User login
Updates in COPD Guidelines and Treatment
Al Wachami N, Guennouni M, Iderdar Y, et al. Estimating the global prevalence of chronic obstructive pulmonary disease (COPD): a systematic review and meta-analysis. BMC Public Health. 2024;24(1):297. doi:10.1186/s12889-024-17686-9
COPD trends brief. American Lung Association. Accessed July 11, 2024. https://www.lung.org/research/trends-in-lung-disease/copd-trends-brief
Chronic obstructive pulmonary disease (COPD). World Health Organization. March 16, 2023. Accessed July 11, 2024. https://www.who.int/news-room/fact-sheets/detail/chronic-obstructive-pulmonary-disease-(copd)
Shalabi MS, Aqdi SW, Alfort OA, et al. Effectiveness and safety of bronchodilators and inhaled corticosteroids in the management of chronic obstructive pulmonary disease. Int J Commun Med Public Health. 2023;10(8):2955-2959. doi:10.18203/2394-6040.ijcmph20232392
McCormick B. FDA approves ensifentrine for maintenance treatment of adult patients with COPD. AJMC. June 26, 2024. Accessed July 11, 2024. https://www.ajmc.com/view/fda-approves-ensifentrine-for-maintenance-treatment-of-adult-patients-with-copd
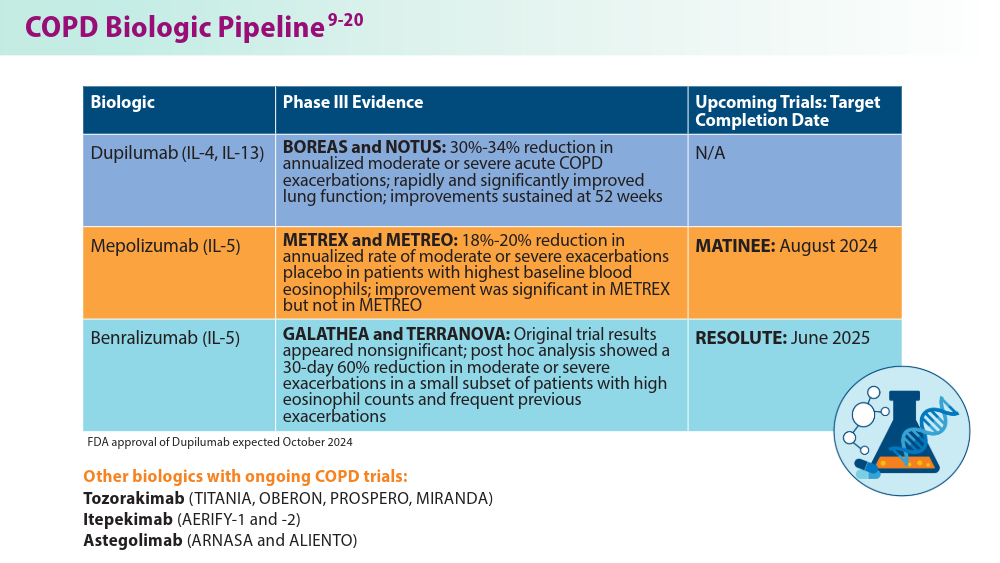
Kersul AL, Cosio BG. Biologics in COPD. Open Resp Arch. 2024;6(2):100306. doi:10.1016/j.opresp.2024.100306
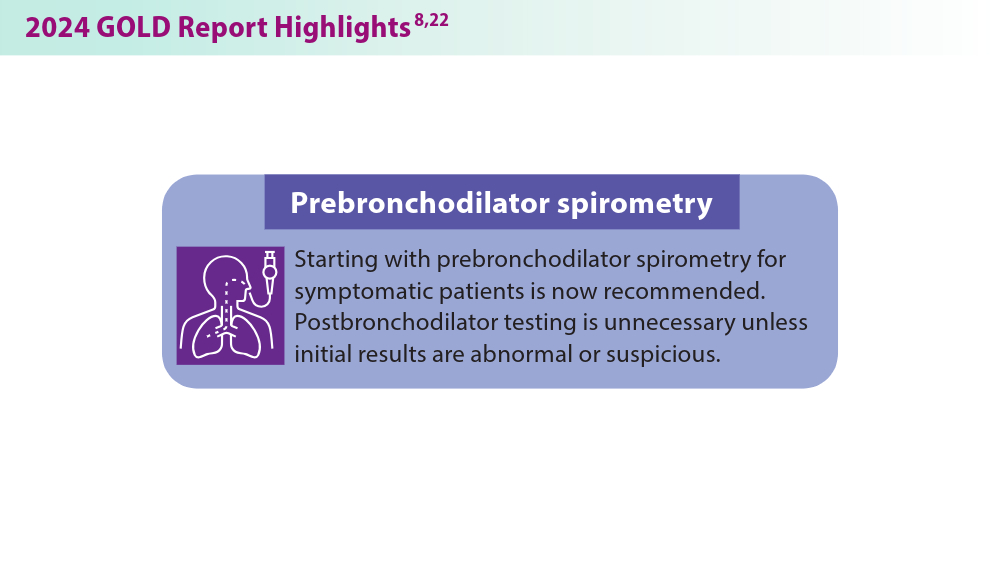
2023 GOLD Report. Global Initiative for Chronic Obstructive Lung Disease. Accessed July 11, 2024. https://goldcopd.org/2023-gold-report-2
2024 GOLD Report. Global Initiative for Chronic Obstructive Lung Disease. Accessed July 11, 2024. https://goldcopd.org/2024-gold-report/
Regeneron Pharmaceuticals Inc. Dupixent® (dupilumab) late-breaking data from NOTUS confirmatory phase 3 COPD trial presented at ATS and published in the New England Journal of Medicine [press release]. May 20, 2024. Accessed July 11, 2024. https://investor.regeneron.com/news-releases/news-release-details/dupixentr-dupilumab-late-breaking-data-notus-confirmatory-phase
Pavord ID, Chapman KR, Bafadhel M, et al. Mepolizumab for eosinophil-associated COPD: analysis of METREX and METREO. Int J Chron Obstruct Pulmon Dis. 2021;16:1755-1770. doi:10.2147/COPD.S294333
Mepolizumab as add-on treatment in participants with COPD characterized by frequent exacerbations and eosinophil level (MATINEE). Clinicaltrials.gov. Updated August 28, 2023. Accessed July 11, 2024. https://clinicaltrials.gov/study/NCT04133909
Singh D, Criner GJ, Agustí A, et al. Benralizumab prevents recurrent exacerbations in patients with chronic obstructive pulmonary disease: a post hoc analysis. Int J Chron Obstruct Pulmon Dis. 2023;18:1595-1599. doi:10.2147/COPD.S418944
Efficacy and safety of benralizumab in moderate to very severe chronic obstructive pulmonary disease (COPD) with a history of frequent exacerbations (RESOLUTE). Clinicaltrials.gov. Updated May 8, 2024. Accessed July 11, 2024. https://clinicaltrials.gov/study/NCT04053634
Efficacy and safety of tozorakimab in symptomatic chronic obstructive pulmonary disease with a history of exacerbations (TITANIA). Clinicaltrials.gov. Updated June 27, 2024. Accessed July 11, 2024. https://clinicaltrials.gov/study/NCT05158387
Efficacy and safety of tozorakimab in symptomatic chronic obstructive pulmonary disease with a history of exacerbations (OBERON). Clinicaltrials.gov. Updated June 21, 2024. Accessed July 11, 2024. https://clinicaltrials.gov/study/NCT05166889
Long-term efficacy and safety of tozorakimab in participants with chronic obstructive pulmonary disease with a history of exacerbations (PROSPERO). Clinicaltrials.gov. Updated June 20, 2024. Accessed July 11, 2024. https://clinicaltrials.gov/study/NCT05742802
Efficacy and safety of tozorakimab in symptomatic chronic obstructive pulmonary disease with a history of exacerbations (MIRANDA). Clinicaltrials.gov. Updated June 4, 2024. Accessed July 11, 2024. https://clinicaltrials.gov/study/NCT06040086
Study to assess the efficacy, safety, and tolerability of SAR440340/REGN3500/itepekimab in chronic obstructive pulmonary disease (COPD) (AERIFY-1). ClinicalTrials.gov. Updated June 21, 2024. Accessed July 11, 2024. https://classic.clinicaltrials.gov/ct2/show/NCT04701983
Study to assess the efficacy, safety, and tolerability of SAR440340/REGN3500/itepekimab in chronic obstructive pulmonary disease (COPD) (AERIFY-2). ClinicalTrials.gov. Updated May 9, 2024. Accessed July 11, 2024. https://classic.clinicaltrials.gov/ct2/show/NCT04751487
ALIENTO and ARNASA: study designs of two randomised, double-blind, placebo-controlled trials of astegolimab in patients with COPD. Medically. 2023. Accessed July 11, 2024. https://medically.gene.com/global/en/unrestricted/respiratory/ERS-2023/ers-2023-poster-brightling-aliento-and-arnasa-study-des.html
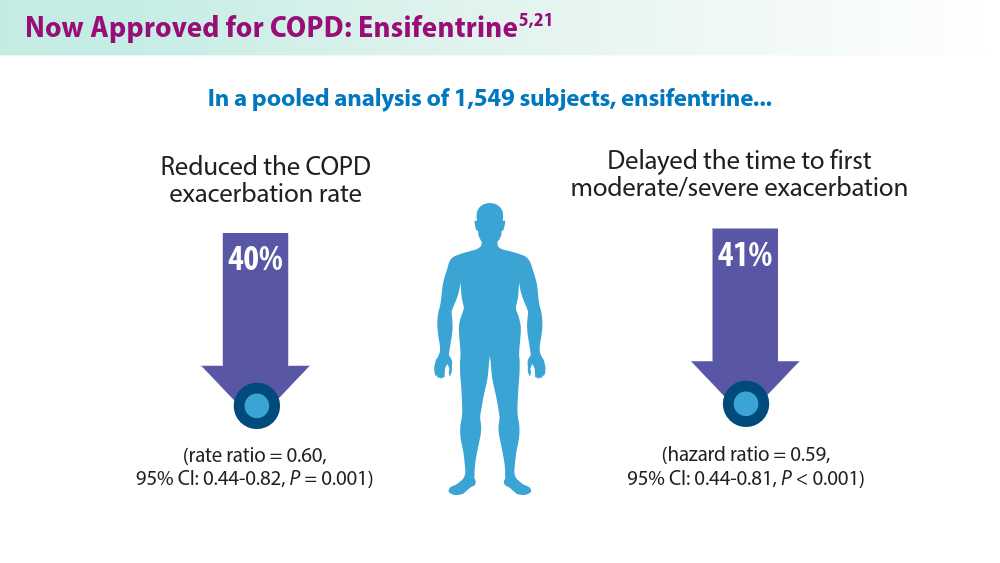
Anzueto A, Barjaktarevic IZ, Siler TM, et al. Ensifentrine, a novel phosphodiesterase 3 and 4 inhibitor for the treatment of chronic obstructive pulmonary disease: randomized, double-blind, placebo-controlled, multicenter phase III trials (the ENHANCE trials). Am J Respir Crit Care Med. 2023;208(4):406-416. doi:10.1164/rccm.202306-0944OC
US Preventive Services Taskforce. Lung cancer: screening. March 9, 2021. Accessed July 11, 2024. https://www.uspreventiveservicestaskforce.org/uspstf/recommendation/lung-cancer-screening
Al Wachami N, Guennouni M, Iderdar Y, et al. Estimating the global prevalence of chronic obstructive pulmonary disease (COPD): a systematic review and meta-analysis. BMC Public Health. 2024;24(1):297. doi:10.1186/s12889-024-17686-9
COPD trends brief. American Lung Association. Accessed July 11, 2024. https://www.lung.org/research/trends-in-lung-disease/copd-trends-brief
Chronic obstructive pulmonary disease (COPD). World Health Organization. March 16, 2023. Accessed July 11, 2024. https://www.who.int/news-room/fact-sheets/detail/chronic-obstructive-pulmonary-disease-(copd)
Shalabi MS, Aqdi SW, Alfort OA, et al. Effectiveness and safety of bronchodilators and inhaled corticosteroids in the management of chronic obstructive pulmonary disease. Int J Commun Med Public Health. 2023;10(8):2955-2959. doi:10.18203/2394-6040.ijcmph20232392
McCormick B. FDA approves ensifentrine for maintenance treatment of adult patients with COPD. AJMC. June 26, 2024. Accessed July 11, 2024. https://www.ajmc.com/view/fda-approves-ensifentrine-for-maintenance-treatment-of-adult-patients-with-copd
Kersul AL, Cosio BG. Biologics in COPD. Open Resp Arch. 2024;6(2):100306. doi:10.1016/j.opresp.2024.100306
2023 GOLD Report. Global Initiative for Chronic Obstructive Lung Disease. Accessed July 11, 2024. https://goldcopd.org/2023-gold-report-2
2024 GOLD Report. Global Initiative for Chronic Obstructive Lung Disease. Accessed July 11, 2024. https://goldcopd.org/2024-gold-report/
Regeneron Pharmaceuticals Inc. Dupixent® (dupilumab) late-breaking data from NOTUS confirmatory phase 3 COPD trial presented at ATS and published in the New England Journal of Medicine [press release]. May 20, 2024. Accessed July 11, 2024. https://investor.regeneron.com/news-releases/news-release-details/dupixentr-dupilumab-late-breaking-data-notus-confirmatory-phase
Pavord ID, Chapman KR, Bafadhel M, et al. Mepolizumab for eosinophil-associated COPD: analysis of METREX and METREO. Int J Chron Obstruct Pulmon Dis. 2021;16:1755-1770. doi:10.2147/COPD.S294333
Mepolizumab as add-on treatment in participants with COPD characterized by frequent exacerbations and eosinophil level (MATINEE). Clinicaltrials.gov. Updated August 28, 2023. Accessed July 11, 2024. https://clinicaltrials.gov/study/NCT04133909
Singh D, Criner GJ, Agustí A, et al. Benralizumab prevents recurrent exacerbations in patients with chronic obstructive pulmonary disease: a post hoc analysis. Int J Chron Obstruct Pulmon Dis. 2023;18:1595-1599. doi:10.2147/COPD.S418944
Efficacy and safety of benralizumab in moderate to very severe chronic obstructive pulmonary disease (COPD) with a history of frequent exacerbations (RESOLUTE). Clinicaltrials.gov. Updated May 8, 2024. Accessed July 11, 2024. https://clinicaltrials.gov/study/NCT04053634
Efficacy and safety of tozorakimab in symptomatic chronic obstructive pulmonary disease with a history of exacerbations (TITANIA). Clinicaltrials.gov. Updated June 27, 2024. Accessed July 11, 2024. https://clinicaltrials.gov/study/NCT05158387
Efficacy and safety of tozorakimab in symptomatic chronic obstructive pulmonary disease with a history of exacerbations (OBERON). Clinicaltrials.gov. Updated June 21, 2024. Accessed July 11, 2024. https://clinicaltrials.gov/study/NCT05166889
Long-term efficacy and safety of tozorakimab in participants with chronic obstructive pulmonary disease with a history of exacerbations (PROSPERO). Clinicaltrials.gov. Updated June 20, 2024. Accessed July 11, 2024. https://clinicaltrials.gov/study/NCT05742802
Efficacy and safety of tozorakimab in symptomatic chronic obstructive pulmonary disease with a history of exacerbations (MIRANDA). Clinicaltrials.gov. Updated June 4, 2024. Accessed July 11, 2024. https://clinicaltrials.gov/study/NCT06040086
Study to assess the efficacy, safety, and tolerability of SAR440340/REGN3500/itepekimab in chronic obstructive pulmonary disease (COPD) (AERIFY-1). ClinicalTrials.gov. Updated June 21, 2024. Accessed July 11, 2024. https://classic.clinicaltrials.gov/ct2/show/NCT04701983
Study to assess the efficacy, safety, and tolerability of SAR440340/REGN3500/itepekimab in chronic obstructive pulmonary disease (COPD) (AERIFY-2). ClinicalTrials.gov. Updated May 9, 2024. Accessed July 11, 2024. https://classic.clinicaltrials.gov/ct2/show/NCT04751487
ALIENTO and ARNASA: study designs of two randomised, double-blind, placebo-controlled trials of astegolimab in patients with COPD. Medically. 2023. Accessed July 11, 2024. https://medically.gene.com/global/en/unrestricted/respiratory/ERS-2023/ers-2023-poster-brightling-aliento-and-arnasa-study-des.html
Anzueto A, Barjaktarevic IZ, Siler TM, et al. Ensifentrine, a novel phosphodiesterase 3 and 4 inhibitor for the treatment of chronic obstructive pulmonary disease: randomized, double-blind, placebo-controlled, multicenter phase III trials (the ENHANCE trials). Am J Respir Crit Care Med. 2023;208(4):406-416. doi:10.1164/rccm.202306-0944OC
US Preventive Services Taskforce. Lung cancer: screening. March 9, 2021. Accessed July 11, 2024. https://www.uspreventiveservicestaskforce.org/uspstf/recommendation/lung-cancer-screening
Al Wachami N, Guennouni M, Iderdar Y, et al. Estimating the global prevalence of chronic obstructive pulmonary disease (COPD): a systematic review and meta-analysis. BMC Public Health. 2024;24(1):297. doi:10.1186/s12889-024-17686-9
COPD trends brief. American Lung Association. Accessed July 11, 2024. https://www.lung.org/research/trends-in-lung-disease/copd-trends-brief
Chronic obstructive pulmonary disease (COPD). World Health Organization. March 16, 2023. Accessed July 11, 2024. https://www.who.int/news-room/fact-sheets/detail/chronic-obstructive-pulmonary-disease-(copd)
Shalabi MS, Aqdi SW, Alfort OA, et al. Effectiveness and safety of bronchodilators and inhaled corticosteroids in the management of chronic obstructive pulmonary disease. Int J Commun Med Public Health. 2023;10(8):2955-2959. doi:10.18203/2394-6040.ijcmph20232392
McCormick B. FDA approves ensifentrine for maintenance treatment of adult patients with COPD. AJMC. June 26, 2024. Accessed July 11, 2024. https://www.ajmc.com/view/fda-approves-ensifentrine-for-maintenance-treatment-of-adult-patients-with-copd
Kersul AL, Cosio BG. Biologics in COPD. Open Resp Arch. 2024;6(2):100306. doi:10.1016/j.opresp.2024.100306
2023 GOLD Report. Global Initiative for Chronic Obstructive Lung Disease. Accessed July 11, 2024. https://goldcopd.org/2023-gold-report-2
2024 GOLD Report. Global Initiative for Chronic Obstructive Lung Disease. Accessed July 11, 2024. https://goldcopd.org/2024-gold-report/
Regeneron Pharmaceuticals Inc. Dupixent® (dupilumab) late-breaking data from NOTUS confirmatory phase 3 COPD trial presented at ATS and published in the New England Journal of Medicine [press release]. May 20, 2024. Accessed July 11, 2024. https://investor.regeneron.com/news-releases/news-release-details/dupixentr-dupilumab-late-breaking-data-notus-confirmatory-phase
Pavord ID, Chapman KR, Bafadhel M, et al. Mepolizumab for eosinophil-associated COPD: analysis of METREX and METREO. Int J Chron Obstruct Pulmon Dis. 2021;16:1755-1770. doi:10.2147/COPD.S294333
Mepolizumab as add-on treatment in participants with COPD characterized by frequent exacerbations and eosinophil level (MATINEE). Clinicaltrials.gov. Updated August 28, 2023. Accessed July 11, 2024. https://clinicaltrials.gov/study/NCT04133909
Singh D, Criner GJ, Agustí A, et al. Benralizumab prevents recurrent exacerbations in patients with chronic obstructive pulmonary disease: a post hoc analysis. Int J Chron Obstruct Pulmon Dis. 2023;18:1595-1599. doi:10.2147/COPD.S418944
Efficacy and safety of benralizumab in moderate to very severe chronic obstructive pulmonary disease (COPD) with a history of frequent exacerbations (RESOLUTE). Clinicaltrials.gov. Updated May 8, 2024. Accessed July 11, 2024. https://clinicaltrials.gov/study/NCT04053634
Efficacy and safety of tozorakimab in symptomatic chronic obstructive pulmonary disease with a history of exacerbations (TITANIA). Clinicaltrials.gov. Updated June 27, 2024. Accessed July 11, 2024. https://clinicaltrials.gov/study/NCT05158387
Efficacy and safety of tozorakimab in symptomatic chronic obstructive pulmonary disease with a history of exacerbations (OBERON). Clinicaltrials.gov. Updated June 21, 2024. Accessed July 11, 2024. https://clinicaltrials.gov/study/NCT05166889
Long-term efficacy and safety of tozorakimab in participants with chronic obstructive pulmonary disease with a history of exacerbations (PROSPERO). Clinicaltrials.gov. Updated June 20, 2024. Accessed July 11, 2024. https://clinicaltrials.gov/study/NCT05742802
Efficacy and safety of tozorakimab in symptomatic chronic obstructive pulmonary disease with a history of exacerbations (MIRANDA). Clinicaltrials.gov. Updated June 4, 2024. Accessed July 11, 2024. https://clinicaltrials.gov/study/NCT06040086
Study to assess the efficacy, safety, and tolerability of SAR440340/REGN3500/itepekimab in chronic obstructive pulmonary disease (COPD) (AERIFY-1). ClinicalTrials.gov. Updated June 21, 2024. Accessed July 11, 2024. https://classic.clinicaltrials.gov/ct2/show/NCT04701983
Study to assess the efficacy, safety, and tolerability of SAR440340/REGN3500/itepekimab in chronic obstructive pulmonary disease (COPD) (AERIFY-2). ClinicalTrials.gov. Updated May 9, 2024. Accessed July 11, 2024. https://classic.clinicaltrials.gov/ct2/show/NCT04751487
ALIENTO and ARNASA: study designs of two randomised, double-blind, placebo-controlled trials of astegolimab in patients with COPD. Medically. 2023. Accessed July 11, 2024. https://medically.gene.com/global/en/unrestricted/respiratory/ERS-2023/ers-2023-poster-brightling-aliento-and-arnasa-study-des.html
Anzueto A, Barjaktarevic IZ, Siler TM, et al. Ensifentrine, a novel phosphodiesterase 3 and 4 inhibitor for the treatment of chronic obstructive pulmonary disease: randomized, double-blind, placebo-controlled, multicenter phase III trials (the ENHANCE trials). Am J Respir Crit Care Med. 2023;208(4):406-416. doi:10.1164/rccm.202306-0944OC
US Preventive Services Taskforce. Lung cancer: screening. March 9, 2021. Accessed July 11, 2024. https://www.uspreventiveservicestaskforce.org/uspstf/recommendation/lung-cancer-screening
Ensifentrine for COPD: Out of reach for many?
