User login
A wise aproach to bipolar depression
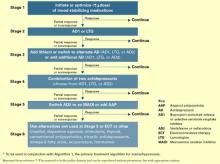
Most of us care for patients with bipolar disorder and face this problem regularly: We start an antidepressant for breakthrough depressive symptoms, and the patient responds. How long do we continue the antidepressant?
In this issue, Robert M. Post, MD, head of the Bipolar Collaborative Network, summarizes the published literature—and some very recent unpublished reports—related to this question and makes systematic recommendations. I won’t attempt to summarize his carefully considered conclusions, but I would like to highlight his two-pronged” approach:
- conservative treatment—no change in medication—when the patient remains well
- aggressive—if not radical—treatment when the illness course remains problematic.
I cannot help but reflect that these recommendations—wise advice for many clinical problems—echo the Hippocratic principles of “first, do no harm” and “extreme illnesses require extreme remedies.” Although, thank goodness, today’s medical treatments bear no resemblance to those used in Hippocrates’ time, our wisdom still bears a resemblance to his.
Conscientious physicians aspire to keep up with the latest literature while growing in professional wisdom. Helping us with those challenging tasks is Current Psychiatry’s goal.
Most of us care for patients with bipolar disorder and face this problem regularly: We start an antidepressant for breakthrough depressive symptoms, and the patient responds. How long do we continue the antidepressant?
In this issue, Robert M. Post, MD, head of the Bipolar Collaborative Network, summarizes the published literature—and some very recent unpublished reports—related to this question and makes systematic recommendations. I won’t attempt to summarize his carefully considered conclusions, but I would like to highlight his two-pronged” approach:
- conservative treatment—no change in medication—when the patient remains well
- aggressive—if not radical—treatment when the illness course remains problematic.
I cannot help but reflect that these recommendations—wise advice for many clinical problems—echo the Hippocratic principles of “first, do no harm” and “extreme illnesses require extreme remedies.” Although, thank goodness, today’s medical treatments bear no resemblance to those used in Hippocrates’ time, our wisdom still bears a resemblance to his.
Conscientious physicians aspire to keep up with the latest literature while growing in professional wisdom. Helping us with those challenging tasks is Current Psychiatry’s goal.
Most of us care for patients with bipolar disorder and face this problem regularly: We start an antidepressant for breakthrough depressive symptoms, and the patient responds. How long do we continue the antidepressant?
In this issue, Robert M. Post, MD, head of the Bipolar Collaborative Network, summarizes the published literature—and some very recent unpublished reports—related to this question and makes systematic recommendations. I won’t attempt to summarize his carefully considered conclusions, but I would like to highlight his two-pronged” approach:
- conservative treatment—no change in medication—when the patient remains well
- aggressive—if not radical—treatment when the illness course remains problematic.
I cannot help but reflect that these recommendations—wise advice for many clinical problems—echo the Hippocratic principles of “first, do no harm” and “extreme illnesses require extreme remedies.” Although, thank goodness, today’s medical treatments bear no resemblance to those used in Hippocrates’ time, our wisdom still bears a resemblance to his.
Conscientious physicians aspire to keep up with the latest literature while growing in professional wisdom. Helping us with those challenging tasks is Current Psychiatry’s goal.
Intramuscular olanzapine: Treating acute agitation in psychosis and bipolar mania
Oral atypical antipsychotics are given to treat a variety of psychiatric illnesses. Intramuscular (IM) preparations of atypicals are increasingly becoming available for emergency use, such as treating acute agitation.
The FDA has approved IM olanzapine for treating acute agitation associated with schizophrenia and bipolar type I mania.
How it works
As with the agent’s oral formulations (tablets, capsules, wafers), IM olanzapine is primarily an antagonist at serotonergic (5-HT2A) and dopaminergic (D2) receptors. Olanzapine is about twice as active at 5-HT2A compared with D2 receptors, which may underlie the agent’s efficacy as an antipsychotic and mood stabilizer without significant extrapyramidal effects.
Olanzapine also shows primarily antagonistic binding affinity at the 5-HT2B/2C, D1/D3/D4/D5, muscarinic, histamine H1 and alpha1-adrenergic receptors.1 This binding profile is comparable to that of clozapine and predicts a similar clinical response.
Pharmacokinetics
On most pharmacokinetic measures, IM olanzapine is nearly identical to its oral formulations, allowing easy comparison when switching to oral dosing as the patient improves.2
Plasma clearance (linear pharmacokinetics), half-life (approximately 30 hours), and volume of distribution are similar for IM and oral olanzapine. Maximum plasma concentrations after one, two, or three 10-mg injections given over 24 hours were similar to steady-state concentrations after daily administration of oral olanzapine, 20 mg.
The one key difference between IM and oral olanzapine is rate of absorption, which influences onset of action. IM olanzapine generally reaches maximum concentration in 15 to 45 minutes, compared with 4 hours after an oral dose. This rapid peak absorption could prove valuable in the first hour of a psychiatric emergency.
Efficacy
Three double-blind, randomized, placebo and active comparator-controlled studies demonstrated IM olanzapine’s safety and efficacy for treating acute agitation in patients with schizophrenia and bipolar type I mania. A fourth study gauged its efficacy in treating acute agitation in dementia.
Schizophrenia. In a study of 285 patients,3 IM olanzapine, 10 mg, was significantly more effective in reducing agitation than IM haloperidol, 7.5 mg, and IM placebo 15, 30, and 45 minutes after injection. Agitation was measured with the Positive and Negative Symptom Scale-Excited Component (PANSS-EC), Agitated Behavior Scale, and Agitation-Calmness Evaluation scale. Olanzapine and haloperidol were similar in efficacy 1 and 2 hours after injection, and both were more effective than placebo.
In another study,4 270 acutely agitated inpatients with schizophrenia received 1 to 3 IM injections of olanzapine (2.5, 5, 7.5, or 10 mg), haloperidol (7.5 mg), or placebo. The higher the olanzapine dose, the greater the PANSS-EC score reduction 2 hours after the first injection. Olanzapine was more effective than haloperidol on some agitation measures at 7.5 and 10 mg, and olanzapine was significantly more effective than haloperidol 24 hours post-injection, based on Agitated Behavior Scale scores.4 Both agents were similarly effective 2 hours after injection.
Bipolar type I mania. Agitated patients (N = 201) received 1 to 3 IM injections of olanzapine (10 mg for the first two injections, 5 mg for the third), lorazepam (2 mg first two, 1 mg third), or placebo.
Two hours after the first injection, agitation was more greatly reduced within the olanzapine group than in the lorazepam or placebo groups based on PANSS-EC, Agitated Behavior Scale, and Agitation-Calmness Evaluation Scale scores. At 24 hours, olanzapine was more effective than placebo but similar in efficacy to lorazepam.5
Table
IM olanzapine: Fast facts
| Drug brand name: Zyprexa IntraMuscular |
| Class Atypical antipsychotic |
| FDA-approved indication: Acute agitation associated with bipolar type I mania and schizophrenia |
| Approval date: March 29, 2004 |
| Manufacturer: Eli Lilly and Co. |
| Dosing form: 10 mg |
| Dosing recommendations: 10 mg for adults with schizophrenia and bipolar type I mania (5 mg ages 65 and older); 2.5 mg for patients who are debilitated, predisposed to hypotensive reactions, or sensitive to olanzapine. Consider 5- or 7.5-mg doses if clinical factors warrant, such as reduced clearance/slower metabolism in older, nonsmoking women. |
Dementia. A total of 272 patients with Alzheimer’s dementia, mixed dementia, or both received IM olanzapine (2.5 mg or 5 mg), IM lorazepam (1 mg), or IM placebo. The 5-mg olanzapine dose significantly reduced agitation 30 minutes post-injection, whereas lorazepam separated from placebo 60 minutes post-injection based on PANSS-EC scores. At 24 hours, both olanzapine doses were more effective than lorazepam or placebo.6
Tolerability
No clinically significant side effects have been reported with IM olanzapine. Incidence of extrapyramidal symptoms and QTc interval changes has been similar to that reported with placebo. Most studies have reported little change in vital signs, although a 7-bpm increase in heart rate and 5- to 7-mm Hg decrease in systolic blood pressure have been noted (Eli Lilly and Co., data on file).
Differences in treatment-emergent somnolence rates among patients receiving IM olanzapine (4% to 13%) and placebo (3% to 6%) were not statistically significant. Analyses of patients without treatment-emergent somnolence suggest that IM olanzapine retains a specific calming effect (as opposed to nonspecific sedation).7
Clinical implications
IM olanzapine offers psychiatrists a fast-acting option for treating agitation in patients with schizophrenia and bipolar type I mania. Its onset of action, measurable at 15 minutes post-injection, should prove valuable in the critical first hour of emergency psychiatric treatment. IM olanzapine’s efficacy and safety profile compare favorably with those of IM haloperidol and IM lorazepam.
IM olanzapine has shown safety and efficacy in treating agitation associated with dementia. Though the FDA has not approved this indication, the agent will likely be used for this purpose.
The only other fast-acting, injectable atypical antipsychotic—IM ziprasidone—is indicated for treatment of acute agitation in schizophrenia. Head-to-head comparisons between IM olanzapine and IM ziprasidone have not been conducted.
Clinical use and research will determine IM olanzapine’s role in treating patients with severe agitation (such as nonconsenting patients), those who are medically compromised, or patients in drug-induced psychotic states.
Related resources
- Zyprexa Web site. www.zyprexa.com.
- American Association for Emergency Psychiatry. http://www.emergencypsychiatry.org
Drug brand names
- Clozapine • Clozaril
- Haloperidol • Haldol
- Lorazepam • Ativan
- Olanzapine • Zyprexa
- Ziprasidone • Geodon
Disclosure
Dr. Battaglia is a consultant to and speaker for Eli Lilly and Co.
1. Bymaster FP, Calligaro DO, Falcone JF, et al. Radioreceptor binding profile of the atypical antipsychotic olanzapine. Neuropsychopharmacology 1996;14:87-96.
2. FDA Psychopharmacological Drugs Advisory Committee. Briefing document for Zyprexa (intramuscular olanzapine), February 13, 2001.
3. Wright P, Birkett M, David SR, et al. Double-blind, placebo-controlled comparison of intramuscular olanzapine and intramuscular haloperidol in the treatment of acute agitation in schizophrenia. Am J Psychiatry 2001;158:1149-51.
4. Breier A, Meehan K, Birkett M, et al. A double-blind, placebo-controlled dose-response comparison of intramuscular olanzapine and haloperidol in the treatment of acute agitation in schizophrenia. Arch Gen Psychiatry 2002;59:441-8.
5. Meehan K, Zhang F, David S, et al. A double-blind, randomized comparison of the efficacy and safety of intramuscular injections of olanzapine, lorazepam, or placebo in treating patients diagnosed with bipolar mania. J Clin Psychopharmacol 2001;21:389-97.
6. Meehan KM, Wang J, David S, et al. Comparison of rapidly acting intramuscular olanzapine, lorazepam, and placebo: A double blind, randomized study in acutely agitated patients with dementia. Neuropsychopharmacology 2002;26:494-504.
7. Battaglia J, Lindborg S, Alaka K, et al. To sleep or not to sleep? Calming versus sedative effects of intramuscular olanzapine in agitated patients. Am J Emerg Med 2003;21:192-8.
Oral atypical antipsychotics are given to treat a variety of psychiatric illnesses. Intramuscular (IM) preparations of atypicals are increasingly becoming available for emergency use, such as treating acute agitation.
The FDA has approved IM olanzapine for treating acute agitation associated with schizophrenia and bipolar type I mania.
How it works
As with the agent’s oral formulations (tablets, capsules, wafers), IM olanzapine is primarily an antagonist at serotonergic (5-HT2A) and dopaminergic (D2) receptors. Olanzapine is about twice as active at 5-HT2A compared with D2 receptors, which may underlie the agent’s efficacy as an antipsychotic and mood stabilizer without significant extrapyramidal effects.
Olanzapine also shows primarily antagonistic binding affinity at the 5-HT2B/2C, D1/D3/D4/D5, muscarinic, histamine H1 and alpha1-adrenergic receptors.1 This binding profile is comparable to that of clozapine and predicts a similar clinical response.
Pharmacokinetics
On most pharmacokinetic measures, IM olanzapine is nearly identical to its oral formulations, allowing easy comparison when switching to oral dosing as the patient improves.2
Plasma clearance (linear pharmacokinetics), half-life (approximately 30 hours), and volume of distribution are similar for IM and oral olanzapine. Maximum plasma concentrations after one, two, or three 10-mg injections given over 24 hours were similar to steady-state concentrations after daily administration of oral olanzapine, 20 mg.
The one key difference between IM and oral olanzapine is rate of absorption, which influences onset of action. IM olanzapine generally reaches maximum concentration in 15 to 45 minutes, compared with 4 hours after an oral dose. This rapid peak absorption could prove valuable in the first hour of a psychiatric emergency.
Efficacy
Three double-blind, randomized, placebo and active comparator-controlled studies demonstrated IM olanzapine’s safety and efficacy for treating acute agitation in patients with schizophrenia and bipolar type I mania. A fourth study gauged its efficacy in treating acute agitation in dementia.
Schizophrenia. In a study of 285 patients,3 IM olanzapine, 10 mg, was significantly more effective in reducing agitation than IM haloperidol, 7.5 mg, and IM placebo 15, 30, and 45 minutes after injection. Agitation was measured with the Positive and Negative Symptom Scale-Excited Component (PANSS-EC), Agitated Behavior Scale, and Agitation-Calmness Evaluation scale. Olanzapine and haloperidol were similar in efficacy 1 and 2 hours after injection, and both were more effective than placebo.
In another study,4 270 acutely agitated inpatients with schizophrenia received 1 to 3 IM injections of olanzapine (2.5, 5, 7.5, or 10 mg), haloperidol (7.5 mg), or placebo. The higher the olanzapine dose, the greater the PANSS-EC score reduction 2 hours after the first injection. Olanzapine was more effective than haloperidol on some agitation measures at 7.5 and 10 mg, and olanzapine was significantly more effective than haloperidol 24 hours post-injection, based on Agitated Behavior Scale scores.4 Both agents were similarly effective 2 hours after injection.
Bipolar type I mania. Agitated patients (N = 201) received 1 to 3 IM injections of olanzapine (10 mg for the first two injections, 5 mg for the third), lorazepam (2 mg first two, 1 mg third), or placebo.
Two hours after the first injection, agitation was more greatly reduced within the olanzapine group than in the lorazepam or placebo groups based on PANSS-EC, Agitated Behavior Scale, and Agitation-Calmness Evaluation Scale scores. At 24 hours, olanzapine was more effective than placebo but similar in efficacy to lorazepam.5
Table
IM olanzapine: Fast facts
| Drug brand name: Zyprexa IntraMuscular |
| Class Atypical antipsychotic |
| FDA-approved indication: Acute agitation associated with bipolar type I mania and schizophrenia |
| Approval date: March 29, 2004 |
| Manufacturer: Eli Lilly and Co. |
| Dosing form: 10 mg |
| Dosing recommendations: 10 mg for adults with schizophrenia and bipolar type I mania (5 mg ages 65 and older); 2.5 mg for patients who are debilitated, predisposed to hypotensive reactions, or sensitive to olanzapine. Consider 5- or 7.5-mg doses if clinical factors warrant, such as reduced clearance/slower metabolism in older, nonsmoking women. |
Dementia. A total of 272 patients with Alzheimer’s dementia, mixed dementia, or both received IM olanzapine (2.5 mg or 5 mg), IM lorazepam (1 mg), or IM placebo. The 5-mg olanzapine dose significantly reduced agitation 30 minutes post-injection, whereas lorazepam separated from placebo 60 minutes post-injection based on PANSS-EC scores. At 24 hours, both olanzapine doses were more effective than lorazepam or placebo.6
Tolerability
No clinically significant side effects have been reported with IM olanzapine. Incidence of extrapyramidal symptoms and QTc interval changes has been similar to that reported with placebo. Most studies have reported little change in vital signs, although a 7-bpm increase in heart rate and 5- to 7-mm Hg decrease in systolic blood pressure have been noted (Eli Lilly and Co., data on file).
Differences in treatment-emergent somnolence rates among patients receiving IM olanzapine (4% to 13%) and placebo (3% to 6%) were not statistically significant. Analyses of patients without treatment-emergent somnolence suggest that IM olanzapine retains a specific calming effect (as opposed to nonspecific sedation).7
Clinical implications
IM olanzapine offers psychiatrists a fast-acting option for treating agitation in patients with schizophrenia and bipolar type I mania. Its onset of action, measurable at 15 minutes post-injection, should prove valuable in the critical first hour of emergency psychiatric treatment. IM olanzapine’s efficacy and safety profile compare favorably with those of IM haloperidol and IM lorazepam.
IM olanzapine has shown safety and efficacy in treating agitation associated with dementia. Though the FDA has not approved this indication, the agent will likely be used for this purpose.
The only other fast-acting, injectable atypical antipsychotic—IM ziprasidone—is indicated for treatment of acute agitation in schizophrenia. Head-to-head comparisons between IM olanzapine and IM ziprasidone have not been conducted.
Clinical use and research will determine IM olanzapine’s role in treating patients with severe agitation (such as nonconsenting patients), those who are medically compromised, or patients in drug-induced psychotic states.
Related resources
- Zyprexa Web site. www.zyprexa.com.
- American Association for Emergency Psychiatry. http://www.emergencypsychiatry.org
Drug brand names
- Clozapine • Clozaril
- Haloperidol • Haldol
- Lorazepam • Ativan
- Olanzapine • Zyprexa
- Ziprasidone • Geodon
Disclosure
Dr. Battaglia is a consultant to and speaker for Eli Lilly and Co.
Oral atypical antipsychotics are given to treat a variety of psychiatric illnesses. Intramuscular (IM) preparations of atypicals are increasingly becoming available for emergency use, such as treating acute agitation.
The FDA has approved IM olanzapine for treating acute agitation associated with schizophrenia and bipolar type I mania.
How it works
As with the agent’s oral formulations (tablets, capsules, wafers), IM olanzapine is primarily an antagonist at serotonergic (5-HT2A) and dopaminergic (D2) receptors. Olanzapine is about twice as active at 5-HT2A compared with D2 receptors, which may underlie the agent’s efficacy as an antipsychotic and mood stabilizer without significant extrapyramidal effects.
Olanzapine also shows primarily antagonistic binding affinity at the 5-HT2B/2C, D1/D3/D4/D5, muscarinic, histamine H1 and alpha1-adrenergic receptors.1 This binding profile is comparable to that of clozapine and predicts a similar clinical response.
Pharmacokinetics
On most pharmacokinetic measures, IM olanzapine is nearly identical to its oral formulations, allowing easy comparison when switching to oral dosing as the patient improves.2
Plasma clearance (linear pharmacokinetics), half-life (approximately 30 hours), and volume of distribution are similar for IM and oral olanzapine. Maximum plasma concentrations after one, two, or three 10-mg injections given over 24 hours were similar to steady-state concentrations after daily administration of oral olanzapine, 20 mg.
The one key difference between IM and oral olanzapine is rate of absorption, which influences onset of action. IM olanzapine generally reaches maximum concentration in 15 to 45 minutes, compared with 4 hours after an oral dose. This rapid peak absorption could prove valuable in the first hour of a psychiatric emergency.
Efficacy
Three double-blind, randomized, placebo and active comparator-controlled studies demonstrated IM olanzapine’s safety and efficacy for treating acute agitation in patients with schizophrenia and bipolar type I mania. A fourth study gauged its efficacy in treating acute agitation in dementia.
Schizophrenia. In a study of 285 patients,3 IM olanzapine, 10 mg, was significantly more effective in reducing agitation than IM haloperidol, 7.5 mg, and IM placebo 15, 30, and 45 minutes after injection. Agitation was measured with the Positive and Negative Symptom Scale-Excited Component (PANSS-EC), Agitated Behavior Scale, and Agitation-Calmness Evaluation scale. Olanzapine and haloperidol were similar in efficacy 1 and 2 hours after injection, and both were more effective than placebo.
In another study,4 270 acutely agitated inpatients with schizophrenia received 1 to 3 IM injections of olanzapine (2.5, 5, 7.5, or 10 mg), haloperidol (7.5 mg), or placebo. The higher the olanzapine dose, the greater the PANSS-EC score reduction 2 hours after the first injection. Olanzapine was more effective than haloperidol on some agitation measures at 7.5 and 10 mg, and olanzapine was significantly more effective than haloperidol 24 hours post-injection, based on Agitated Behavior Scale scores.4 Both agents were similarly effective 2 hours after injection.
Bipolar type I mania. Agitated patients (N = 201) received 1 to 3 IM injections of olanzapine (10 mg for the first two injections, 5 mg for the third), lorazepam (2 mg first two, 1 mg third), or placebo.
Two hours after the first injection, agitation was more greatly reduced within the olanzapine group than in the lorazepam or placebo groups based on PANSS-EC, Agitated Behavior Scale, and Agitation-Calmness Evaluation Scale scores. At 24 hours, olanzapine was more effective than placebo but similar in efficacy to lorazepam.5
Table
IM olanzapine: Fast facts
| Drug brand name: Zyprexa IntraMuscular |
| Class Atypical antipsychotic |
| FDA-approved indication: Acute agitation associated with bipolar type I mania and schizophrenia |
| Approval date: March 29, 2004 |
| Manufacturer: Eli Lilly and Co. |
| Dosing form: 10 mg |
| Dosing recommendations: 10 mg for adults with schizophrenia and bipolar type I mania (5 mg ages 65 and older); 2.5 mg for patients who are debilitated, predisposed to hypotensive reactions, or sensitive to olanzapine. Consider 5- or 7.5-mg doses if clinical factors warrant, such as reduced clearance/slower metabolism in older, nonsmoking women. |
Dementia. A total of 272 patients with Alzheimer’s dementia, mixed dementia, or both received IM olanzapine (2.5 mg or 5 mg), IM lorazepam (1 mg), or IM placebo. The 5-mg olanzapine dose significantly reduced agitation 30 minutes post-injection, whereas lorazepam separated from placebo 60 minutes post-injection based on PANSS-EC scores. At 24 hours, both olanzapine doses were more effective than lorazepam or placebo.6
Tolerability
No clinically significant side effects have been reported with IM olanzapine. Incidence of extrapyramidal symptoms and QTc interval changes has been similar to that reported with placebo. Most studies have reported little change in vital signs, although a 7-bpm increase in heart rate and 5- to 7-mm Hg decrease in systolic blood pressure have been noted (Eli Lilly and Co., data on file).
Differences in treatment-emergent somnolence rates among patients receiving IM olanzapine (4% to 13%) and placebo (3% to 6%) were not statistically significant. Analyses of patients without treatment-emergent somnolence suggest that IM olanzapine retains a specific calming effect (as opposed to nonspecific sedation).7
Clinical implications
IM olanzapine offers psychiatrists a fast-acting option for treating agitation in patients with schizophrenia and bipolar type I mania. Its onset of action, measurable at 15 minutes post-injection, should prove valuable in the critical first hour of emergency psychiatric treatment. IM olanzapine’s efficacy and safety profile compare favorably with those of IM haloperidol and IM lorazepam.
IM olanzapine has shown safety and efficacy in treating agitation associated with dementia. Though the FDA has not approved this indication, the agent will likely be used for this purpose.
The only other fast-acting, injectable atypical antipsychotic—IM ziprasidone—is indicated for treatment of acute agitation in schizophrenia. Head-to-head comparisons between IM olanzapine and IM ziprasidone have not been conducted.
Clinical use and research will determine IM olanzapine’s role in treating patients with severe agitation (such as nonconsenting patients), those who are medically compromised, or patients in drug-induced psychotic states.
Related resources
- Zyprexa Web site. www.zyprexa.com.
- American Association for Emergency Psychiatry. http://www.emergencypsychiatry.org
Drug brand names
- Clozapine • Clozaril
- Haloperidol • Haldol
- Lorazepam • Ativan
- Olanzapine • Zyprexa
- Ziprasidone • Geodon
Disclosure
Dr. Battaglia is a consultant to and speaker for Eli Lilly and Co.
1. Bymaster FP, Calligaro DO, Falcone JF, et al. Radioreceptor binding profile of the atypical antipsychotic olanzapine. Neuropsychopharmacology 1996;14:87-96.
2. FDA Psychopharmacological Drugs Advisory Committee. Briefing document for Zyprexa (intramuscular olanzapine), February 13, 2001.
3. Wright P, Birkett M, David SR, et al. Double-blind, placebo-controlled comparison of intramuscular olanzapine and intramuscular haloperidol in the treatment of acute agitation in schizophrenia. Am J Psychiatry 2001;158:1149-51.
4. Breier A, Meehan K, Birkett M, et al. A double-blind, placebo-controlled dose-response comparison of intramuscular olanzapine and haloperidol in the treatment of acute agitation in schizophrenia. Arch Gen Psychiatry 2002;59:441-8.
5. Meehan K, Zhang F, David S, et al. A double-blind, randomized comparison of the efficacy and safety of intramuscular injections of olanzapine, lorazepam, or placebo in treating patients diagnosed with bipolar mania. J Clin Psychopharmacol 2001;21:389-97.
6. Meehan KM, Wang J, David S, et al. Comparison of rapidly acting intramuscular olanzapine, lorazepam, and placebo: A double blind, randomized study in acutely agitated patients with dementia. Neuropsychopharmacology 2002;26:494-504.
7. Battaglia J, Lindborg S, Alaka K, et al. To sleep or not to sleep? Calming versus sedative effects of intramuscular olanzapine in agitated patients. Am J Emerg Med 2003;21:192-8.
1. Bymaster FP, Calligaro DO, Falcone JF, et al. Radioreceptor binding profile of the atypical antipsychotic olanzapine. Neuropsychopharmacology 1996;14:87-96.
2. FDA Psychopharmacological Drugs Advisory Committee. Briefing document for Zyprexa (intramuscular olanzapine), February 13, 2001.
3. Wright P, Birkett M, David SR, et al. Double-blind, placebo-controlled comparison of intramuscular olanzapine and intramuscular haloperidol in the treatment of acute agitation in schizophrenia. Am J Psychiatry 2001;158:1149-51.
4. Breier A, Meehan K, Birkett M, et al. A double-blind, placebo-controlled dose-response comparison of intramuscular olanzapine and haloperidol in the treatment of acute agitation in schizophrenia. Arch Gen Psychiatry 2002;59:441-8.
5. Meehan K, Zhang F, David S, et al. A double-blind, randomized comparison of the efficacy and safety of intramuscular injections of olanzapine, lorazepam, or placebo in treating patients diagnosed with bipolar mania. J Clin Psychopharmacol 2001;21:389-97.
6. Meehan KM, Wang J, David S, et al. Comparison of rapidly acting intramuscular olanzapine, lorazepam, and placebo: A double blind, randomized study in acutely agitated patients with dementia. Neuropsychopharmacology 2002;26:494-504.
7. Battaglia J, Lindborg S, Alaka K, et al. To sleep or not to sleep? Calming versus sedative effects of intramuscular olanzapine in agitated patients. Am J Emerg Med 2003;21:192-8.
Olanzapine/fluoxetine combination: Evidence for using the first treatment indicated for bipolar depression
Patients with bipolar disorder spend half their lives significantly symptomatic, mainly in the depressive phase.1 Treating bipolar depression poses a clinical challenge, although new research is starting to uncover some answers. Antidepressant drugs are commonly used, but recent data question the effectiveness of this practice.2
An olanzapine-fluoxetine combination (OFC), FDA-approved for treating bipolar type I depression, has demonstrated efficacy in clinical trials.
How it works
Most atypical antipsychotics—including olanzapine—are potent 5-HT2A (serotonin) receptor antagonists. This effect is similar to that of some antidepressants and may mediate some antidepressant and antianxiety effects of these drugs.3
Like most atypicals, olanzapine is also a potent 5-HT2C blocker. While binding to this receptor, serotonin inhibits dopamine release in the nucleus accumbens and frontal cortex.4 Thus, serotonin blockade would increase dopamine release in these areas. One study showed that olanzapine and fluoxetine together increased dopamine and norepinephrine in the frontal cortex of rats, compared with either drug given individually.5 Dopamine is critical to regulating motivation, defined as the ability to exert energy to obtain rewards.6 Olanzapine also interacts with dopaminergic (D1-5), muscarinic (M1-5), alpha1 adrenergic, histamine1, serotonin (5-HT2B,2C,3,6), and glutamate and other receptors.
Pharmacokinetics
Combining olanzapine and fluoxetine in one capsule raises potential kinetic problems. Olanzapine’s mean half-life is 30 hours,7 but fluoxetine’s is 24 to 72 hours and its principal active metabolite, norfluoxetine, has a half-life of 4 to 16 hours.7 Because fluoxetine and norfluoxetine inhibit the cytochrome P (CYP)-450 2D6 enzyme—which is involved in their metabolism—autoinhibition of degradation occurs with chronic dosing, thereby increasing the relative half-life of fluoxetine and norfluoxetine. Therefore, maximum steady-state plasma levels will be achieved with olanzapine and fluoxetine at very different rates, although this has not posed a problem in clinical trials. Still, consider this disparity when evaluating potential side effects or drug-drug interactions.
Table 1
Drugs that may interact with OFC
| Drugs metabolized by CYP 2D6 isoenzymes | Drugs metabolized by CYP 2C isoenzymes |
|---|---|
| Citalopram | Citalopram |
| Codeine | Clomipramine |
| Dextromethorphan | Diazepam |
| Haloperidol | Imipramine |
| Metoprolol | Nonsteroidal |
| Other SSRIs | anti-inflammatory drugs |
| Perphenazine | Omeprazole |
| Propafenone | Phenytoin |
| Propranolol | Proguanil |
| Risperidone | Tolbutamide |
| Thioridazine | Tricyclic antidepressants |
| Trazodone | Warfarin |
| Tricyclic antidepressants (most) | |
| Venlafaxine | |
| Source: reference 8 | |
Both compounds reach maximum concentration in 4 to 6 hours.7 Although food’s effect on OFC’s absorption has not been tested, a clinically important effect is unlikely. Food does not significantly alter absorption kinetics of olanzapine or fluoxetine.7
Avoid giving OFC concomitantly with drugs metabolized by CYP 2D6 and 2C (Table 1), because fluoxetine is a potent inhibitor of these isoenzymes. The resulting altered plasma concentrations could lead to drug-drug interactions.8
Efficacy
In an 8-week, double-blind, multinational trial,9 833 patients with bipolar I disorder in the depressive phase randomly received placebo, olanzapine alone (5 to 20 mg/d), or OFC in several fixed combinations (all shown as olanzapine/fluoxetine): 6/25 mg/d, 6/50 mg/d, or 12/50 mg/d. Dosage titration was allowed.
The researchers found that:
- OFC was significantly more effective than placebo. A mean 18.5-point improvement in Montgomery-Asberg Depression Rating Scale (MADRS) scores was reported in the OFC group, compared with a mean 11.9-point improvement in the placebo group.
- Olanzapine alone produced a mean 15-point MADRS score reduction. Remission criteria were achieved in 24.5%, 32.8%, and 48.8% of patients treated with placebo, olanzapine, and OFC, respectively.
- Both OFC and olanzapine alone produced greater MADRS score reductions than did placebo at every follow-up week. Mania induction rates were low in the olanzapine and OFC treatment groups (5.7% and 6.4%, respectively) as measured with the Young Mania Rating Scale.
Shelton et al3 also compared OFC to olanzapine and fluoxetine alone in treatment-resistant unipolar depression. Thirty-two patients with major depression who responded inadequately to two types of antidepressants were treated with fluoxetine, up to 60 mg/d. After 7 weeks, 28 patients who did not respond to fluoxetine then received fluoxetine alone (mean modal dose: 52 mg/d), olanzapine alone (12.5 mg/d), or OFC (13.5 mg/52 mg/d) for another 8 weeks.
Olanzapine alone produced a transient effect at week 3 with relapse thereafter, possibly because of interactions between olanzapine and falling fluoxetine plasma concentrations over the first 3 weeks. Fluoxetine monotherapy produced minimal results across the 8-week random phase.
The OFC group, however, achieved significant improvement in MADRS scores compared with the placebo group after week one. The effect continued throughout the trial and during a subsequent 8-week open-label phase.3
Recent data suggest continued benefit in treatment- and nontreatment-resistant depressed patients for up to 1 year.10 Two follow-up trials—one using a lead-in with venlafaxine, the second with nortriptyline—produced negative results. In both studies, however, patients achieved a robust effect while continuing the same drug during the double-blind phase, suggesting that initial trials were inadequate.11,12 OFC showed early onset of effect in both studies. Other large-scale attempts at replication are anticipated.
Tolerability
Common side effects of OFC include increased appetite, weight gain, somnolence, fatigue, nausea, diarrhea, and dry mouth—the same effects associated with olanzapine or fluoxetine.
Combining the agents does not lessen the side effects, particularly olanzapine-induced weight gain. Simple, assertive dietary and exercise counseling can counteract olanzapine-induced weight gain.13 Sexual dysfunction was reported infrequently in clinical trials but is possible with exposure to fluoxetine.
