User login
Curbing opioid abuse could be a quality of care issue
WASHINGTON – MedPAC advisors think it might be time to address opioid abuse as a quality of care issue.
Commission member Herb Kuhn, president and CEO of the Missouri Hospital Association, suggested the Centers for Medicare & Medicaid Services develop coding that tracks how opioids are used and what conditions they are treating and see of those treatments line up with standards of care.
“You could begin to look at some of the protocols from some of the medical societies in terms of proper prescription or activities here and begin to look at this more as a quality initiative so that, ultimately, that comes into play in terms of payment,” Mr. Kuhn, a former deputy director at CMS, said at the Oct 9 meeting of the Medicare Payment Advisory Commission.
Commissioner Scott Armstrong, president and CEO of Seattle’s Group Health Cooperative, agreed.
“To me, this is much more a quality of care issue,” Mr. Armstrong said. Currently “what’s so difficult here is that all of our interventions are retrospective.”
He noted that within his organization, once opioid prescribing became an issue, every patient prescribed an opioid was identified.
“We began to monitor what percentage of those patients had a proactive care management plan,” he said. “Every patients’ needs are going to be different, but it was really about are we paying attention to the evidence and the kind of use of opioids that should be appropriate given to every individual patient.”
Commissioner Kathy Buto, former vice president of global health policy at Johnson & Johnson and senior health advisor at the Congressional Budget Office, called on CMS to better understand how Medicare can incentivize better pain management efforts.
One challenge that will need to be overcome in Medicare is that in Part D stand alone plans, there is no direct connection between the drug benefit and the rest of the health care services provided, something that also will need to be resolved as the country shifts to an accountable care model.
MedPAC advises Congress on issues affecting Medicare and makes recommendations on payment and quality issues affecting the program. No recommendations were made at this meeting as commissioners still sought seeking further information on how to address opioid abuse.
Commissioners also suggested CMS find incentives to promote the use of tools such as prescription drug monitoring programs more regularly.
WASHINGTON – MedPAC advisors think it might be time to address opioid abuse as a quality of care issue.
Commission member Herb Kuhn, president and CEO of the Missouri Hospital Association, suggested the Centers for Medicare & Medicaid Services develop coding that tracks how opioids are used and what conditions they are treating and see of those treatments line up with standards of care.
“You could begin to look at some of the protocols from some of the medical societies in terms of proper prescription or activities here and begin to look at this more as a quality initiative so that, ultimately, that comes into play in terms of payment,” Mr. Kuhn, a former deputy director at CMS, said at the Oct 9 meeting of the Medicare Payment Advisory Commission.
Commissioner Scott Armstrong, president and CEO of Seattle’s Group Health Cooperative, agreed.
“To me, this is much more a quality of care issue,” Mr. Armstrong said. Currently “what’s so difficult here is that all of our interventions are retrospective.”
He noted that within his organization, once opioid prescribing became an issue, every patient prescribed an opioid was identified.
“We began to monitor what percentage of those patients had a proactive care management plan,” he said. “Every patients’ needs are going to be different, but it was really about are we paying attention to the evidence and the kind of use of opioids that should be appropriate given to every individual patient.”
Commissioner Kathy Buto, former vice president of global health policy at Johnson & Johnson and senior health advisor at the Congressional Budget Office, called on CMS to better understand how Medicare can incentivize better pain management efforts.
One challenge that will need to be overcome in Medicare is that in Part D stand alone plans, there is no direct connection between the drug benefit and the rest of the health care services provided, something that also will need to be resolved as the country shifts to an accountable care model.
MedPAC advises Congress on issues affecting Medicare and makes recommendations on payment and quality issues affecting the program. No recommendations were made at this meeting as commissioners still sought seeking further information on how to address opioid abuse.
Commissioners also suggested CMS find incentives to promote the use of tools such as prescription drug monitoring programs more regularly.
WASHINGTON – MedPAC advisors think it might be time to address opioid abuse as a quality of care issue.
Commission member Herb Kuhn, president and CEO of the Missouri Hospital Association, suggested the Centers for Medicare & Medicaid Services develop coding that tracks how opioids are used and what conditions they are treating and see of those treatments line up with standards of care.
“You could begin to look at some of the protocols from some of the medical societies in terms of proper prescription or activities here and begin to look at this more as a quality initiative so that, ultimately, that comes into play in terms of payment,” Mr. Kuhn, a former deputy director at CMS, said at the Oct 9 meeting of the Medicare Payment Advisory Commission.
Commissioner Scott Armstrong, president and CEO of Seattle’s Group Health Cooperative, agreed.
“To me, this is much more a quality of care issue,” Mr. Armstrong said. Currently “what’s so difficult here is that all of our interventions are retrospective.”
He noted that within his organization, once opioid prescribing became an issue, every patient prescribed an opioid was identified.
“We began to monitor what percentage of those patients had a proactive care management plan,” he said. “Every patients’ needs are going to be different, but it was really about are we paying attention to the evidence and the kind of use of opioids that should be appropriate given to every individual patient.”
Commissioner Kathy Buto, former vice president of global health policy at Johnson & Johnson and senior health advisor at the Congressional Budget Office, called on CMS to better understand how Medicare can incentivize better pain management efforts.
One challenge that will need to be overcome in Medicare is that in Part D stand alone plans, there is no direct connection between the drug benefit and the rest of the health care services provided, something that also will need to be resolved as the country shifts to an accountable care model.
MedPAC advises Congress on issues affecting Medicare and makes recommendations on payment and quality issues affecting the program. No recommendations were made at this meeting as commissioners still sought seeking further information on how to address opioid abuse.
Commissioners also suggested CMS find incentives to promote the use of tools such as prescription drug monitoring programs more regularly.
AMA study: Wellpoint dominates the insurance market
In many areas of the country, only one or two health insurers dominate the market, leaving physicians and patients with few choices when it comes to dealing with health plans, according to a new analysis from the American Medical Association.
In 41% of metropolitan areas examined in the AMA’s study, a single health insurer holds half or more of the market share. And the AMA found that 72% of the markets they analyzed would be considered “highly concentrated” under guidelines developed by the U.S. Department of Justice and the Federal Trade Commission to assess market competition.
Wellpoint Inc. stood out among insurers as the most dominant across the country. As of Jan. 1, 2012, Wellpoint had the greatest market share in 82 of 388 metropolitan areas analyzed by the AMA, giving it the top market share in more than double the number of areas as the next two insurers (Health Care Service Corp. and UnitedHealth Group).
The lack of competition puts physicians and patients at risk, the AMA said, because it gives health plans the power to raise premiums without increasing benefits, while also cutting payments to providers. The AMA is calling on state and federal regulators to take the lack of competition into account when considering future insurance mergers.
“The dominant market power of big health insurers increases the risk of anticompetitive behavior that harms patients and physicians and presents a significant barrier to the market success of smaller insurance rivals,” Dr. Robert M. Wah, AMA president, said in a statement.
The 10 states with the least competition in their commercial health insurance markets were: Alabama, Hawaii, Michigan, Delaware, Louisiana, South Carolina, Alaska, Illinois, Nebraska, and North Dakota.
On Twitter @maryellenny
In many areas of the country, only one or two health insurers dominate the market, leaving physicians and patients with few choices when it comes to dealing with health plans, according to a new analysis from the American Medical Association.
In 41% of metropolitan areas examined in the AMA’s study, a single health insurer holds half or more of the market share. And the AMA found that 72% of the markets they analyzed would be considered “highly concentrated” under guidelines developed by the U.S. Department of Justice and the Federal Trade Commission to assess market competition.
Wellpoint Inc. stood out among insurers as the most dominant across the country. As of Jan. 1, 2012, Wellpoint had the greatest market share in 82 of 388 metropolitan areas analyzed by the AMA, giving it the top market share in more than double the number of areas as the next two insurers (Health Care Service Corp. and UnitedHealth Group).
The lack of competition puts physicians and patients at risk, the AMA said, because it gives health plans the power to raise premiums without increasing benefits, while also cutting payments to providers. The AMA is calling on state and federal regulators to take the lack of competition into account when considering future insurance mergers.
“The dominant market power of big health insurers increases the risk of anticompetitive behavior that harms patients and physicians and presents a significant barrier to the market success of smaller insurance rivals,” Dr. Robert M. Wah, AMA president, said in a statement.
The 10 states with the least competition in their commercial health insurance markets were: Alabama, Hawaii, Michigan, Delaware, Louisiana, South Carolina, Alaska, Illinois, Nebraska, and North Dakota.
On Twitter @maryellenny
In many areas of the country, only one or two health insurers dominate the market, leaving physicians and patients with few choices when it comes to dealing with health plans, according to a new analysis from the American Medical Association.
In 41% of metropolitan areas examined in the AMA’s study, a single health insurer holds half or more of the market share. And the AMA found that 72% of the markets they analyzed would be considered “highly concentrated” under guidelines developed by the U.S. Department of Justice and the Federal Trade Commission to assess market competition.
Wellpoint Inc. stood out among insurers as the most dominant across the country. As of Jan. 1, 2012, Wellpoint had the greatest market share in 82 of 388 metropolitan areas analyzed by the AMA, giving it the top market share in more than double the number of areas as the next two insurers (Health Care Service Corp. and UnitedHealth Group).
The lack of competition puts physicians and patients at risk, the AMA said, because it gives health plans the power to raise premiums without increasing benefits, while also cutting payments to providers. The AMA is calling on state and federal regulators to take the lack of competition into account when considering future insurance mergers.
“The dominant market power of big health insurers increases the risk of anticompetitive behavior that harms patients and physicians and presents a significant barrier to the market success of smaller insurance rivals,” Dr. Robert M. Wah, AMA president, said in a statement.
