User login
Updated CLL guidelines incorporate a decade of advances
include new and revised recommendations based on major advances in genomics, targeted therapies, and biomarkers that have occurred since the last iteration in 2008.
The guidelines are an update from a consensus document issued a decade ago by the International Workshop on CLL, focusing on the conduct of clinical trials in patients with CLL. The new guidelines are published in Blood.
Major changes or additions include:
Molecular genetics: The updated guidelines recognize the clinical importance of specific genomic alterations/mutations on response to standard chemotherapy or chemoimmunotherapy, including the 17p deletion and mutations in TP53.
“Therefore, the assessment of both del(17p) and TP53 mutation has prognostic and predictive value and should guide therapeutic decisions in routine practice. For clinical trials, it is recommended that molecular genetics be performed prior to treating a patient on protocol,” the guidelines state.
IGHV mutational status: The mutational status of immunoglobulin variable heavy chain (IGHV) genes has been demonstrated to offer important prognostic information, according to the guidelines authors led by Michael Hallek, MD of the University of Cologne, Germany.
Specifically, leukemia with IGHV genes without somatic mutations are associated with worse clinical outcomes, compared with leukemia with IGHV mutations. Patients with mutated IGHV and other prognostic factors such as favorable cytogenetics or minimal residual disease (MRD) negativity generally have excellent outcomes with a chemoimmunotherapy regimen consisting of fludarabine, cyclophosphamide, and rituximab, the authors noted.
Biomarkers: The guidelines call for standardization and use in prospective clinical trials of assays for serum markers such as soluble CD23, thymidine kinase, and beta-2-microglobulin. These markers have been shown in several studies to be associated with overall survival or progression-free survival, and of these markers, beta-2-microglobulin “has retained independent prognostic value in several multiparameter scores,” the guidelines state.
The authors also tip their hats to recently developed or improved prognostic scores, especially the CLL International Prognostic Index (CLL-IPI), which incorporates clinical stage, age, IGHV mutational status, beta-2-microglobulin, and del(17p) and/or TP53 mutations.
Organ function assessment: Not new, but improved in the current version of the guidelines, are recommendations for evaluation of splenomegaly, hepatomegaly, and lymphadenopathy in response assessment. These recommendations were harmonized with the relevant sections of the updated lymphoma response guidelines.
Continuous therapy: The guidelines panel recommends assessment of response duration during continuous therapy with oral agents and after the end of therapy, especially after chemotherapy or chemoimmunotherapy.
“Study protocols should provide detailed specifications of the planned time points for the assessment of the treatment response under continuous therapy. Response durations of less than six months are not considered clinically relevant,” the panel cautioned.
Response assessments for treatments with a maintenance phase should be performed at a minimum of 2 months after patients achieve their best responses.
MRD: The guidelines call for minimal residual disease (MRD) assessment in clinical trials aimed at maximizing remission depth, with emphasis on reporting the sensitivity of the MRD evaluation method used, and the type of tissue assessed.
Antiviral prophylaxis: The guidelines caution that because patients treated with anti-CD20 antibodies, such as rituximab or obinutuzumab, could have reactivation of hepatitis B virus (HBV) infections, patients should be tested for HBV serological status before starting on an anti-CD20 agent.
“Progressive multifocal leukoencephalopathy has been reported in a few CLL patients treated with anti-CD20 antibodies; therefore, infections with John Cunningham (JC) virus should be ruled out in situations of unclear neurological symptoms,” the panel recommended.
They note that patients younger than 65 treated with fludarabine-based therapy in the first line do not require routine monitoring or infection prophylaxis, due to the low reported incidence of infections in this group.
The authors reported having no financial disclosures related to the guidelines.
include new and revised recommendations based on major advances in genomics, targeted therapies, and biomarkers that have occurred since the last iteration in 2008.
The guidelines are an update from a consensus document issued a decade ago by the International Workshop on CLL, focusing on the conduct of clinical trials in patients with CLL. The new guidelines are published in Blood.
Major changes or additions include:
Molecular genetics: The updated guidelines recognize the clinical importance of specific genomic alterations/mutations on response to standard chemotherapy or chemoimmunotherapy, including the 17p deletion and mutations in TP53.
“Therefore, the assessment of both del(17p) and TP53 mutation has prognostic and predictive value and should guide therapeutic decisions in routine practice. For clinical trials, it is recommended that molecular genetics be performed prior to treating a patient on protocol,” the guidelines state.
IGHV mutational status: The mutational status of immunoglobulin variable heavy chain (IGHV) genes has been demonstrated to offer important prognostic information, according to the guidelines authors led by Michael Hallek, MD of the University of Cologne, Germany.
Specifically, leukemia with IGHV genes without somatic mutations are associated with worse clinical outcomes, compared with leukemia with IGHV mutations. Patients with mutated IGHV and other prognostic factors such as favorable cytogenetics or minimal residual disease (MRD) negativity generally have excellent outcomes with a chemoimmunotherapy regimen consisting of fludarabine, cyclophosphamide, and rituximab, the authors noted.
Biomarkers: The guidelines call for standardization and use in prospective clinical trials of assays for serum markers such as soluble CD23, thymidine kinase, and beta-2-microglobulin. These markers have been shown in several studies to be associated with overall survival or progression-free survival, and of these markers, beta-2-microglobulin “has retained independent prognostic value in several multiparameter scores,” the guidelines state.
The authors also tip their hats to recently developed or improved prognostic scores, especially the CLL International Prognostic Index (CLL-IPI), which incorporates clinical stage, age, IGHV mutational status, beta-2-microglobulin, and del(17p) and/or TP53 mutations.
Organ function assessment: Not new, but improved in the current version of the guidelines, are recommendations for evaluation of splenomegaly, hepatomegaly, and lymphadenopathy in response assessment. These recommendations were harmonized with the relevant sections of the updated lymphoma response guidelines.
Continuous therapy: The guidelines panel recommends assessment of response duration during continuous therapy with oral agents and after the end of therapy, especially after chemotherapy or chemoimmunotherapy.
“Study protocols should provide detailed specifications of the planned time points for the assessment of the treatment response under continuous therapy. Response durations of less than six months are not considered clinically relevant,” the panel cautioned.
Response assessments for treatments with a maintenance phase should be performed at a minimum of 2 months after patients achieve their best responses.
MRD: The guidelines call for minimal residual disease (MRD) assessment in clinical trials aimed at maximizing remission depth, with emphasis on reporting the sensitivity of the MRD evaluation method used, and the type of tissue assessed.
Antiviral prophylaxis: The guidelines caution that because patients treated with anti-CD20 antibodies, such as rituximab or obinutuzumab, could have reactivation of hepatitis B virus (HBV) infections, patients should be tested for HBV serological status before starting on an anti-CD20 agent.
“Progressive multifocal leukoencephalopathy has been reported in a few CLL patients treated with anti-CD20 antibodies; therefore, infections with John Cunningham (JC) virus should be ruled out in situations of unclear neurological symptoms,” the panel recommended.
They note that patients younger than 65 treated with fludarabine-based therapy in the first line do not require routine monitoring or infection prophylaxis, due to the low reported incidence of infections in this group.
The authors reported having no financial disclosures related to the guidelines.
include new and revised recommendations based on major advances in genomics, targeted therapies, and biomarkers that have occurred since the last iteration in 2008.
The guidelines are an update from a consensus document issued a decade ago by the International Workshop on CLL, focusing on the conduct of clinical trials in patients with CLL. The new guidelines are published in Blood.
Major changes or additions include:
Molecular genetics: The updated guidelines recognize the clinical importance of specific genomic alterations/mutations on response to standard chemotherapy or chemoimmunotherapy, including the 17p deletion and mutations in TP53.
“Therefore, the assessment of both del(17p) and TP53 mutation has prognostic and predictive value and should guide therapeutic decisions in routine practice. For clinical trials, it is recommended that molecular genetics be performed prior to treating a patient on protocol,” the guidelines state.
IGHV mutational status: The mutational status of immunoglobulin variable heavy chain (IGHV) genes has been demonstrated to offer important prognostic information, according to the guidelines authors led by Michael Hallek, MD of the University of Cologne, Germany.
Specifically, leukemia with IGHV genes without somatic mutations are associated with worse clinical outcomes, compared with leukemia with IGHV mutations. Patients with mutated IGHV and other prognostic factors such as favorable cytogenetics or minimal residual disease (MRD) negativity generally have excellent outcomes with a chemoimmunotherapy regimen consisting of fludarabine, cyclophosphamide, and rituximab, the authors noted.
Biomarkers: The guidelines call for standardization and use in prospective clinical trials of assays for serum markers such as soluble CD23, thymidine kinase, and beta-2-microglobulin. These markers have been shown in several studies to be associated with overall survival or progression-free survival, and of these markers, beta-2-microglobulin “has retained independent prognostic value in several multiparameter scores,” the guidelines state.
The authors also tip their hats to recently developed or improved prognostic scores, especially the CLL International Prognostic Index (CLL-IPI), which incorporates clinical stage, age, IGHV mutational status, beta-2-microglobulin, and del(17p) and/or TP53 mutations.
Organ function assessment: Not new, but improved in the current version of the guidelines, are recommendations for evaluation of splenomegaly, hepatomegaly, and lymphadenopathy in response assessment. These recommendations were harmonized with the relevant sections of the updated lymphoma response guidelines.
Continuous therapy: The guidelines panel recommends assessment of response duration during continuous therapy with oral agents and after the end of therapy, especially after chemotherapy or chemoimmunotherapy.
“Study protocols should provide detailed specifications of the planned time points for the assessment of the treatment response under continuous therapy. Response durations of less than six months are not considered clinically relevant,” the panel cautioned.
Response assessments for treatments with a maintenance phase should be performed at a minimum of 2 months after patients achieve their best responses.
MRD: The guidelines call for minimal residual disease (MRD) assessment in clinical trials aimed at maximizing remission depth, with emphasis on reporting the sensitivity of the MRD evaluation method used, and the type of tissue assessed.