Extrapyramidal side effects, including akathisia, appear to be relatively infrequent. Tardive dyskinesia (TD) is unlikely, although cases putatively associated with olanzapine have been reported.5 Many patients with TD have taken conventional antipsychotics, however, so the causal link with olanzapine is obscure. Still, alert patients and families to the possibility of TD and its emerging features.
Table 2
Olanzapine-fluoxetine: Fast facts
| Drug brand name: Symbyax |
| Class: Combined atypical antipsychotic/selective serotonin reuptake inhibitor |
| FDA-approved indication: Bipolar type I depression |
| Approval date: Dec. 24, 2003 |
| Manufacturer: Eli Lilly and Co. |
| Dosing forms: 6/25 mg/d, 12/50 mg/d, 12/25 mg/d, 12/50 mg/d |
| Dosing recommendations: Start at 6/25 mg at bedtime. Titrate according to tolerability and therapeutic benefit. Once the antidepressant effect is achieved, continue dosage indefinitely if no adverse effects occur. Dosages up to 18/75 mg/d have been used in clinical trials. |
Although considered rare, isolated cases of neuroleptic malignant syndrome have been attributed to olanzapine.14 Cycle induction has not been reported in clinical trials, but be mindful of this possibility with long-term treatment.
Clinical implications
Taking olanzapine and fluoxetine as a single capsule could save the patient substantial cost. OFC comes in four dosing forms (Table 2), allowing for some flexibility.
It is unclear whether clinicians will prefer the single combination capsule or prescribe each drug separately to increase flexibility. Starting treatment with olanzapine and fluoxetine individually allows the psychiatrist to change the dosages independently and in smaller increments. Taken as separate agents, however, the two products are more expensive than the combined formula. OFC costs about the same as olanzapine alone. On the other hand, if the clinician begins the compounds individually, converting to the dosages in the combined product probably will not be exactly 1:1.
Tolerability is another major advantage of OFC; the combined agent exhibited a 10% dropout rate because of adverse effects compared with 4.6% for placebo.7 Moreover, some patients will prefer the convenience of using a single capsule instead of two medications.
Related resources
- Tollefson GD, Sanger TM. Anxious-depressive symptoms in schizophrenia: a new treatment target for pharmacotherapy? Schizophr Res 1999;35(suppl):S13-S21.
- Symbyax Web site. www.symbyax.com
Drug brand names
- Citalopram • Celexa
- Clomipramine • Anafranil
- Diazepam • Valium
- Fluoxetine • Prozac
- Haloperidol • Haldol
- Imipramine • Tofranil
- Metoprolol succinate • Toprol
- Nortriptyline • Aventyl
- Olanzapine • Zyprexa
- Omeprazole • Prilosec
- Phenytoin • Dilantin
- Proguanil • Malarone
- Propafenone • Rythmol
- Propranolol • Inderal
- Risperidone • Risperdal
- Tolbutamide • Orinase
- Venlafaxine • Effexor
- Warfarin • Coumadin
Disclosure
Dr. Shelton receives research grants from Abbott Laboratories, Eli Lilly and Co., GlaxoSmithKline, Janssen Pharmaceutica, Pfizer Inc., and Wyeth Pharmaceuticals; is a consultant to Janssen Pharmaceutica, Pfizer Inc., and Wyeth Pharmaceuticals; and is a speaker for Abbott Laboratories, Eli Lilly and Co., Forest Pharmaceuticals, GlaxoSmithKline, Janssen Pharmaceutica, Pfizer Inc., and Wyeth Pharmaceuticals
1. Judd LL, Akiskal HS, Schettler PJ, et al. The long-term natural history of the weekly symptomatic status of bipolar I disorder. Arch Gen Psychiatry 2002;59:530-7.
2. Nemeroff CB, Evans DL, Gyulai L, et al. Double-blind, placebo-controlled comparison of imipramine and paroxetine in the treatment of bipolar depression. Am J Psychiatry 2001;158:906-12.
3. Shelton RC, Tollefson GD, Tohen M, et al. A novel augmentation strategy for treating resistant major depression. Am J Psychiatry 2001;158:131-4.
4. Shelton RC. The combination of olanzapine and fluoxetine in mood disorders. Expert Opin Pharmacother 2003;4:1175-83.
5. Zhang W, Perry KW, Wong DT, et al. Synergistic effects of olanzapine and other antipsychotic agents in combination with fluoxetine on norepinephrine and dopamine release in rat prefrontal cortex. Neuropsychopharmacology 2000;23:250-62.
6. Salamone JD, Cousins MS, Snyder BJ. Behavioral functions of nucleus accumbens dopamine: empirical and conceptual problems with the anhedonia hypothesis. Neurosci Biobehav Rev 1997;21:341-59.
7. Symbyax package insert. Eli Lilly and Co., 2003.
8. Nemeroff CB, DeVane CL, Pollock BG. Newer antidepressants and the cytochrome P450 system. Am J Psychiatry 1996;153:311-20.
9. Tohen M, Vieta E, Calabrese J, et al. Efficacy of olanzapine and olanzapine-fluoxetine combination in the treatment of bipolar I depression. Arch Gen Psychiatry 2003;60:1079-88.
10. Corya SA, Andersen SW, Detke HC, et al. Long-term antidepressant efficacy and safety of olanzapine/fluoxetine combination: a 76-week open-label study. J Clin Psychiatry 2003;64:1349-56.
11. Dube S. Olanzapine-fluoxetine combination in treatment-resistant depression. Eur Psychiatry 2002;17(suppl 1):98.-
12. Dube S, Corya SA, Andersen SW, et al. Efficacy of olanzapine/fluoxetine combination in treatment resistant depression (presentation). San Juan, PR: American College of Neuropsychopharmacology annual meeting, 2002.
13. Ball MP, Coons VB, Buchanan RW. A program for treating olanzapine-related weight gain. Psychiatr Serv 2001;52:967-9.
14. Kogoj A, Velikonja I. Olanzapine-induced neuroleptic malignant syndrome—a case review. Hum Psychopharmacol 2003;18:301-9.
Patients with bipolar disorder spend half their lives significantly symptomatic, mainly in the depressive phase.1 Treating bipolar depression poses a clinical challenge, although new research is starting to uncover some answers. Antidepressant drugs are commonly used, but recent data question the effectiveness of this practice.2
An olanzapine-fluoxetine combination (OFC), FDA-approved for treating bipolar type I depression, has demonstrated efficacy in clinical trials.
How it works
Most atypical antipsychotics—including olanzapine—are potent 5-HT2A (serotonin) receptor antagonists. This effect is similar to that of some antidepressants and may mediate some antidepressant and antianxiety effects of these drugs.3
Like most atypicals, olanzapine is also a potent 5-HT2C blocker. While binding to this receptor, serotonin inhibits dopamine release in the nucleus accumbens and frontal cortex.4 Thus, serotonin blockade would increase dopamine release in these areas. One study showed that olanzapine and fluoxetine together increased dopamine and norepinephrine in the frontal cortex of rats, compared with either drug given individually.5 Dopamine is critical to regulating motivation, defined as the ability to exert energy to obtain rewards.6 Olanzapine also interacts with dopaminergic (D1-5), muscarinic (M1-5), alpha1 adrenergic, histamine1, serotonin (5-HT2B,2C,3,6), and glutamate and other receptors.
Pharmacokinetics
Combining olanzapine and fluoxetine in one capsule raises potential kinetic problems. Olanzapine’s mean half-life is 30 hours,7 but fluoxetine’s is 24 to 72 hours and its principal active metabolite, norfluoxetine, has a half-life of 4 to 16 hours.7 Because fluoxetine and norfluoxetine inhibit the cytochrome P (CYP)-450 2D6 enzyme—which is involved in their metabolism—autoinhibition of degradation occurs with chronic dosing, thereby increasing the relative half-life of fluoxetine and norfluoxetine. Therefore, maximum steady-state plasma levels will be achieved with olanzapine and fluoxetine at very different rates, although this has not posed a problem in clinical trials. Still, consider this disparity when evaluating potential side effects or drug-drug interactions.
Table 1
Drugs that may interact with OFC
| Drugs metabolized by CYP 2D6 isoenzymes | Drugs metabolized by CYP 2C isoenzymes |
|---|---|
| Citalopram | Citalopram |
| Codeine | Clomipramine |
| Dextromethorphan | Diazepam |
| Haloperidol | Imipramine |
| Metoprolol | Nonsteroidal |
| Other SSRIs | anti-inflammatory drugs |
| Perphenazine | Omeprazole |
| Propafenone | Phenytoin |
| Propranolol | Proguanil |
| Risperidone | Tolbutamide |
| Thioridazine | Tricyclic antidepressants |
| Trazodone | Warfarin |
| Tricyclic antidepressants (most) | |
| Venlafaxine | |
| Source: reference 8 | |
Both compounds reach maximum concentration in 4 to 6 hours.7 Although food’s effect on OFC’s absorption has not been tested, a clinically important effect is unlikely. Food does not significantly alter absorption kinetics of olanzapine or fluoxetine.7
Avoid giving OFC concomitantly with drugs metabolized by CYP 2D6 and 2C (Table 1), because fluoxetine is a potent inhibitor of these isoenzymes. The resulting altered plasma concentrations could lead to drug-drug interactions.8
Efficacy
In an 8-week, double-blind, multinational trial,9 833 patients with bipolar I disorder in the depressive phase randomly received placebo, olanzapine alone (5 to 20 mg/d), or OFC in several fixed combinations (all shown as olanzapine/fluoxetine): 6/25 mg/d, 6/50 mg/d, or 12/50 mg/d. Dosage titration was allowed.
The researchers found that:
- OFC was significantly more effective than placebo. A mean 18.5-point improvement in Montgomery-Asberg Depression Rating Scale (MADRS) scores was reported in the OFC group, compared with a mean 11.9-point improvement in the placebo group.
- Olanzapine alone produced a mean 15-point MADRS score reduction. Remission criteria were achieved in 24.5%, 32.8%, and 48.8% of patients treated with placebo, olanzapine, and OFC, respectively.
- Both OFC and olanzapine alone produced greater MADRS score reductions than did placebo at every follow-up week. Mania induction rates were low in the olanzapine and OFC treatment groups (5.7% and 6.4%, respectively) as measured with the Young Mania Rating Scale.
Shelton et al3 also compared OFC to olanzapine and fluoxetine alone in treatment-resistant unipolar depression. Thirty-two patients with major depression who responded inadequately to two types of antidepressants were treated with fluoxetine, up to 60 mg/d. After 7 weeks, 28 patients who did not respond to fluoxetine then received fluoxetine alone (mean modal dose: 52 mg/d), olanzapine alone (12.5 mg/d), or OFC (13.5 mg/52 mg/d) for another 8 weeks.
Olanzapine alone produced a transient effect at week 3 with relapse thereafter, possibly because of interactions between olanzapine and falling fluoxetine plasma concentrations over the first 3 weeks. Fluoxetine monotherapy produced minimal results across the 8-week random phase.
The OFC group, however, achieved significant improvement in MADRS scores compared with the placebo group after week one. The effect continued throughout the trial and during a subsequent 8-week open-label phase.3
Recent data suggest continued benefit in treatment- and nontreatment-resistant depressed patients for up to 1 year.10 Two follow-up trials—one using a lead-in with venlafaxine, the second with nortriptyline—produced negative results. In both studies, however, patients achieved a robust effect while continuing the same drug during the double-blind phase, suggesting that initial trials were inadequate.11,12 OFC showed early onset of effect in both studies. Other large-scale attempts at replication are anticipated.
Tolerability
Common side effects of OFC include increased appetite, weight gain, somnolence, fatigue, nausea, diarrhea, and dry mouth—the same effects associated with olanzapine or fluoxetine.
Combining the agents does not lessen the side effects, particularly olanzapine-induced weight gain. Simple, assertive dietary and exercise counseling can counteract olanzapine-induced weight gain.13 Sexual dysfunction was reported infrequently in clinical trials but is possible with exposure to fluoxetine.
Extrapyramidal side effects, including akathisia, appear to be relatively infrequent. Tardive dyskinesia (TD) is unlikely, although cases putatively associated with olanzapine have been reported.5 Many patients with TD have taken conventional antipsychotics, however, so the causal link with olanzapine is obscure. Still, alert patients and families to the possibility of TD and its emerging features.
Table 2
Olanzapine-fluoxetine: Fast facts
| Drug brand name: Symbyax |
| Class: Combined atypical antipsychotic/selective serotonin reuptake inhibitor |
| FDA-approved indication: Bipolar type I depression |
| Approval date: Dec. 24, 2003 |
| Manufacturer: Eli Lilly and Co. |
| Dosing forms: 6/25 mg/d, 12/50 mg/d, 12/25 mg/d, 12/50 mg/d |
| Dosing recommendations: Start at 6/25 mg at bedtime. Titrate according to tolerability and therapeutic benefit. Once the antidepressant effect is achieved, continue dosage indefinitely if no adverse effects occur. Dosages up to 18/75 mg/d have been used in clinical trials. |
Although considered rare, isolated cases of neuroleptic malignant syndrome have been attributed to olanzapine.14 Cycle induction has not been reported in clinical trials, but be mindful of this possibility with long-term treatment.
Clinical implications
Taking olanzapine and fluoxetine as a single capsule could save the patient substantial cost. OFC comes in four dosing forms (Table 2), allowing for some flexibility.
It is unclear whether clinicians will prefer the single combination capsule or prescribe each drug separately to increase flexibility. Starting treatment with olanzapine and fluoxetine individually allows the psychiatrist to change the dosages independently and in smaller increments. Taken as separate agents, however, the two products are more expensive than the combined formula. OFC costs about the same as olanzapine alone. On the other hand, if the clinician begins the compounds individually, converting to the dosages in the combined product probably will not be exactly 1:1.
Tolerability is another major advantage of OFC; the combined agent exhibited a 10% dropout rate because of adverse effects compared with 4.6% for placebo.7 Moreover, some patients will prefer the convenience of using a single capsule instead of two medications.
Related resources
- Tollefson GD, Sanger TM. Anxious-depressive symptoms in schizophrenia: a new treatment target for pharmacotherapy? Schizophr Res 1999;35(suppl):S13-S21.
- Symbyax Web site. www.symbyax.com
Drug brand names
- Citalopram • Celexa
- Clomipramine • Anafranil
- Diazepam • Valium
- Fluoxetine • Prozac
- Haloperidol • Haldol
- Imipramine • Tofranil
- Metoprolol succinate • Toprol
- Nortriptyline • Aventyl
- Olanzapine • Zyprexa
- Omeprazole • Prilosec
- Phenytoin • Dilantin
- Proguanil • Malarone
- Propafenone • Rythmol
- Propranolol • Inderal
- Risperidone • Risperdal
- Tolbutamide • Orinase
- Venlafaxine • Effexor
- Warfarin • Coumadin
Disclosure
Dr. Shelton receives research grants from Abbott Laboratories, Eli Lilly and Co., GlaxoSmithKline, Janssen Pharmaceutica, Pfizer Inc., and Wyeth Pharmaceuticals; is a consultant to Janssen Pharmaceutica, Pfizer Inc., and Wyeth Pharmaceuticals; and is a speaker for Abbott Laboratories, Eli Lilly and Co., Forest Pharmaceuticals, GlaxoSmithKline, Janssen Pharmaceutica, Pfizer Inc., and Wyeth Pharmaceuticals
Patients with bipolar disorder spend half their lives significantly symptomatic, mainly in the depressive phase.1 Treating bipolar depression poses a clinical challenge, although new research is starting to uncover some answers. Antidepressant drugs are commonly used, but recent data question the effectiveness of this practice.2
An olanzapine-fluoxetine combination (OFC), FDA-approved for treating bipolar type I depression, has demonstrated efficacy in clinical trials.
How it works
Most atypical antipsychotics—including olanzapine—are potent 5-HT2A (serotonin) receptor antagonists. This effect is similar to that of some antidepressants and may mediate some antidepressant and antianxiety effects of these drugs.3
Like most atypicals, olanzapine is also a potent 5-HT2C blocker. While binding to this receptor, serotonin inhibits dopamine release in the nucleus accumbens and frontal cortex.4 Thus, serotonin blockade would increase dopamine release in these areas. One study showed that olanzapine and fluoxetine together increased dopamine and norepinephrine in the frontal cortex of rats, compared with either drug given individually.5 Dopamine is critical to regulating motivation, defined as the ability to exert energy to obtain rewards.6 Olanzapine also interacts with dopaminergic (D1-5), muscarinic (M1-5), alpha1 adrenergic, histamine1, serotonin (5-HT2B,2C,3,6), and glutamate and other receptors.
Pharmacokinetics
Combining olanzapine and fluoxetine in one capsule raises potential kinetic problems. Olanzapine’s mean half-life is 30 hours,7 but fluoxetine’s is 24 to 72 hours and its principal active metabolite, norfluoxetine, has a half-life of 4 to 16 hours.7 Because fluoxetine and norfluoxetine inhibit the cytochrome P (CYP)-450 2D6 enzyme—which is involved in their metabolism—autoinhibition of degradation occurs with chronic dosing, thereby increasing the relative half-life of fluoxetine and norfluoxetine. Therefore, maximum steady-state plasma levels will be achieved with olanzapine and fluoxetine at very different rates, although this has not posed a problem in clinical trials. Still, consider this disparity when evaluating potential side effects or drug-drug interactions.
Table 1
Drugs that may interact with OFC
| Drugs metabolized by CYP 2D6 isoenzymes | Drugs metabolized by CYP 2C isoenzymes |
|---|---|
| Citalopram | Citalopram |
| Codeine | Clomipramine |
| Dextromethorphan | Diazepam |
| Haloperidol | Imipramine |
| Metoprolol | Nonsteroidal |
| Other SSRIs | anti-inflammatory drugs |
| Perphenazine | Omeprazole |
| Propafenone | Phenytoin |
| Propranolol | Proguanil |
| Risperidone | Tolbutamide |
| Thioridazine | Tricyclic antidepressants |
| Trazodone | Warfarin |
| Tricyclic antidepressants (most) | |
| Venlafaxine | |
| Source: reference 8 | |
Both compounds reach maximum concentration in 4 to 6 hours.7 Although food’s effect on OFC’s absorption has not been tested, a clinically important effect is unlikely. Food does not significantly alter absorption kinetics of olanzapine or fluoxetine.7
Avoid giving OFC concomitantly with drugs metabolized by CYP 2D6 and 2C (Table 1), because fluoxetine is a potent inhibitor of these isoenzymes. The resulting altered plasma concentrations could lead to drug-drug interactions.8
Efficacy
In an 8-week, double-blind, multinational trial,9 833 patients with bipolar I disorder in the depressive phase randomly received placebo, olanzapine alone (5 to 20 mg/d), or OFC in several fixed combinations (all shown as olanzapine/fluoxetine): 6/25 mg/d, 6/50 mg/d, or 12/50 mg/d. Dosage titration was allowed.
The researchers found that:
- OFC was significantly more effective than placebo. A mean 18.5-point improvement in Montgomery-Asberg Depression Rating Scale (MADRS) scores was reported in the OFC group, compared with a mean 11.9-point improvement in the placebo group.
- Olanzapine alone produced a mean 15-point MADRS score reduction. Remission criteria were achieved in 24.5%, 32.8%, and 48.8% of patients treated with placebo, olanzapine, and OFC, respectively.
- Both OFC and olanzapine alone produced greater MADRS score reductions than did placebo at every follow-up week. Mania induction rates were low in the olanzapine and OFC treatment groups (5.7% and 6.4%, respectively) as measured with the Young Mania Rating Scale.
Shelton et al3 also compared OFC to olanzapine and fluoxetine alone in treatment-resistant unipolar depression. Thirty-two patients with major depression who responded inadequately to two types of antidepressants were treated with fluoxetine, up to 60 mg/d. After 7 weeks, 28 patients who did not respond to fluoxetine then received fluoxetine alone (mean modal dose: 52 mg/d), olanzapine alone (12.5 mg/d), or OFC (13.5 mg/52 mg/d) for another 8 weeks.
Olanzapine alone produced a transient effect at week 3 with relapse thereafter, possibly because of interactions between olanzapine and falling fluoxetine plasma concentrations over the first 3 weeks. Fluoxetine monotherapy produced minimal results across the 8-week random phase.
The OFC group, however, achieved significant improvement in MADRS scores compared with the placebo group after week one. The effect continued throughout the trial and during a subsequent 8-week open-label phase.3
Recent data suggest continued benefit in treatment- and nontreatment-resistant depressed patients for up to 1 year.10 Two follow-up trials—one using a lead-in with venlafaxine, the second with nortriptyline—produced negative results. In both studies, however, patients achieved a robust effect while continuing the same drug during the double-blind phase, suggesting that initial trials were inadequate.11,12 OFC showed early onset of effect in both studies. Other large-scale attempts at replication are anticipated.
Tolerability
Common side effects of OFC include increased appetite, weight gain, somnolence, fatigue, nausea, diarrhea, and dry mouth—the same effects associated with olanzapine or fluoxetine.
Combining the agents does not lessen the side effects, particularly olanzapine-induced weight gain. Simple, assertive dietary and exercise counseling can counteract olanzapine-induced weight gain.13 Sexual dysfunction was reported infrequently in clinical trials but is possible with exposure to fluoxetine.
Extrapyramidal side effects, including akathisia, appear to be relatively infrequent. Tardive dyskinesia (TD) is unlikely, although cases putatively associated with olanzapine have been reported.5 Many patients with TD have taken conventional antipsychotics, however, so the causal link with olanzapine is obscure. Still, alert patients and families to the possibility of TD and its emerging features.
Table 2
Olanzapine-fluoxetine: Fast facts
| Drug brand name: Symbyax |
| Class: Combined atypical antipsychotic/selective serotonin reuptake inhibitor |
| FDA-approved indication: Bipolar type I depression |
| Approval date: Dec. 24, 2003 |
| Manufacturer: Eli Lilly and Co. |
| Dosing forms: 6/25 mg/d, 12/50 mg/d, 12/25 mg/d, 12/50 mg/d |
| Dosing recommendations: Start at 6/25 mg at bedtime. Titrate according to tolerability and therapeutic benefit. Once the antidepressant effect is achieved, continue dosage indefinitely if no adverse effects occur. Dosages up to 18/75 mg/d have been used in clinical trials. |
Although considered rare, isolated cases of neuroleptic malignant syndrome have been attributed to olanzapine.14 Cycle induction has not been reported in clinical trials, but be mindful of this possibility with long-term treatment.
Clinical implications
Taking olanzapine and fluoxetine as a single capsule could save the patient substantial cost. OFC comes in four dosing forms (Table 2), allowing for some flexibility.
It is unclear whether clinicians will prefer the single combination capsule or prescribe each drug separately to increase flexibility. Starting treatment with olanzapine and fluoxetine individually allows the psychiatrist to change the dosages independently and in smaller increments. Taken as separate agents, however, the two products are more expensive than the combined formula. OFC costs about the same as olanzapine alone. On the other hand, if the clinician begins the compounds individually, converting to the dosages in the combined product probably will not be exactly 1:1.
Tolerability is another major advantage of OFC; the combined agent exhibited a 10% dropout rate because of adverse effects compared with 4.6% for placebo.7 Moreover, some patients will prefer the convenience of using a single capsule instead of two medications.
Related resources
- Tollefson GD, Sanger TM. Anxious-depressive symptoms in schizophrenia: a new treatment target for pharmacotherapy? Schizophr Res 1999;35(suppl):S13-S21.
- Symbyax Web site. www.symbyax.com
Drug brand names
- Citalopram • Celexa
- Clomipramine • Anafranil
- Diazepam • Valium
- Fluoxetine • Prozac
- Haloperidol • Haldol
- Imipramine • Tofranil
- Metoprolol succinate • Toprol
- Nortriptyline • Aventyl
- Olanzapine • Zyprexa
- Omeprazole • Prilosec
- Phenytoin • Dilantin
- Proguanil • Malarone
- Propafenone • Rythmol
- Propranolol • Inderal
- Risperidone • Risperdal
- Tolbutamide • Orinase
- Venlafaxine • Effexor
- Warfarin • Coumadin
Disclosure
Dr. Shelton receives research grants from Abbott Laboratories, Eli Lilly and Co., GlaxoSmithKline, Janssen Pharmaceutica, Pfizer Inc., and Wyeth Pharmaceuticals; is a consultant to Janssen Pharmaceutica, Pfizer Inc., and Wyeth Pharmaceuticals; and is a speaker for Abbott Laboratories, Eli Lilly and Co., Forest Pharmaceuticals, GlaxoSmithKline, Janssen Pharmaceutica, Pfizer Inc., and Wyeth Pharmaceuticals
1. Judd LL, Akiskal HS, Schettler PJ, et al. The long-term natural history of the weekly symptomatic status of bipolar I disorder. Arch Gen Psychiatry 2002;59:530-7.
2. Nemeroff CB, Evans DL, Gyulai L, et al. Double-blind, placebo-controlled comparison of imipramine and paroxetine in the treatment of bipolar depression. Am J Psychiatry 2001;158:906-12.
3. Shelton RC, Tollefson GD, Tohen M, et al. A novel augmentation strategy for treating resistant major depression. Am J Psychiatry 2001;158:131-4.
4. Shelton RC. The combination of olanzapine and fluoxetine in mood disorders. Expert Opin Pharmacother 2003;4:1175-83.
5. Zhang W, Perry KW, Wong DT, et al. Synergistic effects of olanzapine and other antipsychotic agents in combination with fluoxetine on norepinephrine and dopamine release in rat prefrontal cortex. Neuropsychopharmacology 2000;23:250-62.
6. Salamone JD, Cousins MS, Snyder BJ. Behavioral functions of nucleus accumbens dopamine: empirical and conceptual problems with the anhedonia hypothesis. Neurosci Biobehav Rev 1997;21:341-59.
7. Symbyax package insert. Eli Lilly and Co., 2003.
8. Nemeroff CB, DeVane CL, Pollock BG. Newer antidepressants and the cytochrome P450 system. Am J Psychiatry 1996;153:311-20.
9. Tohen M, Vieta E, Calabrese J, et al. Efficacy of olanzapine and olanzapine-fluoxetine combination in the treatment of bipolar I depression. Arch Gen Psychiatry 2003;60:1079-88.
10. Corya SA, Andersen SW, Detke HC, et al. Long-term antidepressant efficacy and safety of olanzapine/fluoxetine combination: a 76-week open-label study. J Clin Psychiatry 2003;64:1349-56.
11. Dube S. Olanzapine-fluoxetine combination in treatment-resistant depression. Eur Psychiatry 2002;17(suppl 1):98.-
12. Dube S, Corya SA, Andersen SW, et al. Efficacy of olanzapine/fluoxetine combination in treatment resistant depression (presentation). San Juan, PR: American College of Neuropsychopharmacology annual meeting, 2002.
13. Ball MP, Coons VB, Buchanan RW. A program for treating olanzapine-related weight gain. Psychiatr Serv 2001;52:967-9.
14. Kogoj A, Velikonja I. Olanzapine-induced neuroleptic malignant syndrome—a case review. Hum Psychopharmacol 2003;18:301-9.
1. Judd LL, Akiskal HS, Schettler PJ, et al. The long-term natural history of the weekly symptomatic status of bipolar I disorder. Arch Gen Psychiatry 2002;59:530-7.
2. Nemeroff CB, Evans DL, Gyulai L, et al. Double-blind, placebo-controlled comparison of imipramine and paroxetine in the treatment of bipolar depression. Am J Psychiatry 2001;158:906-12.
3. Shelton RC, Tollefson GD, Tohen M, et al. A novel augmentation strategy for treating resistant major depression. Am J Psychiatry 2001;158:131-4.
4. Shelton RC. The combination of olanzapine and fluoxetine in mood disorders. Expert Opin Pharmacother 2003;4:1175-83.
5. Zhang W, Perry KW, Wong DT, et al. Synergistic effects of olanzapine and other antipsychotic agents in combination with fluoxetine on norepinephrine and dopamine release in rat prefrontal cortex. Neuropsychopharmacology 2000;23:250-62.
6. Salamone JD, Cousins MS, Snyder BJ. Behavioral functions of nucleus accumbens dopamine: empirical and conceptual problems with the anhedonia hypothesis. Neurosci Biobehav Rev 1997;21:341-59.
7. Symbyax package insert. Eli Lilly and Co., 2003.
8. Nemeroff CB, DeVane CL, Pollock BG. Newer antidepressants and the cytochrome P450 system. Am J Psychiatry 1996;153:311-20.
9. Tohen M, Vieta E, Calabrese J, et al. Efficacy of olanzapine and olanzapine-fluoxetine combination in the treatment of bipolar I depression. Arch Gen Psychiatry 2003;60:1079-88.
10. Corya SA, Andersen SW, Detke HC, et al. Long-term antidepressant efficacy and safety of olanzapine/fluoxetine combination: a 76-week open-label study. J Clin Psychiatry 2003;64:1349-56.
11. Dube S. Olanzapine-fluoxetine combination in treatment-resistant depression. Eur Psychiatry 2002;17(suppl 1):98.-
12. Dube S, Corya SA, Andersen SW, et al. Efficacy of olanzapine/fluoxetine combination in treatment resistant depression (presentation). San Juan, PR: American College of Neuropsychopharmacology annual meeting, 2002.
13. Ball MP, Coons VB, Buchanan RW. A program for treating olanzapine-related weight gain. Psychiatr Serv 2001;52:967-9.
14. Kogoj A, Velikonja I. Olanzapine-induced neuroleptic malignant syndrome—a case review. Hum Psychopharmacol 2003;18:301-9.
Bipolar maintenance: Are atypical antipsychotics really ‘mood stabilizers’?
Maintenance therapy with mood stabilizers is the most critical phase of bipolar disorder treatment but the stage with the least available evidence about medication risks and benefits. The FDA’s recent approval of olanzapine for bipolar maintenance raises the question of whether atypical antipsychotics are really mood stabilizers. This article attempts to answer that question by:
- describing the “ideal” mood stabilizer
- discussing atypicals’ advantages over conventional antipsychotics in bipolar patients
- comparing efficacy data for the six available atypicals
- recommending strategies to prevent and treat atypicals’ potentially serious side effects during long-term therapy.
What is a ‘mood stabilizer’?
Successful mood stabilizer maintenance therapy decreases the time patients are sick and disabled. Although somewhat dated after only 2 years, the most recent American Psychiatric Association (APA) practice guidelines1 support using mood stabilizers for patients with bipolar I and bipolar II disorders.
Table 1
Bipolar maintenance treatment goals
|
| Adapted from American Psychiatric Association practice guidelines for treating patients with bipolar disorder (reference 1) |
The goals of maintenance therapy are listed in Table 1. The ideal mood stabilizer would work in maintenance and all bipolar phases and treatment stages—from treating acute depression, mania, hypomania, and mixed states to preventing abnormal mood elevations and depressions. It would not precipitate depression or mania, rapid cycling, or cycle acceleration.
In other words, the best “mood stabilizer” would work in all four treatment roles of bipolar disorder: treating highs and lows, and preventing highs and lows. No such mood stabilizer exists, although lithium may come closest to the ideal.2
Most U.S. psychiatrists use combination therapies for bipolar disorder, particularly when treating acute manic states. The most common combination is a “known” mood stabilizer—such as lithium or divalproex—plus an antipsychotic to quickly control mania.
After mania remits, clinicians often try to eliminate the antipsychotic in hopes of maintaining mood stability and euthymia with the mood stabilizer alone. This was especially true before atypical antipsychotics were approved, given the risk for tardive dyskinesia (TD) associated with long-term use of conventional antipsychotics.
Unfortunately, patients frequently relapse with this strategy, so psychiatrists may leave their bipolar patients on atypical antipsychotics during long-term maintenance. But how good are atypicals as mood stabilizers? Perhaps more importantly, how safe is long-term use of atypicals in bipolar patients?
Antipsychotics as mood stabilizers
The 2002 APA practice guidelines discuss efficacy data for using lithium, divalproex or valproate, lamotrigine, carbamazepine, and electroconvulsive therapy for bipolar maintenance treatment. Two sentences on antipsychotic drug use note:
- one placebo-controlled study of a conventional antipsychotic showing no efficacy
- some data supporting clozapine as a prophylactic bipolar treatment.1
A 1998 review of five open trials3 touched on conventional depot antipsychotics’ value in reducing manic or affective illness. However, the authors warned:
- no controlled trials existed
- maintenance antipsychotic treatment may be associated with increased risk for tardive movement disorders
- conventional agents can exacerbate depressive symptoms in some patients.
Using conventional antipsychotics long-term in bipolar disorder is not advisable, with the possible exception of depot preparations in nonadhering patients with severe illness. Long-acting injectable atypicals—such as the recently approved IM risperidone—may displace any use of conventional antipsychotics in bipolar patients.
