User login
VIDEO: Researchers beginning to explore microbiome’s effect on surgical outcomes
SAN DIEGO – Surgery seems to stimulate abrupt changes in both the skin and gut microbiome, which in some patients may increase the risk of surgical-site infections and anastomotic leaks. With that knowledge, researchers are exploring the very first steps toward a presurgical microbiome optimization protocol, Heidi Nelson, MD, FACS, said at the annual clinical congress of the American College of Surgeons.
It’s very early in the journey, said Dr. Nelson, the Fred C. Andersen Professor of Surgery at Mayo Clinic, Rochester, Minn. The path is not straightforward because the human microbiome appears to be nearly as individually unique as the human fingerprint, so presurgical protocols might have to be individually tailored to each patient.
Dr. Nelson comoderated a session exploring this topic with John Alverdy, MD, FACS, of the University of Chicago. The panel discussed human and animal studies suggesting that the stress of surgery, when combined with subclinical ischemia and any baseline physiologic stress (chronic illness or radiation, for example), can cause some commensals to begin producing collagenase – a change that endangers even surgically sound anastomoses. The skin microbiome is altered as well, with areas around abdominal incisions beginning to express gut flora, which increase the risk of a surgical-site infection.
Through diet or other presurgical interventions, Dr. Nelson said in a video interview, it might be possible to optimize the microbiome and reduce the chances of some of these occurrences.
She had no financial disclosures.
On Twitter @Alz_Gal
SAN DIEGO – Surgery seems to stimulate abrupt changes in both the skin and gut microbiome, which in some patients may increase the risk of surgical-site infections and anastomotic leaks. With that knowledge, researchers are exploring the very first steps toward a presurgical microbiome optimization protocol, Heidi Nelson, MD, FACS, said at the annual clinical congress of the American College of Surgeons.
It’s very early in the journey, said Dr. Nelson, the Fred C. Andersen Professor of Surgery at Mayo Clinic, Rochester, Minn. The path is not straightforward because the human microbiome appears to be nearly as individually unique as the human fingerprint, so presurgical protocols might have to be individually tailored to each patient.
Dr. Nelson comoderated a session exploring this topic with John Alverdy, MD, FACS, of the University of Chicago. The panel discussed human and animal studies suggesting that the stress of surgery, when combined with subclinical ischemia and any baseline physiologic stress (chronic illness or radiation, for example), can cause some commensals to begin producing collagenase – a change that endangers even surgically sound anastomoses. The skin microbiome is altered as well, with areas around abdominal incisions beginning to express gut flora, which increase the risk of a surgical-site infection.
Through diet or other presurgical interventions, Dr. Nelson said in a video interview, it might be possible to optimize the microbiome and reduce the chances of some of these occurrences.
She had no financial disclosures.
On Twitter @Alz_Gal
SAN DIEGO – Surgery seems to stimulate abrupt changes in both the skin and gut microbiome, which in some patients may increase the risk of surgical-site infections and anastomotic leaks. With that knowledge, researchers are exploring the very first steps toward a presurgical microbiome optimization protocol, Heidi Nelson, MD, FACS, said at the annual clinical congress of the American College of Surgeons.
It’s very early in the journey, said Dr. Nelson, the Fred C. Andersen Professor of Surgery at Mayo Clinic, Rochester, Minn. The path is not straightforward because the human microbiome appears to be nearly as individually unique as the human fingerprint, so presurgical protocols might have to be individually tailored to each patient.
Dr. Nelson comoderated a session exploring this topic with John Alverdy, MD, FACS, of the University of Chicago. The panel discussed human and animal studies suggesting that the stress of surgery, when combined with subclinical ischemia and any baseline physiologic stress (chronic illness or radiation, for example), can cause some commensals to begin producing collagenase – a change that endangers even surgically sound anastomoses. The skin microbiome is altered as well, with areas around abdominal incisions beginning to express gut flora, which increase the risk of a surgical-site infection.
Through diet or other presurgical interventions, Dr. Nelson said in a video interview, it might be possible to optimize the microbiome and reduce the chances of some of these occurrences.
She had no financial disclosures.
On Twitter @Alz_Gal
AT THE ACS CLINICAL CONGRESS
CDC data show decline in some hospital-acquired infections
SAN DIEGO – There was an encouraging 22% reduction in hospital-acquired infections (HAIs) after adjustment for clinical variables when 2015 and 2011 data from national Centers for Disease Control and Prevention hospital surveys were compared.
“The data suggest that national efforts toward preventing HAIs are succeeding,” reported Shelley S. Magill, MD, PhD, a medical epidemiologist in the Division of Healthcare Quality Promotion at the CDC who summarized the data at an annual scientific meeting on infectious diseases .
The comparative data were drawn from point prevalence surveys conducted in 2011 and 2015 as part of the CDC’s Emerging Infections Program. In this type of survey, the data are collected over 1 day, providing a snapshot in time among selected hospitals. The analysis presented by Dr. Magill was restricted to the 148 hospitals that participated in both the 2011 and 2015 surveys, although the 2015 survey included a total of 199 hospitals, of which other data analyses are planned.
Due to the change in incidence, the rank order of HAIs was different in 2015 relative to 2011. While surgical site infections (SSIs) represented the most frequent HAI in 2011, they fell to the third most frequent HAI in 2015; pneumonia and gastrointestinal (GI) infections assumed the first and second spots, respectively. The GI HAI infection category includes Clostridium difficile infection.
The incidence of SSI HAI among all hospitalized patients in the survey fell by 41% between 2011 and 2015 (from 1.00% to 0.59%; P = .001). The other big contributor to the overall reduction in HAIs was the fall in the incidence of urinary tract infections, which fell 36% (from 0.55% to 0.35%; P = .04). The decrease in pneumonia (from 0.97% to 0.89%) was not significant, nor was the even more modest reduction in bloodstream HAI (from 0.45% to 0.43%). There was a modest increase in GI/Clostridium difficile infections (from 0.56% to 0.59%).
The surveys do not permit the reduction in HAI rates to be attributed to any specific prevention practices, but Dr. Magill pointed out that the overall reductions correlate with reduced use of urinary catheters and central lines; reductions of both have been advocated as a means for improved infection control. Of several factors that might contribute to a reduction in SSI HAI, Dr. Magill speculated that better adherence to guidelines and more rigorous steps at preoperative infection control strategies might be among them.
Detailed analyses of the data collected from all of the hospitals that participated in the 2015 survey are planned, including an evaluation of which antibiotics were used to treat the HAIs found in this survey. Although the findings so far encourage speculation that infection control practices, such as prudent use of urinary catheters, are having a positive effect, Dr. Magill said that the data also point out the challenges.
“Given that pneumonia continues to represent a large proportion of HAIs in hospitals, more work is needed to identify risk factors; understand the factors that are preventable, particularly in the nonventilated patients; and develop better preventive approaches,” Dr. Magill said.
Dr. Magill reported no financial relationships relevant to this study.
SAN DIEGO – There was an encouraging 22% reduction in hospital-acquired infections (HAIs) after adjustment for clinical variables when 2015 and 2011 data from national Centers for Disease Control and Prevention hospital surveys were compared.
“The data suggest that national efforts toward preventing HAIs are succeeding,” reported Shelley S. Magill, MD, PhD, a medical epidemiologist in the Division of Healthcare Quality Promotion at the CDC who summarized the data at an annual scientific meeting on infectious diseases .
The comparative data were drawn from point prevalence surveys conducted in 2011 and 2015 as part of the CDC’s Emerging Infections Program. In this type of survey, the data are collected over 1 day, providing a snapshot in time among selected hospitals. The analysis presented by Dr. Magill was restricted to the 148 hospitals that participated in both the 2011 and 2015 surveys, although the 2015 survey included a total of 199 hospitals, of which other data analyses are planned.
Due to the change in incidence, the rank order of HAIs was different in 2015 relative to 2011. While surgical site infections (SSIs) represented the most frequent HAI in 2011, they fell to the third most frequent HAI in 2015; pneumonia and gastrointestinal (GI) infections assumed the first and second spots, respectively. The GI HAI infection category includes Clostridium difficile infection.
The incidence of SSI HAI among all hospitalized patients in the survey fell by 41% between 2011 and 2015 (from 1.00% to 0.59%; P = .001). The other big contributor to the overall reduction in HAIs was the fall in the incidence of urinary tract infections, which fell 36% (from 0.55% to 0.35%; P = .04). The decrease in pneumonia (from 0.97% to 0.89%) was not significant, nor was the even more modest reduction in bloodstream HAI (from 0.45% to 0.43%). There was a modest increase in GI/Clostridium difficile infections (from 0.56% to 0.59%).
The surveys do not permit the reduction in HAI rates to be attributed to any specific prevention practices, but Dr. Magill pointed out that the overall reductions correlate with reduced use of urinary catheters and central lines; reductions of both have been advocated as a means for improved infection control. Of several factors that might contribute to a reduction in SSI HAI, Dr. Magill speculated that better adherence to guidelines and more rigorous steps at preoperative infection control strategies might be among them.
Detailed analyses of the data collected from all of the hospitals that participated in the 2015 survey are planned, including an evaluation of which antibiotics were used to treat the HAIs found in this survey. Although the findings so far encourage speculation that infection control practices, such as prudent use of urinary catheters, are having a positive effect, Dr. Magill said that the data also point out the challenges.
“Given that pneumonia continues to represent a large proportion of HAIs in hospitals, more work is needed to identify risk factors; understand the factors that are preventable, particularly in the nonventilated patients; and develop better preventive approaches,” Dr. Magill said.
Dr. Magill reported no financial relationships relevant to this study.
SAN DIEGO – There was an encouraging 22% reduction in hospital-acquired infections (HAIs) after adjustment for clinical variables when 2015 and 2011 data from national Centers for Disease Control and Prevention hospital surveys were compared.
“The data suggest that national efforts toward preventing HAIs are succeeding,” reported Shelley S. Magill, MD, PhD, a medical epidemiologist in the Division of Healthcare Quality Promotion at the CDC who summarized the data at an annual scientific meeting on infectious diseases .
The comparative data were drawn from point prevalence surveys conducted in 2011 and 2015 as part of the CDC’s Emerging Infections Program. In this type of survey, the data are collected over 1 day, providing a snapshot in time among selected hospitals. The analysis presented by Dr. Magill was restricted to the 148 hospitals that participated in both the 2011 and 2015 surveys, although the 2015 survey included a total of 199 hospitals, of which other data analyses are planned.
Due to the change in incidence, the rank order of HAIs was different in 2015 relative to 2011. While surgical site infections (SSIs) represented the most frequent HAI in 2011, they fell to the third most frequent HAI in 2015; pneumonia and gastrointestinal (GI) infections assumed the first and second spots, respectively. The GI HAI infection category includes Clostridium difficile infection.
The incidence of SSI HAI among all hospitalized patients in the survey fell by 41% between 2011 and 2015 (from 1.00% to 0.59%; P = .001). The other big contributor to the overall reduction in HAIs was the fall in the incidence of urinary tract infections, which fell 36% (from 0.55% to 0.35%; P = .04). The decrease in pneumonia (from 0.97% to 0.89%) was not significant, nor was the even more modest reduction in bloodstream HAI (from 0.45% to 0.43%). There was a modest increase in GI/Clostridium difficile infections (from 0.56% to 0.59%).
