User login
Lung cancer biomarker moves into the clinic
SEATTLE – A new biomarker for bronchial epithelium that helps identify smokers with suspicious lesions who have lung cancer is now ready for clinical use. And one for nasal epithelium that could be used for screening may not be far behind.
“There is clearly a critical unmet need to develop molecular biomarkers to address some of the challenges that we now face since we have instituted CT screening for lung cancer,” Dr. Avi Spira said at a joint meeting of the Global Biomarkers Consortium and World Cutaneous Malignancies Congress.
Although the National Lung Screening Trial established that annual chest CT among high-risk current and former smokers reduces their risk of death from lung cancer (N Engl J Med. 2011;365:395-409), the vast majority of those who screen positive do not have lung cancer. Also, screening only patients who meet criteria set by the trial will pick up less than half of all lung cancers in the United States.
“That leads to two critical unmet needs for molecular biomarkers in the so-called post–National Lung Screening Trial era,” said Dr. Spira, professor of medicine, pathology and laboratory medicine, and bioinformatics; chief of the division of computational biomedicine; and director of the translational bioinformatics program, Clinical and Translational Science Institute, all at Boston University.
“The first is … we desperately need molecular biomarkers that can distinguish a benign nodule found on CT versus a malignant one,” he said. “The second and arguably longer-term biomarker that we need is to distinguish which smokers would benefit from CT screening annually.”
Much of his team’s research in this area builds on the concept of field of injury. “The idea here is if you smoke, even though lung cancer tends to develop deep within the parenchyma of your lung, all of the epithelial cells that line your respiratory tract have genomic alterations that reflect the presence of that cancer,” Dr. Spira explained. Thus, profiling epithelial cells anywhere in the airway could be used for early detection and risk assessment.
He and his colleagues developed a 23-gene signature for use on bronchial epithelial cells. The biomarker was validated in the Airway Epithelium Gene Expression In the Diagnosis of Lung Cancer (AEGIS) 1 and 2 trials among 639 current and former smokers undergoing bronchoscopy for suspicious nodules seen on CT.
With 1 year of follow-up, biomarker sensitivity was 88%-89%, while specificity was 47% (N Engl J Med. 2015;373:243-251). “However the negative predictive value, which is really what drives the clinical utility of this test, is above 90%. And that’s what we believe will drive physicians to use the test – [determining] who can they avoid sending for an unnecessary [biopsy] procedure,” Dr. Spira said. Bronchoscopy alone had sensitivity of about 75%, but bronchoscopy combined with the gene signature had sensitivity of 97%.
Subgroup analyses showed the biomarker had superior sensitivity for detecting lung cancer when lesions measured no more than 3 cm or were located in the lung periphery, and when patients had early-stage disease. In addition, it performed similarly well across different types of tumors.
Of special note, among patients whose pretest probability of cancer fell in the intermediate range (10%-60%), bronchoscopy had an 83% nondiagnostic rate, but the biomarker had 88% sensitivity and a 91% negative predictive value. “That means if you have a nondiagnostic bronchoscopy in a patient who is at intermediate pretest risk for disease, a negative gene expression test would mean there is a less than 10% chance this is cancer. That’s where a physician might feel, okay, I don’t have to go on and do a biopsy, I can watch that patient serially with CT scans of the chest,” Dr. Spira said.
The biomarker test is now clinically available (Percepta, manufactured by Veracyte). “I think it’s exciting because it’s the first of what I believe are many molecular biomarkers that are going to be emerging in the clinical space for the early detection of lung cancer,” he said.
“The multimillion dollar question is why are we seeing gene expression changes in normal-appearing cells so far away from where the tumor arises? We don’t have the full answer to that yet, but based on the genes that are changing, we have developed some hypotheses,” Dr. Spira said.
Some of the down-regulated genes are involved in antioxidant and DNA repair pathways, suggesting that the smokers who ultimately get cancer have less of a protective response to smoking. And some of the up-regulated genes include ones in the PI3 kinase signaling pathway.
“I would argue that what we are seeing in the proximal airway isn’t necessarily reflecting the presence of the cancer but the susceptibility, and that’s a really important distinguishing factor because then perhaps the test could be used as a screening tool,” Dr. Spira maintained.
As not all smokers at elevated risk for lung cancer will undergo bronchoscopy, one of the investigators’ future goals is to move biomarker testing to a less invasive site. They are currently focusing on the nose, using nasal epithelium collected by brushings from the inferior turbinate.
An analysis of nasal epithelium collected at the time of bronchoscopy in the AEGIS trials has shown that a 200-gene signature performs well for distinguishing between patients with and without lung cancer, Dr. Spira reported. Furthermore, the changes in gene expression profile in the nose were similar to those seen in the bronchus.
Such a biomarker might have best clinical utility in two other settings, he proposed. The first would be in patients having nodules that are clearly not accessible by bronchoscopy, in which case the biomarker would be applied for diagnosis. The second would be in smokers being seen for routine annual exams, in which case it would be used to identify those who should have CT surveillance.
“We are hopeful that the nasal epithelium can serve as a less invasive surrogate for the bronchus and ultimately allow us to move airway profiling into the screening setting for lung cancer in the longer term,” he concluded.
Dr. Spira disclosed that he receives intellectual property rights and consulting fees from, and has an ownership interest in, Veracyte Inc.
SEATTLE – A new biomarker for bronchial epithelium that helps identify smokers with suspicious lesions who have lung cancer is now ready for clinical use. And one for nasal epithelium that could be used for screening may not be far behind.
“There is clearly a critical unmet need to develop molecular biomarkers to address some of the challenges that we now face since we have instituted CT screening for lung cancer,” Dr. Avi Spira said at a joint meeting of the Global Biomarkers Consortium and World Cutaneous Malignancies Congress.
Although the National Lung Screening Trial established that annual chest CT among high-risk current and former smokers reduces their risk of death from lung cancer (N Engl J Med. 2011;365:395-409), the vast majority of those who screen positive do not have lung cancer. Also, screening only patients who meet criteria set by the trial will pick up less than half of all lung cancers in the United States.
“That leads to two critical unmet needs for molecular biomarkers in the so-called post–National Lung Screening Trial era,” said Dr. Spira, professor of medicine, pathology and laboratory medicine, and bioinformatics; chief of the division of computational biomedicine; and director of the translational bioinformatics program, Clinical and Translational Science Institute, all at Boston University.
“The first is … we desperately need molecular biomarkers that can distinguish a benign nodule found on CT versus a malignant one,” he said. “The second and arguably longer-term biomarker that we need is to distinguish which smokers would benefit from CT screening annually.”
Much of his team’s research in this area builds on the concept of field of injury. “The idea here is if you smoke, even though lung cancer tends to develop deep within the parenchyma of your lung, all of the epithelial cells that line your respiratory tract have genomic alterations that reflect the presence of that cancer,” Dr. Spira explained. Thus, profiling epithelial cells anywhere in the airway could be used for early detection and risk assessment.
He and his colleagues developed a 23-gene signature for use on bronchial epithelial cells. The biomarker was validated in the Airway Epithelium Gene Expression In the Diagnosis of Lung Cancer (AEGIS) 1 and 2 trials among 639 current and former smokers undergoing bronchoscopy for suspicious nodules seen on CT.
With 1 year of follow-up, biomarker sensitivity was 88%-89%, while specificity was 47% (N Engl J Med. 2015;373:243-251). “However the negative predictive value, which is really what drives the clinical utility of this test, is above 90%. And that’s what we believe will drive physicians to use the test – [determining] who can they avoid sending for an unnecessary [biopsy] procedure,” Dr. Spira said. Bronchoscopy alone had sensitivity of about 75%, but bronchoscopy combined with the gene signature had sensitivity of 97%.
Subgroup analyses showed the biomarker had superior sensitivity for detecting lung cancer when lesions measured no more than 3 cm or were located in the lung periphery, and when patients had early-stage disease. In addition, it performed similarly well across different types of tumors.
Of special note, among patients whose pretest probability of cancer fell in the intermediate range (10%-60%), bronchoscopy had an 83% nondiagnostic rate, but the biomarker had 88% sensitivity and a 91% negative predictive value. “That means if you have a nondiagnostic bronchoscopy in a patient who is at intermediate pretest risk for disease, a negative gene expression test would mean there is a less than 10% chance this is cancer. That’s where a physician might feel, okay, I don’t have to go on and do a biopsy, I can watch that patient serially with CT scans of the chest,” Dr. Spira said.
The biomarker test is now clinically available (Percepta, manufactured by Veracyte). “I think it’s exciting because it’s the first of what I believe are many molecular biomarkers that are going to be emerging in the clinical space for the early detection of lung cancer,” he said.
“The multimillion dollar question is why are we seeing gene expression changes in normal-appearing cells so far away from where the tumor arises? We don’t have the full answer to that yet, but based on the genes that are changing, we have developed some hypotheses,” Dr. Spira said.
Some of the down-regulated genes are involved in antioxidant and DNA repair pathways, suggesting that the smokers who ultimately get cancer have less of a protective response to smoking. And some of the up-regulated genes include ones in the PI3 kinase signaling pathway.
“I would argue that what we are seeing in the proximal airway isn’t necessarily reflecting the presence of the cancer but the susceptibility, and that’s a really important distinguishing factor because then perhaps the test could be used as a screening tool,” Dr. Spira maintained.
As not all smokers at elevated risk for lung cancer will undergo bronchoscopy, one of the investigators’ future goals is to move biomarker testing to a less invasive site. They are currently focusing on the nose, using nasal epithelium collected by brushings from the inferior turbinate.
An analysis of nasal epithelium collected at the time of bronchoscopy in the AEGIS trials has shown that a 200-gene signature performs well for distinguishing between patients with and without lung cancer, Dr. Spira reported. Furthermore, the changes in gene expression profile in the nose were similar to those seen in the bronchus.
Such a biomarker might have best clinical utility in two other settings, he proposed. The first would be in patients having nodules that are clearly not accessible by bronchoscopy, in which case the biomarker would be applied for diagnosis. The second would be in smokers being seen for routine annual exams, in which case it would be used to identify those who should have CT surveillance.
“We are hopeful that the nasal epithelium can serve as a less invasive surrogate for the bronchus and ultimately allow us to move airway profiling into the screening setting for lung cancer in the longer term,” he concluded.
Dr. Spira disclosed that he receives intellectual property rights and consulting fees from, and has an ownership interest in, Veracyte Inc.
SEATTLE – A new biomarker for bronchial epithelium that helps identify smokers with suspicious lesions who have lung cancer is now ready for clinical use. And one for nasal epithelium that could be used for screening may not be far behind.
“There is clearly a critical unmet need to develop molecular biomarkers to address some of the challenges that we now face since we have instituted CT screening for lung cancer,” Dr. Avi Spira said at a joint meeting of the Global Biomarkers Consortium and World Cutaneous Malignancies Congress.
Although the National Lung Screening Trial established that annual chest CT among high-risk current and former smokers reduces their risk of death from lung cancer (N Engl J Med. 2011;365:395-409), the vast majority of those who screen positive do not have lung cancer. Also, screening only patients who meet criteria set by the trial will pick up less than half of all lung cancers in the United States.
“That leads to two critical unmet needs for molecular biomarkers in the so-called post–National Lung Screening Trial era,” said Dr. Spira, professor of medicine, pathology and laboratory medicine, and bioinformatics; chief of the division of computational biomedicine; and director of the translational bioinformatics program, Clinical and Translational Science Institute, all at Boston University.
“The first is … we desperately need molecular biomarkers that can distinguish a benign nodule found on CT versus a malignant one,” he said. “The second and arguably longer-term biomarker that we need is to distinguish which smokers would benefit from CT screening annually.”
Much of his team’s research in this area builds on the concept of field of injury. “The idea here is if you smoke, even though lung cancer tends to develop deep within the parenchyma of your lung, all of the epithelial cells that line your respiratory tract have genomic alterations that reflect the presence of that cancer,” Dr. Spira explained. Thus, profiling epithelial cells anywhere in the airway could be used for early detection and risk assessment.
He and his colleagues developed a 23-gene signature for use on bronchial epithelial cells. The biomarker was validated in the Airway Epithelium Gene Expression In the Diagnosis of Lung Cancer (AEGIS) 1 and 2 trials among 639 current and former smokers undergoing bronchoscopy for suspicious nodules seen on CT.
With 1 year of follow-up, biomarker sensitivity was 88%-89%, while specificity was 47% (N Engl J Med. 2015;373:243-251). “However the negative predictive value, which is really what drives the clinical utility of this test, is above 90%. And that’s what we believe will drive physicians to use the test – [determining] who can they avoid sending for an unnecessary [biopsy] procedure,” Dr. Spira said. Bronchoscopy alone had sensitivity of about 75%, but bronchoscopy combined with the gene signature had sensitivity of 97%.
Subgroup analyses showed the biomarker had superior sensitivity for detecting lung cancer when lesions measured no more than 3 cm or were located in the lung periphery, and when patients had early-stage disease. In addition, it performed similarly well across different types of tumors.
Of special note, among patients whose pretest probability of cancer fell in the intermediate range (10%-60%), bronchoscopy had an 83% nondiagnostic rate, but the biomarker had 88% sensitivity and a 91% negative predictive value. “That means if you have a nondiagnostic bronchoscopy in a patient who is at intermediate pretest risk for disease, a negative gene expression test would mean there is a less than 10% chance this is cancer. That’s where a physician might feel, okay, I don’t have to go on and do a biopsy, I can watch that patient serially with CT scans of the chest,” Dr. Spira said.
The biomarker test is now clinically available (Percepta, manufactured by Veracyte). “I think it’s exciting because it’s the first of what I believe are many molecular biomarkers that are going to be emerging in the clinical space for the early detection of lung cancer,” he said.
“The multimillion dollar question is why are we seeing gene expression changes in normal-appearing cells so far away from where the tumor arises? We don’t have the full answer to that yet, but based on the genes that are changing, we have developed some hypotheses,” Dr. Spira said.
Some of the down-regulated genes are involved in antioxidant and DNA repair pathways, suggesting that the smokers who ultimately get cancer have less of a protective response to smoking. And some of the up-regulated genes include ones in the PI3 kinase signaling pathway.
“I would argue that what we are seeing in the proximal airway isn’t necessarily reflecting the presence of the cancer but the susceptibility, and that’s a really important distinguishing factor because then perhaps the test could be used as a screening tool,” Dr. Spira maintained.
As not all smokers at elevated risk for lung cancer will undergo bronchoscopy, one of the investigators’ future goals is to move biomarker testing to a less invasive site. They are currently focusing on the nose, using nasal epithelium collected by brushings from the inferior turbinate.
