, a condition that we are reminded is not always accompanied by eosinophilia. Some discussions of the more common conditions include:
- Evaluation of confusion;
- Etiologies of cirrhosis;
- Malignancies associated with hypercalcemia; and
- Work-up for new-onset seizures.
My interest remained high throughout the book, because I never knew what to expect. For example, a patient presenting with acute chest pain caused by esophageal perforation resulting in delayed diagnosis might follow the index case presentation of Whipple’s disease. We are also reminded that, despite the insistence of Gregory House, MD, (Dr. House is the titular character from the television series “House”) that “it’s never lupus,” it sometimes is actually lupus. A couple of interesting lupus cases are presented in a realistically perplexing manner, followed by beneficial discussion.
Analysis
The real value in this book lies in continued reminders of how and why clinicians make diagnostic errors. In fact, an early chapter in the book deals explicitly with improving diagnostic safety.
Robert Wachter, MD, MHM, reminds us in the introductory chapter that diagnostic errors comprise nearly one in five preventable adverse events. Until recently, diagnostic errors have been given relatively little attention, most likely because they are difficult to measure and harder to fix.
As hospital-based providers, the more awareness we have about the “anatomy and physiology” of both good and faulty decision making, the more likely we are to make better decisions. This book can be a crucial resource for any hospital-based care provider.
Dr. Lindsey is medical director of hospital-based physician services at Hospital Corporation of America (HCA).
At A Glance
Series: Hospital Medicine: Current Concepts
Title: Clinical Care Conundrums: Challenging Diagnoses in Hospital Medicine
Edited by: James C. Pile, Thomas E. Baudendistel, Brian Harte
Series Editors: Scott Flanders, Sanjay Saint
Pages: 208
Clinical Care Conundrums is written in 22 chapters, each discussing a clinical case presentation in a format similar to the series by the same name, published frequently in the Journal of Hospital Medicine.
An expert clinician’s approach to the “clinical conundrums” is disclosed using the presentation of an actual patient case in a prototypical “morning report” style. As in a patient care situation, sequential pieces of information are provided to the expert clinician, who is unfamiliar with the case. The focus of each case is the thought processes of both the clinical team caring for the patient and the commentator.
Excerpt
“Clinicians rely heavily on diagnostic test information, yet diagnostic tests are also susceptible to error. About 18% of critical laboratory results are judged nonrepresentative of the patient’s clinical condition after a chart review. …CT scans have 1.7% misinterpretation rate. Pathologic discrepancies occur in 11%-19% of cancer biopsy specimens. These data should remind clinicians to question…”
Each case provides great learning potential, not only in the unusual presentation of common diseases or more typical presentations of unusual diseases, but also in discussions of the possibilities in differential diagnoses. The range of information is wide. Readers are taken through discussions of conditions infrequently encountered but potentially fatal in the event of missed or delayed diagnosis, such as strongyloides hyperinfection, a condition that we are reminded is not always accompanied by eosinophilia. Some discussions of the more common conditions include:
- Evaluation of confusion;
- Etiologies of cirrhosis;
- Malignancies associated with hypercalcemia; and
- Work-up for new-onset seizures.
My interest remained high throughout the book, because I never knew what to expect. For example, a patient presenting with acute chest pain caused by esophageal perforation resulting in delayed diagnosis might follow the index case presentation of Whipple’s disease. We are also reminded that, despite the insistence of Gregory House, MD, (Dr. House is the titular character from the television series “House”) that “it’s never lupus,” it sometimes is actually lupus. A couple of interesting lupus cases are presented in a realistically perplexing manner, followed by beneficial discussion.
Analysis
The real value in this book lies in continued reminders of how and why clinicians make diagnostic errors. In fact, an early chapter in the book deals explicitly with improving diagnostic safety.
Robert Wachter, MD, MHM, reminds us in the introductory chapter that diagnostic errors comprise nearly one in five preventable adverse events. Until recently, diagnostic errors have been given relatively little attention, most likely because they are difficult to measure and harder to fix.
As hospital-based providers, the more awareness we have about the “anatomy and physiology” of both good and faulty decision making, the more likely we are to make better decisions. This book can be a crucial resource for any hospital-based care provider.
Dr. Lindsey is medical director of hospital-based physician services at Hospital Corporation of America (HCA).
Hospitalist-Led Quality Initiatives Plentiful at Community Hospitals
Community hospitals offer multiple opportunities for hospitalists to become involved in both quality assurance and quality improvement. To help steer the right approach and avoid possible missteps, it’s important to acknowledge the differences between the community and academic settings, according to two medical directors with whom we spoke.
For example, in the rural, 47-bed Riverside Tappahannock Hospital where Randy Ferrance, DC, MD, SFHM, is medical director for hospital-based quality, cost effectiveness is king.
“We live on a thin margin, and being sure we provide cost-effective care is the difference between having adequate nursing and not,” he says. It’s a critical difference from academic institutions, he notes, where “there is protected time to do QI, research, and administrative tasks.”
Dr. Ferrance advises those interested in tackling quality projects to “make sure that the project is tied to quality measures and that you’re being cognizant of the cost impact.”
Although much of the work around quality assurance and quality improvement in the community hospital setting is being tackled by nonphysician administrative partners, “those people are usually more than happy to develop a physician partner,” says Colleen A. McCoy, MD, PhD, medical director for hospital medicine at Williamsport (Pa.) Regional Medical Center, a part of the Susquehanna Health System.
“The idea is to look for quality projects where there is a quantifiable financial payoff to the hospital,” she says. That could be a Centers for Medicare and Medicaid Services (CMS) core measure or helping to rewrite an order set for new inpatient guidelines on stroke, as Dr. McCoy did at her hospital.
First Order of Business
Dr. McCoy has been actively engaged in quality initiatives since she joined Williams-port in 2012. She cautions new hospitalists to spend the first six months at their new job developing a reputation for clinical excellence and attention to detail.
“Having a reputation that is respected clinically opens many doors,” she says. As generalists, hospitalists interact with a wider variety of staff than specialists. This leads to broad early exposure to a diverse group of decision makers in your institution. “As a hospitalist, you can get a lot of credibility in your organization much sooner than, for example, a young cardiologist or a young gastroenterologist,” she notes.
It is also important for new hospitalists to be mindful of their position in the organization and to watch how their institutions work and operate, so that when they propose a project they are not doing so from a critical standpoint.
“Unrequested input is often seen as criticism,” she says.
Dr. Ferrance agrees. “It’s always a good idea to make sure we focus on processes and not on people in the process.”
Meeting the Mark
“If you want to leapfrog into doing things quickly, you have to be very savvy about the cost impact of your quality improvement,” continues Dr. McCoy. She and Dr. Ferrance advise those just getting started to consider tackling core measures that are reported to CMS or to identify other quality improvement projects that can be financially quantified.
Early on at Riverside Tappahannock Hospital, Dr. Ferrance participated in root cause analyses and developed (at that time) paper-based standard order sets with quality measures attached to them.

Because of her attention to detail during her orientation at Williamsport, Dr. McCoy, who had been a clinical instructor at Emory University and worked for Kaiser Permanente, quickly spotted some necessary omissions regarding DVT prophylaxis. She helped rewrite the ICU admission order sets, inserting a query for DVT prophylaxis. That one intervention helped to increase compliance on a CMS core measure.
Assess Advancement Ops
Is your community hospital open to QI projects? Dr. McCoy says candidates should ask direct questions during job interviews to assess a prospective employer’s approach to quality. She suggests two fair questions:
- Is it possible, within my first two years here as a junior staff member, to participate in a QI project?
- If I were successful in that venture, is this organization open and able to give me more opportunities in that field?
It is key for the medical director to know who in the administrative organization of the hospital would really appreciate a physician partner or physician champion for new projects. If young hospitalists are interested in such projects, they should make that known to their medical directors.
“Having the senior person in your group make a connection with your [administrative] partner is how things get done in the community medical center,” Dr. McCoy says.
Dr. Ferrance’s HM group comprises four physicians and one nurse practitioner, so “there are plenty of QI projects to go around.”
“I would be more than happy to give them [junior staff hospitalists] any QI project they are interested in taking on,” he adds. “With medicine evolving as it does, we need to revisit processes every two to three years.” For example, drug shortages and cost increases often necessitate formulary cutbacks and the need for a change in administration protocols.
When selecting a QI project, it pays to stay ahead of the game, Dr. McCoy says. She encourages hospitalists to be aware of the next core measures and volunteer to help develop guidelines. She helped create a new protocol for inpatient tissue plasminogen activator (tPa) evaluation for acute stroke, which was a recent recommendation for stroke center certification. This approach was key in helping Williamsport retain its accreditation as a stroke center. The hospital has garnered multiple accolades from the Joint Commission, U.S. News and World Report, and other reporting agencies.
“The community setting is a much smaller world than academia,” she says. But smaller can be good for one’s career advancement. “If you hit a project out of the park and it makes your hospital look better, you can very quickly get a promotion or an increase in other opportunities. These types of projects may lead to the hospital asking, ‘Have you thought about being director of the hospital medicine group or taking a leadership role in hospital operations?’”
Gretchen Henkel is a freelance writer in California.
Community hospitals offer multiple opportunities for hospitalists to become involved in both quality assurance and quality improvement. To help steer the right approach and avoid possible missteps, it’s important to acknowledge the differences between the community and academic settings, according to two medical directors with whom we spoke.
For example, in the rural, 47-bed Riverside Tappahannock Hospital where Randy Ferrance, DC, MD, SFHM, is medical director for hospital-based quality, cost effectiveness is king.
“We live on a thin margin, and being sure we provide cost-effective care is the difference between having adequate nursing and not,” he says. It’s a critical difference from academic institutions, he notes, where “there is protected time to do QI, research, and administrative tasks.”
Dr. Ferrance advises those interested in tackling quality projects to “make sure that the project is tied to quality measures and that you’re being cognizant of the cost impact.”
Although much of the work around quality assurance and quality improvement in the community hospital setting is being tackled by nonphysician administrative partners, “those people are usually more than happy to develop a physician partner,” says Colleen A. McCoy, MD, PhD, medical director for hospital medicine at Williamsport (Pa.) Regional Medical Center, a part of the Susquehanna Health System.
“The idea is to look for quality projects where there is a quantifiable financial payoff to the hospital,” she says. That could be a Centers for Medicare and Medicaid Services (CMS) core measure or helping to rewrite an order set for new inpatient guidelines on stroke, as Dr. McCoy did at her hospital.
First Order of Business
Dr. McCoy has been actively engaged in quality initiatives since she joined Williams-port in 2012. She cautions new hospitalists to spend the first six months at their new job developing a reputation for clinical excellence and attention to detail.
“Having a reputation that is respected clinically opens many doors,” she says. As generalists, hospitalists interact with a wider variety of staff than specialists. This leads to broad early exposure to a diverse group of decision makers in your institution. “As a hospitalist, you can get a lot of credibility in your organization much sooner than, for example, a young cardiologist or a young gastroenterologist,” she notes.
It is also important for new hospitalists to be mindful of their position in the organization and to watch how their institutions work and operate, so that when they propose a project they are not doing so from a critical standpoint.
“Unrequested input is often seen as criticism,” she says.
Dr. Ferrance agrees. “It’s always a good idea to make sure we focus on processes and not on people in the process.”
Meeting the Mark
“If you want to leapfrog into doing things quickly, you have to be very savvy about the cost impact of your quality improvement,” continues Dr. McCoy. She and Dr. Ferrance advise those just getting started to consider tackling core measures that are reported to CMS or to identify other quality improvement projects that can be financially quantified.
Early on at Riverside Tappahannock Hospital, Dr. Ferrance participated in root cause analyses and developed (at that time) paper-based standard order sets with quality measures attached to them.

Because of her attention to detail during her orientation at Williamsport, Dr. McCoy, who had been a clinical instructor at Emory University and worked for Kaiser Permanente, quickly spotted some necessary omissions regarding DVT prophylaxis. She helped rewrite the ICU admission order sets, inserting a query for DVT prophylaxis. That one intervention helped to increase compliance on a CMS core measure.
Assess Advancement Ops
Is your community hospital open to QI projects? Dr. McCoy says candidates should ask direct questions during job interviews to assess a prospective employer’s approach to quality. She suggests two fair questions:
- Is it possible, within my first two years here as a junior staff member, to participate in a QI project?
- If I were successful in that venture, is this organization open and able to give me more opportunities in that field?
It is key for the medical director to know who in the administrative organization of the hospital would really appreciate a physician partner or physician champion for new projects. If young hospitalists are interested in such projects, they should make that known to their medical directors.
“Having the senior person in your group make a connection with your [administrative] partner is how things get done in the community medical center,” Dr. McCoy says.
Dr. Ferrance’s HM group comprises four physicians and one nurse practitioner, so “there are plenty of QI projects to go around.”
“I would be more than happy to give them [junior staff hospitalists] any QI project they are interested in taking on,” he adds. “With medicine evolving as it does, we need to revisit processes every two to three years.” For example, drug shortages and cost increases often necessitate formulary cutbacks and the need for a change in administration protocols.
When selecting a QI project, it pays to stay ahead of the game, Dr. McCoy says. She encourages hospitalists to be aware of the next core measures and volunteer to help develop guidelines. She helped create a new protocol for inpatient tissue plasminogen activator (tPa) evaluation for acute stroke, which was a recent recommendation for stroke center certification. This approach was key in helping Williamsport retain its accreditation as a stroke center. The hospital has garnered multiple accolades from the Joint Commission, U.S. News and World Report, and other reporting agencies.
