User login
Bipolar disorder and substance abuse: Overcome the challenges of ‘dual diagnosis’ patients
After testing positive for cocaine on a recent court-mandated urine drug screen, Mr. M, age 49, is referred by his parole officer for psychiatric and substance abuse treatment. Mr. M has bipolar I disorder and alcohol, cocaine, and opioid dependence. He says he has been hospitalized or incarcerated at least once each year for the past 22 years. Mr. M has seen numerous psychiatrists as an outpatient, but rarely for more than 2 to 3 months and has not taken any psychotropics for more than 5 months.
Approximately 1 week before his recent urine drug screen, Mr. M became euphoric, stopped sleeping for several days, and spent $2,000 on cocaine and “escorts.” He reports that each day he smokes 30 cigarettes and drinks 1 pint of liquor and prefers to use cocaine and opiates by IV injection. Several years ago Mr. M was diagnosed with hepatitis C virus (HCV) but received no further workup or treatment. Although he denies manic or psychotic symptoms, Mr. M is observed speaking to unseen others in the waiting room and has difficulty remaining still during his interview. His chief concern is insomnia, stating, “Doc, I just need something to help me sleep.”
The high prevalence of substance use disorders (SUDs) in persons with bipolar disorder (BD) is well documented.1,2 Up to 60% of bipolar patients develop an SUD at some point in their lives.3-5 Alcohol use disorders are particularly common among BD patients, with a lifetime prevalence of roughly 50%.2-5 Recent epidemiologic data indicate that 38% of persons with bipolar I disorder and 19% of those with bipolar II disorder meet criteria for alcohol dependence.5 Comorbid SUDs in patients with BD are associated with:
- poor treatment compliance
- longer and more frequent mood episodes
- more mixed episodes
- more hospitalizations
- more frequent suicide attempts.1,2
The impact of co-occurring SUDs on suicidality is particularly high among those with bipolar I disorder.6
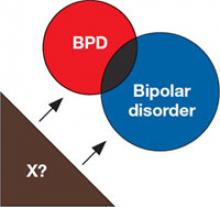
Frequently referred to as “dual diagnosis” conditions, co-occurring BD and SUDs may be more accurately envisioned as multi-morbid, rather than comorbid, illnesses. Data from the Stanley Foundation Bipolar Network suggest that 42% of BD patients have a lifetime history of ≥2 comorbid axis I disorders.7 Rates of generalized anxiety disorder, panic disorder, and posttraumatic stress disorder are particularly high in BD patients with co-occurring SUDs.8,9 In addition, the presence of 1 SUD may mark the presence of other SUDs; for example, alcohol dependence is strongly associated with polysubstance abuse, especially in females with BD.8 Furthermore, medical comorbidities that impact treatment decisions also are highly prevalent in BD patients with comorbid SUDs.10 In particular, HCV rates are higher in persons with BD compared with the general population,11 and are >5 times as likely in bipolar patients with co-occurring SUDs.12
Unfortunately, limited treatment research guides clinical management of comorbid BD and SUDs.2,13,14 Clinical trials of medications for BD traditionally have excluded patients with SUDs, and persons with serious mental illness usually are ineligible for SUD treatment studies.13 Furthermore, the few randomized controlled trials (RCTs) conducted in persons with both illnesses have been constrained by relatively small sample sizes and low retention rates. In the absence of a definitive consensus for optimal treatment, this article outlines general clinical considerations and an integrated approach to assessing and managing this complex patient population.
Birds of a feather
Multiple hypotheses try to account for the high rate of SUDs in patients with BD (Table 1), but none fully explain the complex interaction observed clinically.14,15 Substance dependence and BD are chronic remitting/relapsing disorders with heterogeneous presentations and highly variable natural histories. As with SUDs, BD may go undiagnosed and untreated for years, coming to clinical attention only after substantial disease progression.16
The fluctuating illness course in BD and SUDs makes diagnosis and treatment difficult. Symptomatic periods often are interrupted by spontaneous remissions and longer—although usually temporary—periods of perceived control. Both BD and SUDs may be associated with profound mood instability, increased impulsivity, altered responsiveness to reward, and impaired executive function.17 Finally, the high degree of heritability in BD18 and many SUDs19 may make treatment engagement more difficult if either disorder is present in multiple family members because of:
- potential for greater clinical severity
- reduced psychosocial resources
- altered familial behavioral norms that may impede the patient’s recognition of illness.
Denial of illness is a critical symptom that may fluctuate with disease course in both disorders. Persons with BD or SUDs may be least likely to recognize that they are ill during periods of highest symptom severity. Accordingly, treatment adherence in patients with either disorder may be limited at baseline and decline further when the 2 illnesses co-occur.20
Involvement in the criminal justice system and medical comorbidities, particularly HCV, also complicate diagnosis and treatment of BD patients with SUDs. For more information about these topics, see Box1 and Box2.
Table 1
Why is substance abuse so prevalent among bipolar patients?
| Proposed hypothesis | Selected limitations of this hypothesis |
|---|---|
| Self-medication: substance abuse occurs as an attempt to regulate mood | High rates of substance use during euthymia; high prevalence of alcohol/depressant use during depressive phase, stimulant use during manic phase |
| Common neurobiologic or genetic risk factors | Specific evidence from linkage/association studies currently is lacking |
| Substance use occurs as a symptom of bipolar disorder | High percentage of patients with bipolar disorder do not have SUDs; there is a poor correlation of onset, course of bipolar, and SUD symptoms |
| Substance use unmasks bipolar disorder or a bipolar diathesis | Emergence of mania before SUD is common and predictive of more severe course of bipolar disorder |
| High comorbidity rates are an artifact of misdiagnosis based on overlapping symptoms and poor diagnostic boundaries | Very high prevalence of SUDs also is observed in longitudinal studies of patients initially hospitalized for mania |
| SUDs: substance use disorders | |
| Source: References 14,15 | |
Integrated clinical management
Assessment. Although not intended to be comprehensive, suggestions for routine assessment of patients with suspected SUDs and/or BD are listed in Table 2. Because clinicians may encounter dual diagnosis patients in general psychiatric clinics or specialty (addiction or mood disorder) clinics, it is useful to obtain a thorough substance use history in all patients with known or suspected BD as well as a thorough history of hypomania/mania and depression in all patients with addictive disorders. BD diagnoses by self-report or chart history in patients with SUDs should be considered cautiously because BD often is overdiagnosed in persons engaged in active substance abuse or experiencing withdrawal.21 If past or present mood symptoms and substance use have co-occurred, further focused assessment of mood symptoms before alcohol and drug use or during extended periods of abstinence are necessary to make the diagnosis of bipolar disorder with confidence. Family history of SUDs and/or BD are neither necessary nor sufficient for either diagnosis; however, collateral information from family or significant others could help make the diagnosis and may identify aids and obstacles to treatment planning and engagement.
When a patient’s clinical history strongly supports the diagnoses of BD and co-occurring SUDs, more detailed inquiry is warranted. Determining the patient’s age at onset of each disorder may have prognostic value because onset of mania before SUDs developed, especially in adolescence, may predict a more severe course of both illnesses.22 A complete alcohol use history should include routine questioning about past withdrawal. Previous withdrawal seizures in an actively drinking BD patient may tip the balance toward adding an anticonvulsant for mood stabilization. A thorough SUD history should elicit information about polysubstance abuse or dependence and include screening for injection drug use and other risk factors for HCV and human immunodeficiency virus (HIV), such as hypersexuality during manic or hypomanic episodes. Document the date of the last screening for HCV/ HIV in BD patients at high risk of infection. The U.S. Centers for Disease Control and Prevention recommends that all patients at high risk for HIV consider voluntary screening at least annually.23
Assess your patient’s historical and ongoing alcohol and other drug abuse at the initial visit, and continue to monitor substance use at all subsequent visits, especially in patients with HCV. When feasible, order urine drug screening and laboratory testing for alcohol use biomarkers such as carbohydrate-deficient transferrin and gamma-glutamyltransferase to supplement self-report data, especially in patients with poor insight or low motivation. Assess suicidal ideation and any changes in suicide risk factors at every visit.
Treatment. No biologic therapies have been FDA-approved for treating patients with co-occurring BD and SUDs. Comorbid SUDs in BD patients—as well as rapid cycling and mixed mood episodes, both of which are more common in patients with comorbid SUDs—predict poor response to lithium.17 However, the evidence base for optimal pharmacotherapy remains extremely limited. Published double-blind, placebo-controlled RCTs in persons with BD and co-morbid SUDs are limited to only 1 trial each of lithium, carbamazepine, quetiapine, and naltrexone, and 2 comparisons of lithium plus divalproex vs lithium alone (Table 3).24-29
Salloum et al24 reported that bipolar I disorder patients with alcohol dependence who received divalproex plus lithium as maintenance treatment had fewer heavy drinking days and fewer drinks per heavy drinking day than those receiving lithium plus placebo. However, the addition of divalproex did not improve manic or depressive symptoms, and depression remission rates remained relatively low in both groups. A recent 6-month study comparing lithium vs lithium plus divalproex in patients with SUDs and rapid-cycling BD found no additional benefit of divalproex over lithium monotherapy in retention, mood, or substance use outcomes.28 However, modest evidence that anticonvulsants such as valproic acid and carbamazepine may help treat acute alcohol withdrawal2 could support their preferential use as mood stabilizers over lithium in actively drinking BD patients.
Research underscores the difficulty in keeping dual diagnosis patients in treatment. Salloum et al24 reported that only one-third of randomized subjects completed the 24-week study. In the Kemp study,28 79% of 149 recruited subjects failed to complete the lead-in stabilization phase. Of the 31 remaining subjects who were randomized to lithium or lithium/divalproex combination, only 8 (26% of those randomized, 5% of those recruited) completed the 6-month trial.
Substance abuse is associated with significantly decreased treatment adherence in persons with BD20 and may affect medication choice. For example, caution may be warranted in the use of lamotrigine in substance-abusing patients with poor adherence because re-titration from the starting dose is recommended if the medicine has been missed for a consecutive period exceeding 5 half-lives of the drug.30
Notable progress has been made in developing psychosocial treatments for comorbid SUDs and BD. Integrated group therapy has been designed to address the 2 disorders simultaneously by emphasizing the relationship between the disorders and highlighting similarities in cognitive and behavioral change that promote recovery in both.31 In a recent well-controlled RCT, this approach reduced alcohol and other drug use to approximately one-half the levels observed in those who received only group drug counseling.31
Research suggests that an integrated approach that encompasses psychiatric, medical, psychosocial, and legal dimensions simultaneously may be most effective. For patients such as Mr. M, this would include aggressively treating mood symptoms while employing motivational interviewing techniques to improve engagement in substance dependence treatment. If possible, involving family members, parole officials, housing agencies, and other public assistance workers in the treatment plan may increase treatment adherence and reduce loss of contact during illness exacerbations. Stabilization of substance use and psychiatric morbidity should be accompanied by timely evaluation of HCV and other medical comorbidities in order to improve long-term prognosis.
Table 2
Assessing patients you suspect have comorbid BD and SUDs
| Initial assessment |
|---|
Thorough substance use history in all patients with known or suspected bipolar disorder:
|
Thorough evaluation of any history of hypomania/mania and depression in all patients with known or suspected SUDs:
|
| Assess risk factors, screening status for hepatitis C, HIV |
| Obtain collateral information from family and significant others if feasible and appropriate |
| Detailed assessment of suicide risk |
| Follow-up assessments |
| Substance use since last visit by self-report |
| Consider UDS, CDT, GGT |
| Medication adherence |
| Detailed assessment of suicide risk |
| BD: bipolar disorder; CDT: carbohydrate-deficient transferrin; GGT: gamma-glutamyltransferase; HIV: human immunodeficiency virus; SUDs: substance use disorders; UDS: urine drug screen |
Table 3
Pharmacotherapy for bipolar disorder and co-occurring SUDs
| Study | Diagnoses/N* | Medications | Outcome |
|---|---|---|---|
| Salloum et al, 200524 | BD I, alcohol dependence. N=59 [20] | Divalproex + lithium vs lithium, 24 weeks | Decreased number of heavy drinking days, fewer drinks per heavy drinking day |
| Geller et al, 199825 | BD I, BP II, MDD (adolescents); alcohol, cannabis abuse. N=25 [21] | Lithium, 6 weeks | Decreased cannabis-positive urine drug screen (lithium > placebo) |
| Brady et al, 200226 | BD I, BD II, cyclothymia; cocaine dependence. N=57 | Carbamazepine, 12 weeks | Trend toward longer time to cocaine use |
| Brown et al, 200827 | BD I, BD II; N=102 | Quetiapine, 12 weeks | Decreased HAM-D scores (quetiapine > placebo) |
| Kemp et al, 200928 | BD I, BD II, rapid cycling; alcohol, cannabis, cocaine abuse or dependence. N=31 [8] | Divalproex + lithium vs lithium, 6 months | No group differences |
| Brown et al, 200929 | BD I, BD II; alcohol dependence. N=50 [26] | Naltrexone, 12 weeks | Trend toward increased probability of no drinking days |
| * N=number of subjects randomized to double-blind treatment. Numbers in brackets indicate the number of subjects who completed all study visits (when reported) | |||
| BD: bipolar disorder; HAM-D: 17-item Hamilton Rating Scale for Depression; MDD: major depressive disorder; SUDs: substance use disorders | |||
Related Resources
- International Society for Bipolar Disorders. www.isbd.org.
- National Institute on Alcohol Abuse and Alcoholism. www.niaaa.nih.gov.
- National Institute on Drug Abuse. www.nida.nih.gov.
Drug Brand Names
- Carbamazepine • Tegretol
- Divalproex/valproic acid • Depakote
- Lamotrigine • Lamictal
- Lithium • Lithobid
- Naltrexone • ReVia
- Quetiapine • Seroquel
Disclosure
Dr. Tolliver receives research grant funding from Forest Laboratories and the National Institute on Alcohol Abuse and Alcoholism. Neither source influenced the content or submission of this manuscript.
A recent analysis of data from >65,000 veterans found bipolar patients with comorbid substance use disorders (SUDs) were 7 times more likely to have hepatitis C virus (HCV) than patients with no serious mental illness.a Matthews and colleagues found that 29.6% of persons diagnosed with bipolar disorder (BD) and SUDs tested positive for HCV—roughly 5 times the relative risk of patients without either diagnosis.b The high prevalence of HCV in patients with comorbid BD and SUDs may be the result of injection drug use, increased risky sexual behavior while manic or intoxicated, or both.
HCV has multiple treatment implications for these patients. Alcohol abuse and dependence are the most common SUDs that co-occur with BD,c-e and patients with HCV who drink alcohol excessively have more severe hepatic fibrosis, accelerated disease progression, and higher rates of cirrhosis and hepatocellular carcinoma than HCV patients who do not drink.f Medications commonly used to treat BD or alcohol dependence may have adverse effects on the liver and require more careful monitoring in the presence of HCV infection. For example, valproic acid has been reported to improve drinking outcomes in alcohol-dependent patients with BDg but has been associated with higher rates of marked hepatic transaminase elevation in patients with HCV infection compared with those without HCV.h Marked elevation of hepatic transaminases may be observed in HCV-infected individuals treated with other medications such as lithium or antidepressants,h and valproic acid use is not an absolute contraindication in HCV patients. Nevertheless, the effects of valproic acid in HCV-infected BD patients who drink alcohol are unknown and therefore cautious and frequent monitoring of hepatic enzymes are warranted in this population.
Finally, both SUDs and BD complicate HCV treatment. In a database review of >113,000 veterans with HCV infection, Butt and colleagues found that individuals with BD accounted for 10.4% of the HCV-infected sample but only 5% of those who received HCV treatment.i Similarly, patients with alcohol abuse or dependence made up 44.3% of the HCV-infected sample but only 28.9% of those who received HCV treatment.
Because the rate of liver biopsy in untreated patients was low, the decision not to treat appeared to be based more often on other criteria. This is not surprising; pegylated interferon-alfa—the most effective treatment for chronic HCV—has been associated with multiple neuropsychiatric symptoms observed in BD, including depression, mania, psychosis, and suicidal ideation.j Emergence of severe psychiatric complications usually results in permanent discontinuation of interferon treatment. Likewise, the presence of alcohol abuse or other SUDs is a strong negative predictor of interferon treatment response and retention and generally has been considered a relative contraindication for interferon initiation.f
References
a. Himelhoch S, McCarthy JF, Ganoczy D, et al. Understanding associations between serious mental illness and hepatitis C virus among veterans: a national multivariate analysis. Psychosomatics. 2009;50:30-37.
b. Matthews AM, Huckans MS, Blackwell AD, et al. Hepatitis C testing and infection rates in bipolar patients with and without comorbid substance use disorders. Bipolar Disord. 2008;10:266-270.
c. Grant BF, Stinson FS, Dawson DA, et al. Prevalence and co-occurrence of substance use disorders and independent mood and anxiety disorders. Results from the National Epidemiologic Survey on Alcohol and Related Conditions. Arch Gen Psychiatry. 2004;61:807-816.
d. Hasin DS, Stinson FS, Ogburn E, et al. Prevalence, correlates, disability, and comorbidity of DSM-IV alcohol abuse and dependence in the United States. Results from the National Epidemiologic Survey on Alcohol and Related Conditions. Arch Gen Psychiatry. 2007;64:830-842.
e. Merikangas KR, Akiskal HS, Angst J, et al. Lifetime and 12-month prevalence of bipolar spectrum disorder in the National Comorbidity Survey Replication. Arch Gen Psychiatry. 2007;64:543-552.
f. Bhattacharya R, Shuhart M. Hepatitis C and alcohol. J Clin Gastroenterol. 2003;36:242-252.
g. Salloum IM, Cornelius JR, Daley DC, et al. Efficacy of valproate maintenance in patients with bipolar disorder and alcoholism: a double-blind, placebo-controlled study. Arch Gen Psychiatry. 2005;62:37-45.
h. Felker BL, Sloan KL, Dominitz JA, et al. The safety of valproic acid use for patients with hepatitis C infection. Am J Psychiatry. 2003;160:174-178.
i. Butt AA, Justice AC, Skanderson M, et al. Rate and predictors of treatment prescription for hepatitis C. Gut. 2006;56:385-389.
j. Onyike CU, Bonner JO, Lyketsos CG, et al. Mania during treatment of chronic hepatitis C with pegylated interferon and ribavirin. Am J Psychiatry. 2004;161:429-435.
Long recognized to be more prevalent in forensic populations, bipolar disorder (BD) is especially overrepresented among those with repeat arrests and incarcerations. In a recent study of >79,000 inmates incarcerated in Texas in 2006 and 2007, those with BD were 3.3 times more likely to have had ≥4 previous incarcerations.k
Comorbid substance use disorder (SUD) is a significant risk factor for criminal arrest. For example, in a Los Angeles County (CA) sample of inmates with BD, 75.8% had co-occurring SUDs, compared with 18.5% in a comparison group of hospitalized BD patients.l The association of SUDs with arrest is especially high in females with BD. In the Los Angeles sample mentioned above, incarcerated bipolar women were >38 times more likely to have a SUD than a comparison group of female patients treated in the community.m
References
k. Baillargeon J, Binswanger IA, Penn JV, et al. Psychiatric disorders and repeat incarcerations: the revolving prison door. Am J Psychiatry. 2009;166:103-109.
l. Quanbeck CD, Stone DC, Scott CL, et al. Clinical and legal correlates of inmates with bipolar disorder at time of criminal arrest. J Clin Psychiatry. 2004;65:198-203.
m. McDermott BE, Quanbeck CD, Frye MA. Comorbid substance use disorder in women with bipolar disorder is associated with criminal arrest. Bipolar Disord. 2007;9(5):536-540.
1. Levin FR, Hennessey G. Bipolar disorder and substance abuse. Biol Psychiatry. 2004;56:738-748.
2. Frye MA, Salloum IM. Bipolar disorder and comorbid alcoholism: prevalence rate and treatment considerations. Bipolar Disord. 2006;8:677-685.
3. Grant BF, Stinson FS, Dawson DA, et al. Prevalence and co-occurrence of substance use disorders and independent mood and anxiety disorders. Results from the National Epidemiologic Survey on Alcohol and Related Conditions. Arch Gen Psychiatry. 2004;61:807-816.
4. Hasin DS, Stinson FS, Ogburn E, et al. Prevalence, correlates, disability, and comorbidity of DSM-IV alcohol abuse and dependence in the United States. Results from the National Epidemiologic Survey on Alcohol and Related Conditions. Arch Gen Psychiatry. 2007;64:830-842.
5. Merikangas KR, Akiskal HS, Angst J, et al. Lifetime and 12-month prevalence of bipolar spectrum disorder in the National Comorbidity Survey Replication. Arch Gen Psychiatry. 2007;64:543-552.
6. Sublette EM, Carballo JJ, Moreno C, et al. Substance use disorders and suicide attempts in bipolar subtypes. J Psychiatric Res. 2009;43:230-238.
7. McElroy SL, Altshuler LL, Suppes T, et al. Axis I psychiatric comorbidity and its relationship to historical illness variables in 288 patients with bipolar disorder. Am J Psychiatry. 2001;158:420-426.
8. Frye MA, Altshuler LL, McElroy SL, et al. Gender differences in prevalence, risk, and clinical correlates of alcoholism comorbidity in bipolar disorder. Am J Psychiatry. 2003;160:883-889.
9. Simon NM, Otto MW, Wisniewski SR, et al. Anxiety disorder comorbidity in bipolar disorder patients: data from the first 500 participants in the systematic treatment enhancement program for bipolar disorder (STEP-BD). Am J Psychiatry. 2004;161:2222-2229.
10. Perron BE, Howard MO, Nienhuis JK, et al. Prevalence and burden of general medical conditions among adults with bipolar I disorder: results from the National Epidemiologic Survey on Alcohol and Related Conditions. J Clin Psychiatry. 2009;70:1407-1415.
11. Himelhoch S, McCarthy JF, Ganoczy D, et al. Understanding associations between serious mental illness and hepatitis C virus among veterans: a national multivariate analysis. Psychosomatics. 2009;50:30-37.
12. Matthews AM, Huckans MS, Blackwell AD, et al. Hepatitis C testing and infection rates in bipolar patients with and without comorbid substance use disorders. Bipolar Disord. 2008;10:266-270.
13. Singh JB, Zarate CA. Pharmacological treatment of psychiatric comorbidity in bipolar disorder: a review of controlled trials. Bipolar Disord. 2006;8:696-709.
14. Vornik LA, Brown ES. Management of comorbid bipolar disorder and substance abuse. J Clin Psychiatry. 2006;67(suppl 7):24-30.
15. Strakowski SM, DelBello MP. The co-occurrence of bipolar and substance use disorders. Clin Psych Rev. 2000;20:191-206.
16. Berk M, Dodd S, Callaly P, et al. History of illness prior to a diagnosis of bipolar disorder or schizoaffective disorder. J Affect Disord. 2007;103:181-186.
17. Goodwin FK, Jamison KR. Manic-depressive illness: bipolar disorders and recurrent depression. 2nd ed. New York, NY: Oxford University Press; 2007.
18. McGuffin P, Rijsdijk F, Andrew M, et al. The heritability of bipolar affective disorder and the genetic relationship to unipolar depression. Arch Gen Psychiatry. 2003;60:497-502.
19. Kendler KS, Prescott CA, Myers J, et al. The structure of genetic and environmental risk factors for common psychiatric and substance abuse disorders in men and women. Arch Gen Psychiatry. 2003;60:929-937.
20. Weiss RD, Greenfield SF, Najavits LM, et al. Medication compliance among patients with bipolar disorder and substance use disorder. J Clin Psychiatry. 1998;59:172-174.
21. Goldberg JF, Garno JL, Callahan AM, et al. Overdiagnosis of bipolar disorder among substance use disorder inpatients with mood instability. J Clin Psychiatry. 2008;69:1751-1757.
22. Winokur G, Coryell W, Akiskal HS, et al. Alcoholism in manic-depressive (bipolar) illness: familial illness, course of illness, and the primary-secondary distinction. Am J Psychiatry. 1995;152:365-372.
23. Branson BM, Handsfield HH, Lampe MA, et al. Revised recommendations for HIV testing of adults, adolescents, and pregnant women in health care settings. MMWR. 2006;55(RR14):1-17.
24. Salloum IM, Cornelius JR, Daley DC, et al. Efficacy of valproate maintenance in patients with bipolar disorder and alcoholism: a double-blind, placebo-controlled study. Arch Gen Psychiatry. 2005;62:37-45.
25. Geller B, Cooper TB, Sun K, et al. Double-blind and placebo-controlled study of lithium for adolescent bipolar disorders with secondary substance dependency. J Am Acad Child Adolesc Psychiatry. 1998;37(2):171-178.
26. Brady KT, Sonne SC, Malcolm RJ, et al. Carbamazepine in the treatment of cocaine dependence: subtyping by affective disorder. Exp Clin Psychopharmacol. 2002;10:276-285.
27. Brown ES, Garza M, Carmody TJ. A randomized, double-blind, placebo-controlled add-on trial of quetiapine in outpatients with bipolar disorder and alcohol use disorders. J Clin Psychiatry. 2008;69:701-705.
28. Kemp DE, Gao K, Ganocy S, et al. A 6-month, double-blind, maintenance trial of lithium monotherapy versus the combination of lithium and divalproex for rapid-cycling bipolar disorder and co-occurring substance abuse or dependence. J Clin Psychiatry. 2009;70:113-121.
29. Brown ES, Carmody TJ, Schmitz JM, et al. A randomized, double-blind, placebo-controlled pilot study of naltrexone in outpatients with bipolar disorder and alcohol dependence. Alcohol Clin Exp Res. 2009;3:1863-1869.
30. Lamictal [package insert]. Research Triangle Park, NC: GlaxoSmithKline; 2009.
31. Weiss RD, Griffin ML, Kolodziej MR, et al. A randomized trial of integrated group therapy versus group drug counseling for patients with bipolar disorder and substance dependence. Am J Psychiatry. 2007;164:100-107.
After testing positive for cocaine on a recent court-mandated urine drug screen, Mr. M, age 49, is referred by his parole officer for psychiatric and substance abuse treatment. Mr. M has bipolar I disorder and alcohol, cocaine, and opioid dependence. He says he has been hospitalized or incarcerated at least once each year for the past 22 years. Mr. M has seen numerous psychiatrists as an outpatient, but rarely for more than 2 to 3 months and has not taken any psychotropics for more than 5 months.
Approximately 1 week before his recent urine drug screen, Mr. M became euphoric, stopped sleeping for several days, and spent $2,000 on cocaine and “escorts.” He reports that each day he smokes 30 cigarettes and drinks 1 pint of liquor and prefers to use cocaine and opiates by IV injection. Several years ago Mr. M was diagnosed with hepatitis C virus (HCV) but received no further workup or treatment. Although he denies manic or psychotic symptoms, Mr. M is observed speaking to unseen others in the waiting room and has difficulty remaining still during his interview. His chief concern is insomnia, stating, “Doc, I just need something to help me sleep.”
The high prevalence of substance use disorders (SUDs) in persons with bipolar disorder (BD) is well documented.1,2 Up to 60% of bipolar patients develop an SUD at some point in their lives.3-5 Alcohol use disorders are particularly common among BD patients, with a lifetime prevalence of roughly 50%.2-5 Recent epidemiologic data indicate that 38% of persons with bipolar I disorder and 19% of those with bipolar II disorder meet criteria for alcohol dependence.5 Comorbid SUDs in patients with BD are associated with:
- poor treatment compliance
- longer and more frequent mood episodes
- more mixed episodes
- more hospitalizations
- more frequent suicide attempts.1,2
The impact of co-occurring SUDs on suicidality is particularly high among those with bipolar I disorder.6
Frequently referred to as “dual diagnosis” conditions, co-occurring BD and SUDs may be more accurately envisioned as multi-morbid, rather than comorbid, illnesses. Data from the Stanley Foundation Bipolar Network suggest that 42% of BD patients have a lifetime history of ≥2 comorbid axis I disorders.7 Rates of generalized anxiety disorder, panic disorder, and posttraumatic stress disorder are particularly high in BD patients with co-occurring SUDs.8,9 In addition, the presence of 1 SUD may mark the presence of other SUDs; for example, alcohol dependence is strongly associated with polysubstance abuse, especially in females with BD.8 Furthermore, medical comorbidities that impact treatment decisions also are highly prevalent in BD patients with comorbid SUDs.10 In particular, HCV rates are higher in persons with BD compared with the general population,11 and are >5 times as likely in bipolar patients with co-occurring SUDs.12
Unfortunately, limited treatment research guides clinical management of comorbid BD and SUDs.2,13,14 Clinical trials of medications for BD traditionally have excluded patients with SUDs, and persons with serious mental illness usually are ineligible for SUD treatment studies.13 Furthermore, the few randomized controlled trials (RCTs) conducted in persons with both illnesses have been constrained by relatively small sample sizes and low retention rates. In the absence of a definitive consensus for optimal treatment, this article outlines general clinical considerations and an integrated approach to assessing and managing this complex patient population.
Birds of a feather
Multiple hypotheses try to account for the high rate of SUDs in patients with BD (Table 1), but none fully explain the complex interaction observed clinically.14,15 Substance dependence and BD are chronic remitting/relapsing disorders with heterogeneous presentations and highly variable natural histories. As with SUDs, BD may go undiagnosed and untreated for years, coming to clinical attention only after substantial disease progression.16
The fluctuating illness course in BD and SUDs makes diagnosis and treatment difficult. Symptomatic periods often are interrupted by spontaneous remissions and longer—although usually temporary—periods of perceived control. Both BD and SUDs may be associated with profound mood instability, increased impulsivity, altered responsiveness to reward, and impaired executive function.17 Finally, the high degree of heritability in BD18 and many SUDs19 may make treatment engagement more difficult if either disorder is present in multiple family members because of:
- potential for greater clinical severity
- reduced psychosocial resources
- altered familial behavioral norms that may impede the patient’s recognition of illness.
Denial of illness is a critical symptom that may fluctuate with disease course in both disorders. Persons with BD or SUDs may be least likely to recognize that they are ill during periods of highest symptom severity. Accordingly, treatment adherence in patients with either disorder may be limited at baseline and decline further when the 2 illnesses co-occur.20
Involvement in the criminal justice system and medical comorbidities, particularly HCV, also complicate diagnosis and treatment of BD patients with SUDs. For more information about these topics, see Box1 and Box2.
Table 1
Why is substance abuse so prevalent among bipolar patients?
| Proposed hypothesis | Selected limitations of this hypothesis |
|---|---|
| Self-medication: substance abuse occurs as an attempt to regulate mood | High rates of substance use during euthymia; high prevalence of alcohol/depressant use during depressive phase, stimulant use during manic phase |
| Common neurobiologic or genetic risk factors | Specific evidence from linkage/association studies currently is lacking |
| Substance use occurs as a symptom of bipolar disorder | High percentage of patients with bipolar disorder do not have SUDs; there is a poor correlation of onset, course of bipolar, and SUD symptoms |
| Substance use unmasks bipolar disorder or a bipolar diathesis | Emergence of mania before SUD is common and predictive of more severe course of bipolar disorder |
| High comorbidity rates are an artifact of misdiagnosis based on overlapping symptoms and poor diagnostic boundaries | Very high prevalence of SUDs also is observed in longitudinal studies of patients initially hospitalized for mania |
| SUDs: substance use disorders | |
| Source: References 14,15 | |
Integrated clinical management
Assessment. Although not intended to be comprehensive, suggestions for routine assessment of patients with suspected SUDs and/or BD are listed in Table 2. Because clinicians may encounter dual diagnosis patients in general psychiatric clinics or specialty (addiction or mood disorder) clinics, it is useful to obtain a thorough substance use history in all patients with known or suspected BD as well as a thorough history of hypomania/mania and depression in all patients with addictive disorders. BD diagnoses by self-report or chart history in patients with SUDs should be considered cautiously because BD often is overdiagnosed in persons engaged in active substance abuse or experiencing withdrawal.21 If past or present mood symptoms and substance use have co-occurred, further focused assessment of mood symptoms before alcohol and drug use or during extended periods of abstinence are necessary to make the diagnosis of bipolar disorder with confidence. Family history of SUDs and/or BD are neither necessary nor sufficient for either diagnosis; however, collateral information from family or significant others could help make the diagnosis and may identify aids and obstacles to treatment planning and engagement.
When a patient’s clinical history strongly supports the diagnoses of BD and co-occurring SUDs, more detailed inquiry is warranted. Determining the patient’s age at onset of each disorder may have prognostic value because onset of mania before SUDs developed, especially in adolescence, may predict a more severe course of both illnesses.22 A complete alcohol use history should include routine questioning about past withdrawal. Previous withdrawal seizures in an actively drinking BD patient may tip the balance toward adding an anticonvulsant for mood stabilization. A thorough SUD history should elicit information about polysubstance abuse or dependence and include screening for injection drug use and other risk factors for HCV and human immunodeficiency virus (HIV), such as hypersexuality during manic or hypomanic episodes. Document the date of the last screening for HCV/ HIV in BD patients at high risk of infection. The U.S. Centers for Disease Control and Prevention recommends that all patients at high risk for HIV consider voluntary screening at least annually.23
Assess your patient’s historical and ongoing alcohol and other drug abuse at the initial visit, and continue to monitor substance use at all subsequent visits, especially in patients with HCV. When feasible, order urine drug screening and laboratory testing for alcohol use biomarkers such as carbohydrate-deficient transferrin and gamma-glutamyltransferase to supplement self-report data, especially in patients with poor insight or low motivation. Assess suicidal ideation and any changes in suicide risk factors at every visit.
Treatment. No biologic therapies have been FDA-approved for treating patients with co-occurring BD and SUDs. Comorbid SUDs in BD patients—as well as rapid cycling and mixed mood episodes, both of which are more common in patients with comorbid SUDs—predict poor response to lithium.17 However, the evidence base for optimal pharmacotherapy remains extremely limited. Published double-blind, placebo-controlled RCTs in persons with BD and co-morbid SUDs are limited to only 1 trial each of lithium, carbamazepine, quetiapine, and naltrexone, and 2 comparisons of lithium plus divalproex vs lithium alone (Table 3).24-29
Salloum et al24 reported that bipolar I disorder patients with alcohol dependence who received divalproex plus lithium as maintenance treatment had fewer heavy drinking days and fewer drinks per heavy drinking day than those receiving lithium plus placebo. However, the addition of divalproex did not improve manic or depressive symptoms, and depression remission rates remained relatively low in both groups. A recent 6-month study comparing lithium vs lithium plus divalproex in patients with SUDs and rapid-cycling BD found no additional benefit of divalproex over lithium monotherapy in retention, mood, or substance use outcomes.28 However, modest evidence that anticonvulsants such as valproic acid and carbamazepine may help treat acute alcohol withdrawal2 could support their preferential use as mood stabilizers over lithium in actively drinking BD patients.
Research underscores the difficulty in keeping dual diagnosis patients in treatment. Salloum et al24 reported that only one-third of randomized subjects completed the 24-week study. In the Kemp study,28 79% of 149 recruited subjects failed to complete the lead-in stabilization phase. Of the 31 remaining subjects who were randomized to lithium or lithium/divalproex combination, only 8 (26% of those randomized, 5% of those recruited) completed the 6-month trial.
Substance abuse is associated with significantly decreased treatment adherence in persons with BD20 and may affect medication choice. For example, caution may be warranted in the use of lamotrigine in substance-abusing patients with poor adherence because re-titration from the starting dose is recommended if the medicine has been missed for a consecutive period exceeding 5 half-lives of the drug.30
Notable progress has been made in developing psychosocial treatments for comorbid SUDs and BD. Integrated group therapy has been designed to address the 2 disorders simultaneously by emphasizing the relationship between the disorders and highlighting similarities in cognitive and behavioral change that promote recovery in both.31 In a recent well-controlled RCT, this approach reduced alcohol and other drug use to approximately one-half the levels observed in those who received only group drug counseling.31
Research suggests that an integrated approach that encompasses psychiatric, medical, psychosocial, and legal dimensions simultaneously may be most effective. For patients such as Mr. M, this would include aggressively treating mood symptoms while employing motivational interviewing techniques to improve engagement in substance dependence treatment. If possible, involving family members, parole officials, housing agencies, and other public assistance workers in the treatment plan may increase treatment adherence and reduce loss of contact during illness exacerbations. Stabilization of substance use and psychiatric morbidity should be accompanied by timely evaluation of HCV and other medical comorbidities in order to improve long-term prognosis.
Table 2
Assessing patients you suspect have comorbid BD and SUDs
| Initial assessment |
|---|
Thorough substance use history in all patients with known or suspected bipolar disorder:
|
Thorough evaluation of any history of hypomania/mania and depression in all patients with known or suspected SUDs:
|
| Assess risk factors, screening status for hepatitis C, HIV |
| Obtain collateral information from family and significant others if feasible and appropriate |
| Detailed assessment of suicide risk |
| Follow-up assessments |
| Substance use since last visit by self-report |
| Consider UDS, CDT, GGT |
| Medication adherence |
| Detailed assessment of suicide risk |
| BD: bipolar disorder; CDT: carbohydrate-deficient transferrin; GGT: gamma-glutamyltransferase; HIV: human immunodeficiency virus; SUDs: substance use disorders; UDS: urine drug screen |
Table 3
Pharmacotherapy for bipolar disorder and co-occurring SUDs
| Study | Diagnoses/N* | Medications | Outcome |
|---|---|---|---|
| Salloum et al, 200524 | BD I, alcohol dependence. N=59 [20] | Divalproex + lithium vs lithium, 24 weeks | Decreased number of heavy drinking days, fewer drinks per heavy drinking day |
| Geller et al, 199825 | BD I, BP II, MDD (adolescents); alcohol, cannabis abuse. N=25 [21] | Lithium, 6 weeks | Decreased cannabis-positive urine drug screen (lithium > placebo) |
| Brady et al, 200226 | BD I, BD II, cyclothymia; cocaine dependence. N=57 | Carbamazepine, 12 weeks | Trend toward longer time to cocaine use |
| Brown et al, 200827 | BD I, BD II; N=102 | Quetiapine, 12 weeks | Decreased HAM-D scores (quetiapine > placebo) |
| Kemp et al, 200928 | BD I, BD II, rapid cycling; alcohol, cannabis, cocaine abuse or dependence. N=31 [8] | Divalproex + lithium vs lithium, 6 months | No group differences |
| Brown et al, 200929 | BD I, BD II; alcohol dependence. N=50 [26] | Naltrexone, 12 weeks | Trend toward increased probability of no drinking days |
| * N=number of subjects randomized to double-blind treatment. Numbers in brackets indicate the number of subjects who completed all study visits (when reported) | |||
| BD: bipolar disorder; HAM-D: 17-item Hamilton Rating Scale for Depression; MDD: major depressive disorder; SUDs: substance use disorders | |||
Related Resources
- International Society for Bipolar Disorders. www.isbd.org.
- National Institute on Alcohol Abuse and Alcoholism. www.niaaa.nih.gov.
- National Institute on Drug Abuse. www.nida.nih.gov.
Drug Brand Names
- Carbamazepine • Tegretol
- Divalproex/valproic acid • Depakote
- Lamotrigine • Lamictal
- Lithium • Lithobid
- Naltrexone • ReVia
- Quetiapine • Seroquel
Disclosure
Dr. Tolliver receives research grant funding from Forest Laboratories and the National Institute on Alcohol Abuse and Alcoholism. Neither source influenced the content or submission of this manuscript.
A recent analysis of data from >65,000 veterans found bipolar patients with comorbid substance use disorders (SUDs) were 7 times more likely to have hepatitis C virus (HCV) than patients with no serious mental illness.a Matthews and colleagues found that 29.6% of persons diagnosed with bipolar disorder (BD) and SUDs tested positive for HCV—roughly 5 times the relative risk of patients without either diagnosis.b The high prevalence of HCV in patients with comorbid BD and SUDs may be the result of injection drug use, increased risky sexual behavior while manic or intoxicated, or both.
HCV has multiple treatment implications for these patients. Alcohol abuse and dependence are the most common SUDs that co-occur with BD,c-e and patients with HCV who drink alcohol excessively have more severe hepatic fibrosis, accelerated disease progression, and higher rates of cirrhosis and hepatocellular carcinoma than HCV patients who do not drink.f Medications commonly used to treat BD or alcohol dependence may have adverse effects on the liver and require more careful monitoring in the presence of HCV infection. For example, valproic acid has been reported to improve drinking outcomes in alcohol-dependent patients with BDg but has been associated with higher rates of marked hepatic transaminase elevation in patients with HCV infection compared with those without HCV.h Marked elevation of hepatic transaminases may be observed in HCV-infected individuals treated with other medications such as lithium or antidepressants,h and valproic acid use is not an absolute contraindication in HCV patients. Nevertheless, the effects of valproic acid in HCV-infected BD patients who drink alcohol are unknown and therefore cautious and frequent monitoring of hepatic enzymes are warranted in this population.
Finally, both SUDs and BD complicate HCV treatment. In a database review of >113,000 veterans with HCV infection, Butt and colleagues found that individuals with BD accounted for 10.4% of the HCV-infected sample but only 5% of those who received HCV treatment.i Similarly, patients with alcohol abuse or dependence made up 44.3% of the HCV-infected sample but only 28.9% of those who received HCV treatment.
Because the rate of liver biopsy in untreated patients was low, the decision not to treat appeared to be based more often on other criteria. This is not surprising; pegylated interferon-alfa—the most effective treatment for chronic HCV—has been associated with multiple neuropsychiatric symptoms observed in BD, including depression, mania, psychosis, and suicidal ideation.j Emergence of severe psychiatric complications usually results in permanent discontinuation of interferon treatment. Likewise, the presence of alcohol abuse or other SUDs is a strong negative predictor of interferon treatment response and retention and generally has been considered a relative contraindication for interferon initiation.f
References
a. Himelhoch S, McCarthy JF, Ganoczy D, et al. Understanding associations between serious mental illness and hepatitis C virus among veterans: a national multivariate analysis. Psychosomatics. 2009;50:30-37.
b. Matthews AM, Huckans MS, Blackwell AD, et al. Hepatitis C testing and infection rates in bipolar patients with and without comorbid substance use disorders. Bipolar Disord. 2008;10:266-270.
c. Grant BF, Stinson FS, Dawson DA, et al. Prevalence and co-occurrence of substance use disorders and independent mood and anxiety disorders. Results from the National Epidemiologic Survey on Alcohol and Related Conditions. Arch Gen Psychiatry. 2004;61:807-816.
d. Hasin DS, Stinson FS, Ogburn E, et al. Prevalence, correlates, disability, and comorbidity of DSM-IV alcohol abuse and dependence in the United States. Results from the National Epidemiologic Survey on Alcohol and Related Conditions. Arch Gen Psychiatry. 2007;64:830-842.
e. Merikangas KR, Akiskal HS, Angst J, et al. Lifetime and 12-month prevalence of bipolar spectrum disorder in the National Comorbidity Survey Replication. Arch Gen Psychiatry. 2007;64:543-552.
f. Bhattacharya R, Shuhart M. Hepatitis C and alcohol. J Clin Gastroenterol. 2003;36:242-252.
g. Salloum IM, Cornelius JR, Daley DC, et al. Efficacy of valproate maintenance in patients with bipolar disorder and alcoholism: a double-blind, placebo-controlled study. Arch Gen Psychiatry. 2005;62:37-45.
h. Felker BL, Sloan KL, Dominitz JA, et al. The safety of valproic acid use for patients with hepatitis C infection. Am J Psychiatry. 2003;160:174-178.
i. Butt AA, Justice AC, Skanderson M, et al. Rate and predictors of treatment prescription for hepatitis C. Gut. 2006;56:385-389.
j. Onyike CU, Bonner JO, Lyketsos CG, et al. Mania during treatment of chronic hepatitis C with pegylated interferon and ribavirin. Am J Psychiatry. 2004;161:429-435.
Long recognized to be more prevalent in forensic populations, bipolar disorder (BD) is especially overrepresented among those with repeat arrests and incarcerations. In a recent study of >79,000 inmates incarcerated in Texas in 2006 and 2007, those with BD were 3.3 times more likely to have had ≥4 previous incarcerations.k
Comorbid substance use disorder (SUD) is a significant risk factor for criminal arrest. For example, in a Los Angeles County (CA) sample of inmates with BD, 75.8% had co-occurring SUDs, compared with 18.5% in a comparison group of hospitalized BD patients.l The association of SUDs with arrest is especially high in females with BD. In the Los Angeles sample mentioned above, incarcerated bipolar women were >38 times more likely to have a SUD than a comparison group of female patients treated in the community.m
References
k. Baillargeon J, Binswanger IA, Penn JV, et al. Psychiatric disorders and repeat incarcerations: the revolving prison door. Am J Psychiatry. 2009;166:103-109.
l. Quanbeck CD, Stone DC, Scott CL, et al. Clinical and legal correlates of inmates with bipolar disorder at time of criminal arrest. J Clin Psychiatry. 2004;65:198-203.
m. McDermott BE, Quanbeck CD, Frye MA. Comorbid substance use disorder in women with bipolar disorder is associated with criminal arrest. Bipolar Disord. 2007;9(5):536-540.
After testing positive for cocaine on a recent court-mandated urine drug screen, Mr. M, age 49, is referred by his parole officer for psychiatric and substance abuse treatment. Mr. M has bipolar I disorder and alcohol, cocaine, and opioid dependence. He says he has been hospitalized or incarcerated at least once each year for the past 22 years. Mr. M has seen numerous psychiatrists as an outpatient, but rarely for more than 2 to 3 months and has not taken any psychotropics for more than 5 months.
Approximately 1 week before his recent urine drug screen, Mr. M became euphoric, stopped sleeping for several days, and spent $2,000 on cocaine and “escorts.” He reports that each day he smokes 30 cigarettes and drinks 1 pint of liquor and prefers to use cocaine and opiates by IV injection. Several years ago Mr. M was diagnosed with hepatitis C virus (HCV) but received no further workup or treatment. Although he denies manic or psychotic symptoms, Mr. M is observed speaking to unseen others in the waiting room and has difficulty remaining still during his interview. His chief concern is insomnia, stating, “Doc, I just need something to help me sleep.”
The high prevalence of substance use disorders (SUDs) in persons with bipolar disorder (BD) is well documented.1,2 Up to 60% of bipolar patients develop an SUD at some point in their lives.3-5 Alcohol use disorders are particularly common among BD patients, with a lifetime prevalence of roughly 50%.2-5 Recent epidemiologic data indicate that 38% of persons with bipolar I disorder and 19% of those with bipolar II disorder meet criteria for alcohol dependence.5 Comorbid SUDs in patients with BD are associated with:
- poor treatment compliance
- longer and more frequent mood episodes
- more mixed episodes
- more hospitalizations
- more frequent suicide attempts.1,2
The impact of co-occurring SUDs on suicidality is particularly high among those with bipolar I disorder.6
Frequently referred to as “dual diagnosis” conditions, co-occurring BD and SUDs may be more accurately envisioned as multi-morbid, rather than comorbid, illnesses. Data from the Stanley Foundation Bipolar Network suggest that 42% of BD patients have a lifetime history of ≥2 comorbid axis I disorders.7 Rates of generalized anxiety disorder, panic disorder, and posttraumatic stress disorder are particularly high in BD patients with co-occurring SUDs.8,9 In addition, the presence of 1 SUD may mark the presence of other SUDs; for example, alcohol dependence is strongly associated with polysubstance abuse, especially in females with BD.8 Furthermore, medical comorbidities that impact treatment decisions also are highly prevalent in BD patients with comorbid SUDs.10 In particular, HCV rates are higher in persons with BD compared with the general population,11 and are >5 times as likely in bipolar patients with co-occurring SUDs.12
Unfortunately, limited treatment research guides clinical management of comorbid BD and SUDs.2,13,14 Clinical trials of medications for BD traditionally have excluded patients with SUDs, and persons with serious mental illness usually are ineligible for SUD treatment studies.13 Furthermore, the few randomized controlled trials (RCTs) conducted in persons with both illnesses have been constrained by relatively small sample sizes and low retention rates. In the absence of a definitive consensus for optimal treatment, this article outlines general clinical considerations and an integrated approach to assessing and managing this complex patient population.
Birds of a feather
Multiple hypotheses try to account for the high rate of SUDs in patients with BD (Table 1), but none fully explain the complex interaction observed clinically.14,15 Substance dependence and BD are chronic remitting/relapsing disorders with heterogeneous presentations and highly variable natural histories. As with SUDs, BD may go undiagnosed and untreated for years, coming to clinical attention only after substantial disease progression.16
The fluctuating illness course in BD and SUDs makes diagnosis and treatment difficult. Symptomatic periods often are interrupted by spontaneous remissions and longer—although usually temporary—periods of perceived control. Both BD and SUDs may be associated with profound mood instability, increased impulsivity, altered responsiveness to reward, and impaired executive function.17 Finally, the high degree of heritability in BD18 and many SUDs19 may make treatment engagement more difficult if either disorder is present in multiple family members because of:
- potential for greater clinical severity
- reduced psychosocial resources
- altered familial behavioral norms that may impede the patient’s recognition of illness.
Denial of illness is a critical symptom that may fluctuate with disease course in both disorders. Persons with BD or SUDs may be least likely to recognize that they are ill during periods of highest symptom severity. Accordingly, treatment adherence in patients with either disorder may be limited at baseline and decline further when the 2 illnesses co-occur.20
Involvement in the criminal justice system and medical comorbidities, particularly HCV, also complicate diagnosis and treatment of BD patients with SUDs. For more information about these topics, see Box1 and Box2.
Table 1
Why is substance abuse so prevalent among bipolar patients?
| Proposed hypothesis | Selected limitations of this hypothesis |
|---|---|
| Self-medication: substance abuse occurs as an attempt to regulate mood | High rates of substance use during euthymia; high prevalence of alcohol/depressant use during depressive phase, stimulant use during manic phase |
| Common neurobiologic or genetic risk factors | Specific evidence from linkage/association studies currently is lacking |
| Substance use occurs as a symptom of bipolar disorder | High percentage of patients with bipolar disorder do not have SUDs; there is a poor correlation of onset, course of bipolar, and SUD symptoms |
| Substance use unmasks bipolar disorder or a bipolar diathesis | Emergence of mania before SUD is common and predictive of more severe course of bipolar disorder |
| High comorbidity rates are an artifact of misdiagnosis based on overlapping symptoms and poor diagnostic boundaries | Very high prevalence of SUDs also is observed in longitudinal studies of patients initially hospitalized for mania |
| SUDs: substance use disorders | |
| Source: References 14,15 | |
Integrated clinical management
Assessment. Although not intended to be comprehensive, suggestions for routine assessment of patients with suspected SUDs and/or BD are listed in Table 2. Because clinicians may encounter dual diagnosis patients in general psychiatric clinics or specialty (addiction or mood disorder) clinics, it is useful to obtain a thorough substance use history in all patients with known or suspected BD as well as a thorough history of hypomania/mania and depression in all patients with addictive disorders. BD diagnoses by self-report or chart history in patients with SUDs should be considered cautiously because BD often is overdiagnosed in persons engaged in active substance abuse or experiencing withdrawal.21 If past or present mood symptoms and substance use have co-occurred, further focused assessment of mood symptoms before alcohol and drug use or during extended periods of abstinence are necessary to make the diagnosis of bipolar disorder with confidence. Family history of SUDs and/or BD are neither necessary nor sufficient for either diagnosis; however, collateral information from family or significant others could help make the diagnosis and may identify aids and obstacles to treatment planning and engagement.
When a patient’s clinical history strongly supports the diagnoses of BD and co-occurring SUDs, more detailed inquiry is warranted. Determining the patient’s age at onset of each disorder may have prognostic value because onset of mania before SUDs developed, especially in adolescence, may predict a more severe course of both illnesses.22 A complete alcohol use history should include routine questioning about past withdrawal. Previous withdrawal seizures in an actively drinking BD patient may tip the balance toward adding an anticonvulsant for mood stabilization. A thorough SUD history should elicit information about polysubstance abuse or dependence and include screening for injection drug use and other risk factors for HCV and human immunodeficiency virus (HIV), such as hypersexuality during manic or hypomanic episodes. Document the date of the last screening for HCV/ HIV in BD patients at high risk of infection. The U.S. Centers for Disease Control and Prevention recommends that all patients at high risk for HIV consider voluntary screening at least annually.23
Assess your patient’s historical and ongoing alcohol and other drug abuse at the initial visit, and continue to monitor substance use at all subsequent visits, especially in patients with HCV. When feasible, order urine drug screening and laboratory testing for alcohol use biomarkers such as carbohydrate-deficient transferrin and gamma-glutamyltransferase to supplement self-report data, especially in patients with poor insight or low motivation. Assess suicidal ideation and any changes in suicide risk factors at every visit.
Treatment. No biologic therapies have been FDA-approved for treating patients with co-occurring BD and SUDs. Comorbid SUDs in BD patients—as well as rapid cycling and mixed mood episodes, both of which are more common in patients with comorbid SUDs—predict poor response to lithium.17 However, the evidence base for optimal pharmacotherapy remains extremely limited. Published double-blind, placebo-controlled RCTs in persons with BD and co-morbid SUDs are limited to only 1 trial each of lithium, carbamazepine, quetiapine, and naltrexone, and 2 comparisons of lithium plus divalproex vs lithium alone (Table 3).24-29
Salloum et al24 reported that bipolar I disorder patients with alcohol dependence who received divalproex plus lithium as maintenance treatment had fewer heavy drinking days and fewer drinks per heavy drinking day than those receiving lithium plus placebo. However, the addition of divalproex did not improve manic or depressive symptoms, and depression remission rates remained relatively low in both groups. A recent 6-month study comparing lithium vs lithium plus divalproex in patients with SUDs and rapid-cycling BD found no additional benefit of divalproex over lithium monotherapy in retention, mood, or substance use outcomes.28 However, modest evidence that anticonvulsants such as valproic acid and carbamazepine may help treat acute alcohol withdrawal2 could support their preferential use as mood stabilizers over lithium in actively drinking BD patients.
Research underscores the difficulty in keeping dual diagnosis patients in treatment. Salloum et al24 reported that only one-third of randomized subjects completed the 24-week study. In the Kemp study,28 79% of 149 recruited subjects failed to complete the lead-in stabilization phase. Of the 31 remaining subjects who were randomized to lithium or lithium/divalproex combination, only 8 (26% of those randomized, 5% of those recruited) completed the 6-month trial.
Substance abuse is associated with significantly decreased treatment adherence in persons with BD20 and may affect medication choice. For example, caution may be warranted in the use of lamotrigine in substance-abusing patients with poor adherence because re-titration from the starting dose is recommended if the medicine has been missed for a consecutive period exceeding 5 half-lives of the drug.30
Notable progress has been made in developing psychosocial treatments for comorbid SUDs and BD. Integrated group therapy has been designed to address the 2 disorders simultaneously by emphasizing the relationship between the disorders and highlighting similarities in cognitive and behavioral change that promote recovery in both.31 In a recent well-controlled RCT, this approach reduced alcohol and other drug use to approximately one-half the levels observed in those who received only group drug counseling.31
Research suggests that an integrated approach that encompasses psychiatric, medical, psychosocial, and legal dimensions simultaneously may be most effective. For patients such as Mr. M, this would include aggressively treating mood symptoms while employing motivational interviewing techniques to improve engagement in substance dependence treatment. If possible, involving family members, parole officials, housing agencies, and other public assistance workers in the treatment plan may increase treatment adherence and reduce loss of contact during illness exacerbations. Stabilization of substance use and psychiatric morbidity should be accompanied by timely evaluation of HCV and other medical comorbidities in order to improve long-term prognosis.
Table 2
Assessing patients you suspect have comorbid BD and SUDs
| Initial assessment |
|---|
Thorough substance use history in all patients with known or suspected bipolar disorder:
|
Thorough evaluation of any history of hypomania/mania and depression in all patients with known or suspected SUDs:
|
| Assess risk factors, screening status for hepatitis C, HIV |
| Obtain collateral information from family and significant others if feasible and appropriate |
| Detailed assessment of suicide risk |
| Follow-up assessments |
| Substance use since last visit by self-report |
| Consider UDS, CDT, GGT |
| Medication adherence |
| Detailed assessment of suicide risk |
| BD: bipolar disorder; CDT: carbohydrate-deficient transferrin; GGT: gamma-glutamyltransferase; HIV: human immunodeficiency virus; SUDs: substance use disorders; UDS: urine drug screen |
Table 3
Pharmacotherapy for bipolar disorder and co-occurring SUDs
| Study | Diagnoses/N* | Medications | Outcome |
|---|---|---|---|
| Salloum et al, 200524 | BD I, alcohol dependence. N=59 [20] | Divalproex + lithium vs lithium, 24 weeks | Decreased number of heavy drinking days, fewer drinks per heavy drinking day |
| Geller et al, 199825 | BD I, BP II, MDD (adolescents); alcohol, cannabis abuse. N=25 [21] | Lithium, 6 weeks | Decreased cannabis-positive urine drug screen (lithium > placebo) |
| Brady et al, 200226 | BD I, BD II, cyclothymia; cocaine dependence. N=57 | Carbamazepine, 12 weeks | Trend toward longer time to cocaine use |
| Brown et al, 200827 | BD I, BD II; N=102 | Quetiapine, 12 weeks | Decreased HAM-D scores (quetiapine > placebo) |
| Kemp et al, 200928 | BD I, BD II, rapid cycling; alcohol, cannabis, cocaine abuse or dependence. N=31 [8] | Divalproex + lithium vs lithium, 6 months | No group differences |
| Brown et al, 200929 | BD I, BD II; alcohol dependence. N=50 [26] | Naltrexone, 12 weeks | Trend toward increased probability of no drinking days |
| * N=number of subjects randomized to double-blind treatment. Numbers in brackets indicate the number of subjects who completed all study visits (when reported) | |||
| BD: bipolar disorder; HAM-D: 17-item Hamilton Rating Scale for Depression; MDD: major depressive disorder; SUDs: substance use disorders | |||
Related Resources
- International Society for Bipolar Disorders. www.isbd.org.
- National Institute on Alcohol Abuse and Alcoholism. www.niaaa.nih.gov.
- National Institute on Drug Abuse. www.nida.nih.gov.
Drug Brand Names
- Carbamazepine • Tegretol
- Divalproex/valproic acid • Depakote
- Lamotrigine • Lamictal
- Lithium • Lithobid
- Naltrexone • ReVia
- Quetiapine • Seroquel
Disclosure
Dr. Tolliver receives research grant funding from Forest Laboratories and the National Institute on Alcohol Abuse and Alcoholism. Neither source influenced the content or submission of this manuscript.
A recent analysis of data from >65,000 veterans found bipolar patients with comorbid substance use disorders (SUDs) were 7 times more likely to have hepatitis C virus (HCV) than patients with no serious mental illness.a Matthews and colleagues found that 29.6% of persons diagnosed with bipolar disorder (BD) and SUDs tested positive for HCV—roughly 5 times the relative risk of patients without either diagnosis.b The high prevalence of HCV in patients with comorbid BD and SUDs may be the result of injection drug use, increased risky sexual behavior while manic or intoxicated, or both.