Antiviral prophylaxis: The guidelines caution that because patients treated with anti-CD20 antibodies, such as rituximab or obinutuzumab, could have reactivation of hepatitis B virus (HBV) infections, patients should be tested for HBV serological status before starting on an anti-CD20 agent.
“Progressive multifocal leukoencephalopathy has been reported in a few CLL patients treated with anti-CD20 antibodies; therefore, infections with John Cunningham (JC) virus should be ruled out in situations of unclear neurological symptoms,” the panel recommended.
They note that patients younger than 65 treated with fludarabine-based therapy in the first line do not require routine monitoring or infection prophylaxis, due to the low reported incidence of infections in this group.
The authors reported having no financial disclosures related to the guidelines.
FROM BLOOD
Project provides ‘unprecedented understanding’ of cancers
Through extensive analyses of data from The Cancer Genome Atlas (TCGA), researchers have produced a new resource known as the Pan-Cancer Atlas.
Multiple research groups analyzed data on more than 10,000 tumors spanning 33 types of cancer, including acute myeloid leukemia and diffuse large B-cell lymphoma.
The work revealed new insights regarding cells of origin, oncogenic processes, and signaling pathways.
These insights make up the Pan-Cancer Atlas and are described in 27 papers published in Cell Press journals. The entire collection of papers is available through a portal on cell.com.
The Pan-Cancer Atlas is the final output of TCGA, a joint effort of the National Cancer Institute (NCI) and the National Human Genome Research Institute (NHGRI) to “collect, select, and analyze human tissues for genomic alterations on a very large scale.”
“This project is the culmination of more than a decade of ground-breaking work,” said Francis S. Collins, MD, PhD, director of the National Institutes of Health.
“This analysis provides cancer researchers with unprecedented understanding of how, where, and why tumors arise in humans, enabling better informed clinical trials and future treatments.”
The project focused on genome sequencing as well as other analyses, such as investigating gene and protein expression profiles and associating them with clinical and imaging data.
“The Pan-Cancer Atlas effort complements the over 30 tumor-specific papers that have been published by TCGA in the last decade and expands upon earlier pan-cancer work that was published in 2013,” said Jean Claude Zenklusen, PhD, director of the TCGA Program Office at NCI.
The Pan-Cancer Atlas is divided into 3 main categories—cell of origin, oncogenic processes, and signaling pathways—each anchored by a summary paper that recaps the core findings for the topic. Companion papers report in-depth explorations of individual topics within these categories.
Cell of origin
In the first Pan-Cancer Atlas summary paper, the authors review the findings from analyses using a technique called molecular clustering, which groups tumors by parameters such as genes being expressed, abnormality of chromosome numbers in tumor cells, and DNA modifications.
The analyses suggest that tumor types cluster by their possible cells of origin, a finding that has implications for the classification and treatment of various cancers.
“Rather than the organ of origin, we can now use molecular features to identify the cancer’s cell of origin,” said Li Ding, PhD, of Washington University School of Medicine in St. Louis, Missouri.
“We are looking at what genes are turned on in the tumor, and that brings us to a particular cell type. For example, squamous cell cancers can arise in the lung, bladder, cervix, and some tumors of the head and neck. We traditionally have treated cancers in these areas as completely different diseases, but, [by] studying their molecular features, we now know such cancers are closely related.”
“This new molecular-based classification system should greatly help in the clinic, where it is already explaining some of the similar clinical behavior of what we thought were different tumor types,” said Charles Perou, PhD, of UNC Lineberger Comprehensive Cancer Center in Chapel Hill, North Carolina.
“These findings also provide many new therapeutic opportunities, which can and will be tested in the next phase of human clinical trials.”
Oncogenic processes
The second Pan-Cancer Atlas summary paper presents a broad view of the TCGA findings on the processes that lead to cancer development and progression.
The research revealed insights into 3 critical oncogenic processes—germline and somatic mutations, the influence of the tumor’s underlying genome and epigenome on gene and protein expression, and the interplay of tumor and immune cells.
“For the 10,000 tumors we analyzed, we now know—in detail—the inherited mutations driving cancer and the genetic errors that accumulate as people age, increasing the risk of cancer,” Dr Ding said. “This is the first definitive summary of the genetics behind 33 major types of cancer.”
“TCGA has created a catalogue of alterations that occur in a variety of cancer types,” said Katherine Hoadley, PhD, of University of North Carolina at Chapel Hill.
“Having this catalogue of alterations is really important for us to look, in future studies, at why these alterations are there and to predict outcomes for patients.”
Signaling pathways
The final Pan-Cancer Atlas summary paper details TCGA research on the genomic alterations in the signaling pathways that control cell-cycle progression, cell death, and cell growth. The work highlights the similarities and differences in these processes across a range of cancers.
The researchers believe these studies have revealed new patterns of potential vulnerabilities that might aid the development of targeted and combination therapies.
Through extensive analyses of data from The Cancer Genome Atlas (TCGA), researchers have produced a new resource known as the Pan-Cancer Atlas.
Multiple research groups analyzed data on more than 10,000 tumors spanning 33 types of cancer, including acute myeloid leukemia and diffuse large B-cell lymphoma.
The work revealed new insights regarding cells of origin, oncogenic processes, and signaling pathways.
These insights make up the Pan-Cancer Atlas and are described in 27 papers published in Cell Press journals. The entire collection of papers is available through a portal on cell.com.
The Pan-Cancer Atlas is the final output of TCGA, a joint effort of the National Cancer Institute (NCI) and the National Human Genome Research Institute (NHGRI) to “collect, select, and analyze human tissues for genomic alterations on a very large scale.”
“This project is the culmination of more than a decade of ground-breaking work,” said Francis S. Collins, MD, PhD, director of the National Institutes of Health.
“This analysis provides cancer researchers with unprecedented understanding of how, where, and why tumors arise in humans, enabling better informed clinical trials and future treatments.”
The project focused on genome sequencing as well as other analyses, such as investigating gene and protein expression profiles and associating them with clinical and imaging data.
“The Pan-Cancer Atlas effort complements the over 30 tumor-specific papers that have been published by TCGA in the last decade and expands upon earlier pan-cancer work that was published in 2013,” said Jean Claude Zenklusen, PhD, director of the TCGA Program Office at NCI.
The Pan-Cancer Atlas is divided into 3 main categories—cell of origin, oncogenic processes, and signaling pathways—each anchored by a summary paper that recaps the core findings for the topic. Companion papers report in-depth explorations of individual topics within these categories.
Cell of origin
In the first Pan-Cancer Atlas summary paper, the authors review the findings from analyses using a technique called molecular clustering, which groups tumors by parameters such as genes being expressed, abnormality of chromosome numbers in tumor cells, and DNA modifications.
The analyses suggest that tumor types cluster by their possible cells of origin, a finding that has implications for the classification and treatment of various cancers.
“Rather than the organ of origin, we can now use molecular features to identify the cancer’s cell of origin,” said Li Ding, PhD, of Washington University School of Medicine in St. Louis, Missouri.
“We are looking at what genes are turned on in the tumor, and that brings us to a particular cell type. For example, squamous cell cancers can arise in the lung, bladder, cervix, and some tumors of the head and neck. We traditionally have treated cancers in these areas as completely different diseases, but, [by] studying their molecular features, we now know such cancers are closely related.”
“This new molecular-based classification system should greatly help in the clinic, where it is already explaining some of the similar clinical behavior of what we thought were different tumor types,” said Charles Perou, PhD, of UNC Lineberger Comprehensive Cancer Center in Chapel Hill, North Carolina.
“These findings also provide many new therapeutic opportunities, which can and will be tested in the next phase of human clinical trials.”
Oncogenic processes
The second Pan-Cancer Atlas summary paper presents a broad view of the TCGA findings on the processes that lead to cancer development and progression.
The research revealed insights into 3 critical oncogenic processes—germline and somatic mutations, the influence of the tumor’s underlying genome and epigenome on gene and protein expression, and the interplay of tumor and immune cells.
“For the 10,000 tumors we analyzed, we now know—in detail—the inherited mutations driving cancer and the genetic errors that accumulate as people age, increasing the risk of cancer,” Dr Ding said. “This is the first definitive summary of the genetics behind 33 major types of cancer.”
“TCGA has created a catalogue of alterations that occur in a variety of cancer types,” said Katherine Hoadley, PhD, of University of North Carolina at Chapel Hill.
“Having this catalogue of alterations is really important for us to look, in future studies, at why these alterations are there and to predict outcomes for patients.”
Signaling pathways
The final Pan-Cancer Atlas summary paper details TCGA research on the genomic alterations in the signaling pathways that control cell-cycle progression, cell death, and cell growth. The work highlights the similarities and differences in these processes across a range of cancers.
The researchers believe these studies have revealed new patterns of potential vulnerabilities that might aid the development of targeted and combination therapies.
Through extensive analyses of data from The Cancer Genome Atlas (TCGA), researchers have produced a new resource known as the Pan-Cancer Atlas.
Multiple research groups analyzed data on more than 10,000 tumors spanning 33 types of cancer, including acute myeloid leukemia and diffuse large B-cell lymphoma.
The work revealed new insights regarding cells of origin, oncogenic processes, and signaling pathways.
These insights make up the Pan-Cancer Atlas and are described in 27 papers published in Cell Press journals. The entire collection of papers is available through a portal on cell.com.
The Pan-Cancer Atlas is the final output of TCGA, a joint effort of the National Cancer Institute (NCI) and the National Human Genome Research Institute (NHGRI) to “collect, select, and analyze human tissues for genomic alterations on a very large scale.”
“This project is the culmination of more than a decade of ground-breaking work,” said Francis S. Collins, MD, PhD, director of the National Institutes of Health.
“This analysis provides cancer researchers with unprecedented understanding of how, where, and why tumors arise in humans, enabling better informed clinical trials and future treatments.”
The project focused on genome sequencing as well as other analyses, such as investigating gene and protein expression profiles and associating them with clinical and imaging data.
“The Pan-Cancer Atlas effort complements the over 30 tumor-specific papers that have been published by TCGA in the last decade and expands upon earlier pan-cancer work that was published in 2013,” said Jean Claude Zenklusen, PhD, director of the TCGA Program Office at NCI.
