User login
sNDA gets priority review for CLL/SLL
The U.S. Food and Drug Administration (FDA) has accepted for priority review a supplemental new drug application (sNDA) for ibrutinib (Imbruvica®).
With this sNDA, Pharmacyclics LLC (an AbbVie company) and Janssen Biotech, Inc., are seeking approval for ibrutinib in combination with obinutuzumab (Gazyva®) in previously untreated adults with chronic lymphocytic leukemia (CLL) or small lymphocytic lymphoma (SLL).
The FDA grants priority review to applications for products that may provide significant improvements in the treatment, diagnosis, or prevention of serious conditions.
The agency intends to take action on a priority review application within 6 months of receiving it rather than the standard 10 months.
Ibrutinib is already FDA-approved as monotherapy for adults with CLL/SLL (previously treated or untreated), with and without 17p deletion. Ibrutinib is also approved in combination with bendamustine and rituximab for adults with previously treated CLL/SLL.
Obinutuzumab is FDA-approved for use in combination with chlorambucil to treat previously untreated CLL.
The sNDA for ibrutinib in combination with obinutuzumab is based on results from the phase 3 iLLUMINATE trial (NCT02264574).
The trial is a comparison of ibrutinib plus obinutuzumab and chlorambucil plus obinutuzumab in patients with previously untreated CLL/SLL.
In May, AbbVie announced that the trial’s primary endpoint was met. Specifically, ibrutinib plus obinutuzumab was associated with significantly longer progression-free survival than chlorambucil plus obinutuzumab.
Data from the trial have not been released. Pharmacyclics and Janssen said they plan to present the data in a future publication or at a medical congress.
The U.S. Food and Drug Administration (FDA) has accepted for priority review a supplemental new drug application (sNDA) for ibrutinib (Imbruvica®).
With this sNDA, Pharmacyclics LLC (an AbbVie company) and Janssen Biotech, Inc., are seeking approval for ibrutinib in combination with obinutuzumab (Gazyva®) in previously untreated adults with chronic lymphocytic leukemia (CLL) or small lymphocytic lymphoma (SLL).
The FDA grants priority review to applications for products that may provide significant improvements in the treatment, diagnosis, or prevention of serious conditions.
The agency intends to take action on a priority review application within 6 months of receiving it rather than the standard 10 months.
Ibrutinib is already FDA-approved as monotherapy for adults with CLL/SLL (previously treated or untreated), with and without 17p deletion. Ibrutinib is also approved in combination with bendamustine and rituximab for adults with previously treated CLL/SLL.
Obinutuzumab is FDA-approved for use in combination with chlorambucil to treat previously untreated CLL.
The sNDA for ibrutinib in combination with obinutuzumab is based on results from the phase 3 iLLUMINATE trial (NCT02264574).
The trial is a comparison of ibrutinib plus obinutuzumab and chlorambucil plus obinutuzumab in patients with previously untreated CLL/SLL.
In May, AbbVie announced that the trial’s primary endpoint was met. Specifically, ibrutinib plus obinutuzumab was associated with significantly longer progression-free survival than chlorambucil plus obinutuzumab.
Data from the trial have not been released. Pharmacyclics and Janssen said they plan to present the data in a future publication or at a medical congress.
The U.S. Food and Drug Administration (FDA) has accepted for priority review a supplemental new drug application (sNDA) for ibrutinib (Imbruvica®).
With this sNDA, Pharmacyclics LLC (an AbbVie company) and Janssen Biotech, Inc., are seeking approval for ibrutinib in combination with obinutuzumab (Gazyva®) in previously untreated adults with chronic lymphocytic leukemia (CLL) or small lymphocytic lymphoma (SLL).
The FDA grants priority review to applications for products that may provide significant improvements in the treatment, diagnosis, or prevention of serious conditions.
The agency intends to take action on a priority review application within 6 months of receiving it rather than the standard 10 months.
Ibrutinib is already FDA-approved as monotherapy for adults with CLL/SLL (previously treated or untreated), with and without 17p deletion. Ibrutinib is also approved in combination with bendamustine and rituximab for adults with previously treated CLL/SLL.
Obinutuzumab is FDA-approved for use in combination with chlorambucil to treat previously untreated CLL.
The sNDA for ibrutinib in combination with obinutuzumab is based on results from the phase 3 iLLUMINATE trial (NCT02264574).
The trial is a comparison of ibrutinib plus obinutuzumab and chlorambucil plus obinutuzumab in patients with previously untreated CLL/SLL.
In May, AbbVie announced that the trial’s primary endpoint was met. Specifically, ibrutinib plus obinutuzumab was associated with significantly longer progression-free survival than chlorambucil plus obinutuzumab.
Data from the trial have not been released. Pharmacyclics and Janssen said they plan to present the data in a future publication or at a medical congress.
FDA issues draft guidance on MRD
The U.S. Food and Drug Administration (FDA) has issued a draft guidance on the use of minimal residual disease (MRD) assessment in trials of patients with hematologic malignancies.
The FDA said it developed this guidance to assist sponsors who are planning to use MRD as a biomarker in clinical trials conducted under an investigational new drug application or to support FDA approval of products intended to treat hematologic malignancies.
“As a result of important workshops where we’ve heard from stakeholders and an analysis of marketing applications showing inconsistent quality of MRD data, the FDA identified a need to provide sponsors with guidance on the use of MRD as a biomarker in regulatory submissions,” said FDA Commissioner Scott Gottlieb, MD.
The guidance explains how MRD might be used in clinical trials, highlights considerations for MRD assessment that are specific to certain hematologic malignancies, and lists requirements for regulatory submissions that utilize MRD.
The full document, “Hematologic Malignancies: Regulatory Considerations for Use of Minimal Residual Disease in Development of Drug and Biological Products for Treatment,” is available for download from the FDA website.
How MRD can be used
The guidance notes that MRD could potentially be used as a biomarker in clinical trials, specifically, as a diagnostic, prognostic, predictive, efficacy-response, or monitoring biomarker.
MRD could also be used as a surrogate endpoint, and there are two mechanisms for obtaining FDA feedback on the use of a novel surrogate endpoint to support approval of a product:
- The drug development tool qualification process
- Discussions with the specific Center for Drug Evaluation and Research or Center for Biologics Evaluation and Research review division.
Furthermore, a sponsor can use MRD “to select patients at high risk or to enrich the trial population,” according to the guidance.
Disease specifics
The guidance also details specific considerations for MRD assessment in individual hematologic malignancies. For example:
- In acute lymphoblastic leukemia, a patient with an MRD level of 0.1% or more in first or second complete remission has a high risk of relapse.
- In trials of acute myeloid leukemia, the sponsor should provide data showing that the marker selected to assess MRD “reflects the leukemia and not underlying clonal hematopoiesis.”
- Patients with low-risk acute promyelocytic leukemia who achieve MRD negativity after arsenic/tretinoin-based therapy are generally considered cured.
- In chronic lymphocytic leukemia, MRD can be assessed in the peripheral blood or bone marrow, but the sample source should remain the same throughout a trial.
- In chronic myeloid leukemia, MRD can be used to select and monitor patients who are eligible to discontinue treatment with tyrosine kinase inhibitors.
- In multiple myeloma, imaging techniques may be combined with MRD assessment of the bone marrow to assess patient response to treatment.
Types of technology
The guidance lists the four general technologies used for MRD assessment in hematologic malignancies:
- Multiparametric flow cytometry
- Next-generation sequencing
- Quantitative reverse transcription polymerase chain reaction of specific gene fusions
- Allele-specific oligonucleotide polymerase chain reaction.
The FDA said it does not have a preference as to which technology is used in a trial. However, the sponsor must pre-specify the technology used and should utilize the same technology throughout a trial.
The FDA also said it “does not foresee the need for co-development of an MRD assay with a drug product.” However, the assay must be analytically valid for results important to the trial, and MRD assessment must be a clinically valid biomarker in the context in which it’s used.
If the MRD assay used is not FDA-cleared or -approved, additional information about the assay must be provided to the FDA.
The U.S. Food and Drug Administration (FDA) has issued a draft guidance on the use of minimal residual disease (MRD) assessment in trials of patients with hematologic malignancies.
The FDA said it developed this guidance to assist sponsors who are planning to use MRD as a biomarker in clinical trials conducted under an investigational new drug application or to support FDA approval of products intended to treat hematologic malignancies.
“As a result of important workshops where we’ve heard from stakeholders and an analysis of marketing applications showing inconsistent quality of MRD data, the FDA identified a need to provide sponsors with guidance on the use of MRD as a biomarker in regulatory submissions,” said FDA Commissioner Scott Gottlieb, MD.
The guidance explains how MRD might be used in clinical trials, highlights considerations for MRD assessment that are specific to certain hematologic malignancies, and lists requirements for regulatory submissions that utilize MRD.
The full document, “Hematologic Malignancies: Regulatory Considerations for Use of Minimal Residual Disease in Development of Drug and Biological Products for Treatment,” is available for download from the FDA website.
How MRD can be used
The guidance notes that MRD could potentially be used as a biomarker in clinical trials, specifically, as a diagnostic, prognostic, predictive, efficacy-response, or monitoring biomarker.
MRD could also be used as a surrogate endpoint, and there are two mechanisms for obtaining FDA feedback on the use of a novel surrogate endpoint to support approval of a product:
- The drug development tool qualification process
- Discussions with the specific Center for Drug Evaluation and Research or Center for Biologics Evaluation and Research review division.
Furthermore, a sponsor can use MRD “to select patients at high risk or to enrich the trial population,” according to the guidance.
Disease specifics
The guidance also details specific considerations for MRD assessment in individual hematologic malignancies. For example:
- In acute lymphoblastic leukemia, a patient with an MRD level of 0.1% or more in first or second complete remission has a high risk of relapse.
- In trials of acute myeloid leukemia, the sponsor should provide data showing that the marker selected to assess MRD “reflects the leukemia and not underlying clonal hematopoiesis.”
- Patients with low-risk acute promyelocytic leukemia who achieve MRD negativity after arsenic/tretinoin-based therapy are generally considered cured.
- In chronic lymphocytic leukemia, MRD can be assessed in the peripheral blood or bone marrow, but the sample source should remain the same throughout a trial.
- In chronic myeloid leukemia, MRD can be used to select and monitor patients who are eligible to discontinue treatment with tyrosine kinase inhibitors.
- In multiple myeloma, imaging techniques may be combined with MRD assessment of the bone marrow to assess patient response to treatment.
Types of technology
The guidance lists the four general technologies used for MRD assessment in hematologic malignancies:
- Multiparametric flow cytometry
- Next-generation sequencing
- Quantitative reverse transcription polymerase chain reaction of specific gene fusions
- Allele-specific oligonucleotide polymerase chain reaction.
The FDA said it does not have a preference as to which technology is used in a trial. However, the sponsor must pre-specify the technology used and should utilize the same technology throughout a trial.
The FDA also said it “does not foresee the need for co-development of an MRD assay with a drug product.” However, the assay must be analytically valid for results important to the trial, and MRD assessment must be a clinically valid biomarker in the context in which it’s used.
If the MRD assay used is not FDA-cleared or -approved, additional information about the assay must be provided to the FDA.
The U.S. Food and Drug Administration (FDA) has issued a draft guidance on the use of minimal residual disease (MRD) assessment in trials of patients with hematologic malignancies.
The FDA said it developed this guidance to assist sponsors who are planning to use MRD as a biomarker in clinical trials conducted under an investigational new drug application or to support FDA approval of products intended to treat hematologic malignancies.
“As a result of important workshops where we’ve heard from stakeholders and an analysis of marketing applications showing inconsistent quality of MRD data, the FDA identified a need to provide sponsors with guidance on the use of MRD as a biomarker in regulatory submissions,” said FDA Commissioner Scott Gottlieb, MD.
The guidance explains how MRD might be used in clinical trials, highlights considerations for MRD assessment that are specific to certain hematologic malignancies, and lists requirements for regulatory submissions that utilize MRD.
The full document, “Hematologic Malignancies: Regulatory Considerations for Use of Minimal Residual Disease in Development of Drug and Biological Products for Treatment,” is available for download from the FDA website.
How MRD can be used
The guidance notes that MRD could potentially be used as a biomarker in clinical trials, specifically, as a diagnostic, prognostic, predictive, efficacy-response, or monitoring biomarker.
