User login
Pediatric Hospital Medicine 2014 Conference Draws Record-Setting Crowd
Surrounded by the bucolic grounds of the Disney Yacht and Beach Club Resort in Lake Buena Vista, Fla., more than 800 pediatric hospitalists gathered in July for Pediatric Hospital Medicine 2014 (PHM14). Preceded by the Society for Pediatric Sedation’s pre-course, PHM14 began in earnest with a warm welcome from Doug Carlson, MD, FAAP, chief of pediatric hospital medicine programs at St. Louis (Mo.) Children’s Hospital and chair of the PHM14 organizing committee.
The first day of the conference started with Patrick Conway, MD, MSc, FAAP, MHM, chief medical officer for the Centers for Medicare and Medicaid Services (CMS), who gave an update of ongoing reforms in the U.S. health delivery system, with a focus on pediatrics. With three years of experience as CMS’ top doc, Dr. Conway related the difficulties of going from an unsustainable fee-for-service system to a people-centered, outcomes-driven system.
“Pediatrics,” Dr. Conway said, “is a leader in patient and family engagement and population health.” This practice, he added, means that the six goals of the CMS Quality Strategy align well with ongoing efforts in PHM.
Despite the difficulties of instituting change in a system that handles $3 billion daily, Dr. Conway, formerly a pediatric hospitalist at Cincinnati Children’s Hospital, said he’s witnessed many signs of improvement in the CMS landscape. Preliminary data from 2012-2014, he said, have shown a 9% reduction in hospital-acquired conditions across all measures, and overall hospital utilization is “dropping like a rock.”
While “having a foot in the boat and a foot on the dock” has been difficult, the transition, through its alphabet soup of innovation programs, is now beginning to pay off. Giving providers a pathway through the changing landscape of risk, Dr. Conway said, is an ongoing priority.
Wrapping up the first day, three healthcare system CEOs took the stage to answer questions from the audience, with Mark Shen, MD, SFHM, president of Dell Children’s Medical Center of Central Texas in Austin, Texas, posing questions like a seasoned talk show host. Panel members included David J. Bailey, MD, MBA, president and CEO of the Nemours Foundation; Steve Narang, MD, MHCM, FAAP, CEO of Banner Good Samaritan Medical Center in Phoenix, Ariz.; and Jeff Sperring, MD, FAAP, president and CEO of Riley Hospital for Children at Indiana University Health in Indianapolis.
Questions were wide-ranging.
Q: How did you become a CEO?
“All I had to do was keep on saying ‘yes,’” Dr. Bailey said.
Q: What are you doing as a CEO to move from a fee-for-service system to a population-based system?
“We are still living in two different worlds. …It depends on ACO penetration, whether quality or volume will be the driver over the next three to five years,” Dr. Narang said.
Q: If PHM fellowship becomes a requirement, will your hospital fund them?
“It’s hard to define what we do, but we know there are core competencies. I don’t think we’re going to be at a point where certification will limit being a hospitalist anytime soon,” Dr. Shen said.
Q: What are the three most important things, from a CEO perspective, that a hospitalist should know?
“Know where your organization wants to go,” Dr. Sperring said.
The next day kicked off with an inspiring call to action by Steve Meuthing, MD, vice president for safety at Cincinnati Children’s Hospital Medical Center. He called on pediatric hospitalists to eliminate all serious harm from children’s hospitals in the U.S. As a part of the Children’s Hospitals’ Solutions for Patient Safety (SPS) network, an organization accounting for 25% of all children hospitalized in the U.S., Dr. Meuthing related the need to employ high reliability theory, along with operational and cultural changes, to improve reliability in patient safety.
“If you don’t standardize, the rest is just chaos,” he said. “We have to make it easy to do these things.”
Dr. Meuthing said improving process reliability is key to reducing adverse outcomes, and high reliability organizations have utilized this approach to reduce serious harm events across the 81 SPS hospitals. While prevention of patient harm is the goal, an additional benefit is cost savings. He estimated $27 million of cost savings was realized within SPS network hospitals in 2012-2013.
Oral abstract and conundrum presentations, concurrent with 23 sessions across nine tracks, kept attendees busy. Topics ranged from a PHM circumcision service to decreasing overuse of continuous pulse oximetry. The day’s talks wrapped up with the respective presidents of the meeting’s co-sponsors—the American Academy of Pediatrics, the American Pediatrics Association, and SHM—sharing their organizations’ visions of PHM’s future in a town hall format.
The second full day began with an update of the Joint Council of Pediatric Hospital Medicine’s efforts to further advance PHM as a field. The process of submitting a petition to the American Board of Pediatrics was reviewed, as were the current status and time course of the move toward Accreditation Council for Graduate Medical Education certification.
After lunch, the highly anticipated “Top Articles” session was presented by Robert Dudas, MD, medical director of the pediatric hospitalist program at Johns Hopkins Bayview Medical Center in Baltimore, and Karen Wilson, MD, MPH, section head for pediatric hospital medicine at Children’s Hospital Colorado in Aurora. The presenters reviewed literature from the past year on topics ranging from nebulized hypertonic saline for bronchiolitis to antibiotic prophylaxis in vesicoureteral reflux.
The final day commenced with a talk by Alberto Puig, MD, PhD, FACP, associate director of undergraduate education at Massachusetts General Hospital in Boston, whose experiences as an internist provided insight regarding the history of the physical examination, from the aphorisms of Hippocrates to the family-centered bedside rounding of today.
Dr. Chang is associate clinical professor of medicine and pediatrics at the University of California at San Diego School of Medicine and a hospitalist at both UCSD Medical Center and Rady Children’s Hospital. He is pediatric editor of The Hospitalist.
Dr. O’Callaghan is a clinical assistant professor of pediatrics at the University of Washington and a member of Team Hospitalist.
Dr. Hale is a past member of Team Hospitalist and a pediatric hospitalist at the Floating Hospital for Children at Tufts Medical Center in Boston.
Dr. Pressel is a pediatric hospitalist and inpatient medical director at Nemours/Alfred I. duPont Hospital for Children in Wilmington, Del., and a member of Team Hospitalist.
Surrounded by the bucolic grounds of the Disney Yacht and Beach Club Resort in Lake Buena Vista, Fla., more than 800 pediatric hospitalists gathered in July for Pediatric Hospital Medicine 2014 (PHM14). Preceded by the Society for Pediatric Sedation’s pre-course, PHM14 began in earnest with a warm welcome from Doug Carlson, MD, FAAP, chief of pediatric hospital medicine programs at St. Louis (Mo.) Children’s Hospital and chair of the PHM14 organizing committee.
The first day of the conference started with Patrick Conway, MD, MSc, FAAP, MHM, chief medical officer for the Centers for Medicare and Medicaid Services (CMS), who gave an update of ongoing reforms in the U.S. health delivery system, with a focus on pediatrics. With three years of experience as CMS’ top doc, Dr. Conway related the difficulties of going from an unsustainable fee-for-service system to a people-centered, outcomes-driven system.
“Pediatrics,” Dr. Conway said, “is a leader in patient and family engagement and population health.” This practice, he added, means that the six goals of the CMS Quality Strategy align well with ongoing efforts in PHM.
Despite the difficulties of instituting change in a system that handles $3 billion daily, Dr. Conway, formerly a pediatric hospitalist at Cincinnati Children’s Hospital, said he’s witnessed many signs of improvement in the CMS landscape. Preliminary data from 2012-2014, he said, have shown a 9% reduction in hospital-acquired conditions across all measures, and overall hospital utilization is “dropping like a rock.”
While “having a foot in the boat and a foot on the dock” has been difficult, the transition, through its alphabet soup of innovation programs, is now beginning to pay off. Giving providers a pathway through the changing landscape of risk, Dr. Conway said, is an ongoing priority.
Wrapping up the first day, three healthcare system CEOs took the stage to answer questions from the audience, with Mark Shen, MD, SFHM, president of Dell Children’s Medical Center of Central Texas in Austin, Texas, posing questions like a seasoned talk show host. Panel members included David J. Bailey, MD, MBA, president and CEO of the Nemours Foundation; Steve Narang, MD, MHCM, FAAP, CEO of Banner Good Samaritan Medical Center in Phoenix, Ariz.; and Jeff Sperring, MD, FAAP, president and CEO of Riley Hospital for Children at Indiana University Health in Indianapolis.
Questions were wide-ranging.
Q: How did you become a CEO?
“All I had to do was keep on saying ‘yes,’” Dr. Bailey said.
Q: What are you doing as a CEO to move from a fee-for-service system to a population-based system?
“We are still living in two different worlds. …It depends on ACO penetration, whether quality or volume will be the driver over the next three to five years,” Dr. Narang said.
Q: If PHM fellowship becomes a requirement, will your hospital fund them?
“It’s hard to define what we do, but we know there are core competencies. I don’t think we’re going to be at a point where certification will limit being a hospitalist anytime soon,” Dr. Shen said.
Q: What are the three most important things, from a CEO perspective, that a hospitalist should know?
“Know where your organization wants to go,” Dr. Sperring said.
The next day kicked off with an inspiring call to action by Steve Meuthing, MD, vice president for safety at Cincinnati Children’s Hospital Medical Center. He called on pediatric hospitalists to eliminate all serious harm from children’s hospitals in the U.S. As a part of the Children’s Hospitals’ Solutions for Patient Safety (SPS) network, an organization accounting for 25% of all children hospitalized in the U.S., Dr. Meuthing related the need to employ high reliability theory, along with operational and cultural changes, to improve reliability in patient safety.
“If you don’t standardize, the rest is just chaos,” he said. “We have to make it easy to do these things.”
Dr. Meuthing said improving process reliability is key to reducing adverse outcomes, and high reliability organizations have utilized this approach to reduce serious harm events across the 81 SPS hospitals. While prevention of patient harm is the goal, an additional benefit is cost savings. He estimated $27 million of cost savings was realized within SPS network hospitals in 2012-2013.
Oral abstract and conundrum presentations, concurrent with 23 sessions across nine tracks, kept attendees busy. Topics ranged from a PHM circumcision service to decreasing overuse of continuous pulse oximetry. The day’s talks wrapped up with the respective presidents of the meeting’s co-sponsors—the American Academy of Pediatrics, the American Pediatrics Association, and SHM—sharing their organizations’ visions of PHM’s future in a town hall format.
The second full day began with an update of the Joint Council of Pediatric Hospital Medicine’s efforts to further advance PHM as a field. The process of submitting a petition to the American Board of Pediatrics was reviewed, as were the current status and time course of the move toward Accreditation Council for Graduate Medical Education certification.
After lunch, the highly anticipated “Top Articles” session was presented by Robert Dudas, MD, medical director of the pediatric hospitalist program at Johns Hopkins Bayview Medical Center in Baltimore, and Karen Wilson, MD, MPH, section head for pediatric hospital medicine at Children’s Hospital Colorado in Aurora. The presenters reviewed literature from the past year on topics ranging from nebulized hypertonic saline for bronchiolitis to antibiotic prophylaxis in vesicoureteral reflux.
The final day commenced with a talk by Alberto Puig, MD, PhD, FACP, associate director of undergraduate education at Massachusetts General Hospital in Boston, whose experiences as an internist provided insight regarding the history of the physical examination, from the aphorisms of Hippocrates to the family-centered bedside rounding of today.
Dr. Chang is associate clinical professor of medicine and pediatrics at the University of California at San Diego School of Medicine and a hospitalist at both UCSD Medical Center and Rady Children’s Hospital. He is pediatric editor of The Hospitalist.
Dr. O’Callaghan is a clinical assistant professor of pediatrics at the University of Washington and a member of Team Hospitalist.
Dr. Hale is a past member of Team Hospitalist and a pediatric hospitalist at the Floating Hospital for Children at Tufts Medical Center in Boston.
Dr. Pressel is a pediatric hospitalist and inpatient medical director at Nemours/Alfred I. duPont Hospital for Children in Wilmington, Del., and a member of Team Hospitalist.
Surrounded by the bucolic grounds of the Disney Yacht and Beach Club Resort in Lake Buena Vista, Fla., more than 800 pediatric hospitalists gathered in July for Pediatric Hospital Medicine 2014 (PHM14). Preceded by the Society for Pediatric Sedation’s pre-course, PHM14 began in earnest with a warm welcome from Doug Carlson, MD, FAAP, chief of pediatric hospital medicine programs at St. Louis (Mo.) Children’s Hospital and chair of the PHM14 organizing committee.
The first day of the conference started with Patrick Conway, MD, MSc, FAAP, MHM, chief medical officer for the Centers for Medicare and Medicaid Services (CMS), who gave an update of ongoing reforms in the U.S. health delivery system, with a focus on pediatrics. With three years of experience as CMS’ top doc, Dr. Conway related the difficulties of going from an unsustainable fee-for-service system to a people-centered, outcomes-driven system.
“Pediatrics,” Dr. Conway said, “is a leader in patient and family engagement and population health.” This practice, he added, means that the six goals of the CMS Quality Strategy align well with ongoing efforts in PHM.
Despite the difficulties of instituting change in a system that handles $3 billion daily, Dr. Conway, formerly a pediatric hospitalist at Cincinnati Children’s Hospital, said he’s witnessed many signs of improvement in the CMS landscape. Preliminary data from 2012-2014, he said, have shown a 9% reduction in hospital-acquired conditions across all measures, and overall hospital utilization is “dropping like a rock.”
While “having a foot in the boat and a foot on the dock” has been difficult, the transition, through its alphabet soup of innovation programs, is now beginning to pay off. Giving providers a pathway through the changing landscape of risk, Dr. Conway said, is an ongoing priority.
Wrapping up the first day, three healthcare system CEOs took the stage to answer questions from the audience, with Mark Shen, MD, SFHM, president of Dell Children’s Medical Center of Central Texas in Austin, Texas, posing questions like a seasoned talk show host. Panel members included David J. Bailey, MD, MBA, president and CEO of the Nemours Foundation; Steve Narang, MD, MHCM, FAAP, CEO of Banner Good Samaritan Medical Center in Phoenix, Ariz.; and Jeff Sperring, MD, FAAP, president and CEO of Riley Hospital for Children at Indiana University Health in Indianapolis.
Questions were wide-ranging.
Q: How did you become a CEO?
“All I had to do was keep on saying ‘yes,’” Dr. Bailey said.
Q: What are you doing as a CEO to move from a fee-for-service system to a population-based system?
“We are still living in two different worlds. …It depends on ACO penetration, whether quality or volume will be the driver over the next three to five years,” Dr. Narang said.
Q: If PHM fellowship becomes a requirement, will your hospital fund them?
“It’s hard to define what we do, but we know there are core competencies. I don’t think we’re going to be at a point where certification will limit being a hospitalist anytime soon,” Dr. Shen said.
Q: What are the three most important things, from a CEO perspective, that a hospitalist should know?
“Know where your organization wants to go,” Dr. Sperring said.
The next day kicked off with an inspiring call to action by Steve Meuthing, MD, vice president for safety at Cincinnati Children’s Hospital Medical Center. He called on pediatric hospitalists to eliminate all serious harm from children’s hospitals in the U.S. As a part of the Children’s Hospitals’ Solutions for Patient Safety (SPS) network, an organization accounting for 25% of all children hospitalized in the U.S., Dr. Meuthing related the need to employ high reliability theory, along with operational and cultural changes, to improve reliability in patient safety.
“If you don’t standardize, the rest is just chaos,” he said. “We have to make it easy to do these things.”
Dr. Meuthing said improving process reliability is key to reducing adverse outcomes, and high reliability organizations have utilized this approach to reduce serious harm events across the 81 SPS hospitals. While prevention of patient harm is the goal, an additional benefit is cost savings. He estimated $27 million of cost savings was realized within SPS network hospitals in 2012-2013.
Oral abstract and conundrum presentations, concurrent with 23 sessions across nine tracks, kept attendees busy. Topics ranged from a PHM circumcision service to decreasing overuse of continuous pulse oximetry. The day’s talks wrapped up with the respective presidents of the meeting’s co-sponsors—the American Academy of Pediatrics, the American Pediatrics Association, and SHM—sharing their organizations’ visions of PHM’s future in a town hall format.
The second full day began with an update of the Joint Council of Pediatric Hospital Medicine’s efforts to further advance PHM as a field. The process of submitting a petition to the American Board of Pediatrics was reviewed, as were the current status and time course of the move toward Accreditation Council for Graduate Medical Education certification.
After lunch, the highly anticipated “Top Articles” session was presented by Robert Dudas, MD, medical director of the pediatric hospitalist program at Johns Hopkins Bayview Medical Center in Baltimore, and Karen Wilson, MD, MPH, section head for pediatric hospital medicine at Children’s Hospital Colorado in Aurora. The presenters reviewed literature from the past year on topics ranging from nebulized hypertonic saline for bronchiolitis to antibiotic prophylaxis in vesicoureteral reflux.
The final day commenced with a talk by Alberto Puig, MD, PhD, FACP, associate director of undergraduate education at Massachusetts General Hospital in Boston, whose experiences as an internist provided insight regarding the history of the physical examination, from the aphorisms of Hippocrates to the family-centered bedside rounding of today.
Dr. Chang is associate clinical professor of medicine and pediatrics at the University of California at San Diego School of Medicine and a hospitalist at both UCSD Medical Center and Rady Children’s Hospital. He is pediatric editor of The Hospitalist.
Dr. O’Callaghan is a clinical assistant professor of pediatrics at the University of Washington and a member of Team Hospitalist.
Dr. Hale is a past member of Team Hospitalist and a pediatric hospitalist at the Floating Hospital for Children at Tufts Medical Center in Boston.
