User login
Help your bipolar disorder patients remain employed
Mrs. S, age 34, worked as an office manager with responsibilities for more than 40 employees for 5 years. Starting in her mid 20s she had repeated periods of depression, binge drinking, and risk-taking that were treated ineffectively with antidepressants. Ultimately, she was fired from her job.
Eventually Mrs. S was diagnosed as bipolar and over time responded well to a mood-stabilizing regimen. She now desires to return to work, both for financial reasons and for the sense of accomplishment that comes from working. Initially, personnel managers review her résumé and tell her she would be bored by the routine nature of entry-level positions, or they offer her jobs with major responsibilities. She accepts a high-level position but soon leaves, feeling overwhelmed by the stress.
Bipolar disorder’s long-term course presents a therapeutic challenge when patients desire to remain employed, seek temporary or permanent disability status, or—most commonly—attempt to return to employment after a period of inability to work. As the experience of Mrs. S illustrates, previous capabilities that appear higher than the person’s present or recent work experience are a key issue to address in interpersonal therapy.
Evidence-based research is informative, but ultimately you must apply judgment and flexibility in setting and revising goals with the bipolar individual. Attention to the disorder’s core characteristics can help you equip patients for work that contributes to their pursuit of health.
Obstacles to employment
Role function. Bipolar disorder impairs family and social function in approximately one-half of persons with this diagnosis, a higher impairment rate than in persons with major depression.1
Cognitive function. Bipolar disorder patients have subtle sustained impairments in cognitive function, particularly working memory.2,3 These deficits—although generally much less severe than in persons with schizophrenia—contribute to workplace and educational difficulties.
Unstable mood. Some symptoms associated with elevated mood contribute to functional impairment. These are not limited to mania or hypomania but also can be prominent in mixed states and depression.
A study from the Systematic Treatment Enhancement Program for Bipolar Disorder (STEP-BD) found that two-thirds of 1,380 depressed bipolar I and II patients had ?1 concomitant symptoms principally associated with manic states. The most prominent were distractibility, pressured speech and thoughts, risky behavior, and agitation.4 Each of these—or, more often, all of these—can interfere with work responsibilities.
Circadian rhythm pattern. Sleep disturbances in bipolar disorder differ from those associated with other medical conditions. Bipolar patients’ tendency to increase their activity and interests in the evening may keep them awake into the early morning hours. Insufficient sleep and impaired daytime cognition and alertness related to idio syncratic circadian rhythms can interfere with job requirements.5 The structure of employment can help many bipolar patients maintain effective sleep patterns as well as waking activities (Box 1).
Some individuals recognize their disturbed activity pattern, but many view it simply as the way they approach a day. For the latter group, a sustained treatment effort is needed to help them recognize the adverse consequences of the pattern and develop a more effective daily routine.
Adverse treatment effects. Although important, this core medical issue is not central to the interpersonal focus of this article. The simple tolerability objective in prescribing medications—and less frequently therapies such as electroconvulsive treatment—is to avoid dosages that impair concentration, alertness, or motor speed and accuracy. Similarly, avoid medications that can cause physical changes noticeable to others—such as tremor, sleepiness, or significant weight gain—or adjust dosages to eliminate these side effects.
Work, defined as what we do to make a living, is useful for most individuals. For persons with bipolar disorder, work has additional benefits. Having a job aids in structuring their daily activities, which tend to be skewed by circadian rhythm-linked problems of inadequate sleep or sleep that starts too late and extends into the day. The routine expectations of a work schedule also can counteract the distractibility and unproductive multitasking common in some bipolar disorder patients.
These benefits are not guaranteed and vary considerably across occupational settings, but patients and family members readily understand this aspect of work. Its benefits can serve as an important impetus for patients to persist in efforts to attain employment, even in the face of obstacles.
Bipolar symptom domains
Anxiety is recognized as a separate and major domain in bipolar psychopathology,6 contributing strongly to poor outcomes. Although anxiety is somewhat more predominant in depression and mixed states, it is common in manic and recovered bipolar states as well.
Social anxiety and panic states appear to be most specifically associated with bipolar disorder.7 Because these types of anxiety entail excessive fearful responses, psychotherapeutic techniques including extinction approaches can be helpful.
Depression in bipolar disorder tends to manifest as slowed motor and cognitive function, which is likely to be evident in work situations. Additionally, loss of social interests—one of the most common and severe aspects of depression in bipolar disorders—is likely to be evident to coworkers and to negatively impact work effectiveness.
Irritability occurs most frequently in mixed bipolar states but also is characteristic of—though generally less intense in—depressed and manic clinical states. Even when strictly internal and subjective, irritability can reduce an individual’s confidence and work effectiveness. Expressed irritability, from minor annoyances to explosive outbursts, can have serious employment consequences, including termination.
Manic symptoms. The impulsivity that is common in bipolar mania can interfere with work. Acting without considering consequences, taking undue risks, or reaching conclusions on inadequate information can cause problems, including physical harm to self or coworkers. Excessive talking—usually associated with internally recognized racing thoughts—can be a nuisance when mild or problematic if it interferes with customer or coworker interactions.
Hyperactivity and increased energy may be perceived as behaviors that facilitate productivity at work (Box 2).8-10 The adaptive characteristics of many hypomanic states are infrequent or absent in depressive, manic, and mixed manic clinical states, however.
Psychosis is principally associated with manic episodes, but it can be a component of any symptomatic clinical state. Delusional ideas or persecutory thoughts are rarely compatible with a work environment, in part because of potential risks to others.
For some purposes, bipolar disease confers social and employment advantages. Common, frequently adaptive behavioral characteristics of hypomania include:
- perseverance
- high energy
- heightened perceptual sensitivity
- exuberance and playfulness
- optimism.
Increased energy and mild degrees of hyperactivity—as well as thinking along creative, multisystem lines—can benefit work productivity, customer interactions, and work group relations. Heightened confidence and social interests can be valuable in some sales and marketing activities.
Although these attitudes and behaviors can have constructive effects, patients need to understand their limits and destructive potential. This is not a straightforward issue, as patients may not have self-awareness of some adverse consequences of characteristics such as irritability, risk taking, or inappropriate sexual advances. A phenomenon little described in clinical literature but relatively common in biographical accounts of persons with bipolar disorder is that friends or coworkers may encourage, rationalize, and take advantage of an individual’s hypomanic energy, thwarting effective interventions.
Componential treatment
Bipolar disorder’s multiple symptom domains suggest a componential approach to treatment. It may be useful to convey this concept metaphorically to the patient. When working on a jigsaw puzzle, a section that has been put together can be largely left intact and attention turned to other sections of the puzzle. Similarly, once a particular bipolar component is well managed—whether via medication, lifestyle, attitudes, or combinations of these—that symptom is likely to remain stable, barring a new insult/stressor (such as a medical condition requiring drugs that interfere with the bipolar regimen).
If mood stabilizers control risky behavior, impulsivity, and affective lability, the regimen generally will remain effective. If residual or new problems develop in another area (such as anxiety, sleep cycle, or irritability), choose drug regimens and psychoeducation approaches that are compatible with the mood-stabilizing plan. This attitude toward treatment:
- is reassuring to most patients, who come to see a new or recurring problem in one domain as not inherently a harbinger of complete relapse
- can reduce patient- or clinician-initiated deletions and additions of medications in a regimen that has been established as effective.
Autobiographical accounts of persons with bipolar disorders can be useful in educating patients about the considerations presented here. Actress Patty Duke made these observations in describing the gradual development of an effective treatment for her severe bipolar disorder:
I work at not flying off the handle…and I’m much better at it. My general medical bills dropped by $50,000 a year since my bipolar diagnosis and treatment. Until then, I was always in the hospital for some phantom illness. I was there with real symptoms born of depression. I haven’t been in the hospital since I was diagnosed.
My recovery from manic-depression has been an evolution, not a sudden miracle. For someone who spent 50% of her life screaming and yelling about something, I am now down to, say, 5%.11
Psychosocial factors to consider
Stigma in the workplace. Although most coworkers are tolerant of and fair-minded about the functional difficulties common in symptomatic bipolar disorder, some will have biased, inaccurate views about psychiatric conditions. Advise bipolar individuals to make case-by-case decisions about whether to provide personal information to other employees and, if so, how much.
As with most medical conditions, the default choice will be to not discuss personal information in the workplace. Some coworkers, however, might appreciate learning of the bipolar condition (for example, a supervisor who seems empathic to an employee’s seeming stressed state).
Realistic expectations. Most clinicians recognize that relief from a syndromal bipolar state is achieved more quickly than a sustained recovered status in which symptoms are minimal. Attaining functional capacity in a normal range also lags, both in time and in the proportion of persons who ever achieve sustained good function.12 Patients, their families, and often employers may have unrealistic expectations about early resumption of work after a depressive or manic episode resolves.
Ethnic considerations. Some literature suggests ethnic differences in the initial presentation of bipolar disorder, with more severe manifestations in some populations particularly if psychosis is a component symptom.13 Additionally, some cultural views about stigma from illness can add to patients’ or family members’ reluctance to re-enter the workplace.
Socioeconomic status. Sometimes bipolar illness puts out of reach the occupational activities that an individual has previously undertaken or that are characteristic of the family’s experience and expectations. Resistance to a change in self-concept can add to the difficulty in successfully moving a patient to consider employment that is more routinized and less intellectual or decisional in nature (Box 3).14
Divergence in education vs work status. Persons with bipolar disorders often have substantial divergence between high educational attainment and lower work performance. When this is the case, all or most of the factors reviewed in this article probably have contributed. Mrs. S’s experience illustrates this aspect of our care for persons with bipolar disorders.
An employment barrier for some bipolar patients is that a brief, often long-past period of high intellectual or vocational performance serves as the benchmark for their capabilities. Patients with this characteristic resist revising their self-concept. Some treat the loss of this idealized image as an unfair consequence of their illness or society’s reaction to bipolar disorder. Their stubbornness tends to prevent realistic engagement socially or vocationally at levels that are presently feasible for them.
Resistance to change associated with this characteristic often is difficult to manage effectively with short, relatively infrequent medication-focused visits. Specific psychosocial interventions may be more effective.14
CASE CONTINUED: Finding a new balance
After leaving the stressful high-level job, Mrs. S next resolved to limit her search to half-time positions and took a job with limited responsibilities in a bookstore. Her work productivity was outstanding, but she became easily flustered when asked to assume additional responsibilities. Some of these required quick learning of new skills in inventory re-supply or interacting with dissatisfied customers.
As she became more confident and less fearful of being fired, Mrs. S talked with 2 supervisors about her illness management. This halted their well-intentioned efforts to promote her, based on their perception of her as talented and engaging.
Attention to these workplace issues took up approximately half of the time in her regular psychiatric appointments for more than 1 year. Through this process, Mrs. S developed increasingly effective insight into the complex mix of her accomplishments and resilience on one hand and her fluctuating social and vocational impairment on the other. She also recognized that subsyndromal symptoms continued at times, despite her overall good functional state. These insights and her greater self-confidence helped Mrs. S resolve and manage the divergences in her own and others’ perceptions of her capabilities and potential.
Related Resource
- Coping with depression or bipolar disorder at your job (patient information). Depression and Bipolar Support Alliance. www.dbsalliance.org/site/PageServer?pagename=Employment_Information.
Disclosure
Dr. Bowden reports no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
1. Ware JE, Jr, Kosinski M, Bayliss MS, et al. Comparison of methods for the scoring and statistical analysis of SF-36 health profile and summary measures: summary of results from the Medical Outcomes Study. Med Care. 1995;33(suppl 4):AS264-AS279.
2. Glahn D, Bearden CE, Barguil M, et al. The neurocognitive signature of psychotic bipolar disorder. Biol Psychiatry. 2007;62:910-916.
3. Goodwin G, Martinez-Aran A, Glahn DC, et al. Cognitive impairment in bipolar disorder: neurodevelopment or neurodegeneration? An ECNP expert meeting report. Eur Neuropsychopharm. 2008;18:787-793.
4. Goldberg JF, Perlis RH, Bowden CL, et al. Manic symptoms during depressive episodes in 1,380 patients with bipolar disorder: findings from the STEP-BD. Am J Psychiatry. 2009;166(2):173-181.
5. Mansour HA, Wood J, Chowdari KV, et al. Circadian phase variation in bipolar I disorder. Chronobiol Int. 2005;22(3):571-584.
6. Feske U, Frank E, Mallinger AG, et al. Anxiety as a correlate of response to the acute treatment of bipolar I disorder. Am J Psychiatry. 2000;57:956-962.
7. Mantere O, Melartin TK, Suominen K, et al. Difference in axis I and II comorbidities between bipolar I and II disorder and major depressive disorder. J Clin Psychiatry. 2006;67:584-593.
8. Bowden CL. Bipolar disorder and creativity. In: Shaw MP, Runco MA, eds. Creativity and affect. Norwood, NJ: Ablex Publishing Corp; 1994:73-86.
9. Andreasen N, Powers S. Overinclusive thinking in mania and schizophrenia. Br J Psychiatry. 1974;125:452-456.
10. Solovay MR, Shenton ME, Holzman PS. Comparative studies of thought disorders. I. Mania and schizophrenia. Arch Gen Psychiatry. 1987;44:13-20.
11. Duke P, Hochman G. A brilliant madness: living with manic-depressive illness. New York, NY: Bantam Books; 1997.
12. Coryell W, Scheftner W, Keller M, et al. The enduring psychosocial consequences of mania and depression. Am J Psychiatry. 1993;150:720-727.
13. Kennedy N, Boydell J, van Os J, et al. Ethnic differences in first clinical presentation of bipolar disorder: results from an epidemiological study. J Affect Dis. 2004;83:161-168.
14. Mikowitz DJ, Goldstein MJ. Bipolar disorder: a family-focused approach. New York, NY: Guilford Press; 2006.
Mrs. S, age 34, worked as an office manager with responsibilities for more than 40 employees for 5 years. Starting in her mid 20s she had repeated periods of depression, binge drinking, and risk-taking that were treated ineffectively with antidepressants. Ultimately, she was fired from her job.
Eventually Mrs. S was diagnosed as bipolar and over time responded well to a mood-stabilizing regimen. She now desires to return to work, both for financial reasons and for the sense of accomplishment that comes from working. Initially, personnel managers review her résumé and tell her she would be bored by the routine nature of entry-level positions, or they offer her jobs with major responsibilities. She accepts a high-level position but soon leaves, feeling overwhelmed by the stress.
Bipolar disorder’s long-term course presents a therapeutic challenge when patients desire to remain employed, seek temporary or permanent disability status, or—most commonly—attempt to return to employment after a period of inability to work. As the experience of Mrs. S illustrates, previous capabilities that appear higher than the person’s present or recent work experience are a key issue to address in interpersonal therapy.
Evidence-based research is informative, but ultimately you must apply judgment and flexibility in setting and revising goals with the bipolar individual. Attention to the disorder’s core characteristics can help you equip patients for work that contributes to their pursuit of health.
Obstacles to employment
Role function. Bipolar disorder impairs family and social function in approximately one-half of persons with this diagnosis, a higher impairment rate than in persons with major depression.1
Cognitive function. Bipolar disorder patients have subtle sustained impairments in cognitive function, particularly working memory.2,3 These deficits—although generally much less severe than in persons with schizophrenia—contribute to workplace and educational difficulties.
Unstable mood. Some symptoms associated with elevated mood contribute to functional impairment. These are not limited to mania or hypomania but also can be prominent in mixed states and depression.
A study from the Systematic Treatment Enhancement Program for Bipolar Disorder (STEP-BD) found that two-thirds of 1,380 depressed bipolar I and II patients had ?1 concomitant symptoms principally associated with manic states. The most prominent were distractibility, pressured speech and thoughts, risky behavior, and agitation.4 Each of these—or, more often, all of these—can interfere with work responsibilities.
Circadian rhythm pattern. Sleep disturbances in bipolar disorder differ from those associated with other medical conditions. Bipolar patients’ tendency to increase their activity and interests in the evening may keep them awake into the early morning hours. Insufficient sleep and impaired daytime cognition and alertness related to idio syncratic circadian rhythms can interfere with job requirements.5 The structure of employment can help many bipolar patients maintain effective sleep patterns as well as waking activities (Box 1).
Some individuals recognize their disturbed activity pattern, but many view it simply as the way they approach a day. For the latter group, a sustained treatment effort is needed to help them recognize the adverse consequences of the pattern and develop a more effective daily routine.
Adverse treatment effects. Although important, this core medical issue is not central to the interpersonal focus of this article. The simple tolerability objective in prescribing medications—and less frequently therapies such as electroconvulsive treatment—is to avoid dosages that impair concentration, alertness, or motor speed and accuracy. Similarly, avoid medications that can cause physical changes noticeable to others—such as tremor, sleepiness, or significant weight gain—or adjust dosages to eliminate these side effects.
Work, defined as what we do to make a living, is useful for most individuals. For persons with bipolar disorder, work has additional benefits. Having a job aids in structuring their daily activities, which tend to be skewed by circadian rhythm-linked problems of inadequate sleep or sleep that starts too late and extends into the day. The routine expectations of a work schedule also can counteract the distractibility and unproductive multitasking common in some bipolar disorder patients.
These benefits are not guaranteed and vary considerably across occupational settings, but patients and family members readily understand this aspect of work. Its benefits can serve as an important impetus for patients to persist in efforts to attain employment, even in the face of obstacles.
Bipolar symptom domains
Anxiety is recognized as a separate and major domain in bipolar psychopathology,6 contributing strongly to poor outcomes. Although anxiety is somewhat more predominant in depression and mixed states, it is common in manic and recovered bipolar states as well.
Social anxiety and panic states appear to be most specifically associated with bipolar disorder.7 Because these types of anxiety entail excessive fearful responses, psychotherapeutic techniques including extinction approaches can be helpful.
Depression in bipolar disorder tends to manifest as slowed motor and cognitive function, which is likely to be evident in work situations. Additionally, loss of social interests—one of the most common and severe aspects of depression in bipolar disorders—is likely to be evident to coworkers and to negatively impact work effectiveness.
Irritability occurs most frequently in mixed bipolar states but also is characteristic of—though generally less intense in—depressed and manic clinical states. Even when strictly internal and subjective, irritability can reduce an individual’s confidence and work effectiveness. Expressed irritability, from minor annoyances to explosive outbursts, can have serious employment consequences, including termination.
Manic symptoms. The impulsivity that is common in bipolar mania can interfere with work. Acting without considering consequences, taking undue risks, or reaching conclusions on inadequate information can cause problems, including physical harm to self or coworkers. Excessive talking—usually associated with internally recognized racing thoughts—can be a nuisance when mild or problematic if it interferes with customer or coworker interactions.
Hyperactivity and increased energy may be perceived as behaviors that facilitate productivity at work (Box 2).8-10 The adaptive characteristics of many hypomanic states are infrequent or absent in depressive, manic, and mixed manic clinical states, however.
Psychosis is principally associated with manic episodes, but it can be a component of any symptomatic clinical state. Delusional ideas or persecutory thoughts are rarely compatible with a work environment, in part because of potential risks to others.
For some purposes, bipolar disease confers social and employment advantages. Common, frequently adaptive behavioral characteristics of hypomania include:
- perseverance
- high energy
- heightened perceptual sensitivity
- exuberance and playfulness
- optimism.
Increased energy and mild degrees of hyperactivity—as well as thinking along creative, multisystem lines—can benefit work productivity, customer interactions, and work group relations. Heightened confidence and social interests can be valuable in some sales and marketing activities.
Although these attitudes and behaviors can have constructive effects, patients need to understand their limits and destructive potential. This is not a straightforward issue, as patients may not have self-awareness of some adverse consequences of characteristics such as irritability, risk taking, or inappropriate sexual advances. A phenomenon little described in clinical literature but relatively common in biographical accounts of persons with bipolar disorder is that friends or coworkers may encourage, rationalize, and take advantage of an individual’s hypomanic energy, thwarting effective interventions.
Componential treatment
Bipolar disorder’s multiple symptom domains suggest a componential approach to treatment. It may be useful to convey this concept metaphorically to the patient. When working on a jigsaw puzzle, a section that has been put together can be largely left intact and attention turned to other sections of the puzzle. Similarly, once a particular bipolar component is well managed—whether via medication, lifestyle, attitudes, or combinations of these—that symptom is likely to remain stable, barring a new insult/stressor (such as a medical condition requiring drugs that interfere with the bipolar regimen).
If mood stabilizers control risky behavior, impulsivity, and affective lability, the regimen generally will remain effective. If residual or new problems develop in another area (such as anxiety, sleep cycle, or irritability), choose drug regimens and psychoeducation approaches that are compatible with the mood-stabilizing plan. This attitude toward treatment:
- is reassuring to most patients, who come to see a new or recurring problem in one domain as not inherently a harbinger of complete relapse
- can reduce patient- or clinician-initiated deletions and additions of medications in a regimen that has been established as effective.
Autobiographical accounts of persons with bipolar disorders can be useful in educating patients about the considerations presented here. Actress Patty Duke made these observations in describing the gradual development of an effective treatment for her severe bipolar disorder:
I work at not flying off the handle…and I’m much better at it. My general medical bills dropped by $50,000 a year since my bipolar diagnosis and treatment. Until then, I was always in the hospital for some phantom illness. I was there with real symptoms born of depression. I haven’t been in the hospital since I was diagnosed.
My recovery from manic-depression has been an evolution, not a sudden miracle. For someone who spent 50% of her life screaming and yelling about something, I am now down to, say, 5%.11
Psychosocial factors to consider
Stigma in the workplace. Although most coworkers are tolerant of and fair-minded about the functional difficulties common in symptomatic bipolar disorder, some will have biased, inaccurate views about psychiatric conditions. Advise bipolar individuals to make case-by-case decisions about whether to provide personal information to other employees and, if so, how much.
As with most medical conditions, the default choice will be to not discuss personal information in the workplace. Some coworkers, however, might appreciate learning of the bipolar condition (for example, a supervisor who seems empathic to an employee’s seeming stressed state).
Realistic expectations. Most clinicians recognize that relief from a syndromal bipolar state is achieved more quickly than a sustained recovered status in which symptoms are minimal. Attaining functional capacity in a normal range also lags, both in time and in the proportion of persons who ever achieve sustained good function.12 Patients, their families, and often employers may have unrealistic expectations about early resumption of work after a depressive or manic episode resolves.
Ethnic considerations. Some literature suggests ethnic differences in the initial presentation of bipolar disorder, with more severe manifestations in some populations particularly if psychosis is a component symptom.13 Additionally, some cultural views about stigma from illness can add to patients’ or family members’ reluctance to re-enter the workplace.
Socioeconomic status. Sometimes bipolar illness puts out of reach the occupational activities that an individual has previously undertaken or that are characteristic of the family’s experience and expectations. Resistance to a change in self-concept can add to the difficulty in successfully moving a patient to consider employment that is more routinized and less intellectual or decisional in nature (Box 3).14
Divergence in education vs work status. Persons with bipolar disorders often have substantial divergence between high educational attainment and lower work performance. When this is the case, all or most of the factors reviewed in this article probably have contributed. Mrs. S’s experience illustrates this aspect of our care for persons with bipolar disorders.
An employment barrier for some bipolar patients is that a brief, often long-past period of high intellectual or vocational performance serves as the benchmark for their capabilities. Patients with this characteristic resist revising their self-concept. Some treat the loss of this idealized image as an unfair consequence of their illness or society’s reaction to bipolar disorder. Their stubbornness tends to prevent realistic engagement socially or vocationally at levels that are presently feasible for them.
Resistance to change associated with this characteristic often is difficult to manage effectively with short, relatively infrequent medication-focused visits. Specific psychosocial interventions may be more effective.14
CASE CONTINUED: Finding a new balance
After leaving the stressful high-level job, Mrs. S next resolved to limit her search to half-time positions and took a job with limited responsibilities in a bookstore. Her work productivity was outstanding, but she became easily flustered when asked to assume additional responsibilities. Some of these required quick learning of new skills in inventory re-supply or interacting with dissatisfied customers.
As she became more confident and less fearful of being fired, Mrs. S talked with 2 supervisors about her illness management. This halted their well-intentioned efforts to promote her, based on their perception of her as talented and engaging.
Attention to these workplace issues took up approximately half of the time in her regular psychiatric appointments for more than 1 year. Through this process, Mrs. S developed increasingly effective insight into the complex mix of her accomplishments and resilience on one hand and her fluctuating social and vocational impairment on the other. She also recognized that subsyndromal symptoms continued at times, despite her overall good functional state. These insights and her greater self-confidence helped Mrs. S resolve and manage the divergences in her own and others’ perceptions of her capabilities and potential.
Related Resource
- Coping with depression or bipolar disorder at your job (patient information). Depression and Bipolar Support Alliance. www.dbsalliance.org/site/PageServer?pagename=Employment_Information.
Disclosure
Dr. Bowden reports no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
Mrs. S, age 34, worked as an office manager with responsibilities for more than 40 employees for 5 years. Starting in her mid 20s she had repeated periods of depression, binge drinking, and risk-taking that were treated ineffectively with antidepressants. Ultimately, she was fired from her job.
Eventually Mrs. S was diagnosed as bipolar and over time responded well to a mood-stabilizing regimen. She now desires to return to work, both for financial reasons and for the sense of accomplishment that comes from working. Initially, personnel managers review her résumé and tell her she would be bored by the routine nature of entry-level positions, or they offer her jobs with major responsibilities. She accepts a high-level position but soon leaves, feeling overwhelmed by the stress.
Bipolar disorder’s long-term course presents a therapeutic challenge when patients desire to remain employed, seek temporary or permanent disability status, or—most commonly—attempt to return to employment after a period of inability to work. As the experience of Mrs. S illustrates, previous capabilities that appear higher than the person’s present or recent work experience are a key issue to address in interpersonal therapy.
Evidence-based research is informative, but ultimately you must apply judgment and flexibility in setting and revising goals with the bipolar individual. Attention to the disorder’s core characteristics can help you equip patients for work that contributes to their pursuit of health.
Obstacles to employment
Role function. Bipolar disorder impairs family and social function in approximately one-half of persons with this diagnosis, a higher impairment rate than in persons with major depression.1
Cognitive function. Bipolar disorder patients have subtle sustained impairments in cognitive function, particularly working memory.2,3 These deficits—although generally much less severe than in persons with schizophrenia—contribute to workplace and educational difficulties.
Unstable mood. Some symptoms associated with elevated mood contribute to functional impairment. These are not limited to mania or hypomania but also can be prominent in mixed states and depression.
A study from the Systematic Treatment Enhancement Program for Bipolar Disorder (STEP-BD) found that two-thirds of 1,380 depressed bipolar I and II patients had ?1 concomitant symptoms principally associated with manic states. The most prominent were distractibility, pressured speech and thoughts, risky behavior, and agitation.4 Each of these—or, more often, all of these—can interfere with work responsibilities.
Circadian rhythm pattern. Sleep disturbances in bipolar disorder differ from those associated with other medical conditions. Bipolar patients’ tendency to increase their activity and interests in the evening may keep them awake into the early morning hours. Insufficient sleep and impaired daytime cognition and alertness related to idio syncratic circadian rhythms can interfere with job requirements.5 The structure of employment can help many bipolar patients maintain effective sleep patterns as well as waking activities (Box 1).
Some individuals recognize their disturbed activity pattern, but many view it simply as the way they approach a day. For the latter group, a sustained treatment effort is needed to help them recognize the adverse consequences of the pattern and develop a more effective daily routine.
Adverse treatment effects. Although important, this core medical issue is not central to the interpersonal focus of this article. The simple tolerability objective in prescribing medications—and less frequently therapies such as electroconvulsive treatment—is to avoid dosages that impair concentration, alertness, or motor speed and accuracy. Similarly, avoid medications that can cause physical changes noticeable to others—such as tremor, sleepiness, or significant weight gain—or adjust dosages to eliminate these side effects.
Work, defined as what we do to make a living, is useful for most individuals. For persons with bipolar disorder, work has additional benefits. Having a job aids in structuring their daily activities, which tend to be skewed by circadian rhythm-linked problems of inadequate sleep or sleep that starts too late and extends into the day. The routine expectations of a work schedule also can counteract the distractibility and unproductive multitasking common in some bipolar disorder patients.
These benefits are not guaranteed and vary considerably across occupational settings, but patients and family members readily understand this aspect of work. Its benefits can serve as an important impetus for patients to persist in efforts to attain employment, even in the face of obstacles.
Bipolar symptom domains
Anxiety is recognized as a separate and major domain in bipolar psychopathology,6 contributing strongly to poor outcomes. Although anxiety is somewhat more predominant in depression and mixed states, it is common in manic and recovered bipolar states as well.
Social anxiety and panic states appear to be most specifically associated with bipolar disorder.7 Because these types of anxiety entail excessive fearful responses, psychotherapeutic techniques including extinction approaches can be helpful.
Depression in bipolar disorder tends to manifest as slowed motor and cognitive function, which is likely to be evident in work situations. Additionally, loss of social interests—one of the most common and severe aspects of depression in bipolar disorders—is likely to be evident to coworkers and to negatively impact work effectiveness.
Irritability occurs most frequently in mixed bipolar states but also is characteristic of—though generally less intense in—depressed and manic clinical states. Even when strictly internal and subjective, irritability can reduce an individual’s confidence and work effectiveness. Expressed irritability, from minor annoyances to explosive outbursts, can have serious employment consequences, including termination.
Manic symptoms. The impulsivity that is common in bipolar mania can interfere with work. Acting without considering consequences, taking undue risks, or reaching conclusions on inadequate information can cause problems, including physical harm to self or coworkers. Excessive talking—usually associated with internally recognized racing thoughts—can be a nuisance when mild or problematic if it interferes with customer or coworker interactions.
Hyperactivity and increased energy may be perceived as behaviors that facilitate productivity at work (Box 2).8-10 The adaptive characteristics of many hypomanic states are infrequent or absent in depressive, manic, and mixed manic clinical states, however.
Psychosis is principally associated with manic episodes, but it can be a component of any symptomatic clinical state. Delusional ideas or persecutory thoughts are rarely compatible with a work environment, in part because of potential risks to others.
For some purposes, bipolar disease confers social and employment advantages. Common, frequently adaptive behavioral characteristics of hypomania include:
- perseverance
- high energy
- heightened perceptual sensitivity
- exuberance and playfulness
- optimism.
Increased energy and mild degrees of hyperactivity—as well as thinking along creative, multisystem lines—can benefit work productivity, customer interactions, and work group relations. Heightened confidence and social interests can be valuable in some sales and marketing activities.
Although these attitudes and behaviors can have constructive effects, patients need to understand their limits and destructive potential. This is not a straightforward issue, as patients may not have self-awareness of some adverse consequences of characteristics such as irritability, risk taking, or inappropriate sexual advances. A phenomenon little described in clinical literature but relatively common in biographical accounts of persons with bipolar disorder is that friends or coworkers may encourage, rationalize, and take advantage of an individual’s hypomanic energy, thwarting effective interventions.
Componential treatment
Bipolar disorder’s multiple symptom domains suggest a componential approach to treatment. It may be useful to convey this concept metaphorically to the patient. When working on a jigsaw puzzle, a section that has been put together can be largely left intact and attention turned to other sections of the puzzle. Similarly, once a particular bipolar component is well managed—whether via medication, lifestyle, attitudes, or combinations of these—that symptom is likely to remain stable, barring a new insult/stressor (such as a medical condition requiring drugs that interfere with the bipolar regimen).
If mood stabilizers control risky behavior, impulsivity, and affective lability, the regimen generally will remain effective. If residual or new problems develop in another area (such as anxiety, sleep cycle, or irritability), choose drug regimens and psychoeducation approaches that are compatible with the mood-stabilizing plan. This attitude toward treatment:
- is reassuring to most patients, who come to see a new or recurring problem in one domain as not inherently a harbinger of complete relapse
- can reduce patient- or clinician-initiated deletions and additions of medications in a regimen that has been established as effective.
Autobiographical accounts of persons with bipolar disorders can be useful in educating patients about the considerations presented here. Actress Patty Duke made these observations in describing the gradual development of an effective treatment for her severe bipolar disorder:
I work at not flying off the handle…and I’m much better at it. My general medical bills dropped by $50,000 a year since my bipolar diagnosis and treatment. Until then, I was always in the hospital for some phantom illness. I was there with real symptoms born of depression. I haven’t been in the hospital since I was diagnosed.
My recovery from manic-depression has been an evolution, not a sudden miracle. For someone who spent 50% of her life screaming and yelling about something, I am now down to, say, 5%.11
Psychosocial factors to consider
Stigma in the workplace. Although most coworkers are tolerant of and fair-minded about the functional difficulties common in symptomatic bipolar disorder, some will have biased, inaccurate views about psychiatric conditions. Advise bipolar individuals to make case-by-case decisions about whether to provide personal information to other employees and, if so, how much.
As with most medical conditions, the default choice will be to not discuss personal information in the workplace. Some coworkers, however, might appreciate learning of the bipolar condition (for example, a supervisor who seems empathic to an employee’s seeming stressed state).