“The community setting is a much smaller world than academia,” she says. But smaller can be good for one’s career advancement. “If you hit a project out of the park and it makes your hospital look better, you can very quickly get a promotion or an increase in other opportunities. These types of projects may lead to the hospital asking, ‘Have you thought about being director of the hospital medicine group or taking a leadership role in hospital operations?’”
Gretchen Henkel is a freelance writer in California.
Community hospitals offer multiple opportunities for hospitalists to become involved in both quality assurance and quality improvement. To help steer the right approach and avoid possible missteps, it’s important to acknowledge the differences between the community and academic settings, according to two medical directors with whom we spoke.
For example, in the rural, 47-bed Riverside Tappahannock Hospital where Randy Ferrance, DC, MD, SFHM, is medical director for hospital-based quality, cost effectiveness is king.
“We live on a thin margin, and being sure we provide cost-effective care is the difference between having adequate nursing and not,” he says. It’s a critical difference from academic institutions, he notes, where “there is protected time to do QI, research, and administrative tasks.”
Dr. Ferrance advises those interested in tackling quality projects to “make sure that the project is tied to quality measures and that you’re being cognizant of the cost impact.”
Although much of the work around quality assurance and quality improvement in the community hospital setting is being tackled by nonphysician administrative partners, “those people are usually more than happy to develop a physician partner,” says Colleen A. McCoy, MD, PhD, medical director for hospital medicine at Williamsport (Pa.) Regional Medical Center, a part of the Susquehanna Health System.
“The idea is to look for quality projects where there is a quantifiable financial payoff to the hospital,” she says. That could be a Centers for Medicare and Medicaid Services (CMS) core measure or helping to rewrite an order set for new inpatient guidelines on stroke, as Dr. McCoy did at her hospital.
First Order of Business
Dr. McCoy has been actively engaged in quality initiatives since she joined Williams-port in 2012. She cautions new hospitalists to spend the first six months at their new job developing a reputation for clinical excellence and attention to detail.
“Having a reputation that is respected clinically opens many doors,” she says. As generalists, hospitalists interact with a wider variety of staff than specialists. This leads to broad early exposure to a diverse group of decision makers in your institution. “As a hospitalist, you can get a lot of credibility in your organization much sooner than, for example, a young cardiologist or a young gastroenterologist,” she notes.
It is also important for new hospitalists to be mindful of their position in the organization and to watch how their institutions work and operate, so that when they propose a project they are not doing so from a critical standpoint.
“Unrequested input is often seen as criticism,” she says.
Dr. Ferrance agrees. “It’s always a good idea to make sure we focus on processes and not on people in the process.”
Meeting the Mark
“If you want to leapfrog into doing things quickly, you have to be very savvy about the cost impact of your quality improvement,” continues Dr. McCoy. She and Dr. Ferrance advise those just getting started to consider tackling core measures that are reported to CMS or to identify other quality improvement projects that can be financially quantified.
Early on at Riverside Tappahannock Hospital, Dr. Ferrance participated in root cause analyses and developed (at that time) paper-based standard order sets with quality measures attached to them.

Because of her attention to detail during her orientation at Williamsport, Dr. McCoy, who had been a clinical instructor at Emory University and worked for Kaiser Permanente, quickly spotted some necessary omissions regarding DVT prophylaxis. She helped rewrite the ICU admission order sets, inserting a query for DVT prophylaxis. That one intervention helped to increase compliance on a CMS core measure.
Assess Advancement Ops
Is your community hospital open to QI projects? Dr. McCoy says candidates should ask direct questions during job interviews to assess a prospective employer’s approach to quality. She suggests two fair questions:
- Is it possible, within my first two years here as a junior staff member, to participate in a QI project?
- If I were successful in that venture, is this organization open and able to give me more opportunities in that field?
It is key for the medical director to know who in the administrative organization of the hospital would really appreciate a physician partner or physician champion for new projects. If young hospitalists are interested in such projects, they should make that known to their medical directors.
“Having the senior person in your group make a connection with your [administrative] partner is how things get done in the community medical center,” Dr. McCoy says.
Dr. Ferrance’s HM group comprises four physicians and one nurse practitioner, so “there are plenty of QI projects to go around.”
“I would be more than happy to give them [junior staff hospitalists] any QI project they are interested in taking on,” he adds. “With medicine evolving as it does, we need to revisit processes every two to three years.” For example, drug shortages and cost increases often necessitate formulary cutbacks and the need for a change in administration protocols.
When selecting a QI project, it pays to stay ahead of the game, Dr. McCoy says. She encourages hospitalists to be aware of the next core measures and volunteer to help develop guidelines. She helped create a new protocol for inpatient tissue plasminogen activator (tPa) evaluation for acute stroke, which was a recent recommendation for stroke center certification. This approach was key in helping Williamsport retain its accreditation as a stroke center. The hospital has garnered multiple accolades from the Joint Commission, U.S. News and World Report, and other reporting agencies.
“The community setting is a much smaller world than academia,” she says. But smaller can be good for one’s career advancement. “If you hit a project out of the park and it makes your hospital look better, you can very quickly get a promotion or an increase in other opportunities. These types of projects may lead to the hospital asking, ‘Have you thought about being director of the hospital medicine group or taking a leadership role in hospital operations?’”
Gretchen Henkel is a freelance writer in California.
Hospitalists Play Vital Role in Patients’ View of Hospital Stay
Special Reports
Hospitalists are often perceived as the face of the hospital, whether that is their official responsibility or not. They are on the front lines of hearing, seeing, and understanding where gaps exist in a patient’s experience.
“Whenever I hear a patient complain, I can almost piece together what happened without having to interview other staff,” says Jairy C. Hunter III, MD, MBA, SFHM, associate CMO for care transitions at the Medical University of South Carolina in Charleston.
“Up to this point, there hasn’t been as much accountability regarding customer satisfaction in our industry compared to other industries,” Dr. Hunter says.
The paradigm shift has occurred because payers are demanding it. They want value and satisfaction in what they are paying for. In fact, there is a movement to try to standardize procedures whenever possible, such as the amount of time it takes someone to answer a call bell or the volume of noise in a hallway.
“Patients are being asked questions about such topics in surveys,” Dr. Hunter says. “Although these types of questions don’t involve medical decision-making or a course of treatment, they do include personal interactions that influence how patients feel about their hospital experience.”
Another reason for the shift is the significant increase in the use of electronic communication devices and the explosion of online ratings of consumer products and services. Naturally, consumers want access to accurate and easy-to-use information about the quality of healthcare services.
Patient experience surveys focus on how patients’ experienced or perceived key aspects of their care, not how satisfied they were with their care.1 One way a hospital can measure patient experience is with the Hospital Consumer Assessment of Healthcare Providers and Systems (HCAHPS) survey, which was developed by the Centers for Medicare and Medicaid Services (CMS) and the Agency for Healthcare Research and Quality (AHRQ).2 Although other patient satisfaction/experience vendors offer surveys, the Deficit Reduction Act of 2005 states that all Inpatient Prospective Payment Systems (IPPS) hospitals who wish to receive their full annual payment update must collect and submit HCAHPS data to CMS.
The HCAHPS survey, which employs standardized survey instrument and data collection methodology to measure patients’ perspectives on hospital care, is administered to a random sample of patients throughout the year. CMS cleans, adjusts, and analyzes the data and then publicly reports the results. All CAHPS products are available at no cost at www.cahps.ahrq.gov.2
Christine Crofton, PhD, director of CAHPS in Rockville, Md., notes that the HCAHPS survey focuses on patient experience measures because they are considered more understandable, unambiguous, actionable, and objective compared to general satisfaction ratings. Although CAHPS surveys do ask respondents to provide overall ratings (e.g. rate the physician on a scale of one to 10), their primary focus is to ask patients to report on their experiences with specific aspects of care in order to provide information that is not biased by different expectations.
For example, if a patient doesn’t understand what symptoms or problems to report to his or her provider after leaving the hospital, the lack of understanding could lead to a complication, a worsening condition, or readmission.
“A specific survey question about written discharge instructions will give hospital administrators more actionable information concerning an increase in readmission rates than a response to a 10-point satisfaction scale,” Dr. Crofton explains.
Efforts to Improve
At medical institutions across the nation, hospitalists and their team members are making conscious efforts to improve the patient experience in light of the growing importance of surveys. Baylor Scott and White Health in Round Rock, Texas, offers a lecture series and provider coaching as part of its continuing education program. The training, says Trina E. Dorrah, MD, MPH, a BSWH hospitalist and physician director for quality improvement, encompasses such topics as:
- Dealing with difficult patient scenarios;
- Patient experience improvement tips;
- Tips to improve providers’ explanations; and
- Tips to improve patients’ understanding.
Dr. Dorrah uses one-on-one shadowing to help providers improve the patient experience.
“I accompany the provider when visiting the patient and observe his or her interactions,” she says. “This enables me to help providers to see what skills they can incorporate to positively impact patient experience.”
Interdisciplinary rounds have also helped to improve the patient experience.
“Patients want to know that their entire healthcare team is focused on them and that they are working together to improve their experience,” Dr. Dorrah says. On weekdays, hospitalists lead interdisciplinary rounds with the rest of the care team, including case management, nursing, and therapy. “We discuss our patients and ensure that we are all on the same page regarding the plan.”
In addition, hospitalists round with nurses each morning. “Everyone benefits,” Dr. Dorrah says. “The patient gets more coordinated care and the nurse is better educated about the plan of care for the day. The number of pages from the nurse to the physician is also reduced because the nurse better understands the care plan.”
BSWH, which uses Press Ganey Associates to administer HCAHPS surveys, considers the scores for the doctor communication domain when establishing a hospitalist team goal for the year.
“If our team reaches the goal, the leadership/administrative team rewards the hospitalist team with a financial bonus,” Dr. Dorrah says.
Lawrence General Hospital, in Lawrence, Mass., which also uses Press Ganey Associates to administer and manage its HCAHPS satisfaction surveys, is working to increase the ability of hospitalists and other caregivers to proactively meet and exceed patients’ needs with its Five-to-Thrive program. The program consists of these five strategies:
- Care-Out-Loud: an initiative that charges every clinical and nonclinical staff member to be present, sensitive, and compassionate to the patient and explain each step of the clinical interaction;
- Manager rounding on staff and patients;
- Hourly staff rounding on patients;
- Interdisciplinary bedside rounding; and
- Senior leader rounding.
“It is based on best practice tactics that aim to improve the overall patient and family experience,” says Damaris Valera, MS, CMPE, director of the hospital’s Service Excellence Program.
Cogent Healthcare at University of Florida Health in Jacksonville, Fla., places a large emphasis on AIDET principles—acknowledge, introduce, duration, explanation, and thank you—during each patient encounter, says Larry Sharp, MD, SFHM, system medical director. AIDET principles entail offering a pleasant greeting and introducing yourself to patients, keeping patients abreast of wait times, explaining procedures, and thanking patients for the opportunity to participate in their care.
The medical director makes shadow rounds with providers and then ghost rounds by surveying the patients after rounds to get the patients’ direct feedback about encounters.
“We provide information to our providers from these rounds as a method to improve care,” Dr. Sharp says.
Northwestern University Feinberg School of Medicine in Chicago trains hospitalists on communication skills and consequently saw a trend toward improved satisfaction scores and used physician face cards to improve patients’ knowledge of the names and roles of physicians, which did not impact patient satisfaction, reports Kevin J. O’Leary, MD, MS, SFHM, associate professor of medicine, chief of the division of hospital medicine, and associate chair for quality in the department of medicine at Northwestern.3,4 Findings were published in the Journal of Hospital Medicine.
“These efforts have reinforced the need for multifaceted interventions,” Dr. O’Leary says. “Alone, each one has had little effect, but combined they may have a greater effect. The data is intended to be formative and to identify opportunities to learn.”
Additional improvements have been made due to a better understanding of drivers of low satisfaction.
“Unit medical directors [hospitalists] have started to visit patients to get a qualitative sense of what things affect patient experience,” Dr. O’Leary says. As a result, two previously unidentified issues—ED personnel making promises that can’t be kept to patients and patients receiving conflicting information from specialist consultants and hospitalists—surfaced which could now be addressed.”
Challenges and Limitations
Despite their best efforts to improve the patient experience, hospitalists face myriad obstacles. First, the HCAHPS survey asks about the collective care delivered by doctors during the hospitalization, as opposed to the care given by one particular hospitalist.
“One challenge hospitalists face by not having individual data is not knowing which hospitalists excel at the patient experience and which ones do not,” Dr. Dorrah says. “When no one feels that he or she is the problem, it is difficult to hold individual hospitalists accountable.”

Another problem, Dr. Dorrah reports, stems from the fact that patients may see more than one physician—perhaps several hospitalists or specialists—during their hospitalization. When the HCAHPS survey asks patients to assess the care given by all physicians, patients consider the care given by multiple different physicians.
“Therefore, it is difficult to hold a particular hospitalist accountable for the physician communication domain when he or she is not the only provider influencing patients’ perceptions.”
Some hospital systems still have chosen to attribute HCAHPS doctor communication scores to individual hospitalists. These health systems address the issue by attributing the survey results to the admitting physician, the discharging physician, or all hospitalists who participated in the patient’s care.