The surveys do not permit the reduction in HAI rates to be attributed to any specific prevention practices, but Dr. Magill pointed out that the overall reductions correlate with reduced use of urinary catheters and central lines; reductions of both have been advocated as a means for improved infection control. Of several factors that might contribute to a reduction in SSI HAI, Dr. Magill speculated that better adherence to guidelines and more rigorous steps at preoperative infection control strategies might be among them.
Detailed analyses of the data collected from all of the hospitals that participated in the 2015 survey are planned, including an evaluation of which antibiotics were used to treat the HAIs found in this survey. Although the findings so far encourage speculation that infection control practices, such as prudent use of urinary catheters, are having a positive effect, Dr. Magill said that the data also point out the challenges.
“Given that pneumonia continues to represent a large proportion of HAIs in hospitals, more work is needed to identify risk factors; understand the factors that are preventable, particularly in the nonventilated patients; and develop better preventive approaches,” Dr. Magill said.
Dr. Magill reported no financial relationships relevant to this study.
AT ID WEEK 2017
Key clinical point:
Major finding: In two point prevalence surveys conducted in the same hospitals, the rate of HAI was 22% lower in 2015 (P = .001), compared with 2011.
Data source: CDC national surveys of HAIs in 148 hospitals in two different years (2011 and 2015) were compared.
Disclosures: Dr. Magill reported no financial relationships relevant to this study.
Cases of Legionnaires’ continue to rise in the United States
SAN DIEGO –
“Improved testing and surveillance are needed to improve understanding of disease and outbreak burden,” Laura A. Cooley, MD, said at an annual scientific meeting on infectious diseases. “There is more to learn about environmental sources of Legionella for cases not associated with known outbreaks and about the distribution of Legionella in the environment.”
A Gram-negative bacillus, Legionella is an intracellular parasite of free-living protozoa primarily found in freshwater. “It can live and grow in biofilm, and there are more than 60 species of the bacterium,” she said at the combined annual meetings of the Infectious Diseases Society of America, the Society for Healthcare Epidemiology of America, the HIV Medicine Association, and the Pediatric Infectious Diseases Society.
Cases are higher in the warmer months, and the rates are highest among the elderly, men, and those of black race. Currently, L. pneumophila accounts for about 90% of cases in the United States. “Once it’s transmitted, it has to hit a susceptible population to cause disease, generally older individuals and people with underlying conditions,” Dr. Cooley said.
A separate analysis evaluated Legionella cases reported among U.S. residents between 2005 and 2009 (MMWR. 2011;60[32]:1083-6). It found that only 4% were associated with outbreaks, and 96% were sporadic. “That doesn’t mean that [the cases] weren’t associated with the same kind of source, they just weren’t identified as an outbreak,” Dr. Cooley said. “It shows that there is a lot to learn about transmission of Legionella.”
Data from the National Notifiable Diseases Surveillance System indicate that rates of Legionella continue to rise nationwide, especially in the Midwest and Northeast. “Why? It’s possible that there are differences in testing preferences and reporting preferences in this region of the country,” Dr. Cooley noted. “Maybe people are more tuned in to the potential for outbreaks, but there are reasons why there could be differences in disease, like differences in infrastructure, climate, population density, and cooling tower density.” CDC data from 2015 indicate that most cases are not associated with a known exposure, and that the case fatality rate differs by exposure type: 12% for cases reporting health care exposure during the 10 days before symptom onset (25% for definite cases), 9% for cases reporting assisted or senior living exposure, 7% when no specific exposure is reported, and 4% for cases reporting travel exposure (MMWR. 2017;66[22]:584-9).
The U.S. case definition of Legionnaires’ disease consists of clinical or radiologic pneumonia plus confirmatory laboratory testing, either by urinary antigen test (UAT), lower respiratory culture, or appropriate serological testing. Polymerase chain reaction can be used as a presumptive test for a suspect case. “UAT is easy and it detects L. pneumophila serogroup 1 (Lp1), but it has some gaps,” Dr. Cooley said. “It isn’t completely sensitive for Lp1, and it doesn’t detect any other species or serogroups. That’s why we also recommend that a culture of respiratory secretions on selective media be performed at the same time. That being said, in the U.S., nearly all reported cases of Legionella are diagnosed by UAT only.”
A 2016 CDC MMWR and Vital Signs report found that almost all Legionella outbreaks could be prevented with effective water management, and the CDC has published a step-by-step guide to creating a water management program to reduce Legionella growth and spread in buildings. The 2017 MMWR Report found that definite health care–associated Legionnaires’ disease is deadly for one in four people who get it. The report also found that this issue is widespread; 76% of complete reporting jurisdictions reported at least one definite case of health care–associated Legionella disease in 2015. More recently, the Centers for Medicare & Medicaid Services issued a requirement to reduce risk in health care facility water systems to prevent cases and outbreaks. It applies to hospitals, skilled nursing facilities, and critical access hospitals.
Dr. Cooley reported having no financial disclosures.
SAN DIEGO –
“Improved testing and surveillance are needed to improve understanding of disease and outbreak burden,” Laura A. Cooley, MD, said at an annual scientific meeting on infectious diseases. “There is more to learn about environmental sources of Legionella for cases not associated with known outbreaks and about the distribution of Legionella in the environment.”
A Gram-negative bacillus, Legionella is an intracellular parasite of free-living protozoa primarily found in freshwater. “It can live and grow in biofilm, and there are more than 60 species of the bacterium,” she said at the combined annual meetings of the Infectious Diseases Society of America, the Society for Healthcare Epidemiology of America, the HIV Medicine Association, and the Pediatric Infectious Diseases Society.
Cases are higher in the warmer months, and the rates are highest among the elderly, men, and those of black race. Currently, L. pneumophila accounts for about 90% of cases in the United States. “Once it’s transmitted, it has to hit a susceptible population to cause disease, generally older individuals and people with underlying conditions,” Dr. Cooley said.
A separate analysis evaluated Legionella cases reported among U.S. residents between 2005 and 2009 (MMWR. 2011;60[32]:1083-6). It found that only 4% were associated with outbreaks, and 96% were sporadic. “That doesn’t mean that [the cases] weren’t associated with the same kind of source, they just weren’t identified as an outbreak,” Dr. Cooley said. “It shows that there is a lot to learn about transmission of Legionella.”
Data from the National Notifiable Diseases Surveillance System indicate that rates of Legionella continue to rise nationwide, especially in the Midwest and Northeast. “Why? It’s possible that there are differences in testing preferences and reporting preferences in this region of the country,” Dr. Cooley noted. “Maybe people are more tuned in to the potential for outbreaks, but there are reasons why there could be differences in disease, like differences in infrastructure, climate, population density, and cooling tower density.” CDC data from 2015 indicate that most cases are not associated with a known exposure, and that the case fatality rate differs by exposure type: 12% for cases reporting health care exposure during the 10 days before symptom onset (25% for definite cases), 9% for cases reporting assisted or senior living exposure, 7% when no specific exposure is reported, and 4% for cases reporting travel exposure (MMWR. 2017;66[22]:584-9).
The U.S. case definition of Legionnaires’ disease consists of clinical or radiologic pneumonia plus confirmatory laboratory testing, either by urinary antigen test (UAT), lower respiratory culture, or appropriate serological testing. Polymerase chain reaction can be used as a presumptive test for a suspect case. “UAT is easy and it detects L. pneumophila serogroup 1 (Lp1), but it has some gaps,” Dr. Cooley said. “It isn’t completely sensitive for Lp1, and it doesn’t detect any other species or serogroups. That’s why we also recommend that a culture of respiratory secretions on selective media be performed at the same time. That being said, in the U.S., nearly all reported cases of Legionella are diagnosed by UAT only.”
A 2016 CDC MMWR and Vital Signs report found that almost all Legionella outbreaks could be prevented with effective water management, and the CDC has published a step-by-step guide to creating a water management program to reduce Legionella growth and spread in buildings. The 2017 MMWR Report found that definite health care–associated Legionnaires’ disease is deadly for one in four people who get it. The report also found that this issue is widespread; 76% of complete reporting jurisdictions reported at least one definite case of health care–associated Legionella disease in 2015. More recently, the Centers for Medicare & Medicaid Services issued a requirement to reduce risk in health care facility water systems to prevent cases and outbreaks. It applies to hospitals, skilled nursing facilities, and critical access hospitals.
Dr. Cooley reported having no financial disclosures.
SAN DIEGO –
“Improved testing and surveillance are needed to improve understanding of disease and outbreak burden,” Laura A. Cooley, MD, said at an annual scientific meeting on infectious diseases. “There is more to learn about environmental sources of Legionella for cases not associated with known outbreaks and about the distribution of Legionella in the environment.”
A Gram-negative bacillus, Legionella is an intracellular parasite of free-living protozoa primarily found in freshwater. “It can live and grow in biofilm, and there are more than 60 species of the bacterium,” she said at the combined annual meetings of the Infectious Diseases Society of America, the Society for Healthcare Epidemiology of America, the HIV Medicine Association, and the Pediatric Infectious Diseases Society.
Cases are higher in the warmer months, and the rates are highest among the elderly, men, and those of black race. Currently, L. pneumophila accounts for about 90% of cases in the United States. “Once it’s transmitted, it has to hit a susceptible population to cause disease, generally older individuals and people with underlying conditions,” Dr. Cooley said.
A separate analysis evaluated Legionella cases reported among U.S. residents between 2005 and 2009 (MMWR. 2011;60[32]:1083-6). It found that only 4% were associated with outbreaks, and 96% were sporadic. “That doesn’t mean that [the cases] weren’t associated with the same kind of source, they just weren’t identified as an outbreak,” Dr. Cooley said. “It shows that there is a lot to learn about transmission of Legionella.”
Data from the National Notifiable Diseases Surveillance System indicate that rates of Legionella continue to rise nationwide, especially in the Midwest and Northeast. “Why? It’s possible that there are differences in testing preferences and reporting preferences in this region of the country,” Dr. Cooley noted. “Maybe people are more tuned in to the potential for outbreaks, but there are reasons why there could be differences in disease, like differences in infrastructure, climate, population density, and cooling tower density.” CDC data from 2015 indicate that most cases are not associated with a known exposure, and that the case fatality rate differs by exposure type: 12% for cases reporting health care exposure during the 10 days before symptom onset (25% for definite cases), 9% for cases reporting assisted or senior living exposure, 7% when no specific exposure is reported, and 4% for cases reporting travel exposure (MMWR. 2017;66[22]:584-9).
The U.S. case definition of Legionnaires’ disease consists of clinical or radiologic pneumonia plus confirmatory laboratory testing, either by urinary antigen test (UAT), lower respiratory culture, or appropriate serological testing. Polymerase chain reaction can be used as a presumptive test for a suspect case. “UAT is easy and it detects L. pneumophila serogroup 1 (Lp1), but it has some gaps,” Dr. Cooley said. “It isn’t completely sensitive for Lp1, and it doesn’t detect any other species or serogroups. That’s why we also recommend that a culture of respiratory secretions on selective media be performed at the same time. That being said, in the U.S., nearly all reported cases of Legionella are diagnosed by UAT only.”
