User login
Current Controversies in Mohs Micrographic Surgery
Mohs micrographic surgery (MMS) has been met with controversy since its inception in the 1930s. Current debate centers on the types of tumors treated with MMS, increasing utilization, third-party payer reimbursement, the Appropriate Use Criteria (AUC), and subspecialty certification.
Controversies in Applications
Controversy surrounding treatment with MMS for certain tumor types is abundant, in large part due to a lack of well-designed studies. Perhaps most notably, the surgical management of melanoma has been hotly contested for decades.1 An increasing number of Mohs surgeons advocate the use of MMS for treatment of melanoma. Advocates reason that tumor margins may be ill-defined, necessitating histologic examination of the margin for tumor clearance. In a study by Zitelli et al,2 5-year survival and metastatic rates for 535 patients with melanomas treated by MMS with frozen sections were the same or better when compared to historical controls treated with conventional wide local excision. Melanoma-associated antigen recognized by T cells (MART-1) immunostaining may offer improved diagnostic accuracy.3 Others believe that staged excision with permanent sections processed vertically, en face, or horizontally (“slow Mohs”) is more accurate and efficacious for the treatment of melanoma.1 Advocates of this approach maintain that when compared to MMS with frozen sections, staged excision with permanent sections enables more accurate interpretation of residual melanoma and atypical junctional melanocytic hyperplasia as well as circumvents difficulty in interpreting freeze artifact.4
Although Merkel cell carcinoma has traditionally been treated with wide local excision, MMS with or without adjuvant radiotherapy has gained traction as a treatment option. Advocates for treatment by MMS hold that Merkel cell carcinoma is a contiguous tumor with a high rate of residual tumor persistence, making histologic margin control an ideal characteristic of treatment. However, in the absence of large randomized controlled studies comparing MMS to wide local excision, controversy surrounds the most appropriate surgical approach.1 In a retrospective study of 86 patients by O’Connor et al,5 MMS was demonstrated to compare favorably to standard surgical excision. Standard surgical excision was associated with a 31.7% (13/41) local persistence rate and 48.8% (20/41) regional metastasis rate compared to 8.3% (1/12) and 33.3% (4/12) for MMS, respectively.5
Controversies in Increasing Utilization
The incidence of skin cancers has increased in recent years. As a result, it is reasonable to expect the rates of MMS to increase. Nonetheless, there is escalating concern among groups of third-party payers, the public, and physicians that MMS is being overused.6 Growth of the body of evidence supporting the appropriateness of MMS remains essential. Such studies continue to support reasons for increased MMS usage, demonstrating the stability of the percentage of skin cancers treated with MMS in the setting of increasing skin cancer incidence, the procedure’s superior efficacy for appropriately chosen cases, its expanding application to melanoma and other tumors, and an emphasis of MMS in residency training programs.6-9
A current hot topic of controversy focuses on the wide variation among Mohs surgeons in the mean number of stages used to resect a tumor. Overuse among outliers has been proposed to stem from lack of technical expertise or from abuse of the current fee-for-service payment model, which bases compensation on the number of stages performed. A study by Krishnan et al10 determined that the mean number of stages per tumor in the studied population (all physicians [N=2305] receiving Medicare payments for MMS from January 2012 to December 2014) was 1.74, with a range of 1.09 to 4.11. Persistently high outliers were more likely to perform MMS in a solo practice, with an odds ratio of 2.35.10 In response to the wide variation in mean stages used to resect a skin cancer and its implications on increased financial burden and surgery to individual patients, intervention has been proposed. Notably, it has been demonstrated that mailing out individual reports of practice patterns to high-outlier physicians resulted in a reduction in mean stages per tumor as well as an associated cost savings when compared to outlier physicians who did not receive these reports.11
Controversies in Reimbursement
Mohs micrographic surgery also has been in the spotlight for debate regarding reimbursement. The procedure has been targeted partly in response to its substantial contribution to total Medicare reimbursements paid out. In 2013, primary MMS billing codes constituted nearly 19% of total reimbursements to dermatologists and approximately 0.5% of total reimbursements to all physicians participating in Medicare.12 Mohs micrographic surgery codes have correspondingly received frequent review by the Relative Value Scale Update Committee and remained on a list of potentially misvalued services according to the Centers for Medicare & Medicaid Services for years.13 Due to continued scrutiny and review, especially by the Relative Value Scale Update Committee and Centers for Medicare & Medicaid Services, reimbursement to perform MMS and reconstructive surgery has gone down by more than 20% in the last 15 years.14 Public perception mirrors third-party payer concerns for overcompensation. An article title in the New York Times theatrically postures “Patients’ Costs Skyrocket, Specialists’ Incomes Soar.” The article recounts an MMS patient’s “outrage at charges” associated with treatment of her “minor medical problem” and the simultaneous “sharp climb” in dermatologist income over the last 2 decades.15
However, studies continue to demonstrate the cost-effectiveness of MMS. A study by Ravitskiy et al16 demonstrates the cost-effectiveness of MMS, regardless of place of service or type of tumor. Of 406 tumors studied, MMS was the least expensive surgical procedure evaluated ($805 per tumor) when compared to standard surgical excision with permanent margins ($1026 per tumor), standard surgical excision with frozen margins ($1200 per tumor), and ambulatory surgery center standard surgical excision ($2507 per tumor). Furthermore, adjusted for inflation, the cost of MMS was lower in 2009 vs 1998.16 Similar results have been consistently demonstrated.17
Controversies in the AUC
To provide clinicians, policy makers, and insurers guidance for utilization of MMS in the setting of concerns for overutilization, overcompensation, and inappropriate application, the MMS AUC were established in 2012. The guidelines were developed by a process integrating evidence-based medicine, clinical experience, and expert opinion and is applicable to 270 clinical scenarios.18
A unique set of debate accompanies the guidelines. Namely, controversy has surrounded the classification of most primary superficial basal cell carcinomas as appropriate for treatment by MMS. These tumors have comparable cure rates when treated by MMS or curettage and cryosurgery, are often multifocal and require more Mohs stages than other basal cell carcinoma subtypes, and largely lack data on recurrence and invasion.19 The guidelines also have been scrutinized for including only studies from the United States.20 Furthermore, the report is largely based on expert opinion rather than evidence.
Some Mohs surgeons have concerns that the guidelines will minimize clinical judgment. Nonetheless, deviations from the AUC practiced by Mohs surgeons have been reported where clinical judgment supplants guideline criteria. The most commonly cited reasons for performing MMS on tumors classified as uncertain or inappropriate, according to one study by Ruiz et al,21 included performing multiple MMSs on the same day, tumor location on the lower legs, and incorporation into an adjacent wound. Reported discrepancies in the AUC further emphasize the importance of clinical judgment and call into question the need for future revision of the criteria.22 For example, a primary squamous cell carcinoma in situ greater than or equal to 2 cm located on the trunk and extremities (excluding pretibial surfaces, hands, feet, nail units, and ankles) in a healthy patient is categorized as appropriate, while a recurrent but otherwise identical squamous cell carcinoma in situ is categorized as uncertain. These counterintuitive criteria are unsupported by existing studies.
Controversies in Subspecialty Certification
Recently, debate also has surfaced regarding subspecialty certification. Over the last decade, proponents of subspecialty certification have argued that board certification would bring consistency and decrease divisiveness among dermatologists; help to prevent exclusion of Mohs surgeons from insurance networks and teaching opportunities at the Veterans Administration; and demonstrate competence to patients, the media, and payers. Those in opposition contest that practices may be restricted by insurers using lack of certification to eliminate dermatologists from their networks, economic credentialing may be applied to dermatologists such that those without the subspecialty certification may not be deemed qualified to manage skin cancer, major limitations may be set determining which dermatologists can sit for the certification examination, and subspecialty certification could create disenfranchisement of many dermatologists. A 2017 American Academy of Dermatology member survey demonstrated ambivalence regarding subcertification, with 51% of respondents pro-subcertification and 48% anti-subcertification.23
Nonetheless, after years of debate the American Board of Dermatology proposed subspecialty certification in Micrographic Dermatologic Surgery, which was approved by the American Board of Medical Specialties on October 26, 2018. The first certification examination will likely take place in 2 years, and a maintenance of certification examination will be required every 10 years.24
Final Thoughts
Further investigation is needed to elucidate and optimize solutions to many of the current controversies associated with MMS.
- Levy RM, Hanke CW. Mohs micrographic surgery: facts and controversies. Clin Dermatol. 2010;28:269-274.
- Zitelli JA, Brown C, Hanusa BH. Surgical margins for excision of primary cutaneous melanoma. J Am Acad Dermatol. 1997;37:422-429.
- Albertini JG, Elston DM, Libow LF, et al. Mohs micrographic surgery for melanoma: a case series, a comparative study of immunostains, an informative case report, and a unique mapping technique. Dermatol Surg. 2002;28:656-665.
- Walling HW, Scupham RK, Bean AK, et al. Staged excision versus Mohs micrographic surgery for lentigo maligna and lentigo maligna melanoma. J Am Acad Dermatol. 2007;57:659-664.
- O’Connor WJ, Roenigk RK, Brodland DG. Merkel cell carcinoma. comparison of Mohs micrographic surgery and wide excision in eighty-six patients. Dermatol Surg. 1997;23:929-933.
- Reeder VJ, Gustafson CJ, Mireku K, et al. Trends in Mohs surgery from 1995 to 2010: an analysis of nationally representative data. Dermatol Surg. 2015;41:397-403.
- Mosterd K, Krekels GA, Nieman FH, et al. Surgical excision versus Mohs’ micrographic surgery for primary and recurrent basal-cell carcinoma of the face: a prospective randomised controlled trial with 5-years’ follow-up. Lancet Oncol. 2008;9:1149-1156.
- Viola KV, Rezzadeh KS, Gonsalves L, et al. National utilization patterns of Mohs micrographic surgery for invasive melanoma and melanoma in situ. J Am Acad Dermatol. 2015;72:1060-1065.
- Todd MM, Miller JJ, Ammirati CT. Dermatologic surgery training in residency. Dermatol Surg. 2002;28:547-549.
- Krishnan A, Xu T, Hutfless S, et al; American College of Mohs Surgery Improving Wisely Study Group. Outlier practice patterns in Mohs micrographic surgery: defining the problem and a proposed solution. JAMA Dermatol. 2017;153:565-570.
- Albertini JG, Wang P, Fahim C, et al. Evaluation of a peer-to-peer data transparency intervention for Mohs micrographic surgery overuse [published online May 5, 2019]. JAMA Dermatol. doi:10.1001/jamadermatol.2019.1259.
- Johnstone C, Joiner KA, Pierce J, et al. Mohs micrographic surgery volume and payment patterns among dermatologists in the Medicare population, 2013. Am J Clin Oncol. 2018;41:1199-1203.
- Donaldson MR, Coldiron BM. Mohs micrographic surgery utilization in the Medicare population, 2009. Dermatol Surg. 2012;38:1427-1434.
- Bath C. Dermatologists defend Mohs surgery as effective and cost-efficient with low rate of recurrence. ASCO Post. March 15, 2014. https://www.ascopost.com/issues/march-15-2014/dermatologists-defend-mohs-surgery-as-effective-and-cost-efficient-with-low-rate-of-recurrence. Accessed October 23, 2019.
- Rosenthal E. Patients’ costs skyrocket; specialists’ incomes soar. New York Times. January 18, 2004. https://www.nytimes.com/2014/01/19/health/patients-costs-skyrocket-specialists-incomes-soar.html. Accessed October 23, 2019.
- Ravitskiy L, Brodland DG, Zitelli JA. Cost analysis: Mohs micrographic surgery. Dermatol Surg. 2012;38:585-594.
- Tierney EP, Hanke CW. Cost effectiveness of Mohs micrographic surgery: review of the literature. J Drugs Dermatol. 2009;8:914-922.
- Connolly SM, Baker DR, Coldiron BM, et al. AAD/ACMS/ASDSA/ASMS 2012 appropriate use criteria for Mohs micrographic surgery: a report of the American Academy of Dermatology, American College of Mohs Surgery, American Society for Dermatologic Surgery Association, and the American Society for Mohs Surgery. J Am Acad Dermatol. 2012;67:531-550.
- Steinman HK, Dixon A, Zachary CB. Reevaluating Mohs surgery appropriate use criteria for primary superficial basal cell carcinoma. JAMA Dermatol. 2018;154:755-756.
- Kelleners-Smeets NW, Mosterd K. Comment on 2012 appropriate use criteria for Mohs micrographic surgery. J Am Acad Dermatol. 2013;69:317-318.
- Ruiz ES, Karia PS, Morgan FC, et al. Multiple Mohs micrographic surgery is the most common reason for divergence from the appropriate use criteria: a single institution retrospective cohort study. J Am Acad Dermatol. 2016;75:830-831.
- Croley JA, Joseph AK, Wagner RF Jr. Discrepancies in the Mohs Micrographic Surgery appropriate use criteria [published online December 23, 2018]. J Am Acad Dermatol. doi:10.1016/j.jaad.2018.11.064.
- Weinstein A. The ABD’s push for subspecialty certification in Mohs surgery will fracture dermatology. Pract Dermatol. April 2018:37-39. https://practicaldermatology.com/articles/2018-apr/perspective-the-abds-push-for-subspecialty-certification-in-mohs-surgery-will-fracture-dermatology. Accessed Oc
tober 30, 2019. - ABD Micrographic Dermatologic Surgery (MDS) Subspecialty Certification Questions & Answers. American Board of Dermatology website. https://www.abderm.org/residents-and-fellows/fellowship-training/micrographic-dermatologic-surgery-mds-questions-and-answers-1.aspx. Accessed October 23, 2019.
Mohs micrographic surgery (MMS) has been met with controversy since its inception in the 1930s. Current debate centers on the types of tumors treated with MMS, increasing utilization, third-party payer reimbursement, the Appropriate Use Criteria (AUC), and subspecialty certification.
Controversies in Applications
Controversy surrounding treatment with MMS for certain tumor types is abundant, in large part due to a lack of well-designed studies. Perhaps most notably, the surgical management of melanoma has been hotly contested for decades.1 An increasing number of Mohs surgeons advocate the use of MMS for treatment of melanoma. Advocates reason that tumor margins may be ill-defined, necessitating histologic examination of the margin for tumor clearance. In a study by Zitelli et al,2 5-year survival and metastatic rates for 535 patients with melanomas treated by MMS with frozen sections were the same or better when compared to historical controls treated with conventional wide local excision. Melanoma-associated antigen recognized by T cells (MART-1) immunostaining may offer improved diagnostic accuracy.3 Others believe that staged excision with permanent sections processed vertically, en face, or horizontally (“slow Mohs”) is more accurate and efficacious for the treatment of melanoma.1 Advocates of this approach maintain that when compared to MMS with frozen sections, staged excision with permanent sections enables more accurate interpretation of residual melanoma and atypical junctional melanocytic hyperplasia as well as circumvents difficulty in interpreting freeze artifact.4
Although Merkel cell carcinoma has traditionally been treated with wide local excision, MMS with or without adjuvant radiotherapy has gained traction as a treatment option. Advocates for treatment by MMS hold that Merkel cell carcinoma is a contiguous tumor with a high rate of residual tumor persistence, making histologic margin control an ideal characteristic of treatment. However, in the absence of large randomized controlled studies comparing MMS to wide local excision, controversy surrounds the most appropriate surgical approach.1 In a retrospective study of 86 patients by O’Connor et al,5 MMS was demonstrated to compare favorably to standard surgical excision. Standard surgical excision was associated with a 31.7% (13/41) local persistence rate and 48.8% (20/41) regional metastasis rate compared to 8.3% (1/12) and 33.3% (4/12) for MMS, respectively.5
Controversies in Increasing Utilization
The incidence of skin cancers has increased in recent years. As a result, it is reasonable to expect the rates of MMS to increase. Nonetheless, there is escalating concern among groups of third-party payers, the public, and physicians that MMS is being overused.6 Growth of the body of evidence supporting the appropriateness of MMS remains essential. Such studies continue to support reasons for increased MMS usage, demonstrating the stability of the percentage of skin cancers treated with MMS in the setting of increasing skin cancer incidence, the procedure’s superior efficacy for appropriately chosen cases, its expanding application to melanoma and other tumors, and an emphasis of MMS in residency training programs.6-9
A current hot topic of controversy focuses on the wide variation among Mohs surgeons in the mean number of stages used to resect a tumor. Overuse among outliers has been proposed to stem from lack of technical expertise or from abuse of the current fee-for-service payment model, which bases compensation on the number of stages performed. A study by Krishnan et al10 determined that the mean number of stages per tumor in the studied population (all physicians [N=2305] receiving Medicare payments for MMS from January 2012 to December 2014) was 1.74, with a range of 1.09 to 4.11. Persistently high outliers were more likely to perform MMS in a solo practice, with an odds ratio of 2.35.10 In response to the wide variation in mean stages used to resect a skin cancer and its implications on increased financial burden and surgery to individual patients, intervention has been proposed. Notably, it has been demonstrated that mailing out individual reports of practice patterns to high-outlier physicians resulted in a reduction in mean stages per tumor as well as an associated cost savings when compared to outlier physicians who did not receive these reports.11
Controversies in Reimbursement
Mohs micrographic surgery also has been in the spotlight for debate regarding reimbursement. The procedure has been targeted partly in response to its substantial contribution to total Medicare reimbursements paid out. In 2013, primary MMS billing codes constituted nearly 19% of total reimbursements to dermatologists and approximately 0.5% of total reimbursements to all physicians participating in Medicare.12 Mohs micrographic surgery codes have correspondingly received frequent review by the Relative Value Scale Update Committee and remained on a list of potentially misvalued services according to the Centers for Medicare & Medicaid Services for years.13 Due to continued scrutiny and review, especially by the Relative Value Scale Update Committee and Centers for Medicare & Medicaid Services, reimbursement to perform MMS and reconstructive surgery has gone down by more than 20% in the last 15 years.14 Public perception mirrors third-party payer concerns for overcompensation. An article title in the New York Times theatrically postures “Patients’ Costs Skyrocket, Specialists’ Incomes Soar.” The article recounts an MMS patient’s “outrage at charges” associated with treatment of her “minor medical problem” and the simultaneous “sharp climb” in dermatologist income over the last 2 decades.15
However, studies continue to demonstrate the cost-effectiveness of MMS. A study by Ravitskiy et al16 demonstrates the cost-effectiveness of MMS, regardless of place of service or type of tumor. Of 406 tumors studied, MMS was the least expensive surgical procedure evaluated ($805 per tumor) when compared to standard surgical excision with permanent margins ($1026 per tumor), standard surgical excision with frozen margins ($1200 per tumor), and ambulatory surgery center standard surgical excision ($2507 per tumor). Furthermore, adjusted for inflation, the cost of MMS was lower in 2009 vs 1998.16 Similar results have been consistently demonstrated.17
Controversies in the AUC
To provide clinicians, policy makers, and insurers guidance for utilization of MMS in the setting of concerns for overutilization, overcompensation, and inappropriate application, the MMS AUC were established in 2012. The guidelines were developed by a process integrating evidence-based medicine, clinical experience, and expert opinion and is applicable to 270 clinical scenarios.18
A unique set of debate accompanies the guidelines. Namely, controversy has surrounded the classification of most primary superficial basal cell carcinomas as appropriate for treatment by MMS. These tumors have comparable cure rates when treated by MMS or curettage and cryosurgery, are often multifocal and require more Mohs stages than other basal cell carcinoma subtypes, and largely lack data on recurrence and invasion.19 The guidelines also have been scrutinized for including only studies from the United States.20 Furthermore, the report is largely based on expert opinion rather than evidence.
Some Mohs surgeons have concerns that the guidelines will minimize clinical judgment. Nonetheless, deviations from the AUC practiced by Mohs surgeons have been reported where clinical judgment supplants guideline criteria. The most commonly cited reasons for performing MMS on tumors classified as uncertain or inappropriate, according to one study by Ruiz et al,21 included performing multiple MMSs on the same day, tumor location on the lower legs, and incorporation into an adjacent wound. Reported discrepancies in the AUC further emphasize the importance of clinical judgment and call into question the need for future revision of the criteria.22 For example, a primary squamous cell carcinoma in situ greater than or equal to 2 cm located on the trunk and extremities (excluding pretibial surfaces, hands, feet, nail units, and ankles) in a healthy patient is categorized as appropriate, while a recurrent but otherwise identical squamous cell carcinoma in situ is categorized as uncertain. These counterintuitive criteria are unsupported by existing studies.
Controversies in Subspecialty Certification
Recently, debate also has surfaced regarding subspecialty certification. Over the last decade, proponents of subspecialty certification have argued that board certification would bring consistency and decrease divisiveness among dermatologists; help to prevent exclusion of Mohs surgeons from insurance networks and teaching opportunities at the Veterans Administration; and demonstrate competence to patients, the media, and payers. Those in opposition contest that practices may be restricted by insurers using lack of certification to eliminate dermatologists from their networks, economic credentialing may be applied to dermatologists such that those without the subspecialty certification may not be deemed qualified to manage skin cancer, major limitations may be set determining which dermatologists can sit for the certification examination, and subspecialty certification could create disenfranchisement of many dermatologists. A 2017 American Academy of Dermatology member survey demonstrated ambivalence regarding subcertification, with 51% of respondents pro-subcertification and 48% anti-subcertification.23
Nonetheless, after years of debate the American Board of Dermatology proposed subspecialty certification in Micrographic Dermatologic Surgery, which was approved by the American Board of Medical Specialties on October 26, 2018. The first certification examination will likely take place in 2 years, and a maintenance of certification examination will be required every 10 years.24
Final Thoughts
Further investigation is needed to elucidate and optimize solutions to many of the current controversies associated with MMS.
Mohs micrographic surgery (MMS) has been met with controversy since its inception in the 1930s. Current debate centers on the types of tumors treated with MMS, increasing utilization, third-party payer reimbursement, the Appropriate Use Criteria (AUC), and subspecialty certification.
Controversies in Applications
Controversy surrounding treatment with MMS for certain tumor types is abundant, in large part due to a lack of well-designed studies. Perhaps most notably, the surgical management of melanoma has been hotly contested for decades.1 An increasing number of Mohs surgeons advocate the use of MMS for treatment of melanoma. Advocates reason that tumor margins may be ill-defined, necessitating histologic examination of the margin for tumor clearance. In a study by Zitelli et al,2 5-year survival and metastatic rates for 535 patients with melanomas treated by MMS with frozen sections were the same or better when compared to historical controls treated with conventional wide local excision. Melanoma-associated antigen recognized by T cells (MART-1) immunostaining may offer improved diagnostic accuracy.3 Others believe that staged excision with permanent sections processed vertically, en face, or horizontally (“slow Mohs”) is more accurate and efficacious for the treatment of melanoma.1 Advocates of this approach maintain that when compared to MMS with frozen sections, staged excision with permanent sections enables more accurate interpretation of residual melanoma and atypical junctional melanocytic hyperplasia as well as circumvents difficulty in interpreting freeze artifact.4
Although Merkel cell carcinoma has traditionally been treated with wide local excision, MMS with or without adjuvant radiotherapy has gained traction as a treatment option. Advocates for treatment by MMS hold that Merkel cell carcinoma is a contiguous tumor with a high rate of residual tumor persistence, making histologic margin control an ideal characteristic of treatment. However, in the absence of large randomized controlled studies comparing MMS to wide local excision, controversy surrounds the most appropriate surgical approach.1 In a retrospective study of 86 patients by O’Connor et al,5 MMS was demonstrated to compare favorably to standard surgical excision. Standard surgical excision was associated with a 31.7% (13/41) local persistence rate and 48.8% (20/41) regional metastasis rate compared to 8.3% (1/12) and 33.3% (4/12) for MMS, respectively.5
Controversies in Increasing Utilization
The incidence of skin cancers has increased in recent years. As a result, it is reasonable to expect the rates of MMS to increase. Nonetheless, there is escalating concern among groups of third-party payers, the public, and physicians that MMS is being overused.6 Growth of the body of evidence supporting the appropriateness of MMS remains essential. Such studies continue to support reasons for increased MMS usage, demonstrating the stability of the percentage of skin cancers treated with MMS in the setting of increasing skin cancer incidence, the procedure’s superior efficacy for appropriately chosen cases, its expanding application to melanoma and other tumors, and an emphasis of MMS in residency training programs.6-9
A current hot topic of controversy focuses on the wide variation among Mohs surgeons in the mean number of stages used to resect a tumor. Overuse among outliers has been proposed to stem from lack of technical expertise or from abuse of the current fee-for-service payment model, which bases compensation on the number of stages performed. A study by Krishnan et al10 determined that the mean number of stages per tumor in the studied population (all physicians [N=2305] receiving Medicare payments for MMS from January 2012 to December 2014) was 1.74, with a range of 1.09 to 4.11. Persistently high outliers were more likely to perform MMS in a solo practice, with an odds ratio of 2.35.10 In response to the wide variation in mean stages used to resect a skin cancer and its implications on increased financial burden and surgery to individual patients, intervention has been proposed. Notably, it has been demonstrated that mailing out individual reports of practice patterns to high-outlier physicians resulted in a reduction in mean stages per tumor as well as an associated cost savings when compared to outlier physicians who did not receive these reports.11
Controversies in Reimbursement
Mohs micrographic surgery also has been in the spotlight for debate regarding reimbursement. The procedure has been targeted partly in response to its substantial contribution to total Medicare reimbursements paid out. In 2013, primary MMS billing codes constituted nearly 19% of total reimbursements to dermatologists and approximately 0.5% of total reimbursements to all physicians participating in Medicare.12 Mohs micrographic surgery codes have correspondingly received frequent review by the Relative Value Scale Update Committee and remained on a list of potentially misvalued services according to the Centers for Medicare & Medicaid Services for years.13 Due to continued scrutiny and review, especially by the Relative Value Scale Update Committee and Centers for Medicare & Medicaid Services, reimbursement to perform MMS and reconstructive surgery has gone down by more than 20% in the last 15 years.14 Public perception mirrors third-party payer concerns for overcompensation. An article title in the New York Times theatrically postures “Patients’ Costs Skyrocket, Specialists’ Incomes Soar.” The article recounts an MMS patient’s “outrage at charges” associated with treatment of her “minor medical problem” and the simultaneous “sharp climb” in dermatologist income over the last 2 decades.15
However, studies continue to demonstrate the cost-effectiveness of MMS. A study by Ravitskiy et al16 demonstrates the cost-effectiveness of MMS, regardless of place of service or type of tumor. Of 406 tumors studied, MMS was the least expensive surgical procedure evaluated ($805 per tumor) when compared to standard surgical excision with permanent margins ($1026 per tumor), standard surgical excision with frozen margins ($1200 per tumor), and ambulatory surgery center standard surgical excision ($2507 per tumor). Furthermore, adjusted for inflation, the cost of MMS was lower in 2009 vs 1998.16 Similar results have been consistently demonstrated.17
Controversies in the AUC
To provide clinicians, policy makers, and insurers guidance for utilization of MMS in the setting of concerns for overutilization, overcompensation, and inappropriate application, the MMS AUC were established in 2012. The guidelines were developed by a process integrating evidence-based medicine, clinical experience, and expert opinion and is applicable to 270 clinical scenarios.18
A unique set of debate accompanies the guidelines. Namely, controversy has surrounded the classification of most primary superficial basal cell carcinomas as appropriate for treatment by MMS. These tumors have comparable cure rates when treated by MMS or curettage and cryosurgery, are often multifocal and require more Mohs stages than other basal cell carcinoma subtypes, and largely lack data on recurrence and invasion.19 The guidelines also have been scrutinized for including only studies from the United States.20 Furthermore, the report is largely based on expert opinion rather than evidence.
Some Mohs surgeons have concerns that the guidelines will minimize clinical judgment. Nonetheless, deviations from the AUC practiced by Mohs surgeons have been reported where clinical judgment supplants guideline criteria. The most commonly cited reasons for performing MMS on tumors classified as uncertain or inappropriate, according to one study by Ruiz et al,21 included performing multiple MMSs on the same day, tumor location on the lower legs, and incorporation into an adjacent wound. Reported discrepancies in the AUC further emphasize the importance of clinical judgment and call into question the need for future revision of the criteria.22 For example, a primary squamous cell carcinoma in situ greater than or equal to 2 cm located on the trunk and extremities (excluding pretibial surfaces, hands, feet, nail units, and ankles) in a healthy patient is categorized as appropriate, while a recurrent but otherwise identical squamous cell carcinoma in situ is categorized as uncertain. These counterintuitive criteria are unsupported by existing studies.
Controversies in Subspecialty Certification
Recently, debate also has surfaced regarding subspecialty certification. Over the last decade, proponents of subspecialty certification have argued that board certification would bring consistency and decrease divisiveness among dermatologists; help to prevent exclusion of Mohs surgeons from insurance networks and teaching opportunities at the Veterans Administration; and demonstrate competence to patients, the media, and payers. Those in opposition contest that practices may be restricted by insurers using lack of certification to eliminate dermatologists from their networks, economic credentialing may be applied to dermatologists such that those without the subspecialty certification may not be deemed qualified to manage skin cancer, major limitations may be set determining which dermatologists can sit for the certification examination, and subspecialty certification could create disenfranchisement of many dermatologists. A 2017 American Academy of Dermatology member survey demonstrated ambivalence regarding subcertification, with 51% of respondents pro-subcertification and 48% anti-subcertification.23
Nonetheless, after years of debate the American Board of Dermatology proposed subspecialty certification in Micrographic Dermatologic Surgery, which was approved by the American Board of Medical Specialties on October 26, 2018. The first certification examination will likely take place in 2 years, and a maintenance of certification examination will be required every 10 years.24
Final Thoughts
Further investigation is needed to elucidate and optimize solutions to many of the current controversies associated with MMS.
- Levy RM, Hanke CW. Mohs micrographic surgery: facts and controversies. Clin Dermatol. 2010;28:269-274.
- Zitelli JA, Brown C, Hanusa BH. Surgical margins for excision of primary cutaneous melanoma. J Am Acad Dermatol. 1997;37:422-429.
- Albertini JG, Elston DM, Libow LF, et al. Mohs micrographic surgery for melanoma: a case series, a comparative study of immunostains, an informative case report, and a unique mapping technique. Dermatol Surg. 2002;28:656-665.
- Walling HW, Scupham RK, Bean AK, et al. Staged excision versus Mohs micrographic surgery for lentigo maligna and lentigo maligna melanoma. J Am Acad Dermatol. 2007;57:659-664.
- O’Connor WJ, Roenigk RK, Brodland DG. Merkel cell carcinoma. comparison of Mohs micrographic surgery and wide excision in eighty-six patients. Dermatol Surg. 1997;23:929-933.
- Reeder VJ, Gustafson CJ, Mireku K, et al. Trends in Mohs surgery from 1995 to 2010: an analysis of nationally representative data. Dermatol Surg. 2015;41:397-403.
- Mosterd K, Krekels GA, Nieman FH, et al. Surgical excision versus Mohs’ micrographic surgery for primary and recurrent basal-cell carcinoma of the face: a prospective randomised controlled trial with 5-years’ follow-up. Lancet Oncol. 2008;9:1149-1156.
- Viola KV, Rezzadeh KS, Gonsalves L, et al. National utilization patterns of Mohs micrographic surgery for invasive melanoma and melanoma in situ. J Am Acad Dermatol. 2015;72:1060-1065.
- Todd MM, Miller JJ, Ammirati CT. Dermatologic surgery training in residency. Dermatol Surg. 2002;28:547-549.
- Krishnan A, Xu T, Hutfless S, et al; American College of Mohs Surgery Improving Wisely Study Group. Outlier practice patterns in Mohs micrographic surgery: defining the problem and a proposed solution. JAMA Dermatol. 2017;153:565-570.
- Albertini JG, Wang P, Fahim C, et al. Evaluation of a peer-to-peer data transparency intervention for Mohs micrographic surgery overuse [published online May 5, 2019]. JAMA Dermatol. doi:10.1001/jamadermatol.2019.1259.
- Johnstone C, Joiner KA, Pierce J, et al. Mohs micrographic surgery volume and payment patterns among dermatologists in the Medicare population, 2013. Am J Clin Oncol. 2018;41:1199-1203.
- Donaldson MR, Coldiron BM. Mohs micrographic surgery utilization in the Medicare population, 2009. Dermatol Surg. 2012;38:1427-1434.
- Bath C. Dermatologists defend Mohs surgery as effective and cost-efficient with low rate of recurrence. ASCO Post. March 15, 2014. https://www.ascopost.com/issues/march-15-2014/dermatologists-defend-mohs-surgery-as-effective-and-cost-efficient-with-low-rate-of-recurrence. Accessed October 23, 2019.
- Rosenthal E. Patients’ costs skyrocket; specialists’ incomes soar. New York Times. January 18, 2004. https://www.nytimes.com/2014/01/19/health/patients-costs-skyrocket-specialists-incomes-soar.html. Accessed October 23, 2019.
