User login
Just 20 minutes of vigorous activity daily benefits teens
Vigorous physical activity for 20 minutes a day was enough to maximize cardiorespiratory benefits in adolescents, based on data from more than 300 individuals.
Current recommendations for physical activity in children and adolescents from the World Health Organization call for moderate to vigorous physical activity (MVPA) for an average of 60 minutes a day for physical and mental health; however, guidance on how much physical activity teens need to maximize cardiorespiratory fitness (CRF) has not been determined, Samuel Joseph Burden, BMedSci, of John Radcliffe Hospital Oxford (England), and colleagues wrote.
“Although data in young people are limited, adult studies have shown that regular, brief vigorous physical activity is highly effective at improving health markers, including CRF, which is also an important marker of health in youth,” the researchers wrote.
In a study published in Pediatrics, the researchers examined the associations between physical activity intensity and maximal CRF. The study population included 339 adolescents aged 13-14 years who were evaluated during the 2018-2019 and 2019-2020 school years. Participants wore wrist accelerometers to measure the intensity of physical activity and participated in 20-meter shuttle runs to demonstrate CRF. The researchers used partial multivariable linear regression to assess variables at different intensities including moderate physical activity (MPA), light physical activity (LPA), and sedentary time, as well as vigorous physical activity (VPA).
The wrist monitors measured the intensities of physical activity based on the bandpass-filtered followed by Euclidean norm metric (BFEN), a validated metric. “Previously validated thresholds for BFEN were used to determine the average duration of daily physical activity at each intensity: 0.1 g for LPA, 0.314 g for MPA, and 0.998 g for VPA,” the researchers wrote. Physical activity below the threshold for LPA was categorized as sedentary time.
Participants wore the accelerometers for 1 week; value recording included at least 3 weekdays and 1 weekend day, and each valid day required more than 6 hours of awake time.
Overall, VPA for up to 20 minutes was significantly associated with improved CRF. However, the benefits on CRF plateaued after that time, and longer duration of VPA was not associated with significantly greater improvements in CRF. Neither MPA nor LPA were associated with any improvements in CRF.
Participants who engaged in an average of 14 minutes (range, 12-17 minutes) of VPA per day met the median CRF.
The researchers also conducted independent t tests to assess differences in VPA at different CRF thresholds.
Those in the highest quartile of VPA had CRF z scores 1.03 higher, compared with those in the lower quartiles.
Given that current PA guidelines involve a combination of moderate and vigorous PA that could be met by MPA with no VPA, the current findings have public health implications for improving CRF in adolescents, the researchers wrote.
Even with MPA as an option, most adolescents fail to meet the recommendations of at least 60 minutes of MVPA, they said. “One possible reason is that this duration is quite long, requiring a daily time commitment that some may find difficult to maintain. A shorter target of 20 minutes might be easier to schedule daily and a focus on VPA would simplify messages about the intensity of activity that is likely to improve CRF.”
The study findings were limited by several factors including the use of data from only two schools in the United Kingdom, which may limit generalizability, and future research would ideally include a more direct assessment of VO2 max, the researchers wrote. However, the results were strengthened by the large and diverse study population, including teens with a wide range of body mass index as well as CRF.
Future research is needed to test whether interventions based on a target of 20 minutes of VPA creates significant improvements in adolescent cardiometabolic health, the researchers concluded.
Any activity has value for sedentary teens
The current study suggests that counseling teens about physical activity may be less challenging for clinicians if optimal cardiorespiratory benefits can be reached with shorter bouts of activity, Michele LaBotz, MD, of Intermed Sports Medicine, South Portland, Maine, and Sarah Hoffman, DO, of Tufts University, Boston, wrote in an accompanying editorial.
The results have two key implications for pediatricians, the authors said. First, “optimal CRF can be achieved with much shorter periods of activity than previously recommended.” Second, “current ‘moderate to vigorous’ PA recommendations may not be sufficient to improve CRF in adolescents, if achieved through moderate activity only.”
However, the editorialists emphasized that, although shorter periods of higher-intensity exercise reduce the time burden for teens and families, specific education is needed to explain the extra effort involved in exercising vigorously enough for cardiorespiratory benefits.
Patients can be counseled that activity is vigorous when they start to sweat, their face gets red, and they feel short of breath and unable to talk during activity,” they explained. These sensations may be new and uncomfortable for children and teens who have been quite sedentary or used to low-intensity activity. Dr. LaBotz and Dr. Hoffman advised pediatricians to counsel patients to build intensity gradually, with “exercise snacks,” that involve several minutes of activity that become more challenging over time.
“Exercise snacks can include anything that elevates the heart rate for a minute or more, such as running up and down the stairs a few times; chasing the dog around the backyard; or just putting on some music and dancing hard,” the editorialists wrote.
“Some exercise is better than none, and extrapolating from adult data, the biggest benefit likely occurs when we can help our most sedentary and least fit patients become a bit more active, even if it falls short of currently recommended levels,” they concluded.
The study was supported by grants to various researchers from the British Heart Foundation, the Elizabeth Casson Trust, the U.K. National Institute of Health Research, the Professor Nigel Groome Studentship scheme (Oxford Brookes University), and the U.K. Department of Health. The researchers had no financial conflicts to disclose. The editorialists had no financial conflicts to disclose.
Vigorous physical activity for 20 minutes a day was enough to maximize cardiorespiratory benefits in adolescents, based on data from more than 300 individuals.
Current recommendations for physical activity in children and adolescents from the World Health Organization call for moderate to vigorous physical activity (MVPA) for an average of 60 minutes a day for physical and mental health; however, guidance on how much physical activity teens need to maximize cardiorespiratory fitness (CRF) has not been determined, Samuel Joseph Burden, BMedSci, of John Radcliffe Hospital Oxford (England), and colleagues wrote.
“Although data in young people are limited, adult studies have shown that regular, brief vigorous physical activity is highly effective at improving health markers, including CRF, which is also an important marker of health in youth,” the researchers wrote.
In a study published in Pediatrics, the researchers examined the associations between physical activity intensity and maximal CRF. The study population included 339 adolescents aged 13-14 years who were evaluated during the 2018-2019 and 2019-2020 school years. Participants wore wrist accelerometers to measure the intensity of physical activity and participated in 20-meter shuttle runs to demonstrate CRF. The researchers used partial multivariable linear regression to assess variables at different intensities including moderate physical activity (MPA), light physical activity (LPA), and sedentary time, as well as vigorous physical activity (VPA).
The wrist monitors measured the intensities of physical activity based on the bandpass-filtered followed by Euclidean norm metric (BFEN), a validated metric. “Previously validated thresholds for BFEN were used to determine the average duration of daily physical activity at each intensity: 0.1 g for LPA, 0.314 g for MPA, and 0.998 g for VPA,” the researchers wrote. Physical activity below the threshold for LPA was categorized as sedentary time.
Participants wore the accelerometers for 1 week; value recording included at least 3 weekdays and 1 weekend day, and each valid day required more than 6 hours of awake time.
Overall, VPA for up to 20 minutes was significantly associated with improved CRF. However, the benefits on CRF plateaued after that time, and longer duration of VPA was not associated with significantly greater improvements in CRF. Neither MPA nor LPA were associated with any improvements in CRF.
Participants who engaged in an average of 14 minutes (range, 12-17 minutes) of VPA per day met the median CRF.
The researchers also conducted independent t tests to assess differences in VPA at different CRF thresholds.
Those in the highest quartile of VPA had CRF z scores 1.03 higher, compared with those in the lower quartiles.
Given that current PA guidelines involve a combination of moderate and vigorous PA that could be met by MPA with no VPA, the current findings have public health implications for improving CRF in adolescents, the researchers wrote.
Even with MPA as an option, most adolescents fail to meet the recommendations of at least 60 minutes of MVPA, they said. “One possible reason is that this duration is quite long, requiring a daily time commitment that some may find difficult to maintain. A shorter target of 20 minutes might be easier to schedule daily and a focus on VPA would simplify messages about the intensity of activity that is likely to improve CRF.”
The study findings were limited by several factors including the use of data from only two schools in the United Kingdom, which may limit generalizability, and future research would ideally include a more direct assessment of VO2 max, the researchers wrote. However, the results were strengthened by the large and diverse study population, including teens with a wide range of body mass index as well as CRF.
Future research is needed to test whether interventions based on a target of 20 minutes of VPA creates significant improvements in adolescent cardiometabolic health, the researchers concluded.
Any activity has value for sedentary teens
The current study suggests that counseling teens about physical activity may be less challenging for clinicians if optimal cardiorespiratory benefits can be reached with shorter bouts of activity, Michele LaBotz, MD, of Intermed Sports Medicine, South Portland, Maine, and Sarah Hoffman, DO, of Tufts University, Boston, wrote in an accompanying editorial.
The results have two key implications for pediatricians, the authors said. First, “optimal CRF can be achieved with much shorter periods of activity than previously recommended.” Second, “current ‘moderate to vigorous’ PA recommendations may not be sufficient to improve CRF in adolescents, if achieved through moderate activity only.”
However, the editorialists emphasized that, although shorter periods of higher-intensity exercise reduce the time burden for teens and families, specific education is needed to explain the extra effort involved in exercising vigorously enough for cardiorespiratory benefits.
Patients can be counseled that activity is vigorous when they start to sweat, their face gets red, and they feel short of breath and unable to talk during activity,” they explained. These sensations may be new and uncomfortable for children and teens who have been quite sedentary or used to low-intensity activity. Dr. LaBotz and Dr. Hoffman advised pediatricians to counsel patients to build intensity gradually, with “exercise snacks,” that involve several minutes of activity that become more challenging over time.
“Exercise snacks can include anything that elevates the heart rate for a minute or more, such as running up and down the stairs a few times; chasing the dog around the backyard; or just putting on some music and dancing hard,” the editorialists wrote.
“Some exercise is better than none, and extrapolating from adult data, the biggest benefit likely occurs when we can help our most sedentary and least fit patients become a bit more active, even if it falls short of currently recommended levels,” they concluded.
The study was supported by grants to various researchers from the British Heart Foundation, the Elizabeth Casson Trust, the U.K. National Institute of Health Research, the Professor Nigel Groome Studentship scheme (Oxford Brookes University), and the U.K. Department of Health. The researchers had no financial conflicts to disclose. The editorialists had no financial conflicts to disclose.
Vigorous physical activity for 20 minutes a day was enough to maximize cardiorespiratory benefits in adolescents, based on data from more than 300 individuals.
Current recommendations for physical activity in children and adolescents from the World Health Organization call for moderate to vigorous physical activity (MVPA) for an average of 60 minutes a day for physical and mental health; however, guidance on how much physical activity teens need to maximize cardiorespiratory fitness (CRF) has not been determined, Samuel Joseph Burden, BMedSci, of John Radcliffe Hospital Oxford (England), and colleagues wrote.
“Although data in young people are limited, adult studies have shown that regular, brief vigorous physical activity is highly effective at improving health markers, including CRF, which is also an important marker of health in youth,” the researchers wrote.
In a study published in Pediatrics, the researchers examined the associations between physical activity intensity and maximal CRF. The study population included 339 adolescents aged 13-14 years who were evaluated during the 2018-2019 and 2019-2020 school years. Participants wore wrist accelerometers to measure the intensity of physical activity and participated in 20-meter shuttle runs to demonstrate CRF. The researchers used partial multivariable linear regression to assess variables at different intensities including moderate physical activity (MPA), light physical activity (LPA), and sedentary time, as well as vigorous physical activity (VPA).
The wrist monitors measured the intensities of physical activity based on the bandpass-filtered followed by Euclidean norm metric (BFEN), a validated metric. “Previously validated thresholds for BFEN were used to determine the average duration of daily physical activity at each intensity: 0.1 g for LPA, 0.314 g for MPA, and 0.998 g for VPA,” the researchers wrote. Physical activity below the threshold for LPA was categorized as sedentary time.
Participants wore the accelerometers for 1 week; value recording included at least 3 weekdays and 1 weekend day, and each valid day required more than 6 hours of awake time.
Overall, VPA for up to 20 minutes was significantly associated with improved CRF. However, the benefits on CRF plateaued after that time, and longer duration of VPA was not associated with significantly greater improvements in CRF. Neither MPA nor LPA were associated with any improvements in CRF.
Participants who engaged in an average of 14 minutes (range, 12-17 minutes) of VPA per day met the median CRF.
The researchers also conducted independent t tests to assess differences in VPA at different CRF thresholds.
Those in the highest quartile of VPA had CRF z scores 1.03 higher, compared with those in the lower quartiles.
Given that current PA guidelines involve a combination of moderate and vigorous PA that could be met by MPA with no VPA, the current findings have public health implications for improving CRF in adolescents, the researchers wrote.
Even with MPA as an option, most adolescents fail to meet the recommendations of at least 60 minutes of MVPA, they said. “One possible reason is that this duration is quite long, requiring a daily time commitment that some may find difficult to maintain. A shorter target of 20 minutes might be easier to schedule daily and a focus on VPA would simplify messages about the intensity of activity that is likely to improve CRF.”
The study findings were limited by several factors including the use of data from only two schools in the United Kingdom, which may limit generalizability, and future research would ideally include a more direct assessment of VO2 max, the researchers wrote. However, the results were strengthened by the large and diverse study population, including teens with a wide range of body mass index as well as CRF.
Future research is needed to test whether interventions based on a target of 20 minutes of VPA creates significant improvements in adolescent cardiometabolic health, the researchers concluded.
Any activity has value for sedentary teens
The current study suggests that counseling teens about physical activity may be less challenging for clinicians if optimal cardiorespiratory benefits can be reached with shorter bouts of activity, Michele LaBotz, MD, of Intermed Sports Medicine, South Portland, Maine, and Sarah Hoffman, DO, of Tufts University, Boston, wrote in an accompanying editorial.
The results have two key implications for pediatricians, the authors said. First, “optimal CRF can be achieved with much shorter periods of activity than previously recommended.” Second, “current ‘moderate to vigorous’ PA recommendations may not be sufficient to improve CRF in adolescents, if achieved through moderate activity only.”
However, the editorialists emphasized that, although shorter periods of higher-intensity exercise reduce the time burden for teens and families, specific education is needed to explain the extra effort involved in exercising vigorously enough for cardiorespiratory benefits.
Patients can be counseled that activity is vigorous when they start to sweat, their face gets red, and they feel short of breath and unable to talk during activity,” they explained. These sensations may be new and uncomfortable for children and teens who have been quite sedentary or used to low-intensity activity. Dr. LaBotz and Dr. Hoffman advised pediatricians to counsel patients to build intensity gradually, with “exercise snacks,” that involve several minutes of activity that become more challenging over time.
“Exercise snacks can include anything that elevates the heart rate for a minute or more, such as running up and down the stairs a few times; chasing the dog around the backyard; or just putting on some music and dancing hard,” the editorialists wrote.
“Some exercise is better than none, and extrapolating from adult data, the biggest benefit likely occurs when we can help our most sedentary and least fit patients become a bit more active, even if it falls short of currently recommended levels,” they concluded.
The study was supported by grants to various researchers from the British Heart Foundation, the Elizabeth Casson Trust, the U.K. National Institute of Health Research, the Professor Nigel Groome Studentship scheme (Oxford Brookes University), and the U.K. Department of Health. The researchers had no financial conflicts to disclose. The editorialists had no financial conflicts to disclose.
FROM PEDIATRICS
Asian American teens have highest rate of suicidal ideation
NEW ORLEANS – In an unexpected finding, researchers discovered that According to a weighted analysis, 24% of Asian Americans reported thinking about or planning suicide vs. 22% of Whites and Blacks and 20% of Hispanics (P < .01).
“We were shocked,” said study lead author Esha Hansoti, MD, who conducted the research at UT Southwestern Medical Center, Dallas, and is now a psychiatry resident at Zucker Hillside Hospital Northwell/Hofstra in Glen Oaks, NY. The findings were released at the annual meeting of the American Psychiatric Association.
Dr. Hansoti and colleagues launched the analysis in light of sparse research into Asian American mental health, she said. Even within this population, she said, mental illness “tends to be overlooked” and discussion of the topic may be considered taboo.
For the new study, researchers analyzed the 2019 Youth Risk Behavior Survey, conducted biennially by the Centers for Disease Control and Prevention, which had more than 13,000 participants in grades 9-12.
A weighted bivariate analysis of 618 Asian American adolescents – adjusted for age, sex, and depressive symptoms – found no statistically significant impact on suicidal ideation by gender, age, substance use, sexual/physical dating violence, or fluency in English.
However, several groups had a statistically significant higher risk, including victims of forced sexual intercourse and those who were threatened or bullied at school.
Those who didn’t get mostly A grades were also at high risk: Adolescents with mostly Ds and Fs were more likely to have acknowledged suicidal ideation than those with mostly As (adjusted odds ratio [AOR] = 3.2).
Gays and lesbians (AOR = 7.9 vs. heterosexuals), and bisexuals (AOR = 5.2 vs. heterosexuals) also showed sharply higher rates of suicidal ideation.
It’s not clear why Asian American adolescents may be at higher risk of suicidal ideation. The survey was completed prior to the COVID-19 pandemic, which spawned bigotry against people of Asian descent and an ongoing outbreak of high-profile violence against Asian Americans across the country.
Dr. Hansoti noted that Asian Americans face the pressures to live up to the standards of being a “model minority.” In addition, “very few Asian American adolescents are taken to a therapist, and few mental health providers are Asian Americans.”
She urged fellow psychiatrists “to remember that our perceptions of Asian Americans might hinder some of the diagnoses we could be making. Be thoughtful about how their ethnicity and race affects their presentation and their own perception of their illness.”
She added that Asian Americans may experience mental illness and anxiety “more somatically and physically than emotionally.”
In an interview, Anne Saw, PhD, associate professor of clinical-community psychology at DePaul University, Chicago, said the findings are “helpful for corroborating other studies identifying risk factors of suicidal ideation among Asian American adolescents. Since this research utilizes the Youth Risk Behavior Survey, these findings can be compared with risk factors of suicidal ideation among adolescents from other racial/ethnic backgrounds to pinpoint general as well as specific risk factors, thus informing how we can tailor interventions for specific groups.”
According to Dr. Saw, while it’s clear that suicide is a leading cause of death among Asian American adolescents, it’s still unknown which specific subgroups other than girls and LGBTIA+ individuals are especially vulnerable and which culturally tailored interventions are most effective for decreasing suicide risk.
“Psychiatrists should understand that risk and protective factors for suicidal behavior in Asian American adolescents are multifaceted and require careful attention and intervention across different environments,” she said.
No funding and no disclosures were reported.
NEW ORLEANS – In an unexpected finding, researchers discovered that According to a weighted analysis, 24% of Asian Americans reported thinking about or planning suicide vs. 22% of Whites and Blacks and 20% of Hispanics (P < .01).
“We were shocked,” said study lead author Esha Hansoti, MD, who conducted the research at UT Southwestern Medical Center, Dallas, and is now a psychiatry resident at Zucker Hillside Hospital Northwell/Hofstra in Glen Oaks, NY. The findings were released at the annual meeting of the American Psychiatric Association.
Dr. Hansoti and colleagues launched the analysis in light of sparse research into Asian American mental health, she said. Even within this population, she said, mental illness “tends to be overlooked” and discussion of the topic may be considered taboo.
For the new study, researchers analyzed the 2019 Youth Risk Behavior Survey, conducted biennially by the Centers for Disease Control and Prevention, which had more than 13,000 participants in grades 9-12.
A weighted bivariate analysis of 618 Asian American adolescents – adjusted for age, sex, and depressive symptoms – found no statistically significant impact on suicidal ideation by gender, age, substance use, sexual/physical dating violence, or fluency in English.