“None of these methods are perfect, but health systems are increasingly wanting to ensure their inpatient providers are as invested in the patient experience as their outpatient physicians,” Dr. Dorrah says.
Another obstacle hospitalist groups face is the fact that more attention is given to raising HCAHPS survey scores than to improving the overall patient experience.
“In an effort to raise survey scores, hospitals often lose sight of what truly matters to patients,” Dr. Dorrah says. “Many things contribute to a positive or negative patient experience that are not necessarily measured by the survey. If you only pay attention to the survey, your hospital may overlook things that truly matter to your patients.”
Finally, with the increasing focus on the patient experience, the focus on maintaining a good provider experience can fall short.
“While it’s tempting to ask hospitalists to do more—see more patients, take on more responsibility, and participate in more committees—if hospitals fail to provide a positive environment for their hospitalists, they will have a difficult time fully engaging their hospitalists with the patient experience,” Dr. Dorrah says.
Some situations are out of the hospitalists’ hands. A patient may get upset or angry, and the cause is outside of anyone’s control.
“They may have to spend a night in the emergency department or have an unfavorable outcome,” Dr. Hunter says. “In those instances, employ the art of personal interaction—try to empathize with patients and let them know that you care about them.”
Another limitation, Dr. Sharp says, is that you can’t specifically script encounters to “teach to the test,” by using verbiage with the patient that is verbatim from the satisfaction survey questions.
“Nor can we directly control the temperature in patients’ rooms or the quality of their food,” he says. “We also do not have direct control over a negative experience in the emergency department before patients are referred to us, and many surveys show that it is very difficult to overcome a bad experience.”
Tools at Your Fingertips
As a result of the growing emphasis on patient-centered care, SHM created a Patient Experience Committee this year. SHM defines patient experience as “everything we say and do that affects our patients’ thoughts, feelings, and well-being.” The committee is looking at the issues at hand and defining the patient experience and what makes it good.
“We are looking at success stories, as well as not so successful stories, from some of our members to identify what seems to work and what doesn’t work,” says Dr. Sharp, a member of the committee. “By identifying best practices, we can then share this knowledge with the rest of the society, along with methods to implement these practices. We can centralize the gathered knowledge and data and then analyze and make it available to SHM members for their implementation and use.”
The hospitalist plays a key role in the patient experience. Now, more than ever, it’s important to do what you can to make it positive. Consider initiatives you might want to participate in—and perhaps even start your own.
Karen Appold is a medical writer in Pennsylvania.
References
- Consumer Assessment of Healthcare Providers & Systems (CAHPS). CMS.gov. Accessed August 2, 2015.
- Survey of patients’ experiences (HCAHPS). Medicare.gov/Hospital Compare. Accessed August 2, 2015.
- O’Leary KJ, Darling TA, Rauworth J, Williams MV. Impact of hospitalist communication-skills training on patient-satisfaction scores. J Hosp Med. 2013;8(6):315-320.
- Simons Y, Caprio T, Furiasse N, Kriss M, Williams MV, O’Leary KJ. The impact of facecards on patients’ knowledge, satisfaction, trust, and agreement with hospital physicians: a pilot study. J Hosp Med. 2014;9(3):137-141.
Special Reports
Hospitalists are often perceived as the face of the hospital, whether that is their official responsibility or not. They are on the front lines of hearing, seeing, and understanding where gaps exist in a patient’s experience.
“Whenever I hear a patient complain, I can almost piece together what happened without having to interview other staff,” says Jairy C. Hunter III, MD, MBA, SFHM, associate CMO for care transitions at the Medical University of South Carolina in Charleston.
“Up to this point, there hasn’t been as much accountability regarding customer satisfaction in our industry compared to other industries,” Dr. Hunter says.
The paradigm shift has occurred because payers are demanding it. They want value and satisfaction in what they are paying for. In fact, there is a movement to try to standardize procedures whenever possible, such as the amount of time it takes someone to answer a call bell or the volume of noise in a hallway.
“Patients are being asked questions about such topics in surveys,” Dr. Hunter says. “Although these types of questions don’t involve medical decision-making or a course of treatment, they do include personal interactions that influence how patients feel about their hospital experience.”
Another reason for the shift is the significant increase in the use of electronic communication devices and the explosion of online ratings of consumer products and services. Naturally, consumers want access to accurate and easy-to-use information about the quality of healthcare services.
Patient experience surveys focus on how patients’ experienced or perceived key aspects of their care, not how satisfied they were with their care.1 One way a hospital can measure patient experience is with the Hospital Consumer Assessment of Healthcare Providers and Systems (HCAHPS) survey, which was developed by the Centers for Medicare and Medicaid Services (CMS) and the Agency for Healthcare Research and Quality (AHRQ).2 Although other patient satisfaction/experience vendors offer surveys, the Deficit Reduction Act of 2005 states that all Inpatient Prospective Payment Systems (IPPS) hospitals who wish to receive their full annual payment update must collect and submit HCAHPS data to CMS.
The HCAHPS survey, which employs standardized survey instrument and data collection methodology to measure patients’ perspectives on hospital care, is administered to a random sample of patients throughout the year. CMS cleans, adjusts, and analyzes the data and then publicly reports the results. All CAHPS products are available at no cost at www.cahps.ahrq.gov.2
Christine Crofton, PhD, director of CAHPS in Rockville, Md., notes that the HCAHPS survey focuses on patient experience measures because they are considered more understandable, unambiguous, actionable, and objective compared to general satisfaction ratings. Although CAHPS surveys do ask respondents to provide overall ratings (e.g. rate the physician on a scale of one to 10), their primary focus is to ask patients to report on their experiences with specific aspects of care in order to provide information that is not biased by different expectations.
For example, if a patient doesn’t understand what symptoms or problems to report to his or her provider after leaving the hospital, the lack of understanding could lead to a complication, a worsening condition, or readmission.
“A specific survey question about written discharge instructions will give hospital administrators more actionable information concerning an increase in readmission rates than a response to a 10-point satisfaction scale,” Dr. Crofton explains.
Efforts to Improve
At medical institutions across the nation, hospitalists and their team members are making conscious efforts to improve the patient experience in light of the growing importance of surveys. Baylor Scott and White Health in Round Rock, Texas, offers a lecture series and provider coaching as part of its continuing education program. The training, says Trina E. Dorrah, MD, MPH, a BSWH hospitalist and physician director for quality improvement, encompasses such topics as:
- Dealing with difficult patient scenarios;
- Patient experience improvement tips;
- Tips to improve providers’ explanations; and
- Tips to improve patients’ understanding.
Dr. Dorrah uses one-on-one shadowing to help providers improve the patient experience.
“I accompany the provider when visiting the patient and observe his or her interactions,” she says. “This enables me to help providers to see what skills they can incorporate to positively impact patient experience.”
Interdisciplinary rounds have also helped to improve the patient experience.
“Patients want to know that their entire healthcare team is focused on them and that they are working together to improve their experience,” Dr. Dorrah says. On weekdays, hospitalists lead interdisciplinary rounds with the rest of the care team, including case management, nursing, and therapy. “We discuss our patients and ensure that we are all on the same page regarding the plan.”
In addition, hospitalists round with nurses each morning. “Everyone benefits,” Dr. Dorrah says. “The patient gets more coordinated care and the nurse is better educated about the plan of care for the day. The number of pages from the nurse to the physician is also reduced because the nurse better understands the care plan.”
BSWH, which uses Press Ganey Associates to administer HCAHPS surveys, considers the scores for the doctor communication domain when establishing a hospitalist team goal for the year.
“If our team reaches the goal, the leadership/administrative team rewards the hospitalist team with a financial bonus,” Dr. Dorrah says.
Lawrence General Hospital, in Lawrence, Mass., which also uses Press Ganey Associates to administer and manage its HCAHPS satisfaction surveys, is working to increase the ability of hospitalists and other caregivers to proactively meet and exceed patients’ needs with its Five-to-Thrive program. The program consists of these five strategies:
- Care-Out-Loud: an initiative that charges every clinical and nonclinical staff member to be present, sensitive, and compassionate to the patient and explain each step of the clinical interaction;
- Manager rounding on staff and patients;
- Hourly staff rounding on patients;
- Interdisciplinary bedside rounding; and
- Senior leader rounding.
“It is based on best practice tactics that aim to improve the overall patient and family experience,” says Damaris Valera, MS, CMPE, director of the hospital’s Service Excellence Program.
Cogent Healthcare at University of Florida Health in Jacksonville, Fla., places a large emphasis on AIDET principles—acknowledge, introduce, duration, explanation, and thank you—during each patient encounter, says Larry Sharp, MD, SFHM, system medical director. AIDET principles entail offering a pleasant greeting and introducing yourself to patients, keeping patients abreast of wait times, explaining procedures, and thanking patients for the opportunity to participate in their care.
The medical director makes shadow rounds with providers and then ghost rounds by surveying the patients after rounds to get the patients’ direct feedback about encounters.
“We provide information to our providers from these rounds as a method to improve care,” Dr. Sharp says.
Northwestern University Feinberg School of Medicine in Chicago trains hospitalists on communication skills and consequently saw a trend toward improved satisfaction scores and used physician face cards to improve patients’ knowledge of the names and roles of physicians, which did not impact patient satisfaction, reports Kevin J. O’Leary, MD, MS, SFHM, associate professor of medicine, chief of the division of hospital medicine, and associate chair for quality in the department of medicine at Northwestern.3,4 Findings were published in the Journal of Hospital Medicine.
“These efforts have reinforced the need for multifaceted interventions,” Dr. O’Leary says. “Alone, each one has had little effect, but combined they may have a greater effect. The data is intended to be formative and to identify opportunities to learn.”
Additional improvements have been made due to a better understanding of drivers of low satisfaction.
“Unit medical directors [hospitalists] have started to visit patients to get a qualitative sense of what things affect patient experience,” Dr. O’Leary says. As a result, two previously unidentified issues—ED personnel making promises that can’t be kept to patients and patients receiving conflicting information from specialist consultants and hospitalists—surfaced which could now be addressed.”
Challenges and Limitations
Despite their best efforts to improve the patient experience, hospitalists face myriad obstacles. First, the HCAHPS survey asks about the collective care delivered by doctors during the hospitalization, as opposed to the care given by one particular hospitalist.
“One challenge hospitalists face by not having individual data is not knowing which hospitalists excel at the patient experience and which ones do not,” Dr. Dorrah says. “When no one feels that he or she is the problem, it is difficult to hold individual hospitalists accountable.”

Another problem, Dr. Dorrah reports, stems from the fact that patients may see more than one physician—perhaps several hospitalists or specialists—during their hospitalization. When the HCAHPS survey asks patients to assess the care given by all physicians, patients consider the care given by multiple different physicians.
“Therefore, it is difficult to hold a particular hospitalist accountable for the physician communication domain when he or she is not the only provider influencing patients’ perceptions.”
Some hospital systems still have chosen to attribute HCAHPS doctor communication scores to individual hospitalists. These health systems address the issue by attributing the survey results to the admitting physician, the discharging physician, or all hospitalists who participated in the patient’s care.
“None of these methods are perfect, but health systems are increasingly wanting to ensure their inpatient providers are as invested in the patient experience as their outpatient physicians,” Dr. Dorrah says.
Another obstacle hospitalist groups face is the fact that more attention is given to raising HCAHPS survey scores than to improving the overall patient experience.
“In an effort to raise survey scores, hospitals often lose sight of what truly matters to patients,” Dr. Dorrah says. “Many things contribute to a positive or negative patient experience that are not necessarily measured by the survey. If you only pay attention to the survey, your hospital may overlook things that truly matter to your patients.”
Finally, with the increasing focus on the patient experience, the focus on maintaining a good provider experience can fall short.
“While it’s tempting to ask hospitalists to do more—see more patients, take on more responsibility, and participate in more committees—if hospitals fail to provide a positive environment for their hospitalists, they will have a difficult time fully engaging their hospitalists with the patient experience,” Dr. Dorrah says.
Some situations are out of the hospitalists’ hands. A patient may get upset or angry, and the cause is outside of anyone’s control.
“They may have to spend a night in the emergency department or have an unfavorable outcome,” Dr. Hunter says. “In those instances, employ the art of personal interaction—try to empathize with patients and let them know that you care about them.”
Another limitation, Dr. Sharp says, is that you can’t specifically script encounters to “teach to the test,” by using verbiage with the patient that is verbatim from the satisfaction survey questions.
“Nor can we directly control the temperature in patients’ rooms or the quality of their food,” he says. “We also do not have direct control over a negative experience in the emergency department before patients are referred to us, and many surveys show that it is very difficult to overcome a bad experience.”
Tools at Your Fingertips
As a result of the growing emphasis on patient-centered care, SHM created a Patient Experience Committee this year. SHM defines patient experience as “everything we say and do that affects our patients’ thoughts, feelings, and well-being.” The committee is looking at the issues at hand and defining the patient experience and what makes it good.
“We are looking at success stories, as well as not so successful stories, from some of our members to identify what seems to work and what doesn’t work,” says Dr. Sharp, a member of the committee. “By identifying best practices, we can then share this knowledge with the rest of the society, along with methods to implement these practices. We can centralize the gathered knowledge and data and then analyze and make it available to SHM members for their implementation and use.”
The hospitalist plays a key role in the patient experience. Now, more than ever, it’s important to do what you can to make it positive. Consider initiatives you might want to participate in—and perhaps even start your own.
