User login
Clonal hematopoiesis explored in aplastic anemia
Clonal hematopoiesis was detected in DNA samples from approximately half of 439 patients with aplastic anemia, and a third of the study population carried mutations in candidate genes that correlated with clinical outcomes, according to a report published online July 2 in the New England Journal of Medicine.
Most patients with aplastic anemia respond to immunosuppressive therapy or bone marrow transplantation, but about 15% later develop myelodysplastic syndromes, acute myeloid leukemia (AML), or both. Historically, this has been attributed to “clonal evolution,” but a more accurate term is clonal hematopoiesis. However, not all patients with clonal hematopoiesis go on to develop late myelodysplastic syndromes or AML, said Dr. Tetsuichi Yoshizato of the department of pathology and tumor biology at Kyoto (Japan) University and associates.
To clarify the role of clonal hematopoiesis in aplastic anemia, the investigators analyzed DNA in blood, bone marrow, and buccal samples from 439 patients with bone marrow failure who were treated at three specialized centers in the United States and Japan.
Targeted sequencing of a panel of genes that are recurrently mutated in myeloid cancers was performed; 249 mutations were detected in candidate genes for myelodysplastic syndromes/AML in 36% of the study population. And about one-third of patients whose DNA harbored mutations had multiple (as many as 7) mutations. The most frequently mutated genes were BCOR and BCORL1 (in 9.3% of patients), PIGA (7.5%), DNMT3A (8.4%), and ASXL1 (6.2%), which together accounted for 77% of all mutation-positive patients, the investigators reported.
In addition, 47% of patients had expanded hematopoietic cell clones. Clones carrying certain mutations were associated with a better response to immunosuppressive treatment, while clones carrying several other mutations were associated with a poor treatment response, lower survival, and progression to myelodysplastic syndromes/AML. Mutations in PIGA and BCOR and BCORL1 correlated with a better response to immunosuppressive therapy and better overall and progression-free survival; mutations in a subgroup of genes that included DNMT3A and ASXL1 were associated with worse outcomes.
The pattern of mutations in individual patients, however, varied markedly over time and was often unpredictable. “It should be underscored that the complex dynamics of clonal hematopoiesis are highly variable and not necessarily determinative,” Dr. Yoshizato and associates said (N. Engl. J. Med. 2015 July 2 [doi:10.1056/NEJMoa1414799]).
Although further genetic research is needed before these findings can be applied clinically to guide prognosis and treatment, they already “have implications for bone marrow failure, for early events in leukemogenesis, and for normal aging,” the investigators added.
Clonal hematopoiesis was detected in DNA samples from approximately half of 439 patients with aplastic anemia, and a third of the study population carried mutations in candidate genes that correlated with clinical outcomes, according to a report published online July 2 in the New England Journal of Medicine.
Most patients with aplastic anemia respond to immunosuppressive therapy or bone marrow transplantation, but about 15% later develop myelodysplastic syndromes, acute myeloid leukemia (AML), or both. Historically, this has been attributed to “clonal evolution,” but a more accurate term is clonal hematopoiesis. However, not all patients with clonal hematopoiesis go on to develop late myelodysplastic syndromes or AML, said Dr. Tetsuichi Yoshizato of the department of pathology and tumor biology at Kyoto (Japan) University and associates.
To clarify the role of clonal hematopoiesis in aplastic anemia, the investigators analyzed DNA in blood, bone marrow, and buccal samples from 439 patients with bone marrow failure who were treated at three specialized centers in the United States and Japan.
Targeted sequencing of a panel of genes that are recurrently mutated in myeloid cancers was performed; 249 mutations were detected in candidate genes for myelodysplastic syndromes/AML in 36% of the study population. And about one-third of patients whose DNA harbored mutations had multiple (as many as 7) mutations. The most frequently mutated genes were BCOR and BCORL1 (in 9.3% of patients), PIGA (7.5%), DNMT3A (8.4%), and ASXL1 (6.2%), which together accounted for 77% of all mutation-positive patients, the investigators reported.
In addition, 47% of patients had expanded hematopoietic cell clones. Clones carrying certain mutations were associated with a better response to immunosuppressive treatment, while clones carrying several other mutations were associated with a poor treatment response, lower survival, and progression to myelodysplastic syndromes/AML. Mutations in PIGA and BCOR and BCORL1 correlated with a better response to immunosuppressive therapy and better overall and progression-free survival; mutations in a subgroup of genes that included DNMT3A and ASXL1 were associated with worse outcomes.
The pattern of mutations in individual patients, however, varied markedly over time and was often unpredictable. “It should be underscored that the complex dynamics of clonal hematopoiesis are highly variable and not necessarily determinative,” Dr. Yoshizato and associates said (N. Engl. J. Med. 2015 July 2 [doi:10.1056/NEJMoa1414799]).
Although further genetic research is needed before these findings can be applied clinically to guide prognosis and treatment, they already “have implications for bone marrow failure, for early events in leukemogenesis, and for normal aging,” the investigators added.
Clonal hematopoiesis was detected in DNA samples from approximately half of 439 patients with aplastic anemia, and a third of the study population carried mutations in candidate genes that correlated with clinical outcomes, according to a report published online July 2 in the New England Journal of Medicine.
Most patients with aplastic anemia respond to immunosuppressive therapy or bone marrow transplantation, but about 15% later develop myelodysplastic syndromes, acute myeloid leukemia (AML), or both. Historically, this has been attributed to “clonal evolution,” but a more accurate term is clonal hematopoiesis. However, not all patients with clonal hematopoiesis go on to develop late myelodysplastic syndromes or AML, said Dr. Tetsuichi Yoshizato of the department of pathology and tumor biology at Kyoto (Japan) University and associates.
To clarify the role of clonal hematopoiesis in aplastic anemia, the investigators analyzed DNA in blood, bone marrow, and buccal samples from 439 patients with bone marrow failure who were treated at three specialized centers in the United States and Japan.
Targeted sequencing of a panel of genes that are recurrently mutated in myeloid cancers was performed; 249 mutations were detected in candidate genes for myelodysplastic syndromes/AML in 36% of the study population. And about one-third of patients whose DNA harbored mutations had multiple (as many as 7) mutations. The most frequently mutated genes were BCOR and BCORL1 (in 9.3% of patients), PIGA (7.5%), DNMT3A (8.4%), and ASXL1 (6.2%), which together accounted for 77% of all mutation-positive patients, the investigators reported.
In addition, 47% of patients had expanded hematopoietic cell clones. Clones carrying certain mutations were associated with a better response to immunosuppressive treatment, while clones carrying several other mutations were associated with a poor treatment response, lower survival, and progression to myelodysplastic syndromes/AML. Mutations in PIGA and BCOR and BCORL1 correlated with a better response to immunosuppressive therapy and better overall and progression-free survival; mutations in a subgroup of genes that included DNMT3A and ASXL1 were associated with worse outcomes.
The pattern of mutations in individual patients, however, varied markedly over time and was often unpredictable. “It should be underscored that the complex dynamics of clonal hematopoiesis are highly variable and not necessarily determinative,” Dr. Yoshizato and associates said (N. Engl. J. Med. 2015 July 2 [doi:10.1056/NEJMoa1414799]).
Although further genetic research is needed before these findings can be applied clinically to guide prognosis and treatment, they already “have implications for bone marrow failure, for early events in leukemogenesis, and for normal aging,” the investigators added.
FROM THE NEW ENGLAND JOURNAL OF MEDICINE
Key clinical point: Clonal hematopoiesis was detected in 47% of 439 patients with aplastic anemia, and some of the mutations were related to clinical outcomes.
Major finding: The most frequently mutated genes were BCOR and BCORL1 (in 9.3% of patients), PIGA (7.5%), DNMT3A (8.4%), and ASXL1 (6.2%), which together accounted for 77% of all mutation-positive patients.
Data source: DNA analysis of blood, bone marrow, and buccal samples from 439 patients with aplastic anemia treated at three medical centers in the United States and Japan.
Disclosures: This work was supported by the Ministry of Health, Labor, and Welfare of Japan; the Japan Society for the Promotion of Science; the National Heart, Lung, and Blood Institute; the Aplastic Anemia and MDS International Foundation; and the Scott Hamilton Cancer Alliance for Research, Education, and Survivorship Foundation. Dr. Yoshizato reported having no relevant financial disclosures; an associate reported receiving a grant from Daiichi-Sankyo unrelated to this work.
Nanobody can help treat acquired TTP

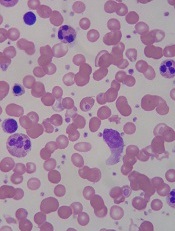
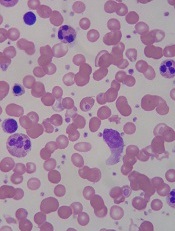
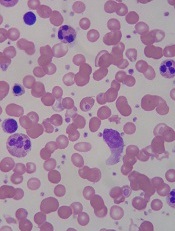
Image by Erhabor Osaro
TORONTO—Adding the anti-von Willebrand factor nanobody caplacizumab to standard therapy can provide clinical benefits for patients with
acquired thrombotic thrombocytopenic purpura (TTP), according to research presented at the 2015 ISTH Congress.
In the phase 2 TITAN trial, patients who received caplacizumab and standard therapy had a significantly shorter time to platelet normalization than patients who received standard therapy and placebo.
Caplacizumab was also associated with a shorter time to troponin, creatinine, and lactate dehydrogenase (LDH) normalization, as well as a reduced need for plasma exchange (PE).
However, some patients relapsed after stopping caplacizumab, and the majority of these relapses could be linked to unresolved disease activity. The drug also increased the risk of mild-to-moderate bleeding compared to placebo.
Flora Peyvandi, MD, PhD, of the University of Milan in Italy, presented data from the TITAN trial at ISTH as abstract LB006. Information on using ADAMTS13 activity for treatment monitoring in the TITAN trial was also presented at the meeting, as abstract OR363.
TITAN was sponsored by Ablynx, the company developing caplacizumab.
The study enrolled 75 patients with acquired TTP from January 2011 to January 2014. Patients were randomized to receive caplacizumab (n=36) or placebo (n=39).
All patients also received the current standard of care, which is, primarily, multiple PEs. The protocol for the study was adapted in September 2013 to allow 1 day of PE prior to study enrollment.
Patients in the caplacizumab arm immediately received an intravenous bolus dose of 10 mg and then a 10 mg subcutaneous dose of the drug daily until 30 days had elapsed after the final PE. Patients in the control arm received placebo at the same time points.
Platelet responses and relapse
The study’s primary endpoint was the time to platelet normalization. And patients in the caplacizumab arm achieved platelet normalization at more than twice the rate of patients in the placebo arm (overall hazard rate ratio=2.2, P=0.005).
Among patients with no prior PE, the median time to platelet normalization was 3 days in caplacizumab-treated patients (n=34) and 4.9 days in controls (n=35). Among patients with 1 prior PE, the median time to platelet normalization was 2.4 days in the caplacizumab arm (n=2) and 4.3 days in the placebo arm (n=4).
In the caplacizumab arm, a higher proportion of patients achieved a complete remission, and fewer patients had exacerbations of TTP. The complete remission rates were 81% and 46%, respectively. And the exacerbation rates were 8% and 28%, respectively.
However, the rate of exacerbation and/or relapse at up to 1 month of follow-up was the same in both arms, at 28%.
Seven patients relapsed within 10 days of stopping caplacizumab. All of these patients had continuous low ADAMTS13 activity (<10%) during and near the end of treatment.
Cardiac, renal, and tissue responses
Additional analyses revealed that patients in the caplacizumab arm had a faster time to troponin normalization than those in the placebo arm. At baseline, 53% of caplacizumab-treated patients and 46% of controls had elevated troponin. The median time to normalization was 9 days and 27 days, respectively.
Patients in the caplacizumab arm also had a faster time to creatinine normalization than those in the placebo arm. At baseline, 31% of caplacizumab-treated patients and 41% of controls had elevated creatinine. The median time to normalization was 4 days and 6 days, respectively.
And patients in the caplacizumab arm had a faster time to LDH normalization than those in the placebo arm. At baseline, 91% of caplacizumab-treated patients and 87% of controls had elevated LDH. The median time to normalization was 3 days and 4 days, respectively.
However, the investigators said they could not rule out a possible effect of PE therapy on LDH, creatinine, and troponin levels.
Need for PE
Results showed that caplacizumab could reduce the need for PE, at least while patients continued to receive the drug.
Patients in the caplacizumab arm required fewer PEs during the daily PE treatment period and the overall treatment period. But this benefit was lost during the 1-month follow-up period, which is reflective of the increased number of relapses, according to the investigators.
During the daily PE treatment period, the mean number of PE days was 5.9 in the caplacizumab arm and 7.9 in the placebo arm. During the overall treatment period, it was 7.7 and 11.7 days, respectively. And during the overall treatment and follow-up period, it was 10.2 and 11.7 days, respectively.
Adverse events
The investigators said caplacizumab increased the risk of bleeding events, but these were readily managed.
Treatment-emergent adverse events (AEs) occurred in 97% of patients in the caplacizumab arm and 100% of patients in the placebo arm. Eight percent of caplacizumab-treated patients discontinued treatment due to AEs, but none of the controls did.
Fifty-four percent of patients in the caplacizumab arm had a bleeding event, as did 38% of patients in the placebo arm. Eighty percent of the bleeding events in the caplacizumab arm were mild. Three patients required drug treatment. None required von Willebrand factor or factor VIII substitution.
Serious AEs occurred in 57% of caplacizumab-treated patients and 51% of controls. Serious bleeding events occurred in 6% and 5%, respectively. ![]()