However, several groups had a statistically significant higher risk, including victims of forced sexual intercourse and those who were threatened or bullied at school.
Those who didn’t get mostly A grades were also at high risk: Adolescents with mostly Ds and Fs were more likely to have acknowledged suicidal ideation than those with mostly As (adjusted odds ratio [AOR] = 3.2).
Gays and lesbians (AOR = 7.9 vs. heterosexuals), and bisexuals (AOR = 5.2 vs. heterosexuals) also showed sharply higher rates of suicidal ideation.
It’s not clear why Asian American adolescents may be at higher risk of suicidal ideation. The survey was completed prior to the COVID-19 pandemic, which spawned bigotry against people of Asian descent and an ongoing outbreak of high-profile violence against Asian Americans across the country.
Dr. Hansoti noted that Asian Americans face the pressures to live up to the standards of being a “model minority.” In addition, “very few Asian American adolescents are taken to a therapist, and few mental health providers are Asian Americans.”
She urged fellow psychiatrists “to remember that our perceptions of Asian Americans might hinder some of the diagnoses we could be making. Be thoughtful about how their ethnicity and race affects their presentation and their own perception of their illness.”
She added that Asian Americans may experience mental illness and anxiety “more somatically and physically than emotionally.”
In an interview, Anne Saw, PhD, associate professor of clinical-community psychology at DePaul University, Chicago, said the findings are “helpful for corroborating other studies identifying risk factors of suicidal ideation among Asian American adolescents. Since this research utilizes the Youth Risk Behavior Survey, these findings can be compared with risk factors of suicidal ideation among adolescents from other racial/ethnic backgrounds to pinpoint general as well as specific risk factors, thus informing how we can tailor interventions for specific groups.”
According to Dr. Saw, while it’s clear that suicide is a leading cause of death among Asian American adolescents, it’s still unknown which specific subgroups other than girls and LGBTIA+ individuals are especially vulnerable and which culturally tailored interventions are most effective for decreasing suicide risk.
“Psychiatrists should understand that risk and protective factors for suicidal behavior in Asian American adolescents are multifaceted and require careful attention and intervention across different environments,” she said.
No funding and no disclosures were reported.
NEW ORLEANS – In an unexpected finding, researchers discovered that According to a weighted analysis, 24% of Asian Americans reported thinking about or planning suicide vs. 22% of Whites and Blacks and 20% of Hispanics (P < .01).
“We were shocked,” said study lead author Esha Hansoti, MD, who conducted the research at UT Southwestern Medical Center, Dallas, and is now a psychiatry resident at Zucker Hillside Hospital Northwell/Hofstra in Glen Oaks, NY. The findings were released at the annual meeting of the American Psychiatric Association.
Dr. Hansoti and colleagues launched the analysis in light of sparse research into Asian American mental health, she said. Even within this population, she said, mental illness “tends to be overlooked” and discussion of the topic may be considered taboo.
For the new study, researchers analyzed the 2019 Youth Risk Behavior Survey, conducted biennially by the Centers for Disease Control and Prevention, which had more than 13,000 participants in grades 9-12.
A weighted bivariate analysis of 618 Asian American adolescents – adjusted for age, sex, and depressive symptoms – found no statistically significant impact on suicidal ideation by gender, age, substance use, sexual/physical dating violence, or fluency in English.
However, several groups had a statistically significant higher risk, including victims of forced sexual intercourse and those who were threatened or bullied at school.
Those who didn’t get mostly A grades were also at high risk: Adolescents with mostly Ds and Fs were more likely to have acknowledged suicidal ideation than those with mostly As (adjusted odds ratio [AOR] = 3.2).
Gays and lesbians (AOR = 7.9 vs. heterosexuals), and bisexuals (AOR = 5.2 vs. heterosexuals) also showed sharply higher rates of suicidal ideation.
It’s not clear why Asian American adolescents may be at higher risk of suicidal ideation. The survey was completed prior to the COVID-19 pandemic, which spawned bigotry against people of Asian descent and an ongoing outbreak of high-profile violence against Asian Americans across the country.
Dr. Hansoti noted that Asian Americans face the pressures to live up to the standards of being a “model minority.” In addition, “very few Asian American adolescents are taken to a therapist, and few mental health providers are Asian Americans.”
She urged fellow psychiatrists “to remember that our perceptions of Asian Americans might hinder some of the diagnoses we could be making. Be thoughtful about how their ethnicity and race affects their presentation and their own perception of their illness.”
She added that Asian Americans may experience mental illness and anxiety “more somatically and physically than emotionally.”
In an interview, Anne Saw, PhD, associate professor of clinical-community psychology at DePaul University, Chicago, said the findings are “helpful for corroborating other studies identifying risk factors of suicidal ideation among Asian American adolescents. Since this research utilizes the Youth Risk Behavior Survey, these findings can be compared with risk factors of suicidal ideation among adolescents from other racial/ethnic backgrounds to pinpoint general as well as specific risk factors, thus informing how we can tailor interventions for specific groups.”
According to Dr. Saw, while it’s clear that suicide is a leading cause of death among Asian American adolescents, it’s still unknown which specific subgroups other than girls and LGBTIA+ individuals are especially vulnerable and which culturally tailored interventions are most effective for decreasing suicide risk.
“Psychiatrists should understand that risk and protective factors for suicidal behavior in Asian American adolescents are multifaceted and require careful attention and intervention across different environments,” she said.
No funding and no disclosures were reported.
AT APA 2022
Youth with bipolar disorder at high risk of eating disorders
Investigators studied close to 200 youth with BD and found that more than 25% had a lifetime ED, which included anorexia nervosa (AN), bulimia nervosa (BN), and an ED not otherwise specified (NOS).
Those with comorbid EDs were more likely to be female and to have BD-II subtype. Their presentations were also more complicated and included a history of suicidality, additional psychiatric conditions, smoking, and a history of sexual abuse, as well as more severe depression and emotional instability.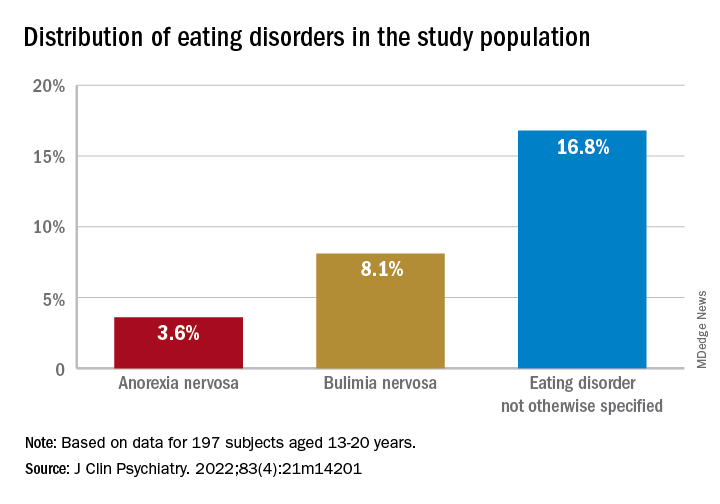
“We think the take-home message is that, in addition to other more recognized psychiatric comorbidities, youth with BD are also vulnerable to developing EDs. Thus, clinicians should be routinely monitoring for eating, appetite, and body image disturbances when working with this population,” lead author Diana Khoubaeva, research analyst at the Centre for Youth Bipolar Disorder, Centre for Addiction and Mental Health, Toronto, and senior author Benjamin Goldstein, MD, PhD, director of the Centre for Youth Bipolar Disorder, wrote in an e-mail to this news organization.
“Given the more complicated clinical picture of youth with co-occurring BD and EDs, this combination warrants careful attention,” the investigators note.
The study was published online May 11 in the Journal of Clinical Psychiatry.
Lack of research
“From the existing literature, we learned that EDs are not uncommon in individuals with BD, and that they are often associated with a more severe clinical profile,” say the researchers. “However, the majority of these studies have been limited to adult samples, and there was a real scarcity of studies that examined this co-occurrence in youth.”
This is “surprising” because EDs often have their onset in adolescence, so the researchers decided to explore the issue in their “fairly large sample of youth with BD.”
To investigate the issue, the researchers studied 197 youth (aged 13-20 years) with a diagnosis of BD (BD-I, BD-II, or BD-NOS) who were recruited between 2009 and 2017 (mean [standard deviation] age, 16.69 [1.50] years; 67.5% female).
ED diagnoses included both current and lifetime AN, BN, and ED-NOS. The researchers used the Kiddie Schedule for Affective Disorders and Schizophrenia for School Age Children, Present and Lifetime Version (K-SADS-PL) to determine the diagnosis of BD.
They also collected information about comorbid psychiatric disorders, as well as substance use disorders and cigarette smoking. The Life Problems Inventory (LPI) was used to identify dimensional borderline personality traits.
Information about physical and sexual abuse, suicidal ideation, nonsuicidal self-injury (NSSI), and affect regulation were obtained from other measurement tools. Participants’ height and weight were measured to calculate body mass index.
Neurobiological and environmental factors
Of the total sample, 24.84% had received a diagnosis of ED in their lifetime.
Moreover, 28.9% had a lifetime history of binge eating. Of these, 17.7% also had been diagnosed with an ED.
Participants with BD-II were significantly more likely than those with BD-I to report both current and lifetime BN. There were no significant differences by BD subtype in AN, ED-NOS, or binge eating.
Higher correlates of clinical characteristics, psychiatric morbidity, treatment history, and dimensional traits in those with vs. those without an ED are detailed in the accompanying table.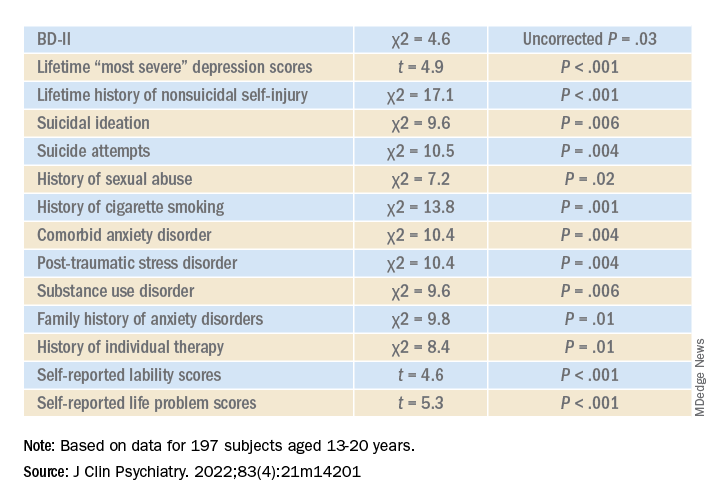
The ED group scored significantly higher on all LPI scores, including impulsivity, emotional dysregulation, identity confusion, and interpersonal problems, compared to those without an ED. They also were less likely to report lifetime lithium use (chi2 = 7.9, P = .01).
Multivariate analysis revealed that lifetime EDs were significantly associated with female sex, history of cigarette smoking, history of individual therapy, family history of anxiety, and LPI total score and were negatively associated with BD-I subtype.
“The comorbidity [between EDs and BD] could be driven by both neurobiological and environmental factors,” Dr. Khoubaeva and Dr. Goldstein noted. EDs and BD “are both illnesses that are fundamentally linked with dysfunction in reward systems – that is, there are imbalances in terms of too much or too little reward seeking.”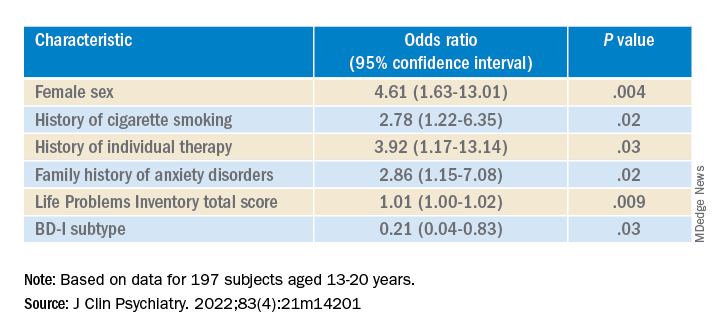
They added that individuals affected by these conditions have “ongoing challenges with instability of emotions and ability to manage emotions; and eating too much or too little can be a manifestation of coping with emotions.”
In addition, medications commonly used to treat BD “are known to have side effects such as weight/appetite/metabolic changes, which may make it harder to regulate eating, and which may exacerbate preexisting body image challenges.”
The researchers recommend implementing trauma-informed care, assessing and addressing suicidality and self-injury, and prioritizing therapies that target emotional dysregulation, such as dialectical behavioral therapy.
‘Clarion call’
Commenting on the study, Roger McIntyre, MD, professor of psychiatry and pharmacology, University of Toronto, and head of the Mood Disorders Psychopharmacology Unit, said the study is “the first of its kind to comprehensively characterize the prevalence of ED in youth living with BD.
“It could be hypothesized that EDs have overlapping domain disturbances of cognitive dysfunction, such as executive function and impulse control, as well as cognitive reward processes,” said Dr. McIntyre, who is the chairman and executive director of the Brain and Cognitive Discover Foundation, Toronto, and was not involved with the study.
“The data are a clarion call for clinicians to routinely screen for EDs in youth with BD and, when present, to be aware of the greater complexity, severity, and risk in this patient subpopulation. The higher prevalence of ED in youth with BD-II is an additional reminder of the severity, morbidity, and complexity of BD-II,” Dr. McIntyre said.
The study received no direct funding. It was supported by philanthropic donations to the Centre for Youth Bipolar Disorder and the CAMH Discovery Fund. Dr. Goldstein reports grant support from Brain Canada, Canadian Institutes of Health Research, Heart and Stroke Foundation, National Institute of Mental Health, and the departments of psychiatry at the University of Toronto and Sunnybrook Health Sciences Centre. He also acknowledges his position as RBC investments chair in Children›s Mental Health and Developmental Psychopathology at CAMH, a joint Hospital-University chair among the University of Toronto, CAMH, and the CAMH Foundation. Ms. Khoubaeva reports no relevant financial relationships. The other authors’ disclosures are listed in the original article. Dr. McIntyre has received research grant support from CIHR/GACD/National Natural Science Foundation of China (NSFC); speaker/consultation fees from Lundbeck, Janssen, Alkermes, Neumora Therapeutics, Mitsubishi Tanabe, Purdue, Pfizer, Otsuka, Takeda, Neurocrine, Sunovion, Bausch Health, Axsome, Novo Nordisk, Kris, Sanofi, Eisai, Intra-Cellular, NewBridge Pharmaceuticals, Abbvie, and Atai Life Sciences. Dr. McIntyre is a CEO of Braxia Scientific.
A version of this article first appeared on Medscape.com.
Investigators studied close to 200 youth with BD and found that more than 25% had a lifetime ED, which included anorexia nervosa (AN), bulimia nervosa (BN), and an ED not otherwise specified (NOS).
Those with comorbid EDs were more likely to be female and to have BD-II subtype. Their presentations were also more complicated and included a history of suicidality, additional psychiatric conditions, smoking, and a history of sexual abuse, as well as more severe depression and emotional instability.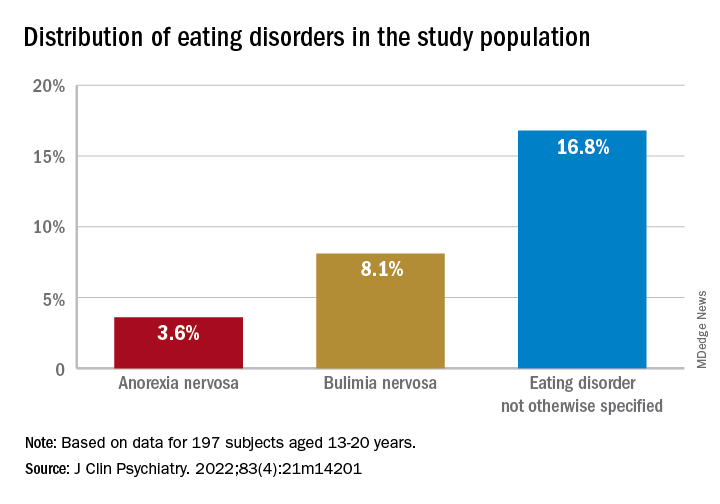
“We think the take-home message is that, in addition to other more recognized psychiatric comorbidities, youth with BD are also vulnerable to developing EDs. Thus, clinicians should be routinely monitoring for eating, appetite, and body image disturbances when working with this population,” lead author Diana Khoubaeva, research analyst at the Centre for Youth Bipolar Disorder, Centre for Addiction and Mental Health, Toronto, and senior author Benjamin Goldstein, MD, PhD, director of the Centre for Youth Bipolar Disorder, wrote in an e-mail to this news organization.
“Given the more complicated clinical picture of youth with co-occurring BD and EDs, this combination warrants careful attention,” the investigators note.
The study was published online May 11 in the Journal of Clinical Psychiatry.
Lack of research
“From the existing literature, we learned that EDs are not uncommon in individuals with BD, and that they are often associated with a more severe clinical profile,” say the researchers. “However, the majority of these studies have been limited to adult samples, and there was a real scarcity of studies that examined this co-occurrence in youth.”
This is “surprising” because EDs often have their onset in adolescence, so the researchers decided to explore the issue in their “fairly large sample of youth with BD.”
To investigate the issue, the researchers studied 197 youth (aged 13-20 years) with a diagnosis of BD (BD-I, BD-II, or BD-NOS) who were recruited between 2009 and 2017 (mean [standard deviation] age, 16.69 [1.50] years; 67.5% female).
ED diagnoses included both current and lifetime AN, BN, and ED-NOS. The researchers used the Kiddie Schedule for Affective Disorders and Schizophrenia for School Age Children, Present and Lifetime Version (K-SADS-PL) to determine the diagnosis of BD.
They also collected information about comorbid psychiatric disorders, as well as substance use disorders and cigarette smoking. The Life Problems Inventory (LPI) was used to identify dimensional borderline personality traits.
Information about physical and sexual abuse, suicidal ideation, nonsuicidal self-injury (NSSI), and affect regulation were obtained from other measurement tools. Participants’ height and weight were measured to calculate body mass index.
Neurobiological and environmental factors
Of the total sample, 24.84% had received a diagnosis of ED in their lifetime.
Moreover, 28.9% had a lifetime history of binge eating. Of these, 17.7% also had been diagnosed with an ED.
Participants with BD-II were significantly more likely than those with BD-I to report both current and lifetime BN. There were no significant differences by BD subtype in AN, ED-NOS, or binge eating.
Higher correlates of clinical characteristics, psychiatric morbidity, treatment history, and dimensional traits in those with vs. those without an ED are detailed in the accompanying table.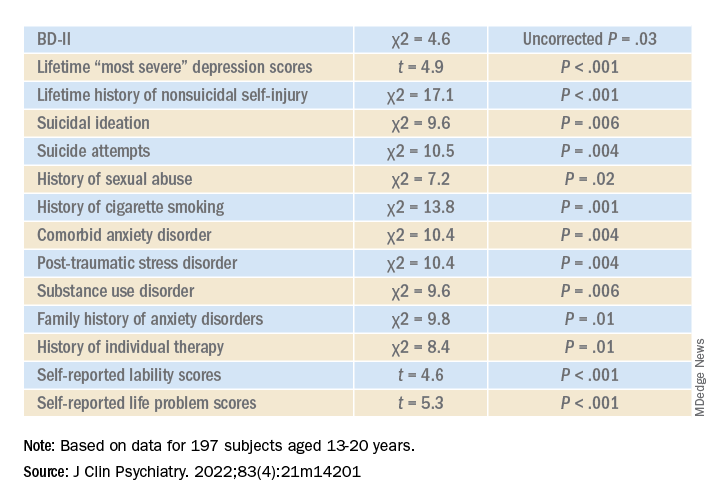
The ED group scored significantly higher on all LPI scores, including impulsivity, emotional dysregulation, identity confusion, and interpersonal problems, compared to those without an ED. They also were less likely to report lifetime lithium use (chi2 = 7.9, P = .01).
