User login
Cord blood product gets orphan designation

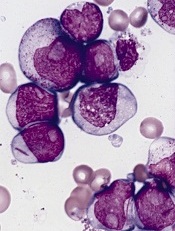
Credit: NHS
The US Food and Drug Administration (FDA) has granted orphan designation to a cord blood product called NiCord for the treatment of acute lymphoblastic leukemia (ALL), acute myeloid leukemia (AML), Hodgkin lymphoma (HL), and myelodysplastic syndromes (MDS).
NiCord consists of cells from a single cord blood unit cultured in nicotinamide—a vitamin B derivative—and cytokines that are typically used for expansion—thrombopoietin, interleukin 6, FLT3 ligand, and stem cell factor.
The FDA’s orphan drug designation for NiCord coincides with the positive opinion of the European Medicines Agency’s (EMA’s) Committee for Orphan Medicinal Products regarding NiCord as a treatment for AML. Gamida Cell, the company developing NiCord, intends to file for orphan drug status with the EMA for other indications as well.
“Receipt of orphan drug status for NiCord in the US and Europe advances Gamida Cell’s commercialization plans a major step further, as both afford significant advantages,” said Yael Margolin, President and CEO of Gamida Cell.
Orphan drug designation provides various regulatory and economic benefits, including 7 years of market exclusivity upon product approval in the US and 10 years in the European Union.
Trials of NiCord
NiCord is currently being tested in a phase 1/2 study as an investigational therapeutic treatment for hematologic malignancies. In this study, NiCord is being used as the sole stem cell source.
In a previous study, presented at the 11th Annual International Cord Blood Symposium, researchers transplanted a NiCord unit and an unmanipulated cord blood unit in patients with ALL, AML, MDS, HL, or non-Hodgkin lymphoma.
A majority of patients in this small, phase 1/2 study achieved early platelet and neutrophil engraftment. And, in some patients, that engraftment persisted for 2 years.
Eight of the 11 patients enrolled achieved engraftment with the NiCord unit, and 2 engrafted with the unmanipulated cord blood unit. One patient had primary graft failure.
There were no adverse events attributable to the NiCord unit, but 4 patients developed grade 1-2 acute GVHD, and 1 patient developed limited chronic GVHD.
For more information on NiCord, visit the Gamida Cell website. ![]()

Credit: NHS
The US Food and Drug Administration (FDA) has granted orphan designation to a cord blood product called NiCord for the treatment of acute lymphoblastic leukemia (ALL), acute myeloid leukemia (AML), Hodgkin lymphoma (HL), and myelodysplastic syndromes (MDS).
NiCord consists of cells from a single cord blood unit cultured in nicotinamide—a vitamin B derivative—and cytokines that are typically used for expansion—thrombopoietin, interleukin 6, FLT3 ligand, and stem cell factor.
The FDA’s orphan drug designation for NiCord coincides with the positive opinion of the European Medicines Agency’s (EMA’s) Committee for Orphan Medicinal Products regarding NiCord as a treatment for AML. Gamida Cell, the company developing NiCord, intends to file for orphan drug status with the EMA for other indications as well.
“Receipt of orphan drug status for NiCord in the US and Europe advances Gamida Cell’s commercialization plans a major step further, as both afford significant advantages,” said Yael Margolin, President and CEO of Gamida Cell.
Orphan drug designation provides various regulatory and economic benefits, including 7 years of market exclusivity upon product approval in the US and 10 years in the European Union.
Trials of NiCord
NiCord is currently being tested in a phase 1/2 study as an investigational therapeutic treatment for hematologic malignancies. In this study, NiCord is being used as the sole stem cell source.
In a previous study, presented at the 11th Annual International Cord Blood Symposium, researchers transplanted a NiCord unit and an unmanipulated cord blood unit in patients with ALL, AML, MDS, HL, or non-Hodgkin lymphoma.
A majority of patients in this small, phase 1/2 study achieved early platelet and neutrophil engraftment. And, in some patients, that engraftment persisted for 2 years.
Eight of the 11 patients enrolled achieved engraftment with the NiCord unit, and 2 engrafted with the unmanipulated cord blood unit. One patient had primary graft failure.
There were no adverse events attributable to the NiCord unit, but 4 patients developed grade 1-2 acute GVHD, and 1 patient developed limited chronic GVHD.
For more information on NiCord, visit the Gamida Cell website. ![]()

Credit: NHS
The US Food and Drug Administration (FDA) has granted orphan designation to a cord blood product called NiCord for the treatment of acute lymphoblastic leukemia (ALL), acute myeloid leukemia (AML), Hodgkin lymphoma (HL), and myelodysplastic syndromes (MDS).
NiCord consists of cells from a single cord blood unit cultured in nicotinamide—a vitamin B derivative—and cytokines that are typically used for expansion—thrombopoietin, interleukin 6, FLT3 ligand, and stem cell factor.
The FDA’s orphan drug designation for NiCord coincides with the positive opinion of the European Medicines Agency’s (EMA’s) Committee for Orphan Medicinal Products regarding NiCord as a treatment for AML. Gamida Cell, the company developing NiCord, intends to file for orphan drug status with the EMA for other indications as well.
“Receipt of orphan drug status for NiCord in the US and Europe advances Gamida Cell’s commercialization plans a major step further, as both afford significant advantages,” said Yael Margolin, President and CEO of Gamida Cell.
Orphan drug designation provides various regulatory and economic benefits, including 7 years of market exclusivity upon product approval in the US and 10 years in the European Union.
Trials of NiCord
NiCord is currently being tested in a phase 1/2 study as an investigational therapeutic treatment for hematologic malignancies. In this study, NiCord is being used as the sole stem cell source.
In a previous study, presented at the 11th Annual International Cord Blood Symposium, researchers transplanted a NiCord unit and an unmanipulated cord blood unit in patients with ALL, AML, MDS, HL, or non-Hodgkin lymphoma.
A majority of patients in this small, phase 1/2 study achieved early platelet and neutrophil engraftment. And, in some patients, that engraftment persisted for 2 years.
Eight of the 11 patients enrolled achieved engraftment with the NiCord unit, and 2 engrafted with the unmanipulated cord blood unit. One patient had primary graft failure.
There were no adverse events attributable to the NiCord unit, but 4 patients developed grade 1-2 acute GVHD, and 1 patient developed limited chronic GVHD.
For more information on NiCord, visit the Gamida Cell website. ![]()
CAR T-cell therapy gets orphan designation for DLBCL

