User login
Role of TET2 in hematologic malignancies
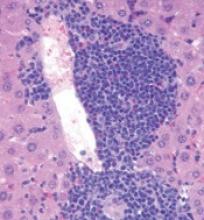
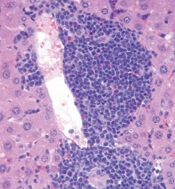
New research appears to explain how TET2 mutations increase the risk of hematologic malignancies.
In studying mouse models and patient samples, researchers found evidence to suggest that loss of TET2 opens the door for mutations that drive lymphoid and myeloid malignancies.
The researchers said loss of TET2 leads to hypermutagenicity in hematopoietic stem and progenitor cells (HSPCs), and although TET2-deficient HSPCs are likely not malignant, the higher mutation rates in these cells may result in additional driver mutations in TET2 target genes over time.
“If you lose TET2, it’s not a malignant state per se,” said Mingjiang Xu, MD, PhD, of the University of Miami Miller School of Medicine in Florida.
“But it’s creating a situation for other mutations to happen, leading to all types of blood cancer.”
Dr Xu and his colleagues reported these findings in Nature Communications.
The researchers found that Tet2-knockout mice developed spontaneous, lethal hematologic malignancies. Most (92%) developed myeloid malignancies, but 3.5% developed T-cell malignancies, and 4.5% developed B-cell malignancies.
In sequencing tumor and non-tumor cells from the Tet2-knockout mice, the researchers observed that loss of Tet2 leads to hypermutagenicity in HSPCs.
The team identified 190 genes with recurrent single-nucleotide variants. This included genes that are recurrently altered in human hematologic malignancies—Apc, Nf1, Flt3, Cbl, Notch1, and Mll2.
The researchers also analyzed samples from patients with acute myeloid leukemia, myeloproliferative neoplasms, and myelodysplastic syndromes.
The team found that patients with TET2 mutations had “significantly more mutational events than patients with wild-type TET2.” And TET2 mutations were associated with subclonal events in APC, NF1, ASXL1, CBL, and ZRSR2, among other genes.
These findings suggest that targeting TET2 could potentially prevent the development of hematologic malignancies.
The researchers noted that TET2 mutations occur in healthy elderly individuals with clonal hematopoiesis, and these individuals would be ideal candidates for a preventive therapy targeting TET2.
“We are developing a method to target TET2,” Dr Xu said. “If we target that population [with TET2 mutations] for early therapy, we could potentially prevent those downstream mutations from happening.” ![]()
New research appears to explain how TET2 mutations increase the risk of hematologic malignancies.
In studying mouse models and patient samples, researchers found evidence to suggest that loss of TET2 opens the door for mutations that drive lymphoid and myeloid malignancies.
The researchers said loss of TET2 leads to hypermutagenicity in hematopoietic stem and progenitor cells (HSPCs), and although TET2-deficient HSPCs are likely not malignant, the higher mutation rates in these cells may result in additional driver mutations in TET2 target genes over time.
“If you lose TET2, it’s not a malignant state per se,” said Mingjiang Xu, MD, PhD, of the University of Miami Miller School of Medicine in Florida.
“But it’s creating a situation for other mutations to happen, leading to all types of blood cancer.”
Dr Xu and his colleagues reported these findings in Nature Communications.
The researchers found that Tet2-knockout mice developed spontaneous, lethal hematologic malignancies. Most (92%) developed myeloid malignancies, but 3.5% developed T-cell malignancies, and 4.5% developed B-cell malignancies.
In sequencing tumor and non-tumor cells from the Tet2-knockout mice, the researchers observed that loss of Tet2 leads to hypermutagenicity in HSPCs.
The team identified 190 genes with recurrent single-nucleotide variants. This included genes that are recurrently altered in human hematologic malignancies—Apc, Nf1, Flt3, Cbl, Notch1, and Mll2.
The researchers also analyzed samples from patients with acute myeloid leukemia, myeloproliferative neoplasms, and myelodysplastic syndromes.
The team found that patients with TET2 mutations had “significantly more mutational events than patients with wild-type TET2.” And TET2 mutations were associated with subclonal events in APC, NF1, ASXL1, CBL, and ZRSR2, among other genes.
These findings suggest that targeting TET2 could potentially prevent the development of hematologic malignancies.
The researchers noted that TET2 mutations occur in healthy elderly individuals with clonal hematopoiesis, and these individuals would be ideal candidates for a preventive therapy targeting TET2.
“We are developing a method to target TET2,” Dr Xu said. “If we target that population [with TET2 mutations] for early therapy, we could potentially prevent those downstream mutations from happening.” ![]()
New research appears to explain how TET2 mutations increase the risk of hematologic malignancies.
In studying mouse models and patient samples, researchers found evidence to suggest that loss of TET2 opens the door for mutations that drive lymphoid and myeloid malignancies.
The researchers said loss of TET2 leads to hypermutagenicity in hematopoietic stem and progenitor cells (HSPCs), and although TET2-deficient HSPCs are likely not malignant, the higher mutation rates in these cells may result in additional driver mutations in TET2 target genes over time.
“If you lose TET2, it’s not a malignant state per se,” said Mingjiang Xu, MD, PhD, of the University of Miami Miller School of Medicine in Florida.
“But it’s creating a situation for other mutations to happen, leading to all types of blood cancer.”
Dr Xu and his colleagues reported these findings in Nature Communications.
The researchers found that Tet2-knockout mice developed spontaneous, lethal hematologic malignancies. Most (92%) developed myeloid malignancies, but 3.5% developed T-cell malignancies, and 4.5% developed B-cell malignancies.
In sequencing tumor and non-tumor cells from the Tet2-knockout mice, the researchers observed that loss of Tet2 leads to hypermutagenicity in HSPCs.
The team identified 190 genes with recurrent single-nucleotide variants. This included genes that are recurrently altered in human hematologic malignancies—Apc, Nf1, Flt3, Cbl, Notch1, and Mll2.
The researchers also analyzed samples from patients with acute myeloid leukemia, myeloproliferative neoplasms, and myelodysplastic syndromes.
The team found that patients with TET2 mutations had “significantly more mutational events than patients with wild-type TET2.” And TET2 mutations were associated with subclonal events in APC, NF1, ASXL1, CBL, and ZRSR2, among other genes.
These findings suggest that targeting TET2 could potentially prevent the development of hematologic malignancies.
The researchers noted that TET2 mutations occur in healthy elderly individuals with clonal hematopoiesis, and these individuals would be ideal candidates for a preventive therapy targeting TET2.
“We are developing a method to target TET2,” Dr Xu said. “If we target that population [with TET2 mutations] for early therapy, we could potentially prevent those downstream mutations from happening.” ![]()
FDA issues warnings about illegal ‘anticancer’ products
The US Food and Drug Administration (FDA) has posted warning letters addressed to 14 US-based companies illegally selling more than 65 products.
The companies are fraudulently claiming that these products prevent, diagnose, treat, or cure cancer.
The products are being marketed and sold without FDA approval, most commonly on websites and social media platforms.
“Consumers should not use these or similar unproven products because they may be unsafe and could prevent a person from seeking an appropriate and potentially life-saving cancer diagnosis or treatment,” said Douglas W. Stearn, director of the Office of Enforcement and Import Operations in the FDA’s Office of Regulatory Affairs.
“We encourage people to remain vigilant whether online or in a store, and avoid purchasing products marketed to treat cancer without any proof they will work. Patients should consult a healthcare professional about proper prevention, diagnosis, and treatment of cancer.”
It is a violation of the Federal Food, Drug and Cosmetic Act to market and sell products that claim to prevent, diagnose, treat, mitigate, or cure diseases without first demonstrating to the FDA that they are safe and effective for their labeled uses.
The illegally sold products cited in the FDA’s warning letters include a variety of product types, such as pills, topical creams, ointments, oils, drops, syrups, teas, and diagnostics (such as thermography devices).
They include products marketed for use by humans or pets that make illegal, unproven claims regarding preventing, reversing, or curing cancer; killing/inhibiting cancer cells or tumors; or other similar anticancer claims.
The FDA has requested responses from the 14 companies stating how the violations will be corrected. Failure to correct the violations promptly may result in legal action, including product seizure, injunction, and/or criminal prosecution.
As part of the FDA’s effort to protect consumers from cancer health fraud, the FDA has issued more than 90 warning letters in the past 10 years to companies marketing hundreds of fraudulent cancer-related products on websites, social media, and in stores.
Although many of these companies have stopped selling the products or making fraudulent claims, numerous unsafe and unapproved products continue to be sold directly to consumers due, in part, to the ease with which companies can move their marketing operations to new websites.
The FDA continues to monitor and take action against companies promoting and selling unproven treatments in an effort to minimize the potential dangers to consumers and to educate consumers about the risks.
The FDA encourages healthcare professionals and consumers to report adverse reactions associated with these or similar products to the FDA’s MedWatch program. ![]()
The US Food and Drug Administration (FDA) has posted warning letters addressed to 14 US-based companies illegally selling more than 65 products.
The companies are fraudulently claiming that these products prevent, diagnose, treat, or cure cancer.
The products are being marketed and sold without FDA approval, most commonly on websites and social media platforms.
“Consumers should not use these or similar unproven products because they may be unsafe and could prevent a person from seeking an appropriate and potentially life-saving cancer diagnosis or treatment,” said Douglas W. Stearn, director of the Office of Enforcement and Import Operations in the FDA’s Office of Regulatory Affairs.
“We encourage people to remain vigilant whether online or in a store, and avoid purchasing products marketed to treat cancer without any proof they will work. Patients should consult a healthcare professional about proper prevention, diagnosis, and treatment of cancer.”
It is a violation of the Federal Food, Drug and Cosmetic Act to market and sell products that claim to prevent, diagnose, treat, mitigate, or cure diseases without first demonstrating to the FDA that they are safe and effective for their labeled uses.
The illegally sold products cited in the FDA’s warning letters include a variety of product types, such as pills, topical creams, ointments, oils, drops, syrups, teas, and diagnostics (such as thermography devices).
They include products marketed for use by humans or pets that make illegal, unproven claims regarding preventing, reversing, or curing cancer; killing/inhibiting cancer cells or tumors; or other similar anticancer claims.
The FDA has requested responses from the 14 companies stating how the violations will be corrected. Failure to correct the violations promptly may result in legal action, including product seizure, injunction, and/or criminal prosecution.
As part of the FDA’s effort to protect consumers from cancer health fraud, the FDA has issued more than 90 warning letters in the past 10 years to companies marketing hundreds of fraudulent cancer-related products on websites, social media, and in stores.
Although many of these companies have stopped selling the products or making fraudulent claims, numerous unsafe and unapproved products continue to be sold directly to consumers due, in part, to the ease with which companies can move their marketing operations to new websites.