Realistic expectations. Most clinicians recognize that relief from a syndromal bipolar state is achieved more quickly than a sustained recovered status in which symptoms are minimal. Attaining functional capacity in a normal range also lags, both in time and in the proportion of persons who ever achieve sustained good function.12 Patients, their families, and often employers may have unrealistic expectations about early resumption of work after a depressive or manic episode resolves.
Ethnic considerations. Some literature suggests ethnic differences in the initial presentation of bipolar disorder, with more severe manifestations in some populations particularly if psychosis is a component symptom.13 Additionally, some cultural views about stigma from illness can add to patients’ or family members’ reluctance to re-enter the workplace.
Socioeconomic status. Sometimes bipolar illness puts out of reach the occupational activities that an individual has previously undertaken or that are characteristic of the family’s experience and expectations. Resistance to a change in self-concept can add to the difficulty in successfully moving a patient to consider employment that is more routinized and less intellectual or decisional in nature (Box 3).14
Divergence in education vs work status. Persons with bipolar disorders often have substantial divergence between high educational attainment and lower work performance. When this is the case, all or most of the factors reviewed in this article probably have contributed. Mrs. S’s experience illustrates this aspect of our care for persons with bipolar disorders.
An employment barrier for some bipolar patients is that a brief, often long-past period of high intellectual or vocational performance serves as the benchmark for their capabilities. Patients with this characteristic resist revising their self-concept. Some treat the loss of this idealized image as an unfair consequence of their illness or society’s reaction to bipolar disorder. Their stubbornness tends to prevent realistic engagement socially or vocationally at levels that are presently feasible for them.
Resistance to change associated with this characteristic often is difficult to manage effectively with short, relatively infrequent medication-focused visits. Specific psychosocial interventions may be more effective.14
CASE CONTINUED: Finding a new balance
After leaving the stressful high-level job, Mrs. S next resolved to limit her search to half-time positions and took a job with limited responsibilities in a bookstore. Her work productivity was outstanding, but she became easily flustered when asked to assume additional responsibilities. Some of these required quick learning of new skills in inventory re-supply or interacting with dissatisfied customers.
As she became more confident and less fearful of being fired, Mrs. S talked with 2 supervisors about her illness management. This halted their well-intentioned efforts to promote her, based on their perception of her as talented and engaging.
Attention to these workplace issues took up approximately half of the time in her regular psychiatric appointments for more than 1 year. Through this process, Mrs. S developed increasingly effective insight into the complex mix of her accomplishments and resilience on one hand and her fluctuating social and vocational impairment on the other. She also recognized that subsyndromal symptoms continued at times, despite her overall good functional state. These insights and her greater self-confidence helped Mrs. S resolve and manage the divergences in her own and others’ perceptions of her capabilities and potential.
Related Resource
- Coping with depression or bipolar disorder at your job (patient information). Depression and Bipolar Support Alliance. www.dbsalliance.org/site/PageServer?pagename=Employment_Information.
Disclosure
Dr. Bowden reports no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
1. Ware JE, Jr, Kosinski M, Bayliss MS, et al. Comparison of methods for the scoring and statistical analysis of SF-36 health profile and summary measures: summary of results from the Medical Outcomes Study. Med Care. 1995;33(suppl 4):AS264-AS279.
2. Glahn D, Bearden CE, Barguil M, et al. The neurocognitive signature of psychotic bipolar disorder. Biol Psychiatry. 2007;62:910-916.
3. Goodwin G, Martinez-Aran A, Glahn DC, et al. Cognitive impairment in bipolar disorder: neurodevelopment or neurodegeneration? An ECNP expert meeting report. Eur Neuropsychopharm. 2008;18:787-793.
4. Goldberg JF, Perlis RH, Bowden CL, et al. Manic symptoms during depressive episodes in 1,380 patients with bipolar disorder: findings from the STEP-BD. Am J Psychiatry. 2009;166(2):173-181.
5. Mansour HA, Wood J, Chowdari KV, et al. Circadian phase variation in bipolar I disorder. Chronobiol Int. 2005;22(3):571-584.
6. Feske U, Frank E, Mallinger AG, et al. Anxiety as a correlate of response to the acute treatment of bipolar I disorder. Am J Psychiatry. 2000;57:956-962.
7. Mantere O, Melartin TK, Suominen K, et al. Difference in axis I and II comorbidities between bipolar I and II disorder and major depressive disorder. J Clin Psychiatry. 2006;67:584-593.
8. Bowden CL. Bipolar disorder and creativity. In: Shaw MP, Runco MA, eds. Creativity and affect. Norwood, NJ: Ablex Publishing Corp; 1994:73-86.
9. Andreasen N, Powers S. Overinclusive thinking in mania and schizophrenia. Br J Psychiatry. 1974;125:452-456.
10. Solovay MR, Shenton ME, Holzman PS. Comparative studies of thought disorders. I. Mania and schizophrenia. Arch Gen Psychiatry. 1987;44:13-20.
11. Duke P, Hochman G. A brilliant madness: living with manic-depressive illness. New York, NY: Bantam Books; 1997.
12. Coryell W, Scheftner W, Keller M, et al. The enduring psychosocial consequences of mania and depression. Am J Psychiatry. 1993;150:720-727.
13. Kennedy N, Boydell J, van Os J, et al. Ethnic differences in first clinical presentation of bipolar disorder: results from an epidemiological study. J Affect Dis. 2004;83:161-168.
14. Mikowitz DJ, Goldstein MJ. Bipolar disorder: a family-focused approach. New York, NY: Guilford Press; 2006.
1. Ware JE, Jr, Kosinski M, Bayliss MS, et al. Comparison of methods for the scoring and statistical analysis of SF-36 health profile and summary measures: summary of results from the Medical Outcomes Study. Med Care. 1995;33(suppl 4):AS264-AS279.
2. Glahn D, Bearden CE, Barguil M, et al. The neurocognitive signature of psychotic bipolar disorder. Biol Psychiatry. 2007;62:910-916.
3. Goodwin G, Martinez-Aran A, Glahn DC, et al. Cognitive impairment in bipolar disorder: neurodevelopment or neurodegeneration? An ECNP expert meeting report. Eur Neuropsychopharm. 2008;18:787-793.
4. Goldberg JF, Perlis RH, Bowden CL, et al. Manic symptoms during depressive episodes in 1,380 patients with bipolar disorder: findings from the STEP-BD. Am J Psychiatry. 2009;166(2):173-181.
5. Mansour HA, Wood J, Chowdari KV, et al. Circadian phase variation in bipolar I disorder. Chronobiol Int. 2005;22(3):571-584.
6. Feske U, Frank E, Mallinger AG, et al. Anxiety as a correlate of response to the acute treatment of bipolar I disorder. Am J Psychiatry. 2000;57:956-962.
7. Mantere O, Melartin TK, Suominen K, et al. Difference in axis I and II comorbidities between bipolar I and II disorder and major depressive disorder. J Clin Psychiatry. 2006;67:584-593.
8. Bowden CL. Bipolar disorder and creativity. In: Shaw MP, Runco MA, eds. Creativity and affect. Norwood, NJ: Ablex Publishing Corp; 1994:73-86.
9. Andreasen N, Powers S. Overinclusive thinking in mania and schizophrenia. Br J Psychiatry. 1974;125:452-456.
10. Solovay MR, Shenton ME, Holzman PS. Comparative studies of thought disorders. I. Mania and schizophrenia. Arch Gen Psychiatry. 1987;44:13-20.
11. Duke P, Hochman G. A brilliant madness: living with manic-depressive illness. New York, NY: Bantam Books; 1997.
12. Coryell W, Scheftner W, Keller M, et al. The enduring psychosocial consequences of mania and depression. Am J Psychiatry. 1993;150:720-727.
13. Kennedy N, Boydell J, van Os J, et al. Ethnic differences in first clinical presentation of bipolar disorder: results from an epidemiological study. J Affect Dis. 2004;83:161-168.
14. Mikowitz DJ, Goldstein MJ. Bipolar disorder: a family-focused approach. New York, NY: Guilford Press; 2006.
Tips to differentiate bipolar II disorder and borderline personality disorder
Unipolar depression or "soft" bipolar disorder? Tips to avoid misdiagnosis
Controversies in bipolar disorder: Trust evidence or experience?
Today’s buzzword in health care is evidence-based medicine. Most clinicians would agree that evidence from clinical research should guide decisions about treating bipolar disorder. In theory, randomized controlled trials should tell us how to manage bipolar patients and achieve therapeutic success. page 40.)
We rarely have encountered a patient with postpartum depression or psychosis who does not have a history of (often undiagnosed and untreated) recurrent mood episodes. For most of these patients, a mood stabilizer may be a better choice than an antidepressant.
The role of thyroid hormones
Adding a thyroid hormone—usually liothyronine—to an antidepressant has been demonstrated to accelerate, page 47.)
Atypical depression and the bipolar spectrum
Depressive episodes are considered either “typical” (a category that includes melancholic depression—in DSM-IV-TR, major depression with melancholic features) or “atypical” (in DSM-IV-TR, major depression with atypical features). Atypical features were originally associated with response to monoamine oxidase inhibitor antidepressants, whereas non atypical depression was thought more likely to respond to tricyclic antidepressants.34 The depression of bipolar disorder is usually atypical ( Box 4 ), especially in patients with softer variants of the illness.35
We believe that depressed patients with atypical symptoms aggregate into groups according to the presence, severity, and character of interdepressive manic or hypomanic episodes. Some patients experience recurrent depressive episodes with intervening euthymia (recurrent major depression), whereas others experience depressive episodes punctuated by brief subthreshold hypomanic episodes. Patients in these groups occasionally tolerate or even benefit from cautiously managed antidepressant monotherapy. Patients with atypical depressive episodes alternating with frank hypomanic, manic, mixed, or manic-psychotic episodes usually require a mood stabilizer and may benefit from cotreatment with an atypical antipsychotic.
Akiskol and Benazzi35 suggest that atypical depression may be a subtype of the bipolar spectrum. Our experience suggests that the bipolar spectrum is a continuum of degrees of risk for mood instability in persons with recurrent atypical depression.
DSM-IV-TR defines atypical depression as depression characterized by mood reactivity and at least 2 of these 4 features:
- hypersomnia
- increased appetite or weight gain
- leaden paralysis
- sensitivity to interpersonal rejection.
The term ‘hypersomnia’ is misleading. Many of these patients do not sleep excessively because work or school attendance prevents oversleeping. Instead, they experience an increased sleep requirement manifested by difficulty getting up in the morning and increased daytime sleepiness.
Increased appetite and weight gain (hyperphagia) often are present, but almost as often our patients report no change in appetite or weight or even anorexia and weight loss.
We rarely see a condition one would term ‘leaden paralysis.’ We also find that ‘sensitivity to interpersonal rejection’ is too narrow a construct. Our patients with atypical depression experience increased sensitivity to every stressor in their lives—work, school, family, and social stressors—not just interpersonal rejection.
Related resources
- Lieber AL. Bipolar spectrum disorder: an overview of the soft bipolar spectrum. www.psycom.net/depression.central.lieber.html.
- Phelps J. Why am I still depressed? Recognizing and managing the ups and downs of bipolar II and soft bipolar disorder. www.psycheducation.org.
- Maier T. Evidence-based psychiatry: understanding the limitations of a method. J Eval Clin Pract. 2006;12(3):325.
Drug brand names
- Liothyronine • Cytomel
- Sertraline • Zoloft
Disclosure
The authors report no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
1. Goldberg JF. What constitutes evidence-based pharmacotherapy for bipolar disorder? Part 1: First-line treatments. J Clin Psychiatry. 2007;68:1982-1983.
2. Goldberg JF. What constitutes evidence-based pharmacotherapy for bipolar disorder? Part 2: Complex presentations and clinical context. J Clin Psychiatry. 2008;69:495-496.
3. Levine R, Fink M. Why evidence-based medicine cannot be applied to psychiatry. Psychiatric Times. 2008;25(4):10.
4. Akiskol HS, Benazzi F. The DSM-IV and ICD-10 categories of recurrent [major] depressive and bipolar II disorders: evidence that they lie on a dimensional spectrum. J Affect Disord. 2006;92:45-54.
5. Goodwin FK, Jamison KR. Manic-depressive illness: bipolar disorders and recurrent depression. 2nd ed. New York, NY: Oxford University Press; 2007:3–27.
6. Hirschfeld RMA, Lewis L, Vornik L. Perceptions and impact of bipolar disorder: how far have we really come? Results of the National Depressive and Manic-Depressive Association 2000 survey of individuals with bipolar disorder. J Clin Psychiatry. 2003;64(2):161-167.
7. Blanco C, Laje G, Olfson M, et al. Trends in the treatment of bipolar disorder by outpatient psychiatrists. Am J Psychiatry. 2002;159:1005-1010.
8. Ghaemi SN, Lenox MS, Baldessarini RJ. Effectiveness and safety of long-term antidepressant treatment in bipolar disorder. J Clin Psychiatry. 2001;62:565-569.
9. Ghaemi SN, Boiman EE, Goodwin FK. Diagnosing bipolar disorder and the effect of antidepressants: a naturalistic study. J Clin Psychiatry. 2000;61:804-808.
10. Gijsman HF, Geddes JR, Rendell JM, et al. Antidepressants for bipolar depression: a systematic review of randomized, controlled trials. Am J Psychiatry. 2005;161:1537-1547.
11. Ghaemi SN, Sachs GS, Chiou AM, et al. Is bipolar disorder still underdiagnosed? Are antidepressants overutilized? J Affect Disord. 1999;52:134-144.
12. Sachs GS, Nierenberg AA, Calabrese JR, et al. Effectiveness of adjunctive antidepressant treatment for bipolar depression. N Engl J Med. 2007;356:1711-1722.
13. Altshuler L, Suppes T, Black D, et al. Impact of antidepressant discontinuation after acute bipolar depression remission on rates of depressive relapse at 1-year follow-up. Am J Psychiatry. 2003;160:1252-1262.
14. Akiskol HS. Developmental pathways to bipolarity: are juvenile-onset depressions pre-bipolar? J Am Acad Child Adolesc Psychiatry. 1995;34(6):754-763.
15. Geller B, Zimmerman B, Williams M, et al. Bipolar disorder at prospective follow-up of adults who had prepubertal major depressive disorder. Am J Psychiatry. 2001;158:125-127.
16. Food and Drug Administration: Center for Drug Evaluation and Research. Revisions to product labeling. Available at: http://www.FDA.gov/cder/drug/antidepressants/default.htm. Accessed January 12, 2009.
17. McElroy S, Strakowski S, West S, et al. Phenomenology of adolescent and adult mania in hospitalized patients with bipolar disorder. Am J Psychiatry. 1997;154:44-49.
18. Olfson M, Marcus SC. A case-control study of antidepressants and attempted suicide during early phase treatment of major depressive episodes. J Clin Psychiatry. 2008;69:425-432.
19. Keck PE, Jr, McElroy SL, Havens JR, et al. Psychosis in bipolar disorder: phenomenology and impact on morbidity and course of illness. Compr Psychiatry. 2003;44:263-269.
20. Jones I, Craddock N. Familiarity of the puerperal trigger in bipolar disorder: results of a family study. Am J Psychiatry. 2001;158:913-917.
21. Chaudron LH, Pies RW. The relationship between postpartum psychosis and bipolar disorder: a review. J Clin Psychiatry. 2003;64:1284-1292.
22. Wisner KL, Peindl KS, Hanusa BH. Psychiatric episodes in women and young children. J Affect Disord. 1995;34:1-11.
23. Sharma V. A cautionary note on the use of antidepressants in postpartum depression. Bipolar Disord. 2006;8:411-414.
24. O’Malley S. “Are you there alone?” The unspeakable crime of Andrea Yates. New York, NY: Simon and Schuster; 2004.
25. Altshuler LL, Bauer M, Frye MA, et al. Does thyroid supplementation accelerate tricyclic antidepressant response? A review and meta-analysis of the literature. Am J Psychiatry. 2001;158:1617-1622.
26. Joffe RT. The use of thyroid supplements to augment antidepressant medication. J Clin Psychiatry. 2008;59:26-29.
27. Cooper-Kazaz R, Apter JT, Cohen R, et al. Combined treatment with sertraline and liothyronine in major depression: a randomized, double-blind, placebo-controlled trial. Arch Gen Psychiatry. 2007;64:679-688.
28. Gold MS, Pottash AL, Extein I. Hypothyroidism and depression: evidence from complete thyroid function evaluation. JAMA. 1981;245:28-31.
29. Kupka RW, Nolen WA, Post RM, et al. High rate of autoimmune thyroiditis in bipolar disorder: lack of association with lithium exposure. Biol Psychiatry. 2002;51:305-311.
30. Szuba MP, Amsterdam JD. Rapid antidepressant response after nocturnal TRH administration in patients with bipolar I and bipolar type II major depression. J Clin Psychopharmacol. 2005;25:325-330.
31. Extein I, Pottash AL, Gold MS. Does subclinical hypothyroidism predispose to tricyclic-induced rapid mood cycles? J Clin Psychiatry. 1982;43:32-33.
32. American Association of Clinical Endocrinologists. Medical guidelines for clinical practice for the evaluation and treatment of hyperthyroidism and hypothyroidism. Endocr Prac. 2002;8:457-469.
33. El-Mallakh RS, Karippott A. Antidepressant-associated chronic irritable dysphoria (ACID) in bipolar disorder. J Affect Disord. 2005;84:267-272.
34. Henkl V, Mergl R, Antje-Kathrin A, et al. Treatment of depression with atypical features: a meta-analytic approach. Psychiatry Res. 2006;141(1):89-101.
35. Perugi G, Akiskal HS, Lattanzi D, et al. The high prevalence of “soft” bipolar (II) features in atypical depression. Compr Psychiatry. 1998;39(2):63-71.
Today’s buzzword in health care is evidence-based medicine. Most clinicians would agree that evidence from clinical research should guide decisions about treating bipolar disorder. In theory, randomized controlled trials should tell us how to manage bipolar patients and achieve therapeutic success. page 40.)
We rarely have encountered a patient with postpartum depression or psychosis who does not have a history of (often undiagnosed and untreated) recurrent mood episodes. For most of these patients, a mood stabilizer may be a better choice than an antidepressant.
The role of thyroid hormones
Adding a thyroid hormone—usually liothyronine—to an antidepressant has been demonstrated to accelerate, page 47.)
Atypical depression and the bipolar spectrum
Depressive episodes are considered either “typical” (a category that includes melancholic depression—in DSM-IV-TR, major depression with melancholic features) or “atypical” (in DSM-IV-TR, major depression with atypical features). Atypical features were originally associated with response to monoamine oxidase inhibitor antidepressants, whereas non atypical depression was thought more likely to respond to tricyclic antidepressants.34 The depression of bipolar disorder is usually atypical ( Box 4 ), especially in patients with softer variants of the illness.35
We believe that depressed patients with atypical symptoms aggregate into groups according to the presence, severity, and character of interdepressive manic or hypomanic episodes. Some patients experience recurrent depressive episodes with intervening euthymia (recurrent major depression), whereas others experience depressive episodes punctuated by brief subthreshold hypomanic episodes. Patients in these groups occasionally tolerate or even benefit from cautiously managed antidepressant monotherapy. Patients with atypical depressive episodes alternating with frank hypomanic, manic, mixed, or manic-psychotic episodes usually require a mood stabilizer and may benefit from cotreatment with an atypical antipsychotic.
Akiskol and Benazzi35 suggest that atypical depression may be a subtype of the bipolar spectrum. Our experience suggests that the bipolar spectrum is a continuum of degrees of risk for mood instability in persons with recurrent atypical depression.
DSM-IV-TR defines atypical depression as depression characterized by mood reactivity and at least 2 of these 4 features:
- hypersomnia
- increased appetite or weight gain
- leaden paralysis
- sensitivity to interpersonal rejection.
The term ‘hypersomnia’ is misleading. Many of these patients do not sleep excessively because work or school attendance prevents oversleeping. Instead, they experience an increased sleep requirement manifested by difficulty getting up in the morning and increased daytime sleepiness.
Increased appetite and weight gain (hyperphagia) often are present, but almost as often our patients report no change in appetite or weight or even anorexia and weight loss.
We rarely see a condition one would term ‘leaden paralysis.’ We also find that ‘sensitivity to interpersonal rejection’ is too narrow a construct. Our patients with atypical depression experience increased sensitivity to every stressor in their lives—work, school, family, and social stressors—not just interpersonal rejection.
Related resources
- Lieber AL. Bipolar spectrum disorder: an overview of the soft bipolar spectrum. www.psycom.net/depression.central.lieber.html.
- Phelps J. Why am I still depressed? Recognizing and managing the ups and downs of bipolar II and soft bipolar disorder. www.psycheducation.org.
- Maier T. Evidence-based psychiatry: understanding the limitations of a method. J Eval Clin Pract. 2006;12(3):325.
Drug brand names
- Liothyronine • Cytomel
- Sertraline • Zoloft
Disclosure
The authors report no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
Today’s buzzword in health care is evidence-based medicine. Most clinicians would agree that evidence from clinical research should guide decisions about treating bipolar disorder. In theory, randomized controlled trials should tell us how to manage bipolar patients and achieve therapeutic success. page 40.)
We rarely have encountered a patient with postpartum depression or psychosis who does not have a history of (often undiagnosed and untreated) recurrent mood episodes. For most of these patients, a mood stabilizer may be a better choice than an antidepressant.
The role of thyroid hormones
Adding a thyroid hormone—usually liothyronine—to an antidepressant has been demonstrated to accelerate, page 47.)
Atypical depression and the bipolar spectrum
Depressive episodes are considered either “typical” (a category that includes melancholic depression—in DSM-IV-TR, major depression with melancholic features) or “atypical” (in DSM-IV-TR, major depression with atypical features). Atypical features were originally associated with response to monoamine oxidase inhibitor antidepressants, whereas non atypical depression was thought more likely to respond to tricyclic antidepressants.34 The depression of bipolar disorder is usually atypical ( Box 4 ), especially in patients with softer variants of the illness.35
We believe that depressed patients with atypical symptoms aggregate into groups according to the presence, severity, and character of interdepressive manic or hypomanic episodes. Some patients experience recurrent depressive episodes with intervening euthymia (recurrent major depression), whereas others experience depressive episodes punctuated by brief subthreshold hypomanic episodes. Patients in these groups occasionally tolerate or even benefit from cautiously managed antidepressant monotherapy. Patients with atypical depressive episodes alternating with frank hypomanic, manic, mixed, or manic-psychotic episodes usually require a mood stabilizer and may benefit from cotreatment with an atypical antipsychotic.
Akiskol and Benazzi35 suggest that atypical depression may be a subtype of the bipolar spectrum. Our experience suggests that the bipolar spectrum is a continuum of degrees of risk for mood instability in persons with recurrent atypical depression.
DSM-IV-TR defines atypical depression as depression characterized by mood reactivity and at least 2 of these 4 features:
- hypersomnia
- increased appetite or weight gain
- leaden paralysis
- sensitivity to interpersonal rejection.
The term ‘hypersomnia’ is misleading. Many of these patients do not sleep excessively because work or school attendance prevents oversleeping. Instead, they experience an increased sleep requirement manifested by difficulty getting up in the morning and increased daytime sleepiness.
Increased appetite and weight gain (hyperphagia) often are present, but almost as often our patients report no change in appetite or weight or even anorexia and weight loss.
We rarely see a condition one would term ‘leaden paralysis.’ We also find that ‘sensitivity to interpersonal rejection’ is too narrow a construct. Our patients with atypical depression experience increased sensitivity to every stressor in their lives—work, school, family, and social stressors—not just interpersonal rejection.
Related resources
- Lieber AL. Bipolar spectrum disorder: an overview of the soft bipolar spectrum. www.psycom.net/depression.central.lieber.html.
- Phelps J. Why am I still depressed? Recognizing and managing the ups and downs of bipolar II and soft bipolar disorder. www.psycheducation.org.
- Maier T. Evidence-based psychiatry: understanding the limitations of a method. J Eval Clin Pract. 2006;12(3):325.
Drug brand names
- Liothyronine • Cytomel
- Sertraline • Zoloft
Disclosure
The authors report no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
1. Goldberg JF. What constitutes evidence-based pharmacotherapy for bipolar disorder? Part 1: First-line treatments. J Clin Psychiatry. 2007;68:1982-1983.
2. Goldberg JF. What constitutes evidence-based pharmacotherapy for bipolar disorder? Part 2: Complex presentations and clinical context. J Clin Psychiatry. 2008;69:495-496.
3. Levine R, Fink M. Why evidence-based medicine cannot be applied to psychiatry. Psychiatric Times. 2008;25(4):10.
4. Akiskol HS, Benazzi F. The DSM-IV and ICD-10 categories of recurrent [major] depressive and bipolar II disorders: evidence that they lie on a dimensional spectrum. J Affect Disord. 2006;92:45-54.
5. Goodwin FK, Jamison KR. Manic-depressive illness: bipolar disorders and recurrent depression. 2nd ed. New York, NY: Oxford University Press; 2007:3–27.
6. Hirschfeld RMA, Lewis L, Vornik L. Perceptions and impact of bipolar disorder: how far have we really come? Results of the National Depressive and Manic-Depressive Association 2000 survey of individuals with bipolar disorder. J Clin Psychiatry. 2003;64(2):161-167.
7. Blanco C, Laje G, Olfson M, et al. Trends in the treatment of bipolar disorder by outpatient psychiatrists. Am J Psychiatry. 2002;159:1005-1010.
8. Ghaemi SN, Lenox MS, Baldessarini RJ. Effectiveness and safety of long-term antidepressant treatment in bipolar disorder. J Clin Psychiatry. 2001;62:565-569.
9. Ghaemi SN, Boiman EE, Goodwin FK. Diagnosing bipolar disorder and the effect of antidepressants: a naturalistic study. J Clin Psychiatry. 2000;61:804-808.
10. Gijsman HF, Geddes JR, Rendell JM, et al. Antidepressants for bipolar depression: a systematic review of randomized, controlled trials. Am J Psychiatry. 2005;161:1537-1547.
11. Ghaemi SN, Sachs GS, Chiou AM, et al. Is bipolar disorder still underdiagnosed? Are antidepressants overutilized? J Affect Disord. 1999;52:134-144.
12. Sachs GS, Nierenberg AA, Calabrese JR, et al. Effectiveness of adjunctive antidepressant treatment for bipolar depression. N Engl J Med. 2007;356:1711-1722.
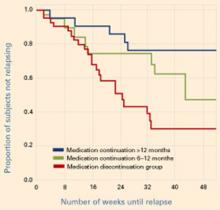
13. Altshuler L, Suppes T, Black D, et al. Impact of antidepressant discontinuation after acute bipolar depression remission on rates of depressive relapse at 1-year follow-up. Am J Psychiatry. 2003;160:1252-1262.
14. Akiskol HS. Developmental pathways to bipolarity: are juvenile-onset depressions pre-bipolar? J Am Acad Child Adolesc Psychiatry. 1995;34(6):754-763.
15. Geller B, Zimmerman B, Williams M, et al. Bipolar disorder at prospective follow-up of adults who had prepubertal major depressive disorder. Am J Psychiatry. 2001;158:125-127.
16. Food and Drug Administration: Center for Drug Evaluation and Research. Revisions to product labeling. Available at: http://www.FDA.gov/cder/drug/antidepressants/default.htm. Accessed January 12, 2009.
17. McElroy S, Strakowski S, West S, et al. Phenomenology of adolescent and adult mania in hospitalized patients with bipolar disorder. Am J Psychiatry. 1997;154:44-49.
18. Olfson M, Marcus SC. A case-control study of antidepressants and attempted suicide during early phase treatment of major depressive episodes. J Clin Psychiatry. 2008;69:425-432.
19. Keck PE, Jr, McElroy SL, Havens JR, et al. Psychosis in bipolar disorder: phenomenology and impact on morbidity and course of illness. Compr Psychiatry. 2003;44:263-269.
20. Jones I, Craddock N. Familiarity of the puerperal trigger in bipolar disorder: results of a family study. Am J Psychiatry. 2001;158:913-917.
21. Chaudron LH, Pies RW. The relationship between postpartum psychosis and bipolar disorder: a review. J Clin Psychiatry. 2003;64:1284-1292.
22. Wisner KL, Peindl KS, Hanusa BH. Psychiatric episodes in women and young children. J Affect Disord. 1995;34:1-11.
23. Sharma V. A cautionary note on the use of antidepressants in postpartum depression. Bipolar Disord. 2006;8:411-414.
24. O’Malley S. “Are you there alone?” The unspeakable crime of Andrea Yates. New York, NY: Simon and Schuster; 2004.
25. Altshuler LL, Bauer M, Frye MA, et al. Does thyroid supplementation accelerate tricyclic antidepressant response? A review and meta-analysis of the literature. Am J Psychiatry. 2001;158:1617-1622.
26. Joffe RT. The use of thyroid supplements to augment antidepressant medication. J Clin Psychiatry. 2008;59:26-29.
27. Cooper-Kazaz R, Apter JT, Cohen R, et al. Combined treatment with sertraline and liothyronine in major depression: a randomized, double-blind, placebo-controlled trial. Arch Gen Psychiatry. 2007;64:679-688.
28. Gold MS, Pottash AL, Extein I. Hypothyroidism and depression: evidence from complete thyroid function evaluation. JAMA. 1981;245:28-31.
29. Kupka RW, Nolen WA, Post RM, et al. High rate of autoimmune thyroiditis in bipolar disorder: lack of association with lithium exposure. Biol Psychiatry. 2002;51:305-311.
30. Szuba MP, Amsterdam JD. Rapid antidepressant response after nocturnal TRH administration in patients with bipolar I and bipolar type II major depression. J Clin Psychopharmacol. 2005;25:325-330.
31. Extein I, Pottash AL, Gold MS. Does subclinical hypothyroidism predispose to tricyclic-induced rapid mood cycles? J Clin Psychiatry. 1982;43:32-33.
32. American Association of Clinical Endocrinologists. Medical guidelines for clinical practice for the evaluation and treatment of hyperthyroidism and hypothyroidism. Endocr Prac. 2002;8:457-469.
33. El-Mallakh RS, Karippott A. Antidepressant-associated chronic irritable dysphoria (ACID) in bipolar disorder. J Affect Disord. 2005;84:267-272.
34. Henkl V, Mergl R, Antje-Kathrin A, et al. Treatment of depression with atypical features: a meta-analytic approach. Psychiatry Res. 2006;141(1):89-101.
35. Perugi G, Akiskal HS, Lattanzi D, et al. The high prevalence of “soft” bipolar (II) features in atypical depression. Compr Psychiatry. 1998;39(2):63-71.
1. Goldberg JF. What constitutes evidence-based pharmacotherapy for bipolar disorder? Part 1: First-line treatments. J Clin Psychiatry. 2007;68:1982-1983.
2. Goldberg JF. What constitutes evidence-based pharmacotherapy for bipolar disorder? Part 2: Complex presentations and clinical context. J Clin Psychiatry. 2008;69:495-496.
3. Levine R, Fink M. Why evidence-based medicine cannot be applied to psychiatry. Psychiatric Times. 2008;25(4):10.
4. Akiskol HS, Benazzi F. The DSM-IV and ICD-10 categories of recurrent [major] depressive and bipolar II disorders: evidence that they lie on a dimensional spectrum. J Affect Disord. 2006;92:45-54.
5. Goodwin FK, Jamison KR. Manic-depressive illness: bipolar disorders and recurrent depression. 2nd ed. New York, NY: Oxford University Press; 2007:3–27.
6. Hirschfeld RMA, Lewis L, Vornik L. Perceptions and impact of bipolar disorder: how far have we really come? Results of the National Depressive and Manic-Depressive Association 2000 survey of individuals with bipolar disorder. J Clin Psychiatry. 2003;64(2):161-167.
7. Blanco C, Laje G, Olfson M, et al. Trends in the treatment of bipolar disorder by outpatient psychiatrists. Am J Psychiatry. 2002;159:1005-1010.
8. Ghaemi SN, Lenox MS, Baldessarini RJ. Effectiveness and safety of long-term antidepressant treatment in bipolar disorder. J Clin Psychiatry. 2001;62:565-569.
9. Ghaemi SN, Boiman EE, Goodwin FK. Diagnosing bipolar disorder and the effect of antidepressants: a naturalistic study. J Clin Psychiatry. 2000;61:804-808.
10. Gijsman HF, Geddes JR, Rendell JM, et al. Antidepressants for bipolar depression: a systematic review of randomized, controlled trials. Am J Psychiatry. 2005;161:1537-1547.
11. Ghaemi SN, Sachs GS, Chiou AM, et al. Is bipolar disorder still underdiagnosed? Are antidepressants overutilized? J Affect Disord. 1999;52:134-144.
12. Sachs GS, Nierenberg AA, Calabrese JR, et al. Effectiveness of adjunctive antidepressant treatment for bipolar depression. N Engl J Med. 2007;356:1711-1722.
13. Altshuler L, Suppes T, Black D, et al. Impact of antidepressant discontinuation after acute bipolar depression remission on rates of depressive relapse at 1-year follow-up. Am J Psychiatry. 2003;160:1252-1262.