An analysis of nasal epithelium collected at the time of bronchoscopy in the AEGIS trials has shown that a 200-gene signature performs well for distinguishing between patients with and without lung cancer, Dr. Spira reported. Furthermore, the changes in gene expression profile in the nose were similar to those seen in the bronchus.
Such a biomarker might have best clinical utility in two other settings, he proposed. The first would be in patients having nodules that are clearly not accessible by bronchoscopy, in which case the biomarker would be applied for diagnosis. The second would be in smokers being seen for routine annual exams, in which case it would be used to identify those who should have CT surveillance.
“We are hopeful that the nasal epithelium can serve as a less invasive surrogate for the bronchus and ultimately allow us to move airway profiling into the screening setting for lung cancer in the longer term,” he concluded.
Dr. Spira disclosed that he receives intellectual property rights and consulting fees from, and has an ownership interest in, Veracyte Inc.
AT THE GLOBAL BIOMARKERS CONSORTIUM CONFERENCE
Similar outcomes for salvage vs. planned surgery after chemoradiotherapy in esophageal cancer
For patients with esophageal cancer, salvage surgery after definitive chemoradiotherapy had similar mortality and morbidity rates, and similar survival outcomes, to the combination of neoadjuvant chemoradiation and planned surgery, according to a study published online in the Journal of Clinical Oncology.
Definitive chemoradiotherapy (dCRT) is an alternative to highly invasive surgical resection, which carries a significant rate of morbidity and mortality; however, recent data indicate that 50% of patients with complete response to dCRT experience tumor recurrence.
“Our study demonstrated a similar survival and recurrence pattern for the SALV [salvage surgery after definitive chemoradiotherapy] and NCRS [neoadjuvant chemoradiation and planned surgery] groups, potentially validating an approach of dCRT with reserved SALV for persistent or recurrent disease. Importantly, there were no differences in oncologic safety of surgery, including extent of nodal dissection, between the SALV and NCRS groups,” wrote Dr. Sheraz Markar, a clinical research fellow from Imperial College, London, and colleagues (Journ. Clin. Onc. 2015 July 20 [doi:10.1200/JCO.2014.59.9092]).
The retrospective study compared 308 patients with esophageal cancer who underwent SALV with 540 patients who received NCRS at European centers from 2000 to 2010. After a median follow up of 54 months, the SALV and NCRS groups had similar rates of 3-year overall survival (43.3% vs. 40.1% ) and disease-free survival (39.2% vs. 32.8%). The two groups also had similar rates tumor recurrence: overall (46.8% vs. 47.9%), locoregional (18.8% vs. 15.9%), distant (24.3% vs. 28.1%) and mixed (13.0% vs. 13.5%).
The SALV and NCRS groups had similar rates of in-hospital mortality (8.4% vs. 9.3%) and morbidity (63.6% vs. 58.9%), but SALV patients had significantly more complications from anastomotic leak (17.2% vs. 10.7%) and surgical site infection (18.5% vs. 12.2%).
Subset analysis of the SALV group showed that patients who received a total radiation dose ≥ 55 Gy (compared with SALV patients who received a lower dose) had significantly increased in-hospital mortality (27.8% vs. 4.3%; P < .001), overall morbidity (75.9% vs. 61%; P = .039), anastomotic leak (27.8% vs. 15%; P = .023), surgical site infection (29.6% vs. 16.1%; P = .02), and pulmonary complications (55.6% vs. 40.2%; P = .038).
“Currently, there is no evidence in terms of locoregional control or survival benefit to support a high total radiation dose (> 50 Gy) in patients receiving dCRT,” according to the researchers, who noted that the findings suggest, “an upper threshold of 50 Gy should be used in these patients to optimize the benefits of dCRT without compromising the safety of SALV, if required.”
Patients who underwent SALV at high-volume centers had significantly lower rates of in-hospital mortality (6.3% vs. 16.2%; P = .009) and overall morbidity (58.8% vs. 80.9%; P = .001) compared with procedures done at low-volume centers.
Compared with recurrent disease, patients with persistent disease after dCRT had poorer long-term prognoses, suggesting a more aggressive tumor biology. Early identification of CRT-resistant tumors to allow early surgical treatment is an important area for future investigation, the investigators said.
For patients with esophageal cancer, salvage surgery after definitive chemoradiotherapy had similar mortality and morbidity rates, and similar survival outcomes, to the combination of neoadjuvant chemoradiation and planned surgery, according to a study published online in the Journal of Clinical Oncology.
Definitive chemoradiotherapy (dCRT) is an alternative to highly invasive surgical resection, which carries a significant rate of morbidity and mortality; however, recent data indicate that 50% of patients with complete response to dCRT experience tumor recurrence.
“Our study demonstrated a similar survival and recurrence pattern for the SALV [salvage surgery after definitive chemoradiotherapy] and NCRS [neoadjuvant chemoradiation and planned surgery] groups, potentially validating an approach of dCRT with reserved SALV for persistent or recurrent disease. Importantly, there were no differences in oncologic safety of surgery, including extent of nodal dissection, between the SALV and NCRS groups,” wrote Dr. Sheraz Markar, a clinical research fellow from Imperial College, London, and colleagues (Journ. Clin. Onc. 2015 July 20 [doi:10.1200/JCO.2014.59.9092]).
The retrospective study compared 308 patients with esophageal cancer who underwent SALV with 540 patients who received NCRS at European centers from 2000 to 2010. After a median follow up of 54 months, the SALV and NCRS groups had similar rates of 3-year overall survival (43.3% vs. 40.1% ) and disease-free survival (39.2% vs. 32.8%). The two groups also had similar rates tumor recurrence: overall (46.8% vs. 47.9%), locoregional (18.8% vs. 15.9%), distant (24.3% vs. 28.1%) and mixed (13.0% vs. 13.5%).
The SALV and NCRS groups had similar rates of in-hospital mortality (8.4% vs. 9.3%) and morbidity (63.6% vs. 58.9%), but SALV patients had significantly more complications from anastomotic leak (17.2% vs. 10.7%) and surgical site infection (18.5% vs. 12.2%).
Subset analysis of the SALV group showed that patients who received a total radiation dose ≥ 55 Gy (compared with SALV patients who received a lower dose) had significantly increased in-hospital mortality (27.8% vs. 4.3%; P < .001), overall morbidity (75.9% vs. 61%; P = .039), anastomotic leak (27.8% vs. 15%; P = .023), surgical site infection (29.6% vs. 16.1%; P = .02), and pulmonary complications (55.6% vs. 40.2%; P = .038).
“Currently, there is no evidence in terms of locoregional control or survival benefit to support a high total radiation dose (> 50 Gy) in patients receiving dCRT,” according to the researchers, who noted that the findings suggest, “an upper threshold of 50 Gy should be used in these patients to optimize the benefits of dCRT without compromising the safety of SALV, if required.”
Patients who underwent SALV at high-volume centers had significantly lower rates of in-hospital mortality (6.3% vs. 16.2%; P = .009) and overall morbidity (58.8% vs. 80.9%; P = .001) compared with procedures done at low-volume centers.
Compared with recurrent disease, patients with persistent disease after dCRT had poorer long-term prognoses, suggesting a more aggressive tumor biology. Early identification of CRT-resistant tumors to allow early surgical treatment is an important area for future investigation, the investigators said.
For patients with esophageal cancer, salvage surgery after definitive chemoradiotherapy had similar mortality and morbidity rates, and similar survival outcomes, to the combination of neoadjuvant chemoradiation and planned surgery, according to a study published online in the Journal of Clinical Oncology.
Definitive chemoradiotherapy (dCRT) is an alternative to highly invasive surgical resection, which carries a significant rate of morbidity and mortality; however, recent data indicate that 50% of patients with complete response to dCRT experience tumor recurrence.
“Our study demonstrated a similar survival and recurrence pattern for the SALV [salvage surgery after definitive chemoradiotherapy] and NCRS [neoadjuvant chemoradiation and planned surgery] groups, potentially validating an approach of dCRT with reserved SALV for persistent or recurrent disease. Importantly, there were no differences in oncologic safety of surgery, including extent of nodal dissection, between the SALV and NCRS groups,” wrote Dr. Sheraz Markar, a clinical research fellow from Imperial College, London, and colleagues (Journ. Clin. Onc. 2015 July 20 [doi:10.1200/JCO.2014.59.9092]).
The retrospective study compared 308 patients with esophageal cancer who underwent SALV with 540 patients who received NCRS at European centers from 2000 to 2010. After a median follow up of 54 months, the SALV and NCRS groups had similar rates of 3-year overall survival (43.3% vs. 40.1% ) and disease-free survival (39.2% vs. 32.8%). The two groups also had similar rates tumor recurrence: overall (46.8% vs. 47.9%), locoregional (18.8% vs. 15.9%), distant (24.3% vs. 28.1%) and mixed (13.0% vs. 13.5%).
The SALV and NCRS groups had similar rates of in-hospital mortality (8.4% vs. 9.3%) and morbidity (63.6% vs. 58.9%), but SALV patients had significantly more complications from anastomotic leak (17.2% vs. 10.7%) and surgical site infection (18.5% vs. 12.2%).
Subset analysis of the SALV group showed that patients who received a total radiation dose ≥ 55 Gy (compared with SALV patients who received a lower dose) had significantly increased in-hospital mortality (27.8% vs. 4.3%; P < .001), overall morbidity (75.9% vs. 61%; P = .039), anastomotic leak (27.8% vs. 15%; P = .023), surgical site infection (29.6% vs. 16.1%; P = .02), and pulmonary complications (55.6% vs. 40.2%; P = .038).
“Currently, there is no evidence in terms of locoregional control or survival benefit to support a high total radiation dose (> 50 Gy) in patients receiving dCRT,” according to the researchers, who noted that the findings suggest, “an upper threshold of 50 Gy should be used in these patients to optimize the benefits of dCRT without compromising the safety of SALV, if required.”
Patients who underwent SALV at high-volume centers had significantly lower rates of in-hospital mortality (6.3% vs. 16.2%; P = .009) and overall morbidity (58.8% vs. 80.9%; P = .001) compared with procedures done at low-volume centers.
Compared with recurrent disease, patients with persistent disease after dCRT had poorer long-term prognoses, suggesting a more aggressive tumor biology. Early identification of CRT-resistant tumors to allow early surgical treatment is an important area for future investigation, the investigators said.
FROM JOURNAL OF CLINICAL ONCOLOGY
Key clinical point: As management for esophageal cancer, salvage esophagectomy after definitive chemoradiotherapy (SALV) produced similar outcomes to the combination of neoadjuvant chemoradiation and planned surgery (NCRS).
Major finding: The SALV and NCRS groups had similar rates of 3-year overall survival (43.3% vs. 40.1% ) and disease-free survival (39.2% vs. 32.8%), tumor recurrence (46.8% vs. 47.9%), and in-hospital mortality (8.4% vs. 9.3%) and morbidity (63.6% vs. 58.9%).
Data source: Retrospective analysis of 848 patients (308 SALV, 540 NCRS) who underwent surgical resection for esophageal cancer in French-speaking European centers from 2000 to 2010.
Disclosures: Dr. Markar reported having no disclosures. Two of his coauthors reported ties to industry.
Dickkopf-3 overexpression linked to tumor traits in esophageal adenocarcinoma
Esophageal adenocarcinoma is fatal to 90% of patients, indicating a profound need for new therapeutic agents, according to Zhuewn Wang and her colleagues.
The search for genes involved in oncogenesis provides one avenue for finding potential targets. Ms. Wang and her colleagues performed a laboratory study at the University of Michigan, Ann Arbor, to examine the results of the overexpression of DKK3 (the gene for the Dickkopf-3 protein [DKK3]) in DKK3-transfected tissue-cultured esophageal adenocarcinoma (EAC) cell lines. They found that DKK3 overexpression correlated with significantly increased proliferation and Matrigel invasion ability – both known to be important oncogenic traits (J. Thorac. Cardiovasc. Surg. 2015;150:377-85).
DKK3 was overexpressed (greater than twofold) in 76% (72/95) of esophageal adenocarcinomas tested. In addition, the DKK3 protein was present at moderate to high levels in 47% (29/62) of esophageal adenocarcinomas as shown by tissue microarray. Nodal metastases were also significantly increased in patients with esophageal adenocarcinomas highly overexpressing DKK3 (28/32) vs. non–highly expressing EAC tumors (42/63).
In vitro studies showed that stable transfection of DKK3 in an EAC cell line significantly increased proliferation and Matrigel invasion. The researchers also found that the levels of SMAD4, a key mediator of the transforming growth factor–beta pathway, increased after activin treatment of the transfected cell line, and siSMAD4 significantly decreased Matrigel invasion, suggesting that DKK3 acts through the transforming growth factor–beta pathway, according to the researchers.
Additionally, the transfected cells showed increased endothelial tube formation, and they were significantly more resistant to 5-fluorouracil and cisplatin. This finding correlates with the fact that DKK3 expression was found to be significantly higher in chemoresistant esophageal adenocarcinomas, the investigators reported.
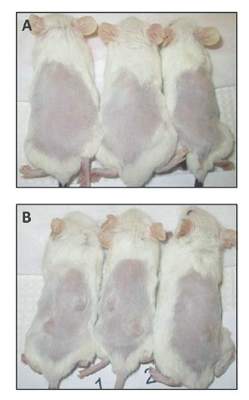
In their animal model system (NOD/SCIDg mice), injection of the transfected cells resulted in tumors at all sites (8/8), whereas vector-only cells grew in only one of eight sites.
“The results of the current study suggest that DKK3 may play an important role in tumor growth and invasion in EAC. DKK3 is overexpressed in a significant number of esophageal adenocarcinomas and targeting DKK3 and its downstream mediators may be beneficial in the prevention and treatment of micrometastatic disease and potentially decreasing disease recurrence,” the researchers concluded.
The authors reported that they had no relevant financial conflicts.
The number of EAC cell lines currently available for study is limited. Despite the fact that the majority of EAC human tumors overexpress Dickkopf-3 in vivo, none of the cell lines used in this study had significant expression. Therefore the authors had to use a forced overexpression transfection strategy to evaluate EAC tumor biology, according to Dr. David R. Jones (J. Thorac. Cardovasc. Surg. 2015;150:288).