The FDA continues to monitor and take action against companies promoting and selling unproven treatments in an effort to minimize the potential dangers to consumers and to educate consumers about the risks.
The FDA encourages healthcare professionals and consumers to report adverse reactions associated with these or similar products to the FDA’s MedWatch program. ![]()
The US Food and Drug Administration (FDA) has posted warning letters addressed to 14 US-based companies illegally selling more than 65 products.
The companies are fraudulently claiming that these products prevent, diagnose, treat, or cure cancer.
The products are being marketed and sold without FDA approval, most commonly on websites and social media platforms.
“Consumers should not use these or similar unproven products because they may be unsafe and could prevent a person from seeking an appropriate and potentially life-saving cancer diagnosis or treatment,” said Douglas W. Stearn, director of the Office of Enforcement and Import Operations in the FDA’s Office of Regulatory Affairs.
“We encourage people to remain vigilant whether online or in a store, and avoid purchasing products marketed to treat cancer without any proof they will work. Patients should consult a healthcare professional about proper prevention, diagnosis, and treatment of cancer.”
It is a violation of the Federal Food, Drug and Cosmetic Act to market and sell products that claim to prevent, diagnose, treat, mitigate, or cure diseases without first demonstrating to the FDA that they are safe and effective for their labeled uses.
The illegally sold products cited in the FDA’s warning letters include a variety of product types, such as pills, topical creams, ointments, oils, drops, syrups, teas, and diagnostics (such as thermography devices).
They include products marketed for use by humans or pets that make illegal, unproven claims regarding preventing, reversing, or curing cancer; killing/inhibiting cancer cells or tumors; or other similar anticancer claims.
The FDA has requested responses from the 14 companies stating how the violations will be corrected. Failure to correct the violations promptly may result in legal action, including product seizure, injunction, and/or criminal prosecution.
As part of the FDA’s effort to protect consumers from cancer health fraud, the FDA has issued more than 90 warning letters in the past 10 years to companies marketing hundreds of fraudulent cancer-related products on websites, social media, and in stores.
Although many of these companies have stopped selling the products or making fraudulent claims, numerous unsafe and unapproved products continue to be sold directly to consumers due, in part, to the ease with which companies can move their marketing operations to new websites.
The FDA continues to monitor and take action against companies promoting and selling unproven treatments in an effort to minimize the potential dangers to consumers and to educate consumers about the risks.
The FDA encourages healthcare professionals and consumers to report adverse reactions associated with these or similar products to the FDA’s MedWatch program. ![]()
MDS genetic analysis identifies allogeneic HSCT candidates
NEW YORK – Genetic mutation analysis of patients with myelodysplastic syndrome (MDS) may have a useful role in routine practice based on recent reports that showed clear links between certain gene mutations and the outcomes of patients who underwent allogeneic hematopoietic stem cell transplantation (HSCT).
Two reports published in 2017 helped strengthen the case for routine mutation analysis in distinguishing patients with MDS or myeloproliferative neoplasms (MDN) who are very likely to have just a brief response to allogeneic HSCT from similar patients who seem likely to have several years of overall survival following transplantation.
Allogeneic HSCT is the only potentially curative procedure for patients with MDS or MDN. Although an increasing number of these patients undergo transplantation, clinicians need to choose the patients they select for the treatment carefully. “Molecular testing is playing an increasing role in selecting the best candidates,” Dr. Zeidan said.
The largest reported genetic study of allogeneic HSCT in MDS patients involved 1,514 patients entered into a U.S.-based dataset during 2005-2015. Testing identified at least one mutation in 1,196 (79%) of these patients.
Analysis of data from these patients found a disparate pattern of posttransplant survival that appeared to link with gene mutations and other risk factors. The highest risk patients were those with a mutation in their TP53 gene, found in 289 patients (19% of the 1,514 tested) who had a median overall survival (OS) of 0.7 years and a 3-year OS of 20% (New Engl J Med. 2017 Feb 9;376[6]:536-47).
Among patients without a TP53 mutation, OS depended on age, with the best survival seen among patients less than 40 years old. Patients in this subgroup who also had no other high-risk features – no therapy-related MDS, a platelet level of at least 30 x 109 at the time of transplantation, and bone marrow blasts less than 15% at diagnosis – had the best OS, 82% at 3-years of follow-up. The studied cohort included 116 patients (8%) who fell into this low-risk, best-outcome category, the optimal population for receiving an allogeneic HSCT, Dr. Zeidan said. Another 98 patients (6%) who had at least one of these high risk feature had a median OS of 2.6 years and a 3-year OS of 49%.
Additional gene mutations further subdivided the older patients in the study, those at least 40 years old, into various risk subgroups. Older patients with a mutation in a ras-pathway gene had a 0.9 year median OS and a 3-year OS of 30%. This subgroup included 129 patients (9%). Among older patients with no mutation in the ras-pathway gene, mutations in the JAK2 gene also linked with worse survival, a median OS of 0.5 years and a 3-year OS of 28% of a subgroup with 28 patients (2%). The largest subgroup in the study was older patients with no mutations in the TP53, JAK2, or ras-pathway genes, a subgroup with 854 patients (56%), who had a median OS of 2.3 years and a 3-year OS of 46%.
The second recent report was a Japanese study of 797 MDS patients who underwent genetic testing and received an allogeneic HSCT through the Japan Marrow Donor Program. The investigators found identifiable mutations in 617 patients (77%) and documented that patients with a TP53 or ras-pathway mutation had a “dismal prognosis” when associated with a complex karyotype and myelodysplastic or myeloproliferative neoplasms. However, among patients with a mutated TP53 gene or complex karyotype alone, long-term survival following transplantation appeared possible (Blood. 2017. doi: org/10.1182/blood-2016-12-754796.
Two smaller, earlier studies (J Clin Oncol. 2014 Sept 1;32[25]:2691-8; J Clin Oncol. 2016 Oct 20;34[30]:2627-37) also implicated mutations in the TET2, DNMT3A, ASXL1, and RUNX1 genes as identifying MDS patients with worse OS following allogeneic HSCT, Dr. Zeidan noted, but the combination of a TP53 gene mutation and a complex karyotype appears to confer the worst prognosis of all. Patients with mutations in more than one of these genes fared much worse than those with single mutations.
Dr. Zeidan had no relevant disclosures.
[email protected]
On Twitter @mitchelzoler
NEW YORK – Genetic mutation analysis of patients with myelodysplastic syndrome (MDS) may have a useful role in routine practice based on recent reports that showed clear links between certain gene mutations and the outcomes of patients who underwent allogeneic hematopoietic stem cell transplantation (HSCT).
Two reports published in 2017 helped strengthen the case for routine mutation analysis in distinguishing patients with MDS or myeloproliferative neoplasms (MDN) who are very likely to have just a brief response to allogeneic HSCT from similar patients who seem likely to have several years of overall survival following transplantation.
Allogeneic HSCT is the only potentially curative procedure for patients with MDS or MDN. Although an increasing number of these patients undergo transplantation, clinicians need to choose the patients they select for the treatment carefully. “Molecular testing is playing an increasing role in selecting the best candidates,” Dr. Zeidan said.
The largest reported genetic study of allogeneic HSCT in MDS patients involved 1,514 patients entered into a U.S.-based dataset during 2005-2015. Testing identified at least one mutation in 1,196 (79%) of these patients.
Analysis of data from these patients found a disparate pattern of posttransplant survival that appeared to link with gene mutations and other risk factors. The highest risk patients were those with a mutation in their TP53 gene, found in 289 patients (19% of the 1,514 tested) who had a median overall survival (OS) of 0.7 years and a 3-year OS of 20% (New Engl J Med. 2017 Feb 9;376[6]:536-47).
Among patients without a TP53 mutation, OS depended on age, with the best survival seen among patients less than 40 years old. Patients in this subgroup who also had no other high-risk features – no therapy-related MDS, a platelet level of at least 30 x 109 at the time of transplantation, and bone marrow blasts less than 15% at diagnosis – had the best OS, 82% at 3-years of follow-up. The studied cohort included 116 patients (8%) who fell into this low-risk, best-outcome category, the optimal population for receiving an allogeneic HSCT, Dr. Zeidan said. Another 98 patients (6%) who had at least one of these high risk feature had a median OS of 2.6 years and a 3-year OS of 49%.
Additional gene mutations further subdivided the older patients in the study, those at least 40 years old, into various risk subgroups. Older patients with a mutation in a ras-pathway gene had a 0.9 year median OS and a 3-year OS of 30%. This subgroup included 129 patients (9%). Among older patients with no mutation in the ras-pathway gene, mutations in the JAK2 gene also linked with worse survival, a median OS of 0.5 years and a 3-year OS of 28% of a subgroup with 28 patients (2%). The largest subgroup in the study was older patients with no mutations in the TP53, JAK2, or ras-pathway genes, a subgroup with 854 patients (56%), who had a median OS of 2.3 years and a 3-year OS of 46%.
The second recent report was a Japanese study of 797 MDS patients who underwent genetic testing and received an allogeneic HSCT through the Japan Marrow Donor Program. The investigators found identifiable mutations in 617 patients (77%) and documented that patients with a TP53 or ras-pathway mutation had a “dismal prognosis” when associated with a complex karyotype and myelodysplastic or myeloproliferative neoplasms. However, among patients with a mutated TP53 gene or complex karyotype alone, long-term survival following transplantation appeared possible (Blood. 2017. doi: org/10.1182/blood-2016-12-754796.
Two smaller, earlier studies (J Clin Oncol. 2014 Sept 1;32[25]:2691-8; J Clin Oncol. 2016 Oct 20;34[30]:2627-37) also implicated mutations in the TET2, DNMT3A, ASXL1, and RUNX1 genes as identifying MDS patients with worse OS following allogeneic HSCT, Dr. Zeidan noted, but the combination of a TP53 gene mutation and a complex karyotype appears to confer the worst prognosis of all. Patients with mutations in more than one of these genes fared much worse than those with single mutations.
Dr. Zeidan had no relevant disclosures.
[email protected]
On Twitter @mitchelzoler
NEW YORK – Genetic mutation analysis of patients with myelodysplastic syndrome (MDS) may have a useful role in routine practice based on recent reports that showed clear links between certain gene mutations and the outcomes of patients who underwent allogeneic hematopoietic stem cell transplantation (HSCT).
Two reports published in 2017 helped strengthen the case for routine mutation analysis in distinguishing patients with MDS or myeloproliferative neoplasms (MDN) who are very likely to have just a brief response to allogeneic HSCT from similar patients who seem likely to have several years of overall survival following transplantation.
Allogeneic HSCT is the only potentially curative procedure for patients with MDS or MDN. Although an increasing number of these patients undergo transplantation, clinicians need to choose the patients they select for the treatment carefully. “Molecular testing is playing an increasing role in selecting the best candidates,” Dr. Zeidan said.
