User login
CAR T-cell ‘cocktail’ may overcome antigen escape relapse
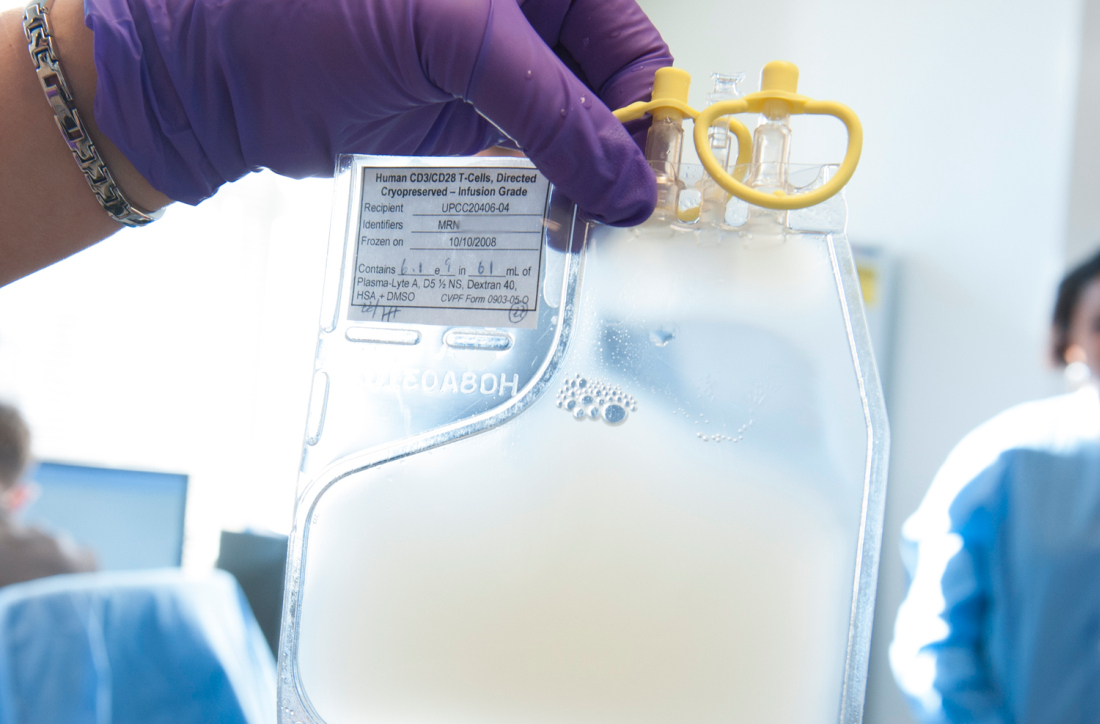
A chimeric antigen receptor (CAR) T-cell “cocktail” targeting both CD19 and CD22 could improve outcomes for patients with refractory or relapsed B-cell malignancies, according to investigators.
This dual approach, which appeared safe and effective, may be able to overcome antigen escape relapse, reported Na Wang, MD, of Huazhong University of Science and Technology in China, and colleagues.
The investigators tested this method in an open-label, single-arm pilot study involving 89 patients with refractory/relapsed B cell malignancies. Of these, 51 patients had B-cell acute lymphoblastic leukemia (B-ALL), while the remaining 38 had non-Hodgkin lymphoma (NHL). All patients had dual expression of CD19 and CD22 on malignant B cells, good performance status, and “essentially” normal organ function, the investigators reported in Blood.
Following lymphodepletion, patients were infused with CAR19 and CAR22 T cells, then evaluated for responses with imaging or bone marrow aspiration on a monthly basis for 6 months, then every 3 months thereafter.
After 30 days, most patients with ALL (96%) achieved a minimal residual disease-negative complete response or complete response with incomplete count recovery. After a median follow-up of 16.7 months, almost half of these responders relapsed (49%), median progression-free survival was 13.6 months, and overall survival was 31 months.
With a minimum follow-up of 3 months, half of the patients with NHL (50%) achieved complete responses, with the caveat that two patients who died of septic shock and severe cytokine release syndrome were excluded from this efficacy analysis. After a median follow-up of 14.4 months, in the NHL group, median progression-free survival was 9.9 months and overall survival was 18 months.
Across disease types, almost all patients (95.5%) experienced cytokine release syndrome, with more than three-quarters (77.6%) categorized as grade 1 or 2. CAR T cell-related encephalopathy syndrome (CRES) occurred in 13.5% of patients; most were low grade, apart from one case that was grade 4. In total, 12 patients died due to adverse events.
“The severe [adverse events] were mostly cytopenias and the most frequent fatal [adverse event] was lung infection, which was attributable in part to the high disease burden and heavy pretreatment of the enrolled patients,” the investigators wrote. “Nearly all the high-grade CRS and CRES were reversible and occurred in similar incidences as previously reported. Thus, the sequential infusion of CAR19/22 T-cell “cocktail” was an efficient and well-tolerated approach to circumvent antigen loss of CD19 or CD22.”
The investigators reported having no conflicts of interest.
SOURCE: Wang N et al. 2019 Oct 29. doi: 10.1182/blood.2019000017.
A chimeric antigen receptor (CAR) T-cell “cocktail” targeting both CD19 and CD22 could improve outcomes for patients with refractory or relapsed B-cell malignancies, according to investigators.
This dual approach, which appeared safe and effective, may be able to overcome antigen escape relapse, reported Na Wang, MD, of Huazhong University of Science and Technology in China, and colleagues.
The investigators tested this method in an open-label, single-arm pilot study involving 89 patients with refractory/relapsed B cell malignancies. Of these, 51 patients had B-cell acute lymphoblastic leukemia (B-ALL), while the remaining 38 had non-Hodgkin lymphoma (NHL). All patients had dual expression of CD19 and CD22 on malignant B cells, good performance status, and “essentially” normal organ function, the investigators reported in Blood.
Following lymphodepletion, patients were infused with CAR19 and CAR22 T cells, then evaluated for responses with imaging or bone marrow aspiration on a monthly basis for 6 months, then every 3 months thereafter.
After 30 days, most patients with ALL (96%) achieved a minimal residual disease-negative complete response or complete response with incomplete count recovery. After a median follow-up of 16.7 months, almost half of these responders relapsed (49%), median progression-free survival was 13.6 months, and overall survival was 31 months.
With a minimum follow-up of 3 months, half of the patients with NHL (50%) achieved complete responses, with the caveat that two patients who died of septic shock and severe cytokine release syndrome were excluded from this efficacy analysis. After a median follow-up of 14.4 months, in the NHL group, median progression-free survival was 9.9 months and overall survival was 18 months.
Across disease types, almost all patients (95.5%) experienced cytokine release syndrome, with more than three-quarters (77.6%) categorized as grade 1 or 2. CAR T cell-related encephalopathy syndrome (CRES) occurred in 13.5% of patients; most were low grade, apart from one case that was grade 4. In total, 12 patients died due to adverse events.
“The severe [adverse events] were mostly cytopenias and the most frequent fatal [adverse event] was lung infection, which was attributable in part to the high disease burden and heavy pretreatment of the enrolled patients,” the investigators wrote. “Nearly all the high-grade CRS and CRES were reversible and occurred in similar incidences as previously reported. Thus, the sequential infusion of CAR19/22 T-cell “cocktail” was an efficient and well-tolerated approach to circumvent antigen loss of CD19 or CD22.”
The investigators reported having no conflicts of interest.
SOURCE: Wang N et al. 2019 Oct 29. doi: 10.1182/blood.2019000017.
A chimeric antigen receptor (CAR) T-cell “cocktail” targeting both CD19 and CD22 could improve outcomes for patients with refractory or relapsed B-cell malignancies, according to investigators.
This dual approach, which appeared safe and effective, may be able to overcome antigen escape relapse, reported Na Wang, MD, of Huazhong University of Science and Technology in China, and colleagues.
The investigators tested this method in an open-label, single-arm pilot study involving 89 patients with refractory/relapsed B cell malignancies. Of these, 51 patients had B-cell acute lymphoblastic leukemia (B-ALL), while the remaining 38 had non-Hodgkin lymphoma (NHL). All patients had dual expression of CD19 and CD22 on malignant B cells, good performance status, and “essentially” normal organ function, the investigators reported in Blood.
Following lymphodepletion, patients were infused with CAR19 and CAR22 T cells, then evaluated for responses with imaging or bone marrow aspiration on a monthly basis for 6 months, then every 3 months thereafter.
After 30 days, most patients with ALL (96%) achieved a minimal residual disease-negative complete response or complete response with incomplete count recovery. After a median follow-up of 16.7 months, almost half of these responders relapsed (49%), median progression-free survival was 13.6 months, and overall survival was 31 months.
With a minimum follow-up of 3 months, half of the patients with NHL (50%) achieved complete responses, with the caveat that two patients who died of septic shock and severe cytokine release syndrome were excluded from this efficacy analysis. After a median follow-up of 14.4 months, in the NHL group, median progression-free survival was 9.9 months and overall survival was 18 months.
Across disease types, almost all patients (95.5%) experienced cytokine release syndrome, with more than three-quarters (77.6%) categorized as grade 1 or 2. CAR T cell-related encephalopathy syndrome (CRES) occurred in 13.5% of patients; most were low grade, apart from one case that was grade 4. In total, 12 patients died due to adverse events.
“The severe [adverse events] were mostly cytopenias and the most frequent fatal [adverse event] was lung infection, which was attributable in part to the high disease burden and heavy pretreatment of the enrolled patients,” the investigators wrote. “Nearly all the high-grade CRS and CRES were reversible and occurred in similar incidences as previously reported. Thus, the sequential infusion of CAR19/22 T-cell “cocktail” was an efficient and well-tolerated approach to circumvent antigen loss of CD19 or CD22.”
The investigators reported having no conflicts of interest.
SOURCE: Wang N et al. 2019 Oct 29. doi: 10.1182/blood.2019000017.
FROM BLOOD
Adding polatuzumab extends survival in relapsed/refractory DLBCL
For patients with relapsed or refractory diffuse large B-cell lymphoma (DLBCL), adding polatuzumab vedotin to bendamustine and rituximab can improve complete response rates and extend overall survival, according to findings from a phase 1b/2 trial.
Adding polatuzumab decreased mortality risk by 58%, reported lead author Laurie H. Sehn, MD, of the University of British Columbia, Vancouver, and colleagues.
“Patients with transplantation-ineligible [relapsed/refractory] DLBCL, including those who experienced treatment failure with [autologous stem cell transplant], have dismal outcomes with limited therapeutic options,” the investigators wrote in the Journal of Clinical Oncology. “To our knowledge, this is the first randomized trial demonstrating an [overall survival] benefit in patients with transplantation-ineligible [relapsed/refractory] DLBCL.”
In the first part of the study, 27 patients were treated with polatuzumab vedotin, bendamustine, and obinutuzumab. After a median follow-up of 27 months, this regimen returned a complete response rate of 29.6%, median progression-free survival of 6.3 months, and median overall survival of 10.8 months.
In the primary analysis, 80 patients were randomized to receive bendamustine and rituximab, with or without polatuzumab. Adding polatuzumab had a significant benefit, as 40.0% of these patients achieved a complete response, compared with 17.5% of patients who did not receive polatuzumab. After a median follow-up of 22.3 months, outcomes also were significantly improved with the addition of polatuzumab for both median progression-free survival (9.5 vs. 3.7 months) and overall survival (12.4 vs. 4.7 months).
Adding polatuzumab did come with some safety trade-offs. Rates of certain grade 3 or 4 adverse events were higher, including thrombocytopenia (41% vs. 23.1%), neutropenia (46.2% vs. 33.3%), and anemia (28.2% vs. 17.9%), while infection rates were comparable. Almost half of the patients treated with polatuzumab (43.6%) developed grade 1 or 2 peripheral neuropathy, but most cases resolved.
