User login
AML trial placed on full clinical hold
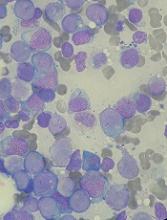
The US Food and Drug Administration (FDA) has placed a full clinical hold on a phase 1/2 trial of SEL24, a dual PIM/FLT3 kinase inhibitor, in patients with relapsed/refractory acute myeloid leukemia (AML).
The hold is due to a fatal cerebral adverse event that is considered possibly related to SEL24.
The clinical hold means no new patients will be enrolled in the trial and enrolled patients will not receive SEL24 until the hold is lifted.
Selvita S.A., the company developing SEL24, received a clinical hold letter from the FDA on October 6 and said it plans to work with the agency to have the hold lifted.
As part of this process, Selvita will provide the FDA with additional data and analysis on patients treated with SEL24 as well as a proposed protocol amendment.
The trial began in the first quarter of 2017. The study is designed to determine the maximum tolerated dose and recommended dose of SEL24 in patients with relapsed and refractory AML. The study began with a 25 mg daily dose, which was then escalated following cohort reviews.
One AML patient started treatment with a 150 mg dose of SEL24 as the third patient in this dose cohort and received 4 doses of the drug. This patient developed a life-threatening, grade 4 venous thrombus in the brain with subsequent intracerebral hemorrhage, which required hospitalization.
The patient died in hospice 4 days later due to the cerebral event. The patient’s death was subsequently evaluated as possibly related to SEL24.
A safety report and a review of data by the trial’s data monitoring committee were submitted to the FDA. The agency then placed a clinical hold on the trial and requested more safety data on patients who have received SEL24, as well as specific protocol changes and additional guidance to the study staff.
Selvita said it plans to comply with the requests and provide additional information to the agency and clinical trial centers, in collaboration with the Menarini Group, its global development partner for SEL24.
The FDA has 30 days from the receipt of Selvita’s response to let the company know whether the clinical hold is lifted. ![]()
The US Food and Drug Administration (FDA) has placed a full clinical hold on a phase 1/2 trial of SEL24, a dual PIM/FLT3 kinase inhibitor, in patients with relapsed/refractory acute myeloid leukemia (AML).
The hold is due to a fatal cerebral adverse event that is considered possibly related to SEL24.
The clinical hold means no new patients will be enrolled in the trial and enrolled patients will not receive SEL24 until the hold is lifted.
Selvita S.A., the company developing SEL24, received a clinical hold letter from the FDA on October 6 and said it plans to work with the agency to have the hold lifted.
As part of this process, Selvita will provide the FDA with additional data and analysis on patients treated with SEL24 as well as a proposed protocol amendment.
The trial began in the first quarter of 2017. The study is designed to determine the maximum tolerated dose and recommended dose of SEL24 in patients with relapsed and refractory AML. The study began with a 25 mg daily dose, which was then escalated following cohort reviews.
One AML patient started treatment with a 150 mg dose of SEL24 as the third patient in this dose cohort and received 4 doses of the drug. This patient developed a life-threatening, grade 4 venous thrombus in the brain with subsequent intracerebral hemorrhage, which required hospitalization.
The patient died in hospice 4 days later due to the cerebral event. The patient’s death was subsequently evaluated as possibly related to SEL24.
A safety report and a review of data by the trial’s data monitoring committee were submitted to the FDA. The agency then placed a clinical hold on the trial and requested more safety data on patients who have received SEL24, as well as specific protocol changes and additional guidance to the study staff.
Selvita said it plans to comply with the requests and provide additional information to the agency and clinical trial centers, in collaboration with the Menarini Group, its global development partner for SEL24.
The FDA has 30 days from the receipt of Selvita’s response to let the company know whether the clinical hold is lifted. ![]()
The US Food and Drug Administration (FDA) has placed a full clinical hold on a phase 1/2 trial of SEL24, a dual PIM/FLT3 kinase inhibitor, in patients with relapsed/refractory acute myeloid leukemia (AML).
The hold is due to a fatal cerebral adverse event that is considered possibly related to SEL24.
The clinical hold means no new patients will be enrolled in the trial and enrolled patients will not receive SEL24 until the hold is lifted.
Selvita S.A., the company developing SEL24, received a clinical hold letter from the FDA on October 6 and said it plans to work with the agency to have the hold lifted.
As part of this process, Selvita will provide the FDA with additional data and analysis on patients treated with SEL24 as well as a proposed protocol amendment.
The trial began in the first quarter of 2017. The study is designed to determine the maximum tolerated dose and recommended dose of SEL24 in patients with relapsed and refractory AML. The study began with a 25 mg daily dose, which was then escalated following cohort reviews.
One AML patient started treatment with a 150 mg dose of SEL24 as the third patient in this dose cohort and received 4 doses of the drug. This patient developed a life-threatening, grade 4 venous thrombus in the brain with subsequent intracerebral hemorrhage, which required hospitalization.
The patient died in hospice 4 days later due to the cerebral event. The patient’s death was subsequently evaluated as possibly related to SEL24.
A safety report and a review of data by the trial’s data monitoring committee were submitted to the FDA. The agency then placed a clinical hold on the trial and requested more safety data on patients who have received SEL24, as well as specific protocol changes and additional guidance to the study staff.
Selvita said it plans to comply with the requests and provide additional information to the agency and clinical trial centers, in collaboration with the Menarini Group, its global development partner for SEL24.
The FDA has 30 days from the receipt of Selvita’s response to let the company know whether the clinical hold is lifted. ![]()
FDA grants drug orphan designation for AML
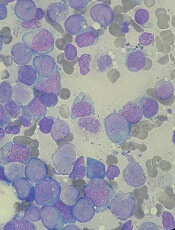
The US Food and Drug Administration (FDA) has granted orphan drug designation to PCM-075 for the treatment of patients with acute myeloid leukemia (AML).
PCM-075 is an oral adenosine triphosphate competitive inhibitor of the serine/threonine Polo-like kinase 1 (PLK1) enzyme, which appears to be overexpressed in several hematologic and solid tumor malignancies.
PCM-075 is being developed by Trovagene, Inc.
The company is initiating a phase 1b/2 trial of PCM-075 in combination with standard care (low-dose cytarabine or decitabine) in patients with AML (NCT03303339).
Trovagene has already completed a phase 1 dose-escalation study of PCM-075 in patients with advanced metastatic solid tumor malignancies. This study was recently published in Investigational New Drugs.
According to Trovagene, preclinical studies have shown that PCM-075 synergizes with more than 10 drugs used to treat hematologic and solid tumor malignancies, including FLT3 and HDAC inhibitors, taxanes, and cytotoxins.
Trovagene believes the combination of PCM-075 with other compounds has the potential for improved clinical efficacy in AML, non-Hodgkin lymphoma, castration-resistant prostate cancer, triple-negative breast cancer, and adrenocortical carcinoma.
About orphan designation
The FDA grants orphan designation to products intended to treat, diagnose, or prevent diseases/disorders that affect fewer than 200,000 people in the US.
The designation provides incentives for sponsors to develop products for rare diseases. This may include tax credits toward the cost of clinical trials, prescription drug user fee waivers, and 7 years of market exclusivity if the product is approved. ![]()
The US Food and Drug Administration (FDA) has granted orphan drug designation to PCM-075 for the treatment of patients with acute myeloid leukemia (AML).
PCM-075 is an oral adenosine triphosphate competitive inhibitor of the serine/threonine Polo-like kinase 1 (PLK1) enzyme, which appears to be overexpressed in several hematologic and solid tumor malignancies.
PCM-075 is being developed by Trovagene, Inc.
The company is initiating a phase 1b/2 trial of PCM-075 in combination with standard care (low-dose cytarabine or decitabine) in patients with AML (NCT03303339).
Trovagene has already completed a phase 1 dose-escalation study of PCM-075 in patients with advanced metastatic solid tumor malignancies. This study was recently published in Investigational New Drugs.
According to Trovagene, preclinical studies have shown that PCM-075 synergizes with more than 10 drugs used to treat hematologic and solid tumor malignancies, including FLT3 and HDAC inhibitors, taxanes, and cytotoxins.
Trovagene believes the combination of PCM-075 with other compounds has the potential for improved clinical efficacy in AML, non-Hodgkin lymphoma, castration-resistant prostate cancer, triple-negative breast cancer, and adrenocortical carcinoma.
About orphan designation
The FDA grants orphan designation to products intended to treat, diagnose, or prevent diseases/disorders that affect fewer than 200,000 people in the US.
The designation provides incentives for sponsors to develop products for rare diseases. This may include tax credits toward the cost of clinical trials, prescription drug user fee waivers, and 7 years of market exclusivity if the product is approved. ![]()
The US Food and Drug Administration (FDA) has granted orphan drug designation to PCM-075 for the treatment of patients with acute myeloid leukemia (AML).
PCM-075 is an oral adenosine triphosphate competitive inhibitor of the serine/threonine Polo-like kinase 1 (PLK1) enzyme, which appears to be overexpressed in several hematologic and solid tumor malignancies.
PCM-075 is being developed by Trovagene, Inc.
The company is initiating a phase 1b/2 trial of PCM-075 in combination with standard care (low-dose cytarabine or decitabine) in patients with AML (NCT03303339).
Trovagene has already completed a phase 1 dose-escalation study of PCM-075 in patients with advanced metastatic solid tumor malignancies. This study was recently published in Investigational New Drugs.
According to Trovagene, preclinical studies have shown that PCM-075 synergizes with more than 10 drugs used to treat hematologic and solid tumor malignancies, including FLT3 and HDAC inhibitors, taxanes, and cytotoxins.
Trovagene believes the combination of PCM-075 with other compounds has the potential for improved clinical efficacy in AML, non-Hodgkin lymphoma, castration-resistant prostate cancer, triple-negative breast cancer, and adrenocortical carcinoma.
About orphan designation
The FDA grants orphan designation to products intended to treat, diagnose, or prevent diseases/disorders that affect fewer than 200,000 people in the US.
The designation provides incentives for sponsors to develop products for rare diseases. This may include tax credits toward the cost of clinical trials, prescription drug user fee waivers, and 7 years of market exclusivity if the product is approved. ![]()
Newer blood cancer drugs may not improve OS, QOL
A study of cancer drugs approved by the European Commission from 2009 to 2013 showed that few hematology drugs were known to provide a benefit in overall survival (OS) or quality of life (QOL) over existing treatments.
Of 12 drugs approved for 17 hematology indications, 3 drugs had been shown to provide a benefit in OS (for 3 indications) at the time of approval.
None of the other hematology drugs were known to provide an OS benefit even after a median follow-up of 5.4 years.
Two hematology drugs were shown to provide a benefit in QOL (for 2 indications) after approval, but none of the drugs were known to provide a QOL benefit at the time of approval.
These findings were published in The BMJ alongside a related editorial, feature article, and patient commentary.
All cancer drugs
Researchers analyzed reports on all cancer drug approvals by the European Commission from 2009 to 2013.
There were 48 drugs approved for 68 cancer indications during this period. Fifty-one of the indications were for solid tumor malignancies, and 17 were for hematologic malignancies.
For 24 indications (35%), research had demonstrated a significant improvement in OS at the time of the drugs’ approval. For 3 indications, an improvement in OS was demonstrated after approval.
There was a known improvement in QOL for 7 of the indications (10%) at the time of approval and for 5 indications after approval.
The median follow-up was 5.4 years (range, 3.3 years to 8.1 years).
Overall, there was a significant improvement in OS or QOL during the study period for 51% of the indications (35/68). For the other half (49%, n=33), it wasn’t clear if the drugs provide any benefits in OS or QOL.
All cancer trials
The 68 approvals of cancer drugs were supported by 72 clinical trials.
Sixty approvals (88%) were supported by at least 1 randomized, controlled trial. Eight approvals (12%) were based on a single-arm study. This included 6 of 10 conditional marketing authorizations and 2 of 58 regular marketing authorizations.