- Ravitskiy L, Brodland DG, Zitelli JA. Cost analysis: Mohs micrographic surgery. Dermatol Surg. 2012;38:585-594.
- Tierney EP, Hanke CW. Cost effectiveness of Mohs micrographic surgery: review of the literature. J Drugs Dermatol. 2009;8:914-922.
- Connolly SM, Baker DR, Coldiron BM, et al. AAD/ACMS/ASDSA/ASMS 2012 appropriate use criteria for Mohs micrographic surgery: a report of the American Academy of Dermatology, American College of Mohs Surgery, American Society for Dermatologic Surgery Association, and the American Society for Mohs Surgery. J Am Acad Dermatol. 2012;67:531-550.
- Steinman HK, Dixon A, Zachary CB. Reevaluating Mohs surgery appropriate use criteria for primary superficial basal cell carcinoma. JAMA Dermatol. 2018;154:755-756.
- Kelleners-Smeets NW, Mosterd K. Comment on 2012 appropriate use criteria for Mohs micrographic surgery. J Am Acad Dermatol. 2013;69:317-318.
- Ruiz ES, Karia PS, Morgan FC, et al. Multiple Mohs micrographic surgery is the most common reason for divergence from the appropriate use criteria: a single institution retrospective cohort study. J Am Acad Dermatol. 2016;75:830-831.
- Croley JA, Joseph AK, Wagner RF Jr. Discrepancies in the Mohs Micrographic Surgery appropriate use criteria [published online December 23, 2018]. J Am Acad Dermatol. doi:10.1016/j.jaad.2018.11.064.
- Weinstein A. The ABD’s push for subspecialty certification in Mohs surgery will fracture dermatology. Pract Dermatol. April 2018:37-39. https://practicaldermatology.com/articles/2018-apr/perspective-the-abds-push-for-subspecialty-certification-in-mohs-surgery-will-fracture-dermatology. Accessed Oc
tober 30, 2019. - ABD Micrographic Dermatologic Surgery (MDS) Subspecialty Certification Questions & Answers. American Board of Dermatology website. https://www.abderm.org/residents-and-fellows/fellowship-training/micrographic-dermatologic-surgery-mds-questions-and-answers-1.aspx. Accessed October 23, 2019.
- Levy RM, Hanke CW. Mohs micrographic surgery: facts and controversies. Clin Dermatol. 2010;28:269-274.
- Zitelli JA, Brown C, Hanusa BH. Surgical margins for excision of primary cutaneous melanoma. J Am Acad Dermatol. 1997;37:422-429.
- Albertini JG, Elston DM, Libow LF, et al. Mohs micrographic surgery for melanoma: a case series, a comparative study of immunostains, an informative case report, and a unique mapping technique. Dermatol Surg. 2002;28:656-665.
- Walling HW, Scupham RK, Bean AK, et al. Staged excision versus Mohs micrographic surgery for lentigo maligna and lentigo maligna melanoma. J Am Acad Dermatol. 2007;57:659-664.
- O’Connor WJ, Roenigk RK, Brodland DG. Merkel cell carcinoma. comparison of Mohs micrographic surgery and wide excision in eighty-six patients. Dermatol Surg. 1997;23:929-933.
- Reeder VJ, Gustafson CJ, Mireku K, et al. Trends in Mohs surgery from 1995 to 2010: an analysis of nationally representative data. Dermatol Surg. 2015;41:397-403.
- Mosterd K, Krekels GA, Nieman FH, et al. Surgical excision versus Mohs’ micrographic surgery for primary and recurrent basal-cell carcinoma of the face: a prospective randomised controlled trial with 5-years’ follow-up. Lancet Oncol. 2008;9:1149-1156.
- Viola KV, Rezzadeh KS, Gonsalves L, et al. National utilization patterns of Mohs micrographic surgery for invasive melanoma and melanoma in situ. J Am Acad Dermatol. 2015;72:1060-1065.
- Todd MM, Miller JJ, Ammirati CT. Dermatologic surgery training in residency. Dermatol Surg. 2002;28:547-549.
- Krishnan A, Xu T, Hutfless S, et al; American College of Mohs Surgery Improving Wisely Study Group. Outlier practice patterns in Mohs micrographic surgery: defining the problem and a proposed solution. JAMA Dermatol. 2017;153:565-570.
- Albertini JG, Wang P, Fahim C, et al. Evaluation of a peer-to-peer data transparency intervention for Mohs micrographic surgery overuse [published online May 5, 2019]. JAMA Dermatol. doi:10.1001/jamadermatol.2019.1259.
- Johnstone C, Joiner KA, Pierce J, et al. Mohs micrographic surgery volume and payment patterns among dermatologists in the Medicare population, 2013. Am J Clin Oncol. 2018;41:1199-1203.
- Donaldson MR, Coldiron BM. Mohs micrographic surgery utilization in the Medicare population, 2009. Dermatol Surg. 2012;38:1427-1434.
- Bath C. Dermatologists defend Mohs surgery as effective and cost-efficient with low rate of recurrence. ASCO Post. March 15, 2014. https://www.ascopost.com/issues/march-15-2014/dermatologists-defend-mohs-surgery-as-effective-and-cost-efficient-with-low-rate-of-recurrence. Accessed October 23, 2019.
- Rosenthal E. Patients’ costs skyrocket; specialists’ incomes soar. New York Times. January 18, 2004. https://www.nytimes.com/2014/01/19/health/patients-costs-skyrocket-specialists-incomes-soar.html. Accessed October 23, 2019.
- Ravitskiy L, Brodland DG, Zitelli JA. Cost analysis: Mohs micrographic surgery. Dermatol Surg. 2012;38:585-594.
- Tierney EP, Hanke CW. Cost effectiveness of Mohs micrographic surgery: review of the literature. J Drugs Dermatol. 2009;8:914-922.
- Connolly SM, Baker DR, Coldiron BM, et al. AAD/ACMS/ASDSA/ASMS 2012 appropriate use criteria for Mohs micrographic surgery: a report of the American Academy of Dermatology, American College of Mohs Surgery, American Society for Dermatologic Surgery Association, and the American Society for Mohs Surgery. J Am Acad Dermatol. 2012;67:531-550.
- Steinman HK, Dixon A, Zachary CB. Reevaluating Mohs surgery appropriate use criteria for primary superficial basal cell carcinoma. JAMA Dermatol. 2018;154:755-756.
- Kelleners-Smeets NW, Mosterd K. Comment on 2012 appropriate use criteria for Mohs micrographic surgery. J Am Acad Dermatol. 2013;69:317-318.
- Ruiz ES, Karia PS, Morgan FC, et al. Multiple Mohs micrographic surgery is the most common reason for divergence from the appropriate use criteria: a single institution retrospective cohort study. J Am Acad Dermatol. 2016;75:830-831.
- Croley JA, Joseph AK, Wagner RF Jr. Discrepancies in the Mohs Micrographic Surgery appropriate use criteria [published online December 23, 2018]. J Am Acad Dermatol. doi:10.1016/j.jaad.2018.11.064.
- Weinstein A. The ABD’s push for subspecialty certification in Mohs surgery will fracture dermatology. Pract Dermatol. April 2018:37-39. https://practicaldermatology.com/articles/2018-apr/perspective-the-abds-push-for-subspecialty-certification-in-mohs-surgery-will-fracture-dermatology. Accessed Oc
tober 30, 2019. - ABD Micrographic Dermatologic Surgery (MDS) Subspecialty Certification Questions & Answers. American Board of Dermatology website. https://www.abderm.org/residents-and-fellows/fellowship-training/micrographic-dermatologic-surgery-mds-questions-and-answers-1.aspx. Accessed October 23, 2019.
Resident Pearl:
• Further investigation is needed to elucidate and optimize solutions to current controversies in Mohs micrographic surgery.
Skin Scores: A Review of Clinical Scoring Systems in Dermatology
The practice of dermatology is rife with bedside tools: swabs, smears, and scoring systems. First popularized in specialties such as emergency medicine and internal medicine, clinical scoring systems are now emerging in dermatology. These evidence-based scores can be calculated quickly at the bedside—often through a free smartphone app—to help guide clinical decision-making regarding diagnosis, prognosis, and management. As with any medical tool, scoring systems have limitations and should be used as a supplement, not substitute, for one’s clinical judgement. This article reviews 4 clinical scoring systems practical for dermatology residents.
SCORTEN Prognosticates Cases of Stevens-Johnson Syndrome/Toxic Epidermal Necrolysis
Perhaps the best-known scoring system in dermatology, the SCORTEN is widely used to predict hospital mortality from Stevens-Johnson syndrome/toxic epidermal necrolysis. The SCORTEN includes 7 variables of equal weight—age of 40 years or older, heart rate of 120 beats per minute or more, cancer/hematologic malignancy, involved body surface area (BSA) greater than 10%, serum urea greater than 10 mmol/L, serum bicarbonate less than 20 mmol/L, and serum glucose greater than 14 mmol/L—each contributing 1 point to the overall score if present.1 The involved BSA is defined as the sum of detached and detachable epidermis.1
The SCORTEN was developed and prospectively validated to be calculated at the end of the first 24 hours of admission; for this calculation, use the BSA affected at that time, and use the most abnormal values during the first 24 hours of admission for the other variables.1 In addition, a follow-up study including some of the original coauthors recommends recalculating the SCORTEN at the end of hospital day 3, having found that the score’s predictive value was better on this day than hospital days 1, 2, 4, or 5.2 Based on the original study, a SCORTEN of 0 to 1 corresponds to a mortality rate of 3.2%, 2 to 12.1%, 3 to 35.3%, 4 to 58.3%, and 5 or greater to 90.0%.1
Limitations of the SCORTEN include its ability to overestimate or underestimate mortality as demonstrated by 2 multi-institutional cohorts.3,4 Recently, the ABCD-10 score was developed as an alternative to the SCORTEN and was found to predict mortality similarly when validated in an internal cohort.5
PEST Screens for Psoriatic Arthritis
Dermatologists play an important role in screening for psoriatic arthritis, as an estimated 1 in 5 patients with psoriasis have psoriatic arthritis.6 To this end, several screening tools have been developed to help differentiate psoriatic arthritis from other arthritides. Joint guidelines from the American Academy of Dermatology and the National Psoriasis Foundation acknowledge that “. . . these screening tools have tended to perform less well when tested in groups of people other than those for which they were originally developed. As such, their usefulness in routine clinical practice remains controversial.”7 Nevertheless, the guidelines state, “[b]ecause screening and early detection of inflammatory arthritis are essential to optimize patient [quality of life] and reduce morbidity, providers may consider using a formal screening tool of their choice.”7
With these limitations in mind, I have found the Psoriasis Epidemiology Screening Tool (PEST) to be the most useful psoriatic arthritis screening tool. One study determined that the PEST has the best trade-off between sensitivity and specificity compared to 2 other psoriatic arthritis screening tools, the Psoriatic Arthritis Screening and Evaluation (PASE) and the Early Arthritis for Psoriatic Patients (EARP).8
The PEST is comprised of 5 questions: (1) Have you ever had a swollen joint (or joints)? (2) Has a doctor ever told you that you have arthritis? (3) Do your fingernails or toenails have holes or pits? (4) Have you had pain in your heel? (5) Have you had a finger or toe that was completely swollen and painful for no apparent reason? According to the PEST, a referral to a rheumatologist should be considered for patients answering yes to 3 or more questions, which is 97% sensitive and 79% specific for psoriatic arthritis.9 Patients who answer yes to fewer than 3 questions should still be referred to a rheumatologist if there is a strong clinical suspicion of psoriatic arthritis.10
The PEST can be accessed for free in 13 languages via the GRAPPA (Group for Research and Assessment of Psoriasis and Psoriatic Arthritis) app as well as downloaded for free from the National Psoriasis Foundation’s website (https://www.psoriasis.org/psa-screening/providers).
ALT-70 Differentiates Cellulitis From Pseudocellulitis
Overdiagnosing cellulitis in the United States has been estimated to result in up to 130,000 unnecessary hospitalizations and up to $515 million in avoidable health care spending.11 Dermatologists are in a unique position to help fix this issue. In one retrospective study of 1430 inpatient dermatology consultations, 74.32% of inpatients evaluated for presumed cellulitis by a dermatologist were instead diagnosed with a cellulitis mimicker (ie, pseudocellulitis), such as stasis dermatitis or contact dermatitis.12
The ALT-70 score was developed and prospectively validated to help differentiate lower extremity cellulitis from pseudocellulitis in adult patients in the emergency department (ED).13 In addition, the score has retrospectively been shown to function similarly in the inpatient setting when calculated at 24 and 48 hours after ED presentation.14 Although the ALT-70 score was designed for use by frontline clinicians prior to dermatology consultation, I also have found it helpful to calculate as a consultant, as it provides an objective measure of risk to communicate to the primary team in support of one diagnosis or another.
ALT-70 is an acronym for the score’s 4 variables: asymmetry, leukocytosis, tachycardia, and age of 70 years or older.15 If present, each variable confers a certain number of points to the final score: 3 points for asymmetry (defined as unilateral leg involvement), 1 point for leukocytosis (white blood cell count ≥10,000/μL), 1 point for tachycardia (≥90 beats per minute), and 2 points for age of 70 years or older. An ALT-70 score of 0 to 2 corresponds to an 83.3% or greater chance of pseudocellulitis, suggesting that the diagnosis of cellulitis be reconsidered. A score of 3 to 4 is indeterminate, and additional information such as a dermatology consultation should be pursued. A score of 5 to 7 corresponds to an 82.2% or greater chance of cellulitis, signifying that empiric treatment with antibiotics be considered.15
The ALT-70 score does not apply to cases involving areas other than the lower extremities; intravenous antibiotic use within 48 hours before ED presentation; surgery within the last 30 days; abscess; penetrating trauma; burn; or known history of osteomyelitis, diabetic ulcer, or indwelling hardware at the site of infection.15 The ALT-70 score is available for free via the MDCalc app and website (https://www.mdcalc.com/alt-70-score-cellulitis).
Mohs AUC Determines the Appropriateness of Mohs Micrographic Surgery
In 2012, the American Academy of Dermatology, American College of Mohs Surgery, American Society for Dermatologic Surgery Association, and American Society for Mohs Surgery published appropriate use criteria (AUC) to guide the decision to pursue Mohs micrographic surgery (MMS) in the United States.16 Based on various tumor and patient characteristics, the Mohs AUC assign scores to 270 different clinical scenarios. A score of 1 to 3 signifies that MMS is inappropriate and generally not considered acceptable. A score 4 to 6 indicates that the appropriateness of MMS is uncertain. A score 7 to 9 means that MMS is appropriate and generally considered acceptable.16
Since publication, the Mohs AUC have been criticized for classifying most primary superficial basal cell carcinomas as appropriate for MMS17 (which an AUC coauthor18 and others19,20 have defended), excluding certain reasons for performing MMS (such as operating on multiple tumors on the same day),21 including counterintuitive scores,22 and omitting trials from Europe23 (which AUC coauthors also have defended24).
Final Thoughts
Scoring systems are emerging in dermatology as evidence-based bedside tools to help guide clinical decision-making. Despite their limitations, these scores have the potential to make a meaningful impact in dermatology as they have in other specialties.
- Bastuji-Garin S, Fouchard N, Bertocchi M, et al. SCORTEN: a severity-of-illness score for toxic epidermal necrolysis. J Invest Dermatol. 2000;115:149-153.
- Guegan S, Bastuji-Garin S, Poszepczynska-Guigne E, et al. Performance of the SCORTEN during the first five days of hospitalization to predict the prognosis of epidermal necrolysis. J Invest Dermatol. 2006;126:272-276.
- Micheletti RG, Chiesa-Fuxench Z, Noe MH, et al. Stevens-Johnson syndrome/toxic epidermal necrolysis: a multicenter retrospective study of 377 adult patients from the United States. J Invest Dermatol. 2018;138:2315-2321.
- Sekula P, Liss Y, Davidovici B, et al. Evaluation of SCORTEN on a cohort of patients with Stevens-Johnson syndrome and toxic epidermal necrolysis included in the RegiSCAR study. J Burn Care Res. 2011;32:237-245.
- Noe MH, Rosenbach M, Hubbard RA, et al. Development and validation of a risk prediction model for in-hospital mortality among patients with Stevens-Johnson syndrome/toxic epidermal necrolysis-ABCD-10. JAMA Dermatol. 2019;155:448-454.
- Alinaghi F, Calov M, Kristensen LE, et al. Prevalence of psoriatic arthritis in patients with psoriasis: a systematic review and meta-analysis of observational and clinical studies. J Am Acad Dermatol. 2019;80:251-265.e219.
- Elmets CA, Leonardi CL, Davis DMR, et al. Joint AAD-NPF guidelines of care for the management and treatment of psoriasis with awareness and attention to comorbidities. J Am Acad Dermatol. 2019;80:1073-1113.
- Karreman MC, Weel A, van der Ven M, et al. Performance of screening tools for psoriatic arthritis: a cross-sectional study in primary care. Rheumatology (Oxford). 2017;56:597-602.
- Ibrahim GH, Buch MH, Lawson C, et al. Evaluation of an existing screening tool for psoriatic arthritis in people with psoriasis and the development of a new instrument: the Psoriasis Epidemiology Screening Tool (PEST) questionnaire. Clin Exp Rheumatol. 2009;27:469-474.
- Zhang A, Kurtzman DJB, Perez-Chada LM, et al. Psoriatic arthritis and the dermatologist: an approach to screening and clinical evaluation. Clin Dermatol. 2018;36:551-560.
- Weng QY, Raff AB, Cohen JM, et al. Costs and consequences associated with misdiagnosed lower extremity cellulitis. JAMA Dermatol. 2017;153:141-146.
- Strazzula L, Cotliar J, Fox LP, et al. Inpatient dermatology consultation aids diagnosis of cellulitis among hospitalized patients: a multi-institutional analysis. J Am Acad Dermatol. 2015;73:70-75.
- Li DG, Dewan AK, Xia FD, et al. The ALT-70 predictive model outperforms thermal imaging for the diagnosis of lower extremity cellulitis: a prospective evaluation. J Am Acad Dermatol. 2018;79:1076-1080.e1071.
- Singer S, Li DG, Gunasekera N, et al. The ALT-70 predictive model maintains predictive value at 24 and 48 hours after presentation [published online March 23, 2019]. J Am Acad Dermatol. doi:10.1016/j.jaad.2019.03.050.
- Raff AB, Weng QY, Cohen JM, et al. A predictive model for diagnosis of lower extremity cellulitis: a cross-sectional study. J Am Acad Dermatol. 2017;76:618-625.e2.
- Connolly SM, Baker DR, Coldiron BM, et al. AAD/ACMS/ASDSA/ASMS 2012 appropriate use criteria for Mohs micrographic surgery: a report of the American Academy of Dermatology, American College of Mohs Surgery, American Society for Dermatologic Surgery Association, and the American Society for Mohs Surgery. J Am Acad Dermatol. 2012;67:531-550.
- Steinman HK, Dixon A, Zachary CB. Reevaluating Mohs surgery appropriate use criteria for primary superficial basal cell carcinoma. JAMA Dermatol. 2018;154:755-756.
- Montuno MA, Coldiron BM. Mohs appropriate use criteria for superficial basal cell carcinoma. JAMA Dermatol. 2019;155:394-395.
- MacFarlane DF, Perlis C. Mohs appropriate use criteria for superficial basal cell carcinoma. JAMA Dermatol. 2019;155:395-396.
- Kantor J. Mohs appropriate use criteria for superficial basal cell carcinoma. JAMA Dermatol. 2019;155:395.
- Ruiz ES, Karia PS, Morgan FC, et al. Multiple Mohs micrographic surgery is the most common reason for divergence from the appropriate use criteria: a single institution retrospective cohort study. J Am Acad Dermatol. 2016;75:830-831.
- Croley JA, Joseph AK, Wagner RF Jr. Discrepancies in the Mohs Micrographic Surgery appropriate use criteria [published online December 23, 2018]. J Am Acad Dermatol. doi:10.1016/j.jaad.2018.11.064.
- Kelleners-Smeets NW, Mosterd K. Comment on 2012 appropriate use criteria for Mohs micrographic surgery. J Am Acad Dermatol. 2013;69:317-318.
- Connolly S, Baker D, Coldiron B, et al. Reply to “comment on 2012 appropriate use criteria for Mohs micrographic surgery.” J Am Acad Dermatol. 2013;69:318.
The practice of dermatology is rife with bedside tools: swabs, smears, and scoring systems. First popularized in specialties such as emergency medicine and internal medicine, clinical scoring systems are now emerging in dermatology. These evidence-based scores can be calculated quickly at the bedside—often through a free smartphone app—to help guide clinical decision-making regarding diagnosis, prognosis, and management. As with any medical tool, scoring systems have limitations and should be used as a supplement, not substitute, for one’s clinical judgement. This article reviews 4 clinical scoring systems practical for dermatology residents.
SCORTEN Prognosticates Cases of Stevens-Johnson Syndrome/Toxic Epidermal Necrolysis
Perhaps the best-known scoring system in dermatology, the SCORTEN is widely used to predict hospital mortality from Stevens-Johnson syndrome/toxic epidermal necrolysis. The SCORTEN includes 7 variables of equal weight—age of 40 years or older, heart rate of 120 beats per minute or more, cancer/hematologic malignancy, involved body surface area (BSA) greater than 10%, serum urea greater than 10 mmol/L, serum bicarbonate less than 20 mmol/L, and serum glucose greater than 14 mmol/L—each contributing 1 point to the overall score if present.1 The involved BSA is defined as the sum of detached and detachable epidermis.1
The SCORTEN was developed and prospectively validated to be calculated at the end of the first 24 hours of admission; for this calculation, use the BSA affected at that time, and use the most abnormal values during the first 24 hours of admission for the other variables.1 In addition, a follow-up study including some of the original coauthors recommends recalculating the SCORTEN at the end of hospital day 3, having found that the score’s predictive value was better on this day than hospital days 1, 2, 4, or 5.2 Based on the original study, a SCORTEN of 0 to 1 corresponds to a mortality rate of 3.2%, 2 to 12.1%, 3 to 35.3%, 4 to 58.3%, and 5 or greater to 90.0%.1
Limitations of the SCORTEN include its ability to overestimate or underestimate mortality as demonstrated by 2 multi-institutional cohorts.3,4 Recently, the ABCD-10 score was developed as an alternative to the SCORTEN and was found to predict mortality similarly when validated in an internal cohort.5
PEST Screens for Psoriatic Arthritis
Dermatologists play an important role in screening for psoriatic arthritis, as an estimated 1 in 5 patients with psoriasis have psoriatic arthritis.6 To this end, several screening tools have been developed to help differentiate psoriatic arthritis from other arthritides. Joint guidelines from the American Academy of Dermatology and the National Psoriasis Foundation acknowledge that “. . . these screening tools have tended to perform less well when tested in groups of people other than those for which they were originally developed. As such, their usefulness in routine clinical practice remains controversial.”7 Nevertheless, the guidelines state, “[b]ecause screening and early detection of inflammatory arthritis are essential to optimize patient [quality of life] and reduce morbidity, providers may consider using a formal screening tool of their choice.”7
With these limitations in mind, I have found the Psoriasis Epidemiology Screening Tool (PEST) to be the most useful psoriatic arthritis screening tool. One study determined that the PEST has the best trade-off between sensitivity and specificity compared to 2 other psoriatic arthritis screening tools, the Psoriatic Arthritis Screening and Evaluation (PASE) and the Early Arthritis for Psoriatic Patients (EARP).8
The PEST is comprised of 5 questions: (1) Have you ever had a swollen joint (or joints)? (2) Has a doctor ever told you that you have arthritis? (3) Do your fingernails or toenails have holes or pits? (4) Have you had pain in your heel? (5) Have you had a finger or toe that was completely swollen and painful for no apparent reason? According to the PEST, a referral to a rheumatologist should be considered for patients answering yes to 3 or more questions, which is 97% sensitive and 79% specific for psoriatic arthritis.9 Patients who answer yes to fewer than 3 questions should still be referred to a rheumatologist if there is a strong clinical suspicion of psoriatic arthritis.10
The PEST can be accessed for free in 13 languages via the GRAPPA (Group for Research and Assessment of Psoriasis and Psoriatic Arthritis) app as well as downloaded for free from the National Psoriasis Foundation’s website (https://www.psoriasis.org/psa-screening/providers).
ALT-70 Differentiates Cellulitis From Pseudocellulitis
Overdiagnosing cellulitis in the United States has been estimated to result in up to 130,000 unnecessary hospitalizations and up to $515 million in avoidable health care spending.11 Dermatologists are in a unique position to help fix this issue. In one retrospective study of 1430 inpatient dermatology consultations, 74.32% of inpatients evaluated for presumed cellulitis by a dermatologist were instead diagnosed with a cellulitis mimicker (ie, pseudocellulitis), such as stasis dermatitis or contact dermatitis.12
The ALT-70 score was developed and prospectively validated to help differentiate lower extremity cellulitis from pseudocellulitis in adult patients in the emergency department (ED).13 In addition, the score has retrospectively been shown to function similarly in the inpatient setting when calculated at 24 and 48 hours after ED presentation.14 Although the ALT-70 score was designed for use by frontline clinicians prior to dermatology consultation, I also have found it helpful to calculate as a consultant, as it provides an objective measure of risk to communicate to the primary team in support of one diagnosis or another.
ALT-70 is an acronym for the score’s 4 variables: asymmetry, leukocytosis, tachycardia, and age of 70 years or older.15 If present, each variable confers a certain number of points to the final score: 3 points for asymmetry (defined as unilateral leg involvement), 1 point for leukocytosis (white blood cell count ≥10,000/μL), 1 point for tachycardia (≥90 beats per minute), and 2 points for age of 70 years or older. An ALT-70 score of 0 to 2 corresponds to an 83.3% or greater chance of pseudocellulitis, suggesting that the diagnosis of cellulitis be reconsidered. A score of 3 to 4 is indeterminate, and additional information such as a dermatology consultation should be pursued. A score of 5 to 7 corresponds to an 82.2% or greater chance of cellulitis, signifying that empiric treatment with antibiotics be considered.15
The ALT-70 score does not apply to cases involving areas other than the lower extremities; intravenous antibiotic use within 48 hours before ED presentation; surgery within the last 30 days; abscess; penetrating trauma; burn; or known history of osteomyelitis, diabetic ulcer, or indwelling hardware at the site of infection.15 The ALT-70 score is available for free via the MDCalc app and website (https://www.mdcalc.com/alt-70-score-cellulitis).
Mohs AUC Determines the Appropriateness of Mohs Micrographic Surgery
In 2012, the American Academy of Dermatology, American College of Mohs Surgery, American Society for Dermatologic Surgery Association, and American Society for Mohs Surgery published appropriate use criteria (AUC) to guide the decision to pursue Mohs micrographic surgery (MMS) in the United States.16 Based on various tumor and patient characteristics, the Mohs AUC assign scores to 270 different clinical scenarios. A score of 1 to 3 signifies that MMS is inappropriate and generally not considered acceptable. A score 4 to 6 indicates that the appropriateness of MMS is uncertain. A score 7 to 9 means that MMS is appropriate and generally considered acceptable.16
Since publication, the Mohs AUC have been criticized for classifying most primary superficial basal cell carcinomas as appropriate for MMS17 (which an AUC coauthor18 and others19,20 have defended), excluding certain reasons for performing MMS (such as operating on multiple tumors on the same day),21 including counterintuitive scores,22 and omitting trials from Europe23 (which AUC coauthors also have defended24).
Final Thoughts
Scoring systems are emerging in dermatology as evidence-based bedside tools to help guide clinical decision-making. Despite their limitations, these scores have the potential to make a meaningful impact in dermatology as they have in other specialties.
The practice of dermatology is rife with bedside tools: swabs, smears, and scoring systems. First popularized in specialties such as emergency medicine and internal medicine, clinical scoring systems are now emerging in dermatology. These evidence-based scores can be calculated quickly at the bedside—often through a free smartphone app—to help guide clinical decision-making regarding diagnosis, prognosis, and management. As with any medical tool, scoring systems have limitations and should be used as a supplement, not substitute, for one’s clinical judgement. This article reviews 4 clinical scoring systems practical for dermatology residents.
SCORTEN Prognosticates Cases of Stevens-Johnson Syndrome/Toxic Epidermal Necrolysis
Perhaps the best-known scoring system in dermatology, the SCORTEN is widely used to predict hospital mortality from Stevens-Johnson syndrome/toxic epidermal necrolysis. The SCORTEN includes 7 variables of equal weight—age of 40 years or older, heart rate of 120 beats per minute or more, cancer/hematologic malignancy, involved body surface area (BSA) greater than 10%, serum urea greater than 10 mmol/L, serum bicarbonate less than 20 mmol/L, and serum glucose greater than 14 mmol/L—each contributing 1 point to the overall score if present.1 The involved BSA is defined as the sum of detached and detachable epidermis.1
The SCORTEN was developed and prospectively validated to be calculated at the end of the first 24 hours of admission; for this calculation, use the BSA affected at that time, and use the most abnormal values during the first 24 hours of admission for the other variables.1 In addition, a follow-up study including some of the original coauthors recommends recalculating the SCORTEN at the end of hospital day 3, having found that the score’s predictive value was better on this day than hospital days 1, 2, 4, or 5.2 Based on the original study, a SCORTEN of 0 to 1 corresponds to a mortality rate of 3.2%, 2 to 12.1%, 3 to 35.3%, 4 to 58.3%, and 5 or greater to 90.0%.1
Limitations of the SCORTEN include its ability to overestimate or underestimate mortality as demonstrated by 2 multi-institutional cohorts.3,4 Recently, the ABCD-10 score was developed as an alternative to the SCORTEN and was found to predict mortality similarly when validated in an internal cohort.5
PEST Screens for Psoriatic Arthritis
Dermatologists play an important role in screening for psoriatic arthritis, as an estimated 1 in 5 patients with psoriasis have psoriatic arthritis.6 To this end, several screening tools have been developed to help differentiate psoriatic arthritis from other arthritides. Joint guidelines from the American Academy of Dermatology and the National Psoriasis Foundation acknowledge that “. . . these screening tools have tended to perform less well when tested in groups of people other than those for which they were originally developed. As such, their usefulness in routine clinical practice remains controversial.”7 Nevertheless, the guidelines state, “[b]ecause screening and early detection of inflammatory arthritis are essential to optimize patient [quality of life] and reduce morbidity, providers may consider using a formal screening tool of their choice.”7
With these limitations in mind, I have found the Psoriasis Epidemiology Screening Tool (PEST) to be the most useful psoriatic arthritis screening tool. One study determined that the PEST has the best trade-off between sensitivity and specificity compared to 2 other psoriatic arthritis screening tools, the Psoriatic Arthritis Screening and Evaluation (PASE) and the Early Arthritis for Psoriatic Patients (EARP).8
The PEST is comprised of 5 questions: (1) Have you ever had a swollen joint (or joints)? (2) Has a doctor ever told you that you have arthritis? (3) Do your fingernails or toenails have holes or pits? (4) Have you had pain in your heel? (5) Have you had a finger or toe that was completely swollen and painful for no apparent reason? According to the PEST, a referral to a rheumatologist should be considered for patients answering yes to 3 or more questions, which is 97% sensitive and 79% specific for psoriatic arthritis.9 Patients who answer yes to fewer than 3 questions should still be referred to a rheumatologist if there is a strong clinical suspicion of psoriatic arthritis.10
The PEST can be accessed for free in 13 languages via the GRAPPA (Group for Research and Assessment of Psoriasis and Psoriatic Arthritis) app as well as downloaded for free from the National Psoriasis Foundation’s website (https://www.psoriasis.org/psa-screening/providers).
ALT-70 Differentiates Cellulitis From Pseudocellulitis
Overdiagnosing cellulitis in the United States has been estimated to result in up to 130,000 unnecessary hospitalizations and up to $515 million in avoidable health care spending.11 Dermatologists are in a unique position to help fix this issue. In one retrospective study of 1430 inpatient dermatology consultations, 74.32% of inpatients evaluated for presumed cellulitis by a dermatologist were instead diagnosed with a cellulitis mimicker (ie, pseudocellulitis), such as stasis dermatitis or contact dermatitis.12
The ALT-70 score was developed and prospectively validated to help differentiate lower extremity cellulitis from pseudocellulitis in adult patients in the emergency department (ED).13 In addition, the score has retrospectively been shown to function similarly in the inpatient setting when calculated at 24 and 48 hours after ED presentation.14 Although the ALT-70 score was designed for use by frontline clinicians prior to dermatology consultation, I also have found it helpful to calculate as a consultant, as it provides an objective measure of risk to communicate to the primary team in support of one diagnosis or another.