The largest reported genetic study of allogeneic HSCT in MDS patients involved 1,514 patients entered into a U.S.-based dataset during 2005-2015. Testing identified at least one mutation in 1,196 (79%) of these patients.
Analysis of data from these patients found a disparate pattern of posttransplant survival that appeared to link with gene mutations and other risk factors. The highest risk patients were those with a mutation in their TP53 gene, found in 289 patients (19% of the 1,514 tested) who had a median overall survival (OS) of 0.7 years and a 3-year OS of 20% (New Engl J Med. 2017 Feb 9;376[6]:536-47).
Among patients without a TP53 mutation, OS depended on age, with the best survival seen among patients less than 40 years old. Patients in this subgroup who also had no other high-risk features – no therapy-related MDS, a platelet level of at least 30 x 109 at the time of transplantation, and bone marrow blasts less than 15% at diagnosis – had the best OS, 82% at 3-years of follow-up. The studied cohort included 116 patients (8%) who fell into this low-risk, best-outcome category, the optimal population for receiving an allogeneic HSCT, Dr. Zeidan said. Another 98 patients (6%) who had at least one of these high risk feature had a median OS of 2.6 years and a 3-year OS of 49%.
Additional gene mutations further subdivided the older patients in the study, those at least 40 years old, into various risk subgroups. Older patients with a mutation in a ras-pathway gene had a 0.9 year median OS and a 3-year OS of 30%. This subgroup included 129 patients (9%). Among older patients with no mutation in the ras-pathway gene, mutations in the JAK2 gene also linked with worse survival, a median OS of 0.5 years and a 3-year OS of 28% of a subgroup with 28 patients (2%). The largest subgroup in the study was older patients with no mutations in the TP53, JAK2, or ras-pathway genes, a subgroup with 854 patients (56%), who had a median OS of 2.3 years and a 3-year OS of 46%.
The second recent report was a Japanese study of 797 MDS patients who underwent genetic testing and received an allogeneic HSCT through the Japan Marrow Donor Program. The investigators found identifiable mutations in 617 patients (77%) and documented that patients with a TP53 or ras-pathway mutation had a “dismal prognosis” when associated with a complex karyotype and myelodysplastic or myeloproliferative neoplasms. However, among patients with a mutated TP53 gene or complex karyotype alone, long-term survival following transplantation appeared possible (Blood. 2017. doi: org/10.1182/blood-2016-12-754796.
Two smaller, earlier studies (J Clin Oncol. 2014 Sept 1;32[25]:2691-8; J Clin Oncol. 2016 Oct 20;34[30]:2627-37) also implicated mutations in the TET2, DNMT3A, ASXL1, and RUNX1 genes as identifying MDS patients with worse OS following allogeneic HSCT, Dr. Zeidan noted, but the combination of a TP53 gene mutation and a complex karyotype appears to confer the worst prognosis of all. Patients with mutations in more than one of these genes fared much worse than those with single mutations.
Dr. Zeidan had no relevant disclosures.
[email protected]
On Twitter @mitchelzoler
WES misses genes associated with leukemia, other diseases
Whole-exome sequencing (WES) may routinely miss genetic variations associated with leukemia and other diseases, according to research published in Scientific Reports.
The study revealed 832 genes that have low coverage across multiple WES platforms.
These genes are associated with leukemia, psoriasis, heart failure, and other diseases, and they may be missed by researchers using WES to study these diseases.
“Although it was known that coverage—the average number of times a given piece of DNA is read during sequencing—could be uneven in whole-exome sequencing, our new methods are the first to really quantify this,” said study author Santhosh Girirajan, MBBS, PhD, of The Pennsylvania State University, University Park.
“Adequate coverage—often as many as 70 or more reads for each piece of DNA—increases our confidence that the sequence is accurate, and, without it, it is nearly impossible to make confident predictions about the relationship between a mutation in a gene and a disease.”
“In our study, we found 832 genes that have systematically low coverage across 3 different sequencing platforms, meaning that these genes would be missed in disease studies.”
The researchers said low-coverage regions may result from limited precision in WES technologies due to certain genomic features.
Highly repetitive stretches of DNA can prevent the sequencer from reading the DNA properly. The study showed that at least 60% of low-coverage genes occur near DNA repeats.
“One solution to this problem is for researchers to use whole-genome sequencing, which examines all base pairs of DNA instead of just the regions that contain genes,” Dr Girirajan said. “Our study found that whole-genome data had significantly fewer low-coverage genes than whole-exome data, and its coverage is more uniformly distributed across all parts of the genome.”
“However, the costs of whole-exome sequencing are still significantly lower than whole-genome sequencing. Until the costs of whole-genome sequencing is no longer a barrier, human genetics researchers should be aware of these limitations in whole-exome sequencing technologies.” ![]()
Whole-exome sequencing (WES) may routinely miss genetic variations associated with leukemia and other diseases, according to research published in Scientific Reports.
The study revealed 832 genes that have low coverage across multiple WES platforms.
These genes are associated with leukemia, psoriasis, heart failure, and other diseases, and they may be missed by researchers using WES to study these diseases.
“Although it was known that coverage—the average number of times a given piece of DNA is read during sequencing—could be uneven in whole-exome sequencing, our new methods are the first to really quantify this,” said study author Santhosh Girirajan, MBBS, PhD, of The Pennsylvania State University, University Park.
“Adequate coverage—often as many as 70 or more reads for each piece of DNA—increases our confidence that the sequence is accurate, and, without it, it is nearly impossible to make confident predictions about the relationship between a mutation in a gene and a disease.”
“In our study, we found 832 genes that have systematically low coverage across 3 different sequencing platforms, meaning that these genes would be missed in disease studies.”
The researchers said low-coverage regions may result from limited precision in WES technologies due to certain genomic features.
Highly repetitive stretches of DNA can prevent the sequencer from reading the DNA properly. The study showed that at least 60% of low-coverage genes occur near DNA repeats.
“One solution to this problem is for researchers to use whole-genome sequencing, which examines all base pairs of DNA instead of just the regions that contain genes,” Dr Girirajan said. “Our study found that whole-genome data had significantly fewer low-coverage genes than whole-exome data, and its coverage is more uniformly distributed across all parts of the genome.”
“However, the costs of whole-exome sequencing are still significantly lower than whole-genome sequencing. Until the costs of whole-genome sequencing is no longer a barrier, human genetics researchers should be aware of these limitations in whole-exome sequencing technologies.” ![]()
Whole-exome sequencing (WES) may routinely miss genetic variations associated with leukemia and other diseases, according to research published in Scientific Reports.
The study revealed 832 genes that have low coverage across multiple WES platforms.
These genes are associated with leukemia, psoriasis, heart failure, and other diseases, and they may be missed by researchers using WES to study these diseases.
“Although it was known that coverage—the average number of times a given piece of DNA is read during sequencing—could be uneven in whole-exome sequencing, our new methods are the first to really quantify this,” said study author Santhosh Girirajan, MBBS, PhD, of The Pennsylvania State University, University Park.
“Adequate coverage—often as many as 70 or more reads for each piece of DNA—increases our confidence that the sequence is accurate, and, without it, it is nearly impossible to make confident predictions about the relationship between a mutation in a gene and a disease.”
“In our study, we found 832 genes that have systematically low coverage across 3 different sequencing platforms, meaning that these genes would be missed in disease studies.”
The researchers said low-coverage regions may result from limited precision in WES technologies due to certain genomic features.
Highly repetitive stretches of DNA can prevent the sequencer from reading the DNA properly. The study showed that at least 60% of low-coverage genes occur near DNA repeats.
“One solution to this problem is for researchers to use whole-genome sequencing, which examines all base pairs of DNA instead of just the regions that contain genes,” Dr Girirajan said. “Our study found that whole-genome data had significantly fewer low-coverage genes than whole-exome data, and its coverage is more uniformly distributed across all parts of the genome.”
“However, the costs of whole-exome sequencing are still significantly lower than whole-genome sequencing. Until the costs of whole-genome sequencing is no longer a barrier, human genetics researchers should be aware of these limitations in whole-exome sequencing technologies.” ![]()
A spouse’s cancer diagnosis can lower household income
A spouse’s cancer diagnosis can significantly diminish family income, according to research published in the Journal of Health Economics.
Investigators tracked changes in employment and income among working-age couples in Canada and found that, on average, a spousal cancer diagnosis results in a 5% decline in household income for men and a 9% decline for women.
“The average annual household income for the working-age couples we studied was about $100,000, so the loss of income per family is about $5000 to $9000, which is a pretty substantial decline,” said study author R. Vincent Pohl, PhD, of the University of Georgia in Athens, Georgia.
“In a situation where one household member has a devastating diagnosis, it leads to the whole household suffering economically.”
One reason for the income decline is attributed to what’s known as the caregiver effect—when one family member reduces his or her own employment to support another.
“We thought that the household’s lessened income could happen in one of two ways,” Dr Pohl said. “One is that the person who is diagnosed might not be able to work because they are getting treatment or they’re too sick to work.”
“The second is what happens to their spouse. Does the spouse work more to make up for the lost income or does the spouse also reduce his or her labor supply in order to take care of the spouse that is diagnosed with cancer? We find the latter, that spouses reduce their labor supply and therefore have lowered income levels, which leads to the household having lower income levels as well.”
The investigators found that, in the 5 years after a spouse’s cancer diagnosis, both husbands and wives reduced their employment rates by about 2.4 percentage points, on average.
The women had lower average employment rates, so the decrease represented a larger relative decline for them.
When a wife was diagnosed with cancer, her husband’s annual earnings decreased by about $2000, or 3.5% of his income.
When a husband was diagnosed with cancer, his wife’s annual earnings decreased by about $1500, or 6% of her income.
Total family income decreased by up to 4.8% among men and 8.5% among women.
The investigators found the declines were due to lower earnings among both cancer patients and their spouses.
“What we need to think about, in terms of policy implications, is how we can protect not just individuals from the consequences of getting sick, but their entire family,” Dr Pohl said. That’s not really something that existing policies do.”
“If you think about disability insurance, it’s a function of an individual’s inability to work. It doesn’t take into account that family members might have to take care of an individual and therefore might also lose their job or reduce their working hours and, thus, their income.”
Dr Pohl said this study allowed the investigators to examine behavior on a level that’s representative for the entire country of Canada, but the findings may not be transferable to the US, where healthcare is handled differently than in many developed nations.
“One reason why we don’t see that the spouse works more, potentially, is that health insurance is not provided through jobs in Canada,” Dr Pohl said. “In the United States, we could expect that if one spouse is diagnosed with a disease, the other spouse has to keep their job in order to keep health insurance for the family.” ![]()
A spouse’s cancer diagnosis can significantly diminish family income, according to research published in the Journal of Health Economics.
Investigators tracked changes in employment and income among working-age couples in Canada and found that, on average, a spousal cancer diagnosis results in a 5% decline in household income for men and a 9% decline for women.