Eighteen of the approvals (26%) were supported by a pivotal study powered to evaluate OS as the primary endpoint. And 37 of the approvals (54%) had a supporting pivotal trial evaluating QOL, but results were not reported for 2 of these trials.
Hematology trials and drugs
Of the 12 drugs approved for 17 hematology indications, 4 were regular approvals, 5 were conditional approvals, and 8 had orphan drug designation.
The approvals were supported by data from 18 trials—13 randomized and 5 single-arm trials.
The study drug was compared to an active comparator in 9 of the trials. The drug was evaluated as an add-on treatment in 4 trials. And the drug was not compared to anything in 5 trials (the single-arm trials).
OS was the primary endpoint in 1 of the trials, and 17 trials had OS or QOL as a secondary endpoint.
There were 3 drugs that had demonstrated an OS benefit at the time of approval but no QOL benefit at any time:
- Decitabine used for first-line treatment of acute myeloid leukemia in adults 65 and older who are ineligible for chemotherapy
- Pomalidomide in combination with dexamethasone as third-line therapy for relapsed/refractory multiple myeloma (MM)
- Rituximab plus chemotherapy for first-line treatment of chronic lymphocytic leukemia (CLL).
There were 2 drugs that had demonstrated a QOL benefit, only after approval, but they were not known to provide an OS benefit at any time:
- Nilotinib as a treatment for adults with newly diagnosed, chronic phase, Ph+ chronic myeloid leukemia (CML)
- Ofatumumab for CLL that is refractory to fludarabine and alemtuzumab
For the remaining drugs, there was no evidence of an OS or QOL benefit at any time during the period studied. The drugs included:
- Bortezomib given alone or in combination with doxorubicin or dexamethasone as second-line therapy for MM patients ineligible for hematopoietic stem cell transplant (HSCT)
- Bortezomib plus dexamethasone with or without thalidomide as first-line therapy in MM patients eligible for HSCT
- Bosutinib as second- or third-line treatment of Ph+ CML (any phase)
- Brentuximab vedotin for relapsed or refractory systemic anaplastic large-cell lymphoma
- Brentuximab vedotin for relapsed or refractory, CD30+ Hodgkin lymphoma after autologous HSCT or as third-line treatment for patients ineligible for autologous HSCT
- Dasatinib for first-line treatment of chronic phase, Ph+ CML
- Pixantrone for multiply relapsed or refractory B-cell non-Hodgkin lymphoma
- Ponatinib for patients with Ph+ acute lymphoblastic leukemia who are ineligible for imatinib or have disease that is resistant or intolerant to dasatinib or characterized by T315I mutation
- Ponatinib for patients with any phase of CML who are ineligible for imatinib or have disease that is resistant or intolerant to dasatinib/nilotinib or characterized by T315I mutation
- Rituximab as maintenance after induction for patients with follicular lymphoma
- Rituximab plus chemotherapy for relapsed or refractory CLL
- Temsirolimus for relapsed or refractory mantle cell lymphoma.

A study of cancer drugs approved by the European Commission from 2009 to 2013 showed that few hematology drugs were known to provide a benefit in overall survival (OS) or quality of life (QOL) over existing treatments.
Of 12 drugs approved for 17 hematology indications, 3 drugs had been shown to provide a benefit in OS (for 3 indications) at the time of approval.
None of the other hematology drugs were known to provide an OS benefit even after a median follow-up of 5.4 years.
Two hematology drugs were shown to provide a benefit in QOL (for 2 indications) after approval, but none of the drugs were known to provide a QOL benefit at the time of approval.
These findings were published in The BMJ alongside a related editorial, feature article, and patient commentary.
All cancer drugs
Researchers analyzed reports on all cancer drug approvals by the European Commission from 2009 to 2013.
There were 48 drugs approved for 68 cancer indications during this period. Fifty-one of the indications were for solid tumor malignancies, and 17 were for hematologic malignancies.
For 24 indications (35%), research had demonstrated a significant improvement in OS at the time of the drugs’ approval. For 3 indications, an improvement in OS was demonstrated after approval.
There was a known improvement in QOL for 7 of the indications (10%) at the time of approval and for 5 indications after approval.
The median follow-up was 5.4 years (range, 3.3 years to 8.1 years).
Overall, there was a significant improvement in OS or QOL during the study period for 51% of the indications (35/68). For the other half (49%, n=33), it wasn’t clear if the drugs provide any benefits in OS or QOL.
All cancer trials
The 68 approvals of cancer drugs were supported by 72 clinical trials.
Sixty approvals (88%) were supported by at least 1 randomized, controlled trial. Eight approvals (12%) were based on a single-arm study. This included 6 of 10 conditional marketing authorizations and 2 of 58 regular marketing authorizations.
Eighteen of the approvals (26%) were supported by a pivotal study powered to evaluate OS as the primary endpoint. And 37 of the approvals (54%) had a supporting pivotal trial evaluating QOL, but results were not reported for 2 of these trials.
Hematology trials and drugs
Of the 12 drugs approved for 17 hematology indications, 4 were regular approvals, 5 were conditional approvals, and 8 had orphan drug designation.
The approvals were supported by data from 18 trials—13 randomized and 5 single-arm trials.
The study drug was compared to an active comparator in 9 of the trials. The drug was evaluated as an add-on treatment in 4 trials. And the drug was not compared to anything in 5 trials (the single-arm trials).
OS was the primary endpoint in 1 of the trials, and 17 trials had OS or QOL as a secondary endpoint.
There were 3 drugs that had demonstrated an OS benefit at the time of approval but no QOL benefit at any time:
- Decitabine used for first-line treatment of acute myeloid leukemia in adults 65 and older who are ineligible for chemotherapy
- Pomalidomide in combination with dexamethasone as third-line therapy for relapsed/refractory multiple myeloma (MM)
- Rituximab plus chemotherapy for first-line treatment of chronic lymphocytic leukemia (CLL).
There were 2 drugs that had demonstrated a QOL benefit, only after approval, but they were not known to provide an OS benefit at any time:
- Nilotinib as a treatment for adults with newly diagnosed, chronic phase, Ph+ chronic myeloid leukemia (CML)
- Ofatumumab for CLL that is refractory to fludarabine and alemtuzumab
For the remaining drugs, there was no evidence of an OS or QOL benefit at any time during the period studied. The drugs included:
- Bortezomib given alone or in combination with doxorubicin or dexamethasone as second-line therapy for MM patients ineligible for hematopoietic stem cell transplant (HSCT)
- Bortezomib plus dexamethasone with or without thalidomide as first-line therapy in MM patients eligible for HSCT
- Bosutinib as second- or third-line treatment of Ph+ CML (any phase)
- Brentuximab vedotin for relapsed or refractory systemic anaplastic large-cell lymphoma
- Brentuximab vedotin for relapsed or refractory, CD30+ Hodgkin lymphoma after autologous HSCT or as third-line treatment for patients ineligible for autologous HSCT
- Dasatinib for first-line treatment of chronic phase, Ph+ CML
- Pixantrone for multiply relapsed or refractory B-cell non-Hodgkin lymphoma
- Ponatinib for patients with Ph+ acute lymphoblastic leukemia who are ineligible for imatinib or have disease that is resistant or intolerant to dasatinib or characterized by T315I mutation
- Ponatinib for patients with any phase of CML who are ineligible for imatinib or have disease that is resistant or intolerant to dasatinib/nilotinib or characterized by T315I mutation
- Rituximab as maintenance after induction for patients with follicular lymphoma
- Rituximab plus chemotherapy for relapsed or refractory CLL
- Temsirolimus for relapsed or refractory mantle cell lymphoma.

A study of cancer drugs approved by the European Commission from 2009 to 2013 showed that few hematology drugs were known to provide a benefit in overall survival (OS) or quality of life (QOL) over existing treatments.
Of 12 drugs approved for 17 hematology indications, 3 drugs had been shown to provide a benefit in OS (for 3 indications) at the time of approval.
None of the other hematology drugs were known to provide an OS benefit even after a median follow-up of 5.4 years.
Two hematology drugs were shown to provide a benefit in QOL (for 2 indications) after approval, but none of the drugs were known to provide a QOL benefit at the time of approval.
These findings were published in The BMJ alongside a related editorial, feature article, and patient commentary.
All cancer drugs
Researchers analyzed reports on all cancer drug approvals by the European Commission from 2009 to 2013.
There were 48 drugs approved for 68 cancer indications during this period. Fifty-one of the indications were for solid tumor malignancies, and 17 were for hematologic malignancies.
For 24 indications (35%), research had demonstrated a significant improvement in OS at the time of the drugs’ approval. For 3 indications, an improvement in OS was demonstrated after approval.
There was a known improvement in QOL for 7 of the indications (10%) at the time of approval and for 5 indications after approval.
The median follow-up was 5.4 years (range, 3.3 years to 8.1 years).
Overall, there was a significant improvement in OS or QOL during the study period for 51% of the indications (35/68). For the other half (49%, n=33), it wasn’t clear if the drugs provide any benefits in OS or QOL.
All cancer trials
The 68 approvals of cancer drugs were supported by 72 clinical trials.
Sixty approvals (88%) were supported by at least 1 randomized, controlled trial. Eight approvals (12%) were based on a single-arm study. This included 6 of 10 conditional marketing authorizations and 2 of 58 regular marketing authorizations.
Eighteen of the approvals (26%) were supported by a pivotal study powered to evaluate OS as the primary endpoint. And 37 of the approvals (54%) had a supporting pivotal trial evaluating QOL, but results were not reported for 2 of these trials.
Hematology trials and drugs
Of the 12 drugs approved for 17 hematology indications, 4 were regular approvals, 5 were conditional approvals, and 8 had orphan drug designation.
The approvals were supported by data from 18 trials—13 randomized and 5 single-arm trials.
The study drug was compared to an active comparator in 9 of the trials. The drug was evaluated as an add-on treatment in 4 trials. And the drug was not compared to anything in 5 trials (the single-arm trials).
OS was the primary endpoint in 1 of the trials, and 17 trials had OS or QOL as a secondary endpoint.
There were 3 drugs that had demonstrated an OS benefit at the time of approval but no QOL benefit at any time:
- Decitabine used for first-line treatment of acute myeloid leukemia in adults 65 and older who are ineligible for chemotherapy
- Pomalidomide in combination with dexamethasone as third-line therapy for relapsed/refractory multiple myeloma (MM)
- Rituximab plus chemotherapy for first-line treatment of chronic lymphocytic leukemia (CLL).
There were 2 drugs that had demonstrated a QOL benefit, only after approval, but they were not known to provide an OS benefit at any time:
- Nilotinib as a treatment for adults with newly diagnosed, chronic phase, Ph+ chronic myeloid leukemia (CML)
- Ofatumumab for CLL that is refractory to fludarabine and alemtuzumab
For the remaining drugs, there was no evidence of an OS or QOL benefit at any time during the period studied. The drugs included:
- Bortezomib given alone or in combination with doxorubicin or dexamethasone as second-line therapy for MM patients ineligible for hematopoietic stem cell transplant (HSCT)
- Bortezomib plus dexamethasone with or without thalidomide as first-line therapy in MM patients eligible for HSCT
- Bosutinib as second- or third-line treatment of Ph+ CML (any phase)
- Brentuximab vedotin for relapsed or refractory systemic anaplastic large-cell lymphoma
- Brentuximab vedotin for relapsed or refractory, CD30+ Hodgkin lymphoma after autologous HSCT or as third-line treatment for patients ineligible for autologous HSCT
- Dasatinib for first-line treatment of chronic phase, Ph+ CML
- Pixantrone for multiply relapsed or refractory B-cell non-Hodgkin lymphoma
- Ponatinib for patients with Ph+ acute lymphoblastic leukemia who are ineligible for imatinib or have disease that is resistant or intolerant to dasatinib or characterized by T315I mutation
- Ponatinib for patients with any phase of CML who are ineligible for imatinib or have disease that is resistant or intolerant to dasatinib/nilotinib or characterized by T315I mutation
- Rituximab as maintenance after induction for patients with follicular lymphoma
- Rituximab plus chemotherapy for relapsed or refractory CLL
- Temsirolimus for relapsed or refractory mantle cell lymphoma.