14. Akiskol HS. Developmental pathways to bipolarity: are juvenile-onset depressions pre-bipolar? J Am Acad Child Adolesc Psychiatry. 1995;34(6):754-763.
15. Geller B, Zimmerman B, Williams M, et al. Bipolar disorder at prospective follow-up of adults who had prepubertal major depressive disorder. Am J Psychiatry. 2001;158:125-127.
16. Food and Drug Administration: Center for Drug Evaluation and Research. Revisions to product labeling. Available at: http://www.FDA.gov/cder/drug/antidepressants/default.htm. Accessed January 12, 2009.
17. McElroy S, Strakowski S, West S, et al. Phenomenology of adolescent and adult mania in hospitalized patients with bipolar disorder. Am J Psychiatry. 1997;154:44-49.
18. Olfson M, Marcus SC. A case-control study of antidepressants and attempted suicide during early phase treatment of major depressive episodes. J Clin Psychiatry. 2008;69:425-432.
19. Keck PE, Jr, McElroy SL, Havens JR, et al. Psychosis in bipolar disorder: phenomenology and impact on morbidity and course of illness. Compr Psychiatry. 2003;44:263-269.
20. Jones I, Craddock N. Familiarity of the puerperal trigger in bipolar disorder: results of a family study. Am J Psychiatry. 2001;158:913-917.
21. Chaudron LH, Pies RW. The relationship between postpartum psychosis and bipolar disorder: a review. J Clin Psychiatry. 2003;64:1284-1292.
22. Wisner KL, Peindl KS, Hanusa BH. Psychiatric episodes in women and young children. J Affect Disord. 1995;34:1-11.
23. Sharma V. A cautionary note on the use of antidepressants in postpartum depression. Bipolar Disord. 2006;8:411-414.
24. O’Malley S. “Are you there alone?” The unspeakable crime of Andrea Yates. New York, NY: Simon and Schuster; 2004.
25. Altshuler LL, Bauer M, Frye MA, et al. Does thyroid supplementation accelerate tricyclic antidepressant response? A review and meta-analysis of the literature. Am J Psychiatry. 2001;158:1617-1622.
26. Joffe RT. The use of thyroid supplements to augment antidepressant medication. J Clin Psychiatry. 2008;59:26-29.
27. Cooper-Kazaz R, Apter JT, Cohen R, et al. Combined treatment with sertraline and liothyronine in major depression: a randomized, double-blind, placebo-controlled trial. Arch Gen Psychiatry. 2007;64:679-688.
28. Gold MS, Pottash AL, Extein I. Hypothyroidism and depression: evidence from complete thyroid function evaluation. JAMA. 1981;245:28-31.
29. Kupka RW, Nolen WA, Post RM, et al. High rate of autoimmune thyroiditis in bipolar disorder: lack of association with lithium exposure. Biol Psychiatry. 2002;51:305-311.
30. Szuba MP, Amsterdam JD. Rapid antidepressant response after nocturnal TRH administration in patients with bipolar I and bipolar type II major depression. J Clin Psychopharmacol. 2005;25:325-330.
31. Extein I, Pottash AL, Gold MS. Does subclinical hypothyroidism predispose to tricyclic-induced rapid mood cycles? J Clin Psychiatry. 1982;43:32-33.
32. American Association of Clinical Endocrinologists. Medical guidelines for clinical practice for the evaluation and treatment of hyperthyroidism and hypothyroidism. Endocr Prac. 2002;8:457-469.
33. El-Mallakh RS, Karippott A. Antidepressant-associated chronic irritable dysphoria (ACID) in bipolar disorder. J Affect Disord. 2005;84:267-272.
34. Henkl V, Mergl R, Antje-Kathrin A, et al. Treatment of depression with atypical features: a meta-analytic approach. Psychiatry Res. 2006;141(1):89-101.
35. Perugi G, Akiskal HS, Lattanzi D, et al. The high prevalence of “soft” bipolar (II) features in atypical depression. Compr Psychiatry. 1998;39(2):63-71.
Bipolar MANIAS: Life events help confirm the diagnosis
Can knowing a patient’s environmental stressors and family history help us more quickly diagnose bipolar mania?
Kessing et al1 studied patients who were diagnosed as having mania or a mixed episode during their first psychiatric hospitalization. They found that certain life events were associated with these diagnoses, reinforcing the belief that environment to some extent influences psychiatric illness.
Although more research is needed, this finding may help psychiatrists reach a diagnosis of bipolar mania when the clinical course is unclear. Life events that may contribute to bipolar mania are remembered with the mnemonic MANIAS:
- Marital status change. The patient recently was married, divorced, or lost a significant other to death.
- Family Admission. The patient’s mother, father, or sibling was hospitalized at some point for a psychiatric disorder. It does not seem to matter whether the patient remembers the family member’s hospitalization.
- No work. The patient is unemployed.
- Inability to work. The patient is disabled or collects disability benefits.
- Abstaining from relationships. The patient does not have a significant other.
- Suicide was completed by the patient’s mother, father, or sibling. It does not matter how long ago or at what point in the patient’s life the suicide happened.
1. Kessing LV, Agerbo E, Mortensen PB. Major stressful life events and other risk factors for first admission with mania. Bipolar Disord 2004;6(2):122-9.
Dr. Wilson is a fellow, division of child and adolescent psychiatry, department of psychiatry, Louisiana State University Health Sciences Center, New Orleans.
Can knowing a patient’s environmental stressors and family history help us more quickly diagnose bipolar mania?
Kessing et al1 studied patients who were diagnosed as having mania or a mixed episode during their first psychiatric hospitalization. They found that certain life events were associated with these diagnoses, reinforcing the belief that environment to some extent influences psychiatric illness.
Although more research is needed, this finding may help psychiatrists reach a diagnosis of bipolar mania when the clinical course is unclear. Life events that may contribute to bipolar mania are remembered with the mnemonic MANIAS:
- Marital status change. The patient recently was married, divorced, or lost a significant other to death.
- Family Admission. The patient’s mother, father, or sibling was hospitalized at some point for a psychiatric disorder. It does not seem to matter whether the patient remembers the family member’s hospitalization.
- No work. The patient is unemployed.
- Inability to work. The patient is disabled or collects disability benefits.
- Abstaining from relationships. The patient does not have a significant other.
- Suicide was completed by the patient’s mother, father, or sibling. It does not matter how long ago or at what point in the patient’s life the suicide happened.
Can knowing a patient’s environmental stressors and family history help us more quickly diagnose bipolar mania?
Kessing et al1 studied patients who were diagnosed as having mania or a mixed episode during their first psychiatric hospitalization. They found that certain life events were associated with these diagnoses, reinforcing the belief that environment to some extent influences psychiatric illness.
Although more research is needed, this finding may help psychiatrists reach a diagnosis of bipolar mania when the clinical course is unclear. Life events that may contribute to bipolar mania are remembered with the mnemonic MANIAS:
- Marital status change. The patient recently was married, divorced, or lost a significant other to death.
- Family Admission. The patient’s mother, father, or sibling was hospitalized at some point for a psychiatric disorder. It does not seem to matter whether the patient remembers the family member’s hospitalization.
- No work. The patient is unemployed.
- Inability to work. The patient is disabled or collects disability benefits.
- Abstaining from relationships. The patient does not have a significant other.
- Suicide was completed by the patient’s mother, father, or sibling. It does not matter how long ago or at what point in the patient’s life the suicide happened.
1. Kessing LV, Agerbo E, Mortensen PB. Major stressful life events and other risk factors for first admission with mania. Bipolar Disord 2004;6(2):122-9.
Dr. Wilson is a fellow, division of child and adolescent psychiatry, department of psychiatry, Louisiana State University Health Sciences Center, New Orleans.
1. Kessing LV, Agerbo E, Mortensen PB. Major stressful life events and other risk factors for first admission with mania. Bipolar Disord 2004;6(2):122-9.
Dr. Wilson is a fellow, division of child and adolescent psychiatry, department of psychiatry, Louisiana State University Health Sciences Center, New Orleans.
What would Confucius say about mood stabilizers?
When Confucius was asked what he would do first should he become minister of the Kingdom of Wei, he replied: “What is necessary is to rectify names.” He further stated, “If names be not correct, language is not in accordance with the truth of things. If language be not in accordance with the truth of things, affairs cannot be carried on to success” (from The Analects of Confucius, James R. Ware translation, 1980: book 13, verse 3).
I am reminded of this aphorism by Dr. Leslie Citrome’s article, “Treatment-resistant schizophrenia: What role for mood stabilizers?”. This article highlights several psychotropic classes whose names badly need rectification, including “mood stabilizers,” “anticonvulsants,” and “antipsychotics.”
A compound’s first use tends to give it its functional name. Sodium valproate was first used to treat seizures, so it is called an anticonvulsant. Lithium was first used to stabilize mood, so it is called a mood stabilizer. Sometimes valproate is now called a mood stabilizer as well. As Dr. Citrome demonstrates, both compounds also may have efficacy as adjuncts in treating schizophrenia. So do we call them antipsychotics, too?
Each compound has a variety of effects, of course, and we start to diverge from the “truth of things” when we get locked into thinking of a compound in just one way. We also make it less likely that affairs can “be carried on to success” for our patients.
When Confucius was asked what he would do first should he become minister of the Kingdom of Wei, he replied: “What is necessary is to rectify names.” He further stated, “If names be not correct, language is not in accordance with the truth of things. If language be not in accordance with the truth of things, affairs cannot be carried on to success” (from The Analects of Confucius, James R. Ware translation, 1980: book 13, verse 3).
I am reminded of this aphorism by Dr. Leslie Citrome’s article, “Treatment-resistant schizophrenia: What role for mood stabilizers?”. This article highlights several psychotropic classes whose names badly need rectification, including “mood stabilizers,” “anticonvulsants,” and “antipsychotics.”
A compound’s first use tends to give it its functional name. Sodium valproate was first used to treat seizures, so it is called an anticonvulsant. Lithium was first used to stabilize mood, so it is called a mood stabilizer. Sometimes valproate is now called a mood stabilizer as well. As Dr. Citrome demonstrates, both compounds also may have efficacy as adjuncts in treating schizophrenia. So do we call them antipsychotics, too?
Each compound has a variety of effects, of course, and we start to diverge from the “truth of things” when we get locked into thinking of a compound in just one way. We also make it less likely that affairs can “be carried on to success” for our patients.
When Confucius was asked what he would do first should he become minister of the Kingdom of Wei, he replied: “What is necessary is to rectify names.” He further stated, “If names be not correct, language is not in accordance with the truth of things. If language be not in accordance with the truth of things, affairs cannot be carried on to success” (from The Analects of Confucius, James R. Ware translation, 1980: book 13, verse 3).
I am reminded of this aphorism by Dr. Leslie Citrome’s article, “Treatment-resistant schizophrenia: What role for mood stabilizers?”. This article highlights several psychotropic classes whose names badly need rectification, including “mood stabilizers,” “anticonvulsants,” and “antipsychotics.”
A compound’s first use tends to give it its functional name. Sodium valproate was first used to treat seizures, so it is called an anticonvulsant. Lithium was first used to stabilize mood, so it is called a mood stabilizer. Sometimes valproate is now called a mood stabilizer as well. As Dr. Citrome demonstrates, both compounds also may have efficacy as adjuncts in treating schizophrenia. So do we call them antipsychotics, too?
Each compound has a variety of effects, of course, and we start to diverge from the “truth of things” when we get locked into thinking of a compound in just one way. We also make it less likely that affairs can “be carried on to success” for our patients.
Commentary: When medical illness complicates schizophrenia and bipolar disorder
Patients with schizophrenia or bipolar disorder face a higher risk of premature death, compared with the general population. Their overall mortality rate is elevated not only by higher suicide rates but also by higher rates of medical comorbidities, including obesity, diabetes mellitus, cardiovascular and pulmonary diseases, HIV infection, and cancer.1,2
Schizophrenia and bipolar disorder are also frequently complicated by psychiatric comorbidities including alcohol and substance use disorders (such as nicotine dependence), anxiety disorders, and eating disorders (such as binge eating).3,4 Even so, the impact of psychiatric comorbidity on medical morbidity and mortality has not been adequately investigated and has—until rather recently—received little attention from clinical researchers.
Within the past 5 years or so, epidemiologic and population studies have shown increased morbidity and mortality from medical illnesses in patients with serious and persistent mental illness.5,6 These findings have sparked renewed interest in behavioral, biological, and psychosocial factors associated with schizophrenia and bipolar disorder that may contribute to comorbid medical illnesses. These factors include:
- negative and depressive symptoms
- physical inactivity and poor diet
- hypothalamic-pituitary-adrenal axis dysregulation associated with acute psychotic and affective episodes
- amotivation
- social isolation
- limited access to primary and preventive health care.7
The degree to which these factors may elevate medical comorbidity rates in patients with Commentary these serious psychiatric illnesses has not been well-studied or described.
TREATMENT IMPLICATIONS
These observations raise concerns about safe and effective use of medications by patients with schizophrenia or bipolar disorder as well as medical illness. Issues for clinicians to consider include:
- possible pharmacokinetic and pharmacodynamic interactions in patients taking concomitant medications for psychiatric and medical illnesses
- potential beneficial and adverse effects of psychotropics on medical illnesses
- and—conversely—potential beneficial and adverse effects on mood and psychotic disorders of medications used to treat medical illnesses.
Being aware of metabolic effects when prescribing psychotropics is not a new idea. Lithium, for example, has long been known to cause weight gain, suppress thyroid hormone, and interact with thiazide diuretics when used to treat bipolar disorder. Thus, therapeutic blood monitoring is recommended for patients receiving acute and maintenance lithium therapy.
More recently, atypical antipsychotics such as olanzapine and clozapine (and risperidone and quetiapine to a lesser extent) have been shown to produce substantial weight gain and other metabolic effects that increase the risk of diabetes and cardiovascular disease.7 As a result, the American Diabetes Association—along with the American Psychiatric Association and other groups—now recommends that psychiatrists and other physicians monitor patients’ body weight and body mass index, vital signs, serum glucose, and lipids when prescribing these agents.7-11 Careful monitoring should improve the medical care of patients with schizophrenia and bipolar disorder and help protect them from the medical risks associated with overweight and obesity.
Similar precautions are needed when schizophrenia and bipolar disorder co-occur with other medical illnesses treated by complex pharmacologic regimens, such as pulmonary disease, cancer, and HIV. Three points to keep in mind are:
- careful selection of treatments for co-occurring medical illnesses, considering potential effects on the primary psychiatric disorder
- the impact of psychotropics on patients’ medical illnesses
- and the potential for drug interactions.
1. Kilbourne AM, Cornelius JR, Han X, et al. Burden of general medical conditions among individuals with bipolar disorder. Bipolar Disord 2004;6:368-73.
2. Meyer JM, Nasrallah HA. Medical illness and schizophrenia Washington, DC: American Psychiatric Press, Inc, 2003.
3. McElroy SL, Altshuler LL, Suppes T, et al. Axis I psychiatric comorbidity and its relationship with historical illness variables in 288 patients with bipolar disorder. Am J Psychiatry 2001;158:420-6.
4. Green AI, Canuso CM, Brenner MJ, et al. Detection and management of comorbidity in patients with schizophrenia. Psychiatr Clin North Am 2003;26:115-39.
5. Buda M, Tsuang MT, Fleming JA. Causes of death in DSM-III schizophrenics and other psychotics (atypical group). Comparison with the general population. Arch Gen Psychiatry 1988;45:283-5.
6. Osby U, Brandt L, Correia N, et al. Excess mortality in bipolar and unipolar disorder in Sweden. Arch Gen Psychiatry 2001;58:844-50.
7. Keck PE, Jr, Buse JB, Dagago-Jack S, et al. Managing metabolic concerns in patients with severe mental illness: a special report (Postgrad Med). Minneapolis, MN: McGraw-Hill, 2003.
8. American Diabetes Association. Consensus Development Conference on Antipsychotic Drugs and Obesity and Diabetes. Diabetes Care 2004;27:596-601.
9. Marder SR, Essock SM, Miller AL, et al. Physical health monitoring of patients with schizophrenia. Am J Psychiatry 2004;161:1334-9.
10. Chue P, Kovacs CS. Safety and tolerability of atypical antipsychotics in patients with bipolar disorder: prevalence, monitoring and management. Bipolar Disord 2003;5(suppl 2):62-79.
11. Nasrallah HA, Newcomer JW. Atypical antipsychotics and metabolic dysregulation. Evaluating the risk/benefit equation and improving standard of care. J Clin Psychopharmacol 2004;24(suppl 2):S7-S14.
Patients with schizophrenia or bipolar disorder face a higher risk of premature death, compared with the general population. Their overall mortality rate is elevated not only by higher suicide rates but also by higher rates of medical comorbidities, including obesity, diabetes mellitus, cardiovascular and pulmonary diseases, HIV infection, and cancer.1,2
Schizophrenia and bipolar disorder are also frequently complicated by psychiatric comorbidities including alcohol and substance use disorders (such as nicotine dependence), anxiety disorders, and eating disorders (such as binge eating).3,4 Even so, the impact of psychiatric comorbidity on medical morbidity and mortality has not been adequately investigated and has—until rather recently—received little attention from clinical researchers.
Within the past 5 years or so, epidemiologic and population studies have shown increased morbidity and mortality from medical illnesses in patients with serious and persistent mental illness.5,6 These findings have sparked renewed interest in behavioral, biological, and psychosocial factors associated with schizophrenia and bipolar disorder that may contribute to comorbid medical illnesses. These factors include:
- negative and depressive symptoms
- physical inactivity and poor diet
- hypothalamic-pituitary-adrenal axis dysregulation associated with acute psychotic and affective episodes
- amotivation
- social isolation
- limited access to primary and preventive health care.7
The degree to which these factors may elevate medical comorbidity rates in patients with Commentary these serious psychiatric illnesses has not been well-studied or described.
TREATMENT IMPLICATIONS
These observations raise concerns about safe and effective use of medications by patients with schizophrenia or bipolar disorder as well as medical illness. Issues for clinicians to consider include:
- possible pharmacokinetic and pharmacodynamic interactions in patients taking concomitant medications for psychiatric and medical illnesses
- potential beneficial and adverse effects of psychotropics on medical illnesses
- and—conversely—potential beneficial and adverse effects on mood and psychotic disorders of medications used to treat medical illnesses.
Being aware of metabolic effects when prescribing psychotropics is not a new idea. Lithium, for example, has long been known to cause weight gain, suppress thyroid hormone, and interact with thiazide diuretics when used to treat bipolar disorder. Thus, therapeutic blood monitoring is recommended for patients receiving acute and maintenance lithium therapy.
More recently, atypical antipsychotics such as olanzapine and clozapine (and risperidone and quetiapine to a lesser extent) have been shown to produce substantial weight gain and other metabolic effects that increase the risk of diabetes and cardiovascular disease.7 As a result, the American Diabetes Association—along with the American Psychiatric Association and other groups—now recommends that psychiatrists and other physicians monitor patients’ body weight and body mass index, vital signs, serum glucose, and lipids when prescribing these agents.7-11 Careful monitoring should improve the medical care of patients with schizophrenia and bipolar disorder and help protect them from the medical risks associated with overweight and obesity.
Similar precautions are needed when schizophrenia and bipolar disorder co-occur with other medical illnesses treated by complex pharmacologic regimens, such as pulmonary disease, cancer, and HIV. Three points to keep in mind are:
- careful selection of treatments for co-occurring medical illnesses, considering potential effects on the primary psychiatric disorder
- the impact of psychotropics on patients’ medical illnesses
- and the potential for drug interactions.
Patients with schizophrenia or bipolar disorder face a higher risk of premature death, compared with the general population. Their overall mortality rate is elevated not only by higher suicide rates but also by higher rates of medical comorbidities, including obesity, diabetes mellitus, cardiovascular and pulmonary diseases, HIV infection, and cancer.1,2
Schizophrenia and bipolar disorder are also frequently complicated by psychiatric comorbidities including alcohol and substance use disorders (such as nicotine dependence), anxiety disorders, and eating disorders (such as binge eating).3,4 Even so, the impact of psychiatric comorbidity on medical morbidity and mortality has not been adequately investigated and has—until rather recently—received little attention from clinical researchers.
Within the past 5 years or so, epidemiologic and population studies have shown increased morbidity and mortality from medical illnesses in patients with serious and persistent mental illness.5,6 These findings have sparked renewed interest in behavioral, biological, and psychosocial factors associated with schizophrenia and bipolar disorder that may contribute to comorbid medical illnesses. These factors include:
- negative and depressive symptoms
- physical inactivity and poor diet
- hypothalamic-pituitary-adrenal axis dysregulation associated with acute psychotic and affective episodes
- amotivation
- social isolation
- limited access to primary and preventive health care.7
The degree to which these factors may elevate medical comorbidity rates in patients with Commentary these serious psychiatric illnesses has not been well-studied or described.
TREATMENT IMPLICATIONS
These observations raise concerns about safe and effective use of medications by patients with schizophrenia or bipolar disorder as well as medical illness. Issues for clinicians to consider include:
- possible pharmacokinetic and pharmacodynamic interactions in patients taking concomitant medications for psychiatric and medical illnesses
- potential beneficial and adverse effects of psychotropics on medical illnesses
- and—conversely—potential beneficial and adverse effects on mood and psychotic disorders of medications used to treat medical illnesses.
Being aware of metabolic effects when prescribing psychotropics is not a new idea. Lithium, for example, has long been known to cause weight gain, suppress thyroid hormone, and interact with thiazide diuretics when used to treat bipolar disorder. Thus, therapeutic blood monitoring is recommended for patients receiving acute and maintenance lithium therapy.
More recently, atypical antipsychotics such as olanzapine and clozapine (and risperidone and quetiapine to a lesser extent) have been shown to produce substantial weight gain and other metabolic effects that increase the risk of diabetes and cardiovascular disease.7 As a result, the American Diabetes Association—along with the American Psychiatric Association and other groups—now recommends that psychiatrists and other physicians monitor patients’ body weight and body mass index, vital signs, serum glucose, and lipids when prescribing these agents.7-11 Careful monitoring should improve the medical care of patients with schizophrenia and bipolar disorder and help protect them from the medical risks associated with overweight and obesity.
Similar precautions are needed when schizophrenia and bipolar disorder co-occur with other medical illnesses treated by complex pharmacologic regimens, such as pulmonary disease, cancer, and HIV. Three points to keep in mind are:
- careful selection of treatments for co-occurring medical illnesses, considering potential effects on the primary psychiatric disorder
- the impact of psychotropics on patients’ medical illnesses
- and the potential for drug interactions.
1. Kilbourne AM, Cornelius JR, Han X, et al. Burden of general medical conditions among individuals with bipolar disorder. Bipolar Disord 2004;6:368-73.
2. Meyer JM, Nasrallah HA. Medical illness and schizophrenia Washington, DC: American Psychiatric Press, Inc, 2003.
3. McElroy SL, Altshuler LL, Suppes T, et al. Axis I psychiatric comorbidity and its relationship with historical illness variables in 288 patients with bipolar disorder. Am J Psychiatry 2001;158:420-6.
4. Green AI, Canuso CM, Brenner MJ, et al. Detection and management of comorbidity in patients with schizophrenia. Psychiatr Clin North Am 2003;26:115-39.
5. Buda M, Tsuang MT, Fleming JA. Causes of death in DSM-III schizophrenics and other psychotics (atypical group). Comparison with the general population. Arch Gen Psychiatry 1988;45:283-5.
6. Osby U, Brandt L, Correia N, et al. Excess mortality in bipolar and unipolar disorder in Sweden. Arch Gen Psychiatry 2001;58:844-50.
7. Keck PE, Jr, Buse JB, Dagago-Jack S, et al. Managing metabolic concerns in patients with severe mental illness: a special report (Postgrad Med). Minneapolis, MN: McGraw-Hill, 2003.
8. American Diabetes Association. Consensus Development Conference on Antipsychotic Drugs and Obesity and Diabetes. Diabetes Care 2004;27:596-601.
9. Marder SR, Essock SM, Miller AL, et al. Physical health monitoring of patients with schizophrenia. Am J Psychiatry 2004;161:1334-9.
10. Chue P, Kovacs CS. Safety and tolerability of atypical antipsychotics in patients with bipolar disorder: prevalence, monitoring and management. Bipolar Disord 2003;5(suppl 2):62-79.
11. Nasrallah HA, Newcomer JW. Atypical antipsychotics and metabolic dysregulation. Evaluating the risk/benefit equation and improving standard of care. J Clin Psychopharmacol 2004;24(suppl 2):S7-S14.
1. Kilbourne AM, Cornelius JR, Han X, et al. Burden of general medical conditions among individuals with bipolar disorder. Bipolar Disord 2004;6:368-73.
2. Meyer JM, Nasrallah HA. Medical illness and schizophrenia Washington, DC: American Psychiatric Press, Inc, 2003.
3. McElroy SL, Altshuler LL, Suppes T, et al. Axis I psychiatric comorbidity and its relationship with historical illness variables in 288 patients with bipolar disorder. Am J Psychiatry 2001;158:420-6.
4. Green AI, Canuso CM, Brenner MJ, et al. Detection and management of comorbidity in patients with schizophrenia. Psychiatr Clin North Am 2003;26:115-39.
5. Buda M, Tsuang MT, Fleming JA. Causes of death in DSM-III schizophrenics and other psychotics (atypical group). Comparison with the general population. Arch Gen Psychiatry 1988;45:283-5.
6. Osby U, Brandt L, Correia N, et al. Excess mortality in bipolar and unipolar disorder in Sweden. Arch Gen Psychiatry 2001;58:844-50.
7. Keck PE, Jr, Buse JB, Dagago-Jack S, et al. Managing metabolic concerns in patients with severe mental illness: a special report (Postgrad Med). Minneapolis, MN: McGraw-Hill, 2003.
8. American Diabetes Association. Consensus Development Conference on Antipsychotic Drugs and Obesity and Diabetes. Diabetes Care 2004;27:596-601.
9. Marder SR, Essock SM, Miller AL, et al. Physical health monitoring of patients with schizophrenia. Am J Psychiatry 2004;161:1334-9.
10. Chue P, Kovacs CS. Safety and tolerability of atypical antipsychotics in patients with bipolar disorder: prevalence, monitoring and management. Bipolar Disord 2003;5(suppl 2):62-79.
11. Nasrallah HA, Newcomer JW. Atypical antipsychotics and metabolic dysregulation. Evaluating the risk/benefit equation and improving standard of care. J Clin Psychopharmacol 2004;24(suppl 2):S7-S14.
Bipolar moving target: Draw a bead on rapid cycling with type-specific therapies
Rapid-cycling bipolar disorder is a moving target, with treatment-resistant depression recurring frequently and alternating with hypomanic/manic episodes (Box).1,2 Can one medication adequately treat these complicated patients, or is combination therapy necessary? If more than one medication is needed, are some combinations more effective than others?
This article attempts to answer these questions by:
- discussing recent treatment trial results
- suggesting an algorithm for managing hypomanic/manic and depressive episodes in rapid-cycling patients with bipolar disorder types I or II.
CLINICAL CHARACTERISTICS
Rapid cycling is associated most consistently with female gender and bipolar II disorder2 (Table); why these two groups are primarily affected is unknown. Results of studies linking rapid cycling with hypothyroidism, gonadal steroid effects, family history, and substance use have been inconsistent and contradictory.2
Age of onset. Recent studies examining bipolar disorder’s age of onset have contradicted earlier rapid-cycling literature. In two large studies, Schneck et al3 and Coryell et al4 found rapid cycling associated with early onset of bipolar illness. The authors note that high rates of rapid cycling in children and adolescents resemble adult rapid cycling and speculate that early-onset bipolar illness might lead to rapid cycling vulnerability.5
Rapid cycling—defined in DSM-IV-TR as four or more depressive, manic, hypomanic, or mixed episodes in the previous 12 months—is considered a longitudinal course specifier for bipolar I or II disorder.1 Episodes must be demarcated by:
- full or partial remission lasting at least 2 months
- or a switch to a mood state of opposite polarity.
Cycling variations include ultra-rapid (1 day to 1 week), ultra-ultra rapid or ultradian (<24 hours), and continuous (no euthymic periods between mood episodes). Rapid cycling occurs in an estimated 15% to 25% of patients with bipolar disorder,2 though psychiatrists in specialty and tertiary referral centers see higher percentages because of the illness’ refractory nature.
Transient vs persistent state. Rapid cycling is thought to be either a transient state in long-term bipolar illness or a more chronic expression of the illness. Several studies6,7 have described rapid cycling as a transient phenomenon, whereas others8-11 have found a more persistent rapid cycling course during follow-up. Interestingly, a recent study11 suggested the mood-cycle pattern may be the most important predictor of rapid cycling. Patients with a depression–hypomania/mania-euthymia course demonstrated more-persistent rapid cycling than did those with a hypomania/mania-depression-euthymia course.
Antidepressants. Antidepressants’ role in initiating or exacerbating rapid cycling also remains unclear. Wehr et al8 found that discontinuing antidepressants contributed to cycling cessation or slowing. However, two prospective studies by Coryell et al4 that controlled for major depression found no association between antidepressant use and rapid cycling.
More recently, Yildiz and Sachs12 found a possible gender-specific relationship between antidepressants and rapid cycling. Women exposed to antidepressants before their first hypomanic/manic episode were more likely to develop rapid cycling than women who were not so exposed. This association was not evident in men.
NO DEFINITIVE CHOICES
Any discussion of treating rapid-cycling bipolar disorder is based on limited data, as few prospective studies of this exclusive cohort exist. Many studies report on mixed cohorts of refractory bipolar patients that include rapid cyclers, but separate analyses of rapid-cycling subgroups are not usually reported. Notable exceptions are recent studies by Calabrese et al, which are discussed below.
Lithium. Dunner and Fieve13 were the first to suggest that rapid-cycling bipolar patients respond poorly to lithium maintenance monotherapy. Later studies, however, suggested that lithium could benefit rapid cyclers, primarily in reducing hypomanic or manic episodes.
Baldessarini et al10 found that lithium was less effective for rapid than nonrapid cyclers only in reducing recurrence of depressive episodes. Kukopulos et al14 reported that lithium response in rapid cyclers increased from 16% to 78% after antidepressants were stopped, suggesting that a positive response to lithium may require more limited antidepressant use (or patients not having been exposed to antidepressants at all).
Thus, lithium prophylaxis has at least partial efficacy in many rapid cyclers, especially when antidepressants are avoided.
Divalproex. As with lithium, divalproex sodium appears more effective in treating and preventing hypomanic/manic episodes than depressive episodes in bipolar patients with rapid-cycling illness. Six open studies showed that patients who had not responded to lithium tended to do better with divalproex.15
Calabrese et al then tested the hypothesis that rapid cycling predicts nonresponse to lithium and positive response to divalproex.16 In a randomized controlled trial, they enrolled 254 recently hypomanic/manic rapid-cycling outpatients in an open-label stabilization phase involving combination lithium and divalproex therapy. Stabilized patients were then randomized to monotherapy with lithium, serum level ≥ 0.8 mEq/L, or divalproex, serum level ≥ 50 mcg/mL. Only 60 patients (24%) met stability criteria for randomization, achieving a persistent bimodal response as measured by continuous weeks of:
- Hamilton depression scale (24-item) score ≤ 20
- Young Mania Rating Scale score ≤ 12.5
- Global Assessment Scale score ≥ 51.
Most nonresponse was attributed to refractory depression.
After 20 months of maintenance therapy, about one-half of patients relapsed on either monotherapy. In the survival analysis, the median time to any mood episode was 45 weeks with divalproex monotherapy and 18 weeks with lithium monotherapy, although this difference was not statistically significant. The small sample size and high dropout rate may have created a false-negative error in this study.
Thus, these data did not show divalproex monotherapy to be more effective than lithium monotherapy in managing rapid-cycling bipolar disorder. The combination proved more effective in treating mania than depression and superior to monotherapy. This finding underscores combination therapy’s importance and the need to use mood stabilizers that also treat the depressed phase of bipolar disorder in rapid cyclers.
Table
Clinical characteristics of rapid cycling
| Prevalence approximately 15% to 25% in patients with bipolar disorder |
| More common in women than men |
| More common with type II than type I bipolar disorder |
| Primarily a depressive disease |
| Low treatment response rates and high recurrence risk |
| Associated with antidepressant use in some cases |
Carbamazepine. Recent data refute earlier reports suggesting that rapid cycling predicted positive response to carbamazepine. Multiple open studies and four controlled studies suggest that carbamazepine—like lithium and divalproex—possesses moderate to marked efficacy in the hypomanic/manic phase but poor to moderate efficacy in the depressed phase of rapid-cycling bipolar disorder.17
Lamotrigine. Lamotrigine is the first mood-stabilizing agent that has shown efficacy in maintenance treatment of bipolar depression and rapid cycling. In a double-blind, prospective, placebo-controlled trial, Calabrese et al18 enrolled 324 rapid-cycling patients with bipolar disorder type I or II in an open-label stabilization phase with lamotrigine. The 182 stabilized patients were then randomly assigned to receive either lamotrigine (mean 288 +/- 94 mg/d) or placebo.