HCV has multiple treatment implications for these patients. Alcohol abuse and dependence are the most common SUDs that co-occur with BD,c-e and patients with HCV who drink alcohol excessively have more severe hepatic fibrosis, accelerated disease progression, and higher rates of cirrhosis and hepatocellular carcinoma than HCV patients who do not drink.f Medications commonly used to treat BD or alcohol dependence may have adverse effects on the liver and require more careful monitoring in the presence of HCV infection. For example, valproic acid has been reported to improve drinking outcomes in alcohol-dependent patients with BDg but has been associated with higher rates of marked hepatic transaminase elevation in patients with HCV infection compared with those without HCV.h Marked elevation of hepatic transaminases may be observed in HCV-infected individuals treated with other medications such as lithium or antidepressants,h and valproic acid use is not an absolute contraindication in HCV patients. Nevertheless, the effects of valproic acid in HCV-infected BD patients who drink alcohol are unknown and therefore cautious and frequent monitoring of hepatic enzymes are warranted in this population.
Finally, both SUDs and BD complicate HCV treatment. In a database review of >113,000 veterans with HCV infection, Butt and colleagues found that individuals with BD accounted for 10.4% of the HCV-infected sample but only 5% of those who received HCV treatment.i Similarly, patients with alcohol abuse or dependence made up 44.3% of the HCV-infected sample but only 28.9% of those who received HCV treatment.
Because the rate of liver biopsy in untreated patients was low, the decision not to treat appeared to be based more often on other criteria. This is not surprising; pegylated interferon-alfa—the most effective treatment for chronic HCV—has been associated with multiple neuropsychiatric symptoms observed in BD, including depression, mania, psychosis, and suicidal ideation.j Emergence of severe psychiatric complications usually results in permanent discontinuation of interferon treatment. Likewise, the presence of alcohol abuse or other SUDs is a strong negative predictor of interferon treatment response and retention and generally has been considered a relative contraindication for interferon initiation.f
References
a. Himelhoch S, McCarthy JF, Ganoczy D, et al. Understanding associations between serious mental illness and hepatitis C virus among veterans: a national multivariate analysis. Psychosomatics. 2009;50:30-37.
b. Matthews AM, Huckans MS, Blackwell AD, et al. Hepatitis C testing and infection rates in bipolar patients with and without comorbid substance use disorders. Bipolar Disord. 2008;10:266-270.
c. Grant BF, Stinson FS, Dawson DA, et al. Prevalence and co-occurrence of substance use disorders and independent mood and anxiety disorders. Results from the National Epidemiologic Survey on Alcohol and Related Conditions. Arch Gen Psychiatry. 2004;61:807-816.
d. Hasin DS, Stinson FS, Ogburn E, et al. Prevalence, correlates, disability, and comorbidity of DSM-IV alcohol abuse and dependence in the United States. Results from the National Epidemiologic Survey on Alcohol and Related Conditions. Arch Gen Psychiatry. 2007;64:830-842.
e. Merikangas KR, Akiskal HS, Angst J, et al. Lifetime and 12-month prevalence of bipolar spectrum disorder in the National Comorbidity Survey Replication. Arch Gen Psychiatry. 2007;64:543-552.
f. Bhattacharya R, Shuhart M. Hepatitis C and alcohol. J Clin Gastroenterol. 2003;36:242-252.
g. Salloum IM, Cornelius JR, Daley DC, et al. Efficacy of valproate maintenance in patients with bipolar disorder and alcoholism: a double-blind, placebo-controlled study. Arch Gen Psychiatry. 2005;62:37-45.
h. Felker BL, Sloan KL, Dominitz JA, et al. The safety of valproic acid use for patients with hepatitis C infection. Am J Psychiatry. 2003;160:174-178.
i. Butt AA, Justice AC, Skanderson M, et al. Rate and predictors of treatment prescription for hepatitis C. Gut. 2006;56:385-389.
j. Onyike CU, Bonner JO, Lyketsos CG, et al. Mania during treatment of chronic hepatitis C with pegylated interferon and ribavirin. Am J Psychiatry. 2004;161:429-435.
Long recognized to be more prevalent in forensic populations, bipolar disorder (BD) is especially overrepresented among those with repeat arrests and incarcerations. In a recent study of >79,000 inmates incarcerated in Texas in 2006 and 2007, those with BD were 3.3 times more likely to have had ≥4 previous incarcerations.k
Comorbid substance use disorder (SUD) is a significant risk factor for criminal arrest. For example, in a Los Angeles County (CA) sample of inmates with BD, 75.8% had co-occurring SUDs, compared with 18.5% in a comparison group of hospitalized BD patients.l The association of SUDs with arrest is especially high in females with BD. In the Los Angeles sample mentioned above, incarcerated bipolar women were >38 times more likely to have a SUD than a comparison group of female patients treated in the community.m
References
k. Baillargeon J, Binswanger IA, Penn JV, et al. Psychiatric disorders and repeat incarcerations: the revolving prison door. Am J Psychiatry. 2009;166:103-109.
l. Quanbeck CD, Stone DC, Scott CL, et al. Clinical and legal correlates of inmates with bipolar disorder at time of criminal arrest. J Clin Psychiatry. 2004;65:198-203.
m. McDermott BE, Quanbeck CD, Frye MA. Comorbid substance use disorder in women with bipolar disorder is associated with criminal arrest. Bipolar Disord. 2007;9(5):536-540.
1. Levin FR, Hennessey G. Bipolar disorder and substance abuse. Biol Psychiatry. 2004;56:738-748.
2. Frye MA, Salloum IM. Bipolar disorder and comorbid alcoholism: prevalence rate and treatment considerations. Bipolar Disord. 2006;8:677-685.
3. Grant BF, Stinson FS, Dawson DA, et al. Prevalence and co-occurrence of substance use disorders and independent mood and anxiety disorders. Results from the National Epidemiologic Survey on Alcohol and Related Conditions. Arch Gen Psychiatry. 2004;61:807-816.
4. Hasin DS, Stinson FS, Ogburn E, et al. Prevalence, correlates, disability, and comorbidity of DSM-IV alcohol abuse and dependence in the United States. Results from the National Epidemiologic Survey on Alcohol and Related Conditions. Arch Gen Psychiatry. 2007;64:830-842.
5. Merikangas KR, Akiskal HS, Angst J, et al. Lifetime and 12-month prevalence of bipolar spectrum disorder in the National Comorbidity Survey Replication. Arch Gen Psychiatry. 2007;64:543-552.
6. Sublette EM, Carballo JJ, Moreno C, et al. Substance use disorders and suicide attempts in bipolar subtypes. J Psychiatric Res. 2009;43:230-238.
7. McElroy SL, Altshuler LL, Suppes T, et al. Axis I psychiatric comorbidity and its relationship to historical illness variables in 288 patients with bipolar disorder. Am J Psychiatry. 2001;158:420-426.
8. Frye MA, Altshuler LL, McElroy SL, et al. Gender differences in prevalence, risk, and clinical correlates of alcoholism comorbidity in bipolar disorder. Am J Psychiatry. 2003;160:883-889.
9. Simon NM, Otto MW, Wisniewski SR, et al. Anxiety disorder comorbidity in bipolar disorder patients: data from the first 500 participants in the systematic treatment enhancement program for bipolar disorder (STEP-BD). Am J Psychiatry. 2004;161:2222-2229.
10. Perron BE, Howard MO, Nienhuis JK, et al. Prevalence and burden of general medical conditions among adults with bipolar I disorder: results from the National Epidemiologic Survey on Alcohol and Related Conditions. J Clin Psychiatry. 2009;70:1407-1415.
11. Himelhoch S, McCarthy JF, Ganoczy D, et al. Understanding associations between serious mental illness and hepatitis C virus among veterans: a national multivariate analysis. Psychosomatics. 2009;50:30-37.
12. Matthews AM, Huckans MS, Blackwell AD, et al. Hepatitis C testing and infection rates in bipolar patients with and without comorbid substance use disorders. Bipolar Disord. 2008;10:266-270.
13. Singh JB, Zarate CA. Pharmacological treatment of psychiatric comorbidity in bipolar disorder: a review of controlled trials. Bipolar Disord. 2006;8:696-709.
14. Vornik LA, Brown ES. Management of comorbid bipolar disorder and substance abuse. J Clin Psychiatry. 2006;67(suppl 7):24-30.
15. Strakowski SM, DelBello MP. The co-occurrence of bipolar and substance use disorders. Clin Psych Rev. 2000;20:191-206.
16. Berk M, Dodd S, Callaly P, et al. History of illness prior to a diagnosis of bipolar disorder or schizoaffective disorder. J Affect Disord. 2007;103:181-186.
17. Goodwin FK, Jamison KR. Manic-depressive illness: bipolar disorders and recurrent depression. 2nd ed. New York, NY: Oxford University Press; 2007.
18. McGuffin P, Rijsdijk F, Andrew M, et al. The heritability of bipolar affective disorder and the genetic relationship to unipolar depression. Arch Gen Psychiatry. 2003;60:497-502.
19. Kendler KS, Prescott CA, Myers J, et al. The structure of genetic and environmental risk factors for common psychiatric and substance abuse disorders in men and women. Arch Gen Psychiatry. 2003;60:929-937.
20. Weiss RD, Greenfield SF, Najavits LM, et al. Medication compliance among patients with bipolar disorder and substance use disorder. J Clin Psychiatry. 1998;59:172-174.
21. Goldberg JF, Garno JL, Callahan AM, et al. Overdiagnosis of bipolar disorder among substance use disorder inpatients with mood instability. J Clin Psychiatry. 2008;69:1751-1757.
22. Winokur G, Coryell W, Akiskal HS, et al. Alcoholism in manic-depressive (bipolar) illness: familial illness, course of illness, and the primary-secondary distinction. Am J Psychiatry. 1995;152:365-372.
23. Branson BM, Handsfield HH, Lampe MA, et al. Revised recommendations for HIV testing of adults, adolescents, and pregnant women in health care settings. MMWR. 2006;55(RR14):1-17.
24. Salloum IM, Cornelius JR, Daley DC, et al. Efficacy of valproate maintenance in patients with bipolar disorder and alcoholism: a double-blind, placebo-controlled study. Arch Gen Psychiatry. 2005;62:37-45.
25. Geller B, Cooper TB, Sun K, et al. Double-blind and placebo-controlled study of lithium for adolescent bipolar disorders with secondary substance dependency. J Am Acad Child Adolesc Psychiatry. 1998;37(2):171-178.
26. Brady KT, Sonne SC, Malcolm RJ, et al. Carbamazepine in the treatment of cocaine dependence: subtyping by affective disorder. Exp Clin Psychopharmacol. 2002;10:276-285.
27. Brown ES, Garza M, Carmody TJ. A randomized, double-blind, placebo-controlled add-on trial of quetiapine in outpatients with bipolar disorder and alcohol use disorders. J Clin Psychiatry. 2008;69:701-705.
28. Kemp DE, Gao K, Ganocy S, et al. A 6-month, double-blind, maintenance trial of lithium monotherapy versus the combination of lithium and divalproex for rapid-cycling bipolar disorder and co-occurring substance abuse or dependence. J Clin Psychiatry. 2009;70:113-121.
29. Brown ES, Carmody TJ, Schmitz JM, et al. A randomized, double-blind, placebo-controlled pilot study of naltrexone in outpatients with bipolar disorder and alcohol dependence. Alcohol Clin Exp Res. 2009;3:1863-1869.
30. Lamictal [package insert]. Research Triangle Park, NC: GlaxoSmithKline; 2009.
31. Weiss RD, Griffin ML, Kolodziej MR, et al. A randomized trial of integrated group therapy versus group drug counseling for patients with bipolar disorder and substance dependence. Am J Psychiatry. 2007;164:100-107.
1. Levin FR, Hennessey G. Bipolar disorder and substance abuse. Biol Psychiatry. 2004;56:738-748.
2. Frye MA, Salloum IM. Bipolar disorder and comorbid alcoholism: prevalence rate and treatment considerations. Bipolar Disord. 2006;8:677-685.
3. Grant BF, Stinson FS, Dawson DA, et al. Prevalence and co-occurrence of substance use disorders and independent mood and anxiety disorders. Results from the National Epidemiologic Survey on Alcohol and Related Conditions. Arch Gen Psychiatry. 2004;61:807-816.
4. Hasin DS, Stinson FS, Ogburn E, et al. Prevalence, correlates, disability, and comorbidity of DSM-IV alcohol abuse and dependence in the United States. Results from the National Epidemiologic Survey on Alcohol and Related Conditions. Arch Gen Psychiatry. 2007;64:830-842.
5. Merikangas KR, Akiskal HS, Angst J, et al. Lifetime and 12-month prevalence of bipolar spectrum disorder in the National Comorbidity Survey Replication. Arch Gen Psychiatry. 2007;64:543-552.
6. Sublette EM, Carballo JJ, Moreno C, et al. Substance use disorders and suicide attempts in bipolar subtypes. J Psychiatric Res. 2009;43:230-238.
7. McElroy SL, Altshuler LL, Suppes T, et al. Axis I psychiatric comorbidity and its relationship to historical illness variables in 288 patients with bipolar disorder. Am J Psychiatry. 2001;158:420-426.
8. Frye MA, Altshuler LL, McElroy SL, et al. Gender differences in prevalence, risk, and clinical correlates of alcoholism comorbidity in bipolar disorder. Am J Psychiatry. 2003;160:883-889.
9. Simon NM, Otto MW, Wisniewski SR, et al. Anxiety disorder comorbidity in bipolar disorder patients: data from the first 500 participants in the systematic treatment enhancement program for bipolar disorder (STEP-BD). Am J Psychiatry. 2004;161:2222-2229.
10. Perron BE, Howard MO, Nienhuis JK, et al. Prevalence and burden of general medical conditions among adults with bipolar I disorder: results from the National Epidemiologic Survey on Alcohol and Related Conditions. J Clin Psychiatry. 2009;70:1407-1415.
11. Himelhoch S, McCarthy JF, Ganoczy D, et al. Understanding associations between serious mental illness and hepatitis C virus among veterans: a national multivariate analysis. Psychosomatics. 2009;50:30-37.
12. Matthews AM, Huckans MS, Blackwell AD, et al. Hepatitis C testing and infection rates in bipolar patients with and without comorbid substance use disorders. Bipolar Disord. 2008;10:266-270.
13. Singh JB, Zarate CA. Pharmacological treatment of psychiatric comorbidity in bipolar disorder: a review of controlled trials. Bipolar Disord. 2006;8:696-709.
14. Vornik LA, Brown ES. Management of comorbid bipolar disorder and substance abuse. J Clin Psychiatry. 2006;67(suppl 7):24-30.
15. Strakowski SM, DelBello MP. The co-occurrence of bipolar and substance use disorders. Clin Psych Rev. 2000;20:191-206.
16. Berk M, Dodd S, Callaly P, et al. History of illness prior to a diagnosis of bipolar disorder or schizoaffective disorder. J Affect Disord. 2007;103:181-186.
17. Goodwin FK, Jamison KR. Manic-depressive illness: bipolar disorders and recurrent depression. 2nd ed. New York, NY: Oxford University Press; 2007.
18. McGuffin P, Rijsdijk F, Andrew M, et al. The heritability of bipolar affective disorder and the genetic relationship to unipolar depression. Arch Gen Psychiatry. 2003;60:497-502.
19. Kendler KS, Prescott CA, Myers J, et al. The structure of genetic and environmental risk factors for common psychiatric and substance abuse disorders in men and women. Arch Gen Psychiatry. 2003;60:929-937.
20. Weiss RD, Greenfield SF, Najavits LM, et al. Medication compliance among patients with bipolar disorder and substance use disorder. J Clin Psychiatry. 1998;59:172-174.
21. Goldberg JF, Garno JL, Callahan AM, et al. Overdiagnosis of bipolar disorder among substance use disorder inpatients with mood instability. J Clin Psychiatry. 2008;69:1751-1757.
22. Winokur G, Coryell W, Akiskal HS, et al. Alcoholism in manic-depressive (bipolar) illness: familial illness, course of illness, and the primary-secondary distinction. Am J Psychiatry. 1995;152:365-372.
23. Branson BM, Handsfield HH, Lampe MA, et al. Revised recommendations for HIV testing of adults, adolescents, and pregnant women in health care settings. MMWR. 2006;55(RR14):1-17.
24. Salloum IM, Cornelius JR, Daley DC, et al. Efficacy of valproate maintenance in patients with bipolar disorder and alcoholism: a double-blind, placebo-controlled study. Arch Gen Psychiatry. 2005;62:37-45.
25. Geller B, Cooper TB, Sun K, et al. Double-blind and placebo-controlled study of lithium for adolescent bipolar disorders with secondary substance dependency. J Am Acad Child Adolesc Psychiatry. 1998;37(2):171-178.
26. Brady KT, Sonne SC, Malcolm RJ, et al. Carbamazepine in the treatment of cocaine dependence: subtyping by affective disorder. Exp Clin Psychopharmacol. 2002;10:276-285.
27. Brown ES, Garza M, Carmody TJ. A randomized, double-blind, placebo-controlled add-on trial of quetiapine in outpatients with bipolar disorder and alcohol use disorders. J Clin Psychiatry. 2008;69:701-705.
28. Kemp DE, Gao K, Ganocy S, et al. A 6-month, double-blind, maintenance trial of lithium monotherapy versus the combination of lithium and divalproex for rapid-cycling bipolar disorder and co-occurring substance abuse or dependence. J Clin Psychiatry. 2009;70:113-121.
29. Brown ES, Carmody TJ, Schmitz JM, et al. A randomized, double-blind, placebo-controlled pilot study of naltrexone in outpatients with bipolar disorder and alcohol dependence. Alcohol Clin Exp Res. 2009;3:1863-1869.
30. Lamictal [package insert]. Research Triangle Park, NC: GlaxoSmithKline; 2009.
31. Weiss RD, Griffin ML, Kolodziej MR, et al. A randomized trial of integrated group therapy versus group drug counseling for patients with bipolar disorder and substance dependence. Am J Psychiatry. 2007;164:100-107.
Is it a mood disorder or menopause?
Consider the neuroendocrinology of menopause when evaluating midlife women for new or worsening mood symptoms. The risk of depression increases during perimenopause, even in women with no history of depression.1 Fluctuating estrogen levels can cause vasomotor symptoms (VMS) and depression, presenting diagnostic and treatment challenges. In addition to conducting a comprehensive psychiatric evaluation, our collaborative rotation between the UCLA-Kern Psychiatry Residency Program and the department of obstetrics and gynecology uses the following approach for women age >40.
Obtain a menstrual history
Ask your patient when her last menstrual period was and if her periods are irregular, heavy, light, or missing. Menopausal transition begins when the length of the menstrual cycle varies and ends with the final menstrual period. Perimenopause begins early in the transition and ends 12 months after the last menses. During this time VMS and mood instability may worsen.
Ask about menopausal symptoms
Hot flashes typically begin as a sudden sensation of heat centered in the upper chest and face that rapidly generalizes. Flashes last 2 to 4 minutes and often are accompanied by profuse perspiration and occasional palpitations. VMS can occur several times during the day and night. Hot flashes—the most common symptom associated with menopausal transition—peak during the 12 months surrounding the last period and can commonly persist up to 5 years or more. Hot flashes affect a woman’s sense of well-being and often are the reason women seek medical attention during midlife.
Insomnia. Sleep disturbance during the menopausal transition is common, sometimes severe, and may be related to nocturnal hot flashes and night sweats. Hot flashes and awakenings are sometimes followed by chills, shivering, anxiety, or panic.
Mood instability. Dysregulation of monoaminergic neurotransmitter systems caused by fluctuating estrogen levels may cause both depression and VMS.2 Perimenopausal women with VMS are more likely to be depressed than those who do not have VMS. VMS may signal the onset or recurrence of major depression.
Sexual changes. Estrogen deficiency may lead to vaginal dryness and urogenital atrophy, resulting in infection, painful intercourse, or decreased sexual desire.
Body aches. Many perimenopausal women complain of stiffness, joint pain, breast pain, menstrual migraines, bladder discomfort, and impaired balance.
Memory changes. Complaints of forgetfulness may reflect aging and effects of sleep disturbance.3
Diagnostic workup
Perimenopause can be diagnosed before clinical symptoms appear if the follicle stimulating hormone (FSH) level is >25 IU/L and estrogen is <40 pg/mL during the early follicular phase (day 3 of the menstrual cycle).3 In women age <45 with irregular bleeding and menopause symptoms, check serum beta human chorionic gonadotropin (to rule out pregnancy), prolactin, thyroid-stimulating hormone, and FSH.
Women of any age with estrogen deficiency—such as those undergoing chemotherapy for breast cancer, treatment with gonadotropin-releasing hormone agonists for endometriosis or in-vitro fertilization, premature ovarian failure, or who have undergone oophorectomy—might experience VMS and other perimenopausal symptoms.
Women age >45 with 12 months of amenorrhea may be diagnosed with menopause clinically without further testing.
Treatment strategies
Fewer women are choosing hormone replacement therapy (HRT) (estrogen alone or estrogen and progesterone) after the landmark Women’s Health Initiative (WHI) study in 2002.4 Reports that HRT may increase the risk of breast cancer and offers no cardiac protection prompted many women to forego or discontinue HRT use. Subsequent interpretation of the WHI data has reduced many of these concerns.5 As a result, estrogen alone currently is the most effective and only FDA-approved treatment for VMS.5 Because of overlap between VMS and depression, treatment for these 2 conditions could be combined. Theoretically, treating VMS could prevent a major depressive episode in vulnerable women and may improve the chance of full remission of depression.1
Although results of studies of HRT for depression are mixed, estrogen alone may be effective for mild depression during perimenopause but not postmenopause. Estrogen also may be appropriate during perimenopause if a depressive disorder represents a first-onset episode of mild to moderate severity.6 Estrogen is not FDA-approved for treating perimenopausal depression. As with all medications, counsel patients on the risks and benefits and administer the medication at the lowest dose and for the shortest time period to effectively treat symptoms.
Consider antidepressants when HRT is contraindicated or declined. Selective norepinephrine reuptake inhibitors such as venlafaxine, desvenlafaxine, and duloxetine have demonstrated efficacy for VMS and depression.2 Selective serotonin reuptake inhibitors (SSRIs) are effective in women age <40 but show inconsistent efficacy for VMS and depression in women age >50. SSRIs combined with estrogen therapy may be useful in postmenopausal women.2
Biopsychosocial factors
Psychosocial attitudes about aging, sexual attractiveness, and children leaving home may contribute to depression during perimenopause. However, many women welcome the freedom from menstrual periods and pregnancy worries.
Some women may not be aware of the impact of menopausal changes on mood. Educating patients with a mood disorder about what to expect and identifying and treating disabling hormonal dysregulation symptoms is an ideal opportunity to enhance the quality of life for patients during menopause and beyond.
1. Cohen LS, Soares CN, Vitonis AF, et al. Risk for new onset of depression during the menopausal transition: the Harvard study of moods and cycles. Arch Gen Psychiatry. 2006;63(4):385-390.
2. Thase ME, Entsuah R, Cantillon M, et al. Relative antidepressant efficacy of venlafaxine and SSRIs: sex-age interactions. J Womens Health (Larchmt). 2005;14:609-616.
3. Aloysi A, Van Dyk K, Sano M. Women’s cognitive and affective health and neuropsychiatry. Mt Sinai J Medicine. 2006;73(7):967-975.
4. Rossouw JE, Anderson GL, Prentice RL, et al. Risks and benefits of estrogen plus progestin in healthy postmenopausal women: principal results from the Women’s Health Initiative randomized controlled trial. JAMA. 2002;288:321-333.
5. Santoro N. Symptoms of menopause: hot flushes. Clinical ObGyn. 2008;51(3):539-548.
6. Joffe H, Soares CN, Cohen LS. Assessment and treatment of hot flushes and menopausal mood disturbance. Psychiatr Clin N Am. 2003;26:563-580.
Consider the neuroendocrinology of menopause when evaluating midlife women for new or worsening mood symptoms. The risk of depression increases during perimenopause, even in women with no history of depression.1 Fluctuating estrogen levels can cause vasomotor symptoms (VMS) and depression, presenting diagnostic and treatment challenges. In addition to conducting a comprehensive psychiatric evaluation, our collaborative rotation between the UCLA-Kern Psychiatry Residency Program and the department of obstetrics and gynecology uses the following approach for women age >40.
Obtain a menstrual history
Ask your patient when her last menstrual period was and if her periods are irregular, heavy, light, or missing. Menopausal transition begins when the length of the menstrual cycle varies and ends with the final menstrual period. Perimenopause begins early in the transition and ends 12 months after the last menses. During this time VMS and mood instability may worsen.
Ask about menopausal symptoms
Hot flashes typically begin as a sudden sensation of heat centered in the upper chest and face that rapidly generalizes. Flashes last 2 to 4 minutes and often are accompanied by profuse perspiration and occasional palpitations. VMS can occur several times during the day and night. Hot flashes—the most common symptom associated with menopausal transition—peak during the 12 months surrounding the last period and can commonly persist up to 5 years or more. Hot flashes affect a woman’s sense of well-being and often are the reason women seek medical attention during midlife.
Insomnia. Sleep disturbance during the menopausal transition is common, sometimes severe, and may be related to nocturnal hot flashes and night sweats. Hot flashes and awakenings are sometimes followed by chills, shivering, anxiety, or panic.
Mood instability. Dysregulation of monoaminergic neurotransmitter systems caused by fluctuating estrogen levels may cause both depression and VMS.2 Perimenopausal women with VMS are more likely to be depressed than those who do not have VMS. VMS may signal the onset or recurrence of major depression.
Sexual changes. Estrogen deficiency may lead to vaginal dryness and urogenital atrophy, resulting in infection, painful intercourse, or decreased sexual desire.
Body aches. Many perimenopausal women complain of stiffness, joint pain, breast pain, menstrual migraines, bladder discomfort, and impaired balance.
Memory changes. Complaints of forgetfulness may reflect aging and effects of sleep disturbance.3
Diagnostic workup
Perimenopause can be diagnosed before clinical symptoms appear if the follicle stimulating hormone (FSH) level is >25 IU/L and estrogen is <40 pg/mL during the early follicular phase (day 3 of the menstrual cycle).3 In women age <45 with irregular bleeding and menopause symptoms, check serum beta human chorionic gonadotropin (to rule out pregnancy), prolactin, thyroid-stimulating hormone, and FSH.
Women of any age with estrogen deficiency—such as those undergoing chemotherapy for breast cancer, treatment with gonadotropin-releasing hormone agonists for endometriosis or in-vitro fertilization, premature ovarian failure, or who have undergone oophorectomy—might experience VMS and other perimenopausal symptoms.
Women age >45 with 12 months of amenorrhea may be diagnosed with menopause clinically without further testing.
Treatment strategies
Fewer women are choosing hormone replacement therapy (HRT) (estrogen alone or estrogen and progesterone) after the landmark Women’s Health Initiative (WHI) study in 2002.4 Reports that HRT may increase the risk of breast cancer and offers no cardiac protection prompted many women to forego or discontinue HRT use. Subsequent interpretation of the WHI data has reduced many of these concerns.5 As a result, estrogen alone currently is the most effective and only FDA-approved treatment for VMS.5 Because of overlap between VMS and depression, treatment for these 2 conditions could be combined. Theoretically, treating VMS could prevent a major depressive episode in vulnerable women and may improve the chance of full remission of depression.1
Although results of studies of HRT for depression are mixed, estrogen alone may be effective for mild depression during perimenopause but not postmenopause. Estrogen also may be appropriate during perimenopause if a depressive disorder represents a first-onset episode of mild to moderate severity.6 Estrogen is not FDA-approved for treating perimenopausal depression. As with all medications, counsel patients on the risks and benefits and administer the medication at the lowest dose and for the shortest time period to effectively treat symptoms.
Consider antidepressants when HRT is contraindicated or declined. Selective norepinephrine reuptake inhibitors such as venlafaxine, desvenlafaxine, and duloxetine have demonstrated efficacy for VMS and depression.2 Selective serotonin reuptake inhibitors (SSRIs) are effective in women age <40 but show inconsistent efficacy for VMS and depression in women age >50. SSRIs combined with estrogen therapy may be useful in postmenopausal women.2
Biopsychosocial factors
Psychosocial attitudes about aging, sexual attractiveness, and children leaving home may contribute to depression during perimenopause. However, many women welcome the freedom from menstrual periods and pregnancy worries.
Some women may not be aware of the impact of menopausal changes on mood. Educating patients with a mood disorder about what to expect and identifying and treating disabling hormonal dysregulation symptoms is an ideal opportunity to enhance the quality of life for patients during menopause and beyond.
Consider the neuroendocrinology of menopause when evaluating midlife women for new or worsening mood symptoms. The risk of depression increases during perimenopause, even in women with no history of depression.1 Fluctuating estrogen levels can cause vasomotor symptoms (VMS) and depression, presenting diagnostic and treatment challenges. In addition to conducting a comprehensive psychiatric evaluation, our collaborative rotation between the UCLA-Kern Psychiatry Residency Program and the department of obstetrics and gynecology uses the following approach for women age >40.
Obtain a menstrual history
Ask your patient when her last menstrual period was and if her periods are irregular, heavy, light, or missing. Menopausal transition begins when the length of the menstrual cycle varies and ends with the final menstrual period. Perimenopause begins early in the transition and ends 12 months after the last menses. During this time VMS and mood instability may worsen.
Ask about menopausal symptoms
Hot flashes typically begin as a sudden sensation of heat centered in the upper chest and face that rapidly generalizes. Flashes last 2 to 4 minutes and often are accompanied by profuse perspiration and occasional palpitations. VMS can occur several times during the day and night. Hot flashes—the most common symptom associated with menopausal transition—peak during the 12 months surrounding the last period and can commonly persist up to 5 years or more. Hot flashes affect a woman’s sense of well-being and often are the reason women seek medical attention during midlife.
Insomnia. Sleep disturbance during the menopausal transition is common, sometimes severe, and may be related to nocturnal hot flashes and night sweats. Hot flashes and awakenings are sometimes followed by chills, shivering, anxiety, or panic.
Mood instability. Dysregulation of monoaminergic neurotransmitter systems caused by fluctuating estrogen levels may cause both depression and VMS.2 Perimenopausal women with VMS are more likely to be depressed than those who do not have VMS. VMS may signal the onset or recurrence of major depression.
Sexual changes. Estrogen deficiency may lead to vaginal dryness and urogenital atrophy, resulting in infection, painful intercourse, or decreased sexual desire.
Body aches. Many perimenopausal women complain of stiffness, joint pain, breast pain, menstrual migraines, bladder discomfort, and impaired balance.
Memory changes. Complaints of forgetfulness may reflect aging and effects of sleep disturbance.3
Diagnostic workup
Perimenopause can be diagnosed before clinical symptoms appear if the follicle stimulating hormone (FSH) level is >25 IU/L and estrogen is <40 pg/mL during the early follicular phase (day 3 of the menstrual cycle).3 In women age <45 with irregular bleeding and menopause symptoms, check serum beta human chorionic gonadotropin (to rule out pregnancy), prolactin, thyroid-stimulating hormone, and FSH.
Women of any age with estrogen deficiency—such as those undergoing chemotherapy for breast cancer, treatment with gonadotropin-releasing hormone agonists for endometriosis or in-vitro fertilization, premature ovarian failure, or who have undergone oophorectomy—might experience VMS and other perimenopausal symptoms.
Women age >45 with 12 months of amenorrhea may be diagnosed with menopause clinically without further testing.
Treatment strategies
Fewer women are choosing hormone replacement therapy (HRT) (estrogen alone or estrogen and progesterone) after the landmark Women’s Health Initiative (WHI) study in 2002.4 Reports that HRT may increase the risk of breast cancer and offers no cardiac protection prompted many women to forego or discontinue HRT use. Subsequent interpretation of the WHI data has reduced many of these concerns.5 As a result, estrogen alone currently is the most effective and only FDA-approved treatment for VMS.5 Because of overlap between VMS and depression, treatment for these 2 conditions could be combined. Theoretically, treating VMS could prevent a major depressive episode in vulnerable women and may improve the chance of full remission of depression.1
Although results of studies of HRT for depression are mixed, estrogen alone may be effective for mild depression during perimenopause but not postmenopause. Estrogen also may be appropriate during perimenopause if a depressive disorder represents a first-onset episode of mild to moderate severity.6 Estrogen is not FDA-approved for treating perimenopausal depression. As with all medications, counsel patients on the risks and benefits and administer the medication at the lowest dose and for the shortest time period to effectively treat symptoms.
Consider antidepressants when HRT is contraindicated or declined. Selective norepinephrine reuptake inhibitors such as venlafaxine, desvenlafaxine, and duloxetine have demonstrated efficacy for VMS and depression.2 Selective serotonin reuptake inhibitors (SSRIs) are effective in women age <40 but show inconsistent efficacy for VMS and depression in women age >50. SSRIs combined with estrogen therapy may be useful in postmenopausal women.2
Biopsychosocial factors
Psychosocial attitudes about aging, sexual attractiveness, and children leaving home may contribute to depression during perimenopause. However, many women welcome the freedom from menstrual periods and pregnancy worries.
Some women may not be aware of the impact of menopausal changes on mood. Educating patients with a mood disorder about what to expect and identifying and treating disabling hormonal dysregulation symptoms is an ideal opportunity to enhance the quality of life for patients during menopause and beyond.
1. Cohen LS, Soares CN, Vitonis AF, et al. Risk for new onset of depression during the menopausal transition: the Harvard study of moods and cycles. Arch Gen Psychiatry. 2006;63(4):385-390.
2. Thase ME, Entsuah R, Cantillon M, et al. Relative antidepressant efficacy of venlafaxine and SSRIs: sex-age interactions. J Womens Health (Larchmt). 2005;14:609-616.
3. Aloysi A, Van Dyk K, Sano M. Women’s cognitive and affective health and neuropsychiatry. Mt Sinai J Medicine. 2006;73(7):967-975.
4. Rossouw JE, Anderson GL, Prentice RL, et al. Risks and benefits of estrogen plus progestin in healthy postmenopausal women: principal results from the Women’s Health Initiative randomized controlled trial. JAMA. 2002;288:321-333.
5. Santoro N. Symptoms of menopause: hot flushes. Clinical ObGyn. 2008;51(3):539-548.
6. Joffe H, Soares CN, Cohen LS. Assessment and treatment of hot flushes and menopausal mood disturbance. Psychiatr Clin N Am. 2003;26:563-580.
1. Cohen LS, Soares CN, Vitonis AF, et al. Risk for new onset of depression during the menopausal transition: the Harvard study of moods and cycles. Arch Gen Psychiatry. 2006;63(4):385-390.
2. Thase ME, Entsuah R, Cantillon M, et al. Relative antidepressant efficacy of venlafaxine and SSRIs: sex-age interactions. J Womens Health (Larchmt). 2005;14:609-616.
3. Aloysi A, Van Dyk K, Sano M. Women’s cognitive and affective health and neuropsychiatry. Mt Sinai J Medicine. 2006;73(7):967-975.
4. Rossouw JE, Anderson GL, Prentice RL, et al. Risks and benefits of estrogen plus progestin in healthy postmenopausal women: principal results from the Women’s Health Initiative randomized controlled trial. JAMA. 2002;288:321-333.
5. Santoro N. Symptoms of menopause: hot flushes. Clinical ObGyn. 2008;51(3):539-548.
6. Joffe H, Soares CN, Cohen LS. Assessment and treatment of hot flushes and menopausal mood disturbance. Psychiatr Clin N Am. 2003;26:563-580.
Antidepressants in bipolar disorder: 7 myths and realities
Few topics are as controversial as the role of antidepressants for patients with bipolar disorder. Although depression usually is the predominant, most enduring mood state in bipolar disorder, clinicians often face uncertainty about using antidepressants because of concerns about safety and efficacy. Whether and when to use antidepressants for bipolar depression hinges on complex parameters that preclude any single, simple rule.
Rather than asking if antidepressants are useful or detrimental for depressed patients with bipolar disorder, a more practical question might be: Under what circumstances are antidepressants likely to be beneficial, deleterious, or ineffective for an individual patient? Because “real world” patients often have idiosyncrasies that defy practice guidelines’ generic treatment recommendations, clinicians who practice in the proverbial trenches need strategies to tailor treatments to each patient that are informed—but not dictated—by evidence-based research.
Early suspicions
Concerns that antidepressants might precipitate mania were first described with tricyclic antidepressant (TCA) use in Europe in the 1960s. After bupropion and selective serotonin reuptake inhibitors (SSRIs) emerged, some clinicians believed they posed a lesser risk for this phenomenon compared with TCAs1,2 or monoamine oxidase inhibitors (MAOIs).3
Antidepressants’ potential to induce short-term mania/hypomania following acute exposure has been weighed against the longer-term risk for worsening illness course by increasing frequency of subsequent episodes (so-called cycle acceleration). In the 1980s, some researchers suggested that rapid cycling might—at least in some instances—represent an iatrogenic phenomenon caused by long-term antidepressant use. These issues remain controversial, but more than 20 years of research suggest that antidepressants induce mania or accelerate cycling in a smaller minority of bipolar disorder patients than was once thought.
Table 1 and Table 2 summarize findings from randomized controlled studies that have examined antidepressants’ efficacy for acute bipolar depression. Except for a study of fluoxetine plus olanzapine,4 no large-scale placebo-controlled trial has demonstrated superior antidepressant response to a mood stabilizer plus antidepressant compared with a mood stabilizer alone.
Table 1
Antidepressants for bipolar depression: SSRIs and SNRIs*
| Acute efficacy | Reported switch risk |
|---|---|
| Fluoxetine (SSRI) | |
| 86% response rate after 3 weeks in 6-week double-blind randomized comparison with imipramine or placeboa | 0% |
| 38% response rate after 8 weeks of placebo-controlled monotherapy in bipolar II or NOS subjectsb | 0% |
| 56% response rate over 8 weeks in combination with olanzapine; significantly better than placebo plus olanzapine (30%)c | 6% |
| Paroxetine (SSRI) | |
| Same as placebo when added to an antimanic drug (STEP-BD) for up to 26 weeksd | 10.1% (reported only jointly for paroxetine or bupropion) |
| 36% response rate (no different from placebo) when coadministered with therapeutically dosed lithium over 10 weekse | 7% |
| Same as divalproex plus lithium when coadministered with divalproex or lithium over 6 weeks (actual response rates not reported)f | 0% |
| 43% response (coadministered with lithium, divalproex, or carbamazepine) over 6 weeksg | 3% (not statistically significantly different from venlafaxine comparison arm) |
| Sertraline (SSRI) | |
| 41% improved (comparable to rates seen with bupropion [33%] or venlafaxine [36%] when coadministered with a mood stabilizer over 10 weeks)h | 12% |
| Venlafaxine (SNRI) | |
| 36% improved (comparable to rates seen with bupropion [33%] or sertraline [41%]) when coadministered with a mood stabilizer over 10 weeksh | 6% |
| 48% response (coadministered with lithium, divalproex, or carbamazepine) over 6 weeksg | 13% (not statistically significantly different from paroxetine comparison arm) |
| *No data are available for citalopram, desvenlafaxine, duloxetine, escitalopram, fluvoxamine, or milnacipran | |
| NOS: not otherwise specified; SNRI: serotonin/norepinephrine reuptake inhibitor; SSRI: selective serotonin reuptake inhibitor; STEP-BD: Systematic Treatment Enhancement Program for Bipolar Disorder | |
| Source: References a. Cohn JB, Collins G, Ashbrook E, et al. A comparison of fluoxetine, imipramine and placebo in patients with bipolar depressive disorder. Int Clin Psychopharmaol. 1989;4:313-322. b. Amsterdam JD, Shults J. Fluoxetine monotherapy of bipolar type II and bipolar NOS major depression: a double-blind, placebo-substitution, continuation study. Int Clin Psychopharmacol. 2005;20:257-264. c. Tohen M, Vieta E, Calabrese J, et al. Efficacy of olanzapine and olanzapine-fluoxetine combination in the treatment of bipolar I depression. Arch Gen Psychiatry. 2003;60:1079-1088. d. Sachs GS, Nierenberg AA, Calabrese JR, et al. Effectiveness of adjunctive antidepressant treatment for bipolar depression. N Engl J Med. 2007;356:1711-1722. e. Nemeroff CB, Evans DL, Gyulai L, et al. Double-blind, placebo-controlled comparison of imipramine and paroxetine in the treatment of bipolar depression. Am J Psychiatry. 2001;158:906-912. f. Young LT, Joffe RT, Robb JC, et al. Double-blind comparison of addition of a second mood stabilizer versus an antidepressant to an initial mood stabilizer for treatment of patients with bipolar depression. Am J Psychiatry. 2000;157:124-126. g. Vieta E, Martinez-Aran A, Goikolea JM. A randomized trial comparing paroxetine and venlafaxine in the treatment of bipolar depressed patients taking mood stabilizers. J Clin Psychiatry. 2002;63:508-512. h. Leverich GS, Altshuler LL, Frye MA, et al. Risk of switch in mood polarity to hypomania or mania in patients with bipolar depression during acute and continuation trials of venlafaxine, sertraline, and bupropion as adjuncts to mood stabilizers. Am J Psychiatry. 2006;163:232-239. | |
Table 2
Antidepressants for bipolar depression: MAOIs, TCAs, and bupropion*
| Acute efficacy | Reported switch risk |
|---|---|
| Tranylcypromine (MAOI) | |
| 81% response (monotherapy) in bipolar I (n=24) or bipolar II (n=32) patients over 16 weeksa | 21% |
| 75% response among imipramine nonresponders (n=12)b | 17% |
| Moclobemide (MAOI) | |
| 46% response over 8 weeks in 156 bipolar patients (some, but not all, took concomitant mood stabilizers), not significantly different from imipramine comparatorc | 4% |
| Imipramine (TCA) | |
| 57% response rate after 3 weeks in a 6-week double-blind randomized comparison with fluoxetine or placebod | Not reported |
| 48% response (monotherapy) in bipolar I (n=24) or bipolar II (N=32) patients over 16 weeksa | 24% |
| 53% response over 8 weeks in 156 bipolar patients (some, but not all, took concomitant mood stabilizers), not significantly different from moclobemide comparatorc | 11% |
| 41% (coadministered with therapeutically dosed lithium)e | 8% |
| Desipramine (TCA) | |
| 50% (5/10) response rate (coadministered with a mood stabilizer over 8 weeks)f | 50% |
| Bupropion | |
| 55% response (5/9) (coadministered with a mood stabilizer over 8 weeks)f | 11% |
| 33% response rate (coadministered with mood stabilizers over 10 weeks)g | 20% |
| *No data are available for isocarboxazid, mirtazapine, nefazodone, phenelzine, or selegiline transdermal | |
| MAOI: monoamine oxidase inhibitor; TCA: tricyclic antidepressant | |
| Source: References a. Himmelhoch JM, Thase ME, Mallinger AG, et al. Tranylcypromine versus imipramine in anergic bipolar depression. Am J Psychiatry. 1991;148:910-916. b. Thase ME, Malinger AG, McKnight D, et al. Treatment of imipramine-resistant recurrent depressions, IV: a double-blind crossover study of tranylcypromine for anergic bipolar depression. Am J Psychiatry. 1992;149:195-198. c. Silverstone T. Moclobemide vs. imipramine in bipolar depression: a multicentre double-blind clinical trial. Acta Psychiatr Scand. 2001;104:104-109. d. Cohn JB, Collins G, Ashbrook E, et al. A comparison of fluoxetine, imipramine and placebo in patients with bipolar depressive disorder. Int Clin Psychopharmaol. 1989;4:313-322. e. Nemeroff CB, Evans DL, Gyulai L, et al. Double-blind, placebo-controlled comparison of imipramine and paroxetine in the treatment of bipolar depression. Am J Psychiatry. 2001;158:906-912. f. Sachs GS, Lafer B, Stoll AL, et al. A double blind trial of bupropion versus desipramine for bipolar depression. J Clin Psychiatry. 1994;55:391-393. g. Leverich GS, Altshuler LL, Frye MA, et al. Risk of switch in mood polarity to hypomania or mania in patients with bipolar depression during acute and continuation trials of venlafaxine, sertraline, and bupropion as adjuncts to mood stabilizers. Am J Psychiatry. 2006;163:232-239. | |
MYTH 1: Antidepressant-induced mania is a highly prevalent, widespread problem.
Reality: Although some might argue that the precise relative risk of antidepressant-induced mania or hypomania is unknown (eg, considering intervening factors such as the natural illness course), recent literature suggests that the emergence of mania or hypomania can be reasonably attributed to antidepressant use in no more than 10% to 25% of patients with bipolar disorder.5,6 Part of the difficulty in estimating the true prevalence of antidepressant-induced mania involves variability and inconsistency in defining mania induction.
A recent consensus statement proposed a graduated series of definitions for treatment-emergent affective switch:7
- “Definite” switch involves fulfilling DSM-IV syndromic criteria for a manic, hypomanic, or mixed episode for at least 2 days, within 8 weeks of antidepressant introduction.
- “Likely” switches call for at least 2 DSM-IV mania or hypomania symptoms plus a Young Mania Rating Scale (YMRS) score >12, occurring for at least 2 days, within 12 weeks of antidepressant introduction.
- “Possible” switches require a “clear change” in mood or energy with a YMRS score >8, persisting ≥4 hours over 2 days, occurring within 12 weeks of antidepressant initiation.
Adverse effects such as agitation typically diminish or remit with dosage reductions or drug cessation, whereas true antidepressant-induced polarity switches persist even after the medication is discontinued. Moreover, it is often difficult—if not impossible—to know with certainty when a polarity switch results from treatment effects vs the natural illness course. In my experience, true manic or hypomanic syndromes soon after antidepressant exposure are less common than heterogeneous, nonspecific symptoms such as agitation, anxiety, insomnia, or worsening depression (ie, lack of efficacy).
MYTH 2: Antidepressant response rates are lower in bipolar depression.
Reality: It is difficult to draw broad conclusions about antidepressant response rates in unipolar vs bipolar depression because:
- few direct comparisons have been reported
- all relevant studies are retrospective
- small sample sizes in most studies may not have satisfactorily controlled for factors that could predispose to mood destabilization (Table 3).
Table 3
What increases risk of antidepressant-induced mania?
| Factor | Findings |
|---|---|
| History of antidepressant-induced mania or hypomania | Confers an approximate 2- to 5-fold increased risk for subsequent antidepressant-induced mania/hypomania, regardless of antidepressanta |
| Recent mania preceding current depressive episode | Higher risk for antidepressant-associated mania if current depressive episode was preceded by manic phaseb |
| Bipolar I vs bipolar II subtype | Greater risk for switch in bipolar Ic,d |
| Comorbid alcohol or substance use disorder | 5- to 7-fold increased risk for antidepressant-associated maniae |
| Noradrenergic vs serotonergic antidepressants | Possible higher risk for mania induction with TCAs or SNRIs than with bupropionf or SSRIsg |
| Concurrent mania symptoms during a depressive episode | Mild or subthreshold mania symptoms during a depressive episode increase risk for maniah,i |
| Hyperthymic temperamental traits | Associated with increased likelihood of antidepressant-induced maniaj |
| SNRIs: serotonin/norepinephrine reuptake inhibitors; SSRIs: selective serotonin reuptake inhibitors; TCAs: tricyclic antidepressants | |
| Source: References a. Truman CJ, Goldberg JF, Ghaemi SN, et al. Self-reported history of manic/hypomanic switch associated with antidepressant use: data from the Systematic Treatment Enhancement Program for Bipolar Disorder (STEP-BD). J Clin Psychiatry. 2007;68:1472-1479. b. MacQueen GM, Young LT, Marriott M, et al. Previous mood state predicts response and switch rates in patients with bipolar depression. Acta Psychiatr Scand. 2002;105:414-418. c. Himmelhoch JM, Thase ME, Mallinger AG, et al. Tranylcypromine versus imipramine in anergic bipolar depression. Am J Psychiatry. 1991;148:910-916. d. Altshuler LL, Suppes T, Black DO, et al. Lower switch rate in depressed patients with bipolar II than bipolar I disorder treated adjunctively with second-generation antidepressants. Am J Psychiatry. 2006;163:313-315. e. Goldberg JF, Truman CJ. Antidepressant-induced mania: an overview of current controversies. Bipolar Disord. 2003;5:407-420. f. Sachs GS, Lafer B, Stoll AL, et al. A double blind trial of bupropion versus desipramine for bipolar depression. J Clin Psychiatry. 1994;55:391-393. g. Peet M. Induction of mania with selective serotonin re-uptake inhibitors and tricyclic antidepressants. Br J Psychiatry. 1994;164:549-550. h. Frye MA, Hellmann G, McElroy SL, et al. Correlates of treatment-emergent mania associated with antidepressant treatment in bipolar depression. Am J Psychiatry. 2009;166:164-172. i. Bottlender R, Rudolf D, Strauss A, et al. Mood-stabilisers reduce the risk of developing antidepressant-induced maniform states in acute treatment of bipolar I depressed patients. J Affect Disord. 2001;63:79-83. j. Henry C, Sorbara F, Lacoste J, et al. Antidepressant-induced mania in bipolar patients: identification of risk factors. J Clin Psychiatry. 2001;62:249-255. | |
A retrospective review of bipolar (n=41) and unipolar (n=37) depressed patients by Ghaemi et al8 found no significant difference in acute nonresponse rates between the groups. Similarly, Bottlender et al9 found no differences in treatment response when comparing naturalistic antidepressant outcomes for 50 unipolar and 50 bipolar patients matched for age, sex, and illness duration. Comparable antidepressant response outcomes also were reported in a retrospective study of 2,032 unipolar and bipolar inpatients conducted by Möller et al,10 and between unipolar (n=31) vs bipolar II (n=17) depressed patients receiving venlafaxine monotherapy for 6 weeks.11
Antidepressant response may depend on factors such as episode chronicity or the number of failed medication trials within a given episode, regardless of illness polarity. This was suggested by the remarkably low response rates after 2 failed initial antidepressant treatments in the Sequenced Treatment Alternatives to Relieve Depression (STAR*D) unipolar depression trials. In my experience, antidepressant efficacy is more often a function of factors in addition to polarity, including:
- illness severity
- chronicity
- psychiatric, medical, or substance use comorbidity
- psychosocial skills, such as the capacity to tolerate distress, utilize effective coping techniques, and maintain appropriate relationships with others.
MYTH 3: Most antidepressants have been systematically studied for treatment of depression in bipolar disorder.
Reality: Only paroxetine,12,13 bupropion,12 and imipramine13 have been studied in randomized, large-scale, adequately powered placebo-controlled trials. Studies of other antidepressants suffer from small sample sizes (inadequate statistical power), lack of placebo controls, or failure to control for possible confounding factors, such as lack of stratification for bipolar I vs II subtype or presence vs absence of rapid cycling.
One large randomized trial showed comparable antidepressant efficacy with a mood stabilizer plus adjunctive venlafaxine (43%) vs sertraline (55%) vs bupropion (49%) over 10 weeks,14 but the lack of a mood stabilizer monotherapy comparison group limits the ability to anticipate whether adjunctive antidepressants increase response or remission rates more than mood stabilizers alone. Adjunctive imipramine,13 paroxetine,12,13,15 and bupropion12 yield no greater improvement in depressive symptoms than is seen with optimally dosed mood stabilizers alone.
Mirtazapine, a serotonergic/noradrenergic antidepressant that is sometimes prescribed off-label as a sleep aid, has not been systematically studied for safety or efficacy in bipolar depression. In case reports, mirtazapine has induced mania in patients with unipolar depression.16-18 Using mirtazapine to counteract insomnia may be safer in patients with unipolar depression than in those with bipolar disorder. Because poor sleep is a core feature of mania, be certain to differentiate complaints that reflect simple insomnia from a loss of need for sleep:
- daytime fatigue is more common in insomnia than loss of need for sleep
- nocturnal hyperactivity is more often associated with loss of need for sleep.
Using an antidepressant to treat sleep problems that may derive from emerging mania or hypomania runs counter to basic pharmacodynamic principles and may pose greater risk than benefit.
Generally, using a medication that has been studied for treating a specific clinical entity such as bipolar depression is preferable to using one that has not. Avoid medications that have multiple negative placebo-controlled trials—such as paroxetine—unless you have evidence of efficacy in an individual patient.
MYTH 4: Risk for inducing mania is higher with noradrenergic antidepressants.
Reality: This popular belief arose from a unifying hypothesis offered by Sachs et al1 and Leverich et al14 to explain higher rates of mania following treatment with desipramine than bupropion,1 SSRIs compared with TCAs,2 or venlafaxine compared with bupropion or sertraline.14 However, while plausible, this hypothesis does not fully account for the putative noradrenergic properties of bupropion—presumably via increased pre-synaptic norepinephrine outflow, rather than noradrenergic reuptake inhibition19—which reportedly has a lower risk of switching than desipramine1 or venlafaxine.14
The risk for venlafaxine monotherapy to induce mania or hypomania in patients with bipolar II depression has been reported to be nonexistent11 or no higher than seen with lithium.20 Also, some noradrenergic agents, such as duloxetine, have not been shown to induce mania in major depression,21 although duloxetine’s potential to destabilize mood is unknown because of the absence of data in bipolar disorder. Finally, although large-scale clinical trials have not examined the safety and efficacy of the noradrenergic reuptake inhibitor atomoxetine, several case reports have suggested its potential for inducing mania or hypomania.22,23
Likely, all-or-none admonitions against using noradrenergic antidepressants are oversimplifications.
MYTH 5: Coadministering an antimanic mood stabilizer reliably prevents antidepressant-induced mania.
Reality: Most practice guidelines advise administering antimanic mood stabilizers before initiating an antidepressant. Clinicians widely interpret this recommendation as reinforcing the assumption that a mood stabilizer will diminish mania risk when introducing an antidepressant. (Less often, clinicians interpret it as meaning that a mood stabilizer itself may provide antidepressant efficacy.) In fact, whether (and which) antimanic agents mitigate the risk for antidepressant-induced mania has received little empirical study. The largest dataset on this topic—the randomized controlled data from Systematic Treatment Enhancement Program for Bipolar Disorder (STEP-BD)12—found that the risk for treatment-emergent manic switch with paroxetine or bupropion was almost identical (about 10%) with or without an FDA-approved antimanic agent.
In a retrospective study, Henry et al6 found that cotherapy with lithium but not divalproex or carbamazepine protects against antidepressant-induced mania, and that switch rates to mania were the same whether or not an antidepressant was taken with an anticonvulsant. In a naturalistic retrospective study (n=158), Bottlender et al24 revealed that mood stabilizers (lithium, carbamazepine, or divalproex) prevented switches from depression to mania during treatment with TCAs but not SSRIs or MAOIs.
I favor incorporating lithium or other antimanic agents in the regimens of patients with bipolar depression not primarily to guard against antidepressant-induced mania but more for pharmacodynamic synergy—complementary mechanisms of action that collectively may produce more substantial antidepressant effects—especially when the patient’s illness course has included manic or hypomanic features in the preceding year.
MYTH 6: Antidepressants cause or worsen rapid cycling.
Reality: Wehr et al25 reported that antidepressants may accelerate cycling frequency (ie, inter-episode durations become shorter) in a small subgroup (N=10) of patients. By contrast, use of TCAs was not more likely in the weeks preceding shifts from depression to mania or hypomania in a 14-year follow-up study of bipolar rapid cycling from the NIMH Collaborative Depression Study.26 In fact, rapid-cycling patients spent more weeks depressed when taking lithium without a TCA than with 1.
Findings from STEP-BD indicate that prospectively observed rapid cycling, as defined by DSM-IV criteria, is relatively rare, although subjects taking antidepressants often had multiple episodes per year.27 These naturalistic data could suggest that antidepressant use leads to more depressive episodes, or that more depressive episodes lead to more antidepressant use. Causal relationships cannot be inferred from the nonrandomized study design. Nevertheless, antidepressant use was not associated with reduced depressive episodes over 1 year.
I believe that, in general, antidepressants are unlikely to improve a truly rapid-cycling illness course. In this scenario, a more “panoramic” understanding of the need to treat multiple relapses and polarity changes over time likely warrants using multiple anti-cycling agents. Rapid cycling is treated over the course of 1 year, rather than 1 episode.
MYTH 7: Antidepressants should never be used without a mood stabilizer for bipolar depression.
Reality: This admonition is widely cited as a general recommendation from modern practice guidelines; however, it mainly pertains to depression treatment in patients with bipolar I disorder, for whom most controlled trial data exist. For example, relatively high rates of treatment-emergent mania have been reported with TCA or MAOI monotherapy in bipolar I disorder patients (Table 2). Yet for bipolar II disorder, controlled trials demonstrate superior outcomes with venlafaxine monotherapy compared with lithium monotherapy, with no increase in mood destabilization.20
Neither the safety nor the efficacy of antidepressants with vs without mood stabilizers has been studied systematically in cyclothymic or mood disorder patients who may fall within the so-called bipolar spectrum but have never met DSM-IV criteria for a lifetime manic or hypomanic episode (ie, bipolar disorder not otherwise specified). Extrapolation from findings based on bipolar I disorder patients may not be valid for all bipolar subtypes.
Clinical strategies
In constructing a rationale-based approach to bipolar depression, consider these steps:
Step 1: Assess candidacy for antidepressant use. A number of key features can help you delineate the current illness state and context in which depressive symptoms arise—features that may influence you patient’s vulnerability to mood destabilization, and therefore are pertinent for gauging the likelihood that antidepressants may help or harm (Table 4).
Step 2: Consider mood stabilizers with antidepressant properties. Determine whether your patient is taking any mood stabilizers that possess robust antidepressant properties, or whether it may be beneficial to introduce one of these agents before initiating adjunctive antidepressants. Mood stabilizers with antidepressant efficacy are compelling options for patients presenting with any of the features listed in the right-hand column of Table 4, as well as those with:
- psychotic features
- marked agitation
- multiple prior antidepressant nonresponses
- high depression recurrence rates regardless of episode duration (ie, cyclicity, irrespective of ≥4 discrete episodes per year).
Table 4
Assessing antidepressant candidacy in bipolar depression
| Favors antidepressant use | Discourages antidepressant use |
|---|---|
| Bipolar II disorder | Bipolar I disordera |
| Depressed (non-mixed) states | Mixed manic and depressive featuresb,c |
| Absence of rapid cycling | Presence of rapid cyclingd,e |
| Absence of recent mania or hypomania (preceding 2 to 3 months) | Mania or hypomania in past 2 to 3 monthsf |
| Absence of comorbid alcohol or substance use disorder | Presence of comorbid alcohol or substance use disorderg,h |
| Prior favorable antidepressant response | Suboptimal responses to prior antidepressants |
| No history of antidepressant-induced mania or hypomania | History of antidepressant-induced mania or hypomaniai |
| Source: References a. Altshuler LL, Suppes T, Black DO, et al. Lower switch rate in depressed patients with bipolar II than bipolar I disorder treated adjunctively with second-generation antidepressants. Am J Psychiatry. 2006;163:313-315. b. Frye MA, Hellmann G, McElroy SL, et al. Correlates of treatment-emergent mania associated with antidepressant treatment in bipolar depression. Am J Psychiatry. 2009;166:164-172. c. Goldberg JF, Perlis RH, Ghaemi SN, et al. Adjunctive antidepressant use and symptomatic recovery among bipolar depressed patients with concomitant manic symptoms: findings from the STEP-BD. Am J Psychiatry. 2007;164(9):1348-1355. d. Schneck CD, Miklowitz DJ, Miyahara S, et al. The prospective course of rapid-cycling bipolar disorder: findings from the STEP-BD. Am J Psychiatry. 2008;165:370-377. e. Ghaemi SN, Ostacher MM, El-Mallakh RS, et al. Antidepressant discontinuation in bipolar depression: a STEP-BD randomized clinical trial of long-term effectiveness and safety. J Clin Psychiatry. In press. f. MacQueen GM, Young LT, Marriott M, et al. Previous mood state predicts response and switch rates in patients with bipolar depression. Acta Psychiatr Scand. 2002;105:414-418. g. Goldberg JF, Whiteside JE. The association between substance abuse and antidepressant-induced mania in bipolar disorder: a preliminary study. J Clin Psychiatry. 2002;63:791-795. h. Manwani SG, Pardo TB, Albanese MJ, et al. Substance use disorder and other predictors of antidepressant-induced mania: a retrospective chart review. J Clin Psychiatry. 2006;67:1341-1345. i. Truman CJ, Goldberg JF, Ghaemi SN, et al. Self-reported history of manic/hypomanic switch associated with antidepressant use: data from the Systematic Treatment Enhancement Program for Bipolar Disorder (STEP-BD). J Clin Psychiatry. 2007;68:1472-1479. | |
Prospective mood charting may help to establish the latter, in which case recurrence (rather than polarity) may cause waxing and waning depressed mood states.