ALT-70 is an acronym for the score’s 4 variables: asymmetry, leukocytosis, tachycardia, and age of 70 years or older.15 If present, each variable confers a certain number of points to the final score: 3 points for asymmetry (defined as unilateral leg involvement), 1 point for leukocytosis (white blood cell count ≥10,000/μL), 1 point for tachycardia (≥90 beats per minute), and 2 points for age of 70 years or older. An ALT-70 score of 0 to 2 corresponds to an 83.3% or greater chance of pseudocellulitis, suggesting that the diagnosis of cellulitis be reconsidered. A score of 3 to 4 is indeterminate, and additional information such as a dermatology consultation should be pursued. A score of 5 to 7 corresponds to an 82.2% or greater chance of cellulitis, signifying that empiric treatment with antibiotics be considered.15
The ALT-70 score does not apply to cases involving areas other than the lower extremities; intravenous antibiotic use within 48 hours before ED presentation; surgery within the last 30 days; abscess; penetrating trauma; burn; or known history of osteomyelitis, diabetic ulcer, or indwelling hardware at the site of infection.15 The ALT-70 score is available for free via the MDCalc app and website (https://www.mdcalc.com/alt-70-score-cellulitis).
Mohs AUC Determines the Appropriateness of Mohs Micrographic Surgery
In 2012, the American Academy of Dermatology, American College of Mohs Surgery, American Society for Dermatologic Surgery Association, and American Society for Mohs Surgery published appropriate use criteria (AUC) to guide the decision to pursue Mohs micrographic surgery (MMS) in the United States.16 Based on various tumor and patient characteristics, the Mohs AUC assign scores to 270 different clinical scenarios. A score of 1 to 3 signifies that MMS is inappropriate and generally not considered acceptable. A score 4 to 6 indicates that the appropriateness of MMS is uncertain. A score 7 to 9 means that MMS is appropriate and generally considered acceptable.16
Since publication, the Mohs AUC have been criticized for classifying most primary superficial basal cell carcinomas as appropriate for MMS17 (which an AUC coauthor18 and others19,20 have defended), excluding certain reasons for performing MMS (such as operating on multiple tumors on the same day),21 including counterintuitive scores,22 and omitting trials from Europe23 (which AUC coauthors also have defended24).
Final Thoughts
Scoring systems are emerging in dermatology as evidence-based bedside tools to help guide clinical decision-making. Despite their limitations, these scores have the potential to make a meaningful impact in dermatology as they have in other specialties.
- Bastuji-Garin S, Fouchard N, Bertocchi M, et al. SCORTEN: a severity-of-illness score for toxic epidermal necrolysis. J Invest Dermatol. 2000;115:149-153.
- Guegan S, Bastuji-Garin S, Poszepczynska-Guigne E, et al. Performance of the SCORTEN during the first five days of hospitalization to predict the prognosis of epidermal necrolysis. J Invest Dermatol. 2006;126:272-276.
- Micheletti RG, Chiesa-Fuxench Z, Noe MH, et al. Stevens-Johnson syndrome/toxic epidermal necrolysis: a multicenter retrospective study of 377 adult patients from the United States. J Invest Dermatol. 2018;138:2315-2321.
- Sekula P, Liss Y, Davidovici B, et al. Evaluation of SCORTEN on a cohort of patients with Stevens-Johnson syndrome and toxic epidermal necrolysis included in the RegiSCAR study. J Burn Care Res. 2011;32:237-245.
- Noe MH, Rosenbach M, Hubbard RA, et al. Development and validation of a risk prediction model for in-hospital mortality among patients with Stevens-Johnson syndrome/toxic epidermal necrolysis-ABCD-10. JAMA Dermatol. 2019;155:448-454.
- Alinaghi F, Calov M, Kristensen LE, et al. Prevalence of psoriatic arthritis in patients with psoriasis: a systematic review and meta-analysis of observational and clinical studies. J Am Acad Dermatol. 2019;80:251-265.e219.
- Elmets CA, Leonardi CL, Davis DMR, et al. Joint AAD-NPF guidelines of care for the management and treatment of psoriasis with awareness and attention to comorbidities. J Am Acad Dermatol. 2019;80:1073-1113.
- Karreman MC, Weel A, van der Ven M, et al. Performance of screening tools for psoriatic arthritis: a cross-sectional study in primary care. Rheumatology (Oxford). 2017;56:597-602.
- Ibrahim GH, Buch MH, Lawson C, et al. Evaluation of an existing screening tool for psoriatic arthritis in people with psoriasis and the development of a new instrument: the Psoriasis Epidemiology Screening Tool (PEST) questionnaire. Clin Exp Rheumatol. 2009;27:469-474.
- Zhang A, Kurtzman DJB, Perez-Chada LM, et al. Psoriatic arthritis and the dermatologist: an approach to screening and clinical evaluation. Clin Dermatol. 2018;36:551-560.
- Weng QY, Raff AB, Cohen JM, et al. Costs and consequences associated with misdiagnosed lower extremity cellulitis. JAMA Dermatol. 2017;153:141-146.
- Strazzula L, Cotliar J, Fox LP, et al. Inpatient dermatology consultation aids diagnosis of cellulitis among hospitalized patients: a multi-institutional analysis. J Am Acad Dermatol. 2015;73:70-75.
- Li DG, Dewan AK, Xia FD, et al. The ALT-70 predictive model outperforms thermal imaging for the diagnosis of lower extremity cellulitis: a prospective evaluation. J Am Acad Dermatol. 2018;79:1076-1080.e1071.
- Singer S, Li DG, Gunasekera N, et al. The ALT-70 predictive model maintains predictive value at 24 and 48 hours after presentation [published online March 23, 2019]. J Am Acad Dermatol. doi:10.1016/j.jaad.2019.03.050.
- Raff AB, Weng QY, Cohen JM, et al. A predictive model for diagnosis of lower extremity cellulitis: a cross-sectional study. J Am Acad Dermatol. 2017;76:618-625.e2.
- Connolly SM, Baker DR, Coldiron BM, et al. AAD/ACMS/ASDSA/ASMS 2012 appropriate use criteria for Mohs micrographic surgery: a report of the American Academy of Dermatology, American College of Mohs Surgery, American Society for Dermatologic Surgery Association, and the American Society for Mohs Surgery. J Am Acad Dermatol. 2012;67:531-550.
- Steinman HK, Dixon A, Zachary CB. Reevaluating Mohs surgery appropriate use criteria for primary superficial basal cell carcinoma. JAMA Dermatol. 2018;154:755-756.
- Montuno MA, Coldiron BM. Mohs appropriate use criteria for superficial basal cell carcinoma. JAMA Dermatol. 2019;155:394-395.
- MacFarlane DF, Perlis C. Mohs appropriate use criteria for superficial basal cell carcinoma. JAMA Dermatol. 2019;155:395-396.
- Kantor J. Mohs appropriate use criteria for superficial basal cell carcinoma. JAMA Dermatol. 2019;155:395.
- Ruiz ES, Karia PS, Morgan FC, et al. Multiple Mohs micrographic surgery is the most common reason for divergence from the appropriate use criteria: a single institution retrospective cohort study. J Am Acad Dermatol. 2016;75:830-831.
- Croley JA, Joseph AK, Wagner RF Jr. Discrepancies in the Mohs Micrographic Surgery appropriate use criteria [published online December 23, 2018]. J Am Acad Dermatol. doi:10.1016/j.jaad.2018.11.064.
- Kelleners-Smeets NW, Mosterd K. Comment on 2012 appropriate use criteria for Mohs micrographic surgery. J Am Acad Dermatol. 2013;69:317-318.
- Connolly S, Baker D, Coldiron B, et al. Reply to “comment on 2012 appropriate use criteria for Mohs micrographic surgery.” J Am Acad Dermatol. 2013;69:318.
- Bastuji-Garin S, Fouchard N, Bertocchi M, et al. SCORTEN: a severity-of-illness score for toxic epidermal necrolysis. J Invest Dermatol. 2000;115:149-153.
- Guegan S, Bastuji-Garin S, Poszepczynska-Guigne E, et al. Performance of the SCORTEN during the first five days of hospitalization to predict the prognosis of epidermal necrolysis. J Invest Dermatol. 2006;126:272-276.
- Micheletti RG, Chiesa-Fuxench Z, Noe MH, et al. Stevens-Johnson syndrome/toxic epidermal necrolysis: a multicenter retrospective study of 377 adult patients from the United States. J Invest Dermatol. 2018;138:2315-2321.
- Sekula P, Liss Y, Davidovici B, et al. Evaluation of SCORTEN on a cohort of patients with Stevens-Johnson syndrome and toxic epidermal necrolysis included in the RegiSCAR study. J Burn Care Res. 2011;32:237-245.
- Noe MH, Rosenbach M, Hubbard RA, et al. Development and validation of a risk prediction model for in-hospital mortality among patients with Stevens-Johnson syndrome/toxic epidermal necrolysis-ABCD-10. JAMA Dermatol. 2019;155:448-454.
- Alinaghi F, Calov M, Kristensen LE, et al. Prevalence of psoriatic arthritis in patients with psoriasis: a systematic review and meta-analysis of observational and clinical studies. J Am Acad Dermatol. 2019;80:251-265.e219.
- Elmets CA, Leonardi CL, Davis DMR, et al. Joint AAD-NPF guidelines of care for the management and treatment of psoriasis with awareness and attention to comorbidities. J Am Acad Dermatol. 2019;80:1073-1113.
- Karreman MC, Weel A, van der Ven M, et al. Performance of screening tools for psoriatic arthritis: a cross-sectional study in primary care. Rheumatology (Oxford). 2017;56:597-602.
- Ibrahim GH, Buch MH, Lawson C, et al. Evaluation of an existing screening tool for psoriatic arthritis in people with psoriasis and the development of a new instrument: the Psoriasis Epidemiology Screening Tool (PEST) questionnaire. Clin Exp Rheumatol. 2009;27:469-474.
- Zhang A, Kurtzman DJB, Perez-Chada LM, et al. Psoriatic arthritis and the dermatologist: an approach to screening and clinical evaluation. Clin Dermatol. 2018;36:551-560.
- Weng QY, Raff AB, Cohen JM, et al. Costs and consequences associated with misdiagnosed lower extremity cellulitis. JAMA Dermatol. 2017;153:141-146.
- Strazzula L, Cotliar J, Fox LP, et al. Inpatient dermatology consultation aids diagnosis of cellulitis among hospitalized patients: a multi-institutional analysis. J Am Acad Dermatol. 2015;73:70-75.
- Li DG, Dewan AK, Xia FD, et al. The ALT-70 predictive model outperforms thermal imaging for the diagnosis of lower extremity cellulitis: a prospective evaluation. J Am Acad Dermatol. 2018;79:1076-1080.e1071.
- Singer S, Li DG, Gunasekera N, et al. The ALT-70 predictive model maintains predictive value at 24 and 48 hours after presentation [published online March 23, 2019]. J Am Acad Dermatol. doi:10.1016/j.jaad.2019.03.050.
- Raff AB, Weng QY, Cohen JM, et al. A predictive model for diagnosis of lower extremity cellulitis: a cross-sectional study. J Am Acad Dermatol. 2017;76:618-625.e2.
- Connolly SM, Baker DR, Coldiron BM, et al. AAD/ACMS/ASDSA/ASMS 2012 appropriate use criteria for Mohs micrographic surgery: a report of the American Academy of Dermatology, American College of Mohs Surgery, American Society for Dermatologic Surgery Association, and the American Society for Mohs Surgery. J Am Acad Dermatol. 2012;67:531-550.
- Steinman HK, Dixon A, Zachary CB. Reevaluating Mohs surgery appropriate use criteria for primary superficial basal cell carcinoma. JAMA Dermatol. 2018;154:755-756.
- Montuno MA, Coldiron BM. Mohs appropriate use criteria for superficial basal cell carcinoma. JAMA Dermatol. 2019;155:394-395.
- MacFarlane DF, Perlis C. Mohs appropriate use criteria for superficial basal cell carcinoma. JAMA Dermatol. 2019;155:395-396.
- Kantor J. Mohs appropriate use criteria for superficial basal cell carcinoma. JAMA Dermatol. 2019;155:395.
- Ruiz ES, Karia PS, Morgan FC, et al. Multiple Mohs micrographic surgery is the most common reason for divergence from the appropriate use criteria: a single institution retrospective cohort study. J Am Acad Dermatol. 2016;75:830-831.
- Croley JA, Joseph AK, Wagner RF Jr. Discrepancies in the Mohs Micrographic Surgery appropriate use criteria [published online December 23, 2018]. J Am Acad Dermatol. doi:10.1016/j.jaad.2018.11.064.
- Kelleners-Smeets NW, Mosterd K. Comment on 2012 appropriate use criteria for Mohs micrographic surgery. J Am Acad Dermatol. 2013;69:317-318.
- Connolly S, Baker D, Coldiron B, et al. Reply to “comment on 2012 appropriate use criteria for Mohs micrographic surgery.” J Am Acad Dermatol. 2013;69:318.
Resident Pearls
- Mortality from Stevens-Johnson syndrome/toxic epidermal necrolysis can be estimated by calculating the SCORTEN at the end of days 1 and 3 of hospitalization.
- The Psoriasis Epidemiology Screening Tool (PEST) assists with triaging which patients with psoriasis should be evaluated for psoriatic arthritis by a rheumatologist.
- The ALT-70 score is helpful to support one’s diagnosis of cellulitis or pseudocellulitis.
- The Mohs appropriate use criteria (AUC) score 270 different clinical scenarios as appropriate, uncertain, or inappropriate for Mohs micrographic surgery.
#Dermlife and the Burned-out Resident
Dermatologist Dr. Jeffrey Benabio quipped, “The phrase ‘dermatologist burnout’ may seem as oxymoronic as jumbo shrimp, yet both are real.”1 Indeed, dermatologists often self-report as among the happiest specialists both at work and home, according to the annual Medscape Physician Lifestyle and Happiness Report.2 Similarly, others in the medical field may perceive dermatologists as low-stress providers—well-groomed, well-rested rays of sunshine, getting out of work every day at 5:00
Burnout in Dermatology Residents
Burnout is a syndrome of emotional exhaustion, depersonalization, and a sense of reduced personal accomplishment that affects residents of all specialties3; however, there is a paucity of literature on burnout as it relates to dermatology. Although long work hours and schedule volatility have captured the focus of resident burnout conversations, a less discussed set of factors may contribute to dermatology resident burnout, such as increasing patient load, intensifying regulations, and an unrelenting pace of clinic. A recent survey study by Shoimer et al3 found that 61% of 116 participating Canadian dermatology residents cited examinations (including the board certifying examination) as their top stressor, followed by work (27%). Other stressors included family, relationships, finances, pressure from staff, research, and moving. More than 50% of dermatology residents surveyed experienced high levels of emotional exhaustion and depersonalization, while 40% demonstrated a low sense of personal accomplishment, all of which are determinants of the burnout syndrome.3
Comparison to Residents in Other Specialties
Although dermatology residents experience lower burnout rates than colleagues in other specialties, the absolute prevalence warrants attention. A recent study published in the Journal of the American Medical Association of 3588 second-year medical residents in the United States found that rates of burnout symptoms across clinical specialties ranged from 29.6% to 63.8%. The highest rates of burnout were found in urology (63.8%), neurology (61.6%), and ophthalmology (55.8%), but the lowest reported rate of burnout was demonstrated in dermatology (29.6%).4 Although dermatology ranked the lowest, that is still nearly a whopping 1 in 3 dermatology residents with burnout symptoms. The absolute prevalence should not be obscured by the ranking among other specialties.
Preventing Burnout
Several burnout prevention and coping strategies across specialties have been suggested.
Mindfulness and Self-awareness
A study by Chaukos et al5 found that mindfulness and self-awareness are resilience factors associated with resident burnout. Counseling is one strategy demonstrated to increase self-awareness. Mindfulness may be practiced through meditation or yoga. Regular meditation has been shown to improve mood and emotional stress.6 Similarly, yoga has been shown to yield physical, emotional, and psychological benefits to resdients.7
Work Factors
A supportive clinical faculty and receiving constructive monthly performance feedback have been negatively correlated with dermatology resident burnout.3 Other workplace interventions demonstrating utility in decreasing resident burnout include increasing staff awareness about burnout, increasing support for health professionals treating challenging populations, and ensuring a reasonable workload.6
Sleep
It has been demonstrated that sleeping less than 7 hours per night also is associated with resident burnout,7 yet it has been reported that 72% of dermatology residents fall into this category.3 Poor sleep quality has been shown to be a predictor of lower academic performance. It has been proposed that to minimize sleep deprivation and poor sleep quality, institutions should focus on programs that promote regular exercise, sleep hygiene, mindfulness, and time-out activities such as meditation.7
Social Support
Focusing on peers may foster the inner strength to endure suffering.1 Venting, laughing, and discussing care with colleagues has been demonstrated to decrease anxiety.6 Work-related social networks may be strengthened through attendance at conferences, lectures, and professional organizations.7 Additionally, social supports and spending quality time with family have been demonstrated as negative predictors of dermatology resident burnout.3
Physical Exercise
Exercise has been demonstrated to improve mood, anxiety, and depression, thereby decreasing resident burnout.6
Final Thoughts
Burnout among dermatology residents warrants awareness, as it does in other medical specialties. Awareness may facilitate identification and prevention, the latter of which is perhaps best summarized by the words of psychologist Dr. Christina Maslach: “If all of the knowledge and advice about how to beat burnout could be summed up in 1 word, that word would be balance—balance between giving and getting, balance between stress and calm, balance between work and home.”8
- Benabio J. Burnout. Dermatology News. November 14, 2017. https://www.mdedge.com/edermatologynews/article/152098/business-medicine/burnout. Accessed August 14, 2019.
- Martin KL. Medscape Physician Lifestyle & Happiness Report 2019. Medscape website. https://www.medscape.com/slideshow/2019-lifestyle-happiness-6011057. Published January 9, 2019. Accessed August 14, 2019.
- Shoimer I, Patten S, Mydlarski P. Burnout in dermatology residents: a Canadian perspective. Br J Dermatol. 2018;178:270-271.
- Dyrbye LN, Burke SE, Hardeman RR, et al. Association of clinical specialty with symptoms of burnout and career choice regret among us resident physicians. JAMA. 2018;320:1114-1130.
- Chaukos D, Chaed-Friedman E, Mehta D, et al. Risk and resilience factors associated with resident burnout. Acad Psychiatry. 2017;41:189-194.
- Ishak WW, Lederer S, Mandili C, et al. Burnout during residency training: a literature review. J Grad Med Educ. 2009;2:236-242.
- Tolentino J, Guo W, Ricca R, et al. What’s new in academic medicine: can we effectively address the burnout epidemic in healthcare? Int J Acad Med. 2017;3.
- Maslach C. Burnout: a multidimensional perspective. In: Schaufeli W, Maslach C, Marek T, eds. Professional Burnout: Recent Developments in Theory and Research. Washington, DC: Taylor and Francis; 1993:19-32.
Dermatologist Dr. Jeffrey Benabio quipped, “The phrase ‘dermatologist burnout’ may seem as oxymoronic as jumbo shrimp, yet both are real.”1 Indeed, dermatologists often self-report as among the happiest specialists both at work and home, according to the annual Medscape Physician Lifestyle and Happiness Report.2 Similarly, others in the medical field may perceive dermatologists as low-stress providers—well-groomed, well-rested rays of sunshine, getting out of work every day at 5:00
Burnout in Dermatology Residents
Burnout is a syndrome of emotional exhaustion, depersonalization, and a sense of reduced personal accomplishment that affects residents of all specialties3; however, there is a paucity of literature on burnout as it relates to dermatology. Although long work hours and schedule volatility have captured the focus of resident burnout conversations, a less discussed set of factors may contribute to dermatology resident burnout, such as increasing patient load, intensifying regulations, and an unrelenting pace of clinic. A recent survey study by Shoimer et al3 found that 61% of 116 participating Canadian dermatology residents cited examinations (including the board certifying examination) as their top stressor, followed by work (27%). Other stressors included family, relationships, finances, pressure from staff, research, and moving. More than 50% of dermatology residents surveyed experienced high levels of emotional exhaustion and depersonalization, while 40% demonstrated a low sense of personal accomplishment, all of which are determinants of the burnout syndrome.3
Comparison to Residents in Other Specialties
Although dermatology residents experience lower burnout rates than colleagues in other specialties, the absolute prevalence warrants attention. A recent study published in the Journal of the American Medical Association of 3588 second-year medical residents in the United States found that rates of burnout symptoms across clinical specialties ranged from 29.6% to 63.8%. The highest rates of burnout were found in urology (63.8%), neurology (61.6%), and ophthalmology (55.8%), but the lowest reported rate of burnout was demonstrated in dermatology (29.6%).4 Although dermatology ranked the lowest, that is still nearly a whopping 1 in 3 dermatology residents with burnout symptoms. The absolute prevalence should not be obscured by the ranking among other specialties.
Preventing Burnout
Several burnout prevention and coping strategies across specialties have been suggested.
Mindfulness and Self-awareness
A study by Chaukos et al5 found that mindfulness and self-awareness are resilience factors associated with resident burnout. Counseling is one strategy demonstrated to increase self-awareness. Mindfulness may be practiced through meditation or yoga. Regular meditation has been shown to improve mood and emotional stress.6 Similarly, yoga has been shown to yield physical, emotional, and psychological benefits to resdients.7
Work Factors
A supportive clinical faculty and receiving constructive monthly performance feedback have been negatively correlated with dermatology resident burnout.3 Other workplace interventions demonstrating utility in decreasing resident burnout include increasing staff awareness about burnout, increasing support for health professionals treating challenging populations, and ensuring a reasonable workload.6
Sleep
It has been demonstrated that sleeping less than 7 hours per night also is associated with resident burnout,7 yet it has been reported that 72% of dermatology residents fall into this category.3 Poor sleep quality has been shown to be a predictor of lower academic performance. It has been proposed that to minimize sleep deprivation and poor sleep quality, institutions should focus on programs that promote regular exercise, sleep hygiene, mindfulness, and time-out activities such as meditation.7
Social Support
Focusing on peers may foster the inner strength to endure suffering.1 Venting, laughing, and discussing care with colleagues has been demonstrated to decrease anxiety.6 Work-related social networks may be strengthened through attendance at conferences, lectures, and professional organizations.7 Additionally, social supports and spending quality time with family have been demonstrated as negative predictors of dermatology resident burnout.3
Physical Exercise
Exercise has been demonstrated to improve mood, anxiety, and depression, thereby decreasing resident burnout.6
Final Thoughts
Burnout among dermatology residents warrants awareness, as it does in other medical specialties. Awareness may facilitate identification and prevention, the latter of which is perhaps best summarized by the words of psychologist Dr. Christina Maslach: “If all of the knowledge and advice about how to beat burnout could be summed up in 1 word, that word would be balance—balance between giving and getting, balance between stress and calm, balance between work and home.”8
Dermatologist Dr. Jeffrey Benabio quipped, “The phrase ‘dermatologist burnout’ may seem as oxymoronic as jumbo shrimp, yet both are real.”1 Indeed, dermatologists often self-report as among the happiest specialists both at work and home, according to the annual Medscape Physician Lifestyle and Happiness Report.2 Similarly, others in the medical field may perceive dermatologists as low-stress providers—well-groomed, well-rested rays of sunshine, getting out of work every day at 5:00
Burnout in Dermatology Residents
Burnout is a syndrome of emotional exhaustion, depersonalization, and a sense of reduced personal accomplishment that affects residents of all specialties3; however, there is a paucity of literature on burnout as it relates to dermatology. Although long work hours and schedule volatility have captured the focus of resident burnout conversations, a less discussed set of factors may contribute to dermatology resident burnout, such as increasing patient load, intensifying regulations, and an unrelenting pace of clinic. A recent survey study by Shoimer et al3 found that 61% of 116 participating Canadian dermatology residents cited examinations (including the board certifying examination) as their top stressor, followed by work (27%). Other stressors included family, relationships, finances, pressure from staff, research, and moving. More than 50% of dermatology residents surveyed experienced high levels of emotional exhaustion and depersonalization, while 40% demonstrated a low sense of personal accomplishment, all of which are determinants of the burnout syndrome.3
Comparison to Residents in Other Specialties
Although dermatology residents experience lower burnout rates than colleagues in other specialties, the absolute prevalence warrants attention. A recent study published in the Journal of the American Medical Association of 3588 second-year medical residents in the United States found that rates of burnout symptoms across clinical specialties ranged from 29.6% to 63.8%. The highest rates of burnout were found in urology (63.8%), neurology (61.6%), and ophthalmology (55.8%), but the lowest reported rate of burnout was demonstrated in dermatology (29.6%).4 Although dermatology ranked the lowest, that is still nearly a whopping 1 in 3 dermatology residents with burnout symptoms. The absolute prevalence should not be obscured by the ranking among other specialties.
Preventing Burnout
Several burnout prevention and coping strategies across specialties have been suggested.
Mindfulness and Self-awareness
A study by Chaukos et al5 found that mindfulness and self-awareness are resilience factors associated with resident burnout. Counseling is one strategy demonstrated to increase self-awareness. Mindfulness may be practiced through meditation or yoga. Regular meditation has been shown to improve mood and emotional stress.6 Similarly, yoga has been shown to yield physical, emotional, and psychological benefits to resdients.7
Work Factors
A supportive clinical faculty and receiving constructive monthly performance feedback have been negatively correlated with dermatology resident burnout.3 Other workplace interventions demonstrating utility in decreasing resident burnout include increasing staff awareness about burnout, increasing support for health professionals treating challenging populations, and ensuring a reasonable workload.6
Sleep
It has been demonstrated that sleeping less than 7 hours per night also is associated with resident burnout,7 yet it has been reported that 72% of dermatology residents fall into this category.3 Poor sleep quality has been shown to be a predictor of lower academic performance. It has been proposed that to minimize sleep deprivation and poor sleep quality, institutions should focus on programs that promote regular exercise, sleep hygiene, mindfulness, and time-out activities such as meditation.7
Social Support
Focusing on peers may foster the inner strength to endure suffering.1 Venting, laughing, and discussing care with colleagues has been demonstrated to decrease anxiety.6 Work-related social networks may be strengthened through attendance at conferences, lectures, and professional organizations.7 Additionally, social supports and spending quality time with family have been demonstrated as negative predictors of dermatology resident burnout.3
Physical Exercise
Exercise has been demonstrated to improve mood, anxiety, and depression, thereby decreasing resident burnout.6
Final Thoughts
Burnout among dermatology residents warrants awareness, as it does in other medical specialties. Awareness may facilitate identification and prevention, the latter of which is perhaps best summarized by the words of psychologist Dr. Christina Maslach: “If all of the knowledge and advice about how to beat burnout could be summed up in 1 word, that word would be balance—balance between giving and getting, balance between stress and calm, balance between work and home.”8
- Benabio J. Burnout. Dermatology News. November 14, 2017. https://www.mdedge.com/edermatologynews/article/152098/business-medicine/burnout. Accessed August 14, 2019.
- Martin KL. Medscape Physician Lifestyle & Happiness Report 2019. Medscape website. https://www.medscape.com/slideshow/2019-lifestyle-happiness-6011057. Published January 9, 2019. Accessed August 14, 2019.
- Shoimer I, Patten S, Mydlarski P. Burnout in dermatology residents: a Canadian perspective. Br J Dermatol. 2018;178:270-271.
- Dyrbye LN, Burke SE, Hardeman RR, et al. Association of clinical specialty with symptoms of burnout and career choice regret among us resident physicians. JAMA. 2018;320:1114-1130.
- Chaukos D, Chaed-Friedman E, Mehta D, et al. Risk and resilience factors associated with resident burnout. Acad Psychiatry. 2017;41:189-194.
- Ishak WW, Lederer S, Mandili C, et al. Burnout during residency training: a literature review. J Grad Med Educ. 2009;2:236-242.
- Tolentino J, Guo W, Ricca R, et al. What’s new in academic medicine: can we effectively address the burnout epidemic in healthcare? Int J Acad Med. 2017;3.
- Maslach C. Burnout: a multidimensional perspective. In: Schaufeli W, Maslach C, Marek T, eds. Professional Burnout: Recent Developments in Theory and Research. Washington, DC: Taylor and Francis; 1993:19-32.
- Benabio J. Burnout. Dermatology News. November 14, 2017. https://www.mdedge.com/edermatologynews/article/152098/business-medicine/burnout. Accessed August 14, 2019.
- Martin KL. Medscape Physician Lifestyle & Happiness Report 2019. Medscape website. https://www.medscape.com/slideshow/2019-lifestyle-happiness-6011057. Published January 9, 2019. Accessed August 14, 2019.
- Shoimer I, Patten S, Mydlarski P. Burnout in dermatology residents: a Canadian perspective. Br J Dermatol. 2018;178:270-271.
- Dyrbye LN, Burke SE, Hardeman RR, et al. Association of clinical specialty with symptoms of burnout and career choice regret among us resident physicians. JAMA. 2018;320:1114-1130.
- Chaukos D, Chaed-Friedman E, Mehta D, et al. Risk and resilience factors associated with resident burnout. Acad Psychiatry. 2017;41:189-194.
- Ishak WW, Lederer S, Mandili C, et al. Burnout during residency training: a literature review. J Grad Med Educ. 2009;2:236-242.
- Tolentino J, Guo W, Ricca R, et al. What’s new in academic medicine: can we effectively address the burnout epidemic in healthcare? Int J Acad Med. 2017;3.
- Maslach C. Burnout: a multidimensional perspective. In: Schaufeli W, Maslach C, Marek T, eds. Professional Burnout: Recent Developments in Theory and Research. Washington, DC: Taylor and Francis; 1993:19-32.
Resident Pearl
- Reported techniques for preventing and coping with resident burnout include mindfulness and self-awareness, optimization of workplace factors, adequate sleep, social support, and physical exercise.
Challenges of Treating Primary Psychiatric Disease in Dermatology
Dermatology patients experience a high burden of mental health disturbance. Psychiatric disease is seen in an estimated 30% to 60% of our patients.1 It can be secondary to or comorbid with dermatologic disorders, or it can be the primary condition that is driving cutaneous disease. Patients with secondary or comorbid psychiatric disorders often are amenable to referral to a mental health provider or are already participating in some form of mental health treatment; however, patients with primary psychiatric disease who present to dermatology generally do not accept these referrals.2 Therefore, if these patients are to receive care anywhere in the health care system, it often must be in the department of dermatology.
What primary psychiatric conditions do we see in dermatology?
Common primary psychiatric conditions seen in dermatology include delusional infestation, obsessive-compulsive disorder and related disorders, and dermatitis artefacta.
Delusional Infestation
Also known as delusions of parasitosis or delusional parasitosis, delusional infestation presents as a fixed false belief that there is an organism or other foreign entity that is present in the skin and is the cause of cutaneous disruption. It often is an isolated delusion but can have a notable psychosocial impact. The term delusional infestation is sometimes preferred, as it is inclusive of delusions focused on any type of organism, not just parasites. It also encompasses delusions of infestation with nonliving matter such as fibers, also known as Morgellons disease.3
Obsessive-Compulsive Disorder and Related Disorders
This broad category includes several conditions encountered in dermatology. Body dysmorphic disorder (BDD), olfactory reference syndrome (ORS), excoriation disorder, and trichotillomania are some of the most common variants. In patients with BDD, skin and hair are the 2 most common preoccupations. It has been estimated that 12% of dermatology patients experience BDD. Unsurprisingly, it is more common in patients presenting to cosmetic dermatology, but general dermatology patients also are affected at a rate of 7%.2 Patients with ORS falsely believe they have body odor and/or halitosis. Excoriation disorder manifests as repetitive skin picking, either of normal skin or of lesions such as pimples and scabs. Trichotillomania presents as repeated hair pulling, and trichophagia (eating the pulled hair) also may be present.
Dermatitis Artefacta
Almost 1 in 4 patients who seek dermatologic evaluation for primarily psychiatric disorders have dermatitis artefacta, the presence of deliberately self-inflicted skin lesions.2 Patients with dermatitis artefacta have unconscious motives for their behavior and should be distinguished from malingering patients who have a conscious goal of secondary gain.
What treatments are available?
Antidepressants
Selective serotonin reuptake inhibitors are one of the first-line treatments for BDD and may be useful in ORS. In excoriation disorder and trichotillomania, selective serotonin reuptake inhibitors are the most commonly prescribed pharmacotherapy, but they have limited efficacy.2
Antipsychotics
The recommended treatment of delusional infestation is antipsychotic pharmacotherapy. Treatment with risperidone and olanzapine has been reported to achieve full or partial remission in more than two-thirds of cases.4 Aripiprazole, a newer antipsychotic, has fewer side effects and has been successful in several case reports.5-7
Cognitive Behavioral Therapy
Psychotherapy, most often in the form of cognitive behavioral therapy, has been reported as effective treatment of several psychocutaneous diseases. Cognitive behavioral therapy is considered first-line treatment of body-focused repetitive behavior disorders such as excoriation disorder and trichotillomania.2 It addresses maladaptive thought patterns to modify behavior.