For 6 months, 41% of patients receiving lamotrigine and 26% of those receiving placebo remained stable without relapse (P = 0.03), although the difference was statistically significant only for the bipolar II subtype. Lamotrigine appeared most effective in patients with the biphasic pattern of depression-hypomania/mania-euthymia.
Topiramate. Most studies of topiramate in rapid cycling have been retrospective and/or small add-on studies to existing mood stabilizers, with topiramate use associated with moderately or markedly improved manic symptoms.19 Evidence supports further controlled investigations, particularly because topiramate’s weight-loss effects may help overweight or obese patients.
Gabapentin. Gabapentin’s efficacy in rapid cycling has not been established. Although open-label studies showed a 67% response rate when gabapentin was used as adjunctive therapy, two double-blind, placebocontrolled studies of bipolar patients failed to show efficacy.20,21
Atypical antipsychotics. Five atypical antipsychotics—aripiprazole, olanzapine, quetiapine, risperidone, and ziprasidone—are FDA-approved for treating acute mania. Olanzapine is also indicated for bipolar maintenance treatment and has the most data showing efficacy in rapid cycling:
- In a 3-week, placebo-controlled study of 139 patients with bipolar I acute mania, olanzapine (median modal 15 mg/d) reduced manic symptoms to a statistically significantly extent in the 45 rapid cyclers.22
- A long-term prospective study followed 23 patients—30% of whom were rapid cyclers—who used olanzapine (mean 8.2 mg/d) as an adjunct to mood stabilizers. Manic and depressive symptoms were reduced significantly in the cohort, which was followed for a mean of 303 days.23
- An 8-week, double-blind, placebo-controlled study24 compared olanzapine monotherapy with the olanzapine/fluoxetine combination (OFC) in 833 depressed bipolar I patients, of whom 315 (37%) had rapid cycling. Mean olanzapine dosage was 9.7 mg in monotherapy and 7.4 mg in combination therapy; mean fluoxetine dosage was 39.3 mg.
A follow-up analysis25 showed that rapid cyclers’ depressive symptoms improved rapidly, and this improvement was sustained with OFC but not olanzapine monotherapy. Nonrapid-cycling patients responded to both treatments.
Other atypicals have shown partial efficacy in rapid-cycling bipolar disorder, although the studies have had methodologic limitations. Suppes et al26 conducted the first controlled trial using clozapine as add-on therapy in a 1-year, randomized evaluation of 38 patients with treatment-refractory bipolar disorder. The 21 rapid cyclers received a mean peak of 234 mg/d. Brief Psychiatric Rating Scale and Clinical Global Improvement scores improved significantly overall, but data specific to the rapid-cycling patients were not reported.
Small, open-label studies using risperidone and quetiapine as adjuncts to mood stabilizers have shown modest efficacy in rapid cycling, usually in treating manic symptoms. A recent 8-week, double-blind, placebo-controlled trial of quetiapine in bipolar depression showed promising results, though its efficacy in rapid cycling was not reported.27
RECOMMENDED TREATMENT
Because coincidental cycling may give the false appearance of efficacy in the short term, we recommend that you treat rapid cyclers methodically and judge outcomes over several months or cycle-lengths. A general approach includes:
- identify and treat underlying medical illnesses, such as hypothyroidism
- identify and treat comorbid alcohol/drug abuse
- taper or discontinue cycle-inducing agents such as antidepressants or sympathomimetics
- use standard mood stabilizers and/or atypical antipsychotics alone or in combination (Algorithm).
Algorithm Managing manic and depressive phases of rapid-cycling bipolar disorder
Treating acute mania in rapid-cycling patients is similar to managing this phase in nonrapid cyclers. First-tier therapy includes established mood stabilizers such as lithium, divalproex, or atypical antipsychotics. Carbamazepine is usually considered second-tier because of its effects on other medications via cytochrome P-450 system induction, and limited data exist on oxcarbazepine’s efficacy. Lamotrigine has not been proven effective in acute mania. If monotherapy is ineffective, try combinations of mood stabilizers and/or atypical antipsychotics.
Treating the depressed phase in rapid cyclers is far more difficult than treating acute mania and may depend on bipolar subtype:
- Bipolar I patients likely will require one or more mood stabilizers (such as lithium, divalproex, olanzapine) plus add-on lamotrigine.
- Bipolar II patients may benefit from lamotrigine alone.
- Atypical antipsychotics that have putative antidepressant effects without apparent cycle-accelerating effects may also be considered. At this time, olanzapine has the most data.
Given depression’s refractory nature in rapid-cycling bipolar illness, you may need to combine any of the above medications, try electroconvulsive therapy, or use more-experimental strategies such as:
- omega-3 fatty acids
- donepezil
- pramipexole
- high-dose levothyroxine/T4.
Antidepressants. Before using antidepressants to treat bipolar depression, consider carefully the risk of initiating or exacerbating rapid cycling. No definitive evidence is available to guide your decision.
Likewise, the optimal duration of antidepressant treatment is unclear, although tapering the antidepressant as tolerated may be prudent after depressive symptoms are in remission.
Psychosocial interventions. Finally, don’t overlook psychosocial interventions. Bipolar-specific psychotherapies can enhance compliance, lessen depression, and improve treatment response.28
CONCLUSION
Standard mood stabilizers appear to show partial efficacy in rapid cycling’s hypomanic/manic phase but only modest efficacy in the depressed phase. Lamotrigine appears more-promising in treating depressive than acute manic episodes and may be particularly effective for bipolar II patients. Evidence is growing that atypical antipsychotics also have partial efficacy in treating rapid cyclers, though whether this effect is phase-specific is unclear. As no single agent provides ideal bimodal treatment, combination therapy is recommended.
Related resources
- Bipolar Clinic and Research Program. Massachusetts General Hospital. Includes tools for clinicians and the clinical site for the Systematic Treatment Enhancement Program for Bipolar Disorder (STEP-BD). www.manicdepressive.org. Accessed Oct. 14, 2004.
- Goodwin FK, Jamison KR. Manic-depressive illness. New York: Oxford University Press, 1990.
- Marneros A, Goodwin FK (eds). Bipolar disorders: Mixed states, rapid cycling and atypical bipolar disorder. Cambridge, UK: Cambridge University Press (in press).
Drug brand names
- Aripiprazole • Abilify
- Carbamazepine • Carbatrol, others
- Clozapine • Clozaril
- Donepezil • Aricept
- Divalproex sodium • Depakote
- Gabapentin • Neurontin
- Lamotrigine • Lamictal
- Levothyroxine • Synthroid, others
- Lithium • Lithobid, others
- Olanzapine • Zyprexa
- Olanzapine/fluoxetine • Symbyax
- Oxcarbazepine • Trileptal
- Pramipexole • Mirapex
- Quetiapine • Seroquel
- Risperidone • Risperdal
- Topiramate • Topamax
- Ziprasidone • Geodon
Disclosures
Dr. Altman is a speaker for Forest Pharmaceuticals, Janssen Pharmaceutica, AstraZeneca Pharmaceuticals, and Abbott Laboratories.
Dr. Schneck is a consultant to AstraZeneca Pharmaceuticals, UCB Pharma, and Bristol-Myers Squibb Co. and a speaker for AstraZeneca Pharmaceuticals.
1. American Psychiatric Association. Diagnostic and statistical manual of mental disorders (4th ed, text rev). Washington, DC: American Psychiatric Association, 2000.
2. Kupka RW, Luckenbaugh DA, Post RM, et al. Rapid and non-rapid cycling bipolar disorder: a meta-analysis of clinical studies. J Clin Psychiatry 2003;64(12):1483-94.
3. Schneck CD, Miklowitz DJ, Calabrese JR, et al. Phenomenology of rapid cycling bipolar disorder: data from the first 500 participants in the Systematic Treatment Enhancement Program. Am J Psychiatry 2004;161(10):1902-8.
4. Coryell W, Solomon D, Turvey C, et al. The long-term course of rapid-cycling bipolar disorder. Arch Gen Psychiatry 2003;60(9):914-20.
5. Findling RL, Gracious BL, McNamara NK, et al. Rapid, continuous cycling and psychiatric comorbidity in pediatric bipolar I disorder. Bipolar Disord 2001;3:202-10.
6. Coryell W, Endicott J, Keller M. Rapidly cycling affective disorder. Demographics, diagnosis, family history, and course. Arch Gen Psychiatry 1992;49:126-31.
7. Maj M, Magliano L, Pirozzi R, et al. Validity of rapid cycling as a course specifier for bipolar disorder. Am J Psychiatry 1994;151:1015-19.
8. Wehr TA, Sack DA, Rosenthal NE, Cowdry RW. Rapid cycling affective disorder: contributing factors and treatment responses in 51 patients. Am J Psychiatry 1988;145:179-84.
9. Bauer MS, Calabrese J, Dunner DL, et al. Multisite data reanalysis of the validity of rapid cycling as a course modifier for bipolar disorder in DSM-IV. Am J Psychiatry 1994;151:506-15.
10. Baldessarini RJ, Tondo L, Floris G, Hennen J. Effects of rapid cycling on response to lithium maintenance treatment in 360 bipolar I and II disorder patients. J Affect Disord 2000;61:13-22.
11. Koukopoulos A, Sani G, Koukopoulos AE, et al. Duration and stability of the rapid-cycling course: a long-term personal follow-up of 109 patients. J Affect Disord 2003;73:75-85.
12. Yildiz A, Sachs GS. Do antidepressants induce rapid cycling? A gender-specific association. J Clin Psychiatry 2003;64:814-18.
13. Dunner DL, Fieve RR. Clinical factors in lithium carbonate prophylaxis failure. Arch Gen Psychiatry 1974;30:229-33.
14. Kukopulos A, Reginaldi D, Laddomada P, et al. Course of the manic-depressive cycle and changes caused by treatments. Pharmakopsychiatr Neuropsychopharmakol 1980;13:156-67.
15. Calabrese JR, Woyshville MJ, Kimmel SE, Rapport DJ. Predictors of valproate response in bipolar rapid cycling. J Clin Psychopharmacol 1993;13:280-3.
16. Calabrese JR, Shelton M, Rapport DJ, et al. A double-blind 20 month maintenance study of lithium vs. divalproex in rapid-cycling bipolar disorder [presentation]. Pittsburgh, PA: Fifth International Conference on Bipolar Disorder, June 12-14, 2003.
17. Calabrese JR, Bowden C, Woyshville MJ. Lithium and anticonvulsants in the treatment of bipolar disorders. In: Bloom E, Kupfer D (eds). Psychopharmacology: The third generation of progress. New York: Raven Press, 1995;1099-1112.
18. Calabrese JR, Suppes T, Bowden CL, et al. A double-blind, placebo-controlled, prophylaxis study of lamotrigine in rapid-cycling bipolar disorder. J Clin Psychiatry 2000;61(11):841-50.
19. Marcotte D. Use of topiramate, a new anti-epileptic as a mood stabilizer. J Affect Disord 1998;50(2-3):245-51.
20. Pande AC, Crockatt JG, Janney CA, et al. Gabapentin in bipolar disorder: a placebo-controlled trial of adjunctive therapy. Gabapentin Bipolar Disorder Study Group. Bipolar Disord 2000;2(3 pt 2):249-55.
21. Frye MA, Ketter TA, Kimbrell TA, et al. A placebo-controlled study of lamotrigine and gabapentin monotherapy in refractory mood disorders. J Clin Psychopharmacol 2000;20(6):607-14.
22. Sanger TM, Tohen M, Vieta E, et al. Olanzapine in the acute treatment of bipolar I disorder with a history of rapid cycling. J Affect Disord 2003;73:155-61.
23. Calabrese JR, Kasper S, Johnson G, et al. International consensus group on bipolar I depression treatment guidelines. J Clin Psychiatry 2004;65:569-79.
24. Tohen M, Vieta E, Calabrese J, et al. Efficacy of olanzapine and olanzapine-fluoxetine combination in the treatment of bipolar I depression. Arch Gen Psychiatry 2003;60:1079-88.
25. Keck P, Corya S, Andersen SW, et al. Analysis of olanzapine/fluoxetine combination in the treatment of rapid-cycling bipolar depression [presentation]. Boca Raton, FL: New Clinical Drug Evaluation Unit, 2003.
26. Suppes T, Webb A, Paul B, et al. Clinical outcome in a randomized 1-year trial of clozapine versus treatment as usual for patients with treatment-resistant illness and a history of mania. Am J Psychiatry 1999;156:1164-9.
27. Calabrese JR, Macfadden W, McCoy R, et al. Double-blind, placebo-controlled study of quetiapine in bipolar depression [presentation]. Phoenix, AZ: New Clinical Drug Evaluation Unit, 2004.
28. Craighead WE, Miklowitz DJ. Psychosocial interventions for bipolar disorder. J Clin Psychiatry 2000;61(suppl 13):58-64.
Rapid-cycling bipolar disorder is a moving target, with treatment-resistant depression recurring frequently and alternating with hypomanic/manic episodes (Box).1,2 Can one medication adequately treat these complicated patients, or is combination therapy necessary? If more than one medication is needed, are some combinations more effective than others?
This article attempts to answer these questions by:
- discussing recent treatment trial results
- suggesting an algorithm for managing hypomanic/manic and depressive episodes in rapid-cycling patients with bipolar disorder types I or II.
CLINICAL CHARACTERISTICS
Rapid cycling is associated most consistently with female gender and bipolar II disorder2 (Table); why these two groups are primarily affected is unknown. Results of studies linking rapid cycling with hypothyroidism, gonadal steroid effects, family history, and substance use have been inconsistent and contradictory.2
Age of onset. Recent studies examining bipolar disorder’s age of onset have contradicted earlier rapid-cycling literature. In two large studies, Schneck et al3 and Coryell et al4 found rapid cycling associated with early onset of bipolar illness. The authors note that high rates of rapid cycling in children and adolescents resemble adult rapid cycling and speculate that early-onset bipolar illness might lead to rapid cycling vulnerability.5
Rapid cycling—defined in DSM-IV-TR as four or more depressive, manic, hypomanic, or mixed episodes in the previous 12 months—is considered a longitudinal course specifier for bipolar I or II disorder.1 Episodes must be demarcated by:
- full or partial remission lasting at least 2 months
- or a switch to a mood state of opposite polarity.
Cycling variations include ultra-rapid (1 day to 1 week), ultra-ultra rapid or ultradian (<24 hours), and continuous (no euthymic periods between mood episodes). Rapid cycling occurs in an estimated 15% to 25% of patients with bipolar disorder,2 though psychiatrists in specialty and tertiary referral centers see higher percentages because of the illness’ refractory nature.
Transient vs persistent state. Rapid cycling is thought to be either a transient state in long-term bipolar illness or a more chronic expression of the illness. Several studies6,7 have described rapid cycling as a transient phenomenon, whereas others8-11 have found a more persistent rapid cycling course during follow-up. Interestingly, a recent study11 suggested the mood-cycle pattern may be the most important predictor of rapid cycling. Patients with a depression–hypomania/mania-euthymia course demonstrated more-persistent rapid cycling than did those with a hypomania/mania-depression-euthymia course.
Antidepressants. Antidepressants’ role in initiating or exacerbating rapid cycling also remains unclear. Wehr et al8 found that discontinuing antidepressants contributed to cycling cessation or slowing. However, two prospective studies by Coryell et al4 that controlled for major depression found no association between antidepressant use and rapid cycling.
More recently, Yildiz and Sachs12 found a possible gender-specific relationship between antidepressants and rapid cycling. Women exposed to antidepressants before their first hypomanic/manic episode were more likely to develop rapid cycling than women who were not so exposed. This association was not evident in men.
NO DEFINITIVE CHOICES
Any discussion of treating rapid-cycling bipolar disorder is based on limited data, as few prospective studies of this exclusive cohort exist. Many studies report on mixed cohorts of refractory bipolar patients that include rapid cyclers, but separate analyses of rapid-cycling subgroups are not usually reported. Notable exceptions are recent studies by Calabrese et al, which are discussed below.
Lithium. Dunner and Fieve13 were the first to suggest that rapid-cycling bipolar patients respond poorly to lithium maintenance monotherapy. Later studies, however, suggested that lithium could benefit rapid cyclers, primarily in reducing hypomanic or manic episodes.
Baldessarini et al10 found that lithium was less effective for rapid than nonrapid cyclers only in reducing recurrence of depressive episodes. Kukopulos et al14 reported that lithium response in rapid cyclers increased from 16% to 78% after antidepressants were stopped, suggesting that a positive response to lithium may require more limited antidepressant use (or patients not having been exposed to antidepressants at all).
Thus, lithium prophylaxis has at least partial efficacy in many rapid cyclers, especially when antidepressants are avoided.
Divalproex. As with lithium, divalproex sodium appears more effective in treating and preventing hypomanic/manic episodes than depressive episodes in bipolar patients with rapid-cycling illness. Six open studies showed that patients who had not responded to lithium tended to do better with divalproex.15
Calabrese et al then tested the hypothesis that rapid cycling predicts nonresponse to lithium and positive response to divalproex.16 In a randomized controlled trial, they enrolled 254 recently hypomanic/manic rapid-cycling outpatients in an open-label stabilization phase involving combination lithium and divalproex therapy. Stabilized patients were then randomized to monotherapy with lithium, serum level ≥ 0.8 mEq/L, or divalproex, serum level ≥ 50 mcg/mL. Only 60 patients (24%) met stability criteria for randomization, achieving a persistent bimodal response as measured by continuous weeks of:
- Hamilton depression scale (24-item) score ≤ 20
- Young Mania Rating Scale score ≤ 12.5
- Global Assessment Scale score ≥ 51.
Most nonresponse was attributed to refractory depression.
After 20 months of maintenance therapy, about one-half of patients relapsed on either monotherapy. In the survival analysis, the median time to any mood episode was 45 weeks with divalproex monotherapy and 18 weeks with lithium monotherapy, although this difference was not statistically significant. The small sample size and high dropout rate may have created a false-negative error in this study.
Thus, these data did not show divalproex monotherapy to be more effective than lithium monotherapy in managing rapid-cycling bipolar disorder. The combination proved more effective in treating mania than depression and superior to monotherapy. This finding underscores combination therapy’s importance and the need to use mood stabilizers that also treat the depressed phase of bipolar disorder in rapid cyclers.
Table
Clinical characteristics of rapid cycling
| Prevalence approximately 15% to 25% in patients with bipolar disorder |
| More common in women than men |
| More common with type II than type I bipolar disorder |
| Primarily a depressive disease |
| Low treatment response rates and high recurrence risk |
| Associated with antidepressant use in some cases |
Carbamazepine. Recent data refute earlier reports suggesting that rapid cycling predicted positive response to carbamazepine. Multiple open studies and four controlled studies suggest that carbamazepine—like lithium and divalproex—possesses moderate to marked efficacy in the hypomanic/manic phase but poor to moderate efficacy in the depressed phase of rapid-cycling bipolar disorder.17
Lamotrigine. Lamotrigine is the first mood-stabilizing agent that has shown efficacy in maintenance treatment of bipolar depression and rapid cycling. In a double-blind, prospective, placebo-controlled trial, Calabrese et al18 enrolled 324 rapid-cycling patients with bipolar disorder type I or II in an open-label stabilization phase with lamotrigine. The 182 stabilized patients were then randomly assigned to receive either lamotrigine (mean 288 +/- 94 mg/d) or placebo.
For 6 months, 41% of patients receiving lamotrigine and 26% of those receiving placebo remained stable without relapse (P = 0.03), although the difference was statistically significant only for the bipolar II subtype. Lamotrigine appeared most effective in patients with the biphasic pattern of depression-hypomania/mania-euthymia.
Topiramate. Most studies of topiramate in rapid cycling have been retrospective and/or small add-on studies to existing mood stabilizers, with topiramate use associated with moderately or markedly improved manic symptoms.19 Evidence supports further controlled investigations, particularly because topiramate’s weight-loss effects may help overweight or obese patients.
Gabapentin. Gabapentin’s efficacy in rapid cycling has not been established. Although open-label studies showed a 67% response rate when gabapentin was used as adjunctive therapy, two double-blind, placebocontrolled studies of bipolar patients failed to show efficacy.20,21
Atypical antipsychotics. Five atypical antipsychotics—aripiprazole, olanzapine, quetiapine, risperidone, and ziprasidone—are FDA-approved for treating acute mania. Olanzapine is also indicated for bipolar maintenance treatment and has the most data showing efficacy in rapid cycling:
- In a 3-week, placebo-controlled study of 139 patients with bipolar I acute mania, olanzapine (median modal 15 mg/d) reduced manic symptoms to a statistically significantly extent in the 45 rapid cyclers.22
- A long-term prospective study followed 23 patients—30% of whom were rapid cyclers—who used olanzapine (mean 8.2 mg/d) as an adjunct to mood stabilizers. Manic and depressive symptoms were reduced significantly in the cohort, which was followed for a mean of 303 days.23
- An 8-week, double-blind, placebo-controlled study24 compared olanzapine monotherapy with the olanzapine/fluoxetine combination (OFC) in 833 depressed bipolar I patients, of whom 315 (37%) had rapid cycling. Mean olanzapine dosage was 9.7 mg in monotherapy and 7.4 mg in combination therapy; mean fluoxetine dosage was 39.3 mg.
A follow-up analysis25 showed that rapid cyclers’ depressive symptoms improved rapidly, and this improvement was sustained with OFC but not olanzapine monotherapy. Nonrapid-cycling patients responded to both treatments.
Other atypicals have shown partial efficacy in rapid-cycling bipolar disorder, although the studies have had methodologic limitations. Suppes et al26 conducted the first controlled trial using clozapine as add-on therapy in a 1-year, randomized evaluation of 38 patients with treatment-refractory bipolar disorder. The 21 rapid cyclers received a mean peak of 234 mg/d. Brief Psychiatric Rating Scale and Clinical Global Improvement scores improved significantly overall, but data specific to the rapid-cycling patients were not reported.
Small, open-label studies using risperidone and quetiapine as adjuncts to mood stabilizers have shown modest efficacy in rapid cycling, usually in treating manic symptoms. A recent 8-week, double-blind, placebo-controlled trial of quetiapine in bipolar depression showed promising results, though its efficacy in rapid cycling was not reported.27
RECOMMENDED TREATMENT
Because coincidental cycling may give the false appearance of efficacy in the short term, we recommend that you treat rapid cyclers methodically and judge outcomes over several months or cycle-lengths. A general approach includes:
- identify and treat underlying medical illnesses, such as hypothyroidism
- identify and treat comorbid alcohol/drug abuse
- taper or discontinue cycle-inducing agents such as antidepressants or sympathomimetics
- use standard mood stabilizers and/or atypical antipsychotics alone or in combination (Algorithm).
Algorithm Managing manic and depressive phases of rapid-cycling bipolar disorder
Treating acute mania in rapid-cycling patients is similar to managing this phase in nonrapid cyclers. First-tier therapy includes established mood stabilizers such as lithium, divalproex, or atypical antipsychotics. Carbamazepine is usually considered second-tier because of its effects on other medications via cytochrome P-450 system induction, and limited data exist on oxcarbazepine’s efficacy. Lamotrigine has not been proven effective in acute mania. If monotherapy is ineffective, try combinations of mood stabilizers and/or atypical antipsychotics.
Treating the depressed phase in rapid cyclers is far more difficult than treating acute mania and may depend on bipolar subtype:
- Bipolar I patients likely will require one or more mood stabilizers (such as lithium, divalproex, olanzapine) plus add-on lamotrigine.
- Bipolar II patients may benefit from lamotrigine alone.
- Atypical antipsychotics that have putative antidepressant effects without apparent cycle-accelerating effects may also be considered. At this time, olanzapine has the most data.
Given depression’s refractory nature in rapid-cycling bipolar illness, you may need to combine any of the above medications, try electroconvulsive therapy, or use more-experimental strategies such as:
- omega-3 fatty acids
- donepezil
- pramipexole
- high-dose levothyroxine/T4.
Antidepressants. Before using antidepressants to treat bipolar depression, consider carefully the risk of initiating or exacerbating rapid cycling. No definitive evidence is available to guide your decision.
Likewise, the optimal duration of antidepressant treatment is unclear, although tapering the antidepressant as tolerated may be prudent after depressive symptoms are in remission.
Psychosocial interventions. Finally, don’t overlook psychosocial interventions. Bipolar-specific psychotherapies can enhance compliance, lessen depression, and improve treatment response.28
CONCLUSION
Standard mood stabilizers appear to show partial efficacy in rapid cycling’s hypomanic/manic phase but only modest efficacy in the depressed phase. Lamotrigine appears more-promising in treating depressive than acute manic episodes and may be particularly effective for bipolar II patients. Evidence is growing that atypical antipsychotics also have partial efficacy in treating rapid cyclers, though whether this effect is phase-specific is unclear. As no single agent provides ideal bimodal treatment, combination therapy is recommended.
Related resources
- Bipolar Clinic and Research Program. Massachusetts General Hospital. Includes tools for clinicians and the clinical site for the Systematic Treatment Enhancement Program for Bipolar Disorder (STEP-BD). www.manicdepressive.org. Accessed Oct. 14, 2004.
- Goodwin FK, Jamison KR. Manic-depressive illness. New York: Oxford University Press, 1990.
- Marneros A, Goodwin FK (eds). Bipolar disorders: Mixed states, rapid cycling and atypical bipolar disorder. Cambridge, UK: Cambridge University Press (in press).
Drug brand names
- Aripiprazole • Abilify
- Carbamazepine • Carbatrol, others
- Clozapine • Clozaril
- Donepezil • Aricept
- Divalproex sodium • Depakote
- Gabapentin • Neurontin
- Lamotrigine • Lamictal
- Levothyroxine • Synthroid, others
- Lithium • Lithobid, others
- Olanzapine • Zyprexa
- Olanzapine/fluoxetine • Symbyax
- Oxcarbazepine • Trileptal
- Pramipexole • Mirapex
- Quetiapine • Seroquel
- Risperidone • Risperdal
- Topiramate • Topamax
- Ziprasidone • Geodon
Disclosures
Dr. Altman is a speaker for Forest Pharmaceuticals, Janssen Pharmaceutica, AstraZeneca Pharmaceuticals, and Abbott Laboratories.
Dr. Schneck is a consultant to AstraZeneca Pharmaceuticals, UCB Pharma, and Bristol-Myers Squibb Co. and a speaker for AstraZeneca Pharmaceuticals.
Rapid-cycling bipolar disorder is a moving target, with treatment-resistant depression recurring frequently and alternating with hypomanic/manic episodes (Box).1,2 Can one medication adequately treat these complicated patients, or is combination therapy necessary? If more than one medication is needed, are some combinations more effective than others?
This article attempts to answer these questions by:
- discussing recent treatment trial results
- suggesting an algorithm for managing hypomanic/manic and depressive episodes in rapid-cycling patients with bipolar disorder types I or II.
CLINICAL CHARACTERISTICS
Rapid cycling is associated most consistently with female gender and bipolar II disorder2 (Table); why these two groups are primarily affected is unknown. Results of studies linking rapid cycling with hypothyroidism, gonadal steroid effects, family history, and substance use have been inconsistent and contradictory.2
Age of onset. Recent studies examining bipolar disorder’s age of onset have contradicted earlier rapid-cycling literature. In two large studies, Schneck et al3 and Coryell et al4 found rapid cycling associated with early onset of bipolar illness. The authors note that high rates of rapid cycling in children and adolescents resemble adult rapid cycling and speculate that early-onset bipolar illness might lead to rapid cycling vulnerability.5
Rapid cycling—defined in DSM-IV-TR as four or more depressive, manic, hypomanic, or mixed episodes in the previous 12 months—is considered a longitudinal course specifier for bipolar I or II disorder.1 Episodes must be demarcated by:
- full or partial remission lasting at least 2 months
- or a switch to a mood state of opposite polarity.
Cycling variations include ultra-rapid (1 day to 1 week), ultra-ultra rapid or ultradian (<24 hours), and continuous (no euthymic periods between mood episodes). Rapid cycling occurs in an estimated 15% to 25% of patients with bipolar disorder,2 though psychiatrists in specialty and tertiary referral centers see higher percentages because of the illness’ refractory nature.
Transient vs persistent state. Rapid cycling is thought to be either a transient state in long-term bipolar illness or a more chronic expression of the illness. Several studies6,7 have described rapid cycling as a transient phenomenon, whereas others8-11 have found a more persistent rapid cycling course during follow-up. Interestingly, a recent study11 suggested the mood-cycle pattern may be the most important predictor of rapid cycling. Patients with a depression–hypomania/mania-euthymia course demonstrated more-persistent rapid cycling than did those with a hypomania/mania-depression-euthymia course.
Antidepressants. Antidepressants’ role in initiating or exacerbating rapid cycling also remains unclear. Wehr et al8 found that discontinuing antidepressants contributed to cycling cessation or slowing. However, two prospective studies by Coryell et al4 that controlled for major depression found no association between antidepressant use and rapid cycling.
More recently, Yildiz and Sachs12 found a possible gender-specific relationship between antidepressants and rapid cycling. Women exposed to antidepressants before their first hypomanic/manic episode were more likely to develop rapid cycling than women who were not so exposed. This association was not evident in men.
NO DEFINITIVE CHOICES
Any discussion of treating rapid-cycling bipolar disorder is based on limited data, as few prospective studies of this exclusive cohort exist. Many studies report on mixed cohorts of refractory bipolar patients that include rapid cyclers, but separate analyses of rapid-cycling subgroups are not usually reported. Notable exceptions are recent studies by Calabrese et al, which are discussed below.
Lithium. Dunner and Fieve13 were the first to suggest that rapid-cycling bipolar patients respond poorly to lithium maintenance monotherapy. Later studies, however, suggested that lithium could benefit rapid cyclers, primarily in reducing hypomanic or manic episodes.
Baldessarini et al10 found that lithium was less effective for rapid than nonrapid cyclers only in reducing recurrence of depressive episodes. Kukopulos et al14 reported that lithium response in rapid cyclers increased from 16% to 78% after antidepressants were stopped, suggesting that a positive response to lithium may require more limited antidepressant use (or patients not having been exposed to antidepressants at all).
Thus, lithium prophylaxis has at least partial efficacy in many rapid cyclers, especially when antidepressants are avoided.
Divalproex. As with lithium, divalproex sodium appears more effective in treating and preventing hypomanic/manic episodes than depressive episodes in bipolar patients with rapid-cycling illness. Six open studies showed that patients who had not responded to lithium tended to do better with divalproex.15
Calabrese et al then tested the hypothesis that rapid cycling predicts nonresponse to lithium and positive response to divalproex.16 In a randomized controlled trial, they enrolled 254 recently hypomanic/manic rapid-cycling outpatients in an open-label stabilization phase involving combination lithium and divalproex therapy. Stabilized patients were then randomized to monotherapy with lithium, serum level ≥ 0.8 mEq/L, or divalproex, serum level ≥ 50 mcg/mL. Only 60 patients (24%) met stability criteria for randomization, achieving a persistent bimodal response as measured by continuous weeks of:
- Hamilton depression scale (24-item) score ≤ 20
- Young Mania Rating Scale score ≤ 12.5
- Global Assessment Scale score ≥ 51.
Most nonresponse was attributed to refractory depression.
After 20 months of maintenance therapy, about one-half of patients relapsed on either monotherapy. In the survival analysis, the median time to any mood episode was 45 weeks with divalproex monotherapy and 18 weeks with lithium monotherapy, although this difference was not statistically significant. The small sample size and high dropout rate may have created a false-negative error in this study.
Thus, these data did not show divalproex monotherapy to be more effective than lithium monotherapy in managing rapid-cycling bipolar disorder. The combination proved more effective in treating mania than depression and superior to monotherapy. This finding underscores combination therapy’s importance and the need to use mood stabilizers that also treat the depressed phase of bipolar disorder in rapid cyclers.
Table
Clinical characteristics of rapid cycling
| Prevalence approximately 15% to 25% in patients with bipolar disorder |
| More common in women than men |
| More common with type II than type I bipolar disorder |
| Primarily a depressive disease |
| Low treatment response rates and high recurrence risk |
| Associated with antidepressant use in some cases |
Carbamazepine. Recent data refute earlier reports suggesting that rapid cycling predicted positive response to carbamazepine. Multiple open studies and four controlled studies suggest that carbamazepine—like lithium and divalproex—possesses moderate to marked efficacy in the hypomanic/manic phase but poor to moderate efficacy in the depressed phase of rapid-cycling bipolar disorder.17
Lamotrigine. Lamotrigine is the first mood-stabilizing agent that has shown efficacy in maintenance treatment of bipolar depression and rapid cycling. In a double-blind, prospective, placebo-controlled trial, Calabrese et al18 enrolled 324 rapid-cycling patients with bipolar disorder type I or II in an open-label stabilization phase with lamotrigine. The 182 stabilized patients were then randomly assigned to receive either lamotrigine (mean 288 +/- 94 mg/d) or placebo.