Combination therapy with polatuzumab, bendamustine, and rituximab “represents a novel, effective therapeutic regimen to address the unmet need of patients with transplantation-ineligible [relapsed/refractory] DLBCL,” the investigators wrote. Since just 25% of polatuzumab combination–treated patients had received prior autologous stem cell transplant, the investigators said they could not make definitive conclusions on this combination’s efficacy in the post-ASCT setting.
Additional trials involving polatuzumab in the relapsed/refractory setting are ongoing. For patients with treatment-naive DLBCL, a phase 3 trial (NCT03274492) is evaluating substitution of polatuzumab for vincristine in the R-CHOP regimen.
The study was funded by F. Hoffmann-La Roche and Genentech. The investigators reported additional relationships with AbbVie, Kite Pharma, Lundbeck, and others.
SOURCE: Sehn LH et al. J Clin Oncol. 2019 Nov 6. doi: 10.1200/JCO.19.00172.
For patients with relapsed or refractory diffuse large B-cell lymphoma (DLBCL), adding polatuzumab vedotin to bendamustine and rituximab can improve complete response rates and extend overall survival, according to findings from a phase 1b/2 trial.
Adding polatuzumab decreased mortality risk by 58%, reported lead author Laurie H. Sehn, MD, of the University of British Columbia, Vancouver, and colleagues.
“Patients with transplantation-ineligible [relapsed/refractory] DLBCL, including those who experienced treatment failure with [autologous stem cell transplant], have dismal outcomes with limited therapeutic options,” the investigators wrote in the Journal of Clinical Oncology. “To our knowledge, this is the first randomized trial demonstrating an [overall survival] benefit in patients with transplantation-ineligible [relapsed/refractory] DLBCL.”
In the first part of the study, 27 patients were treated with polatuzumab vedotin, bendamustine, and obinutuzumab. After a median follow-up of 27 months, this regimen returned a complete response rate of 29.6%, median progression-free survival of 6.3 months, and median overall survival of 10.8 months.
In the primary analysis, 80 patients were randomized to receive bendamustine and rituximab, with or without polatuzumab. Adding polatuzumab had a significant benefit, as 40.0% of these patients achieved a complete response, compared with 17.5% of patients who did not receive polatuzumab. After a median follow-up of 22.3 months, outcomes also were significantly improved with the addition of polatuzumab for both median progression-free survival (9.5 vs. 3.7 months) and overall survival (12.4 vs. 4.7 months).
Adding polatuzumab did come with some safety trade-offs. Rates of certain grade 3 or 4 adverse events were higher, including thrombocytopenia (41% vs. 23.1%), neutropenia (46.2% vs. 33.3%), and anemia (28.2% vs. 17.9%), while infection rates were comparable. Almost half of the patients treated with polatuzumab (43.6%) developed grade 1 or 2 peripheral neuropathy, but most cases resolved.
Combination therapy with polatuzumab, bendamustine, and rituximab “represents a novel, effective therapeutic regimen to address the unmet need of patients with transplantation-ineligible [relapsed/refractory] DLBCL,” the investigators wrote. Since just 25% of polatuzumab combination–treated patients had received prior autologous stem cell transplant, the investigators said they could not make definitive conclusions on this combination’s efficacy in the post-ASCT setting.
Additional trials involving polatuzumab in the relapsed/refractory setting are ongoing. For patients with treatment-naive DLBCL, a phase 3 trial (NCT03274492) is evaluating substitution of polatuzumab for vincristine in the R-CHOP regimen.
The study was funded by F. Hoffmann-La Roche and Genentech. The investigators reported additional relationships with AbbVie, Kite Pharma, Lundbeck, and others.
SOURCE: Sehn LH et al. J Clin Oncol. 2019 Nov 6. doi: 10.1200/JCO.19.00172.
For patients with relapsed or refractory diffuse large B-cell lymphoma (DLBCL), adding polatuzumab vedotin to bendamustine and rituximab can improve complete response rates and extend overall survival, according to findings from a phase 1b/2 trial.
Adding polatuzumab decreased mortality risk by 58%, reported lead author Laurie H. Sehn, MD, of the University of British Columbia, Vancouver, and colleagues.
“Patients with transplantation-ineligible [relapsed/refractory] DLBCL, including those who experienced treatment failure with [autologous stem cell transplant], have dismal outcomes with limited therapeutic options,” the investigators wrote in the Journal of Clinical Oncology. “To our knowledge, this is the first randomized trial demonstrating an [overall survival] benefit in patients with transplantation-ineligible [relapsed/refractory] DLBCL.”
In the first part of the study, 27 patients were treated with polatuzumab vedotin, bendamustine, and obinutuzumab. After a median follow-up of 27 months, this regimen returned a complete response rate of 29.6%, median progression-free survival of 6.3 months, and median overall survival of 10.8 months.
In the primary analysis, 80 patients were randomized to receive bendamustine and rituximab, with or without polatuzumab. Adding polatuzumab had a significant benefit, as 40.0% of these patients achieved a complete response, compared with 17.5% of patients who did not receive polatuzumab. After a median follow-up of 22.3 months, outcomes also were significantly improved with the addition of polatuzumab for both median progression-free survival (9.5 vs. 3.7 months) and overall survival (12.4 vs. 4.7 months).
Adding polatuzumab did come with some safety trade-offs. Rates of certain grade 3 or 4 adverse events were higher, including thrombocytopenia (41% vs. 23.1%), neutropenia (46.2% vs. 33.3%), and anemia (28.2% vs. 17.9%), while infection rates were comparable. Almost half of the patients treated with polatuzumab (43.6%) developed grade 1 or 2 peripheral neuropathy, but most cases resolved.
Combination therapy with polatuzumab, bendamustine, and rituximab “represents a novel, effective therapeutic regimen to address the unmet need of patients with transplantation-ineligible [relapsed/refractory] DLBCL,” the investigators wrote. Since just 25% of polatuzumab combination–treated patients had received prior autologous stem cell transplant, the investigators said they could not make definitive conclusions on this combination’s efficacy in the post-ASCT setting.
Additional trials involving polatuzumab in the relapsed/refractory setting are ongoing. For patients with treatment-naive DLBCL, a phase 3 trial (NCT03274492) is evaluating substitution of polatuzumab for vincristine in the R-CHOP regimen.
The study was funded by F. Hoffmann-La Roche and Genentech. The investigators reported additional relationships with AbbVie, Kite Pharma, Lundbeck, and others.
SOURCE: Sehn LH et al. J Clin Oncol. 2019 Nov 6. doi: 10.1200/JCO.19.00172.
FROM THE JOURNAL OF CLINICAL ONCOLOGY
FDA approves Brukinsa for relapsed, refractory MCL
The Food and Drug Administration has approved zanubrutinib (Brukinsa) for the treatment of mantle cell lymphoma (MCL) in adult patients who have received at least one prior therapy.
The approval is based on results from two separate studies; in a global phase 1/2 trial, patients with relapsed or refractory MCL who received zanubrutinib had an overall response rate of 84%, with 22% experiencing a complete response and 62% experiencing partial response. Median duration of response was 18.5 months. The ORR in the second study – a multicenter phase 2 trial – was also 84%, but with 59% experiencing a complete response and 24% experiencing partial response; duration of response was 19.5 months.
The most common adverse events reported during the trials were decreased neutrophil count, decreased platelet count, upper respiratory tract infection, decreased white blood cell count, decreased hemoglobin, rash, bruising, diarrhea, cough, musculoskeletal pain, pneumonia, urinary tract infection, hematuria, fatigue, constipation, and hemorrhage. The most common serious adverse events were pneumonia and hemorrhage.
Of the 118 patients with MCL treated with zanubrutinib over the two trials, 8 had to be discontinued because of adverse events.
The recommended dose of zanubrutinib is 320 mg, taken orally 160 mg twice daily or 320 mg once daily, with or without food.
“BTK [Bruton kinase] inhibition is an established mode of treatment for patients with MCL, but many patients treated with previously approved BTK inhibitors do not fully respond to BTK therapy or are forced to discontinue treatment early due to side effects. Today we have a new option for our adult patients who have received one prior systemic or targeted therapy and are living with MCL,” Luhua (Michael) Wang, MD, clinical trial investigator and professor in the department of lymphoma and myeloma at the University of Texas MD Anderson Cancer Center, Houston, said in a statement.
The Food and Drug Administration has approved zanubrutinib (Brukinsa) for the treatment of mantle cell lymphoma (MCL) in adult patients who have received at least one prior therapy.
The approval is based on results from two separate studies; in a global phase 1/2 trial, patients with relapsed or refractory MCL who received zanubrutinib had an overall response rate of 84%, with 22% experiencing a complete response and 62% experiencing partial response. Median duration of response was 18.5 months. The ORR in the second study – a multicenter phase 2 trial – was also 84%, but with 59% experiencing a complete response and 24% experiencing partial response; duration of response was 19.5 months.
The most common adverse events reported during the trials were decreased neutrophil count, decreased platelet count, upper respiratory tract infection, decreased white blood cell count, decreased hemoglobin, rash, bruising, diarrhea, cough, musculoskeletal pain, pneumonia, urinary tract infection, hematuria, fatigue, constipation, and hemorrhage. The most common serious adverse events were pneumonia and hemorrhage.
Of the 118 patients with MCL treated with zanubrutinib over the two trials, 8 had to be discontinued because of adverse events.
The recommended dose of zanubrutinib is 320 mg, taken orally 160 mg twice daily or 320 mg once daily, with or without food.
“BTK [Bruton kinase] inhibition is an established mode of treatment for patients with MCL, but many patients treated with previously approved BTK inhibitors do not fully respond to BTK therapy or are forced to discontinue treatment early due to side effects. Today we have a new option for our adult patients who have received one prior systemic or targeted therapy and are living with MCL,” Luhua (Michael) Wang, MD, clinical trial investigator and professor in the department of lymphoma and myeloma at the University of Texas MD Anderson Cancer Center, Houston, said in a statement.
The Food and Drug Administration has approved zanubrutinib (Brukinsa) for the treatment of mantle cell lymphoma (MCL) in adult patients who have received at least one prior therapy.
The approval is based on results from two separate studies; in a global phase 1/2 trial, patients with relapsed or refractory MCL who received zanubrutinib had an overall response rate of 84%, with 22% experiencing a complete response and 62% experiencing partial response. Median duration of response was 18.5 months. The ORR in the second study – a multicenter phase 2 trial – was also 84%, but with 59% experiencing a complete response and 24% experiencing partial response; duration of response was 19.5 months.
The most common adverse events reported during the trials were decreased neutrophil count, decreased platelet count, upper respiratory tract infection, decreased white blood cell count, decreased hemoglobin, rash, bruising, diarrhea, cough, musculoskeletal pain, pneumonia, urinary tract infection, hematuria, fatigue, constipation, and hemorrhage. The most common serious adverse events were pneumonia and hemorrhage.
Of the 118 patients with MCL treated with zanubrutinib over the two trials, 8 had to be discontinued because of adverse events.
The recommended dose of zanubrutinib is 320 mg, taken orally 160 mg twice daily or 320 mg once daily, with or without food.
“BTK [Bruton kinase] inhibition is an established mode of treatment for patients with MCL, but many patients treated with previously approved BTK inhibitors do not fully respond to BTK therapy or are forced to discontinue treatment early due to side effects. Today we have a new option for our adult patients who have received one prior systemic or targeted therapy and are living with MCL,” Luhua (Michael) Wang, MD, clinical trial investigator and professor in the department of lymphoma and myeloma at the University of Texas MD Anderson Cancer Center, Houston, said in a statement.
Gene signature may help guide initial CLL treatment choice
A novel 17-gene expression signature may help guide the choice of initial treatment in patients with IGHV-unmutated chronic lymphocytic leukemia (CLL), according to findings of a retrospective dual cohort study.