Multivariate analysis revealed that lifetime EDs were significantly associated with female sex, history of cigarette smoking, history of individual therapy, family history of anxiety, and LPI total score and were negatively associated with BD-I subtype.
“The comorbidity [between EDs and BD] could be driven by both neurobiological and environmental factors,” Dr. Khoubaeva and Dr. Goldstein noted. EDs and BD “are both illnesses that are fundamentally linked with dysfunction in reward systems – that is, there are imbalances in terms of too much or too little reward seeking.”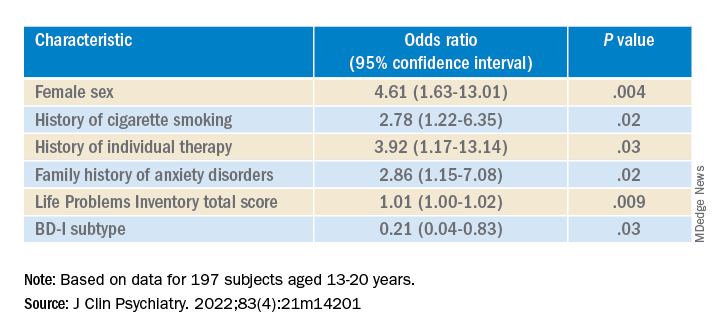
They added that individuals affected by these conditions have “ongoing challenges with instability of emotions and ability to manage emotions; and eating too much or too little can be a manifestation of coping with emotions.”
In addition, medications commonly used to treat BD “are known to have side effects such as weight/appetite/metabolic changes, which may make it harder to regulate eating, and which may exacerbate preexisting body image challenges.”
The researchers recommend implementing trauma-informed care, assessing and addressing suicidality and self-injury, and prioritizing therapies that target emotional dysregulation, such as dialectical behavioral therapy.
‘Clarion call’
Commenting on the study, Roger McIntyre, MD, professor of psychiatry and pharmacology, University of Toronto, and head of the Mood Disorders Psychopharmacology Unit, said the study is “the first of its kind to comprehensively characterize the prevalence of ED in youth living with BD.
“It could be hypothesized that EDs have overlapping domain disturbances of cognitive dysfunction, such as executive function and impulse control, as well as cognitive reward processes,” said Dr. McIntyre, who is the chairman and executive director of the Brain and Cognitive Discover Foundation, Toronto, and was not involved with the study.
“The data are a clarion call for clinicians to routinely screen for EDs in youth with BD and, when present, to be aware of the greater complexity, severity, and risk in this patient subpopulation. The higher prevalence of ED in youth with BD-II is an additional reminder of the severity, morbidity, and complexity of BD-II,” Dr. McIntyre said.
The study received no direct funding. It was supported by philanthropic donations to the Centre for Youth Bipolar Disorder and the CAMH Discovery Fund. Dr. Goldstein reports grant support from Brain Canada, Canadian Institutes of Health Research, Heart and Stroke Foundation, National Institute of Mental Health, and the departments of psychiatry at the University of Toronto and Sunnybrook Health Sciences Centre. He also acknowledges his position as RBC investments chair in Children›s Mental Health and Developmental Psychopathology at CAMH, a joint Hospital-University chair among the University of Toronto, CAMH, and the CAMH Foundation. Ms. Khoubaeva reports no relevant financial relationships. The other authors’ disclosures are listed in the original article. Dr. McIntyre has received research grant support from CIHR/GACD/National Natural Science Foundation of China (NSFC); speaker/consultation fees from Lundbeck, Janssen, Alkermes, Neumora Therapeutics, Mitsubishi Tanabe, Purdue, Pfizer, Otsuka, Takeda, Neurocrine, Sunovion, Bausch Health, Axsome, Novo Nordisk, Kris, Sanofi, Eisai, Intra-Cellular, NewBridge Pharmaceuticals, Abbvie, and Atai Life Sciences. Dr. McIntyre is a CEO of Braxia Scientific.
A version of this article first appeared on Medscape.com.
Investigators studied close to 200 youth with BD and found that more than 25% had a lifetime ED, which included anorexia nervosa (AN), bulimia nervosa (BN), and an ED not otherwise specified (NOS).
Those with comorbid EDs were more likely to be female and to have BD-II subtype. Their presentations were also more complicated and included a history of suicidality, additional psychiatric conditions, smoking, and a history of sexual abuse, as well as more severe depression and emotional instability.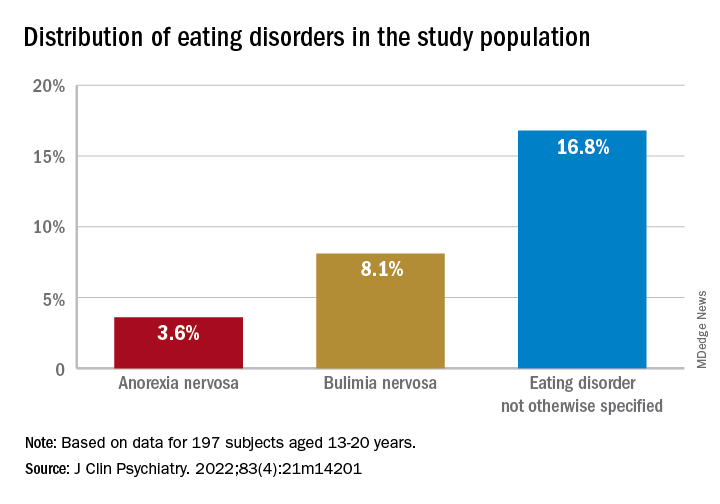
“We think the take-home message is that, in addition to other more recognized psychiatric comorbidities, youth with BD are also vulnerable to developing EDs. Thus, clinicians should be routinely monitoring for eating, appetite, and body image disturbances when working with this population,” lead author Diana Khoubaeva, research analyst at the Centre for Youth Bipolar Disorder, Centre for Addiction and Mental Health, Toronto, and senior author Benjamin Goldstein, MD, PhD, director of the Centre for Youth Bipolar Disorder, wrote in an e-mail to this news organization.
“Given the more complicated clinical picture of youth with co-occurring BD and EDs, this combination warrants careful attention,” the investigators note.
The study was published online May 11 in the Journal of Clinical Psychiatry.
Lack of research
“From the existing literature, we learned that EDs are not uncommon in individuals with BD, and that they are often associated with a more severe clinical profile,” say the researchers. “However, the majority of these studies have been limited to adult samples, and there was a real scarcity of studies that examined this co-occurrence in youth.”
This is “surprising” because EDs often have their onset in adolescence, so the researchers decided to explore the issue in their “fairly large sample of youth with BD.”
To investigate the issue, the researchers studied 197 youth (aged 13-20 years) with a diagnosis of BD (BD-I, BD-II, or BD-NOS) who were recruited between 2009 and 2017 (mean [standard deviation] age, 16.69 [1.50] years; 67.5% female).
ED diagnoses included both current and lifetime AN, BN, and ED-NOS. The researchers used the Kiddie Schedule for Affective Disorders and Schizophrenia for School Age Children, Present and Lifetime Version (K-SADS-PL) to determine the diagnosis of BD.
They also collected information about comorbid psychiatric disorders, as well as substance use disorders and cigarette smoking. The Life Problems Inventory (LPI) was used to identify dimensional borderline personality traits.
Information about physical and sexual abuse, suicidal ideation, nonsuicidal self-injury (NSSI), and affect regulation were obtained from other measurement tools. Participants’ height and weight were measured to calculate body mass index.
Neurobiological and environmental factors
Of the total sample, 24.84% had received a diagnosis of ED in their lifetime.
Moreover, 28.9% had a lifetime history of binge eating. Of these, 17.7% also had been diagnosed with an ED.
Participants with BD-II were significantly more likely than those with BD-I to report both current and lifetime BN. There were no significant differences by BD subtype in AN, ED-NOS, or binge eating.
Higher correlates of clinical characteristics, psychiatric morbidity, treatment history, and dimensional traits in those with vs. those without an ED are detailed in the accompanying table.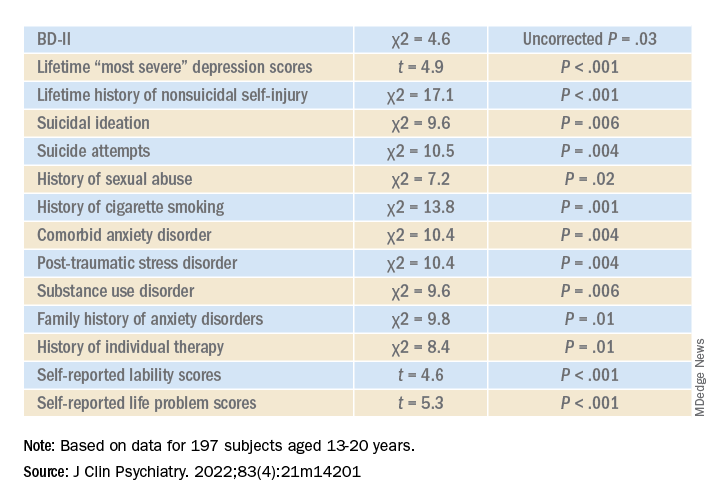
The ED group scored significantly higher on all LPI scores, including impulsivity, emotional dysregulation, identity confusion, and interpersonal problems, compared to those without an ED. They also were less likely to report lifetime lithium use (chi2 = 7.9, P = .01).
Multivariate analysis revealed that lifetime EDs were significantly associated with female sex, history of cigarette smoking, history of individual therapy, family history of anxiety, and LPI total score and were negatively associated with BD-I subtype.
“The comorbidity [between EDs and BD] could be driven by both neurobiological and environmental factors,” Dr. Khoubaeva and Dr. Goldstein noted. EDs and BD “are both illnesses that are fundamentally linked with dysfunction in reward systems – that is, there are imbalances in terms of too much or too little reward seeking.”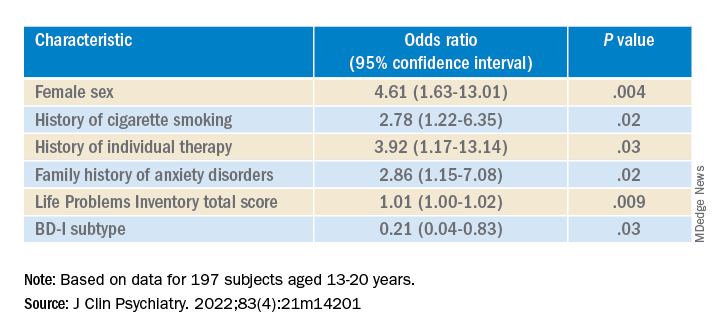
They added that individuals affected by these conditions have “ongoing challenges with instability of emotions and ability to manage emotions; and eating too much or too little can be a manifestation of coping with emotions.”
In addition, medications commonly used to treat BD “are known to have side effects such as weight/appetite/metabolic changes, which may make it harder to regulate eating, and which may exacerbate preexisting body image challenges.”
The researchers recommend implementing trauma-informed care, assessing and addressing suicidality and self-injury, and prioritizing therapies that target emotional dysregulation, such as dialectical behavioral therapy.
‘Clarion call’
Commenting on the study, Roger McIntyre, MD, professor of psychiatry and pharmacology, University of Toronto, and head of the Mood Disorders Psychopharmacology Unit, said the study is “the first of its kind to comprehensively characterize the prevalence of ED in youth living with BD.
“It could be hypothesized that EDs have overlapping domain disturbances of cognitive dysfunction, such as executive function and impulse control, as well as cognitive reward processes,” said Dr. McIntyre, who is the chairman and executive director of the Brain and Cognitive Discover Foundation, Toronto, and was not involved with the study.
“The data are a clarion call for clinicians to routinely screen for EDs in youth with BD and, when present, to be aware of the greater complexity, severity, and risk in this patient subpopulation. The higher prevalence of ED in youth with BD-II is an additional reminder of the severity, morbidity, and complexity of BD-II,” Dr. McIntyre said.
The study received no direct funding. It was supported by philanthropic donations to the Centre for Youth Bipolar Disorder and the CAMH Discovery Fund. Dr. Goldstein reports grant support from Brain Canada, Canadian Institutes of Health Research, Heart and Stroke Foundation, National Institute of Mental Health, and the departments of psychiatry at the University of Toronto and Sunnybrook Health Sciences Centre. He also acknowledges his position as RBC investments chair in Children›s Mental Health and Developmental Psychopathology at CAMH, a joint Hospital-University chair among the University of Toronto, CAMH, and the CAMH Foundation. Ms. Khoubaeva reports no relevant financial relationships. The other authors’ disclosures are listed in the original article. Dr. McIntyre has received research grant support from CIHR/GACD/National Natural Science Foundation of China (NSFC); speaker/consultation fees from Lundbeck, Janssen, Alkermes, Neumora Therapeutics, Mitsubishi Tanabe, Purdue, Pfizer, Otsuka, Takeda, Neurocrine, Sunovion, Bausch Health, Axsome, Novo Nordisk, Kris, Sanofi, Eisai, Intra-Cellular, NewBridge Pharmaceuticals, Abbvie, and Atai Life Sciences. Dr. McIntyre is a CEO of Braxia Scientific.
A version of this article first appeared on Medscape.com.
FROM THE JOURNAL OF CLINICAL PSYCHIATRY
Alcohol, degraded sleep related in young adults
CHARLOTTE, N.C. – Sleep and alcohol consumption in young adults seems to follow a “vicious cycle,” as one observer called it. and those who went to bed earlier and slept longer tended to drink less the next day, a study of drinking and sleeping habits in 21- to 29-year-olds found.
“Sleep is a potential factor that we could intervene on to really identify how to improve drinking behaviors among young adults,” David Reichenberger, a graduate student at Penn State University, University Park, said in an interview after he presented his findings at the annual meeting of the Associated Professional Sleep Societies.
This is one of the few studies of alcohol consumption and sleep patterns that used an objective measure of alcohol consumption, Mr. Reichenberger said. The study evaluated sleep and alcohol consumption patterns in 222 regularly drinking young adults over 6 consecutive days. Study participants completed morning smartphone-based questionnaires, reporting their previous night’s bedtime, sleep duration, sleep quality, and number of drinks consumed. They also wore an alcohol monitor that continuously measured their transdermal alcohol consumption (TAC).
The study analyzed the data using two sets of multilevel models: A linear model that looked at how each drinking predictor was associated with each sleep variable and a Poisson model to determine how sleep predicted next-day alcohol use.
“We found that higher average peak TAC – that is, how intoxicated they got – was associated with a 19-minute later bedtime among young adults,” Mr. Reichenberger said. “Later bedtimes were then associated with a 26% greater TAC among those adults” (P < .02).
Patterns of alcohol consumption and sleep
On days when participants recorded a higher peak TAC, bedtime was delayed, sleep duration was shorter, and subjective sleep quality was worse, he said. However, none of the sleep variables predicted next-day peak TAC.
“We found an association between the duration of the drinking episode and later bedtimes among young adults,” he added. “And on days when the drinking episodes were longer, subsequent sleep was delayed and sleep quality was worse. But we also found that after nights when they had a later bedtime, next-day drinking episodes were about 7% longer.”
Conversely, young adults who had earlier bedtimes and longer sleep durations tended to consume fewer drinks and they achieved lower intoxication levels the next day, Mr. Reichenberger said.
Between-person results showed that young adults who tended to go to bed later drank on average 24% more the next day (P < .01). Also, each extra hour of sleep was associated with a 14% decrease in drinking the next day (P < .03).
Participants who drank more went to bed on average 12-19 minutes later (P < .01) and slept 5 fewer minutes (P < .01). Within-person results showed that on nights when participants drank more than usual they went to bed 8-13 minutes later (P < .01), slept 2-4 fewer minutes (P < .03), and had worse sleep quality (P < .01).
Mr. Reichenberger acknowledged one limitation of the study: Measuring sleep and alcohol consumption patterns over 6 days might not be long enough. Future studies should address that.
A ‘vicious cycle’
Hans P.A. Van Dongen, PhD, director of the Sleep and Performance Research Center at Washington State University, Spokane, said in an interview that the findings imply a “vicious cycle” between sleep and alcohol consumption. “You create a problem and then it perpetuates itself or reinforces itself.”
In older adults, alcohol tends to act as a “sleep aid,” Dr. Van Dongen noted. “Then it disrupts their sleep later on and then the next night they need to use the sleep aid again because they had a really poor night and they’re tired and they want to fall asleep.”
He added: “I think what is new here is that’s not very likely the mechanism that they’re using alcohol as a sleep aid in younger adults that we see in older adults, so I think there is a new element to it. Now does anybody know how that works exactly? No, that’s the next thing.”
The Penn State study identifies “a signal there that needs to be followed up on,” Dr. Van Dongen said. “There’s something nature’s trying to tell us but it’s not exactly clear what it’s trying to tell us.”
The National Institute on Drug Abuse provided funding for the study. Mr. Reichenberger has no relevant disclosures. Dr. Van Dongen has no disclosures to report.
CHARLOTTE, N.C. – Sleep and alcohol consumption in young adults seems to follow a “vicious cycle,” as one observer called it. and those who went to bed earlier and slept longer tended to drink less the next day, a study of drinking and sleeping habits in 21- to 29-year-olds found.
“Sleep is a potential factor that we could intervene on to really identify how to improve drinking behaviors among young adults,” David Reichenberger, a graduate student at Penn State University, University Park, said in an interview after he presented his findings at the annual meeting of the Associated Professional Sleep Societies.
This is one of the few studies of alcohol consumption and sleep patterns that used an objective measure of alcohol consumption, Mr. Reichenberger said. The study evaluated sleep and alcohol consumption patterns in 222 regularly drinking young adults over 6 consecutive days. Study participants completed morning smartphone-based questionnaires, reporting their previous night’s bedtime, sleep duration, sleep quality, and number of drinks consumed. They also wore an alcohol monitor that continuously measured their transdermal alcohol consumption (TAC).
The study analyzed the data using two sets of multilevel models: A linear model that looked at how each drinking predictor was associated with each sleep variable and a Poisson model to determine how sleep predicted next-day alcohol use.
“We found that higher average peak TAC – that is, how intoxicated they got – was associated with a 19-minute later bedtime among young adults,” Mr. Reichenberger said. “Later bedtimes were then associated with a 26% greater TAC among those adults” (P < .02).
Patterns of alcohol consumption and sleep
On days when participants recorded a higher peak TAC, bedtime was delayed, sleep duration was shorter, and subjective sleep quality was worse, he said. However, none of the sleep variables predicted next-day peak TAC.
“We found an association between the duration of the drinking episode and later bedtimes among young adults,” he added. “And on days when the drinking episodes were longer, subsequent sleep was delayed and sleep quality was worse. But we also found that after nights when they had a later bedtime, next-day drinking episodes were about 7% longer.”
Conversely, young adults who had earlier bedtimes and longer sleep durations tended to consume fewer drinks and they achieved lower intoxication levels the next day, Mr. Reichenberger said.
Between-person results showed that young adults who tended to go to bed later drank on average 24% more the next day (P < .01). Also, each extra hour of sleep was associated with a 14% decrease in drinking the next day (P < .03).
Participants who drank more went to bed on average 12-19 minutes later (P < .01) and slept 5 fewer minutes (P < .01). Within-person results showed that on nights when participants drank more than usual they went to bed 8-13 minutes later (P < .01), slept 2-4 fewer minutes (P < .03), and had worse sleep quality (P < .01).
Mr. Reichenberger acknowledged one limitation of the study: Measuring sleep and alcohol consumption patterns over 6 days might not be long enough. Future studies should address that.
