User login
Index discriminates prognostic groups in CLL
An international prognostic index for patients with chronic lymphocytic leukemia (CLL) may help to inform treatment decisions, based on a meta-analysis presented at the International Congress on Malignant Lymphoma in Lugano, Switzerland.
The International Prognostic Index for patients with CLL (CLL-IPI) combines the most important genetic risk factors and traditional clinical stage, age, and serum beta-2-microglobulin measures. By discriminating between prognostic groups, the index may aid in informing treatment of CLL patients, Dr. Jasmin Bahlo of the University Hospital Cologne, Köln, Germany, said.
The CLL-IPI consists of five risk factors – age, clinical stage, IgHV (immunoglobulin heavy-chain variable-region) gene mutation status, serum beta-2-microglobulin measure, and the presence of del(17p) and/or TP53 mutation, Dr. Bahlo said.
To develop the index, Dr. Bahlo and colleagues performed an analysis of 26 possible prognostic factors by using data from eight phase III trials from France, Germany, the United Kingdom, the United States, and Poland. The data included a full analysis set of 3,742 previously untreated patients at early and advanced stages of disease. The median age of the patients was 61 years, the median observation time was 80 months, and the main endpoint was overall survival.
From the 26 variables, the researchers identified five independent predictors for overall survival: age (65 years or more), clinical stage (Binet A/Rai 0 vs. Binet B-C/Rai I-IV), del(17p) and/or TP53 mutation status, IgHV mutation status, and serum beta-2-microglobulin measure (3.5 mg/L or more).
The index was used to identify four risk groups – low risk (score 0-1), intermediate (score 2-3), high (score 4-6), and very high (score 7-10)) – with significantly different overall survival rates at 5 years of 93%, 79%, 64%, and 23%, respectively.
The value of the index was then confirmed in 575 patients, with a 5-year overall survival rate of 91%, 80%, 52%, and 19%, respectively.
Similar findings were seen in an external data set of patients from the Mayo Clinic data set, with 5-year overall survivals of 97%, 91%, 68%, and 21%, respectively. The CLL-IPI also provided accurate estimation regarding time to first treatment; 81%, 47%, 30%, and 19% of patients in the respective risk groups were free from treatment at 5 years.
In the era of more effective treatments for CLL, the established clinical staging systems (Rai and Binet) do not accurately discriminate between prognostic groups because they do not integrate the major clinical, biologic, and genetic variables into one widely accepted prognostic system, Dr. Bahlo noted. The CLL-IPI is, therefore, an important contribution to management of this condition.
The researchers had no relevant financial disclosures.
Until very recently, most treatment decisions in CLL have been based on age, overall fitness of the patient and presence of cytopenias. Biologic prognostic markers have been delineated, but not acted upon, with the recent exception of del17p given the advent of effective novel agents in this setting. This is an admirable attempt to establish a better prognostic index, building upon prior German CLL group data (Pflug et al Blood 2014), but it has limitations. It is a weighted score, heavily dependent on p53 mutation/del17p, which is uncommon at initial diagnosis, and today such patients should be receiving a targeted agent. It would be useful to have a CLL-IPI for patients without del17p. Further, while its ability to predict time to require therapy will remain useful, its survival predictions are likely already outdated given the array of new agents already, or soon to be, available.
Until very recently, most treatment decisions in CLL have been based on age, overall fitness of the patient and presence of cytopenias. Biologic prognostic markers have been delineated, but not acted upon, with the recent exception of del17p given the advent of effective novel agents in this setting. This is an admirable attempt to establish a better prognostic index, building upon prior German CLL group data (Pflug et al Blood 2014), but it has limitations. It is a weighted score, heavily dependent on p53 mutation/del17p, which is uncommon at initial diagnosis, and today such patients should be receiving a targeted agent. It would be useful to have a CLL-IPI for patients without del17p. Further, while its ability to predict time to require therapy will remain useful, its survival predictions are likely already outdated given the array of new agents already, or soon to be, available.
Until very recently, most treatment decisions in CLL have been based on age, overall fitness of the patient and presence of cytopenias. Biologic prognostic markers have been delineated, but not acted upon, with the recent exception of del17p given the advent of effective novel agents in this setting. This is an admirable attempt to establish a better prognostic index, building upon prior German CLL group data (Pflug et al Blood 2014), but it has limitations. It is a weighted score, heavily dependent on p53 mutation/del17p, which is uncommon at initial diagnosis, and today such patients should be receiving a targeted agent. It would be useful to have a CLL-IPI for patients without del17p. Further, while its ability to predict time to require therapy will remain useful, its survival predictions are likely already outdated given the array of new agents already, or soon to be, available.
An international prognostic index for patients with chronic lymphocytic leukemia (CLL) may help to inform treatment decisions, based on a meta-analysis presented at the International Congress on Malignant Lymphoma in Lugano, Switzerland.
The International Prognostic Index for patients with CLL (CLL-IPI) combines the most important genetic risk factors and traditional clinical stage, age, and serum beta-2-microglobulin measures. By discriminating between prognostic groups, the index may aid in informing treatment of CLL patients, Dr. Jasmin Bahlo of the University Hospital Cologne, Köln, Germany, said.
The CLL-IPI consists of five risk factors – age, clinical stage, IgHV (immunoglobulin heavy-chain variable-region) gene mutation status, serum beta-2-microglobulin measure, and the presence of del(17p) and/or TP53 mutation, Dr. Bahlo said.
To develop the index, Dr. Bahlo and colleagues performed an analysis of 26 possible prognostic factors by using data from eight phase III trials from France, Germany, the United Kingdom, the United States, and Poland. The data included a full analysis set of 3,742 previously untreated patients at early and advanced stages of disease. The median age of the patients was 61 years, the median observation time was 80 months, and the main endpoint was overall survival.
From the 26 variables, the researchers identified five independent predictors for overall survival: age (65 years or more), clinical stage (Binet A/Rai 0 vs. Binet B-C/Rai I-IV), del(17p) and/or TP53 mutation status, IgHV mutation status, and serum beta-2-microglobulin measure (3.5 mg/L or more).
The index was used to identify four risk groups – low risk (score 0-1), intermediate (score 2-3), high (score 4-6), and very high (score 7-10)) – with significantly different overall survival rates at 5 years of 93%, 79%, 64%, and 23%, respectively.
The value of the index was then confirmed in 575 patients, with a 5-year overall survival rate of 91%, 80%, 52%, and 19%, respectively.
Similar findings were seen in an external data set of patients from the Mayo Clinic data set, with 5-year overall survivals of 97%, 91%, 68%, and 21%, respectively. The CLL-IPI also provided accurate estimation regarding time to first treatment; 81%, 47%, 30%, and 19% of patients in the respective risk groups were free from treatment at 5 years.
In the era of more effective treatments for CLL, the established clinical staging systems (Rai and Binet) do not accurately discriminate between prognostic groups because they do not integrate the major clinical, biologic, and genetic variables into one widely accepted prognostic system, Dr. Bahlo noted. The CLL-IPI is, therefore, an important contribution to management of this condition.
The researchers had no relevant financial disclosures.
An international prognostic index for patients with chronic lymphocytic leukemia (CLL) may help to inform treatment decisions, based on a meta-analysis presented at the International Congress on Malignant Lymphoma in Lugano, Switzerland.
The International Prognostic Index for patients with CLL (CLL-IPI) combines the most important genetic risk factors and traditional clinical stage, age, and serum beta-2-microglobulin measures. By discriminating between prognostic groups, the index may aid in informing treatment of CLL patients, Dr. Jasmin Bahlo of the University Hospital Cologne, Köln, Germany, said.
The CLL-IPI consists of five risk factors – age, clinical stage, IgHV (immunoglobulin heavy-chain variable-region) gene mutation status, serum beta-2-microglobulin measure, and the presence of del(17p) and/or TP53 mutation, Dr. Bahlo said.
To develop the index, Dr. Bahlo and colleagues performed an analysis of 26 possible prognostic factors by using data from eight phase III trials from France, Germany, the United Kingdom, the United States, and Poland. The data included a full analysis set of 3,742 previously untreated patients at early and advanced stages of disease. The median age of the patients was 61 years, the median observation time was 80 months, and the main endpoint was overall survival.
From the 26 variables, the researchers identified five independent predictors for overall survival: age (65 years or more), clinical stage (Binet A/Rai 0 vs. Binet B-C/Rai I-IV), del(17p) and/or TP53 mutation status, IgHV mutation status, and serum beta-2-microglobulin measure (3.5 mg/L or more).
The index was used to identify four risk groups – low risk (score 0-1), intermediate (score 2-3), high (score 4-6), and very high (score 7-10)) – with significantly different overall survival rates at 5 years of 93%, 79%, 64%, and 23%, respectively.
The value of the index was then confirmed in 575 patients, with a 5-year overall survival rate of 91%, 80%, 52%, and 19%, respectively.
Similar findings were seen in an external data set of patients from the Mayo Clinic data set, with 5-year overall survivals of 97%, 91%, 68%, and 21%, respectively. The CLL-IPI also provided accurate estimation regarding time to first treatment; 81%, 47%, 30%, and 19% of patients in the respective risk groups were free from treatment at 5 years.
In the era of more effective treatments for CLL, the established clinical staging systems (Rai and Binet) do not accurately discriminate between prognostic groups because they do not integrate the major clinical, biologic, and genetic variables into one widely accepted prognostic system, Dr. Bahlo noted. The CLL-IPI is, therefore, an important contribution to management of this condition.
The researchers had no relevant financial disclosures.
FROM 13-ICML
Key clinical point: An international prognostic index for patients with chronic lymphocytic leukemia may help to inform treatment decisions.
