User login
Hydroxyurea well tolerated in longitudinal European study
WASHINGTON – European patients with sickle cell disease (SCD) are tolerating hydroxyurea treatment well, 9 years into a 10-year prospective cohort study.
ESCORT-HU (European Sickle Cell Disease Cohort – Hydroxyurea) is slated to enroll 2,000 children and adults over the study period to assess the long-term safety and efficacy of hydroxyurea (HU) as a treatment for SCD.
“Hydroxyurea is still underused in sickle cell disease” both in Europe and the United States, said Bernard Dauvergne, PharmD, executive director of Addmedica, which markets hydroxyurea as Siklos. In part, fears about toxicity and side effects contribute to this underuse, Dr. Dauvergne said at a top abstracts session of the annual meeting of the Foundation for Sickle Cell Disease Research.
ESCORT-HU was designed as a purely observational, noninterventional study of patients treated with HU. It was initiated as part of the European Medicines Agency risk management plan, conceived at the time of the drug’s approval for SCD, explained Dr. Dauvergne.
“This prospective cohort study could enable the identification of delayed rare adverse events in real life, occurring in between 1 in 10,000 and 1 in 1,000 patients,” Dr. Dauvergne said. However, “no new safety information has been detected ... and no secondary cancer has been reported.”
At the last data analysis cutpoint of June 2017, 1,921 patients had been enrolled. Patients have come from 63 centers in France, Germany, Greece, and Italy, Dr. Dauvergne reported.
Of the 1,829 patients with data available for analysis, 804 were under the age of 18. The pediatric patients were a mean 9 years of age, and the adult patients were a mean 33 years old at enrollment. Most enrollees (84%) have the HbSS genotype.
At baseline, the pediatric patients were dosed at a mean 17.2 mg/kg per day of HU; for adult patients, the figure was 15.54 mg/kg per day. More than one-third (35.4%) of pediatric patients had been on HU at the time of study enrollment, for a mean of 4.5 years. In contrast, more than half (60.4%) of adults had been taking hydroxyurea for a mean of 6.25 years at enrollment.
The 1,002 adult patients with recently reported safety data were on a mean HU dose of 20.2 mg/kg per day. About 40% of adults reported at least one adverse event (AE), and a total of 334 AEs in 16.3% of adult patients were judged to be related to HU.
Skin and subcutaneous tissue reactions occurred in about 1 in 10 patients, with 153 reported incidences of skin dryness, skin reactions, alopecia, or changes in skin pigmentation. The next most common adverse events were blood and lymphatic system disorders, mostly neutropenia or thrombocytopenia, occurring in 9.6% of patients.
Discontinuation rates have been low, with an overall dropout rate of 3.8%.
The ESCORT-HU data “confirm that HU is an efficient and well-tolerated drug in both children and adults,” Dr. Dauvergne said. Over the short term, adverse events are related to the expected dose dependent myelosuppression that’s key to the drug’s mechanism of action. This makes sense given the narrow therapeutic index, with a tight range between an efficacious dose and a cytotoxic one, he said. “And the lower the [patient] weight is, the more sensitive the dose variations become,” Dr. Dauvergne said.
Being flexible about fine-tuning doses is key to finding the balance between tolerability and efficacy, “and consequently, for compliance,” he said.
Data collection for the study will end in 2018, with safety and efficacy data expected in 2019.
WASHINGTON – European patients with sickle cell disease (SCD) are tolerating hydroxyurea treatment well, 9 years into a 10-year prospective cohort study.
ESCORT-HU (European Sickle Cell Disease Cohort – Hydroxyurea) is slated to enroll 2,000 children and adults over the study period to assess the long-term safety and efficacy of hydroxyurea (HU) as a treatment for SCD.
“Hydroxyurea is still underused in sickle cell disease” both in Europe and the United States, said Bernard Dauvergne, PharmD, executive director of Addmedica, which markets hydroxyurea as Siklos. In part, fears about toxicity and side effects contribute to this underuse, Dr. Dauvergne said at a top abstracts session of the annual meeting of the Foundation for Sickle Cell Disease Research.
ESCORT-HU was designed as a purely observational, noninterventional study of patients treated with HU. It was initiated as part of the European Medicines Agency risk management plan, conceived at the time of the drug’s approval for SCD, explained Dr. Dauvergne.
“This prospective cohort study could enable the identification of delayed rare adverse events in real life, occurring in between 1 in 10,000 and 1 in 1,000 patients,” Dr. Dauvergne said. However, “no new safety information has been detected ... and no secondary cancer has been reported.”
At the last data analysis cutpoint of June 2017, 1,921 patients had been enrolled. Patients have come from 63 centers in France, Germany, Greece, and Italy, Dr. Dauvergne reported.
Of the 1,829 patients with data available for analysis, 804 were under the age of 18. The pediatric patients were a mean 9 years of age, and the adult patients were a mean 33 years old at enrollment. Most enrollees (84%) have the HbSS genotype.
At baseline, the pediatric patients were dosed at a mean 17.2 mg/kg per day of HU; for adult patients, the figure was 15.54 mg/kg per day. More than one-third (35.4%) of pediatric patients had been on HU at the time of study enrollment, for a mean of 4.5 years. In contrast, more than half (60.4%) of adults had been taking hydroxyurea for a mean of 6.25 years at enrollment.
The 1,002 adult patients with recently reported safety data were on a mean HU dose of 20.2 mg/kg per day. About 40% of adults reported at least one adverse event (AE), and a total of 334 AEs in 16.3% of adult patients were judged to be related to HU.
Skin and subcutaneous tissue reactions occurred in about 1 in 10 patients, with 153 reported incidences of skin dryness, skin reactions, alopecia, or changes in skin pigmentation. The next most common adverse events were blood and lymphatic system disorders, mostly neutropenia or thrombocytopenia, occurring in 9.6% of patients.
Discontinuation rates have been low, with an overall dropout rate of 3.8%.
The ESCORT-HU data “confirm that HU is an efficient and well-tolerated drug in both children and adults,” Dr. Dauvergne said. Over the short term, adverse events are related to the expected dose dependent myelosuppression that’s key to the drug’s mechanism of action. This makes sense given the narrow therapeutic index, with a tight range between an efficacious dose and a cytotoxic one, he said. “And the lower the [patient] weight is, the more sensitive the dose variations become,” Dr. Dauvergne said.
Being flexible about fine-tuning doses is key to finding the balance between tolerability and efficacy, “and consequently, for compliance,” he said.
Data collection for the study will end in 2018, with safety and efficacy data expected in 2019.
WASHINGTON – European patients with sickle cell disease (SCD) are tolerating hydroxyurea treatment well, 9 years into a 10-year prospective cohort study.
ESCORT-HU (European Sickle Cell Disease Cohort – Hydroxyurea) is slated to enroll 2,000 children and adults over the study period to assess the long-term safety and efficacy of hydroxyurea (HU) as a treatment for SCD.
“Hydroxyurea is still underused in sickle cell disease” both in Europe and the United States, said Bernard Dauvergne, PharmD, executive director of Addmedica, which markets hydroxyurea as Siklos. In part, fears about toxicity and side effects contribute to this underuse, Dr. Dauvergne said at a top abstracts session of the annual meeting of the Foundation for Sickle Cell Disease Research.
ESCORT-HU was designed as a purely observational, noninterventional study of patients treated with HU. It was initiated as part of the European Medicines Agency risk management plan, conceived at the time of the drug’s approval for SCD, explained Dr. Dauvergne.
“This prospective cohort study could enable the identification of delayed rare adverse events in real life, occurring in between 1 in 10,000 and 1 in 1,000 patients,” Dr. Dauvergne said. However, “no new safety information has been detected ... and no secondary cancer has been reported.”
At the last data analysis cutpoint of June 2017, 1,921 patients had been enrolled. Patients have come from 63 centers in France, Germany, Greece, and Italy, Dr. Dauvergne reported.
Of the 1,829 patients with data available for analysis, 804 were under the age of 18. The pediatric patients were a mean 9 years of age, and the adult patients were a mean 33 years old at enrollment. Most enrollees (84%) have the HbSS genotype.
At baseline, the pediatric patients were dosed at a mean 17.2 mg/kg per day of HU; for adult patients, the figure was 15.54 mg/kg per day. More than one-third (35.4%) of pediatric patients had been on HU at the time of study enrollment, for a mean of 4.5 years. In contrast, more than half (60.4%) of adults had been taking hydroxyurea for a mean of 6.25 years at enrollment.
The 1,002 adult patients with recently reported safety data were on a mean HU dose of 20.2 mg/kg per day. About 40% of adults reported at least one adverse event (AE), and a total of 334 AEs in 16.3% of adult patients were judged to be related to HU.
Skin and subcutaneous tissue reactions occurred in about 1 in 10 patients, with 153 reported incidences of skin dryness, skin reactions, alopecia, or changes in skin pigmentation. The next most common adverse events were blood and lymphatic system disorders, mostly neutropenia or thrombocytopenia, occurring in 9.6% of patients.
Discontinuation rates have been low, with an overall dropout rate of 3.8%.
The ESCORT-HU data “confirm that HU is an efficient and well-tolerated drug in both children and adults,” Dr. Dauvergne said. Over the short term, adverse events are related to the expected dose dependent myelosuppression that’s key to the drug’s mechanism of action. This makes sense given the narrow therapeutic index, with a tight range between an efficacious dose and a cytotoxic one, he said. “And the lower the [patient] weight is, the more sensitive the dose variations become,” Dr. Dauvergne said.
Being flexible about fine-tuning doses is key to finding the balance between tolerability and efficacy, “and consequently, for compliance,” he said.
Data collection for the study will end in 2018, with safety and efficacy data expected in 2019.
REPORTING FROM FSCDR 2018
Key clinical point:
Major finding: Of adult participants, 16.9% have experienced hydroxyurea-related adverse events.
Study details: Observational 10-year study of 2,000 adults and children with SCD who were taking hydroxyurea.
Disclosures: The study was sponsored by Addmedica, which markets hydroxyurea as Siklos. Dr. Dauvergne is employed by Addmedica.
Source: Dauvergne B et al. FSCDR 2018, presentation JSCDH-D-18-00052.
FDA lifts hold on trial of MYC inhibitor
The US Food and Drug Administration (FDA) has lifted the clinical hold on a phase 1b trial of APTO-253.
APTO-253 is a small molecule that inhibits expression of the c-Myc oncogene without causing general myelosuppression of the bone marrow, according to Aptose Biosciences Inc., the company developing the drug.
Aptose was testing APTO-253 in a phase 1b trial of patients with relapsed or refractory acute myeloid leukemia (AML) or high-risk myelodysplastic syndromes (MDS) before the FDA put the trial on hold in November 2015.
The hold was placed after an event that occurred during dosing at a clinical site. The event was stoppage of an intravenous infusion pump that was caused by back pressure resulting from clogging of the in-line filter.
Aptose said no drug-related serious adverse events were reported, and the observed pharmacokinetic levels in patients treated with APTO-253 were within the expected range.
However, a review revealed concerns about the documentation records of the manufacturing procedures associated with APTO-253. So Aptose voluntarily stopped dosing in the phase 1b trial, and the FDA placed the trial on hold.
A root cause investigation revealed that the event with the infusion pump resulted from chemistry and manufacturing-based issues.
Therefore, Aptose developed a new formulation of APTO-253 that did not cause filter clogging or pump stoppage during simulated infusion studies.
Now that the FDA has lifted the hold on the phase 1b trial, Aptose said screening and dosing will resume “as soon as practicable.”
“We are eager to return APTO-253 back into the clinic,” said William G. Rice, PhD, chairman, president and chief executive officer of Aptose.
“Our understanding of this molecule has evolved dramatically, and we are excited to deliver a MYC gene expression inhibitor to patients with debilitating hematologic malignancies.”
The phase 1b trial is designed to assess the safety, tolerability, pharmacokinetics, pharmacodynamics, and efficacy of APTO-253 as a single agent and determine the recommended phase 2 dose of the drug.
APTO-253 will be administered once weekly, over a 28-day cycle. The dose-escalation cohort of the study could potentially enroll up to 20 patients with relapsed or refractory AML or high-risk MDS. The study is designed to then transition, as appropriate, to single-agent expansion cohorts in AML and MDS.
The US Food and Drug Administration (FDA) has lifted the clinical hold on a phase 1b trial of APTO-253.
