User login
CMS releases data on $3.5B in industry payments to doctors, teaching hospitals
The federal government publicly released the first data about drug and device industry payments to physicians and hospitals, part of a push toward greater transparency that was mandated under the Affordable Care Act.
On Sept. 30, the Centers for Medicare & Medicaid Services published 4.4 million records of payments to about 546,000 individual physicians and nearly 1,360 teaching hospitals. In total, the records represent $3.5 billion in financial transactions between industry and health care providers.
The Open Payments program, known previously as the Sunshine Act, requires medical device manufacturers and pharmaceutical companies to report payments and transfers of value to physicians and teaching hospitals, including consulting fees, research grants, travel reimbursements, ownership interests, and other gifts.
The data released on Sept. 30 cover only payments made from August through December 2013. Data on payments made in 2014 are slated to be published in June 2015.
“We are taking a big step forward in shining the light on these financial arrangements between physicians and the health care industry,” said Dr. Shantanu Agrawal, director of the CMS Center for Program Integrity. “Using [these] new data, it is now possible to conduct a wide range of analyses of payments made by drug and device manufacturers that were never possible before.”
But the program has been plagued by delays and technical problems. CMS had to extend multiple times the 45-day “review and dispute” period, during which physicians could check the accuracy of data reported about them. It took the agency days to correct technical problems that had caused data to be intermingled, matching the wrong records to physicians with similar names.
Of the 4.4 million records released on Sept. 30, about 40% had to be deidentified either because of data inconsistencies that kept CMS from being able to match them to an individual physician or teaching hospital, or because the data were not available for review for the full 45-day period. CMS expects the data to be fully identified in 2015 once the manufacturers submit corrected information.
Another 199,000 records that were reported to the agency were not published at all, according to CMS. The vast majority of those records were unpublished at the request of the industry, since they related to ongoing research of unapproved treatments. About 9,000 records were not published because they are under active dispute, according to Dr. Agrawal.
While physicians and the industry have been generally supportive of CMS’s move toward greater openness about payments, there has been plenty of criticism of the implementation of the Open Payments program. The American Medical Association has said repeatedly that physicians have not had enough time to review the accuracy of the payments and that CMS is not providing adequate context about what the payments actually say about physician-industry relationships.
“Publicly reporting industry payments to individual physicians can imply, wrongly, that such payments are always inappropriate,” the AMA wrote in a guide for reporters covering the release of Open Payments data. “Some may be, but to be able to make an informed judgment, it is vital to be able to set the financial information in context. Just because a physician has a relationship with industry does not automatically mean that his or her professional judgment has been influenced inappropriately.”
The AMA also said that the process of registering and later reviewing payments was confusing and overly cumbersome for physicians. Only about 26,000 physicians and 400 teaching hospitals registered in the Open Payments system to review their data, according to CMS.
On Twitter @maryellenny
The federal government publicly released the first data about drug and device industry payments to physicians and hospitals, part of a push toward greater transparency that was mandated under the Affordable Care Act.
On Sept. 30, the Centers for Medicare & Medicaid Services published 4.4 million records of payments to about 546,000 individual physicians and nearly 1,360 teaching hospitals. In total, the records represent $3.5 billion in financial transactions between industry and health care providers.
The Open Payments program, known previously as the Sunshine Act, requires medical device manufacturers and pharmaceutical companies to report payments and transfers of value to physicians and teaching hospitals, including consulting fees, research grants, travel reimbursements, ownership interests, and other gifts.
The data released on Sept. 30 cover only payments made from August through December 2013. Data on payments made in 2014 are slated to be published in June 2015.
“We are taking a big step forward in shining the light on these financial arrangements between physicians and the health care industry,” said Dr. Shantanu Agrawal, director of the CMS Center for Program Integrity. “Using [these] new data, it is now possible to conduct a wide range of analyses of payments made by drug and device manufacturers that were never possible before.”
But the program has been plagued by delays and technical problems. CMS had to extend multiple times the 45-day “review and dispute” period, during which physicians could check the accuracy of data reported about them. It took the agency days to correct technical problems that had caused data to be intermingled, matching the wrong records to physicians with similar names.
Of the 4.4 million records released on Sept. 30, about 40% had to be deidentified either because of data inconsistencies that kept CMS from being able to match them to an individual physician or teaching hospital, or because the data were not available for review for the full 45-day period. CMS expects the data to be fully identified in 2015 once the manufacturers submit corrected information.
Another 199,000 records that were reported to the agency were not published at all, according to CMS. The vast majority of those records were unpublished at the request of the industry, since they related to ongoing research of unapproved treatments. About 9,000 records were not published because they are under active dispute, according to Dr. Agrawal.
While physicians and the industry have been generally supportive of CMS’s move toward greater openness about payments, there has been plenty of criticism of the implementation of the Open Payments program. The American Medical Association has said repeatedly that physicians have not had enough time to review the accuracy of the payments and that CMS is not providing adequate context about what the payments actually say about physician-industry relationships.
“Publicly reporting industry payments to individual physicians can imply, wrongly, that such payments are always inappropriate,” the AMA wrote in a guide for reporters covering the release of Open Payments data. “Some may be, but to be able to make an informed judgment, it is vital to be able to set the financial information in context. Just because a physician has a relationship with industry does not automatically mean that his or her professional judgment has been influenced inappropriately.”
The AMA also said that the process of registering and later reviewing payments was confusing and overly cumbersome for physicians. Only about 26,000 physicians and 400 teaching hospitals registered in the Open Payments system to review their data, according to CMS.
On Twitter @maryellenny
The federal government publicly released the first data about drug and device industry payments to physicians and hospitals, part of a push toward greater transparency that was mandated under the Affordable Care Act.
On Sept. 30, the Centers for Medicare & Medicaid Services published 4.4 million records of payments to about 546,000 individual physicians and nearly 1,360 teaching hospitals. In total, the records represent $3.5 billion in financial transactions between industry and health care providers.
The Open Payments program, known previously as the Sunshine Act, requires medical device manufacturers and pharmaceutical companies to report payments and transfers of value to physicians and teaching hospitals, including consulting fees, research grants, travel reimbursements, ownership interests, and other gifts.
The data released on Sept. 30 cover only payments made from August through December 2013. Data on payments made in 2014 are slated to be published in June 2015.
“We are taking a big step forward in shining the light on these financial arrangements between physicians and the health care industry,” said Dr. Shantanu Agrawal, director of the CMS Center for Program Integrity. “Using [these] new data, it is now possible to conduct a wide range of analyses of payments made by drug and device manufacturers that were never possible before.”
But the program has been plagued by delays and technical problems. CMS had to extend multiple times the 45-day “review and dispute” period, during which physicians could check the accuracy of data reported about them. It took the agency days to correct technical problems that had caused data to be intermingled, matching the wrong records to physicians with similar names.
Of the 4.4 million records released on Sept. 30, about 40% had to be deidentified either because of data inconsistencies that kept CMS from being able to match them to an individual physician or teaching hospital, or because the data were not available for review for the full 45-day period. CMS expects the data to be fully identified in 2015 once the manufacturers submit corrected information.
Another 199,000 records that were reported to the agency were not published at all, according to CMS. The vast majority of those records were unpublished at the request of the industry, since they related to ongoing research of unapproved treatments. About 9,000 records were not published because they are under active dispute, according to Dr. Agrawal.
While physicians and the industry have been generally supportive of CMS’s move toward greater openness about payments, there has been plenty of criticism of the implementation of the Open Payments program. The American Medical Association has said repeatedly that physicians have not had enough time to review the accuracy of the payments and that CMS is not providing adequate context about what the payments actually say about physician-industry relationships.
“Publicly reporting industry payments to individual physicians can imply, wrongly, that such payments are always inappropriate,” the AMA wrote in a guide for reporters covering the release of Open Payments data. “Some may be, but to be able to make an informed judgment, it is vital to be able to set the financial information in context. Just because a physician has a relationship with industry does not automatically mean that his or her professional judgment has been influenced inappropriately.”
The AMA also said that the process of registering and later reviewing payments was confusing and overly cumbersome for physicians. Only about 26,000 physicians and 400 teaching hospitals registered in the Open Payments system to review their data, according to CMS.
On Twitter @maryellenny
HHS: ACA drops uncompensated hospital care by $5.7B
Hospitals are projected to save $5.7 billion in 2014 because of a drop in uncompensated care, in large part due to the expansion of Medicaid, according to an analysis by the Department of Health & Human Services.
Hospitals are also benefiting from the growth in private coverage obtained through the Affordable Care Act marketplaces. Overall, hospitals are expected to see a 16% drop in uncompensated care, compared with original projections for the year.
Medicaid, however, is the biggest driver in the savings for hospitals. In states that have expanded eligibility for Medicaid, hospitals could save as much as $4.2 billion, nearly three-quarters of the national savings projected. To date, 27 states plus the District of Columbia have expanded Medicaid, according to HHS.
The American Hospital Association seized on the HHS report as a chance to call on more states to expand their Medicaid eligibility under the ACA.
