User login
Using transcatheter aortic valves for severe mitral annular calcification
PARIS – Transcatheter mitral valve replacement using a repurposed transcatheter aortic valve in patients with severe symptomatic native mitral valve disease and severe mitral annular calcification is feasible and may be an option in carefully selected patients who aren’t candidates for surgery, Mayra Guerrero, MD, said at the annual congress of the European Association of Percutaneous Cardiovascular Interventions.
However, at this early point in development, the procedure is associated with an exceptionally steep learning curve, said Dr. Guerrero, director of cardiac structural interventions at the NorthShore University Health System in Evanston, Ill.
She presented the procedural and 30-day outcomes for the first 104 patients entered into a global registry encompassing 47 centers in 11 countries. Nearly 90% of patients received an Edwards SAPIEN XT or SAPIEN 3 valve. The EuroPCR results update an earlier report on the first 64 patients in the registry (JACC Cardiovasc Interv. 2016 Jul 11;9[13]:1361-71).
The results, she said, are reminiscent of the early days in transcatheter aortic valve replacement, which were marked by an initial very high early mortality rate that fell dramatically as technology and techniques improved.
“We know that there are important things we need to improve. Left ventricular outflow tract obstruction is the Achilles heel of this procedure; we need to work on its prevention and management. We need better annulus sizing methods. We need to find the best delivery method and improve our patient selection in order to avoid taking on patients who are too sick. Still, even during this early experience, the technical success rate has improved, and 30-day mortality continues to drop,” Dr. Guerrero said.
Indeed, the 30-day all-cause mortality rate of 25% in the first 104 patients doesn’t tell the whole story. The rate was 37.5% in the first third of patients, fell to 21.9% in the second tertile, and then to 15% in the most recent tertile.
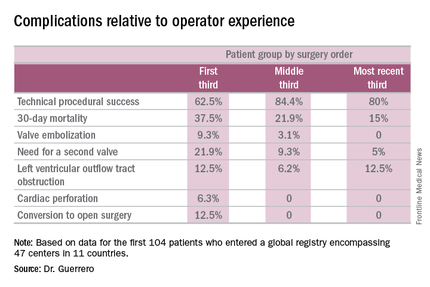
Similarly, the technical success rate of the procedure according to Mitral Valve Academic Research Consortium criteria improved from 62.5% in the first tertile of patients to 84.4% and 80% in the second and third, respectively, she continued.
The rates of almost all complications went down with greater operator experience, too. The notable exception was left ventricular outflow tract obstruction (LVOTO). It occurred in 12.5% of patients in the first tertile and remained unchanged in the third.
It’s noteworthy that the majority of deaths were noncardiac in nature. Patients with mitral annular calcification are a high-risk group even before they develop valvular dysfunction. They are typically older and have multiple comorbidities. Participants in the global registry had a mean Society of Thoracic Surgeons score of 14.4; 38% had diabetes, 45% had chronic obstructive pulmonary disease, 35% had heart failure, 34% had previously undergone coronary artery bypass surgery, and roughly half of patients had a prior aortic valve replacement.
Causes of noncardiac mortality within 30 days included multiorgan failure in 8.6% of subjects, pneumonia in 2.9%, infection in 1.9%, and one fatal thoracentesis-related bleeding complication.
Cardiovascular deaths included two cases due to left ventricular perforation, two fatal strokes, an MI due to air emboli, a lethal complete atrioventricular block, and three deaths owing to LVOTO.
Alcohol ablation met with some success as a bailout treatment in cases of LVOTO with hemodynamic compromise after transmitral valve replacement in the global registry. All six treated patients had significant improvement initially, although the LVOTO recurred the next day in one instance. Four of the six patients were discharged from the hospital. One patient died because of atrioventricular block, and another from multiorgan failure 3 weeks after alcohol ablation of the LVOTO.
Dr. Guerrero has been a leader in this new field. She reported the first percutaneous implantation of a balloon expandable transcatheter valve in a native mitral valve without a surgical incision (Catheter Cardiovasc Interv. 2014 Jun 1;83[7]:E287-91), and more recently, together with coworkers developed a percutaneous alcohol ablation technique for acute reduction of LVOTO due to transcatheter mitral valve replacement (Catheter Cardiovasc Interv. 2016 Jul 5. doi:10.1002/ccd.26649).
She is now the principal investigator in the ongoing Mitral Implantation of Transcatheter Valves (MITRAL) trial, a physician-sponsored, 90-patient pilot study underway at six U.S. sites. MITRAL is recruiting three patient populations for transcatheter mitral valve replacement: patients like those in the global registry, with native mitral valve disease and severe mitral annular calcification; those with a symptomatic failing surgical ring with severe mitral regurgitation or stenosis; and patients with a symptomatic failing surgical bioprosthesis with severe mitral regurgitation or stenosis.
Discussant Nicolo Piazza, MD, of McGill University, Montreal, said transcatheter mitral valve replacement in mitral valve disease with severe mitral annular calcification in patients unsuitable for surgery “definitely represents an unmet clinical need in our practice today.” But he urged caution in interpreting the global registry data.
“This is a real world registry study with inherent selection bias and physician reporting bias,” the cardiologist said.
“We are leveraging a therapy from the aortic field into the mitral field. Of course, we do not have dedicated devices yet to treat these patients. The main finding of this study is that the procedure is actually feasible,” Dr. Piazza said.
Still, it’s sobering that at least 1 in 10 treated patients experiences LVOTO, 1 in 10 requires a second valve, and technical success is achieved in 3 out of 4 patients, he added.
Dr. Piazza predicted that multislice CT scans will be “extremely important” in refining patient selection criteria for the procedure, and echocardiography will be helpful in understanding the optimal procedural techniques and viewing angles. Work also needs to be done on developing optimal anticoagulation protocols in order to avoid valve thrombosis.
Dr. Guerrero reported serving as a consultant to Edwards Lifesciences. Dr. Piazza is a consultant to Medtronic and MicroPort.
PARIS – Transcatheter mitral valve replacement using a repurposed transcatheter aortic valve in patients with severe symptomatic native mitral valve disease and severe mitral annular calcification is feasible and may be an option in carefully selected patients who aren’t candidates for surgery, Mayra Guerrero, MD, said at the annual congress of the European Association of Percutaneous Cardiovascular Interventions.
However, at this early point in development, the procedure is associated with an exceptionally steep learning curve, said Dr. Guerrero, director of cardiac structural interventions at the NorthShore University Health System in Evanston, Ill.
She presented the procedural and 30-day outcomes for the first 104 patients entered into a global registry encompassing 47 centers in 11 countries. Nearly 90% of patients received an Edwards SAPIEN XT or SAPIEN 3 valve. The EuroPCR results update an earlier report on the first 64 patients in the registry (JACC Cardiovasc Interv. 2016 Jul 11;9[13]:1361-71).
The results, she said, are reminiscent of the early days in transcatheter aortic valve replacement, which were marked by an initial very high early mortality rate that fell dramatically as technology and techniques improved.
“We know that there are important things we need to improve. Left ventricular outflow tract obstruction is the Achilles heel of this procedure; we need to work on its prevention and management. We need better annulus sizing methods. We need to find the best delivery method and improve our patient selection in order to avoid taking on patients who are too sick. Still, even during this early experience, the technical success rate has improved, and 30-day mortality continues to drop,” Dr. Guerrero said.
Indeed, the 30-day all-cause mortality rate of 25% in the first 104 patients doesn’t tell the whole story. The rate was 37.5% in the first third of patients, fell to 21.9% in the second tertile, and then to 15% in the most recent tertile.
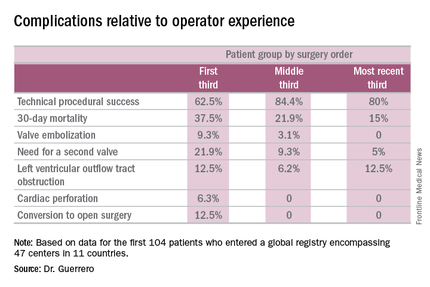
Similarly, the technical success rate of the procedure according to Mitral Valve Academic Research Consortium criteria improved from 62.5% in the first tertile of patients to 84.4% and 80% in the second and third, respectively, she continued.
The rates of almost all complications went down with greater operator experience, too. The notable exception was left ventricular outflow tract obstruction (LVOTO). It occurred in 12.5% of patients in the first tertile and remained unchanged in the third.
It’s noteworthy that the majority of deaths were noncardiac in nature. Patients with mitral annular calcification are a high-risk group even before they develop valvular dysfunction. They are typically older and have multiple comorbidities. Participants in the global registry had a mean Society of Thoracic Surgeons score of 14.4; 38% had diabetes, 45% had chronic obstructive pulmonary disease, 35% had heart failure, 34% had previously undergone coronary artery bypass surgery, and roughly half of patients had a prior aortic valve replacement.
Causes of noncardiac mortality within 30 days included multiorgan failure in 8.6% of subjects, pneumonia in 2.9%, infection in 1.9%, and one fatal thoracentesis-related bleeding complication.
Cardiovascular deaths included two cases due to left ventricular perforation, two fatal strokes, an MI due to air emboli, a lethal complete atrioventricular block, and three deaths owing to LVOTO.
Alcohol ablation met with some success as a bailout treatment in cases of LVOTO with hemodynamic compromise after transmitral valve replacement in the global registry. All six treated patients had significant improvement initially, although the LVOTO recurred the next day in one instance. Four of the six patients were discharged from the hospital. One patient died because of atrioventricular block, and another from multiorgan failure 3 weeks after alcohol ablation of the LVOTO.
Dr. Guerrero has been a leader in this new field. She reported the first percutaneous implantation of a balloon expandable transcatheter valve in a native mitral valve without a surgical incision (Catheter Cardiovasc Interv. 2014 Jun 1;83[7]:E287-91), and more recently, together with coworkers developed a percutaneous alcohol ablation technique for acute reduction of LVOTO due to transcatheter mitral valve replacement (Catheter Cardiovasc Interv. 2016 Jul 5. doi:10.1002/ccd.26649).
She is now the principal investigator in the ongoing Mitral Implantation of Transcatheter Valves (MITRAL) trial, a physician-sponsored, 90-patient pilot study underway at six U.S. sites. MITRAL is recruiting three patient populations for transcatheter mitral valve replacement: patients like those in the global registry, with native mitral valve disease and severe mitral annular calcification; those with a symptomatic failing surgical ring with severe mitral regurgitation or stenosis; and patients with a symptomatic failing surgical bioprosthesis with severe mitral regurgitation or stenosis.
Discussant Nicolo Piazza, MD, of McGill University, Montreal, said transcatheter mitral valve replacement in mitral valve disease with severe mitral annular calcification in patients unsuitable for surgery “definitely represents an unmet clinical need in our practice today.” But he urged caution in interpreting the global registry data.
“This is a real world registry study with inherent selection bias and physician reporting bias,” the cardiologist said.
“We are leveraging a therapy from the aortic field into the mitral field. Of course, we do not have dedicated devices yet to treat these patients. The main finding of this study is that the procedure is actually feasible,” Dr. Piazza said.
Still, it’s sobering that at least 1 in 10 treated patients experiences LVOTO, 1 in 10 requires a second valve, and technical success is achieved in 3 out of 4 patients, he added.
Dr. Piazza predicted that multislice CT scans will be “extremely important” in refining patient selection criteria for the procedure, and echocardiography will be helpful in understanding the optimal procedural techniques and viewing angles. Work also needs to be done on developing optimal anticoagulation protocols in order to avoid valve thrombosis.
Dr. Guerrero reported serving as a consultant to Edwards Lifesciences. Dr. Piazza is a consultant to Medtronic and MicroPort.
PARIS – Transcatheter mitral valve replacement using a repurposed transcatheter aortic valve in patients with severe symptomatic native mitral valve disease and severe mitral annular calcification is feasible and may be an option in carefully selected patients who aren’t candidates for surgery, Mayra Guerrero, MD, said at the annual congress of the European Association of Percutaneous Cardiovascular Interventions.
However, at this early point in development, the procedure is associated with an exceptionally steep learning curve, said Dr. Guerrero, director of cardiac structural interventions at the NorthShore University Health System in Evanston, Ill.
She presented the procedural and 30-day outcomes for the first 104 patients entered into a global registry encompassing 47 centers in 11 countries. Nearly 90% of patients received an Edwards SAPIEN XT or SAPIEN 3 valve. The EuroPCR results update an earlier report on the first 64 patients in the registry (JACC Cardiovasc Interv. 2016 Jul 11;9[13]:1361-71).
The results, she said, are reminiscent of the early days in transcatheter aortic valve replacement, which were marked by an initial very high early mortality rate that fell dramatically as technology and techniques improved.
“We know that there are important things we need to improve. Left ventricular outflow tract obstruction is the Achilles heel of this procedure; we need to work on its prevention and management. We need better annulus sizing methods. We need to find the best delivery method and improve our patient selection in order to avoid taking on patients who are too sick. Still, even during this early experience, the technical success rate has improved, and 30-day mortality continues to drop,” Dr. Guerrero said.
Indeed, the 30-day all-cause mortality rate of 25% in the first 104 patients doesn’t tell the whole story. The rate was 37.5% in the first third of patients, fell to 21.9% in the second tertile, and then to 15% in the most recent tertile.
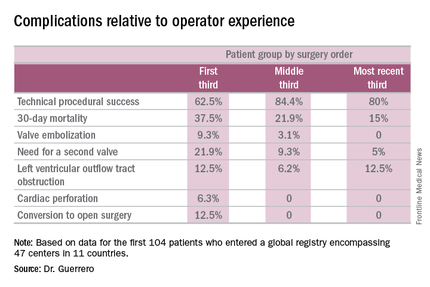
Similarly, the technical success rate of the procedure according to Mitral Valve Academic Research Consortium criteria improved from 62.5% in the first tertile of patients to 84.4% and 80% in the second and third, respectively, she continued.
The rates of almost all complications went down with greater operator experience, too. The notable exception was left ventricular outflow tract obstruction (LVOTO). It occurred in 12.5% of patients in the first tertile and remained unchanged in the third.
It’s noteworthy that the majority of deaths were noncardiac in nature. Patients with mitral annular calcification are a high-risk group even before they develop valvular dysfunction. They are typically older and have multiple comorbidities. Participants in the global registry had a mean Society of Thoracic Surgeons score of 14.4; 38% had diabetes, 45% had chronic obstructive pulmonary disease, 35% had heart failure, 34% had previously undergone coronary artery bypass surgery, and roughly half of patients had a prior aortic valve replacement.
Causes of noncardiac mortality within 30 days included multiorgan failure in 8.6% of subjects, pneumonia in 2.9%, infection in 1.9%, and one fatal thoracentesis-related bleeding complication.
Cardiovascular deaths included two cases due to left ventricular perforation, two fatal strokes, an MI due to air emboli, a lethal complete atrioventricular block, and three deaths owing to LVOTO.
Alcohol ablation met with some success as a bailout treatment in cases of LVOTO with hemodynamic compromise after transmitral valve replacement in the global registry. All six treated patients had significant improvement initially, although the LVOTO recurred the next day in one instance. Four of the six patients were discharged from the hospital. One patient died because of atrioventricular block, and another from multiorgan failure 3 weeks after alcohol ablation of the LVOTO.
Dr. Guerrero has been a leader in this new field. She reported the first percutaneous implantation of a balloon expandable transcatheter valve in a native mitral valve without a surgical incision (Catheter Cardiovasc Interv. 2014 Jun 1;83[7]:E287-91), and more recently, together with coworkers developed a percutaneous alcohol ablation technique for acute reduction of LVOTO due to transcatheter mitral valve replacement (Catheter Cardiovasc Interv. 2016 Jul 5. doi:10.1002/ccd.26649).
She is now the principal investigator in the ongoing Mitral Implantation of Transcatheter Valves (MITRAL) trial, a physician-sponsored, 90-patient pilot study underway at six U.S. sites. MITRAL is recruiting three patient populations for transcatheter mitral valve replacement: patients like those in the global registry, with native mitral valve disease and severe mitral annular calcification; those with a symptomatic failing surgical ring with severe mitral regurgitation or stenosis; and patients with a symptomatic failing surgical bioprosthesis with severe mitral regurgitation or stenosis.
Discussant Nicolo Piazza, MD, of McGill University, Montreal, said transcatheter mitral valve replacement in mitral valve disease with severe mitral annular calcification in patients unsuitable for surgery “definitely represents an unmet clinical need in our practice today.” But he urged caution in interpreting the global registry data.
“This is a real world registry study with inherent selection bias and physician reporting bias,” the cardiologist said.
“We are leveraging a therapy from the aortic field into the mitral field. Of course, we do not have dedicated devices yet to treat these patients. The main finding of this study is that the procedure is actually feasible,” Dr. Piazza said.
Still, it’s sobering that at least 1 in 10 treated patients experiences LVOTO, 1 in 10 requires a second valve, and technical success is achieved in 3 out of 4 patients, he added.
Dr. Piazza predicted that multislice CT scans will be “extremely important” in refining patient selection criteria for the procedure, and echocardiography will be helpful in understanding the optimal procedural techniques and viewing angles. Work also needs to be done on developing optimal anticoagulation protocols in order to avoid valve thrombosis.
Dr. Guerrero reported serving as a consultant to Edwards Lifesciences. Dr. Piazza is a consultant to Medtronic and MicroPort.
AT EUROPCR 2016
Key clinical point: A report from a global registry of transcatheter aortic valve implantation in the mitral position shows the procedure is feasible.
Major finding: Thirty-day mortality fell from 37.5% in the first third of treated patients to 15% in the most recent tertile.
Data source: A real world registry that includes 104 patients at 47 centers in 11 countries to date.