APTO-253 is a small molecule that inhibits expression of the c-Myc oncogene without causing general myelosuppression of the bone marrow, according to Aptose Biosciences Inc., the company developing the drug.
Aptose was testing APTO-253 in a phase 1b trial of patients with relapsed or refractory acute myeloid leukemia (AML) or high-risk myelodysplastic syndromes (MDS) before the FDA put the trial on hold in November 2015.
The hold was placed after an event that occurred during dosing at a clinical site. The event was stoppage of an intravenous infusion pump that was caused by back pressure resulting from clogging of the in-line filter.
Aptose said no drug-related serious adverse events were reported, and the observed pharmacokinetic levels in patients treated with APTO-253 were within the expected range.
However, a review revealed concerns about the documentation records of the manufacturing procedures associated with APTO-253. So Aptose voluntarily stopped dosing in the phase 1b trial, and the FDA placed the trial on hold.
A root cause investigation revealed that the event with the infusion pump resulted from chemistry and manufacturing-based issues.
Therefore, Aptose developed a new formulation of APTO-253 that did not cause filter clogging or pump stoppage during simulated infusion studies.
Now that the FDA has lifted the hold on the phase 1b trial, Aptose said screening and dosing will resume “as soon as practicable.”
“We are eager to return APTO-253 back into the clinic,” said William G. Rice, PhD, chairman, president and chief executive officer of Aptose.
“Our understanding of this molecule has evolved dramatically, and we are excited to deliver a MYC gene expression inhibitor to patients with debilitating hematologic malignancies.”
The phase 1b trial is designed to assess the safety, tolerability, pharmacokinetics, pharmacodynamics, and efficacy of APTO-253 as a single agent and determine the recommended phase 2 dose of the drug.
APTO-253 will be administered once weekly, over a 28-day cycle. The dose-escalation cohort of the study could potentially enroll up to 20 patients with relapsed or refractory AML or high-risk MDS. The study is designed to then transition, as appropriate, to single-agent expansion cohorts in AML and MDS.
The US Food and Drug Administration (FDA) has lifted the clinical hold on a phase 1b trial of APTO-253.
APTO-253 is a small molecule that inhibits expression of the c-Myc oncogene without causing general myelosuppression of the bone marrow, according to Aptose Biosciences Inc., the company developing the drug.
Aptose was testing APTO-253 in a phase 1b trial of patients with relapsed or refractory acute myeloid leukemia (AML) or high-risk myelodysplastic syndromes (MDS) before the FDA put the trial on hold in November 2015.
The hold was placed after an event that occurred during dosing at a clinical site. The event was stoppage of an intravenous infusion pump that was caused by back pressure resulting from clogging of the in-line filter.
Aptose said no drug-related serious adverse events were reported, and the observed pharmacokinetic levels in patients treated with APTO-253 were within the expected range.
However, a review revealed concerns about the documentation records of the manufacturing procedures associated with APTO-253. So Aptose voluntarily stopped dosing in the phase 1b trial, and the FDA placed the trial on hold.
A root cause investigation revealed that the event with the infusion pump resulted from chemistry and manufacturing-based issues.
Therefore, Aptose developed a new formulation of APTO-253 that did not cause filter clogging or pump stoppage during simulated infusion studies.
Now that the FDA has lifted the hold on the phase 1b trial, Aptose said screening and dosing will resume “as soon as practicable.”
“We are eager to return APTO-253 back into the clinic,” said William G. Rice, PhD, chairman, president and chief executive officer of Aptose.
“Our understanding of this molecule has evolved dramatically, and we are excited to deliver a MYC gene expression inhibitor to patients with debilitating hematologic malignancies.”
The phase 1b trial is designed to assess the safety, tolerability, pharmacokinetics, pharmacodynamics, and efficacy of APTO-253 as a single agent and determine the recommended phase 2 dose of the drug.
APTO-253 will be administered once weekly, over a 28-day cycle. The dose-escalation cohort of the study could potentially enroll up to 20 patients with relapsed or refractory AML or high-risk MDS. The study is designed to then transition, as appropriate, to single-agent expansion cohorts in AML and MDS.
Voxelotor cut transfusions in compassionate use sickle cell cohort
WASHINGTON – An investigational drug for sickle cell disease (SCD) boosted hemoglobin levels while reducing hospitalizations and transfusion needs by approximately two-thirds in a small cohort of severely affected patients.
Lanetta Bronté, MD, who presented the findings at the annual meeting of the Foundation for Sickle Cell Disease Research, reviewed the FDA’s requirements for allowing expanded access to an investigational drug. The key point, she said, is that expanded access may be granted “for treatment of patients with serious or immediately life-threatening diseases or conditions that lack therapeutic alternatives.” And, she said, the potential for benefit should outweigh potential risk of taking the investigational drug.
Current treatments don’t really address serious disease-related complications for patients with advanced SCD, she said. Furthermore, these patients will often be excluded from clinical trials of new SCD therapies.
Voxelotor is a novel small molecule that stabilizes the sickle hemoglobin molecule as a monomer in its high oxygen state. Thus, polymerization of the hemoglobin molecules is inhibited, which decreases the amount of red blood cell damage. Other beneficial effects of voxelotor include improved rheology and reduced hemolysis, as well as a boost to the oxygen-carrying capacity of the sickle hemoglobin molecules, Dr. Bronté explained.
For the seven patients in Dr. Bronté’s clinic who were granted expanded access to voxelator, the disease burden of their end-stage SCD was heavy. All participants had iron overload, five were receiving frequent transfusions, two required chronic oxygen supplementation, and four had severe fatigue. One patient had end-stage renal disease, and another had experienced multiple organ failure and prolonged hospitalizations.
None of the patients qualified for participation in ongoing clinical trials of voxelotor, said Dr. Bronté, who is president of the Foundation for Sickle Cell Disease Research. She also maintains a private practice in Hollywood, Fla.
The four women and three men, aged 22-67 years, were treated with voxelotor for a range of 6-17 months under the FDA’s Expanded Access Program. All patients saw rapid increases in serum hemoglobin, with increases of at least 1 g/dL in five of the seven. Across the participants, increases ranged from 0.5-5.4 g/dL at 24 weeks, up from baseline values of 5.2-7.8 g/dL.
One marker of clinical efficacy that Dr. Bronté and her coauthors examined was the number of hospitalizations for pain from vaso-occlusive crises (VOCs). In the 24 weeks before beginning voxelotor, participants had a summed total of 28 hospitalizations. In the first 24 weeks of treatment, there were a total of nine VOC-related hospitalizations among the participants, a 67% decrease.
The total number of red blood cell transfusions required by the study population declined by a similar proportion, from 33 during the 24 weeks before voxelotor treatment to 13 during the first 24 weeks of treatment, a decrease of 60%.
Individual patients saw improvements related to some of their most troublesome SCD complications, Dr. Bronté reported. All four patients whose oxygen saturation levels had been below 95% on room air saw oxygen saturations improve to 98%-99% on voxelotor. The two patients who had moderate or moderately severe depression, as assessed by the Patient Health Questionnaire 9-item, had minimal or no depression on retest after 24 weeks of voxelotor treatment.
Voxelotor was generally well tolerated at a 900-mg once-daily oral dose. One patient developed grade 2 diarrhea after increasing the dose to 1,500 mg, but symptoms resolved after returning to the 900-mg dose. Another patient had transient mild diarrhea on 900 mg of voxelotor; the symptoms resolved without changing or stopping the drug, Dr. Bronté said. There were no serious treatment-related adverse events.
Among this seriously ill population, two patients died after beginning voxelotor treatment, but both deaths were judged to be unrelated to the treatment. Dr. Bronté reported that the two deceased patients, one of whom was on voxelotor for 16 months and the other for 7 months, did experience reduced transfusion needs and reduced VOC-related hospitalizations while on the drug, experiences that were similar to the surviving members of the cohort.
“Voxelotor administered via compassionate use demonstrated large improvements in anemia and hemolysis, including in patients with lower baseline hemoglobin than studied in clinical trials to date,” Dr. Bronté said.
Taken together with clinical improvements and improved patient-focused outcomes among a severely affected population, “these data … support ongoing investigation in controlled clinical trials to confirm the benefits of voxelotor in a broad range of patients with SCD,” she said.
The study was supported by Global Blood Therapeutics, the manufacturer of voxelotor. Dr. Bronté reported having no other conflicts of interest.
WASHINGTON – An investigational drug for sickle cell disease (SCD) boosted hemoglobin levels while reducing hospitalizations and transfusion needs by approximately two-thirds in a small cohort of severely affected patients.
Lanetta Bronté, MD, who presented the findings at the annual meeting of the Foundation for Sickle Cell Disease Research, reviewed the FDA’s requirements for allowing expanded access to an investigational drug. The key point, she said, is that expanded access may be granted “for treatment of patients with serious or immediately life-threatening diseases or conditions that lack therapeutic alternatives.” And, she said, the potential for benefit should outweigh potential risk of taking the investigational drug.
Current treatments don’t really address serious disease-related complications for patients with advanced SCD, she said. Furthermore, these patients will often be excluded from clinical trials of new SCD therapies.
Voxelotor is a novel small molecule that stabilizes the sickle hemoglobin molecule as a monomer in its high oxygen state. Thus, polymerization of the hemoglobin molecules is inhibited, which decreases the amount of red blood cell damage. Other beneficial effects of voxelotor include improved rheology and reduced hemolysis, as well as a boost to the oxygen-carrying capacity of the sickle hemoglobin molecules, Dr. Bronté explained.
For the seven patients in Dr. Bronté’s clinic who were granted expanded access to voxelator, the disease burden of their end-stage SCD was heavy. All participants had iron overload, five were receiving frequent transfusions, two required chronic oxygen supplementation, and four had severe fatigue. One patient had end-stage renal disease, and another had experienced multiple organ failure and prolonged hospitalizations.
None of the patients qualified for participation in ongoing clinical trials of voxelotor, said Dr. Bronté, who is president of the Foundation for Sickle Cell Disease Research. She also maintains a private practice in Hollywood, Fla.
The four women and three men, aged 22-67 years, were treated with voxelotor for a range of 6-17 months under the FDA’s Expanded Access Program. All patients saw rapid increases in serum hemoglobin, with increases of at least 1 g/dL in five of the seven. Across the participants, increases ranged from 0.5-5.4 g/dL at 24 weeks, up from baseline values of 5.2-7.8 g/dL.
One marker of clinical efficacy that Dr. Bronté and her coauthors examined was the number of hospitalizations for pain from vaso-occlusive crises (VOCs). In the 24 weeks before beginning voxelotor, participants had a summed total of 28 hospitalizations. In the first 24 weeks of treatment, there were a total of nine VOC-related hospitalizations among the participants, a 67% decrease.
The total number of red blood cell transfusions required by the study population declined by a similar proportion, from 33 during the 24 weeks before voxelotor treatment to 13 during the first 24 weeks of treatment, a decrease of 60%.
Individual patients saw improvements related to some of their most troublesome SCD complications, Dr. Bronté reported. All four patients whose oxygen saturation levels had been below 95% on room air saw oxygen saturations improve to 98%-99% on voxelotor. The two patients who had moderate or moderately severe depression, as assessed by the Patient Health Questionnaire 9-item, had minimal or no depression on retest after 24 weeks of voxelotor treatment.
Voxelotor was generally well tolerated at a 900-mg once-daily oral dose. One patient developed grade 2 diarrhea after increasing the dose to 1,500 mg, but symptoms resolved after returning to the 900-mg dose. Another patient had transient mild diarrhea on 900 mg of voxelotor; the symptoms resolved without changing or stopping the drug, Dr. Bronté said. There were no serious treatment-related adverse events.
Among this seriously ill population, two patients died after beginning voxelotor treatment, but both deaths were judged to be unrelated to the treatment. Dr. Bronté reported that the two deceased patients, one of whom was on voxelotor for 16 months and the other for 7 months, did experience reduced transfusion needs and reduced VOC-related hospitalizations while on the drug, experiences that were similar to the surviving members of the cohort.
“Voxelotor administered via compassionate use demonstrated large improvements in anemia and hemolysis, including in patients with lower baseline hemoglobin than studied in clinical trials to date,” Dr. Bronté said.
Taken together with clinical improvements and improved patient-focused outcomes among a severely affected population, “these data … support ongoing investigation in controlled clinical trials to confirm the benefits of voxelotor in a broad range of patients with SCD,” she said.