“The ACA is accomplishing its objective in some, but not all states,” said Marie Watteau, an AHA spokeswoman. “Today’s report offers a limited estimate of the level of uncompensated care. As the report states, it’s too early to know what the impact will be on a national level. Our members are counting on uncompensated care reductions and we continue to support the expansion of coverage.”
The decline in uncompensated care was anticipated with the increased insurance coverage under the ACA. As a result, the health law cuts hospital payments that have traditionally been used to offset uncompensated care costs. For instance, federal Medicaid Disproportionate Share Hospital (DSH) payments are scheduled to be cut $1.2 billion in fiscal year 2016 and a total of $17.6 billion by fiscal year 2020.
The HHS estimates are based in part on hospital cost reports from 2011 and 2012. The HHS defined uncompensated care as the combination of charity care to uninsured patients and costs from non-Medicare bad debt.
On Twitter @maryellenny
Hospitals are projected to save $5.7 billion in 2014 because of a drop in uncompensated care, in large part due to the expansion of Medicaid, according to an analysis by the Department of Health & Human Services.
Hospitals are also benefiting from the growth in private coverage obtained through the Affordable Care Act marketplaces. Overall, hospitals are expected to see a 16% drop in uncompensated care, compared with original projections for the year.
Medicaid, however, is the biggest driver in the savings for hospitals. In states that have expanded eligibility for Medicaid, hospitals could save as much as $4.2 billion, nearly three-quarters of the national savings projected. To date, 27 states plus the District of Columbia have expanded Medicaid, according to HHS.
The American Hospital Association seized on the HHS report as a chance to call on more states to expand their Medicaid eligibility under the ACA.
“The ACA is accomplishing its objective in some, but not all states,” said Marie Watteau, an AHA spokeswoman. “Today’s report offers a limited estimate of the level of uncompensated care. As the report states, it’s too early to know what the impact will be on a national level. Our members are counting on uncompensated care reductions and we continue to support the expansion of coverage.”
The decline in uncompensated care was anticipated with the increased insurance coverage under the ACA. As a result, the health law cuts hospital payments that have traditionally been used to offset uncompensated care costs. For instance, federal Medicaid Disproportionate Share Hospital (DSH) payments are scheduled to be cut $1.2 billion in fiscal year 2016 and a total of $17.6 billion by fiscal year 2020.
The HHS estimates are based in part on hospital cost reports from 2011 and 2012. The HHS defined uncompensated care as the combination of charity care to uninsured patients and costs from non-Medicare bad debt.
On Twitter @maryellenny
Hospitals are projected to save $5.7 billion in 2014 because of a drop in uncompensated care, in large part due to the expansion of Medicaid, according to an analysis by the Department of Health & Human Services.
Hospitals are also benefiting from the growth in private coverage obtained through the Affordable Care Act marketplaces. Overall, hospitals are expected to see a 16% drop in uncompensated care, compared with original projections for the year.
Medicaid, however, is the biggest driver in the savings for hospitals. In states that have expanded eligibility for Medicaid, hospitals could save as much as $4.2 billion, nearly three-quarters of the national savings projected. To date, 27 states plus the District of Columbia have expanded Medicaid, according to HHS.
The American Hospital Association seized on the HHS report as a chance to call on more states to expand their Medicaid eligibility under the ACA.
“The ACA is accomplishing its objective in some, but not all states,” said Marie Watteau, an AHA spokeswoman. “Today’s report offers a limited estimate of the level of uncompensated care. As the report states, it’s too early to know what the impact will be on a national level. Our members are counting on uncompensated care reductions and we continue to support the expansion of coverage.”
The decline in uncompensated care was anticipated with the increased insurance coverage under the ACA. As a result, the health law cuts hospital payments that have traditionally been used to offset uncompensated care costs. For instance, federal Medicaid Disproportionate Share Hospital (DSH) payments are scheduled to be cut $1.2 billion in fiscal year 2016 and a total of $17.6 billion by fiscal year 2020.
The HHS estimates are based in part on hospital cost reports from 2011 and 2012. The HHS defined uncompensated care as the combination of charity care to uninsured patients and costs from non-Medicare bad debt.
On Twitter @maryellenny
Watchdog finds security lacking at healthcare.gov, two state marketplaces
Health insurance marketplace websites and databases – including healthcare.gov – need stronger security controls to protect personally identifiable information (PII), according to an audit by the Office of Inspector General (OIG) at the Department of Health & Human Services.
The OIG reviewed information technology (IT) controls within healthcare.gov as well as the state marketplaces in New Mexico and Kentucky. They conducted vulnerability scans and simulated cyberattacks from February to June 2014. While the OIG noted that database administrators had taken steps to ensure PII data protection, auditors identified security vulnerabilities within all three systems.
In a September report summarizing their findings, auditors said healthcare.gov administrators at the Centers for Medicare & Medicaid Services had failed to:
• Implement a process to use automated tools to test database security configuration settings.
• Implement an effective enterprise scanning tool to test for website vulnerabilities.
• Maintain adequate documentation on encryption.
• Detect and defend against website vulnerability scanning and simulated cyberattacks directed at healthcare.gov.
The auditors also found room for improvement in the Kentucky and New Mexico systems. Administrators at the Kentucky Health Benefit Exchange (KHBE) sufficiently protected PII on its websites and databases in accordance with federal requirements, the OIG report found. However, KHBE administrators had not sufficiently restricted user and group access to authorized roles and functions and had not fully addressed federal requirements for its system security planning, risk assessment, and flaw remediation, among others items.
Meanwhile, the OIG found IT policies that control the New Mexico Health Insurance Exchange (NMHIX) website and databases did not always conform to federal requirements and recommendations to secure sensitive information.
The OIG’s public report did not include details of the systems’ vulnerabilities because of the information’s sensitivity; however, detailed information and recommendations was provided to the CMS and the states. The CMS and New Mexico agreed with all of the OIG’s recommendations and described actions they have taken and plan to take to remedy the problems, according to the OIG report. Kentucky leaders concurred with most recommendations and detailed how they would improve their systems.
On Twitter @legal_med
Health insurance marketplace websites and databases – including healthcare.gov – need stronger security controls to protect personally identifiable information (PII), according to an audit by the Office of Inspector General (OIG) at the Department of Health & Human Services.
The OIG reviewed information technology (IT) controls within healthcare.gov as well as the state marketplaces in New Mexico and Kentucky. They conducted vulnerability scans and simulated cyberattacks from February to June 2014. While the OIG noted that database administrators had taken steps to ensure PII data protection, auditors identified security vulnerabilities within all three systems.
In a September report summarizing their findings, auditors said healthcare.gov administrators at the Centers for Medicare & Medicaid Services had failed to:
• Implement a process to use automated tools to test database security configuration settings.
• Implement an effective enterprise scanning tool to test for website vulnerabilities.
• Maintain adequate documentation on encryption.
• Detect and defend against website vulnerability scanning and simulated cyberattacks directed at healthcare.gov.
The auditors also found room for improvement in the Kentucky and New Mexico systems. Administrators at the Kentucky Health Benefit Exchange (KHBE) sufficiently protected PII on its websites and databases in accordance with federal requirements, the OIG report found. However, KHBE administrators had not sufficiently restricted user and group access to authorized roles and functions and had not fully addressed federal requirements for its system security planning, risk assessment, and flaw remediation, among others items.
Meanwhile, the OIG found IT policies that control the New Mexico Health Insurance Exchange (NMHIX) website and databases did not always conform to federal requirements and recommendations to secure sensitive information.
The OIG’s public report did not include details of the systems’ vulnerabilities because of the information’s sensitivity; however, detailed information and recommendations was provided to the CMS and the states. The CMS and New Mexico agreed with all of the OIG’s recommendations and described actions they have taken and plan to take to remedy the problems, according to the OIG report. Kentucky leaders concurred with most recommendations and detailed how they would improve their systems.
On Twitter @legal_med
Health insurance marketplace websites and databases – including healthcare.gov – need stronger security controls to protect personally identifiable information (PII), according to an audit by the Office of Inspector General (OIG) at the Department of Health & Human Services.
The OIG reviewed information technology (IT) controls within healthcare.gov as well as the state marketplaces in New Mexico and Kentucky. They conducted vulnerability scans and simulated cyberattacks from February to June 2014. While the OIG noted that database administrators had taken steps to ensure PII data protection, auditors identified security vulnerabilities within all three systems.
In a September report summarizing their findings, auditors said healthcare.gov administrators at the Centers for Medicare & Medicaid Services had failed to:
• Implement a process to use automated tools to test database security configuration settings.
• Implement an effective enterprise scanning tool to test for website vulnerabilities.
• Maintain adequate documentation on encryption.
• Detect and defend against website vulnerability scanning and simulated cyberattacks directed at healthcare.gov.
The auditors also found room for improvement in the Kentucky and New Mexico systems. Administrators at the Kentucky Health Benefit Exchange (KHBE) sufficiently protected PII on its websites and databases in accordance with federal requirements, the OIG report found. However, KHBE administrators had not sufficiently restricted user and group access to authorized roles and functions and had not fully addressed federal requirements for its system security planning, risk assessment, and flaw remediation, among others items.
