User login
The importance of engaging with local mental health organizations
“Hi Dr. Burke, thanks for coming in today. My daughter struggles with depression and I feel like every time I try to reach out, I hit a dead end with her. How do I connect with someone, who by the nature of their disease, is hard to reach?”
The answer? I’m not quite sure. I stood in front of a classroom of parents, siblings, and persons struggling with mental health issues, lecturing about depression. I can tell you about the complex interplay of biologic, psychological, and social factors that can lead one to become depressed. I can tell you the prevalence of depression in today’s society, and how it is rising among all age groups. I can tell you a myriad of different treatments, from pharmacologic to therapeutic to procedural, for depression. But how, from a parent’s perspective, can you connect with your child struggling with depression when they do not want your help? That I cannot tell you, at least not yet, anyways.
I had connected with the National Alliance on Mental Illness (NAMI) in the Fall of 2018, when a patient of mine was discharged from hospitalization and told by a faith-based substance use treatment program that he would not be allowed to use any “mind-altering” medications when he returned to their program. Concerned about my patient, whom I had just stabilized with the use of medications, I did my best to work through that organization’s resistance to psychotropic medications. When that failed, I reached out to NAMI for help in advocating for persons with mental illness. My involvement escalated to giving a lecture on “Living with Depression” to our local chapter of approximately 25 individuals that night. I had expected to lecture to an engaged crowd about what I thought was my immense knowledge of depression, from diagnosis to development to treatment. What I had not expected, however, was to have a learning experience of my own.
I stood at the front of the room, listening to story after story of persons with depression and their family members discussing their experiences. Throughout the 90-minute lecture, my emotions ranged from being impressed to shocked, scared, and, ultimately, proud. For the past year and 7 months, I had been spending time with persons with mental illness on what was likely the worst days of their lives. I had seen a variety of severe presentations, from grossly psychotic to acutely manic to majorly depressed to highly agitated. With that wealth of experience, I had thought I was becoming an expert; however, at the front of that classroom that night, I realized how little I actually knew. Yes, I had contemplated before how much severe mental illness and hospitalization could affect a person and their loved ones. However, it was a different level of understanding to hear first-hand accounts of the loss of relationships, the struggle to connect, and the fall-out from intensive inpatient treatment.
In residency, we spend what seems like an immeasurable amount of time on inpatient psychiatric units, in outpatient clinics, and everywhere in between. We see so many patients on a daily, weekly, monthly, and yearly basis that it becomes easy to lose the individuality of each patient. We start associating patients with their disorder, rather than with who they are. However, if we take a step back and allow a larger perspective—one that considers not only the patient but their families and communities—we likely would be able to provide greater and more comprehensive care.
My experience at NAMI was one that I will treasure forever. It opened my eyes to struggles that had I failed to even notice, and for that, and many other connections I made, I am grateful to have been blessed with this experience. My greatest recommendation to my fellow residents would be to engage with your local community organizations in the hope that you, too, can have an eye-opening experience that will strengthen your practice.
“Hi Dr. Burke, thanks for coming in today. My daughter struggles with depression and I feel like every time I try to reach out, I hit a dead end with her. How do I connect with someone, who by the nature of their disease, is hard to reach?”
The answer? I’m not quite sure. I stood in front of a classroom of parents, siblings, and persons struggling with mental health issues, lecturing about depression. I can tell you about the complex interplay of biologic, psychological, and social factors that can lead one to become depressed. I can tell you the prevalence of depression in today’s society, and how it is rising among all age groups. I can tell you a myriad of different treatments, from pharmacologic to therapeutic to procedural, for depression. But how, from a parent’s perspective, can you connect with your child struggling with depression when they do not want your help? That I cannot tell you, at least not yet, anyways.
I had connected with the National Alliance on Mental Illness (NAMI) in the Fall of 2018, when a patient of mine was discharged from hospitalization and told by a faith-based substance use treatment program that he would not be allowed to use any “mind-altering” medications when he returned to their program. Concerned about my patient, whom I had just stabilized with the use of medications, I did my best to work through that organization’s resistance to psychotropic medications. When that failed, I reached out to NAMI for help in advocating for persons with mental illness. My involvement escalated to giving a lecture on “Living with Depression” to our local chapter of approximately 25 individuals that night. I had expected to lecture to an engaged crowd about what I thought was my immense knowledge of depression, from diagnosis to development to treatment. What I had not expected, however, was to have a learning experience of my own.
I stood at the front of the room, listening to story after story of persons with depression and their family members discussing their experiences. Throughout the 90-minute lecture, my emotions ranged from being impressed to shocked, scared, and, ultimately, proud. For the past year and 7 months, I had been spending time with persons with mental illness on what was likely the worst days of their lives. I had seen a variety of severe presentations, from grossly psychotic to acutely manic to majorly depressed to highly agitated. With that wealth of experience, I had thought I was becoming an expert; however, at the front of that classroom that night, I realized how little I actually knew. Yes, I had contemplated before how much severe mental illness and hospitalization could affect a person and their loved ones. However, it was a different level of understanding to hear first-hand accounts of the loss of relationships, the struggle to connect, and the fall-out from intensive inpatient treatment.
In residency, we spend what seems like an immeasurable amount of time on inpatient psychiatric units, in outpatient clinics, and everywhere in between. We see so many patients on a daily, weekly, monthly, and yearly basis that it becomes easy to lose the individuality of each patient. We start associating patients with their disorder, rather than with who they are. However, if we take a step back and allow a larger perspective—one that considers not only the patient but their families and communities—we likely would be able to provide greater and more comprehensive care.
My experience at NAMI was one that I will treasure forever. It opened my eyes to struggles that had I failed to even notice, and for that, and many other connections I made, I am grateful to have been blessed with this experience. My greatest recommendation to my fellow residents would be to engage with your local community organizations in the hope that you, too, can have an eye-opening experience that will strengthen your practice.
“Hi Dr. Burke, thanks for coming in today. My daughter struggles with depression and I feel like every time I try to reach out, I hit a dead end with her. How do I connect with someone, who by the nature of their disease, is hard to reach?”
The answer? I’m not quite sure. I stood in front of a classroom of parents, siblings, and persons struggling with mental health issues, lecturing about depression. I can tell you about the complex interplay of biologic, psychological, and social factors that can lead one to become depressed. I can tell you the prevalence of depression in today’s society, and how it is rising among all age groups. I can tell you a myriad of different treatments, from pharmacologic to therapeutic to procedural, for depression. But how, from a parent’s perspective, can you connect with your child struggling with depression when they do not want your help? That I cannot tell you, at least not yet, anyways.
I had connected with the National Alliance on Mental Illness (NAMI) in the Fall of 2018, when a patient of mine was discharged from hospitalization and told by a faith-based substance use treatment program that he would not be allowed to use any “mind-altering” medications when he returned to their program. Concerned about my patient, whom I had just stabilized with the use of medications, I did my best to work through that organization’s resistance to psychotropic medications. When that failed, I reached out to NAMI for help in advocating for persons with mental illness. My involvement escalated to giving a lecture on “Living with Depression” to our local chapter of approximately 25 individuals that night. I had expected to lecture to an engaged crowd about what I thought was my immense knowledge of depression, from diagnosis to development to treatment. What I had not expected, however, was to have a learning experience of my own.
I stood at the front of the room, listening to story after story of persons with depression and their family members discussing their experiences. Throughout the 90-minute lecture, my emotions ranged from being impressed to shocked, scared, and, ultimately, proud. For the past year and 7 months, I had been spending time with persons with mental illness on what was likely the worst days of their lives. I had seen a variety of severe presentations, from grossly psychotic to acutely manic to majorly depressed to highly agitated. With that wealth of experience, I had thought I was becoming an expert; however, at the front of that classroom that night, I realized how little I actually knew. Yes, I had contemplated before how much severe mental illness and hospitalization could affect a person and their loved ones. However, it was a different level of understanding to hear first-hand accounts of the loss of relationships, the struggle to connect, and the fall-out from intensive inpatient treatment.
In residency, we spend what seems like an immeasurable amount of time on inpatient psychiatric units, in outpatient clinics, and everywhere in between. We see so many patients on a daily, weekly, monthly, and yearly basis that it becomes easy to lose the individuality of each patient. We start associating patients with their disorder, rather than with who they are. However, if we take a step back and allow a larger perspective—one that considers not only the patient but their families and communities—we likely would be able to provide greater and more comprehensive care.
My experience at NAMI was one that I will treasure forever. It opened my eyes to struggles that had I failed to even notice, and for that, and many other connections I made, I am grateful to have been blessed with this experience. My greatest recommendation to my fellow residents would be to engage with your local community organizations in the hope that you, too, can have an eye-opening experience that will strengthen your practice.
Paternalism vs autonomy: Why watching our words is important
Two patients were admitted to our unit at the same time: Mr. P, age 27, an architect with unspecified personality disorder, and Mr. D, age 62, a bank manager who has had bipolar disorder for 40 years and was experiencing a moderate depressive episode. Mr. P’s discomfort with the treatment team informing him of his treatment plan was evident, and he discussed at length his terms and stipulations for management. Mr. D, on the other hand, was loath to shoulder the burden of any decision-making, even in minor matters such as what time he should take his daily walk.
Patient autonomy is a central factor in the present-day doctor–patient equation. In psychiatry, this is sometimes further complicated by a patient’s impaired judgment and lowered decision-making capacity (DMC). In our clinical practice, we often notice that younger patients (ie, millennials) prefer to have autonomy rather than being given instructions, which they may find patronizing, whereas the older generation relies more on the doctor for decision-making.
What the decision-making process entails
The decision-making process involves 3 steps:
- information gathering
- deliberation
- implementation.
Decision-making preferences fall on a spectrum that ranges from paternalism at one end to autonomy on the other, with many intervening components, characterized by varying amounts of responsibility shared between doctor and patient.1 This typically comes into play when there is more than one treatment option with similar outcomes.2 Paternalism is defined as an action performed with the intent of promoting another’s good but occurring against the other’s will, or without consent.3 Here, the patient is not privy to the deliberation process, and no explanations are provided.1
Two other decision-making constructs are shared decision-making (SDM) and informed decision-making (IDM). In SDM, the deliberation process involves participation of both patient and doctor, with active discussion and a final decision after both parties reach an agreement. In IDM, the deliberation is conducted solely by the patient, after he or she receives all information. Shared decision-making and IDM are frequently used interchangeably, but in the latter, the doctor has no role other than to provide information.1,5
Before choosing SDM or IDM, it is necessary to assess the patient’s DMC—the ability to understand information about choices, make a judgment that respects personal values, understand potential outcomes, and freely communicate his or her wishes.6
Benefits and risks
The progression from paternalism to autonomy began in the mid-20th century as a consequence of the Nuremberg Trials, from which the concept of “informed consent” first came into existence.7 The Indian value system has always regarded the medical profession and its practitioners with high esteem, as evidenced by the Sanskrit quote “Vaidyo Narayano Harihi,” which translates to “The doctor is God.” A significant chunk of the Indian population still considers the doctor’s word to be law, and they hand over health-related decisions to medical professionals. Here, the expectation of a paternalistic attitude is decidedly unequivocal.
Continue to: Of course...
Of course, there are pros and cons to every approach. Making patients’ independence a priority is the highest virtue of autonomy, but in such cases a patient may have difficulty comprehending medical consequences, and therefore may miss out on the benefits of a sound professional perspective. Paternalism may be superior medically, but the doctor may not be aware of all patient-specific factors, and it would not be prudent to make a decision for a patient without being privy to the entire picture.
The 21st century has witnessed a change in attitudes regarding medical care. With an increasing interest in patient autonomy, it is time for us to adopt these changes and move towards the patient-centred end of the spectrum. However, this should occur only after the patient improves enough symptomatically to regain DMC; autonomy is unlikely to be appropriate for patients with serious mental illness. Ideally, SDM includes the best of both worlds, and results in optimal outcomes. However, when SDM breaks down, a selective, soft paternalistic attitude would be most beneficial, without impinging on the patient’s basic personal rights.
1. Charles C, Gafni A, Whelan T. Decision-making in the physician-patient encounter: revisiting the shared treatment decision-making model. Soc Sci Med. 1999;49(5):651-661.
2. Barry MJ, Edgman-Levitan S. Shared decision making—pinnacle of patient-centered care. N Engl J Med. 2012;366(9):780-781.
3. Sartorius RE. Paternalism. Minneapolis, MN: University of Minnesota Press; 1983.
4. Dong R. Paternalism in medical decision making. Duke University. https://dukespace.lib.duke.edu/dspace/bitstream/handle/10161/3958/Dong_Thesis.pdf. Published 2011. Accessed April 17, 2019.
5. Charles C, Gafni A, Whelan T. Shared decision-making in the medical encounter: what does it mean? (or it takes at least two to tango). Soc Sci Med. 1997;44(5):681-692.
6. Beauchamp TL, Childress JF. Principles of biomedical ethics. 5th ed. New York, NY: Oxford University Press; 2001:57-112.
7. Weindling P. The origins of informed consent: the International Scientific Commission on Medical War Crimes, and the Nuremberg Code. Bull Hist Med. 2001;75(1):37-71.
Two patients were admitted to our unit at the same time: Mr. P, age 27, an architect with unspecified personality disorder, and Mr. D, age 62, a bank manager who has had bipolar disorder for 40 years and was experiencing a moderate depressive episode. Mr. P’s discomfort with the treatment team informing him of his treatment plan was evident, and he discussed at length his terms and stipulations for management. Mr. D, on the other hand, was loath to shoulder the burden of any decision-making, even in minor matters such as what time he should take his daily walk.
Patient autonomy is a central factor in the present-day doctor–patient equation. In psychiatry, this is sometimes further complicated by a patient’s impaired judgment and lowered decision-making capacity (DMC). In our clinical practice, we often notice that younger patients (ie, millennials) prefer to have autonomy rather than being given instructions, which they may find patronizing, whereas the older generation relies more on the doctor for decision-making.
What the decision-making process entails
The decision-making process involves 3 steps:
- information gathering
- deliberation
- implementation.
Decision-making preferences fall on a spectrum that ranges from paternalism at one end to autonomy on the other, with many intervening components, characterized by varying amounts of responsibility shared between doctor and patient.1 This typically comes into play when there is more than one treatment option with similar outcomes.2 Paternalism is defined as an action performed with the intent of promoting another’s good but occurring against the other’s will, or without consent.3 Here, the patient is not privy to the deliberation process, and no explanations are provided.1
Two other decision-making constructs are shared decision-making (SDM) and informed decision-making (IDM). In SDM, the deliberation process involves participation of both patient and doctor, with active discussion and a final decision after both parties reach an agreement. In IDM, the deliberation is conducted solely by the patient, after he or she receives all information. Shared decision-making and IDM are frequently used interchangeably, but in the latter, the doctor has no role other than to provide information.1,5
Before choosing SDM or IDM, it is necessary to assess the patient’s DMC—the ability to understand information about choices, make a judgment that respects personal values, understand potential outcomes, and freely communicate his or her wishes.6
Benefits and risks
The progression from paternalism to autonomy began in the mid-20th century as a consequence of the Nuremberg Trials, from which the concept of “informed consent” first came into existence.7 The Indian value system has always regarded the medical profession and its practitioners with high esteem, as evidenced by the Sanskrit quote “Vaidyo Narayano Harihi,” which translates to “The doctor is God.” A significant chunk of the Indian population still considers the doctor’s word to be law, and they hand over health-related decisions to medical professionals. Here, the expectation of a paternalistic attitude is decidedly unequivocal.
Continue to: Of course...
Of course, there are pros and cons to every approach. Making patients’ independence a priority is the highest virtue of autonomy, but in such cases a patient may have difficulty comprehending medical consequences, and therefore may miss out on the benefits of a sound professional perspective. Paternalism may be superior medically, but the doctor may not be aware of all patient-specific factors, and it would not be prudent to make a decision for a patient without being privy to the entire picture.
The 21st century has witnessed a change in attitudes regarding medical care. With an increasing interest in patient autonomy, it is time for us to adopt these changes and move towards the patient-centred end of the spectrum. However, this should occur only after the patient improves enough symptomatically to regain DMC; autonomy is unlikely to be appropriate for patients with serious mental illness. Ideally, SDM includes the best of both worlds, and results in optimal outcomes. However, when SDM breaks down, a selective, soft paternalistic attitude would be most beneficial, without impinging on the patient’s basic personal rights.
Two patients were admitted to our unit at the same time: Mr. P, age 27, an architect with unspecified personality disorder, and Mr. D, age 62, a bank manager who has had bipolar disorder for 40 years and was experiencing a moderate depressive episode. Mr. P’s discomfort with the treatment team informing him of his treatment plan was evident, and he discussed at length his terms and stipulations for management. Mr. D, on the other hand, was loath to shoulder the burden of any decision-making, even in minor matters such as what time he should take his daily walk.
Patient autonomy is a central factor in the present-day doctor–patient equation. In psychiatry, this is sometimes further complicated by a patient’s impaired judgment and lowered decision-making capacity (DMC). In our clinical practice, we often notice that younger patients (ie, millennials) prefer to have autonomy rather than being given instructions, which they may find patronizing, whereas the older generation relies more on the doctor for decision-making.
What the decision-making process entails
The decision-making process involves 3 steps:
- information gathering
- deliberation
- implementation.
Decision-making preferences fall on a spectrum that ranges from paternalism at one end to autonomy on the other, with many intervening components, characterized by varying amounts of responsibility shared between doctor and patient.1 This typically comes into play when there is more than one treatment option with similar outcomes.2 Paternalism is defined as an action performed with the intent of promoting another’s good but occurring against the other’s will, or without consent.3 Here, the patient is not privy to the deliberation process, and no explanations are provided.1
Two other decision-making constructs are shared decision-making (SDM) and informed decision-making (IDM). In SDM, the deliberation process involves participation of both patient and doctor, with active discussion and a final decision after both parties reach an agreement. In IDM, the deliberation is conducted solely by the patient, after he or she receives all information. Shared decision-making and IDM are frequently used interchangeably, but in the latter, the doctor has no role other than to provide information.1,5
Before choosing SDM or IDM, it is necessary to assess the patient’s DMC—the ability to understand information about choices, make a judgment that respects personal values, understand potential outcomes, and freely communicate his or her wishes.6
Benefits and risks
The progression from paternalism to autonomy began in the mid-20th century as a consequence of the Nuremberg Trials, from which the concept of “informed consent” first came into existence.7 The Indian value system has always regarded the medical profession and its practitioners with high esteem, as evidenced by the Sanskrit quote “Vaidyo Narayano Harihi,” which translates to “The doctor is God.” A significant chunk of the Indian population still considers the doctor’s word to be law, and they hand over health-related decisions to medical professionals. Here, the expectation of a paternalistic attitude is decidedly unequivocal.