The study was supported by Global Blood Therapeutics, the manufacturer of voxelotor. Dr. Bronté reported having no other conflicts of interest.
WASHINGTON – An investigational drug for sickle cell disease (SCD) boosted hemoglobin levels while reducing hospitalizations and transfusion needs by approximately two-thirds in a small cohort of severely affected patients.
Lanetta Bronté, MD, who presented the findings at the annual meeting of the Foundation for Sickle Cell Disease Research, reviewed the FDA’s requirements for allowing expanded access to an investigational drug. The key point, she said, is that expanded access may be granted “for treatment of patients with serious or immediately life-threatening diseases or conditions that lack therapeutic alternatives.” And, she said, the potential for benefit should outweigh potential risk of taking the investigational drug.
Current treatments don’t really address serious disease-related complications for patients with advanced SCD, she said. Furthermore, these patients will often be excluded from clinical trials of new SCD therapies.
Voxelotor is a novel small molecule that stabilizes the sickle hemoglobin molecule as a monomer in its high oxygen state. Thus, polymerization of the hemoglobin molecules is inhibited, which decreases the amount of red blood cell damage. Other beneficial effects of voxelotor include improved rheology and reduced hemolysis, as well as a boost to the oxygen-carrying capacity of the sickle hemoglobin molecules, Dr. Bronté explained.
For the seven patients in Dr. Bronté’s clinic who were granted expanded access to voxelator, the disease burden of their end-stage SCD was heavy. All participants had iron overload, five were receiving frequent transfusions, two required chronic oxygen supplementation, and four had severe fatigue. One patient had end-stage renal disease, and another had experienced multiple organ failure and prolonged hospitalizations.
None of the patients qualified for participation in ongoing clinical trials of voxelotor, said Dr. Bronté, who is president of the Foundation for Sickle Cell Disease Research. She also maintains a private practice in Hollywood, Fla.
The four women and three men, aged 22-67 years, were treated with voxelotor for a range of 6-17 months under the FDA’s Expanded Access Program. All patients saw rapid increases in serum hemoglobin, with increases of at least 1 g/dL in five of the seven. Across the participants, increases ranged from 0.5-5.4 g/dL at 24 weeks, up from baseline values of 5.2-7.8 g/dL.
One marker of clinical efficacy that Dr. Bronté and her coauthors examined was the number of hospitalizations for pain from vaso-occlusive crises (VOCs). In the 24 weeks before beginning voxelotor, participants had a summed total of 28 hospitalizations. In the first 24 weeks of treatment, there were a total of nine VOC-related hospitalizations among the participants, a 67% decrease.
The total number of red blood cell transfusions required by the study population declined by a similar proportion, from 33 during the 24 weeks before voxelotor treatment to 13 during the first 24 weeks of treatment, a decrease of 60%.
Individual patients saw improvements related to some of their most troublesome SCD complications, Dr. Bronté reported. All four patients whose oxygen saturation levels had been below 95% on room air saw oxygen saturations improve to 98%-99% on voxelotor. The two patients who had moderate or moderately severe depression, as assessed by the Patient Health Questionnaire 9-item, had minimal or no depression on retest after 24 weeks of voxelotor treatment.
Voxelotor was generally well tolerated at a 900-mg once-daily oral dose. One patient developed grade 2 diarrhea after increasing the dose to 1,500 mg, but symptoms resolved after returning to the 900-mg dose. Another patient had transient mild diarrhea on 900 mg of voxelotor; the symptoms resolved without changing or stopping the drug, Dr. Bronté said. There were no serious treatment-related adverse events.
Among this seriously ill population, two patients died after beginning voxelotor treatment, but both deaths were judged to be unrelated to the treatment. Dr. Bronté reported that the two deceased patients, one of whom was on voxelotor for 16 months and the other for 7 months, did experience reduced transfusion needs and reduced VOC-related hospitalizations while on the drug, experiences that were similar to the surviving members of the cohort.
“Voxelotor administered via compassionate use demonstrated large improvements in anemia and hemolysis, including in patients with lower baseline hemoglobin than studied in clinical trials to date,” Dr. Bronté said.
Taken together with clinical improvements and improved patient-focused outcomes among a severely affected population, “these data … support ongoing investigation in controlled clinical trials to confirm the benefits of voxelotor in a broad range of patients with SCD,” she said.
The study was supported by Global Blood Therapeutics, the manufacturer of voxelotor. Dr. Bronté reported having no other conflicts of interest.
REPORTING FROM FSCDR 2018
Key clinical point:
Major finding: Transfusion requirements were cut by 60% in the first 24 weeks on voxelotor.
Study details: Open label case series of seven patients with end-stage SCD at a single center.
Disclosures: The study was funded by Global Blood Therapeutics, which manufactures voxelotor. Dr. Bronté reported having no other conflicts of interest.
Voxelotor benefits adolescents with SCD
STOCKHOLM—An ongoing phase 2 study suggests voxelotor (GBT440) can benefit adolescents with sickle cell disease (SCD).
In the HOPE-KIDS 1 study, voxelotor produced sustained improvements in hemoglobin levels and a reduction in clinical measures of hemolysis in a cohort of adolescents with SCD, most of whom were also receiving hydroxyurea (HU).
The most common adverse events (AEs) related to voxelotor were nausea, vomiting, headache, and rash.
These results were presented in a poster (abstract PF709) at the 23rd Congress of the European Hematology Association (EHA).
HOPE-KIDS 1 is sponsored by Global Blood Therapeutics, Inc.
In this study, researchers are evaluating voxelotor in SCD patients ages 6 to 17. In part A, researchers evaluated a 600 mg daily dose of voxelotor. In part B, they are testing voxelotor at daily doses of 900 mg and 1500 mg in patients ages 12 to 17.
At EHA, the researchers presented data on 25 patients who received voxelotor at 900 mg/day for 24 weeks in part B. Eighty-eight percent of the patients (n=22) were also taking HU.
The patients’ median age was 14 (range, 12-17), and 56% were male. Ninety-six percent (n=24) had the HbSS genotype.
Forty-eight percent of patients had 1 to 4 vaso-occlusive crises (VOCs) in the past year, 8% had more than 4 VOCs, and 44% had 0 VOCs.
At baseline, the median hemoglobin was 8.9 g/dL, the median fetal hemoglobin was 10.8 g/dL, and the median time-averaged mean of maximum velocity was 110 cm/s.
All 25 patients were dosed with voxelotor, and 22 completed 24 weeks of dosing. One patient withdrew consent, 1 was lost to follow-up, and 1 patient discontinued due to noncompliance.
Of the 22 patients who completed 24 weeks of voxelotor treatment, all but 3 were receiving concurrent HU.
Results
Voxelotor-related AEs occurring in at least 2 patients included nausea (12%, n=3), vomiting (8%, n=2), headache (8%, n=2), and rash (8%, n=2).
There was 1 case of grade 3 urticaria, which resolved and did not recur with continued dosing. There were no discontinuations of voxelotor due to AEs.
Patients experienced increased hemoglobin levels and improved clinical measures of hemolysis at 24 weeks, as evaluated by changes from baseline in hemoglobin, percent of reticulocytes, and percent of unconjugated bilirubin.
In all, 43% of patients (9/21) achieved a hemoglobin response (>1 g/dL) at 24 weeks. The median hemoglobin change from baseline was 0.7 g/dL, the median reduction in reticulocytes was 22.9%, and the median reduction in unconjugated bilirubin was 38.6%.
Sixty-two percent of patients (13/21) had a reduction in daily symptoms at 24 weeks, as assessed by total symptom scores (TSS). There was a 39% median reduction in TSS from baseline.
Fifty-five percent of patients (11/20) had a numerical decrease in transcranial doppler (TCD) flow at 24 weeks. Among hemoglobin responders (>1 g/dL), 88% (7/8) had a numerical decrease in TCD at 24 weeks.
“We continue to be encouraged by the results of the ongoing HOPE-KIDS 1 study, which are consistent with inhibition of HbS polymerization by voxelotor and support its ongoing clinical evaluation as a potential disease-modifying therapy for both adults and adolescents with SCD,” said Ted W. Love, MD, president and chief executive officer of Global Blood Therapeutics.
“Results to date support our ongoing development of voxelotor in a broad range of patients, including in our phase 3 HOPE study, which is also evaluating voxelotor at doses of 900 mg and 1500 mg per day in adolescents and adults. We continue to expect to announce top-line clinical data from part A of the HOPE study by the end of this quarter.”
STOCKHOLM—An ongoing phase 2 study suggests voxelotor (GBT440) can benefit adolescents with sickle cell disease (SCD).
In the HOPE-KIDS 1 study, voxelotor produced sustained improvements in hemoglobin levels and a reduction in clinical measures of hemolysis in a cohort of adolescents with SCD, most of whom were also receiving hydroxyurea (HU).
The most common adverse events (AEs) related to voxelotor were nausea, vomiting, headache, and rash.
These results were presented in a poster (abstract PF709) at the 23rd Congress of the European Hematology Association (EHA).
HOPE-KIDS 1 is sponsored by Global Blood Therapeutics, Inc.
In this study, researchers are evaluating voxelotor in SCD patients ages 6 to 17. In part A, researchers evaluated a 600 mg daily dose of voxelotor. In part B, they are testing voxelotor at daily doses of 900 mg and 1500 mg in patients ages 12 to 17.
At EHA, the researchers presented data on 25 patients who received voxelotor at 900 mg/day for 24 weeks in part B. Eighty-eight percent of the patients (n=22) were also taking HU.
The patients’ median age was 14 (range, 12-17), and 56% were male. Ninety-six percent (n=24) had the HbSS genotype.
Forty-eight percent of patients had 1 to 4 vaso-occlusive crises (VOCs) in the past year, 8% had more than 4 VOCs, and 44% had 0 VOCs.
At baseline, the median hemoglobin was 8.9 g/dL, the median fetal hemoglobin was 10.8 g/dL, and the median time-averaged mean of maximum velocity was 110 cm/s.
All 25 patients were dosed with voxelotor, and 22 completed 24 weeks of dosing. One patient withdrew consent, 1 was lost to follow-up, and 1 patient discontinued due to noncompliance.
Of the 22 patients who completed 24 weeks of voxelotor treatment, all but 3 were receiving concurrent HU.
Results
Voxelotor-related AEs occurring in at least 2 patients included nausea (12%, n=3), vomiting (8%, n=2), headache (8%, n=2), and rash (8%, n=2).
There was 1 case of grade 3 urticaria, which resolved and did not recur with continued dosing. There were no discontinuations of voxelotor due to AEs.
Patients experienced increased hemoglobin levels and improved clinical measures of hemolysis at 24 weeks, as evaluated by changes from baseline in hemoglobin, percent of reticulocytes, and percent of unconjugated bilirubin.
In all, 43% of patients (9/21) achieved a hemoglobin response (>1 g/dL) at 24 weeks. The median hemoglobin change from baseline was 0.7 g/dL, the median reduction in reticulocytes was 22.9%, and the median reduction in unconjugated bilirubin was 38.6%.
Sixty-two percent of patients (13/21) had a reduction in daily symptoms at 24 weeks, as assessed by total symptom scores (TSS). There was a 39% median reduction in TSS from baseline.
Fifty-five percent of patients (11/20) had a numerical decrease in transcranial doppler (TCD) flow at 24 weeks. Among hemoglobin responders (>1 g/dL), 88% (7/8) had a numerical decrease in TCD at 24 weeks.
“We continue to be encouraged by the results of the ongoing HOPE-KIDS 1 study, which are consistent with inhibition of HbS polymerization by voxelotor and support its ongoing clinical evaluation as a potential disease-modifying therapy for both adults and adolescents with SCD,” said Ted W. Love, MD, president and chief executive officer of Global Blood Therapeutics.
“Results to date support our ongoing development of voxelotor in a broad range of patients, including in our phase 3 HOPE study, which is also evaluating voxelotor at doses of 900 mg and 1500 mg per day in adolescents and adults. We continue to expect to announce top-line clinical data from part A of the HOPE study by the end of this quarter.”
STOCKHOLM—An ongoing phase 2 study suggests voxelotor (GBT440) can benefit adolescents with sickle cell disease (SCD).
In the HOPE-KIDS 1 study, voxelotor produced sustained improvements in hemoglobin levels and a reduction in clinical measures of hemolysis in a cohort of adolescents with SCD, most of whom were also receiving hydroxyurea (HU).