Ensifentrine (Ohtuvayre), a novel medication for the treatment of chronic obstructive pulmonary disease (COPD) recently approved by the Food and Drug Administration, has been shown to reduce COPD exacerbations and may improve the quality of life for patients, but these potential benefits come at an unreasonably high annual cost, authors of a cost and effectiveness analysis say.
Ensifentrine is a first-in-class selective dual inhibitor of both phosphodiesterase 3 (PDE-3) and PDE-4, combining both bronchodilator and nonsteroidal anti-inflammatory effects in a single molecule. The drug is delivered through a standard jet nebulizer.
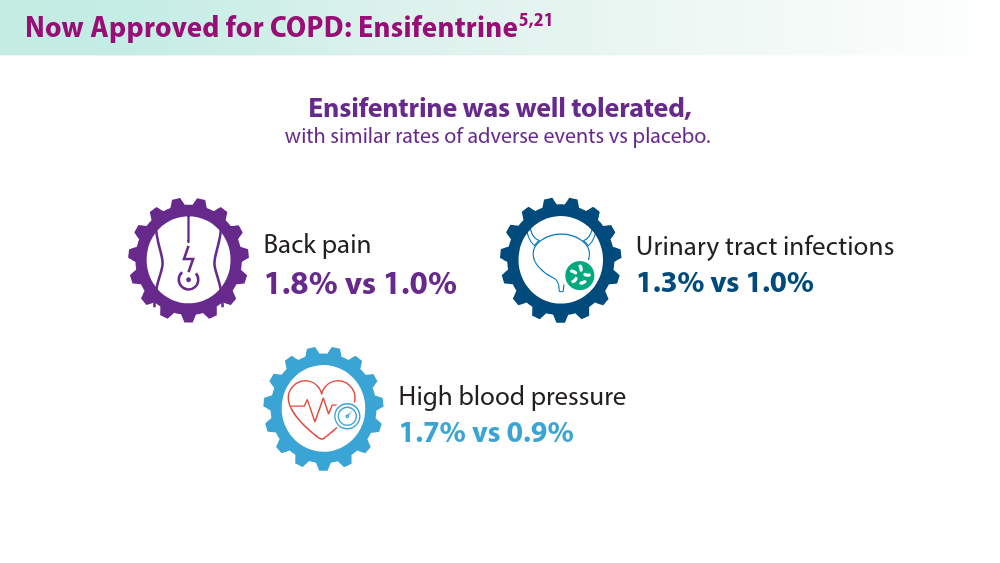
In the phase 3 ENHANCE 1 and 2 trials, ensifentrine significantly improved lung function based on the primary outcome of average forced expiratory volume in 1 second within 0-12 hours of administration, compared with placebo. In addition, patients were reported to tolerate the inhaled treatment well, with similar proportions of ensifentrine- and placebo-assigned patients reporting treatment-emergent adverse events. The most common treatment-emergent adverse events were nasopharyngitis, hypertension, and back pain, reported in < 3% of the ensifentrine group.
High cost barrier
But as authors of the analysis from the Boston, Massachusetts–based Institute for Clinical and Economic Review (ICER) found, the therapeutic edge offered by ensifentrine is outweighed by the annual wholesale acquisition cost that its maker, Vernona Pharma, has established: $35,400, which far exceeds the estimated health-benefit price of $7,500-$12,700, according to ICER. ICER is an independent, nonprofit research institute that conducts evidence-based reviews of healthcare interventions, including prescription drugs, other treatments, and diagnostic tests.
“Current evidence shows that ensifentrine decreases COPD exacerbations when used in combination with some current inhaled therapies, but there are uncertainties about how much benefit it may add to unstudied combinations of inhaled treatments,” said David Rind, MD, chief medical officer of ICER in a statement.
In an interview, Dr. Rind noted that the high price of ensifentrine may lead payers to restrict access to an otherwise promising new therapy. “Obviously many drugs in the US are overpriced, and this one, too, looks like it is overpriced. That causes ongoing financial toxicity for individual patients and it causes problems for the entire US health system, because when we pay too much for drugs we don’t have money for other things. So I’m worried about the fact that this price is too high compared to the benefit it provides.”
As previously reported, as many as one in six persons with COPD in the United States miss or delay COPD medication doses because of high drug costs. “I think that the pricing they chose is going to cause lots of barriers to people getting access and that insurance companies will throw up barriers. Primary care physicians like me won’t even try to get approval for a drug like this given the hoops we will be made to jump through, and so fewer people will get this drug,” Dr. Rind said. He pointed out that a lower wholesale acquisition cost could encourage higher-volume sales, affording the drugmaker a comparable profit with the higher-cost but lower-volume option.
Good drug, high price
An independent appraisal committee for ICER determined that “current evidence is adequate to demonstrate a net health benefit for ensifentrine added to maintenance therapy when compared to maintenance therapy alone.”
But ICER also issued an access and affordability alert “to signal to stakeholders and policymakers that the amount of added healthcare costs associated with a new service may be difficult for the health system to absorb over the short term without displacing other needed services.” ICER recommends that payers should include coverage for smoking cessation therapies, and that drug manufacturers “set prices that will foster affordability and good access for all patients by aligning prices with the patient-centered therapeutic value of their treatments.”
“This looks like a pretty good drug,” Dr. Rind said. “It looks quite safe and I think there will be a lot of patients, particularly those who are having frequent exacerbations, who this would be appropriate for, particularly once they’ve maxed out existing therapies, but maybe even earlier than that. And if the price comes down to the point that patients can really access this and providers can access it, people really should look at this as a potential therapy.”
Drug not yet available?
However, providers have not yet had direct experience with the new medication. “We haven’t been able to prescribe it yet,” said Corinne Young, MSN, FNP-C, FCCP, director of Advance Practice Provider and Clinical Services for Colorado Springs Pulmonary Consultants, president and founder of the Association of Pulmonary Advance Practice Providers, and a member of the CHEST Physician Editorial Board.
She learned “they were going to release it to select specialty pharmacies in the 3rd quarter of 2024. But all the ones we call do not have it and no one knows who does. They haven’t sent any reps into the field in my area so we don’t have any points of contact either,” she said.
Verona Pharma stated it anticipates ensifentrine to be available in the third quarter of 2024 “through an exclusive network of accredited specialty pharmacies.”
Funding for the ICER report came from nonprofit foundations. No funding came from health insurers, pharmacy benefit managers, or life science companies. Dr. Rind had no relevant disclosures.
Ensifentrine (Ohtuvayre), a novel medication for the treatment of chronic obstructive pulmonary disease (COPD) recently approved by the Food and Drug Administration, has been shown to reduce COPD exacerbations and may improve the quality of life for patients, but these potential benefits come at an unreasonably high annual cost, authors of a cost and effectiveness analysis say.
Ensifentrine is a first-in-class selective dual inhibitor of both phosphodiesterase 3 (PDE-3) and PDE-4, combining both bronchodilator and nonsteroidal anti-inflammatory effects in a single molecule. The drug is delivered through a standard jet nebulizer.
In the phase 3 ENHANCE 1 and 2 trials, ensifentrine significantly improved lung function based on the primary outcome of average forced expiratory volume in 1 second within 0-12 hours of administration, compared with placebo. In addition, patients were reported to tolerate the inhaled treatment well, with similar proportions of ensifentrine- and placebo-assigned patients reporting treatment-emergent adverse events. The most common treatment-emergent adverse events were nasopharyngitis, hypertension, and back pain, reported in < 3% of the ensifentrine group.
High cost barrier
But as authors of the analysis from the Boston, Massachusetts–based Institute for Clinical and Economic Review (ICER) found, the therapeutic edge offered by ensifentrine is outweighed by the annual wholesale acquisition cost that its maker, Vernona Pharma, has established: $35,400, which far exceeds the estimated health-benefit price of $7,500-$12,700, according to ICER. ICER is an independent, nonprofit research institute that conducts evidence-based reviews of healthcare interventions, including prescription drugs, other treatments, and diagnostic tests.
“Current evidence shows that ensifentrine decreases COPD exacerbations when used in combination with some current inhaled therapies, but there are uncertainties about how much benefit it may add to unstudied combinations of inhaled treatments,” said David Rind, MD, chief medical officer of ICER in a statement.
In an interview, Dr. Rind noted that the high price of ensifentrine may lead payers to restrict access to an otherwise promising new therapy. “Obviously many drugs in the US are overpriced, and this one, too, looks like it is overpriced. That causes ongoing financial toxicity for individual patients and it causes problems for the entire US health system, because when we pay too much for drugs we don’t have money for other things. So I’m worried about the fact that this price is too high compared to the benefit it provides.”
As previously reported, as many as one in six persons with COPD in the United States miss or delay COPD medication doses because of high drug costs. “I think that the pricing they chose is going to cause lots of barriers to people getting access and that insurance companies will throw up barriers. Primary care physicians like me won’t even try to get approval for a drug like this given the hoops we will be made to jump through, and so fewer people will get this drug,” Dr. Rind said. He pointed out that a lower wholesale acquisition cost could encourage higher-volume sales, affording the drugmaker a comparable profit with the higher-cost but lower-volume option.
Good drug, high price
An independent appraisal committee for ICER determined that “current evidence is adequate to demonstrate a net health benefit for ensifentrine added to maintenance therapy when compared to maintenance therapy alone.”
But ICER also issued an access and affordability alert “to signal to stakeholders and policymakers that the amount of added healthcare costs associated with a new service may be difficult for the health system to absorb over the short term without displacing other needed services.” ICER recommends that payers should include coverage for smoking cessation therapies, and that drug manufacturers “set prices that will foster affordability and good access for all patients by aligning prices with the patient-centered therapeutic value of their treatments.”
“This looks like a pretty good drug,” Dr. Rind said. “It looks quite safe and I think there will be a lot of patients, particularly those who are having frequent exacerbations, who this would be appropriate for, particularly once they’ve maxed out existing therapies, but maybe even earlier than that. And if the price comes down to the point that patients can really access this and providers can access it, people really should look at this as a potential therapy.”
Drug not yet available?
However, providers have not yet had direct experience with the new medication. “We haven’t been able to prescribe it yet,” said Corinne Young, MSN, FNP-C, FCCP, director of Advance Practice Provider and Clinical Services for Colorado Springs Pulmonary Consultants, president and founder of the Association of Pulmonary Advance Practice Providers, and a member of the CHEST Physician Editorial Board.
She learned “they were going to release it to select specialty pharmacies in the 3rd quarter of 2024. But all the ones we call do not have it and no one knows who does. They haven’t sent any reps into the field in my area so we don’t have any points of contact either,” she said.
Verona Pharma stated it anticipates ensifentrine to be available in the third quarter of 2024 “through an exclusive network of accredited specialty pharmacies.”
Funding for the ICER report came from nonprofit foundations. No funding came from health insurers, pharmacy benefit managers, or life science companies. Dr. Rind had no relevant disclosures.
Ensifentrine (Ohtuvayre), a novel medication for the treatment of chronic obstructive pulmonary disease (COPD) recently approved by the Food and Drug Administration, has been shown to reduce COPD exacerbations and may improve the quality of life for patients, but these potential benefits come at an unreasonably high annual cost, authors of a cost and effectiveness analysis say.
Ensifentrine is a first-in-class selective dual inhibitor of both phosphodiesterase 3 (PDE-3) and PDE-4, combining both bronchodilator and nonsteroidal anti-inflammatory effects in a single molecule. The drug is delivered through a standard jet nebulizer.
In the phase 3 ENHANCE 1 and 2 trials, ensifentrine significantly improved lung function based on the primary outcome of average forced expiratory volume in 1 second within 0-12 hours of administration, compared with placebo. In addition, patients were reported to tolerate the inhaled treatment well, with similar proportions of ensifentrine- and placebo-assigned patients reporting treatment-emergent adverse events. The most common treatment-emergent adverse events were nasopharyngitis, hypertension, and back pain, reported in < 3% of the ensifentrine group.
High cost barrier
But as authors of the analysis from the Boston, Massachusetts–based Institute for Clinical and Economic Review (ICER) found, the therapeutic edge offered by ensifentrine is outweighed by the annual wholesale acquisition cost that its maker, Vernona Pharma, has established: $35,400, which far exceeds the estimated health-benefit price of $7,500-$12,700, according to ICER. ICER is an independent, nonprofit research institute that conducts evidence-based reviews of healthcare interventions, including prescription drugs, other treatments, and diagnostic tests.
“Current evidence shows that ensifentrine decreases COPD exacerbations when used in combination with some current inhaled therapies, but there are uncertainties about how much benefit it may add to unstudied combinations of inhaled treatments,” said David Rind, MD, chief medical officer of ICER in a statement.
In an interview, Dr. Rind noted that the high price of ensifentrine may lead payers to restrict access to an otherwise promising new therapy. “Obviously many drugs in the US are overpriced, and this one, too, looks like it is overpriced. That causes ongoing financial toxicity for individual patients and it causes problems for the entire US health system, because when we pay too much for drugs we don’t have money for other things. So I’m worried about the fact that this price is too high compared to the benefit it provides.”
As previously reported, as many as one in six persons with COPD in the United States miss or delay COPD medication doses because of high drug costs. “I think that the pricing they chose is going to cause lots of barriers to people getting access and that insurance companies will throw up barriers. Primary care physicians like me won’t even try to get approval for a drug like this given the hoops we will be made to jump through, and so fewer people will get this drug,” Dr. Rind said. He pointed out that a lower wholesale acquisition cost could encourage higher-volume sales, affording the drugmaker a comparable profit with the higher-cost but lower-volume option.
Good drug, high price
An independent appraisal committee for ICER determined that “current evidence is adequate to demonstrate a net health benefit for ensifentrine added to maintenance therapy when compared to maintenance therapy alone.”
But ICER also issued an access and affordability alert “to signal to stakeholders and policymakers that the amount of added healthcare costs associated with a new service may be difficult for the health system to absorb over the short term without displacing other needed services.” ICER recommends that payers should include coverage for smoking cessation therapies, and that drug manufacturers “set prices that will foster affordability and good access for all patients by aligning prices with the patient-centered therapeutic value of their treatments.”
“This looks like a pretty good drug,” Dr. Rind said. “It looks quite safe and I think there will be a lot of patients, particularly those who are having frequent exacerbations, who this would be appropriate for, particularly once they’ve maxed out existing therapies, but maybe even earlier than that. And if the price comes down to the point that patients can really access this and providers can access it, people really should look at this as a potential therapy.”
Drug not yet available?
However, providers have not yet had direct experience with the new medication. “We haven’t been able to prescribe it yet,” said Corinne Young, MSN, FNP-C, FCCP, director of Advance Practice Provider and Clinical Services for Colorado Springs Pulmonary Consultants, president and founder of the Association of Pulmonary Advance Practice Providers, and a member of the CHEST Physician Editorial Board.
She learned “they were going to release it to select specialty pharmacies in the 3rd quarter of 2024. But all the ones we call do not have it and no one knows who does. They haven’t sent any reps into the field in my area so we don’t have any points of contact either,” she said.
Verona Pharma stated it anticipates ensifentrine to be available in the third quarter of 2024 “through an exclusive network of accredited specialty pharmacies.”
Funding for the ICER report came from nonprofit foundations. No funding came from health insurers, pharmacy benefit managers, or life science companies. Dr. Rind had no relevant disclosures.
Wildfire Pollution May Increase Asthma Hospitalizations
Short-term increases in fine particulate matter (PM2.5) resulting from wildfire smoke are becoming a greater global problem and have been associated with poor asthma and COPD outcomes, wrote Benjamin D. Horne, PhD, of the Intermountain Medical Center Heart Institute, Salt Lake City, Utah, and colleagues. However, the effect of short-term increases in PM2.5 on hospitalizations for asthma and COPD has not been well studied, they noted.
“Our primary reason for studying the association of air pollution in the summer/fall wildfire season separately from the winter is that the drought conditions in the western United States from 2012-2022 resulted in more wildfires and increasingly large wildfires across the west,” Dr. Horne said in an interview. “In part, this provided a chance to measure an increase of fine particulate matter (PM2.5) air pollution from wildfires and also to track what happened to their health when people were exposed to the PM2.5 from wildfire,” he said.
During 2020-2022, the PM2.5 produced during the wildfire season exceeded the PM2.5 levels measured in the winter for the first time, Dr. Horne said. In the part of Utah where the study was conducted, PM2.5 increases in winter because of a combination of concentrated PM2.5 from cars and industry and a weather phenomenon known as a temperature inversion, he said.
A temperature inversion occurs when mountain topography traps pollutants near the ground where the people are, but only during times of cold and snowy weather, Dr. Horne said.
“Past studies in the region were conducted with the assumption that the winter inversion was the primary source of pollution-related health risks, and public and healthcare guidance for health was based on avoiding winter air pollution,” Dr. Horne noted. However, “it may be that the smoke from wildfires requires people to also anticipate how to avoid exposure to PM2.5 during the summer,” he said.
In a study published in CHEST Pulmonary, the researchers reviewed data from 63,976 patients hospitalized with asthma and 18,514 hospitalized with COPD between January 1999 and March 2022 who lived in an area of Utah in which PM2.5 and ozone are measured by the Environmental Protection Agency. The average age of the asthma patients was 22.6 years; 51.0% were women, 16.0% had hypertension, and 10.1% had a history of smoking. The average age of the COPD patients was 63.5 years, 50.3% were women, 69.1% had hypertension, and 42.3% had a history of smoking.
In a regression analysis, the risk for asthma was significantly associated with days of increased PM2.5 during wildfire season and similar to the winter inversion (when cold air traps air pollutants), with odds ratios (ORs) of 1.057 and 1.023 for every 10 µg per m3 of particulate matter, respectively.
Although the risk for asthma hospitalization decreased after a week, a rebound occurred during wildfire season after a 4-week lag, with an OR of 1.098 for every 10 µg per m3 of particulate matter, the researchers wrote. A review of all months showed a significant association between a concurrent day increase in PM2.5 and asthma hospitalization (OR, 1.020 per every 10 µg per m3 of particulate matter, P = .0006).
By contrast, PM2.5 increases had only a weak association with hospitalizations for COPD during either wildfire season or winter inversion season, and ozone was not associated with increased risks for patients with asthma or COPD.
The findings were limited by several factors including the observational design, potential for confounding, and relatively homogeneous study population, the researchers noted.
However, “these findings suggest that people should be aware of the risks from wildfire-generated PM2.5 during the summer and fall, including following best practices for people with asthma such as anticipating symptoms in warm months, carrying medications during summer activities, and expecting to stay indoors to avoid smoke exposure when wildfires have polluted the outdoor air,” Dr. Horne told this news organization.
In the current study, Dr. Horne and colleagues expected to see increases in the risk for asthma and COPD during summer wildfire season. “What was surprising was that the size of the risk of needing care of asthma appeared to occur just as rapidly after the PM2.5 became elevated during wildfire events as it did in the winter,” said Dr. Horne. “Further, the risk in the summer appeared to be greater than during the winter. Increases in hospitalization for asthma occurred on the same day and throughout the first week after a rise in air pollution in summer and early fall, and especially in children that risk remained increased for up to a month after the rise in air pollution,” he said.
Clinicians should be aware of environmental sources of respiratory declines caused by wildfire smoke that may prompt patients to seek care during wildfire events, said Horne. Finally, the general population should recognize the smell of smoke during warm months as an alert that leads to greater caution about spending time outdoors during wildfire events, he said. “Short-term PM2.5 elevations may affect respiratory health and have other effects such as on heart health,” Dr. Horne said. “In general, people should avoid outdoor exercise when air pollution is elevated, since the amount of air that is breathed in during exercise is substantially increased,” he added.
“Further research is needed regarding the mechanisms of effect from PM2.5 on health risk, including effects on respiratory and cardiovascular health,” said Dr. Horne. “This includes evaluating what biomarkers in the blood are changed by air pollution such as inflammatory factors, determining whether some medications may block or reduce the adverse effects of air pollution, and examining whether masks or indoor air purifiers have a meaningful benefit in protecting health during short-term air pollution elevations,” he said.
Data Reveal Respiratory Impact of Wildfires
“Fine particle air pollution has been linked to poor respiratory health outcomes, but relatively little is known about the specific impact of wildfire particulate pollution on patients living in urban population centers,” Alexander S. Rabin, MD, of the University of Michigan, Ann Arbor, said in an interview.
“Although it is known that wildfire risk is increasing throughout the western United States, the increase in the number of days per month with elevated fine particulate matter from 1999 to 2022 was striking,” said Dr. Rabin, who was not involved in the current study. “Over the same period, there was a decrease in the number of high fine particulate matter air pollution days related to the wintertime temperature inversion phenomenon when air pollutants are trapped in Utah’s valleys,” he said. “These data underscore the increased risk of wildfire-related air pollution relative to ‘traditional sources of air pollution from industrial and transportation sources,” he added.
Although the adverse effects of exposure to wildfire smoke and inversion season pollution on asthma were not unexpected, the degree of the effect size of wildfire smoke relative to inversion season was surprising, said Dr. Rabin.