The Pan-Cancer Atlas is divided into 3 main categories—cell of origin, oncogenic processes, and signaling pathways—each anchored by a summary paper that recaps the core findings for the topic. Companion papers report in-depth explorations of individual topics within these categories.
Cell of origin
In the first Pan-Cancer Atlas summary paper, the authors review the findings from analyses using a technique called molecular clustering, which groups tumors by parameters such as genes being expressed, abnormality of chromosome numbers in tumor cells, and DNA modifications.
The analyses suggest that tumor types cluster by their possible cells of origin, a finding that has implications for the classification and treatment of various cancers.
“Rather than the organ of origin, we can now use molecular features to identify the cancer’s cell of origin,” said Li Ding, PhD, of Washington University School of Medicine in St. Louis, Missouri.
“We are looking at what genes are turned on in the tumor, and that brings us to a particular cell type. For example, squamous cell cancers can arise in the lung, bladder, cervix, and some tumors of the head and neck. We traditionally have treated cancers in these areas as completely different diseases, but, [by] studying their molecular features, we now know such cancers are closely related.”
“This new molecular-based classification system should greatly help in the clinic, where it is already explaining some of the similar clinical behavior of what we thought were different tumor types,” said Charles Perou, PhD, of UNC Lineberger Comprehensive Cancer Center in Chapel Hill, North Carolina.
“These findings also provide many new therapeutic opportunities, which can and will be tested in the next phase of human clinical trials.”
Oncogenic processes
The second Pan-Cancer Atlas summary paper presents a broad view of the TCGA findings on the processes that lead to cancer development and progression.
The research revealed insights into 3 critical oncogenic processes—germline and somatic mutations, the influence of the tumor’s underlying genome and epigenome on gene and protein expression, and the interplay of tumor and immune cells.
“For the 10,000 tumors we analyzed, we now know—in detail—the inherited mutations driving cancer and the genetic errors that accumulate as people age, increasing the risk of cancer,” Dr Ding said. “This is the first definitive summary of the genetics behind 33 major types of cancer.”
“TCGA has created a catalogue of alterations that occur in a variety of cancer types,” said Katherine Hoadley, PhD, of University of North Carolina at Chapel Hill.
“Having this catalogue of alterations is really important for us to look, in future studies, at why these alterations are there and to predict outcomes for patients.”
Signaling pathways
The final Pan-Cancer Atlas summary paper details TCGA research on the genomic alterations in the signaling pathways that control cell-cycle progression, cell death, and cell growth. The work highlights the similarities and differences in these processes across a range of cancers.
The researchers believe these studies have revealed new patterns of potential vulnerabilities that might aid the development of targeted and combination therapies.
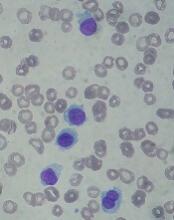
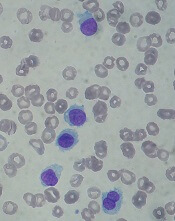
Drug receives priority review for HCL
The US Food and Drug Administration (FDA) has accepted for priority review the biologics license application (BLA) for moxetumomab pasudotox, an investigational anti-CD22 recombinant immunotoxin.
With this BLA, AstraZeneca is seeking approval for moxetumomab pasudotox for the treatment of adults with hairy cell leukemia (HCL) who have received at least 2 prior lines of therapy.
The FDA expects to make a decision on the BLA in the third quarter of this year.
The FDA aims to take action on a priority review application within 6 months of receiving it, rather than the standard 10 months.
The agency grants priority review to applications for products that may provide significant improvements in the treatment, diagnosis, or prevention of serious conditions.
About moxetumomab pasudotox
Moxetumomab pasudotox (formerly CAT-8015 or HA22) is composed of a binding portion of an anti-CD22 antibody fused to a toxin. After binding to CD22, the molecule is internalized, processed, and releases its modified protein toxin, which inhibits protein translation and leads to apoptosis.
In addition to priority review, moxetumomab pasudotox has received orphan drug designation from the FDA.
Moxetumomab pasudotox has been tested in a phase 1 trial. Initial results from this trial were published in the Journal of Clinical Oncology in 2012. Long-term follow-up was presented at the 2017 ASH Annual Meeting.
The ASH data included 49 patients with relapsed/refractory HCL. Their median age was 57 (range, 40-77), most (n=41) were male, and they had a median of 35 (range, 1-60,444) circulating HCL cells/mm3 at baseline (in 48 evaluable patients).
Twenty-eight patients received moxetumomab pasudotox in the dose-escalation portion of the study—at 5, 10, 20, 30, 40, or 50 µg/kg—and 21 received the drug at 50 µg/kg for the extension portion of the study.
Among the 33 patients who received moxetumomab pasudotox at 50 µg/kg, the overall response rate was 88%, and the complete response (CR) rate was 64% (n=21). The median time to CR was 3.6 months, and the median duration of CR was 70.3 months.
The median follow-up was 75 months for the entire study population. At 72 months, the progression-free survival (PFS) rate was 77%.
The researchers found that minimal residual disease (MRD) negativity (via immunohistochemistry) was associated with extended response duration and prolonged PFS.
The MRD evaluation included 19 MRD+ patients and 18 MRD- patients. Forty-seven percent of the MRD+ patients (n=9) and 94% of the MRD- patients (n=17) had a CR as their best response.
The median duration of CR was 13.1 months among the MRD+ patients and was not reached among the MRD- patients (P=0.0002). The median PFS was 82.1 months among the MRD+ patients and not reached among the MRD- patients (P=0.0031).
Moxetumomab pasudotox did not undergo phase 2 testing but proceeded to a phase 3 trial. In this single-arm study, researchers evaluated the drug in HCL patients who had received at least 2 prior therapies.
According to AstraZeneca, the study’s primary endpoint—durable CR—was met. The company said the phase 3 results will be presented at an upcoming medical meeting.
The US Food and Drug Administration (FDA) has accepted for priority review the biologics license application (BLA) for moxetumomab pasudotox, an investigational anti-CD22 recombinant immunotoxin.
With this BLA, AstraZeneca is seeking approval for moxetumomab pasudotox for the treatment of adults with hairy cell leukemia (HCL) who have received at least 2 prior lines of therapy.
The FDA expects to make a decision on the BLA in the third quarter of this year.
The FDA aims to take action on a priority review application within 6 months of receiving it, rather than the standard 10 months.
The agency grants priority review to applications for products that may provide significant improvements in the treatment, diagnosis, or prevention of serious conditions.
About moxetumomab pasudotox
Moxetumomab pasudotox (formerly CAT-8015 or HA22) is composed of a binding portion of an anti-CD22 antibody fused to a toxin. After binding to CD22, the molecule is internalized, processed, and releases its modified protein toxin, which inhibits protein translation and leads to apoptosis.
In addition to priority review, moxetumomab pasudotox has received orphan drug designation from the FDA.
Moxetumomab pasudotox has been tested in a phase 1 trial. Initial results from this trial were published in the Journal of Clinical Oncology in 2012. Long-term follow-up was presented at the 2017 ASH Annual Meeting.
The ASH data included 49 patients with relapsed/refractory HCL. Their median age was 57 (range, 40-77), most (n=41) were male, and they had a median of 35 (range, 1-60,444) circulating HCL cells/mm3 at baseline (in 48 evaluable patients).
Twenty-eight patients received moxetumomab pasudotox in the dose-escalation portion of the study—at 5, 10, 20, 30, 40, or 50 µg/kg—and 21 received the drug at 50 µg/kg for the extension portion of the study.
Among the 33 patients who received moxetumomab pasudotox at 50 µg/kg, the overall response rate was 88%, and the complete response (CR) rate was 64% (n=21). The median time to CR was 3.6 months, and the median duration of CR was 70.3 months.
The median follow-up was 75 months for the entire study population. At 72 months, the progression-free survival (PFS) rate was 77%.
The researchers found that minimal residual disease (MRD) negativity (via immunohistochemistry) was associated with extended response duration and prolonged PFS.
The MRD evaluation included 19 MRD+ patients and 18 MRD- patients. Forty-seven percent of the MRD+ patients (n=9) and 94% of the MRD- patients (n=17) had a CR as their best response.
The median duration of CR was 13.1 months among the MRD+ patients and was not reached among the MRD- patients (P=0.0002). The median PFS was 82.1 months among the MRD+ patients and not reached among the MRD- patients (P=0.0031).
Moxetumomab pasudotox did not undergo phase 2 testing but proceeded to a phase 3 trial. In this single-arm study, researchers evaluated the drug in HCL patients who had received at least 2 prior therapies.
According to AstraZeneca, the study’s primary endpoint—durable CR—was met. The company said the phase 3 results will be presented at an upcoming medical meeting.
The US Food and Drug Administration (FDA) has accepted for priority review the biologics license application (BLA) for moxetumomab pasudotox, an investigational anti-CD22 recombinant immunotoxin.
With this BLA, AstraZeneca is seeking approval for moxetumomab pasudotox for the treatment of adults with hairy cell leukemia (HCL) who have received at least 2 prior lines of therapy.
The FDA expects to make a decision on the BLA in the third quarter of this year.
The FDA aims to take action on a priority review application within 6 months of receiving it, rather than the standard 10 months.
The agency grants priority review to applications for products that may provide significant improvements in the treatment, diagnosis, or prevention of serious conditions.
About moxetumomab pasudotox
Moxetumomab pasudotox (formerly CAT-8015 or HA22) is composed of a binding portion of an anti-CD22 antibody fused to a toxin. After binding to CD22, the molecule is internalized, processed, and releases its modified protein toxin, which inhibits protein translation and leads to apoptosis.
In addition to priority review, moxetumomab pasudotox has received orphan drug designation from the FDA.
Moxetumomab pasudotox has been tested in a phase 1 trial. Initial results from this trial were published in the Journal of Clinical Oncology in 2012. Long-term follow-up was presented at the 2017 ASH Annual Meeting.
