User login
Metastatic breast cancer lesions immunologically depleted compared with primary
The immune microenvironment of metastatic breast cancer lesions is relatively inert and depleted versus primary tumors, results of a recent study suggest.
“These results predict that immune therapy may be more successful in early stage breast cancers rather than in metastatic disease,” Lajos Pusztai, MD, and study coinvestigators reported in Annals of Oncology.
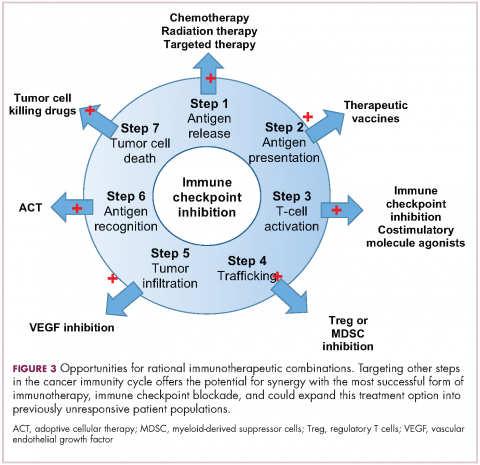
However, metastatic breast cancers showed high expression levels of some targetable molecules that may provide a “foundation for rational immunotherapy combination strategies,” wrote Dr. Pusztai, director of breast cancer translational research at Yale Cancer Center, New Haven, Conn., and his coinvestigators.
The investigators looked at tumor PD-L1 protein expression, tumor infiltrating lymphocyte (TIL) count, and mRNA expression for 730 immune-related genes in both primary and metastatic cancer samples obtained from pathologists at Yale.
The study included one cohort with full sections of paired metastatic and primary tumors from 45 patients, and a second cohort of tissue microarrays from 55 other patients.
Compared with primary lesions, metastatic lesions had substantially lower levels of PD-L1 expression and TIL counts, the investigators found.
Staining of PD-L1 was primarily seen in stromal immune cells, rather than tumor cells, according to investigators. The median stromal PD-L1 positivity was 14% for metastases and 52% for primary tumors in the first cohort (P = .0004), and 7% for metastases and 22% for primary tumors in the second cohort (P = .03).
They also reported significant decreased TIL counts in metastatic lesions for both the first (P = .026) and second (P = .089) cohorts, the report shows.
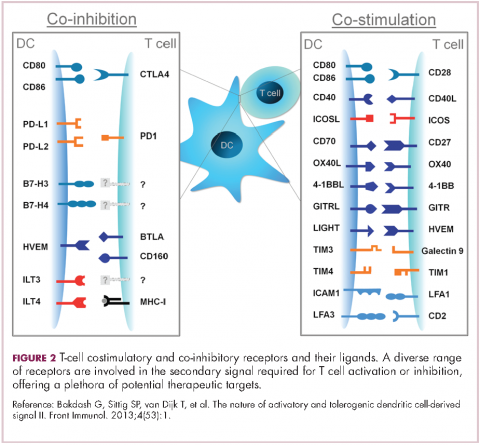
Immune gene expression profiling results, similarly, showed that most immune cell types and functions were “depleted” in the metastatic lesions, including a decreased mRNA expression of CTLA4, Dr. Pusztai and his colleagues reported.
The “lesser immunogenicity” of metastatic breast cancer cells was shown by decreased expression of immune proteasome and MHC class I genes, along with increased expression of HLA-E, which has been shown to suppress immunity, and reduced presence of dendritic cells, they said.
However, they also found high expression of targetable molecules in metastatic lesions. Those included macrophage markers such as CD68 and CD163, cytokine ligand/receptor pairs that mediate pro-tumorigenic effects, such as CCL2/CCR2 and CXCR4/CXCL12, and signaling molecules such as STAT-3 and JAK2, among others.
“We suggest that targeting these molecules may lead to synergy with PD1/PD-L1 blockade in metastatic breast cancer,” they wrote.
The work by Dr. Pusztai and his colleagues was supported by the Breast Cancer Research Foundation, Susan G Komen for the Cure, Department of Defense Breast Cancer Research Program Awards, and the Rosztoczy Foundation. The authors declared no conflicts of interest.
SOURCE: Szekely B, et al. Ann Oncol. 2018 Sep 10. doi: 10.1093/annonc/mdy399.
The immune microenvironment of metastatic breast cancer lesions is relatively inert and depleted versus primary tumors, results of a recent study suggest.
“These results predict that immune therapy may be more successful in early stage breast cancers rather than in metastatic disease,” Lajos Pusztai, MD, and study coinvestigators reported in Annals of Oncology.
However, metastatic breast cancers showed high expression levels of some targetable molecules that may provide a “foundation for rational immunotherapy combination strategies,” wrote Dr. Pusztai, director of breast cancer translational research at Yale Cancer Center, New Haven, Conn., and his coinvestigators.
The investigators looked at tumor PD-L1 protein expression, tumor infiltrating lymphocyte (TIL) count, and mRNA expression for 730 immune-related genes in both primary and metastatic cancer samples obtained from pathologists at Yale.
The study included one cohort with full sections of paired metastatic and primary tumors from 45 patients, and a second cohort of tissue microarrays from 55 other patients.
Compared with primary lesions, metastatic lesions had substantially lower levels of PD-L1 expression and TIL counts, the investigators found.
Staining of PD-L1 was primarily seen in stromal immune cells, rather than tumor cells, according to investigators. The median stromal PD-L1 positivity was 14% for metastases and 52% for primary tumors in the first cohort (P = .0004), and 7% for metastases and 22% for primary tumors in the second cohort (P = .03).
They also reported significant decreased TIL counts in metastatic lesions for both the first (P = .026) and second (P = .089) cohorts, the report shows.
Immune gene expression profiling results, similarly, showed that most immune cell types and functions were “depleted” in the metastatic lesions, including a decreased mRNA expression of CTLA4, Dr. Pusztai and his colleagues reported.
The “lesser immunogenicity” of metastatic breast cancer cells was shown by decreased expression of immune proteasome and MHC class I genes, along with increased expression of HLA-E, which has been shown to suppress immunity, and reduced presence of dendritic cells, they said.
However, they also found high expression of targetable molecules in metastatic lesions. Those included macrophage markers such as CD68 and CD163, cytokine ligand/receptor pairs that mediate pro-tumorigenic effects, such as CCL2/CCR2 and CXCR4/CXCL12, and signaling molecules such as STAT-3 and JAK2, among others.
“We suggest that targeting these molecules may lead to synergy with PD1/PD-L1 blockade in metastatic breast cancer,” they wrote.
The work by Dr. Pusztai and his colleagues was supported by the Breast Cancer Research Foundation, Susan G Komen for the Cure, Department of Defense Breast Cancer Research Program Awards, and the Rosztoczy Foundation. The authors declared no conflicts of interest.
SOURCE: Szekely B, et al. Ann Oncol. 2018 Sep 10. doi: 10.1093/annonc/mdy399.
The immune microenvironment of metastatic breast cancer lesions is relatively inert and depleted versus primary tumors, results of a recent study suggest.
“These results predict that immune therapy may be more successful in early stage breast cancers rather than in metastatic disease,” Lajos Pusztai, MD, and study coinvestigators reported in Annals of Oncology.
However, metastatic breast cancers showed high expression levels of some targetable molecules that may provide a “foundation for rational immunotherapy combination strategies,” wrote Dr. Pusztai, director of breast cancer translational research at Yale Cancer Center, New Haven, Conn., and his coinvestigators.
The investigators looked at tumor PD-L1 protein expression, tumor infiltrating lymphocyte (TIL) count, and mRNA expression for 730 immune-related genes in both primary and metastatic cancer samples obtained from pathologists at Yale.
The study included one cohort with full sections of paired metastatic and primary tumors from 45 patients, and a second cohort of tissue microarrays from 55 other patients.
Compared with primary lesions, metastatic lesions had substantially lower levels of PD-L1 expression and TIL counts, the investigators found.
Staining of PD-L1 was primarily seen in stromal immune cells, rather than tumor cells, according to investigators. The median stromal PD-L1 positivity was 14% for metastases and 52% for primary tumors in the first cohort (P = .0004), and 7% for metastases and 22% for primary tumors in the second cohort (P = .03).
They also reported significant decreased TIL counts in metastatic lesions for both the first (P = .026) and second (P = .089) cohorts, the report shows.
Immune gene expression profiling results, similarly, showed that most immune cell types and functions were “depleted” in the metastatic lesions, including a decreased mRNA expression of CTLA4, Dr. Pusztai and his colleagues reported.
The “lesser immunogenicity” of metastatic breast cancer cells was shown by decreased expression of immune proteasome and MHC class I genes, along with increased expression of HLA-E, which has been shown to suppress immunity, and reduced presence of dendritic cells, they said.
However, they also found high expression of targetable molecules in metastatic lesions. Those included macrophage markers such as CD68 and CD163, cytokine ligand/receptor pairs that mediate pro-tumorigenic effects, such as CCL2/CCR2 and CXCR4/CXCL12, and signaling molecules such as STAT-3 and JAK2, among others.
“We suggest that targeting these molecules may lead to synergy with PD1/PD-L1 blockade in metastatic breast cancer,” they wrote.
The work by Dr. Pusztai and his colleagues was supported by the Breast Cancer Research Foundation, Susan G Komen for the Cure, Department of Defense Breast Cancer Research Program Awards, and the Rosztoczy Foundation. The authors declared no conflicts of interest.
SOURCE: Szekely B, et al. Ann Oncol. 2018 Sep 10. doi: 10.1093/annonc/mdy399.
FROM ANNALS OF ONCOLOGY
Key clinical point: The immune microenvironment of metastatic breast cancer lesions is relatively inert and depleted versus primary tumors.
Major finding: Median stromal PD-L1 positivity was 14% for metastases and 52% for primary tumors in one cohort (P = .0004), and 7% versus 22% in a second (P = .03).
Study details: Analysis of breast cancer tissue samples (primary tumor and metastatic lesions) from 90 patients
Disclosures: The work was supported by the Breast Cancer Research Foundation, the Susan Komen for the Cure, Department of Defense Breast Cancer Research Program Awards, and the Rosztoczy Foundation. The study authors declared no conflicts of interest.
Source: Szekely B et al. Ann Oncol. 2018 Sep 10. doi: 10.1093/annonc/mdy399.
Outcomes similar for concurrent versus sequential treatment in HER2-positive breast cancers
Outcomes for women with operable HER2-positive breast cancer were similar whether they received standard combination chemotherapy with either concurrent or sequential paclitaxel/trastuzumab, long-term results of the phase 3, randomized American College of Surgeons Oncology Group Z1041 trial showed.
Among 280 women with HER-2 positive breast cancer followed for a median of 5.1 years, there were no significant differences in either pathological complete response rates (pCR), disease-free survival (DFS), or overall survival with either concurrent or sequential therapy, wrote Aman U. Buzdar, MD, from the University of Texas MD Anderson Cancer Center, Houston, and his colleagues.
“A previous publication of this study’s primary analysis reported that breast pCR in patients treated with paclitaxel and trastuzumab followed by FEC [fluorouracil, epirubicin, cyclophosphamide] and trastuzumab did not differ significantly from that of patients receiving FEC followed by paclitaxel and trastuzumab. We now report the findings concerning the secondary outcomes, that is, with a median follow-up of approximately 5 years, DFS is similar among the two treatment arms,” they wrote in JAMA Oncology.
The purpose of the current analysis was to evaluate long-term outcomes associated with the two treatment approaches.
In the trial, conducted at 36 centers in the continental United States and Puerto Rico, 280 women (median age, 50 years; range, 28-76 years) were treated with 500 mg/m2 of fluorouracil, 75 mg/m2 epirubicin, and 500 mg/m2 cyclophosphamide every 3 weeks for 12 weeks with concurrent weekly paclitaxel at 80 mg/m2 and trastuzumab at 2 mg/kg – after an initial dose of 4 mg/kg – or the same paclitaxel/trastuzumab combination delivered weekly for 12 weeks, followed by FEC every 3 weeks with weekly trastuzumab for 12 weeks.
Women who also had hormone receptor–positive disease received endocrine therapy. Radiotherapy was delivered at the discretion of the attending physician.
As noted, there were no differences in either DFS rates (adjusted hazard ratio, 1.02; P = .96) or overall survival rates (adjusted HR, 1.17; P = .73) between the trial arms.
The authors concluded that “concurrent administration of trastuzumab with FEC was not found to offer additional clinical benefit and is not warranted.”
The study was supported by grants to participating institutions from the National Cancer Institute. Dr. Buzdar reported no conflicts of interest. Three coauthors reported research support, consulting fees, travel support, and/or other relationships with multiple companies.
SOURCE: Buzdar AU et al. JAMA Oncol. 2018 Sept 6. doi: 10.1001/jamaoncol.2018.3691.
Outcomes for women with operable HER2-positive breast cancer were similar whether they received standard combination chemotherapy with either concurrent or sequential paclitaxel/trastuzumab, long-term results of the phase 3, randomized American College of Surgeons Oncology Group Z1041 trial showed.
Among 280 women with HER-2 positive breast cancer followed for a median of 5.1 years, there were no significant differences in either pathological complete response rates (pCR), disease-free survival (DFS), or overall survival with either concurrent or sequential therapy, wrote Aman U. Buzdar, MD, from the University of Texas MD Anderson Cancer Center, Houston, and his colleagues.
“A previous publication of this study’s primary analysis reported that breast pCR in patients treated with paclitaxel and trastuzumab followed by FEC [fluorouracil, epirubicin, cyclophosphamide] and trastuzumab did not differ significantly from that of patients receiving FEC followed by paclitaxel and trastuzumab. We now report the findings concerning the secondary outcomes, that is, with a median follow-up of approximately 5 years, DFS is similar among the two treatment arms,” they wrote in JAMA Oncology.
The purpose of the current analysis was to evaluate long-term outcomes associated with the two treatment approaches.
In the trial, conducted at 36 centers in the continental United States and Puerto Rico, 280 women (median age, 50 years; range, 28-76 years) were treated with 500 mg/m2 of fluorouracil, 75 mg/m2 epirubicin, and 500 mg/m2 cyclophosphamide every 3 weeks for 12 weeks with concurrent weekly paclitaxel at 80 mg/m2 and trastuzumab at 2 mg/kg – after an initial dose of 4 mg/kg – or the same paclitaxel/trastuzumab combination delivered weekly for 12 weeks, followed by FEC every 3 weeks with weekly trastuzumab for 12 weeks.
Women who also had hormone receptor–positive disease received endocrine therapy. Radiotherapy was delivered at the discretion of the attending physician.
As noted, there were no differences in either DFS rates (adjusted hazard ratio, 1.02; P = .96) or overall survival rates (adjusted HR, 1.17; P = .73) between the trial arms.
The authors concluded that “concurrent administration of trastuzumab with FEC was not found to offer additional clinical benefit and is not warranted.”
The study was supported by grants to participating institutions from the National Cancer Institute. Dr. Buzdar reported no conflicts of interest. Three coauthors reported research support, consulting fees, travel support, and/or other relationships with multiple companies.
SOURCE: Buzdar AU et al. JAMA Oncol. 2018 Sept 6. doi: 10.1001/jamaoncol.2018.3691.
Outcomes for women with operable HER2-positive breast cancer were similar whether they received standard combination chemotherapy with either concurrent or sequential paclitaxel/trastuzumab, long-term results of the phase 3, randomized American College of Surgeons Oncology Group Z1041 trial showed.
Among 280 women with HER-2 positive breast cancer followed for a median of 5.1 years, there were no significant differences in either pathological complete response rates (pCR), disease-free survival (DFS), or overall survival with either concurrent or sequential therapy, wrote Aman U. Buzdar, MD, from the University of Texas MD Anderson Cancer Center, Houston, and his colleagues.
“A previous publication of this study’s primary analysis reported that breast pCR in patients treated with paclitaxel and trastuzumab followed by FEC [fluorouracil, epirubicin, cyclophosphamide] and trastuzumab did not differ significantly from that of patients receiving FEC followed by paclitaxel and trastuzumab. We now report the findings concerning the secondary outcomes, that is, with a median follow-up of approximately 5 years, DFS is similar among the two treatment arms,” they wrote in JAMA Oncology.
The purpose of the current analysis was to evaluate long-term outcomes associated with the two treatment approaches.
In the trial, conducted at 36 centers in the continental United States and Puerto Rico, 280 women (median age, 50 years; range, 28-76 years) were treated with 500 mg/m2 of fluorouracil, 75 mg/m2 epirubicin, and 500 mg/m2 cyclophosphamide every 3 weeks for 12 weeks with concurrent weekly paclitaxel at 80 mg/m2 and trastuzumab at 2 mg/kg – after an initial dose of 4 mg/kg – or the same paclitaxel/trastuzumab combination delivered weekly for 12 weeks, followed by FEC every 3 weeks with weekly trastuzumab for 12 weeks.
Women who also had hormone receptor–positive disease received endocrine therapy. Radiotherapy was delivered at the discretion of the attending physician.
As noted, there were no differences in either DFS rates (adjusted hazard ratio, 1.02; P = .96) or overall survival rates (adjusted HR, 1.17; P = .73) between the trial arms.
The authors concluded that “concurrent administration of trastuzumab with FEC was not found to offer additional clinical benefit and is not warranted.”
The study was supported by grants to participating institutions from the National Cancer Institute. Dr. Buzdar reported no conflicts of interest. Three coauthors reported research support, consulting fees, travel support, and/or other relationships with multiple companies.
SOURCE: Buzdar AU et al. JAMA Oncol. 2018 Sept 6. doi: 10.1001/jamaoncol.2018.3691.
FROM JAMA ONCOLOGY
Key clinical point: Sequencing of chemotherapy, paclitaxel, and trastuzumab did not affect outcomes in women with HER2-positive breast cancers.
Major finding: There were no significant differences in disease-free survival or overall survival among treated with concurrent or sequential therapy.
Study details: A phase 3, randomized trial in 280 women with operable HER2-positive breast cancers.
Disclosures: The study was supported by grants to participating institutions from the National Cancer Institute. Dr. Buzdar reported no conflicts of interest. Three coauthors reported research support, consulting fees, travel support, and/or other relationships with multiple companies.
Source: Buzdar AU et al. JAMA Oncol. 2018 Sept 6. doi: 10.1001/jamaoncol.2018.3691.
Top cancer researcher fails to disclose corporate financial ties in major research journals
This article was produced in partnership with The New York Times.
One of the world’s top breast cancer doctors failed to disclose millions of dollars in payments from drug and health care companies in recent years, omitting his financial ties from dozens of research articles in prestigious publications like the New England Journal of Medicine and the Lancet.
The researcher, José Baselga, MD, a towering figure in the cancer world, is the chief medical officer at Memorial Sloan Kettering Cancer Center in New York. He has held board memberships or advisory roles with Roche and Bristol-Myers Squibb, among other corporations; has had a stake in start-ups testing cancer therapies; and played a key role in the development of breakthrough drugs that have revolutionized treatments for breast cancer.
According to an analysis by ProPublica and the New York Times, Dr. Baselga did not follow financial disclosure rules set by the American Association for Cancer Research when he was president of the group. He also left out payments he received from companies connected to cancer research in his articles published in the group’s journal, Cancer Discovery. At the same time, he has been one of the journal’s two editors in chief.
At a conference this year and before analysts in 2017, he put a positive spin on the results of two Roche-sponsored clinical trials that many others considered disappointments, without disclosing his relationship to the company. Since 2014, he has received more than $3 million from Roche in consulting fees and for his stake in a company it acquired.
Dr. Baselga did not dispute his relationships with at least a dozen companies. In an interview, he said the disclosure lapses were unintentional.
He stressed that much of his industry work was publicly known although he declined to provide payment figures from his involvement with some biotech start-ups. “I acknowledge that there have been inconsistencies, but that’s what it is,” he said. “It’s not that I do not appreciate the importance.”
Dr. Baselga’s extensive corporate relationships – and his frequent failure to disclose them – illustrate how permeable the boundaries remain between academic research and industry, and how weakly reporting requirements are enforced by the medical journals and professional societies charged with policing them.
A decade ago, a series of scandals involving the secret influence of the pharmaceutical industry on drug research prompted the medical community to beef up its conflict-of-interest disclosure requirements. Ethicists worry that outside entanglements can shape the way studies are designed and medications are prescribed to patients, allowing bias to influence medical practice. Disclosing those connections allows the public, other scientists, and doctors to evaluate the research and weigh potential conflicts.
If leaders don’t follow the rules, then we don’t really have rules,” said Walid Gellad, MD, an of the department of medicine at the University of Pittsburgh and director of its Center for Pharmaceutical Policy and Prescribing. “It says that the rules don’t matter.”
The penalties for such ethical lapses are not severe. The cancer research group, the American Association for Cancer Research, warns authors who fill out disclosure forms for its journals that they face a 3-year ban on publishing if they are found to have financial relationships that they did not disclose. But the ban is not included in the conflict-of-interest policy posted on its website, and the group said no author had ever been barred.
Many journals and professional societies do not check conflicts and simply require authors to correct the record.
Officials at the AACR, the American Society of Clinical Oncology and the New England Journal of Medicine said they were looking into Dr. Baselga’s omissions after inquiries from the Times and ProPublica. The Lancet declined to say whether it would look into the matter.
Christine Hickey, a spokeswoman for Memorial Sloan Kettering, said that Dr. Baselga had properly informed the hospital of his outside industry work and that it was Dr. Baselga’s responsibility to disclose such relationships to entities such as medical journals. The cancer center, she said, “has a rigorous and comprehensive compliance program in place to promote honesty and objectivity in scientific research.”
Asked if he planned to correct his disclosures, Dr. Baselga asked reporters what they would recommend. In a statement several days later, he said he would correct his conflict-of-interest reporting for 17 articles, including in the New England Journal of Medicine, the Lancet, and the publication he edits, Cancer Discovery. He said that he did not believe disclosure was required for dozens of other articles detailing early stages of research.
“I have spent my career caring for cancer patients and bringing new therapies to the clinic with the goal of extending and saving lives,” Dr. Baselga said in the statement. “While I have been inconsistent with disclosures and acknowledge that fact, that is a far cry from compromising my responsibilities as a physician, as a scientist and as a clinical leader.”
The corporate imprint on cancer research
Dr. Baselga, 59, supervises clinical operations at Memorial Sloan Kettering, one of the nation’s top cancer centers and wields influence over the lives of patients and companies wishing to conduct trials there. He was paid more than $1.5 million in compensation by the cancer center in 2016, according to the hospital’s latest available tax disclosures, but that does not include his consulting or board fees from outside companies.