“The average annual household income for the working-age couples we studied was about $100,000, so the loss of income per family is about $5000 to $9000, which is a pretty substantial decline,” said study author R. Vincent Pohl, PhD, of the University of Georgia in Athens, Georgia.
“In a situation where one household member has a devastating diagnosis, it leads to the whole household suffering economically.”
One reason for the income decline is attributed to what’s known as the caregiver effect—when one family member reduces his or her own employment to support another.
“We thought that the household’s lessened income could happen in one of two ways,” Dr Pohl said. “One is that the person who is diagnosed might not be able to work because they are getting treatment or they’re too sick to work.”
“The second is what happens to their spouse. Does the spouse work more to make up for the lost income or does the spouse also reduce his or her labor supply in order to take care of the spouse that is diagnosed with cancer? We find the latter, that spouses reduce their labor supply and therefore have lowered income levels, which leads to the household having lower income levels as well.”
The investigators found that, in the 5 years after a spouse’s cancer diagnosis, both husbands and wives reduced their employment rates by about 2.4 percentage points, on average.
The women had lower average employment rates, so the decrease represented a larger relative decline for them.
When a wife was diagnosed with cancer, her husband’s annual earnings decreased by about $2000, or 3.5% of his income.
When a husband was diagnosed with cancer, his wife’s annual earnings decreased by about $1500, or 6% of her income.
Total family income decreased by up to 4.8% among men and 8.5% among women.
The investigators found the declines were due to lower earnings among both cancer patients and their spouses.
“What we need to think about, in terms of policy implications, is how we can protect not just individuals from the consequences of getting sick, but their entire family,” Dr Pohl said. That’s not really something that existing policies do.”
“If you think about disability insurance, it’s a function of an individual’s inability to work. It doesn’t take into account that family members might have to take care of an individual and therefore might also lose their job or reduce their working hours and, thus, their income.”
Dr Pohl said this study allowed the investigators to examine behavior on a level that’s representative for the entire country of Canada, but the findings may not be transferable to the US, where healthcare is handled differently than in many developed nations.
“One reason why we don’t see that the spouse works more, potentially, is that health insurance is not provided through jobs in Canada,” Dr Pohl said. “In the United States, we could expect that if one spouse is diagnosed with a disease, the other spouse has to keep their job in order to keep health insurance for the family.” ![]()
A spouse’s cancer diagnosis can significantly diminish family income, according to research published in the Journal of Health Economics.
Investigators tracked changes in employment and income among working-age couples in Canada and found that, on average, a spousal cancer diagnosis results in a 5% decline in household income for men and a 9% decline for women.
“The average annual household income for the working-age couples we studied was about $100,000, so the loss of income per family is about $5000 to $9000, which is a pretty substantial decline,” said study author R. Vincent Pohl, PhD, of the University of Georgia in Athens, Georgia.
“In a situation where one household member has a devastating diagnosis, it leads to the whole household suffering economically.”
One reason for the income decline is attributed to what’s known as the caregiver effect—when one family member reduces his or her own employment to support another.
“We thought that the household’s lessened income could happen in one of two ways,” Dr Pohl said. “One is that the person who is diagnosed might not be able to work because they are getting treatment or they’re too sick to work.”
“The second is what happens to their spouse. Does the spouse work more to make up for the lost income or does the spouse also reduce his or her labor supply in order to take care of the spouse that is diagnosed with cancer? We find the latter, that spouses reduce their labor supply and therefore have lowered income levels, which leads to the household having lower income levels as well.”
The investigators found that, in the 5 years after a spouse’s cancer diagnosis, both husbands and wives reduced their employment rates by about 2.4 percentage points, on average.
The women had lower average employment rates, so the decrease represented a larger relative decline for them.
When a wife was diagnosed with cancer, her husband’s annual earnings decreased by about $2000, or 3.5% of his income.
When a husband was diagnosed with cancer, his wife’s annual earnings decreased by about $1500, or 6% of her income.
Total family income decreased by up to 4.8% among men and 8.5% among women.
The investigators found the declines were due to lower earnings among both cancer patients and their spouses.
“What we need to think about, in terms of policy implications, is how we can protect not just individuals from the consequences of getting sick, but their entire family,” Dr Pohl said. That’s not really something that existing policies do.”
“If you think about disability insurance, it’s a function of an individual’s inability to work. It doesn’t take into account that family members might have to take care of an individual and therefore might also lose their job or reduce their working hours and, thus, their income.”
Dr Pohl said this study allowed the investigators to examine behavior on a level that’s representative for the entire country of Canada, but the findings may not be transferable to the US, where healthcare is handled differently than in many developed nations.
“One reason why we don’t see that the spouse works more, potentially, is that health insurance is not provided through jobs in Canada,” Dr Pohl said. “In the United States, we could expect that if one spouse is diagnosed with a disease, the other spouse has to keep their job in order to keep health insurance for the family.” ![]()
Targeted drugs transform CLL management
NEW YORK – New, targeted treatments, especially ibrutinib (Imbruvica), have sharply shifted prognosis for patients with chronic lymphocytic leukemia (CLL) and raised new issues for managing these patients now that they survive years longer.
“Ibrutinib has produced a profound change in survival” of patients with CLL, Timothy G. Call, MD, a hematologist/oncologist at the Mayo Clinic in Rochester, Minn., said at a conference held by Imedex. It “has changed the playing field.” No other new agent so far “has produced the same level of progression-free survival in CLL.”
An analysis published in early 2017 projected a greater than 50% jump in U.S. patients living with CLL from 2011, before the advent of targeted oral drugs, to 2025, when the study predicted that there will be nearly 200,000 U.S. patients living with CLL (J Clin Oncol. 2017 January;35[2]:166-74). With targeted drugs like ibrutinib and idelalisib (Zydelig) costing about $130,000 per patient each year, the projected cost for managing the U.S. CLL population is on track to rise to more than $5 billion by 2025, a nearly sixfold increase, compared with CLL patient expenditures in 2011, according to this analysis.
The impact of the higher cost of treatment is already being felt more acutely by many patients because of recent cuts in assistance from the Patient Access Network, which helps patients with copays but recently had to put a lid on CLL assistance availability when its funding availability hit a wall, Dr. Call said.
On the clinical side, there are new considerations triggered by greater patient longevity. “As we make patients live longer with CLL, we need to double down on the diagnosis and treatment of its complications,” such as watching for development of secondary cancers, Dr. Call said in an interview. This stems from the reduced immunosurveillance in patients with CLL and their resulting increased susceptibility to developing environmentally-triggered malignancies like lung and skin cancers. Other long-term implications of impaired immunosurveillance include increased infection susceptibility, an ongoing risk for Richter’s or Hodgkin lymphoma transformation, and a risk for autoimmune complications, such as red blood cell aplasia and transfusion-associated graft versus host disease.
Patients with CLL can also be susceptible to complications from long-term use of the targeted drug they’re on. The new targeted agents can trigger bruising and bleeding, diarrhea, rash, fatigue, muscle and joint aches, and arrhythmia, he noted.
Potential adverse effects, specifically from ibrutinib, include a 3% risk for a major bleed, a 10% rate of new-onset atrial fibrillation, and a 20% risk for new hypertension, Dr. Call said. Before starting ibrutinib, patients should undergo screening for hepatitis B virus infection and receive prophylaxis against herpes zoster activation with acyclovir or valacyclovir. If the patient starts with a CD4 cell count below 200 cells/mm3, it might be prudent to prophylax the patient against Pneumocystis jirovecii pneumonia.
However, even if a toxicity develops on ibrutinib, Dr. Call recommended reducing the dosage rather than discontinuing the drug. “I rarely see a loss in response from a reduced dosage of ibrutinib,” he said.
Because ibrutinib is primarily metabolized via the liver enzyme cytochrome P450 3A (CYP3A), other drugs that enhance or reduce the activity of this enzyme produce significant changes in ibrutinib levels. The Food and Drug Administration considers ibrutinib a “sensitive substrate” for fluctuations in CYP3A activity. Strong CYP3A inhibitors include clarithromycin, ketoconazole, and various anti-HIV medications; moderate CYP3A4 inhibitors include ciprofloxacin, and verapamil; and inducers of CYP3A include phenytoin and rifampin. A more complete list of the drugs that inhibit or induce CYP3A activity can be found at the FDA website: https://www.fda.gov/Drugs/DevelopmentApprovalProcess/DevelopmentResources/DrugInteractionsLabeling/ucm093664.htm#table2-2.
Dr. Call presented the combined experience from several U.S. Mayo Clinic centers for 118 patients treated with ibrutinib after the drug received FDA marketing approval in November 2013. The clinicians identified 75 patients (64%) who were on a concurrent medication that could potentially increase the risk for ibrutinib toxicity and 4 patients (3%) who were on a concurrent drug with the potential to reduce ibrutinib efficacy (Leukemia Lymphoma, 2017;58[6]:1376-83).
“We don’t change the dosage of ibrutinib when the patient is on a CYP3A inducer, but, if the patient is getting a CYP3A inhibitor, we change that to another drug or reduce the ibrutinib dosage,” Dr. Call said.
Dr. Call had no disclosures.
[email protected]
On Twitter @mitchelzoler
NEW YORK – New, targeted treatments, especially ibrutinib (Imbruvica), have sharply shifted prognosis for patients with chronic lymphocytic leukemia (CLL) and raised new issues for managing these patients now that they survive years longer.
“Ibrutinib has produced a profound change in survival” of patients with CLL, Timothy G. Call, MD, a hematologist/oncologist at the Mayo Clinic in Rochester, Minn., said at a conference held by Imedex. It “has changed the playing field.” No other new agent so far “has produced the same level of progression-free survival in CLL.”
An analysis published in early 2017 projected a greater than 50% jump in U.S. patients living with CLL from 2011, before the advent of targeted oral drugs, to 2025, when the study predicted that there will be nearly 200,000 U.S. patients living with CLL (J Clin Oncol. 2017 January;35[2]:166-74). With targeted drugs like ibrutinib and idelalisib (Zydelig) costing about $130,000 per patient each year, the projected cost for managing the U.S. CLL population is on track to rise to more than $5 billion by 2025, a nearly sixfold increase, compared with CLL patient expenditures in 2011, according to this analysis.
The impact of the higher cost of treatment is already being felt more acutely by many patients because of recent cuts in assistance from the Patient Access Network, which helps patients with copays but recently had to put a lid on CLL assistance availability when its funding availability hit a wall, Dr. Call said.
On the clinical side, there are new considerations triggered by greater patient longevity. “As we make patients live longer with CLL, we need to double down on the diagnosis and treatment of its complications,” such as watching for development of secondary cancers, Dr. Call said in an interview. This stems from the reduced immunosurveillance in patients with CLL and their resulting increased susceptibility to developing environmentally-triggered malignancies like lung and skin cancers. Other long-term implications of impaired immunosurveillance include increased infection susceptibility, an ongoing risk for Richter’s or Hodgkin lymphoma transformation, and a risk for autoimmune complications, such as red blood cell aplasia and transfusion-associated graft versus host disease.
