User login
Women Fare Better Than Men Following Total Knee, Hip Replacement
LAS VEGAS—While women may have their first total joint replacement (TJR) at an older age, they are less likely to have complications related to their surgery or require revision surgery, according to a study presented at the 2015 Annual Meeting of the American Academy of Orthopaedic Surgeons (AAOS). The findings contradict the theory that TJR is underutilized in female patients because they have worse outcomes than men.
Researchers reviewed patient databases from an Ontario hospital for first-time primary total hip replacement (THR) and total knee replacement (TKR) patients between 2002 and 2009. There were 37,881 THR surgeries (53.8% female) and 59,564 TKR surgeries (60.5% female). Women who underwent THR were significantly older than males (70 years vs. 65 years); however, there was no difference in age between male and female patients undergoing TKR (median age 68 years for both). A greater proportion of female patients undergoing TJR were defined as frail (6.6% vs. 3.5% for THR; and, 6.7% vs. 4% for TKR).
Following surgery, men were:
• 15% more likely to return to the emergency department within 30 days of hospital discharge following either THR or TKR.
• 60% and 70% more likely to have an acute myocardial infarction within 3 months following THR and TKR, respectively.
• 50% more likely to require a revision arthroplasty within 2 years of TKR.
• 25% more likely to be readmitted to the hospital and 70% more likely to experience an infection or revision surgery within 2 years of TKR, compared to women.
“Despite the fact that women have a higher prevalence of advanced hip and knee arthritis, prior research indicates that North American women with arthritis are less likely to receive joint replacement than men,” said lead study author Bheeshma Ravi, MD, PhD, an orthopedic surgery resident at the University of Toronto. “One possible explanation is that women are less often offered or accept surgery because their risk of serious complications following surgery is greater than that of men.
“In this study, we found that while overall rates of serious complications were low for both groups, they were lower for women than for men for both hip and knee replacement, particularly the latter” said Dr. Ravi. “Thus, the previously documented sex difference utilization of TJR cannot be explained by differential risks of complications following surgery.”
LAS VEGAS—While women may have their first total joint replacement (TJR) at an older age, they are less likely to have complications related to their surgery or require revision surgery, according to a study presented at the 2015 Annual Meeting of the American Academy of Orthopaedic Surgeons (AAOS). The findings contradict the theory that TJR is underutilized in female patients because they have worse outcomes than men.
Researchers reviewed patient databases from an Ontario hospital for first-time primary total hip replacement (THR) and total knee replacement (TKR) patients between 2002 and 2009. There were 37,881 THR surgeries (53.8% female) and 59,564 TKR surgeries (60.5% female). Women who underwent THR were significantly older than males (70 years vs. 65 years); however, there was no difference in age between male and female patients undergoing TKR (median age 68 years for both). A greater proportion of female patients undergoing TJR were defined as frail (6.6% vs. 3.5% for THR; and, 6.7% vs. 4% for TKR).
Following surgery, men were:
• 15% more likely to return to the emergency department within 30 days of hospital discharge following either THR or TKR.
• 60% and 70% more likely to have an acute myocardial infarction within 3 months following THR and TKR, respectively.
• 50% more likely to require a revision arthroplasty within 2 years of TKR.
• 25% more likely to be readmitted to the hospital and 70% more likely to experience an infection or revision surgery within 2 years of TKR, compared to women.
“Despite the fact that women have a higher prevalence of advanced hip and knee arthritis, prior research indicates that North American women with arthritis are less likely to receive joint replacement than men,” said lead study author Bheeshma Ravi, MD, PhD, an orthopedic surgery resident at the University of Toronto. “One possible explanation is that women are less often offered or accept surgery because their risk of serious complications following surgery is greater than that of men.
“In this study, we found that while overall rates of serious complications were low for both groups, they were lower for women than for men for both hip and knee replacement, particularly the latter” said Dr. Ravi. “Thus, the previously documented sex difference utilization of TJR cannot be explained by differential risks of complications following surgery.”
LAS VEGAS—While women may have their first total joint replacement (TJR) at an older age, they are less likely to have complications related to their surgery or require revision surgery, according to a study presented at the 2015 Annual Meeting of the American Academy of Orthopaedic Surgeons (AAOS). The findings contradict the theory that TJR is underutilized in female patients because they have worse outcomes than men.
Researchers reviewed patient databases from an Ontario hospital for first-time primary total hip replacement (THR) and total knee replacement (TKR) patients between 2002 and 2009. There were 37,881 THR surgeries (53.8% female) and 59,564 TKR surgeries (60.5% female). Women who underwent THR were significantly older than males (70 years vs. 65 years); however, there was no difference in age between male and female patients undergoing TKR (median age 68 years for both). A greater proportion of female patients undergoing TJR were defined as frail (6.6% vs. 3.5% for THR; and, 6.7% vs. 4% for TKR).
Following surgery, men were:
• 15% more likely to return to the emergency department within 30 days of hospital discharge following either THR or TKR.
• 60% and 70% more likely to have an acute myocardial infarction within 3 months following THR and TKR, respectively.
• 50% more likely to require a revision arthroplasty within 2 years of TKR.
• 25% more likely to be readmitted to the hospital and 70% more likely to experience an infection or revision surgery within 2 years of TKR, compared to women.
“Despite the fact that women have a higher prevalence of advanced hip and knee arthritis, prior research indicates that North American women with arthritis are less likely to receive joint replacement than men,” said lead study author Bheeshma Ravi, MD, PhD, an orthopedic surgery resident at the University of Toronto. “One possible explanation is that women are less often offered or accept surgery because their risk of serious complications following surgery is greater than that of men.
“In this study, we found that while overall rates of serious complications were low for both groups, they were lower for women than for men for both hip and knee replacement, particularly the latter” said Dr. Ravi. “Thus, the previously documented sex difference utilization of TJR cannot be explained by differential risks of complications following surgery.”
Hip Replacements in Middle-Age Nearly Double From 2002-2011, Outpacing Growth in Elderly Population
LAS VEGAS—The number of total hip replacements (THRs) nearly doubled among middle-age patients between 2002 and 2011, primarily due to the expansion of the middle-age population in the United States, according to a study presented at the 2015 Annual Meeting of the American Academy of Orthopaedic Surgeons (AAOS). Continued growth in utilization of hip replacement surgery in patients ages 45 to 64 years, an increase in revision surgeries for this population as they age, and a nearly 30% decline in the number of surgeons who perform THR could have significant implications for future health care costs, THR demand, and access, researchers said.
The researchers used the Nationwide Inpatient Sample (NIS) to identify primary THRs performed between 2002 and 2011 in patients ages 45 to 64 years, as well as related hospital charges. Population data and projections were obtained from the US Census Bureau and surgeon workforce estimates from the AAOS.
In 2011, 42.3% of THRs were performed in patients ages 45 to 64 years compared to 33.9% in 2002. Utilization of THR in this age group increased 89.2% from 2002 to 2011, from approximately 68,000 THRs in 2002 to 128,000 THRs in 2011. The overall population increased 21.3%. In addition, the authors found that:
• Growth of THR utilization in the 45- to 64-year-old age group grew 2.4 times faster than it did in the Medicare-aged population (age > 65 years).
• A rise in the prevalence of obesity, a known risk factor for hip osteoarthritis, among middle-age Americans was not significantly associated with increased THR utilization.
• Mean hospital charges in the THR 45- to 64-year-old age group declined 5.7% from 2002 to 2011, and declined 2.5% in the Medicare population (age > 65 years).
• Mean physician reimbursement per THR, in 2011 US dollars, declined 26.2% over the same period.
• Concurrently, the number of physicians reporting that they performed THR surgeries declined 28.2%.
“The purpose of this study was to identify potential drivers of THR utilization in the middle-age patient segment,” said lead study author Alexander S. McLawhorn, MD, MBA, an orthopedic surgery resident at the Hospital for Special Surgery in New York City. “Our multivariable statistical model suggested that the observed growth was best explained by an expansion of the middle-age population in the US. This particular age group is projected to continue expanding, and as such the demand for THR in this active group of patients will likely continue to rise as well. Our results underscore concerns about consumption of premium-priced implants in younger patients and the future revision burden this trend implies in the face of a dwindling number of physicians who specialize in hip arthroplasty surgery.”
LAS VEGAS—The number of total hip replacements (THRs) nearly doubled among middle-age patients between 2002 and 2011, primarily due to the expansion of the middle-age population in the United States, according to a study presented at the 2015 Annual Meeting of the American Academy of Orthopaedic Surgeons (AAOS). Continued growth in utilization of hip replacement surgery in patients ages 45 to 64 years, an increase in revision surgeries for this population as they age, and a nearly 30% decline in the number of surgeons who perform THR could have significant implications for future health care costs, THR demand, and access, researchers said.
The researchers used the Nationwide Inpatient Sample (NIS) to identify primary THRs performed between 2002 and 2011 in patients ages 45 to 64 years, as well as related hospital charges. Population data and projections were obtained from the US Census Bureau and surgeon workforce estimates from the AAOS.
In 2011, 42.3% of THRs were performed in patients ages 45 to 64 years compared to 33.9% in 2002. Utilization of THR in this age group increased 89.2% from 2002 to 2011, from approximately 68,000 THRs in 2002 to 128,000 THRs in 2011. The overall population increased 21.3%. In addition, the authors found that:
• Growth of THR utilization in the 45- to 64-year-old age group grew 2.4 times faster than it did in the Medicare-aged population (age > 65 years).
• A rise in the prevalence of obesity, a known risk factor for hip osteoarthritis, among middle-age Americans was not significantly associated with increased THR utilization.
• Mean hospital charges in the THR 45- to 64-year-old age group declined 5.7% from 2002 to 2011, and declined 2.5% in the Medicare population (age > 65 years).
• Mean physician reimbursement per THR, in 2011 US dollars, declined 26.2% over the same period.
• Concurrently, the number of physicians reporting that they performed THR surgeries declined 28.2%.
“The purpose of this study was to identify potential drivers of THR utilization in the middle-age patient segment,” said lead study author Alexander S. McLawhorn, MD, MBA, an orthopedic surgery resident at the Hospital for Special Surgery in New York City. “Our multivariable statistical model suggested that the observed growth was best explained by an expansion of the middle-age population in the US. This particular age group is projected to continue expanding, and as such the demand for THR in this active group of patients will likely continue to rise as well. Our results underscore concerns about consumption of premium-priced implants in younger patients and the future revision burden this trend implies in the face of a dwindling number of physicians who specialize in hip arthroplasty surgery.”
LAS VEGAS—The number of total hip replacements (THRs) nearly doubled among middle-age patients between 2002 and 2011, primarily due to the expansion of the middle-age population in the United States, according to a study presented at the 2015 Annual Meeting of the American Academy of Orthopaedic Surgeons (AAOS). Continued growth in utilization of hip replacement surgery in patients ages 45 to 64 years, an increase in revision surgeries for this population as they age, and a nearly 30% decline in the number of surgeons who perform THR could have significant implications for future health care costs, THR demand, and access, researchers said.
The researchers used the Nationwide Inpatient Sample (NIS) to identify primary THRs performed between 2002 and 2011 in patients ages 45 to 64 years, as well as related hospital charges. Population data and projections were obtained from the US Census Bureau and surgeon workforce estimates from the AAOS.
In 2011, 42.3% of THRs were performed in patients ages 45 to 64 years compared to 33.9% in 2002. Utilization of THR in this age group increased 89.2% from 2002 to 2011, from approximately 68,000 THRs in 2002 to 128,000 THRs in 2011. The overall population increased 21.3%. In addition, the authors found that:
• Growth of THR utilization in the 45- to 64-year-old age group grew 2.4 times faster than it did in the Medicare-aged population (age > 65 years).
• A rise in the prevalence of obesity, a known risk factor for hip osteoarthritis, among middle-age Americans was not significantly associated with increased THR utilization.
• Mean hospital charges in the THR 45- to 64-year-old age group declined 5.7% from 2002 to 2011, and declined 2.5% in the Medicare population (age > 65 years).
• Mean physician reimbursement per THR, in 2011 US dollars, declined 26.2% over the same period.
• Concurrently, the number of physicians reporting that they performed THR surgeries declined 28.2%.
“The purpose of this study was to identify potential drivers of THR utilization in the middle-age patient segment,” said lead study author Alexander S. McLawhorn, MD, MBA, an orthopedic surgery resident at the Hospital for Special Surgery in New York City. “Our multivariable statistical model suggested that the observed growth was best explained by an expansion of the middle-age population in the US. This particular age group is projected to continue expanding, and as such the demand for THR in this active group of patients will likely continue to rise as well. Our results underscore concerns about consumption of premium-priced implants in younger patients and the future revision burden this trend implies in the face of a dwindling number of physicians who specialize in hip arthroplasty surgery.”
Routine Bisphosphonate Treatment for Women Older Than 65 Years Who Sustain a Wrist Fracture Could Prevent Nearly 95,000 Hip Fractures, But at a Significant Cost
LAS VEGAS—Routine bisphosphonate treatment of women older than 65 years who sustain a distal radius fracture could significantly reduce the risk for additional fractures, primarily hip fractures, but at an estimated cost of more than $2 billion annually, according to a study presented at the 2015 Annual Meeting of the American Academy of Orthopaedic Surgeons (AAOS).
More than 50% of men and women older than 80 years meet diagnostic criteria for osteoporosis, placing them at increased risk for bone fractures, including hip fractures, which cause an estimated 300,000 unplanned hospital admissions in the United States each year. The lifetime cost of a hip fracture is estimated at $81,300, of which approximately 44% of the costs are associated with nursing facility expenses. Bisphosphonates, a drug known to increase bone mass and prevent fractures, have been associated with atypical femur fractures in a small, but significant number of patients.
Researchers reviewed existing literature and Medicare data to determine distal radius fracture incidence and age-specific hip fracture rates after distal radius fracture with and without bisphosphonate treatment. A model was then created to determine future fracture rates with and without treatment and related costs.
The model predicted 357,656 lifetime hip fractures following distal radius fracture in all females age 65 years and older in the US. If these patients received regular bisphosphonate treatment following a distal radius fracture, the number of hip fractures would drop to 262,767 over the lifetime of these patients; however, an estimated 19,464 patients would suffer an atypical femur fracture as a result of the treatment.
The cost of routine bisphosphonate treatment, including the cost for treating associated atypical femur fractures, comes to a lifetime total of $19.5 billion, or approximately $205,534 per avoided hip fracture.
“Our study suggests that routine universal utilization of bisphosphonates in elderly women after distal radius fracture would not be economically advantageous despite the cost savings associated with reduction of the hip fracture burden in that population,” said lead study author, Suneel B. Bhat, MD, an orthopedic surgery resident at the Rothman Institute in Philadelphia.
The study authors also hypothesize that the cost of bisphosphonates would need to drop to $70 per patient each year, from the current average annual wholesale cost of $1,485 per patient, to make the treatment affordable to every patient age 65 years and older following a wrist fracture. In addition, selecting patients at lower risk for atypical femur fractures for treatment may reduce the number of bisphosphonate-related fractures. Confirming patient osteoporosis and fracture risk through a DEXA Scan (dual x-ray absorptiometry) before prescribing bisphosphonates remains the most cost-effective method for treating osteoporosis and avoiding subsequent fractures.
LAS VEGAS—Routine bisphosphonate treatment of women older than 65 years who sustain a distal radius fracture could significantly reduce the risk for additional fractures, primarily hip fractures, but at an estimated cost of more than $2 billion annually, according to a study presented at the 2015 Annual Meeting of the American Academy of Orthopaedic Surgeons (AAOS).
More than 50% of men and women older than 80 years meet diagnostic criteria for osteoporosis, placing them at increased risk for bone fractures, including hip fractures, which cause an estimated 300,000 unplanned hospital admissions in the United States each year. The lifetime cost of a hip fracture is estimated at $81,300, of which approximately 44% of the costs are associated with nursing facility expenses. Bisphosphonates, a drug known to increase bone mass and prevent fractures, have been associated with atypical femur fractures in a small, but significant number of patients.
Researchers reviewed existing literature and Medicare data to determine distal radius fracture incidence and age-specific hip fracture rates after distal radius fracture with and without bisphosphonate treatment. A model was then created to determine future fracture rates with and without treatment and related costs.
The model predicted 357,656 lifetime hip fractures following distal radius fracture in all females age 65 years and older in the US. If these patients received regular bisphosphonate treatment following a distal radius fracture, the number of hip fractures would drop to 262,767 over the lifetime of these patients; however, an estimated 19,464 patients would suffer an atypical femur fracture as a result of the treatment.
The cost of routine bisphosphonate treatment, including the cost for treating associated atypical femur fractures, comes to a lifetime total of $19.5 billion, or approximately $205,534 per avoided hip fracture.