Many top medical researchers have ties to the for-profit health care industry, and some overlap is seen as a good thing – after all, these are the companies charged with developing the drugs, medical devices and diagnostic tests of the future.
Dr. Baselga’s relationship to industry is extensive. In addition to sitting on the board of Bristol-Myers Squibb, he is a director of Varian Medical Systems, which sells radiation equipment and for whom Memorial Sloan Kettering is a client.
In all, Dr. Baselga has served on the boards of at least six companies since 2013, positions that have required him to assume a fiduciary responsibility to protect the interests of those companies, even as he oversees the cancer center’s medical operations.
The hospital and Dr. Baselga said steps had been taken to prevent him from having a say in any business between the cancer center and the companies on whose boards he sits.
The chief executive of Memorial Sloan Kettering, Craig B. Thompson, MD, settled lawsuits several years ago that were filed by the University of Pennsylvania, Philadelphia, and an affiliated research center. They contended that he hid research conducted while he was at Penn to start a new company, Agios Pharmaceuticals, and did not share the earnings. Dr. Thompson disputed the allegations. He now sits on the board of Merck, which manufactures Keytruda, a blockbuster cancer therapy.
Ms. Hickey said the cancer center cannot fulfill its charitable mission without working with industry. “We encourage collaboration and are proud that our work has led to the approval of novel, lifesaving cancer treatments for patients around the world,” she said.
Some disclosures are required; others aren’t
After the scandals a decade ago over lack of disclosure, the federal government began requiring drug and device manufacturers to publicly disclose payments to doctors in 2013.
From August 2013 through 2017, Dr. Baselga received nearly $3.5 million from nine companies, according to the federal Open Payments database, which compiles disclosures filed by drug and device companies.
Dr. Baselga has disclosed in other forums investments and advisory roles in biotech start-ups, but he declined to provide a tally of financial interests in those firms. Companies that have not received approval from the Food and Drug Administration for their products – projects still in the testing phases – do not have to report payments they make to doctors.
Serving on boards can be lucrative. In 2017, Dr. Baselga received $260,000 in cash and stock awards to sit on Varian’s board of directors, according to the company’s corporate filings.
ProPublica and the Times analyzed Dr. Baselga’s publications in medical journals since 2013, the year he joined Memorial Sloan Kettering. He failed to disclose any industry relationships in more than 100, or about 60% of the time, a figure that has increased with each passing year. Last year, he did not list any potential conflicts in 87% of the articles that he wrote or cowrote.
Dr. Baselga compiled a color-coded list of his articles and offered a different interpretation. Sixty-two of the papers for which he did not disclose any potential conflict represented “conceptual, basic laboratory or translational work,” and did not require one, he said. Questions could be raised about others, he said, but he added that most “had no clinical nor financial implications.” That left the 17 papers he plans to correct.
Early-stage research often carries financial weight because it helps companies decide whether to move ahead with a product. In about two-thirds of Dr. Baselga’s articles that lacked details of his industry ties, one or more of his coauthors listed theirs.
In 2015, Dr. Baselga published an article in the New England Journal about a Roche-sponsored trial of one of the company’s drugs, Zelboraf. Despite his financial ties to Roche, he declared that he had “nothing to disclose.” Fourteen of his coauthors reported ties to Roche.
Dr. Baselga defended the articles, saying that “these are high-quality manuscripts reporting on important clinical trials that led to a better understanding of cancer treatments.”
The guidelines enacted by most major medical journals and professional societies ask authors and presenters to list recent financial relationships that could pose a conflict.
But much of this reporting still relies on the honor system. A study in August in the journal JAMA Oncology found that one-third of authors in a sample of cancer trials did not report all payments from the studies’ sponsors.
“We don’t routinely check because we don’t have those kind of resources,” said Rita F. Redberg, MD, the editor of JAMA Internal Medicine, who has been critical of the influence of industry on medical practice. “We rely on trust and integrity. It’s kind of an assumed part of the professional relationship.”
Jennifer Zeis, a spokeswoman for the New England Journal of Medicine, said in an email that it had now asked Dr. Baselga to amend his disclosures. She said the journal planned to overhaul its tracking of industry relationships.
The AACR said it had begun an “extensive review” of the disclosure forms submitted by Dr. Baselga.
It said that it had never barred an author from publishing, and that “such an action would be necessary only in cases of egregious, consistent violations of the rules.”
Among the most prominent relationships that Dr. Baselga has often failed to disclose is with the Swiss pharmaceutical giant Roche and its United States subsidiary Genentech.
In June 2017, at the annual meeting of the ASCO in Chicago, Dr. Baselga spoke at a Roche-sponsored investor event about study results that the company had been counting on to persuade oncologists to move patients from Herceptin – which was facing competition from cheaper alternatives – to a combination treatment involving Herceptin and a newer, more expensive drug, Perjeta.
The results were so underwhelming that Roche’s stock fell 5 % on the news. One analyst described the results as a “lead balloon,” and an editorial in the New England Journal called it a “disappointment.”
Dr. Baselga, however, told analysts that critiques were “weird” and “strange.”
This June, at the same cancer conference, Dr. Baselga struck an upbeat note about the results of a Roche trial of the drug taselisib, saying in a blog post published on the cancer center website that the results were “incredibly exciting” while conceding the side effects from the drug were high.
That same day, Roche announced it was scrapping plans to develop the drug. The news was another disappointment involving the class of drugs called PI3K inhibitors, which is a major focus of Dr. Baselga’s current research.
In neither case did Dr. Baselga reveal that his ties to Roche and Genentech went beyond serving as a trial investigator. In 2014, Roche acquired Seragon, a cancer research company in which Dr. Baselga had an ownership stake, for $725 million. Dr. Baselga received more than $3 million in 2014 and 2015 for his stake in the company, according to the federal Open Payments database.
From 2013 to 2017, Roche also paid Dr. Baselga more than $50,000 in consulting fees, according to the database.
These details were not included in the conflict-of-interest statements that are required of all presenters at the ASCO conference, although he did disclose ownership interests and consulting relationships with several other companies in the prior two years.
ASCO said it would conduct an internal review of Dr. Baselga’s disclosures and would refer the findings to a panel.
Dr. Baselga said that he played no role in the Seragon acquisition and that he had cut ties with Roche since joining the board of a competitor, Bristol-Myers, in March. As for his presentations at the ASCO meetings in the last 2 years, he said he had also noted shortcomings in the studies.
The combination of Perjeta with Herceptin was later approved by the FDA for certain high-risk patients. As for taselisib, Dr. Baselga stands by his belief that the PI3K class of drugs will be an important target for fighting cancer.
Katie Thomas covers the pharmaceutical industry for the New York Times.
This article was produced in partnership with The New York Times.
One of the world’s top breast cancer doctors failed to disclose millions of dollars in payments from drug and health care companies in recent years, omitting his financial ties from dozens of research articles in prestigious publications like the New England Journal of Medicine and the Lancet.
The researcher, José Baselga, MD, a towering figure in the cancer world, is the chief medical officer at Memorial Sloan Kettering Cancer Center in New York. He has held board memberships or advisory roles with Roche and Bristol-Myers Squibb, among other corporations; has had a stake in start-ups testing cancer therapies; and played a key role in the development of breakthrough drugs that have revolutionized treatments for breast cancer.
According to an analysis by ProPublica and the New York Times, Dr. Baselga did not follow financial disclosure rules set by the American Association for Cancer Research when he was president of the group. He also left out payments he received from companies connected to cancer research in his articles published in the group’s journal, Cancer Discovery. At the same time, he has been one of the journal’s two editors in chief.
At a conference this year and before analysts in 2017, he put a positive spin on the results of two Roche-sponsored clinical trials that many others considered disappointments, without disclosing his relationship to the company. Since 2014, he has received more than $3 million from Roche in consulting fees and for his stake in a company it acquired.
Dr. Baselga did not dispute his relationships with at least a dozen companies. In an interview, he said the disclosure lapses were unintentional.
He stressed that much of his industry work was publicly known although he declined to provide payment figures from his involvement with some biotech start-ups. “I acknowledge that there have been inconsistencies, but that’s what it is,” he said. “It’s not that I do not appreciate the importance.”
Dr. Baselga’s extensive corporate relationships – and his frequent failure to disclose them – illustrate how permeable the boundaries remain between academic research and industry, and how weakly reporting requirements are enforced by the medical journals and professional societies charged with policing them.
A decade ago, a series of scandals involving the secret influence of the pharmaceutical industry on drug research prompted the medical community to beef up its conflict-of-interest disclosure requirements. Ethicists worry that outside entanglements can shape the way studies are designed and medications are prescribed to patients, allowing bias to influence medical practice. Disclosing those connections allows the public, other scientists, and doctors to evaluate the research and weigh potential conflicts.
If leaders don’t follow the rules, then we don’t really have rules,” said Walid Gellad, MD, an of the department of medicine at the University of Pittsburgh and director of its Center for Pharmaceutical Policy and Prescribing. “It says that the rules don’t matter.”
The penalties for such ethical lapses are not severe. The cancer research group, the American Association for Cancer Research, warns authors who fill out disclosure forms for its journals that they face a 3-year ban on publishing if they are found to have financial relationships that they did not disclose. But the ban is not included in the conflict-of-interest policy posted on its website, and the group said no author had ever been barred.
Many journals and professional societies do not check conflicts and simply require authors to correct the record.
Officials at the AACR, the American Society of Clinical Oncology and the New England Journal of Medicine said they were looking into Dr. Baselga’s omissions after inquiries from the Times and ProPublica. The Lancet declined to say whether it would look into the matter.
Christine Hickey, a spokeswoman for Memorial Sloan Kettering, said that Dr. Baselga had properly informed the hospital of his outside industry work and that it was Dr. Baselga’s responsibility to disclose such relationships to entities such as medical journals. The cancer center, she said, “has a rigorous and comprehensive compliance program in place to promote honesty and objectivity in scientific research.”
Asked if he planned to correct his disclosures, Dr. Baselga asked reporters what they would recommend. In a statement several days later, he said he would correct his conflict-of-interest reporting for 17 articles, including in the New England Journal of Medicine, the Lancet, and the publication he edits, Cancer Discovery. He said that he did not believe disclosure was required for dozens of other articles detailing early stages of research.
“I have spent my career caring for cancer patients and bringing new therapies to the clinic with the goal of extending and saving lives,” Dr. Baselga said in the statement. “While I have been inconsistent with disclosures and acknowledge that fact, that is a far cry from compromising my responsibilities as a physician, as a scientist and as a clinical leader.”
The corporate imprint on cancer research
Dr. Baselga, 59, supervises clinical operations at Memorial Sloan Kettering, one of the nation’s top cancer centers and wields influence over the lives of patients and companies wishing to conduct trials there. He was paid more than $1.5 million in compensation by the cancer center in 2016, according to the hospital’s latest available tax disclosures, but that does not include his consulting or board fees from outside companies.
Many top medical researchers have ties to the for-profit health care industry, and some overlap is seen as a good thing – after all, these are the companies charged with developing the drugs, medical devices and diagnostic tests of the future.
Dr. Baselga’s relationship to industry is extensive. In addition to sitting on the board of Bristol-Myers Squibb, he is a director of Varian Medical Systems, which sells radiation equipment and for whom Memorial Sloan Kettering is a client.
In all, Dr. Baselga has served on the boards of at least six companies since 2013, positions that have required him to assume a fiduciary responsibility to protect the interests of those companies, even as he oversees the cancer center’s medical operations.
The hospital and Dr. Baselga said steps had been taken to prevent him from having a say in any business between the cancer center and the companies on whose boards he sits.
The chief executive of Memorial Sloan Kettering, Craig B. Thompson, MD, settled lawsuits several years ago that were filed by the University of Pennsylvania, Philadelphia, and an affiliated research center. They contended that he hid research conducted while he was at Penn to start a new company, Agios Pharmaceuticals, and did not share the earnings. Dr. Thompson disputed the allegations. He now sits on the board of Merck, which manufactures Keytruda, a blockbuster cancer therapy.
Ms. Hickey said the cancer center cannot fulfill its charitable mission without working with industry. “We encourage collaboration and are proud that our work has led to the approval of novel, lifesaving cancer treatments for patients around the world,” she said.
Some disclosures are required; others aren’t
After the scandals a decade ago over lack of disclosure, the federal government began requiring drug and device manufacturers to publicly disclose payments to doctors in 2013.
From August 2013 through 2017, Dr. Baselga received nearly $3.5 million from nine companies, according to the federal Open Payments database, which compiles disclosures filed by drug and device companies.
Dr. Baselga has disclosed in other forums investments and advisory roles in biotech start-ups, but he declined to provide a tally of financial interests in those firms. Companies that have not received approval from the Food and Drug Administration for their products – projects still in the testing phases – do not have to report payments they make to doctors.
Serving on boards can be lucrative. In 2017, Dr. Baselga received $260,000 in cash and stock awards to sit on Varian’s board of directors, according to the company’s corporate filings.
ProPublica and the Times analyzed Dr. Baselga’s publications in medical journals since 2013, the year he joined Memorial Sloan Kettering. He failed to disclose any industry relationships in more than 100, or about 60% of the time, a figure that has increased with each passing year. Last year, he did not list any potential conflicts in 87% of the articles that he wrote or cowrote.
Dr. Baselga compiled a color-coded list of his articles and offered a different interpretation. Sixty-two of the papers for which he did not disclose any potential conflict represented “conceptual, basic laboratory or translational work,” and did not require one, he said. Questions could be raised about others, he said, but he added that most “had no clinical nor financial implications.” That left the 17 papers he plans to correct.
Early-stage research often carries financial weight because it helps companies decide whether to move ahead with a product. In about two-thirds of Dr. Baselga’s articles that lacked details of his industry ties, one or more of his coauthors listed theirs.
In 2015, Dr. Baselga published an article in the New England Journal about a Roche-sponsored trial of one of the company’s drugs, Zelboraf. Despite his financial ties to Roche, he declared that he had “nothing to disclose.” Fourteen of his coauthors reported ties to Roche.
Dr. Baselga defended the articles, saying that “these are high-quality manuscripts reporting on important clinical trials that led to a better understanding of cancer treatments.”
The guidelines enacted by most major medical journals and professional societies ask authors and presenters to list recent financial relationships that could pose a conflict.
But much of this reporting still relies on the honor system. A study in August in the journal JAMA Oncology found that one-third of authors in a sample of cancer trials did not report all payments from the studies’ sponsors.
“We don’t routinely check because we don’t have those kind of resources,” said Rita F. Redberg, MD, the editor of JAMA Internal Medicine, who has been critical of the influence of industry on medical practice. “We rely on trust and integrity. It’s kind of an assumed part of the professional relationship.”
Jennifer Zeis, a spokeswoman for the New England Journal of Medicine, said in an email that it had now asked Dr. Baselga to amend his disclosures. She said the journal planned to overhaul its tracking of industry relationships.
The AACR said it had begun an “extensive review” of the disclosure forms submitted by Dr. Baselga.
It said that it had never barred an author from publishing, and that “such an action would be necessary only in cases of egregious, consistent violations of the rules.”
Among the most prominent relationships that Dr. Baselga has often failed to disclose is with the Swiss pharmaceutical giant Roche and its United States subsidiary Genentech.
In June 2017, at the annual meeting of the ASCO in Chicago, Dr. Baselga spoke at a Roche-sponsored investor event about study results that the company had been counting on to persuade oncologists to move patients from Herceptin – which was facing competition from cheaper alternatives – to a combination treatment involving Herceptin and a newer, more expensive drug, Perjeta.
The results were so underwhelming that Roche’s stock fell 5 % on the news. One analyst described the results as a “lead balloon,” and an editorial in the New England Journal called it a “disappointment.”
Dr. Baselga, however, told analysts that critiques were “weird” and “strange.”
This June, at the same cancer conference, Dr. Baselga struck an upbeat note about the results of a Roche trial of the drug taselisib, saying in a blog post published on the cancer center website that the results were “incredibly exciting” while conceding the side effects from the drug were high.
That same day, Roche announced it was scrapping plans to develop the drug. The news was another disappointment involving the class of drugs called PI3K inhibitors, which is a major focus of Dr. Baselga’s current research.
In neither case did Dr. Baselga reveal that his ties to Roche and Genentech went beyond serving as a trial investigator. In 2014, Roche acquired Seragon, a cancer research company in which Dr. Baselga had an ownership stake, for $725 million. Dr. Baselga received more than $3 million in 2014 and 2015 for his stake in the company, according to the federal Open Payments database.
From 2013 to 2017, Roche also paid Dr. Baselga more than $50,000 in consulting fees, according to the database.
These details were not included in the conflict-of-interest statements that are required of all presenters at the ASCO conference, although he did disclose ownership interests and consulting relationships with several other companies in the prior two years.
ASCO said it would conduct an internal review of Dr. Baselga’s disclosures and would refer the findings to a panel.
Dr. Baselga said that he played no role in the Seragon acquisition and that he had cut ties with Roche since joining the board of a competitor, Bristol-Myers, in March. As for his presentations at the ASCO meetings in the last 2 years, he said he had also noted shortcomings in the studies.
The combination of Perjeta with Herceptin was later approved by the FDA for certain high-risk patients. As for taselisib, Dr. Baselga stands by his belief that the PI3K class of drugs will be an important target for fighting cancer.
Katie Thomas covers the pharmaceutical industry for the New York Times.
This article was produced in partnership with The New York Times.
One of the world’s top breast cancer doctors failed to disclose millions of dollars in payments from drug and health care companies in recent years, omitting his financial ties from dozens of research articles in prestigious publications like the New England Journal of Medicine and the Lancet.
The researcher, José Baselga, MD, a towering figure in the cancer world, is the chief medical officer at Memorial Sloan Kettering Cancer Center in New York. He has held board memberships or advisory roles with Roche and Bristol-Myers Squibb, among other corporations; has had a stake in start-ups testing cancer therapies; and played a key role in the development of breakthrough drugs that have revolutionized treatments for breast cancer.
According to an analysis by ProPublica and the New York Times, Dr. Baselga did not follow financial disclosure rules set by the American Association for Cancer Research when he was president of the group. He also left out payments he received from companies connected to cancer research in his articles published in the group’s journal, Cancer Discovery. At the same time, he has been one of the journal’s two editors in chief.
At a conference this year and before analysts in 2017, he put a positive spin on the results of two Roche-sponsored clinical trials that many others considered disappointments, without disclosing his relationship to the company. Since 2014, he has received more than $3 million from Roche in consulting fees and for his stake in a company it acquired.
Dr. Baselga did not dispute his relationships with at least a dozen companies. In an interview, he said the disclosure lapses were unintentional.
He stressed that much of his industry work was publicly known although he declined to provide payment figures from his involvement with some biotech start-ups. “I acknowledge that there have been inconsistencies, but that’s what it is,” he said. “It’s not that I do not appreciate the importance.”
Dr. Baselga’s extensive corporate relationships – and his frequent failure to disclose them – illustrate how permeable the boundaries remain between academic research and industry, and how weakly reporting requirements are enforced by the medical journals and professional societies charged with policing them.
A decade ago, a series of scandals involving the secret influence of the pharmaceutical industry on drug research prompted the medical community to beef up its conflict-of-interest disclosure requirements. Ethicists worry that outside entanglements can shape the way studies are designed and medications are prescribed to patients, allowing bias to influence medical practice. Disclosing those connections allows the public, other scientists, and doctors to evaluate the research and weigh potential conflicts.
If leaders don’t follow the rules, then we don’t really have rules,” said Walid Gellad, MD, an of the department of medicine at the University of Pittsburgh and director of its Center for Pharmaceutical Policy and Prescribing. “It says that the rules don’t matter.”
The penalties for such ethical lapses are not severe. The cancer research group, the American Association for Cancer Research, warns authors who fill out disclosure forms for its journals that they face a 3-year ban on publishing if they are found to have financial relationships that they did not disclose. But the ban is not included in the conflict-of-interest policy posted on its website, and the group said no author had ever been barred.
Many journals and professional societies do not check conflicts and simply require authors to correct the record.
Officials at the AACR, the American Society of Clinical Oncology and the New England Journal of Medicine said they were looking into Dr. Baselga’s omissions after inquiries from the Times and ProPublica. The Lancet declined to say whether it would look into the matter.
Christine Hickey, a spokeswoman for Memorial Sloan Kettering, said that Dr. Baselga had properly informed the hospital of his outside industry work and that it was Dr. Baselga’s responsibility to disclose such relationships to entities such as medical journals. The cancer center, she said, “has a rigorous and comprehensive compliance program in place to promote honesty and objectivity in scientific research.”
Asked if he planned to correct his disclosures, Dr. Baselga asked reporters what they would recommend. In a statement several days later, he said he would correct his conflict-of-interest reporting for 17 articles, including in the New England Journal of Medicine, the Lancet, and the publication he edits, Cancer Discovery. He said that he did not believe disclosure was required for dozens of other articles detailing early stages of research.
“I have spent my career caring for cancer patients and bringing new therapies to the clinic with the goal of extending and saving lives,” Dr. Baselga said in the statement. “While I have been inconsistent with disclosures and acknowledge that fact, that is a far cry from compromising my responsibilities as a physician, as a scientist and as a clinical leader.”
The corporate imprint on cancer research
Dr. Baselga, 59, supervises clinical operations at Memorial Sloan Kettering, one of the nation’s top cancer centers and wields influence over the lives of patients and companies wishing to conduct trials there. He was paid more than $1.5 million in compensation by the cancer center in 2016, according to the hospital’s latest available tax disclosures, but that does not include his consulting or board fees from outside companies.
Many top medical researchers have ties to the for-profit health care industry, and some overlap is seen as a good thing – after all, these are the companies charged with developing the drugs, medical devices and diagnostic tests of the future.
Dr. Baselga’s relationship to industry is extensive. In addition to sitting on the board of Bristol-Myers Squibb, he is a director of Varian Medical Systems, which sells radiation equipment and for whom Memorial Sloan Kettering is a client.
In all, Dr. Baselga has served on the boards of at least six companies since 2013, positions that have required him to assume a fiduciary responsibility to protect the interests of those companies, even as he oversees the cancer center’s medical operations.
The hospital and Dr. Baselga said steps had been taken to prevent him from having a say in any business between the cancer center and the companies on whose boards he sits.