This is less than optimal because of an inability to silence Dickkopf-3 to determine if it is sufficient or merely required to drive tumorigenesis or aggressiveness. A more glaring and overarching problem is the lack of an adequate animal model, Dr. Jones added. The xenograft flank model may not recapitulate EAC tumorigenesis or metastases. “Currently there are no well-characterized EAC genetically engineered mouse models that faithfully reproduce EAC,” he pointed out. “The lack of EAC animal models is a major barrier to the preclinical evaluation of novel therapies, target validation, and pathway discovery and confirmation.”
Dr. Jones is a cardiothoracic surgeon at Memorial Sloan Kettering Cancer Center, New York. He made these remarks in his invited commentary.
The number of EAC cell lines currently available for study is limited. Despite the fact that the majority of EAC human tumors overexpress Dickkopf-3 in vivo, none of the cell lines used in this study had significant expression. Therefore the authors had to use a forced overexpression transfection strategy to evaluate EAC tumor biology, according to Dr. David R. Jones (J. Thorac. Cardovasc. Surg. 2015;150:288).
This is less than optimal because of an inability to silence Dickkopf-3 to determine if it is sufficient or merely required to drive tumorigenesis or aggressiveness. A more glaring and overarching problem is the lack of an adequate animal model, Dr. Jones added. The xenograft flank model may not recapitulate EAC tumorigenesis or metastases. “Currently there are no well-characterized EAC genetically engineered mouse models that faithfully reproduce EAC,” he pointed out. “The lack of EAC animal models is a major barrier to the preclinical evaluation of novel therapies, target validation, and pathway discovery and confirmation.”
Dr. Jones is a cardiothoracic surgeon at Memorial Sloan Kettering Cancer Center, New York. He made these remarks in his invited commentary.
The number of EAC cell lines currently available for study is limited. Despite the fact that the majority of EAC human tumors overexpress Dickkopf-3 in vivo, none of the cell lines used in this study had significant expression. Therefore the authors had to use a forced overexpression transfection strategy to evaluate EAC tumor biology, according to Dr. David R. Jones (J. Thorac. Cardovasc. Surg. 2015;150:288).
This is less than optimal because of an inability to silence Dickkopf-3 to determine if it is sufficient or merely required to drive tumorigenesis or aggressiveness. A more glaring and overarching problem is the lack of an adequate animal model, Dr. Jones added. The xenograft flank model may not recapitulate EAC tumorigenesis or metastases. “Currently there are no well-characterized EAC genetically engineered mouse models that faithfully reproduce EAC,” he pointed out. “The lack of EAC animal models is a major barrier to the preclinical evaluation of novel therapies, target validation, and pathway discovery and confirmation.”
Dr. Jones is a cardiothoracic surgeon at Memorial Sloan Kettering Cancer Center, New York. He made these remarks in his invited commentary.
Esophageal adenocarcinoma is fatal to 90% of patients, indicating a profound need for new therapeutic agents, according to Zhuewn Wang and her colleagues.
The search for genes involved in oncogenesis provides one avenue for finding potential targets. Ms. Wang and her colleagues performed a laboratory study at the University of Michigan, Ann Arbor, to examine the results of the overexpression of DKK3 (the gene for the Dickkopf-3 protein [DKK3]) in DKK3-transfected tissue-cultured esophageal adenocarcinoma (EAC) cell lines. They found that DKK3 overexpression correlated with significantly increased proliferation and Matrigel invasion ability – both known to be important oncogenic traits (J. Thorac. Cardiovasc. Surg. 2015;150:377-85).
DKK3 was overexpressed (greater than twofold) in 76% (72/95) of esophageal adenocarcinomas tested. In addition, the DKK3 protein was present at moderate to high levels in 47% (29/62) of esophageal adenocarcinomas as shown by tissue microarray. Nodal metastases were also significantly increased in patients with esophageal adenocarcinomas highly overexpressing DKK3 (28/32) vs. non–highly expressing EAC tumors (42/63).
In vitro studies showed that stable transfection of DKK3 in an EAC cell line significantly increased proliferation and Matrigel invasion. The researchers also found that the levels of SMAD4, a key mediator of the transforming growth factor–beta pathway, increased after activin treatment of the transfected cell line, and siSMAD4 significantly decreased Matrigel invasion, suggesting that DKK3 acts through the transforming growth factor–beta pathway, according to the researchers.
Additionally, the transfected cells showed increased endothelial tube formation, and they were significantly more resistant to 5-fluorouracil and cisplatin. This finding correlates with the fact that DKK3 expression was found to be significantly higher in chemoresistant esophageal adenocarcinomas, the investigators reported.
In their animal model system (NOD/SCIDg mice), injection of the transfected cells resulted in tumors at all sites (8/8), whereas vector-only cells grew in only one of eight sites.
“The results of the current study suggest that DKK3 may play an important role in tumor growth and invasion in EAC. DKK3 is overexpressed in a significant number of esophageal adenocarcinomas and targeting DKK3 and its downstream mediators may be beneficial in the prevention and treatment of micrometastatic disease and potentially decreasing disease recurrence,” the researchers concluded.
The authors reported that they had no relevant financial conflicts.
Esophageal adenocarcinoma is fatal to 90% of patients, indicating a profound need for new therapeutic agents, according to Zhuewn Wang and her colleagues.
The search for genes involved in oncogenesis provides one avenue for finding potential targets. Ms. Wang and her colleagues performed a laboratory study at the University of Michigan, Ann Arbor, to examine the results of the overexpression of DKK3 (the gene for the Dickkopf-3 protein [DKK3]) in DKK3-transfected tissue-cultured esophageal adenocarcinoma (EAC) cell lines. They found that DKK3 overexpression correlated with significantly increased proliferation and Matrigel invasion ability – both known to be important oncogenic traits (J. Thorac. Cardiovasc. Surg. 2015;150:377-85).
DKK3 was overexpressed (greater than twofold) in 76% (72/95) of esophageal adenocarcinomas tested. In addition, the DKK3 protein was present at moderate to high levels in 47% (29/62) of esophageal adenocarcinomas as shown by tissue microarray. Nodal metastases were also significantly increased in patients with esophageal adenocarcinomas highly overexpressing DKK3 (28/32) vs. non–highly expressing EAC tumors (42/63).
In vitro studies showed that stable transfection of DKK3 in an EAC cell line significantly increased proliferation and Matrigel invasion. The researchers also found that the levels of SMAD4, a key mediator of the transforming growth factor–beta pathway, increased after activin treatment of the transfected cell line, and siSMAD4 significantly decreased Matrigel invasion, suggesting that DKK3 acts through the transforming growth factor–beta pathway, according to the researchers.
Additionally, the transfected cells showed increased endothelial tube formation, and they were significantly more resistant to 5-fluorouracil and cisplatin. This finding correlates with the fact that DKK3 expression was found to be significantly higher in chemoresistant esophageal adenocarcinomas, the investigators reported.
In their animal model system (NOD/SCIDg mice), injection of the transfected cells resulted in tumors at all sites (8/8), whereas vector-only cells grew in only one of eight sites.
“The results of the current study suggest that DKK3 may play an important role in tumor growth and invasion in EAC. DKK3 is overexpressed in a significant number of esophageal adenocarcinomas and targeting DKK3 and its downstream mediators may be beneficial in the prevention and treatment of micrometastatic disease and potentially decreasing disease recurrence,” the researchers concluded.
The authors reported that they had no relevant financial conflicts.
FROM THE JOURNAL OF THORACIC AND CARDIOVASCULAR SURGERY
Key clinical point: DKK3 may be important in mediating invasion in esophageal adenocarcinoma and could be a novel target for treating and preventing metastasis.
Major finding: Dickkopf-3 overexpression correlated with tumorigenesis and aggressiveness traits in an esophageal adenocarcinoma cell line, and the gene was overexpressed in primary EAC tumors relative to normal esophageal tissue.
Data source: Laboratory studies using cell culture and a mouse model.
Disclosures: The authors reported that they had no relevant financial conflicts.
FDA panel says benefits of necitumumab for squamous NSCLC outweigh risks
SILVER SPRING, MD. – The majority of a Food and Drug Administration Advisory panel agreed that the benefits of adding necitumumab to gemcitabine and cisplatin for patients with squamous non–small cell lung cancer outweighed the risks.
At the meeting on July 9, the FDA’s Oncologic Drugs Advisory Committee reviewed data from a study that evaluated the anti–epidermal growth factor receptor monoclonal antibody in more than 1,000 patients with stage IV disease. The SQUIRE study was submitted to the FDA by Eli Lilly to support approval of necitumumab for the indication now under review: for use as a first-line treatment, in combination with gemcitabine and cisplatin, for patients with locally advanced or metastatic squamous non–small cell lung cancer (NSCLC). Necitumumab is a recombinant human IgG1 monoclonal antibody that is designed to block the ligand binding site of the human EGFR.
Despite a modest effect on overall survival, a very small but statistically significant effect on progression-free survival, and some safety concerns, 11 of the 12 panelists agreed that the efficacy and safety results of the trial supported a “positive benefit risk assessment” of necitumumab combined with gemcitabine and cisplatin for this group of patients, the main question they were asked by the FDA to discuss. The panel was not asked to specifically vote on whether to recommend approval.
The SQUIRE study, an international phase III study of 1,093 patients with stage IV squamous NSCLC, who had not received chemotherapy for advanced disease, evaluated the safety and efficacy of gemcitabine and cisplatin, with or without necitumumab, administered every 3 weeks, until disease progressed or toxicity became unacceptable, for a maximum of six cycles. The median age of patients was 62 years; they were mostly men and were heavy smokers; 36 patients were enrolled in the United States. (Patients were not selected based on EGFR protein expression but based on tissue pathology.)
Median overall survival (OS), the primary endpoint, was 11.5 months in the necitumumab-treated arm, vs. 9.9 months among controls, a 1.6 month difference that was statistically significant, representing a reduced risk of 16% (hazard ratio, 0.84). Progression-free survival (PFS) was a median of 5.7 months among those in the necitumumab-treated group, vs. 5.5 months, which was also statistically significant and represented a 15% reduced risk (HR, 0.85). There was no significant difference in the objective response rate (ORR), which was 31% among those in the necitumumab arm and 29% among those in the control arm. This is the first study to show an improvement in survival for a first-line treatment for squamous lung cancer, the company officials pointed out.
In the study, there were more venous thromboembolic events (VTEs; 9% vs. 5%) and more cases of sudden death and deaths “not otherwise specified” (2.2% vs. 0.5%) in the necitumumab-treated arm. There were also more cases of hypomagnesemia and skin rashes, and the FDA reviewers pointed out that several cases of sudden death occurred in patients with very low serum magnesium levels. VTEs and sudden or unexplained deaths were also higher among necitumumab-treated patients in another study that evaluated necitumumab in patients with nonsquamous NSCLC, which was stopped early because of the VTE increase; that study found no improvements in OS, PFS or ORR.
Among those agreeing that the risk-benefit assessment was positive, Dr. Michael Menefee of the Mayo Clinic, Jacksonville, Fla., said “Yes was the simple answer, but there are still caveats” regarding toxicity and the magnitude of the overall benefit.
“The survival benefit is modest but it’s real,” said Dr. Deborah Armstrong, the panel chair and professor of oncology, Johns Hopkins University, Baltimore, who also voted positively. She strongly encouraged continuing efforts to manage the toxicities of necitumumab, which she said might improve the risk-benefit balance further.
The panelist who did not agree was Dr. Tito Fojo, a senior investigator and director of the medical oncology fellowship program at the National Cancer Institute. He said that the study did not provide him with enough confidence. Noting it is a very difficult disease to treat, he said, “I just wish the data were much better.” His concerns included the possibility that those in the control arm, who received a median of five treatment cycles may have received less chemotherapy than those in the necitumumab arm, who received a median of six cycles.
Speaking on behalf of Eli Lilly at the meeting, Dr. David Gandara, director of the thoracic oncology program at the University of California Davis Comprehensive Cancer Center, said that although EGFR mutations are rare in squamous NSCLC, “the EGFR pathway itself is biologically relevant.” Necitumumab “attacks that pathway in ways independent of those associated with EGFR tyrosine-kinase inhibitors and independent of EGFR mutation status,” he added.
The FDA usually follows the recommendations of its advisory panels. Panelists have been cleared of potential conflicts of interest related to the topic of the meeting. The FDA decision is expected by the end of 2015, an Eli Lilly spokesperson said.
SILVER SPRING, MD. – The majority of a Food and Drug Administration Advisory panel agreed that the benefits of adding necitumumab to gemcitabine and cisplatin for patients with squamous non–small cell lung cancer outweighed the risks.
At the meeting on July 9, the FDA’s Oncologic Drugs Advisory Committee reviewed data from a study that evaluated the anti–epidermal growth factor receptor monoclonal antibody in more than 1,000 patients with stage IV disease. The SQUIRE study was submitted to the FDA by Eli Lilly to support approval of necitumumab for the indication now under review: for use as a first-line treatment, in combination with gemcitabine and cisplatin, for patients with locally advanced or metastatic squamous non–small cell lung cancer (NSCLC). Necitumumab is a recombinant human IgG1 monoclonal antibody that is designed to block the ligand binding site of the human EGFR.
Despite a modest effect on overall survival, a very small but statistically significant effect on progression-free survival, and some safety concerns, 11 of the 12 panelists agreed that the efficacy and safety results of the trial supported a “positive benefit risk assessment” of necitumumab combined with gemcitabine and cisplatin for this group of patients, the main question they were asked by the FDA to discuss. The panel was not asked to specifically vote on whether to recommend approval.
The SQUIRE study, an international phase III study of 1,093 patients with stage IV squamous NSCLC, who had not received chemotherapy for advanced disease, evaluated the safety and efficacy of gemcitabine and cisplatin, with or without necitumumab, administered every 3 weeks, until disease progressed or toxicity became unacceptable, for a maximum of six cycles. The median age of patients was 62 years; they were mostly men and were heavy smokers; 36 patients were enrolled in the United States. (Patients were not selected based on EGFR protein expression but based on tissue pathology.)
Median overall survival (OS), the primary endpoint, was 11.5 months in the necitumumab-treated arm, vs. 9.9 months among controls, a 1.6 month difference that was statistically significant, representing a reduced risk of 16% (hazard ratio, 0.84). Progression-free survival (PFS) was a median of 5.7 months among those in the necitumumab-treated group, vs. 5.5 months, which was also statistically significant and represented a 15% reduced risk (HR, 0.85). There was no significant difference in the objective response rate (ORR), which was 31% among those in the necitumumab arm and 29% among those in the control arm. This is the first study to show an improvement in survival for a first-line treatment for squamous lung cancer, the company officials pointed out.
