User login
Study reveals potential treatment avenue for DBA, MDS

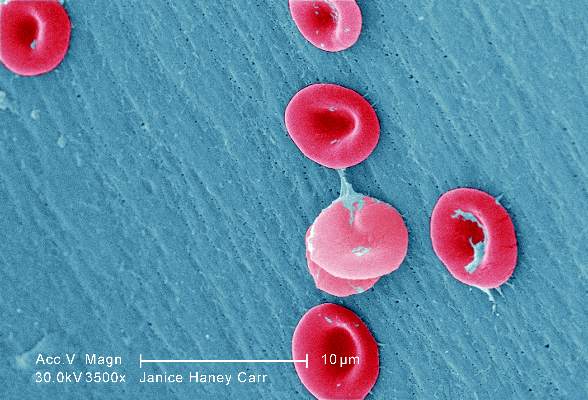
The production of two components of hemoglobin may be out of sync in Diamond Blackfan anemia (DBA) and myelodysplastic syndromes (MDS), according to a new study.
Researchers found that, in samples from patients with DBA or MDS, ribosome dysfunction delayed globin production, while heme synthesis proceeded normally.
This disruption in heme-globin coordination led to a buildup of toxic heme that killed red blood cell (RBC) precursors.
However, treating patient samples with a compound that blocks heme synthesis increased RBC production in both DBA and MDS.
Zhantao Yang, MD, of the University of Washington in Seattle, and his colleagues reported these findings in Science Translational Medicine.
Both DBA and MDS have been linked to defects in ribosome assembly, which is critical to protein production, but how this leads to anemia remains unknown.
To find out, Dr Yang and his colleagues analyzed bone marrow cells from patients with DBA (n=3) or MDS with del(5q) (n=6).
The researchers found that globin translation proceeded slowly in these samples, but heme synthesis proceeded normally.
This resulted in insufficient globin, excess heme, and excess reactive oxygen species in early erythroid precursors and, ultimately, the death of colony-forming unit–erythroid/proerythroblast cells.
The cells that were able to rapidly export heme or slow its synthesis survived and matured into RBCs, but the other colony-forming unit–erythroid cells/early proerythroblasts died.
The researchers noted that it is not clear how excess heme induces cell death in RBC precursors, but they said it likely involves both ferroptosis and apoptosis.
Regardless of the mechanism of cell death, the team found that treating the patients’ cells with succinylacetone (10 mM), a compound that blocks heme synthesis, improved RBC production.
The treatment improved RBC production in DBA and del(5q) MDS marrow cultures by 68% to 95% (P=0.03 to 0.05). In comparison, RBC production in control marrow cultures decreased by 4% to 13%.
The researchers said their experiments revealed additional important findings. First, they found that erythroid differentiation in the marrow cultures “excellently” phenocopied erythroid differentiation in vivo. This suggests these cultures can serve as a reliable platform in preclinical studies.
Second, the team said the fact that epigenetic differences between RBC precursors can lead to their preferential death or survival has broad implications. And querying the cells that preferentially survive could provide important insights. ![]()

The production of two components of hemoglobin may be out of sync in Diamond Blackfan anemia (DBA) and myelodysplastic syndromes (MDS), according to a new study.
Researchers found that, in samples from patients with DBA or MDS, ribosome dysfunction delayed globin production, while heme synthesis proceeded normally.
This disruption in heme-globin coordination led to a buildup of toxic heme that killed red blood cell (RBC) precursors.
However, treating patient samples with a compound that blocks heme synthesis increased RBC production in both DBA and MDS.
Zhantao Yang, MD, of the University of Washington in Seattle, and his colleagues reported these findings in Science Translational Medicine.
Both DBA and MDS have been linked to defects in ribosome assembly, which is critical to protein production, but how this leads to anemia remains unknown.
To find out, Dr Yang and his colleagues analyzed bone marrow cells from patients with DBA (n=3) or MDS with del(5q) (n=6).
The researchers found that globin translation proceeded slowly in these samples, but heme synthesis proceeded normally.
This resulted in insufficient globin, excess heme, and excess reactive oxygen species in early erythroid precursors and, ultimately, the death of colony-forming unit–erythroid/proerythroblast cells.
The cells that were able to rapidly export heme or slow its synthesis survived and matured into RBCs, but the other colony-forming unit–erythroid cells/early proerythroblasts died.
The researchers noted that it is not clear how excess heme induces cell death in RBC precursors, but they said it likely involves both ferroptosis and apoptosis.
Regardless of the mechanism of cell death, the team found that treating the patients’ cells with succinylacetone (10 mM), a compound that blocks heme synthesis, improved RBC production.
The treatment improved RBC production in DBA and del(5q) MDS marrow cultures by 68% to 95% (P=0.03 to 0.05). In comparison, RBC production in control marrow cultures decreased by 4% to 13%.
The researchers said their experiments revealed additional important findings. First, they found that erythroid differentiation in the marrow cultures “excellently” phenocopied erythroid differentiation in vivo. This suggests these cultures can serve as a reliable platform in preclinical studies.
Second, the team said the fact that epigenetic differences between RBC precursors can lead to their preferential death or survival has broad implications. And querying the cells that preferentially survive could provide important insights. ![]()

The production of two components of hemoglobin may be out of sync in Diamond Blackfan anemia (DBA) and myelodysplastic syndromes (MDS), according to a new study.
Researchers found that, in samples from patients with DBA or MDS, ribosome dysfunction delayed globin production, while heme synthesis proceeded normally.
This disruption in heme-globin coordination led to a buildup of toxic heme that killed red blood cell (RBC) precursors.
However, treating patient samples with a compound that blocks heme synthesis increased RBC production in both DBA and MDS.
Zhantao Yang, MD, of the University of Washington in Seattle, and his colleagues reported these findings in Science Translational Medicine.
Both DBA and MDS have been linked to defects in ribosome assembly, which is critical to protein production, but how this leads to anemia remains unknown.
To find out, Dr Yang and his colleagues analyzed bone marrow cells from patients with DBA (n=3) or MDS with del(5q) (n=6).
The researchers found that globin translation proceeded slowly in these samples, but heme synthesis proceeded normally.
This resulted in insufficient globin, excess heme, and excess reactive oxygen species in early erythroid precursors and, ultimately, the death of colony-forming unit–erythroid/proerythroblast cells.
The cells that were able to rapidly export heme or slow its synthesis survived and matured into RBCs, but the other colony-forming unit–erythroid cells/early proerythroblasts died.
The researchers noted that it is not clear how excess heme induces cell death in RBC precursors, but they said it likely involves both ferroptosis and apoptosis.
Regardless of the mechanism of cell death, the team found that treating the patients’ cells with succinylacetone (10 mM), a compound that blocks heme synthesis, improved RBC production.
The treatment improved RBC production in DBA and del(5q) MDS marrow cultures by 68% to 95% (P=0.03 to 0.05). In comparison, RBC production in control marrow cultures decreased by 4% to 13%.
The researchers said their experiments revealed additional important findings. First, they found that erythroid differentiation in the marrow cultures “excellently” phenocopied erythroid differentiation in vivo. This suggests these cultures can serve as a reliable platform in preclinical studies.
Second, the team said the fact that epigenetic differences between RBC precursors can lead to their preferential death or survival has broad implications. And querying the cells that preferentially survive could provide important insights. ![]()
Peptides show promise for treating thalassemia, PV

Preclinical research suggests synthetic peptides called minihepcidins could potentially treat beta-thalassemia and polycythemia vera (PV).
Investigators found that minihepcidin helped to restore normal levels of red blood cells (RBCs) and reduced spleen enlargement in mouse models of beta-thalassemia and PV.
Minihepcidin also controlled the accumulation of excess iron in the mice.
“It seems counterintuitive that one compound could treat two diseases that are quite different, but by restricting iron absorption, it also helps to normalize red blood cell levels in animals,” said study author Stefano Rivella, PhD, of The Children’s Hospital of Philadelphia in Pennsylvania.
“If these preclinical results translate to humans, this could represent a new treatment for both disorders.”
Dr Rivella and his colleagues described the results in Blood.
The investigators used minihepcidins, modified versions of the naturally occurring hormone hepcidin, which regulates iron. Minihepcidins are smaller than the full-length hormone but have long-term stability and long-lasting biological activity when administered to animals.
Previous research showed that minihepcidin treatment can prevent iron overload in mouse models of hemochromatosis.
So Dr Rivella and his colleagues wanted to determine how minihepcidins affect beta-thalassemia and PV in mice separately engineered to model each disease.
The team found that, in young mice that modelled beta-thalassemia, minihepcidin treatment normalized RBC levels and relieved both anemia and iron overload.
In older mice, minihepcidin improved RBC production and did not interfere with a chelating drug used to remove excess iron deposits.
In mice expressing the orthologous JAK2 mutation causing human PV, minihepcidin normalized RBC production.
Because increased iron absorption in PV keeps RBC production in overdrive, when minihepcidin curtailed iron absorption, it lowered the abnormally high numbers of RBCs, which also reduced spleen enlargement.
Dr Rivella noted that if minihepcidins prove successful in clinical trials, they may provide an important tool in treating these blood disorders.
“In animals affected by beta-thalassemia, the compound blocks iron from getting into organs but doesn’t remove excess iron already in organs and tissues,” Dr Rivella said. “If minihepcidins are used in older patients, they would need to be combined with existing chelating drugs that remove the already-accumulated iron.”
However, he added that, in beta-thalassemia, providing minihepcidins in childhood might halt iron accumulation and prevent more severe adult disease.
In PV, minihepcidins may help normalize a patient’s RBC production but, as in beta-thalassemia, would not treat the underlying disease-causing mutations.
Merganser Biotech Inc. is developing minihepcidins as novel therapies for rare hematologic diseases. Merganser’s lead compound, M012, is now under evaluation in a phase 1 clinical program as a potential therapy for beta-thalassemia, low-risk myelodysplasia, PV, alpha-thalassemia, and sickle cell disease.
The company’s chief executive officer, Brian MacDonald, MB ChB, PhD, is a co-author of the current study. Dr Rivella is a paid consultant on Merganser Biotech’s clinical trial, owns restricted stocks in Merganser, and is a member of its scientific advisory board. ![]()

