User login
Two-drug combination targets LSCs in CML

Image by Difu Wu
Targeting a pair of transcription factors might improve the treatment of chronic myeloid leukemia (CML), according to researchers.
The team found that p53 and c-MYC have “defining roles” in the survival of leukemia stem cells (LSCs) in CML.
And by targeting these transcription factors with a pair of investigational drugs, the researchers were able to kill LSCs.
The team described this work in Nature.
“This collaborative study combined proteomics, transcriptomics, and systems biology to identify a novel, precision medicine-based approach for eradicating leukemic stem cells,” said study author Tony Whetton, PhD, of the University of Manchester in the UK.
Dr Whetton and his colleagues first discovered that p53 and c-MYC are “central hubs” in a CML network of deregulated proteins. The team also found that CML cells express increased c-MYC and decreased p53 levels.
So the researchers theorized that simultaneously activating p53 and inhibiting c-MYC could be a method for treating CML.
To that end, the team tested 2 drugs—RITA (or NSC652287), which binds p53 and blocks its degradation, and CPI-203, a BET inhibitor that hinders transcription by disrupting chromatin-dependent signal transduction.
The researchers found that CPI-203 successfully downregulated c-MYC but also reduced p53, while RITA increased p53.
Treating CML CD34+ cells with RITA or CPI-203 for 72 hours reduced cell viability and induced significant apoptosis, the team said. Combining the drugs enhanced these effects.
The researchers also found evidence to suggest that c-MYC inhibition induces differentiation of CML CD34+ cells. The team said that labelling with the cell-division tracker carboxyfluorescein succinimidyl ester (CFSE) and CD34 antibody showed that, as CML cells divided in the presence of CPI-203, there was a clear and rapid loss of CD34 expression that was not seen in the presence of RITA.
The researchers did not observe any differences in the effects of RITA and CPI-203 when they were tested in CML CD34+ cells pretreated with imatinib.
Furthermore, RITA and CPI-203, either alone or in combination, had no significant effects on normal CD34+ cells when tested at lower concentrations. However, when CPI-203 was used alone at higher concentrations (2 or 5 μ M) or with RITA at the highest concentrations tested (RITA at 25 nM, CPI-203 at 5 μ M), apoptosis did occur.
In CML cells, the researchers observed “significant apoptosis” with all concentrations of CPI-203 and RITA tested.
The team also exposed CML LSCs, defined as either CFSEmax or CD34+CD38− cells, to CPI-203 and RITA as well as a pair of tyrosine kinase inhibitors.
The CFSEmax population persisted despite 5 days of treatment with dasatinib or nilotinib, but the cells were “significantly reduced” after 5 days of treatment with CPI-203 alone and in combination with RITA.
Similarly, 72 hours of treatment with RITA with CPI-203 eliminated residual CD34+CD38− cells.
The researchers also assessed LSC engraftment after treatment with RITA and/or CPI-203, as well as dasatinib. They exposed CML CD34+ cells to the drugs for 48 hours before transplanting the cells into sublethally irradiated NSG mice.
The team said dasatinib had no significant effect on NSG-repopulating CML LSCs. However, RITA, CPI-203, and the drugs in combination reduced engraftment, as indicated by decreased CD45+, CD34+, CD33+, CD11b+, CD19+ and CD14+ cells. ![]()

Image by Difu Wu
Targeting a pair of transcription factors might improve the treatment of chronic myeloid leukemia (CML), according to researchers.
The team found that p53 and c-MYC have “defining roles” in the survival of leukemia stem cells (LSCs) in CML.
And by targeting these transcription factors with a pair of investigational drugs, the researchers were able to kill LSCs.
The team described this work in Nature.
“This collaborative study combined proteomics, transcriptomics, and systems biology to identify a novel, precision medicine-based approach for eradicating leukemic stem cells,” said study author Tony Whetton, PhD, of the University of Manchester in the UK.
Dr Whetton and his colleagues first discovered that p53 and c-MYC are “central hubs” in a CML network of deregulated proteins. The team also found that CML cells express increased c-MYC and decreased p53 levels.
So the researchers theorized that simultaneously activating p53 and inhibiting c-MYC could be a method for treating CML.
To that end, the team tested 2 drugs—RITA (or NSC652287), which binds p53 and blocks its degradation, and CPI-203, a BET inhibitor that hinders transcription by disrupting chromatin-dependent signal transduction.
The researchers found that CPI-203 successfully downregulated c-MYC but also reduced p53, while RITA increased p53.
Treating CML CD34+ cells with RITA or CPI-203 for 72 hours reduced cell viability and induced significant apoptosis, the team said. Combining the drugs enhanced these effects.
The researchers also found evidence to suggest that c-MYC inhibition induces differentiation of CML CD34+ cells. The team said that labelling with the cell-division tracker carboxyfluorescein succinimidyl ester (CFSE) and CD34 antibody showed that, as CML cells divided in the presence of CPI-203, there was a clear and rapid loss of CD34 expression that was not seen in the presence of RITA.
The researchers did not observe any differences in the effects of RITA and CPI-203 when they were tested in CML CD34+ cells pretreated with imatinib.
Furthermore, RITA and CPI-203, either alone or in combination, had no significant effects on normal CD34+ cells when tested at lower concentrations. However, when CPI-203 was used alone at higher concentrations (2 or 5 μ M) or with RITA at the highest concentrations tested (RITA at 25 nM, CPI-203 at 5 μ M), apoptosis did occur.
In CML cells, the researchers observed “significant apoptosis” with all concentrations of CPI-203 and RITA tested.
The team also exposed CML LSCs, defined as either CFSEmax or CD34+CD38− cells, to CPI-203 and RITA as well as a pair of tyrosine kinase inhibitors.
The CFSEmax population persisted despite 5 days of treatment with dasatinib or nilotinib, but the cells were “significantly reduced” after 5 days of treatment with CPI-203 alone and in combination with RITA.
Similarly, 72 hours of treatment with RITA with CPI-203 eliminated residual CD34+CD38− cells.
The researchers also assessed LSC engraftment after treatment with RITA and/or CPI-203, as well as dasatinib. They exposed CML CD34+ cells to the drugs for 48 hours before transplanting the cells into sublethally irradiated NSG mice.
The team said dasatinib had no significant effect on NSG-repopulating CML LSCs. However, RITA, CPI-203, and the drugs in combination reduced engraftment, as indicated by decreased CD45+, CD34+, CD33+, CD11b+, CD19+ and CD14+ cells. ![]()

Image by Difu Wu
Targeting a pair of transcription factors might improve the treatment of chronic myeloid leukemia (CML), according to researchers.
The team found that p53 and c-MYC have “defining roles” in the survival of leukemia stem cells (LSCs) in CML.
And by targeting these transcription factors with a pair of investigational drugs, the researchers were able to kill LSCs.
The team described this work in Nature.
“This collaborative study combined proteomics, transcriptomics, and systems biology to identify a novel, precision medicine-based approach for eradicating leukemic stem cells,” said study author Tony Whetton, PhD, of the University of Manchester in the UK.
Dr Whetton and his colleagues first discovered that p53 and c-MYC are “central hubs” in a CML network of deregulated proteins. The team also found that CML cells express increased c-MYC and decreased p53 levels.
So the researchers theorized that simultaneously activating p53 and inhibiting c-MYC could be a method for treating CML.
To that end, the team tested 2 drugs—RITA (or NSC652287), which binds p53 and blocks its degradation, and CPI-203, a BET inhibitor that hinders transcription by disrupting chromatin-dependent signal transduction.
The researchers found that CPI-203 successfully downregulated c-MYC but also reduced p53, while RITA increased p53.
Treating CML CD34+ cells with RITA or CPI-203 for 72 hours reduced cell viability and induced significant apoptosis, the team said. Combining the drugs enhanced these effects.
The researchers also found evidence to suggest that c-MYC inhibition induces differentiation of CML CD34+ cells. The team said that labelling with the cell-division tracker carboxyfluorescein succinimidyl ester (CFSE) and CD34 antibody showed that, as CML cells divided in the presence of CPI-203, there was a clear and rapid loss of CD34 expression that was not seen in the presence of RITA.
The researchers did not observe any differences in the effects of RITA and CPI-203 when they were tested in CML CD34+ cells pretreated with imatinib.
Furthermore, RITA and CPI-203, either alone or in combination, had no significant effects on normal CD34+ cells when tested at lower concentrations. However, when CPI-203 was used alone at higher concentrations (2 or 5 μ M) or with RITA at the highest concentrations tested (RITA at 25 nM, CPI-203 at 5 μ M), apoptosis did occur.
In CML cells, the researchers observed “significant apoptosis” with all concentrations of CPI-203 and RITA tested.
The team also exposed CML LSCs, defined as either CFSEmax or CD34+CD38− cells, to CPI-203 and RITA as well as a pair of tyrosine kinase inhibitors.
The CFSEmax population persisted despite 5 days of treatment with dasatinib or nilotinib, but the cells were “significantly reduced” after 5 days of treatment with CPI-203 alone and in combination with RITA.
Similarly, 72 hours of treatment with RITA with CPI-203 eliminated residual CD34+CD38− cells.
The researchers also assessed LSC engraftment after treatment with RITA and/or CPI-203, as well as dasatinib. They exposed CML CD34+ cells to the drugs for 48 hours before transplanting the cells into sublethally irradiated NSG mice.
The team said dasatinib had no significant effect on NSG-repopulating CML LSCs. However, RITA, CPI-203, and the drugs in combination reduced engraftment, as indicated by decreased CD45+, CD34+, CD33+, CD11b+, CD19+ and CD14+ cells. ![]()
Compound could treat a range of blood cancers