The 10 states with the least competition in their commercial health insurance markets were: Alabama, Hawaii, Michigan, Delaware, Louisiana, South Carolina, Alaska, Illinois, Nebraska, and North Dakota.
On Twitter @maryellenny
MULTIMEDIA: Guide to being a good intern
The first year of residency can be overwhelming. Just ask Dr. Anneliese Beaubrun, an intern at the University of Central Florida College of Medicine’s internal medicine residency program in Orlando.
You’re suddenly responsible for patients, and you definitely don’t want to be the one asking what you think is the wrong question, she says.
But the professors and program directors have a different view.
In a video interview, Dr. Abdo Asmar, associate director of the internal medicine residency program at UCF, shares his advice to first-year residents. Chief resident Olga Karasik, too, looks back at her first year and shares what she’s learned.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
And there’s more.
In her blog, Wellness Rounds, Dr. Mary L. Brandt, professor of surgery, pediatrics and medical ethics and interim senior associate dean of Medical Education at Baylor College of Medicine, Houston, takes a holistic approach to medical school and residency. Her posts cover a wide range of topics, from the type of shoes to wear at the hospital, to advice on preparing for residency interviews.
Being a good intern is among the popular posts on her blog, and in a phone interview she shared some of her top tips and advice for first-year residents.
What are your tips and advice for interns? Leave us a comment.
On Twitter @naseemmiller
The first year of residency can be overwhelming. Just ask Dr. Anneliese Beaubrun, an intern at the University of Central Florida College of Medicine’s internal medicine residency program in Orlando.
You’re suddenly responsible for patients, and you definitely don’t want to be the one asking what you think is the wrong question, she says.
But the professors and program directors have a different view.
In a video interview, Dr. Abdo Asmar, associate director of the internal medicine residency program at UCF, shares his advice to first-year residents. Chief resident Olga Karasik, too, looks back at her first year and shares what she’s learned.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
And there’s more.
In her blog, Wellness Rounds, Dr. Mary L. Brandt, professor of surgery, pediatrics and medical ethics and interim senior associate dean of Medical Education at Baylor College of Medicine, Houston, takes a holistic approach to medical school and residency. Her posts cover a wide range of topics, from the type of shoes to wear at the hospital, to advice on preparing for residency interviews.
Being a good intern is among the popular posts on her blog, and in a phone interview she shared some of her top tips and advice for first-year residents.
What are your tips and advice for interns? Leave us a comment.
On Twitter @naseemmiller
The first year of residency can be overwhelming. Just ask Dr. Anneliese Beaubrun, an intern at the University of Central Florida College of Medicine’s internal medicine residency program in Orlando.
You’re suddenly responsible for patients, and you definitely don’t want to be the one asking what you think is the wrong question, she says.
But the professors and program directors have a different view.
In a video interview, Dr. Abdo Asmar, associate director of the internal medicine residency program at UCF, shares his advice to first-year residents. Chief resident Olga Karasik, too, looks back at her first year and shares what she’s learned.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
And there’s more.
In her blog, Wellness Rounds, Dr. Mary L. Brandt, professor of surgery, pediatrics and medical ethics and interim senior associate dean of Medical Education at Baylor College of Medicine, Houston, takes a holistic approach to medical school and residency. Her posts cover a wide range of topics, from the type of shoes to wear at the hospital, to advice on preparing for residency interviews.
Being a good intern is among the popular posts on her blog, and in a phone interview she shared some of her top tips and advice for first-year residents.
What are your tips and advice for interns? Leave us a comment.
On Twitter @naseemmiller
Auditors collected $57 million from physicians in 2013
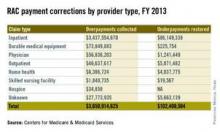
Auditors with the Centers for Medicare & Medicaid Services collected more than $3 billion in overpayments from health providers in 2013, including nearly $57 million from doctors, according to a CMS Sept. 29 annual report to Congress.
Recovery audit contractors (RACs) corrected a total of $3.75 billion in improper payments in fiscal 2013, of which $3.65 billion were in overpayments, the report found. Underpayments made up $102 million of the incorrect fees. Physicians were responsible for $56.8 million of overpayments identified. Underpayments to doctors totaled $1.2 million in 2013. Overpayment recoveries from all health providers were up $1.3 billion from those collected in 2012, according to last year’s report.
After contingency and administrative costs, the RAC program returned $3 billion to the Medicare trust funds. Meanwhile, RACs received from 9% to 12.5% of the inaccurate payments they identified. In fiscal 2013, auditors were paid $301.7 million in contingency fees, according to the report.
The outcome of audit appeals varied widely depending on the type of provider. Appeals decisions were made in 720,416 Medicare Part A claims and 116,433 Part B durable medical equipment (DME) claims in fiscal 2013. Those numbers include first-, second-, third-, and fourth-level appeal decisions, and may count the same claim multiple times. Of total claims appealed, 31% were associated with overpayment findings. Sixty percent of Medicare Part B DME decisions were overturned in providers’ favor, while only 11% of Part A claims were overturned on appeal.
On Twitter @legal_med
Auditors with the Centers for Medicare & Medicaid Services collected more than $3 billion in overpayments from health providers in 2013, including nearly $57 million from doctors, according to a CMS Sept. 29 annual report to Congress.
Recovery audit contractors (RACs) corrected a total of $3.75 billion in improper payments in fiscal 2013, of which $3.65 billion were in overpayments, the report found. Underpayments made up $102 million of the incorrect fees. Physicians were responsible for $56.8 million of overpayments identified. Underpayments to doctors totaled $1.2 million in 2013. Overpayment recoveries from all health providers were up $1.3 billion from those collected in 2012, according to last year’s report.
After contingency and administrative costs, the RAC program returned $3 billion to the Medicare trust funds. Meanwhile, RACs received from 9% to 12.5% of the inaccurate payments they identified. In fiscal 2013, auditors were paid $301.7 million in contingency fees, according to the report.
The outcome of audit appeals varied widely depending on the type of provider. Appeals decisions were made in 720,416 Medicare Part A claims and 116,433 Part B durable medical equipment (DME) claims in fiscal 2013. Those numbers include first-, second-, third-, and fourth-level appeal decisions, and may count the same claim multiple times. Of total claims appealed, 31% were associated with overpayment findings. Sixty percent of Medicare Part B DME decisions were overturned in providers’ favor, while only 11% of Part A claims were overturned on appeal.
On Twitter @legal_med
Auditors with the Centers for Medicare & Medicaid Services collected more than $3 billion in overpayments from health providers in 2013, including nearly $57 million from doctors, according to a CMS Sept. 29 annual report to Congress.
Recovery audit contractors (RACs) corrected a total of $3.75 billion in improper payments in fiscal 2013, of which $3.65 billion were in overpayments, the report found. Underpayments made up $102 million of the incorrect fees. Physicians were responsible for $56.8 million of overpayments identified. Underpayments to doctors totaled $1.2 million in 2013. Overpayment recoveries from all health providers were up $1.3 billion from those collected in 2012, according to last year’s report.
After contingency and administrative costs, the RAC program returned $3 billion to the Medicare trust funds. Meanwhile, RACs received from 9% to 12.5% of the inaccurate payments they identified. In fiscal 2013, auditors were paid $301.7 million in contingency fees, according to the report.
The outcome of audit appeals varied widely depending on the type of provider. Appeals decisions were made in 720,416 Medicare Part A claims and 116,433 Part B durable medical equipment (DME) claims in fiscal 2013. Those numbers include first-, second-, third-, and fourth-level appeal decisions, and may count the same claim multiple times. Of total claims appealed, 31% were associated with overpayment findings. Sixty percent of Medicare Part B DME decisions were overturned in providers’ favor, while only 11% of Part A claims were overturned on appeal.
On Twitter @legal_med
Physician candidates playing key role in midterm elections
Two candidates are playing a role in the GOP push to take control of the U.S. Senate and potentially hamper the further implementation of the Affordable Care Act – and they’re both doctors.
Rep. Bill Cassidy (R-La.) is a physician and congressman who is giving incumbent Sen. Mary Landrieu (D-La.) the fight of her career. And in Oregon, Dr. Monica Wehby, a pediatric neurosurgeon, is challenging Sen. Jeff Merkley (D-Ore.), though she still trails by double digits in the polls.
Both Dr. Wehby and Rep. Cassidy have made their opposition to the Affordable Care Act (ACA) a major component of their campaigns.
Rep. Cassidy, whose wife Laura is also a physician, favors a system that focuses on consumer-driven options such as health savings accounts, as well as moving forward on medical liability reform.
Dr. Wehby, who wants to repeal and replace the ACA, has also called for a federal investigation of the Cover Oregon insurance marketplace.
“It’s not brain surgery; Obamacare is bad for Oregon,” Dr. Wehby said in one of her political ads, which features footage of her in the hospital.
All U.S. Senate races are getting close attention this year because the upper chamber is so closely divided. The GOP needs a net gain of only 6 seats to win control.
Dr. Steve Shogan, a neurosurgeon from Denver, seeks one of Colorado’s Senate seats as an independent, though he’s not considered a contender in the race. Dr. Shogan has also been critical of the ACA, but says that he would prefer to replace it with a two-tiered approach that combines government-provided basic health care coverage with supplemental private insurance.
Several other doctors – mostly Republicans – lost primary bids for the Senate earlier this year.
But while the Senate is getting a lot of attention, there are plenty of physicians who are vying for seats in the House this year. At least 6 doctors are looking to become first-time lawmakers, and another 13 physicians are seeking reelection to the House, according to the American Medical Association.
Currently there are 20 physicians serving in Congress, including 4 Democrats and 16 Republicans.
While the physician candidates come from both parties, the majority are running as Republicans, and their platforms specifically call for repealing the ACA.