Atypical antipsychotics hold several advantages over conventional agents:
- significantly reduced risk for TD and extrapyramidal symptoms (EPS)
- lack of serum prolactin elevation (except with risperidone)
- improved cognition
- possible decreased suicidality, particularly with clozapine.4
Table 2
Tips for managing atypicals’ potentially serious side-effect risks
| Weight gain/obesity | ||
| Assessment | Prevention | Treatment |
| Evaluate comorbid conditions such as eating disorders or substance abuse Take nutritional and exercise history | Check weight and waist circumference at baseline and every visit Calculate body mass index at every visit Prescribe healthy diet and exercise | Patient education, careful monitoring, and prevention are most-effective treatments Drug therapy for persistent weight gain or early rapid gain (>7% in first 6 months). Agents of potential benefit include topiramate, sibutramine, metformin, zonisamide, and orlistat (see Table 3) |
| Glucose control/type 2 diabetes | ||
| Assessment | Prevention | Treatment |
| Take history of glucose intolerance or diabetes Ask about family history of diabetes, obesity, hypertension, heart disease | Check baseline weight and plasma glucose Obtain fasting plasma glucose every 3 months for first year, then annually Prescribe healthy diet and exercise | Primary prevention through careful monitoring is most effective Discontinue atypical antipsychotic; use other mood stabilizer unless atypical is only effective drug for that patient Oral hypoglycemics (metformin, others) |
| Hyperlipidemia | ||
| Assessment | Prevention | Treatment |
| Take history of hyperlipidemia or cardiovascular disease Ask about family history of hyperlipidemia | Check fasting lipid profile including triglycerides at baseline and every 3 months in first year Prescribe healthy diet and exercise | Monitor diet, exercise, weight, lipids regularly Change atypical antipsychotic or use other mood stabilizer (as described above) Oral antilipemics (simvastatin, others) |
Evidence for atypicals
Olanzapine is the only atypical FDA-approved for relapse prevention in bipolar disorder. This approval is supported by several studies, most notably two 1-year, double-blind trials:
- Mean time to any mood relapse was 174 days in patients taking olanzapine, mean 12.5 mg/d (±5 mg), compared with 22 days in a placebo group (Eli Lilly and Co., data on file).
- Manic relapse rate was 14.3% in patients treated with olanzapine, ~12 mg/d, compared with 28% in patients treated with lithium, ~1,100 mg/d (mean 0.76 mEq/L). The two treatments were similarly effective in preventing depressive relapse.5
As a mood stabilizer, olanzapine was as effective as divalproex in a 47-week randomized, double-blind study of 251 adults with bipolar I disorder.6 Patients treated with olanzapine improved more rapidly and had fewer manic symptoms than those treated with divalproex, but bipolar relapse rates were similar in both treatment groups.
Risperidone appears to have a role as a potential maintenance mood stabilizer in bipolar patients, although double-blind trials are lacking.
In a 6-month, open-label investigation, relapse rates were 16% for depression and 7% for mania in bipolar patients receiving risperidone (average 4 mg/d) combined with mood-stabilizing medications.7 These relapse rates are lower than those typically reported for mood-stabilizing monotherapy.
In another 6-month, open-label study, risperidone monotherapy (average 4 mg/d) was effective for treating mania and maintaining euthymia.8
IM risperidone is a useful option for bipolar patients chronically nonadherent with oral medications; it also substantially reduces the risk of neuroleptic side effects compared with older depot antipsychotics.
Quetiapine was recently approved as an antimanic agent and may possess mood-stabilizing properties. In a preliminary study of 10 patients with bipolar disorder, adding quetiapine (mean 200 mg/d) to existing mood stabilizer therapy for 12 weeks improved psychopathology, mania, and depression rating scale scores.9
More-recent unpublished data suggest dosing quetiapine to approximately 600 mg/d as monotherapy or an adjunct to treat acute mania, though controlled maintenance studies are lacking (AstraZeneca Pharmaceuticals, data on file).
Others. Some early evidence supports using ziprasidone and aripiprazole for bipolar mania:
- Ziprasidone monotherapy, 40 to 80 mg bid, was significantly more effective than placebo in reducing acute mania symptoms in a 3-week, double-blind, randomized trial of 197 patients with bipolar I disorder.10
- Aripiprazole monotherapy, 15 to 30 mg/d, had a significantly greater effect than placebo in a 3-week, double-blind, randomized trial of 262 patients in acute manic or mixed bipolar episodes. Response rates among patients with mania were 40% with aripiprazole and 19% with placebo.11
Both ziprasidone and aripiprazole were well-tolerated in these brief trials, although their efficacy as long-term mood-stabilizers in bipolar disorder is unclear.
Using clozapine raises concerns about potentially serious adverse events, although it remains the only agent with proven efficacy in treatment-refractory mania.12,13 Clozapine also appears to reduce hospitalization and affective relapse rates and improve symptoms and quality of life.14,15
Long-term safety
Compared with conventional antipsychotics, EPS are not a major concern with the atypical agents. Except for risperidone, atypicals’ effect on prolactin levels generally is not clinically meaningful. Atypicals appear to be “mood-friendly,” whereas conventional antipsychotics seem to contribute to dysphoria or cause depression in some patients.
Sedation or other annoying side effects such as dry mouth or dizziness can occur with any atypical. Other more-serious side effects may complicate antipsychotic treatment, as we are coming to understand from using atypicals for long-term schizophrenia management.
Table 3
Weight-loss medications for bipolar patients taking atypical antipsychotics
| Drug | Dosage | Side effects | Recommendations |
|---|---|---|---|
| Metformin | 500 to 1,000 mg bid | Hypoglycemia Diarrhea Nausea/vomiting | First-line in patients with comorbid type 2 diabetes |
| Orlistat | 120 mg tid | GI distress Change in bowel habits | Second-line For patients with BMI >27 Supplement fat-soluble vitamins |
| Sibutramine | 5 to 15 mg/d | Dry mouth Anorexia Insomnia Constipation | Second-line For patients with BMI 27 to 30 Risk of serotonin syndrome if given with serotonergic drugs |
| Topiramate | 50 to 250 mg/d | Somnolence Fatigue Paresthesias | Consider first-line for its potential additive mood-stabilizing effect May help comorbid binge-eating or seizure disorders |
| Zonisamide | 100 to 600 mg/d | Somnolence Dizziness Anorexia | Consider first-line for its potential additive mood-stabilizing effect May help comorbid binge-eating or seizure disorders |
Movement disorders. Antipsychotics appear more likely to cause EPS in patients with mood disorders than with schizophrenia. In one study using conventional antipsychotics, bipolar patients were 4 to 5 times more likely than schizophrenia patients to experience acute dystonia.16
Although atypicals pose some small risk for acute EPS and TD, the risk is near placebo-level with clinically relevant and comparable dosages.17 Even so, it is important to educate patients to watch for emerging signs of TD during long-term treatment with any antipsychotic. EPS risk may be dose-dependent, particularly with risperidone.18
Weight gain and obesity. Patients with bipolar disorder are more likely to be overweight or obese (body mass index [BMI] > 30) than the general population,17,19 though the reasons are unknown. Studies suggest an obesity prevalence of 32% to 35% in bipolar patients, compared with 18% in the general population.20,21
All atypicals can cause weight gain, although olanzapine and clozapine are associated with the greatest mean weight gains. In three long-term trials (47 weeks to 18 months), bipolar patients who received olanzapine gained significantly more weight (mean 2 to 3 kg) than those receiving lithium or divalproex.19
Cases with much greater weight gain—even leading to clinical obesity—have been observed, particularly with olanzapine. Although evidence from registration trials and clinical experience show lesser weight gains with risperidone, quetiapine, ziprasidone, and aripiprazole, some of our patients do gain weight while taking these agents—either alone or in combination with lithium or divalproex.
Weight management. Because patients with bipolar disorder may be at increased risk for weight gain and obesity, weight management techniques may improve their health by:
- decreasing morbidity and mortality tied to weight-related physical illnesses
- enhancing psychological well-being.1
In addition to diet and exercise counseling, some bipolar patients taking long-term atypical antipsychotics may benefit from adjunctive weight-loss medications (Table 3). We generally use such medications for bipolar patients who:
- persistently gain weight despite best dietary practices
- gain substantial weight early in treatment with an atypical antipsychotic that is providing effective symptomatic relief.
Early weight gain—particularly gains of >7% within the first 6 weeks—might predict large weight gain over time.
Diabetes. In September 2003, the FDA requested a class-wide labeling change to warn about a possible link between atypical antipsychotics and diabetes. The FDA recommended blood sugar monitoring of patients taking atypicals, especially those with obesity risk factors or family history of diabetes.
Type 2 diabetes develops in some patients taking atypicals, whether or not they gain substantial weight.22 This suggests that weight gain associated with bipolar disorder and the use of atypical antipsychotics may be independent risk factors for diabetes—a clear concern when treating bipolar patients.
Evidence provides no clear answer as to which atypicals may increase diabetes risk. Cautious use and vigilant monitoring of blood glucose are therefore recommended for every patient taking an atypical for long-term therapy. Also watch for increases in triglycerides and cholesterol17 in patients taking atypicals as bipolar maintenance therapy.
Conclusion
Atypical antipsychotics are valuable therapies in preventing bipolar relapses, although olanzapine is the only atypical with this indication so far. Collective data and clinical experience suggest that atypicals are indeed mood stabilizers, although—like other mood stabilizers such as lithium or divalproex—they have limitations. None achieve ideal efficacy in all four bipolar treatment roles: treating the highs and lows, and preventing the highs and lows. Atypicals seem more effective in treating and preventing the highs than the lows, reminding us that effective depression treatment is the greatest unmet need in bipolar disorder.
More double-blind, randomized, controlled trials are needed to fully understand whether all atypicals are mood stabilizers and to determine their safety and side effects in long-term therapy for patients with bipolar disorder.
Related resources
- Depression and Bipolar Support Alliance. www.dbsalliance.org
- Muzina DJ, Calabrese JR. Guidelines for treatment of bipolar disorder.In: Stein DJ, Kupfer DJ, Schatzberg AF (eds). Textbook of mood disorders Washington, DC: American Psychiatric Publishing, 2004 (in press).
Drug brand names
- Aripiprazole • Abilify
- Carbamazepine • Tegretol
- Clozapine • Clozaril
- Divalproex/valproate • Depakote, Depakene
- Lamotrigine • Lamictal
- Lithium • Eskalith, Lithobid, et al
- Metformin • Glucophage
- Olanzapine • Zyprexa
- Orlistat • Xenical
- Quetiapine • Seroquel
- Risperidone • Risperdal, Risperdal Consta
- Sibutramine • Meridia
- Simvastatin • Zocor
- Topiramate • Topamax
- Ziprasidone • Geodon
- Zonisamide • Zonegran
Disclosure
Dr. Muzina receives research grants from AstraZeneca Pharmaceuticals, Eli Lilly and Co., and Abbott Laboratories, is a consultant to AstraZeneca Pharmaceuticals and Pfizer, Inc., and a speaker for AstraZeneca Pharmaceuticals, Pfizer Inc., Eli Lilly and Co., and GlaxoSmithKline.
1. Hirschfeld RM, Bowden CL, Gitlin MJ, et al. Practice guideline for the treatment of patients with bipolar disorder (rev). Am J Psychiatry 2002;159:1-50.
2. Bauer MS, Mitchner L. What is a “mood stabilizer?” An evidence-based response. Am J Psychiatry 2004;161(1):3-18.
3. Keck PE, Jr, McElroy SL, Strakowski SM. Anticonvulsants and antipsychotics in the treatment of bipolar disorder. J Clin Psychiatry 1998;59(suppl 6):74-81.
4. Sharma V. Atypical antipsychotics and suicide in mood and anxiety disorders. Bipolar Disord 2003;5(suppl 2):48-52.
5. Tohen M, Marneros A, Bowden C, et al. Olanzapine versus lithium in relapse prevention in bipolar disorder: a randomized double-blind controlled 12-month clinical trial (presentation). Freiberg, Germany: Stanley Foundation Bipolar Network, Sept. 11-14, 2002.
6. Tohen M, Ketter TA, Zarate CA, et al. Olanzapine versus divalproex sodium for the treatment of acute mania and maintenance of remission: a 47-week study. Am J Psychiatry 2003;160(7):1263-71.
7. Vieta E, Goikolea JM, Corbella B, et al. Risperidone safety and efficacy in the treatment of bipolar and schizoaffective disorders: results from a 6-month, multicenter, open study. J Clin Psychiatry 2001;62(10):818-25.
8. Vieta E, Brugue E, Goikolea JM, et al. Acute and continuation risperidone monotherapy in mania. Hum Psychopharmacol 2004;19(1):41-5.
9. Sajatovic M, Brescan DW, Perez DE, et al. Quetiapine alone and added to a mood stabilizer for serious mood disorders. J Clin Psychiatry 2001;62(9):728-32.
10. Keck PE, Jr, Versiani M, Potkin S, et al. Ziprasidone in the treatment of acute bipolar mania: a three-week, placebo-controlled, double-blind, randomized trial. Am J Psychiatry 2003;160(4):741-8.
11. Keck PE, Jr, Marcus R, Tourkodimitris S, et al. A placebo-controlled, double-blind study of the efficacy and safety of aripiprazole in patients with acute bipolar mania. Am J Psychiatry 2003;160(9):1651-8.
12. Calabrese JR, Kimmel SE, Woyshville MJ, et al. Clozapine for treatment-refractory mania. Am J Psychiatry 1996;153(6):759-64.
13. Green AI, Tohen M, Patel JK, et al. Clozapine in the treatment of refractory psychotic mania. Am J Psychiatry 2000;157(6):982-6.
14. Zarate CA, Jr, Tohen M, Banov MD, et al. Is clozapine a mood stabilizer? J Clin Psychiatry 1995;56(3):108-12.
15. Suppes T, Webb A, Paul B, et al. Clinical outcome in a randomized 1-year trial of clozapine versus treatment as usual for patients with treatment-resistant illness and a history of mania. Am J Psychiatry 1999;156(8):1164-9.
16. Nasrallah HA, Churchill CM, Hamdan-Allan GA. Higher frequency of neuroleptic-induced dystonia in mania than in schizophrenia. Am J Psychiatry 1988;145(11):1455-6.
17. Chue P, Kovacs CS. Safety and tolerability of atypical antipsychotics in patients with bipolar disorder: prevalence, monitoring and management. Bipolar Disord 2003;5(suppl 2):62-79.
18. Simpson GM, Lindenmayer JP. Extrapyramidal symptoms in patients treated with risperidone. J Clin Psychopharmacol 1997;17(3):194-201.
19. Keck PE, Jr, McElroy SL. Bipolar disorder, obesity, and pharmacotherapy-associated weight gain. J Clin Psychiatry 2003;64(12):1426-35.
20. Fagiolini A, Frank E, Houck PR, et al. Prevalence of obesity and weight change during treatment in patients with bipolar I disorder. J Clin Psychiatry 2002;63(6):528-33.
21. Fagiolini A, Kupfer DJ, Houck PR, et al. Obesity as a correlate of outcome in patients with bipolar I disorder. Am J Psychiatry 2003;160(1):112-17.
22. Haupt DW, Newcomer JW. Abnormalities in glucose regulation associated with mental illness and treatment. J Psychosom Res 2002;53(4):925-33.
Maintenance therapy with mood stabilizers is the most critical phase of bipolar disorder treatment but the stage with the least available evidence about medication risks and benefits. The FDA’s recent approval of olanzapine for bipolar maintenance raises the question of whether atypical antipsychotics are really mood stabilizers. This article attempts to answer that question by:
- describing the “ideal” mood stabilizer
- discussing atypicals’ advantages over conventional antipsychotics in bipolar patients
- comparing efficacy data for the six available atypicals
- recommending strategies to prevent and treat atypicals’ potentially serious side effects during long-term therapy.
What is a ‘mood stabilizer’?
Successful mood stabilizer maintenance therapy decreases the time patients are sick and disabled. Although somewhat dated after only 2 years, the most recent American Psychiatric Association (APA) practice guidelines1 support using mood stabilizers for patients with bipolar I and bipolar II disorders.
Table 1
Bipolar maintenance treatment goals
|
| Adapted from American Psychiatric Association practice guidelines for treating patients with bipolar disorder (reference 1) |
The goals of maintenance therapy are listed in Table 1. The ideal mood stabilizer would work in maintenance and all bipolar phases and treatment stages—from treating acute depression, mania, hypomania, and mixed states to preventing abnormal mood elevations and depressions. It would not precipitate depression or mania, rapid cycling, or cycle acceleration.
In other words, the best “mood stabilizer” would work in all four treatment roles of bipolar disorder: treating highs and lows, and preventing highs and lows. No such mood stabilizer exists, although lithium may come closest to the ideal.2
Most U.S. psychiatrists use combination therapies for bipolar disorder, particularly when treating acute manic states. The most common combination is a “known” mood stabilizer—such as lithium or divalproex—plus an antipsychotic to quickly control mania.
After mania remits, clinicians often try to eliminate the antipsychotic in hopes of maintaining mood stability and euthymia with the mood stabilizer alone. This was especially true before atypical antipsychotics were approved, given the risk for tardive dyskinesia (TD) associated with long-term use of conventional antipsychotics.
Unfortunately, patients frequently relapse with this strategy, so psychiatrists may leave their bipolar patients on atypical antipsychotics during long-term maintenance. But how good are atypicals as mood stabilizers? Perhaps more importantly, how safe is long-term use of atypicals in bipolar patients?
Antipsychotics as mood stabilizers
The 2002 APA practice guidelines discuss efficacy data for using lithium, divalproex or valproate, lamotrigine, carbamazepine, and electroconvulsive therapy for bipolar maintenance treatment. Two sentences on antipsychotic drug use note:
- one placebo-controlled study of a conventional antipsychotic showing no efficacy
- some data supporting clozapine as a prophylactic bipolar treatment.1
A 1998 review of five open trials3 touched on conventional depot antipsychotics’ value in reducing manic or affective illness. However, the authors warned:
- no controlled trials existed
- maintenance antipsychotic treatment may be associated with increased risk for tardive movement disorders
- conventional agents can exacerbate depressive symptoms in some patients.
Using conventional antipsychotics long-term in bipolar disorder is not advisable, with the possible exception of depot preparations in nonadhering patients with severe illness. Long-acting injectable atypicals—such as the recently approved IM risperidone—may displace any use of conventional antipsychotics in bipolar patients.
Atypical antipsychotics hold several advantages over conventional agents:
- significantly reduced risk for TD and extrapyramidal symptoms (EPS)
- lack of serum prolactin elevation (except with risperidone)
- improved cognition
- possible decreased suicidality, particularly with clozapine.4
Table 2
Tips for managing atypicals’ potentially serious side-effect risks
| Weight gain/obesity | ||
| Assessment | Prevention | Treatment |
| Evaluate comorbid conditions such as eating disorders or substance abuse Take nutritional and exercise history | Check weight and waist circumference at baseline and every visit Calculate body mass index at every visit Prescribe healthy diet and exercise | Patient education, careful monitoring, and prevention are most-effective treatments Drug therapy for persistent weight gain or early rapid gain (>7% in first 6 months). Agents of potential benefit include topiramate, sibutramine, metformin, zonisamide, and orlistat (see Table 3) |
| Glucose control/type 2 diabetes | ||
| Assessment | Prevention | Treatment |
| Take history of glucose intolerance or diabetes Ask about family history of diabetes, obesity, hypertension, heart disease | Check baseline weight and plasma glucose Obtain fasting plasma glucose every 3 months for first year, then annually Prescribe healthy diet and exercise | Primary prevention through careful monitoring is most effective Discontinue atypical antipsychotic; use other mood stabilizer unless atypical is only effective drug for that patient Oral hypoglycemics (metformin, others) |
| Hyperlipidemia | ||
| Assessment | Prevention | Treatment |
| Take history of hyperlipidemia or cardiovascular disease Ask about family history of hyperlipidemia | Check fasting lipid profile including triglycerides at baseline and every 3 months in first year Prescribe healthy diet and exercise | Monitor diet, exercise, weight, lipids regularly Change atypical antipsychotic or use other mood stabilizer (as described above) Oral antilipemics (simvastatin, others) |
Evidence for atypicals
Olanzapine is the only atypical FDA-approved for relapse prevention in bipolar disorder. This approval is supported by several studies, most notably two 1-year, double-blind trials:
- Mean time to any mood relapse was 174 days in patients taking olanzapine, mean 12.5 mg/d (±5 mg), compared with 22 days in a placebo group (Eli Lilly and Co., data on file).
- Manic relapse rate was 14.3% in patients treated with olanzapine, ~12 mg/d, compared with 28% in patients treated with lithium, ~1,100 mg/d (mean 0.76 mEq/L). The two treatments were similarly effective in preventing depressive relapse.5
As a mood stabilizer, olanzapine was as effective as divalproex in a 47-week randomized, double-blind study of 251 adults with bipolar I disorder.6 Patients treated with olanzapine improved more rapidly and had fewer manic symptoms than those treated with divalproex, but bipolar relapse rates were similar in both treatment groups.
Risperidone appears to have a role as a potential maintenance mood stabilizer in bipolar patients, although double-blind trials are lacking.
In a 6-month, open-label investigation, relapse rates were 16% for depression and 7% for mania in bipolar patients receiving risperidone (average 4 mg/d) combined with mood-stabilizing medications.7 These relapse rates are lower than those typically reported for mood-stabilizing monotherapy.
In another 6-month, open-label study, risperidone monotherapy (average 4 mg/d) was effective for treating mania and maintaining euthymia.8
IM risperidone is a useful option for bipolar patients chronically nonadherent with oral medications; it also substantially reduces the risk of neuroleptic side effects compared with older depot antipsychotics.
Quetiapine was recently approved as an antimanic agent and may possess mood-stabilizing properties. In a preliminary study of 10 patients with bipolar disorder, adding quetiapine (mean 200 mg/d) to existing mood stabilizer therapy for 12 weeks improved psychopathology, mania, and depression rating scale scores.9
More-recent unpublished data suggest dosing quetiapine to approximately 600 mg/d as monotherapy or an adjunct to treat acute mania, though controlled maintenance studies are lacking (AstraZeneca Pharmaceuticals, data on file).
Others. Some early evidence supports using ziprasidone and aripiprazole for bipolar mania:
- Ziprasidone monotherapy, 40 to 80 mg bid, was significantly more effective than placebo in reducing acute mania symptoms in a 3-week, double-blind, randomized trial of 197 patients with bipolar I disorder.10
- Aripiprazole monotherapy, 15 to 30 mg/d, had a significantly greater effect than placebo in a 3-week, double-blind, randomized trial of 262 patients in acute manic or mixed bipolar episodes. Response rates among patients with mania were 40% with aripiprazole and 19% with placebo.11
Both ziprasidone and aripiprazole were well-tolerated in these brief trials, although their efficacy as long-term mood-stabilizers in bipolar disorder is unclear.
Using clozapine raises concerns about potentially serious adverse events, although it remains the only agent with proven efficacy in treatment-refractory mania.12,13 Clozapine also appears to reduce hospitalization and affective relapse rates and improve symptoms and quality of life.14,15
Long-term safety
Compared with conventional antipsychotics, EPS are not a major concern with the atypical agents. Except for risperidone, atypicals’ effect on prolactin levels generally is not clinically meaningful. Atypicals appear to be “mood-friendly,” whereas conventional antipsychotics seem to contribute to dysphoria or cause depression in some patients.
Sedation or other annoying side effects such as dry mouth or dizziness can occur with any atypical. Other more-serious side effects may complicate antipsychotic treatment, as we are coming to understand from using atypicals for long-term schizophrenia management.
Table 3
Weight-loss medications for bipolar patients taking atypical antipsychotics
| Drug | Dosage | Side effects | Recommendations |
|---|---|---|---|
| Metformin | 500 to 1,000 mg bid | Hypoglycemia Diarrhea Nausea/vomiting | First-line in patients with comorbid type 2 diabetes |
| Orlistat | 120 mg tid | GI distress Change in bowel habits | Second-line For patients with BMI >27 Supplement fat-soluble vitamins |
| Sibutramine | 5 to 15 mg/d | Dry mouth Anorexia Insomnia Constipation | Second-line For patients with BMI 27 to 30 Risk of serotonin syndrome if given with serotonergic drugs |
| Topiramate | 50 to 250 mg/d | Somnolence Fatigue Paresthesias | Consider first-line for its potential additive mood-stabilizing effect May help comorbid binge-eating or seizure disorders |
| Zonisamide | 100 to 600 mg/d | Somnolence Dizziness Anorexia | Consider first-line for its potential additive mood-stabilizing effect May help comorbid binge-eating or seizure disorders |
Movement disorders. Antipsychotics appear more likely to cause EPS in patients with mood disorders than with schizophrenia. In one study using conventional antipsychotics, bipolar patients were 4 to 5 times more likely than schizophrenia patients to experience acute dystonia.16
Although atypicals pose some small risk for acute EPS and TD, the risk is near placebo-level with clinically relevant and comparable dosages.17 Even so, it is important to educate patients to watch for emerging signs of TD during long-term treatment with any antipsychotic. EPS risk may be dose-dependent, particularly with risperidone.18
Weight gain and obesity. Patients with bipolar disorder are more likely to be overweight or obese (body mass index [BMI] > 30) than the general population,17,19 though the reasons are unknown. Studies suggest an obesity prevalence of 32% to 35% in bipolar patients, compared with 18% in the general population.20,21
All atypicals can cause weight gain, although olanzapine and clozapine are associated with the greatest mean weight gains. In three long-term trials (47 weeks to 18 months), bipolar patients who received olanzapine gained significantly more weight (mean 2 to 3 kg) than those receiving lithium or divalproex.19
Cases with much greater weight gain—even leading to clinical obesity—have been observed, particularly with olanzapine. Although evidence from registration trials and clinical experience show lesser weight gains with risperidone, quetiapine, ziprasidone, and aripiprazole, some of our patients do gain weight while taking these agents—either alone or in combination with lithium or divalproex.
Weight management. Because patients with bipolar disorder may be at increased risk for weight gain and obesity, weight management techniques may improve their health by:
- decreasing morbidity and mortality tied to weight-related physical illnesses
- enhancing psychological well-being.1
In addition to diet and exercise counseling, some bipolar patients taking long-term atypical antipsychotics may benefit from adjunctive weight-loss medications (Table 3). We generally use such medications for bipolar patients who:
- persistently gain weight despite best dietary practices
- gain substantial weight early in treatment with an atypical antipsychotic that is providing effective symptomatic relief.
Early weight gain—particularly gains of >7% within the first 6 weeks—might predict large weight gain over time.
Diabetes. In September 2003, the FDA requested a class-wide labeling change to warn about a possible link between atypical antipsychotics and diabetes. The FDA recommended blood sugar monitoring of patients taking atypicals, especially those with obesity risk factors or family history of diabetes.
Type 2 diabetes develops in some patients taking atypicals, whether or not they gain substantial weight.22 This suggests that weight gain associated with bipolar disorder and the use of atypical antipsychotics may be independent risk factors for diabetes—a clear concern when treating bipolar patients.
Evidence provides no clear answer as to which atypicals may increase diabetes risk. Cautious use and vigilant monitoring of blood glucose are therefore recommended for every patient taking an atypical for long-term therapy. Also watch for increases in triglycerides and cholesterol17 in patients taking atypicals as bipolar maintenance therapy.
Conclusion
Atypical antipsychotics are valuable therapies in preventing bipolar relapses, although olanzapine is the only atypical with this indication so far. Collective data and clinical experience suggest that atypicals are indeed mood stabilizers, although—like other mood stabilizers such as lithium or divalproex—they have limitations. None achieve ideal efficacy in all four bipolar treatment roles: treating the highs and lows, and preventing the highs and lows. Atypicals seem more effective in treating and preventing the highs than the lows, reminding us that effective depression treatment is the greatest unmet need in bipolar disorder.
More double-blind, randomized, controlled trials are needed to fully understand whether all atypicals are mood stabilizers and to determine their safety and side effects in long-term therapy for patients with bipolar disorder.
Related resources
- Depression and Bipolar Support Alliance. www.dbsalliance.org
- Muzina DJ, Calabrese JR. Guidelines for treatment of bipolar disorder.In: Stein DJ, Kupfer DJ, Schatzberg AF (eds). Textbook of mood disorders Washington, DC: American Psychiatric Publishing, 2004 (in press).
Drug brand names
- Aripiprazole • Abilify
- Carbamazepine • Tegretol
- Clozapine • Clozaril
- Divalproex/valproate • Depakote, Depakene
- Lamotrigine • Lamictal
- Lithium • Eskalith, Lithobid, et al
- Metformin • Glucophage
- Olanzapine • Zyprexa
- Orlistat • Xenical
- Quetiapine • Seroquel
- Risperidone • Risperdal, Risperdal Consta
- Sibutramine • Meridia
- Simvastatin • Zocor
- Topiramate • Topamax
- Ziprasidone • Geodon
- Zonisamide • Zonegran
Disclosure
Dr. Muzina receives research grants from AstraZeneca Pharmaceuticals, Eli Lilly and Co., and Abbott Laboratories, is a consultant to AstraZeneca Pharmaceuticals and Pfizer, Inc., and a speaker for AstraZeneca Pharmaceuticals, Pfizer Inc., Eli Lilly and Co., and GlaxoSmithKline.
Maintenance therapy with mood stabilizers is the most critical phase of bipolar disorder treatment but the stage with the least available evidence about medication risks and benefits. The FDA’s recent approval of olanzapine for bipolar maintenance raises the question of whether atypical antipsychotics are really mood stabilizers. This article attempts to answer that question by:
- describing the “ideal” mood stabilizer
- discussing atypicals’ advantages over conventional antipsychotics in bipolar patients
- comparing efficacy data for the six available atypicals
- recommending strategies to prevent and treat atypicals’ potentially serious side effects during long-term therapy.
What is a ‘mood stabilizer’?
Successful mood stabilizer maintenance therapy decreases the time patients are sick and disabled. Although somewhat dated after only 2 years, the most recent American Psychiatric Association (APA) practice guidelines1 support using mood stabilizers for patients with bipolar I and bipolar II disorders.
Table 1
Bipolar maintenance treatment goals
|
| Adapted from American Psychiatric Association practice guidelines for treating patients with bipolar disorder (reference 1) |
The goals of maintenance therapy are listed in Table 1. The ideal mood stabilizer would work in maintenance and all bipolar phases and treatment stages—from treating acute depression, mania, hypomania, and mixed states to preventing abnormal mood elevations and depressions. It would not precipitate depression or mania, rapid cycling, or cycle acceleration.
In other words, the best “mood stabilizer” would work in all four treatment roles of bipolar disorder: treating highs and lows, and preventing highs and lows. No such mood stabilizer exists, although lithium may come closest to the ideal.2
Most U.S. psychiatrists use combination therapies for bipolar disorder, particularly when treating acute manic states. The most common combination is a “known” mood stabilizer—such as lithium or divalproex—plus an antipsychotic to quickly control mania.
After mania remits, clinicians often try to eliminate the antipsychotic in hopes of maintaining mood stability and euthymia with the mood stabilizer alone. This was especially true before atypical antipsychotics were approved, given the risk for tardive dyskinesia (TD) associated with long-term use of conventional antipsychotics.
Unfortunately, patients frequently relapse with this strategy, so psychiatrists may leave their bipolar patients on atypical antipsychotics during long-term maintenance. But how good are atypicals as mood stabilizers? Perhaps more importantly, how safe is long-term use of atypicals in bipolar patients?
Antipsychotics as mood stabilizers
The 2002 APA practice guidelines discuss efficacy data for using lithium, divalproex or valproate, lamotrigine, carbamazepine, and electroconvulsive therapy for bipolar maintenance treatment. Two sentences on antipsychotic drug use note:
- one placebo-controlled study of a conventional antipsychotic showing no efficacy
- some data supporting clozapine as a prophylactic bipolar treatment.1
A 1998 review of five open trials3 touched on conventional depot antipsychotics’ value in reducing manic or affective illness. However, the authors warned:
- no controlled trials existed
- maintenance antipsychotic treatment may be associated with increased risk for tardive movement disorders
- conventional agents can exacerbate depressive symptoms in some patients.
Using conventional antipsychotics long-term in bipolar disorder is not advisable, with the possible exception of depot preparations in nonadhering patients with severe illness. Long-acting injectable atypicals—such as the recently approved IM risperidone—may displace any use of conventional antipsychotics in bipolar patients.