A ‘vicious cycle’
Hans P.A. Van Dongen, PhD, director of the Sleep and Performance Research Center at Washington State University, Spokane, said in an interview that the findings imply a “vicious cycle” between sleep and alcohol consumption. “You create a problem and then it perpetuates itself or reinforces itself.”
In older adults, alcohol tends to act as a “sleep aid,” Dr. Van Dongen noted. “Then it disrupts their sleep later on and then the next night they need to use the sleep aid again because they had a really poor night and they’re tired and they want to fall asleep.”
He added: “I think what is new here is that’s not very likely the mechanism that they’re using alcohol as a sleep aid in younger adults that we see in older adults, so I think there is a new element to it. Now does anybody know how that works exactly? No, that’s the next thing.”
The Penn State study identifies “a signal there that needs to be followed up on,” Dr. Van Dongen said. “There’s something nature’s trying to tell us but it’s not exactly clear what it’s trying to tell us.”
The National Institute on Drug Abuse provided funding for the study. Mr. Reichenberger has no relevant disclosures. Dr. Van Dongen has no disclosures to report.
CHARLOTTE, N.C. – Sleep and alcohol consumption in young adults seems to follow a “vicious cycle,” as one observer called it. and those who went to bed earlier and slept longer tended to drink less the next day, a study of drinking and sleeping habits in 21- to 29-year-olds found.
“Sleep is a potential factor that we could intervene on to really identify how to improve drinking behaviors among young adults,” David Reichenberger, a graduate student at Penn State University, University Park, said in an interview after he presented his findings at the annual meeting of the Associated Professional Sleep Societies.
This is one of the few studies of alcohol consumption and sleep patterns that used an objective measure of alcohol consumption, Mr. Reichenberger said. The study evaluated sleep and alcohol consumption patterns in 222 regularly drinking young adults over 6 consecutive days. Study participants completed morning smartphone-based questionnaires, reporting their previous night’s bedtime, sleep duration, sleep quality, and number of drinks consumed. They also wore an alcohol monitor that continuously measured their transdermal alcohol consumption (TAC).
The study analyzed the data using two sets of multilevel models: A linear model that looked at how each drinking predictor was associated with each sleep variable and a Poisson model to determine how sleep predicted next-day alcohol use.
“We found that higher average peak TAC – that is, how intoxicated they got – was associated with a 19-minute later bedtime among young adults,” Mr. Reichenberger said. “Later bedtimes were then associated with a 26% greater TAC among those adults” (P < .02).
Patterns of alcohol consumption and sleep
On days when participants recorded a higher peak TAC, bedtime was delayed, sleep duration was shorter, and subjective sleep quality was worse, he said. However, none of the sleep variables predicted next-day peak TAC.
“We found an association between the duration of the drinking episode and later bedtimes among young adults,” he added. “And on days when the drinking episodes were longer, subsequent sleep was delayed and sleep quality was worse. But we also found that after nights when they had a later bedtime, next-day drinking episodes were about 7% longer.”
Conversely, young adults who had earlier bedtimes and longer sleep durations tended to consume fewer drinks and they achieved lower intoxication levels the next day, Mr. Reichenberger said.
Between-person results showed that young adults who tended to go to bed later drank on average 24% more the next day (P < .01). Also, each extra hour of sleep was associated with a 14% decrease in drinking the next day (P < .03).
Participants who drank more went to bed on average 12-19 minutes later (P < .01) and slept 5 fewer minutes (P < .01). Within-person results showed that on nights when participants drank more than usual they went to bed 8-13 minutes later (P < .01), slept 2-4 fewer minutes (P < .03), and had worse sleep quality (P < .01).
Mr. Reichenberger acknowledged one limitation of the study: Measuring sleep and alcohol consumption patterns over 6 days might not be long enough. Future studies should address that.
A ‘vicious cycle’
Hans P.A. Van Dongen, PhD, director of the Sleep and Performance Research Center at Washington State University, Spokane, said in an interview that the findings imply a “vicious cycle” between sleep and alcohol consumption. “You create a problem and then it perpetuates itself or reinforces itself.”
In older adults, alcohol tends to act as a “sleep aid,” Dr. Van Dongen noted. “Then it disrupts their sleep later on and then the next night they need to use the sleep aid again because they had a really poor night and they’re tired and they want to fall asleep.”
He added: “I think what is new here is that’s not very likely the mechanism that they’re using alcohol as a sleep aid in younger adults that we see in older adults, so I think there is a new element to it. Now does anybody know how that works exactly? No, that’s the next thing.”
The Penn State study identifies “a signal there that needs to be followed up on,” Dr. Van Dongen said. “There’s something nature’s trying to tell us but it’s not exactly clear what it’s trying to tell us.”
The National Institute on Drug Abuse provided funding for the study. Mr. Reichenberger has no relevant disclosures. Dr. Van Dongen has no disclosures to report.
At SLEEP 2022
Trans teens less likely to commit acts of sexual violence, says new study
Transgender and nonbinary adolescents are twice as likely to experience sexual violence as their cisgendered peers but are less likely to attempt rape or commit sexual assault, researchers have found.
The study, which was published online in JAMA Network Open, is among the first on the sexual violence that trans, nonbinary, and other gender nonconforming adolescents experience. Previous studies have focused on adults.
“In the busy world of clinical care, it is essential that clinicians be aware of potential disparities their patients are navigating,” said Michele Ybarra, PhD, MPH, president and research director of the Center for Innovative Public Health Research, San Clemente, California, who led the study. “This includes sexual violence victimization for gender minority youth and the need to talk about consent and boundaries for youth of all genders.”
Dr. Ybarra said that while clinicians may be aware that transgender young people face stigma, discrimination, and bullying, they may not be aware that trans youth are also the targets of sexual violence.
Studies indicate that health care providers and communities have significant misconceptions about sexually explicit behavior among trans and nonbinary teens. Misconceptions can lead to discrimination, resulting in higher rates of drug abuse, dropping out of school, suicide, and homelessness.
Dr. Ybarra and her colleagues surveyed 911 trans, nonbinary, or questioning youth on Instagram and Facebook through a collaboration with Growing Up With Media, a national longitudinal survey designed to investigate sexual violence during adolescence.
They also surveyed 3,282 cisgender persons aged 14-16 years who were recruited to the study between June 2018 and March 2020. The term “cisgender” refers to youth who identify with their gender at birth.
The questionnaires asked teens about gender identity, race, economic status, and support systems at home. Factors associated with not experiencing sexual violence included having a strong network of friends, family, and educators; involvement in the community; and having people close who affirm their gender identity.
More than three-fourths (78%) of youth surveyed identified as cisgender, 13.9% identified as questioning, and 7.9% identified as transgender.
Roughly two-thirds (67%) of transgender adolescents said they had experienced serious sexual violence, 73% reported experiencing violence in their communities, and 63% said they had been exposed to aggressive behavior. In contrast, 6.7% of trans youth said they had ever committed sexual violence, while 7.4% of cisgender teens surveyed, or 243 students, said they had done so.
“The relative lack of visibility of gender minority youth in sexual violence research is unacceptable,” Dr. Ybarra told this news organization. “To be counted, one needs to be seen. We aimed to start addressing this exclusion with the current study.”
The findings provide a lens into the levels of sexual violence that LGBTQIA+ youth experience and an opportunity to provide more inclusive care, according to Elizabeth Miller, MD, PhD, FSAHM, Distinguished Professor of Pediatrics, director of the Division of Adolescent and Young Adult Medicine, and medical director of community and population health at UPMC Children’s Hospital of Pittsburgh, who was not involved in the study.
“There are unfortunately pervasive and harmful stereotypes in our society about the ‘sexual deviancy’ attributed to LGBTQIA+ individuals,” Dr. Miller told this news organization. “This study adds to the research literature that counters and challenges these harmful – and inaccurate – perceptions.”
Dr. Miller said clinicians can help this population by offering youth accurate information about relevant support and services, including how to help a friend.
Programs that providers could incorporate include gender transformative approaches, which guide youth to examine gender norms and inequities and that develop leadership skills.
Such programs are more common outside the United States and have been shown to decrease LGBTQIA+ youth exposure to sexual violence, she said.
Dr. Miller said more research is needed to understand the contexts in which gender minority youth experience sexual violence to guide prevention efforts: “We need to move beyond individual-focused interventions to considering community-level interventions to create safer and more inclusive spaces for all youth.”
Dr. Miller has received royalties for writing content for UptoDate Wolters Kluwer outside of the current study. Dr. Ybarra has disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Transgender and nonbinary adolescents are twice as likely to experience sexual violence as their cisgendered peers but are less likely to attempt rape or commit sexual assault, researchers have found.
The study, which was published online in JAMA Network Open, is among the first on the sexual violence that trans, nonbinary, and other gender nonconforming adolescents experience. Previous studies have focused on adults.
“In the busy world of clinical care, it is essential that clinicians be aware of potential disparities their patients are navigating,” said Michele Ybarra, PhD, MPH, president and research director of the Center for Innovative Public Health Research, San Clemente, California, who led the study. “This includes sexual violence victimization for gender minority youth and the need to talk about consent and boundaries for youth of all genders.”
Dr. Ybarra said that while clinicians may be aware that transgender young people face stigma, discrimination, and bullying, they may not be aware that trans youth are also the targets of sexual violence.
Studies indicate that health care providers and communities have significant misconceptions about sexually explicit behavior among trans and nonbinary teens. Misconceptions can lead to discrimination, resulting in higher rates of drug abuse, dropping out of school, suicide, and homelessness.
Dr. Ybarra and her colleagues surveyed 911 trans, nonbinary, or questioning youth on Instagram and Facebook through a collaboration with Growing Up With Media, a national longitudinal survey designed to investigate sexual violence during adolescence.
They also surveyed 3,282 cisgender persons aged 14-16 years who were recruited to the study between June 2018 and March 2020. The term “cisgender” refers to youth who identify with their gender at birth.
The questionnaires asked teens about gender identity, race, economic status, and support systems at home. Factors associated with not experiencing sexual violence included having a strong network of friends, family, and educators; involvement in the community; and having people close who affirm their gender identity.
More than three-fourths (78%) of youth surveyed identified as cisgender, 13.9% identified as questioning, and 7.9% identified as transgender.
Roughly two-thirds (67%) of transgender adolescents said they had experienced serious sexual violence, 73% reported experiencing violence in their communities, and 63% said they had been exposed to aggressive behavior. In contrast, 6.7% of trans youth said they had ever committed sexual violence, while 7.4% of cisgender teens surveyed, or 243 students, said they had done so.
“The relative lack of visibility of gender minority youth in sexual violence research is unacceptable,” Dr. Ybarra told this news organization. “To be counted, one needs to be seen. We aimed to start addressing this exclusion with the current study.”
The findings provide a lens into the levels of sexual violence that LGBTQIA+ youth experience and an opportunity to provide more inclusive care, according to Elizabeth Miller, MD, PhD, FSAHM, Distinguished Professor of Pediatrics, director of the Division of Adolescent and Young Adult Medicine, and medical director of community and population health at UPMC Children’s Hospital of Pittsburgh, who was not involved in the study.
“There are unfortunately pervasive and harmful stereotypes in our society about the ‘sexual deviancy’ attributed to LGBTQIA+ individuals,” Dr. Miller told this news organization. “This study adds to the research literature that counters and challenges these harmful – and inaccurate – perceptions.”
Dr. Miller said clinicians can help this population by offering youth accurate information about relevant support and services, including how to help a friend.
Programs that providers could incorporate include gender transformative approaches, which guide youth to examine gender norms and inequities and that develop leadership skills.
Such programs are more common outside the United States and have been shown to decrease LGBTQIA+ youth exposure to sexual violence, she said.
Dr. Miller said more research is needed to understand the contexts in which gender minority youth experience sexual violence to guide prevention efforts: “We need to move beyond individual-focused interventions to considering community-level interventions to create safer and more inclusive spaces for all youth.”
Dr. Miller has received royalties for writing content for UptoDate Wolters Kluwer outside of the current study. Dr. Ybarra has disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Transgender and nonbinary adolescents are twice as likely to experience sexual violence as their cisgendered peers but are less likely to attempt rape or commit sexual assault, researchers have found.
The study, which was published online in JAMA Network Open, is among the first on the sexual violence that trans, nonbinary, and other gender nonconforming adolescents experience. Previous studies have focused on adults.
“In the busy world of clinical care, it is essential that clinicians be aware of potential disparities their patients are navigating,” said Michele Ybarra, PhD, MPH, president and research director of the Center for Innovative Public Health Research, San Clemente, California, who led the study. “This includes sexual violence victimization for gender minority youth and the need to talk about consent and boundaries for youth of all genders.”
Dr. Ybarra said that while clinicians may be aware that transgender young people face stigma, discrimination, and bullying, they may not be aware that trans youth are also the targets of sexual violence.
Studies indicate that health care providers and communities have significant misconceptions about sexually explicit behavior among trans and nonbinary teens. Misconceptions can lead to discrimination, resulting in higher rates of drug abuse, dropping out of school, suicide, and homelessness.
Dr. Ybarra and her colleagues surveyed 911 trans, nonbinary, or questioning youth on Instagram and Facebook through a collaboration with Growing Up With Media, a national longitudinal survey designed to investigate sexual violence during adolescence.
They also surveyed 3,282 cisgender persons aged 14-16 years who were recruited to the study between June 2018 and March 2020. The term “cisgender” refers to youth who identify with their gender at birth.
The questionnaires asked teens about gender identity, race, economic status, and support systems at home. Factors associated with not experiencing sexual violence included having a strong network of friends, family, and educators; involvement in the community; and having people close who affirm their gender identity.
More than three-fourths (78%) of youth surveyed identified as cisgender, 13.9% identified as questioning, and 7.9% identified as transgender.
Roughly two-thirds (67%) of transgender adolescents said they had experienced serious sexual violence, 73% reported experiencing violence in their communities, and 63% said they had been exposed to aggressive behavior. In contrast, 6.7% of trans youth said they had ever committed sexual violence, while 7.4% of cisgender teens surveyed, or 243 students, said they had done so.
“The relative lack of visibility of gender minority youth in sexual violence research is unacceptable,” Dr. Ybarra told this news organization. “To be counted, one needs to be seen. We aimed to start addressing this exclusion with the current study.”
The findings provide a lens into the levels of sexual violence that LGBTQIA+ youth experience and an opportunity to provide more inclusive care, according to Elizabeth Miller, MD, PhD, FSAHM, Distinguished Professor of Pediatrics, director of the Division of Adolescent and Young Adult Medicine, and medical director of community and population health at UPMC Children’s Hospital of Pittsburgh, who was not involved in the study.
“There are unfortunately pervasive and harmful stereotypes in our society about the ‘sexual deviancy’ attributed to LGBTQIA+ individuals,” Dr. Miller told this news organization. “This study adds to the research literature that counters and challenges these harmful – and inaccurate – perceptions.”
Dr. Miller said clinicians can help this population by offering youth accurate information about relevant support and services, including how to help a friend.
Programs that providers could incorporate include gender transformative approaches, which guide youth to examine gender norms and inequities and that develop leadership skills.
Such programs are more common outside the United States and have been shown to decrease LGBTQIA+ youth exposure to sexual violence, she said.
Dr. Miller said more research is needed to understand the contexts in which gender minority youth experience sexual violence to guide prevention efforts: “We need to move beyond individual-focused interventions to considering community-level interventions to create safer and more inclusive spaces for all youth.”
Dr. Miller has received royalties for writing content for UptoDate Wolters Kluwer outside of the current study. Dr. Ybarra has disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Are teenagers tone deaf?
I suspect that you have heard or read about the recent study in the Journal of Neuroscience that claims to have discovered evidence that as children become teenagers, their brains begin to tune out their mother’s voices. The story appeared in at least 10 Internet news sources including the American Academy of Pediatrics’ daily briefing.
Based on functional MRI studies by a group at Stanford (Calif.) University, the researchers found that while in general, teenagers became more attentive to all voices as they reached puberty, novel voices were favored over the maternal voices that had flooded their environment as younger children. Of course none of this comes as a surprise to anyone who has parented a teenager or spent any time trying to communicate with adolescents. Although we all must be a bit careful not to put too much stock in functional MRI studies, these findings do suggest a physiologic basis for the peer pressure that becomes one of the hallmarks of adolescence. I wouldn’t be surprised if some clever entrepreneur has already begun using MRI to search for just the right tonal qualities that will make the perfect Internet influencer.
But, will these MRI studies help parents who have already thrown up their arms and admitted defeat mumbling, “He’s stopped listening to me?” The more observant parents already realized long ago that their words were often the least effective tools in their tool kit when it comes to modifying behavior.
Just listen in any neighborhood playground or grocery store to how often you hear a parent trying to get a toddler or young child to correct a misbehavior using threats or promises that you and everyone else within earshot knows will never be followed by any consequence. How often do you see a parent modeling behaviors that they expect their children to avoid?
Some more “enlightened” parents will avoid threats and instead attempt to engage in a dialogue with their misbehaving child hoping that a rational discussion with a sleep-deprived toddler in full tantrum mode can convince the youngster to self-correct.
I’m sure you learned and may have even used the playground retort “sticks and stones may break my bones but words will never hurt me.” Of course more untrue words were never spoken. Words can hurt and they can scar. But words and threats can also be hollow and will fall on ears deafened by months and years during which there were no consequences. It is certainly nice to know that there is some physiologic correlation to what we all suspected. The good news is that teenagers are still listening to us, although they are increasingly more interested in what their peers and the rest of the world has to say.
What the study fails to point out is that while teenagers may still be listening to us their behavior is molded not so much by what we say but how we as parents and adults behave. Have we parented in a way in which our words are followed up with appropriate consequences? And, more importantly, have we modeled behavior that matches our words? We need to help parents realize that words can be important but parenting by example is the gold standard.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Other than a Littman stethoscope he accepted as a first-year medical student in 1966, Dr. Wilkoff reports having nothing to disclose. Email him at [email protected].
I suspect that you have heard or read about the recent study in the Journal of Neuroscience that claims to have discovered evidence that as children become teenagers, their brains begin to tune out their mother’s voices. The story appeared in at least 10 Internet news sources including the American Academy of Pediatrics’ daily briefing.
Based on functional MRI studies by a group at Stanford (Calif.) University, the researchers found that while in general, teenagers became more attentive to all voices as they reached puberty, novel voices were favored over the maternal voices that had flooded their environment as younger children. Of course none of this comes as a surprise to anyone who has parented a teenager or spent any time trying to communicate with adolescents. Although we all must be a bit careful not to put too much stock in functional MRI studies, these findings do suggest a physiologic basis for the peer pressure that becomes one of the hallmarks of adolescence. I wouldn’t be surprised if some clever entrepreneur has already begun using MRI to search for just the right tonal qualities that will make the perfect Internet influencer.
But, will these MRI studies help parents who have already thrown up their arms and admitted defeat mumbling, “He’s stopped listening to me?” The more observant parents already realized long ago that their words were often the least effective tools in their tool kit when it comes to modifying behavior.
Just listen in any neighborhood playground or grocery store to how often you hear a parent trying to get a toddler or young child to correct a misbehavior using threats or promises that you and everyone else within earshot knows will never be followed by any consequence. How often do you see a parent modeling behaviors that they expect their children to avoid?
Some more “enlightened” parents will avoid threats and instead attempt to engage in a dialogue with their misbehaving child hoping that a rational discussion with a sleep-deprived toddler in full tantrum mode can convince the youngster to self-correct.
I’m sure you learned and may have even used the playground retort “sticks and stones may break my bones but words will never hurt me.” Of course more untrue words were never spoken. Words can hurt and they can scar. But words and threats can also be hollow and will fall on ears deafened by months and years during which there were no consequences. It is certainly nice to know that there is some physiologic correlation to what we all suspected. The good news is that teenagers are still listening to us, although they are increasingly more interested in what their peers and the rest of the world has to say.