Image by Ed Uthman
A new compound has shown promise for treating hematologic malignancies and other cancers, according to preclinical research published in Nature.
The compound, known as S63845, targets the BCL2 family protein MCL1.
Investigators said their research on S63845 provides the first clear evidence that inhibiting MCL1 is effective in targeting several cancer types, including leukemia, lymphoma, and multiple myeloma (MM).
“MCL1 is important for many cancers because it is a pro-survival protein that allows the cancerous cells to evade the process of programmed cell death that normally removes cancer cells from the body,” said study author Guillaume Lessene, PhD, of the Walter and Eliza Hall Institute in Melbourne, Australia.
“Extensive studies performed in a variety of cancer models have shown that S63845 potently targets cancer cells dependent on MCL1 for their survival.”
About S63845
Dr Lessene and his colleagues said S63845 binds with high affinity to the BH3-binding groove of MCL1. And the compound kills MCL1-dependent cancer cells by activating the BAX/BAK-dependent mitochondrial apoptotic pathway.
In solid tumors, S63845 often wasn’t effective enough on its own. However, when the compound was combined with various kinase inhibitors, it induced a “potent cytotoxic response” in breast cancer, lung cancer, and melanoma cells.
In hematologic malignancies, S63845 proved effective when given alone.
Myeloma
The investigators said 17 of 25 MM cell lines tested were highly sensitive to S63845 (IC50 < 0.1 μ M), 6 cell lines were moderately sensitive (0.1 μ M < IC50 < 1 μ M), and 2 cell lines were insensitive (IC50 > 1 μ M).
The team also administered S63845 (at 25 mg/kg) to mice with MM. Seven of 8 mice had complete regression at 100 days after treatment.
Lymphoma
The investigators tested S63845 in 11 cell lines representative of human lymphomas. Five were highly sensitive to the compound (IC50 < 0.1 μ M), 3 were moderately sensitive (0.1 μ M < IC50 < 1 μ M), and 3 were insensitive (IC50 > 1 μ M).
The team also tested S63845 in 7 c-MYC-driven human Burkitt lymphoma cell lines and found the compound exhibited “potent cytotoxic activity” in all of them.
The investigators then tested S63845 in a c-MYC-driven mouse lymphoma model. They noted that both tumor cells and normal tissues express mouse MCL1 protein in this model.
Treatment with S63845 (25 mg/kg) for 5 consecutive days cured 70% of these mice, and the investigators said there were no evident side effects in normal tissues.
Leukemia
The investigators tested S63845 in 5 chronic myeloid leukemia cell lines, and none of them were sensitive to the compound.
However, the team also tested S63845 in 8 acute myeloid leukemia (AML) cell lines, and all of them were sensitive to the compound (IC50 4–233 nM).
When S63845 was given to mice with AML (25 mg/kg), 6 of the 8 mice achieved complete remission after 80 days.
The investigators also tested S63845 in 25 freshly derived samples from patients with AML. The team said these samples displayed a wide range of responses to S63845.
The most sensitive samples required 100- to 1000-fold less drug (to induce apoptosis) than the resistant samples or normal CD34+ progenitor cells.
Development/funding
S63845 was discovered through a collaboration between 2 pharmaceutical companies—Servier, which is headquartered in France, and Vernalis (R&D), which is based in the UK.
“[C]linical development of a MCL1 inhibitor should be launched in the near future,” said Olivier Geneste, director of oncology research at Servier.
The current research was supported through a collaboration with Servier and through funding from the National Health and Medical Research Council of Australia, the Leukemia and Lymphoma Society, Cancer Council Victoria, the Kay Kendall Leukemia Fund, Victorian Cancer Agency, Australian Cancer Research Foundation, the Victorian Government Operational Infrastructure Scheme, and the estate of Anthony Redstone. ![]()

Image by Ed Uthman
A new compound has shown promise for treating hematologic malignancies and other cancers, according to preclinical research published in Nature.
The compound, known as S63845, targets the BCL2 family protein MCL1.
Investigators said their research on S63845 provides the first clear evidence that inhibiting MCL1 is effective in targeting several cancer types, including leukemia, lymphoma, and multiple myeloma (MM).
“MCL1 is important for many cancers because it is a pro-survival protein that allows the cancerous cells to evade the process of programmed cell death that normally removes cancer cells from the body,” said study author Guillaume Lessene, PhD, of the Walter and Eliza Hall Institute in Melbourne, Australia.
“Extensive studies performed in a variety of cancer models have shown that S63845 potently targets cancer cells dependent on MCL1 for their survival.”
About S63845
Dr Lessene and his colleagues said S63845 binds with high affinity to the BH3-binding groove of MCL1. And the compound kills MCL1-dependent cancer cells by activating the BAX/BAK-dependent mitochondrial apoptotic pathway.
In solid tumors, S63845 often wasn’t effective enough on its own. However, when the compound was combined with various kinase inhibitors, it induced a “potent cytotoxic response” in breast cancer, lung cancer, and melanoma cells.
In hematologic malignancies, S63845 proved effective when given alone.
Myeloma
The investigators said 17 of 25 MM cell lines tested were highly sensitive to S63845 (IC50 < 0.1 μ M), 6 cell lines were moderately sensitive (0.1 μ M < IC50 < 1 μ M), and 2 cell lines were insensitive (IC50 > 1 μ M).
The team also administered S63845 (at 25 mg/kg) to mice with MM. Seven of 8 mice had complete regression at 100 days after treatment.
Lymphoma
The investigators tested S63845 in 11 cell lines representative of human lymphomas. Five were highly sensitive to the compound (IC50 < 0.1 μ M), 3 were moderately sensitive (0.1 μ M < IC50 < 1 μ M), and 3 were insensitive (IC50 > 1 μ M).
The team also tested S63845 in 7 c-MYC-driven human Burkitt lymphoma cell lines and found the compound exhibited “potent cytotoxic activity” in all of them.
The investigators then tested S63845 in a c-MYC-driven mouse lymphoma model. They noted that both tumor cells and normal tissues express mouse MCL1 protein in this model.
Treatment with S63845 (25 mg/kg) for 5 consecutive days cured 70% of these mice, and the investigators said there were no evident side effects in normal tissues.
Leukemia
The investigators tested S63845 in 5 chronic myeloid leukemia cell lines, and none of them were sensitive to the compound.
However, the team also tested S63845 in 8 acute myeloid leukemia (AML) cell lines, and all of them were sensitive to the compound (IC50 4–233 nM).
When S63845 was given to mice with AML (25 mg/kg), 6 of the 8 mice achieved complete remission after 80 days.
The investigators also tested S63845 in 25 freshly derived samples from patients with AML. The team said these samples displayed a wide range of responses to S63845.
The most sensitive samples required 100- to 1000-fold less drug (to induce apoptosis) than the resistant samples or normal CD34+ progenitor cells.
Development/funding
S63845 was discovered through a collaboration between 2 pharmaceutical companies—Servier, which is headquartered in France, and Vernalis (R&D), which is based in the UK.
“[C]linical development of a MCL1 inhibitor should be launched in the near future,” said Olivier Geneste, director of oncology research at Servier.
The current research was supported through a collaboration with Servier and through funding from the National Health and Medical Research Council of Australia, the Leukemia and Lymphoma Society, Cancer Council Victoria, the Kay Kendall Leukemia Fund, Victorian Cancer Agency, Australian Cancer Research Foundation, the Victorian Government Operational Infrastructure Scheme, and the estate of Anthony Redstone. ![]()