A 2016 CDC MMWR and Vital Signs report found that almost all Legionella outbreaks could be prevented with effective water management, and the CDC has published a step-by-step guide to creating a water management program to reduce Legionella growth and spread in buildings. The 2017 MMWR Report found that definite health care–associated Legionnaires’ disease is deadly for one in four people who get it. The report also found that this issue is widespread; 76% of complete reporting jurisdictions reported at least one definite case of health care–associated Legionella disease in 2015. More recently, the Centers for Medicare & Medicaid Services issued a requirement to reduce risk in health care facility water systems to prevent cases and outbreaks. It applies to hospitals, skilled nursing facilities, and critical access hospitals.
Dr. Cooley reported having no financial disclosures.
REPORTING FROM ID WEEK 2017
Nearly 10% of patients with candidemia had CDI
SAN DIEGO – Nearly one in ten adults hospitalized with candidemia had Clostridium difficile coinfections in a large multistate study.
“,” Sharon Tsay, MD, said at an annual scientific meeting on infectious diseases. “In patients with CDI, one in 100 developed candidemia, but in patients with candidemia, nearly one in 10 had CDI,” she said. Patients with diabetes, hemodialysis, solid organ transplantation, or a prior recent hospital stay were significantly more likely to have a CDI coinfection even after the researchers controlled for potential confounders, she reported.
Both candidemia and CDI are serious health care–associated infections that disproportionately affect older, severely ill, and immunosuppressed patients, noted Dr. Tsay, an Epidemic Intelligence Service officer in the mycotic diseases branch at the Centers for Disease Control and Prevention, Atlanta. Every year in the United States, about 50,000 individuals are hospitalized with candidemia, and about 30% die within 30 days of diagnosis. The prevalence of CDI is about tenfold higher, and 30-day mortality rates range between about 1% and 9%.
To understand why candidemia and CDI occur together, consider the effects of oral vancomycin therapy, Dr. Tsay said. Antibiotic pressure disrupts normal gut flora, leading to decreased immunity and Candida colonization. Disrupting the gut microbiome also increases the risk of CDI, which can damage gut mucosa, especially in hypervirulent cases such as C. difficile ribotype 027. Vancomycin can also directly damage the gut mucosa, after which Candida can translocate into the bloodstream.
To better characterize CDI and candidemia coinfections in the United States, Dr. Tsay and her associates analyzed data from CDC’s Emerging Infections Program, which tracks infections of high public health significance in 10 states across the country. Among 2,129 patients with a positive blood culture for Candida from 2014 through 2016, 193 (9%) had a diagnosis of CDI within 90 days. Two-thirds of CDI cases preceded candidemia (median, 10 days) and one-third occurred afterward (median, 7 days). Rates of 30-day mortality rates were 25% in patients with and without CDI. For both groups, Candida albicans was the most commonly identified species, followed by C. glabrata and C. parapsilosis.
A multivariate model identified four risk factors for CDI in patients with candidemia – solid organ transplantation (odds ratio, 3.0), hemodialysis (OR, 1.8), prior hospital stay (OR, 1.7), and diabetes (OR, 1.4). Data were limited to case report forms and did not include information about CDI severity or treatment, Dr. Tsay said.
Dr. Tsay and her associates reported having no conflicts of interest.
SAN DIEGO – Nearly one in ten adults hospitalized with candidemia had Clostridium difficile coinfections in a large multistate study.
“,” Sharon Tsay, MD, said at an annual scientific meeting on infectious diseases. “In patients with CDI, one in 100 developed candidemia, but in patients with candidemia, nearly one in 10 had CDI,” she said. Patients with diabetes, hemodialysis, solid organ transplantation, or a prior recent hospital stay were significantly more likely to have a CDI coinfection even after the researchers controlled for potential confounders, she reported.
Both candidemia and CDI are serious health care–associated infections that disproportionately affect older, severely ill, and immunosuppressed patients, noted Dr. Tsay, an Epidemic Intelligence Service officer in the mycotic diseases branch at the Centers for Disease Control and Prevention, Atlanta. Every year in the United States, about 50,000 individuals are hospitalized with candidemia, and about 30% die within 30 days of diagnosis. The prevalence of CDI is about tenfold higher, and 30-day mortality rates range between about 1% and 9%.
To understand why candidemia and CDI occur together, consider the effects of oral vancomycin therapy, Dr. Tsay said. Antibiotic pressure disrupts normal gut flora, leading to decreased immunity and Candida colonization. Disrupting the gut microbiome also increases the risk of CDI, which can damage gut mucosa, especially in hypervirulent cases such as C. difficile ribotype 027. Vancomycin can also directly damage the gut mucosa, after which Candida can translocate into the bloodstream.
To better characterize CDI and candidemia coinfections in the United States, Dr. Tsay and her associates analyzed data from CDC’s Emerging Infections Program, which tracks infections of high public health significance in 10 states across the country. Among 2,129 patients with a positive blood culture for Candida from 2014 through 2016, 193 (9%) had a diagnosis of CDI within 90 days. Two-thirds of CDI cases preceded candidemia (median, 10 days) and one-third occurred afterward (median, 7 days). Rates of 30-day mortality rates were 25% in patients with and without CDI. For both groups, Candida albicans was the most commonly identified species, followed by C. glabrata and C. parapsilosis.
A multivariate model identified four risk factors for CDI in patients with candidemia – solid organ transplantation (odds ratio, 3.0), hemodialysis (OR, 1.8), prior hospital stay (OR, 1.7), and diabetes (OR, 1.4). Data were limited to case report forms and did not include information about CDI severity or treatment, Dr. Tsay said.
Dr. Tsay and her associates reported having no conflicts of interest.
SAN DIEGO – Nearly one in ten adults hospitalized with candidemia had Clostridium difficile coinfections in a large multistate study.
“,” Sharon Tsay, MD, said at an annual scientific meeting on infectious diseases. “In patients with CDI, one in 100 developed candidemia, but in patients with candidemia, nearly one in 10 had CDI,” she said. Patients with diabetes, hemodialysis, solid organ transplantation, or a prior recent hospital stay were significantly more likely to have a CDI coinfection even after the researchers controlled for potential confounders, she reported.
Both candidemia and CDI are serious health care–associated infections that disproportionately affect older, severely ill, and immunosuppressed patients, noted Dr. Tsay, an Epidemic Intelligence Service officer in the mycotic diseases branch at the Centers for Disease Control and Prevention, Atlanta. Every year in the United States, about 50,000 individuals are hospitalized with candidemia, and about 30% die within 30 days of diagnosis. The prevalence of CDI is about tenfold higher, and 30-day mortality rates range between about 1% and 9%.
To understand why candidemia and CDI occur together, consider the effects of oral vancomycin therapy, Dr. Tsay said. Antibiotic pressure disrupts normal gut flora, leading to decreased immunity and Candida colonization. Disrupting the gut microbiome also increases the risk of CDI, which can damage gut mucosa, especially in hypervirulent cases such as C. difficile ribotype 027. Vancomycin can also directly damage the gut mucosa, after which Candida can translocate into the bloodstream.
To better characterize CDI and candidemia coinfections in the United States, Dr. Tsay and her associates analyzed data from CDC’s Emerging Infections Program, which tracks infections of high public health significance in 10 states across the country. Among 2,129 patients with a positive blood culture for Candida from 2014 through 2016, 193 (9%) had a diagnosis of CDI within 90 days. Two-thirds of CDI cases preceded candidemia (median, 10 days) and one-third occurred afterward (median, 7 days). Rates of 30-day mortality rates were 25% in patients with and without CDI. For both groups, Candida albicans was the most commonly identified species, followed by C. glabrata and C. parapsilosis.
A multivariate model identified four risk factors for CDI in patients with candidemia – solid organ transplantation (odds ratio, 3.0), hemodialysis (OR, 1.8), prior hospital stay (OR, 1.7), and diabetes (OR, 1.4). Data were limited to case report forms and did not include information about CDI severity or treatment, Dr. Tsay said.
Dr. Tsay and her associates reported having no conflicts of interest.
AT IDWEEK 2017
Key clinical point: Look for candidemia and Clostridium difficile infection occurring together.
Major finding: Among 2,129 patients with a positive blood culture for Candida, 193 (9%) had a diagnosis of CDI within 90 days. Risk factors for coinfection included solid organ transplant, hemodialysis, recent hospital stay, and diabetes.
Data source: A multistate analysis of data from the Centers for Disease Control’s Emerging Infections Program.
Disclosures: Dr. Tsay and her associates reported having no conflicts of interest.
Thirty-one percent of multidrug-resistant infections were community acquired
SAN DIEGO – Thirty-one percent of multidrug-resistant infections were acquired from the community in a prospective single-center study of a regional hospital.
“Multidrug-resistant organisms have escaped the hospital,” Nicholas A. Turner, MD, of Duke University Medical Center, Durham, N.C., and his associates wrote in a poster presented at an annual scientific meeting on infectious diseases. “Community acquisition of multidrug-resistant organisms [MDROs] is increasing, not just within referral centers but also community hospitals. Providers will need to be increasingly aware of this trend.”
Infections of MDROs cause about 2,000,000 illnesses and 23,000 deaths annually in the United States, according to the Centers for Disease Control and Prevention. Until recently, MDROs were considered a plague of hospitals. Amid reports of increasing levels of community acquisition, the researchers studied adults admitted to a 202-bed regional hospital between 2013 and 2016. They defined MDROs as infections of methicillin-resistant Staphylococcus aureus (MRSA), gram-negative bacteria resistant to more than three antimicrobial classes, vancomycin-resistant Enterococcus (VRE), or diarrhea with a positive stool culture for Clostridium difficile.
A total of 285 patients had MDROs. Clostridium difficile (45%) and MRSA (35%) were most common. In all, 88 (31%) MDROs were community-acquired – that is, diagnosed within 48 hours of admission in patients who were not on dialysis, did not live in a long-term care facility, and had not been hospitalized for more than 48 hours in the past 90 days. A total of 36% of MRSA and multidrug-resistant gram-negative infections were community acquired, as were 25% of Clostridium difficile infections. There were only 10 VRE infections, of which none were community-acquired.
After the researchers controlled for clinical and demographic variables, the only significant predictor of community-acquired MDRO was cancer (odds ratio [OR], 2.3; 95% confidence interval [CI], 1.02-5.2). Surgery within the previous 12 months was significantly associated with hospital-acquired MDRO (OR, 0.16; 95% CI, 0.05-0.5).
Traditional risk factors for community-acquired MRSA or C. difficile infection did not achieve statistical significance in the multivariable analysis, the researchers noted. “Similar to data from large tertiary care centers, our findings suggest that MDROs are increasingly acquired in the community setting, even at smaller regional hospitals,” they concluded. “Further study is needed to track the expansion of MDROs in the community setting.”
Dr. Turner reported having no conflicts of interest.
SAN DIEGO – Thirty-one percent of multidrug-resistant infections were acquired from the community in a prospective single-center study of a regional hospital.
“Multidrug-resistant organisms have escaped the hospital,” Nicholas A. Turner, MD, of Duke University Medical Center, Durham, N.C., and his associates wrote in a poster presented at an annual scientific meeting on infectious diseases. “Community acquisition of multidrug-resistant organisms [MDROs] is increasing, not just within referral centers but also community hospitals. Providers will need to be increasingly aware of this trend.”