Image by Erhabor Osaro
TORONTO—Adding the anti-von Willebrand factor nanobody caplacizumab to standard therapy can provide clinical benefits for patients with
acquired thrombotic thrombocytopenic purpura (TTP), according to research presented at the 2015 ISTH Congress.
In the phase 2 TITAN trial, patients who received caplacizumab and standard therapy had a significantly shorter time to platelet normalization than patients who received standard therapy and placebo.
Caplacizumab was also associated with a shorter time to troponin, creatinine, and lactate dehydrogenase (LDH) normalization, as well as a reduced need for plasma exchange (PE).
However, some patients relapsed after stopping caplacizumab, and the majority of these relapses could be linked to unresolved disease activity. The drug also increased the risk of mild-to-moderate bleeding compared to placebo.
Flora Peyvandi, MD, PhD, of the University of Milan in Italy, presented data from the TITAN trial at ISTH as abstract LB006. Information on using ADAMTS13 activity for treatment monitoring in the TITAN trial was also presented at the meeting, as abstract OR363.
TITAN was sponsored by Ablynx, the company developing caplacizumab.
The study enrolled 75 patients with acquired TTP from January 2011 to January 2014. Patients were randomized to receive caplacizumab (n=36) or placebo (n=39).
All patients also received the current standard of care, which is, primarily, multiple PEs. The protocol for the study was adapted in September 2013 to allow 1 day of PE prior to study enrollment.
Patients in the caplacizumab arm immediately received an intravenous bolus dose of 10 mg and then a 10 mg subcutaneous dose of the drug daily until 30 days had elapsed after the final PE. Patients in the control arm received placebo at the same time points.
Platelet responses and relapse
The study’s primary endpoint was the time to platelet normalization. And patients in the caplacizumab arm achieved platelet normalization at more than twice the rate of patients in the placebo arm (overall hazard rate ratio=2.2, P=0.005).
Among patients with no prior PE, the median time to platelet normalization was 3 days in caplacizumab-treated patients (n=34) and 4.9 days in controls (n=35). Among patients with 1 prior PE, the median time to platelet normalization was 2.4 days in the caplacizumab arm (n=2) and 4.3 days in the placebo arm (n=4).
In the caplacizumab arm, a higher proportion of patients achieved a complete remission, and fewer patients had exacerbations of TTP. The complete remission rates were 81% and 46%, respectively. And the exacerbation rates were 8% and 28%, respectively.
However, the rate of exacerbation and/or relapse at up to 1 month of follow-up was the same in both arms, at 28%.
Seven patients relapsed within 10 days of stopping caplacizumab. All of these patients had continuous low ADAMTS13 activity (<10%) during and near the end of treatment.
Cardiac, renal, and tissue responses
Additional analyses revealed that patients in the caplacizumab arm had a faster time to troponin normalization than those in the placebo arm. At baseline, 53% of caplacizumab-treated patients and 46% of controls had elevated troponin. The median time to normalization was 9 days and 27 days, respectively.
Patients in the caplacizumab arm also had a faster time to creatinine normalization than those in the placebo arm. At baseline, 31% of caplacizumab-treated patients and 41% of controls had elevated creatinine. The median time to normalization was 4 days and 6 days, respectively.
And patients in the caplacizumab arm had a faster time to LDH normalization than those in the placebo arm. At baseline, 91% of caplacizumab-treated patients and 87% of controls had elevated LDH. The median time to normalization was 3 days and 4 days, respectively.
However, the investigators said they could not rule out a possible effect of PE therapy on LDH, creatinine, and troponin levels.
Need for PE
Results showed that caplacizumab could reduce the need for PE, at least while patients continued to receive the drug.
Patients in the caplacizumab arm required fewer PEs during the daily PE treatment period and the overall treatment period. But this benefit was lost during the 1-month follow-up period, which is reflective of the increased number of relapses, according to the investigators.
During the daily PE treatment period, the mean number of PE days was 5.9 in the caplacizumab arm and 7.9 in the placebo arm. During the overall treatment period, it was 7.7 and 11.7 days, respectively. And during the overall treatment and follow-up period, it was 10.2 and 11.7 days, respectively.
Adverse events
The investigators said caplacizumab increased the risk of bleeding events, but these were readily managed.
Treatment-emergent adverse events (AEs) occurred in 97% of patients in the caplacizumab arm and 100% of patients in the placebo arm. Eight percent of caplacizumab-treated patients discontinued treatment due to AEs, but none of the controls did.
Fifty-four percent of patients in the caplacizumab arm had a bleeding event, as did 38% of patients in the placebo arm. Eighty percent of the bleeding events in the caplacizumab arm were mild. Three patients required drug treatment. None required von Willebrand factor or factor VIII substitution.
Serious AEs occurred in 57% of caplacizumab-treated patients and 51% of controls. Serious bleeding events occurred in 6% and 5%, respectively. ![]()

Image by Erhabor Osaro
TORONTO—Adding the anti-von Willebrand factor nanobody caplacizumab to standard therapy can provide clinical benefits for patients with
acquired thrombotic thrombocytopenic purpura (TTP), according to research presented at the 2015 ISTH Congress.
In the phase 2 TITAN trial, patients who received caplacizumab and standard therapy had a significantly shorter time to platelet normalization than patients who received standard therapy and placebo.
Caplacizumab was also associated with a shorter time to troponin, creatinine, and lactate dehydrogenase (LDH) normalization, as well as a reduced need for plasma exchange (PE).
However, some patients relapsed after stopping caplacizumab, and the majority of these relapses could be linked to unresolved disease activity. The drug also increased the risk of mild-to-moderate bleeding compared to placebo.
Flora Peyvandi, MD, PhD, of the University of Milan in Italy, presented data from the TITAN trial at ISTH as abstract LB006. Information on using ADAMTS13 activity for treatment monitoring in the TITAN trial was also presented at the meeting, as abstract OR363.
TITAN was sponsored by Ablynx, the company developing caplacizumab.
The study enrolled 75 patients with acquired TTP from January 2011 to January 2014. Patients were randomized to receive caplacizumab (n=36) or placebo (n=39).
All patients also received the current standard of care, which is, primarily, multiple PEs. The protocol for the study was adapted in September 2013 to allow 1 day of PE prior to study enrollment.
Patients in the caplacizumab arm immediately received an intravenous bolus dose of 10 mg and then a 10 mg subcutaneous dose of the drug daily until 30 days had elapsed after the final PE. Patients in the control arm received placebo at the same time points.
Platelet responses and relapse
The study’s primary endpoint was the time to platelet normalization. And patients in the caplacizumab arm achieved platelet normalization at more than twice the rate of patients in the placebo arm (overall hazard rate ratio=2.2, P=0.005).
Among patients with no prior PE, the median time to platelet normalization was 3 days in caplacizumab-treated patients (n=34) and 4.9 days in controls (n=35). Among patients with 1 prior PE, the median time to platelet normalization was 2.4 days in the caplacizumab arm (n=2) and 4.3 days in the placebo arm (n=4).
In the caplacizumab arm, a higher proportion of patients achieved a complete remission, and fewer patients had exacerbations of TTP. The complete remission rates were 81% and 46%, respectively. And the exacerbation rates were 8% and 28%, respectively.
However, the rate of exacerbation and/or relapse at up to 1 month of follow-up was the same in both arms, at 28%.
Seven patients relapsed within 10 days of stopping caplacizumab. All of these patients had continuous low ADAMTS13 activity (<10%) during and near the end of treatment.
Cardiac, renal, and tissue responses
Additional analyses revealed that patients in the caplacizumab arm had a faster time to troponin normalization than those in the placebo arm. At baseline, 53% of caplacizumab-treated patients and 46% of controls had elevated troponin. The median time to normalization was 9 days and 27 days, respectively.
Patients in the caplacizumab arm also had a faster time to creatinine normalization than those in the placebo arm. At baseline, 31% of caplacizumab-treated patients and 41% of controls had elevated creatinine. The median time to normalization was 4 days and 6 days, respectively.
And patients in the caplacizumab arm had a faster time to LDH normalization than those in the placebo arm. At baseline, 91% of caplacizumab-treated patients and 87% of controls had elevated LDH. The median time to normalization was 3 days and 4 days, respectively.
However, the investigators said they could not rule out a possible effect of PE therapy on LDH, creatinine, and troponin levels.
Need for PE
Results showed that caplacizumab could reduce the need for PE, at least while patients continued to receive the drug.
Patients in the caplacizumab arm required fewer PEs during the daily PE treatment period and the overall treatment period. But this benefit was lost during the 1-month follow-up period, which is reflective of the increased number of relapses, according to the investigators.
During the daily PE treatment period, the mean number of PE days was 5.9 in the caplacizumab arm and 7.9 in the placebo arm. During the overall treatment period, it was 7.7 and 11.7 days, respectively. And during the overall treatment and follow-up period, it was 10.2 and 11.7 days, respectively.
Adverse events
The investigators said caplacizumab increased the risk of bleeding events, but these were readily managed.
Treatment-emergent adverse events (AEs) occurred in 97% of patients in the caplacizumab arm and 100% of patients in the placebo arm. Eight percent of caplacizumab-treated patients discontinued treatment due to AEs, but none of the controls did.
Fifty-four percent of patients in the caplacizumab arm had a bleeding event, as did 38% of patients in the placebo arm. Eighty percent of the bleeding events in the caplacizumab arm were mild. Three patients required drug treatment. None required von Willebrand factor or factor VIII substitution.
Serious AEs occurred in 57% of caplacizumab-treated patients and 51% of controls. Serious bleeding events occurred in 6% and 5%, respectively. ![]()
Activin receptors continue to show efficacy in ß-thalassemia