Continue to: Of course...
Of course, there are pros and cons to every approach. Making patients’ independence a priority is the highest virtue of autonomy, but in such cases a patient may have difficulty comprehending medical consequences, and therefore may miss out on the benefits of a sound professional perspective. Paternalism may be superior medically, but the doctor may not be aware of all patient-specific factors, and it would not be prudent to make a decision for a patient without being privy to the entire picture.
The 21st century has witnessed a change in attitudes regarding medical care. With an increasing interest in patient autonomy, it is time for us to adopt these changes and move towards the patient-centred end of the spectrum. However, this should occur only after the patient improves enough symptomatically to regain DMC; autonomy is unlikely to be appropriate for patients with serious mental illness. Ideally, SDM includes the best of both worlds, and results in optimal outcomes. However, when SDM breaks down, a selective, soft paternalistic attitude would be most beneficial, without impinging on the patient’s basic personal rights.
1. Charles C, Gafni A, Whelan T. Decision-making in the physician-patient encounter: revisiting the shared treatment decision-making model. Soc Sci Med. 1999;49(5):651-661.
2. Barry MJ, Edgman-Levitan S. Shared decision making—pinnacle of patient-centered care. N Engl J Med. 2012;366(9):780-781.
3. Sartorius RE. Paternalism. Minneapolis, MN: University of Minnesota Press; 1983.
4. Dong R. Paternalism in medical decision making. Duke University. https://dukespace.lib.duke.edu/dspace/bitstream/handle/10161/3958/Dong_Thesis.pdf. Published 2011. Accessed April 17, 2019.
5. Charles C, Gafni A, Whelan T. Shared decision-making in the medical encounter: what does it mean? (or it takes at least two to tango). Soc Sci Med. 1997;44(5):681-692.
6. Beauchamp TL, Childress JF. Principles of biomedical ethics. 5th ed. New York, NY: Oxford University Press; 2001:57-112.
7. Weindling P. The origins of informed consent: the International Scientific Commission on Medical War Crimes, and the Nuremberg Code. Bull Hist Med. 2001;75(1):37-71.
1. Charles C, Gafni A, Whelan T. Decision-making in the physician-patient encounter: revisiting the shared treatment decision-making model. Soc Sci Med. 1999;49(5):651-661.
2. Barry MJ, Edgman-Levitan S. Shared decision making—pinnacle of patient-centered care. N Engl J Med. 2012;366(9):780-781.
3. Sartorius RE. Paternalism. Minneapolis, MN: University of Minnesota Press; 1983.
4. Dong R. Paternalism in medical decision making. Duke University. https://dukespace.lib.duke.edu/dspace/bitstream/handle/10161/3958/Dong_Thesis.pdf. Published 2011. Accessed April 17, 2019.
5. Charles C, Gafni A, Whelan T. Shared decision-making in the medical encounter: what does it mean? (or it takes at least two to tango). Soc Sci Med. 1997;44(5):681-692.
6. Beauchamp TL, Childress JF. Principles of biomedical ethics. 5th ed. New York, NY: Oxford University Press; 2001:57-112.
7. Weindling P. The origins of informed consent: the International Scientific Commission on Medical War Crimes, and the Nuremberg Code. Bull Hist Med. 2001;75(1):37-71.
Treating military members, veterans, and their families
I had the unique opportunity to attend a civilian medical school followed by residency and fellowship training along civilian providers, and I often was asked about my military experience. The more time I spent with civilian providers, the more I realized how unaware they are about the intricacies of military lifestyle and culture.
Of course, this makes sense. During the draft era, almost every family had a member who served, and more people were exposed to the uniqueness of military culture.1 However, with the shift to an all-volunteer military came a decrease in the number of both active duty members and veterans.2 Consequently, today’s society is generally less aware of the realities of the military lifestyle. This is especially true among people born after the Vietnam War, whose knowledge about military life is frequently limited to movies and video games. These movies and games are as accurate a reflection of military life as watching TV series such as ER or The Resident are for learning what it’s like to be a physician. To add to the problem, most medical schools and residency training curricula include little information about military culture.3 As a result, psychiatrists, like many other physicians, often feel unequipped to provide care for veterans, current military personnel, and their loved ones.4 At the very least, most psychiatrists are unaware of the differences between military and civilian cultures.
Veterans, current military members, and their families who seek mental health services outside the Veterans Affairs (VA) and military treatment facilities are more likely to encounter a clinician who does not feel comfortable with the nuances of the military lifestyle and its challenges.3 Facing a physician with limited familiarity with their experiences, and out of fear of being misunderstood, patients may not feel comfortable disclosing pertinent details.
The US military has its own culture, lingo, customs, rules, and regulations. Its structure is hierarchical and mission-oriented. The moment a person joins the military, he or she falls under a set of legal guidelines of the Uniform Code of Military Justice (UCMJ).5 For example, extra-marital sexual conduct, fistfighting (not in combat), disrespecting superior officers, and insubordination are all punishable under UCMJ.5,6 Active duty military members are also prohibited from suing the federal government for injuries.7 The Health Insurance Portability and Accountability Act (HIPAA) permits protected health information of Armed Forces personnel to be disclosed under special circumstances. These include fitness for duty determinations, fitness to perform a particular assignment, or other activities necessary for the military mission.8 A mental health provider’s understanding of the unique aspects of military culture can positively influence the patient-provider relationship whether the patient is still serving, has left the military, or is a family member of a current or former military member.
Not all military veterans qualify for VA health care. For example, those who didn’t serve the required time on active duty, those whose injury existed prior to joining the military and was not worsened by their military service, and those discharged under other-than-honorable, bad conduct, or dishonorable conditions are unlikely to qualify.9 Other veterans simply prefer to be privately treated outside the VA. However, despite where a veteran receives treatment, the clinician’s knowledge of important military concepts can facilitate rapport-building and providing a safe space for disclosure of pertinent history. Obtaining a military history that includes (for example) years of service, number and location of deployments, combat experience, and number of transfers can help with understanding the biopsychosocial factors contributing to the diagnosis and important treatment needs.
While military dependents (spouses and children) don’t wear uniforms, they are also affected by the service and sacrifices of the military member. Spouses have to deal with adjusting to the military lifestyle, searching for new housing and jobs, finding schools for children, and separation and reconnection with a military member. Military children are not spared, either. They, too, have to leave their friends and find new ones, and adjust to new places, routines, and schools, knowing that in 2 to 3 years they likely will have to move again.
As a military member, mother, and spouse of a former military member, I know how life-changing military service can be for the entire family. I encourage all physicians to start routinely asking if their patient or his or her loved ones have ever been in the military, because a positive answer could help you to better understand the patient and provide the most appropriate, person-centered, culturally-informed treatment.
1. Pew Research Center. The military-civilian gap: War and sacrifice in the post-9/11 era. http://www.pewsocialtrends.org/2011/10/05/war-and-sacrifice-in-the-post-911-era. Published October 5, 2011. Accessed March 12, 2019.
2. Bialik K. The changing face of America’s veteran population. http://www.pewresearch.org/fact-tank/2017/11/10/the-changing-face-of-americas-veteran-population. Published November 10, 2017. Accessed March 12, 2019.
3. Meyer EG, Writer BW, Brim W. The importance of military cultural competence. Curr Psychiatry Rep. 2016;18(3):26.
4. Tanielian T, Farris C, Epley C, et al; RAND Corporation. Ready to serve: community-based provider capacity to deliver culturally competent, quality mental health care to veterans and their families. https://www.rand.org/content/dam/rand/pubs/research_reports/RR800/RR806/RAND_RR806.pdf. Accessed December 10, 2018.
5. The Uniform Code of Military Justice. http://www.ucmj.us. Accessed March 4, 2019.
6. Myers M. Here’s what you need to know about the biggest update to UCMJ in decades. Military Times. https://www.militarytimes.com/news/your-army/2019/01/15/heres-what-you-need-to-know-about-the-biggest-update-to-ucmj-in-decades/. Published Jan 15, 2019. Accessed March 12, 2019.
7. Information Institute. Feres Doctrine. https://www.law.cornell.edu/wex/feres_doctrine. Accessed March 12, 2019.
8. Defense Health Agency Privacy and Civil Liberties Office. The military command exception and disclosing PHI of armed forces personnel. https://health.mil/Reference-Center/Fact-Sheets/2015/05/13/Info-Paper-Military-Command-Exception-and-Disclosing-PHI-of-Armed-Forces-Personnel. Published May 13, 2015. Accessed March 12, 2019.
9. Veterans Benefits Administration. Applying for benefits and your character of discharge. https://www.benefits.va.gov/benefits/character_of_discharge.asp. Updated May 19, 2015. Accessed March 12, 2019.
I had the unique opportunity to attend a civilian medical school followed by residency and fellowship training along civilian providers, and I often was asked about my military experience. The more time I spent with civilian providers, the more I realized how unaware they are about the intricacies of military lifestyle and culture.
Of course, this makes sense. During the draft era, almost every family had a member who served, and more people were exposed to the uniqueness of military culture.1 However, with the shift to an all-volunteer military came a decrease in the number of both active duty members and veterans.2 Consequently, today’s society is generally less aware of the realities of the military lifestyle. This is especially true among people born after the Vietnam War, whose knowledge about military life is frequently limited to movies and video games. These movies and games are as accurate a reflection of military life as watching TV series such as ER or The Resident are for learning what it’s like to be a physician. To add to the problem, most medical schools and residency training curricula include little information about military culture.3 As a result, psychiatrists, like many other physicians, often feel unequipped to provide care for veterans, current military personnel, and their loved ones.4 At the very least, most psychiatrists are unaware of the differences between military and civilian cultures.
Veterans, current military members, and their families who seek mental health services outside the Veterans Affairs (VA) and military treatment facilities are more likely to encounter a clinician who does not feel comfortable with the nuances of the military lifestyle and its challenges.3 Facing a physician with limited familiarity with their experiences, and out of fear of being misunderstood, patients may not feel comfortable disclosing pertinent details.
The US military has its own culture, lingo, customs, rules, and regulations. Its structure is hierarchical and mission-oriented. The moment a person joins the military, he or she falls under a set of legal guidelines of the Uniform Code of Military Justice (UCMJ).5 For example, extra-marital sexual conduct, fistfighting (not in combat), disrespecting superior officers, and insubordination are all punishable under UCMJ.5,6 Active duty military members are also prohibited from suing the federal government for injuries.7 The Health Insurance Portability and Accountability Act (HIPAA) permits protected health information of Armed Forces personnel to be disclosed under special circumstances. These include fitness for duty determinations, fitness to perform a particular assignment, or other activities necessary for the military mission.8 A mental health provider’s understanding of the unique aspects of military culture can positively influence the patient-provider relationship whether the patient is still serving, has left the military, or is a family member of a current or former military member.
Not all military veterans qualify for VA health care. For example, those who didn’t serve the required time on active duty, those whose injury existed prior to joining the military and was not worsened by their military service, and those discharged under other-than-honorable, bad conduct, or dishonorable conditions are unlikely to qualify.9 Other veterans simply prefer to be privately treated outside the VA. However, despite where a veteran receives treatment, the clinician’s knowledge of important military concepts can facilitate rapport-building and providing a safe space for disclosure of pertinent history. Obtaining a military history that includes (for example) years of service, number and location of deployments, combat experience, and number of transfers can help with understanding the biopsychosocial factors contributing to the diagnosis and important treatment needs.
While military dependents (spouses and children) don’t wear uniforms, they are also affected by the service and sacrifices of the military member. Spouses have to deal with adjusting to the military lifestyle, searching for new housing and jobs, finding schools for children, and separation and reconnection with a military member. Military children are not spared, either. They, too, have to leave their friends and find new ones, and adjust to new places, routines, and schools, knowing that in 2 to 3 years they likely will have to move again.
As a military member, mother, and spouse of a former military member, I know how life-changing military service can be for the entire family. I encourage all physicians to start routinely asking if their patient or his or her loved ones have ever been in the military, because a positive answer could help you to better understand the patient and provide the most appropriate, person-centered, culturally-informed treatment.
I had the unique opportunity to attend a civilian medical school followed by residency and fellowship training along civilian providers, and I often was asked about my military experience. The more time I spent with civilian providers, the more I realized how unaware they are about the intricacies of military lifestyle and culture.
Of course, this makes sense. During the draft era, almost every family had a member who served, and more people were exposed to the uniqueness of military culture.1 However, with the shift to an all-volunteer military came a decrease in the number of both active duty members and veterans.2 Consequently, today’s society is generally less aware of the realities of the military lifestyle. This is especially true among people born after the Vietnam War, whose knowledge about military life is frequently limited to movies and video games. These movies and games are as accurate a reflection of military life as watching TV series such as ER or The Resident are for learning what it’s like to be a physician. To add to the problem, most medical schools and residency training curricula include little information about military culture.3 As a result, psychiatrists, like many other physicians, often feel unequipped to provide care for veterans, current military personnel, and their loved ones.4 At the very least, most psychiatrists are unaware of the differences between military and civilian cultures.
Veterans, current military members, and their families who seek mental health services outside the Veterans Affairs (VA) and military treatment facilities are more likely to encounter a clinician who does not feel comfortable with the nuances of the military lifestyle and its challenges.3 Facing a physician with limited familiarity with their experiences, and out of fear of being misunderstood, patients may not feel comfortable disclosing pertinent details.
The US military has its own culture, lingo, customs, rules, and regulations. Its structure is hierarchical and mission-oriented. The moment a person joins the military, he or she falls under a set of legal guidelines of the Uniform Code of Military Justice (UCMJ).5 For example, extra-marital sexual conduct, fistfighting (not in combat), disrespecting superior officers, and insubordination are all punishable under UCMJ.5,6 Active duty military members are also prohibited from suing the federal government for injuries.7 The Health Insurance Portability and Accountability Act (HIPAA) permits protected health information of Armed Forces personnel to be disclosed under special circumstances. These include fitness for duty determinations, fitness to perform a particular assignment, or other activities necessary for the military mission.8 A mental health provider’s understanding of the unique aspects of military culture can positively influence the patient-provider relationship whether the patient is still serving, has left the military, or is a family member of a current or former military member.
Not all military veterans qualify for VA health care. For example, those who didn’t serve the required time on active duty, those whose injury existed prior to joining the military and was not worsened by their military service, and those discharged under other-than-honorable, bad conduct, or dishonorable conditions are unlikely to qualify.9 Other veterans simply prefer to be privately treated outside the VA. However, despite where a veteran receives treatment, the clinician’s knowledge of important military concepts can facilitate rapport-building and providing a safe space for disclosure of pertinent history. Obtaining a military history that includes (for example) years of service, number and location of deployments, combat experience, and number of transfers can help with understanding the biopsychosocial factors contributing to the diagnosis and important treatment needs.
While military dependents (spouses and children) don’t wear uniforms, they are also affected by the service and sacrifices of the military member. Spouses have to deal with adjusting to the military lifestyle, searching for new housing and jobs, finding schools for children, and separation and reconnection with a military member. Military children are not spared, either. They, too, have to leave their friends and find new ones, and adjust to new places, routines, and schools, knowing that in 2 to 3 years they likely will have to move again.
As a military member, mother, and spouse of a former military member, I know how life-changing military service can be for the entire family. I encourage all physicians to start routinely asking if their patient or his or her loved ones have ever been in the military, because a positive answer could help you to better understand the patient and provide the most appropriate, person-centered, culturally-informed treatment.
1. Pew Research Center. The military-civilian gap: War and sacrifice in the post-9/11 era. http://www.pewsocialtrends.org/2011/10/05/war-and-sacrifice-in-the-post-911-era. Published October 5, 2011. Accessed March 12, 2019.
2. Bialik K. The changing face of America’s veteran population. http://www.pewresearch.org/fact-tank/2017/11/10/the-changing-face-of-americas-veteran-population. Published November 10, 2017. Accessed March 12, 2019.
3. Meyer EG, Writer BW, Brim W. The importance of military cultural competence. Curr Psychiatry Rep. 2016;18(3):26.
4. Tanielian T, Farris C, Epley C, et al; RAND Corporation. Ready to serve: community-based provider capacity to deliver culturally competent, quality mental health care to veterans and their families. https://www.rand.org/content/dam/rand/pubs/research_reports/RR800/RR806/RAND_RR806.pdf. Accessed December 10, 2018.
5. The Uniform Code of Military Justice. http://www.ucmj.us. Accessed March 4, 2019.
6. Myers M. Here’s what you need to know about the biggest update to UCMJ in decades. Military Times. https://www.militarytimes.com/news/your-army/2019/01/15/heres-what-you-need-to-know-about-the-biggest-update-to-ucmj-in-decades/. Published Jan 15, 2019. Accessed March 12, 2019.
7. Information Institute. Feres Doctrine. https://www.law.cornell.edu/wex/feres_doctrine. Accessed March 12, 2019.
8. Defense Health Agency Privacy and Civil Liberties Office. The military command exception and disclosing PHI of armed forces personnel. https://health.mil/Reference-Center/Fact-Sheets/2015/05/13/Info-Paper-Military-Command-Exception-and-Disclosing-PHI-of-Armed-Forces-Personnel. Published May 13, 2015. Accessed March 12, 2019.
9. Veterans Benefits Administration. Applying for benefits and your character of discharge. https://www.benefits.va.gov/benefits/character_of_discharge.asp. Updated May 19, 2015. Accessed March 12, 2019.
1. Pew Research Center. The military-civilian gap: War and sacrifice in the post-9/11 era. http://www.pewsocialtrends.org/2011/10/05/war-and-sacrifice-in-the-post-911-era. Published October 5, 2011. Accessed March 12, 2019.
