User login
An off-the-shelf drug to rival CAR T cells: ‘very exciting’
ORLANDO – An investigational drug that can achieve the same results as complex cell therapy is creating a buzz at the American Society of Hematology (ASH) meeting.
For the last few years, attention at this meeting has focused on the chimeric antigen receptor (CAR) T cells, mainly “because of their incredible efficacy,” commented ASH Secretary Robert A. Brodsky, MD, professor of medicine and director of the division of hematology at Johns Hopkins University, Baltimore.
But new results with an off-the-shelf product are “very exciting,” he said, because the drug can be given immediately and appears to achieve similar results.
The new product is mosunetuzumab (Genentech/Roche), a bispecific antibody that targets both CD3 (on the surface of T cells) and CD20 (on the surface of B cells). It works by redirecting T cells to engage and eliminate malignant B cells.
“The concept here is that this monoclonal antibody engages T cells and directs their cytotoxicity against B cells – it’s basically an antibody using the patient’s own T cells to do what a CAR T cell would do,” Dr. Brodsky explained.
However, unlike CAR T cells, which are prepared for each individual patient in a complex process that involves genetic engineering that can take several weeks, mosunetuzumab is an off-the-shelf product that can be given to patients immediately (by intravenous infusion).
This is important, commented Dr. Brodsky, because very-poor-prognosis patients can deteriorate rapidly, and some may not survive while the CAR T cells are being made.
Clinical trial results
Clinical results come from a phase 1/1b trial (known as GO29781) conducted in 270 patients with poor-prognosis refractory/relapsed non-Hodgkin’s lymphoma. These patients had previously been treated with a median of three therapies; in addition, 30 patients (11%) were resistant to or had relapsed after an initial response to CAR T-cell therapy, and 77 patients (29%) had progressed after a stem cell transplant.
“These patients had no available therapy that would be expected to improve survival,” noted lead author Stephen J. Schuster, MD, of Abramson Cancer Center at the University of Pennsylvania in Philadelphia.
All patients received mosunetuzumab with an initial treatment of eight cycles. Patients who achieved complete remission (CR) stopped therapy, while patients who had a partial response or had stable disease, continued treatment for 17 cycles.
Two-thirds of patients (n = 180; 67%) had aggressive lymphomas, mainly diffuse large B-cell lymphoma (DLBCL; n = 117), while 85 patients (31%) had indolent disease, mainly follicular lymphoma (FL; n = 82). Objective responses were seen in 46 of 124 patients (37%) with aggressive lymphomas, and 24 (19%) of these patients achieved a CR.
Among patients with indolent lymphoma, objective responses were seen in 42 of 67 patients (63%), and 29 of 67 (43%) had CR.
The complete remissions appear to be long lasting, Dr. Schuster commented. With a median follow-up of 6 months since achieving CR, 17 of 24 patients (71%) with aggressive lymphoma and 24 of 29 patients (83%) with indolent lymphomas remained free of disease.
“Some patients have remained in remission without additional therapy for more than a year,” he commented.
In the subgroup of 30 patients who had previously received CAR T-cell therapy, the objective response rate was 38.9%, and CR was achieved in 4 patients (22%). These rates are similar to what was seen in patients with aggressive lymphoma who had not previously received CAR T-cell therapy, Dr. Schuster commented.
He also noted that in some of these patients, molecular testing showed that the previously administered CAR T cells increased in number. This suggests that, in addition to its ability to kill cancerous B cells, mosunetuzumab may also help augment the effect of the prior CAR T-cell treatment.
Dr. Schuster also highlighted the results of repeat treatment with mosunetuzumab. Patients who achieved CR stopped treatment – but if they relapsed, they were treated again, and the responses seen on this repeat treatment were similar to those seen with initial treatment. “This is not seen with the CAR T cells,” he noted.
Adverse events with mosunetuzumab were similar to those seen with CAR T cells, he noted, namely cytokine release syndrome, which was mostly mild and seen in 29% of patients, and neurologic toxicity, which was moderately severe in 4% patients.
Overall, the results show that “mosunetuzumab generates long-lasting responses with a very tolerable safety profile in patients with B-cell non-Hodgkin lymphomas for whom multiple prior treatments have failed and whose prognosis is poor. Of particular interest, we are seeing durable complete remissions in patients whose lymphomas progressed after CAR T,” Dr. Schuster commented in a statement.
Approached for comment, Peter Martin MD, chief of the Lymphoma Program at Weill Cornell Medicine, New York, and New York-Presbyterian, said he was excited to see these new data. “It’s good news any time we find something with the potential to save lives.”
“The more options that we have to offer to people with lymphoma the better,” he told Medscape Medical News. “There will always be scenarios where one approach might be better than another. I think there is a good chance that bispecific antibodies will have fairly broad approval in previously treated DLBCL. In many centers, it may be that bispecific antibodies are used most frequently post–CAR T cells, while in other areas people who aren’t candidates for CAR T cells or can’t receive them for whatever reason [could benefit from this new approach].”
Laurie Sehn, MD, MPH, medical oncologist at the University of British Columbia in Vancouver, Canada, and chair of the Lymphoma Tumour Group, as well as an associate editor of ASH journal Blood, also commented for Medscape Medical News.
She agreed that the new data are exciting and noted that this abstract was chosen for the plenary session. She thought the data in the 30 patients who had already been treated with CAR T cells was interesting. “This is a patient population with no other options that offer durable benefit, and mosunetuzumab clearly has clinical activity, with encouraging responses.”
Dr. Sehn also noted that toxicity seen with the drug was “far less” than has been seen with CAR T cells, and the risk of high-grade cytokine release syndrome and neurological toxicity is “very low.”
There are several other new products that are using this bispecific technology, she noted. One example is Regeneron’s REGN1979, a bispecific antibody targeting CD20 and CD3, which is also being investigated in a clinical trial in relapsed/refractory B-cell non-Hodgkin’s lymphoma, including in patients who were previously treated with CAR T cells (abstract 762).
How would it be used clinically?
In response to a question from Medscape Medical News, Dr. Schuster suggested that initial use of mosunetuzumab would be in patients who have already tried CAR T-cell therapy and had either not responded or relapsed – in lymphoma, this is about two-thirds of patients who are treated with this approach. This group of patients represents an unmet medical need, and this indication may be the quickest route to approval, he suggested.
Gary Schiller, MD, from UCLA Health, who moderated the press briefing agreed, and said this would be the quickest route to market because it would need only a phase 2 clinical trial in this specific patient population. But this would likely be only the first use for this product, and then it could be expanded to a broader patient population, he added.
Another use would for mosunetuzumab would be to enhance CAR T-cell responses by redirecting the CAR T cells to other antigens without doing any additional gene editing, Dr. Schuster commented. The idea here is to “revive” previously administered CAR T cells that have stopped working, Dr. Schiller added.
This is a chemotherapy-free approach, Dr. Schuster emphasized. “In patients who have not had a lot of chemotherapy, you can see an increase in T cells,” he commented.
Mosunetuzumab “stimulates and invigorates T cells,” and it could be useful as a pretreatment or a bridge to CAR T-cell therapy, he said.
So the product could be used before CAR T-cell therapy, and equally it could be used after CAR T-cell therapy because it could boost responses in both cases.
“Larger, randomized trials are needed to further confirm these promising data and determine whether the treatment benefit of mosunetuzumab is enhanced when it is used earlier in the course of lymphoma therapy or in combination with other agents,” he added.
Genentech says that mosunetuzumab and another bispecific antibody, CD20-TCB, are being evaluated in a robust clinical development program, both as a monotherapies and in combination with other therapies, in both aggressive and indolent non-Hodgkin’s lymphoma.
Dr. Schuster reported relationships with Celgene, Genentech, Merck, Pharmacyclics, Acerta, AbbVie, Gilead, Nordic Nanovector, Pfizer, AstraZeneca, Loxo Oncology, and Novartis. Coauthors also have multiple disclosures, and several are employees of Genentech and Roche. Dr. Sehn consults with several pharmaceutics companies, including Verastem, Roche/Genentech, Morphosys, Takeda, Janssen, Lundbeck, Amgen, Teva, and AbbVie.
A version of this story originally appeared on Medscape.com.
ORLANDO – An investigational drug that can achieve the same results as complex cell therapy is creating a buzz at the American Society of Hematology (ASH) meeting.
For the last few years, attention at this meeting has focused on the chimeric antigen receptor (CAR) T cells, mainly “because of their incredible efficacy,” commented ASH Secretary Robert A. Brodsky, MD, professor of medicine and director of the division of hematology at Johns Hopkins University, Baltimore.
But new results with an off-the-shelf product are “very exciting,” he said, because the drug can be given immediately and appears to achieve similar results.
The new product is mosunetuzumab (Genentech/Roche), a bispecific antibody that targets both CD3 (on the surface of T cells) and CD20 (on the surface of B cells). It works by redirecting T cells to engage and eliminate malignant B cells.
“The concept here is that this monoclonal antibody engages T cells and directs their cytotoxicity against B cells – it’s basically an antibody using the patient’s own T cells to do what a CAR T cell would do,” Dr. Brodsky explained.
However, unlike CAR T cells, which are prepared for each individual patient in a complex process that involves genetic engineering that can take several weeks, mosunetuzumab is an off-the-shelf product that can be given to patients immediately (by intravenous infusion).
This is important, commented Dr. Brodsky, because very-poor-prognosis patients can deteriorate rapidly, and some may not survive while the CAR T cells are being made.
Clinical trial results
Clinical results come from a phase 1/1b trial (known as GO29781) conducted in 270 patients with poor-prognosis refractory/relapsed non-Hodgkin’s lymphoma. These patients had previously been treated with a median of three therapies; in addition, 30 patients (11%) were resistant to or had relapsed after an initial response to CAR T-cell therapy, and 77 patients (29%) had progressed after a stem cell transplant.
“These patients had no available therapy that would be expected to improve survival,” noted lead author Stephen J. Schuster, MD, of Abramson Cancer Center at the University of Pennsylvania in Philadelphia.
All patients received mosunetuzumab with an initial treatment of eight cycles. Patients who achieved complete remission (CR) stopped therapy, while patients who had a partial response or had stable disease, continued treatment for 17 cycles.
Two-thirds of patients (n = 180; 67%) had aggressive lymphomas, mainly diffuse large B-cell lymphoma (DLBCL; n = 117), while 85 patients (31%) had indolent disease, mainly follicular lymphoma (FL; n = 82). Objective responses were seen in 46 of 124 patients (37%) with aggressive lymphomas, and 24 (19%) of these patients achieved a CR.
Among patients with indolent lymphoma, objective responses were seen in 42 of 67 patients (63%), and 29 of 67 (43%) had CR.
The complete remissions appear to be long lasting, Dr. Schuster commented. With a median follow-up of 6 months since achieving CR, 17 of 24 patients (71%) with aggressive lymphoma and 24 of 29 patients (83%) with indolent lymphomas remained free of disease.
“Some patients have remained in remission without additional therapy for more than a year,” he commented.
In the subgroup of 30 patients who had previously received CAR T-cell therapy, the objective response rate was 38.9%, and CR was achieved in 4 patients (22%). These rates are similar to what was seen in patients with aggressive lymphoma who had not previously received CAR T-cell therapy, Dr. Schuster commented.
He also noted that in some of these patients, molecular testing showed that the previously administered CAR T cells increased in number. This suggests that, in addition to its ability to kill cancerous B cells, mosunetuzumab may also help augment the effect of the prior CAR T-cell treatment.
Dr. Schuster also highlighted the results of repeat treatment with mosunetuzumab. Patients who achieved CR stopped treatment – but if they relapsed, they were treated again, and the responses seen on this repeat treatment were similar to those seen with initial treatment. “This is not seen with the CAR T cells,” he noted.
Adverse events with mosunetuzumab were similar to those seen with CAR T cells, he noted, namely cytokine release syndrome, which was mostly mild and seen in 29% of patients, and neurologic toxicity, which was moderately severe in 4% patients.