Credit: Charles Haymond
The European Commission has granted KTE-C19, a chimeric antigen receptor (CAR) T-cell therapy, orphan designation to treat patients with diffuse large B-cell lymphoma (DLBCL) in the European Union (EU).
To create KTE-C19, a patient’s T cells are genetically modified using a gammaretroviral vector to express a CAR designed to target CD19, a protein expressed on B cells.
The product received orphan designation to treat DLBCL in the US last March.
“We are pleased with the approval of orphan drug designation for KTE-C19 in the EU, another important milestone for Kite Pharma and for the progress of our lead program,” said Arie Belldegrun, MD, President and CEO of Kite Pharma, Inc., the company developing KTE-C19.
Orphan designation by the European Commission provides regulatory and financial incentives for companies to develop and market therapies that treat a life-threatening or chronically debilitating condition affecting no more than 5 in 10,000 persons in the EU, and where no satisfactory treatment is available.
In addition to a 10-year period of marketing exclusivity in the EU after product approval, orphan drug designation provides incentives for companies seeking protocol assistance from the European Medicines Agency during the product development phase, and direct access to the centralized authorization procedure.
KTE-C19 in DLBCL
In a study published in the Journal of Clinical Oncology last year, researchers evaluated KTE-C19 in 15 patients with advanced B-cell malignancies.
The patients received a conditioning regimen of cyclophosphamide and fludarabine, followed 1 day later by a single infusion of KTE-C19. The researchers noted that the conditioning regimen is known to be active against B-cell malignancies and could have made a direct contribution to patient responses.
Of the 7 patients with chemotherapy-refractory DLBCL, 4 achieved a complete response to treatment, 2 achieved a partial response, and 1 had stable disease. Three of the complete responses were ongoing at the time of publication, with the duration ranging from 9 months to 22 months.
In the entire patient population, KTE-C19 elicited a number of adverse events, including fever, hypotension, delirium, and other neurologic toxicities. All but 2 patients experienced grade 3/4 adverse events.
Three patients developed unexpected neurologic abnormalities. One patient experienced aphasia and right-sided facial paresis. One patient developed aphasia, confusion, and severe, generalized myoclonus. And 1 patient had aphasia, confusion, hemifacial spasms, apraxia, and gait disturbances.
For more information on KTE-C19, visit Kite Pharma’s website. ![]()

Credit: Charles Haymond
The European Commission has granted KTE-C19, a chimeric antigen receptor (CAR) T-cell therapy, orphan designation to treat patients with diffuse large B-cell lymphoma (DLBCL) in the European Union (EU).
To create KTE-C19, a patient’s T cells are genetically modified using a gammaretroviral vector to express a CAR designed to target CD19, a protein expressed on B cells.
The product received orphan designation to treat DLBCL in the US last March.
“We are pleased with the approval of orphan drug designation for KTE-C19 in the EU, another important milestone for Kite Pharma and for the progress of our lead program,” said Arie Belldegrun, MD, President and CEO of Kite Pharma, Inc., the company developing KTE-C19.
Orphan designation by the European Commission provides regulatory and financial incentives for companies to develop and market therapies that treat a life-threatening or chronically debilitating condition affecting no more than 5 in 10,000 persons in the EU, and where no satisfactory treatment is available.
In addition to a 10-year period of marketing exclusivity in the EU after product approval, orphan drug designation provides incentives for companies seeking protocol assistance from the European Medicines Agency during the product development phase, and direct access to the centralized authorization procedure.
KTE-C19 in DLBCL
In a study published in the Journal of Clinical Oncology last year, researchers evaluated KTE-C19 in 15 patients with advanced B-cell malignancies.
The patients received a conditioning regimen of cyclophosphamide and fludarabine, followed 1 day later by a single infusion of KTE-C19. The researchers noted that the conditioning regimen is known to be active against B-cell malignancies and could have made a direct contribution to patient responses.
Of the 7 patients with chemotherapy-refractory DLBCL, 4 achieved a complete response to treatment, 2 achieved a partial response, and 1 had stable disease. Three of the complete responses were ongoing at the time of publication, with the duration ranging from 9 months to 22 months.
In the entire patient population, KTE-C19 elicited a number of adverse events, including fever, hypotension, delirium, and other neurologic toxicities. All but 2 patients experienced grade 3/4 adverse events.
Three patients developed unexpected neurologic abnormalities. One patient experienced aphasia and right-sided facial paresis. One patient developed aphasia, confusion, and severe, generalized myoclonus. And 1 patient had aphasia, confusion, hemifacial spasms, apraxia, and gait disturbances.
For more information on KTE-C19, visit Kite Pharma’s website. ![]()

Credit: Charles Haymond
The European Commission has granted KTE-C19, a chimeric antigen receptor (CAR) T-cell therapy, orphan designation to treat patients with diffuse large B-cell lymphoma (DLBCL) in the European Union (EU).
To create KTE-C19, a patient’s T cells are genetically modified using a gammaretroviral vector to express a CAR designed to target CD19, a protein expressed on B cells.
The product received orphan designation to treat DLBCL in the US last March.
“We are pleased with the approval of orphan drug designation for KTE-C19 in the EU, another important milestone for Kite Pharma and for the progress of our lead program,” said Arie Belldegrun, MD, President and CEO of Kite Pharma, Inc., the company developing KTE-C19.
Orphan designation by the European Commission provides regulatory and financial incentives for companies to develop and market therapies that treat a life-threatening or chronically debilitating condition affecting no more than 5 in 10,000 persons in the EU, and where no satisfactory treatment is available.
In addition to a 10-year period of marketing exclusivity in the EU after product approval, orphan drug designation provides incentives for companies seeking protocol assistance from the European Medicines Agency during the product development phase, and direct access to the centralized authorization procedure.
KTE-C19 in DLBCL
In a study published in the Journal of Clinical Oncology last year, researchers evaluated KTE-C19 in 15 patients with advanced B-cell malignancies.
The patients received a conditioning regimen of cyclophosphamide and fludarabine, followed 1 day later by a single infusion of KTE-C19. The researchers noted that the conditioning regimen is known to be active against B-cell malignancies and could have made a direct contribution to patient responses.
Of the 7 patients with chemotherapy-refractory DLBCL, 4 achieved a complete response to treatment, 2 achieved a partial response, and 1 had stable disease. Three of the complete responses were ongoing at the time of publication, with the duration ranging from 9 months to 22 months.
In the entire patient population, KTE-C19 elicited a number of adverse events, including fever, hypotension, delirium, and other neurologic toxicities. All but 2 patients experienced grade 3/4 adverse events.
Three patients developed unexpected neurologic abnormalities. One patient experienced aphasia and right-sided facial paresis. One patient developed aphasia, confusion, and severe, generalized myoclonus. And 1 patient had aphasia, confusion, hemifacial spasms, apraxia, and gait disturbances.
For more information on KTE-C19, visit Kite Pharma’s website. ![]()
HIV doesn’t hinder lymphoma patients’ response to ASCT