The ASH data included 49 patients with relapsed/refractory HCL. Their median age was 57 (range, 40-77), most (n=41) were male, and they had a median of 35 (range, 1-60,444) circulating HCL cells/mm3 at baseline (in 48 evaluable patients).
Twenty-eight patients received moxetumomab pasudotox in the dose-escalation portion of the study—at 5, 10, 20, 30, 40, or 50 µg/kg—and 21 received the drug at 50 µg/kg for the extension portion of the study.
Among the 33 patients who received moxetumomab pasudotox at 50 µg/kg, the overall response rate was 88%, and the complete response (CR) rate was 64% (n=21). The median time to CR was 3.6 months, and the median duration of CR was 70.3 months.
The median follow-up was 75 months for the entire study population. At 72 months, the progression-free survival (PFS) rate was 77%.
The researchers found that minimal residual disease (MRD) negativity (via immunohistochemistry) was associated with extended response duration and prolonged PFS.
The MRD evaluation included 19 MRD+ patients and 18 MRD- patients. Forty-seven percent of the MRD+ patients (n=9) and 94% of the MRD- patients (n=17) had a CR as their best response.
The median duration of CR was 13.1 months among the MRD+ patients and was not reached among the MRD- patients (P=0.0002). The median PFS was 82.1 months among the MRD+ patients and not reached among the MRD- patients (P=0.0031).
Moxetumomab pasudotox did not undergo phase 2 testing but proceeded to a phase 3 trial. In this single-arm study, researchers evaluated the drug in HCL patients who had received at least 2 prior therapies.
According to AstraZeneca, the study’s primary endpoint—durable CR—was met. The company said the phase 3 results will be presented at an upcoming medical meeting.
European Commission expands denosumab indication
The , making it is available for the prevention of skeletal-related events in adults with multiple myeloma and other advanced malignancies involving bone.
The European approval is based on the monoclonal antibody’s strong performance in a phase 3, international trial looking specifically at prevention of skeletal-related events in multiple myeloma patients.
During the trial, the drug demonstrated noninferiority to zoledronic acid in delaying the time to first skeletal-related event (hazard ratio, 0.98, 95% confidence interval: 0.85-1.14), according to Amgen, which markets denosumab. The median time to first skeletal-related event was 22.8 months for denosumab versus 24.0 months for zoledronic acid.
The denosumab indication was expanded to include prevention of skeletal-related events by the Food and Drug Administration in the United States in January 2018.
The , making it is available for the prevention of skeletal-related events in adults with multiple myeloma and other advanced malignancies involving bone.
The European approval is based on the monoclonal antibody’s strong performance in a phase 3, international trial looking specifically at prevention of skeletal-related events in multiple myeloma patients.
During the trial, the drug demonstrated noninferiority to zoledronic acid in delaying the time to first skeletal-related event (hazard ratio, 0.98, 95% confidence interval: 0.85-1.14), according to Amgen, which markets denosumab. The median time to first skeletal-related event was 22.8 months for denosumab versus 24.0 months for zoledronic acid.
The denosumab indication was expanded to include prevention of skeletal-related events by the Food and Drug Administration in the United States in January 2018.
The , making it is available for the prevention of skeletal-related events in adults with multiple myeloma and other advanced malignancies involving bone.
The European approval is based on the monoclonal antibody’s strong performance in a phase 3, international trial looking specifically at prevention of skeletal-related events in multiple myeloma patients.
During the trial, the drug demonstrated noninferiority to zoledronic acid in delaying the time to first skeletal-related event (hazard ratio, 0.98, 95% confidence interval: 0.85-1.14), according to Amgen, which markets denosumab. The median time to first skeletal-related event was 22.8 months for denosumab versus 24.0 months for zoledronic acid.
The denosumab indication was expanded to include prevention of skeletal-related events by the Food and Drug Administration in the United States in January 2018.
Agent exhibits activity in leukemias, MDS
The experimental agent prexigebersen (formerly BP1001) was considered well-tolerated and demonstrated early evidence of activity against relapsed/refractory hematologic disorders in a phase 1/1b trial.
The drug reduced blasts in the bone marrow and peripheral blood for patients with acute myeloid leukemia (AML), chronic myeloid leukemia (CML), and myelodysplastic syndrome (MDS).
When given in combination with low-dose cytarabine, prexigebersen produced complete responses (CRs) in patients with AML.
Researchers said that, overall, the toxic effects of prexigebersen were manageable.
There was 1 patient who had dose-limiting toxicities, 1 who discontinued treatment due to possible drug-related toxic effects, and 1 treatment-related death.
Still, the maximum tolerated dose of prexigebersen was not established.
These results were published in The Lancet Haematology. The study was sponsored by Bio-Path Holdings, Inc., the company developing prexigebersen.
Prexigebersen is an anti-sense oligodeoxynucleotide developed to block Grb2 expression and function. Researchers tested the drug in a single-center, dose-escalation, phase 1/1b trial that enrolled and treated 39 patients.
In the phase 1 portion of the trial, patients received prexigebersen monotherapy. In the phase 1b portion, they received the drug in combination with low-dose cytarabine.
There were 32 patients in the phase 1 portion of the trial. Most (n=23) had AML, 5 had CML in blast phase, and 4 had MDS. The patients’ median age was 63 (range, 56-73), and they had received a median of 4 prior therapies.
All 7 patients in the phase 1b portion had AML. They had a median age of 72 (range, 70-76) and had all received 1 prior therapy.
For phase 1, prexigebersen was administered intravenously, twice weekly for 28 days at doses of 5 mg/m² in cohort 1 (n=13), 10 mg/m² in cohort 2 (n=6), 20 mg/m² in cohort 3 (n=3), 40 mg/m² in cohort 4 (n=3), 60 mg/m² in cohort 5 (n=3), and 90 mg/m² in cohort 6 (n=4).
In the phase 1b portion, patients received prexigebersen at 60 mg/m² (n=4) or 90 mg/m² (n=3) in combination with 20 mg of cytarabine (twice-daily subcutaneous injections).
Safety
Twenty-seven patients were evaluable for dose-limiting toxicity—21 from phase 1 and 6 from 1b.
One patient in cohort 1 developed mucositis and hand-foot syndrome, which were considered possibly related to prexigebersen and deemed dose-limiting toxicities. The patient was also receiving hydroxyurea (3 g/day) for CML and had a history of hydroxyurea-induced mucositis.
There were no other dose-limiting toxicities, and the researchers did not identify a maximum tolerated dose of prexigebersen.
The most common grade 3-4 adverse events (AEs) were cardiopulmonary disorders and fevers (including neutropenic fevers and infections).
In the monotherapy group, 17% of patients had grade 3-4 cardiopulmonary AEs, and 11% had fevers. In the prexigebersen-cytarabine combination group, 8% had grade 3-4 cardiopulmonary AEs, and 6% had fevers.
There were 5 grade 5 AEs in 4 patients, all of whom received monotherapy. These included cardiopulmonary disorders (n=2), fevers (n=2), and multi-organ failure (n=1). One patient had both fever (sepsis) and multi-organ failure.
Efficacy
According to the researchers’ assessments, 22% of phase 1 patients (7/32) benefited from prexigebersen monotherapy and therefore received more than 1 cycle of treatment. Five of these patients had AML, and 2 had MDS.
Single-agent activity was observed in other patients as well.
Thirty-three percent (9/27) of patients who had peripheral blood blasts at baseline saw their blasts reduced by 50% or more while receiving monotherapy. One of these patients had CML, and the rest had AML.
Ten percent (3/29) of patients with bone marrow blasts at baseline had a reduction in blasts of 50% or more while receiving monotherapy. Two of these patients had AML, and 1 had MDS.
Of the 7 patients receiving prexigebersen with cytarabine, 2 achieved a CR, and 1 had a CR with incomplete hematological recovery.
Two of the patients had stable disease, and the remaining 2 patients progressed. One of the patients with progressive disease withdrew from the study, and the other died.
Deaths
There were a total of 8 deaths.
One death was considered treatment-related. This patient had progressive CML in blast phase and died of multiple organ failure. This was the first patient treated on the trial, who also had the only dose-limiting toxicities.
Two patients with AML and 1 with MDS died of disease progression. Three AML patients died of sepsis, pneumonia, and cardiac arrest. And a CML patient died of respiratory distress.
The experimental agent prexigebersen (formerly BP1001) was considered well-tolerated and demonstrated early evidence of activity against relapsed/refractory hematologic disorders in a phase 1/1b trial.
The drug reduced blasts in the bone marrow and peripheral blood for patients with acute myeloid leukemia (AML), chronic myeloid leukemia (CML), and myelodysplastic syndrome (MDS).
When given in combination with low-dose cytarabine, prexigebersen produced complete responses (CRs) in patients with AML.
Researchers said that, overall, the toxic effects of prexigebersen were manageable.
There was 1 patient who had dose-limiting toxicities, 1 who discontinued treatment due to possible drug-related toxic effects, and 1 treatment-related death.
Still, the maximum tolerated dose of prexigebersen was not established.
These results were published in The Lancet Haematology. The study was sponsored by Bio-Path Holdings, Inc., the company developing prexigebersen.
Prexigebersen is an anti-sense oligodeoxynucleotide developed to block Grb2 expression and function. Researchers tested the drug in a single-center, dose-escalation, phase 1/1b trial that enrolled and treated 39 patients.
In the phase 1 portion of the trial, patients received prexigebersen monotherapy. In the phase 1b portion, they received the drug in combination with low-dose cytarabine.
There were 32 patients in the phase 1 portion of the trial. Most (n=23) had AML, 5 had CML in blast phase, and 4 had MDS. The patients’ median age was 63 (range, 56-73), and they had received a median of 4 prior therapies.
All 7 patients in the phase 1b portion had AML. They had a median age of 72 (range, 70-76) and had all received 1 prior therapy.
For phase 1, prexigebersen was administered intravenously, twice weekly for 28 days at doses of 5 mg/m² in cohort 1 (n=13), 10 mg/m² in cohort 2 (n=6), 20 mg/m² in cohort 3 (n=3), 40 mg/m² in cohort 4 (n=3), 60 mg/m² in cohort 5 (n=3), and 90 mg/m² in cohort 6 (n=4).