Who treats patients with neurodermatoses?
If a patient presents to dermatology with a rash found to be related to an underlying thyroid disorder, the treatment plan likely would include referral to an endocrinologist. Similarly, patients with primary psychiatric conditions presenting to dermatology should ideally be referred to psychiatrists or psychotherapists, the providers most thoroughly trained and best equipped to treat them. The challenge in psychodermatology is that patients often are resistant to the assessment that the primary pathology is psychiatric. Patients may deny that they are “crazy” and see numerous providers in search of a dermatologist who “believes” them.8
Referral to mental health professionals almost always is refused by patients with primarily psychiatric neurodermatoses, which presents dermatologists with a dilemma. As the authors of the “Psychotropic Agents” chapter of Comprehensive Dermatologic Drug Therapy put it: “A dermatologist has two choices. The first is to try to ‘look the other way’ and pacify the patient by providing relatively benign, but minimally effective treatments. The other option is to try to directly address the psychological/psychiatric problems.” The chapter then provides a thorough guide for the use of psychotropic medications in the dermatology population, advocating for option 2: treatment by dermatologists.9
Should a dermatologist prescribe psychotropic drugs?
In Dermatology, the principle reference textbook in many dermatology training programs, it is stated that “[a]lthough less comprehensive than treatment delivered in collaboration with a psychiatrist, in the authors’ opinion, management of these issues by a dermatologist is better than no treatment at all.”10 Recent reviews in the dermatologic literature of psychiatric diseases and drugs in dermatology agree that dermatologists should feel comfortable with prescribing pharmacologic treatment.2,8,11 Performance of psychotherapy by dermatologists, on the other hand, is not recommended based on time constraints and lack of training.
Despite the apparent agreement in the texts and literature that pharmacotherapy of psychiatric neurodermatoses is within our scope of practice in dermatology, most dermatologists do not prescribe psychotropic agents. Dermatology residencies generally do not provide thorough training in psychopharmacotherapy.9 Unsurprisingly, a survey of 40 dermatologists at one academic institution found that only 11% felt comfortable prescribing an antidepressant and a mere 3% were comfortable prescribing an antipsychotic.12
Final Thoughts
The challenges involved in managing patients with primary psychiatric disease in dermatology are great and many patients are undertreated despite the availability of effective, evidence-based treatment options. We need to continue to work toward providing better access to these treatments in a way that maximizes the chance that our patients will accept our care.
- Korabel H, Dudek D, Jaworek A, et al. Psychodermatology: psychological and psychiatrical aspects of dermatology [in Polish]. Przegl Lek. 2008;65:244-248.
- Krooks JA, Weatherall AG, Holland PJ. Review of epidemiology, clinical presentation, diagnosis, and treatment of common primary psychiatric causes of cutaneous disease. J Dermatolog Treat. 2018;29:418-427.
- Bewley AP, Lepping P, Freundenmann RW, et al. Delusional parasitosis: time to call it delusional infestation. Br J Dermatol. 2018;163:1-2.
- Freudenmann RW, Lepping P. Second-generation antipsychotics in primary and secondary delusional parasitosis: outcome and efficacy. J Clin Psychopharmacol. 2008;28:500-508.
- Miyamoto S, Miyake N, Ogino S, et al. Successful treatment of delusional disorder with low-dose aripiprazole. Psychiatry Clin Neurosci. 2008;62:369.
- Ladizinski B, Busse KL, Bhutani T, et al. Aripiprazole as a viable alternative for treating delusions of parasitosis. J Drugs Dermatol. 2010;9:1531-1532.
- Huang WL, Chang LR. Aripiprazole in the treatment of delusional parasitosis with ocular and dermatologic presentations. J Clin Psychopharmacol. 2013;33:272-273.
- Campbell EH, Elston DM, Hawthorne JD, et al. Diagnosis and management of delusional parasitosis. J Am Acad Dermatol. 2019;80:1428-1434.
- Bhutani T, Lee CS, Koo JYM. Psychotropic agents. In: Wolverton SE, ed. Comprehensive Dermatologic Drug Therapy. 3rd ed. China: Elsevier Saunders; 2013:375-388.
- Duncan KO, Koo JYM. Psychocutaneous diseases. In: Bolognia JL, Schaffer JV, Cerroni L, eds. Dermatology. 4th ed. China: Elsevier; 2018:128-137.
- Shah B, Levenson JL. Use of psychotropic drugs in the dermatology patient: when to start and stop? Clin Dermatol. 2018;36:748-755.
- Gee SN, Zakhary L, Keuthen N, et al. A survey assessment of the recognition and treatment of psychocutaneous disorders in the outpatient dermatology setting: how prepared are we? J Am Acad Dermatol. 2013;68:47-52.
Dermatology patients experience a high burden of mental health disturbance. Psychiatric disease is seen in an estimated 30% to 60% of our patients.1 It can be secondary to or comorbid with dermatologic disorders, or it can be the primary condition that is driving cutaneous disease. Patients with secondary or comorbid psychiatric disorders often are amenable to referral to a mental health provider or are already participating in some form of mental health treatment; however, patients with primary psychiatric disease who present to dermatology generally do not accept these referrals.2 Therefore, if these patients are to receive care anywhere in the health care system, it often must be in the department of dermatology.
What primary psychiatric conditions do we see in dermatology?
Common primary psychiatric conditions seen in dermatology include delusional infestation, obsessive-compulsive disorder and related disorders, and dermatitis artefacta.
Delusional Infestation
Also known as delusions of parasitosis or delusional parasitosis, delusional infestation presents as a fixed false belief that there is an organism or other foreign entity that is present in the skin and is the cause of cutaneous disruption. It often is an isolated delusion but can have a notable psychosocial impact. The term delusional infestation is sometimes preferred, as it is inclusive of delusions focused on any type of organism, not just parasites. It also encompasses delusions of infestation with nonliving matter such as fibers, also known as Morgellons disease.3
Obsessive-Compulsive Disorder and Related Disorders
This broad category includes several conditions encountered in dermatology. Body dysmorphic disorder (BDD), olfactory reference syndrome (ORS), excoriation disorder, and trichotillomania are some of the most common variants. In patients with BDD, skin and hair are the 2 most common preoccupations. It has been estimated that 12% of dermatology patients experience BDD. Unsurprisingly, it is more common in patients presenting to cosmetic dermatology, but general dermatology patients also are affected at a rate of 7%.2 Patients with ORS falsely believe they have body odor and/or halitosis. Excoriation disorder manifests as repetitive skin picking, either of normal skin or of lesions such as pimples and scabs. Trichotillomania presents as repeated hair pulling, and trichophagia (eating the pulled hair) also may be present.
Dermatitis Artefacta
Almost 1 in 4 patients who seek dermatologic evaluation for primarily psychiatric disorders have dermatitis artefacta, the presence of deliberately self-inflicted skin lesions.2 Patients with dermatitis artefacta have unconscious motives for their behavior and should be distinguished from malingering patients who have a conscious goal of secondary gain.
What treatments are available?
Antidepressants
Selective serotonin reuptake inhibitors are one of the first-line treatments for BDD and may be useful in ORS. In excoriation disorder and trichotillomania, selective serotonin reuptake inhibitors are the most commonly prescribed pharmacotherapy, but they have limited efficacy.2
Antipsychotics
The recommended treatment of delusional infestation is antipsychotic pharmacotherapy. Treatment with risperidone and olanzapine has been reported to achieve full or partial remission in more than two-thirds of cases.4 Aripiprazole, a newer antipsychotic, has fewer side effects and has been successful in several case reports.5-7
Cognitive Behavioral Therapy
Psychotherapy, most often in the form of cognitive behavioral therapy, has been reported as effective treatment of several psychocutaneous diseases. Cognitive behavioral therapy is considered first-line treatment of body-focused repetitive behavior disorders such as excoriation disorder and trichotillomania.2 It addresses maladaptive thought patterns to modify behavior.
Who treats patients with neurodermatoses?
If a patient presents to dermatology with a rash found to be related to an underlying thyroid disorder, the treatment plan likely would include referral to an endocrinologist. Similarly, patients with primary psychiatric conditions presenting to dermatology should ideally be referred to psychiatrists or psychotherapists, the providers most thoroughly trained and best equipped to treat them. The challenge in psychodermatology is that patients often are resistant to the assessment that the primary pathology is psychiatric. Patients may deny that they are “crazy” and see numerous providers in search of a dermatologist who “believes” them.8
Referral to mental health professionals almost always is refused by patients with primarily psychiatric neurodermatoses, which presents dermatologists with a dilemma. As the authors of the “Psychotropic Agents” chapter of Comprehensive Dermatologic Drug Therapy put it: “A dermatologist has two choices. The first is to try to ‘look the other way’ and pacify the patient by providing relatively benign, but minimally effective treatments. The other option is to try to directly address the psychological/psychiatric problems.” The chapter then provides a thorough guide for the use of psychotropic medications in the dermatology population, advocating for option 2: treatment by dermatologists.9
Should a dermatologist prescribe psychotropic drugs?
In Dermatology, the principle reference textbook in many dermatology training programs, it is stated that “[a]lthough less comprehensive than treatment delivered in collaboration with a psychiatrist, in the authors’ opinion, management of these issues by a dermatologist is better than no treatment at all.”10 Recent reviews in the dermatologic literature of psychiatric diseases and drugs in dermatology agree that dermatologists should feel comfortable with prescribing pharmacologic treatment.2,8,11 Performance of psychotherapy by dermatologists, on the other hand, is not recommended based on time constraints and lack of training.
Despite the apparent agreement in the texts and literature that pharmacotherapy of psychiatric neurodermatoses is within our scope of practice in dermatology, most dermatologists do not prescribe psychotropic agents. Dermatology residencies generally do not provide thorough training in psychopharmacotherapy.9 Unsurprisingly, a survey of 40 dermatologists at one academic institution found that only 11% felt comfortable prescribing an antidepressant and a mere 3% were comfortable prescribing an antipsychotic.12
Final Thoughts
The challenges involved in managing patients with primary psychiatric disease in dermatology are great and many patients are undertreated despite the availability of effective, evidence-based treatment options. We need to continue to work toward providing better access to these treatments in a way that maximizes the chance that our patients will accept our care.
Dermatology patients experience a high burden of mental health disturbance. Psychiatric disease is seen in an estimated 30% to 60% of our patients.1 It can be secondary to or comorbid with dermatologic disorders, or it can be the primary condition that is driving cutaneous disease. Patients with secondary or comorbid psychiatric disorders often are amenable to referral to a mental health provider or are already participating in some form of mental health treatment; however, patients with primary psychiatric disease who present to dermatology generally do not accept these referrals.2 Therefore, if these patients are to receive care anywhere in the health care system, it often must be in the department of dermatology.
What primary psychiatric conditions do we see in dermatology?
Common primary psychiatric conditions seen in dermatology include delusional infestation, obsessive-compulsive disorder and related disorders, and dermatitis artefacta.
Delusional Infestation
Also known as delusions of parasitosis or delusional parasitosis, delusional infestation presents as a fixed false belief that there is an organism or other foreign entity that is present in the skin and is the cause of cutaneous disruption. It often is an isolated delusion but can have a notable psychosocial impact. The term delusional infestation is sometimes preferred, as it is inclusive of delusions focused on any type of organism, not just parasites. It also encompasses delusions of infestation with nonliving matter such as fibers, also known as Morgellons disease.3
Obsessive-Compulsive Disorder and Related Disorders
This broad category includes several conditions encountered in dermatology. Body dysmorphic disorder (BDD), olfactory reference syndrome (ORS), excoriation disorder, and trichotillomania are some of the most common variants. In patients with BDD, skin and hair are the 2 most common preoccupations. It has been estimated that 12% of dermatology patients experience BDD. Unsurprisingly, it is more common in patients presenting to cosmetic dermatology, but general dermatology patients also are affected at a rate of 7%.2 Patients with ORS falsely believe they have body odor and/or halitosis. Excoriation disorder manifests as repetitive skin picking, either of normal skin or of lesions such as pimples and scabs. Trichotillomania presents as repeated hair pulling, and trichophagia (eating the pulled hair) also may be present.
Dermatitis Artefacta
Almost 1 in 4 patients who seek dermatologic evaluation for primarily psychiatric disorders have dermatitis artefacta, the presence of deliberately self-inflicted skin lesions.2 Patients with dermatitis artefacta have unconscious motives for their behavior and should be distinguished from malingering patients who have a conscious goal of secondary gain.
What treatments are available?
Antidepressants
Selective serotonin reuptake inhibitors are one of the first-line treatments for BDD and may be useful in ORS. In excoriation disorder and trichotillomania, selective serotonin reuptake inhibitors are the most commonly prescribed pharmacotherapy, but they have limited efficacy.2
Antipsychotics
The recommended treatment of delusional infestation is antipsychotic pharmacotherapy. Treatment with risperidone and olanzapine has been reported to achieve full or partial remission in more than two-thirds of cases.4 Aripiprazole, a newer antipsychotic, has fewer side effects and has been successful in several case reports.5-7
Cognitive Behavioral Therapy
Psychotherapy, most often in the form of cognitive behavioral therapy, has been reported as effective treatment of several psychocutaneous diseases. Cognitive behavioral therapy is considered first-line treatment of body-focused repetitive behavior disorders such as excoriation disorder and trichotillomania.2 It addresses maladaptive thought patterns to modify behavior.
Who treats patients with neurodermatoses?
If a patient presents to dermatology with a rash found to be related to an underlying thyroid disorder, the treatment plan likely would include referral to an endocrinologist. Similarly, patients with primary psychiatric conditions presenting to dermatology should ideally be referred to psychiatrists or psychotherapists, the providers most thoroughly trained and best equipped to treat them. The challenge in psychodermatology is that patients often are resistant to the assessment that the primary pathology is psychiatric. Patients may deny that they are “crazy” and see numerous providers in search of a dermatologist who “believes” them.8
Referral to mental health professionals almost always is refused by patients with primarily psychiatric neurodermatoses, which presents dermatologists with a dilemma. As the authors of the “Psychotropic Agents” chapter of Comprehensive Dermatologic Drug Therapy put it: “A dermatologist has two choices. The first is to try to ‘look the other way’ and pacify the patient by providing relatively benign, but minimally effective treatments. The other option is to try to directly address the psychological/psychiatric problems.” The chapter then provides a thorough guide for the use of psychotropic medications in the dermatology population, advocating for option 2: treatment by dermatologists.9
Should a dermatologist prescribe psychotropic drugs?
In Dermatology, the principle reference textbook in many dermatology training programs, it is stated that “[a]lthough less comprehensive than treatment delivered in collaboration with a psychiatrist, in the authors’ opinion, management of these issues by a dermatologist is better than no treatment at all.”10 Recent reviews in the dermatologic literature of psychiatric diseases and drugs in dermatology agree that dermatologists should feel comfortable with prescribing pharmacologic treatment.2,8,11 Performance of psychotherapy by dermatologists, on the other hand, is not recommended based on time constraints and lack of training.
Despite the apparent agreement in the texts and literature that pharmacotherapy of psychiatric neurodermatoses is within our scope of practice in dermatology, most dermatologists do not prescribe psychotropic agents. Dermatology residencies generally do not provide thorough training in psychopharmacotherapy.9 Unsurprisingly, a survey of 40 dermatologists at one academic institution found that only 11% felt comfortable prescribing an antidepressant and a mere 3% were comfortable prescribing an antipsychotic.12
Final Thoughts
The challenges involved in managing patients with primary psychiatric disease in dermatology are great and many patients are undertreated despite the availability of effective, evidence-based treatment options. We need to continue to work toward providing better access to these treatments in a way that maximizes the chance that our patients will accept our care.
- Korabel H, Dudek D, Jaworek A, et al. Psychodermatology: psychological and psychiatrical aspects of dermatology [in Polish]. Przegl Lek. 2008;65:244-248.
- Krooks JA, Weatherall AG, Holland PJ. Review of epidemiology, clinical presentation, diagnosis, and treatment of common primary psychiatric causes of cutaneous disease. J Dermatolog Treat. 2018;29:418-427.
- Bewley AP, Lepping P, Freundenmann RW, et al. Delusional parasitosis: time to call it delusional infestation. Br J Dermatol. 2018;163:1-2.
- Freudenmann RW, Lepping P. Second-generation antipsychotics in primary and secondary delusional parasitosis: outcome and efficacy. J Clin Psychopharmacol. 2008;28:500-508.
- Miyamoto S, Miyake N, Ogino S, et al. Successful treatment of delusional disorder with low-dose aripiprazole. Psychiatry Clin Neurosci. 2008;62:369.
- Ladizinski B, Busse KL, Bhutani T, et al. Aripiprazole as a viable alternative for treating delusions of parasitosis. J Drugs Dermatol. 2010;9:1531-1532.
- Huang WL, Chang LR. Aripiprazole in the treatment of delusional parasitosis with ocular and dermatologic presentations. J Clin Psychopharmacol. 2013;33:272-273.
- Campbell EH, Elston DM, Hawthorne JD, et al. Diagnosis and management of delusional parasitosis. J Am Acad Dermatol. 2019;80:1428-1434.
- Bhutani T, Lee CS, Koo JYM. Psychotropic agents. In: Wolverton SE, ed. Comprehensive Dermatologic Drug Therapy. 3rd ed. China: Elsevier Saunders; 2013:375-388.
- Duncan KO, Koo JYM. Psychocutaneous diseases. In: Bolognia JL, Schaffer JV, Cerroni L, eds. Dermatology. 4th ed. China: Elsevier; 2018:128-137.
- Shah B, Levenson JL. Use of psychotropic drugs in the dermatology patient: when to start and stop? Clin Dermatol. 2018;36:748-755.
- Gee SN, Zakhary L, Keuthen N, et al. A survey assessment of the recognition and treatment of psychocutaneous disorders in the outpatient dermatology setting: how prepared are we? J Am Acad Dermatol. 2013;68:47-52.
- Korabel H, Dudek D, Jaworek A, et al. Psychodermatology: psychological and psychiatrical aspects of dermatology [in Polish]. Przegl Lek. 2008;65:244-248.
- Krooks JA, Weatherall AG, Holland PJ. Review of epidemiology, clinical presentation, diagnosis, and treatment of common primary psychiatric causes of cutaneous disease. J Dermatolog Treat. 2018;29:418-427.
- Bewley AP, Lepping P, Freundenmann RW, et al. Delusional parasitosis: time to call it delusional infestation. Br J Dermatol. 2018;163:1-2.
- Freudenmann RW, Lepping P. Second-generation antipsychotics in primary and secondary delusional parasitosis: outcome and efficacy. J Clin Psychopharmacol. 2008;28:500-508.
- Miyamoto S, Miyake N, Ogino S, et al. Successful treatment of delusional disorder with low-dose aripiprazole. Psychiatry Clin Neurosci. 2008;62:369.
- Ladizinski B, Busse KL, Bhutani T, et al. Aripiprazole as a viable alternative for treating delusions of parasitosis. J Drugs Dermatol. 2010;9:1531-1532.
- Huang WL, Chang LR. Aripiprazole in the treatment of delusional parasitosis with ocular and dermatologic presentations. J Clin Psychopharmacol. 2013;33:272-273.
- Campbell EH, Elston DM, Hawthorne JD, et al. Diagnosis and management of delusional parasitosis. J Am Acad Dermatol. 2019;80:1428-1434.
- Bhutani T, Lee CS, Koo JYM. Psychotropic agents. In: Wolverton SE, ed. Comprehensive Dermatologic Drug Therapy. 3rd ed. China: Elsevier Saunders; 2013:375-388.
- Duncan KO, Koo JYM. Psychocutaneous diseases. In: Bolognia JL, Schaffer JV, Cerroni L, eds. Dermatology. 4th ed. China: Elsevier; 2018:128-137.
- Shah B, Levenson JL. Use of psychotropic drugs in the dermatology patient: when to start and stop? Clin Dermatol. 2018;36:748-755.
- Gee SN, Zakhary L, Keuthen N, et al. A survey assessment of the recognition and treatment of psychocutaneous disorders in the outpatient dermatology setting: how prepared are we? J Am Acad Dermatol. 2013;68:47-52.
Resident Pearl
- Patients often present to dermatology with primary psychologic disorders such as delusional infestation or trichotillomania. Treatment of such conditions with antidepressants and antipsychotics can be highly effective and is within our scope of practice. Increased emphasis on psychopharmacotherapy in dermatology training would increase access to appropriate care for this patient population.
The ABCs of COCs: A Guide for Dermatology Residents on Combined Oral Contraceptives
The American Academy of Dermatology confers combined oral contraceptives (COCs) a strength A recommendation for the treatment of acne based on level I evidence, and 4 COCs are approved for the treatment of acne by the US Food and Drug Administration (FDA).1 Furthermore, when dermatologists prescribe isotretinoin and thalidomide to women of reproductive potential, the iPLEDGE and THALOMID Risk Evaluation and Mitigation Strategy (REMS) programs require 2 concurrent methods of contraception, one of which may be a COC. In addition, COCs have several potential off-label indications in dermatology including idiopathic hirsutism, female pattern hair loss, hidradenitis suppurativa, and autoimmune progesterone dermatitis.
Despite this evidence and opportunity, research suggests that dermatologists underprescribe COCs. The National Ambulatory Medical Care Survey found that between 1993 and 2008, dermatologists in the United States prescribed COCs to only 2.03% of women presenting for acne treatment, which was less often than obstetricians/gynecologists (36.03%) and internists (10.76%).2 More recently, in a survey of 130 US dermatologists conducted from 2014 to 2015, only 55.4% reported prescribing COCs. This survey also found that only 45.8% of dermatologists who prescribed COCs felt very comfortable counseling on how to begin taking them, only 48.6% felt very comfortable counseling patients on side effects, and only 22.2% felt very comfortable managing side effects.3
In light of these data, this article reviews the basics of COCs for dermatology residents, from assessing patient eligibility and selecting a COC to counseling on use and managing risks and side effects. Because there are different approaches to prescribing COCs, readers are encouraged to integrate the information in this article with what they have learned from other sources.
Assess Patient Eligibility
In general, patients should be at least 14 years of age and have waited 2 years after menarche to start COCs. They can be taken until menopause.1,4 Contraindications can be screened for by taking a medical history and measuring a baseline blood pressure (Tables 1 and 2).5 In addition, pregnancy should be excluded with a urine or serum pregnancy test or criteria provided in Box 2 of the 2016 US Selected Practice Recommendations for Contraceptive Use from the Centers for Disease Control and Prevention (CDC).4 Although important for women’s overall health, a pelvic examination is not required to start COCs according to the CDC and the American Academy of Dermatology.1,4
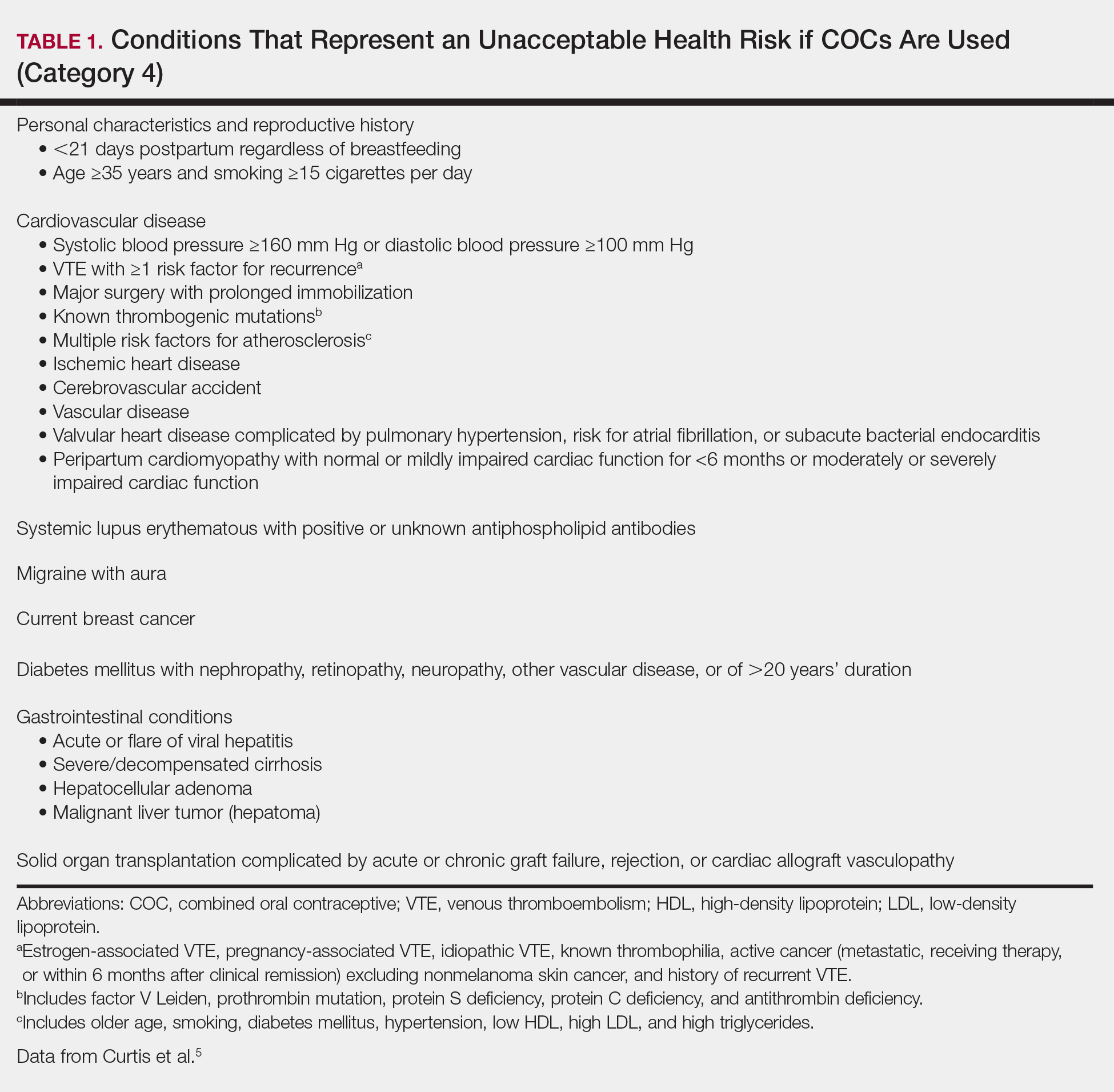
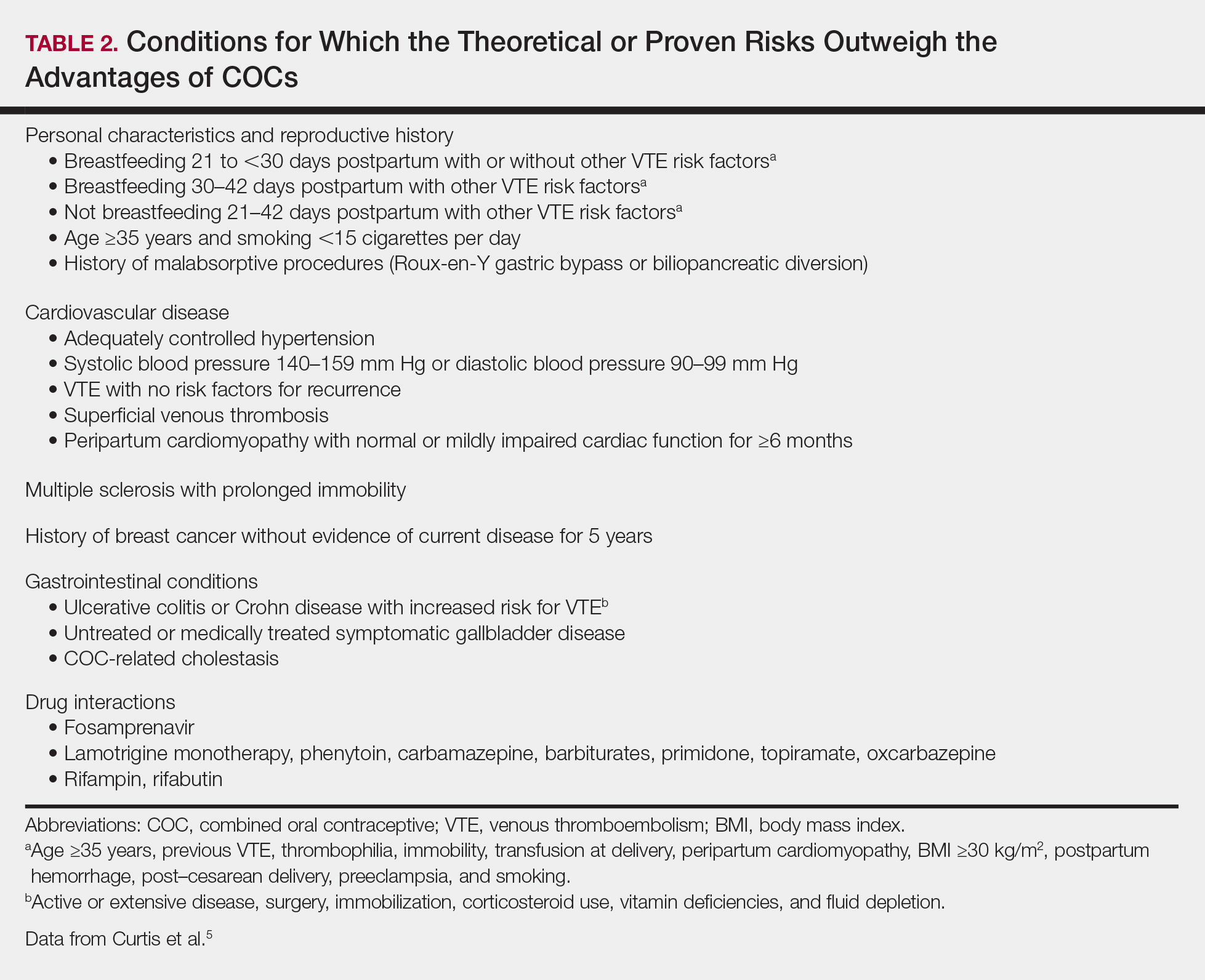
Select the COC
Combined oral contraceptives combine estrogen, usually in the form of ethinyl estradiol, with a progestin. Data suggest that all COCs effectively treat acne, but 4 are specifically FDA approved for acne: ethinyl estradiol–norethindrone acetate–ferrous fumarate, ethinyl estradiol–norgestimate, ethinyl estradiol–drospirenone, and ethinyl estradiol–drospirenone–levomefolate.1 Ethinyl estradiol–desogestrel and ethinyl estradiol–drospirenone are 2 go-to COCs for some of the attending physicians at my residency program. All COCs are FDA approved for contraception. When selecting a COC, one approach is to start with the patient’s drug formulary, then consider the following characteristics.
Monophasic vs Multiphasic
All the hormonally active pills in a monophasic formulation contain the same dose of estrogen and progestin; however, these doses change per pill in a multiphasic formulation, which requires that patients take the pills in a specific order. Given this greater complexity and the fact that multiphasic formulations often are more expensive and lack evidence of superiority, a 2011 Cochrane review recommended monophasic formulations as first line.6 In addition, monophasic formulations are preferred for autoimmune progesterone dermatitis because of the stable progestin dose.
Hormone-Free Interval
Some COCs include placebo pills during which hormone withdrawal symptoms such as bleeding, pelvic pain, mood changes, and headache may occur. If a patient is concerned about these symptoms, choose a COC with no or fewer placebo pills, or have the patient skip the hormone-free interval altogether and start the next pack early7; in this case, the prescription should be written with instructions to allow the patient to get earlier refills from the pharmacy.
Estrogen Dose
To minimize estrogen-related side effects, the lowest possible dose of ethinyl estradiol that is effective and tolerable should be prescribed7,8; 20 μg of ethinyl estradiol generally is the lowest dose available, but it may be associated with more frequent breakthrough bleeding.9 The International Planned Parenthood Federation recommends starting with COCs that contain 30 to 35 μg of estrogen.10 Synthesizing this information, one option is to start with 20 μg of ethinyl estradiol and increase the dose if breakthrough bleeding persists after 3 cycles.
Progestin Type
First-generation progestins (eg, norethindrone), second-generation progestins (eg, norgestrel, levonorgestrel), and third-generation progestins (eg, norgestimate, desogestrel) are derived from testosterone and therefore are variably androgenic; second-generation progestins are the most androgenic, and third-generation progestins are the least. On the other hand, drospirenone, the fourth-generation progestin available in the United States, is derived from 17α-spironolactone and thus is mildly antiandrogenic (3 mg of drospirenone is considered equivalent to 25 mg of spironolactone).