What the study fails to point out is that while teenagers may still be listening to us their behavior is molded not so much by what we say but how we as parents and adults behave. Have we parented in a way in which our words are followed up with appropriate consequences? And, more importantly, have we modeled behavior that matches our words? We need to help parents realize that words can be important but parenting by example is the gold standard.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Other than a Littman stethoscope he accepted as a first-year medical student in 1966, Dr. Wilkoff reports having nothing to disclose. Email him at [email protected].
I suspect that you have heard or read about the recent study in the Journal of Neuroscience that claims to have discovered evidence that as children become teenagers, their brains begin to tune out their mother’s voices. The story appeared in at least 10 Internet news sources including the American Academy of Pediatrics’ daily briefing.
Based on functional MRI studies by a group at Stanford (Calif.) University, the researchers found that while in general, teenagers became more attentive to all voices as they reached puberty, novel voices were favored over the maternal voices that had flooded their environment as younger children. Of course none of this comes as a surprise to anyone who has parented a teenager or spent any time trying to communicate with adolescents. Although we all must be a bit careful not to put too much stock in functional MRI studies, these findings do suggest a physiologic basis for the peer pressure that becomes one of the hallmarks of adolescence. I wouldn’t be surprised if some clever entrepreneur has already begun using MRI to search for just the right tonal qualities that will make the perfect Internet influencer.
But, will these MRI studies help parents who have already thrown up their arms and admitted defeat mumbling, “He’s stopped listening to me?” The more observant parents already realized long ago that their words were often the least effective tools in their tool kit when it comes to modifying behavior.
Just listen in any neighborhood playground or grocery store to how often you hear a parent trying to get a toddler or young child to correct a misbehavior using threats or promises that you and everyone else within earshot knows will never be followed by any consequence. How often do you see a parent modeling behaviors that they expect their children to avoid?
Some more “enlightened” parents will avoid threats and instead attempt to engage in a dialogue with their misbehaving child hoping that a rational discussion with a sleep-deprived toddler in full tantrum mode can convince the youngster to self-correct.
I’m sure you learned and may have even used the playground retort “sticks and stones may break my bones but words will never hurt me.” Of course more untrue words were never spoken. Words can hurt and they can scar. But words and threats can also be hollow and will fall on ears deafened by months and years during which there were no consequences. It is certainly nice to know that there is some physiologic correlation to what we all suspected. The good news is that teenagers are still listening to us, although they are increasingly more interested in what their peers and the rest of the world has to say.
What the study fails to point out is that while teenagers may still be listening to us their behavior is molded not so much by what we say but how we as parents and adults behave. Have we parented in a way in which our words are followed up with appropriate consequences? And, more importantly, have we modeled behavior that matches our words? We need to help parents realize that words can be important but parenting by example is the gold standard.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Other than a Littman stethoscope he accepted as a first-year medical student in 1966, Dr. Wilkoff reports having nothing to disclose. Email him at [email protected].
Abortion debate may affect Rx decisions for pregnant women
Obstetrician Beverly Gray, MD, is already seeing the effects of the Roe v. Wade abortion debate in her North Carolina practice.
The state allows abortion but requires that women get counseling with a qualified health professional 72 hours before the procedure. “Aside from that, we still have patients asking for more efficacious contraceptive methods just in case,” said Dr. Gray, residency director and division director for women’s community and population health and associate professor for obstetrics and gynecology at Duke University, Durham, N.C.
Patients and staff in her clinic have also been approaching her about tubal ligation. “They’re asking about additional birth control methods because they’re concerned about what’s going to happen” with the challenge to the historic Roe v. Wade decision in the Supreme Court and subsequent actions in the states to restrict or ban abortion, she said.
This has implications not just for abortion but for medications known to affect pregnancy. “What I’m really worried about is physicians will be withholding medicine because they’re concerned about teratogenic effects,” said Dr. Gray.
With more states issuing restrictions on abortion, doctors are worried that patients needing certain drugs to maintain their lupus flares, cancer, or other diseases may decide not to take them in the event they accidentally become pregnant. If the drug is known to affect the fetus, the fear is a patient who lives in a state with abortion restrictions will no longer have the option to terminate a pregnancy.
Instead, a scenario may arise in which the patient – and their physician – may opt not to treat at all with an otherwise lifesaving medication, experts told this news organization.
The U.S. landscape on abortion restrictions
A leaked draft of a U.S. Supreme Court opinion on Mississippi’s 15-week abortion ban has sent the medical community into a tailspin. The case, Dobbs v. Jackson Women’s Health Organization, challenges the 1973 Roe v. Wade decision that affirms the constitutional right to abortion. It’s anticipated the high court will decide on the case in June.
Although the upcoming decision is subject to change, the draft indicated the high court would uphold the Mississippi ban. This would essentially overturn the 1973 ruling. An earlier Supreme Court decision allowing a Texas law banning abortion at 6 weeks suggests the court may already be heading in this direction. At the state level, legislatures have been moving on divergent paths – some taking steps to preserve abortion rights, others initiating restrictions.
More than 100 abortion restrictions in 19 states took effect in 2021, according to the Guttmacher Institute, which tracks such metrics. In 2022, “two key themes are anti-abortion policymakers’ continued pursuit of various types of abortion bans and restrictions on medication abortion,” the institute reported.
Forty-six states and the District of Columbia have introduced 2,025 restrictions or proactive measures on sexual and reproductive health and rights so far this year. The latest tally from Guttmacher, updated in late May, revealed that 11 states so far have enacted 42 abortion restrictions. A total of 6 states (Arizona, Florida, Idaho, Kentucky, Oklahoma, and Wyoming) have issued nine bans on abortion.
Comparatively, 11 states have enacted 19 protective abortion measures.
Twenty-two states have introduced 117 restrictions on medication abortions, which account for 54% of U.S. abortions. This includes seven measures that would ban medication abortion outright, according to Guttmacher. Kentucky and South Dakota collectively have enacted 14 restrictions on medication abortion, as well as provisions that ban mailing of abortion pills.
Chilling effect on prescribing
Some physicians anticipate that drugs such as the “morning-after” pill (levonorgestrel) will become less available as restrictions go into effect, since these are medications designed to prevent pregnancy.*
However, the ongoing effort to put a lid on abortion measures has prompted concerns about a trickle-down effect on other medications that are otherwise life-changing or lifesaving to patients but pose a risk to the fetus.
Several drugs are well documented to affect fetal growth and development of the fetus, ranging from mild, transitory effects to severe, permanent birth defects, said Ronald G. Grifka, MD, chief medical officer of University of Michigan Health-West and clinical professor of pediatrics at the University of Michigan Medical School, Ann Arbor. “As new medications are developed, we will need heightened attention to make sure they are safe for the fetus,” he added.
Certain teratogenic medications are associated with a high risk of abortion even though this isn’t their primary use, noted Christina Chambers, PhD, MPH, co-director of the Center for Better Beginnings and associate director with the Altman Clinical & Translational Research Institute at the University of California, San Diego.
“I don’t think anyone would intentionally take these drugs to induce spontaneous abortion. But if the drugs pose a risk for it, I can see how the laws might be stretched” to include them, said Dr. Chambers.
Methotrexate, a medication for autoimmune disorders, has a high risk of spontaneous abortion. So do acne medications such as isotretinoin.
Patients are usually told they’re not supposed to get pregnant on these drugs because there’s a high risk of pregnancy loss and risk of malformations and potential learning problems in the fetus. But many pregnancies aren’t planned, said Dr. Chambers. “Patients may forget about the side effects or think their birth control will protect them. And the next time they refill the medication, they may not hear about the warnings again.”
With a restrictive abortion law or ban in effect, a woman might think: “I won’t take this drug because if there’s any potential that I might get pregnant, I won’t have the option to abort an at-risk pregnancy.” Women and their doctors, for that matter, don’t want to put themselves in this position, said Dr. Chambers.
Rheumatologist Megan Clowse, MD, who prescribes several medications that potentially cause major birth defects and pregnancy loss, worries about the ramifications of these accumulating bans.
“Methotrexate has been a leading drug for us for decades for rheumatoid arthritis. Mycophenolate is a vital drug for lupus,” said Dr. Clowse, associate professor of medicine at Duke University’s division of rheumatology and immunology.
Both methotrexate and mycophenolate pose about a 40% risk of pregnancy loss and significantly increase the risk for birth defects. “I’m definitely concerned that there might be doctors or women who elect not to use those medications in women of reproductive age because of the potential risk for pregnancy and absence of abortion rights,” said Dr. Clowse.
These situations might force women to use contraceptives they don’t want to use, such as hormonal implants or intrauterine devices, she added. Another side effect is that women and their partners may decide to abstain from sex.
The iPLEDGE factor
Some rheumatology drugs like lenalidomide (Revlimid) require a valid negative pregnancy test in a lab every month. Similarly, the iPLEDGE Risk Evaluation and Mitigation Strategy seeks to reduce the teratogenicity of isotretinoin by requiring two types of birth control and regular pregnancy tests by users.
For isotretinoin specifically, abortion restrictions “could lead to increased adherence to pregnancy prevention measures which are already stringent in iPLEDGE. But on the other hand, it could lead to reduced willingness of physicians to prescribe or patients to take the medication,” said Dr. Chambers.
With programs like iPLEDGE in effect, the rate of pregnancies and abortions that occur in dermatology are relatively low, said Jenny Murase, MD, associate clinical professor of dermatology at the University of California, San Francisco.
Nevertheless, as a physician who regularly prescribes medications like isotretinoin in women of childbearing age, “it’s terrifying to me that a woman wouldn’t have the option to terminate the pregnancy if a teratogenic effect from the medication caused a severe birth defect,” said Dr. Murase.
Dermatologists use other teratogenic medications such as thalidomide, mycophenolate mofetil, and methotrexate for chronic dermatologic disease like psoriasis and atopic dermatitis.
The situation is especially tricky for dermatologists since most patients – about 80% – never discuss their pregnancy with their specialist prior to pregnancy initiation. Dr. Murase recalls when a patient with chronic plaque psoriasis on methotrexate in her late 40s became pregnant and had an abortion even before Dr. Murase became aware of the pregnancy.
Because dermatologists routinely prescribe long-term medications for chronic diseases like acne, psoriasis, and atopic dermatitis, it is important to have a conversation regarding the risks and benefits of long-term medication should a pregnancy occur in any woman of childbearing age, she said.
Fewer women in clinical trials?
Abortion restrictions could possibly discourage women of reproductive age to participate in a clinical trial for a new medication, said Dr. Chambers.
A female patient with a chronic disease who’s randomized to receive a new medication may be required to use certain types of birth control because of unknown potential adverse effects the drug may have on the fetus. But in some cases, accidental pregnancies happen.
The participant in the trial may say, “I don’t know enough about the safety of this drug in pregnancy, and I’ve already taken it. I want to terminate the pregnancy,” said Dr. Chambers. Thinking ahead, a woman may decide not to do the trial to avoid the risk of getting pregnant and not having the option to terminate the pregnancy.
This could apply to new drugs such as antiviral treatments, or medications for severe chronic disease that typically have no clinical trial data in pregnancy prior to initial release into the market.
Women may start taking the drug without thinking about getting pregnant, then realize there are no safety data and become concerned about its effects on a future pregnancy.
The question is: Will abortion restrictions have a chilling effect on these new drugs as well? Patients and their doctors may decide not to try it until more data are available. “I can see where abortion restrictions would change the risk or benefit calculation in thinking about what you do or don’t prescribe or take during reproductive age,” said Dr. Chambers.
The upside of restrictions?
If there’s a positive side to these developments with abortion bans, it may encourage women taking new medications or joining clinical trials to think even more carefully about adherence to effective contraception, said Dr. Chambers.
Some methods are more effective than others, she emphasized. “When you have an unplanned pregnancy, it could mean that the method you used wasn’t optimal or you weren’t using it as recommended.” A goal moving forward is to encourage more thoughtful use of highly effective contraceptives, thus reducing the number of unplanned pregnancies, she added.
If patients are taking methotrexate, “the time to think about pregnancy is before getting pregnant so you can switch to a drug that’s compatible with pregnancy,” she said.
This whole thought process regarding pregnancy planning could work toward useful health goals, said Dr. Chambers. “Nobody thinks termination is the preferred method, but planning ahead should involve a discussion of what works best for the patient.”
Patients do have other choices, said Dr. Grifka. “Fortunately, there are many commonly prescribed medications which cross the placenta and have no ill effects on the fetus.”
Talking to patients about choices
Dr. Clowse, who spends a lot of time training rheumatologists, encourages them to have conversations with patients about pregnancy planning. It’s a lot to manage, getting the right drug to a female patient with chronic illness, especially in this current climate of abortion upheaval, she noted.
Her approach is to have an open and honest conversation with patients about their concerns and fears, what the realities are, and what the potential future options are for certain rheumatology drugs in the United States.
Some women who see what’s happening across the country may become so risk averse that they may choose to die rather than take a lifesaving drug that poses certain risks under new restrictions.
“I think that’s tragic,” said Dr. Clowse.
To help their patients, Dr. Gray believes physicians across specialties should better educate themselves about physiology in pregnancy and how to counsel patients on the impact of not taking medications in pregnancy.
In her view, it’s almost coercive to say to a patient, “You really need to have effective contraception if I’m going to give you this lifesaving or quality-of-life-improving medication.”
When confronting such scenarios, Dr. Gray doesn’t think physicians need to change how they counsel patients about contraception. “I don’t think we should be putting pressure on patients to consider other permanent methods just because there’s a lack of abortion options.”
Patients will eventually make those decisions for themselves, she said. “They’re going to want a more efficacious method because they’re worried about not having access to abortion if they get pregnant.”
Dr. Gray reports being a site principal investigator for a phase 3 trial for VeraCept IUD, funded by Sebela Pharmaceuticals. Dr. Clowse reports receiving research funding and doing consulting for GlaxoSmithKline.
*Correction, 6/2/2022: A previous version of this article misstated the intended use of drugs such as the “morning-after” pill (levonorgestrel). They are taken to prevent unintended pregnancy.
A version of this article first appeared on Medscape.com .
Obstetrician Beverly Gray, MD, is already seeing the effects of the Roe v. Wade abortion debate in her North Carolina practice.
The state allows abortion but requires that women get counseling with a qualified health professional 72 hours before the procedure. “Aside from that, we still have patients asking for more efficacious contraceptive methods just in case,” said Dr. Gray, residency director and division director for women’s community and population health and associate professor for obstetrics and gynecology at Duke University, Durham, N.C.
Patients and staff in her clinic have also been approaching her about tubal ligation. “They’re asking about additional birth control methods because they’re concerned about what’s going to happen” with the challenge to the historic Roe v. Wade decision in the Supreme Court and subsequent actions in the states to restrict or ban abortion, she said.
This has implications not just for abortion but for medications known to affect pregnancy. “What I’m really worried about is physicians will be withholding medicine because they’re concerned about teratogenic effects,” said Dr. Gray.
With more states issuing restrictions on abortion, doctors are worried that patients needing certain drugs to maintain their lupus flares, cancer, or other diseases may decide not to take them in the event they accidentally become pregnant. If the drug is known to affect the fetus, the fear is a patient who lives in a state with abortion restrictions will no longer have the option to terminate a pregnancy.
Instead, a scenario may arise in which the patient – and their physician – may opt not to treat at all with an otherwise lifesaving medication, experts told this news organization.
The U.S. landscape on abortion restrictions
A leaked draft of a U.S. Supreme Court opinion on Mississippi’s 15-week abortion ban has sent the medical community into a tailspin. The case, Dobbs v. Jackson Women’s Health Organization, challenges the 1973 Roe v. Wade decision that affirms the constitutional right to abortion. It’s anticipated the high court will decide on the case in June.
Although the upcoming decision is subject to change, the draft indicated the high court would uphold the Mississippi ban. This would essentially overturn the 1973 ruling. An earlier Supreme Court decision allowing a Texas law banning abortion at 6 weeks suggests the court may already be heading in this direction. At the state level, legislatures have been moving on divergent paths – some taking steps to preserve abortion rights, others initiating restrictions.
More than 100 abortion restrictions in 19 states took effect in 2021, according to the Guttmacher Institute, which tracks such metrics. In 2022, “two key themes are anti-abortion policymakers’ continued pursuit of various types of abortion bans and restrictions on medication abortion,” the institute reported.
Forty-six states and the District of Columbia have introduced 2,025 restrictions or proactive measures on sexual and reproductive health and rights so far this year. The latest tally from Guttmacher, updated in late May, revealed that 11 states so far have enacted 42 abortion restrictions. A total of 6 states (Arizona, Florida, Idaho, Kentucky, Oklahoma, and Wyoming) have issued nine bans on abortion.
Comparatively, 11 states have enacted 19 protective abortion measures.
Twenty-two states have introduced 117 restrictions on medication abortions, which account for 54% of U.S. abortions. This includes seven measures that would ban medication abortion outright, according to Guttmacher. Kentucky and South Dakota collectively have enacted 14 restrictions on medication abortion, as well as provisions that ban mailing of abortion pills.
Chilling effect on prescribing
Some physicians anticipate that drugs such as the “morning-after” pill (levonorgestrel) will become less available as restrictions go into effect, since these are medications designed to prevent pregnancy.*
However, the ongoing effort to put a lid on abortion measures has prompted concerns about a trickle-down effect on other medications that are otherwise life-changing or lifesaving to patients but pose a risk to the fetus.
Several drugs are well documented to affect fetal growth and development of the fetus, ranging from mild, transitory effects to severe, permanent birth defects, said Ronald G. Grifka, MD, chief medical officer of University of Michigan Health-West and clinical professor of pediatrics at the University of Michigan Medical School, Ann Arbor. “As new medications are developed, we will need heightened attention to make sure they are safe for the fetus,” he added.
Certain teratogenic medications are associated with a high risk of abortion even though this isn’t their primary use, noted Christina Chambers, PhD, MPH, co-director of the Center for Better Beginnings and associate director with the Altman Clinical & Translational Research Institute at the University of California, San Diego.
“I don’t think anyone would intentionally take these drugs to induce spontaneous abortion. But if the drugs pose a risk for it, I can see how the laws might be stretched” to include them, said Dr. Chambers.
Methotrexate, a medication for autoimmune disorders, has a high risk of spontaneous abortion. So do acne medications such as isotretinoin.
Patients are usually told they’re not supposed to get pregnant on these drugs because there’s a high risk of pregnancy loss and risk of malformations and potential learning problems in the fetus. But many pregnancies aren’t planned, said Dr. Chambers. “Patients may forget about the side effects or think their birth control will protect them. And the next time they refill the medication, they may not hear about the warnings again.”
With a restrictive abortion law or ban in effect, a woman might think: “I won’t take this drug because if there’s any potential that I might get pregnant, I won’t have the option to abort an at-risk pregnancy.” Women and their doctors, for that matter, don’t want to put themselves in this position, said Dr. Chambers.
Rheumatologist Megan Clowse, MD, who prescribes several medications that potentially cause major birth defects and pregnancy loss, worries about the ramifications of these accumulating bans.
“Methotrexate has been a leading drug for us for decades for rheumatoid arthritis. Mycophenolate is a vital drug for lupus,” said Dr. Clowse, associate professor of medicine at Duke University’s division of rheumatology and immunology.
Both methotrexate and mycophenolate pose about a 40% risk of pregnancy loss and significantly increase the risk for birth defects. “I’m definitely concerned that there might be doctors or women who elect not to use those medications in women of reproductive age because of the potential risk for pregnancy and absence of abortion rights,” said Dr. Clowse.