Congress of the European
Hematology Association
VIENNA—Two very similar activin receptors, luspatercept and sotatercept, continue to show efficacy in patients with ß-thalassemia, according to research presented at the 20th Congress of the European Hematology Association (EHA).
The “twin compounds” basically differ from each other in the receptor type, but both can increase hemoglobin levels in non-transfusion-dependent (NTD) patients and reduce transfusion burden in transfusion-dependent (TD) patients.
Luspatercept is a recombinant fusion protein containing a modified extracellular domain of the activin receptor type IIB, while sotatercept is an activin receptor type IIA.
Antonio Piga, MD, of Turin University in Italy, presented the most recent results with luspatercept at EHA as abstract S136*. An update on sotatercept was also presented at the meeting.
Acceleron Pharma Inc. and Celgene Corporation are jointly developing both compounds.
The phase 2, multicenter, open-label trial of luspatercept now has results on 39 patients, 35 of whom were in the dose-escalation cohorts and 4 who are in the expansion cohort that is currently underway.
Adult patients age 18 and older received luspatercept subcutaneously every 3 weeks for 3 months. Doses in the dose-escalation cohorts increased from 0.2 mg/kg to 1.25 mg/kg.
Patients in the expansion cohort received a starting dose of 0.8 mg/kg, with an individual dose titration up to 1.25 mg/kg, for an additional 12 months of treatment. Twenty of 30 patients were enrolled in the expansion cohort as of June 8.
For all patients, the median age was 40, 82% had had a splenectomy, and 49% were male. Twenty-five patients were NTD, and 14 were TD.
NTD patients
NTD patients had a median baseline hemoglobin level of 8.4 g/dL and liver iron concentration (LIC) of 5.8 ± 3.8 mg/g dry weight (dw).
Four of 8 patients who received luspatercept at doses ranging from 0.8 mg/kg to 1.25 mg/kg saw an increase in their hemoglobin levels of 1.5 g/dL or more for 2 weeks or longer, and 3 patients (38%) had a mean hemoglobin increase of 1.5 g/dL for 9 weeks or longer.
Patients on the higher doses of luspatercept had larger hemoglobin increases, and, with continued treatment, patients sustained their hemoglobin increases.
Increases in hemoglobin correlated with reductions in LIC.
“There was a trend to lower liver iron concentration,” Dr Piga said, “a trend that seems important.”
Patients achieved reductions in LIC with and without iron chelation therapy.
Eight of 12 patients with a baseline LIC of 5 mg/g dw or greater had decreases of 1 mg or more at month 4. And 10 of 10 patients with a baseline LIC of less than 5 mg/g dw were able to maintain that concentration.
TD patients
At baseline, TD patients required a median of 7.5 red blood cell (RBC) units every 12 weeks and had an LIC of 5.2 ± 5.7 mg/g dw.
Ten of 14 patients were treated for 12 weeks or longer and were evaluable for changes in transfusion burden. And all 10 patients had a 40% or greater reduction in transfusion burden.
Two of 3 patients with an LIC of 7 mg/g dw had decreases of 1 mg/g dw or more at month 4. And all 7 patients with a baseline LIC less than 7 mg/g dw were able to maintain that level.
Leg ulcers
Three patients with long-term, persistent leg ulcers experienced rapid healing with luspatercept treatment.
One NTD patient on the 0.4 mg/kg dose experienced complete healing after 6 weeks, and 1 TD patient on the 1.0 mg/kg dose experienced complete healing after 18 weeks.
Safety
Bone pain (23%), myalgia (18%), headache (15%), and asthenia (10%) were the most common drug-related adverse events. None of the related adverse events were serious.
Two patients had treatment-related, grade 3 adverse events of bone pain (2 events) and asthenia (1 event). Six of 39 patients discontinued treatment early due to an adverse event of headache, ankle pain, back pain, spider nevi, superficial thrombosis, or bone pain.
The US Food and Drug Administration recently granted luspatercept fast track designation for the treatment of patients with TD or NTD β-thalassemia.
Dr Piga said a pivotal phase 3 trial of luspatercept in patients with β -thalassemia and myelodysplastic syndromes is planned. ![]()
*Data in the abstract differ from the presentation.

Congress of the European
Hematology Association
VIENNA—Two very similar activin receptors, luspatercept and sotatercept, continue to show efficacy in patients with ß-thalassemia, according to research presented at the 20th Congress of the European Hematology Association (EHA).
The “twin compounds” basically differ from each other in the receptor type, but both can increase hemoglobin levels in non-transfusion-dependent (NTD) patients and reduce transfusion burden in transfusion-dependent (TD) patients.
Luspatercept is a recombinant fusion protein containing a modified extracellular domain of the activin receptor type IIB, while sotatercept is an activin receptor type IIA.
Antonio Piga, MD, of Turin University in Italy, presented the most recent results with luspatercept at EHA as abstract S136*. An update on sotatercept was also presented at the meeting.
Acceleron Pharma Inc. and Celgene Corporation are jointly developing both compounds.
The phase 2, multicenter, open-label trial of luspatercept now has results on 39 patients, 35 of whom were in the dose-escalation cohorts and 4 who are in the expansion cohort that is currently underway.
Adult patients age 18 and older received luspatercept subcutaneously every 3 weeks for 3 months. Doses in the dose-escalation cohorts increased from 0.2 mg/kg to 1.25 mg/kg.
Patients in the expansion cohort received a starting dose of 0.8 mg/kg, with an individual dose titration up to 1.25 mg/kg, for an additional 12 months of treatment. Twenty of 30 patients were enrolled in the expansion cohort as of June 8.
For all patients, the median age was 40, 82% had had a splenectomy, and 49% were male. Twenty-five patients were NTD, and 14 were TD.
NTD patients
NTD patients had a median baseline hemoglobin level of 8.4 g/dL and liver iron concentration (LIC) of 5.8 ± 3.8 mg/g dry weight (dw).
Four of 8 patients who received luspatercept at doses ranging from 0.8 mg/kg to 1.25 mg/kg saw an increase in their hemoglobin levels of 1.5 g/dL or more for 2 weeks or longer, and 3 patients (38%) had a mean hemoglobin increase of 1.5 g/dL for 9 weeks or longer.
Patients on the higher doses of luspatercept had larger hemoglobin increases, and, with continued treatment, patients sustained their hemoglobin increases.
Increases in hemoglobin correlated with reductions in LIC.
“There was a trend to lower liver iron concentration,” Dr Piga said, “a trend that seems important.”
Patients achieved reductions in LIC with and without iron chelation therapy.
Eight of 12 patients with a baseline LIC of 5 mg/g dw or greater had decreases of 1 mg or more at month 4. And 10 of 10 patients with a baseline LIC of less than 5 mg/g dw were able to maintain that concentration.
TD patients
At baseline, TD patients required a median of 7.5 red blood cell (RBC) units every 12 weeks and had an LIC of 5.2 ± 5.7 mg/g dw.
Ten of 14 patients were treated for 12 weeks or longer and were evaluable for changes in transfusion burden. And all 10 patients had a 40% or greater reduction in transfusion burden.
Two of 3 patients with an LIC of 7 mg/g dw had decreases of 1 mg/g dw or more at month 4. And all 7 patients with a baseline LIC less than 7 mg/g dw were able to maintain that level.
Leg ulcers
Three patients with long-term, persistent leg ulcers experienced rapid healing with luspatercept treatment.
One NTD patient on the 0.4 mg/kg dose experienced complete healing after 6 weeks, and 1 TD patient on the 1.0 mg/kg dose experienced complete healing after 18 weeks.
Safety
Bone pain (23%), myalgia (18%), headache (15%), and asthenia (10%) were the most common drug-related adverse events. None of the related adverse events were serious.
Two patients had treatment-related, grade 3 adverse events of bone pain (2 events) and asthenia (1 event). Six of 39 patients discontinued treatment early due to an adverse event of headache, ankle pain, back pain, spider nevi, superficial thrombosis, or bone pain.
The US Food and Drug Administration recently granted luspatercept fast track designation for the treatment of patients with TD or NTD β-thalassemia.
Dr Piga said a pivotal phase 3 trial of luspatercept in patients with β -thalassemia and myelodysplastic syndromes is planned. ![]()
*Data in the abstract differ from the presentation.