2. Bialik K. The changing face of America’s veteran population. http://www.pewresearch.org/fact-tank/2017/11/10/the-changing-face-of-americas-veteran-population. Published November 10, 2017. Accessed March 12, 2019.
3. Meyer EG, Writer BW, Brim W. The importance of military cultural competence. Curr Psychiatry Rep. 2016;18(3):26.
4. Tanielian T, Farris C, Epley C, et al; RAND Corporation. Ready to serve: community-based provider capacity to deliver culturally competent, quality mental health care to veterans and their families. https://www.rand.org/content/dam/rand/pubs/research_reports/RR800/RR806/RAND_RR806.pdf. Accessed December 10, 2018.
5. The Uniform Code of Military Justice. http://www.ucmj.us. Accessed March 4, 2019.
6. Myers M. Here’s what you need to know about the biggest update to UCMJ in decades. Military Times. https://www.militarytimes.com/news/your-army/2019/01/15/heres-what-you-need-to-know-about-the-biggest-update-to-ucmj-in-decades/. Published Jan 15, 2019. Accessed March 12, 2019.
7. Information Institute. Feres Doctrine. https://www.law.cornell.edu/wex/feres_doctrine. Accessed March 12, 2019.
8. Defense Health Agency Privacy and Civil Liberties Office. The military command exception and disclosing PHI of armed forces personnel. https://health.mil/Reference-Center/Fact-Sheets/2015/05/13/Info-Paper-Military-Command-Exception-and-Disclosing-PHI-of-Armed-Forces-Personnel. Published May 13, 2015. Accessed March 12, 2019.
9. Veterans Benefits Administration. Applying for benefits and your character of discharge. https://www.benefits.va.gov/benefits/character_of_discharge.asp. Updated May 19, 2015. Accessed March 12, 2019.
Career Choices: Addiction psychiatry
Editor’s note: Career Choices features a psychiatry resident/fellow interviewing a psychiatrist about why he or she has chosen a specific career path. The goal is to inform trainees about the various psychiatric career options, and to give them a feel for the pros and cons of the various paths.
In this Career Choices, Saeed Ahmed, MD, talked with Cornel Stanciu, MD. Dr. Stanciu is an addiction psychiatrist at Dartmouth’s Geisel School of Medicine, where he is an Assistant Professor, and serves as the Director of Addiction Services at New Hampshire Hospital. He provides support to clinicians managing patients with addictive disorders in a multitude of settings, and also assists with policy making and delivery of addiction care at the state level. He is also the author of Deciphering the Addicted Brain, a guide to help families and the general public better understand addictive disorders.
Dr. Ahmed: What attracted you to pursue subspecialty training in addictive disorders?
Dr. Stanciu: In the early stages of my training, I frequently encountered individuals with medical and mental health disorders whose treatment was impacted by underlying substance use. I soon came to realize any attempts at (for example) managing hypertension in someone with cocaine use disorder, or managing schizophrenia in someone with ongoing cannabis use, were futile. Almost all of my patients receiving treatment for mental health disorders were dependent on tobacco or other substances, and most were interested in cessation. Through mentorship from addiction-trained residency faculty members, I was able to get a taste of the neurobiologic complexities of the disease, something that left me with a desire to develop a deeper understanding of the disease process. Witnessing strikingly positive outcomes with implementation of evidence-based treatment modalities further solidified my path to subspecialty training. Even during that early phase, because I expressed interest in managing these conditions, I was immediately put in a position to share and disseminate any newly acquired knowledge to other specialties as well as the public.
Dr. Ahmed: Could one manage addictive disorders with just general psychiatry training, and what are the differences between the different paths to certification that a resident could undertake?
Dr. Stanciu: Addictive disorders fall under the general umbrella of psychiatric care. Most individuals with these disorders exhibit some degree of mental illness. Medical school curriculum offers on average 2 hours of addiction-related didactics during 4 years. General psychiatry training programs vary significantly in the type of exposure to addiction—some residencies have an affiliated addiction fellowship, others have addiction-trained psychiatrists on staff, but most have none. Ultimately, there is great variability in the degree of comfort in working with individuals with addictive disorders post-residency. Being able to prescribe medications for the treatment of addictive disorders is very different from being familiar with the latest evidence-based recommendations and guidelines; the latter is
Addiction medicine is a fairly new route initially intended to allow non-psychiatric specialties access to addictive disorders training and certification. This is offered through the American Board of Preventive Medicine. There are currently 2 routes to sitting for the exam: through completion of a 1-year addiction medicine fellowship, or through the “practice pathway” still available until 2020. To be eligible for the latter, individuals must provide documentation of clinical experience post-residency, which is quantified as number of hours spent treating patients with addictions, plus any additional courses or training, and must be endorsed by a certified addictionologist.
Continue to: What was your fellowship experience link...
Dr. Ahmed: What was your fellowship experience like, and what should one consider when choosing a program?
Dr. Stanciu: I completed my fellowship training through Dartmouth’s Geisel School of Medicine, and the experience was tremendously valuable. In evaluating programs, one of the starting points is whether you have interest in a formal research track, because several programs include an optional year for that. Most programs tend to provide exposure to the Veterans Affairs system. The 1 year should provide you with broad exposure to all possible settings, all addictive disorders and patient populations, and all treatment modalities, in addition to rigorous didactic sessions. The ideal program should include rotations through methadone treatment centers, intensive outpatient programs, pain and interdisciplinary clinics, detoxification units, and centers for treatment of adolescent and young adults, as well as general medical settings and infectious disease clinics. There should also be close collaboration with psychologists who can provide training in evidence-based therapeutic modalities. During this year, it is vital to expand your knowledge of the ethical and legal regulations of treatment programs, state and federal requirements, insurance complexities, and requirements for privacy and protection of health information. The size of these programs can vary significantly, which may limit the one-on-one time devoted to your training, which is something I personally valued. My faculty was very supportive of academic endeavors, providing guidance, funding, and encouragement for attending and presenting at conferences, publishing papers, and other academic pursuits. Additionally, faculty should be current with emerging literature and willing to develop or implement new protocols and evaluate new pharmacologic therapies.
Dr. Ahmed: What are some of the career options and work settings for addiction psychiatrists?
Dr. Stanciu: Addiction psychiatrists work in numerous settings and various capacities. They can provide subspecialty care directly by seeing patients in outpatient clinics or inpatient addiction treatment centers for detoxification or rehabilitation, or they can work with dual-diagnosis populations in inpatient units. The expansion of telemedicine also holds promise for a role through virtual services. Indirectly, they can serve as a resource for expertise in the field through consultations in medical and psychiatric settings, or through policy making by working with the legislature and public health departments. Additionally, they can help create and integrate new knowledge into practice and educate future generations of physicians and the public.
Dr. Ahmed: What are some of the prevalent disorders and reasons for consultation that you encounter in your daily practice?
Continue to: Dr. Stanciu's response...
Dr. Stanciu: This can vary significantly depending on the setting, geographical region, and demographics of the population. My main non-administrative responsibilities are primarily consultative assisting clinicians at a 200-bed psychiatric hospital to address co-occurring addictive disorders. In short-term units, I am primarily asked to provide input on issues related to various toxidromes and withdrawals and the use of relapse prevention medications for alcohol use disorders as well as the use of buprenorphine or other forms of medication-assisted treatment. I work closely with licensed drug and alcohol counselors in implementing brief interventions as well as facilitating outpatient treatment referrals. Clinicians in longer term units may consult on issues related to pain management in individuals who have addictive disorders, the use of evidence-based pharmacologic agents to address cravings, or the use of relapse prevention medications for someone close to discharge. In terms of specific drugs of abuse, although opioids have recently received a tremendous amount of attention due to the visible costs through overdose deaths, the magnitude of individuals who are losing years of quality life through the use of alcohol and tobacco is significant, and hence this is a large portion of the conditions I encounter. I have also seen an abundance of marijuana use due to decreased perception of harm and increased access.
Dr. Ahmed: What are some of the challenges in working in this field?
Dr. Stanciu: Historically, funding for services has been an issue for clinicians working primarily with addictive disorders from the standpoint of reimbursement, patient access to evidence-based pharmacotherapy, and ability to collaborate with existing levels of care. In recent years, federal funding and policies have changed this, and after numerous studies have found increased cost savings, commercial insurances are providing coverage. A significant challenge also has been public stigma and dealing with a condition that is relapsing-remitting, poorly understood by other specialties and the general public, and sometimes labeled as a defect of character. Several efforts in education have lessened this; however, the impact still takes a toll on patients, who may feel ashamed of their disorder and sometimes are hesitant to take medications because they may believe that they are not “clean” if they depend on a medication for remission. Lastly, recent changes in marijuana policies make conversations about this drug quite difficult because patients often view it as harmless, and the laws governing legality and indications for therapeutic use are slightly ahead of the evidence.
Dr. Ahmed: In what direction do you believe the subspecialty is headed?
Dr. Stanciu: Currently, there are approximately 1,000 certified addiction psychiatrists for the 45 million Americans who have addictive disorders. Smoking and other forms of tobacco use pose significant threats to the 2020 Healthy People Tobacco Use objectives. There is a significant demand for addictionologists in both public and private sectors. As with mental health, demand exceeds supply, and efforts are underway to expand downstream education and increase access to specialists. Several federal laws have been put in place to remove barriers and expand access to care and have paved the way to a brighter future. One is the Affordable Care Act, which requires all insurances including Medicaid to cover the cost of treatment. Second is the Mental Health Parity and Addiction Equity Act, which ensures that the duration and dollar amount of coverage for substance use disorders is comparable to that of medical and surgical care.
Continue to: Another exciting possibility...
Another exciting possibility comes from the world of pharmaceuticals. Some medications have modest efficacy for addressing addictive disorders; however, historically these have been poorly utilized. Enhanced understanding of the neurobiology combined with increased insurance reimbursement should prompt research and new drug development. Some promising agents are already in the pipeline. Research into molecular and gene therapy as a way to better individualize care is also underway.
Going forward, I think we will also encounter a different landscape of drugs. Synthetic agents are emerging and increasing in popularity. Alarmingly, public perception of harm is decreasing. When it comes to cannabis use, I see a rise in pathologic use and the ramifications of this will have a drastic impact, particularly on patients with mental health conditions. We will need to undertake better efforts in monitoring, staying updated, and providing public education campaigns.
Dr. Ahmed: What advice do you have for trainees contemplating subspecialty training in addiction psychiatry?
Dr. Stanciu: I cannot emphasize enough the importance of mentorship. The American Academy of Addiction Psychiatry has a robust system for connecting mentees with mentors at all stages in their careers. This can be extremely helpful, especially in situations where the residency program does not have addiction-trained faculty or rotations through treatment centers. Joining such an organization also grants you access to resources that can help further your enthusiasm. Those interested should also familiarize themselves with currently available pharmacotherapeutic treatments that have evidence supporting efficacy for various addictive disorders, and begin to incorporate these medications into general mental health practice, along with attempts at motivational interviewing. For example, begin discussing naltrexone with patients who have comorbid alcohol use disorders and are interested in reducing their drinking; and varenicline with patients who smoke and are interested in quitting. The outcomes should automatically elicit an interest in pursuing further training in the field!
Editor’s note: Career Choices features a psychiatry resident/fellow interviewing a psychiatrist about why he or she has chosen a specific career path. The goal is to inform trainees about the various psychiatric career options, and to give them a feel for the pros and cons of the various paths.
In this Career Choices, Saeed Ahmed, MD, talked with Cornel Stanciu, MD. Dr. Stanciu is an addiction psychiatrist at Dartmouth’s Geisel School of Medicine, where he is an Assistant Professor, and serves as the Director of Addiction Services at New Hampshire Hospital. He provides support to clinicians managing patients with addictive disorders in a multitude of settings, and also assists with policy making and delivery of addiction care at the state level. He is also the author of Deciphering the Addicted Brain, a guide to help families and the general public better understand addictive disorders.
Dr. Ahmed: What attracted you to pursue subspecialty training in addictive disorders?
Dr. Stanciu: In the early stages of my training, I frequently encountered individuals with medical and mental health disorders whose treatment was impacted by underlying substance use. I soon came to realize any attempts at (for example) managing hypertension in someone with cocaine use disorder, or managing schizophrenia in someone with ongoing cannabis use, were futile. Almost all of my patients receiving treatment for mental health disorders were dependent on tobacco or other substances, and most were interested in cessation. Through mentorship from addiction-trained residency faculty members, I was able to get a taste of the neurobiologic complexities of the disease, something that left me with a desire to develop a deeper understanding of the disease process. Witnessing strikingly positive outcomes with implementation of evidence-based treatment modalities further solidified my path to subspecialty training. Even during that early phase, because I expressed interest in managing these conditions, I was immediately put in a position to share and disseminate any newly acquired knowledge to other specialties as well as the public.
Dr. Ahmed: Could one manage addictive disorders with just general psychiatry training, and what are the differences between the different paths to certification that a resident could undertake?
Dr. Stanciu: Addictive disorders fall under the general umbrella of psychiatric care. Most individuals with these disorders exhibit some degree of mental illness. Medical school curriculum offers on average 2 hours of addiction-related didactics during 4 years. General psychiatry training programs vary significantly in the type of exposure to addiction—some residencies have an affiliated addiction fellowship, others have addiction-trained psychiatrists on staff, but most have none. Ultimately, there is great variability in the degree of comfort in working with individuals with addictive disorders post-residency. Being able to prescribe medications for the treatment of addictive disorders is very different from being familiar with the latest evidence-based recommendations and guidelines; the latter is
Addiction medicine is a fairly new route initially intended to allow non-psychiatric specialties access to addictive disorders training and certification. This is offered through the American Board of Preventive Medicine. There are currently 2 routes to sitting for the exam: through completion of a 1-year addiction medicine fellowship, or through the “practice pathway” still available until 2020. To be eligible for the latter, individuals must provide documentation of clinical experience post-residency, which is quantified as number of hours spent treating patients with addictions, plus any additional courses or training, and must be endorsed by a certified addictionologist.
Continue to: What was your fellowship experience link...
Dr. Ahmed: What was your fellowship experience like, and what should one consider when choosing a program?
Dr. Stanciu: I completed my fellowship training through Dartmouth’s Geisel School of Medicine, and the experience was tremendously valuable. In evaluating programs, one of the starting points is whether you have interest in a formal research track, because several programs include an optional year for that. Most programs tend to provide exposure to the Veterans Affairs system. The 1 year should provide you with broad exposure to all possible settings, all addictive disorders and patient populations, and all treatment modalities, in addition to rigorous didactic sessions. The ideal program should include rotations through methadone treatment centers, intensive outpatient programs, pain and interdisciplinary clinics, detoxification units, and centers for treatment of adolescent and young adults, as well as general medical settings and infectious disease clinics. There should also be close collaboration with psychologists who can provide training in evidence-based therapeutic modalities. During this year, it is vital to expand your knowledge of the ethical and legal regulations of treatment programs, state and federal requirements, insurance complexities, and requirements for privacy and protection of health information. The size of these programs can vary significantly, which may limit the one-on-one time devoted to your training, which is something I personally valued. My faculty was very supportive of academic endeavors, providing guidance, funding, and encouragement for attending and presenting at conferences, publishing papers, and other academic pursuits. Additionally, faculty should be current with emerging literature and willing to develop or implement new protocols and evaluate new pharmacologic therapies.
Dr. Ahmed: What are some of the career options and work settings for addiction psychiatrists?
Dr. Stanciu: Addiction psychiatrists work in numerous settings and various capacities. They can provide subspecialty care directly by seeing patients in outpatient clinics or inpatient addiction treatment centers for detoxification or rehabilitation, or they can work with dual-diagnosis populations in inpatient units. The expansion of telemedicine also holds promise for a role through virtual services. Indirectly, they can serve as a resource for expertise in the field through consultations in medical and psychiatric settings, or through policy making by working with the legislature and public health departments. Additionally, they can help create and integrate new knowledge into practice and educate future generations of physicians and the public.
Dr. Ahmed: What are some of the prevalent disorders and reasons for consultation that you encounter in your daily practice?
Continue to: Dr. Stanciu's response...
Dr. Stanciu: This can vary significantly depending on the setting, geographical region, and demographics of the population. My main non-administrative responsibilities are primarily consultative assisting clinicians at a 200-bed psychiatric hospital to address co-occurring addictive disorders. In short-term units, I am primarily asked to provide input on issues related to various toxidromes and withdrawals and the use of relapse prevention medications for alcohol use disorders as well as the use of buprenorphine or other forms of medication-assisted treatment. I work closely with licensed drug and alcohol counselors in implementing brief interventions as well as facilitating outpatient treatment referrals. Clinicians in longer term units may consult on issues related to pain management in individuals who have addictive disorders, the use of evidence-based pharmacologic agents to address cravings, or the use of relapse prevention medications for someone close to discharge. In terms of specific drugs of abuse, although opioids have recently received a tremendous amount of attention due to the visible costs through overdose deaths, the magnitude of individuals who are losing years of quality life through the use of alcohol and tobacco is significant, and hence this is a large portion of the conditions I encounter. I have also seen an abundance of marijuana use due to decreased perception of harm and increased access.
Dr. Ahmed: What are some of the challenges in working in this field?
Dr. Stanciu: Historically, funding for services has been an issue for clinicians working primarily with addictive disorders from the standpoint of reimbursement, patient access to evidence-based pharmacotherapy, and ability to collaborate with existing levels of care. In recent years, federal funding and policies have changed this, and after numerous studies have found increased cost savings, commercial insurances are providing coverage. A significant challenge also has been public stigma and dealing with a condition that is relapsing-remitting, poorly understood by other specialties and the general public, and sometimes labeled as a defect of character. Several efforts in education have lessened this; however, the impact still takes a toll on patients, who may feel ashamed of their disorder and sometimes are hesitant to take medications because they may believe that they are not “clean” if they depend on a medication for remission. Lastly, recent changes in marijuana policies make conversations about this drug quite difficult because patients often view it as harmless, and the laws governing legality and indications for therapeutic use are slightly ahead of the evidence.
Dr. Ahmed: In what direction do you believe the subspecialty is headed?