“[Fludarabine, cyclophosphamide, and rituximab] was the first regimen to improve progression-free survival and overall survival in patients with chronic lymphocytic leukaemia, and has become a gold-standard chemoimmunotherapy regimen in physically fit patients,” wrote the investigators, who were led by Carmen D. Herling, MD, of the Center for Integrated Oncology, Cologne, Germany; and Kevin R. Coombes, PhD, of Ohio State University, Columbus.
While several studies demonstrate that young, fit patients with mutated IGHV gene and no high-risk cytogenetic abnormalities achieve durable remission with the FCR (fludarabine, cyclophosphamide, and rituximab) regimen, there have been no studies to identify if this is true for patients with unmutated IGHV gene, they reported in the Lancet Oncology.
The investigators performed transcriptional profiling using peripheral blood samples collected from two cohorts of patients with CLL who were treated with frontline FCR.
The discovery and training cohort consisted of 101 patients (65% with IGHV-unmutated disease) treated at the MD Anderson Cancer Center who had a median follow-up of about 12 years. The validation cohort consisted of 109 patients with IGHV-unmutated disease treated on the German CLL8 single-arm trial who had a median follow-up of about 6 years.
A total of 1,136 genes showed a significant univariate association with time to progression. Ultimately, 17 of these genes – most of them involved in purine metabolism and oxidative phosphorylation – were included in the expression signature.
Among patients with IGHV-unmutated CLL, the 17-gene signature discriminated between two groups having differing time to progression after their frontline FCR chemoimmunotherapy: an unfavorable prognosis group and an intermediate prognosis group.
The unfavorable prognosis group had a significantly higher relative risk of progression in both the discovery/training cohort (hazard ratio, 3.83; P less than .0001) and the validation cohort (HR, 1.90; P = .008). In the validation cohort, the median time to progression was 39 months among patients with a signature-defined unfavorable prognosis, compared with 59 months among patients with a signature-defined intermediate prognosis.
“We would recommend testing the value of the 17-gene signature in a prospective study that compares FCR treatment with alternative therapies, such as ibrutinib, as part of a randomised clinical trial,” the investigators wrote.
Dr. Herling reported financial disclosures related to Hoffmann-La Roche, and Dr. Coombes reported grants from the National Institutes of Health. The study was funded by the Chronic Lymphocytic Leukaemia Global Research Foundation and the National Institutes of Health/National Cancer Institute.
SOURCE: Herling CD et al. Lancet Oncol. 2019;20(11):1576-86.
A novel 17-gene expression signature may help guide the choice of initial treatment in patients with IGHV-unmutated chronic lymphocytic leukemia (CLL), according to findings of a retrospective dual cohort study.
“[Fludarabine, cyclophosphamide, and rituximab] was the first regimen to improve progression-free survival and overall survival in patients with chronic lymphocytic leukaemia, and has become a gold-standard chemoimmunotherapy regimen in physically fit patients,” wrote the investigators, who were led by Carmen D. Herling, MD, of the Center for Integrated Oncology, Cologne, Germany; and Kevin R. Coombes, PhD, of Ohio State University, Columbus.
While several studies demonstrate that young, fit patients with mutated IGHV gene and no high-risk cytogenetic abnormalities achieve durable remission with the FCR (fludarabine, cyclophosphamide, and rituximab) regimen, there have been no studies to identify if this is true for patients with unmutated IGHV gene, they reported in the Lancet Oncology.
The investigators performed transcriptional profiling using peripheral blood samples collected from two cohorts of patients with CLL who were treated with frontline FCR.
The discovery and training cohort consisted of 101 patients (65% with IGHV-unmutated disease) treated at the MD Anderson Cancer Center who had a median follow-up of about 12 years. The validation cohort consisted of 109 patients with IGHV-unmutated disease treated on the German CLL8 single-arm trial who had a median follow-up of about 6 years.
A total of 1,136 genes showed a significant univariate association with time to progression. Ultimately, 17 of these genes – most of them involved in purine metabolism and oxidative phosphorylation – were included in the expression signature.
Among patients with IGHV-unmutated CLL, the 17-gene signature discriminated between two groups having differing time to progression after their frontline FCR chemoimmunotherapy: an unfavorable prognosis group and an intermediate prognosis group.
The unfavorable prognosis group had a significantly higher relative risk of progression in both the discovery/training cohort (hazard ratio, 3.83; P less than .0001) and the validation cohort (HR, 1.90; P = .008). In the validation cohort, the median time to progression was 39 months among patients with a signature-defined unfavorable prognosis, compared with 59 months among patients with a signature-defined intermediate prognosis.
“We would recommend testing the value of the 17-gene signature in a prospective study that compares FCR treatment with alternative therapies, such as ibrutinib, as part of a randomised clinical trial,” the investigators wrote.
Dr. Herling reported financial disclosures related to Hoffmann-La Roche, and Dr. Coombes reported grants from the National Institutes of Health. The study was funded by the Chronic Lymphocytic Leukaemia Global Research Foundation and the National Institutes of Health/National Cancer Institute.
SOURCE: Herling CD et al. Lancet Oncol. 2019;20(11):1576-86.
A novel 17-gene expression signature may help guide the choice of initial treatment in patients with IGHV-unmutated chronic lymphocytic leukemia (CLL), according to findings of a retrospective dual cohort study.
“[Fludarabine, cyclophosphamide, and rituximab] was the first regimen to improve progression-free survival and overall survival in patients with chronic lymphocytic leukaemia, and has become a gold-standard chemoimmunotherapy regimen in physically fit patients,” wrote the investigators, who were led by Carmen D. Herling, MD, of the Center for Integrated Oncology, Cologne, Germany; and Kevin R. Coombes, PhD, of Ohio State University, Columbus.
While several studies demonstrate that young, fit patients with mutated IGHV gene and no high-risk cytogenetic abnormalities achieve durable remission with the FCR (fludarabine, cyclophosphamide, and rituximab) regimen, there have been no studies to identify if this is true for patients with unmutated IGHV gene, they reported in the Lancet Oncology.
The investigators performed transcriptional profiling using peripheral blood samples collected from two cohorts of patients with CLL who were treated with frontline FCR.
The discovery and training cohort consisted of 101 patients (65% with IGHV-unmutated disease) treated at the MD Anderson Cancer Center who had a median follow-up of about 12 years. The validation cohort consisted of 109 patients with IGHV-unmutated disease treated on the German CLL8 single-arm trial who had a median follow-up of about 6 years.
A total of 1,136 genes showed a significant univariate association with time to progression. Ultimately, 17 of these genes – most of them involved in purine metabolism and oxidative phosphorylation – were included in the expression signature.
Among patients with IGHV-unmutated CLL, the 17-gene signature discriminated between two groups having differing time to progression after their frontline FCR chemoimmunotherapy: an unfavorable prognosis group and an intermediate prognosis group.
The unfavorable prognosis group had a significantly higher relative risk of progression in both the discovery/training cohort (hazard ratio, 3.83; P less than .0001) and the validation cohort (HR, 1.90; P = .008). In the validation cohort, the median time to progression was 39 months among patients with a signature-defined unfavorable prognosis, compared with 59 months among patients with a signature-defined intermediate prognosis.
“We would recommend testing the value of the 17-gene signature in a prospective study that compares FCR treatment with alternative therapies, such as ibrutinib, as part of a randomised clinical trial,” the investigators wrote.
Dr. Herling reported financial disclosures related to Hoffmann-La Roche, and Dr. Coombes reported grants from the National Institutes of Health. The study was funded by the Chronic Lymphocytic Leukaemia Global Research Foundation and the National Institutes of Health/National Cancer Institute.
SOURCE: Herling CD et al. Lancet Oncol. 2019;20(11):1576-86.
FROM LANCET ONCOLOGY
Armored CAR T cells elicit responses in NHL patients
NATIONAL HARBOR, MD – An armored chimeric antigen receptor (CAR) T-cell therapy has demonstrated efficacy in vitro and in patients with relapsed or refractory non-Hodgkin lymphoma (NHL), according to findings presented at the annual meeting of the Society for Immunotherapy of Cancer.
ICTCAR014, a dominant negative PD-1 armored CAR T-cell therapy, proved more cytotoxic than traditional CAR T-cell therapy in vitro and produced responses in 12 of 13 NHL patients who received it.
Xiaobin Victor Lu, PhD, of Innovative Cellular Therapeutics, Shanghai, China, presented results with ICTCAR014 at the meeting.
Dr. Lu explained that ICTCAR014 consists of CD19-targeted CAR T cells genetically engineered to overexpress a PD-1 dominant negative protein with an altered intracellular signaling domain. The dominant negative protein can act as a “decoy receptor” to bind and block the PD-L1/2 inhibitory signal, thereby enhancing the efficacy of CAR T cells.
Innovative Cellular Therapeutics is developing ICTCAR014 because there is “some room to improve” with commercially available CAR T-cell products, Dr. Lu said. Specifically, tisagenlecleucel produced a 52% response rate in the JULIET trial (N Engl J Med. 2019;380:45-56), and axicabtagene ciloleucel produced an 82% response rate in the ZUMA-1 trial (N Engl J Med. 2017;377:2531-44).
There is also evidence to suggest that PD-1 blockade can modulate and “refuel” CAR T cells in relapsed/refractory NHL patients who fail or relapse after traditional anti-CD19 CAR T-cell therapy (Blood. 2017 Feb 23;129[8]:1039-41). This finding has prompted researchers to conduct trials of PD-1 inhibitors in combination with CAR T-cell therapies. But this combination approach may be expensive and cause more side effects than the armored CAR T-cell approach, Dr. Lu said.
In preclinical studies, Dr. Lu and colleagues found that ICTCAR014 was more effective than traditional anti-CD19 CAR T cells in killing Nalm6-PDL1 cells. In addition, the PD-1 dominant negative protein protected CAR T cells from exhaustion.
Dr. Lu also presented results in 13 NHL patients who have received ICTCAR014 in a phase 1 trial in China. Eleven patients had diffuse large B-cell lymphoma (DLBCL), and two had follicular lymphoma.
The objective response rate was 92.3% (12/13), which included five partial responses (38.5%) and seven complete responses (53.8%). Both follicular lymphoma patients and five DLBCL patients achieved a complete response. Five DLBCL patients achieved a partial response, and the remaining DLBCL patient did not respond.
Dr. Lu did not present safety data. However, he reported that there was no increased incidence of cytokine release syndrome or neurotoxicity in these patients, compared with patients receiving traditional CAR T-cell therapy.
Dr. Lu is employed by Innovative Cellular Therapeutics, which funded the research and is developing ICTCAR014.
SOURCE: Lu V et al. SITC 2019, Abstract O25.
NATIONAL HARBOR, MD – An armored chimeric antigen receptor (CAR) T-cell therapy has demonstrated efficacy in vitro and in patients with relapsed or refractory non-Hodgkin lymphoma (NHL), according to findings presented at the annual meeting of the Society for Immunotherapy of Cancer.
ICTCAR014, a dominant negative PD-1 armored CAR T-cell therapy, proved more cytotoxic than traditional CAR T-cell therapy in vitro and produced responses in 12 of 13 NHL patients who received it.
Xiaobin Victor Lu, PhD, of Innovative Cellular Therapeutics, Shanghai, China, presented results with ICTCAR014 at the meeting.
Dr. Lu explained that ICTCAR014 consists of CD19-targeted CAR T cells genetically engineered to overexpress a PD-1 dominant negative protein with an altered intracellular signaling domain. The dominant negative protein can act as a “decoy receptor” to bind and block the PD-L1/2 inhibitory signal, thereby enhancing the efficacy of CAR T cells.
Innovative Cellular Therapeutics is developing ICTCAR014 because there is “some room to improve” with commercially available CAR T-cell products, Dr. Lu said. Specifically, tisagenlecleucel produced a 52% response rate in the JULIET trial (N Engl J Med. 2019;380:45-56), and axicabtagene ciloleucel produced an 82% response rate in the ZUMA-1 trial (N Engl J Med. 2017;377:2531-44).