Dr. Pressel is a pediatric hospitalist and inpatient medical director at Nemours/Alfred I. duPont Hospital for Children in Wilmington, Del., and a member of Team Hospitalist.
Specially-Trained Hospitalists Spearhead SHM’s Quality Improvement Programs
When SHM received the Joint Commission’s John M. Eisenberg Patient Safety and Quality Award for 2011 for innovation in patient safety and quality at the national level, the award represented national recognition for the society’s three major hospital quality improvement initiatives. Moreover, it highlighted the integral role mentors play in each of the programs, helping physicians and hospitals make accelerated progress on important patient safety and quality issues.
Mentored implementation assigns a physician expert to train, guide, and work with the participating facilities’ hospitalist-led, multidisciplinary team through the life cycle of a QI initiative. The three programs focus on VTE prevention, glycemic control, and transitions of care. The first hospital cohort for VTE prevention—the VTE Prevention Collaborative—was in 2007. The care transitions program, known as Project BOOST, started in 2008. The Glycemic Control Mentored Implementation (GCMI) Program began in 2009. A fourth SHM mentored implementation program is MARQUIS, the Multi-Center Medication Reconciliation Quality Improvement Study.
In basic terms, mentoring is “coaching from a physician who has expertise both in the clinical subject matter and in implementing the processes and tools of quality improvement—usually because they’ve done it themselves,” says Gregory Maynard, MD, MSc, SFHM, senior vice president of SHM’s Center for Hospital Innovation and Improvement and a co-founder of two of its mentored implementation programs.
Mentors typically are paired with one or two participating hospitals for 12 to 18 months, conducting monthly conference calls with the team, sharing tools and resources from SHM’s online library, and offering advice on how to navigate the treacherous currents of culture change within a hospital. BOOST mentors also make in-person site visits. They are well versed in protocol and order set design and quality measurement strategies, and they know how to engage frontline professionals and institutional leadership, Dr. Maynard says.
Some mentors have received formal QI training, and many have attended Mentor University, a 1-1/2 day intensive training course offered by SHM that reinforces the nuances of coaching, the contents of SHM’s quality toolkits, and ideas for overcoming common barriers to improvement. SHM’s mentor support provides continuous professional development for the mentors, pairing new mentors with senior mentors to coach them in the process and hosting an online community with other mentors.
“What’s telling to me is that many of the people who have been mentored by SHM’s programs in one topic go on to become mentors in another topic, taking those portable skills and principles and applying them in other quality areas,” Dr. Maynard says. “We’re fostering leadership and quality improvement skills among hospitalists; that’s really one of our main goals. People learn the skill and then spread it within their system.”
Mark Williams, MD, FACP, MHM, Project BOOST principal investigator and a veteran SHM mentor, says that just providing educational materials to health professionals often isn’t enough for them to overcome the barriers to change.
“I’ve seen many large-scale quality projects that didn’t work, as they were simply disseminating information, content, or knowledge,” he says. Mentored implementation as practiced by SHM is “a model for disseminating quality improvement nationally,” he adds. “Pretty much any quality improvement project can be done this way.”
Key to the mentored implementation program’s success is the personalized approach and customized solutions.
“You directly meet with the team in their own setting and begin to see what’s going on,” Dr. Williams says. “You also meet with the hospital’s senior leadership. That’s when you start to see change.”
The Hospitalist connected with eight SHM mentors. The following are snapshots of their work in the mentorship program and some of the lessons they taught—and learned—from the program.
Christine Lum Lung, MD, SFHM
Title: Medical director, Northern Colorado Hospitalists, Fort Collins
Program: VTE Prevention Collaborative
Background: As a practicing hospitalist and medical director of the HM group for a two-hospital system, Dr. Lum Lung chaired its quality committee for VTE protocol development. “It was obvious at our hospitals that we needed to do better at VTE prevention,” she explains.
Dr. Lum Lung’s team received VTE mentorship from Dr. Maynard, who later asked her to become a VTE mentor. She also attended all three levels of SHM’s Leadership Academy and has since become a mentor for the new HP3 (Hospitalist Program Peak Performance) mentored implementation program, a one-year collaboration among SHM, Northwestern University, Blue Cross/Blue Shield of Illinois, and the Illinois Hospital Association that is designed to help hospitalist groups optimize their programs and build healthy group culture.
Teachable moment: The essential qualities of a good mentee, Dr. Lum Lung says, are drive and dedication. “You believe strongly about it, so you can sell it to others. You also need a thick skin to face the adversities that come up. When my mentor gave me tasks and deadlines, I met those deadlines.”
Success story: “I’ve been impressed with how hard groups and individuals can work.” Most of the teams she has worked with were facing significant external stressors—starting a new program, moving into a new hospital, rolling out a new EHR, becoming part of a growing medical group. “Yet each of them has been incredibly engaged in the process and dedicated to completing their projects.”
Lessons learned: “That we all have something to learn from each other. While I am officially the mentor, I have learned a lot about processes, teamwork, and flow issues from the sites that could potentially be incorporated in our program.”
Advice: Working on a project as a team can be very powerful, she says. Even seemingly ‘small’ projects have allowed teams to learn how to work better together on day-to-day issues. With the victory of a small project behind them, they make lists of the next thing that they want to tackle.
“Our profession is constantly changing. We need to be thinking ahead for how we will face those challenges,” Dr. Lum Lung says. “A team that works well together will have an advantage in this new environment. Even if you have people who are new to quality improvement, their participation can still be important.”
Jordan Messler, MD, SFHM
Title: Medical director, Morton Plant Hospitalists, Clearwater, Fla.
Program: GCMI; Project BOOST
Background: Dr. Messler’s interest in QI led him to work with colleagues in SHM who are national leaders in quality. “A couple of years ago, I enrolled in Emory’s Quality Academy, a sister course to Intermountain Health’s course on quality. Then I enrolled our hospital in both the GCMI Program and Project BOOST. My mentors for those programs were terrific guides, which led to my interest in seeing their side of the program as a mentor myself.”
Teachable moment: One program had difficulty implementing a VTE prevention tool and couldn’t get nursing support as it had expected, largely due to lack of nursing engagement on the project team, he says. “We started talking about the history of the projects, and prior interventions. In addition, we talked to the different disciplines separately. It seems there used to be an excellent system where nursing helped out on the project team for risk assessment.”
As VTE prevention became more of a priority, some physicians separately created a new tool to replace the nursing tool without involving the whole team. “And they couldn’t understand why nursing wasn’t buying into the new process.”
Success story: There are similar themes to success and failure. Sites that have strong administrative support (i.e., C-suite representation on the QI team), that have “accountability structure and stick to the basics of QI, with clear goals, ability to gather and report data, and use of a QI model [such as PDSA or Six Sigma] are the ones that succeed,” Dr. Messler says. “And the reverse is consistently true. Sustainable QI needs to be multidisciplinary, involving every voice, considering prior interventions and understanding of the culture.”
Lessons learned: “As mentors, we all continue to say we learn as much or more from these sites as they, hopefully, are learning from us. This collaboration and sharing of ideas has been instrumental to the success of the program.”
Advice: Get started today, and don’t give up. Follow the road map of QI projects, gather support, and get started. You will learn as much from your failures as your successes.
Dr. Messler says hospitals are looking for physician leaders to improve quality, and hospitalists are perfectly positioned to be those QI leaders. These big projects can last for years, so quality teams and hospitals need to be prepared to take the long view.
—Jennifer Quartarolo, MD, SFHM
Stephanie Rennke, MD
Title: Associate clinical professor of medicine, co-director of faculty development, division of hospital medicine, University of California San Francisco Medical Center.
Program: Project BOOST
Background: “When I started as a hospitalist right out of residency, QI had not been part of my training. But I noticed that quality was at the forefront of the academic interests of all the hospitalists at UCSF. I was personally interested in transitions of care. I still do home visits after hours for at-risk patients when they leave the hospital.”
Dr. Rennke started in QI as a member of UCSF’s BOOST team in 2008. “I worked with other faculty in the division who had previous experience in quality improvement and transitions in care. One of the co-principal investigators for BOOST, Dr. Arpana Vidyarthi, suggested that it would be a really rewarding experience to mentor—and it was.”
Teachable moment: “I’ve been so impressed by the diversity of what’s out there. No hospitalist program or hospital is the same. There is no one-size-fits-all for quality improvement or transitions of care, so it is incredibly important that the mentor takes the time to get to know both the team and the hospital.”
Success story: “During a site visit, I had an opportunity to watch one of the nurses, who had received training from a competency-based Teach Back program, practice Teach Back with a patient at the bedside,” Dr. Rennke says. “I was doing a tour of the floor and went into the room of a patient about to be discharged. A young float nurse, not long out of school, sat down with the patient and went through the medications and discharge plan using Teach Back. It didn’t take more time, but the time was spent more constructively, with interaction back and forth. I remember that ‘aha’ moment for the patient and the look in her eyes. For me, as a mentor, it was exciting to think that something I had tried to bring to them had been incorporated by the site and was really working.”
Lessons learned: “I have learned that, while at a large institution like UCSF we tend to work in silos, smaller sites are often more integrated with the various disciplines. You can walk down the hall to the clinical pharmacist or have lunch with the charge nurse. So I’ve tried to bring back home a commitment to really get to know professional colleagues and have them feel that I’m interested in their perspectives.”
Advice: “Work in teams. You cannot do this alone. Include frontline staff. And don’t forget to advertise to others that the program exists. Get the word out—let people know.”
Jennifer Quartarolo, MD, SFHM
Title: Medical director, clinical resource management; associate clinical professor, division of hospital medicine, University of California San Diego Health System
Program: Project BOOST
Background: Dr. Quartarolo has 11 years of clinical experience as an academic hospitalist at two different medical centers, and she completed a training program in healthcare delivery and improvement through the Institute for Health Care Delivery Research in Salt Lake City, Utah. “At my own institution, I had been involved in multiple QI projects,” she says. “Since joining the faculty, I worked with our care transitions team for five years before becoming a mentor. We incorporated many elements from Project BOOST as we worked to improve our care transitions process,” which led to an invitation to be a mentor.
Teachable moment: “I had one site that I worked with that had a great new form they had developed to incorporate into their transition process; however, when they decided to implement the form, they got a lot of pushback from nursing,” she says. “Then they realized that they had not involved any frontline nurses in their planning. This example points out how important it is to have all the key players involved on your team, as improving transitions of care is a complex process requiring multidisciplinary collaboration.”
Success story: Dr. Quartarolo says she has worked with several hospitals that have seen significant improvement in their readmission rates after participating in Project BOOST and implementing its tools.
Lessons learned: “I am constantly impressed by the innovative ideas that teams come up with to deal with the challenges that their hospitals face,” she says. Every hospital is unique and needs to do self-evaluation before deciding what to focus on. “I have also worked with many sites that have challenges getting physicians engaged in their efforts, particularly if they do not have a hospitalist program.”
Advice: “We are in a unique role as hospitalists to identify systems issues and improve quality of care in the inpatient setting, and this is particularly useful in improving care transitions and decreasing readmissions rates.”
Rich Balaban, MD
Title: Medical director, Hospital-to-Home Community Collaboration Program, Cambridge Health Alliance; assistant professor of medicine, Harvard Medical School, Boston
Program: Project BOOST
Background: Dr. Balaban has worked clinically in both the inpatient setting as a hospitalist and the outpatient setting as a primary care doctor. “I have seen hospital discharges as both a receiver and a sender, so [I] have been able to appreciate the challenges facing doctors, nurses, case managers, and patients involved in the care transition process,” he says.
Dr. Balaban also conducted a randomized controlled trial that demonstrated the benefits of engaging nurses at a patient’s primary care site to make outreach phone calls immediately after hospital discharge. Dr. Williams asked him to present on the study.
“It was a great opportunity for me to share the results of our work and for Mark to see my presentation skills,” he says. “When I asked if there were opportunities to get more involved in care transitions work, he invited me to consider becoming a BOOST mentor.”
Teachable moment: “Wearing my primary care hat, I believe that while it is very important to structure an effective discharge for the patient while in the hospital, success or failure ultimately is determined by what happens in the outpatient setting,” Dr. Balaban says. Even if a ‘perfect discharge’ occurs in the hospital, it can all quickly unravel once the patient arrives at home.
Success story: “At several sites, I have encouraged the inpatient care team to invite the outpatient care team to become part of the care transitions team. This has frequently brought an important viewpoint and voice to the care transitions table. While hospitalists have initiated the discussion about care transitions, they need an effective outpatient partner to create a truly effective process.”
Lessons learned: “I have learned to hold judgment until seeing with my own eyes,” Dr. Balaban says. “One of the first sites I visited had developed a post-discharge clinic, which they were excited to show me. From my point of view, I thought that after discharge, patient care should be assumed by the primary care office as soon as possible, and a post-discharge clinic would only delay that process.
“To my great surprise, their post-discharge clinic provided an ideal bridge between the hospital and primary care. The post-discharge clinic really worked and provided patients with a wonderful resource. … I’ve learned that there are many ways to solve problems, often based on the available resources at a specific site.”
Advice: In order to best understand the challenges of hospital discharge, it is critical that you understand what happens to patients after they leave the hospital. Make a home visit to a recently discharged patient to really understand the challenges that patients face when they return home.
Amitkumar R. Patel, MD, MBA, FACP, SFHM
Title: Clinical instructor in hospital medicine, Feinberg School of Medicine, Northwestern University, Chicago
Program: Project BOOST; also working with critical access hospitals in Illinois through PREP (Preventing Readmissions through Effective Partnerships)
Background: Although he now works in an urban teaching hospital, Dr. Patel also did private practice as a community hospitalist and has pursued formal healthcare management-focused training.
“I became a mentor because my experience and interest in quality improvement fit well with Project BOOST,” he says. “I enjoy coaching teams as they face challenges in quality improvement, especially in relation to readmissions reduction. My work with critical access hospitals is the result of my first year as a mentor with the PREP collaborative in Illinois.”
PREP, a collaborative initiative of SHM and the Illinois Hospital Association that is funded by Blue Cross/Blue Shield of Illinois, aims to help hospitals focus on quality initiatives, including BOOST.
Teachable moment/success story: One of Dr. Patel’s BOOST sites believed the team included all appropriate personnel to obtain discharge appointments prior to patients’ discharges. But as they began to work through the process of making sure each appointment was appropriately documented, the various team members assigned to this process could not consistently complete the task within their workflow.
The pilot unit secretaries were not part of the BOOST team initially but saw that they could fulfill this role quickly and easily. They knew who to call at the physicians’ offices to avoid getting stuck in the phone menu trees, and they used this knowledge to reach the schedulers directly. The BOOST team quickly realized the unit secretaries were the most appropriate personnel to capture this information and work with the patients or their families/caregivers to obtain the most convenient appointments. This role was added to the team, and the unit secretaries took ownership of this process. Other teams may also want to look beyond the customary team members to roles that may not be thought of as quality team members.
Lessons learned: “The biggest take-away for me involves the unique culture that exists in many of our urban and rural communities,” he says. Every BOOST site implements the project’s elements in its own unique way, and what works well in one location may not fit the needs of another. The role of the mentor is to balance the need for community-specific advice with unique attributes of the facility and the elements of Project BOOST. “Often, we use our mentor calls to brainstorm solutions, and the teams are teaching me what will work best in their environment.”
Advice: “Responsibility for hospital change management should not be abdicated to administrators or quality improvement staff members,” he says. “QI is not a sometime thing for some staff; it’s an all-the-time process for every staff member, including physicians, to participate in and actively manage.”
—Christopher Kim, MD, MBA, SFHM
Cheryl O’Malley, MD, FHM
Title: Internal medicine residency program director, Banner Good Samaritan Medical Center, Phoenix
Program: GCMI
Background: Banner Good Samaritan has participated in the BOOST, VTE, and GCMI programs. Dr. O’Malley brought her experience from developing, implementing, and leading local glycemic control efforts to mentoring others.
“When I first started working on our hospital’s process, I had so many questions and asked one of my mentors from residency, Dr. Greg Maynard,” she says. “He helped me to see that people around the country were asking the same questions and invited me to join SHM’s glycemic control work group. When the GCMI program started, I was asked to be a mentor.”
Teachable moment: “When I was a new attending on the wards after residency, my patients would ask me why their blood sugars were so much better controlled at home than in the hospital. Usually, the answer was that they were put on a sliding scale when they came into the hospital,” she says, noting that what was done at home wasn’t going to work in the hospital. Patients needed a different regimen—a more proactive approach than just the customary sliding scale.
“I started to learn more about basal rates, nutrition, and correction insulin regimens in the hospital, but I realized that to really have adequate safety and direction for the nursing staff, it would require a formal order set and systematic approach,” she says.
Success story: “One of my sites invited me to come and present grand rounds at the hospital, and the local physician team leader invited the whole quality team to her home. It was a very exciting team and had achieved a lot. Fifteen or 20 of us spent the evening talking about the project but also just enjoying the collegiality,” Dr. O’Malley says. “Even though we had never seen one another, I instantly knew everyone by voice from spending so much time on the phone. And we knew a lot about one another’s personal lives and careers.”
Lessons learned: “Hearing a program describe what they are doing and knowing that they were far ahead of my own hospital in many ways but still being able to provide an insight or a perspective to help them achieve their own next steps. Everyone has something to learn from another hospital or another discipline. We can all leverage our experiences to improve patient care.”
Advice: “Be patient. This is a really long process of constant improvements. I have been working on glycemic control for 10 years now and still feel like we have many opportunities to further improve.”
