User login
AITL responds to 5-azacytidine in small series
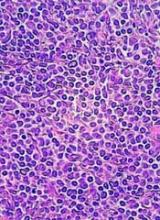
Older patients with refractory angioimmunoblastic T cell lymphoma (AITL) appear to respond well to treatment with 5-azacytidine, regardless of mutations.
Francois Lemonnier, MD, of Henri Mondor University Hospitals in Créteil, France, and his colleagues, reported on a retrospective series of 12 AITL patients who received 5-azacytidine for concomitant myeloid neoplasm or as compassionate therapy for relapsed or refractory AITL. The findings were published in Blood.
Patients were given 5-azacytidine subcutaneously at a dose of 75 mg/m2 daily for 7 consecutive days. The treatment was given every 28 days until progression or unacceptable toxicity for a median of 5.5 cycles. Along with 5-azacytidine, half of the patients received rituximab due to the presence of EBV replication or EBV B-blasts in the lymph node biopsy.
The patients were assessed via CT scan and responses were evaluated by investigators following the Cheson criteria.
This was a heavily pretreated patient population. The median age was 70 years and 11 of the patients had relapsed or refractory disease and had received a median of two lines of therapy. There was only one treatment-naive patient in the series.
Treatment with 5-azacytidine produced an overall response rate of 75%, with six patients achieving a complete response and three patients achieving a partial response. The median progression-free survival was 15 months and median overall survival was 21 months at a median follow-up of 27 months.
The researchers noted that some elderly patients with poor performance status achieved a sustained response after treatment with an acceptable tolerance.
Treatment was well tolerated overall. There were no treatment-related deaths and no patients developed neutropenia. Three patients required transfusion and another had grade 3 diarrhea.
The researchers also performed molecular studies using targeted deep sequencing. They detected TET2 mutations in all 12 patients, with seven patients having two mutations. Four patients had DNMT3A mutations, five patients had RHOA mutations, and four patients had p.G17V substitution. One patient had an IDH2R172 mutation.
Since all patients had a TET2 mutation, the researchers were unable to assess its impact on treatment response. However, they saw no association between the number of TET2 mutations and treatment response, or mutations in DNMT3A, IDH2, and RHOA and treatment response.
The study was funded by a grant from the Leukemia & Lymphoma Society. Three of the coauthors received honoraria from Celgene.
SOURCE: Lemonnier F et al. Blood. 2018 Oct 2. doi: 10.1182/blood-2018-04-840538.
Older patients with refractory angioimmunoblastic T cell lymphoma (AITL) appear to respond well to treatment with 5-azacytidine, regardless of mutations.
Francois Lemonnier, MD, of Henri Mondor University Hospitals in Créteil, France, and his colleagues, reported on a retrospective series of 12 AITL patients who received 5-azacytidine for concomitant myeloid neoplasm or as compassionate therapy for relapsed or refractory AITL. The findings were published in Blood.
Patients were given 5-azacytidine subcutaneously at a dose of 75 mg/m2 daily for 7 consecutive days. The treatment was given every 28 days until progression or unacceptable toxicity for a median of 5.5 cycles. Along with 5-azacytidine, half of the patients received rituximab due to the presence of EBV replication or EBV B-blasts in the lymph node biopsy.
The patients were assessed via CT scan and responses were evaluated by investigators following the Cheson criteria.
This was a heavily pretreated patient population. The median age was 70 years and 11 of the patients had relapsed or refractory disease and had received a median of two lines of therapy. There was only one treatment-naive patient in the series.
Treatment with 5-azacytidine produced an overall response rate of 75%, with six patients achieving a complete response and three patients achieving a partial response. The median progression-free survival was 15 months and median overall survival was 21 months at a median follow-up of 27 months.
The researchers noted that some elderly patients with poor performance status achieved a sustained response after treatment with an acceptable tolerance.
Treatment was well tolerated overall. There were no treatment-related deaths and no patients developed neutropenia. Three patients required transfusion and another had grade 3 diarrhea.
The researchers also performed molecular studies using targeted deep sequencing. They detected TET2 mutations in all 12 patients, with seven patients having two mutations. Four patients had DNMT3A mutations, five patients had RHOA mutations, and four patients had p.G17V substitution. One patient had an IDH2R172 mutation.
Since all patients had a TET2 mutation, the researchers were unable to assess its impact on treatment response. However, they saw no association between the number of TET2 mutations and treatment response, or mutations in DNMT3A, IDH2, and RHOA and treatment response.
The study was funded by a grant from the Leukemia & Lymphoma Society. Three of the coauthors received honoraria from Celgene.
SOURCE: Lemonnier F et al. Blood. 2018 Oct 2. doi: 10.1182/blood-2018-04-840538.
Older patients with refractory angioimmunoblastic T cell lymphoma (AITL) appear to respond well to treatment with 5-azacytidine, regardless of mutations.
Francois Lemonnier, MD, of Henri Mondor University Hospitals in Créteil, France, and his colleagues, reported on a retrospective series of 12 AITL patients who received 5-azacytidine for concomitant myeloid neoplasm or as compassionate therapy for relapsed or refractory AITL. The findings were published in Blood.
Patients were given 5-azacytidine subcutaneously at a dose of 75 mg/m2 daily for 7 consecutive days. The treatment was given every 28 days until progression or unacceptable toxicity for a median of 5.5 cycles. Along with 5-azacytidine, half of the patients received rituximab due to the presence of EBV replication or EBV B-blasts in the lymph node biopsy.
The patients were assessed via CT scan and responses were evaluated by investigators following the Cheson criteria.
This was a heavily pretreated patient population. The median age was 70 years and 11 of the patients had relapsed or refractory disease and had received a median of two lines of therapy. There was only one treatment-naive patient in the series.
Treatment with 5-azacytidine produced an overall response rate of 75%, with six patients achieving a complete response and three patients achieving a partial response. The median progression-free survival was 15 months and median overall survival was 21 months at a median follow-up of 27 months.
The researchers noted that some elderly patients with poor performance status achieved a sustained response after treatment with an acceptable tolerance.
Treatment was well tolerated overall. There were no treatment-related deaths and no patients developed neutropenia. Three patients required transfusion and another had grade 3 diarrhea.
The researchers also performed molecular studies using targeted deep sequencing. They detected TET2 mutations in all 12 patients, with seven patients having two mutations. Four patients had DNMT3A mutations, five patients had RHOA mutations, and four patients had p.G17V substitution. One patient had an IDH2R172 mutation.
Since all patients had a TET2 mutation, the researchers were unable to assess its impact on treatment response. However, they saw no association between the number of TET2 mutations and treatment response, or mutations in DNMT3A, IDH2, and RHOA and treatment response.
The study was funded by a grant from the Leukemia & Lymphoma Society. Three of the coauthors received honoraria from Celgene.
SOURCE: Lemonnier F et al. Blood. 2018 Oct 2. doi: 10.1182/blood-2018-04-840538.
FROM BLOOD
Key clinical point:
Major finding: The overall response rate was 75% among the 12 patients, with 6 patients achieving complete response.
Study details: A retrospective case series of 12 patients with angioimmunoblastic T cell lymphoma.
Disclosures: The study was funded by a grant from the Leukemia & Lymphoma Society. Three of the coauthors received honoraria from Celgene.
Source: Lemonnier F et al. Blood. 2018 Oct 2. doi: 10.1182/blood-2018-04-840538.
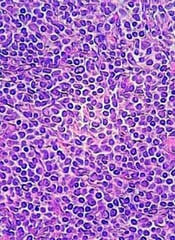
Duvelisib bests ofatumumab as monotherapy for treatment of CLL/SLL
Final analysis of the phase 3 DUO trial has shown monotherapy with oral duvelisib results in a statistically significant improvement in progression-free survival (PFS) and overall response rate (ORR) compared to monotherapy with ofatumumab for patients with relapsed or refractory chronic lymphocytic leukemia/small lympchocytic lymphoma (CLL/SLL).
PFS for all patients as assessed by Independent Review Committee (IRC) was a median 13.3 months with duvelisib compared to 9.9 months with ofatumumab (P<0.0001).
ORR was significantly higher with duvelisib, 74% compared to 45%, P<0.0001, regardless of deletion 17p status.
Duvelisib (Copiktra™) was recently approved by the U.S. Food and Drug Administration for CLL/SLL based in part on this head-to-head trial.
The investigators reported the results in Blood.
"The way we treat patients with CLL is changing rapidly as we move from standard chemotherapy-based approaches to more targeted therapies," said principal investigator Ian W. Flinn, MD, PhD, of Sarah Cannon Research Institute in Nashville.
"Based on these data, duvelisib may offer a new treatment option for patients who otherwise may have limited options."
Duvelisib is an oral, dual inhibitor of phosphoinositide 3-kinase (PI3K)-δ and -γ, which means it blocks the survival and proliferation of malignant B cells and also disrupts the recruitment and differentiation of T cells and macrophages within the tumor microenvironment.
Ofatumumab is a humanized anti-CD20 antibody with single-agent efficacy in refractory CLL. It is approved by the FDA as a treatment option in CLL.
Study design
Investigators randomized 319 relapsed or refractory CLL/SLL patients, 160 to the duvelisib arm and 159 to the ofatumumab arm.
Patients in the duvelisib arm self-administered 25 mg capsules twice daily continuously in 28-day cycles. They could take duvelisib for up to 18 cycles, until disease progression or unacceptable toxicity.
Ofatumumab-treated patients received infusions as approved in the product labeling for monotherapy in relapsed CLL. Dosing of ofatumumab could not exceed 12 doses in 7 cycles.
Prophylaxis for Pneumocystis jirovecci was required for all patients on both treatment arms.
Patients were allowed to crossover to a separate extension study to receive the opposite therapy if they had progressive disease.
They were followed for a median of 22.4 months.
Patient characteristics
According to the investigators, patient characteristics were well balanced between the arms.
The majority (60%) were male and the median age in both arms was 69. Most had an ECOG performance status of 0 or 1; 7% in the duvelisib arm and 10% in the ofatumumab arm had a performance status of 2.
Other patient characteristics in the duvelisib and ofatumumab arms, respectively, were:
- Time from initial diagnosis: 7.5 years, 6.7 years
- CLL/SLL, %: 97/5, 99/2
- Bulky disease: 46%, 45%
- Baseline lymphocyte counts: 38x109/L, 35x109/L
- Deletion 17p and/or TP53 mutation: 31%, 33%
- Median number of prior therapies: 2 in each arm
- Previous alkylating agent: 93%, 95%
- Previous monoclonal antibody: 78%, 83%
- Prior purine analog: 60%, 71%
Of the total patients enrolled, 158 patients in the duvelisib arm and 155 in the ofatumumab arm received treatment, for a median exposure of 50 weeks and 23 weeks, respectively.
Efficacy
In addition to the significantly improved overall PFS and ORR with duvelisib, further analysis revealed that PFS also improved for all predefined subgroups.
High-risk patients with deletion 17p/TP53 mutations also experienced a significant improvement in PFS with duvelisib of 12.7 months compared to 9.0 months with ofatumumab by IRC (P=0.0002).
The estimated probability of being progression-free for these patients at 6 and 12 moths was 73% and 55% with duvelisib and 63% and 30% with ofatumumab.
The investigators pointed out that duvelisib treatment was particularly effective in eliciting a lymph node response—85.0% compared to 15.7% with ofatumumab as assessed by IRC (P<0.0001).
Median overall survival was not reached in either arm. The 12-month probability of survival was 86% for both treatments.
Safety
Median treatment exposure was almost twice as long in the duvelisib arm because ofatumumab treatment was not allowed to exceed 12 doses as specified in the prescribing information.
The investigators explained this resulted in a longer adverse event (AE) reporting period for duvelisib.
One hundred twenty-four duvelisib-treated patients discontinued treatment, most commonly due to AEs (35%), disease progression (22%), subject withdrawal (8%), and death (8%).
All ofatumumab-treated patients discontinued treatment by the time of data cutoff, and 67% had completed treatment as per protocol. Others discontinued due to disease progression (20%), subject withdrawal (5%), and AEs (4%).
Eight (5%) duvelisib patients crossed over to ofatumumab therapy at the time of disease progression, and 89 (57%) ofatumumab-treated patients crossed over to duvelisib.
Nearly all patients in both arms experienced an AE.
The most common hematologic malignancies with duvelisib and ofatumumab, respectively, occurring in 10% or more patients were neutropenia (33%, 21%), anemia (23%, 10%), and thrombocytopenia (15%, 6%).
The most common nonhematologic AES with duvelisib were diarrhea (51%), pyrexia (29%), nausea (23%), and cough (21%).