For 6 months, 41% of patients receiving lamotrigine and 26% of those receiving placebo remained stable without relapse (P = 0.03), although the difference was statistically significant only for the bipolar II subtype. Lamotrigine appeared most effective in patients with the biphasic pattern of depression-hypomania/mania-euthymia.
Topiramate. Most studies of topiramate in rapid cycling have been retrospective and/or small add-on studies to existing mood stabilizers, with topiramate use associated with moderately or markedly improved manic symptoms.19 Evidence supports further controlled investigations, particularly because topiramate’s weight-loss effects may help overweight or obese patients.
Gabapentin. Gabapentin’s efficacy in rapid cycling has not been established. Although open-label studies showed a 67% response rate when gabapentin was used as adjunctive therapy, two double-blind, placebocontrolled studies of bipolar patients failed to show efficacy.20,21
Atypical antipsychotics. Five atypical antipsychotics—aripiprazole, olanzapine, quetiapine, risperidone, and ziprasidone—are FDA-approved for treating acute mania. Olanzapine is also indicated for bipolar maintenance treatment and has the most data showing efficacy in rapid cycling:
- In a 3-week, placebo-controlled study of 139 patients with bipolar I acute mania, olanzapine (median modal 15 mg/d) reduced manic symptoms to a statistically significantly extent in the 45 rapid cyclers.22
- A long-term prospective study followed 23 patients—30% of whom were rapid cyclers—who used olanzapine (mean 8.2 mg/d) as an adjunct to mood stabilizers. Manic and depressive symptoms were reduced significantly in the cohort, which was followed for a mean of 303 days.23
- An 8-week, double-blind, placebo-controlled study24 compared olanzapine monotherapy with the olanzapine/fluoxetine combination (OFC) in 833 depressed bipolar I patients, of whom 315 (37%) had rapid cycling. Mean olanzapine dosage was 9.7 mg in monotherapy and 7.4 mg in combination therapy; mean fluoxetine dosage was 39.3 mg.
A follow-up analysis25 showed that rapid cyclers’ depressive symptoms improved rapidly, and this improvement was sustained with OFC but not olanzapine monotherapy. Nonrapid-cycling patients responded to both treatments.
Other atypicals have shown partial efficacy in rapid-cycling bipolar disorder, although the studies have had methodologic limitations. Suppes et al26 conducted the first controlled trial using clozapine as add-on therapy in a 1-year, randomized evaluation of 38 patients with treatment-refractory bipolar disorder. The 21 rapid cyclers received a mean peak of 234 mg/d. Brief Psychiatric Rating Scale and Clinical Global Improvement scores improved significantly overall, but data specific to the rapid-cycling patients were not reported.
Small, open-label studies using risperidone and quetiapine as adjuncts to mood stabilizers have shown modest efficacy in rapid cycling, usually in treating manic symptoms. A recent 8-week, double-blind, placebo-controlled trial of quetiapine in bipolar depression showed promising results, though its efficacy in rapid cycling was not reported.27
RECOMMENDED TREATMENT
Because coincidental cycling may give the false appearance of efficacy in the short term, we recommend that you treat rapid cyclers methodically and judge outcomes over several months or cycle-lengths. A general approach includes:
- identify and treat underlying medical illnesses, such as hypothyroidism
- identify and treat comorbid alcohol/drug abuse
- taper or discontinue cycle-inducing agents such as antidepressants or sympathomimetics
- use standard mood stabilizers and/or atypical antipsychotics alone or in combination (Algorithm).
Algorithm Managing manic and depressive phases of rapid-cycling bipolar disorder
Treating acute mania in rapid-cycling patients is similar to managing this phase in nonrapid cyclers. First-tier therapy includes established mood stabilizers such as lithium, divalproex, or atypical antipsychotics. Carbamazepine is usually considered second-tier because of its effects on other medications via cytochrome P-450 system induction, and limited data exist on oxcarbazepine’s efficacy. Lamotrigine has not been proven effective in acute mania. If monotherapy is ineffective, try combinations of mood stabilizers and/or atypical antipsychotics.
Treating the depressed phase in rapid cyclers is far more difficult than treating acute mania and may depend on bipolar subtype:
- Bipolar I patients likely will require one or more mood stabilizers (such as lithium, divalproex, olanzapine) plus add-on lamotrigine.
- Bipolar II patients may benefit from lamotrigine alone.
- Atypical antipsychotics that have putative antidepressant effects without apparent cycle-accelerating effects may also be considered. At this time, olanzapine has the most data.
Given depression’s refractory nature in rapid-cycling bipolar illness, you may need to combine any of the above medications, try electroconvulsive therapy, or use more-experimental strategies such as:
- omega-3 fatty acids
- donepezil
- pramipexole
- high-dose levothyroxine/T4.
Antidepressants. Before using antidepressants to treat bipolar depression, consider carefully the risk of initiating or exacerbating rapid cycling. No definitive evidence is available to guide your decision.
Likewise, the optimal duration of antidepressant treatment is unclear, although tapering the antidepressant as tolerated may be prudent after depressive symptoms are in remission.
Psychosocial interventions. Finally, don’t overlook psychosocial interventions. Bipolar-specific psychotherapies can enhance compliance, lessen depression, and improve treatment response.28
CONCLUSION
Standard mood stabilizers appear to show partial efficacy in rapid cycling’s hypomanic/manic phase but only modest efficacy in the depressed phase. Lamotrigine appears more-promising in treating depressive than acute manic episodes and may be particularly effective for bipolar II patients. Evidence is growing that atypical antipsychotics also have partial efficacy in treating rapid cyclers, though whether this effect is phase-specific is unclear. As no single agent provides ideal bimodal treatment, combination therapy is recommended.
Related resources
- Bipolar Clinic and Research Program. Massachusetts General Hospital. Includes tools for clinicians and the clinical site for the Systematic Treatment Enhancement Program for Bipolar Disorder (STEP-BD). www.manicdepressive.org. Accessed Oct. 14, 2004.
- Goodwin FK, Jamison KR. Manic-depressive illness. New York: Oxford University Press, 1990.
- Marneros A, Goodwin FK (eds). Bipolar disorders: Mixed states, rapid cycling and atypical bipolar disorder. Cambridge, UK: Cambridge University Press (in press).
Drug brand names
- Aripiprazole • Abilify
- Carbamazepine • Carbatrol, others
- Clozapine • Clozaril
- Donepezil • Aricept
- Divalproex sodium • Depakote
- Gabapentin • Neurontin
- Lamotrigine • Lamictal
- Levothyroxine • Synthroid, others
- Lithium • Lithobid, others
- Olanzapine • Zyprexa
- Olanzapine/fluoxetine • Symbyax
- Oxcarbazepine • Trileptal
- Pramipexole • Mirapex
- Quetiapine • Seroquel
- Risperidone • Risperdal
- Topiramate • Topamax
- Ziprasidone • Geodon
Disclosures
Dr. Altman is a speaker for Forest Pharmaceuticals, Janssen Pharmaceutica, AstraZeneca Pharmaceuticals, and Abbott Laboratories.
Dr. Schneck is a consultant to AstraZeneca Pharmaceuticals, UCB Pharma, and Bristol-Myers Squibb Co. and a speaker for AstraZeneca Pharmaceuticals.
1. American Psychiatric Association. Diagnostic and statistical manual of mental disorders (4th ed, text rev). Washington, DC: American Psychiatric Association, 2000.
2. Kupka RW, Luckenbaugh DA, Post RM, et al. Rapid and non-rapid cycling bipolar disorder: a meta-analysis of clinical studies. J Clin Psychiatry 2003;64(12):1483-94.
3. Schneck CD, Miklowitz DJ, Calabrese JR, et al. Phenomenology of rapid cycling bipolar disorder: data from the first 500 participants in the Systematic Treatment Enhancement Program. Am J Psychiatry 2004;161(10):1902-8.
4. Coryell W, Solomon D, Turvey C, et al. The long-term course of rapid-cycling bipolar disorder. Arch Gen Psychiatry 2003;60(9):914-20.
5. Findling RL, Gracious BL, McNamara NK, et al. Rapid, continuous cycling and psychiatric comorbidity in pediatric bipolar I disorder. Bipolar Disord 2001;3:202-10.
6. Coryell W, Endicott J, Keller M. Rapidly cycling affective disorder. Demographics, diagnosis, family history, and course. Arch Gen Psychiatry 1992;49:126-31.
7. Maj M, Magliano L, Pirozzi R, et al. Validity of rapid cycling as a course specifier for bipolar disorder. Am J Psychiatry 1994;151:1015-19.
8. Wehr TA, Sack DA, Rosenthal NE, Cowdry RW. Rapid cycling affective disorder: contributing factors and treatment responses in 51 patients. Am J Psychiatry 1988;145:179-84.
9. Bauer MS, Calabrese J, Dunner DL, et al. Multisite data reanalysis of the validity of rapid cycling as a course modifier for bipolar disorder in DSM-IV. Am J Psychiatry 1994;151:506-15.
10. Baldessarini RJ, Tondo L, Floris G, Hennen J. Effects of rapid cycling on response to lithium maintenance treatment in 360 bipolar I and II disorder patients. J Affect Disord 2000;61:13-22.
11. Koukopoulos A, Sani G, Koukopoulos AE, et al. Duration and stability of the rapid-cycling course: a long-term personal follow-up of 109 patients. J Affect Disord 2003;73:75-85.
12. Yildiz A, Sachs GS. Do antidepressants induce rapid cycling? A gender-specific association. J Clin Psychiatry 2003;64:814-18.
13. Dunner DL, Fieve RR. Clinical factors in lithium carbonate prophylaxis failure. Arch Gen Psychiatry 1974;30:229-33.
14. Kukopulos A, Reginaldi D, Laddomada P, et al. Course of the manic-depressive cycle and changes caused by treatments. Pharmakopsychiatr Neuropsychopharmakol 1980;13:156-67.
15. Calabrese JR, Woyshville MJ, Kimmel SE, Rapport DJ. Predictors of valproate response in bipolar rapid cycling. J Clin Psychopharmacol 1993;13:280-3.
16. Calabrese JR, Shelton M, Rapport DJ, et al. A double-blind 20 month maintenance study of lithium vs. divalproex in rapid-cycling bipolar disorder [presentation]. Pittsburgh, PA: Fifth International Conference on Bipolar Disorder, June 12-14, 2003.
17. Calabrese JR, Bowden C, Woyshville MJ. Lithium and anticonvulsants in the treatment of bipolar disorders. In: Bloom E, Kupfer D (eds). Psychopharmacology: The third generation of progress. New York: Raven Press, 1995;1099-1112.
18. Calabrese JR, Suppes T, Bowden CL, et al. A double-blind, placebo-controlled, prophylaxis study of lamotrigine in rapid-cycling bipolar disorder. J Clin Psychiatry 2000;61(11):841-50.
19. Marcotte D. Use of topiramate, a new anti-epileptic as a mood stabilizer. J Affect Disord 1998;50(2-3):245-51.
20. Pande AC, Crockatt JG, Janney CA, et al. Gabapentin in bipolar disorder: a placebo-controlled trial of adjunctive therapy. Gabapentin Bipolar Disorder Study Group. Bipolar Disord 2000;2(3 pt 2):249-55.
21. Frye MA, Ketter TA, Kimbrell TA, et al. A placebo-controlled study of lamotrigine and gabapentin monotherapy in refractory mood disorders. J Clin Psychopharmacol 2000;20(6):607-14.
22. Sanger TM, Tohen M, Vieta E, et al. Olanzapine in the acute treatment of bipolar I disorder with a history of rapid cycling. J Affect Disord 2003;73:155-61.
23. Calabrese JR, Kasper S, Johnson G, et al. International consensus group on bipolar I depression treatment guidelines. J Clin Psychiatry 2004;65:569-79.
24. Tohen M, Vieta E, Calabrese J, et al. Efficacy of olanzapine and olanzapine-fluoxetine combination in the treatment of bipolar I depression. Arch Gen Psychiatry 2003;60:1079-88.
25. Keck P, Corya S, Andersen SW, et al. Analysis of olanzapine/fluoxetine combination in the treatment of rapid-cycling bipolar depression [presentation]. Boca Raton, FL: New Clinical Drug Evaluation Unit, 2003.
26. Suppes T, Webb A, Paul B, et al. Clinical outcome in a randomized 1-year trial of clozapine versus treatment as usual for patients with treatment-resistant illness and a history of mania. Am J Psychiatry 1999;156:1164-9.
27. Calabrese JR, Macfadden W, McCoy R, et al. Double-blind, placebo-controlled study of quetiapine in bipolar depression [presentation]. Phoenix, AZ: New Clinical Drug Evaluation Unit, 2004.
28. Craighead WE, Miklowitz DJ. Psychosocial interventions for bipolar disorder. J Clin Psychiatry 2000;61(suppl 13):58-64.
1. American Psychiatric Association. Diagnostic and statistical manual of mental disorders (4th ed, text rev). Washington, DC: American Psychiatric Association, 2000.
2. Kupka RW, Luckenbaugh DA, Post RM, et al. Rapid and non-rapid cycling bipolar disorder: a meta-analysis of clinical studies. J Clin Psychiatry 2003;64(12):1483-94.
3. Schneck CD, Miklowitz DJ, Calabrese JR, et al. Phenomenology of rapid cycling bipolar disorder: data from the first 500 participants in the Systematic Treatment Enhancement Program. Am J Psychiatry 2004;161(10):1902-8.
4. Coryell W, Solomon D, Turvey C, et al. The long-term course of rapid-cycling bipolar disorder. Arch Gen Psychiatry 2003;60(9):914-20.
5. Findling RL, Gracious BL, McNamara NK, et al. Rapid, continuous cycling and psychiatric comorbidity in pediatric bipolar I disorder. Bipolar Disord 2001;3:202-10.
6. Coryell W, Endicott J, Keller M. Rapidly cycling affective disorder. Demographics, diagnosis, family history, and course. Arch Gen Psychiatry 1992;49:126-31.
7. Maj M, Magliano L, Pirozzi R, et al. Validity of rapid cycling as a course specifier for bipolar disorder. Am J Psychiatry 1994;151:1015-19.
8. Wehr TA, Sack DA, Rosenthal NE, Cowdry RW. Rapid cycling affective disorder: contributing factors and treatment responses in 51 patients. Am J Psychiatry 1988;145:179-84.
9. Bauer MS, Calabrese J, Dunner DL, et al. Multisite data reanalysis of the validity of rapid cycling as a course modifier for bipolar disorder in DSM-IV. Am J Psychiatry 1994;151:506-15.
10. Baldessarini RJ, Tondo L, Floris G, Hennen J. Effects of rapid cycling on response to lithium maintenance treatment in 360 bipolar I and II disorder patients. J Affect Disord 2000;61:13-22.
11. Koukopoulos A, Sani G, Koukopoulos AE, et al. Duration and stability of the rapid-cycling course: a long-term personal follow-up of 109 patients. J Affect Disord 2003;73:75-85.
12. Yildiz A, Sachs GS. Do antidepressants induce rapid cycling? A gender-specific association. J Clin Psychiatry 2003;64:814-18.
13. Dunner DL, Fieve RR. Clinical factors in lithium carbonate prophylaxis failure. Arch Gen Psychiatry 1974;30:229-33.
14. Kukopulos A, Reginaldi D, Laddomada P, et al. Course of the manic-depressive cycle and changes caused by treatments. Pharmakopsychiatr Neuropsychopharmakol 1980;13:156-67.
15. Calabrese JR, Woyshville MJ, Kimmel SE, Rapport DJ. Predictors of valproate response in bipolar rapid cycling. J Clin Psychopharmacol 1993;13:280-3.
16. Calabrese JR, Shelton M, Rapport DJ, et al. A double-blind 20 month maintenance study of lithium vs. divalproex in rapid-cycling bipolar disorder [presentation]. Pittsburgh, PA: Fifth International Conference on Bipolar Disorder, June 12-14, 2003.
17. Calabrese JR, Bowden C, Woyshville MJ. Lithium and anticonvulsants in the treatment of bipolar disorders. In: Bloom E, Kupfer D (eds). Psychopharmacology: The third generation of progress. New York: Raven Press, 1995;1099-1112.
18. Calabrese JR, Suppes T, Bowden CL, et al. A double-blind, placebo-controlled, prophylaxis study of lamotrigine in rapid-cycling bipolar disorder. J Clin Psychiatry 2000;61(11):841-50.
19. Marcotte D. Use of topiramate, a new anti-epileptic as a mood stabilizer. J Affect Disord 1998;50(2-3):245-51.
20. Pande AC, Crockatt JG, Janney CA, et al. Gabapentin in bipolar disorder: a placebo-controlled trial of adjunctive therapy. Gabapentin Bipolar Disorder Study Group. Bipolar Disord 2000;2(3 pt 2):249-55.
21. Frye MA, Ketter TA, Kimbrell TA, et al. A placebo-controlled study of lamotrigine and gabapentin monotherapy in refractory mood disorders. J Clin Psychopharmacol 2000;20(6):607-14.
22. Sanger TM, Tohen M, Vieta E, et al. Olanzapine in the acute treatment of bipolar I disorder with a history of rapid cycling. J Affect Disord 2003;73:155-61.
23. Calabrese JR, Kasper S, Johnson G, et al. International consensus group on bipolar I depression treatment guidelines. J Clin Psychiatry 2004;65:569-79.
24. Tohen M, Vieta E, Calabrese J, et al. Efficacy of olanzapine and olanzapine-fluoxetine combination in the treatment of bipolar I depression. Arch Gen Psychiatry 2003;60:1079-88.
25. Keck P, Corya S, Andersen SW, et al. Analysis of olanzapine/fluoxetine combination in the treatment of rapid-cycling bipolar depression [presentation]. Boca Raton, FL: New Clinical Drug Evaluation Unit, 2003.
26. Suppes T, Webb A, Paul B, et al. Clinical outcome in a randomized 1-year trial of clozapine versus treatment as usual for patients with treatment-resistant illness and a history of mania. Am J Psychiatry 1999;156:1164-9.
27. Calabrese JR, Macfadden W, McCoy R, et al. Double-blind, placebo-controlled study of quetiapine in bipolar depression [presentation]. Phoenix, AZ: New Clinical Drug Evaluation Unit, 2004.
28. Craighead WE, Miklowitz DJ. Psychosocial interventions for bipolar disorder. J Clin Psychiatry 2000;61(suppl 13):58-64.
Acute bipolar mania: Aggressive initial dosing provides faster symptom relief
Evidence on aggressive initial dosing of mood stabilizers and antipsychotics is changing the way acute bipolar mania is treated. To help you apply this information, we searched the literature and meeting abstracts for aggressive strategies tested to date. This article discusses how to:
- identify patients who may benefit from loading or aggressive initial dosing
- calculate mood stabilizer dosages
- dose each atypical antipsychotic
- manage potential antipsychotic side effects during maintenance therapy.
PATIENT SELECTION
Rapidly achieving therapeutic blood levels relieves patient suffering faster than standard titration. It quickly calms the hyperactivity, impulsivity, tension, hostility, and uncooperativeness that distress patients and increase the risk of harm to themselves and others.
The challenge of using higher dosages is to minimize side effects. Loading is not a one-size-fits-all approach, as antimanic drugs’ unique pharmacokinetic and pharmacotherapeutic properties influence how each agent is used.
An interesting body of literature advocates using mood stabilizers plus antipsychotics to treat mania, suggesting greater efficacy than with either agent alone.16 This strategy raises important questions, such as:
- Can two drugs be loaded simultaneously?
- Can patients taking mood stabilizers be treated with antipsychotic loading, and can those taking antipsychotics receive loading dosages of mood stabilizers?
- Would “double loading” improve bipolar mania treatment?
Answers to these questions are needed because of increased demands on clinicians to control hospital costs by rapidly and effectively treating patients with bipolar mania.
Loading doses cannot be standardized but are calculated by multiplying target steady-state plasma concentration by volume of distribution. We suggest aggressive initial schedules for divalproex sodium and atypical antipsychotics in this article with the understanding that practitioners will adjust them based on each patient’s tolerance and response.
Hospitalization. Patients with acute bipolar mania should be supervised closely in the hospital during loading or aggressive initial dosing. Monitor for cardiovascular changes, neurologic disturbances, sensorium changes, and response.
Precautions. Not all patients are candidates for aggressive initial dosing. Contraindications include age <18 or >65 years, pregnancy, breast-feeding, medical illness, and known sensitivity to the medication being given.
Higher-than-usual dosing increases the risk of excessive drug concentrations in sensitive individuals—such as those with a history of sensitivity to lower dosages of similar medications—and toxic levels of drugs with long half-lives can persist. When in doubt, consider giving a smaller amount of the loading dose early in the day, followed later by a larger amount.
DRUG SELECTION
Loading and aggressive initial dosing strategies for bipolar mania were first advanced for divalproex sodium.1 Investigators then examined loading strategies for lithium and carbamazepine, as well as the antipsychotics olanzapine, risperidone, quetiapine, ziprasidone, and aripiprazole, which are known to have antimanic properties.
Olanzapine, quetiapine, and risperidone are FDA-approved for short-term treatment of acute manic episodes associated with bipolar I disorder, and similar indications were being considered for aripiprazole and ziprasidone as this article went to press. We discuss evidence on loading and aggressive initial dosing strategies for each agent.
No studies have compared one loading strategy with another. Thus, when we choose drugs for loading, we consider what each patient needs, available formulations, tolerability, and efficacy for long-term stabilization and maintenance treatment.
LITHIUM
Lithium loading targets the therapeutic range (<1.4 mEq/L), without crossing the toxic threshold (>1.5 mEq/L). Lithium loading has shown antimanic effects, although using >30 mg/kg/d causes severe nausea and vomiting.
Moscovich et al2 reported a case series of 9 adults with acute mania who received lithium loading dosages of 4,050 mg/d. Patients tolerated lithium well at plasma drug levels of approximately 1.2 to 1.4 mEq/L. Their manic symptoms declined significantly within 4 to 5 days, as measured by Clinical Global Impression (CGI) severity of illness, Biegel-Murphy Mania State Rating Scale, and Brief Psychiatric Rating Scale scores.
Table 1
How to calculate divalproex loading for acute bipolar mania*
| Days 1 and 2 |
| Patient weight in pounds x 15 = dosage (mg/d) (Example: 150 lbs x 15 = 1,750 mg/d) |
| Days 3 to 10 |
| Patient weight in pounds x 10 = dosage (mg/d) (Example: 150 lbs. x 10 = 1,500 mg/d) |
| To avoid splitting tablets, make dosage divisible by 125 (round up for young adults, round down for older adults). Divide into bid or tid doses for improved tolerability. |
| Days 4 and 7 |
| Draw blood to monitor valproic acid levels and for other values such as liver function studies. |
| * For use with oral divalproex sodium (delayed-release or extended-release formulations). Do not use valproic acid preparations, as loading is unlikely to be well tolerated. |
| Source: Reference 5 |
Kook et al3 attempted a 30-mg/kg loading dose of slow-release lithium carbonate in 38 patients to evaluate the safety of achieving a therapeutic level in 12 hours. No patient experienced adverse effects during loading or in the 12 hours after loading was completed.
Patients who develop a manic episode while taking lithium pose a therapeutic dilemma. If they stop taking lithium—especially abruptly—manic symptoms can return in as few as 2 days. For these patients, consider increasing the usual dosage by 50% to 100% on the first day of mania treatment,4 then continue a dosage that maintains efficacy and achieves a therapeutic blood level.
To avoid GI upset, avoid any single dose of >1,500 mg; if a greater dosage is needed, divide it for improved tolerance. Obtain lithium blood levels at baseline, after 4 days, and thereafter as clinically relevant to monitor for drug interactions that may affect serum levels.
Side effects—GI irritation, tremor, muscle weakness, thirst, polyuria—are common in the first week, and weight gain may occur after prolonged treatment.
DIVALPROEX
In a study by Keck et al1 of 19 adults with acute bipolar mania, aggressive initial dosing of divalproex sodium, 20 mg/kg/d, was well-tolerated and shortened hospitalization. Side effects including sedation and nausea occurred at a rate similar to that seen with more-gradual titration.
To calculate the initial dose, the authors used a conversion factor of 20 mg/kg/d or added a zero to the patient’s weight in pounds. This amount was given in single or divided doses the first day, then continued for 4 to 7 days. Blood levels were measured on day 4, and all 15 patients who completed the study achieved serum valproate levels >50 mcg/mL.
In a double-blind study by Hirschfeld et al,5 59 adults with Young Mania Rating Scale (YMRS) scores >14 were randomly assigned to receive divalproex oral loading; divalproex nonloading (250 mg tid on days 1 and 2, followed by standard titration on days 3 to 10); or lithium carbonate (300 mg tid, followed by standard titration on days 3 to 10).
Divalproex loading—30 mg/kg/d on days 1 and 2, followed by 20 mg/kg on days 3 to 10— yielded valproate levels >50 mcg/mL in 84% of patients by day 3. Rapid loading appeared to increase antimanic efficacy, as measured by YMRS endpoint scores, without increasing adverse effects. For Table 1, we converted this study’s metric values to patient weight in pounds.
Side effects. Divalproex can inhibit metabolism of other drugs (including anticonvulsants such as lamotrigine) and increase their blood levels. Side effects such as sedation, alopecia, abdominal pain, diarrhea, and tremor may require observation and treatment. Pancreatitis, hepatitis, and allergic reactions are rare but may require discontinuation.
Recommendation. Aggressive initial dosing and loading for patients with acute mania has been reported with enteric-coated delayed-release and extended-release6 divalproex sodium tablets. With identical dosages, the extended-release form produces 11% lower serum levels than the delayed-release form.7
Aggressive dosing of oral valproic acid preparations is not recommended and is likely to be poorly tolerated.8 A pilot study evaluating IV valproate loading in acute mania found no changes in mania in the 2 hours that followed loading.9
CARBAMAZEPINE
Carbamazepine is used off-label to treat mania and mixed phases of bipolar disorder.4,9,10 Excessive absorption rates are associated with dizziness, ataxia, and nausea. Side effects may occur when the plasma level is therapeutic for epilepsy (4 to 12 mcg/mL).11
In mania, the relationship between carbamazepine levels and clinical response is not always clear. Lerer et al12 found a correlation between acute mania response and a serum level of 8.8 mcg/mL (range 4.7 to 14.0 mcg/mL).
Patients with acute mania may require 600 to 1,600 mg/d. Carbamazepine is available in immediate-release and controlled-release preparations. Because generic preparations might not be bio-equivalent,13 use the same formulation throughout treatment to maintain consistent serum levels.
Enzymatic auto-induction—in which carbamazepine gradually increases the activity of its metabolic enzyme—is likely to occur at 3 to 5 weeks of administration, often after hospital discharge. An aggressive initial rescue adjustment can be used if a patient develops mania after having been stabilized on carbamazepine for >6 weeks. Because these patients are past the point of auto-induction, a target blood level of 8.8 mcg/mL can be used and the dosage adjusted proportionally.
For example, if mania recurs in a patient who is stabilized on carbamazepine, 400 mg/d (plasma level 4.5 mcg/mL), carbamazepine can be loaded up to 800 mg/d. Measure the plasma level within 4 days; the target level would be 9.0 mcg/mL (2 times 4.5 mcg/mL), which closely approximates steady state and sets up a ratio to reach the target level of 8.8 mcg/mL.
Side effects include ataxia, diplopia, and dizziness. Complete blood counts, liver function studies, plasma levels, and serum chemistries require regular monitoring.
Recommendation. Carbamazepine is not recommended for oral loading in patients who have never taken it or for those with hyponatremia, hepatic dysfunction, or history of intolerance or agranulocytosis.
OLANZAPINE
Olanzapine has pharmacologic properties favorable for loading.4 The recommended dosage for acute mania is 15 mg/d with standard titration; Karagianis et al14 showed that initial loading doses of >20 mg/d resulted in good control of agitated patients with psychosis. Side effects were uncommon, with sedation occurring in 14% of patients in this case series. The loading dose reduced agitation more effectively than did dosages <20 mg/d given to similar patients.
A multicenter study of 148 acutely agitated inpatients with a variety of psychiatric disorders compared olanzapine rapid initial dose escalation with usual clinical practice.15 Mean aggressive dosages were 28.8 mg/d on day 1, 30.3 mg/d on day 2, and 16.1 mg/d on day 5. Usual-practice dosages were 10 mg/d, plus lorazepam, 0 to 4 mg/d for the first 2 days and 0 to 2 mg/d on days 3 to 4. Based on Positive and Negative Syndrome Scale excited component subscale scores, olanzapine loading controlled agitation more effectively than did usual practice, with similar side-effect rates.
IM olanzapine or the orally dissolving form are bioequivalent to the tablets and may be used for acute agitation associated with bipolar mania in certain clinical settings.14
Table 2
Suggested antipsychotic loading for acute bipolar mania and mixed states*
| Drug | Day(s) | Aggressive initial dosing schedule | Comment |
|---|---|---|---|
| Aripiprazole24,25 | 1 2 to 3 4+ | 30 mg once daily with food 30 mg/d with food Reduce dosage by 10 to 15 mg/d, based on tolerance and response | Nausea and vomiting may occur in first few days; adjust dosage based on tolerance and response |
| Olanzapine14,15 | 1 and 2 3 and 4 5 to 10 | 40 mg in single or divided dosage 20 to 30 mg at bedtime 15 mg once daily (may reduce to 5, 7.5, or 10 mg/d) | Adjust dosage based on tolerance and response; oral or IM formulations may be used |
| Quetiapine19,21 | 1 2 and 3 4 to 10 | 100 mg upon admission and 100 mg at bedtime 100 mg bid (or tid to qid) plus 100 to 200 mg at bedtime 200 mg bid plus 200 to 300 mg at bedtime; may adjust to 400 to 800 mg/d) | Adjust dosage based on tolerance and response |
| Risperidone16,18 | 1 2 3 and 4 | 3 mg in single or divided dosage 4 mg in single or divided dosage 5 mg in single or divided dosage | Adjust dosage by 1 mg up or down, based on tolerance and response; use tablet, rapid-dissolving tablet, or liquid form, but not long-acting IM form |
| Ziprasidone22,23 | 1 2 | 20 mg IM in single dose (may repeat for severe agitation) or 40 mg po bid with food 60 to 80 mg po bid with food | Adjust dosage based on tolerance and response |
| * For hospitalized or partially hospitalized patients, ages18. Not recommended for patients who are pregnant, breastfeeding, medically ill, age >65, or with known sensitivity to the antipsychotic being given. | |||
RISPERIDONE
Sachs et al16 studied 156 inpatients who developed an acute manic or mixed episode while receiving lithium or divalproex. These patients were randomly assigned to begin adjunctive risperidone, 2 mg/d, haloperidol, or placebo. Dosing was flexible, increasing or decreasing by 1 mg/d. Risperidone’s mean modal dosage was 3.8 mg/d across 3 weeks, with mean exposure of 17 days. Risperidone plus a mood stabilizer was more effective than a mood stabilizer alone, and the combination provided rapid, well-tolerated control of manic symptoms.
In a double-blind trial, Hirschfeld et al17 randomly assigned 279 patients with acute bipolar mania to risperidone, 1 to 6 mg/d, or placebo for 3 weeks. As early as day 3, YMRS scores were reduced significantly more with risperidone than with placebo. Somnolence was the most common side effect, and mean modal dosage was 4.1 mg/d.
Table 3
Screening schedule for antipsychotic side effects during bipolar maintenance treatment
| Baseline | |
| Side effect | Recommended screening |
| Weight gain | Weight and body mass index (BMI) monthly for first 3 months; waist circumference |
| Hypertension | Blood pressure |
| Hyperglycemia | Fasting plasma glucose, with glycosylated hemoglobin (Hb A 1c ) if hyperglycemia is detected |
| Hyperlipidemia | Fasting lipid profile |
| Tardive dyskinesia | Abnormal Involuntary Movement Scale (AIMS) or other screen |
| Ophthalmic changes | Ophthalmologic examination for patients taking quetiapine and for all with diabetes mellitus |
| Follow-up schedules | |
| 3 months | |
| Weight and BMI | |
| Blood pressure | |
| Fasting plasma glucose, with Hb A 1c if hyperglycemia is detected; Hb A 1c values may be used to measure interval changes in glucose tolerance | |
| Fasting lipid profile | |
| 6 months | |
| AIMS or other tardive dyskinesia screen | |
| Ophthalmologic examination | |
| Source: Adapted from reference 26. | |
In a multicenter, randomized, double-blind, placebo-controlled study of patients with acute bipolar mania, Khanna et al18 assigned patients to receive risperidone monotherapy (mean modal dosage 5.6 mg/d) or placebo for 3 weeks. Mania scores of patients receiving risperidone were significantly lower at weeks 1 and 2, compared with the placebo group. Risperidone was well-tolerated, with no unexpected adverse events.
Recommendation. Because of a risk of extrapyramidal symptoms (EPS) and orthostatic hypotension, initial risperidone loading dosages >4 mg on day 1 are not recommended.