“Why the wildfire smoke seems to have a worse impact on asthma outcomes could not be determined from this study, but there may be something inherently more dangerous about the cocktail of pollutants released when large wildfires burn uncontrolled,” he said. “I was surprised by the lack of association between wildfire smoke and adverse COPD outcomes; whether this relates to physiological differences or variations in healthcare-seeking behaviors between patients with asthma vs COPD is unknown,” he added.
The current study underscores the harmful effects of fine particulate pollution from wildfire smoke on health, and the increased risk for hospitalization for those with asthma even in urban environments far from the source of the fire, Dr. Rabin said.
However, limitations include the use of estimates of fine particulate pollution taken from monitoring stations that were an average of 14 km from the participants’ primary residences, and air quality measurements may not have accurately reflected exposure, Dr. Rabin noted. “Additionally, the population studied was not reflective of the US population, with approximately 80% of study participants described as non-Hispanic white,” he said. “Patients of color may have increased vulnerability to adverse outcomes from air pollution and therefore additional study is needed in these populations,” Dr. Rabin added.
The study was supported in part by the AIRHEALTH program project and by internal institutional funds. Dr. Horne disclosed serving on the advisory board of Opsis Health, previously consulting for Pfizer regarding risk scores and serving as site principal investigator of a grant funded by the Task Force for Global Health and a grant from the Patient-Centered Outcomes Research Institute and the NIH-funded RECOVER initiative. Dr. Rabin had no financial conflicts to disclose.
A version of this article first appeared on Medscape.com.
Short-term increases in fine particulate matter (PM2.5) resulting from wildfire smoke are becoming a greater global problem and have been associated with poor asthma and COPD outcomes, wrote Benjamin D. Horne, PhD, of the Intermountain Medical Center Heart Institute, Salt Lake City, Utah, and colleagues. However, the effect of short-term increases in PM2.5 on hospitalizations for asthma and COPD has not been well studied, they noted.
“Our primary reason for studying the association of air pollution in the summer/fall wildfire season separately from the winter is that the drought conditions in the western United States from 2012-2022 resulted in more wildfires and increasingly large wildfires across the west,” Dr. Horne said in an interview. “In part, this provided a chance to measure an increase of fine particulate matter (PM2.5) air pollution from wildfires and also to track what happened to their health when people were exposed to the PM2.5 from wildfire,” he said.
During 2020-2022, the PM2.5 produced during the wildfire season exceeded the PM2.5 levels measured in the winter for the first time, Dr. Horne said. In the part of Utah where the study was conducted, PM2.5 increases in winter because of a combination of concentrated PM2.5 from cars and industry and a weather phenomenon known as a temperature inversion, he said.
A temperature inversion occurs when mountain topography traps pollutants near the ground where the people are, but only during times of cold and snowy weather, Dr. Horne said.
“Past studies in the region were conducted with the assumption that the winter inversion was the primary source of pollution-related health risks, and public and healthcare guidance for health was based on avoiding winter air pollution,” Dr. Horne noted. However, “it may be that the smoke from wildfires requires people to also anticipate how to avoid exposure to PM2.5 during the summer,” he said.
In a study published in CHEST Pulmonary, the researchers reviewed data from 63,976 patients hospitalized with asthma and 18,514 hospitalized with COPD between January 1999 and March 2022 who lived in an area of Utah in which PM2.5 and ozone are measured by the Environmental Protection Agency. The average age of the asthma patients was 22.6 years; 51.0% were women, 16.0% had hypertension, and 10.1% had a history of smoking. The average age of the COPD patients was 63.5 years, 50.3% were women, 69.1% had hypertension, and 42.3% had a history of smoking.
In a regression analysis, the risk for asthma was significantly associated with days of increased PM2.5 during wildfire season and similar to the winter inversion (when cold air traps air pollutants), with odds ratios (ORs) of 1.057 and 1.023 for every 10 µg per m3 of particulate matter, respectively.
Although the risk for asthma hospitalization decreased after a week, a rebound occurred during wildfire season after a 4-week lag, with an OR of 1.098 for every 10 µg per m3 of particulate matter, the researchers wrote. A review of all months showed a significant association between a concurrent day increase in PM2.5 and asthma hospitalization (OR, 1.020 per every 10 µg per m3 of particulate matter, P = .0006).
By contrast, PM2.5 increases had only a weak association with hospitalizations for COPD during either wildfire season or winter inversion season, and ozone was not associated with increased risks for patients with asthma or COPD.
The findings were limited by several factors including the observational design, potential for confounding, and relatively homogeneous study population, the researchers noted.
However, “these findings suggest that people should be aware of the risks from wildfire-generated PM2.5 during the summer and fall, including following best practices for people with asthma such as anticipating symptoms in warm months, carrying medications during summer activities, and expecting to stay indoors to avoid smoke exposure when wildfires have polluted the outdoor air,” Dr. Horne told this news organization.
In the current study, Dr. Horne and colleagues expected to see increases in the risk for asthma and COPD during summer wildfire season. “What was surprising was that the size of the risk of needing care of asthma appeared to occur just as rapidly after the PM2.5 became elevated during wildfire events as it did in the winter,” said Dr. Horne. “Further, the risk in the summer appeared to be greater than during the winter. Increases in hospitalization for asthma occurred on the same day and throughout the first week after a rise in air pollution in summer and early fall, and especially in children that risk remained increased for up to a month after the rise in air pollution,” he said.
Clinicians should be aware of environmental sources of respiratory declines caused by wildfire smoke that may prompt patients to seek care during wildfire events, said Horne. Finally, the general population should recognize the smell of smoke during warm months as an alert that leads to greater caution about spending time outdoors during wildfire events, he said. “Short-term PM2.5 elevations may affect respiratory health and have other effects such as on heart health,” Dr. Horne said. “In general, people should avoid outdoor exercise when air pollution is elevated, since the amount of air that is breathed in during exercise is substantially increased,” he added.
“Further research is needed regarding the mechanisms of effect from PM2.5 on health risk, including effects on respiratory and cardiovascular health,” said Dr. Horne. “This includes evaluating what biomarkers in the blood are changed by air pollution such as inflammatory factors, determining whether some medications may block or reduce the adverse effects of air pollution, and examining whether masks or indoor air purifiers have a meaningful benefit in protecting health during short-term air pollution elevations,” he said.
Data Reveal Respiratory Impact of Wildfires
“Fine particle air pollution has been linked to poor respiratory health outcomes, but relatively little is known about the specific impact of wildfire particulate pollution on patients living in urban population centers,” Alexander S. Rabin, MD, of the University of Michigan, Ann Arbor, said in an interview.
“Although it is known that wildfire risk is increasing throughout the western United States, the increase in the number of days per month with elevated fine particulate matter from 1999 to 2022 was striking,” said Dr. Rabin, who was not involved in the current study. “Over the same period, there was a decrease in the number of high fine particulate matter air pollution days related to the wintertime temperature inversion phenomenon when air pollutants are trapped in Utah’s valleys,” he said. “These data underscore the increased risk of wildfire-related air pollution relative to ‘traditional sources of air pollution from industrial and transportation sources,” he added.
Although the adverse effects of exposure to wildfire smoke and inversion season pollution on asthma were not unexpected, the degree of the effect size of wildfire smoke relative to inversion season was surprising, said Dr. Rabin.
“Why the wildfire smoke seems to have a worse impact on asthma outcomes could not be determined from this study, but there may be something inherently more dangerous about the cocktail of pollutants released when large wildfires burn uncontrolled,” he said. “I was surprised by the lack of association between wildfire smoke and adverse COPD outcomes; whether this relates to physiological differences or variations in healthcare-seeking behaviors between patients with asthma vs COPD is unknown,” he added.
The current study underscores the harmful effects of fine particulate pollution from wildfire smoke on health, and the increased risk for hospitalization for those with asthma even in urban environments far from the source of the fire, Dr. Rabin said.
However, limitations include the use of estimates of fine particulate pollution taken from monitoring stations that were an average of 14 km from the participants’ primary residences, and air quality measurements may not have accurately reflected exposure, Dr. Rabin noted. “Additionally, the population studied was not reflective of the US population, with approximately 80% of study participants described as non-Hispanic white,” he said. “Patients of color may have increased vulnerability to adverse outcomes from air pollution and therefore additional study is needed in these populations,” Dr. Rabin added.
The study was supported in part by the AIRHEALTH program project and by internal institutional funds. Dr. Horne disclosed serving on the advisory board of Opsis Health, previously consulting for Pfizer regarding risk scores and serving as site principal investigator of a grant funded by the Task Force for Global Health and a grant from the Patient-Centered Outcomes Research Institute and the NIH-funded RECOVER initiative. Dr. Rabin had no financial conflicts to disclose.
A version of this article first appeared on Medscape.com.
Short-term increases in fine particulate matter (PM2.5) resulting from wildfire smoke are becoming a greater global problem and have been associated with poor asthma and COPD outcomes, wrote Benjamin D. Horne, PhD, of the Intermountain Medical Center Heart Institute, Salt Lake City, Utah, and colleagues. However, the effect of short-term increases in PM2.5 on hospitalizations for asthma and COPD has not been well studied, they noted.
“Our primary reason for studying the association of air pollution in the summer/fall wildfire season separately from the winter is that the drought conditions in the western United States from 2012-2022 resulted in more wildfires and increasingly large wildfires across the west,” Dr. Horne said in an interview. “In part, this provided a chance to measure an increase of fine particulate matter (PM2.5) air pollution from wildfires and also to track what happened to their health when people were exposed to the PM2.5 from wildfire,” he said.
During 2020-2022, the PM2.5 produced during the wildfire season exceeded the PM2.5 levels measured in the winter for the first time, Dr. Horne said. In the part of Utah where the study was conducted, PM2.5 increases in winter because of a combination of concentrated PM2.5 from cars and industry and a weather phenomenon known as a temperature inversion, he said.
A temperature inversion occurs when mountain topography traps pollutants near the ground where the people are, but only during times of cold and snowy weather, Dr. Horne said.
“Past studies in the region were conducted with the assumption that the winter inversion was the primary source of pollution-related health risks, and public and healthcare guidance for health was based on avoiding winter air pollution,” Dr. Horne noted. However, “it may be that the smoke from wildfires requires people to also anticipate how to avoid exposure to PM2.5 during the summer,” he said.
In a study published in CHEST Pulmonary, the researchers reviewed data from 63,976 patients hospitalized with asthma and 18,514 hospitalized with COPD between January 1999 and March 2022 who lived in an area of Utah in which PM2.5 and ozone are measured by the Environmental Protection Agency. The average age of the asthma patients was 22.6 years; 51.0% were women, 16.0% had hypertension, and 10.1% had a history of smoking. The average age of the COPD patients was 63.5 years, 50.3% were women, 69.1% had hypertension, and 42.3% had a history of smoking.
In a regression analysis, the risk for asthma was significantly associated with days of increased PM2.5 during wildfire season and similar to the winter inversion (when cold air traps air pollutants), with odds ratios (ORs) of 1.057 and 1.023 for every 10 µg per m3 of particulate matter, respectively.
Although the risk for asthma hospitalization decreased after a week, a rebound occurred during wildfire season after a 4-week lag, with an OR of 1.098 for every 10 µg per m3 of particulate matter, the researchers wrote. A review of all months showed a significant association between a concurrent day increase in PM2.5 and asthma hospitalization (OR, 1.020 per every 10 µg per m3 of particulate matter, P = .0006).
By contrast, PM2.5 increases had only a weak association with hospitalizations for COPD during either wildfire season or winter inversion season, and ozone was not associated with increased risks for patients with asthma or COPD.
The findings were limited by several factors including the observational design, potential for confounding, and relatively homogeneous study population, the researchers noted.
However, “these findings suggest that people should be aware of the risks from wildfire-generated PM2.5 during the summer and fall, including following best practices for people with asthma such as anticipating symptoms in warm months, carrying medications during summer activities, and expecting to stay indoors to avoid smoke exposure when wildfires have polluted the outdoor air,” Dr. Horne told this news organization.
In the current study, Dr. Horne and colleagues expected to see increases in the risk for asthma and COPD during summer wildfire season. “What was surprising was that the size of the risk of needing care of asthma appeared to occur just as rapidly after the PM2.5 became elevated during wildfire events as it did in the winter,” said Dr. Horne. “Further, the risk in the summer appeared to be greater than during the winter. Increases in hospitalization for asthma occurred on the same day and throughout the first week after a rise in air pollution in summer and early fall, and especially in children that risk remained increased for up to a month after the rise in air pollution,” he said.
Clinicians should be aware of environmental sources of respiratory declines caused by wildfire smoke that may prompt patients to seek care during wildfire events, said Horne. Finally, the general population should recognize the smell of smoke during warm months as an alert that leads to greater caution about spending time outdoors during wildfire events, he said. “Short-term PM2.5 elevations may affect respiratory health and have other effects such as on heart health,” Dr. Horne said. “In general, people should avoid outdoor exercise when air pollution is elevated, since the amount of air that is breathed in during exercise is substantially increased,” he added.
“Further research is needed regarding the mechanisms of effect from PM2.5 on health risk, including effects on respiratory and cardiovascular health,” said Dr. Horne. “This includes evaluating what biomarkers in the blood are changed by air pollution such as inflammatory factors, determining whether some medications may block or reduce the adverse effects of air pollution, and examining whether masks or indoor air purifiers have a meaningful benefit in protecting health during short-term air pollution elevations,” he said.
Data Reveal Respiratory Impact of Wildfires
“Fine particle air pollution has been linked to poor respiratory health outcomes, but relatively little is known about the specific impact of wildfire particulate pollution on patients living in urban population centers,” Alexander S. Rabin, MD, of the University of Michigan, Ann Arbor, said in an interview.
“Although it is known that wildfire risk is increasing throughout the western United States, the increase in the number of days per month with elevated fine particulate matter from 1999 to 2022 was striking,” said Dr. Rabin, who was not involved in the current study. “Over the same period, there was a decrease in the number of high fine particulate matter air pollution days related to the wintertime temperature inversion phenomenon when air pollutants are trapped in Utah’s valleys,” he said. “These data underscore the increased risk of wildfire-related air pollution relative to ‘traditional sources of air pollution from industrial and transportation sources,” he added.
Although the adverse effects of exposure to wildfire smoke and inversion season pollution on asthma were not unexpected, the degree of the effect size of wildfire smoke relative to inversion season was surprising, said Dr. Rabin.
“Why the wildfire smoke seems to have a worse impact on asthma outcomes could not be determined from this study, but there may be something inherently more dangerous about the cocktail of pollutants released when large wildfires burn uncontrolled,” he said. “I was surprised by the lack of association between wildfire smoke and adverse COPD outcomes; whether this relates to physiological differences or variations in healthcare-seeking behaviors between patients with asthma vs COPD is unknown,” he added.
The current study underscores the harmful effects of fine particulate pollution from wildfire smoke on health, and the increased risk for hospitalization for those with asthma even in urban environments far from the source of the fire, Dr. Rabin said.
However, limitations include the use of estimates of fine particulate pollution taken from monitoring stations that were an average of 14 km from the participants’ primary residences, and air quality measurements may not have accurately reflected exposure, Dr. Rabin noted. “Additionally, the population studied was not reflective of the US population, with approximately 80% of study participants described as non-Hispanic white,” he said. “Patients of color may have increased vulnerability to adverse outcomes from air pollution and therefore additional study is needed in these populations,” Dr. Rabin added.
The study was supported in part by the AIRHEALTH program project and by internal institutional funds. Dr. Horne disclosed serving on the advisory board of Opsis Health, previously consulting for Pfizer regarding risk scores and serving as site principal investigator of a grant funded by the Task Force for Global Health and a grant from the Patient-Centered Outcomes Research Institute and the NIH-funded RECOVER initiative. Dr. Rabin had no financial conflicts to disclose.
A version of this article first appeared on Medscape.com.
‘Gift That Keeps Giving’: The Impact of GLP-1 in Asthma
This transcript has been edited for clarity.
Akshay B. Jain, MD: Welcome back to Medscape at ADA 2024, where Dr. James Kim, primary care physician from Calgary, Alberta, will be joining me in deciphering the key highlights at the ADA conference and bringing our own clinical twist into what the relevance would be for people like you and I to take back to our clinics.
Welcome back, Dr. Kim.
James Kim, MBBCh, PgDip, MScCH: Thank you very much. It’s nice to be back.
Dr. Jain: This was a diabetes conference, so obviously we are very pancreas focused. At this conference, we went outside our general area of territory, going outside of the pancreas and delving into other organ states. What I found fascinating were some data regarding the effects of incretin therapy on the lung, and in particular, some of the restrictive lung disorders.
Dr. Kim, you attended these sessions as well. Can you tell us a little bit more about the results that were discussed?
Dr. Kim: This is an interesting field. The moderator of the session went up and said that there has been no time in any previous ADA sessions where the lung issue was actually discussed. This was the first time ever.
They had some of the world leaders in this field, so it was really awesome to see them. Just to paint a picture of these obese asthmatic patients, they are challenging cases because, as you know, the main therapy for any asthmatic patient is inhaled corticosteroid.
Patients who are obese have quite a bit of a steroid resistance. Therefore, they end up being on many medications that sometimes are off label, and many end up on biologics as well. Therefore, the respiratory world has been seeking therapies for these obese asthmatic patients who are likely to be steroid resistant because these people are also likely to end up on an oral steroid as well.
Dr. Jain, you know the effect of the steroids much better than I do, and it’s like a laundry list. We really don’t want our patients to be on oral steroids.
In the past few years, GLP-1 has been studied quite extensively in the lung, especially in the world of asthma, and also in COPD. What’s really fascinating is that the GLP-1 receptors have been found to be quite abundant in the airway. Some studies show that the highest concentration of GLP-1 lies in the airway, whereas some studies have said that it’s the third most common area to find the GLP-1.
It is not a surprise that GLP-1 is being studied in managing the airway, especially airway inflammation in asthma and COPD patients. The preliminary data have been quite encouraging. They also discussed that there are new medications coming out that seem to be incretin based, so we’ll wait to see what those studies show.
There are two current phase 3 trials being held at the moment. One is using semaglutide 2.4 mg subcutaneous and another one is using metformin to reduce the airway inflammation in these asthmatic patients and also in some COPD patients. We’ll look forward to these results.
Dr. Jain: That’s really important to note because we see that there is a high density of these receptors in the airways, and hitherto we had no idea about the overall effect. Now, we’re looking at, as you mentioned, individuals with obesity who have asthma, so there are both the restrictive and obstructive components in the lung coming into play here.
From an endocrinology perspective, I’m thinking that this could be multiple effects of the GLP-1 receptor agonists, where on one hand you’re managing the obesity and you’re working along that line, and on the other hand, it could have local anti-inflammatory effects in the lung. Hence, there could be potential improvement in the overall pulmonary function of these individuals.
Dr. Kim: We are seeing this in primary care. Ever since I found out this information, I have started numerous patients, who are obese, asthmatic patients who do not have diabetes, on GLP-1 therapies, and their pulmonary function tests have improved significantly.
As a matter of fact, one of my personal friends is a severe asthmatic patient. She ends up being on oral steroids about three times a year. There was even one day when I saw her in one of my classes and she was dyspneic. She was short of breath.
I introduced her to one of my colleagues who’s a respirologist and very much into the impact of the incretins and asthma, and she was started on a GLP-1 receptor agonist. She lost about 30 pounds of weight, but now she is labeled as a mild asthmatic. Her pulmonary function test is completely normal. She hasn’t touched an oral steroid for a couple of years now.
That is a huge success story and I’m seeing that even in my own clinic as well. It’s a huge win for the respiratory world.
Dr. Jain: I think from an endocrinology perspective as well, if we are initiating GLP-1 receptor agonists or medications in that class, where we use it for management of obesity, sooner or later we do hit a stage where people will plateau with their weight loss. They won’t have any additional weight loss.
We tell individuals at that time that the fact that they’re able to maintain the weight loss still means that the medication is working from the obesity perspective. For individuals who also have asthma, it would be a good point to tell them that it could still have potential effects on reducing inflammation ongoing. Hence, even though they may not be losing any additional weight, it would still be helpful to continue on these medications from a pulmonary perspective.
Dr. Kim: Right now these pleiotropic effects of GLP-1 agents are absolutely mind-blowing. I mentioned in one of my respiratory presentations to a bunch of respirologists that diabetes is taking over the world, including the respiratory world. Well, you can imagine what their faces were like. However, they were quite impressed at that, and they were very excited with what these two phase 3 trials will show.
Dr. Jain: I think, based on the ADA 2024 conference, GLP-1 receptor agonists continue to be the gift that keeps giving. We have the effects on diabetes, obesity, kidney function, liver protection, lungs, and Alzheimer’s. We saw some sessions about potential use in people with alcohol misuse disorder or gambling problems. Clearly, there’s a large amount of research that›s being done with these agents.
Perhaps when you and I talk about ADA 2025, we might be able to talk about some more pleiotropic benefits outside the pancreas. Until then, please do check out our other videos from ADA 2024. Thanks for joining us again, Dr. Kim.
Dr. Kim: Thank you very much for having me.
Dr. Jain, clinical instructor, Department of Endocrinology, University of British Columbia, and endocrinologist, TLC Diabetes and Endocrinology, Vancouver, British Columbia, Canada, has disclosed ties with Abbott, Acerus, AstraZeneca, Amgen, Bausch Healthcare, Bayer, Boehringer Ingelheim, Care to Know, CCRN, Connected in Motion, CPD Network, Dexcom, Diabetes Canada, Eli Lilly, GSK, HLS Therapeutics, Janssen, Master Clinician Alliance, MDBriefcase, Merck, Medtronic, Moderna, Novartis, Novo Nordisk, Partners in Progressive Medical Education, Pfizer, Sanofi Aventis, Timed Right, WebMD, Gilead Sciences, Insulet, PocketPills, Roche, and Takeda. Dr. Kim, clinical assistant professor, Department of Family Medicine, University of Calgary, Alberta, has disclosed ties with Abbott, AbbVie, AstraZeneca, Bayer, Boehringer Ingelheim, Eisai, Embecta, Eli Lilly, GSK, Janssen, Linpharma, Novo Nordisk, Miravo, Otsuka, Pfizer, Teva, Takeda, and Sanofi, and Partners in Progressive Medical Education.