The chief executive of Memorial Sloan Kettering, Craig B. Thompson, MD, settled lawsuits several years ago that were filed by the University of Pennsylvania, Philadelphia, and an affiliated research center. They contended that he hid research conducted while he was at Penn to start a new company, Agios Pharmaceuticals, and did not share the earnings. Dr. Thompson disputed the allegations. He now sits on the board of Merck, which manufactures Keytruda, a blockbuster cancer therapy.
Ms. Hickey said the cancer center cannot fulfill its charitable mission without working with industry. “We encourage collaboration and are proud that our work has led to the approval of novel, lifesaving cancer treatments for patients around the world,” she said.
Some disclosures are required; others aren’t
After the scandals a decade ago over lack of disclosure, the federal government began requiring drug and device manufacturers to publicly disclose payments to doctors in 2013.
From August 2013 through 2017, Dr. Baselga received nearly $3.5 million from nine companies, according to the federal Open Payments database, which compiles disclosures filed by drug and device companies.
Dr. Baselga has disclosed in other forums investments and advisory roles in biotech start-ups, but he declined to provide a tally of financial interests in those firms. Companies that have not received approval from the Food and Drug Administration for their products – projects still in the testing phases – do not have to report payments they make to doctors.
Serving on boards can be lucrative. In 2017, Dr. Baselga received $260,000 in cash and stock awards to sit on Varian’s board of directors, according to the company’s corporate filings.
ProPublica and the Times analyzed Dr. Baselga’s publications in medical journals since 2013, the year he joined Memorial Sloan Kettering. He failed to disclose any industry relationships in more than 100, or about 60% of the time, a figure that has increased with each passing year. Last year, he did not list any potential conflicts in 87% of the articles that he wrote or cowrote.
Dr. Baselga compiled a color-coded list of his articles and offered a different interpretation. Sixty-two of the papers for which he did not disclose any potential conflict represented “conceptual, basic laboratory or translational work,” and did not require one, he said. Questions could be raised about others, he said, but he added that most “had no clinical nor financial implications.” That left the 17 papers he plans to correct.
Early-stage research often carries financial weight because it helps companies decide whether to move ahead with a product. In about two-thirds of Dr. Baselga’s articles that lacked details of his industry ties, one or more of his coauthors listed theirs.
In 2015, Dr. Baselga published an article in the New England Journal about a Roche-sponsored trial of one of the company’s drugs, Zelboraf. Despite his financial ties to Roche, he declared that he had “nothing to disclose.” Fourteen of his coauthors reported ties to Roche.
Dr. Baselga defended the articles, saying that “these are high-quality manuscripts reporting on important clinical trials that led to a better understanding of cancer treatments.”
The guidelines enacted by most major medical journals and professional societies ask authors and presenters to list recent financial relationships that could pose a conflict.
But much of this reporting still relies on the honor system. A study in August in the journal JAMA Oncology found that one-third of authors in a sample of cancer trials did not report all payments from the studies’ sponsors.
“We don’t routinely check because we don’t have those kind of resources,” said Rita F. Redberg, MD, the editor of JAMA Internal Medicine, who has been critical of the influence of industry on medical practice. “We rely on trust and integrity. It’s kind of an assumed part of the professional relationship.”
Jennifer Zeis, a spokeswoman for the New England Journal of Medicine, said in an email that it had now asked Dr. Baselga to amend his disclosures. She said the journal planned to overhaul its tracking of industry relationships.
The AACR said it had begun an “extensive review” of the disclosure forms submitted by Dr. Baselga.
It said that it had never barred an author from publishing, and that “such an action would be necessary only in cases of egregious, consistent violations of the rules.”
Among the most prominent relationships that Dr. Baselga has often failed to disclose is with the Swiss pharmaceutical giant Roche and its United States subsidiary Genentech.
In June 2017, at the annual meeting of the ASCO in Chicago, Dr. Baselga spoke at a Roche-sponsored investor event about study results that the company had been counting on to persuade oncologists to move patients from Herceptin – which was facing competition from cheaper alternatives – to a combination treatment involving Herceptin and a newer, more expensive drug, Perjeta.
The results were so underwhelming that Roche’s stock fell 5 % on the news. One analyst described the results as a “lead balloon,” and an editorial in the New England Journal called it a “disappointment.”
Dr. Baselga, however, told analysts that critiques were “weird” and “strange.”
This June, at the same cancer conference, Dr. Baselga struck an upbeat note about the results of a Roche trial of the drug taselisib, saying in a blog post published on the cancer center website that the results were “incredibly exciting” while conceding the side effects from the drug were high.
That same day, Roche announced it was scrapping plans to develop the drug. The news was another disappointment involving the class of drugs called PI3K inhibitors, which is a major focus of Dr. Baselga’s current research.
In neither case did Dr. Baselga reveal that his ties to Roche and Genentech went beyond serving as a trial investigator. In 2014, Roche acquired Seragon, a cancer research company in which Dr. Baselga had an ownership stake, for $725 million. Dr. Baselga received more than $3 million in 2014 and 2015 for his stake in the company, according to the federal Open Payments database.
From 2013 to 2017, Roche also paid Dr. Baselga more than $50,000 in consulting fees, according to the database.
These details were not included in the conflict-of-interest statements that are required of all presenters at the ASCO conference, although he did disclose ownership interests and consulting relationships with several other companies in the prior two years.
ASCO said it would conduct an internal review of Dr. Baselga’s disclosures and would refer the findings to a panel.
Dr. Baselga said that he played no role in the Seragon acquisition and that he had cut ties with Roche since joining the board of a competitor, Bristol-Myers, in March. As for his presentations at the ASCO meetings in the last 2 years, he said he had also noted shortcomings in the studies.
The combination of Perjeta with Herceptin was later approved by the FDA for certain high-risk patients. As for taselisib, Dr. Baselga stands by his belief that the PI3K class of drugs will be an important target for fighting cancer.
Katie Thomas covers the pharmaceutical industry for the New York Times.
ESMO scale offers guidance on cancer targets
The European Society for Medical Oncology (ESMO) has published a proposed scale that would rank molecular targets for various cancers by how well they can be treated with new or emerging drugs.
The ESMO Scale of Clinical Actionability for Molecular Targets is designed to “harmonize and standardize the reporting and interpretation of clinically relevant genomics data,” according to Joaquin Mateo, MD, PhD, from the Vall d’Hebron Institute of Oncology in Barcelona, Spain, and his fellow members of the ESMO Translational Research and Precision Medicine Working Group.
“A major challenge for oncologists in the clinic is to distinguish between findings that represent proven clinical value or potential value based on preliminary clinical or preclinical evidence from hypothetical gene-drug matches and findings that are currently irrelevant for clinical practice,” they wrote in Annals of Oncology.
The scale groups targets into one of six tiers based on levels of evidence ranging from the gold standard of prospective, randomized clinical trials to targets for which there are no evidence and only hypothetical actionability. The primary goal is to help oncologists assign priority to potential targets when they review results of gene-sequencing panels for individual patients, according to the developers.
Briefly, the six tiers are:
Tier I includes targets that are agreed to be suitable for routine use and a recommended specific drug when a specific molecular alteration is detected. Examples include trastuzumab for human epidermal growth factor receptor 2 (HER2)–positive breast cancer, and inhibitors of epidermal growth factor receptor (EGFR) in patients with non–small cell lung cancer positive for EGFR mutations.
Tier II includes “investigational targets that likely define a patient population that benefits from a targeted drug but additional data are needed.” This tier includes agents that work in the phosphatidylinostiol 3-kinase pathway.
Tier III is similar to Tier II, in that it includes investigational targets that define a patient population with proven benefit from a targeted therapy, but in this case the target is detected in a different tumor type that has not previously been studied. For example, the targeted agent vemurafenib (Zelboraf), which extends survival of patients with metastatic melanomas carrying the BRAF V600E mutation, has only limited activity against BRAF-mutated colorectal cancers.
Tier IV includes targets with preclinical evidence of actionability.
Tier V includes targets with “evidence of relevant antitumor activity, not resulting in clinical meaningful benefit as single treatment but supporting development of cotargeting approaches.” The authors cite the example of PIK3CA inhibitors in patients with estrogen receptor–positive, HER2-negative breast cancers who also have PIK3CA activating mutations. In clinical trials, this strategy led to objective responses but not change outcomes.
The final tier is not Tier VI, as might be expected, but Tier X, with the X in this case being the unknown – that is, alterations/mutations for which there is neither preclinical nor clinical evidence to support their hypothetical use as a drug target.
“This clinical benefit–centered classification system offers a common language for all the actors involved in clinical cancer drug development. Its implementation in sequencing reports, tumor boards, and scientific communication can enable precise treatment decisions and facilitate discussions with patients about novel therapeutic options,” Dr. Mateo and his associates wrote in their conclusion.
The development process was supported by ESMO. Multiple coauthors reported financial relationships with various companies as well as grants/support from other foundations or charities.
SOURCE: Mateo J et al. Ann Oncol. 2018 Aug 21. doi: 10.1093/annonc/mdy263.
The European Society for Medical Oncology (ESMO) has published a proposed scale that would rank molecular targets for various cancers by how well they can be treated with new or emerging drugs.
The ESMO Scale of Clinical Actionability for Molecular Targets is designed to “harmonize and standardize the reporting and interpretation of clinically relevant genomics data,” according to Joaquin Mateo, MD, PhD, from the Vall d’Hebron Institute of Oncology in Barcelona, Spain, and his fellow members of the ESMO Translational Research and Precision Medicine Working Group.
“A major challenge for oncologists in the clinic is to distinguish between findings that represent proven clinical value or potential value based on preliminary clinical or preclinical evidence from hypothetical gene-drug matches and findings that are currently irrelevant for clinical practice,” they wrote in Annals of Oncology.
The scale groups targets into one of six tiers based on levels of evidence ranging from the gold standard of prospective, randomized clinical trials to targets for which there are no evidence and only hypothetical actionability. The primary goal is to help oncologists assign priority to potential targets when they review results of gene-sequencing panels for individual patients, according to the developers.
Briefly, the six tiers are:
Tier I includes targets that are agreed to be suitable for routine use and a recommended specific drug when a specific molecular alteration is detected. Examples include trastuzumab for human epidermal growth factor receptor 2 (HER2)–positive breast cancer, and inhibitors of epidermal growth factor receptor (EGFR) in patients with non–small cell lung cancer positive for EGFR mutations.
Tier II includes “investigational targets that likely define a patient population that benefits from a targeted drug but additional data are needed.” This tier includes agents that work in the phosphatidylinostiol 3-kinase pathway.
Tier III is similar to Tier II, in that it includes investigational targets that define a patient population with proven benefit from a targeted therapy, but in this case the target is detected in a different tumor type that has not previously been studied. For example, the targeted agent vemurafenib (Zelboraf), which extends survival of patients with metastatic melanomas carrying the BRAF V600E mutation, has only limited activity against BRAF-mutated colorectal cancers.
Tier IV includes targets with preclinical evidence of actionability.
Tier V includes targets with “evidence of relevant antitumor activity, not resulting in clinical meaningful benefit as single treatment but supporting development of cotargeting approaches.” The authors cite the example of PIK3CA inhibitors in patients with estrogen receptor–positive, HER2-negative breast cancers who also have PIK3CA activating mutations. In clinical trials, this strategy led to objective responses but not change outcomes.
The final tier is not Tier VI, as might be expected, but Tier X, with the X in this case being the unknown – that is, alterations/mutations for which there is neither preclinical nor clinical evidence to support their hypothetical use as a drug target.
“This clinical benefit–centered classification system offers a common language for all the actors involved in clinical cancer drug development. Its implementation in sequencing reports, tumor boards, and scientific communication can enable precise treatment decisions and facilitate discussions with patients about novel therapeutic options,” Dr. Mateo and his associates wrote in their conclusion.
The development process was supported by ESMO. Multiple coauthors reported financial relationships with various companies as well as grants/support from other foundations or charities.
SOURCE: Mateo J et al. Ann Oncol. 2018 Aug 21. doi: 10.1093/annonc/mdy263.
The European Society for Medical Oncology (ESMO) has published a proposed scale that would rank molecular targets for various cancers by how well they can be treated with new or emerging drugs.
The ESMO Scale of Clinical Actionability for Molecular Targets is designed to “harmonize and standardize the reporting and interpretation of clinically relevant genomics data,” according to Joaquin Mateo, MD, PhD, from the Vall d’Hebron Institute of Oncology in Barcelona, Spain, and his fellow members of the ESMO Translational Research and Precision Medicine Working Group.
“A major challenge for oncologists in the clinic is to distinguish between findings that represent proven clinical value or potential value based on preliminary clinical or preclinical evidence from hypothetical gene-drug matches and findings that are currently irrelevant for clinical practice,” they wrote in Annals of Oncology.
The scale groups targets into one of six tiers based on levels of evidence ranging from the gold standard of prospective, randomized clinical trials to targets for which there are no evidence and only hypothetical actionability. The primary goal is to help oncologists assign priority to potential targets when they review results of gene-sequencing panels for individual patients, according to the developers.
Briefly, the six tiers are:
Tier I includes targets that are agreed to be suitable for routine use and a recommended specific drug when a specific molecular alteration is detected. Examples include trastuzumab for human epidermal growth factor receptor 2 (HER2)–positive breast cancer, and inhibitors of epidermal growth factor receptor (EGFR) in patients with non–small cell lung cancer positive for EGFR mutations.
Tier II includes “investigational targets that likely define a patient population that benefits from a targeted drug but additional data are needed.” This tier includes agents that work in the phosphatidylinostiol 3-kinase pathway.
Tier III is similar to Tier II, in that it includes investigational targets that define a patient population with proven benefit from a targeted therapy, but in this case the target is detected in a different tumor type that has not previously been studied. For example, the targeted agent vemurafenib (Zelboraf), which extends survival of patients with metastatic melanomas carrying the BRAF V600E mutation, has only limited activity against BRAF-mutated colorectal cancers.
Tier IV includes targets with preclinical evidence of actionability.
Tier V includes targets with “evidence of relevant antitumor activity, not resulting in clinical meaningful benefit as single treatment but supporting development of cotargeting approaches.” The authors cite the example of PIK3CA inhibitors in patients with estrogen receptor–positive, HER2-negative breast cancers who also have PIK3CA activating mutations. In clinical trials, this strategy led to objective responses but not change outcomes.
The final tier is not Tier VI, as might be expected, but Tier X, with the X in this case being the unknown – that is, alterations/mutations for which there is neither preclinical nor clinical evidence to support their hypothetical use as a drug target.
“This clinical benefit–centered classification system offers a common language for all the actors involved in clinical cancer drug development. Its implementation in sequencing reports, tumor boards, and scientific communication can enable precise treatment decisions and facilitate discussions with patients about novel therapeutic options,” Dr. Mateo and his associates wrote in their conclusion.
The development process was supported by ESMO. Multiple coauthors reported financial relationships with various companies as well as grants/support from other foundations or charities.
SOURCE: Mateo J et al. Ann Oncol. 2018 Aug 21. doi: 10.1093/annonc/mdy263.
FROM ANNALS OF ONCOLOGY
Key clinical point: The scale is intended to standardize reporting and interpretation of cancer gene panel results to help oncologists plan treatment.
Major finding: The scale divides current and future therapeutic targets into tiers based on levels of clinical and preclinical evidence.
Study details: Proposed guiding principles for a classification system developed by the Translational Research and Precision Medicine Working Group of the European Society of Medical Oncology.
Disclosures: The development process was supported by ESMO. Multiple coauthors reported financial relationships with various companies as well as grants/support from other foundations or charities.
Source: Mateo J et al. Ann Oncol. 2018 Aug 21. doi: 10.1093/annonc/mdy263.
Delayed diagnosis of breast cancer: $15M award
Delayed diagnosis of breast cancer: $15M award
A woman in her mid-50s had been seen by a breast surgeon for 16 years for regular mammograms and sonograms. In May 2009, the breast surgeon misinterpreted a mammogram as negative, as did a radiologist who re-read the mammogram weeks later. In December 2010, the patient returned to the breast surgeon with nipple discharge. No further testing was conducted. In October 2011, the patient was found to have Stage IIIA breast cancer involving 4 lymph nodes. She underwent left radical mastectomy, chemotherapy, radiation therapy, and breast reconstruction. At time of trial, the cancer had invaded her vertebrae, was Stage IV, and most likely incurable.
PATIENT'S CLAIM: Although the surgeon admittedly did not possess the qualifications required under the Mammography Quality Standards Act, he interpreted about 5,000 mammograms per year in his office. In this case, he failed to detect a small breast tumor in May 2009. He also failed to perform testing when the patient reported nipple discharge. A more timely diagnosis of breast cancer at Stage I would have provided a 90% chance of long-term survival.
DEFENDANTS' DEFENSE: The defense held the radiologist fully liable because the surgeon was not a qualified interpreter of mammography, therefore relying on the radiologist’s interpretation. The radiologist was legally responsible for the missed diagnosis.
VERDICT: A $15M New York verdict was reached, finding the breast surgeon 75% at fault and the radiologist 25%. The radiologist settled before the trial (the jury was not informed of this). The breast surgeon was responsible for $11.25M. The defense indicated intent to appeal.
Alleged failure to evacuate uterus after cesarean delivery
A 37-year-old woman underwent cesarean delivery (CD) performed by 2 ObGyns. After delivery, she began to hemorrhage and the uterus became atonic. Hysterectomy was performed but the bleeding did not stop. The ObGyns called in 3 other ObGyns. During exploratory laparotomy, the bleeding was halted.
PATIENT'S CLAIM: She and her husband had hoped to have more children but the hysterectomy precluded that. She sued all 5 ObGyns, alleging that the delivering ObGyns failed to properly perform the CD and that each physician failed to properly perform the laparotomy, causing a large scar. The claim was discontinued against the 3 surgical ObGyns; trial addressed the 2 delivering ObGyns.
The patient’s expert ObGyn remarked that the hemorrhage was caused by a small placental remnant that remained in the uterus as a result of inadequate evacuation following delivery. The presence of the remnant was indicated by the uterine atony and should have prompted immediate investigation. The physicians’ notes did not document exploration of the uterus prior to closure.
PHYSICIAN'S DEFENSE: The defense’s expert contended that atony would not be a result of a small remnant of placenta. The patient’s uterus was properly evacuated, the hemorrhage was an unforeseeable complication, and the ObGyns properly addressed the hemorrhage.
VERDICT: A New York defense verdict was returned.
Alleged bowel injury during hysterectomy
Two days after a woman underwent a hysterectomy performed by her ObGyn, she went to the emergency department with increasing pain. Her ObGyn admitted her to the hospital. A general surgeon performed an exploratory laparotomy the next day that revealed an abscess; a 1-cm perforation of the patient’s bowel was surgically repaired. The patient had a difficult recovery. She developed pneumonia and respiratory failure. She underwent multiple repair surgeries for recurrent abscesses and fistulas because the wound was slow to heal.
PATIENT'S CLAIM: The ObGyn’s surgical technique was negligent. He injured the bowel when inserting a trocar and did not identify the injury in a timely manner. The expert witness commented that such an injury can sometimes be a surgical complication, but not in this case: the ObGyn rushed the procedure because he had another patient waiting for CD at another hospital.
PHYSICIAN'S DEFENSE: The ObGyn denied negligence and contended that the trocar used in surgery was too blunt to have caused a perforation. It would have been obvious to the ObGyn during surgery if a perforation had occurred. The perforation developed days after surgery within an abscess.
VERDICT: A Mississippi defense verdict was returned.
These cases were selected by the editors of OBG Management from Medical Malpractice Verdicts, Settlements & Experts, with permission of the editor, Lewis Laska (www.verdictslaska.com). The information available to the editors about the cases presented here is sometimes incomplete. Moreover, the cases may or may not have merit. Nevertheless, these cases represent the types of clinical situations that typically result in litigation and are meant to illustrate nationwide variation in jury verdicts and awards.
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
Delayed diagnosis of breast cancer: $15M award
A woman in her mid-50s had been seen by a breast surgeon for 16 years for regular mammograms and sonograms. In May 2009, the breast surgeon misinterpreted a mammogram as negative, as did a radiologist who re-read the mammogram weeks later. In December 2010, the patient returned to the breast surgeon with nipple discharge. No further testing was conducted. In October 2011, the patient was found to have Stage IIIA breast cancer involving 4 lymph nodes. She underwent left radical mastectomy, chemotherapy, radiation therapy, and breast reconstruction. At time of trial, the cancer had invaded her vertebrae, was Stage IV, and most likely incurable.
PATIENT'S CLAIM: Although the surgeon admittedly did not possess the qualifications required under the Mammography Quality Standards Act, he interpreted about 5,000 mammograms per year in his office. In this case, he failed to detect a small breast tumor in May 2009. He also failed to perform testing when the patient reported nipple discharge. A more timely diagnosis of breast cancer at Stage I would have provided a 90% chance of long-term survival.
DEFENDANTS' DEFENSE: The defense held the radiologist fully liable because the surgeon was not a qualified interpreter of mammography, therefore relying on the radiologist’s interpretation. The radiologist was legally responsible for the missed diagnosis.
VERDICT: A $15M New York verdict was reached, finding the breast surgeon 75% at fault and the radiologist 25%. The radiologist settled before the trial (the jury was not informed of this). The breast surgeon was responsible for $11.25M. The defense indicated intent to appeal.
Alleged failure to evacuate uterus after cesarean delivery
A 37-year-old woman underwent cesarean delivery (CD) performed by 2 ObGyns. After delivery, she began to hemorrhage and the uterus became atonic. Hysterectomy was performed but the bleeding did not stop. The ObGyns called in 3 other ObGyns. During exploratory laparotomy, the bleeding was halted.
PATIENT'S CLAIM: She and her husband had hoped to have more children but the hysterectomy precluded that. She sued all 5 ObGyns, alleging that the delivering ObGyns failed to properly perform the CD and that each physician failed to properly perform the laparotomy, causing a large scar. The claim was discontinued against the 3 surgical ObGyns; trial addressed the 2 delivering ObGyns.
The patient’s expert ObGyn remarked that the hemorrhage was caused by a small placental remnant that remained in the uterus as a result of inadequate evacuation following delivery. The presence of the remnant was indicated by the uterine atony and should have prompted immediate investigation. The physicians’ notes did not document exploration of the uterus prior to closure.
PHYSICIAN'S DEFENSE: The defense’s expert contended that atony would not be a result of a small remnant of placenta. The patient’s uterus was properly evacuated, the hemorrhage was an unforeseeable complication, and the ObGyns properly addressed the hemorrhage.
VERDICT: A New York defense verdict was returned.