Meanwhile, the OIG found IT policies that control the New Mexico Health Insurance Exchange (NMHIX) website and databases did not always conform to federal requirements and recommendations to secure sensitive information.
The OIG’s public report did not include details of the systems’ vulnerabilities because of the information’s sensitivity; however, detailed information and recommendations was provided to the CMS and the states. The CMS and New Mexico agreed with all of the OIG’s recommendations and described actions they have taken and plan to take to remedy the problems, according to the OIG report. Kentucky leaders concurred with most recommendations and detailed how they would improve their systems.
On Twitter @legal_med
PROOVIT registry results make case for expansion
PHILADELPHIA – About 7 in 10 patients who enter the trauma bay with vascular injuries are male, and about one-third have an Injury Severity Score of 15 or higher. Penetrating injuries account for more than a third of these cases, and prehospital tourniquet for extremity injuries is used in one in five patients.
These are some of the data from the first year of a registry that is gathering previously uncollected information on management of trauma-related vascular injuries, such as rates of arterial injuries, nonoperative management and amputations. Study coordinator Dr. Joseph DuBose of the University of Texas Health Science Center, Houston, reported on the PROOVIT registry – for Prospective Observational Vascular Injury Treatment – at the annual meeting of the American Association for the Surgery of Trauma (AAST).
PROOVIT grew out of an effort of the AAST leaders, Dr. DuBose said. “We discussed this with the senior leadership of the AAST as well as the AAST Multicenter Committee, recognizing there really is no registry presently that absolutely links the key variables specific to the management of vascular injury and subsequent outcome,” Dr. DuBose said.
While a number of registries exist, including the National Trauma Databank of the American College of Surgeons and the Society for Vascular Surgery Vascular Quality Initiative, along with a number of military registries, they lack key details or are not readily applicable to vascular injury in trauma, he said.
“We desire to establish an aggregate database of information on presentation, diagnosis, management, but to be acutely definitive on surveillance and outcomes in vascular trauma,” Dr. DuBose said.
First-year registry data also looked at secondary outcomes to help establish links between treatments and outcomes specific to vascular trauma, he said. PROOVIT collected data on 542 injuries from 14 trauma centers, 13 of them Level 1 centers, since February 2013. The study population included 484 arterial injuries and 79 major venous injuries (a cohort of patients had both). The most common injury cause was motor vehicle crash, accounting for 28% of all injuries, and the most common types of injuries were blunt trauma (47%) and penetrating trauma (36.5%).
PROOVIT also did a deep dive on the condition of trauma victims. Average Injury Severity Score was 20.7, and was greater than 15 in about a third of patients. A total of 121% of patients were hypotensive with systolic BP of 90 mm Hg or less, and nearly 30% of patients had some sort of vascular injury. The most common method for identifying vascular trauma injuries was CT angiography, used in nearly 40% of cases. “This database provides us an opportunity to look very closely at specific types of injury patterns,” Dr. DuBose said.
“We believe the PROOVIT registry is a viable tool based upon our first year of experience for establishing a much needed link between vascular injury management and subsequent outcome and evolving vascular injury care,” he said. The goal is to develop data out to 7 years of follow-up and beyond. “It would be my hope that we could plan that for 10- to 20-year data to collect much-needed information on long-term outcomes,” he said.
Dr. DuBose acknowledged that securing funding and enrolling more Level 2 trauma centers are goals, and that the registry is integral to quality improvement initiatives. “We can look at individual centers that have better outcomes,” he said. “What practice are they doing better than other people?”
Dr. DuBose said the registry continues to accrue patient data and the PROOVIT investigators invite all trauma centers caring for these patient populations to participate in enrollment. Information is available at the AAST multicenter studies webpage (www.aast.org/Research/MultiInstitutionalStudies.aspx), or by contacting the PROOVIT team at [email protected].
Dr. DuBose reported having no relevant financial disclosures.
This is a splendid initiative and enterprise. One might quibble with this early delivery of results to this audience. It is perhaps a bit premature, but it is clearly post-natal, and the results should engender comments that might increase its influence.
The PROOVIT finding that tourniquets were used in 20% of vascular injuries is heartwarming. This would not have occurred 2 decades ago, and it’s a testament to the influence of tactical combat casualty care, However, cost is a determinant for the future of the registry. The cost must be estimated and it must be borne by some body of support.
Dr. Howard Champion is a trauma surgeon in Annapolis, Md. He was the discussant of the presentation at the meeting.
This is a splendid initiative and enterprise. One might quibble with this early delivery of results to this audience. It is perhaps a bit premature, but it is clearly post-natal, and the results should engender comments that might increase its influence.
The PROOVIT finding that tourniquets were used in 20% of vascular injuries is heartwarming. This would not have occurred 2 decades ago, and it’s a testament to the influence of tactical combat casualty care, However, cost is a determinant for the future of the registry. The cost must be estimated and it must be borne by some body of support.
Dr. Howard Champion is a trauma surgeon in Annapolis, Md. He was the discussant of the presentation at the meeting.
This is a splendid initiative and enterprise. One might quibble with this early delivery of results to this audience. It is perhaps a bit premature, but it is clearly post-natal, and the results should engender comments that might increase its influence.
The PROOVIT finding that tourniquets were used in 20% of vascular injuries is heartwarming. This would not have occurred 2 decades ago, and it’s a testament to the influence of tactical combat casualty care, However, cost is a determinant for the future of the registry. The cost must be estimated and it must be borne by some body of support.
Dr. Howard Champion is a trauma surgeon in Annapolis, Md. He was the discussant of the presentation at the meeting.
PHILADELPHIA – About 7 in 10 patients who enter the trauma bay with vascular injuries are male, and about one-third have an Injury Severity Score of 15 or higher. Penetrating injuries account for more than a third of these cases, and prehospital tourniquet for extremity injuries is used in one in five patients.
These are some of the data from the first year of a registry that is gathering previously uncollected information on management of trauma-related vascular injuries, such as rates of arterial injuries, nonoperative management and amputations. Study coordinator Dr. Joseph DuBose of the University of Texas Health Science Center, Houston, reported on the PROOVIT registry – for Prospective Observational Vascular Injury Treatment – at the annual meeting of the American Association for the Surgery of Trauma (AAST).
PROOVIT grew out of an effort of the AAST leaders, Dr. DuBose said. “We discussed this with the senior leadership of the AAST as well as the AAST Multicenter Committee, recognizing there really is no registry presently that absolutely links the key variables specific to the management of vascular injury and subsequent outcome,” Dr. DuBose said.
While a number of registries exist, including the National Trauma Databank of the American College of Surgeons and the Society for Vascular Surgery Vascular Quality Initiative, along with a number of military registries, they lack key details or are not readily applicable to vascular injury in trauma, he said.
“We desire to establish an aggregate database of information on presentation, diagnosis, management, but to be acutely definitive on surveillance and outcomes in vascular trauma,” Dr. DuBose said.
First-year registry data also looked at secondary outcomes to help establish links between treatments and outcomes specific to vascular trauma, he said. PROOVIT collected data on 542 injuries from 14 trauma centers, 13 of them Level 1 centers, since February 2013. The study population included 484 arterial injuries and 79 major venous injuries (a cohort of patients had both). The most common injury cause was motor vehicle crash, accounting for 28% of all injuries, and the most common types of injuries were blunt trauma (47%) and penetrating trauma (36.5%).
PROOVIT also did a deep dive on the condition of trauma victims. Average Injury Severity Score was 20.7, and was greater than 15 in about a third of patients. A total of 121% of patients were hypotensive with systolic BP of 90 mm Hg or less, and nearly 30% of patients had some sort of vascular injury. The most common method for identifying vascular trauma injuries was CT angiography, used in nearly 40% of cases. “This database provides us an opportunity to look very closely at specific types of injury patterns,” Dr. DuBose said.
“We believe the PROOVIT registry is a viable tool based upon our first year of experience for establishing a much needed link between vascular injury management and subsequent outcome and evolving vascular injury care,” he said. The goal is to develop data out to 7 years of follow-up and beyond. “It would be my hope that we could plan that for 10- to 20-year data to collect much-needed information on long-term outcomes,” he said.
Dr. DuBose acknowledged that securing funding and enrolling more Level 2 trauma centers are goals, and that the registry is integral to quality improvement initiatives. “We can look at individual centers that have better outcomes,” he said. “What practice are they doing better than other people?”
Dr. DuBose said the registry continues to accrue patient data and the PROOVIT investigators invite all trauma centers caring for these patient populations to participate in enrollment. Information is available at the AAST multicenter studies webpage (www.aast.org/Research/MultiInstitutionalStudies.aspx), or by contacting the PROOVIT team at [email protected].
Dr. DuBose reported having no relevant financial disclosures.
PHILADELPHIA – About 7 in 10 patients who enter the trauma bay with vascular injuries are male, and about one-third have an Injury Severity Score of 15 or higher. Penetrating injuries account for more than a third of these cases, and prehospital tourniquet for extremity injuries is used in one in five patients.