Christopher Kim, MD, MBA, SFHM
Title: Clinical associate professor of internal medicine and assistant professor of pediatrics, University of Michigan Health System, Ann Arbor
Program: Project BOOST; Michigan Transitions of Care Collaborative (M-TC2)
Background: Dr. Kim brings clinical, quality improvement, leadership, collaborative learning, and discussion facilitation skills to his work as program director of M-TC2 and as mentor to the sites he works with.
The collaborative is part of a set of state collaborative quality initiatives funded by Blue Cross Blue Shield of Michigan. One of those initiatives is focused on improving care transitions between the hospital setting and ambulatory care providers, using Project BOOST tools—expanded to integrate more closely with primary care providers, physician organizations, and ambulatory care. The eight Michigan-based mentors for M-TC2 have all attended SHM’s Mentor University.
Teachable moment: There are local challenges and there are general challenges—those that are commonly shared by most hospitals, Dr. Kim explains. Both need to be overcome when working on an improvement project such as transitions of care. The local hospitalist brings expertise about the former—which are often more difficult to understand and overcome. The mentor brings knowledge and experience of the universal challenges, as well as the benefit of having seen or heard about what other programs have done. Together, they can work to help the organization become better equipped to improve the initiative at hand.
Success story: “One hospital in the collaborative realized that it could roll out the Teach Back concept to both nurses and physicians,” he says. They started to teach residents how to interact with patients and began using this approach in physician-nurse teams. Subsequently, the team shared with the collaborative how physicians have embraced the concept.
Lessons learned: Every site has its successes and challenges, he says. Sharing both sides of the story can only advance the mission of the collaborative, as each organization learns from the successes and failures of the others.
Mentored implementation really does what it’s intended to do—helping to support the sites and keeping an organization on track and accountable for the work it does, because someone external to the organization is working with it and providing information about what other sites are doing.
Advice: Talk with different disciplines and find out how much they long to work with other care providers, and then have discussions about how to make interdisciplinary practice happen. “At our collaborative meetings over time, many of the 24 participating sites have shared their progress—the good things and the struggles,” Dr. Kim says.
Larry Beresford is a freelance writer in Alameda, Calif.
When SHM received the Joint Commission’s John M. Eisenberg Patient Safety and Quality Award for 2011 for innovation in patient safety and quality at the national level, the award represented national recognition for the society’s three major hospital quality improvement initiatives. Moreover, it highlighted the integral role mentors play in each of the programs, helping physicians and hospitals make accelerated progress on important patient safety and quality issues.
Mentored implementation assigns a physician expert to train, guide, and work with the participating facilities’ hospitalist-led, multidisciplinary team through the life cycle of a QI initiative. The three programs focus on VTE prevention, glycemic control, and transitions of care. The first hospital cohort for VTE prevention—the VTE Prevention Collaborative—was in 2007. The care transitions program, known as Project BOOST, started in 2008. The Glycemic Control Mentored Implementation (GCMI) Program began in 2009. A fourth SHM mentored implementation program is MARQUIS, the Multi-Center Medication Reconciliation Quality Improvement Study.
In basic terms, mentoring is “coaching from a physician who has expertise both in the clinical subject matter and in implementing the processes and tools of quality improvement—usually because they’ve done it themselves,” says Gregory Maynard, MD, MSc, SFHM, senior vice president of SHM’s Center for Hospital Innovation and Improvement and a co-founder of two of its mentored implementation programs.
Mentors typically are paired with one or two participating hospitals for 12 to 18 months, conducting monthly conference calls with the team, sharing tools and resources from SHM’s online library, and offering advice on how to navigate the treacherous currents of culture change within a hospital. BOOST mentors also make in-person site visits. They are well versed in protocol and order set design and quality measurement strategies, and they know how to engage frontline professionals and institutional leadership, Dr. Maynard says.
Some mentors have received formal QI training, and many have attended Mentor University, a 1-1/2 day intensive training course offered by SHM that reinforces the nuances of coaching, the contents of SHM’s quality toolkits, and ideas for overcoming common barriers to improvement. SHM’s mentor support provides continuous professional development for the mentors, pairing new mentors with senior mentors to coach them in the process and hosting an online community with other mentors.
“What’s telling to me is that many of the people who have been mentored by SHM’s programs in one topic go on to become mentors in another topic, taking those portable skills and principles and applying them in other quality areas,” Dr. Maynard says. “We’re fostering leadership and quality improvement skills among hospitalists; that’s really one of our main goals. People learn the skill and then spread it within their system.”
Mark Williams, MD, FACP, MHM, Project BOOST principal investigator and a veteran SHM mentor, says that just providing educational materials to health professionals often isn’t enough for them to overcome the barriers to change.
“I’ve seen many large-scale quality projects that didn’t work, as they were simply disseminating information, content, or knowledge,” he says. Mentored implementation as practiced by SHM is “a model for disseminating quality improvement nationally,” he adds. “Pretty much any quality improvement project can be done this way.”
Key to the mentored implementation program’s success is the personalized approach and customized solutions.
“You directly meet with the team in their own setting and begin to see what’s going on,” Dr. Williams says. “You also meet with the hospital’s senior leadership. That’s when you start to see change.”
The Hospitalist connected with eight SHM mentors. The following are snapshots of their work in the mentorship program and some of the lessons they taught—and learned—from the program.
Christine Lum Lung, MD, SFHM
Title: Medical director, Northern Colorado Hospitalists, Fort Collins
Program: VTE Prevention Collaborative
Background: As a practicing hospitalist and medical director of the HM group for a two-hospital system, Dr. Lum Lung chaired its quality committee for VTE protocol development. “It was obvious at our hospitals that we needed to do better at VTE prevention,” she explains.
Dr. Lum Lung’s team received VTE mentorship from Dr. Maynard, who later asked her to become a VTE mentor. She also attended all three levels of SHM’s Leadership Academy and has since become a mentor for the new HP3 (Hospitalist Program Peak Performance) mentored implementation program, a one-year collaboration among SHM, Northwestern University, Blue Cross/Blue Shield of Illinois, and the Illinois Hospital Association that is designed to help hospitalist groups optimize their programs and build healthy group culture.
Teachable moment: The essential qualities of a good mentee, Dr. Lum Lung says, are drive and dedication. “You believe strongly about it, so you can sell it to others. You also need a thick skin to face the adversities that come up. When my mentor gave me tasks and deadlines, I met those deadlines.”
Success story: “I’ve been impressed with how hard groups and individuals can work.” Most of the teams she has worked with were facing significant external stressors—starting a new program, moving into a new hospital, rolling out a new EHR, becoming part of a growing medical group. “Yet each of them has been incredibly engaged in the process and dedicated to completing their projects.”
Lessons learned: “That we all have something to learn from each other. While I am officially the mentor, I have learned a lot about processes, teamwork, and flow issues from the sites that could potentially be incorporated in our program.”
Advice: Working on a project as a team can be very powerful, she says. Even seemingly ‘small’ projects have allowed teams to learn how to work better together on day-to-day issues. With the victory of a small project behind them, they make lists of the next thing that they want to tackle.
“Our profession is constantly changing. We need to be thinking ahead for how we will face those challenges,” Dr. Lum Lung says. “A team that works well together will have an advantage in this new environment. Even if you have people who are new to quality improvement, their participation can still be important.”
Jordan Messler, MD, SFHM
Title: Medical director, Morton Plant Hospitalists, Clearwater, Fla.
Program: GCMI; Project BOOST
Background: Dr. Messler’s interest in QI led him to work with colleagues in SHM who are national leaders in quality. “A couple of years ago, I enrolled in Emory’s Quality Academy, a sister course to Intermountain Health’s course on quality. Then I enrolled our hospital in both the GCMI Program and Project BOOST. My mentors for those programs were terrific guides, which led to my interest in seeing their side of the program as a mentor myself.”
Teachable moment: One program had difficulty implementing a VTE prevention tool and couldn’t get nursing support as it had expected, largely due to lack of nursing engagement on the project team, he says. “We started talking about the history of the projects, and prior interventions. In addition, we talked to the different disciplines separately. It seems there used to be an excellent system where nursing helped out on the project team for risk assessment.”
As VTE prevention became more of a priority, some physicians separately created a new tool to replace the nursing tool without involving the whole team. “And they couldn’t understand why nursing wasn’t buying into the new process.”
Success story: There are similar themes to success and failure. Sites that have strong administrative support (i.e., C-suite representation on the QI team), that have “accountability structure and stick to the basics of QI, with clear goals, ability to gather and report data, and use of a QI model [such as PDSA or Six Sigma] are the ones that succeed,” Dr. Messler says. “And the reverse is consistently true. Sustainable QI needs to be multidisciplinary, involving every voice, considering prior interventions and understanding of the culture.”
Lessons learned: “As mentors, we all continue to say we learn as much or more from these sites as they, hopefully, are learning from us. This collaboration and sharing of ideas has been instrumental to the success of the program.”
Advice: Get started today, and don’t give up. Follow the road map of QI projects, gather support, and get started. You will learn as much from your failures as your successes.
Dr. Messler says hospitals are looking for physician leaders to improve quality, and hospitalists are perfectly positioned to be those QI leaders. These big projects can last for years, so quality teams and hospitals need to be prepared to take the long view.
—Jennifer Quartarolo, MD, SFHM
Stephanie Rennke, MD
Title: Associate clinical professor of medicine, co-director of faculty development, division of hospital medicine, University of California San Francisco Medical Center.
Program: Project BOOST
Background: “When I started as a hospitalist right out of residency, QI had not been part of my training. But I noticed that quality was at the forefront of the academic interests of all the hospitalists at UCSF. I was personally interested in transitions of care. I still do home visits after hours for at-risk patients when they leave the hospital.”
Dr. Rennke started in QI as a member of UCSF’s BOOST team in 2008. “I worked with other faculty in the division who had previous experience in quality improvement and transitions in care. One of the co-principal investigators for BOOST, Dr. Arpana Vidyarthi, suggested that it would be a really rewarding experience to mentor—and it was.”
Teachable moment: “I’ve been so impressed by the diversity of what’s out there. No hospitalist program or hospital is the same. There is no one-size-fits-all for quality improvement or transitions of care, so it is incredibly important that the mentor takes the time to get to know both the team and the hospital.”
Success story: “During a site visit, I had an opportunity to watch one of the nurses, who had received training from a competency-based Teach Back program, practice Teach Back with a patient at the bedside,” Dr. Rennke says. “I was doing a tour of the floor and went into the room of a patient about to be discharged. A young float nurse, not long out of school, sat down with the patient and went through the medications and discharge plan using Teach Back. It didn’t take more time, but the time was spent more constructively, with interaction back and forth. I remember that ‘aha’ moment for the patient and the look in her eyes. For me, as a mentor, it was exciting to think that something I had tried to bring to them had been incorporated by the site and was really working.”
Lessons learned: “I have learned that, while at a large institution like UCSF we tend to work in silos, smaller sites are often more integrated with the various disciplines. You can walk down the hall to the clinical pharmacist or have lunch with the charge nurse. So I’ve tried to bring back home a commitment to really get to know professional colleagues and have them feel that I’m interested in their perspectives.”
Advice: “Work in teams. You cannot do this alone. Include frontline staff. And don’t forget to advertise to others that the program exists. Get the word out—let people know.”
Jennifer Quartarolo, MD, SFHM
Title: Medical director, clinical resource management; associate clinical professor, division of hospital medicine, University of California San Diego Health System
Program: Project BOOST
Background: Dr. Quartarolo has 11 years of clinical experience as an academic hospitalist at two different medical centers, and she completed a training program in healthcare delivery and improvement through the Institute for Health Care Delivery Research in Salt Lake City, Utah. “At my own institution, I had been involved in multiple QI projects,” she says. “Since joining the faculty, I worked with our care transitions team for five years before becoming a mentor. We incorporated many elements from Project BOOST as we worked to improve our care transitions process,” which led to an invitation to be a mentor.
Teachable moment: “I had one site that I worked with that had a great new form they had developed to incorporate into their transition process; however, when they decided to implement the form, they got a lot of pushback from nursing,” she says. “Then they realized that they had not involved any frontline nurses in their planning. This example points out how important it is to have all the key players involved on your team, as improving transitions of care is a complex process requiring multidisciplinary collaboration.”
Success story: Dr. Quartarolo says she has worked with several hospitals that have seen significant improvement in their readmission rates after participating in Project BOOST and implementing its tools.
Lessons learned: “I am constantly impressed by the innovative ideas that teams come up with to deal with the challenges that their hospitals face,” she says. Every hospital is unique and needs to do self-evaluation before deciding what to focus on. “I have also worked with many sites that have challenges getting physicians engaged in their efforts, particularly if they do not have a hospitalist program.”
Advice: “We are in a unique role as hospitalists to identify systems issues and improve quality of care in the inpatient setting, and this is particularly useful in improving care transitions and decreasing readmissions rates.”
Rich Balaban, MD
Title: Medical director, Hospital-to-Home Community Collaboration Program, Cambridge Health Alliance; assistant professor of medicine, Harvard Medical School, Boston
Program: Project BOOST
Background: Dr. Balaban has worked clinically in both the inpatient setting as a hospitalist and the outpatient setting as a primary care doctor. “I have seen hospital discharges as both a receiver and a sender, so [I] have been able to appreciate the challenges facing doctors, nurses, case managers, and patients involved in the care transition process,” he says.
Dr. Balaban also conducted a randomized controlled trial that demonstrated the benefits of engaging nurses at a patient’s primary care site to make outreach phone calls immediately after hospital discharge. Dr. Williams asked him to present on the study.
“It was a great opportunity for me to share the results of our work and for Mark to see my presentation skills,” he says. “When I asked if there were opportunities to get more involved in care transitions work, he invited me to consider becoming a BOOST mentor.”
Teachable moment: “Wearing my primary care hat, I believe that while it is very important to structure an effective discharge for the patient while in the hospital, success or failure ultimately is determined by what happens in the outpatient setting,” Dr. Balaban says. Even if a ‘perfect discharge’ occurs in the hospital, it can all quickly unravel once the patient arrives at home.
Success story: “At several sites, I have encouraged the inpatient care team to invite the outpatient care team to become part of the care transitions team. This has frequently brought an important viewpoint and voice to the care transitions table. While hospitalists have initiated the discussion about care transitions, they need an effective outpatient partner to create a truly effective process.”
Lessons learned: “I have learned to hold judgment until seeing with my own eyes,” Dr. Balaban says. “One of the first sites I visited had developed a post-discharge clinic, which they were excited to show me. From my point of view, I thought that after discharge, patient care should be assumed by the primary care office as soon as possible, and a post-discharge clinic would only delay that process.
“To my great surprise, their post-discharge clinic provided an ideal bridge between the hospital and primary care. The post-discharge clinic really worked and provided patients with a wonderful resource. … I’ve learned that there are many ways to solve problems, often based on the available resources at a specific site.”
Advice: In order to best understand the challenges of hospital discharge, it is critical that you understand what happens to patients after they leave the hospital. Make a home visit to a recently discharged patient to really understand the challenges that patients face when they return home.
Amitkumar R. Patel, MD, MBA, FACP, SFHM
Title: Clinical instructor in hospital medicine, Feinberg School of Medicine, Northwestern University, Chicago
Program: Project BOOST; also working with critical access hospitals in Illinois through PREP (Preventing Readmissions through Effective Partnerships)
Background: Although he now works in an urban teaching hospital, Dr. Patel also did private practice as a community hospitalist and has pursued formal healthcare management-focused training.
“I became a mentor because my experience and interest in quality improvement fit well with Project BOOST,” he says. “I enjoy coaching teams as they face challenges in quality improvement, especially in relation to readmissions reduction. My work with critical access hospitals is the result of my first year as a mentor with the PREP collaborative in Illinois.”
PREP, a collaborative initiative of SHM and the Illinois Hospital Association that is funded by Blue Cross/Blue Shield of Illinois, aims to help hospitals focus on quality initiatives, including BOOST.
Teachable moment/success story: One of Dr. Patel’s BOOST sites believed the team included all appropriate personnel to obtain discharge appointments prior to patients’ discharges. But as they began to work through the process of making sure each appointment was appropriately documented, the various team members assigned to this process could not consistently complete the task within their workflow.
The pilot unit secretaries were not part of the BOOST team initially but saw that they could fulfill this role quickly and easily. They knew who to call at the physicians’ offices to avoid getting stuck in the phone menu trees, and they used this knowledge to reach the schedulers directly. The BOOST team quickly realized the unit secretaries were the most appropriate personnel to capture this information and work with the patients or their families/caregivers to obtain the most convenient appointments. This role was added to the team, and the unit secretaries took ownership of this process. Other teams may also want to look beyond the customary team members to roles that may not be thought of as quality team members.
Lessons learned: “The biggest take-away for me involves the unique culture that exists in many of our urban and rural communities,” he says. Every BOOST site implements the project’s elements in its own unique way, and what works well in one location may not fit the needs of another. The role of the mentor is to balance the need for community-specific advice with unique attributes of the facility and the elements of Project BOOST. “Often, we use our mentor calls to brainstorm solutions, and the teams are teaching me what will work best in their environment.”
Advice: “Responsibility for hospital change management should not be abdicated to administrators or quality improvement staff members,” he says. “QI is not a sometime thing for some staff; it’s an all-the-time process for every staff member, including physicians, to participate in and actively manage.”