In the study, there were more venous thromboembolic events (VTEs; 9% vs. 5%) and more cases of sudden death and deaths “not otherwise specified” (2.2% vs. 0.5%) in the necitumumab-treated arm. There were also more cases of hypomagnesemia and skin rashes, and the FDA reviewers pointed out that several cases of sudden death occurred in patients with very low serum magnesium levels. VTEs and sudden or unexplained deaths were also higher among necitumumab-treated patients in another study that evaluated necitumumab in patients with nonsquamous NSCLC, which was stopped early because of the VTE increase; that study found no improvements in OS, PFS or ORR.
Among those agreeing that the risk-benefit assessment was positive, Dr. Michael Menefee of the Mayo Clinic, Jacksonville, Fla., said “Yes was the simple answer, but there are still caveats” regarding toxicity and the magnitude of the overall benefit.
“The survival benefit is modest but it’s real,” said Dr. Deborah Armstrong, the panel chair and professor of oncology, Johns Hopkins University, Baltimore, who also voted positively. She strongly encouraged continuing efforts to manage the toxicities of necitumumab, which she said might improve the risk-benefit balance further.
The panelist who did not agree was Dr. Tito Fojo, a senior investigator and director of the medical oncology fellowship program at the National Cancer Institute. He said that the study did not provide him with enough confidence. Noting it is a very difficult disease to treat, he said, “I just wish the data were much better.” His concerns included the possibility that those in the control arm, who received a median of five treatment cycles may have received less chemotherapy than those in the necitumumab arm, who received a median of six cycles.
Speaking on behalf of Eli Lilly at the meeting, Dr. David Gandara, director of the thoracic oncology program at the University of California Davis Comprehensive Cancer Center, said that although EGFR mutations are rare in squamous NSCLC, “the EGFR pathway itself is biologically relevant.” Necitumumab “attacks that pathway in ways independent of those associated with EGFR tyrosine-kinase inhibitors and independent of EGFR mutation status,” he added.
The FDA usually follows the recommendations of its advisory panels. Panelists have been cleared of potential conflicts of interest related to the topic of the meeting. The FDA decision is expected by the end of 2015, an Eli Lilly spokesperson said.
SILVER SPRING, MD. – The majority of a Food and Drug Administration Advisory panel agreed that the benefits of adding necitumumab to gemcitabine and cisplatin for patients with squamous non–small cell lung cancer outweighed the risks.
At the meeting on July 9, the FDA’s Oncologic Drugs Advisory Committee reviewed data from a study that evaluated the anti–epidermal growth factor receptor monoclonal antibody in more than 1,000 patients with stage IV disease. The SQUIRE study was submitted to the FDA by Eli Lilly to support approval of necitumumab for the indication now under review: for use as a first-line treatment, in combination with gemcitabine and cisplatin, for patients with locally advanced or metastatic squamous non–small cell lung cancer (NSCLC). Necitumumab is a recombinant human IgG1 monoclonal antibody that is designed to block the ligand binding site of the human EGFR.
Despite a modest effect on overall survival, a very small but statistically significant effect on progression-free survival, and some safety concerns, 11 of the 12 panelists agreed that the efficacy and safety results of the trial supported a “positive benefit risk assessment” of necitumumab combined with gemcitabine and cisplatin for this group of patients, the main question they were asked by the FDA to discuss. The panel was not asked to specifically vote on whether to recommend approval.
The SQUIRE study, an international phase III study of 1,093 patients with stage IV squamous NSCLC, who had not received chemotherapy for advanced disease, evaluated the safety and efficacy of gemcitabine and cisplatin, with or without necitumumab, administered every 3 weeks, until disease progressed or toxicity became unacceptable, for a maximum of six cycles. The median age of patients was 62 years; they were mostly men and were heavy smokers; 36 patients were enrolled in the United States. (Patients were not selected based on EGFR protein expression but based on tissue pathology.)
Median overall survival (OS), the primary endpoint, was 11.5 months in the necitumumab-treated arm, vs. 9.9 months among controls, a 1.6 month difference that was statistically significant, representing a reduced risk of 16% (hazard ratio, 0.84). Progression-free survival (PFS) was a median of 5.7 months among those in the necitumumab-treated group, vs. 5.5 months, which was also statistically significant and represented a 15% reduced risk (HR, 0.85). There was no significant difference in the objective response rate (ORR), which was 31% among those in the necitumumab arm and 29% among those in the control arm. This is the first study to show an improvement in survival for a first-line treatment for squamous lung cancer, the company officials pointed out.
In the study, there were more venous thromboembolic events (VTEs; 9% vs. 5%) and more cases of sudden death and deaths “not otherwise specified” (2.2% vs. 0.5%) in the necitumumab-treated arm. There were also more cases of hypomagnesemia and skin rashes, and the FDA reviewers pointed out that several cases of sudden death occurred in patients with very low serum magnesium levels. VTEs and sudden or unexplained deaths were also higher among necitumumab-treated patients in another study that evaluated necitumumab in patients with nonsquamous NSCLC, which was stopped early because of the VTE increase; that study found no improvements in OS, PFS or ORR.
Among those agreeing that the risk-benefit assessment was positive, Dr. Michael Menefee of the Mayo Clinic, Jacksonville, Fla., said “Yes was the simple answer, but there are still caveats” regarding toxicity and the magnitude of the overall benefit.
“The survival benefit is modest but it’s real,” said Dr. Deborah Armstrong, the panel chair and professor of oncology, Johns Hopkins University, Baltimore, who also voted positively. She strongly encouraged continuing efforts to manage the toxicities of necitumumab, which she said might improve the risk-benefit balance further.
The panelist who did not agree was Dr. Tito Fojo, a senior investigator and director of the medical oncology fellowship program at the National Cancer Institute. He said that the study did not provide him with enough confidence. Noting it is a very difficult disease to treat, he said, “I just wish the data were much better.” His concerns included the possibility that those in the control arm, who received a median of five treatment cycles may have received less chemotherapy than those in the necitumumab arm, who received a median of six cycles.
Speaking on behalf of Eli Lilly at the meeting, Dr. David Gandara, director of the thoracic oncology program at the University of California Davis Comprehensive Cancer Center, said that although EGFR mutations are rare in squamous NSCLC, “the EGFR pathway itself is biologically relevant.” Necitumumab “attacks that pathway in ways independent of those associated with EGFR tyrosine-kinase inhibitors and independent of EGFR mutation status,” he added.
The FDA usually follows the recommendations of its advisory panels. Panelists have been cleared of potential conflicts of interest related to the topic of the meeting. The FDA decision is expected by the end of 2015, an Eli Lilly spokesperson said.
AT AN FDA ADVISORY COMMITTEE MEETING
Consolidation chemotherapy after concurrent chemoradiation failed to improve outcomes in NSCLC
Results from a large, multinational phase III trial showed that consolidation chemotherapy with docetaxel and cisplatin after concurrent chemoradiation with the same agents failed to improve progression-free survival in patients with locally advanced non–small cell lung cancer (NSCLC), according to a report published online in the Journal of Clinical Oncology.
After a median follow up of 50.7 months, progression-free survival (PFS) for the arm that received consolidation chemotherapy (CC) was 8.1 months, compared with 9.1 months for the arm that did not receive CC (hazard ratio, 0.91; 95% confidence interval, 0.73-1.12; P = .36). Median overall survival (OS) was also similar between groups: 20.6 vs. 21.8 months, respectively (P = .44).
Among patients assigned to the CC arm, only 42.1% received all three planned cycles, 54.1% completed at least two cycles, and 31.6% did not receive any CC.
“The major obstacle in this trial was that many patients could not complete the three planned cycles of CC,” wrote Dr. Jin Seok Ahn of the Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, South Korea, and colleagues. A large proportion of patients failed to start CC because of disease progression or death, and many patients had incomplete recovery from the adverse effects of concurrent chemoradiation. “A full-dose doublet regimen of CC in our trial might have further reduced the rate of completing the three planned cycles of CC,” the investigators noted (J. Clin. Onc. 2015 July 6 [doi:10.1200/JCO.2014.60.0130]).
The randomized phase III trial included 420 patients with inoperable stage IIIA or IIIB non–small cell lung cancer, enrolled from 31 centers in Korea, China, and Taiwan from 2005 to 2011.
Patients older than 60 years, who had similar baseline characteristics to younger patients, experienced significant benefit from CC (HR 0.72), for reasons that remain unexplained.
An exploratory biomarker study indicated the expression of ERCC1 and class III beta-tubulin was not correlated with PFS or OS.
The study was supported in part by Sanofi-Aventis Korea. Dr. Jin Seok Ahn reported financial ties to Eli Lilly, Pfizer, and Roche. Several of his coauthors reported ties to industry sources.
Results from a large, multinational phase III trial showed that consolidation chemotherapy with docetaxel and cisplatin after concurrent chemoradiation with the same agents failed to improve progression-free survival in patients with locally advanced non–small cell lung cancer (NSCLC), according to a report published online in the Journal of Clinical Oncology.
After a median follow up of 50.7 months, progression-free survival (PFS) for the arm that received consolidation chemotherapy (CC) was 8.1 months, compared with 9.1 months for the arm that did not receive CC (hazard ratio, 0.91; 95% confidence interval, 0.73-1.12; P = .36). Median overall survival (OS) was also similar between groups: 20.6 vs. 21.8 months, respectively (P = .44).
Among patients assigned to the CC arm, only 42.1% received all three planned cycles, 54.1% completed at least two cycles, and 31.6% did not receive any CC.
“The major obstacle in this trial was that many patients could not complete the three planned cycles of CC,” wrote Dr. Jin Seok Ahn of the Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, South Korea, and colleagues. A large proportion of patients failed to start CC because of disease progression or death, and many patients had incomplete recovery from the adverse effects of concurrent chemoradiation. “A full-dose doublet regimen of CC in our trial might have further reduced the rate of completing the three planned cycles of CC,” the investigators noted (J. Clin. Onc. 2015 July 6 [doi:10.1200/JCO.2014.60.0130]).
The randomized phase III trial included 420 patients with inoperable stage IIIA or IIIB non–small cell lung cancer, enrolled from 31 centers in Korea, China, and Taiwan from 2005 to 2011.
Patients older than 60 years, who had similar baseline characteristics to younger patients, experienced significant benefit from CC (HR 0.72), for reasons that remain unexplained.
An exploratory biomarker study indicated the expression of ERCC1 and class III beta-tubulin was not correlated with PFS or OS.
The study was supported in part by Sanofi-Aventis Korea. Dr. Jin Seok Ahn reported financial ties to Eli Lilly, Pfizer, and Roche. Several of his coauthors reported ties to industry sources.
Results from a large, multinational phase III trial showed that consolidation chemotherapy with docetaxel and cisplatin after concurrent chemoradiation with the same agents failed to improve progression-free survival in patients with locally advanced non–small cell lung cancer (NSCLC), according to a report published online in the Journal of Clinical Oncology.
After a median follow up of 50.7 months, progression-free survival (PFS) for the arm that received consolidation chemotherapy (CC) was 8.1 months, compared with 9.1 months for the arm that did not receive CC (hazard ratio, 0.91; 95% confidence interval, 0.73-1.12; P = .36). Median overall survival (OS) was also similar between groups: 20.6 vs. 21.8 months, respectively (P = .44).
Among patients assigned to the CC arm, only 42.1% received all three planned cycles, 54.1% completed at least two cycles, and 31.6% did not receive any CC.
“The major obstacle in this trial was that many patients could not complete the three planned cycles of CC,” wrote Dr. Jin Seok Ahn of the Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, South Korea, and colleagues. A large proportion of patients failed to start CC because of disease progression or death, and many patients had incomplete recovery from the adverse effects of concurrent chemoradiation. “A full-dose doublet regimen of CC in our trial might have further reduced the rate of completing the three planned cycles of CC,” the investigators noted (J. Clin. Onc. 2015 July 6 [doi:10.1200/JCO.2014.60.0130]).
The randomized phase III trial included 420 patients with inoperable stage IIIA or IIIB non–small cell lung cancer, enrolled from 31 centers in Korea, China, and Taiwan from 2005 to 2011.
Patients older than 60 years, who had similar baseline characteristics to younger patients, experienced significant benefit from CC (HR 0.72), for reasons that remain unexplained.
An exploratory biomarker study indicated the expression of ERCC1 and class III beta-tubulin was not correlated with PFS or OS.
The study was supported in part by Sanofi-Aventis Korea. Dr. Jin Seok Ahn reported financial ties to Eli Lilly, Pfizer, and Roche. Several of his coauthors reported ties to industry sources.
Key clinical point: Docetaxel and cisplatin consolidation chemotherapy (CC) after concurrent chemoradiation failed to prolong progression-free survival in patients with locally advanced non–small cell lung cancer.
Major finding: PFS was similar for patients who received CC and those who did not, 8.1 vs. 9.1 months, respectively (P = .36).
Data source: The randomized phase III trial included 420 patients with inoperable stage IIIA or IIIB NSCLC, enrolled from 31 centers in Korea, China, and Taiwan.
Disclosures: The study was supported in part by Sanofi-Aventis Korea. Dr. Jin Seok Ahn reported financial ties to Eli Lilly, Pfizer, and Roche. Several of his coauthors reported ties to industry sources.
DDW: LINX device beneficial, safe for GERD
WASHINGTON – Five-year follow-up data on the magnetic device approved for treating gastroesophageal reflux disease confirm its long-term safety and efficacy, Dr. Robert A. Ganz reported at the annual Digestive Disease Week.
Five years after device implantation, the proportion of patients experiencing moderate to severe regurgitation had dropped to about 1%, from almost 60% at baseline, and two-thirds of patients were not taking any proton pump inhibitors (PPIs), said Dr. Ganz, chief of gastroenterology at Abbott Northwestern Hospital, Minneapolis, and one of the study investigators. These were among the results of the study that evaluated the device, the LINX Reflux Management System. The device was approved by the Food and Drug Administration FDA) in 2012 and is for the treatment of people with GERD as defined by abnormal pH testing, who continue to have chronic GERD symptoms that persist despite maximum medical therapy for the treatment of reflux.
“Magnetic sphincter augmentation should be considered first-line surgical therapy for those with gastroesophageal reflux disease, based on the results of this study,” he said.
The 2-year results of the prospective, multicenter study were the basis of the FDA approval of the device, described by the manufacturer, Torax Medical, as a “small implant [composed] of interlinked titanium beads with magnetic cores,” implanted during standard laparoscopy. The magnetic attraction between the beads augments the existing esophageal sphincter’s barrier function to prevent reflux,” according to the company.