There is also evidence to suggest that PD-1 blockade can modulate and “refuel” CAR T cells in relapsed/refractory NHL patients who fail or relapse after traditional anti-CD19 CAR T-cell therapy (Blood. 2017 Feb 23;129[8]:1039-41). This finding has prompted researchers to conduct trials of PD-1 inhibitors in combination with CAR T-cell therapies. But this combination approach may be expensive and cause more side effects than the armored CAR T-cell approach, Dr. Lu said.
In preclinical studies, Dr. Lu and colleagues found that ICTCAR014 was more effective than traditional anti-CD19 CAR T cells in killing Nalm6-PDL1 cells. In addition, the PD-1 dominant negative protein protected CAR T cells from exhaustion.
Dr. Lu also presented results in 13 NHL patients who have received ICTCAR014 in a phase 1 trial in China. Eleven patients had diffuse large B-cell lymphoma (DLBCL), and two had follicular lymphoma.
The objective response rate was 92.3% (12/13), which included five partial responses (38.5%) and seven complete responses (53.8%). Both follicular lymphoma patients and five DLBCL patients achieved a complete response. Five DLBCL patients achieved a partial response, and the remaining DLBCL patient did not respond.
Dr. Lu did not present safety data. However, he reported that there was no increased incidence of cytokine release syndrome or neurotoxicity in these patients, compared with patients receiving traditional CAR T-cell therapy.
Dr. Lu is employed by Innovative Cellular Therapeutics, which funded the research and is developing ICTCAR014.
SOURCE: Lu V et al. SITC 2019, Abstract O25.
NATIONAL HARBOR, MD – An armored chimeric antigen receptor (CAR) T-cell therapy has demonstrated efficacy in vitro and in patients with relapsed or refractory non-Hodgkin lymphoma (NHL), according to findings presented at the annual meeting of the Society for Immunotherapy of Cancer.
ICTCAR014, a dominant negative PD-1 armored CAR T-cell therapy, proved more cytotoxic than traditional CAR T-cell therapy in vitro and produced responses in 12 of 13 NHL patients who received it.
Xiaobin Victor Lu, PhD, of Innovative Cellular Therapeutics, Shanghai, China, presented results with ICTCAR014 at the meeting.
Dr. Lu explained that ICTCAR014 consists of CD19-targeted CAR T cells genetically engineered to overexpress a PD-1 dominant negative protein with an altered intracellular signaling domain. The dominant negative protein can act as a “decoy receptor” to bind and block the PD-L1/2 inhibitory signal, thereby enhancing the efficacy of CAR T cells.
Innovative Cellular Therapeutics is developing ICTCAR014 because there is “some room to improve” with commercially available CAR T-cell products, Dr. Lu said. Specifically, tisagenlecleucel produced a 52% response rate in the JULIET trial (N Engl J Med. 2019;380:45-56), and axicabtagene ciloleucel produced an 82% response rate in the ZUMA-1 trial (N Engl J Med. 2017;377:2531-44).
There is also evidence to suggest that PD-1 blockade can modulate and “refuel” CAR T cells in relapsed/refractory NHL patients who fail or relapse after traditional anti-CD19 CAR T-cell therapy (Blood. 2017 Feb 23;129[8]:1039-41). This finding has prompted researchers to conduct trials of PD-1 inhibitors in combination with CAR T-cell therapies. But this combination approach may be expensive and cause more side effects than the armored CAR T-cell approach, Dr. Lu said.
In preclinical studies, Dr. Lu and colleagues found that ICTCAR014 was more effective than traditional anti-CD19 CAR T cells in killing Nalm6-PDL1 cells. In addition, the PD-1 dominant negative protein protected CAR T cells from exhaustion.
Dr. Lu also presented results in 13 NHL patients who have received ICTCAR014 in a phase 1 trial in China. Eleven patients had diffuse large B-cell lymphoma (DLBCL), and two had follicular lymphoma.
The objective response rate was 92.3% (12/13), which included five partial responses (38.5%) and seven complete responses (53.8%). Both follicular lymphoma patients and five DLBCL patients achieved a complete response. Five DLBCL patients achieved a partial response, and the remaining DLBCL patient did not respond.
Dr. Lu did not present safety data. However, he reported that there was no increased incidence of cytokine release syndrome or neurotoxicity in these patients, compared with patients receiving traditional CAR T-cell therapy.
Dr. Lu is employed by Innovative Cellular Therapeutics, which funded the research and is developing ICTCAR014.
SOURCE: Lu V et al. SITC 2019, Abstract O25.
REPORTING FROM SITC 2019
Consider renal function in TLS risk assessment of venetoclax-treated CLL
EDINBURGH – Impaired renal function may indicate excess risk of tumor lysis syndrome (TLS) in venetoclax-treated chronic lymphocytic leukemia (CLL) patients and should be considered when assessing TLS risk, according to findings from a retrospective cohort study.
Complex karyotype may also affect TLS risk, Anthony Mato, MD, reported at the International Workshop on Chronic Lymphocytic Leukemia.
Of 339 CLL patients who were treated with venetoclax, 38%, 34%, and 28% were considered to have low, medium, or high risk for TLS, respectively, according to the standard definition based on absolute lymphocyte count as a measure of tumor burden and/or lymph node size.
TLS occurred in 35 patients (10%), including 26 cases of laboratory-confirmed TLS and 9 clinical TLS cases; 1 patient required dialysis and 1 death occurred, which was attributable to the TLS, Dr. Mato of Memorial Sloan Kettering Cancer Center, New York, and colleagues reported in a poster at the workshop.
Univariate analysis was performed to “understand baseline factors associated with TLS development during dose escalation,” and it examined sex, creatinine clearance (CrCl), complex karyotype, immunoglobulin heavy chain variable mutation status, prior ibrutinib exposure, venetoclax monotherapy vs. combination therapy, and TLS risk group. The investigators observed no significant difference between the low- and medium-risk patients, therefore those two groups were combined and compared with the high-risk patients.
The univariate analysis showed significant associations between TLS and CrCl (odds ratio, 2.9 for 80 mL/min or less vs. greater than 80 mL/min), complex karyotype (OR, 2.2), and low/medium vs. high TLS risk based on the standard definition (OR, 2.56).
A multivariable analysis of the predictors identified as significant in the univariate analyses showed that standard TLS risk group and CrCl remained independent predictors of TLS.
“Although the odds ratio for complex karyotype suggested potential clinical significance, this did not meet the threshold for statistical significance and was not included in the final model,” they wrote.
The area under the receiver operating characteristic curve for a model including TLS risk group and CrCl was 74.6%, compared with 65% for the area under the ROC curve using the standard tumor burden/lymph node size approach for defining TLS risk, which is described in the venetoclax package insert.
Patients included in the study had a median age of 67 years at venetoclax initiation, 69% were men, 85% were white, and 13% were treated on a clinical trial. Complex karyotype was present in 39%, del(17p) in 43%, and 84% had immunoglobulin heavy chain variable–unmutated disease.
Most patients received venetoclax monotherapy (79%), had relapsed/refractory disease (94%), and had previously received ibrutinib (78%). The median number of prior therapies was 3, but the number ranged from 0-15, the investigators noted.
The findings of this study suggest that, in addition to defining risk based on absolute lymphocyte count and lymph node size, patients with CrCl less than 80 mL/min – indicating impaired renal function – have excess risk of TLS.
Although complex karyotype did not reach statistical significance as an independent predictor of TLS, the findings in this study suggest it “may impact TLS risk and is worthy of further study in larger samples,” they said, concluding that consideration of baseline renal function, and possibly karyotype, could “further guide practitioners in their approach to prophylaxis and patient counseling, allowing for improved safety in the use of this effective agent in CLL.”
Additional planned analyses will focus on TLS risk score development and further refinement of TLS risk stratification, they noted.
Dr. Mato has received grant support, consulting fees, and/or fees for serving on a data and safety monitoring board or advisory board from AbbVie, AstraZeneca, Celgene, Janssen, TG Therapeutics, Pharmacyclics, Loxo, Sunesis, prIME Oncology, Pfizer, Johnson & Johnson, and Regeneron.
EDINBURGH – Impaired renal function may indicate excess risk of tumor lysis syndrome (TLS) in venetoclax-treated chronic lymphocytic leukemia (CLL) patients and should be considered when assessing TLS risk, according to findings from a retrospective cohort study.
Complex karyotype may also affect TLS risk, Anthony Mato, MD, reported at the International Workshop on Chronic Lymphocytic Leukemia.
Of 339 CLL patients who were treated with venetoclax, 38%, 34%, and 28% were considered to have low, medium, or high risk for TLS, respectively, according to the standard definition based on absolute lymphocyte count as a measure of tumor burden and/or lymph node size.
TLS occurred in 35 patients (10%), including 26 cases of laboratory-confirmed TLS and 9 clinical TLS cases; 1 patient required dialysis and 1 death occurred, which was attributable to the TLS, Dr. Mato of Memorial Sloan Kettering Cancer Center, New York, and colleagues reported in a poster at the workshop.
Univariate analysis was performed to “understand baseline factors associated with TLS development during dose escalation,” and it examined sex, creatinine clearance (CrCl), complex karyotype, immunoglobulin heavy chain variable mutation status, prior ibrutinib exposure, venetoclax monotherapy vs. combination therapy, and TLS risk group. The investigators observed no significant difference between the low- and medium-risk patients, therefore those two groups were combined and compared with the high-risk patients.
The univariate analysis showed significant associations between TLS and CrCl (odds ratio, 2.9 for 80 mL/min or less vs. greater than 80 mL/min), complex karyotype (OR, 2.2), and low/medium vs. high TLS risk based on the standard definition (OR, 2.56).
A multivariable analysis of the predictors identified as significant in the univariate analyses showed that standard TLS risk group and CrCl remained independent predictors of TLS.
“Although the odds ratio for complex karyotype suggested potential clinical significance, this did not meet the threshold for statistical significance and was not included in the final model,” they wrote.
The area under the receiver operating characteristic curve for a model including TLS risk group and CrCl was 74.6%, compared with 65% for the area under the ROC curve using the standard tumor burden/lymph node size approach for defining TLS risk, which is described in the venetoclax package insert.
Patients included in the study had a median age of 67 years at venetoclax initiation, 69% were men, 85% were white, and 13% were treated on a clinical trial. Complex karyotype was present in 39%, del(17p) in 43%, and 84% had immunoglobulin heavy chain variable–unmutated disease.
Most patients received venetoclax monotherapy (79%), had relapsed/refractory disease (94%), and had previously received ibrutinib (78%). The median number of prior therapies was 3, but the number ranged from 0-15, the investigators noted.
The findings of this study suggest that, in addition to defining risk based on absolute lymphocyte count and lymph node size, patients with CrCl less than 80 mL/min – indicating impaired renal function – have excess risk of TLS.
Although complex karyotype did not reach statistical significance as an independent predictor of TLS, the findings in this study suggest it “may impact TLS risk and is worthy of further study in larger samples,” they said, concluding that consideration of baseline renal function, and possibly karyotype, could “further guide practitioners in their approach to prophylaxis and patient counseling, allowing for improved safety in the use of this effective agent in CLL.”
Additional planned analyses will focus on TLS risk score development and further refinement of TLS risk stratification, they noted.
Dr. Mato has received grant support, consulting fees, and/or fees for serving on a data and safety monitoring board or advisory board from AbbVie, AstraZeneca, Celgene, Janssen, TG Therapeutics, Pharmacyclics, Loxo, Sunesis, prIME Oncology, Pfizer, Johnson & Johnson, and Regeneron.
EDINBURGH – Impaired renal function may indicate excess risk of tumor lysis syndrome (TLS) in venetoclax-treated chronic lymphocytic leukemia (CLL) patients and should be considered when assessing TLS risk, according to findings from a retrospective cohort study.
Complex karyotype may also affect TLS risk, Anthony Mato, MD, reported at the International Workshop on Chronic Lymphocytic Leukemia.