Karen Appold is a medical writer in Pennsylvania.
References
- Consumer Assessment of Healthcare Providers & Systems (CAHPS). CMS.gov. Accessed August 2, 2015.
- Survey of patients’ experiences (HCAHPS). Medicare.gov/Hospital Compare. Accessed August 2, 2015.
- O’Leary KJ, Darling TA, Rauworth J, Williams MV. Impact of hospitalist communication-skills training on patient-satisfaction scores. J Hosp Med. 2013;8(6):315-320.
- Simons Y, Caprio T, Furiasse N, Kriss M, Williams MV, O’Leary KJ. The impact of facecards on patients’ knowledge, satisfaction, trust, and agreement with hospital physicians: a pilot study. J Hosp Med. 2014;9(3):137-141.
Special Reports
Hospitalists are often perceived as the face of the hospital, whether that is their official responsibility or not. They are on the front lines of hearing, seeing, and understanding where gaps exist in a patient’s experience.
“Whenever I hear a patient complain, I can almost piece together what happened without having to interview other staff,” says Jairy C. Hunter III, MD, MBA, SFHM, associate CMO for care transitions at the Medical University of South Carolina in Charleston.
“Up to this point, there hasn’t been as much accountability regarding customer satisfaction in our industry compared to other industries,” Dr. Hunter says.
The paradigm shift has occurred because payers are demanding it. They want value and satisfaction in what they are paying for. In fact, there is a movement to try to standardize procedures whenever possible, such as the amount of time it takes someone to answer a call bell or the volume of noise in a hallway.
“Patients are being asked questions about such topics in surveys,” Dr. Hunter says. “Although these types of questions don’t involve medical decision-making or a course of treatment, they do include personal interactions that influence how patients feel about their hospital experience.”
Another reason for the shift is the significant increase in the use of electronic communication devices and the explosion of online ratings of consumer products and services. Naturally, consumers want access to accurate and easy-to-use information about the quality of healthcare services.
Patient experience surveys focus on how patients’ experienced or perceived key aspects of their care, not how satisfied they were with their care.1 One way a hospital can measure patient experience is with the Hospital Consumer Assessment of Healthcare Providers and Systems (HCAHPS) survey, which was developed by the Centers for Medicare and Medicaid Services (CMS) and the Agency for Healthcare Research and Quality (AHRQ).2 Although other patient satisfaction/experience vendors offer surveys, the Deficit Reduction Act of 2005 states that all Inpatient Prospective Payment Systems (IPPS) hospitals who wish to receive their full annual payment update must collect and submit HCAHPS data to CMS.
The HCAHPS survey, which employs standardized survey instrument and data collection methodology to measure patients’ perspectives on hospital care, is administered to a random sample of patients throughout the year. CMS cleans, adjusts, and analyzes the data and then publicly reports the results. All CAHPS products are available at no cost at www.cahps.ahrq.gov.2
Christine Crofton, PhD, director of CAHPS in Rockville, Md., notes that the HCAHPS survey focuses on patient experience measures because they are considered more understandable, unambiguous, actionable, and objective compared to general satisfaction ratings. Although CAHPS surveys do ask respondents to provide overall ratings (e.g. rate the physician on a scale of one to 10), their primary focus is to ask patients to report on their experiences with specific aspects of care in order to provide information that is not biased by different expectations.
For example, if a patient doesn’t understand what symptoms or problems to report to his or her provider after leaving the hospital, the lack of understanding could lead to a complication, a worsening condition, or readmission.
“A specific survey question about written discharge instructions will give hospital administrators more actionable information concerning an increase in readmission rates than a response to a 10-point satisfaction scale,” Dr. Crofton explains.
Efforts to Improve
At medical institutions across the nation, hospitalists and their team members are making conscious efforts to improve the patient experience in light of the growing importance of surveys. Baylor Scott and White Health in Round Rock, Texas, offers a lecture series and provider coaching as part of its continuing education program. The training, says Trina E. Dorrah, MD, MPH, a BSWH hospitalist and physician director for quality improvement, encompasses such topics as:
- Dealing with difficult patient scenarios;
- Patient experience improvement tips;
- Tips to improve providers’ explanations; and
- Tips to improve patients’ understanding.
Dr. Dorrah uses one-on-one shadowing to help providers improve the patient experience.
“I accompany the provider when visiting the patient and observe his or her interactions,” she says. “This enables me to help providers to see what skills they can incorporate to positively impact patient experience.”
Interdisciplinary rounds have also helped to improve the patient experience.
“Patients want to know that their entire healthcare team is focused on them and that they are working together to improve their experience,” Dr. Dorrah says. On weekdays, hospitalists lead interdisciplinary rounds with the rest of the care team, including case management, nursing, and therapy. “We discuss our patients and ensure that we are all on the same page regarding the plan.”
In addition, hospitalists round with nurses each morning. “Everyone benefits,” Dr. Dorrah says. “The patient gets more coordinated care and the nurse is better educated about the plan of care for the day. The number of pages from the nurse to the physician is also reduced because the nurse better understands the care plan.”
BSWH, which uses Press Ganey Associates to administer HCAHPS surveys, considers the scores for the doctor communication domain when establishing a hospitalist team goal for the year.
“If our team reaches the goal, the leadership/administrative team rewards the hospitalist team with a financial bonus,” Dr. Dorrah says.
Lawrence General Hospital, in Lawrence, Mass., which also uses Press Ganey Associates to administer and manage its HCAHPS satisfaction surveys, is working to increase the ability of hospitalists and other caregivers to proactively meet and exceed patients’ needs with its Five-to-Thrive program. The program consists of these five strategies:
- Care-Out-Loud: an initiative that charges every clinical and nonclinical staff member to be present, sensitive, and compassionate to the patient and explain each step of the clinical interaction;
- Manager rounding on staff and patients;
- Hourly staff rounding on patients;
- Interdisciplinary bedside rounding; and
- Senior leader rounding.
“It is based on best practice tactics that aim to improve the overall patient and family experience,” says Damaris Valera, MS, CMPE, director of the hospital’s Service Excellence Program.
Cogent Healthcare at University of Florida Health in Jacksonville, Fla., places a large emphasis on AIDET principles—acknowledge, introduce, duration, explanation, and thank you—during each patient encounter, says Larry Sharp, MD, SFHM, system medical director. AIDET principles entail offering a pleasant greeting and introducing yourself to patients, keeping patients abreast of wait times, explaining procedures, and thanking patients for the opportunity to participate in their care.
The medical director makes shadow rounds with providers and then ghost rounds by surveying the patients after rounds to get the patients’ direct feedback about encounters.
“We provide information to our providers from these rounds as a method to improve care,” Dr. Sharp says.
Northwestern University Feinberg School of Medicine in Chicago trains hospitalists on communication skills and consequently saw a trend toward improved satisfaction scores and used physician face cards to improve patients’ knowledge of the names and roles of physicians, which did not impact patient satisfaction, reports Kevin J. O’Leary, MD, MS, SFHM, associate professor of medicine, chief of the division of hospital medicine, and associate chair for quality in the department of medicine at Northwestern.3,4 Findings were published in the Journal of Hospital Medicine.
“These efforts have reinforced the need for multifaceted interventions,” Dr. O’Leary says. “Alone, each one has had little effect, but combined they may have a greater effect. The data is intended to be formative and to identify opportunities to learn.”
Additional improvements have been made due to a better understanding of drivers of low satisfaction.
“Unit medical directors [hospitalists] have started to visit patients to get a qualitative sense of what things affect patient experience,” Dr. O’Leary says. As a result, two previously unidentified issues—ED personnel making promises that can’t be kept to patients and patients receiving conflicting information from specialist consultants and hospitalists—surfaced which could now be addressed.”
Challenges and Limitations
Despite their best efforts to improve the patient experience, hospitalists face myriad obstacles. First, the HCAHPS survey asks about the collective care delivered by doctors during the hospitalization, as opposed to the care given by one particular hospitalist.
“One challenge hospitalists face by not having individual data is not knowing which hospitalists excel at the patient experience and which ones do not,” Dr. Dorrah says. “When no one feels that he or she is the problem, it is difficult to hold individual hospitalists accountable.”

Another problem, Dr. Dorrah reports, stems from the fact that patients may see more than one physician—perhaps several hospitalists or specialists—during their hospitalization. When the HCAHPS survey asks patients to assess the care given by all physicians, patients consider the care given by multiple different physicians.
“Therefore, it is difficult to hold a particular hospitalist accountable for the physician communication domain when he or she is not the only provider influencing patients’ perceptions.”
Some hospital systems still have chosen to attribute HCAHPS doctor communication scores to individual hospitalists. These health systems address the issue by attributing the survey results to the admitting physician, the discharging physician, or all hospitalists who participated in the patient’s care.
“None of these methods are perfect, but health systems are increasingly wanting to ensure their inpatient providers are as invested in the patient experience as their outpatient physicians,” Dr. Dorrah says.
Another obstacle hospitalist groups face is the fact that more attention is given to raising HCAHPS survey scores than to improving the overall patient experience.
“In an effort to raise survey scores, hospitals often lose sight of what truly matters to patients,” Dr. Dorrah says. “Many things contribute to a positive or negative patient experience that are not necessarily measured by the survey. If you only pay attention to the survey, your hospital may overlook things that truly matter to your patients.”
Finally, with the increasing focus on the patient experience, the focus on maintaining a good provider experience can fall short.
“While it’s tempting to ask hospitalists to do more—see more patients, take on more responsibility, and participate in more committees—if hospitals fail to provide a positive environment for their hospitalists, they will have a difficult time fully engaging their hospitalists with the patient experience,” Dr. Dorrah says.
Some situations are out of the hospitalists’ hands. A patient may get upset or angry, and the cause is outside of anyone’s control.
“They may have to spend a night in the emergency department or have an unfavorable outcome,” Dr. Hunter says. “In those instances, employ the art of personal interaction—try to empathize with patients and let them know that you care about them.”
Another limitation, Dr. Sharp says, is that you can’t specifically script encounters to “teach to the test,” by using verbiage with the patient that is verbatim from the satisfaction survey questions.
“Nor can we directly control the temperature in patients’ rooms or the quality of their food,” he says. “We also do not have direct control over a negative experience in the emergency department before patients are referred to us, and many surveys show that it is very difficult to overcome a bad experience.”
Tools at Your Fingertips
As a result of the growing emphasis on patient-centered care, SHM created a Patient Experience Committee this year. SHM defines patient experience as “everything we say and do that affects our patients’ thoughts, feelings, and well-being.” The committee is looking at the issues at hand and defining the patient experience and what makes it good.
“We are looking at success stories, as well as not so successful stories, from some of our members to identify what seems to work and what doesn’t work,” says Dr. Sharp, a member of the committee. “By identifying best practices, we can then share this knowledge with the rest of the society, along with methods to implement these practices. We can centralize the gathered knowledge and data and then analyze and make it available to SHM members for their implementation and use.”
The hospitalist plays a key role in the patient experience. Now, more than ever, it’s important to do what you can to make it positive. Consider initiatives you might want to participate in—and perhaps even start your own.
Karen Appold is a medical writer in Pennsylvania.
References
- Consumer Assessment of Healthcare Providers & Systems (CAHPS). CMS.gov. Accessed August 2, 2015.
- Survey of patients’ experiences (HCAHPS). Medicare.gov/Hospital Compare. Accessed August 2, 2015.
- O’Leary KJ, Darling TA, Rauworth J, Williams MV. Impact of hospitalist communication-skills training on patient-satisfaction scores. J Hosp Med. 2013;8(6):315-320.
- Simons Y, Caprio T, Furiasse N, Kriss M, Williams MV, O’Leary KJ. The impact of facecards on patients’ knowledge, satisfaction, trust, and agreement with hospital physicians: a pilot study. J Hosp Med. 2014;9(3):137-141.
Cognitive, Emotional Memory Disconnect Impacts Patient Satisfaction
There are two types of memory, the cognitive and the emotional, and the latter is more enduring. Maya Angelou characterized the distinction between these two types of memory most eloquently and succinctly when she said, “I’ve learned that people will forget what you said, people will forget what you did, but people will never forget how you made them feel.” She was ahead of her time, because neurocognitive research has objectified with science what Ms. Angelou captured so elegantly in her prose. Emotional events are processed in the sensory systems and then transmitted to the medial-temporal lobe and the amygdale for the formation of an emotional memory. When the memory is cued and retrieved from the amygdale, it triggers an emotional response. Emotional experiences leave strong traces in the brain. Memories about emotional situations are stored in both the conscious and unconscious memory, which is part of the reason emotional memories are so enduring.1 Studies of patients with severe anterograde amnesia following circumscribed bilateral hippocampal brain damage showed enduring memories of emotion despite the absence of conscious memories.2 This has a demonstrably practical application in patients with dementia, who we now know have feelings of happiness and sadness long after they have forgotten what caused the emotion.3
The distinction is important because patients judge the quality of their medical care based on emotions. The patient satisfaction disconnect arises from the fact that physicians live in their cognitive memory, while patients live in their emotional memory. Being cognitive and objective is a critical skill a physician must bring to the bedside every day; the reason we don’t allow physicians to treat family members is that their ability to remain objective will be impaired. I realized that my emotion, my passion, and my empathy for the dying would impair my judgment when I started medical school, and I launched myself on a conscious and systematic discipline to keep those feelings out of my mind during patient care. The effort worked and, for the most part, I have been able to remain objective and unemotional as I care for my patients. Recently, however, I realized that my focus on objectivity negatively impacts patient experience. As a result, I have expanded my view: While I must stay objective and detached with my thinking, I must be emotionally engaged to provide a great patient experience.