a cultured lymphocyte
Credit: CDC
SAN FRANCISCO—Patients with HIV-related lymphoma (HRL) should not be excluded from clinical trials of autologous stem cell transplant (ASCT) due to their HIV status, new research suggests.
Investigators found no significant difference in rates of treatment failure, disease progression, or survival between transplant-treated historical controls who had lymphoma but not HIV and patients with HRL who received the modified BEAM regimen followed by ASCT on a phase 2 trial.
This suggests patients with chemotherapy-sensitive, relapsed/refractory HRL can be treated successfully with the modified BEAM regimen, said study investigator Joseph Alvarnas, MD, of City of Hope National Medical Center in Duarte, California.
“Patients with treatment-responsive HIV infection and HIV-related lymphoma should be considered candidates for autologous transplant if they meet standard transplant criteria,” he added. “And we would argue that exclusion from clinical trials on the basis of HIV infection alone is no longer justified.”
Dr Alvarnas presented this viewpoint and the research to support it at the 2014 ASH Annual Meeting as abstract 674.
The trial enrolled 43 patients with treatable HIV-1 infection, adequate organ function, and aggressive lymphoma. Three patients were excluded because they could not undergo transplant due to lymphoma progression.
Of the 40 remaining patients, 5 were female, and their median age was 46.9 years (range, 22.5-62.2). They had diffuse large B-cell lymphoma (n=16), plasmablastic lymphoma (n=2), Burkitt/Burkitt-like lymphoma (n=7), and Hodgkin lymphoma (n=15).
The pre-ASCT HIV viral load was undetectable in 31 patients. In the patients with detectable HIV, the median viral load pre-ASCT was 84 copies/μL (range, 50-17,455). The median CD4 count was 250.5/µL (range, 39-797).
Before transplant, 30 patients (75%) were in complete remission, 8 (20%) were in partial remission, and 2 (5%) had relapsed/progressive disease.
The patients underwent ASCT after conditioning with the modified BEAM regimen—carmustine at 300 mg/m2 (day -6), etoposide at 100 mg/m2 twice daily (days -5 to -2), cytarabine at 100 mg/m2 (days -5 to -2), and melphalan at 140 mg/m2 (day -1).
Combination antiretroviral therapy (cART) was held during the preparative regimen and resumed after the resolution of gastrointestinal toxicity. The investigators switched efavirenz to an alternative agent 2 or more weeks prior to the planned interruption of cART, as the drug has a long half-life. And AZT was prohibited due to its myelosuppressive effects.
Treatment results
The median follow-up was 24 months. At 100 days post-transplant, the investigators assessed 39 patients for response. One patient was not evaluable due to early death.
Thirty-six of the patients (92.3%) were in complete remission, 1 (2.6%) was in partial remission, and 2 (5.1%) had relapsed or progressive disease.
Fifteen patients reported grade 3 or higher toxicities within a year of transplant. Of the 13 unexpected grade 3-5 adverse events (reported in 9 patients), 5 were infection/sepsis, 1 was acute appendicitis, 1 was acute coronary syndrome, 2 were deep vein thromboses, 2 were gastrointestinal toxicities, and 2 were metabolic abnormalities.
Seventeen patients reported at least 1 infectious episode, 42 events in total, 9 of which were severe. Fourteen patients required readmission to the hospital after transplant.
Within a year of transplant, 5 patients had died—3 from recurrent/persistent disease, 1 due to a fungal infection, and 1 from cardiac arrest. Two additional patients died after the 1-year mark—1 of recurrent/persistent disease and 1 of heart failure.
At 12 months, the rate of overall survival was 86.6%, progression-free survival was 82.3%, progression was 12.5%, and non-relapse mortality was 5.2%.
“In order to place this within context, we had the opportunity to compare our patient experience with 151 matched controls [without HIV] from CIBMTR,” Dr Alvarnas said. “Ninety-three percent of these patients were actually transplanted within 2 years so that they were the time-concordant group, and they were matched for performance score, disease, and disease stage.”
The investigators found no significant difference between their patient group and the HIV-free controls with regard to overall mortality (P=0.56), treatment failure (P=0.10), progression (P=0.06), and treatment-related mortality (P=0.97).
Likewise, there was no significant difference in overall survival between the HRL patients and controls—86.6% and 87.7%, respectively (P=0.56). And the same was true of progression-free survival—82.3% and 69.5%, respectively (P=0.10). ![]()