Dr. Stanciu: Currently, there are approximately 1,000 certified addiction psychiatrists for the 45 million Americans who have addictive disorders. Smoking and other forms of tobacco use pose significant threats to the 2020 Healthy People Tobacco Use objectives. There is a significant demand for addictionologists in both public and private sectors. As with mental health, demand exceeds supply, and efforts are underway to expand downstream education and increase access to specialists. Several federal laws have been put in place to remove barriers and expand access to care and have paved the way to a brighter future. One is the Affordable Care Act, which requires all insurances including Medicaid to cover the cost of treatment. Second is the Mental Health Parity and Addiction Equity Act, which ensures that the duration and dollar amount of coverage for substance use disorders is comparable to that of medical and surgical care.
Continue to: Another exciting possibility...
Another exciting possibility comes from the world of pharmaceuticals. Some medications have modest efficacy for addressing addictive disorders; however, historically these have been poorly utilized. Enhanced understanding of the neurobiology combined with increased insurance reimbursement should prompt research and new drug development. Some promising agents are already in the pipeline. Research into molecular and gene therapy as a way to better individualize care is also underway.
Going forward, I think we will also encounter a different landscape of drugs. Synthetic agents are emerging and increasing in popularity. Alarmingly, public perception of harm is decreasing. When it comes to cannabis use, I see a rise in pathologic use and the ramifications of this will have a drastic impact, particularly on patients with mental health conditions. We will need to undertake better efforts in monitoring, staying updated, and providing public education campaigns.
Dr. Ahmed: What advice do you have for trainees contemplating subspecialty training in addiction psychiatry?
Dr. Stanciu: I cannot emphasize enough the importance of mentorship. The American Academy of Addiction Psychiatry has a robust system for connecting mentees with mentors at all stages in their careers. This can be extremely helpful, especially in situations where the residency program does not have addiction-trained faculty or rotations through treatment centers. Joining such an organization also grants you access to resources that can help further your enthusiasm. Those interested should also familiarize themselves with currently available pharmacotherapeutic treatments that have evidence supporting efficacy for various addictive disorders, and begin to incorporate these medications into general mental health practice, along with attempts at motivational interviewing. For example, begin discussing naltrexone with patients who have comorbid alcohol use disorders and are interested in reducing their drinking; and varenicline with patients who smoke and are interested in quitting. The outcomes should automatically elicit an interest in pursuing further training in the field!
Editor’s note: Career Choices features a psychiatry resident/fellow interviewing a psychiatrist about why he or she has chosen a specific career path. The goal is to inform trainees about the various psychiatric career options, and to give them a feel for the pros and cons of the various paths.
In this Career Choices, Saeed Ahmed, MD, talked with Cornel Stanciu, MD. Dr. Stanciu is an addiction psychiatrist at Dartmouth’s Geisel School of Medicine, where he is an Assistant Professor, and serves as the Director of Addiction Services at New Hampshire Hospital. He provides support to clinicians managing patients with addictive disorders in a multitude of settings, and also assists with policy making and delivery of addiction care at the state level. He is also the author of Deciphering the Addicted Brain, a guide to help families and the general public better understand addictive disorders.
Dr. Ahmed: What attracted you to pursue subspecialty training in addictive disorders?
Dr. Stanciu: In the early stages of my training, I frequently encountered individuals with medical and mental health disorders whose treatment was impacted by underlying substance use. I soon came to realize any attempts at (for example) managing hypertension in someone with cocaine use disorder, or managing schizophrenia in someone with ongoing cannabis use, were futile. Almost all of my patients receiving treatment for mental health disorders were dependent on tobacco or other substances, and most were interested in cessation. Through mentorship from addiction-trained residency faculty members, I was able to get a taste of the neurobiologic complexities of the disease, something that left me with a desire to develop a deeper understanding of the disease process. Witnessing strikingly positive outcomes with implementation of evidence-based treatment modalities further solidified my path to subspecialty training. Even during that early phase, because I expressed interest in managing these conditions, I was immediately put in a position to share and disseminate any newly acquired knowledge to other specialties as well as the public.
Dr. Ahmed: Could one manage addictive disorders with just general psychiatry training, and what are the differences between the different paths to certification that a resident could undertake?
Dr. Stanciu: Addictive disorders fall under the general umbrella of psychiatric care. Most individuals with these disorders exhibit some degree of mental illness. Medical school curriculum offers on average 2 hours of addiction-related didactics during 4 years. General psychiatry training programs vary significantly in the type of exposure to addiction—some residencies have an affiliated addiction fellowship, others have addiction-trained psychiatrists on staff, but most have none. Ultimately, there is great variability in the degree of comfort in working with individuals with addictive disorders post-residency. Being able to prescribe medications for the treatment of addictive disorders is very different from being familiar with the latest evidence-based recommendations and guidelines; the latter is
Addiction medicine is a fairly new route initially intended to allow non-psychiatric specialties access to addictive disorders training and certification. This is offered through the American Board of Preventive Medicine. There are currently 2 routes to sitting for the exam: through completion of a 1-year addiction medicine fellowship, or through the “practice pathway” still available until 2020. To be eligible for the latter, individuals must provide documentation of clinical experience post-residency, which is quantified as number of hours spent treating patients with addictions, plus any additional courses or training, and must be endorsed by a certified addictionologist.
Continue to: What was your fellowship experience link...
Dr. Ahmed: What was your fellowship experience like, and what should one consider when choosing a program?
Dr. Stanciu: I completed my fellowship training through Dartmouth’s Geisel School of Medicine, and the experience was tremendously valuable. In evaluating programs, one of the starting points is whether you have interest in a formal research track, because several programs include an optional year for that. Most programs tend to provide exposure to the Veterans Affairs system. The 1 year should provide you with broad exposure to all possible settings, all addictive disorders and patient populations, and all treatment modalities, in addition to rigorous didactic sessions. The ideal program should include rotations through methadone treatment centers, intensive outpatient programs, pain and interdisciplinary clinics, detoxification units, and centers for treatment of adolescent and young adults, as well as general medical settings and infectious disease clinics. There should also be close collaboration with psychologists who can provide training in evidence-based therapeutic modalities. During this year, it is vital to expand your knowledge of the ethical and legal regulations of treatment programs, state and federal requirements, insurance complexities, and requirements for privacy and protection of health information. The size of these programs can vary significantly, which may limit the one-on-one time devoted to your training, which is something I personally valued. My faculty was very supportive of academic endeavors, providing guidance, funding, and encouragement for attending and presenting at conferences, publishing papers, and other academic pursuits. Additionally, faculty should be current with emerging literature and willing to develop or implement new protocols and evaluate new pharmacologic therapies.
Dr. Ahmed: What are some of the career options and work settings for addiction psychiatrists?
Dr. Stanciu: Addiction psychiatrists work in numerous settings and various capacities. They can provide subspecialty care directly by seeing patients in outpatient clinics or inpatient addiction treatment centers for detoxification or rehabilitation, or they can work with dual-diagnosis populations in inpatient units. The expansion of telemedicine also holds promise for a role through virtual services. Indirectly, they can serve as a resource for expertise in the field through consultations in medical and psychiatric settings, or through policy making by working with the legislature and public health departments. Additionally, they can help create and integrate new knowledge into practice and educate future generations of physicians and the public.
Dr. Ahmed: What are some of the prevalent disorders and reasons for consultation that you encounter in your daily practice?
Continue to: Dr. Stanciu's response...
Dr. Stanciu: This can vary significantly depending on the setting, geographical region, and demographics of the population. My main non-administrative responsibilities are primarily consultative assisting clinicians at a 200-bed psychiatric hospital to address co-occurring addictive disorders. In short-term units, I am primarily asked to provide input on issues related to various toxidromes and withdrawals and the use of relapse prevention medications for alcohol use disorders as well as the use of buprenorphine or other forms of medication-assisted treatment. I work closely with licensed drug and alcohol counselors in implementing brief interventions as well as facilitating outpatient treatment referrals. Clinicians in longer term units may consult on issues related to pain management in individuals who have addictive disorders, the use of evidence-based pharmacologic agents to address cravings, or the use of relapse prevention medications for someone close to discharge. In terms of specific drugs of abuse, although opioids have recently received a tremendous amount of attention due to the visible costs through overdose deaths, the magnitude of individuals who are losing years of quality life through the use of alcohol and tobacco is significant, and hence this is a large portion of the conditions I encounter. I have also seen an abundance of marijuana use due to decreased perception of harm and increased access.
Dr. Ahmed: What are some of the challenges in working in this field?
Dr. Stanciu: Historically, funding for services has been an issue for clinicians working primarily with addictive disorders from the standpoint of reimbursement, patient access to evidence-based pharmacotherapy, and ability to collaborate with existing levels of care. In recent years, federal funding and policies have changed this, and after numerous studies have found increased cost savings, commercial insurances are providing coverage. A significant challenge also has been public stigma and dealing with a condition that is relapsing-remitting, poorly understood by other specialties and the general public, and sometimes labeled as a defect of character. Several efforts in education have lessened this; however, the impact still takes a toll on patients, who may feel ashamed of their disorder and sometimes are hesitant to take medications because they may believe that they are not “clean” if they depend on a medication for remission. Lastly, recent changes in marijuana policies make conversations about this drug quite difficult because patients often view it as harmless, and the laws governing legality and indications for therapeutic use are slightly ahead of the evidence.
Dr. Ahmed: In what direction do you believe the subspecialty is headed?
Dr. Stanciu: Currently, there are approximately 1,000 certified addiction psychiatrists for the 45 million Americans who have addictive disorders. Smoking and other forms of tobacco use pose significant threats to the 2020 Healthy People Tobacco Use objectives. There is a significant demand for addictionologists in both public and private sectors. As with mental health, demand exceeds supply, and efforts are underway to expand downstream education and increase access to specialists. Several federal laws have been put in place to remove barriers and expand access to care and have paved the way to a brighter future. One is the Affordable Care Act, which requires all insurances including Medicaid to cover the cost of treatment. Second is the Mental Health Parity and Addiction Equity Act, which ensures that the duration and dollar amount of coverage for substance use disorders is comparable to that of medical and surgical care.
Continue to: Another exciting possibility...
Another exciting possibility comes from the world of pharmaceuticals. Some medications have modest efficacy for addressing addictive disorders; however, historically these have been poorly utilized. Enhanced understanding of the neurobiology combined with increased insurance reimbursement should prompt research and new drug development. Some promising agents are already in the pipeline. Research into molecular and gene therapy as a way to better individualize care is also underway.
Going forward, I think we will also encounter a different landscape of drugs. Synthetic agents are emerging and increasing in popularity. Alarmingly, public perception of harm is decreasing. When it comes to cannabis use, I see a rise in pathologic use and the ramifications of this will have a drastic impact, particularly on patients with mental health conditions. We will need to undertake better efforts in monitoring, staying updated, and providing public education campaigns.
Dr. Ahmed: What advice do you have for trainees contemplating subspecialty training in addiction psychiatry?
Dr. Stanciu: I cannot emphasize enough the importance of mentorship. The American Academy of Addiction Psychiatry has a robust system for connecting mentees with mentors at all stages in their careers. This can be extremely helpful, especially in situations where the residency program does not have addiction-trained faculty or rotations through treatment centers. Joining such an organization also grants you access to resources that can help further your enthusiasm. Those interested should also familiarize themselves with currently available pharmacotherapeutic treatments that have evidence supporting efficacy for various addictive disorders, and begin to incorporate these medications into general mental health practice, along with attempts at motivational interviewing. For example, begin discussing naltrexone with patients who have comorbid alcohol use disorders and are interested in reducing their drinking; and varenicline with patients who smoke and are interested in quitting. The outcomes should automatically elicit an interest in pursuing further training in the field!
Aerospace medicine and psychiatry
As part of my psychiatry residency training, I had the privilege to work with and learn from an aerospace psychiatrist. Aerospace medicine is a branch of preventive and occupational medicine in which aviators (pilots, aircrew, or astronauts) are subject to evaluation/treatment. The goal is to assess physical and mental health factors to mitigate risks, protect public safety, and ensure the aviators’ well-being.1,2 Aerospace psychiatry is a highly specialized area in which practitioners are trained to perform specific evaluations. In this article, I review those evaluations for those looking to gain insight into the field.
Aviation medical examination
Under Title 14 of the Code of Federal Regulations, the Federal Aviation Administration (FAA) requires aviators to be evaluated for medical certification by undergoing an aviation medical exam.2 In order to be deemed “fit for duty,” aviators must meet strict physical and mental health standards set by the FAA. The extent of these standards varies by the class of licensure (Table 13). Aviation medical exams are performed by any physician who has been designated by the FAA and completed the appropriate FAA aviation medical examiner (AME) training. Aviators who meet the medical standards for their licensure class are recommended for medical certification. If the AME brings up further questions due to the limits of the examination and/or a lack of medical records, the certification will likely be deferred pending further evaluation by an FAA-approved medical specialist and/or the receipt of additional medical records. Questions about a possible psychiatric diagnosis/history or substance use disorder will lead to referral to a psychiatrist familiar with aviation standards for further evaluation.
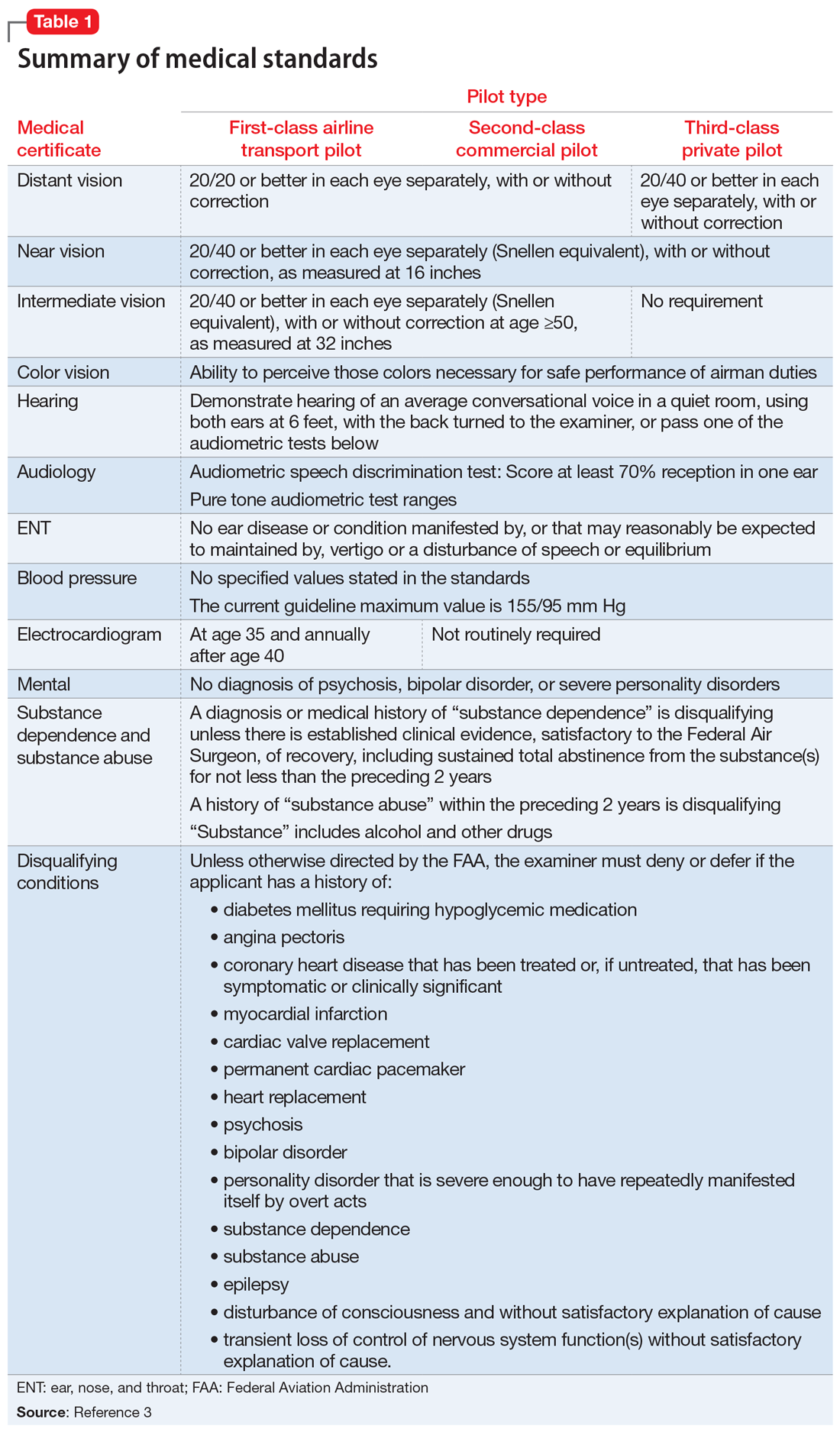
_
Special issuances and Conditions AMEs Can Issue
There are 15 disqualifying conditions for medical certification (Table 13). However, a special issuance of a medical certification may be granted if the aviator shows to the satisfaction of the aviation medical examiner that the duties of the licensure class can be performed without endangering the public safety and that the condition is deemed stable. This may be shown through additional medical evaluations/tests and/or records.
There are certain medical conditions for which an AME can issue a medical certificate without further review from other specialists; thus, an AME can review and follow the Conditions AMEs Can Issue (CACI) worksheet to recommend medical certification (Table 24). The CACI guidelines and worksheets are updated by the FAA regularly to ensure aviators’ health and minimize public risk.
Psychiatric & Psychological Evaluation
Aviators may be referred for Psychiatric and Psychological Evaluation (P&P) if an AME discovers additional concerns about psychiatric and neurocognitive disorders. These cases are not clear-cut. An example would be an aviator who was receiving a psychotropic medication in the past and reported past heavy alcohol use. The P&P includes a thorough psychiatric evaluation by an aerospace psychiatrist and extensive psychological testing by an aerospace psychologist. These clinicians also review collateral information and past medical/AME records. Aviators may be recommended for medical certification with special issuance or may be denied medical certification as a result of these examinations.
Human Intervention Motivation Study program
The Human Intervention Motivation Study (HIMS) program was established to provide an avenue whereby commercial pilots with active substance use disorders can be identified, treated, and successfully returned to active flight status.5 The goal of the HIMS program is to save lives and careers while enhancing flight safety. Physicians trained in HIMS evaluations follow the multifactorial addiction disease model. This evaluation is used to identify active substance use and initiate treatment, and to maintain sobriety and monitor aftercare adherence.