Infections of MDROs cause about 2,000,000 illnesses and 23,000 deaths annually in the United States, according to the Centers for Disease Control and Prevention. Until recently, MDROs were considered a plague of hospitals. Amid reports of increasing levels of community acquisition, the researchers studied adults admitted to a 202-bed regional hospital between 2013 and 2016. They defined MDROs as infections of methicillin-resistant Staphylococcus aureus (MRSA), gram-negative bacteria resistant to more than three antimicrobial classes, vancomycin-resistant Enterococcus (VRE), or diarrhea with a positive stool culture for Clostridium difficile.
A total of 285 patients had MDROs. Clostridium difficile (45%) and MRSA (35%) were most common. In all, 88 (31%) MDROs were community-acquired – that is, diagnosed within 48 hours of admission in patients who were not on dialysis, did not live in a long-term care facility, and had not been hospitalized for more than 48 hours in the past 90 days. A total of 36% of MRSA and multidrug-resistant gram-negative infections were community acquired, as were 25% of Clostridium difficile infections. There were only 10 VRE infections, of which none were community-acquired.
After the researchers controlled for clinical and demographic variables, the only significant predictor of community-acquired MDRO was cancer (odds ratio [OR], 2.3; 95% confidence interval [CI], 1.02-5.2). Surgery within the previous 12 months was significantly associated with hospital-acquired MDRO (OR, 0.16; 95% CI, 0.05-0.5).
Traditional risk factors for community-acquired MRSA or C. difficile infection did not achieve statistical significance in the multivariable analysis, the researchers noted. “Similar to data from large tertiary care centers, our findings suggest that MDROs are increasingly acquired in the community setting, even at smaller regional hospitals,” they concluded. “Further study is needed to track the expansion of MDROs in the community setting.”
Dr. Turner reported having no conflicts of interest.
SAN DIEGO – Thirty-one percent of multidrug-resistant infections were acquired from the community in a prospective single-center study of a regional hospital.
“Multidrug-resistant organisms have escaped the hospital,” Nicholas A. Turner, MD, of Duke University Medical Center, Durham, N.C., and his associates wrote in a poster presented at an annual scientific meeting on infectious diseases. “Community acquisition of multidrug-resistant organisms [MDROs] is increasing, not just within referral centers but also community hospitals. Providers will need to be increasingly aware of this trend.”
Infections of MDROs cause about 2,000,000 illnesses and 23,000 deaths annually in the United States, according to the Centers for Disease Control and Prevention. Until recently, MDROs were considered a plague of hospitals. Amid reports of increasing levels of community acquisition, the researchers studied adults admitted to a 202-bed regional hospital between 2013 and 2016. They defined MDROs as infections of methicillin-resistant Staphylococcus aureus (MRSA), gram-negative bacteria resistant to more than three antimicrobial classes, vancomycin-resistant Enterococcus (VRE), or diarrhea with a positive stool culture for Clostridium difficile.
A total of 285 patients had MDROs. Clostridium difficile (45%) and MRSA (35%) were most common. In all, 88 (31%) MDROs were community-acquired – that is, diagnosed within 48 hours of admission in patients who were not on dialysis, did not live in a long-term care facility, and had not been hospitalized for more than 48 hours in the past 90 days. A total of 36% of MRSA and multidrug-resistant gram-negative infections were community acquired, as were 25% of Clostridium difficile infections. There were only 10 VRE infections, of which none were community-acquired.
After the researchers controlled for clinical and demographic variables, the only significant predictor of community-acquired MDRO was cancer (odds ratio [OR], 2.3; 95% confidence interval [CI], 1.02-5.2). Surgery within the previous 12 months was significantly associated with hospital-acquired MDRO (OR, 0.16; 95% CI, 0.05-0.5).
Traditional risk factors for community-acquired MRSA or C. difficile infection did not achieve statistical significance in the multivariable analysis, the researchers noted. “Similar to data from large tertiary care centers, our findings suggest that MDROs are increasingly acquired in the community setting, even at smaller regional hospitals,” they concluded. “Further study is needed to track the expansion of MDROs in the community setting.”
Dr. Turner reported having no conflicts of interest.
AT IDWEEK 2017
Key clinical point: Multidrug resistant infections are increasingly being acquired in communities.
Major finding:
Data source: A prospective study of 285 patients with multidrug-resistant infections at a 202-bed hospital.
Disclosures: Dr. Turner reported having no conflicts of interest.
Household MRSA contamination predicted human recolonization
SAN DIEGO – Patients who were successfully treated for methicillin-resistant Staphylococcus aureus infections were about four times more likely to become recolonized if their homes contained MRSA, according to the results of a longitudinal household study.
“Many of these homes were contaminated with a classic community strain,” Meghan Frost Davis, DVM, PhD, MPH, said during an oral presentation at an annual meeting on infectious disease. “We need to think about interventions in the home environment to improve our ability to achieve successful decolonization.”
Importantly, Dr. Davis and her associates recently published another study in which biocidal disinfectants failed to eliminate MRSA from homes and appeared to increase the risk of multi-drug resistance (Appl Environ Microbiol. online 22 September 2017, doi: 10.1128/AEM.01369-17). Her team is testing MRSA isolates for resistance to disinfectants and hopes to have more information in about a year, she said. Until then, Dr. Davis suggests advising patients with MRSA to clean sheets and pillowcases frequently.
S. aureus can survive in the environment for long periods. In one case, a MRSA strain tied to an outbreak was cultured from a dry mop that had been locked in a closet for 79 months, Dr. Davis said. “This is concerning because the home is a place that receives bacteria from us,” she said. “A person who was originally colonized or infected with MRSA may clear naturally or through treatment, but the environment may become a reservoir for recolonization and infection.”
To better understand the role of this reservoir, she and her associates recruited 88 index outpatients with MRSA skin and soft tissue infections who were part of a randomized trial of MRSA decolonization strategies. At baseline and 3 months later, the researchers sampled multiple sites in each patient’s home and all household pets. Patients and household members also swabbed themselves in multiple body sites every 2 weeks for up to 3 months. Swabs were cultured in enrichment broth, and positive results were confirmed by PCR (Infect Control Hosp Epidemiol. 2016 Oct;37[10]:1226-33. doi: 10.1017/ice.2016.138. Epub 2016 Jul 28).
Even after accounting for potential confounders, household contamination with MRSA was associated with about a three- to five-fold increase in the odds of human colonization, which was statistically significant. Seventy percent of households had at least one pet, but only 10% had a pet colonized with MRSA. Having such a pet increased the risk of human carriage slightly, but not significantly. However, having more than one pet did predict human colonization, Dr. Davis said. Even if pets aren’t colonized, they still can carry MRSA on “the petting zone” – the top of the head and back, she explained. Thus, pets can serve as reservoirs for MRSA without being colonized.
In all, 53 index patients had at least two consecutive negative cultures and thus were considered decolonized. However, 43% of these individuals were subsequently re-colonized, and those whose homes contained MRSA at baseline were about 4.3 times more likely to become recolonized than those whose households cultured negative (hazard ratio, 4.3; 95% CI, 1.2-16; P less than .03).
A total of six patients were persistently colonized with MRSA, and 62% of contaminated homes tested positive for MRSA Staph protein A (spa) type t008, a common community-onset strain. Living in one of these households significantly increased the chances of persistent colonization (odds ratio, 12.7; 95% CI, 1.33-122; P less than .03).
Pets testing positive for MRSA always came from homes that also tested positive, so these factors couldn’t be disentangled, Dr. Davis said. Repository surfaces in homes – such as the top of a refrigerator – were just as likely to be contaminated with MRSA as high-touch surfaces. However, pillowcases often were most contaminated of all. “If I can give you one take-home message, when you treat people with MRSA, you may want to tell them to clean their sheets and pillowcases a lot.”
Dr. Davis and her associates had no disclosures.
SAN DIEGO – Patients who were successfully treated for methicillin-resistant Staphylococcus aureus infections were about four times more likely to become recolonized if their homes contained MRSA, according to the results of a longitudinal household study.
“Many of these homes were contaminated with a classic community strain,” Meghan Frost Davis, DVM, PhD, MPH, said during an oral presentation at an annual meeting on infectious disease. “We need to think about interventions in the home environment to improve our ability to achieve successful decolonization.”
Importantly, Dr. Davis and her associates recently published another study in which biocidal disinfectants failed to eliminate MRSA from homes and appeared to increase the risk of multi-drug resistance (Appl Environ Microbiol. online 22 September 2017, doi: 10.1128/AEM.01369-17). Her team is testing MRSA isolates for resistance to disinfectants and hopes to have more information in about a year, she said. Until then, Dr. Davis suggests advising patients with MRSA to clean sheets and pillowcases frequently.
S. aureus can survive in the environment for long periods. In one case, a MRSA strain tied to an outbreak was cultured from a dry mop that had been locked in a closet for 79 months, Dr. Davis said. “This is concerning because the home is a place that receives bacteria from us,” she said. “A person who was originally colonized or infected with MRSA may clear naturally or through treatment, but the environment may become a reservoir for recolonization and infection.”
To better understand the role of this reservoir, she and her associates recruited 88 index outpatients with MRSA skin and soft tissue infections who were part of a randomized trial of MRSA decolonization strategies. At baseline and 3 months later, the researchers sampled multiple sites in each patient’s home and all household pets. Patients and household members also swabbed themselves in multiple body sites every 2 weeks for up to 3 months. Swabs were cultured in enrichment broth, and positive results were confirmed by PCR (Infect Control Hosp Epidemiol. 2016 Oct;37[10]:1226-33. doi: 10.1017/ice.2016.138. Epub 2016 Jul 28).
Even after accounting for potential confounders, household contamination with MRSA was associated with about a three- to five-fold increase in the odds of human colonization, which was statistically significant. Seventy percent of households had at least one pet, but only 10% had a pet colonized with MRSA. Having such a pet increased the risk of human carriage slightly, but not significantly. However, having more than one pet did predict human colonization, Dr. Davis said. Even if pets aren’t colonized, they still can carry MRSA on “the petting zone” – the top of the head and back, she explained. Thus, pets can serve as reservoirs for MRSA without being colonized.
In all, 53 index patients had at least two consecutive negative cultures and thus were considered decolonized. However, 43% of these individuals were subsequently re-colonized, and those whose homes contained MRSA at baseline were about 4.3 times more likely to become recolonized than those whose households cultured negative (hazard ratio, 4.3; 95% CI, 1.2-16; P less than .03).
A total of six patients were persistently colonized with MRSA, and 62% of contaminated homes tested positive for MRSA Staph protein A (spa) type t008, a common community-onset strain. Living in one of these households significantly increased the chances of persistent colonization (odds ratio, 12.7; 95% CI, 1.33-122; P less than .03).
Pets testing positive for MRSA always came from homes that also tested positive, so these factors couldn’t be disentangled, Dr. Davis said. Repository surfaces in homes – such as the top of a refrigerator – were just as likely to be contaminated with MRSA as high-touch surfaces. However, pillowcases often were most contaminated of all. “If I can give you one take-home message, when you treat people with MRSA, you may want to tell them to clean their sheets and pillowcases a lot.”
Dr. Davis and her associates had no disclosures.
SAN DIEGO – Patients who were successfully treated for methicillin-resistant Staphylococcus aureus infections were about four times more likely to become recolonized if their homes contained MRSA, according to the results of a longitudinal household study.