Disclosures: The study presenter reported serving as a consultant to Edwards Lifesciences.
Post-AMI death risk model has high predictive accuracy
An updated risk model based on data from patients presenting after acute myocardial infarction to a broad spectrum of U.S. hospitals appears to predict with a high degree of accuracy which patients are at the greatest risk for in-hospital mortality, investigators say.
Created from data on more than 240,000 patients presenting to one of 655 U.S. hospitals in 2012 and 2013 following ST-segment elevation myocardial infarction (STEMI) or non–ST-segment elevation MI (NSTEMI), the model identified the following independent risk factors for in-hospital mortality: age, heart rate, systolic blood pressure, presentation to the hospital after cardiac arrest, presentation in cardiogenic shock, presentation in heart failure, presentation with STEMI, creatinine clearance, and troponin ratio, reported Robert L. McNamara, MD, of Yale University, New Haven, Conn.
The investigators are participants in the ACTION (Acute Coronary Treatment and Intervention Outcomes Network) Registry–GWTG (Get With the Guidelines).
“The new ACTION Registry–GWTG in-hospital mortality risk model and risk score represent robust, parsimonious, and contemporary risk adjustment methodology for use in routine clinical care and hospital quality assessment. The addition of risk adjustment for patients presenting after cardiac arrest is critically important and enables a fairer assessment across hospitals with varied case mix,” they wrote (J Am Coll Cardiol. 2016 Aug 1;68[6]:626-35).
The revised risk model has the potential to facilitate hospital quality assessments and help investigators to identify specific factors that could help clinicians even further lower death rates, the investigators write.
Further mortality reductions?
Although improvements in care of patients with acute MI over the last several decades have driven the in-hospital death rate from 29% in 1969 down to less than 7% today, there are still more than 100,000 AMI-related in-hospital deaths in the United States annually, with wide variations across hospitals, Dr. McNamara and colleagues noted.
A previous risk model published by ACTION Registry–GWTG members included data on patients treated at 306 U.S. hospitals and provided a simple, validated in-hospital mortality and risk score.
Since that model was published, however, the dataset was expanded to include patients presenting after cardiac arrest at the time of AMI presentation.
“Being able to adjust for cardiac arrest is critical because it is a well-documented predictor of mortality. Moreover, continued improvement in AMI care mandates periodic updates to the risk models so that hospitals can assess their quality as contemporary care continues to evolve,” the authors wrote.
To see whether they could develop a new and improved model and risk score, they analyzed data on 243,440 patients treated at one of 655 hospitals in the voluntary network. Data on 145,952 patients (60% of the total), 57,039 of whom presented with STEMI, and 88,913 of whom presented with NSTEMI, were used to for the derivation sample.
Data on the remaining 97,488 (38,060 with STEMI and 59,428 with NSTEMI) were used to create the validation sample.
The authors found that for the total cohort, the in-hospital mortality rate was 4.6%. In multivariate models controlled for demographic and clinical factors, independent risk factors significantly associated with in-hospital mortality (validation cohort) were:
• Presentation after cardiac arrest (odds ratio, 5.15).
• Presentation in cardiogenic shock (OR, 4.22).
• Presentation in heart failure (OR, 1.83).
• STEMI on electrocardiography (OR, 1.81).
• Age, per 5 years (OR, 1.24).
• Systolic BP, per 10 mm Hg decrease (OR, 1.19).
• Creatinine clearance per 5/mL/min/1.73 m2 decrease (OR, 1.11).
• Heart rate per 10 beats/min (OR, 1.09).
• Troponin ratio, per 5 units (OR, 1.05).
The 95% confidence intervals for all of the above factors were significant.
The C-statistic, a standard measure of the predictive accuracy of a logistic regression model, was 0.88, indicating that the final ACTION Registry–GWTG in-hospital mortality model had a high level of discrimination in both the derivation and validation populations, the authors state.
The ACTION Registry–GWTG is a Program of the American College of Cardiology and the American Heart Association, with funding from Schering-Plough and the Bristol-Myers Squibb/Sanofi Pharmaceutical Partnership. Dr. McNamara serves on a clinical trials endpoint adjudication committee for Pfizer. Other coauthors reported multiple financial relationships with pharmaceutical and medical device companies.
Data analyses for the risk models developed by the ACTION Registry generally showed good accuracy and precision. The calibration information showed that patients with a cardiac arrest experienced much greater risk for mortality than did the other major groups (STEMI, NSTEMI, or no cardiac arrest). Until now, clinicians and researchers have generally used either the TIMI [Thrombolysis in Myocardial Infarction] or GRACE [Global Registry of Acute Coronary Events] score to guide therapeutic decisions. With the advent of the ACTION score, which appears to be most helpful for patients with moderate to severe disease, and the HEART [history, ECG, age, risk factor, troponin] score, which targets care for patients with minimal to mild disease, there are other options. Recently, the DAPT (Dual Antiplatelet Therapy) investigators published a prediction algorithm that provides yet another prognostic score to assess risk of ischemic events and risk of bleeding in patients who have undergone percutaneous coronary intervention. The key variables in the DAPT score are age, cigarette smoking, diabetes, MI at presentation, previous percutaneous coronary intervention or previous MI, use of a paclitaxel-eluting stent, stent diameter of less than 3 mm, heart failure or reduced ejection fraction, and use of a vein graft stent.
A comprehensive cross validation and comparison across at least some of the algorithms – TIMI, GRACE, HEART, DAPT, and ACTION – would help at this point. Interventions and decision points have evolved over the past 15 years, and evaluation of relatively contemporary data would be especially helpful. For example, the HEART score is likely to be used in situations in which the negative predictive capabilities are most important. The ACTION score is likely to be most useful in severely ill patients and to provide guidance for newer interventions. If detailed information concerning stents is available, then the DAPT score should prove helpful.
It is likely that one score does not fit all. Each algorithm provides a useful summary of risk to help guide decision making for patients with ischemic symptoms, depending on the severity of the signs and symptoms at presentation and the duration of the follow-up interval. Consensus building would help to move this field forward for hospital-based management of patients evaluated for cardiac ischemia.
Peter W.F. Wilson, MD, of the Atlanta VAMC and Emory Clinical Cardiovascular Research
Institute, Atlanta; and Ralph B. D’Agostino Sr., PhD, of the department of mathematics and statistics, Boston University, made these comments in an accompanying editorial (J Am Coll Cardiol. 2016 Aug 1;68[6]:636-8). They reported no relevant disclosures.
Data analyses for the risk models developed by the ACTION Registry generally showed good accuracy and precision. The calibration information showed that patients with a cardiac arrest experienced much greater risk for mortality than did the other major groups (STEMI, NSTEMI, or no cardiac arrest). Until now, clinicians and researchers have generally used either the TIMI [Thrombolysis in Myocardial Infarction] or GRACE [Global Registry of Acute Coronary Events] score to guide therapeutic decisions. With the advent of the ACTION score, which appears to be most helpful for patients with moderate to severe disease, and the HEART [history, ECG, age, risk factor, troponin] score, which targets care for patients with minimal to mild disease, there are other options. Recently, the DAPT (Dual Antiplatelet Therapy) investigators published a prediction algorithm that provides yet another prognostic score to assess risk of ischemic events and risk of bleeding in patients who have undergone percutaneous coronary intervention. The key variables in the DAPT score are age, cigarette smoking, diabetes, MI at presentation, previous percutaneous coronary intervention or previous MI, use of a paclitaxel-eluting stent, stent diameter of less than 3 mm, heart failure or reduced ejection fraction, and use of a vein graft stent.
A comprehensive cross validation and comparison across at least some of the algorithms – TIMI, GRACE, HEART, DAPT, and ACTION – would help at this point. Interventions and decision points have evolved over the past 15 years, and evaluation of relatively contemporary data would be especially helpful. For example, the HEART score is likely to be used in situations in which the negative predictive capabilities are most important. The ACTION score is likely to be most useful in severely ill patients and to provide guidance for newer interventions. If detailed information concerning stents is available, then the DAPT score should prove helpful.
It is likely that one score does not fit all. Each algorithm provides a useful summary of risk to help guide decision making for patients with ischemic symptoms, depending on the severity of the signs and symptoms at presentation and the duration of the follow-up interval. Consensus building would help to move this field forward for hospital-based management of patients evaluated for cardiac ischemia.
Peter W.F. Wilson, MD, of the Atlanta VAMC and Emory Clinical Cardiovascular Research
Institute, Atlanta; and Ralph B. D’Agostino Sr., PhD, of the department of mathematics and statistics, Boston University, made these comments in an accompanying editorial (J Am Coll Cardiol. 2016 Aug 1;68[6]:636-8). They reported no relevant disclosures.
Data analyses for the risk models developed by the ACTION Registry generally showed good accuracy and precision. The calibration information showed that patients with a cardiac arrest experienced much greater risk for mortality than did the other major groups (STEMI, NSTEMI, or no cardiac arrest). Until now, clinicians and researchers have generally used either the TIMI [Thrombolysis in Myocardial Infarction] or GRACE [Global Registry of Acute Coronary Events] score to guide therapeutic decisions. With the advent of the ACTION score, which appears to be most helpful for patients with moderate to severe disease, and the HEART [history, ECG, age, risk factor, troponin] score, which targets care for patients with minimal to mild disease, there are other options. Recently, the DAPT (Dual Antiplatelet Therapy) investigators published a prediction algorithm that provides yet another prognostic score to assess risk of ischemic events and risk of bleeding in patients who have undergone percutaneous coronary intervention. The key variables in the DAPT score are age, cigarette smoking, diabetes, MI at presentation, previous percutaneous coronary intervention or previous MI, use of a paclitaxel-eluting stent, stent diameter of less than 3 mm, heart failure or reduced ejection fraction, and use of a vein graft stent.
A comprehensive cross validation and comparison across at least some of the algorithms – TIMI, GRACE, HEART, DAPT, and ACTION – would help at this point. Interventions and decision points have evolved over the past 15 years, and evaluation of relatively contemporary data would be especially helpful. For example, the HEART score is likely to be used in situations in which the negative predictive capabilities are most important. The ACTION score is likely to be most useful in severely ill patients and to provide guidance for newer interventions. If detailed information concerning stents is available, then the DAPT score should prove helpful.
It is likely that one score does not fit all. Each algorithm provides a useful summary of risk to help guide decision making for patients with ischemic symptoms, depending on the severity of the signs and symptoms at presentation and the duration of the follow-up interval. Consensus building would help to move this field forward for hospital-based management of patients evaluated for cardiac ischemia.
Peter W.F. Wilson, MD, of the Atlanta VAMC and Emory Clinical Cardiovascular Research
Institute, Atlanta; and Ralph B. D’Agostino Sr., PhD, of the department of mathematics and statistics, Boston University, made these comments in an accompanying editorial (J Am Coll Cardiol. 2016 Aug 1;68[6]:636-8). They reported no relevant disclosures.
An updated risk model based on data from patients presenting after acute myocardial infarction to a broad spectrum of U.S. hospitals appears to predict with a high degree of accuracy which patients are at the greatest risk for in-hospital mortality, investigators say.
Created from data on more than 240,000 patients presenting to one of 655 U.S. hospitals in 2012 and 2013 following ST-segment elevation myocardial infarction (STEMI) or non–ST-segment elevation MI (NSTEMI), the model identified the following independent risk factors for in-hospital mortality: age, heart rate, systolic blood pressure, presentation to the hospital after cardiac arrest, presentation in cardiogenic shock, presentation in heart failure, presentation with STEMI, creatinine clearance, and troponin ratio, reported Robert L. McNamara, MD, of Yale University, New Haven, Conn.
The investigators are participants in the ACTION (Acute Coronary Treatment and Intervention Outcomes Network) Registry–GWTG (Get With the Guidelines).
“The new ACTION Registry–GWTG in-hospital mortality risk model and risk score represent robust, parsimonious, and contemporary risk adjustment methodology for use in routine clinical care and hospital quality assessment. The addition of risk adjustment for patients presenting after cardiac arrest is critically important and enables a fairer assessment across hospitals with varied case mix,” they wrote (J Am Coll Cardiol. 2016 Aug 1;68[6]:626-35).
The revised risk model has the potential to facilitate hospital quality assessments and help investigators to identify specific factors that could help clinicians even further lower death rates, the investigators write.
Further mortality reductions?
Although improvements in care of patients with acute MI over the last several decades have driven the in-hospital death rate from 29% in 1969 down to less than 7% today, there are still more than 100,000 AMI-related in-hospital deaths in the United States annually, with wide variations across hospitals, Dr. McNamara and colleagues noted.
A previous risk model published by ACTION Registry–GWTG members included data on patients treated at 306 U.S. hospitals and provided a simple, validated in-hospital mortality and risk score.
Since that model was published, however, the dataset was expanded to include patients presenting after cardiac arrest at the time of AMI presentation.
“Being able to adjust for cardiac arrest is critical because it is a well-documented predictor of mortality. Moreover, continued improvement in AMI care mandates periodic updates to the risk models so that hospitals can assess their quality as contemporary care continues to evolve,” the authors wrote.
To see whether they could develop a new and improved model and risk score, they analyzed data on 243,440 patients treated at one of 655 hospitals in the voluntary network. Data on 145,952 patients (60% of the total), 57,039 of whom presented with STEMI, and 88,913 of whom presented with NSTEMI, were used to for the derivation sample.
Data on the remaining 97,488 (38,060 with STEMI and 59,428 with NSTEMI) were used to create the validation sample.
The authors found that for the total cohort, the in-hospital mortality rate was 4.6%. In multivariate models controlled for demographic and clinical factors, independent risk factors significantly associated with in-hospital mortality (validation cohort) were:
• Presentation after cardiac arrest (odds ratio, 5.15).
• Presentation in cardiogenic shock (OR, 4.22).
• Presentation in heart failure (OR, 1.83).
• STEMI on electrocardiography (OR, 1.81).
• Age, per 5 years (OR, 1.24).
• Systolic BP, per 10 mm Hg decrease (OR, 1.19).
• Creatinine clearance per 5/mL/min/1.73 m2 decrease (OR, 1.11).
• Heart rate per 10 beats/min (OR, 1.09).
• Troponin ratio, per 5 units (OR, 1.05).
The 95% confidence intervals for all of the above factors were significant.
The C-statistic, a standard measure of the predictive accuracy of a logistic regression model, was 0.88, indicating that the final ACTION Registry–GWTG in-hospital mortality model had a high level of discrimination in both the derivation and validation populations, the authors state.
The ACTION Registry–GWTG is a Program of the American College of Cardiology and the American Heart Association, with funding from Schering-Plough and the Bristol-Myers Squibb/Sanofi Pharmaceutical Partnership. Dr. McNamara serves on a clinical trials endpoint adjudication committee for Pfizer. Other coauthors reported multiple financial relationships with pharmaceutical and medical device companies.
An updated risk model based on data from patients presenting after acute myocardial infarction to a broad spectrum of U.S. hospitals appears to predict with a high degree of accuracy which patients are at the greatest risk for in-hospital mortality, investigators say.
Created from data on more than 240,000 patients presenting to one of 655 U.S. hospitals in 2012 and 2013 following ST-segment elevation myocardial infarction (STEMI) or non–ST-segment elevation MI (NSTEMI), the model identified the following independent risk factors for in-hospital mortality: age, heart rate, systolic blood pressure, presentation to the hospital after cardiac arrest, presentation in cardiogenic shock, presentation in heart failure, presentation with STEMI, creatinine clearance, and troponin ratio, reported Robert L. McNamara, MD, of Yale University, New Haven, Conn.
The investigators are participants in the ACTION (Acute Coronary Treatment and Intervention Outcomes Network) Registry–GWTG (Get With the Guidelines).
“The new ACTION Registry–GWTG in-hospital mortality risk model and risk score represent robust, parsimonious, and contemporary risk adjustment methodology for use in routine clinical care and hospital quality assessment. The addition of risk adjustment for patients presenting after cardiac arrest is critically important and enables a fairer assessment across hospitals with varied case mix,” they wrote (J Am Coll Cardiol. 2016 Aug 1;68[6]:626-35).
The revised risk model has the potential to facilitate hospital quality assessments and help investigators to identify specific factors that could help clinicians even further lower death rates, the investigators write.
Further mortality reductions?
Although improvements in care of patients with acute MI over the last several decades have driven the in-hospital death rate from 29% in 1969 down to less than 7% today, there are still more than 100,000 AMI-related in-hospital deaths in the United States annually, with wide variations across hospitals, Dr. McNamara and colleagues noted.
A previous risk model published by ACTION Registry–GWTG members included data on patients treated at 306 U.S. hospitals and provided a simple, validated in-hospital mortality and risk score.
Since that model was published, however, the dataset was expanded to include patients presenting after cardiac arrest at the time of AMI presentation.
“Being able to adjust for cardiac arrest is critical because it is a well-documented predictor of mortality. Moreover, continued improvement in AMI care mandates periodic updates to the risk models so that hospitals can assess their quality as contemporary care continues to evolve,” the authors wrote.
To see whether they could develop a new and improved model and risk score, they analyzed data on 243,440 patients treated at one of 655 hospitals in the voluntary network. Data on 145,952 patients (60% of the total), 57,039 of whom presented with STEMI, and 88,913 of whom presented with NSTEMI, were used to for the derivation sample.
Data on the remaining 97,488 (38,060 with STEMI and 59,428 with NSTEMI) were used to create the validation sample.
The authors found that for the total cohort, the in-hospital mortality rate was 4.6%. In multivariate models controlled for demographic and clinical factors, independent risk factors significantly associated with in-hospital mortality (validation cohort) were:
• Presentation after cardiac arrest (odds ratio, 5.15).
• Presentation in cardiogenic shock (OR, 4.22).