The study enrolled 100 patients with reflux disease with a median age of 53 years, who had experienced typical heartburn for at least 6 months with or without regurgitation and were taking PPIs daily for at least 3 months (median use 5 years). Patients had GERD for a median of 10 years (range: 1-40 years). People who had any type of previous gastric or esophageal surgery, Barrett’s esophagus, a hiatal hernia greater than 3 cm, a body mass index over 35 kg/m2, or grade C or D esophagitis were excluded.
The device was implanted in all patients, who served as their own controls; 85 patients were followed through 5 years (6 were lost to follow-up, the device was explanted in 6 patients, 2 patients did not consent to extended follow-up, and 1 patient died of an unrelated cancer). The median procedure time was 36 minutes with a range of 7-125 minutes); all procedures were successfully completed with no intraoperative complications and all patients were discharged within 24 hours on an unrestricted diet.
The median total Gastroesophageal Reflux Disease–Health-Related Quality of Life (GERD-HRQL) score at baseline was 27 points among those not on PPIs and 11 points on PPIs, dropping to 4 points at 5 years off PPIs. At baseline, 95% of patients expressed dissatisfaction related to reflux, which dropped to 7% at year 5. Moderate to severe heartburn was reported by 89% at baseline, dropping to about 12% at year 5. The proportion of patients experiencing moderate to severe regurgitation dropped from 57% at baseline to about 1% at 5 years, Dr. Ganz said.
At baseline, 100% were taking PPIs every day, compared with 15% at 5 years. (At 5 years, 75% had discontinued PPIs, and about 9% reported PRN use only). Grade A and B esophagitis decreased from 40% at baseline to 16% at 5 years, at which point most cases were grade A, and there were no patients with grade C or D esophagitis, he said. In addition, at 5 years, 100% of patients “reported the ability to belch, and those needing to vomit – about 16% – reported the ability to vomit,” demonstrating that normal physiology was preserved with the device.
At 5 years, there were no device erosions or migrations, or any significant adverse events other than dysphagia, which “was typically mild and not associated with weight loss and tended to resolve over time,” from about 70% in the first few weeks after surgery to 11% at 1 year and 7% at 5 years, Dr. Ganz said.
In seven cases, the device was removed laparoscopically, with no complications and gastric anatomy was preserved for future treatments. All removals were elective. The device was removed in four patients because of dysphagia, which completely resolved in those patients. One patient had the device removed because of vomiting of unknown cause that persisted after removal. Another two patients who “had the device removed for disease management” continued to experience reflux and had “uneventful” Nissen fundoplication,” he said.
“Five years after magnetic augmentation, we have demonstrated objective evidence of reduction in acid exposure and in the majority of patients, normalized pH [and] we demonstrated significant and durable improvement in all group parameters measured, with preservation of fundic anatomy and normal physiology, with the ability to belch and vomit,” Dr. Ganz concluded. The results also show that the “procedure is reproducible, safe and reversible if necessary,” he added, noting that one of the limitations of the study was that subjects served as their own controls. During the discussion period, he was asked about hiatal hernia repairs, an apparent trend to “decay” from years 1 to 5 in some parameters measured, and dysphagia after the procedure.
About 40% of the patients in the study had a hiatal hernia, and about one-third of these patients had a hernia repair. A subgroup analysis of the data is being performed to evaluate the impact of hernia repair, Dr. Ganz said.
PPI use increased from 8% in year 4, to 15% in year 5. The reason for this s difficult to determine but “even though there is a bit of a decay, patients are still quite satisfied at 5 years,” Dr. Ganz remarked, also referring to the marked impact on regurgitation. Many U.S. patients use PPIs for reasons other than reflux, and studies show that many patients are on PPIs after the Nissen procedure in the absence of pathologic pH scores, he pointed out.
Compared with the type of dysphagia patients experience after the Nissen procedure, which is immediate and improves with time, Dr. Ganz said that the dysphagia associated with the device “seemed to peak around 2 weeks and then it slowly improved with time, so this may be more of a scar tissue–associated dysphagia than an edema dysphagia, but … it does improve with time.
Three-year results of the study were published in 2013 (N. Engl. J. Med. 2013;368:719-72), Dr. Ganz was the lead author.
The study was funded by Torax Medical. Dr. Ganz had no disclosures related to the topic of this presentation.
*This story was updated 7/9/2015.
At DDW this year, Dr. Ganz reported on the 5-year follow-up of the original LINX data that was published in the New England Journal of Medicine in 2013 (368:2039-40). The original study enrolled and followed 100 reflux patients for 3 years after implantation of the magnetic sphincter augmentation device, and it appears that the successful outcomes are sustained over the 5-year period. Most notable are the lasting improvement in regurgitation and the dramatic reduction in requirement for maintenance PPI therapy. These findings led the investigators to suggest that this should be considered a first-line surgical therapy for GERD. Overall, this is not an unreasonable statement when one considers the current model wherein antireflux surgery fits in the treatment of GERD. Medical therapy with proton pump inhibitors is extremely safe and effective for a substantial number of patients with GERD and based on this risk/benefit profile should be the first line therapy (Am. J. Gastroenterol. 2013;108:308-28; quiz 329). However, this treatment is not perfect and there are many patients who continue to have persistent symptoms despite PPI therapy (Clin. Gastroenterol. Hepatol. 2012;10:612-9). Although the majority of PPI nonresponders have a functional etiology, there is a distinct population that continue to have refractory reflux-related symptoms, such as regurgitation, that escape the therapeutic target of PPIs. These patients will require an augmentation of the antireflux barrier and the LINX approach appears to be as effective as fundoplication in this regard (J. Am. Coll. Surg. 2015;221:123-8). The question is whether the side effect profile and durability of LINX is better than fundoplication. The answer here is not clear and I would carefully state that LINX and fundoplication can be considered first-line surgical therapies for GERD patients who have documented pathologic acid gastroesophageal reflux and are intolerant to PPIs or not responding to PPIs.
Dr. John E. Pandolfino is professor of medicine and chief of the division of gastroenterology and hepatology at Northwestern University, Chicago. He is a speaker for Astra Zeneca/Takeda and a consultant for EndoGastric Solutions.
At DDW this year, Dr. Ganz reported on the 5-year follow-up of the original LINX data that was published in the New England Journal of Medicine in 2013 (368:2039-40). The original study enrolled and followed 100 reflux patients for 3 years after implantation of the magnetic sphincter augmentation device, and it appears that the successful outcomes are sustained over the 5-year period. Most notable are the lasting improvement in regurgitation and the dramatic reduction in requirement for maintenance PPI therapy. These findings led the investigators to suggest that this should be considered a first-line surgical therapy for GERD. Overall, this is not an unreasonable statement when one considers the current model wherein antireflux surgery fits in the treatment of GERD. Medical therapy with proton pump inhibitors is extremely safe and effective for a substantial number of patients with GERD and based on this risk/benefit profile should be the first line therapy (Am. J. Gastroenterol. 2013;108:308-28; quiz 329). However, this treatment is not perfect and there are many patients who continue to have persistent symptoms despite PPI therapy (Clin. Gastroenterol. Hepatol. 2012;10:612-9). Although the majority of PPI nonresponders have a functional etiology, there is a distinct population that continue to have refractory reflux-related symptoms, such as regurgitation, that escape the therapeutic target of PPIs. These patients will require an augmentation of the antireflux barrier and the LINX approach appears to be as effective as fundoplication in this regard (J. Am. Coll. Surg. 2015;221:123-8). The question is whether the side effect profile and durability of LINX is better than fundoplication. The answer here is not clear and I would carefully state that LINX and fundoplication can be considered first-line surgical therapies for GERD patients who have documented pathologic acid gastroesophageal reflux and are intolerant to PPIs or not responding to PPIs.
Dr. John E. Pandolfino is professor of medicine and chief of the division of gastroenterology and hepatology at Northwestern University, Chicago. He is a speaker for Astra Zeneca/Takeda and a consultant for EndoGastric Solutions.
At DDW this year, Dr. Ganz reported on the 5-year follow-up of the original LINX data that was published in the New England Journal of Medicine in 2013 (368:2039-40). The original study enrolled and followed 100 reflux patients for 3 years after implantation of the magnetic sphincter augmentation device, and it appears that the successful outcomes are sustained over the 5-year period. Most notable are the lasting improvement in regurgitation and the dramatic reduction in requirement for maintenance PPI therapy. These findings led the investigators to suggest that this should be considered a first-line surgical therapy for GERD. Overall, this is not an unreasonable statement when one considers the current model wherein antireflux surgery fits in the treatment of GERD. Medical therapy with proton pump inhibitors is extremely safe and effective for a substantial number of patients with GERD and based on this risk/benefit profile should be the first line therapy (Am. J. Gastroenterol. 2013;108:308-28; quiz 329). However, this treatment is not perfect and there are many patients who continue to have persistent symptoms despite PPI therapy (Clin. Gastroenterol. Hepatol. 2012;10:612-9). Although the majority of PPI nonresponders have a functional etiology, there is a distinct population that continue to have refractory reflux-related symptoms, such as regurgitation, that escape the therapeutic target of PPIs. These patients will require an augmentation of the antireflux barrier and the LINX approach appears to be as effective as fundoplication in this regard (J. Am. Coll. Surg. 2015;221:123-8). The question is whether the side effect profile and durability of LINX is better than fundoplication. The answer here is not clear and I would carefully state that LINX and fundoplication can be considered first-line surgical therapies for GERD patients who have documented pathologic acid gastroesophageal reflux and are intolerant to PPIs or not responding to PPIs.
Dr. John E. Pandolfino is professor of medicine and chief of the division of gastroenterology and hepatology at Northwestern University, Chicago. He is a speaker for Astra Zeneca/Takeda and a consultant for EndoGastric Solutions.
WASHINGTON – Five-year follow-up data on the magnetic device approved for treating gastroesophageal reflux disease confirm its long-term safety and efficacy, Dr. Robert A. Ganz reported at the annual Digestive Disease Week.
Five years after device implantation, the proportion of patients experiencing moderate to severe regurgitation had dropped to about 1%, from almost 60% at baseline, and two-thirds of patients were not taking any proton pump inhibitors (PPIs), said Dr. Ganz, chief of gastroenterology at Abbott Northwestern Hospital, Minneapolis, and one of the study investigators. These were among the results of the study that evaluated the device, the LINX Reflux Management System. The device was approved by the Food and Drug Administration FDA) in 2012 and is for the treatment of people with GERD as defined by abnormal pH testing, who continue to have chronic GERD symptoms that persist despite maximum medical therapy for the treatment of reflux.
“Magnetic sphincter augmentation should be considered first-line surgical therapy for those with gastroesophageal reflux disease, based on the results of this study,” he said.
The 2-year results of the prospective, multicenter study were the basis of the FDA approval of the device, described by the manufacturer, Torax Medical, as a “small implant [composed] of interlinked titanium beads with magnetic cores,” implanted during standard laparoscopy. The magnetic attraction between the beads augments the existing esophageal sphincter’s barrier function to prevent reflux,” according to the company.
The study enrolled 100 patients with reflux disease with a median age of 53 years, who had experienced typical heartburn for at least 6 months with or without regurgitation and were taking PPIs daily for at least 3 months (median use 5 years). Patients had GERD for a median of 10 years (range: 1-40 years). People who had any type of previous gastric or esophageal surgery, Barrett’s esophagus, a hiatal hernia greater than 3 cm, a body mass index over 35 kg/m2, or grade C or D esophagitis were excluded.
The device was implanted in all patients, who served as their own controls; 85 patients were followed through 5 years (6 were lost to follow-up, the device was explanted in 6 patients, 2 patients did not consent to extended follow-up, and 1 patient died of an unrelated cancer). The median procedure time was 36 minutes with a range of 7-125 minutes); all procedures were successfully completed with no intraoperative complications and all patients were discharged within 24 hours on an unrestricted diet.
The median total Gastroesophageal Reflux Disease–Health-Related Quality of Life (GERD-HRQL) score at baseline was 27 points among those not on PPIs and 11 points on PPIs, dropping to 4 points at 5 years off PPIs. At baseline, 95% of patients expressed dissatisfaction related to reflux, which dropped to 7% at year 5. Moderate to severe heartburn was reported by 89% at baseline, dropping to about 12% at year 5. The proportion of patients experiencing moderate to severe regurgitation dropped from 57% at baseline to about 1% at 5 years, Dr. Ganz said.
At baseline, 100% were taking PPIs every day, compared with 15% at 5 years. (At 5 years, 75% had discontinued PPIs, and about 9% reported PRN use only). Grade A and B esophagitis decreased from 40% at baseline to 16% at 5 years, at which point most cases were grade A, and there were no patients with grade C or D esophagitis, he said. In addition, at 5 years, 100% of patients “reported the ability to belch, and those needing to vomit – about 16% – reported the ability to vomit,” demonstrating that normal physiology was preserved with the device.
At 5 years, there were no device erosions or migrations, or any significant adverse events other than dysphagia, which “was typically mild and not associated with weight loss and tended to resolve over time,” from about 70% in the first few weeks after surgery to 11% at 1 year and 7% at 5 years, Dr. Ganz said.
In seven cases, the device was removed laparoscopically, with no complications and gastric anatomy was preserved for future treatments. All removals were elective. The device was removed in four patients because of dysphagia, which completely resolved in those patients. One patient had the device removed because of vomiting of unknown cause that persisted after removal. Another two patients who “had the device removed for disease management” continued to experience reflux and had “uneventful” Nissen fundoplication,” he said.
“Five years after magnetic augmentation, we have demonstrated objective evidence of reduction in acid exposure and in the majority of patients, normalized pH [and] we demonstrated significant and durable improvement in all group parameters measured, with preservation of fundic anatomy and normal physiology, with the ability to belch and vomit,” Dr. Ganz concluded. The results also show that the “procedure is reproducible, safe and reversible if necessary,” he added, noting that one of the limitations of the study was that subjects served as their own controls. During the discussion period, he was asked about hiatal hernia repairs, an apparent trend to “decay” from years 1 to 5 in some parameters measured, and dysphagia after the procedure.
About 40% of the patients in the study had a hiatal hernia, and about one-third of these patients had a hernia repair. A subgroup analysis of the data is being performed to evaluate the impact of hernia repair, Dr. Ganz said.
PPI use increased from 8% in year 4, to 15% in year 5. The reason for this s difficult to determine but “even though there is a bit of a decay, patients are still quite satisfied at 5 years,” Dr. Ganz remarked, also referring to the marked impact on regurgitation. Many U.S. patients use PPIs for reasons other than reflux, and studies show that many patients are on PPIs after the Nissen procedure in the absence of pathologic pH scores, he pointed out.