A version of this article first appeared on Medscape.com.
This transcript has been edited for clarity.
Akshay B. Jain, MD: Welcome back to Medscape at ADA 2024, where Dr. James Kim, primary care physician from Calgary, Alberta, will be joining me in deciphering the key highlights at the ADA conference and bringing our own clinical twist into what the relevance would be for people like you and I to take back to our clinics.
Welcome back, Dr. Kim.
James Kim, MBBCh, PgDip, MScCH: Thank you very much. It’s nice to be back.
Dr. Jain: This was a diabetes conference, so obviously we are very pancreas focused. At this conference, we went outside our general area of territory, going outside of the pancreas and delving into other organ states. What I found fascinating were some data regarding the effects of incretin therapy on the lung, and in particular, some of the restrictive lung disorders.
Dr. Kim, you attended these sessions as well. Can you tell us a little bit more about the results that were discussed?
Dr. Kim: This is an interesting field. The moderator of the session went up and said that there has been no time in any previous ADA sessions where the lung issue was actually discussed. This was the first time ever.
They had some of the world leaders in this field, so it was really awesome to see them. Just to paint a picture of these obese asthmatic patients, they are challenging cases because, as you know, the main therapy for any asthmatic patient is inhaled corticosteroid.
Patients who are obese have quite a bit of a steroid resistance. Therefore, they end up being on many medications that sometimes are off label, and many end up on biologics as well. Therefore, the respiratory world has been seeking therapies for these obese asthmatic patients who are likely to be steroid resistant because these people are also likely to end up on an oral steroid as well.
Dr. Jain, you know the effect of the steroids much better than I do, and it’s like a laundry list. We really don’t want our patients to be on oral steroids.
In the past few years, GLP-1 has been studied quite extensively in the lung, especially in the world of asthma, and also in COPD. What’s really fascinating is that the GLP-1 receptors have been found to be quite abundant in the airway. Some studies show that the highest concentration of GLP-1 lies in the airway, whereas some studies have said that it’s the third most common area to find the GLP-1.
It is not a surprise that GLP-1 is being studied in managing the airway, especially airway inflammation in asthma and COPD patients. The preliminary data have been quite encouraging. They also discussed that there are new medications coming out that seem to be incretin based, so we’ll wait to see what those studies show.
There are two current phase 3 trials being held at the moment. One is using semaglutide 2.4 mg subcutaneous and another one is using metformin to reduce the airway inflammation in these asthmatic patients and also in some COPD patients. We’ll look forward to these results.
Dr. Jain: That’s really important to note because we see that there is a high density of these receptors in the airways, and hitherto we had no idea about the overall effect. Now, we’re looking at, as you mentioned, individuals with obesity who have asthma, so there are both the restrictive and obstructive components in the lung coming into play here.
From an endocrinology perspective, I’m thinking that this could be multiple effects of the GLP-1 receptor agonists, where on one hand you’re managing the obesity and you’re working along that line, and on the other hand, it could have local anti-inflammatory effects in the lung. Hence, there could be potential improvement in the overall pulmonary function of these individuals.
Dr. Kim: We are seeing this in primary care. Ever since I found out this information, I have started numerous patients, who are obese, asthmatic patients who do not have diabetes, on GLP-1 therapies, and their pulmonary function tests have improved significantly.
As a matter of fact, one of my personal friends is a severe asthmatic patient. She ends up being on oral steroids about three times a year. There was even one day when I saw her in one of my classes and she was dyspneic. She was short of breath.
I introduced her to one of my colleagues who’s a respirologist and very much into the impact of the incretins and asthma, and she was started on a GLP-1 receptor agonist. She lost about 30 pounds of weight, but now she is labeled as a mild asthmatic. Her pulmonary function test is completely normal. She hasn’t touched an oral steroid for a couple of years now.
That is a huge success story and I’m seeing that even in my own clinic as well. It’s a huge win for the respiratory world.
Dr. Jain: I think from an endocrinology perspective as well, if we are initiating GLP-1 receptor agonists or medications in that class, where we use it for management of obesity, sooner or later we do hit a stage where people will plateau with their weight loss. They won’t have any additional weight loss.
We tell individuals at that time that the fact that they’re able to maintain the weight loss still means that the medication is working from the obesity perspective. For individuals who also have asthma, it would be a good point to tell them that it could still have potential effects on reducing inflammation ongoing. Hence, even though they may not be losing any additional weight, it would still be helpful to continue on these medications from a pulmonary perspective.
Dr. Kim: Right now these pleiotropic effects of GLP-1 agents are absolutely mind-blowing. I mentioned in one of my respiratory presentations to a bunch of respirologists that diabetes is taking over the world, including the respiratory world. Well, you can imagine what their faces were like. However, they were quite impressed at that, and they were very excited with what these two phase 3 trials will show.
Dr. Jain: I think, based on the ADA 2024 conference, GLP-1 receptor agonists continue to be the gift that keeps giving. We have the effects on diabetes, obesity, kidney function, liver protection, lungs, and Alzheimer’s. We saw some sessions about potential use in people with alcohol misuse disorder or gambling problems. Clearly, there’s a large amount of research that›s being done with these agents.
Perhaps when you and I talk about ADA 2025, we might be able to talk about some more pleiotropic benefits outside the pancreas. Until then, please do check out our other videos from ADA 2024. Thanks for joining us again, Dr. Kim.
Dr. Kim: Thank you very much for having me.
Dr. Jain, clinical instructor, Department of Endocrinology, University of British Columbia, and endocrinologist, TLC Diabetes and Endocrinology, Vancouver, British Columbia, Canada, has disclosed ties with Abbott, Acerus, AstraZeneca, Amgen, Bausch Healthcare, Bayer, Boehringer Ingelheim, Care to Know, CCRN, Connected in Motion, CPD Network, Dexcom, Diabetes Canada, Eli Lilly, GSK, HLS Therapeutics, Janssen, Master Clinician Alliance, MDBriefcase, Merck, Medtronic, Moderna, Novartis, Novo Nordisk, Partners in Progressive Medical Education, Pfizer, Sanofi Aventis, Timed Right, WebMD, Gilead Sciences, Insulet, PocketPills, Roche, and Takeda. Dr. Kim, clinical assistant professor, Department of Family Medicine, University of Calgary, Alberta, has disclosed ties with Abbott, AbbVie, AstraZeneca, Bayer, Boehringer Ingelheim, Eisai, Embecta, Eli Lilly, GSK, Janssen, Linpharma, Novo Nordisk, Miravo, Otsuka, Pfizer, Teva, Takeda, and Sanofi, and Partners in Progressive Medical Education.
A version of this article first appeared on Medscape.com.
This transcript has been edited for clarity.
Akshay B. Jain, MD: Welcome back to Medscape at ADA 2024, where Dr. James Kim, primary care physician from Calgary, Alberta, will be joining me in deciphering the key highlights at the ADA conference and bringing our own clinical twist into what the relevance would be for people like you and I to take back to our clinics.
Welcome back, Dr. Kim.
James Kim, MBBCh, PgDip, MScCH: Thank you very much. It’s nice to be back.
Dr. Jain: This was a diabetes conference, so obviously we are very pancreas focused. At this conference, we went outside our general area of territory, going outside of the pancreas and delving into other organ states. What I found fascinating were some data regarding the effects of incretin therapy on the lung, and in particular, some of the restrictive lung disorders.
Dr. Kim, you attended these sessions as well. Can you tell us a little bit more about the results that were discussed?
Dr. Kim: This is an interesting field. The moderator of the session went up and said that there has been no time in any previous ADA sessions where the lung issue was actually discussed. This was the first time ever.
They had some of the world leaders in this field, so it was really awesome to see them. Just to paint a picture of these obese asthmatic patients, they are challenging cases because, as you know, the main therapy for any asthmatic patient is inhaled corticosteroid.
Patients who are obese have quite a bit of a steroid resistance. Therefore, they end up being on many medications that sometimes are off label, and many end up on biologics as well. Therefore, the respiratory world has been seeking therapies for these obese asthmatic patients who are likely to be steroid resistant because these people are also likely to end up on an oral steroid as well.
Dr. Jain, you know the effect of the steroids much better than I do, and it’s like a laundry list. We really don’t want our patients to be on oral steroids.
In the past few years, GLP-1 has been studied quite extensively in the lung, especially in the world of asthma, and also in COPD. What’s really fascinating is that the GLP-1 receptors have been found to be quite abundant in the airway. Some studies show that the highest concentration of GLP-1 lies in the airway, whereas some studies have said that it’s the third most common area to find the GLP-1.
It is not a surprise that GLP-1 is being studied in managing the airway, especially airway inflammation in asthma and COPD patients. The preliminary data have been quite encouraging. They also discussed that there are new medications coming out that seem to be incretin based, so we’ll wait to see what those studies show.
There are two current phase 3 trials being held at the moment. One is using semaglutide 2.4 mg subcutaneous and another one is using metformin to reduce the airway inflammation in these asthmatic patients and also in some COPD patients. We’ll look forward to these results.
Dr. Jain: That’s really important to note because we see that there is a high density of these receptors in the airways, and hitherto we had no idea about the overall effect. Now, we’re looking at, as you mentioned, individuals with obesity who have asthma, so there are both the restrictive and obstructive components in the lung coming into play here.
From an endocrinology perspective, I’m thinking that this could be multiple effects of the GLP-1 receptor agonists, where on one hand you’re managing the obesity and you’re working along that line, and on the other hand, it could have local anti-inflammatory effects in the lung. Hence, there could be potential improvement in the overall pulmonary function of these individuals.
Dr. Kim: We are seeing this in primary care. Ever since I found out this information, I have started numerous patients, who are obese, asthmatic patients who do not have diabetes, on GLP-1 therapies, and their pulmonary function tests have improved significantly.
As a matter of fact, one of my personal friends is a severe asthmatic patient. She ends up being on oral steroids about three times a year. There was even one day when I saw her in one of my classes and she was dyspneic. She was short of breath.
I introduced her to one of my colleagues who’s a respirologist and very much into the impact of the incretins and asthma, and she was started on a GLP-1 receptor agonist. She lost about 30 pounds of weight, but now she is labeled as a mild asthmatic. Her pulmonary function test is completely normal. She hasn’t touched an oral steroid for a couple of years now.
That is a huge success story and I’m seeing that even in my own clinic as well. It’s a huge win for the respiratory world.
Dr. Jain: I think from an endocrinology perspective as well, if we are initiating GLP-1 receptor agonists or medications in that class, where we use it for management of obesity, sooner or later we do hit a stage where people will plateau with their weight loss. They won’t have any additional weight loss.
We tell individuals at that time that the fact that they’re able to maintain the weight loss still means that the medication is working from the obesity perspective. For individuals who also have asthma, it would be a good point to tell them that it could still have potential effects on reducing inflammation ongoing. Hence, even though they may not be losing any additional weight, it would still be helpful to continue on these medications from a pulmonary perspective.
Dr. Kim: Right now these pleiotropic effects of GLP-1 agents are absolutely mind-blowing. I mentioned in one of my respiratory presentations to a bunch of respirologists that diabetes is taking over the world, including the respiratory world. Well, you can imagine what their faces were like. However, they were quite impressed at that, and they were very excited with what these two phase 3 trials will show.
Dr. Jain: I think, based on the ADA 2024 conference, GLP-1 receptor agonists continue to be the gift that keeps giving. We have the effects on diabetes, obesity, kidney function, liver protection, lungs, and Alzheimer’s. We saw some sessions about potential use in people with alcohol misuse disorder or gambling problems. Clearly, there’s a large amount of research that›s being done with these agents.
Perhaps when you and I talk about ADA 2025, we might be able to talk about some more pleiotropic benefits outside the pancreas. Until then, please do check out our other videos from ADA 2024. Thanks for joining us again, Dr. Kim.
Dr. Kim: Thank you very much for having me.
Dr. Jain, clinical instructor, Department of Endocrinology, University of British Columbia, and endocrinologist, TLC Diabetes and Endocrinology, Vancouver, British Columbia, Canada, has disclosed ties with Abbott, Acerus, AstraZeneca, Amgen, Bausch Healthcare, Bayer, Boehringer Ingelheim, Care to Know, CCRN, Connected in Motion, CPD Network, Dexcom, Diabetes Canada, Eli Lilly, GSK, HLS Therapeutics, Janssen, Master Clinician Alliance, MDBriefcase, Merck, Medtronic, Moderna, Novartis, Novo Nordisk, Partners in Progressive Medical Education, Pfizer, Sanofi Aventis, Timed Right, WebMD, Gilead Sciences, Insulet, PocketPills, Roche, and Takeda. Dr. Kim, clinical assistant professor, Department of Family Medicine, University of Calgary, Alberta, has disclosed ties with Abbott, AbbVie, AstraZeneca, Bayer, Boehringer Ingelheim, Eisai, Embecta, Eli Lilly, GSK, Janssen, Linpharma, Novo Nordisk, Miravo, Otsuka, Pfizer, Teva, Takeda, and Sanofi, and Partners in Progressive Medical Education.
A version of this article first appeared on Medscape.com.
Alert System Could Warn of Impact of Severe Weather on Health
As more data show potentially dangerous effects of climate and weather on individuals with chronic medical conditions, CVS Health has introduced an initiative that uses technology to provide weather alerts and targeted outreach to those at increased risk, according to a press release from the company. Ultimately, the goals of the initiative are to improve health, reduce emergency department visits, hospital stays, and medical costs, according to the press release.
Extreme weather events such as heat waves are becoming more frequent and severe, but most heat-related deaths are preventable with outreach and intervention, Dan Knecht, MD, vice president and chief clinical innovation officer for CVS Caremark, a division of CVS Health, said in an interview. The approach will combine the company’s services, including care managers, health centers, and data, to aid patients vulnerable to severe weather.
The initiative is starting with a focus on extreme heat events and will expand this fall with alerts about high levels of air pollution for individuals with vulnerability to reduced lung function, asthma, and cardiac problems as a result of exposure to high air-pollution levels, according to Dr. Knecht.
For now, the initiative is available to members of Aetna Medicare, according to Dr. Knecht. “Our goal is to expand to other consumers, including those who visit MinuteClinic and CVS Pharmacy locations, where we can provide timely environment-related recommendations at time of care,” he said.
The alert system uses environmental data analytics to pair highly localized forecasts and real-time insights about air quality, wildfires, and high heat with medical and pharmacy data for high-risk patients in areas affected by extreme weather.
For example, for individuals who are at risk and living in areas facing extreme heat, “registered nurse care managers proactively reach out to vulnerable patients up to several days in advance of an extreme weather event and provide them personalized tips and resources,” said Dr. Knecht.
In addition, he added, “we talk to patients about how to manage their medications during periods of extreme heat and, when delivering medications, take weather data into account to determine appropriate packaging materials for shipments.”
These interventions direct patients to CVS Health–linked resources, such as Oak Street Health clinics available as cooling centers, health services provided at MinuteClinic locations, and medication management at CVS pharmacies. Other interventions include virtual or in-person mental health counseling through MinuteClinic.
Dr. Knecht offered additional guidance for clinicians and patients to help manage heat waves. “Heat and certain medications can impair heat tolerance and the ability to regulate body temperature,” he told this news organization. Extreme heat may affect the performance of some medications and their devices, such as inhalers and diabetes supplies, he added.
Health Alerts Have Potential, But Comprehensive Approach is Needed
“Patients with chronic lung conditions are highly susceptible to the impact of climate change,” MeiLan K. Han, MD, a pulmonologist and professor of internal medicine at the University of Michigan, Ann Arbor, said in an interview. “Increasing dust, hotter temperatures, and higher levels of air pollution make it more difficult for patients to breathe,” she said. Data also suggest that higher levels of air pollution may not only cause chronic lung disease but also cause worsening symptoms among those with existing disease, she added.
A weather-related health alert could be useful for patients so they can be prepared, Dr. Han told this news organization.
“For a patient with chronic lung disease, a hot weather alert may mean that it will be harder for patients to breathe, and [they] may [be] more susceptible to heat stroke and dehydration if they do not have access to air conditioning,” she said. “At a minimum, patients should ensure they are on their controller medications, which often means a daily inhaler for patients with conditions such as asthma and chronic obstructive pulmonary disease (COPD). However, patients also should have access to their short-term reliever medications so they can be prepared for increased shortness of breath that may accompany a hot weather day,” Dr. Han explained.
However, not all patients have access to technology such as smartphones or other devices that will alert them to impending weather events, such as heat waves, said Dr. Han. “For these patients, a standard phone call may be beneficial,” she said.
Looking ahead, “programs for weather-related health alerts will need to be comprehensive, focusing not only on access to needed medications but also climate-controlled settings for temporary relief of heat,” said Dr. Han. “For some of our most vulnerable patients, while they may have air conditioning, they may not be able to afford to run it, so this needs to be considered in developing a comprehensive program,” she emphasized.
Dr. Knecht had no financial conflicts to disclose. Dr. Han disclosed ties with Aerogen, Altesa BioSciences, American Lung Association, Amgen, Apreo Health, AstraZeneca, Biodesix, Boehringer Ingelheim, Chiesi, Cipla, COPD Foundation, DevPro, Gala Therapeutics, Genentech, GlaxoSmithKline, Integrity, MDBriefcase, Medscape, Medtronic, Medwiz, Meissa Vaccines, Merck, Mylan, NACE, National Institutes of Health, Novartis, Nuvaira, Polarian, Pulmonx, Regeneron, Roche, RS Biotherapeutics, Sanofi, Sunovion, Teva, UpToDate, and Verona..
A version of this article first appeared on Medscape.com.
As more data show potentially dangerous effects of climate and weather on individuals with chronic medical conditions, CVS Health has introduced an initiative that uses technology to provide weather alerts and targeted outreach to those at increased risk, according to a press release from the company. Ultimately, the goals of the initiative are to improve health, reduce emergency department visits, hospital stays, and medical costs, according to the press release.
Extreme weather events such as heat waves are becoming more frequent and severe, but most heat-related deaths are preventable with outreach and intervention, Dan Knecht, MD, vice president and chief clinical innovation officer for CVS Caremark, a division of CVS Health, said in an interview. The approach will combine the company’s services, including care managers, health centers, and data, to aid patients vulnerable to severe weather.
The initiative is starting with a focus on extreme heat events and will expand this fall with alerts about high levels of air pollution for individuals with vulnerability to reduced lung function, asthma, and cardiac problems as a result of exposure to high air-pollution levels, according to Dr. Knecht.
For now, the initiative is available to members of Aetna Medicare, according to Dr. Knecht. “Our goal is to expand to other consumers, including those who visit MinuteClinic and CVS Pharmacy locations, where we can provide timely environment-related recommendations at time of care,” he said.
The alert system uses environmental data analytics to pair highly localized forecasts and real-time insights about air quality, wildfires, and high heat with medical and pharmacy data for high-risk patients in areas affected by extreme weather.
For example, for individuals who are at risk and living in areas facing extreme heat, “registered nurse care managers proactively reach out to vulnerable patients up to several days in advance of an extreme weather event and provide them personalized tips and resources,” said Dr. Knecht.
In addition, he added, “we talk to patients about how to manage their medications during periods of extreme heat and, when delivering medications, take weather data into account to determine appropriate packaging materials for shipments.”
These interventions direct patients to CVS Health–linked resources, such as Oak Street Health clinics available as cooling centers, health services provided at MinuteClinic locations, and medication management at CVS pharmacies. Other interventions include virtual or in-person mental health counseling through MinuteClinic.
Dr. Knecht offered additional guidance for clinicians and patients to help manage heat waves. “Heat and certain medications can impair heat tolerance and the ability to regulate body temperature,” he told this news organization. Extreme heat may affect the performance of some medications and their devices, such as inhalers and diabetes supplies, he added.
Health Alerts Have Potential, But Comprehensive Approach is Needed
“Patients with chronic lung conditions are highly susceptible to the impact of climate change,” MeiLan K. Han, MD, a pulmonologist and professor of internal medicine at the University of Michigan, Ann Arbor, said in an interview. “Increasing dust, hotter temperatures, and higher levels of air pollution make it more difficult for patients to breathe,” she said. Data also suggest that higher levels of air pollution may not only cause chronic lung disease but also cause worsening symptoms among those with existing disease, she added.
A weather-related health alert could be useful for patients so they can be prepared, Dr. Han told this news organization.
“For a patient with chronic lung disease, a hot weather alert may mean that it will be harder for patients to breathe, and [they] may [be] more susceptible to heat stroke and dehydration if they do not have access to air conditioning,” she said. “At a minimum, patients should ensure they are on their controller medications, which often means a daily inhaler for patients with conditions such as asthma and chronic obstructive pulmonary disease (COPD). However, patients also should have access to their short-term reliever medications so they can be prepared for increased shortness of breath that may accompany a hot weather day,” Dr. Han explained.
However, not all patients have access to technology such as smartphones or other devices that will alert them to impending weather events, such as heat waves, said Dr. Han. “For these patients, a standard phone call may be beneficial,” she said.
Looking ahead, “programs for weather-related health alerts will need to be comprehensive, focusing not only on access to needed medications but also climate-controlled settings for temporary relief of heat,” said Dr. Han. “For some of our most vulnerable patients, while they may have air conditioning, they may not be able to afford to run it, so this needs to be considered in developing a comprehensive program,” she emphasized.