The most common adverse events (AEs) related to voxelotor were nausea, vomiting, headache, and rash.
These results were presented in a poster (abstract PF709) at the 23rd Congress of the European Hematology Association (EHA).
HOPE-KIDS 1 is sponsored by Global Blood Therapeutics, Inc.
In this study, researchers are evaluating voxelotor in SCD patients ages 6 to 17. In part A, researchers evaluated a 600 mg daily dose of voxelotor. In part B, they are testing voxelotor at daily doses of 900 mg and 1500 mg in patients ages 12 to 17.
At EHA, the researchers presented data on 25 patients who received voxelotor at 900 mg/day for 24 weeks in part B. Eighty-eight percent of the patients (n=22) were also taking HU.
The patients’ median age was 14 (range, 12-17), and 56% were male. Ninety-six percent (n=24) had the HbSS genotype.
Forty-eight percent of patients had 1 to 4 vaso-occlusive crises (VOCs) in the past year, 8% had more than 4 VOCs, and 44% had 0 VOCs.
At baseline, the median hemoglobin was 8.9 g/dL, the median fetal hemoglobin was 10.8 g/dL, and the median time-averaged mean of maximum velocity was 110 cm/s.
All 25 patients were dosed with voxelotor, and 22 completed 24 weeks of dosing. One patient withdrew consent, 1 was lost to follow-up, and 1 patient discontinued due to noncompliance.
Of the 22 patients who completed 24 weeks of voxelotor treatment, all but 3 were receiving concurrent HU.
Results
Voxelotor-related AEs occurring in at least 2 patients included nausea (12%, n=3), vomiting (8%, n=2), headache (8%, n=2), and rash (8%, n=2).
There was 1 case of grade 3 urticaria, which resolved and did not recur with continued dosing. There were no discontinuations of voxelotor due to AEs.
Patients experienced increased hemoglobin levels and improved clinical measures of hemolysis at 24 weeks, as evaluated by changes from baseline in hemoglobin, percent of reticulocytes, and percent of unconjugated bilirubin.
In all, 43% of patients (9/21) achieved a hemoglobin response (>1 g/dL) at 24 weeks. The median hemoglobin change from baseline was 0.7 g/dL, the median reduction in reticulocytes was 22.9%, and the median reduction in unconjugated bilirubin was 38.6%.
Sixty-two percent of patients (13/21) had a reduction in daily symptoms at 24 weeks, as assessed by total symptom scores (TSS). There was a 39% median reduction in TSS from baseline.
Fifty-five percent of patients (11/20) had a numerical decrease in transcranial doppler (TCD) flow at 24 weeks. Among hemoglobin responders (>1 g/dL), 88% (7/8) had a numerical decrease in TCD at 24 weeks.
“We continue to be encouraged by the results of the ongoing HOPE-KIDS 1 study, which are consistent with inhibition of HbS polymerization by voxelotor and support its ongoing clinical evaluation as a potential disease-modifying therapy for both adults and adolescents with SCD,” said Ted W. Love, MD, president and chief executive officer of Global Blood Therapeutics.
“Results to date support our ongoing development of voxelotor in a broad range of patients, including in our phase 3 HOPE study, which is also evaluating voxelotor at doses of 900 mg and 1500 mg per day in adolescents and adults. We continue to expect to announce top-line clinical data from part A of the HOPE study by the end of this quarter.”
Leading researcher in genetics, hematology dies at 84
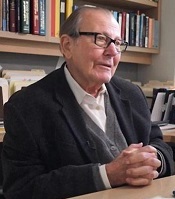
George Stamatoyannopoulos, MD, who conducted important research into hemoglobinopathies, passed away this month at the age of 84.
Dr Stamatoyannopoulos’s research encompassed human genetics and hematology, including the structure and function of hemoglobinopathies, the genetics of thalassemia, and the molecular and cellular control of globin gene switching.
For much of his career, Dr Stamatoyannopoulos focused on the development of gene therapy for hemoglobinopathies and other disorders.
Dr Stamatoyannopoulos was born in Athens, Greece, on March 11, 1934. He entered medical school in Athens at age 17 and graduated at the top of his class 7 years later.
After his medical training, Dr Stamatoyannopoulos pursued thesis research on inherited blood disorders, particularly anemias.
Dr Stamatoyannopoulos performed the first large-scale molecular geographical survey of a genetic trait, which revealed the relationship between malaria and both thalassemia and sickle cell traits.
Dr Stamatoyannopoulos also discovered that fetal hemoglobin could ameliorate the effects of thalassemia. His theory that thalassemia and sickle cell anemia could be treated by re-activating fetal hemoglobin has underpinned decades of efforts to cure these disorders.
As a young investigator, Dr Stamatoyannopoulos expanded genetic studies of blood diseases in Greece, where his work drew the attention of medical genetics pioneer Arno Motulsky, MD.
Dr Motulsky recruited Dr Stamatoyannopoulos to the University of Washington (Seattle) in 1964. Dr Stamatoyannopoulos became a full professor there in 1973, founded the Markey Molecular Medicine Center, and was chief of medical genetics from 1989 to 2005.
Dr Stamatoyannopoulos organized the founding of the American Society of Gene and Cell Therapy. His contributions were recognized by establishment of the Stamatoyannopoulos lecture, the society’s highest award.
Dr Stamatoyannopoulos also served as president of the American Society of Hematology (1992) and president of the American Society of Gene and Cell Therapy (1996). He held leadership positions in other medical and scientific societies as well.
Dr Stamatoyannopoulos authored more than 420 scientific papers and 14 books, including The Molecular Basis of Blood Diseases.
Dr Stamatoyannopoulos died June 16, 2018. He is survived by his wife and collaborator Thalia Papayannopoulou, MD, (a professor of medicine and internationally recognized hematologist), 2 sons, and 3 grandchildren.
George Stamatoyannopoulos, MD, who conducted important research into hemoglobinopathies, passed away this month at the age of 84.
Dr Stamatoyannopoulos’s research encompassed human genetics and hematology, including the structure and function of hemoglobinopathies, the genetics of thalassemia, and the molecular and cellular control of globin gene switching.
For much of his career, Dr Stamatoyannopoulos focused on the development of gene therapy for hemoglobinopathies and other disorders.
Dr Stamatoyannopoulos was born in Athens, Greece, on March 11, 1934. He entered medical school in Athens at age 17 and graduated at the top of his class 7 years later.
After his medical training, Dr Stamatoyannopoulos pursued thesis research on inherited blood disorders, particularly anemias.
Dr Stamatoyannopoulos performed the first large-scale molecular geographical survey of a genetic trait, which revealed the relationship between malaria and both thalassemia and sickle cell traits.
Dr Stamatoyannopoulos also discovered that fetal hemoglobin could ameliorate the effects of thalassemia. His theory that thalassemia and sickle cell anemia could be treated by re-activating fetal hemoglobin has underpinned decades of efforts to cure these disorders.
As a young investigator, Dr Stamatoyannopoulos expanded genetic studies of blood diseases in Greece, where his work drew the attention of medical genetics pioneer Arno Motulsky, MD.
Dr Motulsky recruited Dr Stamatoyannopoulos to the University of Washington (Seattle) in 1964. Dr Stamatoyannopoulos became a full professor there in 1973, founded the Markey Molecular Medicine Center, and was chief of medical genetics from 1989 to 2005.
Dr Stamatoyannopoulos organized the founding of the American Society of Gene and Cell Therapy. His contributions were recognized by establishment of the Stamatoyannopoulos lecture, the society’s highest award.
Dr Stamatoyannopoulos also served as president of the American Society of Hematology (1992) and president of the American Society of Gene and Cell Therapy (1996). He held leadership positions in other medical and scientific societies as well.
Dr Stamatoyannopoulos authored more than 420 scientific papers and 14 books, including The Molecular Basis of Blood Diseases.
Dr Stamatoyannopoulos died June 16, 2018. He is survived by his wife and collaborator Thalia Papayannopoulou, MD, (a professor of medicine and internationally recognized hematologist), 2 sons, and 3 grandchildren.
George Stamatoyannopoulos, MD, who conducted important research into hemoglobinopathies, passed away this month at the age of 84.
Dr Stamatoyannopoulos’s research encompassed human genetics and hematology, including the structure and function of hemoglobinopathies, the genetics of thalassemia, and the molecular and cellular control of globin gene switching.
For much of his career, Dr Stamatoyannopoulos focused on the development of gene therapy for hemoglobinopathies and other disorders.
Dr Stamatoyannopoulos was born in Athens, Greece, on March 11, 1934. He entered medical school in Athens at age 17 and graduated at the top of his class 7 years later.
After his medical training, Dr Stamatoyannopoulos pursued thesis research on inherited blood disorders, particularly anemias.
Dr Stamatoyannopoulos performed the first large-scale molecular geographical survey of a genetic trait, which revealed the relationship between malaria and both thalassemia and sickle cell traits.
Dr Stamatoyannopoulos also discovered that fetal hemoglobin could ameliorate the effects of thalassemia. His theory that thalassemia and sickle cell anemia could be treated by re-activating fetal hemoglobin has underpinned decades of efforts to cure these disorders.
As a young investigator, Dr Stamatoyannopoulos expanded genetic studies of blood diseases in Greece, where his work drew the attention of medical genetics pioneer Arno Motulsky, MD.
Dr Motulsky recruited Dr Stamatoyannopoulos to the University of Washington (Seattle) in 1964. Dr Stamatoyannopoulos became a full professor there in 1973, founded the Markey Molecular Medicine Center, and was chief of medical genetics from 1989 to 2005.
Dr Stamatoyannopoulos organized the founding of the American Society of Gene and Cell Therapy. His contributions were recognized by establishment of the Stamatoyannopoulos lecture, the society’s highest award.
Dr Stamatoyannopoulos also served as president of the American Society of Hematology (1992) and president of the American Society of Gene and Cell Therapy (1996). He held leadership positions in other medical and scientific societies as well.
Dr Stamatoyannopoulos authored more than 420 scientific papers and 14 books, including The Molecular Basis of Blood Diseases.
Dr Stamatoyannopoulos died June 16, 2018. He is survived by his wife and collaborator Thalia Papayannopoulou, MD, (a professor of medicine and internationally recognized hematologist), 2 sons, and 3 grandchildren.
Drug is convenient alternative for PNH, doc says
STOCKHOLM—Results of a phase 3 study suggest the long-acting C5 complement inhibitor ravulizumab produces similar results as eculizumab in patients with paroxysmal nocturnal hemoglobinuria (PNH).
Treatment with ravulizumab every 8 weeks proved noninferior to treatment with eculizumab every 2 weeks for the co-primary endpoints of transfusion avoidance and hemolysis as measured by lactate dehydrogenase (LDH) normalization.
Ravulizumab also proved noninferior with regard to secondary efficacy endpoints and had a safety profile similar to that of eculizumab.
These results suggest ravulizumab could be a more convenient alternative for PNH patients, according to Jong Wook Lee, MD, of Seoul St. Mary’s Hospital in Seoul, South Korea.
Dr Lee presented these results as a late-breaking abstract (LB2603) at the 23rd Congress of the European Hematology Association (EHA).
The study was sponsored by Alexion Pharmaceuticals.
The trial enrolled adults with PNH naive to complement inhibitor therapy. They were randomized to receive ravulizumab (n=125) or eculizumab (n=121) for 183 days.
More than half of patients were male—52% in the ravulizumab arm and 57% in the eculizumab arm. Most patients were Asian (57.6% in the ravulizumab arm and 47.1% in the eculizumab arm) or white (34.4% and 42.1%, respectively).
Patients’ mean age at first infusion was 44.8 in the ravulizumab arm and 46.2 in the eculizumab arm. The mean number of years from PNH diagnosis to consent was 6.7 and 6.4, respectively.
The mean LDH at baseline was 1634 U/L in the ravulizumab arm and 1578 U/L in the eculizumab arm. The mean FACIT-Fatigue score was 36.7 and 36.9, respectively.
All 125 ravulizumab patients completed 26 weeks of treatment, as did 119 of the eculizumab patients. One hundred twenty-four ravulizumab patients entered the extension phase, as did 119 eculizumab patients.
Efficacy
The study’s primary efficacy endpoints were transfusion avoidance and LDH normalization from day 29 to 183. Dr Lee said ravulizumab proved noninferior to eculizumab for both endpoints, and point estimates favored ravulizumab.