Major finding: The index was used to identify four risk groups – low risk (score 0-1), intermediate (score 2-3), high (score 4-6), and very high (score 7-10)) – with significantly different overall survival rates at 5 years of 93%, 79%, 64%, and 23%, respectively.
Data source: A multivariate analysis of 3,742 previously untreated patients at early and advanced CLL stages.
Disclosures: The researchers had no relevant financial disclosures.
VIDEO: Ibrutinib should be therapy ‘backbone’ in relapsed CLL
CHICAGO – Combining ibrutinib with standard chemoimmunotherapy extended progression-free survival in patients with relapsed chronic lymphocytic leukemia (CLL), according to interim results from the HELIOS trial.
In fact, while median progression-free survival was approximately 13 months in the placebo arm, the median progression-free survival had not been reached yet in the study’s ibrutinib arm, explained lead study author Dr. Asher Chanan-Khan.
“I believe that ibrutinib has now become the backbone of treatment of patients with relapsed CLL,” said Dr. Chanan-Khan, professor of medicine at the Mayo Clinic in Jacksonville, Fla.
In a video interview at the annual meeting of the American Society of Clinical Oncology, Dr. Chanan-Khan discussed ibrutinib’s significant impact on the risk of progression and death, even in the presence of factors associated with aggressive disease or poor outcome.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
CHICAGO – Combining ibrutinib with standard chemoimmunotherapy extended progression-free survival in patients with relapsed chronic lymphocytic leukemia (CLL), according to interim results from the HELIOS trial.
In fact, while median progression-free survival was approximately 13 months in the placebo arm, the median progression-free survival had not been reached yet in the study’s ibrutinib arm, explained lead study author Dr. Asher Chanan-Khan.
“I believe that ibrutinib has now become the backbone of treatment of patients with relapsed CLL,” said Dr. Chanan-Khan, professor of medicine at the Mayo Clinic in Jacksonville, Fla.
In a video interview at the annual meeting of the American Society of Clinical Oncology, Dr. Chanan-Khan discussed ibrutinib’s significant impact on the risk of progression and death, even in the presence of factors associated with aggressive disease or poor outcome.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
CHICAGO – Combining ibrutinib with standard chemoimmunotherapy extended progression-free survival in patients with relapsed chronic lymphocytic leukemia (CLL), according to interim results from the HELIOS trial.
In fact, while median progression-free survival was approximately 13 months in the placebo arm, the median progression-free survival had not been reached yet in the study’s ibrutinib arm, explained lead study author Dr. Asher Chanan-Khan.
“I believe that ibrutinib has now become the backbone of treatment of patients with relapsed CLL,” said Dr. Chanan-Khan, professor of medicine at the Mayo Clinic in Jacksonville, Fla.
In a video interview at the annual meeting of the American Society of Clinical Oncology, Dr. Chanan-Khan discussed ibrutinib’s significant impact on the risk of progression and death, even in the presence of factors associated with aggressive disease or poor outcome.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
AT THE 2015 ASCO ANNUAL MEETING
EHA: Venetoclax-rituxumab combo highly active in relapsed/refractory CLL
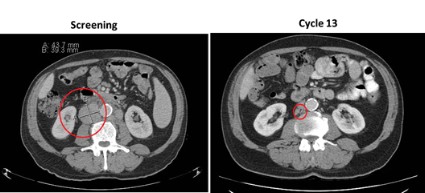
VIENNA – A daily dose of the investigational BCL-2 inhibitor venetoclax plus rituximab induced responses in 84% of patients with relapsed or refractory chronic lymphocytic leukemia in a phase Ib study.
Of the 49 patients, 20 (41%) achieved a complete response by standard assessment and 13 (27%) achieved a complete response with no evidence of residual disease on flow cytometry.
Moreover, six patients elected to stop venetoclax after achieving a complete response and, to date, only one has had recurrence of disease after 24 months without therapy, lead investigator Dr. Andrew W. Roberts reported at the annual congress of the European Hematology Association.
Not only were patients able to come off treatment and continue to remain in complete response, but responses were seen at the same frequencies across all classes of cytogenetic and molecular abnormalities, he noted.
“The greatest advance that this drug brings is for those patients who currently have a terrible prognosis with all other drugs that we now have,” Dr. Roberts of Royal Melbourne Hospital said in a press briefing.
“This is an important step forward in finding chemotherapy-free regimens in these vulnerable, elderly patients,” said press briefing moderator Dr. Anton Hagenbeek of the University Medical Center, Utrecht, the Netherlands.
Patients in the open-label, dose-escalation study had received a median of two prior lines of therapy (range, one to five) for chronic lymphocytic leukemia (CLL); their median age was 68 years (50-88 years). They began treatment with 20 mg or 50 mg venetoclax daily, increasing weekly to final cohort doses of 200 mg to 600 mg. Six cycles of monthly standard rituximab were added after the weekly lead-in phase.
CLL depends on high levels of B-cell lymphoma-2 (BCL-2) to stay alive. Venetoclax binds to and switches off the BCL-2 protein function, triggering the death of the CLL cell.
Grade 3 or 4 adverse events occurring in more than 10% of patients were neutropenia (51%), thrombocytopenia (16%), and anemia (14%). There was one treatment-emergent case of tumor lysis syndrome leading to death early in the trial. This phenomenon can occur when the CLL breaks down very quickly and, as a consequence, the study was redesigned and a lower starting dose is now used, Dr. Roberts said.
“That problem has been eliminated, but we still see a very large improvement in patients in a few weeks,” he said. “Other than that, there is a little bit of neutropenia, but that is very manageable.”
“So do you think you are curing patients with this approach?” Dr. Hagenbeek asked, to which Dr. Roberts replied, “Too early to say.”
Venetoclax is currently being evaluated in less heavily pretreated patients and a phase III trial is comparing the combination of venetoclax and rituximab with standard bendamustine chemotherapy plus rituximab, he said.
In May, the Food and Drug Administration granted venetoclax breakthrough therapy designation for use in relapsed or refractory chronic lymphocytic leukemia with a 17p deletion mutation.
AbbVie, which is developing venetoclax in partnership with Roche and Genentech, plans to submit regulatory applications for venetoclax to the FDA and the European Medicines Agency before the end of 2015.
On Twitter @pwendl
VIENNA – A daily dose of the investigational BCL-2 inhibitor venetoclax plus rituximab induced responses in 84% of patients with relapsed or refractory chronic lymphocytic leukemia in a phase Ib study.
Of the 49 patients, 20 (41%) achieved a complete response by standard assessment and 13 (27%) achieved a complete response with no evidence of residual disease on flow cytometry.
Moreover, six patients elected to stop venetoclax after achieving a complete response and, to date, only one has had recurrence of disease after 24 months without therapy, lead investigator Dr. Andrew W. Roberts reported at the annual congress of the European Hematology Association.
Not only were patients able to come off treatment and continue to remain in complete response, but responses were seen at the same frequencies across all classes of cytogenetic and molecular abnormalities, he noted.
“The greatest advance that this drug brings is for those patients who currently have a terrible prognosis with all other drugs that we now have,” Dr. Roberts of Royal Melbourne Hospital said in a press briefing.
“This is an important step forward in finding chemotherapy-free regimens in these vulnerable, elderly patients,” said press briefing moderator Dr. Anton Hagenbeek of the University Medical Center, Utrecht, the Netherlands.
Patients in the open-label, dose-escalation study had received a median of two prior lines of therapy (range, one to five) for chronic lymphocytic leukemia (CLL); their median age was 68 years (50-88 years). They began treatment with 20 mg or 50 mg venetoclax daily, increasing weekly to final cohort doses of 200 mg to 600 mg. Six cycles of monthly standard rituximab were added after the weekly lead-in phase.
CLL depends on high levels of B-cell lymphoma-2 (BCL-2) to stay alive. Venetoclax binds to and switches off the BCL-2 protein function, triggering the death of the CLL cell.
Grade 3 or 4 adverse events occurring in more than 10% of patients were neutropenia (51%), thrombocytopenia (16%), and anemia (14%). There was one treatment-emergent case of tumor lysis syndrome leading to death early in the trial. This phenomenon can occur when the CLL breaks down very quickly and, as a consequence, the study was redesigned and a lower starting dose is now used, Dr. Roberts said.
“That problem has been eliminated, but we still see a very large improvement in patients in a few weeks,” he said. “Other than that, there is a little bit of neutropenia, but that is very manageable.”
“So do you think you are curing patients with this approach?” Dr. Hagenbeek asked, to which Dr. Roberts replied, “Too early to say.”
Venetoclax is currently being evaluated in less heavily pretreated patients and a phase III trial is comparing the combination of venetoclax and rituximab with standard bendamustine chemotherapy plus rituximab, he said.
In May, the Food and Drug Administration granted venetoclax breakthrough therapy designation for use in relapsed or refractory chronic lymphocytic leukemia with a 17p deletion mutation.
AbbVie, which is developing venetoclax in partnership with Roche and Genentech, plans to submit regulatory applications for venetoclax to the FDA and the European Medicines Agency before the end of 2015.
On Twitter @pwendl
VIENNA – A daily dose of the investigational BCL-2 inhibitor venetoclax plus rituximab induced responses in 84% of patients with relapsed or refractory chronic lymphocytic leukemia in a phase Ib study.
Of the 49 patients, 20 (41%) achieved a complete response by standard assessment and 13 (27%) achieved a complete response with no evidence of residual disease on flow cytometry.
Moreover, six patients elected to stop venetoclax after achieving a complete response and, to date, only one has had recurrence of disease after 24 months without therapy, lead investigator Dr. Andrew W. Roberts reported at the annual congress of the European Hematology Association.