With ofatumumab, the most common nonhematologic AES were infusion-related reaction (19%), cough (14%), and diarrhea, rash, and fatigue (12% each).
Grade 3 or greater AEs occurred in 87% of duvelisib-treated patients and 48% in the ofatumumab arm.
The most common grade 3 or greater events with duvelisib were neutropenia (30%), diarrhea (15%), pneumonia (14%), and anemia (13%).
With ofatumumab, only neutropenia (17%) of grade 3 or higher occurred in 10% or more patients.
Severe immune-related toxicities with duvelisib included colitis (12%) and pneumonitis, alanine transaminase (ALT) or aspartate transaminase (AST) increase (3% each). The events were managed with dose interruptions and steroid therapy for pneumonitis or colitis. All reported events resolved, and none was fatal.
Infectious AEs occurred more frequently with duvelisib, 69% compared to 43% in the ofatumumab arm. Pneumonia (18%) and upper respiratory tract infection (16%) were the most common events.
Three patients in the duvelisib arm and 1 in the ofatumumab arm contracted Pneumocystis jirovecii.
The most frequently reported serious AE was pneumonia (duvelisib 15%; ofatumumab 3%).
Nineteen fatal AEs occurred in patients on the duvelisib arm, 4 of which were related to the study drug: staphylococcal pneumonia (n = 2), sepsis (n=1), and general health deterioration (n = 1).
Seven fatal AEs occurred in patients on the ofatumumab arm, although none was attributed to ofatumumab.
The DUO trial was sponsored by Verastem Oncology and Infinity Pharmaceuticals , Inc.
Final analysis of the phase 3 DUO trial has shown monotherapy with oral duvelisib results in a statistically significant improvement in progression-free survival (PFS) and overall response rate (ORR) compared to monotherapy with ofatumumab for patients with relapsed or refractory chronic lymphocytic leukemia/small lympchocytic lymphoma (CLL/SLL).
PFS for all patients as assessed by Independent Review Committee (IRC) was a median 13.3 months with duvelisib compared to 9.9 months with ofatumumab (P<0.0001).
ORR was significantly higher with duvelisib, 74% compared to 45%, P<0.0001, regardless of deletion 17p status.
Duvelisib (Copiktra™) was recently approved by the U.S. Food and Drug Administration for CLL/SLL based in part on this head-to-head trial.
The investigators reported the results in Blood.
"The way we treat patients with CLL is changing rapidly as we move from standard chemotherapy-based approaches to more targeted therapies," said principal investigator Ian W. Flinn, MD, PhD, of Sarah Cannon Research Institute in Nashville.
"Based on these data, duvelisib may offer a new treatment option for patients who otherwise may have limited options."
Duvelisib is an oral, dual inhibitor of phosphoinositide 3-kinase (PI3K)-δ and -γ, which means it blocks the survival and proliferation of malignant B cells and also disrupts the recruitment and differentiation of T cells and macrophages within the tumor microenvironment.
Ofatumumab is a humanized anti-CD20 antibody with single-agent efficacy in refractory CLL. It is approved by the FDA as a treatment option in CLL.
Study design
Investigators randomized 319 relapsed or refractory CLL/SLL patients, 160 to the duvelisib arm and 159 to the ofatumumab arm.
Patients in the duvelisib arm self-administered 25 mg capsules twice daily continuously in 28-day cycles. They could take duvelisib for up to 18 cycles, until disease progression or unacceptable toxicity.
Ofatumumab-treated patients received infusions as approved in the product labeling for monotherapy in relapsed CLL. Dosing of ofatumumab could not exceed 12 doses in 7 cycles.
Prophylaxis for Pneumocystis jirovecci was required for all patients on both treatment arms.
Patients were allowed to crossover to a separate extension study to receive the opposite therapy if they had progressive disease.
They were followed for a median of 22.4 months.
Patient characteristics
According to the investigators, patient characteristics were well balanced between the arms.
The majority (60%) were male and the median age in both arms was 69. Most had an ECOG performance status of 0 or 1; 7% in the duvelisib arm and 10% in the ofatumumab arm had a performance status of 2.
Other patient characteristics in the duvelisib and ofatumumab arms, respectively, were:
- Time from initial diagnosis: 7.5 years, 6.7 years
- CLL/SLL, %: 97/5, 99/2
- Bulky disease: 46%, 45%
- Baseline lymphocyte counts: 38x109/L, 35x109/L
- Deletion 17p and/or TP53 mutation: 31%, 33%
- Median number of prior therapies: 2 in each arm
- Previous alkylating agent: 93%, 95%
- Previous monoclonal antibody: 78%, 83%
- Prior purine analog: 60%, 71%
Of the total patients enrolled, 158 patients in the duvelisib arm and 155 in the ofatumumab arm received treatment, for a median exposure of 50 weeks and 23 weeks, respectively.
Efficacy
In addition to the significantly improved overall PFS and ORR with duvelisib, further analysis revealed that PFS also improved for all predefined subgroups.
High-risk patients with deletion 17p/TP53 mutations also experienced a significant improvement in PFS with duvelisib of 12.7 months compared to 9.0 months with ofatumumab by IRC (P=0.0002).
The estimated probability of being progression-free for these patients at 6 and 12 moths was 73% and 55% with duvelisib and 63% and 30% with ofatumumab.
The investigators pointed out that duvelisib treatment was particularly effective in eliciting a lymph node response—85.0% compared to 15.7% with ofatumumab as assessed by IRC (P<0.0001).
Median overall survival was not reached in either arm. The 12-month probability of survival was 86% for both treatments.
Safety
Median treatment exposure was almost twice as long in the duvelisib arm because ofatumumab treatment was not allowed to exceed 12 doses as specified in the prescribing information.
The investigators explained this resulted in a longer adverse event (AE) reporting period for duvelisib.
One hundred twenty-four duvelisib-treated patients discontinued treatment, most commonly due to AEs (35%), disease progression (22%), subject withdrawal (8%), and death (8%).
All ofatumumab-treated patients discontinued treatment by the time of data cutoff, and 67% had completed treatment as per protocol. Others discontinued due to disease progression (20%), subject withdrawal (5%), and AEs (4%).
Eight (5%) duvelisib patients crossed over to ofatumumab therapy at the time of disease progression, and 89 (57%) ofatumumab-treated patients crossed over to duvelisib.
Nearly all patients in both arms experienced an AE.
The most common hematologic malignancies with duvelisib and ofatumumab, respectively, occurring in 10% or more patients were neutropenia (33%, 21%), anemia (23%, 10%), and thrombocytopenia (15%, 6%).
The most common nonhematologic AES with duvelisib were diarrhea (51%), pyrexia (29%), nausea (23%), and cough (21%).
With ofatumumab, the most common nonhematologic AES were infusion-related reaction (19%), cough (14%), and diarrhea, rash, and fatigue (12% each).
Grade 3 or greater AEs occurred in 87% of duvelisib-treated patients and 48% in the ofatumumab arm.
The most common grade 3 or greater events with duvelisib were neutropenia (30%), diarrhea (15%), pneumonia (14%), and anemia (13%).
With ofatumumab, only neutropenia (17%) of grade 3 or higher occurred in 10% or more patients.
Severe immune-related toxicities with duvelisib included colitis (12%) and pneumonitis, alanine transaminase (ALT) or aspartate transaminase (AST) increase (3% each). The events were managed with dose interruptions and steroid therapy for pneumonitis or colitis. All reported events resolved, and none was fatal.
Infectious AEs occurred more frequently with duvelisib, 69% compared to 43% in the ofatumumab arm. Pneumonia (18%) and upper respiratory tract infection (16%) were the most common events.
Three patients in the duvelisib arm and 1 in the ofatumumab arm contracted Pneumocystis jirovecii.
The most frequently reported serious AE was pneumonia (duvelisib 15%; ofatumumab 3%).
Nineteen fatal AEs occurred in patients on the duvelisib arm, 4 of which were related to the study drug: staphylococcal pneumonia (n = 2), sepsis (n=1), and general health deterioration (n = 1).
Seven fatal AEs occurred in patients on the ofatumumab arm, although none was attributed to ofatumumab.
The DUO trial was sponsored by Verastem Oncology and Infinity Pharmaceuticals , Inc.
Final analysis of the phase 3 DUO trial has shown monotherapy with oral duvelisib results in a statistically significant improvement in progression-free survival (PFS) and overall response rate (ORR) compared to monotherapy with ofatumumab for patients with relapsed or refractory chronic lymphocytic leukemia/small lympchocytic lymphoma (CLL/SLL).
PFS for all patients as assessed by Independent Review Committee (IRC) was a median 13.3 months with duvelisib compared to 9.9 months with ofatumumab (P<0.0001).
ORR was significantly higher with duvelisib, 74% compared to 45%, P<0.0001, regardless of deletion 17p status.
Duvelisib (Copiktra™) was recently approved by the U.S. Food and Drug Administration for CLL/SLL based in part on this head-to-head trial.
The investigators reported the results in Blood.
"The way we treat patients with CLL is changing rapidly as we move from standard chemotherapy-based approaches to more targeted therapies," said principal investigator Ian W. Flinn, MD, PhD, of Sarah Cannon Research Institute in Nashville.
"Based on these data, duvelisib may offer a new treatment option for patients who otherwise may have limited options."
Duvelisib is an oral, dual inhibitor of phosphoinositide 3-kinase (PI3K)-δ and -γ, which means it blocks the survival and proliferation of malignant B cells and also disrupts the recruitment and differentiation of T cells and macrophages within the tumor microenvironment.
Ofatumumab is a humanized anti-CD20 antibody with single-agent efficacy in refractory CLL. It is approved by the FDA as a treatment option in CLL.
Study design
Investigators randomized 319 relapsed or refractory CLL/SLL patients, 160 to the duvelisib arm and 159 to the ofatumumab arm.
Patients in the duvelisib arm self-administered 25 mg capsules twice daily continuously in 28-day cycles. They could take duvelisib for up to 18 cycles, until disease progression or unacceptable toxicity.
Ofatumumab-treated patients received infusions as approved in the product labeling for monotherapy in relapsed CLL. Dosing of ofatumumab could not exceed 12 doses in 7 cycles.
Prophylaxis for Pneumocystis jirovecci was required for all patients on both treatment arms.
Patients were allowed to crossover to a separate extension study to receive the opposite therapy if they had progressive disease.
They were followed for a median of 22.4 months.
Patient characteristics
According to the investigators, patient characteristics were well balanced between the arms.
The majority (60%) were male and the median age in both arms was 69. Most had an ECOG performance status of 0 or 1; 7% in the duvelisib arm and 10% in the ofatumumab arm had a performance status of 2.
Other patient characteristics in the duvelisib and ofatumumab arms, respectively, were:
- Time from initial diagnosis: 7.5 years, 6.7 years
- CLL/SLL, %: 97/5, 99/2
- Bulky disease: 46%, 45%
- Baseline lymphocyte counts: 38x109/L, 35x109/L
- Deletion 17p and/or TP53 mutation: 31%, 33%
- Median number of prior therapies: 2 in each arm
- Previous alkylating agent: 93%, 95%
- Previous monoclonal antibody: 78%, 83%
- Prior purine analog: 60%, 71%
Of the total patients enrolled, 158 patients in the duvelisib arm and 155 in the ofatumumab arm received treatment, for a median exposure of 50 weeks and 23 weeks, respectively.
Efficacy
In addition to the significantly improved overall PFS and ORR with duvelisib, further analysis revealed that PFS also improved for all predefined subgroups.
High-risk patients with deletion 17p/TP53 mutations also experienced a significant improvement in PFS with duvelisib of 12.7 months compared to 9.0 months with ofatumumab by IRC (P=0.0002).
The estimated probability of being progression-free for these patients at 6 and 12 moths was 73% and 55% with duvelisib and 63% and 30% with ofatumumab.
The investigators pointed out that duvelisib treatment was particularly effective in eliciting a lymph node response—85.0% compared to 15.7% with ofatumumab as assessed by IRC (P<0.0001).
Median overall survival was not reached in either arm. The 12-month probability of survival was 86% for both treatments.
Safety
Median treatment exposure was almost twice as long in the duvelisib arm because ofatumumab treatment was not allowed to exceed 12 doses as specified in the prescribing information.
The investigators explained this resulted in a longer adverse event (AE) reporting period for duvelisib.
One hundred twenty-four duvelisib-treated patients discontinued treatment, most commonly due to AEs (35%), disease progression (22%), subject withdrawal (8%), and death (8%).
All ofatumumab-treated patients discontinued treatment by the time of data cutoff, and 67% had completed treatment as per protocol. Others discontinued due to disease progression (20%), subject withdrawal (5%), and AEs (4%).