Psychotropic agents or combinations that have shown to be effective for bipolar depression (supported by at least 1 randomized controlled trial) without destabilizing mood include quetiapine, olanzapine, olanzapine-fluoxetine combination, lamotrigine, and lithium plus lamotrigine. Those with some—but less robustly demonstrated—antidepressant action include lithium, divalproex, and carbamazepine. Other than quetiapine and olanzapine, second-generation antipsychotics have not demonstrated antidepressant effects in bipolar depression.
In general, optimize therapy with 1 or more mood stabilizers with antidepressant properties before deciding it is necessary to add antidepressants.
Step 3: Use antidepressants in suitable patients. For patients with no risk factors for mood destabilization from antidepressants (Table 3), these drugs may be worth incorporating, keeping in mind the following guiding principles:
- In patients with bipolar I depression, it is preferable to add an antidepressant to an antimanic mood stabilizer (ie, lithium, divalproex, carbamazepine, or an antipsychotic) rather than prescribing antidepressant monotherapy. There is greater diversity of opinion about the safety of antidepressant monotherapy for bipolar II depression.
- Consider using antidepressants that have at least 1 positive randomized controlled trial in bipolar disorder and low risk for mood destabilization (bupropion,12,14 sertraline,14 fluoxetine,4,5 tranylcypromine,3,28 or venlafaxine in bipolar II depression20) before using those with reported increased risk for inducing mania or hypomania (TCAs1,2 or venlafaxine in bipolar I depression14), multiple negative controlled trials (paroxetine12,13), or no controlled data in bipolar depression (citalopram, escitalopram, fluvoxamine, mirtazapine, duloxetine, desvenlafaxine, nefazodone, and selegiline transdermal). Combinations of antidepressants have not been adequately studied in bipolar depression.
- The optimal duration of antidepressant therapy is unknown. However, longer-term treatment may be worthwhile in patients who show robust acute antidepressant response and experience infrequent mania or hypomania. Long-term antidepressant use is less compelling in patients with a poor initial response29 or rapid cycling.30 Abrupt antidepressant cessation also may induce mania, potentially by disrupting homeostasis.31 In the absence of rapid cycling, manic/hypomanic features, or worsening suicidal features, and in the presence of an unequivocal acute response and a greater predisposition to depression than mania, it is reasonable to continue an antidepressant indefinitely until new signs of mania or hypomania emerge.
- Emerging signs of mania or hypomania should signal the need to discontinue the antidepressant. Dosage reductions alone may not diminish emerging manic or hypomanic symptoms, and “counterbalancing” maneuvers (ie, adding antimanic agents while continuing an antidepressant) may not effectively stabilize mood.
Step 4: Consider novel strategies. In the absence of a response to the strategy outlined above—particularly among poor candidates for continued antidepressant therapy—other novel strategies have support from at least 1 randomized controlled trial, including pramipexole,32,33 modafinil,34 riluzole,35 and n-acetyl cysteine.36 Other interventions worth considering include:
- adjunctive thyroid hormone
- cognitive therapy
- light therapy (if a seasonal component is evident)
- electroconvulsive therapy.
Related resources
- Goldberg JF. Treating depression in bipolar disorder. http://thedoctorschannel.com/video/3077.html.
- Goldberg JF. Pharmacologic treatment of acute mania.http://thedoctorschannel.com/video/3032.html.
Drug brand names
- Atomoxetine • Strattera
- Bupropion • Wellbutrin
- Carbamazepine • Tegretol, Equetro
- Citalopram • Celexa
- Desipramine • Norpramin
- Desvenlafaxine • Pristiq
- Divalproex • Depakote, Depakene
- Duloxetine • Cymbalta
- Escitalopram • Lexapro
- Fluoxetine • Prozac
- Fluvoxamine • Luvox
- Imipramine • Tofranil
- Isocarboxazid • Marplan
- Lamotrigine • Lamictal
- Lithium • Lithobid, Eskalith
- Milnacipran • Ixel, Savella
- Mirtazapine • Remeron
- Moclobemide • Aurorix, Manerix
- Modafinil • Provigil
- Nefazodone • Serzone
- Olanzapine • Zyprexa
- Olanzapine-fluoxetine • Symbyax
- Paroxetine • Paxil
- Phenelzine • Nardil
- Pramipexole • Mirapex
- Quetiapine • Seroquel
- Riluzole • Rilutek
- Selegiline transdermal • EMSAM
- Sertraline • Zoloft
- Tranylcypromine • Parnate
- Venlafaxine • Effexor
Disclosures
Dr. Goldberg is a consultant to Eli Lilly and Company and a speaker for AstraZeneca, Eli Lilly and Company, GlaxoSmithKline, Merck, and Pfizer Inc., and has received speaking honoraria from Janssen-Cilag.
1. Sachs GS, Lafer B, Stoll AL, et al. A double blind trial of bupropion versus desipramine for bipolar depression. J Clin Psychiatry. 1994;55:391-393.
2. Peet M. Induction of mania with selective serotonin re-uptake inhibitors and tricyclic antidepressants. Br J Psychiatry. 1994;164:549-550.
3. Himmelhoch JM, Thase ME, Mallinger AG, et al. Tranylcypromine versus imipramine in anergic bipolar depression. Am J Psychiatry. 1991;148:910-916.
4. Tohen M, Vieta E, Calabrese J, et al. Efficacy of olanzapine and olanzapine-fluoxetine combination in the treatment of bipolar I depression. Arch Gen Psychiatry. 2003;60:1079-1088.
5. Goldberg JF, Truman CJ. Antidepressant-induced mania: an overview of current controversies. Bipolar Disord. 2003;5:407-420.
6. Henry C, Sorbara F, Lacoste J, et al. Antidepressant-induced mania in bipolar patients: identification of risk factors. J Clin Psychiatry. 2001;62:249-255.
7. Tohen M, Frank E, Bowden CL, et al. The International Society for Bipolar Disorders (ISBD) Task Force report on the nomenclature of course and outcome in bipolar disorders. Bipolar Disord. 2009;11:453-473.
8. Ghaemi SN, Rosenquist KJ, Ko JY, et al. Antidepressant treatment in bipolar versus unipolar depression. Am J Psychiatry. 2004;161:163-165.
9. Bottlender R, Rudolf D, Jäger M, et al. Are bipolar I depressive patients less responsive to treatment with antidepressants than unipolar depressive patients? Results from a case control study. Eur Psychiatry. 2002;17:200-205.
10. Möller HJ, Bottlender R, Grunze H, et al. Are antidepressants less effective in the acute treatment of bipolar I compared to unipolar depression? J Affect Disord. 2001;67(1-3):141-146.
11. Amsterdam J. Efficacy and safety of venlafaxine in the treatment of bipolar II major depressive episode. J Clin Psychopharmacol. 1998;18:313-317.
12. Sachs GS, Nierenberg AA, Calabrese JR, et al. Effectiveness of adjunctive antidepressant treatment for bipolar depression. N Engl J Med. 2007;356:1711-1722.
13. Nemeroff CB, Evans DL, Gyulai L, et al. Double-blind, placebo-controlled comparison of imipramine and paroxetine in the treatment of bipolar depression. Am J Psychiatry. 2001;158:906-912.
14. Leverich GS, Altshuler LL, Frye MA, et al. Risk of switch in mood polarity to hypomania or mania in patients with bipolar depression during acute and continuation trials of venlafaxine, sertraline, and bupropion as adjuncts to mood stabilizers. Am J Psychiatry. 2006;163:232-239.
15. Young LT, Joffe RT, Robb JC, et al. Double-blind comparison of addition of a second mood stabilizer versus an antidepressant to an initial mood stabilizer for treatment of patients with bipolar depression. Am J Psychiatry. 2000;157:124-126.
16. Soutullo CA, McElroy SL, Keck PE, Jr. Hypomania associated with mirtazapine augmentation of sertraline. J Clin Psychiatry. 1998;59(6):320.-
17. Bhanji NH, Margolese HC, Saint-Laurent M, et al. Dysphoric mania induced by high-dose mirtazapine: a case for “norepinephrine syndrome”? Int Clin Psychopharmacol. 2002;17(6):319-322.
18. Goyal N, Sinha VK. Mirtazapine-induced manic switch in adolescent unipolar depression. Aust N Z J Psychiatry. 2008;42(12):1070-1071.
19. Dong J, Blier P. Modification of norepinephrine and serotonin, but not dopamine, neuron firing by sustained bupropion treatment. Psychopharmacol (Berl). 2001;155:52-57.
20. Amsterdam JD, Wang CH, Shwarz M, et al. Venlafaxine versus lithium monotherapy of rapid and non-rapid cycling patients with bipolar II major depressive disorder: a randomized, parallel group, open-label trial. J Affect Disord. 2009;112(1-3):219-230.
21. Dunner DL, D’Souza DN, Kajdasz DK, et al. Is treatment-associated mania rare with duloxetine: secondary analysis of controlled trials in non-bipolar depression. J Affect Disord. 2005;87:115-119.
22. Henderson TA. Mania induction associated with atomoxetine. J Clin Psychopharmacol. 2004;24(5):567-568.
23. Henderson TA, Hartman K. Aggression, mania, and hypomania induction associated with atomoxetine. Pediatrics. 2004;114(3):895-896.
24. Bottlender R, Rudolf D, Strauss A, et al. Mood-stabilisers reduce the risk of developing antidepressant-induced maniform states in acute treatment of bipolar I depressed patients. J Affect Disord. 2001;63:79-83.
25. Wehr TA, Sack DA, Rosenthal NE, et al. Rapid cycling affective disorder: contributing factors and treatment responses in 51 patients. Am J Psychiatry. 1988;145:179-184.
26. Coryell W, Solomon D, Turvey C, et al. The long-term course of rapid-cycling bipolar disorder. Arch Gen Psychiatry. 2003;60:914-920.
27. Schneck CD, Miklowitz DJ, Miyahara S, et al. The prospective course of rapid-cycling bipolar disorder: findings from the STEP-BD. Am J Psychiatry. 2008;165:370-377.
28. Thase ME, Malinger AG, McKnight D, et al. Treatment of imipramine-resistant recurrent depressions, IV: a double-blind crossover study of tranylcypromine for anergic bipolar depression. Am J Psychiatry. 1992;149:195-198.
29. Altshuler LL, Post RM, Hellemann G, et al. Impact of antidepressant continuation after acute positive or partial treatment response for bipolar depression: a blinded, randomized study. J Clin Psychiatry. 2009;70(4):450-457.
30. Ghaemi SN, Ostacher MM, El-Mallakh RS, et al. Antidepressant discontinuation in bipolar depression: a STEP-BD randomized clinical trial of long-term effectiveness and safety. J Clin Psychiatry. In press.
31. Goldstein TR, Frye MA, Denicoff KD, et al. Antidepressant discontinuation-related mania: critical prospective observation and theoretical implications in bipolar disorder. J Clin Psychiatry. 1999;60(8):563-567.
32. Goldberg JF, Burdick KE, Endick CE. A preliminary randomized, double-blind, placebo-controlled trial of pramipexole added to mood stabilizers for treatment-resistant bipolar depression. Am J Psychiatry. 2004;161:564-566.
33. Zarate CA, Jr, Payne JL, Singh J, et al. Pramipexole for bipolar II depression: a placebo-controlled proof of concept study. Biol Psychiatry. 2004;56:54-60.
34. Frye MA, Grunze H, Suppes T, et al. A placebo-controlled evaluation of adjunctive modafinil in the treatment of bipolar depression. Am J Psychiatry. 2007;164(8):1242-1249.
35. Zarate CA, Jr, Quiroz JA, Singh JB, et al. An open-label trial of the glutamate-modulating agent riluzole in combination with lithium for the treatment of bipolar depression. Biol Psychiatry. 2005;57(4):430-432.
36. Berk M, Copolov DL, Dean O, et al. N-acetyl cysteine for depressive symptoms in bipolar disorder—a double-blind, randomized placebo-controlled trial. Biol Psychiatry. 2008;64(6):468-475.
Few topics are as controversial as the role of antidepressants for patients with bipolar disorder. Although depression usually is the predominant, most enduring mood state in bipolar disorder, clinicians often face uncertainty about using antidepressants because of concerns about safety and efficacy. Whether and when to use antidepressants for bipolar depression hinges on complex parameters that preclude any single, simple rule.
Rather than asking if antidepressants are useful or detrimental for depressed patients with bipolar disorder, a more practical question might be: Under what circumstances are antidepressants likely to be beneficial, deleterious, or ineffective for an individual patient? Because “real world” patients often have idiosyncrasies that defy practice guidelines’ generic treatment recommendations, clinicians who practice in the proverbial trenches need strategies to tailor treatments to each patient that are informed—but not dictated—by evidence-based research.
Early suspicions
Concerns that antidepressants might precipitate mania were first described with tricyclic antidepressant (TCA) use in Europe in the 1960s. After bupropion and selective serotonin reuptake inhibitors (SSRIs) emerged, some clinicians believed they posed a lesser risk for this phenomenon compared with TCAs1,2 or monoamine oxidase inhibitors (MAOIs).3
Antidepressants’ potential to induce short-term mania/hypomania following acute exposure has been weighed against the longer-term risk for worsening illness course by increasing frequency of subsequent episodes (so-called cycle acceleration). In the 1980s, some researchers suggested that rapid cycling might—at least in some instances—represent an iatrogenic phenomenon caused by long-term antidepressant use. These issues remain controversial, but more than 20 years of research suggest that antidepressants induce mania or accelerate cycling in a smaller minority of bipolar disorder patients than was once thought.
Table 1 and Table 2 summarize findings from randomized controlled studies that have examined antidepressants’ efficacy for acute bipolar depression. Except for a study of fluoxetine plus olanzapine,4 no large-scale placebo-controlled trial has demonstrated superior antidepressant response to a mood stabilizer plus antidepressant compared with a mood stabilizer alone.
Table 1
Antidepressants for bipolar depression: SSRIs and SNRIs*
| Acute efficacy | Reported switch risk |
|---|---|
| Fluoxetine (SSRI) | |
| 86% response rate after 3 weeks in 6-week double-blind randomized comparison with imipramine or placeboa | 0% |
| 38% response rate after 8 weeks of placebo-controlled monotherapy in bipolar II or NOS subjectsb | 0% |
| 56% response rate over 8 weeks in combination with olanzapine; significantly better than placebo plus olanzapine (30%)c | 6% |
| Paroxetine (SSRI) | |
| Same as placebo when added to an antimanic drug (STEP-BD) for up to 26 weeksd | 10.1% (reported only jointly for paroxetine or bupropion) |
| 36% response rate (no different from placebo) when coadministered with therapeutically dosed lithium over 10 weekse | 7% |
| Same as divalproex plus lithium when coadministered with divalproex or lithium over 6 weeks (actual response rates not reported)f | 0% |
| 43% response (coadministered with lithium, divalproex, or carbamazepine) over 6 weeksg | 3% (not statistically significantly different from venlafaxine comparison arm) |
| Sertraline (SSRI) | |
| 41% improved (comparable to rates seen with bupropion [33%] or venlafaxine [36%] when coadministered with a mood stabilizer over 10 weeks)h | 12% |
| Venlafaxine (SNRI) | |
| 36% improved (comparable to rates seen with bupropion [33%] or sertraline [41%]) when coadministered with a mood stabilizer over 10 weeksh | 6% |
| 48% response (coadministered with lithium, divalproex, or carbamazepine) over 6 weeksg | 13% (not statistically significantly different from paroxetine comparison arm) |
| *No data are available for citalopram, desvenlafaxine, duloxetine, escitalopram, fluvoxamine, or milnacipran | |
| NOS: not otherwise specified; SNRI: serotonin/norepinephrine reuptake inhibitor; SSRI: selective serotonin reuptake inhibitor; STEP-BD: Systematic Treatment Enhancement Program for Bipolar Disorder | |
| Source: References a. Cohn JB, Collins G, Ashbrook E, et al. A comparison of fluoxetine, imipramine and placebo in patients with bipolar depressive disorder. Int Clin Psychopharmaol. 1989;4:313-322. b. Amsterdam JD, Shults J. Fluoxetine monotherapy of bipolar type II and bipolar NOS major depression: a double-blind, placebo-substitution, continuation study. Int Clin Psychopharmacol. 2005;20:257-264. c. Tohen M, Vieta E, Calabrese J, et al. Efficacy of olanzapine and olanzapine-fluoxetine combination in the treatment of bipolar I depression. Arch Gen Psychiatry. 2003;60:1079-1088. d. Sachs GS, Nierenberg AA, Calabrese JR, et al. Effectiveness of adjunctive antidepressant treatment for bipolar depression. N Engl J Med. 2007;356:1711-1722. e. Nemeroff CB, Evans DL, Gyulai L, et al. Double-blind, placebo-controlled comparison of imipramine and paroxetine in the treatment of bipolar depression. Am J Psychiatry. 2001;158:906-912. f. Young LT, Joffe RT, Robb JC, et al. Double-blind comparison of addition of a second mood stabilizer versus an antidepressant to an initial mood stabilizer for treatment of patients with bipolar depression. Am J Psychiatry. 2000;157:124-126. g. Vieta E, Martinez-Aran A, Goikolea JM. A randomized trial comparing paroxetine and venlafaxine in the treatment of bipolar depressed patients taking mood stabilizers. J Clin Psychiatry. 2002;63:508-512. h. Leverich GS, Altshuler LL, Frye MA, et al. Risk of switch in mood polarity to hypomania or mania in patients with bipolar depression during acute and continuation trials of venlafaxine, sertraline, and bupropion as adjuncts to mood stabilizers. Am J Psychiatry. 2006;163:232-239. | |
Table 2
Antidepressants for bipolar depression: MAOIs, TCAs, and bupropion*
| Acute efficacy | Reported switch risk |
|---|---|
| Tranylcypromine (MAOI) | |
| 81% response (monotherapy) in bipolar I (n=24) or bipolar II (n=32) patients over 16 weeksa | 21% |
| 75% response among imipramine nonresponders (n=12)b | 17% |
| Moclobemide (MAOI) | |
| 46% response over 8 weeks in 156 bipolar patients (some, but not all, took concomitant mood stabilizers), not significantly different from imipramine comparatorc | 4% |
| Imipramine (TCA) | |
| 57% response rate after 3 weeks in a 6-week double-blind randomized comparison with fluoxetine or placebod | Not reported |
| 48% response (monotherapy) in bipolar I (n=24) or bipolar II (N=32) patients over 16 weeksa | 24% |
| 53% response over 8 weeks in 156 bipolar patients (some, but not all, took concomitant mood stabilizers), not significantly different from moclobemide comparatorc | 11% |
| 41% (coadministered with therapeutically dosed lithium)e | 8% |
| Desipramine (TCA) | |
| 50% (5/10) response rate (coadministered with a mood stabilizer over 8 weeks)f | 50% |
| Bupropion | |
| 55% response (5/9) (coadministered with a mood stabilizer over 8 weeks)f | 11% |
| 33% response rate (coadministered with mood stabilizers over 10 weeks)g | 20% |
| *No data are available for isocarboxazid, mirtazapine, nefazodone, phenelzine, or selegiline transdermal | |
| MAOI: monoamine oxidase inhibitor; TCA: tricyclic antidepressant | |
| Source: References a. Himmelhoch JM, Thase ME, Mallinger AG, et al. Tranylcypromine versus imipramine in anergic bipolar depression. Am J Psychiatry. 1991;148:910-916. b. Thase ME, Malinger AG, McKnight D, et al. Treatment of imipramine-resistant recurrent depressions, IV: a double-blind crossover study of tranylcypromine for anergic bipolar depression. Am J Psychiatry. 1992;149:195-198. c. Silverstone T. Moclobemide vs. imipramine in bipolar depression: a multicentre double-blind clinical trial. Acta Psychiatr Scand. 2001;104:104-109. d. Cohn JB, Collins G, Ashbrook E, et al. A comparison of fluoxetine, imipramine and placebo in patients with bipolar depressive disorder. Int Clin Psychopharmaol. 1989;4:313-322. e. Nemeroff CB, Evans DL, Gyulai L, et al. Double-blind, placebo-controlled comparison of imipramine and paroxetine in the treatment of bipolar depression. Am J Psychiatry. 2001;158:906-912. f. Sachs GS, Lafer B, Stoll AL, et al. A double blind trial of bupropion versus desipramine for bipolar depression. J Clin Psychiatry. 1994;55:391-393. g. Leverich GS, Altshuler LL, Frye MA, et al. Risk of switch in mood polarity to hypomania or mania in patients with bipolar depression during acute and continuation trials of venlafaxine, sertraline, and bupropion as adjuncts to mood stabilizers. Am J Psychiatry. 2006;163:232-239. | |
MYTH 1: Antidepressant-induced mania is a highly prevalent, widespread problem.
Reality: Although some might argue that the precise relative risk of antidepressant-induced mania or hypomania is unknown (eg, considering intervening factors such as the natural illness course), recent literature suggests that the emergence of mania or hypomania can be reasonably attributed to antidepressant use in no more than 10% to 25% of patients with bipolar disorder.5,6 Part of the difficulty in estimating the true prevalence of antidepressant-induced mania involves variability and inconsistency in defining mania induction.
A recent consensus statement proposed a graduated series of definitions for treatment-emergent affective switch:7
- “Definite” switch involves fulfilling DSM-IV syndromic criteria for a manic, hypomanic, or mixed episode for at least 2 days, within 8 weeks of antidepressant introduction.
- “Likely” switches call for at least 2 DSM-IV mania or hypomania symptoms plus a Young Mania Rating Scale (YMRS) score >12, occurring for at least 2 days, within 12 weeks of antidepressant introduction.
- “Possible” switches require a “clear change” in mood or energy with a YMRS score >8, persisting ≥4 hours over 2 days, occurring within 12 weeks of antidepressant initiation.
Adverse effects such as agitation typically diminish or remit with dosage reductions or drug cessation, whereas true antidepressant-induced polarity switches persist even after the medication is discontinued. Moreover, it is often difficult—if not impossible—to know with certainty when a polarity switch results from treatment effects vs the natural illness course. In my experience, true manic or hypomanic syndromes soon after antidepressant exposure are less common than heterogeneous, nonspecific symptoms such as agitation, anxiety, insomnia, or worsening depression (ie, lack of efficacy).
MYTH 2: Antidepressant response rates are lower in bipolar depression.
Reality: It is difficult to draw broad conclusions about antidepressant response rates in unipolar vs bipolar depression because:
- few direct comparisons have been reported
- all relevant studies are retrospective
- small sample sizes in most studies may not have satisfactorily controlled for factors that could predispose to mood destabilization (Table 3).
Table 3
What increases risk of antidepressant-induced mania?
| Factor | Findings |
|---|---|
| History of antidepressant-induced mania or hypomania | Confers an approximate 2- to 5-fold increased risk for subsequent antidepressant-induced mania/hypomania, regardless of antidepressanta |
| Recent mania preceding current depressive episode | Higher risk for antidepressant-associated mania if current depressive episode was preceded by manic phaseb |
| Bipolar I vs bipolar II subtype | Greater risk for switch in bipolar Ic,d |
| Comorbid alcohol or substance use disorder | 5- to 7-fold increased risk for antidepressant-associated maniae |
| Noradrenergic vs serotonergic antidepressants | Possible higher risk for mania induction with TCAs or SNRIs than with bupropionf or SSRIsg |
| Concurrent mania symptoms during a depressive episode | Mild or subthreshold mania symptoms during a depressive episode increase risk for maniah,i |
| Hyperthymic temperamental traits | Associated with increased likelihood of antidepressant-induced maniaj |
| SNRIs: serotonin/norepinephrine reuptake inhibitors; SSRIs: selective serotonin reuptake inhibitors; TCAs: tricyclic antidepressants | |
| Source: References a. Truman CJ, Goldberg JF, Ghaemi SN, et al. Self-reported history of manic/hypomanic switch associated with antidepressant use: data from the Systematic Treatment Enhancement Program for Bipolar Disorder (STEP-BD). J Clin Psychiatry. 2007;68:1472-1479. b. MacQueen GM, Young LT, Marriott M, et al. Previous mood state predicts response and switch rates in patients with bipolar depression. Acta Psychiatr Scand. 2002;105:414-418. c. Himmelhoch JM, Thase ME, Mallinger AG, et al. Tranylcypromine versus imipramine in anergic bipolar depression. Am J Psychiatry. 1991;148:910-916. d. Altshuler LL, Suppes T, Black DO, et al. Lower switch rate in depressed patients with bipolar II than bipolar I disorder treated adjunctively with second-generation antidepressants. Am J Psychiatry. 2006;163:313-315. e. Goldberg JF, Truman CJ. Antidepressant-induced mania: an overview of current controversies. Bipolar Disord. 2003;5:407-420. f. Sachs GS, Lafer B, Stoll AL, et al. A double blind trial of bupropion versus desipramine for bipolar depression. J Clin Psychiatry. 1994;55:391-393. g. Peet M. Induction of mania with selective serotonin re-uptake inhibitors and tricyclic antidepressants. Br J Psychiatry. 1994;164:549-550. h. Frye MA, Hellmann G, McElroy SL, et al. Correlates of treatment-emergent mania associated with antidepressant treatment in bipolar depression. Am J Psychiatry. 2009;166:164-172. i. Bottlender R, Rudolf D, Strauss A, et al. Mood-stabilisers reduce the risk of developing antidepressant-induced maniform states in acute treatment of bipolar I depressed patients. J Affect Disord. 2001;63:79-83. j. Henry C, Sorbara F, Lacoste J, et al. Antidepressant-induced mania in bipolar patients: identification of risk factors. J Clin Psychiatry. 2001;62:249-255. | |
A retrospective review of bipolar (n=41) and unipolar (n=37) depressed patients by Ghaemi et al8 found no significant difference in acute nonresponse rates between the groups. Similarly, Bottlender et al9 found no differences in treatment response when comparing naturalistic antidepressant outcomes for 50 unipolar and 50 bipolar patients matched for age, sex, and illness duration. Comparable antidepressant response outcomes also were reported in a retrospective study of 2,032 unipolar and bipolar inpatients conducted by Möller et al,10 and between unipolar (n=31) vs bipolar II (n=17) depressed patients receiving venlafaxine monotherapy for 6 weeks.11
Antidepressant response may depend on factors such as episode chronicity or the number of failed medication trials within a given episode, regardless of illness polarity. This was suggested by the remarkably low response rates after 2 failed initial antidepressant treatments in the Sequenced Treatment Alternatives to Relieve Depression (STAR*D) unipolar depression trials. In my experience, antidepressant efficacy is more often a function of factors in addition to polarity, including:
- illness severity
- chronicity
- psychiatric, medical, or substance use comorbidity
- psychosocial skills, such as the capacity to tolerate distress, utilize effective coping techniques, and maintain appropriate relationships with others.
MYTH 3: Most antidepressants have been systematically studied for treatment of depression in bipolar disorder.
Reality: Only paroxetine,12,13 bupropion,12 and imipramine13 have been studied in randomized, large-scale, adequately powered placebo-controlled trials. Studies of other antidepressants suffer from small sample sizes (inadequate statistical power), lack of placebo controls, or failure to control for possible confounding factors, such as lack of stratification for bipolar I vs II subtype or presence vs absence of rapid cycling.
One large randomized trial showed comparable antidepressant efficacy with a mood stabilizer plus adjunctive venlafaxine (43%) vs sertraline (55%) vs bupropion (49%) over 10 weeks,14 but the lack of a mood stabilizer monotherapy comparison group limits the ability to anticipate whether adjunctive antidepressants increase response or remission rates more than mood stabilizers alone. Adjunctive imipramine,13 paroxetine,12,13,15 and bupropion12 yield no greater improvement in depressive symptoms than is seen with optimally dosed mood stabilizers alone.
Mirtazapine, a serotonergic/noradrenergic antidepressant that is sometimes prescribed off-label as a sleep aid, has not been systematically studied for safety or efficacy in bipolar depression. In case reports, mirtazapine has induced mania in patients with unipolar depression.16-18 Using mirtazapine to counteract insomnia may be safer in patients with unipolar depression than in those with bipolar disorder. Because poor sleep is a core feature of mania, be certain to differentiate complaints that reflect simple insomnia from a loss of need for sleep:
- daytime fatigue is more common in insomnia than loss of need for sleep
- nocturnal hyperactivity is more often associated with loss of need for sleep.
Using an antidepressant to treat sleep problems that may derive from emerging mania or hypomania runs counter to basic pharmacodynamic principles and may pose greater risk than benefit.
Generally, using a medication that has been studied for treating a specific clinical entity such as bipolar depression is preferable to using one that has not. Avoid medications that have multiple negative placebo-controlled trials—such as paroxetine—unless you have evidence of efficacy in an individual patient.
MYTH 4: Risk for inducing mania is higher with noradrenergic antidepressants.
Reality: This popular belief arose from a unifying hypothesis offered by Sachs et al1 and Leverich et al14 to explain higher rates of mania following treatment with desipramine than bupropion,1 SSRIs compared with TCAs,2 or venlafaxine compared with bupropion or sertraline.14 However, while plausible, this hypothesis does not fully account for the putative noradrenergic properties of bupropion—presumably via increased pre-synaptic norepinephrine outflow, rather than noradrenergic reuptake inhibition19—which reportedly has a lower risk of switching than desipramine1 or venlafaxine.14
The risk for venlafaxine monotherapy to induce mania or hypomania in patients with bipolar II depression has been reported to be nonexistent11 or no higher than seen with lithium.20 Also, some noradrenergic agents, such as duloxetine, have not been shown to induce mania in major depression,21 although duloxetine’s potential to destabilize mood is unknown because of the absence of data in bipolar disorder. Finally, although large-scale clinical trials have not examined the safety and efficacy of the noradrenergic reuptake inhibitor atomoxetine, several case reports have suggested its potential for inducing mania or hypomania.22,23
Likely, all-or-none admonitions against using noradrenergic antidepressants are oversimplifications.
MYTH 5: Coadministering an antimanic mood stabilizer reliably prevents antidepressant-induced mania.
Reality: Most practice guidelines advise administering antimanic mood stabilizers before initiating an antidepressant. Clinicians widely interpret this recommendation as reinforcing the assumption that a mood stabilizer will diminish mania risk when introducing an antidepressant. (Less often, clinicians interpret it as meaning that a mood stabilizer itself may provide antidepressant efficacy.) In fact, whether (and which) antimanic agents mitigate the risk for antidepressant-induced mania has received little empirical study. The largest dataset on this topic—the randomized controlled data from Systematic Treatment Enhancement Program for Bipolar Disorder (STEP-BD)12—found that the risk for treatment-emergent manic switch with paroxetine or bupropion was almost identical (about 10%) with or without an FDA-approved antimanic agent.
In a retrospective study, Henry et al6 found that cotherapy with lithium but not divalproex or carbamazepine protects against antidepressant-induced mania, and that switch rates to mania were the same whether or not an antidepressant was taken with an anticonvulsant. In a naturalistic retrospective study (n=158), Bottlender et al24 revealed that mood stabilizers (lithium, carbamazepine, or divalproex) prevented switches from depression to mania during treatment with TCAs but not SSRIs or MAOIs.
I favor incorporating lithium or other antimanic agents in the regimens of patients with bipolar depression not primarily to guard against antidepressant-induced mania but more for pharmacodynamic synergy—complementary mechanisms of action that collectively may produce more substantial antidepressant effects—especially when the patient’s illness course has included manic or hypomanic features in the preceding year.
MYTH 6: Antidepressants cause or worsen rapid cycling.
Reality: Wehr et al25 reported that antidepressants may accelerate cycling frequency (ie, inter-episode durations become shorter) in a small subgroup (N=10) of patients. By contrast, use of TCAs was not more likely in the weeks preceding shifts from depression to mania or hypomania in a 14-year follow-up study of bipolar rapid cycling from the NIMH Collaborative Depression Study.26 In fact, rapid-cycling patients spent more weeks depressed when taking lithium without a TCA than with 1.
Findings from STEP-BD indicate that prospectively observed rapid cycling, as defined by DSM-IV criteria, is relatively rare, although subjects taking antidepressants often had multiple episodes per year.27 These naturalistic data could suggest that antidepressant use leads to more depressive episodes, or that more depressive episodes lead to more antidepressant use. Causal relationships cannot be inferred from the nonrandomized study design. Nevertheless, antidepressant use was not associated with reduced depressive episodes over 1 year.
I believe that, in general, antidepressants are unlikely to improve a truly rapid-cycling illness course. In this scenario, a more “panoramic” understanding of the need to treat multiple relapses and polarity changes over time likely warrants using multiple anti-cycling agents. Rapid cycling is treated over the course of 1 year, rather than 1 episode.
MYTH 7: Antidepressants should never be used without a mood stabilizer for bipolar depression.
Reality: This admonition is widely cited as a general recommendation from modern practice guidelines; however, it mainly pertains to depression treatment in patients with bipolar I disorder, for whom most controlled trial data exist. For example, relatively high rates of treatment-emergent mania have been reported with TCA or MAOI monotherapy in bipolar I disorder patients (Table 2). Yet for bipolar II disorder, controlled trials demonstrate superior outcomes with venlafaxine monotherapy compared with lithium monotherapy, with no increase in mood destabilization.20
Neither the safety nor the efficacy of antidepressants with vs without mood stabilizers has been studied systematically in cyclothymic or mood disorder patients who may fall within the so-called bipolar spectrum but have never met DSM-IV criteria for a lifetime manic or hypomanic episode (ie, bipolar disorder not otherwise specified). Extrapolation from findings based on bipolar I disorder patients may not be valid for all bipolar subtypes.
Clinical strategies
In constructing a rationale-based approach to bipolar depression, consider these steps:
Step 1: Assess candidacy for antidepressant use. A number of key features can help you delineate the current illness state and context in which depressive symptoms arise—features that may influence you patient’s vulnerability to mood destabilization, and therefore are pertinent for gauging the likelihood that antidepressants may help or harm (Table 4).
Step 2: Consider mood stabilizers with antidepressant properties. Determine whether your patient is taking any mood stabilizers that possess robust antidepressant properties, or whether it may be beneficial to introduce one of these agents before initiating adjunctive antidepressants. Mood stabilizers with antidepressant efficacy are compelling options for patients presenting with any of the features listed in the right-hand column of Table 4, as well as those with:
- psychotic features
- marked agitation
- multiple prior antidepressant nonresponses
- high depression recurrence rates regardless of episode duration (ie, cyclicity, irrespective of ≥4 discrete episodes per year).
Table 4
Assessing antidepressant candidacy in bipolar depression
| Favors antidepressant use | Discourages antidepressant use |
|---|---|
| Bipolar II disorder | Bipolar I disordera |
| Depressed (non-mixed) states | Mixed manic and depressive featuresb,c |
| Absence of rapid cycling | Presence of rapid cyclingd,e |
| Absence of recent mania or hypomania (preceding 2 to 3 months) | Mania or hypomania in past 2 to 3 monthsf |
| Absence of comorbid alcohol or substance use disorder | Presence of comorbid alcohol or substance use disorderg,h |
| Prior favorable antidepressant response | Suboptimal responses to prior antidepressants |
| No history of antidepressant-induced mania or hypomania | History of antidepressant-induced mania or hypomaniai |
| Source: References a. Altshuler LL, Suppes T, Black DO, et al. Lower switch rate in depressed patients with bipolar II than bipolar I disorder treated adjunctively with second-generation antidepressants. Am J Psychiatry. 2006;163:313-315. b. Frye MA, Hellmann G, McElroy SL, et al. Correlates of treatment-emergent mania associated with antidepressant treatment in bipolar depression. Am J Psychiatry. 2009;166:164-172. c. Goldberg JF, Perlis RH, Ghaemi SN, et al. Adjunctive antidepressant use and symptomatic recovery among bipolar depressed patients with concomitant manic symptoms: findings from the STEP-BD. Am J Psychiatry. 2007;164(9):1348-1355. d. Schneck CD, Miklowitz DJ, Miyahara S, et al. The prospective course of rapid-cycling bipolar disorder: findings from the STEP-BD. Am J Psychiatry. 2008;165:370-377. e. Ghaemi SN, Ostacher MM, El-Mallakh RS, et al. Antidepressant discontinuation in bipolar depression: a STEP-BD randomized clinical trial of long-term effectiveness and safety. J Clin Psychiatry. In press. f. MacQueen GM, Young LT, Marriott M, et al. Previous mood state predicts response and switch rates in patients with bipolar depression. Acta Psychiatr Scand. 2002;105:414-418. g. Goldberg JF, Whiteside JE. The association between substance abuse and antidepressant-induced mania in bipolar disorder: a preliminary study. J Clin Psychiatry. 2002;63:791-795. h. Manwani SG, Pardo TB, Albanese MJ, et al. Substance use disorder and other predictors of antidepressant-induced mania: a retrospective chart review. J Clin Psychiatry. 2006;67:1341-1345. i. Truman CJ, Goldberg JF, Ghaemi SN, et al. Self-reported history of manic/hypomanic switch associated with antidepressant use: data from the Systematic Treatment Enhancement Program for Bipolar Disorder (STEP-BD). J Clin Psychiatry. 2007;68:1472-1479. | |
Prospective mood charting may help to establish the latter, in which case recurrence (rather than polarity) may cause waxing and waning depressed mood states.
Psychotropic agents or combinations that have shown to be effective for bipolar depression (supported by at least 1 randomized controlled trial) without destabilizing mood include quetiapine, olanzapine, olanzapine-fluoxetine combination, lamotrigine, and lithium plus lamotrigine. Those with some—but less robustly demonstrated—antidepressant action include lithium, divalproex, and carbamazepine. Other than quetiapine and olanzapine, second-generation antipsychotics have not demonstrated antidepressant effects in bipolar depression.
In general, optimize therapy with 1 or more mood stabilizers with antidepressant properties before deciding it is necessary to add antidepressants.
Step 3: Use antidepressants in suitable patients. For patients with no risk factors for mood destabilization from antidepressants (Table 3), these drugs may be worth incorporating, keeping in mind the following guiding principles:
- In patients with bipolar I depression, it is preferable to add an antidepressant to an antimanic mood stabilizer (ie, lithium, divalproex, carbamazepine, or an antipsychotic) rather than prescribing antidepressant monotherapy. There is greater diversity of opinion about the safety of antidepressant monotherapy for bipolar II depression.
- Consider using antidepressants that have at least 1 positive randomized controlled trial in bipolar disorder and low risk for mood destabilization (bupropion,12,14 sertraline,14 fluoxetine,4,5 tranylcypromine,3,28 or venlafaxine in bipolar II depression20) before using those with reported increased risk for inducing mania or hypomania (TCAs1,2 or venlafaxine in bipolar I depression14), multiple negative controlled trials (paroxetine12,13), or no controlled data in bipolar depression (citalopram, escitalopram, fluvoxamine, mirtazapine, duloxetine, desvenlafaxine, nefazodone, and selegiline transdermal). Combinations of antidepressants have not been adequately studied in bipolar depression.
- The optimal duration of antidepressant therapy is unknown. However, longer-term treatment may be worthwhile in patients who show robust acute antidepressant response and experience infrequent mania or hypomania. Long-term antidepressant use is less compelling in patients with a poor initial response29 or rapid cycling.30 Abrupt antidepressant cessation also may induce mania, potentially by disrupting homeostasis.31 In the absence of rapid cycling, manic/hypomanic features, or worsening suicidal features, and in the presence of an unequivocal acute response and a greater predisposition to depression than mania, it is reasonable to continue an antidepressant indefinitely until new signs of mania or hypomania emerge.
- Emerging signs of mania or hypomania should signal the need to discontinue the antidepressant. Dosage reductions alone may not diminish emerging manic or hypomanic symptoms, and “counterbalancing” maneuvers (ie, adding antimanic agents while continuing an antidepressant) may not effectively stabilize mood.
Step 4: Consider novel strategies. In the absence of a response to the strategy outlined above—particularly among poor candidates for continued antidepressant therapy—other novel strategies have support from at least 1 randomized controlled trial, including pramipexole,32,33 modafinil,34 riluzole,35 and n-acetyl cysteine.36 Other interventions worth considering include:
- adjunctive thyroid hormone
- cognitive therapy
- light therapy (if a seasonal component is evident)
- electroconvulsive therapy.
Related resources
- Goldberg JF. Treating depression in bipolar disorder. http://thedoctorschannel.com/video/3077.html.
- Goldberg JF. Pharmacologic treatment of acute mania.http://thedoctorschannel.com/video/3032.html.
Drug brand names
- Atomoxetine • Strattera
- Bupropion • Wellbutrin
- Carbamazepine • Tegretol, Equetro
- Citalopram • Celexa
- Desipramine • Norpramin
- Desvenlafaxine • Pristiq
- Divalproex • Depakote, Depakene
- Duloxetine • Cymbalta
- Escitalopram • Lexapro
- Fluoxetine • Prozac
- Fluvoxamine • Luvox
- Imipramine • Tofranil
- Isocarboxazid • Marplan
- Lamotrigine • Lamictal
- Lithium • Lithobid, Eskalith
- Milnacipran • Ixel, Savella
- Mirtazapine • Remeron
- Moclobemide • Aurorix, Manerix
- Modafinil • Provigil
- Nefazodone • Serzone
- Olanzapine • Zyprexa
- Olanzapine-fluoxetine • Symbyax
- Paroxetine • Paxil
- Phenelzine • Nardil
- Pramipexole • Mirapex
- Quetiapine • Seroquel
- Riluzole • Rilutek
- Selegiline transdermal • EMSAM
- Sertraline • Zoloft
- Tranylcypromine • Parnate
- Venlafaxine • Effexor
Disclosures
Dr. Goldberg is a consultant to Eli Lilly and Company and a speaker for AstraZeneca, Eli Lilly and Company, GlaxoSmithKline, Merck, and Pfizer Inc., and has received speaking honoraria from Janssen-Cilag.
Few topics are as controversial as the role of antidepressants for patients with bipolar disorder. Although depression usually is the predominant, most enduring mood state in bipolar disorder, clinicians often face uncertainty about using antidepressants because of concerns about safety and efficacy. Whether and when to use antidepressants for bipolar depression hinges on complex parameters that preclude any single, simple rule.
Rather than asking if antidepressants are useful or detrimental for depressed patients with bipolar disorder, a more practical question might be: Under what circumstances are antidepressants likely to be beneficial, deleterious, or ineffective for an individual patient? Because “real world” patients often have idiosyncrasies that defy practice guidelines’ generic treatment recommendations, clinicians who practice in the proverbial trenches need strategies to tailor treatments to each patient that are informed—but not dictated—by evidence-based research.
Early suspicions
Concerns that antidepressants might precipitate mania were first described with tricyclic antidepressant (TCA) use in Europe in the 1960s. After bupropion and selective serotonin reuptake inhibitors (SSRIs) emerged, some clinicians believed they posed a lesser risk for this phenomenon compared with TCAs1,2 or monoamine oxidase inhibitors (MAOIs).3
Antidepressants’ potential to induce short-term mania/hypomania following acute exposure has been weighed against the longer-term risk for worsening illness course by increasing frequency of subsequent episodes (so-called cycle acceleration). In the 1980s, some researchers suggested that rapid cycling might—at least in some instances—represent an iatrogenic phenomenon caused by long-term antidepressant use. These issues remain controversial, but more than 20 years of research suggest that antidepressants induce mania or accelerate cycling in a smaller minority of bipolar disorder patients than was once thought.
Table 1 and Table 2 summarize findings from randomized controlled studies that have examined antidepressants’ efficacy for acute bipolar depression. Except for a study of fluoxetine plus olanzapine,4 no large-scale placebo-controlled trial has demonstrated superior antidepressant response to a mood stabilizer plus antidepressant compared with a mood stabilizer alone.
Table 1
Antidepressants for bipolar depression: SSRIs and SNRIs*
| Acute efficacy | Reported switch risk |
|---|---|
| Fluoxetine (SSRI) | |
| 86% response rate after 3 weeks in 6-week double-blind randomized comparison with imipramine or placeboa | 0% |
| 38% response rate after 8 weeks of placebo-controlled monotherapy in bipolar II or NOS subjectsb | 0% |
| 56% response rate over 8 weeks in combination with olanzapine; significantly better than placebo plus olanzapine (30%)c | 6% |
| Paroxetine (SSRI) | |
| Same as placebo when added to an antimanic drug (STEP-BD) for up to 26 weeksd | 10.1% (reported only jointly for paroxetine or bupropion) |
| 36% response rate (no different from placebo) when coadministered with therapeutically dosed lithium over 10 weekse | 7% |
| Same as divalproex plus lithium when coadministered with divalproex or lithium over 6 weeks (actual response rates not reported)f | 0% |
| 43% response (coadministered with lithium, divalproex, or carbamazepine) over 6 weeksg | 3% (not statistically significantly different from venlafaxine comparison arm) |
| Sertraline (SSRI) | |
| 41% improved (comparable to rates seen with bupropion [33%] or venlafaxine [36%] when coadministered with a mood stabilizer over 10 weeks)h | 12% |
| Venlafaxine (SNRI) | |
| 36% improved (comparable to rates seen with bupropion [33%] or sertraline [41%]) when coadministered with a mood stabilizer over 10 weeksh | 6% |
| 48% response (coadministered with lithium, divalproex, or carbamazepine) over 6 weeksg | 13% (not statistically significantly different from paroxetine comparison arm) |
| *No data are available for citalopram, desvenlafaxine, duloxetine, escitalopram, fluvoxamine, or milnacipran | |
| NOS: not otherwise specified; SNRI: serotonin/norepinephrine reuptake inhibitor; SSRI: selective serotonin reuptake inhibitor; STEP-BD: Systematic Treatment Enhancement Program for Bipolar Disorder | |
| Source: References a. Cohn JB, Collins G, Ashbrook E, et al. A comparison of fluoxetine, imipramine and placebo in patients with bipolar depressive disorder. Int Clin Psychopharmaol. 1989;4:313-322. b. Amsterdam JD, Shults J. Fluoxetine monotherapy of bipolar type II and bipolar NOS major depression: a double-blind, placebo-substitution, continuation study. Int Clin Psychopharmacol. 2005;20:257-264. c. Tohen M, Vieta E, Calabrese J, et al. Efficacy of olanzapine and olanzapine-fluoxetine combination in the treatment of bipolar I depression. Arch Gen Psychiatry. 2003;60:1079-1088. d. Sachs GS, Nierenberg AA, Calabrese JR, et al. Effectiveness of adjunctive antidepressant treatment for bipolar depression. N Engl J Med. 2007;356:1711-1722. e. Nemeroff CB, Evans DL, Gyulai L, et al. Double-blind, placebo-controlled comparison of imipramine and paroxetine in the treatment of bipolar depression. Am J Psychiatry. 2001;158:906-912. f. Young LT, Joffe RT, Robb JC, et al. Double-blind comparison of addition of a second mood stabilizer versus an antidepressant to an initial mood stabilizer for treatment of patients with bipolar depression. Am J Psychiatry. 2000;157:124-126. g. Vieta E, Martinez-Aran A, Goikolea JM. A randomized trial comparing paroxetine and venlafaxine in the treatment of bipolar depressed patients taking mood stabilizers. J Clin Psychiatry. 2002;63:508-512. h. Leverich GS, Altshuler LL, Frye MA, et al. Risk of switch in mood polarity to hypomania or mania in patients with bipolar depression during acute and continuation trials of venlafaxine, sertraline, and bupropion as adjuncts to mood stabilizers. Am J Psychiatry. 2006;163:232-239. | |
Table 2
Antidepressants for bipolar depression: MAOIs, TCAs, and bupropion*
| Acute efficacy | Reported switch risk |
|---|---|
| Tranylcypromine (MAOI) | |
| 81% response (monotherapy) in bipolar I (n=24) or bipolar II (n=32) patients over 16 weeksa | 21% |
| 75% response among imipramine nonresponders (n=12)b | 17% |
| Moclobemide (MAOI) | |
| 46% response over 8 weeks in 156 bipolar patients (some, but not all, took concomitant mood stabilizers), not significantly different from imipramine comparatorc | 4% |
| Imipramine (TCA) | |
| 57% response rate after 3 weeks in a 6-week double-blind randomized comparison with fluoxetine or placebod | Not reported |
| 48% response (monotherapy) in bipolar I (n=24) or bipolar II (N=32) patients over 16 weeksa | 24% |
| 53% response over 8 weeks in 156 bipolar patients (some, but not all, took concomitant mood stabilizers), not significantly different from moclobemide comparatorc | 11% |
| 41% (coadministered with therapeutically dosed lithium)e | 8% |
| Desipramine (TCA) | |
| 50% (5/10) response rate (coadministered with a mood stabilizer over 8 weeks)f | 50% |
| Bupropion | |
| 55% response (5/9) (coadministered with a mood stabilizer over 8 weeks)f | 11% |
| 33% response rate (coadministered with mood stabilizers over 10 weeks)g | 20% |
| *No data are available for isocarboxazid, mirtazapine, nefazodone, phenelzine, or selegiline transdermal | |
| MAOI: monoamine oxidase inhibitor; TCA: tricyclic antidepressant | |
| Source: References a. Himmelhoch JM, Thase ME, Mallinger AG, et al. Tranylcypromine versus imipramine in anergic bipolar depression. Am J Psychiatry. 1991;148:910-916. b. Thase ME, Malinger AG, McKnight D, et al. Treatment of imipramine-resistant recurrent depressions, IV: a double-blind crossover study of tranylcypromine for anergic bipolar depression. Am J Psychiatry. 1992;149:195-198. c. Silverstone T. Moclobemide vs. imipramine in bipolar depression: a multicentre double-blind clinical trial. Acta Psychiatr Scand. 2001;104:104-109. d. Cohn JB, Collins G, Ashbrook E, et al. A comparison of fluoxetine, imipramine and placebo in patients with bipolar depressive disorder. Int Clin Psychopharmaol. 1989;4:313-322. e. Nemeroff CB, Evans DL, Gyulai L, et al. Double-blind, placebo-controlled comparison of imipramine and paroxetine in the treatment of bipolar depression. Am J Psychiatry. 2001;158:906-912. f. Sachs GS, Lafer B, Stoll AL, et al. A double blind trial of bupropion versus desipramine for bipolar depression. J Clin Psychiatry. 1994;55:391-393. g. Leverich GS, Altshuler LL, Frye MA, et al. Risk of switch in mood polarity to hypomania or mania in patients with bipolar depression during acute and continuation trials of venlafaxine, sertraline, and bupropion as adjuncts to mood stabilizers. Am J Psychiatry. 2006;163:232-239. | |
MYTH 1: Antidepressant-induced mania is a highly prevalent, widespread problem.
Reality: Although some might argue that the precise relative risk of antidepressant-induced mania or hypomania is unknown (eg, considering intervening factors such as the natural illness course), recent literature suggests that the emergence of mania or hypomania can be reasonably attributed to antidepressant use in no more than 10% to 25% of patients with bipolar disorder.5,6 Part of the difficulty in estimating the true prevalence of antidepressant-induced mania involves variability and inconsistency in defining mania induction.
A recent consensus statement proposed a graduated series of definitions for treatment-emergent affective switch:7
- “Definite” switch involves fulfilling DSM-IV syndromic criteria for a manic, hypomanic, or mixed episode for at least 2 days, within 8 weeks of antidepressant introduction.
- “Likely” switches call for at least 2 DSM-IV mania or hypomania symptoms plus a Young Mania Rating Scale (YMRS) score >12, occurring for at least 2 days, within 12 weeks of antidepressant introduction.
- “Possible” switches require a “clear change” in mood or energy with a YMRS score >8, persisting ≥4 hours over 2 days, occurring within 12 weeks of antidepressant initiation.
Adverse effects such as agitation typically diminish or remit with dosage reductions or drug cessation, whereas true antidepressant-induced polarity switches persist even after the medication is discontinued. Moreover, it is often difficult—if not impossible—to know with certainty when a polarity switch results from treatment effects vs the natural illness course. In my experience, true manic or hypomanic syndromes soon after antidepressant exposure are less common than heterogeneous, nonspecific symptoms such as agitation, anxiety, insomnia, or worsening depression (ie, lack of efficacy).
MYTH 2: Antidepressant response rates are lower in bipolar depression.
Reality: It is difficult to draw broad conclusions about antidepressant response rates in unipolar vs bipolar depression because:
- few direct comparisons have been reported
- all relevant studies are retrospective
- small sample sizes in most studies may not have satisfactorily controlled for factors that could predispose to mood destabilization (Table 3).
Table 3
What increases risk of antidepressant-induced mania?
| Factor | Findings |
|---|---|
| History of antidepressant-induced mania or hypomania | Confers an approximate 2- to 5-fold increased risk for subsequent antidepressant-induced mania/hypomania, regardless of antidepressanta |
| Recent mania preceding current depressive episode | Higher risk for antidepressant-associated mania if current depressive episode was preceded by manic phaseb |
| Bipolar I vs bipolar II subtype | Greater risk for switch in bipolar Ic,d |
| Comorbid alcohol or substance use disorder | 5- to 7-fold increased risk for antidepressant-associated maniae |
| Noradrenergic vs serotonergic antidepressants | Possible higher risk for mania induction with TCAs or SNRIs than with bupropionf or SSRIsg |
| Concurrent mania symptoms during a depressive episode | Mild or subthreshold mania symptoms during a depressive episode increase risk for maniah,i |
| Hyperthymic temperamental traits | Associated with increased likelihood of antidepressant-induced maniaj |
| SNRIs: serotonin/norepinephrine reuptake inhibitors; SSRIs: selective serotonin reuptake inhibitors; TCAs: tricyclic antidepressants | |
| Source: References a. Truman CJ, Goldberg JF, Ghaemi SN, et al. Self-reported history of manic/hypomanic switch associated with antidepressant use: data from the Systematic Treatment Enhancement Program for Bipolar Disorder (STEP-BD). J Clin Psychiatry. 2007;68:1472-1479. b. MacQueen GM, Young LT, Marriott M, et al. Previous mood state predicts response and switch rates in patients with bipolar depression. Acta Psychiatr Scand. 2002;105:414-418. c. Himmelhoch JM, Thase ME, Mallinger AG, et al. Tranylcypromine versus imipramine in anergic bipolar depression. Am J Psychiatry. 1991;148:910-916. d. Altshuler LL, Suppes T, Black DO, et al. Lower switch rate in depressed patients with bipolar II than bipolar I disorder treated adjunctively with second-generation antidepressants. Am J Psychiatry. 2006;163:313-315. e. Goldberg JF, Truman CJ. Antidepressant-induced mania: an overview of current controversies. Bipolar Disord. 2003;5:407-420. f. Sachs GS, Lafer B, Stoll AL, et al. A double blind trial of bupropion versus desipramine for bipolar depression. J Clin Psychiatry. 1994;55:391-393. g. Peet M. Induction of mania with selective serotonin re-uptake inhibitors and tricyclic antidepressants. Br J Psychiatry. 1994;164:549-550. h. Frye MA, Hellmann G, McElroy SL, et al. Correlates of treatment-emergent mania associated with antidepressant treatment in bipolar depression. Am J Psychiatry. 2009;166:164-172. i. Bottlender R, Rudolf D, Strauss A, et al. Mood-stabilisers reduce the risk of developing antidepressant-induced maniform states in acute treatment of bipolar I depressed patients. J Affect Disord. 2001;63:79-83. j. Henry C, Sorbara F, Lacoste J, et al. Antidepressant-induced mania in bipolar patients: identification of risk factors. J Clin Psychiatry. 2001;62:249-255. | |
A retrospective review of bipolar (n=41) and unipolar (n=37) depressed patients by Ghaemi et al8 found no significant difference in acute nonresponse rates between the groups. Similarly, Bottlender et al9 found no differences in treatment response when comparing naturalistic antidepressant outcomes for 50 unipolar and 50 bipolar patients matched for age, sex, and illness duration. Comparable antidepressant response outcomes also were reported in a retrospective study of 2,032 unipolar and bipolar inpatients conducted by Möller et al,10 and between unipolar (n=31) vs bipolar II (n=17) depressed patients receiving venlafaxine monotherapy for 6 weeks.11
Antidepressant response may depend on factors such as episode chronicity or the number of failed medication trials within a given episode, regardless of illness polarity. This was suggested by the remarkably low response rates after 2 failed initial antidepressant treatments in the Sequenced Treatment Alternatives to Relieve Depression (STAR*D) unipolar depression trials. In my experience, antidepressant efficacy is more often a function of factors in addition to polarity, including:
- illness severity
- chronicity
- psychiatric, medical, or substance use comorbidity
- psychosocial skills, such as the capacity to tolerate distress, utilize effective coping techniques, and maintain appropriate relationships with others.
MYTH 3: Most antidepressants have been systematically studied for treatment of depression in bipolar disorder.
Reality: Only paroxetine,12,13 bupropion,12 and imipramine13 have been studied in randomized, large-scale, adequately powered placebo-controlled trials. Studies of other antidepressants suffer from small sample sizes (inadequate statistical power), lack of placebo controls, or failure to control for possible confounding factors, such as lack of stratification for bipolar I vs II subtype or presence vs absence of rapid cycling.
One large randomized trial showed comparable antidepressant efficacy with a mood stabilizer plus adjunctive venlafaxine (43%) vs sertraline (55%) vs bupropion (49%) over 10 weeks,14 but the lack of a mood stabilizer monotherapy comparison group limits the ability to anticipate whether adjunctive antidepressants increase response or remission rates more than mood stabilizers alone. Adjunctive imipramine,13 paroxetine,12,13,15 and bupropion12 yield no greater improvement in depressive symptoms than is seen with optimally dosed mood stabilizers alone.
Mirtazapine, a serotonergic/noradrenergic antidepressant that is sometimes prescribed off-label as a sleep aid, has not been systematically studied for safety or efficacy in bipolar depression. In case reports, mirtazapine has induced mania in patients with unipolar depression.16-18 Using mirtazapine to counteract insomnia may be safer in patients with unipolar depression than in those with bipolar disorder. Because poor sleep is a core feature of mania, be certain to differentiate complaints that reflect simple insomnia from a loss of need for sleep:
- daytime fatigue is more common in insomnia than loss of need for sleep
- nocturnal hyperactivity is more often associated with loss of need for sleep.