Congress of the European
Hematology Association
VIENNA—Two very similar activin receptors, luspatercept and sotatercept, continue to show efficacy in patients with ß-thalassemia, according to research presented at the 20th Congress of the European Hematology Association (EHA).
The “twin compounds” basically differ from each other in the receptor type, but both can increase hemoglobin levels in non-transfusion-dependent (NTD) patients and reduce transfusion burden in transfusion-dependent (TD) patients.
Luspatercept is a recombinant fusion protein containing a modified extracellular domain of the activin receptor type IIB, while sotatercept is an activin receptor type IIA.
Antonio Piga, MD, of Turin University in Italy, presented the most recent results with luspatercept at EHA as abstract S136*. An update on sotatercept was also presented at the meeting.
Acceleron Pharma Inc. and Celgene Corporation are jointly developing both compounds.
The phase 2, multicenter, open-label trial of luspatercept now has results on 39 patients, 35 of whom were in the dose-escalation cohorts and 4 who are in the expansion cohort that is currently underway.
Adult patients age 18 and older received luspatercept subcutaneously every 3 weeks for 3 months. Doses in the dose-escalation cohorts increased from 0.2 mg/kg to 1.25 mg/kg.
Patients in the expansion cohort received a starting dose of 0.8 mg/kg, with an individual dose titration up to 1.25 mg/kg, for an additional 12 months of treatment. Twenty of 30 patients were enrolled in the expansion cohort as of June 8.
For all patients, the median age was 40, 82% had had a splenectomy, and 49% were male. Twenty-five patients were NTD, and 14 were TD.
NTD patients
NTD patients had a median baseline hemoglobin level of 8.4 g/dL and liver iron concentration (LIC) of 5.8 ± 3.8 mg/g dry weight (dw).
Four of 8 patients who received luspatercept at doses ranging from 0.8 mg/kg to 1.25 mg/kg saw an increase in their hemoglobin levels of 1.5 g/dL or more for 2 weeks or longer, and 3 patients (38%) had a mean hemoglobin increase of 1.5 g/dL for 9 weeks or longer.
Patients on the higher doses of luspatercept had larger hemoglobin increases, and, with continued treatment, patients sustained their hemoglobin increases.
Increases in hemoglobin correlated with reductions in LIC.
“There was a trend to lower liver iron concentration,” Dr Piga said, “a trend that seems important.”
Patients achieved reductions in LIC with and without iron chelation therapy.
Eight of 12 patients with a baseline LIC of 5 mg/g dw or greater had decreases of 1 mg or more at month 4. And 10 of 10 patients with a baseline LIC of less than 5 mg/g dw were able to maintain that concentration.
TD patients
At baseline, TD patients required a median of 7.5 red blood cell (RBC) units every 12 weeks and had an LIC of 5.2 ± 5.7 mg/g dw.
Ten of 14 patients were treated for 12 weeks or longer and were evaluable for changes in transfusion burden. And all 10 patients had a 40% or greater reduction in transfusion burden.
Two of 3 patients with an LIC of 7 mg/g dw had decreases of 1 mg/g dw or more at month 4. And all 7 patients with a baseline LIC less than 7 mg/g dw were able to maintain that level.
Leg ulcers
Three patients with long-term, persistent leg ulcers experienced rapid healing with luspatercept treatment.
One NTD patient on the 0.4 mg/kg dose experienced complete healing after 6 weeks, and 1 TD patient on the 1.0 mg/kg dose experienced complete healing after 18 weeks.
Safety
Bone pain (23%), myalgia (18%), headache (15%), and asthenia (10%) were the most common drug-related adverse events. None of the related adverse events were serious.
Two patients had treatment-related, grade 3 adverse events of bone pain (2 events) and asthenia (1 event). Six of 39 patients discontinued treatment early due to an adverse event of headache, ankle pain, back pain, spider nevi, superficial thrombosis, or bone pain.
The US Food and Drug Administration recently granted luspatercept fast track designation for the treatment of patients with TD or NTD β-thalassemia.
Dr Piga said a pivotal phase 3 trial of luspatercept in patients with β -thalassemia and myelodysplastic syndromes is planned. ![]()
*Data in the abstract differ from the presentation.
Drug won’t advance to phase 3 in ß-thalassemia
thalassemia
VIENNA—Data from a phase 2a trial suggest the activin receptor sotatercept can effectively treat patients with ß-thalassemia.
However, the companies developing the drug have decided not to advance sotatercept to phase 3 trials in this patient population.
Instead, the companies are initiating a phase 3 program with sotatercept’s “twin” activin receptor, luspatercept, in patients with ß-thalassemia or myelodysplastic syndromes.
Acceleron Pharma Inc. and Celgene Corporation are jointly developing both compounds. The companies plan to continue developing sotatercept for patients with chronic kidney disease.
Maria Domenica Cappellini, MD, of the University of Milan in Italy, presented results from the phase 2a study of sotatercept in ß-thalassemia at the 20th Congress of the European Hematology Association (abstract S137*).
Phase 2 results with luspatercept in ß-thalassemia were also presented at the meeting.
The dose-finding study of sotatercept had enrolled 46 patients at the time of Dr Cappellini’s presentation. The drug was given subcutaneously at doses ranging from 0.1 mg/kg to 1.0 mg/kg every 3 weeks.
The 30 non-transfusion-dependent (NTD) patients received 4 or fewer red blood cell (RBC) units in the 6 months prior to study enrollment. The 16 transfusion-dependent (TD) patients had received 2 or more RBC units every 30 days for 6 months or more prior to study enrollment.
Twenty-five of the 46 patients remain on treatment, with a median exposure time of 12.4 months.
NTD patients
The patients’ median age was 42, and 53% were female. Fifty-three percent had had a splenectomy, and the median baseline hemoglobin level was 8.4 g/dL.
Treatment with sotatercept produced a dose-dependent hemoglobin increase.
“[W]hat I found quite interesting is that the increase is consistent and persistent, [even] after 1 year,” Dr Cappellini said. “And they are still maintained on treatment, of course, but it is a sustained response.”
At the 0.75 mg/kg dose, 86% of patients had a hemoglobin increase of 1 g/dL for 12 weeks or more, and 71% had an increase of 1.5 g/dL.
TD patients
The patients’ median age was 36 years, and 38% were female. Three-quarters of patients had ß-thalassemia major, and a quarter had ß-thalassemia intermedia.
Nearly a third of patients had had a splenectomy, and their transfusion burden at baseline ranged from 8 RBC units to 35 RBC units every 24 weeks.
The mean reduction in transfusion burden among patients treated with sotatercept at doses of 0.5 mg/kg or higher was 32.25%. And the 1.0 mg/kg dose of sotatercept reduced one patient’s transfusion burden by 61.6%.
Dr Cappellini noted that the pharmacokinetic analysis showed a correlation with exposure. The investigators observed no apparent effects of weight, sex, age, or transfusion burden on drug clearance.
“So the relationship was probably more related to long-term exposure than to the real dosage,” she said.
Safety
Hypertension and bone pain were the most common grade 2-4, treatment-related adverse events.
Seven patients discontinued the study due to adverse events, one patient each with bone pain, superficial thrombophlebitis, ventricular extrasystole, spinal extramedullary erythropoietic tissue, and erythema at the injection site/allergic reaction. Two patients discontinued due to hypertension.
Dr Cappellini concluded that sotatercept and the related molecule, luspatercept, may provide a favorable risk-benefit profile for patients with ß-thalassemia.
“These 2 molecules are merging now for a phase 3 trial in either TD or NTD thalassemia cohorts,” she said. “The two drugs are actually very, very similar, and, in fact, for the trial, we decided to use only one. There is no way to go on with 2 molecules.”
In April, Acceleron and Celgene announced plans to initiate a phase 3 program with luspatercept in myelodysplastic syndromes and β-thalassemia by the end of this year. The companies said they will continue to develop sotatercept for patients with chronic kidney disease. ![]()
*Data in the abstract differ from the presentation.
thalassemia
VIENNA—Data from a phase 2a trial suggest the activin receptor sotatercept can effectively treat patients with ß-thalassemia.
However, the companies developing the drug have decided not to advance sotatercept to phase 3 trials in this patient population.
Instead, the companies are initiating a phase 3 program with sotatercept’s “twin” activin receptor, luspatercept, in patients with ß-thalassemia or myelodysplastic syndromes.
Acceleron Pharma Inc. and Celgene Corporation are jointly developing both compounds. The companies plan to continue developing sotatercept for patients with chronic kidney disease.
Maria Domenica Cappellini, MD, of the University of Milan in Italy, presented results from the phase 2a study of sotatercept in ß-thalassemia at the 20th Congress of the European Hematology Association (abstract S137*).
Phase 2 results with luspatercept in ß-thalassemia were also presented at the meeting.
The dose-finding study of sotatercept had enrolled 46 patients at the time of Dr Cappellini’s presentation. The drug was given subcutaneously at doses ranging from 0.1 mg/kg to 1.0 mg/kg every 3 weeks.
The 30 non-transfusion-dependent (NTD) patients received 4 or fewer red blood cell (RBC) units in the 6 months prior to study enrollment. The 16 transfusion-dependent (TD) patients had received 2 or more RBC units every 30 days for 6 months or more prior to study enrollment.
Twenty-five of the 46 patients remain on treatment, with a median exposure time of 12.4 months.
NTD patients
The patients’ median age was 42, and 53% were female. Fifty-three percent had had a splenectomy, and the median baseline hemoglobin level was 8.4 g/dL.
Treatment with sotatercept produced a dose-dependent hemoglobin increase.
“[W]hat I found quite interesting is that the increase is consistent and persistent, [even] after 1 year,” Dr Cappellini said. “And they are still maintained on treatment, of course, but it is a sustained response.”
At the 0.75 mg/kg dose, 86% of patients had a hemoglobin increase of 1 g/dL for 12 weeks or more, and 71% had an increase of 1.5 g/dL.
TD patients
The patients’ median age was 36 years, and 38% were female. Three-quarters of patients had ß-thalassemia major, and a quarter had ß-thalassemia intermedia.
Nearly a third of patients had had a splenectomy, and their transfusion burden at baseline ranged from 8 RBC units to 35 RBC units every 24 weeks.
The mean reduction in transfusion burden among patients treated with sotatercept at doses of 0.5 mg/kg or higher was 32.25%. And the 1.0 mg/kg dose of sotatercept reduced one patient’s transfusion burden by 61.6%.
Dr Cappellini noted that the pharmacokinetic analysis showed a correlation with exposure. The investigators observed no apparent effects of weight, sex, age, or transfusion burden on drug clearance.
“So the relationship was probably more related to long-term exposure than to the real dosage,” she said.
Safety
Hypertension and bone pain were the most common grade 2-4, treatment-related adverse events.
Seven patients discontinued the study due to adverse events, one patient each with bone pain, superficial thrombophlebitis, ventricular extrasystole, spinal extramedullary erythropoietic tissue, and erythema at the injection site/allergic reaction. Two patients discontinued due to hypertension.
Dr Cappellini concluded that sotatercept and the related molecule, luspatercept, may provide a favorable risk-benefit profile for patients with ß-thalassemia.
“These 2 molecules are merging now for a phase 3 trial in either TD or NTD thalassemia cohorts,” she said. “The two drugs are actually very, very similar, and, in fact, for the trial, we decided to use only one. There is no way to go on with 2 molecules.”
In April, Acceleron and Celgene announced plans to initiate a phase 3 program with luspatercept in myelodysplastic syndromes and β-thalassemia by the end of this year. The companies said they will continue to develop sotatercept for patients with chronic kidney disease. ![]()
*Data in the abstract differ from the presentation.
thalassemia
VIENNA—Data from a phase 2a trial suggest the activin receptor sotatercept can effectively treat patients with ß-thalassemia.
However, the companies developing the drug have decided not to advance sotatercept to phase 3 trials in this patient population.
Instead, the companies are initiating a phase 3 program with sotatercept’s “twin” activin receptor, luspatercept, in patients with ß-thalassemia or myelodysplastic syndromes.
Acceleron Pharma Inc. and Celgene Corporation are jointly developing both compounds. The companies plan to continue developing sotatercept for patients with chronic kidney disease.
Maria Domenica Cappellini, MD, of the University of Milan in Italy, presented results from the phase 2a study of sotatercept in ß-thalassemia at the 20th Congress of the European Hematology Association (abstract S137*).
Phase 2 results with luspatercept in ß-thalassemia were also presented at the meeting.
The dose-finding study of sotatercept had enrolled 46 patients at the time of Dr Cappellini’s presentation. The drug was given subcutaneously at doses ranging from 0.1 mg/kg to 1.0 mg/kg every 3 weeks.
The 30 non-transfusion-dependent (NTD) patients received 4 or fewer red blood cell (RBC) units in the 6 months prior to study enrollment. The 16 transfusion-dependent (TD) patients had received 2 or more RBC units every 30 days for 6 months or more prior to study enrollment.
Twenty-five of the 46 patients remain on treatment, with a median exposure time of 12.4 months.
NTD patients
The patients’ median age was 42, and 53% were female. Fifty-three percent had had a splenectomy, and the median baseline hemoglobin level was 8.4 g/dL.
Treatment with sotatercept produced a dose-dependent hemoglobin increase.
“[W]hat I found quite interesting is that the increase is consistent and persistent, [even] after 1 year,” Dr Cappellini said. “And they are still maintained on treatment, of course, but it is a sustained response.”
At the 0.75 mg/kg dose, 86% of patients had a hemoglobin increase of 1 g/dL for 12 weeks or more, and 71% had an increase of 1.5 g/dL.
TD patients
The patients’ median age was 36 years, and 38% were female. Three-quarters of patients had ß-thalassemia major, and a quarter had ß-thalassemia intermedia.
Nearly a third of patients had had a splenectomy, and their transfusion burden at baseline ranged from 8 RBC units to 35 RBC units every 24 weeks.
The mean reduction in transfusion burden among patients treated with sotatercept at doses of 0.5 mg/kg or higher was 32.25%. And the 1.0 mg/kg dose of sotatercept reduced one patient’s transfusion burden by 61.6%.
Dr Cappellini noted that the pharmacokinetic analysis showed a correlation with exposure. The investigators observed no apparent effects of weight, sex, age, or transfusion burden on drug clearance.
“So the relationship was probably more related to long-term exposure than to the real dosage,” she said.
Safety
Hypertension and bone pain were the most common grade 2-4, treatment-related adverse events.
Seven patients discontinued the study due to adverse events, one patient each with bone pain, superficial thrombophlebitis, ventricular extrasystole, spinal extramedullary erythropoietic tissue, and erythema at the injection site/allergic reaction. Two patients discontinued due to hypertension.
Dr Cappellini concluded that sotatercept and the related molecule, luspatercept, may provide a favorable risk-benefit profile for patients with ß-thalassemia.
“These 2 molecules are merging now for a phase 3 trial in either TD or NTD thalassemia cohorts,” she said. “The two drugs are actually very, very similar, and, in fact, for the trial, we decided to use only one. There is no way to go on with 2 molecules.”
In April, Acceleron and Celgene announced plans to initiate a phase 3 program with luspatercept in myelodysplastic syndromes and β-thalassemia by the end of this year. The companies said they will continue to develop sotatercept for patients with chronic kidney disease. ![]()
*Data in the abstract differ from the presentation.
Unsickling red blood cells