Preclinical research suggests synthetic peptides called minihepcidins could potentially treat beta-thalassemia and polycythemia vera (PV).
Investigators found that minihepcidin helped to restore normal levels of red blood cells (RBCs) and reduced spleen enlargement in mouse models of beta-thalassemia and PV.
Minihepcidin also controlled the accumulation of excess iron in the mice.
“It seems counterintuitive that one compound could treat two diseases that are quite different, but by restricting iron absorption, it also helps to normalize red blood cell levels in animals,” said study author Stefano Rivella, PhD, of The Children’s Hospital of Philadelphia in Pennsylvania.
“If these preclinical results translate to humans, this could represent a new treatment for both disorders.”
Dr Rivella and his colleagues described the results in Blood.
The investigators used minihepcidins, modified versions of the naturally occurring hormone hepcidin, which regulates iron. Minihepcidins are smaller than the full-length hormone but have long-term stability and long-lasting biological activity when administered to animals.
Previous research showed that minihepcidin treatment can prevent iron overload in mouse models of hemochromatosis.
So Dr Rivella and his colleagues wanted to determine how minihepcidins affect beta-thalassemia and PV in mice separately engineered to model each disease.
The team found that, in young mice that modelled beta-thalassemia, minihepcidin treatment normalized RBC levels and relieved both anemia and iron overload.
In older mice, minihepcidin improved RBC production and did not interfere with a chelating drug used to remove excess iron deposits.
In mice expressing the orthologous JAK2 mutation causing human PV, minihepcidin normalized RBC production.
Because increased iron absorption in PV keeps RBC production in overdrive, when minihepcidin curtailed iron absorption, it lowered the abnormally high numbers of RBCs, which also reduced spleen enlargement.
Dr Rivella noted that if minihepcidins prove successful in clinical trials, they may provide an important tool in treating these blood disorders.
“In animals affected by beta-thalassemia, the compound blocks iron from getting into organs but doesn’t remove excess iron already in organs and tissues,” Dr Rivella said. “If minihepcidins are used in older patients, they would need to be combined with existing chelating drugs that remove the already-accumulated iron.”
However, he added that, in beta-thalassemia, providing minihepcidins in childhood might halt iron accumulation and prevent more severe adult disease.
In PV, minihepcidins may help normalize a patient’s RBC production but, as in beta-thalassemia, would not treat the underlying disease-causing mutations.
Merganser Biotech Inc. is developing minihepcidins as novel therapies for rare hematologic diseases. Merganser’s lead compound, M012, is now under evaluation in a phase 1 clinical program as a potential therapy for beta-thalassemia, low-risk myelodysplasia, PV, alpha-thalassemia, and sickle cell disease.
The company’s chief executive officer, Brian MacDonald, MB ChB, PhD, is a co-author of the current study. Dr Rivella is a paid consultant on Merganser Biotech’s clinical trial, owns restricted stocks in Merganser, and is a member of its scientific advisory board. ![]()

Preclinical research suggests synthetic peptides called minihepcidins could potentially treat beta-thalassemia and polycythemia vera (PV).
Investigators found that minihepcidin helped to restore normal levels of red blood cells (RBCs) and reduced spleen enlargement in mouse models of beta-thalassemia and PV.
Minihepcidin also controlled the accumulation of excess iron in the mice.
“It seems counterintuitive that one compound could treat two diseases that are quite different, but by restricting iron absorption, it also helps to normalize red blood cell levels in animals,” said study author Stefano Rivella, PhD, of The Children’s Hospital of Philadelphia in Pennsylvania.
“If these preclinical results translate to humans, this could represent a new treatment for both disorders.”
Dr Rivella and his colleagues described the results in Blood.
The investigators used minihepcidins, modified versions of the naturally occurring hormone hepcidin, which regulates iron. Minihepcidins are smaller than the full-length hormone but have long-term stability and long-lasting biological activity when administered to animals.
Previous research showed that minihepcidin treatment can prevent iron overload in mouse models of hemochromatosis.
So Dr Rivella and his colleagues wanted to determine how minihepcidins affect beta-thalassemia and PV in mice separately engineered to model each disease.
The team found that, in young mice that modelled beta-thalassemia, minihepcidin treatment normalized RBC levels and relieved both anemia and iron overload.
In older mice, minihepcidin improved RBC production and did not interfere with a chelating drug used to remove excess iron deposits.
In mice expressing the orthologous JAK2 mutation causing human PV, minihepcidin normalized RBC production.
Because increased iron absorption in PV keeps RBC production in overdrive, when minihepcidin curtailed iron absorption, it lowered the abnormally high numbers of RBCs, which also reduced spleen enlargement.
Dr Rivella noted that if minihepcidins prove successful in clinical trials, they may provide an important tool in treating these blood disorders.
“In animals affected by beta-thalassemia, the compound blocks iron from getting into organs but doesn’t remove excess iron already in organs and tissues,” Dr Rivella said. “If minihepcidins are used in older patients, they would need to be combined with existing chelating drugs that remove the already-accumulated iron.”
However, he added that, in beta-thalassemia, providing minihepcidins in childhood might halt iron accumulation and prevent more severe adult disease.
In PV, minihepcidins may help normalize a patient’s RBC production but, as in beta-thalassemia, would not treat the underlying disease-causing mutations.
Merganser Biotech Inc. is developing minihepcidins as novel therapies for rare hematologic diseases. Merganser’s lead compound, M012, is now under evaluation in a phase 1 clinical program as a potential therapy for beta-thalassemia, low-risk myelodysplasia, PV, alpha-thalassemia, and sickle cell disease.
The company’s chief executive officer, Brian MacDonald, MB ChB, PhD, is a co-author of the current study. Dr Rivella is a paid consultant on Merganser Biotech’s clinical trial, owns restricted stocks in Merganser, and is a member of its scientific advisory board. ![]()
Tools may aid transition from pediatric to adult care

Photo courtesy of the CDC
WASHINGTON, DC—The American Society of Hematology (ASH) has created a toolkit to help hematologists aid patients who are transitioning from pediatric to adult practices.
The toolkit contains general resources for all hematologic conditions, as well as specific resources for patients with hemophilia and sickle cell disease.
It includes 2 types of forms—a transition-readiness assessment and a clinical summary.
The toolkit was presented at the American College of Physicians (ACP) Internal Medicine Meeting 2016.
“Transitioning from pediatric to adult healthcare practices is often a challenge for patients with chronic medical issues because it can be difficult to adhere to a treatment regimen or attend regular appointments without the assistance of a parent or guardian,” said ASH President Charles S. Abrams, MD, of the University of Pennsylvania in Philadelphia.
“ASH recognizes that understanding a patient’s preparedness to take control of his or her medical condition in adulthood can make a huge difference in quality of care, which is why we are pleased to join the American College of Physicians and partner societies in this important initiative.”
ASH joined more than 2 dozen groups to participate in the ACP’s Pediatric to Adult Care Transition Initiative. The goal of this initiative was to develop guidance and tools that both primary care internal medicine and subspecialty practices can use for patients who are transitioning from pediatric/adolescent practices to adult care.
An ASH Transitions Work Group, made up of society members from pediatric and adult practices, developed 3 segments of the hematology-specific toolkit:
- generic forms for patients with any hematologic condition, with an addendum that includes links to additional condition-specific guidelines and resources
- specific forms for hemophilia
- specific forms for sickle cell disease.
For each segment, there are 2 types of forms— a transition-readiness assessment and a clinical summary.
The transition-readiness assessment should be completed by the patient. It assesses the patient’s readiness for the transition to adult care by evaluating the patient’s understanding of his or her condition and ability to manage medications, appointments, insurance, and medical privacy issues.
This assessment should be used by the adult care team to assess any remaining gaps in the patient’s self-care knowledge or additional issues that should be addressed to ensure optimal care.
The clinical summary is a medical record summary to be completed by the referring provider and the patient. The summary contains essential clinical information regarding the patient’s condition that is to be included in the patient’s medical record upon transfer to the adult practice.
More information on the ACP Pediatric to Adult Care Transitions Initiative is available on the ACP website. The forms for the ASH transitions toolkit are available in the “Hematology” section of the Condition-Specific Tools page. ![]()