Using an antidepressant to treat sleep problems that may derive from emerging mania or hypomania runs counter to basic pharmacodynamic principles and may pose greater risk than benefit.
Generally, using a medication that has been studied for treating a specific clinical entity such as bipolar depression is preferable to using one that has not. Avoid medications that have multiple negative placebo-controlled trials—such as paroxetine—unless you have evidence of efficacy in an individual patient.
MYTH 4: Risk for inducing mania is higher with noradrenergic antidepressants.
Reality: This popular belief arose from a unifying hypothesis offered by Sachs et al1 and Leverich et al14 to explain higher rates of mania following treatment with desipramine than bupropion,1 SSRIs compared with TCAs,2 or venlafaxine compared with bupropion or sertraline.14 However, while plausible, this hypothesis does not fully account for the putative noradrenergic properties of bupropion—presumably via increased pre-synaptic norepinephrine outflow, rather than noradrenergic reuptake inhibition19—which reportedly has a lower risk of switching than desipramine1 or venlafaxine.14
The risk for venlafaxine monotherapy to induce mania or hypomania in patients with bipolar II depression has been reported to be nonexistent11 or no higher than seen with lithium.20 Also, some noradrenergic agents, such as duloxetine, have not been shown to induce mania in major depression,21 although duloxetine’s potential to destabilize mood is unknown because of the absence of data in bipolar disorder. Finally, although large-scale clinical trials have not examined the safety and efficacy of the noradrenergic reuptake inhibitor atomoxetine, several case reports have suggested its potential for inducing mania or hypomania.22,23
Likely, all-or-none admonitions against using noradrenergic antidepressants are oversimplifications.
MYTH 5: Coadministering an antimanic mood stabilizer reliably prevents antidepressant-induced mania.
Reality: Most practice guidelines advise administering antimanic mood stabilizers before initiating an antidepressant. Clinicians widely interpret this recommendation as reinforcing the assumption that a mood stabilizer will diminish mania risk when introducing an antidepressant. (Less often, clinicians interpret it as meaning that a mood stabilizer itself may provide antidepressant efficacy.) In fact, whether (and which) antimanic agents mitigate the risk for antidepressant-induced mania has received little empirical study. The largest dataset on this topic—the randomized controlled data from Systematic Treatment Enhancement Program for Bipolar Disorder (STEP-BD)12—found that the risk for treatment-emergent manic switch with paroxetine or bupropion was almost identical (about 10%) with or without an FDA-approved antimanic agent.
In a retrospective study, Henry et al6 found that cotherapy with lithium but not divalproex or carbamazepine protects against antidepressant-induced mania, and that switch rates to mania were the same whether or not an antidepressant was taken with an anticonvulsant. In a naturalistic retrospective study (n=158), Bottlender et al24 revealed that mood stabilizers (lithium, carbamazepine, or divalproex) prevented switches from depression to mania during treatment with TCAs but not SSRIs or MAOIs.
I favor incorporating lithium or other antimanic agents in the regimens of patients with bipolar depression not primarily to guard against antidepressant-induced mania but more for pharmacodynamic synergy—complementary mechanisms of action that collectively may produce more substantial antidepressant effects—especially when the patient’s illness course has included manic or hypomanic features in the preceding year.
MYTH 6: Antidepressants cause or worsen rapid cycling.
Reality: Wehr et al25 reported that antidepressants may accelerate cycling frequency (ie, inter-episode durations become shorter) in a small subgroup (N=10) of patients. By contrast, use of TCAs was not more likely in the weeks preceding shifts from depression to mania or hypomania in a 14-year follow-up study of bipolar rapid cycling from the NIMH Collaborative Depression Study.26 In fact, rapid-cycling patients spent more weeks depressed when taking lithium without a TCA than with 1.
Findings from STEP-BD indicate that prospectively observed rapid cycling, as defined by DSM-IV criteria, is relatively rare, although subjects taking antidepressants often had multiple episodes per year.27 These naturalistic data could suggest that antidepressant use leads to more depressive episodes, or that more depressive episodes lead to more antidepressant use. Causal relationships cannot be inferred from the nonrandomized study design. Nevertheless, antidepressant use was not associated with reduced depressive episodes over 1 year.
I believe that, in general, antidepressants are unlikely to improve a truly rapid-cycling illness course. In this scenario, a more “panoramic” understanding of the need to treat multiple relapses and polarity changes over time likely warrants using multiple anti-cycling agents. Rapid cycling is treated over the course of 1 year, rather than 1 episode.
MYTH 7: Antidepressants should never be used without a mood stabilizer for bipolar depression.
Reality: This admonition is widely cited as a general recommendation from modern practice guidelines; however, it mainly pertains to depression treatment in patients with bipolar I disorder, for whom most controlled trial data exist. For example, relatively high rates of treatment-emergent mania have been reported with TCA or MAOI monotherapy in bipolar I disorder patients (Table 2). Yet for bipolar II disorder, controlled trials demonstrate superior outcomes with venlafaxine monotherapy compared with lithium monotherapy, with no increase in mood destabilization.20
Neither the safety nor the efficacy of antidepressants with vs without mood stabilizers has been studied systematically in cyclothymic or mood disorder patients who may fall within the so-called bipolar spectrum but have never met DSM-IV criteria for a lifetime manic or hypomanic episode (ie, bipolar disorder not otherwise specified). Extrapolation from findings based on bipolar I disorder patients may not be valid for all bipolar subtypes.
Clinical strategies
In constructing a rationale-based approach to bipolar depression, consider these steps:
Step 1: Assess candidacy for antidepressant use. A number of key features can help you delineate the current illness state and context in which depressive symptoms arise—features that may influence you patient’s vulnerability to mood destabilization, and therefore are pertinent for gauging the likelihood that antidepressants may help or harm (Table 4).
Step 2: Consider mood stabilizers with antidepressant properties. Determine whether your patient is taking any mood stabilizers that possess robust antidepressant properties, or whether it may be beneficial to introduce one of these agents before initiating adjunctive antidepressants. Mood stabilizers with antidepressant efficacy are compelling options for patients presenting with any of the features listed in the right-hand column of Table 4, as well as those with:
- psychotic features
- marked agitation
- multiple prior antidepressant nonresponses
- high depression recurrence rates regardless of episode duration (ie, cyclicity, irrespective of ≥4 discrete episodes per year).
Table 4
Assessing antidepressant candidacy in bipolar depression
| Favors antidepressant use | Discourages antidepressant use |
|---|---|
| Bipolar II disorder | Bipolar I disordera |
| Depressed (non-mixed) states | Mixed manic and depressive featuresb,c |
| Absence of rapid cycling | Presence of rapid cyclingd,e |
| Absence of recent mania or hypomania (preceding 2 to 3 months) | Mania or hypomania in past 2 to 3 monthsf |
| Absence of comorbid alcohol or substance use disorder | Presence of comorbid alcohol or substance use disorderg,h |
| Prior favorable antidepressant response | Suboptimal responses to prior antidepressants |
| No history of antidepressant-induced mania or hypomania | History of antidepressant-induced mania or hypomaniai |
| Source: References a. Altshuler LL, Suppes T, Black DO, et al. Lower switch rate in depressed patients with bipolar II than bipolar I disorder treated adjunctively with second-generation antidepressants. Am J Psychiatry. 2006;163:313-315. b. Frye MA, Hellmann G, McElroy SL, et al. Correlates of treatment-emergent mania associated with antidepressant treatment in bipolar depression. Am J Psychiatry. 2009;166:164-172. c. Goldberg JF, Perlis RH, Ghaemi SN, et al. Adjunctive antidepressant use and symptomatic recovery among bipolar depressed patients with concomitant manic symptoms: findings from the STEP-BD. Am J Psychiatry. 2007;164(9):1348-1355. d. Schneck CD, Miklowitz DJ, Miyahara S, et al. The prospective course of rapid-cycling bipolar disorder: findings from the STEP-BD. Am J Psychiatry. 2008;165:370-377. e. Ghaemi SN, Ostacher MM, El-Mallakh RS, et al. Antidepressant discontinuation in bipolar depression: a STEP-BD randomized clinical trial of long-term effectiveness and safety. J Clin Psychiatry. In press. f. MacQueen GM, Young LT, Marriott M, et al. Previous mood state predicts response and switch rates in patients with bipolar depression. Acta Psychiatr Scand. 2002;105:414-418. g. Goldberg JF, Whiteside JE. The association between substance abuse and antidepressant-induced mania in bipolar disorder: a preliminary study. J Clin Psychiatry. 2002;63:791-795. h. Manwani SG, Pardo TB, Albanese MJ, et al. Substance use disorder and other predictors of antidepressant-induced mania: a retrospective chart review. J Clin Psychiatry. 2006;67:1341-1345. i. Truman CJ, Goldberg JF, Ghaemi SN, et al. Self-reported history of manic/hypomanic switch associated with antidepressant use: data from the Systematic Treatment Enhancement Program for Bipolar Disorder (STEP-BD). J Clin Psychiatry. 2007;68:1472-1479. | |
Prospective mood charting may help to establish the latter, in which case recurrence (rather than polarity) may cause waxing and waning depressed mood states.
Psychotropic agents or combinations that have shown to be effective for bipolar depression (supported by at least 1 randomized controlled trial) without destabilizing mood include quetiapine, olanzapine, olanzapine-fluoxetine combination, lamotrigine, and lithium plus lamotrigine. Those with some—but less robustly demonstrated—antidepressant action include lithium, divalproex, and carbamazepine. Other than quetiapine and olanzapine, second-generation antipsychotics have not demonstrated antidepressant effects in bipolar depression.
In general, optimize therapy with 1 or more mood stabilizers with antidepressant properties before deciding it is necessary to add antidepressants.
Step 3: Use antidepressants in suitable patients. For patients with no risk factors for mood destabilization from antidepressants (Table 3), these drugs may be worth incorporating, keeping in mind the following guiding principles:
- In patients with bipolar I depression, it is preferable to add an antidepressant to an antimanic mood stabilizer (ie, lithium, divalproex, carbamazepine, or an antipsychotic) rather than prescribing antidepressant monotherapy. There is greater diversity of opinion about the safety of antidepressant monotherapy for bipolar II depression.
- Consider using antidepressants that have at least 1 positive randomized controlled trial in bipolar disorder and low risk for mood destabilization (bupropion,12,14 sertraline,14 fluoxetine,4,5 tranylcypromine,3,28 or venlafaxine in bipolar II depression20) before using those with reported increased risk for inducing mania or hypomania (TCAs1,2 or venlafaxine in bipolar I depression14), multiple negative controlled trials (paroxetine12,13), or no controlled data in bipolar depression (citalopram, escitalopram, fluvoxamine, mirtazapine, duloxetine, desvenlafaxine, nefazodone, and selegiline transdermal). Combinations of antidepressants have not been adequately studied in bipolar depression.
- The optimal duration of antidepressant therapy is unknown. However, longer-term treatment may be worthwhile in patients who show robust acute antidepressant response and experience infrequent mania or hypomania. Long-term antidepressant use is less compelling in patients with a poor initial response29 or rapid cycling.30 Abrupt antidepressant cessation also may induce mania, potentially by disrupting homeostasis.31 In the absence of rapid cycling, manic/hypomanic features, or worsening suicidal features, and in the presence of an unequivocal acute response and a greater predisposition to depression than mania, it is reasonable to continue an antidepressant indefinitely until new signs of mania or hypomania emerge.
- Emerging signs of mania or hypomania should signal the need to discontinue the antidepressant. Dosage reductions alone may not diminish emerging manic or hypomanic symptoms, and “counterbalancing” maneuvers (ie, adding antimanic agents while continuing an antidepressant) may not effectively stabilize mood.
Step 4: Consider novel strategies. In the absence of a response to the strategy outlined above—particularly among poor candidates for continued antidepressant therapy—other novel strategies have support from at least 1 randomized controlled trial, including pramipexole,32,33 modafinil,34 riluzole,35 and n-acetyl cysteine.36 Other interventions worth considering include:
- adjunctive thyroid hormone
- cognitive therapy
- light therapy (if a seasonal component is evident)
- electroconvulsive therapy.
Related resources
- Goldberg JF. Treating depression in bipolar disorder. http://thedoctorschannel.com/video/3077.html.
- Goldberg JF. Pharmacologic treatment of acute mania.http://thedoctorschannel.com/video/3032.html.
Drug brand names
- Atomoxetine • Strattera
- Bupropion • Wellbutrin
- Carbamazepine • Tegretol, Equetro
- Citalopram • Celexa
- Desipramine • Norpramin
- Desvenlafaxine • Pristiq
- Divalproex • Depakote, Depakene
- Duloxetine • Cymbalta
- Escitalopram • Lexapro
- Fluoxetine • Prozac
- Fluvoxamine • Luvox
- Imipramine • Tofranil
- Isocarboxazid • Marplan
- Lamotrigine • Lamictal
- Lithium • Lithobid, Eskalith
- Milnacipran • Ixel, Savella
- Mirtazapine • Remeron
- Moclobemide • Aurorix, Manerix
- Modafinil • Provigil
- Nefazodone • Serzone
- Olanzapine • Zyprexa
- Olanzapine-fluoxetine • Symbyax
- Paroxetine • Paxil
- Phenelzine • Nardil
- Pramipexole • Mirapex
- Quetiapine • Seroquel
- Riluzole • Rilutek
- Selegiline transdermal • EMSAM
- Sertraline • Zoloft
- Tranylcypromine • Parnate
- Venlafaxine • Effexor
Disclosures
Dr. Goldberg is a consultant to Eli Lilly and Company and a speaker for AstraZeneca, Eli Lilly and Company, GlaxoSmithKline, Merck, and Pfizer Inc., and has received speaking honoraria from Janssen-Cilag.
1. Sachs GS, Lafer B, Stoll AL, et al. A double blind trial of bupropion versus desipramine for bipolar depression. J Clin Psychiatry. 1994;55:391-393.
2. Peet M. Induction of mania with selective serotonin re-uptake inhibitors and tricyclic antidepressants. Br J Psychiatry. 1994;164:549-550.
3. Himmelhoch JM, Thase ME, Mallinger AG, et al. Tranylcypromine versus imipramine in anergic bipolar depression. Am J Psychiatry. 1991;148:910-916.
4. Tohen M, Vieta E, Calabrese J, et al. Efficacy of olanzapine and olanzapine-fluoxetine combination in the treatment of bipolar I depression. Arch Gen Psychiatry. 2003;60:1079-1088.
5. Goldberg JF, Truman CJ. Antidepressant-induced mania: an overview of current controversies. Bipolar Disord. 2003;5:407-420.
6. Henry C, Sorbara F, Lacoste J, et al. Antidepressant-induced mania in bipolar patients: identification of risk factors. J Clin Psychiatry. 2001;62:249-255.
7. Tohen M, Frank E, Bowden CL, et al. The International Society for Bipolar Disorders (ISBD) Task Force report on the nomenclature of course and outcome in bipolar disorders. Bipolar Disord. 2009;11:453-473.
8. Ghaemi SN, Rosenquist KJ, Ko JY, et al. Antidepressant treatment in bipolar versus unipolar depression. Am J Psychiatry. 2004;161:163-165.
9. Bottlender R, Rudolf D, Jäger M, et al. Are bipolar I depressive patients less responsive to treatment with antidepressants than unipolar depressive patients? Results from a case control study. Eur Psychiatry. 2002;17:200-205.
10. Möller HJ, Bottlender R, Grunze H, et al. Are antidepressants less effective in the acute treatment of bipolar I compared to unipolar depression? J Affect Disord. 2001;67(1-3):141-146.
11. Amsterdam J. Efficacy and safety of venlafaxine in the treatment of bipolar II major depressive episode. J Clin Psychopharmacol. 1998;18:313-317.
12. Sachs GS, Nierenberg AA, Calabrese JR, et al. Effectiveness of adjunctive antidepressant treatment for bipolar depression. N Engl J Med. 2007;356:1711-1722.
13. Nemeroff CB, Evans DL, Gyulai L, et al. Double-blind, placebo-controlled comparison of imipramine and paroxetine in the treatment of bipolar depression. Am J Psychiatry. 2001;158:906-912.
14. Leverich GS, Altshuler LL, Frye MA, et al. Risk of switch in mood polarity to hypomania or mania in patients with bipolar depression during acute and continuation trials of venlafaxine, sertraline, and bupropion as adjuncts to mood stabilizers. Am J Psychiatry. 2006;163:232-239.
15. Young LT, Joffe RT, Robb JC, et al. Double-blind comparison of addition of a second mood stabilizer versus an antidepressant to an initial mood stabilizer for treatment of patients with bipolar depression. Am J Psychiatry. 2000;157:124-126.
16. Soutullo CA, McElroy SL, Keck PE, Jr. Hypomania associated with mirtazapine augmentation of sertraline. J Clin Psychiatry. 1998;59(6):320.-
17. Bhanji NH, Margolese HC, Saint-Laurent M, et al. Dysphoric mania induced by high-dose mirtazapine: a case for “norepinephrine syndrome”? Int Clin Psychopharmacol. 2002;17(6):319-322.
18. Goyal N, Sinha VK. Mirtazapine-induced manic switch in adolescent unipolar depression. Aust N Z J Psychiatry. 2008;42(12):1070-1071.
19. Dong J, Blier P. Modification of norepinephrine and serotonin, but not dopamine, neuron firing by sustained bupropion treatment. Psychopharmacol (Berl). 2001;155:52-57.
20. Amsterdam JD, Wang CH, Shwarz M, et al. Venlafaxine versus lithium monotherapy of rapid and non-rapid cycling patients with bipolar II major depressive disorder: a randomized, parallel group, open-label trial. J Affect Disord. 2009;112(1-3):219-230.
21. Dunner DL, D’Souza DN, Kajdasz DK, et al. Is treatment-associated mania rare with duloxetine: secondary analysis of controlled trials in non-bipolar depression. J Affect Disord. 2005;87:115-119.
22. Henderson TA. Mania induction associated with atomoxetine. J Clin Psychopharmacol. 2004;24(5):567-568.
23. Henderson TA, Hartman K. Aggression, mania, and hypomania induction associated with atomoxetine. Pediatrics. 2004;114(3):895-896.
24. Bottlender R, Rudolf D, Strauss A, et al. Mood-stabilisers reduce the risk of developing antidepressant-induced maniform states in acute treatment of bipolar I depressed patients. J Affect Disord. 2001;63:79-83.
25. Wehr TA, Sack DA, Rosenthal NE, et al. Rapid cycling affective disorder: contributing factors and treatment responses in 51 patients. Am J Psychiatry. 1988;145:179-184.
26. Coryell W, Solomon D, Turvey C, et al. The long-term course of rapid-cycling bipolar disorder. Arch Gen Psychiatry. 2003;60:914-920.
27. Schneck CD, Miklowitz DJ, Miyahara S, et al. The prospective course of rapid-cycling bipolar disorder: findings from the STEP-BD. Am J Psychiatry. 2008;165:370-377.
28. Thase ME, Malinger AG, McKnight D, et al. Treatment of imipramine-resistant recurrent depressions, IV: a double-blind crossover study of tranylcypromine for anergic bipolar depression. Am J Psychiatry. 1992;149:195-198.
29. Altshuler LL, Post RM, Hellemann G, et al. Impact of antidepressant continuation after acute positive or partial treatment response for bipolar depression: a blinded, randomized study. J Clin Psychiatry. 2009;70(4):450-457.
30. Ghaemi SN, Ostacher MM, El-Mallakh RS, et al. Antidepressant discontinuation in bipolar depression: a STEP-BD randomized clinical trial of long-term effectiveness and safety. J Clin Psychiatry. In press.
31. Goldstein TR, Frye MA, Denicoff KD, et al. Antidepressant discontinuation-related mania: critical prospective observation and theoretical implications in bipolar disorder. J Clin Psychiatry. 1999;60(8):563-567.
32. Goldberg JF, Burdick KE, Endick CE. A preliminary randomized, double-blind, placebo-controlled trial of pramipexole added to mood stabilizers for treatment-resistant bipolar depression. Am J Psychiatry. 2004;161:564-566.
33. Zarate CA, Jr, Payne JL, Singh J, et al. Pramipexole for bipolar II depression: a placebo-controlled proof of concept study. Biol Psychiatry. 2004;56:54-60.
34. Frye MA, Grunze H, Suppes T, et al. A placebo-controlled evaluation of adjunctive modafinil in the treatment of bipolar depression. Am J Psychiatry. 2007;164(8):1242-1249.
35. Zarate CA, Jr, Quiroz JA, Singh JB, et al. An open-label trial of the glutamate-modulating agent riluzole in combination with lithium for the treatment of bipolar depression. Biol Psychiatry. 2005;57(4):430-432.
36. Berk M, Copolov DL, Dean O, et al. N-acetyl cysteine for depressive symptoms in bipolar disorder—a double-blind, randomized placebo-controlled trial. Biol Psychiatry. 2008;64(6):468-475.
1. Sachs GS, Lafer B, Stoll AL, et al. A double blind trial of bupropion versus desipramine for bipolar depression. J Clin Psychiatry. 1994;55:391-393.
2. Peet M. Induction of mania with selective serotonin re-uptake inhibitors and tricyclic antidepressants. Br J Psychiatry. 1994;164:549-550.
3. Himmelhoch JM, Thase ME, Mallinger AG, et al. Tranylcypromine versus imipramine in anergic bipolar depression. Am J Psychiatry. 1991;148:910-916.
4. Tohen M, Vieta E, Calabrese J, et al. Efficacy of olanzapine and olanzapine-fluoxetine combination in the treatment of bipolar I depression. Arch Gen Psychiatry. 2003;60:1079-1088.
5. Goldberg JF, Truman CJ. Antidepressant-induced mania: an overview of current controversies. Bipolar Disord. 2003;5:407-420.
6. Henry C, Sorbara F, Lacoste J, et al. Antidepressant-induced mania in bipolar patients: identification of risk factors. J Clin Psychiatry. 2001;62:249-255.
7. Tohen M, Frank E, Bowden CL, et al. The International Society for Bipolar Disorders (ISBD) Task Force report on the nomenclature of course and outcome in bipolar disorders. Bipolar Disord. 2009;11:453-473.
8. Ghaemi SN, Rosenquist KJ, Ko JY, et al. Antidepressant treatment in bipolar versus unipolar depression. Am J Psychiatry. 2004;161:163-165.
9. Bottlender R, Rudolf D, Jäger M, et al. Are bipolar I depressive patients less responsive to treatment with antidepressants than unipolar depressive patients? Results from a case control study. Eur Psychiatry. 2002;17:200-205.
10. Möller HJ, Bottlender R, Grunze H, et al. Are antidepressants less effective in the acute treatment of bipolar I compared to unipolar depression? J Affect Disord. 2001;67(1-3):141-146.
11. Amsterdam J. Efficacy and safety of venlafaxine in the treatment of bipolar II major depressive episode. J Clin Psychopharmacol. 1998;18:313-317.
12. Sachs GS, Nierenberg AA, Calabrese JR, et al. Effectiveness of adjunctive antidepressant treatment for bipolar depression. N Engl J Med. 2007;356:1711-1722.
13. Nemeroff CB, Evans DL, Gyulai L, et al. Double-blind, placebo-controlled comparison of imipramine and paroxetine in the treatment of bipolar depression. Am J Psychiatry. 2001;158:906-912.
14. Leverich GS, Altshuler LL, Frye MA, et al. Risk of switch in mood polarity to hypomania or mania in patients with bipolar depression during acute and continuation trials of venlafaxine, sertraline, and bupropion as adjuncts to mood stabilizers. Am J Psychiatry. 2006;163:232-239.
15. Young LT, Joffe RT, Robb JC, et al. Double-blind comparison of addition of a second mood stabilizer versus an antidepressant to an initial mood stabilizer for treatment of patients with bipolar depression. Am J Psychiatry. 2000;157:124-126.
16. Soutullo CA, McElroy SL, Keck PE, Jr. Hypomania associated with mirtazapine augmentation of sertraline. J Clin Psychiatry. 1998;59(6):320.-
17. Bhanji NH, Margolese HC, Saint-Laurent M, et al. Dysphoric mania induced by high-dose mirtazapine: a case for “norepinephrine syndrome”? Int Clin Psychopharmacol. 2002;17(6):319-322.
18. Goyal N, Sinha VK. Mirtazapine-induced manic switch in adolescent unipolar depression. Aust N Z J Psychiatry. 2008;42(12):1070-1071.
19. Dong J, Blier P. Modification of norepinephrine and serotonin, but not dopamine, neuron firing by sustained bupropion treatment. Psychopharmacol (Berl). 2001;155:52-57.
20. Amsterdam JD, Wang CH, Shwarz M, et al. Venlafaxine versus lithium monotherapy of rapid and non-rapid cycling patients with bipolar II major depressive disorder: a randomized, parallel group, open-label trial. J Affect Disord. 2009;112(1-3):219-230.
21. Dunner DL, D’Souza DN, Kajdasz DK, et al. Is treatment-associated mania rare with duloxetine: secondary analysis of controlled trials in non-bipolar depression. J Affect Disord. 2005;87:115-119.
22. Henderson TA. Mania induction associated with atomoxetine. J Clin Psychopharmacol. 2004;24(5):567-568.
23. Henderson TA, Hartman K. Aggression, mania, and hypomania induction associated with atomoxetine. Pediatrics. 2004;114(3):895-896.
24. Bottlender R, Rudolf D, Strauss A, et al. Mood-stabilisers reduce the risk of developing antidepressant-induced maniform states in acute treatment of bipolar I depressed patients. J Affect Disord. 2001;63:79-83.
25. Wehr TA, Sack DA, Rosenthal NE, et al. Rapid cycling affective disorder: contributing factors and treatment responses in 51 patients. Am J Psychiatry. 1988;145:179-184.
26. Coryell W, Solomon D, Turvey C, et al. The long-term course of rapid-cycling bipolar disorder. Arch Gen Psychiatry. 2003;60:914-920.
27. Schneck CD, Miklowitz DJ, Miyahara S, et al. The prospective course of rapid-cycling bipolar disorder: findings from the STEP-BD. Am J Psychiatry. 2008;165:370-377.
28. Thase ME, Malinger AG, McKnight D, et al. Treatment of imipramine-resistant recurrent depressions, IV: a double-blind crossover study of tranylcypromine for anergic bipolar depression. Am J Psychiatry. 1992;149:195-198.
29. Altshuler LL, Post RM, Hellemann G, et al. Impact of antidepressant continuation after acute positive or partial treatment response for bipolar depression: a blinded, randomized study. J Clin Psychiatry. 2009;70(4):450-457.
30. Ghaemi SN, Ostacher MM, El-Mallakh RS, et al. Antidepressant discontinuation in bipolar depression: a STEP-BD randomized clinical trial of long-term effectiveness and safety. J Clin Psychiatry. In press.
31. Goldstein TR, Frye MA, Denicoff KD, et al. Antidepressant discontinuation-related mania: critical prospective observation and theoretical implications in bipolar disorder. J Clin Psychiatry. 1999;60(8):563-567.
32. Goldberg JF, Burdick KE, Endick CE. A preliminary randomized, double-blind, placebo-controlled trial of pramipexole added to mood stabilizers for treatment-resistant bipolar depression. Am J Psychiatry. 2004;161:564-566.
33. Zarate CA, Jr, Payne JL, Singh J, et al. Pramipexole for bipolar II depression: a placebo-controlled proof of concept study. Biol Psychiatry. 2004;56:54-60.
34. Frye MA, Grunze H, Suppes T, et al. A placebo-controlled evaluation of adjunctive modafinil in the treatment of bipolar depression. Am J Psychiatry. 2007;164(8):1242-1249.
35. Zarate CA, Jr, Quiroz JA, Singh JB, et al. An open-label trial of the glutamate-modulating agent riluzole in combination with lithium for the treatment of bipolar depression. Biol Psychiatry. 2005;57(4):430-432.
36. Berk M, Copolov DL, Dean O, et al. N-acetyl cysteine for depressive symptoms in bipolar disorder—a double-blind, randomized placebo-controlled trial. Biol Psychiatry. 2008;64(6):468-475.
How to treat PTSD in patients with comorbid mood disorders
Major depressive disorder (MDD) and bipolar spectrum disorders are associated with some symptoms of—and fully defined—posttraumatic stress disorder (PTSD). Many traumatic experiences can lead to this comorbidity, the most common being exposure to or witnessing combat for men and rape and sexual molestation for women.1
Trauma has major prognostic and treatment implications for affectively ill patients, including those whose symptoms do not meet PTSD’s full diagnostic criteria. This article aims to help clinicians by:
- presenting evidence characterizing the overlap between affective disorders and PTSD
- reviewing evidence that the bipolar spectrum may be broader than generally thought, an insight that affects PTSD treatment
- making a case for routine PTSD screening for all patients with affective illnesses
- recommending PTSD treatments tailored to the patient’s comorbid affective disorder.
Overlap of trauma and affective illness
PTSD is remarkably comorbid with mood disorders. Americans with MDD and bipolar disorder (BPD) are 7 and 9.4 times, respectively, more likely to meet criteria for PTSD than persons in the general population, according to odds ratios Kessler et al2 calculated from the National Comorbidity Survey database.
I have never seen a patient with PTSD who did not also meet criteria for an affective disorder. The concurrence of PTSD and MDD is not the product of overlapping diagnostic criteria. Rather, evidence indicates these are distinct diagnostic entities.3 A review of diagnostic criteria for PTSD and hypomania/mania leads to the same conclusion.
Bipolar spectrum disorders
DSM-IV-TR assumes that mood disorders fall neatly into boxes. Other data (Table 1)4–8 indicate that these disorders fall along a continuum or—more conservatively—that the scope of bipolarity is much wider than DSM-IV-TR recognizes. This is a controversial topic, and the individual clinician’s position could impact how one manages PTSD patients.
Table 1
Evidence of bipolar spectrum features in major depressive episodes
| Study | Design | Conclusion |
|---|---|---|
| Akiskal and Mallya, 19874 | 200 community mental health clinic patients diagnosed as having MDD | 50% could be classified as having a bipolar disorder |
| Benazzi, 19975 | 203 consecutively presenting patients with depression | 45% met criteria for bipolar II disorder |
| Akiskal and Benazzi, 20056 | 563 consecutive patients presenting with a DSM-IV-diagnosed MDE | 58% showed features of bipolar II disorder |
| Akiskal et al, 20067 | 493 patients in a French national study presenting with MDE | 65% were determined to fall along the ‘bipolar spectrum’ |
| Rabakowski et al, 20058 | 880 Polish outpatients presenting with MDE | 40% met criteria for bipolar disorder |
| MDD: major depressive disorder; MDE: major depressive episode | ||
In this article, I include bipolar I disorder, bipolar II disorder, and mixed depression within the “bipolar spectrum disorders.” If one accepts this—and I do—it follows that 50% to 70% of all major depressive episodes (MDEs) are bipolar in nature.4–9 Depending on your practice setting, you may see a higher or lower base rate of bipolar spectrum disorders.
Mixed depression is not recognized in DSM-IV-TR, and the purpose of this article is not to defend its inclusion as a bipolar spectrum phenomenon. A proposed definition of mixed depression9 requires the presence of an MDE contaminated by ≥3 features of hypomania or mania, without euphoria or inflated self-esteem/grandiosity (Table 2).10
Some experts believe episodes of hypomania and mania frequently occur in the illness course of persons with mixed depression; indeed, mixed depression is a predictor of a bipolar course. It is observed in outpatient9 and inpatient settings.11 Common forms of mixed depression feature combinations of irritability, psychomotor agitation (mild to severe), increased talkativeness (which may fall short of frank pressured speech), racing or “crowded” thoughts (or “mental overactivity”), and distractibility. Other than increased self-esteem/grandiosity, any symptoms within DSM-IV-TR criterion B for a hypomanic or manic episode may be seen in mixed depression. Psychosis is an exclusion criterion for mixed depression.
Mixed depression responds poorly to antidepressant monotherapy. Validation studies suggest that mixed depression is a bipolar variant, as determined by its capacity to predict a bipolar course and its association with a family history of bipolar disorder and age of onset.9
Table 2
Diagnostic characteristics of a hypomanic episode, DSM-IV-TR criteria A and B
| A. A distinct period of persistently elevated, expansive, or irritable mood, lasting throughout at least 4 days, that is clearly different from the usual nondepressed mood. |
| B. During the period of mood disturbance, 3 or more of the following symptoms have persisted (4 if the mood is only irritable) and have been present to a significant degree: 1) inflated self-esteem or grandiosity 2) decreased need for sleep (eg, feels rested after only 3 hours of sleep) 3) more talkative than usual or pressure to keep talking 4) flight of ideas or subjective experience that thoughts are racing 5) distractibility (ie, attention too easily drawn to unimportant or irrelevant external stimuli) 6) increase in goal-directed activity (either socially, at work or school, or sexually) or psychomotor agitation 7) excessive involvement in pleasurable activities that have a high potential for painful consequences (eg, the person engages in unrestrained buying sprees, sexual indiscretions, or foolish business investments). |
| Source: Diagnostic and statistical manual of mental disorders, 4th ed, text rev. Washington, DC: American Psychiatric Association; 2000 |
PTSD risk in affective illness
An adolescent sample. A preliminary cross-sectional study conducted by our group indicates that adolescents with affective disorders may have a much higher risk of developing PTSD than psychiatric comparison subjects.12 We used modules from the Structured Clinical Interview for DSM-IV (SCID) to screen for intra-episode psychopathology (as opposed to lifetime prevalence of disorders) in 79 adolescents with MDD, 34 with BPD as defined in the DSM-IV-TR, and 26 with neither affective disorder (psychiatric controls). We found:
- 38.2% of subjects with BPD met criteria for PTSD, compared with 13.9% of those with MDD (OR 4.9; P =.001)
- 3.8% of adolescents without a mood disorder met criteria for PTSD.
We also found that comorbid PTSD was associated with a 4.5-fold higher risk of a suicide attempt, even after we controlled for BPD diagnosis. When we controlled for the presence of other concurrent anxiety disorders, the likelihood of an adolescent with PTSD having attempted suicide remained significant (OR 3.4; P=.023). This finding suggests that PTSD is an independent risk factor for a suicide attempt.
An adult sample. We then focused on adults meeting criteria for MDD or BPD. In a study of 187 consecutively presenting affectively ill patients, we used the SCID to screen for multiple anxiety disorders including PTSD.13 Lifetime—as opposed to intra-episode—PTSD prevalence was 23.8% among the 118 patients with MDD and 62.3% among the 69 patients with BPD. A patient with BPD was 5 times more likely to have PTSD than a patient with MDD (OR 5.3; P < .0001). The most common cause of trauma leading to PTSD was sexual molestation or rape as a child or adolescent in this predominantly female Latino population.
Populations at risk for PTSD
The prevalence of PTSD in clinical samples varies, depending on the population studied. For instance, women are at much higher risk for developing PTSD than men, even in comparisons where men are exposed to a greater number of traumatic events and analyses control for differences in the prevalence of sexual abuse. The gender difference is greater if the trauma occurs during childhood.14 Essentially all patients in our adolescent and adult studies developed PTSD in response to childhood or adolescent sexual trauma.12,13
A population exposed to a high rate of violent crime would be expected to show a higher PTSD prevalence than one exposed to substantially less violence. The base rate of PTSD also is much higher in affectively ill patients than in the general population.
An analysis by Otto et al15 found a 16% lifetime prevalence of concomitant PTSD in 1,214 persons with BPD (not the manifold forms within the bipolar spectrum). Oquendo et al16 reported a 25.7% lifetime prevalence of PTSD in 230 patients with a history of MDD. Other epidemiologic2 and clinical studies12,13 suggest a considerably higher base rate of PTSD among persons with bipolar disorders than those with MDD.
The method of ascertaining the presence of this disorder may be another variable affecting the reported PTSD prevalence. Persistent avoidance—including “efforts to avoid thoughts, feelings, or conversations associated with the trauma”—is a diagnostic feature of PTSD.10 Researchers and clinicians who do not intentionally screen patients for PTSD are not likely to detect it. Determining the true prevalence of PTSD requires empathic inquiry about exposure to traumatic events.
PTSD screening
Humans are remarkably resilient, and most persons exposed to major trauma are thought not to develop PTSD. However, in my experience, because PTSD appears to be common among persons with affective illness, determining whether such patients have been traumatized is important for prognosis and treatment selection.
To get started, you could create a 1-page form to record traumatic events and identify features of PTSD according to DSM-IV-TR criteria (Checklist).10 PTSD screening without a form can become second nature with practice; an experienced clinician can screen a traumatized patient for the disorder within 3 to 5 minutes.
When screening for a history of trauma, ask patients in a straightforward manner if they have:
- been victims of violent crimes
- witnessed violent crimes
- been exposed to events in which people could have suffered grave injury
- experienced emotional, physical, or sexual abuse.
A person who has experienced emotional abuse but not physical or sexual abuse cannot meet DSM-IV-TR criterion A and therefore does not meet full criteria for PTSD. Many emotionally abused persons meet criteria B through F, however, and they are most reasonably managed similarly to persons who also meet criterion A. When formulating a treatment plan, I recommend using clinical judgment rather than rigid adherence to DSM-IV-TR.
Checklist
DSM-IV-TR diagnostic criteria for posttraumatic stress disorder
| Criterion A. The person has been exposed to a traumatic event in which both of the following have been present: | |
| □ | 1. The person has experienced, witnessed, or been confronted with an event or events that involve actual or threatened death or serious injury, or a threat to the physical integrity of oneself or others |
| □ | 2. The person’s response involved intense fear, helplessness, or horror |
| Criterion B. The traumatic event is persistently re-experienced in at least 1 of the following ways: | |
| □ | 1. Recurrent and intrusive distressing recollections of the event, including images, thoughts, or perceptions |
| □ | 2. Recurrent distressing dreams of the event |
| □ | 3. Acting or feeling as if the traumatic event were recurring (includes a sense of reliving the experience, illusions, hallucinations, and dissociative flashback episodes, including those that occur upon awakening or when intoxicated) |
| □ | 4. Intense psychological distress at exposure to internal or external cues that symbolize or resemble an aspect of the traumatic event |
| □ | 5. Physiologic reactivity upon exposure to internal or external cues that symbolize or resemble an aspect of the traumatic event |
| Criterion C. Persistent avoidance of stimuli associated with the trauma and numbing of general responsiveness (not present before the trauma), as indicated by at least 3 of the following: | |
| □ | 1. Efforts to avoid thoughts, feelings, or conversations associated with the trauma |
| □ | 2. Efforts to avoid activities, places, or people that arouse recollections of the trauma |
| □ | 3. Inability to recall an important aspect of the trauma |
| □ | 4. Markedly diminished interest or participation in significant activities |
| □ | 5. Feeling of detachment or estrangement from others |
| □ | 6. Restricted range of affect |
| □ | 7. Sense of foreshortened future |
| Criterion D. Persistent symptoms of increasing arousal (not present before the trauma), indicated by at least 2 of the following: | |
| □ | 1. Difficulty falling or staying asleep |
| □ | 2. Irritability or outbursts of anger |
| □ | 3. Difficulty concentrating |
| □ | 4. Hypervigilance |
| □ | 5. Exaggerated startle response |
| □ | Criterion E. Duration of disturbance (symptoms in B, C, and D) is >1 month |
| □ | Criterion F. Disturbance causes clinically significant distress or impairment in social, occupational, or other important areas of functioning |
| Source: Adapted from Diagnostic and statistical manual of mental disorders, 4th ed, text rev. Washington, DC: American Psychiatric Association; 2000 | |
Treating PTSD in depression
Pharmacotherapy and psychotherapeutic interventions are important to PTSD patients’ recovery. Limited resources often prevent these patients from receiving expert psychotherapeutic intervention, however, leaving pharmacotherapy as the mainstay of treatment. This is unfortunate, because psychological interventions may be sufficient and preferred in some instances (Box).17–20
Pharmacotherapy for comorbid MDD. Selective serotonin reuptake inhibitors (SSRIs) and venlafaxine are first-line interventions for PTSD in depressed patients who do not meet criteria for a bipolar spectrum disorder. Placebo-controlled studies suggest that sertraline,21,22 fluoxetine,23 and paroxetine,24 are effective; doses higher than those used to treat depression may be required. Extended-release venlafaxine25 in dosages similar to those needed for depressive disorders also can be effective. Bupropion does not appear to be beneficial in treating PTSD.
The monoamine oxidase inhibitor phenelzine was long used successfully in treating PTSD but for the most part has been replaced by SSRIs. Because of its associated dietary restrictions, risk of hypertensive crises, and other side effects, phenelzine probably is best reserved for patients who do not respond to treatment with SSRIs or venlafaxine.
Pharmacotherapy for comorbid bipolar spectrum. If one accepts that most patients meeting criteria for MDE have a bipolar spectrum disorder, then most affectively ill patients with PTSD would need to be treated as if they have bipolar disorder. Oddly enough, this creates difficulties for the use of not only antidepressants and benzodiazepines, but also mood stabilizers:
- Patients with BPD and comorbid anxiety disorders, including PTSD, may be resistant to mood stabilizers.26,27
- Antidepressants can precipitate hypomanic or manic switches or onset of mixed hypomania, a mixed state, or rapid cycling in patients with a bipolar spectrum disorder.28–30
- Benzodiazepines do not appear to relieve acute or chronic PTSD-related distress, and discontinuation could cause rebound symptoms.31
Because no outcome studies have addressed PTSD management in patients with bipolar spectrum disorders, clinicians must rely on their judgment when formulating treatment plans. One strategy is to treat patients with mood stabilizers, then leave well enough alone if both the mood and anxiety symptoms remit (which is possible but unlikely in my experience). I often start treatment for the bipolar spectrum disorder and co-existing PTSD using mood stabilizers (including atypical antipsychotics) and prazosin, an α-1antagonist originally used for treating hypertension.
Prazosin can help diminish nightmares, dreams, and other painful recollections of trauma.32,33 The drug does not affect time to sleep onset. It also has been reported to reduce avoidance behavior and hyperarousal, such as irritability and anger.34 This has been my experience.
Cognitive-behavioral therapy (CBT) involving prolonged exposure (PE) to trauma-related stimuli has been shown to be effective for posttraumatic stress disorder (PTSD) in controlled studies.17,18 PE is an individual CBT designed to help patients process traumatic events and reduce psychological distress. It involves education about reactions to trauma, relaxation techniques, imaginal reliving of the trauma, exposure to cues associated with the trauma, and cognitive restructuring.
Administering D-cycloserine before behavioral treatment sessions facilitates fear extinction, and its use to enhance prolonged PE constitutes state-of-the-art treatment.19 Eye movement desensitization and reprocessing also may be effective.18,20
PE is a reasonable first-line treatment for PTSD patients with comorbid bipolar spectrum disorders when PTSD symptoms persist after pharmacologic treatment for the bipolar spectrum disorder. PE also is a first-line treatment for PTSD in patients with comorbid major depressive disorder. Barriers to PE treatment include its cost and finding professionals who are expert in its use.
Prazosin to treat PTSD-related symptoms in children or adolescents has not been studied, but it can be useful in adults over a wide range of doses. As little as 1 mg at bedtime may confer benefit, although the mean prazosin dose in an 8-week, placebo-controlled study of 40 combat veterans was 13.3 mg in the evening.33
I often initiate prazosin treatment as follows:
- 1 mg on the first night of treatment
- 2 mg on the second night
- 3 mg on the third night
- then, if tolerated, 1 mg upon waking, 1 mg 8 hours later, and 3 mg at bedtime. I then slowly adjust the dose schedule based on the patient’s needs, such as minimizing painful re-experiencing of the trauma. Reducing avoidance and hyperarousal also are reasonable targets. For example, when using prazosin to treat extremely angry men with PTSD stemming from exposure to violent crimes, I have observed that even “murderous” rage ceases with prazosin treatment, only to reappear when prazosin is discontinued.
In treating approximately 100 patients with prazosin, I have not exceeded 16 mg/d. Dosages used for treating hypertension usually are 5 to 20 mg/d. When using prazosin, I always:
- warn patients that faintness or fainting is a side effect and record this caveat in their chart
- obtain sitting and standing blood pressure and pulse before starting treatment and subsequently
- ask patients if they feel dizzy when changing posture before and after initiating treatment.
Most of my PTSD patients are suffering so much that they are willing to accept the risk of fainting associated with prazosin use. For PTSD comorbid with severe panic disorder,12,13 I find that a benzodiazepine with antipanic properties such as alprazolam or clonazepam often works well in conjunction with prazosin.
Some patients with bipolar spectrum disorders might benefit from the addition of an SSRI after mood stabilizer treatment proves effective. However, I have never managed a patient in this manner, and like my own treatment strategy, this has not been subjected to rigorous empiric inquiry. In my view, psychological treatment is much preferred to antidepressant therapy.
Related resource
- Benazzi F. Bipolar disorder—focus on bipolar II disorder and mixed depression. Lancet. 2007;369:935-945.
Drug brand names
- Alprazolam • Xanax
- Bupropion • Wellbutrin
- Clonazepam • Klonopin
- D-cycloserine • Seromycin
- Fluoxetine • Prozac
- Paroxetine • Paxil
- Phenelzine • Nardil
- Prazosin • Minipress
- Sertraline • Zoloft
- Venlafaxine • Effexor
Disclosure
Dr. Dilsaver reports no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
1. Kessler RC, Berglund P, Demler O, et al. The epidemiology of major depressive disorder: results from the National Comorbidity-Replication (NCS-R). JAMA. 2003;289:3095-3105.
2. Kessler RC, Sonnega A, Bromet E, et al. Posttraumatic stress disorder in the National Comorbidity Survey. Arch Gen Psychiatry. 1995;52:1048-1060.
3. Franklin CL, Zimmerman M. Posttraumatic stress disorder and major depressive disorder: investigating the role of overlapping symptoms in diagnostic comorbidity. J Nerv Ment Dis. 2001;189:548-551.
4. Akiskal HS, Mallya G. Criteria for the “soft” bipolar spectrum: treatment implications. Psychopharmacol Bull. 1987;23:68-73.
5. Benazzi F. Prevalence of bipolar II disorder in outpatient depression: a 203-case study in a private practice. J Affect Disord. 1997;43:163-164.
6. Akiskal HS, Benazzi F. Optimizing the detection of bipolar II in outpatient private practice: toward a systematization of clinical diagnostic wisdom. J Clin Psychiatry. 2005;66:914-921.
7. Akiskal HS, Akiskal KK, Lancrenon S, et al. Validating the soft bipolar spectrum in the French National EPIDEP study: the prominence of BP-II. J Affect Disord. 2006;96:207-213.
8. Rabakowski JK, Suwalska D, Lojko D, et al. Bipolar disorders among Polish psychiatric outpatients treated for major depression. J Affect Disord. 2005;84:141-147.
9. Benazzi F. Bipolar disorder—focus on bipolar II disorder and mixed depression. Lancet. 2007;369:935-945.
10. Diagnostic and statistical manual of mental disorders, 4th ed, text rev. Washington, DC: American Psychiatric Association; 2000.
11. Maj M, Pirozzi R, Magliano, et al. Agitated ‘unipolar’ major depression: prevalence, phenomenology, and outcome. J Clin Psychiatry. 2006;67:712-719.
12. Dilsaver SC, Benazzi F, Akiskal HS, et al. Post-traumatic stress disorder among adolescents with bipolar disorder and its relationship to suicidality. Bipolar Disord. 2007;9:649-655.
13. Dilsaver SC, Benazzi F, Akiskal KK, et al. Differential patterns of lifetime multiple anxiety disorder comorbidity between Latino adults with bipolar I and major depressive disorders. Bull Menninger Clinic. 2008;72:130-148.
14. Stein MB, Walker JR, Forde DR. Gender differences in susceptibility to posttraumatic stress disorder. Behav Res Ther. 2000;38:619-628.
15. Otto MW, Perlman CA, Wernicke R, et al. Posttraumatic stress disorder in patients with bipolar disorder: a review of prevalence, correlates, and treatment strategies. Bipolar Disord. 2004;6:470-479.
16. Oquendo M, Brent DA, Birmaher B, et al. Posttraumatic stress disorder comorbid with major depression: factors mediating the association with suicidal behavior. Am J Psychiatry. 2005;162:560-566.
17. Schnurr PP, Friedman MJ, Engel CC, et al. Cognitive behavioral therapy for posttraumatic stress disorder in women: a randomized-controlled trial. JAMA. 2007;297:820-830.
18. Bisson J, Andrew M. Psychological treatment for posttraumatic stress disorder (PTSD). Cochrane Database Syst Rev. 2005;CD003388.-
19. Cukor J, Spitalnick J, Difede J, et al. Emerging treatments for PTSD. Clin Psychol Rev. 2009;29(8):715-726.
20. Hogberg G, Pagani M, Sundin O, et al. Treatment of posttraumatic stress disorder with eye movement desensitization and reprocessing: outcome is stable in 35-month follow-up. Psychiatry Res. 2008;159(1-2):101-108.
21. Brady K, Pearlstein T, Asnis GM, et al. Efficacy and safety of sertraline treatment of posttraumatic stress disorder: a randomized controlled trial. JAMA. 2000;283:1837-1844.
22. Friedman MJ, Marmar CR, Baker DG, et al. Randomized, double-blind comparison of sertraline and placebo for posttraumatic stress disorder in a Department of Veterans Affairs setting. J Clin Psychiatry. 2007;68:711-720.
23. Martenyi F, Brown EB, Zhang H, et al. Fluoxetine versus placebo in posttraumatic stress disorder. J Clin Psychiatry. 2002;63:199-206.
24. Tucker P, Zaninelli R, Yehuda R, et al. Paroxetine in the treatment of chronic posttraumatic stress disorder: results of a placebo-controlled, flexible-dosage trial. J Clin Psychiatry. 2001;62:860-868.
25. Pae CU, Lim HK, Ajwani N, et al. Extended-release formulation of venlafaxine in the treatment of post-traumatic stress disorder. Expert Rev Neurother. 2007;7:603-615.
26. Simon NM, Otto MW, Weiss RD, et al. Pharmacotherapy for bipolar disorder and comorbid conditions: baseline data from the STEP-BD. J Clin Psychopharmacol. 2004;24(5):512-520.
27. Quarantini LC, Miranda-Scippa A, Nery-Fernandes F, et al. The impact of comorbid posttraumatic stress disorder on bipolar patients. Affect Disord. 2009; [Epub ahead of print].
28. Henry C, Sorbara F, Lacoste J, et al. Antidepressant induced mania in bipolar patients: identification and risk factors. J Clin Psychiatry. 2001;62:249-255.
29. Gao K, Kemp DE, Gonocy SJ, et al. Treatment-emergent mania/hypomania during antidepressant monotherapy in patients with rapid cycling bipolar disorder. Bipolar Disord. 2008;10:907-915.
30. Dilsaver SC, Swann AC. Mixed mania: apparent induction by a tricyclic antidepressant in five consecutively treated patients with bipolar depression. Biol Psychiatry. 1995;1:60-62.
31. Braun P, Greenberg D, Dasberg H, et al. Core symptoms of posttraumatic stress disorder unimproved by alprazolam treatment. J Clin Psychiatry. 1990;51:236-238.
32. Taylor FB, Martin P, Thompson C, et al. Prazosin effects on objective sleep measures and clinical symptoms in civilian trauma posttraumatic stress disorder: a placebo-controlled study. Biol Psychiatry. 2008;63:629-632.
33. Raskind MA, Perskind ER, Hoff DJ, et al. A parallel group placebo controlled study of prazosin for trauma nightmares and sleep disturbance in combat veterans with posttraumatic stress disorder. Biol Psychiatry. 2007;61:928-934.
34. Taylor FB, Lowe K, Thompson C, et al. Daytime prazosin reduces psychological distress to trauma specific cues in civilian trauma posttraumatic stress disorder. Biol Psychiatry. 2006;59:577-581.
Major depressive disorder (MDD) and bipolar spectrum disorders are associated with some symptoms of—and fully defined—posttraumatic stress disorder (PTSD). Many traumatic experiences can lead to this comorbidity, the most common being exposure to or witnessing combat for men and rape and sexual molestation for women.1
Trauma has major prognostic and treatment implications for affectively ill patients, including those whose symptoms do not meet PTSD’s full diagnostic criteria. This article aims to help clinicians by:
- presenting evidence characterizing the overlap between affective disorders and PTSD
- reviewing evidence that the bipolar spectrum may be broader than generally thought, an insight that affects PTSD treatment
- making a case for routine PTSD screening for all patients with affective illnesses
- recommending PTSD treatments tailored to the patient’s comorbid affective disorder.
Overlap of trauma and affective illness
PTSD is remarkably comorbid with mood disorders. Americans with MDD and bipolar disorder (BPD) are 7 and 9.4 times, respectively, more likely to meet criteria for PTSD than persons in the general population, according to odds ratios Kessler et al2 calculated from the National Comorbidity Survey database.
I have never seen a patient with PTSD who did not also meet criteria for an affective disorder. The concurrence of PTSD and MDD is not the product of overlapping diagnostic criteria. Rather, evidence indicates these are distinct diagnostic entities.3 A review of diagnostic criteria for PTSD and hypomania/mania leads to the same conclusion.
Bipolar spectrum disorders
DSM-IV-TR assumes that mood disorders fall neatly into boxes. Other data (Table 1)4–8 indicate that these disorders fall along a continuum or—more conservatively—that the scope of bipolarity is much wider than DSM-IV-TR recognizes. This is a controversial topic, and the individual clinician’s position could impact how one manages PTSD patients.
Table 1
Evidence of bipolar spectrum features in major depressive episodes
| Study | Design | Conclusion |
|---|---|---|
| Akiskal and Mallya, 19874 | 200 community mental health clinic patients diagnosed as having MDD | 50% could be classified as having a bipolar disorder |
| Benazzi, 19975 | 203 consecutively presenting patients with depression | 45% met criteria for bipolar II disorder |
| Akiskal and Benazzi, 20056 | 563 consecutive patients presenting with a DSM-IV-diagnosed MDE | 58% showed features of bipolar II disorder |
| Akiskal et al, 20067 | 493 patients in a French national study presenting with MDE | 65% were determined to fall along the ‘bipolar spectrum’ |
| Rabakowski et al, 20058 | 880 Polish outpatients presenting with MDE | 40% met criteria for bipolar disorder |
| MDD: major depressive disorder; MDE: major depressive episode | ||
In this article, I include bipolar I disorder, bipolar II disorder, and mixed depression within the “bipolar spectrum disorders.” If one accepts this—and I do—it follows that 50% to 70% of all major depressive episodes (MDEs) are bipolar in nature.4–9 Depending on your practice setting, you may see a higher or lower base rate of bipolar spectrum disorders.
Mixed depression is not recognized in DSM-IV-TR, and the purpose of this article is not to defend its inclusion as a bipolar spectrum phenomenon. A proposed definition of mixed depression9 requires the presence of an MDE contaminated by ≥3 features of hypomania or mania, without euphoria or inflated self-esteem/grandiosity (Table 2).10
Some experts believe episodes of hypomania and mania frequently occur in the illness course of persons with mixed depression; indeed, mixed depression is a predictor of a bipolar course. It is observed in outpatient9 and inpatient settings.11 Common forms of mixed depression feature combinations of irritability, psychomotor agitation (mild to severe), increased talkativeness (which may fall short of frank pressured speech), racing or “crowded” thoughts (or “mental overactivity”), and distractibility. Other than increased self-esteem/grandiosity, any symptoms within DSM-IV-TR criterion B for a hypomanic or manic episode may be seen in mixed depression. Psychosis is an exclusion criterion for mixed depression.
Mixed depression responds poorly to antidepressant monotherapy. Validation studies suggest that mixed depression is a bipolar variant, as determined by its capacity to predict a bipolar course and its association with a family history of bipolar disorder and age of onset.9
Table 2
Diagnostic characteristics of a hypomanic episode, DSM-IV-TR criteria A and B
| A. A distinct period of persistently elevated, expansive, or irritable mood, lasting throughout at least 4 days, that is clearly different from the usual nondepressed mood. |
| B. During the period of mood disturbance, 3 or more of the following symptoms have persisted (4 if the mood is only irritable) and have been present to a significant degree: 1) inflated self-esteem or grandiosity 2) decreased need for sleep (eg, feels rested after only 3 hours of sleep) 3) more talkative than usual or pressure to keep talking 4) flight of ideas or subjective experience that thoughts are racing 5) distractibility (ie, attention too easily drawn to unimportant or irrelevant external stimuli) 6) increase in goal-directed activity (either socially, at work or school, or sexually) or psychomotor agitation 7) excessive involvement in pleasurable activities that have a high potential for painful consequences (eg, the person engages in unrestrained buying sprees, sexual indiscretions, or foolish business investments). |
| Source: Diagnostic and statistical manual of mental disorders, 4th ed, text rev. Washington, DC: American Psychiatric Association; 2000 |
PTSD risk in affective illness
An adolescent sample. A preliminary cross-sectional study conducted by our group indicates that adolescents with affective disorders may have a much higher risk of developing PTSD than psychiatric comparison subjects.12 We used modules from the Structured Clinical Interview for DSM-IV (SCID) to screen for intra-episode psychopathology (as opposed to lifetime prevalence of disorders) in 79 adolescents with MDD, 34 with BPD as defined in the DSM-IV-TR, and 26 with neither affective disorder (psychiatric controls). We found:
- 38.2% of subjects with BPD met criteria for PTSD, compared with 13.9% of those with MDD (OR 4.9; P =.001)
- 3.8% of adolescents without a mood disorder met criteria for PTSD.
We also found that comorbid PTSD was associated with a 4.5-fold higher risk of a suicide attempt, even after we controlled for BPD diagnosis. When we controlled for the presence of other concurrent anxiety disorders, the likelihood of an adolescent with PTSD having attempted suicide remained significant (OR 3.4; P=.023). This finding suggests that PTSD is an independent risk factor for a suicide attempt.
An adult sample. We then focused on adults meeting criteria for MDD or BPD. In a study of 187 consecutively presenting affectively ill patients, we used the SCID to screen for multiple anxiety disorders including PTSD.13 Lifetime—as opposed to intra-episode—PTSD prevalence was 23.8% among the 118 patients with MDD and 62.3% among the 69 patients with BPD. A patient with BPD was 5 times more likely to have PTSD than a patient with MDD (OR 5.3; P < .0001). The most common cause of trauma leading to PTSD was sexual molestation or rape as a child or adolescent in this predominantly female Latino population.
Populations at risk for PTSD
The prevalence of PTSD in clinical samples varies, depending on the population studied. For instance, women are at much higher risk for developing PTSD than men, even in comparisons where men are exposed to a greater number of traumatic events and analyses control for differences in the prevalence of sexual abuse. The gender difference is greater if the trauma occurs during childhood.14 Essentially all patients in our adolescent and adult studies developed PTSD in response to childhood or adolescent sexual trauma.12,13
A population exposed to a high rate of violent crime would be expected to show a higher PTSD prevalence than one exposed to substantially less violence. The base rate of PTSD also is much higher in affectively ill patients than in the general population.
An analysis by Otto et al15 found a 16% lifetime prevalence of concomitant PTSD in 1,214 persons with BPD (not the manifold forms within the bipolar spectrum). Oquendo et al16 reported a 25.7% lifetime prevalence of PTSD in 230 patients with a history of MDD. Other epidemiologic2 and clinical studies12,13 suggest a considerably higher base rate of PTSD among persons with bipolar disorders than those with MDD.