—Christopher Kim, MD, MBA, SFHM
Cheryl O’Malley, MD, FHM
Title: Internal medicine residency program director, Banner Good Samaritan Medical Center, Phoenix
Program: GCMI
Background: Banner Good Samaritan has participated in the BOOST, VTE, and GCMI programs. Dr. O’Malley brought her experience from developing, implementing, and leading local glycemic control efforts to mentoring others.
“When I first started working on our hospital’s process, I had so many questions and asked one of my mentors from residency, Dr. Greg Maynard,” she says. “He helped me to see that people around the country were asking the same questions and invited me to join SHM’s glycemic control work group. When the GCMI program started, I was asked to be a mentor.”
Teachable moment: “When I was a new attending on the wards after residency, my patients would ask me why their blood sugars were so much better controlled at home than in the hospital. Usually, the answer was that they were put on a sliding scale when they came into the hospital,” she says, noting that what was done at home wasn’t going to work in the hospital. Patients needed a different regimen—a more proactive approach than just the customary sliding scale.
“I started to learn more about basal rates, nutrition, and correction insulin regimens in the hospital, but I realized that to really have adequate safety and direction for the nursing staff, it would require a formal order set and systematic approach,” she says.
Success story: “One of my sites invited me to come and present grand rounds at the hospital, and the local physician team leader invited the whole quality team to her home. It was a very exciting team and had achieved a lot. Fifteen or 20 of us spent the evening talking about the project but also just enjoying the collegiality,” Dr. O’Malley says. “Even though we had never seen one another, I instantly knew everyone by voice from spending so much time on the phone. And we knew a lot about one another’s personal lives and careers.”
Lessons learned: “Hearing a program describe what they are doing and knowing that they were far ahead of my own hospital in many ways but still being able to provide an insight or a perspective to help them achieve their own next steps. Everyone has something to learn from another hospital or another discipline. We can all leverage our experiences to improve patient care.”
Advice: “Be patient. This is a really long process of constant improvements. I have been working on glycemic control for 10 years now and still feel like we have many opportunities to further improve.”
Christopher Kim, MD, MBA, SFHM
Title: Clinical associate professor of internal medicine and assistant professor of pediatrics, University of Michigan Health System, Ann Arbor
Program: Project BOOST; Michigan Transitions of Care Collaborative (M-TC2)
Background: Dr. Kim brings clinical, quality improvement, leadership, collaborative learning, and discussion facilitation skills to his work as program director of M-TC2 and as mentor to the sites he works with.
The collaborative is part of a set of state collaborative quality initiatives funded by Blue Cross Blue Shield of Michigan. One of those initiatives is focused on improving care transitions between the hospital setting and ambulatory care providers, using Project BOOST tools—expanded to integrate more closely with primary care providers, physician organizations, and ambulatory care. The eight Michigan-based mentors for M-TC2 have all attended SHM’s Mentor University.
Teachable moment: There are local challenges and there are general challenges—those that are commonly shared by most hospitals, Dr. Kim explains. Both need to be overcome when working on an improvement project such as transitions of care. The local hospitalist brings expertise about the former—which are often more difficult to understand and overcome. The mentor brings knowledge and experience of the universal challenges, as well as the benefit of having seen or heard about what other programs have done. Together, they can work to help the organization become better equipped to improve the initiative at hand.
Success story: “One hospital in the collaborative realized that it could roll out the Teach Back concept to both nurses and physicians,” he says. They started to teach residents how to interact with patients and began using this approach in physician-nurse teams. Subsequently, the team shared with the collaborative how physicians have embraced the concept.
Lessons learned: Every site has its successes and challenges, he says. Sharing both sides of the story can only advance the mission of the collaborative, as each organization learns from the successes and failures of the others.
Mentored implementation really does what it’s intended to do—helping to support the sites and keeping an organization on track and accountable for the work it does, because someone external to the organization is working with it and providing information about what other sites are doing.
Advice: Talk with different disciplines and find out how much they long to work with other care providers, and then have discussions about how to make interdisciplinary practice happen. “At our collaborative meetings over time, many of the 24 participating sites have shared their progress—the good things and the struggles,” Dr. Kim says.
Larry Beresford is a freelance writer in Alameda, Calif.
When SHM received the Joint Commission’s John M. Eisenberg Patient Safety and Quality Award for 2011 for innovation in patient safety and quality at the national level, the award represented national recognition for the society’s three major hospital quality improvement initiatives. Moreover, it highlighted the integral role mentors play in each of the programs, helping physicians and hospitals make accelerated progress on important patient safety and quality issues.
Mentored implementation assigns a physician expert to train, guide, and work with the participating facilities’ hospitalist-led, multidisciplinary team through the life cycle of a QI initiative. The three programs focus on VTE prevention, glycemic control, and transitions of care. The first hospital cohort for VTE prevention—the VTE Prevention Collaborative—was in 2007. The care transitions program, known as Project BOOST, started in 2008. The Glycemic Control Mentored Implementation (GCMI) Program began in 2009. A fourth SHM mentored implementation program is MARQUIS, the Multi-Center Medication Reconciliation Quality Improvement Study.
In basic terms, mentoring is “coaching from a physician who has expertise both in the clinical subject matter and in implementing the processes and tools of quality improvement—usually because they’ve done it themselves,” says Gregory Maynard, MD, MSc, SFHM, senior vice president of SHM’s Center for Hospital Innovation and Improvement and a co-founder of two of its mentored implementation programs.
Mentors typically are paired with one or two participating hospitals for 12 to 18 months, conducting monthly conference calls with the team, sharing tools and resources from SHM’s online library, and offering advice on how to navigate the treacherous currents of culture change within a hospital. BOOST mentors also make in-person site visits. They are well versed in protocol and order set design and quality measurement strategies, and they know how to engage frontline professionals and institutional leadership, Dr. Maynard says.
Some mentors have received formal QI training, and many have attended Mentor University, a 1-1/2 day intensive training course offered by SHM that reinforces the nuances of coaching, the contents of SHM’s quality toolkits, and ideas for overcoming common barriers to improvement. SHM’s mentor support provides continuous professional development for the mentors, pairing new mentors with senior mentors to coach them in the process and hosting an online community with other mentors.
“What’s telling to me is that many of the people who have been mentored by SHM’s programs in one topic go on to become mentors in another topic, taking those portable skills and principles and applying them in other quality areas,” Dr. Maynard says. “We’re fostering leadership and quality improvement skills among hospitalists; that’s really one of our main goals. People learn the skill and then spread it within their system.”
Mark Williams, MD, FACP, MHM, Project BOOST principal investigator and a veteran SHM mentor, says that just providing educational materials to health professionals often isn’t enough for them to overcome the barriers to change.
“I’ve seen many large-scale quality projects that didn’t work, as they were simply disseminating information, content, or knowledge,” he says. Mentored implementation as practiced by SHM is “a model for disseminating quality improvement nationally,” he adds. “Pretty much any quality improvement project can be done this way.”
Key to the mentored implementation program’s success is the personalized approach and customized solutions.
“You directly meet with the team in their own setting and begin to see what’s going on,” Dr. Williams says. “You also meet with the hospital’s senior leadership. That’s when you start to see change.”
The Hospitalist connected with eight SHM mentors. The following are snapshots of their work in the mentorship program and some of the lessons they taught—and learned—from the program.
Christine Lum Lung, MD, SFHM
Title: Medical director, Northern Colorado Hospitalists, Fort Collins
Program: VTE Prevention Collaborative
Background: As a practicing hospitalist and medical director of the HM group for a two-hospital system, Dr. Lum Lung chaired its quality committee for VTE protocol development. “It was obvious at our hospitals that we needed to do better at VTE prevention,” she explains.
Dr. Lum Lung’s team received VTE mentorship from Dr. Maynard, who later asked her to become a VTE mentor. She also attended all three levels of SHM’s Leadership Academy and has since become a mentor for the new HP3 (Hospitalist Program Peak Performance) mentored implementation program, a one-year collaboration among SHM, Northwestern University, Blue Cross/Blue Shield of Illinois, and the Illinois Hospital Association that is designed to help hospitalist groups optimize their programs and build healthy group culture.
Teachable moment: The essential qualities of a good mentee, Dr. Lum Lung says, are drive and dedication. “You believe strongly about it, so you can sell it to others. You also need a thick skin to face the adversities that come up. When my mentor gave me tasks and deadlines, I met those deadlines.”
Success story: “I’ve been impressed with how hard groups and individuals can work.” Most of the teams she has worked with were facing significant external stressors—starting a new program, moving into a new hospital, rolling out a new EHR, becoming part of a growing medical group. “Yet each of them has been incredibly engaged in the process and dedicated to completing their projects.”
Lessons learned: “That we all have something to learn from each other. While I am officially the mentor, I have learned a lot about processes, teamwork, and flow issues from the sites that could potentially be incorporated in our program.”
Advice: Working on a project as a team can be very powerful, she says. Even seemingly ‘small’ projects have allowed teams to learn how to work better together on day-to-day issues. With the victory of a small project behind them, they make lists of the next thing that they want to tackle.
“Our profession is constantly changing. We need to be thinking ahead for how we will face those challenges,” Dr. Lum Lung says. “A team that works well together will have an advantage in this new environment. Even if you have people who are new to quality improvement, their participation can still be important.”
Jordan Messler, MD, SFHM
Title: Medical director, Morton Plant Hospitalists, Clearwater, Fla.
Program: GCMI; Project BOOST
Background: Dr. Messler’s interest in QI led him to work with colleagues in SHM who are national leaders in quality. “A couple of years ago, I enrolled in Emory’s Quality Academy, a sister course to Intermountain Health’s course on quality. Then I enrolled our hospital in both the GCMI Program and Project BOOST. My mentors for those programs were terrific guides, which led to my interest in seeing their side of the program as a mentor myself.”
Teachable moment: One program had difficulty implementing a VTE prevention tool and couldn’t get nursing support as it had expected, largely due to lack of nursing engagement on the project team, he says. “We started talking about the history of the projects, and prior interventions. In addition, we talked to the different disciplines separately. It seems there used to be an excellent system where nursing helped out on the project team for risk assessment.”
As VTE prevention became more of a priority, some physicians separately created a new tool to replace the nursing tool without involving the whole team. “And they couldn’t understand why nursing wasn’t buying into the new process.”
Success story: There are similar themes to success and failure. Sites that have strong administrative support (i.e., C-suite representation on the QI team), that have “accountability structure and stick to the basics of QI, with clear goals, ability to gather and report data, and use of a QI model [such as PDSA or Six Sigma] are the ones that succeed,” Dr. Messler says. “And the reverse is consistently true. Sustainable QI needs to be multidisciplinary, involving every voice, considering prior interventions and understanding of the culture.”
Lessons learned: “As mentors, we all continue to say we learn as much or more from these sites as they, hopefully, are learning from us. This collaboration and sharing of ideas has been instrumental to the success of the program.”
Advice: Get started today, and don’t give up. Follow the road map of QI projects, gather support, and get started. You will learn as much from your failures as your successes.
Dr. Messler says hospitals are looking for physician leaders to improve quality, and hospitalists are perfectly positioned to be those QI leaders. These big projects can last for years, so quality teams and hospitals need to be prepared to take the long view.
—Jennifer Quartarolo, MD, SFHM
Stephanie Rennke, MD
Title: Associate clinical professor of medicine, co-director of faculty development, division of hospital medicine, University of California San Francisco Medical Center.
Program: Project BOOST
Background: “When I started as a hospitalist right out of residency, QI had not been part of my training. But I noticed that quality was at the forefront of the academic interests of all the hospitalists at UCSF. I was personally interested in transitions of care. I still do home visits after hours for at-risk patients when they leave the hospital.”
Dr. Rennke started in QI as a member of UCSF’s BOOST team in 2008. “I worked with other faculty in the division who had previous experience in quality improvement and transitions in care. One of the co-principal investigators for BOOST, Dr. Arpana Vidyarthi, suggested that it would be a really rewarding experience to mentor—and it was.”
Teachable moment: “I’ve been so impressed by the diversity of what’s out there. No hospitalist program or hospital is the same. There is no one-size-fits-all for quality improvement or transitions of care, so it is incredibly important that the mentor takes the time to get to know both the team and the hospital.”
Success story: “During a site visit, I had an opportunity to watch one of the nurses, who had received training from a competency-based Teach Back program, practice Teach Back with a patient at the bedside,” Dr. Rennke says. “I was doing a tour of the floor and went into the room of a patient about to be discharged. A young float nurse, not long out of school, sat down with the patient and went through the medications and discharge plan using Teach Back. It didn’t take more time, but the time was spent more constructively, with interaction back and forth. I remember that ‘aha’ moment for the patient and the look in her eyes. For me, as a mentor, it was exciting to think that something I had tried to bring to them had been incorporated by the site and was really working.”
Lessons learned: “I have learned that, while at a large institution like UCSF we tend to work in silos, smaller sites are often more integrated with the various disciplines. You can walk down the hall to the clinical pharmacist or have lunch with the charge nurse. So I’ve tried to bring back home a commitment to really get to know professional colleagues and have them feel that I’m interested in their perspectives.”
Advice: “Work in teams. You cannot do this alone. Include frontline staff. And don’t forget to advertise to others that the program exists. Get the word out—let people know.”
Jennifer Quartarolo, MD, SFHM
Title: Medical director, clinical resource management; associate clinical professor, division of hospital medicine, University of California San Diego Health System
Program: Project BOOST
Background: Dr. Quartarolo has 11 years of clinical experience as an academic hospitalist at two different medical centers, and she completed a training program in healthcare delivery and improvement through the Institute for Health Care Delivery Research in Salt Lake City, Utah. “At my own institution, I had been involved in multiple QI projects,” she says. “Since joining the faculty, I worked with our care transitions team for five years before becoming a mentor. We incorporated many elements from Project BOOST as we worked to improve our care transitions process,” which led to an invitation to be a mentor.
Teachable moment: “I had one site that I worked with that had a great new form they had developed to incorporate into their transition process; however, when they decided to implement the form, they got a lot of pushback from nursing,” she says. “Then they realized that they had not involved any frontline nurses in their planning. This example points out how important it is to have all the key players involved on your team, as improving transitions of care is a complex process requiring multidisciplinary collaboration.”
Success story: Dr. Quartarolo says she has worked with several hospitals that have seen significant improvement in their readmission rates after participating in Project BOOST and implementing its tools.
Lessons learned: “I am constantly impressed by the innovative ideas that teams come up with to deal with the challenges that their hospitals face,” she says. Every hospital is unique and needs to do self-evaluation before deciding what to focus on. “I have also worked with many sites that have challenges getting physicians engaged in their efforts, particularly if they do not have a hospitalist program.”
Advice: “We are in a unique role as hospitalists to identify systems issues and improve quality of care in the inpatient setting, and this is particularly useful in improving care transitions and decreasing readmissions rates.”
Rich Balaban, MD
Title: Medical director, Hospital-to-Home Community Collaboration Program, Cambridge Health Alliance; assistant professor of medicine, Harvard Medical School, Boston
Program: Project BOOST
Background: Dr. Balaban has worked clinically in both the inpatient setting as a hospitalist and the outpatient setting as a primary care doctor. “I have seen hospital discharges as both a receiver and a sender, so [I] have been able to appreciate the challenges facing doctors, nurses, case managers, and patients involved in the care transition process,” he says.
Dr. Balaban also conducted a randomized controlled trial that demonstrated the benefits of engaging nurses at a patient’s primary care site to make outreach phone calls immediately after hospital discharge. Dr. Williams asked him to present on the study.
“It was a great opportunity for me to share the results of our work and for Mark to see my presentation skills,” he says. “When I asked if there were opportunities to get more involved in care transitions work, he invited me to consider becoming a BOOST mentor.”
Teachable moment: “Wearing my primary care hat, I believe that while it is very important to structure an effective discharge for the patient while in the hospital, success or failure ultimately is determined by what happens in the outpatient setting,” Dr. Balaban says. Even if a ‘perfect discharge’ occurs in the hospital, it can all quickly unravel once the patient arrives at home.
Success story: “At several sites, I have encouraged the inpatient care team to invite the outpatient care team to become part of the care transitions team. This has frequently brought an important viewpoint and voice to the care transitions table. While hospitalists have initiated the discussion about care transitions, they need an effective outpatient partner to create a truly effective process.”
Lessons learned: “I have learned to hold judgment until seeing with my own eyes,” Dr. Balaban says. “One of the first sites I visited had developed a post-discharge clinic, which they were excited to show me. From my point of view, I thought that after discharge, patient care should be assumed by the primary care office as soon as possible, and a post-discharge clinic would only delay that process.
“To my great surprise, their post-discharge clinic provided an ideal bridge between the hospital and primary care. The post-discharge clinic really worked and provided patients with a wonderful resource. … I’ve learned that there are many ways to solve problems, often based on the available resources at a specific site.”
Advice: In order to best understand the challenges of hospital discharge, it is critical that you understand what happens to patients after they leave the hospital. Make a home visit to a recently discharged patient to really understand the challenges that patients face when they return home.
Amitkumar R. Patel, MD, MBA, FACP, SFHM
Title: Clinical instructor in hospital medicine, Feinberg School of Medicine, Northwestern University, Chicago
Program: Project BOOST; also working with critical access hospitals in Illinois through PREP (Preventing Readmissions through Effective Partnerships)
Background: Although he now works in an urban teaching hospital, Dr. Patel also did private practice as a community hospitalist and has pursued formal healthcare management-focused training.
“I became a mentor because my experience and interest in quality improvement fit well with Project BOOST,” he says. “I enjoy coaching teams as they face challenges in quality improvement, especially in relation to readmissions reduction. My work with critical access hospitals is the result of my first year as a mentor with the PREP collaborative in Illinois.”