Mutations impact outcomes in AML, MDS
Researchers say they have identified genetic mutations that can significantly affect treatment outcomes in patients with acute myeloid leukemia (AML) and myelodysplastic syndromes (MDS).
The findings come from a clinical trial in which the team examined whether combining vorinostat with azacitidine could improve survival in patients with AML and MDS.
The results showed no additional benefit with the combination, when compared to azacitidine alone.
However, researchers did find that patients had significantly shorter survival times if they had mutations in CDKN2A, IDH1, or TP53.
“This important trial . . . has rapidly answered the important question of whether combining azacitidine with vorinostat improves outcomes for people with AML and MDS and emphasizes the need for further studies with new drug partners for azacitidine,” said Charles Craddock, DPhil, of the Queen Elizabeth Hospital in Birmingham, UK.
“Importantly, the linked molecular studies have shed new light on which people will benefit most from azacitidine. Furthermore, discovering that the CDKN2A gene mutation affects treatment response may be hugely valuable in helping doctors to design new treatment combinations in the future.”
Dr Craddock and his colleagues reported their discoveries in Clinical Cancer Research.
Previous, smaller trials had suggested that adding vorinostat to treatment with azacitidine could improve outcomes for patients with AML and MDS.
To test this idea, Dr Craddock and his colleagues enrolled 259 patients in the current trial. Most of these patients (n=217) had AML—111 were newly diagnosed, 73 had relapsed AML, and 33 had refractory disease.
The remaining 42 patients had MDS—36 were newly diagnosed, 5 had relapsed MDS, and 1 had refractory disease.
Half of patients (n=130) received azacitidine and vorinostat, and the other half received azacitidine alone (n=129).
In both arms, azacitidine was given at 75 mg/m2 on a 5-2-2 schedule, beginning on day 1 of a 28-day cycle for up to 6 cycles. In the combination arm, patients also received vorinostat at 300 mg twice daily for 7 consecutive days, beginning on day 3 of each cycle.
Results
The combination did not significantly improve response rates or survival times.
The overall response rate was 41% in the azacitidine arm and 42% in the combination arm (odds ratio [OR]=1.05, P=0.84).
The rate of compete response (CR)/CR with incomplete count recovery/marrow CR was 22% in the azacitidine arm and 26% in the combination arm (OR=0.82, P=0.49).
The median overall survival (OS) was 9.6 months in the azacitidine arm and 11.0 months in the combination arm (hazard ratio[HR]=1.15, P=0.32).
Impact of mutations
In a multivariable analysis adjusted for all clinical variables, mutations in NPM1 were associated with reduced overall response (OR=8.6, P=0.012).
In another multivariate analysis, mutations in CDKN2A, IDH1, and TP53 were associated with decreased OS. The HRs were 10.0 (P<0.001), 3.6 (P=0.001), and 4.7 (P<0.001), respectively.
The median OS was 4.5 months in patients with CDKN2A mutations and 11.0 months in patients without them.
The median OS was 7.6 months in patients with TP53 mutations and 11.3 months in patients without them.
And the median OS was 5.6 months in patients with IDH1 mutations and 11.1 months in patients without them.
The researchers believe that testing patients newly diagnosed with AML and MDS for CDKN2A, IDH1, and TP53 mutations could help doctors tailor treatment for patients who are less likely to do well.
The team also said the information gleaned from this trial will guide the choice of new drug partners with the potential to increase azacitidine’s clinical activity. ![]()
Researchers say they have identified genetic mutations that can significantly affect treatment outcomes in patients with acute myeloid leukemia (AML) and myelodysplastic syndromes (MDS).
The findings come from a clinical trial in which the team examined whether combining vorinostat with azacitidine could improve survival in patients with AML and MDS.
The results showed no additional benefit with the combination, when compared to azacitidine alone.
However, researchers did find that patients had significantly shorter survival times if they had mutations in CDKN2A, IDH1, or TP53.
“This important trial . . . has rapidly answered the important question of whether combining azacitidine with vorinostat improves outcomes for people with AML and MDS and emphasizes the need for further studies with new drug partners for azacitidine,” said Charles Craddock, DPhil, of the Queen Elizabeth Hospital in Birmingham, UK.
“Importantly, the linked molecular studies have shed new light on which people will benefit most from azacitidine. Furthermore, discovering that the CDKN2A gene mutation affects treatment response may be hugely valuable in helping doctors to design new treatment combinations in the future.”
Dr Craddock and his colleagues reported their discoveries in Clinical Cancer Research.
Previous, smaller trials had suggested that adding vorinostat to treatment with azacitidine could improve outcomes for patients with AML and MDS.
To test this idea, Dr Craddock and his colleagues enrolled 259 patients in the current trial. Most of these patients (n=217) had AML—111 were newly diagnosed, 73 had relapsed AML, and 33 had refractory disease.
The remaining 42 patients had MDS—36 were newly diagnosed, 5 had relapsed MDS, and 1 had refractory disease.
Half of patients (n=130) received azacitidine and vorinostat, and the other half received azacitidine alone (n=129).
In both arms, azacitidine was given at 75 mg/m2 on a 5-2-2 schedule, beginning on day 1 of a 28-day cycle for up to 6 cycles. In the combination arm, patients also received vorinostat at 300 mg twice daily for 7 consecutive days, beginning on day 3 of each cycle.
Results
The combination did not significantly improve response rates or survival times.
The overall response rate was 41% in the azacitidine arm and 42% in the combination arm (odds ratio [OR]=1.05, P=0.84).
The rate of compete response (CR)/CR with incomplete count recovery/marrow CR was 22% in the azacitidine arm and 26% in the combination arm (OR=0.82, P=0.49).
The median overall survival (OS) was 9.6 months in the azacitidine arm and 11.0 months in the combination arm (hazard ratio[HR]=1.15, P=0.32).
Impact of mutations
In a multivariable analysis adjusted for all clinical variables, mutations in NPM1 were associated with reduced overall response (OR=8.6, P=0.012).
In another multivariate analysis, mutations in CDKN2A, IDH1, and TP53 were associated with decreased OS. The HRs were 10.0 (P<0.001), 3.6 (P=0.001), and 4.7 (P<0.001), respectively.
The median OS was 4.5 months in patients with CDKN2A mutations and 11.0 months in patients without them.
The median OS was 7.6 months in patients with TP53 mutations and 11.3 months in patients without them.
And the median OS was 5.6 months in patients with IDH1 mutations and 11.1 months in patients without them.
The researchers believe that testing patients newly diagnosed with AML and MDS for CDKN2A, IDH1, and TP53 mutations could help doctors tailor treatment for patients who are less likely to do well.
The team also said the information gleaned from this trial will guide the choice of new drug partners with the potential to increase azacitidine’s clinical activity. ![]()
Researchers say they have identified genetic mutations that can significantly affect treatment outcomes in patients with acute myeloid leukemia (AML) and myelodysplastic syndromes (MDS).
The findings come from a clinical trial in which the team examined whether combining vorinostat with azacitidine could improve survival in patients with AML and MDS.
The results showed no additional benefit with the combination, when compared to azacitidine alone.
However, researchers did find that patients had significantly shorter survival times if they had mutations in CDKN2A, IDH1, or TP53.
“This important trial . . . has rapidly answered the important question of whether combining azacitidine with vorinostat improves outcomes for people with AML and MDS and emphasizes the need for further studies with new drug partners for azacitidine,” said Charles Craddock, DPhil, of the Queen Elizabeth Hospital in Birmingham, UK.
“Importantly, the linked molecular studies have shed new light on which people will benefit most from azacitidine. Furthermore, discovering that the CDKN2A gene mutation affects treatment response may be hugely valuable in helping doctors to design new treatment combinations in the future.”
Dr Craddock and his colleagues reported their discoveries in Clinical Cancer Research.
Previous, smaller trials had suggested that adding vorinostat to treatment with azacitidine could improve outcomes for patients with AML and MDS.
To test this idea, Dr Craddock and his colleagues enrolled 259 patients in the current trial. Most of these patients (n=217) had AML—111 were newly diagnosed, 73 had relapsed AML, and 33 had refractory disease.
The remaining 42 patients had MDS—36 were newly diagnosed, 5 had relapsed MDS, and 1 had refractory disease.
Half of patients (n=130) received azacitidine and vorinostat, and the other half received azacitidine alone (n=129).
In both arms, azacitidine was given at 75 mg/m2 on a 5-2-2 schedule, beginning on day 1 of a 28-day cycle for up to 6 cycles. In the combination arm, patients also received vorinostat at 300 mg twice daily for 7 consecutive days, beginning on day 3 of each cycle.
Results
The combination did not significantly improve response rates or survival times.
The overall response rate was 41% in the azacitidine arm and 42% in the combination arm (odds ratio [OR]=1.05, P=0.84).
The rate of compete response (CR)/CR with incomplete count recovery/marrow CR was 22% in the azacitidine arm and 26% in the combination arm (OR=0.82, P=0.49).
The median overall survival (OS) was 9.6 months in the azacitidine arm and 11.0 months in the combination arm (hazard ratio[HR]=1.15, P=0.32).
Impact of mutations
In a multivariable analysis adjusted for all clinical variables, mutations in NPM1 were associated with reduced overall response (OR=8.6, P=0.012).
In another multivariate analysis, mutations in CDKN2A, IDH1, and TP53 were associated with decreased OS. The HRs were 10.0 (P<0.001), 3.6 (P=0.001), and 4.7 (P<0.001), respectively.
The median OS was 4.5 months in patients with CDKN2A mutations and 11.0 months in patients without them.
The median OS was 7.6 months in patients with TP53 mutations and 11.3 months in patients without them.
And the median OS was 5.6 months in patients with IDH1 mutations and 11.1 months in patients without them.
The researchers believe that testing patients newly diagnosed with AML and MDS for CDKN2A, IDH1, and TP53 mutations could help doctors tailor treatment for patients who are less likely to do well.
The team also said the information gleaned from this trial will guide the choice of new drug partners with the potential to increase azacitidine’s clinical activity. ![]()
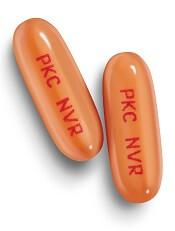
How APL cells evade the immune system
New research has revealed a way in which acute promyelocytic leukemia (APL) cells evade destruction by the immune system.
The study showed how group 2 innate lymphoid cells (ILC2s) are recruited by leukemic cells to suppress an essential anticancer immune response.
Researchers believe this newly discovered immunosuppressive axis likely holds sway in other cancers, and it might be disrupted by therapies already in use to treat other diseases.
Camilla Jandus, MD, PhD, of the Ludwig Institute for Cancer Research in Lausanne, Switzerland, and her colleagues described this research in Nature Communications.
“ILCs are not very abundant in the body, but, when activated, they secrete large amounts of immune factors,” Dr Jandus said. “In this way, they can dictate whether a response will be pro-inflammatory or anti-inflammatory.”
ILC1, 2, and 3 have been shown to play a role in inflammation and autoimmune diseases. However, their role in cancer has remained unclear.
To address that question, Dr Jandus and her colleagues began with the observation that one subtype of the cells, ILC2s, are abnormally abundant and hyperactivated in patients with APL.
The researchers examined ILC2 immunology in patients with active APL and compared it to that of APL patients in remission.
“Our analyses suggest that, in patients with this leukemia, ILC2s are at the beginning of a novel immunosuppressive axis, one that is likely to be active in other types of cancer as well,” Dr Jandus said.
She and her colleagues found that APL cells secrete large quantities of PGD2 and express high levels of B7H6 on their surface. Both of these molecules bind to receptors on ILC2s—CRTH2 and NKp30, respectively—activating the ILC2s and prompting them to secrete interleukin-13 (IL-13).
The IL-13 switches on and expands the population of monocytic myeloid-derived immune cells (M-MDSCs). These cells suppress immune responses and allow leukemic cells to evade immune system attack.