Image by Ed Uthman
A new compound has shown promise for treating hematologic malignancies and other cancers, according to preclinical research published in Nature.
The compound, known as S63845, targets the BCL2 family protein MCL1.
Investigators said their research on S63845 provides the first clear evidence that inhibiting MCL1 is effective in targeting several cancer types, including leukemia, lymphoma, and multiple myeloma (MM).
“MCL1 is important for many cancers because it is a pro-survival protein that allows the cancerous cells to evade the process of programmed cell death that normally removes cancer cells from the body,” said study author Guillaume Lessene, PhD, of the Walter and Eliza Hall Institute in Melbourne, Australia.
“Extensive studies performed in a variety of cancer models have shown that S63845 potently targets cancer cells dependent on MCL1 for their survival.”
About S63845
Dr Lessene and his colleagues said S63845 binds with high affinity to the BH3-binding groove of MCL1. And the compound kills MCL1-dependent cancer cells by activating the BAX/BAK-dependent mitochondrial apoptotic pathway.
In solid tumors, S63845 often wasn’t effective enough on its own. However, when the compound was combined with various kinase inhibitors, it induced a “potent cytotoxic response” in breast cancer, lung cancer, and melanoma cells.
In hematologic malignancies, S63845 proved effective when given alone.
Myeloma
The investigators said 17 of 25 MM cell lines tested were highly sensitive to S63845 (IC50 < 0.1 μ M), 6 cell lines were moderately sensitive (0.1 μ M < IC50 < 1 μ M), and 2 cell lines were insensitive (IC50 > 1 μ M).
The team also administered S63845 (at 25 mg/kg) to mice with MM. Seven of 8 mice had complete regression at 100 days after treatment.
Lymphoma
The investigators tested S63845 in 11 cell lines representative of human lymphomas. Five were highly sensitive to the compound (IC50 < 0.1 μ M), 3 were moderately sensitive (0.1 μ M < IC50 < 1 μ M), and 3 were insensitive (IC50 > 1 μ M).
The team also tested S63845 in 7 c-MYC-driven human Burkitt lymphoma cell lines and found the compound exhibited “potent cytotoxic activity” in all of them.
The investigators then tested S63845 in a c-MYC-driven mouse lymphoma model. They noted that both tumor cells and normal tissues express mouse MCL1 protein in this model.
Treatment with S63845 (25 mg/kg) for 5 consecutive days cured 70% of these mice, and the investigators said there were no evident side effects in normal tissues.
Leukemia
The investigators tested S63845 in 5 chronic myeloid leukemia cell lines, and none of them were sensitive to the compound.
However, the team also tested S63845 in 8 acute myeloid leukemia (AML) cell lines, and all of them were sensitive to the compound (IC50 4–233 nM).
When S63845 was given to mice with AML (25 mg/kg), 6 of the 8 mice achieved complete remission after 80 days.
The investigators also tested S63845 in 25 freshly derived samples from patients with AML. The team said these samples displayed a wide range of responses to S63845.
The most sensitive samples required 100- to 1000-fold less drug (to induce apoptosis) than the resistant samples or normal CD34+ progenitor cells.
Development/funding
S63845 was discovered through a collaboration between 2 pharmaceutical companies—Servier, which is headquartered in France, and Vernalis (R&D), which is based in the UK.
“[C]linical development of a MCL1 inhibitor should be launched in the near future,” said Olivier Geneste, director of oncology research at Servier.
The current research was supported through a collaboration with Servier and through funding from the National Health and Medical Research Council of Australia, the Leukemia and Lymphoma Society, Cancer Council Victoria, the Kay Kendall Leukemia Fund, Victorian Cancer Agency, Australian Cancer Research Foundation, the Victorian Government Operational Infrastructure Scheme, and the estate of Anthony Redstone. ![]()
Legislators question price of leukemia drug
Photo from Business Wire
A pair of US legislators are questioning why ARIAD Pharmaceuticals, Inc. has increased the price of its leukemia drug Iclusig (ponatinib) by more than $80,000 over the last several years.
ARIAD raised the price of Iclusig 4 times in 2016. The drug now costs nearly $199,000 a year.
Senator Bernie Sanders (Vermont) and Congressman Elijah Cummings (Maryland) sent a letter to ARIAD last week requesting information about these price increases.
Cummings and Sanders are also investigating whether ARIAD took additional steps to boost profits by discontinuing sales of certain dosages and quantities of Iclusig in order to charge patients and insurers more in exchange for less medicine.
“These outrageous sales tactics indicate that ARIAD is more concerned with its profit than with its patients,” Sanders and Cummings wrote in the letter.
The US Food and Drug Administration (FDA) approved Iclusig in December 2012 to treat chronic myeloid leukemia (CML) and Philadelphia chromosome-positive acute lymphoblastic leukemia (ALL).
In late 2013, the FDA suspended sales and clinical trials of the drug due to reports of serious adverse events.
The FDA allowed ARIAD to resume selling Iclusig in December 2013, but only to CML/ALL patients who cannot tolerate, or whose disease is resistant to, other tyrosine kinase inhibitors.
“Despite this new evidence showing the drug posed a far greater safety risk to patients than was known when the drug came on the market, ARIAD nonetheless raised the price of Iclusig several times over the subsequent 4 years,” Sanders and Cummings wrote.
“In the interest of patients and taxpayers, we are interested in learning more about the impact that the escalating price and restrictions on product availability have had.”
ARIAD has released a statement acknowledging Cummings’ and Sanders’ letter and defending its decisions to increase the price of Iclusig.
The company said it “makes significant investments in research and development (R&D) to advance breakthrough treatments” for patients with rare cancers.
In fact, ARIAD has invested more than $1.3 billion in R&D and accumulated losses of approximately $1.4 billion, which have not been recovered. In 2015, ARIAD generated $119 million in total revenue and invested $171 million in R&D.
The company said it intends to respond to Cummings’ and Sanders’ request for information. ![]()
Photo from Business Wire
A pair of US legislators are questioning why ARIAD Pharmaceuticals, Inc. has increased the price of its leukemia drug Iclusig (ponatinib) by more than $80,000 over the last several years.
ARIAD raised the price of Iclusig 4 times in 2016. The drug now costs nearly $199,000 a year.
Senator Bernie Sanders (Vermont) and Congressman Elijah Cummings (Maryland) sent a letter to ARIAD last week requesting information about these price increases.
Cummings and Sanders are also investigating whether ARIAD took additional steps to boost profits by discontinuing sales of certain dosages and quantities of Iclusig in order to charge patients and insurers more in exchange for less medicine.
“These outrageous sales tactics indicate that ARIAD is more concerned with its profit than with its patients,” Sanders and Cummings wrote in the letter.
The US Food and Drug Administration (FDA) approved Iclusig in December 2012 to treat chronic myeloid leukemia (CML) and Philadelphia chromosome-positive acute lymphoblastic leukemia (ALL).
In late 2013, the FDA suspended sales and clinical trials of the drug due to reports of serious adverse events.
The FDA allowed ARIAD to resume selling Iclusig in December 2013, but only to CML/ALL patients who cannot tolerate, or whose disease is resistant to, other tyrosine kinase inhibitors.
“Despite this new evidence showing the drug posed a far greater safety risk to patients than was known when the drug came on the market, ARIAD nonetheless raised the price of Iclusig several times over the subsequent 4 years,” Sanders and Cummings wrote.
“In the interest of patients and taxpayers, we are interested in learning more about the impact that the escalating price and restrictions on product availability have had.”
ARIAD has released a statement acknowledging Cummings’ and Sanders’ letter and defending its decisions to increase the price of Iclusig.
The company said it “makes significant investments in research and development (R&D) to advance breakthrough treatments” for patients with rare cancers.
In fact, ARIAD has invested more than $1.3 billion in R&D and accumulated losses of approximately $1.4 billion, which have not been recovered. In 2015, ARIAD generated $119 million in total revenue and invested $171 million in R&D.
The company said it intends to respond to Cummings’ and Sanders’ request for information. ![]()
Photo from Business Wire
A pair of US legislators are questioning why ARIAD Pharmaceuticals, Inc. has increased the price of its leukemia drug Iclusig (ponatinib) by more than $80,000 over the last several years.
ARIAD raised the price of Iclusig 4 times in 2016. The drug now costs nearly $199,000 a year.
Senator Bernie Sanders (Vermont) and Congressman Elijah Cummings (Maryland) sent a letter to ARIAD last week requesting information about these price increases.
Cummings and Sanders are also investigating whether ARIAD took additional steps to boost profits by discontinuing sales of certain dosages and quantities of Iclusig in order to charge patients and insurers more in exchange for less medicine.
“These outrageous sales tactics indicate that ARIAD is more concerned with its profit than with its patients,” Sanders and Cummings wrote in the letter.
The US Food and Drug Administration (FDA) approved Iclusig in December 2012 to treat chronic myeloid leukemia (CML) and Philadelphia chromosome-positive acute lymphoblastic leukemia (ALL).
In late 2013, the FDA suspended sales and clinical trials of the drug due to reports of serious adverse events.
The FDA allowed ARIAD to resume selling Iclusig in December 2013, but only to CML/ALL patients who cannot tolerate, or whose disease is resistant to, other tyrosine kinase inhibitors.
“Despite this new evidence showing the drug posed a far greater safety risk to patients than was known when the drug came on the market, ARIAD nonetheless raised the price of Iclusig several times over the subsequent 4 years,” Sanders and Cummings wrote.
“In the interest of patients and taxpayers, we are interested in learning more about the impact that the escalating price and restrictions on product availability have had.”
ARIAD has released a statement acknowledging Cummings’ and Sanders’ letter and defending its decisions to increase the price of Iclusig.
The company said it “makes significant investments in research and development (R&D) to advance breakthrough treatments” for patients with rare cancers.
In fact, ARIAD has invested more than $1.3 billion in R&D and accumulated losses of approximately $1.4 billion, which have not been recovered. In 2015, ARIAD generated $119 million in total revenue and invested $171 million in R&D.
The company said it intends to respond to Cummings’ and Sanders’ request for information. ![]()
STIM1 long-term follow-up confirms imatinib discontinuation safety
Imatinib discontinuation is safe in patients with chronic myeloid leukemia (CML) who have sustained deep molecular response with no late molecular recurrence, according to long-term follow-up of the French Stop Imatinib Study (STIM1).
Over a median follow-up of 77 months after treatment discontinuation in 100 patients with CML who had undetectable minimal residual disease (UMRD) for at least 2 years, 61 lost UMRD after a median of 2.5 months, and 1 died with UMRD at 10 months, Gabriel Etienne, MD, of Institut Bergonie, Bordeaux, France, and colleagues reported online in the Journal of Clinical Oncology.
Of the 61 patients who lost UMRD, 57 restarted treatment and 55 achieved a second UMRD at a median of 4.3 months. The median time to second UMRD in patients with molecular recurrence with or without loss of major molecular response at the time of relapse was 4.2 months and 5 months, respectively. At a median of 73 months, none of the patients with molecular recurrence experienced CML progression. The rate of molecular recurrence-free survival overall was 43% at 6 months, 40% at 18 months, and 38% at 60 months, the investigators reported (2016 Oct. 3. doi: 10.1200/JCO.2016.68.2914).
These final long-term results of the STIM1 trial confirm the safety of imatinib discontinuation in CML patients with deep molecular response, and “make treatment-free remission legitimate as a criterion of treatment evaluation in the future,” the investigators concluded, noting that the possibility of improved results in patients treated with second-generation tyrosine kinase inhibitors as first- or second-line therapy is currently being evaluated in ongoing discontinuation trials.
Imatinib discontinuation is safe in patients with chronic myeloid leukemia (CML) who have sustained deep molecular response with no late molecular recurrence, according to long-term follow-up of the French Stop Imatinib Study (STIM1).
Over a median follow-up of 77 months after treatment discontinuation in 100 patients with CML who had undetectable minimal residual disease (UMRD) for at least 2 years, 61 lost UMRD after a median of 2.5 months, and 1 died with UMRD at 10 months, Gabriel Etienne, MD, of Institut Bergonie, Bordeaux, France, and colleagues reported online in the Journal of Clinical Oncology.
Of the 61 patients who lost UMRD, 57 restarted treatment and 55 achieved a second UMRD at a median of 4.3 months. The median time to second UMRD in patients with molecular recurrence with or without loss of major molecular response at the time of relapse was 4.2 months and 5 months, respectively. At a median of 73 months, none of the patients with molecular recurrence experienced CML progression. The rate of molecular recurrence-free survival overall was 43% at 6 months, 40% at 18 months, and 38% at 60 months, the investigators reported (2016 Oct. 3. doi: 10.1200/JCO.2016.68.2914).
These final long-term results of the STIM1 trial confirm the safety of imatinib discontinuation in CML patients with deep molecular response, and “make treatment-free remission legitimate as a criterion of treatment evaluation in the future,” the investigators concluded, noting that the possibility of improved results in patients treated with second-generation tyrosine kinase inhibitors as first- or second-line therapy is currently being evaluated in ongoing discontinuation trials.
Imatinib discontinuation is safe in patients with chronic myeloid leukemia (CML) who have sustained deep molecular response with no late molecular recurrence, according to long-term follow-up of the French Stop Imatinib Study (STIM1).
Over a median follow-up of 77 months after treatment discontinuation in 100 patients with CML who had undetectable minimal residual disease (UMRD) for at least 2 years, 61 lost UMRD after a median of 2.5 months, and 1 died with UMRD at 10 months, Gabriel Etienne, MD, of Institut Bergonie, Bordeaux, France, and colleagues reported online in the Journal of Clinical Oncology.
Of the 61 patients who lost UMRD, 57 restarted treatment and 55 achieved a second UMRD at a median of 4.3 months. The median time to second UMRD in patients with molecular recurrence with or without loss of major molecular response at the time of relapse was 4.2 months and 5 months, respectively. At a median of 73 months, none of the patients with molecular recurrence experienced CML progression. The rate of molecular recurrence-free survival overall was 43% at 6 months, 40% at 18 months, and 38% at 60 months, the investigators reported (2016 Oct. 3. doi: 10.1200/JCO.2016.68.2914).
These final long-term results of the STIM1 trial confirm the safety of imatinib discontinuation in CML patients with deep molecular response, and “make treatment-free remission legitimate as a criterion of treatment evaluation in the future,” the investigators concluded, noting that the possibility of improved results in patients treated with second-generation tyrosine kinase inhibitors as first- or second-line therapy is currently being evaluated in ongoing discontinuation trials.
FROM THE JOURNAL OF CLINICAL ONCOLOGY
Key clinical point:
Major finding: The rate of molecular recurrence-free survival overall was 43% at 24 months, 40% at 18 months, and 38% at 60 months.
Data source: Long-term follow-up of 100 patients from the STIM1 trial.
Disclosures: STIM1 was supported by grants from the French Ministry of Health Programme Hospitalier de Recherche and by the Institut National du Cancer. Dr. Etienne reported financial relationships with Novartis, Bristol-Myers Squibb, and ARIAD Pharmaceuticals. Coauthors reported relationships with several pharmaceutical companies.
Cost may hinder timely TKI initiation for CML
Nearly a third of Medicare beneficiaries with chronic myeloid leukemia (CML) did not initiate tyrosine kinase inhibitor therapy within 6 months of diagnosis, according to a review of SEER-Medicare data.
The findings suggest that out-of-pocket costs might be a barrier to timely initiation of tyrosine kinase inhibitor (TKI) therapy in CML patients, Aaron N. Winn of the University of North Carolina at Chapel Hill and his colleagues reported online ahead of print in the Journal of Clinical Oncology.
Of 393 individuals diagnosed with CML between 2007 and 2011, only 68% initiated TKI therapy within 180 days (median, 75 days), and 61% of those patients were adherent. Earlier treatment initiation was associated with receipt of cost-sharing subsidies (hazard ratio, 1.35), more-recent diagnosis (HR, 1.14), and living in a big metropolitan area (HR, 1.80) or metropolitan area vs. an urban area (HR, 1.84), while later treatment initiation was associated with higher levels of comorbidity (HR, 0.81) and age older than 80 years vs. age younger than 70 years (HR, 0.53)
Multivariate analysis showed that therapy initiation within 180 days was significantly more likely among those with more-recent diagnosis (relative risk, 1.06) and those living in a large metropolitan area vs. an urban area (RR, 1.57), and was significantly less likely among those older than age 80 years vs. those younger than age 70 years (RR, 0.71). Adherence within 180 days of therapy initiation was higher for those diagnosed in more-recent years (RR, 1.07) and lower for patients aged 80 years or older vs. 66-69 years (RR, 0.74), the investigators found (J Clin Oncol. 2016 Oct 3. doi: 10/1200/JCO.2016.67.4184).
“Our findings highlight important gaps in TKI use among Medicare beneficiaries with CML and suggest that high cost sharing may result in delays in initiation of these life-saving medications,” they concluded.
This study was supported by a University of North Carolina Clinical and Translational Science award, the UNC School of Medicine, the Royster Society of Fellows at UNC Chapel Hill, and by grants from the National Institutes of Health, North Carolina Translational and Clinical Sciences Institute, and the National Cancer Institute. The authors reported having no disclosures.
Nearly a third of Medicare beneficiaries with chronic myeloid leukemia (CML) did not initiate tyrosine kinase inhibitor therapy within 6 months of diagnosis, according to a review of SEER-Medicare data.
The findings suggest that out-of-pocket costs might be a barrier to timely initiation of tyrosine kinase inhibitor (TKI) therapy in CML patients, Aaron N. Winn of the University of North Carolina at Chapel Hill and his colleagues reported online ahead of print in the Journal of Clinical Oncology.
Of 393 individuals diagnosed with CML between 2007 and 2011, only 68% initiated TKI therapy within 180 days (median, 75 days), and 61% of those patients were adherent. Earlier treatment initiation was associated with receipt of cost-sharing subsidies (hazard ratio, 1.35), more-recent diagnosis (HR, 1.14), and living in a big metropolitan area (HR, 1.80) or metropolitan area vs. an urban area (HR, 1.84), while later treatment initiation was associated with higher levels of comorbidity (HR, 0.81) and age older than 80 years vs. age younger than 70 years (HR, 0.53)
Multivariate analysis showed that therapy initiation within 180 days was significantly more likely among those with more-recent diagnosis (relative risk, 1.06) and those living in a large metropolitan area vs. an urban area (RR, 1.57), and was significantly less likely among those older than age 80 years vs. those younger than age 70 years (RR, 0.71). Adherence within 180 days of therapy initiation was higher for those diagnosed in more-recent years (RR, 1.07) and lower for patients aged 80 years or older vs. 66-69 years (RR, 0.74), the investigators found (J Clin Oncol. 2016 Oct 3. doi: 10/1200/JCO.2016.67.4184).
“Our findings highlight important gaps in TKI use among Medicare beneficiaries with CML and suggest that high cost sharing may result in delays in initiation of these life-saving medications,” they concluded.
This study was supported by a University of North Carolina Clinical and Translational Science award, the UNC School of Medicine, the Royster Society of Fellows at UNC Chapel Hill, and by grants from the National Institutes of Health, North Carolina Translational and Clinical Sciences Institute, and the National Cancer Institute. The authors reported having no disclosures.
Nearly a third of Medicare beneficiaries with chronic myeloid leukemia (CML) did not initiate tyrosine kinase inhibitor therapy within 6 months of diagnosis, according to a review of SEER-Medicare data.
The findings suggest that out-of-pocket costs might be a barrier to timely initiation of tyrosine kinase inhibitor (TKI) therapy in CML patients, Aaron N. Winn of the University of North Carolina at Chapel Hill and his colleagues reported online ahead of print in the Journal of Clinical Oncology.
Of 393 individuals diagnosed with CML between 2007 and 2011, only 68% initiated TKI therapy within 180 days (median, 75 days), and 61% of those patients were adherent. Earlier treatment initiation was associated with receipt of cost-sharing subsidies (hazard ratio, 1.35), more-recent diagnosis (HR, 1.14), and living in a big metropolitan area (HR, 1.80) or metropolitan area vs. an urban area (HR, 1.84), while later treatment initiation was associated with higher levels of comorbidity (HR, 0.81) and age older than 80 years vs. age younger than 70 years (HR, 0.53)
Multivariate analysis showed that therapy initiation within 180 days was significantly more likely among those with more-recent diagnosis (relative risk, 1.06) and those living in a large metropolitan area vs. an urban area (RR, 1.57), and was significantly less likely among those older than age 80 years vs. those younger than age 70 years (RR, 0.71). Adherence within 180 days of therapy initiation was higher for those diagnosed in more-recent years (RR, 1.07) and lower for patients aged 80 years or older vs. 66-69 years (RR, 0.74), the investigators found (J Clin Oncol. 2016 Oct 3. doi: 10/1200/JCO.2016.67.4184).
“Our findings highlight important gaps in TKI use among Medicare beneficiaries with CML and suggest that high cost sharing may result in delays in initiation of these life-saving medications,” they concluded.
This study was supported by a University of North Carolina Clinical and Translational Science award, the UNC School of Medicine, the Royster Society of Fellows at UNC Chapel Hill, and by grants from the National Institutes of Health, North Carolina Translational and Clinical Sciences Institute, and the National Cancer Institute. The authors reported having no disclosures.
FROM THE JOURNAL OF CLINICAL ONCOLOGY
Key clinical point:
Major finding: TKI initiation within 180 days was significantly less likely among those older than age 80 years vs. those under age 70 years (relative risk, 0.71).
Data source: A review of SEER-Medicare data for 393 patients.
Disclosures: This study was supported by a University of North Carolina Clinical and Translational Science award, the UNC School of Medicine, the Royster Society of Fellows at UNC Chapel Hill, and by grants from the National Institutes of Health, North Carolina Translational and Clinical Sciences Institute, and the National Cancer Institute. The authors reported having no disclosures.
Doc offers advice on choosing a frontline TKI