“Many of these homes were contaminated with a classic community strain,” Meghan Frost Davis, DVM, PhD, MPH, said during an oral presentation at an annual meeting on infectious disease. “We need to think about interventions in the home environment to improve our ability to achieve successful decolonization.”
Importantly, Dr. Davis and her associates recently published another study in which biocidal disinfectants failed to eliminate MRSA from homes and appeared to increase the risk of multi-drug resistance (Appl Environ Microbiol. online 22 September 2017, doi: 10.1128/AEM.01369-17). Her team is testing MRSA isolates for resistance to disinfectants and hopes to have more information in about a year, she said. Until then, Dr. Davis suggests advising patients with MRSA to clean sheets and pillowcases frequently.
S. aureus can survive in the environment for long periods. In one case, a MRSA strain tied to an outbreak was cultured from a dry mop that had been locked in a closet for 79 months, Dr. Davis said. “This is concerning because the home is a place that receives bacteria from us,” she said. “A person who was originally colonized or infected with MRSA may clear naturally or through treatment, but the environment may become a reservoir for recolonization and infection.”
To better understand the role of this reservoir, she and her associates recruited 88 index outpatients with MRSA skin and soft tissue infections who were part of a randomized trial of MRSA decolonization strategies. At baseline and 3 months later, the researchers sampled multiple sites in each patient’s home and all household pets. Patients and household members also swabbed themselves in multiple body sites every 2 weeks for up to 3 months. Swabs were cultured in enrichment broth, and positive results were confirmed by PCR (Infect Control Hosp Epidemiol. 2016 Oct;37[10]:1226-33. doi: 10.1017/ice.2016.138. Epub 2016 Jul 28).
Even after accounting for potential confounders, household contamination with MRSA was associated with about a three- to five-fold increase in the odds of human colonization, which was statistically significant. Seventy percent of households had at least one pet, but only 10% had a pet colonized with MRSA. Having such a pet increased the risk of human carriage slightly, but not significantly. However, having more than one pet did predict human colonization, Dr. Davis said. Even if pets aren’t colonized, they still can carry MRSA on “the petting zone” – the top of the head and back, she explained. Thus, pets can serve as reservoirs for MRSA without being colonized.
In all, 53 index patients had at least two consecutive negative cultures and thus were considered decolonized. However, 43% of these individuals were subsequently re-colonized, and those whose homes contained MRSA at baseline were about 4.3 times more likely to become recolonized than those whose households cultured negative (hazard ratio, 4.3; 95% CI, 1.2-16; P less than .03).
A total of six patients were persistently colonized with MRSA, and 62% of contaminated homes tested positive for MRSA Staph protein A (spa) type t008, a common community-onset strain. Living in one of these households significantly increased the chances of persistent colonization (odds ratio, 12.7; 95% CI, 1.33-122; P less than .03).
Pets testing positive for MRSA always came from homes that also tested positive, so these factors couldn’t be disentangled, Dr. Davis said. Repository surfaces in homes – such as the top of a refrigerator – were just as likely to be contaminated with MRSA as high-touch surfaces. However, pillowcases often were most contaminated of all. “If I can give you one take-home message, when you treat people with MRSA, you may want to tell them to clean their sheets and pillowcases a lot.”
Dr. Davis and her associates had no disclosures.
IDWEEK 2017
Key clinical point: Patients who were successfully decolonized of MRSA were significantly more likely to become recolonized if their homes were contaminated with MRSA.
Major finding: The risk of recolonization was about four-fold higher if a home was contaminated at baseline (hazard ratio, 4.3; 95% CI, 1.2-16).
Data source: A nested household study that enrolled 88 index patients with MRSA skin and soft tissue infections.
Disclosures: Dr. Davis and her associates had no disclosures.
High percentage of nursing home residents found to harbor MDROs
SAN DIEGO – Nearly half of nursing home residents harbored multi-drug resistant organisms on their skin, results from a large multi-center surveillance study showed.
“Residents in skilled nursing homes are the most vulnerable patients in the health care system,” lead study author James A. McKinnell, MD, said in an interview in advance of an annual scientific meeting on infectious diseases. “Many residents depend on help from health care workers for routine needs like eating or bathing. Skilled nursing facilities have an obligation to optimize the personal hygiene and environmental cleanliness in skilled nursing facilities.”

The researchers obtained 2,797 body swabs from 1,400 residents in all. Swabs were processed for methicillin-resistant Staphylococcus aureus (MRSA), vancomycin-resistant Enterococcus spp. (VRE), extended spectrum beta-lactamase producers (ESBLs), and carbapenem-resistant Enterobacteriaceae (CRE). “MRSA is a relatively well known bacteria, but CRE is the new pathogen that the CDC has defined as an urgent public health threat,” Dr. McKinnell said.
The researchers also conducted environmental surveillance of commonly touched items in skilled nursing facilities. The five surfaces tested in resident rooms were the bedside table, TV remote, door knobs, light switch, and bathrooms. The five surfaces tested in common areas were the nursing station counter, tables, chairs, hallway hand rails, and drinking fountains.
Overall, 49% of residents harbored MDROs. MRSA was found in 37% of residents, followed by ESBL in 16%, VRE in 7%, and CRE in 1%. Resident MDRO status was known for 11% of MRSA carriers, compared with 18% of ESBL, 4% of VRE, and none of the CRE carriers. Rates of colonization did not differ whether residents had long stays at the facility or postacute stays (49% vs. 48%, respectively), but bed-bound residents were more likely to be MDRO colonized, compared with ambulatory residents (59% vs. 46%; P less than .001). In the analysis of environmental swabs, 93% of common areas and 74% of resident rooms had an MDRO-positive object, with an average of 2.5 and 1.9 objects, respectively, found to be contaminated.
“The fact that about half of patients were carrying a bacteria that could cause infection on their skin was very high,” said Dr. McKinnell, who is a member of the Infectious Disease Clinical Outcome Research Unit at the Los Angeles Biomedical Research Institute at Harbor-UCLA. “Studies conducted in other care settings, we would typically see less than a quarter of patients carry these types of bacteria. I was also surprised to see that 1% of patients were carrying the CRE bacteria on their skin.”
He acknowledged certain limitations of the study, including the fact that the data were taken from a select group of nursing homes that are participating in an interventional study to improve personal hygiene for skilled nursing facility residents. “They may not be representative of all skilled nursing facilities,” he said.
The Agency for Healthcare Research and Quality funded the study. Dr. McKinnell disclosed that he is conducting studies in health care facilities with products supplied from 3M, Clorox, Sage, and Xttrium Laboratories. Many of his coauthors disclosed numerous financial ties to the pharmaceutical industry. The event was the combined annual meetings of the Infectious Diseases Society of America, the Society for Healthcare Epidemiology of America, the HIV Medicine Association, and the Pediatric Infectious Diseases Society.
SAN DIEGO – Nearly half of nursing home residents harbored multi-drug resistant organisms on their skin, results from a large multi-center surveillance study showed.
“Residents in skilled nursing homes are the most vulnerable patients in the health care system,” lead study author James A. McKinnell, MD, said in an interview in advance of an annual scientific meeting on infectious diseases. “Many residents depend on help from health care workers for routine needs like eating or bathing. Skilled nursing facilities have an obligation to optimize the personal hygiene and environmental cleanliness in skilled nursing facilities.”

The researchers obtained 2,797 body swabs from 1,400 residents in all. Swabs were processed for methicillin-resistant Staphylococcus aureus (MRSA), vancomycin-resistant Enterococcus spp. (VRE), extended spectrum beta-lactamase producers (ESBLs), and carbapenem-resistant Enterobacteriaceae (CRE). “MRSA is a relatively well known bacteria, but CRE is the new pathogen that the CDC has defined as an urgent public health threat,” Dr. McKinnell said.
The researchers also conducted environmental surveillance of commonly touched items in skilled nursing facilities. The five surfaces tested in resident rooms were the bedside table, TV remote, door knobs, light switch, and bathrooms. The five surfaces tested in common areas were the nursing station counter, tables, chairs, hallway hand rails, and drinking fountains.
Overall, 49% of residents harbored MDROs. MRSA was found in 37% of residents, followed by ESBL in 16%, VRE in 7%, and CRE in 1%. Resident MDRO status was known for 11% of MRSA carriers, compared with 18% of ESBL, 4% of VRE, and none of the CRE carriers. Rates of colonization did not differ whether residents had long stays at the facility or postacute stays (49% vs. 48%, respectively), but bed-bound residents were more likely to be MDRO colonized, compared with ambulatory residents (59% vs. 46%; P less than .001). In the analysis of environmental swabs, 93% of common areas and 74% of resident rooms had an MDRO-positive object, with an average of 2.5 and 1.9 objects, respectively, found to be contaminated.
“The fact that about half of patients were carrying a bacteria that could cause infection on their skin was very high,” said Dr. McKinnell, who is a member of the Infectious Disease Clinical Outcome Research Unit at the Los Angeles Biomedical Research Institute at Harbor-UCLA. “Studies conducted in other care settings, we would typically see less than a quarter of patients carry these types of bacteria. I was also surprised to see that 1% of patients were carrying the CRE bacteria on their skin.”
He acknowledged certain limitations of the study, including the fact that the data were taken from a select group of nursing homes that are participating in an interventional study to improve personal hygiene for skilled nursing facility residents. “They may not be representative of all skilled nursing facilities,” he said.
The Agency for Healthcare Research and Quality funded the study. Dr. McKinnell disclosed that he is conducting studies in health care facilities with products supplied from 3M, Clorox, Sage, and Xttrium Laboratories. Many of his coauthors disclosed numerous financial ties to the pharmaceutical industry. The event was the combined annual meetings of the Infectious Diseases Society of America, the Society for Healthcare Epidemiology of America, the HIV Medicine Association, and the Pediatric Infectious Diseases Society.
SAN DIEGO – Nearly half of nursing home residents harbored multi-drug resistant organisms on their skin, results from a large multi-center surveillance study showed.
“Residents in skilled nursing homes are the most vulnerable patients in the health care system,” lead study author James A. McKinnell, MD, said in an interview in advance of an annual scientific meeting on infectious diseases. “Many residents depend on help from health care workers for routine needs like eating or bathing. Skilled nursing facilities have an obligation to optimize the personal hygiene and environmental cleanliness in skilled nursing facilities.”

The researchers obtained 2,797 body swabs from 1,400 residents in all. Swabs were processed for methicillin-resistant Staphylococcus aureus (MRSA), vancomycin-resistant Enterococcus spp. (VRE), extended spectrum beta-lactamase producers (ESBLs), and carbapenem-resistant Enterobacteriaceae (CRE). “MRSA is a relatively well known bacteria, but CRE is the new pathogen that the CDC has defined as an urgent public health threat,” Dr. McKinnell said.
The researchers also conducted environmental surveillance of commonly touched items in skilled nursing facilities. The five surfaces tested in resident rooms were the bedside table, TV remote, door knobs, light switch, and bathrooms. The five surfaces tested in common areas were the nursing station counter, tables, chairs, hallway hand rails, and drinking fountains.