Alleged bowel injury during hysterectomy
Two days after a woman underwent a hysterectomy performed by her ObGyn, she went to the emergency department with increasing pain. Her ObGyn admitted her to the hospital. A general surgeon performed an exploratory laparotomy the next day that revealed an abscess; a 1-cm perforation of the patient’s bowel was surgically repaired. The patient had a difficult recovery. She developed pneumonia and respiratory failure. She underwent multiple repair surgeries for recurrent abscesses and fistulas because the wound was slow to heal.
PATIENT'S CLAIM: The ObGyn’s surgical technique was negligent. He injured the bowel when inserting a trocar and did not identify the injury in a timely manner. The expert witness commented that such an injury can sometimes be a surgical complication, but not in this case: the ObGyn rushed the procedure because he had another patient waiting for CD at another hospital.
PHYSICIAN'S DEFENSE: The ObGyn denied negligence and contended that the trocar used in surgery was too blunt to have caused a perforation. It would have been obvious to the ObGyn during surgery if a perforation had occurred. The perforation developed days after surgery within an abscess.
VERDICT: A Mississippi defense verdict was returned.
These cases were selected by the editors of OBG Management from Medical Malpractice Verdicts, Settlements & Experts, with permission of the editor, Lewis Laska (www.verdictslaska.com). The information available to the editors about the cases presented here is sometimes incomplete. Moreover, the cases may or may not have merit. Nevertheless, these cases represent the types of clinical situations that typically result in litigation and are meant to illustrate nationwide variation in jury verdicts and awards.
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
Delayed diagnosis of breast cancer: $15M award
A woman in her mid-50s had been seen by a breast surgeon for 16 years for regular mammograms and sonograms. In May 2009, the breast surgeon misinterpreted a mammogram as negative, as did a radiologist who re-read the mammogram weeks later. In December 2010, the patient returned to the breast surgeon with nipple discharge. No further testing was conducted. In October 2011, the patient was found to have Stage IIIA breast cancer involving 4 lymph nodes. She underwent left radical mastectomy, chemotherapy, radiation therapy, and breast reconstruction. At time of trial, the cancer had invaded her vertebrae, was Stage IV, and most likely incurable.
PATIENT'S CLAIM: Although the surgeon admittedly did not possess the qualifications required under the Mammography Quality Standards Act, he interpreted about 5,000 mammograms per year in his office. In this case, he failed to detect a small breast tumor in May 2009. He also failed to perform testing when the patient reported nipple discharge. A more timely diagnosis of breast cancer at Stage I would have provided a 90% chance of long-term survival.
DEFENDANTS' DEFENSE: The defense held the radiologist fully liable because the surgeon was not a qualified interpreter of mammography, therefore relying on the radiologist’s interpretation. The radiologist was legally responsible for the missed diagnosis.
VERDICT: A $15M New York verdict was reached, finding the breast surgeon 75% at fault and the radiologist 25%. The radiologist settled before the trial (the jury was not informed of this). The breast surgeon was responsible for $11.25M. The defense indicated intent to appeal.
Alleged failure to evacuate uterus after cesarean delivery
A 37-year-old woman underwent cesarean delivery (CD) performed by 2 ObGyns. After delivery, she began to hemorrhage and the uterus became atonic. Hysterectomy was performed but the bleeding did not stop. The ObGyns called in 3 other ObGyns. During exploratory laparotomy, the bleeding was halted.
PATIENT'S CLAIM: She and her husband had hoped to have more children but the hysterectomy precluded that. She sued all 5 ObGyns, alleging that the delivering ObGyns failed to properly perform the CD and that each physician failed to properly perform the laparotomy, causing a large scar. The claim was discontinued against the 3 surgical ObGyns; trial addressed the 2 delivering ObGyns.
The patient’s expert ObGyn remarked that the hemorrhage was caused by a small placental remnant that remained in the uterus as a result of inadequate evacuation following delivery. The presence of the remnant was indicated by the uterine atony and should have prompted immediate investigation. The physicians’ notes did not document exploration of the uterus prior to closure.
PHYSICIAN'S DEFENSE: The defense’s expert contended that atony would not be a result of a small remnant of placenta. The patient’s uterus was properly evacuated, the hemorrhage was an unforeseeable complication, and the ObGyns properly addressed the hemorrhage.
VERDICT: A New York defense verdict was returned.
Alleged bowel injury during hysterectomy
Two days after a woman underwent a hysterectomy performed by her ObGyn, she went to the emergency department with increasing pain. Her ObGyn admitted her to the hospital. A general surgeon performed an exploratory laparotomy the next day that revealed an abscess; a 1-cm perforation of the patient’s bowel was surgically repaired. The patient had a difficult recovery. She developed pneumonia and respiratory failure. She underwent multiple repair surgeries for recurrent abscesses and fistulas because the wound was slow to heal.
PATIENT'S CLAIM: The ObGyn’s surgical technique was negligent. He injured the bowel when inserting a trocar and did not identify the injury in a timely manner. The expert witness commented that such an injury can sometimes be a surgical complication, but not in this case: the ObGyn rushed the procedure because he had another patient waiting for CD at another hospital.
PHYSICIAN'S DEFENSE: The ObGyn denied negligence and contended that the trocar used in surgery was too blunt to have caused a perforation. It would have been obvious to the ObGyn during surgery if a perforation had occurred. The perforation developed days after surgery within an abscess.
VERDICT: A Mississippi defense verdict was returned.
These cases were selected by the editors of OBG Management from Medical Malpractice Verdicts, Settlements & Experts, with permission of the editor, Lewis Laska (www.verdictslaska.com). The information available to the editors about the cases presented here is sometimes incomplete. Moreover, the cases may or may not have merit. Nevertheless, these cases represent the types of clinical situations that typically result in litigation and are meant to illustrate nationwide variation in jury verdicts and awards.
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
Inherited mutations drive 12% of Nigerian breast cancer
About one in eight Nigerian women with breast cancer has an inherited mutation of the BRCA1, BRCA2, PALB2, or TP53 gene.
A new analysis of the Nigerian Breast Cancer Study confirmed that these inherited mutations drive about 12% of the country’s breast cancer cases. The findings could pave the way for the first large-scale national breast cancer gene screening program, wrote Olufunmilayo I. Olopade, MD, and her colleagues. The report is in the Journal of Clinical Oncology.
“We suggest that genomic sequencing to identify women at extremely high risk of breast cancer could be a highly innovative approach to tailored risk management and life-saving interventions,” wrote Dr. Olopade, director of the Center for Clinical Cancer Genetics at the University of Chicago, and her colleagues. “Nigeria now has data to prioritize the integration of genetic testing into its cancer control plan. Women with an extremely high risk of breast cancer because of mutations in these genes can be identified inexpensively and unambiguously and offered interventions to reduce cancer risk.”
And, since about half of the sisters and daughters of affected women will carry the same mutation, such a screening program could reach far beyond every index patient identified, the investigators noted.
“If these women at very high risk can be identified either through their relatives with breast cancer or in the general population, resources can be focused particularly on their behalf. For as-yet unaffected women at high genetic risk, these resources would be intensive surveillance for early detection of breast cancer and, after childbearing is completed, the possibility of preventive salpingo-oophorectomy. Integrated population screening for cancer for all women is the goal, but focused outreach to women at extremely high risk represents an especially efficient use of resources and an attainable evidence-based global health approach.”
The Nigerian Breast Cancer Study enrolled 1,136 women with invasive breast cancer from 1998 to 2014. These were compared with 997 women without cancer, matched from the same communities. Genetic sequencing searched for mutations in both known and breast cancer genes.
Cases and controls were a mean of 47 years old; only 6% of cases reported a family history of breast cancer. Of 577 patients with information on tumor stage, 86% (497) were diagnosed at stage III (241) or IV (256).
Among the cases, 167 (14.7%) carried a mutation in a breast cancer risk gene, compared with 1.8% of controls. BRCA1 was the most common mutation, occurring in 7% of patients; these women were 23 times more likely to develop breast cancer than were those without the gene (odds ratio, 23.4). BRCA2 was the next most common, occurring in 4% of cases and conferring a nearly 11-fold increased risk (OR, 10.76). PALB2 occurred in 11 cases (1%) and no controls, and TP53 in four cases (0.4%).
Women with the BRCA1 mutation were diagnosed at a significantly younger age than were other patients (42.6 vs. 47.9 years), as were carriers of the TP53 mutation (32.8 vs. 47.6 years).
Ten other genes (ATM, BARD1, BRIP1, CHEK1, CHEK2, GEN1, NBN, RAD51C, RAD51D, and XRCC2) carried a mutation in at least one patient each. “When limited to mutations in the four high-risk genes, 11%-12% of cases in this study carried a loss-of-function variant.”
Dr. Olopade had no financial disclosures.
SOURCE: Olopade et al. J Clin Oncol. 2018 Aug 21. doi: 10.1200/JCO.2018.78.3977.
The findings of the Nigerian Breast Cancer Study make a case for large-scale breast cancer gene screening. But even in a wealthy country with good infrastructure, such a program would be dauntingly complex, Ophira Ginsburg, MD, and Paul Brennan, PhD, wrote in an accompanying editorial.
“Given the estimated 40,983 women in Nigeria younger than age 65 years who will be newly diagnosed with breast cancer in 2030, the estimated mutation carrier frequency for a high-risk gene of 11%-12% translates to approximately 5,000 women with breast cancer each year who might benefit directly from tailored risk-reducing strategies. Moreover, 50% of these women’s sisters and daughters would also stand to benefit,” they wrote.
However, 32 million women would need to be screened to find the 220,000 with one of the mutations – a task that is “clearly beyond the scope of most countries.
“Furthermore, women with pathogenic variants would require intensive follow-up and intervention strategies to reduce their risk of developing breast, ovarian/fallopian tube, and potentially other cancers depending on the gene involved. Importantly, this approach would not address the larger problem of the high breast cancer mortality among the vast majority of women without a pathogenic variant but who make up approximately 85% of the breast cancer burden.”
The World Health Organization recognizes this challenge; the agency doesn’t even recommend mammogram-based population screening unless there is a basic, reliable infrastructure including electricity, quality-assurance measures, referral and recall mechanisms, and monitoring and evaluation frameworks. But WHO does suggest some core elements to guide a country’s comprehensive cancer management strategy, including:
• Considering the whole continuum from prevention to palliation.
• Providing a sustainable strategic plan on the basis of the country’s cancer burden, risk factor prevalence, and the resources available to implement the plan.
• Developing an evidence-based approach generated by population-based cancer registries.
“As many countries improve their cancer systems, investing in human resources, infrastructure, monitoring, and evaluation, it is timely to consider how to evaluate readiness to undertake a population-level cancer genetics intervention and consider the core elements that should be in place to make a substantive effect on cancer mortality.”
Dr. Ginsburg is with the Perlmutter Cancer Center of New York University. Dr. Brennan is with the International Agency for Research on Cancer, Lyon, France.
The findings of the Nigerian Breast Cancer Study make a case for large-scale breast cancer gene screening. But even in a wealthy country with good infrastructure, such a program would be dauntingly complex, Ophira Ginsburg, MD, and Paul Brennan, PhD, wrote in an accompanying editorial.
“Given the estimated 40,983 women in Nigeria younger than age 65 years who will be newly diagnosed with breast cancer in 2030, the estimated mutation carrier frequency for a high-risk gene of 11%-12% translates to approximately 5,000 women with breast cancer each year who might benefit directly from tailored risk-reducing strategies. Moreover, 50% of these women’s sisters and daughters would also stand to benefit,” they wrote.
However, 32 million women would need to be screened to find the 220,000 with one of the mutations – a task that is “clearly beyond the scope of most countries.
“Furthermore, women with pathogenic variants would require intensive follow-up and intervention strategies to reduce their risk of developing breast, ovarian/fallopian tube, and potentially other cancers depending on the gene involved. Importantly, this approach would not address the larger problem of the high breast cancer mortality among the vast majority of women without a pathogenic variant but who make up approximately 85% of the breast cancer burden.”
The World Health Organization recognizes this challenge; the agency doesn’t even recommend mammogram-based population screening unless there is a basic, reliable infrastructure including electricity, quality-assurance measures, referral and recall mechanisms, and monitoring and evaluation frameworks. But WHO does suggest some core elements to guide a country’s comprehensive cancer management strategy, including:
• Considering the whole continuum from prevention to palliation.
• Providing a sustainable strategic plan on the basis of the country’s cancer burden, risk factor prevalence, and the resources available to implement the plan.
• Developing an evidence-based approach generated by population-based cancer registries.
“As many countries improve their cancer systems, investing in human resources, infrastructure, monitoring, and evaluation, it is timely to consider how to evaluate readiness to undertake a population-level cancer genetics intervention and consider the core elements that should be in place to make a substantive effect on cancer mortality.”
Dr. Ginsburg is with the Perlmutter Cancer Center of New York University. Dr. Brennan is with the International Agency for Research on Cancer, Lyon, France.
The findings of the Nigerian Breast Cancer Study make a case for large-scale breast cancer gene screening. But even in a wealthy country with good infrastructure, such a program would be dauntingly complex, Ophira Ginsburg, MD, and Paul Brennan, PhD, wrote in an accompanying editorial.
“Given the estimated 40,983 women in Nigeria younger than age 65 years who will be newly diagnosed with breast cancer in 2030, the estimated mutation carrier frequency for a high-risk gene of 11%-12% translates to approximately 5,000 women with breast cancer each year who might benefit directly from tailored risk-reducing strategies. Moreover, 50% of these women’s sisters and daughters would also stand to benefit,” they wrote.
However, 32 million women would need to be screened to find the 220,000 with one of the mutations – a task that is “clearly beyond the scope of most countries.
“Furthermore, women with pathogenic variants would require intensive follow-up and intervention strategies to reduce their risk of developing breast, ovarian/fallopian tube, and potentially other cancers depending on the gene involved. Importantly, this approach would not address the larger problem of the high breast cancer mortality among the vast majority of women without a pathogenic variant but who make up approximately 85% of the breast cancer burden.”
The World Health Organization recognizes this challenge; the agency doesn’t even recommend mammogram-based population screening unless there is a basic, reliable infrastructure including electricity, quality-assurance measures, referral and recall mechanisms, and monitoring and evaluation frameworks. But WHO does suggest some core elements to guide a country’s comprehensive cancer management strategy, including:
• Considering the whole continuum from prevention to palliation.
• Providing a sustainable strategic plan on the basis of the country’s cancer burden, risk factor prevalence, and the resources available to implement the plan.
• Developing an evidence-based approach generated by population-based cancer registries.
“As many countries improve their cancer systems, investing in human resources, infrastructure, monitoring, and evaluation, it is timely to consider how to evaluate readiness to undertake a population-level cancer genetics intervention and consider the core elements that should be in place to make a substantive effect on cancer mortality.”
Dr. Ginsburg is with the Perlmutter Cancer Center of New York University. Dr. Brennan is with the International Agency for Research on Cancer, Lyon, France.
About one in eight Nigerian women with breast cancer has an inherited mutation of the BRCA1, BRCA2, PALB2, or TP53 gene.
A new analysis of the Nigerian Breast Cancer Study confirmed that these inherited mutations drive about 12% of the country’s breast cancer cases. The findings could pave the way for the first large-scale national breast cancer gene screening program, wrote Olufunmilayo I. Olopade, MD, and her colleagues. The report is in the Journal of Clinical Oncology.
“We suggest that genomic sequencing to identify women at extremely high risk of breast cancer could be a highly innovative approach to tailored risk management and life-saving interventions,” wrote Dr. Olopade, director of the Center for Clinical Cancer Genetics at the University of Chicago, and her colleagues. “Nigeria now has data to prioritize the integration of genetic testing into its cancer control plan. Women with an extremely high risk of breast cancer because of mutations in these genes can be identified inexpensively and unambiguously and offered interventions to reduce cancer risk.”
And, since about half of the sisters and daughters of affected women will carry the same mutation, such a screening program could reach far beyond every index patient identified, the investigators noted.
“If these women at very high risk can be identified either through their relatives with breast cancer or in the general population, resources can be focused particularly on their behalf. For as-yet unaffected women at high genetic risk, these resources would be intensive surveillance for early detection of breast cancer and, after childbearing is completed, the possibility of preventive salpingo-oophorectomy. Integrated population screening for cancer for all women is the goal, but focused outreach to women at extremely high risk represents an especially efficient use of resources and an attainable evidence-based global health approach.”
The Nigerian Breast Cancer Study enrolled 1,136 women with invasive breast cancer from 1998 to 2014. These were compared with 997 women without cancer, matched from the same communities. Genetic sequencing searched for mutations in both known and breast cancer genes.
Cases and controls were a mean of 47 years old; only 6% of cases reported a family history of breast cancer. Of 577 patients with information on tumor stage, 86% (497) were diagnosed at stage III (241) or IV (256).
Among the cases, 167 (14.7%) carried a mutation in a breast cancer risk gene, compared with 1.8% of controls. BRCA1 was the most common mutation, occurring in 7% of patients; these women were 23 times more likely to develop breast cancer than were those without the gene (odds ratio, 23.4). BRCA2 was the next most common, occurring in 4% of cases and conferring a nearly 11-fold increased risk (OR, 10.76). PALB2 occurred in 11 cases (1%) and no controls, and TP53 in four cases (0.4%).
Women with the BRCA1 mutation were diagnosed at a significantly younger age than were other patients (42.6 vs. 47.9 years), as were carriers of the TP53 mutation (32.8 vs. 47.6 years).
Ten other genes (ATM, BARD1, BRIP1, CHEK1, CHEK2, GEN1, NBN, RAD51C, RAD51D, and XRCC2) carried a mutation in at least one patient each. “When limited to mutations in the four high-risk genes, 11%-12% of cases in this study carried a loss-of-function variant.”
Dr. Olopade had no financial disclosures.
SOURCE: Olopade et al. J Clin Oncol. 2018 Aug 21. doi: 10.1200/JCO.2018.78.3977.
About one in eight Nigerian women with breast cancer has an inherited mutation of the BRCA1, BRCA2, PALB2, or TP53 gene.
A new analysis of the Nigerian Breast Cancer Study confirmed that these inherited mutations drive about 12% of the country’s breast cancer cases. The findings could pave the way for the first large-scale national breast cancer gene screening program, wrote Olufunmilayo I. Olopade, MD, and her colleagues. The report is in the Journal of Clinical Oncology.
“We suggest that genomic sequencing to identify women at extremely high risk of breast cancer could be a highly innovative approach to tailored risk management and life-saving interventions,” wrote Dr. Olopade, director of the Center for Clinical Cancer Genetics at the University of Chicago, and her colleagues. “Nigeria now has data to prioritize the integration of genetic testing into its cancer control plan. Women with an extremely high risk of breast cancer because of mutations in these genes can be identified inexpensively and unambiguously and offered interventions to reduce cancer risk.”
And, since about half of the sisters and daughters of affected women will carry the same mutation, such a screening program could reach far beyond every index patient identified, the investigators noted.
“If these women at very high risk can be identified either through their relatives with breast cancer or in the general population, resources can be focused particularly on their behalf. For as-yet unaffected women at high genetic risk, these resources would be intensive surveillance for early detection of breast cancer and, after childbearing is completed, the possibility of preventive salpingo-oophorectomy. Integrated population screening for cancer for all women is the goal, but focused outreach to women at extremely high risk represents an especially efficient use of resources and an attainable evidence-based global health approach.”
The Nigerian Breast Cancer Study enrolled 1,136 women with invasive breast cancer from 1998 to 2014. These were compared with 997 women without cancer, matched from the same communities. Genetic sequencing searched for mutations in both known and breast cancer genes.
Cases and controls were a mean of 47 years old; only 6% of cases reported a family history of breast cancer. Of 577 patients with information on tumor stage, 86% (497) were diagnosed at stage III (241) or IV (256).
Among the cases, 167 (14.7%) carried a mutation in a breast cancer risk gene, compared with 1.8% of controls. BRCA1 was the most common mutation, occurring in 7% of patients; these women were 23 times more likely to develop breast cancer than were those without the gene (odds ratio, 23.4). BRCA2 was the next most common, occurring in 4% of cases and conferring a nearly 11-fold increased risk (OR, 10.76). PALB2 occurred in 11 cases (1%) and no controls, and TP53 in four cases (0.4%).
Women with the BRCA1 mutation were diagnosed at a significantly younger age than were other patients (42.6 vs. 47.9 years), as were carriers of the TP53 mutation (32.8 vs. 47.6 years).
Ten other genes (ATM, BARD1, BRIP1, CHEK1, CHEK2, GEN1, NBN, RAD51C, RAD51D, and XRCC2) carried a mutation in at least one patient each. “When limited to mutations in the four high-risk genes, 11%-12% of cases in this study carried a loss-of-function variant.”
Dr. Olopade had no financial disclosures.
SOURCE: Olopade et al. J Clin Oncol. 2018 Aug 21. doi: 10.1200/JCO.2018.78.3977.
FROM THE JOURNAL OF CLINICAL ONCOLOGY
Key clinical point: Loss-of-function mutations in four breast cancer risk genes account for much of the disease among Nigerian women with the disease.
Major finding: Inherited mutations of the BRCA1, BRCA2, PALB2, or TP53 gene account for 12% of breast cancer in Nigerian women.
Study details: The Nigerian Breast Cancer Study comprised 1,136 women with invasive breast cancer and 997 controls.
Disclosures: Dr. Olopade had no financial disclosures. The study was largely funded by the National Institutes of Health and the Susan G Komen Foundation.
Source: Olopade et al. J Clin Oncol. 2018 Aug 21. doi: 10.1200/JCO.2018.78.3977.
Neratinib extends adjuvant treatment of patients with HER2-positive breast cancer
The small-molecule tyrosine kinase inhibitor neratinib is now approved for the extended adjuvant treatment of patients with early-stage HER2 [human epidermal growth factor receptor]-positive breast cancer following postoperative trastuzumab. Trastuzumab is a HER2-targeted monoclonal antibody that has become standard of care in combination with chemotherapy for the treatment of this patient population in which it significantly improves survival. However, disease recurrence will occur in about a quarter of trastuzumab-treated patients owing to the development of resistance.