Overall, the results show that “mosunetuzumab generates long-lasting responses with a very tolerable safety profile in patients with B-cell non-Hodgkin lymphomas for whom multiple prior treatments have failed and whose prognosis is poor. Of particular interest, we are seeing durable complete remissions in patients whose lymphomas progressed after CAR T,” Dr. Schuster commented in a statement.
Approached for comment, Peter Martin MD, chief of the Lymphoma Program at Weill Cornell Medicine, New York, and New York-Presbyterian, said he was excited to see these new data. “It’s good news any time we find something with the potential to save lives.”
“The more options that we have to offer to people with lymphoma the better,” he told Medscape Medical News. “There will always be scenarios where one approach might be better than another. I think there is a good chance that bispecific antibodies will have fairly broad approval in previously treated DLBCL. In many centers, it may be that bispecific antibodies are used most frequently post–CAR T cells, while in other areas people who aren’t candidates for CAR T cells or can’t receive them for whatever reason [could benefit from this new approach].”
Laurie Sehn, MD, MPH, medical oncologist at the University of British Columbia in Vancouver, Canada, and chair of the Lymphoma Tumour Group, as well as an associate editor of ASH journal Blood, also commented for Medscape Medical News.
She agreed that the new data are exciting and noted that this abstract was chosen for the plenary session. She thought the data in the 30 patients who had already been treated with CAR T cells was interesting. “This is a patient population with no other options that offer durable benefit, and mosunetuzumab clearly has clinical activity, with encouraging responses.”
Dr. Sehn also noted that toxicity seen with the drug was “far less” than has been seen with CAR T cells, and the risk of high-grade cytokine release syndrome and neurological toxicity is “very low.”
There are several other new products that are using this bispecific technology, she noted. One example is Regeneron’s REGN1979, a bispecific antibody targeting CD20 and CD3, which is also being investigated in a clinical trial in relapsed/refractory B-cell non-Hodgkin’s lymphoma, including in patients who were previously treated with CAR T cells (abstract 762).
How would it be used clinically?
In response to a question from Medscape Medical News, Dr. Schuster suggested that initial use of mosunetuzumab would be in patients who have already tried CAR T-cell therapy and had either not responded or relapsed – in lymphoma, this is about two-thirds of patients who are treated with this approach. This group of patients represents an unmet medical need, and this indication may be the quickest route to approval, he suggested.
Gary Schiller, MD, from UCLA Health, who moderated the press briefing agreed, and said this would be the quickest route to market because it would need only a phase 2 clinical trial in this specific patient population. But this would likely be only the first use for this product, and then it could be expanded to a broader patient population, he added.
Another use would for mosunetuzumab would be to enhance CAR T-cell responses by redirecting the CAR T cells to other antigens without doing any additional gene editing, Dr. Schuster commented. The idea here is to “revive” previously administered CAR T cells that have stopped working, Dr. Schiller added.
This is a chemotherapy-free approach, Dr. Schuster emphasized. “In patients who have not had a lot of chemotherapy, you can see an increase in T cells,” he commented.
Mosunetuzumab “stimulates and invigorates T cells,” and it could be useful as a pretreatment or a bridge to CAR T-cell therapy, he said.
So the product could be used before CAR T-cell therapy, and equally it could be used after CAR T-cell therapy because it could boost responses in both cases.
“Larger, randomized trials are needed to further confirm these promising data and determine whether the treatment benefit of mosunetuzumab is enhanced when it is used earlier in the course of lymphoma therapy or in combination with other agents,” he added.
Genentech says that mosunetuzumab and another bispecific antibody, CD20-TCB, are being evaluated in a robust clinical development program, both as a monotherapies and in combination with other therapies, in both aggressive and indolent non-Hodgkin’s lymphoma.
Dr. Schuster reported relationships with Celgene, Genentech, Merck, Pharmacyclics, Acerta, AbbVie, Gilead, Nordic Nanovector, Pfizer, AstraZeneca, Loxo Oncology, and Novartis. Coauthors also have multiple disclosures, and several are employees of Genentech and Roche. Dr. Sehn consults with several pharmaceutics companies, including Verastem, Roche/Genentech, Morphosys, Takeda, Janssen, Lundbeck, Amgen, Teva, and AbbVie.
A version of this story originally appeared on Medscape.com.
ORLANDO – An investigational drug that can achieve the same results as complex cell therapy is creating a buzz at the American Society of Hematology (ASH) meeting.
For the last few years, attention at this meeting has focused on the chimeric antigen receptor (CAR) T cells, mainly “because of their incredible efficacy,” commented ASH Secretary Robert A. Brodsky, MD, professor of medicine and director of the division of hematology at Johns Hopkins University, Baltimore.
But new results with an off-the-shelf product are “very exciting,” he said, because the drug can be given immediately and appears to achieve similar results.
The new product is mosunetuzumab (Genentech/Roche), a bispecific antibody that targets both CD3 (on the surface of T cells) and CD20 (on the surface of B cells). It works by redirecting T cells to engage and eliminate malignant B cells.
“The concept here is that this monoclonal antibody engages T cells and directs their cytotoxicity against B cells – it’s basically an antibody using the patient’s own T cells to do what a CAR T cell would do,” Dr. Brodsky explained.
However, unlike CAR T cells, which are prepared for each individual patient in a complex process that involves genetic engineering that can take several weeks, mosunetuzumab is an off-the-shelf product that can be given to patients immediately (by intravenous infusion).
This is important, commented Dr. Brodsky, because very-poor-prognosis patients can deteriorate rapidly, and some may not survive while the CAR T cells are being made.
Clinical trial results
Clinical results come from a phase 1/1b trial (known as GO29781) conducted in 270 patients with poor-prognosis refractory/relapsed non-Hodgkin’s lymphoma. These patients had previously been treated with a median of three therapies; in addition, 30 patients (11%) were resistant to or had relapsed after an initial response to CAR T-cell therapy, and 77 patients (29%) had progressed after a stem cell transplant.
“These patients had no available therapy that would be expected to improve survival,” noted lead author Stephen J. Schuster, MD, of Abramson Cancer Center at the University of Pennsylvania in Philadelphia.
All patients received mosunetuzumab with an initial treatment of eight cycles. Patients who achieved complete remission (CR) stopped therapy, while patients who had a partial response or had stable disease, continued treatment for 17 cycles.
Two-thirds of patients (n = 180; 67%) had aggressive lymphomas, mainly diffuse large B-cell lymphoma (DLBCL; n = 117), while 85 patients (31%) had indolent disease, mainly follicular lymphoma (FL; n = 82). Objective responses were seen in 46 of 124 patients (37%) with aggressive lymphomas, and 24 (19%) of these patients achieved a CR.
Among patients with indolent lymphoma, objective responses were seen in 42 of 67 patients (63%), and 29 of 67 (43%) had CR.
The complete remissions appear to be long lasting, Dr. Schuster commented. With a median follow-up of 6 months since achieving CR, 17 of 24 patients (71%) with aggressive lymphoma and 24 of 29 patients (83%) with indolent lymphomas remained free of disease.
“Some patients have remained in remission without additional therapy for more than a year,” he commented.
In the subgroup of 30 patients who had previously received CAR T-cell therapy, the objective response rate was 38.9%, and CR was achieved in 4 patients (22%). These rates are similar to what was seen in patients with aggressive lymphoma who had not previously received CAR T-cell therapy, Dr. Schuster commented.
He also noted that in some of these patients, molecular testing showed that the previously administered CAR T cells increased in number. This suggests that, in addition to its ability to kill cancerous B cells, mosunetuzumab may also help augment the effect of the prior CAR T-cell treatment.
Dr. Schuster also highlighted the results of repeat treatment with mosunetuzumab. Patients who achieved CR stopped treatment – but if they relapsed, they were treated again, and the responses seen on this repeat treatment were similar to those seen with initial treatment. “This is not seen with the CAR T cells,” he noted.
Adverse events with mosunetuzumab were similar to those seen with CAR T cells, he noted, namely cytokine release syndrome, which was mostly mild and seen in 29% of patients, and neurologic toxicity, which was moderately severe in 4% patients.
Overall, the results show that “mosunetuzumab generates long-lasting responses with a very tolerable safety profile in patients with B-cell non-Hodgkin lymphomas for whom multiple prior treatments have failed and whose prognosis is poor. Of particular interest, we are seeing durable complete remissions in patients whose lymphomas progressed after CAR T,” Dr. Schuster commented in a statement.
Approached for comment, Peter Martin MD, chief of the Lymphoma Program at Weill Cornell Medicine, New York, and New York-Presbyterian, said he was excited to see these new data. “It’s good news any time we find something with the potential to save lives.”
“The more options that we have to offer to people with lymphoma the better,” he told Medscape Medical News. “There will always be scenarios where one approach might be better than another. I think there is a good chance that bispecific antibodies will have fairly broad approval in previously treated DLBCL. In many centers, it may be that bispecific antibodies are used most frequently post–CAR T cells, while in other areas people who aren’t candidates for CAR T cells or can’t receive them for whatever reason [could benefit from this new approach].”
Laurie Sehn, MD, MPH, medical oncologist at the University of British Columbia in Vancouver, Canada, and chair of the Lymphoma Tumour Group, as well as an associate editor of ASH journal Blood, also commented for Medscape Medical News.
She agreed that the new data are exciting and noted that this abstract was chosen for the plenary session. She thought the data in the 30 patients who had already been treated with CAR T cells was interesting. “This is a patient population with no other options that offer durable benefit, and mosunetuzumab clearly has clinical activity, with encouraging responses.”
Dr. Sehn also noted that toxicity seen with the drug was “far less” than has been seen with CAR T cells, and the risk of high-grade cytokine release syndrome and neurological toxicity is “very low.”
There are several other new products that are using this bispecific technology, she noted. One example is Regeneron’s REGN1979, a bispecific antibody targeting CD20 and CD3, which is also being investigated in a clinical trial in relapsed/refractory B-cell non-Hodgkin’s lymphoma, including in patients who were previously treated with CAR T cells (abstract 762).
How would it be used clinically?
In response to a question from Medscape Medical News, Dr. Schuster suggested that initial use of mosunetuzumab would be in patients who have already tried CAR T-cell therapy and had either not responded or relapsed – in lymphoma, this is about two-thirds of patients who are treated with this approach. This group of patients represents an unmet medical need, and this indication may be the quickest route to approval, he suggested.
Gary Schiller, MD, from UCLA Health, who moderated the press briefing agreed, and said this would be the quickest route to market because it would need only a phase 2 clinical trial in this specific patient population. But this would likely be only the first use for this product, and then it could be expanded to a broader patient population, he added.
Another use would for mosunetuzumab would be to enhance CAR T-cell responses by redirecting the CAR T cells to other antigens without doing any additional gene editing, Dr. Schuster commented. The idea here is to “revive” previously administered CAR T cells that have stopped working, Dr. Schiller added.
This is a chemotherapy-free approach, Dr. Schuster emphasized. “In patients who have not had a lot of chemotherapy, you can see an increase in T cells,” he commented.
Mosunetuzumab “stimulates and invigorates T cells,” and it could be useful as a pretreatment or a bridge to CAR T-cell therapy, he said.
So the product could be used before CAR T-cell therapy, and equally it could be used after CAR T-cell therapy because it could boost responses in both cases.
“Larger, randomized trials are needed to further confirm these promising data and determine whether the treatment benefit of mosunetuzumab is enhanced when it is used earlier in the course of lymphoma therapy or in combination with other agents,” he added.
Genentech says that mosunetuzumab and another bispecific antibody, CD20-TCB, are being evaluated in a robust clinical development program, both as a monotherapies and in combination with other therapies, in both aggressive and indolent non-Hodgkin’s lymphoma.
Dr. Schuster reported relationships with Celgene, Genentech, Merck, Pharmacyclics, Acerta, AbbVie, Gilead, Nordic Nanovector, Pfizer, AstraZeneca, Loxo Oncology, and Novartis. Coauthors also have multiple disclosures, and several are employees of Genentech and Roche. Dr. Sehn consults with several pharmaceutics companies, including Verastem, Roche/Genentech, Morphosys, Takeda, Janssen, Lundbeck, Amgen, Teva, and AbbVie.
A version of this story originally appeared on Medscape.com.