The method of ascertaining the presence of this disorder may be another variable affecting the reported PTSD prevalence. Persistent avoidance—including “efforts to avoid thoughts, feelings, or conversations associated with the trauma”—is a diagnostic feature of PTSD.10 Researchers and clinicians who do not intentionally screen patients for PTSD are not likely to detect it. Determining the true prevalence of PTSD requires empathic inquiry about exposure to traumatic events.
PTSD screening
Humans are remarkably resilient, and most persons exposed to major trauma are thought not to develop PTSD. However, in my experience, because PTSD appears to be common among persons with affective illness, determining whether such patients have been traumatized is important for prognosis and treatment selection.
To get started, you could create a 1-page form to record traumatic events and identify features of PTSD according to DSM-IV-TR criteria (Checklist).10 PTSD screening without a form can become second nature with practice; an experienced clinician can screen a traumatized patient for the disorder within 3 to 5 minutes.
When screening for a history of trauma, ask patients in a straightforward manner if they have:
- been victims of violent crimes
- witnessed violent crimes
- been exposed to events in which people could have suffered grave injury
- experienced emotional, physical, or sexual abuse.
A person who has experienced emotional abuse but not physical or sexual abuse cannot meet DSM-IV-TR criterion A and therefore does not meet full criteria for PTSD. Many emotionally abused persons meet criteria B through F, however, and they are most reasonably managed similarly to persons who also meet criterion A. When formulating a treatment plan, I recommend using clinical judgment rather than rigid adherence to DSM-IV-TR.
Checklist
DSM-IV-TR diagnostic criteria for posttraumatic stress disorder
| Criterion A. The person has been exposed to a traumatic event in which both of the following have been present: | |
| □ | 1. The person has experienced, witnessed, or been confronted with an event or events that involve actual or threatened death or serious injury, or a threat to the physical integrity of oneself or others |
| □ | 2. The person’s response involved intense fear, helplessness, or horror |
| Criterion B. The traumatic event is persistently re-experienced in at least 1 of the following ways: | |
| □ | 1. Recurrent and intrusive distressing recollections of the event, including images, thoughts, or perceptions |
| □ | 2. Recurrent distressing dreams of the event |
| □ | 3. Acting or feeling as if the traumatic event were recurring (includes a sense of reliving the experience, illusions, hallucinations, and dissociative flashback episodes, including those that occur upon awakening or when intoxicated) |
| □ | 4. Intense psychological distress at exposure to internal or external cues that symbolize or resemble an aspect of the traumatic event |
| □ | 5. Physiologic reactivity upon exposure to internal or external cues that symbolize or resemble an aspect of the traumatic event |
| Criterion C. Persistent avoidance of stimuli associated with the trauma and numbing of general responsiveness (not present before the trauma), as indicated by at least 3 of the following: | |
| □ | 1. Efforts to avoid thoughts, feelings, or conversations associated with the trauma |
| □ | 2. Efforts to avoid activities, places, or people that arouse recollections of the trauma |
| □ | 3. Inability to recall an important aspect of the trauma |
| □ | 4. Markedly diminished interest or participation in significant activities |
| □ | 5. Feeling of detachment or estrangement from others |
| □ | 6. Restricted range of affect |
| □ | 7. Sense of foreshortened future |
| Criterion D. Persistent symptoms of increasing arousal (not present before the trauma), indicated by at least 2 of the following: | |
| □ | 1. Difficulty falling or staying asleep |
| □ | 2. Irritability or outbursts of anger |
| □ | 3. Difficulty concentrating |
| □ | 4. Hypervigilance |
| □ | 5. Exaggerated startle response |
| □ | Criterion E. Duration of disturbance (symptoms in B, C, and D) is >1 month |
| □ | Criterion F. Disturbance causes clinically significant distress or impairment in social, occupational, or other important areas of functioning |
| Source: Adapted from Diagnostic and statistical manual of mental disorders, 4th ed, text rev. Washington, DC: American Psychiatric Association; 2000 | |
Treating PTSD in depression
Pharmacotherapy and psychotherapeutic interventions are important to PTSD patients’ recovery. Limited resources often prevent these patients from receiving expert psychotherapeutic intervention, however, leaving pharmacotherapy as the mainstay of treatment. This is unfortunate, because psychological interventions may be sufficient and preferred in some instances (Box).17–20
Pharmacotherapy for comorbid MDD. Selective serotonin reuptake inhibitors (SSRIs) and venlafaxine are first-line interventions for PTSD in depressed patients who do not meet criteria for a bipolar spectrum disorder. Placebo-controlled studies suggest that sertraline,21,22 fluoxetine,23 and paroxetine,24 are effective; doses higher than those used to treat depression may be required. Extended-release venlafaxine25 in dosages similar to those needed for depressive disorders also can be effective. Bupropion does not appear to be beneficial in treating PTSD.
The monoamine oxidase inhibitor phenelzine was long used successfully in treating PTSD but for the most part has been replaced by SSRIs. Because of its associated dietary restrictions, risk of hypertensive crises, and other side effects, phenelzine probably is best reserved for patients who do not respond to treatment with SSRIs or venlafaxine.
Pharmacotherapy for comorbid bipolar spectrum. If one accepts that most patients meeting criteria for MDE have a bipolar spectrum disorder, then most affectively ill patients with PTSD would need to be treated as if they have bipolar disorder. Oddly enough, this creates difficulties for the use of not only antidepressants and benzodiazepines, but also mood stabilizers:
- Patients with BPD and comorbid anxiety disorders, including PTSD, may be resistant to mood stabilizers.26,27
- Antidepressants can precipitate hypomanic or manic switches or onset of mixed hypomania, a mixed state, or rapid cycling in patients with a bipolar spectrum disorder.28–30
- Benzodiazepines do not appear to relieve acute or chronic PTSD-related distress, and discontinuation could cause rebound symptoms.31
Because no outcome studies have addressed PTSD management in patients with bipolar spectrum disorders, clinicians must rely on their judgment when formulating treatment plans. One strategy is to treat patients with mood stabilizers, then leave well enough alone if both the mood and anxiety symptoms remit (which is possible but unlikely in my experience). I often start treatment for the bipolar spectrum disorder and co-existing PTSD using mood stabilizers (including atypical antipsychotics) and prazosin, an α-1antagonist originally used for treating hypertension.
Prazosin can help diminish nightmares, dreams, and other painful recollections of trauma.32,33 The drug does not affect time to sleep onset. It also has been reported to reduce avoidance behavior and hyperarousal, such as irritability and anger.34 This has been my experience.
Cognitive-behavioral therapy (CBT) involving prolonged exposure (PE) to trauma-related stimuli has been shown to be effective for posttraumatic stress disorder (PTSD) in controlled studies.17,18 PE is an individual CBT designed to help patients process traumatic events and reduce psychological distress. It involves education about reactions to trauma, relaxation techniques, imaginal reliving of the trauma, exposure to cues associated with the trauma, and cognitive restructuring.
Administering D-cycloserine before behavioral treatment sessions facilitates fear extinction, and its use to enhance prolonged PE constitutes state-of-the-art treatment.19 Eye movement desensitization and reprocessing also may be effective.18,20
PE is a reasonable first-line treatment for PTSD patients with comorbid bipolar spectrum disorders when PTSD symptoms persist after pharmacologic treatment for the bipolar spectrum disorder. PE also is a first-line treatment for PTSD in patients with comorbid major depressive disorder. Barriers to PE treatment include its cost and finding professionals who are expert in its use.
Prazosin to treat PTSD-related symptoms in children or adolescents has not been studied, but it can be useful in adults over a wide range of doses. As little as 1 mg at bedtime may confer benefit, although the mean prazosin dose in an 8-week, placebo-controlled study of 40 combat veterans was 13.3 mg in the evening.33
I often initiate prazosin treatment as follows:
- 1 mg on the first night of treatment
- 2 mg on the second night
- 3 mg on the third night
- then, if tolerated, 1 mg upon waking, 1 mg 8 hours later, and 3 mg at bedtime. I then slowly adjust the dose schedule based on the patient’s needs, such as minimizing painful re-experiencing of the trauma. Reducing avoidance and hyperarousal also are reasonable targets. For example, when using prazosin to treat extremely angry men with PTSD stemming from exposure to violent crimes, I have observed that even “murderous” rage ceases with prazosin treatment, only to reappear when prazosin is discontinued.
In treating approximately 100 patients with prazosin, I have not exceeded 16 mg/d. Dosages used for treating hypertension usually are 5 to 20 mg/d. When using prazosin, I always:
- warn patients that faintness or fainting is a side effect and record this caveat in their chart
- obtain sitting and standing blood pressure and pulse before starting treatment and subsequently
- ask patients if they feel dizzy when changing posture before and after initiating treatment.
Most of my PTSD patients are suffering so much that they are willing to accept the risk of fainting associated with prazosin use. For PTSD comorbid with severe panic disorder,12,13 I find that a benzodiazepine with antipanic properties such as alprazolam or clonazepam often works well in conjunction with prazosin.
Some patients with bipolar spectrum disorders might benefit from the addition of an SSRI after mood stabilizer treatment proves effective. However, I have never managed a patient in this manner, and like my own treatment strategy, this has not been subjected to rigorous empiric inquiry. In my view, psychological treatment is much preferred to antidepressant therapy.
Related resource
- Benazzi F. Bipolar disorder—focus on bipolar II disorder and mixed depression. Lancet. 2007;369:935-945.
Drug brand names
- Alprazolam • Xanax
- Bupropion • Wellbutrin
- Clonazepam • Klonopin
- D-cycloserine • Seromycin
- Fluoxetine • Prozac
- Paroxetine • Paxil
- Phenelzine • Nardil
- Prazosin • Minipress
- Sertraline • Zoloft
- Venlafaxine • Effexor
Disclosure
Dr. Dilsaver reports no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
Major depressive disorder (MDD) and bipolar spectrum disorders are associated with some symptoms of—and fully defined—posttraumatic stress disorder (PTSD). Many traumatic experiences can lead to this comorbidity, the most common being exposure to or witnessing combat for men and rape and sexual molestation for women.1
Trauma has major prognostic and treatment implications for affectively ill patients, including those whose symptoms do not meet PTSD’s full diagnostic criteria. This article aims to help clinicians by:
- presenting evidence characterizing the overlap between affective disorders and PTSD
- reviewing evidence that the bipolar spectrum may be broader than generally thought, an insight that affects PTSD treatment
- making a case for routine PTSD screening for all patients with affective illnesses
- recommending PTSD treatments tailored to the patient’s comorbid affective disorder.
Overlap of trauma and affective illness
PTSD is remarkably comorbid with mood disorders. Americans with MDD and bipolar disorder (BPD) are 7 and 9.4 times, respectively, more likely to meet criteria for PTSD than persons in the general population, according to odds ratios Kessler et al2 calculated from the National Comorbidity Survey database.
I have never seen a patient with PTSD who did not also meet criteria for an affective disorder. The concurrence of PTSD and MDD is not the product of overlapping diagnostic criteria. Rather, evidence indicates these are distinct diagnostic entities.3 A review of diagnostic criteria for PTSD and hypomania/mania leads to the same conclusion.
Bipolar spectrum disorders
DSM-IV-TR assumes that mood disorders fall neatly into boxes. Other data (Table 1)4–8 indicate that these disorders fall along a continuum or—more conservatively—that the scope of bipolarity is much wider than DSM-IV-TR recognizes. This is a controversial topic, and the individual clinician’s position could impact how one manages PTSD patients.
Table 1
Evidence of bipolar spectrum features in major depressive episodes
| Study | Design | Conclusion |
|---|---|---|
| Akiskal and Mallya, 19874 | 200 community mental health clinic patients diagnosed as having MDD | 50% could be classified as having a bipolar disorder |
| Benazzi, 19975 | 203 consecutively presenting patients with depression | 45% met criteria for bipolar II disorder |
| Akiskal and Benazzi, 20056 | 563 consecutive patients presenting with a DSM-IV-diagnosed MDE | 58% showed features of bipolar II disorder |
| Akiskal et al, 20067 | 493 patients in a French national study presenting with MDE | 65% were determined to fall along the ‘bipolar spectrum’ |
| Rabakowski et al, 20058 | 880 Polish outpatients presenting with MDE | 40% met criteria for bipolar disorder |
| MDD: major depressive disorder; MDE: major depressive episode | ||
In this article, I include bipolar I disorder, bipolar II disorder, and mixed depression within the “bipolar spectrum disorders.” If one accepts this—and I do—it follows that 50% to 70% of all major depressive episodes (MDEs) are bipolar in nature.4–9 Depending on your practice setting, you may see a higher or lower base rate of bipolar spectrum disorders.
Mixed depression is not recognized in DSM-IV-TR, and the purpose of this article is not to defend its inclusion as a bipolar spectrum phenomenon. A proposed definition of mixed depression9 requires the presence of an MDE contaminated by ≥3 features of hypomania or mania, without euphoria or inflated self-esteem/grandiosity (Table 2).10
Some experts believe episodes of hypomania and mania frequently occur in the illness course of persons with mixed depression; indeed, mixed depression is a predictor of a bipolar course. It is observed in outpatient9 and inpatient settings.11 Common forms of mixed depression feature combinations of irritability, psychomotor agitation (mild to severe), increased talkativeness (which may fall short of frank pressured speech), racing or “crowded” thoughts (or “mental overactivity”), and distractibility. Other than increased self-esteem/grandiosity, any symptoms within DSM-IV-TR criterion B for a hypomanic or manic episode may be seen in mixed depression. Psychosis is an exclusion criterion for mixed depression.
Mixed depression responds poorly to antidepressant monotherapy. Validation studies suggest that mixed depression is a bipolar variant, as determined by its capacity to predict a bipolar course and its association with a family history of bipolar disorder and age of onset.9
Table 2
Diagnostic characteristics of a hypomanic episode, DSM-IV-TR criteria A and B
| A. A distinct period of persistently elevated, expansive, or irritable mood, lasting throughout at least 4 days, that is clearly different from the usual nondepressed mood. |
| B. During the period of mood disturbance, 3 or more of the following symptoms have persisted (4 if the mood is only irritable) and have been present to a significant degree: 1) inflated self-esteem or grandiosity 2) decreased need for sleep (eg, feels rested after only 3 hours of sleep) 3) more talkative than usual or pressure to keep talking 4) flight of ideas or subjective experience that thoughts are racing 5) distractibility (ie, attention too easily drawn to unimportant or irrelevant external stimuli) 6) increase in goal-directed activity (either socially, at work or school, or sexually) or psychomotor agitation 7) excessive involvement in pleasurable activities that have a high potential for painful consequences (eg, the person engages in unrestrained buying sprees, sexual indiscretions, or foolish business investments). |
| Source: Diagnostic and statistical manual of mental disorders, 4th ed, text rev. Washington, DC: American Psychiatric Association; 2000 |
PTSD risk in affective illness
An adolescent sample. A preliminary cross-sectional study conducted by our group indicates that adolescents with affective disorders may have a much higher risk of developing PTSD than psychiatric comparison subjects.12 We used modules from the Structured Clinical Interview for DSM-IV (SCID) to screen for intra-episode psychopathology (as opposed to lifetime prevalence of disorders) in 79 adolescents with MDD, 34 with BPD as defined in the DSM-IV-TR, and 26 with neither affective disorder (psychiatric controls). We found:
- 38.2% of subjects with BPD met criteria for PTSD, compared with 13.9% of those with MDD (OR 4.9; P =.001)
- 3.8% of adolescents without a mood disorder met criteria for PTSD.
We also found that comorbid PTSD was associated with a 4.5-fold higher risk of a suicide attempt, even after we controlled for BPD diagnosis. When we controlled for the presence of other concurrent anxiety disorders, the likelihood of an adolescent with PTSD having attempted suicide remained significant (OR 3.4; P=.023). This finding suggests that PTSD is an independent risk factor for a suicide attempt.
An adult sample. We then focused on adults meeting criteria for MDD or BPD. In a study of 187 consecutively presenting affectively ill patients, we used the SCID to screen for multiple anxiety disorders including PTSD.13 Lifetime—as opposed to intra-episode—PTSD prevalence was 23.8% among the 118 patients with MDD and 62.3% among the 69 patients with BPD. A patient with BPD was 5 times more likely to have PTSD than a patient with MDD (OR 5.3; P < .0001). The most common cause of trauma leading to PTSD was sexual molestation or rape as a child or adolescent in this predominantly female Latino population.
Populations at risk for PTSD
The prevalence of PTSD in clinical samples varies, depending on the population studied. For instance, women are at much higher risk for developing PTSD than men, even in comparisons where men are exposed to a greater number of traumatic events and analyses control for differences in the prevalence of sexual abuse. The gender difference is greater if the trauma occurs during childhood.14 Essentially all patients in our adolescent and adult studies developed PTSD in response to childhood or adolescent sexual trauma.12,13
A population exposed to a high rate of violent crime would be expected to show a higher PTSD prevalence than one exposed to substantially less violence. The base rate of PTSD also is much higher in affectively ill patients than in the general population.
An analysis by Otto et al15 found a 16% lifetime prevalence of concomitant PTSD in 1,214 persons with BPD (not the manifold forms within the bipolar spectrum). Oquendo et al16 reported a 25.7% lifetime prevalence of PTSD in 230 patients with a history of MDD. Other epidemiologic2 and clinical studies12,13 suggest a considerably higher base rate of PTSD among persons with bipolar disorders than those with MDD.
The method of ascertaining the presence of this disorder may be another variable affecting the reported PTSD prevalence. Persistent avoidance—including “efforts to avoid thoughts, feelings, or conversations associated with the trauma”—is a diagnostic feature of PTSD.10 Researchers and clinicians who do not intentionally screen patients for PTSD are not likely to detect it. Determining the true prevalence of PTSD requires empathic inquiry about exposure to traumatic events.
PTSD screening
Humans are remarkably resilient, and most persons exposed to major trauma are thought not to develop PTSD. However, in my experience, because PTSD appears to be common among persons with affective illness, determining whether such patients have been traumatized is important for prognosis and treatment selection.
To get started, you could create a 1-page form to record traumatic events and identify features of PTSD according to DSM-IV-TR criteria (Checklist).10 PTSD screening without a form can become second nature with practice; an experienced clinician can screen a traumatized patient for the disorder within 3 to 5 minutes.
When screening for a history of trauma, ask patients in a straightforward manner if they have:
- been victims of violent crimes
- witnessed violent crimes
- been exposed to events in which people could have suffered grave injury
- experienced emotional, physical, or sexual abuse.
A person who has experienced emotional abuse but not physical or sexual abuse cannot meet DSM-IV-TR criterion A and therefore does not meet full criteria for PTSD. Many emotionally abused persons meet criteria B through F, however, and they are most reasonably managed similarly to persons who also meet criterion A. When formulating a treatment plan, I recommend using clinical judgment rather than rigid adherence to DSM-IV-TR.
Checklist
DSM-IV-TR diagnostic criteria for posttraumatic stress disorder
| Criterion A. The person has been exposed to a traumatic event in which both of the following have been present: | |
| □ | 1. The person has experienced, witnessed, or been confronted with an event or events that involve actual or threatened death or serious injury, or a threat to the physical integrity of oneself or others |
| □ | 2. The person’s response involved intense fear, helplessness, or horror |
| Criterion B. The traumatic event is persistently re-experienced in at least 1 of the following ways: | |
| □ | 1. Recurrent and intrusive distressing recollections of the event, including images, thoughts, or perceptions |
| □ | 2. Recurrent distressing dreams of the event |
| □ | 3. Acting or feeling as if the traumatic event were recurring (includes a sense of reliving the experience, illusions, hallucinations, and dissociative flashback episodes, including those that occur upon awakening or when intoxicated) |
| □ | 4. Intense psychological distress at exposure to internal or external cues that symbolize or resemble an aspect of the traumatic event |
| □ | 5. Physiologic reactivity upon exposure to internal or external cues that symbolize or resemble an aspect of the traumatic event |
| Criterion C. Persistent avoidance of stimuli associated with the trauma and numbing of general responsiveness (not present before the trauma), as indicated by at least 3 of the following: | |
| □ | 1. Efforts to avoid thoughts, feelings, or conversations associated with the trauma |
| □ | 2. Efforts to avoid activities, places, or people that arouse recollections of the trauma |
| □ | 3. Inability to recall an important aspect of the trauma |
| □ | 4. Markedly diminished interest or participation in significant activities |
| □ | 5. Feeling of detachment or estrangement from others |
| □ | 6. Restricted range of affect |
| □ | 7. Sense of foreshortened future |
| Criterion D. Persistent symptoms of increasing arousal (not present before the trauma), indicated by at least 2 of the following: | |
| □ | 1. Difficulty falling or staying asleep |
| □ | 2. Irritability or outbursts of anger |
| □ | 3. Difficulty concentrating |
| □ | 4. Hypervigilance |
| □ | 5. Exaggerated startle response |
| □ | Criterion E. Duration of disturbance (symptoms in B, C, and D) is >1 month |
| □ | Criterion F. Disturbance causes clinically significant distress or impairment in social, occupational, or other important areas of functioning |
| Source: Adapted from Diagnostic and statistical manual of mental disorders, 4th ed, text rev. Washington, DC: American Psychiatric Association; 2000 | |
Treating PTSD in depression
Pharmacotherapy and psychotherapeutic interventions are important to PTSD patients’ recovery. Limited resources often prevent these patients from receiving expert psychotherapeutic intervention, however, leaving pharmacotherapy as the mainstay of treatment. This is unfortunate, because psychological interventions may be sufficient and preferred in some instances (Box).17–20
Pharmacotherapy for comorbid MDD. Selective serotonin reuptake inhibitors (SSRIs) and venlafaxine are first-line interventions for PTSD in depressed patients who do not meet criteria for a bipolar spectrum disorder. Placebo-controlled studies suggest that sertraline,21,22 fluoxetine,23 and paroxetine,24 are effective; doses higher than those used to treat depression may be required. Extended-release venlafaxine25 in dosages similar to those needed for depressive disorders also can be effective. Bupropion does not appear to be beneficial in treating PTSD.
The monoamine oxidase inhibitor phenelzine was long used successfully in treating PTSD but for the most part has been replaced by SSRIs. Because of its associated dietary restrictions, risk of hypertensive crises, and other side effects, phenelzine probably is best reserved for patients who do not respond to treatment with SSRIs or venlafaxine.
Pharmacotherapy for comorbid bipolar spectrum. If one accepts that most patients meeting criteria for MDE have a bipolar spectrum disorder, then most affectively ill patients with PTSD would need to be treated as if they have bipolar disorder. Oddly enough, this creates difficulties for the use of not only antidepressants and benzodiazepines, but also mood stabilizers:
- Patients with BPD and comorbid anxiety disorders, including PTSD, may be resistant to mood stabilizers.26,27
- Antidepressants can precipitate hypomanic or manic switches or onset of mixed hypomania, a mixed state, or rapid cycling in patients with a bipolar spectrum disorder.28–30
- Benzodiazepines do not appear to relieve acute or chronic PTSD-related distress, and discontinuation could cause rebound symptoms.31
Because no outcome studies have addressed PTSD management in patients with bipolar spectrum disorders, clinicians must rely on their judgment when formulating treatment plans. One strategy is to treat patients with mood stabilizers, then leave well enough alone if both the mood and anxiety symptoms remit (which is possible but unlikely in my experience). I often start treatment for the bipolar spectrum disorder and co-existing PTSD using mood stabilizers (including atypical antipsychotics) and prazosin, an α-1antagonist originally used for treating hypertension.
Prazosin can help diminish nightmares, dreams, and other painful recollections of trauma.32,33 The drug does not affect time to sleep onset. It also has been reported to reduce avoidance behavior and hyperarousal, such as irritability and anger.34 This has been my experience.
Cognitive-behavioral therapy (CBT) involving prolonged exposure (PE) to trauma-related stimuli has been shown to be effective for posttraumatic stress disorder (PTSD) in controlled studies.17,18 PE is an individual CBT designed to help patients process traumatic events and reduce psychological distress. It involves education about reactions to trauma, relaxation techniques, imaginal reliving of the trauma, exposure to cues associated with the trauma, and cognitive restructuring.
Administering D-cycloserine before behavioral treatment sessions facilitates fear extinction, and its use to enhance prolonged PE constitutes state-of-the-art treatment.19 Eye movement desensitization and reprocessing also may be effective.18,20
PE is a reasonable first-line treatment for PTSD patients with comorbid bipolar spectrum disorders when PTSD symptoms persist after pharmacologic treatment for the bipolar spectrum disorder. PE also is a first-line treatment for PTSD in patients with comorbid major depressive disorder. Barriers to PE treatment include its cost and finding professionals who are expert in its use.
Prazosin to treat PTSD-related symptoms in children or adolescents has not been studied, but it can be useful in adults over a wide range of doses. As little as 1 mg at bedtime may confer benefit, although the mean prazosin dose in an 8-week, placebo-controlled study of 40 combat veterans was 13.3 mg in the evening.33
I often initiate prazosin treatment as follows:
- 1 mg on the first night of treatment
- 2 mg on the second night
- 3 mg on the third night
- then, if tolerated, 1 mg upon waking, 1 mg 8 hours later, and 3 mg at bedtime. I then slowly adjust the dose schedule based on the patient’s needs, such as minimizing painful re-experiencing of the trauma. Reducing avoidance and hyperarousal also are reasonable targets. For example, when using prazosin to treat extremely angry men with PTSD stemming from exposure to violent crimes, I have observed that even “murderous” rage ceases with prazosin treatment, only to reappear when prazosin is discontinued.
In treating approximately 100 patients with prazosin, I have not exceeded 16 mg/d. Dosages used for treating hypertension usually are 5 to 20 mg/d. When using prazosin, I always:
- warn patients that faintness or fainting is a side effect and record this caveat in their chart
- obtain sitting and standing blood pressure and pulse before starting treatment and subsequently
- ask patients if they feel dizzy when changing posture before and after initiating treatment.
Most of my PTSD patients are suffering so much that they are willing to accept the risk of fainting associated with prazosin use. For PTSD comorbid with severe panic disorder,12,13 I find that a benzodiazepine with antipanic properties such as alprazolam or clonazepam often works well in conjunction with prazosin.
Some patients with bipolar spectrum disorders might benefit from the addition of an SSRI after mood stabilizer treatment proves effective. However, I have never managed a patient in this manner, and like my own treatment strategy, this has not been subjected to rigorous empiric inquiry. In my view, psychological treatment is much preferred to antidepressant therapy.
Related resource
- Benazzi F. Bipolar disorder—focus on bipolar II disorder and mixed depression. Lancet. 2007;369:935-945.
Drug brand names
- Alprazolam • Xanax
- Bupropion • Wellbutrin
- Clonazepam • Klonopin
- D-cycloserine • Seromycin
- Fluoxetine • Prozac
- Paroxetine • Paxil
- Phenelzine • Nardil
- Prazosin • Minipress
- Sertraline • Zoloft
- Venlafaxine • Effexor
Disclosure
Dr. Dilsaver reports no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
1. Kessler RC, Berglund P, Demler O, et al. The epidemiology of major depressive disorder: results from the National Comorbidity-Replication (NCS-R). JAMA. 2003;289:3095-3105.
2. Kessler RC, Sonnega A, Bromet E, et al. Posttraumatic stress disorder in the National Comorbidity Survey. Arch Gen Psychiatry. 1995;52:1048-1060.
3. Franklin CL, Zimmerman M. Posttraumatic stress disorder and major depressive disorder: investigating the role of overlapping symptoms in diagnostic comorbidity. J Nerv Ment Dis. 2001;189:548-551.
4. Akiskal HS, Mallya G. Criteria for the “soft” bipolar spectrum: treatment implications. Psychopharmacol Bull. 1987;23:68-73.
5. Benazzi F. Prevalence of bipolar II disorder in outpatient depression: a 203-case study in a private practice. J Affect Disord. 1997;43:163-164.
6. Akiskal HS, Benazzi F. Optimizing the detection of bipolar II in outpatient private practice: toward a systematization of clinical diagnostic wisdom. J Clin Psychiatry. 2005;66:914-921.
7. Akiskal HS, Akiskal KK, Lancrenon S, et al. Validating the soft bipolar spectrum in the French National EPIDEP study: the prominence of BP-II. J Affect Disord. 2006;96:207-213.
8. Rabakowski JK, Suwalska D, Lojko D, et al. Bipolar disorders among Polish psychiatric outpatients treated for major depression. J Affect Disord. 2005;84:141-147.
9. Benazzi F. Bipolar disorder—focus on bipolar II disorder and mixed depression. Lancet. 2007;369:935-945.
10. Diagnostic and statistical manual of mental disorders, 4th ed, text rev. Washington, DC: American Psychiatric Association; 2000.
11. Maj M, Pirozzi R, Magliano, et al. Agitated ‘unipolar’ major depression: prevalence, phenomenology, and outcome. J Clin Psychiatry. 2006;67:712-719.
12. Dilsaver SC, Benazzi F, Akiskal HS, et al. Post-traumatic stress disorder among adolescents with bipolar disorder and its relationship to suicidality. Bipolar Disord. 2007;9:649-655.
13. Dilsaver SC, Benazzi F, Akiskal KK, et al. Differential patterns of lifetime multiple anxiety disorder comorbidity between Latino adults with bipolar I and major depressive disorders. Bull Menninger Clinic. 2008;72:130-148.
14. Stein MB, Walker JR, Forde DR. Gender differences in susceptibility to posttraumatic stress disorder. Behav Res Ther. 2000;38:619-628.
15. Otto MW, Perlman CA, Wernicke R, et al. Posttraumatic stress disorder in patients with bipolar disorder: a review of prevalence, correlates, and treatment strategies. Bipolar Disord. 2004;6:470-479.
16. Oquendo M, Brent DA, Birmaher B, et al. Posttraumatic stress disorder comorbid with major depression: factors mediating the association with suicidal behavior. Am J Psychiatry. 2005;162:560-566.
17. Schnurr PP, Friedman MJ, Engel CC, et al. Cognitive behavioral therapy for posttraumatic stress disorder in women: a randomized-controlled trial. JAMA. 2007;297:820-830.
18. Bisson J, Andrew M. Psychological treatment for posttraumatic stress disorder (PTSD). Cochrane Database Syst Rev. 2005;CD003388.-
19. Cukor J, Spitalnick J, Difede J, et al. Emerging treatments for PTSD. Clin Psychol Rev. 2009;29(8):715-726.
20. Hogberg G, Pagani M, Sundin O, et al. Treatment of posttraumatic stress disorder with eye movement desensitization and reprocessing: outcome is stable in 35-month follow-up. Psychiatry Res. 2008;159(1-2):101-108.
21. Brady K, Pearlstein T, Asnis GM, et al. Efficacy and safety of sertraline treatment of posttraumatic stress disorder: a randomized controlled trial. JAMA. 2000;283:1837-1844.
22. Friedman MJ, Marmar CR, Baker DG, et al. Randomized, double-blind comparison of sertraline and placebo for posttraumatic stress disorder in a Department of Veterans Affairs setting. J Clin Psychiatry. 2007;68:711-720.
23. Martenyi F, Brown EB, Zhang H, et al. Fluoxetine versus placebo in posttraumatic stress disorder. J Clin Psychiatry. 2002;63:199-206.
24. Tucker P, Zaninelli R, Yehuda R, et al. Paroxetine in the treatment of chronic posttraumatic stress disorder: results of a placebo-controlled, flexible-dosage trial. J Clin Psychiatry. 2001;62:860-868.
25. Pae CU, Lim HK, Ajwani N, et al. Extended-release formulation of venlafaxine in the treatment of post-traumatic stress disorder. Expert Rev Neurother. 2007;7:603-615.
26. Simon NM, Otto MW, Weiss RD, et al. Pharmacotherapy for bipolar disorder and comorbid conditions: baseline data from the STEP-BD. J Clin Psychopharmacol. 2004;24(5):512-520.
27. Quarantini LC, Miranda-Scippa A, Nery-Fernandes F, et al. The impact of comorbid posttraumatic stress disorder on bipolar patients. Affect Disord. 2009; [Epub ahead of print].
28. Henry C, Sorbara F, Lacoste J, et al. Antidepressant induced mania in bipolar patients: identification and risk factors. J Clin Psychiatry. 2001;62:249-255.
29. Gao K, Kemp DE, Gonocy SJ, et al. Treatment-emergent mania/hypomania during antidepressant monotherapy in patients with rapid cycling bipolar disorder. Bipolar Disord. 2008;10:907-915.
30. Dilsaver SC, Swann AC. Mixed mania: apparent induction by a tricyclic antidepressant in five consecutively treated patients with bipolar depression. Biol Psychiatry. 1995;1:60-62.
31. Braun P, Greenberg D, Dasberg H, et al. Core symptoms of posttraumatic stress disorder unimproved by alprazolam treatment. J Clin Psychiatry. 1990;51:236-238.
32. Taylor FB, Martin P, Thompson C, et al. Prazosin effects on objective sleep measures and clinical symptoms in civilian trauma posttraumatic stress disorder: a placebo-controlled study. Biol Psychiatry. 2008;63:629-632.
33. Raskind MA, Perskind ER, Hoff DJ, et al. A parallel group placebo controlled study of prazosin for trauma nightmares and sleep disturbance in combat veterans with posttraumatic stress disorder. Biol Psychiatry. 2007;61:928-934.
34. Taylor FB, Lowe K, Thompson C, et al. Daytime prazosin reduces psychological distress to trauma specific cues in civilian trauma posttraumatic stress disorder. Biol Psychiatry. 2006;59:577-581.
1. Kessler RC, Berglund P, Demler O, et al. The epidemiology of major depressive disorder: results from the National Comorbidity-Replication (NCS-R). JAMA. 2003;289:3095-3105.
2. Kessler RC, Sonnega A, Bromet E, et al. Posttraumatic stress disorder in the National Comorbidity Survey. Arch Gen Psychiatry. 1995;52:1048-1060.
3. Franklin CL, Zimmerman M. Posttraumatic stress disorder and major depressive disorder: investigating the role of overlapping symptoms in diagnostic comorbidity. J Nerv Ment Dis. 2001;189:548-551.
4. Akiskal HS, Mallya G. Criteria for the “soft” bipolar spectrum: treatment implications. Psychopharmacol Bull. 1987;23:68-73.
5. Benazzi F. Prevalence of bipolar II disorder in outpatient depression: a 203-case study in a private practice. J Affect Disord. 1997;43:163-164.
6. Akiskal HS, Benazzi F. Optimizing the detection of bipolar II in outpatient private practice: toward a systematization of clinical diagnostic wisdom. J Clin Psychiatry. 2005;66:914-921.
7. Akiskal HS, Akiskal KK, Lancrenon S, et al. Validating the soft bipolar spectrum in the French National EPIDEP study: the prominence of BP-II. J Affect Disord. 2006;96:207-213.
8. Rabakowski JK, Suwalska D, Lojko D, et al. Bipolar disorders among Polish psychiatric outpatients treated for major depression. J Affect Disord. 2005;84:141-147.
9. Benazzi F. Bipolar disorder—focus on bipolar II disorder and mixed depression. Lancet. 2007;369:935-945.
10. Diagnostic and statistical manual of mental disorders, 4th ed, text rev. Washington, DC: American Psychiatric Association; 2000.
11. Maj M, Pirozzi R, Magliano, et al. Agitated ‘unipolar’ major depression: prevalence, phenomenology, and outcome. J Clin Psychiatry. 2006;67:712-719.
12. Dilsaver SC, Benazzi F, Akiskal HS, et al. Post-traumatic stress disorder among adolescents with bipolar disorder and its relationship to suicidality. Bipolar Disord. 2007;9:649-655.
13. Dilsaver SC, Benazzi F, Akiskal KK, et al. Differential patterns of lifetime multiple anxiety disorder comorbidity between Latino adults with bipolar I and major depressive disorders. Bull Menninger Clinic. 2008;72:130-148.
14. Stein MB, Walker JR, Forde DR. Gender differences in susceptibility to posttraumatic stress disorder. Behav Res Ther. 2000;38:619-628.
15. Otto MW, Perlman CA, Wernicke R, et al. Posttraumatic stress disorder in patients with bipolar disorder: a review of prevalence, correlates, and treatment strategies. Bipolar Disord. 2004;6:470-479.
16. Oquendo M, Brent DA, Birmaher B, et al. Posttraumatic stress disorder comorbid with major depression: factors mediating the association with suicidal behavior. Am J Psychiatry. 2005;162:560-566.
17. Schnurr PP, Friedman MJ, Engel CC, et al. Cognitive behavioral therapy for posttraumatic stress disorder in women: a randomized-controlled trial. JAMA. 2007;297:820-830.
18. Bisson J, Andrew M. Psychological treatment for posttraumatic stress disorder (PTSD). Cochrane Database Syst Rev. 2005;CD003388.-
19. Cukor J, Spitalnick J, Difede J, et al. Emerging treatments for PTSD. Clin Psychol Rev. 2009;29(8):715-726.
20. Hogberg G, Pagani M, Sundin O, et al. Treatment of posttraumatic stress disorder with eye movement desensitization and reprocessing: outcome is stable in 35-month follow-up. Psychiatry Res. 2008;159(1-2):101-108.
21. Brady K, Pearlstein T, Asnis GM, et al. Efficacy and safety of sertraline treatment of posttraumatic stress disorder: a randomized controlled trial. JAMA. 2000;283:1837-1844.
22. Friedman MJ, Marmar CR, Baker DG, et al. Randomized, double-blind comparison of sertraline and placebo for posttraumatic stress disorder in a Department of Veterans Affairs setting. J Clin Psychiatry. 2007;68:711-720.
23. Martenyi F, Brown EB, Zhang H, et al. Fluoxetine versus placebo in posttraumatic stress disorder. J Clin Psychiatry. 2002;63:199-206.
24. Tucker P, Zaninelli R, Yehuda R, et al. Paroxetine in the treatment of chronic posttraumatic stress disorder: results of a placebo-controlled, flexible-dosage trial. J Clin Psychiatry. 2001;62:860-868.
25. Pae CU, Lim HK, Ajwani N, et al. Extended-release formulation of venlafaxine in the treatment of post-traumatic stress disorder. Expert Rev Neurother. 2007;7:603-615.
26. Simon NM, Otto MW, Weiss RD, et al. Pharmacotherapy for bipolar disorder and comorbid conditions: baseline data from the STEP-BD. J Clin Psychopharmacol. 2004;24(5):512-520.
27. Quarantini LC, Miranda-Scippa A, Nery-Fernandes F, et al. The impact of comorbid posttraumatic stress disorder on bipolar patients. Affect Disord. 2009; [Epub ahead of print].
28. Henry C, Sorbara F, Lacoste J, et al. Antidepressant induced mania in bipolar patients: identification and risk factors. J Clin Psychiatry. 2001;62:249-255.
29. Gao K, Kemp DE, Gonocy SJ, et al. Treatment-emergent mania/hypomania during antidepressant monotherapy in patients with rapid cycling bipolar disorder. Bipolar Disord. 2008;10:907-915.
30. Dilsaver SC, Swann AC. Mixed mania: apparent induction by a tricyclic antidepressant in five consecutively treated patients with bipolar depression. Biol Psychiatry. 1995;1:60-62.
31. Braun P, Greenberg D, Dasberg H, et al. Core symptoms of posttraumatic stress disorder unimproved by alprazolam treatment. J Clin Psychiatry. 1990;51:236-238.
32. Taylor FB, Martin P, Thompson C, et al. Prazosin effects on objective sleep measures and clinical symptoms in civilian trauma posttraumatic stress disorder: a placebo-controlled study. Biol Psychiatry. 2008;63:629-632.
33. Raskind MA, Perskind ER, Hoff DJ, et al. A parallel group placebo controlled study of prazosin for trauma nightmares and sleep disturbance in combat veterans with posttraumatic stress disorder. Biol Psychiatry. 2007;61:928-934.
34. Taylor FB, Lowe K, Thompson C, et al. Daytime prazosin reduces psychological distress to trauma specific cues in civilian trauma posttraumatic stress disorder. Biol Psychiatry. 2006;59:577-581.
Psychosis in women: Consider midlife medical and psychological triggers
Dr. I, a 48-year-old university professor, is brought to the ER by her husband because she has developed an irrational fear of being chased by Nazis. The fears have become increasingly bizarre, her husband reports. She believes her Nazi persecutors are bandaging their arms and using wheelchairs to pretend to be disabled. When out with her husband, Dr. I points to people in wheelchairs, convinced they are after her, will kill her, and are incensed because she left Germany—her country of birth. Her husband brought her to the ER when she started to hear her persecutors addressing her in German at night.
Psychoses of unknown cause usually begin in late adolescence or early adulthood. Less frequently the onset occurs in later adulthood (age ≥40). Late-onset psychosis is much more prevalent in women than in men for reasons that are imperfectly understood.
When you are evaluating a midlife woman with first onset of psychosis, don’t assume an illness of unknown cause (bipolar disorder or schizophrenia) until after you have done a comprehensive search for triggers of her psychotic symptoms. After age 40, women are more likely than men to develop psychosis because of gender-specific medical and psychological precipitants.
Predisposing factors for psychosis
Psychosis is an emergent quality of structural and chemical changes in the brain. As such, it can be expected to surface during:
• brain reorganization or transition (adolescence, senescence, brain trauma, stroke, starvation, inflammation, or brain tumor)
• change in brain chemistry (flux in gonadal, thyroid, or adrenal hormone levels; electrolyte imbalance; fever; exposure to chemical substances; immune response).
Psychological stress impacting the brain via stress hormones also can predispose a person to psychosis.
Because some individuals are more prone than others to develop psychosis during brain alteration, chemical and structural changes in the brain are assumed to interact with genetic propensities to influence gene expression. Once a psychotic event has occurred, it is thought to sensitize the brain so that subsequent events emerge more readily.1
Schizophrenia—though not the only illness in which psychosis plays a role—is a prototype for psychotic illness, and several reported sex differences in this disorder are worth noting.2 The incidence of schizophrenia is approximately the same in both sexes, but women show a later age of onset—a paradox in that the brain develops at a faster pace in females and theoretically should reach the threshold for the first appearance of schizophrenia earlier. Women also require lower doses of antipsychotic medication to recover from an acute psychotic episode and to maintain remission, at least before menopause.3,4 Both of these differences can be explained as an effect of estrogen on a) gene expression5 and b) liver enzymes that metabolize antipsychotics.6
The estrogen hypothesis. Women show a tendency toward premenstrual and postpartum exacerbation of symptoms when estrogen levels are relatively low. These clinical observations, confirmed by some but not all studies, have led to the hypothesis that estrogens are neuroprotective7 and also protect against psychosis.8
Estrogen withdrawal in specific brain cells may release a cascade of events that over time can increase the severity of psychotic and cognitive symptoms. The reason for suspecting such effects is based on what we know about estrogenic effects on neurotransmitter, cognitive, and stress-induction pathways, and—more fundamentally—on neuronal growth and atrophy.
According to the estrogen hypothesis, women are—to some degree—protected against schizophrenia by their relatively high gonadal estrogen production between puberty and and menopause. Women lose this protection with the onset of perimenopausal estrogen fluctuation and decline, accounting for their second peak of illness onset after age 45.
Epidemiologic studies showing a second peak of schizophrenia onset in women (but not men) around the age of menopause support this hypothesis.9,10 Longitudinal outcomes for schizophrenia—which are better in women than in men during late adolescence or early adulthood11—gradually even out after the first 15 years of illness, suggesting that women’s advantage is lost at a time approximating menopause (Box 1).
The question, then, becomes: Is it only because of estrogen loss after age 40 that women become more prone to develop a psychotic illness? Other differences between the sexes that may play roles include immune function, low iron stores, sleep sufficiency, thyroid function, exposure to toxic substances (including therapeutic drugs), societal pressures to be slim while aging (Table), and the experience of stress.12
CASE CONTINUED
Exhausted and confused
Dr. I is a well-groomed, handsome woman, but she hardly speaks when interviewed, looking frightened and somewhat bewildered. She has never had a mental health problem, nor has anyone in her family. She agrees to stay in the hospital but is not sure why. She has slept no more than 1 or 2 hours in the last several days.
Her early history is unremarkable. She did well in school. After earning a PhD at the University of Leipzig, she and her husband immigrated to Canada. Both are university professors. They never decided not to have children, but children hadn’t come. Her menstrual periods stopped 2 years before admission. The question about children is the only 1 that elicits emotion in Dr. I. When I ask about it, tears come to her eyes as she shakes her head.
Her husband reports that she has not been eating well and has, in the last year, started to drink more alcohol than usual—3 to 4 drinks of whiskey a night. She does not smoke cigarettes, and her health generally is good. She uses no medications. Her husband describes their marital relationship as very close, although it has become strained in recent weeks because of her unreasonable fears. He admits that their work is always stressful; competition is fierce, with more and more deadlines and less and less leisure time. The couple has few friends and no hobbies.
Late-onset psychosis symptoms
In late-onset psychosis (after age 45), men appear to suffer substantially milder symptoms and spend less time hospitalized than women.13 Women with late-onset schizophrenia have more severe positive symptoms than men and fewer negative symptoms.14,15 Overall, patients with late-onset schizophrenia have a lower prevalence of looseness of associations and negative symptoms than those with earlier onset.16,17
In addition, individuals with schizophrenia who become ill in middle age have been reported to:
• show better neuropsychological performance (particularly in learning and abstraction/cognitive flexibility) than those with early onset
• possibly have larger thalamic volumes
• respond to lower antipsychotic doses.18
Auditory and visual hallucinations frequently are observed in patients with comorbid late-onset schizophrenia and auditory and visual impairment.16 Palmer et al18 reported no difference in family history of schizophrenia between early and late onset, but this is controversial. Convert et al16 note that most studies reveal a lower lifetime risk of schizophrenia in first-degree relatives of patients with late-onset than early-onset schizophrenia.
CASE CONTINUED
Medical workup
Dr. I’s physical exam is unremarkable. Her thyroid is not enlarged; there are no breast lumps. On mental status exam, her mood is flat. She is preoccupied with fears of the Nazis. Routine blood tests show slight anemia; fasting glucose levels are within normal range.
I give Dr. I zopiclone, 7.5 mg, to help her sleep. The next day she keeps to herself, eats very little, and appears disinterested in her surroundings. Nursing staff report that she often seems frightened. Dr. I asks to use the ward phone to call Germany but is told that she cannot make long distance calls from that phone. This seems to disturb her.
Differential diagnosis
Sensory impairment, substance abuse, and metabolic changes have been implicated in the appearance of psychosis in later life. More specific to women than men, however, are medical and psychiatric precipitants. These include autoimmune disease (and its treatment) and psychiatric disorders, as well as thyroid dysfunction, self-induced starvation (anorexia nervosa) and diet aids, substance use and abuse, insomnia, and iron deficiency (Table).
Autoimmune disease and treatment. Nearly 80% of patients with autoimmune disease are women, and these disorders (as well as their treatment) can manifest as psychosis. Corticosteroids have a well-documented history of triggering psychotic symptoms, which are twice as likely in women than in men. The incidence of severe psychosis while taking oral prednisone ranges from 1.6% to 50% and averages 5.7%. The average daily dose of corticosteroids for patients who develop psychosis is 59.5 mg/d.
Corticosteroid creams absorbed through skin as well as inhaled and intranasal corticosteroids in their more potent formulations can have systemic effects, including psychosis. Nonsteroidal anti-inflammatory drugs such as ibuprofen also can trigger psychosis.19
Psychiatric disorders. Posttraumatic stress disorder with psychotic symptoms may overlap with categories such as psychogenic psychoses, hysterical psychoses, nonaffective remitting psychoses, acute brief psychoses, reactive psychoses, acute and transient psychoses, and bouffées délirantes (in France, the name for transient psychotic reactions).20 Consider these female-predominant conditions in the differential diagnosis, along with micropsychotic episodes in borderline personality disorder, in which the predominance of women is 3:1.
Medical treatment for depression and anxiety also can lead to psychotic symptoms through individual susceptibility to the action of specific drugs or through withdrawal effects.
Clinical assessment
Question all women presenting with psychosis about eating habits and diet pills, and check for hypokalemia and hypocalcemia to rule out starvation effects and reactions to stimulants. Also ask about inhalants, and examine for anemia and thyroid dysfunction. Consider all medications as having the potential to trigger psychotic symptoms.
A family history of illness is important, with a focus on autoimmune disorder and its treatment. A thorough psychiatric history is crucial and needs to include assessment of sleep, mood, and relationships with attachment figures. Do not assume illnesses of unknown cause (bipolar disorder or schizophrenia) until after a comprehensive search for precipitants of psychotic symptoms.
CASE CONTINUED
Guilty feelings
To address her delusions, I start Dr. I on risperidone, 2 mg at bedtime. She goes home for the weekend, and her husband reports that she slept throughout the visit. When she returns, she spends a lot of time in bed but is more communicative.
When I ask Dr. I whether she has called Germany, she says she called her recently widowed father. Dr. I begins to cry when talking of her mother, and tells the nurse she feels guilty for not visiting for the last few years. When her mother died 6 months ago, Dr. I had not seen her in 4 years.
Her fears remit with risperidone, maintained at 2 mg/d, but Dr. I remains depressed and responds slowly to treatment with citalopram, 20 mg/d, and supportive therapy. Her final diagnosis is mood disorder with psychotic features.
Treatment
When treating women with late-onset psychosis, remove all potential triggers and address underlying illness. Cognitive therapy targeting specific symptoms is useful; antipsychotics probably will be necessary. Age-related physiologic changes make older persons more sensitive to the therapeutic and toxic effects of antipsychotics.
Estrogen therapy? Women suffering from schizophrenia show significantly lower estrogen levels than the general population of women, and they experience first-onset or recurrence of a psychotic episode significantly more often in low estrogen phases of the cycle. Estrogens have therefore been postulated to constitute a protective factor against psychosis, which means perimenopause is an at-risk period.21 Although evidence is limited, preliminary studies have found beneficial effects from short-term, off-label use of estrogen therapy in women with psychotic illness (Box 2).
Because continuous use of estrogen plus progestin has been associated with an increased risk of adverse effects,22 off-label use of selective estrogen receptor modulators (SERMs) also is being investigated in women with schizophrenia. SERMs act as tissue-specific estrogen agonists and antagonists because they can either inhibit or enhance estrogen-induced activation of estrogen response element-containing genes.23
Wong et al24 used a crossover design to compare the SERM raloxifene with placebo as adjunctive treatment for 6 postmenopausal women with schizophrenia. Each woman received 8 weeks of raloxifene, 60 mg/d, and 8 weeks of placebo. Three began with placebo and 3 with raloxifene.
Verbal memory was measured weekly with the California Verbal Learning Test, using 5 memory trials, free and cued short-delay recall, and long-delay recall. At baseline, the participants had lower scores than older adults in the general population. Eight weeks of placebo improved scores somewhat, suggesting a practice effect. Eight weeks of raloxifene improved cognitive scores to a level similar to that of schizophrenia-free subjects. After 16 weeks, however, cognitive scores in the 2 groups were indistinguishable.
At present I do not recommend estrogen for women with late-onset schizophrenia because the risk is too high and raloxifene does not enter the brain sufficiently to be a valuable cognitive enhancer. Novel SERMs with more specific efficacy for improving cognitive function may prove useful in the future,25 however, as may phytoestrogens. Adjunctive hormone modulation is a promising area of gender-specific treatment for serious mental illness.26
CASE CONCLUSION
Gradually improving
Dr. I’s depression was triggered by her mother’s death and regrets about not visiting and not being a mother. The content of her delusions was related to her guilt about not having returned to Germany; the delusions were probably triggered by depression, alcohol intake, her relative hypoestrogenic state, stress at work, lack of social supports, and dependence on her husband.
Over the next few years, Dr. I is maintained on a low dose of risperidone (reduced from 2 mg/d to 1 mg/d) and citalopram (reduced from 20 mg/d to 10 mg/d). She becomes increasingly engaged in supportive dynamic therapy, and her symptoms gradually improve.
BOTTOM LINE
Psychosis onset in midlife is mostly a female phenomenon because a perimenopausal estrogen decline increases women’s susceptibility. Seek specific triggers such as medical illness or response to a drug before assuming an illness of unknown cause such as bipolar disorder or schizophrenia. Cognitive therapy targeting specific symptoms is useful; antipsychotics probably will be necessary.
Related Resources
• Women and psychosis: A guide for women and their families. Centre for Addiction and Mental Health. University of Toronto. www.camh.net/About_Addiction_Mental_ Health/Mental_Health_Information/Women_Psychosis.
• Seeman MV. Women and psychosis. www.medscape.com/ viewarticle/408912.
• Chattopadhyay S. Estrogen and schizophrenia: Any link? The Internet Journal of Mental Health. 2004;2(1). www.ispub. com/journal/the_internet_journal_of_mental_health.html.
Drug Brand Names
Citalopram • Celexa Prednisone • Deltasone,
Estradiol • Estrace, Orasone, others
Estrofem, others Raloxifene • Evista
Estradiol transdermal • Risperidone • Risperdal
Estraderm , Climara, others
Methylphenidate • Concerta,
Ritalin, others
Disclosure
Dr. Seeman reports no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
1. Post RM. Kindling and sensitization as models for affective episode recurrence, cyclicity, and tolerance phenomena. Neurosci Biobehav Rev. 2007;31:858-873.
2. Seeman MV. Gender differences in schizophrenia. Can J Psychiatry. 1982;27:107-112.
3. Seeman MV. Interaction of sex, age, and neuroleptic dose. Comp Psychiatry. 1983;24:125-128.
4. Usall J, Suarez D, Haro JM, and the SOHO Study Group. Gender differences in response to antipsychotic treatment in outpatients with schizophrenia. Psychiatry Res. 2007;153: 225-231.
5. Hare E, Glahn DC, Dassori A, et al. Heritability of age of onset of psychosis in schizophrenia. Am J Med Genet B Neuropsychiatr Genet. 2009 Apr 6 [Epub ahead of print].
6. Seeman MV. Gender differences in the prescribing of antipsychotic drugs. Am J Psychiatry. 2004;161:1324-1333.
7. Marin R, Guerra B, Alonso R, et al. Estrogen activates classical and alternative mechanisms to orchestrate neuroprotection. Curr Neurovasc Res. 2005;2:287-301.
8. Seeman MV, Lang M. The role of estrogens in schizophrenia gender differences. Schizophr Bull. 1990;16:185-194.
9. Castle DJ, Abel K, Takei N, et al. Gender differences in schizophrenia: hormonal effect or subtypes? Schizophr Bull. 1995;21:1-12.
10. Häfner H, an der Heiden W. Epidemiology of schizophrenia. Can J Psychiatry. 1997;42:139-151.
11. Grossman LS, Harrow M, Rosen C, et al. Sex differences in schizophrenia and other psychotic disorders: a 20-year longitudinal study of psychosis and recovery. Compr Psychiatry. 2008;49:523-529.
12. Kajantie E, Phillips DI. The effects of sex and hormonal status on the physiological response to acute psychosocial stress. Psychoneuroendocrinology. 2006;31:151-178.
13. Riecher-Rössler A, Löffler W, Munk-Jörgensen P. What do we really know about late-onset schizophrenia? Eur Arch Psychiatry Clin Neurosci. 1997;247:195-208.
14. Lindamer LA, Lohr JB, Harris MJ, et al. Gender-related clinical differences in older patients with schizophrenia. J Clin Psychiatry. 1999;60:61-67.
15. Seeman MV. Does menopause intensify symptoms in schizophrenia? In: Lewis-Hall F, Williams TS, Panetta JA, et al, eds. Psychiatric illness in women: emerging treatments and research. Arlington, VA: American Psychiatric Publishing, Inc.; 2002:239-248.
16. Convert H, Védie C, Paulin P. [Late-onset schizophrenia or chronic delusion]. Encephale. 2006;32:957-961.
17. Sato T, Bottlender R, Schröter A, et al. Psychopathology of early-onset versus late-onset schizophrenia revisited: an observation of 473 neuroleptic-naive patients before and after first-admission treatments. Schizophr Res. 2004;67:175-183.
18. Palmer BW, McClure FS, Jeste DV. Schizophrenia in late life: findings challenge traditional concepts. Harv Rev Psychiatry. 2001;9:51-58.
19. Weiss DB, Dyrud J, House RM, et al. Psychiatric manifestations of autoimmune disorders. Curr Treat Options Neurol. 2005;7:413-417.
20. Castagnini A, Bertelsen A, Munk-Jorgensen P, et al. The relationship of reactive psychosis and ICD-10 acute and transient psychotic disorders: evidence from a case register-based comparison. Psychopathology. 2007;40:47-53.
21. Huber TJ, Rollnik J, Wilhelms J, et al. Estradiol levels in psychotic disorders. Psychoneuroendocrinology. 2001;26: 27-35.
22. Heiss G, Wallace R, Anderson G, et al, for the WHI Investigators. Health risks and benefits 3 years after stopping randomized treatment with estrogen and progestin. JAMA. 2008;299(9):1036-1045.
23. Doncarlos LL, Azcoitia I, Garcia-Segura LM. Neuroprotective actions of selective estrogen receptor modulators. Psychoneuroendocrinology. 2009 May 15 [Epub ahead of print].
24. Wong J, Seeman MV, Shapiro H. Case report: raloxifene in postmenopausal women with psychosis: preliminary findings. Am J Geriatr Psychiatry. 2003;11(6):697-698.
25. Ye L, Chan MY, Leung LK. The soy isoflavone genistein induces estrogen synthesis in an extragonadal pathway. Mol Cell Endocrinol. 2009;302:73-80.
26. Kulkarni J, Gurvich C, Gilbert H, et al. Hormone modulation: a novel therapeutic approach for women with severe mental illness. Aust N Z J Psychiatry. 2008;42:83-88.
Dr. I, a 48-year-old university professor, is brought to the ER by her husband because she has developed an irrational fear of being chased by Nazis. The fears have become increasingly bizarre, her husband reports. She believes her Nazi persecutors are bandaging their arms and using wheelchairs to pretend to be disabled. When out with her husband, Dr. I points to people in wheelchairs, convinced they are after her, will kill her, and are incensed because she left Germany—her country of birth. Her husband brought her to the ER when she started to hear her persecutors addressing her in German at night.
Psychoses of unknown cause usually begin in late adolescence or early adulthood. Less frequently the onset occurs in later adulthood (age ≥40). Late-onset psychosis is much more prevalent in women than in men for reasons that are imperfectly understood.
When you are evaluating a midlife woman with first onset of psychosis, don’t assume an illness of unknown cause (bipolar disorder or schizophrenia) until after you have done a comprehensive search for triggers of her psychotic symptoms. After age 40, women are more likely than men to develop psychosis because of gender-specific medical and psychological precipitants.
Predisposing factors for psychosis
Psychosis is an emergent quality of structural and chemical changes in the brain. As such, it can be expected to surface during:
• brain reorganization or transition (adolescence, senescence, brain trauma, stroke, starvation, inflammation, or brain tumor)
• change in brain chemistry (flux in gonadal, thyroid, or adrenal hormone levels; electrolyte imbalance; fever; exposure to chemical substances; immune response).
Psychological stress impacting the brain via stress hormones also can predispose a person to psychosis.