Of 339 CLL patients who were treated with venetoclax, 38%, 34%, and 28% were considered to have low, medium, or high risk for TLS, respectively, according to the standard definition based on absolute lymphocyte count as a measure of tumor burden and/or lymph node size.
TLS occurred in 35 patients (10%), including 26 cases of laboratory-confirmed TLS and 9 clinical TLS cases; 1 patient required dialysis and 1 death occurred, which was attributable to the TLS, Dr. Mato of Memorial Sloan Kettering Cancer Center, New York, and colleagues reported in a poster at the workshop.
Univariate analysis was performed to “understand baseline factors associated with TLS development during dose escalation,” and it examined sex, creatinine clearance (CrCl), complex karyotype, immunoglobulin heavy chain variable mutation status, prior ibrutinib exposure, venetoclax monotherapy vs. combination therapy, and TLS risk group. The investigators observed no significant difference between the low- and medium-risk patients, therefore those two groups were combined and compared with the high-risk patients.
The univariate analysis showed significant associations between TLS and CrCl (odds ratio, 2.9 for 80 mL/min or less vs. greater than 80 mL/min), complex karyotype (OR, 2.2), and low/medium vs. high TLS risk based on the standard definition (OR, 2.56).
A multivariable analysis of the predictors identified as significant in the univariate analyses showed that standard TLS risk group and CrCl remained independent predictors of TLS.
“Although the odds ratio for complex karyotype suggested potential clinical significance, this did not meet the threshold for statistical significance and was not included in the final model,” they wrote.
The area under the receiver operating characteristic curve for a model including TLS risk group and CrCl was 74.6%, compared with 65% for the area under the ROC curve using the standard tumor burden/lymph node size approach for defining TLS risk, which is described in the venetoclax package insert.
Patients included in the study had a median age of 67 years at venetoclax initiation, 69% were men, 85% were white, and 13% were treated on a clinical trial. Complex karyotype was present in 39%, del(17p) in 43%, and 84% had immunoglobulin heavy chain variable–unmutated disease.
Most patients received venetoclax monotherapy (79%), had relapsed/refractory disease (94%), and had previously received ibrutinib (78%). The median number of prior therapies was 3, but the number ranged from 0-15, the investigators noted.
The findings of this study suggest that, in addition to defining risk based on absolute lymphocyte count and lymph node size, patients with CrCl less than 80 mL/min – indicating impaired renal function – have excess risk of TLS.
Although complex karyotype did not reach statistical significance as an independent predictor of TLS, the findings in this study suggest it “may impact TLS risk and is worthy of further study in larger samples,” they said, concluding that consideration of baseline renal function, and possibly karyotype, could “further guide practitioners in their approach to prophylaxis and patient counseling, allowing for improved safety in the use of this effective agent in CLL.”
Additional planned analyses will focus on TLS risk score development and further refinement of TLS risk stratification, they noted.
Dr. Mato has received grant support, consulting fees, and/or fees for serving on a data and safety monitoring board or advisory board from AbbVie, AstraZeneca, Celgene, Janssen, TG Therapeutics, Pharmacyclics, Loxo, Sunesis, prIME Oncology, Pfizer, Johnson & Johnson, and Regeneron.
REPORTING FROM iwCLL 2019
Pembrolizumab shows promise for relapsed/refractory PMBCL
The programmed death-ligand 1 (PD-L1) inhibitor pembrolizumab showed manageable safety and promising clinical activity in patients with relapsed/refractory primary mediastinal large B-cell lymphoma (PMBCL), according to results from two early-phase studies.
The phase 1b KEYNOTE-013 study included an expansion cohort that evaluated pembrolizumab monotherapy in patients with relapsed/refractory PMBCL. Based on preliminary findings from KEYNOTE-013, the phase 2 KEYNOTE-170 study was initiated to validate these results.
Philippe Armand, MD, PhD, of Dana-Farber Cancer Institute, Boston, and colleagues reported results from 53 patients in KEYNOTE-170 and extended follow-up of 21 patients in KEYNOTE-013. Data from these two trials formed the basis of an accelerated approval by the Food and Drug Administration of pembrolizumab in patients with relapsed/refractory PMBCL in June 2018.
“Frequent amplification and translocation events occur at 9p24.1 in PMBCL, resulting in tumor expression of the programmed cell death-1 (PD-1) ligands PD-L1 and PD-L2. This suggests susceptibility of PMBCL to PD-1 blockade,” the researchers wrote in the Journal of Clinical Oncology.
KEYNOTE-170 included patients with relapsed or refractory disease who were transplant-ineligible and had failed a minimum of two prior lines of treatment. KEYNOTE-013 enrolled patients who relapsed following autologous stem cell transplantation or were ineligible for transplant.
Among patients in KEYNOTE-013 and KEYNOTE-170, the objective response rates were 48% and 45%, respectively. In total, 33% of patients in KEYNOTE-013 and 13% of patients in KEYNOTE-170 achieved a complete response. Among these patients, no disease progression was observed.
The median progression-free survival in KEYNOTE-170 was 5.5 months and 10.4 months in KEYNOTE-013. In KEYNOTE-170, median overall survival was not reached, while in KEYNOTE-013, the median overall survival was 31.4 months.
After a median follow-up time of 29.1 months in KEYNOTE-013 and 12.5 months in KEYNOTE-170, the median duration of response was not reached in either trial, the researchers reported.
With respect to safety, pembrolizumab-related grade 3 or 4 adverse events were observed in 23% and 24% of patients in KEYNOTE-170 and KEYNOTE-013, respectively. The most common adverse event in both trials was neutropenia. No deaths related to pembrolizumab were observed.
Response rates were lower in KEYNOTE-170, compared with KEYNOTE-013, but the researchers noted that longer follow-up could change these results.
“Although the small numbers allow only a tentative hypothesis, they raise the question of whether PD-1 blockade in this setting might resensitize tumors to chemotherapy, as recently suggested. If this can be further validated, it could have profound implication for the management of patients with [relapsed/refractory] PMBCL,” the researchers wrote.
The study was supported by Merck Sharp & Dohme, the Harold and Virginia Lash Foundation, the Leukemia and Lymphoma Society, and the Center for Immuno-Oncology of the Dana-Farber Cancer Institute. The authors reported financial affiliations with Merck Sharp & Dohme and several other companies.
SOURCE: Armand P et al. J Clin Oncol. 2019 Sep 10. doi: 10.1200/JCO.19.01389.
The programmed death-ligand 1 (PD-L1) inhibitor pembrolizumab showed manageable safety and promising clinical activity in patients with relapsed/refractory primary mediastinal large B-cell lymphoma (PMBCL), according to results from two early-phase studies.
The phase 1b KEYNOTE-013 study included an expansion cohort that evaluated pembrolizumab monotherapy in patients with relapsed/refractory PMBCL. Based on preliminary findings from KEYNOTE-013, the phase 2 KEYNOTE-170 study was initiated to validate these results.
Philippe Armand, MD, PhD, of Dana-Farber Cancer Institute, Boston, and colleagues reported results from 53 patients in KEYNOTE-170 and extended follow-up of 21 patients in KEYNOTE-013. Data from these two trials formed the basis of an accelerated approval by the Food and Drug Administration of pembrolizumab in patients with relapsed/refractory PMBCL in June 2018.
“Frequent amplification and translocation events occur at 9p24.1 in PMBCL, resulting in tumor expression of the programmed cell death-1 (PD-1) ligands PD-L1 and PD-L2. This suggests susceptibility of PMBCL to PD-1 blockade,” the researchers wrote in the Journal of Clinical Oncology.
KEYNOTE-170 included patients with relapsed or refractory disease who were transplant-ineligible and had failed a minimum of two prior lines of treatment. KEYNOTE-013 enrolled patients who relapsed following autologous stem cell transplantation or were ineligible for transplant.
Among patients in KEYNOTE-013 and KEYNOTE-170, the objective response rates were 48% and 45%, respectively. In total, 33% of patients in KEYNOTE-013 and 13% of patients in KEYNOTE-170 achieved a complete response. Among these patients, no disease progression was observed.
The median progression-free survival in KEYNOTE-170 was 5.5 months and 10.4 months in KEYNOTE-013. In KEYNOTE-170, median overall survival was not reached, while in KEYNOTE-013, the median overall survival was 31.4 months.
After a median follow-up time of 29.1 months in KEYNOTE-013 and 12.5 months in KEYNOTE-170, the median duration of response was not reached in either trial, the researchers reported.
With respect to safety, pembrolizumab-related grade 3 or 4 adverse events were observed in 23% and 24% of patients in KEYNOTE-170 and KEYNOTE-013, respectively. The most common adverse event in both trials was neutropenia. No deaths related to pembrolizumab were observed.
Response rates were lower in KEYNOTE-170, compared with KEYNOTE-013, but the researchers noted that longer follow-up could change these results.
“Although the small numbers allow only a tentative hypothesis, they raise the question of whether PD-1 blockade in this setting might resensitize tumors to chemotherapy, as recently suggested. If this can be further validated, it could have profound implication for the management of patients with [relapsed/refractory] PMBCL,” the researchers wrote.
The study was supported by Merck Sharp & Dohme, the Harold and Virginia Lash Foundation, the Leukemia and Lymphoma Society, and the Center for Immuno-Oncology of the Dana-Farber Cancer Institute. The authors reported financial affiliations with Merck Sharp & Dohme and several other companies.
SOURCE: Armand P et al. J Clin Oncol. 2019 Sep 10. doi: 10.1200/JCO.19.01389.
The programmed death-ligand 1 (PD-L1) inhibitor pembrolizumab showed manageable safety and promising clinical activity in patients with relapsed/refractory primary mediastinal large B-cell lymphoma (PMBCL), according to results from two early-phase studies.
The phase 1b KEYNOTE-013 study included an expansion cohort that evaluated pembrolizumab monotherapy in patients with relapsed/refractory PMBCL. Based on preliminary findings from KEYNOTE-013, the phase 2 KEYNOTE-170 study was initiated to validate these results.
Philippe Armand, MD, PhD, of Dana-Farber Cancer Institute, Boston, and colleagues reported results from 53 patients in KEYNOTE-170 and extended follow-up of 21 patients in KEYNOTE-013. Data from these two trials formed the basis of an accelerated approval by the Food and Drug Administration of pembrolizumab in patients with relapsed/refractory PMBCL in June 2018.
“Frequent amplification and translocation events occur at 9p24.1 in PMBCL, resulting in tumor expression of the programmed cell death-1 (PD-1) ligands PD-L1 and PD-L2. This suggests susceptibility of PMBCL to PD-1 blockade,” the researchers wrote in the Journal of Clinical Oncology.
KEYNOTE-170 included patients with relapsed or refractory disease who were transplant-ineligible and had failed a minimum of two prior lines of treatment. KEYNOTE-013 enrolled patients who relapsed following autologous stem cell transplantation or were ineligible for transplant.
Among patients in KEYNOTE-013 and KEYNOTE-170, the objective response rates were 48% and 45%, respectively. In total, 33% of patients in KEYNOTE-013 and 13% of patients in KEYNOTE-170 achieved a complete response. Among these patients, no disease progression was observed.
The median progression-free survival in KEYNOTE-170 was 5.5 months and 10.4 months in KEYNOTE-013. In KEYNOTE-170, median overall survival was not reached, while in KEYNOTE-013, the median overall survival was 31.4 months.
After a median follow-up time of 29.1 months in KEYNOTE-013 and 12.5 months in KEYNOTE-170, the median duration of response was not reached in either trial, the researchers reported.
With respect to safety, pembrolizumab-related grade 3 or 4 adverse events were observed in 23% and 24% of patients in KEYNOTE-170 and KEYNOTE-013, respectively. The most common adverse event in both trials was neutropenia. No deaths related to pembrolizumab were observed.
Response rates were lower in KEYNOTE-170, compared with KEYNOTE-013, but the researchers noted that longer follow-up could change these results.