PREP, a collaborative initiative of SHM and the Illinois Hospital Association that is funded by Blue Cross/Blue Shield of Illinois, aims to help hospitals focus on quality initiatives, including BOOST.
Teachable moment/success story: One of Dr. Patel’s BOOST sites believed the team included all appropriate personnel to obtain discharge appointments prior to patients’ discharges. But as they began to work through the process of making sure each appointment was appropriately documented, the various team members assigned to this process could not consistently complete the task within their workflow.
The pilot unit secretaries were not part of the BOOST team initially but saw that they could fulfill this role quickly and easily. They knew who to call at the physicians’ offices to avoid getting stuck in the phone menu trees, and they used this knowledge to reach the schedulers directly. The BOOST team quickly realized the unit secretaries were the most appropriate personnel to capture this information and work with the patients or their families/caregivers to obtain the most convenient appointments. This role was added to the team, and the unit secretaries took ownership of this process. Other teams may also want to look beyond the customary team members to roles that may not be thought of as quality team members.
Lessons learned: “The biggest take-away for me involves the unique culture that exists in many of our urban and rural communities,” he says. Every BOOST site implements the project’s elements in its own unique way, and what works well in one location may not fit the needs of another. The role of the mentor is to balance the need for community-specific advice with unique attributes of the facility and the elements of Project BOOST. “Often, we use our mentor calls to brainstorm solutions, and the teams are teaching me what will work best in their environment.”
Advice: “Responsibility for hospital change management should not be abdicated to administrators or quality improvement staff members,” he says. “QI is not a sometime thing for some staff; it’s an all-the-time process for every staff member, including physicians, to participate in and actively manage.”
—Christopher Kim, MD, MBA, SFHM
Cheryl O’Malley, MD, FHM
Title: Internal medicine residency program director, Banner Good Samaritan Medical Center, Phoenix
Program: GCMI
Background: Banner Good Samaritan has participated in the BOOST, VTE, and GCMI programs. Dr. O’Malley brought her experience from developing, implementing, and leading local glycemic control efforts to mentoring others.
“When I first started working on our hospital’s process, I had so many questions and asked one of my mentors from residency, Dr. Greg Maynard,” she says. “He helped me to see that people around the country were asking the same questions and invited me to join SHM’s glycemic control work group. When the GCMI program started, I was asked to be a mentor.”
Teachable moment: “When I was a new attending on the wards after residency, my patients would ask me why their blood sugars were so much better controlled at home than in the hospital. Usually, the answer was that they were put on a sliding scale when they came into the hospital,” she says, noting that what was done at home wasn’t going to work in the hospital. Patients needed a different regimen—a more proactive approach than just the customary sliding scale.
“I started to learn more about basal rates, nutrition, and correction insulin regimens in the hospital, but I realized that to really have adequate safety and direction for the nursing staff, it would require a formal order set and systematic approach,” she says.
Success story: “One of my sites invited me to come and present grand rounds at the hospital, and the local physician team leader invited the whole quality team to her home. It was a very exciting team and had achieved a lot. Fifteen or 20 of us spent the evening talking about the project but also just enjoying the collegiality,” Dr. O’Malley says. “Even though we had never seen one another, I instantly knew everyone by voice from spending so much time on the phone. And we knew a lot about one another’s personal lives and careers.”
Lessons learned: “Hearing a program describe what they are doing and knowing that they were far ahead of my own hospital in many ways but still being able to provide an insight or a perspective to help them achieve their own next steps. Everyone has something to learn from another hospital or another discipline. We can all leverage our experiences to improve patient care.”
Advice: “Be patient. This is a really long process of constant improvements. I have been working on glycemic control for 10 years now and still feel like we have many opportunities to further improve.”
Christopher Kim, MD, MBA, SFHM
Title: Clinical associate professor of internal medicine and assistant professor of pediatrics, University of Michigan Health System, Ann Arbor
Program: Project BOOST; Michigan Transitions of Care Collaborative (M-TC2)
Background: Dr. Kim brings clinical, quality improvement, leadership, collaborative learning, and discussion facilitation skills to his work as program director of M-TC2 and as mentor to the sites he works with.
The collaborative is part of a set of state collaborative quality initiatives funded by Blue Cross Blue Shield of Michigan. One of those initiatives is focused on improving care transitions between the hospital setting and ambulatory care providers, using Project BOOST tools—expanded to integrate more closely with primary care providers, physician organizations, and ambulatory care. The eight Michigan-based mentors for M-TC2 have all attended SHM’s Mentor University.
Teachable moment: There are local challenges and there are general challenges—those that are commonly shared by most hospitals, Dr. Kim explains. Both need to be overcome when working on an improvement project such as transitions of care. The local hospitalist brings expertise about the former—which are often more difficult to understand and overcome. The mentor brings knowledge and experience of the universal challenges, as well as the benefit of having seen or heard about what other programs have done. Together, they can work to help the organization become better equipped to improve the initiative at hand.
Success story: “One hospital in the collaborative realized that it could roll out the Teach Back concept to both nurses and physicians,” he says. They started to teach residents how to interact with patients and began using this approach in physician-nurse teams. Subsequently, the team shared with the collaborative how physicians have embraced the concept.
Lessons learned: Every site has its successes and challenges, he says. Sharing both sides of the story can only advance the mission of the collaborative, as each organization learns from the successes and failures of the others.
Mentored implementation really does what it’s intended to do—helping to support the sites and keeping an organization on track and accountable for the work it does, because someone external to the organization is working with it and providing information about what other sites are doing.
Advice: Talk with different disciplines and find out how much they long to work with other care providers, and then have discussions about how to make interdisciplinary practice happen. “At our collaborative meetings over time, many of the 24 participating sites have shared their progress—the good things and the struggles,” Dr. Kim says.
Larry Beresford is a freelance writer in Alameda, Calif.
VIDEO: Federal health IT chief DeSalvo talks meaningful use
Dr. Karen DeSalvo is the fifth person to serve as National Coordinator for Health Information Technology at the Health and Human Services Department, but perhaps more than any of her predecessors, she is truly in the thick of the struggle to bring doctors, medical practices, and hospitals into the digital age.
Physicians face a major deadline this year: It’s the last year to sign up for the meaningful use incentive payment program created by the Health Information Technology for Economic and Clinical Health Act (HITECH). If they don’t participate, they lose out on the potential to recoup from the federal government at least a small portion of the money they’ve spent on electronic health record systems. And it’s becoming inevitable that not participating could mean being left behind by insurers, hospitals, and patients.
That’s causing a lot of anxiety. Dr. DeSalvo – a practicing internist – says that she feels doctors’ pain. She recently completed a national listening tour and says that what she learned from those sessions will help inform how the Office of the National Coordinator moves forward.
Dr. Karen DeSalvo is the fifth person to serve as National Coordinator for Health Information Technology at the Health and Human Services Department, but perhaps more than any of her predecessors, she is truly in the thick of the struggle to bring doctors, medical practices, and hospitals into the digital age.
Physicians face a major deadline this year: It’s the last year to sign up for the meaningful use incentive payment program created by the Health Information Technology for Economic and Clinical Health Act (HITECH). If they don’t participate, they lose out on the potential to recoup from the federal government at least a small portion of the money they’ve spent on electronic health record systems. And it’s becoming inevitable that not participating could mean being left behind by insurers, hospitals, and patients.
That’s causing a lot of anxiety. Dr. DeSalvo – a practicing internist – says that she feels doctors’ pain. She recently completed a national listening tour and says that what she learned from those sessions will help inform how the Office of the National Coordinator moves forward.
Dr. Karen DeSalvo is the fifth person to serve as National Coordinator for Health Information Technology at the Health and Human Services Department, but perhaps more than any of her predecessors, she is truly in the thick of the struggle to bring doctors, medical practices, and hospitals into the digital age.
Physicians face a major deadline this year: It’s the last year to sign up for the meaningful use incentive payment program created by the Health Information Technology for Economic and Clinical Health Act (HITECH). If they don’t participate, they lose out on the potential to recoup from the federal government at least a small portion of the money they’ve spent on electronic health record systems. And it’s becoming inevitable that not participating could mean being left behind by insurers, hospitals, and patients.
That’s causing a lot of anxiety. Dr. DeSalvo – a practicing internist – says that she feels doctors’ pain. She recently completed a national listening tour and says that what she learned from those sessions will help inform how the Office of the National Coordinator moves forward.
HHS appoints chief executive to run healthcare.gov
The U.S. Department of Health & Human Services has named a new chief executive officer to run the federal marketplace, which includes the healthcare.gov website.
Kevin Counihan, currently the CEO for Connecticut’s marketplace, has been named to run the federal marketplace. He also will be in charge of the Center for Consumer Information and Insurance Oversight (CCIIO), which regulates health insurance. HHS Secretary Sylvia Mathews Burwell announced in June that the department would be looking for a new CEO.
Mr. Counihan has served as CEO for Health Access CT since June 2012, after having served as chief marketing officer from 2006 to 2011 for the Commonwealth of Massachusetts Health Insurance Connector Authority, which administered that state’s health insurance exchange. Before that, he was a sales and marketing executive for Tufts Health Plan of Massachusetts and regional vice president for CIGNA.
"We are committed to instilling ongoing accountability for reaching milestones, measuring results, and ensuring a successful open enrollment period," Ms. Burwell said in a statement. Mr. Counihan "brings additional operational and technological expertise to the position and will be a clear, single point of contact for streamlined decision making."
Mr. Counihan will report to Centers for Medicare & Medicaid Services Administrator Marilyn Tavenner.
On Twitter @aliciaault
The U.S. Department of Health & Human Services has named a new chief executive officer to run the federal marketplace, which includes the healthcare.gov website.
Kevin Counihan, currently the CEO for Connecticut’s marketplace, has been named to run the federal marketplace. He also will be in charge of the Center for Consumer Information and Insurance Oversight (CCIIO), which regulates health insurance. HHS Secretary Sylvia Mathews Burwell announced in June that the department would be looking for a new CEO.
Mr. Counihan has served as CEO for Health Access CT since June 2012, after having served as chief marketing officer from 2006 to 2011 for the Commonwealth of Massachusetts Health Insurance Connector Authority, which administered that state’s health insurance exchange. Before that, he was a sales and marketing executive for Tufts Health Plan of Massachusetts and regional vice president for CIGNA.
"We are committed to instilling ongoing accountability for reaching milestones, measuring results, and ensuring a successful open enrollment period," Ms. Burwell said in a statement. Mr. Counihan "brings additional operational and technological expertise to the position and will be a clear, single point of contact for streamlined decision making."
Mr. Counihan will report to Centers for Medicare & Medicaid Services Administrator Marilyn Tavenner.
On Twitter @aliciaault
The U.S. Department of Health & Human Services has named a new chief executive officer to run the federal marketplace, which includes the healthcare.gov website.
Kevin Counihan, currently the CEO for Connecticut’s marketplace, has been named to run the federal marketplace. He also will be in charge of the Center for Consumer Information and Insurance Oversight (CCIIO), which regulates health insurance. HHS Secretary Sylvia Mathews Burwell announced in June that the department would be looking for a new CEO.
Mr. Counihan has served as CEO for Health Access CT since June 2012, after having served as chief marketing officer from 2006 to 2011 for the Commonwealth of Massachusetts Health Insurance Connector Authority, which administered that state’s health insurance exchange. Before that, he was a sales and marketing executive for Tufts Health Plan of Massachusetts and regional vice president for CIGNA.
"We are committed to instilling ongoing accountability for reaching milestones, measuring results, and ensuring a successful open enrollment period," Ms. Burwell said in a statement. Mr. Counihan "brings additional operational and technological expertise to the position and will be a clear, single point of contact for streamlined decision making."
Mr. Counihan will report to Centers for Medicare & Medicaid Services Administrator Marilyn Tavenner.
On Twitter @aliciaault
Waiving protections can affect payment investigations
CHICAGO – Accepting poor legal advice or inadvertently waiving the client-attorney privilege may result in tougher judicial scrutiny or have a direct impact the outcome of payment investigations, experts warned at a physicians’ legal issues conference held by the American Bar Association.
"While some audits are relatively minor, others can result in huge reimbursement demands or even more frightening things, including civil or criminal charges being made based on claims of fraud and abuse," said Michael E. Clark, chair of the American Bar Association’s Health Law Section. Legal advisers need to be able to guide physicians through the payment investigation process while protecting their rights.
Bad advice by a lawyer cannot be used as a court defense for a physician’s acts or oversights, health lawyer Eric C. Tostrud said. However, in some instances, poor legal advice can be used as a defense to a fraud claim.
"There are important nuances to the issue," said Mr. Tostrud, an attorney in Minneapolis. For example, a defense of "poor legal advice" depends on the accuracy and completeness of the information the doctor initially disclosed to the attorney as well as whether the physician was completely forthcoming. In addition, courts will review whether health providers disregarded one attorney’s advice for more self-seeking guidance from another lawyer.
The question of bad legal advice arose in the recent case of U.S. v. Tuomey Healthcare System, in which the South Carolina–based health system was accused of submitting Medicare claims that violated the Stark Law. This purported violation included reimbursement claims for services by physicians with whom Tuomey allegedly had financial relationships. As part of its defense, Tuomey said it had relied on attorneys to design and approve the physician contracts. But during the trial, the government presented evidence that Tuomey had dismissed adverse legal and expert opinions when entering into the contracts and had retained subsequent legal opinions that supported the arrangements. A federal jury found the system had violated Stark Law and the False Claims Act, and a federal judge in 2013 ordered Tuomey to pay $237 million in fines.
The attorney-client privilege is another complex concept that can land physicians – and their attorneys – in legal trouble. The privilege protects communications between an attorney and client that are made for the purpose of furnishing or obtaining professional legal advice or assistance. But physicians can waive the privilege by disclosing confidential information through conversations, paper documentation, or e-mails. Doctors who reveal details about such communications to colleagues thus relinquish the protection, Mr. Tostrud said.
"Doctors by their nature are very collaborative," he said in an interview. "They want to talk to other people and consult with others about issues and that includes the advice they might be getting from a lawyer. But the risk of doing that is that they will waive the privilege."
Also, not every communication from or to a lawyer is privileged. The privilege generally protects communications involving legal advice, but does not extend to underlying facts.
In the case of U.S. v. Halifax Hospital Medical Center, a federal court ruled that the Daytona Beach, Fla.–based hospital’s compliance "referral log" was not subject to the privilege even though it was prepared at the instruction of an attorney. The logs merely recorded facts and did not meet the purpose of the privilege. The court concluded also that hundreds of e-mails and other documents relating to Halifax’s compliance and audit activities were not protected. While an attorney may have been included in the e-mails, the lawyer was copied for business purposes, not for legal advice, the court said. Halifax in March agreed to pay the government $85 million to resolve False Claims Act and Stark Law violations.
"E-mail often becomes a lawyer’s nightmare because it’s permanent and clients and people generally tend to treat e-mail like a conversation," Mr. Tostrud said in an interview. "They are not thinking about the permanency of it and are not thinking of the long-term litigation consequences."
One privileged e-mail does not necessarily extend the privilege to an entire string of e-mails, he said. To be protected, each e-mail within a string must be for the purposes of legal advice.
Enlisting the help of an attorney early in an audit or payment investigation is essential, said Mr. Clark, who practices law in Houston. For instance, if it becomes necessary to retain specialized consultants to help review coding and documentation issues, an attorney can help structure a framework whereby the consultants report to the attorney, and the attorney then formulates advice to the physician client.
"Most physicians have a basic understanding about the attorney-client privilege and its scope, but don’t fully understand or appreciate how that legal protection can be lost inadvertently," Mr. Clark said. "Having an attorney on board early in the process of an audit or broader investigation is important to ensuring that the privilege is properly established and protected."
This article was updated Sept. 2, 2014.
On Twitter @legal_med
CHICAGO – Accepting poor legal advice or inadvertently waiving the client-attorney privilege may result in tougher judicial scrutiny or have a direct impact the outcome of payment investigations, experts warned at a physicians’ legal issues conference held by the American Bar Association.
"While some audits are relatively minor, others can result in huge reimbursement demands or even more frightening things, including civil or criminal charges being made based on claims of fraud and abuse," said Michael E. Clark, chair of the American Bar Association’s Health Law Section. Legal advisers need to be able to guide physicians through the payment investigation process while protecting their rights.
Bad advice by a lawyer cannot be used as a court defense for a physician’s acts or oversights, health lawyer Eric C. Tostrud said. However, in some instances, poor legal advice can be used as a defense to a fraud claim.
"There are important nuances to the issue," said Mr. Tostrud, an attorney in Minneapolis. For example, a defense of "poor legal advice" depends on the accuracy and completeness of the information the doctor initially disclosed to the attorney as well as whether the physician was completely forthcoming. In addition, courts will review whether health providers disregarded one attorney’s advice for more self-seeking guidance from another lawyer.
The question of bad legal advice arose in the recent case of U.S. v. Tuomey Healthcare System, in which the South Carolina–based health system was accused of submitting Medicare claims that violated the Stark Law. This purported violation included reimbursement claims for services by physicians with whom Tuomey allegedly had financial relationships. As part of its defense, Tuomey said it had relied on attorneys to design and approve the physician contracts. But during the trial, the government presented evidence that Tuomey had dismissed adverse legal and expert opinions when entering into the contracts and had retained subsequent legal opinions that supported the arrangements. A federal jury found the system had violated Stark Law and the False Claims Act, and a federal judge in 2013 ordered Tuomey to pay $237 million in fines.