1. Bor R, Hubbard T. Aviation mental health: psychological implications for air transportation. Hampshire, England: Ashgate Publishing Limited; 2006.
2. US Department of Transportation Federal Aviation Administration. Medical certification. https://www.faa.gov/licenses_certificates/medical_certification/. Updated February 1, 2019. Accessed February 19, 2019.
3. US Department of Transportation Federal Aviation Administration. Summary of medical standards. https://www.faa.gov/about/office_org/headquarters_offices/avs/offices/aam/ame/guide/media/synopsis.pdf. Revised April 3, 2006. Accessed October 7, 2018.
4. US Department of Transportation Federal Aviation Administration. Guide for aviation medical examiners: CACI conditions. Revised April 3, 2006. https://www.faa.gov/about/office_org/headquarters_offices/avs/offices/aam/ame/guide/certification_ws/. Accessed October 8, 2018.
5. HIMS. About HIMS. http://www.himsprogram.com/Home/About. Accessed February 6, 2019.
As part of my psychiatry residency training, I had the privilege to work with and learn from an aerospace psychiatrist. Aerospace medicine is a branch of preventive and occupational medicine in which aviators (pilots, aircrew, or astronauts) are subject to evaluation/treatment. The goal is to assess physical and mental health factors to mitigate risks, protect public safety, and ensure the aviators’ well-being.1,2 Aerospace psychiatry is a highly specialized area in which practitioners are trained to perform specific evaluations. In this article, I review those evaluations for those looking to gain insight into the field.
Aviation medical examination
Under Title 14 of the Code of Federal Regulations, the Federal Aviation Administration (FAA) requires aviators to be evaluated for medical certification by undergoing an aviation medical exam.2 In order to be deemed “fit for duty,” aviators must meet strict physical and mental health standards set by the FAA. The extent of these standards varies by the class of licensure (Table 13). Aviation medical exams are performed by any physician who has been designated by the FAA and completed the appropriate FAA aviation medical examiner (AME) training. Aviators who meet the medical standards for their licensure class are recommended for medical certification. If the AME brings up further questions due to the limits of the examination and/or a lack of medical records, the certification will likely be deferred pending further evaluation by an FAA-approved medical specialist and/or the receipt of additional medical records. Questions about a possible psychiatric diagnosis/history or substance use disorder will lead to referral to a psychiatrist familiar with aviation standards for further evaluation.
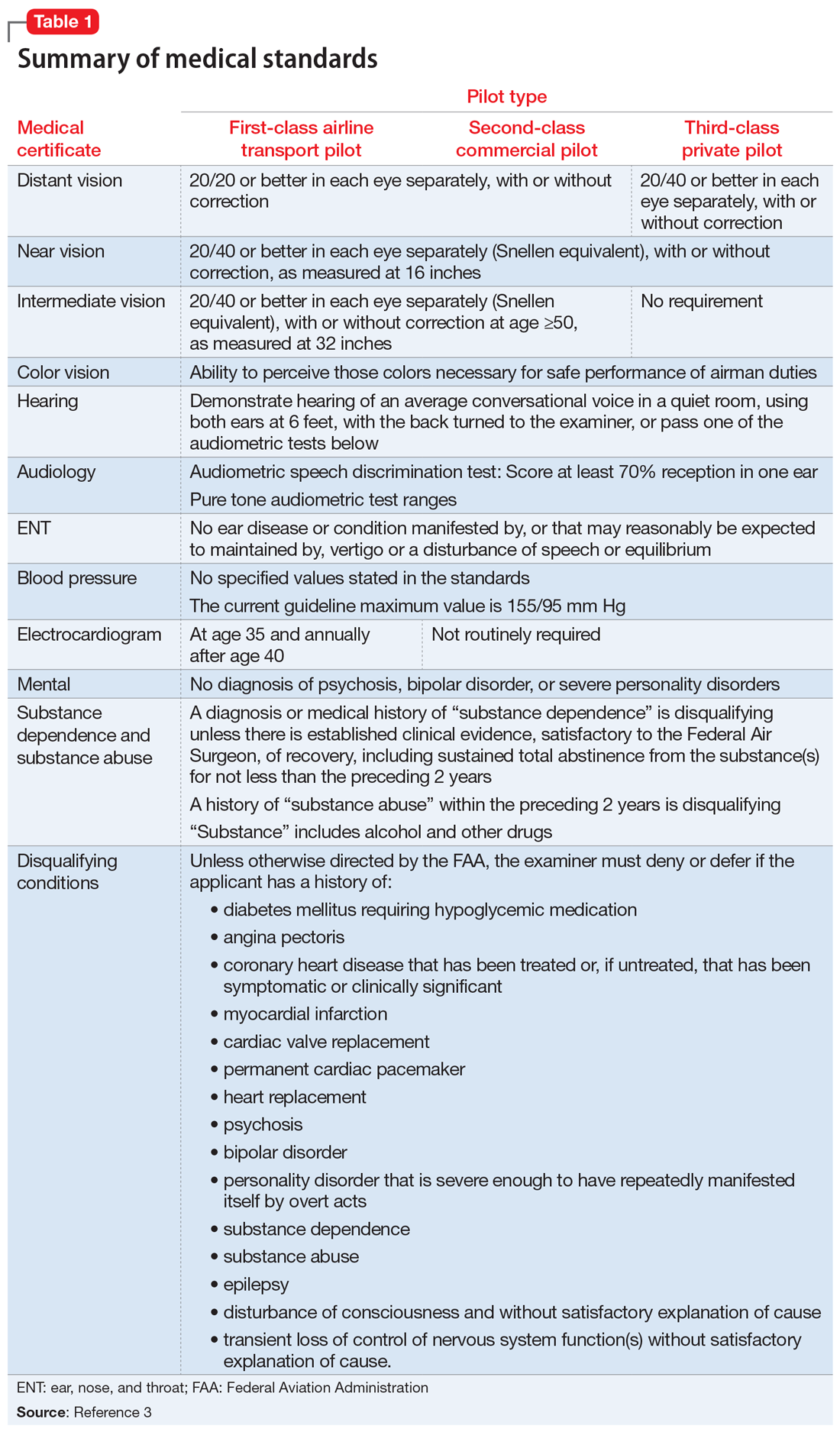
_
Special issuances and Conditions AMEs Can Issue
There are 15 disqualifying conditions for medical certification (Table 13). However, a special issuance of a medical certification may be granted if the aviator shows to the satisfaction of the aviation medical examiner that the duties of the licensure class can be performed without endangering the public safety and that the condition is deemed stable. This may be shown through additional medical evaluations/tests and/or records.
There are certain medical conditions for which an AME can issue a medical certificate without further review from other specialists; thus, an AME can review and follow the Conditions AMEs Can Issue (CACI) worksheet to recommend medical certification (Table 24). The CACI guidelines and worksheets are updated by the FAA regularly to ensure aviators’ health and minimize public risk.
Psychiatric & Psychological Evaluation
Aviators may be referred for Psychiatric and Psychological Evaluation (P&P) if an AME discovers additional concerns about psychiatric and neurocognitive disorders. These cases are not clear-cut. An example would be an aviator who was receiving a psychotropic medication in the past and reported past heavy alcohol use. The P&P includes a thorough psychiatric evaluation by an aerospace psychiatrist and extensive psychological testing by an aerospace psychologist. These clinicians also review collateral information and past medical/AME records. Aviators may be recommended for medical certification with special issuance or may be denied medical certification as a result of these examinations.
Human Intervention Motivation Study program
The Human Intervention Motivation Study (HIMS) program was established to provide an avenue whereby commercial pilots with active substance use disorders can be identified, treated, and successfully returned to active flight status.5 The goal of the HIMS program is to save lives and careers while enhancing flight safety. Physicians trained in HIMS evaluations follow the multifactorial addiction disease model. This evaluation is used to identify active substance use and initiate treatment, and to maintain sobriety and monitor aftercare adherence.
As part of my psychiatry residency training, I had the privilege to work with and learn from an aerospace psychiatrist. Aerospace medicine is a branch of preventive and occupational medicine in which aviators (pilots, aircrew, or astronauts) are subject to evaluation/treatment. The goal is to assess physical and mental health factors to mitigate risks, protect public safety, and ensure the aviators’ well-being.1,2 Aerospace psychiatry is a highly specialized area in which practitioners are trained to perform specific evaluations. In this article, I review those evaluations for those looking to gain insight into the field.
Aviation medical examination
Under Title 14 of the Code of Federal Regulations, the Federal Aviation Administration (FAA) requires aviators to be evaluated for medical certification by undergoing an aviation medical exam.2 In order to be deemed “fit for duty,” aviators must meet strict physical and mental health standards set by the FAA. The extent of these standards varies by the class of licensure (Table 13). Aviation medical exams are performed by any physician who has been designated by the FAA and completed the appropriate FAA aviation medical examiner (AME) training. Aviators who meet the medical standards for their licensure class are recommended for medical certification. If the AME brings up further questions due to the limits of the examination and/or a lack of medical records, the certification will likely be deferred pending further evaluation by an FAA-approved medical specialist and/or the receipt of additional medical records. Questions about a possible psychiatric diagnosis/history or substance use disorder will lead to referral to a psychiatrist familiar with aviation standards for further evaluation.
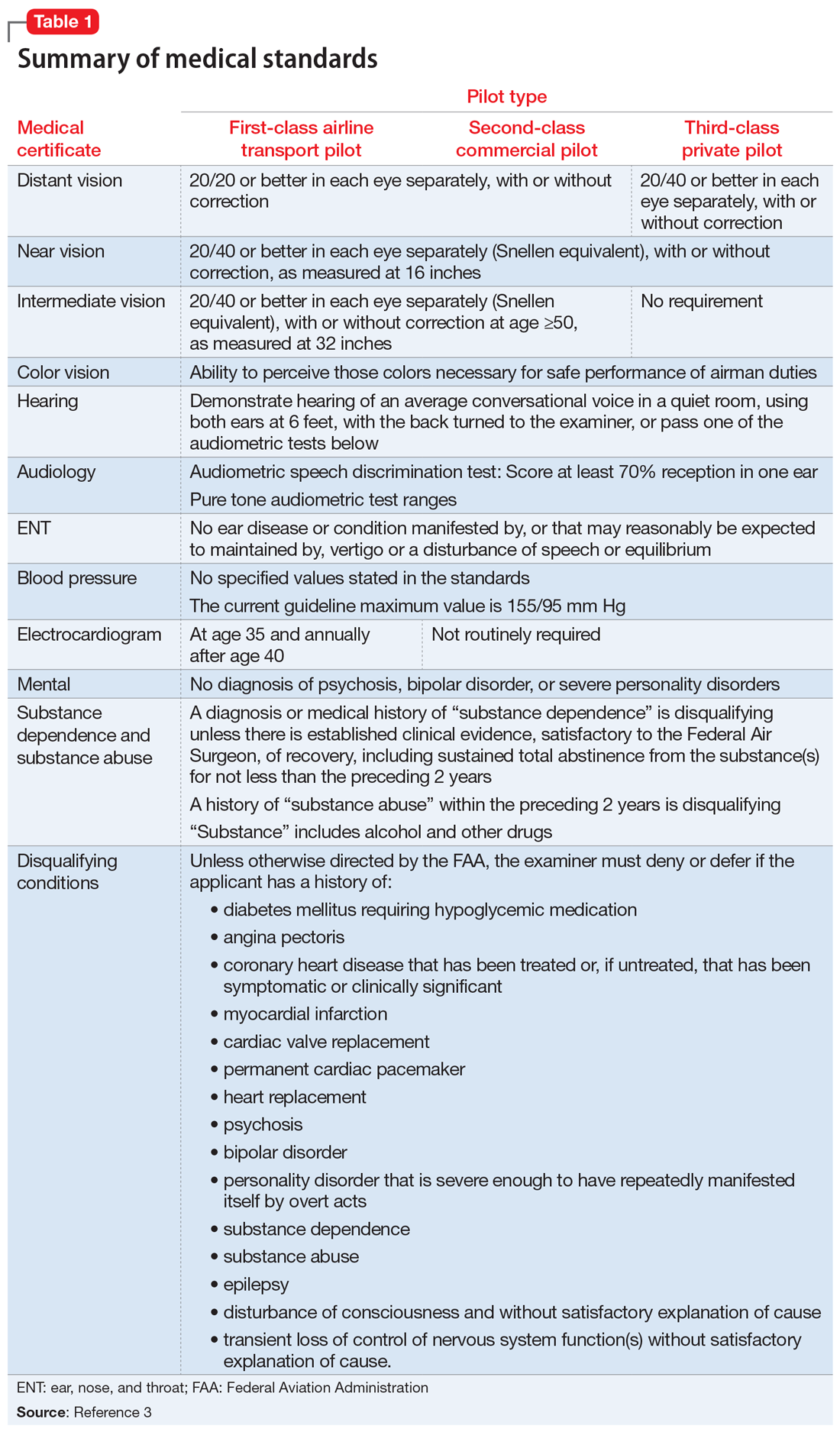
_
Special issuances and Conditions AMEs Can Issue
There are 15 disqualifying conditions for medical certification (Table 13). However, a special issuance of a medical certification may be granted if the aviator shows to the satisfaction of the aviation medical examiner that the duties of the licensure class can be performed without endangering the public safety and that the condition is deemed stable. This may be shown through additional medical evaluations/tests and/or records.
There are certain medical conditions for which an AME can issue a medical certificate without further review from other specialists; thus, an AME can review and follow the Conditions AMEs Can Issue (CACI) worksheet to recommend medical certification (Table 24). The CACI guidelines and worksheets are updated by the FAA regularly to ensure aviators’ health and minimize public risk.
Psychiatric & Psychological Evaluation
Aviators may be referred for Psychiatric and Psychological Evaluation (P&P) if an AME discovers additional concerns about psychiatric and neurocognitive disorders. These cases are not clear-cut. An example would be an aviator who was receiving a psychotropic medication in the past and reported past heavy alcohol use. The P&P includes a thorough psychiatric evaluation by an aerospace psychiatrist and extensive psychological testing by an aerospace psychologist. These clinicians also review collateral information and past medical/AME records. Aviators may be recommended for medical certification with special issuance or may be denied medical certification as a result of these examinations.
Human Intervention Motivation Study program
The Human Intervention Motivation Study (HIMS) program was established to provide an avenue whereby commercial pilots with active substance use disorders can be identified, treated, and successfully returned to active flight status.5 The goal of the HIMS program is to save lives and careers while enhancing flight safety. Physicians trained in HIMS evaluations follow the multifactorial addiction disease model. This evaluation is used to identify active substance use and initiate treatment, and to maintain sobriety and monitor aftercare adherence.
1. Bor R, Hubbard T. Aviation mental health: psychological implications for air transportation. Hampshire, England: Ashgate Publishing Limited; 2006.
2. US Department of Transportation Federal Aviation Administration. Medical certification. https://www.faa.gov/licenses_certificates/medical_certification/. Updated February 1, 2019. Accessed February 19, 2019.
3. US Department of Transportation Federal Aviation Administration. Summary of medical standards. https://www.faa.gov/about/office_org/headquarters_offices/avs/offices/aam/ame/guide/media/synopsis.pdf. Revised April 3, 2006. Accessed October 7, 2018.
4. US Department of Transportation Federal Aviation Administration. Guide for aviation medical examiners: CACI conditions. Revised April 3, 2006. https://www.faa.gov/about/office_org/headquarters_offices/avs/offices/aam/ame/guide/certification_ws/. Accessed October 8, 2018.
5. HIMS. About HIMS. http://www.himsprogram.com/Home/About. Accessed February 6, 2019.
1. Bor R, Hubbard T. Aviation mental health: psychological implications for air transportation. Hampshire, England: Ashgate Publishing Limited; 2006.
2. US Department of Transportation Federal Aviation Administration. Medical certification. https://www.faa.gov/licenses_certificates/medical_certification/. Updated February 1, 2019. Accessed February 19, 2019.
3. US Department of Transportation Federal Aviation Administration. Summary of medical standards. https://www.faa.gov/about/office_org/headquarters_offices/avs/offices/aam/ame/guide/media/synopsis.pdf. Revised April 3, 2006. Accessed October 7, 2018.
4. US Department of Transportation Federal Aviation Administration. Guide for aviation medical examiners: CACI conditions. Revised April 3, 2006. https://www.faa.gov/about/office_org/headquarters_offices/avs/offices/aam/ame/guide/certification_ws/. Accessed October 8, 2018.
5. HIMS. About HIMS. http://www.himsprogram.com/Home/About. Accessed February 6, 2019.
The blinding lies of depression
Numb and empty, I continued to drive home in a daze. My mind focused only on the light ahead changing from yellow to red. “Remember to step on the brake,” commanded the internal boss to my stunned mind. No tears, I continued to drive as green blinked its eye.
Earlier that afternoon as I stepped out of my second outpatient appointment of the day, the office administrator’s assistant gingerly informed me, “The guy who answered the phone for your no-show said she passed.”
“Passed? Like … died?” I asked in shock.
She nodded. “I looked her up in the system. She passed away 2 Saturdays ago.”
That was only 2 days after the last time I met with her when we celebrated her progress.
“Too soon, too soon in your career,” my attending bemoaned as I shared the news.
Gathering my scattered wit, I smoothed my furrowed brow and forced a smile back into my eyes. I had other patients to see.
Continue to: Soothed by the hum of my car...
Soothed by the hum of my car, my mind replayed our last meeting where hope and active plans had replaced broken hopelessness. For the past 2 weeks, I had erroneously dismissed her no-shows as her volatile borderline personality’s decision to fire me. I was wrong.
Holding things together until a silly domestic dispute unleashed the brewing tornado inside, I stormed upstairs to contain the pain. Behind locked doors, my body shuddered from uncontrollable tears that blinded my eyes. She was the first patient I helped through psychotherapy and the first I lost through suicide.