Photo by D. Meyer
NEW YORK—Evaluating treatment goals is essential when choosing which tyrosine kinase inhibitor (TKI) to prescribe for a patient with newly diagnosed chronic myeloid leukemia (CML), according to a speaker at the NCCN 11th Annual Congress: Hematologic Malignancies.
“Deciding what TKI to start people on really depends on what your goals are for that patient,” said the speaker, Jerald Radich, MD, of the Fred Hutchinson Cancer Research Center/Seattle Cancer Care Alliance in Seattle, Washington.
Because the 3 TKIs approved for frontline treatment of CML—imatinib, dasatinib, and nilotinib—produce “amazingly similar” responses, treatment compliance becomes an important factor in patient outcomes, he noted.
“If you take 90% of your imatinib, your MMR [major molecular response] is 90%,” he said. “Your CMR [complete molecular response] is 40%. So taking drug obviously trumps the decision of what drug to take.”
Dr Radich added that the major goal of treatment is to keep patients out of accelerated-phase blast crisis. Once people progress to blast crisis on a TKI, the median survival is less than 1 year.
“So that’s why you treat people aggressively, that’s why you monitor them molecularly, to prevent that from happening,” he said.
Treatment goals
Aside from preventing patients from progressing to blast crisis, treatment goals vary.
Achieving early molecular response (MR) impacts progression and survival, as does achieving a complete cytogenetic response (CCyR).
A major molecular response (MMR) is considered a “safe haven,” Dr Radich said, because once people achieve it, they almost never progress if they stay on drug.
And with a deep/complete molecular response (CMR), patients may potentially discontinue the drug.
So how your response goals line up determines how you use the agents for your treatment course, Dr Radich said.
In all response categories—patients with CCyR, MMR, MR, CMR—survival is virtually within 95% of survival for the general population.
“This is absolutely astonishing,” Dr Radich said.
He emphasized the importance of molecular testing at 3 months and achieving a BCR-ABL level of less than 10%.
Patients who have more than 10% blasts at 3 months have an 88% chance of achieving MMR at 4 years, while those who still have more than 10% blasts at 6 months have a 3.3% chance of achieving MMR at 4 years.
Toxicity
Side effects common to the 3 frontline TKIs are myelosuppression, transaminase elevation, and change in electrolytes. Dr Radich noted that imatinib doesn’t cause much myelosuppression.
“You can give imatinib on day 28 after allogeneic transplant, and it doesn’t affect the counts, which I think is pretty darn good proof that it doesn’t have any primary hematopoietic toxicity,” he said. “You can’t try that trick with the others.”
Venous and arterial cardiovascular events with TKIs are more recently coming to light.
Cardiovascular events with imatinib are about the same as the general population, Dr Radich said.
“[In] fact, some people think it might be protective,” he noted.
Discontinuation
“When we first started treating people with these drugs, we figured that they would be on them for life . . . ,” Dr Radich said. “[Y]ou’d always have a reservoir of CML cells because you can’t extinguish all the stem cells.”
A mathematical model predicted it would take 30 to 40 years to wipe out all CML cells with a TKI. The cumulative cure rate after 15 years of treatment would be 14%. After 30 years, it would be 31%.
Conducting a discontinuation trial would have been out of the question based on these predictions.
“Fortunately, some of the people who did the next trials hadn’t read that literature,” Dr Radich said.
One discontinuation trial (EURO-SKI) included patients who had been on drug for at least 3 years and had CMR for at least 1 year. About half stayed in PCR negativity, now up to 4 years.
A number of trials are now underway evaluating the possibility of TKI discontinuation, and they are showing that between 40% and 50% of patients can remain off drug for years.
Using generic imatinib
While generic imatinib is good for cost-effective, long-term use, second-generation TKIs are better at preventing accelerated-phase blast crisis, Dr Radich said.
The second generation is also better at producing deep remissions, and discontinuation could bring with it a cost savings.
Dr Radich calculated that it cost about $2.5 million for every patient who achieves treatment-free remission using a TKI, while transplant cost $1.31 million per patient who achieves treatment-free remission.
So generic imatinib is good for low- and intermediate-risk patients, as well as for older, sicker patients.
Second-generation TKIs are appropriate for higher-risk patients until they achieve a CCyR or MMR, then they can switch to generic imatinib.
And second-generation TKIs should be used for younger patients in whom drug discontinuation is important.
Frontline treatment observations
In summary, Dr Radich made the following observations about frontline treatment in CML.
- For overall survival, imatinib is equivalent to second-generation TKIs.
- To achieve a deep MR, a second-generation TKI is better than imatinib.
- Discontinuation is equally successful with all TKIs.
- For lower-risk CML, imatinib is equivalent to second-generation TKIs.
- When it comes to progression and possibly high-risk CML, second-generation TKIs are better than imatinib.
- Second-generation TKIs produce more long-term toxicities than imatinib.
- There is substantial cost savings with generics.