The attorney-client privilege is another complex concept that can land physicians – and their attorneys – in legal trouble. The privilege protects communications between an attorney and client that are made for the purpose of furnishing or obtaining professional legal advice or assistance. But physicians can waive the privilege by disclosing confidential information through conversations, paper documentation, or e-mails. Doctors who reveal details about such communications to colleagues thus relinquish the protection, Mr. Tostrud said.
"Doctors by their nature are very collaborative," he said in an interview. "They want to talk to other people and consult with others about issues and that includes the advice they might be getting from a lawyer. But the risk of doing that is that they will waive the privilege."
Also, not every communication from or to a lawyer is privileged. The privilege generally protects communications involving legal advice, but does not extend to underlying facts.
In the case of U.S. v. Halifax Hospital Medical Center, a federal court ruled that the Daytona Beach, Fla.–based hospital’s compliance "referral log" was not subject to the privilege even though it was prepared at the instruction of an attorney. The logs merely recorded facts and did not meet the purpose of the privilege. The court concluded also that hundreds of e-mails and other documents relating to Halifax’s compliance and audit activities were not protected. While an attorney may have been included in the e-mails, the lawyer was copied for business purposes, not for legal advice, the court said. Halifax in March agreed to pay the government $85 million to resolve False Claims Act and Stark Law violations.
"E-mail often becomes a lawyer’s nightmare because it’s permanent and clients and people generally tend to treat e-mail like a conversation," Mr. Tostrud said in an interview. "They are not thinking about the permanency of it and are not thinking of the long-term litigation consequences."
One privileged e-mail does not necessarily extend the privilege to an entire string of e-mails, he said. To be protected, each e-mail within a string must be for the purposes of legal advice.
Enlisting the help of an attorney early in an audit or payment investigation is essential, said Mr. Clark, who practices law in Houston. For instance, if it becomes necessary to retain specialized consultants to help review coding and documentation issues, an attorney can help structure a framework whereby the consultants report to the attorney, and the attorney then formulates advice to the physician client.
"Most physicians have a basic understanding about the attorney-client privilege and its scope, but don’t fully understand or appreciate how that legal protection can be lost inadvertently," Mr. Clark said. "Having an attorney on board early in the process of an audit or broader investigation is important to ensuring that the privilege is properly established and protected."
This article was updated Sept. 2, 2014.
On Twitter @legal_med
CHICAGO – Accepting poor legal advice or inadvertently waiving the client-attorney privilege may result in tougher judicial scrutiny or have a direct impact the outcome of payment investigations, experts warned at a physicians’ legal issues conference held by the American Bar Association.
"While some audits are relatively minor, others can result in huge reimbursement demands or even more frightening things, including civil or criminal charges being made based on claims of fraud and abuse," said Michael E. Clark, chair of the American Bar Association’s Health Law Section. Legal advisers need to be able to guide physicians through the payment investigation process while protecting their rights.
Bad advice by a lawyer cannot be used as a court defense for a physician’s acts or oversights, health lawyer Eric C. Tostrud said. However, in some instances, poor legal advice can be used as a defense to a fraud claim.
"There are important nuances to the issue," said Mr. Tostrud, an attorney in Minneapolis. For example, a defense of "poor legal advice" depends on the accuracy and completeness of the information the doctor initially disclosed to the attorney as well as whether the physician was completely forthcoming. In addition, courts will review whether health providers disregarded one attorney’s advice for more self-seeking guidance from another lawyer.
The question of bad legal advice arose in the recent case of U.S. v. Tuomey Healthcare System, in which the South Carolina–based health system was accused of submitting Medicare claims that violated the Stark Law. This purported violation included reimbursement claims for services by physicians with whom Tuomey allegedly had financial relationships. As part of its defense, Tuomey said it had relied on attorneys to design and approve the physician contracts. But during the trial, the government presented evidence that Tuomey had dismissed adverse legal and expert opinions when entering into the contracts and had retained subsequent legal opinions that supported the arrangements. A federal jury found the system had violated Stark Law and the False Claims Act, and a federal judge in 2013 ordered Tuomey to pay $237 million in fines.
The attorney-client privilege is another complex concept that can land physicians – and their attorneys – in legal trouble. The privilege protects communications between an attorney and client that are made for the purpose of furnishing or obtaining professional legal advice or assistance. But physicians can waive the privilege by disclosing confidential information through conversations, paper documentation, or e-mails. Doctors who reveal details about such communications to colleagues thus relinquish the protection, Mr. Tostrud said.
"Doctors by their nature are very collaborative," he said in an interview. "They want to talk to other people and consult with others about issues and that includes the advice they might be getting from a lawyer. But the risk of doing that is that they will waive the privilege."
Also, not every communication from or to a lawyer is privileged. The privilege generally protects communications involving legal advice, but does not extend to underlying facts.
In the case of U.S. v. Halifax Hospital Medical Center, a federal court ruled that the Daytona Beach, Fla.–based hospital’s compliance "referral log" was not subject to the privilege even though it was prepared at the instruction of an attorney. The logs merely recorded facts and did not meet the purpose of the privilege. The court concluded also that hundreds of e-mails and other documents relating to Halifax’s compliance and audit activities were not protected. While an attorney may have been included in the e-mails, the lawyer was copied for business purposes, not for legal advice, the court said. Halifax in March agreed to pay the government $85 million to resolve False Claims Act and Stark Law violations.
"E-mail often becomes a lawyer’s nightmare because it’s permanent and clients and people generally tend to treat e-mail like a conversation," Mr. Tostrud said in an interview. "They are not thinking about the permanency of it and are not thinking of the long-term litigation consequences."
One privileged e-mail does not necessarily extend the privilege to an entire string of e-mails, he said. To be protected, each e-mail within a string must be for the purposes of legal advice.
Enlisting the help of an attorney early in an audit or payment investigation is essential, said Mr. Clark, who practices law in Houston. For instance, if it becomes necessary to retain specialized consultants to help review coding and documentation issues, an attorney can help structure a framework whereby the consultants report to the attorney, and the attorney then formulates advice to the physician client.
"Most physicians have a basic understanding about the attorney-client privilege and its scope, but don’t fully understand or appreciate how that legal protection can be lost inadvertently," Mr. Clark said. "Having an attorney on board early in the process of an audit or broader investigation is important to ensuring that the privilege is properly established and protected."
This article was updated Sept. 2, 2014.
On Twitter @legal_med
EXPERT ANALYSIS AT AN ABA CONFERENCE
Law discourages drug-addicted pregnant women from seeking care
The enactment of a Tennessee law that criminalizes substance abuse by pregnant women has made patients increasingly hesitant to pursue treatment for their drug addictions, according to Dr. Jessica Young, an obstetrician/gynecologist at Vanderbilt University Medical Center in Nashville, Tenn.
Tennessee’s law, which became effective in July, defines illegal narcotic use by pregnant women as assault, depending on whether the child is born addicted to or is harmed by the narcotic. A 26-year-old woman was among the first to be arrested in mid-July under the law.
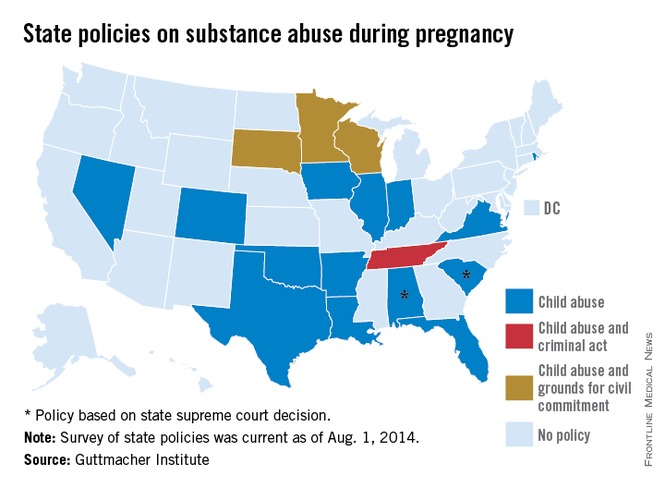
"Since the new law was passed, women . . . often express a fatalistic attitude of, ‘Even if I do the right thing, I will be arrested or have my baby taken away,’ " said Dr. Young, who leads the Vanderbilt Drug Dependency Clinic for pregnant women.
The concern is that women will hide their addictions or self-detox at home, she said. "I think it will require some negative outcomes for this law to be struck down."
Physician associations, including the American Medical Association and ACOG, have long maintained that criminal punishment is not the answer to curbing drug abuse by pregnant women and that such laws create further harm to children. Fear of being reported to police was a primary reason women who abused drugs did not seek prenatal care, a recent study found (Am. J. Obstet. Gynecol. 2009;200:412.e1-10).
Laws that mandate criminal penalties against pregnant women who use drugs can significantly harm the physician-patient relationship, according to Dr. John M. Thorp, professor of obstetrics and gynecology at the University of North Carolina and director of women’s primary health care for UNC Healthcare, both in Chapel Hill.
These laws "put the physician or the clinic or hospital in the role of reporting the crime, which is completely the antithesis of wanting patients to be able to tell physicians what’s wrong with them and being able to offer treatment instead of punishment," Dr. Thorp said in an interview. "These laws are a real setback to the concept that substance abuse addiction is a disease, [and they are] another barrier for women seeking treatment."
Tennessee is the only state to consider drug abuse by pregnant women to be "assault." The law states that a woman may be prosecuted for assault if her child is born addicted or harmed by the drug and for homicide if the child dies from drug exposure. It is an affirmative defense to prosecution if the woman is actively enrolled in an addiction recovery program before the baby is born, remains in the program after delivery, and successfully completes the program.
The American Civil Liberties Union of Tennessee plans to challenge the law in court.
The Tennessee Medical Association opposed the law, but successfully pushed for amendments that would lessen the punitive damages against women, Dave Chaney, TMA director of communications, said in an interview. The medical association successfully lobbied to lower the charging level in the bill to a misdemeanor and helped secure a stipulation that women who enter a treatment program be punished only by a fine.
Various states pursue criminal charges against pregnant women who use narcotics. Eighteen states consider substance abuse during pregnancy to be "child abuse," and three other states consider substance abuse during pregnancy to be grounds for civil commitment, according to an August 2014 analysis by the Guttmacher Institute. Fifteen states require physicians to report suspected prenatal drug abuse to authorities, and four states require health providers to test for prenatal drug exposure if they suspect substance abuse.
Other states could soon follow in Tennessee’s footsteps, Elizabeth Nash, Guttmacher Institute state issues manager, said in an interview. "Legislatures see what’s happening in other states and decide whether it may be right for them."
Meanwhile, a newly proposed federal bill could assist states in addressing the issue of drug-addicted pregnant mothers and babies and drive more effective responses to the crisis. The Protecting Our Infants Act, introduced July 31 by Rep. Mitch McConnell (R-Ky.), aims to better identify and treat opioid use by pregnant women and neonatal abstinence syndrome (NAS) in newborns. The legislation is backed by ACOG.
"Currently, states vary widely in how they mandate and administer screening, diagnosis, and treatment of pregnant women using opioids," ACOG President John C. Jennings said in a statement. The federal "legislation will help identify, compile, and disseminate best practices developed by medical professional organizations, including ACOG, and identify any gaps in best practices that may require additional research or analysis."
The proposed legislation would facilitate the research and dissemination of evidence-informed recommendations for addressing maternal addiction and NAS and provide for NAS studies. The measure also would encourage the Centers for Disease Control and Prevention to work with states to improve the availability and quality of data to more effectively respond to drug-addicted pregnant women. At this article’s deadline, the proposed act was in the Committee on Health, Education, Labor and Pensions.
"My legislation is no silver bullet, but it will help ensure that our public health system is better equipped to prevent and treat opiate addiction in mothers and their newborn children," Mr. McConnell said in a statement. "Together, we can overcome this tragic problem."
Developing resources that promote better medical care for addicted women and their children is a more effective answer than punitive laws, added Hendree Jones, Ph.D., a professor of obstetrics and gynecology at the university and executive director of the UNC Horizons programs. Horizons provides substance abuse treatment and child care to women who are pregnant or parenting young children.
"Incarcerating women to reduce the prevalence of drug use during pregnancy is a misguided solution to the issue," Dr. Jones said in an interview. "Increasing access to high-quality treatment would be a much more fruitful approach."
On Twitter @legal_med
The enactment of a Tennessee law that criminalizes substance abuse by pregnant women has made patients increasingly hesitant to pursue treatment for their drug addictions, according to Dr. Jessica Young, an obstetrician/gynecologist at Vanderbilt University Medical Center in Nashville, Tenn.
Tennessee’s law, which became effective in July, defines illegal narcotic use by pregnant women as assault, depending on whether the child is born addicted to or is harmed by the narcotic. A 26-year-old woman was among the first to be arrested in mid-July under the law.
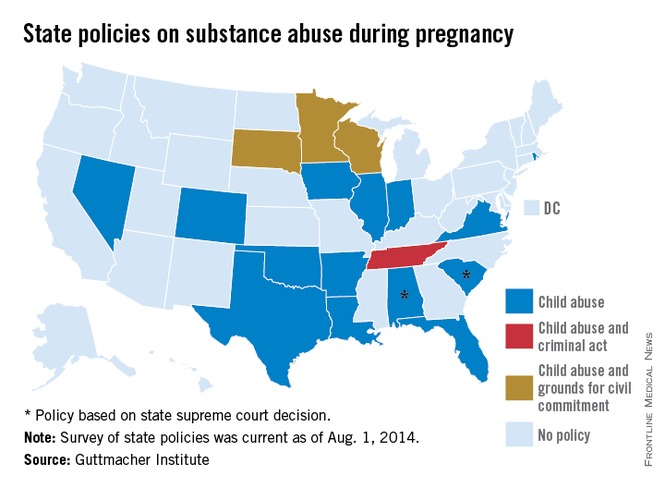
"Since the new law was passed, women . . . often express a fatalistic attitude of, ‘Even if I do the right thing, I will be arrested or have my baby taken away,’ " said Dr. Young, who leads the Vanderbilt Drug Dependency Clinic for pregnant women.
The concern is that women will hide their addictions or self-detox at home, she said. "I think it will require some negative outcomes for this law to be struck down."
Physician associations, including the American Medical Association and ACOG, have long maintained that criminal punishment is not the answer to curbing drug abuse by pregnant women and that such laws create further harm to children. Fear of being reported to police was a primary reason women who abused drugs did not seek prenatal care, a recent study found (Am. J. Obstet. Gynecol. 2009;200:412.e1-10).
Laws that mandate criminal penalties against pregnant women who use drugs can significantly harm the physician-patient relationship, according to Dr. John M. Thorp, professor of obstetrics and gynecology at the University of North Carolina and director of women’s primary health care for UNC Healthcare, both in Chapel Hill.
These laws "put the physician or the clinic or hospital in the role of reporting the crime, which is completely the antithesis of wanting patients to be able to tell physicians what’s wrong with them and being able to offer treatment instead of punishment," Dr. Thorp said in an interview. "These laws are a real setback to the concept that substance abuse addiction is a disease, [and they are] another barrier for women seeking treatment."
Tennessee is the only state to consider drug abuse by pregnant women to be "assault." The law states that a woman may be prosecuted for assault if her child is born addicted or harmed by the drug and for homicide if the child dies from drug exposure. It is an affirmative defense to prosecution if the woman is actively enrolled in an addiction recovery program before the baby is born, remains in the program after delivery, and successfully completes the program.
The American Civil Liberties Union of Tennessee plans to challenge the law in court.
The Tennessee Medical Association opposed the law, but successfully pushed for amendments that would lessen the punitive damages against women, Dave Chaney, TMA director of communications, said in an interview. The medical association successfully lobbied to lower the charging level in the bill to a misdemeanor and helped secure a stipulation that women who enter a treatment program be punished only by a fine.
Various states pursue criminal charges against pregnant women who use narcotics. Eighteen states consider substance abuse during pregnancy to be "child abuse," and three other states consider substance abuse during pregnancy to be grounds for civil commitment, according to an August 2014 analysis by the Guttmacher Institute. Fifteen states require physicians to report suspected prenatal drug abuse to authorities, and four states require health providers to test for prenatal drug exposure if they suspect substance abuse.
Other states could soon follow in Tennessee’s footsteps, Elizabeth Nash, Guttmacher Institute state issues manager, said in an interview. "Legislatures see what’s happening in other states and decide whether it may be right for them."
Meanwhile, a newly proposed federal bill could assist states in addressing the issue of drug-addicted pregnant mothers and babies and drive more effective responses to the crisis. The Protecting Our Infants Act, introduced July 31 by Rep. Mitch McConnell (R-Ky.), aims to better identify and treat opioid use by pregnant women and neonatal abstinence syndrome (NAS) in newborns. The legislation is backed by ACOG.
"Currently, states vary widely in how they mandate and administer screening, diagnosis, and treatment of pregnant women using opioids," ACOG President John C. Jennings said in a statement. The federal "legislation will help identify, compile, and disseminate best practices developed by medical professional organizations, including ACOG, and identify any gaps in best practices that may require additional research or analysis."
The proposed legislation would facilitate the research and dissemination of evidence-informed recommendations for addressing maternal addiction and NAS and provide for NAS studies. The measure also would encourage the Centers for Disease Control and Prevention to work with states to improve the availability and quality of data to more effectively respond to drug-addicted pregnant women. At this article’s deadline, the proposed act was in the Committee on Health, Education, Labor and Pensions.