Orelabrutinib could be ‘preferred’ BTK inhibitor for MCL
ORLANDO – A novel Bruton tyrosine kinase inhibitor has produced favorable results in patients with relapsed or refractory mantle cell lymphoma, according to findings presented at the annual meeting of the American Society of Hematology.
In a phase 2 trial, orelabrutinib produced an overall response rate of 86% and a 12-month progression-free survival rate of 64%. Safety results with orelabrutinib were superior to historical results with ibrutinib.
The efficacy and safety profile of orelabrutinib, as well as its “convenient” dosing, may make it the “preferred therapeutic choice for B-cell malignancy,” said Lijuan Deng, MD, PhD, of Peking University Cancer Hospital & Institute, Beijing, who presented the phase 2 trial of orelabrutinib at ASH 2019.
The trial enrolled 106 patients with relapsed/refractory mantle cell lymphoma who were treated at 22 centers in China. At baseline, the patients had a median age of 62 years (range, 37-73 years), and 79.2% were men. Most patients (94.4%) had stage III-IV disease.
Prior therapies included CHOP (cyclophosphamide, doxorubicin, vincristine, and prednisolone)-based (69.8%), EPOCH (etoposide, prednisone, vincristine, cyclophosphamide, and doxorubicin)-based (22.6%), DHAP (dexamethasone, cytarabine, and cisplatin)-based (22.6%), CVAD (cyclophosphamide, vincristine, doxorubicin, dexamethasone)-based (12.3%), and ESHAP (etoposide, methylprednisolone, cytarabine, and cisplatin)-based (4.7%) regimens, and 88.7% of patients had received prior anti-CD20 therapy.
Patients received orelabrutinib at 100 mg twice daily (n = 20) or 150 mg once a day (n = 86). All 106 patients were evaluable for safety, and 99 were evaluable for efficacy.
Efficacy
“Orelabrutinib achieved high response and durable remissions,” Dr. Deng said.
The overall response rate was 85.9% in the evaluable efficacy population and 83.5% in the 150-mg dosing arm. The complete response rates were 27.3% and 29.1%, respectively. The median time to response, overall, was 1.9 months.
The median duration of response and median progression-free survival were not reached at a median follow-up of 10.5 months. At 12 months, 74.3% of patients were still in response, and the progression-free survival rate was 64%.
Safety
Most adverse events were grade 1-2 in nature. The most common grade 3 or higher events were platelet count decrease (11.3%), neutrophil count decrease (8.5%), anemia (7.5%), hypertension (3.8%), pneumonia (2.8%), white blood count decrease (1.9%), and hypokalemia (1.9%).
Adverse events of interest included grade 3 or higher hypertension (3.8%), diarrhea (6.6%), and infection (10.4%), as well as secondary malignancy (0.9%, n = 1). There were no cases of grade 3 or higher hemorrhage, grade 3 or higher atrial fibrillation/flutter, or grade 5 treatment-related adverse events.
Dr. Deng noted that rates of grade 3 or higher hemorrhage, atrial fibrillation, diarrhea, and infection, as well as rates of secondary malignancies, have historically been higher with ibrutinib (Blood. 2015 Aug 6;126[6]:739-45; Lancet. 2016 Feb 20;387[10020]:770-8).
“Orelabrutinib has an improved safety profile in patients with relapsed or refractory mantle cell lymphoma,” Dr. Deng said. “The most common adverse events were cytopenia and infections, which are considered mechanism based.”
The study was sponsored by InnoCare Pharma. Dr. Deng reported having no conflicts of interest.
SOURCE: Deng L et al. ASH 2019, Abstract 755.
ORLANDO – A novel Bruton tyrosine kinase inhibitor has produced favorable results in patients with relapsed or refractory mantle cell lymphoma, according to findings presented at the annual meeting of the American Society of Hematology.
In a phase 2 trial, orelabrutinib produced an overall response rate of 86% and a 12-month progression-free survival rate of 64%. Safety results with orelabrutinib were superior to historical results with ibrutinib.
The efficacy and safety profile of orelabrutinib, as well as its “convenient” dosing, may make it the “preferred therapeutic choice for B-cell malignancy,” said Lijuan Deng, MD, PhD, of Peking University Cancer Hospital & Institute, Beijing, who presented the phase 2 trial of orelabrutinib at ASH 2019.
The trial enrolled 106 patients with relapsed/refractory mantle cell lymphoma who were treated at 22 centers in China. At baseline, the patients had a median age of 62 years (range, 37-73 years), and 79.2% were men. Most patients (94.4%) had stage III-IV disease.
Prior therapies included CHOP (cyclophosphamide, doxorubicin, vincristine, and prednisolone)-based (69.8%), EPOCH (etoposide, prednisone, vincristine, cyclophosphamide, and doxorubicin)-based (22.6%), DHAP (dexamethasone, cytarabine, and cisplatin)-based (22.6%), CVAD (cyclophosphamide, vincristine, doxorubicin, dexamethasone)-based (12.3%), and ESHAP (etoposide, methylprednisolone, cytarabine, and cisplatin)-based (4.7%) regimens, and 88.7% of patients had received prior anti-CD20 therapy.
Patients received orelabrutinib at 100 mg twice daily (n = 20) or 150 mg once a day (n = 86). All 106 patients were evaluable for safety, and 99 were evaluable for efficacy.
Efficacy
“Orelabrutinib achieved high response and durable remissions,” Dr. Deng said.
The overall response rate was 85.9% in the evaluable efficacy population and 83.5% in the 150-mg dosing arm. The complete response rates were 27.3% and 29.1%, respectively. The median time to response, overall, was 1.9 months.
The median duration of response and median progression-free survival were not reached at a median follow-up of 10.5 months. At 12 months, 74.3% of patients were still in response, and the progression-free survival rate was 64%.
Safety
Most adverse events were grade 1-2 in nature. The most common grade 3 or higher events were platelet count decrease (11.3%), neutrophil count decrease (8.5%), anemia (7.5%), hypertension (3.8%), pneumonia (2.8%), white blood count decrease (1.9%), and hypokalemia (1.9%).
Adverse events of interest included grade 3 or higher hypertension (3.8%), diarrhea (6.6%), and infection (10.4%), as well as secondary malignancy (0.9%, n = 1). There were no cases of grade 3 or higher hemorrhage, grade 3 or higher atrial fibrillation/flutter, or grade 5 treatment-related adverse events.
Dr. Deng noted that rates of grade 3 or higher hemorrhage, atrial fibrillation, diarrhea, and infection, as well as rates of secondary malignancies, have historically been higher with ibrutinib (Blood. 2015 Aug 6;126[6]:739-45; Lancet. 2016 Feb 20;387[10020]:770-8).
“Orelabrutinib has an improved safety profile in patients with relapsed or refractory mantle cell lymphoma,” Dr. Deng said. “The most common adverse events were cytopenia and infections, which are considered mechanism based.”
The study was sponsored by InnoCare Pharma. Dr. Deng reported having no conflicts of interest.
SOURCE: Deng L et al. ASH 2019, Abstract 755.
ORLANDO – A novel Bruton tyrosine kinase inhibitor has produced favorable results in patients with relapsed or refractory mantle cell lymphoma, according to findings presented at the annual meeting of the American Society of Hematology.
In a phase 2 trial, orelabrutinib produced an overall response rate of 86% and a 12-month progression-free survival rate of 64%. Safety results with orelabrutinib were superior to historical results with ibrutinib.
The efficacy and safety profile of orelabrutinib, as well as its “convenient” dosing, may make it the “preferred therapeutic choice for B-cell malignancy,” said Lijuan Deng, MD, PhD, of Peking University Cancer Hospital & Institute, Beijing, who presented the phase 2 trial of orelabrutinib at ASH 2019.
The trial enrolled 106 patients with relapsed/refractory mantle cell lymphoma who were treated at 22 centers in China. At baseline, the patients had a median age of 62 years (range, 37-73 years), and 79.2% were men. Most patients (94.4%) had stage III-IV disease.
Prior therapies included CHOP (cyclophosphamide, doxorubicin, vincristine, and prednisolone)-based (69.8%), EPOCH (etoposide, prednisone, vincristine, cyclophosphamide, and doxorubicin)-based (22.6%), DHAP (dexamethasone, cytarabine, and cisplatin)-based (22.6%), CVAD (cyclophosphamide, vincristine, doxorubicin, dexamethasone)-based (12.3%), and ESHAP (etoposide, methylprednisolone, cytarabine, and cisplatin)-based (4.7%) regimens, and 88.7% of patients had received prior anti-CD20 therapy.
Patients received orelabrutinib at 100 mg twice daily (n = 20) or 150 mg once a day (n = 86). All 106 patients were evaluable for safety, and 99 were evaluable for efficacy.
Efficacy
“Orelabrutinib achieved high response and durable remissions,” Dr. Deng said.
The overall response rate was 85.9% in the evaluable efficacy population and 83.5% in the 150-mg dosing arm. The complete response rates were 27.3% and 29.1%, respectively. The median time to response, overall, was 1.9 months.
The median duration of response and median progression-free survival were not reached at a median follow-up of 10.5 months. At 12 months, 74.3% of patients were still in response, and the progression-free survival rate was 64%.
Safety
Most adverse events were grade 1-2 in nature. The most common grade 3 or higher events were platelet count decrease (11.3%), neutrophil count decrease (8.5%), anemia (7.5%), hypertension (3.8%), pneumonia (2.8%), white blood count decrease (1.9%), and hypokalemia (1.9%).
Adverse events of interest included grade 3 or higher hypertension (3.8%), diarrhea (6.6%), and infection (10.4%), as well as secondary malignancy (0.9%, n = 1). There were no cases of grade 3 or higher hemorrhage, grade 3 or higher atrial fibrillation/flutter, or grade 5 treatment-related adverse events.
Dr. Deng noted that rates of grade 3 or higher hemorrhage, atrial fibrillation, diarrhea, and infection, as well as rates of secondary malignancies, have historically been higher with ibrutinib (Blood. 2015 Aug 6;126[6]:739-45; Lancet. 2016 Feb 20;387[10020]:770-8).
“Orelabrutinib has an improved safety profile in patients with relapsed or refractory mantle cell lymphoma,” Dr. Deng said. “The most common adverse events were cytopenia and infections, which are considered mechanism based.”
The study was sponsored by InnoCare Pharma. Dr. Deng reported having no conflicts of interest.
SOURCE: Deng L et al. ASH 2019, Abstract 755.
REPORTING FROM ASH 2019
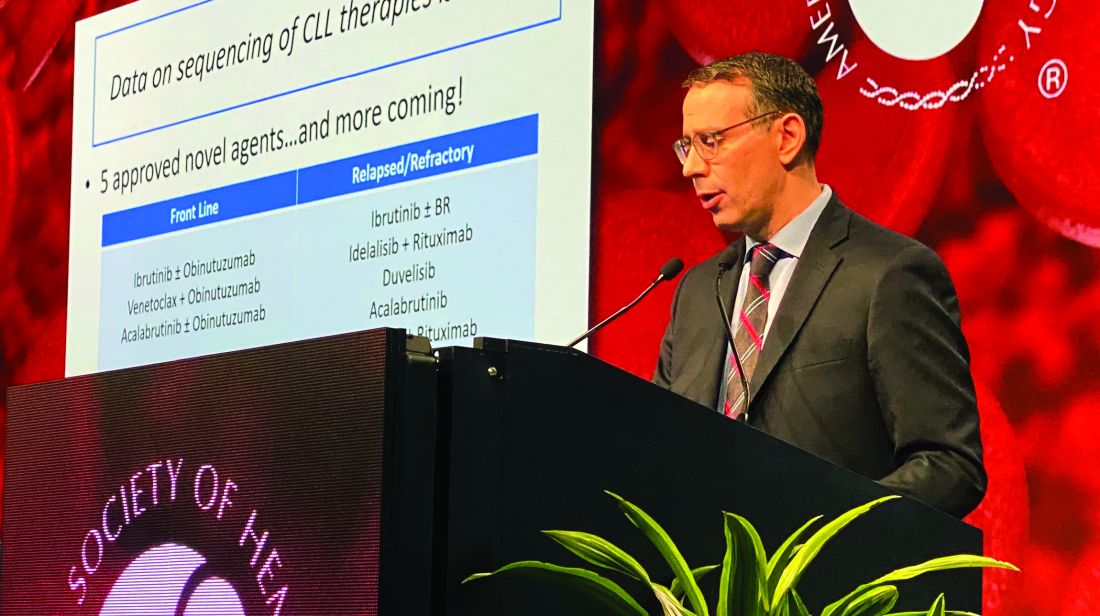
Efficacy of postvenetoclax therapy may depend on prior agent exposure in CLL
ORLANDO – For a patient with chronic lymphocytic leukemia (CLL) who has discontinued venetoclax, choosing the best next therapy may depend on what novel agents the patient was exposed to and why they discontinued them, according to Anthony R. Mato, MD, with the Center for CLL at Memorial Sloan Kettering Cancer Center in New York.