Neratinib may help overcome trastuzumab resistance thanks to its potent inhibition of the downstream phosphorylation of HER2 and other members of the HER family. Its approval was based on the phase 3 ExteNET trial, in which extended adjuvant treatment with neratinib was compared with placebo among 2,840 patients who remained disease free after 1 year of adjuvant trastuzumab.1
The ExteNET trial was performed at 495 centers in Europe, Asia, Australia, New Zealand, and South America. Patients aged 18 years or older (≥20 years in Japan), with stage 1-3 HER2-positive breast cancer, who completed neoadjuvant and adjuvant trastuzumab therapy up to 1 year before randomization were eligible. Patients also had an Eastern Cooperative Oncology Group Performance Status of 0 or 1 (range, 0-5; 0, fully active, and 5, dead), normal organ function, and a left ventricular ejection fraction within normal institutional range. Patients with clinically significant cardiac, gastrointesintal or psychiatric comorbidities and those who were not able to swallow oral medication were excluded from the study.
Patients randomly received oral neratinib 240 mg per day or matching placebo, and randomization was stratified according to HR status (positive or negative), nodal status (0, 1-3, or ≥4) and trastuzumab-adjuvant regimen (sequentially or concurrently with chemotherapy).
The primary outcome was invasive disease-free survival (iDFS). The 2-year iDFS rate was 93.9% for neratinib, compared with 91.6% for placebo (hazard ratio [HR], 0.66; P < .008). Recently, a 5-year analysis of the ExteNET trial showed that after a median follow-up of 5.2 years, the iDFS rates were 90.2% vs 87.7% (HR, 0.73; P = .0083).2
Adverse events
The most common adverse event (AE) was diarrhea, in 95% of patients, 40% of whom had grade 3 diarrhea, leading to dose reduction in 26% of patients and discontinuation in 16.8% of patients. Serious AEs occurred in 7% of patients in the neratinib and 6% of those in the placebo arms. In the 5-year analysis, there was no evidence of increased risk of long-term toxicity or adverse consequences of neratinib-associated diarrhea. Furthermore, the ongoing, open-label phase 2 CONTROL trial suggests that the occurrence and severity of neratinib-associated diarrhea can be effectively controlled with antidiarrheal prophylaxis, with drugs such as loperamide.3
At the January 2017 cut-off, 137 patients treated with neratinib (240 mg/day) for 1 year had also received treatment with loperamide monotherapy, 64 patients had received loperamide and budesonide, and 10 patients had received loperamide and colestipol. The safety data from the loperamide monotherapy arm were compared with the safety data from the ExteNET trial, which was based in a similar population of patients who did not receive antidiarrheal prophylaxis. The incidence of all-grade diarrhea was 77% vs 95%, respectively, for those who received antidiarrheal prophylaxis in the CONTROL trial compared with those in the ExteNET trial who did not, and the repective rates of grade 3 diarrhea were 31% and 40%. The rate of dose reductions and holds owing to diarrhea were also lower among those who received antidiarrheal prophylaxis, but the rate of discontinuation due to diarrhea was higher in the loperamide-treated cohort.
Warnings and precautions
Neratinib is marketed as Nerlynx by Puma Biotechnology Inc. The prescribing information describes warnings and precautions relating to diarrhea, hepatotoxicity, and embryofetal toxicity. Patients should be monitored for diarrhea and treated with antidiarrheals as needed. Severe diarrhea with dehydration should be treated with fluids and electrolytes as needed, treatment should be interrupted and resumed at a reduced dose. For grade 3/4 diarrhea or diarrhea with complicating features (eg, dehydration, fever, neutropenia), stool cultures should be performed to rule out infectious causes.
Total bilirubin, aspartate and alanine aminotransferase, and alkaline phosphatase levels should be measured before starting treatment, every 3 months during treatment, or as clinically indicated. Neratinib can cause fetal harm, so pregnant women should be advised of the risk to the fetus and patients of reproductive potential should be counseled on the need for effective contraception during treatment and for at least 1 month after the last dose.4
1. Chan A, Delaloge S, Holmes FA, et al. Neratinib after trastuzumab-based adjuvant therapy in patients with HER2-positive breast cancer (ExteNET): a multicentre, randomised, double-blind, placebo-controlled, phase 3 trial. Lancet Oncol. 2016;17: 367-377.
2. Martin M, Holmes FA, Ejlertsen B, et al. Neratinib after trastuzumab- based adjuvant therapy in HER2-positive breast cancer (ExteNET): a 5-year analysis of a randomised, double-blind, placebo- controlled, phase 3 trial. Lancet Oncol. 2017;18(12):1688-1700.
3. Ibrahim E, Tripathy D, Wilkinson M, et al. E£ects of adding budesonide or colestipol to loperamide prophylaxis on neratinib-associated diarrhea in patients (pts) with HER2+ early-stage breast cancer (EBC): The CONTROL trial. Cancer Res. 2017; 77(13 supplement): Abstract CT128.
4. Nerlynx (neratinib) tablets, for oral use. Prescribing information. Puma Biotechnology Inc. https://nerlynx.com/pdf/full-prescribinginformation. pdf. Revised July 2017. Accessed November 20th, 2017.
The small-molecule tyrosine kinase inhibitor neratinib is now approved for the extended adjuvant treatment of patients with early-stage HER2 [human epidermal growth factor receptor]-positive breast cancer following postoperative trastuzumab. Trastuzumab is a HER2-targeted monoclonal antibody that has become standard of care in combination with chemotherapy for the treatment of this patient population in which it significantly improves survival. However, disease recurrence will occur in about a quarter of trastuzumab-treated patients owing to the development of resistance.
Neratinib may help overcome trastuzumab resistance thanks to its potent inhibition of the downstream phosphorylation of HER2 and other members of the HER family. Its approval was based on the phase 3 ExteNET trial, in which extended adjuvant treatment with neratinib was compared with placebo among 2,840 patients who remained disease free after 1 year of adjuvant trastuzumab.1
The ExteNET trial was performed at 495 centers in Europe, Asia, Australia, New Zealand, and South America. Patients aged 18 years or older (≥20 years in Japan), with stage 1-3 HER2-positive breast cancer, who completed neoadjuvant and adjuvant trastuzumab therapy up to 1 year before randomization were eligible. Patients also had an Eastern Cooperative Oncology Group Performance Status of 0 or 1 (range, 0-5; 0, fully active, and 5, dead), normal organ function, and a left ventricular ejection fraction within normal institutional range. Patients with clinically significant cardiac, gastrointesintal or psychiatric comorbidities and those who were not able to swallow oral medication were excluded from the study.
Patients randomly received oral neratinib 240 mg per day or matching placebo, and randomization was stratified according to HR status (positive or negative), nodal status (0, 1-3, or ≥4) and trastuzumab-adjuvant regimen (sequentially or concurrently with chemotherapy).
The primary outcome was invasive disease-free survival (iDFS). The 2-year iDFS rate was 93.9% for neratinib, compared with 91.6% for placebo (hazard ratio [HR], 0.66; P < .008). Recently, a 5-year analysis of the ExteNET trial showed that after a median follow-up of 5.2 years, the iDFS rates were 90.2% vs 87.7% (HR, 0.73; P = .0083).2
Adverse events
The most common adverse event (AE) was diarrhea, in 95% of patients, 40% of whom had grade 3 diarrhea, leading to dose reduction in 26% of patients and discontinuation in 16.8% of patients. Serious AEs occurred in 7% of patients in the neratinib and 6% of those in the placebo arms. In the 5-year analysis, there was no evidence of increased risk of long-term toxicity or adverse consequences of neratinib-associated diarrhea. Furthermore, the ongoing, open-label phase 2 CONTROL trial suggests that the occurrence and severity of neratinib-associated diarrhea can be effectively controlled with antidiarrheal prophylaxis, with drugs such as loperamide.3
At the January 2017 cut-off, 137 patients treated with neratinib (240 mg/day) for 1 year had also received treatment with loperamide monotherapy, 64 patients had received loperamide and budesonide, and 10 patients had received loperamide and colestipol. The safety data from the loperamide monotherapy arm were compared with the safety data from the ExteNET trial, which was based in a similar population of patients who did not receive antidiarrheal prophylaxis. The incidence of all-grade diarrhea was 77% vs 95%, respectively, for those who received antidiarrheal prophylaxis in the CONTROL trial compared with those in the ExteNET trial who did not, and the repective rates of grade 3 diarrhea were 31% and 40%. The rate of dose reductions and holds owing to diarrhea were also lower among those who received antidiarrheal prophylaxis, but the rate of discontinuation due to diarrhea was higher in the loperamide-treated cohort.
Warnings and precautions
Neratinib is marketed as Nerlynx by Puma Biotechnology Inc. The prescribing information describes warnings and precautions relating to diarrhea, hepatotoxicity, and embryofetal toxicity. Patients should be monitored for diarrhea and treated with antidiarrheals as needed. Severe diarrhea with dehydration should be treated with fluids and electrolytes as needed, treatment should be interrupted and resumed at a reduced dose. For grade 3/4 diarrhea or diarrhea with complicating features (eg, dehydration, fever, neutropenia), stool cultures should be performed to rule out infectious causes.
Total bilirubin, aspartate and alanine aminotransferase, and alkaline phosphatase levels should be measured before starting treatment, every 3 months during treatment, or as clinically indicated. Neratinib can cause fetal harm, so pregnant women should be advised of the risk to the fetus and patients of reproductive potential should be counseled on the need for effective contraception during treatment and for at least 1 month after the last dose.4
The small-molecule tyrosine kinase inhibitor neratinib is now approved for the extended adjuvant treatment of patients with early-stage HER2 [human epidermal growth factor receptor]-positive breast cancer following postoperative trastuzumab. Trastuzumab is a HER2-targeted monoclonal antibody that has become standard of care in combination with chemotherapy for the treatment of this patient population in which it significantly improves survival. However, disease recurrence will occur in about a quarter of trastuzumab-treated patients owing to the development of resistance.
Neratinib may help overcome trastuzumab resistance thanks to its potent inhibition of the downstream phosphorylation of HER2 and other members of the HER family. Its approval was based on the phase 3 ExteNET trial, in which extended adjuvant treatment with neratinib was compared with placebo among 2,840 patients who remained disease free after 1 year of adjuvant trastuzumab.1
The ExteNET trial was performed at 495 centers in Europe, Asia, Australia, New Zealand, and South America. Patients aged 18 years or older (≥20 years in Japan), with stage 1-3 HER2-positive breast cancer, who completed neoadjuvant and adjuvant trastuzumab therapy up to 1 year before randomization were eligible. Patients also had an Eastern Cooperative Oncology Group Performance Status of 0 or 1 (range, 0-5; 0, fully active, and 5, dead), normal organ function, and a left ventricular ejection fraction within normal institutional range. Patients with clinically significant cardiac, gastrointesintal or psychiatric comorbidities and those who were not able to swallow oral medication were excluded from the study.
Patients randomly received oral neratinib 240 mg per day or matching placebo, and randomization was stratified according to HR status (positive or negative), nodal status (0, 1-3, or ≥4) and trastuzumab-adjuvant regimen (sequentially or concurrently with chemotherapy).
The primary outcome was invasive disease-free survival (iDFS). The 2-year iDFS rate was 93.9% for neratinib, compared with 91.6% for placebo (hazard ratio [HR], 0.66; P < .008). Recently, a 5-year analysis of the ExteNET trial showed that after a median follow-up of 5.2 years, the iDFS rates were 90.2% vs 87.7% (HR, 0.73; P = .0083).2
Adverse events
The most common adverse event (AE) was diarrhea, in 95% of patients, 40% of whom had grade 3 diarrhea, leading to dose reduction in 26% of patients and discontinuation in 16.8% of patients. Serious AEs occurred in 7% of patients in the neratinib and 6% of those in the placebo arms. In the 5-year analysis, there was no evidence of increased risk of long-term toxicity or adverse consequences of neratinib-associated diarrhea. Furthermore, the ongoing, open-label phase 2 CONTROL trial suggests that the occurrence and severity of neratinib-associated diarrhea can be effectively controlled with antidiarrheal prophylaxis, with drugs such as loperamide.3
At the January 2017 cut-off, 137 patients treated with neratinib (240 mg/day) for 1 year had also received treatment with loperamide monotherapy, 64 patients had received loperamide and budesonide, and 10 patients had received loperamide and colestipol. The safety data from the loperamide monotherapy arm were compared with the safety data from the ExteNET trial, which was based in a similar population of patients who did not receive antidiarrheal prophylaxis. The incidence of all-grade diarrhea was 77% vs 95%, respectively, for those who received antidiarrheal prophylaxis in the CONTROL trial compared with those in the ExteNET trial who did not, and the repective rates of grade 3 diarrhea were 31% and 40%. The rate of dose reductions and holds owing to diarrhea were also lower among those who received antidiarrheal prophylaxis, but the rate of discontinuation due to diarrhea was higher in the loperamide-treated cohort.
Warnings and precautions
Neratinib is marketed as Nerlynx by Puma Biotechnology Inc. The prescribing information describes warnings and precautions relating to diarrhea, hepatotoxicity, and embryofetal toxicity. Patients should be monitored for diarrhea and treated with antidiarrheals as needed. Severe diarrhea with dehydration should be treated with fluids and electrolytes as needed, treatment should be interrupted and resumed at a reduced dose. For grade 3/4 diarrhea or diarrhea with complicating features (eg, dehydration, fever, neutropenia), stool cultures should be performed to rule out infectious causes.
Total bilirubin, aspartate and alanine aminotransferase, and alkaline phosphatase levels should be measured before starting treatment, every 3 months during treatment, or as clinically indicated. Neratinib can cause fetal harm, so pregnant women should be advised of the risk to the fetus and patients of reproductive potential should be counseled on the need for effective contraception during treatment and for at least 1 month after the last dose.4
1. Chan A, Delaloge S, Holmes FA, et al. Neratinib after trastuzumab-based adjuvant therapy in patients with HER2-positive breast cancer (ExteNET): a multicentre, randomised, double-blind, placebo-controlled, phase 3 trial. Lancet Oncol. 2016;17: 367-377.
2. Martin M, Holmes FA, Ejlertsen B, et al. Neratinib after trastuzumab- based adjuvant therapy in HER2-positive breast cancer (ExteNET): a 5-year analysis of a randomised, double-blind, placebo- controlled, phase 3 trial. Lancet Oncol. 2017;18(12):1688-1700.
3. Ibrahim E, Tripathy D, Wilkinson M, et al. E£ects of adding budesonide or colestipol to loperamide prophylaxis on neratinib-associated diarrhea in patients (pts) with HER2+ early-stage breast cancer (EBC): The CONTROL trial. Cancer Res. 2017; 77(13 supplement): Abstract CT128.
4. Nerlynx (neratinib) tablets, for oral use. Prescribing information. Puma Biotechnology Inc. https://nerlynx.com/pdf/full-prescribinginformation. pdf. Revised July 2017. Accessed November 20th, 2017.
1. Chan A, Delaloge S, Holmes FA, et al. Neratinib after trastuzumab-based adjuvant therapy in patients with HER2-positive breast cancer (ExteNET): a multicentre, randomised, double-blind, placebo-controlled, phase 3 trial. Lancet Oncol. 2016;17: 367-377.
2. Martin M, Holmes FA, Ejlertsen B, et al. Neratinib after trastuzumab- based adjuvant therapy in HER2-positive breast cancer (ExteNET): a 5-year analysis of a randomised, double-blind, placebo- controlled, phase 3 trial. Lancet Oncol. 2017;18(12):1688-1700.
3. Ibrahim E, Tripathy D, Wilkinson M, et al. E£ects of adding budesonide or colestipol to loperamide prophylaxis on neratinib-associated diarrhea in patients (pts) with HER2+ early-stage breast cancer (EBC): The CONTROL trial. Cancer Res. 2017; 77(13 supplement): Abstract CT128.
4. Nerlynx (neratinib) tablets, for oral use. Prescribing information. Puma Biotechnology Inc. https://nerlynx.com/pdf/full-prescribinginformation. pdf. Revised July 2017. Accessed November 20th, 2017.
Meeting the potential of immunotherapy: new targets provide rational combinations
The relationship between the immune system and tumors is complex and dynamic, and for immunotherapy to reach its full potential it will likely need to attack on multiple fronts. Here, we discuss some of the latest and most promising developments in the immuno-oncology field designed to build on the successes and address limitations.
The anti-tumor immune response
Cancer is a disease of genomic instability, whereby genetic alterations ranging from a single nucleotide to the whole chromosome level frequently occur. Although cancers derive from a patient’s own tissues, these genetic differences can mark the cancer cell as non-self, triggering an immune response to eliminate these cells.
The first hints of this anti-tumor immunity date back more than a century and a half and sparked the concept of mobilizing the immune system to treat patients.1-3 Although early pioneers achieved little progress in this regard, their efforts provided invaluable insights into the complex and dynamic relationship between a tumor and the immune system that are now translating into real clinical successes.
We now understand that the immune system has a dual role in both restraining and promoting cancer development and have translated this understanding into the theory of cancer immunoediting. Immunoediting has three stages: elimination, wherein the tumor is seemingly destroyed by the innate and adaptive immune response; equilibrium, in which cancer cells that were able to escape elimination are selected for growth; and escape, whereby these resistant cancer cells overwhelm the immune system and develop into a symptomatic lesion.4,5
Immuno-oncologists have also described the cancer immunity cycle to capture the steps that are required for an effective anti-tumor immune response and defects in this cycle form the basis of the most common mechanisms used by cancer cells to subvert the anti-tumor immune response. Much like the cancer hallmarks did for molecularly targeted cancer drugs, the cancer immunity cycle serves as the intellectual framework for cancer immunotherapy.6,7
Exploiting nature’s weapon of mass destruction
Initially, attempts at immunotherapy focused on boosting the immune response using adjuvants and cytokines. The characterization of subtle differences between tumor cells and normal cells led to the development of vaccines and cell-based therapies that exploited these tumor-associated antigens (TAAs).1-6
Despite the approval of a therapeutic vaccine, sipuleucel-T, in 2010 for the treatment of metastatic prostate cancer, in general the success of vaccines has been limited. Marketing authorization for sipuleucel-T was recently withdrawn in Europe, and although it is still available in the United States, it is not widely used because of issues with production and administration. Other vaccines, such as GVAX, which looked particularly promising in early-stage clinical trials, failed to show clinical efficacy in subsequent testing.8,9
Cell-based therapies, such as adoptive cellular therapy (ACT), in which immune cells are removed from the host, primed to attack cancer cells, and then reinfused back into the patient, have focused on T cells because they are the major effectors of the adaptive immune response. Clinical success with the most common approach, tumor-infiltrating lymphocyte (TIL)
Two key techniques have been developed (Figure 1). T-cell receptor (TCR) therapy involves genetically modifying the receptor on the surface of T cells that is responsible for recognizing antigens bound to major histocompatibility complex (MHC) molecules on the surface of antigen-presenting cells (APCs). The TCR can be altered to recognize a specific TAA or modified to improve its antigen recognition and binding capabilities. This type of therapy is limited by the fact that the TCRs need to be genetically matched to the patient’s immune type.
Releasing the brakes
To ensure that it is only activated at the appropriate time and not in response to the antigens expressed on the surface of the host’s own tissues or harmless materials, the immune system has developed numerous mechanisms for immunological tolerance. Cancer cells are able to exploit these mechanisms to allow them to evade the anti-tumor immune response. One of the main ways in which they do this is by manipulating the signaling pathways involved in T-cell activation, which play a vital role in tolerance.12
To become fully activated, T cells require a primary signal generated by an interaction between the TCR and the antigen-MHC complex on the surface of an APC, followed by secondary costimulatory signals generated by a range of different receptors present on the T-cell surface binding to their ligands on the APC.
If the second signal is inhibitory rather than stimulatory, then the T cell is deactivated instead of becoming activated. Two key coinhibitory receptors are programmed cell death 1 (PD-1) and cytotoxic T-lymphocyte antigen 4 (CTLA-4) and tumor cells are able to overcome the anti-tumor immune response in part by expressing the ligands that bind these receptors to dampen the activity of tumor-infiltrating T cells and induce tolerance.13
The development of inhibitors of CTLA-4 and PD-1 and their respective ligands has driven some of the most dramatic successes with cancer immunotherapy, particularly with PD-1-targeting drugs which have fewer side effects. Targeting of this pathway has resulted in durable responses, revolutionizing the treatment of metastatic melanoma, with recently published long-term survival data for pembrolizumab showing that 40% of patients were alive 3 years after initiating treatment and, in a separate study, 34% of nivolumab-treated patients were still alive after 5 years.14,15 More recently, PD-1 inhibitors have been slowly expanding into a range of other cancer types and 4 immune checkpoint inhibitors are now approved by the United States Food and Drug Administration (FDA): ipilimumab (Yervoy), nivolumab (Opdivo), pembrolizumab (Keytruda) and atezolizumab (Tecentriq).
Six years on from the first approval in this drug class and an extensive network of coinhibitory receptors has been uncovered – so-called immune checkpoints – many of which are now also serving as therapeutic targets (Table, Figure 2).16 Lymphocyte activation gene 3 (LAG-3) is a member of the immunoglobulin superfamily of receptors that is expressed on a number of different types of immune cell. In addition to negatively regulating cytotoxic T-cell activation like PD-1 and CTLA-4, it is also thought to regulate the immunosuppressive functions of regulatory T cells and the maturation and activation of dendritic cells. T-cell immunoglobulin and mucin domain-containing 3 (TIM-3) is found on the surface of helper and cytotoxic T cells and regulates T-cell inhibition as well as macrophage activation. Inhibitors of both proteins have been developed that are being evaluated in phase 1 or 2 clinical trials in a variety of tumor types.17
Indeed, although T cells have commanded the most attention, there is growing appreciation of the potential for targeting other types of immune cell that play a role in the anti-tumor immune response or in fostering an immunosuppressive microenvironment. NK cells have been a particular focus, since they represent the body’s first line of immune defense and they appear to have analogous inhibitory and activating receptors expressed on their surface that regulate their cytotoxic activity.
The best-defined NK cell receptors are the killer cell immunoglobulin-like receptors (KIRs) that bind to the MHC class I proteins found on the surface of all cells that distinguish them as ‘self’ or ‘non-self’. KIRs can be either activating or inhibitory, depending upon their structure and the ligands to which they bind.19 To date, 2 antibodies targeting inhibitory KIRs have been developed. Though there has been some disappointment with these drugs, most recently a phase 2 trial of lirilumab in elderly patients with acute myeloid leukemia, which missed its primary endpoint, they continue to be evaluated in clinical trials.20
The inhibitory immune checkpoint field has also expanded to include molecules that regulate T-cell activity in other ways. Most prominently, this includes enzymes like indoleamine-2,3 dioxygenase (IDO), which is involved in the metabolism of the essential amino acid tryptophan. IDO-induced depletion of tryptophan and generation of tryptophan metabolites is toxic to cytotoxic T cells, and IDO is also thought to directly activate regulatory T cells, thus the net effect of IDO is immunosuppression. Two IDO inhibitors are currently being developed.21
Stepping on the gas
Despite their unprecedented success, immune checkpoint inhibitors are not effective in all patients or in all tumor types. Their efficacy is limited in large part by the requirement for a pre-existing anti-tumor immune response. If there are no T cells within the tumor microenvironment then releasing the brakes on the immune system won’t help.