These are some of the data from the first year of a registry that is gathering previously uncollected information on management of trauma-related vascular injuries, such as rates of arterial injuries, nonoperative management and amputations. Study coordinator Dr. Joseph DuBose of the University of Texas Health Science Center, Houston, reported on the PROOVIT registry – for Prospective Observational Vascular Injury Treatment – at the annual meeting of the American Association for the Surgery of Trauma (AAST).
PROOVIT grew out of an effort of the AAST leaders, Dr. DuBose said. “We discussed this with the senior leadership of the AAST as well as the AAST Multicenter Committee, recognizing there really is no registry presently that absolutely links the key variables specific to the management of vascular injury and subsequent outcome,” Dr. DuBose said.
While a number of registries exist, including the National Trauma Databank of the American College of Surgeons and the Society for Vascular Surgery Vascular Quality Initiative, along with a number of military registries, they lack key details or are not readily applicable to vascular injury in trauma, he said.
“We desire to establish an aggregate database of information on presentation, diagnosis, management, but to be acutely definitive on surveillance and outcomes in vascular trauma,” Dr. DuBose said.
First-year registry data also looked at secondary outcomes to help establish links between treatments and outcomes specific to vascular trauma, he said. PROOVIT collected data on 542 injuries from 14 trauma centers, 13 of them Level 1 centers, since February 2013. The study population included 484 arterial injuries and 79 major venous injuries (a cohort of patients had both). The most common injury cause was motor vehicle crash, accounting for 28% of all injuries, and the most common types of injuries were blunt trauma (47%) and penetrating trauma (36.5%).
PROOVIT also did a deep dive on the condition of trauma victims. Average Injury Severity Score was 20.7, and was greater than 15 in about a third of patients. A total of 121% of patients were hypotensive with systolic BP of 90 mm Hg or less, and nearly 30% of patients had some sort of vascular injury. The most common method for identifying vascular trauma injuries was CT angiography, used in nearly 40% of cases. “This database provides us an opportunity to look very closely at specific types of injury patterns,” Dr. DuBose said.
“We believe the PROOVIT registry is a viable tool based upon our first year of experience for establishing a much needed link between vascular injury management and subsequent outcome and evolving vascular injury care,” he said. The goal is to develop data out to 7 years of follow-up and beyond. “It would be my hope that we could plan that for 10- to 20-year data to collect much-needed information on long-term outcomes,” he said.
Dr. DuBose acknowledged that securing funding and enrolling more Level 2 trauma centers are goals, and that the registry is integral to quality improvement initiatives. “We can look at individual centers that have better outcomes,” he said. “What practice are they doing better than other people?”
Dr. DuBose said the registry continues to accrue patient data and the PROOVIT investigators invite all trauma centers caring for these patient populations to participate in enrollment. Information is available at the AAST multicenter studies webpage (www.aast.org/Research/MultiInstitutionalStudies.aspx), or by contacting the PROOVIT team at [email protected].
Dr. DuBose reported having no relevant financial disclosures.
AT THE AAST ANNUAL MEETING
Key clinical point: Gathering previously uncollected information on management of trauma-related vascular injuries can inform treatment and may improve outcomes.
Major finding: The most common injury cause was motor vehicle crash, accounting for 28% of all injuries, and the most common types of injuries were blunt trauma (47%) and penetrating trauma (36.5%).
Data source: The AAST PROOVIT registry involving 13 Level 1 and 1 Level 2 trauma centers with data on 542 injuries.
Disclosures: Dr. DuBose reported having no relevant financial disclosures.
CMS website snafu could lead to penalties for meaningful users
First-time meaningful use participants who are using older technology, but who did not get a hardship exemption by July 1, will see their Medicare pay reduced 1% in 2015.
Because of a confluence of factors, a certain subset of physicians who engaged in meaningful use for the first time this year will not be able to attest to their participation by the Oct. 1 deadline set by the Centers for Medicare & Medicaid Services – and thus, will be penalized.
“Physicians are not only frustrated, but perhaps reaching despondency on the topic,” Dr. Steven J. Stack, president-elect of the American Medical Association, said in an interview.
Overall, about half of physicians had not participated in meaningful use as of the beginning of this year. Theoretically, all of them could face the 1% reduction in Medicare pay, though it’s likely that a smaller subset will, Dr. Stack said.
Those who did not meet meaningful use criteria in 2013 and who anticipated that they would not do so again in 2014 could have applied for a hardship exemption by July 1 to avoid a penalty in 2015. Physicians who were starting on the meaningful use process for the first time in 2014 also had until July 1 to apply for that exemption.
After determining that many vendors did not have 2014 software ready for physicians, CMS proposed in late May to give all meaningful users more flexibility. Physicians were told they could use either a 2011 version, a 2014 version, or some combination, and not be penalized in 2015. That proposal was made final in late August.
Applying for that flexibility will be done via the CMS website, which is slated to be ready a few weeks after Oct. 1.
But first-time meaningful use participants must make their attestation to the CMS by Oct. 1.
The bottom line is that first-time participants who are using older technology and did not get the exemption will be penalized.
A CMS spokesman said that they could still receive an incentive payment for 2014 – if they go online in mid-October and apply for the flexibility option.
But Dr. Stack called that little consolation. It is as if the CMS took away $100 of a $1,000 pot and said that there was still $900 left, he said.
“It doesn’t seem reasonable and certainly undermines the premise that they offered any kind of relief,” said Dr. Stack.
Thom Kuhn, a staff member at the American College of Physicians, also said that the CMS explanation was not good enough.
“Failure to have a system ready by the time a final rule is issued is a management failure,” said Mr. Kuhn, in an interview.
Meanwhile, two members of Congress - Rep. Renee Ellmers (R-N.C.) and Rep. Jim Matheson (D-Utah) - have called on the CMS to extend that Oct. 1 deadline. In a letter to the agency, they requested "an administrative delay" for those attempting to attest to meaningful use for the first time in 2014.*
On Twitter @aliciaault
*Correction, 9/24/2014: An earlier version of this article implied that the administrative delay was requested in legislation. It was requested in a letter.
First-time meaningful use participants who are using older technology, but who did not get a hardship exemption by July 1, will see their Medicare pay reduced 1% in 2015.
Because of a confluence of factors, a certain subset of physicians who engaged in meaningful use for the first time this year will not be able to attest to their participation by the Oct. 1 deadline set by the Centers for Medicare & Medicaid Services – and thus, will be penalized.
“Physicians are not only frustrated, but perhaps reaching despondency on the topic,” Dr. Steven J. Stack, president-elect of the American Medical Association, said in an interview.
Overall, about half of physicians had not participated in meaningful use as of the beginning of this year. Theoretically, all of them could face the 1% reduction in Medicare pay, though it’s likely that a smaller subset will, Dr. Stack said.
Those who did not meet meaningful use criteria in 2013 and who anticipated that they would not do so again in 2014 could have applied for a hardship exemption by July 1 to avoid a penalty in 2015. Physicians who were starting on the meaningful use process for the first time in 2014 also had until July 1 to apply for that exemption.
After determining that many vendors did not have 2014 software ready for physicians, CMS proposed in late May to give all meaningful users more flexibility. Physicians were told they could use either a 2011 version, a 2014 version, or some combination, and not be penalized in 2015. That proposal was made final in late August.
Applying for that flexibility will be done via the CMS website, which is slated to be ready a few weeks after Oct. 1.
But first-time meaningful use participants must make their attestation to the CMS by Oct. 1.
The bottom line is that first-time participants who are using older technology and did not get the exemption will be penalized.
A CMS spokesman said that they could still receive an incentive payment for 2014 – if they go online in mid-October and apply for the flexibility option.
But Dr. Stack called that little consolation. It is as if the CMS took away $100 of a $1,000 pot and said that there was still $900 left, he said.
“It doesn’t seem reasonable and certainly undermines the premise that they offered any kind of relief,” said Dr. Stack.
Thom Kuhn, a staff member at the American College of Physicians, also said that the CMS explanation was not good enough.
“Failure to have a system ready by the time a final rule is issued is a management failure,” said Mr. Kuhn, in an interview.
Meanwhile, two members of Congress - Rep. Renee Ellmers (R-N.C.) and Rep. Jim Matheson (D-Utah) - have called on the CMS to extend that Oct. 1 deadline. In a letter to the agency, they requested "an administrative delay" for those attempting to attest to meaningful use for the first time in 2014.*
On Twitter @aliciaault
*Correction, 9/24/2014: An earlier version of this article implied that the administrative delay was requested in legislation. It was requested in a letter.
First-time meaningful use participants who are using older technology, but who did not get a hardship exemption by July 1, will see their Medicare pay reduced 1% in 2015.
Because of a confluence of factors, a certain subset of physicians who engaged in meaningful use for the first time this year will not be able to attest to their participation by the Oct. 1 deadline set by the Centers for Medicare & Medicaid Services – and thus, will be penalized.
“Physicians are not only frustrated, but perhaps reaching despondency on the topic,” Dr. Steven J. Stack, president-elect of the American Medical Association, said in an interview.
Overall, about half of physicians had not participated in meaningful use as of the beginning of this year. Theoretically, all of them could face the 1% reduction in Medicare pay, though it’s likely that a smaller subset will, Dr. Stack said.