Photo by D. Meyer
NEW YORK—Evaluating treatment goals is essential when choosing which tyrosine kinase inhibitor (TKI) to prescribe for a patient with newly diagnosed chronic myeloid leukemia (CML), according to a speaker at the NCCN 11th Annual Congress: Hematologic Malignancies.
“Deciding what TKI to start people on really depends on what your goals are for that patient,” said the speaker, Jerald Radich, MD, of the Fred Hutchinson Cancer Research Center/Seattle Cancer Care Alliance in Seattle, Washington.
Because the 3 TKIs approved for frontline treatment of CML—imatinib, dasatinib, and nilotinib—produce “amazingly similar” responses, treatment compliance becomes an important factor in patient outcomes, he noted.
“If you take 90% of your imatinib, your MMR [major molecular response] is 90%,” he said. “Your CMR [complete molecular response] is 40%. So taking drug obviously trumps the decision of what drug to take.”
Dr Radich added that the major goal of treatment is to keep patients out of accelerated-phase blast crisis. Once people progress to blast crisis on a TKI, the median survival is less than 1 year.
“So that’s why you treat people aggressively, that’s why you monitor them molecularly, to prevent that from happening,” he said.
Treatment goals
Aside from preventing patients from progressing to blast crisis, treatment goals vary.
Achieving early molecular response (MR) impacts progression and survival, as does achieving a complete cytogenetic response (CCyR).
A major molecular response (MMR) is considered a “safe haven,” Dr Radich said, because once people achieve it, they almost never progress if they stay on drug.
And with a deep/complete molecular response (CMR), patients may potentially discontinue the drug.
So how your response goals line up determines how you use the agents for your treatment course, Dr Radich said.
In all response categories—patients with CCyR, MMR, MR, CMR—survival is virtually within 95% of survival for the general population.
“This is absolutely astonishing,” Dr Radich said.
He emphasized the importance of molecular testing at 3 months and achieving a BCR-ABL level of less than 10%.
Patients who have more than 10% blasts at 3 months have an 88% chance of achieving MMR at 4 years, while those who still have more than 10% blasts at 6 months have a 3.3% chance of achieving MMR at 4 years.
Toxicity
Side effects common to the 3 frontline TKIs are myelosuppression, transaminase elevation, and change in electrolytes. Dr Radich noted that imatinib doesn’t cause much myelosuppression.
“You can give imatinib on day 28 after allogeneic transplant, and it doesn’t affect the counts, which I think is pretty darn good proof that it doesn’t have any primary hematopoietic toxicity,” he said. “You can’t try that trick with the others.”
Venous and arterial cardiovascular events with TKIs are more recently coming to light.
Cardiovascular events with imatinib are about the same as the general population, Dr Radich said.
“[In] fact, some people think it might be protective,” he noted.
Discontinuation
“When we first started treating people with these drugs, we figured that they would be on them for life . . . ,” Dr Radich said. “[Y]ou’d always have a reservoir of CML cells because you can’t extinguish all the stem cells.”
A mathematical model predicted it would take 30 to 40 years to wipe out all CML cells with a TKI. The cumulative cure rate after 15 years of treatment would be 14%. After 30 years, it would be 31%.
Conducting a discontinuation trial would have been out of the question based on these predictions.
“Fortunately, some of the people who did the next trials hadn’t read that literature,” Dr Radich said.
One discontinuation trial (EURO-SKI) included patients who had been on drug for at least 3 years and had CMR for at least 1 year. About half stayed in PCR negativity, now up to 4 years.
A number of trials are now underway evaluating the possibility of TKI discontinuation, and they are showing that between 40% and 50% of patients can remain off drug for years.
Using generic imatinib
While generic imatinib is good for cost-effective, long-term use, second-generation TKIs are better at preventing accelerated-phase blast crisis, Dr Radich said.
The second generation is also better at producing deep remissions, and discontinuation could bring with it a cost savings.
Dr Radich calculated that it cost about $2.5 million for every patient who achieves treatment-free remission using a TKI, while transplant cost $1.31 million per patient who achieves treatment-free remission.
So generic imatinib is good for low- and intermediate-risk patients, as well as for older, sicker patients.
Second-generation TKIs are appropriate for higher-risk patients until they achieve a CCyR or MMR, then they can switch to generic imatinib.
And second-generation TKIs should be used for younger patients in whom drug discontinuation is important.
Frontline treatment observations
In summary, Dr Radich made the following observations about frontline treatment in CML.
- For overall survival, imatinib is equivalent to second-generation TKIs.
- To achieve a deep MR, a second-generation TKI is better than imatinib.
- Discontinuation is equally successful with all TKIs.
- For lower-risk CML, imatinib is equivalent to second-generation TKIs.
- When it comes to progression and possibly high-risk CML, second-generation TKIs are better than imatinib.
- Second-generation TKIs produce more long-term toxicities than imatinib.
- There is substantial cost savings with generics.


Photo by D. Meyer
NEW YORK—Evaluating treatment goals is essential when choosing which tyrosine kinase inhibitor (TKI) to prescribe for a patient with newly diagnosed chronic myeloid leukemia (CML), according to a speaker at the NCCN 11th Annual Congress: Hematologic Malignancies.
“Deciding what TKI to start people on really depends on what your goals are for that patient,” said the speaker, Jerald Radich, MD, of the Fred Hutchinson Cancer Research Center/Seattle Cancer Care Alliance in Seattle, Washington.
Because the 3 TKIs approved for frontline treatment of CML—imatinib, dasatinib, and nilotinib—produce “amazingly similar” responses, treatment compliance becomes an important factor in patient outcomes, he noted.
“If you take 90% of your imatinib, your MMR [major molecular response] is 90%,” he said. “Your CMR [complete molecular response] is 40%. So taking drug obviously trumps the decision of what drug to take.”
Dr Radich added that the major goal of treatment is to keep patients out of accelerated-phase blast crisis. Once people progress to blast crisis on a TKI, the median survival is less than 1 year.
“So that’s why you treat people aggressively, that’s why you monitor them molecularly, to prevent that from happening,” he said.
Treatment goals
Aside from preventing patients from progressing to blast crisis, treatment goals vary.
Achieving early molecular response (MR) impacts progression and survival, as does achieving a complete cytogenetic response (CCyR).
A major molecular response (MMR) is considered a “safe haven,” Dr Radich said, because once people achieve it, they almost never progress if they stay on drug.
And with a deep/complete molecular response (CMR), patients may potentially discontinue the drug.
So how your response goals line up determines how you use the agents for your treatment course, Dr Radich said.
In all response categories—patients with CCyR, MMR, MR, CMR—survival is virtually within 95% of survival for the general population.
“This is absolutely astonishing,” Dr Radich said.
He emphasized the importance of molecular testing at 3 months and achieving a BCR-ABL level of less than 10%.
Patients who have more than 10% blasts at 3 months have an 88% chance of achieving MMR at 4 years, while those who still have more than 10% blasts at 6 months have a 3.3% chance of achieving MMR at 4 years.
Toxicity
Side effects common to the 3 frontline TKIs are myelosuppression, transaminase elevation, and change in electrolytes. Dr Radich noted that imatinib doesn’t cause much myelosuppression.
“You can give imatinib on day 28 after allogeneic transplant, and it doesn’t affect the counts, which I think is pretty darn good proof that it doesn’t have any primary hematopoietic toxicity,” he said. “You can’t try that trick with the others.”
Venous and arterial cardiovascular events with TKIs are more recently coming to light.
Cardiovascular events with imatinib are about the same as the general population, Dr Radich said.
“[In] fact, some people think it might be protective,” he noted.
Discontinuation
“When we first started treating people with these drugs, we figured that they would be on them for life . . . ,” Dr Radich said. “[Y]ou’d always have a reservoir of CML cells because you can’t extinguish all the stem cells.”
A mathematical model predicted it would take 30 to 40 years to wipe out all CML cells with a TKI. The cumulative cure rate after 15 years of treatment would be 14%. After 30 years, it would be 31%.
Conducting a discontinuation trial would have been out of the question based on these predictions.
“Fortunately, some of the people who did the next trials hadn’t read that literature,” Dr Radich said.
One discontinuation trial (EURO-SKI) included patients who had been on drug for at least 3 years and had CMR for at least 1 year. About half stayed in PCR negativity, now up to 4 years.
A number of trials are now underway evaluating the possibility of TKI discontinuation, and they are showing that between 40% and 50% of patients can remain off drug for years.
Using generic imatinib
While generic imatinib is good for cost-effective, long-term use, second-generation TKIs are better at preventing accelerated-phase blast crisis, Dr Radich said.
The second generation is also better at producing deep remissions, and discontinuation could bring with it a cost savings.
Dr Radich calculated that it cost about $2.5 million for every patient who achieves treatment-free remission using a TKI, while transplant cost $1.31 million per patient who achieves treatment-free remission.
So generic imatinib is good for low- and intermediate-risk patients, as well as for older, sicker patients.
Second-generation TKIs are appropriate for higher-risk patients until they achieve a CCyR or MMR, then they can switch to generic imatinib.
And second-generation TKIs should be used for younger patients in whom drug discontinuation is important.
Frontline treatment observations
In summary, Dr Radich made the following observations about frontline treatment in CML.
- For overall survival, imatinib is equivalent to second-generation TKIs.
- To achieve a deep MR, a second-generation TKI is better than imatinib.
- Discontinuation is equally successful with all TKIs.
- For lower-risk CML, imatinib is equivalent to second-generation TKIs.
- When it comes to progression and possibly high-risk CML, second-generation TKIs are better than imatinib.
- Second-generation TKIs produce more long-term toxicities than imatinib.
- There is substantial cost savings with generics.