Patients with CLL can also be susceptible to complications from long-term use of the targeted drug they’re on. The new targeted agents can trigger bruising and bleeding, diarrhea, rash, fatigue, muscle and joint aches, and arrhythmia, he noted.
Potential adverse effects, specifically from ibrutinib, include a 3% risk for a major bleed, a 10% rate of new-onset atrial fibrillation, and a 20% risk for new hypertension, Dr. Call said. Before starting ibrutinib, patients should undergo screening for hepatitis B virus infection and receive prophylaxis against herpes zoster activation with acyclovir or valacyclovir. If the patient starts with a CD4 cell count below 200 cells/mm3, it might be prudent to prophylax the patient against Pneumocystis jirovecii pneumonia.
However, even if a toxicity develops on ibrutinib, Dr. Call recommended reducing the dosage rather than discontinuing the drug. “I rarely see a loss in response from a reduced dosage of ibrutinib,” he said.
Because ibrutinib is primarily metabolized via the liver enzyme cytochrome P450 3A (CYP3A), other drugs that enhance or reduce the activity of this enzyme produce significant changes in ibrutinib levels. The Food and Drug Administration considers ibrutinib a “sensitive substrate” for fluctuations in CYP3A activity. Strong CYP3A inhibitors include clarithromycin, ketoconazole, and various anti-HIV medications; moderate CYP3A4 inhibitors include ciprofloxacin, and verapamil; and inducers of CYP3A include phenytoin and rifampin. A more complete list of the drugs that inhibit or induce CYP3A activity can be found at the FDA website: https://www.fda.gov/Drugs/DevelopmentApprovalProcess/DevelopmentResources/DrugInteractionsLabeling/ucm093664.htm#table2-2.
Dr. Call presented the combined experience from several U.S. Mayo Clinic centers for 118 patients treated with ibrutinib after the drug received FDA marketing approval in November 2013. The clinicians identified 75 patients (64%) who were on a concurrent medication that could potentially increase the risk for ibrutinib toxicity and 4 patients (3%) who were on a concurrent drug with the potential to reduce ibrutinib efficacy (Leukemia Lymphoma, 2017;58[6]:1376-83).
“We don’t change the dosage of ibrutinib when the patient is on a CYP3A inducer, but, if the patient is getting a CYP3A inhibitor, we change that to another drug or reduce the ibrutinib dosage,” Dr. Call said.
Dr. Call had no disclosures.
[email protected]
On Twitter @mitchelzoler
NEW YORK – New, targeted treatments, especially ibrutinib (Imbruvica), have sharply shifted prognosis for patients with chronic lymphocytic leukemia (CLL) and raised new issues for managing these patients now that they survive years longer.
“Ibrutinib has produced a profound change in survival” of patients with CLL, Timothy G. Call, MD, a hematologist/oncologist at the Mayo Clinic in Rochester, Minn., said at a conference held by Imedex. It “has changed the playing field.” No other new agent so far “has produced the same level of progression-free survival in CLL.”
An analysis published in early 2017 projected a greater than 50% jump in U.S. patients living with CLL from 2011, before the advent of targeted oral drugs, to 2025, when the study predicted that there will be nearly 200,000 U.S. patients living with CLL (J Clin Oncol. 2017 January;35[2]:166-74). With targeted drugs like ibrutinib and idelalisib (Zydelig) costing about $130,000 per patient each year, the projected cost for managing the U.S. CLL population is on track to rise to more than $5 billion by 2025, a nearly sixfold increase, compared with CLL patient expenditures in 2011, according to this analysis.
The impact of the higher cost of treatment is already being felt more acutely by many patients because of recent cuts in assistance from the Patient Access Network, which helps patients with copays but recently had to put a lid on CLL assistance availability when its funding availability hit a wall, Dr. Call said.
On the clinical side, there are new considerations triggered by greater patient longevity. “As we make patients live longer with CLL, we need to double down on the diagnosis and treatment of its complications,” such as watching for development of secondary cancers, Dr. Call said in an interview. This stems from the reduced immunosurveillance in patients with CLL and their resulting increased susceptibility to developing environmentally-triggered malignancies like lung and skin cancers. Other long-term implications of impaired immunosurveillance include increased infection susceptibility, an ongoing risk for Richter’s or Hodgkin lymphoma transformation, and a risk for autoimmune complications, such as red blood cell aplasia and transfusion-associated graft versus host disease.
Patients with CLL can also be susceptible to complications from long-term use of the targeted drug they’re on. The new targeted agents can trigger bruising and bleeding, diarrhea, rash, fatigue, muscle and joint aches, and arrhythmia, he noted.
Potential adverse effects, specifically from ibrutinib, include a 3% risk for a major bleed, a 10% rate of new-onset atrial fibrillation, and a 20% risk for new hypertension, Dr. Call said. Before starting ibrutinib, patients should undergo screening for hepatitis B virus infection and receive prophylaxis against herpes zoster activation with acyclovir or valacyclovir. If the patient starts with a CD4 cell count below 200 cells/mm3, it might be prudent to prophylax the patient against Pneumocystis jirovecii pneumonia.
However, even if a toxicity develops on ibrutinib, Dr. Call recommended reducing the dosage rather than discontinuing the drug. “I rarely see a loss in response from a reduced dosage of ibrutinib,” he said.
Because ibrutinib is primarily metabolized via the liver enzyme cytochrome P450 3A (CYP3A), other drugs that enhance or reduce the activity of this enzyme produce significant changes in ibrutinib levels. The Food and Drug Administration considers ibrutinib a “sensitive substrate” for fluctuations in CYP3A activity. Strong CYP3A inhibitors include clarithromycin, ketoconazole, and various anti-HIV medications; moderate CYP3A4 inhibitors include ciprofloxacin, and verapamil; and inducers of CYP3A include phenytoin and rifampin. A more complete list of the drugs that inhibit or induce CYP3A activity can be found at the FDA website: https://www.fda.gov/Drugs/DevelopmentApprovalProcess/DevelopmentResources/DrugInteractionsLabeling/ucm093664.htm#table2-2.
Dr. Call presented the combined experience from several U.S. Mayo Clinic centers for 118 patients treated with ibrutinib after the drug received FDA marketing approval in November 2013. The clinicians identified 75 patients (64%) who were on a concurrent medication that could potentially increase the risk for ibrutinib toxicity and 4 patients (3%) who were on a concurrent drug with the potential to reduce ibrutinib efficacy (Leukemia Lymphoma, 2017;58[6]:1376-83).
“We don’t change the dosage of ibrutinib when the patient is on a CYP3A inducer, but, if the patient is getting a CYP3A inhibitor, we change that to another drug or reduce the ibrutinib dosage,” Dr. Call said.
Dr. Call had no disclosures.
[email protected]
On Twitter @mitchelzoler
CHMP recommends inotuzumab ozogamicin for adult ALL
The European Medicines Agency’s Committee for Medicinal Products for Human Use (CHMP) has adopted a positive opinion of inotuzumab ozogamicin (Besponsa®).
The CHMP is recommending approval of inotuzumab ozogamicin for the treatment of adults with relapsed or refractory CD22-positive B-cell precursor acute lymphoblastic leukemia (ALL), including patients with Philadelphia chromosome-positive ALL who have failed treatment with at least one tyrosine kinase inhibitor.
The CHMP’s opinion will be reviewed by the European Commission, which is expected to issue a decision on approval within 67 days from adoption of the opinion.
Inotuzumab ozogamicin is an antibody-drug conjugate that consists of a monoclonal antibody targeting CD22 and a cytotoxic agent known as calicheamicin.
The product originates from a collaboration between Pfizer and Celltech (now UCB), but Pfizer has sole responsibility for all manufacturing and clinical development activities.
The application for inotuzumab ozogamicin is supported by results from a phase 3 trial, which were published in NEJM in June 2016.
The trial enrolled 326 adult patients with relapsed or refractory B-cell ALL and compared inotuzumab ozogamicin to standard of care chemotherapy.
The rate of complete remission, including incomplete hematologic recovery, was 80.7% in the inotuzumab ozogamicin arm and 29.4% in the chemotherapy arm (P<0.001). The median duration of remission was 4.6 months and 3.1 months, respectively (P=0.03).
Forty-one percent of patients treated with inotuzumab ozogamicin and 11% of those who received chemotherapy proceeded to stem cell transplant directly after treatment (P<0.001).
The median progression-free survival was 5.0 months in the inotuzumab ozogamicin arm and 1.8 months in the chemotherapy arm (P<0.001).
The median overall survival was 7.7 months and 6.7 months, respectively (P=0.04). This did not meet the prespecified boundary of significance (P=0.0208).
Liver-related adverse events were more common in the inotuzumab ozogamicin arm than the chemotherapy arm. The most frequent of these were increased aspartate aminotransferase level (20% vs 10%), hyperbilirubinemia (15% vs 10%), and increased alanine aminotransferase level (14% vs 11%).
Veno-occlusive liver disease occurred in 11% of patients in the inotuzumab ozogamicin arm and 1% in the chemotherapy arm.
There were 17 deaths during treatment in the inotuzumab ozogamicin arm and 11 in the chemotherapy arm. Four deaths were considered related to inotuzumab ozogamicin, and 2 were thought to be related to chemotherapy. ![]()
The European Medicines Agency’s Committee for Medicinal Products for Human Use (CHMP) has adopted a positive opinion of inotuzumab ozogamicin (Besponsa®).
The CHMP is recommending approval of inotuzumab ozogamicin for the treatment of adults with relapsed or refractory CD22-positive B-cell precursor acute lymphoblastic leukemia (ALL), including patients with Philadelphia chromosome-positive ALL who have failed treatment with at least one tyrosine kinase inhibitor.
The CHMP’s opinion will be reviewed by the European Commission, which is expected to issue a decision on approval within 67 days from adoption of the opinion.
Inotuzumab ozogamicin is an antibody-drug conjugate that consists of a monoclonal antibody targeting CD22 and a cytotoxic agent known as calicheamicin.
The product originates from a collaboration between Pfizer and Celltech (now UCB), but Pfizer has sole responsibility for all manufacturing and clinical development activities.
The application for inotuzumab ozogamicin is supported by results from a phase 3 trial, which were published in NEJM in June 2016.
The trial enrolled 326 adult patients with relapsed or refractory B-cell ALL and compared inotuzumab ozogamicin to standard of care chemotherapy.
The rate of complete remission, including incomplete hematologic recovery, was 80.7% in the inotuzumab ozogamicin arm and 29.4% in the chemotherapy arm (P<0.001). The median duration of remission was 4.6 months and 3.1 months, respectively (P=0.03).