a cultured lymphocyte
Credit: CDC
SAN FRANCISCO—Patients with HIV-related lymphoma (HRL) should not be excluded from clinical trials of autologous stem cell transplant (ASCT) due to their HIV status, new research suggests.
Investigators found no significant difference in rates of treatment failure, disease progression, or survival between transplant-treated historical controls who had lymphoma but not HIV and patients with HRL who received the modified BEAM regimen followed by ASCT on a phase 2 trial.
This suggests patients with chemotherapy-sensitive, relapsed/refractory HRL can be treated successfully with the modified BEAM regimen, said study investigator Joseph Alvarnas, MD, of City of Hope National Medical Center in Duarte, California.
“Patients with treatment-responsive HIV infection and HIV-related lymphoma should be considered candidates for autologous transplant if they meet standard transplant criteria,” he added. “And we would argue that exclusion from clinical trials on the basis of HIV infection alone is no longer justified.”
Dr Alvarnas presented this viewpoint and the research to support it at the 2014 ASH Annual Meeting as abstract 674.
The trial enrolled 43 patients with treatable HIV-1 infection, adequate organ function, and aggressive lymphoma. Three patients were excluded because they could not undergo transplant due to lymphoma progression.
Of the 40 remaining patients, 5 were female, and their median age was 46.9 years (range, 22.5-62.2). They had diffuse large B-cell lymphoma (n=16), plasmablastic lymphoma (n=2), Burkitt/Burkitt-like lymphoma (n=7), and Hodgkin lymphoma (n=15).
The pre-ASCT HIV viral load was undetectable in 31 patients. In the patients with detectable HIV, the median viral load pre-ASCT was 84 copies/μL (range, 50-17,455). The median CD4 count was 250.5/µL (range, 39-797).
Before transplant, 30 patients (75%) were in complete remission, 8 (20%) were in partial remission, and 2 (5%) had relapsed/progressive disease.
The patients underwent ASCT after conditioning with the modified BEAM regimen—carmustine at 300 mg/m2 (day -6), etoposide at 100 mg/m2 twice daily (days -5 to -2), cytarabine at 100 mg/m2 (days -5 to -2), and melphalan at 140 mg/m2 (day -1).
Combination antiretroviral therapy (cART) was held during the preparative regimen and resumed after the resolution of gastrointestinal toxicity. The investigators switched efavirenz to an alternative agent 2 or more weeks prior to the planned interruption of cART, as the drug has a long half-life. And AZT was prohibited due to its myelosuppressive effects.
Treatment results
The median follow-up was 24 months. At 100 days post-transplant, the investigators assessed 39 patients for response. One patient was not evaluable due to early death.
Thirty-six of the patients (92.3%) were in complete remission, 1 (2.6%) was in partial remission, and 2 (5.1%) had relapsed or progressive disease.
Fifteen patients reported grade 3 or higher toxicities within a year of transplant. Of the 13 unexpected grade 3-5 adverse events (reported in 9 patients), 5 were infection/sepsis, 1 was acute appendicitis, 1 was acute coronary syndrome, 2 were deep vein thromboses, 2 were gastrointestinal toxicities, and 2 were metabolic abnormalities.
Seventeen patients reported at least 1 infectious episode, 42 events in total, 9 of which were severe. Fourteen patients required readmission to the hospital after transplant.
Within a year of transplant, 5 patients had died—3 from recurrent/persistent disease, 1 due to a fungal infection, and 1 from cardiac arrest. Two additional patients died after the 1-year mark—1 of recurrent/persistent disease and 1 of heart failure.
At 12 months, the rate of overall survival was 86.6%, progression-free survival was 82.3%, progression was 12.5%, and non-relapse mortality was 5.2%.
“In order to place this within context, we had the opportunity to compare our patient experience with 151 matched controls [without HIV] from CIBMTR,” Dr Alvarnas said. “Ninety-three percent of these patients were actually transplanted within 2 years so that they were the time-concordant group, and they were matched for performance score, disease, and disease stage.”
The investigators found no significant difference between their patient group and the HIV-free controls with regard to overall mortality (P=0.56), treatment failure (P=0.10), progression (P=0.06), and treatment-related mortality (P=0.97).
Likewise, there was no significant difference in overall survival between the HRL patients and controls—86.6% and 87.7%, respectively (P=0.56). And the same was true of progression-free survival—82.3% and 69.5%, respectively (P=0.10). ![]()

a cultured lymphocyte
Credit: CDC
SAN FRANCISCO—Patients with HIV-related lymphoma (HRL) should not be excluded from clinical trials of autologous stem cell transplant (ASCT) due to their HIV status, new research suggests.
Investigators found no significant difference in rates of treatment failure, disease progression, or survival between transplant-treated historical controls who had lymphoma but not HIV and patients with HRL who received the modified BEAM regimen followed by ASCT on a phase 2 trial.
This suggests patients with chemotherapy-sensitive, relapsed/refractory HRL can be treated successfully with the modified BEAM regimen, said study investigator Joseph Alvarnas, MD, of City of Hope National Medical Center in Duarte, California.
“Patients with treatment-responsive HIV infection and HIV-related lymphoma should be considered candidates for autologous transplant if they meet standard transplant criteria,” he added. “And we would argue that exclusion from clinical trials on the basis of HIV infection alone is no longer justified.”
Dr Alvarnas presented this viewpoint and the research to support it at the 2014 ASH Annual Meeting as abstract 674.
The trial enrolled 43 patients with treatable HIV-1 infection, adequate organ function, and aggressive lymphoma. Three patients were excluded because they could not undergo transplant due to lymphoma progression.
Of the 40 remaining patients, 5 were female, and their median age was 46.9 years (range, 22.5-62.2). They had diffuse large B-cell lymphoma (n=16), plasmablastic lymphoma (n=2), Burkitt/Burkitt-like lymphoma (n=7), and Hodgkin lymphoma (n=15).
The pre-ASCT HIV viral load was undetectable in 31 patients. In the patients with detectable HIV, the median viral load pre-ASCT was 84 copies/μL (range, 50-17,455). The median CD4 count was 250.5/µL (range, 39-797).
Before transplant, 30 patients (75%) were in complete remission, 8 (20%) were in partial remission, and 2 (5%) had relapsed/progressive disease.
The patients underwent ASCT after conditioning with the modified BEAM regimen—carmustine at 300 mg/m2 (day -6), etoposide at 100 mg/m2 twice daily (days -5 to -2), cytarabine at 100 mg/m2 (days -5 to -2), and melphalan at 140 mg/m2 (day -1).
Combination antiretroviral therapy (cART) was held during the preparative regimen and resumed after the resolution of gastrointestinal toxicity. The investigators switched efavirenz to an alternative agent 2 or more weeks prior to the planned interruption of cART, as the drug has a long half-life. And AZT was prohibited due to its myelosuppressive effects.
Treatment results
The median follow-up was 24 months. At 100 days post-transplant, the investigators assessed 39 patients for response. One patient was not evaluable due to early death.
Thirty-six of the patients (92.3%) were in complete remission, 1 (2.6%) was in partial remission, and 2 (5.1%) had relapsed or progressive disease.
Fifteen patients reported grade 3 or higher toxicities within a year of transplant. Of the 13 unexpected grade 3-5 adverse events (reported in 9 patients), 5 were infection/sepsis, 1 was acute appendicitis, 1 was acute coronary syndrome, 2 were deep vein thromboses, 2 were gastrointestinal toxicities, and 2 were metabolic abnormalities.
Seventeen patients reported at least 1 infectious episode, 42 events in total, 9 of which were severe. Fourteen patients required readmission to the hospital after transplant.
Within a year of transplant, 5 patients had died—3 from recurrent/persistent disease, 1 due to a fungal infection, and 1 from cardiac arrest. Two additional patients died after the 1-year mark—1 of recurrent/persistent disease and 1 of heart failure.
At 12 months, the rate of overall survival was 86.6%, progression-free survival was 82.3%, progression was 12.5%, and non-relapse mortality was 5.2%.
“In order to place this within context, we had the opportunity to compare our patient experience with 151 matched controls [without HIV] from CIBMTR,” Dr Alvarnas said. “Ninety-three percent of these patients were actually transplanted within 2 years so that they were the time-concordant group, and they were matched for performance score, disease, and disease stage.”
The investigators found no significant difference between their patient group and the HIV-free controls with regard to overall mortality (P=0.56), treatment failure (P=0.10), progression (P=0.06), and treatment-related mortality (P=0.97).
Likewise, there was no significant difference in overall survival between the HRL patients and controls—86.6% and 87.7%, respectively (P=0.56). And the same was true of progression-free survival—82.3% and 69.5%, respectively (P=0.10). ![]()
Maintenance prolongs PFS, not OS, in relapsed CLL