Although COCs with less androgenic progestins should theoretically treat acne better, a 2012 Cochrane review of COCs and acne concluded that “differences in the comparative effectiveness of COCs containing varying progestin types and dosages were less clear, and data were limited for any particular comparison.”11 As a result, regardless of the progestin, all COCs are believed to have a net antiandrogenic effect due to their estrogen component.1
Counsel on Use
Combined oral contraceptives can be started on any day of the menstrual cycle, including the day the prescription is given. If a patient begins a COC within 5 days of the first day of her most recent period, backup contraception is not needed.4 If she begins the COC more than 5 days after the first day of her most recent period, she needs to use backup contraception or abstain from sexual intercourse for the next 7 days.4 In general, at least 3 months of therapy are required to evaluate the effectiveness of COCs for acne.1
Manage Risks and Side Effects
Breakthrough Bleeding
The most common side effect of breakthrough bleeding can be minimized by taking COCs at approximately the same time every day and avoiding missed pills. If breakthrough bleeding does not stop after 3 cycles, consider increasing the estrogen dose to 30 to 35 μg and/or referring to an obstetrician/gynecologist to rule out other etiologies of bleeding.7,8
Nausea, Headache, Bloating, and Breast Tenderness
These symptoms typically resolve after the first 3 months. To minimize nausea, patients should take COCs in the early evening and eat breakfast the next morning.7,8 For headaches that occur during the hormone-free interval, consider skipping the placebo pills and starting the next pack early. Switching the progestin to drospirenone, which has a mild diuretic effect, can help with bloating as well as breast tenderness.7 For persistent symptoms, consider a lower estrogen dose.7,8
Changes in Libido
In a systemic review including 8422 COC users, 64% reported no change in libido, 22% reported an increase, and 15% reported a decrease.12
Weight Gain
Although patients may be concerned that COCs cause weight gain, a 2014 Cochrane review concluded that “available evidence is insufficient to determine the effect of combination contraceptives on weight, but no large effect is evident.”13 If weight gain does occur, anecdotal evidence suggests it tends to be not more than 5 pounds. If weight gain is an issue, consider a less androgenic progestin.8
Venous Thromboembolism
Use the 3-6-9-12 model to contextualize venous thromboembolism (VTE) risk: a woman’s annual VTE risk is 3 per 10,000 women at baseline, 6 per 10,000 women with nondrospirenone COCs, 9 per 10,000 women with drospirenone-containing COCs, and 12 per 10,000 women when pregnant.14 Patients should be counseled on the signs and symptoms of VTE such as unilateral or bilateral leg or arm swelling, pain, warmth, redness, and/or shortness of breath. The British Society for Haematology recommends maintaining mobility as a reasonable precaution when traveling for more than 3 hours.15
Cardiovascular Disease
A 2015 Cochrane review found that the risk for myocardial infarction or ischemic stroke is increased 1.6‐fold in COC users.16 Despite this increased relative risk, the increased absolute annual risk of myocardial infarction in nonsmoking women remains low: increased from 0.83 to 3.53 per 10,000,000 women younger than 35 years and from 9.45 to 40.4 per 10,000,000 women 35 years and older.17
Breast Cancer and Cervical Cancer
Data are mixed on the effect of COCs on the risk for breast cancer and cervical cancer.1 According to the CDC, COC use for 5 or more years might increase the risk of cervical carcinoma in situ and invasive cervical carcinoma in women with persistent human papillomavirus infection.5 Regardless of COC use, women should undergo age-appropriate screening for breast cancer and cervical cancer.
Melasma
Melasma is an estrogen-mediated side effect of COCs.8 A study from 1967 found that 29% of COC users (N=212) developed melasma; however, they were taking COCs with much higher ethinyl estradiol doses (50–100 μg) than typically used today.18 Nevertheless, as part of an overall skin care regimen, photoprotection should be encouraged with a broad-spectrum, water-resistant sunscreen that has a sun protection factor of at least 30. In addition, sunscreens with iron oxides have been shown to better prevent melasma relapse by protecting against the shorter wavelengths of visible light.19
- Zaenglein AL, Pathy AL, Schlosser BJ, et al. Guidelines of care for the management of acne vulgaris. J Am Acad Dermatol. 2016;74:945-973.e933.
- Landis ET, Levender MM, Davis SA, et al. Isotretinoin and oral contraceptive use in female acne patients varies by physician specialty: analysis of data from the National Ambulatory Medical Care Survey. J Dermatolog Treat. 2012;23:272-277.
- Fitzpatrick L, Mauer E, Chen CL. Oral contraceptives for acne treatment: US dermatologists’ knowledge, comfort, and prescribing practices. Cutis. 2017;99:195-201.
- Curtis KM, Jatlaoui TC, Tepper NK, et al. U.S. Selected Practice Recommendations for Contraceptive Use, 2016. MMWR Recomm Rep. 2016;65:1-66.
- Curtis KM, Tepper NK, Jatlaoui TC, et al. U.S. Medical Eligibility Criteria for Contraceptive Use, 2016. MMWR Recomm Rep. 2016;65:1-103.
- Van Vliet HA, Grimes DA, Lopez LM, et al. Triphasic versus monophasic oral contraceptives for contraception. Cochrane Database Syst Rev. 2011:CD003553.
- Stewart M, Black K. Choosing a combined oral contraceptive pill. Aust Prescr. 2015;38:6-11.
- McKinney K. Understanding the options: a guide to oral contraceptives. https://www.cecentral.com/assets/2097/022%20Oral%20Contraceptives%2010-26-09.pdf. Published November 5, 2009. Accessed June 20, 2019.
- Gallo MF, Nanda K, Grimes DA, et al. 20 microg versus >20 microg estrogen combined oral contraceptives for contraception. Cochrane Database Syst Rev. 2013:CD003989.
- Terki F, Malhotra U. Medical and Service Delivery Guidelines for Sexual and Reproductive Health Services. London, United Kingdom: International Planned Parenthood Federation; 2004.
- Arowojolu AO, Gallo MF, Lopez LM, et al. Combined oral contraceptive pills for treatment of acne. Cochrane Database Syst Rev. 2012:CD004425.
- Pastor Z, Holla K, Chmel R. The influence of combined oral contraceptives on female sexual desire: a systematic review. Eur J Contracept Reprod Health Care. 2013;18:27-43.
- Gallo MF, Lopez LM, Grimes DA, et al. Combination contraceptives: effects on weight. Cochrane Database Syst Rev. 2014:CD003987.
- Birth control pills for acne: tips from Julie Harper at the Summer AAD. Cutis. https://www.mdedge.com/dermatology/article/144550/acne/birth-control-pills-acne-tips-julie-harper-summer-aad. Published August 14, 2017. Accessed June 24, 2019.
- Watson HG, Baglin TP. Guidelines on travel-related venous thrombosis. Br J Haematol. 2011;152:31-34.
- Roach RE, Helmerhorst FM, Lijfering WM, et al. Combined oral contraceptives: the risk of myocardial infarction and ischemic stroke. Cochrane Database Syst Rev. 2015:CD011054.
- Acute myocardial infarction and combined oral contraceptives: results of an international multicentre case-control study. WHO Collaborative Study of Cardiovascular Disease and Steroid Hormone Contraception. Lancet. 1997;349:1202-1209.
- Resnik S. Melasma induced by oral contraceptive drugs. JAMA. 1967;199:601-605.
- Boukari F, Jourdan E, Fontas E, et al. Prevention of melasma relapses with sunscreen combining protection against UV and short wavelengths of visible light: a prospective randomized comparative trial. J Am Acad Dermatol. 2015;72:189-190.e181.
The American Academy of Dermatology confers combined oral contraceptives (COCs) a strength A recommendation for the treatment of acne based on level I evidence, and 4 COCs are approved for the treatment of acne by the US Food and Drug Administration (FDA).1 Furthermore, when dermatologists prescribe isotretinoin and thalidomide to women of reproductive potential, the iPLEDGE and THALOMID Risk Evaluation and Mitigation Strategy (REMS) programs require 2 concurrent methods of contraception, one of which may be a COC. In addition, COCs have several potential off-label indications in dermatology including idiopathic hirsutism, female pattern hair loss, hidradenitis suppurativa, and autoimmune progesterone dermatitis.
Despite this evidence and opportunity, research suggests that dermatologists underprescribe COCs. The National Ambulatory Medical Care Survey found that between 1993 and 2008, dermatologists in the United States prescribed COCs to only 2.03% of women presenting for acne treatment, which was less often than obstetricians/gynecologists (36.03%) and internists (10.76%).2 More recently, in a survey of 130 US dermatologists conducted from 2014 to 2015, only 55.4% reported prescribing COCs. This survey also found that only 45.8% of dermatologists who prescribed COCs felt very comfortable counseling on how to begin taking them, only 48.6% felt very comfortable counseling patients on side effects, and only 22.2% felt very comfortable managing side effects.3
In light of these data, this article reviews the basics of COCs for dermatology residents, from assessing patient eligibility and selecting a COC to counseling on use and managing risks and side effects. Because there are different approaches to prescribing COCs, readers are encouraged to integrate the information in this article with what they have learned from other sources.
Assess Patient Eligibility
In general, patients should be at least 14 years of age and have waited 2 years after menarche to start COCs. They can be taken until menopause.1,4 Contraindications can be screened for by taking a medical history and measuring a baseline blood pressure (Tables 1 and 2).5 In addition, pregnancy should be excluded with a urine or serum pregnancy test or criteria provided in Box 2 of the 2016 US Selected Practice Recommendations for Contraceptive Use from the Centers for Disease Control and Prevention (CDC).4 Although important for women’s overall health, a pelvic examination is not required to start COCs according to the CDC and the American Academy of Dermatology.1,4
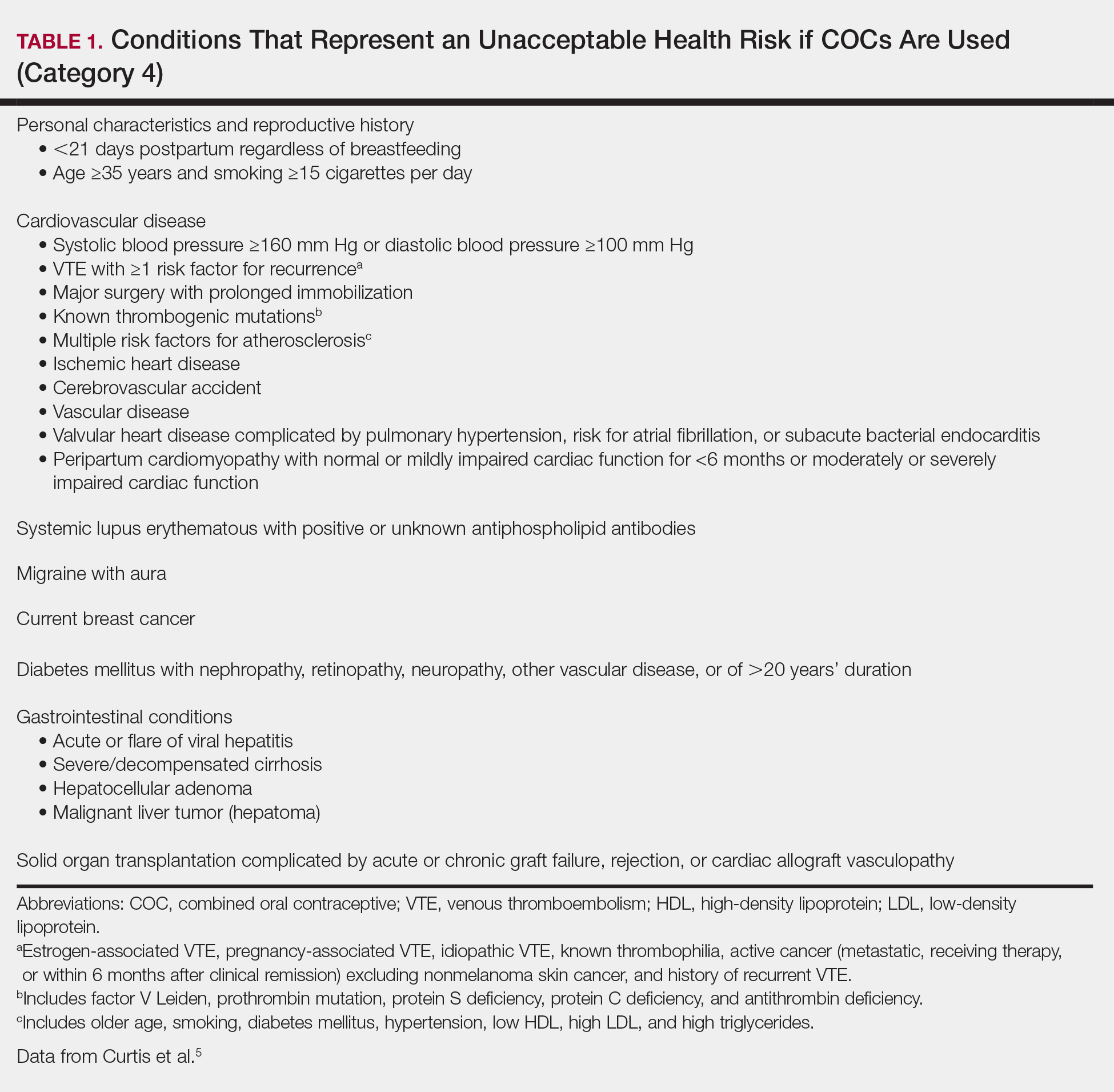
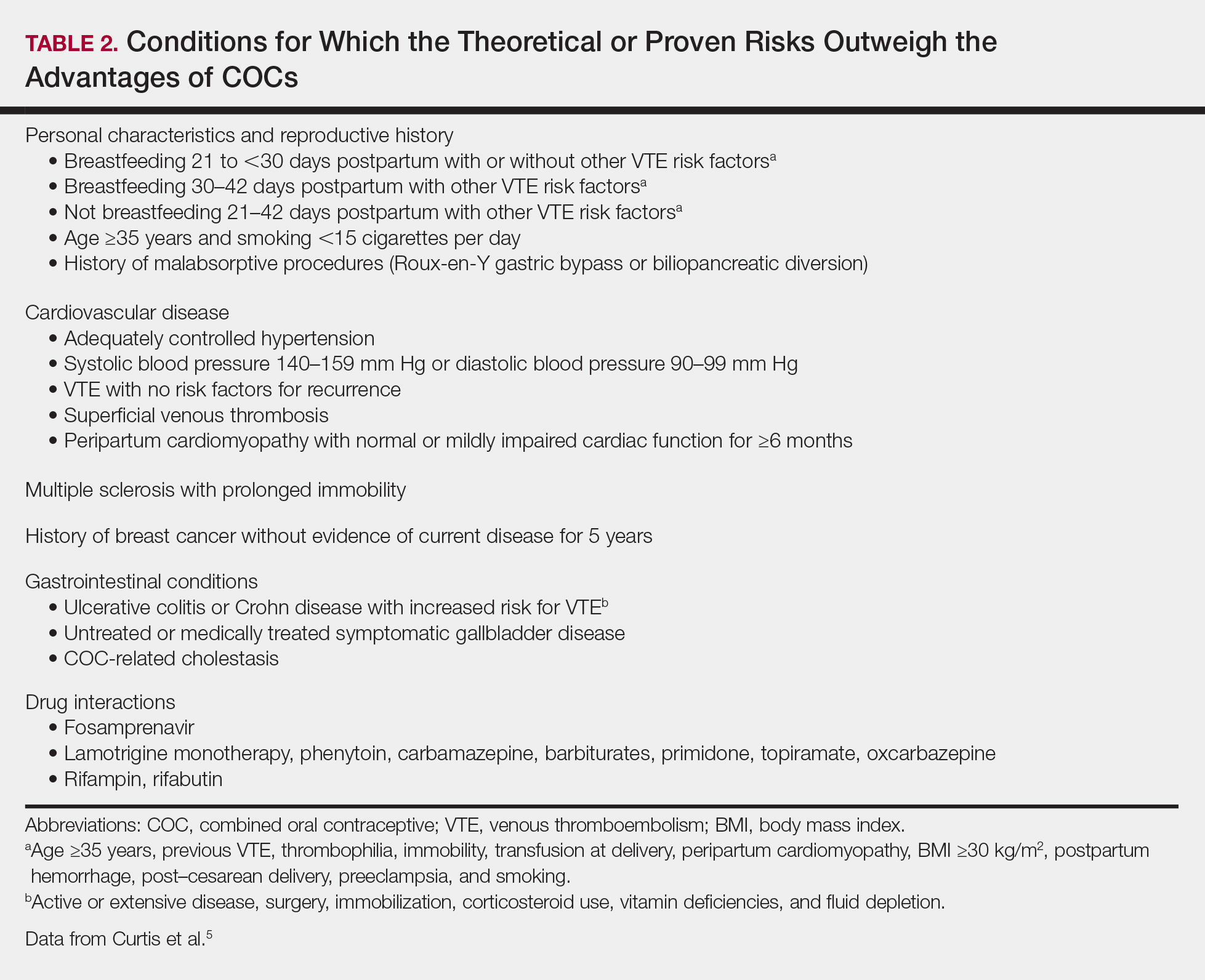
Select the COC
Combined oral contraceptives combine estrogen, usually in the form of ethinyl estradiol, with a progestin. Data suggest that all COCs effectively treat acne, but 4 are specifically FDA approved for acne: ethinyl estradiol–norethindrone acetate–ferrous fumarate, ethinyl estradiol–norgestimate, ethinyl estradiol–drospirenone, and ethinyl estradiol–drospirenone–levomefolate.1 Ethinyl estradiol–desogestrel and ethinyl estradiol–drospirenone are 2 go-to COCs for some of the attending physicians at my residency program. All COCs are FDA approved for contraception. When selecting a COC, one approach is to start with the patient’s drug formulary, then consider the following characteristics.
Monophasic vs Multiphasic
All the hormonally active pills in a monophasic formulation contain the same dose of estrogen and progestin; however, these doses change per pill in a multiphasic formulation, which requires that patients take the pills in a specific order. Given this greater complexity and the fact that multiphasic formulations often are more expensive and lack evidence of superiority, a 2011 Cochrane review recommended monophasic formulations as first line.6 In addition, monophasic formulations are preferred for autoimmune progesterone dermatitis because of the stable progestin dose.
Hormone-Free Interval
Some COCs include placebo pills during which hormone withdrawal symptoms such as bleeding, pelvic pain, mood changes, and headache may occur. If a patient is concerned about these symptoms, choose a COC with no or fewer placebo pills, or have the patient skip the hormone-free interval altogether and start the next pack early7; in this case, the prescription should be written with instructions to allow the patient to get earlier refills from the pharmacy.
Estrogen Dose
To minimize estrogen-related side effects, the lowest possible dose of ethinyl estradiol that is effective and tolerable should be prescribed7,8; 20 μg of ethinyl estradiol generally is the lowest dose available, but it may be associated with more frequent breakthrough bleeding.9 The International Planned Parenthood Federation recommends starting with COCs that contain 30 to 35 μg of estrogen.10 Synthesizing this information, one option is to start with 20 μg of ethinyl estradiol and increase the dose if breakthrough bleeding persists after 3 cycles.
Progestin Type
First-generation progestins (eg, norethindrone), second-generation progestins (eg, norgestrel, levonorgestrel), and third-generation progestins (eg, norgestimate, desogestrel) are derived from testosterone and therefore are variably androgenic; second-generation progestins are the most androgenic, and third-generation progestins are the least. On the other hand, drospirenone, the fourth-generation progestin available in the United States, is derived from 17α-spironolactone and thus is mildly antiandrogenic (3 mg of drospirenone is considered equivalent to 25 mg of spironolactone).
Although COCs with less androgenic progestins should theoretically treat acne better, a 2012 Cochrane review of COCs and acne concluded that “differences in the comparative effectiveness of COCs containing varying progestin types and dosages were less clear, and data were limited for any particular comparison.”11 As a result, regardless of the progestin, all COCs are believed to have a net antiandrogenic effect due to their estrogen component.1
Counsel on Use
Combined oral contraceptives can be started on any day of the menstrual cycle, including the day the prescription is given. If a patient begins a COC within 5 days of the first day of her most recent period, backup contraception is not needed.4 If she begins the COC more than 5 days after the first day of her most recent period, she needs to use backup contraception or abstain from sexual intercourse for the next 7 days.4 In general, at least 3 months of therapy are required to evaluate the effectiveness of COCs for acne.1
Manage Risks and Side Effects
Breakthrough Bleeding
The most common side effect of breakthrough bleeding can be minimized by taking COCs at approximately the same time every day and avoiding missed pills. If breakthrough bleeding does not stop after 3 cycles, consider increasing the estrogen dose to 30 to 35 μg and/or referring to an obstetrician/gynecologist to rule out other etiologies of bleeding.7,8
Nausea, Headache, Bloating, and Breast Tenderness
These symptoms typically resolve after the first 3 months. To minimize nausea, patients should take COCs in the early evening and eat breakfast the next morning.7,8 For headaches that occur during the hormone-free interval, consider skipping the placebo pills and starting the next pack early. Switching the progestin to drospirenone, which has a mild diuretic effect, can help with bloating as well as breast tenderness.7 For persistent symptoms, consider a lower estrogen dose.7,8
Changes in Libido
In a systemic review including 8422 COC users, 64% reported no change in libido, 22% reported an increase, and 15% reported a decrease.12
Weight Gain
Although patients may be concerned that COCs cause weight gain, a 2014 Cochrane review concluded that “available evidence is insufficient to determine the effect of combination contraceptives on weight, but no large effect is evident.”13 If weight gain does occur, anecdotal evidence suggests it tends to be not more than 5 pounds. If weight gain is an issue, consider a less androgenic progestin.8
Venous Thromboembolism
Use the 3-6-9-12 model to contextualize venous thromboembolism (VTE) risk: a woman’s annual VTE risk is 3 per 10,000 women at baseline, 6 per 10,000 women with nondrospirenone COCs, 9 per 10,000 women with drospirenone-containing COCs, and 12 per 10,000 women when pregnant.14 Patients should be counseled on the signs and symptoms of VTE such as unilateral or bilateral leg or arm swelling, pain, warmth, redness, and/or shortness of breath. The British Society for Haematology recommends maintaining mobility as a reasonable precaution when traveling for more than 3 hours.15
Cardiovascular Disease
A 2015 Cochrane review found that the risk for myocardial infarction or ischemic stroke is increased 1.6‐fold in COC users.16 Despite this increased relative risk, the increased absolute annual risk of myocardial infarction in nonsmoking women remains low: increased from 0.83 to 3.53 per 10,000,000 women younger than 35 years and from 9.45 to 40.4 per 10,000,000 women 35 years and older.17
Breast Cancer and Cervical Cancer
Data are mixed on the effect of COCs on the risk for breast cancer and cervical cancer.1 According to the CDC, COC use for 5 or more years might increase the risk of cervical carcinoma in situ and invasive cervical carcinoma in women with persistent human papillomavirus infection.5 Regardless of COC use, women should undergo age-appropriate screening for breast cancer and cervical cancer.
Melasma
Melasma is an estrogen-mediated side effect of COCs.8 A study from 1967 found that 29% of COC users (N=212) developed melasma; however, they were taking COCs with much higher ethinyl estradiol doses (50–100 μg) than typically used today.18 Nevertheless, as part of an overall skin care regimen, photoprotection should be encouraged with a broad-spectrum, water-resistant sunscreen that has a sun protection factor of at least 30. In addition, sunscreens with iron oxides have been shown to better prevent melasma relapse by protecting against the shorter wavelengths of visible light.19
The American Academy of Dermatology confers combined oral contraceptives (COCs) a strength A recommendation for the treatment of acne based on level I evidence, and 4 COCs are approved for the treatment of acne by the US Food and Drug Administration (FDA).1 Furthermore, when dermatologists prescribe isotretinoin and thalidomide to women of reproductive potential, the iPLEDGE and THALOMID Risk Evaluation and Mitigation Strategy (REMS) programs require 2 concurrent methods of contraception, one of which may be a COC. In addition, COCs have several potential off-label indications in dermatology including idiopathic hirsutism, female pattern hair loss, hidradenitis suppurativa, and autoimmune progesterone dermatitis.
Despite this evidence and opportunity, research suggests that dermatologists underprescribe COCs. The National Ambulatory Medical Care Survey found that between 1993 and 2008, dermatologists in the United States prescribed COCs to only 2.03% of women presenting for acne treatment, which was less often than obstetricians/gynecologists (36.03%) and internists (10.76%).2 More recently, in a survey of 130 US dermatologists conducted from 2014 to 2015, only 55.4% reported prescribing COCs. This survey also found that only 45.8% of dermatologists who prescribed COCs felt very comfortable counseling on how to begin taking them, only 48.6% felt very comfortable counseling patients on side effects, and only 22.2% felt very comfortable managing side effects.3
In light of these data, this article reviews the basics of COCs for dermatology residents, from assessing patient eligibility and selecting a COC to counseling on use and managing risks and side effects. Because there are different approaches to prescribing COCs, readers are encouraged to integrate the information in this article with what they have learned from other sources.
Assess Patient Eligibility
In general, patients should be at least 14 years of age and have waited 2 years after menarche to start COCs. They can be taken until menopause.1,4 Contraindications can be screened for by taking a medical history and measuring a baseline blood pressure (Tables 1 and 2).5 In addition, pregnancy should be excluded with a urine or serum pregnancy test or criteria provided in Box 2 of the 2016 US Selected Practice Recommendations for Contraceptive Use from the Centers for Disease Control and Prevention (CDC).4 Although important for women’s overall health, a pelvic examination is not required to start COCs according to the CDC and the American Academy of Dermatology.1,4
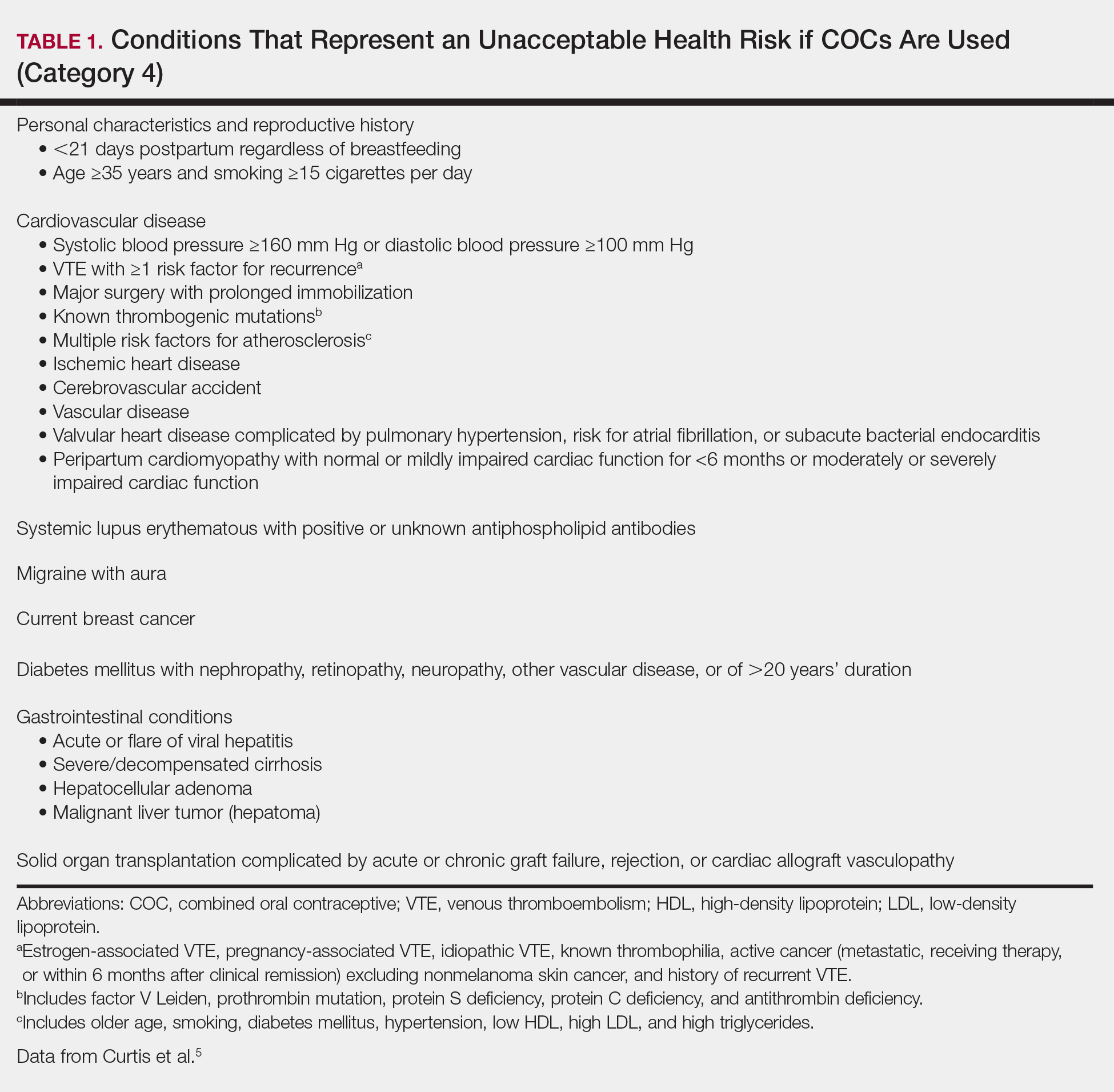
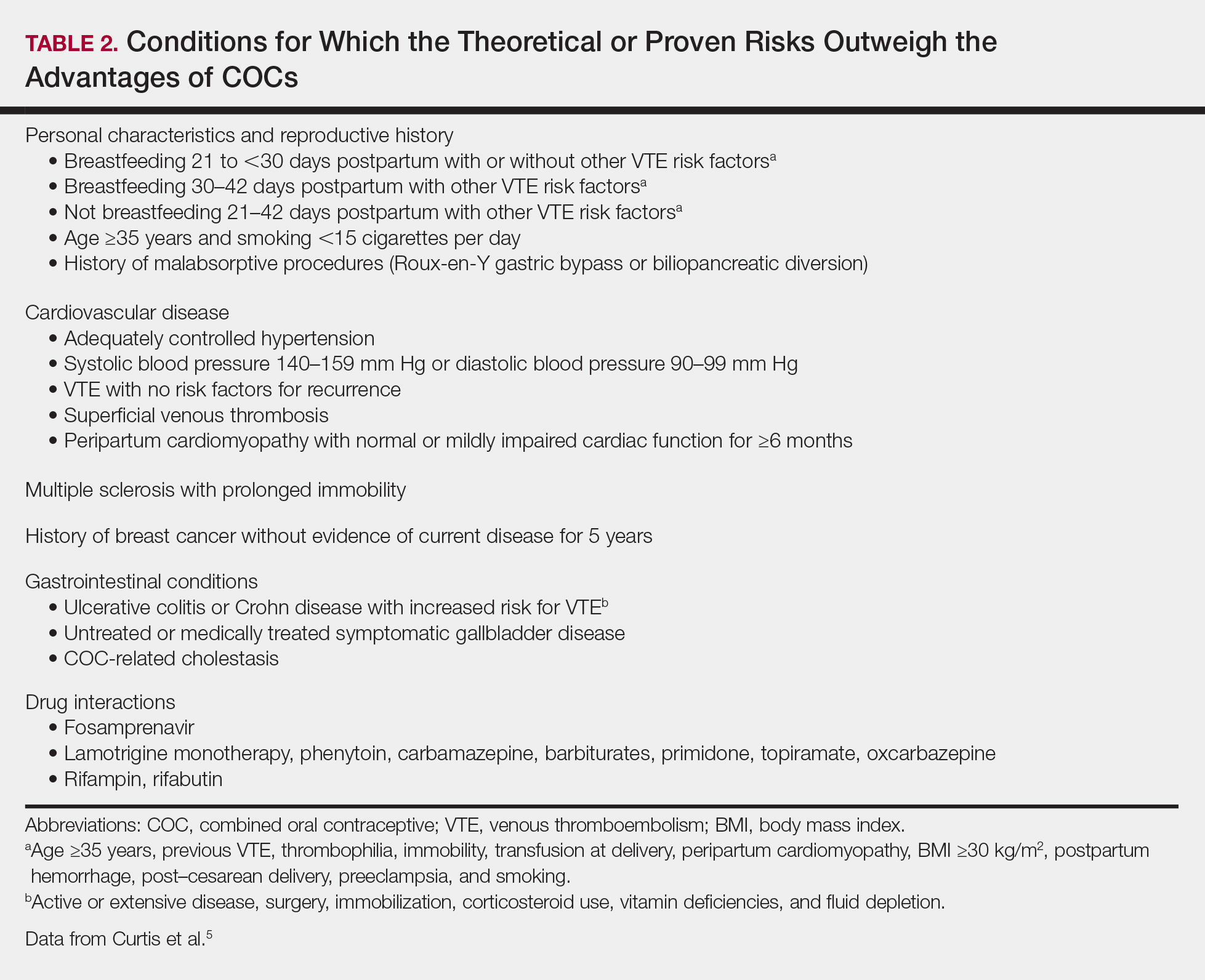
Select the COC
Combined oral contraceptives combine estrogen, usually in the form of ethinyl estradiol, with a progestin. Data suggest that all COCs effectively treat acne, but 4 are specifically FDA approved for acne: ethinyl estradiol–norethindrone acetate–ferrous fumarate, ethinyl estradiol–norgestimate, ethinyl estradiol–drospirenone, and ethinyl estradiol–drospirenone–levomefolate.1 Ethinyl estradiol–desogestrel and ethinyl estradiol–drospirenone are 2 go-to COCs for some of the attending physicians at my residency program. All COCs are FDA approved for contraception. When selecting a COC, one approach is to start with the patient’s drug formulary, then consider the following characteristics.