More recently, researchers have returned to the idea of stimulating an anti-tumor immune response, this time by targeting the other side of the immune checkpoint coin, the costimulatory molecules. These drugs could prove more effective as they aren’t reliant on a pre-existing anti-tumor immune response. A number of agonist antibodies designed to target these receptors have now been developed and are undergoing clinical evaluation.22
Furthest along in development are those targeting OX40, a costimulatory molecule that is upregulated on the surface of T cells once they have been fully activated by the TCR signal and an initial costimulatory signal. OX40 is thought to be involved in a more long-term immune response and in the formation of a memory response. A mouse monoclonal antibody had a potent immune-stimulating effect accompanied by the regression of at least 1 metastatic lesion in 30% of patients treated in a phase 1 clinical trial, but was limited by the generation of anti-mouse antibodies. 7 OX40 agonists are now in clinical development, 6 fully human monoclonal antibodies and 1 OX40 ligand-Fc fusion protein, MEDI-6383.23
Combinations are key
Many researchers are now reaching the conclusion that combination therapy is likely to be key in expanding the scope of immunotherapy into currently unresponsive patient populations. Investigating rational combinations is already becoming a burgeoning area of the immuno-oncology field, with a variety of different strategies being tested.
Now the question becomes what are the optimal combinations and the timing and sequencing of combination therapy is likely to be a paramount consideration. Developing combinations that have distinct mechanisms of action or target multiple steps in the cancer immunity cycle offers the greatest potential for therapeutic synergy since this is most likely to address potential mechanisms of resistance by blocking other paths to immune evasion for cancer cells (Figure 3).
Given the expanding network of immune-checkpoint inhibitors and agonists, the focal point of combination therapy has been combining immune checkpoint-targeting drugs with different mechanisms of action, including those that would simultaneously release the brakes and step on the gas pedal. The vast majority of ongoing clinical trials of approved checkpoint inhibitors and the drugs in development listed in the table are combination trials.
These efforts yielded the first FDA-approved combination immunotherapy regimen in 2015; nivolumab and ipilimumab for the treatment of metastatic melanoma. Approval was based on the demonstration of improved ORR, prolonged response duration, and improved progression-free survival among 142 patients treated with the combination, compared to either drug alone.24
The results of a phase 1/2 trial evaluating the combination of a 4-1BB receptor agonist urelumab with nivolumab in hematologic malignancies and solid tumors found the combination to be safe and particularly effective in patients with advanced/metastatic melanoma, with an ORR of 50%.25 Nivolumab was also combined with the CD27 agonist varlilumab in a phase 1/2 clinical trial of patients with solid tumors, for which data was also recently released. Among 46 patients enrolled, primarily those with colorectal and ovarian cancer the combination had an acceptable safety profile and favorable changes in intratumoral immune biomarkers were observed. The phase 2 portion of the trial is ongoing.26
Meanwhile, Incyte’s IDO inhibitor epacadostat has recently been making waves in combination with pembrolizumab in patients with advanced solid tumors. It demonstrated particularly promising clinical activity in patients with metastatic melanoma, with an overall response rate (ORR) of 57%, including 2 complete responses (CRs), prompting initiation of a phase 3 trial of this combination (NCT02752074).27
1. Adams JL, Smothers J, Srinivasan R, et al. Big opportunities for small molecules in immuno-oncology. Nat Rev Drug Disc. 2015;14:603-622.
2. D’Errico G, Machado HL, Sainz Jr B. A current perspective on cancer immune therapy: step-by-step approach to constructing the magic bullet. Clin Trans Med. 2017;6:3.
3. Farkona S, Diamandis EP, Blaustig IM. Cancer immunotherapy: the beginning of the end of cancer? BMC Med. 2016;14:73.
4. Meiliana A, Dewi NM, Wijaya A. Cancer immunotherapy: a review. Indones Biomed J. 2016;8(1):1-20.
5. Smyth MJ, Ngiow SF, Ribas A, et al. Combination cancer immunotherapies tailored to the tumor microenvironment. Nat Rev Clin Oncol. 2016;13:143-158.
6. de Charette M, Marabelle A, Houot R. Turning tumor cells into antigen presenting cells: The next step to improve cancer immunotherapy? Eur J Cancer 2016;68:134-147.
7. Chen DS and Mellman I. Oncology Meets Immunology: The Cancer-Immunity Cycle. Immunity 2013;39:1-10.
8. Mellman I, Coukos G, Dranoff G. Cancer immunotherapy comes of age. Nature 2011;480:480-489.
9. Le DT, Wang-Gillam A, Picozzi V Jr, et al. A phase 2, randomized trial of GVAX Pancreas and CRS-207 immunotherapy versus GVAX alone in patients with metastatic pancreatic adenocarcinoma: Updated results. Presented at: the ASCO Gastrointestinal Cancers Symposium; January 16-18, 2014; San Francisco, CA. Abstract 177.
10. Sharpe M and Mount N. Genetically modified T cells in cancer therapy: opportunities and challenges. Dis Model Mech. 2015;8(4):337-350.
11. Perica K, Varela JC, Oelke M, et al. Adoptive T Cell Immunotherapy for Cancer. Ram Mai Med J. 2015;6(1):e0004.
12. Xing Y and Hogquist KA. T-Cell Tolerance: Central and Peripheral. Cold Spring Harb Perspect Biol. 2012;4:a006957.
13. Buchbinder EI and Desai A. CTLA-4 and PD-1 Pathways: Similarities, Differences, and Implications of Their Inhibition. Am J Clin Oncol. 2016;39(1):98-106.
14. Robert C, Ribas A, Hamid O, et al. 3-year overall survival for patients with advanced melanoma treated with pembrolizumab in KEYNOTE-001. J Clin Oncol. 2016(suppl;abstr 9503).
15. Hodi SF, Kluger HM, Sznol M, et al. Durable, long-term survival in previously treated patients with advanced melanoma who received nivolumab monotherapy in a phase I trial. Presented at the 2016 AACR Annual Meeting; April 16-20; New Orleans, LA. Abstract CT001.
16. Bakdash G, Sittig SP, van Dijk T, et al. The nature of activatory and tolerogenic dendritic cell-derived signal II. Front Immunol. 2013;4(53):1-18.
17. Sheridan C. Immuno-oncology moves beyond PD-1. Nat Biotechnol. 2015;33(7):673-675.
18. Blake SJ, Dougall WC, Miles JJ, et al. Molecular pathways: targeting CD96 and TIGIT for cancer immunotherapy. Clin Cancer Res. 2016;22(21):5183-5188.
19. Carotta S. Targeting NK cells for anticancer immunotherapy: clinical and preclinical approaches. Front Immunol. 2016;7:152.
20. Innate Pharma Web site. Innate Pharma Announces Top-Line Results from EFFIKIR Trial Evaluating the Efficacy of Lirilumab as a Single Agent in Elderly Patients with Acute Myeloid Leukemia. http://www.innate-pharma.com/en/news-events/press-releases/innate-pharma-announces-top-line-results-effikir-trial-evaluating-efficacy-lirilumab-single-agent-elderly-patients-acute-myeloid-leukemia. Last updated February 6, 2017. Accessed online February 22, 2017.
21. Sheridan C. IDO inhibitors move center stage in immuno-oncology. Nat Biotechnol. 2015;33(4):321-322.
22. Sanmamed MF, Pastor F, Rodriguez A, et al. Agonists of co-stimulation in cancer immunotherapy directed against CD137, OX40, GITR, CD27, CD28, and ICOS. Semin Oncol. 2015;42(4):640-655.
23. Linch SN, McNamara MJ, Redmond WL. OX40 agonists and combination immunotherapy: putting the pedal to the metal. Front Oncol. 2015;5:34.
24. U.S. Food and Drug Administration Web site. Nivolumab in combination with ipilimumab. https://www.fda.gov/Drugs/InformationOnDrugs/ApprovedDrugs/ucm465274.htm. Last updated October 1, 2015. Accessed online February 22, 2017.
25. Massarelli E. Clinical safety and efficacy assessment of the CD137 agonist urelumab alone and in combination with nivolumab in patients with hematologic and solid tumor malignancies. Presented at the 31st Annual Meeting of the Society for the Immunotherapy of Cancer; November 9-13, 2016; National Harbor, MD. Abstract 239.
26. Sanborn RE, Pishvain MJ, Callahan MK, et al. Phase I results from the combination of an immune-activating anti-CD27 antibody (varlilumab) in combination with PD-1 blockade (nivolumab): activation across multiple immune pathways without untoward immune-related adverse events. Clin Cancer Res. 2016;76(14):suppl. Abstract CT023.
27. Gangadhar T, Hamid O, Smith D.C, et al. Epacadostat plus pembrolizumab in patients with advanced melanoma and select solid tumors: updated phase 1 results from ECHO-202/KEYNOTE-037. Ann Oncol. 2016;27(6):379-400.
The relationship between the immune system and tumors is complex and dynamic, and for immunotherapy to reach its full potential it will likely need to attack on multiple fronts. Here, we discuss some of the latest and most promising developments in the immuno-oncology field designed to build on the successes and address limitations.
The anti-tumor immune response
Cancer is a disease of genomic instability, whereby genetic alterations ranging from a single nucleotide to the whole chromosome level frequently occur. Although cancers derive from a patient’s own tissues, these genetic differences can mark the cancer cell as non-self, triggering an immune response to eliminate these cells.
The first hints of this anti-tumor immunity date back more than a century and a half and sparked the concept of mobilizing the immune system to treat patients.1-3 Although early pioneers achieved little progress in this regard, their efforts provided invaluable insights into the complex and dynamic relationship between a tumor and the immune system that are now translating into real clinical successes.
We now understand that the immune system has a dual role in both restraining and promoting cancer development and have translated this understanding into the theory of cancer immunoediting. Immunoediting has three stages: elimination, wherein the tumor is seemingly destroyed by the innate and adaptive immune response; equilibrium, in which cancer cells that were able to escape elimination are selected for growth; and escape, whereby these resistant cancer cells overwhelm the immune system and develop into a symptomatic lesion.4,5
Immuno-oncologists have also described the cancer immunity cycle to capture the steps that are required for an effective anti-tumor immune response and defects in this cycle form the basis of the most common mechanisms used by cancer cells to subvert the anti-tumor immune response. Much like the cancer hallmarks did for molecularly targeted cancer drugs, the cancer immunity cycle serves as the intellectual framework for cancer immunotherapy.6,7
Exploiting nature’s weapon of mass destruction
Initially, attempts at immunotherapy focused on boosting the immune response using adjuvants and cytokines. The characterization of subtle differences between tumor cells and normal cells led to the development of vaccines and cell-based therapies that exploited these tumor-associated antigens (TAAs).1-6
Despite the approval of a therapeutic vaccine, sipuleucel-T, in 2010 for the treatment of metastatic prostate cancer, in general the success of vaccines has been limited. Marketing authorization for sipuleucel-T was recently withdrawn in Europe, and although it is still available in the United States, it is not widely used because of issues with production and administration. Other vaccines, such as GVAX, which looked particularly promising in early-stage clinical trials, failed to show clinical efficacy in subsequent testing.8,9
Cell-based therapies, such as adoptive cellular therapy (ACT), in which immune cells are removed from the host, primed to attack cancer cells, and then reinfused back into the patient, have focused on T cells because they are the major effectors of the adaptive immune response. Clinical success with the most common approach, tumor-infiltrating lymphocyte (TIL)
Two key techniques have been developed (Figure 1). T-cell receptor (TCR) therapy involves genetically modifying the receptor on the surface of T cells that is responsible for recognizing antigens bound to major histocompatibility complex (MHC) molecules on the surface of antigen-presenting cells (APCs). The TCR can be altered to recognize a specific TAA or modified to improve its antigen recognition and binding capabilities. This type of therapy is limited by the fact that the TCRs need to be genetically matched to the patient’s immune type.
Releasing the brakes
To ensure that it is only activated at the appropriate time and not in response to the antigens expressed on the surface of the host’s own tissues or harmless materials, the immune system has developed numerous mechanisms for immunological tolerance. Cancer cells are able to exploit these mechanisms to allow them to evade the anti-tumor immune response. One of the main ways in which they do this is by manipulating the signaling pathways involved in T-cell activation, which play a vital role in tolerance.12
To become fully activated, T cells require a primary signal generated by an interaction between the TCR and the antigen-MHC complex on the surface of an APC, followed by secondary costimulatory signals generated by a range of different receptors present on the T-cell surface binding to their ligands on the APC.
If the second signal is inhibitory rather than stimulatory, then the T cell is deactivated instead of becoming activated. Two key coinhibitory receptors are programmed cell death 1 (PD-1) and cytotoxic T-lymphocyte antigen 4 (CTLA-4) and tumor cells are able to overcome the anti-tumor immune response in part by expressing the ligands that bind these receptors to dampen the activity of tumor-infiltrating T cells and induce tolerance.13
The development of inhibitors of CTLA-4 and PD-1 and their respective ligands has driven some of the most dramatic successes with cancer immunotherapy, particularly with PD-1-targeting drugs which have fewer side effects. Targeting of this pathway has resulted in durable responses, revolutionizing the treatment of metastatic melanoma, with recently published long-term survival data for pembrolizumab showing that 40% of patients were alive 3 years after initiating treatment and, in a separate study, 34% of nivolumab-treated patients were still alive after 5 years.14,15 More recently, PD-1 inhibitors have been slowly expanding into a range of other cancer types and 4 immune checkpoint inhibitors are now approved by the United States Food and Drug Administration (FDA): ipilimumab (Yervoy), nivolumab (Opdivo), pembrolizumab (Keytruda) and atezolizumab (Tecentriq).
Six years on from the first approval in this drug class and an extensive network of coinhibitory receptors has been uncovered – so-called immune checkpoints – many of which are now also serving as therapeutic targets (Table, Figure 2).16 Lymphocyte activation gene 3 (LAG-3) is a member of the immunoglobulin superfamily of receptors that is expressed on a number of different types of immune cell. In addition to negatively regulating cytotoxic T-cell activation like PD-1 and CTLA-4, it is also thought to regulate the immunosuppressive functions of regulatory T cells and the maturation and activation of dendritic cells. T-cell immunoglobulin and mucin domain-containing 3 (TIM-3) is found on the surface of helper and cytotoxic T cells and regulates T-cell inhibition as well as macrophage activation. Inhibitors of both proteins have been developed that are being evaluated in phase 1 or 2 clinical trials in a variety of tumor types.17
Indeed, although T cells have commanded the most attention, there is growing appreciation of the potential for targeting other types of immune cell that play a role in the anti-tumor immune response or in fostering an immunosuppressive microenvironment. NK cells have been a particular focus, since they represent the body’s first line of immune defense and they appear to have analogous inhibitory and activating receptors expressed on their surface that regulate their cytotoxic activity.
The best-defined NK cell receptors are the killer cell immunoglobulin-like receptors (KIRs) that bind to the MHC class I proteins found on the surface of all cells that distinguish them as ‘self’ or ‘non-self’. KIRs can be either activating or inhibitory, depending upon their structure and the ligands to which they bind.19 To date, 2 antibodies targeting inhibitory KIRs have been developed. Though there has been some disappointment with these drugs, most recently a phase 2 trial of lirilumab in elderly patients with acute myeloid leukemia, which missed its primary endpoint, they continue to be evaluated in clinical trials.20
The inhibitory immune checkpoint field has also expanded to include molecules that regulate T-cell activity in other ways. Most prominently, this includes enzymes like indoleamine-2,3 dioxygenase (IDO), which is involved in the metabolism of the essential amino acid tryptophan. IDO-induced depletion of tryptophan and generation of tryptophan metabolites is toxic to cytotoxic T cells, and IDO is also thought to directly activate regulatory T cells, thus the net effect of IDO is immunosuppression. Two IDO inhibitors are currently being developed.21
Stepping on the gas
Despite their unprecedented success, immune checkpoint inhibitors are not effective in all patients or in all tumor types. Their efficacy is limited in large part by the requirement for a pre-existing anti-tumor immune response. If there are no T cells within the tumor microenvironment then releasing the brakes on the immune system won’t help.
More recently, researchers have returned to the idea of stimulating an anti-tumor immune response, this time by targeting the other side of the immune checkpoint coin, the costimulatory molecules. These drugs could prove more effective as they aren’t reliant on a pre-existing anti-tumor immune response. A number of agonist antibodies designed to target these receptors have now been developed and are undergoing clinical evaluation.22
Furthest along in development are those targeting OX40, a costimulatory molecule that is upregulated on the surface of T cells once they have been fully activated by the TCR signal and an initial costimulatory signal. OX40 is thought to be involved in a more long-term immune response and in the formation of a memory response. A mouse monoclonal antibody had a potent immune-stimulating effect accompanied by the regression of at least 1 metastatic lesion in 30% of patients treated in a phase 1 clinical trial, but was limited by the generation of anti-mouse antibodies. 7 OX40 agonists are now in clinical development, 6 fully human monoclonal antibodies and 1 OX40 ligand-Fc fusion protein, MEDI-6383.23
Combinations are key
Many researchers are now reaching the conclusion that combination therapy is likely to be key in expanding the scope of immunotherapy into currently unresponsive patient populations. Investigating rational combinations is already becoming a burgeoning area of the immuno-oncology field, with a variety of different strategies being tested.
Now the question becomes what are the optimal combinations and the timing and sequencing of combination therapy is likely to be a paramount consideration. Developing combinations that have distinct mechanisms of action or target multiple steps in the cancer immunity cycle offers the greatest potential for therapeutic synergy since this is most likely to address potential mechanisms of resistance by blocking other paths to immune evasion for cancer cells (Figure 3).
Given the expanding network of immune-checkpoint inhibitors and agonists, the focal point of combination therapy has been combining immune checkpoint-targeting drugs with different mechanisms of action, including those that would simultaneously release the brakes and step on the gas pedal. The vast majority of ongoing clinical trials of approved checkpoint inhibitors and the drugs in development listed in the table are combination trials.
These efforts yielded the first FDA-approved combination immunotherapy regimen in 2015; nivolumab and ipilimumab for the treatment of metastatic melanoma. Approval was based on the demonstration of improved ORR, prolonged response duration, and improved progression-free survival among 142 patients treated with the combination, compared to either drug alone.24
The results of a phase 1/2 trial evaluating the combination of a 4-1BB receptor agonist urelumab with nivolumab in hematologic malignancies and solid tumors found the combination to be safe and particularly effective in patients with advanced/metastatic melanoma, with an ORR of 50%.25 Nivolumab was also combined with the CD27 agonist varlilumab in a phase 1/2 clinical trial of patients with solid tumors, for which data was also recently released. Among 46 patients enrolled, primarily those with colorectal and ovarian cancer the combination had an acceptable safety profile and favorable changes in intratumoral immune biomarkers were observed. The phase 2 portion of the trial is ongoing.26
Meanwhile, Incyte’s IDO inhibitor epacadostat has recently been making waves in combination with pembrolizumab in patients with advanced solid tumors. It demonstrated particularly promising clinical activity in patients with metastatic melanoma, with an overall response rate (ORR) of 57%, including 2 complete responses (CRs), prompting initiation of a phase 3 trial of this combination (NCT02752074).27
The relationship between the immune system and tumors is complex and dynamic, and for immunotherapy to reach its full potential it will likely need to attack on multiple fronts. Here, we discuss some of the latest and most promising developments in the immuno-oncology field designed to build on the successes and address limitations.
The anti-tumor immune response
Cancer is a disease of genomic instability, whereby genetic alterations ranging from a single nucleotide to the whole chromosome level frequently occur. Although cancers derive from a patient’s own tissues, these genetic differences can mark the cancer cell as non-self, triggering an immune response to eliminate these cells.
The first hints of this anti-tumor immunity date back more than a century and a half and sparked the concept of mobilizing the immune system to treat patients.1-3 Although early pioneers achieved little progress in this regard, their efforts provided invaluable insights into the complex and dynamic relationship between a tumor and the immune system that are now translating into real clinical successes.
We now understand that the immune system has a dual role in both restraining and promoting cancer development and have translated this understanding into the theory of cancer immunoediting. Immunoediting has three stages: elimination, wherein the tumor is seemingly destroyed by the innate and adaptive immune response; equilibrium, in which cancer cells that were able to escape elimination are selected for growth; and escape, whereby these resistant cancer cells overwhelm the immune system and develop into a symptomatic lesion.4,5
Immuno-oncologists have also described the cancer immunity cycle to capture the steps that are required for an effective anti-tumor immune response and defects in this cycle form the basis of the most common mechanisms used by cancer cells to subvert the anti-tumor immune response. Much like the cancer hallmarks did for molecularly targeted cancer drugs, the cancer immunity cycle serves as the intellectual framework for cancer immunotherapy.6,7
Exploiting nature’s weapon of mass destruction
Initially, attempts at immunotherapy focused on boosting the immune response using adjuvants and cytokines. The characterization of subtle differences between tumor cells and normal cells led to the development of vaccines and cell-based therapies that exploited these tumor-associated antigens (TAAs).1-6
Despite the approval of a therapeutic vaccine, sipuleucel-T, in 2010 for the treatment of metastatic prostate cancer, in general the success of vaccines has been limited. Marketing authorization for sipuleucel-T was recently withdrawn in Europe, and although it is still available in the United States, it is not widely used because of issues with production and administration. Other vaccines, such as GVAX, which looked particularly promising in early-stage clinical trials, failed to show clinical efficacy in subsequent testing.8,9
Cell-based therapies, such as adoptive cellular therapy (ACT), in which immune cells are removed from the host, primed to attack cancer cells, and then reinfused back into the patient, have focused on T cells because they are the major effectors of the adaptive immune response. Clinical success with the most common approach, tumor-infiltrating lymphocyte (TIL)
Two key techniques have been developed (Figure 1). T-cell receptor (TCR) therapy involves genetically modifying the receptor on the surface of T cells that is responsible for recognizing antigens bound to major histocompatibility complex (MHC) molecules on the surface of antigen-presenting cells (APCs). The TCR can be altered to recognize a specific TAA or modified to improve its antigen recognition and binding capabilities. This type of therapy is limited by the fact that the TCRs need to be genetically matched to the patient’s immune type.