"My legislation is no silver bullet, but it will help ensure that our public health system is better equipped to prevent and treat opiate addiction in mothers and their newborn children," Mr. McConnell said in a statement. "Together, we can overcome this tragic problem."
Developing resources that promote better medical care for addicted women and their children is a more effective answer than punitive laws, added Hendree Jones, Ph.D., a professor of obstetrics and gynecology at the university and executive director of the UNC Horizons programs. Horizons provides substance abuse treatment and child care to women who are pregnant or parenting young children.
"Incarcerating women to reduce the prevalence of drug use during pregnancy is a misguided solution to the issue," Dr. Jones said in an interview. "Increasing access to high-quality treatment would be a much more fruitful approach."
On Twitter @legal_med
The enactment of a Tennessee law that criminalizes substance abuse by pregnant women has made patients increasingly hesitant to pursue treatment for their drug addictions, according to Dr. Jessica Young, an obstetrician/gynecologist at Vanderbilt University Medical Center in Nashville, Tenn.
Tennessee’s law, which became effective in July, defines illegal narcotic use by pregnant women as assault, depending on whether the child is born addicted to or is harmed by the narcotic. A 26-year-old woman was among the first to be arrested in mid-July under the law.
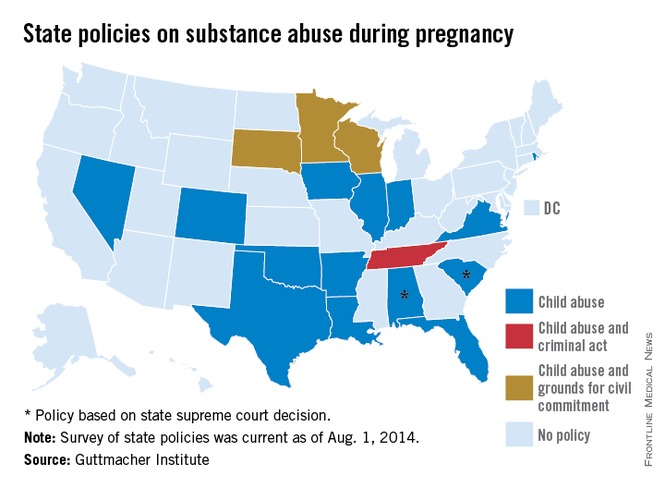
"Since the new law was passed, women . . . often express a fatalistic attitude of, ‘Even if I do the right thing, I will be arrested or have my baby taken away,’ " said Dr. Young, who leads the Vanderbilt Drug Dependency Clinic for pregnant women.
The concern is that women will hide their addictions or self-detox at home, she said. "I think it will require some negative outcomes for this law to be struck down."
Physician associations, including the American Medical Association and ACOG, have long maintained that criminal punishment is not the answer to curbing drug abuse by pregnant women and that such laws create further harm to children. Fear of being reported to police was a primary reason women who abused drugs did not seek prenatal care, a recent study found (Am. J. Obstet. Gynecol. 2009;200:412.e1-10).
Laws that mandate criminal penalties against pregnant women who use drugs can significantly harm the physician-patient relationship, according to Dr. John M. Thorp, professor of obstetrics and gynecology at the University of North Carolina and director of women’s primary health care for UNC Healthcare, both in Chapel Hill.
These laws "put the physician or the clinic or hospital in the role of reporting the crime, which is completely the antithesis of wanting patients to be able to tell physicians what’s wrong with them and being able to offer treatment instead of punishment," Dr. Thorp said in an interview. "These laws are a real setback to the concept that substance abuse addiction is a disease, [and they are] another barrier for women seeking treatment."
Tennessee is the only state to consider drug abuse by pregnant women to be "assault." The law states that a woman may be prosecuted for assault if her child is born addicted or harmed by the drug and for homicide if the child dies from drug exposure. It is an affirmative defense to prosecution if the woman is actively enrolled in an addiction recovery program before the baby is born, remains in the program after delivery, and successfully completes the program.
The American Civil Liberties Union of Tennessee plans to challenge the law in court.
The Tennessee Medical Association opposed the law, but successfully pushed for amendments that would lessen the punitive damages against women, Dave Chaney, TMA director of communications, said in an interview. The medical association successfully lobbied to lower the charging level in the bill to a misdemeanor and helped secure a stipulation that women who enter a treatment program be punished only by a fine.
Various states pursue criminal charges against pregnant women who use narcotics. Eighteen states consider substance abuse during pregnancy to be "child abuse," and three other states consider substance abuse during pregnancy to be grounds for civil commitment, according to an August 2014 analysis by the Guttmacher Institute. Fifteen states require physicians to report suspected prenatal drug abuse to authorities, and four states require health providers to test for prenatal drug exposure if they suspect substance abuse.
Other states could soon follow in Tennessee’s footsteps, Elizabeth Nash, Guttmacher Institute state issues manager, said in an interview. "Legislatures see what’s happening in other states and decide whether it may be right for them."
Meanwhile, a newly proposed federal bill could assist states in addressing the issue of drug-addicted pregnant mothers and babies and drive more effective responses to the crisis. The Protecting Our Infants Act, introduced July 31 by Rep. Mitch McConnell (R-Ky.), aims to better identify and treat opioid use by pregnant women and neonatal abstinence syndrome (NAS) in newborns. The legislation is backed by ACOG.
"Currently, states vary widely in how they mandate and administer screening, diagnosis, and treatment of pregnant women using opioids," ACOG President John C. Jennings said in a statement. The federal "legislation will help identify, compile, and disseminate best practices developed by medical professional organizations, including ACOG, and identify any gaps in best practices that may require additional research or analysis."
The proposed legislation would facilitate the research and dissemination of evidence-informed recommendations for addressing maternal addiction and NAS and provide for NAS studies. The measure also would encourage the Centers for Disease Control and Prevention to work with states to improve the availability and quality of data to more effectively respond to drug-addicted pregnant women. At this article’s deadline, the proposed act was in the Committee on Health, Education, Labor and Pensions.
"My legislation is no silver bullet, but it will help ensure that our public health system is better equipped to prevent and treat opiate addiction in mothers and their newborn children," Mr. McConnell said in a statement. "Together, we can overcome this tragic problem."
Developing resources that promote better medical care for addicted women and their children is a more effective answer than punitive laws, added Hendree Jones, Ph.D., a professor of obstetrics and gynecology at the university and executive director of the UNC Horizons programs. Horizons provides substance abuse treatment and child care to women who are pregnant or parenting young children.
"Incarcerating women to reduce the prevalence of drug use during pregnancy is a misguided solution to the issue," Dr. Jones said in an interview. "Increasing access to high-quality treatment would be a much more fruitful approach."
On Twitter @legal_med
Malpractice caps in flux in Florida
Less than 4 months after the Florida Supreme Court struck down the state’s wrongful death noneconomic damages cap, the fate of the state’s personal injury medical malpractice award limit may also be in jeopardy.
The state’s highest court heard oral arguments in June regarding Myles et al. v. Weingrad, an injury malpractice case that focuses on whether Florida’s $500,000 medical malpractice noneconomic damages cap can be applied retroactively. However, after the court in March ruled that the state’s wrongful death cap was unconstitutional, the plaintiffs in Weingrad now argue the injury limit should be thrown out on constitutional grounds.
The personal injury malpractice cap is indeed in danger of being overturned, said Jeff Scott, general counsel for the Florida Medical Association. The FMA is not directly involved in the case.
"Given the track record of the (Florida) Supreme Court, one would have to conclude the likelihood of a favorable opinion is slim," Mr. Scott said in an interview.
The case stems from leg surgery performed on Kimberly Ann Miles by Aventura, Fla.–based surgeon Dr. Daniel Weingrad. Ms. Miles claimed the surgery to remove residual melanoma was unnecessary and resulted in ongoing pain. A jury awarded Ms. Miles and her husband $1.5 million in noneconomic damages and $16,000 in economic damages.
Dr. Weingrad requested that the trial court reduce the noneconomic damages award to $500,000 in accordance with the state’s cap, enacted in 2003. The plaintiffs argued the statute was implemented after the alleged negligence occurred and should not apply. An appeals court ruled in favor of Dr. Weingrad, and the plaintiffs appealed to the Florida Supreme Court.
Before Florida Supreme Court justices heard the case however, they reviewed McCall v. United States in which they overturned the state’s $1 million wrongful death damages cap. The award limit violated plaintiffs’ equal protection rights, judges said. In the months following the decision, plaintiffs’ attorneys have tried to get the injury award limit struck down by citing language in McCall, said Dinah S. Stein, a malpractice defense attorney who represents Dr. Weingrad.
"The plaintiffs’ bar has become fired up about" the McCall ruling, she said. "It’s our job to explain to the courts it’s not as far reaching as the plaintiffs’ bar would like them to think. (McCall) is limited. It doesn’t apply here; it’s prospective only and only applies to per-claim caps."
In Weingrad, the state Supreme Court has the option of ruling on the injury cap’s constitutionality or deciding only whether the limit can be applied retroactively. Other state courts faced with cap retroactivity questions have declined to immediately address constitutional issues. The Missouri Supreme Court for instance, in 2010 ruled that the state’s noneconomic damages cap in medical malpractices cases could not be applied retroactively in Klotz v. St. Anthonys Medical Center.
"The Supreme Court’s opinion was very limited, and they never addressed the overriding issues of the general constitutionality of caps," said J. Thaddeus Eckenrode, a malpractice defense attorney who represented the defendant in the Missouri case. "To that extent, it was surprising, although I think many people thought the court would rule against the use of the caps. All the court held was that in this particular case, since the plaintiff’s cause of action accrued before the new cap law went into effect, that law could not be applied to his case."
However, the same court held in 2012 that Missouri’s noneconomic damages cap violated a plaintiff’s right to a jury trial and overturned the award limit. Other noneconomic damages caps have faced similar challenges recently. The Georgia Supreme Court in 2010 found unconstitutional the state’s $350,000 cap. A proposed ballot measure in California aims to quadruple that state’s $250,000 cap.
Significant conflicts among court precedents exist across the country about the constitutionality of lawsuit award limits, Mr. Eckenrode said.
"Nearly any state’s highest court can find support for their decision to either uphold or throw out caps," he said in an e-mail. "As you examine the notion of caps around the country, you’ll find a relatively even split of states with caps in place and states that have thrown them out. It seems to be a political hotbed issue and, depending on the philosophical leaning of any state’s legislature and/or Supreme Court, one can take a pretty educated guess as to what the immediate future holds for caps in a given state."
On Twitter @legal_med
Less than 4 months after the Florida Supreme Court struck down the state’s wrongful death noneconomic damages cap, the fate of the state’s personal injury medical malpractice award limit may also be in jeopardy.
The state’s highest court heard oral arguments in June regarding Myles et al. v. Weingrad, an injury malpractice case that focuses on whether Florida’s $500,000 medical malpractice noneconomic damages cap can be applied retroactively. However, after the court in March ruled that the state’s wrongful death cap was unconstitutional, the plaintiffs in Weingrad now argue the injury limit should be thrown out on constitutional grounds.
The personal injury malpractice cap is indeed in danger of being overturned, said Jeff Scott, general counsel for the Florida Medical Association. The FMA is not directly involved in the case.
"Given the track record of the (Florida) Supreme Court, one would have to conclude the likelihood of a favorable opinion is slim," Mr. Scott said in an interview.
The case stems from leg surgery performed on Kimberly Ann Miles by Aventura, Fla.–based surgeon Dr. Daniel Weingrad. Ms. Miles claimed the surgery to remove residual melanoma was unnecessary and resulted in ongoing pain. A jury awarded Ms. Miles and her husband $1.5 million in noneconomic damages and $16,000 in economic damages.
Dr. Weingrad requested that the trial court reduce the noneconomic damages award to $500,000 in accordance with the state’s cap, enacted in 2003. The plaintiffs argued the statute was implemented after the alleged negligence occurred and should not apply. An appeals court ruled in favor of Dr. Weingrad, and the plaintiffs appealed to the Florida Supreme Court.
Before Florida Supreme Court justices heard the case however, they reviewed McCall v. United States in which they overturned the state’s $1 million wrongful death damages cap. The award limit violated plaintiffs’ equal protection rights, judges said. In the months following the decision, plaintiffs’ attorneys have tried to get the injury award limit struck down by citing language in McCall, said Dinah S. Stein, a malpractice defense attorney who represents Dr. Weingrad.
"The plaintiffs’ bar has become fired up about" the McCall ruling, she said. "It’s our job to explain to the courts it’s not as far reaching as the plaintiffs’ bar would like them to think. (McCall) is limited. It doesn’t apply here; it’s prospective only and only applies to per-claim caps."
In Weingrad, the state Supreme Court has the option of ruling on the injury cap’s constitutionality or deciding only whether the limit can be applied retroactively. Other state courts faced with cap retroactivity questions have declined to immediately address constitutional issues. The Missouri Supreme Court for instance, in 2010 ruled that the state’s noneconomic damages cap in medical malpractices cases could not be applied retroactively in Klotz v. St. Anthonys Medical Center.
"The Supreme Court’s opinion was very limited, and they never addressed the overriding issues of the general constitutionality of caps," said J. Thaddeus Eckenrode, a malpractice defense attorney who represented the defendant in the Missouri case. "To that extent, it was surprising, although I think many people thought the court would rule against the use of the caps. All the court held was that in this particular case, since the plaintiff’s cause of action accrued before the new cap law went into effect, that law could not be applied to his case."
However, the same court held in 2012 that Missouri’s noneconomic damages cap violated a plaintiff’s right to a jury trial and overturned the award limit. Other noneconomic damages caps have faced similar challenges recently. The Georgia Supreme Court in 2010 found unconstitutional the state’s $350,000 cap. A proposed ballot measure in California aims to quadruple that state’s $250,000 cap.
Significant conflicts among court precedents exist across the country about the constitutionality of lawsuit award limits, Mr. Eckenrode said.
"Nearly any state’s highest court can find support for their decision to either uphold or throw out caps," he said in an e-mail. "As you examine the notion of caps around the country, you’ll find a relatively even split of states with caps in place and states that have thrown them out. It seems to be a political hotbed issue and, depending on the philosophical leaning of any state’s legislature and/or Supreme Court, one can take a pretty educated guess as to what the immediate future holds for caps in a given state."
On Twitter @legal_med
Less than 4 months after the Florida Supreme Court struck down the state’s wrongful death noneconomic damages cap, the fate of the state’s personal injury medical malpractice award limit may also be in jeopardy.
The state’s highest court heard oral arguments in June regarding Myles et al. v. Weingrad, an injury malpractice case that focuses on whether Florida’s $500,000 medical malpractice noneconomic damages cap can be applied retroactively. However, after the court in March ruled that the state’s wrongful death cap was unconstitutional, the plaintiffs in Weingrad now argue the injury limit should be thrown out on constitutional grounds.
The personal injury malpractice cap is indeed in danger of being overturned, said Jeff Scott, general counsel for the Florida Medical Association. The FMA is not directly involved in the case.
"Given the track record of the (Florida) Supreme Court, one would have to conclude the likelihood of a favorable opinion is slim," Mr. Scott said in an interview.
The case stems from leg surgery performed on Kimberly Ann Miles by Aventura, Fla.–based surgeon Dr. Daniel Weingrad. Ms. Miles claimed the surgery to remove residual melanoma was unnecessary and resulted in ongoing pain. A jury awarded Ms. Miles and her husband $1.5 million in noneconomic damages and $16,000 in economic damages.
Dr. Weingrad requested that the trial court reduce the noneconomic damages award to $500,000 in accordance with the state’s cap, enacted in 2003. The plaintiffs argued the statute was implemented after the alleged negligence occurred and should not apply. An appeals court ruled in favor of Dr. Weingrad, and the plaintiffs appealed to the Florida Supreme Court.
Before Florida Supreme Court justices heard the case however, they reviewed McCall v. United States in which they overturned the state’s $1 million wrongful death damages cap. The award limit violated plaintiffs’ equal protection rights, judges said. In the months following the decision, plaintiffs’ attorneys have tried to get the injury award limit struck down by citing language in McCall, said Dinah S. Stein, a malpractice defense attorney who represents Dr. Weingrad.
"The plaintiffs’ bar has become fired up about" the McCall ruling, she said. "It’s our job to explain to the courts it’s not as far reaching as the plaintiffs’ bar would like them to think. (McCall) is limited. It doesn’t apply here; it’s prospective only and only applies to per-claim caps."
In Weingrad, the state Supreme Court has the option of ruling on the injury cap’s constitutionality or deciding only whether the limit can be applied retroactively. Other state courts faced with cap retroactivity questions have declined to immediately address constitutional issues. The Missouri Supreme Court for instance, in 2010 ruled that the state’s noneconomic damages cap in medical malpractices cases could not be applied retroactively in Klotz v. St. Anthonys Medical Center.
"The Supreme Court’s opinion was very limited, and they never addressed the overriding issues of the general constitutionality of caps," said J. Thaddeus Eckenrode, a malpractice defense attorney who represented the defendant in the Missouri case. "To that extent, it was surprising, although I think many people thought the court would rule against the use of the caps. All the court held was that in this particular case, since the plaintiff’s cause of action accrued before the new cap law went into effect, that law could not be applied to his case."
However, the same court held in 2012 that Missouri’s noneconomic damages cap violated a plaintiff’s right to a jury trial and overturned the award limit. Other noneconomic damages caps have faced similar challenges recently. The Georgia Supreme Court in 2010 found unconstitutional the state’s $350,000 cap. A proposed ballot measure in California aims to quadruple that state’s $250,000 cap.