Medicare doesn’t lower TKI costs enough, study suggests

cut in half with a pill splitter
Photo by Patrick Pelletier
Significant out-of-pocket costs may delay treatment for Medicare beneficiaries with chronic myeloid leukemia (CML), according to a study published in the Journal of Clinical Oncology.
Researchers studied 393 patients with CML who had federally funded health insurance—specifically, a Medicare Part D plan.
Nearly a third of these patients did not start tyrosine kinase inhibitor (TKI) treatment within 6 months of their diagnosis.
However, patients who had access to subsidies that help cover treatment costs had a shorter median time to the start of therapy.
“There are 2 troubling findings here,” said study author Aaron Winn, a doctoral student at the University of North Carolina at Chapel Hill.
“First, we are seeing that more than 30% of people aren’t starting therapy within 6 months. Second, we are seeing long delays in starting drugs for people without subsidies. This is very concerning as these delays may be an indicator that the patient is trying to find funds to pay for their first treatment.”
Medicare Part D and TKIs
Previous studies have shown that patients insured through Medicare Part D have out of-pocket costs of nearly $3000 for the first month’s supply of a TKI.
According to researchers, the high upfront costs are due to the Medicare Part D benefit design, which requires patients to pay a larger share of medication costs until they have paid at least $4850 out-of-pocket in a year (cost in 2016). After that, patients pay 5% of the monthly drug costs.
In order to qualify for Medicare Part D’s low-income subsidy, an individual must have an annual income of less than $17,820 and assets of less than $13,640 (figures for 2016).
“Once you’re on Medicare Part D, there really aren’t ways to minimize these out-of-pocket costs, other than subsidies,” said Stacie Dusetzina, PhD, of the University of North Carolina at Chapel Hill.
“One of the challenges is that when the Medicare benefit was designed, I don’t think they were really considering these very expensive therapies. The benefit design makes a lot more sense when you’re looking at drugs that cost several hundred dollars versus several thousand dollars or more. We really need to think carefully about how much these high out-of-pocket costs are impacting patients’ access to life-saving drugs.”
Study results
For this study, Dr Dusetzina and her colleagues evaluated data on 393 patients who were diagnosed with CML between 2007 and 2011. The patients’ median age was 77, 47% were married, 48% were male, and 85% were white.
All of the patients were enrolled in Medicare Part D, and 40% qualified for subsidies to lower drug costs.
Of all the patients, there were 32% who had not started treatment with a first-line TKI (imatinib, nilotinib, or dasatinib) within 6 months of diagnosis.
However, having access to subsidies was associated with a shorter time to the start of treatment. The median time to the start of treatment was 58 days for patients with subsidies and 108 days for patients without them.
While the gap between the 2 groups widened after diagnosis, eventually, patients without subsidies did catch up, Dr Dusetzina said.
Ninety days from diagnosis, 48% of patients without subsidies had started treatment, compared to 63% of patients with subsidies. At 6 months from diagnosis, 64% of patients without subsidies had started treatment, compared to 65% of patients with subsidies.
Dr Dusetzina said patients without subsidies could be catching up as they find the financial resources to help cover those initial costs. But overall, patients with subsidies were 35% more likely to start TKI treatment faster.
“We recognize that people have a high cost to even start therapy, and this study really demonstrates the difference between people with and without a subsidy in initiating therapy,” Dr Dusetzina said. “The out-of-pocket costs may be delaying people starting these life-saving drugs.” ![]()

cut in half with a pill splitter
Photo by Patrick Pelletier
Significant out-of-pocket costs may delay treatment for Medicare beneficiaries with chronic myeloid leukemia (CML), according to a study published in the Journal of Clinical Oncology.
Researchers studied 393 patients with CML who had federally funded health insurance—specifically, a Medicare Part D plan.
Nearly a third of these patients did not start tyrosine kinase inhibitor (TKI) treatment within 6 months of their diagnosis.
However, patients who had access to subsidies that help cover treatment costs had a shorter median time to the start of therapy.
“There are 2 troubling findings here,” said study author Aaron Winn, a doctoral student at the University of North Carolina at Chapel Hill.
“First, we are seeing that more than 30% of people aren’t starting therapy within 6 months. Second, we are seeing long delays in starting drugs for people without subsidies. This is very concerning as these delays may be an indicator that the patient is trying to find funds to pay for their first treatment.”
Medicare Part D and TKIs
Previous studies have shown that patients insured through Medicare Part D have out of-pocket costs of nearly $3000 for the first month’s supply of a TKI.
According to researchers, the high upfront costs are due to the Medicare Part D benefit design, which requires patients to pay a larger share of medication costs until they have paid at least $4850 out-of-pocket in a year (cost in 2016). After that, patients pay 5% of the monthly drug costs.
In order to qualify for Medicare Part D’s low-income subsidy, an individual must have an annual income of less than $17,820 and assets of less than $13,640 (figures for 2016).
“Once you’re on Medicare Part D, there really aren’t ways to minimize these out-of-pocket costs, other than subsidies,” said Stacie Dusetzina, PhD, of the University of North Carolina at Chapel Hill.
“One of the challenges is that when the Medicare benefit was designed, I don’t think they were really considering these very expensive therapies. The benefit design makes a lot more sense when you’re looking at drugs that cost several hundred dollars versus several thousand dollars or more. We really need to think carefully about how much these high out-of-pocket costs are impacting patients’ access to life-saving drugs.”
Study results
For this study, Dr Dusetzina and her colleagues evaluated data on 393 patients who were diagnosed with CML between 2007 and 2011. The patients’ median age was 77, 47% were married, 48% were male, and 85% were white.
All of the patients were enrolled in Medicare Part D, and 40% qualified for subsidies to lower drug costs.
Of all the patients, there were 32% who had not started treatment with a first-line TKI (imatinib, nilotinib, or dasatinib) within 6 months of diagnosis.
However, having access to subsidies was associated with a shorter time to the start of treatment. The median time to the start of treatment was 58 days for patients with subsidies and 108 days for patients without them.
While the gap between the 2 groups widened after diagnosis, eventually, patients without subsidies did catch up, Dr Dusetzina said.
Ninety days from diagnosis, 48% of patients without subsidies had started treatment, compared to 63% of patients with subsidies. At 6 months from diagnosis, 64% of patients without subsidies had started treatment, compared to 65% of patients with subsidies.
Dr Dusetzina said patients without subsidies could be catching up as they find the financial resources to help cover those initial costs. But overall, patients with subsidies were 35% more likely to start TKI treatment faster.
“We recognize that people have a high cost to even start therapy, and this study really demonstrates the difference between people with and without a subsidy in initiating therapy,” Dr Dusetzina said. “The out-of-pocket costs may be delaying people starting these life-saving drugs.” ![]()