Eight (5%) duvelisib patients crossed over to ofatumumab therapy at the time of disease progression, and 89 (57%) ofatumumab-treated patients crossed over to duvelisib.
Nearly all patients in both arms experienced an AE.
The most common hematologic malignancies with duvelisib and ofatumumab, respectively, occurring in 10% or more patients were neutropenia (33%, 21%), anemia (23%, 10%), and thrombocytopenia (15%, 6%).
The most common nonhematologic AES with duvelisib were diarrhea (51%), pyrexia (29%), nausea (23%), and cough (21%).
With ofatumumab, the most common nonhematologic AES were infusion-related reaction (19%), cough (14%), and diarrhea, rash, and fatigue (12% each).
Grade 3 or greater AEs occurred in 87% of duvelisib-treated patients and 48% in the ofatumumab arm.
The most common grade 3 or greater events with duvelisib were neutropenia (30%), diarrhea (15%), pneumonia (14%), and anemia (13%).
With ofatumumab, only neutropenia (17%) of grade 3 or higher occurred in 10% or more patients.
Severe immune-related toxicities with duvelisib included colitis (12%) and pneumonitis, alanine transaminase (ALT) or aspartate transaminase (AST) increase (3% each). The events were managed with dose interruptions and steroid therapy for pneumonitis or colitis. All reported events resolved, and none was fatal.
Infectious AEs occurred more frequently with duvelisib, 69% compared to 43% in the ofatumumab arm. Pneumonia (18%) and upper respiratory tract infection (16%) were the most common events.
Three patients in the duvelisib arm and 1 in the ofatumumab arm contracted Pneumocystis jirovecii.
The most frequently reported serious AE was pneumonia (duvelisib 15%; ofatumumab 3%).
Nineteen fatal AEs occurred in patients on the duvelisib arm, 4 of which were related to the study drug: staphylococcal pneumonia (n = 2), sepsis (n=1), and general health deterioration (n = 1).
Seven fatal AEs occurred in patients on the ofatumumab arm, although none was attributed to ofatumumab.
The DUO trial was sponsored by Verastem Oncology and Infinity Pharmaceuticals , Inc.
5-year remission rates with combo prove durable in MCL
Long-term results of a phase 2 clinical trial of the lenalidomide and rituximab combination as first-line therapy for mantle cell lymphoma (MCL) show continued durable responses with manageable toxicities after 5 years.
With a median follow-up of 64 months, 21 of 33 patients with initial responses remained in durable, minimal residual disease (MRD)-negative remission following induction with lenalidomide and rituximab and maintenance with those same two agents for at least 3 years.
The patients with durable responses included five who opted to discontinue maintenance after 3 years, reported Jia Ruan, MD, PhD, of Cornell University in New York, and her colleagues.
“Our long-term data provide proof of concept that an outpatient-based induction and maintenance strategy free of conventional chemotherapy is effective, safe, and feasible as first-line therapy for MCL,” they wrote.
Their report was published in Blood.
In the multicenter, phase 2 single-arm study (NCT01472562), 38 patients with untreated MCL were enrolled and treated with lenalidomide 20 mg daily on days 1-21 of each 28-day cycle for 12 cycles during induction, followed by dose reduction to 15 mg during the maintenance phase.
Patients also received standard dose rituximab 375 mg/m2 weekly for 4 weeks during cycle 1, then once every other cycle.
Patients remained on treatment until disease progression, unacceptable toxicities, or study withdrawal. Patients who remained in remission after 3 years, based on routine surveillance CT scans, had the option to discontinue maintenance.
Results
Of the original 38 patients enrolled, 36 were evaluable for response, including 23 with a complete response (CR) and 10 with a partial response.
At the 64-month median follow-up, neither the median progression-free survival (PFS) nor duration of response had been reached.
Overall, 21 of the 33 patients with responses (64%) had ongoing responses, including six patients with responses beyond 6 years.
Estimated 3-year and 5-year PFS rates were 80.3% and 63.9%, respectively. Respective estimated 3- and 5-year overall survival rates were 89.5% and 77.4%.
Mantle cell lymphoma international prognostic index (MIPI) scores were not associated with either response or PFS rates, but patients with high-risk MIPI scores were significantly more likely to have worse overall survival (P=0.04).
Safety
Grade 3 or greater hematologic toxicities included neutropenia in 42% of patients in both induction and maintenance, anemia in 8% and 3%, thrombocytopenia in 11% and 5%, and febrile neutropenia in 3% and 5%.
Secondary primary malignancies occurred in six patients. These included five noninvasive skin cancers requiring only local therapy without the need for study interruption.
Two patients, including one with a skin cancer, died from the secondary malignancies, including one from Merkel cell carcinoma and one from pancreatic cancer.
“The efficacy and survival outcome observed in our study compared favorably to those reported with lenalidomide either as single agent, or in combination with rituximab in relapsed and refractory setting,” the investigators wrote, “lending support for prioritizing novel agents such as lenalidomide early in the treatment sequence, to compare to conventional chemotherapy-based approach.”
The study was supported in part by Celgene Corporation, a Clinical Translational Science Center grant, and the Lymphoma Foundation.
Long-term results of a phase 2 clinical trial of the lenalidomide and rituximab combination as first-line therapy for mantle cell lymphoma (MCL) show continued durable responses with manageable toxicities after 5 years.
With a median follow-up of 64 months, 21 of 33 patients with initial responses remained in durable, minimal residual disease (MRD)-negative remission following induction with lenalidomide and rituximab and maintenance with those same two agents for at least 3 years.
The patients with durable responses included five who opted to discontinue maintenance after 3 years, reported Jia Ruan, MD, PhD, of Cornell University in New York, and her colleagues.
“Our long-term data provide proof of concept that an outpatient-based induction and maintenance strategy free of conventional chemotherapy is effective, safe, and feasible as first-line therapy for MCL,” they wrote.
Their report was published in Blood.
In the multicenter, phase 2 single-arm study (NCT01472562), 38 patients with untreated MCL were enrolled and treated with lenalidomide 20 mg daily on days 1-21 of each 28-day cycle for 12 cycles during induction, followed by dose reduction to 15 mg during the maintenance phase.
Patients also received standard dose rituximab 375 mg/m2 weekly for 4 weeks during cycle 1, then once every other cycle.
Patients remained on treatment until disease progression, unacceptable toxicities, or study withdrawal. Patients who remained in remission after 3 years, based on routine surveillance CT scans, had the option to discontinue maintenance.
Results
Of the original 38 patients enrolled, 36 were evaluable for response, including 23 with a complete response (CR) and 10 with a partial response.
At the 64-month median follow-up, neither the median progression-free survival (PFS) nor duration of response had been reached.
Overall, 21 of the 33 patients with responses (64%) had ongoing responses, including six patients with responses beyond 6 years.
Estimated 3-year and 5-year PFS rates were 80.3% and 63.9%, respectively. Respective estimated 3- and 5-year overall survival rates were 89.5% and 77.4%.
Mantle cell lymphoma international prognostic index (MIPI) scores were not associated with either response or PFS rates, but patients with high-risk MIPI scores were significantly more likely to have worse overall survival (P=0.04).
Safety
Grade 3 or greater hematologic toxicities included neutropenia in 42% of patients in both induction and maintenance, anemia in 8% and 3%, thrombocytopenia in 11% and 5%, and febrile neutropenia in 3% and 5%.
Secondary primary malignancies occurred in six patients. These included five noninvasive skin cancers requiring only local therapy without the need for study interruption.
Two patients, including one with a skin cancer, died from the secondary malignancies, including one from Merkel cell carcinoma and one from pancreatic cancer.
“The efficacy and survival outcome observed in our study compared favorably to those reported with lenalidomide either as single agent, or in combination with rituximab in relapsed and refractory setting,” the investigators wrote, “lending support for prioritizing novel agents such as lenalidomide early in the treatment sequence, to compare to conventional chemotherapy-based approach.”
The study was supported in part by Celgene Corporation, a Clinical Translational Science Center grant, and the Lymphoma Foundation.
Long-term results of a phase 2 clinical trial of the lenalidomide and rituximab combination as first-line therapy for mantle cell lymphoma (MCL) show continued durable responses with manageable toxicities after 5 years.
With a median follow-up of 64 months, 21 of 33 patients with initial responses remained in durable, minimal residual disease (MRD)-negative remission following induction with lenalidomide and rituximab and maintenance with those same two agents for at least 3 years.
The patients with durable responses included five who opted to discontinue maintenance after 3 years, reported Jia Ruan, MD, PhD, of Cornell University in New York, and her colleagues.
“Our long-term data provide proof of concept that an outpatient-based induction and maintenance strategy free of conventional chemotherapy is effective, safe, and feasible as first-line therapy for MCL,” they wrote.
Their report was published in Blood.
In the multicenter, phase 2 single-arm study (NCT01472562), 38 patients with untreated MCL were enrolled and treated with lenalidomide 20 mg daily on days 1-21 of each 28-day cycle for 12 cycles during induction, followed by dose reduction to 15 mg during the maintenance phase.
Patients also received standard dose rituximab 375 mg/m2 weekly for 4 weeks during cycle 1, then once every other cycle.
Patients remained on treatment until disease progression, unacceptable toxicities, or study withdrawal. Patients who remained in remission after 3 years, based on routine surveillance CT scans, had the option to discontinue maintenance.
Results
Of the original 38 patients enrolled, 36 were evaluable for response, including 23 with a complete response (CR) and 10 with a partial response.
At the 64-month median follow-up, neither the median progression-free survival (PFS) nor duration of response had been reached.
Overall, 21 of the 33 patients with responses (64%) had ongoing responses, including six patients with responses beyond 6 years.
Estimated 3-year and 5-year PFS rates were 80.3% and 63.9%, respectively. Respective estimated 3- and 5-year overall survival rates were 89.5% and 77.4%.
Mantle cell lymphoma international prognostic index (MIPI) scores were not associated with either response or PFS rates, but patients with high-risk MIPI scores were significantly more likely to have worse overall survival (P=0.04).
Safety
Grade 3 or greater hematologic toxicities included neutropenia in 42% of patients in both induction and maintenance, anemia in 8% and 3%, thrombocytopenia in 11% and 5%, and febrile neutropenia in 3% and 5%.
Secondary primary malignancies occurred in six patients. These included five noninvasive skin cancers requiring only local therapy without the need for study interruption.
Two patients, including one with a skin cancer, died from the secondary malignancies, including one from Merkel cell carcinoma and one from pancreatic cancer.
“The efficacy and survival outcome observed in our study compared favorably to those reported with lenalidomide either as single agent, or in combination with rituximab in relapsed and refractory setting,” the investigators wrote, “lending support for prioritizing novel agents such as lenalidomide early in the treatment sequence, to compare to conventional chemotherapy-based approach.”
The study was supported in part by Celgene Corporation, a Clinical Translational Science Center grant, and the Lymphoma Foundation.
Brentuximab vendotin plus CHP meets PFS endpoint in ECHELON-2
Takeda Pharmaceuticals and Seattle Genetics announced top-line results in the ECHELON-2 phase 3 trial of brentuximab vedotin plus CHP (cyclophosphamide, doxorubicin, prednisone) in the frontline treatment of CD-30 expressing peripheral T-cell lymphoma (PTCL).
The combination achieved statistically significant improvement in progression-free survival (PFS), compared with the control arm of standard chemotherapy alone using cyclophosphamide, doxorubicin, vincristine, and prednisone (CHOP). The PFS was assessed by an Independent Review Facility (hazard ratio, 0.71; P = .0110).
The combination of brentuximab vedotin plus CHP also outperformed CHOP in overall survival, a secondary endpoint of the trial (hazard ratio, 0.66, P = .0244), according to the drug sponsors.
Full results of ECHELON-2 will be presented in December 2018 at the annual meeting of the American Society of Hematology, according to the announcement from Seattle Genetics and Takeda.
Takeda Pharmaceuticals and Seattle Genetics announced top-line results in the ECHELON-2 phase 3 trial of brentuximab vedotin plus CHP (cyclophosphamide, doxorubicin, prednisone) in the frontline treatment of CD-30 expressing peripheral T-cell lymphoma (PTCL).
The combination achieved statistically significant improvement in progression-free survival (PFS), compared with the control arm of standard chemotherapy alone using cyclophosphamide, doxorubicin, vincristine, and prednisone (CHOP). The PFS was assessed by an Independent Review Facility (hazard ratio, 0.71; P = .0110).