Overall, 49% of residents harbored MDROs. MRSA was found in 37% of residents, followed by ESBL in 16%, VRE in 7%, and CRE in 1%. Resident MDRO status was known for 11% of MRSA carriers, compared with 18% of ESBL, 4% of VRE, and none of the CRE carriers. Rates of colonization did not differ whether residents had long stays at the facility or postacute stays (49% vs. 48%, respectively), but bed-bound residents were more likely to be MDRO colonized, compared with ambulatory residents (59% vs. 46%; P less than .001). In the analysis of environmental swabs, 93% of common areas and 74% of resident rooms had an MDRO-positive object, with an average of 2.5 and 1.9 objects, respectively, found to be contaminated.
“The fact that about half of patients were carrying a bacteria that could cause infection on their skin was very high,” said Dr. McKinnell, who is a member of the Infectious Disease Clinical Outcome Research Unit at the Los Angeles Biomedical Research Institute at Harbor-UCLA. “Studies conducted in other care settings, we would typically see less than a quarter of patients carry these types of bacteria. I was also surprised to see that 1% of patients were carrying the CRE bacteria on their skin.”
He acknowledged certain limitations of the study, including the fact that the data were taken from a select group of nursing homes that are participating in an interventional study to improve personal hygiene for skilled nursing facility residents. “They may not be representative of all skilled nursing facilities,” he said.
The Agency for Healthcare Research and Quality funded the study. Dr. McKinnell disclosed that he is conducting studies in health care facilities with products supplied from 3M, Clorox, Sage, and Xttrium Laboratories. Many of his coauthors disclosed numerous financial ties to the pharmaceutical industry. The event was the combined annual meetings of the Infectious Diseases Society of America, the Society for Healthcare Epidemiology of America, the HIV Medicine Association, and the Pediatric Infectious Diseases Society.
AT ID WEEK 2017
Key clinical point: About one of every two nursing home residents is colonized with multidrug resistant organisms.
Major finding:
Study details: A surveillance study of 1,400 residents at 28 skilled nursing facilities in Southern California.
Disclosures: The Agency for Healthcare Research and Quality funded the study. Dr. McKinnell disclosed that he is conducting studies in health care facilities with products supplied from 3M, Clorox, Sage, and Xttrium Laboratories. Many of his coauthors disclosed numerous financial ties to the pharmaceutical industry.
Postsurgical antibiotics cut infection in obese women after C-section
A 48-hour course of postoperative cephalexin and metronidazole, plus typical preoperative antibiotics, cut surgical site infections by 59% in obese women who had a cesarean delivery.
The benefit of the additional postoperative treatment was driven by a significant, 69% risk reduction among women who had ruptured membranes, Amy M. Valent, DO, and her colleagues reported (JAMA. 2017;318[11]:1026-34). However, the authors noted, “tests for interaction between the intact membranes and [ruptured] subgroups and postpartum cephalexin-metronidazole were not statistically different and should not be interpreted as showing a difference in significance or effect size among the subgroups with and without [rupture].”
The trial comprised 403 obese women who had a cesarean delivery. They were a mean of 28 years old. The mean body mass index was 40 kg/m2, and the mean subcutaneous adipose tissue thickness was about 3.4 cm. About a third of each treatment group was positive for Group B streptococcus; 31% had ruptured membranes at the onset of labor. More than 60% of women in both groups had a scheduled cesarean delivery.
All women had standard preoperative care, including skin prep with a chlorhexidine or povidone-iodine cleansing and an intravenous infusion of 2 g cefazolin. After delivery, they were randomized to placebo or to oral cephalexin 500 mg plus metronidazole 500 mg every 8 hours for 48 hours. The primary outcome was surgical site infection incidence within 30 days.
The overall rate of surgical site infection was 10.9% (44 women). Infections developed in 13 women in the active group and 31 in the placebo group (6.4% vs. 15.4%) – a significant difference, translating to a 59% risk reduction (relative risk, 0.41). Cellulitis was the only secondary outcome that was significantly reduced by prophylactic antibiotics, with infections occurring in 5.9% of the metronidazole-cephalexin group vs. 13.4% of the placebo group (RR, 0.44). The antibiotic regimen didn’t affect the other secondary endpoints, which included rates of incisional morbidity, endometritis, fever of unknown etiology, and wound separation.
The authors conducted a post-hoc analysis to examine the antibiotics’ effects on women who had ruptured and intact membranes at the time of delivery. The benefit was greatest among those with ruptured membranes. There were six infections among the active group and 19 among the placebo group (9.5% vs. 30.2%). This difference translated to a relative risk of 0.31 – a 69% risk reduction.
Among women with intact membranes, there were seven infections in the active group and 12 in the placebo group (5% vs. 8.7%). This translated to a 0.58 relative risk, which was not statistically significant.
“Interaction testing was performed between study groups (cephalexin-metronidazole vs. placebo) and by membrane status (intact vs. ruptured),” the authors noted. “The rate of surgical site infection was highest in those with [ruptured membranes] who received placebo (30.2%) and lowest in those with intact membranes who received antibiotics (5.0%), but the test for interaction did not show statistical significance at P = .30.”
There were no serious adverse events or allergic reactions reported for cephalexin or metronidazole. The authors noted that both drugs are excreted into breast milk in small amounts, but that no study has ever linked them with neonatal harm through breast milk exposure. However, they added, “Long-term childhood or adverse neonatal outcomes specific to cephalexin-metronidazole exposure cannot be determined, as outcome measures were not evaluated for this study protocol. Recognizing the maternal and neonatal benefit of breastfeeding, the lack of known neonatal adverse effects, and maternal reduction in [surgical site infection], the benefit of this antibiotic regimen likely outweighs the theoretical risks of breast milk exposure in the obese population.”
The University of Cincinnati Department of Obstetrics and Gynecology sponsored the trial. None of the authors reported any financial conflicts.
Despite the positive outcomes of this trial, it’s not yet time to tack on yet more antibiotics for every obese woman who undergoes a cesarean delivery, David P. Calfee, MD, and Amos Grünebaum, MD, wrote in an accompanying editorial (JAMA. 2017;318[11]:1012-3).
“When determining if and how the results of this study should alter current clinical practice, it is important to recognize that the results of this study are quite different from those of several previous studies conducted in other surgical patient populations in which no benefit from postoperative antimicrobial prophylaxis was found and on which current clinical guidelines for antimicrobial prophylaxis are based,” they wrote. “The explanation for this difference may be as simple as the identification in the current study of a very specific, high-risk group of patients for which the intervention is effective. However, several questions are worthy of additional consideration and study.”
For instance, the study was conducted over 5 years and may not reflect current practices for managing these patients, such as glycemic control and maintaining normothermia. Additionally, there may be additional risks to women that were not identified in the study, such as infection from antimicrobial-resistant pathogens.
Dr. Calfee and Dr. Grünebaum are at Weill Cornell Medical Center in New York. Dr. Calfee reported receiving grants from Merck, Sharp, and Dohme.
Despite the positive outcomes of this trial, it’s not yet time to tack on yet more antibiotics for every obese woman who undergoes a cesarean delivery, David P. Calfee, MD, and Amos Grünebaum, MD, wrote in an accompanying editorial (JAMA. 2017;318[11]:1012-3).
“When determining if and how the results of this study should alter current clinical practice, it is important to recognize that the results of this study are quite different from those of several previous studies conducted in other surgical patient populations in which no benefit from postoperative antimicrobial prophylaxis was found and on which current clinical guidelines for antimicrobial prophylaxis are based,” they wrote. “The explanation for this difference may be as simple as the identification in the current study of a very specific, high-risk group of patients for which the intervention is effective. However, several questions are worthy of additional consideration and study.”
For instance, the study was conducted over 5 years and may not reflect current practices for managing these patients, such as glycemic control and maintaining normothermia. Additionally, there may be additional risks to women that were not identified in the study, such as infection from antimicrobial-resistant pathogens.
Dr. Calfee and Dr. Grünebaum are at Weill Cornell Medical Center in New York. Dr. Calfee reported receiving grants from Merck, Sharp, and Dohme.
Despite the positive outcomes of this trial, it’s not yet time to tack on yet more antibiotics for every obese woman who undergoes a cesarean delivery, David P. Calfee, MD, and Amos Grünebaum, MD, wrote in an accompanying editorial (JAMA. 2017;318[11]:1012-3).
“When determining if and how the results of this study should alter current clinical practice, it is important to recognize that the results of this study are quite different from those of several previous studies conducted in other surgical patient populations in which no benefit from postoperative antimicrobial prophylaxis was found and on which current clinical guidelines for antimicrobial prophylaxis are based,” they wrote. “The explanation for this difference may be as simple as the identification in the current study of a very specific, high-risk group of patients for which the intervention is effective. However, several questions are worthy of additional consideration and study.”
For instance, the study was conducted over 5 years and may not reflect current practices for managing these patients, such as glycemic control and maintaining normothermia. Additionally, there may be additional risks to women that were not identified in the study, such as infection from antimicrobial-resistant pathogens.
Dr. Calfee and Dr. Grünebaum are at Weill Cornell Medical Center in New York. Dr. Calfee reported receiving grants from Merck, Sharp, and Dohme.
A 48-hour course of postoperative cephalexin and metronidazole, plus typical preoperative antibiotics, cut surgical site infections by 59% in obese women who had a cesarean delivery.
The benefit of the additional postoperative treatment was driven by a significant, 69% risk reduction among women who had ruptured membranes, Amy M. Valent, DO, and her colleagues reported (JAMA. 2017;318[11]:1026-34). However, the authors noted, “tests for interaction between the intact membranes and [ruptured] subgroups and postpartum cephalexin-metronidazole were not statistically different and should not be interpreted as showing a difference in significance or effect size among the subgroups with and without [rupture].”
The trial comprised 403 obese women who had a cesarean delivery. They were a mean of 28 years old. The mean body mass index was 40 kg/m2, and the mean subcutaneous adipose tissue thickness was about 3.4 cm. About a third of each treatment group was positive for Group B streptococcus; 31% had ruptured membranes at the onset of labor. More than 60% of women in both groups had a scheduled cesarean delivery.
All women had standard preoperative care, including skin prep with a chlorhexidine or povidone-iodine cleansing and an intravenous infusion of 2 g cefazolin. After delivery, they were randomized to placebo or to oral cephalexin 500 mg plus metronidazole 500 mg every 8 hours for 48 hours. The primary outcome was surgical site infection incidence within 30 days.
The overall rate of surgical site infection was 10.9% (44 women). Infections developed in 13 women in the active group and 31 in the placebo group (6.4% vs. 15.4%) – a significant difference, translating to a 59% risk reduction (relative risk, 0.41). Cellulitis was the only secondary outcome that was significantly reduced by prophylactic antibiotics, with infections occurring in 5.9% of the metronidazole-cephalexin group vs. 13.4% of the placebo group (RR, 0.44). The antibiotic regimen didn’t affect the other secondary endpoints, which included rates of incisional morbidity, endometritis, fever of unknown etiology, and wound separation.
The authors conducted a post-hoc analysis to examine the antibiotics’ effects on women who had ruptured and intact membranes at the time of delivery. The benefit was greatest among those with ruptured membranes. There were six infections among the active group and 19 among the placebo group (9.5% vs. 30.2%). This difference translated to a relative risk of 0.31 – a 69% risk reduction.
Among women with intact membranes, there were seven infections in the active group and 12 in the placebo group (5% vs. 8.7%). This translated to a 0.58 relative risk, which was not statistically significant.