cut in half with a pill splitter
Photo by Patrick Pelletier
Significant out-of-pocket costs may delay treatment for Medicare beneficiaries with chronic myeloid leukemia (CML), according to a study published in the Journal of Clinical Oncology.
Researchers studied 393 patients with CML who had federally funded health insurance—specifically, a Medicare Part D plan.
Nearly a third of these patients did not start tyrosine kinase inhibitor (TKI) treatment within 6 months of their diagnosis.
However, patients who had access to subsidies that help cover treatment costs had a shorter median time to the start of therapy.
“There are 2 troubling findings here,” said study author Aaron Winn, a doctoral student at the University of North Carolina at Chapel Hill.
“First, we are seeing that more than 30% of people aren’t starting therapy within 6 months. Second, we are seeing long delays in starting drugs for people without subsidies. This is very concerning as these delays may be an indicator that the patient is trying to find funds to pay for their first treatment.”
Medicare Part D and TKIs
Previous studies have shown that patients insured through Medicare Part D have out of-pocket costs of nearly $3000 for the first month’s supply of a TKI.
According to researchers, the high upfront costs are due to the Medicare Part D benefit design, which requires patients to pay a larger share of medication costs until they have paid at least $4850 out-of-pocket in a year (cost in 2016). After that, patients pay 5% of the monthly drug costs.
In order to qualify for Medicare Part D’s low-income subsidy, an individual must have an annual income of less than $17,820 and assets of less than $13,640 (figures for 2016).
“Once you’re on Medicare Part D, there really aren’t ways to minimize these out-of-pocket costs, other than subsidies,” said Stacie Dusetzina, PhD, of the University of North Carolina at Chapel Hill.
“One of the challenges is that when the Medicare benefit was designed, I don’t think they were really considering these very expensive therapies. The benefit design makes a lot more sense when you’re looking at drugs that cost several hundred dollars versus several thousand dollars or more. We really need to think carefully about how much these high out-of-pocket costs are impacting patients’ access to life-saving drugs.”
Study results
For this study, Dr Dusetzina and her colleagues evaluated data on 393 patients who were diagnosed with CML between 2007 and 2011. The patients’ median age was 77, 47% were married, 48% were male, and 85% were white.
All of the patients were enrolled in Medicare Part D, and 40% qualified for subsidies to lower drug costs.
Of all the patients, there were 32% who had not started treatment with a first-line TKI (imatinib, nilotinib, or dasatinib) within 6 months of diagnosis.
However, having access to subsidies was associated with a shorter time to the start of treatment. The median time to the start of treatment was 58 days for patients with subsidies and 108 days for patients without them.
While the gap between the 2 groups widened after diagnosis, eventually, patients without subsidies did catch up, Dr Dusetzina said.
Ninety days from diagnosis, 48% of patients without subsidies had started treatment, compared to 63% of patients with subsidies. At 6 months from diagnosis, 64% of patients without subsidies had started treatment, compared to 65% of patients with subsidies.
Dr Dusetzina said patients without subsidies could be catching up as they find the financial resources to help cover those initial costs. But overall, patients with subsidies were 35% more likely to start TKI treatment faster.
“We recognize that people have a high cost to even start therapy, and this study really demonstrates the difference between people with and without a subsidy in initiating therapy,” Dr Dusetzina said. “The out-of-pocket costs may be delaying people starting these life-saving drugs.” ![]()
Ponatinib approved to treat CML, ALL in Japan
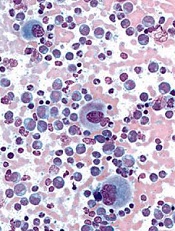
Image from UCSD
The Japanese Pharmaceuticals and Medical Devices Agency (PMDA) has approved 2 uses of the tyrosine kinase inhibitor (TKI) ponatinib (Iclusig®).
The drug is now approved to treat recurrent or refractory Philadelphia chromosome-positive acute lymphoblastic leukemia (Ph+ ALL) and chronic myeloid leukemia (CML) that was resistant to or intolerant of prior treatment.
Ponatinib will be manufactured and sold by Otsuka Pharmaceutical Co., Ltd.
Due to the limited existing treatment options for patients in Japan, Otsuka said it will provide access to ponatinib free of charge as soon as procedures are in place from an ethical standpoint.
This program will be offered at medical institutions where clinical trials of ponatinib were performed and which are amenable to accepting the drug access program until the product is listed on the Japan National Health Insurance price list.
About ponatinib
Ponatinib is a TKI discovered by ARIAD Pharmaceuticals, Inc. The drug has demonstrated activity against native and mutated BCR-ABL and other kinases.
The PMDA’s approval of ponatinib for CML and Ph+ ALL is based on data from a phase 1/2 trial of Japanese patients, a phase 1 trial, and the phase 2 PACE trial.
Extended follow-up data from the PACE trial, collected in 2013, suggested ponatinib can increase the risk of thrombotic events. When these data came to light, officials in the European Union and the US, where ponatinib had already been approved, began to investigate the drug.
Ponatinib was pulled from the US market for a little over 2 months, and trials of the TKI were placed on partial hold while the US Food and Drug Administration evaluated the drug’s safety. Ponatinib went back on the market in January 2014, with new safety measures in place.
Ponatinib was not pulled from the market in the European Union, but the European Medicine’s Agency released recommendations for safer use of the TKI. The Committee for Medicinal Products for Human Use reviewed data on ponatinib and decided its benefits outweigh its risks.
In addition to the European Union and the US, ponatinib has been approved in Australia, Canada, Israel, and Switzerland. ![]()
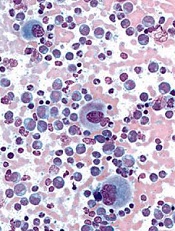
Image from UCSD
The Japanese Pharmaceuticals and Medical Devices Agency (PMDA) has approved 2 uses of the tyrosine kinase inhibitor (TKI) ponatinib (Iclusig®).
The drug is now approved to treat recurrent or refractory Philadelphia chromosome-positive acute lymphoblastic leukemia (Ph+ ALL) and chronic myeloid leukemia (CML) that was resistant to or intolerant of prior treatment.
Ponatinib will be manufactured and sold by Otsuka Pharmaceutical Co., Ltd.
Due to the limited existing treatment options for patients in Japan, Otsuka said it will provide access to ponatinib free of charge as soon as procedures are in place from an ethical standpoint.
This program will be offered at medical institutions where clinical trials of ponatinib were performed and which are amenable to accepting the drug access program until the product is listed on the Japan National Health Insurance price list.
About ponatinib
Ponatinib is a TKI discovered by ARIAD Pharmaceuticals, Inc. The drug has demonstrated activity against native and mutated BCR-ABL and other kinases.
The PMDA’s approval of ponatinib for CML and Ph+ ALL is based on data from a phase 1/2 trial of Japanese patients, a phase 1 trial, and the phase 2 PACE trial.
Extended follow-up data from the PACE trial, collected in 2013, suggested ponatinib can increase the risk of thrombotic events. When these data came to light, officials in the European Union and the US, where ponatinib had already been approved, began to investigate the drug.
Ponatinib was pulled from the US market for a little over 2 months, and trials of the TKI were placed on partial hold while the US Food and Drug Administration evaluated the drug’s safety. Ponatinib went back on the market in January 2014, with new safety measures in place.
Ponatinib was not pulled from the market in the European Union, but the European Medicine’s Agency released recommendations for safer use of the TKI. The Committee for Medicinal Products for Human Use reviewed data on ponatinib and decided its benefits outweigh its risks.
In addition to the European Union and the US, ponatinib has been approved in Australia, Canada, Israel, and Switzerland. ![]()
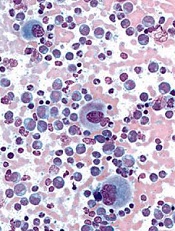
Image from UCSD
The Japanese Pharmaceuticals and Medical Devices Agency (PMDA) has approved 2 uses of the tyrosine kinase inhibitor (TKI) ponatinib (Iclusig®).
The drug is now approved to treat recurrent or refractory Philadelphia chromosome-positive acute lymphoblastic leukemia (Ph+ ALL) and chronic myeloid leukemia (CML) that was resistant to or intolerant of prior treatment.
Ponatinib will be manufactured and sold by Otsuka Pharmaceutical Co., Ltd.
Due to the limited existing treatment options for patients in Japan, Otsuka said it will provide access to ponatinib free of charge as soon as procedures are in place from an ethical standpoint.
This program will be offered at medical institutions where clinical trials of ponatinib were performed and which are amenable to accepting the drug access program until the product is listed on the Japan National Health Insurance price list.
About ponatinib
Ponatinib is a TKI discovered by ARIAD Pharmaceuticals, Inc. The drug has demonstrated activity against native and mutated BCR-ABL and other kinases.
The PMDA’s approval of ponatinib for CML and Ph+ ALL is based on data from a phase 1/2 trial of Japanese patients, a phase 1 trial, and the phase 2 PACE trial.
Extended follow-up data from the PACE trial, collected in 2013, suggested ponatinib can increase the risk of thrombotic events. When these data came to light, officials in the European Union and the US, where ponatinib had already been approved, began to investigate the drug.
Ponatinib was pulled from the US market for a little over 2 months, and trials of the TKI were placed on partial hold while the US Food and Drug Administration evaluated the drug’s safety. Ponatinib went back on the market in January 2014, with new safety measures in place.
Ponatinib was not pulled from the market in the European Union, but the European Medicine’s Agency released recommendations for safer use of the TKI. The Committee for Medicinal Products for Human Use reviewed data on ponatinib and decided its benefits outweigh its risks.
In addition to the European Union and the US, ponatinib has been approved in Australia, Canada, Israel, and Switzerland. ![]()
DNA methylation rises sharply at progression of Ph+ CML
A large uptick in DNA methylation occurs at the time of progression in patients with Philadelphia chromosome–positive chronic myeloid leukemia (CML), according to results from a comparative cohort study. The observation raises the possibility of new therapeutic targets for advanced disease.
Researchers led by Gerwin Heller, PhD, of the Medical University of Vienna’s Clinical Division of Oncology and Comprehensive Cancer Center, Austria, collected peripheral blood mononuclear cells from 23 patients with CML during various disease phases (chronic phase in 17, acute phase in 5, and blast crisis in 9) and from 5 healthy controls.
They isolated DNA and analyzed it with a novel next-generation sequencing approach, known as reduced representation bisulfite sequencing, to identify the presence and extent of methylation.
Compared with the healthy controls, patients in chronic-phase CML had 666 differentially methylated CpG (cytosine-phosphate-guanine) sites, whereas those in blast crisis had 6,912 differentially methylated CpG sites (Leukemia. 2016;30:1861-8). Some 44% of the former but 88% of the latter affected CpG sites showed increased methylation.
Among patients with chronic-phase CML who experienced progression to the accelerated phase or blast crisis, analyses identified between 344 and 897 genes that were methylated at the time of progression but had not been at the time of diagnosis.
RNA sequencing determined that many of these newly methylated genes showed downregulated expression in the samples collected during blast crisis, compared with those collected during chronic phase disease. These genes included some tumor suppressor genes (EPB41L3, PRDX2), regulators of cell proliferation (BCL11B, NDRG2, PID1), and regulators of drug metabolism (CYP1B1), among others.
Treatment of CML cells with the epigenetically active drugs azacitidine (a DNA methyltransferase inhibitor) and trichostatin A (a histone deacetylase inhibitor) led to re-expression of the CYP1B1 gene.
“Together, our results demonstrate that CpG site methylation clearly increases during CML progression and that it may provide a useful basis for revealing new targets of therapy in advanced CML,” wrote Dr. Heller and colleagues, who disclosed that one of them has received research grants from Novartis and Ariad.
“Our findings suggest that investigating the efficacy of [DNA methyltransferase inhibitors] in patients with progressed CML should be considered,” they said.
A large uptick in DNA methylation occurs at the time of progression in patients with Philadelphia chromosome–positive chronic myeloid leukemia (CML), according to results from a comparative cohort study. The observation raises the possibility of new therapeutic targets for advanced disease.
Researchers led by Gerwin Heller, PhD, of the Medical University of Vienna’s Clinical Division of Oncology and Comprehensive Cancer Center, Austria, collected peripheral blood mononuclear cells from 23 patients with CML during various disease phases (chronic phase in 17, acute phase in 5, and blast crisis in 9) and from 5 healthy controls.
They isolated DNA and analyzed it with a novel next-generation sequencing approach, known as reduced representation bisulfite sequencing, to identify the presence and extent of methylation.
Compared with the healthy controls, patients in chronic-phase CML had 666 differentially methylated CpG (cytosine-phosphate-guanine) sites, whereas those in blast crisis had 6,912 differentially methylated CpG sites (Leukemia. 2016;30:1861-8). Some 44% of the former but 88% of the latter affected CpG sites showed increased methylation.
Among patients with chronic-phase CML who experienced progression to the accelerated phase or blast crisis, analyses identified between 344 and 897 genes that were methylated at the time of progression but had not been at the time of diagnosis.
RNA sequencing determined that many of these newly methylated genes showed downregulated expression in the samples collected during blast crisis, compared with those collected during chronic phase disease. These genes included some tumor suppressor genes (EPB41L3, PRDX2), regulators of cell proliferation (BCL11B, NDRG2, PID1), and regulators of drug metabolism (CYP1B1), among others.
Treatment of CML cells with the epigenetically active drugs azacitidine (a DNA methyltransferase inhibitor) and trichostatin A (a histone deacetylase inhibitor) led to re-expression of the CYP1B1 gene.
“Together, our results demonstrate that CpG site methylation clearly increases during CML progression and that it may provide a useful basis for revealing new targets of therapy in advanced CML,” wrote Dr. Heller and colleagues, who disclosed that one of them has received research grants from Novartis and Ariad.
“Our findings suggest that investigating the efficacy of [DNA methyltransferase inhibitors] in patients with progressed CML should be considered,” they said.
A large uptick in DNA methylation occurs at the time of progression in patients with Philadelphia chromosome–positive chronic myeloid leukemia (CML), according to results from a comparative cohort study. The observation raises the possibility of new therapeutic targets for advanced disease.
Researchers led by Gerwin Heller, PhD, of the Medical University of Vienna’s Clinical Division of Oncology and Comprehensive Cancer Center, Austria, collected peripheral blood mononuclear cells from 23 patients with CML during various disease phases (chronic phase in 17, acute phase in 5, and blast crisis in 9) and from 5 healthy controls.
They isolated DNA and analyzed it with a novel next-generation sequencing approach, known as reduced representation bisulfite sequencing, to identify the presence and extent of methylation.
Compared with the healthy controls, patients in chronic-phase CML had 666 differentially methylated CpG (cytosine-phosphate-guanine) sites, whereas those in blast crisis had 6,912 differentially methylated CpG sites (Leukemia. 2016;30:1861-8). Some 44% of the former but 88% of the latter affected CpG sites showed increased methylation.
Among patients with chronic-phase CML who experienced progression to the accelerated phase or blast crisis, analyses identified between 344 and 897 genes that were methylated at the time of progression but had not been at the time of diagnosis.
RNA sequencing determined that many of these newly methylated genes showed downregulated expression in the samples collected during blast crisis, compared with those collected during chronic phase disease. These genes included some tumor suppressor genes (EPB41L3, PRDX2), regulators of cell proliferation (BCL11B, NDRG2, PID1), and regulators of drug metabolism (CYP1B1), among others.
Treatment of CML cells with the epigenetically active drugs azacitidine (a DNA methyltransferase inhibitor) and trichostatin A (a histone deacetylase inhibitor) led to re-expression of the CYP1B1 gene.
“Together, our results demonstrate that CpG site methylation clearly increases during CML progression and that it may provide a useful basis for revealing new targets of therapy in advanced CML,” wrote Dr. Heller and colleagues, who disclosed that one of them has received research grants from Novartis and Ariad.
“Our findings suggest that investigating the efficacy of [DNA methyltransferase inhibitors] in patients with progressed CML should be considered,” they said.
FROM LEUKEMIA
Key clinical point: Increases in DNA methylation occur at progression of Ph+ CML; this realization may enable new therapeutic targets.
Major finding: Patients who progressed from chronic phase to accelerated phase or blast crisis had up to 897 genes that were newly methylated since diagnosis, including some tumor-suppressor genes and regulators of cell proliferation and drug metabolism.
Data source: A cohort study of 23 patients with CML and 5 healthy controls.
Disclosures: The investigators disclosed that one of the authors has received research grants from Novartis and Ariad.
EZH2 inhibitors could improve treatment of CML, studies suggest