Dr. Knecht had no financial conflicts to disclose. Dr. Han disclosed ties with Aerogen, Altesa BioSciences, American Lung Association, Amgen, Apreo Health, AstraZeneca, Biodesix, Boehringer Ingelheim, Chiesi, Cipla, COPD Foundation, DevPro, Gala Therapeutics, Genentech, GlaxoSmithKline, Integrity, MDBriefcase, Medscape, Medtronic, Medwiz, Meissa Vaccines, Merck, Mylan, NACE, National Institutes of Health, Novartis, Nuvaira, Polarian, Pulmonx, Regeneron, Roche, RS Biotherapeutics, Sanofi, Sunovion, Teva, UpToDate, and Verona..
A version of this article first appeared on Medscape.com.
As more data show potentially dangerous effects of climate and weather on individuals with chronic medical conditions, CVS Health has introduced an initiative that uses technology to provide weather alerts and targeted outreach to those at increased risk, according to a press release from the company. Ultimately, the goals of the initiative are to improve health, reduce emergency department visits, hospital stays, and medical costs, according to the press release.
Extreme weather events such as heat waves are becoming more frequent and severe, but most heat-related deaths are preventable with outreach and intervention, Dan Knecht, MD, vice president and chief clinical innovation officer for CVS Caremark, a division of CVS Health, said in an interview. The approach will combine the company’s services, including care managers, health centers, and data, to aid patients vulnerable to severe weather.
The initiative is starting with a focus on extreme heat events and will expand this fall with alerts about high levels of air pollution for individuals with vulnerability to reduced lung function, asthma, and cardiac problems as a result of exposure to high air-pollution levels, according to Dr. Knecht.
For now, the initiative is available to members of Aetna Medicare, according to Dr. Knecht. “Our goal is to expand to other consumers, including those who visit MinuteClinic and CVS Pharmacy locations, where we can provide timely environment-related recommendations at time of care,” he said.
The alert system uses environmental data analytics to pair highly localized forecasts and real-time insights about air quality, wildfires, and high heat with medical and pharmacy data for high-risk patients in areas affected by extreme weather.
For example, for individuals who are at risk and living in areas facing extreme heat, “registered nurse care managers proactively reach out to vulnerable patients up to several days in advance of an extreme weather event and provide them personalized tips and resources,” said Dr. Knecht.
In addition, he added, “we talk to patients about how to manage their medications during periods of extreme heat and, when delivering medications, take weather data into account to determine appropriate packaging materials for shipments.”
These interventions direct patients to CVS Health–linked resources, such as Oak Street Health clinics available as cooling centers, health services provided at MinuteClinic locations, and medication management at CVS pharmacies. Other interventions include virtual or in-person mental health counseling through MinuteClinic.
Dr. Knecht offered additional guidance for clinicians and patients to help manage heat waves. “Heat and certain medications can impair heat tolerance and the ability to regulate body temperature,” he told this news organization. Extreme heat may affect the performance of some medications and their devices, such as inhalers and diabetes supplies, he added.
Health Alerts Have Potential, But Comprehensive Approach is Needed
“Patients with chronic lung conditions are highly susceptible to the impact of climate change,” MeiLan K. Han, MD, a pulmonologist and professor of internal medicine at the University of Michigan, Ann Arbor, said in an interview. “Increasing dust, hotter temperatures, and higher levels of air pollution make it more difficult for patients to breathe,” she said. Data also suggest that higher levels of air pollution may not only cause chronic lung disease but also cause worsening symptoms among those with existing disease, she added.
A weather-related health alert could be useful for patients so they can be prepared, Dr. Han told this news organization.
“For a patient with chronic lung disease, a hot weather alert may mean that it will be harder for patients to breathe, and [they] may [be] more susceptible to heat stroke and dehydration if they do not have access to air conditioning,” she said. “At a minimum, patients should ensure they are on their controller medications, which often means a daily inhaler for patients with conditions such as asthma and chronic obstructive pulmonary disease (COPD). However, patients also should have access to their short-term reliever medications so they can be prepared for increased shortness of breath that may accompany a hot weather day,” Dr. Han explained.
However, not all patients have access to technology such as smartphones or other devices that will alert them to impending weather events, such as heat waves, said Dr. Han. “For these patients, a standard phone call may be beneficial,” she said.
Looking ahead, “programs for weather-related health alerts will need to be comprehensive, focusing not only on access to needed medications but also climate-controlled settings for temporary relief of heat,” said Dr. Han. “For some of our most vulnerable patients, while they may have air conditioning, they may not be able to afford to run it, so this needs to be considered in developing a comprehensive program,” she emphasized.
Dr. Knecht had no financial conflicts to disclose. Dr. Han disclosed ties with Aerogen, Altesa BioSciences, American Lung Association, Amgen, Apreo Health, AstraZeneca, Biodesix, Boehringer Ingelheim, Chiesi, Cipla, COPD Foundation, DevPro, Gala Therapeutics, Genentech, GlaxoSmithKline, Integrity, MDBriefcase, Medscape, Medtronic, Medwiz, Meissa Vaccines, Merck, Mylan, NACE, National Institutes of Health, Novartis, Nuvaira, Polarian, Pulmonx, Regeneron, Roche, RS Biotherapeutics, Sanofi, Sunovion, Teva, UpToDate, and Verona..
A version of this article first appeared on Medscape.com.
Could This COPD Treatment’s Cost Put It Out of Reach for Many?
Ensifentrine (Ohtuvayre), a novel medication for the treatment of chronic obstructive pulmonary disease (COPD) recently approved by the US Food and Drug Administration, has been shown to reduce COPD exacerbations and may improve the quality of life for patients, but these potential benefits come at a high annual cost, authors of a cost-effectiveness analysis say.
Ensifentrine is a first-in-class selective dual inhibitor of both phosphodiesterase 3 (PDE-3) and PDE-4, combining both bronchodilator and nonsteroidal anti-inflammatory effects in a single molecule. The drug is delivered through a standard jet nebulizer.
In the phase 3 ENHANCE 1 and 2 trials, ensifentrine significantly improved lung function based on the primary outcome of average forced expiratory volume in 1 second (FEV1) within 0-12 hours of administration compared with placebo. In addition, patients were found to tolerate the inhaled treatment well, with similar proportions of ensifentrine- and placebo-assigned patients reporting treatment-emergent adverse events. The most common treatment-emergent adverse events were nasopharyngitis, hypertension, and back pain, reported in < 3% of the ensifentrine group.
High Cost Barrier
But as authors of the analysis from the Boston-based Institute for Clinical and Economic Review (ICER) found, ICER is an independent, nonprofit research institute that conducts evidence-based reviews of healthcare interventions, including prescription drugs, other treatments, and diagnostic tests.
“Current evidence shows that ensifentrine decreases COPD exacerbations when used in combination with some current inhaled therapies, but there are uncertainties about how much benefit it may add to unstudied combinations of inhaled treatments,” said David Rind, MD, chief medical officer of ICER, in a statement.
In an interview, Dr. Rind noted that the high price of ensifentrine may lead payers to restrict access to an otherwise promising new therapy. “Obviously many drugs in the US are overpriced, and this one, too, looks like it is overpriced. That causes ongoing financial toxicity for individual patients and it causes problems for the entire US health system, because when we pay too much for drugs we don’t have money for other things. So I’m worried about the fact that this price is too high compared to the benefit it provides,” he said.
As previously reported, as many as 1 in 6 persons with COPD in the United States miss or delay COPD medication doses owing to high drug costs. “I think that the pricing they chose is going to cause lots of barriers to people getting access and that insurance companies will throw up barriers. Primary care physicians like me won’t even try to get approval for a drug like this given the hoops we will be made to jump through, and so fewer people will get this drug,” Dr. Rind said. He pointed out that a lower wholesale acquisition cost could encourage higher volume sales, affording the drug maker a comparable profit to the higher cost but lower volume option.
Good Drug, High Price
An independent appraisal committee for ICER determined that “current evidence is adequate to demonstrate a net health benefit for ensifentrine added to maintenance therapy when compared to maintenance therapy alone.”
But ICER also issued an access and affordability alert “to signal to stakeholders and policymakers that the amount of added health care costs associated with a new service may be difficult for the health system to absorb over the short term without displacing other needed services.” ICER recommends that payers should include coverage for smoking cessation therapies, and that drug manufacturers “set prices that will foster affordability and good access for all patients by aligning prices with the patient-centered therapeutic value of their treatments.”
“This looks like a pretty good drug,” Dr. Rind said. “It looks quite safe, and I think there will be a lot of patients, particularly those who are having frequent exacerbations, who this would be appropriate for, particularly once they’ve maxed out existing therapies, but maybe even earlier than that. And if the price comes down to the point that patients can really access this and providers can access it, people really should look at this as a potential therapy.”
Drug Not Yet Available?
However, providers have not yet had experience to gauge the new medication. “We haven’t been able to prescribe it yet,” said Corinne Young, MSN, FNP-C, FCCP, director of advance practice provider and clinical services for Colorado Springs Pulmonary Consultants and president and founder of the Association of Pulmonary Advanced Practice Providers. She learned that “they were going to release it to select specialty pharmacies in the third quarter of 2024. But all the ones we call do not have it, and no one knows who does. They haven’t sent any reps into the field in my area, so we don’t have any points of contact either,” she said.
Verona Pharma stated it anticipates ensifentrine to be available in the third quarter of 2024 “through an exclusive network of accredited specialty pharmacies.”
Funding for the ICER report came from nonprofit foundations. No funding came from health insurers, pharmacy benefit managers, or life science companies. Dr. Rind had no disclosures relevant to ensifentrine or Verona Pharma. Ms. Young is a member of the CHEST Physician Editorial Board.
A version of this article first appeared on Medscape.com.
Ensifentrine (Ohtuvayre), a novel medication for the treatment of chronic obstructive pulmonary disease (COPD) recently approved by the US Food and Drug Administration, has been shown to reduce COPD exacerbations and may improve the quality of life for patients, but these potential benefits come at a high annual cost, authors of a cost-effectiveness analysis say.
Ensifentrine is a first-in-class selective dual inhibitor of both phosphodiesterase 3 (PDE-3) and PDE-4, combining both bronchodilator and nonsteroidal anti-inflammatory effects in a single molecule. The drug is delivered through a standard jet nebulizer.
In the phase 3 ENHANCE 1 and 2 trials, ensifentrine significantly improved lung function based on the primary outcome of average forced expiratory volume in 1 second (FEV1) within 0-12 hours of administration compared with placebo. In addition, patients were found to tolerate the inhaled treatment well, with similar proportions of ensifentrine- and placebo-assigned patients reporting treatment-emergent adverse events. The most common treatment-emergent adverse events were nasopharyngitis, hypertension, and back pain, reported in < 3% of the ensifentrine group.
High Cost Barrier
But as authors of the analysis from the Boston-based Institute for Clinical and Economic Review (ICER) found, ICER is an independent, nonprofit research institute that conducts evidence-based reviews of healthcare interventions, including prescription drugs, other treatments, and diagnostic tests.
“Current evidence shows that ensifentrine decreases COPD exacerbations when used in combination with some current inhaled therapies, but there are uncertainties about how much benefit it may add to unstudied combinations of inhaled treatments,” said David Rind, MD, chief medical officer of ICER, in a statement.
In an interview, Dr. Rind noted that the high price of ensifentrine may lead payers to restrict access to an otherwise promising new therapy. “Obviously many drugs in the US are overpriced, and this one, too, looks like it is overpriced. That causes ongoing financial toxicity for individual patients and it causes problems for the entire US health system, because when we pay too much for drugs we don’t have money for other things. So I’m worried about the fact that this price is too high compared to the benefit it provides,” he said.
As previously reported, as many as 1 in 6 persons with COPD in the United States miss or delay COPD medication doses owing to high drug costs. “I think that the pricing they chose is going to cause lots of barriers to people getting access and that insurance companies will throw up barriers. Primary care physicians like me won’t even try to get approval for a drug like this given the hoops we will be made to jump through, and so fewer people will get this drug,” Dr. Rind said. He pointed out that a lower wholesale acquisition cost could encourage higher volume sales, affording the drug maker a comparable profit to the higher cost but lower volume option.
Good Drug, High Price
An independent appraisal committee for ICER determined that “current evidence is adequate to demonstrate a net health benefit for ensifentrine added to maintenance therapy when compared to maintenance therapy alone.”
But ICER also issued an access and affordability alert “to signal to stakeholders and policymakers that the amount of added health care costs associated with a new service may be difficult for the health system to absorb over the short term without displacing other needed services.” ICER recommends that payers should include coverage for smoking cessation therapies, and that drug manufacturers “set prices that will foster affordability and good access for all patients by aligning prices with the patient-centered therapeutic value of their treatments.”
“This looks like a pretty good drug,” Dr. Rind said. “It looks quite safe, and I think there will be a lot of patients, particularly those who are having frequent exacerbations, who this would be appropriate for, particularly once they’ve maxed out existing therapies, but maybe even earlier than that. And if the price comes down to the point that patients can really access this and providers can access it, people really should look at this as a potential therapy.”
Drug Not Yet Available?
However, providers have not yet had experience to gauge the new medication. “We haven’t been able to prescribe it yet,” said Corinne Young, MSN, FNP-C, FCCP, director of advance practice provider and clinical services for Colorado Springs Pulmonary Consultants and president and founder of the Association of Pulmonary Advanced Practice Providers. She learned that “they were going to release it to select specialty pharmacies in the third quarter of 2024. But all the ones we call do not have it, and no one knows who does. They haven’t sent any reps into the field in my area, so we don’t have any points of contact either,” she said.
Verona Pharma stated it anticipates ensifentrine to be available in the third quarter of 2024 “through an exclusive network of accredited specialty pharmacies.”
Funding for the ICER report came from nonprofit foundations. No funding came from health insurers, pharmacy benefit managers, or life science companies. Dr. Rind had no disclosures relevant to ensifentrine or Verona Pharma. Ms. Young is a member of the CHEST Physician Editorial Board.
A version of this article first appeared on Medscape.com.
Ensifentrine (Ohtuvayre), a novel medication for the treatment of chronic obstructive pulmonary disease (COPD) recently approved by the US Food and Drug Administration, has been shown to reduce COPD exacerbations and may improve the quality of life for patients, but these potential benefits come at a high annual cost, authors of a cost-effectiveness analysis say.
Ensifentrine is a first-in-class selective dual inhibitor of both phosphodiesterase 3 (PDE-3) and PDE-4, combining both bronchodilator and nonsteroidal anti-inflammatory effects in a single molecule. The drug is delivered through a standard jet nebulizer.
In the phase 3 ENHANCE 1 and 2 trials, ensifentrine significantly improved lung function based on the primary outcome of average forced expiratory volume in 1 second (FEV1) within 0-12 hours of administration compared with placebo. In addition, patients were found to tolerate the inhaled treatment well, with similar proportions of ensifentrine- and placebo-assigned patients reporting treatment-emergent adverse events. The most common treatment-emergent adverse events were nasopharyngitis, hypertension, and back pain, reported in < 3% of the ensifentrine group.
High Cost Barrier
But as authors of the analysis from the Boston-based Institute for Clinical and Economic Review (ICER) found, ICER is an independent, nonprofit research institute that conducts evidence-based reviews of healthcare interventions, including prescription drugs, other treatments, and diagnostic tests.
“Current evidence shows that ensifentrine decreases COPD exacerbations when used in combination with some current inhaled therapies, but there are uncertainties about how much benefit it may add to unstudied combinations of inhaled treatments,” said David Rind, MD, chief medical officer of ICER, in a statement.
In an interview, Dr. Rind noted that the high price of ensifentrine may lead payers to restrict access to an otherwise promising new therapy. “Obviously many drugs in the US are overpriced, and this one, too, looks like it is overpriced. That causes ongoing financial toxicity for individual patients and it causes problems for the entire US health system, because when we pay too much for drugs we don’t have money for other things. So I’m worried about the fact that this price is too high compared to the benefit it provides,” he said.
As previously reported, as many as 1 in 6 persons with COPD in the United States miss or delay COPD medication doses owing to high drug costs. “I think that the pricing they chose is going to cause lots of barriers to people getting access and that insurance companies will throw up barriers. Primary care physicians like me won’t even try to get approval for a drug like this given the hoops we will be made to jump through, and so fewer people will get this drug,” Dr. Rind said. He pointed out that a lower wholesale acquisition cost could encourage higher volume sales, affording the drug maker a comparable profit to the higher cost but lower volume option.
Good Drug, High Price
An independent appraisal committee for ICER determined that “current evidence is adequate to demonstrate a net health benefit for ensifentrine added to maintenance therapy when compared to maintenance therapy alone.”
But ICER also issued an access and affordability alert “to signal to stakeholders and policymakers that the amount of added health care costs associated with a new service may be difficult for the health system to absorb over the short term without displacing other needed services.” ICER recommends that payers should include coverage for smoking cessation therapies, and that drug manufacturers “set prices that will foster affordability and good access for all patients by aligning prices with the patient-centered therapeutic value of their treatments.”
“This looks like a pretty good drug,” Dr. Rind said. “It looks quite safe, and I think there will be a lot of patients, particularly those who are having frequent exacerbations, who this would be appropriate for, particularly once they’ve maxed out existing therapies, but maybe even earlier than that. And if the price comes down to the point that patients can really access this and providers can access it, people really should look at this as a potential therapy.”
Drug Not Yet Available?
However, providers have not yet had experience to gauge the new medication. “We haven’t been able to prescribe it yet,” said Corinne Young, MSN, FNP-C, FCCP, director of advance practice provider and clinical services for Colorado Springs Pulmonary Consultants and president and founder of the Association of Pulmonary Advanced Practice Providers. She learned that “they were going to release it to select specialty pharmacies in the third quarter of 2024. But all the ones we call do not have it, and no one knows who does. They haven’t sent any reps into the field in my area, so we don’t have any points of contact either,” she said.
Verona Pharma stated it anticipates ensifentrine to be available in the third quarter of 2024 “through an exclusive network of accredited specialty pharmacies.”
Funding for the ICER report came from nonprofit foundations. No funding came from health insurers, pharmacy benefit managers, or life science companies. Dr. Rind had no disclosures relevant to ensifentrine or Verona Pharma. Ms. Young is a member of the CHEST Physician Editorial Board.
A version of this article first appeared on Medscape.com.
Could Mobile Tech Help to Minimize COPD Exacerbations?
Could mobile technology help patients with chronic obstructive pulmonary disease (COPD) who may not seek care until they experience an exacerbation?
Self-management interventions for COPD can potentially improve quality of life and reduce hospitalizations, wrote Robert Wu, MD, associate professor in the Department of Medicine at the University of Toronto, and colleagues. However, data on the use of devices and apps to manage COPD by providing reminders for self-care, predicting early exacerbations, and facilitating communication with healthcare providers are limited, they said.
In a study published in COPD: Journal of Chronic Obstructive Pulmonary Disease, the researchers reported details from interviews with 26 adult patients with COPD who used a wearable device and app for 6 months to help manage their condition. The interviews were part of a larger cohort study.
“The motivation for this study was to understand the patient perspective on using wearables to help support their chronic lung condition,” Dr. Wu said in an interview. “People with COPD can be at high risk of being admitted to hospital, so it is important to see if innovative technology like wearables or remote monitoring can help them,” he said.
Individuals with COPD tend to be older and less technologically adept, and they may be less willing to adopt new technology, he added. “We wanted to understand what would make people use a self-management app,” he said.
On enrollment in the study, patients received a smartwatch and a smartphone with a preinstalled app for COPD management. The app included daily reminders to take medication, perform guided breathing sessions, check blood oxygen on the smartwatch or an oximeter, and complete a symptom questionnaire. The app also allowed participants to record when they exercised and provided feedback on heart rate and daily activity, including passive step counts. Participants earned stars for meeting daily exercise goals of active minutes and total steps.
Participants received training in the use of the app from members of the research team and completed semi-structured interviews after using the items for 6 months.
The researchers divided their findings into four main themes: information, support and reassurance; barriers to adoption; impact on communication with healthcare providers; and opportunities for improvement.
Overall, most patients reported that the feedback they received through the app was useful. In particular, participants reported that the app and smartwatch provided reassurance and feedback about stable vitals during exercise, which encouraged some to adhere to regular exercise routines. Approximately two thirds (65%) said that the daily exercise reminders were motivational. In addition, 20% reported that they interpreted vital data, including heart rate, as a signal to slow down.
Participants rated medication reminders and the option to create an action plan for COPD management as the least useful features; 69% said that they already had medication reminders in place.
A total of four patients experienced technical difficulties with the app that kept it from impacting their disease management. Some of the suggestions from participants for improvement included adding information about food intake, weight, blood pressure, and temperature to the health information being tracked, as well as restoring the oxygen saturation measure, which had been disabled because of accuracy concerns. Barriers to use of the device and app included the bulkiness of the device as well as the reported technical malfunctions.
The findings were limited by several factors, including the small sample size and likely focus on early adopters of technology, which may not represent most patients with COPD, the researchers noted. Other limitations included the recruitment of most patients after the start of the COVID-19 pandemic, which may have affected their experience and also limited the assessment of the app on communication with healthcare providers, the researchers noted. The study also did not address financial or social barriers.
However, the results suggest that patients with COPD identified the potential value of wearable devices for disease management and that improved technology could promote patient empowerment and lifestyle changes, the researchers concluded.
Technology Can Augment Care and Connections
“As clinicians and researchers, we have ideas about what patients would want, but it is always better to get their feedback of what they really want and what they would use,” Dr. Wu told this news organization. “We thought older adults with COPD would be less likely to engage with the technology. We found that many wanted to have their data to help make connections with their condition, and some purchased smartwatches after the study to make these connections,” he said.
The takeaway message from the current study is that people with COPD may benefit from self-management apps, but they would like to use them in collaboration with their healthcare team, said Dr. Wu. “Clinicians may see more of their patients bringing in data from wearables and apps,” he noted.
Concerns persist that using technology to help support people with COPD could increase the “digital divide” and that those with lower digital literacy, financial insecurity, or English as a second language could be left behind, and it is important to remain attentive to equity in pursuing the use of devices and apps, Dr. Wu told this news organization.