Those who did not meet meaningful use criteria in 2013 and who anticipated that they would not do so again in 2014 could have applied for a hardship exemption by July 1 to avoid a penalty in 2015. Physicians who were starting on the meaningful use process for the first time in 2014 also had until July 1 to apply for that exemption.
After determining that many vendors did not have 2014 software ready for physicians, CMS proposed in late May to give all meaningful users more flexibility. Physicians were told they could use either a 2011 version, a 2014 version, or some combination, and not be penalized in 2015. That proposal was made final in late August.
Applying for that flexibility will be done via the CMS website, which is slated to be ready a few weeks after Oct. 1.
But first-time meaningful use participants must make their attestation to the CMS by Oct. 1.
The bottom line is that first-time participants who are using older technology and did not get the exemption will be penalized.
A CMS spokesman said that they could still receive an incentive payment for 2014 – if they go online in mid-October and apply for the flexibility option.
But Dr. Stack called that little consolation. It is as if the CMS took away $100 of a $1,000 pot and said that there was still $900 left, he said.
“It doesn’t seem reasonable and certainly undermines the premise that they offered any kind of relief,” said Dr. Stack.
Thom Kuhn, a staff member at the American College of Physicians, also said that the CMS explanation was not good enough.
“Failure to have a system ready by the time a final rule is issued is a management failure,” said Mr. Kuhn, in an interview.
Meanwhile, two members of Congress - Rep. Renee Ellmers (R-N.C.) and Rep. Jim Matheson (D-Utah) - have called on the CMS to extend that Oct. 1 deadline. In a letter to the agency, they requested "an administrative delay" for those attempting to attest to meaningful use for the first time in 2014.*
On Twitter @aliciaault
*Correction, 9/24/2014: An earlier version of this article implied that the administrative delay was requested in legislation. It was requested in a letter.
Congress poised to act on 2015 meaningful use full year reporting requirement
WASHINGTON – Members of Congress are moving to push legislation through that would shorten the reporting period for stage 2 meaningful use in 2015 if the Centers for Medicare & Medicaid Services does not act.
At issue is the requirement that eligible physicians, hospitals, and other providers must attest that they meet stage 2 requirements for the full 365-day period in 2015 (beginning Oct. 1, 2014, for hospitals and Jan 1, 2015, for physicians) or face a 1% reduction in Medicare payments as a penalty for not adopting the stage 2 requirements.
“Only 9% of hospitals in this country right now are up to the [stage 2] mandate on meaningful use,” Rep. Renee Ellmers (R-N.C.) said Sept. 18 at the HIMSS Policy Summit. “There’s only 1% of physician offices in this country that are up to the meaningful use mandate.”
Rep. Ellmers and Rep. Jim Matheson (D-Utah), have introduced the Flexibility in Health IT Reporting Act (H.R. 5481), which would alter those reporting requirements so eligible providers and hospitals would have to attest that they met stage 2 requirements for a 3-month period for 2015 rather than meeting the current regulations, which call for a full year. This would give doctors and hospitals extra time to ensure electronic health record systems are properly upgraded for the next level of requirements.
“My hope is that CMS is going to hear from so many of you, so many from industry that they will actually end up making the change on their own without us actually having to vote on it,” Rep. Ellmers said. “If we do have to vote on it, it will be when we come back in the lame-duck session. I don’t want to have to wait that long.”
She suggested that hospitals could question whether it is worth it to press for stage 2 attestation or just take the 1% penalty.
“There will already have been $24 billion of hard-earned taxpayer dollars that have been invested in this,” she said. “That is going by the wayside if hospitals are not participating in meaningful use,”
Robert Tennant, senior policy adviser at the Medical Group Management Association, made a similar observation about the physician community. He noted that physicians who are eligible to receive incentive bonuses under the meaningful use program and have been participating since the program began in 2011 have already received $38,000 of the $44,000 maximum bonus.
“To move to stage 2 will only allow you to receive a maximum of $6,000, so the money is somewhat less now and so what we don’t want to do is add further discouragement for [eligible providers] to move to stage 2 of the program,” Mr. Tennant said in an interview.
The American Medical Association voiced its support for the bill in a letter to Rep. Ellmers.
At a separate press conference Sept. 18 as part of National Health IT Week, Rep. Phil Gingrey (R-Ga.), also voiced his support for the bill.
WASHINGTON – Members of Congress are moving to push legislation through that would shorten the reporting period for stage 2 meaningful use in 2015 if the Centers for Medicare & Medicaid Services does not act.
At issue is the requirement that eligible physicians, hospitals, and other providers must attest that they meet stage 2 requirements for the full 365-day period in 2015 (beginning Oct. 1, 2014, for hospitals and Jan 1, 2015, for physicians) or face a 1% reduction in Medicare payments as a penalty for not adopting the stage 2 requirements.
“Only 9% of hospitals in this country right now are up to the [stage 2] mandate on meaningful use,” Rep. Renee Ellmers (R-N.C.) said Sept. 18 at the HIMSS Policy Summit. “There’s only 1% of physician offices in this country that are up to the meaningful use mandate.”
Rep. Ellmers and Rep. Jim Matheson (D-Utah), have introduced the Flexibility in Health IT Reporting Act (H.R. 5481), which would alter those reporting requirements so eligible providers and hospitals would have to attest that they met stage 2 requirements for a 3-month period for 2015 rather than meeting the current regulations, which call for a full year. This would give doctors and hospitals extra time to ensure electronic health record systems are properly upgraded for the next level of requirements.
“My hope is that CMS is going to hear from so many of you, so many from industry that they will actually end up making the change on their own without us actually having to vote on it,” Rep. Ellmers said. “If we do have to vote on it, it will be when we come back in the lame-duck session. I don’t want to have to wait that long.”
She suggested that hospitals could question whether it is worth it to press for stage 2 attestation or just take the 1% penalty.
“There will already have been $24 billion of hard-earned taxpayer dollars that have been invested in this,” she said. “That is going by the wayside if hospitals are not participating in meaningful use,”
Robert Tennant, senior policy adviser at the Medical Group Management Association, made a similar observation about the physician community. He noted that physicians who are eligible to receive incentive bonuses under the meaningful use program and have been participating since the program began in 2011 have already received $38,000 of the $44,000 maximum bonus.
“To move to stage 2 will only allow you to receive a maximum of $6,000, so the money is somewhat less now and so what we don’t want to do is add further discouragement for [eligible providers] to move to stage 2 of the program,” Mr. Tennant said in an interview.
The American Medical Association voiced its support for the bill in a letter to Rep. Ellmers.
At a separate press conference Sept. 18 as part of National Health IT Week, Rep. Phil Gingrey (R-Ga.), also voiced his support for the bill.
WASHINGTON – Members of Congress are moving to push legislation through that would shorten the reporting period for stage 2 meaningful use in 2015 if the Centers for Medicare & Medicaid Services does not act.
At issue is the requirement that eligible physicians, hospitals, and other providers must attest that they meet stage 2 requirements for the full 365-day period in 2015 (beginning Oct. 1, 2014, for hospitals and Jan 1, 2015, for physicians) or face a 1% reduction in Medicare payments as a penalty for not adopting the stage 2 requirements.
“Only 9% of hospitals in this country right now are up to the [stage 2] mandate on meaningful use,” Rep. Renee Ellmers (R-N.C.) said Sept. 18 at the HIMSS Policy Summit. “There’s only 1% of physician offices in this country that are up to the meaningful use mandate.”
Rep. Ellmers and Rep. Jim Matheson (D-Utah), have introduced the Flexibility in Health IT Reporting Act (H.R. 5481), which would alter those reporting requirements so eligible providers and hospitals would have to attest that they met stage 2 requirements for a 3-month period for 2015 rather than meeting the current regulations, which call for a full year. This would give doctors and hospitals extra time to ensure electronic health record systems are properly upgraded for the next level of requirements.
“My hope is that CMS is going to hear from so many of you, so many from industry that they will actually end up making the change on their own without us actually having to vote on it,” Rep. Ellmers said. “If we do have to vote on it, it will be when we come back in the lame-duck session. I don’t want to have to wait that long.”
She suggested that hospitals could question whether it is worth it to press for stage 2 attestation or just take the 1% penalty.
“There will already have been $24 billion of hard-earned taxpayer dollars that have been invested in this,” she said. “That is going by the wayside if hospitals are not participating in meaningful use,”
Robert Tennant, senior policy adviser at the Medical Group Management Association, made a similar observation about the physician community. He noted that physicians who are eligible to receive incentive bonuses under the meaningful use program and have been participating since the program began in 2011 have already received $38,000 of the $44,000 maximum bonus.
“To move to stage 2 will only allow you to receive a maximum of $6,000, so the money is somewhat less now and so what we don’t want to do is add further discouragement for [eligible providers] to move to stage 2 of the program,” Mr. Tennant said in an interview.
The American Medical Association voiced its support for the bill in a letter to Rep. Ellmers.