The combination of brentuximab vedotin plus CHP also outperformed CHOP in overall survival, a secondary endpoint of the trial (hazard ratio, 0.66, P = .0244), according to the drug sponsors.
Full results of ECHELON-2 will be presented in December 2018 at the annual meeting of the American Society of Hematology, according to the announcement from Seattle Genetics and Takeda.
Takeda Pharmaceuticals and Seattle Genetics announced top-line results in the ECHELON-2 phase 3 trial of brentuximab vedotin plus CHP (cyclophosphamide, doxorubicin, prednisone) in the frontline treatment of CD-30 expressing peripheral T-cell lymphoma (PTCL).
The combination achieved statistically significant improvement in progression-free survival (PFS), compared with the control arm of standard chemotherapy alone using cyclophosphamide, doxorubicin, vincristine, and prednisone (CHOP). The PFS was assessed by an Independent Review Facility (hazard ratio, 0.71; P = .0110).
The combination of brentuximab vedotin plus CHP also outperformed CHOP in overall survival, a secondary endpoint of the trial (hazard ratio, 0.66, P = .0244), according to the drug sponsors.
Full results of ECHELON-2 will be presented in December 2018 at the annual meeting of the American Society of Hematology, according to the announcement from Seattle Genetics and Takeda.
Ground-breaking therapy comes with distinct challenges
NEW YORK—Two chimeric antigen receptor (CAR) T-cell therapies—axicabtagene ciloleucel (Yescarta ®) and tisagenlecleucel (Kymriah™)—are already approved in B-cell lymphoma by the U.S. Food and Drug Administration.
A third, lisocabtagene maraleucel, will most likely be approved before too long.
Despite differences in their costimulatory molecules, persistence, efficacy, and toxicity profiles, they all have high overall response rates and a fall-out of response during the first 3 to 6 months.
Longer-term follow-up is necessary to determine whether CAR T-cell therapy is actually curative.
“But based on the way things are looking,” said Reem Karmali, MD, of Robert H. Lurie Comprehensive Cancer Center of Northwestern University, “it seems this might be a realistic expectation.”
“CAR T-cell therapy is clearly effective and has been a ground-breaking form of therapy,” she said, “but there seems to be two sides to the coin. There are a number of challenges that we face with CAR T-cell therapy.”
Dr. Karmali outlined those challenges in a presentation at the NCCN 13th Annual Congress: Hematologic Malignancies.
Patient selection
One of the biggest challenges, according to Dr. Karmali, is patient selection.
First, patients must have an adequate hematopoietic reserve to ensure successful CAR T-cell manufacture.
Dr. Karmali referred to the JULIET study, in which 7% of patients failed the manufacturing process due to insufficient apheresis.
Second, the patient’s disease must be stable enough to make it through the time it takes to manufacturing the CAR product, which is typically 2 to 4 weeks.
Third, the patient’s overall health must be good enough to tolerate CAR T toxicities. "The patient needs good major organ function as well as preserved neurologic function,” she explained, “to withstand the unique toxicities that come with CAR T-cell therapy, specifically CRS [cytokine release syndrome] and neurotoxicity.”
Toxicities
The major toxicities are CRS and CAR‑T‑cell‑related encephalopathy syndrome (CRES).
Dr. Karmali pointed out there is also a theoretical risk of insertional oncogenesis from viral transduction used in manufacturing the T cells, and an off-tumor on target-effect that can result in B-cell aplasia and hypogammaglobulinemia.
The profiles of inflammatory cytokines and inflammation markers differ for each CAR construct and are driven in different ways. However, IL-6 is an important mediator for CRS and IL-6 receptor blockade is effective in managing the toxicity.
The drug of choice is tocilizumab, Dr. Karmali said, and for patients who are refractory to tocilizumab, siltuximab can be used.
“Steroids are extremely useful for CRS,” she added, “because they hold down inflammation and prevent immune activation.”
Steroids are also the mainstay for managing the neurotoxicity of CAR T-cell therapy because they help stabilize the blood-brain barrier.
“It’s important to make a note,” she said, “that there actually have been a number of analyses that have looked at the impact of using IL-6 receptor blockade and steroids on CAR T-cell expansion and persistence and there really doesn’t seem to be an impact.”
“So we really ought to use these quite liberally for grade 2 or higher toxicity without worrying about dampening the effect of CAR T-cell therapy,” she emphasized.
The Lee grading criteria for the management of CRS and the CTCAE 4.03 and CARTOX-10 for CRES provide guidance in assessing and managing the toxicities.
Future directions
Dr. Karmali outlined a few new directions to address the challenges with CAR T-cell therapy, such as switchable CARs that can be turned on or off and potentially improve safety; development of new constructs that may improve homing; improvement in persistence; use of combination and sequencing strategies; and improved antigen selection that may be effective with other lymphoproliferative diseases.
“A provocative question is whether CAR T-cell therapy can actually replace autologous stem cell transplant as second-line therapy,” she said. “This is actually being actively evaluated in a number of clinical trials including ZUMA-7 (NCT03391466).”
“I think another provocative question is whether CAR T-cell therapy can be used as consolidation in CR1 [first complete remission],” she added.
The rationale for using CAR Ts as either a replacement for autologous stem cell transplant or in CR1 is that there may be minimal residual disease present that would be enough to elicit a CAR T-cell effect, she explained.
“Ultimately, one envisions the following paradigm for the treatment of lymphomas across the board,” Dr. Karmali concluded.
“Specifically, chemotherapy with a targeted agent for rapid cytoreduction, followed by CAR T-cell consolidation in combination with either other cellular therapies or immunotherapy as a means of eradicating the minimal residual disease and ensuring a pathway to cure.”
NEW YORK—Two chimeric antigen receptor (CAR) T-cell therapies—axicabtagene ciloleucel (Yescarta ®) and tisagenlecleucel (Kymriah™)—are already approved in B-cell lymphoma by the U.S. Food and Drug Administration.
A third, lisocabtagene maraleucel, will most likely be approved before too long.
Despite differences in their costimulatory molecules, persistence, efficacy, and toxicity profiles, they all have high overall response rates and a fall-out of response during the first 3 to 6 months.
Longer-term follow-up is necessary to determine whether CAR T-cell therapy is actually curative.
“But based on the way things are looking,” said Reem Karmali, MD, of Robert H. Lurie Comprehensive Cancer Center of Northwestern University, “it seems this might be a realistic expectation.”
“CAR T-cell therapy is clearly effective and has been a ground-breaking form of therapy,” she said, “but there seems to be two sides to the coin. There are a number of challenges that we face with CAR T-cell therapy.”
Dr. Karmali outlined those challenges in a presentation at the NCCN 13th Annual Congress: Hematologic Malignancies.
Patient selection
One of the biggest challenges, according to Dr. Karmali, is patient selection.
First, patients must have an adequate hematopoietic reserve to ensure successful CAR T-cell manufacture.
Dr. Karmali referred to the JULIET study, in which 7% of patients failed the manufacturing process due to insufficient apheresis.
Second, the patient’s disease must be stable enough to make it through the time it takes to manufacturing the CAR product, which is typically 2 to 4 weeks.
Third, the patient’s overall health must be good enough to tolerate CAR T toxicities. "The patient needs good major organ function as well as preserved neurologic function,” she explained, “to withstand the unique toxicities that come with CAR T-cell therapy, specifically CRS [cytokine release syndrome] and neurotoxicity.”
Toxicities
The major toxicities are CRS and CAR‑T‑cell‑related encephalopathy syndrome (CRES).
Dr. Karmali pointed out there is also a theoretical risk of insertional oncogenesis from viral transduction used in manufacturing the T cells, and an off-tumor on target-effect that can result in B-cell aplasia and hypogammaglobulinemia.
The profiles of inflammatory cytokines and inflammation markers differ for each CAR construct and are driven in different ways. However, IL-6 is an important mediator for CRS and IL-6 receptor blockade is effective in managing the toxicity.
The drug of choice is tocilizumab, Dr. Karmali said, and for patients who are refractory to tocilizumab, siltuximab can be used.
“Steroids are extremely useful for CRS,” she added, “because they hold down inflammation and prevent immune activation.”
Steroids are also the mainstay for managing the neurotoxicity of CAR T-cell therapy because they help stabilize the blood-brain barrier.
“It’s important to make a note,” she said, “that there actually have been a number of analyses that have looked at the impact of using IL-6 receptor blockade and steroids on CAR T-cell expansion and persistence and there really doesn’t seem to be an impact.”
“So we really ought to use these quite liberally for grade 2 or higher toxicity without worrying about dampening the effect of CAR T-cell therapy,” she emphasized.
The Lee grading criteria for the management of CRS and the CTCAE 4.03 and CARTOX-10 for CRES provide guidance in assessing and managing the toxicities.
Future directions
Dr. Karmali outlined a few new directions to address the challenges with CAR T-cell therapy, such as switchable CARs that can be turned on or off and potentially improve safety; development of new constructs that may improve homing; improvement in persistence; use of combination and sequencing strategies; and improved antigen selection that may be effective with other lymphoproliferative diseases.
“A provocative question is whether CAR T-cell therapy can actually replace autologous stem cell transplant as second-line therapy,” she said. “This is actually being actively evaluated in a number of clinical trials including ZUMA-7 (NCT03391466).”
“I think another provocative question is whether CAR T-cell therapy can be used as consolidation in CR1 [first complete remission],” she added.
The rationale for using CAR Ts as either a replacement for autologous stem cell transplant or in CR1 is that there may be minimal residual disease present that would be enough to elicit a CAR T-cell effect, she explained.
“Ultimately, one envisions the following paradigm for the treatment of lymphomas across the board,” Dr. Karmali concluded.
“Specifically, chemotherapy with a targeted agent for rapid cytoreduction, followed by CAR T-cell consolidation in combination with either other cellular therapies or immunotherapy as a means of eradicating the minimal residual disease and ensuring a pathway to cure.”
NEW YORK—Two chimeric antigen receptor (CAR) T-cell therapies—axicabtagene ciloleucel (Yescarta ®) and tisagenlecleucel (Kymriah™)—are already approved in B-cell lymphoma by the U.S. Food and Drug Administration.
A third, lisocabtagene maraleucel, will most likely be approved before too long.
Despite differences in their costimulatory molecules, persistence, efficacy, and toxicity profiles, they all have high overall response rates and a fall-out of response during the first 3 to 6 months.
Longer-term follow-up is necessary to determine whether CAR T-cell therapy is actually curative.
“But based on the way things are looking,” said Reem Karmali, MD, of Robert H. Lurie Comprehensive Cancer Center of Northwestern University, “it seems this might be a realistic expectation.”
“CAR T-cell therapy is clearly effective and has been a ground-breaking form of therapy,” she said, “but there seems to be two sides to the coin. There are a number of challenges that we face with CAR T-cell therapy.”
Dr. Karmali outlined those challenges in a presentation at the NCCN 13th Annual Congress: Hematologic Malignancies.
Patient selection
One of the biggest challenges, according to Dr. Karmali, is patient selection.
First, patients must have an adequate hematopoietic reserve to ensure successful CAR T-cell manufacture.
Dr. Karmali referred to the JULIET study, in which 7% of patients failed the manufacturing process due to insufficient apheresis.
Second, the patient’s disease must be stable enough to make it through the time it takes to manufacturing the CAR product, which is typically 2 to 4 weeks.
Third, the patient’s overall health must be good enough to tolerate CAR T toxicities. "The patient needs good major organ function as well as preserved neurologic function,” she explained, “to withstand the unique toxicities that come with CAR T-cell therapy, specifically CRS [cytokine release syndrome] and neurotoxicity.”
Toxicities
The major toxicities are CRS and CAR‑T‑cell‑related encephalopathy syndrome (CRES).
Dr. Karmali pointed out there is also a theoretical risk of insertional oncogenesis from viral transduction used in manufacturing the T cells, and an off-tumor on target-effect that can result in B-cell aplasia and hypogammaglobulinemia.
The profiles of inflammatory cytokines and inflammation markers differ for each CAR construct and are driven in different ways. However, IL-6 is an important mediator for CRS and IL-6 receptor blockade is effective in managing the toxicity.
The drug of choice is tocilizumab, Dr. Karmali said, and for patients who are refractory to tocilizumab, siltuximab can be used.
“Steroids are extremely useful for CRS,” she added, “because they hold down inflammation and prevent immune activation.”
Steroids are also the mainstay for managing the neurotoxicity of CAR T-cell therapy because they help stabilize the blood-brain barrier.
“It’s important to make a note,” she said, “that there actually have been a number of analyses that have looked at the impact of using IL-6 receptor blockade and steroids on CAR T-cell expansion and persistence and there really doesn’t seem to be an impact.”