The proportion of patients who remained transfusion-free was 73.6% in the ravulizumab arm and 66.1% in the eculizumab arm (difference, 6.8; 95% CI, -4.66, 18.14).
The proportion of patients who achieved LDH normalization was 53.6% and 49.4%, respectively (difference, 1.19; 95% CI, 0.8, 1.77).
Secondary efficacy endpoints included the percentage change in LDH from baseline, change in FACIT-Fatigue score from baseline, and the proportions of patients with breakthrough hemolysis and stabilized hemoglobin.
Again, ravulizumab was noninferior to eculizumab for all endpoints, with point estimates favoring ravulizumab.
The LDH percentage change was -76.84% in the ravulizumab arm and -76.02% in the eculizumab arm (difference, 0.83; 95% CI, -3.56, 5.21).
The change (improvement) in FACIT-Fatigue score was 7.07 and 6.40, respectively (difference, 0.67; 95% CI, -1.21, 2.55).
The percentage of patients with hemoglobin stabilization was 68.0% in the ravulizumab arm and 64.5% in the eculizumab arm (difference, 2.9; 95% CI, -8.80, 14.64).
The percentage of patients with breakthrough hemolysis was 4.0% and 10.7%, respectively (difference, 6.7; 95% CI, -0.18, 14.21).
Dr Lee noted that the proportion of patients with breakthrough hemolysis was more than 2.5-fold higher in the eculizumab arm than the ravulizumab arm—13 patients with 15 events and 5 patients with 5 events, respectively.
He said this was likely due to the immediate, complete, and sustained inhibition of C5 (mean free C5 <0.5 μg/mL) achieved by ravulizumab. Complete inhibition was observed after the first ravulizumab infusion and was sustained throughout the 26-week treatment period.
Safety
Dr Lee said ravulizumab had a similar safety profile to eculizumab, and both drugs were well tolerated.
Most patients experienced a treatment-emergent adverse event (TEAE)—88% in the ravulizumab arm and 86.8% in the eculizumab arm.
The most common TEAEs (in the ravulizumab and eculizumab arms, respectively) were headache (36.0% and 33.1%), nasopharyngitis (8.8% and 14.9%), upper respiratory tract infection (10.4% and 5.8%), and pyrexia (4.8% and 10.7%).
Serious AEs occurred in 8.8% of patients in the ravulizumab arm and 7.4% of those in the eculizumab arm.
Major adverse vascular events occurred in 2 patients in the ravulizumab arm and 1 in the eculizumab arm. There were no meningococcal infections in either arm.
One patient in the eculizumab arm was discontinued from the study and died of lung cancer (which was unrelated to treatment).
STOCKHOLM—Results of a phase 3 study suggest the long-acting C5 complement inhibitor ravulizumab produces similar results as eculizumab in patients with paroxysmal nocturnal hemoglobinuria (PNH).
Treatment with ravulizumab every 8 weeks proved noninferior to treatment with eculizumab every 2 weeks for the co-primary endpoints of transfusion avoidance and hemolysis as measured by lactate dehydrogenase (LDH) normalization.
Ravulizumab also proved noninferior with regard to secondary efficacy endpoints and had a safety profile similar to that of eculizumab.
These results suggest ravulizumab could be a more convenient alternative for PNH patients, according to Jong Wook Lee, MD, of Seoul St. Mary’s Hospital in Seoul, South Korea.
Dr Lee presented these results as a late-breaking abstract (LB2603) at the 23rd Congress of the European Hematology Association (EHA).
The study was sponsored by Alexion Pharmaceuticals.
The trial enrolled adults with PNH naive to complement inhibitor therapy. They were randomized to receive ravulizumab (n=125) or eculizumab (n=121) for 183 days.
More than half of patients were male—52% in the ravulizumab arm and 57% in the eculizumab arm. Most patients were Asian (57.6% in the ravulizumab arm and 47.1% in the eculizumab arm) or white (34.4% and 42.1%, respectively).
Patients’ mean age at first infusion was 44.8 in the ravulizumab arm and 46.2 in the eculizumab arm. The mean number of years from PNH diagnosis to consent was 6.7 and 6.4, respectively.
The mean LDH at baseline was 1634 U/L in the ravulizumab arm and 1578 U/L in the eculizumab arm. The mean FACIT-Fatigue score was 36.7 and 36.9, respectively.
All 125 ravulizumab patients completed 26 weeks of treatment, as did 119 of the eculizumab patients. One hundred twenty-four ravulizumab patients entered the extension phase, as did 119 eculizumab patients.
Efficacy
The study’s primary efficacy endpoints were transfusion avoidance and LDH normalization from day 29 to 183. Dr Lee said ravulizumab proved noninferior to eculizumab for both endpoints, and point estimates favored ravulizumab.
The proportion of patients who remained transfusion-free was 73.6% in the ravulizumab arm and 66.1% in the eculizumab arm (difference, 6.8; 95% CI, -4.66, 18.14).
The proportion of patients who achieved LDH normalization was 53.6% and 49.4%, respectively (difference, 1.19; 95% CI, 0.8, 1.77).
Secondary efficacy endpoints included the percentage change in LDH from baseline, change in FACIT-Fatigue score from baseline, and the proportions of patients with breakthrough hemolysis and stabilized hemoglobin.
Again, ravulizumab was noninferior to eculizumab for all endpoints, with point estimates favoring ravulizumab.
The LDH percentage change was -76.84% in the ravulizumab arm and -76.02% in the eculizumab arm (difference, 0.83; 95% CI, -3.56, 5.21).
The change (improvement) in FACIT-Fatigue score was 7.07 and 6.40, respectively (difference, 0.67; 95% CI, -1.21, 2.55).
The percentage of patients with hemoglobin stabilization was 68.0% in the ravulizumab arm and 64.5% in the eculizumab arm (difference, 2.9; 95% CI, -8.80, 14.64).
The percentage of patients with breakthrough hemolysis was 4.0% and 10.7%, respectively (difference, 6.7; 95% CI, -0.18, 14.21).
Dr Lee noted that the proportion of patients with breakthrough hemolysis was more than 2.5-fold higher in the eculizumab arm than the ravulizumab arm—13 patients with 15 events and 5 patients with 5 events, respectively.
He said this was likely due to the immediate, complete, and sustained inhibition of C5 (mean free C5 <0.5 μg/mL) achieved by ravulizumab. Complete inhibition was observed after the first ravulizumab infusion and was sustained throughout the 26-week treatment period.
Safety
Dr Lee said ravulizumab had a similar safety profile to eculizumab, and both drugs were well tolerated.
Most patients experienced a treatment-emergent adverse event (TEAE)—88% in the ravulizumab arm and 86.8% in the eculizumab arm.
The most common TEAEs (in the ravulizumab and eculizumab arms, respectively) were headache (36.0% and 33.1%), nasopharyngitis (8.8% and 14.9%), upper respiratory tract infection (10.4% and 5.8%), and pyrexia (4.8% and 10.7%).
Serious AEs occurred in 8.8% of patients in the ravulizumab arm and 7.4% of those in the eculizumab arm.
Major adverse vascular events occurred in 2 patients in the ravulizumab arm and 1 in the eculizumab arm. There were no meningococcal infections in either arm.
One patient in the eculizumab arm was discontinued from the study and died of lung cancer (which was unrelated to treatment).
STOCKHOLM—Results of a phase 3 study suggest the long-acting C5 complement inhibitor ravulizumab produces similar results as eculizumab in patients with paroxysmal nocturnal hemoglobinuria (PNH).
Treatment with ravulizumab every 8 weeks proved noninferior to treatment with eculizumab every 2 weeks for the co-primary endpoints of transfusion avoidance and hemolysis as measured by lactate dehydrogenase (LDH) normalization.
Ravulizumab also proved noninferior with regard to secondary efficacy endpoints and had a safety profile similar to that of eculizumab.
These results suggest ravulizumab could be a more convenient alternative for PNH patients, according to Jong Wook Lee, MD, of Seoul St. Mary’s Hospital in Seoul, South Korea.
Dr Lee presented these results as a late-breaking abstract (LB2603) at the 23rd Congress of the European Hematology Association (EHA).
The study was sponsored by Alexion Pharmaceuticals.
The trial enrolled adults with PNH naive to complement inhibitor therapy. They were randomized to receive ravulizumab (n=125) or eculizumab (n=121) for 183 days.
More than half of patients were male—52% in the ravulizumab arm and 57% in the eculizumab arm. Most patients were Asian (57.6% in the ravulizumab arm and 47.1% in the eculizumab arm) or white (34.4% and 42.1%, respectively).
Patients’ mean age at first infusion was 44.8 in the ravulizumab arm and 46.2 in the eculizumab arm. The mean number of years from PNH diagnosis to consent was 6.7 and 6.4, respectively.
The mean LDH at baseline was 1634 U/L in the ravulizumab arm and 1578 U/L in the eculizumab arm. The mean FACIT-Fatigue score was 36.7 and 36.9, respectively.
All 125 ravulizumab patients completed 26 weeks of treatment, as did 119 of the eculizumab patients. One hundred twenty-four ravulizumab patients entered the extension phase, as did 119 eculizumab patients.
Efficacy
The study’s primary efficacy endpoints were transfusion avoidance and LDH normalization from day 29 to 183. Dr Lee said ravulizumab proved noninferior to eculizumab for both endpoints, and point estimates favored ravulizumab.
The proportion of patients who remained transfusion-free was 73.6% in the ravulizumab arm and 66.1% in the eculizumab arm (difference, 6.8; 95% CI, -4.66, 18.14).
The proportion of patients who achieved LDH normalization was 53.6% and 49.4%, respectively (difference, 1.19; 95% CI, 0.8, 1.77).
Secondary efficacy endpoints included the percentage change in LDH from baseline, change in FACIT-Fatigue score from baseline, and the proportions of patients with breakthrough hemolysis and stabilized hemoglobin.
Again, ravulizumab was noninferior to eculizumab for all endpoints, with point estimates favoring ravulizumab.
The LDH percentage change was -76.84% in the ravulizumab arm and -76.02% in the eculizumab arm (difference, 0.83; 95% CI, -3.56, 5.21).
The change (improvement) in FACIT-Fatigue score was 7.07 and 6.40, respectively (difference, 0.67; 95% CI, -1.21, 2.55).
The percentage of patients with hemoglobin stabilization was 68.0% in the ravulizumab arm and 64.5% in the eculizumab arm (difference, 2.9; 95% CI, -8.80, 14.64).
The percentage of patients with breakthrough hemolysis was 4.0% and 10.7%, respectively (difference, 6.7; 95% CI, -0.18, 14.21).
Dr Lee noted that the proportion of patients with breakthrough hemolysis was more than 2.5-fold higher in the eculizumab arm than the ravulizumab arm—13 patients with 15 events and 5 patients with 5 events, respectively.
He said this was likely due to the immediate, complete, and sustained inhibition of C5 (mean free C5 <0.5 μg/mL) achieved by ravulizumab. Complete inhibition was observed after the first ravulizumab infusion and was sustained throughout the 26-week treatment period.
Safety
Dr Lee said ravulizumab had a similar safety profile to eculizumab, and both drugs were well tolerated.
Most patients experienced a treatment-emergent adverse event (TEAE)—88% in the ravulizumab arm and 86.8% in the eculizumab arm.
The most common TEAEs (in the ravulizumab and eculizumab arms, respectively) were headache (36.0% and 33.1%), nasopharyngitis (8.8% and 14.9%), upper respiratory tract infection (10.4% and 5.8%), and pyrexia (4.8% and 10.7%).
Serious AEs occurred in 8.8% of patients in the ravulizumab arm and 7.4% of those in the eculizumab arm.
Major adverse vascular events occurred in 2 patients in the ravulizumab arm and 1 in the eculizumab arm. There were no meningococcal infections in either arm.
One patient in the eculizumab arm was discontinued from the study and died of lung cancer (which was unrelated to treatment).
Sickle cell disease exacts a heavy vocational toll
WASHINGTON – Three-quarters of patients with sickle cell disease (SCD) reported missing work in the last year because of disease symptoms, according to results from a single-center study.
While the direct costs of SCD are easy to measure, it’s harder to capture the indirect costs patients may incur from this chronic, progressive disease, which range from lost days at work to the downstream consequences of “presenteeism.”