MRD could also be used as a surrogate endpoint, and there are two mechanisms for obtaining FDA feedback on the use of a novel surrogate endpoint to support approval of a product:
- The drug development tool qualification process
- Discussions with the specific Center for Drug Evaluation and Research or Center for Biologics Evaluation and Research review division.
Furthermore, a sponsor can use MRD “to select patients at high risk or to enrich the trial population,” according to the guidance.
Disease specifics
The guidance also details specific considerations for MRD assessment in individual hematologic malignancies. For example:
- In acute lymphoblastic leukemia, a patient with an MRD level of 0.1% or more in first or second complete remission has a high risk of relapse.
- In trials of acute myeloid leukemia, the sponsor should provide data showing that the marker selected to assess MRD “reflects the leukemia and not underlying clonal hematopoiesis.”
- Patients with low-risk acute promyelocytic leukemia who achieve MRD negativity after arsenic/tretinoin-based therapy are generally considered cured.
- In chronic lymphocytic leukemia, MRD can be assessed in the peripheral blood or bone marrow, but the sample source should remain the same throughout a trial.
- In chronic myeloid leukemia, MRD can be used to select and monitor patients who are eligible to discontinue treatment with tyrosine kinase inhibitors.
- In multiple myeloma, imaging techniques may be combined with MRD assessment of the bone marrow to assess patient response to treatment.
Types of technology
The guidance lists the four general technologies used for MRD assessment in hematologic malignancies:
- Multiparametric flow cytometry
- Next-generation sequencing
- Quantitative reverse transcription polymerase chain reaction of specific gene fusions
- Allele-specific oligonucleotide polymerase chain reaction.
The FDA said it does not have a preference as to which technology is used in a trial. However, the sponsor must pre-specify the technology used and should utilize the same technology throughout a trial.
The FDA also said it “does not foresee the need for co-development of an MRD assay with a drug product.” However, the assay must be analytically valid for results important to the trial, and MRD assessment must be a clinically valid biomarker in the context in which it’s used.
If the MRD assay used is not FDA-cleared or -approved, additional information about the assay must be provided to the FDA.
Entospletinib falls short in relapsed/refractory DLBCL
Entospletinib, a selective inhibitor of spleen tyrosine kinase (Syk), showed a dismal rate of progression-free survival and a high rate of adverse events in a cohort of previously treated patients with diffuse large B-cell lymphoma (DLBCL).
Entospletinib was evaluated in an open-label, single-agent, phase 2 trial (NCT01799889) with five relapsed/refractory patient cohorts: chronic lymphocytic leukemia (CLL), follicular lymphoma, other indolent non-Hodgkin lymphomas, mantle cell lymphoma, and DLBCL.
John M. Burke, MD, of Rocky Mountain Cancer Centers in Aurora, Colo., and his colleagues reported on the current analysis, which looked specifically at the 43 patients in the trial with previously treated DLBCL. Patients received at least one starting dose of 800 mg of entospletinib orally twice daily. The findings were published in Clinical Lymphoma, Myeloma & Leukemia.
In a previous report on the relapsed/refractory CLL cohort, the investigational agent demonstrated clinical activity with acceptable toxicity (Blood. 2015 Apr 9;125[15]:2336-43).
In the current report, the rate of progression-free survival (PFS) at 16 weeks was 3.6% and the median PFS was 1.5 months. None of the patients in the study achieved a complete or partial response to treatment, and just five patients had stable disease.
All patients in the study eventually discontinued treatment and the median treatment duration was 1 month.
“The lack of activity of Syk inhibition in patients with relapsed DLBCL is in contrast to what would have been expected from preclinical data,” the investigators wrote. “Although it is unclear why entospletinib monotherapy lacked activity in the present study, it is possible that resistance to Syk inhibition played a role. Potential mechanisms of resistance of DLBCL to Syk inhibition include transcriptional upregulation of Syk mediated by FOXO1 and PTEN depletion.”
The investigators said that Syk inhibition in combination with BCL2 inhibitors could potentially overcome this resistance. Another approach, they suggested, would be to offer entospletinib in combination with Janus kinase (JAK) 1/3 inhibition.
“Based on results of the preclinical data, the efficacy of entospletinib in combination will be evaluated in future clinical trials,” the investigators wrote.
The rate of adverse events was high in the DLBCL cohort. Forty-two patients (98%) experienced an adverse event and nearly three-quarters experienced a grade 3 event. Overall, 30% of the grade 3 adverse events were related to treatment. More than 40% of patients interrupted treatment because of adverse events, and 19% discontinued. Four patients experienced an adverse event that led to death.
While the lack of clinical activity may have surprised investigators, the safety profile was in line with other patient cohorts in the phase 2 study. In the CLL and indolent non-Hodgkin lymphoma cohorts, the rates of treatment interruption were 45% and 54%, respectively.
The study was supported by Gilead Sciences. Dr. Burke reported relationships with Gilead and other companies.
SOURCE: Burke JM et al. Clin Lymphoma Myeloma Leuk. 2018 Aug;18(8):e327-e331.
Entospletinib, a selective inhibitor of spleen tyrosine kinase (Syk), showed a dismal rate of progression-free survival and a high rate of adverse events in a cohort of previously treated patients with diffuse large B-cell lymphoma (DLBCL).
Entospletinib was evaluated in an open-label, single-agent, phase 2 trial (NCT01799889) with five relapsed/refractory patient cohorts: chronic lymphocytic leukemia (CLL), follicular lymphoma, other indolent non-Hodgkin lymphomas, mantle cell lymphoma, and DLBCL.
John M. Burke, MD, of Rocky Mountain Cancer Centers in Aurora, Colo., and his colleagues reported on the current analysis, which looked specifically at the 43 patients in the trial with previously treated DLBCL. Patients received at least one starting dose of 800 mg of entospletinib orally twice daily. The findings were published in Clinical Lymphoma, Myeloma & Leukemia.
In a previous report on the relapsed/refractory CLL cohort, the investigational agent demonstrated clinical activity with acceptable toxicity (Blood. 2015 Apr 9;125[15]:2336-43).
In the current report, the rate of progression-free survival (PFS) at 16 weeks was 3.6% and the median PFS was 1.5 months. None of the patients in the study achieved a complete or partial response to treatment, and just five patients had stable disease.
All patients in the study eventually discontinued treatment and the median treatment duration was 1 month.
“The lack of activity of Syk inhibition in patients with relapsed DLBCL is in contrast to what would have been expected from preclinical data,” the investigators wrote. “Although it is unclear why entospletinib monotherapy lacked activity in the present study, it is possible that resistance to Syk inhibition played a role. Potential mechanisms of resistance of DLBCL to Syk inhibition include transcriptional upregulation of Syk mediated by FOXO1 and PTEN depletion.”
The investigators said that Syk inhibition in combination with BCL2 inhibitors could potentially overcome this resistance. Another approach, they suggested, would be to offer entospletinib in combination with Janus kinase (JAK) 1/3 inhibition.
“Based on results of the preclinical data, the efficacy of entospletinib in combination will be evaluated in future clinical trials,” the investigators wrote.
The rate of adverse events was high in the DLBCL cohort. Forty-two patients (98%) experienced an adverse event and nearly three-quarters experienced a grade 3 event. Overall, 30% of the grade 3 adverse events were related to treatment. More than 40% of patients interrupted treatment because of adverse events, and 19% discontinued. Four patients experienced an adverse event that led to death.
While the lack of clinical activity may have surprised investigators, the safety profile was in line with other patient cohorts in the phase 2 study. In the CLL and indolent non-Hodgkin lymphoma cohorts, the rates of treatment interruption were 45% and 54%, respectively.
The study was supported by Gilead Sciences. Dr. Burke reported relationships with Gilead and other companies.
SOURCE: Burke JM et al. Clin Lymphoma Myeloma Leuk. 2018 Aug;18(8):e327-e331.
Entospletinib, a selective inhibitor of spleen tyrosine kinase (Syk), showed a dismal rate of progression-free survival and a high rate of adverse events in a cohort of previously treated patients with diffuse large B-cell lymphoma (DLBCL).
Entospletinib was evaluated in an open-label, single-agent, phase 2 trial (NCT01799889) with five relapsed/refractory patient cohorts: chronic lymphocytic leukemia (CLL), follicular lymphoma, other indolent non-Hodgkin lymphomas, mantle cell lymphoma, and DLBCL.
John M. Burke, MD, of Rocky Mountain Cancer Centers in Aurora, Colo., and his colleagues reported on the current analysis, which looked specifically at the 43 patients in the trial with previously treated DLBCL. Patients received at least one starting dose of 800 mg of entospletinib orally twice daily. The findings were published in Clinical Lymphoma, Myeloma & Leukemia.
In a previous report on the relapsed/refractory CLL cohort, the investigational agent demonstrated clinical activity with acceptable toxicity (Blood. 2015 Apr 9;125[15]:2336-43).
In the current report, the rate of progression-free survival (PFS) at 16 weeks was 3.6% and the median PFS was 1.5 months. None of the patients in the study achieved a complete or partial response to treatment, and just five patients had stable disease.
All patients in the study eventually discontinued treatment and the median treatment duration was 1 month.
“The lack of activity of Syk inhibition in patients with relapsed DLBCL is in contrast to what would have been expected from preclinical data,” the investigators wrote. “Although it is unclear why entospletinib monotherapy lacked activity in the present study, it is possible that resistance to Syk inhibition played a role. Potential mechanisms of resistance of DLBCL to Syk inhibition include transcriptional upregulation of Syk mediated by FOXO1 and PTEN depletion.”
The investigators said that Syk inhibition in combination with BCL2 inhibitors could potentially overcome this resistance. Another approach, they suggested, would be to offer entospletinib in combination with Janus kinase (JAK) 1/3 inhibition.
“Based on results of the preclinical data, the efficacy of entospletinib in combination will be evaluated in future clinical trials,” the investigators wrote.
The rate of adverse events was high in the DLBCL cohort. Forty-two patients (98%) experienced an adverse event and nearly three-quarters experienced a grade 3 event. Overall, 30% of the grade 3 adverse events were related to treatment. More than 40% of patients interrupted treatment because of adverse events, and 19% discontinued. Four patients experienced an adverse event that led to death.
While the lack of clinical activity may have surprised investigators, the safety profile was in line with other patient cohorts in the phase 2 study. In the CLL and indolent non-Hodgkin lymphoma cohorts, the rates of treatment interruption were 45% and 54%, respectively.
The study was supported by Gilead Sciences. Dr. Burke reported relationships with Gilead and other companies.
SOURCE: Burke JM et al. Clin Lymphoma Myeloma Leuk. 2018 Aug;18(8):e327-e331.
FROM CLINICAL LYMPHOMA, MYELOMA & LEUKEMIA
Key clinical point:
Major finding: The rate of progression-free survival at 16 weeks was 3.6% with a median PFS of 1.5 months.
Study details: An analysis of 43 relapsed/refractory DLBCL patients who received single-agent entospletinib.
Disclosures: The study was supported by Gilead Sciences. Dr. Burke reported relationships with Gilead and other companies.
Source: Burke JM et al. Clin Lymphoma Myeloma Leuk. 2018 Aug;18(8):e327-e331.
Updated ThroLy system predicts need for thromboprophylaxis
DUBROVNIK, CROATIA – An updated scoring system can more accurately identify lymphoma patients who may require thromboprophylaxis, according to researchers.
The revised scoring system, ThroLy, proved more effective than other systems for predicting thromboembolic events in lymphoma patients, with a positive predictive value of 22%-25%, a negative predictive value of 96%, sensitivity of 56%-57%, and specificity of 85%-87%.
Darko Antic, MD, PhD, of the University of Belgrade in Serbia, presented these findings at Leukemia and Lymphoma, a meeting jointly sponsored by the University of Texas MD Anderson Cancer Center and the School of Medicine at the University of Zagreb, Croatia.
Dr. Antic said that he and his colleagues developed ThroLy because other systems used to predict venous thromboembolism (VTE) are not quite right for lymphoma. He noted that the Padua score is not designed for cancer patients and the Khorana score is predominantly used for solid tumor malignancies.
The ThroLy scoring system is based on variables used in the Padua and Khorana systems, as well as variables that are specific to lymphoma patients.