Photo courtesy of the CDC
WASHINGTON, DC—The American Society of Hematology (ASH) has created a toolkit to help hematologists aid patients who are transitioning from pediatric to adult practices.
The toolkit contains general resources for all hematologic conditions, as well as specific resources for patients with hemophilia and sickle cell disease.
It includes 2 types of forms—a transition-readiness assessment and a clinical summary.
The toolkit was presented at the American College of Physicians (ACP) Internal Medicine Meeting 2016.
“Transitioning from pediatric to adult healthcare practices is often a challenge for patients with chronic medical issues because it can be difficult to adhere to a treatment regimen or attend regular appointments without the assistance of a parent or guardian,” said ASH President Charles S. Abrams, MD, of the University of Pennsylvania in Philadelphia.
“ASH recognizes that understanding a patient’s preparedness to take control of his or her medical condition in adulthood can make a huge difference in quality of care, which is why we are pleased to join the American College of Physicians and partner societies in this important initiative.”
ASH joined more than 2 dozen groups to participate in the ACP’s Pediatric to Adult Care Transition Initiative. The goal of this initiative was to develop guidance and tools that both primary care internal medicine and subspecialty practices can use for patients who are transitioning from pediatric/adolescent practices to adult care.
An ASH Transitions Work Group, made up of society members from pediatric and adult practices, developed 3 segments of the hematology-specific toolkit:
- generic forms for patients with any hematologic condition, with an addendum that includes links to additional condition-specific guidelines and resources
- specific forms for hemophilia
- specific forms for sickle cell disease.
For each segment, there are 2 types of forms— a transition-readiness assessment and a clinical summary.
The transition-readiness assessment should be completed by the patient. It assesses the patient’s readiness for the transition to adult care by evaluating the patient’s understanding of his or her condition and ability to manage medications, appointments, insurance, and medical privacy issues.
This assessment should be used by the adult care team to assess any remaining gaps in the patient’s self-care knowledge or additional issues that should be addressed to ensure optimal care.
The clinical summary is a medical record summary to be completed by the referring provider and the patient. The summary contains essential clinical information regarding the patient’s condition that is to be included in the patient’s medical record upon transfer to the adult practice.
More information on the ACP Pediatric to Adult Care Transitions Initiative is available on the ACP website. The forms for the ASH transitions toolkit are available in the “Hematology” section of the Condition-Specific Tools page. ![]()

Photo courtesy of the CDC
WASHINGTON, DC—The American Society of Hematology (ASH) has created a toolkit to help hematologists aid patients who are transitioning from pediatric to adult practices.
The toolkit contains general resources for all hematologic conditions, as well as specific resources for patients with hemophilia and sickle cell disease.
It includes 2 types of forms—a transition-readiness assessment and a clinical summary.
The toolkit was presented at the American College of Physicians (ACP) Internal Medicine Meeting 2016.
“Transitioning from pediatric to adult healthcare practices is often a challenge for patients with chronic medical issues because it can be difficult to adhere to a treatment regimen or attend regular appointments without the assistance of a parent or guardian,” said ASH President Charles S. Abrams, MD, of the University of Pennsylvania in Philadelphia.
“ASH recognizes that understanding a patient’s preparedness to take control of his or her medical condition in adulthood can make a huge difference in quality of care, which is why we are pleased to join the American College of Physicians and partner societies in this important initiative.”
ASH joined more than 2 dozen groups to participate in the ACP’s Pediatric to Adult Care Transition Initiative. The goal of this initiative was to develop guidance and tools that both primary care internal medicine and subspecialty practices can use for patients who are transitioning from pediatric/adolescent practices to adult care.
An ASH Transitions Work Group, made up of society members from pediatric and adult practices, developed 3 segments of the hematology-specific toolkit:
- generic forms for patients with any hematologic condition, with an addendum that includes links to additional condition-specific guidelines and resources
- specific forms for hemophilia
- specific forms for sickle cell disease.
For each segment, there are 2 types of forms— a transition-readiness assessment and a clinical summary.
The transition-readiness assessment should be completed by the patient. It assesses the patient’s readiness for the transition to adult care by evaluating the patient’s understanding of his or her condition and ability to manage medications, appointments, insurance, and medical privacy issues.
This assessment should be used by the adult care team to assess any remaining gaps in the patient’s self-care knowledge or additional issues that should be addressed to ensure optimal care.
The clinical summary is a medical record summary to be completed by the referring provider and the patient. The summary contains essential clinical information regarding the patient’s condition that is to be included in the patient’s medical record upon transfer to the adult practice.
More information on the ACP Pediatric to Adult Care Transitions Initiative is available on the ACP website. The forms for the ASH transitions toolkit are available in the “Hematology” section of the Condition-Specific Tools page. ![]()
Team identifies new function of Fanconi anemia genes

Image by Sarah Pfau
Research published in Cell has revealed a new function of genes in the Fanconi anemia (FA) pathway, and investigators believe this finding could have
implications for the treatment of FA and related disorders.
The team found that FA genes are required for selective autophagy.
In particular, the FANCC gene plays a key role in 2 types of selective autophagy: virophagy (the removal of viruses inside the cell) and mitophagy (the removal of mitochondria).
Experiments in mice showed that genetic deletion of FANCC blocks virophagy and increases the animals’ susceptibility to lethal viral encephalitis.
The investigators also found that FANCC protein is required for the clearance of damaged mitochondria and decreases the production of mitochondrial reactive oxygen species and inflammasome activation.
And other genes in the FA pathway are required for mitophagy as well—FANCA, FANCF, FANCL, FANCD2, BRCA1, and BRCA2.
“There’s increasing evidence that the failure of cells to appropriately clear damaged mitochondria leads to abnormal activation of the inflammasome—a process that is emerging as an important contributor to many different diseases,” said study author Beth Levine, MD, of UT Southwestern Medical Center in Dallas, Texas.
“The finding that FA genes function in clearing mitochondria and decreasing inflammasome activation provides a potential new inflammasome-targeted avenue of therapy for patients with diseases related to mutations in the FA genes.”
FA pathway genes were already known to play a role in DNA repair. The investigators said this new link to autophagy opens up unexplored horizons for understanding the function of these genes in human health and disease.
“Our findings suggest a novel mechanism by which mutations in FA genes may lead to the clinical manifestations in patients with FA and to cancers in patients with mutations in FA genes,” said study author Rhea Sumpter, MD, PhD, of UT Southwestern Medical Center.
“We’ve shown that this new function of the FA genes in the selective autophagy pathways does not depend on their role in DNA repair.”
In addition, the autophagy function may partly explain why patients with FA are highly susceptible to infection and cancer, Dr Levine said.
While further research is needed to understand how these findings may be used to treat disease, the investigators said they have identified a novel avenue for developing potential therapies for FA and cancer patients.
“I believe the clearest therapeutic possibilities to come from our study results are the development of new FA agents that target the inflammasome and production of interleukin 1 beta (IL-1β), a pro-inflammatory cytokine,” Dr Sumpter said.
“Clinically, IL-1β signaling has been targeted with FDA-approved drugs very successfully in several auto-inflammatory diseases that involve excessive inflammasome activation. Our results suggest that FA patients may also benefit from these therapies.” ![]()

Image by Sarah Pfau
Research published in Cell has revealed a new function of genes in the Fanconi anemia (FA) pathway, and investigators believe this finding could have
implications for the treatment of FA and related disorders.
The team found that FA genes are required for selective autophagy.
In particular, the FANCC gene plays a key role in 2 types of selective autophagy: virophagy (the removal of viruses inside the cell) and mitophagy (the removal of mitochondria).
Experiments in mice showed that genetic deletion of FANCC blocks virophagy and increases the animals’ susceptibility to lethal viral encephalitis.
The investigators also found that FANCC protein is required for the clearance of damaged mitochondria and decreases the production of mitochondrial reactive oxygen species and inflammasome activation.
And other genes in the FA pathway are required for mitophagy as well—FANCA, FANCF, FANCL, FANCD2, BRCA1, and BRCA2.
“There’s increasing evidence that the failure of cells to appropriately clear damaged mitochondria leads to abnormal activation of the inflammasome—a process that is emerging as an important contributor to many different diseases,” said study author Beth Levine, MD, of UT Southwestern Medical Center in Dallas, Texas.
“The finding that FA genes function in clearing mitochondria and decreasing inflammasome activation provides a potential new inflammasome-targeted avenue of therapy for patients with diseases related to mutations in the FA genes.”
FA pathway genes were already known to play a role in DNA repair. The investigators said this new link to autophagy opens up unexplored horizons for understanding the function of these genes in human health and disease.
“Our findings suggest a novel mechanism by which mutations in FA genes may lead to the clinical manifestations in patients with FA and to cancers in patients with mutations in FA genes,” said study author Rhea Sumpter, MD, PhD, of UT Southwestern Medical Center.
“We’ve shown that this new function of the FA genes in the selective autophagy pathways does not depend on their role in DNA repair.”
In addition, the autophagy function may partly explain why patients with FA are highly susceptible to infection and cancer, Dr Levine said.
While further research is needed to understand how these findings may be used to treat disease, the investigators said they have identified a novel avenue for developing potential therapies for FA and cancer patients.
“I believe the clearest therapeutic possibilities to come from our study results are the development of new FA agents that target the inflammasome and production of interleukin 1 beta (IL-1β), a pro-inflammatory cytokine,” Dr Sumpter said.
“Clinically, IL-1β signaling has been targeted with FDA-approved drugs very successfully in several auto-inflammatory diseases that involve excessive inflammasome activation. Our results suggest that FA patients may also benefit from these therapies.” ![]()