At a separate press conference Sept. 18 as part of National Health IT Week, Rep. Phil Gingrey (R-Ga.), also voiced his support for the bill.
Survey: Many physicians plan to reduce their workload
Nearly 45% of physicians plan to cut back on seeing patients, to take on fewer patients, to retire, or to restrict new patients within the next 3 years.
Increased workloads, regulatory burdens and ongoing changes to the health care system are drivers of the anticipated career moves, according to a survey of 20,088 physicians commissioned by the Physicians Foundation, a nonprofit research organization.
The 2014 Survey of America’s Physicians: Practice Patterns and Perspectives, released Sept. 16, was conducted by Merritt Hawkins and is based on responses from physicians across the United States from March 2014 to June 2014. The survey found 81% of physicians described themselves as overextended or at full capacity, up from 75% in 2012. Within the next 1-3 years, 18% of doctors said they plan to reduce their hours, 10% plan to seek a nonclinical job, 9% will retire, and 8% plan to reduce the number of patients seen. Also, 39% said they will accelerate their retirement plans due to changes in the health care system.
Some of those changes include the Affordable Care Act. Of doctors surveyed, 29% gave the ACA a C grade as a vehicle for health reform; 21% gave the ACA a D, and 25% said the law deserves an F. Just 4% gave the law an A grade and 22% said it deserved a B.
Dr. Walker Ray, vice president of the Physicians Foundation and chair of its research committee, said the survey results suggest a looming physician shortage and decreased quality care for patients.
“America’s physician workforce is undergoing significant changes,” Dr. Ray said in a statement. “Physicians are younger, more are working in employed practice settings, and more are leaving private practice. This new guard of physicians report having less capacity to take on additional patients. With more physicians retiring and an increasing number of doctors, particularly younger physicians, planning to switch in whole or in part to concierge medicine, we could see a limiting effect on physician supply and, ultimately, on the ability of the U.S. health care system to properly care for millions of new patients.”
Electronic medical records have been adopted by 85% of physicians, up from 70% in 2012, the survey found. However, 46% of respondents indicated EMRs have reduced their efficiency, while 24% say the systems have improved their efficiency. Meanwhile, 26% of doctors now participate in accountable care organizations, but only 13% believe ACOs will enhance quality and decrease costs.
As for workload, physicians worked an average of 53 hours a week in 2014, the same number of hours doctors reported working in 2012. Aside from treating patients, physicians spent an average of 20% of their time on nonclinical paperwork in 2014.
Additionally, the study found that 53% of physicians were hospital or medical group employees, up from 44% in 2012 and 38% in 2008. In 2014, 35% said they were independent practice owners, down from 49% in 2012.
“The physician workforce, and medicine in general, is experiencing a period of massive transition,” Lou Goodman, Ph.D., Texas Medical Association CEO and president of the Physicians Foundation, said in a statement. “As such, the growing diversity of the physician workforce will reflect different perspectives and sentiments surrounding the state of medicine. While I am troubled that a majority of physicians are pessimistic about the state of medicine, I am heartened by the fact that 71% of physicians would still choose to be a physician if they had to do it over, while nearly 80% describe patient relationships as the most satisfying factor about practicing medicine.”
On Twitter @legal_med
This article was updated on October 1, 2014.
Nearly 45% of physicians plan to cut back on seeing patients, to take on fewer patients, to retire, or to restrict new patients within the next 3 years.
Increased workloads, regulatory burdens and ongoing changes to the health care system are drivers of the anticipated career moves, according to a survey of 20,088 physicians commissioned by the Physicians Foundation, a nonprofit research organization.
The 2014 Survey of America’s Physicians: Practice Patterns and Perspectives, released Sept. 16, was conducted by Merritt Hawkins and is based on responses from physicians across the United States from March 2014 to June 2014. The survey found 81% of physicians described themselves as overextended or at full capacity, up from 75% in 2012. Within the next 1-3 years, 18% of doctors said they plan to reduce their hours, 10% plan to seek a nonclinical job, 9% will retire, and 8% plan to reduce the number of patients seen. Also, 39% said they will accelerate their retirement plans due to changes in the health care system.
Some of those changes include the Affordable Care Act. Of doctors surveyed, 29% gave the ACA a C grade as a vehicle for health reform; 21% gave the ACA a D, and 25% said the law deserves an F. Just 4% gave the law an A grade and 22% said it deserved a B.
Dr. Walker Ray, vice president of the Physicians Foundation and chair of its research committee, said the survey results suggest a looming physician shortage and decreased quality care for patients.
“America’s physician workforce is undergoing significant changes,” Dr. Ray said in a statement. “Physicians are younger, more are working in employed practice settings, and more are leaving private practice. This new guard of physicians report having less capacity to take on additional patients. With more physicians retiring and an increasing number of doctors, particularly younger physicians, planning to switch in whole or in part to concierge medicine, we could see a limiting effect on physician supply and, ultimately, on the ability of the U.S. health care system to properly care for millions of new patients.”
Electronic medical records have been adopted by 85% of physicians, up from 70% in 2012, the survey found. However, 46% of respondents indicated EMRs have reduced their efficiency, while 24% say the systems have improved their efficiency. Meanwhile, 26% of doctors now participate in accountable care organizations, but only 13% believe ACOs will enhance quality and decrease costs.
As for workload, physicians worked an average of 53 hours a week in 2014, the same number of hours doctors reported working in 2012. Aside from treating patients, physicians spent an average of 20% of their time on nonclinical paperwork in 2014.
Additionally, the study found that 53% of physicians were hospital or medical group employees, up from 44% in 2012 and 38% in 2008. In 2014, 35% said they were independent practice owners, down from 49% in 2012.
“The physician workforce, and medicine in general, is experiencing a period of massive transition,” Lou Goodman, Ph.D., Texas Medical Association CEO and president of the Physicians Foundation, said in a statement. “As such, the growing diversity of the physician workforce will reflect different perspectives and sentiments surrounding the state of medicine. While I am troubled that a majority of physicians are pessimistic about the state of medicine, I am heartened by the fact that 71% of physicians would still choose to be a physician if they had to do it over, while nearly 80% describe patient relationships as the most satisfying factor about practicing medicine.”
On Twitter @legal_med
This article was updated on October 1, 2014.
Nearly 45% of physicians plan to cut back on seeing patients, to take on fewer patients, to retire, or to restrict new patients within the next 3 years.
Increased workloads, regulatory burdens and ongoing changes to the health care system are drivers of the anticipated career moves, according to a survey of 20,088 physicians commissioned by the Physicians Foundation, a nonprofit research organization.
The 2014 Survey of America’s Physicians: Practice Patterns and Perspectives, released Sept. 16, was conducted by Merritt Hawkins and is based on responses from physicians across the United States from March 2014 to June 2014. The survey found 81% of physicians described themselves as overextended or at full capacity, up from 75% in 2012. Within the next 1-3 years, 18% of doctors said they plan to reduce their hours, 10% plan to seek a nonclinical job, 9% will retire, and 8% plan to reduce the number of patients seen. Also, 39% said they will accelerate their retirement plans due to changes in the health care system.
Some of those changes include the Affordable Care Act. Of doctors surveyed, 29% gave the ACA a C grade as a vehicle for health reform; 21% gave the ACA a D, and 25% said the law deserves an F. Just 4% gave the law an A grade and 22% said it deserved a B.
Dr. Walker Ray, vice president of the Physicians Foundation and chair of its research committee, said the survey results suggest a looming physician shortage and decreased quality care for patients.
“America’s physician workforce is undergoing significant changes,” Dr. Ray said in a statement. “Physicians are younger, more are working in employed practice settings, and more are leaving private practice. This new guard of physicians report having less capacity to take on additional patients. With more physicians retiring and an increasing number of doctors, particularly younger physicians, planning to switch in whole or in part to concierge medicine, we could see a limiting effect on physician supply and, ultimately, on the ability of the U.S. health care system to properly care for millions of new patients.”
Electronic medical records have been adopted by 85% of physicians, up from 70% in 2012, the survey found. However, 46% of respondents indicated EMRs have reduced their efficiency, while 24% say the systems have improved their efficiency. Meanwhile, 26% of doctors now participate in accountable care organizations, but only 13% believe ACOs will enhance quality and decrease costs.
As for workload, physicians worked an average of 53 hours a week in 2014, the same number of hours doctors reported working in 2012. Aside from treating patients, physicians spent an average of 20% of their time on nonclinical paperwork in 2014.
Additionally, the study found that 53% of physicians were hospital or medical group employees, up from 44% in 2012 and 38% in 2008. In 2014, 35% said they were independent practice owners, down from 49% in 2012.
“The physician workforce, and medicine in general, is experiencing a period of massive transition,” Lou Goodman, Ph.D., Texas Medical Association CEO and president of the Physicians Foundation, said in a statement. “As such, the growing diversity of the physician workforce will reflect different perspectives and sentiments surrounding the state of medicine. While I am troubled that a majority of physicians are pessimistic about the state of medicine, I am heartened by the fact that 71% of physicians would still choose to be a physician if they had to do it over, while nearly 80% describe patient relationships as the most satisfying factor about practicing medicine.”