“Indirect costs are related to things that have value, but it’s a little bit harder to apply an exact value to it,” said Nicholas Vendetti of Pfizer. But this is a critical piece for understanding SCD, he said. “The burden of illness is unknown without productivity costs.”
Mr. Vendetti and his collaborators attempted to capture the indirect costs of SCD, and reported the results of a single-site study at the annual meeting of the Foundation for Sickle Cell Disease Research.
They recruited patients from Virginia Commonwealth University’s adult sickle cell clinic and trained interviewers to conduct structured interviews using the Institute for Medical Technology Assessment Productivity Cost Questionnaire. The interviewers asked about absenteeism, lost work, unpaid work activity, and “presenteeism,” defined as days when participants were at work but experienced decreased work output because of disease symptoms.
In the end, the study enrolled 186 patients aged 18 and older, a figure that “really exceeded what we expected when we started the protocol,” Mr. Vendetti said. Most participants were between the ages of 20 and 60 years – the most productive working years.
About 58% of participants were female. Nearly half (46%) had the HbSS genotype, while 30% had the HbSC genotype. About half (52%) were high school graduates, and about a third had some college. There were no advanced degrees earned in the study population, and 11.5% had not finished high school.
Initial questions about educational status and employment status “highlighted a very interesting aspect of the disease: 43.8% reported that they were currently unable to work as part of their disease process,” Mr. Vendetti said. Just 28% were employed for wages, 3% were self-employed, and about 7% reported being homemakers. The remainder were out of work, were students, or were retired.
Three-quarters of patients reported missing work in the last year because of SCD symptoms. This group reported missing a mean 36.75 days yearly. Assuming the average Virginia hourly wage of $25.53 per hour, this comes to an average of $7,506 in lost wages each year, Mr. Vendetti said.
Presenteeism had a large impact as well. Nearly 73% of patients said they were bothered at work – either psychologically or physically – by their symptoms in the last 4 weeks, and 90% over the past year. These patients estimated they were affected for about 100 working days yearly.
When asked on a scale of 0-10 how much work they were able to get done on days when their SCD was affecting productivity, “most patients are falling into that middle range” of a score of 4-6, Mr. Vendetti said. “Most patients are moderately affected.
“It’s hard to apply a dollar value to that, but it’s easy to see how it could affect the trajectory of your career,” he added.
Another aspect of the indirect cost of the sickle cell disease burden that’s even harder to tease out is whether those affected are unable to complete a significant amount of unpaid work. Again, about three-quarters of patients reported that SCD had affected their ability to do this kind of work, and these patients said this happened on an average 105 days each year.
Even though patients may not be hiring others to do housework they’re unable to complete, or to care for children on days when they’re too unwell to do so, that doesn’t mean there’s no impact on the patient and those around them, Mr. Vendetti said. “If you ask a family member or a friend for help, that creates a strain in the relationship.”
In terms of resources to address the indirect burden of SCD on careers, Mr. Vendetti pointed out that many states have vocational rehabilitation programs that offer a significant amount of support and assistance to help find a productive work path that still accommodates a chronic illness such as SCD. In Virginia, he said, individuals need to be on disability to avail themselves of the program.
Health care providers can educate themselves about these and other programs. “Most adult sickle cell disease patients didn’t even know they might be eligible” for vocational assistance, he said.
During discussion after the presentation, an audience member pointed out that parents and caregivers of children with SCD are probably also incurring significant indirect costs because of their care-giving burden and that this population should also be studied. Mr. Vendetti agreed. “This is potential that isn’t fulfilled” for all patients and families whose work and personal lives are so profoundly affected by SCD, he said. “This is a dream deferred.”
Mr. Vendetti is employed by Pfizer and is a Pfizer stockholder. A coauthor of the study is a Pfizer consultant.
WASHINGTON – Three-quarters of patients with sickle cell disease (SCD) reported missing work in the last year because of disease symptoms, according to results from a single-center study.
While the direct costs of SCD are easy to measure, it’s harder to capture the indirect costs patients may incur from this chronic, progressive disease, which range from lost days at work to the downstream consequences of “presenteeism.”
“Indirect costs are related to things that have value, but it’s a little bit harder to apply an exact value to it,” said Nicholas Vendetti of Pfizer. But this is a critical piece for understanding SCD, he said. “The burden of illness is unknown without productivity costs.”
Mr. Vendetti and his collaborators attempted to capture the indirect costs of SCD, and reported the results of a single-site study at the annual meeting of the Foundation for Sickle Cell Disease Research.
They recruited patients from Virginia Commonwealth University’s adult sickle cell clinic and trained interviewers to conduct structured interviews using the Institute for Medical Technology Assessment Productivity Cost Questionnaire. The interviewers asked about absenteeism, lost work, unpaid work activity, and “presenteeism,” defined as days when participants were at work but experienced decreased work output because of disease symptoms.
In the end, the study enrolled 186 patients aged 18 and older, a figure that “really exceeded what we expected when we started the protocol,” Mr. Vendetti said. Most participants were between the ages of 20 and 60 years – the most productive working years.
About 58% of participants were female. Nearly half (46%) had the HbSS genotype, while 30% had the HbSC genotype. About half (52%) were high school graduates, and about a third had some college. There were no advanced degrees earned in the study population, and 11.5% had not finished high school.
Initial questions about educational status and employment status “highlighted a very interesting aspect of the disease: 43.8% reported that they were currently unable to work as part of their disease process,” Mr. Vendetti said. Just 28% were employed for wages, 3% were self-employed, and about 7% reported being homemakers. The remainder were out of work, were students, or were retired.
Three-quarters of patients reported missing work in the last year because of SCD symptoms. This group reported missing a mean 36.75 days yearly. Assuming the average Virginia hourly wage of $25.53 per hour, this comes to an average of $7,506 in lost wages each year, Mr. Vendetti said.
Presenteeism had a large impact as well. Nearly 73% of patients said they were bothered at work – either psychologically or physically – by their symptoms in the last 4 weeks, and 90% over the past year. These patients estimated they were affected for about 100 working days yearly.
When asked on a scale of 0-10 how much work they were able to get done on days when their SCD was affecting productivity, “most patients are falling into that middle range” of a score of 4-6, Mr. Vendetti said. “Most patients are moderately affected.
“It’s hard to apply a dollar value to that, but it’s easy to see how it could affect the trajectory of your career,” he added.
Another aspect of the indirect cost of the sickle cell disease burden that’s even harder to tease out is whether those affected are unable to complete a significant amount of unpaid work. Again, about three-quarters of patients reported that SCD had affected their ability to do this kind of work, and these patients said this happened on an average 105 days each year.
Even though patients may not be hiring others to do housework they’re unable to complete, or to care for children on days when they’re too unwell to do so, that doesn’t mean there’s no impact on the patient and those around them, Mr. Vendetti said. “If you ask a family member or a friend for help, that creates a strain in the relationship.”
In terms of resources to address the indirect burden of SCD on careers, Mr. Vendetti pointed out that many states have vocational rehabilitation programs that offer a significant amount of support and assistance to help find a productive work path that still accommodates a chronic illness such as SCD. In Virginia, he said, individuals need to be on disability to avail themselves of the program.
Health care providers can educate themselves about these and other programs. “Most adult sickle cell disease patients didn’t even know they might be eligible” for vocational assistance, he said.
During discussion after the presentation, an audience member pointed out that parents and caregivers of children with SCD are probably also incurring significant indirect costs because of their care-giving burden and that this population should also be studied. Mr. Vendetti agreed. “This is potential that isn’t fulfilled” for all patients and families whose work and personal lives are so profoundly affected by SCD, he said. “This is a dream deferred.”
Mr. Vendetti is employed by Pfizer and is a Pfizer stockholder. A coauthor of the study is a Pfizer consultant.
WASHINGTON – Three-quarters of patients with sickle cell disease (SCD) reported missing work in the last year because of disease symptoms, according to results from a single-center study.
While the direct costs of SCD are easy to measure, it’s harder to capture the indirect costs patients may incur from this chronic, progressive disease, which range from lost days at work to the downstream consequences of “presenteeism.”
“Indirect costs are related to things that have value, but it’s a little bit harder to apply an exact value to it,” said Nicholas Vendetti of Pfizer. But this is a critical piece for understanding SCD, he said. “The burden of illness is unknown without productivity costs.”
Mr. Vendetti and his collaborators attempted to capture the indirect costs of SCD, and reported the results of a single-site study at the annual meeting of the Foundation for Sickle Cell Disease Research.
They recruited patients from Virginia Commonwealth University’s adult sickle cell clinic and trained interviewers to conduct structured interviews using the Institute for Medical Technology Assessment Productivity Cost Questionnaire. The interviewers asked about absenteeism, lost work, unpaid work activity, and “presenteeism,” defined as days when participants were at work but experienced decreased work output because of disease symptoms.
In the end, the study enrolled 186 patients aged 18 and older, a figure that “really exceeded what we expected when we started the protocol,” Mr. Vendetti said. Most participants were between the ages of 20 and 60 years – the most productive working years.
About 58% of participants were female. Nearly half (46%) had the HbSS genotype, while 30% had the HbSC genotype. About half (52%) were high school graduates, and about a third had some college. There were no advanced degrees earned in the study population, and 11.5% had not finished high school.
Initial questions about educational status and employment status “highlighted a very interesting aspect of the disease: 43.8% reported that they were currently unable to work as part of their disease process,” Mr. Vendetti said. Just 28% were employed for wages, 3% were self-employed, and about 7% reported being homemakers. The remainder were out of work, were students, or were retired.
Three-quarters of patients reported missing work in the last year because of SCD symptoms. This group reported missing a mean 36.75 days yearly. Assuming the average Virginia hourly wage of $25.53 per hour, this comes to an average of $7,506 in lost wages each year, Mr. Vendetti said.
Presenteeism had a large impact as well. Nearly 73% of patients said they were bothered at work – either psychologically or physically – by their symptoms in the last 4 weeks, and 90% over the past year. These patients estimated they were affected for about 100 working days yearly.
When asked on a scale of 0-10 how much work they were able to get done on days when their SCD was affecting productivity, “most patients are falling into that middle range” of a score of 4-6, Mr. Vendetti said. “Most patients are moderately affected.
“It’s hard to apply a dollar value to that, but it’s easy to see how it could affect the trajectory of your career,” he added.
Another aspect of the indirect cost of the sickle cell disease burden that’s even harder to tease out is whether those affected are unable to complete a significant amount of unpaid work. Again, about three-quarters of patients reported that SCD had affected their ability to do this kind of work, and these patients said this happened on an average 105 days each year.
Even though patients may not be hiring others to do housework they’re unable to complete, or to care for children on days when they’re too unwell to do so, that doesn’t mean there’s no impact on the patient and those around them, Mr. Vendetti said. “If you ask a family member or a friend for help, that creates a strain in the relationship.”
In terms of resources to address the indirect burden of SCD on careers, Mr. Vendetti pointed out that many states have vocational rehabilitation programs that offer a significant amount of support and assistance to help find a productive work path that still accommodates a chronic illness such as SCD. In Virginia, he said, individuals need to be on disability to avail themselves of the program.
Health care providers can educate themselves about these and other programs. “Most adult sickle cell disease patients didn’t even know they might be eligible” for vocational assistance, he said.
During discussion after the presentation, an audience member pointed out that parents and caregivers of children with SCD are probably also incurring significant indirect costs because of their care-giving burden and that this population should also be studied. Mr. Vendetti agreed. “This is potential that isn’t fulfilled” for all patients and families whose work and personal lives are so profoundly affected by SCD, he said. “This is a dream deferred.”
Mr. Vendetti is employed by Pfizer and is a Pfizer stockholder. A coauthor of the study is a Pfizer consultant.
REPORTING FROM FSCDR 2018
Key clinical point:
Major finding: Three-quarters of patients reported missing work in the last year because of SCD symptoms. This group reported missing a mean 37 days yearly.
Study details: Single-site survey-based study of 186 adults with SCD.
Disclosures: Pfizer sponsored the study. Mr. Vendetti is employed by Pfizer and holds Pfizer stock. A study coauthor is a Pfizer consultant.
Family engagement can buffer early cognitive hit from SCD
WASHINGTON – Can early family interventions help children with sickle cell disease (SCD) stay on track for normal cognitive development?
Given the stakes – even young children with SCD have a high risk of ischemic cerebral insults, with significant downstream cognitive deficits – these interventions are sorely needed, said Allison King, MD, PhD, of Washington University, St. Louis.