Image by Sarah Pfau
Research published in Cell has revealed a new function of genes in the Fanconi anemia (FA) pathway, and investigators believe this finding could have
implications for the treatment of FA and related disorders.
The team found that FA genes are required for selective autophagy.
In particular, the FANCC gene plays a key role in 2 types of selective autophagy: virophagy (the removal of viruses inside the cell) and mitophagy (the removal of mitochondria).
Experiments in mice showed that genetic deletion of FANCC blocks virophagy and increases the animals’ susceptibility to lethal viral encephalitis.
The investigators also found that FANCC protein is required for the clearance of damaged mitochondria and decreases the production of mitochondrial reactive oxygen species and inflammasome activation.
And other genes in the FA pathway are required for mitophagy as well—FANCA, FANCF, FANCL, FANCD2, BRCA1, and BRCA2.
“There’s increasing evidence that the failure of cells to appropriately clear damaged mitochondria leads to abnormal activation of the inflammasome—a process that is emerging as an important contributor to many different diseases,” said study author Beth Levine, MD, of UT Southwestern Medical Center in Dallas, Texas.
“The finding that FA genes function in clearing mitochondria and decreasing inflammasome activation provides a potential new inflammasome-targeted avenue of therapy for patients with diseases related to mutations in the FA genes.”
FA pathway genes were already known to play a role in DNA repair. The investigators said this new link to autophagy opens up unexplored horizons for understanding the function of these genes in human health and disease.
“Our findings suggest a novel mechanism by which mutations in FA genes may lead to the clinical manifestations in patients with FA and to cancers in patients with mutations in FA genes,” said study author Rhea Sumpter, MD, PhD, of UT Southwestern Medical Center.
“We’ve shown that this new function of the FA genes in the selective autophagy pathways does not depend on their role in DNA repair.”
In addition, the autophagy function may partly explain why patients with FA are highly susceptible to infection and cancer, Dr Levine said.
While further research is needed to understand how these findings may be used to treat disease, the investigators said they have identified a novel avenue for developing potential therapies for FA and cancer patients.
“I believe the clearest therapeutic possibilities to come from our study results are the development of new FA agents that target the inflammasome and production of interleukin 1 beta (IL-1β), a pro-inflammatory cytokine,” Dr Sumpter said.
“Clinically, IL-1β signaling has been targeted with FDA-approved drugs very successfully in several auto-inflammatory diseases that involve excessive inflammasome activation. Our results suggest that FA patients may also benefit from these therapies.” ![]()
Product approved for hemoglobin maintenance

Image courtesy of NHLBI
The US Food and Drug Administration (FDA) has approved the use of a powder formulation of ferric pyrophosphate citrate (Triferic powder packet) to maintain hemoglobin in adult patients with hemodialysis-dependent chronic kidney disease.
The FDA previously approved ferric pyrophosphate citrate solution (Triferic) in ampule form. It is an iron-replacement drug intended to treat anemia in chronic kidney disease patients receiving hemodialysis.
Triferic is delivered to hemodialysis patients via dialysate, replacing the ongoing iron loss that occurs during their dialysis treatment. The drug is added to the bicarbonate concentrate on-site at the dialysis clinic.
Once in dialysate, Triferic crosses the dialyzer membrane and enters the blood, where it immediately binds to transferrin and is transported to the erythroid precursor cells to be incorporated into hemoglobin.
Triferic is designed to deliver sufficient iron to the bone marrow and maintain hemoglobin without increasing iron stores.
“We are pleased to obtain this FDA approval for the Triferic powder packet,” said Robert L. Chioini, founder, chairman, and chief executive officer of Rockwell Medical, Inc., makers of Triferic.
“The Triferic powder packet is similar to the size of a packet of sugar. It is much smaller and lighter than the current Triferic liquid ampule, and it enables us to place 3-times greater the number of units in an even smaller carton.”
“This presentation is much more convenient for customers, as it reduces storage space and requires fewer reorders to maintain inventory. We expect it to be commercially available shortly.” ![]()

Image courtesy of NHLBI
The US Food and Drug Administration (FDA) has approved the use of a powder formulation of ferric pyrophosphate citrate (Triferic powder packet) to maintain hemoglobin in adult patients with hemodialysis-dependent chronic kidney disease.
The FDA previously approved ferric pyrophosphate citrate solution (Triferic) in ampule form. It is an iron-replacement drug intended to treat anemia in chronic kidney disease patients receiving hemodialysis.
Triferic is delivered to hemodialysis patients via dialysate, replacing the ongoing iron loss that occurs during their dialysis treatment. The drug is added to the bicarbonate concentrate on-site at the dialysis clinic.
Once in dialysate, Triferic crosses the dialyzer membrane and enters the blood, where it immediately binds to transferrin and is transported to the erythroid precursor cells to be incorporated into hemoglobin.
Triferic is designed to deliver sufficient iron to the bone marrow and maintain hemoglobin without increasing iron stores.
“We are pleased to obtain this FDA approval for the Triferic powder packet,” said Robert L. Chioini, founder, chairman, and chief executive officer of Rockwell Medical, Inc., makers of Triferic.
“The Triferic powder packet is similar to the size of a packet of sugar. It is much smaller and lighter than the current Triferic liquid ampule, and it enables us to place 3-times greater the number of units in an even smaller carton.”
“This presentation is much more convenient for customers, as it reduces storage space and requires fewer reorders to maintain inventory. We expect it to be commercially available shortly.” ![]()

Image courtesy of NHLBI
The US Food and Drug Administration (FDA) has approved the use of a powder formulation of ferric pyrophosphate citrate (Triferic powder packet) to maintain hemoglobin in adult patients with hemodialysis-dependent chronic kidney disease.
The FDA previously approved ferric pyrophosphate citrate solution (Triferic) in ampule form. It is an iron-replacement drug intended to treat anemia in chronic kidney disease patients receiving hemodialysis.
Triferic is delivered to hemodialysis patients via dialysate, replacing the ongoing iron loss that occurs during their dialysis treatment. The drug is added to the bicarbonate concentrate on-site at the dialysis clinic.
Once in dialysate, Triferic crosses the dialyzer membrane and enters the blood, where it immediately binds to transferrin and is transported to the erythroid precursor cells to be incorporated into hemoglobin.
Triferic is designed to deliver sufficient iron to the bone marrow and maintain hemoglobin without increasing iron stores.
“We are pleased to obtain this FDA approval for the Triferic powder packet,” said Robert L. Chioini, founder, chairman, and chief executive officer of Rockwell Medical, Inc., makers of Triferic.
“The Triferic powder packet is similar to the size of a packet of sugar. It is much smaller and lighter than the current Triferic liquid ampule, and it enables us to place 3-times greater the number of units in an even smaller carton.”
“This presentation is much more convenient for customers, as it reduces storage space and requires fewer reorders to maintain inventory. We expect it to be commercially available shortly.” ![]()
Team designs ‘targeted EPO’

Researchers say they have used a rational design approach to create a safer variant of the drug erythropoietin (EPO).
This “targeted EPO” effectively stimulated red blood cell production in mice and had a minimal impact on platelets.
The team believes this approach could allow for the use of higher restorative doses of EPO without platelet-mediated side effects, and it might improve drug pharmacokinetics.
Devin Burrill, PhD, of the Wyss Institute for Biologically Inspired Engineering at Harvard University in Boston, Massachusetts, and his colleagues described the approach in PNAS.
The researchers noted that EPO has been widely used to treat anemia, but the drug also poses a risk of thrombotic complications. To combat this problem, the team set out to design a more effective, multi-part drug molecule.
“Compared to currently available EPO drugs, our molecule is engineered to prevent EPO from binding to and activating cells that promote side effects such as blood clotting or tumor growth,” said Jeffrey Way, PhD, also of the Wyss Institute.
“This cell-targeted EPO approach demonstrates a new theoretical basis for the rational design of engineered protein fusion drugs.”
To create their drug, the researchers first mutated EPO to reduce its ability to bind to EPO receptors.
Then, using a chain of amino acids as a flexible linker, they attached mutated EPO to an antibody fragment that specifically binds the human red blood cell marker glycophorin A (huGYPA). This antibody fragment binds to red blood cell precursors while avoiding other types of blood cells.
When the team’s fusion protein molecules were delivered to huGYPA transgenic mice, the antibody fragments piloted toward and bound to the membranes of red blood cell precursors, towing along EPO molecules on the other end of their linkers.
In such close proximity to the surface of the cells, a high concentration of tethered EPO bounced around until it ultimately toggled into place on the cells’ receptors. In this way, red blood cell production was increased with only minimal effects on platelets.
“Our rational design strategy is unique compared to current industry approaches,” Dr Burrill said. “Our goal is to use our method to advance predictive drug design and minimize the time between drug concept and commercialization.”
“The principles of synthetic biology influenced our efforts,” added James Collins, PhD, of the Wyss Institute.
“In drug development, the focus is typically on increasing the strength of interaction with a drug target, but, here, we found that weakening an interaction was useful. This illustrates how we need to adopt alternative, non-traditional approaches if we want to build complex, multi-part therapeutics.”
The researchers said this specific, cell-targeted approach could be applied quite broadly. In addition to “targeted EPO,” the team has developed “targeted interferon-alfa.” ![]()