Dr. Jane Orient, an internist and executive director of the Association of American Physicians and Surgeons, said that she isn’t surprised. Not only do most physicians tend to be conservative, she said, but frustration with the ACA and other health care regulations is bubbling over.
“Physicians are seeing that their profession is being destroyed,” she said. “If they don’t fight for our rights to practice medicine according to our best judgment and according to our professional ethics, and without constantly being clerks for the third-party payers and the government, then we really have to get politically active.”
The ACA has prompted more physicians to get engaged in politics this year, according to Mark A. Peterson, Ph.D., professor of public policy and political science at the University of California, Los Angeles. While Dr. Peterson said that he agrees that most physicians identify with the Republican party, he added that there are still plenty of physicians who favor the ACA or even single-payer approaches, but they seem to have largely stayed out of politics.
“I don’t know why more of them haven’t taken up the charge to run for office, but it certainly didn’t help Democrats in recruitment that 2014 has been long perceived as a Republican year,” he said.
On Twitter @maryellenny
Two candidates are playing a role in the GOP push to take control of the U.S. Senate and potentially hamper the further implementation of the Affordable Care Act – and they’re both doctors.
Rep. Bill Cassidy (R-La.) is a physician and congressman who is giving incumbent Sen. Mary Landrieu (D-La.) the fight of her career. And in Oregon, Dr. Monica Wehby, a pediatric neurosurgeon, is challenging Sen. Jeff Merkley (D-Ore.), though she still trails by double digits in the polls.
Both Dr. Wehby and Rep. Cassidy have made their opposition to the Affordable Care Act (ACA) a major component of their campaigns.
Rep. Cassidy, whose wife Laura is also a physician, favors a system that focuses on consumer-driven options such as health savings accounts, as well as moving forward on medical liability reform.
Dr. Wehby, who wants to repeal and replace the ACA, has also called for a federal investigation of the Cover Oregon insurance marketplace.
“It’s not brain surgery; Obamacare is bad for Oregon,” Dr. Wehby said in one of her political ads, which features footage of her in the hospital.
All U.S. Senate races are getting close attention this year because the upper chamber is so closely divided. The GOP needs a net gain of only 6 seats to win control.
Dr. Steve Shogan, a neurosurgeon from Denver, seeks one of Colorado’s Senate seats as an independent, though he’s not considered a contender in the race. Dr. Shogan has also been critical of the ACA, but says that he would prefer to replace it with a two-tiered approach that combines government-provided basic health care coverage with supplemental private insurance.
Several other doctors – mostly Republicans – lost primary bids for the Senate earlier this year.
But while the Senate is getting a lot of attention, there are plenty of physicians who are vying for seats in the House this year. At least 6 doctors are looking to become first-time lawmakers, and another 13 physicians are seeking reelection to the House, according to the American Medical Association.
Currently there are 20 physicians serving in Congress, including 4 Democrats and 16 Republicans.
While the physician candidates come from both parties, the majority are running as Republicans, and their platforms specifically call for repealing the ACA.
Dr. Jane Orient, an internist and executive director of the Association of American Physicians and Surgeons, said that she isn’t surprised. Not only do most physicians tend to be conservative, she said, but frustration with the ACA and other health care regulations is bubbling over.
“Physicians are seeing that their profession is being destroyed,” she said. “If they don’t fight for our rights to practice medicine according to our best judgment and according to our professional ethics, and without constantly being clerks for the third-party payers and the government, then we really have to get politically active.”
The ACA has prompted more physicians to get engaged in politics this year, according to Mark A. Peterson, Ph.D., professor of public policy and political science at the University of California, Los Angeles. While Dr. Peterson said that he agrees that most physicians identify with the Republican party, he added that there are still plenty of physicians who favor the ACA or even single-payer approaches, but they seem to have largely stayed out of politics.
“I don’t know why more of them haven’t taken up the charge to run for office, but it certainly didn’t help Democrats in recruitment that 2014 has been long perceived as a Republican year,” he said.
On Twitter @maryellenny
Two candidates are playing a role in the GOP push to take control of the U.S. Senate and potentially hamper the further implementation of the Affordable Care Act – and they’re both doctors.
Rep. Bill Cassidy (R-La.) is a physician and congressman who is giving incumbent Sen. Mary Landrieu (D-La.) the fight of her career. And in Oregon, Dr. Monica Wehby, a pediatric neurosurgeon, is challenging Sen. Jeff Merkley (D-Ore.), though she still trails by double digits in the polls.
Both Dr. Wehby and Rep. Cassidy have made their opposition to the Affordable Care Act (ACA) a major component of their campaigns.
Rep. Cassidy, whose wife Laura is also a physician, favors a system that focuses on consumer-driven options such as health savings accounts, as well as moving forward on medical liability reform.
Dr. Wehby, who wants to repeal and replace the ACA, has also called for a federal investigation of the Cover Oregon insurance marketplace.
“It’s not brain surgery; Obamacare is bad for Oregon,” Dr. Wehby said in one of her political ads, which features footage of her in the hospital.
All U.S. Senate races are getting close attention this year because the upper chamber is so closely divided. The GOP needs a net gain of only 6 seats to win control.
Dr. Steve Shogan, a neurosurgeon from Denver, seeks one of Colorado’s Senate seats as an independent, though he’s not considered a contender in the race. Dr. Shogan has also been critical of the ACA, but says that he would prefer to replace it with a two-tiered approach that combines government-provided basic health care coverage with supplemental private insurance.
Several other doctors – mostly Republicans – lost primary bids for the Senate earlier this year.
But while the Senate is getting a lot of attention, there are plenty of physicians who are vying for seats in the House this year. At least 6 doctors are looking to become first-time lawmakers, and another 13 physicians are seeking reelection to the House, according to the American Medical Association.
Currently there are 20 physicians serving in Congress, including 4 Democrats and 16 Republicans.
While the physician candidates come from both parties, the majority are running as Republicans, and their platforms specifically call for repealing the ACA.
Dr. Jane Orient, an internist and executive director of the Association of American Physicians and Surgeons, said that she isn’t surprised. Not only do most physicians tend to be conservative, she said, but frustration with the ACA and other health care regulations is bubbling over.
“Physicians are seeing that their profession is being destroyed,” she said. “If they don’t fight for our rights to practice medicine according to our best judgment and according to our professional ethics, and without constantly being clerks for the third-party payers and the government, then we really have to get politically active.”
The ACA has prompted more physicians to get engaged in politics this year, according to Mark A. Peterson, Ph.D., professor of public policy and political science at the University of California, Los Angeles. While Dr. Peterson said that he agrees that most physicians identify with the Republican party, he added that there are still plenty of physicians who favor the ACA or even single-payer approaches, but they seem to have largely stayed out of politics.
“I don’t know why more of them haven’t taken up the charge to run for office, but it certainly didn’t help Democrats in recruitment that 2014 has been long perceived as a Republican year,” he said.
On Twitter @maryellenny
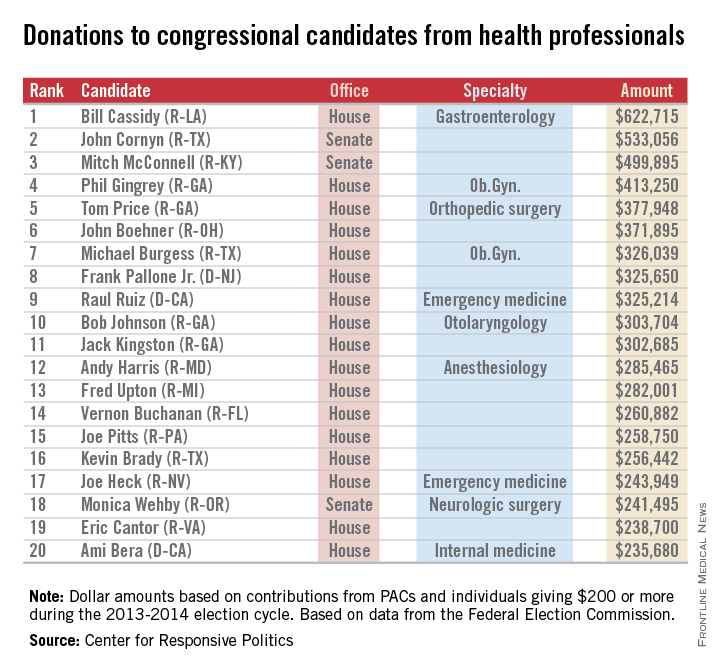
Doctors share the wealth with congressional candidates
Doctors and other health professionals are contributing generously to candidates from both parties in this year’s mid-term election, OpenSecrets.org reported.
Rep. Bill Cassidy (R-La.), a gastroenterologist, has reaped almost $623,000 from his fellow health professionals – more money than any other candidate in the 2013-2014 election cycle. On the other side of Capitol Hill, Sen. John Cornyn (R-Tex.) has taken in the most in donations, totalling just over $533,000 in this election cycle. Senate Minority Leader Mitch McConnell (R-Ky.) has received just under $500,000, according to the Center for Responsive Politics, which operates OpenSecrets.com.
In the House, Rep. Phil Gingrey (R-Ga.), an ob.gyn., has seen about $413,000 in donations. Ten physician-legislators are included in the top 20 candidates most generously supported by health professionals.
The report from the Center for Responsive Politics is based on data released by the Federal Election Commission on Sept. 8, 2014, and covers contributions of $200 or more from political action committees and individuals.
The health professionals category includes physicians, dentists, nurses, physician assistants, other health professionals, and the political action committees that represent them.

Doctors and other health professionals are contributing generously to candidates from both parties in this year’s mid-term election, OpenSecrets.org reported.