Speaking at the annual meeting of the Foundation for Sickle Cell Disease Research, Dr. King shared her institution’s suite of interventions, which are aimed at giving infants and toddlers early home enrichment through parent education and engagement.
Dr. King reviewed some of the factors that are known to be associated with intelligence quotient (IQ) changes in individuals with SCD. The single largest impact comes with an overt stroke, which drops IQ by an average 10 points. A “silent” subclinical stroke is associated with a mean 5-point decrease, while hypoxemia is associated with diminution in IQ of about 0.75 points.
On the other hand, having a parent with at least some college education is associated with a robust 6-point boost in IQ, Dr. King said.
Even if the disease results in a mean 5-point drop in IQ for the national population of children with SCD, this would result in the bell curve of intellectual ability for this cohort shifting significantly to the left, Dr. King said. Instead of 6 million children with SCD falling into the “intellectually disabled” category of those with IQs less than 70, the number would climb to 9.4 million, a 57% increase.
Cognitive impairment can be evident by the toddler years. Across the literature, 46%-58% of young children with SCD have been found to have risk for developmental delay or to show frank delay by 12-36 months of age, Dr. King said. Factors associated with risk of delay include low hemoglobin level, disease phenotype, positive transcranial Doppler findings, and – importantly – parental education, income, and perceived helplessness.
Dr. King and her collaborators have tackled the home environment to address some of these potentially remediable social factors. They hypothesized that a parent education program that boosts the quality of parent-child interactions would help children with SCD have better developmental outcomes.
She and her colleagues designed a prospective single-arm pilot study that enrolled children with SCD from birth to 36 months of age, along with a parent or caregiver (Pediatr Blood Cancer. 2016 Dec;63[12]:2131-8).
Over a period of continuous enrollment of up to 2 years, the families received a monthly visit from a home educator. During these visits, the educators delivered a validated “Born to Learn” curriculum that uses a parents-as-teachers model.
Of the 35 children, 15 (43%) were female. At enrollment, the children were a mean 5 months of age and their primary caregiver was a mean 25 years old. The children’s mean age of exit from the study was 26 months. Most patients had either the HbSS (46%) or the HbSC (43%) phenotype. At enrollment, the mean peripheral oxygen saturation was 100%, and hematocrit was a mean 27.9%.
“The parenting intervention improved cognition and language,” Dr. King said, especially in the domains of cognitive performance and expressive language, which both saw significant age-normed score improvements over the course of the study (P = .016 and .002, respectively).
Among the pre- and poststudy measures that were used was the Home Observation for Measurement of Environment tool, said Dr. King. This observer-completed scale measures parent/caregiver responsivity, acceptance, and organization. Also, the parent’s level of organization and involvement is assessed, as are available learning materials and variety of resources and enrichment.
Scores improved here, too, particularly in the domains of organization and the amount of learning materials available at home (P less than .05 for both). There was a numeric improvement in the overall score, but the figure wasn’t statistically significant.
Dr. King used recent research to bring home the importance of early intervention to support cognitive development in children with SCD. A recent meta-analysis found that 50.3% of SCD patients will have had a silent brain infarct by 30 years of age (Blood. 2016 Apr 21;127[16]:2038-40). The same publication, she said, cited work that found a prevalence of silent infarcts ranging from more than 25% by the age of 5 years to 19%-28% at 8 years.
But “parent education impacts IQ more than silent infarcts,” she said. In her work, the highest predicted IQs are seen in young patients with no infarcts and whose parents have had some college education. Perhaps surprisingly, she said, the next highest IQ tier consists of patients who have detectable infarcts, but whose parents have had at least some college education. These patients’ predicted IQs were higher than those who had no infarcts but whose parents had no more than a high school education, as well as children with the double hit of an infarct and parents with no college education.
Putting these puzzle pieces together matters for long-term outcomes, Dr. King said. Socioeconomic status is the strongest predictor of grade retention for children with SCD, with the poorest quartile in a study of 536 pediatric SCD patients having an odds ratio of 6.4 for grade retention, compared with the highest quartile (P = .001). Notably, children in the lowest quartile lived in homes where the per capita income was less than $3,000 (Am J Hematol. 2014;89[10]:e188-92). This highlights the “abject poverty” many of these families face, Dr. King said.
Children in this poorest quartile, especially boys, fared poorly going forward. “By age 15, 65% of poor males with sickle cell anemia fail a grade,” Dr. King said. The frequent absenteeism occasioned by hospital stays, clinic visits, and days at home with pain mount to an average of 15-22 missed school days annually, she said, adding that “absenteeism is an important predictor of dropout.”
These trends are brought forward into the workplace, with adults who have SCD being less likely to be employed if their IQs are lower. The association is particularly strong for processing speed, according to one study (J Clin Exp Neuropsychol. 2016 Aug;38[6]:661-71).
Dr. King outlined some concrete steps that those caring for children with SCD can take to maximize their chances for school success, acknowledging that time and resource constraints will vary by practice setting. These include completing an in-clinic educational inventory, asking about recent school performance, and if indicated, referring for neuropsychology evaluation to be shared with the school.
Physicians also can work to engage institutional resources for advocacy and communication with the school.
Parents can be encouraged to request a 504 plan, a federally mandated set of accommodations. For children with SCD, these might include setting up tutoring for periods when the child is homebound, allowing a water bottle and frequent bathroom breaks since hydration is critical for children with SCD, and allowing extra time for testing if processing speed is an issue.
An additional education step is the individualized education plan, or IEP, which can include instruction in smaller groups or teaching that’s modified for special learning needs; alternative methods of assessments; and, for older children, consideration of a vocational education path to complete high school.
Dr. King reported having no conflicts of interest.
WASHINGTON – Can early family interventions help children with sickle cell disease (SCD) stay on track for normal cognitive development?
Given the stakes – even young children with SCD have a high risk of ischemic cerebral insults, with significant downstream cognitive deficits – these interventions are sorely needed, said Allison King, MD, PhD, of Washington University, St. Louis.
Speaking at the annual meeting of the Foundation for Sickle Cell Disease Research, Dr. King shared her institution’s suite of interventions, which are aimed at giving infants and toddlers early home enrichment through parent education and engagement.
Dr. King reviewed some of the factors that are known to be associated with intelligence quotient (IQ) changes in individuals with SCD. The single largest impact comes with an overt stroke, which drops IQ by an average 10 points. A “silent” subclinical stroke is associated with a mean 5-point decrease, while hypoxemia is associated with diminution in IQ of about 0.75 points.
On the other hand, having a parent with at least some college education is associated with a robust 6-point boost in IQ, Dr. King said.
Even if the disease results in a mean 5-point drop in IQ for the national population of children with SCD, this would result in the bell curve of intellectual ability for this cohort shifting significantly to the left, Dr. King said. Instead of 6 million children with SCD falling into the “intellectually disabled” category of those with IQs less than 70, the number would climb to 9.4 million, a 57% increase.
Cognitive impairment can be evident by the toddler years. Across the literature, 46%-58% of young children with SCD have been found to have risk for developmental delay or to show frank delay by 12-36 months of age, Dr. King said. Factors associated with risk of delay include low hemoglobin level, disease phenotype, positive transcranial Doppler findings, and – importantly – parental education, income, and perceived helplessness.
Dr. King and her collaborators have tackled the home environment to address some of these potentially remediable social factors. They hypothesized that a parent education program that boosts the quality of parent-child interactions would help children with SCD have better developmental outcomes.
She and her colleagues designed a prospective single-arm pilot study that enrolled children with SCD from birth to 36 months of age, along with a parent or caregiver (Pediatr Blood Cancer. 2016 Dec;63[12]:2131-8).
Over a period of continuous enrollment of up to 2 years, the families received a monthly visit from a home educator. During these visits, the educators delivered a validated “Born to Learn” curriculum that uses a parents-as-teachers model.
Of the 35 children, 15 (43%) were female. At enrollment, the children were a mean 5 months of age and their primary caregiver was a mean 25 years old. The children’s mean age of exit from the study was 26 months. Most patients had either the HbSS (46%) or the HbSC (43%) phenotype. At enrollment, the mean peripheral oxygen saturation was 100%, and hematocrit was a mean 27.9%.
“The parenting intervention improved cognition and language,” Dr. King said, especially in the domains of cognitive performance and expressive language, which both saw significant age-normed score improvements over the course of the study (P = .016 and .002, respectively).
Among the pre- and poststudy measures that were used was the Home Observation for Measurement of Environment tool, said Dr. King. This observer-completed scale measures parent/caregiver responsivity, acceptance, and organization. Also, the parent’s level of organization and involvement is assessed, as are available learning materials and variety of resources and enrichment.
Scores improved here, too, particularly in the domains of organization and the amount of learning materials available at home (P less than .05 for both). There was a numeric improvement in the overall score, but the figure wasn’t statistically significant.
Dr. King used recent research to bring home the importance of early intervention to support cognitive development in children with SCD. A recent meta-analysis found that 50.3% of SCD patients will have had a silent brain infarct by 30 years of age (Blood. 2016 Apr 21;127[16]:2038-40). The same publication, she said, cited work that found a prevalence of silent infarcts ranging from more than 25% by the age of 5 years to 19%-28% at 8 years.
But “parent education impacts IQ more than silent infarcts,” she said. In her work, the highest predicted IQs are seen in young patients with no infarcts and whose parents have had some college education. Perhaps surprisingly, she said, the next highest IQ tier consists of patients who have detectable infarcts, but whose parents have had at least some college education. These patients’ predicted IQs were higher than those who had no infarcts but whose parents had no more than a high school education, as well as children with the double hit of an infarct and parents with no college education.
Putting these puzzle pieces together matters for long-term outcomes, Dr. King said. Socioeconomic status is the strongest predictor of grade retention for children with SCD, with the poorest quartile in a study of 536 pediatric SCD patients having an odds ratio of 6.4 for grade retention, compared with the highest quartile (P = .001). Notably, children in the lowest quartile lived in homes where the per capita income was less than $3,000 (Am J Hematol. 2014;89[10]:e188-92). This highlights the “abject poverty” many of these families face, Dr. King said.
Children in this poorest quartile, especially boys, fared poorly going forward. “By age 15, 65% of poor males with sickle cell anemia fail a grade,” Dr. King said. The frequent absenteeism occasioned by hospital stays, clinic visits, and days at home with pain mount to an average of 15-22 missed school days annually, she said, adding that “absenteeism is an important predictor of dropout.”
These trends are brought forward into the workplace, with adults who have SCD being less likely to be employed if their IQs are lower. The association is particularly strong for processing speed, according to one study (J Clin Exp Neuropsychol. 2016 Aug;38[6]:661-71).
Dr. King outlined some concrete steps that those caring for children with SCD can take to maximize their chances for school success, acknowledging that time and resource constraints will vary by practice setting. These include completing an in-clinic educational inventory, asking about recent school performance, and if indicated, referring for neuropsychology evaluation to be shared with the school.
Physicians also can work to engage institutional resources for advocacy and communication with the school.
Parents can be encouraged to request a 504 plan, a federally mandated set of accommodations. For children with SCD, these might include setting up tutoring for periods when the child is homebound, allowing a water bottle and frequent bathroom breaks since hydration is critical for children with SCD, and allowing extra time for testing if processing speed is an issue.
An additional education step is the individualized education plan, or IEP, which can include instruction in smaller groups or teaching that’s modified for special learning needs; alternative methods of assessments; and, for older children, consideration of a vocational education path to complete high school.
Dr. King reported having no conflicts of interest.
WASHINGTON – Can early family interventions help children with sickle cell disease (SCD) stay on track for normal cognitive development?
Given the stakes – even young children with SCD have a high risk of ischemic cerebral insults, with significant downstream cognitive deficits – these interventions are sorely needed, said Allison King, MD, PhD, of Washington University, St. Louis.
Speaking at the annual meeting of the Foundation for Sickle Cell Disease Research, Dr. King shared her institution’s suite of interventions, which are aimed at giving infants and toddlers early home enrichment through parent education and engagement.
Dr. King reviewed some of the factors that are known to be associated with intelligence quotient (IQ) changes in individuals with SCD. The single largest impact comes with an overt stroke, which drops IQ by an average 10 points. A “silent” subclinical stroke is associated with a mean 5-point decrease, while hypoxemia is associated with diminution in IQ of about 0.75 points.