“Interaction testing was performed between study groups (cephalexin-metronidazole vs. placebo) and by membrane status (intact vs. ruptured),” the authors noted. “The rate of surgical site infection was highest in those with [ruptured membranes] who received placebo (30.2%) and lowest in those with intact membranes who received antibiotics (5.0%), but the test for interaction did not show statistical significance at P = .30.”
There were no serious adverse events or allergic reactions reported for cephalexin or metronidazole. The authors noted that both drugs are excreted into breast milk in small amounts, but that no study has ever linked them with neonatal harm through breast milk exposure. However, they added, “Long-term childhood or adverse neonatal outcomes specific to cephalexin-metronidazole exposure cannot be determined, as outcome measures were not evaluated for this study protocol. Recognizing the maternal and neonatal benefit of breastfeeding, the lack of known neonatal adverse effects, and maternal reduction in [surgical site infection], the benefit of this antibiotic regimen likely outweighs the theoretical risks of breast milk exposure in the obese population.”
The University of Cincinnati Department of Obstetrics and Gynecology sponsored the trial. None of the authors reported any financial conflicts.
A 48-hour course of postoperative cephalexin and metronidazole, plus typical preoperative antibiotics, cut surgical site infections by 59% in obese women who had a cesarean delivery.
The benefit of the additional postoperative treatment was driven by a significant, 69% risk reduction among women who had ruptured membranes, Amy M. Valent, DO, and her colleagues reported (JAMA. 2017;318[11]:1026-34). However, the authors noted, “tests for interaction between the intact membranes and [ruptured] subgroups and postpartum cephalexin-metronidazole were not statistically different and should not be interpreted as showing a difference in significance or effect size among the subgroups with and without [rupture].”
The trial comprised 403 obese women who had a cesarean delivery. They were a mean of 28 years old. The mean body mass index was 40 kg/m2, and the mean subcutaneous adipose tissue thickness was about 3.4 cm. About a third of each treatment group was positive for Group B streptococcus; 31% had ruptured membranes at the onset of labor. More than 60% of women in both groups had a scheduled cesarean delivery.
All women had standard preoperative care, including skin prep with a chlorhexidine or povidone-iodine cleansing and an intravenous infusion of 2 g cefazolin. After delivery, they were randomized to placebo or to oral cephalexin 500 mg plus metronidazole 500 mg every 8 hours for 48 hours. The primary outcome was surgical site infection incidence within 30 days.
The overall rate of surgical site infection was 10.9% (44 women). Infections developed in 13 women in the active group and 31 in the placebo group (6.4% vs. 15.4%) – a significant difference, translating to a 59% risk reduction (relative risk, 0.41). Cellulitis was the only secondary outcome that was significantly reduced by prophylactic antibiotics, with infections occurring in 5.9% of the metronidazole-cephalexin group vs. 13.4% of the placebo group (RR, 0.44). The antibiotic regimen didn’t affect the other secondary endpoints, which included rates of incisional morbidity, endometritis, fever of unknown etiology, and wound separation.
The authors conducted a post-hoc analysis to examine the antibiotics’ effects on women who had ruptured and intact membranes at the time of delivery. The benefit was greatest among those with ruptured membranes. There were six infections among the active group and 19 among the placebo group (9.5% vs. 30.2%). This difference translated to a relative risk of 0.31 – a 69% risk reduction.
Among women with intact membranes, there were seven infections in the active group and 12 in the placebo group (5% vs. 8.7%). This translated to a 0.58 relative risk, which was not statistically significant.
“Interaction testing was performed between study groups (cephalexin-metronidazole vs. placebo) and by membrane status (intact vs. ruptured),” the authors noted. “The rate of surgical site infection was highest in those with [ruptured membranes] who received placebo (30.2%) and lowest in those with intact membranes who received antibiotics (5.0%), but the test for interaction did not show statistical significance at P = .30.”
There were no serious adverse events or allergic reactions reported for cephalexin or metronidazole. The authors noted that both drugs are excreted into breast milk in small amounts, but that no study has ever linked them with neonatal harm through breast milk exposure. However, they added, “Long-term childhood or adverse neonatal outcomes specific to cephalexin-metronidazole exposure cannot be determined, as outcome measures were not evaluated for this study protocol. Recognizing the maternal and neonatal benefit of breastfeeding, the lack of known neonatal adverse effects, and maternal reduction in [surgical site infection], the benefit of this antibiotic regimen likely outweighs the theoretical risks of breast milk exposure in the obese population.”
The University of Cincinnati Department of Obstetrics and Gynecology sponsored the trial. None of the authors reported any financial conflicts.
FROM JAMA
Key clinical point:
Major finding: Infections developed in 13 women in the active group and 31 in the placebo group (6.4% vs. 15.4%) – a significant difference, translating to a 59% risk reduction (relative risk, 0.41).
Data source: The randomized, placebo-controlled study comprised 403 women.
Disclosures: The University of Cincinnati Department of Obstetrics and Gynecology sponsored the study. None of the authors reported any financial conflicts.
Increase in sepsis incidence stable from 2009 to 2014
The trend for sepsis incidence from 2009 to 2014, “calculated relative to the observed 2014 rates,” was a stable increase of 0.6% per year using the more accurate of two forms of analysis, investigators reported.
The incidence of sepsis was an adjusted 5.9% among hospitalized adults in 2014, with in-hospital mortality of 15%, according to a retrospective cohort study published online Sept. 13 in JAMA.
“Most studies [of sepsis incidence] have used claims data, but increasing clinical awareness, changes in diagnosis and coding practices, and variable definitions have led to uncertainty about the accuracy of reported trends,” wrote Chanu Rhee, MD, of Harvard Medical School, Boston, and his associates (JAMA. 2017 Sep 13. doi: 10.1001/jama.2017.13836).
They used two methods – one involving claims-based estimates using ICD-9-CM codes and the other based on clinical data from electronic health records (EHRs) – to analyze data for more than 2.9 million adults admitted to 409 U.S. academic, community, and federal acute-care hospitals in 2014. The claims-based “explicit-codes” approach used discharge diagnoses of severe sepsis (995.92) or septic shock (785.52), while the EHR-based, clinical-criteria method included blood cultures, antibiotics, and concurrent organ dysfunction with or without the criterion of a lactate level of 2.0 mmol/L or greater, the investigators said.
The explicit-codes approach produced an increase of 10.3% per year in sepsis incidence from 2009 to 2014, compared with 0.6% per year for the clinical-criteria approach, while in-hospital mortality declined by 7% a year using explicit codes and 3.3% using clinical criteria, Dr. Rhee and his associates reported.
“EHR-based criteria were more sensitive than explicit sepsis codes on medical record review, with comparable [positive predictive value]; EHR-based criteria had similar sensitivity to implicit or explicit codes combined but higher [positive predictive value],” they said.
The estimates provided by Dr. Rhee and his associates provide “a clearer understanding of trends in the incidence and mortality of sepsis in the United States but also a better understanding of the challenges in improving ICD coding to accurately document the global burden of sepsis,” Kristina E. Rudd, MD, of the University of Washington, Seattle, and her associates said in an editorial (JAMA 2017 Sep 13. doi: 10.1001/jama.2017.13697).
The study was funded by the Centers for Disease Control and Prevention, Agency for Healthcare Research and Quality, National Institutes of Health, Department of Veterans Affairs, National Institutes of Health Clinical Center, and National Institute of Allergy and Infectious Diseases. Three of Dr. Rhee’s associates reported receiving personal fees from private companies or serving on advisory boards or as consultants. No other authors reported disclosures. Dr. Rudd and her associates had no conflicts of interest to report.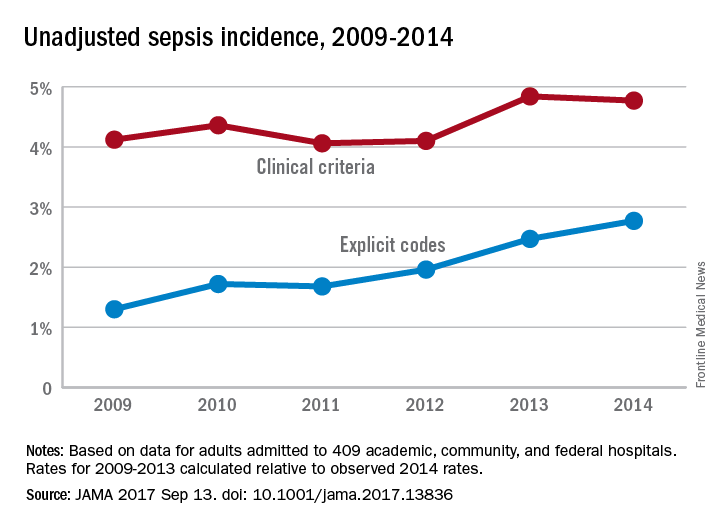
The trend for sepsis incidence from 2009 to 2014, “calculated relative to the observed 2014 rates,” was a stable increase of 0.6% per year using the more accurate of two forms of analysis, investigators reported.
The incidence of sepsis was an adjusted 5.9% among hospitalized adults in 2014, with in-hospital mortality of 15%, according to a retrospective cohort study published online Sept. 13 in JAMA.
“Most studies [of sepsis incidence] have used claims data, but increasing clinical awareness, changes in diagnosis and coding practices, and variable definitions have led to uncertainty about the accuracy of reported trends,” wrote Chanu Rhee, MD, of Harvard Medical School, Boston, and his associates (JAMA. 2017 Sep 13. doi: 10.1001/jama.2017.13836).
They used two methods – one involving claims-based estimates using ICD-9-CM codes and the other based on clinical data from electronic health records (EHRs) – to analyze data for more than 2.9 million adults admitted to 409 U.S. academic, community, and federal acute-care hospitals in 2014. The claims-based “explicit-codes” approach used discharge diagnoses of severe sepsis (995.92) or septic shock (785.52), while the EHR-based, clinical-criteria method included blood cultures, antibiotics, and concurrent organ dysfunction with or without the criterion of a lactate level of 2.0 mmol/L or greater, the investigators said.
The explicit-codes approach produced an increase of 10.3% per year in sepsis incidence from 2009 to 2014, compared with 0.6% per year for the clinical-criteria approach, while in-hospital mortality declined by 7% a year using explicit codes and 3.3% using clinical criteria, Dr. Rhee and his associates reported.
“EHR-based criteria were more sensitive than explicit sepsis codes on medical record review, with comparable [positive predictive value]; EHR-based criteria had similar sensitivity to implicit or explicit codes combined but higher [positive predictive value],” they said.
The estimates provided by Dr. Rhee and his associates provide “a clearer understanding of trends in the incidence and mortality of sepsis in the United States but also a better understanding of the challenges in improving ICD coding to accurately document the global burden of sepsis,” Kristina E. Rudd, MD, of the University of Washington, Seattle, and her associates said in an editorial (JAMA 2017 Sep 13. doi: 10.1001/jama.2017.13697).
The study was funded by the Centers for Disease Control and Prevention, Agency for Healthcare Research and Quality, National Institutes of Health, Department of Veterans Affairs, National Institutes of Health Clinical Center, and National Institute of Allergy and Infectious Diseases. Three of Dr. Rhee’s associates reported receiving personal fees from private companies or serving on advisory boards or as consultants. No other authors reported disclosures. Dr. Rudd and her associates had no conflicts of interest to report.