Atypical antipsychotics hold several advantages over conventional agents:
- significantly reduced risk for TD and extrapyramidal symptoms (EPS)
- lack of serum prolactin elevation (except with risperidone)
- improved cognition
- possible decreased suicidality, particularly with clozapine.4
Table 2
Tips for managing atypicals’ potentially serious side-effect risks
| Weight gain/obesity | ||
| Assessment | Prevention | Treatment |
| Evaluate comorbid conditions such as eating disorders or substance abuse Take nutritional and exercise history | Check weight and waist circumference at baseline and every visit Calculate body mass index at every visit Prescribe healthy diet and exercise | Patient education, careful monitoring, and prevention are most-effective treatments Drug therapy for persistent weight gain or early rapid gain (>7% in first 6 months). Agents of potential benefit include topiramate, sibutramine, metformin, zonisamide, and orlistat (see Table 3) |
| Glucose control/type 2 diabetes | ||
| Assessment | Prevention | Treatment |
| Take history of glucose intolerance or diabetes Ask about family history of diabetes, obesity, hypertension, heart disease | Check baseline weight and plasma glucose Obtain fasting plasma glucose every 3 months for first year, then annually Prescribe healthy diet and exercise | Primary prevention through careful monitoring is most effective Discontinue atypical antipsychotic; use other mood stabilizer unless atypical is only effective drug for that patient Oral hypoglycemics (metformin, others) |
| Hyperlipidemia | ||
| Assessment | Prevention | Treatment |
| Take history of hyperlipidemia or cardiovascular disease Ask about family history of hyperlipidemia | Check fasting lipid profile including triglycerides at baseline and every 3 months in first year Prescribe healthy diet and exercise | Monitor diet, exercise, weight, lipids regularly Change atypical antipsychotic or use other mood stabilizer (as described above) Oral antilipemics (simvastatin, others) |
Evidence for atypicals
Olanzapine is the only atypical FDA-approved for relapse prevention in bipolar disorder. This approval is supported by several studies, most notably two 1-year, double-blind trials:
- Mean time to any mood relapse was 174 days in patients taking olanzapine, mean 12.5 mg/d (±5 mg), compared with 22 days in a placebo group (Eli Lilly and Co., data on file).
- Manic relapse rate was 14.3% in patients treated with olanzapine, ~12 mg/d, compared with 28% in patients treated with lithium, ~1,100 mg/d (mean 0.76 mEq/L). The two treatments were similarly effective in preventing depressive relapse.5
As a mood stabilizer, olanzapine was as effective as divalproex in a 47-week randomized, double-blind study of 251 adults with bipolar I disorder.6 Patients treated with olanzapine improved more rapidly and had fewer manic symptoms than those treated with divalproex, but bipolar relapse rates were similar in both treatment groups.
Risperidone appears to have a role as a potential maintenance mood stabilizer in bipolar patients, although double-blind trials are lacking.
In a 6-month, open-label investigation, relapse rates were 16% for depression and 7% for mania in bipolar patients receiving risperidone (average 4 mg/d) combined with mood-stabilizing medications.7 These relapse rates are lower than those typically reported for mood-stabilizing monotherapy.
In another 6-month, open-label study, risperidone monotherapy (average 4 mg/d) was effective for treating mania and maintaining euthymia.8
IM risperidone is a useful option for bipolar patients chronically nonadherent with oral medications; it also substantially reduces the risk of neuroleptic side effects compared with older depot antipsychotics.
Quetiapine was recently approved as an antimanic agent and may possess mood-stabilizing properties. In a preliminary study of 10 patients with bipolar disorder, adding quetiapine (mean 200 mg/d) to existing mood stabilizer therapy for 12 weeks improved psychopathology, mania, and depression rating scale scores.9
More-recent unpublished data suggest dosing quetiapine to approximately 600 mg/d as monotherapy or an adjunct to treat acute mania, though controlled maintenance studies are lacking (AstraZeneca Pharmaceuticals, data on file).
Others. Some early evidence supports using ziprasidone and aripiprazole for bipolar mania:
- Ziprasidone monotherapy, 40 to 80 mg bid, was significantly more effective than placebo in reducing acute mania symptoms in a 3-week, double-blind, randomized trial of 197 patients with bipolar I disorder.10
- Aripiprazole monotherapy, 15 to 30 mg/d, had a significantly greater effect than placebo in a 3-week, double-blind, randomized trial of 262 patients in acute manic or mixed bipolar episodes. Response rates among patients with mania were 40% with aripiprazole and 19% with placebo.11
Both ziprasidone and aripiprazole were well-tolerated in these brief trials, although their efficacy as long-term mood-stabilizers in bipolar disorder is unclear.
Using clozapine raises concerns about potentially serious adverse events, although it remains the only agent with proven efficacy in treatment-refractory mania.12,13 Clozapine also appears to reduce hospitalization and affective relapse rates and improve symptoms and quality of life.14,15
Long-term safety
Compared with conventional antipsychotics, EPS are not a major concern with the atypical agents. Except for risperidone, atypicals’ effect on prolactin levels generally is not clinically meaningful. Atypicals appear to be “mood-friendly,” whereas conventional antipsychotics seem to contribute to dysphoria or cause depression in some patients.
Sedation or other annoying side effects such as dry mouth or dizziness can occur with any atypical. Other more-serious side effects may complicate antipsychotic treatment, as we are coming to understand from using atypicals for long-term schizophrenia management.
Table 3
Weight-loss medications for bipolar patients taking atypical antipsychotics
| Drug | Dosage | Side effects | Recommendations |
|---|---|---|---|
| Metformin | 500 to 1,000 mg bid | Hypoglycemia Diarrhea Nausea/vomiting | First-line in patients with comorbid type 2 diabetes |
| Orlistat | 120 mg tid | GI distress Change in bowel habits | Second-line For patients with BMI >27 Supplement fat-soluble vitamins |
| Sibutramine | 5 to 15 mg/d | Dry mouth Anorexia Insomnia Constipation | Second-line For patients with BMI 27 to 30 Risk of serotonin syndrome if given with serotonergic drugs |
| Topiramate | 50 to 250 mg/d | Somnolence Fatigue Paresthesias | Consider first-line for its potential additive mood-stabilizing effect May help comorbid binge-eating or seizure disorders |
| Zonisamide | 100 to 600 mg/d | Somnolence Dizziness Anorexia | Consider first-line for its potential additive mood-stabilizing effect May help comorbid binge-eating or seizure disorders |
Movement disorders. Antipsychotics appear more likely to cause EPS in patients with mood disorders than with schizophrenia. In one study using conventional antipsychotics, bipolar patients were 4 to 5 times more likely than schizophrenia patients to experience acute dystonia.16
Although atypicals pose some small risk for acute EPS and TD, the risk is near placebo-level with clinically relevant and comparable dosages.17 Even so, it is important to educate patients to watch for emerging signs of TD during long-term treatment with any antipsychotic. EPS risk may be dose-dependent, particularly with risperidone.18
Weight gain and obesity. Patients with bipolar disorder are more likely to be overweight or obese (body mass index [BMI] > 30) than the general population,17,19 though the reasons are unknown. Studies suggest an obesity prevalence of 32% to 35% in bipolar patients, compared with 18% in the general population.20,21
All atypicals can cause weight gain, although olanzapine and clozapine are associated with the greatest mean weight gains. In three long-term trials (47 weeks to 18 months), bipolar patients who received olanzapine gained significantly more weight (mean 2 to 3 kg) than those receiving lithium or divalproex.19
Cases with much greater weight gain—even leading to clinical obesity—have been observed, particularly with olanzapine. Although evidence from registration trials and clinical experience show lesser weight gains with risperidone, quetiapine, ziprasidone, and aripiprazole, some of our patients do gain weight while taking these agents—either alone or in combination with lithium or divalproex.
Weight management. Because patients with bipolar disorder may be at increased risk for weight gain and obesity, weight management techniques may improve their health by:
- decreasing morbidity and mortality tied to weight-related physical illnesses
- enhancing psychological well-being.1
In addition to diet and exercise counseling, some bipolar patients taking long-term atypical antipsychotics may benefit from adjunctive weight-loss medications (Table 3). We generally use such medications for bipolar patients who:
- persistently gain weight despite best dietary practices
- gain substantial weight early in treatment with an atypical antipsychotic that is providing effective symptomatic relief.
Early weight gain—particularly gains of >7% within the first 6 weeks—might predict large weight gain over time.
Diabetes. In September 2003, the FDA requested a class-wide labeling change to warn about a possible link between atypical antipsychotics and diabetes. The FDA recommended blood sugar monitoring of patients taking atypicals, especially those with obesity risk factors or family history of diabetes.
Type 2 diabetes develops in some patients taking atypicals, whether or not they gain substantial weight.22 This suggests that weight gain associated with bipolar disorder and the use of atypical antipsychotics may be independent risk factors for diabetes—a clear concern when treating bipolar patients.
Evidence provides no clear answer as to which atypicals may increase diabetes risk. Cautious use and vigilant monitoring of blood glucose are therefore recommended for every patient taking an atypical for long-term therapy. Also watch for increases in triglycerides and cholesterol17 in patients taking atypicals as bipolar maintenance therapy.
Conclusion
Atypical antipsychotics are valuable therapies in preventing bipolar relapses, although olanzapine is the only atypical with this indication so far. Collective data and clinical experience suggest that atypicals are indeed mood stabilizers, although—like other mood stabilizers such as lithium or divalproex—they have limitations. None achieve ideal efficacy in all four bipolar treatment roles: treating the highs and lows, and preventing the highs and lows. Atypicals seem more effective in treating and preventing the highs than the lows, reminding us that effective depression treatment is the greatest unmet need in bipolar disorder.
More double-blind, randomized, controlled trials are needed to fully understand whether all atypicals are mood stabilizers and to determine their safety and side effects in long-term therapy for patients with bipolar disorder.
Related resources
- Depression and Bipolar Support Alliance. www.dbsalliance.org
- Muzina DJ, Calabrese JR. Guidelines for treatment of bipolar disorder.In: Stein DJ, Kupfer DJ, Schatzberg AF (eds). Textbook of mood disorders Washington, DC: American Psychiatric Publishing, 2004 (in press).
Drug brand names
- Aripiprazole • Abilify
- Carbamazepine • Tegretol
- Clozapine • Clozaril
- Divalproex/valproate • Depakote, Depakene
- Lamotrigine • Lamictal
- Lithium • Eskalith, Lithobid, et al
- Metformin • Glucophage
- Olanzapine • Zyprexa
- Orlistat • Xenical
- Quetiapine • Seroquel
- Risperidone • Risperdal, Risperdal Consta
- Sibutramine • Meridia
- Simvastatin • Zocor
- Topiramate • Topamax
- Ziprasidone • Geodon
- Zonisamide • Zonegran
Disclosure
Dr. Muzina receives research grants from AstraZeneca Pharmaceuticals, Eli Lilly and Co., and Abbott Laboratories, is a consultant to AstraZeneca Pharmaceuticals and Pfizer, Inc., and a speaker for AstraZeneca Pharmaceuticals, Pfizer Inc., Eli Lilly and Co., and GlaxoSmithKline.
1. Hirschfeld RM, Bowden CL, Gitlin MJ, et al. Practice guideline for the treatment of patients with bipolar disorder (rev). Am J Psychiatry 2002;159:1-50.
2. Bauer MS, Mitchner L. What is a “mood stabilizer?” An evidence-based response. Am J Psychiatry 2004;161(1):3-18.
3. Keck PE, Jr, McElroy SL, Strakowski SM. Anticonvulsants and antipsychotics in the treatment of bipolar disorder. J Clin Psychiatry 1998;59(suppl 6):74-81.
4. Sharma V. Atypical antipsychotics and suicide in mood and anxiety disorders. Bipolar Disord 2003;5(suppl 2):48-52.
5. Tohen M, Marneros A, Bowden C, et al. Olanzapine versus lithium in relapse prevention in bipolar disorder: a randomized double-blind controlled 12-month clinical trial (presentation). Freiberg, Germany: Stanley Foundation Bipolar Network, Sept. 11-14, 2002.
6. Tohen M, Ketter TA, Zarate CA, et al. Olanzapine versus divalproex sodium for the treatment of acute mania and maintenance of remission: a 47-week study. Am J Psychiatry 2003;160(7):1263-71.
7. Vieta E, Goikolea JM, Corbella B, et al. Risperidone safety and efficacy in the treatment of bipolar and schizoaffective disorders: results from a 6-month, multicenter, open study. J Clin Psychiatry 2001;62(10):818-25.
8. Vieta E, Brugue E, Goikolea JM, et al. Acute and continuation risperidone monotherapy in mania. Hum Psychopharmacol 2004;19(1):41-5.
9. Sajatovic M, Brescan DW, Perez DE, et al. Quetiapine alone and added to a mood stabilizer for serious mood disorders. J Clin Psychiatry 2001;62(9):728-32.
10. Keck PE, Jr, Versiani M, Potkin S, et al. Ziprasidone in the treatment of acute bipolar mania: a three-week, placebo-controlled, double-blind, randomized trial. Am J Psychiatry 2003;160(4):741-8.
11. Keck PE, Jr, Marcus R, Tourkodimitris S, et al. A placebo-controlled, double-blind study of the efficacy and safety of aripiprazole in patients with acute bipolar mania. Am J Psychiatry 2003;160(9):1651-8.
12. Calabrese JR, Kimmel SE, Woyshville MJ, et al. Clozapine for treatment-refractory mania. Am J Psychiatry 1996;153(6):759-64.
13. Green AI, Tohen M, Patel JK, et al. Clozapine in the treatment of refractory psychotic mania. Am J Psychiatry 2000;157(6):982-6.
14. Zarate CA, Jr, Tohen M, Banov MD, et al. Is clozapine a mood stabilizer? J Clin Psychiatry 1995;56(3):108-12.
15. Suppes T, Webb A, Paul B, et al. Clinical outcome in a randomized 1-year trial of clozapine versus treatment as usual for patients with treatment-resistant illness and a history of mania. Am J Psychiatry 1999;156(8):1164-9.
16. Nasrallah HA, Churchill CM, Hamdan-Allan GA. Higher frequency of neuroleptic-induced dystonia in mania than in schizophrenia. Am J Psychiatry 1988;145(11):1455-6.
17. Chue P, Kovacs CS. Safety and tolerability of atypical antipsychotics in patients with bipolar disorder: prevalence, monitoring and management. Bipolar Disord 2003;5(suppl 2):62-79.
18. Simpson GM, Lindenmayer JP. Extrapyramidal symptoms in patients treated with risperidone. J Clin Psychopharmacol 1997;17(3):194-201.
19. Keck PE, Jr, McElroy SL. Bipolar disorder, obesity, and pharmacotherapy-associated weight gain. J Clin Psychiatry 2003;64(12):1426-35.
20. Fagiolini A, Frank E, Houck PR, et al. Prevalence of obesity and weight change during treatment in patients with bipolar I disorder. J Clin Psychiatry 2002;63(6):528-33.
21. Fagiolini A, Kupfer DJ, Houck PR, et al. Obesity as a correlate of outcome in patients with bipolar I disorder. Am J Psychiatry 2003;160(1):112-17.
22. Haupt DW, Newcomer JW. Abnormalities in glucose regulation associated with mental illness and treatment. J Psychosom Res 2002;53(4):925-33.
1. Hirschfeld RM, Bowden CL, Gitlin MJ, et al. Practice guideline for the treatment of patients with bipolar disorder (rev). Am J Psychiatry 2002;159:1-50.
2. Bauer MS, Mitchner L. What is a “mood stabilizer?” An evidence-based response. Am J Psychiatry 2004;161(1):3-18.
3. Keck PE, Jr, McElroy SL, Strakowski SM. Anticonvulsants and antipsychotics in the treatment of bipolar disorder. J Clin Psychiatry 1998;59(suppl 6):74-81.
4. Sharma V. Atypical antipsychotics and suicide in mood and anxiety disorders. Bipolar Disord 2003;5(suppl 2):48-52.
5. Tohen M, Marneros A, Bowden C, et al. Olanzapine versus lithium in relapse prevention in bipolar disorder: a randomized double-blind controlled 12-month clinical trial (presentation). Freiberg, Germany: Stanley Foundation Bipolar Network, Sept. 11-14, 2002.
6. Tohen M, Ketter TA, Zarate CA, et al. Olanzapine versus divalproex sodium for the treatment of acute mania and maintenance of remission: a 47-week study. Am J Psychiatry 2003;160(7):1263-71.
7. Vieta E, Goikolea JM, Corbella B, et al. Risperidone safety and efficacy in the treatment of bipolar and schizoaffective disorders: results from a 6-month, multicenter, open study. J Clin Psychiatry 2001;62(10):818-25.
8. Vieta E, Brugue E, Goikolea JM, et al. Acute and continuation risperidone monotherapy in mania. Hum Psychopharmacol 2004;19(1):41-5.
9. Sajatovic M, Brescan DW, Perez DE, et al. Quetiapine alone and added to a mood stabilizer for serious mood disorders. J Clin Psychiatry 2001;62(9):728-32.
10. Keck PE, Jr, Versiani M, Potkin S, et al. Ziprasidone in the treatment of acute bipolar mania: a three-week, placebo-controlled, double-blind, randomized trial. Am J Psychiatry 2003;160(4):741-8.
11. Keck PE, Jr, Marcus R, Tourkodimitris S, et al. A placebo-controlled, double-blind study of the efficacy and safety of aripiprazole in patients with acute bipolar mania. Am J Psychiatry 2003;160(9):1651-8.
12. Calabrese JR, Kimmel SE, Woyshville MJ, et al. Clozapine for treatment-refractory mania. Am J Psychiatry 1996;153(6):759-64.
13. Green AI, Tohen M, Patel JK, et al. Clozapine in the treatment of refractory psychotic mania. Am J Psychiatry 2000;157(6):982-6.
14. Zarate CA, Jr, Tohen M, Banov MD, et al. Is clozapine a mood stabilizer? J Clin Psychiatry 1995;56(3):108-12.
15. Suppes T, Webb A, Paul B, et al. Clinical outcome in a randomized 1-year trial of clozapine versus treatment as usual for patients with treatment-resistant illness and a history of mania. Am J Psychiatry 1999;156(8):1164-9.
16. Nasrallah HA, Churchill CM, Hamdan-Allan GA. Higher frequency of neuroleptic-induced dystonia in mania than in schizophrenia. Am J Psychiatry 1988;145(11):1455-6.
17. Chue P, Kovacs CS. Safety and tolerability of atypical antipsychotics in patients with bipolar disorder: prevalence, monitoring and management. Bipolar Disord 2003;5(suppl 2):62-79.
18. Simpson GM, Lindenmayer JP. Extrapyramidal symptoms in patients treated with risperidone. J Clin Psychopharmacol 1997;17(3):194-201.
19. Keck PE, Jr, McElroy SL. Bipolar disorder, obesity, and pharmacotherapy-associated weight gain. J Clin Psychiatry 2003;64(12):1426-35.
20. Fagiolini A, Frank E, Houck PR, et al. Prevalence of obesity and weight change during treatment in patients with bipolar I disorder. J Clin Psychiatry 2002;63(6):528-33.
21. Fagiolini A, Kupfer DJ, Houck PR, et al. Obesity as a correlate of outcome in patients with bipolar I disorder. Am J Psychiatry 2003;160(1):112-17.
22. Haupt DW, Newcomer JW. Abnormalities in glucose regulation associated with mental illness and treatment. J Psychosom Res 2002;53(4):925-33.
Bipolar I vs. Bipolar II
I agree with most of the points in Dr. Shivakumar and Dr. Suppes’ article on the Texas Medical Algorithm Project (TMAP) and with the algorithms they mentioned (Current Psychiatry, February 2004).
However, the article does not address the difference between bipolar type I and bipolar type II disorder. While this may at first seem trivial, recognizing the difference is crucial to planning treatment. Since rapid cycling and depression are more prevalent than hypomania in bipolar type II, patients with this form of the disorder often require different medication(s) than do those with bipolar type I.
Also, some psychotropics are appropriate for outpatient treatment but not for inpatients and vice-versa. For example, lamotrigine takes time to work up to an effective dosage without significantly increasing the risk for rash; this would be reasonable treatment for an outpatient with bipolar type II but is not practical for an inpatient, especially with bipolar type I.
Michael S. Wilson, II, MD
Louisiana State University Health Sciences Center
New Orleans
Dr. Suppes responds
Dr. Wilson raises the issue of treatment recommendations for bipolar I versus bipolar II disorder.
All treatment guidelines—including the American Psychiatric Association Guidelines, Texas Algorithms, and others—are based on evidence gathered from studies of bipolar I patients. The full article from the TMAP consensus conference discusses this issue as well as the paucity of data available to make treatment recommendations for patients with bipolar II disorder.1
Unfortunately, this has not changed dramatically over the last 4 years. The good news is that numerous ongoing studies will reveal how best to treat bipolar II patients.
Dr. Wilson also notes that time to response makes a medication appropriate for use in one setting but not in another. Given today’s brief inpatient stays, any antidepressant or maintenance medication started during hospitalization will not begin to work until after discharge. Following titration guidelines with lamotrigine is critical, but as with antidepressants the time to response is a few weeks. Thus, these medications will require outpatient monitoring to assess efficacy and tolerability.
Delineating treatment for patients with bipolar II disorder is important. No matter how the prevalence is evaluated, bipolar II disorder affects many individuals. We recently reviewed the evidence in this area2 and were struck by how little attention this patient group has received to date.
Trisha Suppes, MD, PhD
Associate professor, department of psychiatry
Director, Bipolar Disorder Research Program
University of Texas Southwestern Medical Center
Dallas
- Suppes T, Dennehy EB, Swann AC, et al. Report of the Texas consensus conference panel on medication treatment of bipolar disorder 2000. J Clin Psychiatry 2002;63:288–99.
- Suppes T, Dennehy EB. Evidence-based long term treatment of bipolar II disorder. J Clin Psychiatry 2002;63(suppl 10):29–33.
I agree with most of the points in Dr. Shivakumar and Dr. Suppes’ article on the Texas Medical Algorithm Project (TMAP) and with the algorithms they mentioned (Current Psychiatry, February 2004).
However, the article does not address the difference between bipolar type I and bipolar type II disorder. While this may at first seem trivial, recognizing the difference is crucial to planning treatment. Since rapid cycling and depression are more prevalent than hypomania in bipolar type II, patients with this form of the disorder often require different medication(s) than do those with bipolar type I.
Also, some psychotropics are appropriate for outpatient treatment but not for inpatients and vice-versa. For example, lamotrigine takes time to work up to an effective dosage without significantly increasing the risk for rash; this would be reasonable treatment for an outpatient with bipolar type II but is not practical for an inpatient, especially with bipolar type I.
Michael S. Wilson, II, MD
Louisiana State University Health Sciences Center
New Orleans
Dr. Suppes responds
Dr. Wilson raises the issue of treatment recommendations for bipolar I versus bipolar II disorder.
All treatment guidelines—including the American Psychiatric Association Guidelines, Texas Algorithms, and others—are based on evidence gathered from studies of bipolar I patients. The full article from the TMAP consensus conference discusses this issue as well as the paucity of data available to make treatment recommendations for patients with bipolar II disorder.1
Unfortunately, this has not changed dramatically over the last 4 years. The good news is that numerous ongoing studies will reveal how best to treat bipolar II patients.
Dr. Wilson also notes that time to response makes a medication appropriate for use in one setting but not in another. Given today’s brief inpatient stays, any antidepressant or maintenance medication started during hospitalization will not begin to work until after discharge. Following titration guidelines with lamotrigine is critical, but as with antidepressants the time to response is a few weeks. Thus, these medications will require outpatient monitoring to assess efficacy and tolerability.
Delineating treatment for patients with bipolar II disorder is important. No matter how the prevalence is evaluated, bipolar II disorder affects many individuals. We recently reviewed the evidence in this area2 and were struck by how little attention this patient group has received to date.
Trisha Suppes, MD, PhD
Associate professor, department of psychiatry
Director, Bipolar Disorder Research Program
University of Texas Southwestern Medical Center
Dallas
- Suppes T, Dennehy EB, Swann AC, et al. Report of the Texas consensus conference panel on medication treatment of bipolar disorder 2000. J Clin Psychiatry 2002;63:288–99.
- Suppes T, Dennehy EB. Evidence-based long term treatment of bipolar II disorder. J Clin Psychiatry 2002;63(suppl 10):29–33.
I agree with most of the points in Dr. Shivakumar and Dr. Suppes’ article on the Texas Medical Algorithm Project (TMAP) and with the algorithms they mentioned (Current Psychiatry, February 2004).
However, the article does not address the difference between bipolar type I and bipolar type II disorder. While this may at first seem trivial, recognizing the difference is crucial to planning treatment. Since rapid cycling and depression are more prevalent than hypomania in bipolar type II, patients with this form of the disorder often require different medication(s) than do those with bipolar type I.
Also, some psychotropics are appropriate for outpatient treatment but not for inpatients and vice-versa. For example, lamotrigine takes time to work up to an effective dosage without significantly increasing the risk for rash; this would be reasonable treatment for an outpatient with bipolar type II but is not practical for an inpatient, especially with bipolar type I.
Michael S. Wilson, II, MD
Louisiana State University Health Sciences Center
New Orleans
Dr. Suppes responds
Dr. Wilson raises the issue of treatment recommendations for bipolar I versus bipolar II disorder.
All treatment guidelines—including the American Psychiatric Association Guidelines, Texas Algorithms, and others—are based on evidence gathered from studies of bipolar I patients. The full article from the TMAP consensus conference discusses this issue as well as the paucity of data available to make treatment recommendations for patients with bipolar II disorder.1
Unfortunately, this has not changed dramatically over the last 4 years. The good news is that numerous ongoing studies will reveal how best to treat bipolar II patients.
Dr. Wilson also notes that time to response makes a medication appropriate for use in one setting but not in another. Given today’s brief inpatient stays, any antidepressant or maintenance medication started during hospitalization will not begin to work until after discharge. Following titration guidelines with lamotrigine is critical, but as with antidepressants the time to response is a few weeks. Thus, these medications will require outpatient monitoring to assess efficacy and tolerability.
Delineating treatment for patients with bipolar II disorder is important. No matter how the prevalence is evaluated, bipolar II disorder affects many individuals. We recently reviewed the evidence in this area2 and were struck by how little attention this patient group has received to date.
Trisha Suppes, MD, PhD
Associate professor, department of psychiatry
Director, Bipolar Disorder Research Program
University of Texas Southwestern Medical Center
Dallas
- Suppes T, Dennehy EB, Swann AC, et al. Report of the Texas consensus conference panel on medication treatment of bipolar disorder 2000. J Clin Psychiatry 2002;63:288–99.
- Suppes T, Dennehy EB. Evidence-based long term treatment of bipolar II disorder. J Clin Psychiatry 2002;63(suppl 10):29–33.
Bipolar treatment update: Evidence is driving change in mania, depression algorithms
Many well-controlled trials in the past 4 years have evaluated new medications for treating bipolar disorder. It’s time to build a consensus on how this data may apply to clinical practice.
This year, our group will re-examine the Texas Medication Algorithm Project (TMAP) treatment algorithms for bipolar I disorder.
What makes TMAP unique? It is the first project to evaluate treatment algorithm use in community mental health settings for patients with a history of mania (see Box).1-5 Severely, persistently ill outpatients such as these are seldom included in research but are frequently seen in clinical practice.
To preview for psychiatrists the changes expected in 2004, this article describes the goals of TMAP and the controlled study on which the medication algorithms are based. We review the medication algorithms of 2000 as a starting point and present the evidence that is changing clinical practice.
Guiding principles of TMAP
A treatment algorithm is no substitute for clinical judgment; rather, medication guidelines and algorithms are guideposts to help the clinician and patient collaboratively develop the most effective medication strategy with the fewest side effects.
The Texas Medication Algorithm Project (TMAP)1-3 is a public and academic collaboration started in 1996 to develop evidence- and consensus-based medication treatment algorithms for schizophrenia, major depressive disorder, and bipolar disorder.
TMAP’s goal is to establish “best practices” to encourage uniformity of care, achieve the best possible patient outcomes, and use mental health care dollars most efficiently. The project includes four phases, in which the treatment algorithms were developed, compared with treatment-as-usual, put into practice, and will undergo periodic updates.4 The next update begins this year.
The comparison of algorithms for treating bipolar mania/hypomania and depression included 409 patients (mean age 38 to 40) with bipolar I disorder or schizoaffective disorder, bipolar type. These patients were severely and persistently mentally ill, from a diverse ethnic population, and significantly impaired in functioning.
During 12 months of treatment, psychiatric symptoms diminished more rapidly in patients in the algorithm group—as measured by the Brief Psychiatric Rating Scale (BPRS-24)—compared with those receiving usual treatment. After the first 3 months, the usual-treatment patients also showed diminished symptoms. At study’s end, symptom severity between the groups was not significantly different; both groups showed improvement.
Manic and psychotic symptoms—measured by Clinician-Administered Rating Scale subscales (CARS-M)5—improved significantly more in the algorithm group in the first 3 months, and this gap between the two groups was sustained for 12 months. Depressive symptoms declined, but no overall differences were noted between the two groups. Side effect rates and functioning were also similar.
TMAP’s treatment manual (see Related resources) describes clinicians’ preferred tactics and decision points, which we summarize here. The guidelines are an ongoing effort to apply evidence-based medicine to everyday practice and are meant to be adapted to patient needs.
Treatment goals that guided TMAP algorithm development are:
- symptomatic remission
- full return of psychosocial functioning
- prevention of relapse and recurrence.
Suggestions came from controlled clinical trials, open trials, retrospective data analyses, expert clinical consensus, and input from consumers.
Treatment selection. Initial algorithm stages recommend simple treatments (in terms of safety, tolerability, and side effects), whereas later stages recommend more-complicated regimens. A patient’s symptoms, comorbid conditions, and treatment history guide treatment selection. Patients may enter an algorithm at any stage, depending on their clinical presentation and medication history.
The clinician may consider patient preference when deciding among equivalent medications. The algorithm strongly encourages patients and families to participate, such as by keeping daily mood charts and completing symptom and side-effect checklists. When clinicians face a choice among medication brands, generics, or forms (such as immediate- versus slow-release), agents with greater tolerability are preferred.
Patient management. When patients enter the algorithm, clinic visits are frequent (such as every 2 weeks). Follow-up appointments address medication adherence, dosage adjustments, and side effects or adverse reactions.
If a patient’s symptoms show no change after two treatment stages, re-evaluate the diagnosis and consider mitigating factors such as substance abuse. Patients who complete acute treatment should receive continuation treatment.
Documentation. Clinicians are advised to document decision points and the rationale for treatment choices made outside the algorithm package.
Treating mania or hypomania
After clinical evaluation confirms the diagnosis of bipolar illness,4 the TMAP mania/hypomania algorithm (Algorithm 1) splits into three treatment pathways:
- euphoric mania/hypomania
- mixed or dysphoric mania/hypomania
- psychotic mania.
These pathways recognize the need for differing approaches to initial monotherapy and later two-drug combinations. If a patient develops persistent or severe depressive symptoms, the bipolar algorithm for a major depressive episode (Algorithm 2) is used during depressive periods with the primary mania algorithm.
Treatment recommendations. The key to using mood stabilizers is to achieve the optimum response—assuming good tolerability—before switching to another agent. Adjust medication dosages one at a time to allow adequate response and assessment.
When switching medications, use an overlap-and-taper strategy, assuming there is no medical necessity to stop a drug abruptly. Add the new medication, then gradually taper the one that is being discontinued. Monitor serum levels.
Discontinue antidepressants when appropriate in patients with hypomania/mania or rapid cycling, and continually evaluate suicide and homicide potential of patients in mixed or depressive states.
Stage 1: Monotherapy. First medication choices are lithium, divalproex, or olanzapine. For mixed or dysphoric mania, the algorithm recommends divalproex (preferred over valproic acid because of tolerability and side effects) or olanzapine.6 Data suggest dysphoric manic patients are less likely to respond to lithium.7 A Consensus Panel minority expressed concern about using olanzapine as first-line monotherapy for acute mania because of limited data on the drug’s long-term safety. Patients with partial response or residual symptoms may move to stage 2 or switch to other medication options within stage 1.
Patients with psychotic mania move directly to stage 4 for a broader range of combination therapy.
Stage 2: Combination therapy. Combination therapy has become the standard of care in treating most patients with bipolar disorder. The algorithm recommends using two agents:
- lithium or an anticonvulsant plus another anticonvulsant ([Li or AC]+AC)
- or lithium or an anticonvulsant plus an atypical antipsychotic ([Li or AC]+AAP).8
Recommended agents include lithium, divalproex, oxcarbazepine, olanzapine, or risperidone. The experts recommended oxcarbazepine as first choice because it is better tolerated and interacts with fewer drugs than carbamazepine and does not require serum level monitoring.9
A Consensus Panel minority expressed concern that few studies had examined using oxcarbazepine in bipolar disorder. Carbamazepine was also considered an option.
Stages 3 and 4: Other two-drug combinations. Other two-drug combinations are tried at these stages, drawing from the same pool of medication classes described in stage 2.
Stage 4 broadens the choice of atypical antipsychotic by adding quetiapine10 and ziprasidone11 to the recommended stage-2 agents olanzapine and risperidone. When the 2000 algorithm was developed, limited data were available on using some newer atypicals in patients with bipolar mania. Based on recent, high-quality studies of mono- and combination therapy—including quetiapine,10 ziprasidone,11 risperidone,12,13 and aripiprazole14 —the 2004 algorithm update panel will likely recommend using atypicals earlier, including at stage 1.
Algorithm 1 Treating mania/hypomania in patients with bipolar I disorder
Stage 5: Triple-drug combination. Lithium, an anticonvulsant (divalproex or oxcarbazepine), and an atypical antipsychotic (olanzapine, risperidone, quetiapine, or ziprasidone) is a recommended triple-drug combination. In the 2004 update, the choices will likely expand to include all the newer atypicals and will list carbamazepine as an option.