Compared with the type of dysphagia patients experience after the Nissen procedure, which is immediate and improves with time, Dr. Ganz said that the dysphagia associated with the device “seemed to peak around 2 weeks and then it slowly improved with time, so this may be more of a scar tissue–associated dysphagia than an edema dysphagia, but … it does improve with time.
Three-year results of the study were published in 2013 (N. Engl. J. Med. 2013;368:719-72), Dr. Ganz was the lead author.
The study was funded by Torax Medical. Dr. Ganz had no disclosures related to the topic of this presentation.
*This story was updated 7/9/2015.
WASHINGTON – Five-year follow-up data on the magnetic device approved for treating gastroesophageal reflux disease confirm its long-term safety and efficacy, Dr. Robert A. Ganz reported at the annual Digestive Disease Week.
Five years after device implantation, the proportion of patients experiencing moderate to severe regurgitation had dropped to about 1%, from almost 60% at baseline, and two-thirds of patients were not taking any proton pump inhibitors (PPIs), said Dr. Ganz, chief of gastroenterology at Abbott Northwestern Hospital, Minneapolis, and one of the study investigators. These were among the results of the study that evaluated the device, the LINX Reflux Management System. The device was approved by the Food and Drug Administration FDA) in 2012 and is for the treatment of people with GERD as defined by abnormal pH testing, who continue to have chronic GERD symptoms that persist despite maximum medical therapy for the treatment of reflux.
“Magnetic sphincter augmentation should be considered first-line surgical therapy for those with gastroesophageal reflux disease, based on the results of this study,” he said.
The 2-year results of the prospective, multicenter study were the basis of the FDA approval of the device, described by the manufacturer, Torax Medical, as a “small implant [composed] of interlinked titanium beads with magnetic cores,” implanted during standard laparoscopy. The magnetic attraction between the beads augments the existing esophageal sphincter’s barrier function to prevent reflux,” according to the company.
The study enrolled 100 patients with reflux disease with a median age of 53 years, who had experienced typical heartburn for at least 6 months with or without regurgitation and were taking PPIs daily for at least 3 months (median use 5 years). Patients had GERD for a median of 10 years (range: 1-40 years). People who had any type of previous gastric or esophageal surgery, Barrett’s esophagus, a hiatal hernia greater than 3 cm, a body mass index over 35 kg/m2, or grade C or D esophagitis were excluded.
The device was implanted in all patients, who served as their own controls; 85 patients were followed through 5 years (6 were lost to follow-up, the device was explanted in 6 patients, 2 patients did not consent to extended follow-up, and 1 patient died of an unrelated cancer). The median procedure time was 36 minutes with a range of 7-125 minutes); all procedures were successfully completed with no intraoperative complications and all patients were discharged within 24 hours on an unrestricted diet.
The median total Gastroesophageal Reflux Disease–Health-Related Quality of Life (GERD-HRQL) score at baseline was 27 points among those not on PPIs and 11 points on PPIs, dropping to 4 points at 5 years off PPIs. At baseline, 95% of patients expressed dissatisfaction related to reflux, which dropped to 7% at year 5. Moderate to severe heartburn was reported by 89% at baseline, dropping to about 12% at year 5. The proportion of patients experiencing moderate to severe regurgitation dropped from 57% at baseline to about 1% at 5 years, Dr. Ganz said.
At baseline, 100% were taking PPIs every day, compared with 15% at 5 years. (At 5 years, 75% had discontinued PPIs, and about 9% reported PRN use only). Grade A and B esophagitis decreased from 40% at baseline to 16% at 5 years, at which point most cases were grade A, and there were no patients with grade C or D esophagitis, he said. In addition, at 5 years, 100% of patients “reported the ability to belch, and those needing to vomit – about 16% – reported the ability to vomit,” demonstrating that normal physiology was preserved with the device.
At 5 years, there were no device erosions or migrations, or any significant adverse events other than dysphagia, which “was typically mild and not associated with weight loss and tended to resolve over time,” from about 70% in the first few weeks after surgery to 11% at 1 year and 7% at 5 years, Dr. Ganz said.
In seven cases, the device was removed laparoscopically, with no complications and gastric anatomy was preserved for future treatments. All removals were elective. The device was removed in four patients because of dysphagia, which completely resolved in those patients. One patient had the device removed because of vomiting of unknown cause that persisted after removal. Another two patients who “had the device removed for disease management” continued to experience reflux and had “uneventful” Nissen fundoplication,” he said.
“Five years after magnetic augmentation, we have demonstrated objective evidence of reduction in acid exposure and in the majority of patients, normalized pH [and] we demonstrated significant and durable improvement in all group parameters measured, with preservation of fundic anatomy and normal physiology, with the ability to belch and vomit,” Dr. Ganz concluded. The results also show that the “procedure is reproducible, safe and reversible if necessary,” he added, noting that one of the limitations of the study was that subjects served as their own controls. During the discussion period, he was asked about hiatal hernia repairs, an apparent trend to “decay” from years 1 to 5 in some parameters measured, and dysphagia after the procedure.
About 40% of the patients in the study had a hiatal hernia, and about one-third of these patients had a hernia repair. A subgroup analysis of the data is being performed to evaluate the impact of hernia repair, Dr. Ganz said.
PPI use increased from 8% in year 4, to 15% in year 5. The reason for this s difficult to determine but “even though there is a bit of a decay, patients are still quite satisfied at 5 years,” Dr. Ganz remarked, also referring to the marked impact on regurgitation. Many U.S. patients use PPIs for reasons other than reflux, and studies show that many patients are on PPIs after the Nissen procedure in the absence of pathologic pH scores, he pointed out.
Compared with the type of dysphagia patients experience after the Nissen procedure, which is immediate and improves with time, Dr. Ganz said that the dysphagia associated with the device “seemed to peak around 2 weeks and then it slowly improved with time, so this may be more of a scar tissue–associated dysphagia than an edema dysphagia, but … it does improve with time.
Three-year results of the study were published in 2013 (N. Engl. J. Med. 2013;368:719-72), Dr. Ganz was the lead author.
The study was funded by Torax Medical. Dr. Ganz had no disclosures related to the topic of this presentation.
*This story was updated 7/9/2015.
AT DDW 2015
Key clinical point: A magnetic device designed to augment the lower esophageal sphincter is a surgical option that can be expected to provide long-term control of reflux symptoms in patients with GERD.
Major finding: Improvements 5 years after treatment with the Linx Reflux Management System include a drop from 60% experiencing regurgitation to 1%, and two-third of patients no longer taking PPIs.
Data source: The multicenter, prospective study evaluated the long-term safety and efficacy of the device over 5 years in 100 patients with GERD, who served as their own controls; 85 were included in the 5-year follow-up.
Disclosures: The study was funded by the device manufacturer, Torax Medical. Dr. Ganz had no disclosures related to the topic of this presentation.
Invasive approaches ‘overused’ for evaluating pulmonary nodules
One in four intermediate-sized (8-20 mm) pulmonary nodules were found to be malignant, based on results from a retrospective study of 377 patients seen in 18 community pulmonology practices.
Malignant nodules were more likely to be found in current or former smokers and to be larger than the benign nodules.
Further, despite guideline recommendations for surveillance of pulmonary nodules with less than a 5% pretest probability of malignancy, 44% of 36 patients with low-risk pulmonary nodules underwent at least one invasive procedure.
“To our knowledge, this is the first study that documents the prevalence of cancer (25%) in patients with intermediate-sized nodules referred to community-based pulmonologists,” wrote Dr. Nichole T. Tanner of the Medical University of South Carolina, Charleston, and her coauthors in the study published online (Chest 2015 June 18 [doi:10.1378/chest.15-0630]). “This finding has implications for managing pulmonary nodules in the community; because the risk of cancer is substantial, patients should be managed based on their individualized risk for malignancy.”
Biopsy – either by transthoracic needle aspiration or bronchoscopy – was performed in 33% (125) of patients, of whom 35% were found to have a malignancy and 57% had a specific benign diagnosis; biopsies in 8% were nondiagnostic and those patients were followed for 2 years.
Referrals for surgery were given to 20% (77) of patients; 19 had previously undergone a biopsy, with 11 having a nondiagnostic biopsy and eight having a received a benign result. Of patients who underwent surgery, 65% were diagnosed with a malignancy, and 35% had benign disease. However, the rate of surgical resection was similar regardless of patients’ pretest probability of malignancy.
PET scanning, performed in 37% of patients, was more likely in those who had a biopsy or surgery. The overall accuracy of PET was 74%, and the false-negative rate decreased slightly as the size of the nodule increased.
“Guidelines recommend surgery if the pretest probability of cancer is high (pCA > 65%) because a negative biopsy would not dissuade the clinician from pursuing a definitive diagnosis and a positive biopsy would lead to surgery anyway.”
The researchers pointed out that there are a range of noninvasive options now available to determine the likelihood that a nodule is malignant, such as CT scanning with the use of volumetric software to measure diameter and volume-doubling time of a nodule in between scans.
The study was supported by Integrated Diagnostics. All but one study author declared consulting fees, grant funding, stock options, or employment with Integrated Diagnostics.
One in four intermediate-sized (8-20 mm) pulmonary nodules were found to be malignant, based on results from a retrospective study of 377 patients seen in 18 community pulmonology practices.
Malignant nodules were more likely to be found in current or former smokers and to be larger than the benign nodules.
Further, despite guideline recommendations for surveillance of pulmonary nodules with less than a 5% pretest probability of malignancy, 44% of 36 patients with low-risk pulmonary nodules underwent at least one invasive procedure.
“To our knowledge, this is the first study that documents the prevalence of cancer (25%) in patients with intermediate-sized nodules referred to community-based pulmonologists,” wrote Dr. Nichole T. Tanner of the Medical University of South Carolina, Charleston, and her coauthors in the study published online (Chest 2015 June 18 [doi:10.1378/chest.15-0630]). “This finding has implications for managing pulmonary nodules in the community; because the risk of cancer is substantial, patients should be managed based on their individualized risk for malignancy.”
Biopsy – either by transthoracic needle aspiration or bronchoscopy – was performed in 33% (125) of patients, of whom 35% were found to have a malignancy and 57% had a specific benign diagnosis; biopsies in 8% were nondiagnostic and those patients were followed for 2 years.
Referrals for surgery were given to 20% (77) of patients; 19 had previously undergone a biopsy, with 11 having a nondiagnostic biopsy and eight having a received a benign result. Of patients who underwent surgery, 65% were diagnosed with a malignancy, and 35% had benign disease. However, the rate of surgical resection was similar regardless of patients’ pretest probability of malignancy.
PET scanning, performed in 37% of patients, was more likely in those who had a biopsy or surgery. The overall accuracy of PET was 74%, and the false-negative rate decreased slightly as the size of the nodule increased.
“Guidelines recommend surgery if the pretest probability of cancer is high (pCA > 65%) because a negative biopsy would not dissuade the clinician from pursuing a definitive diagnosis and a positive biopsy would lead to surgery anyway.”
The researchers pointed out that there are a range of noninvasive options now available to determine the likelihood that a nodule is malignant, such as CT scanning with the use of volumetric software to measure diameter and volume-doubling time of a nodule in between scans.
The study was supported by Integrated Diagnostics. All but one study author declared consulting fees, grant funding, stock options, or employment with Integrated Diagnostics.
One in four intermediate-sized (8-20 mm) pulmonary nodules were found to be malignant, based on results from a retrospective study of 377 patients seen in 18 community pulmonology practices.
Malignant nodules were more likely to be found in current or former smokers and to be larger than the benign nodules.
Further, despite guideline recommendations for surveillance of pulmonary nodules with less than a 5% pretest probability of malignancy, 44% of 36 patients with low-risk pulmonary nodules underwent at least one invasive procedure.
“To our knowledge, this is the first study that documents the prevalence of cancer (25%) in patients with intermediate-sized nodules referred to community-based pulmonologists,” wrote Dr. Nichole T. Tanner of the Medical University of South Carolina, Charleston, and her coauthors in the study published online (Chest 2015 June 18 [doi:10.1378/chest.15-0630]). “This finding has implications for managing pulmonary nodules in the community; because the risk of cancer is substantial, patients should be managed based on their individualized risk for malignancy.”
Biopsy – either by transthoracic needle aspiration or bronchoscopy – was performed in 33% (125) of patients, of whom 35% were found to have a malignancy and 57% had a specific benign diagnosis; biopsies in 8% were nondiagnostic and those patients were followed for 2 years.
Referrals for surgery were given to 20% (77) of patients; 19 had previously undergone a biopsy, with 11 having a nondiagnostic biopsy and eight having a received a benign result. Of patients who underwent surgery, 65% were diagnosed with a malignancy, and 35% had benign disease. However, the rate of surgical resection was similar regardless of patients’ pretest probability of malignancy.
PET scanning, performed in 37% of patients, was more likely in those who had a biopsy or surgery. The overall accuracy of PET was 74%, and the false-negative rate decreased slightly as the size of the nodule increased.
“Guidelines recommend surgery if the pretest probability of cancer is high (pCA > 65%) because a negative biopsy would not dissuade the clinician from pursuing a definitive diagnosis and a positive biopsy would lead to surgery anyway.”
The researchers pointed out that there are a range of noninvasive options now available to determine the likelihood that a nodule is malignant, such as CT scanning with the use of volumetric software to measure diameter and volume-doubling time of a nodule in between scans.
The study was supported by Integrated Diagnostics. All but one study author declared consulting fees, grant funding, stock options, or employment with Integrated Diagnostics.
FROM CHEST
Key clinical point: One in four pulmonary nodules 8-20 mm in size are malignant, and invasive tests are being overused in low-risk patients in community settings.
Major finding: Despite guidelines recommending pulmonary nodes with a less than 5% pretest probability of malignancy be managed with surveillance only, 44% of low-risk patients in the study underwent at least one invasive procedure for what proved to be a benign nodule.
Data source: A multicenter, retrospective study in 377 patients.
Disclosures: The study was supported by Integrated Diagnostics. All but one author declared consulting fees, grant funding, stock options, or employment with Integrated Diagnostics.
Barrett’s esophagus increasing in frequency
Patients with Barrett’s esophagus, a condition in which cells lining the esophagus are replaced by the type of cells that normally line the intestine, need to be monitored carefully to prevent the development of esophageal cancer, a gastroenterologist expert in the condition said here at Digestive Diseases: New Advances. The condition can occur following exposure to stomach acids and bile from gastroesophageal reflux disease (GERD).