Not only were patients able to come off treatment and continue to remain in complete response, but responses were seen at the same frequencies across all classes of cytogenetic and molecular abnormalities, he noted.
“The greatest advance that this drug brings is for those patients who currently have a terrible prognosis with all other drugs that we now have,” Dr. Roberts of Royal Melbourne Hospital said in a press briefing.
“This is an important step forward in finding chemotherapy-free regimens in these vulnerable, elderly patients,” said press briefing moderator Dr. Anton Hagenbeek of the University Medical Center, Utrecht, the Netherlands.
Patients in the open-label, dose-escalation study had received a median of two prior lines of therapy (range, one to five) for chronic lymphocytic leukemia (CLL); their median age was 68 years (50-88 years). They began treatment with 20 mg or 50 mg venetoclax daily, increasing weekly to final cohort doses of 200 mg to 600 mg. Six cycles of monthly standard rituximab were added after the weekly lead-in phase.
CLL depends on high levels of B-cell lymphoma-2 (BCL-2) to stay alive. Venetoclax binds to and switches off the BCL-2 protein function, triggering the death of the CLL cell.
Grade 3 or 4 adverse events occurring in more than 10% of patients were neutropenia (51%), thrombocytopenia (16%), and anemia (14%). There was one treatment-emergent case of tumor lysis syndrome leading to death early in the trial. This phenomenon can occur when the CLL breaks down very quickly and, as a consequence, the study was redesigned and a lower starting dose is now used, Dr. Roberts said.
“That problem has been eliminated, but we still see a very large improvement in patients in a few weeks,” he said. “Other than that, there is a little bit of neutropenia, but that is very manageable.”
“So do you think you are curing patients with this approach?” Dr. Hagenbeek asked, to which Dr. Roberts replied, “Too early to say.”
Venetoclax is currently being evaluated in less heavily pretreated patients and a phase III trial is comparing the combination of venetoclax and rituximab with standard bendamustine chemotherapy plus rituximab, he said.
In May, the Food and Drug Administration granted venetoclax breakthrough therapy designation for use in relapsed or refractory chronic lymphocytic leukemia with a 17p deletion mutation.
AbbVie, which is developing venetoclax in partnership with Roche and Genentech, plans to submit regulatory applications for venetoclax to the FDA and the European Medicines Agency before the end of 2015.
On Twitter @pwendl
AT THE EHA CONGRESS
Key clinical point: Venetoclax plus rituximab is a highly active nonchemotherapy combination for patients with relapsed or refractory chronic lymphocytic leukemia.
Major finding: Overall, 84% of patients responded to venetoclax plus rituximab.
Data source: Phase Ib trial in 49 patients with relapsed or refractory chronic lymphocytic leukemia.
Disclosures: AbbVie sponsored the study. Dr. Roberts’ financial disclosures were not available at press time.
Chronic lymphocytic leukemia prognosis relatively good after transplantation failure
Unlike for those with acute leukemia, patients with chronic lymphocytic leukemia who had disease progression after undergoing transplantation had a relatively good prognosis, with 2- and 5-year overall survival rates of 67% and 38%, investigators reported online April 6 in the Journal of Clinical Oncology.*
Patients with chronic lymphocytic leukemia (CLL) who experienced acute or chronic graft-versus-host disease (GVHD) had significantly longer overall survival (OS) than those who did not have GVHD (P = .04 and P = .05, respectively). “Nearly half our patients with active CLL after transplantation had chronic GVHD, and the association of chronic GVHD with achieving cure and its power to predict OS among patients for whom transplantation failed suggests that the GVL (graft-versus-leukemia) effect contributes to prolonged survival even in patients with a high burden of disease,” wrote Dr. Uri Rozovski and associates at the University of Texas MD Anderson Cancer Center, Houston (J. Clin. Oncol. 2015 Apr. 6 [doi:10.1200/JCO.2014.58.6750]).
A matched-pair analysis showed that patients who underwent allogeneic stem cell transplant (SCT) about the same time and did not relapse also had higher rates of acute and chronic GVHD (P = .004 and P = .011, respectively).
The retrospective review of the Bone Marrow Transplantation Program database identified 358 patients with CLL or RT who underwent SCT from 1998 to 2011. The study evaluated 72 patients who had disease progression at a median 74 months after SCT, most of whom received one to eight lines of treatment after relapse and had a median OS of almost 3 years from the time of progression. Multivariate analysis showed that low hemoglobin levels and the presence of Richter’s transformation (RT) were associated with shorter OS; chronic GVHD and response to the first post-SCT treatment predicted longer OS.
Patients with RT had a worse prognosis, with a median OS of 15 months (95% confidence interval, 2-28 months) and 2- and 5-year survival rates of 36% and 0%. Transplantation carried a significant risk for transformation: 16 (30%) patients with CLL developed RT after allogeneic SCT. Conversely, four patients with RT developed CLL after transplantation.
The authors note that even in patients who did not maintain a durable response, SCT was beneficial. The study cohort received a variety of salvage treatments, and patients who received ibrutinib responded well. “Because of the favorable outcomes with ibrutinib in relapsed/refractory CLL, we believe that ibrutinib might have a role in the treatment of disease progression following transplantation failure,” they wrote.
*Correction, 4/8/2015: A previous version of this article misstated the type of leukemia referenced in the study.
Unlike for those with acute leukemia, patients with chronic lymphocytic leukemia who had disease progression after undergoing transplantation had a relatively good prognosis, with 2- and 5-year overall survival rates of 67% and 38%, investigators reported online April 6 in the Journal of Clinical Oncology.*
Patients with chronic lymphocytic leukemia (CLL) who experienced acute or chronic graft-versus-host disease (GVHD) had significantly longer overall survival (OS) than those who did not have GVHD (P = .04 and P = .05, respectively). “Nearly half our patients with active CLL after transplantation had chronic GVHD, and the association of chronic GVHD with achieving cure and its power to predict OS among patients for whom transplantation failed suggests that the GVL (graft-versus-leukemia) effect contributes to prolonged survival even in patients with a high burden of disease,” wrote Dr. Uri Rozovski and associates at the University of Texas MD Anderson Cancer Center, Houston (J. Clin. Oncol. 2015 Apr. 6 [doi:10.1200/JCO.2014.58.6750]).
A matched-pair analysis showed that patients who underwent allogeneic stem cell transplant (SCT) about the same time and did not relapse also had higher rates of acute and chronic GVHD (P = .004 and P = .011, respectively).
The retrospective review of the Bone Marrow Transplantation Program database identified 358 patients with CLL or RT who underwent SCT from 1998 to 2011. The study evaluated 72 patients who had disease progression at a median 74 months after SCT, most of whom received one to eight lines of treatment after relapse and had a median OS of almost 3 years from the time of progression. Multivariate analysis showed that low hemoglobin levels and the presence of Richter’s transformation (RT) were associated with shorter OS; chronic GVHD and response to the first post-SCT treatment predicted longer OS.
Patients with RT had a worse prognosis, with a median OS of 15 months (95% confidence interval, 2-28 months) and 2- and 5-year survival rates of 36% and 0%. Transplantation carried a significant risk for transformation: 16 (30%) patients with CLL developed RT after allogeneic SCT. Conversely, four patients with RT developed CLL after transplantation.
The authors note that even in patients who did not maintain a durable response, SCT was beneficial. The study cohort received a variety of salvage treatments, and patients who received ibrutinib responded well. “Because of the favorable outcomes with ibrutinib in relapsed/refractory CLL, we believe that ibrutinib might have a role in the treatment of disease progression following transplantation failure,” they wrote.
*Correction, 4/8/2015: A previous version of this article misstated the type of leukemia referenced in the study.
Unlike for those with acute leukemia, patients with chronic lymphocytic leukemia who had disease progression after undergoing transplantation had a relatively good prognosis, with 2- and 5-year overall survival rates of 67% and 38%, investigators reported online April 6 in the Journal of Clinical Oncology.*
Patients with chronic lymphocytic leukemia (CLL) who experienced acute or chronic graft-versus-host disease (GVHD) had significantly longer overall survival (OS) than those who did not have GVHD (P = .04 and P = .05, respectively). “Nearly half our patients with active CLL after transplantation had chronic GVHD, and the association of chronic GVHD with achieving cure and its power to predict OS among patients for whom transplantation failed suggests that the GVL (graft-versus-leukemia) effect contributes to prolonged survival even in patients with a high burden of disease,” wrote Dr. Uri Rozovski and associates at the University of Texas MD Anderson Cancer Center, Houston (J. Clin. Oncol. 2015 Apr. 6 [doi:10.1200/JCO.2014.58.6750]).
A matched-pair analysis showed that patients who underwent allogeneic stem cell transplant (SCT) about the same time and did not relapse also had higher rates of acute and chronic GVHD (P = .004 and P = .011, respectively).
The retrospective review of the Bone Marrow Transplantation Program database identified 358 patients with CLL or RT who underwent SCT from 1998 to 2011. The study evaluated 72 patients who had disease progression at a median 74 months after SCT, most of whom received one to eight lines of treatment after relapse and had a median OS of almost 3 years from the time of progression. Multivariate analysis showed that low hemoglobin levels and the presence of Richter’s transformation (RT) were associated with shorter OS; chronic GVHD and response to the first post-SCT treatment predicted longer OS.
Patients with RT had a worse prognosis, with a median OS of 15 months (95% confidence interval, 2-28 months) and 2- and 5-year survival rates of 36% and 0%. Transplantation carried a significant risk for transformation: 16 (30%) patients with CLL developed RT after allogeneic SCT. Conversely, four patients with RT developed CLL after transplantation.