Monophasic vs Multiphasic
All the hormonally active pills in a monophasic formulation contain the same dose of estrogen and progestin; however, these doses change per pill in a multiphasic formulation, which requires that patients take the pills in a specific order. Given this greater complexity and the fact that multiphasic formulations often are more expensive and lack evidence of superiority, a 2011 Cochrane review recommended monophasic formulations as first line.6 In addition, monophasic formulations are preferred for autoimmune progesterone dermatitis because of the stable progestin dose.
Hormone-Free Interval
Some COCs include placebo pills during which hormone withdrawal symptoms such as bleeding, pelvic pain, mood changes, and headache may occur. If a patient is concerned about these symptoms, choose a COC with no or fewer placebo pills, or have the patient skip the hormone-free interval altogether and start the next pack early7; in this case, the prescription should be written with instructions to allow the patient to get earlier refills from the pharmacy.
Estrogen Dose
To minimize estrogen-related side effects, the lowest possible dose of ethinyl estradiol that is effective and tolerable should be prescribed7,8; 20 μg of ethinyl estradiol generally is the lowest dose available, but it may be associated with more frequent breakthrough bleeding.9 The International Planned Parenthood Federation recommends starting with COCs that contain 30 to 35 μg of estrogen.10 Synthesizing this information, one option is to start with 20 μg of ethinyl estradiol and increase the dose if breakthrough bleeding persists after 3 cycles.
Progestin Type
First-generation progestins (eg, norethindrone), second-generation progestins (eg, norgestrel, levonorgestrel), and third-generation progestins (eg, norgestimate, desogestrel) are derived from testosterone and therefore are variably androgenic; second-generation progestins are the most androgenic, and third-generation progestins are the least. On the other hand, drospirenone, the fourth-generation progestin available in the United States, is derived from 17α-spironolactone and thus is mildly antiandrogenic (3 mg of drospirenone is considered equivalent to 25 mg of spironolactone).
Although COCs with less androgenic progestins should theoretically treat acne better, a 2012 Cochrane review of COCs and acne concluded that “differences in the comparative effectiveness of COCs containing varying progestin types and dosages were less clear, and data were limited for any particular comparison.”11 As a result, regardless of the progestin, all COCs are believed to have a net antiandrogenic effect due to their estrogen component.1
Counsel on Use
Combined oral contraceptives can be started on any day of the menstrual cycle, including the day the prescription is given. If a patient begins a COC within 5 days of the first day of her most recent period, backup contraception is not needed.4 If she begins the COC more than 5 days after the first day of her most recent period, she needs to use backup contraception or abstain from sexual intercourse for the next 7 days.4 In general, at least 3 months of therapy are required to evaluate the effectiveness of COCs for acne.1
Manage Risks and Side Effects
Breakthrough Bleeding
The most common side effect of breakthrough bleeding can be minimized by taking COCs at approximately the same time every day and avoiding missed pills. If breakthrough bleeding does not stop after 3 cycles, consider increasing the estrogen dose to 30 to 35 μg and/or referring to an obstetrician/gynecologist to rule out other etiologies of bleeding.7,8
Nausea, Headache, Bloating, and Breast Tenderness
These symptoms typically resolve after the first 3 months. To minimize nausea, patients should take COCs in the early evening and eat breakfast the next morning.7,8 For headaches that occur during the hormone-free interval, consider skipping the placebo pills and starting the next pack early. Switching the progestin to drospirenone, which has a mild diuretic effect, can help with bloating as well as breast tenderness.7 For persistent symptoms, consider a lower estrogen dose.7,8
Changes in Libido
In a systemic review including 8422 COC users, 64% reported no change in libido, 22% reported an increase, and 15% reported a decrease.12
Weight Gain
Although patients may be concerned that COCs cause weight gain, a 2014 Cochrane review concluded that “available evidence is insufficient to determine the effect of combination contraceptives on weight, but no large effect is evident.”13 If weight gain does occur, anecdotal evidence suggests it tends to be not more than 5 pounds. If weight gain is an issue, consider a less androgenic progestin.8
Venous Thromboembolism
Use the 3-6-9-12 model to contextualize venous thromboembolism (VTE) risk: a woman’s annual VTE risk is 3 per 10,000 women at baseline, 6 per 10,000 women with nondrospirenone COCs, 9 per 10,000 women with drospirenone-containing COCs, and 12 per 10,000 women when pregnant.14 Patients should be counseled on the signs and symptoms of VTE such as unilateral or bilateral leg or arm swelling, pain, warmth, redness, and/or shortness of breath. The British Society for Haematology recommends maintaining mobility as a reasonable precaution when traveling for more than 3 hours.15
Cardiovascular Disease
A 2015 Cochrane review found that the risk for myocardial infarction or ischemic stroke is increased 1.6‐fold in COC users.16 Despite this increased relative risk, the increased absolute annual risk of myocardial infarction in nonsmoking women remains low: increased from 0.83 to 3.53 per 10,000,000 women younger than 35 years and from 9.45 to 40.4 per 10,000,000 women 35 years and older.17
Breast Cancer and Cervical Cancer
Data are mixed on the effect of COCs on the risk for breast cancer and cervical cancer.1 According to the CDC, COC use for 5 or more years might increase the risk of cervical carcinoma in situ and invasive cervical carcinoma in women with persistent human papillomavirus infection.5 Regardless of COC use, women should undergo age-appropriate screening for breast cancer and cervical cancer.
Melasma
Melasma is an estrogen-mediated side effect of COCs.8 A study from 1967 found that 29% of COC users (N=212) developed melasma; however, they were taking COCs with much higher ethinyl estradiol doses (50–100 μg) than typically used today.18 Nevertheless, as part of an overall skin care regimen, photoprotection should be encouraged with a broad-spectrum, water-resistant sunscreen that has a sun protection factor of at least 30. In addition, sunscreens with iron oxides have been shown to better prevent melasma relapse by protecting against the shorter wavelengths of visible light.19
- Zaenglein AL, Pathy AL, Schlosser BJ, et al. Guidelines of care for the management of acne vulgaris. J Am Acad Dermatol. 2016;74:945-973.e933.
- Landis ET, Levender MM, Davis SA, et al. Isotretinoin and oral contraceptive use in female acne patients varies by physician specialty: analysis of data from the National Ambulatory Medical Care Survey. J Dermatolog Treat. 2012;23:272-277.
- Fitzpatrick L, Mauer E, Chen CL. Oral contraceptives for acne treatment: US dermatologists’ knowledge, comfort, and prescribing practices. Cutis. 2017;99:195-201.
- Curtis KM, Jatlaoui TC, Tepper NK, et al. U.S. Selected Practice Recommendations for Contraceptive Use, 2016. MMWR Recomm Rep. 2016;65:1-66.
- Curtis KM, Tepper NK, Jatlaoui TC, et al. U.S. Medical Eligibility Criteria for Contraceptive Use, 2016. MMWR Recomm Rep. 2016;65:1-103.
- Van Vliet HA, Grimes DA, Lopez LM, et al. Triphasic versus monophasic oral contraceptives for contraception. Cochrane Database Syst Rev. 2011:CD003553.
- Stewart M, Black K. Choosing a combined oral contraceptive pill. Aust Prescr. 2015;38:6-11.
- McKinney K. Understanding the options: a guide to oral contraceptives. https://www.cecentral.com/assets/2097/022%20Oral%20Contraceptives%2010-26-09.pdf. Published November 5, 2009. Accessed June 20, 2019.
- Gallo MF, Nanda K, Grimes DA, et al. 20 microg versus >20 microg estrogen combined oral contraceptives for contraception. Cochrane Database Syst Rev. 2013:CD003989.
- Terki F, Malhotra U. Medical and Service Delivery Guidelines for Sexual and Reproductive Health Services. London, United Kingdom: International Planned Parenthood Federation; 2004.
- Arowojolu AO, Gallo MF, Lopez LM, et al. Combined oral contraceptive pills for treatment of acne. Cochrane Database Syst Rev. 2012:CD004425.
- Pastor Z, Holla K, Chmel R. The influence of combined oral contraceptives on female sexual desire: a systematic review. Eur J Contracept Reprod Health Care. 2013;18:27-43.
- Gallo MF, Lopez LM, Grimes DA, et al. Combination contraceptives: effects on weight. Cochrane Database Syst Rev. 2014:CD003987.
- Birth control pills for acne: tips from Julie Harper at the Summer AAD. Cutis. https://www.mdedge.com/dermatology/article/144550/acne/birth-control-pills-acne-tips-julie-harper-summer-aad. Published August 14, 2017. Accessed June 24, 2019.
- Watson HG, Baglin TP. Guidelines on travel-related venous thrombosis. Br J Haematol. 2011;152:31-34.
- Roach RE, Helmerhorst FM, Lijfering WM, et al. Combined oral contraceptives: the risk of myocardial infarction and ischemic stroke. Cochrane Database Syst Rev. 2015:CD011054.
- Acute myocardial infarction and combined oral contraceptives: results of an international multicentre case-control study. WHO Collaborative Study of Cardiovascular Disease and Steroid Hormone Contraception. Lancet. 1997;349:1202-1209.
- Resnik S. Melasma induced by oral contraceptive drugs. JAMA. 1967;199:601-605.
- Boukari F, Jourdan E, Fontas E, et al. Prevention of melasma relapses with sunscreen combining protection against UV and short wavelengths of visible light: a prospective randomized comparative trial. J Am Acad Dermatol. 2015;72:189-190.e181.
- Zaenglein AL, Pathy AL, Schlosser BJ, et al. Guidelines of care for the management of acne vulgaris. J Am Acad Dermatol. 2016;74:945-973.e933.
- Landis ET, Levender MM, Davis SA, et al. Isotretinoin and oral contraceptive use in female acne patients varies by physician specialty: analysis of data from the National Ambulatory Medical Care Survey. J Dermatolog Treat. 2012;23:272-277.
- Fitzpatrick L, Mauer E, Chen CL. Oral contraceptives for acne treatment: US dermatologists’ knowledge, comfort, and prescribing practices. Cutis. 2017;99:195-201.
- Curtis KM, Jatlaoui TC, Tepper NK, et al. U.S. Selected Practice Recommendations for Contraceptive Use, 2016. MMWR Recomm Rep. 2016;65:1-66.
- Curtis KM, Tepper NK, Jatlaoui TC, et al. U.S. Medical Eligibility Criteria for Contraceptive Use, 2016. MMWR Recomm Rep. 2016;65:1-103.
- Van Vliet HA, Grimes DA, Lopez LM, et al. Triphasic versus monophasic oral contraceptives for contraception. Cochrane Database Syst Rev. 2011:CD003553.
- Stewart M, Black K. Choosing a combined oral contraceptive pill. Aust Prescr. 2015;38:6-11.
- McKinney K. Understanding the options: a guide to oral contraceptives. https://www.cecentral.com/assets/2097/022%20Oral%20Contraceptives%2010-26-09.pdf. Published November 5, 2009. Accessed June 20, 2019.
- Gallo MF, Nanda K, Grimes DA, et al. 20 microg versus >20 microg estrogen combined oral contraceptives for contraception. Cochrane Database Syst Rev. 2013:CD003989.
- Terki F, Malhotra U. Medical and Service Delivery Guidelines for Sexual and Reproductive Health Services. London, United Kingdom: International Planned Parenthood Federation; 2004.
- Arowojolu AO, Gallo MF, Lopez LM, et al. Combined oral contraceptive pills for treatment of acne. Cochrane Database Syst Rev. 2012:CD004425.
- Pastor Z, Holla K, Chmel R. The influence of combined oral contraceptives on female sexual desire: a systematic review. Eur J Contracept Reprod Health Care. 2013;18:27-43.
- Gallo MF, Lopez LM, Grimes DA, et al. Combination contraceptives: effects on weight. Cochrane Database Syst Rev. 2014:CD003987.
- Birth control pills for acne: tips from Julie Harper at the Summer AAD. Cutis. https://www.mdedge.com/dermatology/article/144550/acne/birth-control-pills-acne-tips-julie-harper-summer-aad. Published August 14, 2017. Accessed June 24, 2019.
- Watson HG, Baglin TP. Guidelines on travel-related venous thrombosis. Br J Haematol. 2011;152:31-34.
- Roach RE, Helmerhorst FM, Lijfering WM, et al. Combined oral contraceptives: the risk of myocardial infarction and ischemic stroke. Cochrane Database Syst Rev. 2015:CD011054.
- Acute myocardial infarction and combined oral contraceptives: results of an international multicentre case-control study. WHO Collaborative Study of Cardiovascular Disease and Steroid Hormone Contraception. Lancet. 1997;349:1202-1209.
- Resnik S. Melasma induced by oral contraceptive drugs. JAMA. 1967;199:601-605.
- Boukari F, Jourdan E, Fontas E, et al. Prevention of melasma relapses with sunscreen combining protection against UV and short wavelengths of visible light: a prospective randomized comparative trial. J Am Acad Dermatol. 2015;72:189-190.e181.
Resident Pearls
- Screen for contraindications to combined oral contraceptives (COCs) by taking a medical history, measuring a baseline blood pressure, and excluding pregnancy. A baseline pelvic examination is unnecessary.
- Characteristics to consider when selecting a COC include the formulation, hormone-free interval, estrogen dose, and progestin type.
- Combined oral contraceptives can be initiated on any day of the menstrual cycle, with the need for backup contraception based on the number of days since the first day of the patient’s most recent period.
- Management of risks and side effects includes simple lifestyle changes, skipping the hormone-free interval, switching the COC, and referring to an obstetrician/gynecologist.
Surgical Dermatoethics for the Trainee
It is an uncomfortable and unavoidable reality as physicians that for every procedure we learn, there must be a first time we perform it. As with any type of skill, it takes practice to become proficient. The unique challenge in medicine is that the practice involves performing procedures on real patients. We cannot avoid the hands-on nature of the training process; we can, however, approach its ethical challenges mindfully. Herein, I will discuss some of the ethical considerations in providing care as a trainee and identify potential barriers to best practices, particularly as they relate to procedural dermatology.
Tell Patients You Are in Training
In every patient encounter, we must introduce ourselves as a trainee. The principle of right to the truth dictates that we are transparent about our level of training and do not misrepresent ourselves to our patients. A statement released by the American Medical Association (AMA) Council on Ethical and Judicial Affairs asserts that “[p]atients should be informed of the identity and training status of individuals involved in their care.”1
Although straightforward in theory, this mandate is not always simple in practice. With patients unfamiliar with the health care system, it could be more onerous to clearly communicate training status than simply introducing oneself as a resident. A study conducted in the emergency department at Vanderbilt University Hospital (Nashville, Tennessee) found that many patients and their family members (N=430) did not understand the various roles and responsibilities of physicians in the teaching hospital setting. For example, 30% believed an attending physician requires supervision by a resident, and an additional 17% of those surveyed were not sure.2 The AMA requests we “refrain from using terms that may be confusing when describing the training status of the students,”1 which evidently is audience specific. Thus, as with any type of patient education, a thorough introduction may require assessment of understanding.
Disclosure of Experience Level With a Particular Procedure
There is a clear professional expectation that we disclose to patients that we are in training; however, a universal standard does not exist for disclosure of our exact level of experience in a particular procedure. Do we need to tell patients if it is our first time performing a given procedure? What if it is our tenth? Multiple studies have found that patients want specifics. In one study of bariatric surgery patients (N=108), 93% felt that they should always be informed if it was the first time a trainee was performing a particular procedure.3 A study conducted in the emergency department setting (N=202) also found that the majority of patients thought they should be informed if a resident was performing a procedure for the first time, but the distribution differed by procedure (66% for suturing vs 82% for lumbar puncture).4
Despite these findings, this degree of specificity is not always discussed with patients and perhaps does not need to be. LaRosa and Grant-Kels5 analyzed a hypothetical scenario in which a dermatology resident is to perform his first excision under attending supervision and concluded that broad disclosure of training status would suffice in the given scenario, as it would not be necessary to state that it was his first time performing an excision. It is unclear if the same conclusion could be drawn for all procedures and levels of experience. Outcome data would help inform the analysis, but the available data are from other specialties including general surgery, gynecology, and urology. Some studies demonstrate an increased risk of adverse outcomes with trainee involvement in procedures such as bariatric surgery and emergency general surgery, but the data are mixed and may not be generalizable to dermatologic procedures.6-8
The appropriate level of detail to disclose regarding a physician’s experience may need to be assessed on a case-by-case basis, and the principles of informed consent can help. Informed consent requires understanding of the diagnosis, the treatment options including nonintervention, and the risks and benefits of each alternative. In obtaining informed consent, we must disclose “any facts which are necessary to form the basis of an intelligent consent by the patient to the proposed treatment.”9 Providers must determine what aspects of a trainee’s experience level are relevant to the risk-benefit analysis in a given set of circumstances. Surely, there is a large degree of subjectivity in this determination as data are limited, but information deemed relevant must be shared. Information that is inconsequential, on the other hand, may be omitted. It could even be argued that more detailed information, especially if it may cause anxiety, would be detrimental to share. For example, we would not list the chemical name of every preservative in every vaccine we recommend for children if there is no evidence of inflicting harm. If the information has not been shown to have clinical impact or affect safety concerns, the anxiety may be undue.
Withholding Information Can Violate Ethical Principles
We must be careful not to withhold details of our experience level with a particular procedure for the wrong reasons. It would be wrong, for example, to withhold information simply to avoid causing anxiety, which could be seen as an invocation of therapeutic privilege, a controversial practice of withholding important information that poses a psychological threat to the patient. A classic example is the physician who defers disclosure of a terminal diagnosis to preserve hope. Although therapeutic privilege theoretically promotes the principle of beneficence, it violates the principles of autonomy and right to truth and therefore generally is regarded as unethically paternalistic in modern medical ethics.9
Patients Can Refuse Trainee Participation
It also is unethical to withhold information to obtain consent and avoid refusal of our care. Refusal of trainee participation is not uncommon. In the aforementioned study of bariatric surgery patients, 92.4% supported their procedure being performed at a teaching hospital, but only 56% would consent to a resident assisting staff during the procedure. A mere 33% of those patients would consent to a resident primarily performing with staff assisting.3 Although the proportion of patients who refuse certainly depends on the type of procedure among other factors, it is a reality in any teaching environment. The training paradigm in medicine depends on being able to practice procedures with supervision before we are independent providers. If patients refuse our care, our training suffers. However, the AMA maintains that “[p]atients are free to choose from whom they receive treatment,”1 and we must respect this aspect of patient autonomy.
Final Thoughts
When it comes to the performance of procedures, there are a few basic principles to keep in mind to provide ethical care to our patients while we are in training. Although we must accept that a crucial part of learning dermatologic procedures is hands on with real patients, we also need to come prepared having learned what we can through reading and practice with cadavers or skin substitutes. Procedures we execute as residents should be performed with adequate supervision, and as we progress through residency, we should be given increased autonomy and graded responsibility to prepare us for independent practice at graduation. Although it is the responsibility of the attending physician to provide appropriate oversight for the resident’s level of training, we should feel empowered to ask for help and have the humility to know when we need it.
- Medical student involvement in patient care: report of the council on ethical and judicial affairs. Virtual Mentor. 2001;3. doi:10.1001/virtualmentor.2001.3.3.code1-0103.
- Santen S, Hemphill RR, Prough E, et al. Do patients understand their physician’s level of training? a survey of emergency department patients. Acad Med. 2004;79:139-143.
- McClellan JM, Nelson D, Porta CR, et al. Bariatric surgery patient perceptions and willingness to consent to resident participation. Surg Obes Relat Dis. 2016;12:1065-1071.
- Santen SA, Hemphill RR, McDonald MF, et al. Patients’ willingness to allow residents to learn to practice medical procedures. Acad Med. 2004;79:144-147.
- LaRosa C, Grant-Kels JM. See one, do one, teach one: the ethical dilemma of residents performing their first procedure on patients. J Am Acad Dermatol. 2016;75:845-848.
- Can MF. The trainee effect on early postoperative surgical outcomes: reflects the effect of resident involvement or hospital capacity to overcome complications? J Invest Surg. 2017;31:67-68.
- Goldberg I, Yang J, Park J, et al. Surgical trainee impact on bariatric surgery safety [published online November 13, 2018]. Surg Endosc. doi:10.1007/s00464-018-6587-0.
- Kasotakis G, Lakha A, Sarkar B, et al. Trainee participation is associated with adverse outcomes in emergency general surgery: an analysis of the National Surgical Quality Improvement Program database. Ann Surg. 2014;3:483-490.
- Richard C, Lajeunesse Y, Lussier MT. Therapeutic privilege: between the ethics of lying and the practice of truth. J Med Ethics. 2010;36:353-357.
It is an uncomfortable and unavoidable reality as physicians that for every procedure we learn, there must be a first time we perform it. As with any type of skill, it takes practice to become proficient. The unique challenge in medicine is that the practice involves performing procedures on real patients. We cannot avoid the hands-on nature of the training process; we can, however, approach its ethical challenges mindfully. Herein, I will discuss some of the ethical considerations in providing care as a trainee and identify potential barriers to best practices, particularly as they relate to procedural dermatology.
Tell Patients You Are in Training
In every patient encounter, we must introduce ourselves as a trainee. The principle of right to the truth dictates that we are transparent about our level of training and do not misrepresent ourselves to our patients. A statement released by the American Medical Association (AMA) Council on Ethical and Judicial Affairs asserts that “[p]atients should be informed of the identity and training status of individuals involved in their care.”1
Although straightforward in theory, this mandate is not always simple in practice. With patients unfamiliar with the health care system, it could be more onerous to clearly communicate training status than simply introducing oneself as a resident. A study conducted in the emergency department at Vanderbilt University Hospital (Nashville, Tennessee) found that many patients and their family members (N=430) did not understand the various roles and responsibilities of physicians in the teaching hospital setting. For example, 30% believed an attending physician requires supervision by a resident, and an additional 17% of those surveyed were not sure.2 The AMA requests we “refrain from using terms that may be confusing when describing the training status of the students,”1 which evidently is audience specific. Thus, as with any type of patient education, a thorough introduction may require assessment of understanding.
Disclosure of Experience Level With a Particular Procedure
There is a clear professional expectation that we disclose to patients that we are in training; however, a universal standard does not exist for disclosure of our exact level of experience in a particular procedure. Do we need to tell patients if it is our first time performing a given procedure? What if it is our tenth? Multiple studies have found that patients want specifics. In one study of bariatric surgery patients (N=108), 93% felt that they should always be informed if it was the first time a trainee was performing a particular procedure.3 A study conducted in the emergency department setting (N=202) also found that the majority of patients thought they should be informed if a resident was performing a procedure for the first time, but the distribution differed by procedure (66% for suturing vs 82% for lumbar puncture).4
Despite these findings, this degree of specificity is not always discussed with patients and perhaps does not need to be. LaRosa and Grant-Kels5 analyzed a hypothetical scenario in which a dermatology resident is to perform his first excision under attending supervision and concluded that broad disclosure of training status would suffice in the given scenario, as it would not be necessary to state that it was his first time performing an excision. It is unclear if the same conclusion could be drawn for all procedures and levels of experience. Outcome data would help inform the analysis, but the available data are from other specialties including general surgery, gynecology, and urology. Some studies demonstrate an increased risk of adverse outcomes with trainee involvement in procedures such as bariatric surgery and emergency general surgery, but the data are mixed and may not be generalizable to dermatologic procedures.6-8
The appropriate level of detail to disclose regarding a physician’s experience may need to be assessed on a case-by-case basis, and the principles of informed consent can help. Informed consent requires understanding of the diagnosis, the treatment options including nonintervention, and the risks and benefits of each alternative. In obtaining informed consent, we must disclose “any facts which are necessary to form the basis of an intelligent consent by the patient to the proposed treatment.”9 Providers must determine what aspects of a trainee’s experience level are relevant to the risk-benefit analysis in a given set of circumstances. Surely, there is a large degree of subjectivity in this determination as data are limited, but information deemed relevant must be shared. Information that is inconsequential, on the other hand, may be omitted. It could even be argued that more detailed information, especially if it may cause anxiety, would be detrimental to share. For example, we would not list the chemical name of every preservative in every vaccine we recommend for children if there is no evidence of inflicting harm. If the information has not been shown to have clinical impact or affect safety concerns, the anxiety may be undue.
Withholding Information Can Violate Ethical Principles
We must be careful not to withhold details of our experience level with a particular procedure for the wrong reasons. It would be wrong, for example, to withhold information simply to avoid causing anxiety, which could be seen as an invocation of therapeutic privilege, a controversial practice of withholding important information that poses a psychological threat to the patient. A classic example is the physician who defers disclosure of a terminal diagnosis to preserve hope. Although therapeutic privilege theoretically promotes the principle of beneficence, it violates the principles of autonomy and right to truth and therefore generally is regarded as unethically paternalistic in modern medical ethics.9
Patients Can Refuse Trainee Participation
It also is unethical to withhold information to obtain consent and avoid refusal of our care. Refusal of trainee participation is not uncommon. In the aforementioned study of bariatric surgery patients, 92.4% supported their procedure being performed at a teaching hospital, but only 56% would consent to a resident assisting staff during the procedure. A mere 33% of those patients would consent to a resident primarily performing with staff assisting.3 Although the proportion of patients who refuse certainly depends on the type of procedure among other factors, it is a reality in any teaching environment. The training paradigm in medicine depends on being able to practice procedures with supervision before we are independent providers. If patients refuse our care, our training suffers. However, the AMA maintains that “[p]atients are free to choose from whom they receive treatment,”1 and we must respect this aspect of patient autonomy.
Final Thoughts
When it comes to the performance of procedures, there are a few basic principles to keep in mind to provide ethical care to our patients while we are in training. Although we must accept that a crucial part of learning dermatologic procedures is hands on with real patients, we also need to come prepared having learned what we can through reading and practice with cadavers or skin substitutes. Procedures we execute as residents should be performed with adequate supervision, and as we progress through residency, we should be given increased autonomy and graded responsibility to prepare us for independent practice at graduation. Although it is the responsibility of the attending physician to provide appropriate oversight for the resident’s level of training, we should feel empowered to ask for help and have the humility to know when we need it.
It is an uncomfortable and unavoidable reality as physicians that for every procedure we learn, there must be a first time we perform it. As with any type of skill, it takes practice to become proficient. The unique challenge in medicine is that the practice involves performing procedures on real patients. We cannot avoid the hands-on nature of the training process; we can, however, approach its ethical challenges mindfully. Herein, I will discuss some of the ethical considerations in providing care as a trainee and identify potential barriers to best practices, particularly as they relate to procedural dermatology.
Tell Patients You Are in Training
In every patient encounter, we must introduce ourselves as a trainee. The principle of right to the truth dictates that we are transparent about our level of training and do not misrepresent ourselves to our patients. A statement released by the American Medical Association (AMA) Council on Ethical and Judicial Affairs asserts that “[p]atients should be informed of the identity and training status of individuals involved in their care.”1
Although straightforward in theory, this mandate is not always simple in practice. With patients unfamiliar with the health care system, it could be more onerous to clearly communicate training status than simply introducing oneself as a resident. A study conducted in the emergency department at Vanderbilt University Hospital (Nashville, Tennessee) found that many patients and their family members (N=430) did not understand the various roles and responsibilities of physicians in the teaching hospital setting. For example, 30% believed an attending physician requires supervision by a resident, and an additional 17% of those surveyed were not sure.2 The AMA requests we “refrain from using terms that may be confusing when describing the training status of the students,”1 which evidently is audience specific. Thus, as with any type of patient education, a thorough introduction may require assessment of understanding.
Disclosure of Experience Level With a Particular Procedure
There is a clear professional expectation that we disclose to patients that we are in training; however, a universal standard does not exist for disclosure of our exact level of experience in a particular procedure. Do we need to tell patients if it is our first time performing a given procedure? What if it is our tenth? Multiple studies have found that patients want specifics. In one study of bariatric surgery patients (N=108), 93% felt that they should always be informed if it was the first time a trainee was performing a particular procedure.3 A study conducted in the emergency department setting (N=202) also found that the majority of patients thought they should be informed if a resident was performing a procedure for the first time, but the distribution differed by procedure (66% for suturing vs 82% for lumbar puncture).4
Despite these findings, this degree of specificity is not always discussed with patients and perhaps does not need to be. LaRosa and Grant-Kels5 analyzed a hypothetical scenario in which a dermatology resident is to perform his first excision under attending supervision and concluded that broad disclosure of training status would suffice in the given scenario, as it would not be necessary to state that it was his first time performing an excision. It is unclear if the same conclusion could be drawn for all procedures and levels of experience. Outcome data would help inform the analysis, but the available data are from other specialties including general surgery, gynecology, and urology. Some studies demonstrate an increased risk of adverse outcomes with trainee involvement in procedures such as bariatric surgery and emergency general surgery, but the data are mixed and may not be generalizable to dermatologic procedures.6-8
The appropriate level of detail to disclose regarding a physician’s experience may need to be assessed on a case-by-case basis, and the principles of informed consent can help. Informed consent requires understanding of the diagnosis, the treatment options including nonintervention, and the risks and benefits of each alternative. In obtaining informed consent, we must disclose “any facts which are necessary to form the basis of an intelligent consent by the patient to the proposed treatment.”9 Providers must determine what aspects of a trainee’s experience level are relevant to the risk-benefit analysis in a given set of circumstances. Surely, there is a large degree of subjectivity in this determination as data are limited, but information deemed relevant must be shared. Information that is inconsequential, on the other hand, may be omitted. It could even be argued that more detailed information, especially if it may cause anxiety, would be detrimental to share. For example, we would not list the chemical name of every preservative in every vaccine we recommend for children if there is no evidence of inflicting harm. If the information has not been shown to have clinical impact or affect safety concerns, the anxiety may be undue.
Withholding Information Can Violate Ethical Principles
We must be careful not to withhold details of our experience level with a particular procedure for the wrong reasons. It would be wrong, for example, to withhold information simply to avoid causing anxiety, which could be seen as an invocation of therapeutic privilege, a controversial practice of withholding important information that poses a psychological threat to the patient. A classic example is the physician who defers disclosure of a terminal diagnosis to preserve hope. Although therapeutic privilege theoretically promotes the principle of beneficence, it violates the principles of autonomy and right to truth and therefore generally is regarded as unethically paternalistic in modern medical ethics.9
Patients Can Refuse Trainee Participation
It also is unethical to withhold information to obtain consent and avoid refusal of our care. Refusal of trainee participation is not uncommon. In the aforementioned study of bariatric surgery patients, 92.4% supported their procedure being performed at a teaching hospital, but only 56% would consent to a resident assisting staff during the procedure. A mere 33% of those patients would consent to a resident primarily performing with staff assisting.3 Although the proportion of patients who refuse certainly depends on the type of procedure among other factors, it is a reality in any teaching environment. The training paradigm in medicine depends on being able to practice procedures with supervision before we are independent providers. If patients refuse our care, our training suffers. However, the AMA maintains that “[p]atients are free to choose from whom they receive treatment,”1 and we must respect this aspect of patient autonomy.
Final Thoughts
When it comes to the performance of procedures, there are a few basic principles to keep in mind to provide ethical care to our patients while we are in training. Although we must accept that a crucial part of learning dermatologic procedures is hands on with real patients, we also need to come prepared having learned what we can through reading and practice with cadavers or skin substitutes. Procedures we execute as residents should be performed with adequate supervision, and as we progress through residency, we should be given increased autonomy and graded responsibility to prepare us for independent practice at graduation. Although it is the responsibility of the attending physician to provide appropriate oversight for the resident’s level of training, we should feel empowered to ask for help and have the humility to know when we need it.
- Medical student involvement in patient care: report of the council on ethical and judicial affairs. Virtual Mentor. 2001;3. doi:10.1001/virtualmentor.2001.3.3.code1-0103.
- Santen S, Hemphill RR, Prough E, et al. Do patients understand their physician’s level of training? a survey of emergency department patients. Acad Med. 2004;79:139-143.
- McClellan JM, Nelson D, Porta CR, et al. Bariatric surgery patient perceptions and willingness to consent to resident participation. Surg Obes Relat Dis. 2016;12:1065-1071.
- Santen SA, Hemphill RR, McDonald MF, et al. Patients’ willingness to allow residents to learn to practice medical procedures. Acad Med. 2004;79:144-147.