The researchers tested these findings in a mouse model of APL. Like patients, mice with APL displayed abnormal activation of ILC2s and M-MDSCs.
However, interfering with all the signals of the immunosuppressive axis restored anti-cancer immunity and prolonged survival in the mice.
Treating mice with a PGD2 inhibitor, an NKp30-blocking antibody, and an anti-IL-13 antibody resulted in reduced APL cell engraftment and a decrease in PGD2, ILC2s, and M-MDSCs. These mice also had significantly longer survival than untreated control mice (P<0.05).
Dr Jandus and her colleagues noted that antibodies against IL-13 and inhibitors of PGD2 are already in clinical use for other diseases, and antibodies that interfere with NKp30-B7H6 binding are in clinical development.
“We also found that this immunosuppressive axis may be operating in other types of cancer; in particular, prostate cancer,” Dr Jandus said. “We believe that some ILCs, like ILC2s, might suppress immune responses, while others might stimulate them. That’s what we are investigating in other types of tumors now.”
This research was supported by the Novartis Foundation for Medical-Biological Research, Ludwig Cancer Research, the Swiss National Science Foundation, Fondazione San Salvatore, ProFemmes UNIL, Fondation Pierre Mercier pour la Science, the Swiss Cancer League, and the Foundation for the Fight against Cancer. ![]()
New research has revealed a way in which acute promyelocytic leukemia (APL) cells evade destruction by the immune system.
The study showed how group 2 innate lymphoid cells (ILC2s) are recruited by leukemic cells to suppress an essential anticancer immune response.
Researchers believe this newly discovered immunosuppressive axis likely holds sway in other cancers, and it might be disrupted by therapies already in use to treat other diseases.
Camilla Jandus, MD, PhD, of the Ludwig Institute for Cancer Research in Lausanne, Switzerland, and her colleagues described this research in Nature Communications.
“ILCs are not very abundant in the body, but, when activated, they secrete large amounts of immune factors,” Dr Jandus said. “In this way, they can dictate whether a response will be pro-inflammatory or anti-inflammatory.”
ILC1, 2, and 3 have been shown to play a role in inflammation and autoimmune diseases. However, their role in cancer has remained unclear.
To address that question, Dr Jandus and her colleagues began with the observation that one subtype of the cells, ILC2s, are abnormally abundant and hyperactivated in patients with APL.
The researchers examined ILC2 immunology in patients with active APL and compared it to that of APL patients in remission.
“Our analyses suggest that, in patients with this leukemia, ILC2s are at the beginning of a novel immunosuppressive axis, one that is likely to be active in other types of cancer as well,” Dr Jandus said.
She and her colleagues found that APL cells secrete large quantities of PGD2 and express high levels of B7H6 on their surface. Both of these molecules bind to receptors on ILC2s—CRTH2 and NKp30, respectively—activating the ILC2s and prompting them to secrete interleukin-13 (IL-13).
The IL-13 switches on and expands the population of monocytic myeloid-derived immune cells (M-MDSCs). These cells suppress immune responses and allow leukemic cells to evade immune system attack.
The researchers tested these findings in a mouse model of APL. Like patients, mice with APL displayed abnormal activation of ILC2s and M-MDSCs.
However, interfering with all the signals of the immunosuppressive axis restored anti-cancer immunity and prolonged survival in the mice.
Treating mice with a PGD2 inhibitor, an NKp30-blocking antibody, and an anti-IL-13 antibody resulted in reduced APL cell engraftment and a decrease in PGD2, ILC2s, and M-MDSCs. These mice also had significantly longer survival than untreated control mice (P<0.05).
Dr Jandus and her colleagues noted that antibodies against IL-13 and inhibitors of PGD2 are already in clinical use for other diseases, and antibodies that interfere with NKp30-B7H6 binding are in clinical development.
“We also found that this immunosuppressive axis may be operating in other types of cancer; in particular, prostate cancer,” Dr Jandus said. “We believe that some ILCs, like ILC2s, might suppress immune responses, while others might stimulate them. That’s what we are investigating in other types of tumors now.”
This research was supported by the Novartis Foundation for Medical-Biological Research, Ludwig Cancer Research, the Swiss National Science Foundation, Fondazione San Salvatore, ProFemmes UNIL, Fondation Pierre Mercier pour la Science, the Swiss Cancer League, and the Foundation for the Fight against Cancer. ![]()
New research has revealed a way in which acute promyelocytic leukemia (APL) cells evade destruction by the immune system.
The study showed how group 2 innate lymphoid cells (ILC2s) are recruited by leukemic cells to suppress an essential anticancer immune response.
Researchers believe this newly discovered immunosuppressive axis likely holds sway in other cancers, and it might be disrupted by therapies already in use to treat other diseases.
Camilla Jandus, MD, PhD, of the Ludwig Institute for Cancer Research in Lausanne, Switzerland, and her colleagues described this research in Nature Communications.
“ILCs are not very abundant in the body, but, when activated, they secrete large amounts of immune factors,” Dr Jandus said. “In this way, they can dictate whether a response will be pro-inflammatory or anti-inflammatory.”
ILC1, 2, and 3 have been shown to play a role in inflammation and autoimmune diseases. However, their role in cancer has remained unclear.
To address that question, Dr Jandus and her colleagues began with the observation that one subtype of the cells, ILC2s, are abnormally abundant and hyperactivated in patients with APL.
The researchers examined ILC2 immunology in patients with active APL and compared it to that of APL patients in remission.
“Our analyses suggest that, in patients with this leukemia, ILC2s are at the beginning of a novel immunosuppressive axis, one that is likely to be active in other types of cancer as well,” Dr Jandus said.
She and her colleagues found that APL cells secrete large quantities of PGD2 and express high levels of B7H6 on their surface. Both of these molecules bind to receptors on ILC2s—CRTH2 and NKp30, respectively—activating the ILC2s and prompting them to secrete interleukin-13 (IL-13).
The IL-13 switches on and expands the population of monocytic myeloid-derived immune cells (M-MDSCs). These cells suppress immune responses and allow leukemic cells to evade immune system attack.
The researchers tested these findings in a mouse model of APL. Like patients, mice with APL displayed abnormal activation of ILC2s and M-MDSCs.
However, interfering with all the signals of the immunosuppressive axis restored anti-cancer immunity and prolonged survival in the mice.
Treating mice with a PGD2 inhibitor, an NKp30-blocking antibody, and an anti-IL-13 antibody resulted in reduced APL cell engraftment and a decrease in PGD2, ILC2s, and M-MDSCs. These mice also had significantly longer survival than untreated control mice (P<0.05).
Dr Jandus and her colleagues noted that antibodies against IL-13 and inhibitors of PGD2 are already in clinical use for other diseases, and antibodies that interfere with NKp30-B7H6 binding are in clinical development.
“We also found that this immunosuppressive axis may be operating in other types of cancer; in particular, prostate cancer,” Dr Jandus said. “We believe that some ILCs, like ILC2s, might suppress immune responses, while others might stimulate them. That’s what we are investigating in other types of tumors now.”
This research was supported by the Novartis Foundation for Medical-Biological Research, Ludwig Cancer Research, the Swiss National Science Foundation, Fondazione San Salvatore, ProFemmes UNIL, Fondation Pierre Mercier pour la Science, the Swiss Cancer League, and the Foundation for the Fight against Cancer. ![]()
Flotetuzumab for AML passes phase 1 test
MADRID – Flotetuzumab, a novel bispecific monoclonal antibody that employs a proprietary technology to redirect T lymphocytes to kill CD123-expressing cells, was safe and demonstrated efficacy in patients with acute myeloid leukemia in a phase 1 trial, based on data presented at the European Society for Medical Oncology (ESMO) Congress.
Flotetuzumab combines a portion of antibody recognizing CD3, which is an activating molecule expressed by T cells, and an arm that recognizes CD123 on the cancer cell, explained Norbert Vey, MD, PhD, Head, Leukemia Treatment Unit, Institut Paoli-Calmettes, Marseille, France. This bispecific quality, produced through a proprietary technology called Dual-Affinity ReTargeting, is considered promising because CD123 is expressed by more than 90% of AML cells and is highly expressed on stem cells involved in initiating myelodysplastic syndrome (MDS).
In this dose-ranging study (NCT02152956), 42 patients with AML and 5 patients with MDS were treated in the first cycle with infusions of flotetuzumab on either a continuous 7-day or a 4-days-on, 3-days-off schedule. For subsequent cycles, patients received the 4-days-on, 3-days-off schedule. Continuous infusion is employed due to the short half-life of flotetuzumab.
The most common adverse events were infusion-related reactions, which were observed in 76.6% of patients. Pyrexia, a potential sign of cytokine release syndrome (CRS), was observed in 23.4% of patients, who were given tocilizumab at the earliest sign of CRS. Two patients had grade 3 CRS, and one discontinued therapy. There was also one case of grade 3 myalgia. Dr. Vey characterized the overall level of adverse events as “acceptable.”
In addition to its relative safety, flotetuzumab was associated with “encouraging antileukemic activity,” Dr. Vey said. Six of 14 patients receiving doses that exceeded 500 ng/kg per day had objective responses and two of these patients had complete responses. Again, toxicity at these dose levels was considered manageable.
“This rate of clinical response is exciting,” commented Tim Somervaille, MD, Senior Group Leader, Leukemia Biology Laboratory, Cancer Research UK Institute, Manchester (England). An ESMO-invited discussant on this paper, Dr. Somervaille expressed enthusiasm in general about a growing role for bispecific T-cell engagers. Blinatumomab, the first of these agents, received regulatory approval for refractory AML in 2014.
“There are a number of these bispecific T cell antibodies that are in early-phase trials,” said Dr. Somervaille, citing several that also target CD123 within the context of a different partner antigen than that employed by flotetuzumab. He also mentioned ongoing efforts to develop bispecific natural killer cell engagers that target malignant cells through immune activation.
As for flotetuzumab, the phase 1 trial provided adequate data to encourage further development.
“A cohort expansion is now ongoing and enrolling patients at 11 sites in the United States and Europe,” Dr. Vey reported. “A clinical update on these results is expected by the end of the year.”
Dr. Vey reported financial relationships with Bristol-Myers Squibb, Novartis, and Servier.
MacroGenics retains full development and commercialization rights to flotetuzumab in the United States, Canada, Mexico, Japan, South Korea, and India. Servier participates in the development and has rights to flotetuzumab in all other countries. The U.S. Food and Drug Administration has granted orphan drug designation to flotetuzumab for the investigational treatment of AML, according to a press release from MacroGenics.
MADRID – Flotetuzumab, a novel bispecific monoclonal antibody that employs a proprietary technology to redirect T lymphocytes to kill CD123-expressing cells, was safe and demonstrated efficacy in patients with acute myeloid leukemia in a phase 1 trial, based on data presented at the European Society for Medical Oncology (ESMO) Congress.
Flotetuzumab combines a portion of antibody recognizing CD3, which is an activating molecule expressed by T cells, and an arm that recognizes CD123 on the cancer cell, explained Norbert Vey, MD, PhD, Head, Leukemia Treatment Unit, Institut Paoli-Calmettes, Marseille, France. This bispecific quality, produced through a proprietary technology called Dual-Affinity ReTargeting, is considered promising because CD123 is expressed by more than 90% of AML cells and is highly expressed on stem cells involved in initiating myelodysplastic syndrome (MDS).
In this dose-ranging study (NCT02152956), 42 patients with AML and 5 patients with MDS were treated in the first cycle with infusions of flotetuzumab on either a continuous 7-day or a 4-days-on, 3-days-off schedule. For subsequent cycles, patients received the 4-days-on, 3-days-off schedule. Continuous infusion is employed due to the short half-life of flotetuzumab.
The most common adverse events were infusion-related reactions, which were observed in 76.6% of patients. Pyrexia, a potential sign of cytokine release syndrome (CRS), was observed in 23.4% of patients, who were given tocilizumab at the earliest sign of CRS. Two patients had grade 3 CRS, and one discontinued therapy. There was also one case of grade 3 myalgia. Dr. Vey characterized the overall level of adverse events as “acceptable.”