The authors note that even in patients who did not maintain a durable response, SCT was beneficial. The study cohort received a variety of salvage treatments, and patients who received ibrutinib responded well. “Because of the favorable outcomes with ibrutinib in relapsed/refractory CLL, we believe that ibrutinib might have a role in the treatment of disease progression following transplantation failure,” they wrote.
*Correction, 4/8/2015: A previous version of this article misstated the type of leukemia referenced in the study.
FROM JOURNAL OF CLINICAL ONCOLOGY
Key clinical point: The prognosis for patients with chronic lymphocytic* leukemia who have undergone failed stem cell transplantation (SCT) is relatively good.
Major finding: From the time of progression after SCT, median OS was 36 months (95% CI, 24-48) for patients with CLL, and 38% survived 5 or more years.
Data source: The retrospective database review identified 72 patients with CLL or Richter’s transformation who underwent allogenic SCT from 1998 to 2011 and progressed after transplantation.
Disclosures: Dr. Rozovski reported having no disclosures. Two of the coauthors reported ties to several industry sources.
Ofatumumab maintenance halves risk of progression in relapsed CLL
SAN FRANCISCO – Ofatumumab maintenance therapy nearly doubled progression-free survival in patients with relapsed CLL, according to a preplanned interim analysis of the phase III PROLONG study.
At a median follow-up of 19.1 months, progression-free survival was 15.2 months with the standard approach of observation alone and 29.4 months with maintenance ofatumumab (Hazard ratio, 0.50; P < .0001).
Ofatumumab (Arzerra) also significantly increased the median time to next treatment from 31.1 months to 38 months (HR, 0.66; P = .0108), Dr. Marinus van Oers reported at the annual meeting of the American Society of Hematology.
The benefit in progression-free survival (PFS) with maintenance was “statistically significant and clinical relevant” and was present in all subgroups, he said. It was independent of age, gender, number and type of prior treatment, minimal residual disease status at study entry, and “response at study entry, although we have the impression that it’s more effective in patients on PR [partial response] than in patients on CR [complete response],” he added.
The rationale for the trial lies in the fact that despite recent advances, there is still no curative treatment for chronic lymphocytic leukemia (CLL). Ofatumumab, a type 1 CD20 monoclonal antibody, has a role as maintenance in follicular lymphoma (FL), which shares similarities in biological behavior with CLL. This role is debated, but a recent meta-analysis shows ofatumumab maintenance prolongs PFS and tends to prolong overall survival in relapsed patients with FL, Dr. van Oers of the Academic Medical Center in Amsterdam, The Netherlands, observed.
PROLONG randomized 474 patients with relapsed CLL to observation or ofatumumab 300 mg in week 1 and 1,000 mg in week 2, and every 8 weeks for 2 years. All patients were in second or third remission and within 3 months of response assessment after the last reinduction treatment. Patients with refractory disease or prior maintenance therapy or stem cell transplantation were excluded.
At baseline, the median age was about 65 years, 70% had at least two prior treatments, 80% were in partial remission from their last CLL treatment, and less than 10% had poor-risk cytogenetics 11p or 17p deletions. At the time of the analysis, 25% of patients had received all 13 cycles of ofatumumab.
Adverse events of any grade were increased with the addition of ofatumumab versus placebo (86% vs. 72%; P < .0001). Sixty percent were related to study treatment, but none resulted in study withdrawal, Dr. van Oers said. In all, 17 patients on the experimental arm dropped out due to physician decision or patient wish.
Among grade 3 events, neutropenia was significantly increased with maintenance therapy versus placebo (24% vs. 10%; P < .0001) and there was a non-significant increase in infections (13% vs. 8%). Five deaths occurred in the observation arm and two in the ofatumumab arm, one due to sepsis two months after the end of treatment and the other due to unrelated GI obstruction.
Median overall survival has not been reached for either arm (HR, 0.85; P = .487), he reported on behalf of HOVON and the NORDIC CLL group, co-developers of the study.
SAN FRANCISCO – Ofatumumab maintenance therapy nearly doubled progression-free survival in patients with relapsed CLL, according to a preplanned interim analysis of the phase III PROLONG study.
At a median follow-up of 19.1 months, progression-free survival was 15.2 months with the standard approach of observation alone and 29.4 months with maintenance ofatumumab (Hazard ratio, 0.50; P < .0001).
Ofatumumab (Arzerra) also significantly increased the median time to next treatment from 31.1 months to 38 months (HR, 0.66; P = .0108), Dr. Marinus van Oers reported at the annual meeting of the American Society of Hematology.
The benefit in progression-free survival (PFS) with maintenance was “statistically significant and clinical relevant” and was present in all subgroups, he said. It was independent of age, gender, number and type of prior treatment, minimal residual disease status at study entry, and “response at study entry, although we have the impression that it’s more effective in patients on PR [partial response] than in patients on CR [complete response],” he added.
The rationale for the trial lies in the fact that despite recent advances, there is still no curative treatment for chronic lymphocytic leukemia (CLL). Ofatumumab, a type 1 CD20 monoclonal antibody, has a role as maintenance in follicular lymphoma (FL), which shares similarities in biological behavior with CLL. This role is debated, but a recent meta-analysis shows ofatumumab maintenance prolongs PFS and tends to prolong overall survival in relapsed patients with FL, Dr. van Oers of the Academic Medical Center in Amsterdam, The Netherlands, observed.
PROLONG randomized 474 patients with relapsed CLL to observation or ofatumumab 300 mg in week 1 and 1,000 mg in week 2, and every 8 weeks for 2 years. All patients were in second or third remission and within 3 months of response assessment after the last reinduction treatment. Patients with refractory disease or prior maintenance therapy or stem cell transplantation were excluded.
At baseline, the median age was about 65 years, 70% had at least two prior treatments, 80% were in partial remission from their last CLL treatment, and less than 10% had poor-risk cytogenetics 11p or 17p deletions. At the time of the analysis, 25% of patients had received all 13 cycles of ofatumumab.
Adverse events of any grade were increased with the addition of ofatumumab versus placebo (86% vs. 72%; P < .0001). Sixty percent were related to study treatment, but none resulted in study withdrawal, Dr. van Oers said. In all, 17 patients on the experimental arm dropped out due to physician decision or patient wish.
Among grade 3 events, neutropenia was significantly increased with maintenance therapy versus placebo (24% vs. 10%; P < .0001) and there was a non-significant increase in infections (13% vs. 8%). Five deaths occurred in the observation arm and two in the ofatumumab arm, one due to sepsis two months after the end of treatment and the other due to unrelated GI obstruction.
Median overall survival has not been reached for either arm (HR, 0.85; P = .487), he reported on behalf of HOVON and the NORDIC CLL group, co-developers of the study.
SAN FRANCISCO – Ofatumumab maintenance therapy nearly doubled progression-free survival in patients with relapsed CLL, according to a preplanned interim analysis of the phase III PROLONG study.
At a median follow-up of 19.1 months, progression-free survival was 15.2 months with the standard approach of observation alone and 29.4 months with maintenance ofatumumab (Hazard ratio, 0.50; P < .0001).
Ofatumumab (Arzerra) also significantly increased the median time to next treatment from 31.1 months to 38 months (HR, 0.66; P = .0108), Dr. Marinus van Oers reported at the annual meeting of the American Society of Hematology.
The benefit in progression-free survival (PFS) with maintenance was “statistically significant and clinical relevant” and was present in all subgroups, he said. It was independent of age, gender, number and type of prior treatment, minimal residual disease status at study entry, and “response at study entry, although we have the impression that it’s more effective in patients on PR [partial response] than in patients on CR [complete response],” he added.
The rationale for the trial lies in the fact that despite recent advances, there is still no curative treatment for chronic lymphocytic leukemia (CLL). Ofatumumab, a type 1 CD20 monoclonal antibody, has a role as maintenance in follicular lymphoma (FL), which shares similarities in biological behavior with CLL. This role is debated, but a recent meta-analysis shows ofatumumab maintenance prolongs PFS and tends to prolong overall survival in relapsed patients with FL, Dr. van Oers of the Academic Medical Center in Amsterdam, The Netherlands, observed.
PROLONG randomized 474 patients with relapsed CLL to observation or ofatumumab 300 mg in week 1 and 1,000 mg in week 2, and every 8 weeks for 2 years. All patients were in second or third remission and within 3 months of response assessment after the last reinduction treatment. Patients with refractory disease or prior maintenance therapy or stem cell transplantation were excluded.
At baseline, the median age was about 65 years, 70% had at least two prior treatments, 80% were in partial remission from their last CLL treatment, and less than 10% had poor-risk cytogenetics 11p or 17p deletions. At the time of the analysis, 25% of patients had received all 13 cycles of ofatumumab.
Adverse events of any grade were increased with the addition of ofatumumab versus placebo (86% vs. 72%; P < .0001). Sixty percent were related to study treatment, but none resulted in study withdrawal, Dr. van Oers said. In all, 17 patients on the experimental arm dropped out due to physician decision or patient wish.
Among grade 3 events, neutropenia was significantly increased with maintenance therapy versus placebo (24% vs. 10%; P < .0001) and there was a non-significant increase in infections (13% vs. 8%). Five deaths occurred in the observation arm and two in the ofatumumab arm, one due to sepsis two months after the end of treatment and the other due to unrelated GI obstruction.
Median overall survival has not been reached for either arm (HR, 0.85; P = .487), he reported on behalf of HOVON and the NORDIC CLL group, co-developers of the study.
AT ASH 2014
Key clinical point: Maintenance ofatumumab cuts the risk of progression in half among patients with relapsed CLL.