“Although the small numbers allow only a tentative hypothesis, they raise the question of whether PD-1 blockade in this setting might resensitize tumors to chemotherapy, as recently suggested. If this can be further validated, it could have profound implication for the management of patients with [relapsed/refractory] PMBCL,” the researchers wrote.
The study was supported by Merck Sharp & Dohme, the Harold and Virginia Lash Foundation, the Leukemia and Lymphoma Society, and the Center for Immuno-Oncology of the Dana-Farber Cancer Institute. The authors reported financial affiliations with Merck Sharp & Dohme and several other companies.
SOURCE: Armand P et al. J Clin Oncol. 2019 Sep 10. doi: 10.1200/JCO.19.01389.
FROM JOURNAL OF CLINICAL ONCOLOGY
Primary CNS lymphoma: R-CHOP hits back
Primary central nervous system lymphoma (PCNSL) is a rare and aggressive form of non-Hodgkin lymphoma solely confined to the CNS. The majority of PCNSL histologically presents as diffuse large B-cell lymphoma (DLBCL). However, outcomes in these patients are notably inferior, compared with nodal or other extranodal DLBCL. In order to achieve long-term progression-free survival, high-dose methotrexate (HD-MTX)–based chemotherapy followed by consolidation is needed. However, this treatment is associated with high toxicity burden and it is restricted to a select patient population – the young and fit – and requires administration at specialized hematological centers.
In the 1990s, the conventional DLBCL treatment regimen with CHOP (cyclophosphamide, doxorubicin, vincristine, and prednisone) was tested in PCNSL patients. The results were rather disappointing. The addition of CHOP to whole brain radiation or HD-MTX could not improve survival.1-3 The reason for CHOP failure was poor CNS penetration of doxorubicin and cyclophosphamide because of their high molecular weight. Consequently, it was concluded that there is no role for CHOP-like chemotherapy in the treatment of PCNSL.4
But is this really the case? Twenty years later, this traditional view has been challenged by Andres J.M. Ferreri, MD, and colleagues in the INGRID trial.5 Dr. Ferreri presented findings from the trial at the International Conference on Malignant Lymphoma in Lugano, Switzerland, which was greeted with much excitement.6
INGRID is a phase 2 trial conducted on patients with refractory/relapsed PCNSL. It consisted of a CHOP plus rituximab (R-CHOP) regimen, which was upgraded by engineered tumor necrosis factor–alpha (TNF-alpha). The idea was to enhance the blood-brain barrier (BBB) permeability and consequently improve the efficacy of R-CHOP in PCNSL. The use of human TNF-alpha is limited by relevant toxicities. In order to avoid that, a fusion of human TNF-alpha and CNGRCG peptide (called NGR-TNF) was developed.
CNGRCG peptide is a ligand of CD13, an aminopeptidase that is expressed almost exclusively on tumor blood vessels. Preclinical data showed that binding of CNGRCG to CD13 results in targeted – local, not systemic – delivery of TNF-alpha to the tumor blood vessels. Consequently, TNF-alpha led to increased vascular permeability in tumor tissue and enabled higher penetration of chemotherapeutic agents.7,8
Altogether, 12 heavily pretreated PCNSL patients were included in the INGRID trial. Seven patients had two or more previous treatment regimens. Within this trial, patients received R-CHOP with NGR-TNF (0.8 mcg/m2) applied 2 hours prior to R-CHOP. The great majority of grade 3/4 adverse events were hematological toxicities. Importantly, no neurological side effects of any grade occurred.
The primary aim of this study was to investigate the CD13 expression on tumor tissue and provide a proof of concept for the use of NGR-TNF/R-CHOP. Indeed, CD13 expression was observed on tumor vessels in all patients. Consequently, increased BBB permeability in tumor tissue after NGR-TNF infusion was observed using dynamic contrast-enhanced MRI and by brain scintigraphy (SPECT). This was assessed 1 day after NGR-TNF/R-CHOP treatment. More importantly, this effect on BBB seems to be sustained because it was also observed after the last cycle of NGR-TNF/R-CHOP. The fact that there was no change of drug concentrations of R-CHOP components in plasma or cerebrospinal fluid suggests that the effect of NGR-TNF is restricted to tumor vessels.
The authors also reported preliminary results regarding response rates to NGR-TNF/R-CHOP. The overall response rate was 75%. Of note, six patients achieved complete remission and one patient achieved a partial remission. The median duration of response was 10 months (range, 7-14 months), and nine patients were able to proceed to consolidation treatment.
These preliminary results are encouraging and open a new window for the treatment strategies in PCNSL patients. NGR-TNF/R-CHOP treatment induced responses in 75% of these heavily pretreated patients. The low toxicity profile and feasibility of this regimen could allow clinicians to carry out this treatment approach in outpatient settings, as well as in older and comorbid patients. Extensive supportive therapy – such as intensive hydration or leucovorin-rescue by HD-MTX – is not needed.
These results will need to be confirmed through testing in a larger patient population. Dr. Ferreri and colleagues are currently conducting the extended phase of this study and aim to recruit 28 patients. If they report positive results from that study, evaluation of NGR-TNF/R-CHOP as a first-line treatment of PCNSL seems to be the next reasonable step.
Dr. Zeremski and Dr. Fischer are both in the department of hematology/oncology and affiliated with the Health Campus Immunology, Infectiology and Inflammation at Otto-von-Guericke University Magdeburg (Germany). Dr. Fischer is a member of the editorial advisory board of Hematology News. The authors reported having no conflicts of interest.
References
1. J Clin Oncol. 1996;14:556-64.
2. Cancer. 2000;89:1359-70.
3. J Neurooncol. 1996;30:257-65.
4. Guidelines on the diagnosis and management of adult patients with primary CNS lymphoma (PCNSL) and primary intra-ocular lymphoma (PIOL). British Society for Haematology/British Committee for Standards in Haematology; HO/016, 2009.
5. Blood. 2019;134:252-62.
6. Hematol Oncol. 2019; 37:159.
7. BioDrugs. 2013;27:591-603.
8. J Clin Invest. 2002;110:475-82.
Primary central nervous system lymphoma (PCNSL) is a rare and aggressive form of non-Hodgkin lymphoma solely confined to the CNS. The majority of PCNSL histologically presents as diffuse large B-cell lymphoma (DLBCL). However, outcomes in these patients are notably inferior, compared with nodal or other extranodal DLBCL. In order to achieve long-term progression-free survival, high-dose methotrexate (HD-MTX)–based chemotherapy followed by consolidation is needed. However, this treatment is associated with high toxicity burden and it is restricted to a select patient population – the young and fit – and requires administration at specialized hematological centers.
In the 1990s, the conventional DLBCL treatment regimen with CHOP (cyclophosphamide, doxorubicin, vincristine, and prednisone) was tested in PCNSL patients. The results were rather disappointing. The addition of CHOP to whole brain radiation or HD-MTX could not improve survival.1-3 The reason for CHOP failure was poor CNS penetration of doxorubicin and cyclophosphamide because of their high molecular weight. Consequently, it was concluded that there is no role for CHOP-like chemotherapy in the treatment of PCNSL.4
But is this really the case? Twenty years later, this traditional view has been challenged by Andres J.M. Ferreri, MD, and colleagues in the INGRID trial.5 Dr. Ferreri presented findings from the trial at the International Conference on Malignant Lymphoma in Lugano, Switzerland, which was greeted with much excitement.6
INGRID is a phase 2 trial conducted on patients with refractory/relapsed PCNSL. It consisted of a CHOP plus rituximab (R-CHOP) regimen, which was upgraded by engineered tumor necrosis factor–alpha (TNF-alpha). The idea was to enhance the blood-brain barrier (BBB) permeability and consequently improve the efficacy of R-CHOP in PCNSL. The use of human TNF-alpha is limited by relevant toxicities. In order to avoid that, a fusion of human TNF-alpha and CNGRCG peptide (called NGR-TNF) was developed.
CNGRCG peptide is a ligand of CD13, an aminopeptidase that is expressed almost exclusively on tumor blood vessels. Preclinical data showed that binding of CNGRCG to CD13 results in targeted – local, not systemic – delivery of TNF-alpha to the tumor blood vessels. Consequently, TNF-alpha led to increased vascular permeability in tumor tissue and enabled higher penetration of chemotherapeutic agents.7,8
Altogether, 12 heavily pretreated PCNSL patients were included in the INGRID trial. Seven patients had two or more previous treatment regimens. Within this trial, patients received R-CHOP with NGR-TNF (0.8 mcg/m2) applied 2 hours prior to R-CHOP. The great majority of grade 3/4 adverse events were hematological toxicities. Importantly, no neurological side effects of any grade occurred.
The primary aim of this study was to investigate the CD13 expression on tumor tissue and provide a proof of concept for the use of NGR-TNF/R-CHOP. Indeed, CD13 expression was observed on tumor vessels in all patients. Consequently, increased BBB permeability in tumor tissue after NGR-TNF infusion was observed using dynamic contrast-enhanced MRI and by brain scintigraphy (SPECT). This was assessed 1 day after NGR-TNF/R-CHOP treatment. More importantly, this effect on BBB seems to be sustained because it was also observed after the last cycle of NGR-TNF/R-CHOP. The fact that there was no change of drug concentrations of R-CHOP components in plasma or cerebrospinal fluid suggests that the effect of NGR-TNF is restricted to tumor vessels.
The authors also reported preliminary results regarding response rates to NGR-TNF/R-CHOP. The overall response rate was 75%. Of note, six patients achieved complete remission and one patient achieved a partial remission. The median duration of response was 10 months (range, 7-14 months), and nine patients were able to proceed to consolidation treatment.
These preliminary results are encouraging and open a new window for the treatment strategies in PCNSL patients. NGR-TNF/R-CHOP treatment induced responses in 75% of these heavily pretreated patients. The low toxicity profile and feasibility of this regimen could allow clinicians to carry out this treatment approach in outpatient settings, as well as in older and comorbid patients. Extensive supportive therapy – such as intensive hydration or leucovorin-rescue by HD-MTX – is not needed.
These results will need to be confirmed through testing in a larger patient population. Dr. Ferreri and colleagues are currently conducting the extended phase of this study and aim to recruit 28 patients. If they report positive results from that study, evaluation of NGR-TNF/R-CHOP as a first-line treatment of PCNSL seems to be the next reasonable step.
Dr. Zeremski and Dr. Fischer are both in the department of hematology/oncology and affiliated with the Health Campus Immunology, Infectiology and Inflammation at Otto-von-Guericke University Magdeburg (Germany). Dr. Fischer is a member of the editorial advisory board of Hematology News. The authors reported having no conflicts of interest.
References
1. J Clin Oncol. 1996;14:556-64.
2. Cancer. 2000;89:1359-70.
3. J Neurooncol. 1996;30:257-65.
4. Guidelines on the diagnosis and management of adult patients with primary CNS lymphoma (PCNSL) and primary intra-ocular lymphoma (PIOL). British Society for Haematology/British Committee for Standards in Haematology; HO/016, 2009.
5. Blood. 2019;134:252-62.
6. Hematol Oncol. 2019; 37:159.
7. BioDrugs. 2013;27:591-603.
8. J Clin Invest. 2002;110:475-82.
Primary central nervous system lymphoma (PCNSL) is a rare and aggressive form of non-Hodgkin lymphoma solely confined to the CNS. The majority of PCNSL histologically presents as diffuse large B-cell lymphoma (DLBCL). However, outcomes in these patients are notably inferior, compared with nodal or other extranodal DLBCL. In order to achieve long-term progression-free survival, high-dose methotrexate (HD-MTX)–based chemotherapy followed by consolidation is needed. However, this treatment is associated with high toxicity burden and it is restricted to a select patient population – the young and fit – and requires administration at specialized hematological centers.