In addition to its relative safety, flotetuzumab was associated with “encouraging antileukemic activity,” Dr. Vey said. Six of 14 patients receiving doses that exceeded 500 ng/kg per day had objective responses and two of these patients had complete responses. Again, toxicity at these dose levels was considered manageable.
“This rate of clinical response is exciting,” commented Tim Somervaille, MD, Senior Group Leader, Leukemia Biology Laboratory, Cancer Research UK Institute, Manchester (England). An ESMO-invited discussant on this paper, Dr. Somervaille expressed enthusiasm in general about a growing role for bispecific T-cell engagers. Blinatumomab, the first of these agents, received regulatory approval for refractory AML in 2014.
“There are a number of these bispecific T cell antibodies that are in early-phase trials,” said Dr. Somervaille, citing several that also target CD123 within the context of a different partner antigen than that employed by flotetuzumab. He also mentioned ongoing efforts to develop bispecific natural killer cell engagers that target malignant cells through immune activation.
As for flotetuzumab, the phase 1 trial provided adequate data to encourage further development.
“A cohort expansion is now ongoing and enrolling patients at 11 sites in the United States and Europe,” Dr. Vey reported. “A clinical update on these results is expected by the end of the year.”
Dr. Vey reported financial relationships with Bristol-Myers Squibb, Novartis, and Servier.
MacroGenics retains full development and commercialization rights to flotetuzumab in the United States, Canada, Mexico, Japan, South Korea, and India. Servier participates in the development and has rights to flotetuzumab in all other countries. The U.S. Food and Drug Administration has granted orphan drug designation to flotetuzumab for the investigational treatment of AML, according to a press release from MacroGenics.
MADRID – Flotetuzumab, a novel bispecific monoclonal antibody that employs a proprietary technology to redirect T lymphocytes to kill CD123-expressing cells, was safe and demonstrated efficacy in patients with acute myeloid leukemia in a phase 1 trial, based on data presented at the European Society for Medical Oncology (ESMO) Congress.
Flotetuzumab combines a portion of antibody recognizing CD3, which is an activating molecule expressed by T cells, and an arm that recognizes CD123 on the cancer cell, explained Norbert Vey, MD, PhD, Head, Leukemia Treatment Unit, Institut Paoli-Calmettes, Marseille, France. This bispecific quality, produced through a proprietary technology called Dual-Affinity ReTargeting, is considered promising because CD123 is expressed by more than 90% of AML cells and is highly expressed on stem cells involved in initiating myelodysplastic syndrome (MDS).
In this dose-ranging study (NCT02152956), 42 patients with AML and 5 patients with MDS were treated in the first cycle with infusions of flotetuzumab on either a continuous 7-day or a 4-days-on, 3-days-off schedule. For subsequent cycles, patients received the 4-days-on, 3-days-off schedule. Continuous infusion is employed due to the short half-life of flotetuzumab.
The most common adverse events were infusion-related reactions, which were observed in 76.6% of patients. Pyrexia, a potential sign of cytokine release syndrome (CRS), was observed in 23.4% of patients, who were given tocilizumab at the earliest sign of CRS. Two patients had grade 3 CRS, and one discontinued therapy. There was also one case of grade 3 myalgia. Dr. Vey characterized the overall level of adverse events as “acceptable.”
In addition to its relative safety, flotetuzumab was associated with “encouraging antileukemic activity,” Dr. Vey said. Six of 14 patients receiving doses that exceeded 500 ng/kg per day had objective responses and two of these patients had complete responses. Again, toxicity at these dose levels was considered manageable.
“This rate of clinical response is exciting,” commented Tim Somervaille, MD, Senior Group Leader, Leukemia Biology Laboratory, Cancer Research UK Institute, Manchester (England). An ESMO-invited discussant on this paper, Dr. Somervaille expressed enthusiasm in general about a growing role for bispecific T-cell engagers. Blinatumomab, the first of these agents, received regulatory approval for refractory AML in 2014.
“There are a number of these bispecific T cell antibodies that are in early-phase trials,” said Dr. Somervaille, citing several that also target CD123 within the context of a different partner antigen than that employed by flotetuzumab. He also mentioned ongoing efforts to develop bispecific natural killer cell engagers that target malignant cells through immune activation.
As for flotetuzumab, the phase 1 trial provided adequate data to encourage further development.
“A cohort expansion is now ongoing and enrolling patients at 11 sites in the United States and Europe,” Dr. Vey reported. “A clinical update on these results is expected by the end of the year.”
Dr. Vey reported financial relationships with Bristol-Myers Squibb, Novartis, and Servier.
MacroGenics retains full development and commercialization rights to flotetuzumab in the United States, Canada, Mexico, Japan, South Korea, and India. Servier participates in the development and has rights to flotetuzumab in all other countries. The U.S. Food and Drug Administration has granted orphan drug designation to flotetuzumab for the investigational treatment of AML, according to a press release from MacroGenics.
AT ESMO 2017
Key clinical point: The phase 1 trial provided adequate data to encourage further development of flotetuzumab for patients with acute myeloid leukemia.
Major finding: Six of 14 patients receiving doses that exceeded 500 ng/kg per day had objective responses and two of these patients had complete responses.
Data source: Phase 1 dose-escalation study in 42 patients with AML and 5 patients with MDS.
Disclosures: Dr. Vey reported financial relationships with Bristol-Myers Squibb, Novartis, and Servier.
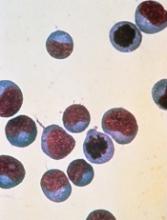
Midostaurin approved to treat AML, SM in Europe
The European Commission has approved the multi-targeted kinase inhibitor midostaurin (Rydapt®) to treat acute myeloid leukemia (AML) and 3 types of advanced systemic mastocytosis (SM).
Midostaurin is approved to treat adults with newly diagnosed acute myeloid leukemia (AML) who are FLT3 mutation-positive. In these patients, midostaurin can be used in combination with standard daunorubicin and cytarabine induction, followed by high-dose cytarabine consolidation. Patients who achieve a complete response can then receive midostaurin as maintenance therapy.
Midostaurin is also approved as monotherapy for adults with aggressive SM (ASM), SM with associated hematological neoplasm (SM-AHN), and mast cell leukemia (MCL).
Midostaurin in AML
The approval of midostaurin in AML is based on results from the phase 3 RATIFY trial, which were published in NEJM last month.
In RATIFY, researchers compared midostaurin plus standard chemotherapy to placebo plus standard chemotherapy in 717 adults younger than age 60 who had FLT3-mutated AML.
The median overall survival was significantly longer in the midostaurin arm than the placebo arm—74.7 months and 25.6 months, respectively (hazard ratio=0.77, P=0.016).
And the median event-free survival was significantly longer in the midostaurin arm than the placebo arm—8.2 months and 3.0 months, respectively (hazard ratio=0.78, P=0.004).
The most frequent adverse events (AEs) in the midostaurin arm (occurring in at least 20% of patients) were febrile neutropenia, nausea, vomiting, mucositis, headache, musculoskeletal pain, petechiae, device-related infection, epistaxis, hyperglycemia, and upper respiratory tract infection.
The most frequent grade 3/4 AEs (occurring in at least 10% of patients) were febrile neutropenia, device-related infection, and mucositis. Nine percent of patients in the midostaurin arm stopped treatment due to AEs, as did 6% in the placebo arm.
Midostaurin in advanced SM
The approval of midostaurin in advanced SM is based on results from a pair of phase 2, single-arm studies, hereafter referred to as Study 2 and Study 3. Data from Study 2 were published in NEJM in June 2016, and data from Study 3 were presented at the 2010 ASH Annual Meeting.
Study 2 included 116 patients, 115 of whom were evaluable for response.
The overall response rate (ORR) was 17% in the entire cohort, 31% among patients with ASM, 11% among patients with SM-AHN, and 19% among patients with MCL. The complete response rates were 2%, 6%, 0%, and 5%, respectively.
Study 3 included 26 patients with advanced SM. In 3 of the patients, the subtype of SM was unconfirmed.
Among the 17 patients with SM-AHN, there were 10 responses (ORR=59%), including 1 partial response and 9 major responses. In the 6 patients with MCL, there were 2 responses (ORR=33%), which included 1 partial response and 1 major response.
In both studies combined, there were 142 adults with ASM, SM-AHN, or MCL.
The most frequent AEs (excluding laboratory abnormalities) that occurred in at least 20% of these patients were nausea, vomiting, diarrhea, edema, musculoskeletal pain, abdominal pain, fatigue, upper respiratory tract infection, constipation, pyrexia, headache, and dyspnea.
The most frequent grade 3 or higher AEs (excluding laboratory abnormalities) that occurred in at least 5% of patients were fatigue, sepsis, gastrointestinal hemorrhage, pneumonia, diarrhea, febrile neutropenia, edema, dyspnea, nausea, vomiting, abdominal pain, and renal insufficiency.
Serious AEs occurred in 68% of patients, most commonly infections and gastrointestinal disorders.
Twenty-one percent of patients discontinued treatment due to AEs, the most frequent of which were infection, nausea or vomiting, QT prolongation, and gastrointestinal hemorrhage. ![]()
The European Commission has approved the multi-targeted kinase inhibitor midostaurin (Rydapt®) to treat acute myeloid leukemia (AML) and 3 types of advanced systemic mastocytosis (SM).
Midostaurin is approved to treat adults with newly diagnosed acute myeloid leukemia (AML) who are FLT3 mutation-positive. In these patients, midostaurin can be used in combination with standard daunorubicin and cytarabine induction, followed by high-dose cytarabine consolidation. Patients who achieve a complete response can then receive midostaurin as maintenance therapy.
Midostaurin is also approved as monotherapy for adults with aggressive SM (ASM), SM with associated hematological neoplasm (SM-AHN), and mast cell leukemia (MCL).
Midostaurin in AML
The approval of midostaurin in AML is based on results from the phase 3 RATIFY trial, which were published in NEJM last month.
In RATIFY, researchers compared midostaurin plus standard chemotherapy to placebo plus standard chemotherapy in 717 adults younger than age 60 who had FLT3-mutated AML.
The median overall survival was significantly longer in the midostaurin arm than the placebo arm—74.7 months and 25.6 months, respectively (hazard ratio=0.77, P=0.016).
And the median event-free survival was significantly longer in the midostaurin arm than the placebo arm—8.2 months and 3.0 months, respectively (hazard ratio=0.78, P=0.004).
The most frequent adverse events (AEs) in the midostaurin arm (occurring in at least 20% of patients) were febrile neutropenia, nausea, vomiting, mucositis, headache, musculoskeletal pain, petechiae, device-related infection, epistaxis, hyperglycemia, and upper respiratory tract infection.
The most frequent grade 3/4 AEs (occurring in at least 10% of patients) were febrile neutropenia, device-related infection, and mucositis. Nine percent of patients in the midostaurin arm stopped treatment due to AEs, as did 6% in the placebo arm.
Midostaurin in advanced SM
The approval of midostaurin in advanced SM is based on results from a pair of phase 2, single-arm studies, hereafter referred to as Study 2 and Study 3. Data from Study 2 were published in NEJM in June 2016, and data from Study 3 were presented at the 2010 ASH Annual Meeting.
Study 2 included 116 patients, 115 of whom were evaluable for response.
The overall response rate (ORR) was 17% in the entire cohort, 31% among patients with ASM, 11% among patients with SM-AHN, and 19% among patients with MCL. The complete response rates were 2%, 6%, 0%, and 5%, respectively.
Study 3 included 26 patients with advanced SM. In 3 of the patients, the subtype of SM was unconfirmed.
Among the 17 patients with SM-AHN, there were 10 responses (ORR=59%), including 1 partial response and 9 major responses. In the 6 patients with MCL, there were 2 responses (ORR=33%), which included 1 partial response and 1 major response.
In both studies combined, there were 142 adults with ASM, SM-AHN, or MCL.