These situations might force women to use contraceptives they don’t want to use, such as hormonal implants or intrauterine devices, she added. Another side effect is that women and their partners may decide to abstain from sex.
The iPLEDGE factor
Some rheumatology drugs like lenalidomide (Revlimid) require a valid negative pregnancy test in a lab every month. Similarly, the iPLEDGE Risk Evaluation and Mitigation Strategy seeks to reduce the teratogenicity of isotretinoin by requiring two types of birth control and regular pregnancy tests by users.
For isotretinoin specifically, abortion restrictions “could lead to increased adherence to pregnancy prevention measures which are already stringent in iPLEDGE. But on the other hand, it could lead to reduced willingness of physicians to prescribe or patients to take the medication,” said Dr. Chambers.
With programs like iPLEDGE in effect, the rate of pregnancies and abortions that occur in dermatology are relatively low, said Jenny Murase, MD, associate clinical professor of dermatology at the University of California, San Francisco.
Nevertheless, as a physician who regularly prescribes medications like isotretinoin in women of childbearing age, “it’s terrifying to me that a woman wouldn’t have the option to terminate the pregnancy if a teratogenic effect from the medication caused a severe birth defect,” said Dr. Murase.
Dermatologists use other teratogenic medications such as thalidomide, mycophenolate mofetil, and methotrexate for chronic dermatologic disease like psoriasis and atopic dermatitis.
The situation is especially tricky for dermatologists since most patients – about 80% – never discuss their pregnancy with their specialist prior to pregnancy initiation. Dr. Murase recalls when a patient with chronic plaque psoriasis on methotrexate in her late 40s became pregnant and had an abortion even before Dr. Murase became aware of the pregnancy.
Because dermatologists routinely prescribe long-term medications for chronic diseases like acne, psoriasis, and atopic dermatitis, it is important to have a conversation regarding the risks and benefits of long-term medication should a pregnancy occur in any woman of childbearing age, she said.
Fewer women in clinical trials?
Abortion restrictions could possibly discourage women of reproductive age to participate in a clinical trial for a new medication, said Dr. Chambers.
A female patient with a chronic disease who’s randomized to receive a new medication may be required to use certain types of birth control because of unknown potential adverse effects the drug may have on the fetus. But in some cases, accidental pregnancies happen.
The participant in the trial may say, “I don’t know enough about the safety of this drug in pregnancy, and I’ve already taken it. I want to terminate the pregnancy,” said Dr. Chambers. Thinking ahead, a woman may decide not to do the trial to avoid the risk of getting pregnant and not having the option to terminate the pregnancy.
This could apply to new drugs such as antiviral treatments, or medications for severe chronic disease that typically have no clinical trial data in pregnancy prior to initial release into the market.
Women may start taking the drug without thinking about getting pregnant, then realize there are no safety data and become concerned about its effects on a future pregnancy.
The question is: Will abortion restrictions have a chilling effect on these new drugs as well? Patients and their doctors may decide not to try it until more data are available. “I can see where abortion restrictions would change the risk or benefit calculation in thinking about what you do or don’t prescribe or take during reproductive age,” said Dr. Chambers.
The upside of restrictions?
If there’s a positive side to these developments with abortion bans, it may encourage women taking new medications or joining clinical trials to think even more carefully about adherence to effective contraception, said Dr. Chambers.
Some methods are more effective than others, she emphasized. “When you have an unplanned pregnancy, it could mean that the method you used wasn’t optimal or you weren’t using it as recommended.” A goal moving forward is to encourage more thoughtful use of highly effective contraceptives, thus reducing the number of unplanned pregnancies, she added.
If patients are taking methotrexate, “the time to think about pregnancy is before getting pregnant so you can switch to a drug that’s compatible with pregnancy,” she said.
This whole thought process regarding pregnancy planning could work toward useful health goals, said Dr. Chambers. “Nobody thinks termination is the preferred method, but planning ahead should involve a discussion of what works best for the patient.”
Patients do have other choices, said Dr. Grifka. “Fortunately, there are many commonly prescribed medications which cross the placenta and have no ill effects on the fetus.”
Talking to patients about choices
Dr. Clowse, who spends a lot of time training rheumatologists, encourages them to have conversations with patients about pregnancy planning. It’s a lot to manage, getting the right drug to a female patient with chronic illness, especially in this current climate of abortion upheaval, she noted.
Her approach is to have an open and honest conversation with patients about their concerns and fears, what the realities are, and what the potential future options are for certain rheumatology drugs in the United States.
Some women who see what’s happening across the country may become so risk averse that they may choose to die rather than take a lifesaving drug that poses certain risks under new restrictions.
“I think that’s tragic,” said Dr. Clowse.
To help their patients, Dr. Gray believes physicians across specialties should better educate themselves about physiology in pregnancy and how to counsel patients on the impact of not taking medications in pregnancy.
In her view, it’s almost coercive to say to a patient, “You really need to have effective contraception if I’m going to give you this lifesaving or quality-of-life-improving medication.”
When confronting such scenarios, Dr. Gray doesn’t think physicians need to change how they counsel patients about contraception. “I don’t think we should be putting pressure on patients to consider other permanent methods just because there’s a lack of abortion options.”
Patients will eventually make those decisions for themselves, she said. “They’re going to want a more efficacious method because they’re worried about not having access to abortion if they get pregnant.”
Dr. Gray reports being a site principal investigator for a phase 3 trial for VeraCept IUD, funded by Sebela Pharmaceuticals. Dr. Clowse reports receiving research funding and doing consulting for GlaxoSmithKline.
*Correction, 6/2/2022: A previous version of this article misstated the intended use of drugs such as the “morning-after” pill (levonorgestrel). They are taken to prevent unintended pregnancy.
A version of this article first appeared on Medscape.com .
Obstetrician Beverly Gray, MD, is already seeing the effects of the Roe v. Wade abortion debate in her North Carolina practice.
The state allows abortion but requires that women get counseling with a qualified health professional 72 hours before the procedure. “Aside from that, we still have patients asking for more efficacious contraceptive methods just in case,” said Dr. Gray, residency director and division director for women’s community and population health and associate professor for obstetrics and gynecology at Duke University, Durham, N.C.
Patients and staff in her clinic have also been approaching her about tubal ligation. “They’re asking about additional birth control methods because they’re concerned about what’s going to happen” with the challenge to the historic Roe v. Wade decision in the Supreme Court and subsequent actions in the states to restrict or ban abortion, she said.
This has implications not just for abortion but for medications known to affect pregnancy. “What I’m really worried about is physicians will be withholding medicine because they’re concerned about teratogenic effects,” said Dr. Gray.
With more states issuing restrictions on abortion, doctors are worried that patients needing certain drugs to maintain their lupus flares, cancer, or other diseases may decide not to take them in the event they accidentally become pregnant. If the drug is known to affect the fetus, the fear is a patient who lives in a state with abortion restrictions will no longer have the option to terminate a pregnancy.
Instead, a scenario may arise in which the patient – and their physician – may opt not to treat at all with an otherwise lifesaving medication, experts told this news organization.
The U.S. landscape on abortion restrictions
A leaked draft of a U.S. Supreme Court opinion on Mississippi’s 15-week abortion ban has sent the medical community into a tailspin. The case, Dobbs v. Jackson Women’s Health Organization, challenges the 1973 Roe v. Wade decision that affirms the constitutional right to abortion. It’s anticipated the high court will decide on the case in June.
Although the upcoming decision is subject to change, the draft indicated the high court would uphold the Mississippi ban. This would essentially overturn the 1973 ruling. An earlier Supreme Court decision allowing a Texas law banning abortion at 6 weeks suggests the court may already be heading in this direction. At the state level, legislatures have been moving on divergent paths – some taking steps to preserve abortion rights, others initiating restrictions.
More than 100 abortion restrictions in 19 states took effect in 2021, according to the Guttmacher Institute, which tracks such metrics. In 2022, “two key themes are anti-abortion policymakers’ continued pursuit of various types of abortion bans and restrictions on medication abortion,” the institute reported.
Forty-six states and the District of Columbia have introduced 2,025 restrictions or proactive measures on sexual and reproductive health and rights so far this year. The latest tally from Guttmacher, updated in late May, revealed that 11 states so far have enacted 42 abortion restrictions. A total of 6 states (Arizona, Florida, Idaho, Kentucky, Oklahoma, and Wyoming) have issued nine bans on abortion.
Comparatively, 11 states have enacted 19 protective abortion measures.
Twenty-two states have introduced 117 restrictions on medication abortions, which account for 54% of U.S. abortions. This includes seven measures that would ban medication abortion outright, according to Guttmacher. Kentucky and South Dakota collectively have enacted 14 restrictions on medication abortion, as well as provisions that ban mailing of abortion pills.
Chilling effect on prescribing
Some physicians anticipate that drugs such as the “morning-after” pill (levonorgestrel) will become less available as restrictions go into effect, since these are medications designed to prevent pregnancy.*
However, the ongoing effort to put a lid on abortion measures has prompted concerns about a trickle-down effect on other medications that are otherwise life-changing or lifesaving to patients but pose a risk to the fetus.
Several drugs are well documented to affect fetal growth and development of the fetus, ranging from mild, transitory effects to severe, permanent birth defects, said Ronald G. Grifka, MD, chief medical officer of University of Michigan Health-West and clinical professor of pediatrics at the University of Michigan Medical School, Ann Arbor. “As new medications are developed, we will need heightened attention to make sure they are safe for the fetus,” he added.
Certain teratogenic medications are associated with a high risk of abortion even though this isn’t their primary use, noted Christina Chambers, PhD, MPH, co-director of the Center for Better Beginnings and associate director with the Altman Clinical & Translational Research Institute at the University of California, San Diego.
“I don’t think anyone would intentionally take these drugs to induce spontaneous abortion. But if the drugs pose a risk for it, I can see how the laws might be stretched” to include them, said Dr. Chambers.
Methotrexate, a medication for autoimmune disorders, has a high risk of spontaneous abortion. So do acne medications such as isotretinoin.
Patients are usually told they’re not supposed to get pregnant on these drugs because there’s a high risk of pregnancy loss and risk of malformations and potential learning problems in the fetus. But many pregnancies aren’t planned, said Dr. Chambers. “Patients may forget about the side effects or think their birth control will protect them. And the next time they refill the medication, they may not hear about the warnings again.”
With a restrictive abortion law or ban in effect, a woman might think: “I won’t take this drug because if there’s any potential that I might get pregnant, I won’t have the option to abort an at-risk pregnancy.” Women and their doctors, for that matter, don’t want to put themselves in this position, said Dr. Chambers.
Rheumatologist Megan Clowse, MD, who prescribes several medications that potentially cause major birth defects and pregnancy loss, worries about the ramifications of these accumulating bans.
“Methotrexate has been a leading drug for us for decades for rheumatoid arthritis. Mycophenolate is a vital drug for lupus,” said Dr. Clowse, associate professor of medicine at Duke University’s division of rheumatology and immunology.
Both methotrexate and mycophenolate pose about a 40% risk of pregnancy loss and significantly increase the risk for birth defects. “I’m definitely concerned that there might be doctors or women who elect not to use those medications in women of reproductive age because of the potential risk for pregnancy and absence of abortion rights,” said Dr. Clowse.
These situations might force women to use contraceptives they don’t want to use, such as hormonal implants or intrauterine devices, she added. Another side effect is that women and their partners may decide to abstain from sex.
The iPLEDGE factor
Some rheumatology drugs like lenalidomide (Revlimid) require a valid negative pregnancy test in a lab every month. Similarly, the iPLEDGE Risk Evaluation and Mitigation Strategy seeks to reduce the teratogenicity of isotretinoin by requiring two types of birth control and regular pregnancy tests by users.
For isotretinoin specifically, abortion restrictions “could lead to increased adherence to pregnancy prevention measures which are already stringent in iPLEDGE. But on the other hand, it could lead to reduced willingness of physicians to prescribe or patients to take the medication,” said Dr. Chambers.
With programs like iPLEDGE in effect, the rate of pregnancies and abortions that occur in dermatology are relatively low, said Jenny Murase, MD, associate clinical professor of dermatology at the University of California, San Francisco.
Nevertheless, as a physician who regularly prescribes medications like isotretinoin in women of childbearing age, “it’s terrifying to me that a woman wouldn’t have the option to terminate the pregnancy if a teratogenic effect from the medication caused a severe birth defect,” said Dr. Murase.
Dermatologists use other teratogenic medications such as thalidomide, mycophenolate mofetil, and methotrexate for chronic dermatologic disease like psoriasis and atopic dermatitis.
The situation is especially tricky for dermatologists since most patients – about 80% – never discuss their pregnancy with their specialist prior to pregnancy initiation. Dr. Murase recalls when a patient with chronic plaque psoriasis on methotrexate in her late 40s became pregnant and had an abortion even before Dr. Murase became aware of the pregnancy.
Because dermatologists routinely prescribe long-term medications for chronic diseases like acne, psoriasis, and atopic dermatitis, it is important to have a conversation regarding the risks and benefits of long-term medication should a pregnancy occur in any woman of childbearing age, she said.
Fewer women in clinical trials?
Abortion restrictions could possibly discourage women of reproductive age to participate in a clinical trial for a new medication, said Dr. Chambers.
A female patient with a chronic disease who’s randomized to receive a new medication may be required to use certain types of birth control because of unknown potential adverse effects the drug may have on the fetus. But in some cases, accidental pregnancies happen.
The participant in the trial may say, “I don’t know enough about the safety of this drug in pregnancy, and I’ve already taken it. I want to terminate the pregnancy,” said Dr. Chambers. Thinking ahead, a woman may decide not to do the trial to avoid the risk of getting pregnant and not having the option to terminate the pregnancy.
This could apply to new drugs such as antiviral treatments, or medications for severe chronic disease that typically have no clinical trial data in pregnancy prior to initial release into the market.
Women may start taking the drug without thinking about getting pregnant, then realize there are no safety data and become concerned about its effects on a future pregnancy.
The question is: Will abortion restrictions have a chilling effect on these new drugs as well? Patients and their doctors may decide not to try it until more data are available. “I can see where abortion restrictions would change the risk or benefit calculation in thinking about what you do or don’t prescribe or take during reproductive age,” said Dr. Chambers.
The upside of restrictions?
If there’s a positive side to these developments with abortion bans, it may encourage women taking new medications or joining clinical trials to think even more carefully about adherence to effective contraception, said Dr. Chambers.
Some methods are more effective than others, she emphasized. “When you have an unplanned pregnancy, it could mean that the method you used wasn’t optimal or you weren’t using it as recommended.” A goal moving forward is to encourage more thoughtful use of highly effective contraceptives, thus reducing the number of unplanned pregnancies, she added.
If patients are taking methotrexate, “the time to think about pregnancy is before getting pregnant so you can switch to a drug that’s compatible with pregnancy,” she said.
This whole thought process regarding pregnancy planning could work toward useful health goals, said Dr. Chambers. “Nobody thinks termination is the preferred method, but planning ahead should involve a discussion of what works best for the patient.”
Patients do have other choices, said Dr. Grifka. “Fortunately, there are many commonly prescribed medications which cross the placenta and have no ill effects on the fetus.”
Talking to patients about choices
Dr. Clowse, who spends a lot of time training rheumatologists, encourages them to have conversations with patients about pregnancy planning. It’s a lot to manage, getting the right drug to a female patient with chronic illness, especially in this current climate of abortion upheaval, she noted.
Her approach is to have an open and honest conversation with patients about their concerns and fears, what the realities are, and what the potential future options are for certain rheumatology drugs in the United States.
Some women who see what’s happening across the country may become so risk averse that they may choose to die rather than take a lifesaving drug that poses certain risks under new restrictions.
“I think that’s tragic,” said Dr. Clowse.
To help their patients, Dr. Gray believes physicians across specialties should better educate themselves about physiology in pregnancy and how to counsel patients on the impact of not taking medications in pregnancy.
In her view, it’s almost coercive to say to a patient, “You really need to have effective contraception if I’m going to give you this lifesaving or quality-of-life-improving medication.”
When confronting such scenarios, Dr. Gray doesn’t think physicians need to change how they counsel patients about contraception. “I don’t think we should be putting pressure on patients to consider other permanent methods just because there’s a lack of abortion options.”
Patients will eventually make those decisions for themselves, she said. “They’re going to want a more efficacious method because they’re worried about not having access to abortion if they get pregnant.”
Dr. Gray reports being a site principal investigator for a phase 3 trial for VeraCept IUD, funded by Sebela Pharmaceuticals. Dr. Clowse reports receiving research funding and doing consulting for GlaxoSmithKline.
*Correction, 6/2/2022: A previous version of this article misstated the intended use of drugs such as the “morning-after” pill (levonorgestrel). They are taken to prevent unintended pregnancy.
A version of this article first appeared on Medscape.com .
Exploding e-cigarettes cause traumatic injuries in teens
A study shows that, over a 4-year period, 15 teenagers were injured from exploding e-cigarettes, according to surgeons who have treated young people at nine hospitals in the United States.
“It definitely was an injury we were seeing frequently,” Shannon Acker, MD, an assistant professor of pediatric surgery at the University of Colorado at Denver, Aurora, and a pediatric surgeon at Children’s Hospital Colorado, said in a statement.
Reporting in the Journal of Surgical Research, doctors detail injuries from e-cigarette explosions from January 2016 through December 2019. Ten teens were hospitalized, including three who were admitted to ICUs.
“When we think about e-cigarettes, vaping, and the problems of marketing cigarettes to teenagers, it usually has to do with addiction and lung injury,” said Dr. Acker, a coauthor of the new study. “Whereas we, as trauma surgeons, were seeing these other traumatic injuries.”
Six of the teens had facial burns, five of them lost multiple teeth, five had burns around the thighs and groin, four burned their hands, and four burned their eyes. One teen injured their radial nerve, which runs through the arm. Another cut their face, and one fractured their jaw.
Overall, six teens needed surgery, including one who needed multiple operations for a severe hand injury.
Three of the teenagers had never used e-cigarettes before the day they were hurt.
Vaping has become far more common than smoking traditional cigarettes among U.S. teens in recent years. More than 2 million of them currently use e-cigarettes, according to the Food and Drug Administration, including more than 11% of high school students and almost 3% of middle schoolers.
Most e-cigarettes contain nicotine, which is highly addictive and can impair healthy brain development in adolescents, according to the CDC. Other chemicals and flavorings in the liquids that are heated during vaping can also damage the lungs. Fires and explosions, while rare, are also a risk that’s been previously documented by the FDA, the Centers for Disease Control and Prevention, and the Federal Emergency Management Agency.
Nationwide, there were 195 reported explosions and fires involving e-cigarettes in all ages between 2009 and 2016, according to a FEMA report. While no deaths were reported, 29% of these cases involved severe injuries.
“The shape and construction of electronic cigarettes” can make them behave like “flaming rockets when a battery fails,” according to FEMA.
Vaping devices typically use a rechargeable lithium-ion battery that vaporizes the liquid nicotine solution, Dr. Acker said. “They are not highly regulated, and the batteries may be of inferior quality and prone to explosion.”
A version of this article first appeared on WebMD.com.
A study shows that, over a 4-year period, 15 teenagers were injured from exploding e-cigarettes, according to surgeons who have treated young people at nine hospitals in the United States.
“It definitely was an injury we were seeing frequently,” Shannon Acker, MD, an assistant professor of pediatric surgery at the University of Colorado at Denver, Aurora, and a pediatric surgeon at Children’s Hospital Colorado, said in a statement.
Reporting in the Journal of Surgical Research, doctors detail injuries from e-cigarette explosions from January 2016 through December 2019. Ten teens were hospitalized, including three who were admitted to ICUs.