VIENNA—Researchers say they have found a way to unsickle red blood cells (RBCs), at least in vitro.
Using pegylated carboxyhemoglobin bovine gas transfer, the team restored sickled RBCs to a more normal, rounder shape in as little as 5 minutes.
Ronald Jubin, PhD, of Prolong Pharmaceuticals, the company developing carboxyhemoglobin, described this process at the 20th Congress of the European Hematology Association (abstract S140).
Pegylated carboxyhemoglobin bovine (Sanguinate [SG]) was designed to reduce vasoconstriction, counteract inflammatory responses, and deliver oxygen to hypoxic cells by releasing carbon monoxide.
The investigators contend that using SG early in a vasooclusive crisis (VOC) can limit the crisis and reduce pain severity.
They evaluated SG treatment using RBCs from healthy volunteers and patients with sickle cell disease (SCD).
The researchers monitored carboxyhemoglobin and oxyhemoglobin levels and analyzed patient samples using light microscopy and image capture flow cytometry. In this manner, they were able to visualize and quantify the effects of SG treatment on reversing the sickling of RBCs.
The investigators found that SG rapidly transferred its carbon monoxide component to oxygenated RBCs along with oxygen loading of SG.
“SG restored more normal RBC shape in as little as 5 minutes,” Dr Jubin said.
SG was also able to continually facilitate gas transfer through multiple exposure events and limited inflammatory marker expression in SCD blood samples.
The researchers concluded that SG can serve as an active gas transport agent, providing either carbon monoxide or oxygen to sickled RBCs. They also noted that image capture flow cytometry allowed for a quantitative measurement of decreased sickling and may provide a way to monitor SG treatment effects on SCD patients in future studies.
Dr Jubin said phase 1 safety trials of SG have been completed, and phase 2 trials are in development for VOC, SCD leg ulcers, delayed cerebral ischemia, prevention of delayed kidney graft function, and pulmonary hypertension in beta-thalassemia.
SG was recently awarded orphan drug status by the US Food and Drug Administration.
Orphan designation provides the company developing a drug with certain benefits and incentives, including a 7-year period of marketing exclusivity upon regulatory approval, potential tax credits for certain activities, eligibility for orphan drug grants, and the waiver of certain administrative fees. ![]()

VIENNA—Researchers say they have found a way to unsickle red blood cells (RBCs), at least in vitro.
Using pegylated carboxyhemoglobin bovine gas transfer, the team restored sickled RBCs to a more normal, rounder shape in as little as 5 minutes.
Ronald Jubin, PhD, of Prolong Pharmaceuticals, the company developing carboxyhemoglobin, described this process at the 20th Congress of the European Hematology Association (abstract S140).
Pegylated carboxyhemoglobin bovine (Sanguinate [SG]) was designed to reduce vasoconstriction, counteract inflammatory responses, and deliver oxygen to hypoxic cells by releasing carbon monoxide.
The investigators contend that using SG early in a vasooclusive crisis (VOC) can limit the crisis and reduce pain severity.
They evaluated SG treatment using RBCs from healthy volunteers and patients with sickle cell disease (SCD).
The researchers monitored carboxyhemoglobin and oxyhemoglobin levels and analyzed patient samples using light microscopy and image capture flow cytometry. In this manner, they were able to visualize and quantify the effects of SG treatment on reversing the sickling of RBCs.
The investigators found that SG rapidly transferred its carbon monoxide component to oxygenated RBCs along with oxygen loading of SG.
“SG restored more normal RBC shape in as little as 5 minutes,” Dr Jubin said.
SG was also able to continually facilitate gas transfer through multiple exposure events and limited inflammatory marker expression in SCD blood samples.
The researchers concluded that SG can serve as an active gas transport agent, providing either carbon monoxide or oxygen to sickled RBCs. They also noted that image capture flow cytometry allowed for a quantitative measurement of decreased sickling and may provide a way to monitor SG treatment effects on SCD patients in future studies.
Dr Jubin said phase 1 safety trials of SG have been completed, and phase 2 trials are in development for VOC, SCD leg ulcers, delayed cerebral ischemia, prevention of delayed kidney graft function, and pulmonary hypertension in beta-thalassemia.
SG was recently awarded orphan drug status by the US Food and Drug Administration.
Orphan designation provides the company developing a drug with certain benefits and incentives, including a 7-year period of marketing exclusivity upon regulatory approval, potential tax credits for certain activities, eligibility for orphan drug grants, and the waiver of certain administrative fees. ![]()

VIENNA—Researchers say they have found a way to unsickle red blood cells (RBCs), at least in vitro.
Using pegylated carboxyhemoglobin bovine gas transfer, the team restored sickled RBCs to a more normal, rounder shape in as little as 5 minutes.
Ronald Jubin, PhD, of Prolong Pharmaceuticals, the company developing carboxyhemoglobin, described this process at the 20th Congress of the European Hematology Association (abstract S140).
Pegylated carboxyhemoglobin bovine (Sanguinate [SG]) was designed to reduce vasoconstriction, counteract inflammatory responses, and deliver oxygen to hypoxic cells by releasing carbon monoxide.
The investigators contend that using SG early in a vasooclusive crisis (VOC) can limit the crisis and reduce pain severity.
They evaluated SG treatment using RBCs from healthy volunteers and patients with sickle cell disease (SCD).
The researchers monitored carboxyhemoglobin and oxyhemoglobin levels and analyzed patient samples using light microscopy and image capture flow cytometry. In this manner, they were able to visualize and quantify the effects of SG treatment on reversing the sickling of RBCs.
The investigators found that SG rapidly transferred its carbon monoxide component to oxygenated RBCs along with oxygen loading of SG.
“SG restored more normal RBC shape in as little as 5 minutes,” Dr Jubin said.
SG was also able to continually facilitate gas transfer through multiple exposure events and limited inflammatory marker expression in SCD blood samples.
The researchers concluded that SG can serve as an active gas transport agent, providing either carbon monoxide or oxygen to sickled RBCs. They also noted that image capture flow cytometry allowed for a quantitative measurement of decreased sickling and may provide a way to monitor SG treatment effects on SCD patients in future studies.
Dr Jubin said phase 1 safety trials of SG have been completed, and phase 2 trials are in development for VOC, SCD leg ulcers, delayed cerebral ischemia, prevention of delayed kidney graft function, and pulmonary hypertension in beta-thalassemia.
SG was recently awarded orphan drug status by the US Food and Drug Administration.
Orphan designation provides the company developing a drug with certain benefits and incentives, including a 7-year period of marketing exclusivity upon regulatory approval, potential tax credits for certain activities, eligibility for orphan drug grants, and the waiver of certain administrative fees. ![]()
FDA extends approval of ITP drug to kids

Photo courtesy of the FDA
The US Food and Drug Administration (FDA) has approved eltrombopag (Promacta) to treat children age 6 and older with chronic immune thrombocytopenia (ITP) who have had an insufficient response to corticosteroids, immunoglobulins, or splenectomy.
Eltrombopag is an oral thrombopoietin receptor agonist that works by inducing the stimulation and differentiation of megakaryocytes to increase platelet production.
The drug is already FDA-approved to treat adults with ITP.
The FDA’s latest approval of eltrombopag was based on data from the phase 2 PETIT trial and the phase 3 PETIT2 trial.
“Young patients with chronic ITP who have either an insufficient response to or side effects from standard therapies have limited treatment options, making this FDA approval of eltrombopag for children 6 years and older particularly important,” said James B. Bussel, MD, a professor at Weill Cornell Medical College in New York and lead investigator of the PETIT study.
“Through the eltrombopag studies, one of which is the largest randomized trial ever performed in children with chronic ITP, we discovered that Promacta—a treatment that can be taken once daily by mouth and shown to be well tolerated—can manage this disorder and help these young patients.”
PETIT trials: Efficacy
The PETIT trial included 67 ITP patients stratified by age cohort (12-17 years, 6-11 years, and 1-5 years). They were randomized (2:1) to receive eltrombopag or placebo for 7 weeks. Eltrombopag dose was titrated to a target platelet count of 50-200 x109/L.
The primary efficacy endpoint was the proportion of subjects achieving platelet counts of 50 x109/L or higher at least once between days 8 and 43 of the randomized period of the study.
Significantly more patients in the eltrombopag arm met this endpoint—62.2%—compared to 31.8% in the placebo arm (P=0.011).
The PETIT2 trial enrolled 92 patients with chronic ITP who were randomized (2:1) to receive eltrombopag or placebo for 13 weeks. The eltrombopag
dose was titrated to a target platelet count of 50-200 x109/L.
The primary efficacy endpoint was the proportion of subjects who achieve platelet counts of 50 x109/L or higher for at least 6 out of 8 weeks, between weeks 5 and 12 of the randomized period.
Significantly more patients in the eltrombopag arm met this endpoint—41.3%—compared to 3.4% of patients in the placebo arm (P<0.001).
PETIT trials: Safety
For both trials, there were 107 eltrombopag-treated patients evaluable for safety.
The most common adverse events occurring more frequently in the eltrombopag arms than the placebo arms were upper respiratory tract infection,
nasopharyngitis, cough, diarrhea, pyrexia, rhinitis, abdominal pain, oropharyngeal pain, toothache, increased ALT or AST, rash, and rhinorrhea.
Serious adverse events were reported in 8% of patients during the randomized part of both trials, although no serious adverse event occurred in more than 1 patient (1%).
An ALT elevation of at least 3 times the upper limit of normal occurred in 5% of eltrombopag-treated patients. Of those patients, 2% had ALT increases
of at least 5 times the upper limit of normal.
There were no deaths or thromboembolic events during either study.
Eltrombopag is marketed as Promacta in the US and Revolade in most countries outside the US. For more information on the drug, see the full prescribing information. ![]()