In a previous study, the researchers found several variables that were independently associated with risk for VTE in lymphoma, including previous VTE, previous acute MI or stroke, mediastinal involvement, high body mass index, reduced mobility, extranodal localization, neutropenia, and hemoglobin less than 100 g/L (Am J Hematol. 2016 Oct;91[10]:1014-9).
In an initial version of the ThroLy scoring system, previous VTE, previous acute MI/stroke, obesity, and mediastinal involvement were all worth two points, and the other factors were worth a single point in the ThroLy system.
Patients with scores of 0 to 1 were considered low risk, patients with scores of 2 to 3 were considered intermediate risk, and patients with scores of 4 or greater were considered high risk.
To validate and refine ThroLy, Dr. Antic and his colleagues used it to assess 1,723 lymphoma patients treated at eight institutions in Austria, Croatia, France, Jordan, Macedonia, Spain, Switzerland, and the United States.
Patients had indolent non-Hodgkin lymphoma, aggressive non-Hodgkin lymphoma, chronic lymphocytic leukemia/small lymphocytic lymphoma, and Hodgkin lymphoma. Most subjects (84%) were outpatients. A total of 9%of patients had thrombosis, with 7% having VTE.
ThroLy had a positive predictive value of 17%, compared with 11% with Khorana and 13% with Padua. The negative predictive value was 93%, 92%, and 95%, respectively. The sensitivity was 51% with ThroLy, 42% with Khorana, and 70% with Padua; specificity was 72%, 64%, and 52%, respectively.
“The positive predictive value was low [with ThroLy] but definitely higher than the positive predictive value of the other two [scoring systems],” Dr. Antic noted.
Updated models
To further improve ThroLy, the researchers updated the system, creating two new models. Model 1 included the type of lymphoma/clinical stage (1 point), previous VTE (5 points), reduced mobility (2 points), hemoglobin less than 100 g/L (1 point), and the presence of vascular devices (1 point). Model 2 included all of the variables in Model 1 plus the thrombophilic condition, which was worth 1 point.
Patients were considered low risk if they scored 2 points or lower and high risk if they scored more than 2 points.
For Model 1, the positive predictive value was 22%, the negative predictive value was 96%, the sensitivity was 56%, and the specificity was 85%. For Model 2, the positive predictive value was 25%, the negative predictive value was 96%, the sensitivity was 57%, and the specificity was 87%.
There were no major differences in model discrimination and calibration based on the country in which a patient was treated or whether the patient was treated in an inpatient or outpatient setting.
Dr. Antic did not report any conflicts of interest. The Leukemia and Lymphoma meeting is organized by Jonathan Wood & Association, which is owned by the parent company of this news organization.
DUBROVNIK, CROATIA – An updated scoring system can more accurately identify lymphoma patients who may require thromboprophylaxis, according to researchers.
The revised scoring system, ThroLy, proved more effective than other systems for predicting thromboembolic events in lymphoma patients, with a positive predictive value of 22%-25%, a negative predictive value of 96%, sensitivity of 56%-57%, and specificity of 85%-87%.
Darko Antic, MD, PhD, of the University of Belgrade in Serbia, presented these findings at Leukemia and Lymphoma, a meeting jointly sponsored by the University of Texas MD Anderson Cancer Center and the School of Medicine at the University of Zagreb, Croatia.
Dr. Antic said that he and his colleagues developed ThroLy because other systems used to predict venous thromboembolism (VTE) are not quite right for lymphoma. He noted that the Padua score is not designed for cancer patients and the Khorana score is predominantly used for solid tumor malignancies.
The ThroLy scoring system is based on variables used in the Padua and Khorana systems, as well as variables that are specific to lymphoma patients.
In a previous study, the researchers found several variables that were independently associated with risk for VTE in lymphoma, including previous VTE, previous acute MI or stroke, mediastinal involvement, high body mass index, reduced mobility, extranodal localization, neutropenia, and hemoglobin less than 100 g/L (Am J Hematol. 2016 Oct;91[10]:1014-9).
In an initial version of the ThroLy scoring system, previous VTE, previous acute MI/stroke, obesity, and mediastinal involvement were all worth two points, and the other factors were worth a single point in the ThroLy system.
Patients with scores of 0 to 1 were considered low risk, patients with scores of 2 to 3 were considered intermediate risk, and patients with scores of 4 or greater were considered high risk.
To validate and refine ThroLy, Dr. Antic and his colleagues used it to assess 1,723 lymphoma patients treated at eight institutions in Austria, Croatia, France, Jordan, Macedonia, Spain, Switzerland, and the United States.
Patients had indolent non-Hodgkin lymphoma, aggressive non-Hodgkin lymphoma, chronic lymphocytic leukemia/small lymphocytic lymphoma, and Hodgkin lymphoma. Most subjects (84%) were outpatients. A total of 9%of patients had thrombosis, with 7% having VTE.
ThroLy had a positive predictive value of 17%, compared with 11% with Khorana and 13% with Padua. The negative predictive value was 93%, 92%, and 95%, respectively. The sensitivity was 51% with ThroLy, 42% with Khorana, and 70% with Padua; specificity was 72%, 64%, and 52%, respectively.
“The positive predictive value was low [with ThroLy] but definitely higher than the positive predictive value of the other two [scoring systems],” Dr. Antic noted.
Updated models
To further improve ThroLy, the researchers updated the system, creating two new models. Model 1 included the type of lymphoma/clinical stage (1 point), previous VTE (5 points), reduced mobility (2 points), hemoglobin less than 100 g/L (1 point), and the presence of vascular devices (1 point). Model 2 included all of the variables in Model 1 plus the thrombophilic condition, which was worth 1 point.
Patients were considered low risk if they scored 2 points or lower and high risk if they scored more than 2 points.
For Model 1, the positive predictive value was 22%, the negative predictive value was 96%, the sensitivity was 56%, and the specificity was 85%. For Model 2, the positive predictive value was 25%, the negative predictive value was 96%, the sensitivity was 57%, and the specificity was 87%.
There were no major differences in model discrimination and calibration based on the country in which a patient was treated or whether the patient was treated in an inpatient or outpatient setting.
Dr. Antic did not report any conflicts of interest. The Leukemia and Lymphoma meeting is organized by Jonathan Wood & Association, which is owned by the parent company of this news organization.
DUBROVNIK, CROATIA – An updated scoring system can more accurately identify lymphoma patients who may require thromboprophylaxis, according to researchers.
The revised scoring system, ThroLy, proved more effective than other systems for predicting thromboembolic events in lymphoma patients, with a positive predictive value of 22%-25%, a negative predictive value of 96%, sensitivity of 56%-57%, and specificity of 85%-87%.
Darko Antic, MD, PhD, of the University of Belgrade in Serbia, presented these findings at Leukemia and Lymphoma, a meeting jointly sponsored by the University of Texas MD Anderson Cancer Center and the School of Medicine at the University of Zagreb, Croatia.
Dr. Antic said that he and his colleagues developed ThroLy because other systems used to predict venous thromboembolism (VTE) are not quite right for lymphoma. He noted that the Padua score is not designed for cancer patients and the Khorana score is predominantly used for solid tumor malignancies.
The ThroLy scoring system is based on variables used in the Padua and Khorana systems, as well as variables that are specific to lymphoma patients.
In a previous study, the researchers found several variables that were independently associated with risk for VTE in lymphoma, including previous VTE, previous acute MI or stroke, mediastinal involvement, high body mass index, reduced mobility, extranodal localization, neutropenia, and hemoglobin less than 100 g/L (Am J Hematol. 2016 Oct;91[10]:1014-9).
In an initial version of the ThroLy scoring system, previous VTE, previous acute MI/stroke, obesity, and mediastinal involvement were all worth two points, and the other factors were worth a single point in the ThroLy system.
Patients with scores of 0 to 1 were considered low risk, patients with scores of 2 to 3 were considered intermediate risk, and patients with scores of 4 or greater were considered high risk.
To validate and refine ThroLy, Dr. Antic and his colleagues used it to assess 1,723 lymphoma patients treated at eight institutions in Austria, Croatia, France, Jordan, Macedonia, Spain, Switzerland, and the United States.
Patients had indolent non-Hodgkin lymphoma, aggressive non-Hodgkin lymphoma, chronic lymphocytic leukemia/small lymphocytic lymphoma, and Hodgkin lymphoma. Most subjects (84%) were outpatients. A total of 9%of patients had thrombosis, with 7% having VTE.
ThroLy had a positive predictive value of 17%, compared with 11% with Khorana and 13% with Padua. The negative predictive value was 93%, 92%, and 95%, respectively. The sensitivity was 51% with ThroLy, 42% with Khorana, and 70% with Padua; specificity was 72%, 64%, and 52%, respectively.
“The positive predictive value was low [with ThroLy] but definitely higher than the positive predictive value of the other two [scoring systems],” Dr. Antic noted.
Updated models
To further improve ThroLy, the researchers updated the system, creating two new models. Model 1 included the type of lymphoma/clinical stage (1 point), previous VTE (5 points), reduced mobility (2 points), hemoglobin less than 100 g/L (1 point), and the presence of vascular devices (1 point). Model 2 included all of the variables in Model 1 plus the thrombophilic condition, which was worth 1 point.
Patients were considered low risk if they scored 2 points or lower and high risk if they scored more than 2 points.
For Model 1, the positive predictive value was 22%, the negative predictive value was 96%, the sensitivity was 56%, and the specificity was 85%. For Model 2, the positive predictive value was 25%, the negative predictive value was 96%, the sensitivity was 57%, and the specificity was 87%.
There were no major differences in model discrimination and calibration based on the country in which a patient was treated or whether the patient was treated in an inpatient or outpatient setting.
Dr. Antic did not report any conflicts of interest. The Leukemia and Lymphoma meeting is organized by Jonathan Wood & Association, which is owned by the parent company of this news organization.
REPORTING FROM LEUKEMIA AND LYMPHOMA 2018
Key clinical point:
Major finding: The updated ThroLy had a positive predictive value of 22%-25%, a negative predictive value of 96%, sensitivity of 56%-57%, and specificity of 85%-87%.
Study details: The scoring system was validated on 1,723 lymphoma patients treated at eight institutions worldwide.
Disclosures: Dr. Antic reported having no conflicts of interest.
MCL treatment choices depend partly on age
CHICAGO – Treatment for mantle cell lymphoma (MCL) depends at least in part on patient age, with some important differences in those aged 65 years or younger versus those over age 65, according to Kristie A. Blum, MD.
“For the [younger] early-stage patients I’ll think about radiation and maybe observation, although I think [observation] is pretty uncommon,” Dr. Blum, acting hematology and medical oncology professor at Emory University in Atlanta, said at the American Society of Hematology Meeting on Hematologic Malignancies.
For advanced-stage patients, a number of options, including observation, can be considered, she said.
Observation
Observation is acceptable in highly selected advanced stage cases. In a 2009 study of 97 mantle cell patients, 31 were observed for more than 3 months before treatment was initiated (median time to treatment, 12 months), and at median follow-up of 55 months, overall survival (OS) was significantly better in the observation group (not reached vs. 64 months in treated patients), she said (J Clin Oncol. 2009 Mar 10;27[8]:1209-13).
Observed patients had better performance status and lower-risk standard International Prognostic Index scores, compared with treated patients, and the authors concluded that a “watch-and-wait” approach is acceptable in select patients.
“In addition, if you looked at their overall survival from the time of first treatment, there was no difference in the groups, suggesting you really weren’t hurting people by delaying their therapy,” Dr. Blum said.
In a more recent series of 440 favorable-risk MCL patients, 17% were observed for at least 3 months (median time to treatment, 35 months), 80% were observed for at least 12 months, and 13% were observed for 5 years.
Again, median OS was better for observed patients than for those treated initially, at 72 months vs. 52.5 months (Ann Oncol. 2017;28[10]:2489-95).
“So I do think there is a subset of patients that can safely be observed with mantle cell [lymphoma],” she said.
Transplant-based approaches
Transplant-based approaches in younger patients with advanced disease include the Nordic regimen plus autologous stem cell transplant (ASCT), R-CHOP/R-DHAP plus ASCT, and R-bendamustine/R-cytarabine – all with post-ASCT maintenance rituximab, Dr. Blum said.