“Our study suggests that routine universal utilization of bisphosphonates in elderly women after distal radius fracture would not be economically advantageous despite the cost savings associated with reduction of the hip fracture burden in that population,” said lead study author, Suneel B. Bhat, MD, an orthopedic surgery resident at the Rothman Institute in Philadelphia.
The study authors also hypothesize that the cost of bisphosphonates would need to drop to $70 per patient each year, from the current average annual wholesale cost of $1,485 per patient, to make the treatment affordable to every patient age 65 years and older following a wrist fracture. In addition, selecting patients at lower risk for atypical femur fractures for treatment may reduce the number of bisphosphonate-related fractures. Confirming patient osteoporosis and fracture risk through a DEXA Scan (dual x-ray absorptiometry) before prescribing bisphosphonates remains the most cost-effective method for treating osteoporosis and avoiding subsequent fractures.
LAS VEGAS—Routine bisphosphonate treatment of women older than 65 years who sustain a distal radius fracture could significantly reduce the risk for additional fractures, primarily hip fractures, but at an estimated cost of more than $2 billion annually, according to a study presented at the 2015 Annual Meeting of the American Academy of Orthopaedic Surgeons (AAOS).
More than 50% of men and women older than 80 years meet diagnostic criteria for osteoporosis, placing them at increased risk for bone fractures, including hip fractures, which cause an estimated 300,000 unplanned hospital admissions in the United States each year. The lifetime cost of a hip fracture is estimated at $81,300, of which approximately 44% of the costs are associated with nursing facility expenses. Bisphosphonates, a drug known to increase bone mass and prevent fractures, have been associated with atypical femur fractures in a small, but significant number of patients.
Researchers reviewed existing literature and Medicare data to determine distal radius fracture incidence and age-specific hip fracture rates after distal radius fracture with and without bisphosphonate treatment. A model was then created to determine future fracture rates with and without treatment and related costs.
The model predicted 357,656 lifetime hip fractures following distal radius fracture in all females age 65 years and older in the US. If these patients received regular bisphosphonate treatment following a distal radius fracture, the number of hip fractures would drop to 262,767 over the lifetime of these patients; however, an estimated 19,464 patients would suffer an atypical femur fracture as a result of the treatment.
The cost of routine bisphosphonate treatment, including the cost for treating associated atypical femur fractures, comes to a lifetime total of $19.5 billion, or approximately $205,534 per avoided hip fracture.
“Our study suggests that routine universal utilization of bisphosphonates in elderly women after distal radius fracture would not be economically advantageous despite the cost savings associated with reduction of the hip fracture burden in that population,” said lead study author, Suneel B. Bhat, MD, an orthopedic surgery resident at the Rothman Institute in Philadelphia.
The study authors also hypothesize that the cost of bisphosphonates would need to drop to $70 per patient each year, from the current average annual wholesale cost of $1,485 per patient, to make the treatment affordable to every patient age 65 years and older following a wrist fracture. In addition, selecting patients at lower risk for atypical femur fractures for treatment may reduce the number of bisphosphonate-related fractures. Confirming patient osteoporosis and fracture risk through a DEXA Scan (dual x-ray absorptiometry) before prescribing bisphosphonates remains the most cost-effective method for treating osteoporosis and avoiding subsequent fractures.
Nearly Half of Patients Have Delirium Before and After Hip Fracture Surgery, Diminishing Outcomes and Increasing Health Care Costs
LAS VEGAS─Nearly 50% of hip fracture patients, age 65 years and older, had delirium before, during, and after surgery, resulting in significantly longer hospital stays and higher costs for care, according to data presented at the 2015 Annual Meeting of the American Academy of Orthopaedic Surgeons (AAOS). Delirium was associated with 7.4 additional hospital days and approximately $8,000 more in hospital costs.
Approximately 300,000 Americans are hospitalized with hip fractures each year. The risk is particularly high in post-menopausal women who face an increased risk for osteoporosis. Delirium is common among older hip fracture patients, and multiple studies have found that patients with postoperative delirium are more likely to have complications, including infections, and less likely to return to their pre-injury level of function. Delirium patients also are more frequently placed in nursing homes following surgery and have an increased rate of mortality.
In this study, researchers at the University of Toronto sought to determine the economic implications of perioperative delirium in older orthopedic patients by reviewing hip fracture records between January 2011 and December 2012. A total of 242 hip fracture patients with a mean age of 82 years (ages 65 to 103 years) were studied. Demographic, clinical, surgical, and adverse events data were analyzed. Perioperative delirium was assessed using the Confusion Assessment Method (CAM).
The study found that 116 patients (48%) experienced delirium during hospital admission. The patients with delirium were significantly older (mean age 85 years), and were more likely to have a higher American Society of Anesthesiologists (ASA) score (1 represents a completely healthy fit patient, and 5 represents a patient not expected to live beyond 24 hours without surgery). After controlling for these differences, perioperative delirium was associated with 7.4 additional hospital days and $8,282 ($8,649 in US dollars) in additional hospital costs (1.5 times the cost of patients who did not experience delirium).
There were no differences in mean time between triage or admission and surgery, length of surgery, or anesthesia type between groups. A significantly greater proportion of patients who experienced perioperative delirium required long-term and/or skilled care facility admission following their hospital stay than did those who did not experience delirium (8% versus 0%).
“Older patients are at high risk of developing delirium during hospitalization for a hip fracture, which is associated with worse outcomes,” said orthopedic surgeon and lead study author Michael G. Zywiel, MD. “Our work demonstrates that delirium also markedly increases the cost of elderly patient care while in the hospital. Given the high number of patients hospitalized every year with a hip fracture, there is a real need to develop and fund improved interventions to prevent in-hospital delirium in these patients.
“Our research suggests that reducing the rate of delirium would simultaneously increase the quality of care while decreasing costs, presenting hospitals, surgeons, and other stakeholders with promising opportunities to improve the value of hip fracture care,” said Dr. Zywiel.
The AAOS’s new clinical practice guideline, “Management of Hip Fractures in the Elderly,” makes a series of recommendations to reduce delirium in older hip fracture patients. They include:
• Preoperative regional analgesia to reduce pain.
• Hip fracture surgery within 48 hours of hospital admission.
• Intensive physical therapy following hospital discharge to improve functional outcomes.
• An osteoporosis evaluation, as well as vitamin D and calcium supplements, for patients following a hip fracture.
LAS VEGAS─Nearly 50% of hip fracture patients, age 65 years and older, had delirium before, during, and after surgery, resulting in significantly longer hospital stays and higher costs for care, according to data presented at the 2015 Annual Meeting of the American Academy of Orthopaedic Surgeons (AAOS). Delirium was associated with 7.4 additional hospital days and approximately $8,000 more in hospital costs.
Approximately 300,000 Americans are hospitalized with hip fractures each year. The risk is particularly high in post-menopausal women who face an increased risk for osteoporosis. Delirium is common among older hip fracture patients, and multiple studies have found that patients with postoperative delirium are more likely to have complications, including infections, and less likely to return to their pre-injury level of function. Delirium patients also are more frequently placed in nursing homes following surgery and have an increased rate of mortality.
In this study, researchers at the University of Toronto sought to determine the economic implications of perioperative delirium in older orthopedic patients by reviewing hip fracture records between January 2011 and December 2012. A total of 242 hip fracture patients with a mean age of 82 years (ages 65 to 103 years) were studied. Demographic, clinical, surgical, and adverse events data were analyzed. Perioperative delirium was assessed using the Confusion Assessment Method (CAM).
The study found that 116 patients (48%) experienced delirium during hospital admission. The patients with delirium were significantly older (mean age 85 years), and were more likely to have a higher American Society of Anesthesiologists (ASA) score (1 represents a completely healthy fit patient, and 5 represents a patient not expected to live beyond 24 hours without surgery). After controlling for these differences, perioperative delirium was associated with 7.4 additional hospital days and $8,282 ($8,649 in US dollars) in additional hospital costs (1.5 times the cost of patients who did not experience delirium).
There were no differences in mean time between triage or admission and surgery, length of surgery, or anesthesia type between groups. A significantly greater proportion of patients who experienced perioperative delirium required long-term and/or skilled care facility admission following their hospital stay than did those who did not experience delirium (8% versus 0%).
“Older patients are at high risk of developing delirium during hospitalization for a hip fracture, which is associated with worse outcomes,” said orthopedic surgeon and lead study author Michael G. Zywiel, MD. “Our work demonstrates that delirium also markedly increases the cost of elderly patient care while in the hospital. Given the high number of patients hospitalized every year with a hip fracture, there is a real need to develop and fund improved interventions to prevent in-hospital delirium in these patients.
“Our research suggests that reducing the rate of delirium would simultaneously increase the quality of care while decreasing costs, presenting hospitals, surgeons, and other stakeholders with promising opportunities to improve the value of hip fracture care,” said Dr. Zywiel.
The AAOS’s new clinical practice guideline, “Management of Hip Fractures in the Elderly,” makes a series of recommendations to reduce delirium in older hip fracture patients. They include:
• Preoperative regional analgesia to reduce pain.
• Hip fracture surgery within 48 hours of hospital admission.
• Intensive physical therapy following hospital discharge to improve functional outcomes.
• An osteoporosis evaluation, as well as vitamin D and calcium supplements, for patients following a hip fracture.
LAS VEGAS─Nearly 50% of hip fracture patients, age 65 years and older, had delirium before, during, and after surgery, resulting in significantly longer hospital stays and higher costs for care, according to data presented at the 2015 Annual Meeting of the American Academy of Orthopaedic Surgeons (AAOS). Delirium was associated with 7.4 additional hospital days and approximately $8,000 more in hospital costs.
Approximately 300,000 Americans are hospitalized with hip fractures each year. The risk is particularly high in post-menopausal women who face an increased risk for osteoporosis. Delirium is common among older hip fracture patients, and multiple studies have found that patients with postoperative delirium are more likely to have complications, including infections, and less likely to return to their pre-injury level of function. Delirium patients also are more frequently placed in nursing homes following surgery and have an increased rate of mortality.
In this study, researchers at the University of Toronto sought to determine the economic implications of perioperative delirium in older orthopedic patients by reviewing hip fracture records between January 2011 and December 2012. A total of 242 hip fracture patients with a mean age of 82 years (ages 65 to 103 years) were studied. Demographic, clinical, surgical, and adverse events data were analyzed. Perioperative delirium was assessed using the Confusion Assessment Method (CAM).
The study found that 116 patients (48%) experienced delirium during hospital admission. The patients with delirium were significantly older (mean age 85 years), and were more likely to have a higher American Society of Anesthesiologists (ASA) score (1 represents a completely healthy fit patient, and 5 represents a patient not expected to live beyond 24 hours without surgery). After controlling for these differences, perioperative delirium was associated with 7.4 additional hospital days and $8,282 ($8,649 in US dollars) in additional hospital costs (1.5 times the cost of patients who did not experience delirium).
There were no differences in mean time between triage or admission and surgery, length of surgery, or anesthesia type between groups. A significantly greater proportion of patients who experienced perioperative delirium required long-term and/or skilled care facility admission following their hospital stay than did those who did not experience delirium (8% versus 0%).
“Older patients are at high risk of developing delirium during hospitalization for a hip fracture, which is associated with worse outcomes,” said orthopedic surgeon and lead study author Michael G. Zywiel, MD. “Our work demonstrates that delirium also markedly increases the cost of elderly patient care while in the hospital. Given the high number of patients hospitalized every year with a hip fracture, there is a real need to develop and fund improved interventions to prevent in-hospital delirium in these patients.
“Our research suggests that reducing the rate of delirium would simultaneously increase the quality of care while decreasing costs, presenting hospitals, surgeons, and other stakeholders with promising opportunities to improve the value of hip fracture care,” said Dr. Zywiel.
The AAOS’s new clinical practice guideline, “Management of Hip Fractures in the Elderly,” makes a series of recommendations to reduce delirium in older hip fracture patients. They include:
• Preoperative regional analgesia to reduce pain.
• Hip fracture surgery within 48 hours of hospital admission.
• Intensive physical therapy following hospital discharge to improve functional outcomes.
• An osteoporosis evaluation, as well as vitamin D and calcium supplements, for patients following a hip fracture.
Hip Replacement Patients May Safely Drive as Early As Two Weeks Following Surgery
LAS VEGAS—Improved surgical, pain management, and rehabilitation procedures can allow patients who undergo a total hip replacement (THR) to safely drive as early as 2 weeks following surgery, according to new research presented at the 2015 Annual Meeting of the American Academy of Orthopaedic Surgeons (AAOS).
Each year, more than 322,000 patients undergo hip replacement surgery in the United States. Previous studies, conducted more than a decade ago, recommended between 6 and 8 weeks of recovery before driving; however, recent advances in surgical treatment and care may have shortened this time frame. A shorter driving ban would allow patients to more quickly resume daily activities and return to work.
In this study, which appeared online November 2014 in the Journal of Arthroplasty, researchers evaluated 38 patients who underwent right THR between 2013 and 2014. Driving performance was evaluated using the Brake Reaction Test (BRT), which measures brake time reaction after a stimulus. All patients underwent preoperative assessment to establish a baseline reaction time, and then agreed to be retested at 2, 4, and 6 weeks after surgery. Patients were allowed to drive when their postoperative reaction time was equal to or less than their preoperative baseline reaction time. At each testing session patients were asked if they felt ready to drive again.
Of the 38 patients, 33 (87%) reached their baseline time within 2 weeks. The remaining patients (13%) reached their baseline at 4 weeks. Among the other findings of the study:
• There were no differences with respect to age, gender, or the use of assistance devices in terms of driving readiness.
• Of the 33 patients who tested ready to drive at 2 weeks, 24 (73%) stated that they felt ready to drive while 5 (15%) were not sure. Four patients (12%) reported that they did not feel ready to drive.
• Of the 5 patients who returned to driving at 4 weeks, 3 agreed that they were not able to drive at the 2-week mark, and the other 2 thought they were able to drive by 2 weeks.
“We found that brake reaction time returned to baseline or better in the vast majority of patients undergoing contemporary THR by 2 weeks following surgery, and all patients achieved a safe brake reaction time according to nationally recognized guidelines,” said lead study author and orthopedic surgeon Victor Hugo Hernandez, MD.
Dr. Hernandez said the “findings have allowed us to encourage patients to re-evaluate their driving ability as soon as 2 weeks after THR,” but warned that the study results “are based on our particular population, and caution should be taken in translating these results to the regular population.” In addition, patients should never drive if they are still taking narcotic pain medication.
LAS VEGAS—Improved surgical, pain management, and rehabilitation procedures can allow patients who undergo a total hip replacement (THR) to safely drive as early as 2 weeks following surgery, according to new research presented at the 2015 Annual Meeting of the American Academy of Orthopaedic Surgeons (AAOS).
Each year, more than 322,000 patients undergo hip replacement surgery in the United States. Previous studies, conducted more than a decade ago, recommended between 6 and 8 weeks of recovery before driving; however, recent advances in surgical treatment and care may have shortened this time frame. A shorter driving ban would allow patients to more quickly resume daily activities and return to work.
In this study, which appeared online November 2014 in the Journal of Arthroplasty, researchers evaluated 38 patients who underwent right THR between 2013 and 2014. Driving performance was evaluated using the Brake Reaction Test (BRT), which measures brake time reaction after a stimulus. All patients underwent preoperative assessment to establish a baseline reaction time, and then agreed to be retested at 2, 4, and 6 weeks after surgery. Patients were allowed to drive when their postoperative reaction time was equal to or less than their preoperative baseline reaction time. At each testing session patients were asked if they felt ready to drive again.
Of the 38 patients, 33 (87%) reached their baseline time within 2 weeks. The remaining patients (13%) reached their baseline at 4 weeks. Among the other findings of the study:
• There were no differences with respect to age, gender, or the use of assistance devices in terms of driving readiness.
• Of the 33 patients who tested ready to drive at 2 weeks, 24 (73%) stated that they felt ready to drive while 5 (15%) were not sure. Four patients (12%) reported that they did not feel ready to drive.
• Of the 5 patients who returned to driving at 4 weeks, 3 agreed that they were not able to drive at the 2-week mark, and the other 2 thought they were able to drive by 2 weeks.
“We found that brake reaction time returned to baseline or better in the vast majority of patients undergoing contemporary THR by 2 weeks following surgery, and all patients achieved a safe brake reaction time according to nationally recognized guidelines,” said lead study author and orthopedic surgeon Victor Hugo Hernandez, MD.
Dr. Hernandez said the “findings have allowed us to encourage patients to re-evaluate their driving ability as soon as 2 weeks after THR,” but warned that the study results “are based on our particular population, and caution should be taken in translating these results to the regular population.” In addition, patients should never drive if they are still taking narcotic pain medication.
LAS VEGAS—Improved surgical, pain management, and rehabilitation procedures can allow patients who undergo a total hip replacement (THR) to safely drive as early as 2 weeks following surgery, according to new research presented at the 2015 Annual Meeting of the American Academy of Orthopaedic Surgeons (AAOS).