“So we really ought to use these quite liberally for grade 2 or higher toxicity without worrying about dampening the effect of CAR T-cell therapy,” she emphasized.
The Lee grading criteria for the management of CRS and the CTCAE 4.03 and CARTOX-10 for CRES provide guidance in assessing and managing the toxicities.
Future directions
Dr. Karmali outlined a few new directions to address the challenges with CAR T-cell therapy, such as switchable CARs that can be turned on or off and potentially improve safety; development of new constructs that may improve homing; improvement in persistence; use of combination and sequencing strategies; and improved antigen selection that may be effective with other lymphoproliferative diseases.
“A provocative question is whether CAR T-cell therapy can actually replace autologous stem cell transplant as second-line therapy,” she said. “This is actually being actively evaluated in a number of clinical trials including ZUMA-7 (NCT03391466).”
“I think another provocative question is whether CAR T-cell therapy can be used as consolidation in CR1 [first complete remission],” she added.
The rationale for using CAR Ts as either a replacement for autologous stem cell transplant or in CR1 is that there may be minimal residual disease present that would be enough to elicit a CAR T-cell effect, she explained.
“Ultimately, one envisions the following paradigm for the treatment of lymphomas across the board,” Dr. Karmali concluded.
“Specifically, chemotherapy with a targeted agent for rapid cytoreduction, followed by CAR T-cell consolidation in combination with either other cellular therapies or immunotherapy as a means of eradicating the minimal residual disease and ensuring a pathway to cure.”
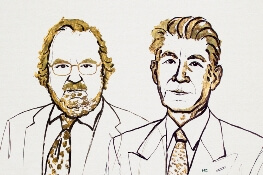
Two immunologists receive Nobel Prize in medicine
Two immunologists have been awarded the Nobel Prize in Physiology or Medicine for discoveries that represent a “paradigmatic shift in the fight against cancer,” the Nobel committee said.
James P. Allison, PhD, of MD Anderson Cancer Center, and Tasuku Honjo, MD, PhD, of Kyoto University, shared the prize for their discovery of cancer therapies that work by inhibiting negative immune regulation.
Dr. Allison studied the protein CTLA-4 found on T cells, which acts as a T-cell brake, and Dr. Honjo discovered a protein on immune cells called PD-1 that also acts as a T-cell brake.
In addition to sharing the honor, the scientists will split the 9 million Swedish kronor ($1.01 million) that comes with the prize.
Drs. Allison and Honjo, working in parallel, pursued different strategies for inhibiting the brakes on the immune system. Both strategies produced effective checkpoint inhibitors in the treatment of cancer.
James P. Allison
Dr. Allison was one of several scientists during the 1990s who noticed that CTLA-4 functions as a brake on T cells. Unlike other scientists, however, he set out to investigate whether blocking CTLA-4 with an antibody he had already developed could release the brake on the immune system.
The antibody had “spectacular” effects in curing mice with cancer. Despite little interest from the pharmaceutical industry, Dr. Allison continued efforts to develop the antibody therapy for humans.
The antibody turned out to be ipilimumab, which was approved in 2011 by the U.S. Food and Drug Administration (FDA) for the treatment of advanced melanoma.
Tasuko Honjo
A few years prior to Dr. Allison’s finding, Dr. Honjo discovered PD-1 and set out to determine its function. PD-1 also operates as a T-cell brake, but it uses a different mechanism than does CTLA-4.
Dr. Honjo and others demonstrated in animal experiments that PD-1 blockade could be an effective anticancer therapy. Over the years he demonstrated the efficacy of targeting PD-1 in different types of human cancers.
The first two PD-1 checkpoint inhibitors—pembrolizumab and nivolumab—were approved by the FDA in 2014 for the treatment of melanoma.
Nivolumab is also approved to treat classical Hodgkin lymphoma (HL), non-small cell lung cancer (NSCLC), small cell lung cancer, squamous cell carcinoma of the head and neck, colorectal cancer, hepatocellular carcinoma, renal cell carcinoma, urothelial carcinoma, and microsatellite instability-high or mismatch repair deficient colorectal cancer.
Pembrolizumab is also approved to treat primary mediastinal large B-cell lymphoma, advanced NSCLC, classical HL, advanced gastric cancer, advanced cervical cancer, head and neck squamous cell cancer, advanced urothelial bladder cancer, and microsatellite instability-high cancer.
And targeting both CTLA-4 and PD-1 in combination therapy together may prove to be even more effective in eliminating cancer cells than either strategy alone, as is being demonstrated in patients with melanoma.
The Nobel organization wrote in a press release, “Checkpoint therapy has now revolutionized cancer treatment and has fundamentally changed the way we view how cancer can be managed.”
Two immunologists have been awarded the Nobel Prize in Physiology or Medicine for discoveries that represent a “paradigmatic shift in the fight against cancer,” the Nobel committee said.
James P. Allison, PhD, of MD Anderson Cancer Center, and Tasuku Honjo, MD, PhD, of Kyoto University, shared the prize for their discovery of cancer therapies that work by inhibiting negative immune regulation.
Dr. Allison studied the protein CTLA-4 found on T cells, which acts as a T-cell brake, and Dr. Honjo discovered a protein on immune cells called PD-1 that also acts as a T-cell brake.
In addition to sharing the honor, the scientists will split the 9 million Swedish kronor ($1.01 million) that comes with the prize.
Drs. Allison and Honjo, working in parallel, pursued different strategies for inhibiting the brakes on the immune system. Both strategies produced effective checkpoint inhibitors in the treatment of cancer.
James P. Allison
Dr. Allison was one of several scientists during the 1990s who noticed that CTLA-4 functions as a brake on T cells. Unlike other scientists, however, he set out to investigate whether blocking CTLA-4 with an antibody he had already developed could release the brake on the immune system.
The antibody had “spectacular” effects in curing mice with cancer. Despite little interest from the pharmaceutical industry, Dr. Allison continued efforts to develop the antibody therapy for humans.
The antibody turned out to be ipilimumab, which was approved in 2011 by the U.S. Food and Drug Administration (FDA) for the treatment of advanced melanoma.
Tasuko Honjo
A few years prior to Dr. Allison’s finding, Dr. Honjo discovered PD-1 and set out to determine its function. PD-1 also operates as a T-cell brake, but it uses a different mechanism than does CTLA-4.
Dr. Honjo and others demonstrated in animal experiments that PD-1 blockade could be an effective anticancer therapy. Over the years he demonstrated the efficacy of targeting PD-1 in different types of human cancers.
The first two PD-1 checkpoint inhibitors—pembrolizumab and nivolumab—were approved by the FDA in 2014 for the treatment of melanoma.
Nivolumab is also approved to treat classical Hodgkin lymphoma (HL), non-small cell lung cancer (NSCLC), small cell lung cancer, squamous cell carcinoma of the head and neck, colorectal cancer, hepatocellular carcinoma, renal cell carcinoma, urothelial carcinoma, and microsatellite instability-high or mismatch repair deficient colorectal cancer.
Pembrolizumab is also approved to treat primary mediastinal large B-cell lymphoma, advanced NSCLC, classical HL, advanced gastric cancer, advanced cervical cancer, head and neck squamous cell cancer, advanced urothelial bladder cancer, and microsatellite instability-high cancer.
And targeting both CTLA-4 and PD-1 in combination therapy together may prove to be even more effective in eliminating cancer cells than either strategy alone, as is being demonstrated in patients with melanoma.
The Nobel organization wrote in a press release, “Checkpoint therapy has now revolutionized cancer treatment and has fundamentally changed the way we view how cancer can be managed.”
Two immunologists have been awarded the Nobel Prize in Physiology or Medicine for discoveries that represent a “paradigmatic shift in the fight against cancer,” the Nobel committee said.
James P. Allison, PhD, of MD Anderson Cancer Center, and Tasuku Honjo, MD, PhD, of Kyoto University, shared the prize for their discovery of cancer therapies that work by inhibiting negative immune regulation.
Dr. Allison studied the protein CTLA-4 found on T cells, which acts as a T-cell brake, and Dr. Honjo discovered a protein on immune cells called PD-1 that also acts as a T-cell brake.
In addition to sharing the honor, the scientists will split the 9 million Swedish kronor ($1.01 million) that comes with the prize.
Drs. Allison and Honjo, working in parallel, pursued different strategies for inhibiting the brakes on the immune system. Both strategies produced effective checkpoint inhibitors in the treatment of cancer.
James P. Allison
Dr. Allison was one of several scientists during the 1990s who noticed that CTLA-4 functions as a brake on T cells. Unlike other scientists, however, he set out to investigate whether blocking CTLA-4 with an antibody he had already developed could release the brake on the immune system.
The antibody had “spectacular” effects in curing mice with cancer. Despite little interest from the pharmaceutical industry, Dr. Allison continued efforts to develop the antibody therapy for humans.
The antibody turned out to be ipilimumab, which was approved in 2011 by the U.S. Food and Drug Administration (FDA) for the treatment of advanced melanoma.
Tasuko Honjo
A few years prior to Dr. Allison’s finding, Dr. Honjo discovered PD-1 and set out to determine its function. PD-1 also operates as a T-cell brake, but it uses a different mechanism than does CTLA-4.
Dr. Honjo and others demonstrated in animal experiments that PD-1 blockade could be an effective anticancer therapy. Over the years he demonstrated the efficacy of targeting PD-1 in different types of human cancers.
The first two PD-1 checkpoint inhibitors—pembrolizumab and nivolumab—were approved by the FDA in 2014 for the treatment of melanoma.
Nivolumab is also approved to treat classical Hodgkin lymphoma (HL), non-small cell lung cancer (NSCLC), small cell lung cancer, squamous cell carcinoma of the head and neck, colorectal cancer, hepatocellular carcinoma, renal cell carcinoma, urothelial carcinoma, and microsatellite instability-high or mismatch repair deficient colorectal cancer.
Pembrolizumab is also approved to treat primary mediastinal large B-cell lymphoma, advanced NSCLC, classical HL, advanced gastric cancer, advanced cervical cancer, head and neck squamous cell cancer, advanced urothelial bladder cancer, and microsatellite instability-high cancer.
And targeting both CTLA-4 and PD-1 in combination therapy together may prove to be even more effective in eliminating cancer cells than either strategy alone, as is being demonstrated in patients with melanoma.
The Nobel organization wrote in a press release, “Checkpoint therapy has now revolutionized cancer treatment and has fundamentally changed the way we view how cancer can be managed.”
Brentuximab improves survival in older HL patients
Older patients with untreated Hodgkin lymphoma (HL) can achieve significantly improved survival by adding brentuximab vedotin to their treatment before and after standard chemotherapy, a recent study found.
In patients with low comorbidity scores, responses were even more robust, reported lead author Andrew M. Evens, DO, of the Rutgers Cancer Institute of New Jersey, and colleagues.
“Causes of poor outcomes for older patients with HL are not fully understood but have been attributed to a combination of factors, including presence of comorbidities, poorer performance status, disease and biological differences, inability to tolerate chemotherapy at the full dose, and increased treatment-related toxicities,” the authors wrote in the Journal of Clinical Oncology.
The primary goal of the study was to improve outcomes for untreated, older patients, a group that’s historically been a difficult-to-treat patient population.
The phase 2 trial included 48 HL patients with a median age of 69 (range, 60 – 88).
All patients underwent geriatric assessment for comorbidities and loss of activities of daily living.
Treatment consisted of two doses of brentuximab followed by six cycles of doxorubicin, vinblastine, and dacarbazine (AVD), then four more doses of brentuximab (consolidation doses).
The primary endpoint was complete remission at completion of AVD.
Secondary outcomes included overall response rate, 2-year progression-free survival, 2-year overall survival, and safety.
Just over half the patients (52%) completed all cycles of therapy, and almost three quarters (73%) received at least one consolidation dose of brentuximab.
Among the first 23 evaluable patients, both the complete remission rate and overall response rate were 96%. Intention-to-treat survival rates for all 48 patients were 84% for 2-year progression-free survival and 93% for 2-year overall survival.
Historical 2-year progression-free survival rates in similar older patients is poor, at 50%, so the progression-free survival rate of 84% in this study represents a significant improvement.
Of note, patients with fewer comorbidities and without loss of instrumental activities of daily living showed more robust responses.
Patients with Cumulative Illness Rating Scale for Geriatrics (CIRS-G) comorbidity scores of less than 10 had a 2-year progression-free survival rate of 100% versus 45% for those with higher scores.
Similarly, patients without loss of instrumental activities achieved a progression-free survival rate of 94% versus 25% for those who had lost some instrumental activities.