Releasing the brakes
To ensure that it is only activated at the appropriate time and not in response to the antigens expressed on the surface of the host’s own tissues or harmless materials, the immune system has developed numerous mechanisms for immunological tolerance. Cancer cells are able to exploit these mechanisms to allow them to evade the anti-tumor immune response. One of the main ways in which they do this is by manipulating the signaling pathways involved in T-cell activation, which play a vital role in tolerance.12
To become fully activated, T cells require a primary signal generated by an interaction between the TCR and the antigen-MHC complex on the surface of an APC, followed by secondary costimulatory signals generated by a range of different receptors present on the T-cell surface binding to their ligands on the APC.
If the second signal is inhibitory rather than stimulatory, then the T cell is deactivated instead of becoming activated. Two key coinhibitory receptors are programmed cell death 1 (PD-1) and cytotoxic T-lymphocyte antigen 4 (CTLA-4) and tumor cells are able to overcome the anti-tumor immune response in part by expressing the ligands that bind these receptors to dampen the activity of tumor-infiltrating T cells and induce tolerance.13
The development of inhibitors of CTLA-4 and PD-1 and their respective ligands has driven some of the most dramatic successes with cancer immunotherapy, particularly with PD-1-targeting drugs which have fewer side effects. Targeting of this pathway has resulted in durable responses, revolutionizing the treatment of metastatic melanoma, with recently published long-term survival data for pembrolizumab showing that 40% of patients were alive 3 years after initiating treatment and, in a separate study, 34% of nivolumab-treated patients were still alive after 5 years.14,15 More recently, PD-1 inhibitors have been slowly expanding into a range of other cancer types and 4 immune checkpoint inhibitors are now approved by the United States Food and Drug Administration (FDA): ipilimumab (Yervoy), nivolumab (Opdivo), pembrolizumab (Keytruda) and atezolizumab (Tecentriq).
Six years on from the first approval in this drug class and an extensive network of coinhibitory receptors has been uncovered – so-called immune checkpoints – many of which are now also serving as therapeutic targets (Table, Figure 2).16 Lymphocyte activation gene 3 (LAG-3) is a member of the immunoglobulin superfamily of receptors that is expressed on a number of different types of immune cell. In addition to negatively regulating cytotoxic T-cell activation like PD-1 and CTLA-4, it is also thought to regulate the immunosuppressive functions of regulatory T cells and the maturation and activation of dendritic cells. T-cell immunoglobulin and mucin domain-containing 3 (TIM-3) is found on the surface of helper and cytotoxic T cells and regulates T-cell inhibition as well as macrophage activation. Inhibitors of both proteins have been developed that are being evaluated in phase 1 or 2 clinical trials in a variety of tumor types.17
Indeed, although T cells have commanded the most attention, there is growing appreciation of the potential for targeting other types of immune cell that play a role in the anti-tumor immune response or in fostering an immunosuppressive microenvironment. NK cells have been a particular focus, since they represent the body’s first line of immune defense and they appear to have analogous inhibitory and activating receptors expressed on their surface that regulate their cytotoxic activity.
The best-defined NK cell receptors are the killer cell immunoglobulin-like receptors (KIRs) that bind to the MHC class I proteins found on the surface of all cells that distinguish them as ‘self’ or ‘non-self’. KIRs can be either activating or inhibitory, depending upon their structure and the ligands to which they bind.19 To date, 2 antibodies targeting inhibitory KIRs have been developed. Though there has been some disappointment with these drugs, most recently a phase 2 trial of lirilumab in elderly patients with acute myeloid leukemia, which missed its primary endpoint, they continue to be evaluated in clinical trials.20
The inhibitory immune checkpoint field has also expanded to include molecules that regulate T-cell activity in other ways. Most prominently, this includes enzymes like indoleamine-2,3 dioxygenase (IDO), which is involved in the metabolism of the essential amino acid tryptophan. IDO-induced depletion of tryptophan and generation of tryptophan metabolites is toxic to cytotoxic T cells, and IDO is also thought to directly activate regulatory T cells, thus the net effect of IDO is immunosuppression. Two IDO inhibitors are currently being developed.21
Stepping on the gas
Despite their unprecedented success, immune checkpoint inhibitors are not effective in all patients or in all tumor types. Their efficacy is limited in large part by the requirement for a pre-existing anti-tumor immune response. If there are no T cells within the tumor microenvironment then releasing the brakes on the immune system won’t help.
More recently, researchers have returned to the idea of stimulating an anti-tumor immune response, this time by targeting the other side of the immune checkpoint coin, the costimulatory molecules. These drugs could prove more effective as they aren’t reliant on a pre-existing anti-tumor immune response. A number of agonist antibodies designed to target these receptors have now been developed and are undergoing clinical evaluation.22
Furthest along in development are those targeting OX40, a costimulatory molecule that is upregulated on the surface of T cells once they have been fully activated by the TCR signal and an initial costimulatory signal. OX40 is thought to be involved in a more long-term immune response and in the formation of a memory response. A mouse monoclonal antibody had a potent immune-stimulating effect accompanied by the regression of at least 1 metastatic lesion in 30% of patients treated in a phase 1 clinical trial, but was limited by the generation of anti-mouse antibodies. 7 OX40 agonists are now in clinical development, 6 fully human monoclonal antibodies and 1 OX40 ligand-Fc fusion protein, MEDI-6383.23
Combinations are key
Many researchers are now reaching the conclusion that combination therapy is likely to be key in expanding the scope of immunotherapy into currently unresponsive patient populations. Investigating rational combinations is already becoming a burgeoning area of the immuno-oncology field, with a variety of different strategies being tested.
Now the question becomes what are the optimal combinations and the timing and sequencing of combination therapy is likely to be a paramount consideration. Developing combinations that have distinct mechanisms of action or target multiple steps in the cancer immunity cycle offers the greatest potential for therapeutic synergy since this is most likely to address potential mechanisms of resistance by blocking other paths to immune evasion for cancer cells (Figure 3).
Given the expanding network of immune-checkpoint inhibitors and agonists, the focal point of combination therapy has been combining immune checkpoint-targeting drugs with different mechanisms of action, including those that would simultaneously release the brakes and step on the gas pedal. The vast majority of ongoing clinical trials of approved checkpoint inhibitors and the drugs in development listed in the table are combination trials.
These efforts yielded the first FDA-approved combination immunotherapy regimen in 2015; nivolumab and ipilimumab for the treatment of metastatic melanoma. Approval was based on the demonstration of improved ORR, prolonged response duration, and improved progression-free survival among 142 patients treated with the combination, compared to either drug alone.24
The results of a phase 1/2 trial evaluating the combination of a 4-1BB receptor agonist urelumab with nivolumab in hematologic malignancies and solid tumors found the combination to be safe and particularly effective in patients with advanced/metastatic melanoma, with an ORR of 50%.25 Nivolumab was also combined with the CD27 agonist varlilumab in a phase 1/2 clinical trial of patients with solid tumors, for which data was also recently released. Among 46 patients enrolled, primarily those with colorectal and ovarian cancer the combination had an acceptable safety profile and favorable changes in intratumoral immune biomarkers were observed. The phase 2 portion of the trial is ongoing.26
Meanwhile, Incyte’s IDO inhibitor epacadostat has recently been making waves in combination with pembrolizumab in patients with advanced solid tumors. It demonstrated particularly promising clinical activity in patients with metastatic melanoma, with an overall response rate (ORR) of 57%, including 2 complete responses (CRs), prompting initiation of a phase 3 trial of this combination (NCT02752074).27
1. Adams JL, Smothers J, Srinivasan R, et al. Big opportunities for small molecules in immuno-oncology. Nat Rev Drug Disc. 2015;14:603-622.
2. D’Errico G, Machado HL, Sainz Jr B. A current perspective on cancer immune therapy: step-by-step approach to constructing the magic bullet. Clin Trans Med. 2017;6:3.
3. Farkona S, Diamandis EP, Blaustig IM. Cancer immunotherapy: the beginning of the end of cancer? BMC Med. 2016;14:73.
4. Meiliana A, Dewi NM, Wijaya A. Cancer immunotherapy: a review. Indones Biomed J. 2016;8(1):1-20.
5. Smyth MJ, Ngiow SF, Ribas A, et al. Combination cancer immunotherapies tailored to the tumor microenvironment. Nat Rev Clin Oncol. 2016;13:143-158.
6. de Charette M, Marabelle A, Houot R. Turning tumor cells into antigen presenting cells: The next step to improve cancer immunotherapy? Eur J Cancer 2016;68:134-147.
7. Chen DS and Mellman I. Oncology Meets Immunology: The Cancer-Immunity Cycle. Immunity 2013;39:1-10.
8. Mellman I, Coukos G, Dranoff G. Cancer immunotherapy comes of age. Nature 2011;480:480-489.
9. Le DT, Wang-Gillam A, Picozzi V Jr, et al. A phase 2, randomized trial of GVAX Pancreas and CRS-207 immunotherapy versus GVAX alone in patients with metastatic pancreatic adenocarcinoma: Updated results. Presented at: the ASCO Gastrointestinal Cancers Symposium; January 16-18, 2014; San Francisco, CA. Abstract 177.
10. Sharpe M and Mount N. Genetically modified T cells in cancer therapy: opportunities and challenges. Dis Model Mech. 2015;8(4):337-350.
11. Perica K, Varela JC, Oelke M, et al. Adoptive T Cell Immunotherapy for Cancer. Ram Mai Med J. 2015;6(1):e0004.
12. Xing Y and Hogquist KA. T-Cell Tolerance: Central and Peripheral. Cold Spring Harb Perspect Biol. 2012;4:a006957.
13. Buchbinder EI and Desai A. CTLA-4 and PD-1 Pathways: Similarities, Differences, and Implications of Their Inhibition. Am J Clin Oncol. 2016;39(1):98-106.
14. Robert C, Ribas A, Hamid O, et al. 3-year overall survival for patients with advanced melanoma treated with pembrolizumab in KEYNOTE-001. J Clin Oncol. 2016(suppl;abstr 9503).
15. Hodi SF, Kluger HM, Sznol M, et al. Durable, long-term survival in previously treated patients with advanced melanoma who received nivolumab monotherapy in a phase I trial. Presented at the 2016 AACR Annual Meeting; April 16-20; New Orleans, LA. Abstract CT001.
16. Bakdash G, Sittig SP, van Dijk T, et al. The nature of activatory and tolerogenic dendritic cell-derived signal II. Front Immunol. 2013;4(53):1-18.
17. Sheridan C. Immuno-oncology moves beyond PD-1. Nat Biotechnol. 2015;33(7):673-675.
18. Blake SJ, Dougall WC, Miles JJ, et al. Molecular pathways: targeting CD96 and TIGIT for cancer immunotherapy. Clin Cancer Res. 2016;22(21):5183-5188.
19. Carotta S. Targeting NK cells for anticancer immunotherapy: clinical and preclinical approaches. Front Immunol. 2016;7:152.
20. Innate Pharma Web site. Innate Pharma Announces Top-Line Results from EFFIKIR Trial Evaluating the Efficacy of Lirilumab as a Single Agent in Elderly Patients with Acute Myeloid Leukemia. http://www.innate-pharma.com/en/news-events/press-releases/innate-pharma-announces-top-line-results-effikir-trial-evaluating-efficacy-lirilumab-single-agent-elderly-patients-acute-myeloid-leukemia. Last updated February 6, 2017. Accessed online February 22, 2017.
21. Sheridan C. IDO inhibitors move center stage in immuno-oncology. Nat Biotechnol. 2015;33(4):321-322.
22. Sanmamed MF, Pastor F, Rodriguez A, et al. Agonists of co-stimulation in cancer immunotherapy directed against CD137, OX40, GITR, CD27, CD28, and ICOS. Semin Oncol. 2015;42(4):640-655.
23. Linch SN, McNamara MJ, Redmond WL. OX40 agonists and combination immunotherapy: putting the pedal to the metal. Front Oncol. 2015;5:34.
24. U.S. Food and Drug Administration Web site. Nivolumab in combination with ipilimumab. https://www.fda.gov/Drugs/InformationOnDrugs/ApprovedDrugs/ucm465274.htm. Last updated October 1, 2015. Accessed online February 22, 2017.
25. Massarelli E. Clinical safety and efficacy assessment of the CD137 agonist urelumab alone and in combination with nivolumab in patients with hematologic and solid tumor malignancies. Presented at the 31st Annual Meeting of the Society for the Immunotherapy of Cancer; November 9-13, 2016; National Harbor, MD. Abstract 239.
26. Sanborn RE, Pishvain MJ, Callahan MK, et al. Phase I results from the combination of an immune-activating anti-CD27 antibody (varlilumab) in combination with PD-1 blockade (nivolumab): activation across multiple immune pathways without untoward immune-related adverse events. Clin Cancer Res. 2016;76(14):suppl. Abstract CT023.
27. Gangadhar T, Hamid O, Smith D.C, et al. Epacadostat plus pembrolizumab in patients with advanced melanoma and select solid tumors: updated phase 1 results from ECHO-202/KEYNOTE-037. Ann Oncol. 2016;27(6):379-400.
1. Adams JL, Smothers J, Srinivasan R, et al. Big opportunities for small molecules in immuno-oncology. Nat Rev Drug Disc. 2015;14:603-622.
2. D’Errico G, Machado HL, Sainz Jr B. A current perspective on cancer immune therapy: step-by-step approach to constructing the magic bullet. Clin Trans Med. 2017;6:3.
3. Farkona S, Diamandis EP, Blaustig IM. Cancer immunotherapy: the beginning of the end of cancer? BMC Med. 2016;14:73.
4. Meiliana A, Dewi NM, Wijaya A. Cancer immunotherapy: a review. Indones Biomed J. 2016;8(1):1-20.
5. Smyth MJ, Ngiow SF, Ribas A, et al. Combination cancer immunotherapies tailored to the tumor microenvironment. Nat Rev Clin Oncol. 2016;13:143-158.
6. de Charette M, Marabelle A, Houot R. Turning tumor cells into antigen presenting cells: The next step to improve cancer immunotherapy? Eur J Cancer 2016;68:134-147.
7. Chen DS and Mellman I. Oncology Meets Immunology: The Cancer-Immunity Cycle. Immunity 2013;39:1-10.
8. Mellman I, Coukos G, Dranoff G. Cancer immunotherapy comes of age. Nature 2011;480:480-489.
9. Le DT, Wang-Gillam A, Picozzi V Jr, et al. A phase 2, randomized trial of GVAX Pancreas and CRS-207 immunotherapy versus GVAX alone in patients with metastatic pancreatic adenocarcinoma: Updated results. Presented at: the ASCO Gastrointestinal Cancers Symposium; January 16-18, 2014; San Francisco, CA. Abstract 177.
10. Sharpe M and Mount N. Genetically modified T cells in cancer therapy: opportunities and challenges. Dis Model Mech. 2015;8(4):337-350.
11. Perica K, Varela JC, Oelke M, et al. Adoptive T Cell Immunotherapy for Cancer. Ram Mai Med J. 2015;6(1):e0004.
12. Xing Y and Hogquist KA. T-Cell Tolerance: Central and Peripheral. Cold Spring Harb Perspect Biol. 2012;4:a006957.
13. Buchbinder EI and Desai A. CTLA-4 and PD-1 Pathways: Similarities, Differences, and Implications of Their Inhibition. Am J Clin Oncol. 2016;39(1):98-106.
14. Robert C, Ribas A, Hamid O, et al. 3-year overall survival for patients with advanced melanoma treated with pembrolizumab in KEYNOTE-001. J Clin Oncol. 2016(suppl;abstr 9503).
15. Hodi SF, Kluger HM, Sznol M, et al. Durable, long-term survival in previously treated patients with advanced melanoma who received nivolumab monotherapy in a phase I trial. Presented at the 2016 AACR Annual Meeting; April 16-20; New Orleans, LA. Abstract CT001.
16. Bakdash G, Sittig SP, van Dijk T, et al. The nature of activatory and tolerogenic dendritic cell-derived signal II. Front Immunol. 2013;4(53):1-18.
17. Sheridan C. Immuno-oncology moves beyond PD-1. Nat Biotechnol. 2015;33(7):673-675.
18. Blake SJ, Dougall WC, Miles JJ, et al. Molecular pathways: targeting CD96 and TIGIT for cancer immunotherapy. Clin Cancer Res. 2016;22(21):5183-5188.
19. Carotta S. Targeting NK cells for anticancer immunotherapy: clinical and preclinical approaches. Front Immunol. 2016;7:152.
20. Innate Pharma Web site. Innate Pharma Announces Top-Line Results from EFFIKIR Trial Evaluating the Efficacy of Lirilumab as a Single Agent in Elderly Patients with Acute Myeloid Leukemia. http://www.innate-pharma.com/en/news-events/press-releases/innate-pharma-announces-top-line-results-effikir-trial-evaluating-efficacy-lirilumab-single-agent-elderly-patients-acute-myeloid-leukemia. Last updated February 6, 2017. Accessed online February 22, 2017.
21. Sheridan C. IDO inhibitors move center stage in immuno-oncology. Nat Biotechnol. 2015;33(4):321-322.
22. Sanmamed MF, Pastor F, Rodriguez A, et al. Agonists of co-stimulation in cancer immunotherapy directed against CD137, OX40, GITR, CD27, CD28, and ICOS. Semin Oncol. 2015;42(4):640-655.
23. Linch SN, McNamara MJ, Redmond WL. OX40 agonists and combination immunotherapy: putting the pedal to the metal. Front Oncol. 2015;5:34.
24. U.S. Food and Drug Administration Web site. Nivolumab in combination with ipilimumab. https://www.fda.gov/Drugs/InformationOnDrugs/ApprovedDrugs/ucm465274.htm. Last updated October 1, 2015. Accessed online February 22, 2017.
25. Massarelli E. Clinical safety and efficacy assessment of the CD137 agonist urelumab alone and in combination with nivolumab in patients with hematologic and solid tumor malignancies. Presented at the 31st Annual Meeting of the Society for the Immunotherapy of Cancer; November 9-13, 2016; National Harbor, MD. Abstract 239.
26. Sanborn RE, Pishvain MJ, Callahan MK, et al. Phase I results from the combination of an immune-activating anti-CD27 antibody (varlilumab) in combination with PD-1 blockade (nivolumab): activation across multiple immune pathways without untoward immune-related adverse events. Clin Cancer Res. 2016;76(14):suppl. Abstract CT023.
27. Gangadhar T, Hamid O, Smith D.C, et al. Epacadostat plus pembrolizumab in patients with advanced melanoma and select solid tumors: updated phase 1 results from ECHO-202/KEYNOTE-037. Ann Oncol. 2016;27(6):379-400.
Variants in five genes signal TNBC risk
Women with germline pathogenic variants in five genes are at high risk for developing triple-negative breast cancer, and have a greater than 20% lifetime risk for breast cancer in general, results of a large study suggest.
Multigene testing of nearly 11,000 women with triple-negative breast cancer (TNBC; lacking estrogen, progesterone, and human epidermal growth factor receptors) showed that germline pathogenic variants in BARD1, BRCA1, BRCA2, PALB2, and RAD51D were associated with risk for clinical TNBC ranging from nearly sixfold to more than 16-fold higher than that of women without the genetic variants, reported Fergus J. Couch, PhD, of the Mayo Clinic, Rochester, Minn., and his colleagues.
“The results suggest that all TNBC patients should undergo multigene panel testing, regardless of age at diagnosis or family history of cancer, for improved cancer risk assessment and because of the ongoing development of targeted therapeutic approaches for TNBC patients with mutations in predisposition genes,” they wrote. Their report is in the Journal of the National Cancer Institute.
Although National Comprehensive Cancer Network guidelines recommend testing for the cancer predisposition genes BRCA1 and BRCA2 in women with a TNBC diagnosis at age 60 or younger or those with a family history of breast and/or ovarian cancer, the picture is less clear regarding genetic predisposition to TNBC, the authors noted.
“[R]ecommendations for testing of other genes are not fully established because the risks of TNBC associated with mutations in cancer predisposition genes have not been established. Thus, a better understanding of gene-specific risks for TNBC is needed to identify the genes that should be tested in the setting of TNBC,” they wrote.
The investigators looked for associations between deleterious mutations in cancer predisposition genes and TNBC among 8,753 patients with TNBC testing with a 21-gene assay, and among 2,148 women tested for 17 genes in studies conducted by the Triple Negative Breast Cancer Consortium.
They found that among white women, germline pathogenic variants were associated with the following odds ratios (OR) for TNBC (all P values less than .0001):
- BRCA2 = 5.42
- BARD1 = 5.92
- RAD51D = 6.97
- PALB2 = 14.41
- BRCA1 = 16.27
Although there were insufficient data on the risks for African American women, an exploratory analysis showed that risks for TNBC associated with specific pathogenic variants were similar to those for white women, the authors said.
The pathogenic variants were detected in 12% of all patients in the study.
“Continued study of gene-specific risks for breast cancer subtypes may lead to tailored medical management recommendations for PV [pathogenic variant] carriers. Consistent with this hypothesis, initial studies evaluating intensified screening in high-risk women have suggested that a decrease in mortality from TNBC can be achieved,” they wrote.
The study was supported in part by the National Institutes of Health and the Breast Cancer Research Foundation, and was sponsored by Ambry Genetics Inc. The authors reported having no conflicts of interest.
SOURCE: Shimelis H et al. J Natl Cancer Inst. 2018 Aug 7. doi: 10.1093/jnci/djy106.
Women with germline pathogenic variants in five genes are at high risk for developing triple-negative breast cancer, and have a greater than 20% lifetime risk for breast cancer in general, results of a large study suggest.
Multigene testing of nearly 11,000 women with triple-negative breast cancer (TNBC; lacking estrogen, progesterone, and human epidermal growth factor receptors) showed that germline pathogenic variants in BARD1, BRCA1, BRCA2, PALB2, and RAD51D were associated with risk for clinical TNBC ranging from nearly sixfold to more than 16-fold higher than that of women without the genetic variants, reported Fergus J. Couch, PhD, of the Mayo Clinic, Rochester, Minn., and his colleagues.
“The results suggest that all TNBC patients should undergo multigene panel testing, regardless of age at diagnosis or family history of cancer, for improved cancer risk assessment and because of the ongoing development of targeted therapeutic approaches for TNBC patients with mutations in predisposition genes,” they wrote. Their report is in the Journal of the National Cancer Institute.