“When we think about e-cigarettes, vaping, and the problems of marketing cigarettes to teenagers, it usually has to do with addiction and lung injury,” said Dr. Acker, a coauthor of the new study. “Whereas we, as trauma surgeons, were seeing these other traumatic injuries.”
Six of the teens had facial burns, five of them lost multiple teeth, five had burns around the thighs and groin, four burned their hands, and four burned their eyes. One teen injured their radial nerve, which runs through the arm. Another cut their face, and one fractured their jaw.
Overall, six teens needed surgery, including one who needed multiple operations for a severe hand injury.
Three of the teenagers had never used e-cigarettes before the day they were hurt.
Vaping has become far more common than smoking traditional cigarettes among U.S. teens in recent years. More than 2 million of them currently use e-cigarettes, according to the Food and Drug Administration, including more than 11% of high school students and almost 3% of middle schoolers.
Most e-cigarettes contain nicotine, which is highly addictive and can impair healthy brain development in adolescents, according to the CDC. Other chemicals and flavorings in the liquids that are heated during vaping can also damage the lungs. Fires and explosions, while rare, are also a risk that’s been previously documented by the FDA, the Centers for Disease Control and Prevention, and the Federal Emergency Management Agency.
Nationwide, there were 195 reported explosions and fires involving e-cigarettes in all ages between 2009 and 2016, according to a FEMA report. While no deaths were reported, 29% of these cases involved severe injuries.
“The shape and construction of electronic cigarettes” can make them behave like “flaming rockets when a battery fails,” according to FEMA.
Vaping devices typically use a rechargeable lithium-ion battery that vaporizes the liquid nicotine solution, Dr. Acker said. “They are not highly regulated, and the batteries may be of inferior quality and prone to explosion.”
A version of this article first appeared on WebMD.com.
A study shows that, over a 4-year period, 15 teenagers were injured from exploding e-cigarettes, according to surgeons who have treated young people at nine hospitals in the United States.
“It definitely was an injury we were seeing frequently,” Shannon Acker, MD, an assistant professor of pediatric surgery at the University of Colorado at Denver, Aurora, and a pediatric surgeon at Children’s Hospital Colorado, said in a statement.
Reporting in the Journal of Surgical Research, doctors detail injuries from e-cigarette explosions from January 2016 through December 2019. Ten teens were hospitalized, including three who were admitted to ICUs.
“When we think about e-cigarettes, vaping, and the problems of marketing cigarettes to teenagers, it usually has to do with addiction and lung injury,” said Dr. Acker, a coauthor of the new study. “Whereas we, as trauma surgeons, were seeing these other traumatic injuries.”
Six of the teens had facial burns, five of them lost multiple teeth, five had burns around the thighs and groin, four burned their hands, and four burned their eyes. One teen injured their radial nerve, which runs through the arm. Another cut their face, and one fractured their jaw.
Overall, six teens needed surgery, including one who needed multiple operations for a severe hand injury.
Three of the teenagers had never used e-cigarettes before the day they were hurt.
Vaping has become far more common than smoking traditional cigarettes among U.S. teens in recent years. More than 2 million of them currently use e-cigarettes, according to the Food and Drug Administration, including more than 11% of high school students and almost 3% of middle schoolers.
Most e-cigarettes contain nicotine, which is highly addictive and can impair healthy brain development in adolescents, according to the CDC. Other chemicals and flavorings in the liquids that are heated during vaping can also damage the lungs. Fires and explosions, while rare, are also a risk that’s been previously documented by the FDA, the Centers for Disease Control and Prevention, and the Federal Emergency Management Agency.
Nationwide, there were 195 reported explosions and fires involving e-cigarettes in all ages between 2009 and 2016, according to a FEMA report. While no deaths were reported, 29% of these cases involved severe injuries.
“The shape and construction of electronic cigarettes” can make them behave like “flaming rockets when a battery fails,” according to FEMA.
Vaping devices typically use a rechargeable lithium-ion battery that vaporizes the liquid nicotine solution, Dr. Acker said. “They are not highly regulated, and the batteries may be of inferior quality and prone to explosion.”
A version of this article first appeared on WebMD.com.
FROM THE JOURNAL OF SURGICAL RESEARCH
Cannabis vaping continues its rise in teens
More teenagers in the United States reported cannabis use with vaping in 2019, compared with 2017, while cannabis use without vaping declined, based on annual survey data from more than 50,000 teens.
“With vaping prevalence rising so quickly among teens, getting a clearer picture of how cannabis use is shifting helps inform prevention and cessation efforts,” corresponding author Noah T. Kreski, MPH, of Columbia University, New York, said in an interview.
“In just 2 years, the most common cannabis use pattern changed from ‘occasional use without vaping’ to ‘frequent use with vaping,’ said Mx. Kreski, who uses the honorific Mx. and the pronouns they/them. “Knowing that, as well as the high overlap of cannabis vaping with nicotine use and binge drinking, adds to the urgency of reducing adolescent vaping.”
To quantify the trends in cannabis vaping, the researchers reviewed data from Monitoring the Future, an annual survey of high school students across the United States. The study population included 51,052 individuals; approximately 49% were male and 49% were non-Hispanic White. The researchers examined frequency of cannabis use, trends across demographic groups, and concurrent use of cannabis and other substances such as alcohol and tobacco. The findings were published in the journal Addiction.
Frequent cannabis use was defined as six or more times in the past 30 days; occasional use was defined as one to five times in the past 30 days.
Frequent cannabis use with vaping increased from 2.1% in 2017 to 5.4% in 2019. Occasional cannabis use with vaping also increased, though less dramatically, from less than 2% in 2017 to approximately 3.5% in 2019.
By contrast, both frequent and occasional cannabis use without vaping declined from 2017 to 2019 (from 3.8% to 2.1% and from 6.9% to 4.4%, respectively).
Overall, the prevalence of any level of cannabis use increased from 13.9% in 2017 to 15.4% in 2019. Both males and females showed a similar increase in reported frequent cannabis use with vaping of approximately 3%.
The results document that vaping cannabis has become more common than smoking alone among U.S. teens across almost all demographic groups, and across sex, race, urbanicity, and level of parent education; however, the increased was especially marked among Hispanic/Latinx teens and those of lower socioeconomic status, the researchers wrote.
The researchers also examined the associations between cannabis use with and without vaping and concurrent nicotine and alcohol use. Overall, the strongest association was between smoking or vaping nicotine and vaping cannabis; teens who smoked or vaped nicotine were 42 times more likely than nonnicotine users to report vaping cannabis in the past 30 days (adjusted odds ratio, 42.28). In addition, more occasions of binge drinking were more strongly associated with cannabis use with vaping (up to 10 times more likely), compared with cannabis use without vaping, (aORs, 4.48-10.09).
The study findings were limited by several factors, including the lack of questions on tetrahydrocannabinol (THC) or cannabidiol content of the cannabis products used, although evidence suggests that the potency of cannabis products in the United States is increasing, the researchers noted. Other limitations included the cross-sectional design, which prevents making associations about causality, and lack of data on the quantity of cannabis used; only data on frequency of use were recorded.
However, the results reflect a rise in cannabis use with vaping among teens in the United States, along with an increased risk of tobacco use, e-cigarette use, and binge drinking, the researchers said.
As cannabis legalization expands across the United States, policies are needed to deter use among adolescents, the researchers wrote. “These policies should be crafted to reduce an emphasis on criminalization in preference for public health promotion given the history of unequal application of punitive consequences of drug use for racialized minorities in the United States. As products, delivery systems, potency, and marketing proliferate within a for-profit industry, increased attention to youth trends, including investment in sustained and evidence-based prevention and intervention, is increasingly necessary.”
The take-home message for clinicians is to ask whether your patients are vaping, because the prevalence is not only up, but fairly universal, Mx. Kreski said. “Have a discussion that covers a broad range of substance use topics and informs teens of the potential risks of vaping, while avoiding stigma.”
The message for parents is “to talk to your kids about the risks of vaping,” said Mx. Kreski. “Prioritize open communication rather than punishment, and work together with your teens to prevent or reduce vaping.” The message for teens: “Understand that vaping has risks. You should feel empowered to talk to your parents or doctor about those risks. While it may seem like everyone’s vaping, the majority don’t. Keeping communication open between parents/caregivers, teens, and health care providers is one of the best ways to address these trends in vaping.”
Beware more powerful cannabis products
“While drug use in general is declining in adolescents, marijuana use remains very common,” Kelly A. Curran, MD, of the University of Oklahoma Health Sciences Center, Oklahoma City, said in an interview.
“There is growing evidence that marijuana is now the first drug used by adolescents – replacing alcohol and nicotine – and frequent use can lead to substance abuse,” said Dr. Curran, who specializes in adolescent medicine but was involved in the study. “Cannabis use patterns have evolved over time. As I frequently tell my patients and their families, new strains and hybrids of marijuana have higher potencies of THC. Many adolescents are eschewing smoking and in its place using marijuana concentrates (wax, oil, shatter) via vape, dab pen, or rig. Use of these methods puts adolescents at high risk of social and health complications such as [e-cigarette or vaping use-associated lung injury], cannabis hyperemesis syndrome, and psychosis – and understanding these patterns and associated drug use helps health care professionals and parents keep adolescents safe.”
The take-home message for clinicians is that marijuana use via vaping continues to rise and to become more common than “traditional” marijuana smoking, Dr. Curran said. “This increase is across genders, in nearly all race/ethnicities (especially in Latinx youth), and in youth from lower socioeconomic status.” Vaping marijuana is associated with other substance abuse, so health care professionals should include questions about different forms of marijuana use, such as vape, dab pen, or rig, when working with patients, and counsel patients and families about the risks associated with use of any of these products.
The study was supported by the National Center for Injury Prevention and Control and by the National Institute on Drug Abuse. The researchers had no financial conflicts to disclose. Dr. Curran had no financial conflicts to disclose and serves on the editorial advisory board of Pediatric News.
More teenagers in the United States reported cannabis use with vaping in 2019, compared with 2017, while cannabis use without vaping declined, based on annual survey data from more than 50,000 teens.
“With vaping prevalence rising so quickly among teens, getting a clearer picture of how cannabis use is shifting helps inform prevention and cessation efforts,” corresponding author Noah T. Kreski, MPH, of Columbia University, New York, said in an interview.
“In just 2 years, the most common cannabis use pattern changed from ‘occasional use without vaping’ to ‘frequent use with vaping,’ said Mx. Kreski, who uses the honorific Mx. and the pronouns they/them. “Knowing that, as well as the high overlap of cannabis vaping with nicotine use and binge drinking, adds to the urgency of reducing adolescent vaping.”
To quantify the trends in cannabis vaping, the researchers reviewed data from Monitoring the Future, an annual survey of high school students across the United States. The study population included 51,052 individuals; approximately 49% were male and 49% were non-Hispanic White. The researchers examined frequency of cannabis use, trends across demographic groups, and concurrent use of cannabis and other substances such as alcohol and tobacco. The findings were published in the journal Addiction.
Frequent cannabis use was defined as six or more times in the past 30 days; occasional use was defined as one to five times in the past 30 days.
Frequent cannabis use with vaping increased from 2.1% in 2017 to 5.4% in 2019. Occasional cannabis use with vaping also increased, though less dramatically, from less than 2% in 2017 to approximately 3.5% in 2019.
By contrast, both frequent and occasional cannabis use without vaping declined from 2017 to 2019 (from 3.8% to 2.1% and from 6.9% to 4.4%, respectively).
Overall, the prevalence of any level of cannabis use increased from 13.9% in 2017 to 15.4% in 2019. Both males and females showed a similar increase in reported frequent cannabis use with vaping of approximately 3%.
The results document that vaping cannabis has become more common than smoking alone among U.S. teens across almost all demographic groups, and across sex, race, urbanicity, and level of parent education; however, the increased was especially marked among Hispanic/Latinx teens and those of lower socioeconomic status, the researchers wrote.
The researchers also examined the associations between cannabis use with and without vaping and concurrent nicotine and alcohol use. Overall, the strongest association was between smoking or vaping nicotine and vaping cannabis; teens who smoked or vaped nicotine were 42 times more likely than nonnicotine users to report vaping cannabis in the past 30 days (adjusted odds ratio, 42.28). In addition, more occasions of binge drinking were more strongly associated with cannabis use with vaping (up to 10 times more likely), compared with cannabis use without vaping, (aORs, 4.48-10.09).
The study findings were limited by several factors, including the lack of questions on tetrahydrocannabinol (THC) or cannabidiol content of the cannabis products used, although evidence suggests that the potency of cannabis products in the United States is increasing, the researchers noted. Other limitations included the cross-sectional design, which prevents making associations about causality, and lack of data on the quantity of cannabis used; only data on frequency of use were recorded.
However, the results reflect a rise in cannabis use with vaping among teens in the United States, along with an increased risk of tobacco use, e-cigarette use, and binge drinking, the researchers said.
As cannabis legalization expands across the United States, policies are needed to deter use among adolescents, the researchers wrote. “These policies should be crafted to reduce an emphasis on criminalization in preference for public health promotion given the history of unequal application of punitive consequences of drug use for racialized minorities in the United States. As products, delivery systems, potency, and marketing proliferate within a for-profit industry, increased attention to youth trends, including investment in sustained and evidence-based prevention and intervention, is increasingly necessary.”
The take-home message for clinicians is to ask whether your patients are vaping, because the prevalence is not only up, but fairly universal, Mx. Kreski said. “Have a discussion that covers a broad range of substance use topics and informs teens of the potential risks of vaping, while avoiding stigma.”
The message for parents is “to talk to your kids about the risks of vaping,” said Mx. Kreski. “Prioritize open communication rather than punishment, and work together with your teens to prevent or reduce vaping.” The message for teens: “Understand that vaping has risks. You should feel empowered to talk to your parents or doctor about those risks. While it may seem like everyone’s vaping, the majority don’t. Keeping communication open between parents/caregivers, teens, and health care providers is one of the best ways to address these trends in vaping.”
Beware more powerful cannabis products
“While drug use in general is declining in adolescents, marijuana use remains very common,” Kelly A. Curran, MD, of the University of Oklahoma Health Sciences Center, Oklahoma City, said in an interview.
“There is growing evidence that marijuana is now the first drug used by adolescents – replacing alcohol and nicotine – and frequent use can lead to substance abuse,” said Dr. Curran, who specializes in adolescent medicine but was involved in the study. “Cannabis use patterns have evolved over time. As I frequently tell my patients and their families, new strains and hybrids of marijuana have higher potencies of THC. Many adolescents are eschewing smoking and in its place using marijuana concentrates (wax, oil, shatter) via vape, dab pen, or rig. Use of these methods puts adolescents at high risk of social and health complications such as [e-cigarette or vaping use-associated lung injury], cannabis hyperemesis syndrome, and psychosis – and understanding these patterns and associated drug use helps health care professionals and parents keep adolescents safe.”
The take-home message for clinicians is that marijuana use via vaping continues to rise and to become more common than “traditional” marijuana smoking, Dr. Curran said. “This increase is across genders, in nearly all race/ethnicities (especially in Latinx youth), and in youth from lower socioeconomic status.” Vaping marijuana is associated with other substance abuse, so health care professionals should include questions about different forms of marijuana use, such as vape, dab pen, or rig, when working with patients, and counsel patients and families about the risks associated with use of any of these products.
The study was supported by the National Center for Injury Prevention and Control and by the National Institute on Drug Abuse. The researchers had no financial conflicts to disclose. Dr. Curran had no financial conflicts to disclose and serves on the editorial advisory board of Pediatric News.
More teenagers in the United States reported cannabis use with vaping in 2019, compared with 2017, while cannabis use without vaping declined, based on annual survey data from more than 50,000 teens.
“With vaping prevalence rising so quickly among teens, getting a clearer picture of how cannabis use is shifting helps inform prevention and cessation efforts,” corresponding author Noah T. Kreski, MPH, of Columbia University, New York, said in an interview.
“In just 2 years, the most common cannabis use pattern changed from ‘occasional use without vaping’ to ‘frequent use with vaping,’ said Mx. Kreski, who uses the honorific Mx. and the pronouns they/them. “Knowing that, as well as the high overlap of cannabis vaping with nicotine use and binge drinking, adds to the urgency of reducing adolescent vaping.”
To quantify the trends in cannabis vaping, the researchers reviewed data from Monitoring the Future, an annual survey of high school students across the United States. The study population included 51,052 individuals; approximately 49% were male and 49% were non-Hispanic White. The researchers examined frequency of cannabis use, trends across demographic groups, and concurrent use of cannabis and other substances such as alcohol and tobacco. The findings were published in the journal Addiction.
Frequent cannabis use was defined as six or more times in the past 30 days; occasional use was defined as one to five times in the past 30 days.
Frequent cannabis use with vaping increased from 2.1% in 2017 to 5.4% in 2019. Occasional cannabis use with vaping also increased, though less dramatically, from less than 2% in 2017 to approximately 3.5% in 2019.
By contrast, both frequent and occasional cannabis use without vaping declined from 2017 to 2019 (from 3.8% to 2.1% and from 6.9% to 4.4%, respectively).
Overall, the prevalence of any level of cannabis use increased from 13.9% in 2017 to 15.4% in 2019. Both males and females showed a similar increase in reported frequent cannabis use with vaping of approximately 3%.
The results document that vaping cannabis has become more common than smoking alone among U.S. teens across almost all demographic groups, and across sex, race, urbanicity, and level of parent education; however, the increased was especially marked among Hispanic/Latinx teens and those of lower socioeconomic status, the researchers wrote.
The researchers also examined the associations between cannabis use with and without vaping and concurrent nicotine and alcohol use. Overall, the strongest association was between smoking or vaping nicotine and vaping cannabis; teens who smoked or vaped nicotine were 42 times more likely than nonnicotine users to report vaping cannabis in the past 30 days (adjusted odds ratio, 42.28). In addition, more occasions of binge drinking were more strongly associated with cannabis use with vaping (up to 10 times more likely), compared with cannabis use without vaping, (aORs, 4.48-10.09).
The study findings were limited by several factors, including the lack of questions on tetrahydrocannabinol (THC) or cannabidiol content of the cannabis products used, although evidence suggests that the potency of cannabis products in the United States is increasing, the researchers noted. Other limitations included the cross-sectional design, which prevents making associations about causality, and lack of data on the quantity of cannabis used; only data on frequency of use were recorded.
However, the results reflect a rise in cannabis use with vaping among teens in the United States, along with an increased risk of tobacco use, e-cigarette use, and binge drinking, the researchers said.
As cannabis legalization expands across the United States, policies are needed to deter use among adolescents, the researchers wrote. “These policies should be crafted to reduce an emphasis on criminalization in preference for public health promotion given the history of unequal application of punitive consequences of drug use for racialized minorities in the United States. As products, delivery systems, potency, and marketing proliferate within a for-profit industry, increased attention to youth trends, including investment in sustained and evidence-based prevention and intervention, is increasingly necessary.”
The take-home message for clinicians is to ask whether your patients are vaping, because the prevalence is not only up, but fairly universal, Mx. Kreski said. “Have a discussion that covers a broad range of substance use topics and informs teens of the potential risks of vaping, while avoiding stigma.”
The message for parents is “to talk to your kids about the risks of vaping,” said Mx. Kreski. “Prioritize open communication rather than punishment, and work together with your teens to prevent or reduce vaping.” The message for teens: “Understand that vaping has risks. You should feel empowered to talk to your parents or doctor about those risks. While it may seem like everyone’s vaping, the majority don’t. Keeping communication open between parents/caregivers, teens, and health care providers is one of the best ways to address these trends in vaping.”
Beware more powerful cannabis products
“While drug use in general is declining in adolescents, marijuana use remains very common,” Kelly A. Curran, MD, of the University of Oklahoma Health Sciences Center, Oklahoma City, said in an interview.