Stage 6: ECT or clozapine. For patients with inadequate response to triple-drug combinations, the algorithm recommends adding electroconvulsive therapy (ECT) or clozapine.
ECT15 is recommended three times a week until the patient achieves remission of manic symptoms or fails to achieve a sustained response over three to six treatment cycles. Treatment resistance is declared if no response is seen after 6 to 10 treatment cycles.
Clozapine’s16 recommendation at this stage is consistent with its use in patients who fail to respond to other atypical antipsychotics. Blood monitoring for agranulocytosis is required; other adverse effects include an increased risk of seizures, myocarditis, and orthostatic hypotension.
Stage 7: Other. Treatment options such as topiramate17,18 and lamotrigine19 are recommended at this stage. These recommendations also will be reviewed and likely revised.
Treating bipolar depression
The TMAP algorithm for treating depression in bipolar disorder (Algorithm 2) assumes that anti-depressants will be used only with optimum mood-stabilizer levels because of the risk of inducing manic symptoms. The bipolar depression algorithm is always used with the primary algorithm for mania/hypomania.
The patient’s clinical presentation guides medication selection. For the “pure” bipolar I patient with a major depressive episode but little mood lability or hypomania, starting an antide-pressant is a clear decision. On the other hand, patients with predominant depressive symptoms plus dysphoric hypomania, mood lability, and irritability need a balance of mood-stabilizing drugs and antidepressants.
Stage 1: Mood stabilizer. Initiate a mood stabilizer and optimize the dosage. Choices are the same mood stabilizers listed in the hypomania/mania treatment algorithm.
Stage 2: Antidepressant. Adding an antidepressant implies that depressive symptoms are severe enough to change treatment. Antidepressant options include a selective serotonin reuptake inhibitor (SSRI), sustained-release bupropion, or lamotrigine.20
Using SSRIs is supported by widespread clinical experience and offers the convenience of once-daily dosing. Recommended SSRIs include fluoxetine, paroxetine, fluvoxamine, sertraline, and citalopram. The SSRI escitalopram was introduced after the 2000 algorithms were published; evidence for using it and other newer medications will be reviewed for the 2004 update.
The recommendation for sustained-release bupropion is consistent with the algorithm principle to use medications in the most well-tolerated form when accessible and available.
With lamotrigine, review with patients the risk of serious rash. To minimize rash risk, start lamotrigine slowly and follow the recommended titration schedule.
Stage 3: Multiple choices. At this stage, no definitive studies, safety data, or tolerability issues are available to rank the medication choices. The algorithm suggests:
- adding lithium21 or a second antidepressant
- or switching to an alternate antidepressant such as venlafaxine or nefazodone.
If a patient moves to stage 3 because of side effects with one antidepressant class, a different class—preferably with a contrasting side-effect profile—is recommended.
Algorithm 2 Treating depression in bipolar I disorder*
Stage 4: Two antidepressants. To enhance clinical response, the algorithm recommends combining two antidepressants, preferably from different classes. Monitor patients closely for side effects.
Stage 5. Antipsychotic or MAOI. At this stage, the algorithm recommends adding an atypical antipsychotic22 or switching to a monoamine oxidase inhibitor (MAOI).
Early evidence supported the efficacy of MAOIs in bipolar depression. However, the panel ranked MAOIs lower in the algorithm because they are associated with more bothersome side effects than SSRIs and other antidepressants. When using MAOIs, provide patients with dietary restriction guidelines.
Stage 6. Other therapies. Therapies such as ECT or “other” interventions are recommended at this stage. ECT has proven efficacy in bipolar depression and is appropriate for patients with limited medication response. The panel gave ECT a low ranking because of limited availability, lack of patient acceptance, and newer options.
Medication options include experimental treatments with limited evidence, such as inositol, dopamine agonists, stimulants, thyroid supplementation, conventional antipsychotics, and tri-cyclic antidepressants.
Acute to maintenance treatment
Adjunctive treatments for agitation, insomnia, GI upset, sedation, headache, and tremor are recommended in the physician manual supporting the TMAP guidelines (see Related resources). The manual also suggests ways to manage medication side effects and modify the algorithms for inpatients.
Patient and family psychoeducation plays an important role in helping the patient:
- identify prodromal bipolar symptoms
- understand the need to take medications as prescribed.
Continuation treatment. After mania or hypomania remits, continue medication(s) at the effective acute-phase dosages for at least 3 months. Use follow-up visits to enhance patient adherence, detect early symptoms of relapse, and monitor for side effects.
During the late continuation phase, after a period of sustained stability, clinicians can try to simplify the medications. When discontinuing a medication, taper the dosage by no more than 25% per week. If symptoms recur, promptly return to acute-phase treatment. Consider restarting medications and titrating up to the dosage(s) that resulted in remission.
In a depressive episode, continue the antidepressant(s) for 1 to 3 months at the effective acutephase dosage(s). Follow up frequently, and educate patients to watch for symptom recurrence and to communicate with you to assess when medication changes are needed.
Maintenance treatment. Relatively few well-controlled studies on long-term management of bipolar patients were available for the 2000 algorithm update.23 In general, all patients need mood stabilizer(s) to prevent relapse, using the lowest dosage that maintains therapeutic efficacy. Based on new evidence for lamotrigine and atypical antipsychotics—including FDAapproval of olanzapine for bipolar maintenace therapy—we anticipate recommendations will be expanded and more delineated in the 2004 update.
Discontinuing antidepressants after 3 to 6 months of initial treatment is now recommended. However, a recent retrospective case series suggests that continuing antidepressants at least 1 year after initial successful therapy may protect against depressive relapse. During this study, continuing antidepressants more than 3 to 6 months did not appear to increase the risk of switching to mania.24
Should antidepressants be continued or discontinued after successful acute treatment of a bipolar I depressive episode? This is an active area of research and debate as to the most appropriate strategy. The 2004 algorithm update panel will consider recent evidence that supports continuing antidepressants after symptom remission.24
- Texas Medication Algorithm Project algorithms and physician manual. Texas Department of Mental Health and Mental Retardation. http://www.mhmr.state.tx.us/centraloffice/medicaldirector/TIMA.html
- American Psychiatric Association. Practice guidelines for the treatment of patients with bipolar disorder. Am J Psychiatry 2002; 159(4):suppl 2.
- Depression and Bipolar Support Alliance. www.dbsalliance.org
Drug brand names
- Bupropion • Wellbutrin SR
- Carbamazepine • Tegretol
- Citalopram • Celexa
- Clozapine • Clozaril
- Divalproex sodium • Depakote
- Escitalopram • Lexapro
- Fluoxetine • Prozac
- Fluvoxamine • Luvox
- Inositol • Various
- Lamotrigine • Lamictal
- Nefazodone • Serzone
- Olanzapine • Zyprexa
- Oxcarbazepine • Trileptal
- Paroxetine • Paxil
- Quetiapine • Seroquel
- Risperidone • Risperdal
- Sertraline • Zoloft
- Topiramate • Topamax
- Tranylcypromine • Parnate
- Valproic acid • Depakene
- Venlafaxine • Effexor
- Ziprasidone • Geodon
Disclosure
Dr. Shivakumar reports no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
Dr. Suppes receives research support from or is a consultant to Abbott Laboratories, AstraZeneca Pharmaceuticals, Bristol-Myers Squibb, Eli Lilly and Co., GlaxoSmithKline, Janssen Pharmaceutica, Johnson & Johnson, National Institutes of Mental Health, Novartis Pharmaceuticals Corp., Pfizer Inc., Pharmaceutical Research Institute, Ortho-McNeil Pharmaceutical, Robert Wood Johnson Pharmaceutical Research Institute, The Stanley Medical Research Institute, and UCB Pharma.
1. Gilbert DA, Altshuler KZ, Rago WV, et al. Texas Medication Algorithm Project: definitions, rationale, and methods to develop medication algorithms. J Clin Psychiatry 1998;59:345-51.
2. Altshuler KZ, Rush AJ. Computerized Texas Medication Algorithm Project undergoes testing. Outcomes Accountability Alert 1999;4(1):10-11.
3. Rush AJ, Crismon ML, Kashner TM, et al. Texas Medication Algorithm Project, Phase 3 (TMAP-3): rationale and study design. J Clin Psychiatry 2003;64(4):357-69.
4. Altman E, Hedeker D, Janicak P, et al. The Clinician-Administered Rating Scale For Mania (CARS-M): development, reliability, and validity. Biol Psychiatry 1994;36:124-34.
5. Suppes T, Dennehy EB, Swann AC, et al. Report of the Texas consensus conference panel on medication treatment of bipolar disorder 2000. J Clin Psychiatry 2002;63:288-99.
6. Dennehy EB, Doyle K, Suppes T. The efficacy of olanzapine monotherapy for acute hypomania or mania in an outpatient setting. Int Clin Psychopharmacol 2003;18(3):143-5.
7. Dilsaver SC, Swann AC, Shoaib AM, et al. The manic syndrome: factors which may predict a patient’s response to lithium, carbamazepine and valproate. J Psych Neurosci 1993;18:61-6.
8. Tohen M, Chengappa KNR, Suppes T, et al. Efficacy of olanzapine in combination with valproate or lithium in the treatment of mania in patients partially nonresponsive to valproate or lithium monotherapy. Arch Gen Psychiatry 2002;59(1):62-9.
9. Emrich HM. Studies with oxcarbazepine (Trileptal) in acute mania. Int Clin Psychopharmacol 1990;190(5,suppl):83-8.
10. Vieta E, Parramon G, Padrell E, et al. Quetiapine in the treatment of rapid cycling bipolar disorder. Bipolar Disord 2002;4(5):335-40.
11. Keck PE, Versiani M, Potkin S, et al. Ziprasidone in the treatment of acute bipolar mania: a three week placebo-controlled, double-blinded randomized trial. Am J Psychiatry 2003;160(4):741-8.
12. Yatham LN, Grossman F, Augustyns I, et al. Mood stabilisers plus risperidone or placebo in the treatment of acute mania. International, double-blinded, randomised controlled trial. Br J Psychiatry 2003;182:141-7.
13. Sachs GS, Grossman F, Ghaemi SN, et al. Combination of a mood stabilizer with risperidone or haloperidol for treatment of acute mania: a double-blind, placebo-controlled comparison of efficacy and safety. Am J Psychiatry 2002;159(7):1146-54.
14. Keck PE, Jr, Marcus R, Tourkodimitris S, et al. Aripiprazole study group. A placebo-controlled, double-blind study of the efficacy and safety of aripiprazole in patients with acute bipolar mania. Am J Psychiatry 2003;160(9):1651-8.
15. Mukherjee S, Sackeim HA, Schnur DB. Electroconvulsive therapy of acute manic episode: a review of 50 years’ experience. Am J Psychiatry 1988;45:727-32.
16. Suppes T, Webb A, Paul B, et al. Clinical outcome in a randomized 1-year trail of clozapine versus treatment as usual for patients with treatment-resistant illness and a history of mania. Am J Psychiatry 1999;156(8):1164-9.
17. Guille C, Sachs G. Clinical outcome of adjunctive topiramate treatment in a sample of refractory bipolar patients with comorbid conditions. Prog Neuropsychopharmacol Biol Psychiatry 2002;26(6):1035-9.
18. Vieta E, Torrent C, Garcia-Ribas G, et al. Use of topiramate in treatment-resistant bipolar spectrum disorders. J Clin Psychopharmacol 2002;22(4):431-5.
19. Calabrese JR, Suppes T, Bowden CL, et al. A double blinded, placebo-controlled, prophylaxis study of lamotrigine in rapid-cycling bipolar disorder. J Clin Psychiatry 2000;61:841-50.
20. Calabrese JR, Bowden CL, Sachs GS, et al. A placebo-controlled 18-month trial of lamotrigine and lithium maintenance treatment in recently depressed patients with bipolar I disorder. J Clin Psychiatry 2003;64(9):1013-24.
21. Bauer M, Dopfmer S. Lithium augmentation in treatment-resistant depression: meta-analysis of placebo-controlled studies. J Clin Psychopharmacology 1999;19:427-34.
22. Shelton RC, Tollefson GD, Tohen M, et al. A novel augmentation strategy for treating resistant major depression. Am J Psychiatry 2001;158:131-4.
23. Baldessarini RJ, Tohen M, Tondo L. Maintenance treatment in bipolar disorder (comment). Arch Gen Psychiatry 2000;57:490-2.
24. Altshuler L, Suppes T, Black D, et al. Impact of antidepressant discontinuation after acute bipolar depression remission on rates of depressive relapse at 1-year follow-up. Am J Psychiatry 2003;160:1252-62.
Many well-controlled trials in the past 4 years have evaluated new medications for treating bipolar disorder. It’s time to build a consensus on how this data may apply to clinical practice.
This year, our group will re-examine the Texas Medication Algorithm Project (TMAP) treatment algorithms for bipolar I disorder.
What makes TMAP unique? It is the first project to evaluate treatment algorithm use in community mental health settings for patients with a history of mania (see Box).1-5 Severely, persistently ill outpatients such as these are seldom included in research but are frequently seen in clinical practice.
To preview for psychiatrists the changes expected in 2004, this article describes the goals of TMAP and the controlled study on which the medication algorithms are based. We review the medication algorithms of 2000 as a starting point and present the evidence that is changing clinical practice.
Guiding principles of TMAP
A treatment algorithm is no substitute for clinical judgment; rather, medication guidelines and algorithms are guideposts to help the clinician and patient collaboratively develop the most effective medication strategy with the fewest side effects.
The Texas Medication Algorithm Project (TMAP)1-3 is a public and academic collaboration started in 1996 to develop evidence- and consensus-based medication treatment algorithms for schizophrenia, major depressive disorder, and bipolar disorder.
TMAP’s goal is to establish “best practices” to encourage uniformity of care, achieve the best possible patient outcomes, and use mental health care dollars most efficiently. The project includes four phases, in which the treatment algorithms were developed, compared with treatment-as-usual, put into practice, and will undergo periodic updates.4 The next update begins this year.
The comparison of algorithms for treating bipolar mania/hypomania and depression included 409 patients (mean age 38 to 40) with bipolar I disorder or schizoaffective disorder, bipolar type. These patients were severely and persistently mentally ill, from a diverse ethnic population, and significantly impaired in functioning.
During 12 months of treatment, psychiatric symptoms diminished more rapidly in patients in the algorithm group—as measured by the Brief Psychiatric Rating Scale (BPRS-24)—compared with those receiving usual treatment. After the first 3 months, the usual-treatment patients also showed diminished symptoms. At study’s end, symptom severity between the groups was not significantly different; both groups showed improvement.
Manic and psychotic symptoms—measured by Clinician-Administered Rating Scale subscales (CARS-M)5—improved significantly more in the algorithm group in the first 3 months, and this gap between the two groups was sustained for 12 months. Depressive symptoms declined, but no overall differences were noted between the two groups. Side effect rates and functioning were also similar.
TMAP’s treatment manual (see Related resources) describes clinicians’ preferred tactics and decision points, which we summarize here. The guidelines are an ongoing effort to apply evidence-based medicine to everyday practice and are meant to be adapted to patient needs.
Treatment goals that guided TMAP algorithm development are:
- symptomatic remission
- full return of psychosocial functioning
- prevention of relapse and recurrence.
Suggestions came from controlled clinical trials, open trials, retrospective data analyses, expert clinical consensus, and input from consumers.
Treatment selection. Initial algorithm stages recommend simple treatments (in terms of safety, tolerability, and side effects), whereas later stages recommend more-complicated regimens. A patient’s symptoms, comorbid conditions, and treatment history guide treatment selection. Patients may enter an algorithm at any stage, depending on their clinical presentation and medication history.
The clinician may consider patient preference when deciding among equivalent medications. The algorithm strongly encourages patients and families to participate, such as by keeping daily mood charts and completing symptom and side-effect checklists. When clinicians face a choice among medication brands, generics, or forms (such as immediate- versus slow-release), agents with greater tolerability are preferred.
Patient management. When patients enter the algorithm, clinic visits are frequent (such as every 2 weeks). Follow-up appointments address medication adherence, dosage adjustments, and side effects or adverse reactions.
If a patient’s symptoms show no change after two treatment stages, re-evaluate the diagnosis and consider mitigating factors such as substance abuse. Patients who complete acute treatment should receive continuation treatment.
Documentation. Clinicians are advised to document decision points and the rationale for treatment choices made outside the algorithm package.
Treating mania or hypomania
After clinical evaluation confirms the diagnosis of bipolar illness,4 the TMAP mania/hypomania algorithm (Algorithm 1) splits into three treatment pathways:
- euphoric mania/hypomania
- mixed or dysphoric mania/hypomania
- psychotic mania.
These pathways recognize the need for differing approaches to initial monotherapy and later two-drug combinations. If a patient develops persistent or severe depressive symptoms, the bipolar algorithm for a major depressive episode (Algorithm 2) is used during depressive periods with the primary mania algorithm.
Treatment recommendations. The key to using mood stabilizers is to achieve the optimum response—assuming good tolerability—before switching to another agent. Adjust medication dosages one at a time to allow adequate response and assessment.
When switching medications, use an overlap-and-taper strategy, assuming there is no medical necessity to stop a drug abruptly. Add the new medication, then gradually taper the one that is being discontinued. Monitor serum levels.
Discontinue antidepressants when appropriate in patients with hypomania/mania or rapid cycling, and continually evaluate suicide and homicide potential of patients in mixed or depressive states.
Stage 1: Monotherapy. First medication choices are lithium, divalproex, or olanzapine. For mixed or dysphoric mania, the algorithm recommends divalproex (preferred over valproic acid because of tolerability and side effects) or olanzapine.6 Data suggest dysphoric manic patients are less likely to respond to lithium.7 A Consensus Panel minority expressed concern about using olanzapine as first-line monotherapy for acute mania because of limited data on the drug’s long-term safety. Patients with partial response or residual symptoms may move to stage 2 or switch to other medication options within stage 1.
Patients with psychotic mania move directly to stage 4 for a broader range of combination therapy.
Stage 2: Combination therapy. Combination therapy has become the standard of care in treating most patients with bipolar disorder. The algorithm recommends using two agents:
- lithium or an anticonvulsant plus another anticonvulsant ([Li or AC]+AC)
- or lithium or an anticonvulsant plus an atypical antipsychotic ([Li or AC]+AAP).8
Recommended agents include lithium, divalproex, oxcarbazepine, olanzapine, or risperidone. The experts recommended oxcarbazepine as first choice because it is better tolerated and interacts with fewer drugs than carbamazepine and does not require serum level monitoring.9
A Consensus Panel minority expressed concern that few studies had examined using oxcarbazepine in bipolar disorder. Carbamazepine was also considered an option.
Stages 3 and 4: Other two-drug combinations. Other two-drug combinations are tried at these stages, drawing from the same pool of medication classes described in stage 2.
Stage 4 broadens the choice of atypical antipsychotic by adding quetiapine10 and ziprasidone11 to the recommended stage-2 agents olanzapine and risperidone. When the 2000 algorithm was developed, limited data were available on using some newer atypicals in patients with bipolar mania. Based on recent, high-quality studies of mono- and combination therapy—including quetiapine,10 ziprasidone,11 risperidone,12,13 and aripiprazole14 —the 2004 algorithm update panel will likely recommend using atypicals earlier, including at stage 1.
Algorithm 1 Treating mania/hypomania in patients with bipolar I disorder
Stage 5: Triple-drug combination. Lithium, an anticonvulsant (divalproex or oxcarbazepine), and an atypical antipsychotic (olanzapine, risperidone, quetiapine, or ziprasidone) is a recommended triple-drug combination. In the 2004 update, the choices will likely expand to include all the newer atypicals and will list carbamazepine as an option.
Stage 6: ECT or clozapine. For patients with inadequate response to triple-drug combinations, the algorithm recommends adding electroconvulsive therapy (ECT) or clozapine.
ECT15 is recommended three times a week until the patient achieves remission of manic symptoms or fails to achieve a sustained response over three to six treatment cycles. Treatment resistance is declared if no response is seen after 6 to 10 treatment cycles.
Clozapine’s16 recommendation at this stage is consistent with its use in patients who fail to respond to other atypical antipsychotics. Blood monitoring for agranulocytosis is required; other adverse effects include an increased risk of seizures, myocarditis, and orthostatic hypotension.
Stage 7: Other. Treatment options such as topiramate17,18 and lamotrigine19 are recommended at this stage. These recommendations also will be reviewed and likely revised.
Treating bipolar depression
The TMAP algorithm for treating depression in bipolar disorder (Algorithm 2) assumes that anti-depressants will be used only with optimum mood-stabilizer levels because of the risk of inducing manic symptoms. The bipolar depression algorithm is always used with the primary algorithm for mania/hypomania.
The patient’s clinical presentation guides medication selection. For the “pure” bipolar I patient with a major depressive episode but little mood lability or hypomania, starting an antide-pressant is a clear decision. On the other hand, patients with predominant depressive symptoms plus dysphoric hypomania, mood lability, and irritability need a balance of mood-stabilizing drugs and antidepressants.
Stage 1: Mood stabilizer. Initiate a mood stabilizer and optimize the dosage. Choices are the same mood stabilizers listed in the hypomania/mania treatment algorithm.
Stage 2: Antidepressant. Adding an antidepressant implies that depressive symptoms are severe enough to change treatment. Antidepressant options include a selective serotonin reuptake inhibitor (SSRI), sustained-release bupropion, or lamotrigine.20
Using SSRIs is supported by widespread clinical experience and offers the convenience of once-daily dosing. Recommended SSRIs include fluoxetine, paroxetine, fluvoxamine, sertraline, and citalopram. The SSRI escitalopram was introduced after the 2000 algorithms were published; evidence for using it and other newer medications will be reviewed for the 2004 update.
The recommendation for sustained-release bupropion is consistent with the algorithm principle to use medications in the most well-tolerated form when accessible and available.
With lamotrigine, review with patients the risk of serious rash. To minimize rash risk, start lamotrigine slowly and follow the recommended titration schedule.
Stage 3: Multiple choices. At this stage, no definitive studies, safety data, or tolerability issues are available to rank the medication choices. The algorithm suggests:
- adding lithium21 or a second antidepressant
- or switching to an alternate antidepressant such as venlafaxine or nefazodone.
If a patient moves to stage 3 because of side effects with one antidepressant class, a different class—preferably with a contrasting side-effect profile—is recommended.
Algorithm 2 Treating depression in bipolar I disorder*
Stage 4: Two antidepressants. To enhance clinical response, the algorithm recommends combining two antidepressants, preferably from different classes. Monitor patients closely for side effects.
Stage 5. Antipsychotic or MAOI. At this stage, the algorithm recommends adding an atypical antipsychotic22 or switching to a monoamine oxidase inhibitor (MAOI).
Early evidence supported the efficacy of MAOIs in bipolar depression. However, the panel ranked MAOIs lower in the algorithm because they are associated with more bothersome side effects than SSRIs and other antidepressants. When using MAOIs, provide patients with dietary restriction guidelines.
Stage 6. Other therapies. Therapies such as ECT or “other” interventions are recommended at this stage. ECT has proven efficacy in bipolar depression and is appropriate for patients with limited medication response. The panel gave ECT a low ranking because of limited availability, lack of patient acceptance, and newer options.
Medication options include experimental treatments with limited evidence, such as inositol, dopamine agonists, stimulants, thyroid supplementation, conventional antipsychotics, and tri-cyclic antidepressants.
Acute to maintenance treatment
Adjunctive treatments for agitation, insomnia, GI upset, sedation, headache, and tremor are recommended in the physician manual supporting the TMAP guidelines (see Related resources). The manual also suggests ways to manage medication side effects and modify the algorithms for inpatients.
Patient and family psychoeducation plays an important role in helping the patient:
- identify prodromal bipolar symptoms
- understand the need to take medications as prescribed.
Continuation treatment. After mania or hypomania remits, continue medication(s) at the effective acute-phase dosages for at least 3 months. Use follow-up visits to enhance patient adherence, detect early symptoms of relapse, and monitor for side effects.
During the late continuation phase, after a period of sustained stability, clinicians can try to simplify the medications. When discontinuing a medication, taper the dosage by no more than 25% per week. If symptoms recur, promptly return to acute-phase treatment. Consider restarting medications and titrating up to the dosage(s) that resulted in remission.
In a depressive episode, continue the antidepressant(s) for 1 to 3 months at the effective acutephase dosage(s). Follow up frequently, and educate patients to watch for symptom recurrence and to communicate with you to assess when medication changes are needed.
Maintenance treatment. Relatively few well-controlled studies on long-term management of bipolar patients were available for the 2000 algorithm update.23 In general, all patients need mood stabilizer(s) to prevent relapse, using the lowest dosage that maintains therapeutic efficacy. Based on new evidence for lamotrigine and atypical antipsychotics—including FDAapproval of olanzapine for bipolar maintenace therapy—we anticipate recommendations will be expanded and more delineated in the 2004 update.
Discontinuing antidepressants after 3 to 6 months of initial treatment is now recommended. However, a recent retrospective case series suggests that continuing antidepressants at least 1 year after initial successful therapy may protect against depressive relapse. During this study, continuing antidepressants more than 3 to 6 months did not appear to increase the risk of switching to mania.24
Should antidepressants be continued or discontinued after successful acute treatment of a bipolar I depressive episode? This is an active area of research and debate as to the most appropriate strategy. The 2004 algorithm update panel will consider recent evidence that supports continuing antidepressants after symptom remission.24
- Texas Medication Algorithm Project algorithms and physician manual. Texas Department of Mental Health and Mental Retardation. http://www.mhmr.state.tx.us/centraloffice/medicaldirector/TIMA.html
- American Psychiatric Association. Practice guidelines for the treatment of patients with bipolar disorder. Am J Psychiatry 2002; 159(4):suppl 2.
- Depression and Bipolar Support Alliance. www.dbsalliance.org
Drug brand names
- Bupropion • Wellbutrin SR
- Carbamazepine • Tegretol
- Citalopram • Celexa
- Clozapine • Clozaril
- Divalproex sodium • Depakote
- Escitalopram • Lexapro
- Fluoxetine • Prozac
- Fluvoxamine • Luvox
- Inositol • Various
- Lamotrigine • Lamictal
- Nefazodone • Serzone
- Olanzapine • Zyprexa
- Oxcarbazepine • Trileptal
- Paroxetine • Paxil
- Quetiapine • Seroquel
- Risperidone • Risperdal
- Sertraline • Zoloft
- Topiramate • Topamax
- Tranylcypromine • Parnate
- Valproic acid • Depakene
- Venlafaxine • Effexor
- Ziprasidone • Geodon
Disclosure
Dr. Shivakumar reports no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
Dr. Suppes receives research support from or is a consultant to Abbott Laboratories, AstraZeneca Pharmaceuticals, Bristol-Myers Squibb, Eli Lilly and Co., GlaxoSmithKline, Janssen Pharmaceutica, Johnson & Johnson, National Institutes of Mental Health, Novartis Pharmaceuticals Corp., Pfizer Inc., Pharmaceutical Research Institute, Ortho-McNeil Pharmaceutical, Robert Wood Johnson Pharmaceutical Research Institute, The Stanley Medical Research Institute, and UCB Pharma.
Many well-controlled trials in the past 4 years have evaluated new medications for treating bipolar disorder. It’s time to build a consensus on how this data may apply to clinical practice.
This year, our group will re-examine the Texas Medication Algorithm Project (TMAP) treatment algorithms for bipolar I disorder.
What makes TMAP unique? It is the first project to evaluate treatment algorithm use in community mental health settings for patients with a history of mania (see Box).1-5 Severely, persistently ill outpatients such as these are seldom included in research but are frequently seen in clinical practice.
To preview for psychiatrists the changes expected in 2004, this article describes the goals of TMAP and the controlled study on which the medication algorithms are based. We review the medication algorithms of 2000 as a starting point and present the evidence that is changing clinical practice.
Guiding principles of TMAP
A treatment algorithm is no substitute for clinical judgment; rather, medication guidelines and algorithms are guideposts to help the clinician and patient collaboratively develop the most effective medication strategy with the fewest side effects.
The Texas Medication Algorithm Project (TMAP)1-3 is a public and academic collaboration started in 1996 to develop evidence- and consensus-based medication treatment algorithms for schizophrenia, major depressive disorder, and bipolar disorder.
TMAP’s goal is to establish “best practices” to encourage uniformity of care, achieve the best possible patient outcomes, and use mental health care dollars most efficiently. The project includes four phases, in which the treatment algorithms were developed, compared with treatment-as-usual, put into practice, and will undergo periodic updates.4 The next update begins this year.
The comparison of algorithms for treating bipolar mania/hypomania and depression included 409 patients (mean age 38 to 40) with bipolar I disorder or schizoaffective disorder, bipolar type. These patients were severely and persistently mentally ill, from a diverse ethnic population, and significantly impaired in functioning.
During 12 months of treatment, psychiatric symptoms diminished more rapidly in patients in the algorithm group—as measured by the Brief Psychiatric Rating Scale (BPRS-24)—compared with those receiving usual treatment. After the first 3 months, the usual-treatment patients also showed diminished symptoms. At study’s end, symptom severity between the groups was not significantly different; both groups showed improvement.
Manic and psychotic symptoms—measured by Clinician-Administered Rating Scale subscales (CARS-M)5—improved significantly more in the algorithm group in the first 3 months, and this gap between the two groups was sustained for 12 months. Depressive symptoms declined, but no overall differences were noted between the two groups. Side effect rates and functioning were also similar.
TMAP’s treatment manual (see Related resources) describes clinicians’ preferred tactics and decision points, which we summarize here. The guidelines are an ongoing effort to apply evidence-based medicine to everyday practice and are meant to be adapted to patient needs.
Treatment goals that guided TMAP algorithm development are:
- symptomatic remission
- full return of psychosocial functioning
- prevention of relapse and recurrence.
Suggestions came from controlled clinical trials, open trials, retrospective data analyses, expert clinical consensus, and input from consumers.
Treatment selection. Initial algorithm stages recommend simple treatments (in terms of safety, tolerability, and side effects), whereas later stages recommend more-complicated regimens. A patient’s symptoms, comorbid conditions, and treatment history guide treatment selection. Patients may enter an algorithm at any stage, depending on their clinical presentation and medication history.
The clinician may consider patient preference when deciding among equivalent medications. The algorithm strongly encourages patients and families to participate, such as by keeping daily mood charts and completing symptom and side-effect checklists. When clinicians face a choice among medication brands, generics, or forms (such as immediate- versus slow-release), agents with greater tolerability are preferred.
Patient management. When patients enter the algorithm, clinic visits are frequent (such as every 2 weeks). Follow-up appointments address medication adherence, dosage adjustments, and side effects or adverse reactions.
If a patient’s symptoms show no change after two treatment stages, re-evaluate the diagnosis and consider mitigating factors such as substance abuse. Patients who complete acute treatment should receive continuation treatment.
Documentation. Clinicians are advised to document decision points and the rationale for treatment choices made outside the algorithm package.
Treating mania or hypomania
After clinical evaluation confirms the diagnosis of bipolar illness,4 the TMAP mania/hypomania algorithm (Algorithm 1) splits into three treatment pathways:
- euphoric mania/hypomania
- mixed or dysphoric mania/hypomania
- psychotic mania.
These pathways recognize the need for differing approaches to initial monotherapy and later two-drug combinations. If a patient develops persistent or severe depressive symptoms, the bipolar algorithm for a major depressive episode (Algorithm 2) is used during depressive periods with the primary mania algorithm.
Treatment recommendations. The key to using mood stabilizers is to achieve the optimum response—assuming good tolerability—before switching to another agent. Adjust medication dosages one at a time to allow adequate response and assessment.
When switching medications, use an overlap-and-taper strategy, assuming there is no medical necessity to stop a drug abruptly. Add the new medication, then gradually taper the one that is being discontinued. Monitor serum levels.
Discontinue antidepressants when appropriate in patients with hypomania/mania or rapid cycling, and continually evaluate suicide and homicide potential of patients in mixed or depressive states.
Stage 1: Monotherapy. First medication choices are lithium, divalproex, or olanzapine. For mixed or dysphoric mania, the algorithm recommends divalproex (preferred over valproic acid because of tolerability and side effects) or olanzapine.6 Data suggest dysphoric manic patients are less likely to respond to lithium.7 A Consensus Panel minority expressed concern about using olanzapine as first-line monotherapy for acute mania because of limited data on the drug’s long-term safety. Patients with partial response or residual symptoms may move to stage 2 or switch to other medication options within stage 1.
Patients with psychotic mania move directly to stage 4 for a broader range of combination therapy.