QUETIAPINE
Quetiapine has shown antimanic efficacy as monotherapy and as adjunctive therapy to mood stabilizers.19,20 The effective dosage was a mean 600 mg/d (range 400 to 800 mg/d) in monotherapy and adjunctive treatment. These studies achieved 400 mg/d within the first 4 days (100 mg on day 1, 200 mg on day 2, 300 mg on day 3, and 400 mg on day 4).
These data combined with revised prescribing information suggest aggressive initial dose escalation of quetiapine within the first 4 days for selected patients. A titration study in patients with schizophrenia used a more-rapid escalation rate of 400 mg within 2 days.21 Dizziness, orthostatic hypotension, and sedation were not more frequent in this high-dose group than in the two lower-dose titration groups. In our experience, 200 to 400 mg can be given the first day of treatment.
ZIPRASIDONE
In a randomized, double-blind, controlled trial, Keck et al22 assigned 210 patients with a manic or mixed bipolar episode to 3 weeks of ziprasidone, 40 to 80 mg bid, or placebo. Ziprasidone produced rapid, sustained improvement in manic symptoms on all primary and most secondary efficacy measures, such as the YMRS and CGI.
Significant improvements seen within 2 days were maintained. Ziprasidone was well tolerated and was associated with a low EPS rate; neither weight gain nor clinically significant changes in vital signs were seen.
IM ziprasidone, which is approved for use in schizophrenia, may also have efficacy in bipolar mania.23 The recommended dose of 20 mg IM is equivalent to 120 to 160 mg orally, so a single injection may reach the target antimanic dosage.
Recommendation. Ziprasidone could be an option for aggressive initial dosing for a patient who has previously received ziprasidone IM and is not at risk for QTc prolongation.
ARIPIPRAZOLE
In a randomized controlled trial, Keck et al24 assigned 262 patients with acute bipolar mania or mixed states to aripiprazole, 30 mg/d, or placebo for 3 weeks. By day 4, manic symptoms were improved significantly more in patients receiving aripiprazole, and discontinuation rates were similar.
Similarly, in a randomized, controlled multi-center study, Sachs et al25 used 30 mg/d in 272 patients with bipolar mania or mixed states. Compared with placebo, aripiprazole produced significant improvement by day 4, with similar discontinuation rates.
Recommendation. Aggressive initial dosing of aripiprazole could be useful for a patient who does not require an IM or rapidly dissolvable medication.
Table 4
Suggested response to metabolic changes during bipolar maintenance therapy
| Metabolic change | Therapeutic action |
|---|---|
| ≥5% increase in total body weight | Consider weight-reduction strategies or medication adjustment |
| Fasting glucose: ≥126 mg/mL ≥300 mg/mL or ≤60 mg/mL | Consider evaluation for diabetes mellitus Seek immediate consultation |
| Total cholesterol ≥200 mg/dL or triglycerides ≥165 mg/dL | Consider lipid-lowering with dietary and/or medication changes |
| Source: Adapted from reference 26. | |
MAINTENANCE THERAPY
Ideally, if a medication stabilizes a patient’s acute bipolar mania, that medication is continued for further stabilization and maintenance. Aggressive initial dosing befits this approach because it establishes a therapeutic blood level and usually reveals any side effects within days. Moreover, patients often prefer to continue the medication that provided relief when they felt most distressed.
Weight gain. Long-term use of atypical antipsychotics may be associated with weight gain, dyslipidemia, and the development of metabolic syndromes and diabetes mellitus. Weight gain risk may be further elevated in patients taking both antipsychotics and lithium or valproic acid.26 When atypical antipsychotics are used for bipolar maintenance therapy, the American Diabetes Association and American Psychiatric Association recommend close monitoring (Tables 3 and 4).
Abnormal movements. Though tardive dyskinesia risk is very low with atypical antipsychotics, we recommend screening during the first year of treatment. The development of diabetes mellitus may precipitate or worsen abnormal movements.
Related resources
- American Diabetes Association. www.diabetes.org
- American Obesity Association. www.obesity.org
- Expert Consensus Treatment Guidelines for Bipolar Disorder: A Guide for Patients and Families. Task Force for the APA Practice Guideline for the Treatment of Patients with Bipolar Disorder. www.psychguides.com/pfg3.php
Drug brand names
- Aripiprazole • Abilify
- Carbamazepine • Tegretol
- Divalproex sodium • Depakote
- Haloperidol • Haldol
- Olanzapine • Zyprexa
- Quetiapine • Seroquel
- Risperidone • Risperdal
- Valproic acid • Depakene
- Ziprasidone • Geodon
Disclosures
Dr. Carroll is a consultant to Abbott Laboratories, Bristol-Myers Squibb Co., AstraZeneca Pharmaceuticals, Eli Lilly and Co., Janssen Pharmaceutica, and Pfizer Inc.
Dr. Fawver is a consultant to Eli Lilly and Co. and Pfizer Inc.
Dr. Thalassinos is a consultant for AstraZeneca Pharamaceuticals, Eli Lilly and Co., and Pfizer Inc.
Acknowledgment
The authors thank Donald R. Schmitt, PharmD, Christopher Thomas, PharmD, and Tina Fore, Library Service, Chillicothe VA Medical Center, for their help in identifying articles used in this review.
1. Keck PE, Jr, McElroy SL, Tugrul KC, et al. Valproate oral loading in the treatment of acute mania. J Clin Psychiatry. 1993;54:305-8.
2. Moscovich DG, Shapira B, Lerer B, et al. Rapid lithiumization in acute manic patients. Hum Psychopharmacol. 1992;7:343-5.
3. Kook KA, Stimmel GL, Wilkins JN, et al. Accuracy and safety of a priori lithium loading. J Clin Psychiatry. 1985;46:49-51.
4. Carroll BT, Thalassinos A, Fawver JD. Loading strategies in acute mania. CNS Spectrums. 2001;6:919-30.
5. Hirschfeld RMA, Allen MH, McEvoy J, et al. Safety and tolerability of oral loading divalproex sodium in acutely manic bipolar patients. J Clin Psychiatry. 1999;60:815-18.
6. Miller BP, et al. Oral loading of extended-release divalproex in acute mania (presentation). New Orleans: American Psychiatric Association annual meeting, 2001.
7. Thibault M, Blume WT, Saint-Hilaire JM, et al. Divalproex extended-release versus the original divalproex tablet: results of a randomized, crossover study of well-controlled epileptic patients with primary generalized seizures. Epilepsy Res. 2002;50:243-9.
8. Hirschfeld RMA, Baker JD, Wozniak P, et al. The safety and early efficacy of oral-loaded divalproex versus standard-titration divalproex, lithium, olanzapine, and placebo in the treatment of acute mania associated with bipolar disorder. J Clin Psychiatry. 2003;64:841-6.
9. Phrolov K, Applebaum J, Levine J, et al. Single-dose intravenous valproate in acute mania. J Clin Psychiatry. 2004;65:68-70.
10. Keck PE, Jr, McElroy SL, Bennet TA. Pharmacologic loading in the treatment of acute mania. Bipolar Disord. 2000;2:42-6.
11. Dunn RT, Frye MS, Tim KA, et al. The efficacy and use of anticonvulsants in mood disorders. Clin Neuropharmacol. 1998;21:215-35.
12. Lerer B, Moore N, Meyendor E, et al. Carbamazepine versus lithium in mania a double-blind study. J Clin Psychiatry. 1987;48:89-93.
13. Brown B. The use of generic mood stabilizers: carbamazepine (monograph). J Clin Psychiatry. 1997;15(4):11-17.
14. Karagianis JL, Dawe IC, Thakur A, et al. Rapid tranquilization with olanzapine in acute psychosis: a case series. J Clin Psychiatry. 2001;62(suppl 2):12-16.
15. Baker RW, Kinon BJ, Maguire GA, et al. Effectiveness of rapid initial dose escalation of up to 40 milligrams per day of oral olanzapine in acute agitation. J Clin Psychopharmacol. 2003;23(4):342-8.
16. Sachs GS, Grossman F, Ghaemi SN, et al. Combination of mood stabilizer with risperidone or haloperidol for the treatment of acute mania: a double-blind, placebo controlled comparison of efficacy and safety. Am J Psychiatry. 2002;159:1146-54.
17. Hirschfeld RMA, Keck PE, Jr, Karcher K, et al. Rapid antimanic effect of risperidone monotherapy: a 3-week multicenter, randomized, double-blind, placebo-controlled trial. Am J Psychiatry. 2004;161:1057-65.
18. Khanna S, Vieta E, Lyons B, et al. Risperidone monotherapy in acute bipolar mania (abstract P219). Pittsburgh: Fifth International Conference on Bipolar Disorder, 2003.
19. Jones MW, Huizar K, et al. Quetiapine monotherapy for acute mania associated with bipolar disorder (poster presentation). San Francisco: American Psychiatric Association annual meeting, 2003.
20. Sachs G, Mullen JA, Devine NA, Sweitzer DE. Quetiapine versus placebo as adjunct to mood stabilizer for the treatment of acute mania (abstract). Bipolar Disord. 2002;4(suppl 1):133.-
21. Smith MA, McCoy R, Hamer J, Brecher M. Optimal titration for quetiapine (poster presentation): Boca Raton, FL: National Clinical Drug Evaluation Unit annual meeting, 2002.
22. Keck PE, Jr, Versiani M, Potkin S, et al. Ziprasidone in the treatment of acute bipolar mania: a three-week, placebo-controlled, double-blind, randomized trial. Am J Psychiatry. 2003;160:741-8.
23. Holtzheimer PE, Neumaier JF. Treatment of acute mania. CNS Spectrums. 2003;8(12):917-28.
24. Keck PE, Jr, Marcus R, Tourkodimitris S, et al. A placebo-controlled, double-blind study of the efficacy and safety of aripiprazole in patients with acute bipolar mania. Am J Psychiatry. 2003;160(9):1651-8.
25. Sachs G, Sanchez R, Marcus R, et al. Aripiprazole vs placebo with an acute manic or mixed episode. New York: American Psychiatric Association annual meeting, 2004.
26. American Diabetes Association, American Psychiatric Association, American Association of Clinical Endocrinologists, North American Association for the Study of Obesity. Consensus Development Conference on Antipsychotic Drugs and Obesity and Diabetes. Diabetes Care. 2004;27:596-601.
Evidence on aggressive initial dosing of mood stabilizers and antipsychotics is changing the way acute bipolar mania is treated. To help you apply this information, we searched the literature and meeting abstracts for aggressive strategies tested to date. This article discusses how to:
- identify patients who may benefit from loading or aggressive initial dosing
- calculate mood stabilizer dosages
- dose each atypical antipsychotic
- manage potential antipsychotic side effects during maintenance therapy.
PATIENT SELECTION
Rapidly achieving therapeutic blood levels relieves patient suffering faster than standard titration. It quickly calms the hyperactivity, impulsivity, tension, hostility, and uncooperativeness that distress patients and increase the risk of harm to themselves and others.
The challenge of using higher dosages is to minimize side effects. Loading is not a one-size-fits-all approach, as antimanic drugs’ unique pharmacokinetic and pharmacotherapeutic properties influence how each agent is used.
An interesting body of literature advocates using mood stabilizers plus antipsychotics to treat mania, suggesting greater efficacy than with either agent alone.16 This strategy raises important questions, such as:
- Can two drugs be loaded simultaneously?
- Can patients taking mood stabilizers be treated with antipsychotic loading, and can those taking antipsychotics receive loading dosages of mood stabilizers?
- Would “double loading” improve bipolar mania treatment?
Answers to these questions are needed because of increased demands on clinicians to control hospital costs by rapidly and effectively treating patients with bipolar mania.
Loading doses cannot be standardized but are calculated by multiplying target steady-state plasma concentration by volume of distribution. We suggest aggressive initial schedules for divalproex sodium and atypical antipsychotics in this article with the understanding that practitioners will adjust them based on each patient’s tolerance and response.
Hospitalization. Patients with acute bipolar mania should be supervised closely in the hospital during loading or aggressive initial dosing. Monitor for cardiovascular changes, neurologic disturbances, sensorium changes, and response.
Precautions. Not all patients are candidates for aggressive initial dosing. Contraindications include age <18 or >65 years, pregnancy, breast-feeding, medical illness, and known sensitivity to the medication being given.
Higher-than-usual dosing increases the risk of excessive drug concentrations in sensitive individuals—such as those with a history of sensitivity to lower dosages of similar medications—and toxic levels of drugs with long half-lives can persist. When in doubt, consider giving a smaller amount of the loading dose early in the day, followed later by a larger amount.
DRUG SELECTION
Loading and aggressive initial dosing strategies for bipolar mania were first advanced for divalproex sodium.1 Investigators then examined loading strategies for lithium and carbamazepine, as well as the antipsychotics olanzapine, risperidone, quetiapine, ziprasidone, and aripiprazole, which are known to have antimanic properties.
Olanzapine, quetiapine, and risperidone are FDA-approved for short-term treatment of acute manic episodes associated with bipolar I disorder, and similar indications were being considered for aripiprazole and ziprasidone as this article went to press. We discuss evidence on loading and aggressive initial dosing strategies for each agent.
No studies have compared one loading strategy with another. Thus, when we choose drugs for loading, we consider what each patient needs, available formulations, tolerability, and efficacy for long-term stabilization and maintenance treatment.
LITHIUM
Lithium loading targets the therapeutic range (<1.4 mEq/L), without crossing the toxic threshold (>1.5 mEq/L). Lithium loading has shown antimanic effects, although using >30 mg/kg/d causes severe nausea and vomiting.
Moscovich et al2 reported a case series of 9 adults with acute mania who received lithium loading dosages of 4,050 mg/d. Patients tolerated lithium well at plasma drug levels of approximately 1.2 to 1.4 mEq/L. Their manic symptoms declined significantly within 4 to 5 days, as measured by Clinical Global Impression (CGI) severity of illness, Biegel-Murphy Mania State Rating Scale, and Brief Psychiatric Rating Scale scores.
Table 1
How to calculate divalproex loading for acute bipolar mania*
| Days 1 and 2 |
| Patient weight in pounds x 15 = dosage (mg/d) (Example: 150 lbs x 15 = 1,750 mg/d) |
| Days 3 to 10 |
| Patient weight in pounds x 10 = dosage (mg/d) (Example: 150 lbs. x 10 = 1,500 mg/d) |
| To avoid splitting tablets, make dosage divisible by 125 (round up for young adults, round down for older adults). Divide into bid or tid doses for improved tolerability. |
| Days 4 and 7 |
| Draw blood to monitor valproic acid levels and for other values such as liver function studies. |
| * For use with oral divalproex sodium (delayed-release or extended-release formulations). Do not use valproic acid preparations, as loading is unlikely to be well tolerated. |
| Source: Reference 5 |
Kook et al3 attempted a 30-mg/kg loading dose of slow-release lithium carbonate in 38 patients to evaluate the safety of achieving a therapeutic level in 12 hours. No patient experienced adverse effects during loading or in the 12 hours after loading was completed.
Patients who develop a manic episode while taking lithium pose a therapeutic dilemma. If they stop taking lithium—especially abruptly—manic symptoms can return in as few as 2 days. For these patients, consider increasing the usual dosage by 50% to 100% on the first day of mania treatment,4 then continue a dosage that maintains efficacy and achieves a therapeutic blood level.
To avoid GI upset, avoid any single dose of >1,500 mg; if a greater dosage is needed, divide it for improved tolerance. Obtain lithium blood levels at baseline, after 4 days, and thereafter as clinically relevant to monitor for drug interactions that may affect serum levels.
Side effects—GI irritation, tremor, muscle weakness, thirst, polyuria—are common in the first week, and weight gain may occur after prolonged treatment.
DIVALPROEX
In a study by Keck et al1 of 19 adults with acute bipolar mania, aggressive initial dosing of divalproex sodium, 20 mg/kg/d, was well-tolerated and shortened hospitalization. Side effects including sedation and nausea occurred at a rate similar to that seen with more-gradual titration.
To calculate the initial dose, the authors used a conversion factor of 20 mg/kg/d or added a zero to the patient’s weight in pounds. This amount was given in single or divided doses the first day, then continued for 4 to 7 days. Blood levels were measured on day 4, and all 15 patients who completed the study achieved serum valproate levels >50 mcg/mL.
In a double-blind study by Hirschfeld et al,5 59 adults with Young Mania Rating Scale (YMRS) scores >14 were randomly assigned to receive divalproex oral loading; divalproex nonloading (250 mg tid on days 1 and 2, followed by standard titration on days 3 to 10); or lithium carbonate (300 mg tid, followed by standard titration on days 3 to 10).
Divalproex loading—30 mg/kg/d on days 1 and 2, followed by 20 mg/kg on days 3 to 10— yielded valproate levels >50 mcg/mL in 84% of patients by day 3. Rapid loading appeared to increase antimanic efficacy, as measured by YMRS endpoint scores, without increasing adverse effects. For Table 1, we converted this study’s metric values to patient weight in pounds.
Side effects. Divalproex can inhibit metabolism of other drugs (including anticonvulsants such as lamotrigine) and increase their blood levels. Side effects such as sedation, alopecia, abdominal pain, diarrhea, and tremor may require observation and treatment. Pancreatitis, hepatitis, and allergic reactions are rare but may require discontinuation.
Recommendation. Aggressive initial dosing and loading for patients with acute mania has been reported with enteric-coated delayed-release and extended-release6 divalproex sodium tablets. With identical dosages, the extended-release form produces 11% lower serum levels than the delayed-release form.7
Aggressive dosing of oral valproic acid preparations is not recommended and is likely to be poorly tolerated.8 A pilot study evaluating IV valproate loading in acute mania found no changes in mania in the 2 hours that followed loading.9
CARBAMAZEPINE
Carbamazepine is used off-label to treat mania and mixed phases of bipolar disorder.4,9,10 Excessive absorption rates are associated with dizziness, ataxia, and nausea. Side effects may occur when the plasma level is therapeutic for epilepsy (4 to 12 mcg/mL).11
In mania, the relationship between carbamazepine levels and clinical response is not always clear. Lerer et al12 found a correlation between acute mania response and a serum level of 8.8 mcg/mL (range 4.7 to 14.0 mcg/mL).
Patients with acute mania may require 600 to 1,600 mg/d. Carbamazepine is available in immediate-release and controlled-release preparations. Because generic preparations might not be bio-equivalent,13 use the same formulation throughout treatment to maintain consistent serum levels.
Enzymatic auto-induction—in which carbamazepine gradually increases the activity of its metabolic enzyme—is likely to occur at 3 to 5 weeks of administration, often after hospital discharge. An aggressive initial rescue adjustment can be used if a patient develops mania after having been stabilized on carbamazepine for >6 weeks. Because these patients are past the point of auto-induction, a target blood level of 8.8 mcg/mL can be used and the dosage adjusted proportionally.
For example, if mania recurs in a patient who is stabilized on carbamazepine, 400 mg/d (plasma level 4.5 mcg/mL), carbamazepine can be loaded up to 800 mg/d. Measure the plasma level within 4 days; the target level would be 9.0 mcg/mL (2 times 4.5 mcg/mL), which closely approximates steady state and sets up a ratio to reach the target level of 8.8 mcg/mL.
Side effects include ataxia, diplopia, and dizziness. Complete blood counts, liver function studies, plasma levels, and serum chemistries require regular monitoring.
Recommendation. Carbamazepine is not recommended for oral loading in patients who have never taken it or for those with hyponatremia, hepatic dysfunction, or history of intolerance or agranulocytosis.
OLANZAPINE
Olanzapine has pharmacologic properties favorable for loading.4 The recommended dosage for acute mania is 15 mg/d with standard titration; Karagianis et al14 showed that initial loading doses of >20 mg/d resulted in good control of agitated patients with psychosis. Side effects were uncommon, with sedation occurring in 14% of patients in this case series. The loading dose reduced agitation more effectively than did dosages <20 mg/d given to similar patients.
A multicenter study of 148 acutely agitated inpatients with a variety of psychiatric disorders compared olanzapine rapid initial dose escalation with usual clinical practice.15 Mean aggressive dosages were 28.8 mg/d on day 1, 30.3 mg/d on day 2, and 16.1 mg/d on day 5. Usual-practice dosages were 10 mg/d, plus lorazepam, 0 to 4 mg/d for the first 2 days and 0 to 2 mg/d on days 3 to 4. Based on Positive and Negative Syndrome Scale excited component subscale scores, olanzapine loading controlled agitation more effectively than did usual practice, with similar side-effect rates.
IM olanzapine or the orally dissolving form are bioequivalent to the tablets and may be used for acute agitation associated with bipolar mania in certain clinical settings.14
Table 2
Suggested antipsychotic loading for acute bipolar mania and mixed states*
| Drug | Day(s) | Aggressive initial dosing schedule | Comment |
|---|---|---|---|
| Aripiprazole24,25 | 1 2 to 3 4+ | 30 mg once daily with food 30 mg/d with food Reduce dosage by 10 to 15 mg/d, based on tolerance and response | Nausea and vomiting may occur in first few days; adjust dosage based on tolerance and response |
| Olanzapine14,15 | 1 and 2 3 and 4 5 to 10 | 40 mg in single or divided dosage 20 to 30 mg at bedtime 15 mg once daily (may reduce to 5, 7.5, or 10 mg/d) | Adjust dosage based on tolerance and response; oral or IM formulations may be used |
| Quetiapine19,21 | 1 2 and 3 4 to 10 | 100 mg upon admission and 100 mg at bedtime 100 mg bid (or tid to qid) plus 100 to 200 mg at bedtime 200 mg bid plus 200 to 300 mg at bedtime; may adjust to 400 to 800 mg/d) | Adjust dosage based on tolerance and response |
| Risperidone16,18 | 1 2 3 and 4 | 3 mg in single or divided dosage 4 mg in single or divided dosage 5 mg in single or divided dosage | Adjust dosage by 1 mg up or down, based on tolerance and response; use tablet, rapid-dissolving tablet, or liquid form, but not long-acting IM form |
| Ziprasidone22,23 | 1 2 | 20 mg IM in single dose (may repeat for severe agitation) or 40 mg po bid with food 60 to 80 mg po bid with food | Adjust dosage based on tolerance and response |
| * For hospitalized or partially hospitalized patients, ages18. Not recommended for patients who are pregnant, breastfeeding, medically ill, age >65, or with known sensitivity to the antipsychotic being given. | |||
RISPERIDONE
Sachs et al16 studied 156 inpatients who developed an acute manic or mixed episode while receiving lithium or divalproex. These patients were randomly assigned to begin adjunctive risperidone, 2 mg/d, haloperidol, or placebo. Dosing was flexible, increasing or decreasing by 1 mg/d. Risperidone’s mean modal dosage was 3.8 mg/d across 3 weeks, with mean exposure of 17 days. Risperidone plus a mood stabilizer was more effective than a mood stabilizer alone, and the combination provided rapid, well-tolerated control of manic symptoms.
In a double-blind trial, Hirschfeld et al17 randomly assigned 279 patients with acute bipolar mania to risperidone, 1 to 6 mg/d, or placebo for 3 weeks. As early as day 3, YMRS scores were reduced significantly more with risperidone than with placebo. Somnolence was the most common side effect, and mean modal dosage was 4.1 mg/d.
Table 3
Screening schedule for antipsychotic side effects during bipolar maintenance treatment
| Baseline | |
| Side effect | Recommended screening |
| Weight gain | Weight and body mass index (BMI) monthly for first 3 months; waist circumference |
| Hypertension | Blood pressure |
| Hyperglycemia | Fasting plasma glucose, with glycosylated hemoglobin (Hb A 1c ) if hyperglycemia is detected |
| Hyperlipidemia | Fasting lipid profile |
| Tardive dyskinesia | Abnormal Involuntary Movement Scale (AIMS) or other screen |
| Ophthalmic changes | Ophthalmologic examination for patients taking quetiapine and for all with diabetes mellitus |
| Follow-up schedules | |
| 3 months | |
| Weight and BMI | |
| Blood pressure | |
| Fasting plasma glucose, with Hb A 1c if hyperglycemia is detected; Hb A 1c values may be used to measure interval changes in glucose tolerance | |
| Fasting lipid profile | |
| 6 months | |
| AIMS or other tardive dyskinesia screen | |
| Ophthalmologic examination | |
| Source: Adapted from reference 26. | |
In a multicenter, randomized, double-blind, placebo-controlled study of patients with acute bipolar mania, Khanna et al18 assigned patients to receive risperidone monotherapy (mean modal dosage 5.6 mg/d) or placebo for 3 weeks. Mania scores of patients receiving risperidone were significantly lower at weeks 1 and 2, compared with the placebo group. Risperidone was well-tolerated, with no unexpected adverse events.
Recommendation. Because of a risk of extrapyramidal symptoms (EPS) and orthostatic hypotension, initial risperidone loading dosages >4 mg on day 1 are not recommended.
QUETIAPINE
Quetiapine has shown antimanic efficacy as monotherapy and as adjunctive therapy to mood stabilizers.19,20 The effective dosage was a mean 600 mg/d (range 400 to 800 mg/d) in monotherapy and adjunctive treatment. These studies achieved 400 mg/d within the first 4 days (100 mg on day 1, 200 mg on day 2, 300 mg on day 3, and 400 mg on day 4).
These data combined with revised prescribing information suggest aggressive initial dose escalation of quetiapine within the first 4 days for selected patients. A titration study in patients with schizophrenia used a more-rapid escalation rate of 400 mg within 2 days.21 Dizziness, orthostatic hypotension, and sedation were not more frequent in this high-dose group than in the two lower-dose titration groups. In our experience, 200 to 400 mg can be given the first day of treatment.
ZIPRASIDONE
In a randomized, double-blind, controlled trial, Keck et al22 assigned 210 patients with a manic or mixed bipolar episode to 3 weeks of ziprasidone, 40 to 80 mg bid, or placebo. Ziprasidone produced rapid, sustained improvement in manic symptoms on all primary and most secondary efficacy measures, such as the YMRS and CGI.
Significant improvements seen within 2 days were maintained. Ziprasidone was well tolerated and was associated with a low EPS rate; neither weight gain nor clinically significant changes in vital signs were seen.
IM ziprasidone, which is approved for use in schizophrenia, may also have efficacy in bipolar mania.23 The recommended dose of 20 mg IM is equivalent to 120 to 160 mg orally, so a single injection may reach the target antimanic dosage.
Recommendation. Ziprasidone could be an option for aggressive initial dosing for a patient who has previously received ziprasidone IM and is not at risk for QTc prolongation.
ARIPIPRAZOLE
In a randomized controlled trial, Keck et al24 assigned 262 patients with acute bipolar mania or mixed states to aripiprazole, 30 mg/d, or placebo for 3 weeks. By day 4, manic symptoms were improved significantly more in patients receiving aripiprazole, and discontinuation rates were similar.
Similarly, in a randomized, controlled multi-center study, Sachs et al25 used 30 mg/d in 272 patients with bipolar mania or mixed states. Compared with placebo, aripiprazole produced significant improvement by day 4, with similar discontinuation rates.
Recommendation. Aggressive initial dosing of aripiprazole could be useful for a patient who does not require an IM or rapidly dissolvable medication.
Table 4
Suggested response to metabolic changes during bipolar maintenance therapy
| Metabolic change | Therapeutic action |
|---|---|
| ≥5% increase in total body weight | Consider weight-reduction strategies or medication adjustment |
| Fasting glucose: ≥126 mg/mL ≥300 mg/mL or ≤60 mg/mL | Consider evaluation for diabetes mellitus Seek immediate consultation |
| Total cholesterol ≥200 mg/dL or triglycerides ≥165 mg/dL | Consider lipid-lowering with dietary and/or medication changes |
| Source: Adapted from reference 26. | |
MAINTENANCE THERAPY
Ideally, if a medication stabilizes a patient’s acute bipolar mania, that medication is continued for further stabilization and maintenance. Aggressive initial dosing befits this approach because it establishes a therapeutic blood level and usually reveals any side effects within days. Moreover, patients often prefer to continue the medication that provided relief when they felt most distressed.
Weight gain. Long-term use of atypical antipsychotics may be associated with weight gain, dyslipidemia, and the development of metabolic syndromes and diabetes mellitus. Weight gain risk may be further elevated in patients taking both antipsychotics and lithium or valproic acid.26 When atypical antipsychotics are used for bipolar maintenance therapy, the American Diabetes Association and American Psychiatric Association recommend close monitoring (Tables 3 and 4).
Abnormal movements. Though tardive dyskinesia risk is very low with atypical antipsychotics, we recommend screening during the first year of treatment. The development of diabetes mellitus may precipitate or worsen abnormal movements.
Related resources
- American Diabetes Association. www.diabetes.org
- American Obesity Association. www.obesity.org
- Expert Consensus Treatment Guidelines for Bipolar Disorder: A Guide for Patients and Families. Task Force for the APA Practice Guideline for the Treatment of Patients with Bipolar Disorder. www.psychguides.com/pfg3.php
Drug brand names
- Aripiprazole • Abilify
- Carbamazepine • Tegretol
- Divalproex sodium • Depakote
- Haloperidol • Haldol
- Olanzapine • Zyprexa
- Quetiapine • Seroquel
- Risperidone • Risperdal
- Valproic acid • Depakene
- Ziprasidone • Geodon
Disclosures
Dr. Carroll is a consultant to Abbott Laboratories, Bristol-Myers Squibb Co., AstraZeneca Pharmaceuticals, Eli Lilly and Co., Janssen Pharmaceutica, and Pfizer Inc.
Dr. Fawver is a consultant to Eli Lilly and Co. and Pfizer Inc.
Dr. Thalassinos is a consultant for AstraZeneca Pharamaceuticals, Eli Lilly and Co., and Pfizer Inc.
Acknowledgment
The authors thank Donald R. Schmitt, PharmD, Christopher Thomas, PharmD, and Tina Fore, Library Service, Chillicothe VA Medical Center, for their help in identifying articles used in this review.
Evidence on aggressive initial dosing of mood stabilizers and antipsychotics is changing the way acute bipolar mania is treated. To help you apply this information, we searched the literature and meeting abstracts for aggressive strategies tested to date. This article discusses how to:
- identify patients who may benefit from loading or aggressive initial dosing
- calculate mood stabilizer dosages
- dose each atypical antipsychotic
- manage potential antipsychotic side effects during maintenance therapy.
PATIENT SELECTION
Rapidly achieving therapeutic blood levels relieves patient suffering faster than standard titration. It quickly calms the hyperactivity, impulsivity, tension, hostility, and uncooperativeness that distress patients and increase the risk of harm to themselves and others.
The challenge of using higher dosages is to minimize side effects. Loading is not a one-size-fits-all approach, as antimanic drugs’ unique pharmacokinetic and pharmacotherapeutic properties influence how each agent is used.
An interesting body of literature advocates using mood stabilizers plus antipsychotics to treat mania, suggesting greater efficacy than with either agent alone.16 This strategy raises important questions, such as:
- Can two drugs be loaded simultaneously?
- Can patients taking mood stabilizers be treated with antipsychotic loading, and can those taking antipsychotics receive loading dosages of mood stabilizers?
- Would “double loading” improve bipolar mania treatment?
Answers to these questions are needed because of increased demands on clinicians to control hospital costs by rapidly and effectively treating patients with bipolar mania.
Loading doses cannot be standardized but are calculated by multiplying target steady-state plasma concentration by volume of distribution. We suggest aggressive initial schedules for divalproex sodium and atypical antipsychotics in this article with the understanding that practitioners will adjust them based on each patient’s tolerance and response.
Hospitalization. Patients with acute bipolar mania should be supervised closely in the hospital during loading or aggressive initial dosing. Monitor for cardiovascular changes, neurologic disturbances, sensorium changes, and response.
Precautions. Not all patients are candidates for aggressive initial dosing. Contraindications include age <18 or >65 years, pregnancy, breast-feeding, medical illness, and known sensitivity to the medication being given.
Higher-than-usual dosing increases the risk of excessive drug concentrations in sensitive individuals—such as those with a history of sensitivity to lower dosages of similar medications—and toxic levels of drugs with long half-lives can persist. When in doubt, consider giving a smaller amount of the loading dose early in the day, followed later by a larger amount.
DRUG SELECTION
Loading and aggressive initial dosing strategies for bipolar mania were first advanced for divalproex sodium.1 Investigators then examined loading strategies for lithium and carbamazepine, as well as the antipsychotics olanzapine, risperidone, quetiapine, ziprasidone, and aripiprazole, which are known to have antimanic properties.
Olanzapine, quetiapine, and risperidone are FDA-approved for short-term treatment of acute manic episodes associated with bipolar I disorder, and similar indications were being considered for aripiprazole and ziprasidone as this article went to press. We discuss evidence on loading and aggressive initial dosing strategies for each agent.
No studies have compared one loading strategy with another. Thus, when we choose drugs for loading, we consider what each patient needs, available formulations, tolerability, and efficacy for long-term stabilization and maintenance treatment.
LITHIUM
Lithium loading targets the therapeutic range (<1.4 mEq/L), without crossing the toxic threshold (>1.5 mEq/L). Lithium loading has shown antimanic effects, although using >30 mg/kg/d causes severe nausea and vomiting.