Major finding: Progression-free survival was 15.2 months with observation alone and 29.4 months with maintenance ofatumumab (Hazard ratio, 0.50; P < .0001).
Data source: Randomized phase III trial in 474 patients with relapsed CLL.
Disclosures: GlaxoSmithKline sponsored the study. Dr. van Oers reported having no financial disclosures.
VIDEO: Are chemo-free regimens possible for CLL?
MILAN – The Food and Drug Administration has given full approval for ibrutinib for patients with chronic lymphocytic leukemia who have received at least one prior therapy and for those who have a deletion in chromosome 17 (17p deletion) and may or may not have received previous treatment.
At the annual congress of the European Hematology Association, Dr. Peter Hillmen discusses the results he presented from RESONATE, the study used to convert conditional, accelerated approval to full approval. The study evaluated daily ibrutinib monotherapy versus the anti-CD20 antibody ofatumumab, for patients with relapsed or refractory chronic lymphocytic leukemia (CLL).
Dr. Hillmen, professor of experimental hematology at the University of Leeds, England, also outlines some of the research in the works to evaluate ibrutinib as frontline therapy for patients with CLL and the possibility of chemotherapy-free regimens. He disclosed a consultancy role and honoraria from Pharmacyclics.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
MILAN – The Food and Drug Administration has given full approval for ibrutinib for patients with chronic lymphocytic leukemia who have received at least one prior therapy and for those who have a deletion in chromosome 17 (17p deletion) and may or may not have received previous treatment.
At the annual congress of the European Hematology Association, Dr. Peter Hillmen discusses the results he presented from RESONATE, the study used to convert conditional, accelerated approval to full approval. The study evaluated daily ibrutinib monotherapy versus the anti-CD20 antibody ofatumumab, for patients with relapsed or refractory chronic lymphocytic leukemia (CLL).
Dr. Hillmen, professor of experimental hematology at the University of Leeds, England, also outlines some of the research in the works to evaluate ibrutinib as frontline therapy for patients with CLL and the possibility of chemotherapy-free regimens. He disclosed a consultancy role and honoraria from Pharmacyclics.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
MILAN – The Food and Drug Administration has given full approval for ibrutinib for patients with chronic lymphocytic leukemia who have received at least one prior therapy and for those who have a deletion in chromosome 17 (17p deletion) and may or may not have received previous treatment.
At the annual congress of the European Hematology Association, Dr. Peter Hillmen discusses the results he presented from RESONATE, the study used to convert conditional, accelerated approval to full approval. The study evaluated daily ibrutinib monotherapy versus the anti-CD20 antibody ofatumumab, for patients with relapsed or refractory chronic lymphocytic leukemia (CLL).
Dr. Hillmen, professor of experimental hematology at the University of Leeds, England, also outlines some of the research in the works to evaluate ibrutinib as frontline therapy for patients with CLL and the possibility of chemotherapy-free regimens. He disclosed a consultancy role and honoraria from Pharmacyclics.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
AT THE EHA CONGRESS
VIDEO: ABT-199 alone and in combination shows promise against advanced CLL
MILAN – Dr. Andrew W. Roberts discusses the high response rates that have occurred with the Bcl-2 inhibitor ABT-199, alone and in combination, against refractory or relapsed chronic lymphocytic leukemia.
Drug-induced tumor lysis syndrome in some patients appears to have been avoided with a new modified dosing regimen, said Dr. Roberts, who presented phase Ib study results of ABT-199 in combination with rituximab at the annual congress of the European Hematology Association. In the interview, Dr. Roberts of the Royal Melbourne Hospital and Walter and Eliza Hall Institute of Medical Research, Parkville, Victoria, Australia, describes the study results and future plans for ABT-199 research.
On Twitter @nikolaideslaura
MILAN – Dr. Andrew W. Roberts discusses the high response rates that have occurred with the Bcl-2 inhibitor ABT-199, alone and in combination, against refractory or relapsed chronic lymphocytic leukemia.
Drug-induced tumor lysis syndrome in some patients appears to have been avoided with a new modified dosing regimen, said Dr. Roberts, who presented phase Ib study results of ABT-199 in combination with rituximab at the annual congress of the European Hematology Association. In the interview, Dr. Roberts of the Royal Melbourne Hospital and Walter and Eliza Hall Institute of Medical Research, Parkville, Victoria, Australia, describes the study results and future plans for ABT-199 research.
On Twitter @nikolaideslaura
MILAN – Dr. Andrew W. Roberts discusses the high response rates that have occurred with the Bcl-2 inhibitor ABT-199, alone and in combination, against refractory or relapsed chronic lymphocytic leukemia.
Drug-induced tumor lysis syndrome in some patients appears to have been avoided with a new modified dosing regimen, said Dr. Roberts, who presented phase Ib study results of ABT-199 in combination with rituximab at the annual congress of the European Hematology Association. In the interview, Dr. Roberts of the Royal Melbourne Hospital and Walter and Eliza Hall Institute of Medical Research, Parkville, Victoria, Australia, describes the study results and future plans for ABT-199 research.
On Twitter @nikolaideslaura
AT THE EHA CONGRESS
FDA gives full approval to ibrutinib for CLL
The Food and Drug Administration has given full approval for ibrutinib (Imbruvica) for patients with chronic lymphocytic leukemia who have received at least one prior therapy and for those who have a deletion in chromosome 17 (17p deletion) and may or may not have received previous treatment.
The drug received conditional, accelerated approval from the FDA in February for CLL. The agency said that new trial results that looked at overall survival and progression-free survival confirmed the drug’s benefit. Ibrutinib’s label will be updated to show that it has a confirmed survival benefit.
The FDA also designated ibrutinib as a breakthrough therapy for CLL with 17p deletion.
"Imbruvica is the fourth drug approved to treat CLL that received a breakthrough therapy designation, reflecting the promise of the breakthrough therapy designation program and demonstrating the FDA’s commitment to working cooperatively with companies to expedite the development, review, and approval of these important new drugs," said Dr. Richard Pazdur, director of the Office of Hematology and Oncology Products in the FDA’s Center for Drug Evaluation and Research, in a statement.
"This FDA approval for Imbruvica is a major step toward chemo-free treatment in CLL," said Dr. John Byrd, director of the hematology division at the Ohio State University Comprehensive Cancer Center, Columbus, in a statement issued by Pharmacyclics, the Sunnyvale, Calif.–based company that is comarketing the drug with Janssen Biotech.
"I continue to be awed by the duration of my patients’ responses to Imbruvica and am grateful Imbruvica now is available to a broader group of CLL patients," said Dr. Byrd, who was a lead investigator for the main trial evaluating ibrutinib, RESONATE.
Three other drugs for CLL have also received breakthrough designations: obinutuzumab (Gazyva), ofatumumab (Arzerra), and most recently, idelalisib (Zydelig), earlier in July.
CLL is a non-Hodgkin’s lymphoma that primarily affects older individuals. The National Cancer Institute estimates that 15,720 Americans will be diagnosed and 4,600 will die from CLL in 2014, the FDA said.
In RESONATE, 391 previously treated patients received either ibrutinib or ofatumumab. Of those, 127 patients had a 17p deletion. The trial was stopped early because overall, patients receiving ibrutinib had a 78% reduction in the risk of disease progression or death, and a 57% reduction in risk of death. For the patients with 17p, there was a 75% reduction in the risk of disease progression or death.
This is the third FDA approval for ibrutinib. In addition to the accelerated approval for CLL in February, the drug was approved for mantle cell lymphoma in November 2013.
Dr. Byrd has served as an unpaid adviser to both Pharmacyclics and Janssen. He reported no financial interest in either company.
On Twitter @aliciaault
The Food and Drug Administration has given full approval for ibrutinib (Imbruvica) for patients with chronic lymphocytic leukemia who have received at least one prior therapy and for those who have a deletion in chromosome 17 (17p deletion) and may or may not have received previous treatment.
The drug received conditional, accelerated approval from the FDA in February for CLL. The agency said that new trial results that looked at overall survival and progression-free survival confirmed the drug’s benefit. Ibrutinib’s label will be updated to show that it has a confirmed survival benefit.
The FDA also designated ibrutinib as a breakthrough therapy for CLL with 17p deletion.
"Imbruvica is the fourth drug approved to treat CLL that received a breakthrough therapy designation, reflecting the promise of the breakthrough therapy designation program and demonstrating the FDA’s commitment to working cooperatively with companies to expedite the development, review, and approval of these important new drugs," said Dr. Richard Pazdur, director of the Office of Hematology and Oncology Products in the FDA’s Center for Drug Evaluation and Research, in a statement.
"This FDA approval for Imbruvica is a major step toward chemo-free treatment in CLL," said Dr. John Byrd, director of the hematology division at the Ohio State University Comprehensive Cancer Center, Columbus, in a statement issued by Pharmacyclics, the Sunnyvale, Calif.–based company that is comarketing the drug with Janssen Biotech.
"I continue to be awed by the duration of my patients’ responses to Imbruvica and am grateful Imbruvica now is available to a broader group of CLL patients," said Dr. Byrd, who was a lead investigator for the main trial evaluating ibrutinib, RESONATE.
Three other drugs for CLL have also received breakthrough designations: obinutuzumab (Gazyva), ofatumumab (Arzerra), and most recently, idelalisib (Zydelig), earlier in July.
CLL is a non-Hodgkin’s lymphoma that primarily affects older individuals. The National Cancer Institute estimates that 15,720 Americans will be diagnosed and 4,600 will die from CLL in 2014, the FDA said.