In the phase 1b portion, patients received prexigebersen at 60 mg/m² (n=4) or 90 mg/m² (n=3) in combination with 20 mg of cytarabine (twice-daily subcutaneous injections).
Safety
Twenty-seven patients were evaluable for dose-limiting toxicity—21 from phase 1 and 6 from 1b.
One patient in cohort 1 developed mucositis and hand-foot syndrome, which were considered possibly related to prexigebersen and deemed dose-limiting toxicities. The patient was also receiving hydroxyurea (3 g/day) for CML and had a history of hydroxyurea-induced mucositis.
There were no other dose-limiting toxicities, and the researchers did not identify a maximum tolerated dose of prexigebersen.
The most common grade 3-4 adverse events (AEs) were cardiopulmonary disorders and fevers (including neutropenic fevers and infections).
In the monotherapy group, 17% of patients had grade 3-4 cardiopulmonary AEs, and 11% had fevers. In the prexigebersen-cytarabine combination group, 8% had grade 3-4 cardiopulmonary AEs, and 6% had fevers.
There were 5 grade 5 AEs in 4 patients, all of whom received monotherapy. These included cardiopulmonary disorders (n=2), fevers (n=2), and multi-organ failure (n=1). One patient had both fever (sepsis) and multi-organ failure.
Efficacy
According to the researchers’ assessments, 22% of phase 1 patients (7/32) benefited from prexigebersen monotherapy and therefore received more than 1 cycle of treatment. Five of these patients had AML, and 2 had MDS.
Single-agent activity was observed in other patients as well.
Thirty-three percent (9/27) of patients who had peripheral blood blasts at baseline saw their blasts reduced by 50% or more while receiving monotherapy. One of these patients had CML, and the rest had AML.
Ten percent (3/29) of patients with bone marrow blasts at baseline had a reduction in blasts of 50% or more while receiving monotherapy. Two of these patients had AML, and 1 had MDS.
Of the 7 patients receiving prexigebersen with cytarabine, 2 achieved a CR, and 1 had a CR with incomplete hematological recovery.
Two of the patients had stable disease, and the remaining 2 patients progressed. One of the patients with progressive disease withdrew from the study, and the other died.
Deaths
There were a total of 8 deaths.
One death was considered treatment-related. This patient had progressive CML in blast phase and died of multiple organ failure. This was the first patient treated on the trial, who also had the only dose-limiting toxicities.
Two patients with AML and 1 with MDS died of disease progression. Three AML patients died of sepsis, pneumonia, and cardiac arrest. And a CML patient died of respiratory distress.
The experimental agent prexigebersen (formerly BP1001) was considered well-tolerated and demonstrated early evidence of activity against relapsed/refractory hematologic disorders in a phase 1/1b trial.
The drug reduced blasts in the bone marrow and peripheral blood for patients with acute myeloid leukemia (AML), chronic myeloid leukemia (CML), and myelodysplastic syndrome (MDS).
When given in combination with low-dose cytarabine, prexigebersen produced complete responses (CRs) in patients with AML.
Researchers said that, overall, the toxic effects of prexigebersen were manageable.
There was 1 patient who had dose-limiting toxicities, 1 who discontinued treatment due to possible drug-related toxic effects, and 1 treatment-related death.
Still, the maximum tolerated dose of prexigebersen was not established.
These results were published in The Lancet Haematology. The study was sponsored by Bio-Path Holdings, Inc., the company developing prexigebersen.
Prexigebersen is an anti-sense oligodeoxynucleotide developed to block Grb2 expression and function. Researchers tested the drug in a single-center, dose-escalation, phase 1/1b trial that enrolled and treated 39 patients.
In the phase 1 portion of the trial, patients received prexigebersen monotherapy. In the phase 1b portion, they received the drug in combination with low-dose cytarabine.
There were 32 patients in the phase 1 portion of the trial. Most (n=23) had AML, 5 had CML in blast phase, and 4 had MDS. The patients’ median age was 63 (range, 56-73), and they had received a median of 4 prior therapies.
All 7 patients in the phase 1b portion had AML. They had a median age of 72 (range, 70-76) and had all received 1 prior therapy.
For phase 1, prexigebersen was administered intravenously, twice weekly for 28 days at doses of 5 mg/m² in cohort 1 (n=13), 10 mg/m² in cohort 2 (n=6), 20 mg/m² in cohort 3 (n=3), 40 mg/m² in cohort 4 (n=3), 60 mg/m² in cohort 5 (n=3), and 90 mg/m² in cohort 6 (n=4).
In the phase 1b portion, patients received prexigebersen at 60 mg/m² (n=4) or 90 mg/m² (n=3) in combination with 20 mg of cytarabine (twice-daily subcutaneous injections).
Safety
Twenty-seven patients were evaluable for dose-limiting toxicity—21 from phase 1 and 6 from 1b.
One patient in cohort 1 developed mucositis and hand-foot syndrome, which were considered possibly related to prexigebersen and deemed dose-limiting toxicities. The patient was also receiving hydroxyurea (3 g/day) for CML and had a history of hydroxyurea-induced mucositis.
There were no other dose-limiting toxicities, and the researchers did not identify a maximum tolerated dose of prexigebersen.
The most common grade 3-4 adverse events (AEs) were cardiopulmonary disorders and fevers (including neutropenic fevers and infections).
In the monotherapy group, 17% of patients had grade 3-4 cardiopulmonary AEs, and 11% had fevers. In the prexigebersen-cytarabine combination group, 8% had grade 3-4 cardiopulmonary AEs, and 6% had fevers.
There were 5 grade 5 AEs in 4 patients, all of whom received monotherapy. These included cardiopulmonary disorders (n=2), fevers (n=2), and multi-organ failure (n=1). One patient had both fever (sepsis) and multi-organ failure.
Efficacy
According to the researchers’ assessments, 22% of phase 1 patients (7/32) benefited from prexigebersen monotherapy and therefore received more than 1 cycle of treatment. Five of these patients had AML, and 2 had MDS.
Single-agent activity was observed in other patients as well.
Thirty-three percent (9/27) of patients who had peripheral blood blasts at baseline saw their blasts reduced by 50% or more while receiving monotherapy. One of these patients had CML, and the rest had AML.
Ten percent (3/29) of patients with bone marrow blasts at baseline had a reduction in blasts of 50% or more while receiving monotherapy. Two of these patients had AML, and 1 had MDS.
Of the 7 patients receiving prexigebersen with cytarabine, 2 achieved a CR, and 1 had a CR with incomplete hematological recovery.
Two of the patients had stable disease, and the remaining 2 patients progressed. One of the patients with progressive disease withdrew from the study, and the other died.
Deaths
There were a total of 8 deaths.
One death was considered treatment-related. This patient had progressive CML in blast phase and died of multiple organ failure. This was the first patient treated on the trial, who also had the only dose-limiting toxicities.
Two patients with AML and 1 with MDS died of disease progression. Three AML patients died of sepsis, pneumonia, and cardiac arrest. And a CML patient died of respiratory distress.
FDA approves blinatumomab to treat MRD+ BCP-ALL
The US Food and Drug Administration (FDA) has expanded the approved indication for blinatumomab (Blincyto®).
The drug is now approved to treat adults and children with B-cell precursor acute lymphoblastic leukemia (BCP-ALL) in first or second complete remission (CR) with minimal residual disease (MRD) greater than or equal to 0.1%.
Blinatumomab received accelerated approval for this indication because the drug has not yet shown a clinical benefit in these patients.
The FDA’s accelerated approval program allows conditional approval of a drug that fills an unmet medical need for a serious condition.
Accelerated approval is based on surrogate or intermediate endpoints—in this case, MRD response rate and hematologic relapse-free survival (RFS)—that are reasonably likely to predict clinical benefit.
Continued approval of blinatumomab for the aforementioned indication may be contingent upon verification of clinical benefit in confirmatory trials.
“This is the first FDA-approved treatment for patients with MRD-positive ALL,” said Richard Pazdur, MD, director of the FDA’s Oncology Center of Excellence.
“Because patients who have MRD are more likely to relapse, having a treatment option that eliminates even very low amounts of residual leukemia cells may help keep the cancer in remission longer. We look forward to furthering our understanding about the reduction in MRD after treatment with Blincyto. Studies are being conducted to assess how Blincyto affects long-term survival outcomes in patients with MRD.”
About blinatumomab
Blinatumomab is a bispecific, CD19-directed, CD3 T-cell engager (BiTE®) antibody construct that binds to CD19 expressed on the surface of cells of B-lineage origin and CD3 expressed on the surface of T cells.
In 2014, the FDA granted blinatumomab accelerated approval to treat adults with Philadelphia chromosome-negative (Ph-) relapsed/refractory BCP-ALL.
In 2016, the FDA granted the therapy accelerated approval for pediatric patients with Ph- relapsed/refractory BCP-ALL.
Last year, the FDA granted blinatumomab full approval for pediatric and adult patients with Ph- or Ph+ relapsed/refractory BCP-ALL.
The FDA-approved prescribing information for blinatumomab includes a boxed warning for cytokine release syndrome and neurologic toxicities. Blinatumomab is also under a risk evaluation and mitigation strategy program in the US.
BLAST study
The new accelerated approval for blinatumomab was supported by results from the phase 2 BLAST study, which were published in Blood in January.
The study enrolled adults with MRD-positive BCP-ALL in complete hematologic remission after 3 or more cycles of intensive chemotherapy.
Patients received continuous intravenous infusions of blinatumomab at 15 μg/m2/day for 4 weeks, followed by 2 weeks off. They received up to 4 cycles of treatment and could undergo hematopoietic stem cell transplant (HSCT) at any time after the first cycle.
In all, there were 116 patients who received at least 1 infusion of blinatumomab. Seventy-six patients went on to HSCT while in continuous CR after cycle 1 (n=27), 2 (n=36), or 3/4 (n=13).
The study’s primary endpoint was the rate of complete MRD response within the first treatment cycle, and 78% of evaluable patients (88/113) achieved this endpoint.