• Presentation in heart failure (OR, 1.83).
• STEMI on electrocardiography (OR, 1.81).
• Age, per 5 years (OR, 1.24).
• Systolic BP, per 10 mm Hg decrease (OR, 1.19).
• Creatinine clearance per 5/mL/min/1.73 m2 decrease (OR, 1.11).
• Heart rate per 10 beats/min (OR, 1.09).
• Troponin ratio, per 5 units (OR, 1.05).
The 95% confidence intervals for all of the above factors were significant.
The C-statistic, a standard measure of the predictive accuracy of a logistic regression model, was 0.88, indicating that the final ACTION Registry–GWTG in-hospital mortality model had a high level of discrimination in both the derivation and validation populations, the authors state.
The ACTION Registry–GWTG is a Program of the American College of Cardiology and the American Heart Association, with funding from Schering-Plough and the Bristol-Myers Squibb/Sanofi Pharmaceutical Partnership. Dr. McNamara serves on a clinical trials endpoint adjudication committee for Pfizer. Other coauthors reported multiple financial relationships with pharmaceutical and medical device companies.
FROM JOURNAL OF THE AMERICAN COLLEGE OF CARDIOLOGY
Key clinical point: An updated cardiac mortality risk model may help to further reduce in-hospital deaths following acute myocardial infarction.
Major finding: The C-statistic for the model, a measure of predictive accuracy, was 0.88.
Data source: Updated risk model and in-hospital mortality score based on data from 243,440 patients following an AMI in 655 U.S. hospitals.
Disclosures: The ACTION Registry-GWTG is a Program of the American College of Cardiology and the American Heart Association, with funding from Schering-Plough and the Bristol-Myers Squibb/Sanofi Pharmaceutical Partnership. Dr. McNamara serves on a clinical trials endpoint adjudication committee for Pfizer. Other coauthors reported multiple financial relationships with pharmaceutical and medical device companies.
Making the case for CABG using bilateral thoracic arteries
Cardiac surgeons have been slow to embrace bilateral internal thoracic arteries (ITAs) for coronary artery bypass grafting (CABG) despite accumulating evidence that this technique achieves better long-term survival than the single-artery technique, perhaps because they think the bilateral technique is more difficult. However, investigators from Johns Hopkins University have found no difference in results between four different bilateral ITAs techniques regardless of complexity.
Their single-center study analyzed outcomes from 762 patients at Johns Hopkins who had CABG by way of one of four different bilateral ITA (BITA) techniques between 1997 and 2014. The results are in the July issue of the Journal of Thoracic and Cardiovascular Surgery (2016;152:120-7).
“We found no significant difference in terms of long-term survival or freedom from repeat revascularization between different configurations of BITA use,” wrote J. Trent Magruder, MD, and his colleagues.
Dr. Magruder and his coauthors cited 13 reports that found BITA achieved better graft patency and long-term survival than did single internal thoracic arteries, but they noted the lack of reports comparing different BITA techniques. “Given the paucity of comparative data on long-term outcomes of various BITA configurations, we sought to study differences in mortality and the need for repeat revascularization among patients receiving varying BITA graft configurations at our institution,” they said.
The four groups and types of BITA procedures they analyzed were:
LL/RL group, in situ left ITA (LITA) anastomosed to the left anterior descending artery (LAD) with in situ right ITA (RITA) anastomosed to the left coronary circulation (n = 239).
LL/RR group, in situ LITA-LAD and in situ RITA-right coronary circulation (n = 239 patients).
RL/LL group, in situ RITA-LAD with in situ LITA-left coronary circulation (n = 185 patients).
Y group, in situ LITA-LAD with a free RITA as a composite graft with inflow from the LITA or a saphenous vein graft (n = 99 patients).
BITA cases comprised 5.7% of all 14,502 CABG procedures Johns Hopkins cardiac surgeons performed through the study period (60 BITA cases were dropped from the analysis because of incomplete data). That rate is about in line with a previously reported use rate of 4% of CABG procedures in the United States (Circulation. 2009;120:935-40).
Among the reasons Dr. Magruder and his coauthors cited for the lack of uptake of BITA among cardiac surgeons are discrepancies in survival data, a perceived high risk of complications such as sternal surgical site infections in patients with diabetes or chronic obstructive pulmonary disease or in those who are obese, and increased operative time and risk of bleeding.
With regard to the operation itself, the mean cross-clamp and coronary bypass times and number of bypass grafts were similar among all four groups, the latter ranging from 3.0 for the RL/LL group to 3.4 for the Y group. However, the researchers did find appreciable differences in rates of transfusions during the operation and skeletonization of the RITA at harvest. The Y group had the highest rates for both – 57.6% had transfusions and 72.7% had skeletonized RITA at harvest – followed by the RL/LL with rates of 43.2% for transfusions and 31.4% with skeletonized RITA. Rates for both intraoperative transfusion and RITA skeletonization were 24.7% and 8%, respectively, in the LL/RL group; and 37.7% and 18%, respectively, in the LL/RR group.
In-hospital complications, including reintervention for bleeding, heart attack, stroke, inflammation of the mediastinum, and death, were similar among all four groups. There were no in-hospital heart attacks. The only statistically significant difference was in hospital stay, ranging from an average of 6.1 days for the LL/RL group to 7.4 for both the LL/RR and RL/LL groups.
Through the duration of follow-up, the overall rate for repeat percutaneous coronary intervention was 7.6% – highest among the RL/LL (9.2%) and Y groups (9%). Those in the LL/RR group had the highest rates of repeat CABG: 1.7% vs. 0.8% for LL/RL group, 0.5% for the RL/LL group and 0% for group Y. Rates of late cardiac death were around 5% for the first three groups, but none were reported in group Y.
Dr. Magruder and colleagues acknowledged their study used a limited sample size for each procedure, but that their findings show that cardiac surgeons should choose their BITA configuration based on individual patient factors. “In general, the technically simplest operations should be selected because more complex procedures offer no additional benefit,” they said.
Dr. Magruder and his coauthors had no financial disclosures.
The take-home message of the study by Dr. Magruder and colleagues is that using bilateral internal thoracic arteries (BITA) is more important than the specific configuration, Saswata Deb, MD, BSc, and Stephen E. Fremes, MD, MSc, BSc, of the University of Toronto wrote in their invited commentary (J Thorac Cardiovasc Surg. 2016;152:128-30). “In other words: BITA – just do it!” they wrote.
Because the survival advantage of BITA in CABG typically becomes apparent 10 years or more after the operation, the Johns Hopkins study, along with the Arterial Revascularization Trial that compares BITA with single ITA (Semin Thorac Cardiovasc Surg. 2014;26:76-94), can help redefine how cardiac surgeons select conduits for CABG, the commentators said.
“What does this particular study add?” they asked. “Point estimates for the adjusted hazard ratio of death or repeat revascularization were close to unity for each of the primary grafting hypothesis comparisons.”
Dr. Deb and Dr. Fremes had no financial relationships to disclose.
The take-home message of the study by Dr. Magruder and colleagues is that using bilateral internal thoracic arteries (BITA) is more important than the specific configuration, Saswata Deb, MD, BSc, and Stephen E. Fremes, MD, MSc, BSc, of the University of Toronto wrote in their invited commentary (J Thorac Cardiovasc Surg. 2016;152:128-30). “In other words: BITA – just do it!” they wrote.
Because the survival advantage of BITA in CABG typically becomes apparent 10 years or more after the operation, the Johns Hopkins study, along with the Arterial Revascularization Trial that compares BITA with single ITA (Semin Thorac Cardiovasc Surg. 2014;26:76-94), can help redefine how cardiac surgeons select conduits for CABG, the commentators said.
“What does this particular study add?” they asked. “Point estimates for the adjusted hazard ratio of death or repeat revascularization were close to unity for each of the primary grafting hypothesis comparisons.”
Dr. Deb and Dr. Fremes had no financial relationships to disclose.
The take-home message of the study by Dr. Magruder and colleagues is that using bilateral internal thoracic arteries (BITA) is more important than the specific configuration, Saswata Deb, MD, BSc, and Stephen E. Fremes, MD, MSc, BSc, of the University of Toronto wrote in their invited commentary (J Thorac Cardiovasc Surg. 2016;152:128-30). “In other words: BITA – just do it!” they wrote.
Because the survival advantage of BITA in CABG typically becomes apparent 10 years or more after the operation, the Johns Hopkins study, along with the Arterial Revascularization Trial that compares BITA with single ITA (Semin Thorac Cardiovasc Surg. 2014;26:76-94), can help redefine how cardiac surgeons select conduits for CABG, the commentators said.
“What does this particular study add?” they asked. “Point estimates for the adjusted hazard ratio of death or repeat revascularization were close to unity for each of the primary grafting hypothesis comparisons.”
Dr. Deb and Dr. Fremes had no financial relationships to disclose.
Cardiac surgeons have been slow to embrace bilateral internal thoracic arteries (ITAs) for coronary artery bypass grafting (CABG) despite accumulating evidence that this technique achieves better long-term survival than the single-artery technique, perhaps because they think the bilateral technique is more difficult. However, investigators from Johns Hopkins University have found no difference in results between four different bilateral ITAs techniques regardless of complexity.
Their single-center study analyzed outcomes from 762 patients at Johns Hopkins who had CABG by way of one of four different bilateral ITA (BITA) techniques between 1997 and 2014. The results are in the July issue of the Journal of Thoracic and Cardiovascular Surgery (2016;152:120-7).
“We found no significant difference in terms of long-term survival or freedom from repeat revascularization between different configurations of BITA use,” wrote J. Trent Magruder, MD, and his colleagues.
Dr. Magruder and his coauthors cited 13 reports that found BITA achieved better graft patency and long-term survival than did single internal thoracic arteries, but they noted the lack of reports comparing different BITA techniques. “Given the paucity of comparative data on long-term outcomes of various BITA configurations, we sought to study differences in mortality and the need for repeat revascularization among patients receiving varying BITA graft configurations at our institution,” they said.
The four groups and types of BITA procedures they analyzed were:
LL/RL group, in situ left ITA (LITA) anastomosed to the left anterior descending artery (LAD) with in situ right ITA (RITA) anastomosed to the left coronary circulation (n = 239).
LL/RR group, in situ LITA-LAD and in situ RITA-right coronary circulation (n = 239 patients).
RL/LL group, in situ RITA-LAD with in situ LITA-left coronary circulation (n = 185 patients).
Y group, in situ LITA-LAD with a free RITA as a composite graft with inflow from the LITA or a saphenous vein graft (n = 99 patients).
BITA cases comprised 5.7% of all 14,502 CABG procedures Johns Hopkins cardiac surgeons performed through the study period (60 BITA cases were dropped from the analysis because of incomplete data). That rate is about in line with a previously reported use rate of 4% of CABG procedures in the United States (Circulation. 2009;120:935-40).
Among the reasons Dr. Magruder and his coauthors cited for the lack of uptake of BITA among cardiac surgeons are discrepancies in survival data, a perceived high risk of complications such as sternal surgical site infections in patients with diabetes or chronic obstructive pulmonary disease or in those who are obese, and increased operative time and risk of bleeding.
With regard to the operation itself, the mean cross-clamp and coronary bypass times and number of bypass grafts were similar among all four groups, the latter ranging from 3.0 for the RL/LL group to 3.4 for the Y group. However, the researchers did find appreciable differences in rates of transfusions during the operation and skeletonization of the RITA at harvest. The Y group had the highest rates for both – 57.6% had transfusions and 72.7% had skeletonized RITA at harvest – followed by the RL/LL with rates of 43.2% for transfusions and 31.4% with skeletonized RITA. Rates for both intraoperative transfusion and RITA skeletonization were 24.7% and 8%, respectively, in the LL/RL group; and 37.7% and 18%, respectively, in the LL/RR group.
In-hospital complications, including reintervention for bleeding, heart attack, stroke, inflammation of the mediastinum, and death, were similar among all four groups. There were no in-hospital heart attacks. The only statistically significant difference was in hospital stay, ranging from an average of 6.1 days for the LL/RL group to 7.4 for both the LL/RR and RL/LL groups.
Through the duration of follow-up, the overall rate for repeat percutaneous coronary intervention was 7.6% – highest among the RL/LL (9.2%) and Y groups (9%). Those in the LL/RR group had the highest rates of repeat CABG: 1.7% vs. 0.8% for LL/RL group, 0.5% for the RL/LL group and 0% for group Y. Rates of late cardiac death were around 5% for the first three groups, but none were reported in group Y.
Dr. Magruder and colleagues acknowledged their study used a limited sample size for each procedure, but that their findings show that cardiac surgeons should choose their BITA configuration based on individual patient factors. “In general, the technically simplest operations should be selected because more complex procedures offer no additional benefit,” they said.
Dr. Magruder and his coauthors had no financial disclosures.
Cardiac surgeons have been slow to embrace bilateral internal thoracic arteries (ITAs) for coronary artery bypass grafting (CABG) despite accumulating evidence that this technique achieves better long-term survival than the single-artery technique, perhaps because they think the bilateral technique is more difficult. However, investigators from Johns Hopkins University have found no difference in results between four different bilateral ITAs techniques regardless of complexity.
Their single-center study analyzed outcomes from 762 patients at Johns Hopkins who had CABG by way of one of four different bilateral ITA (BITA) techniques between 1997 and 2014. The results are in the July issue of the Journal of Thoracic and Cardiovascular Surgery (2016;152:120-7).
“We found no significant difference in terms of long-term survival or freedom from repeat revascularization between different configurations of BITA use,” wrote J. Trent Magruder, MD, and his colleagues.
Dr. Magruder and his coauthors cited 13 reports that found BITA achieved better graft patency and long-term survival than did single internal thoracic arteries, but they noted the lack of reports comparing different BITA techniques. “Given the paucity of comparative data on long-term outcomes of various BITA configurations, we sought to study differences in mortality and the need for repeat revascularization among patients receiving varying BITA graft configurations at our institution,” they said.
The four groups and types of BITA procedures they analyzed were:
LL/RL group, in situ left ITA (LITA) anastomosed to the left anterior descending artery (LAD) with in situ right ITA (RITA) anastomosed to the left coronary circulation (n = 239).
LL/RR group, in situ LITA-LAD and in situ RITA-right coronary circulation (n = 239 patients).
RL/LL group, in situ RITA-LAD with in situ LITA-left coronary circulation (n = 185 patients).
Y group, in situ LITA-LAD with a free RITA as a composite graft with inflow from the LITA or a saphenous vein graft (n = 99 patients).
BITA cases comprised 5.7% of all 14,502 CABG procedures Johns Hopkins cardiac surgeons performed through the study period (60 BITA cases were dropped from the analysis because of incomplete data). That rate is about in line with a previously reported use rate of 4% of CABG procedures in the United States (Circulation. 2009;120:935-40).
Among the reasons Dr. Magruder and his coauthors cited for the lack of uptake of BITA among cardiac surgeons are discrepancies in survival data, a perceived high risk of complications such as sternal surgical site infections in patients with diabetes or chronic obstructive pulmonary disease or in those who are obese, and increased operative time and risk of bleeding.
With regard to the operation itself, the mean cross-clamp and coronary bypass times and number of bypass grafts were similar among all four groups, the latter ranging from 3.0 for the RL/LL group to 3.4 for the Y group. However, the researchers did find appreciable differences in rates of transfusions during the operation and skeletonization of the RITA at harvest. The Y group had the highest rates for both – 57.6% had transfusions and 72.7% had skeletonized RITA at harvest – followed by the RL/LL with rates of 43.2% for transfusions and 31.4% with skeletonized RITA. Rates for both intraoperative transfusion and RITA skeletonization were 24.7% and 8%, respectively, in the LL/RL group; and 37.7% and 18%, respectively, in the LL/RR group.
In-hospital complications, including reintervention for bleeding, heart attack, stroke, inflammation of the mediastinum, and death, were similar among all four groups. There were no in-hospital heart attacks. The only statistically significant difference was in hospital stay, ranging from an average of 6.1 days for the LL/RL group to 7.4 for both the LL/RR and RL/LL groups.
Through the duration of follow-up, the overall rate for repeat percutaneous coronary intervention was 7.6% – highest among the RL/LL (9.2%) and Y groups (9%). Those in the LL/RR group had the highest rates of repeat CABG: 1.7% vs. 0.8% for LL/RL group, 0.5% for the RL/LL group and 0% for group Y. Rates of late cardiac death were around 5% for the first three groups, but none were reported in group Y.
Dr. Magruder and colleagues acknowledged their study used a limited sample size for each procedure, but that their findings show that cardiac surgeons should choose their BITA configuration based on individual patient factors. “In general, the technically simplest operations should be selected because more complex procedures offer no additional benefit,” they said.
Dr. Magruder and his coauthors had no financial disclosures.
FROM THE JOURNAL OF THORACIC AND CARDIOVASCULAR SURGERY
Key clinical point: No specific technique for bilateral internal thoracic artery (BITA) graft in coronary artery bypass grafting (CABG) has an advantage over other techniques.
Major finding: Among four different BITA configurations, no in-hospital deaths occurred and the late cardiac death rate was around 5% for three of the four groups and 0% for the fourth group.
Data source: Single-center, retrospective study of 762 patients who had CABG with use of BITA from 1997 to 2014.
Disclosures: Dr. Magruder and colleagues reported having no financial disclosures.
Four-branched arch replacement gets acceptable results
NEW YORK – A total aortic arch replacement approach that uses a four-branched graft with antegrade cerebral perfusion can be done with low rates of in-hospital death and complications, a large series from two institutions in Japan showed.
Kenji Minatoya, MD, of the National Cerebral and Cardiovascular Center in Osaka, Japan, reported that his institution’s approach for total arch replacement (TAR) had an in-hospital death rate of 5.2%.