Researchers say they have used a rational design approach to create a safer variant of the drug erythropoietin (EPO).
This “targeted EPO” effectively stimulated red blood cell production in mice and had a minimal impact on platelets.
The team believes this approach could allow for the use of higher restorative doses of EPO without platelet-mediated side effects, and it might improve drug pharmacokinetics.
Devin Burrill, PhD, of the Wyss Institute for Biologically Inspired Engineering at Harvard University in Boston, Massachusetts, and his colleagues described the approach in PNAS.
The researchers noted that EPO has been widely used to treat anemia, but the drug also poses a risk of thrombotic complications. To combat this problem, the team set out to design a more effective, multi-part drug molecule.
“Compared to currently available EPO drugs, our molecule is engineered to prevent EPO from binding to and activating cells that promote side effects such as blood clotting or tumor growth,” said Jeffrey Way, PhD, also of the Wyss Institute.
“This cell-targeted EPO approach demonstrates a new theoretical basis for the rational design of engineered protein fusion drugs.”
To create their drug, the researchers first mutated EPO to reduce its ability to bind to EPO receptors.
Then, using a chain of amino acids as a flexible linker, they attached mutated EPO to an antibody fragment that specifically binds the human red blood cell marker glycophorin A (huGYPA). This antibody fragment binds to red blood cell precursors while avoiding other types of blood cells.
When the team’s fusion protein molecules were delivered to huGYPA transgenic mice, the antibody fragments piloted toward and bound to the membranes of red blood cell precursors, towing along EPO molecules on the other end of their linkers.
In such close proximity to the surface of the cells, a high concentration of tethered EPO bounced around until it ultimately toggled into place on the cells’ receptors. In this way, red blood cell production was increased with only minimal effects on platelets.
“Our rational design strategy is unique compared to current industry approaches,” Dr Burrill said. “Our goal is to use our method to advance predictive drug design and minimize the time between drug concept and commercialization.”
“The principles of synthetic biology influenced our efforts,” added James Collins, PhD, of the Wyss Institute.
“In drug development, the focus is typically on increasing the strength of interaction with a drug target, but, here, we found that weakening an interaction was useful. This illustrates how we need to adopt alternative, non-traditional approaches if we want to build complex, multi-part therapeutics.”
The researchers said this specific, cell-targeted approach could be applied quite broadly. In addition to “targeted EPO,” the team has developed “targeted interferon-alfa.” ![]()

Researchers say they have used a rational design approach to create a safer variant of the drug erythropoietin (EPO).
This “targeted EPO” effectively stimulated red blood cell production in mice and had a minimal impact on platelets.
The team believes this approach could allow for the use of higher restorative doses of EPO without platelet-mediated side effects, and it might improve drug pharmacokinetics.
Devin Burrill, PhD, of the Wyss Institute for Biologically Inspired Engineering at Harvard University in Boston, Massachusetts, and his colleagues described the approach in PNAS.
The researchers noted that EPO has been widely used to treat anemia, but the drug also poses a risk of thrombotic complications. To combat this problem, the team set out to design a more effective, multi-part drug molecule.
“Compared to currently available EPO drugs, our molecule is engineered to prevent EPO from binding to and activating cells that promote side effects such as blood clotting or tumor growth,” said Jeffrey Way, PhD, also of the Wyss Institute.
“This cell-targeted EPO approach demonstrates a new theoretical basis for the rational design of engineered protein fusion drugs.”
To create their drug, the researchers first mutated EPO to reduce its ability to bind to EPO receptors.
Then, using a chain of amino acids as a flexible linker, they attached mutated EPO to an antibody fragment that specifically binds the human red blood cell marker glycophorin A (huGYPA). This antibody fragment binds to red blood cell precursors while avoiding other types of blood cells.
When the team’s fusion protein molecules were delivered to huGYPA transgenic mice, the antibody fragments piloted toward and bound to the membranes of red blood cell precursors, towing along EPO molecules on the other end of their linkers.
In such close proximity to the surface of the cells, a high concentration of tethered EPO bounced around until it ultimately toggled into place on the cells’ receptors. In this way, red blood cell production was increased with only minimal effects on platelets.
“Our rational design strategy is unique compared to current industry approaches,” Dr Burrill said. “Our goal is to use our method to advance predictive drug design and minimize the time between drug concept and commercialization.”
“The principles of synthetic biology influenced our efforts,” added James Collins, PhD, of the Wyss Institute.
“In drug development, the focus is typically on increasing the strength of interaction with a drug target, but, here, we found that weakening an interaction was useful. This illustrates how we need to adopt alternative, non-traditional approaches if we want to build complex, multi-part therapeutics.”
The researchers said this specific, cell-targeted approach could be applied quite broadly. In addition to “targeted EPO,” the team has developed “targeted interferon-alfa.” ![]()
Drug corrects anemia in CKD patients

The investigational therapy roxadustat can effectively treat anemia in patients with chronic kidney disease (CKD) who are not on dialysis, according to a phase 2 study.
Roxadustat increased and maintained hemoglobin levels and decreased hepcidin levels in these patients, who had not received previous treatment with
erythropoiesis-stimulating agents and were treated with roxadustat regardless of their baseline iron repletion status.
In addition, researchers said there were no serious adverse events related to roxadustat.
Robert Provenzano, MD, of St. John Hospital and Medical Center in Detroit, Michigan, and his colleagues reported these results in the Clinical Journal of the American Society of Nephrology.
The study was sponsored by FibroGen, Inc., the company developing roxadustat in collaboration with AstraZeneca.
Roxadustat (FG-4592) is an oral, small-molecule inhibitor of hypoxia-inducible factor (HIF) prolyl hydroxylase activity. HIF is a transcription factor that induces the natural physiological response to conditions of low oxygen, “turning on” erythropoiesis and other protective pathways.
In this randomized, phase 2 study of roxadustat, 145 patients with anemia (hemoglobin < 10.5 g/dL at baseline) and non-dialysis CKD were randomized into 1 of 6 cohorts of approximately 24 patients.
The cohorts had varying roxadustat starting doses (tiered weight and fixed amounts) and frequencies (2 and 3 times weekly), followed by hemoglobin maintenance with roxadustat 1 to 3 times weekly. The treatment duration was 16 or 24 weeks.
Results
Of the 143 patients evaluable for efficacy, 92% achieved a hemoglobin response—defined as a hemoglobin increase of > 1.0 g/dL from baseline and a hemoglobin of > 11.0 g/dL by the end of treatment (up to 16 weeks of treatment in 47 patients, and up to 24 weeks of treatment in 96 patients).
Generally, patients in all cohorts who received higher starting doses of roxadustat demonstrated earlier achievement of the hemoglobin response.
Roxadustat increased hemoglobin independently of the patients’ baseline iron repletion and inflammatory status, as measured by baseline C–reactive protein levels. Intravenous iron was not permitted throughout the study period, and 52.4% of patients were iron-replete at baseline.
Over 16 weeks of treatment, roxadustat decreased hepcidin levels by 16.9% (P=0.004), maintained reticulocyte hemoglobin content, and increased hemoglobin by a mean (±SD) of 1.83 (±0.09) g/dL (P<0.001).
After 8 weeks of roxadustat, total cholesterol levels decreased by a mean (±SD) of 26 (±30) mg/dL (P<0.001).
“In this study, anemia correction was achieved under a range of treatment options, including tiered-weight as well as fixed-starting-dose strategies,” Dr Provenzano said. “Correction of anemia and maintenance of hemoglobin response were seen at different dose frequencies—2 or 3 times weekly for achievement of hemoglobin response; 1, 2, or 3 times weekly for maintenance.”
“Secondary analyses showing decreases in hepcidin and increased iron utilization, as well as reductions in total cholesterol levels, suggest roxadustat consistently affects these parameters.”
Treatment-emergent adverse events were reported in 80% of all patients.
The most common events that occurred in more than 5% of patients were nausea (9.7%), diarrhea (8.3%), constipation (6.2%), vomiting (5.5%), peripheral edema (12.4%), urinary tract infection (9.7%), nasopharyngitis (9.0%), sinusitis (5.5%), dizziness (6.2%), headache (5.5%), and hypertension (7.6%). ![]()