Forty-one percent of patients treated with inotuzumab ozogamicin and 11% of those who received chemotherapy proceeded to stem cell transplant directly after treatment (P<0.001).
The median progression-free survival was 5.0 months in the inotuzumab ozogamicin arm and 1.8 months in the chemotherapy arm (P<0.001).
The median overall survival was 7.7 months and 6.7 months, respectively (P=0.04). This did not meet the prespecified boundary of significance (P=0.0208).
Liver-related adverse events were more common in the inotuzumab ozogamicin arm than the chemotherapy arm. The most frequent of these were increased aspartate aminotransferase level (20% vs 10%), hyperbilirubinemia (15% vs 10%), and increased alanine aminotransferase level (14% vs 11%).
Veno-occlusive liver disease occurred in 11% of patients in the inotuzumab ozogamicin arm and 1% in the chemotherapy arm.
There were 17 deaths during treatment in the inotuzumab ozogamicin arm and 11 in the chemotherapy arm. Four deaths were considered related to inotuzumab ozogamicin, and 2 were thought to be related to chemotherapy. ![]()
The European Medicines Agency’s Committee for Medicinal Products for Human Use (CHMP) has adopted a positive opinion of inotuzumab ozogamicin (Besponsa®).
The CHMP is recommending approval of inotuzumab ozogamicin for the treatment of adults with relapsed or refractory CD22-positive B-cell precursor acute lymphoblastic leukemia (ALL), including patients with Philadelphia chromosome-positive ALL who have failed treatment with at least one tyrosine kinase inhibitor.
The CHMP’s opinion will be reviewed by the European Commission, which is expected to issue a decision on approval within 67 days from adoption of the opinion.
Inotuzumab ozogamicin is an antibody-drug conjugate that consists of a monoclonal antibody targeting CD22 and a cytotoxic agent known as calicheamicin.
The product originates from a collaboration between Pfizer and Celltech (now UCB), but Pfizer has sole responsibility for all manufacturing and clinical development activities.
The application for inotuzumab ozogamicin is supported by results from a phase 3 trial, which were published in NEJM in June 2016.
The trial enrolled 326 adult patients with relapsed or refractory B-cell ALL and compared inotuzumab ozogamicin to standard of care chemotherapy.
The rate of complete remission, including incomplete hematologic recovery, was 80.7% in the inotuzumab ozogamicin arm and 29.4% in the chemotherapy arm (P<0.001). The median duration of remission was 4.6 months and 3.1 months, respectively (P=0.03).
Forty-one percent of patients treated with inotuzumab ozogamicin and 11% of those who received chemotherapy proceeded to stem cell transplant directly after treatment (P<0.001).
The median progression-free survival was 5.0 months in the inotuzumab ozogamicin arm and 1.8 months in the chemotherapy arm (P<0.001).
The median overall survival was 7.7 months and 6.7 months, respectively (P=0.04). This did not meet the prespecified boundary of significance (P=0.0208).
Liver-related adverse events were more common in the inotuzumab ozogamicin arm than the chemotherapy arm. The most frequent of these were increased aspartate aminotransferase level (20% vs 10%), hyperbilirubinemia (15% vs 10%), and increased alanine aminotransferase level (14% vs 11%).
Veno-occlusive liver disease occurred in 11% of patients in the inotuzumab ozogamicin arm and 1% in the chemotherapy arm.
There were 17 deaths during treatment in the inotuzumab ozogamicin arm and 11 in the chemotherapy arm. Four deaths were considered related to inotuzumab ozogamicin, and 2 were thought to be related to chemotherapy. ![]()
ALL, HL guidelines added to radiation therapy resource
The National Comprehensive Cancer Network® (NCCN) has added 9 disease sites to its NCCN Radiation Therapy Compendium™, a resource that provides a single access point for NCCN recommendations pertaining to radiation therapy (RT).
The compendium provides guidance on all RT modalities recommended within NCCN guidelines, including intensity modulated RT, intra-operative RT, stereotactic radiosurgery/stereotactic body RT/stereotactic ablative RT, image-guided RT, low dose-rate brachytherapy/high dose-rate brachytherapy, radioisotope, and particle therapy.
The NCCN Radiation Therapy Compendium was launched with recommendations pertaining to 24 cancer types.
Now, NCCN has added RT recommendations from an additional 9 NCCN Clinical Practice Guidelines in Oncology:
Acute lymphoblastic leukemia (ALL), Version 2.2016
Basal cell skin cancer, Version 1.2017
Dermatofibrosarcoma protuberans, Version 1.2017
Gastric cancer, Version 1.2017
Hodgkin lymphoma (HL), Version 1.2017
Merkel cell carcinoma, Version 1.2017
Ovarian cancer, Version 1.2017
Squamous cell skin cancer, Version 1.2017
Thymomas and thymic carcinomas, Version 1.2017
The first 24 disease sites included in the NCCN Radiation Therapy Compendium were:
Acute myeloid leukemia
Anal cancer
B-cell lymphomas
Bladder cancer
Breast cancer
Chronic lymphocytic leukemia/small lymphoblastic lymphoma
Colon cancer
Hepatobiliary cancers
Kidney cancer
Malignant pleural mesothelioma
Melanoma
Multiple myeloma
Neuroendocrine tumors
Non-small cell lung cancer
Occult primary cancer
Pancreatic adenocarcinoma
Penile cancer
Primary cutaneous B-cell lymphomas
Prostate cancer
Rectal cancer
Small cell lung cancer
Soft tissue sarcoma
T-cell lymphomas
Testicular cancer
The NCCN said additional cancer types will be added to the NCCN Radiation Therapy Compendium on a rolling basis over the coming months.
For more information and to access the NCCN Radiation Therapy Compendium, visit NCCN.org/RTCompendium. ![]()
The National Comprehensive Cancer Network® (NCCN) has added 9 disease sites to its NCCN Radiation Therapy Compendium™, a resource that provides a single access point for NCCN recommendations pertaining to radiation therapy (RT).
The compendium provides guidance on all RT modalities recommended within NCCN guidelines, including intensity modulated RT, intra-operative RT, stereotactic radiosurgery/stereotactic body RT/stereotactic ablative RT, image-guided RT, low dose-rate brachytherapy/high dose-rate brachytherapy, radioisotope, and particle therapy.
The NCCN Radiation Therapy Compendium was launched with recommendations pertaining to 24 cancer types.
Now, NCCN has added RT recommendations from an additional 9 NCCN Clinical Practice Guidelines in Oncology:
Acute lymphoblastic leukemia (ALL), Version 2.2016
Basal cell skin cancer, Version 1.2017
Dermatofibrosarcoma protuberans, Version 1.2017
Gastric cancer, Version 1.2017
Hodgkin lymphoma (HL), Version 1.2017
Merkel cell carcinoma, Version 1.2017
Ovarian cancer, Version 1.2017
Squamous cell skin cancer, Version 1.2017
Thymomas and thymic carcinomas, Version 1.2017
The first 24 disease sites included in the NCCN Radiation Therapy Compendium were:
Acute myeloid leukemia
Anal cancer
B-cell lymphomas
Bladder cancer
Breast cancer
Chronic lymphocytic leukemia/small lymphoblastic lymphoma
Colon cancer
Hepatobiliary cancers
Kidney cancer
Malignant pleural mesothelioma
Melanoma
Multiple myeloma
Neuroendocrine tumors
Non-small cell lung cancer
Occult primary cancer
Pancreatic adenocarcinoma
Penile cancer
Primary cutaneous B-cell lymphomas
Prostate cancer
Rectal cancer
Small cell lung cancer
Soft tissue sarcoma
T-cell lymphomas
Testicular cancer
The NCCN said additional cancer types will be added to the NCCN Radiation Therapy Compendium on a rolling basis over the coming months.
For more information and to access the NCCN Radiation Therapy Compendium, visit NCCN.org/RTCompendium. ![]()
The National Comprehensive Cancer Network® (NCCN) has added 9 disease sites to its NCCN Radiation Therapy Compendium™, a resource that provides a single access point for NCCN recommendations pertaining to radiation therapy (RT).
The compendium provides guidance on all RT modalities recommended within NCCN guidelines, including intensity modulated RT, intra-operative RT, stereotactic radiosurgery/stereotactic body RT/stereotactic ablative RT, image-guided RT, low dose-rate brachytherapy/high dose-rate brachytherapy, radioisotope, and particle therapy.
The NCCN Radiation Therapy Compendium was launched with recommendations pertaining to 24 cancer types.
Now, NCCN has added RT recommendations from an additional 9 NCCN Clinical Practice Guidelines in Oncology:
Acute lymphoblastic leukemia (ALL), Version 2.2016
Basal cell skin cancer, Version 1.2017
Dermatofibrosarcoma protuberans, Version 1.2017
Gastric cancer, Version 1.2017
Hodgkin lymphoma (HL), Version 1.2017
Merkel cell carcinoma, Version 1.2017
Ovarian cancer, Version 1.2017
Squamous cell skin cancer, Version 1.2017
Thymomas and thymic carcinomas, Version 1.2017
The first 24 disease sites included in the NCCN Radiation Therapy Compendium were:
Acute myeloid leukemia
Anal cancer
B-cell lymphomas
Bladder cancer
Breast cancer
Chronic lymphocytic leukemia/small lymphoblastic lymphoma
Colon cancer
Hepatobiliary cancers
Kidney cancer
Malignant pleural mesothelioma
Melanoma
Multiple myeloma
Neuroendocrine tumors
Non-small cell lung cancer
Occult primary cancer
Pancreatic adenocarcinoma
Penile cancer
Primary cutaneous B-cell lymphomas
Prostate cancer
Rectal cancer
Small cell lung cancer
Soft tissue sarcoma
T-cell lymphomas
Testicular cancer
The NCCN said additional cancer types will be added to the NCCN Radiation Therapy Compendium on a rolling basis over the coming months.
For more information and to access the NCCN Radiation Therapy Compendium, visit NCCN.org/RTCompendium. ![]()
Optimum antithymocyte globulin exposure after HTC affects survival
Optimum antithymocyte globulin exposure after allogeneic hemopoietic cell transplantation (HTC) is associated with a higher probability of survival as a result of reductions in transplant-related and relapse-related deaths, based on findings from a retrospective multicenter cohort study.
The findings come from a pharmacokinetic-pharmacodynamic analysis of data from 146 patients with acute lymphoid leukemia, acute myeloid leukemia, or myelodysplastic syndrome. All were receiving their first T cell–repleted allogeneic peripheral blood stem cell HCT with antithymocyte globulin (ATG) as part of their nonmyeloablative conditioning regimen. Based on hazard ratios for overall survival, nonrelapse mortality, and relapse-related mortality, the optimum range of ATG exposure was 60-95 arbitrary units per day/mL, Rick Admiraal, MD, of the University Medical Centre Utrecht, Netherlands, and his colleagues reported in the Lancet Haematology (Lancet Haematol. 2017 Apr;4[4]:e183-91).