Photo courtesy of the FDA
The US Food and Drug Administration (FDA) has approved eltrombopag (Promacta) to treat children age 6 and older with chronic immune thrombocytopenia (ITP) who have had an insufficient response to corticosteroids, immunoglobulins, or splenectomy.
Eltrombopag is an oral thrombopoietin receptor agonist that works by inducing the stimulation and differentiation of megakaryocytes to increase platelet production.
The drug is already FDA-approved to treat adults with ITP.
The FDA’s latest approval of eltrombopag was based on data from the phase 2 PETIT trial and the phase 3 PETIT2 trial.
“Young patients with chronic ITP who have either an insufficient response to or side effects from standard therapies have limited treatment options, making this FDA approval of eltrombopag for children 6 years and older particularly important,” said James B. Bussel, MD, a professor at Weill Cornell Medical College in New York and lead investigator of the PETIT study.
“Through the eltrombopag studies, one of which is the largest randomized trial ever performed in children with chronic ITP, we discovered that Promacta—a treatment that can be taken once daily by mouth and shown to be well tolerated—can manage this disorder and help these young patients.”
PETIT trials: Efficacy
The PETIT trial included 67 ITP patients stratified by age cohort (12-17 years, 6-11 years, and 1-5 years). They were randomized (2:1) to receive eltrombopag or placebo for 7 weeks. Eltrombopag dose was titrated to a target platelet count of 50-200 x109/L.
The primary efficacy endpoint was the proportion of subjects achieving platelet counts of 50 x109/L or higher at least once between days 8 and 43 of the randomized period of the study.
Significantly more patients in the eltrombopag arm met this endpoint—62.2%—compared to 31.8% in the placebo arm (P=0.011).
The PETIT2 trial enrolled 92 patients with chronic ITP who were randomized (2:1) to receive eltrombopag or placebo for 13 weeks. The eltrombopag
dose was titrated to a target platelet count of 50-200 x109/L.
The primary efficacy endpoint was the proportion of subjects who achieve platelet counts of 50 x109/L or higher for at least 6 out of 8 weeks, between weeks 5 and 12 of the randomized period.
Significantly more patients in the eltrombopag arm met this endpoint—41.3%—compared to 3.4% of patients in the placebo arm (P<0.001).
PETIT trials: Safety
For both trials, there were 107 eltrombopag-treated patients evaluable for safety.
The most common adverse events occurring more frequently in the eltrombopag arms than the placebo arms were upper respiratory tract infection,
nasopharyngitis, cough, diarrhea, pyrexia, rhinitis, abdominal pain, oropharyngeal pain, toothache, increased ALT or AST, rash, and rhinorrhea.
Serious adverse events were reported in 8% of patients during the randomized part of both trials, although no serious adverse event occurred in more than 1 patient (1%).
An ALT elevation of at least 3 times the upper limit of normal occurred in 5% of eltrombopag-treated patients. Of those patients, 2% had ALT increases
of at least 5 times the upper limit of normal.
There were no deaths or thromboembolic events during either study.
Eltrombopag is marketed as Promacta in the US and Revolade in most countries outside the US. For more information on the drug, see the full prescribing information. ![]()

Photo courtesy of the FDA
The US Food and Drug Administration (FDA) has approved eltrombopag (Promacta) to treat children age 6 and older with chronic immune thrombocytopenia (ITP) who have had an insufficient response to corticosteroids, immunoglobulins, or splenectomy.
Eltrombopag is an oral thrombopoietin receptor agonist that works by inducing the stimulation and differentiation of megakaryocytes to increase platelet production.
The drug is already FDA-approved to treat adults with ITP.
The FDA’s latest approval of eltrombopag was based on data from the phase 2 PETIT trial and the phase 3 PETIT2 trial.
“Young patients with chronic ITP who have either an insufficient response to or side effects from standard therapies have limited treatment options, making this FDA approval of eltrombopag for children 6 years and older particularly important,” said James B. Bussel, MD, a professor at Weill Cornell Medical College in New York and lead investigator of the PETIT study.
“Through the eltrombopag studies, one of which is the largest randomized trial ever performed in children with chronic ITP, we discovered that Promacta—a treatment that can be taken once daily by mouth and shown to be well tolerated—can manage this disorder and help these young patients.”
PETIT trials: Efficacy
The PETIT trial included 67 ITP patients stratified by age cohort (12-17 years, 6-11 years, and 1-5 years). They were randomized (2:1) to receive eltrombopag or placebo for 7 weeks. Eltrombopag dose was titrated to a target platelet count of 50-200 x109/L.
The primary efficacy endpoint was the proportion of subjects achieving platelet counts of 50 x109/L or higher at least once between days 8 and 43 of the randomized period of the study.
Significantly more patients in the eltrombopag arm met this endpoint—62.2%—compared to 31.8% in the placebo arm (P=0.011).
The PETIT2 trial enrolled 92 patients with chronic ITP who were randomized (2:1) to receive eltrombopag or placebo for 13 weeks. The eltrombopag
dose was titrated to a target platelet count of 50-200 x109/L.
The primary efficacy endpoint was the proportion of subjects who achieve platelet counts of 50 x109/L or higher for at least 6 out of 8 weeks, between weeks 5 and 12 of the randomized period.
Significantly more patients in the eltrombopag arm met this endpoint—41.3%—compared to 3.4% of patients in the placebo arm (P<0.001).
PETIT trials: Safety
For both trials, there were 107 eltrombopag-treated patients evaluable for safety.
The most common adverse events occurring more frequently in the eltrombopag arms than the placebo arms were upper respiratory tract infection,
nasopharyngitis, cough, diarrhea, pyrexia, rhinitis, abdominal pain, oropharyngeal pain, toothache, increased ALT or AST, rash, and rhinorrhea.
Serious adverse events were reported in 8% of patients during the randomized part of both trials, although no serious adverse event occurred in more than 1 patient (1%).
An ALT elevation of at least 3 times the upper limit of normal occurred in 5% of eltrombopag-treated patients. Of those patients, 2% had ALT increases
of at least 5 times the upper limit of normal.
There were no deaths or thromboembolic events during either study.
Eltrombopag is marketed as Promacta in the US and Revolade in most countries outside the US. For more information on the drug, see the full prescribing information. ![]()
Resolution draws attention to sickle cell trait

and a normal one
Image by Betty Pace
Two members of the US House of Representatives have introduced a resolution calling for expanded government efforts to increase sickle cell trait (SCT) research and improve access to SCT screening and education.
Barbara Lee (D-CA) and Michael C. Burgess (R-TX) introduced the resolution, which was assigned to a congressional committee that will consider it before possibly sending it on to the House or Senate as a whole.
The resolution, H.Res.296, encourages the medical community as well as state and federal governments to work to ensure that all individuals are made aware of their SCT status by developing a common strategy for disseminating screening results and providing education and counseling to parents and families in collaboration with all 50 states’ newborn screening programs.
The resolution calls on the US Department of Health and Human Services to develop a public awareness campaign stressing the importance of knowing your SCT status and to expand access for screening and appropriate counseling for SCT carriers.
The resolution also says the House commits to ensuring support for research that expands our understanding of SCT and sickle cell disease.
The American Society of Hematology (ASH) said it applauds this bipartisan effort to advance public understanding of SCT, which is estimated to affect more than 300,000 people in the US, many of whom are unaware of their status.
ASH also said it has identified several priorities for research in this area and has collaborated with the US Centers for Disease Control and Prevention and the Sickle Cell Disease Association of America to develop a Sickle Cell Trait Toolkit for SCT carriers and their families.
To follow the progress of the resolution, H.Res.296 – Calling for Sickle Cell Trait Research, visit Congress.gov. ![]()

and a normal one
Image by Betty Pace
Two members of the US House of Representatives have introduced a resolution calling for expanded government efforts to increase sickle cell trait (SCT) research and improve access to SCT screening and education.
Barbara Lee (D-CA) and Michael C. Burgess (R-TX) introduced the resolution, which was assigned to a congressional committee that will consider it before possibly sending it on to the House or Senate as a whole.
The resolution, H.Res.296, encourages the medical community as well as state and federal governments to work to ensure that all individuals are made aware of their SCT status by developing a common strategy for disseminating screening results and providing education and counseling to parents and families in collaboration with all 50 states’ newborn screening programs.
The resolution calls on the US Department of Health and Human Services to develop a public awareness campaign stressing the importance of knowing your SCT status and to expand access for screening and appropriate counseling for SCT carriers.
The resolution also says the House commits to ensuring support for research that expands our understanding of SCT and sickle cell disease.
The American Society of Hematology (ASH) said it applauds this bipartisan effort to advance public understanding of SCT, which is estimated to affect more than 300,000 people in the US, many of whom are unaware of their status.
ASH also said it has identified several priorities for research in this area and has collaborated with the US Centers for Disease Control and Prevention and the Sickle Cell Disease Association of America to develop a Sickle Cell Trait Toolkit for SCT carriers and their families.
To follow the progress of the resolution, H.Res.296 – Calling for Sickle Cell Trait Research, visit Congress.gov. ![]()

and a normal one
Image by Betty Pace
Two members of the US House of Representatives have introduced a resolution calling for expanded government efforts to increase sickle cell trait (SCT) research and improve access to SCT screening and education.
Barbara Lee (D-CA) and Michael C. Burgess (R-TX) introduced the resolution, which was assigned to a congressional committee that will consider it before possibly sending it on to the House or Senate as a whole.
The resolution, H.Res.296, encourages the medical community as well as state and federal governments to work to ensure that all individuals are made aware of their SCT status by developing a common strategy for disseminating screening results and providing education and counseling to parents and families in collaboration with all 50 states’ newborn screening programs.
The resolution calls on the US Department of Health and Human Services to develop a public awareness campaign stressing the importance of knowing your SCT status and to expand access for screening and appropriate counseling for SCT carriers.
The resolution also says the House commits to ensuring support for research that expands our understanding of SCT and sickle cell disease.
The American Society of Hematology (ASH) said it applauds this bipartisan effort to advance public understanding of SCT, which is estimated to affect more than 300,000 people in the US, many of whom are unaware of their status.
ASH also said it has identified several priorities for research in this area and has collaborated with the US Centers for Disease Control and Prevention and the Sickle Cell Disease Association of America to develop a Sickle Cell Trait Toolkit for SCT carriers and their families.
To follow the progress of the resolution, H.Res.296 – Calling for Sickle Cell Trait Research, visit Congress.gov. ![]()
Drug on fast track to treat β-thalassemia