Credit: Linda Bartlett
SAN FRANCISCO—Maintenance therapy with the anti-CD20 monoclonal antibody ofatumumab improves progression-free survival (PFS), but not overall survival (OS), in patients with relapsed chronic lymphocytic leukemia (CLL), according to an interim analysis of the PROLONG study.
The median PFS was about 29 months in patients who received ofatumumab and about 15 months for patients who did not receive maintenance (P<0.0001).
But there was no significant difference in the median OS, which was not reached in either treatment arm.
Marinus H.J. van Oers, MD, PhD, of the Academisch Medisch Centrum and HOVON in Amsterdam, The Netherlands, reported these results at the 2014 ASH Annual Meeting (abstract 21*). The study was sponsored by GlaxoSmithKline, makers of ofatumumab.
“[A]s of 2014, still we cannot say that we are able to cure CLL,” Dr van Oers noted. “And CLL is characterized by decreasing response duration with subsequent lines of treatment. In this respect, but also a number of other respects, there are similarities in biological behavior between CLL and follicular lymphoma.”
“There is definitely a role—although it’s somewhat debated—for maintenance treatment in follicular lymphoma. Therefore, it is rational to explore safe and effective maintenance treatment in CLL as well.”
To that end, Dr van Oers and his colleagues compared ofatumumab maintenance to observation in patients who were in remission after induction treatment for relapsed CLL. The team enrolled 474 patients who were in complete or partial remission after their 2nd- or 3rd-line treatment for CLL.
Patients were randomized to observation (n=236) or to receive ofatumumab (n=238) at 300 mg, followed 1 week later by 1000 mg every 8 weeks for up to 2 years. Patients on ofatumumab also received premedication with acetaminophen, antihistamine, and glucocorticoid.
The patients were stratified by the number and type of prior therapy, as well as remission status after induction treatment, and baseline characteristics were similar between the two treatment arms.
“The median age was about 65, and about 30% of patients were older than 70 years,” Dr van Oers noted. “[There was] a male preponderance, as you would expect, and the time since diagnosis was somewhere between 5 and 6 years.”
“Most patients were in [partial response], actually 80%, and most patients had received 2 prior regimens, about 70%. As for prior treatments, 80% of patients had received effective immuno-chemotherapy.”
“In both arms, there were only a few patients with unfavorable cytogenetics—11q and 17p deletion. [As for] β2 microglobulin, two-thirds [of patients in both arms] had low levels. And, in both arms, there were almost twice as many IGVH-mutated as unmutated patients.”
Patient outcomes
The median follow-up was 19.1 months. The study’s primary endpoint was PFS, which was defined as the time from randomization to the date of disease progression or death from any cause.
The median PFS was significantly longer in the ofatumumab arm than in the observation arm, at 29.4 months and 15.2 months, respectively (hazard ratio [HR]=0.50; P<0.0001).
Similarly, the time to the start of patients’ next therapy was significantly longer in the ofatumumab arm than in the in observation arm—a median of 38 months and 31.1 months, respectively (HR=0.66, P=0.108).
However, there was no significant difference in OS, which was not reached in either arm (HR=0.85, P=0.4877).
Adverse events (AEs) occurred in 86% of patients in the ofatumumab arm and 72% of patients in the observation arm (P<0.001). Sixty percent of AEs were considered related to ofatumumab. None of the AEs led to study withdrawal.
Grade 3 or higher AEs occurred in 46% of patients in the ofatumumab arm and 28% in the observation arm. They included neutropenia (24% and 10%, respectively; P<0.001), infections (13% and 8%, respectively), thrombocytopenia (2% and 3%, respectively), and infusion-related reactions (1% and 0%, respectively).
There were 5 deaths in the observation arm—1 due to progression and 4 due to causes other than progression, infection, or secondary malignancy. There were 2 deaths in the ofatumumab arm—1 due to infection/sepsis and 1 due to an “other” cause.
“So based on this planned interim analysis, we can conclude that ofatumumab maintenance in relapsed CLL results in a highly significant and clinically meaningful improvement of progression-free survival,” Dr van Oers said in closing.
“It significantly prolongs time to next treatment, it’s well-tolerated, and it’s associated with an adverse event profile which is quite characteristic of anti-CD20 monoclonal antibodies.” ![]()
*Information in the abstract differs from that presented at the meeting.