If the patient is Bruton tyrosine kinase (BTK) inhibitor naive, then use of a BTK inhibitor after venetoclax would be supported, Dr. Mato said, by the high overall response rates and durable remissions that he and his coinvestigators documented in a retrospective, multicenter study designed specifically to address the gap in knowledge regarding what to use after venetoclax.
If the patient is BTK inhibitor exposed, then the reason for discontinuation needs to be considered before going with that venetoclax-to-BTK inhibitor sequence, Dr. Mato said during an oral presentation at the annual meeting of the American Society of Hematology.
“In patients with resistance to a BTK inhibitor, the sequence was not supported – it did not appear to be effective,” he said. “However, in the setting of intolerance, an alternate BTK inhibitor could be considered.”
The study did not support a venetoclax-to-PI3K inhibitor sequence in PI3K-naive patients, he added, noting that remissions did not appear to be durable, suggesting a potential overlap in resistance mechanisms between agents.
All told, the most effective therapies for in the postvenetoclax setting included the use of a BTK inhibitor in BTK inhibitor–naive or previously responsive patients, and allogeneic transplant following double novel-agent exposure.
“These data may provide support for venetoclax’s earlier use in the course of CLL, and may guide clinical practice and aid in the design of future clinical trials to address sequencing of novel agents,” Dr. Mato told attendees.
While prospective and real-world data clearly show that venetoclax is active in ibrutinib- or idelalisib-exposed patients, data are conversely “variable and limited” with regard to outcomes for next therapies following venetoclax.
“Current data addressing this key sequencing question, I feel, is a major limitation in supporting the sequence of venetoclax to a BTK inhibitor,” Dr. Mato said.
Accordingly, Dr. Mato and colleagues at 31 centers internationally planned and conducted this study, which included data on 326 patients treated with venetoclax who then discontinued for any reason.
“I wanted to highlight that 50% of the sites for this trial were recruited by a single tweet,” said Dr. Mato, adding that he and his coauthors received no funding to conduct this study and volunteered their time to complete it.
They found that, in BTK inhibitor–naive patients who discontinued venetoclax, subsequent BTK inhibitor treatment was associated with a high overall response rate and durable remissions, with a median progression-free survival (PFS) of 32 months.
In BTK inhibitor–exposed patients, response to postvenetoclax BTK inhibitor treatment depended on the reason for discontinuation, with a favorable result (PFS not reached with a mean follow-up of 7.7 months) in patients who were intolerant of the prior BTK inhibitor. By contrast, median PFS was only about 4 months for patients who were resistant to the prior BTK inhibitor.
PI3K inhibitors did not produce durable remissions after venetoclax, with a median PFS also of just 4 months, Dr. Mato reported.
However, cellular therapies appeared to be effective after venetoclax. Allogeneic hematopoietic stem cell transplantation was particularly effective, with the median PFS not reached, while chimeric antigen receptor T-cell therapy produced a PFS of 9 months.
Dr. Mato emphasized that the results of the retrospective trial were “hypothesis generating” and noted that patients in the study had received a median of 3, and up to 11, prior therapies. “This population are probably not our patients receiving venetoclax in clinical practice. They’re more heavily pretreated.”
Dr. Mato reported disclosures related to Gilead, AstraZeneca, AbbVie, Sunesis, Johnson & Johnson, TG Therapeutics, Loxo Oncology, DTRM Biopharma, Genentech, Janssen, Acerta Pharma, Pharmacyclics, and Celgene.
SOURCE: Mato AR et al. ASH 2019, Abstract 502.
ORLANDO – For a patient with chronic lymphocytic leukemia (CLL) who has discontinued venetoclax, choosing the best next therapy may depend on what novel agents the patient was exposed to and why they discontinued them, according to Anthony R. Mato, MD, with the Center for CLL at Memorial Sloan Kettering Cancer Center in New York.
If the patient is Bruton tyrosine kinase (BTK) inhibitor naive, then use of a BTK inhibitor after venetoclax would be supported, Dr. Mato said, by the high overall response rates and durable remissions that he and his coinvestigators documented in a retrospective, multicenter study designed specifically to address the gap in knowledge regarding what to use after venetoclax.
If the patient is BTK inhibitor exposed, then the reason for discontinuation needs to be considered before going with that venetoclax-to-BTK inhibitor sequence, Dr. Mato said during an oral presentation at the annual meeting of the American Society of Hematology.
“In patients with resistance to a BTK inhibitor, the sequence was not supported – it did not appear to be effective,” he said. “However, in the setting of intolerance, an alternate BTK inhibitor could be considered.”
The study did not support a venetoclax-to-PI3K inhibitor sequence in PI3K-naive patients, he added, noting that remissions did not appear to be durable, suggesting a potential overlap in resistance mechanisms between agents.
All told, the most effective therapies for in the postvenetoclax setting included the use of a BTK inhibitor in BTK inhibitor–naive or previously responsive patients, and allogeneic transplant following double novel-agent exposure.
“These data may provide support for venetoclax’s earlier use in the course of CLL, and may guide clinical practice and aid in the design of future clinical trials to address sequencing of novel agents,” Dr. Mato told attendees.
While prospective and real-world data clearly show that venetoclax is active in ibrutinib- or idelalisib-exposed patients, data are conversely “variable and limited” with regard to outcomes for next therapies following venetoclax.
“Current data addressing this key sequencing question, I feel, is a major limitation in supporting the sequence of venetoclax to a BTK inhibitor,” Dr. Mato said.
Accordingly, Dr. Mato and colleagues at 31 centers internationally planned and conducted this study, which included data on 326 patients treated with venetoclax who then discontinued for any reason.
“I wanted to highlight that 50% of the sites for this trial were recruited by a single tweet,” said Dr. Mato, adding that he and his coauthors received no funding to conduct this study and volunteered their time to complete it.
They found that, in BTK inhibitor–naive patients who discontinued venetoclax, subsequent BTK inhibitor treatment was associated with a high overall response rate and durable remissions, with a median progression-free survival (PFS) of 32 months.
In BTK inhibitor–exposed patients, response to postvenetoclax BTK inhibitor treatment depended on the reason for discontinuation, with a favorable result (PFS not reached with a mean follow-up of 7.7 months) in patients who were intolerant of the prior BTK inhibitor. By contrast, median PFS was only about 4 months for patients who were resistant to the prior BTK inhibitor.
PI3K inhibitors did not produce durable remissions after venetoclax, with a median PFS also of just 4 months, Dr. Mato reported.
However, cellular therapies appeared to be effective after venetoclax. Allogeneic hematopoietic stem cell transplantation was particularly effective, with the median PFS not reached, while chimeric antigen receptor T-cell therapy produced a PFS of 9 months.
Dr. Mato emphasized that the results of the retrospective trial were “hypothesis generating” and noted that patients in the study had received a median of 3, and up to 11, prior therapies. “This population are probably not our patients receiving venetoclax in clinical practice. They’re more heavily pretreated.”
Dr. Mato reported disclosures related to Gilead, AstraZeneca, AbbVie, Sunesis, Johnson & Johnson, TG Therapeutics, Loxo Oncology, DTRM Biopharma, Genentech, Janssen, Acerta Pharma, Pharmacyclics, and Celgene.
SOURCE: Mato AR et al. ASH 2019, Abstract 502.
ORLANDO – For a patient with chronic lymphocytic leukemia (CLL) who has discontinued venetoclax, choosing the best next therapy may depend on what novel agents the patient was exposed to and why they discontinued them, according to Anthony R. Mato, MD, with the Center for CLL at Memorial Sloan Kettering Cancer Center in New York.
If the patient is Bruton tyrosine kinase (BTK) inhibitor naive, then use of a BTK inhibitor after venetoclax would be supported, Dr. Mato said, by the high overall response rates and durable remissions that he and his coinvestigators documented in a retrospective, multicenter study designed specifically to address the gap in knowledge regarding what to use after venetoclax.
If the patient is BTK inhibitor exposed, then the reason for discontinuation needs to be considered before going with that venetoclax-to-BTK inhibitor sequence, Dr. Mato said during an oral presentation at the annual meeting of the American Society of Hematology.
“In patients with resistance to a BTK inhibitor, the sequence was not supported – it did not appear to be effective,” he said. “However, in the setting of intolerance, an alternate BTK inhibitor could be considered.”
The study did not support a venetoclax-to-PI3K inhibitor sequence in PI3K-naive patients, he added, noting that remissions did not appear to be durable, suggesting a potential overlap in resistance mechanisms between agents.
All told, the most effective therapies for in the postvenetoclax setting included the use of a BTK inhibitor in BTK inhibitor–naive or previously responsive patients, and allogeneic transplant following double novel-agent exposure.
“These data may provide support for venetoclax’s earlier use in the course of CLL, and may guide clinical practice and aid in the design of future clinical trials to address sequencing of novel agents,” Dr. Mato told attendees.
While prospective and real-world data clearly show that venetoclax is active in ibrutinib- or idelalisib-exposed patients, data are conversely “variable and limited” with regard to outcomes for next therapies following venetoclax.
“Current data addressing this key sequencing question, I feel, is a major limitation in supporting the sequence of venetoclax to a BTK inhibitor,” Dr. Mato said.
Accordingly, Dr. Mato and colleagues at 31 centers internationally planned and conducted this study, which included data on 326 patients treated with venetoclax who then discontinued for any reason.
“I wanted to highlight that 50% of the sites for this trial were recruited by a single tweet,” said Dr. Mato, adding that he and his coauthors received no funding to conduct this study and volunteered their time to complete it.
They found that, in BTK inhibitor–naive patients who discontinued venetoclax, subsequent BTK inhibitor treatment was associated with a high overall response rate and durable remissions, with a median progression-free survival (PFS) of 32 months.
In BTK inhibitor–exposed patients, response to postvenetoclax BTK inhibitor treatment depended on the reason for discontinuation, with a favorable result (PFS not reached with a mean follow-up of 7.7 months) in patients who were intolerant of the prior BTK inhibitor. By contrast, median PFS was only about 4 months for patients who were resistant to the prior BTK inhibitor.
PI3K inhibitors did not produce durable remissions after venetoclax, with a median PFS also of just 4 months, Dr. Mato reported.
However, cellular therapies appeared to be effective after venetoclax. Allogeneic hematopoietic stem cell transplantation was particularly effective, with the median PFS not reached, while chimeric antigen receptor T-cell therapy produced a PFS of 9 months.
Dr. Mato emphasized that the results of the retrospective trial were “hypothesis generating” and noted that patients in the study had received a median of 3, and up to 11, prior therapies. “This population are probably not our patients receiving venetoclax in clinical practice. They’re more heavily pretreated.”
Dr. Mato reported disclosures related to Gilead, AstraZeneca, AbbVie, Sunesis, Johnson & Johnson, TG Therapeutics, Loxo Oncology, DTRM Biopharma, Genentech, Janssen, Acerta Pharma, Pharmacyclics, and Celgene.
SOURCE: Mato AR et al. ASH 2019, Abstract 502.
REPORTING FROM ASH 2019
Off-the-shelf cellular therapy shows promise in the lab
ORLANDO – A cellular therapy called FT596 is active against B-cell malignancies and, when combined with rituximab, can be more effective than traditional chimeric antigen receptor (CAR) T cells, preclinical research findings suggest.