- LaRosa C, Grant-Kels JM. See one, do one, teach one: the ethical dilemma of residents performing their first procedure on patients. J Am Acad Dermatol. 2016;75:845-848.
- Can MF. The trainee effect on early postoperative surgical outcomes: reflects the effect of resident involvement or hospital capacity to overcome complications? J Invest Surg. 2017;31:67-68.
- Goldberg I, Yang J, Park J, et al. Surgical trainee impact on bariatric surgery safety [published online November 13, 2018]. Surg Endosc. doi:10.1007/s00464-018-6587-0.
- Kasotakis G, Lakha A, Sarkar B, et al. Trainee participation is associated with adverse outcomes in emergency general surgery: an analysis of the National Surgical Quality Improvement Program database. Ann Surg. 2014;3:483-490.
- Richard C, Lajeunesse Y, Lussier MT. Therapeutic privilege: between the ethics of lying and the practice of truth. J Med Ethics. 2010;36:353-357.
- Medical student involvement in patient care: report of the council on ethical and judicial affairs. Virtual Mentor. 2001;3. doi:10.1001/virtualmentor.2001.3.3.code1-0103.
- Santen S, Hemphill RR, Prough E, et al. Do patients understand their physician’s level of training? a survey of emergency department patients. Acad Med. 2004;79:139-143.
- McClellan JM, Nelson D, Porta CR, et al. Bariatric surgery patient perceptions and willingness to consent to resident participation. Surg Obes Relat Dis. 2016;12:1065-1071.
- Santen SA, Hemphill RR, McDonald MF, et al. Patients’ willingness to allow residents to learn to practice medical procedures. Acad Med. 2004;79:144-147.
- LaRosa C, Grant-Kels JM. See one, do one, teach one: the ethical dilemma of residents performing their first procedure on patients. J Am Acad Dermatol. 2016;75:845-848.
- Can MF. The trainee effect on early postoperative surgical outcomes: reflects the effect of resident involvement or hospital capacity to overcome complications? J Invest Surg. 2017;31:67-68.
- Goldberg I, Yang J, Park J, et al. Surgical trainee impact on bariatric surgery safety [published online November 13, 2018]. Surg Endosc. doi:10.1007/s00464-018-6587-0.
- Kasotakis G, Lakha A, Sarkar B, et al. Trainee participation is associated with adverse outcomes in emergency general surgery: an analysis of the National Surgical Quality Improvement Program database. Ann Surg. 2014;3:483-490.
- Richard C, Lajeunesse Y, Lussier MT. Therapeutic privilege: between the ethics of lying and the practice of truth. J Med Ethics. 2010;36:353-357.
Resident Pearl
- As residents, we must gain experience performing procedures on real patients to enter independent practice as proficient dermatologists. It is important to be mindful of the ethical challenges inherent to the hands-on training process and to understand the ethical principles that guide best practices.
The Evolution of the Micrographic Surgery and Dermatologic Oncology Fellowship
Originating in 1968, the dermatologic surgery fellowship is as young as many dermatologists in practice today. Not surprisingly, the blossoming fellowship has undergone its fair share of both growth and growing pains over the last 5 decades.
A Brief History
The first dermatologic surgery fellowship was born in 1968 when Dr. Perry Robins established a program at the New York University Medical Center for training in chemosurgery.1 The fellowship quickly underwent notable change with the rising popularity of the fresh tissue technique, which was first performed by Dr. Fred Mohs in 1953 and made popular following publication of a series of landmark articles on the technique by Drs. Sam Stegman and Theodore Tromovitch in the late 1960s and early 1970s. The fellowship correspondingly saw a rise in fresh tissue technique training, accompanied by a decline in chemosurgery training. In 1974, Dr. Daniel Jones coined the term micrographic surgery to describe the favored technique, and at the 1985 annual meeting of the American College of Chemosurgery, the name of the technique was changed to Mohs micrographic surgery.1
By 1995, the fellowship was officially named Procedural Dermatology, and programs were exclusively accredited by the American College of Mohs Surgery (ACMS). A 1-year Procedural Dermatology fellowship gained accreditation by the Accreditation Council for Graduate Medical Education (ACGME) in 2003.2 Beginning in July 2013, all fellowship programs in the United States fell under the governance of the ACGME; however, the ACMS has remained the sponsor of the matching process.3 In 2014, the ACGME changed the name of the fellowship to Micrographic Surgery and Dermatologic Oncology (MSDO).2 Fellowship training today is centered on the core elements of cutaneous oncologic surgery, cutaneous reconstructive surgery, and dermatologic oncology; however, the scope of training in technologies and techniques offered has continued to broaden.4 Many programs now offer additional training in cosmetic and other procedural dermatology. To date, there are 76 accredited MSDO fellowship training programs in the United States and more than 1500 fellowship-trained micrographic surgeons.2,4
Trends in Program and Match Statistics
As the role of dermatologic surgery within the field of dermatology continues to expand, the MSDO fellowship has become increasingly popular over the last decade. From 2005 to 2018, applicants participating in the fellowship match increased by 34%.3 Despite the fellowship’s growing popularity, programs participating in the match have remained largely stable from 2005 to 2018, with 50 positions offered in 2005 and 58 in 2018. The match rate has correspondingly decreased from 66.2% in 2005 to 61.1% in 2018.3
Changes in the Match Process
The fellowship match is processed by the SF Match and sponsored by the ACMS. Over the last decade, programs have increasingly opted for exemptions from participation in the SF Match. In 2005, there were 8 match exemptions. In 2018, there were 20.4 Despite the increasing popularity of match exemptions, in October 2018 the ACMS Board of Directors approved a new policy that eliminated match exemptions, with the exception of applicants on active military duty and international (non-Canadian) applicants. All other applicants applying for a fellowship position for the 2020-2021 academic year must participate in the match.4 This new policy attempts to ensure a fair match process, especially for applicants who have trained at a program without an affiliated MSDO fellowship.
The Road to Board Certification
Further growth during the fellowship’s mid-adult years centered on the long-contested debate on subspecialty board certification. In 2009, an American Society for Dermatologic Surgery membership survey demonstrated an overwhelming majority in opposition. In 2014, the debate resurfaced. At the 2016 American Society for Dermatologic Surgery annual meeting, former American Academy of Dermatology presidents Brett Coldiron, MD, and Darrell S. Rigel, MD, MS, conveyed opposing positions, after which an audience survey demonstrated a 69% opposition rate. Proponents continued to argue that board certification would decrease divisiveness in the specialty, create a better brand, help to obtain a Medicare specialty designation that could help prevent exclusion of Mohs surgeons from insurance networks, give allopathic dermatologists the same opportunity for certification as osteopathic counterparts, and demonstrate competence to the public. Those in opposition argued that the term dermatologic oncology erroneously suggests general dermatologists are not experts in the treatment of skin cancers, practices may be restricted by carriers misusing the new credential, and subspecialty certification would actually create division among practicing dermatologists.5
Following years of debate, the American Board of Dermatology’s proposal to offer subspecialty certification in Micrographic Dermatologic Surgery was submitted to the American Board of Medical Specialties and approved on October 26, 2018. The name of the new subspecialty (Micrographic Dermatologic Surgery) is different than that of the fellowship (Micrographic Surgery and Dermatologic Oncology), a decision reached in response to diplomats indicating discomfort with the term oncology potentially misleading the public that general dermatologists do not treat skin cancer. Per the American Board of Dermatology official website, the first certification examination likely will take place in about 2 years. A maintenance of certification examination for the subspecialty will be required every 10 years.6
Final Thoughts
During its short history, the MSDO fellowship has undergone a notable evolution in recognition, popularity among residents, match process, and board certification, which attests to its adaptability over time and growing prominence.
- Robins P, Ebede TL, Hale EK. The evolution of Mohs micrographic surgery. Skin Cancer Foundation website. https://www.skincancer.org/skin-cancer-information/mohs-surgery/evolution-of-mohs. Updated July 13, 2016. Accessed April 17, 2019.
- Micrographic surgery and dermatologic oncology. American Board of Dermatology website. https://www.abderm.org/residents-and-fellows/fellowship-training/micrographic-surgery-and-dermatologic-oncology.aspx. Accessed April 9, 2019.
- Micrographic Surgery and Dermatologic Oncology Fellowship. San Francisco Match website. https://sfmatch.org/SpecialtyInsideAll.aspx?id=10&typ=1&name=Micrographic%20Surgery%20and%20Dermatologic%20Oncology. Accessed April 9, 2019.
- ACMS fellowship training. American College of Mohs Surgery website. https://www.mohscollege.org/fellowship-training. Accessed April 9, 2019.
- Should the ABD offer a Mohs surgery sub-certification? Dermatology World. April 26, 2017. https://www.aad.org/dw/dw-weekly/should-the-abd-offer-a-mohs-surgery-sub-certification. Accessed April 9, 2019.
- ABD Micrographic Dermatologic Surgery (MDS) subspecialty certification. American Board of Dermatology website. https://www.abderm.org/residents-and-fellows/fellowship-training/micrographic-dermatologic-surgery-mds-questions-and-answers-1.aspx. Accessed April 9, 2019.
Originating in 1968, the dermatologic surgery fellowship is as young as many dermatologists in practice today. Not surprisingly, the blossoming fellowship has undergone its fair share of both growth and growing pains over the last 5 decades.
A Brief History
The first dermatologic surgery fellowship was born in 1968 when Dr. Perry Robins established a program at the New York University Medical Center for training in chemosurgery.1 The fellowship quickly underwent notable change with the rising popularity of the fresh tissue technique, which was first performed by Dr. Fred Mohs in 1953 and made popular following publication of a series of landmark articles on the technique by Drs. Sam Stegman and Theodore Tromovitch in the late 1960s and early 1970s. The fellowship correspondingly saw a rise in fresh tissue technique training, accompanied by a decline in chemosurgery training. In 1974, Dr. Daniel Jones coined the term micrographic surgery to describe the favored technique, and at the 1985 annual meeting of the American College of Chemosurgery, the name of the technique was changed to Mohs micrographic surgery.1
By 1995, the fellowship was officially named Procedural Dermatology, and programs were exclusively accredited by the American College of Mohs Surgery (ACMS). A 1-year Procedural Dermatology fellowship gained accreditation by the Accreditation Council for Graduate Medical Education (ACGME) in 2003.2 Beginning in July 2013, all fellowship programs in the United States fell under the governance of the ACGME; however, the ACMS has remained the sponsor of the matching process.3 In 2014, the ACGME changed the name of the fellowship to Micrographic Surgery and Dermatologic Oncology (MSDO).2 Fellowship training today is centered on the core elements of cutaneous oncologic surgery, cutaneous reconstructive surgery, and dermatologic oncology; however, the scope of training in technologies and techniques offered has continued to broaden.4 Many programs now offer additional training in cosmetic and other procedural dermatology. To date, there are 76 accredited MSDO fellowship training programs in the United States and more than 1500 fellowship-trained micrographic surgeons.2,4
Trends in Program and Match Statistics
As the role of dermatologic surgery within the field of dermatology continues to expand, the MSDO fellowship has become increasingly popular over the last decade. From 2005 to 2018, applicants participating in the fellowship match increased by 34%.3 Despite the fellowship’s growing popularity, programs participating in the match have remained largely stable from 2005 to 2018, with 50 positions offered in 2005 and 58 in 2018. The match rate has correspondingly decreased from 66.2% in 2005 to 61.1% in 2018.3
Changes in the Match Process
The fellowship match is processed by the SF Match and sponsored by the ACMS. Over the last decade, programs have increasingly opted for exemptions from participation in the SF Match. In 2005, there were 8 match exemptions. In 2018, there were 20.4 Despite the increasing popularity of match exemptions, in October 2018 the ACMS Board of Directors approved a new policy that eliminated match exemptions, with the exception of applicants on active military duty and international (non-Canadian) applicants. All other applicants applying for a fellowship position for the 2020-2021 academic year must participate in the match.4 This new policy attempts to ensure a fair match process, especially for applicants who have trained at a program without an affiliated MSDO fellowship.
The Road to Board Certification
Further growth during the fellowship’s mid-adult years centered on the long-contested debate on subspecialty board certification. In 2009, an American Society for Dermatologic Surgery membership survey demonstrated an overwhelming majority in opposition. In 2014, the debate resurfaced. At the 2016 American Society for Dermatologic Surgery annual meeting, former American Academy of Dermatology presidents Brett Coldiron, MD, and Darrell S. Rigel, MD, MS, conveyed opposing positions, after which an audience survey demonstrated a 69% opposition rate. Proponents continued to argue that board certification would decrease divisiveness in the specialty, create a better brand, help to obtain a Medicare specialty designation that could help prevent exclusion of Mohs surgeons from insurance networks, give allopathic dermatologists the same opportunity for certification as osteopathic counterparts, and demonstrate competence to the public. Those in opposition argued that the term dermatologic oncology erroneously suggests general dermatologists are not experts in the treatment of skin cancers, practices may be restricted by carriers misusing the new credential, and subspecialty certification would actually create division among practicing dermatologists.5
Following years of debate, the American Board of Dermatology’s proposal to offer subspecialty certification in Micrographic Dermatologic Surgery was submitted to the American Board of Medical Specialties and approved on October 26, 2018. The name of the new subspecialty (Micrographic Dermatologic Surgery) is different than that of the fellowship (Micrographic Surgery and Dermatologic Oncology), a decision reached in response to diplomats indicating discomfort with the term oncology potentially misleading the public that general dermatologists do not treat skin cancer. Per the American Board of Dermatology official website, the first certification examination likely will take place in about 2 years. A maintenance of certification examination for the subspecialty will be required every 10 years.6
Final Thoughts
During its short history, the MSDO fellowship has undergone a notable evolution in recognition, popularity among residents, match process, and board certification, which attests to its adaptability over time and growing prominence.
Originating in 1968, the dermatologic surgery fellowship is as young as many dermatologists in practice today. Not surprisingly, the blossoming fellowship has undergone its fair share of both growth and growing pains over the last 5 decades.
A Brief History
The first dermatologic surgery fellowship was born in 1968 when Dr. Perry Robins established a program at the New York University Medical Center for training in chemosurgery.1 The fellowship quickly underwent notable change with the rising popularity of the fresh tissue technique, which was first performed by Dr. Fred Mohs in 1953 and made popular following publication of a series of landmark articles on the technique by Drs. Sam Stegman and Theodore Tromovitch in the late 1960s and early 1970s. The fellowship correspondingly saw a rise in fresh tissue technique training, accompanied by a decline in chemosurgery training. In 1974, Dr. Daniel Jones coined the term micrographic surgery to describe the favored technique, and at the 1985 annual meeting of the American College of Chemosurgery, the name of the technique was changed to Mohs micrographic surgery.1
By 1995, the fellowship was officially named Procedural Dermatology, and programs were exclusively accredited by the American College of Mohs Surgery (ACMS). A 1-year Procedural Dermatology fellowship gained accreditation by the Accreditation Council for Graduate Medical Education (ACGME) in 2003.2 Beginning in July 2013, all fellowship programs in the United States fell under the governance of the ACGME; however, the ACMS has remained the sponsor of the matching process.3 In 2014, the ACGME changed the name of the fellowship to Micrographic Surgery and Dermatologic Oncology (MSDO).2 Fellowship training today is centered on the core elements of cutaneous oncologic surgery, cutaneous reconstructive surgery, and dermatologic oncology; however, the scope of training in technologies and techniques offered has continued to broaden.4 Many programs now offer additional training in cosmetic and other procedural dermatology. To date, there are 76 accredited MSDO fellowship training programs in the United States and more than 1500 fellowship-trained micrographic surgeons.2,4
Trends in Program and Match Statistics
As the role of dermatologic surgery within the field of dermatology continues to expand, the MSDO fellowship has become increasingly popular over the last decade. From 2005 to 2018, applicants participating in the fellowship match increased by 34%.3 Despite the fellowship’s growing popularity, programs participating in the match have remained largely stable from 2005 to 2018, with 50 positions offered in 2005 and 58 in 2018. The match rate has correspondingly decreased from 66.2% in 2005 to 61.1% in 2018.3
Changes in the Match Process
The fellowship match is processed by the SF Match and sponsored by the ACMS. Over the last decade, programs have increasingly opted for exemptions from participation in the SF Match. In 2005, there were 8 match exemptions. In 2018, there were 20.4 Despite the increasing popularity of match exemptions, in October 2018 the ACMS Board of Directors approved a new policy that eliminated match exemptions, with the exception of applicants on active military duty and international (non-Canadian) applicants. All other applicants applying for a fellowship position for the 2020-2021 academic year must participate in the match.4 This new policy attempts to ensure a fair match process, especially for applicants who have trained at a program without an affiliated MSDO fellowship.
The Road to Board Certification
Further growth during the fellowship’s mid-adult years centered on the long-contested debate on subspecialty board certification. In 2009, an American Society for Dermatologic Surgery membership survey demonstrated an overwhelming majority in opposition. In 2014, the debate resurfaced. At the 2016 American Society for Dermatologic Surgery annual meeting, former American Academy of Dermatology presidents Brett Coldiron, MD, and Darrell S. Rigel, MD, MS, conveyed opposing positions, after which an audience survey demonstrated a 69% opposition rate. Proponents continued to argue that board certification would decrease divisiveness in the specialty, create a better brand, help to obtain a Medicare specialty designation that could help prevent exclusion of Mohs surgeons from insurance networks, give allopathic dermatologists the same opportunity for certification as osteopathic counterparts, and demonstrate competence to the public. Those in opposition argued that the term dermatologic oncology erroneously suggests general dermatologists are not experts in the treatment of skin cancers, practices may be restricted by carriers misusing the new credential, and subspecialty certification would actually create division among practicing dermatologists.5
Following years of debate, the American Board of Dermatology’s proposal to offer subspecialty certification in Micrographic Dermatologic Surgery was submitted to the American Board of Medical Specialties and approved on October 26, 2018. The name of the new subspecialty (Micrographic Dermatologic Surgery) is different than that of the fellowship (Micrographic Surgery and Dermatologic Oncology), a decision reached in response to diplomats indicating discomfort with the term oncology potentially misleading the public that general dermatologists do not treat skin cancer. Per the American Board of Dermatology official website, the first certification examination likely will take place in about 2 years. A maintenance of certification examination for the subspecialty will be required every 10 years.6
Final Thoughts
During its short history, the MSDO fellowship has undergone a notable evolution in recognition, popularity among residents, match process, and board certification, which attests to its adaptability over time and growing prominence.
- Robins P, Ebede TL, Hale EK. The evolution of Mohs micrographic surgery. Skin Cancer Foundation website. https://www.skincancer.org/skin-cancer-information/mohs-surgery/evolution-of-mohs. Updated July 13, 2016. Accessed April 17, 2019.
- Micrographic surgery and dermatologic oncology. American Board of Dermatology website. https://www.abderm.org/residents-and-fellows/fellowship-training/micrographic-surgery-and-dermatologic-oncology.aspx. Accessed April 9, 2019.
- Micrographic Surgery and Dermatologic Oncology Fellowship. San Francisco Match website. https://sfmatch.org/SpecialtyInsideAll.aspx?id=10&typ=1&name=Micrographic%20Surgery%20and%20Dermatologic%20Oncology. Accessed April 9, 2019.
- ACMS fellowship training. American College of Mohs Surgery website. https://www.mohscollege.org/fellowship-training. Accessed April 9, 2019.
- Should the ABD offer a Mohs surgery sub-certification? Dermatology World. April 26, 2017. https://www.aad.org/dw/dw-weekly/should-the-abd-offer-a-mohs-surgery-sub-certification. Accessed April 9, 2019.
- ABD Micrographic Dermatologic Surgery (MDS) subspecialty certification. American Board of Dermatology website. https://www.abderm.org/residents-and-fellows/fellowship-training/micrographic-dermatologic-surgery-mds-questions-and-answers-1.aspx. Accessed April 9, 2019.
- Robins P, Ebede TL, Hale EK. The evolution of Mohs micrographic surgery. Skin Cancer Foundation website. https://www.skincancer.org/skin-cancer-information/mohs-surgery/evolution-of-mohs. Updated July 13, 2016. Accessed April 17, 2019.
- Micrographic surgery and dermatologic oncology. American Board of Dermatology website. https://www.abderm.org/residents-and-fellows/fellowship-training/micrographic-surgery-and-dermatologic-oncology.aspx. Accessed April 9, 2019.
- Micrographic Surgery and Dermatologic Oncology Fellowship. San Francisco Match website. https://sfmatch.org/SpecialtyInsideAll.aspx?id=10&typ=1&name=Micrographic%20Surgery%20and%20Dermatologic%20Oncology. Accessed April 9, 2019.
- ACMS fellowship training. American College of Mohs Surgery website. https://www.mohscollege.org/fellowship-training. Accessed April 9, 2019.
- Should the ABD offer a Mohs surgery sub-certification? Dermatology World. April 26, 2017. https://www.aad.org/dw/dw-weekly/should-the-abd-offer-a-mohs-surgery-sub-certification. Accessed April 9, 2019.
- ABD Micrographic Dermatologic Surgery (MDS) subspecialty certification. American Board of Dermatology website. https://www.abderm.org/residents-and-fellows/fellowship-training/micrographic-dermatologic-surgery-mds-questions-and-answers-1.aspx. Accessed April 9, 2019.
Resident Pearl
- Residents should be aware of recent changes to the Micrographic Surgery and Dermatologic Oncology fellowship: the elimination of fellowship match exemptions for most applicants for the upcoming 2019-2020 academic year, the American Board of Medical Specialties approval of subspecialty certification in Micrographic Dermatologic Surgery, and the likelihood of the first subspecialty certification examination in the next 2 years.
Supercharge Your On-Call Bag: 4 Must-Have Items for Dermatology Residents
It is no secret that a well-stocked on-call bag is one of the keys to providing inpatient care as a dermatology resident. Beyond the basic items that should never be left at home, there are some lesser-known tools that I have learned about from my book- and street-smart attendings and co-residents in the Department of Dermatology at the State University of New York Downstate Medical Center (referred to here as Downstate). Here are our top 4 items to pack the next time you are on call. (Bonus: you will find them helpful in clinic, too.)
Item 1: WoundSeal Powder
The most valuable player in my on-call bag, WoundSeal Powder (Biolife) is an over-the-counter hemostatic agent that I learned about from Daniel M. Siegel, MD, MS, a Mohs surgeon at Downstate and former president of the American Academy of Dermatology. The powder consists of a hydrophilic polymer and potassium ferrate.1 When poured over a bleeding wound and pressed in place (eg, with a sterile cotton-tipped swab), the hydrophilic polymer absorbs plasma while the iron in potassium ferrate agglomerates blood solids. The result is a scablike seal that is safe to leave in place until the wound has healed.1
Since Dr. Siegel introduced WoundSeal to Downstate about a decade ago, it has become our department’s go-to hemostatic agent for most punch biopsies performed in the inpatient setting. In our experience, achieving hemostasis in the hospital usually is easier, safer, and faster with WoundSeal than suture. Furthermore, using WoundSeal eliminates the need for patients to follow up for suture removal. From a practical perspective, WoundSeal works best when the biopsy defect is positioned parallel to the ground so the powder can be poured directly over and into the defect. From a cosmetic perspective, we have found that WoundSeal and suture have similar outcomes when used for punch biopsies up to 4 mm in size on the trunk and extremities in both adult and pediatric patients. Working with other dermatology attendings such as Sharon A. Glick, MD; Eve Lowenstein, MD, PhD; and Jeannette Jakus, MD, MBA, I also have found WoundSeal helpful when taking care of suture-phobic children or patients with lesions that are less amenable to suture, such as an ulcer or indurated plaque.
Item 2: Purple Surgical Marker
Another tip I have learned from Drs. Siegel and Jakus: If you are ever in a bind for a topical antibacterial or antifungal agent, look no further than a sterile purple surgical marker. These markers are a surprising source of gentian violet, the same purple dye that is the basis of Gram staining and sold as an over-the-counter antiseptic in 1% to 2% concentrations. Purple surgical markers, on the other hand, are 2.5% to 10% gentian violet.2
Gentian violet has been shown to have antibacterial, antifungal, antiviral, antihelminthic, and antitrypanosomal properties, but its efficacy has been mostly demonstrated against Streptococcus, methicillin-sensitive and methicillin-resistant Staphylococcus aureus, and Candida.3 Given the dermatologic relevance of these organisms, gentian violet is a favorite among attendings at my residency program; it is not uncommon to remove a patient’s dressing and uncover an iatrogenically purple wound. Best of all, pediatric patients are invariably amused when they see someone drawing on their skin with a purple marker.
When using a sterile surgical marker to apply gentian violet to the skin, we use either the marker tip or the ink core, which Dr. Siegel taught me can be easily accessed by snapping most plastic markers in half.
Item 3: Handheld Blacklight
The Wood lamp is a useful tool in the diagnosis of various infectious diseases and pigmentary disorders,4 but it is not always practical to use when on call, as standard ones are relatively large and corded, so they must be plugged into an electric outlet to work. You can therefore imagine the gratitude I have for my co-residents Miriam Lieberman, MD; Jaime Alexander, MD; Nicole Weiler, MD; and Alessandra Haskin, MD, for introducing me to the most convenient Wood lamp: the handheld blacklight. For less than $10, this gadget combines the diagnostic power of UV light with the portability of a pocket-sized, battery-powered flashlight. You will never want to use another Wood lamp again.
Item 4: Normal Saline Flush
Normal saline can be used for more than storing specimens for frozen section or tissue culture; it also can substitute for Michel solution when storing specimens for direct immunofluorescence (DIF) studies. I learned this tip from Edward Heilman, MD, a dermatopathologist at Downstate. For the last 20 years, Dr. Heilman has been successfully storing DIF specimens in refrigerated normal saline for up to 24 hours when Michel solution is unavailable, after which the specimen is processed or transferred to Michel solution for further storage while being transported to an immunofluorescence laboratory.
In 2004, Vodegel et al5 formally studied this technique in 25 patients with autoimmune skin diseases such as pemphigus and pemphigoid. (Thanks to Dr. Lieberman for telling me about this study.) The experiment involved taking 4 punch biopsies from each patient and placing them in either normal saline at −80°C for 24 or 48 hours, room temperature Michel solution for 48 hours, or liquid nitrogen for up to 2 weeks before being processed for DIF and analyzed by a blinded interpreter. Interestingly, specimens stored in normal saline for 24 hours were the most diagnostic, with a conclusive diagnosis reached in 21 of 25 specimens (84%). This result was attributed to the statistically significant reduction (P<.01) in background fluorescence with normal saline compared to Michel solution and liquid nitrogen, which in turn allowed for easier detection of diagnostic immunoreactants. Similar to Dr. Heilman, the authors cautioned against placing DIF specimens in normal saline for more than 24 hours; in their experience, the risk for an artefactual split developing at the dermoepidermal junction increases with this practice.5
- Biolife. How WoundSeal works. WoundSeal website. http://woundseal.com/how-it-works. Accessed March 7, 2019.
- Viscot Medical, LLC. Safety data sheet. http://www.viscot.com/download/MSDS%20Gentian%20Violet%20Ink.pdf. Published September 11, 2014. Accessed March 7, 2019.
- Maley AM, Arbiser JL. Gentian violet: a 19th century drug re-emerges in the 21st century. Exp Dermatol. 2013;22:775-780.
- Klatte JL, van der Beek N, Kemperman PM. 100 years of Wood’s lamp revised. J Eur Acad Dermatol Venereol. 2015;29:842-847.
- Vodegel RM, de Jong MC, Meijer HJ, et al. Enhanced diagnostic immunofluorescence using biopsies transported in saline. BMC Dermatol. 2004;4:10.
It is no secret that a well-stocked on-call bag is one of the keys to providing inpatient care as a dermatology resident. Beyond the basic items that should never be left at home, there are some lesser-known tools that I have learned about from my book- and street-smart attendings and co-residents in the Department of Dermatology at the State University of New York Downstate Medical Center (referred to here as Downstate). Here are our top 4 items to pack the next time you are on call. (Bonus: you will find them helpful in clinic, too.)
Item 1: WoundSeal Powder
The most valuable player in my on-call bag, WoundSeal Powder (Biolife) is an over-the-counter hemostatic agent that I learned about from Daniel M. Siegel, MD, MS, a Mohs surgeon at Downstate and former president of the American Academy of Dermatology. The powder consists of a hydrophilic polymer and potassium ferrate.1 When poured over a bleeding wound and pressed in place (eg, with a sterile cotton-tipped swab), the hydrophilic polymer absorbs plasma while the iron in potassium ferrate agglomerates blood solids. The result is a scablike seal that is safe to leave in place until the wound has healed.1
Since Dr. Siegel introduced WoundSeal to Downstate about a decade ago, it has become our department’s go-to hemostatic agent for most punch biopsies performed in the inpatient setting. In our experience, achieving hemostasis in the hospital usually is easier, safer, and faster with WoundSeal than suture. Furthermore, using WoundSeal eliminates the need for patients to follow up for suture removal. From a practical perspective, WoundSeal works best when the biopsy defect is positioned parallel to the ground so the powder can be poured directly over and into the defect. From a cosmetic perspective, we have found that WoundSeal and suture have similar outcomes when used for punch biopsies up to 4 mm in size on the trunk and extremities in both adult and pediatric patients. Working with other dermatology attendings such as Sharon A. Glick, MD; Eve Lowenstein, MD, PhD; and Jeannette Jakus, MD, MBA, I also have found WoundSeal helpful when taking care of suture-phobic children or patients with lesions that are less amenable to suture, such as an ulcer or indurated plaque.
Item 2: Purple Surgical Marker
Another tip I have learned from Drs. Siegel and Jakus: If you are ever in a bind for a topical antibacterial or antifungal agent, look no further than a sterile purple surgical marker. These markers are a surprising source of gentian violet, the same purple dye that is the basis of Gram staining and sold as an over-the-counter antiseptic in 1% to 2% concentrations. Purple surgical markers, on the other hand, are 2.5% to 10% gentian violet.2
Gentian violet has been shown to have antibacterial, antifungal, antiviral, antihelminthic, and antitrypanosomal properties, but its efficacy has been mostly demonstrated against Streptococcus, methicillin-sensitive and methicillin-resistant Staphylococcus aureus, and Candida.3 Given the dermatologic relevance of these organisms, gentian violet is a favorite among attendings at my residency program; it is not uncommon to remove a patient’s dressing and uncover an iatrogenically purple wound. Best of all, pediatric patients are invariably amused when they see someone drawing on their skin with a purple marker.
When using a sterile surgical marker to apply gentian violet to the skin, we use either the marker tip or the ink core, which Dr. Siegel taught me can be easily accessed by snapping most plastic markers in half.
Item 3: Handheld Blacklight
The Wood lamp is a useful tool in the diagnosis of various infectious diseases and pigmentary disorders,4 but it is not always practical to use when on call, as standard ones are relatively large and corded, so they must be plugged into an electric outlet to work. You can therefore imagine the gratitude I have for my co-residents Miriam Lieberman, MD; Jaime Alexander, MD; Nicole Weiler, MD; and Alessandra Haskin, MD, for introducing me to the most convenient Wood lamp: the handheld blacklight. For less than $10, this gadget combines the diagnostic power of UV light with the portability of a pocket-sized, battery-powered flashlight. You will never want to use another Wood lamp again.
Item 4: Normal Saline Flush
Normal saline can be used for more than storing specimens for frozen section or tissue culture; it also can substitute for Michel solution when storing specimens for direct immunofluorescence (DIF) studies. I learned this tip from Edward Heilman, MD, a dermatopathologist at Downstate. For the last 20 years, Dr. Heilman has been successfully storing DIF specimens in refrigerated normal saline for up to 24 hours when Michel solution is unavailable, after which the specimen is processed or transferred to Michel solution for further storage while being transported to an immunofluorescence laboratory.
In 2004, Vodegel et al5 formally studied this technique in 25 patients with autoimmune skin diseases such as pemphigus and pemphigoid. (Thanks to Dr. Lieberman for telling me about this study.) The experiment involved taking 4 punch biopsies from each patient and placing them in either normal saline at −80°C for 24 or 48 hours, room temperature Michel solution for 48 hours, or liquid nitrogen for up to 2 weeks before being processed for DIF and analyzed by a blinded interpreter. Interestingly, specimens stored in normal saline for 24 hours were the most diagnostic, with a conclusive diagnosis reached in 21 of 25 specimens (84%). This result was attributed to the statistically significant reduction (P<.01) in background fluorescence with normal saline compared to Michel solution and liquid nitrogen, which in turn allowed for easier detection of diagnostic immunoreactants. Similar to Dr. Heilman, the authors cautioned against placing DIF specimens in normal saline for more than 24 hours; in their experience, the risk for an artefactual split developing at the dermoepidermal junction increases with this practice.5
It is no secret that a well-stocked on-call bag is one of the keys to providing inpatient care as a dermatology resident. Beyond the basic items that should never be left at home, there are some lesser-known tools that I have learned about from my book- and street-smart attendings and co-residents in the Department of Dermatology at the State University of New York Downstate Medical Center (referred to here as Downstate). Here are our top 4 items to pack the next time you are on call. (Bonus: you will find them helpful in clinic, too.)