Cytarabine-containing induction was established as the pretransplant standard of care by the 474-patient MCL Younger trial, which demonstrated significantly prolonged time to treatment failure (9.1 vs. 3.9 years), with alternating pretransplant R-CHOP/R-DHAP versus R-CHOP for six cycles, though this was associated with increased toxicity. (Lancet. 2016 Aug 6;388[10044]:565-75).
For example, grade 3-4 thrombocytopenia occurred in 73% vs. 9% of patients, she noted.
The Nordic MCL2 trial showed that an intensive regimen involving alternating Maxi-CHOP and AraC followed by transplant results in median OS of about 12 years and PFS of about 8 years.
“I do want to highlight, though, that again, the high-risk patients don’t do very well,” she said, noting that median PFS even with this intensive approach was only 2.5 years in those at high risk based on MCL International Prognostic Index (MIPI) score, compared with 12.7 years for patients with a low-risk MIPI score.
Newer induction regimens also show some promise and appear feasible in younger patients based on early data, she said, noting that the SWOG S1106 trial comparing R-bendamustine and R-HyperCVAD showed a minimal residual disease (MRD) negativity rate of 78% in the R-bendamustine group. Another study evaluating R-bendamustine followed by AraC showed a 96% complete remission and PFS at 13 months of 96%, with MRD-negativity of 93% (Br J Haematol. 2016 Apr;173[1]:89-95).
Transplant also is an option in advanced stage patients aged 66-70 years who are fit and willing, Dr. Blum said.
“I spend a long time talking to these patients about whether they want a transplant or not,” she said.
For induction in those patients who choose transplant, Dr. Blum said she prefers bendamustine-based regimens, “because these have been published in patients up to the age of 70.”
Transplant timing is usually at the first complete remission.
Data show that 5-year OS after such early ASCT in patients with no more than two prior lines of chemotherapy is about 60%, compared with about 44% with late ASCT. For reduced intensity conditioning allogeneic stem cell transplant in that study, the 5-year OS was 62% for early transplant and 31% for late transplant (J Clin Oncol. 2014 Feb 1;32[4]:273-81).
R-HyperCVAD
R-HyperCVAD is another option in younger patients, and is usually given for eight cycles, followed by transplant only in those who aren’t in complete remission, Dr. Blum said.
Median failure-free survival among patients aged 65 years and younger in one study of this regimen was 6.5 years and OS was 13.4 years. In those over age 65, median failure-free survival was about 3 years (Br J Haematol. 2016 Jan;172[1]:80-88).
The SWOG 0213 study looked at this in a multicenter fashion, she said, noting that 39% of patients – 48% of whom were aged 65 and older – could not complete all eight cycles.
“Again, there was a high rate of this sort of infectious toxicity,” she said.
Median PFS was about 5 years in this study as well, and OS was nearly 7 years. For those over age 65, median PFS was just 1.6 years.
“So I don’t typically recommend this for the 65- to 70-year-olds,” she said.
Older nontransplant candidates
When treating patients who are unfit for transplant, Dr. Blum pointed to the results of the StiL and BRIGHT studies, which both showed that R-bendamustine was noninferior to R-CHOP as first-line treatment.
In addition, recent data on combined bendamustine and cytarabine (R-BAC500) showed that in 57 patients with a median age of 71 years, 95% received at least four cycles, and 67% completed six cycles. CR was 91% , and 2-year OS and PFS were 86% and 81%, respectively.
However, grade 3-4 neutropenia and thrombocytopenia occurred in 49% and 52% of patients, respectively (Lancet Haematol. 2017 Jan 1;4[1]:e15-e23).
The bortezomib-containing regimen VR-CAP has also been shown to be of benefit for older MCL patients not eligible for transplant, she said.
Median PFS with VR-CAP in a study of 487 newly diagnosed MCL patients was about 25 months vs. 14 months with R-CHOP (N Engl J Med. 2015 Mar 5;372:944-53).
“R-lenalidomide has activity in the front-line setting as well,” Dr. Blum said, citing a multicenter phase 2 study of 38 patients with a mean age of 65 years. The intention-to-treat analysis showed an overall response rate of 87%, CR rate of 61%, and 2-year PFS of 85% (N Engl J Med. 2015;373:1835-44).
Maintenance therapy
As for maintenance therapy in younger patients, a phase 3 study of 299 patients showed that rituximab maintenance was associated with significantly better 4-year PFS (83% vs. 64% with observation), and 4-year OS (89% vs. 80% with observation), she said (N Engl J Med. 2017 Sep 28;377:1250-60).
“I do think that rituximab maintenance is the standard of care now, based on this study,” Dr. Blum said, adding that there is also a role for rituximab maintenance in older patients.
A European Mantle Cell Network study of patients aged 60 and older (median age of 70) showed an OS of 62% with R-CHOP vs. 47% with R-FC (rituximab, fludarabine, and cyclophosphamide), and – among those then randomized to maintenance rituximab or interferon alpha – 4-year PFS of 58% vs. 29%, respectively (N Engl J Med. 2012;367:520-31).
“Now I will tell you that most of these patients are getting bendamustine. We don’t really know the role for rituximab maintenance after bendamustine-based induction, but at this point I think it’s reasonable to consider adding it,” she said.
Dr. Blum is a consultant for Acerta, AstraZeneca, and Molecular Templates and has received research funding from Acerta, AstraZeneca, Celgene, Cephalon, Immunomedics, Janssen, Merck, Millennium, Molecular Templates, Novartis, Pharmacyclics, and Seattle Genetics.
CHICAGO – Treatment for mantle cell lymphoma (MCL) depends at least in part on patient age, with some important differences in those aged 65 years or younger versus those over age 65, according to Kristie A. Blum, MD.
“For the [younger] early-stage patients I’ll think about radiation and maybe observation, although I think [observation] is pretty uncommon,” Dr. Blum, acting hematology and medical oncology professor at Emory University in Atlanta, said at the American Society of Hematology Meeting on Hematologic Malignancies.
For advanced-stage patients, a number of options, including observation, can be considered, she said.
Observation
Observation is acceptable in highly selected advanced stage cases. In a 2009 study of 97 mantle cell patients, 31 were observed for more than 3 months before treatment was initiated (median time to treatment, 12 months), and at median follow-up of 55 months, overall survival (OS) was significantly better in the observation group (not reached vs. 64 months in treated patients), she said (J Clin Oncol. 2009 Mar 10;27[8]:1209-13).
Observed patients had better performance status and lower-risk standard International Prognostic Index scores, compared with treated patients, and the authors concluded that a “watch-and-wait” approach is acceptable in select patients.
“In addition, if you looked at their overall survival from the time of first treatment, there was no difference in the groups, suggesting you really weren’t hurting people by delaying their therapy,” Dr. Blum said.
In a more recent series of 440 favorable-risk MCL patients, 17% were observed for at least 3 months (median time to treatment, 35 months), 80% were observed for at least 12 months, and 13% were observed for 5 years.
Again, median OS was better for observed patients than for those treated initially, at 72 months vs. 52.5 months (Ann Oncol. 2017;28[10]:2489-95).
“So I do think there is a subset of patients that can safely be observed with mantle cell [lymphoma],” she said.
Transplant-based approaches
Transplant-based approaches in younger patients with advanced disease include the Nordic regimen plus autologous stem cell transplant (ASCT), R-CHOP/R-DHAP plus ASCT, and R-bendamustine/R-cytarabine – all with post-ASCT maintenance rituximab, Dr. Blum said.
Cytarabine-containing induction was established as the pretransplant standard of care by the 474-patient MCL Younger trial, which demonstrated significantly prolonged time to treatment failure (9.1 vs. 3.9 years), with alternating pretransplant R-CHOP/R-DHAP versus R-CHOP for six cycles, though this was associated with increased toxicity. (Lancet. 2016 Aug 6;388[10044]:565-75).
For example, grade 3-4 thrombocytopenia occurred in 73% vs. 9% of patients, she noted.
The Nordic MCL2 trial showed that an intensive regimen involving alternating Maxi-CHOP and AraC followed by transplant results in median OS of about 12 years and PFS of about 8 years.
“I do want to highlight, though, that again, the high-risk patients don’t do very well,” she said, noting that median PFS even with this intensive approach was only 2.5 years in those at high risk based on MCL International Prognostic Index (MIPI) score, compared with 12.7 years for patients with a low-risk MIPI score.
Newer induction regimens also show some promise and appear feasible in younger patients based on early data, she said, noting that the SWOG S1106 trial comparing R-bendamustine and R-HyperCVAD showed a minimal residual disease (MRD) negativity rate of 78% in the R-bendamustine group. Another study evaluating R-bendamustine followed by AraC showed a 96% complete remission and PFS at 13 months of 96%, with MRD-negativity of 93% (Br J Haematol. 2016 Apr;173[1]:89-95).
Transplant also is an option in advanced stage patients aged 66-70 years who are fit and willing, Dr. Blum said.
“I spend a long time talking to these patients about whether they want a transplant or not,” she said.
For induction in those patients who choose transplant, Dr. Blum said she prefers bendamustine-based regimens, “because these have been published in patients up to the age of 70.”
Transplant timing is usually at the first complete remission.
Data show that 5-year OS after such early ASCT in patients with no more than two prior lines of chemotherapy is about 60%, compared with about 44% with late ASCT. For reduced intensity conditioning allogeneic stem cell transplant in that study, the 5-year OS was 62% for early transplant and 31% for late transplant (J Clin Oncol. 2014 Feb 1;32[4]:273-81).
R-HyperCVAD
R-HyperCVAD is another option in younger patients, and is usually given for eight cycles, followed by transplant only in those who aren’t in complete remission, Dr. Blum said.
Median failure-free survival among patients aged 65 years and younger in one study of this regimen was 6.5 years and OS was 13.4 years. In those over age 65, median failure-free survival was about 3 years (Br J Haematol. 2016 Jan;172[1]:80-88).
The SWOG 0213 study looked at this in a multicenter fashion, she said, noting that 39% of patients – 48% of whom were aged 65 and older – could not complete all eight cycles.
“Again, there was a high rate of this sort of infectious toxicity,” she said.
Median PFS was about 5 years in this study as well, and OS was nearly 7 years. For those over age 65, median PFS was just 1.6 years.
“So I don’t typically recommend this for the 65- to 70-year-olds,” she said.
Older nontransplant candidates
When treating patients who are unfit for transplant, Dr. Blum pointed to the results of the StiL and BRIGHT studies, which both showed that R-bendamustine was noninferior to R-CHOP as first-line treatment.
In addition, recent data on combined bendamustine and cytarabine (R-BAC500) showed that in 57 patients with a median age of 71 years, 95% received at least four cycles, and 67% completed six cycles. CR was 91% , and 2-year OS and PFS were 86% and 81%, respectively.
However, grade 3-4 neutropenia and thrombocytopenia occurred in 49% and 52% of patients, respectively (Lancet Haematol. 2017 Jan 1;4[1]:e15-e23).
The bortezomib-containing regimen VR-CAP has also been shown to be of benefit for older MCL patients not eligible for transplant, she said.
Median PFS with VR-CAP in a study of 487 newly diagnosed MCL patients was about 25 months vs. 14 months with R-CHOP (N Engl J Med. 2015 Mar 5;372:944-53).
“R-lenalidomide has activity in the front-line setting as well,” Dr. Blum said, citing a multicenter phase 2 study of 38 patients with a mean age of 65 years. The intention-to-treat analysis showed an overall response rate of 87%, CR rate of 61%, and 2-year PFS of 85% (N Engl J Med. 2015;373:1835-44).
Maintenance therapy
As for maintenance therapy in younger patients, a phase 3 study of 299 patients showed that rituximab maintenance was associated with significantly better 4-year PFS (83% vs. 64% with observation), and 4-year OS (89% vs. 80% with observation), she said (N Engl J Med. 2017 Sep 28;377:1250-60).
“I do think that rituximab maintenance is the standard of care now, based on this study,” Dr. Blum said, adding that there is also a role for rituximab maintenance in older patients.
A European Mantle Cell Network study of patients aged 60 and older (median age of 70) showed an OS of 62% with R-CHOP vs. 47% with R-FC (rituximab, fludarabine, and cyclophosphamide), and – among those then randomized to maintenance rituximab or interferon alpha – 4-year PFS of 58% vs. 29%, respectively (N Engl J Med. 2012;367:520-31).