The investigational therapy roxadustat can effectively treat anemia in patients with chronic kidney disease (CKD) who are not on dialysis, according to a phase 2 study.
Roxadustat increased and maintained hemoglobin levels and decreased hepcidin levels in these patients, who had not received previous treatment with
erythropoiesis-stimulating agents and were treated with roxadustat regardless of their baseline iron repletion status.
In addition, researchers said there were no serious adverse events related to roxadustat.
Robert Provenzano, MD, of St. John Hospital and Medical Center in Detroit, Michigan, and his colleagues reported these results in the Clinical Journal of the American Society of Nephrology.
The study was sponsored by FibroGen, Inc., the company developing roxadustat in collaboration with AstraZeneca.
Roxadustat (FG-4592) is an oral, small-molecule inhibitor of hypoxia-inducible factor (HIF) prolyl hydroxylase activity. HIF is a transcription factor that induces the natural physiological response to conditions of low oxygen, “turning on” erythropoiesis and other protective pathways.
In this randomized, phase 2 study of roxadustat, 145 patients with anemia (hemoglobin < 10.5 g/dL at baseline) and non-dialysis CKD were randomized into 1 of 6 cohorts of approximately 24 patients.
The cohorts had varying roxadustat starting doses (tiered weight and fixed amounts) and frequencies (2 and 3 times weekly), followed by hemoglobin maintenance with roxadustat 1 to 3 times weekly. The treatment duration was 16 or 24 weeks.
Results
Of the 143 patients evaluable for efficacy, 92% achieved a hemoglobin response—defined as a hemoglobin increase of > 1.0 g/dL from baseline and a hemoglobin of > 11.0 g/dL by the end of treatment (up to 16 weeks of treatment in 47 patients, and up to 24 weeks of treatment in 96 patients).
Generally, patients in all cohorts who received higher starting doses of roxadustat demonstrated earlier achievement of the hemoglobin response.
Roxadustat increased hemoglobin independently of the patients’ baseline iron repletion and inflammatory status, as measured by baseline C–reactive protein levels. Intravenous iron was not permitted throughout the study period, and 52.4% of patients were iron-replete at baseline.
Over 16 weeks of treatment, roxadustat decreased hepcidin levels by 16.9% (P=0.004), maintained reticulocyte hemoglobin content, and increased hemoglobin by a mean (±SD) of 1.83 (±0.09) g/dL (P<0.001).
After 8 weeks of roxadustat, total cholesterol levels decreased by a mean (±SD) of 26 (±30) mg/dL (P<0.001).
“In this study, anemia correction was achieved under a range of treatment options, including tiered-weight as well as fixed-starting-dose strategies,” Dr Provenzano said. “Correction of anemia and maintenance of hemoglobin response were seen at different dose frequencies—2 or 3 times weekly for achievement of hemoglobin response; 1, 2, or 3 times weekly for maintenance.”
“Secondary analyses showing decreases in hepcidin and increased iron utilization, as well as reductions in total cholesterol levels, suggest roxadustat consistently affects these parameters.”
Treatment-emergent adverse events were reported in 80% of all patients.
The most common events that occurred in more than 5% of patients were nausea (9.7%), diarrhea (8.3%), constipation (6.2%), vomiting (5.5%), peripheral edema (12.4%), urinary tract infection (9.7%), nasopharyngitis (9.0%), sinusitis (5.5%), dizziness (6.2%), headache (5.5%), and hypertension (7.6%). ![]()

The investigational therapy roxadustat can effectively treat anemia in patients with chronic kidney disease (CKD) who are not on dialysis, according to a phase 2 study.
Roxadustat increased and maintained hemoglobin levels and decreased hepcidin levels in these patients, who had not received previous treatment with
erythropoiesis-stimulating agents and were treated with roxadustat regardless of their baseline iron repletion status.
In addition, researchers said there were no serious adverse events related to roxadustat.
Robert Provenzano, MD, of St. John Hospital and Medical Center in Detroit, Michigan, and his colleagues reported these results in the Clinical Journal of the American Society of Nephrology.
The study was sponsored by FibroGen, Inc., the company developing roxadustat in collaboration with AstraZeneca.
Roxadustat (FG-4592) is an oral, small-molecule inhibitor of hypoxia-inducible factor (HIF) prolyl hydroxylase activity. HIF is a transcription factor that induces the natural physiological response to conditions of low oxygen, “turning on” erythropoiesis and other protective pathways.
In this randomized, phase 2 study of roxadustat, 145 patients with anemia (hemoglobin < 10.5 g/dL at baseline) and non-dialysis CKD were randomized into 1 of 6 cohorts of approximately 24 patients.
The cohorts had varying roxadustat starting doses (tiered weight and fixed amounts) and frequencies (2 and 3 times weekly), followed by hemoglobin maintenance with roxadustat 1 to 3 times weekly. The treatment duration was 16 or 24 weeks.
Results
Of the 143 patients evaluable for efficacy, 92% achieved a hemoglobin response—defined as a hemoglobin increase of > 1.0 g/dL from baseline and a hemoglobin of > 11.0 g/dL by the end of treatment (up to 16 weeks of treatment in 47 patients, and up to 24 weeks of treatment in 96 patients).
Generally, patients in all cohorts who received higher starting doses of roxadustat demonstrated earlier achievement of the hemoglobin response.
Roxadustat increased hemoglobin independently of the patients’ baseline iron repletion and inflammatory status, as measured by baseline C–reactive protein levels. Intravenous iron was not permitted throughout the study period, and 52.4% of patients were iron-replete at baseline.
Over 16 weeks of treatment, roxadustat decreased hepcidin levels by 16.9% (P=0.004), maintained reticulocyte hemoglobin content, and increased hemoglobin by a mean (±SD) of 1.83 (±0.09) g/dL (P<0.001).
After 8 weeks of roxadustat, total cholesterol levels decreased by a mean (±SD) of 26 (±30) mg/dL (P<0.001).
“In this study, anemia correction was achieved under a range of treatment options, including tiered-weight as well as fixed-starting-dose strategies,” Dr Provenzano said. “Correction of anemia and maintenance of hemoglobin response were seen at different dose frequencies—2 or 3 times weekly for achievement of hemoglobin response; 1, 2, or 3 times weekly for maintenance.”
“Secondary analyses showing decreases in hepcidin and increased iron utilization, as well as reductions in total cholesterol levels, suggest roxadustat consistently affects these parameters.”
Treatment-emergent adverse events were reported in 80% of all patients.
The most common events that occurred in more than 5% of patients were nausea (9.7%), diarrhea (8.3%), constipation (6.2%), vomiting (5.5%), peripheral edema (12.4%), urinary tract infection (9.7%), nasopharyngitis (9.0%), sinusitis (5.5%), dizziness (6.2%), headache (5.5%), and hypertension (7.6%).
Drug bests placebo in kids with chronic ITP

Photo by Bill Branson
The thrombopoietin receptor agonist romiplostim can produce durable platelet responses in children with symptomatic chronic immune thrombocytopenia (ITP), according to a phase 3 study.
Fifty-two percent of patients who received romiplostim achieved a durable platelet response, compared to 10% of placebo-treated patients.
Investigators said these results suggest romiplostim may be a treatment option for this patient population.
“The results of this study suggest that romiplostim could reduce the frequency and severity of bleeding events for children suffering from symptomatic ITP, thus providing them with another potential treatment option,” said Michael D. Tarantino, MD, of the University of Illinois College of Medicine-Peoria.
Dr Tarantino and his colleagues reported the results in The Lancet. The study was supported by Amgen, which markets romiplostim (Nplate) as a treatment for adults with chronic ITP.
This double-blind study included 62 children (ages 6 to 14) who had ITP for more than 6 months and were randomized to weekly romiplostim (n=42) or placebo (n=20) for 24 weeks. Baseline characteristics were well-balanced between the treatment arms.
The median time since ITP diagnosis was about 2 years for both arms, and the median age at diagnosis was about 7. The median baseline platelet counts were 17.8 x 109/L in the romiplostim arm and 17.7 x 109/L in the placebo arm.
Durable platelet response, the primary endpoint of the study, was defined as achieving weekly platelet responses without rescue medication in at least 6 of the final 8 weeks of the study.
The rates of durable platelet response were 52% (22/42) in the romiplostim arm and 10% (2/20) in the placebo arm (P=0.002, odds ratio 9.1, 95% CI: 1.9, 43.2).
The rates of overall platelet response were 71% (30/42) in the romiplostim arm and 20% in the placebo arm (P=0.0002, odds ratio 9.0, 95% CI: 2.5, 32.3), and the rates of any platelet response were 81% (34/42) and 55% (11/20), respectively (P=0.0313).
The most frequently reported adverse events (AEs) observed in patients receiving romiplostim were contusion (50%), epistaxis (48%), headache (43%), and upper respiratory tract infection (38%).
Oropharyngeal pain occurred more frequently with romiplostim than placebo—26.2% (11/42) and 5.3% (1/19), respectively.
In the 11 romiplostim-treated patients with oropharyngeal pain, streptococcal pharyngitis (n=2), allergic rhinitis (n=2), gastroesophageal reflux (n=1), and serum sickness from IVIg (n=1) were also reported. No oropharyngeal pain AEs were serious or considered treatment-related.
Serious AEs occurred in 23.8% of romiplostim-treated patients and 5.3% of placebo-treated patients.
Serious AEs in the romiplostim arm included epistaxis (n=2), contusion (n=2), headache (n=2), bronchiolitis (n=1), nausea (n=1), petechiae (n=1), epilepsy (n=1), fever (n=1), thrombocytosis (n=1), urinary tract infection (n=1), and vomiting (n=1).
One subject with treatment-related serious AEs experienced headache and thrombocytosis, which did not recur when romiplostim was restarted.
There were no thrombotic events, none of the patients withdrew due to AEs, and none died.
“These data are important in understanding how Nplate may play a role in helping children manage this disease,” said Sean E. Harper, MD, executive vice president of research and development at Amgen.
“We will work with regulatory authorities towards an approval for Nplate for pediatric patients.”