Looking ahead, research involving self-management, remote monitoring, and wearable devices has focused on other conditions such as heart failure and diabetes, and more work is needed to examine how these technologies can improve care for patients with COPD, said Dr. Wu. “We see this study as one important step — to understand what will motivate people to use self-management apps and wearables,” he said.
“Acute exacerbations of COPD are very important events that can alter quality of life, lung function, and even mortality in COPD,” said Nathaniel Marchetti, DO, medical director of the Respiratory Intensive Care Unit at Temple University Hospital, Philadelphia, in an interview.
“Many of these exacerbations are not recognized by clinicians or even patients until they present late and end up in an urgent office visit with a physician or in the emergency room [ER], so addressing exacerbations earlier has the potential to avoid ER visits or hospitalizations,” he said.
The study identified areas for further research, Dr. Marchetti said. “More information would be needed to determine if the use of an app to monitor heart rate, symptoms, and oxygen saturation could alter important outcomes in COPD such as exacerbations,” he noted.
As for limitations, “no one wants to carry two smartphones,” said Dr. Marchetti. “Future devices need to be easy to use and available on the patient’s own phone,” he said. Patients should be able to choose a smartwatch or possibly a bracelet that can be synced to a smartphone, he added. The current study also failed to address what would be done with collected data, such as link them to health professionals who would offer treatment when needed, he said.
Overall, the data from the current study suggest that patients with COPD would like some device that monitors symptoms and vital signs and offers suggestions/incentives to exercise and take medications, Dr. Marchetti told this news organization. “A larger study will be needed that compares how such a device could improve outcomes of COPD; outcomes could include admissions/ER visits, exercise performance, or compliance with medication,” he said. In addition, clinical algorithms for the identification and treatment of acute exacerbations of COPD would be needed, Dr. Marchetti noted. These algorithms would determine whether treatment decisions would be initiated by a clinical team of health professionals or whether clinicians would provide medications that the patients would then decide to take based on data collected on the app, using the investigator-provided algorithms, he said.
The study was supported in part by Samsung Research America (SRA) and was initiated by Dr. Wu with input from SRA, but the company had no role in the methods or results. The study also was supported by grants from the National Natural Science Foundation of China.
Dr. Marchetti had no relevant financial conflicts to disclose.
A version of this article appeared on Medscape.com.
Could mobile technology help patients with chronic obstructive pulmonary disease (COPD) who may not seek care until they experience an exacerbation?
Self-management interventions for COPD can potentially improve quality of life and reduce hospitalizations, wrote Robert Wu, MD, associate professor in the Department of Medicine at the University of Toronto, and colleagues. However, data on the use of devices and apps to manage COPD by providing reminders for self-care, predicting early exacerbations, and facilitating communication with healthcare providers are limited, they said.
In a study published in COPD: Journal of Chronic Obstructive Pulmonary Disease, the researchers reported details from interviews with 26 adult patients with COPD who used a wearable device and app for 6 months to help manage their condition. The interviews were part of a larger cohort study.
“The motivation for this study was to understand the patient perspective on using wearables to help support their chronic lung condition,” Dr. Wu said in an interview. “People with COPD can be at high risk of being admitted to hospital, so it is important to see if innovative technology like wearables or remote monitoring can help them,” he said.
Individuals with COPD tend to be older and less technologically adept, and they may be less willing to adopt new technology, he added. “We wanted to understand what would make people use a self-management app,” he said.
On enrollment in the study, patients received a smartwatch and a smartphone with a preinstalled app for COPD management. The app included daily reminders to take medication, perform guided breathing sessions, check blood oxygen on the smartwatch or an oximeter, and complete a symptom questionnaire. The app also allowed participants to record when they exercised and provided feedback on heart rate and daily activity, including passive step counts. Participants earned stars for meeting daily exercise goals of active minutes and total steps.
Participants received training in the use of the app from members of the research team and completed semi-structured interviews after using the items for 6 months.
The researchers divided their findings into four main themes: information, support and reassurance; barriers to adoption; impact on communication with healthcare providers; and opportunities for improvement.
Overall, most patients reported that the feedback they received through the app was useful. In particular, participants reported that the app and smartwatch provided reassurance and feedback about stable vitals during exercise, which encouraged some to adhere to regular exercise routines. Approximately two thirds (65%) said that the daily exercise reminders were motivational. In addition, 20% reported that they interpreted vital data, including heart rate, as a signal to slow down.
Participants rated medication reminders and the option to create an action plan for COPD management as the least useful features; 69% said that they already had medication reminders in place.
A total of four patients experienced technical difficulties with the app that kept it from impacting their disease management. Some of the suggestions from participants for improvement included adding information about food intake, weight, blood pressure, and temperature to the health information being tracked, as well as restoring the oxygen saturation measure, which had been disabled because of accuracy concerns. Barriers to use of the device and app included the bulkiness of the device as well as the reported technical malfunctions.
The findings were limited by several factors, including the small sample size and likely focus on early adopters of technology, which may not represent most patients with COPD, the researchers noted. Other limitations included the recruitment of most patients after the start of the COVID-19 pandemic, which may have affected their experience and also limited the assessment of the app on communication with healthcare providers, the researchers noted. The study also did not address financial or social barriers.
However, the results suggest that patients with COPD identified the potential value of wearable devices for disease management and that improved technology could promote patient empowerment and lifestyle changes, the researchers concluded.
Technology Can Augment Care and Connections
“As clinicians and researchers, we have ideas about what patients would want, but it is always better to get their feedback of what they really want and what they would use,” Dr. Wu told this news organization. “We thought older adults with COPD would be less likely to engage with the technology. We found that many wanted to have their data to help make connections with their condition, and some purchased smartwatches after the study to make these connections,” he said.
The takeaway message from the current study is that people with COPD may benefit from self-management apps, but they would like to use them in collaboration with their healthcare team, said Dr. Wu. “Clinicians may see more of their patients bringing in data from wearables and apps,” he noted.
Concerns persist that using technology to help support people with COPD could increase the “digital divide” and that those with lower digital literacy, financial insecurity, or English as a second language could be left behind, and it is important to remain attentive to equity in pursuing the use of devices and apps, Dr. Wu told this news organization.
Looking ahead, research involving self-management, remote monitoring, and wearable devices has focused on other conditions such as heart failure and diabetes, and more work is needed to examine how these technologies can improve care for patients with COPD, said Dr. Wu. “We see this study as one important step — to understand what will motivate people to use self-management apps and wearables,” he said.
“Acute exacerbations of COPD are very important events that can alter quality of life, lung function, and even mortality in COPD,” said Nathaniel Marchetti, DO, medical director of the Respiratory Intensive Care Unit at Temple University Hospital, Philadelphia, in an interview.
“Many of these exacerbations are not recognized by clinicians or even patients until they present late and end up in an urgent office visit with a physician or in the emergency room [ER], so addressing exacerbations earlier has the potential to avoid ER visits or hospitalizations,” he said.
The study identified areas for further research, Dr. Marchetti said. “More information would be needed to determine if the use of an app to monitor heart rate, symptoms, and oxygen saturation could alter important outcomes in COPD such as exacerbations,” he noted.
As for limitations, “no one wants to carry two smartphones,” said Dr. Marchetti. “Future devices need to be easy to use and available on the patient’s own phone,” he said. Patients should be able to choose a smartwatch or possibly a bracelet that can be synced to a smartphone, he added. The current study also failed to address what would be done with collected data, such as link them to health professionals who would offer treatment when needed, he said.
Overall, the data from the current study suggest that patients with COPD would like some device that monitors symptoms and vital signs and offers suggestions/incentives to exercise and take medications, Dr. Marchetti told this news organization. “A larger study will be needed that compares how such a device could improve outcomes of COPD; outcomes could include admissions/ER visits, exercise performance, or compliance with medication,” he said. In addition, clinical algorithms for the identification and treatment of acute exacerbations of COPD would be needed, Dr. Marchetti noted. These algorithms would determine whether treatment decisions would be initiated by a clinical team of health professionals or whether clinicians would provide medications that the patients would then decide to take based on data collected on the app, using the investigator-provided algorithms, he said.
The study was supported in part by Samsung Research America (SRA) and was initiated by Dr. Wu with input from SRA, but the company had no role in the methods or results. The study also was supported by grants from the National Natural Science Foundation of China.
Dr. Marchetti had no relevant financial conflicts to disclose.
A version of this article appeared on Medscape.com.
Could mobile technology help patients with chronic obstructive pulmonary disease (COPD) who may not seek care until they experience an exacerbation?
Self-management interventions for COPD can potentially improve quality of life and reduce hospitalizations, wrote Robert Wu, MD, associate professor in the Department of Medicine at the University of Toronto, and colleagues. However, data on the use of devices and apps to manage COPD by providing reminders for self-care, predicting early exacerbations, and facilitating communication with healthcare providers are limited, they said.
In a study published in COPD: Journal of Chronic Obstructive Pulmonary Disease, the researchers reported details from interviews with 26 adult patients with COPD who used a wearable device and app for 6 months to help manage their condition. The interviews were part of a larger cohort study.
“The motivation for this study was to understand the patient perspective on using wearables to help support their chronic lung condition,” Dr. Wu said in an interview. “People with COPD can be at high risk of being admitted to hospital, so it is important to see if innovative technology like wearables or remote monitoring can help them,” he said.
Individuals with COPD tend to be older and less technologically adept, and they may be less willing to adopt new technology, he added. “We wanted to understand what would make people use a self-management app,” he said.
On enrollment in the study, patients received a smartwatch and a smartphone with a preinstalled app for COPD management. The app included daily reminders to take medication, perform guided breathing sessions, check blood oxygen on the smartwatch or an oximeter, and complete a symptom questionnaire. The app also allowed participants to record when they exercised and provided feedback on heart rate and daily activity, including passive step counts. Participants earned stars for meeting daily exercise goals of active minutes and total steps.
Participants received training in the use of the app from members of the research team and completed semi-structured interviews after using the items for 6 months.
The researchers divided their findings into four main themes: information, support and reassurance; barriers to adoption; impact on communication with healthcare providers; and opportunities for improvement.
Overall, most patients reported that the feedback they received through the app was useful. In particular, participants reported that the app and smartwatch provided reassurance and feedback about stable vitals during exercise, which encouraged some to adhere to regular exercise routines. Approximately two thirds (65%) said that the daily exercise reminders were motivational. In addition, 20% reported that they interpreted vital data, including heart rate, as a signal to slow down.
Participants rated medication reminders and the option to create an action plan for COPD management as the least useful features; 69% said that they already had medication reminders in place.
A total of four patients experienced technical difficulties with the app that kept it from impacting their disease management. Some of the suggestions from participants for improvement included adding information about food intake, weight, blood pressure, and temperature to the health information being tracked, as well as restoring the oxygen saturation measure, which had been disabled because of accuracy concerns. Barriers to use of the device and app included the bulkiness of the device as well as the reported technical malfunctions.
The findings were limited by several factors, including the small sample size and likely focus on early adopters of technology, which may not represent most patients with COPD, the researchers noted. Other limitations included the recruitment of most patients after the start of the COVID-19 pandemic, which may have affected their experience and also limited the assessment of the app on communication with healthcare providers, the researchers noted. The study also did not address financial or social barriers.
However, the results suggest that patients with COPD identified the potential value of wearable devices for disease management and that improved technology could promote patient empowerment and lifestyle changes, the researchers concluded.
Technology Can Augment Care and Connections
“As clinicians and researchers, we have ideas about what patients would want, but it is always better to get their feedback of what they really want and what they would use,” Dr. Wu told this news organization. “We thought older adults with COPD would be less likely to engage with the technology. We found that many wanted to have their data to help make connections with their condition, and some purchased smartwatches after the study to make these connections,” he said.
The takeaway message from the current study is that people with COPD may benefit from self-management apps, but they would like to use them in collaboration with their healthcare team, said Dr. Wu. “Clinicians may see more of their patients bringing in data from wearables and apps,” he noted.
Concerns persist that using technology to help support people with COPD could increase the “digital divide” and that those with lower digital literacy, financial insecurity, or English as a second language could be left behind, and it is important to remain attentive to equity in pursuing the use of devices and apps, Dr. Wu told this news organization.
Looking ahead, research involving self-management, remote monitoring, and wearable devices has focused on other conditions such as heart failure and diabetes, and more work is needed to examine how these technologies can improve care for patients with COPD, said Dr. Wu. “We see this study as one important step — to understand what will motivate people to use self-management apps and wearables,” he said.
“Acute exacerbations of COPD are very important events that can alter quality of life, lung function, and even mortality in COPD,” said Nathaniel Marchetti, DO, medical director of the Respiratory Intensive Care Unit at Temple University Hospital, Philadelphia, in an interview.
“Many of these exacerbations are not recognized by clinicians or even patients until they present late and end up in an urgent office visit with a physician or in the emergency room [ER], so addressing exacerbations earlier has the potential to avoid ER visits or hospitalizations,” he said.
The study identified areas for further research, Dr. Marchetti said. “More information would be needed to determine if the use of an app to monitor heart rate, symptoms, and oxygen saturation could alter important outcomes in COPD such as exacerbations,” he noted.
As for limitations, “no one wants to carry two smartphones,” said Dr. Marchetti. “Future devices need to be easy to use and available on the patient’s own phone,” he said. Patients should be able to choose a smartwatch or possibly a bracelet that can be synced to a smartphone, he added. The current study also failed to address what would be done with collected data, such as link them to health professionals who would offer treatment when needed, he said.
Overall, the data from the current study suggest that patients with COPD would like some device that monitors symptoms and vital signs and offers suggestions/incentives to exercise and take medications, Dr. Marchetti told this news organization. “A larger study will be needed that compares how such a device could improve outcomes of COPD; outcomes could include admissions/ER visits, exercise performance, or compliance with medication,” he said. In addition, clinical algorithms for the identification and treatment of acute exacerbations of COPD would be needed, Dr. Marchetti noted. These algorithms would determine whether treatment decisions would be initiated by a clinical team of health professionals or whether clinicians would provide medications that the patients would then decide to take based on data collected on the app, using the investigator-provided algorithms, he said.
The study was supported in part by Samsung Research America (SRA) and was initiated by Dr. Wu with input from SRA, but the company had no role in the methods or results. The study also was supported by grants from the National Natural Science Foundation of China.
Dr. Marchetti had no relevant financial conflicts to disclose.
A version of this article appeared on Medscape.com.
Will Hospital-at-Home Go Mainstream?
Jordan Stohler, a 42-year-old nurse in Knoxville, Tennessee, was readmitted to Fort Sanders Medical Center in June 2023 with sepsis after a double mastectomy.
She spent 5 days in the hospital after surgery to clear up the infection. Then she was offered a choice: She could either stay in the hospital while she received IV antibiotics, or she could go home and have the antibiotics given to her there under the Advanced Care at Home program of Covenant Health, the nine-hospital system to which Fort Sanders belongs.
She opted to go home, where she knew she’d be more comfortable and would be close to her beloved dog. In the end, she was very glad she did.
“I received great care in the hospital, but to be allowed to be in the comfort of your own home, to be around my dog, who I think is therapeutic, to be able to cook my own meals, and to have the same one-on-one nursing care that I would have gotten in the hospital was great,” Ms. Stohler said. “
Being cared for at home helped her heal, she said. “I probably would have gotten a little stir crazy if I’d stayed in the hospital any longer. I received excellent care at home.”
Currently, 322 hospitals in 37 states have Medicare waivers for these kinds of programs, although not all of them are currently functioning.
A recent survey published in JAMA found that nearly half of consumers would accept hospital-at-home, and more than a third were neutral on it. Only 17% said they’d rather be cared for in a brick-and-mortar hospital.
The findings of the JAMA survey confirm those of earlier studies, said Bruce Leff, MD, a professor at Johns Hopkins Medical School in Baltimore, who has researched hospital-at-home since the 1990s. Like the new study, those trials found that the results had no relationship to individual traits, such as socioeconomic status, medical conditions, age, gender, or race.
Whether a person felt comfortable with the idea of hospital-at-home boiled down “to a preference for receiving care at home or in the hospital,” he said. Some people distrust hospitals, and others feel insecure about receiving care at home, even if it is provided by qualified health care professionals.
How Patients Are Selected
While the details of hospital-at-home vary from program to program, the basic scenario is that patients who need certain kinds of acute care can be sent home from hospitals, emergency departments, or clinics to receive that care at home. Among the kinds of conditions that make stable patients eligible are heart failure, COPD, pneumonia, cellulitis, and COVID-19, said John Busigin, MD, a hospitalist and medical director of Covenant Advanced Care at Home.
When a patient is admitted to hospital-at-home, the hospital will send along whatever equipment and medications that person needs. In some cases, this may include a hospital bed, although Ms. Stohler used her own. An IV line was put into her arm, and the IV stand was placed next to the bed.
Ms. Stohler received a computer tablet that she used to communicate with doctors and nurses in Covenant’s “command center” in Knoxville. She also wore a watch with a button she could push in case of an emergency. And she had a telephone line that went directly to her medical team, in case she had an issue and the tablet didn’t work.
Twice a day, or as needed, specially trained paramedics came to Ms. Stohler’s home. They checked on the IV line, changed the IV bag, performed tests, and uploaded vital signs from monitoring equipment to Ms. Stohler’s tablet so it could be transmitted to the command center. A physician assistant came in on the second and fourth days of her weeklong stay in the program, and she saw a hospitalist remotely every day.
While some hospital-at-home programs have registered nurses visit patients at home, RNs are in short supply. To fill this gap, Covenant’s program uses community paramedics who have been in the field for at least 5 years, doing everything from intubating patients and placing them on ventilators to providing advanced cardiac life support, Dr. Busigin said. To get certified as community paramedics, they go through a 3-month training program.
Shortly after Ms. Stohler went into hospital-at-home, she had another crisis. Excess fluid had built up in her body because of all the IV fluids she’d received in the hospital while fighting the sepsis. As a result, she became short of breath. If she had been discharged to home rather than hospital-at-home, she said, she would have had to go to the emergency room. Instead, she sent out a distress call. One of the paramedics rushed to her house and gave her an IV diuretic medication, which helped her urinate to get rid of the excess fluid.
A small number of the estimated 300 people who have gone through the program had to be admitted to the hospital, Dr. Busigin said. Nationally, he said, about 5%-10% are admitted. But readmissions among the patients in the Covenant program have been 25% lower than for patients who received conventional hospital care and had the same conditions as those in hospital-at-home.
Studies have shown that these programs not only reduce readmissions, but also cost less, on average, and create a better patient experience than traditional hospital care does. And, according to the JAMA survey, most consumers like the idea. Fifty-six percent of people who took the survey agreed with the statement that people recover faster at home than in the hospital. Fifty-nine percent agreed they’d feel safe being treated at home, and 49% said they’d be more comfortable if treated at home.
The 1134 people who took the survey were also asked about their comfort level with providing various kinds of care to their loved ones during a hospital-at-home episode. The results varied with the type of task: For example, 82% of the respondents agreed or strongly agreed they could manage a patient’s medications, while just 41% said they’d be willing to change a feeding tube. Smaller percentages were willing to change an IV bag or a catheter or do wound care.
However, hospital-at-home programs don’t allow caregivers to take part in clinical care, which is prohibited by Medicare waivers and state licensing regulations. None of the 22 health systems that use the hospital-at-home services of Medically Home, including Covenant, ask caregivers to do anything along this line, said Pippa Shulman, DO, medical director of the company, which provides equipment, technology, and protocols for hospital programs
The only exception at Covenant, Dr. Busigin said, is that the hospital may train family members to do wound care when a patient is discharged from the hospital to Advanced Care at Home. They may also prepare meals for their loved ones, although the program provides balanced meals to patients if they want them. Ms. Stohler had some of these meals, which just had to be heated up, for the first few days of hospital-at-home, and later her relatives brought meals to her house.
Challenges for the Future
The number of Medicare hospital-at-home waivers has nearly doubled since 2021. A year earlier, when Medicare began reimbursing hospitals for acute care at home to help them cope with the overflow of COVID patients, there were only about 15-20 programs in the United States, said Dr. Leff of Johns Hopkins.
A big reason for the lack of use before the pandemic, Dr. Leff said, is that there was no payment system for hospitals that offered hospital-at-home. Now, they can get paid by Medicare and 10 state Medicaid programs, and a number of private payers are also coming on board. Ms. Stohler’s private insurer covered her hospital-at-home stay, and Dr. Busigin said several plans that contract with Covenant will pay for it.
Dr. Leff said he’s cautiously optimistic Congress will extend the Medicare waiver program, which is scheduled to end in December, for another 5 years. A couple of key House committees have signed off on a bill to do that, he said, and a Congressional Budget Office report found that the program did not cost Medicare more money.
But even if the waiver is renewed, some health systems may find it tough to deliver the service. The current version of this model depends a lot on technology, because telemedicine is used and reliable communication is needed for patients in hospital-at-home. That’s why many of the hospitals hire outside vendors like Medically Home to provide the infrastructure they need.
Medically Home manages the tablets given to patients and all connection and networking services, including internet and cellphone connections. It also provides technical services in the command centers that hospitals set up for the doctors and nurses who provide care remotely.
And the firm figures out how to deliver the standard care for each condition in each hospital-at-home. “We need to make sure that the patient is going to get what they need in the time frame it needs to be delivered in, and that it’s safe and effective for the patient,” Dr. Shulman said. “So we’ve developed logistical protocols for a multitude of disease states that allow us to provide high-acuity care in the home to a variety of complex patients.”
The health care workers use the hospital electronic health record for hospital-at-home patients, and vital signs uploaded from patient tablets flow directly into the electronic health record, she said.
Rural Areas Need Help
The use of hospital-at-home in rural areas holds a lot of promise, Dr. Leff said.