Rep. Bill Cassidy (R-La.), a gastroenterologist, has reaped almost $623,000 from his fellow health professionals – more money than any other candidate in the 2013-2014 election cycle. On the other side of Capitol Hill, Sen. John Cornyn (R-Tex.) has taken in the most in donations, totalling just over $533,000 in this election cycle. Senate Minority Leader Mitch McConnell (R-Ky.) has received just under $500,000, according to the Center for Responsive Politics, which operates OpenSecrets.com.
In the House, Rep. Phil Gingrey (R-Ga.), an ob.gyn., has seen about $413,000 in donations. Ten physician-legislators are included in the top 20 candidates most generously supported by health professionals.
The report from the Center for Responsive Politics is based on data released by the Federal Election Commission on Sept. 8, 2014, and covers contributions of $200 or more from political action committees and individuals.
The health professionals category includes physicians, dentists, nurses, physician assistants, other health professionals, and the political action committees that represent them.

Doctors and other health professionals are contributing generously to candidates from both parties in this year’s mid-term election, OpenSecrets.org reported.
Rep. Bill Cassidy (R-La.), a gastroenterologist, has reaped almost $623,000 from his fellow health professionals – more money than any other candidate in the 2013-2014 election cycle. On the other side of Capitol Hill, Sen. John Cornyn (R-Tex.) has taken in the most in donations, totalling just over $533,000 in this election cycle. Senate Minority Leader Mitch McConnell (R-Ky.) has received just under $500,000, according to the Center for Responsive Politics, which operates OpenSecrets.com.
In the House, Rep. Phil Gingrey (R-Ga.), an ob.gyn., has seen about $413,000 in donations. Ten physician-legislators are included in the top 20 candidates most generously supported by health professionals.
The report from the Center for Responsive Politics is based on data released by the Federal Election Commission on Sept. 8, 2014, and covers contributions of $200 or more from political action committees and individuals.
The health professionals category includes physicians, dentists, nurses, physician assistants, other health professionals, and the political action committees that represent them.

Industry payments to docs, hospitals top $4.5 billion
The drug and device industry made about $4.6 billion in payments to physicians and teaching hospitals in the last 5 months of 2013, according to updated data from the government.
The Centers for Medicare & Medicaid Services (CMS) recently released a massive data set detailing payments from industry to health care providers as part of the new Open Payments program, a transparency initiative mandated under the Affordable Care Act. In the initial data release on Sept. 30, the agency said that industry payments totaled $3.5 billion across 4.4 million published payment records. But updated figures, released by the agency Oct. 6, show that the industry spent an additional $1.1 billion for 199,000 payment records that have yet to be published.
The CMS held off on publishing payment data for two reasons: Either there was an unresolved dispute at the end of the 45-day review period, or the manufacturer requested a delay in publication because the payments were related to a drug or device that was still under development.
The bulk of the unpublished payment data – about 190,000 records – falls into the “delay in publication” category. In total, manufacturers made $551 million in payments related to products in development. Under the regulations governing the Open Payments program, the delay cannot exceed 4 years or the date when the product is approved by the Food and Drug Administration.
The rest of the unpublished payment data relate to about 9,000 payments totaling $514 million that are still under active dispute. About 91% of the total payments in question are associated with only 40 disputes, according to the CMS.
The next round of Open Payments data, which will include payments from all of 2014, will be published in June 2015.
On Twitter @maryellenny
The drug and device industry made about $4.6 billion in payments to physicians and teaching hospitals in the last 5 months of 2013, according to updated data from the government.
The Centers for Medicare & Medicaid Services (CMS) recently released a massive data set detailing payments from industry to health care providers as part of the new Open Payments program, a transparency initiative mandated under the Affordable Care Act. In the initial data release on Sept. 30, the agency said that industry payments totaled $3.5 billion across 4.4 million published payment records. But updated figures, released by the agency Oct. 6, show that the industry spent an additional $1.1 billion for 199,000 payment records that have yet to be published.
The CMS held off on publishing payment data for two reasons: Either there was an unresolved dispute at the end of the 45-day review period, or the manufacturer requested a delay in publication because the payments were related to a drug or device that was still under development.
The bulk of the unpublished payment data – about 190,000 records – falls into the “delay in publication” category. In total, manufacturers made $551 million in payments related to products in development. Under the regulations governing the Open Payments program, the delay cannot exceed 4 years or the date when the product is approved by the Food and Drug Administration.
The rest of the unpublished payment data relate to about 9,000 payments totaling $514 million that are still under active dispute. About 91% of the total payments in question are associated with only 40 disputes, according to the CMS.
The next round of Open Payments data, which will include payments from all of 2014, will be published in June 2015.
On Twitter @maryellenny
The drug and device industry made about $4.6 billion in payments to physicians and teaching hospitals in the last 5 months of 2013, according to updated data from the government.
The Centers for Medicare & Medicaid Services (CMS) recently released a massive data set detailing payments from industry to health care providers as part of the new Open Payments program, a transparency initiative mandated under the Affordable Care Act. In the initial data release on Sept. 30, the agency said that industry payments totaled $3.5 billion across 4.4 million published payment records. But updated figures, released by the agency Oct. 6, show that the industry spent an additional $1.1 billion for 199,000 payment records that have yet to be published.
The CMS held off on publishing payment data for two reasons: Either there was an unresolved dispute at the end of the 45-day review period, or the manufacturer requested a delay in publication because the payments were related to a drug or device that was still under development.
The bulk of the unpublished payment data – about 190,000 records – falls into the “delay in publication” category. In total, manufacturers made $551 million in payments related to products in development. Under the regulations governing the Open Payments program, the delay cannot exceed 4 years or the date when the product is approved by the Food and Drug Administration.
The rest of the unpublished payment data relate to about 9,000 payments totaling $514 million that are still under active dispute. About 91% of the total payments in question are associated with only 40 disputes, according to the CMS.
The next round of Open Payments data, which will include payments from all of 2014, will be published in June 2015.
On Twitter @maryellenny
Some docs get another chance at 'meaningful use' hardship exemption
Doctors and hospitals are getting another chance to apply for relief from the federal EHR meaningful use program and avoid penalties, officials at the Centers for Medicare & Medicaid Services announced.
The agency is reopening the application period for hardship exemptions, specifically for physicians and hospitals that are attesting to their meaningful use of electronic health records (EHRs) for the first time, and who have been using older technology.
The new deadline for hardship applications is 11:59 p.m. EST on Nov. 30.
The deadline to apply for a hardship exemption originally closed on April 1 for hospitals and July 1 for physicians. But the Centers for Medicare & Medicaid Services (CMS) reopened the process after it became clear that a subset of physicians who were attesting to meaningful use for the first time could see a 1% penalty due to a government website problem.
At the center of the problem is a backlog in the availability of newly certified EHR products. Knowing that many physicians and hospitals would be unable to attest to using newly certified products in time for this year’s meaningful use deadline, the CMS proposed in May to allow them to attest to using older technology during 2014.
The final rule, released in August, gives physicians the flexibility to use either a 2011 certified product, a newer 2014 certified product, or a combination of both, without being penalized. But the website where physicians must apply for the flexibility was not ready in time for the Oct. 1 attestation deadline.
The mismatch in deadlines raised the ire of physician groups and members of Congress, who called on the CMS to find some pathway for physicians to avoid penalties earned through no fault of their own.
On Oct. 7, the CMS announced that it would reopen the hardship application period for physicians and hospitals that had been unable to fully implement 2014 certified EHRs due to delays in their availability, as well as those who were unable to attest to meaningful use by the deadline and were using the flexibility options outlined by the CMS.
The announcement was praised by the American Medical Association. AMA President Robert M. Wah said the change will allow more physicians to avoid an “unfair” penalty in 2015.
“Giving physicians more time to file for a hardship exemption provides necessary relief as many physicians are struggling to meet a number of reporting mandates to avoid multiple penalties,” Dr. Wah said in a statement.
On Twitter @maryellenny
Doctors and hospitals are getting another chance to apply for relief from the federal EHR meaningful use program and avoid penalties, officials at the Centers for Medicare & Medicaid Services announced.
The agency is reopening the application period for hardship exemptions, specifically for physicians and hospitals that are attesting to their meaningful use of electronic health records (EHRs) for the first time, and who have been using older technology.
The new deadline for hardship applications is 11:59 p.m. EST on Nov. 30.
The deadline to apply for a hardship exemption originally closed on April 1 for hospitals and July 1 for physicians. But the Centers for Medicare & Medicaid Services (CMS) reopened the process after it became clear that a subset of physicians who were attesting to meaningful use for the first time could see a 1% penalty due to a government website problem.
At the center of the problem is a backlog in the availability of newly certified EHR products. Knowing that many physicians and hospitals would be unable to attest to using newly certified products in time for this year’s meaningful use deadline, the CMS proposed in May to allow them to attest to using older technology during 2014.
The final rule, released in August, gives physicians the flexibility to use either a 2011 certified product, a newer 2014 certified product, or a combination of both, without being penalized. But the website where physicians must apply for the flexibility was not ready in time for the Oct. 1 attestation deadline.
The mismatch in deadlines raised the ire of physician groups and members of Congress, who called on the CMS to find some pathway for physicians to avoid penalties earned through no fault of their own.
On Oct. 7, the CMS announced that it would reopen the hardship application period for physicians and hospitals that had been unable to fully implement 2014 certified EHRs due to delays in their availability, as well as those who were unable to attest to meaningful use by the deadline and were using the flexibility options outlined by the CMS.
The announcement was praised by the American Medical Association. AMA President Robert M. Wah said the change will allow more physicians to avoid an “unfair” penalty in 2015.
“Giving physicians more time to file for a hardship exemption provides necessary relief as many physicians are struggling to meet a number of reporting mandates to avoid multiple penalties,” Dr. Wah said in a statement.