A key secondary endpoint was RFS at 18 months. There were 110 patients evaluable for this endpoint. They all had Ph- BCP-ALL and <5% blasts at baseline.
The estimated RFS at 18 months was 54%, and the median RFS was 18.9 months. The median RFS was 24.6 months for patients treated in first CR and 11.0 months for patients treated in a later CR (P=0.004).
Another key endpoint was overall survival (OS). The median OS was 36.5 months, both for the 110 patients in the RFS analysis and for the entire study population.
In a landmark analysis, complete MRD responders had longer OS than MRD nonresponders—38.9 months and 12.5 months, respectively (P=0.002). And complete MRD responders had longer RFS than nonresponders—23.6 months and 5.7 months, respectively (P=0.002).
All 116 patients who started cycle 1 had at least 1 adverse event (AE). The rate of grade 3 AEs was 33%, and the rate of grade 4 AEs was 27%. These AEs were considered treatment-related in 29% (grade 3) and 22% (grade 4) of patients.
Four (3%) patients developed cytokine release syndrome—2 with grade 1 and 2 with grade 3. All of these events occurred during cycle 1.
Fifty-three percent of patients (n=61) had neurologic events. In most cases (97%, n=59), these events resolved.
There were 2 fatal AEs during the treatment period, both in cycle 1. One of these events—atypical pneumonitis with H1N1 influenza—was considered treatment-related. The other event—subdural hemorrhage—was considered unrelated to treatment.
There were 4 fatal AEs reported after blinatumomab treatment. Two of these deaths—due to multifocal CNS lesions and graft-versus-host disease—occurred in HSCT recipients. The other 2 deaths—due to disease progression and multi-organ failure—occurred in nontransplanted patients after relapse.
The US Food and Drug Administration (FDA) has expanded the approved indication for blinatumomab (Blincyto®).
The drug is now approved to treat adults and children with B-cell precursor acute lymphoblastic leukemia (BCP-ALL) in first or second complete remission (CR) with minimal residual disease (MRD) greater than or equal to 0.1%.
Blinatumomab received accelerated approval for this indication because the drug has not yet shown a clinical benefit in these patients.
The FDA’s accelerated approval program allows conditional approval of a drug that fills an unmet medical need for a serious condition.
Accelerated approval is based on surrogate or intermediate endpoints—in this case, MRD response rate and hematologic relapse-free survival (RFS)—that are reasonably likely to predict clinical benefit.
Continued approval of blinatumomab for the aforementioned indication may be contingent upon verification of clinical benefit in confirmatory trials.
“This is the first FDA-approved treatment for patients with MRD-positive ALL,” said Richard Pazdur, MD, director of the FDA’s Oncology Center of Excellence.
“Because patients who have MRD are more likely to relapse, having a treatment option that eliminates even very low amounts of residual leukemia cells may help keep the cancer in remission longer. We look forward to furthering our understanding about the reduction in MRD after treatment with Blincyto. Studies are being conducted to assess how Blincyto affects long-term survival outcomes in patients with MRD.”
About blinatumomab
Blinatumomab is a bispecific, CD19-directed, CD3 T-cell engager (BiTE®) antibody construct that binds to CD19 expressed on the surface of cells of B-lineage origin and CD3 expressed on the surface of T cells.
In 2014, the FDA granted blinatumomab accelerated approval to treat adults with Philadelphia chromosome-negative (Ph-) relapsed/refractory BCP-ALL.
In 2016, the FDA granted the therapy accelerated approval for pediatric patients with Ph- relapsed/refractory BCP-ALL.
Last year, the FDA granted blinatumomab full approval for pediatric and adult patients with Ph- or Ph+ relapsed/refractory BCP-ALL.
The FDA-approved prescribing information for blinatumomab includes a boxed warning for cytokine release syndrome and neurologic toxicities. Blinatumomab is also under a risk evaluation and mitigation strategy program in the US.
BLAST study
The new accelerated approval for blinatumomab was supported by results from the phase 2 BLAST study, which were published in Blood in January.
The study enrolled adults with MRD-positive BCP-ALL in complete hematologic remission after 3 or more cycles of intensive chemotherapy.
Patients received continuous intravenous infusions of blinatumomab at 15 μg/m2/day for 4 weeks, followed by 2 weeks off. They received up to 4 cycles of treatment and could undergo hematopoietic stem cell transplant (HSCT) at any time after the first cycle.
In all, there were 116 patients who received at least 1 infusion of blinatumomab. Seventy-six patients went on to HSCT while in continuous CR after cycle 1 (n=27), 2 (n=36), or 3/4 (n=13).
The study’s primary endpoint was the rate of complete MRD response within the first treatment cycle, and 78% of evaluable patients (88/113) achieved this endpoint.
A key secondary endpoint was RFS at 18 months. There were 110 patients evaluable for this endpoint. They all had Ph- BCP-ALL and <5% blasts at baseline.
The estimated RFS at 18 months was 54%, and the median RFS was 18.9 months. The median RFS was 24.6 months for patients treated in first CR and 11.0 months for patients treated in a later CR (P=0.004).
Another key endpoint was overall survival (OS). The median OS was 36.5 months, both for the 110 patients in the RFS analysis and for the entire study population.
In a landmark analysis, complete MRD responders had longer OS than MRD nonresponders—38.9 months and 12.5 months, respectively (P=0.002). And complete MRD responders had longer RFS than nonresponders—23.6 months and 5.7 months, respectively (P=0.002).
All 116 patients who started cycle 1 had at least 1 adverse event (AE). The rate of grade 3 AEs was 33%, and the rate of grade 4 AEs was 27%. These AEs were considered treatment-related in 29% (grade 3) and 22% (grade 4) of patients.
Four (3%) patients developed cytokine release syndrome—2 with grade 1 and 2 with grade 3. All of these events occurred during cycle 1.
Fifty-three percent of patients (n=61) had neurologic events. In most cases (97%, n=59), these events resolved.
There were 2 fatal AEs during the treatment period, both in cycle 1. One of these events—atypical pneumonitis with H1N1 influenza—was considered treatment-related. The other event—subdural hemorrhage—was considered unrelated to treatment.
There were 4 fatal AEs reported after blinatumomab treatment. Two of these deaths—due to multifocal CNS lesions and graft-versus-host disease—occurred in HSCT recipients. The other 2 deaths—due to disease progression and multi-organ failure—occurred in nontransplanted patients after relapse.
The US Food and Drug Administration (FDA) has expanded the approved indication for blinatumomab (Blincyto®).
The drug is now approved to treat adults and children with B-cell precursor acute lymphoblastic leukemia (BCP-ALL) in first or second complete remission (CR) with minimal residual disease (MRD) greater than or equal to 0.1%.
Blinatumomab received accelerated approval for this indication because the drug has not yet shown a clinical benefit in these patients.
The FDA’s accelerated approval program allows conditional approval of a drug that fills an unmet medical need for a serious condition.
Accelerated approval is based on surrogate or intermediate endpoints—in this case, MRD response rate and hematologic relapse-free survival (RFS)—that are reasonably likely to predict clinical benefit.
Continued approval of blinatumomab for the aforementioned indication may be contingent upon verification of clinical benefit in confirmatory trials.
“This is the first FDA-approved treatment for patients with MRD-positive ALL,” said Richard Pazdur, MD, director of the FDA’s Oncology Center of Excellence.
“Because patients who have MRD are more likely to relapse, having a treatment option that eliminates even very low amounts of residual leukemia cells may help keep the cancer in remission longer. We look forward to furthering our understanding about the reduction in MRD after treatment with Blincyto. Studies are being conducted to assess how Blincyto affects long-term survival outcomes in patients with MRD.”
About blinatumomab
Blinatumomab is a bispecific, CD19-directed, CD3 T-cell engager (BiTE®) antibody construct that binds to CD19 expressed on the surface of cells of B-lineage origin and CD3 expressed on the surface of T cells.
In 2014, the FDA granted blinatumomab accelerated approval to treat adults with Philadelphia chromosome-negative (Ph-) relapsed/refractory BCP-ALL.
In 2016, the FDA granted the therapy accelerated approval for pediatric patients with Ph- relapsed/refractory BCP-ALL.
Last year, the FDA granted blinatumomab full approval for pediatric and adult patients with Ph- or Ph+ relapsed/refractory BCP-ALL.
The FDA-approved prescribing information for blinatumomab includes a boxed warning for cytokine release syndrome and neurologic toxicities. Blinatumomab is also under a risk evaluation and mitigation strategy program in the US.
BLAST study
The new accelerated approval for blinatumomab was supported by results from the phase 2 BLAST study, which were published in Blood in January.
The study enrolled adults with MRD-positive BCP-ALL in complete hematologic remission after 3 or more cycles of intensive chemotherapy.
Patients received continuous intravenous infusions of blinatumomab at 15 μg/m2/day for 4 weeks, followed by 2 weeks off. They received up to 4 cycles of treatment and could undergo hematopoietic stem cell transplant (HSCT) at any time after the first cycle.
In all, there were 116 patients who received at least 1 infusion of blinatumomab. Seventy-six patients went on to HSCT while in continuous CR after cycle 1 (n=27), 2 (n=36), or 3/4 (n=13).
The study’s primary endpoint was the rate of complete MRD response within the first treatment cycle, and 78% of evaluable patients (88/113) achieved this endpoint.
A key secondary endpoint was RFS at 18 months. There were 110 patients evaluable for this endpoint. They all had Ph- BCP-ALL and <5% blasts at baseline.
The estimated RFS at 18 months was 54%, and the median RFS was 18.9 months. The median RFS was 24.6 months for patients treated in first CR and 11.0 months for patients treated in a later CR (P=0.004).
Another key endpoint was overall survival (OS). The median OS was 36.5 months, both for the 110 patients in the RFS analysis and for the entire study population.
In a landmark analysis, complete MRD responders had longer OS than MRD nonresponders—38.9 months and 12.5 months, respectively (P=0.002). And complete MRD responders had longer RFS than nonresponders—23.6 months and 5.7 months, respectively (P=0.002).