Image courtesy of NHLBI
The US Food and Drug Administration (FDA) has granted fast track designation to luspatercept for the treatment of patients with transfusion-dependent (TD) or non-transfusion-dependent (NTD) β-thalassemia.
Luspatercept is a modified activin receptor type IIB fusion protein that acts as a ligand trap for members of the transforming growth factor-β (TGF-β) superfamily involved in the late stages of erythropoiesis.
The drug regulates late-stage erythrocyte precursor differentiation and maturation. This mechanism of action is distinct from that of erythropoietin, which stimulates the proliferation of early stage erythrocyte precursor cells.
Luspatercept is currently in phase 2 trials in patients with β-thalassemia and individuals with myelodysplastic syndromes (MDS). Data from the trial in β-thalassemia were presented at the 2014 ASH Annual Meeting, and results from the MDS trial were recently presented at the 13th International Symposium on Myelodysplastic Syndromes.
Acceleron Pharma Inc. and Celgene Corporation are jointly developing luspatercept.
About fast track designation
The FDA’s fast track program is designed to facilitate the development of new drugs that are intended to treat serious or life-threatening conditions and that demonstrate the potential to address unmet medical needs.
The designation provides pharmaceutical companies with the opportunity for more frequent interaction with the FDA while developing a drug. It also allows a sponsor to submit sections of a biologics license application on a rolling basis, as they are finalized.
“The FDA’s fast track designation for the luspatercept development program recognizes the serious unmet medical needs of patients with β-thalassemia and the potential for luspatercept in this area,” said Jacqualyn A. Fouse, president of hematology/oncology for Celgene.
“Celgene and Acceleron are working diligently to initiate a phase 3 clinical program in 2015 to treat patients with β-thalassemia, and we look forward to continuing to work closely with health authorities and other important stakeholders to advance this program.”
Phase 2 trial in β-thalassemia
At ASH 2014, researchers presented results of a phase 2 trial in which they investigated whether luspatercept could increase hemoglobin levels and decrease transfusion dependence.
The goal was to increase hemoglobin levels 1.5 g/dL or more for at least 2 weeks in NTD patients and decrease the transfusion burden by 20% or more over 12 weeks in TD patients.
Thirty patients, 7 TD and 23 NTD, received an injection of luspatercept every 3 weeks for 3 months at doses ranging from 0.2 mg/kg to 1.0 mg/kg.
Three-quarters of patients who received 0.8 mg/kg to 1.0 mg/kg of luspatercept experienced an increase in their hemoglobin levels or a reduction in their transfusion burden.
Of the NTD patients, 8 of 12 with iron overload at baseline experienced a reduction in liver iron concentration of 1 mg or more at 16 weeks.
TD patients had a more than 60% reduction in transfusion burden over 12 weeks. This included 2 patients with β0 β0 genotype, who experienced a 79% and 75% reduction.
Luspatercept did not cause any treatment-related serious or severe adverse events. The most common adverse events were bone pain (20%), headache (17%), myalgia (13%), and asthenia (10%).
There was 1 grade 3 dose-limiting toxicity of worsening lumbar spine bone pain. And 3 patients discontinued treatment early, 1 each with occipital headache, ankle pain, and back pain. ![]()

Image courtesy of NHLBI
The US Food and Drug Administration (FDA) has granted fast track designation to luspatercept for the treatment of patients with transfusion-dependent (TD) or non-transfusion-dependent (NTD) β-thalassemia.
Luspatercept is a modified activin receptor type IIB fusion protein that acts as a ligand trap for members of the transforming growth factor-β (TGF-β) superfamily involved in the late stages of erythropoiesis.
The drug regulates late-stage erythrocyte precursor differentiation and maturation. This mechanism of action is distinct from that of erythropoietin, which stimulates the proliferation of early stage erythrocyte precursor cells.
Luspatercept is currently in phase 2 trials in patients with β-thalassemia and individuals with myelodysplastic syndromes (MDS). Data from the trial in β-thalassemia were presented at the 2014 ASH Annual Meeting, and results from the MDS trial were recently presented at the 13th International Symposium on Myelodysplastic Syndromes.
Acceleron Pharma Inc. and Celgene Corporation are jointly developing luspatercept.
About fast track designation
The FDA’s fast track program is designed to facilitate the development of new drugs that are intended to treat serious or life-threatening conditions and that demonstrate the potential to address unmet medical needs.
The designation provides pharmaceutical companies with the opportunity for more frequent interaction with the FDA while developing a drug. It also allows a sponsor to submit sections of a biologics license application on a rolling basis, as they are finalized.
“The FDA’s fast track designation for the luspatercept development program recognizes the serious unmet medical needs of patients with β-thalassemia and the potential for luspatercept in this area,” said Jacqualyn A. Fouse, president of hematology/oncology for Celgene.
“Celgene and Acceleron are working diligently to initiate a phase 3 clinical program in 2015 to treat patients with β-thalassemia, and we look forward to continuing to work closely with health authorities and other important stakeholders to advance this program.”
Phase 2 trial in β-thalassemia
At ASH 2014, researchers presented results of a phase 2 trial in which they investigated whether luspatercept could increase hemoglobin levels and decrease transfusion dependence.
The goal was to increase hemoglobin levels 1.5 g/dL or more for at least 2 weeks in NTD patients and decrease the transfusion burden by 20% or more over 12 weeks in TD patients.
Thirty patients, 7 TD and 23 NTD, received an injection of luspatercept every 3 weeks for 3 months at doses ranging from 0.2 mg/kg to 1.0 mg/kg.
Three-quarters of patients who received 0.8 mg/kg to 1.0 mg/kg of luspatercept experienced an increase in their hemoglobin levels or a reduction in their transfusion burden.
Of the NTD patients, 8 of 12 with iron overload at baseline experienced a reduction in liver iron concentration of 1 mg or more at 16 weeks.
TD patients had a more than 60% reduction in transfusion burden over 12 weeks. This included 2 patients with β0 β0 genotype, who experienced a 79% and 75% reduction.
Luspatercept did not cause any treatment-related serious or severe adverse events. The most common adverse events were bone pain (20%), headache (17%), myalgia (13%), and asthenia (10%).
There was 1 grade 3 dose-limiting toxicity of worsening lumbar spine bone pain. And 3 patients discontinued treatment early, 1 each with occipital headache, ankle pain, and back pain. ![]()

Image courtesy of NHLBI
The US Food and Drug Administration (FDA) has granted fast track designation to luspatercept for the treatment of patients with transfusion-dependent (TD) or non-transfusion-dependent (NTD) β-thalassemia.
Luspatercept is a modified activin receptor type IIB fusion protein that acts as a ligand trap for members of the transforming growth factor-β (TGF-β) superfamily involved in the late stages of erythropoiesis.
The drug regulates late-stage erythrocyte precursor differentiation and maturation. This mechanism of action is distinct from that of erythropoietin, which stimulates the proliferation of early stage erythrocyte precursor cells.
Luspatercept is currently in phase 2 trials in patients with β-thalassemia and individuals with myelodysplastic syndromes (MDS). Data from the trial in β-thalassemia were presented at the 2014 ASH Annual Meeting, and results from the MDS trial were recently presented at the 13th International Symposium on Myelodysplastic Syndromes.
Acceleron Pharma Inc. and Celgene Corporation are jointly developing luspatercept.
About fast track designation
The FDA’s fast track program is designed to facilitate the development of new drugs that are intended to treat serious or life-threatening conditions and that demonstrate the potential to address unmet medical needs.
The designation provides pharmaceutical companies with the opportunity for more frequent interaction with the FDA while developing a drug. It also allows a sponsor to submit sections of a biologics license application on a rolling basis, as they are finalized.
“The FDA’s fast track designation for the luspatercept development program recognizes the serious unmet medical needs of patients with β-thalassemia and the potential for luspatercept in this area,” said Jacqualyn A. Fouse, president of hematology/oncology for Celgene.
“Celgene and Acceleron are working diligently to initiate a phase 3 clinical program in 2015 to treat patients with β-thalassemia, and we look forward to continuing to work closely with health authorities and other important stakeholders to advance this program.”
Phase 2 trial in β-thalassemia
At ASH 2014, researchers presented results of a phase 2 trial in which they investigated whether luspatercept could increase hemoglobin levels and decrease transfusion dependence.
The goal was to increase hemoglobin levels 1.5 g/dL or more for at least 2 weeks in NTD patients and decrease the transfusion burden by 20% or more over 12 weeks in TD patients.
Thirty patients, 7 TD and 23 NTD, received an injection of luspatercept every 3 weeks for 3 months at doses ranging from 0.2 mg/kg to 1.0 mg/kg.
Three-quarters of patients who received 0.8 mg/kg to 1.0 mg/kg of luspatercept experienced an increase in their hemoglobin levels or a reduction in their transfusion burden.
Of the NTD patients, 8 of 12 with iron overload at baseline experienced a reduction in liver iron concentration of 1 mg or more at 16 weeks.
TD patients had a more than 60% reduction in transfusion burden over 12 weeks. This included 2 patients with β0 β0 genotype, who experienced a 79% and 75% reduction.
Luspatercept did not cause any treatment-related serious or severe adverse events. The most common adverse events were bone pain (20%), headache (17%), myalgia (13%), and asthenia (10%).
There was 1 grade 3 dose-limiting toxicity of worsening lumbar spine bone pain. And 3 patients discontinued treatment early, 1 each with occipital headache, ankle pain, and back pain.
Genome editing increases hemoglobin production

Scientists have found they can use a genome-editing technique to increase hemoglobin production, and they described this method in Nature Communications.
The team used transcription activator-like effector nucleases (TALENs) to introduce the hereditary persistence of fetal hemoglobin (HPFH)-175T4C point mutation into erythroid cell lines.
This served to switch on the fetal hemoglobin gene and increase hemoglobin production.
“Our laboratory study provides a proof of concept that changing just one letter of DNA in a gene could alleviate the symptoms of sickle cell anemia and thalassemia—inherited diseases in which people have damaged hemoglobin,” said Merlin Crossley, PhD, of the University of New South Wales in Sydney, Australia.
“Because the good genetic variation we introduced already exists in nature, this approach should be effective and safe. However, more research is needed before it can be tested in people as a possible cure for serious blood diseases.”
Dr Crossley and his colleagues introduced the HPFH-175T4C point mutation into erythroid cell lines using TALENs, which can be designed to cut a gene at a specific point, as well as provide the desired piece of donor DNA for insertion.
“Breaks in DNA can be lethal to cells, so they have in-built machinery to repair any nicks as soon as possible, by grabbing any spare DNA that seems to match . . . ,” Dr Crossley explained.
“We exploited this effect. When our genome-editing protein cuts the DNA, the cell quickly replaces it with the donor DNA that we have also provided.”
The researchers pointed out that the HPFH-175T4C point mutation increased fetal globin expression via de novo recruitment of the activator TAL1, which promoted chromatin looping of distal enhancers to the modified γ-globin promoter.
The team also said that, if their editing technique proves safe and effective in hematopoietic stem cells, it could offer significant advantages over other approaches used to treat hemoglobin disorders, such as conventional gene therapy.

Scientists have found they can use a genome-editing technique to increase hemoglobin production, and they described this method in Nature Communications.
The team used transcription activator-like effector nucleases (TALENs) to introduce the hereditary persistence of fetal hemoglobin (HPFH)-175T4C point mutation into erythroid cell lines.
This served to switch on the fetal hemoglobin gene and increase hemoglobin production.
“Our laboratory study provides a proof of concept that changing just one letter of DNA in a gene could alleviate the symptoms of sickle cell anemia and thalassemia—inherited diseases in which people have damaged hemoglobin,” said Merlin Crossley, PhD, of the University of New South Wales in Sydney, Australia.
“Because the good genetic variation we introduced already exists in nature, this approach should be effective and safe. However, more research is needed before it can be tested in people as a possible cure for serious blood diseases.”
Dr Crossley and his colleagues introduced the HPFH-175T4C point mutation into erythroid cell lines using TALENs, which can be designed to cut a gene at a specific point, as well as provide the desired piece of donor DNA for insertion.
“Breaks in DNA can be lethal to cells, so they have in-built machinery to repair any nicks as soon as possible, by grabbing any spare DNA that seems to match . . . ,” Dr Crossley explained.
“We exploited this effect. When our genome-editing protein cuts the DNA, the cell quickly replaces it with the donor DNA that we have also provided.”
The researchers pointed out that the HPFH-175T4C point mutation increased fetal globin expression via de novo recruitment of the activator TAL1, which promoted chromatin looping of distal enhancers to the modified γ-globin promoter.
The team also said that, if their editing technique proves safe and effective in hematopoietic stem cells, it could offer significant advantages over other approaches used to treat hemoglobin disorders, such as conventional gene therapy.