Moscovich et al2 reported a case series of 9 adults with acute mania who received lithium loading dosages of 4,050 mg/d. Patients tolerated lithium well at plasma drug levels of approximately 1.2 to 1.4 mEq/L. Their manic symptoms declined significantly within 4 to 5 days, as measured by Clinical Global Impression (CGI) severity of illness, Biegel-Murphy Mania State Rating Scale, and Brief Psychiatric Rating Scale scores.
Table 1
How to calculate divalproex loading for acute bipolar mania*
| Days 1 and 2 |
| Patient weight in pounds x 15 = dosage (mg/d) (Example: 150 lbs x 15 = 1,750 mg/d) |
| Days 3 to 10 |
| Patient weight in pounds x 10 = dosage (mg/d) (Example: 150 lbs. x 10 = 1,500 mg/d) |
| To avoid splitting tablets, make dosage divisible by 125 (round up for young adults, round down for older adults). Divide into bid or tid doses for improved tolerability. |
| Days 4 and 7 |
| Draw blood to monitor valproic acid levels and for other values such as liver function studies. |
| * For use with oral divalproex sodium (delayed-release or extended-release formulations). Do not use valproic acid preparations, as loading is unlikely to be well tolerated. |
| Source: Reference 5 |
Kook et al3 attempted a 30-mg/kg loading dose of slow-release lithium carbonate in 38 patients to evaluate the safety of achieving a therapeutic level in 12 hours. No patient experienced adverse effects during loading or in the 12 hours after loading was completed.
Patients who develop a manic episode while taking lithium pose a therapeutic dilemma. If they stop taking lithium—especially abruptly—manic symptoms can return in as few as 2 days. For these patients, consider increasing the usual dosage by 50% to 100% on the first day of mania treatment,4 then continue a dosage that maintains efficacy and achieves a therapeutic blood level.
To avoid GI upset, avoid any single dose of >1,500 mg; if a greater dosage is needed, divide it for improved tolerance. Obtain lithium blood levels at baseline, after 4 days, and thereafter as clinically relevant to monitor for drug interactions that may affect serum levels.
Side effects—GI irritation, tremor, muscle weakness, thirst, polyuria—are common in the first week, and weight gain may occur after prolonged treatment.
DIVALPROEX
In a study by Keck et al1 of 19 adults with acute bipolar mania, aggressive initial dosing of divalproex sodium, 20 mg/kg/d, was well-tolerated and shortened hospitalization. Side effects including sedation and nausea occurred at a rate similar to that seen with more-gradual titration.
To calculate the initial dose, the authors used a conversion factor of 20 mg/kg/d or added a zero to the patient’s weight in pounds. This amount was given in single or divided doses the first day, then continued for 4 to 7 days. Blood levels were measured on day 4, and all 15 patients who completed the study achieved serum valproate levels >50 mcg/mL.
In a double-blind study by Hirschfeld et al,5 59 adults with Young Mania Rating Scale (YMRS) scores >14 were randomly assigned to receive divalproex oral loading; divalproex nonloading (250 mg tid on days 1 and 2, followed by standard titration on days 3 to 10); or lithium carbonate (300 mg tid, followed by standard titration on days 3 to 10).
Divalproex loading—30 mg/kg/d on days 1 and 2, followed by 20 mg/kg on days 3 to 10— yielded valproate levels >50 mcg/mL in 84% of patients by day 3. Rapid loading appeared to increase antimanic efficacy, as measured by YMRS endpoint scores, without increasing adverse effects. For Table 1, we converted this study’s metric values to patient weight in pounds.
Side effects. Divalproex can inhibit metabolism of other drugs (including anticonvulsants such as lamotrigine) and increase their blood levels. Side effects such as sedation, alopecia, abdominal pain, diarrhea, and tremor may require observation and treatment. Pancreatitis, hepatitis, and allergic reactions are rare but may require discontinuation.
Recommendation. Aggressive initial dosing and loading for patients with acute mania has been reported with enteric-coated delayed-release and extended-release6 divalproex sodium tablets. With identical dosages, the extended-release form produces 11% lower serum levels than the delayed-release form.7
Aggressive dosing of oral valproic acid preparations is not recommended and is likely to be poorly tolerated.8 A pilot study evaluating IV valproate loading in acute mania found no changes in mania in the 2 hours that followed loading.9
CARBAMAZEPINE
Carbamazepine is used off-label to treat mania and mixed phases of bipolar disorder.4,9,10 Excessive absorption rates are associated with dizziness, ataxia, and nausea. Side effects may occur when the plasma level is therapeutic for epilepsy (4 to 12 mcg/mL).11
In mania, the relationship between carbamazepine levels and clinical response is not always clear. Lerer et al12 found a correlation between acute mania response and a serum level of 8.8 mcg/mL (range 4.7 to 14.0 mcg/mL).
Patients with acute mania may require 600 to 1,600 mg/d. Carbamazepine is available in immediate-release and controlled-release preparations. Because generic preparations might not be bio-equivalent,13 use the same formulation throughout treatment to maintain consistent serum levels.
Enzymatic auto-induction—in which carbamazepine gradually increases the activity of its metabolic enzyme—is likely to occur at 3 to 5 weeks of administration, often after hospital discharge. An aggressive initial rescue adjustment can be used if a patient develops mania after having been stabilized on carbamazepine for >6 weeks. Because these patients are past the point of auto-induction, a target blood level of 8.8 mcg/mL can be used and the dosage adjusted proportionally.
For example, if mania recurs in a patient who is stabilized on carbamazepine, 400 mg/d (plasma level 4.5 mcg/mL), carbamazepine can be loaded up to 800 mg/d. Measure the plasma level within 4 days; the target level would be 9.0 mcg/mL (2 times 4.5 mcg/mL), which closely approximates steady state and sets up a ratio to reach the target level of 8.8 mcg/mL.
Side effects include ataxia, diplopia, and dizziness. Complete blood counts, liver function studies, plasma levels, and serum chemistries require regular monitoring.
Recommendation. Carbamazepine is not recommended for oral loading in patients who have never taken it or for those with hyponatremia, hepatic dysfunction, or history of intolerance or agranulocytosis.
OLANZAPINE
Olanzapine has pharmacologic properties favorable for loading.4 The recommended dosage for acute mania is 15 mg/d with standard titration; Karagianis et al14 showed that initial loading doses of >20 mg/d resulted in good control of agitated patients with psychosis. Side effects were uncommon, with sedation occurring in 14% of patients in this case series. The loading dose reduced agitation more effectively than did dosages <20 mg/d given to similar patients.
A multicenter study of 148 acutely agitated inpatients with a variety of psychiatric disorders compared olanzapine rapid initial dose escalation with usual clinical practice.15 Mean aggressive dosages were 28.8 mg/d on day 1, 30.3 mg/d on day 2, and 16.1 mg/d on day 5. Usual-practice dosages were 10 mg/d, plus lorazepam, 0 to 4 mg/d for the first 2 days and 0 to 2 mg/d on days 3 to 4. Based on Positive and Negative Syndrome Scale excited component subscale scores, olanzapine loading controlled agitation more effectively than did usual practice, with similar side-effect rates.
IM olanzapine or the orally dissolving form are bioequivalent to the tablets and may be used for acute agitation associated with bipolar mania in certain clinical settings.14
Table 2
Suggested antipsychotic loading for acute bipolar mania and mixed states*
| Drug | Day(s) | Aggressive initial dosing schedule | Comment |
|---|---|---|---|
| Aripiprazole24,25 | 1 2 to 3 4+ | 30 mg once daily with food 30 mg/d with food Reduce dosage by 10 to 15 mg/d, based on tolerance and response | Nausea and vomiting may occur in first few days; adjust dosage based on tolerance and response |
| Olanzapine14,15 | 1 and 2 3 and 4 5 to 10 | 40 mg in single or divided dosage 20 to 30 mg at bedtime 15 mg once daily (may reduce to 5, 7.5, or 10 mg/d) | Adjust dosage based on tolerance and response; oral or IM formulations may be used |
| Quetiapine19,21 | 1 2 and 3 4 to 10 | 100 mg upon admission and 100 mg at bedtime 100 mg bid (or tid to qid) plus 100 to 200 mg at bedtime 200 mg bid plus 200 to 300 mg at bedtime; may adjust to 400 to 800 mg/d) | Adjust dosage based on tolerance and response |
| Risperidone16,18 | 1 2 3 and 4 | 3 mg in single or divided dosage 4 mg in single or divided dosage 5 mg in single or divided dosage | Adjust dosage by 1 mg up or down, based on tolerance and response; use tablet, rapid-dissolving tablet, or liquid form, but not long-acting IM form |
| Ziprasidone22,23 | 1 2 | 20 mg IM in single dose (may repeat for severe agitation) or 40 mg po bid with food 60 to 80 mg po bid with food | Adjust dosage based on tolerance and response |
| * For hospitalized or partially hospitalized patients, ages18. Not recommended for patients who are pregnant, breastfeeding, medically ill, age >65, or with known sensitivity to the antipsychotic being given. | |||
RISPERIDONE
Sachs et al16 studied 156 inpatients who developed an acute manic or mixed episode while receiving lithium or divalproex. These patients were randomly assigned to begin adjunctive risperidone, 2 mg/d, haloperidol, or placebo. Dosing was flexible, increasing or decreasing by 1 mg/d. Risperidone’s mean modal dosage was 3.8 mg/d across 3 weeks, with mean exposure of 17 days. Risperidone plus a mood stabilizer was more effective than a mood stabilizer alone, and the combination provided rapid, well-tolerated control of manic symptoms.
In a double-blind trial, Hirschfeld et al17 randomly assigned 279 patients with acute bipolar mania to risperidone, 1 to 6 mg/d, or placebo for 3 weeks. As early as day 3, YMRS scores were reduced significantly more with risperidone than with placebo. Somnolence was the most common side effect, and mean modal dosage was 4.1 mg/d.
Table 3
Screening schedule for antipsychotic side effects during bipolar maintenance treatment
| Baseline | |
| Side effect | Recommended screening |
| Weight gain | Weight and body mass index (BMI) monthly for first 3 months; waist circumference |
| Hypertension | Blood pressure |
| Hyperglycemia | Fasting plasma glucose, with glycosylated hemoglobin (Hb A 1c ) if hyperglycemia is detected |
| Hyperlipidemia | Fasting lipid profile |
| Tardive dyskinesia | Abnormal Involuntary Movement Scale (AIMS) or other screen |
| Ophthalmic changes | Ophthalmologic examination for patients taking quetiapine and for all with diabetes mellitus |
| Follow-up schedules | |
| 3 months | |
| Weight and BMI | |
| Blood pressure | |
| Fasting plasma glucose, with Hb A 1c if hyperglycemia is detected; Hb A 1c values may be used to measure interval changes in glucose tolerance | |
| Fasting lipid profile | |
| 6 months | |
| AIMS or other tardive dyskinesia screen | |
| Ophthalmologic examination | |
| Source: Adapted from reference 26. | |
In a multicenter, randomized, double-blind, placebo-controlled study of patients with acute bipolar mania, Khanna et al18 assigned patients to receive risperidone monotherapy (mean modal dosage 5.6 mg/d) or placebo for 3 weeks. Mania scores of patients receiving risperidone were significantly lower at weeks 1 and 2, compared with the placebo group. Risperidone was well-tolerated, with no unexpected adverse events.
Recommendation. Because of a risk of extrapyramidal symptoms (EPS) and orthostatic hypotension, initial risperidone loading dosages >4 mg on day 1 are not recommended.
QUETIAPINE
Quetiapine has shown antimanic efficacy as monotherapy and as adjunctive therapy to mood stabilizers.19,20 The effective dosage was a mean 600 mg/d (range 400 to 800 mg/d) in monotherapy and adjunctive treatment. These studies achieved 400 mg/d within the first 4 days (100 mg on day 1, 200 mg on day 2, 300 mg on day 3, and 400 mg on day 4).
These data combined with revised prescribing information suggest aggressive initial dose escalation of quetiapine within the first 4 days for selected patients. A titration study in patients with schizophrenia used a more-rapid escalation rate of 400 mg within 2 days.21 Dizziness, orthostatic hypotension, and sedation were not more frequent in this high-dose group than in the two lower-dose titration groups. In our experience, 200 to 400 mg can be given the first day of treatment.
ZIPRASIDONE
In a randomized, double-blind, controlled trial, Keck et al22 assigned 210 patients with a manic or mixed bipolar episode to 3 weeks of ziprasidone, 40 to 80 mg bid, or placebo. Ziprasidone produced rapid, sustained improvement in manic symptoms on all primary and most secondary efficacy measures, such as the YMRS and CGI.
Significant improvements seen within 2 days were maintained. Ziprasidone was well tolerated and was associated with a low EPS rate; neither weight gain nor clinically significant changes in vital signs were seen.
IM ziprasidone, which is approved for use in schizophrenia, may also have efficacy in bipolar mania.23 The recommended dose of 20 mg IM is equivalent to 120 to 160 mg orally, so a single injection may reach the target antimanic dosage.
Recommendation. Ziprasidone could be an option for aggressive initial dosing for a patient who has previously received ziprasidone IM and is not at risk for QTc prolongation.
ARIPIPRAZOLE
In a randomized controlled trial, Keck et al24 assigned 262 patients with acute bipolar mania or mixed states to aripiprazole, 30 mg/d, or placebo for 3 weeks. By day 4, manic symptoms were improved significantly more in patients receiving aripiprazole, and discontinuation rates were similar.
Similarly, in a randomized, controlled multi-center study, Sachs et al25 used 30 mg/d in 272 patients with bipolar mania or mixed states. Compared with placebo, aripiprazole produced significant improvement by day 4, with similar discontinuation rates.
Recommendation. Aggressive initial dosing of aripiprazole could be useful for a patient who does not require an IM or rapidly dissolvable medication.
Table 4
Suggested response to metabolic changes during bipolar maintenance therapy
| Metabolic change | Therapeutic action |
|---|---|
| ≥5% increase in total body weight | Consider weight-reduction strategies or medication adjustment |
| Fasting glucose: ≥126 mg/mL ≥300 mg/mL or ≤60 mg/mL | Consider evaluation for diabetes mellitus Seek immediate consultation |
| Total cholesterol ≥200 mg/dL or triglycerides ≥165 mg/dL | Consider lipid-lowering with dietary and/or medication changes |
| Source: Adapted from reference 26. | |
MAINTENANCE THERAPY
Ideally, if a medication stabilizes a patient’s acute bipolar mania, that medication is continued for further stabilization and maintenance. Aggressive initial dosing befits this approach because it establishes a therapeutic blood level and usually reveals any side effects within days. Moreover, patients often prefer to continue the medication that provided relief when they felt most distressed.
Weight gain. Long-term use of atypical antipsychotics may be associated with weight gain, dyslipidemia, and the development of metabolic syndromes and diabetes mellitus. Weight gain risk may be further elevated in patients taking both antipsychotics and lithium or valproic acid.26 When atypical antipsychotics are used for bipolar maintenance therapy, the American Diabetes Association and American Psychiatric Association recommend close monitoring (Tables 3 and 4).
Abnormal movements. Though tardive dyskinesia risk is very low with atypical antipsychotics, we recommend screening during the first year of treatment. The development of diabetes mellitus may precipitate or worsen abnormal movements.
Related resources
- American Diabetes Association. www.diabetes.org
- American Obesity Association. www.obesity.org
- Expert Consensus Treatment Guidelines for Bipolar Disorder: A Guide for Patients and Families. Task Force for the APA Practice Guideline for the Treatment of Patients with Bipolar Disorder. www.psychguides.com/pfg3.php
Drug brand names
- Aripiprazole • Abilify
- Carbamazepine • Tegretol
- Divalproex sodium • Depakote
- Haloperidol • Haldol
- Olanzapine • Zyprexa
- Quetiapine • Seroquel
- Risperidone • Risperdal
- Valproic acid • Depakene
- Ziprasidone • Geodon
Disclosures
Dr. Carroll is a consultant to Abbott Laboratories, Bristol-Myers Squibb Co., AstraZeneca Pharmaceuticals, Eli Lilly and Co., Janssen Pharmaceutica, and Pfizer Inc.
Dr. Fawver is a consultant to Eli Lilly and Co. and Pfizer Inc.
Dr. Thalassinos is a consultant for AstraZeneca Pharamaceuticals, Eli Lilly and Co., and Pfizer Inc.
Acknowledgment
The authors thank Donald R. Schmitt, PharmD, Christopher Thomas, PharmD, and Tina Fore, Library Service, Chillicothe VA Medical Center, for their help in identifying articles used in this review.
1. Keck PE, Jr, McElroy SL, Tugrul KC, et al. Valproate oral loading in the treatment of acute mania. J Clin Psychiatry. 1993;54:305-8.
2. Moscovich DG, Shapira B, Lerer B, et al. Rapid lithiumization in acute manic patients. Hum Psychopharmacol. 1992;7:343-5.
3. Kook KA, Stimmel GL, Wilkins JN, et al. Accuracy and safety of a priori lithium loading. J Clin Psychiatry. 1985;46:49-51.
4. Carroll BT, Thalassinos A, Fawver JD. Loading strategies in acute mania. CNS Spectrums. 2001;6:919-30.
5. Hirschfeld RMA, Allen MH, McEvoy J, et al. Safety and tolerability of oral loading divalproex sodium in acutely manic bipolar patients. J Clin Psychiatry. 1999;60:815-18.
6. Miller BP, et al. Oral loading of extended-release divalproex in acute mania (presentation). New Orleans: American Psychiatric Association annual meeting, 2001.
7. Thibault M, Blume WT, Saint-Hilaire JM, et al. Divalproex extended-release versus the original divalproex tablet: results of a randomized, crossover study of well-controlled epileptic patients with primary generalized seizures. Epilepsy Res. 2002;50:243-9.
8. Hirschfeld RMA, Baker JD, Wozniak P, et al. The safety and early efficacy of oral-loaded divalproex versus standard-titration divalproex, lithium, olanzapine, and placebo in the treatment of acute mania associated with bipolar disorder. J Clin Psychiatry. 2003;64:841-6.
9. Phrolov K, Applebaum J, Levine J, et al. Single-dose intravenous valproate in acute mania. J Clin Psychiatry. 2004;65:68-70.
10. Keck PE, Jr, McElroy SL, Bennet TA. Pharmacologic loading in the treatment of acute mania. Bipolar Disord. 2000;2:42-6.
11. Dunn RT, Frye MS, Tim KA, et al. The efficacy and use of anticonvulsants in mood disorders. Clin Neuropharmacol. 1998;21:215-35.
12. Lerer B, Moore N, Meyendor E, et al. Carbamazepine versus lithium in mania a double-blind study. J Clin Psychiatry. 1987;48:89-93.
13. Brown B. The use of generic mood stabilizers: carbamazepine (monograph). J Clin Psychiatry. 1997;15(4):11-17.
14. Karagianis JL, Dawe IC, Thakur A, et al. Rapid tranquilization with olanzapine in acute psychosis: a case series. J Clin Psychiatry. 2001;62(suppl 2):12-16.
15. Baker RW, Kinon BJ, Maguire GA, et al. Effectiveness of rapid initial dose escalation of up to 40 milligrams per day of oral olanzapine in acute agitation. J Clin Psychopharmacol. 2003;23(4):342-8.
16. Sachs GS, Grossman F, Ghaemi SN, et al. Combination of mood stabilizer with risperidone or haloperidol for the treatment of acute mania: a double-blind, placebo controlled comparison of efficacy and safety. Am J Psychiatry. 2002;159:1146-54.
17. Hirschfeld RMA, Keck PE, Jr, Karcher K, et al. Rapid antimanic effect of risperidone monotherapy: a 3-week multicenter, randomized, double-blind, placebo-controlled trial. Am J Psychiatry. 2004;161:1057-65.
18. Khanna S, Vieta E, Lyons B, et al. Risperidone monotherapy in acute bipolar mania (abstract P219). Pittsburgh: Fifth International Conference on Bipolar Disorder, 2003.
19. Jones MW, Huizar K, et al. Quetiapine monotherapy for acute mania associated with bipolar disorder (poster presentation). San Francisco: American Psychiatric Association annual meeting, 2003.
20. Sachs G, Mullen JA, Devine NA, Sweitzer DE. Quetiapine versus placebo as adjunct to mood stabilizer for the treatment of acute mania (abstract). Bipolar Disord. 2002;4(suppl 1):133.-
21. Smith MA, McCoy R, Hamer J, Brecher M. Optimal titration for quetiapine (poster presentation): Boca Raton, FL: National Clinical Drug Evaluation Unit annual meeting, 2002.
22. Keck PE, Jr, Versiani M, Potkin S, et al. Ziprasidone in the treatment of acute bipolar mania: a three-week, placebo-controlled, double-blind, randomized trial. Am J Psychiatry. 2003;160:741-8.
23. Holtzheimer PE, Neumaier JF. Treatment of acute mania. CNS Spectrums. 2003;8(12):917-28.
24. Keck PE, Jr, Marcus R, Tourkodimitris S, et al. A placebo-controlled, double-blind study of the efficacy and safety of aripiprazole in patients with acute bipolar mania. Am J Psychiatry. 2003;160(9):1651-8.
25. Sachs G, Sanchez R, Marcus R, et al. Aripiprazole vs placebo with an acute manic or mixed episode. New York: American Psychiatric Association annual meeting, 2004.
26. American Diabetes Association, American Psychiatric Association, American Association of Clinical Endocrinologists, North American Association for the Study of Obesity. Consensus Development Conference on Antipsychotic Drugs and Obesity and Diabetes. Diabetes Care. 2004;27:596-601.
1. Keck PE, Jr, McElroy SL, Tugrul KC, et al. Valproate oral loading in the treatment of acute mania. J Clin Psychiatry. 1993;54:305-8.
2. Moscovich DG, Shapira B, Lerer B, et al. Rapid lithiumization in acute manic patients. Hum Psychopharmacol. 1992;7:343-5.
3. Kook KA, Stimmel GL, Wilkins JN, et al. Accuracy and safety of a priori lithium loading. J Clin Psychiatry. 1985;46:49-51.
4. Carroll BT, Thalassinos A, Fawver JD. Loading strategies in acute mania. CNS Spectrums. 2001;6:919-30.
5. Hirschfeld RMA, Allen MH, McEvoy J, et al. Safety and tolerability of oral loading divalproex sodium in acutely manic bipolar patients. J Clin Psychiatry. 1999;60:815-18.
6. Miller BP, et al. Oral loading of extended-release divalproex in acute mania (presentation). New Orleans: American Psychiatric Association annual meeting, 2001.
7. Thibault M, Blume WT, Saint-Hilaire JM, et al. Divalproex extended-release versus the original divalproex tablet: results of a randomized, crossover study of well-controlled epileptic patients with primary generalized seizures. Epilepsy Res. 2002;50:243-9.
8. Hirschfeld RMA, Baker JD, Wozniak P, et al. The safety and early efficacy of oral-loaded divalproex versus standard-titration divalproex, lithium, olanzapine, and placebo in the treatment of acute mania associated with bipolar disorder. J Clin Psychiatry. 2003;64:841-6.
9. Phrolov K, Applebaum J, Levine J, et al. Single-dose intravenous valproate in acute mania. J Clin Psychiatry. 2004;65:68-70.
10. Keck PE, Jr, McElroy SL, Bennet TA. Pharmacologic loading in the treatment of acute mania. Bipolar Disord. 2000;2:42-6.
11. Dunn RT, Frye MS, Tim KA, et al. The efficacy and use of anticonvulsants in mood disorders. Clin Neuropharmacol. 1998;21:215-35.
12. Lerer B, Moore N, Meyendor E, et al. Carbamazepine versus lithium in mania a double-blind study. J Clin Psychiatry. 1987;48:89-93.
13. Brown B. The use of generic mood stabilizers: carbamazepine (monograph). J Clin Psychiatry. 1997;15(4):11-17.
14. Karagianis JL, Dawe IC, Thakur A, et al. Rapid tranquilization with olanzapine in acute psychosis: a case series. J Clin Psychiatry. 2001;62(suppl 2):12-16.
15. Baker RW, Kinon BJ, Maguire GA, et al. Effectiveness of rapid initial dose escalation of up to 40 milligrams per day of oral olanzapine in acute agitation. J Clin Psychopharmacol. 2003;23(4):342-8.
16. Sachs GS, Grossman F, Ghaemi SN, et al. Combination of mood stabilizer with risperidone or haloperidol for the treatment of acute mania: a double-blind, placebo controlled comparison of efficacy and safety. Am J Psychiatry. 2002;159:1146-54.
17. Hirschfeld RMA, Keck PE, Jr, Karcher K, et al. Rapid antimanic effect of risperidone monotherapy: a 3-week multicenter, randomized, double-blind, placebo-controlled trial. Am J Psychiatry. 2004;161:1057-65.
18. Khanna S, Vieta E, Lyons B, et al. Risperidone monotherapy in acute bipolar mania (abstract P219). Pittsburgh: Fifth International Conference on Bipolar Disorder, 2003.
19. Jones MW, Huizar K, et al. Quetiapine monotherapy for acute mania associated with bipolar disorder (poster presentation). San Francisco: American Psychiatric Association annual meeting, 2003.
20. Sachs G, Mullen JA, Devine NA, Sweitzer DE. Quetiapine versus placebo as adjunct to mood stabilizer for the treatment of acute mania (abstract). Bipolar Disord. 2002;4(suppl 1):133.-
21. Smith MA, McCoy R, Hamer J, Brecher M. Optimal titration for quetiapine (poster presentation): Boca Raton, FL: National Clinical Drug Evaluation Unit annual meeting, 2002.
22. Keck PE, Jr, Versiani M, Potkin S, et al. Ziprasidone in the treatment of acute bipolar mania: a three-week, placebo-controlled, double-blind, randomized trial. Am J Psychiatry. 2003;160:741-8.
23. Holtzheimer PE, Neumaier JF. Treatment of acute mania. CNS Spectrums. 2003;8(12):917-28.
24. Keck PE, Jr, Marcus R, Tourkodimitris S, et al. A placebo-controlled, double-blind study of the efficacy and safety of aripiprazole in patients with acute bipolar mania. Am J Psychiatry. 2003;160(9):1651-8.
25. Sachs G, Sanchez R, Marcus R, et al. Aripiprazole vs placebo with an acute manic or mixed episode. New York: American Psychiatric Association annual meeting, 2004.
26. American Diabetes Association, American Psychiatric Association, American Association of Clinical Endocrinologists, North American Association for the Study of Obesity. Consensus Development Conference on Antipsychotic Drugs and Obesity and Diabetes. Diabetes Care. 2004;27:596-601.
Bipolar depression dilemma: Continue antidepressants after remission—or not?
Psychiatrists in the trenches are not alone in being unsure how to treat breakthrough bipolar depression. No panelist or other expert attending a recent American College of Neuropsychopharmacology symposium could definitively recommend:
- when to add an antidepressant to mood-stabilizer therapy
- whether to discontinue antidepressants after bipolar depression is stabilized.
Until controlled trials address these issues, we must use limited evidence to treat patients with bipolar depression. To help you meet this challenge, this article offers provisional suggestions based on recent published and unpublished reports.
Evidence for continuing
No published, randomized studies have examined how long to continue antidepressants after bipolar depression has stabilized. Until recently, conventional wisdom has been to discontinue antidepressants as soon as possible because of worries about antidepressant-induced mania. Then two case-controlled studies—one retrospective and one prospective—challenged that assumption.
Figure Reduced relapse rates in patients whose antidepressants were continued
In a prospective case-controlled study, patients with bipolar disorder who continued antidepressant treatment for 6 to 12 months or >12 months after depressive episode remission had lower relapse rates than those who discontinued antidepressants within 6 months.
Source: Reprinted with permission from reference 2. Copyright 2003. American Psychiatric AssociationUsing similar methodologies, Altshuler et al1,2 examined bipolar patients who remained in remission for 6 weeks on mood stabilizers plus adjunctive antidepressants. Those who continued the antidepressants were less likely to relapse into depression (without an increase in manic episodes) than those whose antidepressants were discontinued (Figure).
Relapse rates in the first study1 were 35% at 1 year in those who continued antidepressants and 68% in those who did not. In the second study,2 36% and 70% of patients, respectively, had relapsed at 1 year. In the latter study, those who continued to take antidepressants for at least 6 months—instead of at least 12 months—had intermediate depressive relapse rates (53% for 6 months vs. 24% for 12 months).
When interpreting these data, keep several caveats in mind. For one, patients were not randomly assigned to continue or discontinue antidepressants but were designated by patient and clinician choice. When comparing the two patient groups, however, the authors found no inherent differences in illness characteristics that might have biased the results.
More importantly, few patients initially treated with antidepressant augmentation responded well and remained in remission. In the prospective study, 549 of 1,078 patients in the Stanley Foundation Bipolar Network received an antidepressant for breakthrough depressive symptoms.2 Only 189 remained on antidepressants for 2 months, and only 84 (15%) of the original population remained in remission for 2 months.
Summary. A small subgroup of patients appears to respond well to antidepressants and sustains this response for 6 to 8 weeks. For this subset, continuing antidepressant therapy would appear to be an appropriate strategy, based on:
- a significantly reduced risk for depressive relapse
- no increased risk of switching to mania, which is the usual reason to terminate antidepressants early.
Subsequent evidence
One needs to assess these observations in light of an interim analysis reported halfway through a small, open, randomized study. Ghaemi et al3 found no significant difference in outcomes—regardless of rapid-cycling status—among 14 bipolar patients who remained on antidepressants and 19 who discontinued across an average 60 and 50 weeks, respectively.
Table
Evidence on continuing antidepressants in breakthrough bipolar depression
| Study | Design | Results |
|---|---|---|
| Altshuler et al 1 | Retrospective, case-control, 39 patients (1 year) | Relapse rates: 35% in patients who continued antidepressants after mood stabilization and and 68% in those who did not; study included no rapid-cyclers |
| Altshuler et al 2 | Prospective, case control 84 patients (1 year) | Relapse rates: 36% in patients who continued antidepressants after mood stabilization and 70% in those who did not; study included no rapid cyclers |
| Ghaemi et al 3 (unpublished) | Open, randomized 33 patients (approx. 1 yr) | Relapse rate: 50% within 20 weeks, whether or not patients continued antidepressants; one-third of patients were rapid cyclers |
A survival analysis initially suggested some benefit for continuing antidepressants, but this disappeared when the authors adjusted for potential confounding factors—which was not done in the Altshuler et al studies. Patients receiving short-term or long-term antidepressants had a similar number of depressive episodes per year (1.00 vs. 0.75 episodes/year, respectively). For some reason, nonrapid-cycling patients showed greater depressive morbidity than those with rapid cycling.
Rapid cyclers comprised 30% of patients who continued antidepressants and 37% of those who discontinued. This may explain the 50% relapse rate within 20 weeks in both groups. By comparison, the Altshuler et al studies included no rapid cyclers.1,2 More details on this unpublished data are expected.
Are antidepressants the answer?
The high relapse rate in patients taking mood stabilizers—with or without an antidepressant—and the Ghaemi et al data3 suggest that we need alternate antidepressant approaches to bipolar depression. Potential regimens—anticonvulsants, atypical antipsychotics, and other agents—merit further study. So far the evidence is mixed, and the most effective approaches are not well-delineated.
Anticonvulsants. Sachs et al4 reported that adding lamotrigine or lamotrigine plus an antidepressant to mood stabilizer therapy did not appear more effective in treating bipolar depression than simply maintaining the mood stabilizers.
Similarly, a small randomized, double-blind study in the Systematic Treatment Enhancement Program for Bipolar Disorder (STEP-BD) was stopped early because of low total response. Adjunctive lamotrigine (24%) and inositol (17%) appeared more effective than risperidone (5%) for refractory bipolar depression.
Antipsychotics. In an 8-week randomized trial by Tohen et al,5 833 patients with moderate to severe bipolar I depression were treated with olanzapine, olanzapine plus fluoxetine, or placebo. Core depression symptoms improved significantly more with olanzapine alone or with fluoxetine compared with placebo, as measured by mean changes in the Montgomery-Asberg Depression Rating Scale.
In a 6-month open trial, 192 patients whose bipolar I depression remitted with any of the three treatments6 continued olanzapine and then, if needed after the first week, the olanzapine/fluoxetine combination (OFC). Nearly two-thirds of patients (62%) remained without a depressive recurrence, and 94% remained without a manic recurrence while taking the OFC. These unpublished data indicate that the OFC provided greater prophylactic antimanic than antidepressant effects.
Calabrese et al7 recently presented unpublished data comparing the effects of quetiapine monotherapy, 300 or 600 mg/d, with placebo in patients with bipolar depression. Beginning in the first week of treatment, both quetiapine dosages produced significantly greater antidepressant, antianxiety, and anti-insomnia effects than placebo (P < 0.001). Remission rates with both dosages were >50%.
Summary. These first controlled studies of atypical antipsychotics in bipolar depression suggest that this drug class may have antidepressant as well as their demonstrated antimanic effects.