On Twitter @maryellenny
Doctors and hospitals are getting another chance to apply for relief from the federal EHR meaningful use program and avoid penalties, officials at the Centers for Medicare & Medicaid Services announced.
The agency is reopening the application period for hardship exemptions, specifically for physicians and hospitals that are attesting to their meaningful use of electronic health records (EHRs) for the first time, and who have been using older technology.
The new deadline for hardship applications is 11:59 p.m. EST on Nov. 30.
The deadline to apply for a hardship exemption originally closed on April 1 for hospitals and July 1 for physicians. But the Centers for Medicare & Medicaid Services (CMS) reopened the process after it became clear that a subset of physicians who were attesting to meaningful use for the first time could see a 1% penalty due to a government website problem.
At the center of the problem is a backlog in the availability of newly certified EHR products. Knowing that many physicians and hospitals would be unable to attest to using newly certified products in time for this year’s meaningful use deadline, the CMS proposed in May to allow them to attest to using older technology during 2014.
The final rule, released in August, gives physicians the flexibility to use either a 2011 certified product, a newer 2014 certified product, or a combination of both, without being penalized. But the website where physicians must apply for the flexibility was not ready in time for the Oct. 1 attestation deadline.
The mismatch in deadlines raised the ire of physician groups and members of Congress, who called on the CMS to find some pathway for physicians to avoid penalties earned through no fault of their own.
On Oct. 7, the CMS announced that it would reopen the hardship application period for physicians and hospitals that had been unable to fully implement 2014 certified EHRs due to delays in their availability, as well as those who were unable to attest to meaningful use by the deadline and were using the flexibility options outlined by the CMS.
The announcement was praised by the American Medical Association. AMA President Robert M. Wah said the change will allow more physicians to avoid an “unfair” penalty in 2015.
“Giving physicians more time to file for a hardship exemption provides necessary relief as many physicians are struggling to meet a number of reporting mandates to avoid multiple penalties,” Dr. Wah said in a statement.
On Twitter @maryellenny
Malpractice Counsel
Aortic Rupture
A 59-year-old woman involved in a motor vehicle crash presented to the ED via emergency medical services. The patient had been the front-seat passenger and was wearing a seat belt. She complained of chest wall pain, but denied head injury, loss of consciousness, neck pain, abdominal pain, or shortness of breath. Her past medical history was unremarkable.
A chest X-ray was performed and interpreted as normal by the attending radiologist. Laboratory studies were normal except for mild anemia. The patient was discharged from the hospital with a diagnosis of chest wall contusion. She died 36 hours later from a ruptured thoracic aorta. The family of the patient brought a malpractice suit against the emergency physician (EP) for failing to diagnose and treat acute aortic rupture. At trial, a defense verdict was returned.
Discussion
Aortic rupture from blunt trauma is a devastating injury. More than 90% of patients who have sustained this type of injury in a motor vehicle crash die at the scene.1 For the remaining 10%, 50% die within the following 24 hours.1 The injury occurs in the proximal descending aorta, secondary to the fixation of the vessels between the left subclavian artery and the ligamentum arteriosum; the cause in approximately 80% to 90% of cases is due to blunt trauma. Involvement of the ascending aorta is much less common. Many patients, such as the one in this case, exhibit no external physical findings of injury. Chest pain is the most frequent complaint, followed by dyspnea—both fairly nonspecific symptoms. Physical findings that should raise a suspicion for a thoracic aortic injury include hypotension, hypertension in the upper extremity and hypotension in the lower extremity, unequal BPs in the extremities, external evidence of chest wall trauma, and palpable fractures of the sternum and ribs.2 While it is unclear if this patient had unequal extremity BPs, she did not have any of the other classic findings of aortic rupture. Associated neurological, abdominal, or orthopedic injuries are frequently present as well, and can mask the subtle signs of aortic rupture.
A chest radiograph is often the initial screening test used to evaluate for possible thoracic aortic injury. Suspicious findings include a widened mediastinum (greater than 8 cm), right-sided deviation of the esophagus, depression of the left mainstem bronchus, loss of the aortic knob, and an apical pleural cap. Unfortunately, chest X-ray can be normal, and a normal mediastinum on the radiograph does not exclude the diagnosis.
For patients with suspected thoracic aortic injury, helical computed tomography with angiography is the study of choice. It can accurately identify operative and nonoperative lesions, as well as associated injuries (eg, small pneumothorax, rib fractures). Magnetic resonance angiography provides similar sensitivity and specificity, but is not practical for the majority of trauma patients. Occasionally, aortography can be considered when the CT scan results are indeterminate and when thought to be needed to plan operative intervention. Finally, transesophageal echocardiography can be considered in hemodynamically unstable patients unable to be transferred to the radiology suite.
For most patients, immediate operative intervention is the definitive treatment. For patients with suspected thoracic aortic injury and hypertension, shear forces need to be decreased just as they are for patients with aortic dissection. A short-acting β-blocker like intravenous (IV) esmolol can be used initially to slow HR. Then, an IV arterial vasodilator can be given to decrease BP. To prevent rebound tachycardia and increased shear forces, the β-blocker should always be initiated before the vasodilator is given. Vital-sign targets include an HR of 60 beats/minute and a systolic BP in the range of 100 to 120 mm Hg.
This was a very atypical presentation of a devastating injury. Given the benign presentation, lack of associated injuries, and the normal chest X-ray, a defense verdict appears to be the correct one in this very unfortunate case.
Foot Drop
A 20-year-old woman presented to the ED complaining of severe numbness, tingling, and pain in her left calf. According to the patient, she had attended a New Year’s Eve party, where she spent much of the time dancing. She was awakened by calf pain on the following morning and sought treatment at the ED.
On physical examination, the patient’s vital signs were normal. Examination of the left calf revealed tenderness to palpation; no swelling was noted. The patient was unable to lift her left foot or bear weight on the left leg. She had normal dorsalis pedis and posterior tibial pulses in the affected leg. The remainder of her examination was normal and no testing was performed. The patient was diagnosed with “floppy foot syndrome” and discharged home with a prescription for a nonsteroidal anti-inflammatory drug.
The next day, the patient presented to a different ED because of worsening pain and swelling of the calf. She was admitted to the hospital and the orthopedic service was consulted. The patient was diagnosed with compartment syndrome; however, by that time her condition was complicated by rhabdomyolysis, resulting in acute renal failure.
The patient underwent a fasciotomy. After surgery, she required hemodialysis until her kidney function returned. She had damage to the nerves in her left calf and leg resulting in a permanent foot drop that required prolonged physical therapy following her hospitalization.
The patient sued the initial EP for failure to diagnose compartment syndrome, which resulted in permanent nerve damage and foot drop. A $750,000 settlement was reached.
Discussion
The EP did not appear to have taken this case seriously, as “floppy foot syndrome” is not a recognized diagnosis. No significance was attached to the presence of the foot drop, which is an objective and concerning physical finding.
The differential diagnoses of foot drop are relatively small: a nerve injury, which is the most common cause; a central nervous system event, such as a stroke; or a muscular disorder.3 An injury or problem with the peroneal nerve is the most common cause of foot drop.
While the patient’s history was not typical for the development of compartment syndrome, she potentially participated in strenuous physical activity, which can result in muscle swelling and subsequent compartment syndrome.4 The pain from compartment syndrome is typically described as out of proportion to physical findings; this seems to have been the case for this patient.
The symptoms and findings of compartment syndrome are classically taught as the five “Ps”: pain, paresthesias, paralysis, pallor, and pulselessness, with the symptoms typically presenting in this order. The patient had the first three symptoms, but they were not appreciated in the initial evaluation. Pulselessness is usually the last finding to develop, and tissue damage is frequently present at that point.
Interestingly, approximately 40% of compartment syndromes occur at the level of the tibia and fibula. The lower leg has four compartments: the anterior, which contains the anterior tibial artery and deep peroneal nerve; the lateral, which contains the superficial peroneal nerve; the superficial posterior, which contains the sural nerve; and the deep posterior, which contains the posterior tibial artery and nerve.
As pressure within the enclosed space increases due to swelling, hemorrhage, fracture, etc, the blood supply as well as nerve and muscle functions become compromised. Left untreated, the increased pressure can result in permanent tissue and nerve damage.
Compartment syndrome is a time sensitive diagnosis because of the need for surgical intervention to open the compartment. The EP can measure compartment pressures if he or she has the right equipment and training. A normal compartment pressure is less than 10 mm Hg. When the compartment pressure begins to exceed 30 mm Hg, tissue damage can occur. If unable to measure compartment pressure, an emergent orthopedic consult is indicated.
- Chiesa R, de Moura MR, Lucci C, et al. Traumatic rupture of the thoracic aorta. Acta Chir Belq. 2003;103(4):364-374.
- Ross C, Schwab TM. Cardiac trauma. In: Tintinalli JE, Stapczynski JS, Cline DM, Ma OJ, Cydulka RK, Meckler GD. Ross C. In: Tintinalli’s Emergency Medicine: A Comprehensive Study Guide. 7th ed. New York, NY: McGraw Hill Medical; 2011:1758-1765.
- Ricarte IF, Figueiredo MM, Fukuda TG, Pedroso JL, Silva GS. Acute foot drop syndrome mimicking peroneal nerve injury: an atypical presentation of ischemic stroke. J Stroke Cerebrovasc Dis. 2014:23(5):1229-1231.
- Aliano K, Gulati S, Stavrides S, Davenport T, Hines G. Low-impact trauma causing acute compartment syndrome of the lower extremities. Am J Emerg Med. 2013;31(5):890.e3-e4.