Each year, more than 322,000 patients undergo hip replacement surgery in the United States. Previous studies, conducted more than a decade ago, recommended between 6 and 8 weeks of recovery before driving; however, recent advances in surgical treatment and care may have shortened this time frame. A shorter driving ban would allow patients to more quickly resume daily activities and return to work.
In this study, which appeared online November 2014 in the Journal of Arthroplasty, researchers evaluated 38 patients who underwent right THR between 2013 and 2014. Driving performance was evaluated using the Brake Reaction Test (BRT), which measures brake time reaction after a stimulus. All patients underwent preoperative assessment to establish a baseline reaction time, and then agreed to be retested at 2, 4, and 6 weeks after surgery. Patients were allowed to drive when their postoperative reaction time was equal to or less than their preoperative baseline reaction time. At each testing session patients were asked if they felt ready to drive again.
Of the 38 patients, 33 (87%) reached their baseline time within 2 weeks. The remaining patients (13%) reached their baseline at 4 weeks. Among the other findings of the study:
• There were no differences with respect to age, gender, or the use of assistance devices in terms of driving readiness.
• Of the 33 patients who tested ready to drive at 2 weeks, 24 (73%) stated that they felt ready to drive while 5 (15%) were not sure. Four patients (12%) reported that they did not feel ready to drive.
• Of the 5 patients who returned to driving at 4 weeks, 3 agreed that they were not able to drive at the 2-week mark, and the other 2 thought they were able to drive by 2 weeks.
“We found that brake reaction time returned to baseline or better in the vast majority of patients undergoing contemporary THR by 2 weeks following surgery, and all patients achieved a safe brake reaction time according to nationally recognized guidelines,” said lead study author and orthopedic surgeon Victor Hugo Hernandez, MD.
Dr. Hernandez said the “findings have allowed us to encourage patients to re-evaluate their driving ability as soon as 2 weeks after THR,” but warned that the study results “are based on our particular population, and caution should be taken in translating these results to the regular population.” In addition, patients should never drive if they are still taking narcotic pain medication.
Harrington Rod Revision After Failed Total Hip Arthroplasty Due to Missed Acetabular Metastasis
We report the case of a patient who was treated with total hip arthroplasty (THA) for osteoarthritis but was found to have a large acetabular defect caused by pulmonary metastasis. She was promptly referred to our orthopedic oncology clinic for revision because she had experienced no improvement in her symptoms. The patient provided written informed consent for print and electronic publication of this case report.
Case Report
A 61-year-old woman was referred to us for evaluation of a large right supra-acetabular lesion after undergoing a right THA at another hospital 3 weeks earlier. Preoperative radiographs showed severe osteoarthritis of the right hip but there was no diagnosis of an acetabular lesion in her medical history. During the operation, the surgeon noted poor acetabulum bone quality and sent acetabular reamings for histopathologic analysis, which revealed adenocarcinoma. The arthroplasty was completed in a normal fashion, and the patient was discharged. Postoperatively, her pain did not resolve, and her functional status deteriorated from ambulating with a walker to very limited activity and weight-bearing.
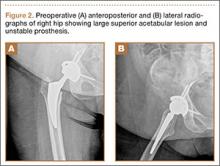
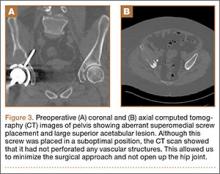
When the patient came to our clinic, we learned she underwent a lobectomy in 2011 for lung cancer resulting from her 40-pack-year history of smoking and had a strong family history of breast cancer. She also had a history of coronary artery disease, hypertension, hyperlipidemia, morbid obesity, and depression. We obtained plain films and a computed tomography (CT) scan that showed a 6.5×7.1×6.5-cm lytic lesion arising from the right acetabulum with cortical penetration and an extraosseous soft-tissue component. Two smaller 10-mm to 12-mm lesions were also found superior and medial to the large lesion. These radiographs and CT images are shown in Figures 1-3.
We discussed nonoperative and operative options for treatment with the patient and her family, and she elected to undergo palliative surgical curettage and fixation. Significant bone erosion of the acetabulum and a resultant lack of mechanical support for the acetabular cup were found intraoperatively. An unusual surgical approach was selected in order to minimize morbidity and avoid performing a revision acetabular component if the cup was found to be stable from the standpoint of osseointegration. We approached from the superior side of the ilium, removing the abductors in the superperiosteal fashion extending down from the supra-acetabular ilium, sparing the hip capsule. When the acetabular component was exposed and stressed under fluoroscopy, there was no evidence of loosening. We decided to reconstruct the mechanical defect without revision of the acetabular component and to leave the screw in place. After partial excision of the right supra-acetabular ilium, specimens were sent to pathology. We placed five 4.8-mm and four 4.0-mm threaded Steinmann pins intraosseously through the iliac wing to abut the acetabular cup. In this way, the Steinmann pins provided a stable roof to the cup for weight-bearing and scaffolding for methylmethacrylate cement impregnated with tobramycin. A postoperative radiograph of the patient’s pelvis is shown in Figure 4.
Immediately after her surgery, the patient was bearing weight as tolerated and participating in physical therapy 3 times a day. Two months postoperatively, she was able to walk 1 block with use of a walker, and her pain was controlled with oral pain medication. At her 1-year visit, she was walking without pain for prolonged distances. She had a mild limp but did not need ambulatory aids. She had full range of motion, was able to perform all of her desired activities, and was quite pleased with her result. One-year postoperative radiographs (Figure 5) show stable placement of her acetabular cup with her pins and cement in an unchanged position without recurrence of her destructive lesion. There was no evidence of progression of her cancer, although she had some heterotopic bone in her lateral soft tissues.
Discussion
Many cases have been reported in the literature of metastases to the pelvis and acetabulum; almost 10% of bone metastases are in the pelvis.1 Although many are seen on radiographs, pelvic metastases, especially if they involve the acetabulum, can present with hip pain, decreased joint range of motion, and reduced ambulatory function, all symptoms that are similar to osteoarthritis. While the presence of metastases indicates late-stage disease, many patients still live for years with hip symptoms before succumbing to cancer.1 Palliative treatment initially consists of protected weight-bearing, analgesics, antineoplastic medications ,and radiation. When these first-line therapies fail, palliative operative treatment can be considered, with goals to maintain stability and to preserve mobility, independence, and comfort.2 Patients should be offered this only if there is a reasonable chance that structural stability can be achieved via reconstruction and if the patient will live long enough to realize the functional improvement.3 Harrington4 described patterns of acetabular metastases and surgical treatments in his classic series of 58 patients. For class II and III lesions, he concluded it was necessary to provide additional structural support to the acetabular component of a THA, either in the form of a protrusion shell or with Steinmann pins and bone cement.4 Antiprotrusion cages combined with arthroplasty have been used with modest success for cases where implant bone integration is unlikely.5-6 Several studies since Harrington have shown that constructs with cement reinforced with Steinmann pins can provide reduced pain and improved mobility with a low failure rate for the remainder of the patient’s life.7-9
In addition, a few cases have been reported of metastases to endoprostheses, which were implanted long before the diagnosis of cancer.10 To an unsuspecting surgeon, the lytic periprosthetic metastases may look like osteolysis or pseudotumor. Fabbri and colleagues11 presented 4 cases showing how sarcoma around a joint endoprosthesis can easily be mistaken for pseudotumor. A patient considering primary or revision THA for bone loss caused by osteolysis would be given different options than if the bone loss were secondary to metastases. Revision techniques in the setting of acetabular osteolysis include acetabular liner exchanges, cementless hemispherical components and jumbo cups, structural allografts, metal augments, impaction grafting, and acetabular cages and cup-cage constructs. Rarely are “Harrington” reconstructions performed for this reason.12
This case is unusual because the diagnosis of metastatic disease was missed and THA was performed under the presumptive diagnosis of osteoarthritis. While a malignant process was recognized intraoperatively, the joint replacement was completed nonetheless, with revision surgery inevitably occurring within a few weeks. Our patient’s history of lung cancer reinforces the importance of preoperative history taking, and the missed diagnosis highlights the need for clinicians to maintain a broad differential, even in seemingly simple arthritis cases. Proper preoperative imaging, biopsies, and cultures are also paramount. Lesions that are painful, involve the whole cortex, appear soon after implementation, and are rapidly progressing should raise concern for malignancy.10 If there is concern for osteolysis, quantitative CT with 3-dimensional reconstructions can help visualize the lesions and help in planning surgery.13 Had a timely diagnosis been made, the proper reconstruction could have been planned before the index procedure, and our patient could have been spared the pain, risk, and morbidity of a second operation.
The second lesson of this case is that, as long as the cup was stable, the etiology of the hip pain was lack of mechanical support. Once corrected, the total hip functioned as planned. A minimally invasive approach that allowed for observation of the cup without exposing the entire hip saved a patient a significant amount of morbidity and led to an acceptable outcome.
1. Ho L, Ahlmann ER, Menendez LR. Modified Harrington reconstruction for advanced periacetabular metastatic disease. J Surg Oncol. 2010;101(2):170-174.
2. Papagelopoulos PJ, Mavrogenis AF, Soucacos PN. Evaluation and treatment of pelvic metastases. Injury. 2007;38(4):509-520.
3. Allan DG, Bell RS, Davis A, Langer F. Complex acetabular reconstruction for metastatic tumor. J Arthroplasty. 1995;10(3):301-306.
4. Harrington KD. The management of acetabular insufficiency secondary to metastatic malignant disease. J Bone Joint Surg Am. 1981;63(4):653-64.
5. Hoell S, Dedy N, Gosheger G, Dieckmann R, Daniilidis K, Hardes J. The Burch-Schneider cage for reconstruction after metastatic destruction of the acetabulum: outcome and complications. Arch Orthop Trauma Surg. 2012;132(3):405-410.
6. Clayer M. The survivorship of protrusio cages for metastatic disease involving the acetabulum. Clin Orthop. 2010;468(11):2980-2984.
7. Marco RA, Sheth DS, Boland PJ, Wunder JS, Siegel JA, Healey JH. Functional and oncological outcome of acetabular reconstruction for the treatment of metastatic disease. J Bone Joint Surg Am. 2000;82(5):642-651.
8. Tillman RM, Myers GJ, Abudu AT, Carter SR, Grimer RJ. The three-pin modified ‘Harrington’ procedure for advanced metastatic destruction of the acetabulum. J Bone Joint Surg Br. 2008;90(1):84-87.
9. Walker RH. Pelvic reconstruction/total hip arthroplasty for metastatic acetabular insufficiency. Clin Orthop. 1993;294:170-175.
10. Dramis A, Desai AS, Board TN, Hekal WE, Panezai JR. Periprosthetic osteolysis due to metastatic renal cell carcinoma: a case report. Cases J. 2008;1(1):297.
11. Fabbri N, Rustemi E, Masetti C, et al. Severe osteolysis and soft tissue mass around total hip arthroplasty: description of four cases and review of the literature with respect to clinico-radiographic and pathologic differential diagnosis. Eur J Radiol. 2011;77(1):43-50.
12. Deirmengian GK, Zmistowski B, O’Neil JT, Hozack WJ. Management of acetabular bone loss in revision total hip arthroplasty. J Bone Joint Surg Am. 2011;93(19):1842-1852.
13. Kitamura N, Leung SB, Engh CA Sr. Characteristics of pelvic osteolysis on computed tomography after total hip arthroplasty. Clin Orthop. 2005;441:291-297.
We report the case of a patient who was treated with total hip arthroplasty (THA) for osteoarthritis but was found to have a large acetabular defect caused by pulmonary metastasis. She was promptly referred to our orthopedic oncology clinic for revision because she had experienced no improvement in her symptoms. The patient provided written informed consent for print and electronic publication of this case report.
Case Report
A 61-year-old woman was referred to us for evaluation of a large right supra-acetabular lesion after undergoing a right THA at another hospital 3 weeks earlier. Preoperative radiographs showed severe osteoarthritis of the right hip but there was no diagnosis of an acetabular lesion in her medical history. During the operation, the surgeon noted poor acetabulum bone quality and sent acetabular reamings for histopathologic analysis, which revealed adenocarcinoma. The arthroplasty was completed in a normal fashion, and the patient was discharged. Postoperatively, her pain did not resolve, and her functional status deteriorated from ambulating with a walker to very limited activity and weight-bearing.
When the patient came to our clinic, we learned she underwent a lobectomy in 2011 for lung cancer resulting from her 40-pack-year history of smoking and had a strong family history of breast cancer. She also had a history of coronary artery disease, hypertension, hyperlipidemia, morbid obesity, and depression. We obtained plain films and a computed tomography (CT) scan that showed a 6.5×7.1×6.5-cm lytic lesion arising from the right acetabulum with cortical penetration and an extraosseous soft-tissue component. Two smaller 10-mm to 12-mm lesions were also found superior and medial to the large lesion. These radiographs and CT images are shown in Figures 1-3.
We discussed nonoperative and operative options for treatment with the patient and her family, and she elected to undergo palliative surgical curettage and fixation. Significant bone erosion of the acetabulum and a resultant lack of mechanical support for the acetabular cup were found intraoperatively. An unusual surgical approach was selected in order to minimize morbidity and avoid performing a revision acetabular component if the cup was found to be stable from the standpoint of osseointegration. We approached from the superior side of the ilium, removing the abductors in the superperiosteal fashion extending down from the supra-acetabular ilium, sparing the hip capsule. When the acetabular component was exposed and stressed under fluoroscopy, there was no evidence of loosening. We decided to reconstruct the mechanical defect without revision of the acetabular component and to leave the screw in place. After partial excision of the right supra-acetabular ilium, specimens were sent to pathology. We placed five 4.8-mm and four 4.0-mm threaded Steinmann pins intraosseously through the iliac wing to abut the acetabular cup. In this way, the Steinmann pins provided a stable roof to the cup for weight-bearing and scaffolding for methylmethacrylate cement impregnated with tobramycin. A postoperative radiograph of the patient’s pelvis is shown in Figure 4.
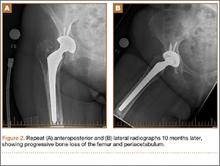
Immediately after her surgery, the patient was bearing weight as tolerated and participating in physical therapy 3 times a day. Two months postoperatively, she was able to walk 1 block with use of a walker, and her pain was controlled with oral pain medication. At her 1-year visit, she was walking without pain for prolonged distances. She had a mild limp but did not need ambulatory aids. She had full range of motion, was able to perform all of her desired activities, and was quite pleased with her result. One-year postoperative radiographs (Figure 5) show stable placement of her acetabular cup with her pins and cement in an unchanged position without recurrence of her destructive lesion. There was no evidence of progression of her cancer, although she had some heterotopic bone in her lateral soft tissues.
Discussion
Many cases have been reported in the literature of metastases to the pelvis and acetabulum; almost 10% of bone metastases are in the pelvis.1 Although many are seen on radiographs, pelvic metastases, especially if they involve the acetabulum, can present with hip pain, decreased joint range of motion, and reduced ambulatory function, all symptoms that are similar to osteoarthritis. While the presence of metastases indicates late-stage disease, many patients still live for years with hip symptoms before succumbing to cancer.1 Palliative treatment initially consists of protected weight-bearing, analgesics, antineoplastic medications ,and radiation. When these first-line therapies fail, palliative operative treatment can be considered, with goals to maintain stability and to preserve mobility, independence, and comfort.2 Patients should be offered this only if there is a reasonable chance that structural stability can be achieved via reconstruction and if the patient will live long enough to realize the functional improvement.3 Harrington4 described patterns of acetabular metastases and surgical treatments in his classic series of 58 patients. For class II and III lesions, he concluded it was necessary to provide additional structural support to the acetabular component of a THA, either in the form of a protrusion shell or with Steinmann pins and bone cement.4 Antiprotrusion cages combined with arthroplasty have been used with modest success for cases where implant bone integration is unlikely.5-6 Several studies since Harrington have shown that constructs with cement reinforced with Steinmann pins can provide reduced pain and improved mobility with a low failure rate for the remainder of the patient’s life.7-9
In addition, a few cases have been reported of metastases to endoprostheses, which were implanted long before the diagnosis of cancer.10 To an unsuspecting surgeon, the lytic periprosthetic metastases may look like osteolysis or pseudotumor. Fabbri and colleagues11 presented 4 cases showing how sarcoma around a joint endoprosthesis can easily be mistaken for pseudotumor. A patient considering primary or revision THA for bone loss caused by osteolysis would be given different options than if the bone loss were secondary to metastases. Revision techniques in the setting of acetabular osteolysis include acetabular liner exchanges, cementless hemispherical components and jumbo cups, structural allografts, metal augments, impaction grafting, and acetabular cages and cup-cage constructs. Rarely are “Harrington” reconstructions performed for this reason.12
This case is unusual because the diagnosis of metastatic disease was missed and THA was performed under the presumptive diagnosis of osteoarthritis. While a malignant process was recognized intraoperatively, the joint replacement was completed nonetheless, with revision surgery inevitably occurring within a few weeks. Our patient’s history of lung cancer reinforces the importance of preoperative history taking, and the missed diagnosis highlights the need for clinicians to maintain a broad differential, even in seemingly simple arthritis cases. Proper preoperative imaging, biopsies, and cultures are also paramount. Lesions that are painful, involve the whole cortex, appear soon after implementation, and are rapidly progressing should raise concern for malignancy.10 If there is concern for osteolysis, quantitative CT with 3-dimensional reconstructions can help visualize the lesions and help in planning surgery.13 Had a timely diagnosis been made, the proper reconstruction could have been planned before the index procedure, and our patient could have been spared the pain, risk, and morbidity of a second operation.