Dr. Minatoya and his colleagues started using four-branch TAR in the 1980s, switching from retrograde to antegrade cerebral perfusion to protect the brain later on. “The study purpose was to investigate the results of total arch replacement using the four-branch graft as a benchmark in the endovascular era,” he said at the meeting, sponsored by the American Association for Thoracic Surgery.
The study involved 1,005 cases of total arch replacement performed at Dr. Minatoya’s center and at Tokyo Medical University from 2001 to 2016.
The study population included a cohort of 152 people in their 80s. The in-hospital death rate in this group was 11.8%, Dr. Minatoya said. The over-80 group mostly underwent thoracic endovascular aortic repair (TEVAR) beginning in 2008, he said, but in recent years some had open total arch replacement operations.
The univariate analysis showed that chronic kidney disease, long operation times, long durations for coronary bypass and circulatory arrest, and extended time on mechanical ventilation were risk factors for in-hospital death in octogenarians, Dr. Minatoya said. The multivariate analysis showed that male gender along with extended mechanical ventilation were risk factors for in-hospital death in this group, he said.
The overall population included 252 emergent operations, 224 of which were for acute aortic dissections, Dr. Minatoya said. The in-hospital death rate was 4.5% for elective operations and 7.1% for emergent cases, he said. The death rate for isolated, elective total arch replacement was 3.4%.
Focusing on acute aortic dissections, Dr. Minatoya said, “We have adopted an aggressive strategy for entry-site resection, including total arch replacement, in patients with arch tears.” Almost 50% of patients with acute aortic dissection had total arch replacement, he said, with identical 4.9% rates for in-hospital mortality rate and permanent neurological deficit in this group.
The leading overall causes of in-hospital death were low-output syndrome (38.5%), sepsis (25%), respiratory failure (21%) and rupture of the residual aneurysm (9%), Dr. Minatoya said.
Fifteen patients (1.5%) underwent second operations for arch grafts, he said: 11 for pseudoaneurysm; three for hemolysis and one for infection. Other overall measures in the analysis were a permanent neurological dysfunction rate of 3.6%, a temporary neurological dysfunction rate of 6.4%, and no spinal cord complications. Overall 5-year survival was 80.7% and 10-year survival was 63.1%, Dr. Minatoya said.
A total of 311 patients had concomitant procedures. They included aortic valve operations (64); aortic root replacement (38); mitral valve replacement (13); and coronary artery bypass grafting (196).
The typical operation in the study population took about 8 hours, Dr. Minatoya said (482 minutes). Timing of key operative steps were cardiopulmonary time of 254 minutes, cardiac arrest time of 146 minutes, antegrade cerebral perfusion time of 160 minutes and lower-body circulatory arrest time of 62 minutes.
“Since the mean age was 70 years old, we think the survival rate was acceptable,” Dr. Minatoya said, regarding overall study results. Overall risk factors for in-hospital death were short stature, long pump time, chronic kidney disease, and age of 80 and up, he said. Short stature was a risk factor for permanent neurological deficit, and males over age 80 had a higher risk for total arch replacement.
“Total arch replacement using the four-branched graft with antegrade cerebral perfusion could be accomplished with acceptable early and late results,” Dr. Minatoya said. “The branched-arch TEVAR may be a good option for octogenarians and patients with chronic kidney disease.”
Dr. Minatoya had no financial relationships to disclose.
NEW YORK – A total aortic arch replacement approach that uses a four-branched graft with antegrade cerebral perfusion can be done with low rates of in-hospital death and complications, a large series from two institutions in Japan showed.
Kenji Minatoya, MD, of the National Cerebral and Cardiovascular Center in Osaka, Japan, reported that his institution’s approach for total arch replacement (TAR) had an in-hospital death rate of 5.2%.
Dr. Minatoya and his colleagues started using four-branch TAR in the 1980s, switching from retrograde to antegrade cerebral perfusion to protect the brain later on. “The study purpose was to investigate the results of total arch replacement using the four-branch graft as a benchmark in the endovascular era,” he said at the meeting, sponsored by the American Association for Thoracic Surgery.
The study involved 1,005 cases of total arch replacement performed at Dr. Minatoya’s center and at Tokyo Medical University from 2001 to 2016.
The study population included a cohort of 152 people in their 80s. The in-hospital death rate in this group was 11.8%, Dr. Minatoya said. The over-80 group mostly underwent thoracic endovascular aortic repair (TEVAR) beginning in 2008, he said, but in recent years some had open total arch replacement operations.
The univariate analysis showed that chronic kidney disease, long operation times, long durations for coronary bypass and circulatory arrest, and extended time on mechanical ventilation were risk factors for in-hospital death in octogenarians, Dr. Minatoya said. The multivariate analysis showed that male gender along with extended mechanical ventilation were risk factors for in-hospital death in this group, he said.
The overall population included 252 emergent operations, 224 of which were for acute aortic dissections, Dr. Minatoya said. The in-hospital death rate was 4.5% for elective operations and 7.1% for emergent cases, he said. The death rate for isolated, elective total arch replacement was 3.4%.
Focusing on acute aortic dissections, Dr. Minatoya said, “We have adopted an aggressive strategy for entry-site resection, including total arch replacement, in patients with arch tears.” Almost 50% of patients with acute aortic dissection had total arch replacement, he said, with identical 4.9% rates for in-hospital mortality rate and permanent neurological deficit in this group.
The leading overall causes of in-hospital death were low-output syndrome (38.5%), sepsis (25%), respiratory failure (21%) and rupture of the residual aneurysm (9%), Dr. Minatoya said.
Fifteen patients (1.5%) underwent second operations for arch grafts, he said: 11 for pseudoaneurysm; three for hemolysis and one for infection. Other overall measures in the analysis were a permanent neurological dysfunction rate of 3.6%, a temporary neurological dysfunction rate of 6.4%, and no spinal cord complications. Overall 5-year survival was 80.7% and 10-year survival was 63.1%, Dr. Minatoya said.
A total of 311 patients had concomitant procedures. They included aortic valve operations (64); aortic root replacement (38); mitral valve replacement (13); and coronary artery bypass grafting (196).
The typical operation in the study population took about 8 hours, Dr. Minatoya said (482 minutes). Timing of key operative steps were cardiopulmonary time of 254 minutes, cardiac arrest time of 146 minutes, antegrade cerebral perfusion time of 160 minutes and lower-body circulatory arrest time of 62 minutes.
“Since the mean age was 70 years old, we think the survival rate was acceptable,” Dr. Minatoya said, regarding overall study results. Overall risk factors for in-hospital death were short stature, long pump time, chronic kidney disease, and age of 80 and up, he said. Short stature was a risk factor for permanent neurological deficit, and males over age 80 had a higher risk for total arch replacement.
“Total arch replacement using the four-branched graft with antegrade cerebral perfusion could be accomplished with acceptable early and late results,” Dr. Minatoya said. “The branched-arch TEVAR may be a good option for octogenarians and patients with chronic kidney disease.”
Dr. Minatoya had no financial relationships to disclose.
NEW YORK – A total aortic arch replacement approach that uses a four-branched graft with antegrade cerebral perfusion can be done with low rates of in-hospital death and complications, a large series from two institutions in Japan showed.
Kenji Minatoya, MD, of the National Cerebral and Cardiovascular Center in Osaka, Japan, reported that his institution’s approach for total arch replacement (TAR) had an in-hospital death rate of 5.2%.
Dr. Minatoya and his colleagues started using four-branch TAR in the 1980s, switching from retrograde to antegrade cerebral perfusion to protect the brain later on. “The study purpose was to investigate the results of total arch replacement using the four-branch graft as a benchmark in the endovascular era,” he said at the meeting, sponsored by the American Association for Thoracic Surgery.
The study involved 1,005 cases of total arch replacement performed at Dr. Minatoya’s center and at Tokyo Medical University from 2001 to 2016.
The study population included a cohort of 152 people in their 80s. The in-hospital death rate in this group was 11.8%, Dr. Minatoya said. The over-80 group mostly underwent thoracic endovascular aortic repair (TEVAR) beginning in 2008, he said, but in recent years some had open total arch replacement operations.
The univariate analysis showed that chronic kidney disease, long operation times, long durations for coronary bypass and circulatory arrest, and extended time on mechanical ventilation were risk factors for in-hospital death in octogenarians, Dr. Minatoya said. The multivariate analysis showed that male gender along with extended mechanical ventilation were risk factors for in-hospital death in this group, he said.
The overall population included 252 emergent operations, 224 of which were for acute aortic dissections, Dr. Minatoya said. The in-hospital death rate was 4.5% for elective operations and 7.1% for emergent cases, he said. The death rate for isolated, elective total arch replacement was 3.4%.
Focusing on acute aortic dissections, Dr. Minatoya said, “We have adopted an aggressive strategy for entry-site resection, including total arch replacement, in patients with arch tears.” Almost 50% of patients with acute aortic dissection had total arch replacement, he said, with identical 4.9% rates for in-hospital mortality rate and permanent neurological deficit in this group.
The leading overall causes of in-hospital death were low-output syndrome (38.5%), sepsis (25%), respiratory failure (21%) and rupture of the residual aneurysm (9%), Dr. Minatoya said.
Fifteen patients (1.5%) underwent second operations for arch grafts, he said: 11 for pseudoaneurysm; three for hemolysis and one for infection. Other overall measures in the analysis were a permanent neurological dysfunction rate of 3.6%, a temporary neurological dysfunction rate of 6.4%, and no spinal cord complications. Overall 5-year survival was 80.7% and 10-year survival was 63.1%, Dr. Minatoya said.
A total of 311 patients had concomitant procedures. They included aortic valve operations (64); aortic root replacement (38); mitral valve replacement (13); and coronary artery bypass grafting (196).
The typical operation in the study population took about 8 hours, Dr. Minatoya said (482 minutes). Timing of key operative steps were cardiopulmonary time of 254 minutes, cardiac arrest time of 146 minutes, antegrade cerebral perfusion time of 160 minutes and lower-body circulatory arrest time of 62 minutes.
“Since the mean age was 70 years old, we think the survival rate was acceptable,” Dr. Minatoya said, regarding overall study results. Overall risk factors for in-hospital death were short stature, long pump time, chronic kidney disease, and age of 80 and up, he said. Short stature was a risk factor for permanent neurological deficit, and males over age 80 had a higher risk for total arch replacement.
“Total arch replacement using the four-branched graft with antegrade cerebral perfusion could be accomplished with acceptable early and late results,” Dr. Minatoya said. “The branched-arch TEVAR may be a good option for octogenarians and patients with chronic kidney disease.”
Dr. Minatoya had no financial relationships to disclose.
AT THE AATS AORTIC SYMPOSIUM 2016
Key clinical point: Four-branched total aortic arch replacement can achieve acceptable early and late results.
Major finding: Overall in-hospital mortality was 5.2% and 5-year survival was 80.7%.
Data source: Consecutive series of 1,005 patients who had total arch replacement between 2001 and 2016 at two centers in Japan.
Disclosures: Dr. Minatoya reported having no financial disclosures.
Pediatric autologous aortic repair built to last
NEW YORK – With more than 1 million adults living today with congenital aortic disease, cardiovascular surgeons must think of outcomes in terms of decades, not years, when performing aortic arch repair in newborns, infants, and children, according to Charles D. Fraser Jr., M.D.
To that end, an all-autologous approach to aortic arch repair is key in preserving problem-free aortic function in adulthood, said Dr. Fraser, surgeon-in-chief at Texas Children’s Hospital in Houston.
Dr. Fraser reported on his center’s experience with all-autologous aortic arch repair techniques. He reviewed the following five principles that guide aortic arch repair in newborns, infants, and children at Texas Children’s Hospital:
• Use of autologous tissue reconstruction and avoidance of prosthetic material.
• Concomitant intracardiac repair.
• Use of anatomic reconstruction.
• Optimization of ventriculoarterial coupling.
• Preservation of laryngeal nerve function.
“The principles we developed at Texas Children’s Hospital we hope will translate into fewer of these patients that surgeons caring for adults with aortic disease will have to take care of later in life,” Dr. Fraser said at the meeting sponsored by the American Association for Thoracic Surgery. He reviewed cases in which he explained techniques he and his colleagues developed to address long-term outcomes.
The first challenge is to determine when to perform aortic repair in pediatric patients. “A question often asked is how small is too small when assessing the aortic arch in association with significant periductal coarctation?” he said. “Our rule of thumb has been that the arch diameter measured in millimeters should be at least the patient’s weight in kilograms plus one.” In other words, a 3-kg baby should have an aortic arch of at least 4 mm in diameter, he said.
He described the case of a 3.8-kg male baby on prostaglandin E1 who had aortic arch advancement repair and closure of atrial and ventricular septal defects at 8 days of age. The patient had an early origin of the left common carotid artery and a small proximal aortic arch. “This is the kind of patient in which we would do a complete aortic arch reconstruction, again with the autologous technique,” Dr. Fraser said.
In such a patient, Dr. Fraser and his colleagues at Texas Children’s Hospital support the circulation to the brain with antegrade cerebral perfusion, using transcranial Doppler and near-infrared spectroscopy to guide their profusion strategy, before putting the child on cardiac bypass and “profound” hypothermia. Careful planning before cannulation is important to perform the aortic transection at the correct level, he said
He also explained the ascending sliding arch aortoplasty, also known as the “Texas slide,” first described by E. Dean McKenzie, M.D., at Texas Children’s Hospital in 2011 (Ann. Thorac. Surg. 2011;91:805-10) This technique involves sliding a tongue-shaped piece of the ascending aorta underneath the aortic arch to construct an all-autologous repair.
“In patients with bicuspid aortic valves, we often observe that the ascending aorta is extremely elongated,” he said. “The idea is to take advantage of that and slide the ascending aorta completely up underneath the aortic arch and construct an all-autologous arch advancement type of repair.”
He presented the case of a 4-year-old boy with coarctation of the aorta in whom the Texas slide was indicated. “If this patient were treated with a simple coarctectomy, the patient would be subject to a life with a moderately hypoplastic aortic arch, and over the course of time, this could be problematic,” Dr. Fraser said. “The sliding reconstruction has relevance not only to the status of the aortic arch over the long term but it also has a profound effect on ventricular function.”
He noted a single-center, retrospective study from the United Kingdom that demonstrated that the quality of the aortic arch reconstruction, and the related opportunity for ventricular arterial coupling, directly correlate with long-term performance of the aortic arch in patients with hypoplastic left heart syndrome (J Thorac Cardiovasc Surg. 2014;148:1526-33).
“This is very important as part of the growing population of these patients who need long-term management, most of whom we’re anticipating managing not just for years, but for decades,” Dr. Fraser said.
He said he had no relevant financial disclosures.
NEW YORK – With more than 1 million adults living today with congenital aortic disease, cardiovascular surgeons must think of outcomes in terms of decades, not years, when performing aortic arch repair in newborns, infants, and children, according to Charles D. Fraser Jr., M.D.
To that end, an all-autologous approach to aortic arch repair is key in preserving problem-free aortic function in adulthood, said Dr. Fraser, surgeon-in-chief at Texas Children’s Hospital in Houston.
Dr. Fraser reported on his center’s experience with all-autologous aortic arch repair techniques. He reviewed the following five principles that guide aortic arch repair in newborns, infants, and children at Texas Children’s Hospital:
• Use of autologous tissue reconstruction and avoidance of prosthetic material.
• Concomitant intracardiac repair.
• Use of anatomic reconstruction.
• Optimization of ventriculoarterial coupling.
• Preservation of laryngeal nerve function.
“The principles we developed at Texas Children’s Hospital we hope will translate into fewer of these patients that surgeons caring for adults with aortic disease will have to take care of later in life,” Dr. Fraser said at the meeting sponsored by the American Association for Thoracic Surgery. He reviewed cases in which he explained techniques he and his colleagues developed to address long-term outcomes.
The first challenge is to determine when to perform aortic repair in pediatric patients. “A question often asked is how small is too small when assessing the aortic arch in association with significant periductal coarctation?” he said. “Our rule of thumb has been that the arch diameter measured in millimeters should be at least the patient’s weight in kilograms plus one.” In other words, a 3-kg baby should have an aortic arch of at least 4 mm in diameter, he said.
He described the case of a 3.8-kg male baby on prostaglandin E1 who had aortic arch advancement repair and closure of atrial and ventricular septal defects at 8 days of age. The patient had an early origin of the left common carotid artery and a small proximal aortic arch. “This is the kind of patient in which we would do a complete aortic arch reconstruction, again with the autologous technique,” Dr. Fraser said.
In such a patient, Dr. Fraser and his colleagues at Texas Children’s Hospital support the circulation to the brain with antegrade cerebral perfusion, using transcranial Doppler and near-infrared spectroscopy to guide their profusion strategy, before putting the child on cardiac bypass and “profound” hypothermia. Careful planning before cannulation is important to perform the aortic transection at the correct level, he said
He also explained the ascending sliding arch aortoplasty, also known as the “Texas slide,” first described by E. Dean McKenzie, M.D., at Texas Children’s Hospital in 2011 (Ann. Thorac. Surg. 2011;91:805-10) This technique involves sliding a tongue-shaped piece of the ascending aorta underneath the aortic arch to construct an all-autologous repair.
“In patients with bicuspid aortic valves, we often observe that the ascending aorta is extremely elongated,” he said. “The idea is to take advantage of that and slide the ascending aorta completely up underneath the aortic arch and construct an all-autologous arch advancement type of repair.”