“There is growing evidence that marijuana is now the first drug used by adolescents – replacing alcohol and nicotine – and frequent use can lead to substance abuse,” said Dr. Curran, who specializes in adolescent medicine but was involved in the study. “Cannabis use patterns have evolved over time. As I frequently tell my patients and their families, new strains and hybrids of marijuana have higher potencies of THC. Many adolescents are eschewing smoking and in its place using marijuana concentrates (wax, oil, shatter) via vape, dab pen, or rig. Use of these methods puts adolescents at high risk of social and health complications such as [e-cigarette or vaping use-associated lung injury], cannabis hyperemesis syndrome, and psychosis – and understanding these patterns and associated drug use helps health care professionals and parents keep adolescents safe.”
The take-home message for clinicians is that marijuana use via vaping continues to rise and to become more common than “traditional” marijuana smoking, Dr. Curran said. “This increase is across genders, in nearly all race/ethnicities (especially in Latinx youth), and in youth from lower socioeconomic status.” Vaping marijuana is associated with other substance abuse, so health care professionals should include questions about different forms of marijuana use, such as vape, dab pen, or rig, when working with patients, and counsel patients and families about the risks associated with use of any of these products.
The study was supported by the National Center for Injury Prevention and Control and by the National Institute on Drug Abuse. The researchers had no financial conflicts to disclose. Dr. Curran had no financial conflicts to disclose and serves on the editorial advisory board of Pediatric News.
FROM ADDICTION
Four mental health trajectories in youth: Predicting persistent psychopathology
A study that tracked psychopathology in 13,000 children and adolescents found that
Investigators also found a strong correlation between new incidence of high psychopathology and externalizing problems such as hyperactivity. “It is of paramount importance to identify factors that distinguish those with persisting problems and escalating trajectories so that resources can be appropriately directed,” wrote the authors of the study published online in JAMA Network Open.
Recent studies have shown that concurrent and sequential comorbidity of psychiatric disorders are very common in adult populations, lead author Colm Healy, PhD, a postdoctoral researcher for psychiatry with the University of Medicine and Health Sciences, Ireland, said in an interview.
The speculation is that this occurs in early life when psychiatry symptoms experience high fluidity. “This presents a complex scenario to model, where young people’s mental health appears to shift and change across development. Few investigations to date have had the data available to examine these trajectories over the full range of child development,” said Dr. Healy.
He and his colleagues attempted to map the profiles and trajectories of psychopathology in children and adolescents, using latent profile transition analysis (LPTA), a person-centered method, to assess comorbidity and movement in the various phases of childhood development.
“The idea behind person-centered methods such as LTPA is that it identifies unobserved subgroups of participants who respond similarly to specific variables – in this case responses to a broad measure of psychopathology,” explained Dr. Healy.
The study included 7,507 children from the child sample (ages 3, 5, and 9 years) and 6,039 children from the adolescent sample (ages 9, 13, and 17 or 18 years). Data analysis took place from October 2020 to September 2021.
Dr. Healy and colleagues in a supplementary investigation compared cohorts at age 9 years to look for sex and generational differences.
Four developmental profiles
Researchers identified 4 distinct developmental profies for person-centered psychopathological trajectories: no psychopathology (incidence range, 60%-70%), high psychopathology (incidence range, 3%-5%), externalizing problems (incidence range, 15%-25%), and internalizing problems (incidence range, 7%-12%).
Internalizing problems reflect issues with peers and emotional problems whereas externalizing problems more closely associate with hyperactivity and conduct.
Less than 5% of the youth studied experienced persistent symptoms. However, 48.6% in the child cohort and 44.1% in the adolescent cohort moved into one of the 3 psychopathology profiles (high psychopathology, externalizing, internalizing problems) at some point in development.
The spread of trajectories was more diverse in the child cohort, said Dr. Healy. “Children ebbed and flowed between the different profiles over time with a large proportion falling into one of the psychopathology categories and then switching between these profiles.” Switching was also evident in the adolescent cohort but to a lesser extent, he said.
Externalizing problems link to high psychopathology
Rates of remittance were higher among individuals in both cohorts for internalizing problems, compared with externalizing problems.
It’s possible that for some of these young people, internalizing problems are a reaction to environmental stressors such as bullying,” said Dr. Healy. “When that stress is relieved, the internalizing problems may dissipate.”
In a clinically relevant finding, children with externalizing problems (age 5, 129 [61.3%] and age 9, 95 [74.3%]) were more likely to present with new incidents of high psychopathology. This was also true in the adolescent group (age 13, 129 [91.1%] and age 17, 146 [89.9%]).
This suggests that a proportion of youth with externalizing problems have an escalating trajectory of psychopathology. “Thus, it may be possible to distinguish those with an escalating trajectory from a stable or remitting trajectory. The specific distinguishing factors require further investigation, but it has been observed before that some of those reporting externalizing problems in early life continue to have difficulties into later life,” noted Dr. Healy.
A combination of environmental or biological factors may explain this escalation, which could respond to early intervention, he said.
Overall, few children in the study transitioned directly from no psychopathology to high psychopathology.
Differences between boys, girls
In both cohorts, investigators noticed significant differences between the sexes.
Boys in childhood made up a larger proportion of the three psychopathology profiles. But by late adolescence, girls made up a larger proportion of the internalizing profile whereas boys made up a larger proportion of the externalizing profile. “These differences were in line with our expectations,” said Dr. Healy.
Trajectories also differed among boys and girls. In childhood, girls had a higher percentage of de-escalating trajectories relative to boys. “More girls than boys in the psychopathology profiles switched to a non or less severe profile. In adolescence, differences in trajectories were less obvious, with the exception that girls were more likely than boys to transition to internalizing problems from all of the other profiles at age 17,” said Dr. Healy.
Most young people who experience psychopathology will eventually see an improvement in symptoms, noted Dr. Healy. Next steps are to identify markers that distinguish individuals with persistent trajectories from remitting trajectories at the different phases of development, he said.
Study draws mixed reviews
Clinical psychiatrists not involved in the study had varying reactions to the results.
“This study is notable for its data-driven and powerful illustration of how childhood and adolescence are dynamic periods during which psychiatric symptoms can emerge and evolve,” said Sunny X. Tang, MD, a psychiatrist and an assistant professor at the Institute of Behavioral Science and the Feinstein Institutes for Medical Research, Manhasset, New York.
The clinical call for action is for person-centered mental health screening to be a routine part of pediatric and adolescent primary care or school-based services, noted Dr. Tang.
Paul S. Nestadt, MD, an assistant professor and public mental health researcher at Johns Hopkins University, Baltimore, did not think the study would have a significant impact on clinical practice.
He noted that Dr. Healy and coauthors found that some children stayed true to type, but many fluctuated between the four profile groups. The finding that fluctuation occurred more frequently in younger children is not surprising “and is consistent with what we know about the ‘moving targets’ that make diagnosing children so difficult,” said Dr. Nestadt.
“It would have been helpful to have identified clinical indicators of likely persistence in psychopathology, but the measure employed here did not allow that. It is also frustrating to not have any information on treatment, such that we cannot know whether the children who shifted to ‘no psychopathology’ did so because of treatment or spontaneously,” he added.
Victor M. Fornari, MD, MS, director of the Division of Child & Adolescent Psychiatry at The Zucker Hillside Hospital and Cohen’s Children’s Medical Center, New York, said the study is an important contribution to understanding the development of psychopathology during childhood.
“Generally, it is felt that nearly one in five youth will meet criteria for at least one psychiatric disorder by the age of 18. It is well known that externalizing disorders like ADHD manifest earlier in childhood and that depression often manifests later in adolescence,” he said.
No disclosures were reported.
A study that tracked psychopathology in 13,000 children and adolescents found that
Investigators also found a strong correlation between new incidence of high psychopathology and externalizing problems such as hyperactivity. “It is of paramount importance to identify factors that distinguish those with persisting problems and escalating trajectories so that resources can be appropriately directed,” wrote the authors of the study published online in JAMA Network Open.
Recent studies have shown that concurrent and sequential comorbidity of psychiatric disorders are very common in adult populations, lead author Colm Healy, PhD, a postdoctoral researcher for psychiatry with the University of Medicine and Health Sciences, Ireland, said in an interview.
The speculation is that this occurs in early life when psychiatry symptoms experience high fluidity. “This presents a complex scenario to model, where young people’s mental health appears to shift and change across development. Few investigations to date have had the data available to examine these trajectories over the full range of child development,” said Dr. Healy.
He and his colleagues attempted to map the profiles and trajectories of psychopathology in children and adolescents, using latent profile transition analysis (LPTA), a person-centered method, to assess comorbidity and movement in the various phases of childhood development.
“The idea behind person-centered methods such as LTPA is that it identifies unobserved subgroups of participants who respond similarly to specific variables – in this case responses to a broad measure of psychopathology,” explained Dr. Healy.
The study included 7,507 children from the child sample (ages 3, 5, and 9 years) and 6,039 children from the adolescent sample (ages 9, 13, and 17 or 18 years). Data analysis took place from October 2020 to September 2021.
Dr. Healy and colleagues in a supplementary investigation compared cohorts at age 9 years to look for sex and generational differences.
Four developmental profiles
Researchers identified 4 distinct developmental profies for person-centered psychopathological trajectories: no psychopathology (incidence range, 60%-70%), high psychopathology (incidence range, 3%-5%), externalizing problems (incidence range, 15%-25%), and internalizing problems (incidence range, 7%-12%).
Internalizing problems reflect issues with peers and emotional problems whereas externalizing problems more closely associate with hyperactivity and conduct.
Less than 5% of the youth studied experienced persistent symptoms. However, 48.6% in the child cohort and 44.1% in the adolescent cohort moved into one of the 3 psychopathology profiles (high psychopathology, externalizing, internalizing problems) at some point in development.
The spread of trajectories was more diverse in the child cohort, said Dr. Healy. “Children ebbed and flowed between the different profiles over time with a large proportion falling into one of the psychopathology categories and then switching between these profiles.” Switching was also evident in the adolescent cohort but to a lesser extent, he said.
Externalizing problems link to high psychopathology
Rates of remittance were higher among individuals in both cohorts for internalizing problems, compared with externalizing problems.
It’s possible that for some of these young people, internalizing problems are a reaction to environmental stressors such as bullying,” said Dr. Healy. “When that stress is relieved, the internalizing problems may dissipate.”
In a clinically relevant finding, children with externalizing problems (age 5, 129 [61.3%] and age 9, 95 [74.3%]) were more likely to present with new incidents of high psychopathology. This was also true in the adolescent group (age 13, 129 [91.1%] and age 17, 146 [89.9%]).
This suggests that a proportion of youth with externalizing problems have an escalating trajectory of psychopathology. “Thus, it may be possible to distinguish those with an escalating trajectory from a stable or remitting trajectory. The specific distinguishing factors require further investigation, but it has been observed before that some of those reporting externalizing problems in early life continue to have difficulties into later life,” noted Dr. Healy.
A combination of environmental or biological factors may explain this escalation, which could respond to early intervention, he said.
Overall, few children in the study transitioned directly from no psychopathology to high psychopathology.
Differences between boys, girls
In both cohorts, investigators noticed significant differences between the sexes.
Boys in childhood made up a larger proportion of the three psychopathology profiles. But by late adolescence, girls made up a larger proportion of the internalizing profile whereas boys made up a larger proportion of the externalizing profile. “These differences were in line with our expectations,” said Dr. Healy.
Trajectories also differed among boys and girls. In childhood, girls had a higher percentage of de-escalating trajectories relative to boys. “More girls than boys in the psychopathology profiles switched to a non or less severe profile. In adolescence, differences in trajectories were less obvious, with the exception that girls were more likely than boys to transition to internalizing problems from all of the other profiles at age 17,” said Dr. Healy.
Most young people who experience psychopathology will eventually see an improvement in symptoms, noted Dr. Healy. Next steps are to identify markers that distinguish individuals with persistent trajectories from remitting trajectories at the different phases of development, he said.
Study draws mixed reviews
Clinical psychiatrists not involved in the study had varying reactions to the results.
“This study is notable for its data-driven and powerful illustration of how childhood and adolescence are dynamic periods during which psychiatric symptoms can emerge and evolve,” said Sunny X. Tang, MD, a psychiatrist and an assistant professor at the Institute of Behavioral Science and the Feinstein Institutes for Medical Research, Manhasset, New York.
The clinical call for action is for person-centered mental health screening to be a routine part of pediatric and adolescent primary care or school-based services, noted Dr. Tang.
Paul S. Nestadt, MD, an assistant professor and public mental health researcher at Johns Hopkins University, Baltimore, did not think the study would have a significant impact on clinical practice.
He noted that Dr. Healy and coauthors found that some children stayed true to type, but many fluctuated between the four profile groups. The finding that fluctuation occurred more frequently in younger children is not surprising “and is consistent with what we know about the ‘moving targets’ that make diagnosing children so difficult,” said Dr. Nestadt.
“It would have been helpful to have identified clinical indicators of likely persistence in psychopathology, but the measure employed here did not allow that. It is also frustrating to not have any information on treatment, such that we cannot know whether the children who shifted to ‘no psychopathology’ did so because of treatment or spontaneously,” he added.
Victor M. Fornari, MD, MS, director of the Division of Child & Adolescent Psychiatry at The Zucker Hillside Hospital and Cohen’s Children’s Medical Center, New York, said the study is an important contribution to understanding the development of psychopathology during childhood.
“Generally, it is felt that nearly one in five youth will meet criteria for at least one psychiatric disorder by the age of 18. It is well known that externalizing disorders like ADHD manifest earlier in childhood and that depression often manifests later in adolescence,” he said.
No disclosures were reported.
A study that tracked psychopathology in 13,000 children and adolescents found that
Investigators also found a strong correlation between new incidence of high psychopathology and externalizing problems such as hyperactivity. “It is of paramount importance to identify factors that distinguish those with persisting problems and escalating trajectories so that resources can be appropriately directed,” wrote the authors of the study published online in JAMA Network Open.
Recent studies have shown that concurrent and sequential comorbidity of psychiatric disorders are very common in adult populations, lead author Colm Healy, PhD, a postdoctoral researcher for psychiatry with the University of Medicine and Health Sciences, Ireland, said in an interview.
The speculation is that this occurs in early life when psychiatry symptoms experience high fluidity. “This presents a complex scenario to model, where young people’s mental health appears to shift and change across development. Few investigations to date have had the data available to examine these trajectories over the full range of child development,” said Dr. Healy.
He and his colleagues attempted to map the profiles and trajectories of psychopathology in children and adolescents, using latent profile transition analysis (LPTA), a person-centered method, to assess comorbidity and movement in the various phases of childhood development.
“The idea behind person-centered methods such as LTPA is that it identifies unobserved subgroups of participants who respond similarly to specific variables – in this case responses to a broad measure of psychopathology,” explained Dr. Healy.
The study included 7,507 children from the child sample (ages 3, 5, and 9 years) and 6,039 children from the adolescent sample (ages 9, 13, and 17 or 18 years). Data analysis took place from October 2020 to September 2021.
Dr. Healy and colleagues in a supplementary investigation compared cohorts at age 9 years to look for sex and generational differences.
Four developmental profiles
Researchers identified 4 distinct developmental profies for person-centered psychopathological trajectories: no psychopathology (incidence range, 60%-70%), high psychopathology (incidence range, 3%-5%), externalizing problems (incidence range, 15%-25%), and internalizing problems (incidence range, 7%-12%).
Internalizing problems reflect issues with peers and emotional problems whereas externalizing problems more closely associate with hyperactivity and conduct.
Less than 5% of the youth studied experienced persistent symptoms. However, 48.6% in the child cohort and 44.1% in the adolescent cohort moved into one of the 3 psychopathology profiles (high psychopathology, externalizing, internalizing problems) at some point in development.
The spread of trajectories was more diverse in the child cohort, said Dr. Healy. “Children ebbed and flowed between the different profiles over time with a large proportion falling into one of the psychopathology categories and then switching between these profiles.” Switching was also evident in the adolescent cohort but to a lesser extent, he said.
Externalizing problems link to high psychopathology
Rates of remittance were higher among individuals in both cohorts for internalizing problems, compared with externalizing problems.
It’s possible that for some of these young people, internalizing problems are a reaction to environmental stressors such as bullying,” said Dr. Healy. “When that stress is relieved, the internalizing problems may dissipate.”
In a clinically relevant finding, children with externalizing problems (age 5, 129 [61.3%] and age 9, 95 [74.3%]) were more likely to present with new incidents of high psychopathology. This was also true in the adolescent group (age 13, 129 [91.1%] and age 17, 146 [89.9%]).
This suggests that a proportion of youth with externalizing problems have an escalating trajectory of psychopathology. “Thus, it may be possible to distinguish those with an escalating trajectory from a stable or remitting trajectory. The specific distinguishing factors require further investigation, but it has been observed before that some of those reporting externalizing problems in early life continue to have difficulties into later life,” noted Dr. Healy.
A combination of environmental or biological factors may explain this escalation, which could respond to early intervention, he said.
Overall, few children in the study transitioned directly from no psychopathology to high psychopathology.
Differences between boys, girls
In both cohorts, investigators noticed significant differences between the sexes.
Boys in childhood made up a larger proportion of the three psychopathology profiles. But by late adolescence, girls made up a larger proportion of the internalizing profile whereas boys made up a larger proportion of the externalizing profile. “These differences were in line with our expectations,” said Dr. Healy.
Trajectories also differed among boys and girls. In childhood, girls had a higher percentage of de-escalating trajectories relative to boys. “More girls than boys in the psychopathology profiles switched to a non or less severe profile. In adolescence, differences in trajectories were less obvious, with the exception that girls were more likely than boys to transition to internalizing problems from all of the other profiles at age 17,” said Dr. Healy.
Most young people who experience psychopathology will eventually see an improvement in symptoms, noted Dr. Healy. Next steps are to identify markers that distinguish individuals with persistent trajectories from remitting trajectories at the different phases of development, he said.
Study draws mixed reviews
Clinical psychiatrists not involved in the study had varying reactions to the results.
“This study is notable for its data-driven and powerful illustration of how childhood and adolescence are dynamic periods during which psychiatric symptoms can emerge and evolve,” said Sunny X. Tang, MD, a psychiatrist and an assistant professor at the Institute of Behavioral Science and the Feinstein Institutes for Medical Research, Manhasset, New York.
The clinical call for action is for person-centered mental health screening to be a routine part of pediatric and adolescent primary care or school-based services, noted Dr. Tang.
Paul S. Nestadt, MD, an assistant professor and public mental health researcher at Johns Hopkins University, Baltimore, did not think the study would have a significant impact on clinical practice.
He noted that Dr. Healy and coauthors found that some children stayed true to type, but many fluctuated between the four profile groups. The finding that fluctuation occurred more frequently in younger children is not surprising “and is consistent with what we know about the ‘moving targets’ that make diagnosing children so difficult,” said Dr. Nestadt.
“It would have been helpful to have identified clinical indicators of likely persistence in psychopathology, but the measure employed here did not allow that. It is also frustrating to not have any information on treatment, such that we cannot know whether the children who shifted to ‘no psychopathology’ did so because of treatment or spontaneously,” he added.
Victor M. Fornari, MD, MS, director of the Division of Child & Adolescent Psychiatry at The Zucker Hillside Hospital and Cohen’s Children’s Medical Center, New York, said the study is an important contribution to understanding the development of psychopathology during childhood.
“Generally, it is felt that nearly one in five youth will meet criteria for at least one psychiatric disorder by the age of 18. It is well known that externalizing disorders like ADHD manifest earlier in childhood and that depression often manifests later in adolescence,” he said.
No disclosures were reported.
FROM JAMA NETWORK OPEN