Credit: Linda Bartlett
SAN FRANCISCO—Maintenance therapy with the anti-CD20 monoclonal antibody ofatumumab improves progression-free survival (PFS), but not overall survival (OS), in patients with relapsed chronic lymphocytic leukemia (CLL), according to an interim analysis of the PROLONG study.
The median PFS was about 29 months in patients who received ofatumumab and about 15 months for patients who did not receive maintenance (P<0.0001).
But there was no significant difference in the median OS, which was not reached in either treatment arm.
Marinus H.J. van Oers, MD, PhD, of the Academisch Medisch Centrum and HOVON in Amsterdam, The Netherlands, reported these results at the 2014 ASH Annual Meeting (abstract 21*). The study was sponsored by GlaxoSmithKline, makers of ofatumumab.
“[A]s of 2014, still we cannot say that we are able to cure CLL,” Dr van Oers noted. “And CLL is characterized by decreasing response duration with subsequent lines of treatment. In this respect, but also a number of other respects, there are similarities in biological behavior between CLL and follicular lymphoma.”
“There is definitely a role—although it’s somewhat debated—for maintenance treatment in follicular lymphoma. Therefore, it is rational to explore safe and effective maintenance treatment in CLL as well.”
To that end, Dr van Oers and his colleagues compared ofatumumab maintenance to observation in patients who were in remission after induction treatment for relapsed CLL. The team enrolled 474 patients who were in complete or partial remission after their 2nd- or 3rd-line treatment for CLL.
Patients were randomized to observation (n=236) or to receive ofatumumab (n=238) at 300 mg, followed 1 week later by 1000 mg every 8 weeks for up to 2 years. Patients on ofatumumab also received premedication with acetaminophen, antihistamine, and glucocorticoid.
The patients were stratified by the number and type of prior therapy, as well as remission status after induction treatment, and baseline characteristics were similar between the two treatment arms.
“The median age was about 65, and about 30% of patients were older than 70 years,” Dr van Oers noted. “[There was] a male preponderance, as you would expect, and the time since diagnosis was somewhere between 5 and 6 years.”
“Most patients were in [partial response], actually 80%, and most patients had received 2 prior regimens, about 70%. As for prior treatments, 80% of patients had received effective immuno-chemotherapy.”
“In both arms, there were only a few patients with unfavorable cytogenetics—11q and 17p deletion. [As for] β2 microglobulin, two-thirds [of patients in both arms] had low levels. And, in both arms, there were almost twice as many IGVH-mutated as unmutated patients.”
Patient outcomes
The median follow-up was 19.1 months. The study’s primary endpoint was PFS, which was defined as the time from randomization to the date of disease progression or death from any cause.
The median PFS was significantly longer in the ofatumumab arm than in the observation arm, at 29.4 months and 15.2 months, respectively (hazard ratio [HR]=0.50; P<0.0001).
Similarly, the time to the start of patients’ next therapy was significantly longer in the ofatumumab arm than in the in observation arm—a median of 38 months and 31.1 months, respectively (HR=0.66, P=0.108).
However, there was no significant difference in OS, which was not reached in either arm (HR=0.85, P=0.4877).
Adverse events (AEs) occurred in 86% of patients in the ofatumumab arm and 72% of patients in the observation arm (P<0.001). Sixty percent of AEs were considered related to ofatumumab. None of the AEs led to study withdrawal.
Grade 3 or higher AEs occurred in 46% of patients in the ofatumumab arm and 28% in the observation arm. They included neutropenia (24% and 10%, respectively; P<0.001), infections (13% and 8%, respectively), thrombocytopenia (2% and 3%, respectively), and infusion-related reactions (1% and 0%, respectively).
There were 5 deaths in the observation arm—1 due to progression and 4 due to causes other than progression, infection, or secondary malignancy. There were 2 deaths in the ofatumumab arm—1 due to infection/sepsis and 1 due to an “other” cause.
“So based on this planned interim analysis, we can conclude that ofatumumab maintenance in relapsed CLL results in a highly significant and clinically meaningful improvement of progression-free survival,” Dr van Oers said in closing.
“It significantly prolongs time to next treatment, it’s well-tolerated, and it’s associated with an adverse event profile which is quite characteristic of anti-CD20 monoclonal antibodies.” ![]()
*Information in the abstract differs from that presented at the meeting.

Credit: Linda Bartlett
SAN FRANCISCO—Maintenance therapy with the anti-CD20 monoclonal antibody ofatumumab improves progression-free survival (PFS), but not overall survival (OS), in patients with relapsed chronic lymphocytic leukemia (CLL), according to an interim analysis of the PROLONG study.
The median PFS was about 29 months in patients who received ofatumumab and about 15 months for patients who did not receive maintenance (P<0.0001).
But there was no significant difference in the median OS, which was not reached in either treatment arm.
Marinus H.J. van Oers, MD, PhD, of the Academisch Medisch Centrum and HOVON in Amsterdam, The Netherlands, reported these results at the 2014 ASH Annual Meeting (abstract 21*). The study was sponsored by GlaxoSmithKline, makers of ofatumumab.
“[A]s of 2014, still we cannot say that we are able to cure CLL,” Dr van Oers noted. “And CLL is characterized by decreasing response duration with subsequent lines of treatment. In this respect, but also a number of other respects, there are similarities in biological behavior between CLL and follicular lymphoma.”
“There is definitely a role—although it’s somewhat debated—for maintenance treatment in follicular lymphoma. Therefore, it is rational to explore safe and effective maintenance treatment in CLL as well.”
To that end, Dr van Oers and his colleagues compared ofatumumab maintenance to observation in patients who were in remission after induction treatment for relapsed CLL. The team enrolled 474 patients who were in complete or partial remission after their 2nd- or 3rd-line treatment for CLL.
Patients were randomized to observation (n=236) or to receive ofatumumab (n=238) at 300 mg, followed 1 week later by 1000 mg every 8 weeks for up to 2 years. Patients on ofatumumab also received premedication with acetaminophen, antihistamine, and glucocorticoid.
The patients were stratified by the number and type of prior therapy, as well as remission status after induction treatment, and baseline characteristics were similar between the two treatment arms.
“The median age was about 65, and about 30% of patients were older than 70 years,” Dr van Oers noted. “[There was] a male preponderance, as you would expect, and the time since diagnosis was somewhere between 5 and 6 years.”
“Most patients were in [partial response], actually 80%, and most patients had received 2 prior regimens, about 70%. As for prior treatments, 80% of patients had received effective immuno-chemotherapy.”
“In both arms, there were only a few patients with unfavorable cytogenetics—11q and 17p deletion. [As for] β2 microglobulin, two-thirds [of patients in both arms] had low levels. And, in both arms, there were almost twice as many IGVH-mutated as unmutated patients.”
Patient outcomes
The median follow-up was 19.1 months. The study’s primary endpoint was PFS, which was defined as the time from randomization to the date of disease progression or death from any cause.
The median PFS was significantly longer in the ofatumumab arm than in the observation arm, at 29.4 months and 15.2 months, respectively (hazard ratio [HR]=0.50; P<0.0001).
Similarly, the time to the start of patients’ next therapy was significantly longer in the ofatumumab arm than in the in observation arm—a median of 38 months and 31.1 months, respectively (HR=0.66, P=0.108).
However, there was no significant difference in OS, which was not reached in either arm (HR=0.85, P=0.4877).
Adverse events (AEs) occurred in 86% of patients in the ofatumumab arm and 72% of patients in the observation arm (P<0.001). Sixty percent of AEs were considered related to ofatumumab. None of the AEs led to study withdrawal.
Grade 3 or higher AEs occurred in 46% of patients in the ofatumumab arm and 28% in the observation arm. They included neutropenia (24% and 10%, respectively; P<0.001), infections (13% and 8%, respectively), thrombocytopenia (2% and 3%, respectively), and infusion-related reactions (1% and 0%, respectively).
There were 5 deaths in the observation arm—1 due to progression and 4 due to causes other than progression, infection, or secondary malignancy. There were 2 deaths in the ofatumumab arm—1 due to infection/sepsis and 1 due to an “other” cause.
“So based on this planned interim analysis, we can conclude that ofatumumab maintenance in relapsed CLL results in a highly significant and clinically meaningful improvement of progression-free survival,” Dr van Oers said in closing.
“It significantly prolongs time to next treatment, it’s well-tolerated, and it’s associated with an adverse event profile which is quite characteristic of anti-CD20 monoclonal antibodies.” ![]()
*Information in the abstract differs from that presented at the meeting.
Older patients benefit from brentuximab treatment