Photo by Bill Branson
The thrombopoietin receptor agonist romiplostim can produce durable platelet responses in children with symptomatic chronic immune thrombocytopenia (ITP), according to a phase 3 study.
Fifty-two percent of patients who received romiplostim achieved a durable platelet response, compared to 10% of placebo-treated patients.
Investigators said these results suggest romiplostim may be a treatment option for this patient population.
“The results of this study suggest that romiplostim could reduce the frequency and severity of bleeding events for children suffering from symptomatic ITP, thus providing them with another potential treatment option,” said Michael D. Tarantino, MD, of the University of Illinois College of Medicine-Peoria.
Dr Tarantino and his colleagues reported the results in The Lancet. The study was supported by Amgen, which markets romiplostim (Nplate) as a treatment for adults with chronic ITP.
This double-blind study included 62 children (ages 6 to 14) who had ITP for more than 6 months and were randomized to weekly romiplostim (n=42) or placebo (n=20) for 24 weeks. Baseline characteristics were well-balanced between the treatment arms.
The median time since ITP diagnosis was about 2 years for both arms, and the median age at diagnosis was about 7. The median baseline platelet counts were 17.8 x 109/L in the romiplostim arm and 17.7 x 109/L in the placebo arm.
Durable platelet response, the primary endpoint of the study, was defined as achieving weekly platelet responses without rescue medication in at least 6 of the final 8 weeks of the study.
The rates of durable platelet response were 52% (22/42) in the romiplostim arm and 10% (2/20) in the placebo arm (P=0.002, odds ratio 9.1, 95% CI: 1.9, 43.2).
The rates of overall platelet response were 71% (30/42) in the romiplostim arm and 20% in the placebo arm (P=0.0002, odds ratio 9.0, 95% CI: 2.5, 32.3), and the rates of any platelet response were 81% (34/42) and 55% (11/20), respectively (P=0.0313).
The most frequently reported adverse events (AEs) observed in patients receiving romiplostim were contusion (50%), epistaxis (48%), headache (43%), and upper respiratory tract infection (38%).
Oropharyngeal pain occurred more frequently with romiplostim than placebo—26.2% (11/42) and 5.3% (1/19), respectively.
In the 11 romiplostim-treated patients with oropharyngeal pain, streptococcal pharyngitis (n=2), allergic rhinitis (n=2), gastroesophageal reflux (n=1), and serum sickness from IVIg (n=1) were also reported. No oropharyngeal pain AEs were serious or considered treatment-related.
Serious AEs occurred in 23.8% of romiplostim-treated patients and 5.3% of placebo-treated patients.
Serious AEs in the romiplostim arm included epistaxis (n=2), contusion (n=2), headache (n=2), bronchiolitis (n=1), nausea (n=1), petechiae (n=1), epilepsy (n=1), fever (n=1), thrombocytosis (n=1), urinary tract infection (n=1), and vomiting (n=1).
One subject with treatment-related serious AEs experienced headache and thrombocytosis, which did not recur when romiplostim was restarted.
There were no thrombotic events, none of the patients withdrew due to AEs, and none died.
“These data are important in understanding how Nplate may play a role in helping children manage this disease,” said Sean E. Harper, MD, executive vice president of research and development at Amgen.
“We will work with regulatory authorities towards an approval for Nplate for pediatric patients.”

Photo by Bill Branson
The thrombopoietin receptor agonist romiplostim can produce durable platelet responses in children with symptomatic chronic immune thrombocytopenia (ITP), according to a phase 3 study.
Fifty-two percent of patients who received romiplostim achieved a durable platelet response, compared to 10% of placebo-treated patients.
Investigators said these results suggest romiplostim may be a treatment option for this patient population.
“The results of this study suggest that romiplostim could reduce the frequency and severity of bleeding events for children suffering from symptomatic ITP, thus providing them with another potential treatment option,” said Michael D. Tarantino, MD, of the University of Illinois College of Medicine-Peoria.
Dr Tarantino and his colleagues reported the results in The Lancet. The study was supported by Amgen, which markets romiplostim (Nplate) as a treatment for adults with chronic ITP.
This double-blind study included 62 children (ages 6 to 14) who had ITP for more than 6 months and were randomized to weekly romiplostim (n=42) or placebo (n=20) for 24 weeks. Baseline characteristics were well-balanced between the treatment arms.
The median time since ITP diagnosis was about 2 years for both arms, and the median age at diagnosis was about 7. The median baseline platelet counts were 17.8 x 109/L in the romiplostim arm and 17.7 x 109/L in the placebo arm.
Durable platelet response, the primary endpoint of the study, was defined as achieving weekly platelet responses without rescue medication in at least 6 of the final 8 weeks of the study.
The rates of durable platelet response were 52% (22/42) in the romiplostim arm and 10% (2/20) in the placebo arm (P=0.002, odds ratio 9.1, 95% CI: 1.9, 43.2).
The rates of overall platelet response were 71% (30/42) in the romiplostim arm and 20% in the placebo arm (P=0.0002, odds ratio 9.0, 95% CI: 2.5, 32.3), and the rates of any platelet response were 81% (34/42) and 55% (11/20), respectively (P=0.0313).
The most frequently reported adverse events (AEs) observed in patients receiving romiplostim were contusion (50%), epistaxis (48%), headache (43%), and upper respiratory tract infection (38%).
Oropharyngeal pain occurred more frequently with romiplostim than placebo—26.2% (11/42) and 5.3% (1/19), respectively.
In the 11 romiplostim-treated patients with oropharyngeal pain, streptococcal pharyngitis (n=2), allergic rhinitis (n=2), gastroesophageal reflux (n=1), and serum sickness from IVIg (n=1) were also reported. No oropharyngeal pain AEs were serious or considered treatment-related.
Serious AEs occurred in 23.8% of romiplostim-treated patients and 5.3% of placebo-treated patients.
Serious AEs in the romiplostim arm included epistaxis (n=2), contusion (n=2), headache (n=2), bronchiolitis (n=1), nausea (n=1), petechiae (n=1), epilepsy (n=1), fever (n=1), thrombocytosis (n=1), urinary tract infection (n=1), and vomiting (n=1).
One subject with treatment-related serious AEs experienced headache and thrombocytosis, which did not recur when romiplostim was restarted.
There were no thrombotic events, none of the patients withdrew due to AEs, and none died.
“These data are important in understanding how Nplate may play a role in helping children manage this disease,” said Sean E. Harper, MD, executive vice president of research and development at Amgen.
“We will work with regulatory authorities towards an approval for Nplate for pediatric patients.”
TCD screening underused in sickle cell patients

with sickle cell anemia
Photo courtesy of St. Jude
Results of a large, retrospective study suggest the use of transcranial Doppler (TCD) screening is on the rise in US children and adolescents with sickle cell anemia.
However, the rate of TCD screening in these patients falls well below national recommendations.
In addition, TCD screening rates vary greatly by state, and the use of screening tends to decrease as patients grow older.
Sarah L. Reeves, PhD, of University of Michigan, Ann Arbor, and her colleagues reported these findings in JAMA Pediatrics.
The researchers noted that guidelines from the National Heart, Lung, and Blood Institute recommend that patients with sickle cell anemia receive annual TCD screenings from age 2 to 16 to identify those patients at the highest risk of stroke.
Dr Reeves and her colleagues wanted to determine if this recommendation is being followed. So they analyzed Medicaid claims data from 2005 through 2010 for Florida, Illinois, Louisiana, Michigan, South Carolina, and Texas.
The data included 4775 patients, ages 2 to 16, with sickle cell anemia. For these patients, TCD screening rates increased from 22% in 2005 to 44% in 2010 (P<0.001).
The researchers found that TCD screening rates varied significantly by state (P=0.004), and Texas had the lowest screening rate at any time point (7% in 2005).
The team also analyzed a subset of 2388 patients who were enrolled for 2 or more consecutive years to examine potential predictors of TCD screening.
This analysis revealed that, with each year of increasing age, a patient’s odds of receiving TCD screening decreased (odds ratio=0.97, P=0.002).
On the other hand, an increasing number of well-child visits was associated with higher odds of receiving TCD screening (odds ratio=1.10, P=0.007).
And the odds of receiving TCD screening were higher for patients who previously underwent TCD screening (odds ratio=2.44, P<0.001).
The researchers said these results suggest that, despite national recommendations, TCD screening rates remain low in young patients with sickle cell anemia in the US.