The news of her death triggered anguish from past suicides of dear friends. Chopper, who blew off his face during our sophomore y
A few years later, another classmate, Aaron, sank into depression. He, too, shot himself. Just months before I’d received the call requesting my presence at his funeral, he had asked me if I would be his Valentine. Jokingly, I agreed, knowing our paths would never cross after our graduation. At his funeral, his parents insisted that I sat as a member of his immediate family.
Oh … the blinding lies of depression. Those who have fallen prey to suicide never knew the truth: Their lives and their deaths matter.
Even strangers weep.
Numb and empty, I continued to drive home in a daze. My mind focused only on the light ahead changing from yellow to red. “Remember to step on the brake,” commanded the internal boss to my stunned mind. No tears, I continued to drive as green blinked its eye.
Earlier that afternoon as I stepped out of my second outpatient appointment of the day, the office administrator’s assistant gingerly informed me, “The guy who answered the phone for your no-show said she passed.”
“Passed? Like … died?” I asked in shock.
She nodded. “I looked her up in the system. She passed away 2 Saturdays ago.”
That was only 2 days after the last time I met with her when we celebrated her progress.
“Too soon, too soon in your career,” my attending bemoaned as I shared the news.
Gathering my scattered wit, I smoothed my furrowed brow and forced a smile back into my eyes. I had other patients to see.
Continue to: Soothed by the hum of my car...
Soothed by the hum of my car, my mind replayed our last meeting where hope and active plans had replaced broken hopelessness. For the past 2 weeks, I had erroneously dismissed her no-shows as her volatile borderline personality’s decision to fire me. I was wrong.
Holding things together until a silly domestic dispute unleashed the brewing tornado inside, I stormed upstairs to contain the pain. Behind locked doors, my body shuddered from uncontrollable tears that blinded my eyes. She was the first patient I helped through psychotherapy and the first I lost through suicide.
The news of her death triggered anguish from past suicides of dear friends. Chopper, who blew off his face during our sophomore y
A few years later, another classmate, Aaron, sank into depression. He, too, shot himself. Just months before I’d received the call requesting my presence at his funeral, he had asked me if I would be his Valentine. Jokingly, I agreed, knowing our paths would never cross after our graduation. At his funeral, his parents insisted that I sat as a member of his immediate family.
Oh … the blinding lies of depression. Those who have fallen prey to suicide never knew the truth: Their lives and their deaths matter.
Even strangers weep.
Numb and empty, I continued to drive home in a daze. My mind focused only on the light ahead changing from yellow to red. “Remember to step on the brake,” commanded the internal boss to my stunned mind. No tears, I continued to drive as green blinked its eye.
Earlier that afternoon as I stepped out of my second outpatient appointment of the day, the office administrator’s assistant gingerly informed me, “The guy who answered the phone for your no-show said she passed.”
“Passed? Like … died?” I asked in shock.
She nodded. “I looked her up in the system. She passed away 2 Saturdays ago.”
That was only 2 days after the last time I met with her when we celebrated her progress.
“Too soon, too soon in your career,” my attending bemoaned as I shared the news.
Gathering my scattered wit, I smoothed my furrowed brow and forced a smile back into my eyes. I had other patients to see.
Continue to: Soothed by the hum of my car...
Soothed by the hum of my car, my mind replayed our last meeting where hope and active plans had replaced broken hopelessness. For the past 2 weeks, I had erroneously dismissed her no-shows as her volatile borderline personality’s decision to fire me. I was wrong.
Holding things together until a silly domestic dispute unleashed the brewing tornado inside, I stormed upstairs to contain the pain. Behind locked doors, my body shuddered from uncontrollable tears that blinded my eyes. She was the first patient I helped through psychotherapy and the first I lost through suicide.
The news of her death triggered anguish from past suicides of dear friends. Chopper, who blew off his face during our sophomore y
A few years later, another classmate, Aaron, sank into depression. He, too, shot himself. Just months before I’d received the call requesting my presence at his funeral, he had asked me if I would be his Valentine. Jokingly, I agreed, knowing our paths would never cross after our graduation. At his funeral, his parents insisted that I sat as a member of his immediate family.
Oh … the blinding lies of depression. Those who have fallen prey to suicide never knew the truth: Their lives and their deaths matter.
Even strangers weep.
The effect of collateral information on involuntary psychiatric commitment
Collateral information is a key component obtained during the psych
Here I describe a case in which collateral information obtained about a patient was a primary factor in that patient’s involuntary commitment. However, the patient’s subsequent behavior observed on an inpatient psychiatric unit was entirely inconsistent with those behaviors described by the collateral informant to be “continuous and dangerous.”
CASE
Mr. M, age 18, presented to an emergency psychiatric center for evaluation of dangerous and aggressive behavior. He had a history of autism spectrum disorder (ASD), which was well managed with oral risperidone. He was petitioned for an involuntary psychiatric admission by his foster mother, who reported that Mr. M was aggressive and dangerous, often punching holes in the walls of their home, and that he threatened to assault his foster siblings on several occasions. She detailed a progressively declining history for Mr. M and said that he was “constantly talking to voices in his head that absolutely consume him,” to the extent that Mr. M could not pay attention to his daily tasks. The admitting psychiatrist upheld the petition for involuntary admission, citing that based on the foster’s mother collateral information, Mr. M was deemed to be a danger to others and therefore fulfilled criteria for involuntary psychiatric admission.
Once admitted to the inpatient psychiatric unit, Mr. M was observed to be pleasant, cooperative, and fully engaged in the milieu. At no point during his 7-day admission was he observed to be internally preoccupied or remotely disorganized. Mr. M was switched from oral risperidone to oral haloperidol because he developed acute gynecomastia, and was discharged home.
Does collateral information lead to unfair bias?
The importance of collateral information on the psychiatric admission process must not be understated. It is an opportunity to hear a first-hand account of behaviors consistent with an acute psychiatric disturbance, and guides us in formulating a clinically appropriate assessment and plan. But what happens when our patients’ close contacts or informants provide misleading or unintentionally suboptimal collateral information? How must we reconcile the ethical and legal obligation we have to balance patient autonomy with beneficence?
Studies examining patients’ attitudes toward involuntary admissions have routinely found that patients are less likely than clinical staff to view the involuntary admission as clinically justified.2 Consistent with these findings, Mr. M did not view his admission as necessary. At first, he seemed to lack insight regarding the events precipitating his involuntary admission, describing himself not as responding to internal stimuli, but rather, “imaginative because I have autism.” As time went on, though, it was clear that his account of his behavior was in fact correct.
Mr. M’s diagnosis of ASD further complicated the over-reliance on misleading collateral information provided by his foster mother, because the admitting psychiatrist invariably perceived Mr. M as a poor historian. A study examining how subjective histories described by patients with neurologic or psychiatric disorders are perceived by clinicians found physicians had a tendency for negative stereotyping and placed less credence on those patients’ subjective histories.3 Other literature has similarly concluded that there is an urgent need to carefully weigh information supplied to us by collateral informants because the first-hand accounts of perceivably dangerous behavior often are incomplete or misleading.4-5
Continue to: Ideas for improvement...
Ideas for improvement: respecting patient autonomy
These issues underscore the need for a more thorough review of collateral information to ensure that patient autonomy is not unjustly violated. How do we implement these necessary ideas without creating further undue burden during the admission process? Certainly, I am not suggesting that we evaluate the collateral informant to the degree that we evaluate the patient. However, I have outlined some suggestions for ensuring we act in our patients’ best interest when processing collateral information during an admission:
- Until proven otherwise, the patient’s story is true. If our patient maintains descriptions of his behavior that exist in stark opposition to the collateral information we obtain, we should only not believe the patient if his presentation suggests he may be acutely impaired or a poor historian (such as profound disorganization, overt psychosis, or failing to have capacity).
- Treat symptoms, not diagnoses. In this case, Mr. M was described by his foster mother to be psychotic in addition to having ASD, and an inexperienced psychiatrist may have initiated a titration to a higher antipsychotic dose. However, in the absence of any observable signs of aggression or psychosis, there was simply no indication for further titration of his antipsychotic.
- Document, document, document. When collateral information is supplied to us, it is crucial that we maintain a detailed account of this information. If we have a reason to believe that a patient poses an immediate danger to himself or others, we should carefully document our reasoning so that changes in behavior (if any) can be observed on a day-to-day basis.
1. Testa M, West SG. Civil commitment in the United States. Psychiatry (Edgmont). 2010;7(10):30-40.
2. Roe D, Weishut DJ, Jaglom M, et al. Patients’ and staff members’ attitudes about the rights of hospitalized psychiatric patients. Psychiatr Serv. 2002;53(1):87-91.
3. Crichton P, Carel H, Kidd IJ. Epistemic injustice in psychiatry. BJPsych Bull. 2017;41(2):65-70.
4. Marett C, Mossman D. What is your liability for involuntary commitment based on fault information? Current Psychiatry. 2017;16(3):21-25,33.
5. Lincoln AL, Allen M. The influence of collateral information on access to inpatient psychiatric services. International Journal of Psychosocial Rehabilitation. 2002;6:99-108.
Collateral information is a key component obtained during the psych
Here I describe a case in which collateral information obtained about a patient was a primary factor in that patient’s involuntary commitment. However, the patient’s subsequent behavior observed on an inpatient psychiatric unit was entirely inconsistent with those behaviors described by the collateral informant to be “continuous and dangerous.”
CASE
Mr. M, age 18, presented to an emergency psychiatric center for evaluation of dangerous and aggressive behavior. He had a history of autism spectrum disorder (ASD), which was well managed with oral risperidone. He was petitioned for an involuntary psychiatric admission by his foster mother, who reported that Mr. M was aggressive and dangerous, often punching holes in the walls of their home, and that he threatened to assault his foster siblings on several occasions. She detailed a progressively declining history for Mr. M and said that he was “constantly talking to voices in his head that absolutely consume him,” to the extent that Mr. M could not pay attention to his daily tasks. The admitting psychiatrist upheld the petition for involuntary admission, citing that based on the foster’s mother collateral information, Mr. M was deemed to be a danger to others and therefore fulfilled criteria for involuntary psychiatric admission.
Once admitted to the inpatient psychiatric unit, Mr. M was observed to be pleasant, cooperative, and fully engaged in the milieu. At no point during his 7-day admission was he observed to be internally preoccupied or remotely disorganized. Mr. M was switched from oral risperidone to oral haloperidol because he developed acute gynecomastia, and was discharged home.
Does collateral information lead to unfair bias?
The importance of collateral information on the psychiatric admission process must not be understated. It is an opportunity to hear a first-hand account of behaviors consistent with an acute psychiatric disturbance, and guides us in formulating a clinically appropriate assessment and plan. But what happens when our patients’ close contacts or informants provide misleading or unintentionally suboptimal collateral information? How must we reconcile the ethical and legal obligation we have to balance patient autonomy with beneficence?
Studies examining patients’ attitudes toward involuntary admissions have routinely found that patients are less likely than clinical staff to view the involuntary admission as clinically justified.2 Consistent with these findings, Mr. M did not view his admission as necessary. At first, he seemed to lack insight regarding the events precipitating his involuntary admission, describing himself not as responding to internal stimuli, but rather, “imaginative because I have autism.” As time went on, though, it was clear that his account of his behavior was in fact correct.
Mr. M’s diagnosis of ASD further complicated the over-reliance on misleading collateral information provided by his foster mother, because the admitting psychiatrist invariably perceived Mr. M as a poor historian. A study examining how subjective histories described by patients with neurologic or psychiatric disorders are perceived by clinicians found physicians had a tendency for negative stereotyping and placed less credence on those patients’ subjective histories.3 Other literature has similarly concluded that there is an urgent need to carefully weigh information supplied to us by collateral informants because the first-hand accounts of perceivably dangerous behavior often are incomplete or misleading.4-5
Continue to: Ideas for improvement...
Ideas for improvement: respecting patient autonomy
These issues underscore the need for a more thorough review of collateral information to ensure that patient autonomy is not unjustly violated. How do we implement these necessary ideas without creating further undue burden during the admission process? Certainly, I am not suggesting that we evaluate the collateral informant to the degree that we evaluate the patient. However, I have outlined some suggestions for ensuring we act in our patients’ best interest when processing collateral information during an admission:
- Until proven otherwise, the patient’s story is true. If our patient maintains descriptions of his behavior that exist in stark opposition to the collateral information we obtain, we should only not believe the patient if his presentation suggests he may be acutely impaired or a poor historian (such as profound disorganization, overt psychosis, or failing to have capacity).
- Treat symptoms, not diagnoses. In this case, Mr. M was described by his foster mother to be psychotic in addition to having ASD, and an inexperienced psychiatrist may have initiated a titration to a higher antipsychotic dose. However, in the absence of any observable signs of aggression or psychosis, there was simply no indication for further titration of his antipsychotic.
- Document, document, document. When collateral information is supplied to us, it is crucial that we maintain a detailed account of this information. If we have a reason to believe that a patient poses an immediate danger to himself or others, we should carefully document our reasoning so that changes in behavior (if any) can be observed on a day-to-day basis.
Collateral information is a key component obtained during the psych
Here I describe a case in which collateral information obtained about a patient was a primary factor in that patient’s involuntary commitment. However, the patient’s subsequent behavior observed on an inpatient psychiatric unit was entirely inconsistent with those behaviors described by the collateral informant to be “continuous and dangerous.”
CASE
Mr. M, age 18, presented to an emergency psychiatric center for evaluation of dangerous and aggressive behavior. He had a history of autism spectrum disorder (ASD), which was well managed with oral risperidone. He was petitioned for an involuntary psychiatric admission by his foster mother, who reported that Mr. M was aggressive and dangerous, often punching holes in the walls of their home, and that he threatened to assault his foster siblings on several occasions. She detailed a progressively declining history for Mr. M and said that he was “constantly talking to voices in his head that absolutely consume him,” to the extent that Mr. M could not pay attention to his daily tasks. The admitting psychiatrist upheld the petition for involuntary admission, citing that based on the foster’s mother collateral information, Mr. M was deemed to be a danger to others and therefore fulfilled criteria for involuntary psychiatric admission.
Once admitted to the inpatient psychiatric unit, Mr. M was observed to be pleasant, cooperative, and fully engaged in the milieu. At no point during his 7-day admission was he observed to be internally preoccupied or remotely disorganized. Mr. M was switched from oral risperidone to oral haloperidol because he developed acute gynecomastia, and was discharged home.
Does collateral information lead to unfair bias?
The importance of collateral information on the psychiatric admission process must not be understated. It is an opportunity to hear a first-hand account of behaviors consistent with an acute psychiatric disturbance, and guides us in formulating a clinically appropriate assessment and plan. But what happens when our patients’ close contacts or informants provide misleading or unintentionally suboptimal collateral information? How must we reconcile the ethical and legal obligation we have to balance patient autonomy with beneficence?
Studies examining patients’ attitudes toward involuntary admissions have routinely found that patients are less likely than clinical staff to view the involuntary admission as clinically justified.2 Consistent with these findings, Mr. M did not view his admission as necessary. At first, he seemed to lack insight regarding the events precipitating his involuntary admission, describing himself not as responding to internal stimuli, but rather, “imaginative because I have autism.” As time went on, though, it was clear that his account of his behavior was in fact correct.
Mr. M’s diagnosis of ASD further complicated the over-reliance on misleading collateral information provided by his foster mother, because the admitting psychiatrist invariably perceived Mr. M as a poor historian. A study examining how subjective histories described by patients with neurologic or psychiatric disorders are perceived by clinicians found physicians had a tendency for negative stereotyping and placed less credence on those patients’ subjective histories.3 Other literature has similarly concluded that there is an urgent need to carefully weigh information supplied to us by collateral informants because the first-hand accounts of perceivably dangerous behavior often are incomplete or misleading.4-5
Continue to: Ideas for improvement...
Ideas for improvement: respecting patient autonomy
These issues underscore the need for a more thorough review of collateral information to ensure that patient autonomy is not unjustly violated. How do we implement these necessary ideas without creating further undue burden during the admission process? Certainly, I am not suggesting that we evaluate the collateral informant to the degree that we evaluate the patient. However, I have outlined some suggestions for ensuring we act in our patients’ best interest when processing collateral information during an admission:
- Until proven otherwise, the patient’s story is true. If our patient maintains descriptions of his behavior that exist in stark opposition to the collateral information we obtain, we should only not believe the patient if his presentation suggests he may be acutely impaired or a poor historian (such as profound disorganization, overt psychosis, or failing to have capacity).
- Treat symptoms, not diagnoses. In this case, Mr. M was described by his foster mother to be psychotic in addition to having ASD, and an inexperienced psychiatrist may have initiated a titration to a higher antipsychotic dose. However, in the absence of any observable signs of aggression or psychosis, there was simply no indication for further titration of his antipsychotic.
- Document, document, document. When collateral information is supplied to us, it is crucial that we maintain a detailed account of this information. If we have a reason to believe that a patient poses an immediate danger to himself or others, we should carefully document our reasoning so that changes in behavior (if any) can be observed on a day-to-day basis.
1. Testa M, West SG. Civil commitment in the United States. Psychiatry (Edgmont). 2010;7(10):30-40.
2. Roe D, Weishut DJ, Jaglom M, et al. Patients’ and staff members’ attitudes about the rights of hospitalized psychiatric patients. Psychiatr Serv. 2002;53(1):87-91.
3. Crichton P, Carel H, Kidd IJ. Epistemic injustice in psychiatry. BJPsych Bull. 2017;41(2):65-70.
4. Marett C, Mossman D. What is your liability for involuntary commitment based on fault information? Current Psychiatry. 2017;16(3):21-25,33.
5. Lincoln AL, Allen M. The influence of collateral information on access to inpatient psychiatric services. International Journal of Psychosocial Rehabilitation. 2002;6:99-108.
1. Testa M, West SG. Civil commitment in the United States. Psychiatry (Edgmont). 2010;7(10):30-40.
2. Roe D, Weishut DJ, Jaglom M, et al. Patients’ and staff members’ attitudes about the rights of hospitalized psychiatric patients. Psychiatr Serv. 2002;53(1):87-91.
3. Crichton P, Carel H, Kidd IJ. Epistemic injustice in psychiatry. BJPsych Bull. 2017;41(2):65-70.
4. Marett C, Mossman D. What is your liability for involuntary commitment based on fault information? Current Psychiatry. 2017;16(3):21-25,33.