On Twitter @legal_med
This article was updated on October 1, 2014.
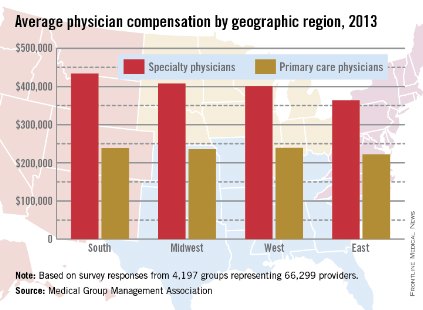
Physician income in 2013: The East earned least
Both primary care and specialty care physicians in the Eastern United States had the lowest total compensation of any region in 2013, the Medical Group Management Association reported.
Specialists in the East earned an average of $364,000, and primary care physicians earned $222,000. Compensation for specialists was highest in the South, at $434,000, with primary care physicians there earning $238,611. Primary care physicians in the West earned slightly more, reporting the highest total at $239,968, with specialists earning an average of $401,000. In the Midwest, specialists earned almost $408,000, and primary care physicians averaged $236,000, according to the MGMA.
Nonmetropolitan areas reported the lowest compensation rates by population, with primary physicians earning more than $223,000 and specialists earning $337,000 in areas with less than 50,000 residents. The highest-earning areas by population were metropolitan areas of 50,000 to 250,000 people, where primary care physicians earned $241,000 and specialty physicians earned $422,000. Both specialists and nonspecialists in metropolitan areas of more than 1,000,000 people averaged marginally more than physicians in areas of between 250,001 and 1,000,000 people.
Compensation rates for certified registered nurse anesthetists, physician assistants, and nurse practitioners were highest in the Midwest and West, and lowest in the East, except for nurse practitioners.
The MGMA data were collected from almost 4,200 medical groups representing more than 66,000 providers.
Both primary care and specialty care physicians in the Eastern United States had the lowest total compensation of any region in 2013, the Medical Group Management Association reported.
Specialists in the East earned an average of $364,000, and primary care physicians earned $222,000. Compensation for specialists was highest in the South, at $434,000, with primary care physicians there earning $238,611. Primary care physicians in the West earned slightly more, reporting the highest total at $239,968, with specialists earning an average of $401,000. In the Midwest, specialists earned almost $408,000, and primary care physicians averaged $236,000, according to the MGMA.
Nonmetropolitan areas reported the lowest compensation rates by population, with primary physicians earning more than $223,000 and specialists earning $337,000 in areas with less than 50,000 residents. The highest-earning areas by population were metropolitan areas of 50,000 to 250,000 people, where primary care physicians earned $241,000 and specialty physicians earned $422,000. Both specialists and nonspecialists in metropolitan areas of more than 1,000,000 people averaged marginally more than physicians in areas of between 250,001 and 1,000,000 people.
Compensation rates for certified registered nurse anesthetists, physician assistants, and nurse practitioners were highest in the Midwest and West, and lowest in the East, except for nurse practitioners.
The MGMA data were collected from almost 4,200 medical groups representing more than 66,000 providers.
Both primary care and specialty care physicians in the Eastern United States had the lowest total compensation of any region in 2013, the Medical Group Management Association reported.
Specialists in the East earned an average of $364,000, and primary care physicians earned $222,000. Compensation for specialists was highest in the South, at $434,000, with primary care physicians there earning $238,611. Primary care physicians in the West earned slightly more, reporting the highest total at $239,968, with specialists earning an average of $401,000. In the Midwest, specialists earned almost $408,000, and primary care physicians averaged $236,000, according to the MGMA.
Nonmetropolitan areas reported the lowest compensation rates by population, with primary physicians earning more than $223,000 and specialists earning $337,000 in areas with less than 50,000 residents. The highest-earning areas by population were metropolitan areas of 50,000 to 250,000 people, where primary care physicians earned $241,000 and specialty physicians earned $422,000. Both specialists and nonspecialists in metropolitan areas of more than 1,000,000 people averaged marginally more than physicians in areas of between 250,001 and 1,000,000 people.
Compensation rates for certified registered nurse anesthetists, physician assistants, and nurse practitioners were highest in the Midwest and West, and lowest in the East, except for nurse practitioners.
The MGMA data were collected from almost 4,200 medical groups representing more than 66,000 providers.
EHRs rob physicians of 4 hours of free time per week
Using an electronic health records eats 48 minutes of doctors’ free time daily – or 4 hours per week – according to a survey of family physicians.
At least one data management function took more time when using an EHR than when using a paper-based system, according to 411 family physicians who responded to a survey conducted by the National Library of Medicine (NLM) and the American College of Physicians. The results were published Sept. 8 in JAMA Internal Medicine (2014 Sept. 8 [doi:10.1001/jamainternmed.2014.4506]).
Functions that took longer with an EHR included returning telephone calls; managing messages, refill requests, or new test results; writing visit notes; ordering and scheduling tests; finding and reviewing medical records; writing prescriptions; and reading colleagues; clinical notes.
Nearly 64% of respondents, all of whom were experienced EHR users, reported that "note writing took longer," according to Dr. Clement McDonald of NLM and his associates. "Surprisingly, a third (34%) reported that it took longer to find and review medical record data with the [EHR] than without, and a similar proportion, 32%, [reported] that it was slower to read other clinicians’ notes."
Respondents reported using a wide variety of systems, with 61 distinct EHR systems being identified. However, nine systems were used by 20 or more respondents and accounted for 79% (324) of all users responding to the survey. Of these nine, the Veterans Affairs’ Computer Patient Record System was associated with lowest amount of free time loss at less than 20 minutes per day.
"The loss of free time that our respondents reported was large and pervasive and could decrease access or increase the cost of care" Dr. McDonald wrote. "Policy makers should consider these time costs in future [EHR] mandates."
The authors reported no conflicts of interest.
The study was funded by the National Library of Medicine and the American College of Physicians. The authors reported no conflicts of interest.
Using an electronic health records eats 48 minutes of doctors’ free time daily – or 4 hours per week – according to a survey of family physicians.
At least one data management function took more time when using an EHR than when using a paper-based system, according to 411 family physicians who responded to a survey conducted by the National Library of Medicine (NLM) and the American College of Physicians. The results were published Sept. 8 in JAMA Internal Medicine (2014 Sept. 8 [doi:10.1001/jamainternmed.2014.4506]).
Functions that took longer with an EHR included returning telephone calls; managing messages, refill requests, or new test results; writing visit notes; ordering and scheduling tests; finding and reviewing medical records; writing prescriptions; and reading colleagues; clinical notes.
Nearly 64% of respondents, all of whom were experienced EHR users, reported that "note writing took longer," according to Dr. Clement McDonald of NLM and his associates. "Surprisingly, a third (34%) reported that it took longer to find and review medical record data with the [EHR] than without, and a similar proportion, 32%, [reported] that it was slower to read other clinicians’ notes."
Respondents reported using a wide variety of systems, with 61 distinct EHR systems being identified. However, nine systems were used by 20 or more respondents and accounted for 79% (324) of all users responding to the survey. Of these nine, the Veterans Affairs’ Computer Patient Record System was associated with lowest amount of free time loss at less than 20 minutes per day.
"The loss of free time that our respondents reported was large and pervasive and could decrease access or increase the cost of care" Dr. McDonald wrote. "Policy makers should consider these time costs in future [EHR] mandates."
The authors reported no conflicts of interest.
The study was funded by the National Library of Medicine and the American College of Physicians. The authors reported no conflicts of interest.
Using an electronic health records eats 48 minutes of doctors’ free time daily – or 4 hours per week – according to a survey of family physicians.
At least one data management function took more time when using an EHR than when using a paper-based system, according to 411 family physicians who responded to a survey conducted by the National Library of Medicine (NLM) and the American College of Physicians. The results were published Sept. 8 in JAMA Internal Medicine (2014 Sept. 8 [doi:10.1001/jamainternmed.2014.4506]).
Functions that took longer with an EHR included returning telephone calls; managing messages, refill requests, or new test results; writing visit notes; ordering and scheduling tests; finding and reviewing medical records; writing prescriptions; and reading colleagues; clinical notes.
Nearly 64% of respondents, all of whom were experienced EHR users, reported that "note writing took longer," according to Dr. Clement McDonald of NLM and his associates. "Surprisingly, a third (34%) reported that it took longer to find and review medical record data with the [EHR] than without, and a similar proportion, 32%, [reported] that it was slower to read other clinicians’ notes."
Respondents reported using a wide variety of systems, with 61 distinct EHR systems being identified. However, nine systems were used by 20 or more respondents and accounted for 79% (324) of all users responding to the survey. Of these nine, the Veterans Affairs’ Computer Patient Record System was associated with lowest amount of free time loss at less than 20 minutes per day.
"The loss of free time that our respondents reported was large and pervasive and could decrease access or increase the cost of care" Dr. McDonald wrote. "Policy makers should consider these time costs in future [EHR] mandates."
The authors reported no conflicts of interest.
The study was funded by the National Library of Medicine and the American College of Physicians. The authors reported no conflicts of interest.