He presented the case of a 4-year-old boy with coarctation of the aorta in whom the Texas slide was indicated. “If this patient were treated with a simple coarctectomy, the patient would be subject to a life with a moderately hypoplastic aortic arch, and over the course of time, this could be problematic,” Dr. Fraser said. “The sliding reconstruction has relevance not only to the status of the aortic arch over the long term but it also has a profound effect on ventricular function.”
He noted a single-center, retrospective study from the United Kingdom that demonstrated that the quality of the aortic arch reconstruction, and the related opportunity for ventricular arterial coupling, directly correlate with long-term performance of the aortic arch in patients with hypoplastic left heart syndrome (J Thorac Cardiovasc Surg. 2014;148:1526-33).
“This is very important as part of the growing population of these patients who need long-term management, most of whom we’re anticipating managing not just for years, but for decades,” Dr. Fraser said.
He said he had no relevant financial disclosures.
NEW YORK – With more than 1 million adults living today with congenital aortic disease, cardiovascular surgeons must think of outcomes in terms of decades, not years, when performing aortic arch repair in newborns, infants, and children, according to Charles D. Fraser Jr., M.D.
To that end, an all-autologous approach to aortic arch repair is key in preserving problem-free aortic function in adulthood, said Dr. Fraser, surgeon-in-chief at Texas Children’s Hospital in Houston.
Dr. Fraser reported on his center’s experience with all-autologous aortic arch repair techniques. He reviewed the following five principles that guide aortic arch repair in newborns, infants, and children at Texas Children’s Hospital:
• Use of autologous tissue reconstruction and avoidance of prosthetic material.
• Concomitant intracardiac repair.
• Use of anatomic reconstruction.
• Optimization of ventriculoarterial coupling.
• Preservation of laryngeal nerve function.
“The principles we developed at Texas Children’s Hospital we hope will translate into fewer of these patients that surgeons caring for adults with aortic disease will have to take care of later in life,” Dr. Fraser said at the meeting sponsored by the American Association for Thoracic Surgery. He reviewed cases in which he explained techniques he and his colleagues developed to address long-term outcomes.
The first challenge is to determine when to perform aortic repair in pediatric patients. “A question often asked is how small is too small when assessing the aortic arch in association with significant periductal coarctation?” he said. “Our rule of thumb has been that the arch diameter measured in millimeters should be at least the patient’s weight in kilograms plus one.” In other words, a 3-kg baby should have an aortic arch of at least 4 mm in diameter, he said.
He described the case of a 3.8-kg male baby on prostaglandin E1 who had aortic arch advancement repair and closure of atrial and ventricular septal defects at 8 days of age. The patient had an early origin of the left common carotid artery and a small proximal aortic arch. “This is the kind of patient in which we would do a complete aortic arch reconstruction, again with the autologous technique,” Dr. Fraser said.
In such a patient, Dr. Fraser and his colleagues at Texas Children’s Hospital support the circulation to the brain with antegrade cerebral perfusion, using transcranial Doppler and near-infrared spectroscopy to guide their profusion strategy, before putting the child on cardiac bypass and “profound” hypothermia. Careful planning before cannulation is important to perform the aortic transection at the correct level, he said
He also explained the ascending sliding arch aortoplasty, also known as the “Texas slide,” first described by E. Dean McKenzie, M.D., at Texas Children’s Hospital in 2011 (Ann. Thorac. Surg. 2011;91:805-10) This technique involves sliding a tongue-shaped piece of the ascending aorta underneath the aortic arch to construct an all-autologous repair.
“In patients with bicuspid aortic valves, we often observe that the ascending aorta is extremely elongated,” he said. “The idea is to take advantage of that and slide the ascending aorta completely up underneath the aortic arch and construct an all-autologous arch advancement type of repair.”
He presented the case of a 4-year-old boy with coarctation of the aorta in whom the Texas slide was indicated. “If this patient were treated with a simple coarctectomy, the patient would be subject to a life with a moderately hypoplastic aortic arch, and over the course of time, this could be problematic,” Dr. Fraser said. “The sliding reconstruction has relevance not only to the status of the aortic arch over the long term but it also has a profound effect on ventricular function.”
He noted a single-center, retrospective study from the United Kingdom that demonstrated that the quality of the aortic arch reconstruction, and the related opportunity for ventricular arterial coupling, directly correlate with long-term performance of the aortic arch in patients with hypoplastic left heart syndrome (J Thorac Cardiovasc Surg. 2014;148:1526-33).
“This is very important as part of the growing population of these patients who need long-term management, most of whom we’re anticipating managing not just for years, but for decades,” Dr. Fraser said.
He said he had no relevant financial disclosures.
AT AATS AORTIC SYMPOSIUM 2016
Key clinical point: Surgeons must think of outcomes for operations to correct aortic arch disease in children in the context of decades, not years.
Major finding: Five principles should guide autologous aortic arch repair in newborns, infants, and children.
Data source: Case studies from Texas Children’s Hospital.
Disclosures: Dr. Fraser reported having no relevant financial disclosures.
Protective hypothermia during arch surgery lacked benefit, study shows
NEW YORK – Deep hypothermia may affect long-term survival in individuals who have aortic arch surgery with antegrade cerebral perfusion (ACP), but not short-term outcomes in terms of death and major morbidities, according to a Baylor College of Medicine study.
The study evaluated outcomes of 544 consecutive patients who had proximal and total aortic arch surgery and received ACP for more than 30 minutes over a 10-year period, said lead investigator Ourania Preventza, MD, of the division of cardiothoracic surgery at the college in Houston. The researchers compared results of three different hypothermia levels: deep hypothermia at 14.1°-20° C; low-moderate at 20.1°-23.9° C; and high-moderate at 24°-28° C. The study also classified ACP time in two levels: 31-45 minutes for 238 patients (43.8%); and 45 minutes or more in 306 patients (56.3%).
“The different temperature levels did not significantly affect the short-term mortality and major morbidity rates,” Dr. Preventza said. “Reoperation for bleeding was associated with lower temperature (14.1°-20° C). The long-term survival rate in patients who underwent proximal arch surgery involving ACP for more than 30 minutes and use of moderate hypothermia (20.1°-28° C) were actually improved.”
While the outcomes showed small variations between the three groups, with deep hypothermia being associated with a higher percentage of adverse outcomes, Dr. Preventza said the differences were not statistically significant. The overall operative mortality rate was 12.5% (68 patients): 15.5% (18 patients) in the deep-hypothermia group; 11.8% (31 patients) in the low-moderate group; and 11.5% (19 patients) in the high-moderate group (P = 0.54).
The patients who underwent deep hypothermia were more likely to receive unilateral ACP, and those who underwent moderate hypothermia were more likely to have bilateral ACP, Dr. Preventza said at the meeting sponsored by the American Association for Thoracic Surgery. The deep-hypothermia group had higher transfusion rates, but, again, the researchers did not consider this variation to be statistically significant.
In the deep-hypothermia group, 20.9% of patients had a reoperation for bleeding, compared with 11.3% in the overall group and 7.7% and 10.2% in the low- and high-moderate groups, respectively, Dr. Preventza reported. Multivariate analysis revealed that higher temperature was associated with less bleeding, with an odds ratio of 0.61 (P = 0.015).
Deep hypothermia was related to statistically significant differences in the rates of permanent stroke and permanent neurologic events in the univariate analysis only, Dr. Preventza said: 6.3% and 7.2%, respectively, in the overall analysis vs. 12.2% for both events in the deep-hypothermia group. In the propensity score analysis, the rates of permanent stroke and permanent neurologic events in the moderate-hypothermia group were 7.6% and 8.5%, respectively, vs. 11.3% for both events in the deep-hypothermia group, a nonsignificant difference.
“With regard to permanent stoke and permanent neurological events, the multivariate analysis showed that preoperatively a neurologic deficit as well as acute type I aortic dissection were associated with adverse neurological events,” she said.
“However,” Dr. Preventza added, “the surprising thing is that when we looked at long-term survival for the entire cohort, we saw that the patients with moderate hypothermia did better.”
Kaplan-Meier analysis for the propensity pairs showed that the probability of survival at 8 years was 55.3% for the deep-hypothermia group vs. 68.5% for the moderate-hypothermia group.
The approach the Baylor researchers used involved cannulating the axillary or innominate artery in most patients before administering ACP, although a few patients had femoral or direct aortic cannulation, Dr. Preventza said. For bilateral ACP, the researchers delivered cerebral perfusion via a 9-French Pruitt balloon-tip catheter (LeMaitre Vascular) in the left common carotid artery. To protect the brain, they administered perfusion at 8-12 cc/kg per min and maintained a perfusion pressure of 50-70 mm Hg, as measured via the radial arterial line and guided by near-infrared spectroscopy.
Dr. Preventza had no relevant disclosures.
NEW YORK – Deep hypothermia may affect long-term survival in individuals who have aortic arch surgery with antegrade cerebral perfusion (ACP), but not short-term outcomes in terms of death and major morbidities, according to a Baylor College of Medicine study.
The study evaluated outcomes of 544 consecutive patients who had proximal and total aortic arch surgery and received ACP for more than 30 minutes over a 10-year period, said lead investigator Ourania Preventza, MD, of the division of cardiothoracic surgery at the college in Houston. The researchers compared results of three different hypothermia levels: deep hypothermia at 14.1°-20° C; low-moderate at 20.1°-23.9° C; and high-moderate at 24°-28° C. The study also classified ACP time in two levels: 31-45 minutes for 238 patients (43.8%); and 45 minutes or more in 306 patients (56.3%).
“The different temperature levels did not significantly affect the short-term mortality and major morbidity rates,” Dr. Preventza said. “Reoperation for bleeding was associated with lower temperature (14.1°-20° C). The long-term survival rate in patients who underwent proximal arch surgery involving ACP for more than 30 minutes and use of moderate hypothermia (20.1°-28° C) were actually improved.”
While the outcomes showed small variations between the three groups, with deep hypothermia being associated with a higher percentage of adverse outcomes, Dr. Preventza said the differences were not statistically significant. The overall operative mortality rate was 12.5% (68 patients): 15.5% (18 patients) in the deep-hypothermia group; 11.8% (31 patients) in the low-moderate group; and 11.5% (19 patients) in the high-moderate group (P = 0.54).
The patients who underwent deep hypothermia were more likely to receive unilateral ACP, and those who underwent moderate hypothermia were more likely to have bilateral ACP, Dr. Preventza said at the meeting sponsored by the American Association for Thoracic Surgery. The deep-hypothermia group had higher transfusion rates, but, again, the researchers did not consider this variation to be statistically significant.
In the deep-hypothermia group, 20.9% of patients had a reoperation for bleeding, compared with 11.3% in the overall group and 7.7% and 10.2% in the low- and high-moderate groups, respectively, Dr. Preventza reported. Multivariate analysis revealed that higher temperature was associated with less bleeding, with an odds ratio of 0.61 (P = 0.015).
Deep hypothermia was related to statistically significant differences in the rates of permanent stroke and permanent neurologic events in the univariate analysis only, Dr. Preventza said: 6.3% and 7.2%, respectively, in the overall analysis vs. 12.2% for both events in the deep-hypothermia group. In the propensity score analysis, the rates of permanent stroke and permanent neurologic events in the moderate-hypothermia group were 7.6% and 8.5%, respectively, vs. 11.3% for both events in the deep-hypothermia group, a nonsignificant difference.
“With regard to permanent stoke and permanent neurological events, the multivariate analysis showed that preoperatively a neurologic deficit as well as acute type I aortic dissection were associated with adverse neurological events,” she said.
“However,” Dr. Preventza added, “the surprising thing is that when we looked at long-term survival for the entire cohort, we saw that the patients with moderate hypothermia did better.”
Kaplan-Meier analysis for the propensity pairs showed that the probability of survival at 8 years was 55.3% for the deep-hypothermia group vs. 68.5% for the moderate-hypothermia group.
The approach the Baylor researchers used involved cannulating the axillary or innominate artery in most patients before administering ACP, although a few patients had femoral or direct aortic cannulation, Dr. Preventza said. For bilateral ACP, the researchers delivered cerebral perfusion via a 9-French Pruitt balloon-tip catheter (LeMaitre Vascular) in the left common carotid artery. To protect the brain, they administered perfusion at 8-12 cc/kg per min and maintained a perfusion pressure of 50-70 mm Hg, as measured via the radial arterial line and guided by near-infrared spectroscopy.
Dr. Preventza had no relevant disclosures.
NEW YORK – Deep hypothermia may affect long-term survival in individuals who have aortic arch surgery with antegrade cerebral perfusion (ACP), but not short-term outcomes in terms of death and major morbidities, according to a Baylor College of Medicine study.
The study evaluated outcomes of 544 consecutive patients who had proximal and total aortic arch surgery and received ACP for more than 30 minutes over a 10-year period, said lead investigator Ourania Preventza, MD, of the division of cardiothoracic surgery at the college in Houston. The researchers compared results of three different hypothermia levels: deep hypothermia at 14.1°-20° C; low-moderate at 20.1°-23.9° C; and high-moderate at 24°-28° C. The study also classified ACP time in two levels: 31-45 minutes for 238 patients (43.8%); and 45 minutes or more in 306 patients (56.3%).
“The different temperature levels did not significantly affect the short-term mortality and major morbidity rates,” Dr. Preventza said. “Reoperation for bleeding was associated with lower temperature (14.1°-20° C). The long-term survival rate in patients who underwent proximal arch surgery involving ACP for more than 30 minutes and use of moderate hypothermia (20.1°-28° C) were actually improved.”
While the outcomes showed small variations between the three groups, with deep hypothermia being associated with a higher percentage of adverse outcomes, Dr. Preventza said the differences were not statistically significant. The overall operative mortality rate was 12.5% (68 patients): 15.5% (18 patients) in the deep-hypothermia group; 11.8% (31 patients) in the low-moderate group; and 11.5% (19 patients) in the high-moderate group (P = 0.54).
The patients who underwent deep hypothermia were more likely to receive unilateral ACP, and those who underwent moderate hypothermia were more likely to have bilateral ACP, Dr. Preventza said at the meeting sponsored by the American Association for Thoracic Surgery. The deep-hypothermia group had higher transfusion rates, but, again, the researchers did not consider this variation to be statistically significant.
In the deep-hypothermia group, 20.9% of patients had a reoperation for bleeding, compared with 11.3% in the overall group and 7.7% and 10.2% in the low- and high-moderate groups, respectively, Dr. Preventza reported. Multivariate analysis revealed that higher temperature was associated with less bleeding, with an odds ratio of 0.61 (P = 0.015).
Deep hypothermia was related to statistically significant differences in the rates of permanent stroke and permanent neurologic events in the univariate analysis only, Dr. Preventza said: 6.3% and 7.2%, respectively, in the overall analysis vs. 12.2% for both events in the deep-hypothermia group. In the propensity score analysis, the rates of permanent stroke and permanent neurologic events in the moderate-hypothermia group were 7.6% and 8.5%, respectively, vs. 11.3% for both events in the deep-hypothermia group, a nonsignificant difference.
“With regard to permanent stoke and permanent neurological events, the multivariate analysis showed that preoperatively a neurologic deficit as well as acute type I aortic dissection were associated with adverse neurological events,” she said.
“However,” Dr. Preventza added, “the surprising thing is that when we looked at long-term survival for the entire cohort, we saw that the patients with moderate hypothermia did better.”
Kaplan-Meier analysis for the propensity pairs showed that the probability of survival at 8 years was 55.3% for the deep-hypothermia group vs. 68.5% for the moderate-hypothermia group.
The approach the Baylor researchers used involved cannulating the axillary or innominate artery in most patients before administering ACP, although a few patients had femoral or direct aortic cannulation, Dr. Preventza said. For bilateral ACP, the researchers delivered cerebral perfusion via a 9-French Pruitt balloon-tip catheter (LeMaitre Vascular) in the left common carotid artery. To protect the brain, they administered perfusion at 8-12 cc/kg per min and maintained a perfusion pressure of 50-70 mm Hg, as measured via the radial arterial line and guided by near-infrared spectroscopy.
Dr. Preventza had no relevant disclosures.
AT AATS AORTIC SYMPOSIUM 2016
Key clinical point: Differing temperatures of hypothermia did not affect death or morbidity in patients who had aortic arch surgery with more than 30 minutes of antegrade cerebral perfusion.
Major finding: The overall operative death rate in the study was 12.4% with no statistically significant differences between three different hypothermia groups.
Data source: Series of 510 consecutive patients who had proximal and total arch surgery and received antegrade cerebral perfusion for more than 30 minutes over a 10-year period.
Disclosures: Dr. Preventza reported having no financial disclosures.
Surgery for acute type A dissection shows 20-year shift to valve sparing, biological valves
NEW YORK – A study of an international database of individuals who have had open repair for acute type A aortic dissection (ATAAD) has revealed that in the past 20 years, cardiovascular surgeons have widely embraced valve-sparing procedures, bioprosthetic valves, and cerebral profusion strategies, according to a report here on the latest analysis of the database.
The most telling result is the decline in overall mortality, Santi Trimarchi, MD, PhD, of the University of Milan IRCCS Policlinico San Donato in Italy reported on behalf of the International Registry of Acute Aortic Dissection (IRAD) Interventional Cohort (IVC). The cohort analyzed surgery techniques and outcomes of 1,732 patients who had open repair from 1996 to 2016, clustering results in three time intervals: 1996-2003; 2004-2009; and 2010-2015.
“We noted in the registry that the overall in-hospital mortality rate was 14.3%, and this mortality decreased over time from 17.5% in the first six-year time span to 12.2% in the last six years,” Dr. Trimarchi said.

Among other trends the study identified are greater reliance on biological vs. mechanical valves, an increase in valve-sparing procedures, and steady use of Bentall procedures throughout the study period. “Operative techniques for redo aortic valve repair have been improving over the time, and that’s why we see more frequent use of biologic valves,” he said at the meeting, sponsored by the American Association for Thoracic Surgery.