I can remain objective and detached in my clinical judgment as I engage and connect emotionally during my patient encounters. This delicate balancing act has taken years of trial and error, however. I recently cared for a woman in her 60s who had fallen and broke her hip. Everyone was pleased that a top orthopedic surgeon was on call and able to give her the first-rate care she needed to begin walking again. The surgery went smoothly, and she was transferred to the medical/surgical ward, where things took a turn for the worse. She had a lot of anxiety in addition to her osteoporosis. Objectively, she was doing great, and we had a big success on our hands; however, she remained anxious, and she peppered the surgeon with fears that, while unfounded, were very real in her mind. The surgeon brushed them off, saying that her fears were not real and that he didn’t need to address them; his response made her emotional state spiral out of control. Her nurse notified me of the situation, and I came to her bedside. She was very agitated. I sat down at a low level and just started listening. She got all of her anxieties out in words. I held her hand, looked her in the eye, and assured her that I would be there for her and that things were going to be alright. Subsequently, she wrote letters of gratitude and proclaimed to any medical staff who would listen what a talented and great doctor I was. I did not have the skill to fix her broken hip; if it had been left to me alone, she would still be bed-bound. But I did have the human skills to connect with her and fix her agitated mind. If we remember the enduring power of the emotional memory, we can create great patient experiences.
The importance of these experiences was illustrated to me at the 2014 Dignity Health Patient Experience Summit, a powerful event featuring motivational speakers and leaders from across the country. The most powerful speakers, however, were patients. These patients had received terrible diagnoses that committed them to a prolonged interaction with the healthcare system. They were scared of what their diagnoses would mean for their future, they were subjected to uncomfortable procedures in which they struggled to maintain their dignity, and they repeatedly met the indifference of healthcare providers and clerical people who were only there to do a job. They related how the lack of caring and empathy made fears and anxiety much worse. But each of them had a story about that one person, that one care provider, who took the time to reassure them, to show that they cared, and to ensure that the patient did not feel alone. In most of these stories, the stand-out care providers took the time to hold their hands and reassure the patients. They took the time to connect with the patient’s emotional memory in a positive way, and that simple gesture of empathy had a powerful and lasting impact on the patient.
Invariably, the care provider at the heart of the patients’ stories was a nurse. Nurses have the reputation for being angels of mercy because they do the simple, empathetic gestures that let a patient know they are being cared for. These feelings endure in the patients’ memories long after the treatment is over. Doctors can, and should, be that type of care provider. It requires us to recognize that patients are scared and anxious, even though they may do their best not to show it. We, as physicians, often don’t see their anxiety, and we are so focused on the cognitive memory that we don’t address the anxiety and fear that is just under the surface. But taking just a few minutes to acknowledge their emotions, to explore them, and to reassure the patient that we are there for them has a lasting impact. In my group, we talk about the “human-business-human” encounter with patients. We begin all interactions with a human interaction (“Hello, I am Dr. McIlraith…”), conduct the business we came to provide (“Now I am going to examine you…”), and end with a human interaction (“What else can I do for you today?”). Patients expect physical contact with us during the “business” part of that interaction. I find that respectful, reassuring, and appropriate physical contact during the final “human” portion of that interaction helps solidify my patients’ experience. It helps make them feel that they have been cared for, particularly if the visit includes bad news.
Much of the recent focus on patient satisfaction has been driven by financial incentives. In 2013, CMS began penalizing hospitals 1.25% for poor HCAHPS scores as a part of the Affordable Care Act. In 2014, the maximum penalty increased to 2%, and to 3% in 2015. Hospitals have notoriously high overhead costs and slim profit margins, so these penalties can have a profound impact on the financial viability of an institution. But, while hospitals across the country have taken notice (see related article in this edition of The Hospitalist), I find doctors are more motivated by the well-being of their patients than are their hospital administrators. Satisfied patients are more compliant with treatment plans and have better outcomes.4,5 Hospitalists spend a lot of effort making sure their heart failure patients are on an ACE inhibitor, and their heart attack patients are discharged on aspirin, beta blockers, and statins so that they will have a good outcome following treatment for their acute illness. The same outcome-driven, evidence-based practice of medicine relates to patient satisfaction, however. Success in HCAHPS is as important as core measures when it comes to patient outcomes. And if I can’t convince you patient satisfaction is important because of the good it does for hospitals and patients, think about yourself for a minute. Satisfied patients are much less likely to sue their physicians.6 Practicing quality, evidence-based medicine will keep you out of peer review; however, satisfied patients will keep you out of the courtroom.
I frequently hear the comment that “we can do great on patient satisfaction, but then it gets busy, and patient satisfaction goes out the window.” My own experience contradicts this maxim, however. It is not how much time you spend with your patient but, rather, what you do with the time you have. One of the most powerful things we can do is listen. I used to make the mistake that I only wanted to hear the information I needed to figure out my patients’ problems so I could start treating them; however, I have come to learn that being heard is, in itself, therapy for my patients. It is often quoted that physicians interrupt their patients within 18 seconds of starting the interview.7 A lot of physicians dispense with attentive listening when they are under time pressure, when they should instead dispense with lengthy discourses on the patient treatment plan. It is important to educate our patients on their illness and treatment, I admit. I find a lot of hospitalists want to impart their knowledge and their treatment rationale to their patients; however, they frequently give patients and families much more information than they can hold in their cognitive memory. And time pressures are not the only anxieties hospitalists carry with them to the bedside. Our increasingly metric-driven profession means that we not only have to worry about morning discharges, interdisciplinary rounds, length of stay, and so on, but we also have to consider patient experience. It is not easy to hide all the stress we are under when we come to the bedside of a patient, but we have to. The easiest way to do that is to take a deep breath, sit next to the patient, ask an open-ended question, and then say nothing until the patient is done speaking. Active listening with good eye contact and encouragement to continue solidifies the patient’s experience of being heard. There are extreme cases when a patient is in a manic phase and won’t ever stop speaking; bend the rules a bit in those circumstances. However, the above rule works very effectively in the majority of physician-patient interactions. Being heard leaves an enduring emotional memory with our patients.
Hospital medicine often looks to other industries for inspiration on how we can improve. The airline industry is often held up as an example of how we can model patient safety, for instance, but these comparisons oversimplify the challenges we face. The same is true with patient satisfaction. In the business world, adages like “The customer is always right” are central to customer satisfaction, yet completely irrelevant to HM practice. Patients and families frequently have inappropriate and unrealistic expectations of their hospitalist physicians. We cannot, and should not, tell the patient addicted to narcotics that they can have as much IV Dilaudid as they would like. We cannot fix the patient with end-stage cancer, heart failure, or dementia. This is where we have to part ways with comparisons to principles that guide other industries if we are going to find a way forward with patient experience in hospital medicine. Because we have to set limits for patients, we often have to give our patients and families bad news, and because we have to tell them things they don’t like to hear, like “You can’t have any salt in your diet,” or “You must quit drinking alcohol,” we must develop our own principles on patient experience and satisfaction. Otherwise our options are either delivering inappropriate medical care or abandoning the pursuit of patient satisfaction all together. This is when we must remember that emotional memories are more enduring. We can’t always give our patients what they want, and we can’t always tell them what they want to hear, but we can always show them that we care. When we show our patients that we care in a palpable way, we leave them with the feeling that they have been cared for regardless of their condition, and the positive memory will endure despite the negative information we may have to convey. Maybe they won’t cut down on their salt or quit drinking alcohol, but they will never forget that their hospitalist physician cared.
And if they remember that the physician cared, it is much more likely that they will cut down on the salt or quit drinking alcohol when they go home. To paraphrase Maya Angelou, “I can’t always tell my patients what they want to hear, I can’t always tell them that their lifestyle is appropriate, but I can always show them that I care.”
Dr. McIlraith is chairman of the department of hospital medicine of Mercy Medical Group in Sacramento, Calif.
References
- LeDoux JE. Emotional memory. Scholarpedia. Accessed August 2, 2015.
- Feinstein JS, Duff MC, D Tranel D. Sustained experience of emotion after loss of memory in patients with amnesia. Proc Natl Acad Sci. 2010:107(17):7674-7679.
- Guzmán-Vélez E, Feinstein JS, Tranel D. Feelings without memory in Alzheimer disease. Cogn Behav Neurol. 2014;27(3):117-129.
- Institute of Medicine. Crossing the quality chasm: a new health system for the 21st century. March 2001. Accessed August 2, 2015.
- Bertakis KD, Azari R. Patient-centered care is associated with decreased health care utilization. J Am Board Fam Med. 2011;24(3):229-239.
- Stelfox HT, Gandhi TK, Orav EJ, Gustafson ML. The relation of patient statisfaction with complaints against physicians and malpractice lawsuits. Am J Med. 2005;118(10):1126-1133.
- Beckman HB, Frankel RM. The effect of physician behavior on the collection of data. Ann Intern Med. 1984;101(5):692-696.
There are two types of memory, the cognitive and the emotional, and the latter is more enduring. Maya Angelou characterized the distinction between these two types of memory most eloquently and succinctly when she said, “I’ve learned that people will forget what you said, people will forget what you did, but people will never forget how you made them feel.” She was ahead of her time, because neurocognitive research has objectified with science what Ms. Angelou captured so elegantly in her prose. Emotional events are processed in the sensory systems and then transmitted to the medial-temporal lobe and the amygdale for the formation of an emotional memory. When the memory is cued and retrieved from the amygdale, it triggers an emotional response. Emotional experiences leave strong traces in the brain. Memories about emotional situations are stored in both the conscious and unconscious memory, which is part of the reason emotional memories are so enduring.1 Studies of patients with severe anterograde amnesia following circumscribed bilateral hippocampal brain damage showed enduring memories of emotion despite the absence of conscious memories.2 This has a demonstrably practical application in patients with dementia, who we now know have feelings of happiness and sadness long after they have forgotten what caused the emotion.3
The distinction is important because patients judge the quality of their medical care based on emotions. The patient satisfaction disconnect arises from the fact that physicians live in their cognitive memory, while patients live in their emotional memory. Being cognitive and objective is a critical skill a physician must bring to the bedside every day; the reason we don’t allow physicians to treat family members is that their ability to remain objective will be impaired. I realized that my emotion, my passion, and my empathy for the dying would impair my judgment when I started medical school, and I launched myself on a conscious and systematic discipline to keep those feelings out of my mind during patient care. The effort worked and, for the most part, I have been able to remain objective and unemotional as I care for my patients. Recently, however, I realized that my focus on objectivity negatively impacts patient experience. As a result, I have expanded my view: While I must stay objective and detached with my thinking, I must be emotionally engaged to provide a great patient experience.
I can remain objective and detached in my clinical judgment as I engage and connect emotionally during my patient encounters. This delicate balancing act has taken years of trial and error, however. I recently cared for a woman in her 60s who had fallen and broke her hip. Everyone was pleased that a top orthopedic surgeon was on call and able to give her the first-rate care she needed to begin walking again. The surgery went smoothly, and she was transferred to the medical/surgical ward, where things took a turn for the worse. She had a lot of anxiety in addition to her osteoporosis. Objectively, she was doing great, and we had a big success on our hands; however, she remained anxious, and she peppered the surgeon with fears that, while unfounded, were very real in her mind. The surgeon brushed them off, saying that her fears were not real and that he didn’t need to address them; his response made her emotional state spiral out of control. Her nurse notified me of the situation, and I came to her bedside. She was very agitated. I sat down at a low level and just started listening. She got all of her anxieties out in words. I held her hand, looked her in the eye, and assured her that I would be there for her and that things were going to be alright. Subsequently, she wrote letters of gratitude and proclaimed to any medical staff who would listen what a talented and great doctor I was. I did not have the skill to fix her broken hip; if it had been left to me alone, she would still be bed-bound. But I did have the human skills to connect with her and fix her agitated mind. If we remember the enduring power of the emotional memory, we can create great patient experiences.
The importance of these experiences was illustrated to me at the 2014 Dignity Health Patient Experience Summit, a powerful event featuring motivational speakers and leaders from across the country. The most powerful speakers, however, were patients. These patients had received terrible diagnoses that committed them to a prolonged interaction with the healthcare system. They were scared of what their diagnoses would mean for their future, they were subjected to uncomfortable procedures in which they struggled to maintain their dignity, and they repeatedly met the indifference of healthcare providers and clerical people who were only there to do a job. They related how the lack of caring and empathy made fears and anxiety much worse. But each of them had a story about that one person, that one care provider, who took the time to reassure them, to show that they cared, and to ensure that the patient did not feel alone. In most of these stories, the stand-out care providers took the time to hold their hands and reassure the patients. They took the time to connect with the patient’s emotional memory in a positive way, and that simple gesture of empathy had a powerful and lasting impact on the patient.