The estimated 5-year survival was significantly greater with optimum ATG exposure than with below-optimum exposure (69% vs. 32%; hazard ratio, 2.41) or with above-optimum exposure (69% vs. 48%; hazard ratio, 2.11).
Optimum ATG exposure also was associated with a greater likelihood of event-free survival: The hazard ratio was 2.54 for those with below-optimum exposure and 1.83 for those with above-optimum exposure, the researchers said. Further, above-optimum exposure was associated with higher relapse-related mortality (hazard ratio, 2.66). Below-optimum exposure was associated with higher non-relapse mortality (hazard ratio, 4.36) as well as with a higher risk for grade 3-4 acute graft-versus-host disease (hazard ratio, 3.09), but not for chronic graft-versus-host disease (hazard ratio, 2.38).
Optimum target attainment was better with modeled dosing based on absolute lymphocyte counts than with weight-based dosing, the authors said.
The findings underscore the importance of optimum ATG dosing, as “survival after HCT is highly affected by ATG exposure after HCT,” and they suggest that survival chances may be improved with individualized dosing based on lymphocyte counts–a finding that requires assessment in a prospective study, they concluded.
This study was funded by the Dutch Organization for Scientific Research and the Queen Wilhelmina Fund for Cancer Research. Dr. Admiraal reported having no relevant disclosures.
The study by Dr. Admiraal and his associates introduces important concepts regarding ATG dosing, but the suggestion that dosing should be individualized based on lymphocyte count and should target the area under the time-versus-thymoglobulin-concentration curve of 60-95 arbitrary units per day/mL after HCT should not yet become the standard of care.
“As the authors correctly point out, first a prospective study is needed,” Dr. Storek wrote.
However, even if such a study confirms this approach – which the authors previously showed to be of benefit in children – it would apply only to the setting in which it was developed. The problem is that there are numerous HCT settings, each requiring a different dose. Further, there is no universally accepted assay for measuring thymoglobulin concentrations, he noted.
“Following the seminal observations in the paper … much work remains to be done,” he wrote.
Jan Storek, MD, is with the University of Calgary (Alta.) and Alberta Health Services, Calgary. He made his comments in an editorial (Lancet Haematol. 2017 Apr;4[4]:e154-5) published with the study and reported having no disclosures.
The study by Dr. Admiraal and his associates introduces important concepts regarding ATG dosing, but the suggestion that dosing should be individualized based on lymphocyte count and should target the area under the time-versus-thymoglobulin-concentration curve of 60-95 arbitrary units per day/mL after HCT should not yet become the standard of care.
“As the authors correctly point out, first a prospective study is needed,” Dr. Storek wrote.
However, even if such a study confirms this approach – which the authors previously showed to be of benefit in children – it would apply only to the setting in which it was developed. The problem is that there are numerous HCT settings, each requiring a different dose. Further, there is no universally accepted assay for measuring thymoglobulin concentrations, he noted.
“Following the seminal observations in the paper … much work remains to be done,” he wrote.
Jan Storek, MD, is with the University of Calgary (Alta.) and Alberta Health Services, Calgary. He made his comments in an editorial (Lancet Haematol. 2017 Apr;4[4]:e154-5) published with the study and reported having no disclosures.
The study by Dr. Admiraal and his associates introduces important concepts regarding ATG dosing, but the suggestion that dosing should be individualized based on lymphocyte count and should target the area under the time-versus-thymoglobulin-concentration curve of 60-95 arbitrary units per day/mL after HCT should not yet become the standard of care.
“As the authors correctly point out, first a prospective study is needed,” Dr. Storek wrote.
However, even if such a study confirms this approach – which the authors previously showed to be of benefit in children – it would apply only to the setting in which it was developed. The problem is that there are numerous HCT settings, each requiring a different dose. Further, there is no universally accepted assay for measuring thymoglobulin concentrations, he noted.
“Following the seminal observations in the paper … much work remains to be done,” he wrote.
Jan Storek, MD, is with the University of Calgary (Alta.) and Alberta Health Services, Calgary. He made his comments in an editorial (Lancet Haematol. 2017 Apr;4[4]:e154-5) published with the study and reported having no disclosures.
Optimum antithymocyte globulin exposure after allogeneic hemopoietic cell transplantation (HTC) is associated with a higher probability of survival as a result of reductions in transplant-related and relapse-related deaths, based on findings from a retrospective multicenter cohort study.
The findings come from a pharmacokinetic-pharmacodynamic analysis of data from 146 patients with acute lymphoid leukemia, acute myeloid leukemia, or myelodysplastic syndrome. All were receiving their first T cell–repleted allogeneic peripheral blood stem cell HCT with antithymocyte globulin (ATG) as part of their nonmyeloablative conditioning regimen. Based on hazard ratios for overall survival, nonrelapse mortality, and relapse-related mortality, the optimum range of ATG exposure was 60-95 arbitrary units per day/mL, Rick Admiraal, MD, of the University Medical Centre Utrecht, Netherlands, and his colleagues reported in the Lancet Haematology (Lancet Haematol. 2017 Apr;4[4]:e183-91).
The estimated 5-year survival was significantly greater with optimum ATG exposure than with below-optimum exposure (69% vs. 32%; hazard ratio, 2.41) or with above-optimum exposure (69% vs. 48%; hazard ratio, 2.11).
Optimum ATG exposure also was associated with a greater likelihood of event-free survival: The hazard ratio was 2.54 for those with below-optimum exposure and 1.83 for those with above-optimum exposure, the researchers said. Further, above-optimum exposure was associated with higher relapse-related mortality (hazard ratio, 2.66). Below-optimum exposure was associated with higher non-relapse mortality (hazard ratio, 4.36) as well as with a higher risk for grade 3-4 acute graft-versus-host disease (hazard ratio, 3.09), but not for chronic graft-versus-host disease (hazard ratio, 2.38).
Optimum target attainment was better with modeled dosing based on absolute lymphocyte counts than with weight-based dosing, the authors said.
The findings underscore the importance of optimum ATG dosing, as “survival after HCT is highly affected by ATG exposure after HCT,” and they suggest that survival chances may be improved with individualized dosing based on lymphocyte counts–a finding that requires assessment in a prospective study, they concluded.
This study was funded by the Dutch Organization for Scientific Research and the Queen Wilhelmina Fund for Cancer Research. Dr. Admiraal reported having no relevant disclosures.
Optimum antithymocyte globulin exposure after allogeneic hemopoietic cell transplantation (HTC) is associated with a higher probability of survival as a result of reductions in transplant-related and relapse-related deaths, based on findings from a retrospective multicenter cohort study.
The findings come from a pharmacokinetic-pharmacodynamic analysis of data from 146 patients with acute lymphoid leukemia, acute myeloid leukemia, or myelodysplastic syndrome. All were receiving their first T cell–repleted allogeneic peripheral blood stem cell HCT with antithymocyte globulin (ATG) as part of their nonmyeloablative conditioning regimen. Based on hazard ratios for overall survival, nonrelapse mortality, and relapse-related mortality, the optimum range of ATG exposure was 60-95 arbitrary units per day/mL, Rick Admiraal, MD, of the University Medical Centre Utrecht, Netherlands, and his colleagues reported in the Lancet Haematology (Lancet Haematol. 2017 Apr;4[4]:e183-91).
The estimated 5-year survival was significantly greater with optimum ATG exposure than with below-optimum exposure (69% vs. 32%; hazard ratio, 2.41) or with above-optimum exposure (69% vs. 48%; hazard ratio, 2.11).
Optimum ATG exposure also was associated with a greater likelihood of event-free survival: The hazard ratio was 2.54 for those with below-optimum exposure and 1.83 for those with above-optimum exposure, the researchers said. Further, above-optimum exposure was associated with higher relapse-related mortality (hazard ratio, 2.66). Below-optimum exposure was associated with higher non-relapse mortality (hazard ratio, 4.36) as well as with a higher risk for grade 3-4 acute graft-versus-host disease (hazard ratio, 3.09), but not for chronic graft-versus-host disease (hazard ratio, 2.38).
Optimum target attainment was better with modeled dosing based on absolute lymphocyte counts than with weight-based dosing, the authors said.
The findings underscore the importance of optimum ATG dosing, as “survival after HCT is highly affected by ATG exposure after HCT,” and they suggest that survival chances may be improved with individualized dosing based on lymphocyte counts–a finding that requires assessment in a prospective study, they concluded.
This study was funded by the Dutch Organization for Scientific Research and the Queen Wilhelmina Fund for Cancer Research. Dr. Admiraal reported having no relevant disclosures.
FROM THE LANCET HAEMATOLOGY
Key clinical point:
Major finding: The estimated 5-year survival with optimum ATG exposure was 69% vs. 32% and 48% with below- and above-optimum exposure (hazard ratios, 2.41 and 2.11, respectively).
Data source: A retrospective cohort study of 146 patients receiving their first T-cell repleted allogeneic peripheral blood stem cell HCT.
Disclosures: This study was funded by the Dutch Organization for Scientific Research and the Queen Wilhelmina Fund for Cancer Research. Dr. Admiraal reported having no disclosures.
Second cancers take greater toll on younger patients
Second cancers take a greater toll on patients under the age of 40, according to research published in JAMA Oncology.
Researchers studied 14 types of cancer occurring in more than 1 million patients.
For nearly all of the cancers studied, 5-year survival rates were much higher if the cancer occurred as a first malignancy rather than a second cancer.
These survival differences were more pronounced in pediatric patients and adolescents and young adults (AYAs) than they were in patients age 40 and older.
Researchers hope these findings will help guide clinicians in providing age-specific recommendations on cancer prevention, screening, treatment, and survivorship, especially among the AYA population.
“Although the increased incidence of second cancers is well known among cancer survivors, less is known about outcomes of these cancers or the influence of age,” said Theresa Keegan, PhD, of the UC Davis Comprehensive Cancer Center in Sacramento, California.
With this in mind, Dr Keegan and her colleagues analyzed data on patients diagnosed with either a single cancer or a first and second malignancy during 1992 through 2008. The researchers used Surveillance, Epidemiology and End Results program data collected from 13 cancer registries.
The team collected data on the 14 most common cancer types that affect AYAs: acute lymphoblastic leukemia (ALL), acute myeloid leukemia (AML), Hodgkin lymphoma (HL), non-Hodgkin lymphoma (NHL), soft tissue sarcoma, and bone sarcoma, as well as female breast, thyroid, testicular, colorectal, central nervous system, cervical, and ovarian cancers.
There were a total of 15,954 pediatric patients (younger than 15 years at diagnosis), 125,750 AYAs (ages 15 to 39), and 878,370 older adult patients (age 40 and older).
Survival rates
For pediatric patients, the 5-year relative survival was 80% for a first cancer and 47% for a second primary malignancy.