Stage 2: Combination therapy. Combination therapy has become the standard of care in treating most patients with bipolar disorder. The algorithm recommends using two agents:
- lithium or an anticonvulsant plus another anticonvulsant ([Li or AC]+AC)
- or lithium or an anticonvulsant plus an atypical antipsychotic ([Li or AC]+AAP).8
Recommended agents include lithium, divalproex, oxcarbazepine, olanzapine, or risperidone. The experts recommended oxcarbazepine as first choice because it is better tolerated and interacts with fewer drugs than carbamazepine and does not require serum level monitoring.9
A Consensus Panel minority expressed concern that few studies had examined using oxcarbazepine in bipolar disorder. Carbamazepine was also considered an option.
Stages 3 and 4: Other two-drug combinations. Other two-drug combinations are tried at these stages, drawing from the same pool of medication classes described in stage 2.
Stage 4 broadens the choice of atypical antipsychotic by adding quetiapine10 and ziprasidone11 to the recommended stage-2 agents olanzapine and risperidone. When the 2000 algorithm was developed, limited data were available on using some newer atypicals in patients with bipolar mania. Based on recent, high-quality studies of mono- and combination therapy—including quetiapine,10 ziprasidone,11 risperidone,12,13 and aripiprazole14 —the 2004 algorithm update panel will likely recommend using atypicals earlier, including at stage 1.
Algorithm 1 Treating mania/hypomania in patients with bipolar I disorder
Stage 5: Triple-drug combination. Lithium, an anticonvulsant (divalproex or oxcarbazepine), and an atypical antipsychotic (olanzapine, risperidone, quetiapine, or ziprasidone) is a recommended triple-drug combination. In the 2004 update, the choices will likely expand to include all the newer atypicals and will list carbamazepine as an option.
Stage 6: ECT or clozapine. For patients with inadequate response to triple-drug combinations, the algorithm recommends adding electroconvulsive therapy (ECT) or clozapine.
ECT15 is recommended three times a week until the patient achieves remission of manic symptoms or fails to achieve a sustained response over three to six treatment cycles. Treatment resistance is declared if no response is seen after 6 to 10 treatment cycles.
Clozapine’s16 recommendation at this stage is consistent with its use in patients who fail to respond to other atypical antipsychotics. Blood monitoring for agranulocytosis is required; other adverse effects include an increased risk of seizures, myocarditis, and orthostatic hypotension.
Stage 7: Other. Treatment options such as topiramate17,18 and lamotrigine19 are recommended at this stage. These recommendations also will be reviewed and likely revised.
Treating bipolar depression
The TMAP algorithm for treating depression in bipolar disorder (Algorithm 2) assumes that anti-depressants will be used only with optimum mood-stabilizer levels because of the risk of inducing manic symptoms. The bipolar depression algorithm is always used with the primary algorithm for mania/hypomania.
The patient’s clinical presentation guides medication selection. For the “pure” bipolar I patient with a major depressive episode but little mood lability or hypomania, starting an antide-pressant is a clear decision. On the other hand, patients with predominant depressive symptoms plus dysphoric hypomania, mood lability, and irritability need a balance of mood-stabilizing drugs and antidepressants.
Stage 1: Mood stabilizer. Initiate a mood stabilizer and optimize the dosage. Choices are the same mood stabilizers listed in the hypomania/mania treatment algorithm.
Stage 2: Antidepressant. Adding an antidepressant implies that depressive symptoms are severe enough to change treatment. Antidepressant options include a selective serotonin reuptake inhibitor (SSRI), sustained-release bupropion, or lamotrigine.20
Using SSRIs is supported by widespread clinical experience and offers the convenience of once-daily dosing. Recommended SSRIs include fluoxetine, paroxetine, fluvoxamine, sertraline, and citalopram. The SSRI escitalopram was introduced after the 2000 algorithms were published; evidence for using it and other newer medications will be reviewed for the 2004 update.
The recommendation for sustained-release bupropion is consistent with the algorithm principle to use medications in the most well-tolerated form when accessible and available.
With lamotrigine, review with patients the risk of serious rash. To minimize rash risk, start lamotrigine slowly and follow the recommended titration schedule.
Stage 3: Multiple choices. At this stage, no definitive studies, safety data, or tolerability issues are available to rank the medication choices. The algorithm suggests:
- adding lithium21 or a second antidepressant
- or switching to an alternate antidepressant such as venlafaxine or nefazodone.
If a patient moves to stage 3 because of side effects with one antidepressant class, a different class—preferably with a contrasting side-effect profile—is recommended.
Algorithm 2 Treating depression in bipolar I disorder*
Stage 4: Two antidepressants. To enhance clinical response, the algorithm recommends combining two antidepressants, preferably from different classes. Monitor patients closely for side effects.
Stage 5. Antipsychotic or MAOI. At this stage, the algorithm recommends adding an atypical antipsychotic22 or switching to a monoamine oxidase inhibitor (MAOI).
Early evidence supported the efficacy of MAOIs in bipolar depression. However, the panel ranked MAOIs lower in the algorithm because they are associated with more bothersome side effects than SSRIs and other antidepressants. When using MAOIs, provide patients with dietary restriction guidelines.
Stage 6. Other therapies. Therapies such as ECT or “other” interventions are recommended at this stage. ECT has proven efficacy in bipolar depression and is appropriate for patients with limited medication response. The panel gave ECT a low ranking because of limited availability, lack of patient acceptance, and newer options.
Medication options include experimental treatments with limited evidence, such as inositol, dopamine agonists, stimulants, thyroid supplementation, conventional antipsychotics, and tri-cyclic antidepressants.
Acute to maintenance treatment
Adjunctive treatments for agitation, insomnia, GI upset, sedation, headache, and tremor are recommended in the physician manual supporting the TMAP guidelines (see Related resources). The manual also suggests ways to manage medication side effects and modify the algorithms for inpatients.
Patient and family psychoeducation plays an important role in helping the patient:
- identify prodromal bipolar symptoms
- understand the need to take medications as prescribed.
Continuation treatment. After mania or hypomania remits, continue medication(s) at the effective acute-phase dosages for at least 3 months. Use follow-up visits to enhance patient adherence, detect early symptoms of relapse, and monitor for side effects.
During the late continuation phase, after a period of sustained stability, clinicians can try to simplify the medications. When discontinuing a medication, taper the dosage by no more than 25% per week. If symptoms recur, promptly return to acute-phase treatment. Consider restarting medications and titrating up to the dosage(s) that resulted in remission.
In a depressive episode, continue the antidepressant(s) for 1 to 3 months at the effective acutephase dosage(s). Follow up frequently, and educate patients to watch for symptom recurrence and to communicate with you to assess when medication changes are needed.
Maintenance treatment. Relatively few well-controlled studies on long-term management of bipolar patients were available for the 2000 algorithm update.23 In general, all patients need mood stabilizer(s) to prevent relapse, using the lowest dosage that maintains therapeutic efficacy. Based on new evidence for lamotrigine and atypical antipsychotics—including FDAapproval of olanzapine for bipolar maintenace therapy—we anticipate recommendations will be expanded and more delineated in the 2004 update.
Discontinuing antidepressants after 3 to 6 months of initial treatment is now recommended. However, a recent retrospective case series suggests that continuing antidepressants at least 1 year after initial successful therapy may protect against depressive relapse. During this study, continuing antidepressants more than 3 to 6 months did not appear to increase the risk of switching to mania.24
Should antidepressants be continued or discontinued after successful acute treatment of a bipolar I depressive episode? This is an active area of research and debate as to the most appropriate strategy. The 2004 algorithm update panel will consider recent evidence that supports continuing antidepressants after symptom remission.24
- Texas Medication Algorithm Project algorithms and physician manual. Texas Department of Mental Health and Mental Retardation. http://www.mhmr.state.tx.us/centraloffice/medicaldirector/TIMA.html
- American Psychiatric Association. Practice guidelines for the treatment of patients with bipolar disorder. Am J Psychiatry 2002; 159(4):suppl 2.
- Depression and Bipolar Support Alliance. www.dbsalliance.org
Drug brand names
- Bupropion • Wellbutrin SR
- Carbamazepine • Tegretol
- Citalopram • Celexa
- Clozapine • Clozaril
- Divalproex sodium • Depakote
- Escitalopram • Lexapro
- Fluoxetine • Prozac
- Fluvoxamine • Luvox
- Inositol • Various
- Lamotrigine • Lamictal
- Nefazodone • Serzone
- Olanzapine • Zyprexa
- Oxcarbazepine • Trileptal
- Paroxetine • Paxil
- Quetiapine • Seroquel
- Risperidone • Risperdal
- Sertraline • Zoloft
- Topiramate • Topamax
- Tranylcypromine • Parnate
- Valproic acid • Depakene
- Venlafaxine • Effexor
- Ziprasidone • Geodon
Disclosure
Dr. Shivakumar reports no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
Dr. Suppes receives research support from or is a consultant to Abbott Laboratories, AstraZeneca Pharmaceuticals, Bristol-Myers Squibb, Eli Lilly and Co., GlaxoSmithKline, Janssen Pharmaceutica, Johnson & Johnson, National Institutes of Mental Health, Novartis Pharmaceuticals Corp., Pfizer Inc., Pharmaceutical Research Institute, Ortho-McNeil Pharmaceutical, Robert Wood Johnson Pharmaceutical Research Institute, The Stanley Medical Research Institute, and UCB Pharma.
1. Gilbert DA, Altshuler KZ, Rago WV, et al. Texas Medication Algorithm Project: definitions, rationale, and methods to develop medication algorithms. J Clin Psychiatry 1998;59:345-51.
2. Altshuler KZ, Rush AJ. Computerized Texas Medication Algorithm Project undergoes testing. Outcomes Accountability Alert 1999;4(1):10-11.
3. Rush AJ, Crismon ML, Kashner TM, et al. Texas Medication Algorithm Project, Phase 3 (TMAP-3): rationale and study design. J Clin Psychiatry 2003;64(4):357-69.
4. Altman E, Hedeker D, Janicak P, et al. The Clinician-Administered Rating Scale For Mania (CARS-M): development, reliability, and validity. Biol Psychiatry 1994;36:124-34.
5. Suppes T, Dennehy EB, Swann AC, et al. Report of the Texas consensus conference panel on medication treatment of bipolar disorder 2000. J Clin Psychiatry 2002;63:288-99.
6. Dennehy EB, Doyle K, Suppes T. The efficacy of olanzapine monotherapy for acute hypomania or mania in an outpatient setting. Int Clin Psychopharmacol 2003;18(3):143-5.
7. Dilsaver SC, Swann AC, Shoaib AM, et al. The manic syndrome: factors which may predict a patient’s response to lithium, carbamazepine and valproate. J Psych Neurosci 1993;18:61-6.
8. Tohen M, Chengappa KNR, Suppes T, et al. Efficacy of olanzapine in combination with valproate or lithium in the treatment of mania in patients partially nonresponsive to valproate or lithium monotherapy. Arch Gen Psychiatry 2002;59(1):62-9.
9. Emrich HM. Studies with oxcarbazepine (Trileptal) in acute mania. Int Clin Psychopharmacol 1990;190(5,suppl):83-8.
10. Vieta E, Parramon G, Padrell E, et al. Quetiapine in the treatment of rapid cycling bipolar disorder. Bipolar Disord 2002;4(5):335-40.
11. Keck PE, Versiani M, Potkin S, et al. Ziprasidone in the treatment of acute bipolar mania: a three week placebo-controlled, double-blinded randomized trial. Am J Psychiatry 2003;160(4):741-8.
12. Yatham LN, Grossman F, Augustyns I, et al. Mood stabilisers plus risperidone or placebo in the treatment of acute mania. International, double-blinded, randomised controlled trial. Br J Psychiatry 2003;182:141-7.
13. Sachs GS, Grossman F, Ghaemi SN, et al. Combination of a mood stabilizer with risperidone or haloperidol for treatment of acute mania: a double-blind, placebo-controlled comparison of efficacy and safety. Am J Psychiatry 2002;159(7):1146-54.
14. Keck PE, Jr, Marcus R, Tourkodimitris S, et al. Aripiprazole study group. A placebo-controlled, double-blind study of the efficacy and safety of aripiprazole in patients with acute bipolar mania. Am J Psychiatry 2003;160(9):1651-8.
15. Mukherjee S, Sackeim HA, Schnur DB. Electroconvulsive therapy of acute manic episode: a review of 50 years’ experience. Am J Psychiatry 1988;45:727-32.
16. Suppes T, Webb A, Paul B, et al. Clinical outcome in a randomized 1-year trail of clozapine versus treatment as usual for patients with treatment-resistant illness and a history of mania. Am J Psychiatry 1999;156(8):1164-9.
17. Guille C, Sachs G. Clinical outcome of adjunctive topiramate treatment in a sample of refractory bipolar patients with comorbid conditions. Prog Neuropsychopharmacol Biol Psychiatry 2002;26(6):1035-9.
18. Vieta E, Torrent C, Garcia-Ribas G, et al. Use of topiramate in treatment-resistant bipolar spectrum disorders. J Clin Psychopharmacol 2002;22(4):431-5.
19. Calabrese JR, Suppes T, Bowden CL, et al. A double blinded, placebo-controlled, prophylaxis study of lamotrigine in rapid-cycling bipolar disorder. J Clin Psychiatry 2000;61:841-50.
20. Calabrese JR, Bowden CL, Sachs GS, et al. A placebo-controlled 18-month trial of lamotrigine and lithium maintenance treatment in recently depressed patients with bipolar I disorder. J Clin Psychiatry 2003;64(9):1013-24.
21. Bauer M, Dopfmer S. Lithium augmentation in treatment-resistant depression: meta-analysis of placebo-controlled studies. J Clin Psychopharmacology 1999;19:427-34.
22. Shelton RC, Tollefson GD, Tohen M, et al. A novel augmentation strategy for treating resistant major depression. Am J Psychiatry 2001;158:131-4.
23. Baldessarini RJ, Tohen M, Tondo L. Maintenance treatment in bipolar disorder (comment). Arch Gen Psychiatry 2000;57:490-2.
24. Altshuler L, Suppes T, Black D, et al. Impact of antidepressant discontinuation after acute bipolar depression remission on rates of depressive relapse at 1-year follow-up. Am J Psychiatry 2003;160:1252-62.
1. Gilbert DA, Altshuler KZ, Rago WV, et al. Texas Medication Algorithm Project: definitions, rationale, and methods to develop medication algorithms. J Clin Psychiatry 1998;59:345-51.
2. Altshuler KZ, Rush AJ. Computerized Texas Medication Algorithm Project undergoes testing. Outcomes Accountability Alert 1999;4(1):10-11.
3. Rush AJ, Crismon ML, Kashner TM, et al. Texas Medication Algorithm Project, Phase 3 (TMAP-3): rationale and study design. J Clin Psychiatry 2003;64(4):357-69.
4. Altman E, Hedeker D, Janicak P, et al. The Clinician-Administered Rating Scale For Mania (CARS-M): development, reliability, and validity. Biol Psychiatry 1994;36:124-34.
5. Suppes T, Dennehy EB, Swann AC, et al. Report of the Texas consensus conference panel on medication treatment of bipolar disorder 2000. J Clin Psychiatry 2002;63:288-99.
6. Dennehy EB, Doyle K, Suppes T. The efficacy of olanzapine monotherapy for acute hypomania or mania in an outpatient setting. Int Clin Psychopharmacol 2003;18(3):143-5.
7. Dilsaver SC, Swann AC, Shoaib AM, et al. The manic syndrome: factors which may predict a patient’s response to lithium, carbamazepine and valproate. J Psych Neurosci 1993;18:61-6.
8. Tohen M, Chengappa KNR, Suppes T, et al. Efficacy of olanzapine in combination with valproate or lithium in the treatment of mania in patients partially nonresponsive to valproate or lithium monotherapy. Arch Gen Psychiatry 2002;59(1):62-9.
9. Emrich HM. Studies with oxcarbazepine (Trileptal) in acute mania. Int Clin Psychopharmacol 1990;190(5,suppl):83-8.
10. Vieta E, Parramon G, Padrell E, et al. Quetiapine in the treatment of rapid cycling bipolar disorder. Bipolar Disord 2002;4(5):335-40.
11. Keck PE, Versiani M, Potkin S, et al. Ziprasidone in the treatment of acute bipolar mania: a three week placebo-controlled, double-blinded randomized trial. Am J Psychiatry 2003;160(4):741-8.
12. Yatham LN, Grossman F, Augustyns I, et al. Mood stabilisers plus risperidone or placebo in the treatment of acute mania. International, double-blinded, randomised controlled trial. Br J Psychiatry 2003;182:141-7.
13. Sachs GS, Grossman F, Ghaemi SN, et al. Combination of a mood stabilizer with risperidone or haloperidol for treatment of acute mania: a double-blind, placebo-controlled comparison of efficacy and safety. Am J Psychiatry 2002;159(7):1146-54.
14. Keck PE, Jr, Marcus R, Tourkodimitris S, et al. Aripiprazole study group. A placebo-controlled, double-blind study of the efficacy and safety of aripiprazole in patients with acute bipolar mania. Am J Psychiatry 2003;160(9):1651-8.
15. Mukherjee S, Sackeim HA, Schnur DB. Electroconvulsive therapy of acute manic episode: a review of 50 years’ experience. Am J Psychiatry 1988;45:727-32.
16. Suppes T, Webb A, Paul B, et al. Clinical outcome in a randomized 1-year trail of clozapine versus treatment as usual for patients with treatment-resistant illness and a history of mania. Am J Psychiatry 1999;156(8):1164-9.
17. Guille C, Sachs G. Clinical outcome of adjunctive topiramate treatment in a sample of refractory bipolar patients with comorbid conditions. Prog Neuropsychopharmacol Biol Psychiatry 2002;26(6):1035-9.
18. Vieta E, Torrent C, Garcia-Ribas G, et al. Use of topiramate in treatment-resistant bipolar spectrum disorders. J Clin Psychopharmacol 2002;22(4):431-5.
19. Calabrese JR, Suppes T, Bowden CL, et al. A double blinded, placebo-controlled, prophylaxis study of lamotrigine in rapid-cycling bipolar disorder. J Clin Psychiatry 2000;61:841-50.
20. Calabrese JR, Bowden CL, Sachs GS, et al. A placebo-controlled 18-month trial of lamotrigine and lithium maintenance treatment in recently depressed patients with bipolar I disorder. J Clin Psychiatry 2003;64(9):1013-24.
21. Bauer M, Dopfmer S. Lithium augmentation in treatment-resistant depression: meta-analysis of placebo-controlled studies. J Clin Psychopharmacology 1999;19:427-34.
22. Shelton RC, Tollefson GD, Tohen M, et al. A novel augmentation strategy for treating resistant major depression. Am J Psychiatry 2001;158:131-4.
23. Baldessarini RJ, Tohen M, Tondo L. Maintenance treatment in bipolar disorder (comment). Arch Gen Psychiatry 2000;57:490-2.
24. Altshuler L, Suppes T, Black D, et al. Impact of antidepressant discontinuation after acute bipolar depression remission on rates of depressive relapse at 1-year follow-up. Am J Psychiatry 2003;160:1252-62.
TMP bipolar algorithms: Not ‘cookbook’ medicine
How do you feel about the state, insurance companies, or professional societies telling you how to practice medicine? Most of us would take strong exception to that idea, almost as if we had been asked, “How do you feel about the butcher of Baghdad?” One reason we became doctors—in addition to wanting to heal the sick—was that we do not like anyone telling us what to do.
Let me rephrase the question: “How do you feel about evidence-based guidelines that could help you make increasingly complex decisions about which medications to use under which circumstances?” At worst, most of us would respond, “Well, I don’t really need them, but I refer to them from time to time. And I certainly know a lot of practitioners who could benefit from them.”
Two ways to ask the same question, with a big difference in response. I resist anyone’s attempts to write a “cookbook” for my clinical practice, but I am interested in anything that helps me practice rationally.
This year, Trisha Suppes, MD, PhD, and the other the Texas Medication Algorithm Project (TMAP) collaborators will update their treatment algorithms to include evidence published since 2000. In this issue, Dr. Suppes and Geetha Shivakumar, MD, of the University of Texas/Southwestern Medical Center’s department of psychiatry preview potential updates in the TMAP bipolar mania and bipolar depression algorithms. They make it clear that algorithms can be valuable tools when carefully designed and implemented.
Despite my wariness about practice guidelines, I found this article quite palatable and—I must admit—useful. I hope you do, too.
How do you feel about the state, insurance companies, or professional societies telling you how to practice medicine? Most of us would take strong exception to that idea, almost as if we had been asked, “How do you feel about the butcher of Baghdad?” One reason we became doctors—in addition to wanting to heal the sick—was that we do not like anyone telling us what to do.
Let me rephrase the question: “How do you feel about evidence-based guidelines that could help you make increasingly complex decisions about which medications to use under which circumstances?” At worst, most of us would respond, “Well, I don’t really need them, but I refer to them from time to time. And I certainly know a lot of practitioners who could benefit from them.”
Two ways to ask the same question, with a big difference in response. I resist anyone’s attempts to write a “cookbook” for my clinical practice, but I am interested in anything that helps me practice rationally.
This year, Trisha Suppes, MD, PhD, and the other the Texas Medication Algorithm Project (TMAP) collaborators will update their treatment algorithms to include evidence published since 2000. In this issue, Dr. Suppes and Geetha Shivakumar, MD, of the University of Texas/Southwestern Medical Center’s department of psychiatry preview potential updates in the TMAP bipolar mania and bipolar depression algorithms. They make it clear that algorithms can be valuable tools when carefully designed and implemented.
Despite my wariness about practice guidelines, I found this article quite palatable and—I must admit—useful. I hope you do, too.
How do you feel about the state, insurance companies, or professional societies telling you how to practice medicine? Most of us would take strong exception to that idea, almost as if we had been asked, “How do you feel about the butcher of Baghdad?” One reason we became doctors—in addition to wanting to heal the sick—was that we do not like anyone telling us what to do.
Let me rephrase the question: “How do you feel about evidence-based guidelines that could help you make increasingly complex decisions about which medications to use under which circumstances?” At worst, most of us would respond, “Well, I don’t really need them, but I refer to them from time to time. And I certainly know a lot of practitioners who could benefit from them.”
Two ways to ask the same question, with a big difference in response. I resist anyone’s attempts to write a “cookbook” for my clinical practice, but I am interested in anything that helps me practice rationally.
This year, Trisha Suppes, MD, PhD, and the other the Texas Medication Algorithm Project (TMAP) collaborators will update their treatment algorithms to include evidence published since 2000. In this issue, Dr. Suppes and Geetha Shivakumar, MD, of the University of Texas/Southwestern Medical Center’s department of psychiatry preview potential updates in the TMAP bipolar mania and bipolar depression algorithms. They make it clear that algorithms can be valuable tools when carefully designed and implemented.
Despite my wariness about practice guidelines, I found this article quite palatable and—I must admit—useful. I hope you do, too.
Omega-3 fatty acids: Do ‘fish oils’ have a therapeutic role in psychiatry?
Fourteen clinical trials in the past 3 years have examined the potential of omega-3 fatty acids in treating psychiatric disorders. Preliminary findings in at least 700 patients suggest that:
- omega-3 fatty acids used as adjuncts or monotherapy appear well-tolerated and safe in psychiatric disorders
- efficacy data vary by disorder
- the two marine omega-3 fatty acids may differ in efficacy.
Although we cannot offer specific guidance for using omega-3 fatty acids at this time, we can update you on recent trials of these “fish oils” in depression, bipolar disorder, schizophrenia, and other psychiatric disorders.
Treating depression
Prevalence rates of major depression1,2 and suicidal ideation3 decrease in populations as fish consumption increases. Some studies4,5 have shown omega-3 fatty acid deficiency in erythrocyte membranes and serum of depressed patients. This putative deficiency has been hypothesized to lead to:
- alterations in membrane fluidity, which affect monoamine (particularly serotonin) neurotransmission6,7
- an imbalance between omega-6 and omega-3 fatty acids, which affects the inflammatory response system (Box).5-12
- Nemets et al. 13 Twenty patients with recurrent major depression taking maintenance antidepressants were randomly assigned to adjunctive ethyl-EPA, 2 grams/d, or placebo for 4 weeks. Patients given ethyl-EPA showed significantly greater improvement than the placebo group in depressive symptoms, as measured by the Hamilton Rating Scale for Depression (HRSD).13
- Peet and Horrobin. 14 Seventy depressed patients taking antidepressants were randomly assigned to adjunctive ethyl-EPA (1, 2, or 4 grams/d) or placebo for 12 weeks. Only the group taking ethyl-EPA, 1 gram/d, showed significantly greater improvement than the placebo group.
- Su et al. 15 Twenty-eight patients taking antidepressants for major depression were randomly assigned to adjunctive omega-3 fatty acids (4.4 grams/d of EPA plus 2.2 grams/d of DHA) or placebo. After 8 weeks, depressive symptoms improved significantly more in the adjunctive treatment group.
- Marangell et al. 16 Thirty-six patients with mild to moderate depression (defined as a score of 17 on the 28-item HRSD) were randomly assigned to monotherapy with DHA, 2 grams/d, or placebo. Response rates after 6 weeks were comparable (27.8% with DHA versus 23.5% with placebo).
Polyunsaturated fatty acids contain a hydrocarbon chain with two or more double bonds. They are divided into families based on the location of their first double bond relative to the methyl end carbon—the “omega” carbon. Polyunsaturated fatty acids of interest in psychiatry include:
- omega-6 fatty acids—arachidonic acid (AA) and linoleic acid (LA)
- omega-3 fatty acids—eicosapentaenoic acid (EPA), docosahexaenoic acid (DHA), and alpha-linolenic acid (ALA).
Omega-3 and omega-6 fatty acids are called “essential” because they must be obtained from dietary sources. EPA and DHA are derived largely from wild—not farm-raised—fish, including sea bass, mackerel, pike, sardines, salmon, trout, herring, and cod liver oil.8 ALA, a precursor to both EPA and DHA, is derived from plant sources such as flaxseed oil, canola oil, walnuts, and soybean oil.
Polyunsaturated fatty acids, particularly AA and DHA, are important components of the phospholipid bilayer of neuronal cell membranes.They increase the ability of phospholipids to move “fluidly” within the membrane and modulate neurotransmission6,7 and signal transduction pathways9,10 thought to be important in psychiatric disorders. They also are precursors for eicosanoid molecules (such as prostaglandins and leukotrienes) and cytokines. Thus, an imbalance favoring omega-6 fatty acids over omega-3 fatty acids may lead to overproduction of pro-inflammatory cytokines.11
Omega-3 fatty acids are thought to be beneficial in numerous inflammatory and cardiovascular diseases. The American Heart Association’s dietary guidelines include dietary sources of omega-3 fatty acids as part of a healthy diet.12 Unfortunately, typical Western culture diets disproportionately favor foods rich in cholesterol and omega-6 fatty acids instead.
Table 1
Controlled trials of omega-3 fatty acids in treating major depression
| Author, year of publication | Duration and dosages | Number of patients | Results |
|---|---|---|---|
| Adjunctive therapy | |||
| Nemets et al, 2002 13 | 4 weeks, 2 grams/d of ethyl-EPA in recurrent depression | 20 | Significantly greater reduction in mean HRSD scores in ethyl-EPA group(-12.4) compared with placebo group (-1.6) 6 of 10 patients in ethyl-EPA group achieved 50% reduction in HRSD scores, compared with 1 in 10 patients in placebo group |
| Peet and Horrobin, 2002 14 | 12 weeks, 1, 2, or 4 grams/d of ethyl-EPA | 70 | Patients receiving 1 gram/d of ethyl-EPA showed significantly greater reduction in:
|
| Su et al, 2003 15 | 8 weeks, 4.4 grams/d of EPA and 2.2 grams/d of DHA | 28 | Treatment group showed significantly greater reduction in HRSD scores from baseline at weeks 4, 6, and 8 than placebo group |
| Monotherapy | |||
| Marangell et al, 2003 16 | 6 weeks, 2 grams/d of DHA | 36 | Little difference between response rates in DHA group (27.8%) and placebo group (23.5%) |
| BDI: Beck Depression Inventory | |||
| DHA: docosahexaenoic acid | |||
| EPA: eicosapentaenoic acid | |||
| HRSD: Hamilton Rating Scale for Depression | |||
| MADRS: Montgomery-Åsberg Depression Rating Scale | |||
Analysis. For patients with unipolar depression who were treated with omega-3 fatty acids:
- the most promisingresults have been seen with adjunctive EPA
- safety and tolerability have been good across studies.
No positive monotherapy studies have been published. Studies are needed to confirm EPA’s efficacy in unipolar depression and to determine the most effective dosage.
Treating bipolar disorder
EPA and DHA have been studied in bipolar disorder (Table 2) because their actions in modulating signal transduction pathways resemble those of lithium and valproate.10,17 Biochemical studies also have shown decreased AA and DHA in erythrocyte membranes of manic patients compared with controls.18
- Stoll et al. 19 Thirty patients receiving usual treatment for bipolar disorder were randomly assigned to adjunctive omega-3 fatty acids (6.2 grams/d of EPA plus 3.4 grams/d of DHA) or placebo for 4 months. Results were promising; patients receiving the omega-3 fatty acids remained in remission significantly longer than the placebo group.
- Keck et al. 20,21 On the other hand, two more-recent studies were disappointing. Both were 4-month, randomized, controlled trials in which patients received adjunctive EPA, 6 grams/d, or placebo. One study enrolled 59 patients with acute bipolar depression;20 the other enrolled 62 patients with rapid-cycling bipolar disorder.21 EPA was well-tolerated, but both studies found little difference in effectiveness between EPA and placebo.
Table 2
Controlled trials of adjunctive omega-3 fatty acids in treating bipolar disorder
| Author, year of publication | Duration and dosages | Number of patients | Results |
|---|---|---|---|
| Stoll et al, 1999 19 | 4 months, maintenance therapy (6.2 grams/d of EPA and 3.4 grams/d of DHA) in patients with bipolar I or II disorder | 30 | Significantly longer remission in omega-3 fatty acid group compared with placebo group |
| Keck et al, 2003 20 | 4 months, 6 grams/d of EPA in patients with acute bipolar depression | 59 | No significant difference in mean change from baseline to endpoint between EPA and placebo groups |
| Keck et al, 2003 21 | 4 months, 6 grams/d of EPA in patients with rapid-cycling bipolar disorder | 62 | Little difference in mean change from baseline to endpoint between EPA and placebo groups |
| DHA: docosahexaenoic acid | |||
| EPA: eicosapentaenoic acid | |||
Analysis. Further studies are needed to determine omega-3 fatty acids’ usefulness in treating bipolar illness.
Treating schizophrenia
Essential fatty acid deficiency and resulting lipid membrane abnormalities have been hypothesized to play a role in schizophrenia onset.22 Moreover, epidemiologic data suggest an association between high fish consumption and positive outcomes in patients with schizophrenia.23
Open-label trials, adjunctive therapy
- Mellor et al. 24 Twenty patients receiving antipsychotics for schizophrenia were treated for 6 weeks with 10 grams/d of a fish oil formulation containing 1.7 grams of EPA and 1.1 grams of DHA (Table 3). Psychotic symptoms improved significantly and were correlated with increased omega-3 fatty acid levels in erythrocyte membranes. Tardive dyskinesia also improved significantly, as measured by Abnormal Involuntary Movement Scale (AIMS) scores.
- Arvindakshan et al. 25 Thirty-three patients receiving antipsychotics for schizophrenia were given omega-3 fatty acids (360 mg/d of EPA and 240 mg/d of DHA) plus antioxidants (800 IU vitamin E and 1,000 IU vitamin C) for 4 months. Symptom and quality-of-life measures improved significantly, and clinical improvement was retained after 4 months of supplement washout.
Table 3
Clinical trials of omega-3 fatty acids in treating schizophrenia
| Authors, year of publication | Duration and dosages | Number of patients | Results |
|---|---|---|---|
| Open-label trials, adjunctive therapy | |||
| Mellor et al, 1995 24 | 6 weeks, 10 grams/d of fish oil (1.7 grams EPA and 1.1 grams DHA) | 20 | Significant improvement on PANSS and AIMS scores from baseline to endpoint |
| Arvindakshan et al, 2003 25 | 4 months, 360 mg/d of EPA and 240 mg/d of DHA, plus antioxidants (1,000 IU of vitamin C and 800 IU of vitamin E) | 33 | Significant improvements on total BPRS, PANSS, and Henrich’s Quality of Life Scale scores; improvements sustained after 4 months of supplementation washout |
| Controlled trials, adjunctive therapy | |||
| Peet et al, 2001 26 | 3 months, 2 grams/d of EPA or DHA | 45 | Greater improvement in total PANSS scores with EPA compared with DHA and placebo; EPA more effective than DHA in treating positive symptoms |
| Fenton et al, 2001 27 | 16 weeks, 3 grams/d of ethyl-EPA in patients with schizophrenia or schizoaffective disorder | 87 | No difference between ethyl-EPA and placebo groups in positive or negative symptoms, cognition, mood, or EPS |
| Peet et al, 2002 28 | 12 weeks, 1, 2, or 4 grams/d of ethyl-EPA with typical and atypical antipsychotics, including clozapine | 115 | Significantly greater improvement in mean total PANSS scores in clozapine-treated patients taking ethyl-EPA, 2 grams/d, compared with placebo; no difference between ethyl-EPAand placebo in patients taking typical or atypical antipsychotics |
| Emsley et al, 2002 29 | 12 weeks, 3 grams/d of ethyl-EPA | 40 | Significantly greater reduction in total PANSS and EPS Rating Scale dyskinesia scores in ethyl-EPA group compared with placebo |
| Controlled trial, monotherapy | |||
| Peet et al, 2001 26 | 3 months, 2 grams/d of EPA | 26 | EPA-treated patients had significantly lower PANSS scores at endpoint, compared with placebo; significantly more patients on placebo required antipsychotics (12 of 12) than did those on EPA (8 of 14) |
| AIMS: Abnormal Involuntary Movement Scale | |||
| BPRS: Brief Psychiatric Rating Scale | |||
| DHA: docosahexaenoic acid | |||
| EPA: eicosapentaenoic acid | |||
| EPS: extrapyramidal symptoms | |||
| PANSS: Positive and Negative Syndrome Scale | |||
Controlled trials, adjunctive therapy
- Peet et al. 26 In a 3-month study, 45 patients with schizophrenia were randomly assigned to adjunctive EPA or DHA (2 grams/d) or placebo. Those receiving EPA showed significantly greater improvement as measured by the Positive and Negative Syndrome Scale (PANSS), compared with DHA or placebo.