FT596 is a universal, anti-CD19 CAR natural killer (NK) cell therapy derived from a master induced pluripotent stem cell (iPSC) line.
FT596 reduced tumor growth in mouse models of leukemia and lymphoma. When combined with rituximab, FT596 was able to overcome CD19 antigen escape.
Jode P. Goodridge, PhD, of Fate Therapeutics in San Diego, presented these results at the annual meeting of the American Society of Hematology.
Dr. Goodridge explained that FT596 begins with a source material, such as a fibroblast, that is reprogrammed into an iPSC progenitor cell. That cell is sorted and expanded into a renewable, homogeneous, pluripotent master iPSC line. The iPSCs are differentiated into CD34 cells, which are differentiated into NK cells. The iPSC-derived NK cells are then modified with the following:
- An anti-CD19 CAR that is optimized for NK-cell biology and contains an NKG2D transmembrane domain, a 2B4 costimulatory domain, and a CD3-zeta signaling domain.
- An interleukin-15 receptor fusion that promotes cell survival and reduces the need for cytokine support.
- A high-affinity 158V, noncleavable CD16 Fc receptor that enhances antibody-dependent cellular cytotoxicity when FT596 is combined with a monoclonal antibody such as rituximab.
Dr. Goodridge presented results with FT596, both alone and in combination with rituximab, in vitro and in vivo.
When compared with no treatment, three doses of FT596 monotherapy reduced tumor growth in a mouse model of leukemia (Nalm6). FT596 plus rituximab reduced tumor growth in a mouse model of lymphoma (Raji), when compared with no treatment or rituximab alone.
Three doses of FT596 proved more effective than a single dose of CD19 CAR T-cell therapy in a mouse model of lymphoma (Raji). FT596 both reduced tumor growth and prolonged survival in the mice.
Lastly, in vitro experiments in Raji cells showed that FT596 plus rituximab can produce deeper responses than primary CAR-T cells, and the combination can prevent antigen escape.
Dr. Goodridge said these results support the phase 1 study of FT596, given as monotherapy or in combination with rituximab or obinutuzumab, in patients with relapsed/refractory B-cell lymphomas or chronic lymphocytic leukemia.
Dr. Goodridge is employed by Fate Therapeutics, the company developing FT596.
SOURCE: Goodridge JP et al. ASH 2019. Abstract 301.
ORLANDO – A cellular therapy called FT596 is active against B-cell malignancies and, when combined with rituximab, can be more effective than traditional chimeric antigen receptor (CAR) T cells, preclinical research findings suggest.
FT596 is a universal, anti-CD19 CAR natural killer (NK) cell therapy derived from a master induced pluripotent stem cell (iPSC) line.
FT596 reduced tumor growth in mouse models of leukemia and lymphoma. When combined with rituximab, FT596 was able to overcome CD19 antigen escape.
Jode P. Goodridge, PhD, of Fate Therapeutics in San Diego, presented these results at the annual meeting of the American Society of Hematology.
Dr. Goodridge explained that FT596 begins with a source material, such as a fibroblast, that is reprogrammed into an iPSC progenitor cell. That cell is sorted and expanded into a renewable, homogeneous, pluripotent master iPSC line. The iPSCs are differentiated into CD34 cells, which are differentiated into NK cells. The iPSC-derived NK cells are then modified with the following:
- An anti-CD19 CAR that is optimized for NK-cell biology and contains an NKG2D transmembrane domain, a 2B4 costimulatory domain, and a CD3-zeta signaling domain.
- An interleukin-15 receptor fusion that promotes cell survival and reduces the need for cytokine support.
- A high-affinity 158V, noncleavable CD16 Fc receptor that enhances antibody-dependent cellular cytotoxicity when FT596 is combined with a monoclonal antibody such as rituximab.
Dr. Goodridge presented results with FT596, both alone and in combination with rituximab, in vitro and in vivo.
When compared with no treatment, three doses of FT596 monotherapy reduced tumor growth in a mouse model of leukemia (Nalm6). FT596 plus rituximab reduced tumor growth in a mouse model of lymphoma (Raji), when compared with no treatment or rituximab alone.
Three doses of FT596 proved more effective than a single dose of CD19 CAR T-cell therapy in a mouse model of lymphoma (Raji). FT596 both reduced tumor growth and prolonged survival in the mice.
Lastly, in vitro experiments in Raji cells showed that FT596 plus rituximab can produce deeper responses than primary CAR-T cells, and the combination can prevent antigen escape.
Dr. Goodridge said these results support the phase 1 study of FT596, given as monotherapy or in combination with rituximab or obinutuzumab, in patients with relapsed/refractory B-cell lymphomas or chronic lymphocytic leukemia.
Dr. Goodridge is employed by Fate Therapeutics, the company developing FT596.
SOURCE: Goodridge JP et al. ASH 2019. Abstract 301.
ORLANDO – A cellular therapy called FT596 is active against B-cell malignancies and, when combined with rituximab, can be more effective than traditional chimeric antigen receptor (CAR) T cells, preclinical research findings suggest.
FT596 is a universal, anti-CD19 CAR natural killer (NK) cell therapy derived from a master induced pluripotent stem cell (iPSC) line.
FT596 reduced tumor growth in mouse models of leukemia and lymphoma. When combined with rituximab, FT596 was able to overcome CD19 antigen escape.
Jode P. Goodridge, PhD, of Fate Therapeutics in San Diego, presented these results at the annual meeting of the American Society of Hematology.
Dr. Goodridge explained that FT596 begins with a source material, such as a fibroblast, that is reprogrammed into an iPSC progenitor cell. That cell is sorted and expanded into a renewable, homogeneous, pluripotent master iPSC line. The iPSCs are differentiated into CD34 cells, which are differentiated into NK cells. The iPSC-derived NK cells are then modified with the following:
- An anti-CD19 CAR that is optimized for NK-cell biology and contains an NKG2D transmembrane domain, a 2B4 costimulatory domain, and a CD3-zeta signaling domain.
- An interleukin-15 receptor fusion that promotes cell survival and reduces the need for cytokine support.
- A high-affinity 158V, noncleavable CD16 Fc receptor that enhances antibody-dependent cellular cytotoxicity when FT596 is combined with a monoclonal antibody such as rituximab.
Dr. Goodridge presented results with FT596, both alone and in combination with rituximab, in vitro and in vivo.
When compared with no treatment, three doses of FT596 monotherapy reduced tumor growth in a mouse model of leukemia (Nalm6). FT596 plus rituximab reduced tumor growth in a mouse model of lymphoma (Raji), when compared with no treatment or rituximab alone.
Three doses of FT596 proved more effective than a single dose of CD19 CAR T-cell therapy in a mouse model of lymphoma (Raji). FT596 both reduced tumor growth and prolonged survival in the mice.
Lastly, in vitro experiments in Raji cells showed that FT596 plus rituximab can produce deeper responses than primary CAR-T cells, and the combination can prevent antigen escape.
Dr. Goodridge said these results support the phase 1 study of FT596, given as monotherapy or in combination with rituximab or obinutuzumab, in patients with relapsed/refractory B-cell lymphomas or chronic lymphocytic leukemia.
Dr. Goodridge is employed by Fate Therapeutics, the company developing FT596.
SOURCE: Goodridge JP et al. ASH 2019. Abstract 301.
REPORTING FROM ASH 2019
Newly identified genetic changes contribute to transformation of follicular lymphoma
A molecular analysis of a patient with follicular lymphoma (FL) that became B-lymphoblastic leukemia/lymphoma (B-ALL/LBL) uncovered genetic changes that may improve understanding of this transformation.
“The study provides new insights into the pathogenesis of FL-B-ALL/LBL transformation and suggests novel, disease biology–based therapeutic approaches to this aggressive and currently incurable disease,” wrote Jonathan Belman, MD, PhD, of the Hospital of the University of Pennsylvania, Philadelphia, and coauthors. Their findings were published in Cold Spring Harbor Molecular Case Studies.
To further understand the rare occasions when FL transforms into a more aggressive form of lymphoma, the researchers investigated a 36-year-old man with low-grade FL that became B-ALL/LBL roughly 1 year after diagnosis. Their analysis included immunoglobulin (Ig) gene rearrangement studies, cytogenetic analysis, and whole exome sequencing of the patient’s FL, B-ALL/LBL, and normal cells.
Next generation sequencing of Ig rearrangements from normal, FL, and B-ALL/LBL specimens revealed considerable somatic hypermutation (SHM) in a single neoplastic clone – IgHV4-34_JH6 – in the FL cells. By comparison, though no dominant clone was found in the B-ALL/LBL specimen, there was even more extensive SHM, along with clones that could be traced to the FL lineage.
In addition, fluorescence in situ hybridization (FISH) studies on the FL specimen were positive for rearrangements of BCL2 and BCL6 genes; a rearrangement of BCL6 is associated with clinical aggressiveness. Those same two rearrangements were found in the B-ALL/LBL specimen, along with a MYC gene rearrangement unseen in the FL.
“MYC translocations are well known to contribute to high aggressiveness of lymphomas, and are hallmark of FL-B-ALL/LBL transformation,” the researchers wrote.
Finally, comparative whole exome sequencing of normal tissue plus the cancerous specimens identified 751 single nucleotide variants. The normal tissue contained 111 of those mutations, while the FL specimens contained 116 mutations – 11 of which were shared solely with B-ALL/LBL – and the B-ALL/LBL specimens contained a striking 575 unique mutations. Notably, a nonsense mutation in the KMT2D gene that was shared by FL and B-ALL/LBL may have contributed to lymphomagenesis.
The study was funded by a grant from the National Institutes of Health, the Abramson Cancer Center Translational Center in Lymphoma, the Daniel B. Allanoff Foundation, and a Hematopathology Divisional Training grant.
SOURCE: Belman JP et al. Cold Spring Harb Mol Case Stud. 2019 Nov 27. doi: 10.1101/mcs.a004614.
A molecular analysis of a patient with follicular lymphoma (FL) that became B-lymphoblastic leukemia/lymphoma (B-ALL/LBL) uncovered genetic changes that may improve understanding of this transformation.
“The study provides new insights into the pathogenesis of FL-B-ALL/LBL transformation and suggests novel, disease biology–based therapeutic approaches to this aggressive and currently incurable disease,” wrote Jonathan Belman, MD, PhD, of the Hospital of the University of Pennsylvania, Philadelphia, and coauthors. Their findings were published in Cold Spring Harbor Molecular Case Studies.
To further understand the rare occasions when FL transforms into a more aggressive form of lymphoma, the researchers investigated a 36-year-old man with low-grade FL that became B-ALL/LBL roughly 1 year after diagnosis. Their analysis included immunoglobulin (Ig) gene rearrangement studies, cytogenetic analysis, and whole exome sequencing of the patient’s FL, B-ALL/LBL, and normal cells.
Next generation sequencing of Ig rearrangements from normal, FL, and B-ALL/LBL specimens revealed considerable somatic hypermutation (SHM) in a single neoplastic clone – IgHV4-34_JH6 – in the FL cells. By comparison, though no dominant clone was found in the B-ALL/LBL specimen, there was even more extensive SHM, along with clones that could be traced to the FL lineage.
In addition, fluorescence in situ hybridization (FISH) studies on the FL specimen were positive for rearrangements of BCL2 and BCL6 genes; a rearrangement of BCL6 is associated with clinical aggressiveness. Those same two rearrangements were found in the B-ALL/LBL specimen, along with a MYC gene rearrangement unseen in the FL.
“MYC translocations are well known to contribute to high aggressiveness of lymphomas, and are hallmark of FL-B-ALL/LBL transformation,” the researchers wrote.
Finally, comparative whole exome sequencing of normal tissue plus the cancerous specimens identified 751 single nucleotide variants. The normal tissue contained 111 of those mutations, while the FL specimens contained 116 mutations – 11 of which were shared solely with B-ALL/LBL – and the B-ALL/LBL specimens contained a striking 575 unique mutations. Notably, a nonsense mutation in the KMT2D gene that was shared by FL and B-ALL/LBL may have contributed to lymphomagenesis.