Aortic Rupture
A 59-year-old woman involved in a motor vehicle crash presented to the ED via emergency medical services. The patient had been the front-seat passenger and was wearing a seat belt. She complained of chest wall pain, but denied head injury, loss of consciousness, neck pain, abdominal pain, or shortness of breath. Her past medical history was unremarkable.
A chest X-ray was performed and interpreted as normal by the attending radiologist. Laboratory studies were normal except for mild anemia. The patient was discharged from the hospital with a diagnosis of chest wall contusion. She died 36 hours later from a ruptured thoracic aorta. The family of the patient brought a malpractice suit against the emergency physician (EP) for failing to diagnose and treat acute aortic rupture. At trial, a defense verdict was returned.
Discussion
Aortic rupture from blunt trauma is a devastating injury. More than 90% of patients who have sustained this type of injury in a motor vehicle crash die at the scene.1 For the remaining 10%, 50% die within the following 24 hours.1 The injury occurs in the proximal descending aorta, secondary to the fixation of the vessels between the left subclavian artery and the ligamentum arteriosum; the cause in approximately 80% to 90% of cases is due to blunt trauma. Involvement of the ascending aorta is much less common. Many patients, such as the one in this case, exhibit no external physical findings of injury. Chest pain is the most frequent complaint, followed by dyspnea—both fairly nonspecific symptoms. Physical findings that should raise a suspicion for a thoracic aortic injury include hypotension, hypertension in the upper extremity and hypotension in the lower extremity, unequal BPs in the extremities, external evidence of chest wall trauma, and palpable fractures of the sternum and ribs.2 While it is unclear if this patient had unequal extremity BPs, she did not have any of the other classic findings of aortic rupture. Associated neurological, abdominal, or orthopedic injuries are frequently present as well, and can mask the subtle signs of aortic rupture.
A chest radiograph is often the initial screening test used to evaluate for possible thoracic aortic injury. Suspicious findings include a widened mediastinum (greater than 8 cm), right-sided deviation of the esophagus, depression of the left mainstem bronchus, loss of the aortic knob, and an apical pleural cap. Unfortunately, chest X-ray can be normal, and a normal mediastinum on the radiograph does not exclude the diagnosis.
For patients with suspected thoracic aortic injury, helical computed tomography with angiography is the study of choice. It can accurately identify operative and nonoperative lesions, as well as associated injuries (eg, small pneumothorax, rib fractures). Magnetic resonance angiography provides similar sensitivity and specificity, but is not practical for the majority of trauma patients. Occasionally, aortography can be considered when the CT scan results are indeterminate and when thought to be needed to plan operative intervention. Finally, transesophageal echocardiography can be considered in hemodynamically unstable patients unable to be transferred to the radiology suite.
For most patients, immediate operative intervention is the definitive treatment. For patients with suspected thoracic aortic injury and hypertension, shear forces need to be decreased just as they are for patients with aortic dissection. A short-acting β-blocker like intravenous (IV) esmolol can be used initially to slow HR. Then, an IV arterial vasodilator can be given to decrease BP. To prevent rebound tachycardia and increased shear forces, the β-blocker should always be initiated before the vasodilator is given. Vital-sign targets include an HR of 60 beats/minute and a systolic BP in the range of 100 to 120 mm Hg.
This was a very atypical presentation of a devastating injury. Given the benign presentation, lack of associated injuries, and the normal chest X-ray, a defense verdict appears to be the correct one in this very unfortunate case.
Foot Drop
A 20-year-old woman presented to the ED complaining of severe numbness, tingling, and pain in her left calf. According to the patient, she had attended a New Year’s Eve party, where she spent much of the time dancing. She was awakened by calf pain on the following morning and sought treatment at the ED.
On physical examination, the patient’s vital signs were normal. Examination of the left calf revealed tenderness to palpation; no swelling was noted. The patient was unable to lift her left foot or bear weight on the left leg. She had normal dorsalis pedis and posterior tibial pulses in the affected leg. The remainder of her examination was normal and no testing was performed. The patient was diagnosed with “floppy foot syndrome” and discharged home with a prescription for a nonsteroidal anti-inflammatory drug.
The next day, the patient presented to a different ED because of worsening pain and swelling of the calf. She was admitted to the hospital and the orthopedic service was consulted. The patient was diagnosed with compartment syndrome; however, by that time her condition was complicated by rhabdomyolysis, resulting in acute renal failure.
The patient underwent a fasciotomy. After surgery, she required hemodialysis until her kidney function returned. She had damage to the nerves in her left calf and leg resulting in a permanent foot drop that required prolonged physical therapy following her hospitalization.
The patient sued the initial EP for failure to diagnose compartment syndrome, which resulted in permanent nerve damage and foot drop. A $750,000 settlement was reached.
Discussion
The EP did not appear to have taken this case seriously, as “floppy foot syndrome” is not a recognized diagnosis. No significance was attached to the presence of the foot drop, which is an objective and concerning physical finding.
The differential diagnoses of foot drop are relatively small: a nerve injury, which is the most common cause; a central nervous system event, such as a stroke; or a muscular disorder.3 An injury or problem with the peroneal nerve is the most common cause of foot drop.
While the patient’s history was not typical for the development of compartment syndrome, she potentially participated in strenuous physical activity, which can result in muscle swelling and subsequent compartment syndrome.4 The pain from compartment syndrome is typically described as out of proportion to physical findings; this seems to have been the case for this patient.
The symptoms and findings of compartment syndrome are classically taught as the five “Ps”: pain, paresthesias, paralysis, pallor, and pulselessness, with the symptoms typically presenting in this order. The patient had the first three symptoms, but they were not appreciated in the initial evaluation. Pulselessness is usually the last finding to develop, and tissue damage is frequently present at that point.
Interestingly, approximately 40% of compartment syndromes occur at the level of the tibia and fibula. The lower leg has four compartments: the anterior, which contains the anterior tibial artery and deep peroneal nerve; the lateral, which contains the superficial peroneal nerve; the superficial posterior, which contains the sural nerve; and the deep posterior, which contains the posterior tibial artery and nerve.
As pressure within the enclosed space increases due to swelling, hemorrhage, fracture, etc, the blood supply as well as nerve and muscle functions become compromised. Left untreated, the increased pressure can result in permanent tissue and nerve damage.
Compartment syndrome is a time sensitive diagnosis because of the need for surgical intervention to open the compartment. The EP can measure compartment pressures if he or she has the right equipment and training. A normal compartment pressure is less than 10 mm Hg. When the compartment pressure begins to exceed 30 mm Hg, tissue damage can occur. If unable to measure compartment pressure, an emergent orthopedic consult is indicated.
Aortic Rupture
A 59-year-old woman involved in a motor vehicle crash presented to the ED via emergency medical services. The patient had been the front-seat passenger and was wearing a seat belt. She complained of chest wall pain, but denied head injury, loss of consciousness, neck pain, abdominal pain, or shortness of breath. Her past medical history was unremarkable.
A chest X-ray was performed and interpreted as normal by the attending radiologist. Laboratory studies were normal except for mild anemia. The patient was discharged from the hospital with a diagnosis of chest wall contusion. She died 36 hours later from a ruptured thoracic aorta. The family of the patient brought a malpractice suit against the emergency physician (EP) for failing to diagnose and treat acute aortic rupture. At trial, a defense verdict was returned.
Discussion
Aortic rupture from blunt trauma is a devastating injury. More than 90% of patients who have sustained this type of injury in a motor vehicle crash die at the scene.1 For the remaining 10%, 50% die within the following 24 hours.1 The injury occurs in the proximal descending aorta, secondary to the fixation of the vessels between the left subclavian artery and the ligamentum arteriosum; the cause in approximately 80% to 90% of cases is due to blunt trauma. Involvement of the ascending aorta is much less common. Many patients, such as the one in this case, exhibit no external physical findings of injury. Chest pain is the most frequent complaint, followed by dyspnea—both fairly nonspecific symptoms. Physical findings that should raise a suspicion for a thoracic aortic injury include hypotension, hypertension in the upper extremity and hypotension in the lower extremity, unequal BPs in the extremities, external evidence of chest wall trauma, and palpable fractures of the sternum and ribs.2 While it is unclear if this patient had unequal extremity BPs, she did not have any of the other classic findings of aortic rupture. Associated neurological, abdominal, or orthopedic injuries are frequently present as well, and can mask the subtle signs of aortic rupture.
A chest radiograph is often the initial screening test used to evaluate for possible thoracic aortic injury. Suspicious findings include a widened mediastinum (greater than 8 cm), right-sided deviation of the esophagus, depression of the left mainstem bronchus, loss of the aortic knob, and an apical pleural cap. Unfortunately, chest X-ray can be normal, and a normal mediastinum on the radiograph does not exclude the diagnosis.
For patients with suspected thoracic aortic injury, helical computed tomography with angiography is the study of choice. It can accurately identify operative and nonoperative lesions, as well as associated injuries (eg, small pneumothorax, rib fractures). Magnetic resonance angiography provides similar sensitivity and specificity, but is not practical for the majority of trauma patients. Occasionally, aortography can be considered when the CT scan results are indeterminate and when thought to be needed to plan operative intervention. Finally, transesophageal echocardiography can be considered in hemodynamically unstable patients unable to be transferred to the radiology suite.
For most patients, immediate operative intervention is the definitive treatment. For patients with suspected thoracic aortic injury and hypertension, shear forces need to be decreased just as they are for patients with aortic dissection. A short-acting β-blocker like intravenous (IV) esmolol can be used initially to slow HR. Then, an IV arterial vasodilator can be given to decrease BP. To prevent rebound tachycardia and increased shear forces, the β-blocker should always be initiated before the vasodilator is given. Vital-sign targets include an HR of 60 beats/minute and a systolic BP in the range of 100 to 120 mm Hg.