All 116 patients who started cycle 1 had at least 1 adverse event (AE). The rate of grade 3 AEs was 33%, and the rate of grade 4 AEs was 27%. These AEs were considered treatment-related in 29% (grade 3) and 22% (grade 4) of patients.
Four (3%) patients developed cytokine release syndrome—2 with grade 1 and 2 with grade 3. All of these events occurred during cycle 1.
Fifty-three percent of patients (n=61) had neurologic events. In most cases (97%, n=59), these events resolved.
There were 2 fatal AEs during the treatment period, both in cycle 1. One of these events—atypical pneumonitis with H1N1 influenza—was considered treatment-related. The other event—subdural hemorrhage—was considered unrelated to treatment.
There were 4 fatal AEs reported after blinatumomab treatment. Two of these deaths—due to multifocal CNS lesions and graft-versus-host disease—occurred in HSCT recipients. The other 2 deaths—due to disease progression and multi-organ failure—occurred in nontransplanted patients after relapse.
Drug receives orphan designation for AML
The US Food and Drug Administration (FDA) has granted orphan designation to MAX-40279 for the treatment of acute myeloid leukemia (AML).
MAX-40279 is a multi-target kinase inhibitor being developed by MaxiNovel Pharmaceuticals, Inc.
The drug mainly targets FMS-related tyrosine kinase 3 (FLT3) and fibroblast growth factor receptor (FGFR).
MAX-40279 demonstrated “potent” inhibition of FLT3 and FGFR in preclinical testing, according to MaxiNovel Pharmaceuticals, Inc.
The company is currently testing MAX-40279 in a phase 1 trial of patients with AML (NCT03412292).
About orphan designation
The FDA grants orphan designation to products intended to treat, diagnose, or prevent diseases/disorders that affect fewer than 200,000 people in the US.
The designation provides incentives for sponsors to develop products for rare diseases. This may include tax credits toward the cost of clinical trials, prescription drug user fee waivers, and 7 years of market exclusivity if the product is approved.
The US Food and Drug Administration (FDA) has granted orphan designation to MAX-40279 for the treatment of acute myeloid leukemia (AML).
MAX-40279 is a multi-target kinase inhibitor being developed by MaxiNovel Pharmaceuticals, Inc.
The drug mainly targets FMS-related tyrosine kinase 3 (FLT3) and fibroblast growth factor receptor (FGFR).
MAX-40279 demonstrated “potent” inhibition of FLT3 and FGFR in preclinical testing, according to MaxiNovel Pharmaceuticals, Inc.
The company is currently testing MAX-40279 in a phase 1 trial of patients with AML (NCT03412292).
About orphan designation
The FDA grants orphan designation to products intended to treat, diagnose, or prevent diseases/disorders that affect fewer than 200,000 people in the US.
The designation provides incentives for sponsors to develop products for rare diseases. This may include tax credits toward the cost of clinical trials, prescription drug user fee waivers, and 7 years of market exclusivity if the product is approved.
The US Food and Drug Administration (FDA) has granted orphan designation to MAX-40279 for the treatment of acute myeloid leukemia (AML).
MAX-40279 is a multi-target kinase inhibitor being developed by MaxiNovel Pharmaceuticals, Inc.
The drug mainly targets FMS-related tyrosine kinase 3 (FLT3) and fibroblast growth factor receptor (FGFR).
MAX-40279 demonstrated “potent” inhibition of FLT3 and FGFR in preclinical testing, according to MaxiNovel Pharmaceuticals, Inc.
The company is currently testing MAX-40279 in a phase 1 trial of patients with AML (NCT03412292).
About orphan designation
The FDA grants orphan designation to products intended to treat, diagnose, or prevent diseases/disorders that affect fewer than 200,000 people in the US.
The designation provides incentives for sponsors to develop products for rare diseases. This may include tax credits toward the cost of clinical trials, prescription drug user fee waivers, and 7 years of market exclusivity if the product is approved.
MRD may indicate relapse risk in AML
Detecting molecular minimal residual disease among patients in complete remission was a significant independent predictor of relapse and survival in acute myeloid leukemia (AML), findings from a new study suggest.
Mojca Jongen-Lavrencic, MD, PhD, of the Erasmus University in the Netherlands, and colleagues conducted targeted next-generation sequencing on bone marrow or peripheral blood samples to detect minimal residual disease in 482 newly diagnosed AML patients aged 18-65 years. The sampling was conducted at diagnosis and again after induction therapy. The study endpoints included 4-year rates of relapse, relapse-free survival, and overall survival. The findings are reported in the New England Journal of Medicine.
Overall, at least one mutation was found in 430 patients (89.2%). Persistent DTA mutations, which are associated with age-related hematopoiesis, were not significantly associated with higher 4-year relapse rates, compared with no detection of DTA mutations (P = .29). However, having a persistent DTA mutation and a coexisting persistent non-DTA mutation was a significant predictor of relapse, with a 4-year relapse rate of 66.7% versus 39.4% for no detection (P = .002).
Similarly, having a persistent non-DTA mutation at any allele frequency was linked to an increase risk of relapse at 4 years (55.7% with detection versus 34.6% without detection, P = .001). Non-DTA mutation was also significantly associated with reduced relapsed-free survival and reduced overall survival.
The study was funded by the Queen Wilhelmina Fund Foundation of the Dutch Cancer, among others. There was no commercial funding for the study.
SOURCE: Jongen-Lavrencic M et al. N Engl J Med. 2018 Mar 29;378:1189-99.
Detecting molecular minimal residual disease among patients in complete remission was a significant independent predictor of relapse and survival in acute myeloid leukemia (AML), findings from a new study suggest.
Mojca Jongen-Lavrencic, MD, PhD, of the Erasmus University in the Netherlands, and colleagues conducted targeted next-generation sequencing on bone marrow or peripheral blood samples to detect minimal residual disease in 482 newly diagnosed AML patients aged 18-65 years. The sampling was conducted at diagnosis and again after induction therapy. The study endpoints included 4-year rates of relapse, relapse-free survival, and overall survival. The findings are reported in the New England Journal of Medicine.
Overall, at least one mutation was found in 430 patients (89.2%). Persistent DTA mutations, which are associated with age-related hematopoiesis, were not significantly associated with higher 4-year relapse rates, compared with no detection of DTA mutations (P = .29). However, having a persistent DTA mutation and a coexisting persistent non-DTA mutation was a significant predictor of relapse, with a 4-year relapse rate of 66.7% versus 39.4% for no detection (P = .002).
Similarly, having a persistent non-DTA mutation at any allele frequency was linked to an increase risk of relapse at 4 years (55.7% with detection versus 34.6% without detection, P = .001). Non-DTA mutation was also significantly associated with reduced relapsed-free survival and reduced overall survival.
The study was funded by the Queen Wilhelmina Fund Foundation of the Dutch Cancer, among others. There was no commercial funding for the study.
SOURCE: Jongen-Lavrencic M et al. N Engl J Med. 2018 Mar 29;378:1189-99.
Detecting molecular minimal residual disease among patients in complete remission was a significant independent predictor of relapse and survival in acute myeloid leukemia (AML), findings from a new study suggest.
Mojca Jongen-Lavrencic, MD, PhD, of the Erasmus University in the Netherlands, and colleagues conducted targeted next-generation sequencing on bone marrow or peripheral blood samples to detect minimal residual disease in 482 newly diagnosed AML patients aged 18-65 years. The sampling was conducted at diagnosis and again after induction therapy. The study endpoints included 4-year rates of relapse, relapse-free survival, and overall survival. The findings are reported in the New England Journal of Medicine.
Overall, at least one mutation was found in 430 patients (89.2%). Persistent DTA mutations, which are associated with age-related hematopoiesis, were not significantly associated with higher 4-year relapse rates, compared with no detection of DTA mutations (P = .29). However, having a persistent DTA mutation and a coexisting persistent non-DTA mutation was a significant predictor of relapse, with a 4-year relapse rate of 66.7% versus 39.4% for no detection (P = .002).
Similarly, having a persistent non-DTA mutation at any allele frequency was linked to an increase risk of relapse at 4 years (55.7% with detection versus 34.6% without detection, P = .001). Non-DTA mutation was also significantly associated with reduced relapsed-free survival and reduced overall survival.
The study was funded by the Queen Wilhelmina Fund Foundation of the Dutch Cancer, among others. There was no commercial funding for the study.
SOURCE: Jongen-Lavrencic M et al. N Engl J Med. 2018 Mar 29;378:1189-99.
FROM NEW ENGLAND JOURNAL OF MEDICINE
Disease, genetics contribute to neurocognitive decline in ALL
Chemotherapeutic agents have been associated with neurocognitive side effects in survivors of pediatric acute lymphoblastic leukemia (ALL).
Now, researchers have found evidence to suggest that genetics and ALL itself can increase the risk for long-term problems with attention, organization, and related neurocognitive skills.
The researchers reported these findings in JAMA Oncology.
The team evaluated patients enrolled in the Total XV St. Jude clinical trial, analyzing the cerebrospinal fluid (CSF) of 235 pediatric ALL patients treated with chemotherapy alone.
The CSF had been collected at 5 times before and during treatment (between 2000 and 2010). The analysis included neurocognitive testing and brain imaging of 138 ALL survivors who were at least 8 years old and 5 years from their cancer diagnosis.
The researchers found that, even before treatment began, some patients had proteins in their CSF that suggested injury to glial cells.
“This was a surprise,” said study author Kevin Krull, PhD, of St. Jude Children’s Research Hospital in Memphis, Tennessee.
“Until now, we had not suspected that leukemia by itself or the inflammatory response to the disease may lead to changes that leave ALL survivors at risk for problems with executive functioning and processing speed later.”
Previously, researchers had assumed neurocognitive problems were a side effect of ALL therapy, particularly treatment with methotrexate.
So finding elevated biomarkers in the CSF of some patients during methotrexate treatment was not surprising, but, previously, little was known about the neurotoxic mechanism involved. The biomarkers identified were indicative of injury to neurons, axons, and glial cells.
The researchers checked patients’ CSF for 5 proteins and other biomarkers of brain cell damage related to treatment with either high-dose intravenous methotrexate or intrathecal methotrexate.