In the 1990s, the conventional DLBCL treatment regimen with CHOP (cyclophosphamide, doxorubicin, vincristine, and prednisone) was tested in PCNSL patients. The results were rather disappointing. The addition of CHOP to whole brain radiation or HD-MTX could not improve survival.1-3 The reason for CHOP failure was poor CNS penetration of doxorubicin and cyclophosphamide because of their high molecular weight. Consequently, it was concluded that there is no role for CHOP-like chemotherapy in the treatment of PCNSL.4
But is this really the case? Twenty years later, this traditional view has been challenged by Andres J.M. Ferreri, MD, and colleagues in the INGRID trial.5 Dr. Ferreri presented findings from the trial at the International Conference on Malignant Lymphoma in Lugano, Switzerland, which was greeted with much excitement.6
INGRID is a phase 2 trial conducted on patients with refractory/relapsed PCNSL. It consisted of a CHOP plus rituximab (R-CHOP) regimen, which was upgraded by engineered tumor necrosis factor–alpha (TNF-alpha). The idea was to enhance the blood-brain barrier (BBB) permeability and consequently improve the efficacy of R-CHOP in PCNSL. The use of human TNF-alpha is limited by relevant toxicities. In order to avoid that, a fusion of human TNF-alpha and CNGRCG peptide (called NGR-TNF) was developed.
CNGRCG peptide is a ligand of CD13, an aminopeptidase that is expressed almost exclusively on tumor blood vessels. Preclinical data showed that binding of CNGRCG to CD13 results in targeted – local, not systemic – delivery of TNF-alpha to the tumor blood vessels. Consequently, TNF-alpha led to increased vascular permeability in tumor tissue and enabled higher penetration of chemotherapeutic agents.7,8
Altogether, 12 heavily pretreated PCNSL patients were included in the INGRID trial. Seven patients had two or more previous treatment regimens. Within this trial, patients received R-CHOP with NGR-TNF (0.8 mcg/m2) applied 2 hours prior to R-CHOP. The great majority of grade 3/4 adverse events were hematological toxicities. Importantly, no neurological side effects of any grade occurred.
The primary aim of this study was to investigate the CD13 expression on tumor tissue and provide a proof of concept for the use of NGR-TNF/R-CHOP. Indeed, CD13 expression was observed on tumor vessels in all patients. Consequently, increased BBB permeability in tumor tissue after NGR-TNF infusion was observed using dynamic contrast-enhanced MRI and by brain scintigraphy (SPECT). This was assessed 1 day after NGR-TNF/R-CHOP treatment. More importantly, this effect on BBB seems to be sustained because it was also observed after the last cycle of NGR-TNF/R-CHOP. The fact that there was no change of drug concentrations of R-CHOP components in plasma or cerebrospinal fluid suggests that the effect of NGR-TNF is restricted to tumor vessels.
The authors also reported preliminary results regarding response rates to NGR-TNF/R-CHOP. The overall response rate was 75%. Of note, six patients achieved complete remission and one patient achieved a partial remission. The median duration of response was 10 months (range, 7-14 months), and nine patients were able to proceed to consolidation treatment.
These preliminary results are encouraging and open a new window for the treatment strategies in PCNSL patients. NGR-TNF/R-CHOP treatment induced responses in 75% of these heavily pretreated patients. The low toxicity profile and feasibility of this regimen could allow clinicians to carry out this treatment approach in outpatient settings, as well as in older and comorbid patients. Extensive supportive therapy – such as intensive hydration or leucovorin-rescue by HD-MTX – is not needed.
These results will need to be confirmed through testing in a larger patient population. Dr. Ferreri and colleagues are currently conducting the extended phase of this study and aim to recruit 28 patients. If they report positive results from that study, evaluation of NGR-TNF/R-CHOP as a first-line treatment of PCNSL seems to be the next reasonable step.
Dr. Zeremski and Dr. Fischer are both in the department of hematology/oncology and affiliated with the Health Campus Immunology, Infectiology and Inflammation at Otto-von-Guericke University Magdeburg (Germany). Dr. Fischer is a member of the editorial advisory board of Hematology News. The authors reported having no conflicts of interest.
References
1. J Clin Oncol. 1996;14:556-64.
2. Cancer. 2000;89:1359-70.
3. J Neurooncol. 1996;30:257-65.
4. Guidelines on the diagnosis and management of adult patients with primary CNS lymphoma (PCNSL) and primary intra-ocular lymphoma (PIOL). British Society for Haematology/British Committee for Standards in Haematology; HO/016, 2009.
5. Blood. 2019;134:252-62.
6. Hematol Oncol. 2019; 37:159.
7. BioDrugs. 2013;27:591-603.
8. J Clin Invest. 2002;110:475-82.
PJP prophylaxis may be unnecessary for CLL patients on BTK inhibitors
EDINBURGH – Routine empiric prophylaxis against pneumocystis jiroveci pneumonia (PJP) may be unwarranted in chronic lymphocytic leukemia patients initiating Bruton tyrosine kinase (BTK) inhibitor therapy, a retrospective chart review suggests.
Among 212 patients with chronic lymphocytic leukemia (CLL) who were treated with ibrutinib or acalabrutinib either as monotherapy or as part of a combination regimen for at least 30 days between Jan. 1, 2010, and Feb. 1, 2019, at Dana-Farber Cancer Institute and Brigham and Women’s Hospital in Boston, 125 (59%) received PJP prophylaxis, including either trimethoprim-sulfamethoxazole (74%) or atovaquone (26%), Christine Ryan, MD, reported at the International Workshop on CLL.
Two PJP cases occurred in the 120 patients on single-agent ibrutinib, including one in a previously untreated patient and one in a patient with relapsed/refractory CLL. Neither patient had received PJP prophylaxis, said Dr. Ryan, a senior resident at Brigham and Women’s Hospital.
No PJP cases occurred in the 21 patients who received acalabrutinib monotherapy or in the 14 patients who received acalabrutinib combination therapy, and 1 occurred in a trial cohort of 57 patients receiving frontline ibrutinib plus fludarabine-based chemotherapy (FCR). The latter had been prescribed PJP prophylaxis, but “unfortunately self-discontinued the prophylaxis” 2 months prior to the infection, Dr. Ryan said.
“The overall prevalence of PJP in patients not on prophylaxis was 3.4%, there were no cases of PJP in patients on prophylaxis, and the incidence rate in patients not on prophylaxis was 1.9 per 100 person-years, with a number needed to treat to prevent 1 case of PJP calculated to be 42 patients,” she said.
In addition to PJP, three cases of proven or probable invasive fungal infections (IFI) occurred, including one case of pulmonary histoplasmosis in the ibrutinib plus FCR trial cohort and two cases of aspergillosis, including a pulmonary case and a brain abscess, in an ibrutinib plus umbralisib trial cohort.
“The overall prevalence of aspergillosis or histoplasmosis in our entire cohort was 1.4%, and notably there were no cases of IFI in the single-agent therapy cohort, but the prevalence in the ibrutinib-combination therapy patients was 4.2%,” Dr. Ryan said.
Patients included in the review were adults with a median age of 64.8 years, and 64% were men. The median duration of BTK inhibitor therapy was 23.2 months.
“We know that CLL patients treated with fludarabine have an increased risk of PJP,” she said. “As such, it is routinely recommended that patients receiving fludarabine-containing chemotherapy regimens are prescribed PJP prophylaxis.”
Additionally, the increasing use of oral BTK inhibitors has raised concerns about the potential risk of PJP or other IFIs in patients on those agents, Dr. Ryan explained, noting that existing case reports and case series looking at PJP have shown varying prevalence rates, and little is known about the effects of prophylaxis.
“At present, there are no international guidelines regarding the use of antimicrobial prophylaxis in CLL patients treated with BTK inhibitors, and prophylaxis practices vary widely across countries and institutions,” she said.
The findings of the current study demonstrate that such variation exists “even within our own institution,” Dr. Ryan added.
The findings also show an overall low PJP prevalence of 3.4% in patients not receiving prophylaxis, which falls below the “commonly accepted threshold of 5%, above which routine prophylaxis becomes recommended,” she said.
“Overall, our data suggest that routine PJP or IFI prophylaxis in patients receiving BTK inhibitors may not be needed, but this is definitely an area that requires further study, ideally with a prospective trial with a larger sample size and multiple institutions, to support the development of consensus guidelines on this issue,” she said.
Dr. Ryan reported having no financial disclosures.
EDINBURGH – Routine empiric prophylaxis against pneumocystis jiroveci pneumonia (PJP) may be unwarranted in chronic lymphocytic leukemia patients initiating Bruton tyrosine kinase (BTK) inhibitor therapy, a retrospective chart review suggests.
Among 212 patients with chronic lymphocytic leukemia (CLL) who were treated with ibrutinib or acalabrutinib either as monotherapy or as part of a combination regimen for at least 30 days between Jan. 1, 2010, and Feb. 1, 2019, at Dana-Farber Cancer Institute and Brigham and Women’s Hospital in Boston, 125 (59%) received PJP prophylaxis, including either trimethoprim-sulfamethoxazole (74%) or atovaquone (26%), Christine Ryan, MD, reported at the International Workshop on CLL.
Two PJP cases occurred in the 120 patients on single-agent ibrutinib, including one in a previously untreated patient and one in a patient with relapsed/refractory CLL. Neither patient had received PJP prophylaxis, said Dr. Ryan, a senior resident at Brigham and Women’s Hospital.
No PJP cases occurred in the 21 patients who received acalabrutinib monotherapy or in the 14 patients who received acalabrutinib combination therapy, and 1 occurred in a trial cohort of 57 patients receiving frontline ibrutinib plus fludarabine-based chemotherapy (FCR). The latter had been prescribed PJP prophylaxis, but “unfortunately self-discontinued the prophylaxis” 2 months prior to the infection, Dr. Ryan said.
“The overall prevalence of PJP in patients not on prophylaxis was 3.4%, there were no cases of PJP in patients on prophylaxis, and the incidence rate in patients not on prophylaxis was 1.9 per 100 person-years, with a number needed to treat to prevent 1 case of PJP calculated to be 42 patients,” she said.
In addition to PJP, three cases of proven or probable invasive fungal infections (IFI) occurred, including one case of pulmonary histoplasmosis in the ibrutinib plus FCR trial cohort and two cases of aspergillosis, including a pulmonary case and a brain abscess, in an ibrutinib plus umbralisib trial cohort.
“The overall prevalence of aspergillosis or histoplasmosis in our entire cohort was 1.4%, and notably there were no cases of IFI in the single-agent therapy cohort, but the prevalence in the ibrutinib-combination therapy patients was 4.2%,” Dr. Ryan said.
Patients included in the review were adults with a median age of 64.8 years, and 64% were men. The median duration of BTK inhibitor therapy was 23.2 months.
“We know that CLL patients treated with fludarabine have an increased risk of PJP,” she said. “As such, it is routinely recommended that patients receiving fludarabine-containing chemotherapy regimens are prescribed PJP prophylaxis.”
Additionally, the increasing use of oral BTK inhibitors has raised concerns about the potential risk of PJP or other IFIs in patients on those agents, Dr. Ryan explained, noting that existing case reports and case series looking at PJP have shown varying prevalence rates, and little is known about the effects of prophylaxis.
“At present, there are no international guidelines regarding the use of antimicrobial prophylaxis in CLL patients treated with BTK inhibitors, and prophylaxis practices vary widely across countries and institutions,” she said.
The findings of the current study demonstrate that such variation exists “even within our own institution,” Dr. Ryan added.
The findings also show an overall low PJP prevalence of 3.4% in patients not receiving prophylaxis, which falls below the “commonly accepted threshold of 5%, above which routine prophylaxis becomes recommended,” she said.
“Overall, our data suggest that routine PJP or IFI prophylaxis in patients receiving BTK inhibitors may not be needed, but this is definitely an area that requires further study, ideally with a prospective trial with a larger sample size and multiple institutions, to support the development of consensus guidelines on this issue,” she said.