Grade 3 or 4 adverse events occurred in 42% of patients, with neutropenia being the most common (44%).
“This study represents among the best-reported outcomes to date for untreated older patients with HL,” the investigators concluded.
Seattle Genetics supported the investigator-initiated trial.
Older patients with untreated Hodgkin lymphoma (HL) can achieve significantly improved survival by adding brentuximab vedotin to their treatment before and after standard chemotherapy, a recent study found.
In patients with low comorbidity scores, responses were even more robust, reported lead author Andrew M. Evens, DO, of the Rutgers Cancer Institute of New Jersey, and colleagues.
“Causes of poor outcomes for older patients with HL are not fully understood but have been attributed to a combination of factors, including presence of comorbidities, poorer performance status, disease and biological differences, inability to tolerate chemotherapy at the full dose, and increased treatment-related toxicities,” the authors wrote in the Journal of Clinical Oncology.
The primary goal of the study was to improve outcomes for untreated, older patients, a group that’s historically been a difficult-to-treat patient population.
The phase 2 trial included 48 HL patients with a median age of 69 (range, 60 – 88).
All patients underwent geriatric assessment for comorbidities and loss of activities of daily living.
Treatment consisted of two doses of brentuximab followed by six cycles of doxorubicin, vinblastine, and dacarbazine (AVD), then four more doses of brentuximab (consolidation doses).
The primary endpoint was complete remission at completion of AVD.
Secondary outcomes included overall response rate, 2-year progression-free survival, 2-year overall survival, and safety.
Just over half the patients (52%) completed all cycles of therapy, and almost three quarters (73%) received at least one consolidation dose of brentuximab.
Among the first 23 evaluable patients, both the complete remission rate and overall response rate were 96%. Intention-to-treat survival rates for all 48 patients were 84% for 2-year progression-free survival and 93% for 2-year overall survival.
Historical 2-year progression-free survival rates in similar older patients is poor, at 50%, so the progression-free survival rate of 84% in this study represents a significant improvement.
Of note, patients with fewer comorbidities and without loss of instrumental activities of daily living showed more robust responses.
Patients with Cumulative Illness Rating Scale for Geriatrics (CIRS-G) comorbidity scores of less than 10 had a 2-year progression-free survival rate of 100% versus 45% for those with higher scores.
Similarly, patients without loss of instrumental activities achieved a progression-free survival rate of 94% versus 25% for those who had lost some instrumental activities.
Grade 3 or 4 adverse events occurred in 42% of patients, with neutropenia being the most common (44%).
“This study represents among the best-reported outcomes to date for untreated older patients with HL,” the investigators concluded.
Seattle Genetics supported the investigator-initiated trial.
Older patients with untreated Hodgkin lymphoma (HL) can achieve significantly improved survival by adding brentuximab vedotin to their treatment before and after standard chemotherapy, a recent study found.
In patients with low comorbidity scores, responses were even more robust, reported lead author Andrew M. Evens, DO, of the Rutgers Cancer Institute of New Jersey, and colleagues.
“Causes of poor outcomes for older patients with HL are not fully understood but have been attributed to a combination of factors, including presence of comorbidities, poorer performance status, disease and biological differences, inability to tolerate chemotherapy at the full dose, and increased treatment-related toxicities,” the authors wrote in the Journal of Clinical Oncology.
The primary goal of the study was to improve outcomes for untreated, older patients, a group that’s historically been a difficult-to-treat patient population.
The phase 2 trial included 48 HL patients with a median age of 69 (range, 60 – 88).
All patients underwent geriatric assessment for comorbidities and loss of activities of daily living.
Treatment consisted of two doses of brentuximab followed by six cycles of doxorubicin, vinblastine, and dacarbazine (AVD), then four more doses of brentuximab (consolidation doses).
The primary endpoint was complete remission at completion of AVD.
Secondary outcomes included overall response rate, 2-year progression-free survival, 2-year overall survival, and safety.
Just over half the patients (52%) completed all cycles of therapy, and almost three quarters (73%) received at least one consolidation dose of brentuximab.
Among the first 23 evaluable patients, both the complete remission rate and overall response rate were 96%. Intention-to-treat survival rates for all 48 patients were 84% for 2-year progression-free survival and 93% for 2-year overall survival.
Historical 2-year progression-free survival rates in similar older patients is poor, at 50%, so the progression-free survival rate of 84% in this study represents a significant improvement.
Of note, patients with fewer comorbidities and without loss of instrumental activities of daily living showed more robust responses.
Patients with Cumulative Illness Rating Scale for Geriatrics (CIRS-G) comorbidity scores of less than 10 had a 2-year progression-free survival rate of 100% versus 45% for those with higher scores.
Similarly, patients without loss of instrumental activities achieved a progression-free survival rate of 94% versus 25% for those who had lost some instrumental activities.
Grade 3 or 4 adverse events occurred in 42% of patients, with neutropenia being the most common (44%).
“This study represents among the best-reported outcomes to date for untreated older patients with HL,” the investigators concluded.
Seattle Genetics supported the investigator-initiated trial.
FDA lifts partial hold on tazemetostat trials
The U.S. Food and Drug Administration has lifted the partial clinical hold on trials of tazemetostat, an EZH2 inhibitor being developed to treat solid tumors and lymphomas, according to a press release from the drug’s developer Epizyme.
The patient had been on study for approximately 15 months and had achieved a confirmed partial response. The patient has since discontinued tazemetostat and responded to treatment for T-LBL.
“This remains the only case of T-LBL we’ve seen in more than 750 patients treated with tazemetostat,” Robert Bazemore, president and chief executive officer of Epizyme, said in a webcast on Sept. 24.
Epizyme assessed the risk of secondary malignancies, including T-LBL, as well as the overall risks and benefits of tazemetostat treatment, conducting a review of the published literature and an examination of efficacy and safety data across all of its tazemetostat trials. A panel of external scientific and medical experts who reviewed the findings concluded that T-LBL risks appear to be confined to pediatric patients who received higher doses of the drug. The phase 1 pediatric study in which the patient developed T-LBL included higher doses of tazemetostat than those used in the phase 2 adult studies.
“The team at Epizyme has worked diligently in collaboration with external experts and the FDA over the past several months,” Mr. Bazemore said.
The company is not making any substantial changes to trial designs or the patient populations involved in tazemetostat trials. However, Epizyme is modifying dosing in the pediatric studies, improving patient monitoring, and making changes to exclusion criteria to reduce the potential risk of T-LBL and other secondary malignancies. Mr. Bazemore said Epizyme hopes to submit a New Drug Application for tazemetostat in the treatment of epithelioid sarcoma.
Tazemetostat is under investigation as monotherapy in phase 2 trials of follicular lymphoma and solid-tumor malignancies. The drug is also being studied as part of combination therapy for non–small cell lung cancer and diffuse large B-cell lymphoma (DLBCL).
In August, Epizyme announced its decision to stop developing tazemetostat for use as monotherapy or in combination with prednisolone for patients with DLBCL. However, tazemetostat is still under investigation as a potential treatment for DLBCL as part of other combination regimens.
Epizyme is now working to resolve partial clinical holds placed on tazemetostat in France and Germany in order to resume trial enrollment in those countries.
The U.S. Food and Drug Administration has lifted the partial clinical hold on trials of tazemetostat, an EZH2 inhibitor being developed to treat solid tumors and lymphomas, according to a press release from the drug’s developer Epizyme.
The patient had been on study for approximately 15 months and had achieved a confirmed partial response. The patient has since discontinued tazemetostat and responded to treatment for T-LBL.
“This remains the only case of T-LBL we’ve seen in more than 750 patients treated with tazemetostat,” Robert Bazemore, president and chief executive officer of Epizyme, said in a webcast on Sept. 24.
Epizyme assessed the risk of secondary malignancies, including T-LBL, as well as the overall risks and benefits of tazemetostat treatment, conducting a review of the published literature and an examination of efficacy and safety data across all of its tazemetostat trials. A panel of external scientific and medical experts who reviewed the findings concluded that T-LBL risks appear to be confined to pediatric patients who received higher doses of the drug. The phase 1 pediatric study in which the patient developed T-LBL included higher doses of tazemetostat than those used in the phase 2 adult studies.
“The team at Epizyme has worked diligently in collaboration with external experts and the FDA over the past several months,” Mr. Bazemore said.
The company is not making any substantial changes to trial designs or the patient populations involved in tazemetostat trials. However, Epizyme is modifying dosing in the pediatric studies, improving patient monitoring, and making changes to exclusion criteria to reduce the potential risk of T-LBL and other secondary malignancies. Mr. Bazemore said Epizyme hopes to submit a New Drug Application for tazemetostat in the treatment of epithelioid sarcoma.
Tazemetostat is under investigation as monotherapy in phase 2 trials of follicular lymphoma and solid-tumor malignancies. The drug is also being studied as part of combination therapy for non–small cell lung cancer and diffuse large B-cell lymphoma (DLBCL).
In August, Epizyme announced its decision to stop developing tazemetostat for use as monotherapy or in combination with prednisolone for patients with DLBCL. However, tazemetostat is still under investigation as a potential treatment for DLBCL as part of other combination regimens.
Epizyme is now working to resolve partial clinical holds placed on tazemetostat in France and Germany in order to resume trial enrollment in those countries.
The U.S. Food and Drug Administration has lifted the partial clinical hold on trials of tazemetostat, an EZH2 inhibitor being developed to treat solid tumors and lymphomas, according to a press release from the drug’s developer Epizyme.
The patient had been on study for approximately 15 months and had achieved a confirmed partial response. The patient has since discontinued tazemetostat and responded to treatment for T-LBL.
“This remains the only case of T-LBL we’ve seen in more than 750 patients treated with tazemetostat,” Robert Bazemore, president and chief executive officer of Epizyme, said in a webcast on Sept. 24.
Epizyme assessed the risk of secondary malignancies, including T-LBL, as well as the overall risks and benefits of tazemetostat treatment, conducting a review of the published literature and an examination of efficacy and safety data across all of its tazemetostat trials. A panel of external scientific and medical experts who reviewed the findings concluded that T-LBL risks appear to be confined to pediatric patients who received higher doses of the drug. The phase 1 pediatric study in which the patient developed T-LBL included higher doses of tazemetostat than those used in the phase 2 adult studies.
“The team at Epizyme has worked diligently in collaboration with external experts and the FDA over the past several months,” Mr. Bazemore said.
The company is not making any substantial changes to trial designs or the patient populations involved in tazemetostat trials. However, Epizyme is modifying dosing in the pediatric studies, improving patient monitoring, and making changes to exclusion criteria to reduce the potential risk of T-LBL and other secondary malignancies. Mr. Bazemore said Epizyme hopes to submit a New Drug Application for tazemetostat in the treatment of epithelioid sarcoma.
Tazemetostat is under investigation as monotherapy in phase 2 trials of follicular lymphoma and solid-tumor malignancies. The drug is also being studied as part of combination therapy for non–small cell lung cancer and diffuse large B-cell lymphoma (DLBCL).
In August, Epizyme announced its decision to stop developing tazemetostat for use as monotherapy or in combination with prednisolone for patients with DLBCL. However, tazemetostat is still under investigation as a potential treatment for DLBCL as part of other combination regimens.
Epizyme is now working to resolve partial clinical holds placed on tazemetostat in France and Germany in order to resume trial enrollment in those countries.
Prognostic factors guide mantle cell treatment decisions
CHICAGO – The treatment options for patients with mantle cell lymphoma (MCL) vary based on age, but several prognostic factors can help guide treatment decision making in all patients, according to Kristie A. Blum, MD.
These include age, disease stage, disease sites, Mantle Cell Lymphoma International Prognostic Index (MIPI), biologic factors, and histology, Dr. Blum said during a presentation at the American Society of Hematology Meeting on Hematologic Malignancies.
Age
“I think the most important thing to recognize is there really isn’t any randomized transplant data for patients that are over 65. … There are very few transplant studies for patients [aged] 66-70,” said Dr. Blum, acting professor of hematology and medical oncology at Emory University in Atlanta.
The SWOG 0213 study did examine rituximab-hyperCVAD (R-HCVAD) in this age group, and showed that it has higher toxicity and lower efficacy in older versus younger patients, she said.
“Of course this is not typically a transplant approach, but an intensive-therapy approach,” she said, noting that progression-free and overall survival in patients aged 66-70 years were just 29% and 57%, respectively (Ann Oncol. 2013 Jun; 24[6]:1587-93).
The CALGB 59909 and 50403 studies of chemoimmunotherapy and autologous stem cell transplant (ASCT), with or without bortezomib, included only adults up to age 70.