“A lot of rural hospitals have been closing, and hospital-at-home could be a mechanism to create hospital-level care where facilities have closed down. It’s easier to do this in urban areas, but it can be done in rural environments as well.”
Rami Karjian, CEO of Medically Home, agreed. The firm services hospital-at-home programs in rural areas of Oklahoma and California, using cellphones and paramedics in areas that lack broadband connections and nurses, he pointed out.
“Hospital-at-home can’t just be available to people who live in big cities,” he said. “The access problems in health care are pervasive, and this is part of how we solve access problems in rural areas.”
A version of this article first appeared on WebMD.com.
Jordan Stohler, a 42-year-old nurse in Knoxville, Tennessee, was readmitted to Fort Sanders Medical Center in June 2023 with sepsis after a double mastectomy.
She spent 5 days in the hospital after surgery to clear up the infection. Then she was offered a choice: She could either stay in the hospital while she received IV antibiotics, or she could go home and have the antibiotics given to her there under the Advanced Care at Home program of Covenant Health, the nine-hospital system to which Fort Sanders belongs.
She opted to go home, where she knew she’d be more comfortable and would be close to her beloved dog. In the end, she was very glad she did.
“I received great care in the hospital, but to be allowed to be in the comfort of your own home, to be around my dog, who I think is therapeutic, to be able to cook my own meals, and to have the same one-on-one nursing care that I would have gotten in the hospital was great,” Ms. Stohler said. “
Being cared for at home helped her heal, she said. “I probably would have gotten a little stir crazy if I’d stayed in the hospital any longer. I received excellent care at home.”
Currently, 322 hospitals in 37 states have Medicare waivers for these kinds of programs, although not all of them are currently functioning.
A recent survey published in JAMA found that nearly half of consumers would accept hospital-at-home, and more than a third were neutral on it. Only 17% said they’d rather be cared for in a brick-and-mortar hospital.
The findings of the JAMA survey confirm those of earlier studies, said Bruce Leff, MD, a professor at Johns Hopkins Medical School in Baltimore, who has researched hospital-at-home since the 1990s. Like the new study, those trials found that the results had no relationship to individual traits, such as socioeconomic status, medical conditions, age, gender, or race.
Whether a person felt comfortable with the idea of hospital-at-home boiled down “to a preference for receiving care at home or in the hospital,” he said. Some people distrust hospitals, and others feel insecure about receiving care at home, even if it is provided by qualified health care professionals.
How Patients Are Selected
While the details of hospital-at-home vary from program to program, the basic scenario is that patients who need certain kinds of acute care can be sent home from hospitals, emergency departments, or clinics to receive that care at home. Among the kinds of conditions that make stable patients eligible are heart failure, COPD, pneumonia, cellulitis, and COVID-19, said John Busigin, MD, a hospitalist and medical director of Covenant Advanced Care at Home.
When a patient is admitted to hospital-at-home, the hospital will send along whatever equipment and medications that person needs. In some cases, this may include a hospital bed, although Ms. Stohler used her own. An IV line was put into her arm, and the IV stand was placed next to the bed.
Ms. Stohler received a computer tablet that she used to communicate with doctors and nurses in Covenant’s “command center” in Knoxville. She also wore a watch with a button she could push in case of an emergency. And she had a telephone line that went directly to her medical team, in case she had an issue and the tablet didn’t work.
Twice a day, or as needed, specially trained paramedics came to Ms. Stohler’s home. They checked on the IV line, changed the IV bag, performed tests, and uploaded vital signs from monitoring equipment to Ms. Stohler’s tablet so it could be transmitted to the command center. A physician assistant came in on the second and fourth days of her weeklong stay in the program, and she saw a hospitalist remotely every day.
While some hospital-at-home programs have registered nurses visit patients at home, RNs are in short supply. To fill this gap, Covenant’s program uses community paramedics who have been in the field for at least 5 years, doing everything from intubating patients and placing them on ventilators to providing advanced cardiac life support, Dr. Busigin said. To get certified as community paramedics, they go through a 3-month training program.
Shortly after Ms. Stohler went into hospital-at-home, she had another crisis. Excess fluid had built up in her body because of all the IV fluids she’d received in the hospital while fighting the sepsis. As a result, she became short of breath. If she had been discharged to home rather than hospital-at-home, she said, she would have had to go to the emergency room. Instead, she sent out a distress call. One of the paramedics rushed to her house and gave her an IV diuretic medication, which helped her urinate to get rid of the excess fluid.
A small number of the estimated 300 people who have gone through the program had to be admitted to the hospital, Dr. Busigin said. Nationally, he said, about 5%-10% are admitted. But readmissions among the patients in the Covenant program have been 25% lower than for patients who received conventional hospital care and had the same conditions as those in hospital-at-home.
Studies have shown that these programs not only reduce readmissions, but also cost less, on average, and create a better patient experience than traditional hospital care does. And, according to the JAMA survey, most consumers like the idea. Fifty-six percent of people who took the survey agreed with the statement that people recover faster at home than in the hospital. Fifty-nine percent agreed they’d feel safe being treated at home, and 49% said they’d be more comfortable if treated at home.
The 1134 people who took the survey were also asked about their comfort level with providing various kinds of care to their loved ones during a hospital-at-home episode. The results varied with the type of task: For example, 82% of the respondents agreed or strongly agreed they could manage a patient’s medications, while just 41% said they’d be willing to change a feeding tube. Smaller percentages were willing to change an IV bag or a catheter or do wound care.
However, hospital-at-home programs don’t allow caregivers to take part in clinical care, which is prohibited by Medicare waivers and state licensing regulations. None of the 22 health systems that use the hospital-at-home services of Medically Home, including Covenant, ask caregivers to do anything along this line, said Pippa Shulman, DO, medical director of the company, which provides equipment, technology, and protocols for hospital programs
The only exception at Covenant, Dr. Busigin said, is that the hospital may train family members to do wound care when a patient is discharged from the hospital to Advanced Care at Home. They may also prepare meals for their loved ones, although the program provides balanced meals to patients if they want them. Ms. Stohler had some of these meals, which just had to be heated up, for the first few days of hospital-at-home, and later her relatives brought meals to her house.
Challenges for the Future
The number of Medicare hospital-at-home waivers has nearly doubled since 2021. A year earlier, when Medicare began reimbursing hospitals for acute care at home to help them cope with the overflow of COVID patients, there were only about 15-20 programs in the United States, said Dr. Leff of Johns Hopkins.
A big reason for the lack of use before the pandemic, Dr. Leff said, is that there was no payment system for hospitals that offered hospital-at-home. Now, they can get paid by Medicare and 10 state Medicaid programs, and a number of private payers are also coming on board. Ms. Stohler’s private insurer covered her hospital-at-home stay, and Dr. Busigin said several plans that contract with Covenant will pay for it.
Dr. Leff said he’s cautiously optimistic Congress will extend the Medicare waiver program, which is scheduled to end in December, for another 5 years. A couple of key House committees have signed off on a bill to do that, he said, and a Congressional Budget Office report found that the program did not cost Medicare more money.
But even if the waiver is renewed, some health systems may find it tough to deliver the service. The current version of this model depends a lot on technology, because telemedicine is used and reliable communication is needed for patients in hospital-at-home. That’s why many of the hospitals hire outside vendors like Medically Home to provide the infrastructure they need.
Medically Home manages the tablets given to patients and all connection and networking services, including internet and cellphone connections. It also provides technical services in the command centers that hospitals set up for the doctors and nurses who provide care remotely.
And the firm figures out how to deliver the standard care for each condition in each hospital-at-home. “We need to make sure that the patient is going to get what they need in the time frame it needs to be delivered in, and that it’s safe and effective for the patient,” Dr. Shulman said. “So we’ve developed logistical protocols for a multitude of disease states that allow us to provide high-acuity care in the home to a variety of complex patients.”
The health care workers use the hospital electronic health record for hospital-at-home patients, and vital signs uploaded from patient tablets flow directly into the electronic health record, she said.
Rural Areas Need Help
The use of hospital-at-home in rural areas holds a lot of promise, Dr. Leff said.
“A lot of rural hospitals have been closing, and hospital-at-home could be a mechanism to create hospital-level care where facilities have closed down. It’s easier to do this in urban areas, but it can be done in rural environments as well.”
Rami Karjian, CEO of Medically Home, agreed. The firm services hospital-at-home programs in rural areas of Oklahoma and California, using cellphones and paramedics in areas that lack broadband connections and nurses, he pointed out.
“Hospital-at-home can’t just be available to people who live in big cities,” he said. “The access problems in health care are pervasive, and this is part of how we solve access problems in rural areas.”
A version of this article first appeared on WebMD.com.
Jordan Stohler, a 42-year-old nurse in Knoxville, Tennessee, was readmitted to Fort Sanders Medical Center in June 2023 with sepsis after a double mastectomy.
She spent 5 days in the hospital after surgery to clear up the infection. Then she was offered a choice: She could either stay in the hospital while she received IV antibiotics, or she could go home and have the antibiotics given to her there under the Advanced Care at Home program of Covenant Health, the nine-hospital system to which Fort Sanders belongs.
She opted to go home, where she knew she’d be more comfortable and would be close to her beloved dog. In the end, she was very glad she did.
“I received great care in the hospital, but to be allowed to be in the comfort of your own home, to be around my dog, who I think is therapeutic, to be able to cook my own meals, and to have the same one-on-one nursing care that I would have gotten in the hospital was great,” Ms. Stohler said. “
Being cared for at home helped her heal, she said. “I probably would have gotten a little stir crazy if I’d stayed in the hospital any longer. I received excellent care at home.”
Currently, 322 hospitals in 37 states have Medicare waivers for these kinds of programs, although not all of them are currently functioning.
A recent survey published in JAMA found that nearly half of consumers would accept hospital-at-home, and more than a third were neutral on it. Only 17% said they’d rather be cared for in a brick-and-mortar hospital.
The findings of the JAMA survey confirm those of earlier studies, said Bruce Leff, MD, a professor at Johns Hopkins Medical School in Baltimore, who has researched hospital-at-home since the 1990s. Like the new study, those trials found that the results had no relationship to individual traits, such as socioeconomic status, medical conditions, age, gender, or race.
Whether a person felt comfortable with the idea of hospital-at-home boiled down “to a preference for receiving care at home or in the hospital,” he said. Some people distrust hospitals, and others feel insecure about receiving care at home, even if it is provided by qualified health care professionals.
How Patients Are Selected
While the details of hospital-at-home vary from program to program, the basic scenario is that patients who need certain kinds of acute care can be sent home from hospitals, emergency departments, or clinics to receive that care at home. Among the kinds of conditions that make stable patients eligible are heart failure, COPD, pneumonia, cellulitis, and COVID-19, said John Busigin, MD, a hospitalist and medical director of Covenant Advanced Care at Home.
When a patient is admitted to hospital-at-home, the hospital will send along whatever equipment and medications that person needs. In some cases, this may include a hospital bed, although Ms. Stohler used her own. An IV line was put into her arm, and the IV stand was placed next to the bed.
Ms. Stohler received a computer tablet that she used to communicate with doctors and nurses in Covenant’s “command center” in Knoxville. She also wore a watch with a button she could push in case of an emergency. And she had a telephone line that went directly to her medical team, in case she had an issue and the tablet didn’t work.
Twice a day, or as needed, specially trained paramedics came to Ms. Stohler’s home. They checked on the IV line, changed the IV bag, performed tests, and uploaded vital signs from monitoring equipment to Ms. Stohler’s tablet so it could be transmitted to the command center. A physician assistant came in on the second and fourth days of her weeklong stay in the program, and she saw a hospitalist remotely every day.
While some hospital-at-home programs have registered nurses visit patients at home, RNs are in short supply. To fill this gap, Covenant’s program uses community paramedics who have been in the field for at least 5 years, doing everything from intubating patients and placing them on ventilators to providing advanced cardiac life support, Dr. Busigin said. To get certified as community paramedics, they go through a 3-month training program.
Shortly after Ms. Stohler went into hospital-at-home, she had another crisis. Excess fluid had built up in her body because of all the IV fluids she’d received in the hospital while fighting the sepsis. As a result, she became short of breath. If she had been discharged to home rather than hospital-at-home, she said, she would have had to go to the emergency room. Instead, she sent out a distress call. One of the paramedics rushed to her house and gave her an IV diuretic medication, which helped her urinate to get rid of the excess fluid.
A small number of the estimated 300 people who have gone through the program had to be admitted to the hospital, Dr. Busigin said. Nationally, he said, about 5%-10% are admitted. But readmissions among the patients in the Covenant program have been 25% lower than for patients who received conventional hospital care and had the same conditions as those in hospital-at-home.
Studies have shown that these programs not only reduce readmissions, but also cost less, on average, and create a better patient experience than traditional hospital care does. And, according to the JAMA survey, most consumers like the idea. Fifty-six percent of people who took the survey agreed with the statement that people recover faster at home than in the hospital. Fifty-nine percent agreed they’d feel safe being treated at home, and 49% said they’d be more comfortable if treated at home.
The 1134 people who took the survey were also asked about their comfort level with providing various kinds of care to their loved ones during a hospital-at-home episode. The results varied with the type of task: For example, 82% of the respondents agreed or strongly agreed they could manage a patient’s medications, while just 41% said they’d be willing to change a feeding tube. Smaller percentages were willing to change an IV bag or a catheter or do wound care.
However, hospital-at-home programs don’t allow caregivers to take part in clinical care, which is prohibited by Medicare waivers and state licensing regulations. None of the 22 health systems that use the hospital-at-home services of Medically Home, including Covenant, ask caregivers to do anything along this line, said Pippa Shulman, DO, medical director of the company, which provides equipment, technology, and protocols for hospital programs
The only exception at Covenant, Dr. Busigin said, is that the hospital may train family members to do wound care when a patient is discharged from the hospital to Advanced Care at Home. They may also prepare meals for their loved ones, although the program provides balanced meals to patients if they want them. Ms. Stohler had some of these meals, which just had to be heated up, for the first few days of hospital-at-home, and later her relatives brought meals to her house.
Challenges for the Future
The number of Medicare hospital-at-home waivers has nearly doubled since 2021. A year earlier, when Medicare began reimbursing hospitals for acute care at home to help them cope with the overflow of COVID patients, there were only about 15-20 programs in the United States, said Dr. Leff of Johns Hopkins.
A big reason for the lack of use before the pandemic, Dr. Leff said, is that there was no payment system for hospitals that offered hospital-at-home. Now, they can get paid by Medicare and 10 state Medicaid programs, and a number of private payers are also coming on board. Ms. Stohler’s private insurer covered her hospital-at-home stay, and Dr. Busigin said several plans that contract with Covenant will pay for it.
Dr. Leff said he’s cautiously optimistic Congress will extend the Medicare waiver program, which is scheduled to end in December, for another 5 years. A couple of key House committees have signed off on a bill to do that, he said, and a Congressional Budget Office report found that the program did not cost Medicare more money.
But even if the waiver is renewed, some health systems may find it tough to deliver the service. The current version of this model depends a lot on technology, because telemedicine is used and reliable communication is needed for patients in hospital-at-home. That’s why many of the hospitals hire outside vendors like Medically Home to provide the infrastructure they need.
Medically Home manages the tablets given to patients and all connection and networking services, including internet and cellphone connections. It also provides technical services in the command centers that hospitals set up for the doctors and nurses who provide care remotely.
And the firm figures out how to deliver the standard care for each condition in each hospital-at-home. “We need to make sure that the patient is going to get what they need in the time frame it needs to be delivered in, and that it’s safe and effective for the patient,” Dr. Shulman said. “So we’ve developed logistical protocols for a multitude of disease states that allow us to provide high-acuity care in the home to a variety of complex patients.”
The health care workers use the hospital electronic health record for hospital-at-home patients, and vital signs uploaded from patient tablets flow directly into the electronic health record, she said.
Rural Areas Need Help
The use of hospital-at-home in rural areas holds a lot of promise, Dr. Leff said.
“A lot of rural hospitals have been closing, and hospital-at-home could be a mechanism to create hospital-level care where facilities have closed down. It’s easier to do this in urban areas, but it can be done in rural environments as well.”
Rami Karjian, CEO of Medically Home, agreed. The firm services hospital-at-home programs in rural areas of Oklahoma and California, using cellphones and paramedics in areas that lack broadband connections and nurses, he pointed out.
“Hospital-at-home can’t just be available to people who live in big cities,” he said. “The access problems in health care are pervasive, and this is part of how we solve access problems in rural areas.”
A version of this article first appeared on WebMD.com.
Are Beta-Blockers Safe for COPD?
Everyone takes a pharmacology class in medical school that includes a lecture on beta receptors. They’re in the heart (beta-1) and lungs (beta-2), and drug compounds agonize or antagonize one or both. The professor will caution against using antagonists (beta blockade) for patients with chronic obstructive pulmonary disease (COPD) lest they further impair the patient’s irreversibly narrowed airways. Obsequious students mature into obsequious doctors, intent on “doing no harm.” For better or worse, you withhold beta-blockers from your patient with COPD and comorbid cardiac disease.
Perhaps because the pulmonologist isn’t usually the one who decides whether a beta-blocker is prescribed, I’ve been napping on this topic since training. Early in fellowship, I read an ACP Journal Club article about a Cochrane systematic review (yes, I read a review of a review) that concluded that beta-blockers are fine in patients with COPD. The summary appealed to my bias towards evidence-based medicine (EBM) supplanting physiology, medical school, and everything else. I was more apt to believe my stodgy residency attendings than the stodgy pharmacology professor. Even though COPD and cardiovascular disease share multiple risk factors, I had never reinvestigated the relationship between beta-blockers and COPD.
Turns out that while I was sleeping, the debate continued. Go figure. Just last month a prospective, observational study published in JAMA Network Open found that beta-blockers did not increase the risk for cardiovascular or respiratory events among patients with COPD being discharged after hospitalization for acute myocardial infarction. Although this could be viewed as a triumph for EBM over physiology and a validation of my decade-plus of intellectual laziness, the results are actually pretty thin. These studies, in which patients with an indication for a therapy (a beta-blocker in this case) are analyzed by whether or not they received it, are problematic. The fanciest statistics — in this case, they used propensity scores — can’t control for residual confounding. What drove the physicians to prescribe in some cases but not others? We can only guess.
This might be okay if there hadn’t been a randomized controlled trial (RCT) published in 2019 in The New England Journal of Medicine that found that beta-blockers increase the risk for severe COPD exacerbations. In EBM, the RCT trumps all. Ironically, this trial was designed to test whether beta-blockers reduce severe COPD exacerbations. Yes, we’d come full circle. There was enough biologic plausibility to support a positive effect, or so thought the study authors and the Department of Defense (DOD) — for reasons I can’t possibly guess, the DOD funded this RCT. My pharmacology professor must be rolling over in his tenure.
The RCT did leave beta-blockers some wiggle room. The authors purposely excluded anyone with a cardiovascular indication for a beta-blocker. The intent was to ensure beneficial effects were isolated to respiratory and not cardiovascular outcomes. Of course, the reason I’m writing and you’re reading this is that COPD and cardiovascular disease co-occur at a high rate. The RCT notwithstanding, we prescribe beta-blockers to patients with COPD because they have a cardiac indication, not to reduce acute COPD exacerbations. So, it’s possible there’d be a net beta-blocker benefit in patients with COPD and comorbid heart disease.
That’s where the JAMA Network Open study comes in, but as discussed, methodologic weaknesses preclude its being the final word. That said, I think it’s unlikely we’ll see a COPD with comorbid cardiac disease RCT performed to assess whether beta-blockers provide a net benefit, unless maybe the DOD wants to fund another one of these. In the meantime, I’m calling clinical equipoise and punting. Fortunately for me, I don’t have to prescribe beta-blockers.
Dr. Holley is professor of medicine at Uniformed Services University in Bethesda, Maryland, and a pulmonary/sleep and critical care medicine physician at MedStar Washington Hospital Center in Washington, DC. He reported conflicts of interest with Metapharm, CHEST College, and WebMD.
A version of this article first appeared on Medscape.com.
Everyone takes a pharmacology class in medical school that includes a lecture on beta receptors. They’re in the heart (beta-1) and lungs (beta-2), and drug compounds agonize or antagonize one or both. The professor will caution against using antagonists (beta blockade) for patients with chronic obstructive pulmonary disease (COPD) lest they further impair the patient’s irreversibly narrowed airways. Obsequious students mature into obsequious doctors, intent on “doing no harm.” For better or worse, you withhold beta-blockers from your patient with COPD and comorbid cardiac disease.
Perhaps because the pulmonologist isn’t usually the one who decides whether a beta-blocker is prescribed, I’ve been napping on this topic since training. Early in fellowship, I read an ACP Journal Club article about a Cochrane systematic review (yes, I read a review of a review) that concluded that beta-blockers are fine in patients with COPD. The summary appealed to my bias towards evidence-based medicine (EBM) supplanting physiology, medical school, and everything else. I was more apt to believe my stodgy residency attendings than the stodgy pharmacology professor. Even though COPD and cardiovascular disease share multiple risk factors, I had never reinvestigated the relationship between beta-blockers and COPD.
Turns out that while I was sleeping, the debate continued. Go figure. Just last month a prospective, observational study published in JAMA Network Open found that beta-blockers did not increase the risk for cardiovascular or respiratory events among patients with COPD being discharged after hospitalization for acute myocardial infarction. Although this could be viewed as a triumph for EBM over physiology and a validation of my decade-plus of intellectual laziness, the results are actually pretty thin. These studies, in which patients with an indication for a therapy (a beta-blocker in this case) are analyzed by whether or not they received it, are problematic. The fanciest statistics — in this case, they used propensity scores — can’t control for residual confounding. What drove the physicians to prescribe in some cases but not others? We can only guess.