with sickle cell anemia
Photo courtesy of St. Jude
Results of a large, retrospective study suggest the use of transcranial Doppler (TCD) screening is on the rise in US children and adolescents with sickle cell anemia.
However, the rate of TCD screening in these patients falls well below national recommendations.
In addition, TCD screening rates vary greatly by state, and the use of screening tends to decrease as patients grow older.
Sarah L. Reeves, PhD, of University of Michigan, Ann Arbor, and her colleagues reported these findings in JAMA Pediatrics.
The researchers noted that guidelines from the National Heart, Lung, and Blood Institute recommend that patients with sickle cell anemia receive annual TCD screenings from age 2 to 16 to identify those patients at the highest risk of stroke.
Dr Reeves and her colleagues wanted to determine if this recommendation is being followed. So they analyzed Medicaid claims data from 2005 through 2010 for Florida, Illinois, Louisiana, Michigan, South Carolina, and Texas.
The data included 4775 patients, ages 2 to 16, with sickle cell anemia. For these patients, TCD screening rates increased from 22% in 2005 to 44% in 2010 (P<0.001).
The researchers found that TCD screening rates varied significantly by state (P=0.004), and Texas had the lowest screening rate at any time point (7% in 2005).
The team also analyzed a subset of 2388 patients who were enrolled for 2 or more consecutive years to examine potential predictors of TCD screening.
This analysis revealed that, with each year of increasing age, a patient’s odds of receiving TCD screening decreased (odds ratio=0.97, P=0.002).
On the other hand, an increasing number of well-child visits was associated with higher odds of receiving TCD screening (odds ratio=1.10, P=0.007).
And the odds of receiving TCD screening were higher for patients who previously underwent TCD screening (odds ratio=2.44, P<0.001).
The researchers said these results suggest that, despite national recommendations, TCD screening rates remain low in young patients with sickle cell anemia in the US.

with sickle cell anemia
Photo courtesy of St. Jude
Results of a large, retrospective study suggest the use of transcranial Doppler (TCD) screening is on the rise in US children and adolescents with sickle cell anemia.
However, the rate of TCD screening in these patients falls well below national recommendations.
In addition, TCD screening rates vary greatly by state, and the use of screening tends to decrease as patients grow older.
Sarah L. Reeves, PhD, of University of Michigan, Ann Arbor, and her colleagues reported these findings in JAMA Pediatrics.
The researchers noted that guidelines from the National Heart, Lung, and Blood Institute recommend that patients with sickle cell anemia receive annual TCD screenings from age 2 to 16 to identify those patients at the highest risk of stroke.
Dr Reeves and her colleagues wanted to determine if this recommendation is being followed. So they analyzed Medicaid claims data from 2005 through 2010 for Florida, Illinois, Louisiana, Michigan, South Carolina, and Texas.
The data included 4775 patients, ages 2 to 16, with sickle cell anemia. For these patients, TCD screening rates increased from 22% in 2005 to 44% in 2010 (P<0.001).
The researchers found that TCD screening rates varied significantly by state (P=0.004), and Texas had the lowest screening rate at any time point (7% in 2005).
The team also analyzed a subset of 2388 patients who were enrolled for 2 or more consecutive years to examine potential predictors of TCD screening.
This analysis revealed that, with each year of increasing age, a patient’s odds of receiving TCD screening decreased (odds ratio=0.97, P=0.002).
On the other hand, an increasing number of well-child visits was associated with higher odds of receiving TCD screening (odds ratio=1.10, P=0.007).
And the odds of receiving TCD screening were higher for patients who previously underwent TCD screening (odds ratio=2.44, P<0.001).
The researchers said these results suggest that, despite national recommendations, TCD screening rates remain low in young patients with sickle cell anemia in the US.
Sickle cell anemia: Stroke screening still underused
Children and adolescents with sickle cell anemia still are not being screened for stroke risk using transcranial Doppler, despite clinical guidelines that strongly recommend annual screening and despite these patients’ frequent health care encounters, according to a report published online April 11 in JAMA Pediatrics.
Approximately 10% of children and adolescents with sickle cell anemia experience stroke before the age of 20 years, unless those at high risk are identified and treated preemptively with blood transfusions, which reduces stroke risk by 92%. The National Heart, Lung, and Blood Institute clinical practice guideline on treating sickle cell disease calls for patients aged 2-16 years to undergo transcranial Doppler every year to detect any elevated velocity of cerebral blood flow, which indicates high stroke risk, said Sarah L. Reeves, Ph.D., of the Child Health Evaluation and Research Unit, University of Michigan, Ann Arbor, and her associates.
To assess screening rates, the investigators performed a retrospective cross-sectional analysis of administrative claims data for 4,775 affected children and adolescents treated during a 5-year period in Florida, Illinois, Louisiana, Michigan, South Carolina, and Texas. This yielded 10,787 person-years of data.
Overall, screening rates increased somewhat across all six states during the study period – from 22% to 44% – but “even the highest rates we report are suboptimal,” Dr. Reeves and her associates noted (JAMA Ped. 2016 Apr 11. doi: 10.1001/jamapediatrics.2015.4859).
This is especially true given that the average patient had 20.0 disease-related outpatient visits, 2.1 disease-related hospitalizations, 3.7 emergency department visits, and 1 well-child visit each year – numerous missed opportunities when they could have been referred for screening.
One way to improve screening rates would be to integrate transcranial Doppler exams into comprehensive sickle-cell healthcare, rather than requiring separate scheduled appointments at imaging facilities, they added.
This study was funded by the Agency for Healthcare Research and Quality and the Centers for Medicare & Medicaid Services. Dr. Reeves and her associates reported having no relevant financial disclosures.
Children and adolescents with sickle cell anemia still are not being screened for stroke risk using transcranial Doppler, despite clinical guidelines that strongly recommend annual screening and despite these patients’ frequent health care encounters, according to a report published online April 11 in JAMA Pediatrics.
Approximately 10% of children and adolescents with sickle cell anemia experience stroke before the age of 20 years, unless those at high risk are identified and treated preemptively with blood transfusions, which reduces stroke risk by 92%. The National Heart, Lung, and Blood Institute clinical practice guideline on treating sickle cell disease calls for patients aged 2-16 years to undergo transcranial Doppler every year to detect any elevated velocity of cerebral blood flow, which indicates high stroke risk, said Sarah L. Reeves, Ph.D., of the Child Health Evaluation and Research Unit, University of Michigan, Ann Arbor, and her associates.
To assess screening rates, the investigators performed a retrospective cross-sectional analysis of administrative claims data for 4,775 affected children and adolescents treated during a 5-year period in Florida, Illinois, Louisiana, Michigan, South Carolina, and Texas. This yielded 10,787 person-years of data.
Overall, screening rates increased somewhat across all six states during the study period – from 22% to 44% – but “even the highest rates we report are suboptimal,” Dr. Reeves and her associates noted (JAMA Ped. 2016 Apr 11. doi: 10.1001/jamapediatrics.2015.4859).
This is especially true given that the average patient had 20.0 disease-related outpatient visits, 2.1 disease-related hospitalizations, 3.7 emergency department visits, and 1 well-child visit each year – numerous missed opportunities when they could have been referred for screening.
One way to improve screening rates would be to integrate transcranial Doppler exams into comprehensive sickle-cell healthcare, rather than requiring separate scheduled appointments at imaging facilities, they added.
This study was funded by the Agency for Healthcare Research and Quality and the Centers for Medicare & Medicaid Services. Dr. Reeves and her associates reported having no relevant financial disclosures.
Children and adolescents with sickle cell anemia still are not being screened for stroke risk using transcranial Doppler, despite clinical guidelines that strongly recommend annual screening and despite these patients’ frequent health care encounters, according to a report published online April 11 in JAMA Pediatrics.
Approximately 10% of children and adolescents with sickle cell anemia experience stroke before the age of 20 years, unless those at high risk are identified and treated preemptively with blood transfusions, which reduces stroke risk by 92%. The National Heart, Lung, and Blood Institute clinical practice guideline on treating sickle cell disease calls for patients aged 2-16 years to undergo transcranial Doppler every year to detect any elevated velocity of cerebral blood flow, which indicates high stroke risk, said Sarah L. Reeves, Ph.D., of the Child Health Evaluation and Research Unit, University of Michigan, Ann Arbor, and her associates.
To assess screening rates, the investigators performed a retrospective cross-sectional analysis of administrative claims data for 4,775 affected children and adolescents treated during a 5-year period in Florida, Illinois, Louisiana, Michigan, South Carolina, and Texas. This yielded 10,787 person-years of data.
Overall, screening rates increased somewhat across all six states during the study period – from 22% to 44% – but “even the highest rates we report are suboptimal,” Dr. Reeves and her associates noted (JAMA Ped. 2016 Apr 11. doi: 10.1001/jamapediatrics.2015.4859).
This is especially true given that the average patient had 20.0 disease-related outpatient visits, 2.1 disease-related hospitalizations, 3.7 emergency department visits, and 1 well-child visit each year – numerous missed opportunities when they could have been referred for screening.
One way to improve screening rates would be to integrate transcranial Doppler exams into comprehensive sickle-cell healthcare, rather than requiring separate scheduled appointments at imaging facilities, they added.
This study was funded by the Agency for Healthcare Research and Quality and the Centers for Medicare & Medicaid Services. Dr. Reeves and her associates reported having no relevant financial disclosures.
FROM JAMA PEDIATRICS
Key clinical point: Transcranial Doppler screening for stroke risk is still underused among children and adolescents with sickle cell anemia, despite clinical guidelines that strongly recommend annual screening.
Major finding: Screening rates increased somewhat across all six states studied, from 22% to 44%, but even the highest rates were suboptimal.
Data source: A retrospective cross-sectional analysis of administrative claims data for 4,775 pediatric patients treated in a 5-year period.
Disclosures: This study was funded by the Agency for Healthcare Research and Quality and the Centers for Medicare & Medicaid Services. Dr. Reeves and her associates reported having no relevant financial disclosures.