For AYAs, the 5-year relative survival was 81% for a first cancer and 60% for a second primary malignancy.
For older adults, the 5-year relative survival was 70% for a first cancer and 61% for a second primary malignancy.
When the researchers looked at 5-year survival by age and individual cancer types, they found striking differences depending on whether it was a first or second malignancy in all but 2 of the 14 cancer types, testicular cancer and melanoma.
“For almost every type of cancer, the AYA population did worse with a secondary cancer,” said study author Melanie Goldfarb, MD, of John Wayne Cancer Institute at Providence Saint John’s Health Center in Santa Monica, California.
“What struck us was that the second cancer caused such an increased risk of death.”
Lymphomas
For pediatric patients with HL, the 5-year relative survival was 95% when patients had HL as a first cancer. There were no data on HL as a second primary malignancy.
For AYAs, the 5-year relative survival was 93% when patients had HL as a first cancer and 72% when they had HL as a second primary malignancy.
For older adults, the 5-year relative survival was 69% when patients had HL as a first cancer and 54% when they had HL as a second primary malignancy.
For pediatric patients with NHL, the 5-year relative survival was 84% when patients had NHL as a first cancer and 63% when they had NHL as a second primary malignancy.
For AYAs, the 5-year relative survival was 64% when patients had NHL as a first cancer and 22% when they had NHL as a second primary malignancy.
For older adults, the 5-year relative survival was 57% when patients had NHL as a first cancer and 54% when they had NHL as a second primary malignancy.
Leukemias
For pediatric patients with ALL, the 5-year relative survival was 87% when patients had ALL as a first cancer and 63% when they had ALL as a second primary malignancy.
For AYAs, the 5-year relative survival was 48% when patients had ALL as a first cancer and 26% when they had ALL as a second primary malignancy.
For older adults, the 5-year relative survival was 17% when patients had ALL as a first cancer and 11% when they had ALL as a second primary malignancy.
For pediatric patients with AML, the 5-year relative survival was 57% when patients had AML as a first cancer and 29% when they had AML as a second primary malignancy.
For AYAs, the 5-year relative survival was 46% when patients had AML as a first cancer and 23% when they had AML as a second primary malignancy.
For older adults, the 5-year relative survival was 12% when patients had AML as a first cancer and 10% when they had AML as a second primary malignancy.
Why younger patients tend to fare worse after a second cancer than older patients is not fully understood or specifically addressed in the current study, the researchers noted.
Now, the team plans to examine how the time between getting a first and second cancer affects survival and whether the type of treatment for the first cancer influences the outcome of a second cancer. ![]()
Second cancers take a greater toll on patients under the age of 40, according to research published in JAMA Oncology.
Researchers studied 14 types of cancer occurring in more than 1 million patients.
For nearly all of the cancers studied, 5-year survival rates were much higher if the cancer occurred as a first malignancy rather than a second cancer.
These survival differences were more pronounced in pediatric patients and adolescents and young adults (AYAs) than they were in patients age 40 and older.
Researchers hope these findings will help guide clinicians in providing age-specific recommendations on cancer prevention, screening, treatment, and survivorship, especially among the AYA population.
“Although the increased incidence of second cancers is well known among cancer survivors, less is known about outcomes of these cancers or the influence of age,” said Theresa Keegan, PhD, of the UC Davis Comprehensive Cancer Center in Sacramento, California.
With this in mind, Dr Keegan and her colleagues analyzed data on patients diagnosed with either a single cancer or a first and second malignancy during 1992 through 2008. The researchers used Surveillance, Epidemiology and End Results program data collected from 13 cancer registries.
The team collected data on the 14 most common cancer types that affect AYAs: acute lymphoblastic leukemia (ALL), acute myeloid leukemia (AML), Hodgkin lymphoma (HL), non-Hodgkin lymphoma (NHL), soft tissue sarcoma, and bone sarcoma, as well as female breast, thyroid, testicular, colorectal, central nervous system, cervical, and ovarian cancers.
There were a total of 15,954 pediatric patients (younger than 15 years at diagnosis), 125,750 AYAs (ages 15 to 39), and 878,370 older adult patients (age 40 and older).
Survival rates
For pediatric patients, the 5-year relative survival was 80% for a first cancer and 47% for a second primary malignancy.
For AYAs, the 5-year relative survival was 81% for a first cancer and 60% for a second primary malignancy.
For older adults, the 5-year relative survival was 70% for a first cancer and 61% for a second primary malignancy.
When the researchers looked at 5-year survival by age and individual cancer types, they found striking differences depending on whether it was a first or second malignancy in all but 2 of the 14 cancer types, testicular cancer and melanoma.
“For almost every type of cancer, the AYA population did worse with a secondary cancer,” said study author Melanie Goldfarb, MD, of John Wayne Cancer Institute at Providence Saint John’s Health Center in Santa Monica, California.
“What struck us was that the second cancer caused such an increased risk of death.”
Lymphomas
For pediatric patients with HL, the 5-year relative survival was 95% when patients had HL as a first cancer. There were no data on HL as a second primary malignancy.
For AYAs, the 5-year relative survival was 93% when patients had HL as a first cancer and 72% when they had HL as a second primary malignancy.
For older adults, the 5-year relative survival was 69% when patients had HL as a first cancer and 54% when they had HL as a second primary malignancy.
For pediatric patients with NHL, the 5-year relative survival was 84% when patients had NHL as a first cancer and 63% when they had NHL as a second primary malignancy.
For AYAs, the 5-year relative survival was 64% when patients had NHL as a first cancer and 22% when they had NHL as a second primary malignancy.
For older adults, the 5-year relative survival was 57% when patients had NHL as a first cancer and 54% when they had NHL as a second primary malignancy.
Leukemias
For pediatric patients with ALL, the 5-year relative survival was 87% when patients had ALL as a first cancer and 63% when they had ALL as a second primary malignancy.
For AYAs, the 5-year relative survival was 48% when patients had ALL as a first cancer and 26% when they had ALL as a second primary malignancy.
For older adults, the 5-year relative survival was 17% when patients had ALL as a first cancer and 11% when they had ALL as a second primary malignancy.
For pediatric patients with AML, the 5-year relative survival was 57% when patients had AML as a first cancer and 29% when they had AML as a second primary malignancy.
For AYAs, the 5-year relative survival was 46% when patients had AML as a first cancer and 23% when they had AML as a second primary malignancy.
For older adults, the 5-year relative survival was 12% when patients had AML as a first cancer and 10% when they had AML as a second primary malignancy.
Why younger patients tend to fare worse after a second cancer than older patients is not fully understood or specifically addressed in the current study, the researchers noted.
Now, the team plans to examine how the time between getting a first and second cancer affects survival and whether the type of treatment for the first cancer influences the outcome of a second cancer. ![]()
Second cancers take a greater toll on patients under the age of 40, according to research published in JAMA Oncology.
Researchers studied 14 types of cancer occurring in more than 1 million patients.
For nearly all of the cancers studied, 5-year survival rates were much higher if the cancer occurred as a first malignancy rather than a second cancer.
These survival differences were more pronounced in pediatric patients and adolescents and young adults (AYAs) than they were in patients age 40 and older.
Researchers hope these findings will help guide clinicians in providing age-specific recommendations on cancer prevention, screening, treatment, and survivorship, especially among the AYA population.
“Although the increased incidence of second cancers is well known among cancer survivors, less is known about outcomes of these cancers or the influence of age,” said Theresa Keegan, PhD, of the UC Davis Comprehensive Cancer Center in Sacramento, California.
With this in mind, Dr Keegan and her colleagues analyzed data on patients diagnosed with either a single cancer or a first and second malignancy during 1992 through 2008. The researchers used Surveillance, Epidemiology and End Results program data collected from 13 cancer registries.
The team collected data on the 14 most common cancer types that affect AYAs: acute lymphoblastic leukemia (ALL), acute myeloid leukemia (AML), Hodgkin lymphoma (HL), non-Hodgkin lymphoma (NHL), soft tissue sarcoma, and bone sarcoma, as well as female breast, thyroid, testicular, colorectal, central nervous system, cervical, and ovarian cancers.
There were a total of 15,954 pediatric patients (younger than 15 years at diagnosis), 125,750 AYAs (ages 15 to 39), and 878,370 older adult patients (age 40 and older).
Survival rates
For pediatric patients, the 5-year relative survival was 80% for a first cancer and 47% for a second primary malignancy.
For AYAs, the 5-year relative survival was 81% for a first cancer and 60% for a second primary malignancy.
For older adults, the 5-year relative survival was 70% for a first cancer and 61% for a second primary malignancy.
When the researchers looked at 5-year survival by age and individual cancer types, they found striking differences depending on whether it was a first or second malignancy in all but 2 of the 14 cancer types, testicular cancer and melanoma.
“For almost every type of cancer, the AYA population did worse with a secondary cancer,” said study author Melanie Goldfarb, MD, of John Wayne Cancer Institute at Providence Saint John’s Health Center in Santa Monica, California.
“What struck us was that the second cancer caused such an increased risk of death.”
Lymphomas
For pediatric patients with HL, the 5-year relative survival was 95% when patients had HL as a first cancer. There were no data on HL as a second primary malignancy.
For AYAs, the 5-year relative survival was 93% when patients had HL as a first cancer and 72% when they had HL as a second primary malignancy.
For older adults, the 5-year relative survival was 69% when patients had HL as a first cancer and 54% when they had HL as a second primary malignancy.
For pediatric patients with NHL, the 5-year relative survival was 84% when patients had NHL as a first cancer and 63% when they had NHL as a second primary malignancy.
For AYAs, the 5-year relative survival was 64% when patients had NHL as a first cancer and 22% when they had NHL as a second primary malignancy.
For older adults, the 5-year relative survival was 57% when patients had NHL as a first cancer and 54% when they had NHL as a second primary malignancy.
Leukemias
For pediatric patients with ALL, the 5-year relative survival was 87% when patients had ALL as a first cancer and 63% when they had ALL as a second primary malignancy.
For AYAs, the 5-year relative survival was 48% when patients had ALL as a first cancer and 26% when they had ALL as a second primary malignancy.
For older adults, the 5-year relative survival was 17% when patients had ALL as a first cancer and 11% when they had ALL as a second primary malignancy.
For pediatric patients with AML, the 5-year relative survival was 57% when patients had AML as a first cancer and 29% when they had AML as a second primary malignancy.
For AYAs, the 5-year relative survival was 46% when patients had AML as a first cancer and 23% when they had AML as a second primary malignancy.
For older adults, the 5-year relative survival was 12% when patients had AML as a first cancer and 10% when they had AML as a second primary malignancy.
Why younger patients tend to fare worse after a second cancer than older patients is not fully understood or specifically addressed in the current study, the researchers noted.
Now, the team plans to examine how the time between getting a first and second cancer affects survival and whether the type of treatment for the first cancer influences the outcome of a second cancer.