In RESONATE, 391 previously treated patients received either ibrutinib or ofatumumab. Of those, 127 patients had a 17p deletion. The trial was stopped early because overall, patients receiving ibrutinib had a 78% reduction in the risk of disease progression or death, and a 57% reduction in risk of death. For the patients with 17p, there was a 75% reduction in the risk of disease progression or death.
This is the third FDA approval for ibrutinib. In addition to the accelerated approval for CLL in February, the drug was approved for mantle cell lymphoma in November 2013.
Dr. Byrd has served as an unpaid adviser to both Pharmacyclics and Janssen. He reported no financial interest in either company.
On Twitter @aliciaault
The Food and Drug Administration has given full approval for ibrutinib (Imbruvica) for patients with chronic lymphocytic leukemia who have received at least one prior therapy and for those who have a deletion in chromosome 17 (17p deletion) and may or may not have received previous treatment.
The drug received conditional, accelerated approval from the FDA in February for CLL. The agency said that new trial results that looked at overall survival and progression-free survival confirmed the drug’s benefit. Ibrutinib’s label will be updated to show that it has a confirmed survival benefit.
The FDA also designated ibrutinib as a breakthrough therapy for CLL with 17p deletion.
"Imbruvica is the fourth drug approved to treat CLL that received a breakthrough therapy designation, reflecting the promise of the breakthrough therapy designation program and demonstrating the FDA’s commitment to working cooperatively with companies to expedite the development, review, and approval of these important new drugs," said Dr. Richard Pazdur, director of the Office of Hematology and Oncology Products in the FDA’s Center for Drug Evaluation and Research, in a statement.
"This FDA approval for Imbruvica is a major step toward chemo-free treatment in CLL," said Dr. John Byrd, director of the hematology division at the Ohio State University Comprehensive Cancer Center, Columbus, in a statement issued by Pharmacyclics, the Sunnyvale, Calif.–based company that is comarketing the drug with Janssen Biotech.
"I continue to be awed by the duration of my patients’ responses to Imbruvica and am grateful Imbruvica now is available to a broader group of CLL patients," said Dr. Byrd, who was a lead investigator for the main trial evaluating ibrutinib, RESONATE.
Three other drugs for CLL have also received breakthrough designations: obinutuzumab (Gazyva), ofatumumab (Arzerra), and most recently, idelalisib (Zydelig), earlier in July.
CLL is a non-Hodgkin’s lymphoma that primarily affects older individuals. The National Cancer Institute estimates that 15,720 Americans will be diagnosed and 4,600 will die from CLL in 2014, the FDA said.
In RESONATE, 391 previously treated patients received either ibrutinib or ofatumumab. Of those, 127 patients had a 17p deletion. The trial was stopped early because overall, patients receiving ibrutinib had a 78% reduction in the risk of disease progression or death, and a 57% reduction in risk of death. For the patients with 17p, there was a 75% reduction in the risk of disease progression or death.
This is the third FDA approval for ibrutinib. In addition to the accelerated approval for CLL in February, the drug was approved for mantle cell lymphoma in November 2013.
Dr. Byrd has served as an unpaid adviser to both Pharmacyclics and Janssen. He reported no financial interest in either company.
On Twitter @aliciaault
ABT-199 rebounds in advanced CLL after tackling tumor lysis syndrome
MILAN – The investigational Bcl-2 inhibitor ABT-199 continues to impress with substantial activity as single-agent or combination therapy in relapsed or refractory chronic lymphocytic leukemia, following dose-scheduling modifications to address the risk of tumor lysis syndrome.
ABT-199 monotherapy
Updated data from all 105 CLL patients in the phase I trial show the overall response rate remains high at 77%, with 23% of patients achieving complete remission.
Seven of 11 complete responders assessed had no detectable minimal residual disease, Dr. John F. Seymour said at the annual congress of the European Hematology Association.
Overall response rates were sustained in the 75%-80% range for high-risk patients with deletion 17p, fludarabine-refractory, or immunoglobulin heavy-chain variable (IGHV)-unmutated CLL; and complete response rates in these subgroups also did not differ from the overall group at 22% to 29%.
Prior results from the first-in-human trial dazzled the leukemia community, but tumor lysis syndrome (TLS) complications, including two fatal events, temporarily halted ABT-199 clinical trials and gave the advantage to its closest competitor, the recently approved and more tolerable CLL drug ibrutinib (Imbruvica).
Use of a modified, ramp-up dosing scheme and aggressive TLS prophylaxis appear to have ameliorated the risk of TLS, with no further clinically significant or grade 3 or 4 events reported in the 49 patients treated with this schema, said Dr. Seymour, director of hematology and cancer medicine at the Peter MacCallum Cancer Centre, East Melbourne, Australia.
Rather than using a 3-week schedule and 50-mg starting dose, the safety expansion cohort received once-daily oral ABT-199 beginning at 20 mg, with weekly adjustments to 50 mg, 100 mg, 200 mg, and 400 mg over 5 weeks.
The 400-mg dose has been identified as the phase II dose, with 59% of patients free of progression at 18 months and beyond on this dose, he said.
As of April 2014, 37 of the 105 patients discontinued treatment, 22 due to progressive disease and 12 for adverse events; in addition, two proceeded to allogeneic hematopoietic cell transplantation, and one needed Coumadin, which is not permitted on protocol.
The median duration of response has not yet been reached for patients treated at doses of 400 mg or above, he said.
The most common treatment-emergent adverse events of any grade were diarrhea (40% of patients), neutropenia (36%), and nausea (35%).
Neutropenia was the only grade 3/4 event occurring in more than 10% of patients (33%), followed by anemia in 10%.
Combination ABT-199
Of substantial interest to many was a second phase Ib study presented in the same session, evaluating the role of ABT-199 with the anti-CD20 antibody rituximab (Rituxan) in relapsed or refractory CLL.
After a median time on study of just 7.5 months, the overall response rate was 84% among 25 evaluable patients, including 9 complete responses (36%) and 12 partial responses (48%), said Dr. Andrew W. Roberts, with the Royal Melbourne (Australia) Hospital and Walter and Eliza Hall Institute of Medical Research.
Six of eight complete responders tested were negative for minimal residual disease by flow cytometry.
Preliminary pharmacokinetic results suggest no apparent effect of rituximab on ABT-199 exposure, he said.
Three patients discontinued ABT-199 after achieving a complete remission, including one with fludarabine-refractory disease, and all remain in complete remission at 8.6, 8.8, and 11.6 months after cessation.
Dose modifications were also made in this study following a fatal TLS event in December 2012 after a first dose of ABT-199 at 50 mg. Under the modified step-up dosing, ABT-199 was started at 20 mg, escalating up to 600 mg daily over 5 weeks, with rituximab 375 mg/m2 added on day 1 of week 5 and rituximab 500 mg/m2 added on day 1 of months 2-6.
The combination was well tolerated, and no new safety concerns were identified, Dr. Roberts said. The most common grade 3/4 adverse events among 45 patients evaluable for safety were neutropenia in 47%, anemia in 16%, thrombocytopenia in 13%, and febrile neutropenia in 7%. Grade 3/4 neutropenia was more common at 600 mg, with the 400-mg dose selected for the ongoing safety expansion cohort. Two serious TLS events occurred, but both were prior to schedule modifications, he said.
One patient in the combination study and 13 in the monotherapy study received treatment for small lymphocytic lymphoma. Response rates and tolerability were similar between CLL and SLL patients in the monotherapy study, Dr. Roberts said in an interview.
During a press briefing at the meeting, Dr. Seymour said ABT-199 potentially could be combined with ibrutinib and that the combination was very potent in laboratory tests in both CLL and some forms of mantle cell lymphoma. Negotiations with the various companies involved are intricate, but there is agreement and commitment "to begin clinical trials of the combination later this year," he added.
ABT-199 is currently being evaluated in a phase II trial as monotherapy in deletion 17p relapsed CLL, as combination therapy with rituximab versus bendamustine plus rituximab in a phase III trial in relapsed/refractory CLL, and in combination trials with bendamustine/rituximab and obinutuzumab in relapsed/refractory CLL.
AbbVie and Genentech sponsored the trials. Dr. Seymour is a consultant and adviser for AbbVie, Genentech, and Roche. Dr. Roberts reported research funding from AbbVie and Genentech and milestone payments to his institution related to ABT-199.
MILAN – The investigational Bcl-2 inhibitor ABT-199 continues to impress with substantial activity as single-agent or combination therapy in relapsed or refractory chronic lymphocytic leukemia, following dose-scheduling modifications to address the risk of tumor lysis syndrome.
ABT-199 monotherapy
Updated data from all 105 CLL patients in the phase I trial show the overall response rate remains high at 77%, with 23% of patients achieving complete remission.
Seven of 11 complete responders assessed had no detectable minimal residual disease, Dr. John F. Seymour said at the annual congress of the European Hematology Association.
Overall response rates were sustained in the 75%-80% range for high-risk patients with deletion 17p, fludarabine-refractory, or immunoglobulin heavy-chain variable (IGHV)-unmutated CLL; and complete response rates in these subgroups also did not differ from the overall group at 22% to 29%.
Prior results from the first-in-human trial dazzled the leukemia community, but tumor lysis syndrome (TLS) complications, including two fatal events, temporarily halted ABT-199 clinical trials and gave the advantage to its closest competitor, the recently approved and more tolerable CLL drug ibrutinib (Imbruvica).
Use of a modified, ramp-up dosing scheme and aggressive TLS prophylaxis appear to have ameliorated the risk of TLS, with no further clinically significant or grade 3 or 4 events reported in the 49 patients treated with this schema, said Dr. Seymour, director of hematology and cancer medicine at the Peter MacCallum Cancer Centre, East Melbourne, Australia.