Scientists have found they can use a genome-editing technique to increase hemoglobin production, and they described this method in Nature Communications.
The team used transcription activator-like effector nucleases (TALENs) to introduce the hereditary persistence of fetal hemoglobin (HPFH)-175T4C point mutation into erythroid cell lines.
This served to switch on the fetal hemoglobin gene and increase hemoglobin production.
“Our laboratory study provides a proof of concept that changing just one letter of DNA in a gene could alleviate the symptoms of sickle cell anemia and thalassemia—inherited diseases in which people have damaged hemoglobin,” said Merlin Crossley, PhD, of the University of New South Wales in Sydney, Australia.
“Because the good genetic variation we introduced already exists in nature, this approach should be effective and safe. However, more research is needed before it can be tested in people as a possible cure for serious blood diseases.”
Dr Crossley and his colleagues introduced the HPFH-175T4C point mutation into erythroid cell lines using TALENs, which can be designed to cut a gene at a specific point, as well as provide the desired piece of donor DNA for insertion.
“Breaks in DNA can be lethal to cells, so they have in-built machinery to repair any nicks as soon as possible, by grabbing any spare DNA that seems to match . . . ,” Dr Crossley explained.
“We exploited this effect. When our genome-editing protein cuts the DNA, the cell quickly replaces it with the donor DNA that we have also provided.”
The researchers pointed out that the HPFH-175T4C point mutation increased fetal globin expression via de novo recruitment of the activator TAL1, which promoted chromatin looping of distal enhancers to the modified γ-globin promoter.
The team also said that, if their editing technique proves safe and effective in hematopoietic stem cells, it could offer significant advantages over other approaches used to treat hemoglobin disorders, such as conventional gene therapy.
Modified T cells may treat GVHD
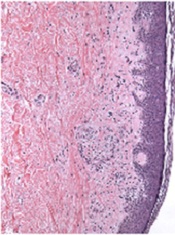
Image from PLOS ONE
A T-cell therapy designed to mitigate graft-vs-host disease (GVHD) is both feasible and safe, according to results of a pilot study published in Molecular Therapy.
To create this therapy, researchers transduced donor T cells with γ-retroviruses carrying a CD34-TK75 fusion gene.
The team said this allows them to track the cells via PET/CT and induce apoptosis by administering the antiviral drug ganciclovir if patients begin showing signs of GVHD.
“If donor T cells expand and cause severe graft-vs-host disease, we can give the patient ganciclovir, and it should kill the T cells and stop the process,” said study author John F. DiPersio, MD, PhD, of the Washington University School of Medicine in St Louis, Missouri.
Dr DiPersio and his colleagues tested the CD34-TK75-enriched T cells in 8 patients—4 with acute myeloid leukemia and 4 with myelodysplastic syndromes—who relapsed after allogeneic transplant. Six patients underwent [18F]FHBG PET/CT to track the T cells at several time points after infusion.
Patients received T-cell infusions ranging from 0.1 × 106 cells/kg to 1.3 × 106 cells/kg. Seven of the 8 patients received chemotherapy before T-cell infusion.
Four patients achieved a complete remission, 1 had progressive disease, and 3 patients died before the researchers could evaluate them for response.
Two patients developed GVHD—1 before T-cell infusion and 1 after. The patient who developed GVHD before infusion had grade 2 liver GVHD that resolved after an increased dose of steroids. The patient ultimately died of relapsed leukemia.
The patient who developed GVHD after T-cell infusion did not respond to chemotherapy or T-cell infusion. At 64 days after infusion, he exhibited symptoms consistent with grade 4 liver GVHD. He was treated with high-dose steroids and ganciclovir but did not respond. His primary cause of death was relapsed/progressive disease.
The mean overall survival after T-cell infusion was 165 days, 4 patients were still alive at 6 months, and 1 patient lived 408 days. All of the patients ultimately died.
The researchers said they did not detect any replication competent retrovirus or any antibodies against CD34-TK in any of the patients. The team also said there were no toxicities related to the CD34-TK75-enriched T cells.
Among patients who underwent imaging, there was no clear distinction between the [18F]FHBG biodistribution at baseline and later time points. And there was no difference between images in the patient who developed GVHD after infusion and patients who did not.
Past work from Dr DiPersio’s lab showed that leukemic mice that receive donor T cells and go on to develop GVHD show a characteristic migration pattern of the T cells through the body. When the cells gather early in the thymus, the mice develop GVHD. When T cells don’t migrate to the thymus, GVHD doesn’t occur.
In the current study, the patients received a relatively small number of CD34-TK75-enriched T cells, so the researchers were not able to show whether the migration patterns in mice were similar in humans.
However, based on the results of this study, Dr DiPersio and his colleagues are participating in a larger trial in partnership with a company based in Italy. The researchers are planning to include patients from multiple medical centers, and each participant should receive about 50 times more of the CD34-TK75-enriched T cells than were administered in this trial.
Washington University is the only center in the new trial that will be able to perform the imaging studies examining migration patterns of the T cells.
Image from PLOS ONE
A T-cell therapy designed to mitigate graft-vs-host disease (GVHD) is both feasible and safe, according to results of a pilot study published in Molecular Therapy.
To create this therapy, researchers transduced donor T cells with γ-retroviruses carrying a CD34-TK75 fusion gene.
The team said this allows them to track the cells via PET/CT and induce apoptosis by administering the antiviral drug ganciclovir if patients begin showing signs of GVHD.
“If donor T cells expand and cause severe graft-vs-host disease, we can give the patient ganciclovir, and it should kill the T cells and stop the process,” said study author John F. DiPersio, MD, PhD, of the Washington University School of Medicine in St Louis, Missouri.
Dr DiPersio and his colleagues tested the CD34-TK75-enriched T cells in 8 patients—4 with acute myeloid leukemia and 4 with myelodysplastic syndromes—who relapsed after allogeneic transplant. Six patients underwent [18F]FHBG PET/CT to track the T cells at several time points after infusion.
Patients received T-cell infusions ranging from 0.1 × 106 cells/kg to 1.3 × 106 cells/kg. Seven of the 8 patients received chemotherapy before T-cell infusion.
Four patients achieved a complete remission, 1 had progressive disease, and 3 patients died before the researchers could evaluate them for response.
Two patients developed GVHD—1 before T-cell infusion and 1 after. The patient who developed GVHD before infusion had grade 2 liver GVHD that resolved after an increased dose of steroids. The patient ultimately died of relapsed leukemia.
The patient who developed GVHD after T-cell infusion did not respond to chemotherapy or T-cell infusion. At 64 days after infusion, he exhibited symptoms consistent with grade 4 liver GVHD. He was treated with high-dose steroids and ganciclovir but did not respond. His primary cause of death was relapsed/progressive disease.
The mean overall survival after T-cell infusion was 165 days, 4 patients were still alive at 6 months, and 1 patient lived 408 days. All of the patients ultimately died.
The researchers said they did not detect any replication competent retrovirus or any antibodies against CD34-TK in any of the patients. The team also said there were no toxicities related to the CD34-TK75-enriched T cells.
Among patients who underwent imaging, there was no clear distinction between the [18F]FHBG biodistribution at baseline and later time points. And there was no difference between images in the patient who developed GVHD after infusion and patients who did not.
Past work from Dr DiPersio’s lab showed that leukemic mice that receive donor T cells and go on to develop GVHD show a characteristic migration pattern of the T cells through the body. When the cells gather early in the thymus, the mice develop GVHD. When T cells don’t migrate to the thymus, GVHD doesn’t occur.
In the current study, the patients received a relatively small number of CD34-TK75-enriched T cells, so the researchers were not able to show whether the migration patterns in mice were similar in humans.
However, based on the results of this study, Dr DiPersio and his colleagues are participating in a larger trial in partnership with a company based in Italy. The researchers are planning to include patients from multiple medical centers, and each participant should receive about 50 times more of the CD34-TK75-enriched T cells than were administered in this trial.
Washington University is the only center in the new trial that will be able to perform the imaging studies examining migration patterns of the T cells.
Image from PLOS ONE
A T-cell therapy designed to mitigate graft-vs-host disease (GVHD) is both feasible and safe, according to results of a pilot study published in Molecular Therapy.
To create this therapy, researchers transduced donor T cells with γ-retroviruses carrying a CD34-TK75 fusion gene.
The team said this allows them to track the cells via PET/CT and induce apoptosis by administering the antiviral drug ganciclovir if patients begin showing signs of GVHD.
“If donor T cells expand and cause severe graft-vs-host disease, we can give the patient ganciclovir, and it should kill the T cells and stop the process,” said study author John F. DiPersio, MD, PhD, of the Washington University School of Medicine in St Louis, Missouri.
Dr DiPersio and his colleagues tested the CD34-TK75-enriched T cells in 8 patients—4 with acute myeloid leukemia and 4 with myelodysplastic syndromes—who relapsed after allogeneic transplant. Six patients underwent [18F]FHBG PET/CT to track the T cells at several time points after infusion.
Patients received T-cell infusions ranging from 0.1 × 106 cells/kg to 1.3 × 106 cells/kg. Seven of the 8 patients received chemotherapy before T-cell infusion.
Four patients achieved a complete remission, 1 had progressive disease, and 3 patients died before the researchers could evaluate them for response.
Two patients developed GVHD—1 before T-cell infusion and 1 after. The patient who developed GVHD before infusion had grade 2 liver GVHD that resolved after an increased dose of steroids. The patient ultimately died of relapsed leukemia.
The patient who developed GVHD after T-cell infusion did not respond to chemotherapy or T-cell infusion. At 64 days after infusion, he exhibited symptoms consistent with grade 4 liver GVHD. He was treated with high-dose steroids and ganciclovir but did not respond. His primary cause of death was relapsed/progressive disease.
The mean overall survival after T-cell infusion was 165 days, 4 patients were still alive at 6 months, and 1 patient lived 408 days. All of the patients ultimately died.
The researchers said they did not detect any replication competent retrovirus or any antibodies against CD34-TK in any of the patients. The team also said there were no toxicities related to the CD34-TK75-enriched T cells.
Among patients who underwent imaging, there was no clear distinction between the [18F]FHBG biodistribution at baseline and later time points. And there was no difference between images in the patient who developed GVHD after infusion and patients who did not.
Past work from Dr DiPersio’s lab showed that leukemic mice that receive donor T cells and go on to develop GVHD show a characteristic migration pattern of the T cells through the body. When the cells gather early in the thymus, the mice develop GVHD. When T cells don’t migrate to the thymus, GVHD doesn’t occur.
In the current study, the patients received a relatively small number of CD34-TK75-enriched T cells, so the researchers were not able to show whether the migration patterns in mice were similar in humans.
However, based on the results of this study, Dr DiPersio and his colleagues are participating in a larger trial in partnership with a company based in Italy. The researchers are planning to include patients from multiple medical centers, and each participant should receive about 50 times more of the CD34-TK75-enriched T cells than were administered in this trial.
Washington University is the only center in the new trial that will be able to perform the imaging studies examining migration patterns of the T cells.