“Now I will tell you that most of these patients are getting bendamustine. We don’t really know the role for rituximab maintenance after bendamustine-based induction, but at this point I think it’s reasonable to consider adding it,” she said.
Dr. Blum is a consultant for Acerta, AstraZeneca, and Molecular Templates and has received research funding from Acerta, AstraZeneca, Celgene, Cephalon, Immunomedics, Janssen, Merck, Millennium, Molecular Templates, Novartis, Pharmacyclics, and Seattle Genetics.
CHICAGO – Treatment for mantle cell lymphoma (MCL) depends at least in part on patient age, with some important differences in those aged 65 years or younger versus those over age 65, according to Kristie A. Blum, MD.
“For the [younger] early-stage patients I’ll think about radiation and maybe observation, although I think [observation] is pretty uncommon,” Dr. Blum, acting hematology and medical oncology professor at Emory University in Atlanta, said at the American Society of Hematology Meeting on Hematologic Malignancies.
For advanced-stage patients, a number of options, including observation, can be considered, she said.
Observation
Observation is acceptable in highly selected advanced stage cases. In a 2009 study of 97 mantle cell patients, 31 were observed for more than 3 months before treatment was initiated (median time to treatment, 12 months), and at median follow-up of 55 months, overall survival (OS) was significantly better in the observation group (not reached vs. 64 months in treated patients), she said (J Clin Oncol. 2009 Mar 10;27[8]:1209-13).
Observed patients had better performance status and lower-risk standard International Prognostic Index scores, compared with treated patients, and the authors concluded that a “watch-and-wait” approach is acceptable in select patients.
“In addition, if you looked at their overall survival from the time of first treatment, there was no difference in the groups, suggesting you really weren’t hurting people by delaying their therapy,” Dr. Blum said.
In a more recent series of 440 favorable-risk MCL patients, 17% were observed for at least 3 months (median time to treatment, 35 months), 80% were observed for at least 12 months, and 13% were observed for 5 years.
Again, median OS was better for observed patients than for those treated initially, at 72 months vs. 52.5 months (Ann Oncol. 2017;28[10]:2489-95).
“So I do think there is a subset of patients that can safely be observed with mantle cell [lymphoma],” she said.
Transplant-based approaches
Transplant-based approaches in younger patients with advanced disease include the Nordic regimen plus autologous stem cell transplant (ASCT), R-CHOP/R-DHAP plus ASCT, and R-bendamustine/R-cytarabine – all with post-ASCT maintenance rituximab, Dr. Blum said.
Cytarabine-containing induction was established as the pretransplant standard of care by the 474-patient MCL Younger trial, which demonstrated significantly prolonged time to treatment failure (9.1 vs. 3.9 years), with alternating pretransplant R-CHOP/R-DHAP versus R-CHOP for six cycles, though this was associated with increased toxicity. (Lancet. 2016 Aug 6;388[10044]:565-75).
For example, grade 3-4 thrombocytopenia occurred in 73% vs. 9% of patients, she noted.
The Nordic MCL2 trial showed that an intensive regimen involving alternating Maxi-CHOP and AraC followed by transplant results in median OS of about 12 years and PFS of about 8 years.
“I do want to highlight, though, that again, the high-risk patients don’t do very well,” she said, noting that median PFS even with this intensive approach was only 2.5 years in those at high risk based on MCL International Prognostic Index (MIPI) score, compared with 12.7 years for patients with a low-risk MIPI score.
Newer induction regimens also show some promise and appear feasible in younger patients based on early data, she said, noting that the SWOG S1106 trial comparing R-bendamustine and R-HyperCVAD showed a minimal residual disease (MRD) negativity rate of 78% in the R-bendamustine group. Another study evaluating R-bendamustine followed by AraC showed a 96% complete remission and PFS at 13 months of 96%, with MRD-negativity of 93% (Br J Haematol. 2016 Apr;173[1]:89-95).
Transplant also is an option in advanced stage patients aged 66-70 years who are fit and willing, Dr. Blum said.
“I spend a long time talking to these patients about whether they want a transplant or not,” she said.
For induction in those patients who choose transplant, Dr. Blum said she prefers bendamustine-based regimens, “because these have been published in patients up to the age of 70.”
Transplant timing is usually at the first complete remission.
Data show that 5-year OS after such early ASCT in patients with no more than two prior lines of chemotherapy is about 60%, compared with about 44% with late ASCT. For reduced intensity conditioning allogeneic stem cell transplant in that study, the 5-year OS was 62% for early transplant and 31% for late transplant (J Clin Oncol. 2014 Feb 1;32[4]:273-81).
R-HyperCVAD
R-HyperCVAD is another option in younger patients, and is usually given for eight cycles, followed by transplant only in those who aren’t in complete remission, Dr. Blum said.
Median failure-free survival among patients aged 65 years and younger in one study of this regimen was 6.5 years and OS was 13.4 years. In those over age 65, median failure-free survival was about 3 years (Br J Haematol. 2016 Jan;172[1]:80-88).
The SWOG 0213 study looked at this in a multicenter fashion, she said, noting that 39% of patients – 48% of whom were aged 65 and older – could not complete all eight cycles.
“Again, there was a high rate of this sort of infectious toxicity,” she said.
Median PFS was about 5 years in this study as well, and OS was nearly 7 years. For those over age 65, median PFS was just 1.6 years.
“So I don’t typically recommend this for the 65- to 70-year-olds,” she said.
Older nontransplant candidates
When treating patients who are unfit for transplant, Dr. Blum pointed to the results of the StiL and BRIGHT studies, which both showed that R-bendamustine was noninferior to R-CHOP as first-line treatment.
In addition, recent data on combined bendamustine and cytarabine (R-BAC500) showed that in 57 patients with a median age of 71 years, 95% received at least four cycles, and 67% completed six cycles. CR was 91% , and 2-year OS and PFS were 86% and 81%, respectively.
However, grade 3-4 neutropenia and thrombocytopenia occurred in 49% and 52% of patients, respectively (Lancet Haematol. 2017 Jan 1;4[1]:e15-e23).
The bortezomib-containing regimen VR-CAP has also been shown to be of benefit for older MCL patients not eligible for transplant, she said.
Median PFS with VR-CAP in a study of 487 newly diagnosed MCL patients was about 25 months vs. 14 months with R-CHOP (N Engl J Med. 2015 Mar 5;372:944-53).
“R-lenalidomide has activity in the front-line setting as well,” Dr. Blum said, citing a multicenter phase 2 study of 38 patients with a mean age of 65 years. The intention-to-treat analysis showed an overall response rate of 87%, CR rate of 61%, and 2-year PFS of 85% (N Engl J Med. 2015;373:1835-44).
Maintenance therapy
As for maintenance therapy in younger patients, a phase 3 study of 299 patients showed that rituximab maintenance was associated with significantly better 4-year PFS (83% vs. 64% with observation), and 4-year OS (89% vs. 80% with observation), she said (N Engl J Med. 2017 Sep 28;377:1250-60).
“I do think that rituximab maintenance is the standard of care now, based on this study,” Dr. Blum said, adding that there is also a role for rituximab maintenance in older patients.
A European Mantle Cell Network study of patients aged 60 and older (median age of 70) showed an OS of 62% with R-CHOP vs. 47% with R-FC (rituximab, fludarabine, and cyclophosphamide), and – among those then randomized to maintenance rituximab or interferon alpha – 4-year PFS of 58% vs. 29%, respectively (N Engl J Med. 2012;367:520-31).
“Now I will tell you that most of these patients are getting bendamustine. We don’t really know the role for rituximab maintenance after bendamustine-based induction, but at this point I think it’s reasonable to consider adding it,” she said.
Dr. Blum is a consultant for Acerta, AstraZeneca, and Molecular Templates and has received research funding from Acerta, AstraZeneca, Celgene, Cephalon, Immunomedics, Janssen, Merck, Millennium, Molecular Templates, Novartis, Pharmacyclics, and Seattle Genetics.
EXPERT ANALYSIS FROM MHM 2018
Phase 1 NHL, ALL trials placed on clinical hold
Update: On October 12, 2018, Affimed N.V. received a notification from the U.S. Food and Drug Administration (FDA) saying the agency concurred with Affimed’s decision and formally placed the investigational new drug application for AFM11 on full clinical hold. Affimed said it will comply with the FDA and other global health authorities’ requests for information to resolve the clinical hold.
Affimed N.V. has placed trials of AFM11 on clinical hold and notified the global health authorities of its decision.
AFM11 is a CD19/CD3-targeting T-cell engager being evaluated in two phase 1 trials—one in patients with relapsed or refractory, CD19-positive B-cell non-Hodgkin lymphoma (NHL) and one in adults with relapsed or refractory B-precursor acute lymphoblastic leukemia (ALL).
Affimed initiated the clinical hold on these trials after serious adverse events occurred in three patients treated with AFM11.
This included a death in the ALL study and two life-threatening events in the NHL study.
The serious adverse events occurred in patients enrolled in the highest dose cohorts of each study.
A total of 33 patients have been treated in the two studies (NCT02848911 and NCT02106091), and preliminary signs of clinical activity have been observed in several patients.
Affimed said it will be working closely with the global health authorities, safety monitoring committees, and the studies’ clinical investigators to review the adverse events, assess all the data, and determine next steps for the AFM11 program.
Affimed intends to provide an update on AFM11 upon completing the evaluation.
Update: On October 12, 2018, Affimed N.V. received a notification from the U.S. Food and Drug Administration (FDA) saying the agency concurred with Affimed’s decision and formally placed the investigational new drug application for AFM11 on full clinical hold. Affimed said it will comply with the FDA and other global health authorities’ requests for information to resolve the clinical hold.
Affimed N.V. has placed trials of AFM11 on clinical hold and notified the global health authorities of its decision.
AFM11 is a CD19/CD3-targeting T-cell engager being evaluated in two phase 1 trials—one in patients with relapsed or refractory, CD19-positive B-cell non-Hodgkin lymphoma (NHL) and one in adults with relapsed or refractory B-precursor acute lymphoblastic leukemia (ALL).
Affimed initiated the clinical hold on these trials after serious adverse events occurred in three patients treated with AFM11.
This included a death in the ALL study and two life-threatening events in the NHL study.
The serious adverse events occurred in patients enrolled in the highest dose cohorts of each study.
A total of 33 patients have been treated in the two studies (NCT02848911 and NCT02106091), and preliminary signs of clinical activity have been observed in several patients.
Affimed said it will be working closely with the global health authorities, safety monitoring committees, and the studies’ clinical investigators to review the adverse events, assess all the data, and determine next steps for the AFM11 program.
Affimed intends to provide an update on AFM11 upon completing the evaluation.
Update: On October 12, 2018, Affimed N.V. received a notification from the U.S. Food and Drug Administration (FDA) saying the agency concurred with Affimed’s decision and formally placed the investigational new drug application for AFM11 on full clinical hold. Affimed said it will comply with the FDA and other global health authorities’ requests for information to resolve the clinical hold.
Affimed N.V. has placed trials of AFM11 on clinical hold and notified the global health authorities of its decision.
AFM11 is a CD19/CD3-targeting T-cell engager being evaluated in two phase 1 trials—one in patients with relapsed or refractory, CD19-positive B-cell non-Hodgkin lymphoma (NHL) and one in adults with relapsed or refractory B-precursor acute lymphoblastic leukemia (ALL).
Affimed initiated the clinical hold on these trials after serious adverse events occurred in three patients treated with AFM11.
This included a death in the ALL study and two life-threatening events in the NHL study.
The serious adverse events occurred in patients enrolled in the highest dose cohorts of each study.
A total of 33 patients have been treated in the two studies (NCT02848911 and NCT02106091), and preliminary signs of clinical activity have been observed in several patients.
Affimed said it will be working closely with the global health authorities, safety monitoring committees, and the studies’ clinical investigators to review the adverse events, assess all the data, and determine next steps for the AFM11 program.
Affimed intends to provide an update on AFM11 upon completing the evaluation.
Variant not associated with CLL, AIHA, or ITP in certain patients
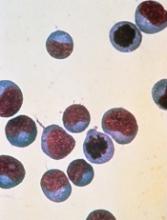
DUBROVNIK, CROATIA—New research suggests there is no association between the PTPN22 R620W polymorphism and chronic lymphocytic leukemia (CLL) or autoimmune hematologic disorders in patients from the Republic of Macedonia.