Rather than using a 3-week schedule and 50-mg starting dose, the safety expansion cohort received once-daily oral ABT-199 beginning at 20 mg, with weekly adjustments to 50 mg, 100 mg, 200 mg, and 400 mg over 5 weeks.
The 400-mg dose has been identified as the phase II dose, with 59% of patients free of progression at 18 months and beyond on this dose, he said.
As of April 2014, 37 of the 105 patients discontinued treatment, 22 due to progressive disease and 12 for adverse events; in addition, two proceeded to allogeneic hematopoietic cell transplantation, and one needed Coumadin, which is not permitted on protocol.
The median duration of response has not yet been reached for patients treated at doses of 400 mg or above, he said.
The most common treatment-emergent adverse events of any grade were diarrhea (40% of patients), neutropenia (36%), and nausea (35%).
Neutropenia was the only grade 3/4 event occurring in more than 10% of patients (33%), followed by anemia in 10%.
Combination ABT-199
Of substantial interest to many was a second phase Ib study presented in the same session, evaluating the role of ABT-199 with the anti-CD20 antibody rituximab (Rituxan) in relapsed or refractory CLL.
After a median time on study of just 7.5 months, the overall response rate was 84% among 25 evaluable patients, including 9 complete responses (36%) and 12 partial responses (48%), said Dr. Andrew W. Roberts, with the Royal Melbourne (Australia) Hospital and Walter and Eliza Hall Institute of Medical Research.
Six of eight complete responders tested were negative for minimal residual disease by flow cytometry.
Preliminary pharmacokinetic results suggest no apparent effect of rituximab on ABT-199 exposure, he said.
Three patients discontinued ABT-199 after achieving a complete remission, including one with fludarabine-refractory disease, and all remain in complete remission at 8.6, 8.8, and 11.6 months after cessation.
Dose modifications were also made in this study following a fatal TLS event in December 2012 after a first dose of ABT-199 at 50 mg. Under the modified step-up dosing, ABT-199 was started at 20 mg, escalating up to 600 mg daily over 5 weeks, with rituximab 375 mg/m2 added on day 1 of week 5 and rituximab 500 mg/m2 added on day 1 of months 2-6.
The combination was well tolerated, and no new safety concerns were identified, Dr. Roberts said. The most common grade 3/4 adverse events among 45 patients evaluable for safety were neutropenia in 47%, anemia in 16%, thrombocytopenia in 13%, and febrile neutropenia in 7%. Grade 3/4 neutropenia was more common at 600 mg, with the 400-mg dose selected for the ongoing safety expansion cohort. Two serious TLS events occurred, but both were prior to schedule modifications, he said.
One patient in the combination study and 13 in the monotherapy study received treatment for small lymphocytic lymphoma. Response rates and tolerability were similar between CLL and SLL patients in the monotherapy study, Dr. Roberts said in an interview.
During a press briefing at the meeting, Dr. Seymour said ABT-199 potentially could be combined with ibrutinib and that the combination was very potent in laboratory tests in both CLL and some forms of mantle cell lymphoma. Negotiations with the various companies involved are intricate, but there is agreement and commitment "to begin clinical trials of the combination later this year," he added.
ABT-199 is currently being evaluated in a phase II trial as monotherapy in deletion 17p relapsed CLL, as combination therapy with rituximab versus bendamustine plus rituximab in a phase III trial in relapsed/refractory CLL, and in combination trials with bendamustine/rituximab and obinutuzumab in relapsed/refractory CLL.
AbbVie and Genentech sponsored the trials. Dr. Seymour is a consultant and adviser for AbbVie, Genentech, and Roche. Dr. Roberts reported research funding from AbbVie and Genentech and milestone payments to his institution related to ABT-199.
MILAN – The investigational Bcl-2 inhibitor ABT-199 continues to impress with substantial activity as single-agent or combination therapy in relapsed or refractory chronic lymphocytic leukemia, following dose-scheduling modifications to address the risk of tumor lysis syndrome.
ABT-199 monotherapy
Updated data from all 105 CLL patients in the phase I trial show the overall response rate remains high at 77%, with 23% of patients achieving complete remission.
Seven of 11 complete responders assessed had no detectable minimal residual disease, Dr. John F. Seymour said at the annual congress of the European Hematology Association.
Overall response rates were sustained in the 75%-80% range for high-risk patients with deletion 17p, fludarabine-refractory, or immunoglobulin heavy-chain variable (IGHV)-unmutated CLL; and complete response rates in these subgroups also did not differ from the overall group at 22% to 29%.
Prior results from the first-in-human trial dazzled the leukemia community, but tumor lysis syndrome (TLS) complications, including two fatal events, temporarily halted ABT-199 clinical trials and gave the advantage to its closest competitor, the recently approved and more tolerable CLL drug ibrutinib (Imbruvica).
Use of a modified, ramp-up dosing scheme and aggressive TLS prophylaxis appear to have ameliorated the risk of TLS, with no further clinically significant or grade 3 or 4 events reported in the 49 patients treated with this schema, said Dr. Seymour, director of hematology and cancer medicine at the Peter MacCallum Cancer Centre, East Melbourne, Australia.
Rather than using a 3-week schedule and 50-mg starting dose, the safety expansion cohort received once-daily oral ABT-199 beginning at 20 mg, with weekly adjustments to 50 mg, 100 mg, 200 mg, and 400 mg over 5 weeks.
The 400-mg dose has been identified as the phase II dose, with 59% of patients free of progression at 18 months and beyond on this dose, he said.
As of April 2014, 37 of the 105 patients discontinued treatment, 22 due to progressive disease and 12 for adverse events; in addition, two proceeded to allogeneic hematopoietic cell transplantation, and one needed Coumadin, which is not permitted on protocol.
The median duration of response has not yet been reached for patients treated at doses of 400 mg or above, he said.
The most common treatment-emergent adverse events of any grade were diarrhea (40% of patients), neutropenia (36%), and nausea (35%).
Neutropenia was the only grade 3/4 event occurring in more than 10% of patients (33%), followed by anemia in 10%.
Combination ABT-199
Of substantial interest to many was a second phase Ib study presented in the same session, evaluating the role of ABT-199 with the anti-CD20 antibody rituximab (Rituxan) in relapsed or refractory CLL.
After a median time on study of just 7.5 months, the overall response rate was 84% among 25 evaluable patients, including 9 complete responses (36%) and 12 partial responses (48%), said Dr. Andrew W. Roberts, with the Royal Melbourne (Australia) Hospital and Walter and Eliza Hall Institute of Medical Research.
Six of eight complete responders tested were negative for minimal residual disease by flow cytometry.
Preliminary pharmacokinetic results suggest no apparent effect of rituximab on ABT-199 exposure, he said.
Three patients discontinued ABT-199 after achieving a complete remission, including one with fludarabine-refractory disease, and all remain in complete remission at 8.6, 8.8, and 11.6 months after cessation.
Dose modifications were also made in this study following a fatal TLS event in December 2012 after a first dose of ABT-199 at 50 mg. Under the modified step-up dosing, ABT-199 was started at 20 mg, escalating up to 600 mg daily over 5 weeks, with rituximab 375 mg/m2 added on day 1 of week 5 and rituximab 500 mg/m2 added on day 1 of months 2-6.
The combination was well tolerated, and no new safety concerns were identified, Dr. Roberts said. The most common grade 3/4 adverse events among 45 patients evaluable for safety were neutropenia in 47%, anemia in 16%, thrombocytopenia in 13%, and febrile neutropenia in 7%. Grade 3/4 neutropenia was more common at 600 mg, with the 400-mg dose selected for the ongoing safety expansion cohort. Two serious TLS events occurred, but both were prior to schedule modifications, he said.
One patient in the combination study and 13 in the monotherapy study received treatment for small lymphocytic lymphoma. Response rates and tolerability were similar between CLL and SLL patients in the monotherapy study, Dr. Roberts said in an interview.
During a press briefing at the meeting, Dr. Seymour said ABT-199 potentially could be combined with ibrutinib and that the combination was very potent in laboratory tests in both CLL and some forms of mantle cell lymphoma. Negotiations with the various companies involved are intricate, but there is agreement and commitment "to begin clinical trials of the combination later this year," he added.
ABT-199 is currently being evaluated in a phase II trial as monotherapy in deletion 17p relapsed CLL, as combination therapy with rituximab versus bendamustine plus rituximab in a phase III trial in relapsed/refractory CLL, and in combination trials with bendamustine/rituximab and obinutuzumab in relapsed/refractory CLL.
AbbVie and Genentech sponsored the trials. Dr. Seymour is a consultant and adviser for AbbVie, Genentech, and Roche. Dr. Roberts reported research funding from AbbVie and Genentech and milestone payments to his institution related to ABT-199.
AT THE EHA CONGRESS
Major finding: The overall response rate was 77% with ABT-199 monotherapy and 84% with the addition of rituximab in relapsed or refractory CLL.
Key clinical point: ABT-199 alone or as combination therapy with rituximab has substantial activity in relapsed/refractory CLL.
Data source: Two phase I trials in patients with CLL.
Disclosures: AbbVie and Genentech, codevelopers of ABT-199, sponsored the trials. Dr. Seymour is a consultant and adviser for AbbVie, Genentech, and Roche. Dr. Roberts reported research funding from AbbVie and Genentech and milestone payments to his institution related to ABT-199.
ONO-4059 delivered hit to relapsed/refractory CLL
MILAN – Monotherapy with the oral BTK inhibitor ONO-4059 showed good efficacy over a range of doses in relapsed or refractory and high-risk chronic lymphocytic leukemia, with a best overall response rate of 84% in a phase I trial.