“Cerebral profusion management has been widely adopted,” Dr. Trimarchi said. “Also there is an important trend showing an increasing utilization of antegrade cerebral profusion while we see a negative trend of the utilization of retrograde brain protection.”
Dr. Trimarchi attributed the detail the study generated to the survey form sent to the 26 IRAD-IVC sites around the world. The form measures 131 different variables, he said.
“Using this new specific surgical data form, we think we can address some surgical issues and report better data from the IRAD registry results on acute dissection,” he said. “These analyses have shown there have been significant changes in operative strategy over time in terms of managing such patients, and more importantly, a significant decrease in in-hospital mortality was observed in a 20-year time period.”
Dr. Trimarchi disclosed that he has received speaking and consulting fees and research support from W.L. Gore & Associates and Medtronic. IRAD is supported by W.L. Gore, Active Sites, Medtronic, Varbedian Aortic Research Fund, the Hewlett Foundation, the Mardigian Foundation, UM Faculty Group Practice, Terumo, and Ann and Bob Aikens.
NEW YORK – A study of an international database of individuals who have had open repair for acute type A aortic dissection (ATAAD) has revealed that in the past 20 years, cardiovascular surgeons have widely embraced valve-sparing procedures, bioprosthetic valves, and cerebral profusion strategies, according to a report here on the latest analysis of the database.
The most telling result is the decline in overall mortality, Santi Trimarchi, MD, PhD, of the University of Milan IRCCS Policlinico San Donato in Italy reported on behalf of the International Registry of Acute Aortic Dissection (IRAD) Interventional Cohort (IVC). The cohort analyzed surgery techniques and outcomes of 1,732 patients who had open repair from 1996 to 2016, clustering results in three time intervals: 1996-2003; 2004-2009; and 2010-2015.
“We noted in the registry that the overall in-hospital mortality rate was 14.3%, and this mortality decreased over time from 17.5% in the first six-year time span to 12.2% in the last six years,” Dr. Trimarchi said.

Among other trends the study identified are greater reliance on biological vs. mechanical valves, an increase in valve-sparing procedures, and steady use of Bentall procedures throughout the study period. “Operative techniques for redo aortic valve repair have been improving over the time, and that’s why we see more frequent use of biologic valves,” he said at the meeting, sponsored by the American Association for Thoracic Surgery.
“Cerebral profusion management has been widely adopted,” Dr. Trimarchi said. “Also there is an important trend showing an increasing utilization of antegrade cerebral profusion while we see a negative trend of the utilization of retrograde brain protection.”
Dr. Trimarchi attributed the detail the study generated to the survey form sent to the 26 IRAD-IVC sites around the world. The form measures 131 different variables, he said.
“Using this new specific surgical data form, we think we can address some surgical issues and report better data from the IRAD registry results on acute dissection,” he said. “These analyses have shown there have been significant changes in operative strategy over time in terms of managing such patients, and more importantly, a significant decrease in in-hospital mortality was observed in a 20-year time period.”
Dr. Trimarchi disclosed that he has received speaking and consulting fees and research support from W.L. Gore & Associates and Medtronic. IRAD is supported by W.L. Gore, Active Sites, Medtronic, Varbedian Aortic Research Fund, the Hewlett Foundation, the Mardigian Foundation, UM Faculty Group Practice, Terumo, and Ann and Bob Aikens.
NEW YORK – A study of an international database of individuals who have had open repair for acute type A aortic dissection (ATAAD) has revealed that in the past 20 years, cardiovascular surgeons have widely embraced valve-sparing procedures, bioprosthetic valves, and cerebral profusion strategies, according to a report here on the latest analysis of the database.
The most telling result is the decline in overall mortality, Santi Trimarchi, MD, PhD, of the University of Milan IRCCS Policlinico San Donato in Italy reported on behalf of the International Registry of Acute Aortic Dissection (IRAD) Interventional Cohort (IVC). The cohort analyzed surgery techniques and outcomes of 1,732 patients who had open repair from 1996 to 2016, clustering results in three time intervals: 1996-2003; 2004-2009; and 2010-2015.
“We noted in the registry that the overall in-hospital mortality rate was 14.3%, and this mortality decreased over time from 17.5% in the first six-year time span to 12.2% in the last six years,” Dr. Trimarchi said.

Among other trends the study identified are greater reliance on biological vs. mechanical valves, an increase in valve-sparing procedures, and steady use of Bentall procedures throughout the study period. “Operative techniques for redo aortic valve repair have been improving over the time, and that’s why we see more frequent use of biologic valves,” he said at the meeting, sponsored by the American Association for Thoracic Surgery.
“Cerebral profusion management has been widely adopted,” Dr. Trimarchi said. “Also there is an important trend showing an increasing utilization of antegrade cerebral profusion while we see a negative trend of the utilization of retrograde brain protection.”
Dr. Trimarchi attributed the detail the study generated to the survey form sent to the 26 IRAD-IVC sites around the world. The form measures 131 different variables, he said.
“Using this new specific surgical data form, we think we can address some surgical issues and report better data from the IRAD registry results on acute dissection,” he said. “These analyses have shown there have been significant changes in operative strategy over time in terms of managing such patients, and more importantly, a significant decrease in in-hospital mortality was observed in a 20-year time period.”
Dr. Trimarchi disclosed that he has received speaking and consulting fees and research support from W.L. Gore & Associates and Medtronic. IRAD is supported by W.L. Gore, Active Sites, Medtronic, Varbedian Aortic Research Fund, the Hewlett Foundation, the Mardigian Foundation, UM Faculty Group Practice, Terumo, and Ann and Bob Aikens.
AT AATS AORTIC SYMPOSIUM 2016
Key clinical point: Operations for acute type A aortic dissection (ATAAD) have seen significant changes in technique over the past 20 years.
Major finding: Use of biological valves increased from 35.6% of procedures to 52% over the study period while reliance of mechanical valves declined from 57.6% to 45.4%.
Data source: Interventional Cohort database of 1,732 patients enrolled in the International Registry of Acute Aortic Dissection database who had open surgery for ATAAD from February 1996 to March 2015.
Disclosures: Dr. Trimarchi disclosed having receive speaking and consulting fees from W.L. Gore & Associates and Medtronic as well as research support from the two companies. IRAD is supported by W.L. Gore, Active Sites, Medtronic, Varbedian Aortic Research Fund, the Hewlett Foundation, the Mardigian Foundation, UM Faculty Group Practice, Terumo, and Ann and Bob Aikens.
Study quantifies volume disparities for ATAD repair in the U.K.
NEW YORK – Mastery is the product of repetition, and it has long been taken for granted that surgeons and centers that perform a high volume of an operation will have better results than those who don’t do the operation as often, but a study out of the United Kingdom has determined just how much better high-volume centers are when it comes to repair of acute type A aortic dissection (ATAD) – and what the in-hospital mortality odds ratio is for lower-volume surgeons.
Specifically, that odds ratio is 1.64 (P = .030), Mohamad Bashir, MD, PhD, MRCS, a research fellow at Liverpool Heart and Chest Hospital, said in reporting early results of the study here. Lower-volume surgeons had worse outcomes in 12 of 14 different operative metrics the study evaluated, most notably in-hospital mortality: 20.2% for lower-volume surgeons vs. 15.2% for higher-volume surgeons. “There is an initiative in the U.K. to change the trend,” Dr. Bashir said. Full study results will be published in an upcoming issue of BMJ, he said.
“In-hospital mortality for surgeons who operate on 20 or more procedures is very good at 13.2%, and the same follows for 90-day mortality, one-year mortality and three-year mortality,” Dr. Bashir said.
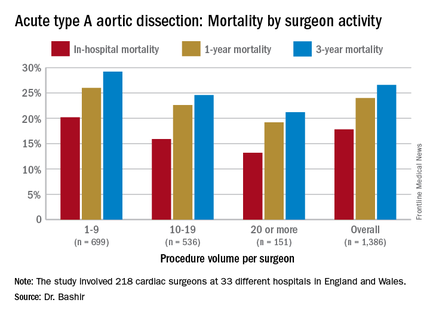
The study evaluated 1,386 ATAD procedures in the National Institute for Cardiovascular Outcomes Research database by 218 different cardiac surgeons at 33 different hospitals in England and Wales from April 2007 to March 2013. That would make the average number of procedures per surgeon 6.4, Dr. Bashir said, but a closer look at each surgeon’s case load reveals some disconcerting trends: almost 80% of the surgeons performed fewer than 10 ATAD repairs in the 6-year span of the study, and 34 surgeons, or about 15%, just did a single procedure in that time. The highest-volume surgeon did 32 procedures. The minimum hospital volume was 8 ATAD operations and the maximum was 103.
The study stratified lower- and higher-volume surgeon groups by characteristics of the patients they operated on. “The differences between these two groups are pretty interesting because we noticed that the lower-volume surgeons are actually operating on patients who are diabetic, who are smokers, who use inotropic support prior to anesthesia and who also have an injection fraction that is significant,” Dr. Bashir said.
In drilling down into those characteristics, people with diabetes made up 6% of the lower-volume surgeons’ cases vs. 3.1% of the higher-volume surgeons’ cases, despite an almost 50-50 split in share of procedures between the two surgeon groups. Current smokers comprised 20.5% of the lower-volume surgeons’ patients vs. 15.5% of their high-volume counterparts’ patients. Operative characteristics in terms of urgency of surgery were similar between the two groups. However Dr. Bashir noted, lower-volume surgeons had longer times for cardiopulmonary bypass, aortic cross-clamping, and circulatory arrest.
The study investigators applied a multivariable logistic regression model to determine predictors of in-hospital mortality for ATAD. “The odds ratio (OR) of mortality for lower-volume surgeons is 1.64, which is statistically significant,” Dr. Bashir said. Odds ratios for other predictors are: previous cardiac surgery, 2.51; peripheral vascular disease, 2.15; preoperative cardiogenic shock, 2.05; salvage operation, 5.57; and concomitant coronary artery bypass procedure, 2.98. For 5-year mortality, the odds ratio was 1.37 for the lower-volume surgeons.
Dr. Bashir laid out how the National Health Service can use the study results. “Concentration of expertise and volume to the appropriate surgeons and centers who perform increasingly more work and more complex aortic cases would be required to change the paradigm of acute type A aortic dissection outcomes in the U.K.,” he said. “It is reasonable to suggest that there should be a national standardization mandate and a quality-improvement framework of acute aortic dissection treatment.”
Dr. Bashir had no financial relationships to disclose.
NEW YORK – Mastery is the product of repetition, and it has long been taken for granted that surgeons and centers that perform a high volume of an operation will have better results than those who don’t do the operation as often, but a study out of the United Kingdom has determined just how much better high-volume centers are when it comes to repair of acute type A aortic dissection (ATAD) – and what the in-hospital mortality odds ratio is for lower-volume surgeons.
Specifically, that odds ratio is 1.64 (P = .030), Mohamad Bashir, MD, PhD, MRCS, a research fellow at Liverpool Heart and Chest Hospital, said in reporting early results of the study here. Lower-volume surgeons had worse outcomes in 12 of 14 different operative metrics the study evaluated, most notably in-hospital mortality: 20.2% for lower-volume surgeons vs. 15.2% for higher-volume surgeons. “There is an initiative in the U.K. to change the trend,” Dr. Bashir said. Full study results will be published in an upcoming issue of BMJ, he said.
“In-hospital mortality for surgeons who operate on 20 or more procedures is very good at 13.2%, and the same follows for 90-day mortality, one-year mortality and three-year mortality,” Dr. Bashir said.
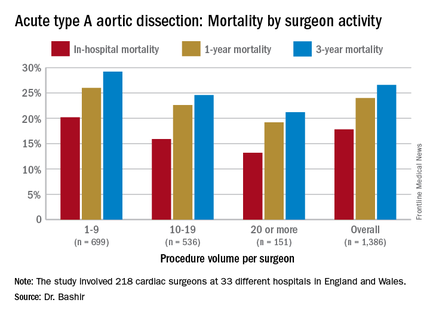
The study evaluated 1,386 ATAD procedures in the National Institute for Cardiovascular Outcomes Research database by 218 different cardiac surgeons at 33 different hospitals in England and Wales from April 2007 to March 2013. That would make the average number of procedures per surgeon 6.4, Dr. Bashir said, but a closer look at each surgeon’s case load reveals some disconcerting trends: almost 80% of the surgeons performed fewer than 10 ATAD repairs in the 6-year span of the study, and 34 surgeons, or about 15%, just did a single procedure in that time. The highest-volume surgeon did 32 procedures. The minimum hospital volume was 8 ATAD operations and the maximum was 103.
The study stratified lower- and higher-volume surgeon groups by characteristics of the patients they operated on. “The differences between these two groups are pretty interesting because we noticed that the lower-volume surgeons are actually operating on patients who are diabetic, who are smokers, who use inotropic support prior to anesthesia and who also have an injection fraction that is significant,” Dr. Bashir said.
In drilling down into those characteristics, people with diabetes made up 6% of the lower-volume surgeons’ cases vs. 3.1% of the higher-volume surgeons’ cases, despite an almost 50-50 split in share of procedures between the two surgeon groups. Current smokers comprised 20.5% of the lower-volume surgeons’ patients vs. 15.5% of their high-volume counterparts’ patients. Operative characteristics in terms of urgency of surgery were similar between the two groups. However Dr. Bashir noted, lower-volume surgeons had longer times for cardiopulmonary bypass, aortic cross-clamping, and circulatory arrest.
The study investigators applied a multivariable logistic regression model to determine predictors of in-hospital mortality for ATAD. “The odds ratio (OR) of mortality for lower-volume surgeons is 1.64, which is statistically significant,” Dr. Bashir said. Odds ratios for other predictors are: previous cardiac surgery, 2.51; peripheral vascular disease, 2.15; preoperative cardiogenic shock, 2.05; salvage operation, 5.57; and concomitant coronary artery bypass procedure, 2.98. For 5-year mortality, the odds ratio was 1.37 for the lower-volume surgeons.
Dr. Bashir laid out how the National Health Service can use the study results. “Concentration of expertise and volume to the appropriate surgeons and centers who perform increasingly more work and more complex aortic cases would be required to change the paradigm of acute type A aortic dissection outcomes in the U.K.,” he said. “It is reasonable to suggest that there should be a national standardization mandate and a quality-improvement framework of acute aortic dissection treatment.”
Dr. Bashir had no financial relationships to disclose.
NEW YORK – Mastery is the product of repetition, and it has long been taken for granted that surgeons and centers that perform a high volume of an operation will have better results than those who don’t do the operation as often, but a study out of the United Kingdom has determined just how much better high-volume centers are when it comes to repair of acute type A aortic dissection (ATAD) – and what the in-hospital mortality odds ratio is for lower-volume surgeons.
Specifically, that odds ratio is 1.64 (P = .030), Mohamad Bashir, MD, PhD, MRCS, a research fellow at Liverpool Heart and Chest Hospital, said in reporting early results of the study here. Lower-volume surgeons had worse outcomes in 12 of 14 different operative metrics the study evaluated, most notably in-hospital mortality: 20.2% for lower-volume surgeons vs. 15.2% for higher-volume surgeons. “There is an initiative in the U.K. to change the trend,” Dr. Bashir said. Full study results will be published in an upcoming issue of BMJ, he said.
“In-hospital mortality for surgeons who operate on 20 or more procedures is very good at 13.2%, and the same follows for 90-day mortality, one-year mortality and three-year mortality,” Dr. Bashir said.
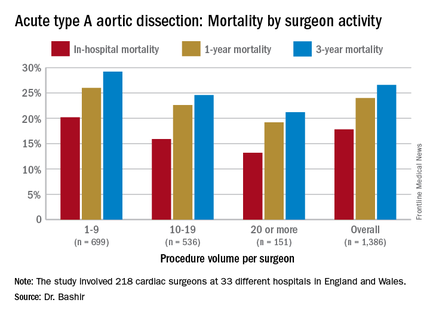
The study evaluated 1,386 ATAD procedures in the National Institute for Cardiovascular Outcomes Research database by 218 different cardiac surgeons at 33 different hospitals in England and Wales from April 2007 to March 2013. That would make the average number of procedures per surgeon 6.4, Dr. Bashir said, but a closer look at each surgeon’s case load reveals some disconcerting trends: almost 80% of the surgeons performed fewer than 10 ATAD repairs in the 6-year span of the study, and 34 surgeons, or about 15%, just did a single procedure in that time. The highest-volume surgeon did 32 procedures. The minimum hospital volume was 8 ATAD operations and the maximum was 103.
The study stratified lower- and higher-volume surgeon groups by characteristics of the patients they operated on. “The differences between these two groups are pretty interesting because we noticed that the lower-volume surgeons are actually operating on patients who are diabetic, who are smokers, who use inotropic support prior to anesthesia and who also have an injection fraction that is significant,” Dr. Bashir said.
In drilling down into those characteristics, people with diabetes made up 6% of the lower-volume surgeons’ cases vs. 3.1% of the higher-volume surgeons’ cases, despite an almost 50-50 split in share of procedures between the two surgeon groups. Current smokers comprised 20.5% of the lower-volume surgeons’ patients vs. 15.5% of their high-volume counterparts’ patients. Operative characteristics in terms of urgency of surgery were similar between the two groups. However Dr. Bashir noted, lower-volume surgeons had longer times for cardiopulmonary bypass, aortic cross-clamping, and circulatory arrest.