Because some individuals are more prone than others to develop psychosis during brain alteration, chemical and structural changes in the brain are assumed to interact with genetic propensities to influence gene expression. Once a psychotic event has occurred, it is thought to sensitize the brain so that subsequent events emerge more readily.1
Schizophrenia—though not the only illness in which psychosis plays a role—is a prototype for psychotic illness, and several reported sex differences in this disorder are worth noting.2 The incidence of schizophrenia is approximately the same in both sexes, but women show a later age of onset—a paradox in that the brain develops at a faster pace in females and theoretically should reach the threshold for the first appearance of schizophrenia earlier. Women also require lower doses of antipsychotic medication to recover from an acute psychotic episode and to maintain remission, at least before menopause.3,4 Both of these differences can be explained as an effect of estrogen on a) gene expression5 and b) liver enzymes that metabolize antipsychotics.6
The estrogen hypothesis. Women show a tendency toward premenstrual and postpartum exacerbation of symptoms when estrogen levels are relatively low. These clinical observations, confirmed by some but not all studies, have led to the hypothesis that estrogens are neuroprotective7 and also protect against psychosis.8
Estrogen withdrawal in specific brain cells may release a cascade of events that over time can increase the severity of psychotic and cognitive symptoms. The reason for suspecting such effects is based on what we know about estrogenic effects on neurotransmitter, cognitive, and stress-induction pathways, and—more fundamentally—on neuronal growth and atrophy.
According to the estrogen hypothesis, women are—to some degree—protected against schizophrenia by their relatively high gonadal estrogen production between puberty and and menopause. Women lose this protection with the onset of perimenopausal estrogen fluctuation and decline, accounting for their second peak of illness onset after age 45.
Epidemiologic studies showing a second peak of schizophrenia onset in women (but not men) around the age of menopause support this hypothesis.9,10 Longitudinal outcomes for schizophrenia—which are better in women than in men during late adolescence or early adulthood11—gradually even out after the first 15 years of illness, suggesting that women’s advantage is lost at a time approximating menopause (Box 1).
The question, then, becomes: Is it only because of estrogen loss after age 40 that women become more prone to develop a psychotic illness? Other differences between the sexes that may play roles include immune function, low iron stores, sleep sufficiency, thyroid function, exposure to toxic substances (including therapeutic drugs), societal pressures to be slim while aging (Table), and the experience of stress.12
CASE CONTINUED
Exhausted and confused
Dr. I is a well-groomed, handsome woman, but she hardly speaks when interviewed, looking frightened and somewhat bewildered. She has never had a mental health problem, nor has anyone in her family. She agrees to stay in the hospital but is not sure why. She has slept no more than 1 or 2 hours in the last several days.
Her early history is unremarkable. She did well in school. After earning a PhD at the University of Leipzig, she and her husband immigrated to Canada. Both are university professors. They never decided not to have children, but children hadn’t come. Her menstrual periods stopped 2 years before admission. The question about children is the only 1 that elicits emotion in Dr. I. When I ask about it, tears come to her eyes as she shakes her head.
Her husband reports that she has not been eating well and has, in the last year, started to drink more alcohol than usual—3 to 4 drinks of whiskey a night. She does not smoke cigarettes, and her health generally is good. She uses no medications. Her husband describes their marital relationship as very close, although it has become strained in recent weeks because of her unreasonable fears. He admits that their work is always stressful; competition is fierce, with more and more deadlines and less and less leisure time. The couple has few friends and no hobbies.
Late-onset psychosis symptoms
In late-onset psychosis (after age 45), men appear to suffer substantially milder symptoms and spend less time hospitalized than women.13 Women with late-onset schizophrenia have more severe positive symptoms than men and fewer negative symptoms.14,15 Overall, patients with late-onset schizophrenia have a lower prevalence of looseness of associations and negative symptoms than those with earlier onset.16,17
In addition, individuals with schizophrenia who become ill in middle age have been reported to:
• show better neuropsychological performance (particularly in learning and abstraction/cognitive flexibility) than those with early onset
• possibly have larger thalamic volumes
• respond to lower antipsychotic doses.18
Auditory and visual hallucinations frequently are observed in patients with comorbid late-onset schizophrenia and auditory and visual impairment.16 Palmer et al18 reported no difference in family history of schizophrenia between early and late onset, but this is controversial. Convert et al16 note that most studies reveal a lower lifetime risk of schizophrenia in first-degree relatives of patients with late-onset than early-onset schizophrenia.
CASE CONTINUED
Medical workup
Dr. I’s physical exam is unremarkable. Her thyroid is not enlarged; there are no breast lumps. On mental status exam, her mood is flat. She is preoccupied with fears of the Nazis. Routine blood tests show slight anemia; fasting glucose levels are within normal range.
I give Dr. I zopiclone, 7.5 mg, to help her sleep. The next day she keeps to herself, eats very little, and appears disinterested in her surroundings. Nursing staff report that she often seems frightened. Dr. I asks to use the ward phone to call Germany but is told that she cannot make long distance calls from that phone. This seems to disturb her.
Differential diagnosis
Sensory impairment, substance abuse, and metabolic changes have been implicated in the appearance of psychosis in later life. More specific to women than men, however, are medical and psychiatric precipitants. These include autoimmune disease (and its treatment) and psychiatric disorders, as well as thyroid dysfunction, self-induced starvation (anorexia nervosa) and diet aids, substance use and abuse, insomnia, and iron deficiency (Table).
Autoimmune disease and treatment. Nearly 80% of patients with autoimmune disease are women, and these disorders (as well as their treatment) can manifest as psychosis. Corticosteroids have a well-documented history of triggering psychotic symptoms, which are twice as likely in women than in men. The incidence of severe psychosis while taking oral prednisone ranges from 1.6% to 50% and averages 5.7%. The average daily dose of corticosteroids for patients who develop psychosis is 59.5 mg/d.
Corticosteroid creams absorbed through skin as well as inhaled and intranasal corticosteroids in their more potent formulations can have systemic effects, including psychosis. Nonsteroidal anti-inflammatory drugs such as ibuprofen also can trigger psychosis.19
Psychiatric disorders. Posttraumatic stress disorder with psychotic symptoms may overlap with categories such as psychogenic psychoses, hysterical psychoses, nonaffective remitting psychoses, acute brief psychoses, reactive psychoses, acute and transient psychoses, and bouffées délirantes (in France, the name for transient psychotic reactions).20 Consider these female-predominant conditions in the differential diagnosis, along with micropsychotic episodes in borderline personality disorder, in which the predominance of women is 3:1.
Medical treatment for depression and anxiety also can lead to psychotic symptoms through individual susceptibility to the action of specific drugs or through withdrawal effects.
Clinical assessment
Question all women presenting with psychosis about eating habits and diet pills, and check for hypokalemia and hypocalcemia to rule out starvation effects and reactions to stimulants. Also ask about inhalants, and examine for anemia and thyroid dysfunction. Consider all medications as having the potential to trigger psychotic symptoms.
A family history of illness is important, with a focus on autoimmune disorder and its treatment. A thorough psychiatric history is crucial and needs to include assessment of sleep, mood, and relationships with attachment figures. Do not assume illnesses of unknown cause (bipolar disorder or schizophrenia) until after a comprehensive search for precipitants of psychotic symptoms.
CASE CONTINUED
Guilty feelings
To address her delusions, I start Dr. I on risperidone, 2 mg at bedtime. She goes home for the weekend, and her husband reports that she slept throughout the visit. When she returns, she spends a lot of time in bed but is more communicative.
When I ask Dr. I whether she has called Germany, she says she called her recently widowed father. Dr. I begins to cry when talking of her mother, and tells the nurse she feels guilty for not visiting for the last few years. When her mother died 6 months ago, Dr. I had not seen her in 4 years.
Her fears remit with risperidone, maintained at 2 mg/d, but Dr. I remains depressed and responds slowly to treatment with citalopram, 20 mg/d, and supportive therapy. Her final diagnosis is mood disorder with psychotic features.
Treatment
When treating women with late-onset psychosis, remove all potential triggers and address underlying illness. Cognitive therapy targeting specific symptoms is useful; antipsychotics probably will be necessary. Age-related physiologic changes make older persons more sensitive to the therapeutic and toxic effects of antipsychotics.
Estrogen therapy? Women suffering from schizophrenia show significantly lower estrogen levels than the general population of women, and they experience first-onset or recurrence of a psychotic episode significantly more often in low estrogen phases of the cycle. Estrogens have therefore been postulated to constitute a protective factor against psychosis, which means perimenopause is an at-risk period.21 Although evidence is limited, preliminary studies have found beneficial effects from short-term, off-label use of estrogen therapy in women with psychotic illness (Box 2).
Because continuous use of estrogen plus progestin has been associated with an increased risk of adverse effects,22 off-label use of selective estrogen receptor modulators (SERMs) also is being investigated in women with schizophrenia. SERMs act as tissue-specific estrogen agonists and antagonists because they can either inhibit or enhance estrogen-induced activation of estrogen response element-containing genes.23
Wong et al24 used a crossover design to compare the SERM raloxifene with placebo as adjunctive treatment for 6 postmenopausal women with schizophrenia. Each woman received 8 weeks of raloxifene, 60 mg/d, and 8 weeks of placebo. Three began with placebo and 3 with raloxifene.
Verbal memory was measured weekly with the California Verbal Learning Test, using 5 memory trials, free and cued short-delay recall, and long-delay recall. At baseline, the participants had lower scores than older adults in the general population. Eight weeks of placebo improved scores somewhat, suggesting a practice effect. Eight weeks of raloxifene improved cognitive scores to a level similar to that of schizophrenia-free subjects. After 16 weeks, however, cognitive scores in the 2 groups were indistinguishable.
At present I do not recommend estrogen for women with late-onset schizophrenia because the risk is too high and raloxifene does not enter the brain sufficiently to be a valuable cognitive enhancer. Novel SERMs with more specific efficacy for improving cognitive function may prove useful in the future,25 however, as may phytoestrogens. Adjunctive hormone modulation is a promising area of gender-specific treatment for serious mental illness.26
CASE CONCLUSION
Gradually improving
Dr. I’s depression was triggered by her mother’s death and regrets about not visiting and not being a mother. The content of her delusions was related to her guilt about not having returned to Germany; the delusions were probably triggered by depression, alcohol intake, her relative hypoestrogenic state, stress at work, lack of social supports, and dependence on her husband.
Over the next few years, Dr. I is maintained on a low dose of risperidone (reduced from 2 mg/d to 1 mg/d) and citalopram (reduced from 20 mg/d to 10 mg/d). She becomes increasingly engaged in supportive dynamic therapy, and her symptoms gradually improve.
BOTTOM LINE
Psychosis onset in midlife is mostly a female phenomenon because a perimenopausal estrogen decline increases women’s susceptibility. Seek specific triggers such as medical illness or response to a drug before assuming an illness of unknown cause such as bipolar disorder or schizophrenia. Cognitive therapy targeting specific symptoms is useful; antipsychotics probably will be necessary.
Related Resources
• Women and psychosis: A guide for women and their families. Centre for Addiction and Mental Health. University of Toronto. www.camh.net/About_Addiction_Mental_ Health/Mental_Health_Information/Women_Psychosis.
• Seeman MV. Women and psychosis. www.medscape.com/ viewarticle/408912.
• Chattopadhyay S. Estrogen and schizophrenia: Any link? The Internet Journal of Mental Health. 2004;2(1). www.ispub. com/journal/the_internet_journal_of_mental_health.html.
Drug Brand Names
Citalopram • Celexa Prednisone • Deltasone,
Estradiol • Estrace, Orasone, others
Estrofem, others Raloxifene • Evista
Estradiol transdermal • Risperidone • Risperdal
Estraderm , Climara, others
Methylphenidate • Concerta,
Ritalin, others
Disclosure
Dr. Seeman reports no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
Dr. I, a 48-year-old university professor, is brought to the ER by her husband because she has developed an irrational fear of being chased by Nazis. The fears have become increasingly bizarre, her husband reports. She believes her Nazi persecutors are bandaging their arms and using wheelchairs to pretend to be disabled. When out with her husband, Dr. I points to people in wheelchairs, convinced they are after her, will kill her, and are incensed because she left Germany—her country of birth. Her husband brought her to the ER when she started to hear her persecutors addressing her in German at night.
Psychoses of unknown cause usually begin in late adolescence or early adulthood. Less frequently the onset occurs in later adulthood (age ≥40). Late-onset psychosis is much more prevalent in women than in men for reasons that are imperfectly understood.
When you are evaluating a midlife woman with first onset of psychosis, don’t assume an illness of unknown cause (bipolar disorder or schizophrenia) until after you have done a comprehensive search for triggers of her psychotic symptoms. After age 40, women are more likely than men to develop psychosis because of gender-specific medical and psychological precipitants.
Predisposing factors for psychosis
Psychosis is an emergent quality of structural and chemical changes in the brain. As such, it can be expected to surface during:
• brain reorganization or transition (adolescence, senescence, brain trauma, stroke, starvation, inflammation, or brain tumor)
• change in brain chemistry (flux in gonadal, thyroid, or adrenal hormone levels; electrolyte imbalance; fever; exposure to chemical substances; immune response).
Psychological stress impacting the brain via stress hormones also can predispose a person to psychosis.
Because some individuals are more prone than others to develop psychosis during brain alteration, chemical and structural changes in the brain are assumed to interact with genetic propensities to influence gene expression. Once a psychotic event has occurred, it is thought to sensitize the brain so that subsequent events emerge more readily.1
Schizophrenia—though not the only illness in which psychosis plays a role—is a prototype for psychotic illness, and several reported sex differences in this disorder are worth noting.2 The incidence of schizophrenia is approximately the same in both sexes, but women show a later age of onset—a paradox in that the brain develops at a faster pace in females and theoretically should reach the threshold for the first appearance of schizophrenia earlier. Women also require lower doses of antipsychotic medication to recover from an acute psychotic episode and to maintain remission, at least before menopause.3,4 Both of these differences can be explained as an effect of estrogen on a) gene expression5 and b) liver enzymes that metabolize antipsychotics.6
The estrogen hypothesis. Women show a tendency toward premenstrual and postpartum exacerbation of symptoms when estrogen levels are relatively low. These clinical observations, confirmed by some but not all studies, have led to the hypothesis that estrogens are neuroprotective7 and also protect against psychosis.8
Estrogen withdrawal in specific brain cells may release a cascade of events that over time can increase the severity of psychotic and cognitive symptoms. The reason for suspecting such effects is based on what we know about estrogenic effects on neurotransmitter, cognitive, and stress-induction pathways, and—more fundamentally—on neuronal growth and atrophy.
According to the estrogen hypothesis, women are—to some degree—protected against schizophrenia by their relatively high gonadal estrogen production between puberty and and menopause. Women lose this protection with the onset of perimenopausal estrogen fluctuation and decline, accounting for their second peak of illness onset after age 45.
Epidemiologic studies showing a second peak of schizophrenia onset in women (but not men) around the age of menopause support this hypothesis.9,10 Longitudinal outcomes for schizophrenia—which are better in women than in men during late adolescence or early adulthood11—gradually even out after the first 15 years of illness, suggesting that women’s advantage is lost at a time approximating menopause (Box 1).
The question, then, becomes: Is it only because of estrogen loss after age 40 that women become more prone to develop a psychotic illness? Other differences between the sexes that may play roles include immune function, low iron stores, sleep sufficiency, thyroid function, exposure to toxic substances (including therapeutic drugs), societal pressures to be slim while aging (Table), and the experience of stress.12
CASE CONTINUED
Exhausted and confused
Dr. I is a well-groomed, handsome woman, but she hardly speaks when interviewed, looking frightened and somewhat bewildered. She has never had a mental health problem, nor has anyone in her family. She agrees to stay in the hospital but is not sure why. She has slept no more than 1 or 2 hours in the last several days.
Her early history is unremarkable. She did well in school. After earning a PhD at the University of Leipzig, she and her husband immigrated to Canada. Both are university professors. They never decided not to have children, but children hadn’t come. Her menstrual periods stopped 2 years before admission. The question about children is the only 1 that elicits emotion in Dr. I. When I ask about it, tears come to her eyes as she shakes her head.
Her husband reports that she has not been eating well and has, in the last year, started to drink more alcohol than usual—3 to 4 drinks of whiskey a night. She does not smoke cigarettes, and her health generally is good. She uses no medications. Her husband describes their marital relationship as very close, although it has become strained in recent weeks because of her unreasonable fears. He admits that their work is always stressful; competition is fierce, with more and more deadlines and less and less leisure time. The couple has few friends and no hobbies.
Late-onset psychosis symptoms
In late-onset psychosis (after age 45), men appear to suffer substantially milder symptoms and spend less time hospitalized than women.13 Women with late-onset schizophrenia have more severe positive symptoms than men and fewer negative symptoms.14,15 Overall, patients with late-onset schizophrenia have a lower prevalence of looseness of associations and negative symptoms than those with earlier onset.16,17
In addition, individuals with schizophrenia who become ill in middle age have been reported to:
• show better neuropsychological performance (particularly in learning and abstraction/cognitive flexibility) than those with early onset
• possibly have larger thalamic volumes
• respond to lower antipsychotic doses.18
Auditory and visual hallucinations frequently are observed in patients with comorbid late-onset schizophrenia and auditory and visual impairment.16 Palmer et al18 reported no difference in family history of schizophrenia between early and late onset, but this is controversial. Convert et al16 note that most studies reveal a lower lifetime risk of schizophrenia in first-degree relatives of patients with late-onset than early-onset schizophrenia.
CASE CONTINUED
Medical workup
Dr. I’s physical exam is unremarkable. Her thyroid is not enlarged; there are no breast lumps. On mental status exam, her mood is flat. She is preoccupied with fears of the Nazis. Routine blood tests show slight anemia; fasting glucose levels are within normal range.
I give Dr. I zopiclone, 7.5 mg, to help her sleep. The next day she keeps to herself, eats very little, and appears disinterested in her surroundings. Nursing staff report that she often seems frightened. Dr. I asks to use the ward phone to call Germany but is told that she cannot make long distance calls from that phone. This seems to disturb her.
Differential diagnosis
Sensory impairment, substance abuse, and metabolic changes have been implicated in the appearance of psychosis in later life. More specific to women than men, however, are medical and psychiatric precipitants. These include autoimmune disease (and its treatment) and psychiatric disorders, as well as thyroid dysfunction, self-induced starvation (anorexia nervosa) and diet aids, substance use and abuse, insomnia, and iron deficiency (Table).
Autoimmune disease and treatment. Nearly 80% of patients with autoimmune disease are women, and these disorders (as well as their treatment) can manifest as psychosis. Corticosteroids have a well-documented history of triggering psychotic symptoms, which are twice as likely in women than in men. The incidence of severe psychosis while taking oral prednisone ranges from 1.6% to 50% and averages 5.7%. The average daily dose of corticosteroids for patients who develop psychosis is 59.5 mg/d.
Corticosteroid creams absorbed through skin as well as inhaled and intranasal corticosteroids in their more potent formulations can have systemic effects, including psychosis. Nonsteroidal anti-inflammatory drugs such as ibuprofen also can trigger psychosis.19
Psychiatric disorders. Posttraumatic stress disorder with psychotic symptoms may overlap with categories such as psychogenic psychoses, hysterical psychoses, nonaffective remitting psychoses, acute brief psychoses, reactive psychoses, acute and transient psychoses, and bouffées délirantes (in France, the name for transient psychotic reactions).20 Consider these female-predominant conditions in the differential diagnosis, along with micropsychotic episodes in borderline personality disorder, in which the predominance of women is 3:1.
Medical treatment for depression and anxiety also can lead to psychotic symptoms through individual susceptibility to the action of specific drugs or through withdrawal effects.
Clinical assessment
Question all women presenting with psychosis about eating habits and diet pills, and check for hypokalemia and hypocalcemia to rule out starvation effects and reactions to stimulants. Also ask about inhalants, and examine for anemia and thyroid dysfunction. Consider all medications as having the potential to trigger psychotic symptoms.
A family history of illness is important, with a focus on autoimmune disorder and its treatment. A thorough psychiatric history is crucial and needs to include assessment of sleep, mood, and relationships with attachment figures. Do not assume illnesses of unknown cause (bipolar disorder or schizophrenia) until after a comprehensive search for precipitants of psychotic symptoms.
CASE CONTINUED
Guilty feelings
To address her delusions, I start Dr. I on risperidone, 2 mg at bedtime. She goes home for the weekend, and her husband reports that she slept throughout the visit. When she returns, she spends a lot of time in bed but is more communicative.
When I ask Dr. I whether she has called Germany, she says she called her recently widowed father. Dr. I begins to cry when talking of her mother, and tells the nurse she feels guilty for not visiting for the last few years. When her mother died 6 months ago, Dr. I had not seen her in 4 years.
Her fears remit with risperidone, maintained at 2 mg/d, but Dr. I remains depressed and responds slowly to treatment with citalopram, 20 mg/d, and supportive therapy. Her final diagnosis is mood disorder with psychotic features.
Treatment
When treating women with late-onset psychosis, remove all potential triggers and address underlying illness. Cognitive therapy targeting specific symptoms is useful; antipsychotics probably will be necessary. Age-related physiologic changes make older persons more sensitive to the therapeutic and toxic effects of antipsychotics.
Estrogen therapy? Women suffering from schizophrenia show significantly lower estrogen levels than the general population of women, and they experience first-onset or recurrence of a psychotic episode significantly more often in low estrogen phases of the cycle. Estrogens have therefore been postulated to constitute a protective factor against psychosis, which means perimenopause is an at-risk period.21 Although evidence is limited, preliminary studies have found beneficial effects from short-term, off-label use of estrogen therapy in women with psychotic illness (Box 2).
Because continuous use of estrogen plus progestin has been associated with an increased risk of adverse effects,22 off-label use of selective estrogen receptor modulators (SERMs) also is being investigated in women with schizophrenia. SERMs act as tissue-specific estrogen agonists and antagonists because they can either inhibit or enhance estrogen-induced activation of estrogen response element-containing genes.23
Wong et al24 used a crossover design to compare the SERM raloxifene with placebo as adjunctive treatment for 6 postmenopausal women with schizophrenia. Each woman received 8 weeks of raloxifene, 60 mg/d, and 8 weeks of placebo. Three began with placebo and 3 with raloxifene.
Verbal memory was measured weekly with the California Verbal Learning Test, using 5 memory trials, free and cued short-delay recall, and long-delay recall. At baseline, the participants had lower scores than older adults in the general population. Eight weeks of placebo improved scores somewhat, suggesting a practice effect. Eight weeks of raloxifene improved cognitive scores to a level similar to that of schizophrenia-free subjects. After 16 weeks, however, cognitive scores in the 2 groups were indistinguishable.
At present I do not recommend estrogen for women with late-onset schizophrenia because the risk is too high and raloxifene does not enter the brain sufficiently to be a valuable cognitive enhancer. Novel SERMs with more specific efficacy for improving cognitive function may prove useful in the future,25 however, as may phytoestrogens. Adjunctive hormone modulation is a promising area of gender-specific treatment for serious mental illness.26
CASE CONCLUSION
Gradually improving
Dr. I’s depression was triggered by her mother’s death and regrets about not visiting and not being a mother. The content of her delusions was related to her guilt about not having returned to Germany; the delusions were probably triggered by depression, alcohol intake, her relative hypoestrogenic state, stress at work, lack of social supports, and dependence on her husband.
Over the next few years, Dr. I is maintained on a low dose of risperidone (reduced from 2 mg/d to 1 mg/d) and citalopram (reduced from 20 mg/d to 10 mg/d). She becomes increasingly engaged in supportive dynamic therapy, and her symptoms gradually improve.
BOTTOM LINE
Psychosis onset in midlife is mostly a female phenomenon because a perimenopausal estrogen decline increases women’s susceptibility. Seek specific triggers such as medical illness or response to a drug before assuming an illness of unknown cause such as bipolar disorder or schizophrenia. Cognitive therapy targeting specific symptoms is useful; antipsychotics probably will be necessary.
Related Resources
• Women and psychosis: A guide for women and their families. Centre for Addiction and Mental Health. University of Toronto. www.camh.net/About_Addiction_Mental_ Health/Mental_Health_Information/Women_Psychosis.
• Seeman MV. Women and psychosis. www.medscape.com/ viewarticle/408912.
• Chattopadhyay S. Estrogen and schizophrenia: Any link? The Internet Journal of Mental Health. 2004;2(1). www.ispub. com/journal/the_internet_journal_of_mental_health.html.
Drug Brand Names
Citalopram • Celexa Prednisone • Deltasone,
Estradiol • Estrace, Orasone, others
Estrofem, others Raloxifene • Evista
Estradiol transdermal • Risperidone • Risperdal
Estraderm , Climara, others
Methylphenidate • Concerta,
Ritalin, others
Disclosure
Dr. Seeman reports no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
1. Post RM. Kindling and sensitization as models for affective episode recurrence, cyclicity, and tolerance phenomena. Neurosci Biobehav Rev. 2007;31:858-873.
2. Seeman MV. Gender differences in schizophrenia. Can J Psychiatry. 1982;27:107-112.
3. Seeman MV. Interaction of sex, age, and neuroleptic dose. Comp Psychiatry. 1983;24:125-128.
4. Usall J, Suarez D, Haro JM, and the SOHO Study Group. Gender differences in response to antipsychotic treatment in outpatients with schizophrenia. Psychiatry Res. 2007;153: 225-231.
5. Hare E, Glahn DC, Dassori A, et al. Heritability of age of onset of psychosis in schizophrenia. Am J Med Genet B Neuropsychiatr Genet. 2009 Apr 6 [Epub ahead of print].
6. Seeman MV. Gender differences in the prescribing of antipsychotic drugs. Am J Psychiatry. 2004;161:1324-1333.
7. Marin R, Guerra B, Alonso R, et al. Estrogen activates classical and alternative mechanisms to orchestrate neuroprotection. Curr Neurovasc Res. 2005;2:287-301.
8. Seeman MV, Lang M. The role of estrogens in schizophrenia gender differences. Schizophr Bull. 1990;16:185-194.
9. Castle DJ, Abel K, Takei N, et al. Gender differences in schizophrenia: hormonal effect or subtypes? Schizophr Bull. 1995;21:1-12.
10. Häfner H, an der Heiden W. Epidemiology of schizophrenia. Can J Psychiatry. 1997;42:139-151.
11. Grossman LS, Harrow M, Rosen C, et al. Sex differences in schizophrenia and other psychotic disorders: a 20-year longitudinal study of psychosis and recovery. Compr Psychiatry. 2008;49:523-529.
12. Kajantie E, Phillips DI. The effects of sex and hormonal status on the physiological response to acute psychosocial stress. Psychoneuroendocrinology. 2006;31:151-178.
13. Riecher-Rössler A, Löffler W, Munk-Jörgensen P. What do we really know about late-onset schizophrenia? Eur Arch Psychiatry Clin Neurosci. 1997;247:195-208.
14. Lindamer LA, Lohr JB, Harris MJ, et al. Gender-related clinical differences in older patients with schizophrenia. J Clin Psychiatry. 1999;60:61-67.
15. Seeman MV. Does menopause intensify symptoms in schizophrenia? In: Lewis-Hall F, Williams TS, Panetta JA, et al, eds. Psychiatric illness in women: emerging treatments and research. Arlington, VA: American Psychiatric Publishing, Inc.; 2002:239-248.
16. Convert H, Védie C, Paulin P. [Late-onset schizophrenia or chronic delusion]. Encephale. 2006;32:957-961.
17. Sato T, Bottlender R, Schröter A, et al. Psychopathology of early-onset versus late-onset schizophrenia revisited: an observation of 473 neuroleptic-naive patients before and after first-admission treatments. Schizophr Res. 2004;67:175-183.
18. Palmer BW, McClure FS, Jeste DV. Schizophrenia in late life: findings challenge traditional concepts. Harv Rev Psychiatry. 2001;9:51-58.
19. Weiss DB, Dyrud J, House RM, et al. Psychiatric manifestations of autoimmune disorders. Curr Treat Options Neurol. 2005;7:413-417.
20. Castagnini A, Bertelsen A, Munk-Jorgensen P, et al. The relationship of reactive psychosis and ICD-10 acute and transient psychotic disorders: evidence from a case register-based comparison. Psychopathology. 2007;40:47-53.
21. Huber TJ, Rollnik J, Wilhelms J, et al. Estradiol levels in psychotic disorders. Psychoneuroendocrinology. 2001;26: 27-35.
22. Heiss G, Wallace R, Anderson G, et al, for the WHI Investigators. Health risks and benefits 3 years after stopping randomized treatment with estrogen and progestin. JAMA. 2008;299(9):1036-1045.
23. Doncarlos LL, Azcoitia I, Garcia-Segura LM. Neuroprotective actions of selective estrogen receptor modulators. Psychoneuroendocrinology. 2009 May 15 [Epub ahead of print].
24. Wong J, Seeman MV, Shapiro H. Case report: raloxifene in postmenopausal women with psychosis: preliminary findings. Am J Geriatr Psychiatry. 2003;11(6):697-698.
25. Ye L, Chan MY, Leung LK. The soy isoflavone genistein induces estrogen synthesis in an extragonadal pathway. Mol Cell Endocrinol. 2009;302:73-80.
26. Kulkarni J, Gurvich C, Gilbert H, et al. Hormone modulation: a novel therapeutic approach for women with severe mental illness. Aust N Z J Psychiatry. 2008;42:83-88.
1. Post RM. Kindling and sensitization as models for affective episode recurrence, cyclicity, and tolerance phenomena. Neurosci Biobehav Rev. 2007;31:858-873.
2. Seeman MV. Gender differences in schizophrenia. Can J Psychiatry. 1982;27:107-112.
3. Seeman MV. Interaction of sex, age, and neuroleptic dose. Comp Psychiatry. 1983;24:125-128.
4. Usall J, Suarez D, Haro JM, and the SOHO Study Group. Gender differences in response to antipsychotic treatment in outpatients with schizophrenia. Psychiatry Res. 2007;153: 225-231.
5. Hare E, Glahn DC, Dassori A, et al. Heritability of age of onset of psychosis in schizophrenia. Am J Med Genet B Neuropsychiatr Genet. 2009 Apr 6 [Epub ahead of print].
6. Seeman MV. Gender differences in the prescribing of antipsychotic drugs. Am J Psychiatry. 2004;161:1324-1333.
7. Marin R, Guerra B, Alonso R, et al. Estrogen activates classical and alternative mechanisms to orchestrate neuroprotection. Curr Neurovasc Res. 2005;2:287-301.
8. Seeman MV, Lang M. The role of estrogens in schizophrenia gender differences. Schizophr Bull. 1990;16:185-194.
9. Castle DJ, Abel K, Takei N, et al. Gender differences in schizophrenia: hormonal effect or subtypes? Schizophr Bull. 1995;21:1-12.
10. Häfner H, an der Heiden W. Epidemiology of schizophrenia. Can J Psychiatry. 1997;42:139-151.
11. Grossman LS, Harrow M, Rosen C, et al. Sex differences in schizophrenia and other psychotic disorders: a 20-year longitudinal study of psychosis and recovery. Compr Psychiatry. 2008;49:523-529.
12. Kajantie E, Phillips DI. The effects of sex and hormonal status on the physiological response to acute psychosocial stress. Psychoneuroendocrinology. 2006;31:151-178.
13. Riecher-Rössler A, Löffler W, Munk-Jörgensen P. What do we really know about late-onset schizophrenia? Eur Arch Psychiatry Clin Neurosci. 1997;247:195-208.
14. Lindamer LA, Lohr JB, Harris MJ, et al. Gender-related clinical differences in older patients with schizophrenia. J Clin Psychiatry. 1999;60:61-67.
15. Seeman MV. Does menopause intensify symptoms in schizophrenia? In: Lewis-Hall F, Williams TS, Panetta JA, et al, eds. Psychiatric illness in women: emerging treatments and research. Arlington, VA: American Psychiatric Publishing, Inc.; 2002:239-248.
16. Convert H, Védie C, Paulin P. [Late-onset schizophrenia or chronic delusion]. Encephale. 2006;32:957-961.
17. Sato T, Bottlender R, Schröter A, et al. Psychopathology of early-onset versus late-onset schizophrenia revisited: an observation of 473 neuroleptic-naive patients before and after first-admission treatments. Schizophr Res. 2004;67:175-183.
18. Palmer BW, McClure FS, Jeste DV. Schizophrenia in late life: findings challenge traditional concepts. Harv Rev Psychiatry. 2001;9:51-58.
19. Weiss DB, Dyrud J, House RM, et al. Psychiatric manifestations of autoimmune disorders. Curr Treat Options Neurol. 2005;7:413-417.
20. Castagnini A, Bertelsen A, Munk-Jorgensen P, et al. The relationship of reactive psychosis and ICD-10 acute and transient psychotic disorders: evidence from a case register-based comparison. Psychopathology. 2007;40:47-53.
21. Huber TJ, Rollnik J, Wilhelms J, et al. Estradiol levels in psychotic disorders. Psychoneuroendocrinology. 2001;26: 27-35.
22. Heiss G, Wallace R, Anderson G, et al, for the WHI Investigators. Health risks and benefits 3 years after stopping randomized treatment with estrogen and progestin. JAMA. 2008;299(9):1036-1045.
23. Doncarlos LL, Azcoitia I, Garcia-Segura LM. Neuroprotective actions of selective estrogen receptor modulators. Psychoneuroendocrinology. 2009 May 15 [Epub ahead of print].
24. Wong J, Seeman MV, Shapiro H. Case report: raloxifene in postmenopausal women with psychosis: preliminary findings. Am J Geriatr Psychiatry. 2003;11(6):697-698.
25. Ye L, Chan MY, Leung LK. The soy isoflavone genistein induces estrogen synthesis in an extragonadal pathway. Mol Cell Endocrinol. 2009;302:73-80.
26. Kulkarni J, Gurvich C, Gilbert H, et al. Hormone modulation: a novel therapeutic approach for women with severe mental illness. Aust N Z J Psychiatry. 2008;42:83-88.
Borderline or bipolar? Don't skimp on the life story
Borderline, bipolar, or both? Frame your diagnosis on the patient history
Borderline personality disorder (BPD) and bipolar disorder are frequently confused with each other, in part because of their considerable symptomatic overlap. This redundancy occurs despite the different ways these disorders are conceptualized: BPD as a personality disorder and bipolar disorder as a brain disease among Axis I clinical disorders.
BPD and bipolar disorder—especially bipolar II—often co-occur ( Box ) and are frequently misidentified, as shown by clinical and epidemiologic studies. Misdiagnosis creates problems for clinicians and patients. When diagnosed with BPD, patients with bipolar disorder may be deprived of potentially effective pharmacologic treatments.1 Conversely, the stigma that BPD carries—particularly in the mental health community—may lead clinicians to:
- not even disclose the BPD diagnosis to patients2
- lean in the direction of diagnosing BPD as bipolar disorder, potentially resulting in treatments that have little relevance or failure to refer for more appropriate psychosocial treatments.
To help you avoid confusion and the pitfalls of misdiagnosis, this article clarifies the distinctions between bipolar disorder and BPD. We discuss symptom overlap, highlight key differences between the constructs, outline diagnostic differences, and provide useful suggestions to discern the differential diagnosis.
between BPD and bipolar disorder*
1. Inability of current nosology to separate 2 distinct conditions
Relatively indistinct diagnostic boundaries confuse the differentiation of borderline personality disorder (BPD) and bipolar disorder (5 of 9 BPD criteria may occur with mania or hypomania). In this model, the person has 1 disorder but because of symptom overlap receives a diagnosis of both. Because structured interviews do not allow for subjective judgment or expert opinion, the result is the generation of 2 diagnoses when 1 may provide a more parsimonious and valid explanation.
2. BPD exists on a spectrum with bipolar disorder
The mood lability of BPD may be viewed as not unlike that seen with bipolar disorder.1 Behaviors displayed by patients with BPD are subsequently conceptualized as arising from their unstable mood. Supporting arguments cite family study data and evidence from pharmacotherapy trials of anticonvulsants, including divalproex, for rapid cycling bipolar disorder and BPD.2 Family studies have been notable for their failure to directly characterize family members, however, and clinical trials have been quite small. Further, treatment response may have very limited nosologic implications.
3. Bipolar disorder is a risk factor for BPD
4. BPD is a risk factor for bipolar disorder
Early emergence of a bipolar disorder (in preadolescent or adolescent patients) has been proposed to disrupt psychological development, leading to BPD. This adverse impact on personality development—the “scar hypothesis”3 —is supported by data showing greater risk of co-occurring BPD with earlier onset bipolar disorder.4 More important, prospective studies of patients with bipolar disorder show a greater risk for developing BPD.5
BPD also may be a risk factor for the development of bipolar disorder—the “vulnerability hypothesis.”3 Patients with BPD are more likely to develop bipolar disorder, even compared to patients with other personality disorders.5
5. Shared risk factors
BPD and bipolar disorder may be linked by shared risk factors, such as shared genes or trait neuroticism.3
*Some evidence supports each potential explanation, and they are not necessarily mutually exclusive
References
a. Akiskal HS. Demystifying borderline personality: critique of the concept and unorthodox reflections on its natural kinship with the bipolar spectrum. Acta Psychiatr Scand. 2004;110(6):401-407.
b. Mackinnon DF, Pies R. Affective instability as rapid cycling: theoretical and clinical implications for borderline personality and bipolar spectrum disorders. Bipolar Disord. 2006;8(1):1-14.
c. Christensen MV, Kessing LV. Do personality traits predict first onset in depressive and bipolar disorder? Nord J Psychiatry. 2006;60(2):79-88.
d. Goldberg JF, Garno JL. Age at onset of bipolar disorder and risk for comorbid borderline personality disorder. Bipolar Disord. 2009;11(2):205-208.
e. Gunderson JG, Weinberg I, Daversa MT, et al. Descriptive and longitudinal observations on the relationship of borderline personality disorder and bipolar disorder. Am J Psychiatry. 2006;163(7):1173-1178.
Overlapping symptoms
Bipolar disorder is generally considered a clinical disorder or brain disease that can be understood as a broken mood “thermostat.” The lifetime prevalence of bipolar types I and II is approximately 2%.3 Approximately one-half of patients have a family history of illness, and multiple genes are believed to influence inheritance. Mania is the disorder’s hallmark,4 although overactivity has alternatively been proposed as a core feature.5 Most patients with mania ultimately experience depression6 ( Table 1 ).
No dimensional personality correlates have been consistently demonstrated in bipolar disorder, although co-occurring personality disorders—often the “dramatic” Cluster B type—are common4,7 and may adversely affect treatment response and suicide risk.8,9
Both bipolar disorder and BPD are associated with considerable risk of suicide or suicide attempts.10,11 Self-mutilation or self-injurious behavior without suicidal intent are particularly common in BPD.12 Threats of suicide—which may be manipulative or help-seeking—also are common in BPD and tend to be acute rather than chronic.13
Borderline personality disorder is characterized by an enduring and inflexible pattern of thoughts, feelings, and behaviors that impairs an individual’s psychosocial or vocational function. Its estimated prevalence is approximately 1%,14 although recent community estimates approach 6%.15 Genetic influences play a lesser etiologic role in BPD than in bipolar disorder.
Several of BPD’s common features ( Table 2 )—impulsivity, mood instability, inappropriate anger, suicidal behavior, and unstable relationships—are shared with bipolar disorder, but patients with BPD tend to show higher levels of impulsiveness and hostility than patients with bipolar disorder.16 Dimensional assessments of personality traits suggest that BPD is characterized by high neuroticism and low agreeableness.17 BPD also has been more strongly associated with a childhood history of abuse, even when compared with control groups having other personality disorders or major depression.18 The male-to-female ratio for bipolar disorder approximates 1:1;3 in BPD this ratio has been estimated at 1:4 in clinical samples19 and near 1:1 in community samples.15
BPD and bipolar disorder often co-occur. Evidence indicates ≤20% of patients with BPD have comorbid bipolar disorder20 and 15% of patients with bipolar disorder have comorbid BPD.21 Co-occurrence happens much more often than would be expected by chance. These similar bidirectional comorbidity estimates (15% to 20%) would not be expected for conditions of such differing prevalence (<1% vs 2% or more). This suggests:
- the estimated prevalence of bipolar disorder in BPD is too low
- the estimated prevalence of BPD in bipolar disorder samples is too high
- borderline personality disorder is present in >1% of the population
- bipolar disorder is less common
- some combination of the above.
Among these possibilities, the prevalence estimates of bipolar disorder are the most consistent. Several studies suggest that BPD may be much more common, with some estimates exceeding 5%.15
Table 1
Common signs and symptoms
associated with mania and depression in bipolar disorder
| (Hypo)mania | Depression |
|---|---|
| Elevated mood | Decreased mood |
| Irritability | Irritability |
| Decreased need for sleep | Anhedonia |
| Grandiosity | Decreased self-attitude |
| Talkativeness | Insomnia/hypersomnia |
| Racing thoughts | Change in appetite/weight |
| Increased motor activity | Fatigue |
| Increased sex drive | Hopelessness |
| Religiosity | Suicidal thoughts |
| Distractibility | Impaired concentration |
Table 2
Borderline personality disorder: Commonly reported features
| Impulsivity |
| Unstable relationships |
| Unstable self-image |
| Affective instability |
| Fear of abandonment |
| Recurrent self-injurious or suicidal behavior |
| Feelings of emptiness |
| Intense anger or hostility |
| Transient paranoia or dissociative symptoms |
Roots of misdiagnosis
The presence of bipolar disorder or BPD may increase the risk that the other will be misdiagnosed. When symptoms of both are present, those suggesting 1 diagnosis may reflect the consequences of the other. A diagnosis of BPD could represent a partially treated or treatment-resistant bipolar disorder, or a BPD diagnosis could be the result of several years of disruption by a mood disorder.
Characteristics of bipolar disorder have contributed to clinician bias in favor of that diagnosis rather than BPD ( Table 3 ).22,23 Bipolar disorder also may be misdiagnosed as BPD. This error may most likely occur when the history focuses excessively on cross-sectional symptoms, such as when a patient with bipolar disorder shows prominent mood lability or interpersonal sensitivity during a mood episode but not when euthymic.
Bipolar II disorder. The confusion between bipolar disorder and BPD may be particularly problematic for patients with bipolar II disorder or subthreshold bipolar disorders. The manias of bipolar I disorder are much more readily distinguishable from the mood instability or reactivity of BPD. The manic symptoms of bipolar I are more florid, more pronounced, and lead to more obvious impairment.
The milder highs of bipolar II may resemble the mood fluctuations seen in BPD. Further, bipolar II is characterized by a greater chronicity and affective morbidity than bipolar I, and episodes of illness may be characterized by irritability, anger, and racing thoughts.24 Whereas impulsivity or aggression are more characteristic of BPD, bipolar II is similar to BPD on dimensions of affective instability.24,25
When present in BPD, affective instability or lability is conceptualized as ultra-rapid or ultradian, with a frequency of hours to days. BPD is less likely than bipolar II to show affective lability between depression and euthymia or elation and more likely to show fluctuations into anger and anxiety.26
Nonetheless, because of the increased prominence of shared features and reduced distinguishing features, bipolar II and BPD are prone to misdiagnosis and commonly co-occur.
Table 3
Clinician biases that may favor a bipolar disorder diagnosis, rather than BPD
| Bipolar disorder is supported by decades of research |
| Patients with bipolar disorder are often considered more “likeable” than those with BPD |
| Bipolar disorder is more treatable and has a better long-term outcome than BPD (although BPD is generally characterized by clinical improvement, whereas bipolar disorder is more stable with perhaps some increase in depressive symptom burden) |
| Widely thought to have a biologic basis, the bipolar diagnosis conveys less stigma than BPD, which often is less empathically attributed to the patient’s own failings |
| A bipolar diagnosis is easier to explain to patients than BPD; many psychiatrists have difficulty explaining personality disorders in terms patients understand |
| BPD: borderline personality disorder |
| Source: References 22,23 |
History, the diagnostic key
A thorough and rigorous psychiatric history is essential to distinguish BPD from bipolar disorder. Supplementing the patient’s history with an informant interview is often helpful.
Because personality disorders are considered a chronic and enduring pattern of maladaptive behavior, focus the history on longitudinal course and not simply cross-sectional symptoms. Thus, symptoms suggestive of BPD that are confined only to clearly defined episodes of mood disturbance and are absent during euthymia would not warrant a BPD diagnosis.
Temporal relationship. A detailed chronologic history can help determine the temporal relationship between any borderline features and mood episodes. When the patient’s life story is used as a scaffold for the phenomenologic portions of the psychiatric history, one can determine whether any such functional impairment is confined to episodes of mood disorder or appears as an enduring pattern of thinking, acting, and relating. Exploring what happened at notable life transitions—leaving school, loss of job, divorce/separation—may be similarly helpful.
Family history of psychiatric illness may provide a clue to an individual’s genetic predisposition but, of course, does not determine diagnosis. A detailed family and social history that provides evidence of an individual’s function in school, work, and interpersonal relationships is more relevant.
Abandonment and identity issues. Essential to BPD is fear of abandonment, often an undue fear that those important to patients will leave them. Patients may go to extremes to avoid being “abandoned,” even when this threat is not genuine.27,28 Their insecure attachments often lead them to fear being alone. The patient with BPD may:
- make frantic phone calls or send text messages to a friend or lover seeking reassurance
- take extreme measures such as refusing to leave the person’s home or pleading with them not to leave.
Patients with BPD often struggle with identity disturbance, leading them to wonder who they are and what their beliefs and core values are.29 Although occasionally patients with bipolar disorder may have these symptoms, they are not characteristic of bipolar disorder.
Mood lability. The time course of changes in affect or mood swings also may help distinguish BPD from bipolar disorder.
- With bipolar disorder the shift typically is from depression to elation or the reverse, and moods are sustained. Manias or hypomanias are often immediately followed by a “crash” into depression.
- With BPD, “roller-coaster moods” are typical, mood shifts are nonsustained, and the poles often are anxiety, anger, or desperation.
Patients with BPD often report moods shifting rapidly over minutes or hours, but they rarely describe moods sustained for days or weeks on end—other than perhaps depression. Mood lability of BPD often is produced by interpersonal sensitivity, whereas mood lability in bipolar disorder tends to be autonomous and persistent.
Young patients. Assessment can be particularly challenging in young adults and adolescents because symptoms of an emerging bipolar disorder can be more difficult to distinguish from BPD.30 Patients this young also may have less longitudinal history to distinguish an enduring pattern of thinking and relating from a mood disorder. For these cases, it may be particularly important to classify the frequency and pattern of mood symptoms.
Affective dysregulation is a core feature of BPD and is variably defined as a mood reactivity, typically of short duration (often hours). Cycling in bipolar disorder classically involves a periodicity of weeks to months. Even the broadest definitions include a minimum duration of 2 days for hypomania.5
Mood reactivity can occur within episodes of bipolar disorder, although episodes may occur spontaneously and without an obvious precipitant or stressor. Impulsivity may represent more of an essential feature of BPD than affective instability or mood reactivity and may be of particular diagnostic relevance.
Treatment implications
When you are unable to make a clear diagnosis, describe your clinical reasoning and differential diagnosis in the assessment or formulation. With close follow-up, the longitudinal history and course of illness may eventually lead you to an accurate diagnosis.
There are good reasons to acknowledge both conditions when bipolar disorder and BPD are present. Proper recognition of bipolar disorder is a prerequisite to taking full advantage of proven pharmacologic treatments. The evidence base for pharmacologic management of BPD remains limited,31 but recognizing this disorder may help the patient understand his or her psychiatric history and encourage the use of effective psychosocial treatments.
Psychosocial treatments for bipolar disorder may target demoralization and circadian rhythms with sleep hygiene or social rhythms therapy. Acknowledging BPD:
- helps both clinician and patient to better understand the condition
- facilitates setting realistic treatment goals because BPD tends to respond to medication less robustly than bipolar disorder.
Recognizing BPD also allows for referral to targeted psychosocial treatments, including dialectical behavior therapy, mentalization-based treatment, or Systems Training for Emotional Predictability and Problem Solving (STEPPS).32-34
Related resources
- National Institute of Mental Health. Overview on borderline personality disorder. www.nimh.nih.gov/health/publications/borderline-personality-disorder-fact-sheet/index.shtml.
- National Institute of Mental Health. Bipolar disorder. www.nimh.nih.gov/health/publications/bipolar-disorder/index.shtml.
- Systems Training for Emotional Predictability and Problem Solving (STEPPS). www.uihealthcare.com/topics/medicaldepartments/psychiatry/stepps/index.html.
Drug brand name
- Divalproex • Depakote, Depakene, others
Disclosures
Dr. Fiedorowicz reports no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
Dr. Black receives research/grant support from AstraZeneca and Forest Laboratories and is a consultant to Jazz Pharmaceuticals.
Acknowledgment
The authors would like to thank Nancee Blum, MSW, and Nancy Hale, RN, for their assistance and expertise in the preparation of this article.
1. John H, Sharma V. Misdiagnosis of bipolar disorder as borderline personality disorder: clinical and economic consequences. World J Biol Psychiatry. 2007;1-4[epub ahead of print].
2. Lequesne ER, Hersh RG. Disclosure of a diagnosis of borderline personality disorder. J Psychiatr Pract. 2004;10(3):170-176.
3. Merikangas KR, Akiskal HS, Angst J, et al. Lifetime and 12-month prevalence of bipolar spectrum disorder in the National Comorbidity Survey replication. Arch Gen Psychiatry. 2007;64(5):543-552.
4. Belmaker RH. Bipolar disorder. N Engl J Med. 2004;351(5):476-486.
5. Benazzi F. Testing new diagnostic criteria for hypomania. Ann Clin Psychiatry. 2007;19(2):99-104.
6. Solomon DA, Leon AC, Endicott J, et al. Unipolar mania over the course of a 20-year follow-up study. Am J Psychiatry. 2003;160(11):2049-2051.
7. Schiavone P, Dorz S, Conforti D, et al. Comorbidity of DSM-IV personality disorders in unipolar and bipolar affective disorders: a comparative study. Psychol Rep. 2004;95(1):121-128.
8. Fan AH, Hassell J. Bipolar disorder and comorbid personality psychopathology: a review of the literature. J Clin Psychiatry. 2008;69(11):1794-1803.
9. Garno JL, Goldberg JF, Ramirez PM, et al. Bipolar disorder with comorbid cluster B personality disorder features: impact on suicidality. J Clin Psychiatry. 2005;66(3):339-345.
10. Black DW, Blum N, Pfohl B, et al. Suicidal behavior in borderline personality disorder: prevalence, risk factors, prediction, and prevention. J Pers Disord. 2004;18(3):226-239.
11. Fiedorowicz JG, Leon AC, Keller MB, et al. Do risk factors for suicidal behavior differ by affective disorder polarity? Psychol Med. 2009;39(5):763-771.
12. Paris J. Understanding self-mutilation in borderline personality disorder. Harv Rev Psychiatry. 2005;13(3):179-185.
13. Zanarini MC, Frankenburg FR, Hennen J, et al. The McLean Study of Adult Development (MSAD): overview and implications of the first six years of prospective follow-up. J Pers Disord. 2005;19(5):505-523.
14. Torgersen S, Kringlen E, Cramer V. The prevalence of personality disorders in a community sample. Arch Gen Psychiatry. 2001;58(6):590-596.
15. Grant BF, Chou SP, Goldstein RB, et al. Prevalence, correlates, disability, and comorbidity of DSM-IV borderline personality disorder: results from the Wave 2 National Epidemiologic Survey on Alcohol and Related Conditions. J Clin Psychiatry. 2008;69(4):533-545.
16. Wilson ST, Stanley B, Oquendo MA, et al. Comparing impulsiveness, hostility, and depression in borderline personality disorder and bipolar II disorder. J Clin Psychiatry. 2007;68(10):1533-1539.
17. Zweig-Frank H, Paris J. The five-factor model of personality in borderline and nonborderline personality disorders. Can J Psychiatry. 1995;40(9):523-526.
18. Zanarini MC, Frankenburg FR, Reich DB, et al. Adult experiences of abuse reported by borderline patients and Axis II comparison subjects over six years of prospective follow-up. J Nerv Ment Dis. 2005;193(6):412-416.
19. Zanarini MC, Frankenburg FR, Reich DB, et al. Violence in the lives of adult borderline patients. J Nerv Ment Dis. 1999;187(2):65-71.
20. McCormick B, Blum N, Hansel R, et al. Relationship of sex to symptom severity, psychiatric comorbidity, and health care utilization in 163 subjects with borderline personality disorder. Compr Psychiatry. 2007;48(5):406-412.
21. Brieger P, Ehrt U, Marneros A. Frequency of comorbid personality disorders in bipolar and unipolar affective disorders. Compr Psychiatry. 2003;44(1):28-34.
22. Paris J, Zweig-Frank H. A 27-year follow-up of patients with borderline personality disorder. Compr Psychiatry. 2001;42(6):482-487.
23. Coryell WH, Fiedorowicz JG, Solomon D, et al. Age transitions in the course of bipolar I disorder. Psychol Med. 2009;39(8):1247-1252.
24. Benazzi F. Borderline personality-bipolar spectrum relationship. Prog Neuropsychopharmacol Biol Psychiatry. 2006;30(1):68-74.
25. Critchfield KL, Levy KN, Clarkin JF. The relationship between impulsivity, aggression, and impulsive-aggression in borderline personality disorder: an empirical analysis of self-report measures. J Pers Disord. 2004;18(6):555-570.
26. Henry C, Mitropoulou V, New AS, et al. Affective instability and impulsivity in borderline personality and bipolar II disorders: similarities and differences. J Psychiatr Res. 2001;35(6):307-312.
27. Bray A. The extended mind and borderline personality disorder. Australas Psychiatry. 2008;16(1):8-12.
28. Gunderson JG. The borderline patient’s intolerance of aloneness: insecure attachments and therapist availability. Am J Psychiatry. 1996;153(6):752-758.
29. Jorgensen CR. Disturbed sense of identity in borderline personality disorder. J Pers Disord. 2006;20(6):618-644.
30. Smith DJ, Muir WJ, Blackwood DH. Borderline personality disorder characteristics in young adults with recurrent mood disorders: a comparison of bipolar and unipolar depression. J Affect Disord. 2005;87(1):17-23.
31. Binks CA, Fenton M, McCarthy L, et al. Pharmacological interventions for people with borderline personality disorder. Cochrane Database Syst Rev. 2006(1);CD005653.-
32. Lynch TR, Trost WT, Salsman N, et al. Dialectical behavior therapy for borderline personality disorder. Annu Rev Clin Psychol. 2007;3:181-205.
33. Bateman AW, Fonagy P. Mentalization-based treatment of BPD. J Pers Disord. 2004;18(1):36-51.
34. Blum N, St John D, Pfohl B, et al. Systems Training for Emotional Predictability and Problem Solving (STEPPS) for outpatients with borderline personality disorder: a randomized controlled trial and 1-year follow-up. Am J Psychiatry. 2008;165(4):468-478.
Borderline personality disorder (BPD) and bipolar disorder are frequently confused with each other, in part because of their considerable symptomatic overlap. This redundancy occurs despite the different ways these disorders are conceptualized: BPD as a personality disorder and bipolar disorder as a brain disease among Axis I clinical disorders.
BPD and bipolar disorder—especially bipolar II—often co-occur ( Box ) and are frequently misidentified, as shown by clinical and epidemiologic studies. Misdiagnosis creates problems for clinicians and patients. When diagnosed with BPD, patients with bipolar disorder may be deprived of potentially effective pharmacologic treatments.1 Conversely, the stigma that BPD carries—particularly in the mental health community—may lead clinicians to:
- not even disclose the BPD diagnosis to patients2
- lean in the direction of diagnosing BPD as bipolar disorder, potentially resulting in treatments that have little relevance or failure to refer for more appropriate psychosocial treatments.
To help you avoid confusion and the pitfalls of misdiagnosis, this article clarifies the distinctions between bipolar disorder and BPD. We discuss symptom overlap, highlight key differences between the constructs, outline diagnostic differences, and provide useful suggestions to discern the differential diagnosis.
between BPD and bipolar disorder*
1. Inability of current nosology to separate 2 distinct conditions
Relatively indistinct diagnostic boundaries confuse the differentiation of borderline personality disorder (BPD) and bipolar disorder (5 of 9 BPD criteria may occur with mania or hypomania). In this model, the person has 1 disorder but because of symptom overlap receives a diagnosis of both. Because structured interviews do not allow for subjective judgment or expert opinion, the result is the generation of 2 diagnoses when 1 may provide a more parsimonious and valid explanation.
2. BPD exists on a spectrum with bipolar disorder
The mood lability of BPD may be viewed as not unlike that seen with bipolar disorder.1 Behaviors displayed by patients with BPD are subsequently conceptualized as arising from their unstable mood. Supporting arguments cite family study data and evidence from pharmacotherapy trials of anticonvulsants, including divalproex, for rapid cycling bipolar disorder and BPD.2 Family studies have been notable for their failure to directly characterize family members, however, and clinical trials have been quite small. Further, treatment response may have very limited nosologic implications.
3. Bipolar disorder is a risk factor for BPD
4. BPD is a risk factor for bipolar disorder
Early emergence of a bipolar disorder (in preadolescent or adolescent patients) has been proposed to disrupt psychological development, leading to BPD. This adverse impact on personality development—the “scar hypothesis”3 —is supported by data showing greater risk of co-occurring BPD with earlier onset bipolar disorder.4 More important, prospective studies of patients with bipolar disorder show a greater risk for developing BPD.5
BPD also may be a risk factor for the development of bipolar disorder—the “vulnerability hypothesis.”3 Patients with BPD are more likely to develop bipolar disorder, even compared to patients with other personality disorders.5
5. Shared risk factors
BPD and bipolar disorder may be linked by shared risk factors, such as shared genes or trait neuroticism.3
*Some evidence supports each potential explanation, and they are not necessarily mutually exclusive
References
a. Akiskal HS. Demystifying borderline personality: critique of the concept and unorthodox reflections on its natural kinship with the bipolar spectrum. Acta Psychiatr Scand. 2004;110(6):401-407.
b. Mackinnon DF, Pies R. Affective instability as rapid cycling: theoretical and clinical implications for borderline personality and bipolar spectrum disorders. Bipolar Disord. 2006;8(1):1-14.
c. Christensen MV, Kessing LV. Do personality traits predict first onset in depressive and bipolar disorder? Nord J Psychiatry. 2006;60(2):79-88.
d. Goldberg JF, Garno JL. Age at onset of bipolar disorder and risk for comorbid borderline personality disorder. Bipolar Disord. 2009;11(2):205-208.
e. Gunderson JG, Weinberg I, Daversa MT, et al. Descriptive and longitudinal observations on the relationship of borderline personality disorder and bipolar disorder. Am J Psychiatry. 2006;163(7):1173-1178.
Overlapping symptoms
Bipolar disorder is generally considered a clinical disorder or brain disease that can be understood as a broken mood “thermostat.” The lifetime prevalence of bipolar types I and II is approximately 2%.3 Approximately one-half of patients have a family history of illness, and multiple genes are believed to influence inheritance. Mania is the disorder’s hallmark,4 although overactivity has alternatively been proposed as a core feature.5 Most patients with mania ultimately experience depression6 ( Table 1 ).