Credit: NIH
SAN FRANCISCO—Younger patients with Hodgkin lymphoma fare well on brentuximab vedotin, experiencing an overall objective response rate (ORR) of 75% and a complete response (CR) rate of 34% in the pivotal phase 2 study of patients with relapsed/refractory disease.
And a retrospective study of patients older than 60 years showed that single-agent therapy was well tolerated, prompting an ORR of 53% and a CR rate of 40% in a relapsed or refractory population.
So investigators decided to explore in a prospective study whether patients 60 years or older could benefit from up-front treatment with brentuximab as a single agent or in combination.
Andres Forero-Torres, MD, of the University of Alabama in Birmingham, presented the results of this trial at the 2014 ASH Annual Meeting (abstract 294).*
Enrolled patients had classic Hodgkin lymphoma, were treatment-naïve, and were ineligible for or declined conventional front-line treatment. The primary endpoint was ORR.
The study is being conducted in 3 parts—brentuximab as a single agent, brentuximab plus dacarbazine, and brentuximab plus bendamustine. At the time of the ASH presentation, data for the brentuximab-bendamustine combination were not available.
Single-agent brentuximab
Twenty-seven patients on the single-agent arm were evaluable for efficacy and safety. They were a median age of 78 (range, 64 to 92). About half (52%) were male, and 78% had an ECOG performance status of grade 0 or 1.
Forty-four percent had moderate renal function impairment with a creatinine clearance between 30 and 60 mL/min. Thirty percent had B symptoms, 22% had bulky disease, and 52% had extra-nodal involvement.
Patients received 1.8 mg/kg of brentuximab intravenously on day 1 of a 21-day cycle. Response was assessed by CT scan during cycles 2, 4, 8, and 16, and by CT plus PET scan during cycles 2 and 8.
The median follow-up was 8.7 months. Dr Forero-Torres pointed out that, initially, “there were no progressions,” and all patients achieved tumor reduction.
The ORR was 93%, the CR rate was 70%, the partial response rate was 22%, and the rate of stable disease was 7%.
The median duration of response was 9.1 months (range, 0.03 to 13.14), and the median progression-free survival was 10.5 months (range, 2.6 to 14.3). For patients who had a CR, the median progression-free survival was about 12 months, Dr Forero-Torres said.
The median number of treatment cycles administered per patient was 8 (range, 3 to 23). Patients discontinued treatment primarily because of progressive disease (41%) or adverse events (AEs, 37%).
AEs occurring in 20% or more of patients were constipation, decreased appetite, diarrhea, peripheral edema, nausea, fatigue, and peripheral sensory neuropathy. All were grade 1 or 2, except for peripheral sensory neuropathy, which also had about 20% grade 3 events.
Grade 3 or higher treatment-related AEs included peripheral sensory neuropathy (n=7), peripheral motor neuropathy (n=2), rash (n=2), and 1 patient each with anemia, increased aspartate aminotransferase, asthenia, neutropenia, orthostatic hypotension, generalized rash, and maculopapular rash.
Serious AEs (SAEs) were minimal, Dr Forero-Torres said, and included 1 patient each with pyrexia, orthostatic hypotension, asthenia and rash, and deep vein thrombosis.
Seven patients discontinued treatment due to peripheral sensory neuropathy, 2 due to peripheral motor neuropathy, and 1 due to orthostatic hypotension.
Dr Forero-Torres emphasized that there were no grade 4 AEs, no AE-related deaths, and no deaths within 30 days of the last dose of medication.
Brentuximab plus dacarbazine
Fourteen of 18 patients in the combination arm were evaluable for efficacy and safety. Their median age was 72.5 (range, 62 to 87), 72% were male, 67% had an ECOG status of grade 0 or 1, and 56% had normal renal function with a creatinine clearance greater than 80 mL/min.
Forty-four percent exhibited B symptoms, 11% had bulky disease, and 50% had extra-nodal involvement.
They received brentuximab at 1.8 mg/kg plus dacarbazine at 375 mg/m2 for cycles 1-12, followed by monotherapy for cycles 13-16.
At the time of the interim analysis, 83% of patients were still on treatment, “so this is very early preliminary data,” Dr Forero-Torres noted.
All of the patients achieved tumor reduction, and 4 patients achieved a CR.
They had a median treatment duration of 16.7 weeks (range, 3 to 36), received a median of 5.5 cycles (range, 1 to 12), and had a median follow-up time of 19.1 weeks (range, 6.1 to 36.1).
The most common grade 1 or 2 AEs were peripheral sensory neuropathy (33%), nausea (33%), diarrhea (28%), constipation (28%), fatigue (22%), alopecia (22%), arthralgia (22%), and headache (22%).
Grade 3 AEs or SAEs, with 1 patient each, were C difficile colitis (SAE), hypotension (SAE), and hyperglycemia.
Dr Forero-Torres noted that investigators observed “robust antitumor activity” among these older patients receiving front-line brentuximab.
The cohort combining brentuximab with bendamustine is currently enrolling patients.
The study is sponsored by Seattle Genetics, Inc., developer of brentuximab vedotin (Adcetris).![]()
*Information in the abstract differs from that presented at the meeting.