Image by Difu Wu
Two preclinical studies published in Cancer Discovery suggest that EZH2 inhibitors might enhance the efficacy of treatment with tyrosine kinase inhibitors (TKIs) in patients with chronic myeloid leukemia (CML).
One study showed that CML leukemic stem cells (LSCs) are dependent upon EZH2.
The other study revealed that epigenetic reprogramming sensitizes CML LSCs to combined treatment with an EZH2 inhibitor and a TKI.
EZH2 dependence
In the first study, in vitro experiments revealed that LSCs have an overabundance of EZH2. In fact, the researchers found that EZH2 helps LSCs survive and give rise to full-fledged CML cells.
Experiments in mice showed that inactivating EZH2 through gene-editing techniques caused LSCs to die, halting CML at its source.
“The stem cells’ dependence on EZH2 suggests they will be especially vulnerable to drugs that target the protein,” said study author Stuart Orkin, MD, of Boston Children’s Hospital in Massachusetts.
“Our findings suggest inhibition of EZH2 should be considered as a way to eradicate CML when used in combination with current targeted therapies. It offers a promising approach to shortening the duration of therapy in order to achieve a cure. If successful, the cost savings of such an approach could also be significant.”
Combination treatment
The second study supports the idea that combining EZH2 inhibitors and TKIs could benefit patients with CML.
Mary T. Scott, of the University of Glasgow in the UK, and her colleagues found that EZH2 and H3K27me3 reprogramming is important for LSC survival and renders the cells sensitive to combined treatment with an EZH2 inhibitor and a TKI.
The researchers treated CML CD34+ cells, normal CD34+ cells, and LSCs with the EZH2 inhibitor GSK343 and the TKI dasatinib, both alone and in combination. The team said that GSK343 selectively targeted the loss of H3K27me3 in the presence of dasatinib.
In addition, combination treatment led to a significant reduction in cell viability (even in “TKI-persistent” cells), an increase in apoptosis, and a reduction in colony-forming cell and granulocyte/erythroid/macrophage/megakaryocyte outputs, when compared to dasatinib alone.
The researchers also evaluated a TKI and an EZH2 inhibitor in a mouse model of CML. The mice received nilotinib and EPZ-6438, both alone and in combination, for either 14 days or 25 days.
After 14 days of treatment, mice that received the combination had significant reductions in levels of leukemic (Ph+) human CD45+ cells, CD45+CD34+ progenitor cells, and primitive CD45+CD34+CD38− stem cells in the bone marrow, when compared to mice that received nilotinib alone.
After 25 days of treatment, mice that received the combination had near-complete elimination of CD45+CD34+ progenitor cells and a greater than 70% reduction of CD45+CD34+CD38− cells, when compared to mice that received nilotinib alone.
The researchers said these results demonstrate a clear rationale for combining TKI treatment with an EZH2 inhibitor, as an EZH2 inhibitor can target primitive CML cells not eradicated by a TKI alone. ![]()

Image by Difu Wu
Two preclinical studies published in Cancer Discovery suggest that EZH2 inhibitors might enhance the efficacy of treatment with tyrosine kinase inhibitors (TKIs) in patients with chronic myeloid leukemia (CML).
One study showed that CML leukemic stem cells (LSCs) are dependent upon EZH2.
The other study revealed that epigenetic reprogramming sensitizes CML LSCs to combined treatment with an EZH2 inhibitor and a TKI.
EZH2 dependence
In the first study, in vitro experiments revealed that LSCs have an overabundance of EZH2. In fact, the researchers found that EZH2 helps LSCs survive and give rise to full-fledged CML cells.
Experiments in mice showed that inactivating EZH2 through gene-editing techniques caused LSCs to die, halting CML at its source.
“The stem cells’ dependence on EZH2 suggests they will be especially vulnerable to drugs that target the protein,” said study author Stuart Orkin, MD, of Boston Children’s Hospital in Massachusetts.
“Our findings suggest inhibition of EZH2 should be considered as a way to eradicate CML when used in combination with current targeted therapies. It offers a promising approach to shortening the duration of therapy in order to achieve a cure. If successful, the cost savings of such an approach could also be significant.”
Combination treatment
The second study supports the idea that combining EZH2 inhibitors and TKIs could benefit patients with CML.
Mary T. Scott, of the University of Glasgow in the UK, and her colleagues found that EZH2 and H3K27me3 reprogramming is important for LSC survival and renders the cells sensitive to combined treatment with an EZH2 inhibitor and a TKI.
The researchers treated CML CD34+ cells, normal CD34+ cells, and LSCs with the EZH2 inhibitor GSK343 and the TKI dasatinib, both alone and in combination. The team said that GSK343 selectively targeted the loss of H3K27me3 in the presence of dasatinib.
In addition, combination treatment led to a significant reduction in cell viability (even in “TKI-persistent” cells), an increase in apoptosis, and a reduction in colony-forming cell and granulocyte/erythroid/macrophage/megakaryocyte outputs, when compared to dasatinib alone.
The researchers also evaluated a TKI and an EZH2 inhibitor in a mouse model of CML. The mice received nilotinib and EPZ-6438, both alone and in combination, for either 14 days or 25 days.
After 14 days of treatment, mice that received the combination had significant reductions in levels of leukemic (Ph+) human CD45+ cells, CD45+CD34+ progenitor cells, and primitive CD45+CD34+CD38− stem cells in the bone marrow, when compared to mice that received nilotinib alone.
After 25 days of treatment, mice that received the combination had near-complete elimination of CD45+CD34+ progenitor cells and a greater than 70% reduction of CD45+CD34+CD38− cells, when compared to mice that received nilotinib alone.
The researchers said these results demonstrate a clear rationale for combining TKI treatment with an EZH2 inhibitor, as an EZH2 inhibitor can target primitive CML cells not eradicated by a TKI alone. ![]()

Image by Difu Wu
Two preclinical studies published in Cancer Discovery suggest that EZH2 inhibitors might enhance the efficacy of treatment with tyrosine kinase inhibitors (TKIs) in patients with chronic myeloid leukemia (CML).
One study showed that CML leukemic stem cells (LSCs) are dependent upon EZH2.
The other study revealed that epigenetic reprogramming sensitizes CML LSCs to combined treatment with an EZH2 inhibitor and a TKI.
EZH2 dependence
In the first study, in vitro experiments revealed that LSCs have an overabundance of EZH2. In fact, the researchers found that EZH2 helps LSCs survive and give rise to full-fledged CML cells.
Experiments in mice showed that inactivating EZH2 through gene-editing techniques caused LSCs to die, halting CML at its source.
“The stem cells’ dependence on EZH2 suggests they will be especially vulnerable to drugs that target the protein,” said study author Stuart Orkin, MD, of Boston Children’s Hospital in Massachusetts.
“Our findings suggest inhibition of EZH2 should be considered as a way to eradicate CML when used in combination with current targeted therapies. It offers a promising approach to shortening the duration of therapy in order to achieve a cure. If successful, the cost savings of such an approach could also be significant.”
Combination treatment
The second study supports the idea that combining EZH2 inhibitors and TKIs could benefit patients with CML.
Mary T. Scott, of the University of Glasgow in the UK, and her colleagues found that EZH2 and H3K27me3 reprogramming is important for LSC survival and renders the cells sensitive to combined treatment with an EZH2 inhibitor and a TKI.
The researchers treated CML CD34+ cells, normal CD34+ cells, and LSCs with the EZH2 inhibitor GSK343 and the TKI dasatinib, both alone and in combination. The team said that GSK343 selectively targeted the loss of H3K27me3 in the presence of dasatinib.
In addition, combination treatment led to a significant reduction in cell viability (even in “TKI-persistent” cells), an increase in apoptosis, and a reduction in colony-forming cell and granulocyte/erythroid/macrophage/megakaryocyte outputs, when compared to dasatinib alone.
The researchers also evaluated a TKI and an EZH2 inhibitor in a mouse model of CML. The mice received nilotinib and EPZ-6438, both alone and in combination, for either 14 days or 25 days.
After 14 days of treatment, mice that received the combination had significant reductions in levels of leukemic (Ph+) human CD45+ cells, CD45+CD34+ progenitor cells, and primitive CD45+CD34+CD38− stem cells in the bone marrow, when compared to mice that received nilotinib alone.
After 25 days of treatment, mice that received the combination had near-complete elimination of CD45+CD34+ progenitor cells and a greater than 70% reduction of CD45+CD34+CD38− cells, when compared to mice that received nilotinib alone.
The researchers said these results demonstrate a clear rationale for combining TKI treatment with an EZH2 inhibitor, as an EZH2 inhibitor can target primitive CML cells not eradicated by a TKI alone.