The study was funded by a grant from the National Institutes of Health, the Abramson Cancer Center Translational Center in Lymphoma, the Daniel B. Allanoff Foundation, and a Hematopathology Divisional Training grant.
SOURCE: Belman JP et al. Cold Spring Harb Mol Case Stud. 2019 Nov 27. doi: 10.1101/mcs.a004614.
A molecular analysis of a patient with follicular lymphoma (FL) that became B-lymphoblastic leukemia/lymphoma (B-ALL/LBL) uncovered genetic changes that may improve understanding of this transformation.
“The study provides new insights into the pathogenesis of FL-B-ALL/LBL transformation and suggests novel, disease biology–based therapeutic approaches to this aggressive and currently incurable disease,” wrote Jonathan Belman, MD, PhD, of the Hospital of the University of Pennsylvania, Philadelphia, and coauthors. Their findings were published in Cold Spring Harbor Molecular Case Studies.
To further understand the rare occasions when FL transforms into a more aggressive form of lymphoma, the researchers investigated a 36-year-old man with low-grade FL that became B-ALL/LBL roughly 1 year after diagnosis. Their analysis included immunoglobulin (Ig) gene rearrangement studies, cytogenetic analysis, and whole exome sequencing of the patient’s FL, B-ALL/LBL, and normal cells.
Next generation sequencing of Ig rearrangements from normal, FL, and B-ALL/LBL specimens revealed considerable somatic hypermutation (SHM) in a single neoplastic clone – IgHV4-34_JH6 – in the FL cells. By comparison, though no dominant clone was found in the B-ALL/LBL specimen, there was even more extensive SHM, along with clones that could be traced to the FL lineage.
In addition, fluorescence in situ hybridization (FISH) studies on the FL specimen were positive for rearrangements of BCL2 and BCL6 genes; a rearrangement of BCL6 is associated with clinical aggressiveness. Those same two rearrangements were found in the B-ALL/LBL specimen, along with a MYC gene rearrangement unseen in the FL.
“MYC translocations are well known to contribute to high aggressiveness of lymphomas, and are hallmark of FL-B-ALL/LBL transformation,” the researchers wrote.
Finally, comparative whole exome sequencing of normal tissue plus the cancerous specimens identified 751 single nucleotide variants. The normal tissue contained 111 of those mutations, while the FL specimens contained 116 mutations – 11 of which were shared solely with B-ALL/LBL – and the B-ALL/LBL specimens contained a striking 575 unique mutations. Notably, a nonsense mutation in the KMT2D gene that was shared by FL and B-ALL/LBL may have contributed to lymphomagenesis.
The study was funded by a grant from the National Institutes of Health, the Abramson Cancer Center Translational Center in Lymphoma, the Daniel B. Allanoff Foundation, and a Hematopathology Divisional Training grant.
SOURCE: Belman JP et al. Cold Spring Harb Mol Case Stud. 2019 Nov 27. doi: 10.1101/mcs.a004614.
FROM COLD SPRING HARBOR MOLECULAR CASE STUDIES
SOX11 shows value as diagnostic marker in MCL
SOX11 may be an accurate diagnostic marker for mantle cell lymphoma (MCL), allowing clinicians to distinguish it from other lymphoproliferative disorders, according to findings from a meta-analysis of 14 case-control studies.
Woojoo Lee, PhD, of Inha University, Incheon, Republic of Korea, and coinvestigators, evaluated the diagnostic accuracy of SOX11 immunohistochemistry for the diagnosis of MCL. The results were published in PLoS One.
The researchers searched major databases for studies that evaluated the use of SOX11 immunohistochemistry in patients with MCL and other lymphoproliferative disorders. After applying the search parameters, the team identified 383 studies, 14 of which were included in the meta-analysis. Various data were extracted from eligible studies, including the type and clonality of anti-SOX11 antibody, number of SOX11-positive lymphomas (MCLs and other lymphoproliferative disorders), specificity, sensitivity, and others. After combining the data, the investigators calculated pooled sensitivity, specificity, and area under the curve. Among the included studies, hairy cell leukemia, Burkitt’s lymphoma, and lymphoblastic lymphoma were common among patient populations. In total, clone MRQ-58 mouse antibodies were used in five study populations.
The researchers found that the pooled specificity was 0.95 (95% CI, 0.9-0.97), and sensitivity was 0.9 (95% CI, 0.86-0.92). There was statistically significant substantial heterogeneity observed for specificity, but not for sensitivity, the investigators reported.
“The results demonstrated that SOX11 was a potential diagnostic marker for MCL,” they wrote. “Meta-regression revealed a significant inverse relationship between specificity and proportions of [Burkitt’s lymphoma, lymphoblastic lymphoma, and hairy cell leukemia].”
With respect to antibody type, the clone MRQ-58 mouse antibody showed consistently high specificity in the clinical setting, despite observed heterogeneity.
“Future studies using MRQ-58 are needed to improve our understanding of the diagnostic accuracy of SOX11 immunohistochemistry for MCL,” the investigators wrote.
The study was funded by the Next-Generation BioGreen 21 program (Republic of Korea). The authors reported having no conflicts of interest.
SOURCE: Lee W et al. PLoS One. 2019 Nov 12. doi: 10.1371/journal.pone.0225096.
SOX11 may be an accurate diagnostic marker for mantle cell lymphoma (MCL), allowing clinicians to distinguish it from other lymphoproliferative disorders, according to findings from a meta-analysis of 14 case-control studies.
Woojoo Lee, PhD, of Inha University, Incheon, Republic of Korea, and coinvestigators, evaluated the diagnostic accuracy of SOX11 immunohistochemistry for the diagnosis of MCL. The results were published in PLoS One.
The researchers searched major databases for studies that evaluated the use of SOX11 immunohistochemistry in patients with MCL and other lymphoproliferative disorders. After applying the search parameters, the team identified 383 studies, 14 of which were included in the meta-analysis. Various data were extracted from eligible studies, including the type and clonality of anti-SOX11 antibody, number of SOX11-positive lymphomas (MCLs and other lymphoproliferative disorders), specificity, sensitivity, and others. After combining the data, the investigators calculated pooled sensitivity, specificity, and area under the curve. Among the included studies, hairy cell leukemia, Burkitt’s lymphoma, and lymphoblastic lymphoma were common among patient populations. In total, clone MRQ-58 mouse antibodies were used in five study populations.
The researchers found that the pooled specificity was 0.95 (95% CI, 0.9-0.97), and sensitivity was 0.9 (95% CI, 0.86-0.92). There was statistically significant substantial heterogeneity observed for specificity, but not for sensitivity, the investigators reported.
“The results demonstrated that SOX11 was a potential diagnostic marker for MCL,” they wrote. “Meta-regression revealed a significant inverse relationship between specificity and proportions of [Burkitt’s lymphoma, lymphoblastic lymphoma, and hairy cell leukemia].”
With respect to antibody type, the clone MRQ-58 mouse antibody showed consistently high specificity in the clinical setting, despite observed heterogeneity.
“Future studies using MRQ-58 are needed to improve our understanding of the diagnostic accuracy of SOX11 immunohistochemistry for MCL,” the investigators wrote.
The study was funded by the Next-Generation BioGreen 21 program (Republic of Korea). The authors reported having no conflicts of interest.
SOURCE: Lee W et al. PLoS One. 2019 Nov 12. doi: 10.1371/journal.pone.0225096.
SOX11 may be an accurate diagnostic marker for mantle cell lymphoma (MCL), allowing clinicians to distinguish it from other lymphoproliferative disorders, according to findings from a meta-analysis of 14 case-control studies.
Woojoo Lee, PhD, of Inha University, Incheon, Republic of Korea, and coinvestigators, evaluated the diagnostic accuracy of SOX11 immunohistochemistry for the diagnosis of MCL. The results were published in PLoS One.
The researchers searched major databases for studies that evaluated the use of SOX11 immunohistochemistry in patients with MCL and other lymphoproliferative disorders. After applying the search parameters, the team identified 383 studies, 14 of which were included in the meta-analysis. Various data were extracted from eligible studies, including the type and clonality of anti-SOX11 antibody, number of SOX11-positive lymphomas (MCLs and other lymphoproliferative disorders), specificity, sensitivity, and others. After combining the data, the investigators calculated pooled sensitivity, specificity, and area under the curve. Among the included studies, hairy cell leukemia, Burkitt’s lymphoma, and lymphoblastic lymphoma were common among patient populations. In total, clone MRQ-58 mouse antibodies were used in five study populations.
The researchers found that the pooled specificity was 0.95 (95% CI, 0.9-0.97), and sensitivity was 0.9 (95% CI, 0.86-0.92). There was statistically significant substantial heterogeneity observed for specificity, but not for sensitivity, the investigators reported.
“The results demonstrated that SOX11 was a potential diagnostic marker for MCL,” they wrote. “Meta-regression revealed a significant inverse relationship between specificity and proportions of [Burkitt’s lymphoma, lymphoblastic lymphoma, and hairy cell leukemia].”
With respect to antibody type, the clone MRQ-58 mouse antibody showed consistently high specificity in the clinical setting, despite observed heterogeneity.
“Future studies using MRQ-58 are needed to improve our understanding of the diagnostic accuracy of SOX11 immunohistochemistry for MCL,” the investigators wrote.
The study was funded by the Next-Generation BioGreen 21 program (Republic of Korea). The authors reported having no conflicts of interest.
SOURCE: Lee W et al. PLoS One. 2019 Nov 12. doi: 10.1371/journal.pone.0225096.
FROM PLOS ONE
Acalabrutinib may outperform other targeted therapies in MCL
For patients with relapsed or refractory mantle cell lymphoma (MCL), second generation Bruton’s tyrosine kinase (BTK) inhibitor acalabrutinib may offer increased response rates and better tolerability compared with other single-agent targeted therapies, based on a recent analysis.
Improved safety could lead to long-term benefits resulting from extended treatment duration, according to lead author Claire Telford, PhD, of AstraZeneca in Gaithersburg, Md., and colleagues. AstraZeneca manufactures acalabrutinib (Calquence).
Currently, treatment for MCL is guided by a number of clinical considerations, the investigators explained in Clinical Therapeutics.
“The type of treatment recommended for relapsed/refractory MCL depends on multiple factors, namely time to the relapse, extent of disease, previous regimens, candidacy for allogeneic stem cell transplantation, and the patient’s overall health,” they wrote.
To determine how acalabrutinib stacks up with other options, the investigators drew data from the phase 2 ACE-LY-004 trial, which tested acalabrutinib in 124 patients with relapsed or refractory MCL. After matching, the investigators compared the ACE-LY-004 outcomes from 12 other trials, in which patients received different targeted therapies.
Results pointed to higher overall response and complete response rates for acalabrutinib, compared with other single-agent targeted therapy. Specifically, acalabrutinib had a higher overall response rate, compared with ibrutinib (9.3% higher), lenalidomide (38.1% higher), temsirolimus (40.7% higher), and bortezomib (50.6% higher). For each of these, complete responses also were higher.
There was no significant difference in overall response or complete response rates between acalabrutinib and rituximab combinations – bendamustine plus rituximab, ibrutinib plus rituximab, and lenalidomide plus rituximab.
The investigators also highlighted a number of safety advantages. Compared with ibrutinib, acalabrutinib was associated with significantly fewer instances of grade 3 or 4 atrial fibrillation. Risk of grade 3 or 4 thrombocytopenia was significantly lower with acalabrutinib than with ibrutinib, bortezomib, lenalidomide, and temsirolimus.
Still, in some instances, acalabrutinib was comparatively less tolerable. It was associated with a higher risk of grade 3 or 4 infections than bendamustine plus rituximab; and anemia was more common among patients receiving acalabrutinib than among those who had lenalidomide plus rituximab or ibrutinib plus rituximab.
“This comparison of targeted therapies used in the treatment of relapsed/refractory MCL has shown that acalabrutinib has the potential to provide higher response rates, with trends for longer [progression-free survival] and [overall survival], and an improved safety profile,” the investigators wrote.
The study was funded by AstraZeneca. Dr. Telford is an employee of AstraZeneca and other authors reported financial relationships with the company.