Invariably, the care provider at the heart of the patients’ stories was a nurse. Nurses have the reputation for being angels of mercy because they do the simple, empathetic gestures that let a patient know they are being cared for. These feelings endure in the patients’ memories long after the treatment is over. Doctors can, and should, be that type of care provider. It requires us to recognize that patients are scared and anxious, even though they may do their best not to show it. We, as physicians, often don’t see their anxiety, and we are so focused on the cognitive memory that we don’t address the anxiety and fear that is just under the surface. But taking just a few minutes to acknowledge their emotions, to explore them, and to reassure the patient that we are there for them has a lasting impact. In my group, we talk about the “human-business-human” encounter with patients. We begin all interactions with a human interaction (“Hello, I am Dr. McIlraith…”), conduct the business we came to provide (“Now I am going to examine you…”), and end with a human interaction (“What else can I do for you today?”). Patients expect physical contact with us during the “business” part of that interaction. I find that respectful, reassuring, and appropriate physical contact during the final “human” portion of that interaction helps solidify my patients’ experience. It helps make them feel that they have been cared for, particularly if the visit includes bad news.
Much of the recent focus on patient satisfaction has been driven by financial incentives. In 2013, CMS began penalizing hospitals 1.25% for poor HCAHPS scores as a part of the Affordable Care Act. In 2014, the maximum penalty increased to 2%, and to 3% in 2015. Hospitals have notoriously high overhead costs and slim profit margins, so these penalties can have a profound impact on the financial viability of an institution. But, while hospitals across the country have taken notice (see related article in this edition of The Hospitalist), I find doctors are more motivated by the well-being of their patients than are their hospital administrators. Satisfied patients are more compliant with treatment plans and have better outcomes.4,5 Hospitalists spend a lot of effort making sure their heart failure patients are on an ACE inhibitor, and their heart attack patients are discharged on aspirin, beta blockers, and statins so that they will have a good outcome following treatment for their acute illness. The same outcome-driven, evidence-based practice of medicine relates to patient satisfaction, however. Success in HCAHPS is as important as core measures when it comes to patient outcomes. And if I can’t convince you patient satisfaction is important because of the good it does for hospitals and patients, think about yourself for a minute. Satisfied patients are much less likely to sue their physicians.6 Practicing quality, evidence-based medicine will keep you out of peer review; however, satisfied patients will keep you out of the courtroom.
I frequently hear the comment that “we can do great on patient satisfaction, but then it gets busy, and patient satisfaction goes out the window.” My own experience contradicts this maxim, however. It is not how much time you spend with your patient but, rather, what you do with the time you have. One of the most powerful things we can do is listen. I used to make the mistake that I only wanted to hear the information I needed to figure out my patients’ problems so I could start treating them; however, I have come to learn that being heard is, in itself, therapy for my patients. It is often quoted that physicians interrupt their patients within 18 seconds of starting the interview.7 A lot of physicians dispense with attentive listening when they are under time pressure, when they should instead dispense with lengthy discourses on the patient treatment plan. It is important to educate our patients on their illness and treatment, I admit. I find a lot of hospitalists want to impart their knowledge and their treatment rationale to their patients; however, they frequently give patients and families much more information than they can hold in their cognitive memory. And time pressures are not the only anxieties hospitalists carry with them to the bedside. Our increasingly metric-driven profession means that we not only have to worry about morning discharges, interdisciplinary rounds, length of stay, and so on, but we also have to consider patient experience. It is not easy to hide all the stress we are under when we come to the bedside of a patient, but we have to. The easiest way to do that is to take a deep breath, sit next to the patient, ask an open-ended question, and then say nothing until the patient is done speaking. Active listening with good eye contact and encouragement to continue solidifies the patient’s experience of being heard. There are extreme cases when a patient is in a manic phase and won’t ever stop speaking; bend the rules a bit in those circumstances. However, the above rule works very effectively in the majority of physician-patient interactions. Being heard leaves an enduring emotional memory with our patients.
Hospital medicine often looks to other industries for inspiration on how we can improve. The airline industry is often held up as an example of how we can model patient safety, for instance, but these comparisons oversimplify the challenges we face. The same is true with patient satisfaction. In the business world, adages like “The customer is always right” are central to customer satisfaction, yet completely irrelevant to HM practice. Patients and families frequently have inappropriate and unrealistic expectations of their hospitalist physicians. We cannot, and should not, tell the patient addicted to narcotics that they can have as much IV Dilaudid as they would like. We cannot fix the patient with end-stage cancer, heart failure, or dementia. This is where we have to part ways with comparisons to principles that guide other industries if we are going to find a way forward with patient experience in hospital medicine. Because we have to set limits for patients, we often have to give our patients and families bad news, and because we have to tell them things they don’t like to hear, like “You can’t have any salt in your diet,” or “You must quit drinking alcohol,” we must develop our own principles on patient experience and satisfaction. Otherwise our options are either delivering inappropriate medical care or abandoning the pursuit of patient satisfaction all together. This is when we must remember that emotional memories are more enduring. We can’t always give our patients what they want, and we can’t always tell them what they want to hear, but we can always show them that we care. When we show our patients that we care in a palpable way, we leave them with the feeling that they have been cared for regardless of their condition, and the positive memory will endure despite the negative information we may have to convey. Maybe they won’t cut down on their salt or quit drinking alcohol, but they will never forget that their hospitalist physician cared.
And if they remember that the physician cared, it is much more likely that they will cut down on the salt or quit drinking alcohol when they go home. To paraphrase Maya Angelou, “I can’t always tell my patients what they want to hear, I can’t always tell them that their lifestyle is appropriate, but I can always show them that I care.”
Dr. McIlraith is chairman of the department of hospital medicine of Mercy Medical Group in Sacramento, Calif.
References
- LeDoux JE. Emotional memory. Scholarpedia. Accessed August 2, 2015.
- Feinstein JS, Duff MC, D Tranel D. Sustained experience of emotion after loss of memory in patients with amnesia. Proc Natl Acad Sci. 2010:107(17):7674-7679.
- Guzmán-Vélez E, Feinstein JS, Tranel D. Feelings without memory in Alzheimer disease. Cogn Behav Neurol. 2014;27(3):117-129.
- Institute of Medicine. Crossing the quality chasm: a new health system for the 21st century. March 2001. Accessed August 2, 2015.
- Bertakis KD, Azari R. Patient-centered care is associated with decreased health care utilization. J Am Board Fam Med. 2011;24(3):229-239.
- Stelfox HT, Gandhi TK, Orav EJ, Gustafson ML. The relation of patient statisfaction with complaints against physicians and malpractice lawsuits. Am J Med. 2005;118(10):1126-1133.
- Beckman HB, Frankel RM. The effect of physician behavior on the collection of data. Ann Intern Med. 1984;101(5):692-696.
There are two types of memory, the cognitive and the emotional, and the latter is more enduring. Maya Angelou characterized the distinction between these two types of memory most eloquently and succinctly when she said, “I’ve learned that people will forget what you said, people will forget what you did, but people will never forget how you made them feel.” She was ahead of her time, because neurocognitive research has objectified with science what Ms. Angelou captured so elegantly in her prose. Emotional events are processed in the sensory systems and then transmitted to the medial-temporal lobe and the amygdale for the formation of an emotional memory. When the memory is cued and retrieved from the amygdale, it triggers an emotional response. Emotional experiences leave strong traces in the brain. Memories about emotional situations are stored in both the conscious and unconscious memory, which is part of the reason emotional memories are so enduring.1 Studies of patients with severe anterograde amnesia following circumscribed bilateral hippocampal brain damage showed enduring memories of emotion despite the absence of conscious memories.2 This has a demonstrably practical application in patients with dementia, who we now know have feelings of happiness and sadness long after they have forgotten what caused the emotion.3
The distinction is important because patients judge the quality of their medical care based on emotions. The patient satisfaction disconnect arises from the fact that physicians live in their cognitive memory, while patients live in their emotional memory. Being cognitive and objective is a critical skill a physician must bring to the bedside every day; the reason we don’t allow physicians to treat family members is that their ability to remain objective will be impaired. I realized that my emotion, my passion, and my empathy for the dying would impair my judgment when I started medical school, and I launched myself on a conscious and systematic discipline to keep those feelings out of my mind during patient care. The effort worked and, for the most part, I have been able to remain objective and unemotional as I care for my patients. Recently, however, I realized that my focus on objectivity negatively impacts patient experience. As a result, I have expanded my view: While I must stay objective and detached with my thinking, I must be emotionally engaged to provide a great patient experience.
I can remain objective and detached in my clinical judgment as I engage and connect emotionally during my patient encounters. This delicate balancing act has taken years of trial and error, however. I recently cared for a woman in her 60s who had fallen and broke her hip. Everyone was pleased that a top orthopedic surgeon was on call and able to give her the first-rate care she needed to begin walking again. The surgery went smoothly, and she was transferred to the medical/surgical ward, where things took a turn for the worse. She had a lot of anxiety in addition to her osteoporosis. Objectively, she was doing great, and we had a big success on our hands; however, she remained anxious, and she peppered the surgeon with fears that, while unfounded, were very real in her mind. The surgeon brushed them off, saying that her fears were not real and that he didn’t need to address them; his response made her emotional state spiral out of control. Her nurse notified me of the situation, and I came to her bedside. She was very agitated. I sat down at a low level and just started listening. She got all of her anxieties out in words. I held her hand, looked her in the eye, and assured her that I would be there for her and that things were going to be alright. Subsequently, she wrote letters of gratitude and proclaimed to any medical staff who would listen what a talented and great doctor I was. I did not have the skill to fix her broken hip; if it had been left to me alone, she would still be bed-bound. But I did have the human skills to connect with her and fix her agitated mind. If we remember the enduring power of the emotional memory, we can create great patient experiences.
The importance of these experiences was illustrated to me at the 2014 Dignity Health Patient Experience Summit, a powerful event featuring motivational speakers and leaders from across the country. The most powerful speakers, however, were patients. These patients had received terrible diagnoses that committed them to a prolonged interaction with the healthcare system. They were scared of what their diagnoses would mean for their future, they were subjected to uncomfortable procedures in which they struggled to maintain their dignity, and they repeatedly met the indifference of healthcare providers and clerical people who were only there to do a job. They related how the lack of caring and empathy made fears and anxiety much worse. But each of them had a story about that one person, that one care provider, who took the time to reassure them, to show that they cared, and to ensure that the patient did not feel alone. In most of these stories, the stand-out care providers took the time to hold their hands and reassure the patients. They took the time to connect with the patient’s emotional memory in a positive way, and that simple gesture of empathy had a powerful and lasting impact on the patient.
Invariably, the care provider at the heart of the patients’ stories was a nurse. Nurses have the reputation for being angels of mercy because they do the simple, empathetic gestures that let a patient know they are being cared for. These feelings endure in the patients’ memories long after the treatment is over. Doctors can, and should, be that type of care provider. It requires us to recognize that patients are scared and anxious, even though they may do their best not to show it. We, as physicians, often don’t see their anxiety, and we are so focused on the cognitive memory that we don’t address the anxiety and fear that is just under the surface. But taking just a few minutes to acknowledge their emotions, to explore them, and to reassure the patient that we are there for them has a lasting impact. In my group, we talk about the “human-business-human” encounter with patients. We begin all interactions with a human interaction (“Hello, I am Dr. McIlraith…”), conduct the business we came to provide (“Now I am going to examine you…”), and end with a human interaction (“What else can I do for you today?”). Patients expect physical contact with us during the “business” part of that interaction. I find that respectful, reassuring, and appropriate physical contact during the final “human” portion of that interaction helps solidify my patients’ experience. It helps make them feel that they have been cared for, particularly if the visit includes bad news.
Much of the recent focus on patient satisfaction has been driven by financial incentives. In 2013, CMS began penalizing hospitals 1.25% for poor HCAHPS scores as a part of the Affordable Care Act. In 2014, the maximum penalty increased to 2%, and to 3% in 2015. Hospitals have notoriously high overhead costs and slim profit margins, so these penalties can have a profound impact on the financial viability of an institution. But, while hospitals across the country have taken notice (see related article in this edition of The Hospitalist), I find doctors are more motivated by the well-being of their patients than are their hospital administrators. Satisfied patients are more compliant with treatment plans and have better outcomes.4,5 Hospitalists spend a lot of effort making sure their heart failure patients are on an ACE inhibitor, and their heart attack patients are discharged on aspirin, beta blockers, and statins so that they will have a good outcome following treatment for their acute illness. The same outcome-driven, evidence-based practice of medicine relates to patient satisfaction, however. Success in HCAHPS is as important as core measures when it comes to patient outcomes. And if I can’t convince you patient satisfaction is important because of the good it does for hospitals and patients, think about yourself for a minute. Satisfied patients are much less likely to sue their physicians.6 Practicing quality, evidence-based medicine will keep you out of peer review; however, satisfied patients will keep you out of the courtroom.
I frequently hear the comment that “we can do great on patient satisfaction, but then it gets busy, and patient satisfaction goes out the window.” My own experience contradicts this maxim, however. It is not how much time you spend with your patient but, rather, what you do with the time you have. One of the most powerful things we can do is listen. I used to make the mistake that I only wanted to hear the information I needed to figure out my patients’ problems so I could start treating them; however, I have come to learn that being heard is, in itself, therapy for my patients. It is often quoted that physicians interrupt their patients within 18 seconds of starting the interview.7 A lot of physicians dispense with attentive listening when they are under time pressure, when they should instead dispense with lengthy discourses on the patient treatment plan. It is important to educate our patients on their illness and treatment, I admit. I find a lot of hospitalists want to impart their knowledge and their treatment rationale to their patients; however, they frequently give patients and families much more information than they can hold in their cognitive memory. And time pressures are not the only anxieties hospitalists carry with them to the bedside. Our increasingly metric-driven profession means that we not only have to worry about morning discharges, interdisciplinary rounds, length of stay, and so on, but we also have to consider patient experience. It is not easy to hide all the stress we are under when we come to the bedside of a patient, but we have to. The easiest way to do that is to take a deep breath, sit next to the patient, ask an open-ended question, and then say nothing until the patient is done speaking. Active listening with good eye contact and encouragement to continue solidifies the patient’s experience of being heard. There are extreme cases when a patient is in a manic phase and won’t ever stop speaking; bend the rules a bit in those circumstances. However, the above rule works very effectively in the majority of physician-patient interactions. Being heard leaves an enduring emotional memory with our patients.