On the other hand, having a parent with at least some college education is associated with a robust 6-point boost in IQ, Dr. King said.
Even if the disease results in a mean 5-point drop in IQ for the national population of children with SCD, this would result in the bell curve of intellectual ability for this cohort shifting significantly to the left, Dr. King said. Instead of 6 million children with SCD falling into the “intellectually disabled” category of those with IQs less than 70, the number would climb to 9.4 million, a 57% increase.
Cognitive impairment can be evident by the toddler years. Across the literature, 46%-58% of young children with SCD have been found to have risk for developmental delay or to show frank delay by 12-36 months of age, Dr. King said. Factors associated with risk of delay include low hemoglobin level, disease phenotype, positive transcranial Doppler findings, and – importantly – parental education, income, and perceived helplessness.
Dr. King and her collaborators have tackled the home environment to address some of these potentially remediable social factors. They hypothesized that a parent education program that boosts the quality of parent-child interactions would help children with SCD have better developmental outcomes.
She and her colleagues designed a prospective single-arm pilot study that enrolled children with SCD from birth to 36 months of age, along with a parent or caregiver (Pediatr Blood Cancer. 2016 Dec;63[12]:2131-8).
Over a period of continuous enrollment of up to 2 years, the families received a monthly visit from a home educator. During these visits, the educators delivered a validated “Born to Learn” curriculum that uses a parents-as-teachers model.
Of the 35 children, 15 (43%) were female. At enrollment, the children were a mean 5 months of age and their primary caregiver was a mean 25 years old. The children’s mean age of exit from the study was 26 months. Most patients had either the HbSS (46%) or the HbSC (43%) phenotype. At enrollment, the mean peripheral oxygen saturation was 100%, and hematocrit was a mean 27.9%.
“The parenting intervention improved cognition and language,” Dr. King said, especially in the domains of cognitive performance and expressive language, which both saw significant age-normed score improvements over the course of the study (P = .016 and .002, respectively).
Among the pre- and poststudy measures that were used was the Home Observation for Measurement of Environment tool, said Dr. King. This observer-completed scale measures parent/caregiver responsivity, acceptance, and organization. Also, the parent’s level of organization and involvement is assessed, as are available learning materials and variety of resources and enrichment.
Scores improved here, too, particularly in the domains of organization and the amount of learning materials available at home (P less than .05 for both). There was a numeric improvement in the overall score, but the figure wasn’t statistically significant.
Dr. King used recent research to bring home the importance of early intervention to support cognitive development in children with SCD. A recent meta-analysis found that 50.3% of SCD patients will have had a silent brain infarct by 30 years of age (Blood. 2016 Apr 21;127[16]:2038-40). The same publication, she said, cited work that found a prevalence of silent infarcts ranging from more than 25% by the age of 5 years to 19%-28% at 8 years.
But “parent education impacts IQ more than silent infarcts,” she said. In her work, the highest predicted IQs are seen in young patients with no infarcts and whose parents have had some college education. Perhaps surprisingly, she said, the next highest IQ tier consists of patients who have detectable infarcts, but whose parents have had at least some college education. These patients’ predicted IQs were higher than those who had no infarcts but whose parents had no more than a high school education, as well as children with the double hit of an infarct and parents with no college education.
Putting these puzzle pieces together matters for long-term outcomes, Dr. King said. Socioeconomic status is the strongest predictor of grade retention for children with SCD, with the poorest quartile in a study of 536 pediatric SCD patients having an odds ratio of 6.4 for grade retention, compared with the highest quartile (P = .001). Notably, children in the lowest quartile lived in homes where the per capita income was less than $3,000 (Am J Hematol. 2014;89[10]:e188-92). This highlights the “abject poverty” many of these families face, Dr. King said.
Children in this poorest quartile, especially boys, fared poorly going forward. “By age 15, 65% of poor males with sickle cell anemia fail a grade,” Dr. King said. The frequent absenteeism occasioned by hospital stays, clinic visits, and days at home with pain mount to an average of 15-22 missed school days annually, she said, adding that “absenteeism is an important predictor of dropout.”
These trends are brought forward into the workplace, with adults who have SCD being less likely to be employed if their IQs are lower. The association is particularly strong for processing speed, according to one study (J Clin Exp Neuropsychol. 2016 Aug;38[6]:661-71).
Dr. King outlined some concrete steps that those caring for children with SCD can take to maximize their chances for school success, acknowledging that time and resource constraints will vary by practice setting. These include completing an in-clinic educational inventory, asking about recent school performance, and if indicated, referring for neuropsychology evaluation to be shared with the school.
Physicians also can work to engage institutional resources for advocacy and communication with the school.
Parents can be encouraged to request a 504 plan, a federally mandated set of accommodations. For children with SCD, these might include setting up tutoring for periods when the child is homebound, allowing a water bottle and frequent bathroom breaks since hydration is critical for children with SCD, and allowing extra time for testing if processing speed is an issue.
An additional education step is the individualized education plan, or IEP, which can include instruction in smaller groups or teaching that’s modified for special learning needs; alternative methods of assessments; and, for older children, consideration of a vocational education path to complete high school.
Dr. King reported having no conflicts of interest.
EXPERT ANALYSIS FROM FSCDR 2018
Mircera approved for anemia in pediatric patients with CKD
Mircera®, methoxy polyethylene glycol-epoetin beta, was approved by the US Food and Drug Administration (FDA) to treat anemia in pediatric patients who have chronic kidney disease (CKD).
The drug is indicated for patients ages 5 to 17 years on hemodialysis who are switching from another erythropoiesis-stimulating agent (ESA) after their hemoglobin levels have stabilized.
The FDA also approved the agent to treat adult patients with CKD-associated anemia.
However, the drug is not approved to treat anemia caused by cancer chemotherapy.
The FDA based its approval on data from an open-label, multiple-dose, multicenter, dose-finding trial (NCT00717366).
Investigators enrolled 64 pediatric patients with CKD on hemodialysis. The patients had to have stable hemoglobin levels while receiving another ESA, such as epoetin alfa/beta or darbepoetin alfa.
Patients received Mircera intravenously once every 4 weeks for 20 weeks. Investigators adjusted the dosages, if necessary, after the first administration to maintain target hemoglobin levels.
Efficacy was based on the patients’ ability to maintain target hemoglobin levels and also on data extrapolated from trials of Mircera in adults with CKD.
Patients who received Mircera had a mean change in hemoglobin concentration from baseline of -0.15g/dL and 75% maintained hemoglobin values within ± 1g/dL of baseline.
Eighty-one percent maintained hemoglobin values within 10–12g/dL during the evaluation period.
The safety findings in pediatric patients were consistent with those previously reported in adults.
The most common adverse reactions occurring in 10% or more patients, as indicated in the prescribing information, are hypertension, diarrhea, and nasopharyngitis.
The drug carries a black box warning for increased risk of death, myocardial infarction, stroke, venous thromboembolism, thrombosis of vascular access, and tumor progression of recurrence.
Mircera is an erythropoietin receptor activator with greater activity in vivo as well as increased half-life, compared to erythropoietin.
Mircera is manufactured by Vifor (International) Inc.
Mircera®, methoxy polyethylene glycol-epoetin beta, was approved by the US Food and Drug Administration (FDA) to treat anemia in pediatric patients who have chronic kidney disease (CKD).
The drug is indicated for patients ages 5 to 17 years on hemodialysis who are switching from another erythropoiesis-stimulating agent (ESA) after their hemoglobin levels have stabilized.
The FDA also approved the agent to treat adult patients with CKD-associated anemia.
However, the drug is not approved to treat anemia caused by cancer chemotherapy.
The FDA based its approval on data from an open-label, multiple-dose, multicenter, dose-finding trial (NCT00717366).
Investigators enrolled 64 pediatric patients with CKD on hemodialysis. The patients had to have stable hemoglobin levels while receiving another ESA, such as epoetin alfa/beta or darbepoetin alfa.
Patients received Mircera intravenously once every 4 weeks for 20 weeks. Investigators adjusted the dosages, if necessary, after the first administration to maintain target hemoglobin levels.
Efficacy was based on the patients’ ability to maintain target hemoglobin levels and also on data extrapolated from trials of Mircera in adults with CKD.
Patients who received Mircera had a mean change in hemoglobin concentration from baseline of -0.15g/dL and 75% maintained hemoglobin values within ± 1g/dL of baseline.
Eighty-one percent maintained hemoglobin values within 10–12g/dL during the evaluation period.
The safety findings in pediatric patients were consistent with those previously reported in adults.
The most common adverse reactions occurring in 10% or more patients, as indicated in the prescribing information, are hypertension, diarrhea, and nasopharyngitis.
The drug carries a black box warning for increased risk of death, myocardial infarction, stroke, venous thromboembolism, thrombosis of vascular access, and tumor progression of recurrence.
Mircera is an erythropoietin receptor activator with greater activity in vivo as well as increased half-life, compared to erythropoietin.
Mircera is manufactured by Vifor (International) Inc.
Mircera®, methoxy polyethylene glycol-epoetin beta, was approved by the US Food and Drug Administration (FDA) to treat anemia in pediatric patients who have chronic kidney disease (CKD).
The drug is indicated for patients ages 5 to 17 years on hemodialysis who are switching from another erythropoiesis-stimulating agent (ESA) after their hemoglobin levels have stabilized.
The FDA also approved the agent to treat adult patients with CKD-associated anemia.
However, the drug is not approved to treat anemia caused by cancer chemotherapy.
The FDA based its approval on data from an open-label, multiple-dose, multicenter, dose-finding trial (NCT00717366).
Investigators enrolled 64 pediatric patients with CKD on hemodialysis. The patients had to have stable hemoglobin levels while receiving another ESA, such as epoetin alfa/beta or darbepoetin alfa.
Patients received Mircera intravenously once every 4 weeks for 20 weeks. Investigators adjusted the dosages, if necessary, after the first administration to maintain target hemoglobin levels.
Efficacy was based on the patients’ ability to maintain target hemoglobin levels and also on data extrapolated from trials of Mircera in adults with CKD.
Patients who received Mircera had a mean change in hemoglobin concentration from baseline of -0.15g/dL and 75% maintained hemoglobin values within ± 1g/dL of baseline.
Eighty-one percent maintained hemoglobin values within 10–12g/dL during the evaluation period.
The safety findings in pediatric patients were consistent with those previously reported in adults.
The most common adverse reactions occurring in 10% or more patients, as indicated in the prescribing information, are hypertension, diarrhea, and nasopharyngitis.
The drug carries a black box warning for increased risk of death, myocardial infarction, stroke, venous thromboembolism, thrombosis of vascular access, and tumor progression of recurrence.
Mircera is an erythropoietin receptor activator with greater activity in vivo as well as increased half-life, compared to erythropoietin.
Mircera is manufactured by Vifor (International) Inc.
FDA approves long-acting ESA for dialysis-related anemia in children, adolescents
The patients aged 5-17 years with chronic kidney disease whose hemoglobin had been stabilized with an erythropoiesis-stimulating agent (ESA).
Efficacy was based partly on how well target hemoglobin levels were maintained in this trial, but also on extrapolation from results of trials in adults. The safety profile in these pediatric patients was consistent with those previously observed in adults. Mircera is manufactured by Vifor Pharma.
More information on the approval of Mircera in this population can be found in the FDA release. The prescribing information for Mircera, initially approved in 2007, has also been updated.
The patients aged 5-17 years with chronic kidney disease whose hemoglobin had been stabilized with an erythropoiesis-stimulating agent (ESA).
Efficacy was based partly on how well target hemoglobin levels were maintained in this trial, but also on extrapolation from results of trials in adults. The safety profile in these pediatric patients was consistent with those previously observed in adults. Mircera is manufactured by Vifor Pharma.
More information on the approval of Mircera in this population can be found in the FDA release. The prescribing information for Mircera, initially approved in 2007, has also been updated.
The patients aged 5-17 years with chronic kidney disease whose hemoglobin had been stabilized with an erythropoiesis-stimulating agent (ESA).
Efficacy was based partly on how well target hemoglobin levels were maintained in this trial, but also on extrapolation from results of trials in adults. The safety profile in these pediatric patients was consistent with those previously observed in adults. Mircera is manufactured by Vifor Pharma.
More information on the approval of Mircera in this population can be found in the FDA release. The prescribing information for Mircera, initially approved in 2007, has also been updated.