The trend for sepsis incidence from 2009 to 2014, “calculated relative to the observed 2014 rates,” was a stable increase of 0.6% per year using the more accurate of two forms of analysis, investigators reported.
The incidence of sepsis was an adjusted 5.9% among hospitalized adults in 2014, with in-hospital mortality of 15%, according to a retrospective cohort study published online Sept. 13 in JAMA.
“Most studies [of sepsis incidence] have used claims data, but increasing clinical awareness, changes in diagnosis and coding practices, and variable definitions have led to uncertainty about the accuracy of reported trends,” wrote Chanu Rhee, MD, of Harvard Medical School, Boston, and his associates (JAMA. 2017 Sep 13. doi: 10.1001/jama.2017.13836).
They used two methods – one involving claims-based estimates using ICD-9-CM codes and the other based on clinical data from electronic health records (EHRs) – to analyze data for more than 2.9 million adults admitted to 409 U.S. academic, community, and federal acute-care hospitals in 2014. The claims-based “explicit-codes” approach used discharge diagnoses of severe sepsis (995.92) or septic shock (785.52), while the EHR-based, clinical-criteria method included blood cultures, antibiotics, and concurrent organ dysfunction with or without the criterion of a lactate level of 2.0 mmol/L or greater, the investigators said.
The explicit-codes approach produced an increase of 10.3% per year in sepsis incidence from 2009 to 2014, compared with 0.6% per year for the clinical-criteria approach, while in-hospital mortality declined by 7% a year using explicit codes and 3.3% using clinical criteria, Dr. Rhee and his associates reported.
“EHR-based criteria were more sensitive than explicit sepsis codes on medical record review, with comparable [positive predictive value]; EHR-based criteria had similar sensitivity to implicit or explicit codes combined but higher [positive predictive value],” they said.
The estimates provided by Dr. Rhee and his associates provide “a clearer understanding of trends in the incidence and mortality of sepsis in the United States but also a better understanding of the challenges in improving ICD coding to accurately document the global burden of sepsis,” Kristina E. Rudd, MD, of the University of Washington, Seattle, and her associates said in an editorial (JAMA 2017 Sep 13. doi: 10.1001/jama.2017.13697).
The study was funded by the Centers for Disease Control and Prevention, Agency for Healthcare Research and Quality, National Institutes of Health, Department of Veterans Affairs, National Institutes of Health Clinical Center, and National Institute of Allergy and Infectious Diseases. Three of Dr. Rhee’s associates reported receiving personal fees from private companies or serving on advisory boards or as consultants. No other authors reported disclosures. Dr. Rudd and her associates had no conflicts of interest to report.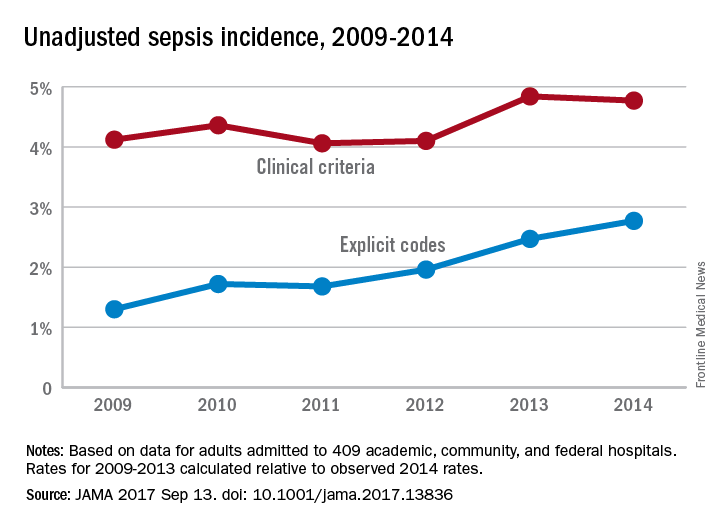
FROM JAMA
Capillary leakage predicts hysterectomy in postpartum group A strep
PARK CITY, UTAH – Systemic capillary leakage – which involves acute respiratory distress, ascites, pleural effusion, and abdominal distention – significantly increases the risk of hysterectomy in women with postpartum group A Streptococcus infection, according to findings from a single-site study.
The investigators at the University of Utah in Salt Lake City analyzed 71 cases of culture-proven infection at the university since 1991. They compared the 33 women who had hysterectomies, ICU admissions, pressor support, or mechanical ventilation with the 38 women who did not.
The goal was to identify predictors of poor outcomes and clarify when hysterectomy is the appropriate clinical decision. “These are young women, and it might have been their first pregnancy. You don’t want to remove their uterus if they don’t need it, but we know if women get really sick, they need that source control within 6-12 hours of presentation,” said Jennifer Kaiser, MD, the study’s lead investigator and an ob.gyn. fellow at the University of Utah.
“Capillary leak is an important objective clinical parameter that should be evaluated and considered with due exigency. I think this has not been well recognized,” Dr. Kaiser said at the annual scientific meeting of the Infectious Diseases Society for Obstetrics and Gynecology. The finding “should prompt you to mobilize a team for hysterectomy, or if you are at a smaller hospital, to think about transporting the patient to a higher level hospital that can perform hysterectomy and offer ICU care,” she added.
The investigators also found that a traditional marker for severe infection – uterine and cervical motion tenderness – did not predict adverse outcomes among the 71 women. Many patients with severe disease don’t actually have tenderness, Dr. Kaiser said.
It also didn’t matter whether the organism was isolated from the uterus or the blood. It’s sometimes thought uterine positivity predicts “worse prognosis, but that didn’t pan out,” she said.
Capillary leakage was a concern in 27 (82%) of the 33 women who had adverse outcomes, compared with 7 (18%) of the women who fared better, and included acute respiratory distress (30% versus 0%); ascites (73% versus 3%); pleural effusion (58% versus 5%), and abdominal distention (61% versus 18%). In total, 21 of the 33 women with adverse outcomes (64%) had hysterectomies. There were no deaths in the group.
Postpartum group A Streptococcus infections are more common in Utah than in other parts of the country, and it’s not known why. The next step for the investigators is to look at genealogies and genetic factors that may predispose women to severe infections, Dr. Kaiser said.
There was no industry funding for the work and Dr. Kaiser reported having no relevant financial disclosures.
PARK CITY, UTAH – Systemic capillary leakage – which involves acute respiratory distress, ascites, pleural effusion, and abdominal distention – significantly increases the risk of hysterectomy in women with postpartum group A Streptococcus infection, according to findings from a single-site study.
The investigators at the University of Utah in Salt Lake City analyzed 71 cases of culture-proven infection at the university since 1991. They compared the 33 women who had hysterectomies, ICU admissions, pressor support, or mechanical ventilation with the 38 women who did not.
The goal was to identify predictors of poor outcomes and clarify when hysterectomy is the appropriate clinical decision. “These are young women, and it might have been their first pregnancy. You don’t want to remove their uterus if they don’t need it, but we know if women get really sick, they need that source control within 6-12 hours of presentation,” said Jennifer Kaiser, MD, the study’s lead investigator and an ob.gyn. fellow at the University of Utah.
“Capillary leak is an important objective clinical parameter that should be evaluated and considered with due exigency. I think this has not been well recognized,” Dr. Kaiser said at the annual scientific meeting of the Infectious Diseases Society for Obstetrics and Gynecology. The finding “should prompt you to mobilize a team for hysterectomy, or if you are at a smaller hospital, to think about transporting the patient to a higher level hospital that can perform hysterectomy and offer ICU care,” she added.
The investigators also found that a traditional marker for severe infection – uterine and cervical motion tenderness – did not predict adverse outcomes among the 71 women. Many patients with severe disease don’t actually have tenderness, Dr. Kaiser said.
It also didn’t matter whether the organism was isolated from the uterus or the blood. It’s sometimes thought uterine positivity predicts “worse prognosis, but that didn’t pan out,” she said.
Capillary leakage was a concern in 27 (82%) of the 33 women who had adverse outcomes, compared with 7 (18%) of the women who fared better, and included acute respiratory distress (30% versus 0%); ascites (73% versus 3%); pleural effusion (58% versus 5%), and abdominal distention (61% versus 18%). In total, 21 of the 33 women with adverse outcomes (64%) had hysterectomies. There were no deaths in the group.
Postpartum group A Streptococcus infections are more common in Utah than in other parts of the country, and it’s not known why. The next step for the investigators is to look at genealogies and genetic factors that may predispose women to severe infections, Dr. Kaiser said.
There was no industry funding for the work and Dr. Kaiser reported having no relevant financial disclosures.
PARK CITY, UTAH – Systemic capillary leakage – which involves acute respiratory distress, ascites, pleural effusion, and abdominal distention – significantly increases the risk of hysterectomy in women with postpartum group A Streptococcus infection, according to findings from a single-site study.
The investigators at the University of Utah in Salt Lake City analyzed 71 cases of culture-proven infection at the university since 1991. They compared the 33 women who had hysterectomies, ICU admissions, pressor support, or mechanical ventilation with the 38 women who did not.
The goal was to identify predictors of poor outcomes and clarify when hysterectomy is the appropriate clinical decision. “These are young women, and it might have been their first pregnancy. You don’t want to remove their uterus if they don’t need it, but we know if women get really sick, they need that source control within 6-12 hours of presentation,” said Jennifer Kaiser, MD, the study’s lead investigator and an ob.gyn. fellow at the University of Utah.
“Capillary leak is an important objective clinical parameter that should be evaluated and considered with due exigency. I think this has not been well recognized,” Dr. Kaiser said at the annual scientific meeting of the Infectious Diseases Society for Obstetrics and Gynecology. The finding “should prompt you to mobilize a team for hysterectomy, or if you are at a smaller hospital, to think about transporting the patient to a higher level hospital that can perform hysterectomy and offer ICU care,” she added.
The investigators also found that a traditional marker for severe infection – uterine and cervical motion tenderness – did not predict adverse outcomes among the 71 women. Many patients with severe disease don’t actually have tenderness, Dr. Kaiser said.
It also didn’t matter whether the organism was isolated from the uterus or the blood. It’s sometimes thought uterine positivity predicts “worse prognosis, but that didn’t pan out,” she said.
Capillary leakage was a concern in 27 (82%) of the 33 women who had adverse outcomes, compared with 7 (18%) of the women who fared better, and included acute respiratory distress (30% versus 0%); ascites (73% versus 3%); pleural effusion (58% versus 5%), and abdominal distention (61% versus 18%). In total, 21 of the 33 women with adverse outcomes (64%) had hysterectomies. There were no deaths in the group.
Postpartum group A Streptococcus infections are more common in Utah than in other parts of the country, and it’s not known why. The next step for the investigators is to look at genealogies and genetic factors that may predispose women to severe infections, Dr. Kaiser said.
There was no industry funding for the work and Dr. Kaiser reported having no relevant financial disclosures.
AT IDSOG
Key clinical point:
Major finding: Signs of capillary leakage were predictive of adverse outcomes (OR 19.93, 95% CI 5.96-66.57, P less than .0001), specifically hysterectomy (OR 51.43, 95% CI 6.29-420.41, P less than .002).
Data source: A review of 71 cases of culture-proven infection at the University of Utah.
Disclosures: There was no industry funding for the work and the lead investigator reported having no relevant financial disclosures.