Although National Comprehensive Cancer Network guidelines recommend testing for the cancer predisposition genes BRCA1 and BRCA2 in women with a TNBC diagnosis at age 60 or younger or those with a family history of breast and/or ovarian cancer, the picture is less clear regarding genetic predisposition to TNBC, the authors noted.
“[R]ecommendations for testing of other genes are not fully established because the risks of TNBC associated with mutations in cancer predisposition genes have not been established. Thus, a better understanding of gene-specific risks for TNBC is needed to identify the genes that should be tested in the setting of TNBC,” they wrote.
The investigators looked for associations between deleterious mutations in cancer predisposition genes and TNBC among 8,753 patients with TNBC testing with a 21-gene assay, and among 2,148 women tested for 17 genes in studies conducted by the Triple Negative Breast Cancer Consortium.
They found that among white women, germline pathogenic variants were associated with the following odds ratios (OR) for TNBC (all P values less than .0001):
- BRCA2 = 5.42
- BARD1 = 5.92
- RAD51D = 6.97
- PALB2 = 14.41
- BRCA1 = 16.27
Although there were insufficient data on the risks for African American women, an exploratory analysis showed that risks for TNBC associated with specific pathogenic variants were similar to those for white women, the authors said.
The pathogenic variants were detected in 12% of all patients in the study.
“Continued study of gene-specific risks for breast cancer subtypes may lead to tailored medical management recommendations for PV [pathogenic variant] carriers. Consistent with this hypothesis, initial studies evaluating intensified screening in high-risk women have suggested that a decrease in mortality from TNBC can be achieved,” they wrote.
The study was supported in part by the National Institutes of Health and the Breast Cancer Research Foundation, and was sponsored by Ambry Genetics Inc. The authors reported having no conflicts of interest.
SOURCE: Shimelis H et al. J Natl Cancer Inst. 2018 Aug 7. doi: 10.1093/jnci/djy106.
Women with germline pathogenic variants in five genes are at high risk for developing triple-negative breast cancer, and have a greater than 20% lifetime risk for breast cancer in general, results of a large study suggest.
Multigene testing of nearly 11,000 women with triple-negative breast cancer (TNBC; lacking estrogen, progesterone, and human epidermal growth factor receptors) showed that germline pathogenic variants in BARD1, BRCA1, BRCA2, PALB2, and RAD51D were associated with risk for clinical TNBC ranging from nearly sixfold to more than 16-fold higher than that of women without the genetic variants, reported Fergus J. Couch, PhD, of the Mayo Clinic, Rochester, Minn., and his colleagues.
“The results suggest that all TNBC patients should undergo multigene panel testing, regardless of age at diagnosis or family history of cancer, for improved cancer risk assessment and because of the ongoing development of targeted therapeutic approaches for TNBC patients with mutations in predisposition genes,” they wrote. Their report is in the Journal of the National Cancer Institute.
Although National Comprehensive Cancer Network guidelines recommend testing for the cancer predisposition genes BRCA1 and BRCA2 in women with a TNBC diagnosis at age 60 or younger or those with a family history of breast and/or ovarian cancer, the picture is less clear regarding genetic predisposition to TNBC, the authors noted.
“[R]ecommendations for testing of other genes are not fully established because the risks of TNBC associated with mutations in cancer predisposition genes have not been established. Thus, a better understanding of gene-specific risks for TNBC is needed to identify the genes that should be tested in the setting of TNBC,” they wrote.
The investigators looked for associations between deleterious mutations in cancer predisposition genes and TNBC among 8,753 patients with TNBC testing with a 21-gene assay, and among 2,148 women tested for 17 genes in studies conducted by the Triple Negative Breast Cancer Consortium.
They found that among white women, germline pathogenic variants were associated with the following odds ratios (OR) for TNBC (all P values less than .0001):
- BRCA2 = 5.42
- BARD1 = 5.92
- RAD51D = 6.97
- PALB2 = 14.41
- BRCA1 = 16.27
Although there were insufficient data on the risks for African American women, an exploratory analysis showed that risks for TNBC associated with specific pathogenic variants were similar to those for white women, the authors said.
The pathogenic variants were detected in 12% of all patients in the study.
“Continued study of gene-specific risks for breast cancer subtypes may lead to tailored medical management recommendations for PV [pathogenic variant] carriers. Consistent with this hypothesis, initial studies evaluating intensified screening in high-risk women have suggested that a decrease in mortality from TNBC can be achieved,” they wrote.
The study was supported in part by the National Institutes of Health and the Breast Cancer Research Foundation, and was sponsored by Ambry Genetics Inc. The authors reported having no conflicts of interest.
SOURCE: Shimelis H et al. J Natl Cancer Inst. 2018 Aug 7. doi: 10.1093/jnci/djy106.
FROM JOURNAL OF THE NATIONAL CANCER INSTITUTE
Key clinical point: Pathogenic variants in five cancer predisposition genes are associated with significantly increased risk for triple negative breast cancer (TNBC).
Major finding: Pathogenic variants in BRCA1 were associated with a more than 16-fold risk for TNBC.
Study details: Retrospective review of multigene assay testing in 10,901 women with TNBC.
Disclosures: The study was supported in part by the National Institutes of Health and the Breast Cancer Research Foundation, and was sponsored by Ambry Genetics Inc. The authors reported having no conflicts of interest.
Source: Shimelis H et al. J Natl Cancer Inst. 2018 Aug 7. doi: 10.1093/jnci/djy106.
RT linked with better survival in DCIS
Treatment with lumpectomy and radiotherapy was associated with a significant reduction in breast cancer mortality in patients with ductal carcinoma in situ (DCIS), compared with a lumpectomy alone or a mastectomy alone, investigators reported in JAMA Oncology.
Among women who received adjuvant radiation, there was an associated 23% reduced risk of dying of breast cancer. This extrapolated to a cumulative mortality of 2.33% for those treated with lumpectomy alone and 1.74% for women treated with lumpectomy and radiotherapy at 15 years (adjusted hazard ratio, 0.77; 95% confidence interval, 0.67-0.88; P less than .001).
“Although the clinical benefit is small, it is intriguing that radiotherapy has this effect, which appears to be attributable to systemic activity rather than local control,” wrote Vasily Giannakeas, MPH, of the Women’s College Research Institute, Toronto, and colleagues.
Emerging evidence suggests that adding radiotherapy to breast conserving surgery can reduce the risk of breast cancer mortality among women with DCIS and lower the risk of local recurrence. Because of the low rate of mortality associated with DCIS, the authors noted that it has been difficult to investigate deaths related to DCIS. The association of adjuvant radiotherapy with breast cancer survival in this population has also not yet been clearly established.
To determine the extent to which radiotherapy is associated with reduced risk of breast cancer mortality in patients treated for DCIS and identify patient subgroups who might derive the most benefit from radiotherapy, the authors conducted a historical cohort study using the Surveillance, Epidemiology, and End Results database. A total of 140,366 women diagnosed with first primary DCIS between 1998 and 2014 were identified, and three separate comparisons were made using 1:1 matching: lumpectomy with radiation versus lumpectomy alone, lumpectomy alone versus mastectomy, and lumpectomy with radiation therapy versus mastectomy.
A total of 35,070 women (25.0%) were treated with lumpectomy alone, 65,301 (46.5%) were treated with lumpectomy and radiotherapy, and 39,995 (28.5%) were treated with mastectomy.
The overall cumulative mortality for the entire cohort from breast cancer at 15 years was 2.03%. The actuarial 15-year mortality rate for the mastectomy group (2.26%) was similar to those who had lumpectomy without radiotherapy (2.33%).
The adjusted HR for death for mastectomy versus lumpectomy alone (based on 20,832 propensity-matched pairs) was 0.91 (95% CI, 0.78-1.05). The adjusted hazard ratios for death were 0.77 (95% CI, 0.67-0.88) for lumpectomy and radiotherapy versus lumpectomy alone (29,465 propensity-matched pairs), 0.91 (95% CI, 0.78-1.05) for mastectomy alone versus lumpectomy alone (20,832 propensity-matched pairs), and 0.75 (95% CI, 0.65-0.87) for lumpectomy and radiotherapy versus mastectomy (29,865 propensity-matched pairs).
When looking at subgroups and the effect of radiotherapy on mortality, the authors found the following: The HR was 0.59 (95% CI, 0.43-0.80) for patients aged younger than 50 years and 0.86 (95% CI, 0.73- 1.01) for those aged 50 years and older; it was 0.67 (95% CI, 0.51-0.87) for patients with ER-positive cancers, 0.50 (95% CI, 0.32-0.78) for ER-negative cancers, and 0.93 (95% CI, 0.77-1.13) for those with unknown ER status.
“How exactly radiotherapy affects survival is an important question that should be explored in future studies,” the authors concluded.
There was no outside funding source reported. Mr. Giannakeas is supported by the Canadian Institutes of Health Research Frederick Banting and Charles Best Doctoral Research Award.
SOURCE: Giannakeas V et al. JAMA Network Open. 2018 Aug 10. doi:10.1001/jamanetworkopen.2018.1100.
In an accompanying editorial, Mira Goldberg, MD, and Timothy J. Whelan, BM, BCh, of the department of oncology at McMaster University, Hamilton, Ont., noted that the primary goal of using adjuvant radiotherapy in patients with ductal carcinoma in situ (DCIS) is to reduce the risk of local recurrence of DCIS or of invasive breast cancer.
Despite widespread screening with mammography, along with improvements in technology so as to detect even smaller lesions, “there is increased concern about the overdiagnosis of DCIS,” they wrote. Results from recent studies generally suggest that patients with good prognostic factors and who have a low risk of local recurrence at 10 years (10%) are unlikely to gain any major benefit from being treated with radiotherapy.
They also pointed out that there is growing interest in the use of molecular markers as a means to help detect patients who are at a lower risk of recurrence and thus who may not benefit from radiotherapy.
“The results of the study by Giannakeas and colleagues are reassuring,” the editorialists wrote, as it demonstrated that the risk of breast cancer mortality in patients with DCIS is very low, and the potential absolute benefit of radiotherapy is also quite small. (The number of patients that need to be treated to prevent a breast cancer death was 370.) These data continue to support a strategy for low-risk DCIS of omitting radiotherapy after lumpectomy. This is especially pertinent when “one considers the negative effects of treatment: the cost and inconvenience of 5-6 weeks of daily treatments, acute adverse effects such as breast pain and fatigue, and potential long-term toxic effects of cardiac disease and second cancers.”
The editorialists also highlighted the authors’ speculation that there could be additional systemic effects of radiotherapy, possibly resulting from an elicited immune response or radiation scatter to distant tissues. While this hypothesis is theoretically possible, their results could also be explained by confounding factors, such as a higher use of endocrine therapy in patients who received adjuvant radiotherapy.
Dr. Whelan has received research support from Genomic Health. This editorial accompanied the article by Giannakeas et al. (JAMA Network Open. 2018;1[4]e181102). No other disclosures were reported.
In an accompanying editorial, Mira Goldberg, MD, and Timothy J. Whelan, BM, BCh, of the department of oncology at McMaster University, Hamilton, Ont., noted that the primary goal of using adjuvant radiotherapy in patients with ductal carcinoma in situ (DCIS) is to reduce the risk of local recurrence of DCIS or of invasive breast cancer.
Despite widespread screening with mammography, along with improvements in technology so as to detect even smaller lesions, “there is increased concern about the overdiagnosis of DCIS,” they wrote. Results from recent studies generally suggest that patients with good prognostic factors and who have a low risk of local recurrence at 10 years (10%) are unlikely to gain any major benefit from being treated with radiotherapy.
They also pointed out that there is growing interest in the use of molecular markers as a means to help detect patients who are at a lower risk of recurrence and thus who may not benefit from radiotherapy.
“The results of the study by Giannakeas and colleagues are reassuring,” the editorialists wrote, as it demonstrated that the risk of breast cancer mortality in patients with DCIS is very low, and the potential absolute benefit of radiotherapy is also quite small. (The number of patients that need to be treated to prevent a breast cancer death was 370.) These data continue to support a strategy for low-risk DCIS of omitting radiotherapy after lumpectomy. This is especially pertinent when “one considers the negative effects of treatment: the cost and inconvenience of 5-6 weeks of daily treatments, acute adverse effects such as breast pain and fatigue, and potential long-term toxic effects of cardiac disease and second cancers.”
The editorialists also highlighted the authors’ speculation that there could be additional systemic effects of radiotherapy, possibly resulting from an elicited immune response or radiation scatter to distant tissues. While this hypothesis is theoretically possible, their results could also be explained by confounding factors, such as a higher use of endocrine therapy in patients who received adjuvant radiotherapy.
Dr. Whelan has received research support from Genomic Health. This editorial accompanied the article by Giannakeas et al. (JAMA Network Open. 2018;1[4]e181102). No other disclosures were reported.
In an accompanying editorial, Mira Goldberg, MD, and Timothy J. Whelan, BM, BCh, of the department of oncology at McMaster University, Hamilton, Ont., noted that the primary goal of using adjuvant radiotherapy in patients with ductal carcinoma in situ (DCIS) is to reduce the risk of local recurrence of DCIS or of invasive breast cancer.
Despite widespread screening with mammography, along with improvements in technology so as to detect even smaller lesions, “there is increased concern about the overdiagnosis of DCIS,” they wrote. Results from recent studies generally suggest that patients with good prognostic factors and who have a low risk of local recurrence at 10 years (10%) are unlikely to gain any major benefit from being treated with radiotherapy.
They also pointed out that there is growing interest in the use of molecular markers as a means to help detect patients who are at a lower risk of recurrence and thus who may not benefit from radiotherapy.
“The results of the study by Giannakeas and colleagues are reassuring,” the editorialists wrote, as it demonstrated that the risk of breast cancer mortality in patients with DCIS is very low, and the potential absolute benefit of radiotherapy is also quite small. (The number of patients that need to be treated to prevent a breast cancer death was 370.) These data continue to support a strategy for low-risk DCIS of omitting radiotherapy after lumpectomy. This is especially pertinent when “one considers the negative effects of treatment: the cost and inconvenience of 5-6 weeks of daily treatments, acute adverse effects such as breast pain and fatigue, and potential long-term toxic effects of cardiac disease and second cancers.”
The editorialists also highlighted the authors’ speculation that there could be additional systemic effects of radiotherapy, possibly resulting from an elicited immune response or radiation scatter to distant tissues. While this hypothesis is theoretically possible, their results could also be explained by confounding factors, such as a higher use of endocrine therapy in patients who received adjuvant radiotherapy.
Dr. Whelan has received research support from Genomic Health. This editorial accompanied the article by Giannakeas et al. (JAMA Network Open. 2018;1[4]e181102). No other disclosures were reported.
Treatment with lumpectomy and radiotherapy was associated with a significant reduction in breast cancer mortality in patients with ductal carcinoma in situ (DCIS), compared with a lumpectomy alone or a mastectomy alone, investigators reported in JAMA Oncology.
Among women who received adjuvant radiation, there was an associated 23% reduced risk of dying of breast cancer. This extrapolated to a cumulative mortality of 2.33% for those treated with lumpectomy alone and 1.74% for women treated with lumpectomy and radiotherapy at 15 years (adjusted hazard ratio, 0.77; 95% confidence interval, 0.67-0.88; P less than .001).
“Although the clinical benefit is small, it is intriguing that radiotherapy has this effect, which appears to be attributable to systemic activity rather than local control,” wrote Vasily Giannakeas, MPH, of the Women’s College Research Institute, Toronto, and colleagues.
Emerging evidence suggests that adding radiotherapy to breast conserving surgery can reduce the risk of breast cancer mortality among women with DCIS and lower the risk of local recurrence. Because of the low rate of mortality associated with DCIS, the authors noted that it has been difficult to investigate deaths related to DCIS. The association of adjuvant radiotherapy with breast cancer survival in this population has also not yet been clearly established.
To determine the extent to which radiotherapy is associated with reduced risk of breast cancer mortality in patients treated for DCIS and identify patient subgroups who might derive the most benefit from radiotherapy, the authors conducted a historical cohort study using the Surveillance, Epidemiology, and End Results database. A total of 140,366 women diagnosed with first primary DCIS between 1998 and 2014 were identified, and three separate comparisons were made using 1:1 matching: lumpectomy with radiation versus lumpectomy alone, lumpectomy alone versus mastectomy, and lumpectomy with radiation therapy versus mastectomy.
A total of 35,070 women (25.0%) were treated with lumpectomy alone, 65,301 (46.5%) were treated with lumpectomy and radiotherapy, and 39,995 (28.5%) were treated with mastectomy.
The overall cumulative mortality for the entire cohort from breast cancer at 15 years was 2.03%. The actuarial 15-year mortality rate for the mastectomy group (2.26%) was similar to those who had lumpectomy without radiotherapy (2.33%).
The adjusted HR for death for mastectomy versus lumpectomy alone (based on 20,832 propensity-matched pairs) was 0.91 (95% CI, 0.78-1.05). The adjusted hazard ratios for death were 0.77 (95% CI, 0.67-0.88) for lumpectomy and radiotherapy versus lumpectomy alone (29,465 propensity-matched pairs), 0.91 (95% CI, 0.78-1.05) for mastectomy alone versus lumpectomy alone (20,832 propensity-matched pairs), and 0.75 (95% CI, 0.65-0.87) for lumpectomy and radiotherapy versus mastectomy (29,865 propensity-matched pairs).
When looking at subgroups and the effect of radiotherapy on mortality, the authors found the following: The HR was 0.59 (95% CI, 0.43-0.80) for patients aged younger than 50 years and 0.86 (95% CI, 0.73- 1.01) for those aged 50 years and older; it was 0.67 (95% CI, 0.51-0.87) for patients with ER-positive cancers, 0.50 (95% CI, 0.32-0.78) for ER-negative cancers, and 0.93 (95% CI, 0.77-1.13) for those with unknown ER status.
“How exactly radiotherapy affects survival is an important question that should be explored in future studies,” the authors concluded.
There was no outside funding source reported. Mr. Giannakeas is supported by the Canadian Institutes of Health Research Frederick Banting and Charles Best Doctoral Research Award.
SOURCE: Giannakeas V et al. JAMA Network Open. 2018 Aug 10. doi:10.1001/jamanetworkopen.2018.1100.
Treatment with lumpectomy and radiotherapy was associated with a significant reduction in breast cancer mortality in patients with ductal carcinoma in situ (DCIS), compared with a lumpectomy alone or a mastectomy alone, investigators reported in JAMA Oncology.
Among women who received adjuvant radiation, there was an associated 23% reduced risk of dying of breast cancer. This extrapolated to a cumulative mortality of 2.33% for those treated with lumpectomy alone and 1.74% for women treated with lumpectomy and radiotherapy at 15 years (adjusted hazard ratio, 0.77; 95% confidence interval, 0.67-0.88; P less than .001).
“Although the clinical benefit is small, it is intriguing that radiotherapy has this effect, which appears to be attributable to systemic activity rather than local control,” wrote Vasily Giannakeas, MPH, of the Women’s College Research Institute, Toronto, and colleagues.
Emerging evidence suggests that adding radiotherapy to breast conserving surgery can reduce the risk of breast cancer mortality among women with DCIS and lower the risk of local recurrence. Because of the low rate of mortality associated with DCIS, the authors noted that it has been difficult to investigate deaths related to DCIS. The association of adjuvant radiotherapy with breast cancer survival in this population has also not yet been clearly established.
To determine the extent to which radiotherapy is associated with reduced risk of breast cancer mortality in patients treated for DCIS and identify patient subgroups who might derive the most benefit from radiotherapy, the authors conducted a historical cohort study using the Surveillance, Epidemiology, and End Results database. A total of 140,366 women diagnosed with first primary DCIS between 1998 and 2014 were identified, and three separate comparisons were made using 1:1 matching: lumpectomy with radiation versus lumpectomy alone, lumpectomy alone versus mastectomy, and lumpectomy with radiation therapy versus mastectomy.
A total of 35,070 women (25.0%) were treated with lumpectomy alone, 65,301 (46.5%) were treated with lumpectomy and radiotherapy, and 39,995 (28.5%) were treated with mastectomy.
The overall cumulative mortality for the entire cohort from breast cancer at 15 years was 2.03%. The actuarial 15-year mortality rate for the mastectomy group (2.26%) was similar to those who had lumpectomy without radiotherapy (2.33%).
The adjusted HR for death for mastectomy versus lumpectomy alone (based on 20,832 propensity-matched pairs) was 0.91 (95% CI, 0.78-1.05). The adjusted hazard ratios for death were 0.77 (95% CI, 0.67-0.88) for lumpectomy and radiotherapy versus lumpectomy alone (29,465 propensity-matched pairs), 0.91 (95% CI, 0.78-1.05) for mastectomy alone versus lumpectomy alone (20,832 propensity-matched pairs), and 0.75 (95% CI, 0.65-0.87) for lumpectomy and radiotherapy versus mastectomy (29,865 propensity-matched pairs).
When looking at subgroups and the effect of radiotherapy on mortality, the authors found the following: The HR was 0.59 (95% CI, 0.43-0.80) for patients aged younger than 50 years and 0.86 (95% CI, 0.73- 1.01) for those aged 50 years and older; it was 0.67 (95% CI, 0.51-0.87) for patients with ER-positive cancers, 0.50 (95% CI, 0.32-0.78) for ER-negative cancers, and 0.93 (95% CI, 0.77-1.13) for those with unknown ER status.
“How exactly radiotherapy affects survival is an important question that should be explored in future studies,” the authors concluded.
There was no outside funding source reported. Mr. Giannakeas is supported by the Canadian Institutes of Health Research Frederick Banting and Charles Best Doctoral Research Award.
SOURCE: Giannakeas V et al. JAMA Network Open. 2018 Aug 10. doi:10.1001/jamanetworkopen.2018.1100.
FROM JAMA ONCOLOGY
Key clinical point: Lumpectomy and adjuvant radiotherapy together was superior to lumpectomy or mastectomy alone.
Major finding: The 15-year breast cancer mortality rate was 2.33% for lumpectomy alone, 1.74% for lumpectomy and radiation, and 2.26% for mastectomy.
Study details: A historical cohort study using Surveillance, Epidemiology, and End Results data that included 140,366 women diagnosed with first primary ductal carcinoma in situ.
Disclosures: There was no outside funding source reported. Mr. Giannakeas is supported by the Canadian Institutes of Health Research Frederick Banting and Charles Best Doctoral Research Award. No other disclosures were reported.
Source: Giannakeas V et al. JAMA Network Open. 2018 Aug 10. doi: 10.1001/jamanetworkopen.2018.1100.