Past studies have shown an association between the PTPN22 R620W variant and both CLL1 and autoimmune diseases2 in patients from Northwest Europe.
However, a study of Macedonian patients suggests there is no association between the variant and CLL, autoimmune hemolytic anemia (AIHA), or idiopathic thrombocytopenic purpura (ITP) for patients from Southeast Europe.
Irina Panovska-Stavridis, PhD, of Ss. Cyril and Methodius University in Skopje, Republic of Macedonia, and her colleagues presented this finding at Leukemia and Lymphoma: Europe and the USA, Linking Knowledge and Practice.
“A lot of data from the literature suggests [the PTPN22 R620W variant ] has a role in developing multiple immune diseases, but it is validated just in patients from Northwest Europe,” Dr. Panovska-Stavridis noted.
Therefore, she and her colleagues decided to assess the frequency of the PTPN22 R620W variant (C1858T, rs2476601) in individuals from Southeast Europe, particularly the Republic of Macedonia.
The researchers evaluated 320 patients—168 with CLL, 66 with AIHA, and 86 with ITP—and 182 age- and sex-matched control subjects with no history of malignant or autoimmune disease.
The team found a similar frequency of the minor T allele and genotype distribution in control subjects and patients.
| CLL | AIHA | ITP | Controls | |
| Minor T allele | 0.107 | 0.067 | 0.036 | 0.05 |
| CC genotype | 0.809 | 0.166 | 0.023 | 0.901 |
| CT genotype | 0.9 | 0.067 | 0.033 | 0.099 |
| TT genotype | 0.928 | 0.072 | 0 | 0 |
Dr. Panovska-Stavridis said these results suggest the PTPN22 R620W variant is not a risk factor for the development of CLL, AIHA, or ITP in patients from Southeast Europe.
She also said the results suggest the influence of the variant on lymphocytic homeostasis is affected by certain genetic and environmental factors, and the development of CLL and autoimmune diseases is influenced by race/ethnicity-based variations in the germline composition of the IGHV locus in correlation with environmental factors.
Dr. Panovska-Stavridis did not declare any conflicts of interest.
1. Hebbring S et al. Blood. 2013 121:237-238; doi: https://doi.org/10.1182/blood-2012-08-450221
2. Burb GL et al. FEBS Lett. 2011 Dec 1;585(23):3689-98. doi: 10.1016/j.febslet.2011.04.032
DUBROVNIK, CROATIA—New research suggests there is no association between the PTPN22 R620W polymorphism and chronic lymphocytic leukemia (CLL) or autoimmune hematologic disorders in patients from the Republic of Macedonia.
Past studies have shown an association between the PTPN22 R620W variant and both CLL1 and autoimmune diseases2 in patients from Northwest Europe.
However, a study of Macedonian patients suggests there is no association between the variant and CLL, autoimmune hemolytic anemia (AIHA), or idiopathic thrombocytopenic purpura (ITP) for patients from Southeast Europe.
Irina Panovska-Stavridis, PhD, of Ss. Cyril and Methodius University in Skopje, Republic of Macedonia, and her colleagues presented this finding at Leukemia and Lymphoma: Europe and the USA, Linking Knowledge and Practice.
“A lot of data from the literature suggests [the PTPN22 R620W variant ] has a role in developing multiple immune diseases, but it is validated just in patients from Northwest Europe,” Dr. Panovska-Stavridis noted.
Therefore, she and her colleagues decided to assess the frequency of the PTPN22 R620W variant (C1858T, rs2476601) in individuals from Southeast Europe, particularly the Republic of Macedonia.
The researchers evaluated 320 patients—168 with CLL, 66 with AIHA, and 86 with ITP—and 182 age- and sex-matched control subjects with no history of malignant or autoimmune disease.
The team found a similar frequency of the minor T allele and genotype distribution in control subjects and patients.
| CLL | AIHA | ITP | Controls | |
| Minor T allele | 0.107 | 0.067 | 0.036 | 0.05 |
| CC genotype | 0.809 | 0.166 | 0.023 | 0.901 |
| CT genotype | 0.9 | 0.067 | 0.033 | 0.099 |
| TT genotype | 0.928 | 0.072 | 0 | 0 |
Dr. Panovska-Stavridis said these results suggest the PTPN22 R620W variant is not a risk factor for the development of CLL, AIHA, or ITP in patients from Southeast Europe.
She also said the results suggest the influence of the variant on lymphocytic homeostasis is affected by certain genetic and environmental factors, and the development of CLL and autoimmune diseases is influenced by race/ethnicity-based variations in the germline composition of the IGHV locus in correlation with environmental factors.
Dr. Panovska-Stavridis did not declare any conflicts of interest.
1. Hebbring S et al. Blood. 2013 121:237-238; doi: https://doi.org/10.1182/blood-2012-08-450221
2. Burb GL et al. FEBS Lett. 2011 Dec 1;585(23):3689-98. doi: 10.1016/j.febslet.2011.04.032
DUBROVNIK, CROATIA—New research suggests there is no association between the PTPN22 R620W polymorphism and chronic lymphocytic leukemia (CLL) or autoimmune hematologic disorders in patients from the Republic of Macedonia.
Past studies have shown an association between the PTPN22 R620W variant and both CLL1 and autoimmune diseases2 in patients from Northwest Europe.
However, a study of Macedonian patients suggests there is no association between the variant and CLL, autoimmune hemolytic anemia (AIHA), or idiopathic thrombocytopenic purpura (ITP) for patients from Southeast Europe.
Irina Panovska-Stavridis, PhD, of Ss. Cyril and Methodius University in Skopje, Republic of Macedonia, and her colleagues presented this finding at Leukemia and Lymphoma: Europe and the USA, Linking Knowledge and Practice.
“A lot of data from the literature suggests [the PTPN22 R620W variant ] has a role in developing multiple immune diseases, but it is validated just in patients from Northwest Europe,” Dr. Panovska-Stavridis noted.
Therefore, she and her colleagues decided to assess the frequency of the PTPN22 R620W variant (C1858T, rs2476601) in individuals from Southeast Europe, particularly the Republic of Macedonia.
The researchers evaluated 320 patients—168 with CLL, 66 with AIHA, and 86 with ITP—and 182 age- and sex-matched control subjects with no history of malignant or autoimmune disease.
The team found a similar frequency of the minor T allele and genotype distribution in control subjects and patients.
| CLL | AIHA | ITP | Controls | |
| Minor T allele | 0.107 | 0.067 | 0.036 | 0.05 |
| CC genotype | 0.809 | 0.166 | 0.023 | 0.901 |
| CT genotype | 0.9 | 0.067 | 0.033 | 0.099 |
| TT genotype | 0.928 | 0.072 | 0 | 0 |
Dr. Panovska-Stavridis said these results suggest the PTPN22 R620W variant is not a risk factor for the development of CLL, AIHA, or ITP in patients from Southeast Europe.
She also said the results suggest the influence of the variant on lymphocytic homeostasis is affected by certain genetic and environmental factors, and the development of CLL and autoimmune diseases is influenced by race/ethnicity-based variations in the germline composition of the IGHV locus in correlation with environmental factors.
Dr. Panovska-Stavridis did not declare any conflicts of interest.
1. Hebbring S et al. Blood. 2013 121:237-238; doi: https://doi.org/10.1182/blood-2012-08-450221
2. Burb GL et al. FEBS Lett. 2011 Dec 1;585(23):3689-98. doi: 10.1016/j.febslet.2011.04.032
System may better predict thrombosis in lymphoma
DUBROVNIK, CROATIA—An updated scoring system can more accurately identify lymphoma patients who may require thromboprophylaxis, according to researchers.
The revised scoring system, ThroLy, proved more effective than other systems for predicting thromboembolic events in lymphoma patients.
Researchers found the updated ThroLy had a positive predictive value of 22% to 25%, a negative predictive value of 96%, sensitivity of 56% to 57%, and specificity of 85% to 87%.
Darko Antić, MD, PhD, of the University of Belgrade in Serbia, presented these findings at Leukemia and Lymphoma: Europe and the USA, Linking Knowledge and Practice.
Dr. Antić said he and his colleagues developed ThroLy because other systems used to predict venous thromboembolism (VTE) are not quite right for lymphoma. He noted that the Padua score is not designed for cancer patients, and the Khorana score is predominantly for solid tumor malignancies.
“It’s good . . . , but it’s not specific for lymphoma patients,” Dr. Antić said.
With this in mind, he and his colleagues developed ThroLy. They based the scoring system on variables used in the Padua and Khorana systems as well as variables that are specific to lymphoma patients.
In a past study*, the researchers found several variables that were independently associated with risk for VTE in lymphoma:
- Previous VTE
- Previous acute myocardial infarction/stroke
- Mediastinal involvement
- Body mass index > 30 kg/m2
- Reduced mobility
- Extranodal localization
- Development of neutropenia
- Hemoglobin level < 100g/L.
Previous VTE, previous acute myocardial infarction/stroke, obesity, and mediastinal involvement were all worth 2 points, and the other factors were worth a single point.
Patients with scores of 0 to 1 were considered low-risk, patients with scores of 2 to 3 were considered intermediate-risk, and patients with scores of 4 or greater were considered high-risk.
Prospective validation
To validate and refine ThroLy, Dr. Antić and his colleagues used it to assess 1723 lymphoma patients treated at 8 institutions in Austria, Croatia, France, Jordan, Macedonia, Spain, Switzerland, and the United States.
Patients had indolent non-Hodgkin lymphoma (n=467), aggressive non-Hodgkin lymphoma (n=647), chronic lymphocytic leukemia/small lymphocytic lymphoma (n=235), and Hodgkin lymphoma (n=366). Most subjects (84%) were outpatients.
Nine percent of patients had thrombosis (n=142), with 7% having VTE (n=121).
ThroLy had a positive predictive value of 17%, compared to 11% with Khorana and 13% with Padua. The negative predictive value was 93%, 92%, and 95%, respectively.
The sensitivity was 51% with ThroLy, 42% with Khorana, and 70% with Padua. The specificity was 72%, 64%, and 52%, respectively.
“The positive predictive value was low [with ThroLy] but definitely higher than the positive predictive value of the other two [scoring systems],” Dr. Antić noted.
Updated models
To further improve ThroLy, the researchers updated the system, creating two new models.
Model 1 included the following variables:
- Type of lymphoma/clinical stage (aggressive/advanced)—1 point
- Previous VTE—5 points
- Reduced mobility—2 points
- Hemoglobin level < 100 g/L—1 point
- Presence of vascular devices—1 point.
Model 2 included all of the aforementioned variables as well as thrombophilic condition, which was worth 1 point.
With these models, patients were divided into two risk groups—low-risk (≤ 2 points) and high-risk (>2 points).
For Model 1, the positive predictive value was 22%, the negative predictive value was 96%, the sensitivity was 56%, and the specificity was 85%.
For Model 2, the positive predictive value was 25%, the negative predictive value was 96%, the sensitivity was 57%, and the specificity was 87%.
Dr. Antić said there were no major differences in model discrimination and calibration according to the country in which a patient was treated or whether patients were treated in inpatient or outpatient settings.
Dr. Antić did not report any conflicts of interest.
*Antić D et al. Am J Hematol. 2016 Oct;91(10):1014-9. doi: 10.1002/ajh.24466.
DUBROVNIK, CROATIA—An updated scoring system can more accurately identify lymphoma patients who may require thromboprophylaxis, according to researchers.
The revised scoring system, ThroLy, proved more effective than other systems for predicting thromboembolic events in lymphoma patients.
Researchers found the updated ThroLy had a positive predictive value of 22% to 25%, a negative predictive value of 96%, sensitivity of 56% to 57%, and specificity of 85% to 87%.
Darko Antić, MD, PhD, of the University of Belgrade in Serbia, presented these findings at Leukemia and Lymphoma: Europe and the USA, Linking Knowledge and Practice.
Dr. Antić said he and his colleagues developed ThroLy because other systems used to predict venous thromboembolism (VTE) are not quite right for lymphoma. He noted that the Padua score is not designed for cancer patients, and the Khorana score is predominantly for solid tumor malignancies.
“It’s good . . . , but it’s not specific for lymphoma patients,” Dr. Antić said.
With this in mind, he and his colleagues developed ThroLy. They based the scoring system on variables used in the Padua and Khorana systems as well as variables that are specific to lymphoma patients.