Among 25 evaluable patients, 2 achieved complete responses with incomplete blood count recovery, 12 had partial responses, and 7 had partial responses with lymphocytosis.
One patient had stable disease and another progressive disease. Two patients withdrew due to adverse events.
ONO-4059 showed particularly good efficacy in patients with the deleterious 17p deletion (89%, or 8/9 patients) and in those refractory to their last therapy (91.6% or 11/12 patients), Dr. Franck Morschhauser, reported at the annual congress of the European Hematology Association.
ONO-4059 is a selective Bruton’s tyrosine kinase (BTK) inhibitor that has demonstrated greater than 90% inhibition of BTK at 12 hours in chronic lymphocytic leukemia (CLL) cells in vivo and antitumor activity in non-Hodgkin’s lymphoma.
In relapsed or refractory B-cell lymphoma, the same investigators reported a best overall response rate of 42% with ONO-4059 at doses of 40, 80, and 160 mg among 12 patients in a phase I study.
The current dose-escalation study evaluated the safety and tolerability of once-daily ONO-4059 at doses ranging from 20 to 600 mg for up to 2 years in patients with relapsed/refractory or high-risk CLL for whom no therapy of higher priority was available. Dose escalation was permitted upon completion of 6 months of treatment. The median duration of treatment was 11.5 cycles.
The 25 evaluable patients (median age, 67 years) had received a median of four prior therapies (range 2-9); 92% had prior exposure to rituximab (Rituxan) and 92% to fludarabine (Fludara); and 48% were refractory to their last therapy.
Lymph node reduction occurred early, between day 1 and 28 of the first cycle, and was accompanied by an improvement in hemoglobin and platelet counts within 3-4 months, said Dr. Morschhauser, head of the lymphoma unit, Centre Hospitalier Régional Universitaire–Claude Huriez Hospital, Lille, France.
"So far we do not have evidence that there is a dose-efficacy relationship, although there is quicker tumor shrinkage when you increase the dose," he said.
The majority of adverse events were grade 1 and 2, with a low incidence of diarrhea, fatigue, bruising, and rash and no dose-limiting toxicities, Dr. Morschhauser said. Five patients experienced grade 3/4 neutropenia: two grade 3 events at 20 and 40 mg and three grade 4 events at 20, 80, and 320 mg.
Eight ONO-4059–related serious adverse events were reported, including febrile neutropenia in the patient with grade 4 neutropenia at the 20-mg dose, pyrexia at 20 mg, rash at 80 mg, hepatitis E reactivation and neutropenia at 320 mg, lymphocytic infiltration of the right dorsal muscle and purpura at 400 mg, and spontaneous psoas hematoma at 500 mg. All events resolved, and four patients remain on study, he reported on behalf of lead author Dr. Christopher Fegan, clinical director of CLL, University Hospital of Wales, Cardiff.
The study was supported by Ono Pharmaceutical. The study authors reported no relevant financial disclosures.
MILAN – Monotherapy with the oral BTK inhibitor ONO-4059 showed good efficacy over a range of doses in relapsed or refractory and high-risk chronic lymphocytic leukemia, with a best overall response rate of 84% in a phase I trial.
Among 25 evaluable patients, 2 achieved complete responses with incomplete blood count recovery, 12 had partial responses, and 7 had partial responses with lymphocytosis.
One patient had stable disease and another progressive disease. Two patients withdrew due to adverse events.
ONO-4059 showed particularly good efficacy in patients with the deleterious 17p deletion (89%, or 8/9 patients) and in those refractory to their last therapy (91.6% or 11/12 patients), Dr. Franck Morschhauser, reported at the annual congress of the European Hematology Association.
ONO-4059 is a selective Bruton’s tyrosine kinase (BTK) inhibitor that has demonstrated greater than 90% inhibition of BTK at 12 hours in chronic lymphocytic leukemia (CLL) cells in vivo and antitumor activity in non-Hodgkin’s lymphoma.
In relapsed or refractory B-cell lymphoma, the same investigators reported a best overall response rate of 42% with ONO-4059 at doses of 40, 80, and 160 mg among 12 patients in a phase I study.
The current dose-escalation study evaluated the safety and tolerability of once-daily ONO-4059 at doses ranging from 20 to 600 mg for up to 2 years in patients with relapsed/refractory or high-risk CLL for whom no therapy of higher priority was available. Dose escalation was permitted upon completion of 6 months of treatment. The median duration of treatment was 11.5 cycles.
The 25 evaluable patients (median age, 67 years) had received a median of four prior therapies (range 2-9); 92% had prior exposure to rituximab (Rituxan) and 92% to fludarabine (Fludara); and 48% were refractory to their last therapy.
Lymph node reduction occurred early, between day 1 and 28 of the first cycle, and was accompanied by an improvement in hemoglobin and platelet counts within 3-4 months, said Dr. Morschhauser, head of the lymphoma unit, Centre Hospitalier Régional Universitaire–Claude Huriez Hospital, Lille, France.
"So far we do not have evidence that there is a dose-efficacy relationship, although there is quicker tumor shrinkage when you increase the dose," he said.
The majority of adverse events were grade 1 and 2, with a low incidence of diarrhea, fatigue, bruising, and rash and no dose-limiting toxicities, Dr. Morschhauser said. Five patients experienced grade 3/4 neutropenia: two grade 3 events at 20 and 40 mg and three grade 4 events at 20, 80, and 320 mg.
Eight ONO-4059–related serious adverse events were reported, including febrile neutropenia in the patient with grade 4 neutropenia at the 20-mg dose, pyrexia at 20 mg, rash at 80 mg, hepatitis E reactivation and neutropenia at 320 mg, lymphocytic infiltration of the right dorsal muscle and purpura at 400 mg, and spontaneous psoas hematoma at 500 mg. All events resolved, and four patients remain on study, he reported on behalf of lead author Dr. Christopher Fegan, clinical director of CLL, University Hospital of Wales, Cardiff.
The study was supported by Ono Pharmaceutical. The study authors reported no relevant financial disclosures.
MILAN – Monotherapy with the oral BTK inhibitor ONO-4059 showed good efficacy over a range of doses in relapsed or refractory and high-risk chronic lymphocytic leukemia, with a best overall response rate of 84% in a phase I trial.
Among 25 evaluable patients, 2 achieved complete responses with incomplete blood count recovery, 12 had partial responses, and 7 had partial responses with lymphocytosis.
One patient had stable disease and another progressive disease. Two patients withdrew due to adverse events.
ONO-4059 showed particularly good efficacy in patients with the deleterious 17p deletion (89%, or 8/9 patients) and in those refractory to their last therapy (91.6% or 11/12 patients), Dr. Franck Morschhauser, reported at the annual congress of the European Hematology Association.
ONO-4059 is a selective Bruton’s tyrosine kinase (BTK) inhibitor that has demonstrated greater than 90% inhibition of BTK at 12 hours in chronic lymphocytic leukemia (CLL) cells in vivo and antitumor activity in non-Hodgkin’s lymphoma.
In relapsed or refractory B-cell lymphoma, the same investigators reported a best overall response rate of 42% with ONO-4059 at doses of 40, 80, and 160 mg among 12 patients in a phase I study.
The current dose-escalation study evaluated the safety and tolerability of once-daily ONO-4059 at doses ranging from 20 to 600 mg for up to 2 years in patients with relapsed/refractory or high-risk CLL for whom no therapy of higher priority was available. Dose escalation was permitted upon completion of 6 months of treatment. The median duration of treatment was 11.5 cycles.
The 25 evaluable patients (median age, 67 years) had received a median of four prior therapies (range 2-9); 92% had prior exposure to rituximab (Rituxan) and 92% to fludarabine (Fludara); and 48% were refractory to their last therapy.
Lymph node reduction occurred early, between day 1 and 28 of the first cycle, and was accompanied by an improvement in hemoglobin and platelet counts within 3-4 months, said Dr. Morschhauser, head of the lymphoma unit, Centre Hospitalier Régional Universitaire–Claude Huriez Hospital, Lille, France.
"So far we do not have evidence that there is a dose-efficacy relationship, although there is quicker tumor shrinkage when you increase the dose," he said.
The majority of adverse events were grade 1 and 2, with a low incidence of diarrhea, fatigue, bruising, and rash and no dose-limiting toxicities, Dr. Morschhauser said. Five patients experienced grade 3/4 neutropenia: two grade 3 events at 20 and 40 mg and three grade 4 events at 20, 80, and 320 mg.
Eight ONO-4059–related serious adverse events were reported, including febrile neutropenia in the patient with grade 4 neutropenia at the 20-mg dose, pyrexia at 20 mg, rash at 80 mg, hepatitis E reactivation and neutropenia at 320 mg, lymphocytic infiltration of the right dorsal muscle and purpura at 400 mg, and spontaneous psoas hematoma at 500 mg. All events resolved, and four patients remain on study, he reported on behalf of lead author Dr. Christopher Fegan, clinical director of CLL, University Hospital of Wales, Cardiff.
The study was supported by Ono Pharmaceutical. The study authors reported no relevant financial disclosures.
AT THE EHA CONGRESS
Key clinical point: ONO-4059 induced responses in most patients with relapsed/refractory CLL, including those with a 17p deletion.
Major finding: The best response rate was 84% overall, 89% in 17p deletion patients, and 91.6% in refractory disease.
Data source: A phase I trial in 25 patients with relapsed/refractory or high-risk chronic lymphocytic leukemia.
Disclosures: The study was supported by Ono Pharmaceutical. The study authors reported no relevant financial disclosures.