The most frequent AEs (excluding laboratory abnormalities) that occurred in at least 20% of these patients were nausea, vomiting, diarrhea, edema, musculoskeletal pain, abdominal pain, fatigue, upper respiratory tract infection, constipation, pyrexia, headache, and dyspnea.
The most frequent grade 3 or higher AEs (excluding laboratory abnormalities) that occurred in at least 5% of patients were fatigue, sepsis, gastrointestinal hemorrhage, pneumonia, diarrhea, febrile neutropenia, edema, dyspnea, nausea, vomiting, abdominal pain, and renal insufficiency.
Serious AEs occurred in 68% of patients, most commonly infections and gastrointestinal disorders.
Twenty-one percent of patients discontinued treatment due to AEs, the most frequent of which were infection, nausea or vomiting, QT prolongation, and gastrointestinal hemorrhage. ![]()
The European Commission has approved the multi-targeted kinase inhibitor midostaurin (Rydapt®) to treat acute myeloid leukemia (AML) and 3 types of advanced systemic mastocytosis (SM).
Midostaurin is approved to treat adults with newly diagnosed acute myeloid leukemia (AML) who are FLT3 mutation-positive. In these patients, midostaurin can be used in combination with standard daunorubicin and cytarabine induction, followed by high-dose cytarabine consolidation. Patients who achieve a complete response can then receive midostaurin as maintenance therapy.
Midostaurin is also approved as monotherapy for adults with aggressive SM (ASM), SM with associated hematological neoplasm (SM-AHN), and mast cell leukemia (MCL).
Midostaurin in AML
The approval of midostaurin in AML is based on results from the phase 3 RATIFY trial, which were published in NEJM last month.
In RATIFY, researchers compared midostaurin plus standard chemotherapy to placebo plus standard chemotherapy in 717 adults younger than age 60 who had FLT3-mutated AML.
The median overall survival was significantly longer in the midostaurin arm than the placebo arm—74.7 months and 25.6 months, respectively (hazard ratio=0.77, P=0.016).
And the median event-free survival was significantly longer in the midostaurin arm than the placebo arm—8.2 months and 3.0 months, respectively (hazard ratio=0.78, P=0.004).
The most frequent adverse events (AEs) in the midostaurin arm (occurring in at least 20% of patients) were febrile neutropenia, nausea, vomiting, mucositis, headache, musculoskeletal pain, petechiae, device-related infection, epistaxis, hyperglycemia, and upper respiratory tract infection.
The most frequent grade 3/4 AEs (occurring in at least 10% of patients) were febrile neutropenia, device-related infection, and mucositis. Nine percent of patients in the midostaurin arm stopped treatment due to AEs, as did 6% in the placebo arm.
Midostaurin in advanced SM
The approval of midostaurin in advanced SM is based on results from a pair of phase 2, single-arm studies, hereafter referred to as Study 2 and Study 3. Data from Study 2 were published in NEJM in June 2016, and data from Study 3 were presented at the 2010 ASH Annual Meeting.
Study 2 included 116 patients, 115 of whom were evaluable for response.
The overall response rate (ORR) was 17% in the entire cohort, 31% among patients with ASM, 11% among patients with SM-AHN, and 19% among patients with MCL. The complete response rates were 2%, 6%, 0%, and 5%, respectively.
Study 3 included 26 patients with advanced SM. In 3 of the patients, the subtype of SM was unconfirmed.
Among the 17 patients with SM-AHN, there were 10 responses (ORR=59%), including 1 partial response and 9 major responses. In the 6 patients with MCL, there were 2 responses (ORR=33%), which included 1 partial response and 1 major response.
In both studies combined, there were 142 adults with ASM, SM-AHN, or MCL.
The most frequent AEs (excluding laboratory abnormalities) that occurred in at least 20% of these patients were nausea, vomiting, diarrhea, edema, musculoskeletal pain, abdominal pain, fatigue, upper respiratory tract infection, constipation, pyrexia, headache, and dyspnea.
The most frequent grade 3 or higher AEs (excluding laboratory abnormalities) that occurred in at least 5% of patients were fatigue, sepsis, gastrointestinal hemorrhage, pneumonia, diarrhea, febrile neutropenia, edema, dyspnea, nausea, vomiting, abdominal pain, and renal insufficiency.
Serious AEs occurred in 68% of patients, most commonly infections and gastrointestinal disorders.
Twenty-one percent of patients discontinued treatment due to AEs, the most frequent of which were infection, nausea or vomiting, QT prolongation, and gastrointestinal hemorrhage. ![]()
FDA grants RMAT designation to HSCT adjunct
The US Food and Drug Administration (FDA) has granted Regenerative Medicine Advanced Therapy (RMAT) designation to ATIR101™, which is intended to be used as an adjunct to haploidentical hematopoietic stem cell transplant (HSCT).
ATIR101 is a personalized T-cell immunotherapy—a donor lymphocyte preparation selectively depleted of host-alloreactive T cells through the use of photo-dynamic therapy.
Recipient-reactive T cells from the donor are activated in a unidirectional mixed-lymphocyte reaction. The cells are then treated with TH9402 (a rhodamide-like dye), which is selectively retained in activated T cells.
Subsequent light exposure eliminates the activated recipient-reactive T cells but preserves the other T cells.
The final product is infused after CD34-selected haploidentical HSCT with the goal of preventing infectious complications, graft-versus-host disease (GVHD), and relapse.
About RMAT designation
The RMAT pathway is analogous to the breakthrough therapy designation designed for traditional drug candidates and medical devices. RMAT designation was specifically created by the US Congress in 2016 in the hopes of getting new cell therapies and advanced medicinal products to patients earlier.
Just like breakthrough designation, RMAT designation allows companies developing regenerative medicine therapies to interact with the FDA more frequently in the clinical testing process. In addition, RMAT-designated products may be eligible for priority review and accelerated approval.
A regenerative medicine is eligible for RMAT designation if it is intended to treat, modify, reverse, or cure a serious or life-threatening disease or condition, and if preliminary clinical evidence indicates the treatment has the potential to address unmet medical needs for such a disease or condition.
“To receive the RMAT designation from the FDA is an important milestone for Kiadis Pharma and a recognition by the FDA of the significant potential for ATIR101 to help patients receive safer and more effective bone marrow transplantations,” said Arthur Lahr, CEO of Kiadis Pharma, the company developing ATIR101.
“We are now going to work even closer with the FDA to agree a path to make this cell therapy treatment available for patients in the US as soon as possible. In Europe, ATIR101 was filed for registration in April 2017, and we continue to prepare the company for the potential European launch in 2019.”
ATIR101 trials
Results of a phase 2 trial of ATIR101 were presented at the 42nd Annual Meeting of the European Society of Blood and Marrow Transplantation in 2016.
Patients who received ATIR101 after haploidentical HSCT had significant improvements in transplant-related mortality and overall survival when compared to historical controls who received a T-cell-depleted haploidentical HSCT without ATIR101.
None of the patients who received ATIR101 developed grade 3-4 GVHD, but a few patients did develop grade 2 GVHD.
A phase 3 trial of ATIR101 is now underway. The trial is expected to enroll 200 patients with acute myeloid leukemia, acute lymphoblastic leukemia, or myelodysplastic syndrome.
The patients will receive a haploidentical HSCT with either a T-cell-depleted graft and adjunctive treatment with ATIR101 or a T-cell-replete graft and post-transplant cyclophosphamide. ![]()
The US Food and Drug Administration (FDA) has granted Regenerative Medicine Advanced Therapy (RMAT) designation to ATIR101™, which is intended to be used as an adjunct to haploidentical hematopoietic stem cell transplant (HSCT).
ATIR101 is a personalized T-cell immunotherapy—a donor lymphocyte preparation selectively depleted of host-alloreactive T cells through the use of photo-dynamic therapy.
Recipient-reactive T cells from the donor are activated in a unidirectional mixed-lymphocyte reaction. The cells are then treated with TH9402 (a rhodamide-like dye), which is selectively retained in activated T cells.
Subsequent light exposure eliminates the activated recipient-reactive T cells but preserves the other T cells.
The final product is infused after CD34-selected haploidentical HSCT with the goal of preventing infectious complications, graft-versus-host disease (GVHD), and relapse.
About RMAT designation
The RMAT pathway is analogous to the breakthrough therapy designation designed for traditional drug candidates and medical devices. RMAT designation was specifically created by the US Congress in 2016 in the hopes of getting new cell therapies and advanced medicinal products to patients earlier.
Just like breakthrough designation, RMAT designation allows companies developing regenerative medicine therapies to interact with the FDA more frequently in the clinical testing process. In addition, RMAT-designated products may be eligible for priority review and accelerated approval.
A regenerative medicine is eligible for RMAT designation if it is intended to treat, modify, reverse, or cure a serious or life-threatening disease or condition, and if preliminary clinical evidence indicates the treatment has the potential to address unmet medical needs for such a disease or condition.
“To receive the RMAT designation from the FDA is an important milestone for Kiadis Pharma and a recognition by the FDA of the significant potential for ATIR101 to help patients receive safer and more effective bone marrow transplantations,” said Arthur Lahr, CEO of Kiadis Pharma, the company developing ATIR101.
“We are now going to work even closer with the FDA to agree a path to make this cell therapy treatment available for patients in the US as soon as possible. In Europe, ATIR101 was filed for registration in April 2017, and we continue to prepare the company for the potential European launch in 2019.”
ATIR101 trials
Results of a phase 2 trial of ATIR101 were presented at the 42nd Annual Meeting of the European Society of Blood and Marrow Transplantation in 2016.
Patients who received ATIR101 after haploidentical HSCT had significant improvements in transplant-related mortality and overall survival when compared to historical controls who received a T-cell-depleted haploidentical HSCT without ATIR101.
None of the patients who received ATIR101 developed grade 3-4 GVHD, but a few patients did develop grade 2 GVHD.
A phase 3 trial of ATIR101 is now underway. The trial is expected to enroll 200 patients with acute myeloid leukemia, acute lymphoblastic leukemia, or myelodysplastic syndrome.
The patients will receive a haploidentical HSCT with either a T-cell-depleted graft and adjunctive treatment with ATIR101 or a T-cell-replete graft and post-transplant cyclophosphamide. ![]()
The US Food and Drug Administration (FDA) has granted Regenerative Medicine Advanced Therapy (RMAT) designation to ATIR101™, which is intended to be used as an adjunct to haploidentical hematopoietic stem cell transplant (HSCT).
ATIR101 is a personalized T-cell immunotherapy—a donor lymphocyte preparation selectively depleted of host-alloreactive T cells through the use of photo-dynamic therapy.
Recipient-reactive T cells from the donor are activated in a unidirectional mixed-lymphocyte reaction. The cells are then treated with TH9402 (a rhodamide-like dye), which is selectively retained in activated T cells.
Subsequent light exposure eliminates the activated recipient-reactive T cells but preserves the other T cells.
The final product is infused after CD34-selected haploidentical HSCT with the goal of preventing infectious complications, graft-versus-host disease (GVHD), and relapse.
About RMAT designation
The RMAT pathway is analogous to the breakthrough therapy designation designed for traditional drug candidates and medical devices. RMAT designation was specifically created by the US Congress in 2016 in the hopes of getting new cell therapies and advanced medicinal products to patients earlier.
Just like breakthrough designation, RMAT designation allows companies developing regenerative medicine therapies to interact with the FDA more frequently in the clinical testing process. In addition, RMAT-designated products may be eligible for priority review and accelerated approval.
A regenerative medicine is eligible for RMAT designation if it is intended to treat, modify, reverse, or cure a serious or life-threatening disease or condition, and if preliminary clinical evidence indicates the treatment has the potential to address unmet medical needs for such a disease or condition.
“To receive the RMAT designation from the FDA is an important milestone for Kiadis Pharma and a recognition by the FDA of the significant potential for ATIR101 to help patients receive safer and more effective bone marrow transplantations,” said Arthur Lahr, CEO of Kiadis Pharma, the company developing ATIR101.
“We are now going to work even closer with the FDA to agree a path to make this cell therapy treatment available for patients in the US as soon as possible. In Europe, ATIR101 was filed for registration in April 2017, and we continue to prepare the company for the potential European launch in 2019.”