The second lesson of this case is that, as long as the cup was stable, the etiology of the hip pain was lack of mechanical support. Once corrected, the total hip functioned as planned. A minimally invasive approach that allowed for observation of the cup without exposing the entire hip saved a patient a significant amount of morbidity and led to an acceptable outcome.
We report the case of a patient who was treated with total hip arthroplasty (THA) for osteoarthritis but was found to have a large acetabular defect caused by pulmonary metastasis. She was promptly referred to our orthopedic oncology clinic for revision because she had experienced no improvement in her symptoms. The patient provided written informed consent for print and electronic publication of this case report.
Case Report
A 61-year-old woman was referred to us for evaluation of a large right supra-acetabular lesion after undergoing a right THA at another hospital 3 weeks earlier. Preoperative radiographs showed severe osteoarthritis of the right hip but there was no diagnosis of an acetabular lesion in her medical history. During the operation, the surgeon noted poor acetabulum bone quality and sent acetabular reamings for histopathologic analysis, which revealed adenocarcinoma. The arthroplasty was completed in a normal fashion, and the patient was discharged. Postoperatively, her pain did not resolve, and her functional status deteriorated from ambulating with a walker to very limited activity and weight-bearing.
When the patient came to our clinic, we learned she underwent a lobectomy in 2011 for lung cancer resulting from her 40-pack-year history of smoking and had a strong family history of breast cancer. She also had a history of coronary artery disease, hypertension, hyperlipidemia, morbid obesity, and depression. We obtained plain films and a computed tomography (CT) scan that showed a 6.5×7.1×6.5-cm lytic lesion arising from the right acetabulum with cortical penetration and an extraosseous soft-tissue component. Two smaller 10-mm to 12-mm lesions were also found superior and medial to the large lesion. These radiographs and CT images are shown in Figures 1-3.
We discussed nonoperative and operative options for treatment with the patient and her family, and she elected to undergo palliative surgical curettage and fixation. Significant bone erosion of the acetabulum and a resultant lack of mechanical support for the acetabular cup were found intraoperatively. An unusual surgical approach was selected in order to minimize morbidity and avoid performing a revision acetabular component if the cup was found to be stable from the standpoint of osseointegration. We approached from the superior side of the ilium, removing the abductors in the superperiosteal fashion extending down from the supra-acetabular ilium, sparing the hip capsule. When the acetabular component was exposed and stressed under fluoroscopy, there was no evidence of loosening. We decided to reconstruct the mechanical defect without revision of the acetabular component and to leave the screw in place. After partial excision of the right supra-acetabular ilium, specimens were sent to pathology. We placed five 4.8-mm and four 4.0-mm threaded Steinmann pins intraosseously through the iliac wing to abut the acetabular cup. In this way, the Steinmann pins provided a stable roof to the cup for weight-bearing and scaffolding for methylmethacrylate cement impregnated with tobramycin. A postoperative radiograph of the patient’s pelvis is shown in Figure 4.
Immediately after her surgery, the patient was bearing weight as tolerated and participating in physical therapy 3 times a day. Two months postoperatively, she was able to walk 1 block with use of a walker, and her pain was controlled with oral pain medication. At her 1-year visit, she was walking without pain for prolonged distances. She had a mild limp but did not need ambulatory aids. She had full range of motion, was able to perform all of her desired activities, and was quite pleased with her result. One-year postoperative radiographs (Figure 5) show stable placement of her acetabular cup with her pins and cement in an unchanged position without recurrence of her destructive lesion. There was no evidence of progression of her cancer, although she had some heterotopic bone in her lateral soft tissues.
Discussion
Many cases have been reported in the literature of metastases to the pelvis and acetabulum; almost 10% of bone metastases are in the pelvis.1 Although many are seen on radiographs, pelvic metastases, especially if they involve the acetabulum, can present with hip pain, decreased joint range of motion, and reduced ambulatory function, all symptoms that are similar to osteoarthritis. While the presence of metastases indicates late-stage disease, many patients still live for years with hip symptoms before succumbing to cancer.1 Palliative treatment initially consists of protected weight-bearing, analgesics, antineoplastic medications ,and radiation. When these first-line therapies fail, palliative operative treatment can be considered, with goals to maintain stability and to preserve mobility, independence, and comfort.2 Patients should be offered this only if there is a reasonable chance that structural stability can be achieved via reconstruction and if the patient will live long enough to realize the functional improvement.3 Harrington4 described patterns of acetabular metastases and surgical treatments in his classic series of 58 patients. For class II and III lesions, he concluded it was necessary to provide additional structural support to the acetabular component of a THA, either in the form of a protrusion shell or with Steinmann pins and bone cement.4 Antiprotrusion cages combined with arthroplasty have been used with modest success for cases where implant bone integration is unlikely.5-6 Several studies since Harrington have shown that constructs with cement reinforced with Steinmann pins can provide reduced pain and improved mobility with a low failure rate for the remainder of the patient’s life.7-9
In addition, a few cases have been reported of metastases to endoprostheses, which were implanted long before the diagnosis of cancer.10 To an unsuspecting surgeon, the lytic periprosthetic metastases may look like osteolysis or pseudotumor. Fabbri and colleagues11 presented 4 cases showing how sarcoma around a joint endoprosthesis can easily be mistaken for pseudotumor. A patient considering primary or revision THA for bone loss caused by osteolysis would be given different options than if the bone loss were secondary to metastases. Revision techniques in the setting of acetabular osteolysis include acetabular liner exchanges, cementless hemispherical components and jumbo cups, structural allografts, metal augments, impaction grafting, and acetabular cages and cup-cage constructs. Rarely are “Harrington” reconstructions performed for this reason.12
This case is unusual because the diagnosis of metastatic disease was missed and THA was performed under the presumptive diagnosis of osteoarthritis. While a malignant process was recognized intraoperatively, the joint replacement was completed nonetheless, with revision surgery inevitably occurring within a few weeks. Our patient’s history of lung cancer reinforces the importance of preoperative history taking, and the missed diagnosis highlights the need for clinicians to maintain a broad differential, even in seemingly simple arthritis cases. Proper preoperative imaging, biopsies, and cultures are also paramount. Lesions that are painful, involve the whole cortex, appear soon after implementation, and are rapidly progressing should raise concern for malignancy.10 If there is concern for osteolysis, quantitative CT with 3-dimensional reconstructions can help visualize the lesions and help in planning surgery.13 Had a timely diagnosis been made, the proper reconstruction could have been planned before the index procedure, and our patient could have been spared the pain, risk, and morbidity of a second operation.
The second lesson of this case is that, as long as the cup was stable, the etiology of the hip pain was lack of mechanical support. Once corrected, the total hip functioned as planned. A minimally invasive approach that allowed for observation of the cup without exposing the entire hip saved a patient a significant amount of morbidity and led to an acceptable outcome.
1. Ho L, Ahlmann ER, Menendez LR. Modified Harrington reconstruction for advanced periacetabular metastatic disease. J Surg Oncol. 2010;101(2):170-174.
2. Papagelopoulos PJ, Mavrogenis AF, Soucacos PN. Evaluation and treatment of pelvic metastases. Injury. 2007;38(4):509-520.
3. Allan DG, Bell RS, Davis A, Langer F. Complex acetabular reconstruction for metastatic tumor. J Arthroplasty. 1995;10(3):301-306.
4. Harrington KD. The management of acetabular insufficiency secondary to metastatic malignant disease. J Bone Joint Surg Am. 1981;63(4):653-64.
5. Hoell S, Dedy N, Gosheger G, Dieckmann R, Daniilidis K, Hardes J. The Burch-Schneider cage for reconstruction after metastatic destruction of the acetabulum: outcome and complications. Arch Orthop Trauma Surg. 2012;132(3):405-410.
6. Clayer M. The survivorship of protrusio cages for metastatic disease involving the acetabulum. Clin Orthop. 2010;468(11):2980-2984.
7. Marco RA, Sheth DS, Boland PJ, Wunder JS, Siegel JA, Healey JH. Functional and oncological outcome of acetabular reconstruction for the treatment of metastatic disease. J Bone Joint Surg Am. 2000;82(5):642-651.
8. Tillman RM, Myers GJ, Abudu AT, Carter SR, Grimer RJ. The three-pin modified ‘Harrington’ procedure for advanced metastatic destruction of the acetabulum. J Bone Joint Surg Br. 2008;90(1):84-87.
9. Walker RH. Pelvic reconstruction/total hip arthroplasty for metastatic acetabular insufficiency. Clin Orthop. 1993;294:170-175.
10. Dramis A, Desai AS, Board TN, Hekal WE, Panezai JR. Periprosthetic osteolysis due to metastatic renal cell carcinoma: a case report. Cases J. 2008;1(1):297.
11. Fabbri N, Rustemi E, Masetti C, et al. Severe osteolysis and soft tissue mass around total hip arthroplasty: description of four cases and review of the literature with respect to clinico-radiographic and pathologic differential diagnosis. Eur J Radiol. 2011;77(1):43-50.
12. Deirmengian GK, Zmistowski B, O’Neil JT, Hozack WJ. Management of acetabular bone loss in revision total hip arthroplasty. J Bone Joint Surg Am. 2011;93(19):1842-1852.
13. Kitamura N, Leung SB, Engh CA Sr. Characteristics of pelvic osteolysis on computed tomography after total hip arthroplasty. Clin Orthop. 2005;441:291-297.
1. Ho L, Ahlmann ER, Menendez LR. Modified Harrington reconstruction for advanced periacetabular metastatic disease. J Surg Oncol. 2010;101(2):170-174.
2. Papagelopoulos PJ, Mavrogenis AF, Soucacos PN. Evaluation and treatment of pelvic metastases. Injury. 2007;38(4):509-520.
3. Allan DG, Bell RS, Davis A, Langer F. Complex acetabular reconstruction for metastatic tumor. J Arthroplasty. 1995;10(3):301-306.
4. Harrington KD. The management of acetabular insufficiency secondary to metastatic malignant disease. J Bone Joint Surg Am. 1981;63(4):653-64.
5. Hoell S, Dedy N, Gosheger G, Dieckmann R, Daniilidis K, Hardes J. The Burch-Schneider cage for reconstruction after metastatic destruction of the acetabulum: outcome and complications. Arch Orthop Trauma Surg. 2012;132(3):405-410.
6. Clayer M. The survivorship of protrusio cages for metastatic disease involving the acetabulum. Clin Orthop. 2010;468(11):2980-2984.
7. Marco RA, Sheth DS, Boland PJ, Wunder JS, Siegel JA, Healey JH. Functional and oncological outcome of acetabular reconstruction for the treatment of metastatic disease. J Bone Joint Surg Am. 2000;82(5):642-651.
8. Tillman RM, Myers GJ, Abudu AT, Carter SR, Grimer RJ. The three-pin modified ‘Harrington’ procedure for advanced metastatic destruction of the acetabulum. J Bone Joint Surg Br. 2008;90(1):84-87.
9. Walker RH. Pelvic reconstruction/total hip arthroplasty for metastatic acetabular insufficiency. Clin Orthop. 1993;294:170-175.
10. Dramis A, Desai AS, Board TN, Hekal WE, Panezai JR. Periprosthetic osteolysis due to metastatic renal cell carcinoma: a case report. Cases J. 2008;1(1):297.
11. Fabbri N, Rustemi E, Masetti C, et al. Severe osteolysis and soft tissue mass around total hip arthroplasty: description of four cases and review of the literature with respect to clinico-radiographic and pathologic differential diagnosis. Eur J Radiol. 2011;77(1):43-50.
12. Deirmengian GK, Zmistowski B, O’Neil JT, Hozack WJ. Management of acetabular bone loss in revision total hip arthroplasty. J Bone Joint Surg Am. 2011;93(19):1842-1852.
13. Kitamura N, Leung SB, Engh CA Sr. Characteristics of pelvic osteolysis on computed tomography after total hip arthroplasty. Clin Orthop. 2005;441:291-297.
Failure of Total Hip Arthroplasty Secondary to Infection Caused by Brucella abortus and the Risk of Transmission to Operative Staff
Brucellosis is a zoonotic disease transmitted to humans through contact with animal hosts or animal products. Infection of total knee or hip arthroplasty by Brucella species is a rare complication with only 18 cases reported in the English literature.1-12 We describe a case of an infected total hip replacement, its treatment, and 2-year follow-up and review the available literature. The patient provided written informed consent for print and electronic publication of this case report.
Case Report
A 67-year-old Spanish-speaking woman, a native of Mexico, presented with a painful right total hip arthroplasty (THA) 2 years after implantation in Chihuahua, Mexico. The patient reported 1 year of increasing thigh pain with recent onset of start-up pain, and also mild groin pain. The patient reported an uneventful postoperative course without wound drainage and denied any history of fevers, chills, or night sweats after the procedure. Preoperative notes and radiographs were unavailable for review. Radiographic evaluation showed a hybrid construct with a well-fixed–appearing, uncemented acetabular component but a failed cemented femoral stem (Figures 1A, 1B). Although we discussed revision surgery, the patient elected not to proceed with surgery or to undergo evaluation to rule out infection. Nine months later, she returned with worsening pain and requested revision surgery; radiographs showed progressive bone loss around the cement mantle (Figures 2A, 2B).
Hematologic evaluation showed an erythrocyte sedimentation rate (ESR) of 54 mm/h (normal, 0-27 mm/h) and C-reactive protein (CRP) level of 0.24 mg/L (normal, <0.8). An aspiration of the hip with fluoroscopic guidance produced a small sample (0.2 mL) of yellow synovial fluid. There was not enough fluid for cell count, but fluid culture was negative.
The patient was taken to the operating room for revision THA. Because of concern about progressive bone loss and elevated infectious indices, the administration of antibiotics was delayed until we obtained sufficient deep-tissue specimens. Before opening the capsule, we introduced a syringe into the joint and aspirated 10 mL of cloudy yellow synovial fluid that was sent for cell count. Additional findings at surgery included a grossly loose stem with a fragmented cement mantle surrounded by poor bone stock with anterior cortical bone loss and a loose acetabular component with pockets of cavitary bone loss. Frozen section showed up to 5 nucleated cells per high power field, and the cell count showed 1480 nucleated cells/µL (50% polymorphonuclear cells). The equivocal intraoperative findings (cell count and frozen section) and the loose femoral and acetabular components with significant bone loss were sufficiently concerning that we removed the components and placed a cement spacer rather than proceed with revision arthroplasty (Figures 3A, 3B). The surgeon, first assistant, and scrub technician wore body exhaust suits. We performed irrigation of the wound bed with pulse lavage.
Intraoperative cultures (synovial fluid, joint capsule synovium, and femur pseudocapsule) were positive after 8 days and growing B abortus. Infectious disease consultants prescribed rifampin 300 mg twice daily and doxycycline 100 mg twice daily for 5 months. Follow-up ESR and CRP returned to normal range. A preoperative aspiration of the hip was negative as well. The patient returned to the operating room at 6 months for re-implantation using uncemented components; synovial fluid and tissue cultures taken at this time were negative. Two years after re-implantation, the patient is doing well without evidence of infection (Figures 4A, 4B). Additional follow-up will be required to monitor for infection and implant survival. Additional history taken from the patient after the culture results revealed that her development of hip pain was preceded by a febrile illness consistent with brucellosis.
Because of the nature of the procedure (irrigation and débridement using pulse lavage), we were concerned about aerosolization of Brucella bacteria and possible transmission to all staff present during the procedure. After consulting with the New Mexico Department of Health (NMDOH) and the Centers for Disease Control and Prevention (CDC), all surgical, anesthesia, and support personnel present in the operative suite and staff who cleaned the room after the procedure were treated prophylactically (rifampin 600 mg daily, doxycycline 100 mg twice daily for 3 weeks) to prevent development of brucellosis.13 All 15 operating room personnel who were exposed elected to proceed with antibiotic prophylaxis. In addition to prophylactic antibiotics, serial serologic testing for anti-Brucella antibodies was conducted at baseline and 2, 4, 6, and 24 weeks postexposure to monitor for the development of Brucella infection. There were no conversions to positive antibody status. No personnel complained of symptoms that would indicate development of brucellosis. At the recommendation of NMDOH and CDC, all staff in the operating room during and immediately after the re-implantation procedure wore properly fitting N-95 disposable respiratory masks (3M, St. Paul, Minnesota) to guard against the potential risk of further exposure.