“So while most of us think that transplant is probably okay and safe in patients up to 70, the question is what induction regimen to use,” she said.
Dr. Blum noted that a retrospective study from the Mayo Clinic looked at all 63 patients aged 65 years and older with MCL who underwent ASCT there (including 22 patients over age 70), and most (60%) were treated with R-CHOP. Just 19% received cytarabine-based regimens (Blood. 2017:130:4536).
Median overall survival after ASCT was 5 years, and median relapse-free survival was 3.2 years.
Stage
Like age, disease stage in MCL patients has not been well studied, Dr. Blum said.
“Most of the randomized transplant studies have been conducted in patients stage II-IV, so we don’t have a lot of data about the early-stage patients,” she said, adding, however, that there are some retrospective data on radiation therapy for stage I-II MCL in older adults.
An International Lymphoma Radiation Oncology Group study of 179 patients, for example, showed that overall survival was “really the same whether they got chemo, chemo plus radiation, or radiation alone,” she said.
The 10-year freedom from progression was 46%, 43%, and 31%, respectively (P = .64).
Location
“What about where the disease presents? We’ve all heard about indolent mantle cell – so there’s this leukemic ‘non-nodal’ variant that’s been described,” she said, noting that this variant has a chronic lymphocytic leukemia–like presentation (no nodal disease, blood and marrow involvement, and splenic involvement). “And they tend to be SOX11-negative with mutated [immunoglobulin variable region heavy chain gene].”
Another variant involves primarily nodal disease that typically presents without elevated white blood cell count, with low Ki-67 (10% or lower), with SOX11 positivity, and without TP53 mutations.
“But I would caution you that this is really not very well defined; there’s no clear marker that predicts for indolent disease,” Dr. Blum said. “If you have one of these patients and you’re thinking about observing them, my experience has been that the most important thing to do is make sure you look at their [gastrointestinal] tract. I’ve had a lot of these patients progress with colon masses over time.”
MIPI
MIPI is basically a risk score calculated based on age, performance status, lactate dehydrogenase levels, and white cell count, she said.
MIPI less than 5.70 indicates low risk, MIPI of 5.70-6.2 is considered intermediate risk, and MIPI greater than 6.2 is considered high risk. High-risk patients who were transplanted in one study had a median overall survival of about 2.8 years and a median time to treatment failure of 1.4 years (J Clin Oncol. 2014 May 1;32[13]:1338-46). Even among patients under age 65 with high risk, the median time to treatment failure was 2 years, she said.
“So I do wonder, are we really helping these patients by transplanting them?” she added. “Similarly, the low-risk patients had a median time to treatment failure of 6 years; I wonder if they didn’t need a transplant.”
Biology
Ki-67 protein, a cellular marker for proliferation, is another important prognostic factor. A European Mantle Cell network study showed that median overall survival for patients with a Ki-67 proliferation index of less than 30% was not reached, and 5-year survival was 75%. At the same time, the median overall survival (OS) for those with Ki-67 proliferation index of 30% or greater was just 3.4 years, and 5-year OS was only 41% (J Clin Oncol. 2016 Apr 20;34[12]:1386-94).
The prognostic effect was independent of induction treatment, Dr. Blum said.
Combining MIPI and the Ki-67 index (MIPI-C) provides further value in defining a very high-risk group; those with both high MIPI and high Ki-67 had a median overall survival of only 1.5 years, and those with both, but who were under age 65, had median OS of only 1.7 years.
Histology
Patients with blastoid MCL variants were shown in that same study to have median OS of about 2.8 years, compared with 8 years in those with nonblastoid variants. The 5-year OS and progression-free survival (PFS) for blastoid variants were 35% and 29%, respectively, and for nonblastoid variants were 68% and 44%, respectively.
“But when you look at this with respect to the Ki-67 – so those patients that were called nonblastoid, that had a high Ki-67 index – their median overall survival is still lower at 5 years,” she said, noting that median OS was not reached in blastic variant (low-Ki-67) patients. “So it seems like the prognostic effect of cytology is largely explained by the Ki-67 index.”
In terms of karyotype, several studies have shown that complex karyotype is associated with poorer outcomes. One recent multicenter study of 274 patients showed that median OS in 53 patients with at least three cytogenetic abnormalities versus the remaining patients was 4.5 years vs. 11.6 years, and median PFS was 1.9 vs. 4.4 years (Cancer. 2018 Jun 1;124[11]:2306-15).
TP53 deletions (which affect about 20% of MCL patients) and mutations (which affect about 10%), are also useful prognostic factors, she said, noting that each is associated with inferior outcomes, and in one study patients with both appeared to have the worst outcomes (Blood. 2017;130:1903-10).
Another study showed that high TP53 staining (greater than 50% positive) is also associated with inferior outcomes, including reduced time to treatment failure and lower overall survival (Blood. 2018;131:417-20).
Finally, the most important factor is the patient’s wishes, Dr. Blum said, noting that she has “a lot of long discussions with these patients.”
“I consider all of these factors with each patient that I see with mantle cell,” she said.
Dr. Blum is a consultant for Acerta, AstraZeneca, and Molecular Templates and has received research funding from Acerta, AstraZeneca, Celgene, Cephalon, Immunomedics, Janssen, Merck, Millennium, Molecular Templates, Novartis, Pharmacyclics, and Seattle Genetics.
CHICAGO – The treatment options for patients with mantle cell lymphoma (MCL) vary based on age, but several prognostic factors can help guide treatment decision making in all patients, according to Kristie A. Blum, MD.
These include age, disease stage, disease sites, Mantle Cell Lymphoma International Prognostic Index (MIPI), biologic factors, and histology, Dr. Blum said during a presentation at the American Society of Hematology Meeting on Hematologic Malignancies.
Age
“I think the most important thing to recognize is there really isn’t any randomized transplant data for patients that are over 65. … There are very few transplant studies for patients [aged] 66-70,” said Dr. Blum, acting professor of hematology and medical oncology at Emory University in Atlanta.
The SWOG 0213 study did examine rituximab-hyperCVAD (R-HCVAD) in this age group, and showed that it has higher toxicity and lower efficacy in older versus younger patients, she said.
“Of course this is not typically a transplant approach, but an intensive-therapy approach,” she said, noting that progression-free and overall survival in patients aged 66-70 years were just 29% and 57%, respectively (Ann Oncol. 2013 Jun; 24[6]:1587-93).
The CALGB 59909 and 50403 studies of chemoimmunotherapy and autologous stem cell transplant (ASCT), with or without bortezomib, included only adults up to age 70.
“So while most of us think that transplant is probably okay and safe in patients up to 70, the question is what induction regimen to use,” she said.
Dr. Blum noted that a retrospective study from the Mayo Clinic looked at all 63 patients aged 65 years and older with MCL who underwent ASCT there (including 22 patients over age 70), and most (60%) were treated with R-CHOP. Just 19% received cytarabine-based regimens (Blood. 2017:130:4536).
Median overall survival after ASCT was 5 years, and median relapse-free survival was 3.2 years.
Stage
Like age, disease stage in MCL patients has not been well studied, Dr. Blum said.
“Most of the randomized transplant studies have been conducted in patients stage II-IV, so we don’t have a lot of data about the early-stage patients,” she said, adding, however, that there are some retrospective data on radiation therapy for stage I-II MCL in older adults.
An International Lymphoma Radiation Oncology Group study of 179 patients, for example, showed that overall survival was “really the same whether they got chemo, chemo plus radiation, or radiation alone,” she said.
The 10-year freedom from progression was 46%, 43%, and 31%, respectively (P = .64).
Location
“What about where the disease presents? We’ve all heard about indolent mantle cell – so there’s this leukemic ‘non-nodal’ variant that’s been described,” she said, noting that this variant has a chronic lymphocytic leukemia–like presentation (no nodal disease, blood and marrow involvement, and splenic involvement). “And they tend to be SOX11-negative with mutated [immunoglobulin variable region heavy chain gene].”
Another variant involves primarily nodal disease that typically presents without elevated white blood cell count, with low Ki-67 (10% or lower), with SOX11 positivity, and without TP53 mutations.
“But I would caution you that this is really not very well defined; there’s no clear marker that predicts for indolent disease,” Dr. Blum said. “If you have one of these patients and you’re thinking about observing them, my experience has been that the most important thing to do is make sure you look at their [gastrointestinal] tract. I’ve had a lot of these patients progress with colon masses over time.”
MIPI
MIPI is basically a risk score calculated based on age, performance status, lactate dehydrogenase levels, and white cell count, she said.
MIPI less than 5.70 indicates low risk, MIPI of 5.70-6.2 is considered intermediate risk, and MIPI greater than 6.2 is considered high risk. High-risk patients who were transplanted in one study had a median overall survival of about 2.8 years and a median time to treatment failure of 1.4 years (J Clin Oncol. 2014 May 1;32[13]:1338-46). Even among patients under age 65 with high risk, the median time to treatment failure was 2 years, she said.
“So I do wonder, are we really helping these patients by transplanting them?” she added. “Similarly, the low-risk patients had a median time to treatment failure of 6 years; I wonder if they didn’t need a transplant.”
Biology
Ki-67 protein, a cellular marker for proliferation, is another important prognostic factor. A European Mantle Cell network study showed that median overall survival for patients with a Ki-67 proliferation index of less than 30% was not reached, and 5-year survival was 75%. At the same time, the median overall survival (OS) for those with Ki-67 proliferation index of 30% or greater was just 3.4 years, and 5-year OS was only 41% (J Clin Oncol. 2016 Apr 20;34[12]:1386-94).
The prognostic effect was independent of induction treatment, Dr. Blum said.
Combining MIPI and the Ki-67 index (MIPI-C) provides further value in defining a very high-risk group; those with both high MIPI and high Ki-67 had a median overall survival of only 1.5 years, and those with both, but who were under age 65, had median OS of only 1.7 years.
Histology
Patients with blastoid MCL variants were shown in that same study to have median OS of about 2.8 years, compared with 8 years in those with nonblastoid variants. The 5-year OS and progression-free survival (PFS) for blastoid variants were 35% and 29%, respectively, and for nonblastoid variants were 68% and 44%, respectively.
“But when you look at this with respect to the Ki-67 – so those patients that were called nonblastoid, that had a high Ki-67 index – their median overall survival is still lower at 5 years,” she said, noting that median OS was not reached in blastic variant (low-Ki-67) patients. “So it seems like the prognostic effect of cytology is largely explained by the Ki-67 index.”
In terms of karyotype, several studies have shown that complex karyotype is associated with poorer outcomes. One recent multicenter study of 274 patients showed that median OS in 53 patients with at least three cytogenetic abnormalities versus the remaining patients was 4.5 years vs. 11.6 years, and median PFS was 1.9 vs. 4.4 years (Cancer. 2018 Jun 1;124[11]:2306-15).
TP53 deletions (which affect about 20% of MCL patients) and mutations (which affect about 10%), are also useful prognostic factors, she said, noting that each is associated with inferior outcomes, and in one study patients with both appeared to have the worst outcomes (Blood. 2017;130:1903-10).
Another study showed that high TP53 staining (greater than 50% positive) is also associated with inferior outcomes, including reduced time to treatment failure and lower overall survival (Blood. 2018;131:417-20).
Finally, the most important factor is the patient’s wishes, Dr. Blum said, noting that she has “a lot of long discussions with these patients.”
“I consider all of these factors with each patient that I see with mantle cell,” she said.
Dr. Blum is a consultant for Acerta, AstraZeneca, and Molecular Templates and has received research funding from Acerta, AstraZeneca, Celgene, Cephalon, Immunomedics, Janssen, Merck, Millennium, Molecular Templates, Novartis, Pharmacyclics, and Seattle Genetics.
CHICAGO – The treatment options for patients with mantle cell lymphoma (MCL) vary based on age, but several prognostic factors can help guide treatment decision making in all patients, according to Kristie A. Blum, MD.
These include age, disease stage, disease sites, Mantle Cell Lymphoma International Prognostic Index (MIPI), biologic factors, and histology, Dr. Blum said during a presentation at the American Society of Hematology Meeting on Hematologic Malignancies.
Age
“I think the most important thing to recognize is there really isn’t any randomized transplant data for patients that are over 65. … There are very few transplant studies for patients [aged] 66-70,” said Dr. Blum, acting professor of hematology and medical oncology at Emory University in Atlanta.
The SWOG 0213 study did examine rituximab-hyperCVAD (R-HCVAD) in this age group, and showed that it has higher toxicity and lower efficacy in older versus younger patients, she said.