5. Lincoln AL, Allen M. The influence of collateral information on access to inpatient psychiatric services. International Journal of Psychosocial Rehabilitation. 2002;6:99-108.
The gift of misery
On the first day of my psychiatry clerkship, I sat at a table with another student, 2 residents, and our attending physician. This wasn’t my first clinical rotation, but it was my first formal exposure to psychiatry, and I was excited and a bit anxious because I was considering psychiatry as an area of specialty training for myself. I’d been assigned 1 patient that morning: a 42-year-old man admitted for alcohol withdrawal. Our team, the psychiatry consultation-liaison team, was asked to evaluate the patient’s depressed mood in the context of withdrawal. As I began to present the patient’s story, I spoke of how terrible this man’s life had been, and how depressed he had recently become; this depression, I said, was likely exacerbated by alcohol use, but he was dealing with his depression by drinking more. He now wanted to quit for good. My attending, whom I had just met, interrupted me: “Misery,” she said with an intense look, “is a gift to an addicted person.”
I have ruminated on those surprising words ever since, and in that time I have begun to understand something about misery through the eyes of my patients. Sick people often are miserable; physical ailments can wreck hopes and plans and suck the joy from seemingly everything. Individuals who are ill or in pain often are suffering psychologically as well as physically. This suffering has been especially apparent to me in patients withdrawing from addictive substances: alcohol, cocaine, heroin, nicotine. I have been begged, cursed, praised, thanked, and more based on my ability or inability to relieve someone’s suffering caused by the lack of a certain substance: Please, just one cigarette. Please, something for this pain. Please, something to drink. As a medical student, I did one of 2 things: stood there helpless, or promised I would do the best I could, knowing my resident or attending would likely tell them no.
Withdrawal from addictive substances is, unsurprisingly, not pleasant. Alcohol withdrawal is one of the few that can be fatal, due to its ability to cause autonomic instability and seizures. Withdrawing from alcohol is also unpleasant due to hallucinosis and tremors, on top of the very real cravings for the substance itself. My patient knew this; he had withdrawn from alcohol in the past. As he talked to me, though, it became clear he had finally decided this was the end. In the past, others encouraged him to stop drinking; this time he was doing it for himself. His life had become so dismal that he was willing to undergo the agony of withdrawal to be free from his addiction.
Was his suffering, then, his misery, a gift? As I came to know my attending better, I also came to understand what these jarring words meant to her. They were her version of the old adage: It’s only when you hit rock bottom that you can start climbing back out. It isn’t the misery of withdrawing, but the misery inflicted by the substance that might provide an unexpected opportunity to start fixing things. For my patient, this particular trip to the hospital—which happened to intersect in space and time with me, a third-year medical student keen to learn and to help—was rock bottom, and he knew it. His life had been destroyed by his addiction, and here, at this intersection, the destruction was so great that he was finally willing to make a change for the better.
It is counterintuitive to think of misery as a gift, but then again, this patient—and more broadly, all patients whose lives are tormented by addiction and substance abuse—are often on the receiving end of counterintuitive advice, and it is frequently the only way to enact lasting change. Consider, for example, Alcoholics’ Anonymous, which works for far more individuals than one might expect. It does not seem possible that a small group without formal training could keep people sober simply by talking openly about their struggles; yet every day throughout the world, it does just that.
Patients struggling with addiction—labeled as addicts and drug-seekers by most of the world—are often written off as “difficult patients.” Perhaps because of my inexperience, I didn’t see this man as difficult, or as just another case of alcohol withdrawal. Although it may often be easier to define someone by his or her disease, I believe in choosing to see the human underneath the label. To me, these patients are not difficult; they are broken and miserable, and they desperately need help. Knowing this, I am forced to consider just how bad things have gotten for them, and how hard it must be to make a change. Their brokenness may be an opportunity to start down a new path, but only if we extend that invitation. Such an invitation may be the first step to turning genuine misery into a gift.
When I’m asked why I have chosen psychiatry, willingly entering such a “difficult field,” I think about my experience on that consult service and this patient. I know that I’m still just beginning my journey, and that even more difficult moments and patients lie ahead. But difficulty depends on one’s perspective; certainly that patient, trying to free himself from addiction’s grasp, was “going through a difficult time.” This is of course a platitude; the word “misery” gets much closer to the truth. I usually answer with some variation of the following: Medicine, especially psychiatry, is about caring for those who need it most: hurting, vulnera
On the first day of my psychiatry clerkship, I sat at a table with another student, 2 residents, and our attending physician. This wasn’t my first clinical rotation, but it was my first formal exposure to psychiatry, and I was excited and a bit anxious because I was considering psychiatry as an area of specialty training for myself. I’d been assigned 1 patient that morning: a 42-year-old man admitted for alcohol withdrawal. Our team, the psychiatry consultation-liaison team, was asked to evaluate the patient’s depressed mood in the context of withdrawal. As I began to present the patient’s story, I spoke of how terrible this man’s life had been, and how depressed he had recently become; this depression, I said, was likely exacerbated by alcohol use, but he was dealing with his depression by drinking more. He now wanted to quit for good. My attending, whom I had just met, interrupted me: “Misery,” she said with an intense look, “is a gift to an addicted person.”
I have ruminated on those surprising words ever since, and in that time I have begun to understand something about misery through the eyes of my patients. Sick people often are miserable; physical ailments can wreck hopes and plans and suck the joy from seemingly everything. Individuals who are ill or in pain often are suffering psychologically as well as physically. This suffering has been especially apparent to me in patients withdrawing from addictive substances: alcohol, cocaine, heroin, nicotine. I have been begged, cursed, praised, thanked, and more based on my ability or inability to relieve someone’s suffering caused by the lack of a certain substance: Please, just one cigarette. Please, something for this pain. Please, something to drink. As a medical student, I did one of 2 things: stood there helpless, or promised I would do the best I could, knowing my resident or attending would likely tell them no.
Withdrawal from addictive substances is, unsurprisingly, not pleasant. Alcohol withdrawal is one of the few that can be fatal, due to its ability to cause autonomic instability and seizures. Withdrawing from alcohol is also unpleasant due to hallucinosis and tremors, on top of the very real cravings for the substance itself. My patient knew this; he had withdrawn from alcohol in the past. As he talked to me, though, it became clear he had finally decided this was the end. In the past, others encouraged him to stop drinking; this time he was doing it for himself. His life had become so dismal that he was willing to undergo the agony of withdrawal to be free from his addiction.
Was his suffering, then, his misery, a gift? As I came to know my attending better, I also came to understand what these jarring words meant to her. They were her version of the old adage: It’s only when you hit rock bottom that you can start climbing back out. It isn’t the misery of withdrawing, but the misery inflicted by the substance that might provide an unexpected opportunity to start fixing things. For my patient, this particular trip to the hospital—which happened to intersect in space and time with me, a third-year medical student keen to learn and to help—was rock bottom, and he knew it. His life had been destroyed by his addiction, and here, at this intersection, the destruction was so great that he was finally willing to make a change for the better.
It is counterintuitive to think of misery as a gift, but then again, this patient—and more broadly, all patients whose lives are tormented by addiction and substance abuse—are often on the receiving end of counterintuitive advice, and it is frequently the only way to enact lasting change. Consider, for example, Alcoholics’ Anonymous, which works for far more individuals than one might expect. It does not seem possible that a small group without formal training could keep people sober simply by talking openly about their struggles; yet every day throughout the world, it does just that.
Patients struggling with addiction—labeled as addicts and drug-seekers by most of the world—are often written off as “difficult patients.” Perhaps because of my inexperience, I didn’t see this man as difficult, or as just another case of alcohol withdrawal. Although it may often be easier to define someone by his or her disease, I believe in choosing to see the human underneath the label. To me, these patients are not difficult; they are broken and miserable, and they desperately need help. Knowing this, I am forced to consider just how bad things have gotten for them, and how hard it must be to make a change. Their brokenness may be an opportunity to start down a new path, but only if we extend that invitation. Such an invitation may be the first step to turning genuine misery into a gift.
When I’m asked why I have chosen psychiatry, willingly entering such a “difficult field,” I think about my experience on that consult service and this patient. I know that I’m still just beginning my journey, and that even more difficult moments and patients lie ahead. But difficulty depends on one’s perspective; certainly that patient, trying to free himself from addiction’s grasp, was “going through a difficult time.” This is of course a platitude; the word “misery” gets much closer to the truth. I usually answer with some variation of the following: Medicine, especially psychiatry, is about caring for those who need it most: hurting, vulnera
On the first day of my psychiatry clerkship, I sat at a table with another student, 2 residents, and our attending physician. This wasn’t my first clinical rotation, but it was my first formal exposure to psychiatry, and I was excited and a bit anxious because I was considering psychiatry as an area of specialty training for myself. I’d been assigned 1 patient that morning: a 42-year-old man admitted for alcohol withdrawal. Our team, the psychiatry consultation-liaison team, was asked to evaluate the patient’s depressed mood in the context of withdrawal. As I began to present the patient’s story, I spoke of how terrible this man’s life had been, and how depressed he had recently become; this depression, I said, was likely exacerbated by alcohol use, but he was dealing with his depression by drinking more. He now wanted to quit for good. My attending, whom I had just met, interrupted me: “Misery,” she said with an intense look, “is a gift to an addicted person.”
I have ruminated on those surprising words ever since, and in that time I have begun to understand something about misery through the eyes of my patients. Sick people often are miserable; physical ailments can wreck hopes and plans and suck the joy from seemingly everything. Individuals who are ill or in pain often are suffering psychologically as well as physically. This suffering has been especially apparent to me in patients withdrawing from addictive substances: alcohol, cocaine, heroin, nicotine. I have been begged, cursed, praised, thanked, and more based on my ability or inability to relieve someone’s suffering caused by the lack of a certain substance: Please, just one cigarette. Please, something for this pain. Please, something to drink. As a medical student, I did one of 2 things: stood there helpless, or promised I would do the best I could, knowing my resident or attending would likely tell them no.
Withdrawal from addictive substances is, unsurprisingly, not pleasant. Alcohol withdrawal is one of the few that can be fatal, due to its ability to cause autonomic instability and seizures. Withdrawing from alcohol is also unpleasant due to hallucinosis and tremors, on top of the very real cravings for the substance itself. My patient knew this; he had withdrawn from alcohol in the past. As he talked to me, though, it became clear he had finally decided this was the end. In the past, others encouraged him to stop drinking; this time he was doing it for himself. His life had become so dismal that he was willing to undergo the agony of withdrawal to be free from his addiction.
Was his suffering, then, his misery, a gift? As I came to know my attending better, I also came to understand what these jarring words meant to her. They were her version of the old adage: It’s only when you hit rock bottom that you can start climbing back out. It isn’t the misery of withdrawing, but the misery inflicted by the substance that might provide an unexpected opportunity to start fixing things. For my patient, this particular trip to the hospital—which happened to intersect in space and time with me, a third-year medical student keen to learn and to help—was rock bottom, and he knew it. His life had been destroyed by his addiction, and here, at this intersection, the destruction was so great that he was finally willing to make a change for the better.
It is counterintuitive to think of misery as a gift, but then again, this patient—and more broadly, all patients whose lives are tormented by addiction and substance abuse—are often on the receiving end of counterintuitive advice, and it is frequently the only way to enact lasting change. Consider, for example, Alcoholics’ Anonymous, which works for far more individuals than one might expect. It does not seem possible that a small group without formal training could keep people sober simply by talking openly about their struggles; yet every day throughout the world, it does just that.
Patients struggling with addiction—labeled as addicts and drug-seekers by most of the world—are often written off as “difficult patients.” Perhaps because of my inexperience, I didn’t see this man as difficult, or as just another case of alcohol withdrawal. Although it may often be easier to define someone by his or her disease, I believe in choosing to see the human underneath the label. To me, these patients are not difficult; they are broken and miserable, and they desperately need help. Knowing this, I am forced to consider just how bad things have gotten for them, and how hard it must be to make a change. Their brokenness may be an opportunity to start down a new path, but only if we extend that invitation. Such an invitation may be the first step to turning genuine misery into a gift.
When I’m asked why I have chosen psychiatry, willingly entering such a “difficult field,” I think about my experience on that consult service and this patient. I know that I’m still just beginning my journey, and that even more difficult moments and patients lie ahead. But difficulty depends on one’s perspective; certainly that patient, trying to free himself from addiction’s grasp, was “going through a difficult time.” This is of course a platitude; the word “misery” gets much closer to the truth. I usually answer with some variation of the following: Medicine, especially psychiatry, is about caring for those who need it most: hurting, vulnera
Fulfillment within success: A physician’s dilemma
They say success without fulfillment is of little value in life. Whether this concept is actually driving the spate of depression and substance abuse currently experienced by youth and middle-aged adults in developed countries is rarely discussed and needs to be explored.
We have all reflected on the tragic ends of Anthony Bourdain, Kate Spade, and Robin Williams. Much has been said about the accolades they achieved and the heights they scaled, and just as much about their struggles with substance abuse over the years. Sensational portrayals by the media also encouraged youth to spend time dissecting the details of these high-profile deaths, lending popularity to the notion of suicide contagion. But somewhere in the myriad theories and conclusions, we still seem baffled by the questions of why these suicides occurred, and why no one had seen them coming.
As humans, we are designed to build. For many people, including physicians, the final product is a rewarding career built on years of hard work, or a flourishing family to look back on be proud of. Sometimes, however, these larger ideas barely intersect with our pictures of success.
As physicians and high achievers, we dream of goals and ambitions and set stringent deadlines for achieving them. Falling short sometimes finds us grappling with self-punishment and doubt. When one goal is achieved, another one is automatically created, or the goal post is pushed further. And the cycle continues.
Having said this, I will ask: What are you looking for? What is it that will give you a sense of purpose?
This is not a redundant question, nor is it an easy one. So are you really taking the time to think about it? Does any of this border on self-reflection and self-awareness for you? If it does, then developing that insight into yourself is perhaps a better way of serving your patients.
Peace and gratification often lie in the little things; not everything you do has to be acknowledged with an award. There is a sense of fulfillment that comes from developing others. The key is to realize that there is never a moment to start doing that—it is an ongoing journey. Therefore, give generously, of your time, of your skills, of your knowledge, but above all, of your kindness. Do it because in the end, you will have something to look back on and be proud of. Do it because maybe somewhere you will find meaning in it. And your success may not be bereft of fulfillment.
They say success without fulfillment is of little value in life. Whether this concept is actually driving the spate of depression and substance abuse currently experienced by youth and middle-aged adults in developed countries is rarely discussed and needs to be explored.
We have all reflected on the tragic ends of Anthony Bourdain, Kate Spade, and Robin Williams. Much has been said about the accolades they achieved and the heights they scaled, and just as much about their struggles with substance abuse over the years. Sensational portrayals by the media also encouraged youth to spend time dissecting the details of these high-profile deaths, lending popularity to the notion of suicide contagion. But somewhere in the myriad theories and conclusions, we still seem baffled by the questions of why these suicides occurred, and why no one had seen them coming.
As humans, we are designed to build. For many people, including physicians, the final product is a rewarding career built on years of hard work, or a flourishing family to look back on be proud of. Sometimes, however, these larger ideas barely intersect with our pictures of success.
As physicians and high achievers, we dream of goals and ambitions and set stringent deadlines for achieving them. Falling short sometimes finds us grappling with self-punishment and doubt. When one goal is achieved, another one is automatically created, or the goal post is pushed further. And the cycle continues.
Having said this, I will ask: What are you looking for? What is it that will give you a sense of purpose?
This is not a redundant question, nor is it an easy one. So are you really taking the time to think about it? Does any of this border on self-reflection and self-awareness for you? If it does, then developing that insight into yourself is perhaps a better way of serving your patients.
Peace and gratification often lie in the little things; not everything you do has to be acknowledged with an award. There is a sense of fulfillment that comes from developing others. The key is to realize that there is never a moment to start doing that—it is an ongoing journey. Therefore, give generously, of your time, of your skills, of your knowledge, but above all, of your kindness. Do it because in the end, you will have something to look back on and be proud of. Do it because maybe somewhere you will find meaning in it. And your success may not be bereft of fulfillment.
They say success without fulfillment is of little value in life. Whether this concept is actually driving the spate of depression and substance abuse currently experienced by youth and middle-aged adults in developed countries is rarely discussed and needs to be explored.
We have all reflected on the tragic ends of Anthony Bourdain, Kate Spade, and Robin Williams. Much has been said about the accolades they achieved and the heights they scaled, and just as much about their struggles with substance abuse over the years. Sensational portrayals by the media also encouraged youth to spend time dissecting the details of these high-profile deaths, lending popularity to the notion of suicide contagion. But somewhere in the myriad theories and conclusions, we still seem baffled by the questions of why these suicides occurred, and why no one had seen them coming.
As humans, we are designed to build. For many people, including physicians, the final product is a rewarding career built on years of hard work, or a flourishing family to look back on be proud of. Sometimes, however, these larger ideas barely intersect with our pictures of success.
As physicians and high achievers, we dream of goals and ambitions and set stringent deadlines for achieving them. Falling short sometimes finds us grappling with self-punishment and doubt. When one goal is achieved, another one is automatically created, or the goal post is pushed further. And the cycle continues.
Having said this, I will ask: What are you looking for? What is it that will give you a sense of purpose?
This is not a redundant question, nor is it an easy one. So are you really taking the time to think about it? Does any of this border on self-reflection and self-awareness for you? If it does, then developing that insight into yourself is perhaps a better way of serving your patients.
Peace and gratification often lie in the little things; not everything you do has to be acknowledged with an award. There is a sense of fulfillment that comes from developing others. The key is to realize that there is never a moment to start doing that—it is an ongoing journey. Therefore, give generously, of your time, of your skills, of your knowledge, but above all, of your kindness. Do it because in the end, you will have something to look back on and be proud of. Do it because maybe somewhere you will find meaning in it. And your success may not be bereft of fulfillment.