The study investigators applied a multivariable logistic regression model to determine predictors of in-hospital mortality for ATAD. “The odds ratio (OR) of mortality for lower-volume surgeons is 1.64, which is statistically significant,” Dr. Bashir said. Odds ratios for other predictors are: previous cardiac surgery, 2.51; peripheral vascular disease, 2.15; preoperative cardiogenic shock, 2.05; salvage operation, 5.57; and concomitant coronary artery bypass procedure, 2.98. For 5-year mortality, the odds ratio was 1.37 for the lower-volume surgeons.
Dr. Bashir laid out how the National Health Service can use the study results. “Concentration of expertise and volume to the appropriate surgeons and centers who perform increasingly more work and more complex aortic cases would be required to change the paradigm of acute type A aortic dissection outcomes in the U.K.,” he said. “It is reasonable to suggest that there should be a national standardization mandate and a quality-improvement framework of acute aortic dissection treatment.”
Dr. Bashir had no financial relationships to disclose.
AT THE AMERICAN ASSOCIATION FOR THORACIC SURGERY AORTIC SYMPOSIUM
Key clinical point: Patients undergoing repair of acute type A aortic dissection (ATAD) by lower-volume surgeons have high mortality in comparison with those undergoing repair by the highest-volume surgeons.
Major finding: In-hospital mortality for ATAD repair was 20.2% for lower-volume surgeons and 15.3% for higher-volume surgeons.
Data source: Analysis of 1,386 ATAD procedures from April 2007 to March 2013 in the National Institute for Cardiovascular Outcomes Research data.
Disclosures: Dr. Bashir reported having no financial disclosures.
Guideline tweak addresses conflicting recommendations on BAV
NEW YORK – While overall guidelines for aortic repair surgery have not changed significantly in the past 5 years, guidelines for the timing of surgery in patients with bicuspid aortic valves and enlarged aortas have undergone some updating in an attempt to clear up disparities in different guidelines on when to operate on those patients.
Lars G. Svensson, MD, PhD, chairman of the Cleveland Clinic Heart and Vascular Institute, coauthor of the clarification statement by the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines (J Thorac Cardiovasc Surg. 2016;151:959-66), reported on the guidelines clarification at the meeting sponsored by the American Association for Thoracic Surgery. He noted that five different clinical guidelines between 2010 and 2014 recommended five different size thresholds for prophylactic aortic root or ascending aortic surgery in the setting of bicuspid aortic valve (BAV), ranging from 4 cm to greater than 5.5 cm. “This created a bit of a quandary and controversy between different guidelines and time periods,” he said.
Dr. Svensson and Loren Hiratzka, MD, medical director of cardiac surgery for TriHealth in Cincinnati, and their colleagues drafted the guideline clarification that makes the following recommendations for aortic root and ascending aorta repair or replacement when patients have BAV (strength of recommendation):
• Surgery is indicated to replace the aortic root or ascending aorta in asymptomatic patients with BAV if the diameter of the aortic root or ascending aorta is 5.5 cm or greater (Class 1).
• Surgical repair is indicated for asymptomatic patients with BAV if the root or ascending aorta diameter is 5 cm or greater in two scenarios: if the patient has an additional risk factor for dissection, such as family history or excessive aortic growth rate; or if the patient is a low surgical risk and has access to an experienced surgeon at a high-volume center (Class IIa).
The guideline update also addresses BAV in patients with Turner syndrome. The 2010 joint guidelines of 10 societies left some questions with regard to surgery in these patients, Dr. Svensson said. The established guidelines included a Class IIb recommendation for imaging of the heart and aorta to help determine the aorta risk in patients with Turner syndrome who had additional risk factors, including BAV, aortic coarctation and/or hypertension, or were planning a pregnancy.
The updated guideline includes Class IIa recommendation that in short-statured patients with Turner syndrome and BAV, measurement of the aortic root or ascending aorta diameter may not predict the dissection risk as well as aortic diameter index greater than 2.5 cm/m2. The updated recommendations also draw on one study that reported that in patients with BAV, a maximum aortic cross-sectional area-to-height ratio of 10 cm2/m or greater was also predictive of aortic dissection. (Ann Thorac Surg. 2015;100:1666-73)
The updated recommendations for open surgery for ascending aortic aneurysm include separate valve and ascending aortic replacement in patients without significant aortic root dilatation or in elderly patients, or in younger patients with minimal dilatation who have aortic valve disease; and excision of the sinuses of Valsalva with a modified David reimplantation when technically feasible in patients with connective tissue disease and others with dilatation of the aortic root and sinuses. For patients in whom the latter procedure is not feasible, root replacement with valved graft conduit would be indicated, Dr. Svensson said.
Dr. Svensson also reported on recent studies that validated recommendations in established guidelines.
Studies of circulatory arrest practices in aortic arch surgery as prescribed by established guidelines showed confirmatory results, he said. “The one point I would make about circulatory arrest is that we found in a fairly large study of 1,352 circulatory arrest patients that we reduced the risk of stroke by 40% when we used the axillary artery with a side a graft,” he said (Ann Thorac Surg. 2004;78:1274-84). His own institution’s clinical trial of 121 patients who received antegrade or retrograde brain perfusion showed rates of 0.8% for each stroke and operative death, he said (J Thorac Cardiovasc Surg. 2015;150:1140-7).
“What was also of interest there was no difference in outcomes with antegrade vs. retrograde brain profusion,” he said. “I think protection of the brain is pretty good if you follow the fundamental principles of brain protection.”
He also reported on a recent study at his institution that documented the benefits of intrathecal papaverine (IP) for spinal cord protection during descending open and endovascular aortic repairs. In 398 aortic repairs from 2001-2009, the rates of spinal cord injury were 23% in the non-IP group vs. 7% in the IP group (P = .07) in a matched cohort.
He noted that the clinical guidelines of the American Association for Thoracic Surgery as well as AATS/Society of Thoracic Surgeons joint guidelines are open to input. “If you have areas where you think guideline should be written about, please let me or other members of the committee know,” he said.
Dr. Svensson had no disclosures relevant to his presentation.
NEW YORK – While overall guidelines for aortic repair surgery have not changed significantly in the past 5 years, guidelines for the timing of surgery in patients with bicuspid aortic valves and enlarged aortas have undergone some updating in an attempt to clear up disparities in different guidelines on when to operate on those patients.
Lars G. Svensson, MD, PhD, chairman of the Cleveland Clinic Heart and Vascular Institute, coauthor of the clarification statement by the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines (J Thorac Cardiovasc Surg. 2016;151:959-66), reported on the guidelines clarification at the meeting sponsored by the American Association for Thoracic Surgery. He noted that five different clinical guidelines between 2010 and 2014 recommended five different size thresholds for prophylactic aortic root or ascending aortic surgery in the setting of bicuspid aortic valve (BAV), ranging from 4 cm to greater than 5.5 cm. “This created a bit of a quandary and controversy between different guidelines and time periods,” he said.
Dr. Svensson and Loren Hiratzka, MD, medical director of cardiac surgery for TriHealth in Cincinnati, and their colleagues drafted the guideline clarification that makes the following recommendations for aortic root and ascending aorta repair or replacement when patients have BAV (strength of recommendation):
• Surgery is indicated to replace the aortic root or ascending aorta in asymptomatic patients with BAV if the diameter of the aortic root or ascending aorta is 5.5 cm or greater (Class 1).
• Surgical repair is indicated for asymptomatic patients with BAV if the root or ascending aorta diameter is 5 cm or greater in two scenarios: if the patient has an additional risk factor for dissection, such as family history or excessive aortic growth rate; or if the patient is a low surgical risk and has access to an experienced surgeon at a high-volume center (Class IIa).
The guideline update also addresses BAV in patients with Turner syndrome. The 2010 joint guidelines of 10 societies left some questions with regard to surgery in these patients, Dr. Svensson said. The established guidelines included a Class IIb recommendation for imaging of the heart and aorta to help determine the aorta risk in patients with Turner syndrome who had additional risk factors, including BAV, aortic coarctation and/or hypertension, or were planning a pregnancy.
The updated guideline includes Class IIa recommendation that in short-statured patients with Turner syndrome and BAV, measurement of the aortic root or ascending aorta diameter may not predict the dissection risk as well as aortic diameter index greater than 2.5 cm/m2. The updated recommendations also draw on one study that reported that in patients with BAV, a maximum aortic cross-sectional area-to-height ratio of 10 cm2/m or greater was also predictive of aortic dissection. (Ann Thorac Surg. 2015;100:1666-73)
The updated recommendations for open surgery for ascending aortic aneurysm include separate valve and ascending aortic replacement in patients without significant aortic root dilatation or in elderly patients, or in younger patients with minimal dilatation who have aortic valve disease; and excision of the sinuses of Valsalva with a modified David reimplantation when technically feasible in patients with connective tissue disease and others with dilatation of the aortic root and sinuses. For patients in whom the latter procedure is not feasible, root replacement with valved graft conduit would be indicated, Dr. Svensson said.
Dr. Svensson also reported on recent studies that validated recommendations in established guidelines.
Studies of circulatory arrest practices in aortic arch surgery as prescribed by established guidelines showed confirmatory results, he said. “The one point I would make about circulatory arrest is that we found in a fairly large study of 1,352 circulatory arrest patients that we reduced the risk of stroke by 40% when we used the axillary artery with a side a graft,” he said (Ann Thorac Surg. 2004;78:1274-84). His own institution’s clinical trial of 121 patients who received antegrade or retrograde brain perfusion showed rates of 0.8% for each stroke and operative death, he said (J Thorac Cardiovasc Surg. 2015;150:1140-7).
“What was also of interest there was no difference in outcomes with antegrade vs. retrograde brain profusion,” he said. “I think protection of the brain is pretty good if you follow the fundamental principles of brain protection.”
He also reported on a recent study at his institution that documented the benefits of intrathecal papaverine (IP) for spinal cord protection during descending open and endovascular aortic repairs. In 398 aortic repairs from 2001-2009, the rates of spinal cord injury were 23% in the non-IP group vs. 7% in the IP group (P = .07) in a matched cohort.
He noted that the clinical guidelines of the American Association for Thoracic Surgery as well as AATS/Society of Thoracic Surgeons joint guidelines are open to input. “If you have areas where you think guideline should be written about, please let me or other members of the committee know,” he said.
Dr. Svensson had no disclosures relevant to his presentation.
NEW YORK – While overall guidelines for aortic repair surgery have not changed significantly in the past 5 years, guidelines for the timing of surgery in patients with bicuspid aortic valves and enlarged aortas have undergone some updating in an attempt to clear up disparities in different guidelines on when to operate on those patients.
Lars G. Svensson, MD, PhD, chairman of the Cleveland Clinic Heart and Vascular Institute, coauthor of the clarification statement by the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines (J Thorac Cardiovasc Surg. 2016;151:959-66), reported on the guidelines clarification at the meeting sponsored by the American Association for Thoracic Surgery. He noted that five different clinical guidelines between 2010 and 2014 recommended five different size thresholds for prophylactic aortic root or ascending aortic surgery in the setting of bicuspid aortic valve (BAV), ranging from 4 cm to greater than 5.5 cm. “This created a bit of a quandary and controversy between different guidelines and time periods,” he said.
Dr. Svensson and Loren Hiratzka, MD, medical director of cardiac surgery for TriHealth in Cincinnati, and their colleagues drafted the guideline clarification that makes the following recommendations for aortic root and ascending aorta repair or replacement when patients have BAV (strength of recommendation):
• Surgery is indicated to replace the aortic root or ascending aorta in asymptomatic patients with BAV if the diameter of the aortic root or ascending aorta is 5.5 cm or greater (Class 1).
• Surgical repair is indicated for asymptomatic patients with BAV if the root or ascending aorta diameter is 5 cm or greater in two scenarios: if the patient has an additional risk factor for dissection, such as family history or excessive aortic growth rate; or if the patient is a low surgical risk and has access to an experienced surgeon at a high-volume center (Class IIa).
The guideline update also addresses BAV in patients with Turner syndrome. The 2010 joint guidelines of 10 societies left some questions with regard to surgery in these patients, Dr. Svensson said. The established guidelines included a Class IIb recommendation for imaging of the heart and aorta to help determine the aorta risk in patients with Turner syndrome who had additional risk factors, including BAV, aortic coarctation and/or hypertension, or were planning a pregnancy.
The updated guideline includes Class IIa recommendation that in short-statured patients with Turner syndrome and BAV, measurement of the aortic root or ascending aorta diameter may not predict the dissection risk as well as aortic diameter index greater than 2.5 cm/m2. The updated recommendations also draw on one study that reported that in patients with BAV, a maximum aortic cross-sectional area-to-height ratio of 10 cm2/m or greater was also predictive of aortic dissection. (Ann Thorac Surg. 2015;100:1666-73)
The updated recommendations for open surgery for ascending aortic aneurysm include separate valve and ascending aortic replacement in patients without significant aortic root dilatation or in elderly patients, or in younger patients with minimal dilatation who have aortic valve disease; and excision of the sinuses of Valsalva with a modified David reimplantation when technically feasible in patients with connective tissue disease and others with dilatation of the aortic root and sinuses. For patients in whom the latter procedure is not feasible, root replacement with valved graft conduit would be indicated, Dr. Svensson said.
Dr. Svensson also reported on recent studies that validated recommendations in established guidelines.
Studies of circulatory arrest practices in aortic arch surgery as prescribed by established guidelines showed confirmatory results, he said. “The one point I would make about circulatory arrest is that we found in a fairly large study of 1,352 circulatory arrest patients that we reduced the risk of stroke by 40% when we used the axillary artery with a side a graft,” he said (Ann Thorac Surg. 2004;78:1274-84). His own institution’s clinical trial of 121 patients who received antegrade or retrograde brain perfusion showed rates of 0.8% for each stroke and operative death, he said (J Thorac Cardiovasc Surg. 2015;150:1140-7).
“What was also of interest there was no difference in outcomes with antegrade vs. retrograde brain profusion,” he said. “I think protection of the brain is pretty good if you follow the fundamental principles of brain protection.”
He also reported on a recent study at his institution that documented the benefits of intrathecal papaverine (IP) for spinal cord protection during descending open and endovascular aortic repairs. In 398 aortic repairs from 2001-2009, the rates of spinal cord injury were 23% in the non-IP group vs. 7% in the IP group (P = .07) in a matched cohort.
He noted that the clinical guidelines of the American Association for Thoracic Surgery as well as AATS/Society of Thoracic Surgeons joint guidelines are open to input. “If you have areas where you think guideline should be written about, please let me or other members of the committee know,” he said.
Dr. Svensson had no disclosures relevant to his presentation.
AT THE AATS AORTIC SYMPOSIUM 2016
Key clinical point: Various clinical guidelines provided five different recommendations for the timing of aortic repair surgery in patients with bicuspid aortic valves.
Major finding: Recent updates in guidelines provide clarity on when an aortic repair is needed in the setting of aortic bicuspid valve.
Data source: American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines.
Disclosures: Dr. Svensson had no relevant financial relationships to disclose.
FDA panel narrowly endorses empagliflozin’s cardiovascular mortality benefit
ROCKVILLE, MD. – In a 12-11 vote, a Food and Drug Administration advisory panel just barely came down in favor of the agency adding a new labeling entry to the already-approved diabetes drug empagliflozin (Jardiance) that would say the drug reduces cardiovascular mortality.
While several members of the panel wished the FDA’s staff good luck in weighing both the evidence and the advisory committee’s closely split endorsement when deciding whether to grant this unprecedented labeling to a diabetes drug, the fact that a majority of panelists favored this course marked a watershed moment in the development of new agents for treating hyperglycemia.
“It’s the first time we have evidence that a diabetes drug can reduce cardiovascular risk. That’s never been seen before, and it’s huge,” said Marvin A. Konstam, MD, a temporary member of the Endocrinologic and Metabolic Drugs Advisory Committee (EMDAC) and chief physician executive of the cardiovascular center at Tufts Medical Center in Boston. “The question is whether or not this effect is real, and the vote was 50-50, but I think there is a good chance it’s real, and, if so, it’s a game changer,” Dr. Konstam said in an interview. He voted in favor of the new labeling, and, like many of his colleagues on the panel, he admitted to agonizing over the decision during the postvote comment period.
What he and the other committee members struggled with was a remarkably strong effect by empagliflozin on reducing cardiovascular mortality by a relative 38%, compared with placebo, in more than 7,000 patients with type 2 diabetes selected for their high cardiovascular disease risk. The major sticking point was that the study enrolled patients into a randomized, placebo-controlled trial that was primarily designed to test the drug’s cardiovascular safety and not its efficacy, and where cardiovascular death was not even a prespecified secondary endpoint.
“It’s very hard to go from safety to superiority in one study,” said Peter W.F. Wilson, MD, who voted against the added indication. Like many panel members who voted no, Dr. Wilson said that any claim to preventing cardiovascular mortality with empagliflozin should meet the standard FDA requirement to have consistent results from at least two studies. “This is the first drug in its class [the sodium-glucose cotransporter 2 inhibitors], and we should have a high bar for the quality of the evidence,” said Dr. Wilson, professor of medicine and public health at Emory University in Atlanta.
“There is substantial evidence [to support the mortality claim], but not yet to the extent to put it on the label,” said another voter on the no side, Judith Fradkin, MD, also a temporary committee member and director of the division of diabetes, endocrinology and metabolic diseases at the National Institutes of Health. The data collected so far in favor of the mortality claim “are very compelling, but what I couldn’t get past is my long-standing belief that a positive result to a study’s secondary outcome is hypothesis generating. We need a second study to put this on the label,” Dr. Fradkin said.
That dramatic and highly meaningful clinical effect of empagliflozin on cardiovascular mortality jumped out at the investigators who ran the EMPA-REG OUTCOME trial as well as to many others from the moment the results had their unveiling less than a year ago, at the annual meeting of the European Association for the Study of Diabetes in Stockholm, and in a concurrently published article (N Engl J Med. 2015 Nov 26;373[22]:2117-28).