FROM JAMA INTERNAL MEDICINE
Key clinical point: Physicians may balk at using EHR systems because they consume rather than save time.
Major finding: EHR usage is accounting for 48 minutes of lost free time per day.
Data source: An analysis of 411 responses to a survey.
Disclosures: The study was funded by the National Library of Medicine and the American College of Physicians. The authors reported no conflicts of interest.
Open Payments may help drive malpractice claims; review period closes Sept. 11
While data glitches and delays with the Open Payments program have caused headaches, legal experts warn of a larger looming problem: Financial relationships disclosed through the program could be used to fuel malpractice lawsuits.
"The law of unintended consequences could result in these types of disclosures causing further pressure on the system by encouraging plaintiffs’ attorneys to use reported data against doctors and to strengthen a plaintiff’s case," John E. Hall Jr., an Atlanta-based medical liability defense attorney, said in an interview.
The Open Payments program, adopted as part of the Affordable Care Act and often referred to as the Sunshine Act, requires makers of drugs, devices, and biologics who participate in federal health care programs to report payments and items of value provided to physicians and teaching hospitals. The information is scheduled to be made publicly available in a searchable database beginning Sept. 30.
The program has been rife with delays due to technical and data concerns. Most recently, the Centers for Medicare & Medicaid Services extended the review and dispute one additional day to midnight on Sept. 11 because of a maintenance and upgrade outage. The period for correcting disputed data will begin Sept. 15 and will last a minimum of 15 days, the agency said.
During medical malpractice cases, it’s not uncommon for plaintiffs to sift through a physician’s history to find information that might reinforce a negligence claim, Mr. Hall said.
"Plaintiffs’ attorneys already search for conflicts of interest in a physician’s background or other historical information that will make physicians look bad in court and attempt to tarnish their credibility," he said.
The Open Payments database may provide additional fodder. The plaintiffs’ bar already is promoting how trial attorneys can use the disclosures in medical malpractice cases, said Stefanie A. Doebler, special counsel for a Washington-based law firm’s health care and food and drug practice groups. Information about the law and how financial relationships can sway doctors’ medical decisions are popping up in articles and on plaintiffs’ attorney websites.
Possible arguments by trial attorneys include that a physician prescribed the wrong drug, downplayed a drug’s risks, or did not reveal an adverse event linked to a medication because of the doctor’s financial relationships, Ms. Doebler said.
"The allegation would be that a financial relationship between a maker and a doctor caused [the doctor] to act in [his or her] own interest, rather than in the interest of the patient," she said.
Conversely, Ms. Doebler pointed out that physician defendants could argue that they were better informed about a drug or device specifically because of their relationship with a manufacturer.
To mitigate the potential legal risks, make it a point to discuss payments or benefits from manufacturers with patients, counseled Carolyn M. Bruguera, general counsel and vice president for consulting services for a Princeton, N.J.–based health care compliance and software consulting firm. That way, the physician has a chance to explain his or her relationships before patients are surprised by online data. Additionally, drug and device makers can help doctors avoid the appearance of impropriety by providing contextual information in Open Payments reports, she said.
Ms. Doebler urged physicians to verify all reported information on the Open Payments website. Doctors also should have a full understanding of all data that applies to their practices and be able to articulate its details and purpose.
It’s critical, she said, to "know what the payment refers to so they can talk about the information intelligently and completely."
On Twitter @legal_med
While data glitches and delays with the Open Payments program have caused headaches, legal experts warn of a larger looming problem: Financial relationships disclosed through the program could be used to fuel malpractice lawsuits.
"The law of unintended consequences could result in these types of disclosures causing further pressure on the system by encouraging plaintiffs’ attorneys to use reported data against doctors and to strengthen a plaintiff’s case," John E. Hall Jr., an Atlanta-based medical liability defense attorney, said in an interview.
The Open Payments program, adopted as part of the Affordable Care Act and often referred to as the Sunshine Act, requires makers of drugs, devices, and biologics who participate in federal health care programs to report payments and items of value provided to physicians and teaching hospitals. The information is scheduled to be made publicly available in a searchable database beginning Sept. 30.
The program has been rife with delays due to technical and data concerns. Most recently, the Centers for Medicare & Medicaid Services extended the review and dispute one additional day to midnight on Sept. 11 because of a maintenance and upgrade outage. The period for correcting disputed data will begin Sept. 15 and will last a minimum of 15 days, the agency said.
During medical malpractice cases, it’s not uncommon for plaintiffs to sift through a physician’s history to find information that might reinforce a negligence claim, Mr. Hall said.
"Plaintiffs’ attorneys already search for conflicts of interest in a physician’s background or other historical information that will make physicians look bad in court and attempt to tarnish their credibility," he said.
The Open Payments database may provide additional fodder. The plaintiffs’ bar already is promoting how trial attorneys can use the disclosures in medical malpractice cases, said Stefanie A. Doebler, special counsel for a Washington-based law firm’s health care and food and drug practice groups. Information about the law and how financial relationships can sway doctors’ medical decisions are popping up in articles and on plaintiffs’ attorney websites.
Possible arguments by trial attorneys include that a physician prescribed the wrong drug, downplayed a drug’s risks, or did not reveal an adverse event linked to a medication because of the doctor’s financial relationships, Ms. Doebler said.
"The allegation would be that a financial relationship between a maker and a doctor caused [the doctor] to act in [his or her] own interest, rather than in the interest of the patient," she said.
Conversely, Ms. Doebler pointed out that physician defendants could argue that they were better informed about a drug or device specifically because of their relationship with a manufacturer.
To mitigate the potential legal risks, make it a point to discuss payments or benefits from manufacturers with patients, counseled Carolyn M. Bruguera, general counsel and vice president for consulting services for a Princeton, N.J.–based health care compliance and software consulting firm. That way, the physician has a chance to explain his or her relationships before patients are surprised by online data. Additionally, drug and device makers can help doctors avoid the appearance of impropriety by providing contextual information in Open Payments reports, she said.
Ms. Doebler urged physicians to verify all reported information on the Open Payments website. Doctors also should have a full understanding of all data that applies to their practices and be able to articulate its details and purpose.
It’s critical, she said, to "know what the payment refers to so they can talk about the information intelligently and completely."
On Twitter @legal_med
While data glitches and delays with the Open Payments program have caused headaches, legal experts warn of a larger looming problem: Financial relationships disclosed through the program could be used to fuel malpractice lawsuits.
"The law of unintended consequences could result in these types of disclosures causing further pressure on the system by encouraging plaintiffs’ attorneys to use reported data against doctors and to strengthen a plaintiff’s case," John E. Hall Jr., an Atlanta-based medical liability defense attorney, said in an interview.
The Open Payments program, adopted as part of the Affordable Care Act and often referred to as the Sunshine Act, requires makers of drugs, devices, and biologics who participate in federal health care programs to report payments and items of value provided to physicians and teaching hospitals. The information is scheduled to be made publicly available in a searchable database beginning Sept. 30.
The program has been rife with delays due to technical and data concerns. Most recently, the Centers for Medicare & Medicaid Services extended the review and dispute one additional day to midnight on Sept. 11 because of a maintenance and upgrade outage. The period for correcting disputed data will begin Sept. 15 and will last a minimum of 15 days, the agency said.
During medical malpractice cases, it’s not uncommon for plaintiffs to sift through a physician’s history to find information that might reinforce a negligence claim, Mr. Hall said.
"Plaintiffs’ attorneys already search for conflicts of interest in a physician’s background or other historical information that will make physicians look bad in court and attempt to tarnish their credibility," he said.
The Open Payments database may provide additional fodder. The plaintiffs’ bar already is promoting how trial attorneys can use the disclosures in medical malpractice cases, said Stefanie A. Doebler, special counsel for a Washington-based law firm’s health care and food and drug practice groups. Information about the law and how financial relationships can sway doctors’ medical decisions are popping up in articles and on plaintiffs’ attorney websites.
Possible arguments by trial attorneys include that a physician prescribed the wrong drug, downplayed a drug’s risks, or did not reveal an adverse event linked to a medication because of the doctor’s financial relationships, Ms. Doebler said.
"The allegation would be that a financial relationship between a maker and a doctor caused [the doctor] to act in [his or her] own interest, rather than in the interest of the patient," she said.
Conversely, Ms. Doebler pointed out that physician defendants could argue that they were better informed about a drug or device specifically because of their relationship with a manufacturer.
To mitigate the potential legal risks, make it a point to discuss payments or benefits from manufacturers with patients, counseled Carolyn M. Bruguera, general counsel and vice president for consulting services for a Princeton, N.J.–based health care compliance and software consulting firm. That way, the physician has a chance to explain his or her relationships before patients are surprised by online data. Additionally, drug and device makers can help doctors avoid the appearance of impropriety by providing contextual information in Open Payments reports, she said.
Ms. Doebler urged physicians to verify all reported information on the Open Payments website. Doctors also should have a full understanding of all data that applies to their practices and be able to articulate its details and purpose.
It’s critical, she said, to "know what the payment refers to so they can talk about the information intelligently and completely."
On Twitter @legal_med