In a past study*, the researchers found several variables that were independently associated with risk for VTE in lymphoma:
- Previous VTE
- Previous acute myocardial infarction/stroke
- Mediastinal involvement
- Body mass index > 30 kg/m2
- Reduced mobility
- Extranodal localization
- Development of neutropenia
- Hemoglobin level < 100g/L.
Previous VTE, previous acute myocardial infarction/stroke, obesity, and mediastinal involvement were all worth 2 points, and the other factors were worth a single point.
Patients with scores of 0 to 1 were considered low-risk, patients with scores of 2 to 3 were considered intermediate-risk, and patients with scores of 4 or greater were considered high-risk.
Prospective validation
To validate and refine ThroLy, Dr. Antić and his colleagues used it to assess 1723 lymphoma patients treated at 8 institutions in Austria, Croatia, France, Jordan, Macedonia, Spain, Switzerland, and the United States.
Patients had indolent non-Hodgkin lymphoma (n=467), aggressive non-Hodgkin lymphoma (n=647), chronic lymphocytic leukemia/small lymphocytic lymphoma (n=235), and Hodgkin lymphoma (n=366). Most subjects (84%) were outpatients.
Nine percent of patients had thrombosis (n=142), with 7% having VTE (n=121).
ThroLy had a positive predictive value of 17%, compared to 11% with Khorana and 13% with Padua. The negative predictive value was 93%, 92%, and 95%, respectively.
The sensitivity was 51% with ThroLy, 42% with Khorana, and 70% with Padua. The specificity was 72%, 64%, and 52%, respectively.
“The positive predictive value was low [with ThroLy] but definitely higher than the positive predictive value of the other two [scoring systems],” Dr. Antić noted.
Updated models
To further improve ThroLy, the researchers updated the system, creating two new models.
Model 1 included the following variables:
- Type of lymphoma/clinical stage (aggressive/advanced)—1 point
- Previous VTE—5 points
- Reduced mobility—2 points
- Hemoglobin level < 100 g/L—1 point
- Presence of vascular devices—1 point.
Model 2 included all of the aforementioned variables as well as thrombophilic condition, which was worth 1 point.
With these models, patients were divided into two risk groups—low-risk (≤ 2 points) and high-risk (>2 points).
For Model 1, the positive predictive value was 22%, the negative predictive value was 96%, the sensitivity was 56%, and the specificity was 85%.
For Model 2, the positive predictive value was 25%, the negative predictive value was 96%, the sensitivity was 57%, and the specificity was 87%.
Dr. Antić said there were no major differences in model discrimination and calibration according to the country in which a patient was treated or whether patients were treated in inpatient or outpatient settings.
Dr. Antić did not report any conflicts of interest.
*Antić D et al. Am J Hematol. 2016 Oct;91(10):1014-9. doi: 10.1002/ajh.24466.
DUBROVNIK, CROATIA—An updated scoring system can more accurately identify lymphoma patients who may require thromboprophylaxis, according to researchers.
The revised scoring system, ThroLy, proved more effective than other systems for predicting thromboembolic events in lymphoma patients.
Researchers found the updated ThroLy had a positive predictive value of 22% to 25%, a negative predictive value of 96%, sensitivity of 56% to 57%, and specificity of 85% to 87%.
Darko Antić, MD, PhD, of the University of Belgrade in Serbia, presented these findings at Leukemia and Lymphoma: Europe and the USA, Linking Knowledge and Practice.
Dr. Antić said he and his colleagues developed ThroLy because other systems used to predict venous thromboembolism (VTE) are not quite right for lymphoma. He noted that the Padua score is not designed for cancer patients, and the Khorana score is predominantly for solid tumor malignancies.
“It’s good . . . , but it’s not specific for lymphoma patients,” Dr. Antić said.
With this in mind, he and his colleagues developed ThroLy. They based the scoring system on variables used in the Padua and Khorana systems as well as variables that are specific to lymphoma patients.
In a past study*, the researchers found several variables that were independently associated with risk for VTE in lymphoma:
- Previous VTE
- Previous acute myocardial infarction/stroke
- Mediastinal involvement
- Body mass index > 30 kg/m2
- Reduced mobility
- Extranodal localization
- Development of neutropenia
- Hemoglobin level < 100g/L.
Previous VTE, previous acute myocardial infarction/stroke, obesity, and mediastinal involvement were all worth 2 points, and the other factors were worth a single point.
Patients with scores of 0 to 1 were considered low-risk, patients with scores of 2 to 3 were considered intermediate-risk, and patients with scores of 4 or greater were considered high-risk.
Prospective validation
To validate and refine ThroLy, Dr. Antić and his colleagues used it to assess 1723 lymphoma patients treated at 8 institutions in Austria, Croatia, France, Jordan, Macedonia, Spain, Switzerland, and the United States.
Patients had indolent non-Hodgkin lymphoma (n=467), aggressive non-Hodgkin lymphoma (n=647), chronic lymphocytic leukemia/small lymphocytic lymphoma (n=235), and Hodgkin lymphoma (n=366). Most subjects (84%) were outpatients.
Nine percent of patients had thrombosis (n=142), with 7% having VTE (n=121).
ThroLy had a positive predictive value of 17%, compared to 11% with Khorana and 13% with Padua. The negative predictive value was 93%, 92%, and 95%, respectively.
The sensitivity was 51% with ThroLy, 42% with Khorana, and 70% with Padua. The specificity was 72%, 64%, and 52%, respectively.
“The positive predictive value was low [with ThroLy] but definitely higher than the positive predictive value of the other two [scoring systems],” Dr. Antić noted.
Updated models
To further improve ThroLy, the researchers updated the system, creating two new models.
Model 1 included the following variables:
- Type of lymphoma/clinical stage (aggressive/advanced)—1 point
- Previous VTE—5 points
- Reduced mobility—2 points
- Hemoglobin level < 100 g/L—1 point
- Presence of vascular devices—1 point.
Model 2 included all of the aforementioned variables as well as thrombophilic condition, which was worth 1 point.
With these models, patients were divided into two risk groups—low-risk (≤ 2 points) and high-risk (>2 points).
For Model 1, the positive predictive value was 22%, the negative predictive value was 96%, the sensitivity was 56%, and the specificity was 85%.
For Model 2, the positive predictive value was 25%, the negative predictive value was 96%, the sensitivity was 57%, and the specificity was 87%.
Dr. Antić said there were no major differences in model discrimination and calibration according to the country in which a patient was treated or whether patients were treated in inpatient or outpatient settings.
Dr. Antić did not report any conflicts of interest.
*Antić D et al. Am J Hematol. 2016 Oct;91(10):1014-9. doi: 10.1002/ajh.24466.
Weighing the costs of CAR T-cell therapy
The cost-effectiveness of tisagenlecleucel (Kymriah) depends on long-term clinical outcomes, which are presently unknown, according to investigators.
If the long-term outcomes are more modest than clinical trials suggest, then payers may be unwilling to cover the costly therapy, reported John K. Lin, MD, of Stanford University, and his colleagues.
Lowering the price or setting up an outcomes-based pricing structure may be necessary to get insurers to cover the therapy.
Tisagenlecleucel is an anti-CD19 chimeric antigen receptor (CAR) T-cell therapy that was approved by the U.S. Food and Drug Administration in August 2017 for relapsed or refractory pediatric B-cell acute lymphoblastic leukemia (ALL).
In 2018, the FDA expanded the indication for tisagenlecleucel to include adults with relapsed or refractory large B-cell lymphoma, though outcomes from lymphoma trials are not analyzed in the current study.
At a wholesale acquisition cost of $475,000 per infusion, it is the most expensive existing oncology therapy to date, and can be accompanied by expensive, potentially fatal adverse effects.
However, clinical trials suggest that tisagenlecleucel can offer years of relapse-free remission, thereby allowing patients to forgo other expensive therapies such as hematopoietic stem cell transplantation (HSCT).
“Although tisagenlecleucel-induced remission rates are promising, compared with those of established therapies (greater than 80% vs. less than 50%), only short-term follow-up data currently exist,” the investigators wrote in the Journal of Clinical Oncology.
“Given the high cost and broad applicability in other malignancies of tisagenlecleucel, a pressing question for policy makers, payers, patients, and clinicians is whether the cost of therapy represents reasonable value.”
The study used a Markov model to assess various long-term clinical outcome rates and cost thresholds of tisagenlecleucel. The lifetime cost of therapy was assessed and compared with costs of existing therapies.
The results showed that a 5-year relapse free survival rate of 40% would make the present cost ($475,000) of tisagenlecleucel economically reasonable. In this scenario, the increased life expectancy would be 12.1 years and would result in an additional 5.07 quality-adjusted life years (QALY) gained at a cost of $61,000 per QALY, compared with blinatumomab.
But if long-term outcomes are less favorable, tisagenlecleucel becomes much less cost effective. A 5-year relapse-free survival rate of 20% would drop increased life expectancy to 3.8 years, resulting in 1.80 QALYs gained and raising the cost to $151,000 per QALY.
“Our results suggest that at tisagenlecleucel’s current price and payment structure, its economic value is uncertain,” the investigators wrote.
They suggested a price drop to $200,000 or $350,000, which would allow the drug to remain cost effective even in a worse-case scenario, in which patients relapse and tisagenlecleucel is a bridge to transplant.
Another option is to move to outcomes-based pricing. Making payment conditional on 7 months of remission would make the treatment cost effective, according to the analysis.
“Price reductions of tisagenlecleucel or payment only for longer-term remissions would favorably influence cost-effectiveness, even if long-term clinical outcomes are modest,” the investigators wrote.
The study was funded by a Veterans Affairs Office of Academic Affiliations advanced fellowship in health service and research development, and a National Center for Advancing Translational Science Clinical and Translational Science Award.
One of the study coauthors reported consulting and research funding from Novartis.
The cost-effectiveness of tisagenlecleucel (Kymriah) depends on long-term clinical outcomes, which are presently unknown, according to investigators.
If the long-term outcomes are more modest than clinical trials suggest, then payers may be unwilling to cover the costly therapy, reported John K. Lin, MD, of Stanford University, and his colleagues.
Lowering the price or setting up an outcomes-based pricing structure may be necessary to get insurers to cover the therapy.
Tisagenlecleucel is an anti-CD19 chimeric antigen receptor (CAR) T-cell therapy that was approved by the U.S. Food and Drug Administration in August 2017 for relapsed or refractory pediatric B-cell acute lymphoblastic leukemia (ALL).
In 2018, the FDA expanded the indication for tisagenlecleucel to include adults with relapsed or refractory large B-cell lymphoma, though outcomes from lymphoma trials are not analyzed in the current study.
At a wholesale acquisition cost of $475,000 per infusion, it is the most expensive existing oncology therapy to date, and can be accompanied by expensive, potentially fatal adverse effects.
However, clinical trials suggest that tisagenlecleucel can offer years of relapse-free remission, thereby allowing patients to forgo other expensive therapies such as hematopoietic stem cell transplantation (HSCT).
“Although tisagenlecleucel-induced remission rates are promising, compared with those of established therapies (greater than 80% vs. less than 50%), only short-term follow-up data currently exist,” the investigators wrote in the Journal of Clinical Oncology.
“Given the high cost and broad applicability in other malignancies of tisagenlecleucel, a pressing question for policy makers, payers, patients, and clinicians is whether the cost of therapy represents reasonable value.”
The study used a Markov model to assess various long-term clinical outcome rates and cost thresholds of tisagenlecleucel. The lifetime cost of therapy was assessed and compared with costs of existing therapies.
The results showed that a 5-year relapse free survival rate of 40% would make the present cost ($475,000) of tisagenlecleucel economically reasonable. In this scenario, the increased life expectancy would be 12.1 years and would result in an additional 5.07 quality-adjusted life years (QALY) gained at a cost of $61,000 per QALY, compared with blinatumomab.
But if long-term outcomes are less favorable, tisagenlecleucel becomes much less cost effective. A 5-year relapse-free survival rate of 20% would drop increased life expectancy to 3.8 years, resulting in 1.80 QALYs gained and raising the cost to $151,000 per QALY.
“Our results suggest that at tisagenlecleucel’s current price and payment structure, its economic value is uncertain,” the investigators wrote.
They suggested a price drop to $200,000 or $350,000, which would allow the drug to remain cost effective even in a worse-case scenario, in which patients relapse and tisagenlecleucel is a bridge to transplant.