A transgender adolescent with chronic pain, depression, and PTSD
X, a 17-year-old Mexican-American transgender male (assigned female at birth) experienced a traumatic brain injury (TBI) 4 years ago and subsequently developed posttraumatic stress disorder (PTSD). I came to treat X at a pediatric outpatient psychiatric clinic after he developed physiologic dysregulation of his nervous system and began to experience panic attacks, major depressive disorder, and auditory hallucinations. X also developed chronic widespread pain during the next few years, including migraines, abdominal pain, and back pain, which significantly impaired his ability to function socially and academically. X was treated by a child and adolescent psychiatrist who used an integrative approach of traditional and complementary medical practices in a pediatric chronic pain clinic.
X’s treatment course at the pediatric psychiatric clinic included 2 years of field capable mental health services. During this time, fluoxetine was started and titrated up to 40 mg/d to target anxiety and depressive symptoms such as pervasive sadness, poor self-esteem, poor concentration, physiologic arousal, and sleep disruption. Risperidone, 2 mg/d, was temporarily added to address residual mood symptoms and the auditory hallucinations X experienced at school. Neuropsychological testing did not indicate that X had cognitive impairments from the TBI. In the pain clinic, X was encouraged to continue with psychotherapy and the selective serotonin reuptake inhibitor. Another recommendation was to seek out acupuncture and yoga. Over the course of 1 year, X’s pain symptoms began to resolve, and his functioning improved significantly. It was during this year that X came out as transgender, first to his friends, and then to his family and his physicians.
The link between PTSD and chronic pain
X’s PTSD presented as nightmares, hypervigilance, and anxiety, especially when he was in school. He would often describe how his chronic pain symptoms prevented him from functioning academically and socially. I wondered if X’s presentation of PTSD indicated a predisposition for chronic widespread pain symptoms or pain syndromes. This theory could be approximated by an association, but research suggests there is a significant temporal relationship between PTSD and widespread pain symptoms, such as in fibromyalgia.
One multicenter study of patients with fibromyalgia found that the prevalence of comorbid PTSD was 45%.1 In two-thirds of patients with fibromyalgia, traumatic life events and PTSD symptoms preceded the onset of chronic widespread pain, while in roughly one-third, traumatic life events and PTSD symptoms followed the onset of chronic widespread pain.1 This study suggests that PTSD could be viewed as a marker of stress vulnerability in which individuals susceptible to stress are more likely to develop chronic widespread pain and other health problems, including fibromyalgia, when a traumatic event occurs.
Benefits of transgender-specific care
During the course of X’s psychiatric treatment, he eventually revealed that he had been experiencing gender dysphoria for many years. His gender transition was occurring during adolescence; during this time, identity formation is a central developmental task.2 X was not comfortable asking others to use his preferred pronouns until he had physiologically transitioned. Any further delay to accessing transgender-specific services would increase the likelihood of a poor prognosis, both behaviorally and medically, because sexual minority adolescents are 3 to 4 times more likely to meet criteria for an internalizing disorder and 2 to 5 times more likely to meet criteria for externalizing disorders.3 My understanding of the minority stress model raised concerns that if X did not get appropriate treatment, the interdependence of stressors of being a sexual minority as well as an ethnic minority would further burden his mental health.
Now that X had access to transgender-specific care, how would management affect his pain symptoms or response to treatment? While some of his pain symptoms began to remit before he came out as transgender, I considered whether hormone therapy might improve his subjective pain. Little research has been conducted in transgender patients to determine whether sex-steroid administration might alter nociception. One study that examined daily fluctuations of sex hormones in 8 women with fibromyalgia found trends suggesting progesterone and testosterone are inversely associated with pain, with peaks of those hormones occurring on days with lower reported pain.4 A small study of female-to-male transgender patients found that administration of sex steroids was associated with relief from chronic painful conditions (headaches, musculoskeletal pain) in 6 of 16 patients who received testosterone injections.5 What little evidence I found in regards to an association between gender-affirming hormone therapy and chronic pain left me feeling optimistic that hormone therapy would not negatively affect the prognosis of X’s chronic pain.
Another consideration in treating X was the practice of chest binding, the compression of chest tissue for masculine gender expression among people who were assigned female sex at birth. One study found that chest binding can improve mood; decrease suicidality, anxiety, and dysphoria; and increase self-esteem.6 However, 97.2% of participants reported at least one negative outcome they attributed to binding. The most common was back pain (53.8%), which X had been experiencing before he began chest binding. I found it notable that X’s primary doctors in the transgender clinic kept this adverse effect in mind when they recommended that he take breaks and limit daily hours of chest binding to minimize the risk of increased chronic back pain.
This particular case spanned several specialized services and required coordination and careful consideration to address X’s developmental and gender-related needs. X experienced significant symptoms incited by a TBI; however, the manifestation of his chronic pain symptoms were more than likely influenced by several overlapping stressors, including belonging to an ethnic minority, transitioning into adulthood, transitioning publicly as a male, and mood symptoms. While it pleased me to see how X responded positively to the integrative and holistic treatment he received, I remain concerned that simply not enough research exists that addresses how transgender individuals are affected, physically and affectively, by chronic levels of stress attributable to their minority status.
1. Häuser W, Galek A, Erbslöh-Möller B, et al. Posttraumatic stress disorder in fibromyalgia syndrome: prevalence, temporal relationship between posttraumatic stress and fibromyalgia symptoms, and impact on clinical outcome. Pain. 2013;154(8):1216-1223.
2. Erikson EH. Identity: Youth and crisis. New York, NY: W.W. Norton & Company; 1968.
3. Fergusson DM, Horwood LJ, Beautrais AL. Is sexual orientation related to mental health problems and suicidality in young people? Arch Gen Psychiatry. 1999;56(10):876-880.
4. Schertzinger M, Wesson-Sides K, Parkitny L, et al. Daily fluctuations of progesterone and testosterone are associated with fibromyalgia pain severity. J Pain. 2018;19(4):410-417.
5. Aloisi AM, Bachiocco V, Costantino A, et al. Cross-sex hormone administration changes pain in transsexual women and men. Pain. 2007;132(suppl 1):S60-S67.
6. Peitzmeier S, Gardner I, Weinand J et al. Health impact of chest binding among transgender adults: a community-engaged, cross-sectional study. Cult Health Sex. 2017;19(1):64-75.
X, a 17-year-old Mexican-American transgender male (assigned female at birth) experienced a traumatic brain injury (TBI) 4 years ago and subsequently developed posttraumatic stress disorder (PTSD). I came to treat X at a pediatric outpatient psychiatric clinic after he developed physiologic dysregulation of his nervous system and began to experience panic attacks, major depressive disorder, and auditory hallucinations. X also developed chronic widespread pain during the next few years, including migraines, abdominal pain, and back pain, which significantly impaired his ability to function socially and academically. X was treated by a child and adolescent psychiatrist who used an integrative approach of traditional and complementary medical practices in a pediatric chronic pain clinic.
X’s treatment course at the pediatric psychiatric clinic included 2 years of field capable mental health services. During this time, fluoxetine was started and titrated up to 40 mg/d to target anxiety and depressive symptoms such as pervasive sadness, poor self-esteem, poor concentration, physiologic arousal, and sleep disruption. Risperidone, 2 mg/d, was temporarily added to address residual mood symptoms and the auditory hallucinations X experienced at school. Neuropsychological testing did not indicate that X had cognitive impairments from the TBI. In the pain clinic, X was encouraged to continue with psychotherapy and the selective serotonin reuptake inhibitor. Another recommendation was to seek out acupuncture and yoga. Over the course of 1 year, X’s pain symptoms began to resolve, and his functioning improved significantly. It was during this year that X came out as transgender, first to his friends, and then to his family and his physicians.
The link between PTSD and chronic pain
X’s PTSD presented as nightmares, hypervigilance, and anxiety, especially when he was in school. He would often describe how his chronic pain symptoms prevented him from functioning academically and socially. I wondered if X’s presentation of PTSD indicated a predisposition for chronic widespread pain symptoms or pain syndromes. This theory could be approximated by an association, but research suggests there is a significant temporal relationship between PTSD and widespread pain symptoms, such as in fibromyalgia.
One multicenter study of patients with fibromyalgia found that the prevalence of comorbid PTSD was 45%.1 In two-thirds of patients with fibromyalgia, traumatic life events and PTSD symptoms preceded the onset of chronic widespread pain, while in roughly one-third, traumatic life events and PTSD symptoms followed the onset of chronic widespread pain.1 This study suggests that PTSD could be viewed as a marker of stress vulnerability in which individuals susceptible to stress are more likely to develop chronic widespread pain and other health problems, including fibromyalgia, when a traumatic event occurs.
Benefits of transgender-specific care
During the course of X’s psychiatric treatment, he eventually revealed that he had been experiencing gender dysphoria for many years. His gender transition was occurring during adolescence; during this time, identity formation is a central developmental task.2 X was not comfortable asking others to use his preferred pronouns until he had physiologically transitioned. Any further delay to accessing transgender-specific services would increase the likelihood of a poor prognosis, both behaviorally and medically, because sexual minority adolescents are 3 to 4 times more likely to meet criteria for an internalizing disorder and 2 to 5 times more likely to meet criteria for externalizing disorders.3 My understanding of the minority stress model raised concerns that if X did not get appropriate treatment, the interdependence of stressors of being a sexual minority as well as an ethnic minority would further burden his mental health.
Now that X had access to transgender-specific care, how would management affect his pain symptoms or response to treatment? While some of his pain symptoms began to remit before he came out as transgender, I considered whether hormone therapy might improve his subjective pain. Little research has been conducted in transgender patients to determine whether sex-steroid administration might alter nociception. One study that examined daily fluctuations of sex hormones in 8 women with fibromyalgia found trends suggesting progesterone and testosterone are inversely associated with pain, with peaks of those hormones occurring on days with lower reported pain.4 A small study of female-to-male transgender patients found that administration of sex steroids was associated with relief from chronic painful conditions (headaches, musculoskeletal pain) in 6 of 16 patients who received testosterone injections.5 What little evidence I found in regards to an association between gender-affirming hormone therapy and chronic pain left me feeling optimistic that hormone therapy would not negatively affect the prognosis of X’s chronic pain.
Another consideration in treating X was the practice of chest binding, the compression of chest tissue for masculine gender expression among people who were assigned female sex at birth. One study found that chest binding can improve mood; decrease suicidality, anxiety, and dysphoria; and increase self-esteem.6 However, 97.2% of participants reported at least one negative outcome they attributed to binding. The most common was back pain (53.8%), which X had been experiencing before he began chest binding. I found it notable that X’s primary doctors in the transgender clinic kept this adverse effect in mind when they recommended that he take breaks and limit daily hours of chest binding to minimize the risk of increased chronic back pain.
This particular case spanned several specialized services and required coordination and careful consideration to address X’s developmental and gender-related needs. X experienced significant symptoms incited by a TBI; however, the manifestation of his chronic pain symptoms were more than likely influenced by several overlapping stressors, including belonging to an ethnic minority, transitioning into adulthood, transitioning publicly as a male, and mood symptoms. While it pleased me to see how X responded positively to the integrative and holistic treatment he received, I remain concerned that simply not enough research exists that addresses how transgender individuals are affected, physically and affectively, by chronic levels of stress attributable to their minority status.
X, a 17-year-old Mexican-American transgender male (assigned female at birth) experienced a traumatic brain injury (TBI) 4 years ago and subsequently developed posttraumatic stress disorder (PTSD). I came to treat X at a pediatric outpatient psychiatric clinic after he developed physiologic dysregulation of his nervous system and began to experience panic attacks, major depressive disorder, and auditory hallucinations. X also developed chronic widespread pain during the next few years, including migraines, abdominal pain, and back pain, which significantly impaired his ability to function socially and academically. X was treated by a child and adolescent psychiatrist who used an integrative approach of traditional and complementary medical practices in a pediatric chronic pain clinic.
X’s treatment course at the pediatric psychiatric clinic included 2 years of field capable mental health services. During this time, fluoxetine was started and titrated up to 40 mg/d to target anxiety and depressive symptoms such as pervasive sadness, poor self-esteem, poor concentration, physiologic arousal, and sleep disruption. Risperidone, 2 mg/d, was temporarily added to address residual mood symptoms and the auditory hallucinations X experienced at school. Neuropsychological testing did not indicate that X had cognitive impairments from the TBI. In the pain clinic, X was encouraged to continue with psychotherapy and the selective serotonin reuptake inhibitor. Another recommendation was to seek out acupuncture and yoga. Over the course of 1 year, X’s pain symptoms began to resolve, and his functioning improved significantly. It was during this year that X came out as transgender, first to his friends, and then to his family and his physicians.
The link between PTSD and chronic pain
X’s PTSD presented as nightmares, hypervigilance, and anxiety, especially when he was in school. He would often describe how his chronic pain symptoms prevented him from functioning academically and socially. I wondered if X’s presentation of PTSD indicated a predisposition for chronic widespread pain symptoms or pain syndromes. This theory could be approximated by an association, but research suggests there is a significant temporal relationship between PTSD and widespread pain symptoms, such as in fibromyalgia.
One multicenter study of patients with fibromyalgia found that the prevalence of comorbid PTSD was 45%.1 In two-thirds of patients with fibromyalgia, traumatic life events and PTSD symptoms preceded the onset of chronic widespread pain, while in roughly one-third, traumatic life events and PTSD symptoms followed the onset of chronic widespread pain.1 This study suggests that PTSD could be viewed as a marker of stress vulnerability in which individuals susceptible to stress are more likely to develop chronic widespread pain and other health problems, including fibromyalgia, when a traumatic event occurs.
Benefits of transgender-specific care
During the course of X’s psychiatric treatment, he eventually revealed that he had been experiencing gender dysphoria for many years. His gender transition was occurring during adolescence; during this time, identity formation is a central developmental task.2 X was not comfortable asking others to use his preferred pronouns until he had physiologically transitioned. Any further delay to accessing transgender-specific services would increase the likelihood of a poor prognosis, both behaviorally and medically, because sexual minority adolescents are 3 to 4 times more likely to meet criteria for an internalizing disorder and 2 to 5 times more likely to meet criteria for externalizing disorders.3 My understanding of the minority stress model raised concerns that if X did not get appropriate treatment, the interdependence of stressors of being a sexual minority as well as an ethnic minority would further burden his mental health.
Now that X had access to transgender-specific care, how would management affect his pain symptoms or response to treatment? While some of his pain symptoms began to remit before he came out as transgender, I considered whether hormone therapy might improve his subjective pain. Little research has been conducted in transgender patients to determine whether sex-steroid administration might alter nociception. One study that examined daily fluctuations of sex hormones in 8 women with fibromyalgia found trends suggesting progesterone and testosterone are inversely associated with pain, with peaks of those hormones occurring on days with lower reported pain.4 A small study of female-to-male transgender patients found that administration of sex steroids was associated with relief from chronic painful conditions (headaches, musculoskeletal pain) in 6 of 16 patients who received testosterone injections.5 What little evidence I found in regards to an association between gender-affirming hormone therapy and chronic pain left me feeling optimistic that hormone therapy would not negatively affect the prognosis of X’s chronic pain.
Another consideration in treating X was the practice of chest binding, the compression of chest tissue for masculine gender expression among people who were assigned female sex at birth. One study found that chest binding can improve mood; decrease suicidality, anxiety, and dysphoria; and increase self-esteem.6 However, 97.2% of participants reported at least one negative outcome they attributed to binding. The most common was back pain (53.8%), which X had been experiencing before he began chest binding. I found it notable that X’s primary doctors in the transgender clinic kept this adverse effect in mind when they recommended that he take breaks and limit daily hours of chest binding to minimize the risk of increased chronic back pain.
This particular case spanned several specialized services and required coordination and careful consideration to address X’s developmental and gender-related needs. X experienced significant symptoms incited by a TBI; however, the manifestation of his chronic pain symptoms were more than likely influenced by several overlapping stressors, including belonging to an ethnic minority, transitioning into adulthood, transitioning publicly as a male, and mood symptoms. While it pleased me to see how X responded positively to the integrative and holistic treatment he received, I remain concerned that simply not enough research exists that addresses how transgender individuals are affected, physically and affectively, by chronic levels of stress attributable to their minority status.
1. Häuser W, Galek A, Erbslöh-Möller B, et al. Posttraumatic stress disorder in fibromyalgia syndrome: prevalence, temporal relationship between posttraumatic stress and fibromyalgia symptoms, and impact on clinical outcome. Pain. 2013;154(8):1216-1223.
2. Erikson EH. Identity: Youth and crisis. New York, NY: W.W. Norton & Company; 1968.
3. Fergusson DM, Horwood LJ, Beautrais AL. Is sexual orientation related to mental health problems and suicidality in young people? Arch Gen Psychiatry. 1999;56(10):876-880.
4. Schertzinger M, Wesson-Sides K, Parkitny L, et al. Daily fluctuations of progesterone and testosterone are associated with fibromyalgia pain severity. J Pain. 2018;19(4):410-417.
5. Aloisi AM, Bachiocco V, Costantino A, et al. Cross-sex hormone administration changes pain in transsexual women and men. Pain. 2007;132(suppl 1):S60-S67.
6. Peitzmeier S, Gardner I, Weinand J et al. Health impact of chest binding among transgender adults: a community-engaged, cross-sectional study. Cult Health Sex. 2017;19(1):64-75.
1. Häuser W, Galek A, Erbslöh-Möller B, et al. Posttraumatic stress disorder in fibromyalgia syndrome: prevalence, temporal relationship between posttraumatic stress and fibromyalgia symptoms, and impact on clinical outcome. Pain. 2013;154(8):1216-1223.
2. Erikson EH. Identity: Youth and crisis. New York, NY: W.W. Norton & Company; 1968.
3. Fergusson DM, Horwood LJ, Beautrais AL. Is sexual orientation related to mental health problems and suicidality in young people? Arch Gen Psychiatry. 1999;56(10):876-880.
4. Schertzinger M, Wesson-Sides K, Parkitny L, et al. Daily fluctuations of progesterone and testosterone are associated with fibromyalgia pain severity. J Pain. 2018;19(4):410-417.
5. Aloisi AM, Bachiocco V, Costantino A, et al. Cross-sex hormone administration changes pain in transsexual women and men. Pain. 2007;132(suppl 1):S60-S67.
6. Peitzmeier S, Gardner I, Weinand J et al. Health impact of chest binding among transgender adults: a community-engaged, cross-sectional study. Cult Health Sex. 2017;19(1):64-75.