ATIR101 trials
Results of a phase 2 trial of ATIR101 were presented at the 42nd Annual Meeting of the European Society of Blood and Marrow Transplantation in 2016.
Patients who received ATIR101 after haploidentical HSCT had significant improvements in transplant-related mortality and overall survival when compared to historical controls who received a T-cell-depleted haploidentical HSCT without ATIR101.
None of the patients who received ATIR101 developed grade 3-4 GVHD, but a few patients did develop grade 2 GVHD.
A phase 3 trial of ATIR101 is now underway. The trial is expected to enroll 200 patients with acute myeloid leukemia, acute lymphoblastic leukemia, or myelodysplastic syndrome.
The patients will receive a haploidentical HSCT with either a T-cell-depleted graft and adjunctive treatment with ATIR101 or a T-cell-replete graft and post-transplant cyclophosphamide.
Team creates guidelines on CAR T-cell-related toxicity
Researchers say they have created guidelines for managing the unique toxicities associated with chimeric antigen receptor (CAR) T-cell therapy.
The guidelines focus on cytokine release syndrome (CRS); neurological toxicity, which the researchers have dubbed “CAR-T-cell-related encephalopathy syndrome (CRES);” and adverse effects related to these syndromes.
“The toxicities are unique, and every member of the care team needs to be trained to recognize them and act accordingly,” said Sattva Neelapu, MD, of University of Texas MD Anderson Cancer Center in Houston.
Dr Neelapu and his colleagues described the toxicities and related recommendations in Nature Reviews Clinical Oncology.
The team’s guidelines include supportive-care considerations for patients receiving CAR T‑cell therapy. For example, they recommend:
- Baseline brain MRI to rule out central nervous system disease
- Cardiac monitoring starting on the day of CAR T‑cell infusion
- Assessing a patient’s vital signs every 4 hours after CAR T-cell infusion
- Assessing and grading CRS at least twice daily and whenever the patient’s status changes
- Assessing and grading CRES at least every 8 hours.
CRS
One section of the guidelines is dedicated to CRS, with subsections on pathophysiology, precautions and supportive care, the use of corticosteroids and IL‑6/IL‑6R antagonists, and grading CRS.
The researchers noted that CRS typically manifests with constitutional symptoms, such as fever, malaise, anorexia, and myalgias. However, CRS can affect any organ system in the body.
The team recommends managing CRS according to grade. For example, patients with grade 1 CRS should typically receive supportive care. However, physicians should consider giving tocilizumab or siltuximab to grade 1 patients who have a refractory fever lasting more than 3 days.
The researchers also noted that CRS can evolve into fulminant hemophagocytic lymphohistiocytosis (HLH), also known as macrophage-activation syndrome (MAS).
The team said HLH/MAS encompasses a group of severe immunological disorders characterized by hyperactivation of macrophages and lymphocytes, proinflammatory cytokine production, lymphohistiocytic tissue infiltration, and immune-mediated multi-organ failure.
The guidelines include diagnostic criteria for CAR T‑cell-related HLH/MAS and recommendations for managing the condition.
CRES
One section of the guidelines is dedicated to the grading and treatment of CRES, which typically manifests as a toxic encephalopathy.
The researchers said the earliest signs of CRES are diminished attention, language disturbance, and impaired handwriting. Other symptoms include confusion, disorientation, agitation, aphasia, somnolence, and tremors.
Patients with severe CRES (grade >2) may experience seizures, motor weakness, incontinence, mental obtundation, increased intracranial pressure, papilledema, and cerebral edema.
Therefore, the guidelines include recommendations for the management of status epilepticus and raised intracranial pressure after CAR T‑cell therapy.
The researchers also devised an algorithm, known as CARTOX-10, for identifying neurotoxicity. (An existing general method didn’t effectively quantify the neurological effects caused by CAR T-cell therapies.)
CARTOX-10 is a 10-point test in which patients are asked to do the following:
- Name the current month (1 point) and year (1 point)
- Name the city (1 point) and hospital they are in (1 point)
- Name the president/prime minister of their home country (1 point)
- Name 3 nearby objects (3 points)
- Write a standard sentence (1 point)
- Count backward from 100 by tens (1 point).
A perfect score indicates normal cognitive function. A patient has mild to severe impairment depending on the number of questions or activities missed.
Dr Neelapu and his colleagues believe their recommendations will be applicable to other types of cell-based immunotherapy as well, including CAR natural killer cells, T-cell receptor engineered T cells, and combination drugs that use an antibody to connect T cells to targets on cancer cells.
Researchers involved in this work have received funding from companies developing/marketing CAR T-cell therapies.
Researchers say they have created guidelines for managing the unique toxicities associated with chimeric antigen receptor (CAR) T-cell therapy.
The guidelines focus on cytokine release syndrome (CRS); neurological toxicity, which the researchers have dubbed “CAR-T-cell-related encephalopathy syndrome (CRES);” and adverse effects related to these syndromes.
“The toxicities are unique, and every member of the care team needs to be trained to recognize them and act accordingly,” said Sattva Neelapu, MD, of University of Texas MD Anderson Cancer Center in Houston.
Dr Neelapu and his colleagues described the toxicities and related recommendations in Nature Reviews Clinical Oncology.
The team’s guidelines include supportive-care considerations for patients receiving CAR T‑cell therapy. For example, they recommend:
- Baseline brain MRI to rule out central nervous system disease
- Cardiac monitoring starting on the day of CAR T‑cell infusion
- Assessing a patient’s vital signs every 4 hours after CAR T-cell infusion
- Assessing and grading CRS at least twice daily and whenever the patient’s status changes
- Assessing and grading CRES at least every 8 hours.
CRS
One section of the guidelines is dedicated to CRS, with subsections on pathophysiology, precautions and supportive care, the use of corticosteroids and IL‑6/IL‑6R antagonists, and grading CRS.
The researchers noted that CRS typically manifests with constitutional symptoms, such as fever, malaise, anorexia, and myalgias. However, CRS can affect any organ system in the body.
The team recommends managing CRS according to grade. For example, patients with grade 1 CRS should typically receive supportive care. However, physicians should consider giving tocilizumab or siltuximab to grade 1 patients who have a refractory fever lasting more than 3 days.
The researchers also noted that CRS can evolve into fulminant hemophagocytic lymphohistiocytosis (HLH), also known as macrophage-activation syndrome (MAS).
The team said HLH/MAS encompasses a group of severe immunological disorders characterized by hyperactivation of macrophages and lymphocytes, proinflammatory cytokine production, lymphohistiocytic tissue infiltration, and immune-mediated multi-organ failure.
The guidelines include diagnostic criteria for CAR T‑cell-related HLH/MAS and recommendations for managing the condition.
CRES
One section of the guidelines is dedicated to the grading and treatment of CRES, which typically manifests as a toxic encephalopathy.
The researchers said the earliest signs of CRES are diminished attention, language disturbance, and impaired handwriting. Other symptoms include confusion, disorientation, agitation, aphasia, somnolence, and tremors.
Patients with severe CRES (grade >2) may experience seizures, motor weakness, incontinence, mental obtundation, increased intracranial pressure, papilledema, and cerebral edema.
Therefore, the guidelines include recommendations for the management of status epilepticus and raised intracranial pressure after CAR T‑cell therapy.
The researchers also devised an algorithm, known as CARTOX-10, for identifying neurotoxicity. (An existing general method didn’t effectively quantify the neurological effects caused by CAR T-cell therapies.)
CARTOX-10 is a 10-point test in which patients are asked to do the following:
- Name the current month (1 point) and year (1 point)
- Name the city (1 point) and hospital they are in (1 point)
- Name the president/prime minister of their home country (1 point)
- Name 3 nearby objects (3 points)
- Write a standard sentence (1 point)
- Count backward from 100 by tens (1 point).
A perfect score indicates normal cognitive function. A patient has mild to severe impairment depending on the number of questions or activities missed.
Dr Neelapu and his colleagues believe their recommendations will be applicable to other types of cell-based immunotherapy as well, including CAR natural killer cells, T-cell receptor engineered T cells, and combination drugs that use an antibody to connect T cells to targets on cancer cells.
Researchers involved in this work have received funding from companies developing/marketing CAR T-cell therapies.
Researchers say they have created guidelines for managing the unique toxicities associated with chimeric antigen receptor (CAR) T-cell therapy.
The guidelines focus on cytokine release syndrome (CRS); neurological toxicity, which the researchers have dubbed “CAR-T-cell-related encephalopathy syndrome (CRES);” and adverse effects related to these syndromes.
“The toxicities are unique, and every member of the care team needs to be trained to recognize them and act accordingly,” said Sattva Neelapu, MD, of University of Texas MD Anderson Cancer Center in Houston.
Dr Neelapu and his colleagues described the toxicities and related recommendations in Nature Reviews Clinical Oncology.
The team’s guidelines include supportive-care considerations for patients receiving CAR T‑cell therapy. For example, they recommend:
- Baseline brain MRI to rule out central nervous system disease
- Cardiac monitoring starting on the day of CAR T‑cell infusion
- Assessing a patient’s vital signs every 4 hours after CAR T-cell infusion
- Assessing and grading CRS at least twice daily and whenever the patient’s status changes
- Assessing and grading CRES at least every 8 hours.
CRS
One section of the guidelines is dedicated to CRS, with subsections on pathophysiology, precautions and supportive care, the use of corticosteroids and IL‑6/IL‑6R antagonists, and grading CRS.
The researchers noted that CRS typically manifests with constitutional symptoms, such as fever, malaise, anorexia, and myalgias. However, CRS can affect any organ system in the body.
The team recommends managing CRS according to grade. For example, patients with grade 1 CRS should typically receive supportive care. However, physicians should consider giving tocilizumab or siltuximab to grade 1 patients who have a refractory fever lasting more than 3 days.
The researchers also noted that CRS can evolve into fulminant hemophagocytic lymphohistiocytosis (HLH), also known as macrophage-activation syndrome (MAS).
The team said HLH/MAS encompasses a group of severe immunological disorders characterized by hyperactivation of macrophages and lymphocytes, proinflammatory cytokine production, lymphohistiocytic tissue infiltration, and immune-mediated multi-organ failure.
The guidelines include diagnostic criteria for CAR T‑cell-related HLH/MAS and recommendations for managing the condition.
CRES
One section of the guidelines is dedicated to the grading and treatment of CRES, which typically manifests as a toxic encephalopathy.
The researchers said the earliest signs of CRES are diminished attention, language disturbance, and impaired handwriting. Other symptoms include confusion, disorientation, agitation, aphasia, somnolence, and tremors.
Patients with severe CRES (grade >2) may experience seizures, motor weakness, incontinence, mental obtundation, increased intracranial pressure, papilledema, and cerebral edema.
Therefore, the guidelines include recommendations for the management of status epilepticus and raised intracranial pressure after CAR T‑cell therapy.
The researchers also devised an algorithm, known as CARTOX-10, for identifying neurotoxicity. (An existing general method didn’t effectively quantify the neurological effects caused by CAR T-cell therapies.)
CARTOX-10 is a 10-point test in which patients are asked to do the following:
- Name the current month (1 point) and year (1 point)
- Name the city (1 point) and hospital they are in (1 point)
- Name the president/prime minister of their home country (1 point)
- Name 3 nearby objects (3 points)
- Write a standard sentence (1 point)
- Count backward from 100 by tens (1 point).
A perfect score indicates normal cognitive function. A patient has mild to severe impairment depending on the number of questions or activities missed.
Dr Neelapu and his colleagues believe their recommendations will be applicable to other types of cell-based immunotherapy as well, including CAR natural killer cells, T-cell receptor engineered T cells, and combination drugs that use an antibody to connect T cells to targets on cancer cells.
Researchers involved in this work have received funding from companies developing/marketing CAR T-cell therapies.
Antibody shows early promise in AML/MDS trial
MADRID—Interim results of a phase 1 study suggest flotetuzumab, a CD123 and CD3 bispecific antibody, may be a feasible treatment option for relapsed or refractory acute myeloid leukemia (AML) or intermediate/high-risk myelodysplastic syndromes (MDS).