- Fenton et al. 27 In a 16-week study, 87 patients with schizophrenia or schizoaffective disorder were randomly assigned to adjunctive ethyl-EPA, 3 grams/d, or placebo. Little difference was noted in outcome measures of psychotic symptoms, mood, cognition, or extrapyramidal symptoms.
- Peet et al. 28 In a 12-week study. 115 patients with schizophrenia receiving typical antipsychotics, clozapine, or other atypical antipsychotics were randomly assigned to adjunctive ethyl-EPA (1, 2, or 4 grams/d) or placebo. Those taking clozapine improved significantly more with 2 grams/d of ethyl-EPA compared with patients receiving placebo. Little difference was noted between ethyl-EPA and placebo among patients taking typical or atypical antipsychotics.
- Emsley et al. 29 Forty patients with schizophrenia were randomly assigned to adjunctive ethyl-EPA, 3 grams/d, or placebo across 12 weeks. The ethyl-EPA group showed greater improvement in total PANSS scores and reduced dyskinesia, compared with placebo. Further analysis suggested, however, that the reduced dyskinesia scores at least partially accounted for the PANSS changes.
Controlled trial, monotherapy
- Peet et al. 26 Twenty-six patients with schizophrenia were randomly assigned to EPA, 2 grams/d, or placebo. After 3 months, those receiving EPA had significantly lower PANSS scores, and fewer (8 of 14) required antipsychotics than did those receiving placebo (12 of 12).
Analysis. Adjunctive ethyl-EPA (and perhaps combinations of EPA and DHA) may help patients with schizophrenia who are taking typical or atypical antipsychotics. EPA monotherapy also may be useful. Data are limited, however, and studies are needed before such use could be recommended.
Treating other disorders
Postpartum depression. The developing fetus and neonate require DHA from maternal stores for neurologic development. Maternal DHA depletion30 has been hypothesized to put mothers at risk for postpartum depression.31 An ecological study with data from 23 countries found that higher concentrations of DHA in maternal breast milk and greater seafood consumption predicted lower postpartum depression rates.32
In a randomized, controlled trial, giving DHA, 200 mg/d, to breastfeeding women during the first 4 months postpartum increased maternal plasma phospholipid content by 8%, compared with a 31% decrease in women given placebo.33
Data from randomized, controlled trials are needed to assess whether omega-3 fatty acid supplementation during pregnancy and the postpartum protects against postpartum depression.
Borderline personality disorder. In an 8-week controlled trial, Zanarini and Frankenburg34 randomly assigned 20 subjects with borderline personality disorder to monotherapy with ethyl-EPA, 1 gram/d, or placebo. Depressive symptoms improved and aggression decreased significantly in the ethyl-EPA group, suggesting the need for further research.
ADHD. Low DHA levels have been found in serum35 and erythrocytes36 of hyperactive children when compared with controls. Limited data in boys ages 6 to 12 also suggest an inverse relationship between plasma omega-3 fatty acids and behavior problems, as measured by the Connors’ Rating Scale.37
More research is needed into omega-3 fatty acids’ potential role in treating attention-deficit/hyperactivity disorder (ADHD), even though results of one controlled trial of adjunctive DHA in ADHD were disappointing.38
Dementia. Some large, prospective, epidemiologic studies39-41—but not others42—found an inverse relationship between dietary intake of omega-3 fatty acids and risk of cognitive decline or dementia.
Related resources
- USDA Nutrient Data Laboratory. http://www.nalusda.gov/fnic/foodcomp (accessed Dec. 1, 2003)
- Stoll AL. The omega-3 connection: the groundbreaking omega-3 antidepression diet and brain program. New York: Simon and Schuster, 2001.
Drug brand names
- Clozapine • Clozaril
Disclosure
The authors report no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
1. Hibbeln JR. Fish consumption and major depression. Lancet 1998;351(9110):1213.-
2. Tanskanen A, Hibbeln JR, Tuomilehto J, et al. Fish consumption and depressive symptoms in the general population in Finland. Psychiatr Serv 2001;52(4):529-31.
3. Tanskanen A, Hibelln JR, Hintikka J, et al. Fish consumption, depression, and suicidality in a general population. Arch Gen Psychiatry 2001;58(5):512-3.
4. Edwards R, Peet M, Shay J, Horrobin D. Omega-3 polyunsaturated fatty acid levels in the diet and in red blood cell membranes of depressed patients. J Affect Disord 1998;48(2-3):149-55.
5. Maes M, Christophe A, Delanghe J, et al. Lowered omega-3 polyunsaturated fatty acids in serum phospholipids and cholesterol esters of depressed patients. Psychiatry Res 1999;85(3):275-91.
6. Lundbaek JA, Andersen OS. Lysophospholipids modulate channel function by altering the mechanical properties of lipid bilayers. J Gen Physiol 1994;104(4):645-73.
7. Delion S, Chalon S, Guilloteau D, et al. Alpha-linolenic acid dietary deficiency alters age-related changes of dopaminergic and serotonergic neurotransmission in the rat frontal cortex. J Neurochem 1996;66(4):1582-91.
8. Passi S, Cataudella S, Di Marco P, et al. Fatty acid composition and antioxidant levels in muscle tissue of different Mediterranean marine species of fish and shellfish. J Agric Food Chem 2002;50(25):7314-22.
9. Hudson CJ, Young LT, Li PP, Warsh JJ. CNS signal transduction in the pathophysiology and pharmacology of affective disorders and schizophrenia. Synapse 1993;13(3):278-93.
10. Sperling RI, Benincaso AI, Knoell CT, et al. Dietary omega-3 polyunsaturated fatty acids inhibit phosphoinositide formation and chemotaxis in neutrophils. J Clin Invest 1993;91(2):651-60.
11. Endres S. Messengers and mediators: interactions among lipids, eicosanoids and cytokines. Am J Clin Nutr 1993;57(5 suppl):798S-800S.
12. Kris-Etherton PM, Harris WS, Appel LJ. Fish consumption, fish oil, omega-3 fatty acids, and cardiovascular disease. Arterioscler Thromb Vasc Biol 2003;23(2):e20-e30.
13. Nemets B, Stahl Z, Belmaker RH. Addition of omega-3 fatty acid to maintenance medication treatment for recurrent unipolar depressive disorder. Am J Psychiatry 2002;159(3):477-9.
14. Peet M, Horrobin DF. A dose-ranging study of the effects of ethyl-eicosapentaenoate in patients with ongoing depression despite apparently adequate treatment with standard drugs. Arch Gen Psychiatry 2002;59(10):913-9.
15. Su K-P, Huang S-Y, Chiu C-C, Shen WW. Omega-3 fatty acids in major depressive disorder: a preliminary double-blind, placebo-con-trolled trial. Eur Neuropsychopharmacol 2003;13(4):267-71.
16. Marangell LB, Martinez JM, Zboyan HA, et al. A double-blind, placebo-controlled study of the omega-3 fatty acid docosahexaenoic acid in the treatment of major depression. Am J Psychiatry 2003;160(5):996-8.
17. Stoll AL, Severus WE. Mood stabilizers: shared mechanisms of action at postsynaptic signal transduction and kindling processes. Harv Rev Psychiatry 1996;4(2):77-89.
18. Chiu CC, Huang SY, Su KP, et al. Polyunsaturated fatty acid deficit in patients with bipolar disorder. Eur Neuropsychopharmacol 2003;13(2):99-103.
19. Stoll AL, Severus WE, Freeman MP, et al. Omega-3 fatty acids in bipolar disorder: a preliminary double-blind, placebo-controlled trial. Arch Gen Psychiatry 1999;56(5):407-12.
20. Keck PE, Jr, McElroy SL, Freeman MP, et al. Randomized, placebo-controlled trial of eicosapentaenoic acid in bipolar depression. Bipolar Disord 2003;5(suppl 1):58.-
21. Keck PE, Jr, McElroy SL, Freeman MP, et al. Randomized, placebo-controlled trial of eicosapentaenoic acid in rapid cycling bipolar disorder. Bipolar Disord 2003;5(suppl 1):58.-
22. Horrobin DF. The membrane phospholipid hypothesis as a biochemical basis for the neurodevelopmental concept of schizophrenia. Schizophr Res 1998;30(3):193-208.
23. Christensen O, Christensen E. Fat consumption and schizophrenia. Acta Psychiatr Scand 1988;78(5):587-591
24. Mellor JE, Laugharne JD, Peet M. Schizophrenic symptoms and dietary intake of n-3 fatty acids. Schizophr Res 1995;18(1):85-6.
25. Arvindakshan M, Ghate M, Ranjekar PK, et al. Supplementation with a combination of omega-3 fatty acids and antioxidants (vitamins E and C) improves the outcome of schizophrenia. Schizophr Res 2003;62(3):195-204.
26. Peet M, Brind J, Ramchand CN, et al. Two double-blind placebo-controlled pilot studies of eicosapentaenoic acid in the treatment of schizophrenia. Schizophr Res 2001;49(3):243-51.
27. Fenton WS, Dickerson F, Boronow J, et al. A placebo-controlled trial of omega-3 fatty acid (ethyl eicosapentaenoic acid) supplementation for residual symptoms and cognitive impairment in schizophrenia. Am J Psychiatry 2001;158(12):2071-4.
28. Peet M, Horrobin DF. E-E Multicentre Study Group. A dose-ranging exploratory study of the effects of ethyl-eicosapentaenoate in patients with persistent schizophrenic symptoms. J Psychiatr Res 2002;36(1):7-18.
29. Emsley R, Myburgh C, Oosthuizen P, Van Rensburg SJ. Randomized, placebo-controlled study of ethyl-eicosapentaenoic acid as supplemental treatment in schizophrenia. Am J Psychiatry 2002;159(9):1596-8.
30. Al MD, van Houwelingen AC, Kester AD, et al. Maternal essential fatty acid patterns during normal pregnancy and their relationship to neonatal essential fatty acid status. Br J Nutr 1995;74(1):55-68.
31. Hibbeln JR, Salem N, Jr. Dietary polyunsaturated fatty acids and depression: when cholesterol does not satisfy. Am J Clin Nutr 1995;62(1):1-9.
32. Hibbeln JR. Seafood consumption, the DHA content of mothers’ milk and prevalence rates of postpartum depression: a cross-national, ecological analysis. J Affect Disord 2002;69(1-3):15-29.
33. Llorente AM, Jensen CL, Voigt RG, et al. Effect of maternal docosahexaenoic acid supplementation on postpartum depression and information processing. Am J Obstet Gynecol 2003;188(5):1348-53.
34. Zanarini MC, Frankenburg FR. Omega-3 fatty acid treatment of women with borderline personality disorder: a double-blind, placebo-controlled pilot study. Am J Psychiatry 2003;160(1):167-9.
35. Mitchell EA, Aman MG, Turbott SH, Manku M. Clinical characteristics and serum essential fatty acid levels in hyperactive children. Clin Pediatr 1987;26(8):406-11.
36. Stevens LJ, Zentall SS, Deck JL, et al. Essential fatty acid metabolism in boys with attention-deficit hyperactivity disorder. Am J Clin Nutr 1995;62(4):761-8.
37. Stevens LJ, Zentall SS, Abate ML, et al. Omega-3 fatty acids in boys with behavior, learning, and health problems. Physiol Behav 1996;59(4-5):915-20.
38. Voigt RG, Llorente AM, Jensen CL, et al. A randomized, double-blind, placebo-controlled trial of docosahexaenoic acid supplementation in children with attention-deficit/hyperactivity disorder. J Pediatr 2001;139(2):189-96.
39. Kalmijn S, Launer LJ, Ott A, et al. Dietary fat intake and the risk of incident dementia in the Rotterdam Study. Ann Neurol 1997;42(5):776-82.
40. Barberger-Gateau P, Letenneur L, Deschamps V, et al. Fish, meat, and risk of dementia: cohort study. BMJ 2002;325(7370):932-3.
41. Morris MC, Evans DA, Bienias JL, et al. Consumption of fish and n-3 fatty acids and risk of incident Alzheimer disease. Arch Neurol 2003;60(7):940-6.
42. Engelhart MJ, Geerlings MI, Ruitenberg A, et al. Diet and risk of dementia: does fat matter? The Rotterdam Study. Neurology 2002;59(12):1915-21.
Fourteen clinical trials in the past 3 years have examined the potential of omega-3 fatty acids in treating psychiatric disorders. Preliminary findings in at least 700 patients suggest that:
- omega-3 fatty acids used as adjuncts or monotherapy appear well-tolerated and safe in psychiatric disorders
- efficacy data vary by disorder
- the two marine omega-3 fatty acids may differ in efficacy.
Although we cannot offer specific guidance for using omega-3 fatty acids at this time, we can update you on recent trials of these “fish oils” in depression, bipolar disorder, schizophrenia, and other psychiatric disorders.
Treating depression
Prevalence rates of major depression1,2 and suicidal ideation3 decrease in populations as fish consumption increases. Some studies4,5 have shown omega-3 fatty acid deficiency in erythrocyte membranes and serum of depressed patients. This putative deficiency has been hypothesized to lead to:
- alterations in membrane fluidity, which affect monoamine (particularly serotonin) neurotransmission6,7
- an imbalance between omega-6 and omega-3 fatty acids, which affects the inflammatory response system (Box).5-12
- Nemets et al. 13 Twenty patients with recurrent major depression taking maintenance antidepressants were randomly assigned to adjunctive ethyl-EPA, 2 grams/d, or placebo for 4 weeks. Patients given ethyl-EPA showed significantly greater improvement than the placebo group in depressive symptoms, as measured by the Hamilton Rating Scale for Depression (HRSD).13
- Peet and Horrobin. 14 Seventy depressed patients taking antidepressants were randomly assigned to adjunctive ethyl-EPA (1, 2, or 4 grams/d) or placebo for 12 weeks. Only the group taking ethyl-EPA, 1 gram/d, showed significantly greater improvement than the placebo group.
- Su et al. 15 Twenty-eight patients taking antidepressants for major depression were randomly assigned to adjunctive omega-3 fatty acids (4.4 grams/d of EPA plus 2.2 grams/d of DHA) or placebo. After 8 weeks, depressive symptoms improved significantly more in the adjunctive treatment group.
- Marangell et al. 16 Thirty-six patients with mild to moderate depression (defined as a score of 17 on the 28-item HRSD) were randomly assigned to monotherapy with DHA, 2 grams/d, or placebo. Response rates after 6 weeks were comparable (27.8% with DHA versus 23.5% with placebo).
Polyunsaturated fatty acids contain a hydrocarbon chain with two or more double bonds. They are divided into families based on the location of their first double bond relative to the methyl end carbon—the “omega” carbon. Polyunsaturated fatty acids of interest in psychiatry include:
- omega-6 fatty acids—arachidonic acid (AA) and linoleic acid (LA)
- omega-3 fatty acids—eicosapentaenoic acid (EPA), docosahexaenoic acid (DHA), and alpha-linolenic acid (ALA).
Omega-3 and omega-6 fatty acids are called “essential” because they must be obtained from dietary sources. EPA and DHA are derived largely from wild—not farm-raised—fish, including sea bass, mackerel, pike, sardines, salmon, trout, herring, and cod liver oil.8 ALA, a precursor to both EPA and DHA, is derived from plant sources such as flaxseed oil, canola oil, walnuts, and soybean oil.
Polyunsaturated fatty acids, particularly AA and DHA, are important components of the phospholipid bilayer of neuronal cell membranes.They increase the ability of phospholipids to move “fluidly” within the membrane and modulate neurotransmission6,7 and signal transduction pathways9,10 thought to be important in psychiatric disorders. They also are precursors for eicosanoid molecules (such as prostaglandins and leukotrienes) and cytokines. Thus, an imbalance favoring omega-6 fatty acids over omega-3 fatty acids may lead to overproduction of pro-inflammatory cytokines.11
Omega-3 fatty acids are thought to be beneficial in numerous inflammatory and cardiovascular diseases. The American Heart Association’s dietary guidelines include dietary sources of omega-3 fatty acids as part of a healthy diet.12 Unfortunately, typical Western culture diets disproportionately favor foods rich in cholesterol and omega-6 fatty acids instead.
Table 1
Controlled trials of omega-3 fatty acids in treating major depression
| Author, year of publication | Duration and dosages | Number of patients | Results |
|---|---|---|---|
| Adjunctive therapy | |||
| Nemets et al, 2002 13 | 4 weeks, 2 grams/d of ethyl-EPA in recurrent depression | 20 | Significantly greater reduction in mean HRSD scores in ethyl-EPA group(-12.4) compared with placebo group (-1.6) 6 of 10 patients in ethyl-EPA group achieved 50% reduction in HRSD scores, compared with 1 in 10 patients in placebo group |
| Peet and Horrobin, 2002 14 | 12 weeks, 1, 2, or 4 grams/d of ethyl-EPA | 70 | Patients receiving 1 gram/d of ethyl-EPA showed significantly greater reduction in:
|
| Su et al, 2003 15 | 8 weeks, 4.4 grams/d of EPA and 2.2 grams/d of DHA | 28 | Treatment group showed significantly greater reduction in HRSD scores from baseline at weeks 4, 6, and 8 than placebo group |
| Monotherapy | |||
| Marangell et al, 2003 16 | 6 weeks, 2 grams/d of DHA | 36 | Little difference between response rates in DHA group (27.8%) and placebo group (23.5%) |
| BDI: Beck Depression Inventory | |||
| DHA: docosahexaenoic acid | |||
| EPA: eicosapentaenoic acid | |||
| HRSD: Hamilton Rating Scale for Depression | |||
| MADRS: Montgomery-Åsberg Depression Rating Scale | |||
Analysis. For patients with unipolar depression who were treated with omega-3 fatty acids:
- the most promisingresults have been seen with adjunctive EPA
- safety and tolerability have been good across studies.
No positive monotherapy studies have been published. Studies are needed to confirm EPA’s efficacy in unipolar depression and to determine the most effective dosage.
Treating bipolar disorder
EPA and DHA have been studied in bipolar disorder (Table 2) because their actions in modulating signal transduction pathways resemble those of lithium and valproate.10,17 Biochemical studies also have shown decreased AA and DHA in erythrocyte membranes of manic patients compared with controls.18
- Stoll et al. 19 Thirty patients receiving usual treatment for bipolar disorder were randomly assigned to adjunctive omega-3 fatty acids (6.2 grams/d of EPA plus 3.4 grams/d of DHA) or placebo for 4 months. Results were promising; patients receiving the omega-3 fatty acids remained in remission significantly longer than the placebo group.
- Keck et al. 20,21 On the other hand, two more-recent studies were disappointing. Both were 4-month, randomized, controlled trials in which patients received adjunctive EPA, 6 grams/d, or placebo. One study enrolled 59 patients with acute bipolar depression;20 the other enrolled 62 patients with rapid-cycling bipolar disorder.21 EPA was well-tolerated, but both studies found little difference in effectiveness between EPA and placebo.
Table 2
Controlled trials of adjunctive omega-3 fatty acids in treating bipolar disorder
| Author, year of publication | Duration and dosages | Number of patients | Results |
|---|---|---|---|
| Stoll et al, 1999 19 | 4 months, maintenance therapy (6.2 grams/d of EPA and 3.4 grams/d of DHA) in patients with bipolar I or II disorder | 30 | Significantly longer remission in omega-3 fatty acid group compared with placebo group |
| Keck et al, 2003 20 | 4 months, 6 grams/d of EPA in patients with acute bipolar depression | 59 | No significant difference in mean change from baseline to endpoint between EPA and placebo groups |
| Keck et al, 2003 21 | 4 months, 6 grams/d of EPA in patients with rapid-cycling bipolar disorder | 62 | Little difference in mean change from baseline to endpoint between EPA and placebo groups |
| DHA: docosahexaenoic acid | |||
| EPA: eicosapentaenoic acid | |||
Analysis. Further studies are needed to determine omega-3 fatty acids’ usefulness in treating bipolar illness.
Treating schizophrenia
Essential fatty acid deficiency and resulting lipid membrane abnormalities have been hypothesized to play a role in schizophrenia onset.22 Moreover, epidemiologic data suggest an association between high fish consumption and positive outcomes in patients with schizophrenia.23
Open-label trials, adjunctive therapy
- Mellor et al. 24 Twenty patients receiving antipsychotics for schizophrenia were treated for 6 weeks with 10 grams/d of a fish oil formulation containing 1.7 grams of EPA and 1.1 grams of DHA (Table 3). Psychotic symptoms improved significantly and were correlated with increased omega-3 fatty acid levels in erythrocyte membranes. Tardive dyskinesia also improved significantly, as measured by Abnormal Involuntary Movement Scale (AIMS) scores.
- Arvindakshan et al. 25 Thirty-three patients receiving antipsychotics for schizophrenia were given omega-3 fatty acids (360 mg/d of EPA and 240 mg/d of DHA) plus antioxidants (800 IU vitamin E and 1,000 IU vitamin C) for 4 months. Symptom and quality-of-life measures improved significantly, and clinical improvement was retained after 4 months of supplement washout.
Table 3
Clinical trials of omega-3 fatty acids in treating schizophrenia
| Authors, year of publication | Duration and dosages | Number of patients | Results |
|---|---|---|---|
| Open-label trials, adjunctive therapy | |||
| Mellor et al, 1995 24 | 6 weeks, 10 grams/d of fish oil (1.7 grams EPA and 1.1 grams DHA) | 20 | Significant improvement on PANSS and AIMS scores from baseline to endpoint |
| Arvindakshan et al, 2003 25 | 4 months, 360 mg/d of EPA and 240 mg/d of DHA, plus antioxidants (1,000 IU of vitamin C and 800 IU of vitamin E) | 33 | Significant improvements on total BPRS, PANSS, and Henrich’s Quality of Life Scale scores; improvements sustained after 4 months of supplementation washout |
| Controlled trials, adjunctive therapy | |||
| Peet et al, 2001 26 | 3 months, 2 grams/d of EPA or DHA | 45 | Greater improvement in total PANSS scores with EPA compared with DHA and placebo; EPA more effective than DHA in treating positive symptoms |
| Fenton et al, 2001 27 | 16 weeks, 3 grams/d of ethyl-EPA in patients with schizophrenia or schizoaffective disorder | 87 | No difference between ethyl-EPA and placebo groups in positive or negative symptoms, cognition, mood, or EPS |
| Peet et al, 2002 28 | 12 weeks, 1, 2, or 4 grams/d of ethyl-EPA with typical and atypical antipsychotics, including clozapine | 115 | Significantly greater improvement in mean total PANSS scores in clozapine-treated patients taking ethyl-EPA, 2 grams/d, compared with placebo; no difference between ethyl-EPAand placebo in patients taking typical or atypical antipsychotics |
| Emsley et al, 2002 29 | 12 weeks, 3 grams/d of ethyl-EPA | 40 | Significantly greater reduction in total PANSS and EPS Rating Scale dyskinesia scores in ethyl-EPA group compared with placebo |
| Controlled trial, monotherapy | |||
| Peet et al, 2001 26 | 3 months, 2 grams/d of EPA | 26 | EPA-treated patients had significantly lower PANSS scores at endpoint, compared with placebo; significantly more patients on placebo required antipsychotics (12 of 12) than did those on EPA (8 of 14) |
| AIMS: Abnormal Involuntary Movement Scale | |||
| BPRS: Brief Psychiatric Rating Scale | |||
| DHA: docosahexaenoic acid | |||
| EPA: eicosapentaenoic acid | |||
| EPS: extrapyramidal symptoms | |||
| PANSS: Positive and Negative Syndrome Scale | |||
Controlled trials, adjunctive therapy
- Peet et al. 26 In a 3-month study, 45 patients with schizophrenia were randomly assigned to adjunctive EPA or DHA (2 grams/d) or placebo. Those receiving EPA showed significantly greater improvement as measured by the Positive and Negative Syndrome Scale (PANSS), compared with DHA or placebo.
- Fenton et al. 27 In a 16-week study, 87 patients with schizophrenia or schizoaffective disorder were randomly assigned to adjunctive ethyl-EPA, 3 grams/d, or placebo. Little difference was noted in outcome measures of psychotic symptoms, mood, cognition, or extrapyramidal symptoms.
- Peet et al. 28 In a 12-week study. 115 patients with schizophrenia receiving typical antipsychotics, clozapine, or other atypical antipsychotics were randomly assigned to adjunctive ethyl-EPA (1, 2, or 4 grams/d) or placebo. Those taking clozapine improved significantly more with 2 grams/d of ethyl-EPA compared with patients receiving placebo. Little difference was noted between ethyl-EPA and placebo among patients taking typical or atypical antipsychotics.
- Emsley et al. 29 Forty patients with schizophrenia were randomly assigned to adjunctive ethyl-EPA, 3 grams/d, or placebo across 12 weeks. The ethyl-EPA group showed greater improvement in total PANSS scores and reduced dyskinesia, compared with placebo. Further analysis suggested, however, that the reduced dyskinesia scores at least partially accounted for the PANSS changes.
Controlled trial, monotherapy
- Peet et al. 26 Twenty-six patients with schizophrenia were randomly assigned to EPA, 2 grams/d, or placebo. After 3 months, those receiving EPA had significantly lower PANSS scores, and fewer (8 of 14) required antipsychotics than did those receiving placebo (12 of 12).
Analysis. Adjunctive ethyl-EPA (and perhaps combinations of EPA and DHA) may help patients with schizophrenia who are taking typical or atypical antipsychotics. EPA monotherapy also may be useful. Data are limited, however, and studies are needed before such use could be recommended.
Treating other disorders
Postpartum depression. The developing fetus and neonate require DHA from maternal stores for neurologic development. Maternal DHA depletion30 has been hypothesized to put mothers at risk for postpartum depression.31 An ecological study with data from 23 countries found that higher concentrations of DHA in maternal breast milk and greater seafood consumption predicted lower postpartum depression rates.32
In a randomized, controlled trial, giving DHA, 200 mg/d, to breastfeeding women during the first 4 months postpartum increased maternal plasma phospholipid content by 8%, compared with a 31% decrease in women given placebo.33
Data from randomized, controlled trials are needed to assess whether omega-3 fatty acid supplementation during pregnancy and the postpartum protects against postpartum depression.
Borderline personality disorder. In an 8-week controlled trial, Zanarini and Frankenburg34 randomly assigned 20 subjects with borderline personality disorder to monotherapy with ethyl-EPA, 1 gram/d, or placebo. Depressive symptoms improved and aggression decreased significantly in the ethyl-EPA group, suggesting the need for further research.
ADHD. Low DHA levels have been found in serum35 and erythrocytes36 of hyperactive children when compared with controls. Limited data in boys ages 6 to 12 also suggest an inverse relationship between plasma omega-3 fatty acids and behavior problems, as measured by the Connors’ Rating Scale.37
More research is needed into omega-3 fatty acids’ potential role in treating attention-deficit/hyperactivity disorder (ADHD), even though results of one controlled trial of adjunctive DHA in ADHD were disappointing.38
Dementia. Some large, prospective, epidemiologic studies39-41—but not others42—found an inverse relationship between dietary intake of omega-3 fatty acids and risk of cognitive decline or dementia.
Related resources
- USDA Nutrient Data Laboratory. http://www.nalusda.gov/fnic/foodcomp (accessed Dec. 1, 2003)
- Stoll AL. The omega-3 connection: the groundbreaking omega-3 antidepression diet and brain program. New York: Simon and Schuster, 2001.
Drug brand names
- Clozapine • Clozaril
Disclosure
The authors report no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
Fourteen clinical trials in the past 3 years have examined the potential of omega-3 fatty acids in treating psychiatric disorders. Preliminary findings in at least 700 patients suggest that:
- omega-3 fatty acids used as adjuncts or monotherapy appear well-tolerated and safe in psychiatric disorders
- efficacy data vary by disorder
- the two marine omega-3 fatty acids may differ in efficacy.
Although we cannot offer specific guidance for using omega-3 fatty acids at this time, we can update you on recent trials of these “fish oils” in depression, bipolar disorder, schizophrenia, and other psychiatric disorders.
Treating depression
Prevalence rates of major depression1,2 and suicidal ideation3 decrease in populations as fish consumption increases. Some studies4,5 have shown omega-3 fatty acid deficiency in erythrocyte membranes and serum of depressed patients. This putative deficiency has been hypothesized to lead to:
- alterations in membrane fluidity, which affect monoamine (particularly serotonin) neurotransmission6,7
- an imbalance between omega-6 and omega-3 fatty acids, which affects the inflammatory response system (Box).5-12
- Nemets et al. 13 Twenty patients with recurrent major depression taking maintenance antidepressants were randomly assigned to adjunctive ethyl-EPA, 2 grams/d, or placebo for 4 weeks. Patients given ethyl-EPA showed significantly greater improvement than the placebo group in depressive symptoms, as measured by the Hamilton Rating Scale for Depression (HRSD).13
- Peet and Horrobin. 14 Seventy depressed patients taking antidepressants were randomly assigned to adjunctive ethyl-EPA (1, 2, or 4 grams/d) or placebo for 12 weeks. Only the group taking ethyl-EPA, 1 gram/d, showed significantly greater improvement than the placebo group.
- Su et al. 15 Twenty-eight patients taking antidepressants for major depression were randomly assigned to adjunctive omega-3 fatty acids (4.4 grams/d of EPA plus 2.2 grams/d of DHA) or placebo. After 8 weeks, depressive symptoms improved significantly more in the adjunctive treatment group.
- Marangell et al. 16 Thirty-six patients with mild to moderate depression (defined as a score of 17 on the 28-item HRSD) were randomly assigned to monotherapy with DHA, 2 grams/d, or placebo. Response rates after 6 weeks were comparable (27.8% with DHA versus 23.5% with placebo).
Polyunsaturated fatty acids contain a hydrocarbon chain with two or more double bonds. They are divided into families based on the location of their first double bond relative to the methyl end carbon—the “omega” carbon. Polyunsaturated fatty acids of interest in psychiatry include:
- omega-6 fatty acids—arachidonic acid (AA) and linoleic acid (LA)
- omega-3 fatty acids—eicosapentaenoic acid (EPA), docosahexaenoic acid (DHA), and alpha-linolenic acid (ALA).
Omega-3 and omega-6 fatty acids are called “essential” because they must be obtained from dietary sources. EPA and DHA are derived largely from wild—not farm-raised—fish, including sea bass, mackerel, pike, sardines, salmon, trout, herring, and cod liver oil.8 ALA, a precursor to both EPA and DHA, is derived from plant sources such as flaxseed oil, canola oil, walnuts, and soybean oil.
Polyunsaturated fatty acids, particularly AA and DHA, are important components of the phospholipid bilayer of neuronal cell membranes.They increase the ability of phospholipids to move “fluidly” within the membrane and modulate neurotransmission6,7 and signal transduction pathways9,10 thought to be important in psychiatric disorders. They also are precursors for eicosanoid molecules (such as prostaglandins and leukotrienes) and cytokines. Thus, an imbalance favoring omega-6 fatty acids over omega-3 fatty acids may lead to overproduction of pro-inflammatory cytokines.11
Omega-3 fatty acids are thought to be beneficial in numerous inflammatory and cardiovascular diseases. The American Heart Association’s dietary guidelines include dietary sources of omega-3 fatty acids as part of a healthy diet.12 Unfortunately, typical Western culture diets disproportionately favor foods rich in cholesterol and omega-6 fatty acids instead.