This was a very atypical presentation of a devastating injury. Given the benign presentation, lack of associated injuries, and the normal chest X-ray, a defense verdict appears to be the correct one in this very unfortunate case.
Foot Drop
A 20-year-old woman presented to the ED complaining of severe numbness, tingling, and pain in her left calf. According to the patient, she had attended a New Year’s Eve party, where she spent much of the time dancing. She was awakened by calf pain on the following morning and sought treatment at the ED.
On physical examination, the patient’s vital signs were normal. Examination of the left calf revealed tenderness to palpation; no swelling was noted. The patient was unable to lift her left foot or bear weight on the left leg. She had normal dorsalis pedis and posterior tibial pulses in the affected leg. The remainder of her examination was normal and no testing was performed. The patient was diagnosed with “floppy foot syndrome” and discharged home with a prescription for a nonsteroidal anti-inflammatory drug.
The next day, the patient presented to a different ED because of worsening pain and swelling of the calf. She was admitted to the hospital and the orthopedic service was consulted. The patient was diagnosed with compartment syndrome; however, by that time her condition was complicated by rhabdomyolysis, resulting in acute renal failure.
The patient underwent a fasciotomy. After surgery, she required hemodialysis until her kidney function returned. She had damage to the nerves in her left calf and leg resulting in a permanent foot drop that required prolonged physical therapy following her hospitalization.
The patient sued the initial EP for failure to diagnose compartment syndrome, which resulted in permanent nerve damage and foot drop. A $750,000 settlement was reached.
Discussion
The EP did not appear to have taken this case seriously, as “floppy foot syndrome” is not a recognized diagnosis. No significance was attached to the presence of the foot drop, which is an objective and concerning physical finding.
The differential diagnoses of foot drop are relatively small: a nerve injury, which is the most common cause; a central nervous system event, such as a stroke; or a muscular disorder.3 An injury or problem with the peroneal nerve is the most common cause of foot drop.
While the patient’s history was not typical for the development of compartment syndrome, she potentially participated in strenuous physical activity, which can result in muscle swelling and subsequent compartment syndrome.4 The pain from compartment syndrome is typically described as out of proportion to physical findings; this seems to have been the case for this patient.
The symptoms and findings of compartment syndrome are classically taught as the five “Ps”: pain, paresthesias, paralysis, pallor, and pulselessness, with the symptoms typically presenting in this order. The patient had the first three symptoms, but they were not appreciated in the initial evaluation. Pulselessness is usually the last finding to develop, and tissue damage is frequently present at that point.
Interestingly, approximately 40% of compartment syndromes occur at the level of the tibia and fibula. The lower leg has four compartments: the anterior, which contains the anterior tibial artery and deep peroneal nerve; the lateral, which contains the superficial peroneal nerve; the superficial posterior, which contains the sural nerve; and the deep posterior, which contains the posterior tibial artery and nerve.
As pressure within the enclosed space increases due to swelling, hemorrhage, fracture, etc, the blood supply as well as nerve and muscle functions become compromised. Left untreated, the increased pressure can result in permanent tissue and nerve damage.
Compartment syndrome is a time sensitive diagnosis because of the need for surgical intervention to open the compartment. The EP can measure compartment pressures if he or she has the right equipment and training. A normal compartment pressure is less than 10 mm Hg. When the compartment pressure begins to exceed 30 mm Hg, tissue damage can occur. If unable to measure compartment pressure, an emergent orthopedic consult is indicated.
- Chiesa R, de Moura MR, Lucci C, et al. Traumatic rupture of the thoracic aorta. Acta Chir Belq. 2003;103(4):364-374.
- Ross C, Schwab TM. Cardiac trauma. In: Tintinalli JE, Stapczynski JS, Cline DM, Ma OJ, Cydulka RK, Meckler GD. Ross C. In: Tintinalli’s Emergency Medicine: A Comprehensive Study Guide. 7th ed. New York, NY: McGraw Hill Medical; 2011:1758-1765.
- Ricarte IF, Figueiredo MM, Fukuda TG, Pedroso JL, Silva GS. Acute foot drop syndrome mimicking peroneal nerve injury: an atypical presentation of ischemic stroke. J Stroke Cerebrovasc Dis. 2014:23(5):1229-1231.
- Aliano K, Gulati S, Stavrides S, Davenport T, Hines G. Low-impact trauma causing acute compartment syndrome of the lower extremities. Am J Emerg Med. 2013;31(5):890.e3-e4.
- Chiesa R, de Moura MR, Lucci C, et al. Traumatic rupture of the thoracic aorta. Acta Chir Belq. 2003;103(4):364-374.
- Ross C, Schwab TM. Cardiac trauma. In: Tintinalli JE, Stapczynski JS, Cline DM, Ma OJ, Cydulka RK, Meckler GD. Ross C. In: Tintinalli’s Emergency Medicine: A Comprehensive Study Guide. 7th ed. New York, NY: McGraw Hill Medical; 2011:1758-1765.
- Ricarte IF, Figueiredo MM, Fukuda TG, Pedroso JL, Silva GS. Acute foot drop syndrome mimicking peroneal nerve injury: an atypical presentation of ischemic stroke. J Stroke Cerebrovasc Dis. 2014:23(5):1229-1231.
- Aliano K, Gulati S, Stavrides S, Davenport T, Hines G. Low-impact trauma causing acute compartment syndrome of the lower extremities. Am J Emerg Med. 2013;31(5):890.e3-e4.
Calif. ballot question would drug test docs after adverse event
A coalition of California physicians and business leaders are striving to defeat a proposed law that would force doctors to be drug tested after adverse events or risk losing their license.
Proposition 46 requires that doctors submit to drug and alcohol testing at random and within 12 hours after an adverse event has been identified. Positive results or failure to appear for testing would result in a medical board investigation and a license suspension until findings are complete, according to the proposed initiative. Californians vote on the ballot item on Nov. 4.
If passed, the proposed law would unreasonably penalize doctors unable to meet testing rules and lead to excessive suspensions, said Dr. Theodore M. Mazer, a San Diego-based otolaryngologist in private practice and past president of the San Diego County Medical Society.
“It’s poorly worded and poorly thought out, and it was simply put there to deceive the voters into thinking they were doing something for patient safety,” Dr. Mazer said in an interview. “It will actually result in questions about privacy invasion for doctors and could take doctors who are doing nothing wrong out of practice temporarily with suspended licenses because they couldn’t report in a timely fashion.”
The drug-testing provision is one of three components of Prop. 46, a ballot initiative backed by the state’s trial bar and consumer interest group, Consumer Watchdog. Another provision of the proposal would raise California’s $250,000 medical malpractice cap on noneconomic damages to $1.1 million. A third measure would require physicians to check a statewide database before prescribing Schedule II and Schedule III drugs. The drug-testing provision would apply only to doctors who practice in hospitals or who have hospital privileges.
A spokesman with Consumer Attorneys of California referred questions to Consumer Watchdog. At this article’s deadline, messages left with Consumer Watchdog had not been returned. In a statement, the organization said Prop. 46’s drug and alcohol testing procedures are in line with other industries charged with protecting people’s lives.
“Millions of Californians in safety-sensitive positions are already drug tested at work, such as police officers, firefighters, construction workers, and truck and bus drivers,” the statement said. “Currently, doctors are not tested, although they practice medicine on tens of thousands of California patients every year.”
California physicians have long faced attacks to the state’s medical malpractice award limit, but the drug-testing proposal is new, said Dr. Richard Thorp, who is president of the California Medical Association. If approved, California would become the first state to mandate such testing of doctors. The proposed law could encourage other states to follow in California’s footsteps, opponents said.
“California’s first in a lot of things,” Dr. Mazer said. “This is not a smart first to be.”
The drug-testing provision raises more questions than answers and would likely cause more harm than good, noted Dr. Yul D. Ejnes in a Sept. 30 Annals of Internal Medicine article. The initiative does not specify the time frame in which a medical board must complete its investigation of a doctor’s positive drug result. Additionally, the proposal targets all physicians with admitting privileges, regardless of access to controlled substances, specialty, or impairment risk.
“Randomly testing physicians without some form of risk stratification will likely result in many false-positive results,” said Dr. Ejnes, an internist in private practice in Cranston, R.I., who is immediate past chair of the American College of Physicians Board of Regents. “Prop. 46 addresses verification of positive results, but, as we see in clinical practice, that process only adds to the intrusiveness, expense, and stress that should not have occurred in the first place.”
Dr. Thorp added that the database measure of the proposal, as it’s written, would be detrimental to doctors and patients. The state’s drug monitoring database, called the Controlled Substance Utilization Review and Evaluation System (CURES), currently lacks funding and staff to fully operate the system, he said. Glitches and accessibility problems led to a 2013 law that raised licensing fees for health providers to better fund the database. Physicians are required to register with the system by 2016, according to the law.
“It’s a huge database,” Dr. Thorp said in an interview. “It takes time to get that moving. To mandate this for every doctor and pharmacist is just a recipe for disaster.”
The database and drug-testing components of the initiative were merely included to sway voters into striking down the malpractice cap, said Dr. Richard E. Anderson, chair and CEO of the Doctors Company, a national liability insurer. The company is among the coalition of health care and business leaders against the proposed law.
“These unrelated provisions were added to try to draw voter support for the [medical malpractice damages cap] increase, which did not poll well by itself,” Dr. Anderson said in an interview. “The result is a cynical and manipulative ballot measure, opposed by an unprecedented coalition of medical providers, insurers, businesses, organized labor, civil liberties and senior groups, local governments, teachers, and school districts.”
Dr. Ejnes emphasized that remedies to physician drug and alcohol abuse are still needed. An estimated 8%-18% of physicians are impaired by drugs or alcohol at some point in their careers, according to the Annals article. But the proposed initiative is not the answer, Dr. Ejnes said.