No dimensional personality correlates have been consistently demonstrated in bipolar disorder, although co-occurring personality disorders—often the “dramatic” Cluster B type—are common4,7 and may adversely affect treatment response and suicide risk.8,9
Both bipolar disorder and BPD are associated with considerable risk of suicide or suicide attempts.10,11 Self-mutilation or self-injurious behavior without suicidal intent are particularly common in BPD.12 Threats of suicide—which may be manipulative or help-seeking—also are common in BPD and tend to be acute rather than chronic.13
Borderline personality disorder is characterized by an enduring and inflexible pattern of thoughts, feelings, and behaviors that impairs an individual’s psychosocial or vocational function. Its estimated prevalence is approximately 1%,14 although recent community estimates approach 6%.15 Genetic influences play a lesser etiologic role in BPD than in bipolar disorder.
Several of BPD’s common features ( Table 2 )—impulsivity, mood instability, inappropriate anger, suicidal behavior, and unstable relationships—are shared with bipolar disorder, but patients with BPD tend to show higher levels of impulsiveness and hostility than patients with bipolar disorder.16 Dimensional assessments of personality traits suggest that BPD is characterized by high neuroticism and low agreeableness.17 BPD also has been more strongly associated with a childhood history of abuse, even when compared with control groups having other personality disorders or major depression.18 The male-to-female ratio for bipolar disorder approximates 1:1;3 in BPD this ratio has been estimated at 1:4 in clinical samples19 and near 1:1 in community samples.15
BPD and bipolar disorder often co-occur. Evidence indicates ≤20% of patients with BPD have comorbid bipolar disorder20 and 15% of patients with bipolar disorder have comorbid BPD.21 Co-occurrence happens much more often than would be expected by chance. These similar bidirectional comorbidity estimates (15% to 20%) would not be expected for conditions of such differing prevalence (<1% vs 2% or more). This suggests:
- the estimated prevalence of bipolar disorder in BPD is too low
- the estimated prevalence of BPD in bipolar disorder samples is too high
- borderline personality disorder is present in >1% of the population
- bipolar disorder is less common
- some combination of the above.
Among these possibilities, the prevalence estimates of bipolar disorder are the most consistent. Several studies suggest that BPD may be much more common, with some estimates exceeding 5%.15
Table 1
Common signs and symptoms
associated with mania and depression in bipolar disorder
| (Hypo)mania | Depression |
|---|---|
| Elevated mood | Decreased mood |
| Irritability | Irritability |
| Decreased need for sleep | Anhedonia |
| Grandiosity | Decreased self-attitude |
| Talkativeness | Insomnia/hypersomnia |
| Racing thoughts | Change in appetite/weight |
| Increased motor activity | Fatigue |
| Increased sex drive | Hopelessness |
| Religiosity | Suicidal thoughts |
| Distractibility | Impaired concentration |
Table 2
Borderline personality disorder: Commonly reported features
| Impulsivity |
| Unstable relationships |
| Unstable self-image |
| Affective instability |
| Fear of abandonment |
| Recurrent self-injurious or suicidal behavior |
| Feelings of emptiness |
| Intense anger or hostility |
| Transient paranoia or dissociative symptoms |
Roots of misdiagnosis
The presence of bipolar disorder or BPD may increase the risk that the other will be misdiagnosed. When symptoms of both are present, those suggesting 1 diagnosis may reflect the consequences of the other. A diagnosis of BPD could represent a partially treated or treatment-resistant bipolar disorder, or a BPD diagnosis could be the result of several years of disruption by a mood disorder.
Characteristics of bipolar disorder have contributed to clinician bias in favor of that diagnosis rather than BPD ( Table 3 ).22,23 Bipolar disorder also may be misdiagnosed as BPD. This error may most likely occur when the history focuses excessively on cross-sectional symptoms, such as when a patient with bipolar disorder shows prominent mood lability or interpersonal sensitivity during a mood episode but not when euthymic.
Bipolar II disorder. The confusion between bipolar disorder and BPD may be particularly problematic for patients with bipolar II disorder or subthreshold bipolar disorders. The manias of bipolar I disorder are much more readily distinguishable from the mood instability or reactivity of BPD. The manic symptoms of bipolar I are more florid, more pronounced, and lead to more obvious impairment.
The milder highs of bipolar II may resemble the mood fluctuations seen in BPD. Further, bipolar II is characterized by a greater chronicity and affective morbidity than bipolar I, and episodes of illness may be characterized by irritability, anger, and racing thoughts.24 Whereas impulsivity or aggression are more characteristic of BPD, bipolar II is similar to BPD on dimensions of affective instability.24,25
When present in BPD, affective instability or lability is conceptualized as ultra-rapid or ultradian, with a frequency of hours to days. BPD is less likely than bipolar II to show affective lability between depression and euthymia or elation and more likely to show fluctuations into anger and anxiety.26
Nonetheless, because of the increased prominence of shared features and reduced distinguishing features, bipolar II and BPD are prone to misdiagnosis and commonly co-occur.
Table 3
Clinician biases that may favor a bipolar disorder diagnosis, rather than BPD
| Bipolar disorder is supported by decades of research |
| Patients with bipolar disorder are often considered more “likeable” than those with BPD |
| Bipolar disorder is more treatable and has a better long-term outcome than BPD (although BPD is generally characterized by clinical improvement, whereas bipolar disorder is more stable with perhaps some increase in depressive symptom burden) |
| Widely thought to have a biologic basis, the bipolar diagnosis conveys less stigma than BPD, which often is less empathically attributed to the patient’s own failings |
| A bipolar diagnosis is easier to explain to patients than BPD; many psychiatrists have difficulty explaining personality disorders in terms patients understand |
| BPD: borderline personality disorder |
| Source: References 22,23 |
History, the diagnostic key
A thorough and rigorous psychiatric history is essential to distinguish BPD from bipolar disorder. Supplementing the patient’s history with an informant interview is often helpful.
Because personality disorders are considered a chronic and enduring pattern of maladaptive behavior, focus the history on longitudinal course and not simply cross-sectional symptoms. Thus, symptoms suggestive of BPD that are confined only to clearly defined episodes of mood disturbance and are absent during euthymia would not warrant a BPD diagnosis.
Temporal relationship. A detailed chronologic history can help determine the temporal relationship between any borderline features and mood episodes. When the patient’s life story is used as a scaffold for the phenomenologic portions of the psychiatric history, one can determine whether any such functional impairment is confined to episodes of mood disorder or appears as an enduring pattern of thinking, acting, and relating. Exploring what happened at notable life transitions—leaving school, loss of job, divorce/separation—may be similarly helpful.
Family history of psychiatric illness may provide a clue to an individual’s genetic predisposition but, of course, does not determine diagnosis. A detailed family and social history that provides evidence of an individual’s function in school, work, and interpersonal relationships is more relevant.
Abandonment and identity issues. Essential to BPD is fear of abandonment, often an undue fear that those important to patients will leave them. Patients may go to extremes to avoid being “abandoned,” even when this threat is not genuine.27,28 Their insecure attachments often lead them to fear being alone. The patient with BPD may:
- make frantic phone calls or send text messages to a friend or lover seeking reassurance
- take extreme measures such as refusing to leave the person’s home or pleading with them not to leave.
Patients with BPD often struggle with identity disturbance, leading them to wonder who they are and what their beliefs and core values are.29 Although occasionally patients with bipolar disorder may have these symptoms, they are not characteristic of bipolar disorder.
Mood lability. The time course of changes in affect or mood swings also may help distinguish BPD from bipolar disorder.
- With bipolar disorder the shift typically is from depression to elation or the reverse, and moods are sustained. Manias or hypomanias are often immediately followed by a “crash” into depression.
- With BPD, “roller-coaster moods” are typical, mood shifts are nonsustained, and the poles often are anxiety, anger, or desperation.
Patients with BPD often report moods shifting rapidly over minutes or hours, but they rarely describe moods sustained for days or weeks on end—other than perhaps depression. Mood lability of BPD often is produced by interpersonal sensitivity, whereas mood lability in bipolar disorder tends to be autonomous and persistent.
Young patients. Assessment can be particularly challenging in young adults and adolescents because symptoms of an emerging bipolar disorder can be more difficult to distinguish from BPD.30 Patients this young also may have less longitudinal history to distinguish an enduring pattern of thinking and relating from a mood disorder. For these cases, it may be particularly important to classify the frequency and pattern of mood symptoms.
Affective dysregulation is a core feature of BPD and is variably defined as a mood reactivity, typically of short duration (often hours). Cycling in bipolar disorder classically involves a periodicity of weeks to months. Even the broadest definitions include a minimum duration of 2 days for hypomania.5
Mood reactivity can occur within episodes of bipolar disorder, although episodes may occur spontaneously and without an obvious precipitant or stressor. Impulsivity may represent more of an essential feature of BPD than affective instability or mood reactivity and may be of particular diagnostic relevance.
Treatment implications
When you are unable to make a clear diagnosis, describe your clinical reasoning and differential diagnosis in the assessment or formulation. With close follow-up, the longitudinal history and course of illness may eventually lead you to an accurate diagnosis.
There are good reasons to acknowledge both conditions when bipolar disorder and BPD are present. Proper recognition of bipolar disorder is a prerequisite to taking full advantage of proven pharmacologic treatments. The evidence base for pharmacologic management of BPD remains limited,31 but recognizing this disorder may help the patient understand his or her psychiatric history and encourage the use of effective psychosocial treatments.
Psychosocial treatments for bipolar disorder may target demoralization and circadian rhythms with sleep hygiene or social rhythms therapy. Acknowledging BPD:
- helps both clinician and patient to better understand the condition
- facilitates setting realistic treatment goals because BPD tends to respond to medication less robustly than bipolar disorder.
Recognizing BPD also allows for referral to targeted psychosocial treatments, including dialectical behavior therapy, mentalization-based treatment, or Systems Training for Emotional Predictability and Problem Solving (STEPPS).32-34
Related resources
- National Institute of Mental Health. Overview on borderline personality disorder. www.nimh.nih.gov/health/publications/borderline-personality-disorder-fact-sheet/index.shtml.
- National Institute of Mental Health. Bipolar disorder. www.nimh.nih.gov/health/publications/bipolar-disorder/index.shtml.
- Systems Training for Emotional Predictability and Problem Solving (STEPPS). www.uihealthcare.com/topics/medicaldepartments/psychiatry/stepps/index.html.
Drug brand name
- Divalproex • Depakote, Depakene, others
Disclosures
Dr. Fiedorowicz reports no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
Dr. Black receives research/grant support from AstraZeneca and Forest Laboratories and is a consultant to Jazz Pharmaceuticals.
Acknowledgment
The authors would like to thank Nancee Blum, MSW, and Nancy Hale, RN, for their assistance and expertise in the preparation of this article.
Borderline personality disorder (BPD) and bipolar disorder are frequently confused with each other, in part because of their considerable symptomatic overlap. This redundancy occurs despite the different ways these disorders are conceptualized: BPD as a personality disorder and bipolar disorder as a brain disease among Axis I clinical disorders.
BPD and bipolar disorder—especially bipolar II—often co-occur ( Box ) and are frequently misidentified, as shown by clinical and epidemiologic studies. Misdiagnosis creates problems for clinicians and patients. When diagnosed with BPD, patients with bipolar disorder may be deprived of potentially effective pharmacologic treatments.1 Conversely, the stigma that BPD carries—particularly in the mental health community—may lead clinicians to:
- not even disclose the BPD diagnosis to patients2
- lean in the direction of diagnosing BPD as bipolar disorder, potentially resulting in treatments that have little relevance or failure to refer for more appropriate psychosocial treatments.
To help you avoid confusion and the pitfalls of misdiagnosis, this article clarifies the distinctions between bipolar disorder and BPD. We discuss symptom overlap, highlight key differences between the constructs, outline diagnostic differences, and provide useful suggestions to discern the differential diagnosis.
between BPD and bipolar disorder*
1. Inability of current nosology to separate 2 distinct conditions
Relatively indistinct diagnostic boundaries confuse the differentiation of borderline personality disorder (BPD) and bipolar disorder (5 of 9 BPD criteria may occur with mania or hypomania). In this model, the person has 1 disorder but because of symptom overlap receives a diagnosis of both. Because structured interviews do not allow for subjective judgment or expert opinion, the result is the generation of 2 diagnoses when 1 may provide a more parsimonious and valid explanation.
2. BPD exists on a spectrum with bipolar disorder
The mood lability of BPD may be viewed as not unlike that seen with bipolar disorder.1 Behaviors displayed by patients with BPD are subsequently conceptualized as arising from their unstable mood. Supporting arguments cite family study data and evidence from pharmacotherapy trials of anticonvulsants, including divalproex, for rapid cycling bipolar disorder and BPD.2 Family studies have been notable for their failure to directly characterize family members, however, and clinical trials have been quite small. Further, treatment response may have very limited nosologic implications.
3. Bipolar disorder is a risk factor for BPD
4. BPD is a risk factor for bipolar disorder
Early emergence of a bipolar disorder (in preadolescent or adolescent patients) has been proposed to disrupt psychological development, leading to BPD. This adverse impact on personality development—the “scar hypothesis”3 —is supported by data showing greater risk of co-occurring BPD with earlier onset bipolar disorder.4 More important, prospective studies of patients with bipolar disorder show a greater risk for developing BPD.5
BPD also may be a risk factor for the development of bipolar disorder—the “vulnerability hypothesis.”3 Patients with BPD are more likely to develop bipolar disorder, even compared to patients with other personality disorders.5
5. Shared risk factors
BPD and bipolar disorder may be linked by shared risk factors, such as shared genes or trait neuroticism.3
*Some evidence supports each potential explanation, and they are not necessarily mutually exclusive
References
a. Akiskal HS. Demystifying borderline personality: critique of the concept and unorthodox reflections on its natural kinship with the bipolar spectrum. Acta Psychiatr Scand. 2004;110(6):401-407.
b. Mackinnon DF, Pies R. Affective instability as rapid cycling: theoretical and clinical implications for borderline personality and bipolar spectrum disorders. Bipolar Disord. 2006;8(1):1-14.
c. Christensen MV, Kessing LV. Do personality traits predict first onset in depressive and bipolar disorder? Nord J Psychiatry. 2006;60(2):79-88.
d. Goldberg JF, Garno JL. Age at onset of bipolar disorder and risk for comorbid borderline personality disorder. Bipolar Disord. 2009;11(2):205-208.
e. Gunderson JG, Weinberg I, Daversa MT, et al. Descriptive and longitudinal observations on the relationship of borderline personality disorder and bipolar disorder. Am J Psychiatry. 2006;163(7):1173-1178.
Overlapping symptoms
Bipolar disorder is generally considered a clinical disorder or brain disease that can be understood as a broken mood “thermostat.” The lifetime prevalence of bipolar types I and II is approximately 2%.3 Approximately one-half of patients have a family history of illness, and multiple genes are believed to influence inheritance. Mania is the disorder’s hallmark,4 although overactivity has alternatively been proposed as a core feature.5 Most patients with mania ultimately experience depression6 ( Table 1 ).
No dimensional personality correlates have been consistently demonstrated in bipolar disorder, although co-occurring personality disorders—often the “dramatic” Cluster B type—are common4,7 and may adversely affect treatment response and suicide risk.8,9
Both bipolar disorder and BPD are associated with considerable risk of suicide or suicide attempts.10,11 Self-mutilation or self-injurious behavior without suicidal intent are particularly common in BPD.12 Threats of suicide—which may be manipulative or help-seeking—also are common in BPD and tend to be acute rather than chronic.13
Borderline personality disorder is characterized by an enduring and inflexible pattern of thoughts, feelings, and behaviors that impairs an individual’s psychosocial or vocational function. Its estimated prevalence is approximately 1%,14 although recent community estimates approach 6%.15 Genetic influences play a lesser etiologic role in BPD than in bipolar disorder.
Several of BPD’s common features ( Table 2 )—impulsivity, mood instability, inappropriate anger, suicidal behavior, and unstable relationships—are shared with bipolar disorder, but patients with BPD tend to show higher levels of impulsiveness and hostility than patients with bipolar disorder.16 Dimensional assessments of personality traits suggest that BPD is characterized by high neuroticism and low agreeableness.17 BPD also has been more strongly associated with a childhood history of abuse, even when compared with control groups having other personality disorders or major depression.18 The male-to-female ratio for bipolar disorder approximates 1:1;3 in BPD this ratio has been estimated at 1:4 in clinical samples19 and near 1:1 in community samples.15
BPD and bipolar disorder often co-occur. Evidence indicates ≤20% of patients with BPD have comorbid bipolar disorder20 and 15% of patients with bipolar disorder have comorbid BPD.21 Co-occurrence happens much more often than would be expected by chance. These similar bidirectional comorbidity estimates (15% to 20%) would not be expected for conditions of such differing prevalence (<1% vs 2% or more). This suggests:
- the estimated prevalence of bipolar disorder in BPD is too low
- the estimated prevalence of BPD in bipolar disorder samples is too high
- borderline personality disorder is present in >1% of the population
- bipolar disorder is less common
- some combination of the above.
Among these possibilities, the prevalence estimates of bipolar disorder are the most consistent. Several studies suggest that BPD may be much more common, with some estimates exceeding 5%.15
Table 1
Common signs and symptoms
associated with mania and depression in bipolar disorder
| (Hypo)mania | Depression |
|---|---|
| Elevated mood | Decreased mood |
| Irritability | Irritability |
| Decreased need for sleep | Anhedonia |
| Grandiosity | Decreased self-attitude |
| Talkativeness | Insomnia/hypersomnia |
| Racing thoughts | Change in appetite/weight |
| Increased motor activity | Fatigue |
| Increased sex drive | Hopelessness |
| Religiosity | Suicidal thoughts |
| Distractibility | Impaired concentration |
Table 2
Borderline personality disorder: Commonly reported features
| Impulsivity |
| Unstable relationships |
| Unstable self-image |
| Affective instability |
| Fear of abandonment |
| Recurrent self-injurious or suicidal behavior |
| Feelings of emptiness |
| Intense anger or hostility |
| Transient paranoia or dissociative symptoms |
Roots of misdiagnosis
The presence of bipolar disorder or BPD may increase the risk that the other will be misdiagnosed. When symptoms of both are present, those suggesting 1 diagnosis may reflect the consequences of the other. A diagnosis of BPD could represent a partially treated or treatment-resistant bipolar disorder, or a BPD diagnosis could be the result of several years of disruption by a mood disorder.
Characteristics of bipolar disorder have contributed to clinician bias in favor of that diagnosis rather than BPD ( Table 3 ).22,23 Bipolar disorder also may be misdiagnosed as BPD. This error may most likely occur when the history focuses excessively on cross-sectional symptoms, such as when a patient with bipolar disorder shows prominent mood lability or interpersonal sensitivity during a mood episode but not when euthymic.
Bipolar II disorder. The confusion between bipolar disorder and BPD may be particularly problematic for patients with bipolar II disorder or subthreshold bipolar disorders. The manias of bipolar I disorder are much more readily distinguishable from the mood instability or reactivity of BPD. The manic symptoms of bipolar I are more florid, more pronounced, and lead to more obvious impairment.
The milder highs of bipolar II may resemble the mood fluctuations seen in BPD. Further, bipolar II is characterized by a greater chronicity and affective morbidity than bipolar I, and episodes of illness may be characterized by irritability, anger, and racing thoughts.24 Whereas impulsivity or aggression are more characteristic of BPD, bipolar II is similar to BPD on dimensions of affective instability.24,25
When present in BPD, affective instability or lability is conceptualized as ultra-rapid or ultradian, with a frequency of hours to days. BPD is less likely than bipolar II to show affective lability between depression and euthymia or elation and more likely to show fluctuations into anger and anxiety.26
Nonetheless, because of the increased prominence of shared features and reduced distinguishing features, bipolar II and BPD are prone to misdiagnosis and commonly co-occur.
Table 3
Clinician biases that may favor a bipolar disorder diagnosis, rather than BPD
| Bipolar disorder is supported by decades of research |
| Patients with bipolar disorder are often considered more “likeable” than those with BPD |
| Bipolar disorder is more treatable and has a better long-term outcome than BPD (although BPD is generally characterized by clinical improvement, whereas bipolar disorder is more stable with perhaps some increase in depressive symptom burden) |
| Widely thought to have a biologic basis, the bipolar diagnosis conveys less stigma than BPD, which often is less empathically attributed to the patient’s own failings |
| A bipolar diagnosis is easier to explain to patients than BPD; many psychiatrists have difficulty explaining personality disorders in terms patients understand |
| BPD: borderline personality disorder |
| Source: References 22,23 |
History, the diagnostic key
A thorough and rigorous psychiatric history is essential to distinguish BPD from bipolar disorder. Supplementing the patient’s history with an informant interview is often helpful.
Because personality disorders are considered a chronic and enduring pattern of maladaptive behavior, focus the history on longitudinal course and not simply cross-sectional symptoms. Thus, symptoms suggestive of BPD that are confined only to clearly defined episodes of mood disturbance and are absent during euthymia would not warrant a BPD diagnosis.
Temporal relationship. A detailed chronologic history can help determine the temporal relationship between any borderline features and mood episodes. When the patient’s life story is used as a scaffold for the phenomenologic portions of the psychiatric history, one can determine whether any such functional impairment is confined to episodes of mood disorder or appears as an enduring pattern of thinking, acting, and relating. Exploring what happened at notable life transitions—leaving school, loss of job, divorce/separation—may be similarly helpful.
Family history of psychiatric illness may provide a clue to an individual’s genetic predisposition but, of course, does not determine diagnosis. A detailed family and social history that provides evidence of an individual’s function in school, work, and interpersonal relationships is more relevant.
Abandonment and identity issues. Essential to BPD is fear of abandonment, often an undue fear that those important to patients will leave them. Patients may go to extremes to avoid being “abandoned,” even when this threat is not genuine.27,28 Their insecure attachments often lead them to fear being alone. The patient with BPD may:
- make frantic phone calls or send text messages to a friend or lover seeking reassurance
- take extreme measures such as refusing to leave the person’s home or pleading with them not to leave.
Patients with BPD often struggle with identity disturbance, leading them to wonder who they are and what their beliefs and core values are.29 Although occasionally patients with bipolar disorder may have these symptoms, they are not characteristic of bipolar disorder.
Mood lability. The time course of changes in affect or mood swings also may help distinguish BPD from bipolar disorder.
- With bipolar disorder the shift typically is from depression to elation or the reverse, and moods are sustained. Manias or hypomanias are often immediately followed by a “crash” into depression.
- With BPD, “roller-coaster moods” are typical, mood shifts are nonsustained, and the poles often are anxiety, anger, or desperation.
Patients with BPD often report moods shifting rapidly over minutes or hours, but they rarely describe moods sustained for days or weeks on end—other than perhaps depression. Mood lability of BPD often is produced by interpersonal sensitivity, whereas mood lability in bipolar disorder tends to be autonomous and persistent.
Young patients. Assessment can be particularly challenging in young adults and adolescents because symptoms of an emerging bipolar disorder can be more difficult to distinguish from BPD.30 Patients this young also may have less longitudinal history to distinguish an enduring pattern of thinking and relating from a mood disorder. For these cases, it may be particularly important to classify the frequency and pattern of mood symptoms.
Affective dysregulation is a core feature of BPD and is variably defined as a mood reactivity, typically of short duration (often hours). Cycling in bipolar disorder classically involves a periodicity of weeks to months. Even the broadest definitions include a minimum duration of 2 days for hypomania.5
Mood reactivity can occur within episodes of bipolar disorder, although episodes may occur spontaneously and without an obvious precipitant or stressor. Impulsivity may represent more of an essential feature of BPD than affective instability or mood reactivity and may be of particular diagnostic relevance.
Treatment implications
When you are unable to make a clear diagnosis, describe your clinical reasoning and differential diagnosis in the assessment or formulation. With close follow-up, the longitudinal history and course of illness may eventually lead you to an accurate diagnosis.
There are good reasons to acknowledge both conditions when bipolar disorder and BPD are present. Proper recognition of bipolar disorder is a prerequisite to taking full advantage of proven pharmacologic treatments. The evidence base for pharmacologic management of BPD remains limited,31 but recognizing this disorder may help the patient understand his or her psychiatric history and encourage the use of effective psychosocial treatments.
Psychosocial treatments for bipolar disorder may target demoralization and circadian rhythms with sleep hygiene or social rhythms therapy. Acknowledging BPD:
- helps both clinician and patient to better understand the condition
- facilitates setting realistic treatment goals because BPD tends to respond to medication less robustly than bipolar disorder.
Recognizing BPD also allows for referral to targeted psychosocial treatments, including dialectical behavior therapy, mentalization-based treatment, or Systems Training for Emotional Predictability and Problem Solving (STEPPS).32-34
Related resources
- National Institute of Mental Health. Overview on borderline personality disorder. www.nimh.nih.gov/health/publications/borderline-personality-disorder-fact-sheet/index.shtml.
- National Institute of Mental Health. Bipolar disorder. www.nimh.nih.gov/health/publications/bipolar-disorder/index.shtml.
- Systems Training for Emotional Predictability and Problem Solving (STEPPS). www.uihealthcare.com/topics/medicaldepartments/psychiatry/stepps/index.html.
Drug brand name
- Divalproex • Depakote, Depakene, others
Disclosures
Dr. Fiedorowicz reports no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
Dr. Black receives research/grant support from AstraZeneca and Forest Laboratories and is a consultant to Jazz Pharmaceuticals.
Acknowledgment
The authors would like to thank Nancee Blum, MSW, and Nancy Hale, RN, for their assistance and expertise in the preparation of this article.
1. John H, Sharma V. Misdiagnosis of bipolar disorder as borderline personality disorder: clinical and economic consequences. World J Biol Psychiatry. 2007;1-4[epub ahead of print].
2. Lequesne ER, Hersh RG. Disclosure of a diagnosis of borderline personality disorder. J Psychiatr Pract. 2004;10(3):170-176.
3. Merikangas KR, Akiskal HS, Angst J, et al. Lifetime and 12-month prevalence of bipolar spectrum disorder in the National Comorbidity Survey replication. Arch Gen Psychiatry. 2007;64(5):543-552.
4. Belmaker RH. Bipolar disorder. N Engl J Med. 2004;351(5):476-486.
5. Benazzi F. Testing new diagnostic criteria for hypomania. Ann Clin Psychiatry. 2007;19(2):99-104.
6. Solomon DA, Leon AC, Endicott J, et al. Unipolar mania over the course of a 20-year follow-up study. Am J Psychiatry. 2003;160(11):2049-2051.
7. Schiavone P, Dorz S, Conforti D, et al. Comorbidity of DSM-IV personality disorders in unipolar and bipolar affective disorders: a comparative study. Psychol Rep. 2004;95(1):121-128.
8. Fan AH, Hassell J. Bipolar disorder and comorbid personality psychopathology: a review of the literature. J Clin Psychiatry. 2008;69(11):1794-1803.
9. Garno JL, Goldberg JF, Ramirez PM, et al. Bipolar disorder with comorbid cluster B personality disorder features: impact on suicidality. J Clin Psychiatry. 2005;66(3):339-345.
10. Black DW, Blum N, Pfohl B, et al. Suicidal behavior in borderline personality disorder: prevalence, risk factors, prediction, and prevention. J Pers Disord. 2004;18(3):226-239.
11. Fiedorowicz JG, Leon AC, Keller MB, et al. Do risk factors for suicidal behavior differ by affective disorder polarity? Psychol Med. 2009;39(5):763-771.
12. Paris J. Understanding self-mutilation in borderline personality disorder. Harv Rev Psychiatry. 2005;13(3):179-185.
13. Zanarini MC, Frankenburg FR, Hennen J, et al. The McLean Study of Adult Development (MSAD): overview and implications of the first six years of prospective follow-up. J Pers Disord. 2005;19(5):505-523.
14. Torgersen S, Kringlen E, Cramer V. The prevalence of personality disorders in a community sample. Arch Gen Psychiatry. 2001;58(6):590-596.
15. Grant BF, Chou SP, Goldstein RB, et al. Prevalence, correlates, disability, and comorbidity of DSM-IV borderline personality disorder: results from the Wave 2 National Epidemiologic Survey on Alcohol and Related Conditions. J Clin Psychiatry. 2008;69(4):533-545.
16. Wilson ST, Stanley B, Oquendo MA, et al. Comparing impulsiveness, hostility, and depression in borderline personality disorder and bipolar II disorder. J Clin Psychiatry. 2007;68(10):1533-1539.
17. Zweig-Frank H, Paris J. The five-factor model of personality in borderline and nonborderline personality disorders. Can J Psychiatry. 1995;40(9):523-526.
18. Zanarini MC, Frankenburg FR, Reich DB, et al. Adult experiences of abuse reported by borderline patients and Axis II comparison subjects over six years of prospective follow-up. J Nerv Ment Dis. 2005;193(6):412-416.
19. Zanarini MC, Frankenburg FR, Reich DB, et al. Violence in the lives of adult borderline patients. J Nerv Ment Dis. 1999;187(2):65-71.
20. McCormick B, Blum N, Hansel R, et al. Relationship of sex to symptom severity, psychiatric comorbidity, and health care utilization in 163 subjects with borderline personality disorder. Compr Psychiatry. 2007;48(5):406-412.
21. Brieger P, Ehrt U, Marneros A. Frequency of comorbid personality disorders in bipolar and unipolar affective disorders. Compr Psychiatry. 2003;44(1):28-34.
22. Paris J, Zweig-Frank H. A 27-year follow-up of patients with borderline personality disorder. Compr Psychiatry. 2001;42(6):482-487.
23. Coryell WH, Fiedorowicz JG, Solomon D, et al. Age transitions in the course of bipolar I disorder. Psychol Med. 2009;39(8):1247-1252.
24. Benazzi F. Borderline personality-bipolar spectrum relationship. Prog Neuropsychopharmacol Biol Psychiatry. 2006;30(1):68-74.
25. Critchfield KL, Levy KN, Clarkin JF. The relationship between impulsivity, aggression, and impulsive-aggression in borderline personality disorder: an empirical analysis of self-report measures. J Pers Disord. 2004;18(6):555-570.
26. Henry C, Mitropoulou V, New AS, et al. Affective instability and impulsivity in borderline personality and bipolar II disorders: similarities and differences. J Psychiatr Res. 2001;35(6):307-312.
27. Bray A. The extended mind and borderline personality disorder. Australas Psychiatry. 2008;16(1):8-12.
28. Gunderson JG. The borderline patient’s intolerance of aloneness: insecure attachments and therapist availability. Am J Psychiatry. 1996;153(6):752-758.
29. Jorgensen CR. Disturbed sense of identity in borderline personality disorder. J Pers Disord. 2006;20(6):618-644.
30. Smith DJ, Muir WJ, Blackwood DH. Borderline personality disorder characteristics in young adults with recurrent mood disorders: a comparison of bipolar and unipolar depression. J Affect Disord. 2005;87(1):17-23.
31. Binks CA, Fenton M, McCarthy L, et al. Pharmacological interventions for people with borderline personality disorder. Cochrane Database Syst Rev. 2006(1);CD005653.-
32. Lynch TR, Trost WT, Salsman N, et al. Dialectical behavior therapy for borderline personality disorder. Annu Rev Clin Psychol. 2007;3:181-205.
33. Bateman AW, Fonagy P. Mentalization-based treatment of BPD. J Pers Disord. 2004;18(1):36-51.
34. Blum N, St John D, Pfohl B, et al. Systems Training for Emotional Predictability and Problem Solving (STEPPS) for outpatients with borderline personality disorder: a randomized controlled trial and 1-year follow-up. Am J Psychiatry. 2008;165(4):468-478.
1. John H, Sharma V. Misdiagnosis of bipolar disorder as borderline personality disorder: clinical and economic consequences. World J Biol Psychiatry. 2007;1-4[epub ahead of print].
2. Lequesne ER, Hersh RG. Disclosure of a diagnosis of borderline personality disorder. J Psychiatr Pract. 2004;10(3):170-176.
3. Merikangas KR, Akiskal HS, Angst J, et al. Lifetime and 12-month prevalence of bipolar spectrum disorder in the National Comorbidity Survey replication. Arch Gen Psychiatry. 2007;64(5):543-552.
4. Belmaker RH. Bipolar disorder. N Engl J Med. 2004;351(5):476-486.
5. Benazzi F. Testing new diagnostic criteria for hypomania. Ann Clin Psychiatry. 2007;19(2):99-104.
6. Solomon DA, Leon AC, Endicott J, et al. Unipolar mania over the course of a 20-year follow-up study. Am J Psychiatry. 2003;160(11):2049-2051.
7. Schiavone P, Dorz S, Conforti D, et al. Comorbidity of DSM-IV personality disorders in unipolar and bipolar affective disorders: a comparative study. Psychol Rep. 2004;95(1):121-128.
8. Fan AH, Hassell J. Bipolar disorder and comorbid personality psychopathology: a review of the literature. J Clin Psychiatry. 2008;69(11):1794-1803.
9. Garno JL, Goldberg JF, Ramirez PM, et al. Bipolar disorder with comorbid cluster B personality disorder features: impact on suicidality. J Clin Psychiatry. 2005;66(3):339-345.
10. Black DW, Blum N, Pfohl B, et al. Suicidal behavior in borderline personality disorder: prevalence, risk factors, prediction, and prevention. J Pers Disord. 2004;18(3):226-239.
11. Fiedorowicz JG, Leon AC, Keller MB, et al. Do risk factors for suicidal behavior differ by affective disorder polarity? Psychol Med. 2009;39(5):763-771.
12. Paris J. Understanding self-mutilation in borderline personality disorder. Harv Rev Psychiatry. 2005;13(3):179-185.
13. Zanarini MC, Frankenburg FR, Hennen J, et al. The McLean Study of Adult Development (MSAD): overview and implications of the first six years of prospective follow-up. J Pers Disord. 2005;19(5):505-523.
14. Torgersen S, Kringlen E, Cramer V. The prevalence of personality disorders in a community sample. Arch Gen Psychiatry. 2001;58(6):590-596.
15. Grant BF, Chou SP, Goldstein RB, et al. Prevalence, correlates, disability, and comorbidity of DSM-IV borderline personality disorder: results from the Wave 2 National Epidemiologic Survey on Alcohol and Related Conditions. J Clin Psychiatry. 2008;69(4):533-545.
16. Wilson ST, Stanley B, Oquendo MA, et al. Comparing impulsiveness, hostility, and depression in borderline personality disorder and bipolar II disorder. J Clin Psychiatry. 2007;68(10):1533-1539.
17. Zweig-Frank H, Paris J. The five-factor model of personality in borderline and nonborderline personality disorders. Can J Psychiatry. 1995;40(9):523-526.
18. Zanarini MC, Frankenburg FR, Reich DB, et al. Adult experiences of abuse reported by borderline patients and Axis II comparison subjects over six years of prospective follow-up. J Nerv Ment Dis. 2005;193(6):412-416.
19. Zanarini MC, Frankenburg FR, Reich DB, et al. Violence in the lives of adult borderline patients. J Nerv Ment Dis. 1999;187(2):65-71.
20. McCormick B, Blum N, Hansel R, et al. Relationship of sex to symptom severity, psychiatric comorbidity, and health care utilization in 163 subjects with borderline personality disorder. Compr Psychiatry. 2007;48(5):406-412.
21. Brieger P, Ehrt U, Marneros A. Frequency of comorbid personality disorders in bipolar and unipolar affective disorders. Compr Psychiatry. 2003;44(1):28-34.
22. Paris J, Zweig-Frank H. A 27-year follow-up of patients with borderline personality disorder. Compr Psychiatry. 2001;42(6):482-487.
23. Coryell WH, Fiedorowicz JG, Solomon D, et al. Age transitions in the course of bipolar I disorder. Psychol Med. 2009;39(8):1247-1252.
24. Benazzi F. Borderline personality-bipolar spectrum relationship. Prog Neuropsychopharmacol Biol Psychiatry. 2006;30(1):68-74.
25. Critchfield KL, Levy KN, Clarkin JF. The relationship between impulsivity, aggression, and impulsive-aggression in borderline personality disorder: an empirical analysis of self-report measures. J Pers Disord. 2004;18(6):555-570.
26. Henry C, Mitropoulou V, New AS, et al. Affective instability and impulsivity in borderline personality and bipolar II disorders: similarities and differences. J Psychiatr Res. 2001;35(6):307-312.
27. Bray A. The extended mind and borderline personality disorder. Australas Psychiatry. 2008;16(1):8-12.
28. Gunderson JG. The borderline patient’s intolerance of aloneness: insecure attachments and therapist availability. Am J Psychiatry. 1996;153(6):752-758.
29. Jorgensen CR. Disturbed sense of identity in borderline personality disorder. J Pers Disord. 2006;20(6):618-644.
30. Smith DJ, Muir WJ, Blackwood DH. Borderline personality disorder characteristics in young adults with recurrent mood disorders: a comparison of bipolar and unipolar depression. J Affect Disord. 2005;87(1):17-23.
31. Binks CA, Fenton M, McCarthy L, et al. Pharmacological interventions for people with borderline personality disorder. Cochrane Database Syst Rev. 2006(1);CD005653.-
32. Lynch TR, Trost WT, Salsman N, et al. Dialectical behavior therapy for borderline personality disorder. Annu Rev Clin Psychol. 2007;3:181-205.
33. Bateman AW, Fonagy P. Mentalization-based treatment of BPD. J Pers Disord. 2004;18(1):36-51.
34. Blum N, St John D, Pfohl B, et al. Systems Training for Emotional Predictability and Problem Solving (STEPPS) for outpatients with borderline personality disorder: a randomized controlled trial and 1-year follow-up. Am J Psychiatry. 2008;165(4):468-478.
Combo Therapy Is the Rule in Pediatric Bipolar
Even the experts say it's a tough call to diagnose a child–particularly a young child–with bipolar disorder, making for enigmatic medication decisions in the pediatric population.
“It's always difficult, and the diagnosis is the most important thing before beginning treatment,” said Dr. Kiki Chang, founder and director of the Pediatric Bipolar Disorders Program at Stanford (Calif.) University.
“It's a diagnosis I've been looking at for the better part of 35 years, and I still find it very hard,” agreed Dr. Gabrielle Carlson, professor of psychiatry and behavioral science at the State University of New York at Stony Brook. When it comes to very young children–under the age of 10–“you get into really dicey territory.”
The problem is that diagnostic criteria for bipolar I, bipolar II, and bipolar disorder not otherwise specified in the DSM-IV were developed based on research in adults and may be exceedingly difficult to apply to children.
It's been said that all normal 4-year-olds look a bit bipolar, with wild mood swings, euphoria, racing thoughts, grandiosity, periods of extreme creative and physical energy, reports of monsters under their beds, and a seemingly reduced need for sleep (by parental report).
Clinical experience and many longitudinal studies do point to profoundly troubled behavior in some children that does have a flavor of bipolar disorder, and many of these children do go on to have unequivocal bipolar disorder in adulthood.
In the most recently published report from Dr. Barbara Geller's group at Washington University, St. Louis, 44% of young adults identified in childhood with bipolar I disorder symptoms had a manic episode after the age of 18, a rate 13–44 times higher than in the general population (Arch. Gen. Psychiatry 2008;65:1125–33).
However, community diagnoses are notoriously fallible, illustrated by the fact that half of the children referred to the Pediatric Bipolar Disorders Program at Stanford do not have the disease. Often, they prove to have unipolar depression marked by irritability. Or pervasive developmental disorder. Or autism, Dr. Chang said.
Significant language impairment and developmental delays complicated the diagnosis of one of Dr. Carlson's patients who, at age 5, nearly got killed running alongside cars because he thought he could run faster than anyone else. He jumped out of a tree, and displayed other examples of “clearly grandiose” behavior. When he was 7, she asked him about chasing traffic and he said, “I was little at the time.” The tree? “I never did that again,” he said. Later, he boasted he could swim across Long Island Sound–a claim he later traced to his grandfather's musing that he could “swim like a fish.”
By age 10, it was clear that child's diagnosis was autism. “He always had interesting ways of putting the world together. But he wasn't delusional when pressed,” said Dr. Carlson.
Being precise about a diagnosis in children with unusual, shocking, and/or harmful behaviors would make little difference if medication management was the same whether a child has bipolar disorder or one of the many differential diagnoses masquerading as bipolar disorder, such as depression, attention-deficit/hyperactivity disorder (ADHD), pervasive developmental disorder, anxiety disorders, Tourette syndrome, or the autism spectrum disorders. But it's not.
“The question of diagnosis makes a big difference,” Dr. Carlson said. In the case of “diagnostic ambiguity” between severe ADHD and bipolar disorder, she chooses to treat the ADHD first, unless there are clear signs of mania.
One advantage of treating ADHD with stimulants is their quick action, sometimes providing rapid evidence of improvement. Plus, their use over many years in multiple clinical trials in children provides reassurance of their safety and guidance about dosing.
It can be difficult to start on a conservative course of action in the face of extreme behavior and symptoms, but Dr. Carlson remembers the lesson she learned from an adolescent who had been unsuccessfully treated with anticonvulsants and atypical antipsychotics for 5 years.
So frightening were the child's early meltdowns that the mother and a community psychiatrist feared that stimulant medication would be contraindicated, with the potential of making a “nightmare” situation worse. But after years of treatment, the youth's symptoms worsened and he was hospitalized. She decided to taper his medications and try traditional stimulants for ADHD, along with time-outs and consistent behavior-modification strategies. “He responded very nicely,” she said. “What was heartwarming was how proud he was that he had control of himself. The mother told me, 'I was able to be a regular mom.'”
Dr. Chang also favors treating ADHD when the diagnosis tends to lean that way (and doesn't include frank mania). He starts with standard doses of short-acting methylphenidate, even when one or more parents has a history of bipolar disorder.
Whereas experts once believed that stimulants would “tip” most children with undiagnosed bipolar disorder into manic episodes, the consensus now is that this is a rare occurrence and fairly easily managed, he said. “Just stop the stimulants.”
An alternative therapy for ADHD symptoms might be atomoxetine (Strattera), a hydrochloride salt, which Dr. Chang considers if stimulants aggravate hyperactive behavior.
If a traditional therapy for ADHD reduces symptoms, both specialists said they feel comfortable in closely monitoring a child through adolescence, when more typical symptoms of bipolar disorder may emerge.
In looking at studies of patients under the age of 10, Dr. Carlson today sees few data to support the use of “powerful, fat-making antipsychotics” for the rest of the child's life (assuming the child proves to have bipolar disorder). She believes there is support in the literature for the short-term use of atypical antipsychotics for management of aggression associated with many diagnoses, however.
Of note, an international review of five longitudinal studies of the children of parents with bipolar disorder found little evidence of classically defined mania in prepubertal children (J. Can. Acad. Child Adoles. Psychiatry 2009;18:200–5).
In the study by Dr. Anne Duffy of Dalhousie University in Halifax, Nova Scotia, children who went on to develop mood disorders seemed to follow a fairly predictable course leading to a first activated episode in adolescence or early adulthood–nonspecific anxiety and sleep problems in childhood, then mood swings in adolescence, with depressive episodes predating mania by several years.
Dr. Chang said while prepubertal mania has been described, it is likely less common than postpubertal mania, “and harder to diagnose given the natural neurodevelopmental propensity of young children to rapidly cycle with their moods.”
Many experts have called for an evaluation of what symptoms constitute a diagnosis of bipolar disorder in children, rather than trying to shade adult-oriented symptoms to fit children. A precise definition would tailor subjects enrolled in clinical trials so that findings would be meaningful and applicable to the children seen in clinical practice, hopefully pointing the way to an evidence-based approach to pharmacotherapy.
In the meantime, treatment guidelines developed by an expert consensus panel that included Dr. Carlson and Dr. Chang offer diagnostic support and provide algorithms for treatment of bipolar I disorder with or without psychosis in children and adolescents (J. Amer. Acad. Child Adolesc. Psychiatry 2005;44:213–35).
A practice parameter with 11 specific recommendations also offers comprehensive guidance to clinicians (J. Am. Acad. Child Adolesc. Psychiatry 2007; 46:107–25).
Dr. Carlson and Dr. Chang describe personal prescribing patterns that conform to these guidelines, most often selecting lithium or another mood stabilizer or an atypical antipsychotic as first line monotherapy, but sometimes recommending combination therapy.
Lithium, valproate, aripiprazole, and quetiapine all figure prominently in his initial treatment strategies, with quetiapine edging out the others if sleep regulation is a particular problem.
A child presenting with rather classic euphoric mania might make Dr. Chang prescribe lithium first, whereas a more chronic picture of predominantly irritable mania or a mixed state would make him lean toward an atypical antipsychotic.
Depression remains a challenge in youthful populations as well as in adults, and Dr. Chang is generally reluctant to prescribe selective serotonin reuptake inhibitors if there is a reasonable suspicion that the child has bipolar disorder.
“We stay away from them if at all possible,” concerned that they may precipitate a manic episode.
He might consider lamotrigine for a child who is already overweight, dosing it very cautiously at first, especially in smaller children, and being cognizant of the risk of a severe rash. He also now considers adding metformin to the regimen of any child or adolescent who gains considerable weight on the atypicals.
Dr. Carlson cited the same sorts of considerations. Atypical antipsychotics, for example, might be her treatment of choice for a child whose most concerning symptoms are aggression and emotional lability, because these drugs tend to ameliorate these symptoms regardless of whether the ultimate diagnosis is bipolar disorder.
Most children with bipolar disorder end up requiring combination therapy for their symptoms, plus occasional agents to manage side effects.
As the regimens grow more complex, the already limited evidence base shrinks to nearly nil, Dr. Chang said. Side effect patterns in children are also poorly understood. “Cognitive side effects have not really been studied at all. We don't have much evidence to guide us, and compared with adults, the cognitive piece is really important,” he said.
When the adult literature suggests a problematic cognitive picture, as in the case of topiramate, Dr. Chang tends to avoid prescribing that drug.
Both clinicians emphasized the need to address the child's environment within the context of his or her symptoms, incorporating psychotherapeutic and educational interventions in any treatment strategy. “Medication in the absence of the others [interventions] is rarely successful,” Dr. Chang said.
Dr. Carlson reported that she is a consultant for many of the pharmaceutical companies conducting research into bipolar disorder and ADHD and is currently participating in a study of lamotrigine (GlaxoSmithKline). Dr. Chang said he has received research or grant support from, or served on the speakers bureau for, AstraZeneca Pharmaceuticals, Bristol-Myers Squibb, Eli Lilly & Co., Otsuka America Pharmaceutical Inc., and GlaxoSmithKline.
By Betsy Bates. Share your thoughts and suggestions at [email protected]
Few data support the use of 'powerful, fat-making antipsychotics' for the rest of the child's life.
Source DR. CARLSON
Even the experts say it's a tough call to diagnose a child–particularly a young child–with bipolar disorder, making for enigmatic medication decisions in the pediatric population.
“It's always difficult, and the diagnosis is the most important thing before beginning treatment,” said Dr. Kiki Chang, founder and director of the Pediatric Bipolar Disorders Program at Stanford (Calif.) University.
“It's a diagnosis I've been looking at for the better part of 35 years, and I still find it very hard,” agreed Dr. Gabrielle Carlson, professor of psychiatry and behavioral science at the State University of New York at Stony Brook. When it comes to very young children–under the age of 10–“you get into really dicey territory.”
The problem is that diagnostic criteria for bipolar I, bipolar II, and bipolar disorder not otherwise specified in the DSM-IV were developed based on research in adults and may be exceedingly difficult to apply to children.
It's been said that all normal 4-year-olds look a bit bipolar, with wild mood swings, euphoria, racing thoughts, grandiosity, periods of extreme creative and physical energy, reports of monsters under their beds, and a seemingly reduced need for sleep (by parental report).
Clinical experience and many longitudinal studies do point to profoundly troubled behavior in some children that does have a flavor of bipolar disorder, and many of these children do go on to have unequivocal bipolar disorder in adulthood.
In the most recently published report from Dr. Barbara Geller's group at Washington University, St. Louis, 44% of young adults identified in childhood with bipolar I disorder symptoms had a manic episode after the age of 18, a rate 13–44 times higher than in the general population (Arch. Gen. Psychiatry 2008;65:1125–33).
However, community diagnoses are notoriously fallible, illustrated by the fact that half of the children referred to the Pediatric Bipolar Disorders Program at Stanford do not have the disease. Often, they prove to have unipolar depression marked by irritability. Or pervasive developmental disorder. Or autism, Dr. Chang said.
Significant language impairment and developmental delays complicated the diagnosis of one of Dr. Carlson's patients who, at age 5, nearly got killed running alongside cars because he thought he could run faster than anyone else. He jumped out of a tree, and displayed other examples of “clearly grandiose” behavior. When he was 7, she asked him about chasing traffic and he said, “I was little at the time.” The tree? “I never did that again,” he said. Later, he boasted he could swim across Long Island Sound–a claim he later traced to his grandfather's musing that he could “swim like a fish.”
By age 10, it was clear that child's diagnosis was autism. “He always had interesting ways of putting the world together. But he wasn't delusional when pressed,” said Dr. Carlson.
Being precise about a diagnosis in children with unusual, shocking, and/or harmful behaviors would make little difference if medication management was the same whether a child has bipolar disorder or one of the many differential diagnoses masquerading as bipolar disorder, such as depression, attention-deficit/hyperactivity disorder (ADHD), pervasive developmental disorder, anxiety disorders, Tourette syndrome, or the autism spectrum disorders. But it's not.
“The question of diagnosis makes a big difference,” Dr. Carlson said. In the case of “diagnostic ambiguity” between severe ADHD and bipolar disorder, she chooses to treat the ADHD first, unless there are clear signs of mania.
One advantage of treating ADHD with stimulants is their quick action, sometimes providing rapid evidence of improvement. Plus, their use over many years in multiple clinical trials in children provides reassurance of their safety and guidance about dosing.
It can be difficult to start on a conservative course of action in the face of extreme behavior and symptoms, but Dr. Carlson remembers the lesson she learned from an adolescent who had been unsuccessfully treated with anticonvulsants and atypical antipsychotics for 5 years.
So frightening were the child's early meltdowns that the mother and a community psychiatrist feared that stimulant medication would be contraindicated, with the potential of making a “nightmare” situation worse. But after years of treatment, the youth's symptoms worsened and he was hospitalized. She decided to taper his medications and try traditional stimulants for ADHD, along with time-outs and consistent behavior-modification strategies. “He responded very nicely,” she said. “What was heartwarming was how proud he was that he had control of himself. The mother told me, 'I was able to be a regular mom.'”
Dr. Chang also favors treating ADHD when the diagnosis tends to lean that way (and doesn't include frank mania). He starts with standard doses of short-acting methylphenidate, even when one or more parents has a history of bipolar disorder.
Whereas experts once believed that stimulants would “tip” most children with undiagnosed bipolar disorder into manic episodes, the consensus now is that this is a rare occurrence and fairly easily managed, he said. “Just stop the stimulants.”
An alternative therapy for ADHD symptoms might be atomoxetine (Strattera), a hydrochloride salt, which Dr. Chang considers if stimulants aggravate hyperactive behavior.
If a traditional therapy for ADHD reduces symptoms, both specialists said they feel comfortable in closely monitoring a child through adolescence, when more typical symptoms of bipolar disorder may emerge.
In looking at studies of patients under the age of 10, Dr. Carlson today sees few data to support the use of “powerful, fat-making antipsychotics” for the rest of the child's life (assuming the child proves to have bipolar disorder). She believes there is support in the literature for the short-term use of atypical antipsychotics for management of aggression associated with many diagnoses, however.
Of note, an international review of five longitudinal studies of the children of parents with bipolar disorder found little evidence of classically defined mania in prepubertal children (J. Can. Acad. Child Adoles. Psychiatry 2009;18:200–5).
In the study by Dr. Anne Duffy of Dalhousie University in Halifax, Nova Scotia, children who went on to develop mood disorders seemed to follow a fairly predictable course leading to a first activated episode in adolescence or early adulthood–nonspecific anxiety and sleep problems in childhood, then mood swings in adolescence, with depressive episodes predating mania by several years.
Dr. Chang said while prepubertal mania has been described, it is likely less common than postpubertal mania, “and harder to diagnose given the natural neurodevelopmental propensity of young children to rapidly cycle with their moods.”
Many experts have called for an evaluation of what symptoms constitute a diagnosis of bipolar disorder in children, rather than trying to shade adult-oriented symptoms to fit children. A precise definition would tailor subjects enrolled in clinical trials so that findings would be meaningful and applicable to the children seen in clinical practice, hopefully pointing the way to an evidence-based approach to pharmacotherapy.
In the meantime, treatment guidelines developed by an expert consensus panel that included Dr. Carlson and Dr. Chang offer diagnostic support and provide algorithms for treatment of bipolar I disorder with or without psychosis in children and adolescents (J. Amer. Acad. Child Adolesc. Psychiatry 2005;44:213–35).
A practice parameter with 11 specific recommendations also offers comprehensive guidance to clinicians (J. Am. Acad. Child Adolesc. Psychiatry 2007; 46:107–25).
Dr. Carlson and Dr. Chang describe personal prescribing patterns that conform to these guidelines, most often selecting lithium or another mood stabilizer or an atypical antipsychotic as first line monotherapy, but sometimes recommending combination therapy.
Lithium, valproate, aripiprazole, and quetiapine all figure prominently in his initial treatment strategies, with quetiapine edging out the others if sleep regulation is a particular problem.
A child presenting with rather classic euphoric mania might make Dr. Chang prescribe lithium first, whereas a more chronic picture of predominantly irritable mania or a mixed state would make him lean toward an atypical antipsychotic.
Depression remains a challenge in youthful populations as well as in adults, and Dr. Chang is generally reluctant to prescribe selective serotonin reuptake inhibitors if there is a reasonable suspicion that the child has bipolar disorder.
“We stay away from them if at all possible,” concerned that they may precipitate a manic episode.
He might consider lamotrigine for a child who is already overweight, dosing it very cautiously at first, especially in smaller children, and being cognizant of the risk of a severe rash. He also now considers adding metformin to the regimen of any child or adolescent who gains considerable weight on the atypicals.
Dr. Carlson cited the same sorts of considerations. Atypical antipsychotics, for example, might be her treatment of choice for a child whose most concerning symptoms are aggression and emotional lability, because these drugs tend to ameliorate these symptoms regardless of whether the ultimate diagnosis is bipolar disorder.
Most children with bipolar disorder end up requiring combination therapy for their symptoms, plus occasional agents to manage side effects.
As the regimens grow more complex, the already limited evidence base shrinks to nearly nil, Dr. Chang said. Side effect patterns in children are also poorly understood. “Cognitive side effects have not really been studied at all. We don't have much evidence to guide us, and compared with adults, the cognitive piece is really important,” he said.
When the adult literature suggests a problematic cognitive picture, as in the case of topiramate, Dr. Chang tends to avoid prescribing that drug.
Both clinicians emphasized the need to address the child's environment within the context of his or her symptoms, incorporating psychotherapeutic and educational interventions in any treatment strategy. “Medication in the absence of the others [interventions] is rarely successful,” Dr. Chang said.
Dr. Carlson reported that she is a consultant for many of the pharmaceutical companies conducting research into bipolar disorder and ADHD and is currently participating in a study of lamotrigine (GlaxoSmithKline). Dr. Chang said he has received research or grant support from, or served on the speakers bureau for, AstraZeneca Pharmaceuticals, Bristol-Myers Squibb, Eli Lilly & Co., Otsuka America Pharmaceutical Inc., and GlaxoSmithKline.
By Betsy Bates. Share your thoughts and suggestions at [email protected]
Few data support the use of 'powerful, fat-making antipsychotics' for the rest of the child's life.
Source DR. CARLSON
Even the experts say it's a tough call to diagnose a child–particularly a young child–with bipolar disorder, making for enigmatic medication decisions in the pediatric population.
“It's always difficult, and the diagnosis is the most important thing before beginning treatment,” said Dr. Kiki Chang, founder and director of the Pediatric Bipolar Disorders Program at Stanford (Calif.) University.
“It's a diagnosis I've been looking at for the better part of 35 years, and I still find it very hard,” agreed Dr. Gabrielle Carlson, professor of psychiatry and behavioral science at the State University of New York at Stony Brook. When it comes to very young children–under the age of 10–“you get into really dicey territory.”
The problem is that diagnostic criteria for bipolar I, bipolar II, and bipolar disorder not otherwise specified in the DSM-IV were developed based on research in adults and may be exceedingly difficult to apply to children.
It's been said that all normal 4-year-olds look a bit bipolar, with wild mood swings, euphoria, racing thoughts, grandiosity, periods of extreme creative and physical energy, reports of monsters under their beds, and a seemingly reduced need for sleep (by parental report).
Clinical experience and many longitudinal studies do point to profoundly troubled behavior in some children that does have a flavor of bipolar disorder, and many of these children do go on to have unequivocal bipolar disorder in adulthood.
In the most recently published report from Dr. Barbara Geller's group at Washington University, St. Louis, 44% of young adults identified in childhood with bipolar I disorder symptoms had a manic episode after the age of 18, a rate 13–44 times higher than in the general population (Arch. Gen. Psychiatry 2008;65:1125–33).
However, community diagnoses are notoriously fallible, illustrated by the fact that half of the children referred to the Pediatric Bipolar Disorders Program at Stanford do not have the disease. Often, they prove to have unipolar depression marked by irritability. Or pervasive developmental disorder. Or autism, Dr. Chang said.
Significant language impairment and developmental delays complicated the diagnosis of one of Dr. Carlson's patients who, at age 5, nearly got killed running alongside cars because he thought he could run faster than anyone else. He jumped out of a tree, and displayed other examples of “clearly grandiose” behavior. When he was 7, she asked him about chasing traffic and he said, “I was little at the time.” The tree? “I never did that again,” he said. Later, he boasted he could swim across Long Island Sound–a claim he later traced to his grandfather's musing that he could “swim like a fish.”
By age 10, it was clear that child's diagnosis was autism. “He always had interesting ways of putting the world together. But he wasn't delusional when pressed,” said Dr. Carlson.
Being precise about a diagnosis in children with unusual, shocking, and/or harmful behaviors would make little difference if medication management was the same whether a child has bipolar disorder or one of the many differential diagnoses masquerading as bipolar disorder, such as depression, attention-deficit/hyperactivity disorder (ADHD), pervasive developmental disorder, anxiety disorders, Tourette syndrome, or the autism spectrum disorders. But it's not.
“The question of diagnosis makes a big difference,” Dr. Carlson said. In the case of “diagnostic ambiguity” between severe ADHD and bipolar disorder, she chooses to treat the ADHD first, unless there are clear signs of mania.
One advantage of treating ADHD with stimulants is their quick action, sometimes providing rapid evidence of improvement. Plus, their use over many years in multiple clinical trials in children provides reassurance of their safety and guidance about dosing.
It can be difficult to start on a conservative course of action in the face of extreme behavior and symptoms, but Dr. Carlson remembers the lesson she learned from an adolescent who had been unsuccessfully treated with anticonvulsants and atypical antipsychotics for 5 years.
So frightening were the child's early meltdowns that the mother and a community psychiatrist feared that stimulant medication would be contraindicated, with the potential of making a “nightmare” situation worse. But after years of treatment, the youth's symptoms worsened and he was hospitalized. She decided to taper his medications and try traditional stimulants for ADHD, along with time-outs and consistent behavior-modification strategies. “He responded very nicely,” she said. “What was heartwarming was how proud he was that he had control of himself. The mother told me, 'I was able to be a regular mom.'”