Significant conflicts among court precedents exist across the country about the constitutionality of lawsuit award limits, Mr. Eckenrode said.
"Nearly any state’s highest court can find support for their decision to either uphold or throw out caps," he said in an e-mail. "As you examine the notion of caps around the country, you’ll find a relatively even split of states with caps in place and states that have thrown them out. It seems to be a political hotbed issue and, depending on the philosophical leaning of any state’s legislature and/or Supreme Court, one can take a pretty educated guess as to what the immediate future holds for caps in a given state."
On Twitter @legal_med
Better access to primary care proposed to cut nonurgent ED visits
A weak tie to a regular physician was seen in Medicaid patients who were high users of emergency departments, according to a recent analysis by the Medicaid and CHIP Payment and Access Commission.
"Expanding the availability of primary care could lead to more efficient use of the ED," a new report by MACPAC states. "However, ED use is likely to remain relatively high in Medicaid until new delivery models are in place to address the needs of frequent users."
The report, released July 31, estimates that nonurgent care accounts for 10% of all Medicaid-covered ED visits for nonelderly patients, a rate that is comparable with the one seen among privately insured patients.
Nearly all Medicaid enrollees report having a usual place of care other than the ED. Approximately one-third of adult and 13% of child enrollees have reported barriers to finding a doctor or delays in getting needed care, MACPAC’s research found. "Medicaid enrollees who report more primary care barriers are more likely to report ED use."
The analysis suggests that frequent ED use could be avoided with better access to primary care. "Some frequent ED users appear to receive inadequate primary or specialty care (while others use those services frequently). Among Medicaid enrollees with 10 or more ED visits in 1 year (who accounted for 12% of all ED visits), about half had weak ties to a regular physician."
Another factor is primary care physicians referring their patients to emergency departments because of the ability to rapidly utilize diagnostics. There has been "a sharp decline in direct admissions to the hospital by office-based physicians and an even sharper increase in the number of submissions through the ED: now, almost one-half of all nonelective admissions go through the ED," the report states
States have pursued a variety of paths to reduce ED visits, including diverting patients with complaints deemed to be nonemergencies to lower-cost settings, charging copayments for so-called nonemergency ED use, and focusing those considered "super utilizers" to other settings. The results of those initiatives have been mixed.
"Given Medicaid’s historically low reimbursement rates, the shortage of primary care physicians accepting these patients isn't surprising," Dr. Alex Rosenau, president of the American College of Emergency Physicians, said in a statement, adding that "efforts to deny payment for Medicaid visits to emergency departments are dangerous and wrong."
A weak tie to a regular physician was seen in Medicaid patients who were high users of emergency departments, according to a recent analysis by the Medicaid and CHIP Payment and Access Commission.
"Expanding the availability of primary care could lead to more efficient use of the ED," a new report by MACPAC states. "However, ED use is likely to remain relatively high in Medicaid until new delivery models are in place to address the needs of frequent users."
The report, released July 31, estimates that nonurgent care accounts for 10% of all Medicaid-covered ED visits for nonelderly patients, a rate that is comparable with the one seen among privately insured patients.
Nearly all Medicaid enrollees report having a usual place of care other than the ED. Approximately one-third of adult and 13% of child enrollees have reported barriers to finding a doctor or delays in getting needed care, MACPAC’s research found. "Medicaid enrollees who report more primary care barriers are more likely to report ED use."
The analysis suggests that frequent ED use could be avoided with better access to primary care. "Some frequent ED users appear to receive inadequate primary or specialty care (while others use those services frequently). Among Medicaid enrollees with 10 or more ED visits in 1 year (who accounted for 12% of all ED visits), about half had weak ties to a regular physician."
Another factor is primary care physicians referring their patients to emergency departments because of the ability to rapidly utilize diagnostics. There has been "a sharp decline in direct admissions to the hospital by office-based physicians and an even sharper increase in the number of submissions through the ED: now, almost one-half of all nonelective admissions go through the ED," the report states
States have pursued a variety of paths to reduce ED visits, including diverting patients with complaints deemed to be nonemergencies to lower-cost settings, charging copayments for so-called nonemergency ED use, and focusing those considered "super utilizers" to other settings. The results of those initiatives have been mixed.
"Given Medicaid’s historically low reimbursement rates, the shortage of primary care physicians accepting these patients isn't surprising," Dr. Alex Rosenau, president of the American College of Emergency Physicians, said in a statement, adding that "efforts to deny payment for Medicaid visits to emergency departments are dangerous and wrong."
A weak tie to a regular physician was seen in Medicaid patients who were high users of emergency departments, according to a recent analysis by the Medicaid and CHIP Payment and Access Commission.
"Expanding the availability of primary care could lead to more efficient use of the ED," a new report by MACPAC states. "However, ED use is likely to remain relatively high in Medicaid until new delivery models are in place to address the needs of frequent users."
The report, released July 31, estimates that nonurgent care accounts for 10% of all Medicaid-covered ED visits for nonelderly patients, a rate that is comparable with the one seen among privately insured patients.
Nearly all Medicaid enrollees report having a usual place of care other than the ED. Approximately one-third of adult and 13% of child enrollees have reported barriers to finding a doctor or delays in getting needed care, MACPAC’s research found. "Medicaid enrollees who report more primary care barriers are more likely to report ED use."
The analysis suggests that frequent ED use could be avoided with better access to primary care. "Some frequent ED users appear to receive inadequate primary or specialty care (while others use those services frequently). Among Medicaid enrollees with 10 or more ED visits in 1 year (who accounted for 12% of all ED visits), about half had weak ties to a regular physician."
Another factor is primary care physicians referring their patients to emergency departments because of the ability to rapidly utilize diagnostics. There has been "a sharp decline in direct admissions to the hospital by office-based physicians and an even sharper increase in the number of submissions through the ED: now, almost one-half of all nonelective admissions go through the ED," the report states
States have pursued a variety of paths to reduce ED visits, including diverting patients with complaints deemed to be nonemergencies to lower-cost settings, charging copayments for so-called nonemergency ED use, and focusing those considered "super utilizers" to other settings. The results of those initiatives have been mixed.
"Given Medicaid’s historically low reimbursement rates, the shortage of primary care physicians accepting these patients isn't surprising," Dr. Alex Rosenau, president of the American College of Emergency Physicians, said in a statement, adding that "efforts to deny payment for Medicaid visits to emergency departments are dangerous and wrong."
Know your risks when selling your practice
CHICAGO – Legal pitfalls lie along the path of transitioning from an independent practice to hospital employment, an accountable care organization, a medical home, or a merger to build a multispecialty group practice, legal experts warned at a physicians’ legal issues conference held by the American Bar Association.
"As a seller, you need to know what you’re getting into when you’re selling" your practice, said Hal Katz, an attorney in Austin, Tex. "Due diligence for you is just as important as it is for the buyer. The business structure you move into is going to be something you’re going to have to live with for the long term. You want to make sure it’s a good fit."
At the due-diligence stage, doctors partnering with another entity should ensure that they review a number of critical records from the other organization, such as corporate records, financial information, payer contracts, and real estate information, he said. Additionally, physician sellers should be aware of any litigation against their future partner and be knowledgeable about their affiliated entities and financial relationships.
Financial troubles or issues with federal regulation compliance are possible red flags for physician sellers. Examples include overpayments, repayments, audits, investigations, subpoenas or corporate integrity agreements.
Medicare providers changing ownership must inform federal authorities. A change of ownership (CHOW) generally happens when a Medicare provider is being purchased or leased by another entity. The CHOW results in the transfer of the former owner’s Medicare identification number and provider agreement to the new owner.
Adequately valuing the practice is another essential – albeit complex – process for physician sellers, Clinton Flome said at the ABA conference.
"Understanding price, understanding value, and most importantly understanding what physicians’ compensation is going to be going forward," are crucial, said Mr. Flome, senior manager at VMG Health in Dallas, a business valuation company. Knowing those criteria is "going to determine whether you have available" funds.
The three primary practice valuation methods include income, asset, and market approaches. The income approach examines historical financial and production information to estimate the future level of cash flows, Mr. Flome said. The asset approach takes into consideration the cost of replicating a comparable asset, security, or service with the same level of utility. The market approach estimates value by comparing the value of similar assets, securities, or services traded in a free and open market and the subject asset, security, or service.
"Everybody (should) be on the same page as to what the transaction is going to look like," Mr. Flome said. "Is this a 100% asset transaction or are you looking at some other alternatives?"
On Twitter @legal_med
CHICAGO – Legal pitfalls lie along the path of transitioning from an independent practice to hospital employment, an accountable care organization, a medical home, or a merger to build a multispecialty group practice, legal experts warned at a physicians’ legal issues conference held by the American Bar Association.
"As a seller, you need to know what you’re getting into when you’re selling" your practice, said Hal Katz, an attorney in Austin, Tex. "Due diligence for you is just as important as it is for the buyer. The business structure you move into is going to be something you’re going to have to live with for the long term. You want to make sure it’s a good fit."
At the due-diligence stage, doctors partnering with another entity should ensure that they review a number of critical records from the other organization, such as corporate records, financial information, payer contracts, and real estate information, he said. Additionally, physician sellers should be aware of any litigation against their future partner and be knowledgeable about their affiliated entities and financial relationships.
Financial troubles or issues with federal regulation compliance are possible red flags for physician sellers. Examples include overpayments, repayments, audits, investigations, subpoenas or corporate integrity agreements.
Medicare providers changing ownership must inform federal authorities. A change of ownership (CHOW) generally happens when a Medicare provider is being purchased or leased by another entity. The CHOW results in the transfer of the former owner’s Medicare identification number and provider agreement to the new owner.
Adequately valuing the practice is another essential – albeit complex – process for physician sellers, Clinton Flome said at the ABA conference.
"Understanding price, understanding value, and most importantly understanding what physicians’ compensation is going to be going forward," are crucial, said Mr. Flome, senior manager at VMG Health in Dallas, a business valuation company. Knowing those criteria is "going to determine whether you have available" funds.
The three primary practice valuation methods include income, asset, and market approaches. The income approach examines historical financial and production information to estimate the future level of cash flows, Mr. Flome said. The asset approach takes into consideration the cost of replicating a comparable asset, security, or service with the same level of utility. The market approach estimates value by comparing the value of similar assets, securities, or services traded in a free and open market and the subject asset, security, or service.
"Everybody (should) be on the same page as to what the transaction is going to look like," Mr. Flome said. "Is this a 100% asset transaction or are you looking at some other alternatives?"
On Twitter @legal_med
CHICAGO – Legal pitfalls lie along the path of transitioning from an independent practice to hospital employment, an accountable care organization, a medical home, or a merger to build a multispecialty group practice, legal experts warned at a physicians’ legal issues conference held by the American Bar Association.
"As a seller, you need to know what you’re getting into when you’re selling" your practice, said Hal Katz, an attorney in Austin, Tex. "Due diligence for you is just as important as it is for the buyer. The business structure you move into is going to be something you’re going to have to live with for the long term. You want to make sure it’s a good fit."
At the due-diligence stage, doctors partnering with another entity should ensure that they review a number of critical records from the other organization, such as corporate records, financial information, payer contracts, and real estate information, he said. Additionally, physician sellers should be aware of any litigation against their future partner and be knowledgeable about their affiliated entities and financial relationships.
Financial troubles or issues with federal regulation compliance are possible red flags for physician sellers. Examples include overpayments, repayments, audits, investigations, subpoenas or corporate integrity agreements.
Medicare providers changing ownership must inform federal authorities. A change of ownership (CHOW) generally happens when a Medicare provider is being purchased or leased by another entity. The CHOW results in the transfer of the former owner’s Medicare identification number and provider agreement to the new owner.
Adequately valuing the practice is another essential – albeit complex – process for physician sellers, Clinton Flome said at the ABA conference.
"Understanding price, understanding value, and most importantly understanding what physicians’ compensation is going to be going forward," are crucial, said Mr. Flome, senior manager at VMG Health in Dallas, a business valuation company. Knowing those criteria is "going to determine whether you have available" funds.
The three primary practice valuation methods include income, asset, and market approaches. The income approach examines historical financial and production information to estimate the future level of cash flows, Mr. Flome said. The asset approach takes into consideration the cost of replicating a comparable asset, security, or service with the same level of utility. The market approach estimates value by comparing the value of similar assets, securities, or services traded in a free and open market and the subject asset, security, or service.
"Everybody (should) be on the same page as to what the transaction is going to look like," Mr. Flome said. "Is this a 100% asset transaction or are you looking at some other alternatives?"
On Twitter @legal_med
EXPERT ANALYSIS AT AN ABA CONFERENCE
Huge chunk of data excluded from Open Payments website
When the government publishes information on the financial relationships between physicians, teaching hospitals, and the pharmaceutical and device industries on Sept. 30 as part of the Open Payments Program, about one-third of the available payment data will be missing.
Officials at the Centers for Medicare & Medicaid Services recently confirmed that they are returning about one-third of the payment records already submitted by manufacturers and group purchasing organizations (GPOs) because of problems of "intermingled data." Those records will be included in the next public data release, scheduled for June 2015. The CMS did not provide information on the exact number of records that were being sent back for corrections.
Delaying the release of these records will allow manufacturers and GPOs to make corrections and give physicians and teaching hospitals time to review and dispute the data, according to the CMS.
But the American Medical Association said that doubts about the accuracy of one-third of the data being reported to the Open Payments system is a clear sign that more time is needed to revamp the program.
"The publication of inaccurate data can potentially harm the physician-patient relationship, which is why the AMA maintains its call for a 6-month delay of the data release," Dr. Robert M. Wah, AMA president, said in a statement.
The AMA, along with about 100 other state medical and specialty societies, has been on CMS officials to delay the start of the program, not only because of data accuracy issues, but because the registration and review processes have been confusing and time consuming.
The Open Payments program, which was mandated under the Affordable Care Act, has had a rocky rollout so far. The CMS was forced to delay the period for teaching hospitals and physicians to review and dispute payments after receiving reports that payment data were being attributed to the wrong physicians. The agency took the system offline for almost 2 weeks in early August to investigate the problems and implement fixes.
The CMS extended the deadline for physician and teaching hospitals to review and dispute data from Aug. 27 to Sept. 8, but is sticking to its plan to publish the first round of payment data on Sept. 30.
On Twitter @maryellenny
When the government publishes information on the financial relationships between physicians, teaching hospitals, and the pharmaceutical and device industries on Sept. 30 as part of the Open Payments Program, about one-third of the available payment data will be missing.
Officials at the Centers for Medicare & Medicaid Services recently confirmed that they are returning about one-third of the payment records already submitted by manufacturers and group purchasing organizations (GPOs) because of problems of "intermingled data." Those records will be included in the next public data release, scheduled for June 2015. The CMS did not provide information on the exact number of records that were being sent back for corrections.
Delaying the release of these records will allow manufacturers and GPOs to make corrections and give physicians and teaching hospitals time to review and dispute the data, according to the CMS.
But the American Medical Association said that doubts about the accuracy of one-third of the data being reported to the Open Payments system is a clear sign that more time is needed to revamp the program.
"The publication of inaccurate data can potentially harm the physician-patient relationship, which is why the AMA maintains its call for a 6-month delay of the data release," Dr. Robert M. Wah, AMA president, said in a statement.
The AMA, along with about 100 other state medical and specialty societies, has been on CMS officials to delay the start of the program, not only because of data accuracy issues, but because the registration and review processes have been confusing and time consuming.
The Open Payments program, which was mandated under the Affordable Care Act, has had a rocky rollout so far. The CMS was forced to delay the period for teaching hospitals and physicians to review and dispute payments after receiving reports that payment data were being attributed to the wrong physicians. The agency took the system offline for almost 2 weeks in early August to investigate the problems and implement fixes.
The CMS extended the deadline for physician and teaching hospitals to review and dispute data from Aug. 27 to Sept. 8, but is sticking to its plan to publish the first round of payment data on Sept. 30.
On Twitter @maryellenny
When the government publishes information on the financial relationships between physicians, teaching hospitals, and the pharmaceutical and device industries on Sept. 30 as part of the Open Payments Program, about one-third of the available payment data will be missing.
Officials at the Centers for Medicare & Medicaid Services recently confirmed that they are returning about one-third of the payment records already submitted by manufacturers and group purchasing organizations (GPOs) because of problems of "intermingled data." Those records will be included in the next public data release, scheduled for June 2015. The CMS did not provide information on the exact number of records that were being sent back for corrections.
Delaying the release of these records will allow manufacturers and GPOs to make corrections and give physicians and teaching hospitals time to review and dispute the data, according to the CMS.
But the American Medical Association said that doubts about the accuracy of one-third of the data being reported to the Open Payments system is a clear sign that more time is needed to revamp the program.
"The publication of inaccurate data can potentially harm the physician-patient relationship, which is why the AMA maintains its call for a 6-month delay of the data release," Dr. Robert M. Wah, AMA president, said in a statement.
The AMA, along with about 100 other state medical and specialty societies, has been on CMS officials to delay the start of the program, not only because of data accuracy issues, but because the registration and review processes have been confusing and time consuming.
The Open Payments program, which was mandated under the Affordable Care Act, has had a rocky rollout so far. The CMS was forced to delay the period for teaching hospitals and physicians to review and dispute payments after receiving reports that payment data were being attributed to the wrong physicians. The agency took the system offline for almost 2 weeks in early August to investigate the problems and implement fixes.
The CMS extended the deadline for physician and teaching hospitals to review and dispute data from Aug. 27 to Sept. 8, but is sticking to its plan to publish the first round of payment data on Sept. 30.
On Twitter @maryellenny