Discussion
Brucellosis is a zoonotic disease transmitted to humans through contact with animal hosts. Transmission can occur via breaks in the skin in direct contact, through the ingestion of unpasteurized dairy products or raw meat, or through ingestion of aerosolized bacteria. Transmission via aerosolization has been described during medical procedures.
Brucella is endemic in India, Middle Eastern and Mediterranean countries, Central Asia, and South America. Brucella species are gram-negative coccobacilli that are capable of surviving within phagocytic cells, making antibiotic treatment difficult. Brucellosis is a febrile illness that occurs after a 1- to 3-week incubation period and is often accompanied by headache, arthralgias, and hepatosplenomegaly. Osteoarticular infection is the most common complication, occurring in 10% to 85% of cases and usually involves the sacroiliac joint and the large joints of the lower extremity. Spondylitis, bursitis, tenosynovitis, endocarditis, colitis, meningitis, and osteomyelitis have also been described.7,14-17
As mentioned previously, 18 cases of infected THAs and total knee arthroplasties (TKAs) in 16 patients were identified in the English literature: 9 THAs and 9 TKAs.1-12 With the exception of 1 case reported in Texas, all others were from the Middle East or the Mediterranean region. In these patients, symptom onset occurred from 2 months to 14 years from the time of the index surgery, and symptom duration ranged from 1 month to 2 years prior to presentation. The exposure was not reported in 2 cases, but the remaining patients either ingested unpasteurized dairy products or worked closely with livestock. Laboratory evaluation revealed elevated ESR or CRP in 8 cases. In 7 cases, no laboratory results were reported, although 1 had a draining sinus. In 1 case, the ESR was normal, but a bone scan was positive. Joint aspiration yielded Brucella species in 8 cases, was negative in 3, and not reported in 5 cases (one aspirate yielded Acinetobacter baumanii). Only 3 cases reported a time-to-culture positivity (1 “prolonged” and 2 took 7 days).
Eight cases presented with loose components, while 1 case was not reported, and the remaining were presumed to be well-fixed. In cases that were identified as loose, 5 underwent a 2-stage revision and 2 underwent a 1-stage revision (in one of the 1-stage revisions, the infection was identified only after the revision from intra-operative cultures). Of those with well-fixed components, 7 patients with 9 infected joints (including the case where no preoperative description of the components was reported) were treated with oral antibiotics only (range, 6 weeks to 26 months) and 1 with irrigation and débridement and oral antibiotics. Among those treated only with antibiotics, there were 2 failures (2 joints) leading to revision surgery. The other 5 cases were reportedly doing well between 8 months and 5 years after treatment. There were no reports of transmission to hospital or laboratory personnel in any of these cases nor were there reports of precautions to limit exposure for operating room staff or hospital personnel.
Failure of TKA or THA secondary to periprosthetic infection by Brucella species is rare, and this represents only the second reported case in the United States.4 This case highlights several important principles. Maintaining a high level of suspicion for infection in cases of failed joint arthroplasty is important. In addition, as more international travel occurs and patients are seen from areas where Brucella is endemic, the possibility of this infectious etiology should be considered. Based on reported cases, patients will usually have elevated ESR or CRP; all (except 2 cases in which no exposure was reported) had known exposure to unpasteurized dairy products or livestock. Joint aspiration yielded Brucella species in 8 cases, was negative in 3, and not reported in 5 cases (1 aspirate yielded Acinetobacter baumanii). In this case, ESR and CRP were elevated, and infection was suspected but joint aspiration was negative. The initial aspiration was cultured for 5 days and previous data, as well as that presented here, suggest that prolonged culture may provide diagnostic value.18 The patient had resided in an endemic area and had exposure to unpasteurized dairy products, but Brucella infection was not considered and, therefore, no precautions were taken.
Of the reported cases, only 1 met major criteria for periprosthetic joint infection (draining sinus) while 10 of the remaining 15 cases were positive for minor criteria of periprosthetic joint infection (elevated ESR or CRP, or positive culture from joint aspiration).19 Unfortunately, the available case reports did not detail the extent to which preoperative periprosthetic joint infection could be established based on minor criteria for periprosthetic joint infection (elevated joint synovial white blood cell count or neutrophil percentage, intra-articular purulence, or elevated neutrophil count on periprosthetic tissue histologic analysis).19
Periprosthetic joint infection by Brucella species is so rare that specific recommendations for this infectious etiology based on 18 reported cases would be overreaching. However, Brucella should be considered when evaluating a potentially infected joint replacement where the possibility of exposure exists (eg, travel to or previous residence in endemic areas, close contact with livestock, or ingestion of unpasteurized dairy products in endemic regions), with the potential for transmission to operating room and hospital personnel also considered. If there is concern about Brucella involvement, tissue and fluid specimens should be labeled so that laboratory personnel can take appropriate precautions. Brucella can be cultured using routine techniques on standard, nonselective media, but the culture time-to-growth may be prolonged. Culture plates should be held for 14 days before reporting no growth of Brucella if it is suspected; the New Mexico Department of Health Microbiology Laboratory holds routine cultures for 1 week after a report of no growth. Thus, a suspicion of Brucella should be communicated in order for culture time to be adjusted if the holding of culture plates after an initial report of no growth is not standard practice. If operative intervention is planned and brucellosis is known, personnel should be notified of the possibility of exposure and appropriate measures taken (ie, wearing N-95 respiratory masks during the procedure and considering other methods of irrigation less likely to aerosolize particulates). It is not known if preoperative antibiotic therapy can sufficiently lower the bacterial load to make aerosolization less likely. If brucellosis is suspected but not identified preoperatively, wearing N-95 respiratory masks should be considered during any open procedures.
Conclusion
In cases of Brucella infection and loose components, 1- or 2-stage revision with appropriate antibiotic therapy is indicated. (There is not enough data to recommend either 1- or 2-stage revision.) Several reports comment on the ability to treat periprosthetic joint infection in the setting of well-fixed components with antibiotic therapy alone. While this appears to have been successful in 7 of 9 infected joints reported in the literature, length of follow-up ranged from 8 months to 5 years, with no report of length of follow-up in some cases. Antibiotic therapy duration ranged from 6 weeks to 26 months, and the antibiotic treatment involved combination therapy with multiple agents reported but, most commonly, doxycycline, rifampin, and streptomycin. With 2 of 9 (22%) joints failing antibiotic therapy alone and those reported to be successful having relatively short-term follow-up, this treatment strategy should be approached with caution.
1. Agarwal S, Kadhi SK, Rooney RJ. Brucellosis complicating bilateral total knee arthroplasty. Clin Orthop. 1991;267:179-181.
2. Cairó M, Calbo E, Gomez L, et al. Foreign-body osteoarticular infection by Brucella melitensis: A report of three cases. J Bone Joint Surg Am. 2006; 88(1):202-204.
3. Erdogan H, Cakmak G, Erdogan A, Arslan H. Brucella melitensis infection in total knee arthroplasty: a case report. Knee Surg Sports Traumatol Arthrosc. 2010;18(7):908-910.
4. Jones RE, Berryhill WH, Smith J, Hofman A, Rogers D. Secondary infection of a total hip replacement with Brucella abortus. Orthopedics. 1983; 6(2):184-186.
5. Kasim RA, Araj GF, Afeiche NE, Tabbarah ZA. Brucella infection in total hip replacement: case report and review of the literature. Scand J Infect Dis. 2004;36(1):65-67.
6. Malizos KN, Makris CA, Soucacos PN. Total knee arthroplasties infected by Brucella melitensis: a case report. Am J Orthop. 1997;26(4):283-285.
7. Ortega-Andreu M, Rodriguez-Merchan EC, Aguera-Gavalda M. Brucellosis as a cause of septic loosening of total hip arthroplasty. J Arthroplasty. 2002;17(3):384-387.
8. Orti A, Alcala R, Navarro V, et al. Brucellar arthritis in a total knee replacement. Eur J Clin Microbiol Infect Dis. 1997;16(11):843-845.
9. Ruiz-Iban MA, Crespo P, Diaz-Peletier R, Rozado AM, Lopez-Pardo A. Total hip arthroplasty infected by Brucella: a report of two cases. J Orthop Surg (Hong Kong). 2006;14(1):99-103.
10. Tassinari E, Di Motta D, Giardina F, Traina F, Fine MD, Toni A. Brucella infection in total knee arthroplasty. Case report and revision of the literature. Chir Organi Mov. 2008;92(1):55-59.
11. Tena D, Romanillos O, Rodriguez-Zapata M, et al. Prosthetic hip infection due to Brucella melitensis: case report and literature review. Diagn Microbiol Infect Dis. 2007;58(4):481-485.
12. Weil Y, Mattan Y, Liebergall M, Rahav G. Brucella prosthetic joint infection: a report of 3 cases and a review of the literature. Clin Infect Dis. 2003;36(7):e81-e86.
13. Brucellosis. Centers for Disease Control and Prevention website. http://www.cdc.gov/nczved/divisions/dfbmd/diseases/brucellosis/recommendations.html. Updated November 12, 2012. Accessed December 22, 2014.
14. Franco MP, Mulder M, Gilman RH, Smits HL. Human brucellosis. Lancet Infect Dis. 2007;7(12):775-786.
15. Khateeb MI, Araj GF, Majeed SA, Lulu AR. Brucella arthritis: a study of 96 cases in Kuwait. Ann Rheum Dis. 1990;49(12):994-998.
16. Luna-Martinez JE, Mejía-Terán C. Brucellosis in Mexico: current status and trends. Vet Microbiol. 2002;90(1-4):19-30.
17. Pappas G, Papadimitriou P, Akritidis N, Christou L, Tsianos EV. The new global map of human brucellosis. Lancet Infect Dis. 2006;6(2):91-99.
18. Schafer P, Fink B, Margull A, Berger I, Frommelt L. Prolonged bacterial culture to identify late periprosthetic joint infection: a promising strategy. Clin Infect Disease. 2008;47(11):1403-1409.
19. Parvizi J, Zmistowski B, Berbari EF, et al. New definition for periprosthetic joint infection: from the Workgroup of the Musculoskeletal Infection Society. Clin Orthop. 2011;469(11):2992-2994.
Brucellosis is a zoonotic disease transmitted to humans through contact with animal hosts or animal products. Infection of total knee or hip arthroplasty by Brucella species is a rare complication with only 18 cases reported in the English literature.1-12 We describe a case of an infected total hip replacement, its treatment, and 2-year follow-up and review the available literature. The patient provided written informed consent for print and electronic publication of this case report.
Case Report
A 67-year-old Spanish-speaking woman, a native of Mexico, presented with a painful right total hip arthroplasty (THA) 2 years after implantation in Chihuahua, Mexico. The patient reported 1 year of increasing thigh pain with recent onset of start-up pain, and also mild groin pain. The patient reported an uneventful postoperative course without wound drainage and denied any history of fevers, chills, or night sweats after the procedure. Preoperative notes and radiographs were unavailable for review. Radiographic evaluation showed a hybrid construct with a well-fixed–appearing, uncemented acetabular component but a failed cemented femoral stem (Figures 1A, 1B). Although we discussed revision surgery, the patient elected not to proceed with surgery or to undergo evaluation to rule out infection. Nine months later, she returned with worsening pain and requested revision surgery; radiographs showed progressive bone loss around the cement mantle (Figures 2A, 2B).
Hematologic evaluation showed an erythrocyte sedimentation rate (ESR) of 54 mm/h (normal, 0-27 mm/h) and C-reactive protein (CRP) level of 0.24 mg/L (normal, <0.8). An aspiration of the hip with fluoroscopic guidance produced a small sample (0.2 mL) of yellow synovial fluid. There was not enough fluid for cell count, but fluid culture was negative.
The patient was taken to the operating room for revision THA. Because of concern about progressive bone loss and elevated infectious indices, the administration of antibiotics was delayed until we obtained sufficient deep-tissue specimens. Before opening the capsule, we introduced a syringe into the joint and aspirated 10 mL of cloudy yellow synovial fluid that was sent for cell count. Additional findings at surgery included a grossly loose stem with a fragmented cement mantle surrounded by poor bone stock with anterior cortical bone loss and a loose acetabular component with pockets of cavitary bone loss. Frozen section showed up to 5 nucleated cells per high power field, and the cell count showed 1480 nucleated cells/µL (50% polymorphonuclear cells). The equivocal intraoperative findings (cell count and frozen section) and the loose femoral and acetabular components with significant bone loss were sufficiently concerning that we removed the components and placed a cement spacer rather than proceed with revision arthroplasty (Figures 3A, 3B). The surgeon, first assistant, and scrub technician wore body exhaust suits. We performed irrigation of the wound bed with pulse lavage.
Intraoperative cultures (synovial fluid, joint capsule synovium, and femur pseudocapsule) were positive after 8 days and growing B abortus. Infectious disease consultants prescribed rifampin 300 mg twice daily and doxycycline 100 mg twice daily for 5 months. Follow-up ESR and CRP returned to normal range. A preoperative aspiration of the hip was negative as well. The patient returned to the operating room at 6 months for re-implantation using uncemented components; synovial fluid and tissue cultures taken at this time were negative. Two years after re-implantation, the patient is doing well without evidence of infection (Figures 4A, 4B). Additional follow-up will be required to monitor for infection and implant survival. Additional history taken from the patient after the culture results revealed that her development of hip pain was preceded by a febrile illness consistent with brucellosis.
Because of the nature of the procedure (irrigation and débridement using pulse lavage), we were concerned about aerosolization of Brucella bacteria and possible transmission to all staff present during the procedure. After consulting with the New Mexico Department of Health (NMDOH) and the Centers for Disease Control and Prevention (CDC), all surgical, anesthesia, and support personnel present in the operative suite and staff who cleaned the room after the procedure were treated prophylactically (rifampin 600 mg daily, doxycycline 100 mg twice daily for 3 weeks) to prevent development of brucellosis.13 All 15 operating room personnel who were exposed elected to proceed with antibiotic prophylaxis. In addition to prophylactic antibiotics, serial serologic testing for anti-Brucella antibodies was conducted at baseline and 2, 4, 6, and 24 weeks postexposure to monitor for the development of Brucella infection. There were no conversions to positive antibody status. No personnel complained of symptoms that would indicate development of brucellosis. At the recommendation of NMDOH and CDC, all staff in the operating room during and immediately after the re-implantation procedure wore properly fitting N-95 disposable respiratory masks (3M, St. Paul, Minnesota) to guard against the potential risk of further exposure.
Discussion
Brucellosis is a zoonotic disease transmitted to humans through contact with animal hosts. Transmission can occur via breaks in the skin in direct contact, through the ingestion of unpasteurized dairy products or raw meat, or through ingestion of aerosolized bacteria. Transmission via aerosolization has been described during medical procedures.
Brucella is endemic in India, Middle Eastern and Mediterranean countries, Central Asia, and South America. Brucella species are gram-negative coccobacilli that are capable of surviving within phagocytic cells, making antibiotic treatment difficult. Brucellosis is a febrile illness that occurs after a 1- to 3-week incubation period and is often accompanied by headache, arthralgias, and hepatosplenomegaly. Osteoarticular infection is the most common complication, occurring in 10% to 85% of cases and usually involves the sacroiliac joint and the large joints of the lower extremity. Spondylitis, bursitis, tenosynovitis, endocarditis, colitis, meningitis, and osteomyelitis have also been described.7,14-17
As mentioned previously, 18 cases of infected THAs and total knee arthroplasties (TKAs) in 16 patients were identified in the English literature: 9 THAs and 9 TKAs.1-12 With the exception of 1 case reported in Texas, all others were from the Middle East or the Mediterranean region. In these patients, symptom onset occurred from 2 months to 14 years from the time of the index surgery, and symptom duration ranged from 1 month to 2 years prior to presentation. The exposure was not reported in 2 cases, but the remaining patients either ingested unpasteurized dairy products or worked closely with livestock. Laboratory evaluation revealed elevated ESR or CRP in 8 cases. In 7 cases, no laboratory results were reported, although 1 had a draining sinus. In 1 case, the ESR was normal, but a bone scan was positive. Joint aspiration yielded Brucella species in 8 cases, was negative in 3, and not reported in 5 cases (one aspirate yielded Acinetobacter baumanii). Only 3 cases reported a time-to-culture positivity (1 “prolonged” and 2 took 7 days).