Dr. Chang also favors treating ADHD when the diagnosis tends to lean that way (and doesn't include frank mania). He starts with standard doses of short-acting methylphenidate, even when one or more parents has a history of bipolar disorder.
Whereas experts once believed that stimulants would “tip” most children with undiagnosed bipolar disorder into manic episodes, the consensus now is that this is a rare occurrence and fairly easily managed, he said. “Just stop the stimulants.”
An alternative therapy for ADHD symptoms might be atomoxetine (Strattera), a hydrochloride salt, which Dr. Chang considers if stimulants aggravate hyperactive behavior.
If a traditional therapy for ADHD reduces symptoms, both specialists said they feel comfortable in closely monitoring a child through adolescence, when more typical symptoms of bipolar disorder may emerge.
In looking at studies of patients under the age of 10, Dr. Carlson today sees few data to support the use of “powerful, fat-making antipsychotics” for the rest of the child's life (assuming the child proves to have bipolar disorder). She believes there is support in the literature for the short-term use of atypical antipsychotics for management of aggression associated with many diagnoses, however.
Of note, an international review of five longitudinal studies of the children of parents with bipolar disorder found little evidence of classically defined mania in prepubertal children (J. Can. Acad. Child Adoles. Psychiatry 2009;18:200–5).
In the study by Dr. Anne Duffy of Dalhousie University in Halifax, Nova Scotia, children who went on to develop mood disorders seemed to follow a fairly predictable course leading to a first activated episode in adolescence or early adulthood–nonspecific anxiety and sleep problems in childhood, then mood swings in adolescence, with depressive episodes predating mania by several years.
Dr. Chang said while prepubertal mania has been described, it is likely less common than postpubertal mania, “and harder to diagnose given the natural neurodevelopmental propensity of young children to rapidly cycle with their moods.”
Many experts have called for an evaluation of what symptoms constitute a diagnosis of bipolar disorder in children, rather than trying to shade adult-oriented symptoms to fit children. A precise definition would tailor subjects enrolled in clinical trials so that findings would be meaningful and applicable to the children seen in clinical practice, hopefully pointing the way to an evidence-based approach to pharmacotherapy.
In the meantime, treatment guidelines developed by an expert consensus panel that included Dr. Carlson and Dr. Chang offer diagnostic support and provide algorithms for treatment of bipolar I disorder with or without psychosis in children and adolescents (J. Amer. Acad. Child Adolesc. Psychiatry 2005;44:213–35).
A practice parameter with 11 specific recommendations also offers comprehensive guidance to clinicians (J. Am. Acad. Child Adolesc. Psychiatry 2007; 46:107–25).
Dr. Carlson and Dr. Chang describe personal prescribing patterns that conform to these guidelines, most often selecting lithium or another mood stabilizer or an atypical antipsychotic as first line monotherapy, but sometimes recommending combination therapy.
Lithium, valproate, aripiprazole, and quetiapine all figure prominently in his initial treatment strategies, with quetiapine edging out the others if sleep regulation is a particular problem.
A child presenting with rather classic euphoric mania might make Dr. Chang prescribe lithium first, whereas a more chronic picture of predominantly irritable mania or a mixed state would make him lean toward an atypical antipsychotic.
Depression remains a challenge in youthful populations as well as in adults, and Dr. Chang is generally reluctant to prescribe selective serotonin reuptake inhibitors if there is a reasonable suspicion that the child has bipolar disorder.
“We stay away from them if at all possible,” concerned that they may precipitate a manic episode.
He might consider lamotrigine for a child who is already overweight, dosing it very cautiously at first, especially in smaller children, and being cognizant of the risk of a severe rash. He also now considers adding metformin to the regimen of any child or adolescent who gains considerable weight on the atypicals.
Dr. Carlson cited the same sorts of considerations. Atypical antipsychotics, for example, might be her treatment of choice for a child whose most concerning symptoms are aggression and emotional lability, because these drugs tend to ameliorate these symptoms regardless of whether the ultimate diagnosis is bipolar disorder.
Most children with bipolar disorder end up requiring combination therapy for their symptoms, plus occasional agents to manage side effects.
As the regimens grow more complex, the already limited evidence base shrinks to nearly nil, Dr. Chang said. Side effect patterns in children are also poorly understood. “Cognitive side effects have not really been studied at all. We don't have much evidence to guide us, and compared with adults, the cognitive piece is really important,” he said.
When the adult literature suggests a problematic cognitive picture, as in the case of topiramate, Dr. Chang tends to avoid prescribing that drug.
Both clinicians emphasized the need to address the child's environment within the context of his or her symptoms, incorporating psychotherapeutic and educational interventions in any treatment strategy. “Medication in the absence of the others [interventions] is rarely successful,” Dr. Chang said.
Dr. Carlson reported that she is a consultant for many of the pharmaceutical companies conducting research into bipolar disorder and ADHD and is currently participating in a study of lamotrigine (GlaxoSmithKline). Dr. Chang said he has received research or grant support from, or served on the speakers bureau for, AstraZeneca Pharmaceuticals, Bristol-Myers Squibb, Eli Lilly & Co., Otsuka America Pharmaceutical Inc., and GlaxoSmithKline.
By Betsy Bates. Share your thoughts and suggestions at [email protected]
Few data support the use of 'powerful, fat-making antipsychotics' for the rest of the child's life.
Source DR. CARLSON
Ziprasidone Appears Safe, Effective in Pediatric Bipolar
ISTANBUL, TURKEY – Flexibly dosed ziprasidone displayed favorable safety and efficacy in children and adolescents with bipolar I disorder in a double-blind, placebo-controlled, randomized clinical trial.
The study involved 238 bipolar I patients aged 6–17 years with a manic or mixed episode who were randomized 2:1 to ziprasidone (Geodon) at 60–160 mg/day or placebo at 36 U.S. centers. Sixty-five percent of patients in the ziprasidone arm and 58% assigned to placebo completed the 4-week trial, Dr. Robert L. Findling reported at the annual congress of the European College of Neuropsychopharmacology.
The primary study end point was change in the Young Mania Rating Scale total score over the course of 4 weeks. The ziprasidone group had a mean 13.8-point drop, significantly greater than the 8.6-point decrease with placebo, according to Dr. Findling, professor of psychiatry and pediatrics at Case Western Reserve University, Cleveland.
The secondary end point was change over time in the Clinical Global Impression of Severity score: a mean reduction of 1.43 points from baseline in the ziprasidone group, compared with a 0.74-point decrease in controls.
The efficacy curves began separating within the first week, while ziprasidone was still being titrated toward a target dose of 60–80 mg/day in children weighing less than 45 kg, or 120–160 mg in those weighing more. The second-generation antipsychotic was given twice daily with food.
Side effects of ziprasidone were similar to those encountered in adult therapy. Sedation occurred in one-third of patients; somnolence in one-quarter; and nausea, fatigue, and dizziness each in 11%–13% of patients.
Weight gain occurred in one patient in each study arm. Prolongation of the QT interval on ECG was noted in a single patient in the ziprasidone arm, whose peak was 478 milliseconds (msec). The mean increase in QT interval in the ziprasidone group at 4 weeks was 8.3 msec, compared with a mean 2.9 msec decrease in the placebo arm.
This is an important study because of the limited safety and efficacy data available on the use of antipsychotic agents among pediatric patients, along with the documented importance of initiating treatment as early in the disease course as possible to achieve the best possible outcomes, according to the psychiatrist.
The trial was supported by Pfizer Inc., manufacturer of ziprasidone. Dr. Findling disclosed having received research grants and/or serving as a consultant to or on the speakers bureau for Pfizer and roughly a dozen other pharmaceutical companies.
With ziprasidone, the mean drop in the score was 13.8 points, compared with 8.6 in the placebo group.
Source DR. FINDLING
ISTANBUL, TURKEY – Flexibly dosed ziprasidone displayed favorable safety and efficacy in children and adolescents with bipolar I disorder in a double-blind, placebo-controlled, randomized clinical trial.
The study involved 238 bipolar I patients aged 6–17 years with a manic or mixed episode who were randomized 2:1 to ziprasidone (Geodon) at 60–160 mg/day or placebo at 36 U.S. centers. Sixty-five percent of patients in the ziprasidone arm and 58% assigned to placebo completed the 4-week trial, Dr. Robert L. Findling reported at the annual congress of the European College of Neuropsychopharmacology.
The primary study end point was change in the Young Mania Rating Scale total score over the course of 4 weeks. The ziprasidone group had a mean 13.8-point drop, significantly greater than the 8.6-point decrease with placebo, according to Dr. Findling, professor of psychiatry and pediatrics at Case Western Reserve University, Cleveland.
The secondary end point was change over time in the Clinical Global Impression of Severity score: a mean reduction of 1.43 points from baseline in the ziprasidone group, compared with a 0.74-point decrease in controls.
The efficacy curves began separating within the first week, while ziprasidone was still being titrated toward a target dose of 60–80 mg/day in children weighing less than 45 kg, or 120–160 mg in those weighing more. The second-generation antipsychotic was given twice daily with food.
Side effects of ziprasidone were similar to those encountered in adult therapy. Sedation occurred in one-third of patients; somnolence in one-quarter; and nausea, fatigue, and dizziness each in 11%–13% of patients.
Weight gain occurred in one patient in each study arm. Prolongation of the QT interval on ECG was noted in a single patient in the ziprasidone arm, whose peak was 478 milliseconds (msec). The mean increase in QT interval in the ziprasidone group at 4 weeks was 8.3 msec, compared with a mean 2.9 msec decrease in the placebo arm.
This is an important study because of the limited safety and efficacy data available on the use of antipsychotic agents among pediatric patients, along with the documented importance of initiating treatment as early in the disease course as possible to achieve the best possible outcomes, according to the psychiatrist.
The trial was supported by Pfizer Inc., manufacturer of ziprasidone. Dr. Findling disclosed having received research grants and/or serving as a consultant to or on the speakers bureau for Pfizer and roughly a dozen other pharmaceutical companies.
With ziprasidone, the mean drop in the score was 13.8 points, compared with 8.6 in the placebo group.
Source DR. FINDLING
ISTANBUL, TURKEY – Flexibly dosed ziprasidone displayed favorable safety and efficacy in children and adolescents with bipolar I disorder in a double-blind, placebo-controlled, randomized clinical trial.
The study involved 238 bipolar I patients aged 6–17 years with a manic or mixed episode who were randomized 2:1 to ziprasidone (Geodon) at 60–160 mg/day or placebo at 36 U.S. centers. Sixty-five percent of patients in the ziprasidone arm and 58% assigned to placebo completed the 4-week trial, Dr. Robert L. Findling reported at the annual congress of the European College of Neuropsychopharmacology.
The primary study end point was change in the Young Mania Rating Scale total score over the course of 4 weeks. The ziprasidone group had a mean 13.8-point drop, significantly greater than the 8.6-point decrease with placebo, according to Dr. Findling, professor of psychiatry and pediatrics at Case Western Reserve University, Cleveland.
The secondary end point was change over time in the Clinical Global Impression of Severity score: a mean reduction of 1.43 points from baseline in the ziprasidone group, compared with a 0.74-point decrease in controls.
The efficacy curves began separating within the first week, while ziprasidone was still being titrated toward a target dose of 60–80 mg/day in children weighing less than 45 kg, or 120–160 mg in those weighing more. The second-generation antipsychotic was given twice daily with food.
Side effects of ziprasidone were similar to those encountered in adult therapy. Sedation occurred in one-third of patients; somnolence in one-quarter; and nausea, fatigue, and dizziness each in 11%–13% of patients.
Weight gain occurred in one patient in each study arm. Prolongation of the QT interval on ECG was noted in a single patient in the ziprasidone arm, whose peak was 478 milliseconds (msec). The mean increase in QT interval in the ziprasidone group at 4 weeks was 8.3 msec, compared with a mean 2.9 msec decrease in the placebo arm.
This is an important study because of the limited safety and efficacy data available on the use of antipsychotic agents among pediatric patients, along with the documented importance of initiating treatment as early in the disease course as possible to achieve the best possible outcomes, according to the psychiatrist.
The trial was supported by Pfizer Inc., manufacturer of ziprasidone. Dr. Findling disclosed having received research grants and/or serving as a consultant to or on the speakers bureau for Pfizer and roughly a dozen other pharmaceutical companies.
With ziprasidone, the mean drop in the score was 13.8 points, compared with 8.6 in the placebo group.
Source DR. FINDLING
Asenapine for schizophrenia and bipolar I disorder
In August 2009, the FDA approved asenapine for treating acute exacerbation of schizophrenia and acute manic or mixed episodes of bipolar disorder with or without psychosis in adults (Table 1). Asenapine is the first psychotropic to obtain simultaneous FDA approval for schizophrenia and bipolar disorder. The drug’s unique receptor binding profile shows promise in treatment of positive and negative symptoms of schizophrenia with a low risk of extrapyramidal and anticholinergic side effects.
Table 1
Asenapine: Fast facts
| Brand name: Saphris |
| Indications: Acute schizophrenia in adults; acute mixed or manic episodes with or without psychosis associated with bipolar I disorder in adults |
| Approval date: August 2009 |
| Availability date: Late 2009 |
| Manufacturer: Schering-Plough |
| Dosing forms: 5-mg and 10-mg sublingual dissolvable tablets |
| Recommended dose: Schizophrenia: 5 mg twice daily; bipolar disorder: 10 mg twice daily |
How it works
Asenapine is an atypical antipsychotic. Although the exact mechanism of these medications’ efficacy is unknown, their antipsychotic and antimanic activity is thought to be the result of antagonism of central dopamine receptors. According to dopamine theory proposed in the 1960s:
- dopaminergic hyperactivity in mesolimbic dopaminergic pathways contributes to positive symptoms of schizophrenia—hallucinations, delusions, disorganized thoughts and behaviors, and catatonia
- dopaminergic hypoactivity in mesocortical dopaminergic pathways (prefrontal cortex) contributes to negative symptoms of schizophrenia—alogia, avolition, anhedonia, autism, social withdrawal, attention problems, blunted affect, and abstract thinking difficulty.
Asenapine has high affinity for multiple dopamine, serotonin, noradrenergic α1 and α2, and histamine H1 receptors, where it works as an antagonist. Asenapine’s affinity for several serotonin, noradrenergic, and dopaminergic D3 and D4 receptors is higher than its affinity for D2 receptors (Table 2),1 which distinguishes asenapine from other atypical antipsychotics except clozapine.
Blockade of 5-HT2A and 5-HT2C receptors in prefrontal cortex increases dopamine release in this area; theoretically, this effect should improve negative symptoms. Another mechanism that possibly improves cognition and negative symptoms is asenapine’s antagonism at central α2 noradrenergic receptors. Central α1 noradrenergic receptor antagonism also might be helpful in improving positive symptoms of schizophrenia.1
Asenapine’s affinity for the muscarinic-1 cholinergic receptors is quite low, and adverse effects associated with antagonism at these receptors—dry mouth, blurred vision, constipation, and urinary retention—are minimal.2
Table 2
Asenapine’s binding affinity for receptor subtypes*
| Receptor substype | Affinity [Ki (nM)] |
|---|---|
| 5-HT2A | 0.06 |
| 5-HT2C | 0.03 |
| D1 | 1.4 |
| D2 | 1.3 |
| D3 | 0.42 |
| D4 | 1.1 |
| α1 | 1.2 |
| α2 | 1.2 |
| H1 | 1.0 |
| M1 | 8128 |
| *Lower numbers indicate higher affinity | |
| 5-HT: serotonin receptors; D1-4: dopamine receptors; α1, α2: noradrenergic receptors; H1: histamine receptor; M1: muscarinic (cholinergic) receptor | |
| Source: Reference 1 | |
Pharmacokinetics
Absorption of asenapine after oral (swallowed) administration is 2%. To increase total bioavailability to 35%, the drug is manufactured as sublingual dissolvable tablets. After sublingual administration, asenapine is readily absorbed and achieves peak plasma concentration in approximately 1 hour. After absorption, 95% of asenapine binds to transport proteins albumin and α1 acid glycoprotein. The half-life of the medication is approximately 24 hours, and steady state usually is achieved in 3 days.
Metabolism creates about 40 metabolites via multiple metabolic pathways; the main ones are glucuronidation by UGT1A4 and oxidative metabolism by cytochrome P450 (CYP)1A2. Asenapine is a weak inhibitor of CYP2D6, so coadministration of asenapine with other drugs that are substrates or inhibitors of CYP1A2 (eg, fluvoxamine) or CYP2D6 (eg, paroxetine, fluoxetine) should be done cautiously. Because asenapine elimination is biphasic, twice-daily dosing is recommended.3
Efficacy in clinical trials
Schizophrenia. Asenapine’s efficacy for treating schizophrenia was evaluated in 3 fixed-dose, 6-week, randomized, double-blind, placebo- and active- (haloperidol, olanzapine, and risperidone) controlled clinical trials in adults.3-5 Subjects in these studies met DSM-IV criteria for schizophrenia and had acute exacerbation of their illness, with Positive and Negative Syndrome Scale (PANSS) total scores ≥60. Symptom improvement was measured after 6 weeks by PANSS total score, PANSS positive subscale, and Clinical Global Impression scale (CGI).
The first trial (n=174) compared asenapine, 5 mg twice daily, to placebo and risperidone, 3 mg twice daily.3-5 Asenapine was superior to placebo as demonstrated by symptom improvement on all 3 scales. Risperidone showed statistically significant symptom improvement on PANSS positive subscale and CGI but not on PANSS total score.
In the second trial (n=448), 2 fixed doses of asenapine (5 mg twice daily and 10 mg twice daily) and olanzapine, 15 mg/d, were compared with placebo.3,5 The only statistically significant symptom improvement in the asenapine group compared with placebo was on the PANSS positive subscale among subjects receiving 5 mg twice daily. Improvements measured by CGI and PANSS total score were not statistically significant.
Olanzapine showed statistically significant symptom improvement on all 3 scales compared with placebo. This study is a negative trial for asenapine; asenapine failed to separate from placebo, whereas olanzapine—the active comparator—did.
The third trial (n=448) compared asenapine, 5 mg twice daily and 10 mg twice daily, with placebo and haloperidol, 4 mg twice daily.3,5 Compared with placebo, asenapine at both doses and haloperidol improved symptoms on all 3 scales. The 10-mg twice-daily dosage did not provide any additional benefits compared with the 5 mg twice-daily dosage.
Bipolar disorder. Asenapine’s efficacy for bipolar disorder was established in two 3-week, randomized, double-blind, placebo- and olanzapine-controlled studies in adults with acute manic or mixed episodes with or without psychosis.3,6-9 Symptoms were assessed using the Young Mania Rating Scale (YMRS) and Clinical Global Impression-Bipolar (CGI-BP) scale.
In both studies, subjects were randomly assigned to receive asenapine, 10 mg twice daily; olanzapine, 5 to 20 mg/d; or placebo. Depending on efficacy and tolerability, the asenapine dose could be adjusted within the dosing range of 5 mg to 10 mg twice daily starting on day 2. Ninety percent of subjects stayed on the 10 mg twice-daily dose. In both studies, asenapine and olanzapine were statistically superior to placebo on YMRS and CGI-BP severity of illness scores.
Currently no evidence supports asenapine’s efficacy for maintenance treatment of schizophrenia or bipolar disorder. American Psychiatric Association practice guidelines recommend continuing treatment for a minimum of 6 months after stabilization of acute episodes of schizophrenia or bipolar disorder to prevent recurrence.10
Tolerability in clinical trials
Tolerability information provided in this article was obtained from a Clinical Trial Database consisting of 3,350 subjects:11
- 1,953 patients participated in multiple dose effectiveness trials (1,480 with schizophrenia and 473 with bipolar disorder manic/mixed episodes)
- 486 subjects were treated for at least 24 weeks
- 293 subjects were treated for at least 52 weeks.
Overall, asenapine was well tolerated (Table 3).11 The most common adverse effects in schizophrenia trials were akathisia, oral hypoesthesia, and somnolence. The discontinuation rate due to adverse effects in schizophrenia trials was 9% in the asenapine group vs 10% in the placebo group.
Among patients with bipolar disorder, the most common side effects were somnolence, dizziness, extrapyramidal symptoms other than akathisia, and increased weight. The discontinuation rate for subjects treated with asenapine was 10% vs 6% with placebo. The most common adverse reactions associated with discontinuation were anxiety and oral hypoesthesia. Oral hypoesthesia did not occur in the placebo group, and akathisia was the only dose-dependent adverse reaction.
Dizziness and weight gain. Clinically important adverse effects of asenapine include dizziness and weight gain. Dizziness is possibly related to orthostatic hypotension caused by the drug’s activity at the α1 receptor (antagonist). To prevent ischemic events or falls with subsequent injuries, use asenapine with caution in hypotensive patients and those with cardiovascular or cerebrovascular problems.
In clinical trials investigating asenapine’s efficacy, mean weight gain was greater in patients receiving asenapine than those receiving placebo. In short-term studies, mean weight gain in patients treated with asenapine was 1.1 kg for subjects with schizophrenia and 1.3 kg for subjects with bipolar mania.3 Mean weight gain in patients treated with placebo was 0.1 kg for subjects with schizophrenia and 0.2 kg for those with bipolar mania.
In a 52-week comparator study of patients with schizophrenia and schizoaffective disorder, mean weight gain was 0.9 kg in the asenapine group vs 4.2 kg in the olanzapine group.3 In both groups, the greatest weight increase occurred in subjects with body mass index <23.
There were no clinically relevant mean changes in serum fasting glucose, serum fasting triglycerides, fasting cholesterol, transaminases, and prolactin. Thrombocytopenia, anemia, tachycardia, temporary bundle branch block, visual accommodation disorder, oral paresthesia, glossodynia, swollen tongue, hyponatremia, and dysarthria occurred in 1 in 100 to 1 in 1,000 patients.
Table 3
Percentages of clinical trial patients who experienced adverse effects with asenapine vs placebo
| Schizophrenia | Bipolar disorder (mania/mixed) | |||||
|---|---|---|---|---|---|---|
| Adverse effect | Placebo (n=378) | Asenapine, 5 mg bid (n=274) | Asenapine, 10 mg bid (n=208) | Asenapine, 5 or 10 mg bid (n=572) | Placebo (n=203) | Asenapine, 5 or 10 mg bid (n=379) |
| Oral hypoesthesia | 1 | 6 | 7 | 5 | <1 | 4 |
| Weight gain | <1 | 2 | 2 | 3 | <1 | 5 |
| Increased appetite | <1 | 3 | 0 | 2 | 1 | 4 |
| Anxiety | 2 | 4 | ||||
| Akathisia | 3 | 4 | 11 | 6 | 2 | 4 |
| Other EPS (excluding akathisia) | 7 | 9 | 12 | 10 | 2 | 7 |
| Insomnia | 13 | 16 | 15 | 15 | 5 | 6 |
| Somnolence | 7 | 15 | 13 | 13 | 6 | 24 |
| Dizziness | 4 | 7 | 3 | 5 | 3 | 11 |
| EPS: extrapyramidal symptoms | ||||||
| Source: Reference 11 | ||||||
Contraindications
There are no absolute contraindications to asenapine use; however, the medication is not recommended for treating:
- women who are pregnant if the risks of treatment outweigh the benefits (pregnancy risk C)
- breast-feeding mothers
- patients with severe hepatic impairment (Child-Pugh C).
Asenapine carries the same class warnings and precautions as other antipsychotic medications, including a “black box” warning of increased mortality risk in elderly patients with dementia-related psychosis. Other class warnings include an increased risk of transient ischemic attack and cerebrovascular accidents in elderly patients with dementia-related psychosis; neuroleptic malignant syndrome; tardive dyskinesia; glycemia/diabetes mellitus; hyperprolactinemia; leukopenia; neutropenia; and agranulocytosis.
Because asenapine is associated with QT prolongation, do not administer it with other QT-prolonging agents, such as procainamide, sotalol, quinidine, erythromycin, clarithromycin, methadone, or other antipsychotics.
Dosing
Asenapine is manufactured as 5-mg and 10-mg sublingual tablets. Advise patients to avoid eating or drinking for 10 minutes after taking asenapine.
The recommended starting and target dosage for patients with schizophrenia is 5 mg twice daily. The recommended starting dosage for patients with an acute mixed or manic episode of bipolar I disorder is 10 mg twice daily; however, this can be reduced to 5 mg twice daily if the patient experiences intolerable side effects.
Related resource
- Asenapine (Saphris) prescribing information. www.spfiles.com/pisaphrisv1.pdf.
Drug brand names
- Asenapine • Saphris
- Clarithromycin • Biaxin
- Clozapine • Clozaril
- Erythromycin • ERY-C, Ery-Tab
- Fluoxetine • Prozac
- Fluvoxamine • Luvox
- Haloperidol • Haldol
- Methadone • Dolophine, Methadose
- Olanzapine • Zyprexa
- Paroxetine • Paxil
- Procainamide • Procanbid
- Quinidine • Quinidine
- Risperidone • Risperdal
- Sotalol • Betapace, Sorine
Disclosures
Dr. Lincoln reports no financial relationship with any company whose products are mentioned in this article, or with manufacturers of competing products.
Dr. Preskorn receives grant/research support from AstraZeneca, Biovail, Boehringer-Ingleheim, Cyberonics, Eli Lilly and Company, EnVivo, GlaxoSmithKline, UNC Chapel Hill, and Wyeth. He is a consultant to Allergan, Covidien, Eli Lilly and Company, Evotec, Lundbeck/Takeda, Transcept, and Wyeth.
1. Bishara D, Taylor D. Upcoming agents for the treatment of schizophrenia: mechanism of action, efficacy and tolerability. Drugs. 2008;68(16):2269-2292.
2. Shahid M, Walker GB, Zorn SH, et al. Asenapine: a novel psychopharmacologic agent with a unique human receptor signature. J Psychopharmacol. 2009;23(1):65-73.
3. Kowalski R, Potkin S, Szeged A, et al. Psychopharmacologic Drugs Advisory Committee: Saphris (asenapine) sublingual tablets. NDA 22-117. Available at: http://www.fda.gov/downloads/AdvisoryCommittees/CommitteesMeetingMaterials/Drugs/PsychopharmacologicDrugsAdvisoryCommittee/UCM179975.pdf. Accessed November 3, 2009.
4. Potkin SG, Cohen M, Panagides J. Efficacy and tolerability of asenapine in acute schizophrenia: a placebo- and risperidone-controlled trial. J Clin Psychiatry. 2007;68(10):1492-1500.
5. Potkin SG, Kane JM, Emsley RA, et al. Asenapine in schizophrenia: an overview of clinical trials in the Olympia program. Abstract 80. Presented at: Annual Meeting of the American Psychiatric Association; May 8, 2008; Washington, DC.
6. McIntyre RS, Hirschfeld R, Calabrese J, et al. Asenapine in bipolar disorder: an overview of clinical trials in the Olympia program. Abstract 44. Presented at: Annual Meeting of the American Psychiatric Association; May 6, 2008; Washington, DC.
7. McIntyre RS, Cohen M, Zhao J, et al. A 3-week, randomized, placebo-controlled trial of asenapine in the treatment of acute mania in bipolar mania and mixed states. Bipolar Disord. 2009;11(7):673-686.
8. McIntyre R, Hirschfeld R, Alphs L, et al. Asenapine in the treatment of acute mania in bipolar I disorder: outcomes from two randomized and placebo-controlled trials. J Affect Disord. 2008;107(suppl 1):S56.-
9. McIntyre R, Panagides J, Alphs L, et al. Treatment of mania in bipolar I disorder: a placebo and olanzapine-controlled trial of asenapine (ARES 7501005). Eur Neuropsychopharmacol. 2007;17(suppl 4):S383.-
10. American Psychiatric Association Work Group on Bipolar Disorder. Practice guideline for the treatment of patients with bipolar disorder. 2nd ed. Arlington, VA: American Psychiatric Association; 2002. Available at: http://www.psychiatryonline.com/pracGuide/loadGuidelinePdf.aspx?file=Bipolar2e_Inactivated_04-16-09. Accessed November 3, 2009.
11. Saphris [package insert]. Kenilworth, NJ: Schering-Plough; 2009.
In August 2009, the FDA approved asenapine for treating acute exacerbation of schizophrenia and acute manic or mixed episodes of bipolar disorder with or without psychosis in adults (Table 1). Asenapine is the first psychotropic to obtain simultaneous FDA approval for schizophrenia and bipolar disorder. The drug’s unique receptor binding profile shows promise in treatment of positive and negative symptoms of schizophrenia with a low risk of extrapyramidal and anticholinergic side effects.
Table 1
Asenapine: Fast facts
| Brand name: Saphris |
| Indications: Acute schizophrenia in adults; acute mixed or manic episodes with or without psychosis associated with bipolar I disorder in adults |
| Approval date: August 2009 |
| Availability date: Late 2009 |
| Manufacturer: Schering-Plough |
| Dosing forms: 5-mg and 10-mg sublingual dissolvable tablets |
| Recommended dose: Schizophrenia: 5 mg twice daily; bipolar disorder: 10 mg twice daily |
How it works
Asenapine is an atypical antipsychotic. Although the exact mechanism of these medications’ efficacy is unknown, their antipsychotic and antimanic activity is thought to be the result of antagonism of central dopamine receptors. According to dopamine theory proposed in the 1960s:
- dopaminergic hyperactivity in mesolimbic dopaminergic pathways contributes to positive symptoms of schizophrenia—hallucinations, delusions, disorganized thoughts and behaviors, and catatonia
- dopaminergic hypoactivity in mesocortical dopaminergic pathways (prefrontal cortex) contributes to negative symptoms of schizophrenia—alogia, avolition, anhedonia, autism, social withdrawal, attention problems, blunted affect, and abstract thinking difficulty.
Asenapine has high affinity for multiple dopamine, serotonin, noradrenergic α1 and α2, and histamine H1 receptors, where it works as an antagonist. Asenapine’s affinity for several serotonin, noradrenergic, and dopaminergic D3 and D4 receptors is higher than its affinity for D2 receptors (Table 2),1 which distinguishes asenapine from other atypical antipsychotics except clozapine.
Blockade of 5-HT2A and 5-HT2C receptors in prefrontal cortex increases dopamine release in this area; theoretically, this effect should improve negative symptoms. Another mechanism that possibly improves cognition and negative symptoms is asenapine’s antagonism at central α2 noradrenergic receptors. Central α1 noradrenergic receptor antagonism also might be helpful in improving positive symptoms of schizophrenia.1
Asenapine’s affinity for the muscarinic-1 cholinergic receptors is quite low, and adverse effects associated with antagonism at these receptors—dry mouth, blurred vision, constipation, and urinary retention—are minimal.2
Table 2
Asenapine’s binding affinity for receptor subtypes*
| Receptor substype | Affinity [Ki (nM)] |
|---|---|
| 5-HT2A | 0.06 |
| 5-HT2C | 0.03 |
| D1 | 1.4 |
| D2 | 1.3 |
| D3 | 0.42 |
| D4 | 1.1 |
| α1 | 1.2 |
| α2 | 1.2 |
| H1 | 1.0 |
| M1 | 8128 |
| *Lower numbers indicate higher affinity | |
| 5-HT: serotonin receptors; D1-4: dopamine receptors; α1, α2: noradrenergic receptors; H1: histamine receptor; M1: muscarinic (cholinergic) receptor | |
| Source: Reference 1 | |
Pharmacokinetics
Absorption of asenapine after oral (swallowed) administration is 2%. To increase total bioavailability to 35%, the drug is manufactured as sublingual dissolvable tablets. After sublingual administration, asenapine is readily absorbed and achieves peak plasma concentration in approximately 1 hour. After absorption, 95% of asenapine binds to transport proteins albumin and α1 acid glycoprotein. The half-life of the medication is approximately 24 hours, and steady state usually is achieved in 3 days.
Metabolism creates about 40 metabolites via multiple metabolic pathways; the main ones are glucuronidation by UGT1A4 and oxidative metabolism by cytochrome P450 (CYP)1A2. Asenapine is a weak inhibitor of CYP2D6, so coadministration of asenapine with other drugs that are substrates or inhibitors of CYP1A2 (eg, fluvoxamine) or CYP2D6 (eg, paroxetine, fluoxetine) should be done cautiously. Because asenapine elimination is biphasic, twice-daily dosing is recommended.3
Efficacy in clinical trials
Schizophrenia. Asenapine’s efficacy for treating schizophrenia was evaluated in 3 fixed-dose, 6-week, randomized, double-blind, placebo- and active- (haloperidol, olanzapine, and risperidone) controlled clinical trials in adults.3-5 Subjects in these studies met DSM-IV criteria for schizophrenia and had acute exacerbation of their illness, with Positive and Negative Syndrome Scale (PANSS) total scores ≥60. Symptom improvement was measured after 6 weeks by PANSS total score, PANSS positive subscale, and Clinical Global Impression scale (CGI).
The first trial (n=174) compared asenapine, 5 mg twice daily, to placebo and risperidone, 3 mg twice daily.3-5 Asenapine was superior to placebo as demonstrated by symptom improvement on all 3 scales. Risperidone showed statistically significant symptom improvement on PANSS positive subscale and CGI but not on PANSS total score.
In the second trial (n=448), 2 fixed doses of asenapine (5 mg twice daily and 10 mg twice daily) and olanzapine, 15 mg/d, were compared with placebo.3,5 The only statistically significant symptom improvement in the asenapine group compared with placebo was on the PANSS positive subscale among subjects receiving 5 mg twice daily. Improvements measured by CGI and PANSS total score were not statistically significant.
Olanzapine showed statistically significant symptom improvement on all 3 scales compared with placebo. This study is a negative trial for asenapine; asenapine failed to separate from placebo, whereas olanzapine—the active comparator—did.
The third trial (n=448) compared asenapine, 5 mg twice daily and 10 mg twice daily, with placebo and haloperidol, 4 mg twice daily.3,5 Compared with placebo, asenapine at both doses and haloperidol improved symptoms on all 3 scales. The 10-mg twice-daily dosage did not provide any additional benefits compared with the 5 mg twice-daily dosage.
Bipolar disorder. Asenapine’s efficacy for bipolar disorder was established in two 3-week, randomized, double-blind, placebo- and olanzapine-controlled studies in adults with acute manic or mixed episodes with or without psychosis.3,6-9 Symptoms were assessed using the Young Mania Rating Scale (YMRS) and Clinical Global Impression-Bipolar (CGI-BP) scale.
In both studies, subjects were randomly assigned to receive asenapine, 10 mg twice daily; olanzapine, 5 to 20 mg/d; or placebo. Depending on efficacy and tolerability, the asenapine dose could be adjusted within the dosing range of 5 mg to 10 mg twice daily starting on day 2. Ninety percent of subjects stayed on the 10 mg twice-daily dose. In both studies, asenapine and olanzapine were statistically superior to placebo on YMRS and CGI-BP severity of illness scores.
Currently no evidence supports asenapine’s efficacy for maintenance treatment of schizophrenia or bipolar disorder. American Psychiatric Association practice guidelines recommend continuing treatment for a minimum of 6 months after stabilization of acute episodes of schizophrenia or bipolar disorder to prevent recurrence.10
Tolerability in clinical trials
Tolerability information provided in this article was obtained from a Clinical Trial Database consisting of 3,350 subjects:11
- 1,953 patients participated in multiple dose effectiveness trials (1,480 with schizophrenia and 473 with bipolar disorder manic/mixed episodes)
- 486 subjects were treated for at least 24 weeks
- 293 subjects were treated for at least 52 weeks.
Overall, asenapine was well tolerated (Table 3).11 The most common adverse effects in schizophrenia trials were akathisia, oral hypoesthesia, and somnolence. The discontinuation rate due to adverse effects in schizophrenia trials was 9% in the asenapine group vs 10% in the placebo group.
Among patients with bipolar disorder, the most common side effects were somnolence, dizziness, extrapyramidal symptoms other than akathisia, and increased weight. The discontinuation rate for subjects treated with asenapine was 10% vs 6% with placebo. The most common adverse reactions associated with discontinuation were anxiety and oral hypoesthesia. Oral hypoesthesia did not occur in the placebo group, and akathisia was the only dose-dependent adverse reaction.
Dizziness and weight gain. Clinically important adverse effects of asenapine include dizziness and weight gain. Dizziness is possibly related to orthostatic hypotension caused by the drug’s activity at the α1 receptor (antagonist). To prevent ischemic events or falls with subsequent injuries, use asenapine with caution in hypotensive patients and those with cardiovascular or cerebrovascular problems.
In clinical trials investigating asenapine’s efficacy, mean weight gain was greater in patients receiving asenapine than those receiving placebo. In short-term studies, mean weight gain in patients treated with asenapine was 1.1 kg for subjects with schizophrenia and 1.3 kg for subjects with bipolar mania.3 Mean weight gain in patients treated with placebo was 0.1 kg for subjects with schizophrenia and 0.2 kg for those with bipolar mania.
In a 52-week comparator study of patients with schizophrenia and schizoaffective disorder, mean weight gain was 0.9 kg in the asenapine group vs 4.2 kg in the olanzapine group.3 In both groups, the greatest weight increase occurred in subjects with body mass index <23.
There were no clinically relevant mean changes in serum fasting glucose, serum fasting triglycerides, fasting cholesterol, transaminases, and prolactin. Thrombocytopenia, anemia, tachycardia, temporary bundle branch block, visual accommodation disorder, oral paresthesia, glossodynia, swollen tongue, hyponatremia, and dysarthria occurred in 1 in 100 to 1 in 1,000 patients.
Table 3
Percentages of clinical trial patients who experienced adverse effects with asenapine vs placebo
| Schizophrenia | Bipolar disorder (mania/mixed) | |||||
|---|---|---|---|---|---|---|
| Adverse effect | Placebo (n=378) | Asenapine, 5 mg bid (n=274) | Asenapine, 10 mg bid (n=208) | Asenapine, 5 or 10 mg bid (n=572) | Placebo (n=203) | Asenapine, 5 or 10 mg bid (n=379) |
| Oral hypoesthesia | 1 | 6 | 7 | 5 | <1 | 4 |
| Weight gain | <1 | 2 | 2 | 3 | <1 | 5 |
| Increased appetite | <1 | 3 | 0 | 2 | 1 | 4 |
| Anxiety | 2 | 4 | ||||
| Akathisia | 3 | 4 | 11 | 6 | 2 | 4 |
| Other EPS (excluding akathisia) | 7 | 9 | 12 | 10 | 2 | 7 |
| Insomnia | 13 | 16 | 15 | 15 | 5 | 6 |
| Somnolence | 7 | 15 | 13 | 13 | 6 | 24 |
| Dizziness | 4 | 7 | 3 | 5 | 3 | 11 |
| EPS: extrapyramidal symptoms | ||||||
| Source: Reference 11 | ||||||
Contraindications
There are no absolute contraindications to asenapine use; however, the medication is not recommended for treating:
- women who are pregnant if the risks of treatment outweigh the benefits (pregnancy risk C)
- breast-feeding mothers
- patients with severe hepatic impairment (Child-Pugh C).
Asenapine carries the same class warnings and precautions as other antipsychotic medications, including a “black box” warning of increased mortality risk in elderly patients with dementia-related psychosis. Other class warnings include an increased risk of transient ischemic attack and cerebrovascular accidents in elderly patients with dementia-related psychosis; neuroleptic malignant syndrome; tardive dyskinesia; glycemia/diabetes mellitus; hyperprolactinemia; leukopenia; neutropenia; and agranulocytosis.
Because asenapine is associated with QT prolongation, do not administer it with other QT-prolonging agents, such as procainamide, sotalol, quinidine, erythromycin, clarithromycin, methadone, or other antipsychotics.
Dosing
Asenapine is manufactured as 5-mg and 10-mg sublingual tablets. Advise patients to avoid eating or drinking for 10 minutes after taking asenapine.
The recommended starting and target dosage for patients with schizophrenia is 5 mg twice daily. The recommended starting dosage for patients with an acute mixed or manic episode of bipolar I disorder is 10 mg twice daily; however, this can be reduced to 5 mg twice daily if the patient experiences intolerable side effects.
Related resource
- Asenapine (Saphris) prescribing information. www.spfiles.com/pisaphrisv1.pdf.
Drug brand names
- Asenapine • Saphris
- Clarithromycin • Biaxin
- Clozapine • Clozaril
- Erythromycin • ERY-C, Ery-Tab
- Fluoxetine • Prozac
- Fluvoxamine • Luvox
- Haloperidol • Haldol
- Methadone • Dolophine, Methadose
- Olanzapine • Zyprexa
- Paroxetine • Paxil
- Procainamide • Procanbid
- Quinidine • Quinidine
- Risperidone • Risperdal
- Sotalol • Betapace, Sorine
Disclosures
Dr. Lincoln reports no financial relationship with any company whose products are mentioned in this article, or with manufacturers of competing products.
Dr. Preskorn receives grant/research support from AstraZeneca, Biovail, Boehringer-Ingleheim, Cyberonics, Eli Lilly and Company, EnVivo, GlaxoSmithKline, UNC Chapel Hill, and Wyeth. He is a consultant to Allergan, Covidien, Eli Lilly and Company, Evotec, Lundbeck/Takeda, Transcept, and Wyeth.
In August 2009, the FDA approved asenapine for treating acute exacerbation of schizophrenia and acute manic or mixed episodes of bipolar disorder with or without psychosis in adults (Table 1). Asenapine is the first psychotropic to obtain simultaneous FDA approval for schizophrenia and bipolar disorder. The drug’s unique receptor binding profile shows promise in treatment of positive and negative symptoms of schizophrenia with a low risk of extrapyramidal and anticholinergic side effects.
Table 1
Asenapine: Fast facts
| Brand name: Saphris |
| Indications: Acute schizophrenia in adults; acute mixed or manic episodes with or without psychosis associated with bipolar I disorder in adults |
| Approval date: August 2009 |
| Availability date: Late 2009 |
| Manufacturer: Schering-Plough |
| Dosing forms: 5-mg and 10-mg sublingual dissolvable tablets |
| Recommended dose: Schizophrenia: 5 mg twice daily; bipolar disorder: 10 mg twice daily |
How it works
Asenapine is an atypical antipsychotic. Although the exact mechanism of these medications’ efficacy is unknown, their antipsychotic and antimanic activity is thought to be the result of antagonism of central dopamine receptors. According to dopamine theory proposed in the 1960s:
- dopaminergic hyperactivity in mesolimbic dopaminergic pathways contributes to positive symptoms of schizophrenia—hallucinations, delusions, disorganized thoughts and behaviors, and catatonia
- dopaminergic hypoactivity in mesocortical dopaminergic pathways (prefrontal cortex) contributes to negative symptoms of schizophrenia—alogia, avolition, anhedonia, autism, social withdrawal, attention problems, blunted affect, and abstract thinking difficulty.
Asenapine has high affinity for multiple dopamine, serotonin, noradrenergic α1 and α2, and histamine H1 receptors, where it works as an antagonist. Asenapine’s affinity for several serotonin, noradrenergic, and dopaminergic D3 and D4 receptors is higher than its affinity for D2 receptors (Table 2),1 which distinguishes asenapine from other atypical antipsychotics except clozapine.
Blockade of 5-HT2A and 5-HT2C receptors in prefrontal cortex increases dopamine release in this area; theoretically, this effect should improve negative symptoms. Another mechanism that possibly improves cognition and negative symptoms is asenapine’s antagonism at central α2 noradrenergic receptors. Central α1 noradrenergic receptor antagonism also might be helpful in improving positive symptoms of schizophrenia.1
Asenapine’s affinity for the muscarinic-1 cholinergic receptors is quite low, and adverse effects associated with antagonism at these receptors—dry mouth, blurred vision, constipation, and urinary retention—are minimal.2
Table 2
Asenapine’s binding affinity for receptor subtypes*
| Receptor substype | Affinity [Ki (nM)] |
|---|---|
| 5-HT2A | 0.06 |
| 5-HT2C | 0.03 |
| D1 | 1.4 |
| D2 | 1.3 |
| D3 | 0.42 |
| D4 | 1.1 |
| α1 | 1.2 |
| α2 | 1.2 |
| H1 | 1.0 |
| M1 | 8128 |
| *Lower numbers indicate higher affinity | |
| 5-HT: serotonin receptors; D1-4: dopamine receptors; α1, α2: noradrenergic receptors; H1: histamine receptor; M1: muscarinic (cholinergic) receptor | |
| Source: Reference 1 | |
Pharmacokinetics
Absorption of asenapine after oral (swallowed) administration is 2%. To increase total bioavailability to 35%, the drug is manufactured as sublingual dissolvable tablets. After sublingual administration, asenapine is readily absorbed and achieves peak plasma concentration in approximately 1 hour. After absorption, 95% of asenapine binds to transport proteins albumin and α1 acid glycoprotein. The half-life of the medication is approximately 24 hours, and steady state usually is achieved in 3 days.
Metabolism creates about 40 metabolites via multiple metabolic pathways; the main ones are glucuronidation by UGT1A4 and oxidative metabolism by cytochrome P450 (CYP)1A2. Asenapine is a weak inhibitor of CYP2D6, so coadministration of asenapine with other drugs that are substrates or inhibitors of CYP1A2 (eg, fluvoxamine) or CYP2D6 (eg, paroxetine, fluoxetine) should be done cautiously. Because asenapine elimination is biphasic, twice-daily dosing is recommended.3
Efficacy in clinical trials
Schizophrenia. Asenapine’s efficacy for treating schizophrenia was evaluated in 3 fixed-dose, 6-week, randomized, double-blind, placebo- and active- (haloperidol, olanzapine, and risperidone) controlled clinical trials in adults.3-5 Subjects in these studies met DSM-IV criteria for schizophrenia and had acute exacerbation of their illness, with Positive and Negative Syndrome Scale (PANSS) total scores ≥60. Symptom improvement was measured after 6 weeks by PANSS total score, PANSS positive subscale, and Clinical Global Impression scale (CGI).
The first trial (n=174) compared asenapine, 5 mg twice daily, to placebo and risperidone, 3 mg twice daily.3-5 Asenapine was superior to placebo as demonstrated by symptom improvement on all 3 scales. Risperidone showed statistically significant symptom improvement on PANSS positive subscale and CGI but not on PANSS total score.
In the second trial (n=448), 2 fixed doses of asenapine (5 mg twice daily and 10 mg twice daily) and olanzapine, 15 mg/d, were compared with placebo.3,5 The only statistically significant symptom improvement in the asenapine group compared with placebo was on the PANSS positive subscale among subjects receiving 5 mg twice daily. Improvements measured by CGI and PANSS total score were not statistically significant.
Olanzapine showed statistically significant symptom improvement on all 3 scales compared with placebo. This study is a negative trial for asenapine; asenapine failed to separate from placebo, whereas olanzapine—the active comparator—did.
The third trial (n=448) compared asenapine, 5 mg twice daily and 10 mg twice daily, with placebo and haloperidol, 4 mg twice daily.3,5 Compared with placebo, asenapine at both doses and haloperidol improved symptoms on all 3 scales. The 10-mg twice-daily dosage did not provide any additional benefits compared with the 5 mg twice-daily dosage.
Bipolar disorder. Asenapine’s efficacy for bipolar disorder was established in two 3-week, randomized, double-blind, placebo- and olanzapine-controlled studies in adults with acute manic or mixed episodes with or without psychosis.3,6-9 Symptoms were assessed using the Young Mania Rating Scale (YMRS) and Clinical Global Impression-Bipolar (CGI-BP) scale.
In both studies, subjects were randomly assigned to receive asenapine, 10 mg twice daily; olanzapine, 5 to 20 mg/d; or placebo. Depending on efficacy and tolerability, the asenapine dose could be adjusted within the dosing range of 5 mg to 10 mg twice daily starting on day 2. Ninety percent of subjects stayed on the 10 mg twice-daily dose. In both studies, asenapine and olanzapine were statistically superior to placebo on YMRS and CGI-BP severity of illness scores.
Currently no evidence supports asenapine’s efficacy for maintenance treatment of schizophrenia or bipolar disorder. American Psychiatric Association practice guidelines recommend continuing treatment for a minimum of 6 months after stabilization of acute episodes of schizophrenia or bipolar disorder to prevent recurrence.10
Tolerability in clinical trials
Tolerability information provided in this article was obtained from a Clinical Trial Database consisting of 3,350 subjects:11
- 1,953 patients participated in multiple dose effectiveness trials (1,480 with schizophrenia and 473 with bipolar disorder manic/mixed episodes)
- 486 subjects were treated for at least 24 weeks
- 293 subjects were treated for at least 52 weeks.
Overall, asenapine was well tolerated (Table 3).11 The most common adverse effects in schizophrenia trials were akathisia, oral hypoesthesia, and somnolence. The discontinuation rate due to adverse effects in schizophrenia trials was 9% in the asenapine group vs 10% in the placebo group.
Among patients with bipolar disorder, the most common side effects were somnolence, dizziness, extrapyramidal symptoms other than akathisia, and increased weight. The discontinuation rate for subjects treated with asenapine was 10% vs 6% with placebo. The most common adverse reactions associated with discontinuation were anxiety and oral hypoesthesia. Oral hypoesthesia did not occur in the placebo group, and akathisia was the only dose-dependent adverse reaction.
Dizziness and weight gain. Clinically important adverse effects of asenapine include dizziness and weight gain. Dizziness is possibly related to orthostatic hypotension caused by the drug’s activity at the α1 receptor (antagonist). To prevent ischemic events or falls with subsequent injuries, use asenapine with caution in hypotensive patients and those with cardiovascular or cerebrovascular problems.
In clinical trials investigating asenapine’s efficacy, mean weight gain was greater in patients receiving asenapine than those receiving placebo. In short-term studies, mean weight gain in patients treated with asenapine was 1.1 kg for subjects with schizophrenia and 1.3 kg for subjects with bipolar mania.3 Mean weight gain in patients treated with placebo was 0.1 kg for subjects with schizophrenia and 0.2 kg for those with bipolar mania.
In a 52-week comparator study of patients with schizophrenia and schizoaffective disorder, mean weight gain was 0.9 kg in the asenapine group vs 4.2 kg in the olanzapine group.3 In both groups, the greatest weight increase occurred in subjects with body mass index <23.
There were no clinically relevant mean changes in serum fasting glucose, serum fasting triglycerides, fasting cholesterol, transaminases, and prolactin. Thrombocytopenia, anemia, tachycardia, temporary bundle branch block, visual accommodation disorder, oral paresthesia, glossodynia, swollen tongue, hyponatremia, and dysarthria occurred in 1 in 100 to 1 in 1,000 patients.
Table 3
Percentages of clinical trial patients who experienced adverse effects with asenapine vs placebo
| Schizophrenia | Bipolar disorder (mania/mixed) | |||||
|---|---|---|---|---|---|---|
| Adverse effect | Placebo (n=378) | Asenapine, 5 mg bid (n=274) | Asenapine, 10 mg bid (n=208) | Asenapine, 5 or 10 mg bid (n=572) | Placebo (n=203) | Asenapine, 5 or 10 mg bid (n=379) |
| Oral hypoesthesia | 1 | 6 | 7 | 5 | <1 | 4 |
| Weight gain | <1 | 2 | 2 | 3 | <1 | 5 |
| Increased appetite | <1 | 3 | 0 | 2 | 1 | 4 |
| Anxiety | 2 | 4 | ||||
| Akathisia | 3 | 4 | 11 | 6 | 2 | 4 |
| Other EPS (excluding akathisia) | 7 | 9 | 12 | 10 | 2 | 7 |
| Insomnia | 13 | 16 | 15 | 15 | 5 | 6 |
| Somnolence | 7 | 15 | 13 | 13 | 6 | 24 |
| Dizziness | 4 | 7 | 3 | 5 | 3 | 11 |
| EPS: extrapyramidal symptoms | ||||||
| Source: Reference 11 | ||||||
Contraindications
There are no absolute contraindications to asenapine use; however, the medication is not recommended for treating:
- women who are pregnant if the risks of treatment outweigh the benefits (pregnancy risk C)
- breast-feeding mothers
- patients with severe hepatic impairment (Child-Pugh C).
Asenapine carries the same class warnings and precautions as other antipsychotic medications, including a “black box” warning of increased mortality risk in elderly patients with dementia-related psychosis. Other class warnings include an increased risk of transient ischemic attack and cerebrovascular accidents in elderly patients with dementia-related psychosis; neuroleptic malignant syndrome; tardive dyskinesia; glycemia/diabetes mellitus; hyperprolactinemia; leukopenia; neutropenia; and agranulocytosis.
Because asenapine is associated with QT prolongation, do not administer it with other QT-prolonging agents, such as procainamide, sotalol, quinidine, erythromycin, clarithromycin, methadone, or other antipsychotics.
Dosing
Asenapine is manufactured as 5-mg and 10-mg sublingual tablets. Advise patients to avoid eating or drinking for 10 minutes after taking asenapine.
The recommended starting and target dosage for patients with schizophrenia is 5 mg twice daily. The recommended starting dosage for patients with an acute mixed or manic episode of bipolar I disorder is 10 mg twice daily; however, this can be reduced to 5 mg twice daily if the patient experiences intolerable side effects.
Related resource
- Asenapine (Saphris) prescribing information. www.spfiles.com/pisaphrisv1.pdf.
Drug brand names
- Asenapine • Saphris
- Clarithromycin • Biaxin
- Clozapine • Clozaril
- Erythromycin • ERY-C, Ery-Tab
- Fluoxetine • Prozac
- Fluvoxamine • Luvox
- Haloperidol • Haldol
- Methadone • Dolophine, Methadose
- Olanzapine • Zyprexa
- Paroxetine • Paxil
- Procainamide • Procanbid
- Quinidine • Quinidine
- Risperidone • Risperdal
- Sotalol • Betapace, Sorine
Disclosures
Dr. Lincoln reports no financial relationship with any company whose products are mentioned in this article, or with manufacturers of competing products.
Dr. Preskorn receives grant/research support from AstraZeneca, Biovail, Boehringer-Ingleheim, Cyberonics, Eli Lilly and Company, EnVivo, GlaxoSmithKline, UNC Chapel Hill, and Wyeth. He is a consultant to Allergan, Covidien, Eli Lilly and Company, Evotec, Lundbeck/Takeda, Transcept, and Wyeth.
1. Bishara D, Taylor D. Upcoming agents for the treatment of schizophrenia: mechanism of action, efficacy and tolerability. Drugs. 2008;68(16):2269-2292.
2. Shahid M, Walker GB, Zorn SH, et al. Asenapine: a novel psychopharmacologic agent with a unique human receptor signature. J Psychopharmacol. 2009;23(1):65-73.
3. Kowalski R, Potkin S, Szeged A, et al. Psychopharmacologic Drugs Advisory Committee: Saphris (asenapine) sublingual tablets. NDA 22-117. Available at: http://www.fda.gov/downloads/AdvisoryCommittees/CommitteesMeetingMaterials/Drugs/PsychopharmacologicDrugsAdvisoryCommittee/UCM179975.pdf. Accessed November 3, 2009.
4. Potkin SG, Cohen M, Panagides J. Efficacy and tolerability of asenapine in acute schizophrenia: a placebo- and risperidone-controlled trial. J Clin Psychiatry. 2007;68(10):1492-1500.
5. Potkin SG, Kane JM, Emsley RA, et al. Asenapine in schizophrenia: an overview of clinical trials in the Olympia program. Abstract 80. Presented at: Annual Meeting of the American Psychiatric Association; May 8, 2008; Washington, DC.
6. McIntyre RS, Hirschfeld R, Calabrese J, et al. Asenapine in bipolar disorder: an overview of clinical trials in the Olympia program. Abstract 44. Presented at: Annual Meeting of the American Psychiatric Association; May 6, 2008; Washington, DC.
7. McIntyre RS, Cohen M, Zhao J, et al. A 3-week, randomized, placebo-controlled trial of asenapine in the treatment of acute mania in bipolar mania and mixed states. Bipolar Disord. 2009;11(7):673-686.
8. McIntyre R, Hirschfeld R, Alphs L, et al. Asenapine in the treatment of acute mania in bipolar I disorder: outcomes from two randomized and placebo-controlled trials. J Affect Disord. 2008;107(suppl 1):S56.-
9. McIntyre R, Panagides J, Alphs L, et al. Treatment of mania in bipolar I disorder: a placebo and olanzapine-controlled trial of asenapine (ARES 7501005). Eur Neuropsychopharmacol. 2007;17(suppl 4):S383.-
10. American Psychiatric Association Work Group on Bipolar Disorder. Practice guideline for the treatment of patients with bipolar disorder. 2nd ed. Arlington, VA: American Psychiatric Association; 2002. Available at: http://www.psychiatryonline.com/pracGuide/loadGuidelinePdf.aspx?file=Bipolar2e_Inactivated_04-16-09. Accessed November 3, 2009.
11. Saphris [package insert]. Kenilworth, NJ: Schering-Plough; 2009.
1. Bishara D, Taylor D. Upcoming agents for the treatment of schizophrenia: mechanism of action, efficacy and tolerability. Drugs. 2008;68(16):2269-2292.
2. Shahid M, Walker GB, Zorn SH, et al. Asenapine: a novel psychopharmacologic agent with a unique human receptor signature. J Psychopharmacol. 2009;23(1):65-73.
3. Kowalski R, Potkin S, Szeged A, et al. Psychopharmacologic Drugs Advisory Committee: Saphris (asenapine) sublingual tablets. NDA 22-117. Available at: http://www.fda.gov/downloads/AdvisoryCommittees/CommitteesMeetingMaterials/Drugs/PsychopharmacologicDrugsAdvisoryCommittee/UCM179975.pdf. Accessed November 3, 2009.
4. Potkin SG, Cohen M, Panagides J. Efficacy and tolerability of asenapine in acute schizophrenia: a placebo- and risperidone-controlled trial. J Clin Psychiatry. 2007;68(10):1492-1500.
5. Potkin SG, Kane JM, Emsley RA, et al. Asenapine in schizophrenia: an overview of clinical trials in the Olympia program. Abstract 80. Presented at: Annual Meeting of the American Psychiatric Association; May 8, 2008; Washington, DC.
6. McIntyre RS, Hirschfeld R, Calabrese J, et al. Asenapine in bipolar disorder: an overview of clinical trials in the Olympia program. Abstract 44. Presented at: Annual Meeting of the American Psychiatric Association; May 6, 2008; Washington, DC.
7. McIntyre RS, Cohen M, Zhao J, et al. A 3-week, randomized, placebo-controlled trial of asenapine in the treatment of acute mania in bipolar mania and mixed states. Bipolar Disord. 2009;11(7):673-686.
8. McIntyre R, Hirschfeld R, Alphs L, et al. Asenapine in the treatment of acute mania in bipolar I disorder: outcomes from two randomized and placebo-controlled trials. J Affect Disord. 2008;107(suppl 1):S56.-
9. McIntyre R, Panagides J, Alphs L, et al. Treatment of mania in bipolar I disorder: a placebo and olanzapine-controlled trial of asenapine (ARES 7501005). Eur Neuropsychopharmacol. 2007;17(suppl 4):S383.-
10. American Psychiatric Association Work Group on Bipolar Disorder. Practice guideline for the treatment of patients with bipolar disorder. 2nd ed. Arlington, VA: American Psychiatric Association; 2002. Available at: http://www.psychiatryonline.com/pracGuide/loadGuidelinePdf.aspx?file=Bipolar2e_Inactivated_04-16-09. Accessed November 3, 2009.
11. Saphris [package insert]. Kenilworth, NJ: Schering-Plough; 2009.