Recommendations—for now
Controlled clinical trials have not been conducted, and the evidence on using adjunctive antidepressants in bipolar depression is ambiguous.8-11 As a result, it is unclear when or how long to use antidepressants, and many of the inferences and suggestions in this paper remain highly provisional.
Initiating antidepressants. My personal treatment guidelines—and those of many other clinicians—are to use the unimodal antidepressants to augment mood stabilizers in bipolar patients experiencing breakthrough depression, as long as they have not had:
- ultra-rapid cycling (>4 episodes/week)
- antidepressant-induced cycle acceleration
- or multiple episodes of antidepressant-induced mania, despite co-treatment with mood stabilizers.
If any of these variables is present, I would instead add another mood stabilizer or an atypical antipsychotic.
Continuing antidepressants. If the patient remains stable for 2 months after the antidepressant is added—with no depression or manic occurrence—I would continue the antidepressant indefinitely, based on the Altshuler et al data.12
Mood charting.I also recommend that clinicians help patients develop an individual method for mood charting, such as that used in the National Institute of Mental Health Life Chart Method (NIMH-LCM)12,13 or the STEP-BD program.14 Goals of the 5-year STEP-BD are to:
- determine the most effective treatments and relapse prevention strategies for bipolar disorder
- evaluate the psychotropic benefit of anticonvulsants, atypical antipsychotics, cholinesterase inhibitors, and neurotransmitter precursors
- determine the benefit of psychotropic combinations.
Mood charts can provide a retrospective and prospective overview of a patient’s illness course and response to medications. Compared with patient recall, mood charts help clinicians evaluate more precisely the risk of switching and the risks and benefits of starting, continuing, or discontinuing antidepressants. Mood charts may be your most effective tool for managing a patient’s bipolar depression and achieving and maintaining long-term remission.
Summary. In the absence of consensus or guidelines for treating bipolar depression, I suggest:
- a conservative approach—ie, no changes in medication—when the patient remains well on a given regimen
- an aggressive—if not radical—series of treatments and revisions when the illness course remains problematic.
Many medication classes and adjunctive strategies are available for treating bipolar illness.15-18 I recommend that you continue to systematically explore adjunctive treatments and combinations until the patient improves or—even better—attains remission. Good response can be achieved—even in treatment-refractory patients ill for long periods or with recurrent bipolar depression—although complex combination therapy is often required.
Related resources
- National Institute of Mental Health-Life Chart Method. Retrospective and prospective mood-tracking charts for patients with bipolar disorder. www.bipolarnews.org
- Systematic Treatment Enhancement Program for Bipolar Depression (STEP-BD). National Institute of Mental Health. www.stepbd.org/research/
Drug brand names
- Fluoxetine • Prozac
- Lamotrigine • Lamictal
- Olanzapine • Zyprexa
- Olanzapine/fluoxetine • Symbyax
- Quetiapine • Seroquel
- Risperidone • Risperdal
Disclosure
Dr. Post is a consultant to Abbott Laboratories, Astra-Zeneca Pharmaceuticals, Bristol-Myers Squibb Co., Elan Pharmaceuticals, GlaxoSmithKline, Janssen Pharmaceutica, Novartis Pharmaceuticals Corp., Shire Pharmaceuticals, and UCB Pharma.
1. Altshuler L, Kiriakos L, Calcagno J, et al. The impact of antidepressant discontinuation versus antidepressant continuation on 1-year risk for relapse of bipolar depression: a retrospective chart review. J Clin Psychiatry 2001;62:612-16.
2. Altshuler L, Suppes T, Black D, et al. Impact of antidepressant discontinuation after acute bipolar depression remission on rates of depressive relapse at 1-year follow-up. Am J Psychiatry 2003;160:1252-62.
3. Ghaemi S, El-Mallakh R, Baldassano CF, et al. Antidepressant treatment in bipolar depression: Long-term outcome (abstract). San Juan, PR: American College of Neuropsychopharmacology annual meeting, 2003.
4. Sachs GS. Mood stabilizers alone vs.mood stabilizers plus antidepressant in bipolar depression (symposium). San Juan, PR: American College of Neuropsychopharmacology annual meeting, 2003.
5. Tohen M, Vieta E, Calabrese J, et al. Efficacy of olanzapine and olanzapine-fluoxetine combination in the treatment of bipolar I depression. Arch Gen Psychiatry 2003;60:1079-88.
6. Tohen M, Vieta E, Ketter TA, et al. Acute and long-term efficacy of olanzapine and olanzapine/fluoxetine combination for bipolar depression (abstract). San Juan, PR: American College of Neuropsychopharmacology annual meeting, 2003.
7. Calabrese JR, Macfadden W, McCoy R, et al. Double-blind, placebo-controlled study of quetiapine in bipolar depression (abstract). New York: American Psychiatric Association annual meeting, 2004.
8. Post RM, Denicoff KD, Leverich GS, et al. Presentations of depression in bipolar illness. Clin Neurosci Res 2002a;2:142-57.
9. Post RM, Leverich GS, Nolen WA, et al. A re-evaluation of the role of antidepressants in the treatment of bipolar depression: data from the Stanley Bipolar Treatment Network. Bipolar Disord 2003a;5:396-406.
10. Post RM, Speer AM, Leverich GS. Bipolar illness: Which critical treatment issues need studying? Clinical Approaches in Bipolar Disorders 2003b;2:24-30.
11. Goodwin GM. Bipolar disorder: is psychiatry’s Cinderella starting to get out a little more? Acta Neuropsychiatry 2000;12:105.-
12. Leverich GS, Post RM. Life charting the course of bipolar disorder. Current Review of Mood and Anxiety Disorders 1996;1:48-61.
13. Leverich GS, Post RM. Life charting of affective disorders. CNS Spectrums 1998;3:21-37.
14. Sachs GS, Thase ME, Otto MW, et al. Rationale, design, and methods of the Systematic Treatment Enhancement Program for Bipolar Disorder (STEP-BD). Biol Psychiatry 2003;53:1028-42.
15. Post RM, Speer AM, Obrocea GV, Leverich GS. Acute and prophylactic effects of anticonvulsants in bipolar depression. Clin Neurosci Res 2002;2:228-51.
16. Post RM, Speer AM. A brief history of anticonvulsant use in affective disorders. In: Trimble MR, Schmitz B (eds). Seizures, affective disorders and anticonvulsant drugs Surrey, UK: Clarius Press 2002;53:81.-
17. Post RM, Speer AM, Leverich GS. Complex combination therapy: the evolution toward rational polypharmacy in lithium-resistant bipolar illness, In: Akiskal H, Tohen M (eds). 50 years: the psychopharmacology of bipolar illness London: John Wiley & Sons Ltd. 2004 (in press).
18. Post RM, Altshuler LL. Mood disorders: treatment of bipolar disorders. Sadock BJ, Sadock VA (eds). Kaplan & Sadock’s comprehensive textbook of psychiatry (8th ed) New York: Lippincott Williams & Wilkins, 2004 (in press).
Psychiatrists in the trenches are not alone in being unsure how to treat breakthrough bipolar depression. No panelist or other expert attending a recent American College of Neuropsychopharmacology symposium could definitively recommend:
- when to add an antidepressant to mood-stabilizer therapy
- whether to discontinue antidepressants after bipolar depression is stabilized.
Until controlled trials address these issues, we must use limited evidence to treat patients with bipolar depression. To help you meet this challenge, this article offers provisional suggestions based on recent published and unpublished reports.
Evidence for continuing
No published, randomized studies have examined how long to continue antidepressants after bipolar depression has stabilized. Until recently, conventional wisdom has been to discontinue antidepressants as soon as possible because of worries about antidepressant-induced mania. Then two case-controlled studies—one retrospective and one prospective—challenged that assumption.
Figure Reduced relapse rates in patients whose antidepressants were continued
In a prospective case-controlled study, patients with bipolar disorder who continued antidepressant treatment for 6 to 12 months or >12 months after depressive episode remission had lower relapse rates than those who discontinued antidepressants within 6 months.
Source: Reprinted with permission from reference 2. Copyright 2003. American Psychiatric AssociationUsing similar methodologies, Altshuler et al1,2 examined bipolar patients who remained in remission for 6 weeks on mood stabilizers plus adjunctive antidepressants. Those who continued the antidepressants were less likely to relapse into depression (without an increase in manic episodes) than those whose antidepressants were discontinued (Figure).
Relapse rates in the first study1 were 35% at 1 year in those who continued antidepressants and 68% in those who did not. In the second study,2 36% and 70% of patients, respectively, had relapsed at 1 year. In the latter study, those who continued to take antidepressants for at least 6 months—instead of at least 12 months—had intermediate depressive relapse rates (53% for 6 months vs. 24% for 12 months).
When interpreting these data, keep several caveats in mind. For one, patients were not randomly assigned to continue or discontinue antidepressants but were designated by patient and clinician choice. When comparing the two patient groups, however, the authors found no inherent differences in illness characteristics that might have biased the results.
More importantly, few patients initially treated with antidepressant augmentation responded well and remained in remission. In the prospective study, 549 of 1,078 patients in the Stanley Foundation Bipolar Network received an antidepressant for breakthrough depressive symptoms.2 Only 189 remained on antidepressants for 2 months, and only 84 (15%) of the original population remained in remission for 2 months.
Summary. A small subgroup of patients appears to respond well to antidepressants and sustains this response for 6 to 8 weeks. For this subset, continuing antidepressant therapy would appear to be an appropriate strategy, based on:
- a significantly reduced risk for depressive relapse
- no increased risk of switching to mania, which is the usual reason to terminate antidepressants early.
Subsequent evidence
One needs to assess these observations in light of an interim analysis reported halfway through a small, open, randomized study. Ghaemi et al3 found no significant difference in outcomes—regardless of rapid-cycling status—among 14 bipolar patients who remained on antidepressants and 19 who discontinued across an average 60 and 50 weeks, respectively.
Table
Evidence on continuing antidepressants in breakthrough bipolar depression
| Study | Design | Results |
|---|---|---|
| Altshuler et al 1 | Retrospective, case-control, 39 patients (1 year) | Relapse rates: 35% in patients who continued antidepressants after mood stabilization and and 68% in those who did not; study included no rapid-cyclers |
| Altshuler et al 2 | Prospective, case control 84 patients (1 year) | Relapse rates: 36% in patients who continued antidepressants after mood stabilization and 70% in those who did not; study included no rapid cyclers |
| Ghaemi et al 3 (unpublished) | Open, randomized 33 patients (approx. 1 yr) | Relapse rate: 50% within 20 weeks, whether or not patients continued antidepressants; one-third of patients were rapid cyclers |
A survival analysis initially suggested some benefit for continuing antidepressants, but this disappeared when the authors adjusted for potential confounding factors—which was not done in the Altshuler et al studies. Patients receiving short-term or long-term antidepressants had a similar number of depressive episodes per year (1.00 vs. 0.75 episodes/year, respectively). For some reason, nonrapid-cycling patients showed greater depressive morbidity than those with rapid cycling.
Rapid cyclers comprised 30% of patients who continued antidepressants and 37% of those who discontinued. This may explain the 50% relapse rate within 20 weeks in both groups. By comparison, the Altshuler et al studies included no rapid cyclers.1,2 More details on this unpublished data are expected.
Are antidepressants the answer?
The high relapse rate in patients taking mood stabilizers—with or without an antidepressant—and the Ghaemi et al data3 suggest that we need alternate antidepressant approaches to bipolar depression. Potential regimens—anticonvulsants, atypical antipsychotics, and other agents—merit further study. So far the evidence is mixed, and the most effective approaches are not well-delineated.
Anticonvulsants. Sachs et al4 reported that adding lamotrigine or lamotrigine plus an antidepressant to mood stabilizer therapy did not appear more effective in treating bipolar depression than simply maintaining the mood stabilizers.
Similarly, a small randomized, double-blind study in the Systematic Treatment Enhancement Program for Bipolar Disorder (STEP-BD) was stopped early because of low total response. Adjunctive lamotrigine (24%) and inositol (17%) appeared more effective than risperidone (5%) for refractory bipolar depression.
Antipsychotics. In an 8-week randomized trial by Tohen et al,5 833 patients with moderate to severe bipolar I depression were treated with olanzapine, olanzapine plus fluoxetine, or placebo. Core depression symptoms improved significantly more with olanzapine alone or with fluoxetine compared with placebo, as measured by mean changes in the Montgomery-Asberg Depression Rating Scale.
In a 6-month open trial, 192 patients whose bipolar I depression remitted with any of the three treatments6 continued olanzapine and then, if needed after the first week, the olanzapine/fluoxetine combination (OFC). Nearly two-thirds of patients (62%) remained without a depressive recurrence, and 94% remained without a manic recurrence while taking the OFC. These unpublished data indicate that the OFC provided greater prophylactic antimanic than antidepressant effects.
Calabrese et al7 recently presented unpublished data comparing the effects of quetiapine monotherapy, 300 or 600 mg/d, with placebo in patients with bipolar depression. Beginning in the first week of treatment, both quetiapine dosages produced significantly greater antidepressant, antianxiety, and anti-insomnia effects than placebo (P < 0.001). Remission rates with both dosages were >50%.
Summary. These first controlled studies of atypical antipsychotics in bipolar depression suggest that this drug class may have antidepressant as well as their demonstrated antimanic effects.
Recommendations—for now
Controlled clinical trials have not been conducted, and the evidence on using adjunctive antidepressants in bipolar depression is ambiguous.8-11 As a result, it is unclear when or how long to use antidepressants, and many of the inferences and suggestions in this paper remain highly provisional.
Initiating antidepressants. My personal treatment guidelines—and those of many other clinicians—are to use the unimodal antidepressants to augment mood stabilizers in bipolar patients experiencing breakthrough depression, as long as they have not had:
- ultra-rapid cycling (>4 episodes/week)
- antidepressant-induced cycle acceleration
- or multiple episodes of antidepressant-induced mania, despite co-treatment with mood stabilizers.
If any of these variables is present, I would instead add another mood stabilizer or an atypical antipsychotic.
Continuing antidepressants. If the patient remains stable for 2 months after the antidepressant is added—with no depression or manic occurrence—I would continue the antidepressant indefinitely, based on the Altshuler et al data.12
Mood charting.I also recommend that clinicians help patients develop an individual method for mood charting, such as that used in the National Institute of Mental Health Life Chart Method (NIMH-LCM)12,13 or the STEP-BD program.14 Goals of the 5-year STEP-BD are to:
- determine the most effective treatments and relapse prevention strategies for bipolar disorder
- evaluate the psychotropic benefit of anticonvulsants, atypical antipsychotics, cholinesterase inhibitors, and neurotransmitter precursors
- determine the benefit of psychotropic combinations.
Mood charts can provide a retrospective and prospective overview of a patient’s illness course and response to medications. Compared with patient recall, mood charts help clinicians evaluate more precisely the risk of switching and the risks and benefits of starting, continuing, or discontinuing antidepressants. Mood charts may be your most effective tool for managing a patient’s bipolar depression and achieving and maintaining long-term remission.
Summary. In the absence of consensus or guidelines for treating bipolar depression, I suggest:
- a conservative approach—ie, no changes in medication—when the patient remains well on a given regimen
- an aggressive—if not radical—series of treatments and revisions when the illness course remains problematic.
Many medication classes and adjunctive strategies are available for treating bipolar illness.15-18 I recommend that you continue to systematically explore adjunctive treatments and combinations until the patient improves or—even better—attains remission. Good response can be achieved—even in treatment-refractory patients ill for long periods or with recurrent bipolar depression—although complex combination therapy is often required.
Related resources
- National Institute of Mental Health-Life Chart Method. Retrospective and prospective mood-tracking charts for patients with bipolar disorder. www.bipolarnews.org
- Systematic Treatment Enhancement Program for Bipolar Depression (STEP-BD). National Institute of Mental Health. www.stepbd.org/research/
Drug brand names
- Fluoxetine • Prozac
- Lamotrigine • Lamictal
- Olanzapine • Zyprexa
- Olanzapine/fluoxetine • Symbyax
- Quetiapine • Seroquel
- Risperidone • Risperdal
Disclosure
Dr. Post is a consultant to Abbott Laboratories, Astra-Zeneca Pharmaceuticals, Bristol-Myers Squibb Co., Elan Pharmaceuticals, GlaxoSmithKline, Janssen Pharmaceutica, Novartis Pharmaceuticals Corp., Shire Pharmaceuticals, and UCB Pharma.
Psychiatrists in the trenches are not alone in being unsure how to treat breakthrough bipolar depression. No panelist or other expert attending a recent American College of Neuropsychopharmacology symposium could definitively recommend:
- when to add an antidepressant to mood-stabilizer therapy
- whether to discontinue antidepressants after bipolar depression is stabilized.
Until controlled trials address these issues, we must use limited evidence to treat patients with bipolar depression. To help you meet this challenge, this article offers provisional suggestions based on recent published and unpublished reports.
Evidence for continuing
No published, randomized studies have examined how long to continue antidepressants after bipolar depression has stabilized. Until recently, conventional wisdom has been to discontinue antidepressants as soon as possible because of worries about antidepressant-induced mania. Then two case-controlled studies—one retrospective and one prospective—challenged that assumption.
Figure Reduced relapse rates in patients whose antidepressants were continued
In a prospective case-controlled study, patients with bipolar disorder who continued antidepressant treatment for 6 to 12 months or >12 months after depressive episode remission had lower relapse rates than those who discontinued antidepressants within 6 months.
Source: Reprinted with permission from reference 2. Copyright 2003. American Psychiatric AssociationUsing similar methodologies, Altshuler et al1,2 examined bipolar patients who remained in remission for 6 weeks on mood stabilizers plus adjunctive antidepressants. Those who continued the antidepressants were less likely to relapse into depression (without an increase in manic episodes) than those whose antidepressants were discontinued (Figure).
Relapse rates in the first study1 were 35% at 1 year in those who continued antidepressants and 68% in those who did not. In the second study,2 36% and 70% of patients, respectively, had relapsed at 1 year. In the latter study, those who continued to take antidepressants for at least 6 months—instead of at least 12 months—had intermediate depressive relapse rates (53% for 6 months vs. 24% for 12 months).
When interpreting these data, keep several caveats in mind. For one, patients were not randomly assigned to continue or discontinue antidepressants but were designated by patient and clinician choice. When comparing the two patient groups, however, the authors found no inherent differences in illness characteristics that might have biased the results.
More importantly, few patients initially treated with antidepressant augmentation responded well and remained in remission. In the prospective study, 549 of 1,078 patients in the Stanley Foundation Bipolar Network received an antidepressant for breakthrough depressive symptoms.2 Only 189 remained on antidepressants for 2 months, and only 84 (15%) of the original population remained in remission for 2 months.
Summary. A small subgroup of patients appears to respond well to antidepressants and sustains this response for 6 to 8 weeks. For this subset, continuing antidepressant therapy would appear to be an appropriate strategy, based on:
- a significantly reduced risk for depressive relapse
- no increased risk of switching to mania, which is the usual reason to terminate antidepressants early.
Subsequent evidence
One needs to assess these observations in light of an interim analysis reported halfway through a small, open, randomized study. Ghaemi et al3 found no significant difference in outcomes—regardless of rapid-cycling status—among 14 bipolar patients who remained on antidepressants and 19 who discontinued across an average 60 and 50 weeks, respectively.
Table
Evidence on continuing antidepressants in breakthrough bipolar depression
| Study | Design | Results |
|---|---|---|
| Altshuler et al 1 | Retrospective, case-control, 39 patients (1 year) | Relapse rates: 35% in patients who continued antidepressants after mood stabilization and and 68% in those who did not; study included no rapid-cyclers |
| Altshuler et al 2 | Prospective, case control 84 patients (1 year) | Relapse rates: 36% in patients who continued antidepressants after mood stabilization and 70% in those who did not; study included no rapid cyclers |
| Ghaemi et al 3 (unpublished) | Open, randomized 33 patients (approx. 1 yr) | Relapse rate: 50% within 20 weeks, whether or not patients continued antidepressants; one-third of patients were rapid cyclers |
A survival analysis initially suggested some benefit for continuing antidepressants, but this disappeared when the authors adjusted for potential confounding factors—which was not done in the Altshuler et al studies. Patients receiving short-term or long-term antidepressants had a similar number of depressive episodes per year (1.00 vs. 0.75 episodes/year, respectively). For some reason, nonrapid-cycling patients showed greater depressive morbidity than those with rapid cycling.
Rapid cyclers comprised 30% of patients who continued antidepressants and 37% of those who discontinued. This may explain the 50% relapse rate within 20 weeks in both groups. By comparison, the Altshuler et al studies included no rapid cyclers.1,2 More details on this unpublished data are expected.
Are antidepressants the answer?
The high relapse rate in patients taking mood stabilizers—with or without an antidepressant—and the Ghaemi et al data3 suggest that we need alternate antidepressant approaches to bipolar depression. Potential regimens—anticonvulsants, atypical antipsychotics, and other agents—merit further study. So far the evidence is mixed, and the most effective approaches are not well-delineated.
Anticonvulsants. Sachs et al4 reported that adding lamotrigine or lamotrigine plus an antidepressant to mood stabilizer therapy did not appear more effective in treating bipolar depression than simply maintaining the mood stabilizers.
Similarly, a small randomized, double-blind study in the Systematic Treatment Enhancement Program for Bipolar Disorder (STEP-BD) was stopped early because of low total response. Adjunctive lamotrigine (24%) and inositol (17%) appeared more effective than risperidone (5%) for refractory bipolar depression.
Antipsychotics. In an 8-week randomized trial by Tohen et al,5 833 patients with moderate to severe bipolar I depression were treated with olanzapine, olanzapine plus fluoxetine, or placebo. Core depression symptoms improved significantly more with olanzapine alone or with fluoxetine compared with placebo, as measured by mean changes in the Montgomery-Asberg Depression Rating Scale.
In a 6-month open trial, 192 patients whose bipolar I depression remitted with any of the three treatments6 continued olanzapine and then, if needed after the first week, the olanzapine/fluoxetine combination (OFC). Nearly two-thirds of patients (62%) remained without a depressive recurrence, and 94% remained without a manic recurrence while taking the OFC. These unpublished data indicate that the OFC provided greater prophylactic antimanic than antidepressant effects.
Calabrese et al7 recently presented unpublished data comparing the effects of quetiapine monotherapy, 300 or 600 mg/d, with placebo in patients with bipolar depression. Beginning in the first week of treatment, both quetiapine dosages produced significantly greater antidepressant, antianxiety, and anti-insomnia effects than placebo (P < 0.001). Remission rates with both dosages were >50%.
Summary. These first controlled studies of atypical antipsychotics in bipolar depression suggest that this drug class may have antidepressant as well as their demonstrated antimanic effects.
Recommendations—for now
Controlled clinical trials have not been conducted, and the evidence on using adjunctive antidepressants in bipolar depression is ambiguous.8-11 As a result, it is unclear when or how long to use antidepressants, and many of the inferences and suggestions in this paper remain highly provisional.
Initiating antidepressants. My personal treatment guidelines—and those of many other clinicians—are to use the unimodal antidepressants to augment mood stabilizers in bipolar patients experiencing breakthrough depression, as long as they have not had:
- ultra-rapid cycling (>4 episodes/week)
- antidepressant-induced cycle acceleration
- or multiple episodes of antidepressant-induced mania, despite co-treatment with mood stabilizers.
If any of these variables is present, I would instead add another mood stabilizer or an atypical antipsychotic.
Continuing antidepressants. If the patient remains stable for 2 months after the antidepressant is added—with no depression or manic occurrence—I would continue the antidepressant indefinitely, based on the Altshuler et al data.12
Mood charting.I also recommend that clinicians help patients develop an individual method for mood charting, such as that used in the National Institute of Mental Health Life Chart Method (NIMH-LCM)12,13 or the STEP-BD program.14 Goals of the 5-year STEP-BD are to:
- determine the most effective treatments and relapse prevention strategies for bipolar disorder
- evaluate the psychotropic benefit of anticonvulsants, atypical antipsychotics, cholinesterase inhibitors, and neurotransmitter precursors
- determine the benefit of psychotropic combinations.
Mood charts can provide a retrospective and prospective overview of a patient’s illness course and response to medications. Compared with patient recall, mood charts help clinicians evaluate more precisely the risk of switching and the risks and benefits of starting, continuing, or discontinuing antidepressants. Mood charts may be your most effective tool for managing a patient’s bipolar depression and achieving and maintaining long-term remission.
Summary. In the absence of consensus or guidelines for treating bipolar depression, I suggest:
- a conservative approach—ie, no changes in medication—when the patient remains well on a given regimen
- an aggressive—if not radical—series of treatments and revisions when the illness course remains problematic.
Many medication classes and adjunctive strategies are available for treating bipolar illness.15-18 I recommend that you continue to systematically explore adjunctive treatments and combinations until the patient improves or—even better—attains remission. Good response can be achieved—even in treatment-refractory patients ill for long periods or with recurrent bipolar depression—although complex combination therapy is often required.
Related resources
- National Institute of Mental Health-Life Chart Method. Retrospective and prospective mood-tracking charts for patients with bipolar disorder. www.bipolarnews.org
- Systematic Treatment Enhancement Program for Bipolar Depression (STEP-BD). National Institute of Mental Health. www.stepbd.org/research/
Drug brand names
- Fluoxetine • Prozac
- Lamotrigine • Lamictal
- Olanzapine • Zyprexa
- Olanzapine/fluoxetine • Symbyax
- Quetiapine • Seroquel
- Risperidone • Risperdal
Disclosure
Dr. Post is a consultant to Abbott Laboratories, Astra-Zeneca Pharmaceuticals, Bristol-Myers Squibb Co., Elan Pharmaceuticals, GlaxoSmithKline, Janssen Pharmaceutica, Novartis Pharmaceuticals Corp., Shire Pharmaceuticals, and UCB Pharma.
1. Altshuler L, Kiriakos L, Calcagno J, et al. The impact of antidepressant discontinuation versus antidepressant continuation on 1-year risk for relapse of bipolar depression: a retrospective chart review. J Clin Psychiatry 2001;62:612-16.
2. Altshuler L, Suppes T, Black D, et al. Impact of antidepressant discontinuation after acute bipolar depression remission on rates of depressive relapse at 1-year follow-up. Am J Psychiatry 2003;160:1252-62.
3. Ghaemi S, El-Mallakh R, Baldassano CF, et al. Antidepressant treatment in bipolar depression: Long-term outcome (abstract). San Juan, PR: American College of Neuropsychopharmacology annual meeting, 2003.
4. Sachs GS. Mood stabilizers alone vs.mood stabilizers plus antidepressant in bipolar depression (symposium). San Juan, PR: American College of Neuropsychopharmacology annual meeting, 2003.
5. Tohen M, Vieta E, Calabrese J, et al. Efficacy of olanzapine and olanzapine-fluoxetine combination in the treatment of bipolar I depression. Arch Gen Psychiatry 2003;60:1079-88.
6. Tohen M, Vieta E, Ketter TA, et al. Acute and long-term efficacy of olanzapine and olanzapine/fluoxetine combination for bipolar depression (abstract). San Juan, PR: American College of Neuropsychopharmacology annual meeting, 2003.
7. Calabrese JR, Macfadden W, McCoy R, et al. Double-blind, placebo-controlled study of quetiapine in bipolar depression (abstract). New York: American Psychiatric Association annual meeting, 2004.
8. Post RM, Denicoff KD, Leverich GS, et al. Presentations of depression in bipolar illness. Clin Neurosci Res 2002a;2:142-57.
9. Post RM, Leverich GS, Nolen WA, et al. A re-evaluation of the role of antidepressants in the treatment of bipolar depression: data from the Stanley Bipolar Treatment Network. Bipolar Disord 2003a;5:396-406.
10. Post RM, Speer AM, Leverich GS. Bipolar illness: Which critical treatment issues need studying? Clinical Approaches in Bipolar Disorders 2003b;2:24-30.
11. Goodwin GM. Bipolar disorder: is psychiatry’s Cinderella starting to get out a little more? Acta Neuropsychiatry 2000;12:105.-
12. Leverich GS, Post RM. Life charting the course of bipolar disorder. Current Review of Mood and Anxiety Disorders 1996;1:48-61.
13. Leverich GS, Post RM. Life charting of affective disorders. CNS Spectrums 1998;3:21-37.
14. Sachs GS, Thase ME, Otto MW, et al. Rationale, design, and methods of the Systematic Treatment Enhancement Program for Bipolar Disorder (STEP-BD). Biol Psychiatry 2003;53:1028-42.
15. Post RM, Speer AM, Obrocea GV, Leverich GS. Acute and prophylactic effects of anticonvulsants in bipolar depression. Clin Neurosci Res 2002;2:228-51.
16. Post RM, Speer AM. A brief history of anticonvulsant use in affective disorders. In: Trimble MR, Schmitz B (eds). Seizures, affective disorders and anticonvulsant drugs Surrey, UK: Clarius Press 2002;53:81.-
17. Post RM, Speer AM, Leverich GS. Complex combination therapy: the evolution toward rational polypharmacy in lithium-resistant bipolar illness, In: Akiskal H, Tohen M (eds). 50 years: the psychopharmacology of bipolar illness London: John Wiley & Sons Ltd. 2004 (in press).
18. Post RM, Altshuler LL. Mood disorders: treatment of bipolar disorders. Sadock BJ, Sadock VA (eds). Kaplan & Sadock’s comprehensive textbook of psychiatry (8th ed) New York: Lippincott Williams & Wilkins, 2004 (in press).
1. Altshuler L, Kiriakos L, Calcagno J, et al. The impact of antidepressant discontinuation versus antidepressant continuation on 1-year risk for relapse of bipolar depression: a retrospective chart review. J Clin Psychiatry 2001;62:612-16.
2. Altshuler L, Suppes T, Black D, et al. Impact of antidepressant discontinuation after acute bipolar depression remission on rates of depressive relapse at 1-year follow-up. Am J Psychiatry 2003;160:1252-62.
3. Ghaemi S, El-Mallakh R, Baldassano CF, et al. Antidepressant treatment in bipolar depression: Long-term outcome (abstract). San Juan, PR: American College of Neuropsychopharmacology annual meeting, 2003.
4. Sachs GS. Mood stabilizers alone vs.mood stabilizers plus antidepressant in bipolar depression (symposium). San Juan, PR: American College of Neuropsychopharmacology annual meeting, 2003.
5. Tohen M, Vieta E, Calabrese J, et al. Efficacy of olanzapine and olanzapine-fluoxetine combination in the treatment of bipolar I depression. Arch Gen Psychiatry 2003;60:1079-88.
6. Tohen M, Vieta E, Ketter TA, et al. Acute and long-term efficacy of olanzapine and olanzapine/fluoxetine combination for bipolar depression (abstract). San Juan, PR: American College of Neuropsychopharmacology annual meeting, 2003.
7. Calabrese JR, Macfadden W, McCoy R, et al. Double-blind, placebo-controlled study of quetiapine in bipolar depression (abstract). New York: American Psychiatric Association annual meeting, 2004.
8. Post RM, Denicoff KD, Leverich GS, et al. Presentations of depression in bipolar illness. Clin Neurosci Res 2002a;2:142-57.
9. Post RM, Leverich GS, Nolen WA, et al. A re-evaluation of the role of antidepressants in the treatment of bipolar depression: data from the Stanley Bipolar Treatment Network. Bipolar Disord 2003a;5:396-406.
10. Post RM, Speer AM, Leverich GS. Bipolar illness: Which critical treatment issues need studying? Clinical Approaches in Bipolar Disorders 2003b;2:24-30.
11. Goodwin GM. Bipolar disorder: is psychiatry’s Cinderella starting to get out a little more? Acta Neuropsychiatry 2000;12:105.-
12. Leverich GS, Post RM. Life charting the course of bipolar disorder. Current Review of Mood and Anxiety Disorders 1996;1:48-61.
13. Leverich GS, Post RM. Life charting of affective disorders. CNS Spectrums 1998;3:21-37.
14. Sachs GS, Thase ME, Otto MW, et al. Rationale, design, and methods of the Systematic Treatment Enhancement Program for Bipolar Disorder (STEP-BD). Biol Psychiatry 2003;53:1028-42.
15. Post RM, Speer AM, Obrocea GV, Leverich GS. Acute and prophylactic effects of anticonvulsants in bipolar depression. Clin Neurosci Res 2002;2:228-51.
16. Post RM, Speer AM. A brief history of anticonvulsant use in affective disorders. In: Trimble MR, Schmitz B (eds). Seizures, affective disorders and anticonvulsant drugs Surrey, UK: Clarius Press 2002;53:81.-
17. Post RM, Speer AM, Leverich GS. Complex combination therapy: the evolution toward rational polypharmacy in lithium-resistant bipolar illness, In: Akiskal H, Tohen M (eds). 50 years: the psychopharmacology of bipolar illness London: John Wiley & Sons Ltd. 2004 (in press).
18. Post RM, Altshuler LL. Mood disorders: treatment of bipolar disorders. Sadock BJ, Sadock VA (eds). Kaplan & Sadock’s comprehensive textbook of psychiatry (8th ed) New York: Lippincott Williams & Wilkins, 2004 (in press).