Eight cases presented with loose components, while 1 case was not reported, and the remaining were presumed to be well-fixed. In cases that were identified as loose, 5 underwent a 2-stage revision and 2 underwent a 1-stage revision (in one of the 1-stage revisions, the infection was identified only after the revision from intra-operative cultures). Of those with well-fixed components, 7 patients with 9 infected joints (including the case where no preoperative description of the components was reported) were treated with oral antibiotics only (range, 6 weeks to 26 months) and 1 with irrigation and débridement and oral antibiotics. Among those treated only with antibiotics, there were 2 failures (2 joints) leading to revision surgery. The other 5 cases were reportedly doing well between 8 months and 5 years after treatment. There were no reports of transmission to hospital or laboratory personnel in any of these cases nor were there reports of precautions to limit exposure for operating room staff or hospital personnel.
Failure of TKA or THA secondary to periprosthetic infection by Brucella species is rare, and this represents only the second reported case in the United States.4 This case highlights several important principles. Maintaining a high level of suspicion for infection in cases of failed joint arthroplasty is important. In addition, as more international travel occurs and patients are seen from areas where Brucella is endemic, the possibility of this infectious etiology should be considered. Based on reported cases, patients will usually have elevated ESR or CRP; all (except 2 cases in which no exposure was reported) had known exposure to unpasteurized dairy products or livestock. Joint aspiration yielded Brucella species in 8 cases, was negative in 3, and not reported in 5 cases (1 aspirate yielded Acinetobacter baumanii). In this case, ESR and CRP were elevated, and infection was suspected but joint aspiration was negative. The initial aspiration was cultured for 5 days and previous data, as well as that presented here, suggest that prolonged culture may provide diagnostic value.18 The patient had resided in an endemic area and had exposure to unpasteurized dairy products, but Brucella infection was not considered and, therefore, no precautions were taken.
Of the reported cases, only 1 met major criteria for periprosthetic joint infection (draining sinus) while 10 of the remaining 15 cases were positive for minor criteria of periprosthetic joint infection (elevated ESR or CRP, or positive culture from joint aspiration).19 Unfortunately, the available case reports did not detail the extent to which preoperative periprosthetic joint infection could be established based on minor criteria for periprosthetic joint infection (elevated joint synovial white blood cell count or neutrophil percentage, intra-articular purulence, or elevated neutrophil count on periprosthetic tissue histologic analysis).19
Periprosthetic joint infection by Brucella species is so rare that specific recommendations for this infectious etiology based on 18 reported cases would be overreaching. However, Brucella should be considered when evaluating a potentially infected joint replacement where the possibility of exposure exists (eg, travel to or previous residence in endemic areas, close contact with livestock, or ingestion of unpasteurized dairy products in endemic regions), with the potential for transmission to operating room and hospital personnel also considered. If there is concern about Brucella involvement, tissue and fluid specimens should be labeled so that laboratory personnel can take appropriate precautions. Brucella can be cultured using routine techniques on standard, nonselective media, but the culture time-to-growth may be prolonged. Culture plates should be held for 14 days before reporting no growth of Brucella if it is suspected; the New Mexico Department of Health Microbiology Laboratory holds routine cultures for 1 week after a report of no growth. Thus, a suspicion of Brucella should be communicated in order for culture time to be adjusted if the holding of culture plates after an initial report of no growth is not standard practice. If operative intervention is planned and brucellosis is known, personnel should be notified of the possibility of exposure and appropriate measures taken (ie, wearing N-95 respiratory masks during the procedure and considering other methods of irrigation less likely to aerosolize particulates). It is not known if preoperative antibiotic therapy can sufficiently lower the bacterial load to make aerosolization less likely. If brucellosis is suspected but not identified preoperatively, wearing N-95 respiratory masks should be considered during any open procedures.
Conclusion
In cases of Brucella infection and loose components, 1- or 2-stage revision with appropriate antibiotic therapy is indicated. (There is not enough data to recommend either 1- or 2-stage revision.) Several reports comment on the ability to treat periprosthetic joint infection in the setting of well-fixed components with antibiotic therapy alone. While this appears to have been successful in 7 of 9 infected joints reported in the literature, length of follow-up ranged from 8 months to 5 years, with no report of length of follow-up in some cases. Antibiotic therapy duration ranged from 6 weeks to 26 months, and the antibiotic treatment involved combination therapy with multiple agents reported but, most commonly, doxycycline, rifampin, and streptomycin. With 2 of 9 (22%) joints failing antibiotic therapy alone and those reported to be successful having relatively short-term follow-up, this treatment strategy should be approached with caution.
Brucellosis is a zoonotic disease transmitted to humans through contact with animal hosts or animal products. Infection of total knee or hip arthroplasty by Brucella species is a rare complication with only 18 cases reported in the English literature.1-12 We describe a case of an infected total hip replacement, its treatment, and 2-year follow-up and review the available literature. The patient provided written informed consent for print and electronic publication of this case report.
Case Report
A 67-year-old Spanish-speaking woman, a native of Mexico, presented with a painful right total hip arthroplasty (THA) 2 years after implantation in Chihuahua, Mexico. The patient reported 1 year of increasing thigh pain with recent onset of start-up pain, and also mild groin pain. The patient reported an uneventful postoperative course without wound drainage and denied any history of fevers, chills, or night sweats after the procedure. Preoperative notes and radiographs were unavailable for review. Radiographic evaluation showed a hybrid construct with a well-fixed–appearing, uncemented acetabular component but a failed cemented femoral stem (Figures 1A, 1B). Although we discussed revision surgery, the patient elected not to proceed with surgery or to undergo evaluation to rule out infection. Nine months later, she returned with worsening pain and requested revision surgery; radiographs showed progressive bone loss around the cement mantle (Figures 2A, 2B).
Hematologic evaluation showed an erythrocyte sedimentation rate (ESR) of 54 mm/h (normal, 0-27 mm/h) and C-reactive protein (CRP) level of 0.24 mg/L (normal, <0.8). An aspiration of the hip with fluoroscopic guidance produced a small sample (0.2 mL) of yellow synovial fluid. There was not enough fluid for cell count, but fluid culture was negative.
The patient was taken to the operating room for revision THA. Because of concern about progressive bone loss and elevated infectious indices, the administration of antibiotics was delayed until we obtained sufficient deep-tissue specimens. Before opening the capsule, we introduced a syringe into the joint and aspirated 10 mL of cloudy yellow synovial fluid that was sent for cell count. Additional findings at surgery included a grossly loose stem with a fragmented cement mantle surrounded by poor bone stock with anterior cortical bone loss and a loose acetabular component with pockets of cavitary bone loss. Frozen section showed up to 5 nucleated cells per high power field, and the cell count showed 1480 nucleated cells/µL (50% polymorphonuclear cells). The equivocal intraoperative findings (cell count and frozen section) and the loose femoral and acetabular components with significant bone loss were sufficiently concerning that we removed the components and placed a cement spacer rather than proceed with revision arthroplasty (Figures 3A, 3B). The surgeon, first assistant, and scrub technician wore body exhaust suits. We performed irrigation of the wound bed with pulse lavage.
Intraoperative cultures (synovial fluid, joint capsule synovium, and femur pseudocapsule) were positive after 8 days and growing B abortus. Infectious disease consultants prescribed rifampin 300 mg twice daily and doxycycline 100 mg twice daily for 5 months. Follow-up ESR and CRP returned to normal range. A preoperative aspiration of the hip was negative as well. The patient returned to the operating room at 6 months for re-implantation using uncemented components; synovial fluid and tissue cultures taken at this time were negative. Two years after re-implantation, the patient is doing well without evidence of infection (Figures 4A, 4B). Additional follow-up will be required to monitor for infection and implant survival. Additional history taken from the patient after the culture results revealed that her development of hip pain was preceded by a febrile illness consistent with brucellosis.
Because of the nature of the procedure (irrigation and débridement using pulse lavage), we were concerned about aerosolization of Brucella bacteria and possible transmission to all staff present during the procedure. After consulting with the New Mexico Department of Health (NMDOH) and the Centers for Disease Control and Prevention (CDC), all surgical, anesthesia, and support personnel present in the operative suite and staff who cleaned the room after the procedure were treated prophylactically (rifampin 600 mg daily, doxycycline 100 mg twice daily for 3 weeks) to prevent development of brucellosis.13 All 15 operating room personnel who were exposed elected to proceed with antibiotic prophylaxis. In addition to prophylactic antibiotics, serial serologic testing for anti-Brucella antibodies was conducted at baseline and 2, 4, 6, and 24 weeks postexposure to monitor for the development of Brucella infection. There were no conversions to positive antibody status. No personnel complained of symptoms that would indicate development of brucellosis. At the recommendation of NMDOH and CDC, all staff in the operating room during and immediately after the re-implantation procedure wore properly fitting N-95 disposable respiratory masks (3M, St. Paul, Minnesota) to guard against the potential risk of further exposure.
Discussion
Brucellosis is a zoonotic disease transmitted to humans through contact with animal hosts. Transmission can occur via breaks in the skin in direct contact, through the ingestion of unpasteurized dairy products or raw meat, or through ingestion of aerosolized bacteria. Transmission via aerosolization has been described during medical procedures.
Brucella is endemic in India, Middle Eastern and Mediterranean countries, Central Asia, and South America. Brucella species are gram-negative coccobacilli that are capable of surviving within phagocytic cells, making antibiotic treatment difficult. Brucellosis is a febrile illness that occurs after a 1- to 3-week incubation period and is often accompanied by headache, arthralgias, and hepatosplenomegaly. Osteoarticular infection is the most common complication, occurring in 10% to 85% of cases and usually involves the sacroiliac joint and the large joints of the lower extremity. Spondylitis, bursitis, tenosynovitis, endocarditis, colitis, meningitis, and osteomyelitis have also been described.7,14-17
As mentioned previously, 18 cases of infected THAs and total knee arthroplasties (TKAs) in 16 patients were identified in the English literature: 9 THAs and 9 TKAs.1-12 With the exception of 1 case reported in Texas, all others were from the Middle East or the Mediterranean region. In these patients, symptom onset occurred from 2 months to 14 years from the time of the index surgery, and symptom duration ranged from 1 month to 2 years prior to presentation. The exposure was not reported in 2 cases, but the remaining patients either ingested unpasteurized dairy products or worked closely with livestock. Laboratory evaluation revealed elevated ESR or CRP in 8 cases. In 7 cases, no laboratory results were reported, although 1 had a draining sinus. In 1 case, the ESR was normal, but a bone scan was positive. Joint aspiration yielded Brucella species in 8 cases, was negative in 3, and not reported in 5 cases (one aspirate yielded Acinetobacter baumanii). Only 3 cases reported a time-to-culture positivity (1 “prolonged” and 2 took 7 days).
Eight cases presented with loose components, while 1 case was not reported, and the remaining were presumed to be well-fixed. In cases that were identified as loose, 5 underwent a 2-stage revision and 2 underwent a 1-stage revision (in one of the 1-stage revisions, the infection was identified only after the revision from intra-operative cultures). Of those with well-fixed components, 7 patients with 9 infected joints (including the case where no preoperative description of the components was reported) were treated with oral antibiotics only (range, 6 weeks to 26 months) and 1 with irrigation and débridement and oral antibiotics. Among those treated only with antibiotics, there were 2 failures (2 joints) leading to revision surgery. The other 5 cases were reportedly doing well between 8 months and 5 years after treatment. There were no reports of transmission to hospital or laboratory personnel in any of these cases nor were there reports of precautions to limit exposure for operating room staff or hospital personnel.
Failure of TKA or THA secondary to periprosthetic infection by Brucella species is rare, and this represents only the second reported case in the United States.4 This case highlights several important principles. Maintaining a high level of suspicion for infection in cases of failed joint arthroplasty is important. In addition, as more international travel occurs and patients are seen from areas where Brucella is endemic, the possibility of this infectious etiology should be considered. Based on reported cases, patients will usually have elevated ESR or CRP; all (except 2 cases in which no exposure was reported) had known exposure to unpasteurized dairy products or livestock. Joint aspiration yielded Brucella species in 8 cases, was negative in 3, and not reported in 5 cases (1 aspirate yielded Acinetobacter baumanii). In this case, ESR and CRP were elevated, and infection was suspected but joint aspiration was negative. The initial aspiration was cultured for 5 days and previous data, as well as that presented here, suggest that prolonged culture may provide diagnostic value.18 The patient had resided in an endemic area and had exposure to unpasteurized dairy products, but Brucella infection was not considered and, therefore, no precautions were taken.
Of the reported cases, only 1 met major criteria for periprosthetic joint infection (draining sinus) while 10 of the remaining 15 cases were positive for minor criteria of periprosthetic joint infection (elevated ESR or CRP, or positive culture from joint aspiration).19 Unfortunately, the available case reports did not detail the extent to which preoperative periprosthetic joint infection could be established based on minor criteria for periprosthetic joint infection (elevated joint synovial white blood cell count or neutrophil percentage, intra-articular purulence, or elevated neutrophil count on periprosthetic tissue histologic analysis).19
Periprosthetic joint infection by Brucella species is so rare that specific recommendations for this infectious etiology based on 18 reported cases would be overreaching. However, Brucella should be considered when evaluating a potentially infected joint replacement where the possibility of exposure exists (eg, travel to or previous residence in endemic areas, close contact with livestock, or ingestion of unpasteurized dairy products in endemic regions), with the potential for transmission to operating room and hospital personnel also considered. If there is concern about Brucella involvement, tissue and fluid specimens should be labeled so that laboratory personnel can take appropriate precautions. Brucella can be cultured using routine techniques on standard, nonselective media, but the culture time-to-growth may be prolonged. Culture plates should be held for 14 days before reporting no growth of Brucella if it is suspected; the New Mexico Department of Health Microbiology Laboratory holds routine cultures for 1 week after a report of no growth. Thus, a suspicion of Brucella should be communicated in order for culture time to be adjusted if the holding of culture plates after an initial report of no growth is not standard practice. If operative intervention is planned and brucellosis is known, personnel should be notified of the possibility of exposure and appropriate measures taken (ie, wearing N-95 respiratory masks during the procedure and considering other methods of irrigation less likely to aerosolize particulates). It is not known if preoperative antibiotic therapy can sufficiently lower the bacterial load to make aerosolization less likely. If brucellosis is suspected but not identified preoperatively, wearing N-95 respiratory masks should be considered during any open procedures.
Conclusion
In cases of Brucella infection and loose components, 1- or 2-stage revision with appropriate antibiotic therapy is indicated. (There is not enough data to recommend either 1- or 2-stage revision.) Several reports comment on the ability to treat periprosthetic joint infection in the setting of well-fixed components with antibiotic therapy alone. While this appears to have been successful in 7 of 9 infected joints reported in the literature, length of follow-up ranged from 8 months to 5 years, with no report of length of follow-up in some cases. Antibiotic therapy duration ranged from 6 weeks to 26 months, and the antibiotic treatment involved combination therapy with multiple agents reported but, most commonly, doxycycline, rifampin, and streptomycin. With 2 of 9 (22%) joints failing antibiotic therapy alone and those reported to be successful having relatively short-term follow-up, this treatment strategy should be approached with caution.
1. Agarwal S, Kadhi SK, Rooney RJ. Brucellosis complicating bilateral total knee arthroplasty. Clin Orthop. 1991;267:179-181.
2. Cairó M, Calbo E, Gomez L, et al. Foreign-body osteoarticular infection by Brucella melitensis: A report of three cases. J Bone Joint Surg Am. 2006; 88(1):202-204.
3. Erdogan H, Cakmak G, Erdogan A, Arslan H. Brucella melitensis infection in total knee arthroplasty: a case report. Knee Surg Sports Traumatol Arthrosc. 2010;18(7):908-910.
4. Jones RE, Berryhill WH, Smith J, Hofman A, Rogers D. Secondary infection of a total hip replacement with Brucella abortus. Orthopedics. 1983; 6(2):184-186.
5. Kasim RA, Araj GF, Afeiche NE, Tabbarah ZA. Brucella infection in total hip replacement: case report and review of the literature. Scand J Infect Dis. 2004;36(1):65-67.
6. Malizos KN, Makris CA, Soucacos PN. Total knee arthroplasties infected by Brucella melitensis: a case report. Am J Orthop. 1997;26(4):283-285.
7. Ortega-Andreu M, Rodriguez-Merchan EC, Aguera-Gavalda M. Brucellosis as a cause of septic loosening of total hip arthroplasty. J Arthroplasty. 2002;17(3):384-387.
8. Orti A, Alcala R, Navarro V, et al. Brucellar arthritis in a total knee replacement. Eur J Clin Microbiol Infect Dis. 1997;16(11):843-845.
9. Ruiz-Iban MA, Crespo P, Diaz-Peletier R, Rozado AM, Lopez-Pardo A. Total hip arthroplasty infected by Brucella: a report of two cases. J Orthop Surg (Hong Kong). 2006;14(1):99-103.
10. Tassinari E, Di Motta D, Giardina F, Traina F, Fine MD, Toni A. Brucella infection in total knee arthroplasty. Case report and revision of the literature. Chir Organi Mov. 2008;92(1):55-59.