SOURCE: Telford C et al. Clin Ther. 2019 Nov 4. doi: 10.1016/j.clinthera.2019.09.012 .
For patients with relapsed or refractory mantle cell lymphoma (MCL), second generation Bruton’s tyrosine kinase (BTK) inhibitor acalabrutinib may offer increased response rates and better tolerability compared with other single-agent targeted therapies, based on a recent analysis.
Improved safety could lead to long-term benefits resulting from extended treatment duration, according to lead author Claire Telford, PhD, of AstraZeneca in Gaithersburg, Md., and colleagues. AstraZeneca manufactures acalabrutinib (Calquence).
Currently, treatment for MCL is guided by a number of clinical considerations, the investigators explained in Clinical Therapeutics.
“The type of treatment recommended for relapsed/refractory MCL depends on multiple factors, namely time to the relapse, extent of disease, previous regimens, candidacy for allogeneic stem cell transplantation, and the patient’s overall health,” they wrote.
To determine how acalabrutinib stacks up with other options, the investigators drew data from the phase 2 ACE-LY-004 trial, which tested acalabrutinib in 124 patients with relapsed or refractory MCL. After matching, the investigators compared the ACE-LY-004 outcomes from 12 other trials, in which patients received different targeted therapies.
Results pointed to higher overall response and complete response rates for acalabrutinib, compared with other single-agent targeted therapy. Specifically, acalabrutinib had a higher overall response rate, compared with ibrutinib (9.3% higher), lenalidomide (38.1% higher), temsirolimus (40.7% higher), and bortezomib (50.6% higher). For each of these, complete responses also were higher.
There was no significant difference in overall response or complete response rates between acalabrutinib and rituximab combinations – bendamustine plus rituximab, ibrutinib plus rituximab, and lenalidomide plus rituximab.
The investigators also highlighted a number of safety advantages. Compared with ibrutinib, acalabrutinib was associated with significantly fewer instances of grade 3 or 4 atrial fibrillation. Risk of grade 3 or 4 thrombocytopenia was significantly lower with acalabrutinib than with ibrutinib, bortezomib, lenalidomide, and temsirolimus.
Still, in some instances, acalabrutinib was comparatively less tolerable. It was associated with a higher risk of grade 3 or 4 infections than bendamustine plus rituximab; and anemia was more common among patients receiving acalabrutinib than among those who had lenalidomide plus rituximab or ibrutinib plus rituximab.
“This comparison of targeted therapies used in the treatment of relapsed/refractory MCL has shown that acalabrutinib has the potential to provide higher response rates, with trends for longer [progression-free survival] and [overall survival], and an improved safety profile,” the investigators wrote.
The study was funded by AstraZeneca. Dr. Telford is an employee of AstraZeneca and other authors reported financial relationships with the company.
SOURCE: Telford C et al. Clin Ther. 2019 Nov 4. doi: 10.1016/j.clinthera.2019.09.012 .
For patients with relapsed or refractory mantle cell lymphoma (MCL), second generation Bruton’s tyrosine kinase (BTK) inhibitor acalabrutinib may offer increased response rates and better tolerability compared with other single-agent targeted therapies, based on a recent analysis.
Improved safety could lead to long-term benefits resulting from extended treatment duration, according to lead author Claire Telford, PhD, of AstraZeneca in Gaithersburg, Md., and colleagues. AstraZeneca manufactures acalabrutinib (Calquence).
Currently, treatment for MCL is guided by a number of clinical considerations, the investigators explained in Clinical Therapeutics.
“The type of treatment recommended for relapsed/refractory MCL depends on multiple factors, namely time to the relapse, extent of disease, previous regimens, candidacy for allogeneic stem cell transplantation, and the patient’s overall health,” they wrote.
To determine how acalabrutinib stacks up with other options, the investigators drew data from the phase 2 ACE-LY-004 trial, which tested acalabrutinib in 124 patients with relapsed or refractory MCL. After matching, the investigators compared the ACE-LY-004 outcomes from 12 other trials, in which patients received different targeted therapies.
Results pointed to higher overall response and complete response rates for acalabrutinib, compared with other single-agent targeted therapy. Specifically, acalabrutinib had a higher overall response rate, compared with ibrutinib (9.3% higher), lenalidomide (38.1% higher), temsirolimus (40.7% higher), and bortezomib (50.6% higher). For each of these, complete responses also were higher.
There was no significant difference in overall response or complete response rates between acalabrutinib and rituximab combinations – bendamustine plus rituximab, ibrutinib plus rituximab, and lenalidomide plus rituximab.
The investigators also highlighted a number of safety advantages. Compared with ibrutinib, acalabrutinib was associated with significantly fewer instances of grade 3 or 4 atrial fibrillation. Risk of grade 3 or 4 thrombocytopenia was significantly lower with acalabrutinib than with ibrutinib, bortezomib, lenalidomide, and temsirolimus.
Still, in some instances, acalabrutinib was comparatively less tolerable. It was associated with a higher risk of grade 3 or 4 infections than bendamustine plus rituximab; and anemia was more common among patients receiving acalabrutinib than among those who had lenalidomide plus rituximab or ibrutinib plus rituximab.
“This comparison of targeted therapies used in the treatment of relapsed/refractory MCL has shown that acalabrutinib has the potential to provide higher response rates, with trends for longer [progression-free survival] and [overall survival], and an improved safety profile,” the investigators wrote.
The study was funded by AstraZeneca. Dr. Telford is an employee of AstraZeneca and other authors reported financial relationships with the company.
SOURCE: Telford C et al. Clin Ther. 2019 Nov 4. doi: 10.1016/j.clinthera.2019.09.012 .
FROM CLINICAL THERAPEUTICS
FDA approves acalabrutinib for CLL, SLL treatment
The Food and Drug Administration has approved acalabrutinib (Calquence) as initial or subsequent treatment for adults with chronic lymphocytic leukemia (CLL) or small lymphocytic leukemia (SLL).
The approval came as part of Project Orbis, a collaboration among the FDA, the Australian Therapeutic Goods Administration, and Health Canada. The program allows for the concurrent submission of review of oncology drug applications among the various agencies.
Acalabrutinib, a bruton tyrosin kinase inhibitor, is already approved in the United States for the treatment of adults with mantle cell lymphoma who have received at least one prior therapy. The FDA granted breakthrough therapy designation to acalabrutinib as a monotherapy for adults with CLL in August 2019, allowing for an expedited review.
The approval in CLL/SLL was based on results from two randomized clinical trials comparing acalabrutinib with other standard treatments. In the first trial, patients with previously untreated CLL who received acalabrutinib had a longer progression-free survival time, compared with patients who received standard treatment. A similar result was seen in the second trial among patients with previously treated CLL.
The most common adverse events associated with acalabrutinib include anemia, neutropenia, upper respiratory tract infection, thrombocytopenia, headache, diarrhea, and musculoskeletal pain. Patients receiving the drug should be monitored for symptoms of arrhythmia, serious infection, bleeding, and low blood count. Full prescribing information can be found on the FDA website.
The Food and Drug Administration has approved acalabrutinib (Calquence) as initial or subsequent treatment for adults with chronic lymphocytic leukemia (CLL) or small lymphocytic leukemia (SLL).
The approval came as part of Project Orbis, a collaboration among the FDA, the Australian Therapeutic Goods Administration, and Health Canada. The program allows for the concurrent submission of review of oncology drug applications among the various agencies.
Acalabrutinib, a bruton tyrosin kinase inhibitor, is already approved in the United States for the treatment of adults with mantle cell lymphoma who have received at least one prior therapy. The FDA granted breakthrough therapy designation to acalabrutinib as a monotherapy for adults with CLL in August 2019, allowing for an expedited review.
The approval in CLL/SLL was based on results from two randomized clinical trials comparing acalabrutinib with other standard treatments. In the first trial, patients with previously untreated CLL who received acalabrutinib had a longer progression-free survival time, compared with patients who received standard treatment. A similar result was seen in the second trial among patients with previously treated CLL.
The most common adverse events associated with acalabrutinib include anemia, neutropenia, upper respiratory tract infection, thrombocytopenia, headache, diarrhea, and musculoskeletal pain. Patients receiving the drug should be monitored for symptoms of arrhythmia, serious infection, bleeding, and low blood count. Full prescribing information can be found on the FDA website.
The Food and Drug Administration has approved acalabrutinib (Calquence) as initial or subsequent treatment for adults with chronic lymphocytic leukemia (CLL) or small lymphocytic leukemia (SLL).
The approval came as part of Project Orbis, a collaboration among the FDA, the Australian Therapeutic Goods Administration, and Health Canada. The program allows for the concurrent submission of review of oncology drug applications among the various agencies.
Acalabrutinib, a bruton tyrosin kinase inhibitor, is already approved in the United States for the treatment of adults with mantle cell lymphoma who have received at least one prior therapy. The FDA granted breakthrough therapy designation to acalabrutinib as a monotherapy for adults with CLL in August 2019, allowing for an expedited review.
The approval in CLL/SLL was based on results from two randomized clinical trials comparing acalabrutinib with other standard treatments. In the first trial, patients with previously untreated CLL who received acalabrutinib had a longer progression-free survival time, compared with patients who received standard treatment. A similar result was seen in the second trial among patients with previously treated CLL.
The most common adverse events associated with acalabrutinib include anemia, neutropenia, upper respiratory tract infection, thrombocytopenia, headache, diarrhea, and musculoskeletal pain. Patients receiving the drug should be monitored for symptoms of arrhythmia, serious infection, bleeding, and low blood count. Full prescribing information can be found on the FDA website.
Frontline ibrutinib saves money over chemoimmunotherapy
Ibrutinib monotherapy was associated with lower total health care costs compared with chemoimmunotherapy in the frontline treatment of patients with chronic lymphocytic leukemia (CLL), according to a retrospective study.
“This study compared time to next treatment, health care resource utilization, and total direct costs among patients with CLL initiating front-line ibrutinib single agent or chemoimmunotherapy,” wrote Bruno Emond, of Analysis Group, Montreal, and colleagues. Their report is in Clinical Lymphoma, Myeloma & Leukemia.
The researchers retrospectively analyzed data from 1,161 patients with CLL who were started on ibrutinib monotherapy or chemoimmunotherapy from 2014 to 2017. Data were collected from the Optum Clinformatics Extended DataMart De-Identified Databases.
Between the two groups, differences in baseline characteristics were controlled for by way of inverse probability of treatment weighting. Two treatment periods were included in the study: the initial 6 months of treatment and entire duration of frontline therapy.
The team also conducted a subgroup analysis of patients treated with bendamustine and rituximab. This cohort was analyzed independently since the regimen is commonly used in clinical practice.
After analysis, the researchers found that ibrutinib monotherapy was associated with net monthly cost savings of $3,766 (P less than .0001), compared with chemoimmunotherapy and bendamustine/rituximab over the frontline therapy period.
Ibrutinib patients had fewer monthly days with outpatient services (rate ratio, 0.75; 95% confidence interval, 0.60-0.94; P = .0200), compared with those on chemoimmunotherapy; and were less likely to initiate a next line of treatment, compared with chemoimmunotherapy patients (hazard ratio, 0.54; 95% CI, 0.33-0.90; P = .0163).
“Cost savings and reductions in health care resource utilization were even more pronounced when considering only the first 6 months of front-line treatment,” the researchers wrote.
The researchers acknowledged that two key limitations of the study were the potential influence of unobserved confounding factors and the use of claims data, which could include errors and omissions.
“These results suggest that ibrutinib single-agent is associated with lower total costs driven by lower medical costs, despite higher pharmacy costs, compared with chemoimmunotherapy and bendamustine/rituximab,” they concluded.
The authors reported financial affiliations with Janssen Scientific Affairs, which funded the study, and other companies.
SOURCE: Emond B et al. Clin Lymphoma Myeloma Leuk. 2019 Aug 26. doi: 10.1016/j.clml.2019.08.004.
Ibrutinib monotherapy was associated with lower total health care costs compared with chemoimmunotherapy in the frontline treatment of patients with chronic lymphocytic leukemia (CLL), according to a retrospective study.