This might be okay if there hadn’t been a randomized controlled trial (RCT) published in 2019 in The New England Journal of Medicine that found that beta-blockers increase the risk for severe COPD exacerbations. In EBM, the RCT trumps all. Ironically, this trial was designed to test whether beta-blockers reduce severe COPD exacerbations. Yes, we’d come full circle. There was enough biologic plausibility to support a positive effect, or so thought the study authors and the Department of Defense (DOD) — for reasons I can’t possibly guess, the DOD funded this RCT. My pharmacology professor must be rolling over in his tenure.
The RCT did leave beta-blockers some wiggle room. The authors purposely excluded anyone with a cardiovascular indication for a beta-blocker. The intent was to ensure beneficial effects were isolated to respiratory and not cardiovascular outcomes. Of course, the reason I’m writing and you’re reading this is that COPD and cardiovascular disease co-occur at a high rate. The RCT notwithstanding, we prescribe beta-blockers to patients with COPD because they have a cardiac indication, not to reduce acute COPD exacerbations. So, it’s possible there’d be a net beta-blocker benefit in patients with COPD and comorbid heart disease.
That’s where the JAMA Network Open study comes in, but as discussed, methodologic weaknesses preclude its being the final word. That said, I think it’s unlikely we’ll see a COPD with comorbid cardiac disease RCT performed to assess whether beta-blockers provide a net benefit, unless maybe the DOD wants to fund another one of these. In the meantime, I’m calling clinical equipoise and punting. Fortunately for me, I don’t have to prescribe beta-blockers.
Dr. Holley is professor of medicine at Uniformed Services University in Bethesda, Maryland, and a pulmonary/sleep and critical care medicine physician at MedStar Washington Hospital Center in Washington, DC. He reported conflicts of interest with Metapharm, CHEST College, and WebMD.
A version of this article first appeared on Medscape.com.
Everyone takes a pharmacology class in medical school that includes a lecture on beta receptors. They’re in the heart (beta-1) and lungs (beta-2), and drug compounds agonize or antagonize one or both. The professor will caution against using antagonists (beta blockade) for patients with chronic obstructive pulmonary disease (COPD) lest they further impair the patient’s irreversibly narrowed airways. Obsequious students mature into obsequious doctors, intent on “doing no harm.” For better or worse, you withhold beta-blockers from your patient with COPD and comorbid cardiac disease.
Perhaps because the pulmonologist isn’t usually the one who decides whether a beta-blocker is prescribed, I’ve been napping on this topic since training. Early in fellowship, I read an ACP Journal Club article about a Cochrane systematic review (yes, I read a review of a review) that concluded that beta-blockers are fine in patients with COPD. The summary appealed to my bias towards evidence-based medicine (EBM) supplanting physiology, medical school, and everything else. I was more apt to believe my stodgy residency attendings than the stodgy pharmacology professor. Even though COPD and cardiovascular disease share multiple risk factors, I had never reinvestigated the relationship between beta-blockers and COPD.
Turns out that while I was sleeping, the debate continued. Go figure. Just last month a prospective, observational study published in JAMA Network Open found that beta-blockers did not increase the risk for cardiovascular or respiratory events among patients with COPD being discharged after hospitalization for acute myocardial infarction. Although this could be viewed as a triumph for EBM over physiology and a validation of my decade-plus of intellectual laziness, the results are actually pretty thin. These studies, in which patients with an indication for a therapy (a beta-blocker in this case) are analyzed by whether or not they received it, are problematic. The fanciest statistics — in this case, they used propensity scores — can’t control for residual confounding. What drove the physicians to prescribe in some cases but not others? We can only guess.
This might be okay if there hadn’t been a randomized controlled trial (RCT) published in 2019 in The New England Journal of Medicine that found that beta-blockers increase the risk for severe COPD exacerbations. In EBM, the RCT trumps all. Ironically, this trial was designed to test whether beta-blockers reduce severe COPD exacerbations. Yes, we’d come full circle. There was enough biologic plausibility to support a positive effect, or so thought the study authors and the Department of Defense (DOD) — for reasons I can’t possibly guess, the DOD funded this RCT. My pharmacology professor must be rolling over in his tenure.
The RCT did leave beta-blockers some wiggle room. The authors purposely excluded anyone with a cardiovascular indication for a beta-blocker. The intent was to ensure beneficial effects were isolated to respiratory and not cardiovascular outcomes. Of course, the reason I’m writing and you’re reading this is that COPD and cardiovascular disease co-occur at a high rate. The RCT notwithstanding, we prescribe beta-blockers to patients with COPD because they have a cardiac indication, not to reduce acute COPD exacerbations. So, it’s possible there’d be a net beta-blocker benefit in patients with COPD and comorbid heart disease.
That’s where the JAMA Network Open study comes in, but as discussed, methodologic weaknesses preclude its being the final word. That said, I think it’s unlikely we’ll see a COPD with comorbid cardiac disease RCT performed to assess whether beta-blockers provide a net benefit, unless maybe the DOD wants to fund another one of these. In the meantime, I’m calling clinical equipoise and punting. Fortunately for me, I don’t have to prescribe beta-blockers.
Dr. Holley is professor of medicine at Uniformed Services University in Bethesda, Maryland, and a pulmonary/sleep and critical care medicine physician at MedStar Washington Hospital Center in Washington, DC. He reported conflicts of interest with Metapharm, CHEST College, and WebMD.
A version of this article first appeared on Medscape.com.
Cost of Drugs Can Be Breathtaking for COPD Patients
For patients with chronic obstructive pulmonary disease (COPD), the Global Initiative on Obstructive Lung Disease recommends long-term term pharmacologic and nonpharmacologic therapies based on each patient’s symptoms and disease severity.
Yet even the most effective drugs work only when patients take them as directed, and according to the World Health Organization, fewer than half of all patients worldwide are fully compliant with long-term COPD drug regimens.
And as a recent cross-sectional study showed, nearly one in six patients in the United States reported missing a COPD drug dose, lowering the dose, or delaying filling a prescription for financial reasons.
“I care for patients with COPD as their pulmonologist, and this is a very common problem that we see in clinical practice,” said Meredith McCormack, MD, a pulmonary and critical care medicine physician and associate director of the Pulmonary & Critical Care Medicine Division at Johns Hopkins University in Baltimore.
Dr. McCormack, a national spokesperson for The American Lung Association, said that she shows new patients the photos of all available inhalers and asks which ones they have and how they take them.
“I would say that a majority of the time people are taking their medicines slightly differently than prescribed, and often, this is due to cost,” she said.
Serious Consequences
Cost-related medication nonadherence (CRN), as investigators term it, can have major health effects and can be significantly more costly in the long run due to increased hospitalization rates, higher morbidity, and greater risk for COPD-related death associated with suboptimal care.
“For some patients even a month or two of being off medications increases the risk of having exacerbations, having more symptoms, [and] having a decline in their lung function,” said Douglas M. Beach, MD, a pulmonologist at Beth Israel Deaconess Medical Center in Boston.
In the aforementioned cross-sectional study, published in the open access journal BMC Public Health, Xin Wen, MD, from the Jiamusi (China) University School of Public Health, and colleagues looked at data on a representative sample of US adults who participated in the US National Health Interview Survey from 2013 through 2020.
The sample included 15,928 persons aged 18 years or older with a self-reported history of COPD who completed a CRN survey including the following questions:
During the past 12 months, have you
- Skipped medication doses to save money?
- Taken less medicine than prescribed to save money?
- Delayed filling a prescription to save money?
The investigators found that a weighted 18.56% of participants representing 2.39 million persons with COPD answered “yes” to one of the questions.
Translated into representative population numbers, that works out to an estimated 1.61 million persons with COPD missing doses, 1.72 million taking lower doses than those prescribed, and 2.03 million delaying filling prescriptions to save money.
A multivariable logistic regression analysis showed that those who were most likely to be nonadherent for financial reasons were patients younger than 65 years, women, persons with low family income, those who lacked health insurance, and patients with multiple comorbidities, the authors found.
Financial Barriers
One of the biggest barriers to COPD medication adherence is, somewhat paradoxically, insurance status, particularly Medicare, said Corinne Young, MSN, FNP-C, FCCP, from Colorado Springs Pulmonary Consultants.
“What’s so unfair about Medicare is that patients have to buy a drug plan, so they have to already pay for an extra plan to have access to drugs, and the plans vary because there are so many choices,” she said in an interview.
Elderly patients may be confused about the available options and may choose the Medicare Advantage plan with the lowest monthly premiums, which have the highest annual deductibles, usually in the $5000-and-up range, she said.
In addition, the Medicare Part D prescription coverage gap, commonly known as the “donut hole,” requires patients to pay a percentage of drug costs above a certain limit ($5030 in 2024) until a yearly out-of-pocket limit (currently $8000) is reached, after which the plan will again pick up most of the costs.
Although makers of inhalers have voluntarily agreed to limit monthly co-pays to $35 for uninsured patients, Medicare plans require insured patients to shell out considerably more, with 30 days of Trelegy Ellipta (fluticasone furoate, umeclidinium, and vilanterol) setting patients back nearly $350 per month, according to a recent search of costs for a United Healthcare Medicare Advantage plan.
Chasing Lower-Cost Options
“I have a lot of patients who use Canadian pharmacies to try to get around it, and I have a lot of patients who make a trip to Mexico every year and load up. I have patients who don’t take their inhalers as they are supposed to in order to make them last longer, and I have patients who take the inhalers of other family members,” Ms. Young said.
Humayun Anjum, MD, FCCP, from Dallas Pulmonary and Critical Care in Dallas, Texas, said in an interview that when patients claim that a prescribed drug isn’t working as expected for them, financial pressures may be partly to blame.
“When you investigate a little bit more, that’s where things become a bit more clear, and the patient may say ‘yeah, I stopped using this inhaler because it was costing me 200 bucks a month and I’m already on other medications,’ ” he said.
He noted that, when possible, he will steer patients toward discount prescription services such as GoodRx, which offers discounts at local pharmacies, or Mark Cuban Cost Plus Drugs, an online pharmacy that offers generic versions of Advair Diskus (fluticasone propionate/salmeterol) at a 100-50 mcg dose for $94.70, a savings of $307.30 over retail pharmacies, according to the company’s website.
Dr. Beach noted that Beth Israel Deaconess has a pharmacist embedded in the pulmonary clinic who can help eligible patients get financial assistance to pay for their medications.
“The influencing factors of CRN are multifaceted and necessitating more rigorous research. Health policy interventions focusing on reducing drug costs, delaying disease progression, preventing exacerbations, and reducing the risk of comorbidities may improve the economic burden of COPD and its outcomes,” Dr. Wen and colleagues wrote.
The study by Dr. Wen and colleagues was funded by grants from Chinese national and academic sources. Dr. McCormack has served as a consultant to Aridis, Boehringer Ingelheim, GlaxoSmithKline, MCG Diagnostics, ndd Medical Technologies, and UpToDate. Ms. Young, Dr. Anjum, and Dr. Beach reported no conflicts of interest.
A version of this article first appeared on Medscape.com.
For patients with chronic obstructive pulmonary disease (COPD), the Global Initiative on Obstructive Lung Disease recommends long-term term pharmacologic and nonpharmacologic therapies based on each patient’s symptoms and disease severity.
Yet even the most effective drugs work only when patients take them as directed, and according to the World Health Organization, fewer than half of all patients worldwide are fully compliant with long-term COPD drug regimens.
And as a recent cross-sectional study showed, nearly one in six patients in the United States reported missing a COPD drug dose, lowering the dose, or delaying filling a prescription for financial reasons.
“I care for patients with COPD as their pulmonologist, and this is a very common problem that we see in clinical practice,” said Meredith McCormack, MD, a pulmonary and critical care medicine physician and associate director of the Pulmonary & Critical Care Medicine Division at Johns Hopkins University in Baltimore.
Dr. McCormack, a national spokesperson for The American Lung Association, said that she shows new patients the photos of all available inhalers and asks which ones they have and how they take them.
“I would say that a majority of the time people are taking their medicines slightly differently than prescribed, and often, this is due to cost,” she said.
Serious Consequences
Cost-related medication nonadherence (CRN), as investigators term it, can have major health effects and can be significantly more costly in the long run due to increased hospitalization rates, higher morbidity, and greater risk for COPD-related death associated with suboptimal care.
“For some patients even a month or two of being off medications increases the risk of having exacerbations, having more symptoms, [and] having a decline in their lung function,” said Douglas M. Beach, MD, a pulmonologist at Beth Israel Deaconess Medical Center in Boston.
In the aforementioned cross-sectional study, published in the open access journal BMC Public Health, Xin Wen, MD, from the Jiamusi (China) University School of Public Health, and colleagues looked at data on a representative sample of US adults who participated in the US National Health Interview Survey from 2013 through 2020.
The sample included 15,928 persons aged 18 years or older with a self-reported history of COPD who completed a CRN survey including the following questions:
During the past 12 months, have you
- Skipped medication doses to save money?
- Taken less medicine than prescribed to save money?
- Delayed filling a prescription to save money?
The investigators found that a weighted 18.56% of participants representing 2.39 million persons with COPD answered “yes” to one of the questions.
Translated into representative population numbers, that works out to an estimated 1.61 million persons with COPD missing doses, 1.72 million taking lower doses than those prescribed, and 2.03 million delaying filling prescriptions to save money.
A multivariable logistic regression analysis showed that those who were most likely to be nonadherent for financial reasons were patients younger than 65 years, women, persons with low family income, those who lacked health insurance, and patients with multiple comorbidities, the authors found.
Financial Barriers
One of the biggest barriers to COPD medication adherence is, somewhat paradoxically, insurance status, particularly Medicare, said Corinne Young, MSN, FNP-C, FCCP, from Colorado Springs Pulmonary Consultants.
“What’s so unfair about Medicare is that patients have to buy a drug plan, so they have to already pay for an extra plan to have access to drugs, and the plans vary because there are so many choices,” she said in an interview.
Elderly patients may be confused about the available options and may choose the Medicare Advantage plan with the lowest monthly premiums, which have the highest annual deductibles, usually in the $5000-and-up range, she said.
In addition, the Medicare Part D prescription coverage gap, commonly known as the “donut hole,” requires patients to pay a percentage of drug costs above a certain limit ($5030 in 2024) until a yearly out-of-pocket limit (currently $8000) is reached, after which the plan will again pick up most of the costs.
Although makers of inhalers have voluntarily agreed to limit monthly co-pays to $35 for uninsured patients, Medicare plans require insured patients to shell out considerably more, with 30 days of Trelegy Ellipta (fluticasone furoate, umeclidinium, and vilanterol) setting patients back nearly $350 per month, according to a recent search of costs for a United Healthcare Medicare Advantage plan.
Chasing Lower-Cost Options
“I have a lot of patients who use Canadian pharmacies to try to get around it, and I have a lot of patients who make a trip to Mexico every year and load up. I have patients who don’t take their inhalers as they are supposed to in order to make them last longer, and I have patients who take the inhalers of other family members,” Ms. Young said.
Humayun Anjum, MD, FCCP, from Dallas Pulmonary and Critical Care in Dallas, Texas, said in an interview that when patients claim that a prescribed drug isn’t working as expected for them, financial pressures may be partly to blame.
“When you investigate a little bit more, that’s where things become a bit more clear, and the patient may say ‘yeah, I stopped using this inhaler because it was costing me 200 bucks a month and I’m already on other medications,’ ” he said.
He noted that, when possible, he will steer patients toward discount prescription services such as GoodRx, which offers discounts at local pharmacies, or Mark Cuban Cost Plus Drugs, an online pharmacy that offers generic versions of Advair Diskus (fluticasone propionate/salmeterol) at a 100-50 mcg dose for $94.70, a savings of $307.30 over retail pharmacies, according to the company’s website.
Dr. Beach noted that Beth Israel Deaconess has a pharmacist embedded in the pulmonary clinic who can help eligible patients get financial assistance to pay for their medications.
“The influencing factors of CRN are multifaceted and necessitating more rigorous research. Health policy interventions focusing on reducing drug costs, delaying disease progression, preventing exacerbations, and reducing the risk of comorbidities may improve the economic burden of COPD and its outcomes,” Dr. Wen and colleagues wrote.
The study by Dr. Wen and colleagues was funded by grants from Chinese national and academic sources. Dr. McCormack has served as a consultant to Aridis, Boehringer Ingelheim, GlaxoSmithKline, MCG Diagnostics, ndd Medical Technologies, and UpToDate. Ms. Young, Dr. Anjum, and Dr. Beach reported no conflicts of interest.
A version of this article first appeared on Medscape.com.
For patients with chronic obstructive pulmonary disease (COPD), the Global Initiative on Obstructive Lung Disease recommends long-term term pharmacologic and nonpharmacologic therapies based on each patient’s symptoms and disease severity.
Yet even the most effective drugs work only when patients take them as directed, and according to the World Health Organization, fewer than half of all patients worldwide are fully compliant with long-term COPD drug regimens.
And as a recent cross-sectional study showed, nearly one in six patients in the United States reported missing a COPD drug dose, lowering the dose, or delaying filling a prescription for financial reasons.
“I care for patients with COPD as their pulmonologist, and this is a very common problem that we see in clinical practice,” said Meredith McCormack, MD, a pulmonary and critical care medicine physician and associate director of the Pulmonary & Critical Care Medicine Division at Johns Hopkins University in Baltimore.
Dr. McCormack, a national spokesperson for The American Lung Association, said that she shows new patients the photos of all available inhalers and asks which ones they have and how they take them.
“I would say that a majority of the time people are taking their medicines slightly differently than prescribed, and often, this is due to cost,” she said.
Serious Consequences
Cost-related medication nonadherence (CRN), as investigators term it, can have major health effects and can be significantly more costly in the long run due to increased hospitalization rates, higher morbidity, and greater risk for COPD-related death associated with suboptimal care.
“For some patients even a month or two of being off medications increases the risk of having exacerbations, having more symptoms, [and] having a decline in their lung function,” said Douglas M. Beach, MD, a pulmonologist at Beth Israel Deaconess Medical Center in Boston.
In the aforementioned cross-sectional study, published in the open access journal BMC Public Health, Xin Wen, MD, from the Jiamusi (China) University School of Public Health, and colleagues looked at data on a representative sample of US adults who participated in the US National Health Interview Survey from 2013 through 2020.
The sample included 15,928 persons aged 18 years or older with a self-reported history of COPD who completed a CRN survey including the following questions:
During the past 12 months, have you
- Skipped medication doses to save money?
- Taken less medicine than prescribed to save money?
- Delayed filling a prescription to save money?
The investigators found that a weighted 18.56% of participants representing 2.39 million persons with COPD answered “yes” to one of the questions.
Translated into representative population numbers, that works out to an estimated 1.61 million persons with COPD missing doses, 1.72 million taking lower doses than those prescribed, and 2.03 million delaying filling prescriptions to save money.
A multivariable logistic regression analysis showed that those who were most likely to be nonadherent for financial reasons were patients younger than 65 years, women, persons with low family income, those who lacked health insurance, and patients with multiple comorbidities, the authors found.
Financial Barriers
One of the biggest barriers to COPD medication adherence is, somewhat paradoxically, insurance status, particularly Medicare, said Corinne Young, MSN, FNP-C, FCCP, from Colorado Springs Pulmonary Consultants.
“What’s so unfair about Medicare is that patients have to buy a drug plan, so they have to already pay for an extra plan to have access to drugs, and the plans vary because there are so many choices,” she said in an interview.
Elderly patients may be confused about the available options and may choose the Medicare Advantage plan with the lowest monthly premiums, which have the highest annual deductibles, usually in the $5000-and-up range, she said.
In addition, the Medicare Part D prescription coverage gap, commonly known as the “donut hole,” requires patients to pay a percentage of drug costs above a certain limit ($5030 in 2024) until a yearly out-of-pocket limit (currently $8000) is reached, after which the plan will again pick up most of the costs.
Although makers of inhalers have voluntarily agreed to limit monthly co-pays to $35 for uninsured patients, Medicare plans require insured patients to shell out considerably more, with 30 days of Trelegy Ellipta (fluticasone furoate, umeclidinium, and vilanterol) setting patients back nearly $350 per month, according to a recent search of costs for a United Healthcare Medicare Advantage plan.
Chasing Lower-Cost Options
“I have a lot of patients who use Canadian pharmacies to try to get around it, and I have a lot of patients who make a trip to Mexico every year and load up. I have patients who don’t take their inhalers as they are supposed to in order to make them last longer, and I have patients who take the inhalers of other family members,” Ms. Young said.
Humayun Anjum, MD, FCCP, from Dallas Pulmonary and Critical Care in Dallas, Texas, said in an interview that when patients claim that a prescribed drug isn’t working as expected for them, financial pressures may be partly to blame.
“When you investigate a little bit more, that’s where things become a bit more clear, and the patient may say ‘yeah, I stopped using this inhaler because it was costing me 200 bucks a month and I’m already on other medications,’ ” he said.
He noted that, when possible, he will steer patients toward discount prescription services such as GoodRx, which offers discounts at local pharmacies, or Mark Cuban Cost Plus Drugs, an online pharmacy that offers generic versions of Advair Diskus (fluticasone propionate/salmeterol) at a 100-50 mcg dose for $94.70, a savings of $307.30 over retail pharmacies, according to the company’s website.
Dr. Beach noted that Beth Israel Deaconess has a pharmacist embedded in the pulmonary clinic who can help eligible patients get financial assistance to pay for their medications.
“The influencing factors of CRN are multifaceted and necessitating more rigorous research. Health policy interventions focusing on reducing drug costs, delaying disease progression, preventing exacerbations, and reducing the risk of comorbidities may improve the economic burden of COPD and its outcomes,” Dr. Wen and colleagues wrote.
The study by Dr. Wen and colleagues was funded by grants from Chinese national and academic sources. Dr. McCormack has served as a consultant to Aridis, Boehringer Ingelheim, GlaxoSmithKline, MCG Diagnostics, ndd Medical Technologies, and UpToDate. Ms. Young, Dr. Anjum, and Dr. Beach reported no conflicts of interest.
A version of this article first appeared on Medscape.com.