Hospital medicine often looks to other industries for inspiration on how we can improve. The airline industry is often held up as an example of how we can model patient safety, for instance, but these comparisons oversimplify the challenges we face. The same is true with patient satisfaction. In the business world, adages like “The customer is always right” are central to customer satisfaction, yet completely irrelevant to HM practice. Patients and families frequently have inappropriate and unrealistic expectations of their hospitalist physicians. We cannot, and should not, tell the patient addicted to narcotics that they can have as much IV Dilaudid as they would like. We cannot fix the patient with end-stage cancer, heart failure, or dementia. This is where we have to part ways with comparisons to principles that guide other industries if we are going to find a way forward with patient experience in hospital medicine. Because we have to set limits for patients, we often have to give our patients and families bad news, and because we have to tell them things they don’t like to hear, like “You can’t have any salt in your diet,” or “You must quit drinking alcohol,” we must develop our own principles on patient experience and satisfaction. Otherwise our options are either delivering inappropriate medical care or abandoning the pursuit of patient satisfaction all together. This is when we must remember that emotional memories are more enduring. We can’t always give our patients what they want, and we can’t always tell them what they want to hear, but we can always show them that we care. When we show our patients that we care in a palpable way, we leave them with the feeling that they have been cared for regardless of their condition, and the positive memory will endure despite the negative information we may have to convey. Maybe they won’t cut down on their salt or quit drinking alcohol, but they will never forget that their hospitalist physician cared.
And if they remember that the physician cared, it is much more likely that they will cut down on the salt or quit drinking alcohol when they go home. To paraphrase Maya Angelou, “I can’t always tell my patients what they want to hear, I can’t always tell them that their lifestyle is appropriate, but I can always show them that I care.”
Dr. McIlraith is chairman of the department of hospital medicine of Mercy Medical Group in Sacramento, Calif.
References
- LeDoux JE. Emotional memory. Scholarpedia. Accessed August 2, 2015.
- Feinstein JS, Duff MC, D Tranel D. Sustained experience of emotion after loss of memory in patients with amnesia. Proc Natl Acad Sci. 2010:107(17):7674-7679.
- Guzmán-Vélez E, Feinstein JS, Tranel D. Feelings without memory in Alzheimer disease. Cogn Behav Neurol. 2014;27(3):117-129.
- Institute of Medicine. Crossing the quality chasm: a new health system for the 21st century. March 2001. Accessed August 2, 2015.
- Bertakis KD, Azari R. Patient-centered care is associated with decreased health care utilization. J Am Board Fam Med. 2011;24(3):229-239.
- Stelfox HT, Gandhi TK, Orav EJ, Gustafson ML. The relation of patient statisfaction with complaints against physicians and malpractice lawsuits. Am J Med. 2005;118(10):1126-1133.
- Beckman HB, Frankel RM. The effect of physician behavior on the collection of data. Ann Intern Med. 1984;101(5):692-696.
HHS: Expand antidiscrimination protections to transgender patients
Transgender patients who receive health care via government programs or funding must receive equal access to treatments and insurance coverage, according to a proposed rule issued Sept. 3 by the Health and Human Services department. The rule would extend antidiscrimination policies under the Affordable Care Act to include gender identity.
The rule would apply to health providers who accept patients covered by Medicare and Medicaid as well as insurance purchased via the health insurance marketplaces.
“The proposed rule clarifies and harmonizes existing well-established federal civil rights laws and clarifies the standards that HHS and in particular, the Office of Civil Rights, will apply in implementing [ACA] Section 1557,” Jocelyn Samuels, OCR director, said in a press conference. “Prior laws enforced by the Office of Civil Rights barred discrimination based only on race, color, national origin, age, or disability. All of the protections against sex discrimination that will be incorporated into the rule are new in this space.”
Section 1557 of the ACA extends civil rights protections to ban sex discrimination in federal health care programs and activities. The new proposed rule establishes that the prohibition on sex discrimination includes discrimination based on gender identity. The rule also includes requirements for effective communication for patients with disabilities and enhanced language assistance for patients with limited English proficiency.
Specifics of the proposed rule include:
• Patients must be treated equally and consistent with their gender identity by health providers. Insurers must provide fair access to coverage regardless of gender identity. For example, some insurers have historically excluded coverage of all care related to gender transition. Such categorical exclusions are prohibited under the proposed rule.
• Women must be treated equally with men in the health care they receive, not only in the health coverage they obtain but in the services they seek from providers.
• For patients with disabilities, the rule contains requirements for the provision of auxiliary aids and services, including alternative formats and sign language interpreters and the accessibility of programs offered through electronic and information technology.
• The rule bolsters language assistance for people with limited English proficiency so that patients are able to more effectively communicate with their providers to describe their symptoms and understand treatment.
During the press conference, Ms. Samuels clarified that the rule does not mean that health insurers must cover any specific treatments or procedures, rather they must apply nondiscriminatory criteria when assessing coverage requests.
The proposed extension of protections is, in part, driven by ongoing cases of sex and identity discrimination by some health providers. In one case, a hospital denied a transgender patient a room assignment consistent with her gender identity. In another, a male domestic violence victim was denied services at a hospital because he did not fit the traditional profile of a domestic violence victim, Ms. Samuels said. In another case, a health provider required that a husband be the guarantor for his wife’s medical bills but did not require the same for male patients and their spouses.
“There continue to be serious problems of discrimination in the health care arena,” she said. “This proposed rule provides very valuable tools for us to be able to appropriately address them.”
HHS is requesting comments on whether Section 1557 should include exemptions for religious organizations and, if so, to what extent. The administration notes that nothing in the proposed rule would affect the application of existing protections for religious beliefs and practices, such as provider conscience laws and regulations under the ACA involving preventive health services.
Comments on the rule will be accepted at www.regulations.gov until Nov. 6.
On Twitter @legal_med
Transgender patients who receive health care via government programs or funding must receive equal access to treatments and insurance coverage, according to a proposed rule issued Sept. 3 by the Health and Human Services department. The rule would extend antidiscrimination policies under the Affordable Care Act to include gender identity.
The rule would apply to health providers who accept patients covered by Medicare and Medicaid as well as insurance purchased via the health insurance marketplaces.
“The proposed rule clarifies and harmonizes existing well-established federal civil rights laws and clarifies the standards that HHS and in particular, the Office of Civil Rights, will apply in implementing [ACA] Section 1557,” Jocelyn Samuels, OCR director, said in a press conference. “Prior laws enforced by the Office of Civil Rights barred discrimination based only on race, color, national origin, age, or disability. All of the protections against sex discrimination that will be incorporated into the rule are new in this space.”
Section 1557 of the ACA extends civil rights protections to ban sex discrimination in federal health care programs and activities. The new proposed rule establishes that the prohibition on sex discrimination includes discrimination based on gender identity. The rule also includes requirements for effective communication for patients with disabilities and enhanced language assistance for patients with limited English proficiency.
Specifics of the proposed rule include:
• Patients must be treated equally and consistent with their gender identity by health providers. Insurers must provide fair access to coverage regardless of gender identity. For example, some insurers have historically excluded coverage of all care related to gender transition. Such categorical exclusions are prohibited under the proposed rule.
• Women must be treated equally with men in the health care they receive, not only in the health coverage they obtain but in the services they seek from providers.
• For patients with disabilities, the rule contains requirements for the provision of auxiliary aids and services, including alternative formats and sign language interpreters and the accessibility of programs offered through electronic and information technology.
• The rule bolsters language assistance for people with limited English proficiency so that patients are able to more effectively communicate with their providers to describe their symptoms and understand treatment.
During the press conference, Ms. Samuels clarified that the rule does not mean that health insurers must cover any specific treatments or procedures, rather they must apply nondiscriminatory criteria when assessing coverage requests.
The proposed extension of protections is, in part, driven by ongoing cases of sex and identity discrimination by some health providers. In one case, a hospital denied a transgender patient a room assignment consistent with her gender identity. In another, a male domestic violence victim was denied services at a hospital because he did not fit the traditional profile of a domestic violence victim, Ms. Samuels said. In another case, a health provider required that a husband be the guarantor for his wife’s medical bills but did not require the same for male patients and their spouses.
“There continue to be serious problems of discrimination in the health care arena,” she said. “This proposed rule provides very valuable tools for us to be able to appropriately address them.”
HHS is requesting comments on whether Section 1557 should include exemptions for religious organizations and, if so, to what extent. The administration notes that nothing in the proposed rule would affect the application of existing protections for religious beliefs and practices, such as provider conscience laws and regulations under the ACA involving preventive health services.
Comments on the rule will be accepted at www.regulations.gov until Nov. 6.
On Twitter @legal_med
Transgender patients who receive health care via government programs or funding must receive equal access to treatments and insurance coverage, according to a proposed rule issued Sept. 3 by the Health and Human Services department. The rule would extend antidiscrimination policies under the Affordable Care Act to include gender identity.
The rule would apply to health providers who accept patients covered by Medicare and Medicaid as well as insurance purchased via the health insurance marketplaces.
“The proposed rule clarifies and harmonizes existing well-established federal civil rights laws and clarifies the standards that HHS and in particular, the Office of Civil Rights, will apply in implementing [ACA] Section 1557,” Jocelyn Samuels, OCR director, said in a press conference. “Prior laws enforced by the Office of Civil Rights barred discrimination based only on race, color, national origin, age, or disability. All of the protections against sex discrimination that will be incorporated into the rule are new in this space.”
Section 1557 of the ACA extends civil rights protections to ban sex discrimination in federal health care programs and activities. The new proposed rule establishes that the prohibition on sex discrimination includes discrimination based on gender identity. The rule also includes requirements for effective communication for patients with disabilities and enhanced language assistance for patients with limited English proficiency.
Specifics of the proposed rule include:
• Patients must be treated equally and consistent with their gender identity by health providers. Insurers must provide fair access to coverage regardless of gender identity. For example, some insurers have historically excluded coverage of all care related to gender transition. Such categorical exclusions are prohibited under the proposed rule.
• Women must be treated equally with men in the health care they receive, not only in the health coverage they obtain but in the services they seek from providers.
• For patients with disabilities, the rule contains requirements for the provision of auxiliary aids and services, including alternative formats and sign language interpreters and the accessibility of programs offered through electronic and information technology.
• The rule bolsters language assistance for people with limited English proficiency so that patients are able to more effectively communicate with their providers to describe their symptoms and understand treatment.
During the press conference, Ms. Samuels clarified that the rule does not mean that health insurers must cover any specific treatments or procedures, rather they must apply nondiscriminatory criteria when assessing coverage requests.
The proposed extension of protections is, in part, driven by ongoing cases of sex and identity discrimination by some health providers. In one case, a hospital denied a transgender patient a room assignment consistent with her gender identity. In another, a male domestic violence victim was denied services at a hospital because he did not fit the traditional profile of a domestic violence victim, Ms. Samuels said. In another case, a health provider required that a husband be the guarantor for his wife’s medical bills but did not require the same for male patients and their spouses.
“There continue to be serious problems of discrimination in the health care arena,” she said. “This proposed rule provides very valuable tools for us to be able to appropriately address them.”
HHS is requesting comments on whether Section 1557 should include exemptions for religious organizations and, if so, to what extent. The administration notes that nothing in the proposed rule would affect the application of existing protections for religious beliefs and practices, such as provider conscience laws and regulations under the ACA involving preventive health services.
Comments on the rule will be accepted at www.regulations.gov until Nov. 6.
On Twitter @legal_med
Why Hospitalist Morale is Declining and Ways to Improve It
Using quotes to ensure that the results were only those that include the two words adjacent to one another, rather than separated, I entered the following phrases into my Google search engine:
- “hospitalist burnout” = 1,580 results
- “hospitalist morale” = 208 results
- “hospitalist well-being” = 0 results
I think the number of results suggests the level of interest in each topic and, if that is the case, clearly thinking about how hospitalists are doing in their careers is more commonly done through the paradigm of burnout than the other two terms. (Of course, there may be other terms that I didn’t consider.) In fact, there have been a handful of published studies of hospitalist burnout and job satisfaction.1,2
Those studies generally have shown both reasonably high levels of job satisfaction and troubling levels of burnout.
But I’ve been thinking about hospitalist morale for a while. I think morale is reasonably distinct from both burnout and job satisfaction.
Causes of a National Decline in Hospitalist Morale
I think hospitalist morale has declined some over the past two or three years across the country. This observation is meaningful because it comes from my experience working with a lot of hospitalist groups coast to coast. But I’m the first to admit it is just anecdotal and is subject to my own biases.
I can think of several things contributing to a decline in morale.