“Of course this is not typically a transplant approach, but an intensive-therapy approach,” she said, noting that progression-free and overall survival in patients aged 66-70 years were just 29% and 57%, respectively (Ann Oncol. 2013 Jun; 24[6]:1587-93).
The CALGB 59909 and 50403 studies of chemoimmunotherapy and autologous stem cell transplant (ASCT), with or without bortezomib, included only adults up to age 70.
“So while most of us think that transplant is probably okay and safe in patients up to 70, the question is what induction regimen to use,” she said.
Dr. Blum noted that a retrospective study from the Mayo Clinic looked at all 63 patients aged 65 years and older with MCL who underwent ASCT there (including 22 patients over age 70), and most (60%) were treated with R-CHOP. Just 19% received cytarabine-based regimens (Blood. 2017:130:4536).
Median overall survival after ASCT was 5 years, and median relapse-free survival was 3.2 years.
Stage
Like age, disease stage in MCL patients has not been well studied, Dr. Blum said.
“Most of the randomized transplant studies have been conducted in patients stage II-IV, so we don’t have a lot of data about the early-stage patients,” she said, adding, however, that there are some retrospective data on radiation therapy for stage I-II MCL in older adults.
An International Lymphoma Radiation Oncology Group study of 179 patients, for example, showed that overall survival was “really the same whether they got chemo, chemo plus radiation, or radiation alone,” she said.
The 10-year freedom from progression was 46%, 43%, and 31%, respectively (P = .64).
Location
“What about where the disease presents? We’ve all heard about indolent mantle cell – so there’s this leukemic ‘non-nodal’ variant that’s been described,” she said, noting that this variant has a chronic lymphocytic leukemia–like presentation (no nodal disease, blood and marrow involvement, and splenic involvement). “And they tend to be SOX11-negative with mutated [immunoglobulin variable region heavy chain gene].”
Another variant involves primarily nodal disease that typically presents without elevated white blood cell count, with low Ki-67 (10% or lower), with SOX11 positivity, and without TP53 mutations.
“But I would caution you that this is really not very well defined; there’s no clear marker that predicts for indolent disease,” Dr. Blum said. “If you have one of these patients and you’re thinking about observing them, my experience has been that the most important thing to do is make sure you look at their [gastrointestinal] tract. I’ve had a lot of these patients progress with colon masses over time.”
MIPI
MIPI is basically a risk score calculated based on age, performance status, lactate dehydrogenase levels, and white cell count, she said.
MIPI less than 5.70 indicates low risk, MIPI of 5.70-6.2 is considered intermediate risk, and MIPI greater than 6.2 is considered high risk. High-risk patients who were transplanted in one study had a median overall survival of about 2.8 years and a median time to treatment failure of 1.4 years (J Clin Oncol. 2014 May 1;32[13]:1338-46). Even among patients under age 65 with high risk, the median time to treatment failure was 2 years, she said.
“So I do wonder, are we really helping these patients by transplanting them?” she added. “Similarly, the low-risk patients had a median time to treatment failure of 6 years; I wonder if they didn’t need a transplant.”
Biology
Ki-67 protein, a cellular marker for proliferation, is another important prognostic factor. A European Mantle Cell network study showed that median overall survival for patients with a Ki-67 proliferation index of less than 30% was not reached, and 5-year survival was 75%. At the same time, the median overall survival (OS) for those with Ki-67 proliferation index of 30% or greater was just 3.4 years, and 5-year OS was only 41% (J Clin Oncol. 2016 Apr 20;34[12]:1386-94).
The prognostic effect was independent of induction treatment, Dr. Blum said.
Combining MIPI and the Ki-67 index (MIPI-C) provides further value in defining a very high-risk group; those with both high MIPI and high Ki-67 had a median overall survival of only 1.5 years, and those with both, but who were under age 65, had median OS of only 1.7 years.
Histology
Patients with blastoid MCL variants were shown in that same study to have median OS of about 2.8 years, compared with 8 years in those with nonblastoid variants. The 5-year OS and progression-free survival (PFS) for blastoid variants were 35% and 29%, respectively, and for nonblastoid variants were 68% and 44%, respectively.
“But when you look at this with respect to the Ki-67 – so those patients that were called nonblastoid, that had a high Ki-67 index – their median overall survival is still lower at 5 years,” she said, noting that median OS was not reached in blastic variant (low-Ki-67) patients. “So it seems like the prognostic effect of cytology is largely explained by the Ki-67 index.”
In terms of karyotype, several studies have shown that complex karyotype is associated with poorer outcomes. One recent multicenter study of 274 patients showed that median OS in 53 patients with at least three cytogenetic abnormalities versus the remaining patients was 4.5 years vs. 11.6 years, and median PFS was 1.9 vs. 4.4 years (Cancer. 2018 Jun 1;124[11]:2306-15).
TP53 deletions (which affect about 20% of MCL patients) and mutations (which affect about 10%), are also useful prognostic factors, she said, noting that each is associated with inferior outcomes, and in one study patients with both appeared to have the worst outcomes (Blood. 2017;130:1903-10).
Another study showed that high TP53 staining (greater than 50% positive) is also associated with inferior outcomes, including reduced time to treatment failure and lower overall survival (Blood. 2018;131:417-20).
Finally, the most important factor is the patient’s wishes, Dr. Blum said, noting that she has “a lot of long discussions with these patients.”
“I consider all of these factors with each patient that I see with mantle cell,” she said.
Dr. Blum is a consultant for Acerta, AstraZeneca, and Molecular Templates and has received research funding from Acerta, AstraZeneca, Celgene, Cephalon, Immunomedics, Janssen, Merck, Millennium, Molecular Templates, Novartis, Pharmacyclics, and Seattle Genetics.
REPORTING FROM MHM 2018
CAR T-cell studies dominate ongoing cellular therapy trials
NEW YORK – The cell therapy landscape increasingly involves strategies beyond chimeric antigen receptor (CAR) T-cell therapy, but those studies still predominate among investigational trials, according to Frederick L. Locke, MD, of Moffitt Cancer Center in Tampa.
Researchers are looking at CAR T-cell therapy for earlier lines of treatment, especially in patients with aggressive lymphomas, Dr. Locke said at the annual congress on Hematologic Malignancies held by the National Comprehensive Cancer Network.
Of 753 trials examining cell therapies and listed at ClinicalTrials.gov as of March 30, 2018, about half (404) were CAR T-cell therapies. The others included T-cell receptor therapies, tumor infiltrating lymphocyte therapies, dendritic cell vaccines, and natural killer cell–based therapies, according to an article in Nature Reviews.
“The development isn’t just here in the United States,” Dr. Locke said. “It’s really global. We see a lot of activity in Europe, but also in China. We’re seeing medical advances across the world through molecular biology and gene engineering of T cells and other immune cells which can be adoptively transferred into patients.”
That activity includes studies seeking to move CAR T-cell therapy earlier in the treatment paradigm for some diseases, he added. “CAR T-cell therapy in non-Hodgkin lymphoma is really beginning a paradigm shift, at least in my mind.”
Several large, randomized trials that are now comparing CD19 CAR T-cell therapy with second-line standard-of-care therapies for patients with aggressive B-cell lymphomas. Among those trials is ZUMA-7, a phase 3, randomized trial comparing axicabtagene ciloleucel with standard-of-care treatment in patients with relapsed or refractory diffuse large B-cell lymphoma.
While prognosis remains poor for relapsed or progressing aggressive B-cell lymphomas treated with chemotherapy, data to date suggest CAR T-cell therapy produces durable, long-term remissions in about 40% of patients at “a year out and counting,” Dr. Locke said.
He presented a proposed treatment algorithm that included R-CHOP chemotherapy up front and CAR T-cell therapy in later lines of treatment, an approach that Dr. Locke speculated could result in a cure rate of perhaps 80% in large-cell lymphomas.
Encouraging longer-term data is emerging, with some patients with aggressive T-cell lymphomas now without recurrence for 5 years or more following a single infusion of CAR T-cell therapy, he said.
Dr. Locke reported a financial disclosure related to Cellular Biomedicine Group.
NEW YORK – The cell therapy landscape increasingly involves strategies beyond chimeric antigen receptor (CAR) T-cell therapy, but those studies still predominate among investigational trials, according to Frederick L. Locke, MD, of Moffitt Cancer Center in Tampa.
Researchers are looking at CAR T-cell therapy for earlier lines of treatment, especially in patients with aggressive lymphomas, Dr. Locke said at the annual congress on Hematologic Malignancies held by the National Comprehensive Cancer Network.
Of 753 trials examining cell therapies and listed at ClinicalTrials.gov as of March 30, 2018, about half (404) were CAR T-cell therapies. The others included T-cell receptor therapies, tumor infiltrating lymphocyte therapies, dendritic cell vaccines, and natural killer cell–based therapies, according to an article in Nature Reviews.
“The development isn’t just here in the United States,” Dr. Locke said. “It’s really global. We see a lot of activity in Europe, but also in China. We’re seeing medical advances across the world through molecular biology and gene engineering of T cells and other immune cells which can be adoptively transferred into patients.”
That activity includes studies seeking to move CAR T-cell therapy earlier in the treatment paradigm for some diseases, he added. “CAR T-cell therapy in non-Hodgkin lymphoma is really beginning a paradigm shift, at least in my mind.”
Several large, randomized trials that are now comparing CD19 CAR T-cell therapy with second-line standard-of-care therapies for patients with aggressive B-cell lymphomas. Among those trials is ZUMA-7, a phase 3, randomized trial comparing axicabtagene ciloleucel with standard-of-care treatment in patients with relapsed or refractory diffuse large B-cell lymphoma.
While prognosis remains poor for relapsed or progressing aggressive B-cell lymphomas treated with chemotherapy, data to date suggest CAR T-cell therapy produces durable, long-term remissions in about 40% of patients at “a year out and counting,” Dr. Locke said.
He presented a proposed treatment algorithm that included R-CHOP chemotherapy up front and CAR T-cell therapy in later lines of treatment, an approach that Dr. Locke speculated could result in a cure rate of perhaps 80% in large-cell lymphomas.
Encouraging longer-term data is emerging, with some patients with aggressive T-cell lymphomas now without recurrence for 5 years or more following a single infusion of CAR T-cell therapy, he said.
Dr. Locke reported a financial disclosure related to Cellular Biomedicine Group.
NEW YORK – The cell therapy landscape increasingly involves strategies beyond chimeric antigen receptor (CAR) T-cell therapy, but those studies still predominate among investigational trials, according to Frederick L. Locke, MD, of Moffitt Cancer Center in Tampa.
Researchers are looking at CAR T-cell therapy for earlier lines of treatment, especially in patients with aggressive lymphomas, Dr. Locke said at the annual congress on Hematologic Malignancies held by the National Comprehensive Cancer Network.
Of 753 trials examining cell therapies and listed at ClinicalTrials.gov as of March 30, 2018, about half (404) were CAR T-cell therapies. The others included T-cell receptor therapies, tumor infiltrating lymphocyte therapies, dendritic cell vaccines, and natural killer cell–based therapies, according to an article in Nature Reviews.
“The development isn’t just here in the United States,” Dr. Locke said. “It’s really global. We see a lot of activity in Europe, but also in China. We’re seeing medical advances across the world through molecular biology and gene engineering of T cells and other immune cells which can be adoptively transferred into patients.”
That activity includes studies seeking to move CAR T-cell therapy earlier in the treatment paradigm for some diseases, he added. “CAR T-cell therapy in non-Hodgkin lymphoma is really beginning a paradigm shift, at least in my mind.”
Several large, randomized trials that are now comparing CD19 CAR T-cell therapy with second-line standard-of-care therapies for patients with aggressive B-cell lymphomas. Among those trials is ZUMA-7, a phase 3, randomized trial comparing axicabtagene ciloleucel with standard-of-care treatment in patients with relapsed or refractory diffuse large B-cell lymphoma.
While prognosis remains poor for relapsed or progressing aggressive B-cell lymphomas treated with chemotherapy, data to date suggest CAR T-cell therapy produces durable, long-term remissions in about 40% of patients at “a year out and counting,” Dr. Locke said.
He presented a proposed treatment algorithm that included R-CHOP chemotherapy up front and CAR T-cell therapy in later lines of treatment, an approach that Dr. Locke speculated could result in a cure rate of perhaps 80% in large-cell lymphomas.
Encouraging longer-term data is emerging, with some patients with aggressive T-cell lymphomas now without recurrence for 5 years or more following a single infusion of CAR T-cell therapy, he said.
Dr. Locke reported a financial disclosure related to Cellular Biomedicine Group.
EXPERT ANALYSIS FROM THE NCCN HEMATOLOGIC MALIGNANCIES CONGRESS