Table 1
Controlled trials of omega-3 fatty acids in treating major depression
| Author, year of publication | Duration and dosages | Number of patients | Results |
|---|---|---|---|
| Adjunctive therapy | |||
| Nemets et al, 2002 13 | 4 weeks, 2 grams/d of ethyl-EPA in recurrent depression | 20 | Significantly greater reduction in mean HRSD scores in ethyl-EPA group(-12.4) compared with placebo group (-1.6) 6 of 10 patients in ethyl-EPA group achieved 50% reduction in HRSD scores, compared with 1 in 10 patients in placebo group |
| Peet and Horrobin, 2002 14 | 12 weeks, 1, 2, or 4 grams/d of ethyl-EPA | 70 | Patients receiving 1 gram/d of ethyl-EPA showed significantly greater reduction in:
|
| Su et al, 2003 15 | 8 weeks, 4.4 grams/d of EPA and 2.2 grams/d of DHA | 28 | Treatment group showed significantly greater reduction in HRSD scores from baseline at weeks 4, 6, and 8 than placebo group |
| Monotherapy | |||
| Marangell et al, 2003 16 | 6 weeks, 2 grams/d of DHA | 36 | Little difference between response rates in DHA group (27.8%) and placebo group (23.5%) |
| BDI: Beck Depression Inventory | |||
| DHA: docosahexaenoic acid | |||
| EPA: eicosapentaenoic acid | |||
| HRSD: Hamilton Rating Scale for Depression | |||
| MADRS: Montgomery-Åsberg Depression Rating Scale | |||
Analysis. For patients with unipolar depression who were treated with omega-3 fatty acids:
- the most promisingresults have been seen with adjunctive EPA
- safety and tolerability have been good across studies.
No positive monotherapy studies have been published. Studies are needed to confirm EPA’s efficacy in unipolar depression and to determine the most effective dosage.
Treating bipolar disorder
EPA and DHA have been studied in bipolar disorder (Table 2) because their actions in modulating signal transduction pathways resemble those of lithium and valproate.10,17 Biochemical studies also have shown decreased AA and DHA in erythrocyte membranes of manic patients compared with controls.18
- Stoll et al. 19 Thirty patients receiving usual treatment for bipolar disorder were randomly assigned to adjunctive omega-3 fatty acids (6.2 grams/d of EPA plus 3.4 grams/d of DHA) or placebo for 4 months. Results were promising; patients receiving the omega-3 fatty acids remained in remission significantly longer than the placebo group.
- Keck et al. 20,21 On the other hand, two more-recent studies were disappointing. Both were 4-month, randomized, controlled trials in which patients received adjunctive EPA, 6 grams/d, or placebo. One study enrolled 59 patients with acute bipolar depression;20 the other enrolled 62 patients with rapid-cycling bipolar disorder.21 EPA was well-tolerated, but both studies found little difference in effectiveness between EPA and placebo.
Table 2
Controlled trials of adjunctive omega-3 fatty acids in treating bipolar disorder
| Author, year of publication | Duration and dosages | Number of patients | Results |
|---|---|---|---|
| Stoll et al, 1999 19 | 4 months, maintenance therapy (6.2 grams/d of EPA and 3.4 grams/d of DHA) in patients with bipolar I or II disorder | 30 | Significantly longer remission in omega-3 fatty acid group compared with placebo group |
| Keck et al, 2003 20 | 4 months, 6 grams/d of EPA in patients with acute bipolar depression | 59 | No significant difference in mean change from baseline to endpoint between EPA and placebo groups |
| Keck et al, 2003 21 | 4 months, 6 grams/d of EPA in patients with rapid-cycling bipolar disorder | 62 | Little difference in mean change from baseline to endpoint between EPA and placebo groups |
| DHA: docosahexaenoic acid | |||
| EPA: eicosapentaenoic acid | |||
Analysis. Further studies are needed to determine omega-3 fatty acids’ usefulness in treating bipolar illness.
Treating schizophrenia
Essential fatty acid deficiency and resulting lipid membrane abnormalities have been hypothesized to play a role in schizophrenia onset.22 Moreover, epidemiologic data suggest an association between high fish consumption and positive outcomes in patients with schizophrenia.23
Open-label trials, adjunctive therapy
- Mellor et al. 24 Twenty patients receiving antipsychotics for schizophrenia were treated for 6 weeks with 10 grams/d of a fish oil formulation containing 1.7 grams of EPA and 1.1 grams of DHA (Table 3). Psychotic symptoms improved significantly and were correlated with increased omega-3 fatty acid levels in erythrocyte membranes. Tardive dyskinesia also improved significantly, as measured by Abnormal Involuntary Movement Scale (AIMS) scores.
- Arvindakshan et al. 25 Thirty-three patients receiving antipsychotics for schizophrenia were given omega-3 fatty acids (360 mg/d of EPA and 240 mg/d of DHA) plus antioxidants (800 IU vitamin E and 1,000 IU vitamin C) for 4 months. Symptom and quality-of-life measures improved significantly, and clinical improvement was retained after 4 months of supplement washout.
Table 3
Clinical trials of omega-3 fatty acids in treating schizophrenia
| Authors, year of publication | Duration and dosages | Number of patients | Results |
|---|---|---|---|
| Open-label trials, adjunctive therapy | |||
| Mellor et al, 1995 24 | 6 weeks, 10 grams/d of fish oil (1.7 grams EPA and 1.1 grams DHA) | 20 | Significant improvement on PANSS and AIMS scores from baseline to endpoint |
| Arvindakshan et al, 2003 25 | 4 months, 360 mg/d of EPA and 240 mg/d of DHA, plus antioxidants (1,000 IU of vitamin C and 800 IU of vitamin E) | 33 | Significant improvements on total BPRS, PANSS, and Henrich’s Quality of Life Scale scores; improvements sustained after 4 months of supplementation washout |
| Controlled trials, adjunctive therapy | |||
| Peet et al, 2001 26 | 3 months, 2 grams/d of EPA or DHA | 45 | Greater improvement in total PANSS scores with EPA compared with DHA and placebo; EPA more effective than DHA in treating positive symptoms |
| Fenton et al, 2001 27 | 16 weeks, 3 grams/d of ethyl-EPA in patients with schizophrenia or schizoaffective disorder | 87 | No difference between ethyl-EPA and placebo groups in positive or negative symptoms, cognition, mood, or EPS |
| Peet et al, 2002 28 | 12 weeks, 1, 2, or 4 grams/d of ethyl-EPA with typical and atypical antipsychotics, including clozapine | 115 | Significantly greater improvement in mean total PANSS scores in clozapine-treated patients taking ethyl-EPA, 2 grams/d, compared with placebo; no difference between ethyl-EPAand placebo in patients taking typical or atypical antipsychotics |
| Emsley et al, 2002 29 | 12 weeks, 3 grams/d of ethyl-EPA | 40 | Significantly greater reduction in total PANSS and EPS Rating Scale dyskinesia scores in ethyl-EPA group compared with placebo |
| Controlled trial, monotherapy | |||
| Peet et al, 2001 26 | 3 months, 2 grams/d of EPA | 26 | EPA-treated patients had significantly lower PANSS scores at endpoint, compared with placebo; significantly more patients on placebo required antipsychotics (12 of 12) than did those on EPA (8 of 14) |
| AIMS: Abnormal Involuntary Movement Scale | |||
| BPRS: Brief Psychiatric Rating Scale | |||
| DHA: docosahexaenoic acid | |||
| EPA: eicosapentaenoic acid | |||
| EPS: extrapyramidal symptoms | |||
| PANSS: Positive and Negative Syndrome Scale | |||
Controlled trials, adjunctive therapy
- Peet et al. 26 In a 3-month study, 45 patients with schizophrenia were randomly assigned to adjunctive EPA or DHA (2 grams/d) or placebo. Those receiving EPA showed significantly greater improvement as measured by the Positive and Negative Syndrome Scale (PANSS), compared with DHA or placebo.
- Fenton et al. 27 In a 16-week study, 87 patients with schizophrenia or schizoaffective disorder were randomly assigned to adjunctive ethyl-EPA, 3 grams/d, or placebo. Little difference was noted in outcome measures of psychotic symptoms, mood, cognition, or extrapyramidal symptoms.
- Peet et al. 28 In a 12-week study. 115 patients with schizophrenia receiving typical antipsychotics, clozapine, or other atypical antipsychotics were randomly assigned to adjunctive ethyl-EPA (1, 2, or 4 grams/d) or placebo. Those taking clozapine improved significantly more with 2 grams/d of ethyl-EPA compared with patients receiving placebo. Little difference was noted between ethyl-EPA and placebo among patients taking typical or atypical antipsychotics.
- Emsley et al. 29 Forty patients with schizophrenia were randomly assigned to adjunctive ethyl-EPA, 3 grams/d, or placebo across 12 weeks. The ethyl-EPA group showed greater improvement in total PANSS scores and reduced dyskinesia, compared with placebo. Further analysis suggested, however, that the reduced dyskinesia scores at least partially accounted for the PANSS changes.
Controlled trial, monotherapy
- Peet et al. 26 Twenty-six patients with schizophrenia were randomly assigned to EPA, 2 grams/d, or placebo. After 3 months, those receiving EPA had significantly lower PANSS scores, and fewer (8 of 14) required antipsychotics than did those receiving placebo (12 of 12).
Analysis. Adjunctive ethyl-EPA (and perhaps combinations of EPA and DHA) may help patients with schizophrenia who are taking typical or atypical antipsychotics. EPA monotherapy also may be useful. Data are limited, however, and studies are needed before such use could be recommended.
Treating other disorders
Postpartum depression. The developing fetus and neonate require DHA from maternal stores for neurologic development. Maternal DHA depletion30 has been hypothesized to put mothers at risk for postpartum depression.31 An ecological study with data from 23 countries found that higher concentrations of DHA in maternal breast milk and greater seafood consumption predicted lower postpartum depression rates.32
In a randomized, controlled trial, giving DHA, 200 mg/d, to breastfeeding women during the first 4 months postpartum increased maternal plasma phospholipid content by 8%, compared with a 31% decrease in women given placebo.33
Data from randomized, controlled trials are needed to assess whether omega-3 fatty acid supplementation during pregnancy and the postpartum protects against postpartum depression.
Borderline personality disorder. In an 8-week controlled trial, Zanarini and Frankenburg34 randomly assigned 20 subjects with borderline personality disorder to monotherapy with ethyl-EPA, 1 gram/d, or placebo. Depressive symptoms improved and aggression decreased significantly in the ethyl-EPA group, suggesting the need for further research.
ADHD. Low DHA levels have been found in serum35 and erythrocytes36 of hyperactive children when compared with controls. Limited data in boys ages 6 to 12 also suggest an inverse relationship between plasma omega-3 fatty acids and behavior problems, as measured by the Connors’ Rating Scale.37
More research is needed into omega-3 fatty acids’ potential role in treating attention-deficit/hyperactivity disorder (ADHD), even though results of one controlled trial of adjunctive DHA in ADHD were disappointing.38
Dementia. Some large, prospective, epidemiologic studies39-41—but not others42—found an inverse relationship between dietary intake of omega-3 fatty acids and risk of cognitive decline or dementia.
Related resources
- USDA Nutrient Data Laboratory. http://www.nalusda.gov/fnic/foodcomp (accessed Dec. 1, 2003)
- Stoll AL. The omega-3 connection: the groundbreaking omega-3 antidepression diet and brain program. New York: Simon and Schuster, 2001.
Drug brand names
- Clozapine • Clozaril
Disclosure
The authors report no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
1. Hibbeln JR. Fish consumption and major depression. Lancet 1998;351(9110):1213.-
2. Tanskanen A, Hibbeln JR, Tuomilehto J, et al. Fish consumption and depressive symptoms in the general population in Finland. Psychiatr Serv 2001;52(4):529-31.
3. Tanskanen A, Hibelln JR, Hintikka J, et al. Fish consumption, depression, and suicidality in a general population. Arch Gen Psychiatry 2001;58(5):512-3.
4. Edwards R, Peet M, Shay J, Horrobin D. Omega-3 polyunsaturated fatty acid levels in the diet and in red blood cell membranes of depressed patients. J Affect Disord 1998;48(2-3):149-55.
5. Maes M, Christophe A, Delanghe J, et al. Lowered omega-3 polyunsaturated fatty acids in serum phospholipids and cholesterol esters of depressed patients. Psychiatry Res 1999;85(3):275-91.
6. Lundbaek JA, Andersen OS. Lysophospholipids modulate channel function by altering the mechanical properties of lipid bilayers. J Gen Physiol 1994;104(4):645-73.
7. Delion S, Chalon S, Guilloteau D, et al. Alpha-linolenic acid dietary deficiency alters age-related changes of dopaminergic and serotonergic neurotransmission in the rat frontal cortex. J Neurochem 1996;66(4):1582-91.
8. Passi S, Cataudella S, Di Marco P, et al. Fatty acid composition and antioxidant levels in muscle tissue of different Mediterranean marine species of fish and shellfish. J Agric Food Chem 2002;50(25):7314-22.
9. Hudson CJ, Young LT, Li PP, Warsh JJ. CNS signal transduction in the pathophysiology and pharmacology of affective disorders and schizophrenia. Synapse 1993;13(3):278-93.
10. Sperling RI, Benincaso AI, Knoell CT, et al. Dietary omega-3 polyunsaturated fatty acids inhibit phosphoinositide formation and chemotaxis in neutrophils. J Clin Invest 1993;91(2):651-60.
11. Endres S. Messengers and mediators: interactions among lipids, eicosanoids and cytokines. Am J Clin Nutr 1993;57(5 suppl):798S-800S.
12. Kris-Etherton PM, Harris WS, Appel LJ. Fish consumption, fish oil, omega-3 fatty acids, and cardiovascular disease. Arterioscler Thromb Vasc Biol 2003;23(2):e20-e30.
13. Nemets B, Stahl Z, Belmaker RH. Addition of omega-3 fatty acid to maintenance medication treatment for recurrent unipolar depressive disorder. Am J Psychiatry 2002;159(3):477-9.
14. Peet M, Horrobin DF. A dose-ranging study of the effects of ethyl-eicosapentaenoate in patients with ongoing depression despite apparently adequate treatment with standard drugs. Arch Gen Psychiatry 2002;59(10):913-9.
15. Su K-P, Huang S-Y, Chiu C-C, Shen WW. Omega-3 fatty acids in major depressive disorder: a preliminary double-blind, placebo-con-trolled trial. Eur Neuropsychopharmacol 2003;13(4):267-71.
16. Marangell LB, Martinez JM, Zboyan HA, et al. A double-blind, placebo-controlled study of the omega-3 fatty acid docosahexaenoic acid in the treatment of major depression. Am J Psychiatry 2003;160(5):996-8.
17. Stoll AL, Severus WE. Mood stabilizers: shared mechanisms of action at postsynaptic signal transduction and kindling processes. Harv Rev Psychiatry 1996;4(2):77-89.
18. Chiu CC, Huang SY, Su KP, et al. Polyunsaturated fatty acid deficit in patients with bipolar disorder. Eur Neuropsychopharmacol 2003;13(2):99-103.
19. Stoll AL, Severus WE, Freeman MP, et al. Omega-3 fatty acids in bipolar disorder: a preliminary double-blind, placebo-controlled trial. Arch Gen Psychiatry 1999;56(5):407-12.
20. Keck PE, Jr, McElroy SL, Freeman MP, et al. Randomized, placebo-controlled trial of eicosapentaenoic acid in bipolar depression. Bipolar Disord 2003;5(suppl 1):58.-
21. Keck PE, Jr, McElroy SL, Freeman MP, et al. Randomized, placebo-controlled trial of eicosapentaenoic acid in rapid cycling bipolar disorder. Bipolar Disord 2003;5(suppl 1):58.-
22. Horrobin DF. The membrane phospholipid hypothesis as a biochemical basis for the neurodevelopmental concept of schizophrenia. Schizophr Res 1998;30(3):193-208.
23. Christensen O, Christensen E. Fat consumption and schizophrenia. Acta Psychiatr Scand 1988;78(5):587-591
24. Mellor JE, Laugharne JD, Peet M. Schizophrenic symptoms and dietary intake of n-3 fatty acids. Schizophr Res 1995;18(1):85-6.
25. Arvindakshan M, Ghate M, Ranjekar PK, et al. Supplementation with a combination of omega-3 fatty acids and antioxidants (vitamins E and C) improves the outcome of schizophrenia. Schizophr Res 2003;62(3):195-204.
26. Peet M, Brind J, Ramchand CN, et al. Two double-blind placebo-controlled pilot studies of eicosapentaenoic acid in the treatment of schizophrenia. Schizophr Res 2001;49(3):243-51.
27. Fenton WS, Dickerson F, Boronow J, et al. A placebo-controlled trial of omega-3 fatty acid (ethyl eicosapentaenoic acid) supplementation for residual symptoms and cognitive impairment in schizophrenia. Am J Psychiatry 2001;158(12):2071-4.
28. Peet M, Horrobin DF. E-E Multicentre Study Group. A dose-ranging exploratory study of the effects of ethyl-eicosapentaenoate in patients with persistent schizophrenic symptoms. J Psychiatr Res 2002;36(1):7-18.
29. Emsley R, Myburgh C, Oosthuizen P, Van Rensburg SJ. Randomized, placebo-controlled study of ethyl-eicosapentaenoic acid as supplemental treatment in schizophrenia. Am J Psychiatry 2002;159(9):1596-8.
30. Al MD, van Houwelingen AC, Kester AD, et al. Maternal essential fatty acid patterns during normal pregnancy and their relationship to neonatal essential fatty acid status. Br J Nutr 1995;74(1):55-68.
31. Hibbeln JR, Salem N, Jr. Dietary polyunsaturated fatty acids and depression: when cholesterol does not satisfy. Am J Clin Nutr 1995;62(1):1-9.
32. Hibbeln JR. Seafood consumption, the DHA content of mothers’ milk and prevalence rates of postpartum depression: a cross-national, ecological analysis. J Affect Disord 2002;69(1-3):15-29.
33. Llorente AM, Jensen CL, Voigt RG, et al. Effect of maternal docosahexaenoic acid supplementation on postpartum depression and information processing. Am J Obstet Gynecol 2003;188(5):1348-53.
34. Zanarini MC, Frankenburg FR. Omega-3 fatty acid treatment of women with borderline personality disorder: a double-blind, placebo-controlled pilot study. Am J Psychiatry 2003;160(1):167-9.
35. Mitchell EA, Aman MG, Turbott SH, Manku M. Clinical characteristics and serum essential fatty acid levels in hyperactive children. Clin Pediatr 1987;26(8):406-11.
36. Stevens LJ, Zentall SS, Deck JL, et al. Essential fatty acid metabolism in boys with attention-deficit hyperactivity disorder. Am J Clin Nutr 1995;62(4):761-8.
37. Stevens LJ, Zentall SS, Abate ML, et al. Omega-3 fatty acids in boys with behavior, learning, and health problems. Physiol Behav 1996;59(4-5):915-20.
38. Voigt RG, Llorente AM, Jensen CL, et al. A randomized, double-blind, placebo-controlled trial of docosahexaenoic acid supplementation in children with attention-deficit/hyperactivity disorder. J Pediatr 2001;139(2):189-96.
39. Kalmijn S, Launer LJ, Ott A, et al. Dietary fat intake and the risk of incident dementia in the Rotterdam Study. Ann Neurol 1997;42(5):776-82.
40. Barberger-Gateau P, Letenneur L, Deschamps V, et al. Fish, meat, and risk of dementia: cohort study. BMJ 2002;325(7370):932-3.
41. Morris MC, Evans DA, Bienias JL, et al. Consumption of fish and n-3 fatty acids and risk of incident Alzheimer disease. Arch Neurol 2003;60(7):940-6.
42. Engelhart MJ, Geerlings MI, Ruitenberg A, et al. Diet and risk of dementia: does fat matter? The Rotterdam Study. Neurology 2002;59(12):1915-21.
1. Hibbeln JR. Fish consumption and major depression. Lancet 1998;351(9110):1213.-
2. Tanskanen A, Hibbeln JR, Tuomilehto J, et al. Fish consumption and depressive symptoms in the general population in Finland. Psychiatr Serv 2001;52(4):529-31.
3. Tanskanen A, Hibelln JR, Hintikka J, et al. Fish consumption, depression, and suicidality in a general population. Arch Gen Psychiatry 2001;58(5):512-3.
4. Edwards R, Peet M, Shay J, Horrobin D. Omega-3 polyunsaturated fatty acid levels in the diet and in red blood cell membranes of depressed patients. J Affect Disord 1998;48(2-3):149-55.
5. Maes M, Christophe A, Delanghe J, et al. Lowered omega-3 polyunsaturated fatty acids in serum phospholipids and cholesterol esters of depressed patients. Psychiatry Res 1999;85(3):275-91.
6. Lundbaek JA, Andersen OS. Lysophospholipids modulate channel function by altering the mechanical properties of lipid bilayers. J Gen Physiol 1994;104(4):645-73.
7. Delion S, Chalon S, Guilloteau D, et al. Alpha-linolenic acid dietary deficiency alters age-related changes of dopaminergic and serotonergic neurotransmission in the rat frontal cortex. J Neurochem 1996;66(4):1582-91.
8. Passi S, Cataudella S, Di Marco P, et al. Fatty acid composition and antioxidant levels in muscle tissue of different Mediterranean marine species of fish and shellfish. J Agric Food Chem 2002;50(25):7314-22.
9. Hudson CJ, Young LT, Li PP, Warsh JJ. CNS signal transduction in the pathophysiology and pharmacology of affective disorders and schizophrenia. Synapse 1993;13(3):278-93.
10. Sperling RI, Benincaso AI, Knoell CT, et al. Dietary omega-3 polyunsaturated fatty acids inhibit phosphoinositide formation and chemotaxis in neutrophils. J Clin Invest 1993;91(2):651-60.
11. Endres S. Messengers and mediators: interactions among lipids, eicosanoids and cytokines. Am J Clin Nutr 1993;57(5 suppl):798S-800S.
12. Kris-Etherton PM, Harris WS, Appel LJ. Fish consumption, fish oil, omega-3 fatty acids, and cardiovascular disease. Arterioscler Thromb Vasc Biol 2003;23(2):e20-e30.
13. Nemets B, Stahl Z, Belmaker RH. Addition of omega-3 fatty acid to maintenance medication treatment for recurrent unipolar depressive disorder. Am J Psychiatry 2002;159(3):477-9.
14. Peet M, Horrobin DF. A dose-ranging study of the effects of ethyl-eicosapentaenoate in patients with ongoing depression despite apparently adequate treatment with standard drugs. Arch Gen Psychiatry 2002;59(10):913-9.
15. Su K-P, Huang S-Y, Chiu C-C, Shen WW. Omega-3 fatty acids in major depressive disorder: a preliminary double-blind, placebo-con-trolled trial. Eur Neuropsychopharmacol 2003;13(4):267-71.
16. Marangell LB, Martinez JM, Zboyan HA, et al. A double-blind, placebo-controlled study of the omega-3 fatty acid docosahexaenoic acid in the treatment of major depression. Am J Psychiatry 2003;160(5):996-8.
17. Stoll AL, Severus WE. Mood stabilizers: shared mechanisms of action at postsynaptic signal transduction and kindling processes. Harv Rev Psychiatry 1996;4(2):77-89.
18. Chiu CC, Huang SY, Su KP, et al. Polyunsaturated fatty acid deficit in patients with bipolar disorder. Eur Neuropsychopharmacol 2003;13(2):99-103.
19. Stoll AL, Severus WE, Freeman MP, et al. Omega-3 fatty acids in bipolar disorder: a preliminary double-blind, placebo-controlled trial. Arch Gen Psychiatry 1999;56(5):407-12.
20. Keck PE, Jr, McElroy SL, Freeman MP, et al. Randomized, placebo-controlled trial of eicosapentaenoic acid in bipolar depression. Bipolar Disord 2003;5(suppl 1):58.-
21. Keck PE, Jr, McElroy SL, Freeman MP, et al. Randomized, placebo-controlled trial of eicosapentaenoic acid in rapid cycling bipolar disorder. Bipolar Disord 2003;5(suppl 1):58.-
22. Horrobin DF. The membrane phospholipid hypothesis as a biochemical basis for the neurodevelopmental concept of schizophrenia. Schizophr Res 1998;30(3):193-208.
23. Christensen O, Christensen E. Fat consumption and schizophrenia. Acta Psychiatr Scand 1988;78(5):587-591
24. Mellor JE, Laugharne JD, Peet M. Schizophrenic symptoms and dietary intake of n-3 fatty acids. Schizophr Res 1995;18(1):85-6.
25. Arvindakshan M, Ghate M, Ranjekar PK, et al. Supplementation with a combination of omega-3 fatty acids and antioxidants (vitamins E and C) improves the outcome of schizophrenia. Schizophr Res 2003;62(3):195-204.
26. Peet M, Brind J, Ramchand CN, et al. Two double-blind placebo-controlled pilot studies of eicosapentaenoic acid in the treatment of schizophrenia. Schizophr Res 2001;49(3):243-51.
27. Fenton WS, Dickerson F, Boronow J, et al. A placebo-controlled trial of omega-3 fatty acid (ethyl eicosapentaenoic acid) supplementation for residual symptoms and cognitive impairment in schizophrenia. Am J Psychiatry 2001;158(12):2071-4.
28. Peet M, Horrobin DF. E-E Multicentre Study Group. A dose-ranging exploratory study of the effects of ethyl-eicosapentaenoate in patients with persistent schizophrenic symptoms. J Psychiatr Res 2002;36(1):7-18.
29. Emsley R, Myburgh C, Oosthuizen P, Van Rensburg SJ. Randomized, placebo-controlled study of ethyl-eicosapentaenoic acid as supplemental treatment in schizophrenia. Am J Psychiatry 2002;159(9):1596-8.
30. Al MD, van Houwelingen AC, Kester AD, et al. Maternal essential fatty acid patterns during normal pregnancy and their relationship to neonatal essential fatty acid status. Br J Nutr 1995;74(1):55-68.
31. Hibbeln JR, Salem N, Jr. Dietary polyunsaturated fatty acids and depression: when cholesterol does not satisfy. Am J Clin Nutr 1995;62(1):1-9.
32. Hibbeln JR. Seafood consumption, the DHA content of mothers’ milk and prevalence rates of postpartum depression: a cross-national, ecological analysis. J Affect Disord 2002;69(1-3):15-29.
33. Llorente AM, Jensen CL, Voigt RG, et al. Effect of maternal docosahexaenoic acid supplementation on postpartum depression and information processing. Am J Obstet Gynecol 2003;188(5):1348-53.
34. Zanarini MC, Frankenburg FR. Omega-3 fatty acid treatment of women with borderline personality disorder: a double-blind, placebo-controlled pilot study. Am J Psychiatry 2003;160(1):167-9.
35. Mitchell EA, Aman MG, Turbott SH, Manku M. Clinical characteristics and serum essential fatty acid levels in hyperactive children. Clin Pediatr 1987;26(8):406-11.
36. Stevens LJ, Zentall SS, Deck JL, et al. Essential fatty acid metabolism in boys with attention-deficit hyperactivity disorder. Am J Clin Nutr 1995;62(4):761-8.
37. Stevens LJ, Zentall SS, Abate ML, et al. Omega-3 fatty acids in boys with behavior, learning, and health problems. Physiol Behav 1996;59(4-5):915-20.
38. Voigt RG, Llorente AM, Jensen CL, et al. A randomized, double-blind, placebo-controlled trial of docosahexaenoic acid supplementation in children with attention-deficit/hyperactivity disorder. J Pediatr 2001;139(2):189-96.
39. Kalmijn S, Launer LJ, Ott A, et al. Dietary fat intake and the risk of incident dementia in the Rotterdam Study. Ann Neurol 1997;42(5):776-82.
40. Barberger-Gateau P, Letenneur L, Deschamps V, et al. Fish, meat, and risk of dementia: cohort study. BMJ 2002;325(7370):932-3.
41. Morris MC, Evans DA, Bienias JL, et al. Consumption of fish and n-3 fatty acids and risk of incident Alzheimer disease. Arch Neurol 2003;60(7):940-6.
42. Engelhart MJ, Geerlings MI, Ruitenberg A, et al. Diet and risk of dementia: does fat matter? The Rotterdam Study. Neurology 2002;59(12):1915-21.
Lithium in bipolar disorder
“Tips for using lithium in bipolar disorder” by West Magnon, MD (Pearls, CURRENT PSYCHIATRY, September 2003) was right on track.
I, too, have found that repeatedly measuring lithium levels is rarely warranted. The exception is when a manic patient is leaving the office and feels compelled to tell a joke. To me, this is suspiciously indicative of a bipolar illness and uncovers the need for a new lithium level determination in a previously diagnosed bipolar individual.
Leonard R. Friedman MD Revere, MA
“Tips for using lithium in bipolar disorder” by West Magnon, MD (Pearls, CURRENT PSYCHIATRY, September 2003) was right on track.
I, too, have found that repeatedly measuring lithium levels is rarely warranted. The exception is when a manic patient is leaving the office and feels compelled to tell a joke. To me, this is suspiciously indicative of a bipolar illness and uncovers the need for a new lithium level determination in a previously diagnosed bipolar individual.
Leonard R. Friedman MD Revere, MA
“Tips for using lithium in bipolar disorder” by West Magnon, MD (Pearls, CURRENT PSYCHIATRY, September 2003) was right on track.
I, too, have found that repeatedly measuring lithium levels is rarely warranted. The exception is when a manic patient is leaving the office and feels compelled to tell a joke. To me, this is suspiciously indicative of a bipolar illness and uncovers the need for a new lithium level determination in a previously diagnosed bipolar individual.
Leonard R. Friedman MD Revere, MA
Using lithium in bipolar disorder
“Tips for Using Lithium in Bipolar Disorder” by West B. Magnon, MD, (Pearls, Current Psychiatry, September 2003) had some “do not try this at home” aspects to it.
For example, when Dr. Magnon said “Lithium, 900 mg/d, works fine,” I believe he was referring to 900 mg/d of lithium carbonate, because 900 mg of lithium is equivalent to 4,791 mg of lithium carbonate, a generally toxic dose. Also, to suggest that one dosage fits all flies in the face of decades of research.
More important, to say that “Gauging lithium blood levels is a waste of time, assuming you have checked for kidney disease” is a dangerous statement. Numerous examples exist of lithium toxicity induced by drug interactions or dehydration in patients without kidney disease.
James W. Jefferson, MD
Distinguished senior scientist, Madison Institute of Medicine
Clinical professor of psychiatry,
University of Wisconsin Medical School
Dr. Magnon responds
Dr. Jefferson’s comments reflect the standard thinking about use of lithium carbonate.
My points are:
- I have not seen these so-called extensive studies about lithium toxicity
- When given in reasonable, effective dosages, the patient responds without toxic effects.
Lithium does have some unpleasant side effects, such as tremor, and weight gain is common in some patients, especially women. Continuous lab testing is just not necessary, however.
West B. Magnon, MD Bradenton, FL
“Tips for Using Lithium in Bipolar Disorder” by West B. Magnon, MD, (Pearls, Current Psychiatry, September 2003) had some “do not try this at home” aspects to it.
For example, when Dr. Magnon said “Lithium, 900 mg/d, works fine,” I believe he was referring to 900 mg/d of lithium carbonate, because 900 mg of lithium is equivalent to 4,791 mg of lithium carbonate, a generally toxic dose. Also, to suggest that one dosage fits all flies in the face of decades of research.
More important, to say that “Gauging lithium blood levels is a waste of time, assuming you have checked for kidney disease” is a dangerous statement. Numerous examples exist of lithium toxicity induced by drug interactions or dehydration in patients without kidney disease.
James W. Jefferson, MD
Distinguished senior scientist, Madison Institute of Medicine
Clinical professor of psychiatry,
University of Wisconsin Medical School
Dr. Magnon responds
Dr. Jefferson’s comments reflect the standard thinking about use of lithium carbonate.
My points are:
- I have not seen these so-called extensive studies about lithium toxicity
- When given in reasonable, effective dosages, the patient responds without toxic effects.
Lithium does have some unpleasant side effects, such as tremor, and weight gain is common in some patients, especially women. Continuous lab testing is just not necessary, however.
West B. Magnon, MD Bradenton, FL
“Tips for Using Lithium in Bipolar Disorder” by West B. Magnon, MD, (Pearls, Current Psychiatry, September 2003) had some “do not try this at home” aspects to it.
For example, when Dr. Magnon said “Lithium, 900 mg/d, works fine,” I believe he was referring to 900 mg/d of lithium carbonate, because 900 mg of lithium is equivalent to 4,791 mg of lithium carbonate, a generally toxic dose. Also, to suggest that one dosage fits all flies in the face of decades of research.
More important, to say that “Gauging lithium blood levels is a waste of time, assuming you have checked for kidney disease” is a dangerous statement. Numerous examples exist of lithium toxicity induced by drug interactions or dehydration in patients without kidney disease.
James W. Jefferson, MD
Distinguished senior scientist, Madison Institute of Medicine
Clinical professor of psychiatry,
University of Wisconsin Medical School
Dr. Magnon responds
Dr. Jefferson’s comments reflect the standard thinking about use of lithium carbonate.
My points are:
- I have not seen these so-called extensive studies about lithium toxicity
- When given in reasonable, effective dosages, the patient responds without toxic effects.
Lithium does have some unpleasant side effects, such as tremor, and weight gain is common in some patients, especially women. Continuous lab testing is just not necessary, however.
West B. Magnon, MD Bradenton, FL