The primary efficacy endpoint placed into the EMPA-REG OUTCOME safety trial as the study developed following the 2008 FDA mandate for cardiovascular safety trials for all new hypoglycemic drugs was a three-part, combined-outcome endpoint of cardiovascular death, nonfatal MI, and nonfatal stroke. Although this primary, combined endpoint had a statistically significant but much more modest benefit with a 14% relative risk reduction, compared with placebo, “the benefit was all driven by the reduction in cardiovascular death that had an astonishing P value of less than .0001 with no suggestion of benefit or risk for MI or stroke,” said Stuart Pocock, PhD, professor of medical statistics at the London School of Hygiene and Tropical Medicine who appeared before the committee as a consultant brought in by the applicant, Boehringer Ingelheim.
The total 309 cardiovascular deaths seen during the study that led to this finding provided more data than most cardiovascular trials, and while in some respects, the cardiovascular benefit seemed “too good to be true,” it also turned out that “the data were so strong that they overwhelm skepticism,” Dr. Pocock told the panel while presenting some advanced statistical test results to prove this assertion. The trial results showed “overwhelming evidence of benefit, beyond a reasonable doubt,” and while cardiovascular death was just one part of the efficacy endpoint, “mortality merits special attention,” he said. The statistical analyses also showed an equally robust 32% relative risk reduction in all-cause mortality, and both the cardiovascular and all-cause death benefits seen in EMPA-REG OUTCOME were consistent across both dosages of empagliflozin tested in the study (10 mg and 25 mg daily) and across the sensitivity analyses applied by the investigators.
“These are convincing data, but I’m not comfortable enough that these robust data would be reproduced in a second trial,” said panel chair Robert J. Smith, MD, who voted against the indication.
An additional limitation acting against the proposed new labeling, according to several panel members, is that the mechanism by which empagliflozin might exert protection against cardiovascular death remains unknown, with no suggestion in the trial results that it acts by protecting patients against ischemic disease.
Current opinion also splits among clinicians on how empagliflozin, which has had FDA approval since 2014 as an option for treating type 2 diabetes, should be used in routine practice to treat diabetes patients with high cardiovascular risk who match those enrolled in the EMPA-REG OUTCOME trial. Dr. Smith urged a cautious approach.
“I think it’s important [for prescribers] to wait to hear from the FDA. If the cardiovascular mortality benefit was proven, then it would be an important option given the magnitude of cardiovascular disease and death as a consequence of type 2 diabetes. But people should be cautious in drawing their own interpretations of the data,” Dr. Smith, professor of medicine at Brown University in Providence, R.I., said in an interview. For the time being, metformin remains the top oral drug for most of these patients because of its proven effectiveness and low cost, he added.
But others have already been active in prescribing empagliflozin to at-risk patients with type 2 diabetes based on last year’s EMPA-REG OUTCOME report.
“I am using it in addition to metformin and aggressive lifestyle changes in patients with established cardiovascular disease and uncontrolled type 2 diabetes,” commented Alison L. Bailey, MD, a cardiologist at the Erlanger Health System and University of Tennessee in Chattanooga. “A patient’s health insurance status must be taken into account as empagliflozin can be a significant financial burden, but if all other things are equal and cost is not prohibitive, I am definitely using this in my patients with type 2 diabetes and cardiovascular disease. I think there are enough data to warrant its use first line in patients who can get the drug without a financial burden,” she said in an interview.
Dr. Konstam cautioned that “just because empagliflozin may have a cardiovascular effect does not make it a cardiovascular drug. As a cardiologist I am not comfortable prescribing this drug. When it comes to diabetes management ,you need to take many things into consideration, most notably blood sugar and hemoglobin A1c,” which are usually best managed by a diabetologist or experienced primary care physician, he said.
Dr. Konstam, Dr. Wilson, Dr. Fradkin, and Dr. Smith had no relevant financial disclosures. Dr. Pocock is a consultant to Boehringer Ingelheim. Dr. Bailey has received research grants from CSL Behring.
On Twitter@mitchelzoler
ROCKVILLE, MD. – In a 12-11 vote, a Food and Drug Administration advisory panel just barely came down in favor of the agency adding a new labeling entry to the already-approved diabetes drug empagliflozin (Jardiance) that would say the drug reduces cardiovascular mortality.
While several members of the panel wished the FDA’s staff good luck in weighing both the evidence and the advisory committee’s closely split endorsement when deciding whether to grant this unprecedented labeling to a diabetes drug, the fact that a majority of panelists favored this course marked a watershed moment in the development of new agents for treating hyperglycemia.
“It’s the first time we have evidence that a diabetes drug can reduce cardiovascular risk. That’s never been seen before, and it’s huge,” said Marvin A. Konstam, MD, a temporary member of the Endocrinologic and Metabolic Drugs Advisory Committee (EMDAC) and chief physician executive of the cardiovascular center at Tufts Medical Center in Boston. “The question is whether or not this effect is real, and the vote was 50-50, but I think there is a good chance it’s real, and, if so, it’s a game changer,” Dr. Konstam said in an interview. He voted in favor of the new labeling, and, like many of his colleagues on the panel, he admitted to agonizing over the decision during the postvote comment period.
What he and the other committee members struggled with was a remarkably strong effect by empagliflozin on reducing cardiovascular mortality by a relative 38%, compared with placebo, in more than 7,000 patients with type 2 diabetes selected for their high cardiovascular disease risk. The major sticking point was that the study enrolled patients into a randomized, placebo-controlled trial that was primarily designed to test the drug’s cardiovascular safety and not its efficacy, and where cardiovascular death was not even a prespecified secondary endpoint.
“It’s very hard to go from safety to superiority in one study,” said Peter W.F. Wilson, MD, who voted against the added indication. Like many panel members who voted no, Dr. Wilson said that any claim to preventing cardiovascular mortality with empagliflozin should meet the standard FDA requirement to have consistent results from at least two studies. “This is the first drug in its class [the sodium-glucose cotransporter 2 inhibitors], and we should have a high bar for the quality of the evidence,” said Dr. Wilson, professor of medicine and public health at Emory University in Atlanta.
“There is substantial evidence [to support the mortality claim], but not yet to the extent to put it on the label,” said another voter on the no side, Judith Fradkin, MD, also a temporary committee member and director of the division of diabetes, endocrinology and metabolic diseases at the National Institutes of Health. The data collected so far in favor of the mortality claim “are very compelling, but what I couldn’t get past is my long-standing belief that a positive result to a study’s secondary outcome is hypothesis generating. We need a second study to put this on the label,” Dr. Fradkin said.
That dramatic and highly meaningful clinical effect of empagliflozin on cardiovascular mortality jumped out at the investigators who ran the EMPA-REG OUTCOME trial as well as to many others from the moment the results had their unveiling less than a year ago, at the annual meeting of the European Association for the Study of Diabetes in Stockholm, and in a concurrently published article (N Engl J Med. 2015 Nov 26;373[22]:2117-28).
The primary efficacy endpoint placed into the EMPA-REG OUTCOME safety trial as the study developed following the 2008 FDA mandate for cardiovascular safety trials for all new hypoglycemic drugs was a three-part, combined-outcome endpoint of cardiovascular death, nonfatal MI, and nonfatal stroke. Although this primary, combined endpoint had a statistically significant but much more modest benefit with a 14% relative risk reduction, compared with placebo, “the benefit was all driven by the reduction in cardiovascular death that had an astonishing P value of less than .0001 with no suggestion of benefit or risk for MI or stroke,” said Stuart Pocock, PhD, professor of medical statistics at the London School of Hygiene and Tropical Medicine who appeared before the committee as a consultant brought in by the applicant, Boehringer Ingelheim.
The total 309 cardiovascular deaths seen during the study that led to this finding provided more data than most cardiovascular trials, and while in some respects, the cardiovascular benefit seemed “too good to be true,” it also turned out that “the data were so strong that they overwhelm skepticism,” Dr. Pocock told the panel while presenting some advanced statistical test results to prove this assertion. The trial results showed “overwhelming evidence of benefit, beyond a reasonable doubt,” and while cardiovascular death was just one part of the efficacy endpoint, “mortality merits special attention,” he said. The statistical analyses also showed an equally robust 32% relative risk reduction in all-cause mortality, and both the cardiovascular and all-cause death benefits seen in EMPA-REG OUTCOME were consistent across both dosages of empagliflozin tested in the study (10 mg and 25 mg daily) and across the sensitivity analyses applied by the investigators.
“These are convincing data, but I’m not comfortable enough that these robust data would be reproduced in a second trial,” said panel chair Robert J. Smith, MD, who voted against the indication.
An additional limitation acting against the proposed new labeling, according to several panel members, is that the mechanism by which empagliflozin might exert protection against cardiovascular death remains unknown, with no suggestion in the trial results that it acts by protecting patients against ischemic disease.
Current opinion also splits among clinicians on how empagliflozin, which has had FDA approval since 2014 as an option for treating type 2 diabetes, should be used in routine practice to treat diabetes patients with high cardiovascular risk who match those enrolled in the EMPA-REG OUTCOME trial. Dr. Smith urged a cautious approach.
“I think it’s important [for prescribers] to wait to hear from the FDA. If the cardiovascular mortality benefit was proven, then it would be an important option given the magnitude of cardiovascular disease and death as a consequence of type 2 diabetes. But people should be cautious in drawing their own interpretations of the data,” Dr. Smith, professor of medicine at Brown University in Providence, R.I., said in an interview. For the time being, metformin remains the top oral drug for most of these patients because of its proven effectiveness and low cost, he added.
But others have already been active in prescribing empagliflozin to at-risk patients with type 2 diabetes based on last year’s EMPA-REG OUTCOME report.
“I am using it in addition to metformin and aggressive lifestyle changes in patients with established cardiovascular disease and uncontrolled type 2 diabetes,” commented Alison L. Bailey, MD, a cardiologist at the Erlanger Health System and University of Tennessee in Chattanooga. “A patient’s health insurance status must be taken into account as empagliflozin can be a significant financial burden, but if all other things are equal and cost is not prohibitive, I am definitely using this in my patients with type 2 diabetes and cardiovascular disease. I think there are enough data to warrant its use first line in patients who can get the drug without a financial burden,” she said in an interview.
Dr. Konstam cautioned that “just because empagliflozin may have a cardiovascular effect does not make it a cardiovascular drug. As a cardiologist I am not comfortable prescribing this drug. When it comes to diabetes management ,you need to take many things into consideration, most notably blood sugar and hemoglobin A1c,” which are usually best managed by a diabetologist or experienced primary care physician, he said.
Dr. Konstam, Dr. Wilson, Dr. Fradkin, and Dr. Smith had no relevant financial disclosures. Dr. Pocock is a consultant to Boehringer Ingelheim. Dr. Bailey has received research grants from CSL Behring.
On Twitter@mitchelzoler
ROCKVILLE, MD. – In a 12-11 vote, a Food and Drug Administration advisory panel just barely came down in favor of the agency adding a new labeling entry to the already-approved diabetes drug empagliflozin (Jardiance) that would say the drug reduces cardiovascular mortality.
While several members of the panel wished the FDA’s staff good luck in weighing both the evidence and the advisory committee’s closely split endorsement when deciding whether to grant this unprecedented labeling to a diabetes drug, the fact that a majority of panelists favored this course marked a watershed moment in the development of new agents for treating hyperglycemia.
“It’s the first time we have evidence that a diabetes drug can reduce cardiovascular risk. That’s never been seen before, and it’s huge,” said Marvin A. Konstam, MD, a temporary member of the Endocrinologic and Metabolic Drugs Advisory Committee (EMDAC) and chief physician executive of the cardiovascular center at Tufts Medical Center in Boston. “The question is whether or not this effect is real, and the vote was 50-50, but I think there is a good chance it’s real, and, if so, it’s a game changer,” Dr. Konstam said in an interview. He voted in favor of the new labeling, and, like many of his colleagues on the panel, he admitted to agonizing over the decision during the postvote comment period.
What he and the other committee members struggled with was a remarkably strong effect by empagliflozin on reducing cardiovascular mortality by a relative 38%, compared with placebo, in more than 7,000 patients with type 2 diabetes selected for their high cardiovascular disease risk. The major sticking point was that the study enrolled patients into a randomized, placebo-controlled trial that was primarily designed to test the drug’s cardiovascular safety and not its efficacy, and where cardiovascular death was not even a prespecified secondary endpoint.
“It’s very hard to go from safety to superiority in one study,” said Peter W.F. Wilson, MD, who voted against the added indication. Like many panel members who voted no, Dr. Wilson said that any claim to preventing cardiovascular mortality with empagliflozin should meet the standard FDA requirement to have consistent results from at least two studies. “This is the first drug in its class [the sodium-glucose cotransporter 2 inhibitors], and we should have a high bar for the quality of the evidence,” said Dr. Wilson, professor of medicine and public health at Emory University in Atlanta.
“There is substantial evidence [to support the mortality claim], but not yet to the extent to put it on the label,” said another voter on the no side, Judith Fradkin, MD, also a temporary committee member and director of the division of diabetes, endocrinology and metabolic diseases at the National Institutes of Health. The data collected so far in favor of the mortality claim “are very compelling, but what I couldn’t get past is my long-standing belief that a positive result to a study’s secondary outcome is hypothesis generating. We need a second study to put this on the label,” Dr. Fradkin said.
That dramatic and highly meaningful clinical effect of empagliflozin on cardiovascular mortality jumped out at the investigators who ran the EMPA-REG OUTCOME trial as well as to many others from the moment the results had their unveiling less than a year ago, at the annual meeting of the European Association for the Study of Diabetes in Stockholm, and in a concurrently published article (N Engl J Med. 2015 Nov 26;373[22]:2117-28).
The primary efficacy endpoint placed into the EMPA-REG OUTCOME safety trial as the study developed following the 2008 FDA mandate for cardiovascular safety trials for all new hypoglycemic drugs was a three-part, combined-outcome endpoint of cardiovascular death, nonfatal MI, and nonfatal stroke. Although this primary, combined endpoint had a statistically significant but much more modest benefit with a 14% relative risk reduction, compared with placebo, “the benefit was all driven by the reduction in cardiovascular death that had an astonishing P value of less than .0001 with no suggestion of benefit or risk for MI or stroke,” said Stuart Pocock, PhD, professor of medical statistics at the London School of Hygiene and Tropical Medicine who appeared before the committee as a consultant brought in by the applicant, Boehringer Ingelheim.
The total 309 cardiovascular deaths seen during the study that led to this finding provided more data than most cardiovascular trials, and while in some respects, the cardiovascular benefit seemed “too good to be true,” it also turned out that “the data were so strong that they overwhelm skepticism,” Dr. Pocock told the panel while presenting some advanced statistical test results to prove this assertion. The trial results showed “overwhelming evidence of benefit, beyond a reasonable doubt,” and while cardiovascular death was just one part of the efficacy endpoint, “mortality merits special attention,” he said. The statistical analyses also showed an equally robust 32% relative risk reduction in all-cause mortality, and both the cardiovascular and all-cause death benefits seen in EMPA-REG OUTCOME were consistent across both dosages of empagliflozin tested in the study (10 mg and 25 mg daily) and across the sensitivity analyses applied by the investigators.
“These are convincing data, but I’m not comfortable enough that these robust data would be reproduced in a second trial,” said panel chair Robert J. Smith, MD, who voted against the indication.
An additional limitation acting against the proposed new labeling, according to several panel members, is that the mechanism by which empagliflozin might exert protection against cardiovascular death remains unknown, with no suggestion in the trial results that it acts by protecting patients against ischemic disease.
Current opinion also splits among clinicians on how empagliflozin, which has had FDA approval since 2014 as an option for treating type 2 diabetes, should be used in routine practice to treat diabetes patients with high cardiovascular risk who match those enrolled in the EMPA-REG OUTCOME trial. Dr. Smith urged a cautious approach.
“I think it’s important [for prescribers] to wait to hear from the FDA. If the cardiovascular mortality benefit was proven, then it would be an important option given the magnitude of cardiovascular disease and death as a consequence of type 2 diabetes. But people should be cautious in drawing their own interpretations of the data,” Dr. Smith, professor of medicine at Brown University in Providence, R.I., said in an interview. For the time being, metformin remains the top oral drug for most of these patients because of its proven effectiveness and low cost, he added.
But others have already been active in prescribing empagliflozin to at-risk patients with type 2 diabetes based on last year’s EMPA-REG OUTCOME report.
“I am using it in addition to metformin and aggressive lifestyle changes in patients with established cardiovascular disease and uncontrolled type 2 diabetes,” commented Alison L. Bailey, MD, a cardiologist at the Erlanger Health System and University of Tennessee in Chattanooga. “A patient’s health insurance status must be taken into account as empagliflozin can be a significant financial burden, but if all other things are equal and cost is not prohibitive, I am definitely using this in my patients with type 2 diabetes and cardiovascular disease. I think there are enough data to warrant its use first line in patients who can get the drug without a financial burden,” she said in an interview.
Dr. Konstam cautioned that “just because empagliflozin may have a cardiovascular effect does not make it a cardiovascular drug. As a cardiologist I am not comfortable prescribing this drug. When it comes to diabetes management ,you need to take many things into consideration, most notably blood sugar and hemoglobin A1c,” which are usually best managed by a diabetologist or experienced primary care physician, he said.
Dr. Konstam, Dr. Wilson, Dr. Fradkin, and Dr. Smith had no relevant financial disclosures. Dr. Pocock is a consultant to Boehringer Ingelheim. Dr. Bailey has received research grants from CSL Behring.
On Twitter@mitchelzoler
AT AN FDA EMDAC MEETING