11. Tena D, Romanillos O, Rodriguez-Zapata M, et al. Prosthetic hip infection due to Brucella melitensis: case report and literature review. Diagn Microbiol Infect Dis. 2007;58(4):481-485.
12. Weil Y, Mattan Y, Liebergall M, Rahav G. Brucella prosthetic joint infection: a report of 3 cases and a review of the literature. Clin Infect Dis. 2003;36(7):e81-e86.
13. Brucellosis. Centers for Disease Control and Prevention website. http://www.cdc.gov/nczved/divisions/dfbmd/diseases/brucellosis/recommendations.html. Updated November 12, 2012. Accessed December 22, 2014.
14. Franco MP, Mulder M, Gilman RH, Smits HL. Human brucellosis. Lancet Infect Dis. 2007;7(12):775-786.
15. Khateeb MI, Araj GF, Majeed SA, Lulu AR. Brucella arthritis: a study of 96 cases in Kuwait. Ann Rheum Dis. 1990;49(12):994-998.
16. Luna-Martinez JE, Mejía-Terán C. Brucellosis in Mexico: current status and trends. Vet Microbiol. 2002;90(1-4):19-30.
17. Pappas G, Papadimitriou P, Akritidis N, Christou L, Tsianos EV. The new global map of human brucellosis. Lancet Infect Dis. 2006;6(2):91-99.
18. Schafer P, Fink B, Margull A, Berger I, Frommelt L. Prolonged bacterial culture to identify late periprosthetic joint infection: a promising strategy. Clin Infect Disease. 2008;47(11):1403-1409.
19. Parvizi J, Zmistowski B, Berbari EF, et al. New definition for periprosthetic joint infection: from the Workgroup of the Musculoskeletal Infection Society. Clin Orthop. 2011;469(11):2992-2994.
1. Agarwal S, Kadhi SK, Rooney RJ. Brucellosis complicating bilateral total knee arthroplasty. Clin Orthop. 1991;267:179-181.
2. Cairó M, Calbo E, Gomez L, et al. Foreign-body osteoarticular infection by Brucella melitensis: A report of three cases. J Bone Joint Surg Am. 2006; 88(1):202-204.
3. Erdogan H, Cakmak G, Erdogan A, Arslan H. Brucella melitensis infection in total knee arthroplasty: a case report. Knee Surg Sports Traumatol Arthrosc. 2010;18(7):908-910.
4. Jones RE, Berryhill WH, Smith J, Hofman A, Rogers D. Secondary infection of a total hip replacement with Brucella abortus. Orthopedics. 1983; 6(2):184-186.
5. Kasim RA, Araj GF, Afeiche NE, Tabbarah ZA. Brucella infection in total hip replacement: case report and review of the literature. Scand J Infect Dis. 2004;36(1):65-67.
6. Malizos KN, Makris CA, Soucacos PN. Total knee arthroplasties infected by Brucella melitensis: a case report. Am J Orthop. 1997;26(4):283-285.
7. Ortega-Andreu M, Rodriguez-Merchan EC, Aguera-Gavalda M. Brucellosis as a cause of septic loosening of total hip arthroplasty. J Arthroplasty. 2002;17(3):384-387.
8. Orti A, Alcala R, Navarro V, et al. Brucellar arthritis in a total knee replacement. Eur J Clin Microbiol Infect Dis. 1997;16(11):843-845.
9. Ruiz-Iban MA, Crespo P, Diaz-Peletier R, Rozado AM, Lopez-Pardo A. Total hip arthroplasty infected by Brucella: a report of two cases. J Orthop Surg (Hong Kong). 2006;14(1):99-103.
10. Tassinari E, Di Motta D, Giardina F, Traina F, Fine MD, Toni A. Brucella infection in total knee arthroplasty. Case report and revision of the literature. Chir Organi Mov. 2008;92(1):55-59.
11. Tena D, Romanillos O, Rodriguez-Zapata M, et al. Prosthetic hip infection due to Brucella melitensis: case report and literature review. Diagn Microbiol Infect Dis. 2007;58(4):481-485.
12. Weil Y, Mattan Y, Liebergall M, Rahav G. Brucella prosthetic joint infection: a report of 3 cases and a review of the literature. Clin Infect Dis. 2003;36(7):e81-e86.
13. Brucellosis. Centers for Disease Control and Prevention website. http://www.cdc.gov/nczved/divisions/dfbmd/diseases/brucellosis/recommendations.html. Updated November 12, 2012. Accessed December 22, 2014.
14. Franco MP, Mulder M, Gilman RH, Smits HL. Human brucellosis. Lancet Infect Dis. 2007;7(12):775-786.
15. Khateeb MI, Araj GF, Majeed SA, Lulu AR. Brucella arthritis: a study of 96 cases in Kuwait. Ann Rheum Dis. 1990;49(12):994-998.
16. Luna-Martinez JE, Mejía-Terán C. Brucellosis in Mexico: current status and trends. Vet Microbiol. 2002;90(1-4):19-30.
17. Pappas G, Papadimitriou P, Akritidis N, Christou L, Tsianos EV. The new global map of human brucellosis. Lancet Infect Dis. 2006;6(2):91-99.
18. Schafer P, Fink B, Margull A, Berger I, Frommelt L. Prolonged bacterial culture to identify late periprosthetic joint infection: a promising strategy. Clin Infect Disease. 2008;47(11):1403-1409.
19. Parvizi J, Zmistowski B, Berbari EF, et al. New definition for periprosthetic joint infection: from the Workgroup of the Musculoskeletal Infection Society. Clin Orthop. 2011;469(11):2992-2994.
Orthopaedic surgeons’ ‘Choosing Wisely’ list centers on osteoarthritis treatments
Three of the five recommendations in the first-ever list developed by the American Academy of Orthopaedic Surgeons for the American Board of Internal Medicine Foundation’s "Choosing Wisely" campaign focus primarily on treatments for symptomatic osteoarthritis.
The campaign is meant to educate patients and physicians about unnecessary and potentially harmful testing and treatment.
According to the Choosing Wisely website, the AAOS’s list was formed based on a review of the most recent approved clinical practice guidelines previously developed by AAOS physician volunteer work groups and a selection of a variety of topics frequently used in orthopaedic surgical practice with input from specialty society leaders and the Academy’s presidential leadership and board of directors. The list was created with the intent to "serve as an educational tool based on an assessment of the current scientific and clinical information and accepted approaches to treatment."
However, some specialists find fault with the recommendations. For example, Dr. Roy Altman, a professor of medicine in the division of rheumatology and immunology at the University of California, Los Angeles, said the methodology used to create the guidelines overlooks a number of treatments, including multimodal therapy, and could have the unintended consequence of allowing specialists to deny effective care to patients.
"These guidelines are not consistent with my clinical experience," Dr. Altman said. In particular, he noted that many of his patients react positively to injection treatments for osteoarthritis (OA), which the Choosing Wisely recommendations specifically discourage.
AAOS’s recommendations are as follows:
• Avoid using postoperative ultrasonography screening for deep vein thrombosis on patients receiving hip or knee arthroplasty because it is not effective at diagnosing unsuspected cases.
• Don’t use needle lavage for long-term relief in symptomatic OA treatment, as the procedure "does not lead to measurable improvements in pain, function, 50-foot walking time, stiffness, tenderness, or swelling."
• Do not use glucosamine and chondroitin sulfate to treat patients with symptomatic knee OA.
• Lateral wedge or neutral insoles do not improve pain or functional outcomes in patients; on the contrary, patients with OA of the knee may experience fewer symptoms without insoles.
• Routine postoperative splinting of the wrist after the carpal tunnel release procedure does not improve subjective outcomes, and may lead to detrimental effects, including adhesion formation, stiffness, and prevention of nerve and tendon movement.
Three of the five recommendations in the first-ever list developed by the American Academy of Orthopaedic Surgeons for the American Board of Internal Medicine Foundation’s "Choosing Wisely" campaign focus primarily on treatments for symptomatic osteoarthritis.
The campaign is meant to educate patients and physicians about unnecessary and potentially harmful testing and treatment.
According to the Choosing Wisely website, the AAOS’s list was formed based on a review of the most recent approved clinical practice guidelines previously developed by AAOS physician volunteer work groups and a selection of a variety of topics frequently used in orthopaedic surgical practice with input from specialty society leaders and the Academy’s presidential leadership and board of directors. The list was created with the intent to "serve as an educational tool based on an assessment of the current scientific and clinical information and accepted approaches to treatment."
However, some specialists find fault with the recommendations. For example, Dr. Roy Altman, a professor of medicine in the division of rheumatology and immunology at the University of California, Los Angeles, said the methodology used to create the guidelines overlooks a number of treatments, including multimodal therapy, and could have the unintended consequence of allowing specialists to deny effective care to patients.
"These guidelines are not consistent with my clinical experience," Dr. Altman said. In particular, he noted that many of his patients react positively to injection treatments for osteoarthritis (OA), which the Choosing Wisely recommendations specifically discourage.
AAOS’s recommendations are as follows:
• Avoid using postoperative ultrasonography screening for deep vein thrombosis on patients receiving hip or knee arthroplasty because it is not effective at diagnosing unsuspected cases.
• Don’t use needle lavage for long-term relief in symptomatic OA treatment, as the procedure "does not lead to measurable improvements in pain, function, 50-foot walking time, stiffness, tenderness, or swelling."
• Do not use glucosamine and chondroitin sulfate to treat patients with symptomatic knee OA.
• Lateral wedge or neutral insoles do not improve pain or functional outcomes in patients; on the contrary, patients with OA of the knee may experience fewer symptoms without insoles.
• Routine postoperative splinting of the wrist after the carpal tunnel release procedure does not improve subjective outcomes, and may lead to detrimental effects, including adhesion formation, stiffness, and prevention of nerve and tendon movement.
Three of the five recommendations in the first-ever list developed by the American Academy of Orthopaedic Surgeons for the American Board of Internal Medicine Foundation’s "Choosing Wisely" campaign focus primarily on treatments for symptomatic osteoarthritis.
The campaign is meant to educate patients and physicians about unnecessary and potentially harmful testing and treatment.
According to the Choosing Wisely website, the AAOS’s list was formed based on a review of the most recent approved clinical practice guidelines previously developed by AAOS physician volunteer work groups and a selection of a variety of topics frequently used in orthopaedic surgical practice with input from specialty society leaders and the Academy’s presidential leadership and board of directors. The list was created with the intent to "serve as an educational tool based on an assessment of the current scientific and clinical information and accepted approaches to treatment."
However, some specialists find fault with the recommendations. For example, Dr. Roy Altman, a professor of medicine in the division of rheumatology and immunology at the University of California, Los Angeles, said the methodology used to create the guidelines overlooks a number of treatments, including multimodal therapy, and could have the unintended consequence of allowing specialists to deny effective care to patients.
"These guidelines are not consistent with my clinical experience," Dr. Altman said. In particular, he noted that many of his patients react positively to injection treatments for osteoarthritis (OA), which the Choosing Wisely recommendations specifically discourage.
AAOS’s recommendations are as follows:
• Avoid using postoperative ultrasonography screening for deep vein thrombosis on patients receiving hip or knee arthroplasty because it is not effective at diagnosing unsuspected cases.
• Don’t use needle lavage for long-term relief in symptomatic OA treatment, as the procedure "does not lead to measurable improvements in pain, function, 50-foot walking time, stiffness, tenderness, or swelling."
• Do not use glucosamine and chondroitin sulfate to treat patients with symptomatic knee OA.
• Lateral wedge or neutral insoles do not improve pain or functional outcomes in patients; on the contrary, patients with OA of the knee may experience fewer symptoms without insoles.
• Routine postoperative splinting of the wrist after the carpal tunnel release procedure does not improve subjective outcomes, and may lead to detrimental effects, including adhesion formation, stiffness, and prevention of nerve and tendon movement.
Aspirin better than heparin at VTE prevention after total hip arthroplasty
Aspirin is an effective, safe, convenient, and inexpensive alternative to low-molecular-weight heparin for extended thromboprophylaxis after total hip arthroplasty, according to a report published online June 3 in Annals of Internal Medicine.
In a multicenter randomized trial involving 786 patients undergoing elective total hip replacement in Canada during a 3-year period, 28 days of oral aspirin prophylaxis was noninferior to and as safe as 28 days of subcutaneous dalteparin injections for preventing venous thromboembolism (VTE), according to Dr. David R. Anderson, who is professor of medicine, pathology, and community health and epidemiology of Dalhousie University, Halifax, N.S., and his associates in the EPCAT (Extended Prophylaxis Comparing Low-Molecular-Weight Heparin to Aspirin in Total Hip Arthroplasty) study.
During this trial, the novel oral anticoagulant rivaroxaban was approved for this indication in Canada, which prompted "a major shift" away from using dalteparin and toward using the new drug in clinical practice. In light of this development, it will be important to "evaluate the benefits and risks of aspirin as extended prophylaxis after [total hip replacement], compared with the new oral anticoagulant agents," noted the EPCAT investigators.
Their findings on the benefits of aspirin also indicate that its role for venous thromboprophylaxis in other settings should now be reconsidered as well, Dr. Anderson and his colleagues added.
In the EPCAT study, patients underwent elective unilateral total hip replacement at 12 university-affiliated tertiary medical centers and received thromboprophylaxis in the form of subcutaneous injections of dalteparin for 10 days. They were randomly assigned to continue receiving dalteparin injections and take placebo oral aspirin tablets (400 patients) or to receive placebo injections and begin taking oral aspirin (81 mg) every day for 28 days (386 patients).
The demographic, medical, and surgical characteristics of the two study groups were comparable. Patients, physicians, study coordinators, and members of the health care teams all were blinded to study assignment.
The introduction of rivaroxaban during the course of the study severely affected ongoing recruitment of subjects, because both patients and orthopedic surgeons became increasingly reluctant to participate in a study requiring daily injections for 38 days when a new oral agent was available. The EPCAT study was terminated early when completion of the intended enrollment appeared "unfeasible" and an interim analysis showed that the primary objective – establishing the noninferiority of aspirin – had been reached.
The primary efficacy outcome was the development of symptomatic proximal deep vein thrombosis (DVT) or pulmonary embolism (PE), confirmed by objective testing, during the 90 days after randomization. This outcome occurred in only 0.3% of the aspirin group, compared with 1.3% of the dalteparin group, establishing the noninferiority of aspirin therapy.
There was a single case of proximal DVT in the aspirin group, compared with two cases of proximal DVT and three of PE in the dalteparin group. Another patient in the dalteparin group developed a symptomatic distal DVT in her calf, "but this was not considered an outcome event," the investigators said.
No major bleeding events developed in the aspirin group, but there was one such event in the dalteparin group for an overall rate of 0.3%. Similarly, there were two clinically significant nonmajor bleeding events for aspirin (0.5% rate), compared with four for dalteparin (1.0% rate). And there were eight minor bleeding events for aspirin (2.1% rate), compared with 18 for dalteparin (4.5% rate).
"In a composite analysis of net clinical benefit that combined VTE and clinically relevant major and nonmajor bleeding complications as outcomes," 0.8% of patients receiving aspirin had complications, compared with 2.5% of patients receiving dalteparin.
There were no differences between the two study groups in secondary outcomes such as wound infections, arterial vascular events, MI, stroke, or deaths.
The EPCAT trial was supported by the Canadian Institutes for Health Research. Aspirin was provided by Bayer HealthCare and dalteparin by Pfizer Pharmaceuticals, but neither Bayer nor Pfizer was involved in the design, conduct, or analysis of the study.
Aspirin is an effective, safe, convenient, and inexpensive alternative to low-molecular-weight heparin for extended thromboprophylaxis after total hip arthroplasty, according to a report published online June 3 in Annals of Internal Medicine.
In a multicenter randomized trial involving 786 patients undergoing elective total hip replacement in Canada during a 3-year period, 28 days of oral aspirin prophylaxis was noninferior to and as safe as 28 days of subcutaneous dalteparin injections for preventing venous thromboembolism (VTE), according to Dr. David R. Anderson, who is professor of medicine, pathology, and community health and epidemiology of Dalhousie University, Halifax, N.S., and his associates in the EPCAT (Extended Prophylaxis Comparing Low-Molecular-Weight Heparin to Aspirin in Total Hip Arthroplasty) study.
During this trial, the novel oral anticoagulant rivaroxaban was approved for this indication in Canada, which prompted "a major shift" away from using dalteparin and toward using the new drug in clinical practice. In light of this development, it will be important to "evaluate the benefits and risks of aspirin as extended prophylaxis after [total hip replacement], compared with the new oral anticoagulant agents," noted the EPCAT investigators.
Their findings on the benefits of aspirin also indicate that its role for venous thromboprophylaxis in other settings should now be reconsidered as well, Dr. Anderson and his colleagues added.