“The reason we worry about Barrett’s is because it’s a major risk factor for developing esophageal adenocarcinoma, and that’s a tumor that has been experiencing an enormous increase in frequency over the past few decades,” said Dr. Stuart Spechler, chief of gastroenterology for the VA North Texas Healthcare System and co-director of the Esophageal Diseases Center at the University of Texas Southwestern Medical Center in Dallas.
The incidence of esophageal adenocarcinoma increased more than sevenfold over 33 years, going from 3.6 per million in 1973 to 25.6 per million in 2006. Barrett’s esophagus affects about 5.6% of U.S. adults, he noted.
Endoscopic screening for Barrett’s esophagus is recommended for patients with multiple risk factors for esophageal cancer, including chronic GERD (having GERD for more than 5 years), hiatal hernia, age of at least 50 years, male gender, white race, and an elevated body mass index, especially if there’s an intra-abdominal body fat distribution, Dr. Spechler said.
Barrett’s esophagus traditionally is treated with proton pump inhibitors because of their ability to decrease gastric acid production and acid reflux and heal reflux esophagitis. “We also recommend that these patients have regular endoscopic surveillance to look for precancerous changes,” most notably dysplasia, he said. If no dysplasia is found, patients should receive a repeat endoscopy every 3-5 years. Patients with high-grade dysplasia should be treated with endoscopic eradication therapy. The risk of developing cancer in patients with high-grade dysplasia is about 6% per year, he said, which is “sufficient to warrant intervention.”
For patients with visible mucosal irregularities, endoscopic mucosal resection can determine how far the neoplasms have spread, Dr. Spechler said.
For those neoplasms confined to the mucosa, like high-grade dysplasia, radiofrequency ablation can be used to burn the abnormal mucosa away. As the esophagus heals, normal cells grow back. The procedure is safe and effective and has been shown to prevent neoplastic progression at 1 year, he said – the most serious complication is esophageal stricture (N. Engl. J. Med. 2009;360:2277-88). Radiofrequency ablation also can be considered in patients with low-grade dysplasia, and even for highly selected patients with nondysplastic Barrett’s esophagus deemed to be at increased risk for progression to high-grade dysplasia or cancer.
“We do worry about Barrett’s esophagus recurring after endoscopic eradication, and there is a rate of recurrence, but this newer treatment seems to be very effective, at least in the short term, for preventing progression to cancer,” he said.
More advanced cancers can be treated by surgery and chemotherapy or radiation therapy.
Overall, “this is a condition that’s increasing in frequency, and we do worry about it, but as long as you are treating patients, screening for Barrett’s esophagus, and following them regularly with surveillance, the prognosis for any individual patient is really excellent,” he said at the meeting, which was held by Global Academy for Medical Education and Rutgers, the State University of New Jersey. Global Academy and this news organization are owned by the same company.
Dr. Spechler has served a consultant for Takeda Pharmaceuticals and is currently a consultant for Interpace Diagnostics.
Patients with Barrett’s esophagus, a condition in which cells lining the esophagus are replaced by the type of cells that normally line the intestine, need to be monitored carefully to prevent the development of esophageal cancer, a gastroenterologist expert in the condition said here at Digestive Diseases: New Advances. The condition can occur following exposure to stomach acids and bile from gastroesophageal reflux disease (GERD).
“The reason we worry about Barrett’s is because it’s a major risk factor for developing esophageal adenocarcinoma, and that’s a tumor that has been experiencing an enormous increase in frequency over the past few decades,” said Dr. Stuart Spechler, chief of gastroenterology for the VA North Texas Healthcare System and co-director of the Esophageal Diseases Center at the University of Texas Southwestern Medical Center in Dallas.
The incidence of esophageal adenocarcinoma increased more than sevenfold over 33 years, going from 3.6 per million in 1973 to 25.6 per million in 2006. Barrett’s esophagus affects about 5.6% of U.S. adults, he noted.
Endoscopic screening for Barrett’s esophagus is recommended for patients with multiple risk factors for esophageal cancer, including chronic GERD (having GERD for more than 5 years), hiatal hernia, age of at least 50 years, male gender, white race, and an elevated body mass index, especially if there’s an intra-abdominal body fat distribution, Dr. Spechler said.
Barrett’s esophagus traditionally is treated with proton pump inhibitors because of their ability to decrease gastric acid production and acid reflux and heal reflux esophagitis. “We also recommend that these patients have regular endoscopic surveillance to look for precancerous changes,” most notably dysplasia, he said. If no dysplasia is found, patients should receive a repeat endoscopy every 3-5 years. Patients with high-grade dysplasia should be treated with endoscopic eradication therapy. The risk of developing cancer in patients with high-grade dysplasia is about 6% per year, he said, which is “sufficient to warrant intervention.”
For patients with visible mucosal irregularities, endoscopic mucosal resection can determine how far the neoplasms have spread, Dr. Spechler said.
For those neoplasms confined to the mucosa, like high-grade dysplasia, radiofrequency ablation can be used to burn the abnormal mucosa away. As the esophagus heals, normal cells grow back. The procedure is safe and effective and has been shown to prevent neoplastic progression at 1 year, he said – the most serious complication is esophageal stricture (N. Engl. J. Med. 2009;360:2277-88). Radiofrequency ablation also can be considered in patients with low-grade dysplasia, and even for highly selected patients with nondysplastic Barrett’s esophagus deemed to be at increased risk for progression to high-grade dysplasia or cancer.
“We do worry about Barrett’s esophagus recurring after endoscopic eradication, and there is a rate of recurrence, but this newer treatment seems to be very effective, at least in the short term, for preventing progression to cancer,” he said.
More advanced cancers can be treated by surgery and chemotherapy or radiation therapy.
Overall, “this is a condition that’s increasing in frequency, and we do worry about it, but as long as you are treating patients, screening for Barrett’s esophagus, and following them regularly with surveillance, the prognosis for any individual patient is really excellent,” he said at the meeting, which was held by Global Academy for Medical Education and Rutgers, the State University of New Jersey. Global Academy and this news organization are owned by the same company.
Dr. Spechler has served a consultant for Takeda Pharmaceuticals and is currently a consultant for Interpace Diagnostics.
Patients with Barrett’s esophagus, a condition in which cells lining the esophagus are replaced by the type of cells that normally line the intestine, need to be monitored carefully to prevent the development of esophageal cancer, a gastroenterologist expert in the condition said here at Digestive Diseases: New Advances. The condition can occur following exposure to stomach acids and bile from gastroesophageal reflux disease (GERD).
“The reason we worry about Barrett’s is because it’s a major risk factor for developing esophageal adenocarcinoma, and that’s a tumor that has been experiencing an enormous increase in frequency over the past few decades,” said Dr. Stuart Spechler, chief of gastroenterology for the VA North Texas Healthcare System and co-director of the Esophageal Diseases Center at the University of Texas Southwestern Medical Center in Dallas.
The incidence of esophageal adenocarcinoma increased more than sevenfold over 33 years, going from 3.6 per million in 1973 to 25.6 per million in 2006. Barrett’s esophagus affects about 5.6% of U.S. adults, he noted.
Endoscopic screening for Barrett’s esophagus is recommended for patients with multiple risk factors for esophageal cancer, including chronic GERD (having GERD for more than 5 years), hiatal hernia, age of at least 50 years, male gender, white race, and an elevated body mass index, especially if there’s an intra-abdominal body fat distribution, Dr. Spechler said.
Barrett’s esophagus traditionally is treated with proton pump inhibitors because of their ability to decrease gastric acid production and acid reflux and heal reflux esophagitis. “We also recommend that these patients have regular endoscopic surveillance to look for precancerous changes,” most notably dysplasia, he said. If no dysplasia is found, patients should receive a repeat endoscopy every 3-5 years. Patients with high-grade dysplasia should be treated with endoscopic eradication therapy. The risk of developing cancer in patients with high-grade dysplasia is about 6% per year, he said, which is “sufficient to warrant intervention.”
For patients with visible mucosal irregularities, endoscopic mucosal resection can determine how far the neoplasms have spread, Dr. Spechler said.
For those neoplasms confined to the mucosa, like high-grade dysplasia, radiofrequency ablation can be used to burn the abnormal mucosa away. As the esophagus heals, normal cells grow back. The procedure is safe and effective and has been shown to prevent neoplastic progression at 1 year, he said – the most serious complication is esophageal stricture (N. Engl. J. Med. 2009;360:2277-88). Radiofrequency ablation also can be considered in patients with low-grade dysplasia, and even for highly selected patients with nondysplastic Barrett’s esophagus deemed to be at increased risk for progression to high-grade dysplasia or cancer.
“We do worry about Barrett’s esophagus recurring after endoscopic eradication, and there is a rate of recurrence, but this newer treatment seems to be very effective, at least in the short term, for preventing progression to cancer,” he said.
More advanced cancers can be treated by surgery and chemotherapy or radiation therapy.
Overall, “this is a condition that’s increasing in frequency, and we do worry about it, but as long as you are treating patients, screening for Barrett’s esophagus, and following them regularly with surveillance, the prognosis for any individual patient is really excellent,” he said at the meeting, which was held by Global Academy for Medical Education and Rutgers, the State University of New Jersey. Global Academy and this news organization are owned by the same company.
Dr. Spechler has served a consultant for Takeda Pharmaceuticals and is currently a consultant for Interpace Diagnostics.
AATS: No postpneumonectomy survival benefit in adding radiation to chemotherapy for NSCLC
SEATTLE – Adding radiotherapy to neoadjuvant chemotherapy does not improve long-term survival after pneumonectomy for non–small cell lung cancer, according to a Turkish investigation of 140 patients.
In the study, 100 (71.4%) patients had two to six cycles of platinum-based chemotherapy at least 3 weeks before surgery; 40 (28.6%) others underwent the same regimen with the addition of radiotherapy dosed at 45-66 Gy 6-8 weeks before surgery.
Five-year survival was 48% in the chemotherapy group and 50% in the chemoradiation group, an insignificant difference (P = .7).
“Chemotherapy before surgery is definitely beneficial, but I think we will get rid of the radiotherapy” in patients with operable tumors, said lead investigator Dr. Cengiz Gebitekin, professor and head of thoracic surgery at Uludag University in Bursa, Turkey.
“It does not provide any survival benefit,” and it might cause harm, he noted, adding that “the benefit of neoadjuvant treatment comes from the chemotherapy.”
The chemoradiation group showed a tendency toward tumor down-staging and higher complete response rates, but also a trend toward more radiation-induced tissue damage. The rate of bronchopleural fistula was 3% in the chemotherapy group and 5% in the chemoradiation group, although the difference was not significant. Even so, “some of these patients had pneumonectomies because of lung damage from the radiotherapy,” Dr. Gebitekin said at the annual meeting of the American Association for Thoracic Surgery.
It’s uncertain why radiation didn’t improve survival. The investigators excluded patients with known metastases or other malignancies, but it’s possible that some patients had occult metastases that had spread beyond the field of their localized neoadjuvant radiation, he said.
The patients were treated between 2000 and 2013 at Uludag University, Istanbul University, and Zurich University Hospital. They were 55 years old on average, and 84% were men.
About 40% of patients in both the chemotherapy and chemoradiation groups had right pneumonectomies; the rest had left pneumonectomies. Bronchopleural fistulas and other comorbidities were more common after right pneumonectomies, but not significantly so.
Seven patients (5%) in the chemotherapy group but none in the chemoradiation group died within 90 days of surgery.
About 32% of chemotherapy patients and 28% of chemoradiation patients (P = .6) developed major morbidities following surgery, including arrhythmias, pneumonia, empyema, and other problems.
Staples were used to close the bronchus in almost all patients, with the stump covered with live tissue in about 70%.
The majority of patients had stage IIb or IIIa disease on postop staging; postop staging was the only factor predictive of long-term survival, with higher-stage patients doing worse.
Dr. Gebitekin said that he had no relevant disclosures.
SEATTLE – Adding radiotherapy to neoadjuvant chemotherapy does not improve long-term survival after pneumonectomy for non–small cell lung cancer, according to a Turkish investigation of 140 patients.
In the study, 100 (71.4%) patients had two to six cycles of platinum-based chemotherapy at least 3 weeks before surgery; 40 (28.6%) others underwent the same regimen with the addition of radiotherapy dosed at 45-66 Gy 6-8 weeks before surgery.
Five-year survival was 48% in the chemotherapy group and 50% in the chemoradiation group, an insignificant difference (P = .7).
“Chemotherapy before surgery is definitely beneficial, but I think we will get rid of the radiotherapy” in patients with operable tumors, said lead investigator Dr. Cengiz Gebitekin, professor and head of thoracic surgery at Uludag University in Bursa, Turkey.
“It does not provide any survival benefit,” and it might cause harm, he noted, adding that “the benefit of neoadjuvant treatment comes from the chemotherapy.”
The chemoradiation group showed a tendency toward tumor down-staging and higher complete response rates, but also a trend toward more radiation-induced tissue damage. The rate of bronchopleural fistula was 3% in the chemotherapy group and 5% in the chemoradiation group, although the difference was not significant. Even so, “some of these patients had pneumonectomies because of lung damage from the radiotherapy,” Dr. Gebitekin said at the annual meeting of the American Association for Thoracic Surgery.
It’s uncertain why radiation didn’t improve survival. The investigators excluded patients with known metastases or other malignancies, but it’s possible that some patients had occult metastases that had spread beyond the field of their localized neoadjuvant radiation, he said.
The patients were treated between 2000 and 2013 at Uludag University, Istanbul University, and Zurich University Hospital. They were 55 years old on average, and 84% were men.
About 40% of patients in both the chemotherapy and chemoradiation groups had right pneumonectomies; the rest had left pneumonectomies. Bronchopleural fistulas and other comorbidities were more common after right pneumonectomies, but not significantly so.
Seven patients (5%) in the chemotherapy group but none in the chemoradiation group died within 90 days of surgery.
About 32% of chemotherapy patients and 28% of chemoradiation patients (P = .6) developed major morbidities following surgery, including arrhythmias, pneumonia, empyema, and other problems.
Staples were used to close the bronchus in almost all patients, with the stump covered with live tissue in about 70%.
The majority of patients had stage IIb or IIIa disease on postop staging; postop staging was the only factor predictive of long-term survival, with higher-stage patients doing worse.
Dr. Gebitekin said that he had no relevant disclosures.
SEATTLE – Adding radiotherapy to neoadjuvant chemotherapy does not improve long-term survival after pneumonectomy for non–small cell lung cancer, according to a Turkish investigation of 140 patients.
In the study, 100 (71.4%) patients had two to six cycles of platinum-based chemotherapy at least 3 weeks before surgery; 40 (28.6%) others underwent the same regimen with the addition of radiotherapy dosed at 45-66 Gy 6-8 weeks before surgery.