Researchers said flotetuzumab demonstrated acceptable tolerability in the dose-escalation portion of the study, with infusion-related reactions (IRRs) and cytokine release syndrome (CRS) being the most common adverse events (AEs).
In addition, flotetuzumab exhibited anti-leukemic activity in 8 of 14 response-evaluable patients, with 6 patients achieving a response.
Norbert Vey, MD, of Institut Paoli-Calmettes in Marseille, France, presented these results at the ESMO 2017 Congress (abstract 995O*). The study is sponsored by MacroGenics, Inc., the company developing flotetuzumab.
Flotetuzumab (MGD006) recognizes CD123 and CD3. The primary mechanism of flotetuzumab is thought to be its ability to redirect T cells to kill CD123-expressing cells. To achieve this, the molecule combines a portion of an antibody recognizing CD3 (an activating molecule expressed by T cells) with an arm that recognizes CD123 on the target cancer cells.
In this ongoing phase 1 study of flotetuzumab, researchers have enrolled 47 patients with a median age of 64 (range, 29-84). About 89% of these patients had AML (n=42), and the rest (n=5) had MDS.
Twenty-four percent had relapsed AML (n=10), 55% had refractory AML (n=23), and 21% had failed treatment with hypomethylating agents (n=9). One patient had intermediate-1-risk MDS, 2 had intermediate-2-risk, and 2 had high-risk MDS.
Treatment
The study began with single patients receiving flotetuzumab at escalating doses—3 ng/kg/day, 10 ng/kg/day, 30 ng/kg/day, and 100 ng/kg/day.
Then, patients received a range of doses on 2 different schedules for cycle 1. One group received treatment 7 days a week. The other had a 4-days-on/3-days-off schedule.
All patients received a lead-in dose during the first week of cycle 1. They received 30 ng/kg/day for 3 days, then 100 ng/kg/day for 4 days.
For the rest of cycle 1, patients in the 4 days/3 days group received doses of 500 ng/kg, 700 ng/kg, 900 ng/kg, or 1000 ng/kg. Patients in the daily dosing group received doses of 300 ng/kg, 500 ng/kg, 700 ng/kg, 900 ng/kg, or 1000 ng/kg.
For cycle 2 and beyond, all patients were on the 4-days-on/3-days-off schedule.
Safety
The maximum tolerated dose and schedule was 500 ng/kg/day for 7 days.
Dose-limiting toxicities occurring at the 700 ng/kg/day dose included grade 2 IRRs/CRS in 2 patients and grade 3 myalgia in 1 patient. There was 1 drug-related central nervous system AE that led to treatment discontinuation.
IRRs/CRS occurred in 77% of patients, with 13% of patients having grade 3 events and 8.5% of patients discontinuing treatment due to IRRs/CRS.
The researchers said they found ways to decrease the incidence and severity of CRS. One is early intervention with tocilizumab. The other is a 2-step lead-in dose during week 1. So patients first receive 30 ng/kg, then 100 ng/kg, and then their target dose.
Other grade 3 AEs occurring in this trial include febrile neutropenia (11%), anemia (11%), and decreases in platelets (13%), white blood cells (11%), and lymphocytes (13%).
Efficacy
The researchers said they observed encouraging anti-leukemic activity in patients treated at 500 ng/kg/day or greater.
As of the data cut-off, 14 patients treated at this dose were evaluable for response. Eight (57%) patients had anti-leukemic activity, with 6 (43%) of these patients experiencing an objective response.
One patient achieved a complete response (CR), 2 had a CR with incomplete count recovery, and 1 had a molecular CR.
In most responders, anti-leukemic activity was observed after a single cycle of therapy.
MacroGenics is currently enrolling patients in dose-expansion cohorts. The company plans to present updated results from this trial at another scientific conference later this year.
*Slides from this presentation are available on the MacroGenics website at http://ir.macrogenics.com/events.cfm.
MADRID—Interim results of a phase 1 study suggest flotetuzumab, a CD123 and CD3 bispecific antibody, may be a feasible treatment option for relapsed or refractory acute myeloid leukemia (AML) or intermediate/high-risk myelodysplastic syndromes (MDS).
Researchers said flotetuzumab demonstrated acceptable tolerability in the dose-escalation portion of the study, with infusion-related reactions (IRRs) and cytokine release syndrome (CRS) being the most common adverse events (AEs).
In addition, flotetuzumab exhibited anti-leukemic activity in 8 of 14 response-evaluable patients, with 6 patients achieving a response.
Norbert Vey, MD, of Institut Paoli-Calmettes in Marseille, France, presented these results at the ESMO 2017 Congress (abstract 995O*). The study is sponsored by MacroGenics, Inc., the company developing flotetuzumab.
Flotetuzumab (MGD006) recognizes CD123 and CD3. The primary mechanism of flotetuzumab is thought to be its ability to redirect T cells to kill CD123-expressing cells. To achieve this, the molecule combines a portion of an antibody recognizing CD3 (an activating molecule expressed by T cells) with an arm that recognizes CD123 on the target cancer cells.
In this ongoing phase 1 study of flotetuzumab, researchers have enrolled 47 patients with a median age of 64 (range, 29-84). About 89% of these patients had AML (n=42), and the rest (n=5) had MDS.
Twenty-four percent had relapsed AML (n=10), 55% had refractory AML (n=23), and 21% had failed treatment with hypomethylating agents (n=9). One patient had intermediate-1-risk MDS, 2 had intermediate-2-risk, and 2 had high-risk MDS.
Treatment
The study began with single patients receiving flotetuzumab at escalating doses—3 ng/kg/day, 10 ng/kg/day, 30 ng/kg/day, and 100 ng/kg/day.
Then, patients received a range of doses on 2 different schedules for cycle 1. One group received treatment 7 days a week. The other had a 4-days-on/3-days-off schedule.
All patients received a lead-in dose during the first week of cycle 1. They received 30 ng/kg/day for 3 days, then 100 ng/kg/day for 4 days.
For the rest of cycle 1, patients in the 4 days/3 days group received doses of 500 ng/kg, 700 ng/kg, 900 ng/kg, or 1000 ng/kg. Patients in the daily dosing group received doses of 300 ng/kg, 500 ng/kg, 700 ng/kg, 900 ng/kg, or 1000 ng/kg.
For cycle 2 and beyond, all patients were on the 4-days-on/3-days-off schedule.
Safety
The maximum tolerated dose and schedule was 500 ng/kg/day for 7 days.
Dose-limiting toxicities occurring at the 700 ng/kg/day dose included grade 2 IRRs/CRS in 2 patients and grade 3 myalgia in 1 patient. There was 1 drug-related central nervous system AE that led to treatment discontinuation.
IRRs/CRS occurred in 77% of patients, with 13% of patients having grade 3 events and 8.5% of patients discontinuing treatment due to IRRs/CRS.
The researchers said they found ways to decrease the incidence and severity of CRS. One is early intervention with tocilizumab. The other is a 2-step lead-in dose during week 1. So patients first receive 30 ng/kg, then 100 ng/kg, and then their target dose.
Other grade 3 AEs occurring in this trial include febrile neutropenia (11%), anemia (11%), and decreases in platelets (13%), white blood cells (11%), and lymphocytes (13%).
Efficacy
The researchers said they observed encouraging anti-leukemic activity in patients treated at 500 ng/kg/day or greater.
As of the data cut-off, 14 patients treated at this dose were evaluable for response. Eight (57%) patients had anti-leukemic activity, with 6 (43%) of these patients experiencing an objective response.
One patient achieved a complete response (CR), 2 had a CR with incomplete count recovery, and 1 had a molecular CR.
In most responders, anti-leukemic activity was observed after a single cycle of therapy.
MacroGenics is currently enrolling patients in dose-expansion cohorts. The company plans to present updated results from this trial at another scientific conference later this year.
*Slides from this presentation are available on the MacroGenics website at http://ir.macrogenics.com/events.cfm.
MADRID—Interim results of a phase 1 study suggest flotetuzumab, a CD123 and CD3 bispecific antibody, may be a feasible treatment option for relapsed or refractory acute myeloid leukemia (AML) or intermediate/high-risk myelodysplastic syndromes (MDS).
Researchers said flotetuzumab demonstrated acceptable tolerability in the dose-escalation portion of the study, with infusion-related reactions (IRRs) and cytokine release syndrome (CRS) being the most common adverse events (AEs).
In addition, flotetuzumab exhibited anti-leukemic activity in 8 of 14 response-evaluable patients, with 6 patients achieving a response.
Norbert Vey, MD, of Institut Paoli-Calmettes in Marseille, France, presented these results at the ESMO 2017 Congress (abstract 995O*). The study is sponsored by MacroGenics, Inc., the company developing flotetuzumab.
Flotetuzumab (MGD006) recognizes CD123 and CD3. The primary mechanism of flotetuzumab is thought to be its ability to redirect T cells to kill CD123-expressing cells. To achieve this, the molecule combines a portion of an antibody recognizing CD3 (an activating molecule expressed by T cells) with an arm that recognizes CD123 on the target cancer cells.
In this ongoing phase 1 study of flotetuzumab, researchers have enrolled 47 patients with a median age of 64 (range, 29-84). About 89% of these patients had AML (n=42), and the rest (n=5) had MDS.
Twenty-four percent had relapsed AML (n=10), 55% had refractory AML (n=23), and 21% had failed treatment with hypomethylating agents (n=9). One patient had intermediate-1-risk MDS, 2 had intermediate-2-risk, and 2 had high-risk MDS.
Treatment
The study began with single patients receiving flotetuzumab at escalating doses—3 ng/kg/day, 10 ng/kg/day, 30 ng/kg/day, and 100 ng/kg/day.
Then, patients received a range of doses on 2 different schedules for cycle 1. One group received treatment 7 days a week. The other had a 4-days-on/3-days-off schedule.
All patients received a lead-in dose during the first week of cycle 1. They received 30 ng/kg/day for 3 days, then 100 ng/kg/day for 4 days.
For the rest of cycle 1, patients in the 4 days/3 days group received doses of 500 ng/kg, 700 ng/kg, 900 ng/kg, or 1000 ng/kg. Patients in the daily dosing group received doses of 300 ng/kg, 500 ng/kg, 700 ng/kg, 900 ng/kg, or 1000 ng/kg.
For cycle 2 and beyond, all patients were on the 4-days-on/3-days-off schedule.
Safety
The maximum tolerated dose and schedule was 500 ng/kg/day for 7 days.
Dose-limiting toxicities occurring at the 700 ng/kg/day dose included grade 2 IRRs/CRS in 2 patients and grade 3 myalgia in 1 patient. There was 1 drug-related central nervous system AE that led to treatment discontinuation.
IRRs/CRS occurred in 77% of patients, with 13% of patients having grade 3 events and 8.5% of patients discontinuing treatment due to IRRs/CRS.
The researchers said they found ways to decrease the incidence and severity of CRS. One is early intervention with tocilizumab. The other is a 2-step lead-in dose during week 1. So patients first receive 30 ng/kg, then 100 ng/kg, and then their target dose.
Other grade 3 AEs occurring in this trial include febrile neutropenia (11%), anemia (11%), and decreases in platelets (13%), white blood cells (11%), and lymphocytes (13%).
Efficacy
The researchers said they observed encouraging anti-leukemic activity in patients treated at 500 ng/kg/day or greater.
As of the data cut-off, 14 patients treated at this dose were evaluable for response. Eight (57%) patients had anti-leukemic activity, with 6 (43%) of these patients experiencing an objective response.
One patient achieved a complete response (CR), 2 had a CR with incomplete count recovery, and 1 had a molecular CR.
In most responders, anti-leukemic activity was observed after a single cycle of therapy.
MacroGenics is currently enrolling patients in dose-expansion cohorts. The company plans to present updated results from this trial at another scientific conference later this year.
*Slides from this presentation are available on the MacroGenics website at http://ir.macrogenics.com/events.cfm.