In the EPCAT study, patients underwent elective unilateral total hip replacement at 12 university-affiliated tertiary medical centers and received thromboprophylaxis in the form of subcutaneous injections of dalteparin for 10 days. They were randomly assigned to continue receiving dalteparin injections and take placebo oral aspirin tablets (400 patients) or to receive placebo injections and begin taking oral aspirin (81 mg) every day for 28 days (386 patients).
The demographic, medical, and surgical characteristics of the two study groups were comparable. Patients, physicians, study coordinators, and members of the health care teams all were blinded to study assignment.
The introduction of rivaroxaban during the course of the study severely affected ongoing recruitment of subjects, because both patients and orthopedic surgeons became increasingly reluctant to participate in a study requiring daily injections for 38 days when a new oral agent was available. The EPCAT study was terminated early when completion of the intended enrollment appeared "unfeasible" and an interim analysis showed that the primary objective – establishing the noninferiority of aspirin – had been reached.
The primary efficacy outcome was the development of symptomatic proximal deep vein thrombosis (DVT) or pulmonary embolism (PE), confirmed by objective testing, during the 90 days after randomization. This outcome occurred in only 0.3% of the aspirin group, compared with 1.3% of the dalteparin group, establishing the noninferiority of aspirin therapy.
There was a single case of proximal DVT in the aspirin group, compared with two cases of proximal DVT and three of PE in the dalteparin group. Another patient in the dalteparin group developed a symptomatic distal DVT in her calf, "but this was not considered an outcome event," the investigators said.
No major bleeding events developed in the aspirin group, but there was one such event in the dalteparin group for an overall rate of 0.3%. Similarly, there were two clinically significant nonmajor bleeding events for aspirin (0.5% rate), compared with four for dalteparin (1.0% rate). And there were eight minor bleeding events for aspirin (2.1% rate), compared with 18 for dalteparin (4.5% rate).
"In a composite analysis of net clinical benefit that combined VTE and clinically relevant major and nonmajor bleeding complications as outcomes," 0.8% of patients receiving aspirin had complications, compared with 2.5% of patients receiving dalteparin.
There were no differences between the two study groups in secondary outcomes such as wound infections, arterial vascular events, MI, stroke, or deaths.
The EPCAT trial was supported by the Canadian Institutes for Health Research. Aspirin was provided by Bayer HealthCare and dalteparin by Pfizer Pharmaceuticals, but neither Bayer nor Pfizer was involved in the design, conduct, or analysis of the study.
Aspirin is an effective, safe, convenient, and inexpensive alternative to low-molecular-weight heparin for extended thromboprophylaxis after total hip arthroplasty, according to a report published online June 3 in Annals of Internal Medicine.
In a multicenter randomized trial involving 786 patients undergoing elective total hip replacement in Canada during a 3-year period, 28 days of oral aspirin prophylaxis was noninferior to and as safe as 28 days of subcutaneous dalteparin injections for preventing venous thromboembolism (VTE), according to Dr. David R. Anderson, who is professor of medicine, pathology, and community health and epidemiology of Dalhousie University, Halifax, N.S., and his associates in the EPCAT (Extended Prophylaxis Comparing Low-Molecular-Weight Heparin to Aspirin in Total Hip Arthroplasty) study.
During this trial, the novel oral anticoagulant rivaroxaban was approved for this indication in Canada, which prompted "a major shift" away from using dalteparin and toward using the new drug in clinical practice. In light of this development, it will be important to "evaluate the benefits and risks of aspirin as extended prophylaxis after [total hip replacement], compared with the new oral anticoagulant agents," noted the EPCAT investigators.
Their findings on the benefits of aspirin also indicate that its role for venous thromboprophylaxis in other settings should now be reconsidered as well, Dr. Anderson and his colleagues added.
In the EPCAT study, patients underwent elective unilateral total hip replacement at 12 university-affiliated tertiary medical centers and received thromboprophylaxis in the form of subcutaneous injections of dalteparin for 10 days. They were randomly assigned to continue receiving dalteparin injections and take placebo oral aspirin tablets (400 patients) or to receive placebo injections and begin taking oral aspirin (81 mg) every day for 28 days (386 patients).
The demographic, medical, and surgical characteristics of the two study groups were comparable. Patients, physicians, study coordinators, and members of the health care teams all were blinded to study assignment.
The introduction of rivaroxaban during the course of the study severely affected ongoing recruitment of subjects, because both patients and orthopedic surgeons became increasingly reluctant to participate in a study requiring daily injections for 38 days when a new oral agent was available. The EPCAT study was terminated early when completion of the intended enrollment appeared "unfeasible" and an interim analysis showed that the primary objective – establishing the noninferiority of aspirin – had been reached.
The primary efficacy outcome was the development of symptomatic proximal deep vein thrombosis (DVT) or pulmonary embolism (PE), confirmed by objective testing, during the 90 days after randomization. This outcome occurred in only 0.3% of the aspirin group, compared with 1.3% of the dalteparin group, establishing the noninferiority of aspirin therapy.
There was a single case of proximal DVT in the aspirin group, compared with two cases of proximal DVT and three of PE in the dalteparin group. Another patient in the dalteparin group developed a symptomatic distal DVT in her calf, "but this was not considered an outcome event," the investigators said.
No major bleeding events developed in the aspirin group, but there was one such event in the dalteparin group for an overall rate of 0.3%. Similarly, there were two clinically significant nonmajor bleeding events for aspirin (0.5% rate), compared with four for dalteparin (1.0% rate). And there were eight minor bleeding events for aspirin (2.1% rate), compared with 18 for dalteparin (4.5% rate).
"In a composite analysis of net clinical benefit that combined VTE and clinically relevant major and nonmajor bleeding complications as outcomes," 0.8% of patients receiving aspirin had complications, compared with 2.5% of patients receiving dalteparin.
There were no differences between the two study groups in secondary outcomes such as wound infections, arterial vascular events, MI, stroke, or deaths.
The EPCAT trial was supported by the Canadian Institutes for Health Research. Aspirin was provided by Bayer HealthCare and dalteparin by Pfizer Pharmaceuticals, but neither Bayer nor Pfizer was involved in the design, conduct, or analysis of the study.
FROM ANNALS OF INTERNAL MEDICINE
Major finding: The primary efficacy outcome – development of symptomatic proximal DVT or PE during the 90 days after total hip arthroplasty – occurred in only 0.3% of the aspirin group, compared with 1.3% of the dalteparin group, establishing the noninferiority of aspirin therapy.
Data source: A randomized multicenter double-blind trial comparing the effectiveness and safety of aspirin and dalteparin for thromboprophylaxis in 786 patients undergoing elective total hip replacement in Canada during a 3-year period.
Disclosures: The EPCAT trial was supported by the Canadian Institutes for Health Research. Aspirin was provided by Bayer HealthCare and dalteparin by Pfizer Pharmaceuticals, but neither Bayer nor Pfizer was involved in the design, conduct, or analysis of the study.
Osteoarthritis patients survive longer after hip resurfacing than replacement
BIRMINGHAM, ENGLAND – Contrary to expectations, metal-on-metal hip resurfacing for osteoarthritis was associated with higher patient survival at 10 years than was total hip arthroplasty in a large, population-based study.
Cumulative mortality rates were 2.8% for hip resurfacing versus 7.3% for cemented total hip replacement (THR; hazard ratio, 0.51). Ten-year mortality rates comparing hip resurfacing to uncemented THR were 2.6% and 3.2%, respectively (HR, 0.64).
Furthermore, the number needed to treat with hip resurfacing to prevent 1 excess death was 29 when compared to cemented THR, and it was 88 when compared to uncemented THR.
"Patients who received a metal-on-metal resurfacing [MoMR] procedure seem to have a long-term survival advantage compared to patients receiving cemented or an uncemented THR," said Dr. Adrian Kendal of the National Institute for Health Research (NIHR) Musculoskeletal Biomedical Research Unit at the University of Oxford, England.
"Our findings were robust after adjustment for known confounders," Dr. Kendal said at the British Society for Rheumatology annual conference. Propensity matching was used in the trial, which took age, gender, comorbidity, rurality, and social deprivation into account.
For the study, data from the English Hospital Episode Statistics database were obtained and linked to Office for National Statistics mortality records for all adults (over age 18) undergoing elective primary hip replacement for osteoarthritis in National Health Service hospitals in England and Wales between April 1999 and March 2012.
After propensity score matching, there were 91,633 procedures performed, of which 12,580 were MoMR, 37,740 were cemented THR, and 41,312 were uncemented THR.
In response to a comment that perhaps people opting for MoMR were more likely to be younger, more active, and hence more likely to exercise, Dr. Kendal conceded that other factors might exist that could have affected survival.
Speculating about why there might be such a difference in survival, he said: "I personally don’t think it’s just the use of cement, because that doesn’t explain the group that received an uncemented total hip replacement."
He added that the way the femur is prepared during THR might be important, regardless of whether or not cement is used. The known risk of thrombotic consequences also could affect survival. In addition, health care inequality might be important, as resurfacing procedures are less common than THR, perhaps because of the lack of specialized centers or dedicated teams.
Commenting on the findings after their presentation, consultant rheumatologist Dr. Alex MacGregor, of the University of East Anglia, Norwich, England, noted that similar data were published on this topic last year (BMJ 2012;344:e3319), but the results had proved somewhat controversial as the authors had a conflict of interest in favor of hip resurfacing.
Dr. MacGregor, who is a member of the National Joint Registry Steering Committee, has been involved in a subsequent reanalysis of the paper’s findings and said that the results will be made public later in the year.
"One of my concerns [with this study] is the use of the 10-year mortality endpoint. If these resurfacing procedures are saving lives, then you would expect to see a survival benefit sooner, say at 90 days," Dr. MacGregor said.
Dr. Kendal responded that they tried to account for this, but the answer will need to come from a properly organized, randomized controlled trial.
"We don’t have a conflict of interest here. If anything, we were perhaps looking for the opposite effect; we were expecting to see an increased mortality rate in the resurfacing group," Dr. Kendal said. "That was not the case as it turned out, so I am reasonably confident that our data support the findings of that BMJ article."
Dr. Kendal and Dr. MacGregor reported no conflicts of interest.
BIRMINGHAM, ENGLAND – Contrary to expectations, metal-on-metal hip resurfacing for osteoarthritis was associated with higher patient survival at 10 years than was total hip arthroplasty in a large, population-based study.
Cumulative mortality rates were 2.8% for hip resurfacing versus 7.3% for cemented total hip replacement (THR; hazard ratio, 0.51). Ten-year mortality rates comparing hip resurfacing to uncemented THR were 2.6% and 3.2%, respectively (HR, 0.64).
Furthermore, the number needed to treat with hip resurfacing to prevent 1 excess death was 29 when compared to cemented THR, and it was 88 when compared to uncemented THR.
"Patients who received a metal-on-metal resurfacing [MoMR] procedure seem to have a long-term survival advantage compared to patients receiving cemented or an uncemented THR," said Dr. Adrian Kendal of the National Institute for Health Research (NIHR) Musculoskeletal Biomedical Research Unit at the University of Oxford, England.
"Our findings were robust after adjustment for known confounders," Dr. Kendal said at the British Society for Rheumatology annual conference. Propensity matching was used in the trial, which took age, gender, comorbidity, rurality, and social deprivation into account.
For the study, data from the English Hospital Episode Statistics database were obtained and linked to Office for National Statistics mortality records for all adults (over age 18) undergoing elective primary hip replacement for osteoarthritis in National Health Service hospitals in England and Wales between April 1999 and March 2012.
After propensity score matching, there were 91,633 procedures performed, of which 12,580 were MoMR, 37,740 were cemented THR, and 41,312 were uncemented THR.
In response to a comment that perhaps people opting for MoMR were more likely to be younger, more active, and hence more likely to exercise, Dr. Kendal conceded that other factors might exist that could have affected survival.
Speculating about why there might be such a difference in survival, he said: "I personally don’t think it’s just the use of cement, because that doesn’t explain the group that received an uncemented total hip replacement."
He added that the way the femur is prepared during THR might be important, regardless of whether or not cement is used. The known risk of thrombotic consequences also could affect survival. In addition, health care inequality might be important, as resurfacing procedures are less common than THR, perhaps because of the lack of specialized centers or dedicated teams.
Commenting on the findings after their presentation, consultant rheumatologist Dr. Alex MacGregor, of the University of East Anglia, Norwich, England, noted that similar data were published on this topic last year (BMJ 2012;344:e3319), but the results had proved somewhat controversial as the authors had a conflict of interest in favor of hip resurfacing.
Dr. MacGregor, who is a member of the National Joint Registry Steering Committee, has been involved in a subsequent reanalysis of the paper’s findings and said that the results will be made public later in the year.
"One of my concerns [with this study] is the use of the 10-year mortality endpoint. If these resurfacing procedures are saving lives, then you would expect to see a survival benefit sooner, say at 90 days," Dr. MacGregor said.
Dr. Kendal responded that they tried to account for this, but the answer will need to come from a properly organized, randomized controlled trial.
"We don’t have a conflict of interest here. If anything, we were perhaps looking for the opposite effect; we were expecting to see an increased mortality rate in the resurfacing group," Dr. Kendal said. "That was not the case as it turned out, so I am reasonably confident that our data support the findings of that BMJ article."
Dr. Kendal and Dr. MacGregor reported no conflicts of interest.
BIRMINGHAM, ENGLAND – Contrary to expectations, metal-on-metal hip resurfacing for osteoarthritis was associated with higher patient survival at 10 years than was total hip arthroplasty in a large, population-based study.
Cumulative mortality rates were 2.8% for hip resurfacing versus 7.3% for cemented total hip replacement (THR; hazard ratio, 0.51). Ten-year mortality rates comparing hip resurfacing to uncemented THR were 2.6% and 3.2%, respectively (HR, 0.64).
Furthermore, the number needed to treat with hip resurfacing to prevent 1 excess death was 29 when compared to cemented THR, and it was 88 when compared to uncemented THR.
"Patients who received a metal-on-metal resurfacing [MoMR] procedure seem to have a long-term survival advantage compared to patients receiving cemented or an uncemented THR," said Dr. Adrian Kendal of the National Institute for Health Research (NIHR) Musculoskeletal Biomedical Research Unit at the University of Oxford, England.
"Our findings were robust after adjustment for known confounders," Dr. Kendal said at the British Society for Rheumatology annual conference. Propensity matching was used in the trial, which took age, gender, comorbidity, rurality, and social deprivation into account.
For the study, data from the English Hospital Episode Statistics database were obtained and linked to Office for National Statistics mortality records for all adults (over age 18) undergoing elective primary hip replacement for osteoarthritis in National Health Service hospitals in England and Wales between April 1999 and March 2012.
After propensity score matching, there were 91,633 procedures performed, of which 12,580 were MoMR, 37,740 were cemented THR, and 41,312 were uncemented THR.
In response to a comment that perhaps people opting for MoMR were more likely to be younger, more active, and hence more likely to exercise, Dr. Kendal conceded that other factors might exist that could have affected survival.
Speculating about why there might be such a difference in survival, he said: "I personally don’t think it’s just the use of cement, because that doesn’t explain the group that received an uncemented total hip replacement."
He added that the way the femur is prepared during THR might be important, regardless of whether or not cement is used. The known risk of thrombotic consequences also could affect survival. In addition, health care inequality might be important, as resurfacing procedures are less common than THR, perhaps because of the lack of specialized centers or dedicated teams.
Commenting on the findings after their presentation, consultant rheumatologist Dr. Alex MacGregor, of the University of East Anglia, Norwich, England, noted that similar data were published on this topic last year (BMJ 2012;344:e3319), but the results had proved somewhat controversial as the authors had a conflict of interest in favor of hip resurfacing.
Dr. MacGregor, who is a member of the National Joint Registry Steering Committee, has been involved in a subsequent reanalysis of the paper’s findings and said that the results will be made public later in the year.
"One of my concerns [with this study] is the use of the 10-year mortality endpoint. If these resurfacing procedures are saving lives, then you would expect to see a survival benefit sooner, say at 90 days," Dr. MacGregor said.
Dr. Kendal responded that they tried to account for this, but the answer will need to come from a properly organized, randomized controlled trial.
"We don’t have a conflict of interest here. If anything, we were perhaps looking for the opposite effect; we were expecting to see an increased mortality rate in the resurfacing group," Dr. Kendal said. "That was not the case as it turned out, so I am reasonably confident that our data support the findings of that BMJ article."
Dr. Kendal and Dr. MacGregor reported no conflicts of interest.
AT RHEUMATOLOGY 2013
Major finding: The number needed to treat with hip resurfacing to prevent 1 excess death was 29 when compared to cemented total hip replacement, and it was 88 when compared to uncemented total hip replacement.
Data source: Retrospective, population-based, observational cohort study of 91,633 osteoarthritis patients who had metal-on-metal resurfacing or total hip replacement between April 1999 and March 2012.
Disclosures: Dr. Kendal and Dr. MacGregor reported no conflicts of interest.