“This study compared time to next treatment, health care resource utilization, and total direct costs among patients with CLL initiating front-line ibrutinib single agent or chemoimmunotherapy,” wrote Bruno Emond, of Analysis Group, Montreal, and colleagues. Their report is in Clinical Lymphoma, Myeloma & Leukemia.
The researchers retrospectively analyzed data from 1,161 patients with CLL who were started on ibrutinib monotherapy or chemoimmunotherapy from 2014 to 2017. Data were collected from the Optum Clinformatics Extended DataMart De-Identified Databases.
Between the two groups, differences in baseline characteristics were controlled for by way of inverse probability of treatment weighting. Two treatment periods were included in the study: the initial 6 months of treatment and entire duration of frontline therapy.
The team also conducted a subgroup analysis of patients treated with bendamustine and rituximab. This cohort was analyzed independently since the regimen is commonly used in clinical practice.
After analysis, the researchers found that ibrutinib monotherapy was associated with net monthly cost savings of $3,766 (P less than .0001), compared with chemoimmunotherapy and bendamustine/rituximab over the frontline therapy period.
Ibrutinib patients had fewer monthly days with outpatient services (rate ratio, 0.75; 95% confidence interval, 0.60-0.94; P = .0200), compared with those on chemoimmunotherapy; and were less likely to initiate a next line of treatment, compared with chemoimmunotherapy patients (hazard ratio, 0.54; 95% CI, 0.33-0.90; P = .0163).
“Cost savings and reductions in health care resource utilization were even more pronounced when considering only the first 6 months of front-line treatment,” the researchers wrote.
The researchers acknowledged that two key limitations of the study were the potential influence of unobserved confounding factors and the use of claims data, which could include errors and omissions.
“These results suggest that ibrutinib single-agent is associated with lower total costs driven by lower medical costs, despite higher pharmacy costs, compared with chemoimmunotherapy and bendamustine/rituximab,” they concluded.
The authors reported financial affiliations with Janssen Scientific Affairs, which funded the study, and other companies.
SOURCE: Emond B et al. Clin Lymphoma Myeloma Leuk. 2019 Aug 26. doi: 10.1016/j.clml.2019.08.004.
Ibrutinib monotherapy was associated with lower total health care costs compared with chemoimmunotherapy in the frontline treatment of patients with chronic lymphocytic leukemia (CLL), according to a retrospective study.
“This study compared time to next treatment, health care resource utilization, and total direct costs among patients with CLL initiating front-line ibrutinib single agent or chemoimmunotherapy,” wrote Bruno Emond, of Analysis Group, Montreal, and colleagues. Their report is in Clinical Lymphoma, Myeloma & Leukemia.
The researchers retrospectively analyzed data from 1,161 patients with CLL who were started on ibrutinib monotherapy or chemoimmunotherapy from 2014 to 2017. Data were collected from the Optum Clinformatics Extended DataMart De-Identified Databases.
Between the two groups, differences in baseline characteristics were controlled for by way of inverse probability of treatment weighting. Two treatment periods were included in the study: the initial 6 months of treatment and entire duration of frontline therapy.
The team also conducted a subgroup analysis of patients treated with bendamustine and rituximab. This cohort was analyzed independently since the regimen is commonly used in clinical practice.
After analysis, the researchers found that ibrutinib monotherapy was associated with net monthly cost savings of $3,766 (P less than .0001), compared with chemoimmunotherapy and bendamustine/rituximab over the frontline therapy period.
Ibrutinib patients had fewer monthly days with outpatient services (rate ratio, 0.75; 95% confidence interval, 0.60-0.94; P = .0200), compared with those on chemoimmunotherapy; and were less likely to initiate a next line of treatment, compared with chemoimmunotherapy patients (hazard ratio, 0.54; 95% CI, 0.33-0.90; P = .0163).
“Cost savings and reductions in health care resource utilization were even more pronounced when considering only the first 6 months of front-line treatment,” the researchers wrote.
The researchers acknowledged that two key limitations of the study were the potential influence of unobserved confounding factors and the use of claims data, which could include errors and omissions.
“These results suggest that ibrutinib single-agent is associated with lower total costs driven by lower medical costs, despite higher pharmacy costs, compared with chemoimmunotherapy and bendamustine/rituximab,” they concluded.
The authors reported financial affiliations with Janssen Scientific Affairs, which funded the study, and other companies.
SOURCE: Emond B et al. Clin Lymphoma Myeloma Leuk. 2019 Aug 26. doi: 10.1016/j.clml.2019.08.004.
FROM CLINICAL LYMPHOMA, MYELOMA & LEUKEMIA
Rituximab maintenance has a durable benefit in follicular lymphoma
The benefit of rituximab maintenance therapy in follicular lymphoma is long lasting and evident out to at least 9 years, according to the final efficacy analysis of the PRIMA phase 3, randomized, controlled trial.
Previously reported results of this pivotal trial showed prolongation of progression-free survival and time to next treatment with rituximab maintenance at a follow-up of 3 years and 6 years.
“Rituximab maintenance is now widely recommended for patients with follicular lymphoma responding to first-line rituximab-based immunochemotherapy,” Emmanuel Bachy, MD, PhD, of Institut National de la Santé et de la Recherche Médicale in Pierre-Bénite, France, and colleagues reported in the Journal of Clinical Oncology.
In PRIMA, patients with previously untreated high–tumor burden follicular lymphoma received any of three immunochemotherapy induction regimens. The 1,018 patients having a response were then randomly assigned to receive 2 years of rituximab (Rituxan) maintenance or observation only.
Dr. Bachy and colleagues performed the trial’s final efficacy analyses, now at a median follow-up of 9 years.
Among the 607 patients consenting to the extended follow-up, median progression-free survival was 10.5 years in the rituximab-maintenance group, compared with 4.1 years in the observation group (hazard ratio, 0.61; P less than .001).
“Subgroup analyses showed the substantial progression-free survival improvement associated with rituximab maintenance was independent of age, sex, induction immunochemotherapy regimen, response to induction, or [Follicular Lymphoma International Prognostic Index] risk score,” the investigators wrote.
Rituximab maintenance also prolonged the median time to next antilymphoma treatment (not reached vs. 6.1 years; hazard ratio, 0.66; P less than .001) and time to next chemotherapy treatment (not reached vs. 9.3 years; hazard ratio, 0.71; P less than .001).
But there was no significant difference in overall survival. Median overall survival was not reached in either group (hazard ratio, 1.04; P = .7948). The estimated 10-year overall survival rate was about 80% in both groups.
“This 9-year follow-up of the PRIMA study demonstrates that rituximab maintenance after induction immunochemotherapy provides a significant long-term [progression-free survival] benefit over observation,” the investigators wrote. “Despite the lack of [overall survival] advantage, it is noteworthy that more than half of the patients in the rituximab maintenance arm remain free of disease progression and have not required new antilymphoma treatment beyond 10 years.”
The trial was sponsored by the Lymphoma Study Association and supported by F. Hoffmann–La Roche and Biogen. Dr. Bachy reported financial disclosures related to Roche and other companies.
SOURCE: Bachy E et al. J Clin Oncol. 2019 Nov 1;37(31):2815-24.
The benefit of rituximab maintenance therapy in follicular lymphoma is long lasting and evident out to at least 9 years, according to the final efficacy analysis of the PRIMA phase 3, randomized, controlled trial.
Previously reported results of this pivotal trial showed prolongation of progression-free survival and time to next treatment with rituximab maintenance at a follow-up of 3 years and 6 years.
“Rituximab maintenance is now widely recommended for patients with follicular lymphoma responding to first-line rituximab-based immunochemotherapy,” Emmanuel Bachy, MD, PhD, of Institut National de la Santé et de la Recherche Médicale in Pierre-Bénite, France, and colleagues reported in the Journal of Clinical Oncology.
In PRIMA, patients with previously untreated high–tumor burden follicular lymphoma received any of three immunochemotherapy induction regimens. The 1,018 patients having a response were then randomly assigned to receive 2 years of rituximab (Rituxan) maintenance or observation only.
Dr. Bachy and colleagues performed the trial’s final efficacy analyses, now at a median follow-up of 9 years.
Among the 607 patients consenting to the extended follow-up, median progression-free survival was 10.5 years in the rituximab-maintenance group, compared with 4.1 years in the observation group (hazard ratio, 0.61; P less than .001).
“Subgroup analyses showed the substantial progression-free survival improvement associated with rituximab maintenance was independent of age, sex, induction immunochemotherapy regimen, response to induction, or [Follicular Lymphoma International Prognostic Index] risk score,” the investigators wrote.
Rituximab maintenance also prolonged the median time to next antilymphoma treatment (not reached vs. 6.1 years; hazard ratio, 0.66; P less than .001) and time to next chemotherapy treatment (not reached vs. 9.3 years; hazard ratio, 0.71; P less than .001).
But there was no significant difference in overall survival. Median overall survival was not reached in either group (hazard ratio, 1.04; P = .7948). The estimated 10-year overall survival rate was about 80% in both groups.
“This 9-year follow-up of the PRIMA study demonstrates that rituximab maintenance after induction immunochemotherapy provides a significant long-term [progression-free survival] benefit over observation,” the investigators wrote. “Despite the lack of [overall survival] advantage, it is noteworthy that more than half of the patients in the rituximab maintenance arm remain free of disease progression and have not required new antilymphoma treatment beyond 10 years.”
The trial was sponsored by the Lymphoma Study Association and supported by F. Hoffmann–La Roche and Biogen. Dr. Bachy reported financial disclosures related to Roche and other companies.
SOURCE: Bachy E et al. J Clin Oncol. 2019 Nov 1;37(31):2815-24.
The benefit of rituximab maintenance therapy in follicular lymphoma is long lasting and evident out to at least 9 years, according to the final efficacy analysis of the PRIMA phase 3, randomized, controlled trial.
Previously reported results of this pivotal trial showed prolongation of progression-free survival and time to next treatment with rituximab maintenance at a follow-up of 3 years and 6 years.
“Rituximab maintenance is now widely recommended for patients with follicular lymphoma responding to first-line rituximab-based immunochemotherapy,” Emmanuel Bachy, MD, PhD, of Institut National de la Santé et de la Recherche Médicale in Pierre-Bénite, France, and colleagues reported in the Journal of Clinical Oncology.
In PRIMA, patients with previously untreated high–tumor burden follicular lymphoma received any of three immunochemotherapy induction regimens. The 1,018 patients having a response were then randomly assigned to receive 2 years of rituximab (Rituxan) maintenance or observation only.
Dr. Bachy and colleagues performed the trial’s final efficacy analyses, now at a median follow-up of 9 years.
Among the 607 patients consenting to the extended follow-up, median progression-free survival was 10.5 years in the rituximab-maintenance group, compared with 4.1 years in the observation group (hazard ratio, 0.61; P less than .001).
“Subgroup analyses showed the substantial progression-free survival improvement associated with rituximab maintenance was independent of age, sex, induction immunochemotherapy regimen, response to induction, or [Follicular Lymphoma International Prognostic Index] risk score,” the investigators wrote.
Rituximab maintenance also prolonged the median time to next antilymphoma treatment (not reached vs. 6.1 years; hazard ratio, 0.66; P less than .001) and time to next chemotherapy treatment (not reached vs. 9.3 years; hazard ratio, 0.71; P less than .001).
But there was no significant difference in overall survival. Median overall survival was not reached in either group (hazard ratio, 1.04; P = .7948). The estimated 10-year overall survival rate was about 80% in both groups.
“This 9-year follow-up of the PRIMA study demonstrates that rituximab maintenance after induction immunochemotherapy provides a significant long-term [progression-free survival] benefit over observation,” the investigators wrote. “Despite the lack of [overall survival] advantage, it is noteworthy that more than half of the patients in the rituximab maintenance arm remain free of disease progression and have not required new antilymphoma treatment beyond 10 years.”
The trial was sponsored by the Lymphoma Study Association and supported by F. Hoffmann–La Roche and Biogen. Dr. Bachy reported financial disclosures related to Roche and other companies.
SOURCE: Bachy E et al. J Clin Oncol. 2019 Nov 1;37(31):2815-24.
FROM THE JOURNAL OF CLINICAL ONCOLOGY