Item 1: WoundSeal Powder
The most valuable player in my on-call bag, WoundSeal Powder (Biolife) is an over-the-counter hemostatic agent that I learned about from Daniel M. Siegel, MD, MS, a Mohs surgeon at Downstate and former president of the American Academy of Dermatology. The powder consists of a hydrophilic polymer and potassium ferrate.1 When poured over a bleeding wound and pressed in place (eg, with a sterile cotton-tipped swab), the hydrophilic polymer absorbs plasma while the iron in potassium ferrate agglomerates blood solids. The result is a scablike seal that is safe to leave in place until the wound has healed.1
Since Dr. Siegel introduced WoundSeal to Downstate about a decade ago, it has become our department’s go-to hemostatic agent for most punch biopsies performed in the inpatient setting. In our experience, achieving hemostasis in the hospital usually is easier, safer, and faster with WoundSeal than suture. Furthermore, using WoundSeal eliminates the need for patients to follow up for suture removal. From a practical perspective, WoundSeal works best when the biopsy defect is positioned parallel to the ground so the powder can be poured directly over and into the defect. From a cosmetic perspective, we have found that WoundSeal and suture have similar outcomes when used for punch biopsies up to 4 mm in size on the trunk and extremities in both adult and pediatric patients. Working with other dermatology attendings such as Sharon A. Glick, MD; Eve Lowenstein, MD, PhD; and Jeannette Jakus, MD, MBA, I also have found WoundSeal helpful when taking care of suture-phobic children or patients with lesions that are less amenable to suture, such as an ulcer or indurated plaque.
Item 2: Purple Surgical Marker
Another tip I have learned from Drs. Siegel and Jakus: If you are ever in a bind for a topical antibacterial or antifungal agent, look no further than a sterile purple surgical marker. These markers are a surprising source of gentian violet, the same purple dye that is the basis of Gram staining and sold as an over-the-counter antiseptic in 1% to 2% concentrations. Purple surgical markers, on the other hand, are 2.5% to 10% gentian violet.2
Gentian violet has been shown to have antibacterial, antifungal, antiviral, antihelminthic, and antitrypanosomal properties, but its efficacy has been mostly demonstrated against Streptococcus, methicillin-sensitive and methicillin-resistant Staphylococcus aureus, and Candida.3 Given the dermatologic relevance of these organisms, gentian violet is a favorite among attendings at my residency program; it is not uncommon to remove a patient’s dressing and uncover an iatrogenically purple wound. Best of all, pediatric patients are invariably amused when they see someone drawing on their skin with a purple marker.
When using a sterile surgical marker to apply gentian violet to the skin, we use either the marker tip or the ink core, which Dr. Siegel taught me can be easily accessed by snapping most plastic markers in half.
Item 3: Handheld Blacklight
The Wood lamp is a useful tool in the diagnosis of various infectious diseases and pigmentary disorders,4 but it is not always practical to use when on call, as standard ones are relatively large and corded, so they must be plugged into an electric outlet to work. You can therefore imagine the gratitude I have for my co-residents Miriam Lieberman, MD; Jaime Alexander, MD; Nicole Weiler, MD; and Alessandra Haskin, MD, for introducing me to the most convenient Wood lamp: the handheld blacklight. For less than $10, this gadget combines the diagnostic power of UV light with the portability of a pocket-sized, battery-powered flashlight. You will never want to use another Wood lamp again.
Item 4: Normal Saline Flush
Normal saline can be used for more than storing specimens for frozen section or tissue culture; it also can substitute for Michel solution when storing specimens for direct immunofluorescence (DIF) studies. I learned this tip from Edward Heilman, MD, a dermatopathologist at Downstate. For the last 20 years, Dr. Heilman has been successfully storing DIF specimens in refrigerated normal saline for up to 24 hours when Michel solution is unavailable, after which the specimen is processed or transferred to Michel solution for further storage while being transported to an immunofluorescence laboratory.
In 2004, Vodegel et al5 formally studied this technique in 25 patients with autoimmune skin diseases such as pemphigus and pemphigoid. (Thanks to Dr. Lieberman for telling me about this study.) The experiment involved taking 4 punch biopsies from each patient and placing them in either normal saline at −80°C for 24 or 48 hours, room temperature Michel solution for 48 hours, or liquid nitrogen for up to 2 weeks before being processed for DIF and analyzed by a blinded interpreter. Interestingly, specimens stored in normal saline for 24 hours were the most diagnostic, with a conclusive diagnosis reached in 21 of 25 specimens (84%). This result was attributed to the statistically significant reduction (P<.01) in background fluorescence with normal saline compared to Michel solution and liquid nitrogen, which in turn allowed for easier detection of diagnostic immunoreactants. Similar to Dr. Heilman, the authors cautioned against placing DIF specimens in normal saline for more than 24 hours; in their experience, the risk for an artefactual split developing at the dermoepidermal junction increases with this practice.5
- Biolife. How WoundSeal works. WoundSeal website. http://woundseal.com/how-it-works. Accessed March 7, 2019.
- Viscot Medical, LLC. Safety data sheet. http://www.viscot.com/download/MSDS%20Gentian%20Violet%20Ink.pdf. Published September 11, 2014. Accessed March 7, 2019.
- Maley AM, Arbiser JL. Gentian violet: a 19th century drug re-emerges in the 21st century. Exp Dermatol. 2013;22:775-780.
- Klatte JL, van der Beek N, Kemperman PM. 100 years of Wood’s lamp revised. J Eur Acad Dermatol Venereol. 2015;29:842-847.
- Vodegel RM, de Jong MC, Meijer HJ, et al. Enhanced diagnostic immunofluorescence using biopsies transported in saline. BMC Dermatol. 2004;4:10.
- Biolife. How WoundSeal works. WoundSeal website. http://woundseal.com/how-it-works. Accessed March 7, 2019.
- Viscot Medical, LLC. Safety data sheet. http://www.viscot.com/download/MSDS%20Gentian%20Violet%20Ink.pdf. Published September 11, 2014. Accessed March 7, 2019.
- Maley AM, Arbiser JL. Gentian violet: a 19th century drug re-emerges in the 21st century. Exp Dermatol. 2013;22:775-780.
- Klatte JL, van der Beek N, Kemperman PM. 100 years of Wood’s lamp revised. J Eur Acad Dermatol Venereol. 2015;29:842-847.
- Vodegel RM, de Jong MC, Meijer HJ, et al. Enhanced diagnostic immunofluorescence using biopsies transported in saline. BMC Dermatol. 2004;4:10.
Resident Pearl
- The following unconventional items will come in handy the next time you are on call (or in clinic) and need an alternative to a suture, topical antimicrobial, Wood lamp, or Michel solution.
Miscommunication With Dermatology Patients: Are We Speaking the Same Language?
I was a third-year medical student, dutifully reviewing discharge instructions with a patient and her family. The patient’s adult daughter asked, “What about that diet you put her on?” As they looked at me quizzically, I looked back equally confused, until it clicked: We needed to talk about the word diet. In everyday conversation, diet generally is understood to mean restriction of food to lose weight, which is what the family hoped would be prescribed for their obese family member. I needed to tell them that I was sorry for the misunderstanding. If they overheard us “ordering a diet,” we simply meant providing trays of hospital food.
We become so familiar with the language of our profession that we do not remember it may be foreign to our patients. In dermatology, we are aware that our specialty is full of esoteric jargon and complex concepts that need to be carefully explained to our patients in simpler terms. But since that incident in medical school, I have been interested in the more insidious potential misunderstandings that can arise from words as seemingly simple as diet. There are many examples in dermatology, particularly in the way we prescribe topical therapy and use trade names.
Topical Therapy
Instructions for systemic medications may be as simple as “take 1 pill twice daily.” Prescriptions for topical medications can be written with an equally simple patient signature such as “apply twice daily to affected area,” but the simplicity is deceptive. The direction to “apply” may seem intuitive to the prescriber, but we do not always specify the amount. Sunscreen, for example, is notoriously underapplied when the actual amount of product needed for protection is not demonstrated.1 One study of new dermatology patients given a prescription for a new topical medication found that the majority of patients underdosed.2
Determination of an “affected area,” regardless of whether the site is indicated, can be even less straightforward. In acne treatment, the affected area is the whole region prone to acne breakouts, whereas in psoriasis it may be discrete psoriatic plaques. We may believe our explanations are perfectly clear, but we have all seen patients spot treating their acne or psoriasis patients covering entire territories of normal skin with topical steroids, despite our education. One study of eczema action plans found that there was considerable variability in the way different providers described disease flares that require treatment. For example, redness was only used as a descriptor of an eczema flare in 68.2% of eczema action plans studied.3 Ensuring our patients understand our criteria for skin requiring topical treatment may mean the difference between treatment success and failure and also may help to avoid unnecessary side effects.
Adherence to topical medication regimens is poor, and inadequate patient education is only one factor.4,5 One study found that more than one-third of new prescriptions for topical medications were never even filled.6 However, improving our communication about application of topical drugs is one way we must address the complicated issue of adherence.
Trade Names
In dermatology, we often use trade names to refer to our medications, even if we do not intend to reference the brand name of the drug specifically. We may tell a patient to use Lidex (Medicis Pharmaceutical Corporation) for her hands but then send an escript to her pharmacy for fluocinonide. Trade names are designed to roll off the tongue, in contrast to the unwieldy, clumsily long generic names assigned to many of our medications.
Substituting trade names may facilitate more natural conversation to promote patient understanding in some cases; however, there are pitfalls associated with this habit. First, we may be doing our patients a disservice if we do not clarify when it would be acceptable to substitute with the generic when the medication is available over-the-counter. If we decide to treat with Rogaine (Johnson & Johnson Consumer Inc) but do not suggest the option of purchasing the generic minoxidil, the patient could be unnecessarily overpaying for a brand name by following our instructions.
Conversely, there are scenarios in which the use of a brand name is actually not specific enough. A patient once told me she was using Differin (Galderma Laboratories, LP) as discussed at her prior visit, but she revealed she was washing it off after application. I initially assumed she misunderstood that adapalene was a gel to be applied and left on. After additional questioning, however, it became clear that she purchased the Differin gentle cleanser, a nonmedicated facial wash, rather than the retinoid we had intended for her. I had not considered that Differin would market an entire line of skin care products but now realize we must be cautious using Differin and adapalene interchangeably. Other examples include popular over-the-counter antihistamine brands such as Allegra (Chattem, a Sanofi company) or Benadryl (Johnson & Johnson Consumer Inc) that market multiple products with different active ingredients.
Final Thoughts
The smooth transfer of information between physician and patient is key to a healthy therapeutic relationship. In residency and throughout our careers, we will continue to develop and refine our communication skills to best serve our patients. We should pay particular attention to the unexpected and surprising ways in which we fail to adequately communicate, make note of these patterns, and share with our colleagues so that we can all learn from our collective experiences.
- Schneider, J. The teaspoon rule of applying sunscreen. Arch Dermatol. 2002;138:838-839.
- Storm A, Benfeldt E, Andersen SE, et al. A prospective study of patient adherence to topical treatments: 95% of patients underdose. J Am Acad Dermatol. 2008;59:975-980.
- Stringer T, Yin HS, Gittler J, et al. The readability, suitability, and content features of eczema action plans in the United States. Pediatr Dermatol. 2018;35:800-807.
- Hougeir FG, Cook-Bolden FE, Rodriguez D, et al. Critical considerations on optimizing topical corticosteroid therapy. J Clin Aesthet Dermatol. 2015;8(suppl 1):S2-S14.
- Savary J, Ortonne JP, Aractingi S. The right dose in the right place: an overview of current prescription, instruction and application modalities for topical psoriasis treatments. J Eur Acad Dermatol Venereol. 2005;19:14-17.
- Storm A, Anderson SE, Benfeldt E, et al. One in 3 prescriptions are never redeemed: primary nonadherence in an outpatient clinic. J Am Acad Dermatol. 2008;59:27-33.
I was a third-year medical student, dutifully reviewing discharge instructions with a patient and her family. The patient’s adult daughter asked, “What about that diet you put her on?” As they looked at me quizzically, I looked back equally confused, until it clicked: We needed to talk about the word diet. In everyday conversation, diet generally is understood to mean restriction of food to lose weight, which is what the family hoped would be prescribed for their obese family member. I needed to tell them that I was sorry for the misunderstanding. If they overheard us “ordering a diet,” we simply meant providing trays of hospital food.
We become so familiar with the language of our profession that we do not remember it may be foreign to our patients. In dermatology, we are aware that our specialty is full of esoteric jargon and complex concepts that need to be carefully explained to our patients in simpler terms. But since that incident in medical school, I have been interested in the more insidious potential misunderstandings that can arise from words as seemingly simple as diet. There are many examples in dermatology, particularly in the way we prescribe topical therapy and use trade names.
Topical Therapy
Instructions for systemic medications may be as simple as “take 1 pill twice daily.” Prescriptions for topical medications can be written with an equally simple patient signature such as “apply twice daily to affected area,” but the simplicity is deceptive. The direction to “apply” may seem intuitive to the prescriber, but we do not always specify the amount. Sunscreen, for example, is notoriously underapplied when the actual amount of product needed for protection is not demonstrated.1 One study of new dermatology patients given a prescription for a new topical medication found that the majority of patients underdosed.2
Determination of an “affected area,” regardless of whether the site is indicated, can be even less straightforward. In acne treatment, the affected area is the whole region prone to acne breakouts, whereas in psoriasis it may be discrete psoriatic plaques. We may believe our explanations are perfectly clear, but we have all seen patients spot treating their acne or psoriasis patients covering entire territories of normal skin with topical steroids, despite our education. One study of eczema action plans found that there was considerable variability in the way different providers described disease flares that require treatment. For example, redness was only used as a descriptor of an eczema flare in 68.2% of eczema action plans studied.3 Ensuring our patients understand our criteria for skin requiring topical treatment may mean the difference between treatment success and failure and also may help to avoid unnecessary side effects.
Adherence to topical medication regimens is poor, and inadequate patient education is only one factor.4,5 One study found that more than one-third of new prescriptions for topical medications were never even filled.6 However, improving our communication about application of topical drugs is one way we must address the complicated issue of adherence.
Trade Names
In dermatology, we often use trade names to refer to our medications, even if we do not intend to reference the brand name of the drug specifically. We may tell a patient to use Lidex (Medicis Pharmaceutical Corporation) for her hands but then send an escript to her pharmacy for fluocinonide. Trade names are designed to roll off the tongue, in contrast to the unwieldy, clumsily long generic names assigned to many of our medications.
Substituting trade names may facilitate more natural conversation to promote patient understanding in some cases; however, there are pitfalls associated with this habit. First, we may be doing our patients a disservice if we do not clarify when it would be acceptable to substitute with the generic when the medication is available over-the-counter. If we decide to treat with Rogaine (Johnson & Johnson Consumer Inc) but do not suggest the option of purchasing the generic minoxidil, the patient could be unnecessarily overpaying for a brand name by following our instructions.
Conversely, there are scenarios in which the use of a brand name is actually not specific enough. A patient once told me she was using Differin (Galderma Laboratories, LP) as discussed at her prior visit, but she revealed she was washing it off after application. I initially assumed she misunderstood that adapalene was a gel to be applied and left on. After additional questioning, however, it became clear that she purchased the Differin gentle cleanser, a nonmedicated facial wash, rather than the retinoid we had intended for her. I had not considered that Differin would market an entire line of skin care products but now realize we must be cautious using Differin and adapalene interchangeably. Other examples include popular over-the-counter antihistamine brands such as Allegra (Chattem, a Sanofi company) or Benadryl (Johnson & Johnson Consumer Inc) that market multiple products with different active ingredients.
Final Thoughts
The smooth transfer of information between physician and patient is key to a healthy therapeutic relationship. In residency and throughout our careers, we will continue to develop and refine our communication skills to best serve our patients. We should pay particular attention to the unexpected and surprising ways in which we fail to adequately communicate, make note of these patterns, and share with our colleagues so that we can all learn from our collective experiences.
I was a third-year medical student, dutifully reviewing discharge instructions with a patient and her family. The patient’s adult daughter asked, “What about that diet you put her on?” As they looked at me quizzically, I looked back equally confused, until it clicked: We needed to talk about the word diet. In everyday conversation, diet generally is understood to mean restriction of food to lose weight, which is what the family hoped would be prescribed for their obese family member. I needed to tell them that I was sorry for the misunderstanding. If they overheard us “ordering a diet,” we simply meant providing trays of hospital food.
We become so familiar with the language of our profession that we do not remember it may be foreign to our patients. In dermatology, we are aware that our specialty is full of esoteric jargon and complex concepts that need to be carefully explained to our patients in simpler terms. But since that incident in medical school, I have been interested in the more insidious potential misunderstandings that can arise from words as seemingly simple as diet. There are many examples in dermatology, particularly in the way we prescribe topical therapy and use trade names.
Topical Therapy
Instructions for systemic medications may be as simple as “take 1 pill twice daily.” Prescriptions for topical medications can be written with an equally simple patient signature such as “apply twice daily to affected area,” but the simplicity is deceptive. The direction to “apply” may seem intuitive to the prescriber, but we do not always specify the amount. Sunscreen, for example, is notoriously underapplied when the actual amount of product needed for protection is not demonstrated.1 One study of new dermatology patients given a prescription for a new topical medication found that the majority of patients underdosed.2
Determination of an “affected area,” regardless of whether the site is indicated, can be even less straightforward. In acne treatment, the affected area is the whole region prone to acne breakouts, whereas in psoriasis it may be discrete psoriatic plaques. We may believe our explanations are perfectly clear, but we have all seen patients spot treating their acne or psoriasis patients covering entire territories of normal skin with topical steroids, despite our education. One study of eczema action plans found that there was considerable variability in the way different providers described disease flares that require treatment. For example, redness was only used as a descriptor of an eczema flare in 68.2% of eczema action plans studied.3 Ensuring our patients understand our criteria for skin requiring topical treatment may mean the difference between treatment success and failure and also may help to avoid unnecessary side effects.
Adherence to topical medication regimens is poor, and inadequate patient education is only one factor.4,5 One study found that more than one-third of new prescriptions for topical medications were never even filled.6 However, improving our communication about application of topical drugs is one way we must address the complicated issue of adherence.
Trade Names
In dermatology, we often use trade names to refer to our medications, even if we do not intend to reference the brand name of the drug specifically. We may tell a patient to use Lidex (Medicis Pharmaceutical Corporation) for her hands but then send an escript to her pharmacy for fluocinonide. Trade names are designed to roll off the tongue, in contrast to the unwieldy, clumsily long generic names assigned to many of our medications.
Substituting trade names may facilitate more natural conversation to promote patient understanding in some cases; however, there are pitfalls associated with this habit. First, we may be doing our patients a disservice if we do not clarify when it would be acceptable to substitute with the generic when the medication is available over-the-counter. If we decide to treat with Rogaine (Johnson & Johnson Consumer Inc) but do not suggest the option of purchasing the generic minoxidil, the patient could be unnecessarily overpaying for a brand name by following our instructions.
Conversely, there are scenarios in which the use of a brand name is actually not specific enough. A patient once told me she was using Differin (Galderma Laboratories, LP) as discussed at her prior visit, but she revealed she was washing it off after application. I initially assumed she misunderstood that adapalene was a gel to be applied and left on. After additional questioning, however, it became clear that she purchased the Differin gentle cleanser, a nonmedicated facial wash, rather than the retinoid we had intended for her. I had not considered that Differin would market an entire line of skin care products but now realize we must be cautious using Differin and adapalene interchangeably. Other examples include popular over-the-counter antihistamine brands such as Allegra (Chattem, a Sanofi company) or Benadryl (Johnson & Johnson Consumer Inc) that market multiple products with different active ingredients.
Final Thoughts
The smooth transfer of information between physician and patient is key to a healthy therapeutic relationship. In residency and throughout our careers, we will continue to develop and refine our communication skills to best serve our patients. We should pay particular attention to the unexpected and surprising ways in which we fail to adequately communicate, make note of these patterns, and share with our colleagues so that we can all learn from our collective experiences.
- Schneider, J. The teaspoon rule of applying sunscreen. Arch Dermatol. 2002;138:838-839.
- Storm A, Benfeldt E, Andersen SE, et al. A prospective study of patient adherence to topical treatments: 95% of patients underdose. J Am Acad Dermatol. 2008;59:975-980.
- Stringer T, Yin HS, Gittler J, et al. The readability, suitability, and content features of eczema action plans in the United States. Pediatr Dermatol. 2018;35:800-807.
- Hougeir FG, Cook-Bolden FE, Rodriguez D, et al. Critical considerations on optimizing topical corticosteroid therapy. J Clin Aesthet Dermatol. 2015;8(suppl 1):S2-S14.
- Savary J, Ortonne JP, Aractingi S. The right dose in the right place: an overview of current prescription, instruction and application modalities for topical psoriasis treatments. J Eur Acad Dermatol Venereol. 2005;19:14-17.
- Storm A, Anderson SE, Benfeldt E, et al. One in 3 prescriptions are never redeemed: primary nonadherence in an outpatient clinic. J Am Acad Dermatol. 2008;59:27-33.
- Schneider, J. The teaspoon rule of applying sunscreen. Arch Dermatol. 2002;138:838-839.
- Storm A, Benfeldt E, Andersen SE, et al. A prospective study of patient adherence to topical treatments: 95% of patients underdose. J Am Acad Dermatol. 2008;59:975-980.
- Stringer T, Yin HS, Gittler J, et al. The readability, suitability, and content features of eczema action plans in the United States. Pediatr Dermatol. 2018;35:800-807.
- Hougeir FG, Cook-Bolden FE, Rodriguez D, et al. Critical considerations on optimizing topical corticosteroid therapy. J Clin Aesthet Dermatol. 2015;8(suppl 1):S2-S14.
- Savary J, Ortonne JP, Aractingi S. The right dose in the right place: an overview of current prescription, instruction and application modalities for topical psoriasis treatments. J Eur Acad Dermatol Venereol. 2005;19:14-17.
- Storm A, Anderson SE, Benfeldt E, et al. One in 3 prescriptions are never redeemed: primary nonadherence in an outpatient clinic. J Am Acad Dermatol. 2008;59:27-33.
Resident Pearl
- It is not just the esoteric jargon and complex pathophysiologic concepts in dermatology that can challenge effective communication with our patients. We face potential for misunderstanding even in situations that may seem straightforward. Vigilance in avoiding ambiguity in all our exchanges with patients can help foster therapeutic relationships and optimize patient care.
Survey: Barriers discourage diverse students from dermatology career
A .
Yssra S. Soliman of the division of dermatology, in the department of medicine, Albert Einstein College of Medicine, New York, and colleagues surveyed 155 students from 28 different medical schools between January and April 2018 about barriers to applying for a dermatology residency. Of total participants, 43% expressed an interest in applying for a dermatology residency. Of the 155 survey respondents, 58% were nonwhite.
Students of ethnic minorities and students with lower incomes cited lack of diversity in dermatology as a top barrier to applying for a dermatology residency, according to a research letter published in JAMA Dermatology.Other primary barriers reported by students of color were negative perceptions of minority students by residencies, such as lower performance expectations; socioeconomic factors, such as lack of loan forgiveness; and a lack of mentors. (Minorities in the study were defined as nonwhite students and lower-income students were defined as those with annual household incomes below $40,000.)
Study authors wrote that the results highlight the need to recruit and mentor students of all backgrounds. Furthermore, efforts should be made to increase minority students’ exposure to dermatology through curriculum, providing research opportunities, and reducing the cost of visiting electives by providing stipends, they concluded.
The survey results are not surprising, said Susan C. Taylor, MD, cofounder of the Skin of Color Center at St. Luke’s-Roosevelt Hospital in New York and a Philadelphia-based dermatologist. “I think that [the survey] is accurate and reflects the most common barriers for minority students,” Dr. Taylor said in an interview.
While recent progress has been made in discussing the subject of diversity in dermatology and identifying ways to improve, there has been little change in the actual numbers of diverse dermatologists, she noted.
Dermatology remains the least diverse medical field, after orthopedics. Blacks for example, compose 13% of the U.S. population and Hispanics compose 16% of the population, but each group represents less than 5% of dermatologists, according to the JAMA Dermatology article. At the same time, data show that race-concordant visits are longer and have higher ratings of patient satisfaction. In addition, minority physicians are more likely to care for patients of their own race or ethnic group, practice in underserved areas, care for poor patients and those with Medicaid, and treat patients who report poor health status, studies have found.
Amit Pandya, MD, chair of the American Academy of Dermatology membership committee, said that, while the response rate for the JAMA Dermatology survey was small, the results add important new information about the views of medical students regarding a career in dermatology.
“More research in a larger population of students is needed to learn more about the barriers to matching in dermatology, particularly for students from an under-represented minority background,” Dr. Pandya, professor of dermatology at the University of Texas Southwestern Medical Center, Dallas, said in an interview.
He added that AAD is making marked efforts to improve diversity in dermatology through its diversity committee. AAD diversity initiatives include an intersociety Work Group on Diversity in Dermatology, a diversity mentorship program for medical students, sponsorship of Nth Dimension bioskill workshops, and the Diversity Champion program, which promotes mentorship, volunteerism, and educational activities for students underrepresented in medicine.
It’s too early to tell if the efforts are working, Dr. Pandya said. It will take a few years to see if the efforts result in more minority applicants being interviewed or accepted to a dermatology residency program.
The AAD will hold a Diversity Champion conference in September in Chicago, which is open to “diversity champions” from dermatology residency programs across the United States. The conference is sponsored by the AAD, Association of Professors of Dermatology, Women’s Dermatologic Society, Skin of Color Society, and Society of Investigative Dermatology.
“It will be an annual conference with the goal of improving diversity in our field,” said Dr. Pandya, conference cochair.
SOURCE: Soliman YS et al. JAMA Dermatol. 2019 Jan 9. doi: 10.1001/jamadermatol.2018.4813.
A .
Yssra S. Soliman of the division of dermatology, in the department of medicine, Albert Einstein College of Medicine, New York, and colleagues surveyed 155 students from 28 different medical schools between January and April 2018 about barriers to applying for a dermatology residency. Of total participants, 43% expressed an interest in applying for a dermatology residency. Of the 155 survey respondents, 58% were nonwhite.
Students of ethnic minorities and students with lower incomes cited lack of diversity in dermatology as a top barrier to applying for a dermatology residency, according to a research letter published in JAMA Dermatology.Other primary barriers reported by students of color were negative perceptions of minority students by residencies, such as lower performance expectations; socioeconomic factors, such as lack of loan forgiveness; and a lack of mentors. (Minorities in the study were defined as nonwhite students and lower-income students were defined as those with annual household incomes below $40,000.)
Study authors wrote that the results highlight the need to recruit and mentor students of all backgrounds. Furthermore, efforts should be made to increase minority students’ exposure to dermatology through curriculum, providing research opportunities, and reducing the cost of visiting electives by providing stipends, they concluded.
The survey results are not surprising, said Susan C. Taylor, MD, cofounder of the Skin of Color Center at St. Luke’s-Roosevelt Hospital in New York and a Philadelphia-based dermatologist. “I think that [the survey] is accurate and reflects the most common barriers for minority students,” Dr. Taylor said in an interview.
While recent progress has been made in discussing the subject of diversity in dermatology and identifying ways to improve, there has been little change in the actual numbers of diverse dermatologists, she noted.
Dermatology remains the least diverse medical field, after orthopedics. Blacks for example, compose 13% of the U.S. population and Hispanics compose 16% of the population, but each group represents less than 5% of dermatologists, according to the JAMA Dermatology article. At the same time, data show that race-concordant visits are longer and have higher ratings of patient satisfaction. In addition, minority physicians are more likely to care for patients of their own race or ethnic group, practice in underserved areas, care for poor patients and those with Medicaid, and treat patients who report poor health status, studies have found.
Amit Pandya, MD, chair of the American Academy of Dermatology membership committee, said that, while the response rate for the JAMA Dermatology survey was small, the results add important new information about the views of medical students regarding a career in dermatology.
“More research in a larger population of students is needed to learn more about the barriers to matching in dermatology, particularly for students from an under-represented minority background,” Dr. Pandya, professor of dermatology at the University of Texas Southwestern Medical Center, Dallas, said in an interview.
He added that AAD is making marked efforts to improve diversity in dermatology through its diversity committee. AAD diversity initiatives include an intersociety Work Group on Diversity in Dermatology, a diversity mentorship program for medical students, sponsorship of Nth Dimension bioskill workshops, and the Diversity Champion program, which promotes mentorship, volunteerism, and educational activities for students underrepresented in medicine.
It’s too early to tell if the efforts are working, Dr. Pandya said. It will take a few years to see if the efforts result in more minority applicants being interviewed or accepted to a dermatology residency program.
The AAD will hold a Diversity Champion conference in September in Chicago, which is open to “diversity champions” from dermatology residency programs across the United States. The conference is sponsored by the AAD, Association of Professors of Dermatology, Women’s Dermatologic Society, Skin of Color Society, and Society of Investigative Dermatology.
“It will be an annual conference with the goal of improving diversity in our field,” said Dr. Pandya, conference cochair.
SOURCE: Soliman YS et al. JAMA Dermatol. 2019 Jan 9. doi: 10.1001/jamadermatol.2018.4813.
A .
Yssra S. Soliman of the division of dermatology, in the department of medicine, Albert Einstein College of Medicine, New York, and colleagues surveyed 155 students from 28 different medical schools between January and April 2018 about barriers to applying for a dermatology residency. Of total participants, 43% expressed an interest in applying for a dermatology residency. Of the 155 survey respondents, 58% were nonwhite.
Students of ethnic minorities and students with lower incomes cited lack of diversity in dermatology as a top barrier to applying for a dermatology residency, according to a research letter published in JAMA Dermatology.Other primary barriers reported by students of color were negative perceptions of minority students by residencies, such as lower performance expectations; socioeconomic factors, such as lack of loan forgiveness; and a lack of mentors. (Minorities in the study were defined as nonwhite students and lower-income students were defined as those with annual household incomes below $40,000.)
Study authors wrote that the results highlight the need to recruit and mentor students of all backgrounds. Furthermore, efforts should be made to increase minority students’ exposure to dermatology through curriculum, providing research opportunities, and reducing the cost of visiting electives by providing stipends, they concluded.
The survey results are not surprising, said Susan C. Taylor, MD, cofounder of the Skin of Color Center at St. Luke’s-Roosevelt Hospital in New York and a Philadelphia-based dermatologist. “I think that [the survey] is accurate and reflects the most common barriers for minority students,” Dr. Taylor said in an interview.
While recent progress has been made in discussing the subject of diversity in dermatology and identifying ways to improve, there has been little change in the actual numbers of diverse dermatologists, she noted.
Dermatology remains the least diverse medical field, after orthopedics. Blacks for example, compose 13% of the U.S. population and Hispanics compose 16% of the population, but each group represents less than 5% of dermatologists, according to the JAMA Dermatology article. At the same time, data show that race-concordant visits are longer and have higher ratings of patient satisfaction. In addition, minority physicians are more likely to care for patients of their own race or ethnic group, practice in underserved areas, care for poor patients and those with Medicaid, and treat patients who report poor health status, studies have found.
Amit Pandya, MD, chair of the American Academy of Dermatology membership committee, said that, while the response rate for the JAMA Dermatology survey was small, the results add important new information about the views of medical students regarding a career in dermatology.
“More research in a larger population of students is needed to learn more about the barriers to matching in dermatology, particularly for students from an under-represented minority background,” Dr. Pandya, professor of dermatology at the University of Texas Southwestern Medical Center, Dallas, said in an interview.
He added that AAD is making marked efforts to improve diversity in dermatology through its diversity committee. AAD diversity initiatives include an intersociety Work Group on Diversity in Dermatology, a diversity mentorship program for medical students, sponsorship of Nth Dimension bioskill workshops, and the Diversity Champion program, which promotes mentorship, volunteerism, and educational activities for students underrepresented in medicine.
It’s too early to tell if the efforts are working, Dr. Pandya said. It will take a few years to see if the efforts result in more minority applicants being interviewed or accepted to a dermatology residency program.
The AAD will hold a Diversity Champion conference in September in Chicago, which is open to “diversity champions” from dermatology residency programs across the United States. The conference is sponsored by the AAD, Association of Professors of Dermatology, Women’s Dermatologic Society, Skin of Color Society, and Society of Investigative Dermatology.
“It will be an annual conference with the goal of improving diversity in our field,” said Dr. Pandya, conference cochair.
SOURCE: Soliman YS et al. JAMA Dermatol. 2019 Jan 9. doi: 10.1001/jamadermatol.2018.4813.