Another option is to move to outcomes-based pricing. Making payment conditional on 7 months of remission would make the treatment cost effective, according to the analysis.
“Price reductions of tisagenlecleucel or payment only for longer-term remissions would favorably influence cost-effectiveness, even if long-term clinical outcomes are modest,” the investigators wrote.
The study was funded by a Veterans Affairs Office of Academic Affiliations advanced fellowship in health service and research development, and a National Center for Advancing Translational Science Clinical and Translational Science Award.
One of the study coauthors reported consulting and research funding from Novartis.
The cost-effectiveness of tisagenlecleucel (Kymriah) depends on long-term clinical outcomes, which are presently unknown, according to investigators.
If the long-term outcomes are more modest than clinical trials suggest, then payers may be unwilling to cover the costly therapy, reported John K. Lin, MD, of Stanford University, and his colleagues.
Lowering the price or setting up an outcomes-based pricing structure may be necessary to get insurers to cover the therapy.
Tisagenlecleucel is an anti-CD19 chimeric antigen receptor (CAR) T-cell therapy that was approved by the U.S. Food and Drug Administration in August 2017 for relapsed or refractory pediatric B-cell acute lymphoblastic leukemia (ALL).
In 2018, the FDA expanded the indication for tisagenlecleucel to include adults with relapsed or refractory large B-cell lymphoma, though outcomes from lymphoma trials are not analyzed in the current study.
At a wholesale acquisition cost of $475,000 per infusion, it is the most expensive existing oncology therapy to date, and can be accompanied by expensive, potentially fatal adverse effects.
However, clinical trials suggest that tisagenlecleucel can offer years of relapse-free remission, thereby allowing patients to forgo other expensive therapies such as hematopoietic stem cell transplantation (HSCT).
“Although tisagenlecleucel-induced remission rates are promising, compared with those of established therapies (greater than 80% vs. less than 50%), only short-term follow-up data currently exist,” the investigators wrote in the Journal of Clinical Oncology.
“Given the high cost and broad applicability in other malignancies of tisagenlecleucel, a pressing question for policy makers, payers, patients, and clinicians is whether the cost of therapy represents reasonable value.”
The study used a Markov model to assess various long-term clinical outcome rates and cost thresholds of tisagenlecleucel. The lifetime cost of therapy was assessed and compared with costs of existing therapies.
The results showed that a 5-year relapse free survival rate of 40% would make the present cost ($475,000) of tisagenlecleucel economically reasonable. In this scenario, the increased life expectancy would be 12.1 years and would result in an additional 5.07 quality-adjusted life years (QALY) gained at a cost of $61,000 per QALY, compared with blinatumomab.
But if long-term outcomes are less favorable, tisagenlecleucel becomes much less cost effective. A 5-year relapse-free survival rate of 20% would drop increased life expectancy to 3.8 years, resulting in 1.80 QALYs gained and raising the cost to $151,000 per QALY.
“Our results suggest that at tisagenlecleucel’s current price and payment structure, its economic value is uncertain,” the investigators wrote.
They suggested a price drop to $200,000 or $350,000, which would allow the drug to remain cost effective even in a worse-case scenario, in which patients relapse and tisagenlecleucel is a bridge to transplant.
Another option is to move to outcomes-based pricing. Making payment conditional on 7 months of remission would make the treatment cost effective, according to the analysis.
“Price reductions of tisagenlecleucel or payment only for longer-term remissions would favorably influence cost-effectiveness, even if long-term clinical outcomes are modest,” the investigators wrote.
The study was funded by a Veterans Affairs Office of Academic Affiliations advanced fellowship in health service and research development, and a National Center for Advancing Translational Science Clinical and Translational Science Award.
One of the study coauthors reported consulting and research funding from Novartis.
CAR T therapy being explored in Hodgkin lymphoma
New York—Although the data set is small and not yet mature, chimeric antigen receptor (CAR) T-cell therapy appears to be a promising approach for Hodgkin lymphoma, according to Philippe Armand, MD, PhD, of Dana-Farber/Brigham and Women’s Cancer Center and the Massachusetts General Hospital Cancer Center.
While based on a handful of patients, the data do suggest this approach may play a role either by targeting CD30 or Epstein Barr virus (EBV), Dr. Armand said in a presentation at the NCCN 13th Annual Congress: Hematologic Malignancies.
“Most importantly perhaps, like it's experience outside of Hodgkin lymphoma, it may really have curative potential, based on the long CR rates that have been already exhibited,” he told attendees at the NCCN conference.
Much of the published clinical experience to date is with CD30-directed CAR Ts, Dr. Armand said, noting that in Hodgkin lymphoma, results so far show promise for this particular approach.
In a recent phase 1 dose escalation study, 9 patients with relapsed/refractory Hodgkin lymphoma or anaplastic large-cell lymphoma (ALCL) received infusions of autologous T cells modified to express CD30-specific CAR T cells encoding the CD28 costimulatory domain, with no conditioning regimen.
Out of 7 relapsed Hodgkin patients, one had a complete response (CR) lasting beyond 2.5 years following a second infusion. Another had a CR persisting almost 2 years and 3 had transient stable disease.
One of the 2 ALCL patients had a CR lasting 9 months after a fourth infusion. No toxicities attributable to the therapy were seen, according to investigators.
The CD30 CAR T cells are being evaluated with a conditioning regimen in the phase 1 RELY-30 trial. According to Dr. Armand, preliminary results presented at the EBMT 2018 meeting showed better expansion of CAR T cells and responses in 3 out of 5 patients, including 2 CRs.
A CD30-directed CAR T-cell therapy with a 4-1bb costimulatory domain has also been tested in a small group of Hodgkin patients with a response rate of 35%, including some CRs. Response rates were lower in patients with extranodal involvement, although that needs to be validated with further study, according to Dr. Armand.
A considerable amount of active research is ongoing in China, Dr. Armand said, while a phase 1 study of T cells expressing a fully human anti-CD30 CAR is being evaluated in the United States in CD30-expressing lymphomas, he added.
Among non-CD30-targeted products, a CD19 CAR-T approach has been tried in Hodgkin lymphoma, though preliminary results suggest only transient activity.
An interesting approach has been the targeting of EBV, Dr. Armand noted. Recently reported results showed that two doses of T cells with specificity for EBV-derived tumor antigens induced clinical responses in patients with EBV-positive Hodgkin lymphoma.
The cells were engineered to express dominant-negative TGF-β receptor type 2 (DNRII).
“We know that TGF-β provides a strong immunosuppressant signal in the tumor microenvironment,” Dr. Armand said, noting that some of the responses in the 7 evaluable patients lasted 4 years or more.
New York—Although the data set is small and not yet mature, chimeric antigen receptor (CAR) T-cell therapy appears to be a promising approach for Hodgkin lymphoma, according to Philippe Armand, MD, PhD, of Dana-Farber/Brigham and Women’s Cancer Center and the Massachusetts General Hospital Cancer Center.
While based on a handful of patients, the data do suggest this approach may play a role either by targeting CD30 or Epstein Barr virus (EBV), Dr. Armand said in a presentation at the NCCN 13th Annual Congress: Hematologic Malignancies.
“Most importantly perhaps, like it's experience outside of Hodgkin lymphoma, it may really have curative potential, based on the long CR rates that have been already exhibited,” he told attendees at the NCCN conference.
Much of the published clinical experience to date is with CD30-directed CAR Ts, Dr. Armand said, noting that in Hodgkin lymphoma, results so far show promise for this particular approach.
In a recent phase 1 dose escalation study, 9 patients with relapsed/refractory Hodgkin lymphoma or anaplastic large-cell lymphoma (ALCL) received infusions of autologous T cells modified to express CD30-specific CAR T cells encoding the CD28 costimulatory domain, with no conditioning regimen.
Out of 7 relapsed Hodgkin patients, one had a complete response (CR) lasting beyond 2.5 years following a second infusion. Another had a CR persisting almost 2 years and 3 had transient stable disease.
One of the 2 ALCL patients had a CR lasting 9 months after a fourth infusion. No toxicities attributable to the therapy were seen, according to investigators.
The CD30 CAR T cells are being evaluated with a conditioning regimen in the phase 1 RELY-30 trial. According to Dr. Armand, preliminary results presented at the EBMT 2018 meeting showed better expansion of CAR T cells and responses in 3 out of 5 patients, including 2 CRs.
A CD30-directed CAR T-cell therapy with a 4-1bb costimulatory domain has also been tested in a small group of Hodgkin patients with a response rate of 35%, including some CRs. Response rates were lower in patients with extranodal involvement, although that needs to be validated with further study, according to Dr. Armand.
A considerable amount of active research is ongoing in China, Dr. Armand said, while a phase 1 study of T cells expressing a fully human anti-CD30 CAR is being evaluated in the United States in CD30-expressing lymphomas, he added.
Among non-CD30-targeted products, a CD19 CAR-T approach has been tried in Hodgkin lymphoma, though preliminary results suggest only transient activity.
An interesting approach has been the targeting of EBV, Dr. Armand noted. Recently reported results showed that two doses of T cells with specificity for EBV-derived tumor antigens induced clinical responses in patients with EBV-positive Hodgkin lymphoma.
The cells were engineered to express dominant-negative TGF-β receptor type 2 (DNRII).
“We know that TGF-β provides a strong immunosuppressant signal in the tumor microenvironment,” Dr. Armand said, noting that some of the responses in the 7 evaluable patients lasted 4 years or more.
New York—Although the data set is small and not yet mature, chimeric antigen receptor (CAR) T-cell therapy appears to be a promising approach for Hodgkin lymphoma, according to Philippe Armand, MD, PhD, of Dana-Farber/Brigham and Women’s Cancer Center and the Massachusetts General Hospital Cancer Center.
While based on a handful of patients, the data do suggest this approach may play a role either by targeting CD30 or Epstein Barr virus (EBV), Dr. Armand said in a presentation at the NCCN 13th Annual Congress: Hematologic Malignancies.
“Most importantly perhaps, like it's experience outside of Hodgkin lymphoma, it may really have curative potential, based on the long CR rates that have been already exhibited,” he told attendees at the NCCN conference.
Much of the published clinical experience to date is with CD30-directed CAR Ts, Dr. Armand said, noting that in Hodgkin lymphoma, results so far show promise for this particular approach.
In a recent phase 1 dose escalation study, 9 patients with relapsed/refractory Hodgkin lymphoma or anaplastic large-cell lymphoma (ALCL) received infusions of autologous T cells modified to express CD30-specific CAR T cells encoding the CD28 costimulatory domain, with no conditioning regimen.
Out of 7 relapsed Hodgkin patients, one had a complete response (CR) lasting beyond 2.5 years following a second infusion. Another had a CR persisting almost 2 years and 3 had transient stable disease.
One of the 2 ALCL patients had a CR lasting 9 months after a fourth infusion. No toxicities attributable to the therapy were seen, according to investigators.
The CD30 CAR T cells are being evaluated with a conditioning regimen in the phase 1 RELY-30 trial. According to Dr. Armand, preliminary results presented at the EBMT 2018 meeting showed better expansion of CAR T cells and responses in 3 out of 5 patients, including 2 CRs.
A CD30-directed CAR T-cell therapy with a 4-1bb costimulatory domain has also been tested in a small group of Hodgkin patients with a response rate of 35%, including some CRs. Response rates were lower in patients with extranodal involvement, although that needs to be validated with further study, according to Dr. Armand.
A considerable amount of active research is ongoing in China, Dr. Armand said, while a phase 1 study of T cells expressing a fully human anti-CD30 CAR is being evaluated in the United States in CD30-expressing lymphomas, he added.
Among non-CD30-targeted products, a CD19 CAR-T approach has been tried in Hodgkin lymphoma, though preliminary results suggest only transient activity.
An interesting approach has been the targeting of EBV, Dr. Armand noted. Recently reported results showed that two doses of T cells with specificity for EBV-derived tumor antigens induced clinical responses in patients with EBV-positive Hodgkin lymphoma.
The cells were engineered to express dominant-negative TGF-β receptor type 2 (DNRII).
“We know that TGF-β provides a strong immunosuppressant signal in the tumor microenvironment,” Dr. Armand said, noting that some of the responses in the 7 evaluable patients lasted 4 years or more.