The biomarkers were present early on but changed and varied throughout treatment. For example, biomarkers of demyelination were present in some patients newly diagnosed with ALL and then decreased during treatment.
Others, including biomarkers of inflammation and neuronal damage, increased as treatment progressed.
Overall, methotrexate treatment was associated with biomarkers that signaled as much as a 70% increased risk for reduced neurocognitive functioning in long-term ALL survivors.
The researchers also looked for evidence that genetic variation might influence the susceptibility of pediatric ALL patients to methotrexate injury.
The team checked patients’ DNA for 42 gene variants known to influence drug metabolism, neurodevelopment, and oxidative stress.
The analysis identified a variant of the COMT gene that was associated with higher biomarker levels following methotrexate treatment. The gene encodes instructions for a protein involved in processing the neurotransmitter dopamine in the frontal regions of the brain.
“Dopamine is the primary neurotransmitter in executive functioning,” Dr Krull noted. “This suggests that 2 independent processes might be coming together in some patients that influence their risk for diminished executive functioning.”
“Taken together, the results suggest that survivors’ neurocognitive deficits are multifactorial and reflect a complex interaction among genetics, treatment intensity, and other factors. Monitoring CSF biomarkers and screening for genetic mediators of brain injury may help identify and intervene with survivors at risk for neurocognitive problems.”
Chemotherapeutic agents have been associated with neurocognitive side effects in survivors of pediatric acute lymphoblastic leukemia (ALL).
Now, researchers have found evidence to suggest that genetics and ALL itself can increase the risk for long-term problems with attention, organization, and related neurocognitive skills.
The researchers reported these findings in JAMA Oncology.
The team evaluated patients enrolled in the Total XV St. Jude clinical trial, analyzing the cerebrospinal fluid (CSF) of 235 pediatric ALL patients treated with chemotherapy alone.
The CSF had been collected at 5 times before and during treatment (between 2000 and 2010). The analysis included neurocognitive testing and brain imaging of 138 ALL survivors who were at least 8 years old and 5 years from their cancer diagnosis.
The researchers found that, even before treatment began, some patients had proteins in their CSF that suggested injury to glial cells.
“This was a surprise,” said study author Kevin Krull, PhD, of St. Jude Children’s Research Hospital in Memphis, Tennessee.
“Until now, we had not suspected that leukemia by itself or the inflammatory response to the disease may lead to changes that leave ALL survivors at risk for problems with executive functioning and processing speed later.”
Previously, researchers had assumed neurocognitive problems were a side effect of ALL therapy, particularly treatment with methotrexate.
So finding elevated biomarkers in the CSF of some patients during methotrexate treatment was not surprising, but, previously, little was known about the neurotoxic mechanism involved. The biomarkers identified were indicative of injury to neurons, axons, and glial cells.
The researchers checked patients’ CSF for 5 proteins and other biomarkers of brain cell damage related to treatment with either high-dose intravenous methotrexate or intrathecal methotrexate.
The biomarkers were present early on but changed and varied throughout treatment. For example, biomarkers of demyelination were present in some patients newly diagnosed with ALL and then decreased during treatment.
Others, including biomarkers of inflammation and neuronal damage, increased as treatment progressed.
Overall, methotrexate treatment was associated with biomarkers that signaled as much as a 70% increased risk for reduced neurocognitive functioning in long-term ALL survivors.
The researchers also looked for evidence that genetic variation might influence the susceptibility of pediatric ALL patients to methotrexate injury.
The team checked patients’ DNA for 42 gene variants known to influence drug metabolism, neurodevelopment, and oxidative stress.
The analysis identified a variant of the COMT gene that was associated with higher biomarker levels following methotrexate treatment. The gene encodes instructions for a protein involved in processing the neurotransmitter dopamine in the frontal regions of the brain.
“Dopamine is the primary neurotransmitter in executive functioning,” Dr Krull noted. “This suggests that 2 independent processes might be coming together in some patients that influence their risk for diminished executive functioning.”
“Taken together, the results suggest that survivors’ neurocognitive deficits are multifactorial and reflect a complex interaction among genetics, treatment intensity, and other factors. Monitoring CSF biomarkers and screening for genetic mediators of brain injury may help identify and intervene with survivors at risk for neurocognitive problems.”
Chemotherapeutic agents have been associated with neurocognitive side effects in survivors of pediatric acute lymphoblastic leukemia (ALL).
Now, researchers have found evidence to suggest that genetics and ALL itself can increase the risk for long-term problems with attention, organization, and related neurocognitive skills.
The researchers reported these findings in JAMA Oncology.
The team evaluated patients enrolled in the Total XV St. Jude clinical trial, analyzing the cerebrospinal fluid (CSF) of 235 pediatric ALL patients treated with chemotherapy alone.
The CSF had been collected at 5 times before and during treatment (between 2000 and 2010). The analysis included neurocognitive testing and brain imaging of 138 ALL survivors who were at least 8 years old and 5 years from their cancer diagnosis.
The researchers found that, even before treatment began, some patients had proteins in their CSF that suggested injury to glial cells.
“This was a surprise,” said study author Kevin Krull, PhD, of St. Jude Children’s Research Hospital in Memphis, Tennessee.
“Until now, we had not suspected that leukemia by itself or the inflammatory response to the disease may lead to changes that leave ALL survivors at risk for problems with executive functioning and processing speed later.”
Previously, researchers had assumed neurocognitive problems were a side effect of ALL therapy, particularly treatment with methotrexate.
So finding elevated biomarkers in the CSF of some patients during methotrexate treatment was not surprising, but, previously, little was known about the neurotoxic mechanism involved. The biomarkers identified were indicative of injury to neurons, axons, and glial cells.
The researchers checked patients’ CSF for 5 proteins and other biomarkers of brain cell damage related to treatment with either high-dose intravenous methotrexate or intrathecal methotrexate.
The biomarkers were present early on but changed and varied throughout treatment. For example, biomarkers of demyelination were present in some patients newly diagnosed with ALL and then decreased during treatment.
Others, including biomarkers of inflammation and neuronal damage, increased as treatment progressed.
Overall, methotrexate treatment was associated with biomarkers that signaled as much as a 70% increased risk for reduced neurocognitive functioning in long-term ALL survivors.
The researchers also looked for evidence that genetic variation might influence the susceptibility of pediatric ALL patients to methotrexate injury.
The team checked patients’ DNA for 42 gene variants known to influence drug metabolism, neurodevelopment, and oxidative stress.
The analysis identified a variant of the COMT gene that was associated with higher biomarker levels following methotrexate treatment. The gene encodes instructions for a protein involved in processing the neurotransmitter dopamine in the frontal regions of the brain.
“Dopamine is the primary neurotransmitter in executive functioning,” Dr Krull noted. “This suggests that 2 independent processes might be coming together in some patients that influence their risk for diminished executive functioning.”
“Taken together, the results suggest that survivors’ neurocognitive deficits are multifactorial and reflect a complex interaction among genetics, treatment intensity, and other factors. Monitoring CSF biomarkers and screening for genetic mediators of brain injury may help identify and intervene with survivors at risk for neurocognitive problems.”
FDA expands indication for blinatumomab in treating ALL
The Food and Drug Administration has granted accelerated who are in remission but still have minimal residual disease (MRD).
This is the first FDA-approved treatment for those with MRD, the FDA said in a statement.
The current approval was based on a single-arm clinical trial of 86 patients in first or second complete remission who had detectable MRD in at least 1 out of 1,000 cells in their bone marrow. Undetectable MRD was achieved by 70 patients after one cycle of blinatumomab treatment. More than half of the patients remained alive and in remission for at least 22.3 months, the FDA said.
Common side effects include bacterial and pathogen-unspecified infections, pyrexia, headache, infusion-related reactions, neutropenia, anemia, febrile neutropenia, and thrombocytopenia. The drug carries a boxed warning about cytokine release syndrome at the start of the first treatment. The FDA also warns that children weighing less than 22 kg should receive the drug prepared with preservative-free saline because of the risk of serious adverse reactions in pediatric patients from a benzyl alcohol preservative.
Blinatumomab is marketed as Blincyto by Amgen.
The Food and Drug Administration has granted accelerated who are in remission but still have minimal residual disease (MRD).
This is the first FDA-approved treatment for those with MRD, the FDA said in a statement.
The current approval was based on a single-arm clinical trial of 86 patients in first or second complete remission who had detectable MRD in at least 1 out of 1,000 cells in their bone marrow. Undetectable MRD was achieved by 70 patients after one cycle of blinatumomab treatment. More than half of the patients remained alive and in remission for at least 22.3 months, the FDA said.
Common side effects include bacterial and pathogen-unspecified infections, pyrexia, headache, infusion-related reactions, neutropenia, anemia, febrile neutropenia, and thrombocytopenia. The drug carries a boxed warning about cytokine release syndrome at the start of the first treatment. The FDA also warns that children weighing less than 22 kg should receive the drug prepared with preservative-free saline because of the risk of serious adverse reactions in pediatric patients from a benzyl alcohol preservative.
Blinatumomab is marketed as Blincyto by Amgen.
The Food and Drug Administration has granted accelerated who are in remission but still have minimal residual disease (MRD).
This is the first FDA-approved treatment for those with MRD, the FDA said in a statement.
The current approval was based on a single-arm clinical trial of 86 patients in first or second complete remission who had detectable MRD in at least 1 out of 1,000 cells in their bone marrow. Undetectable MRD was achieved by 70 patients after one cycle of blinatumomab treatment. More than half of the patients remained alive and in remission for at least 22.3 months, the FDA said.
Common side effects include bacterial and pathogen-unspecified infections, pyrexia, headache, infusion-related reactions, neutropenia, anemia, febrile neutropenia, and thrombocytopenia. The drug carries a boxed warning about cytokine release syndrome at the start of the first treatment. The FDA also warns that children weighing less than 22 kg should receive the drug prepared with preservative-free saline because of the risk of serious adverse reactions in pediatric patients from a benzyl alcohol preservative.
Blinatumomab is marketed as Blincyto by Amgen.