Dr. Ryan reported having no financial disclosures.
EDINBURGH – Routine empiric prophylaxis against pneumocystis jiroveci pneumonia (PJP) may be unwarranted in chronic lymphocytic leukemia patients initiating Bruton tyrosine kinase (BTK) inhibitor therapy, a retrospective chart review suggests.
Among 212 patients with chronic lymphocytic leukemia (CLL) who were treated with ibrutinib or acalabrutinib either as monotherapy or as part of a combination regimen for at least 30 days between Jan. 1, 2010, and Feb. 1, 2019, at Dana-Farber Cancer Institute and Brigham and Women’s Hospital in Boston, 125 (59%) received PJP prophylaxis, including either trimethoprim-sulfamethoxazole (74%) or atovaquone (26%), Christine Ryan, MD, reported at the International Workshop on CLL.
Two PJP cases occurred in the 120 patients on single-agent ibrutinib, including one in a previously untreated patient and one in a patient with relapsed/refractory CLL. Neither patient had received PJP prophylaxis, said Dr. Ryan, a senior resident at Brigham and Women’s Hospital.
No PJP cases occurred in the 21 patients who received acalabrutinib monotherapy or in the 14 patients who received acalabrutinib combination therapy, and 1 occurred in a trial cohort of 57 patients receiving frontline ibrutinib plus fludarabine-based chemotherapy (FCR). The latter had been prescribed PJP prophylaxis, but “unfortunately self-discontinued the prophylaxis” 2 months prior to the infection, Dr. Ryan said.
“The overall prevalence of PJP in patients not on prophylaxis was 3.4%, there were no cases of PJP in patients on prophylaxis, and the incidence rate in patients not on prophylaxis was 1.9 per 100 person-years, with a number needed to treat to prevent 1 case of PJP calculated to be 42 patients,” she said.
In addition to PJP, three cases of proven or probable invasive fungal infections (IFI) occurred, including one case of pulmonary histoplasmosis in the ibrutinib plus FCR trial cohort and two cases of aspergillosis, including a pulmonary case and a brain abscess, in an ibrutinib plus umbralisib trial cohort.
“The overall prevalence of aspergillosis or histoplasmosis in our entire cohort was 1.4%, and notably there were no cases of IFI in the single-agent therapy cohort, but the prevalence in the ibrutinib-combination therapy patients was 4.2%,” Dr. Ryan said.
Patients included in the review were adults with a median age of 64.8 years, and 64% were men. The median duration of BTK inhibitor therapy was 23.2 months.
“We know that CLL patients treated with fludarabine have an increased risk of PJP,” she said. “As such, it is routinely recommended that patients receiving fludarabine-containing chemotherapy regimens are prescribed PJP prophylaxis.”
Additionally, the increasing use of oral BTK inhibitors has raised concerns about the potential risk of PJP or other IFIs in patients on those agents, Dr. Ryan explained, noting that existing case reports and case series looking at PJP have shown varying prevalence rates, and little is known about the effects of prophylaxis.
“At present, there are no international guidelines regarding the use of antimicrobial prophylaxis in CLL patients treated with BTK inhibitors, and prophylaxis practices vary widely across countries and institutions,” she said.
The findings of the current study demonstrate that such variation exists “even within our own institution,” Dr. Ryan added.
The findings also show an overall low PJP prevalence of 3.4% in patients not receiving prophylaxis, which falls below the “commonly accepted threshold of 5%, above which routine prophylaxis becomes recommended,” she said.
“Overall, our data suggest that routine PJP or IFI prophylaxis in patients receiving BTK inhibitors may not be needed, but this is definitely an area that requires further study, ideally with a prospective trial with a larger sample size and multiple institutions, to support the development of consensus guidelines on this issue,” she said.
Dr. Ryan reported having no financial disclosures.
REPORTING FROM IWCLL 2019
Ibrutinib linked to hypertension in B-cell malignancies
The incidence and severity of hypertension was considerably higher in patients with B-cell malignancies treated with ibrutinib, according to a retrospective analysis.
Additionally, new or worsening hypertension was associated with a greater risk of major adverse cardiac events (MACE), including stroke, myocardial infarction, and cardiovascular-related death (hazard ratio, 2.17; 95% confidence interval, 1.08-4.38; P = .03).
“Despite ibrutinib’s benefits, cardiotoxicity has emerged as an increasingly important complication of this life-saving therapy,” Tyler Dickerson, PhD, of the Ohio State University, Columbus, and colleagues wrote in Blood.
The researchers retrospectively studied 562 consecutive patients with a lymphoid malignancy who received ibrutinib. Data was collected from patients treated at The Ohio State University’s Comprehensive Cancer Center during 2009-2016.
The mean age of study participants was 63.8 years, with a mean body mass index of 28.0 kg/m2. Most of the patients included in the analysis were men.
The team assessed rates of new or worsening hypertension, as well as rates of other MACE. The observed rates were compared with Framingham Heart Study–predicted incident-hypertension rates. The effects of various antihypertensive drugs on ibrutinib-linked hypertension were also evaluated.
After a median follow-up of 30 months, 78.3% of patients who received ibrutinib had new or worsening hypertension using a systolic blood pressure cutoff of 130 mm Hg. Of these, 84.8% of cases had an “at least probable association with ibrutinib,” they reported.
Among the 215 patients with no baseline hypertension, 71.6% developed hypertension while on ibrutinib, with a mean increase in systolic blood pressure of 13.4 mm Hg. Among the 347 patients with baseline hypertension, 82.4% experienced a worsening of their hypertension.
“This relationship remained even after accounting for ibrutinib dose, and was not attenuated by the use of any specific anti-hypertensive class,” the researchers wrote.
The researchers observed MACE among 93 patients. This included 84 patients with new or worsening hypertension and 9 patients with stable or no hypertension. Most MACE events were of at least probable ibrutinib association, the researchers reported.
Overall, the cumulative incidence of new hypertension at 1 year was 442 per 1,000 person-years in the current study. This value is 12.9-fold higher than the Framingham Heart Study risk–predicted rate of 34 per 1,000 person-years.
“Given the expected continued increase in ibrutinib use, further studies characterizing the mechanisms, treatment, and implications of [hypertension] during ibrutinib use are needed,” the researchers wrote.
The study was funded by the National Institutes of Health, the D. Warren Brown Family Foundation, the Four Winds Foundation, and the Connie Brown CLL Research Fund. The authors reported financial affiliations with Janssen, Pharmacyclics, and other companies.
SOURCE: Dickerson T et al. Blood. 2019 Oct 3. doi: 10.1182/blood.2019000840.
The incidence and severity of hypertension was considerably higher in patients with B-cell malignancies treated with ibrutinib, according to a retrospective analysis.
Additionally, new or worsening hypertension was associated with a greater risk of major adverse cardiac events (MACE), including stroke, myocardial infarction, and cardiovascular-related death (hazard ratio, 2.17; 95% confidence interval, 1.08-4.38; P = .03).
“Despite ibrutinib’s benefits, cardiotoxicity has emerged as an increasingly important complication of this life-saving therapy,” Tyler Dickerson, PhD, of the Ohio State University, Columbus, and colleagues wrote in Blood.
The researchers retrospectively studied 562 consecutive patients with a lymphoid malignancy who received ibrutinib. Data was collected from patients treated at The Ohio State University’s Comprehensive Cancer Center during 2009-2016.
The mean age of study participants was 63.8 years, with a mean body mass index of 28.0 kg/m2. Most of the patients included in the analysis were men.
The team assessed rates of new or worsening hypertension, as well as rates of other MACE. The observed rates were compared with Framingham Heart Study–predicted incident-hypertension rates. The effects of various antihypertensive drugs on ibrutinib-linked hypertension were also evaluated.
After a median follow-up of 30 months, 78.3% of patients who received ibrutinib had new or worsening hypertension using a systolic blood pressure cutoff of 130 mm Hg. Of these, 84.8% of cases had an “at least probable association with ibrutinib,” they reported.
Among the 215 patients with no baseline hypertension, 71.6% developed hypertension while on ibrutinib, with a mean increase in systolic blood pressure of 13.4 mm Hg. Among the 347 patients with baseline hypertension, 82.4% experienced a worsening of their hypertension.
“This relationship remained even after accounting for ibrutinib dose, and was not attenuated by the use of any specific anti-hypertensive class,” the researchers wrote.
The researchers observed MACE among 93 patients. This included 84 patients with new or worsening hypertension and 9 patients with stable or no hypertension. Most MACE events were of at least probable ibrutinib association, the researchers reported.
Overall, the cumulative incidence of new hypertension at 1 year was 442 per 1,000 person-years in the current study. This value is 12.9-fold higher than the Framingham Heart Study risk–predicted rate of 34 per 1,000 person-years.
“Given the expected continued increase in ibrutinib use, further studies characterizing the mechanisms, treatment, and implications of [hypertension] during ibrutinib use are needed,” the researchers wrote.
The study was funded by the National Institutes of Health, the D. Warren Brown Family Foundation, the Four Winds Foundation, and the Connie Brown CLL Research Fund. The authors reported financial affiliations with Janssen, Pharmacyclics, and other companies.
SOURCE: Dickerson T et al. Blood. 2019 Oct 3. doi: 10.1182/blood.2019000840.
The incidence and severity of hypertension was considerably higher in patients with B-cell malignancies treated with ibrutinib, according to a retrospective analysis.
Additionally, new or worsening hypertension was associated with a greater risk of major adverse cardiac events (MACE), including stroke, myocardial infarction, and cardiovascular-related death (hazard ratio, 2.17; 95% confidence interval, 1.08-4.38; P = .03).
“Despite ibrutinib’s benefits, cardiotoxicity has emerged as an increasingly important complication of this life-saving therapy,” Tyler Dickerson, PhD, of the Ohio State University, Columbus, and colleagues wrote in Blood.
The researchers retrospectively studied 562 consecutive patients with a lymphoid malignancy who received ibrutinib. Data was collected from patients treated at The Ohio State University’s Comprehensive Cancer Center during 2009-2016.
The mean age of study participants was 63.8 years, with a mean body mass index of 28.0 kg/m2. Most of the patients included in the analysis were men.
The team assessed rates of new or worsening hypertension, as well as rates of other MACE. The observed rates were compared with Framingham Heart Study–predicted incident-hypertension rates. The effects of various antihypertensive drugs on ibrutinib-linked hypertension were also evaluated.
After a median follow-up of 30 months, 78.3% of patients who received ibrutinib had new or worsening hypertension using a systolic blood pressure cutoff of 130 mm Hg. Of these, 84.8% of cases had an “at least probable association with ibrutinib,” they reported.
Among the 215 patients with no baseline hypertension, 71.6% developed hypertension while on ibrutinib, with a mean increase in systolic blood pressure of 13.4 mm Hg. Among the 347 patients with baseline hypertension, 82.4% experienced a worsening of their hypertension.
“This relationship remained even after accounting for ibrutinib dose, and was not attenuated by the use of any specific anti-hypertensive class,” the researchers wrote.
The researchers observed MACE among 93 patients. This included 84 patients with new or worsening hypertension and 9 patients with stable or no hypertension. Most MACE events were of at least probable ibrutinib association, the researchers reported.
Overall, the cumulative incidence of new hypertension at 1 year was 442 per 1,000 person-years in the current study. This value is 12.9-fold higher than the Framingham Heart Study risk–predicted rate of 34 per 1,000 person-years.
“Given the expected continued increase in ibrutinib use, further studies characterizing the mechanisms, treatment, and implications of [hypertension] during ibrutinib use are needed,” the researchers wrote.
The study was funded by the National Institutes of Health, the D. Warren Brown Family Foundation, the Four Winds Foundation, and the Connie Brown CLL Research Fund. The authors reported financial affiliations with Janssen, Pharmacyclics, and other companies.
SOURCE: Dickerson T et al. Blood. 2019 Oct 3. doi: 10.1182/blood.2019000840.
FROM BLOOD