Five-year survival was 48% in the chemotherapy group and 50% in the chemoradiation group, an insignificant difference (P = .7).
“Chemotherapy before surgery is definitely beneficial, but I think we will get rid of the radiotherapy” in patients with operable tumors, said lead investigator Dr. Cengiz Gebitekin, professor and head of thoracic surgery at Uludag University in Bursa, Turkey.
“It does not provide any survival benefit,” and it might cause harm, he noted, adding that “the benefit of neoadjuvant treatment comes from the chemotherapy.”
The chemoradiation group showed a tendency toward tumor down-staging and higher complete response rates, but also a trend toward more radiation-induced tissue damage. The rate of bronchopleural fistula was 3% in the chemotherapy group and 5% in the chemoradiation group, although the difference was not significant. Even so, “some of these patients had pneumonectomies because of lung damage from the radiotherapy,” Dr. Gebitekin said at the annual meeting of the American Association for Thoracic Surgery.
It’s uncertain why radiation didn’t improve survival. The investigators excluded patients with known metastases or other malignancies, but it’s possible that some patients had occult metastases that had spread beyond the field of their localized neoadjuvant radiation, he said.
The patients were treated between 2000 and 2013 at Uludag University, Istanbul University, and Zurich University Hospital. They were 55 years old on average, and 84% were men.
About 40% of patients in both the chemotherapy and chemoradiation groups had right pneumonectomies; the rest had left pneumonectomies. Bronchopleural fistulas and other comorbidities were more common after right pneumonectomies, but not significantly so.
Seven patients (5%) in the chemotherapy group but none in the chemoradiation group died within 90 days of surgery.
About 32% of chemotherapy patients and 28% of chemoradiation patients (P = .6) developed major morbidities following surgery, including arrhythmias, pneumonia, empyema, and other problems.
Staples were used to close the bronchus in almost all patients, with the stump covered with live tissue in about 70%.
The majority of patients had stage IIb or IIIa disease on postop staging; postop staging was the only factor predictive of long-term survival, with higher-stage patients doing worse.
Dr. Gebitekin said that he had no relevant disclosures.
AT THE AATS ANNUAL MEETING
Key clinical point: Limit neoadjuvant treatment to chemotherapy for non–small cell lung cancer patients.
Major finding: About half of patients were alive 5 years after pneumonectomies for lung cancer, whether they had neoadjuvant chemotherapy or chemoradiation.
Data source: Retrospective study of 140 pneumonectomy patients.
Disclosures: Dr. Gebitekin had no disclosures.
DDW: Barrett’s ‘indefinite for dysplasia’ may be cancer harbinger
WASHINGTON – A diagnosis of Barrett’s esophagus “indefinite for dysplasia” doesn’t mean that the patient is home free; it may, in fact, be an indicator of increased risk for progression to high-grade dysplasia or esophageal adenocarcinoma, investigators suggest.
Among 87 patients who had follow-up endoscopies and biopsies within a year of a diagnosis of Barrett’s indefinite for dysplasia (IND), 7 had progression of disease, including 5 who developed high-grade dysplasia or adenocarcinoma, and 2 who developed low-grade disease.
Of these seven patients, four had disease progression with 6 months of a diagnosis of Barrett’s IND, Dr, Michelle Ma reported at the annual Digestive Disease Week.
“Indefinite for dysplasia is an important diagnostic category that is associated with an increased risk for prevalent dysplasia, particularly within the first 6 months after diagnosis. After 12 months, the risk for progressing to advanced neoplasia is low, and similar to other studies,” said Dr. Ma of the University of Pennsylvania, Philadelphia.
Although there is fairly strong evidence to guide the management of patients with low-grade and high-grade dysplasia, it’s less clear whether Barrett’s IND is risk marker for progression. Dr. Ma said, citing a somewhat fuzzy definition of the term: “Epithelial abnormalities insufficient to diagnose dysplasia, or epithelial abnormalities unclear due to inflammation or sampling.”
Uncertainty about the natural history of IND is reflected in practice guidelines, which either don’t address it, call for repeat endoscopy in 6 months, or call for an expert gastrointestinal pathology review with repeat endoscopy to clarify dysplasia status if the evidence is of low quality, Dr. Ma said.
To determine the rate of, and risk factors for, neoplastic progression of IND, the authors took a retrospective look at patients in their center’s pathology database and Barrett’s esophagus register with a histopathologic diagnosis of IND from 2000 through 2014. They excluded patients with frank dysplasia or carcinoma on diagnosis, and those who did not have follow-up endoscopies.
The investigatoes factored demographic variables into their analysis, including age, gender, body-mass index, smoking history, use of proton-pump inhibitors (PPI), nonsteroidal anti-inflammatory drugs, and family history of Barrett’s or esophageal adenocarcinoma. They also considered endoscopic/pathologic characteristics such as hiatal hernia size, Barrett’s segment length, muscosal nodularity, and multifocal IND.
A total of 106 patients with IND were eligible for the analysis, 87 of whom had follow-up endoscopy and biopsy within a year of diagnosis. As noted before, 7 of these patients had prevalent disease, with prevalence rates of 2.3% for low-grade dysplasia, 4.6% for high-grade dysplasia, and 1.1% for esophageal adenocarcinoma.
To determine the incidence of dysplasia, the authors first excluded the 7 patients with prevealent dysplasia and 33 patients who did not have a surveillance endoscopy in the first year following a diagnosis of IND, leaving 66 patients for analysis. Of this group, 3 developed incident dysplasia or adenocarcinoma, yielding an incidence of 4.5% over a median of 32 months of follow-up.
An analysis of risk factors for prevalent dysplasia showed that none of the variables was significant, although Barrett’s segment length approached statistical significance. Looking at risk factors for incident dysplasia, both smoking status (P = .0207) and segment length (P = .0253) were significant predictors.
A pathologist who was not involved in the study pointed out that a diagnosis of IND can mean many things to many people.
“Indefinite for dysplasia is really not an entity, it’s about 5,000 things that we choose to put into that category. It’s a horribly non-reproducible diagnosis,” commented Dr. Henry D. Appelman, a professor of anatomic pathology at the University of Michigan in Ann Arbor, during a aquestion-and-answer period.
He questioned whether the diagnoses of IND were subject to review at her center.
Dr. Ma noted that Barrett’s specimens at her institution are routinely reviewed by pathologists specializing in Barrett’s, who will also review slides of patients referred to the center from other institutions.
The study was internally funded. The authors reported no conflicts of interest.
WASHINGTON – A diagnosis of Barrett’s esophagus “indefinite for dysplasia” doesn’t mean that the patient is home free; it may, in fact, be an indicator of increased risk for progression to high-grade dysplasia or esophageal adenocarcinoma, investigators suggest.
Among 87 patients who had follow-up endoscopies and biopsies within a year of a diagnosis of Barrett’s indefinite for dysplasia (IND), 7 had progression of disease, including 5 who developed high-grade dysplasia or adenocarcinoma, and 2 who developed low-grade disease.
Of these seven patients, four had disease progression with 6 months of a diagnosis of Barrett’s IND, Dr, Michelle Ma reported at the annual Digestive Disease Week.
“Indefinite for dysplasia is an important diagnostic category that is associated with an increased risk for prevalent dysplasia, particularly within the first 6 months after diagnosis. After 12 months, the risk for progressing to advanced neoplasia is low, and similar to other studies,” said Dr. Ma of the University of Pennsylvania, Philadelphia.
Although there is fairly strong evidence to guide the management of patients with low-grade and high-grade dysplasia, it’s less clear whether Barrett’s IND is risk marker for progression. Dr. Ma said, citing a somewhat fuzzy definition of the term: “Epithelial abnormalities insufficient to diagnose dysplasia, or epithelial abnormalities unclear due to inflammation or sampling.”
Uncertainty about the natural history of IND is reflected in practice guidelines, which either don’t address it, call for repeat endoscopy in 6 months, or call for an expert gastrointestinal pathology review with repeat endoscopy to clarify dysplasia status if the evidence is of low quality, Dr. Ma said.
To determine the rate of, and risk factors for, neoplastic progression of IND, the authors took a retrospective look at patients in their center’s pathology database and Barrett’s esophagus register with a histopathologic diagnosis of IND from 2000 through 2014. They excluded patients with frank dysplasia or carcinoma on diagnosis, and those who did not have follow-up endoscopies.
The investigatoes factored demographic variables into their analysis, including age, gender, body-mass index, smoking history, use of proton-pump inhibitors (PPI), nonsteroidal anti-inflammatory drugs, and family history of Barrett’s or esophageal adenocarcinoma. They also considered endoscopic/pathologic characteristics such as hiatal hernia size, Barrett’s segment length, muscosal nodularity, and multifocal IND.
A total of 106 patients with IND were eligible for the analysis, 87 of whom had follow-up endoscopy and biopsy within a year of diagnosis. As noted before, 7 of these patients had prevalent disease, with prevalence rates of 2.3% for low-grade dysplasia, 4.6% for high-grade dysplasia, and 1.1% for esophageal adenocarcinoma.
To determine the incidence of dysplasia, the authors first excluded the 7 patients with prevealent dysplasia and 33 patients who did not have a surveillance endoscopy in the first year following a diagnosis of IND, leaving 66 patients for analysis. Of this group, 3 developed incident dysplasia or adenocarcinoma, yielding an incidence of 4.5% over a median of 32 months of follow-up.
An analysis of risk factors for prevalent dysplasia showed that none of the variables was significant, although Barrett’s segment length approached statistical significance. Looking at risk factors for incident dysplasia, both smoking status (P = .0207) and segment length (P = .0253) were significant predictors.
A pathologist who was not involved in the study pointed out that a diagnosis of IND can mean many things to many people.
“Indefinite for dysplasia is really not an entity, it’s about 5,000 things that we choose to put into that category. It’s a horribly non-reproducible diagnosis,” commented Dr. Henry D. Appelman, a professor of anatomic pathology at the University of Michigan in Ann Arbor, during a aquestion-and-answer period.
He questioned whether the diagnoses of IND were subject to review at her center.
Dr. Ma noted that Barrett’s specimens at her institution are routinely reviewed by pathologists specializing in Barrett’s, who will also review slides of patients referred to the center from other institutions.
The study was internally funded. The authors reported no conflicts of interest.
WASHINGTON – A diagnosis of Barrett’s esophagus “indefinite for dysplasia” doesn’t mean that the patient is home free; it may, in fact, be an indicator of increased risk for progression to high-grade dysplasia or esophageal adenocarcinoma, investigators suggest.
Among 87 patients who had follow-up endoscopies and biopsies within a year of a diagnosis of Barrett’s indefinite for dysplasia (IND), 7 had progression of disease, including 5 who developed high-grade dysplasia or adenocarcinoma, and 2 who developed low-grade disease.
Of these seven patients, four had disease progression with 6 months of a diagnosis of Barrett’s IND, Dr, Michelle Ma reported at the annual Digestive Disease Week.
“Indefinite for dysplasia is an important diagnostic category that is associated with an increased risk for prevalent dysplasia, particularly within the first 6 months after diagnosis. After 12 months, the risk for progressing to advanced neoplasia is low, and similar to other studies,” said Dr. Ma of the University of Pennsylvania, Philadelphia.
Although there is fairly strong evidence to guide the management of patients with low-grade and high-grade dysplasia, it’s less clear whether Barrett’s IND is risk marker for progression. Dr. Ma said, citing a somewhat fuzzy definition of the term: “Epithelial abnormalities insufficient to diagnose dysplasia, or epithelial abnormalities unclear due to inflammation or sampling.”
Uncertainty about the natural history of IND is reflected in practice guidelines, which either don’t address it, call for repeat endoscopy in 6 months, or call for an expert gastrointestinal pathology review with repeat endoscopy to clarify dysplasia status if the evidence is of low quality, Dr. Ma said.
To determine the rate of, and risk factors for, neoplastic progression of IND, the authors took a retrospective look at patients in their center’s pathology database and Barrett’s esophagus register with a histopathologic diagnosis of IND from 2000 through 2014. They excluded patients with frank dysplasia or carcinoma on diagnosis, and those who did not have follow-up endoscopies.
The investigatoes factored demographic variables into their analysis, including age, gender, body-mass index, smoking history, use of proton-pump inhibitors (PPI), nonsteroidal anti-inflammatory drugs, and family history of Barrett’s or esophageal adenocarcinoma. They also considered endoscopic/pathologic characteristics such as hiatal hernia size, Barrett’s segment length, muscosal nodularity, and multifocal IND.
A total of 106 patients with IND were eligible for the analysis, 87 of whom had follow-up endoscopy and biopsy within a year of diagnosis. As noted before, 7 of these patients had prevalent disease, with prevalence rates of 2.3% for low-grade dysplasia, 4.6% for high-grade dysplasia, and 1.1% for esophageal adenocarcinoma.
To determine the incidence of dysplasia, the authors first excluded the 7 patients with prevealent dysplasia and 33 patients who did not have a surveillance endoscopy in the first year following a diagnosis of IND, leaving 66 patients for analysis. Of this group, 3 developed incident dysplasia or adenocarcinoma, yielding an incidence of 4.5% over a median of 32 months of follow-up.
An analysis of risk factors for prevalent dysplasia showed that none of the variables was significant, although Barrett’s segment length approached statistical significance. Looking at risk factors for incident dysplasia, both smoking status (P = .0207) and segment length (P = .0253) were significant predictors.
A pathologist who was not involved in the study pointed out that a diagnosis of IND can mean many things to many people.
“Indefinite for dysplasia is really not an entity, it’s about 5,000 things that we choose to put into that category. It’s a horribly non-reproducible diagnosis,” commented Dr. Henry D. Appelman, a professor of anatomic pathology at the University of Michigan in Ann Arbor, during a aquestion-and-answer period.
He questioned whether the diagnoses of IND were subject to review at her center.
Dr. Ma noted that Barrett’s specimens at her institution are routinely reviewed by pathologists specializing in Barrett’s, who will also review slides of patients referred to the center from other institutions.
The study was internally funded. The authors reported no conflicts of interest.
AT DDW 2015
Key clinical point: Barrett’s esophagus indefinite for dysplasia may progress to dysplasia or adenocarcinoma within a year of diagnosis.
Major finding: Seven of 87 patients with a diagnosis of Barrett’s indefinite for dysplasia (IND) had disease progression within 1 year.
Data source: Retrospective case series of 87 patients who had follow-up endoscopies and biopsies within a year of a diagnosis of Barrett’s IND.
Disclosures: The study was internally funded. The authors reported no conflicts of interest.