“Developing a system that achieves the goal of detecting and preventing physician impairment requires a thoughtful dialogue among all stakeholders, led by the medical profession,” he said. “A ballot initiative intended to win votes, debated in sound bites and Tweets and creating more problems than it solves, is not the right solution.”
On Twitter @legal_med
A coalition of California physicians and business leaders are striving to defeat a proposed law that would force doctors to be drug tested after adverse events or risk losing their license.
Proposition 46 requires that doctors submit to drug and alcohol testing at random and within 12 hours after an adverse event has been identified. Positive results or failure to appear for testing would result in a medical board investigation and a license suspension until findings are complete, according to the proposed initiative. Californians vote on the ballot item on Nov. 4.
If passed, the proposed law would unreasonably penalize doctors unable to meet testing rules and lead to excessive suspensions, said Dr. Theodore M. Mazer, a San Diego-based otolaryngologist in private practice and past president of the San Diego County Medical Society.
“It’s poorly worded and poorly thought out, and it was simply put there to deceive the voters into thinking they were doing something for patient safety,” Dr. Mazer said in an interview. “It will actually result in questions about privacy invasion for doctors and could take doctors who are doing nothing wrong out of practice temporarily with suspended licenses because they couldn’t report in a timely fashion.”
The drug-testing provision is one of three components of Prop. 46, a ballot initiative backed by the state’s trial bar and consumer interest group, Consumer Watchdog. Another provision of the proposal would raise California’s $250,000 medical malpractice cap on noneconomic damages to $1.1 million. A third measure would require physicians to check a statewide database before prescribing Schedule II and Schedule III drugs. The drug-testing provision would apply only to doctors who practice in hospitals or who have hospital privileges.
A spokesman with Consumer Attorneys of California referred questions to Consumer Watchdog. At this article’s deadline, messages left with Consumer Watchdog had not been returned. In a statement, the organization said Prop. 46’s drug and alcohol testing procedures are in line with other industries charged with protecting people’s lives.
“Millions of Californians in safety-sensitive positions are already drug tested at work, such as police officers, firefighters, construction workers, and truck and bus drivers,” the statement said. “Currently, doctors are not tested, although they practice medicine on tens of thousands of California patients every year.”
California physicians have long faced attacks to the state’s medical malpractice award limit, but the drug-testing proposal is new, said Dr. Richard Thorp, who is president of the California Medical Association. If approved, California would become the first state to mandate such testing of doctors. The proposed law could encourage other states to follow in California’s footsteps, opponents said.
“California’s first in a lot of things,” Dr. Mazer said. “This is not a smart first to be.”
The drug-testing provision raises more questions than answers and would likely cause more harm than good, noted Dr. Yul D. Ejnes in a Sept. 30 Annals of Internal Medicine article. The initiative does not specify the time frame in which a medical board must complete its investigation of a doctor’s positive drug result. Additionally, the proposal targets all physicians with admitting privileges, regardless of access to controlled substances, specialty, or impairment risk.
“Randomly testing physicians without some form of risk stratification will likely result in many false-positive results,” said Dr. Ejnes, an internist in private practice in Cranston, R.I., who is immediate past chair of the American College of Physicians Board of Regents. “Prop. 46 addresses verification of positive results, but, as we see in clinical practice, that process only adds to the intrusiveness, expense, and stress that should not have occurred in the first place.”
Dr. Thorp added that the database measure of the proposal, as it’s written, would be detrimental to doctors and patients. The state’s drug monitoring database, called the Controlled Substance Utilization Review and Evaluation System (CURES), currently lacks funding and staff to fully operate the system, he said. Glitches and accessibility problems led to a 2013 law that raised licensing fees for health providers to better fund the database. Physicians are required to register with the system by 2016, according to the law.
“It’s a huge database,” Dr. Thorp said in an interview. “It takes time to get that moving. To mandate this for every doctor and pharmacist is just a recipe for disaster.”
The database and drug-testing components of the initiative were merely included to sway voters into striking down the malpractice cap, said Dr. Richard E. Anderson, chair and CEO of the Doctors Company, a national liability insurer. The company is among the coalition of health care and business leaders against the proposed law.
“These unrelated provisions were added to try to draw voter support for the [medical malpractice damages cap] increase, which did not poll well by itself,” Dr. Anderson said in an interview. “The result is a cynical and manipulative ballot measure, opposed by an unprecedented coalition of medical providers, insurers, businesses, organized labor, civil liberties and senior groups, local governments, teachers, and school districts.”
Dr. Ejnes emphasized that remedies to physician drug and alcohol abuse are still needed. An estimated 8%-18% of physicians are impaired by drugs or alcohol at some point in their careers, according to the Annals article. But the proposed initiative is not the answer, Dr. Ejnes said.
“Developing a system that achieves the goal of detecting and preventing physician impairment requires a thoughtful dialogue among all stakeholders, led by the medical profession,” he said. “A ballot initiative intended to win votes, debated in sound bites and Tweets and creating more problems than it solves, is not the right solution.”
On Twitter @legal_med
A coalition of California physicians and business leaders are striving to defeat a proposed law that would force doctors to be drug tested after adverse events or risk losing their license.
Proposition 46 requires that doctors submit to drug and alcohol testing at random and within 12 hours after an adverse event has been identified. Positive results or failure to appear for testing would result in a medical board investigation and a license suspension until findings are complete, according to the proposed initiative. Californians vote on the ballot item on Nov. 4.
If passed, the proposed law would unreasonably penalize doctors unable to meet testing rules and lead to excessive suspensions, said Dr. Theodore M. Mazer, a San Diego-based otolaryngologist in private practice and past president of the San Diego County Medical Society.
“It’s poorly worded and poorly thought out, and it was simply put there to deceive the voters into thinking they were doing something for patient safety,” Dr. Mazer said in an interview. “It will actually result in questions about privacy invasion for doctors and could take doctors who are doing nothing wrong out of practice temporarily with suspended licenses because they couldn’t report in a timely fashion.”
The drug-testing provision is one of three components of Prop. 46, a ballot initiative backed by the state’s trial bar and consumer interest group, Consumer Watchdog. Another provision of the proposal would raise California’s $250,000 medical malpractice cap on noneconomic damages to $1.1 million. A third measure would require physicians to check a statewide database before prescribing Schedule II and Schedule III drugs. The drug-testing provision would apply only to doctors who practice in hospitals or who have hospital privileges.
A spokesman with Consumer Attorneys of California referred questions to Consumer Watchdog. At this article’s deadline, messages left with Consumer Watchdog had not been returned. In a statement, the organization said Prop. 46’s drug and alcohol testing procedures are in line with other industries charged with protecting people’s lives.
“Millions of Californians in safety-sensitive positions are already drug tested at work, such as police officers, firefighters, construction workers, and truck and bus drivers,” the statement said. “Currently, doctors are not tested, although they practice medicine on tens of thousands of California patients every year.”
California physicians have long faced attacks to the state’s medical malpractice award limit, but the drug-testing proposal is new, said Dr. Richard Thorp, who is president of the California Medical Association. If approved, California would become the first state to mandate such testing of doctors. The proposed law could encourage other states to follow in California’s footsteps, opponents said.
“California’s first in a lot of things,” Dr. Mazer said. “This is not a smart first to be.”
The drug-testing provision raises more questions than answers and would likely cause more harm than good, noted Dr. Yul D. Ejnes in a Sept. 30 Annals of Internal Medicine article. The initiative does not specify the time frame in which a medical board must complete its investigation of a doctor’s positive drug result. Additionally, the proposal targets all physicians with admitting privileges, regardless of access to controlled substances, specialty, or impairment risk.
“Randomly testing physicians without some form of risk stratification will likely result in many false-positive results,” said Dr. Ejnes, an internist in private practice in Cranston, R.I., who is immediate past chair of the American College of Physicians Board of Regents. “Prop. 46 addresses verification of positive results, but, as we see in clinical practice, that process only adds to the intrusiveness, expense, and stress that should not have occurred in the first place.”
Dr. Thorp added that the database measure of the proposal, as it’s written, would be detrimental to doctors and patients. The state’s drug monitoring database, called the Controlled Substance Utilization Review and Evaluation System (CURES), currently lacks funding and staff to fully operate the system, he said. Glitches and accessibility problems led to a 2013 law that raised licensing fees for health providers to better fund the database. Physicians are required to register with the system by 2016, according to the law.
“It’s a huge database,” Dr. Thorp said in an interview. “It takes time to get that moving. To mandate this for every doctor and pharmacist is just a recipe for disaster.”
The database and drug-testing components of the initiative were merely included to sway voters into striking down the malpractice cap, said Dr. Richard E. Anderson, chair and CEO of the Doctors Company, a national liability insurer. The company is among the coalition of health care and business leaders against the proposed law.
“These unrelated provisions were added to try to draw voter support for the [medical malpractice damages cap] increase, which did not poll well by itself,” Dr. Anderson said in an interview. “The result is a cynical and manipulative ballot measure, opposed by an unprecedented coalition of medical providers, insurers, businesses, organized labor, civil liberties and senior groups, local governments, teachers, and school districts.”
Dr. Ejnes emphasized that remedies to physician drug and alcohol abuse are still needed. An estimated 8%-18% of physicians are impaired by drugs or alcohol at some point in their careers, according to the Annals article. But the proposed initiative is not the answer, Dr. Ejnes said.
“Developing a system that achieves the goal of detecting and preventing physician impairment requires a thoughtful dialogue among all stakeholders, led by the medical profession,” he said. “A ballot initiative intended to win votes, debated in sound bites and Tweets and creating more problems than it solves, is not the right solution.”
On Twitter @legal_med