EHR adoption. Near the top of the list is the adoption of EHRs in many hospitals, which typically leads doctors in other specialties to seek hospitalist assistance with EHR-related tasks (e.g. medicine reconciliation and order writing) even in cases where there is little or no clinical reason for hospitalist involvement. Lots of hospitalists complain about this. To be clear, in many hospitals the hospitalists are reasonably content with using the EHR, but they experience ongoing frustration and low morale resulting from nonclinical work other doctors pressure them to take over.
Observation status. Many hospitals began classifying a larger portion of patients as observation status over the last few years; at the same time, patients and families have become more aware of how much of a disadvantage this is. In many cases, it is the hospitalist who takes the brunt of patient and family frustration. This can get awfully stressful and frustrating, and I think it is a contributor to allegations of malpractice.
Budgetary stress. Ever since SHM began collecting survey data in the late 1990s, the financial support hospitals have been providing to hospitalists has increased dramatically. The most recent State of Hospital Medicine report, published in 2104, showed median support provided by hospitals of $156,063 per FTE hospitalist, per year. Some hospitals have begun to resist providing more support, and this translates into stress and lower morale for hospitalists. This is far from a universal issue, but it does lead to lower morale for hospitalists who face it.
Many other factors may be contributing to a national decline in morale, but I think these are some of the most important.
What Can Be Done?
Some hospitalist groups have great morale now and don’t need to do much of anything right now, but some groups should think about a deliberate strategy to improve it.
Sadly, there isn’t a prescription that is sure to work. But there are some things you can try.
Self-care. The field of palliative care has thought a lot about caring for caregivers, and hospitalist groups might want to adopt some of their practices. Search the Internet on “self-care” + “palliative care,” and you’ll find a lot of interesting things. The group I’m part of launched a deliberate program of professionally led and facilitated hospitalist self-care, with high hopes that included mindful meditation, among other things. As soon as we had designed our program, the Mayo Clinic published their favorable experience with a program that was very similar to what we had planned, and I thought we would see similar benefits.3
But, while all who attended the sessions thought they were valuable, attendance was so poor that we ended up cancelling the program. The hospitalists were interested in attending but were either on service and busy seeing patients, or were off and didn’t want to drive in to work solely for the purpose of reducing work stress.
I’m convinced a self-care program is valuable but very tricky to schedule effectively. Maybe others have come up with effective ways of overcoming this problem.
Social connections. Some hospitalist groups seem to have little social and personal connection to other physicians and hospital leaders. I think this results in lower hospitalist morale and tends to be self-reinforcing. If you’re in such a group, you and your hospitalist colleagues should deliberately seek better relationships with other doctors and hospital administrative leaders. Ensure that you visit with others at lunch, talk with them at committee meetings, ask about their vacation and personal activities, and pursue activities with them outside of work.
When these sorts of social connections are strong, work is far more satisfying and you’re much more likely to be treated as a peer by other doctors. I think this is really important and shouldn’t be overlooked if your group is suffering from low morale.
Adaptive work. Lastly, you might want to approach changes to your work and morale as “adaptive work,” rather than “technical work.” Space doesn’t permit a description of these, but it is worth reading about how they differ. Many groups will find value in reframing their approach to aspects of work they don’t like as adaptive work.

References
- Hinami K, Whelan CT, Wolosin RJ, Miller JA, Wetterneck TB. Worklife and satisfaction of hospitalists: toward flourishing careers. J Gen Intern Med. 2012;27(1):28-36.
- Hoff TH, Whitcomb WF, Williams K, Nelson JR, Cheesman RA. Characteristics and work experiences of hospitalists in the United States. Arch Intern Med. 2001;161(6):851-858.
- West CP, Dyrbye LN, Rabatin JT, et al. Intervention to promote physician well-being, job satisfaction, and professionalism: a randomized clinical trial. JAMA Intern Med. 2014;174(4):527-533.
Using quotes to ensure that the results were only those that include the two words adjacent to one another, rather than separated, I entered the following phrases into my Google search engine:
- “hospitalist burnout” = 1,580 results
- “hospitalist morale” = 208 results
- “hospitalist well-being” = 0 results
I think the number of results suggests the level of interest in each topic and, if that is the case, clearly thinking about how hospitalists are doing in their careers is more commonly done through the paradigm of burnout than the other two terms. (Of course, there may be other terms that I didn’t consider.) In fact, there have been a handful of published studies of hospitalist burnout and job satisfaction.1,2
Those studies generally have shown both reasonably high levels of job satisfaction and troubling levels of burnout.
But I’ve been thinking about hospitalist morale for a while. I think morale is reasonably distinct from both burnout and job satisfaction.
Causes of a National Decline in Hospitalist Morale
I think hospitalist morale has declined some over the past two or three years across the country. This observation is meaningful because it comes from my experience working with a lot of hospitalist groups coast to coast. But I’m the first to admit it is just anecdotal and is subject to my own biases.
I can think of several things contributing to a decline in morale.
EHR adoption. Near the top of the list is the adoption of EHRs in many hospitals, which typically leads doctors in other specialties to seek hospitalist assistance with EHR-related tasks (e.g. medicine reconciliation and order writing) even in cases where there is little or no clinical reason for hospitalist involvement. Lots of hospitalists complain about this. To be clear, in many hospitals the hospitalists are reasonably content with using the EHR, but they experience ongoing frustration and low morale resulting from nonclinical work other doctors pressure them to take over.
Observation status. Many hospitals began classifying a larger portion of patients as observation status over the last few years; at the same time, patients and families have become more aware of how much of a disadvantage this is. In many cases, it is the hospitalist who takes the brunt of patient and family frustration. This can get awfully stressful and frustrating, and I think it is a contributor to allegations of malpractice.
Budgetary stress. Ever since SHM began collecting survey data in the late 1990s, the financial support hospitals have been providing to hospitalists has increased dramatically. The most recent State of Hospital Medicine report, published in 2104, showed median support provided by hospitals of $156,063 per FTE hospitalist, per year. Some hospitals have begun to resist providing more support, and this translates into stress and lower morale for hospitalists. This is far from a universal issue, but it does lead to lower morale for hospitalists who face it.
Many other factors may be contributing to a national decline in morale, but I think these are some of the most important.
What Can Be Done?
Some hospitalist groups have great morale now and don’t need to do much of anything right now, but some groups should think about a deliberate strategy to improve it.
Sadly, there isn’t a prescription that is sure to work. But there are some things you can try.
Self-care. The field of palliative care has thought a lot about caring for caregivers, and hospitalist groups might want to adopt some of their practices. Search the Internet on “self-care” + “palliative care,” and you’ll find a lot of interesting things. The group I’m part of launched a deliberate program of professionally led and facilitated hospitalist self-care, with high hopes that included mindful meditation, among other things. As soon as we had designed our program, the Mayo Clinic published their favorable experience with a program that was very similar to what we had planned, and I thought we would see similar benefits.3
But, while all who attended the sessions thought they were valuable, attendance was so poor that we ended up cancelling the program. The hospitalists were interested in attending but were either on service and busy seeing patients, or were off and didn’t want to drive in to work solely for the purpose of reducing work stress.
I’m convinced a self-care program is valuable but very tricky to schedule effectively. Maybe others have come up with effective ways of overcoming this problem.
Social connections. Some hospitalist groups seem to have little social and personal connection to other physicians and hospital leaders. I think this results in lower hospitalist morale and tends to be self-reinforcing. If you’re in such a group, you and your hospitalist colleagues should deliberately seek better relationships with other doctors and hospital administrative leaders. Ensure that you visit with others at lunch, talk with them at committee meetings, ask about their vacation and personal activities, and pursue activities with them outside of work.
When these sorts of social connections are strong, work is far more satisfying and you’re much more likely to be treated as a peer by other doctors. I think this is really important and shouldn’t be overlooked if your group is suffering from low morale.
Adaptive work. Lastly, you might want to approach changes to your work and morale as “adaptive work,” rather than “technical work.” Space doesn’t permit a description of these, but it is worth reading about how they differ. Many groups will find value in reframing their approach to aspects of work they don’t like as adaptive work.

References
- Hinami K, Whelan CT, Wolosin RJ, Miller JA, Wetterneck TB. Worklife and satisfaction of hospitalists: toward flourishing careers. J Gen Intern Med. 2012;27(1):28-36.
- Hoff TH, Whitcomb WF, Williams K, Nelson JR, Cheesman RA. Characteristics and work experiences of hospitalists in the United States. Arch Intern Med. 2001;161(6):851-858.
- West CP, Dyrbye LN, Rabatin JT, et al. Intervention to promote physician well-being, job satisfaction, and professionalism: a randomized clinical trial. JAMA Intern Med. 2014;174(4):527-533.
Using quotes to ensure that the results were only those that include the two words adjacent to one another, rather than separated, I entered the following phrases into my Google search engine:
- “hospitalist burnout” = 1,580 results
- “hospitalist morale” = 208 results
- “hospitalist well-being” = 0 results
I think the number of results suggests the level of interest in each topic and, if that is the case, clearly thinking about how hospitalists are doing in their careers is more commonly done through the paradigm of burnout than the other two terms. (Of course, there may be other terms that I didn’t consider.) In fact, there have been a handful of published studies of hospitalist burnout and job satisfaction.1,2
Those studies generally have shown both reasonably high levels of job satisfaction and troubling levels of burnout.
But I’ve been thinking about hospitalist morale for a while. I think morale is reasonably distinct from both burnout and job satisfaction.
Causes of a National Decline in Hospitalist Morale
I think hospitalist morale has declined some over the past two or three years across the country. This observation is meaningful because it comes from my experience working with a lot of hospitalist groups coast to coast. But I’m the first to admit it is just anecdotal and is subject to my own biases.
I can think of several things contributing to a decline in morale.
EHR adoption. Near the top of the list is the adoption of EHRs in many hospitals, which typically leads doctors in other specialties to seek hospitalist assistance with EHR-related tasks (e.g. medicine reconciliation and order writing) even in cases where there is little or no clinical reason for hospitalist involvement. Lots of hospitalists complain about this. To be clear, in many hospitals the hospitalists are reasonably content with using the EHR, but they experience ongoing frustration and low morale resulting from nonclinical work other doctors pressure them to take over.
Observation status. Many hospitals began classifying a larger portion of patients as observation status over the last few years; at the same time, patients and families have become more aware of how much of a disadvantage this is. In many cases, it is the hospitalist who takes the brunt of patient and family frustration. This can get awfully stressful and frustrating, and I think it is a contributor to allegations of malpractice.
Budgetary stress. Ever since SHM began collecting survey data in the late 1990s, the financial support hospitals have been providing to hospitalists has increased dramatically. The most recent State of Hospital Medicine report, published in 2104, showed median support provided by hospitals of $156,063 per FTE hospitalist, per year. Some hospitals have begun to resist providing more support, and this translates into stress and lower morale for hospitalists. This is far from a universal issue, but it does lead to lower morale for hospitalists who face it.
Many other factors may be contributing to a national decline in morale, but I think these are some of the most important.
What Can Be Done?
Some hospitalist groups have great morale now and don’t need to do much of anything right now, but some groups should think about a deliberate strategy to improve it.
Sadly, there isn’t a prescription that is sure to work. But there are some things you can try.
Self-care. The field of palliative care has thought a lot about caring for caregivers, and hospitalist groups might want to adopt some of their practices. Search the Internet on “self-care” + “palliative care,” and you’ll find a lot of interesting things. The group I’m part of launched a deliberate program of professionally led and facilitated hospitalist self-care, with high hopes that included mindful meditation, among other things. As soon as we had designed our program, the Mayo Clinic published their favorable experience with a program that was very similar to what we had planned, and I thought we would see similar benefits.3
But, while all who attended the sessions thought they were valuable, attendance was so poor that we ended up cancelling the program. The hospitalists were interested in attending but were either on service and busy seeing patients, or were off and didn’t want to drive in to work solely for the purpose of reducing work stress.
I’m convinced a self-care program is valuable but very tricky to schedule effectively. Maybe others have come up with effective ways of overcoming this problem.
Social connections. Some hospitalist groups seem to have little social and personal connection to other physicians and hospital leaders. I think this results in lower hospitalist morale and tends to be self-reinforcing. If you’re in such a group, you and your hospitalist colleagues should deliberately seek better relationships with other doctors and hospital administrative leaders. Ensure that you visit with others at lunch, talk with them at committee meetings, ask about their vacation and personal activities, and pursue activities with them outside of work.
When these sorts of social connections are strong, work is far more satisfying and you’re much more likely to be treated as a peer by other doctors. I think this is really important and shouldn’t be overlooked if your group is suffering from low morale.
Adaptive work. Lastly, you might want to approach changes to your work and morale as “adaptive work,” rather than “technical work.” Space doesn’t permit a description of these, but it is worth reading about how they differ. Many groups will find value in reframing their approach to aspects of work they don’t like as adaptive work.

References
- Hinami K, Whelan CT, Wolosin RJ, Miller JA, Wetterneck TB. Worklife and satisfaction of hospitalists: toward flourishing careers. J Gen Intern Med. 2012;27(1):28-36.
- Hoff TH, Whitcomb WF, Williams K, Nelson JR, Cheesman RA. Characteristics and work experiences of hospitalists in the United States. Arch Intern Med. 2001;161(6):851-858.
- West CP, Dyrbye LN, Rabatin JT, et al. Intervention to promote physician well-being, job satisfaction, and professionalism: a randomized clinical trial. JAMA Intern Med. 2014;174(4):527-533.