Credit: NIH
SAN FRANCISCO—Younger patients with Hodgkin lymphoma fare well on brentuximab vedotin, experiencing an overall objective response rate (ORR) of 75% and a complete response (CR) rate of 34% in the pivotal phase 2 study of patients with relapsed/refractory disease.
And a retrospective study of patients older than 60 years showed that single-agent therapy was well tolerated, prompting an ORR of 53% and a CR rate of 40% in a relapsed or refractory population.
So investigators decided to explore in a prospective study whether patients 60 years or older could benefit from up-front treatment with brentuximab as a single agent or in combination.
Andres Forero-Torres, MD, of the University of Alabama in Birmingham, presented the results of this trial at the 2014 ASH Annual Meeting (abstract 294).*
Enrolled patients had classic Hodgkin lymphoma, were treatment-naïve, and were ineligible for or declined conventional front-line treatment. The primary endpoint was ORR.
The study is being conducted in 3 parts—brentuximab as a single agent, brentuximab plus dacarbazine, and brentuximab plus bendamustine. At the time of the ASH presentation, data for the brentuximab-bendamustine combination were not available.
Single-agent brentuximab
Twenty-seven patients on the single-agent arm were evaluable for efficacy and safety. They were a median age of 78 (range, 64 to 92). About half (52%) were male, and 78% had an ECOG performance status of grade 0 or 1.
Forty-four percent had moderate renal function impairment with a creatinine clearance between 30 and 60 mL/min. Thirty percent had B symptoms, 22% had bulky disease, and 52% had extra-nodal involvement.
Patients received 1.8 mg/kg of brentuximab intravenously on day 1 of a 21-day cycle. Response was assessed by CT scan during cycles 2, 4, 8, and 16, and by CT plus PET scan during cycles 2 and 8.
The median follow-up was 8.7 months. Dr Forero-Torres pointed out that, initially, “there were no progressions,” and all patients achieved tumor reduction.
The ORR was 93%, the CR rate was 70%, the partial response rate was 22%, and the rate of stable disease was 7%.
The median duration of response was 9.1 months (range, 0.03 to 13.14), and the median progression-free survival was 10.5 months (range, 2.6 to 14.3). For patients who had a CR, the median progression-free survival was about 12 months, Dr Forero-Torres said.
The median number of treatment cycles administered per patient was 8 (range, 3 to 23). Patients discontinued treatment primarily because of progressive disease (41%) or adverse events (AEs, 37%).
AEs occurring in 20% or more of patients were constipation, decreased appetite, diarrhea, peripheral edema, nausea, fatigue, and peripheral sensory neuropathy. All were grade 1 or 2, except for peripheral sensory neuropathy, which also had about 20% grade 3 events.
Grade 3 or higher treatment-related AEs included peripheral sensory neuropathy (n=7), peripheral motor neuropathy (n=2), rash (n=2), and 1 patient each with anemia, increased aspartate aminotransferase, asthenia, neutropenia, orthostatic hypotension, generalized rash, and maculopapular rash.
Serious AEs (SAEs) were minimal, Dr Forero-Torres said, and included 1 patient each with pyrexia, orthostatic hypotension, asthenia and rash, and deep vein thrombosis.
Seven patients discontinued treatment due to peripheral sensory neuropathy, 2 due to peripheral motor neuropathy, and 1 due to orthostatic hypotension.
Dr Forero-Torres emphasized that there were no grade 4 AEs, no AE-related deaths, and no deaths within 30 days of the last dose of medication.
Brentuximab plus dacarbazine
Fourteen of 18 patients in the combination arm were evaluable for efficacy and safety. Their median age was 72.5 (range, 62 to 87), 72% were male, 67% had an ECOG status of grade 0 or 1, and 56% had normal renal function with a creatinine clearance greater than 80 mL/min.
Forty-four percent exhibited B symptoms, 11% had bulky disease, and 50% had extra-nodal involvement.
They received brentuximab at 1.8 mg/kg plus dacarbazine at 375 mg/m2 for cycles 1-12, followed by monotherapy for cycles 13-16.
At the time of the interim analysis, 83% of patients were still on treatment, “so this is very early preliminary data,” Dr Forero-Torres noted.
All of the patients achieved tumor reduction, and 4 patients achieved a CR.
They had a median treatment duration of 16.7 weeks (range, 3 to 36), received a median of 5.5 cycles (range, 1 to 12), and had a median follow-up time of 19.1 weeks (range, 6.1 to 36.1).
The most common grade 1 or 2 AEs were peripheral sensory neuropathy (33%), nausea (33%), diarrhea (28%), constipation (28%), fatigue (22%), alopecia (22%), arthralgia (22%), and headache (22%).
Grade 3 AEs or SAEs, with 1 patient each, were C difficile colitis (SAE), hypotension (SAE), and hyperglycemia.
Dr Forero-Torres noted that investigators observed “robust antitumor activity” among these older patients receiving front-line brentuximab.
The cohort combining brentuximab with bendamustine is currently enrolling patients.
The study is sponsored by Seattle Genetics, Inc., developer of brentuximab vedotin (Adcetris).![]()
*Information in the abstract differs from that presented at the meeting.

Credit: NIH
SAN FRANCISCO—Younger patients with Hodgkin lymphoma fare well on brentuximab vedotin, experiencing an overall objective response rate (ORR) of 75% and a complete response (CR) rate of 34% in the pivotal phase 2 study of patients with relapsed/refractory disease.
And a retrospective study of patients older than 60 years showed that single-agent therapy was well tolerated, prompting an ORR of 53% and a CR rate of 40% in a relapsed or refractory population.
So investigators decided to explore in a prospective study whether patients 60 years or older could benefit from up-front treatment with brentuximab as a single agent or in combination.
Andres Forero-Torres, MD, of the University of Alabama in Birmingham, presented the results of this trial at the 2014 ASH Annual Meeting (abstract 294).*
Enrolled patients had classic Hodgkin lymphoma, were treatment-naïve, and were ineligible for or declined conventional front-line treatment. The primary endpoint was ORR.
The study is being conducted in 3 parts—brentuximab as a single agent, brentuximab plus dacarbazine, and brentuximab plus bendamustine. At the time of the ASH presentation, data for the brentuximab-bendamustine combination were not available.
Single-agent brentuximab
Twenty-seven patients on the single-agent arm were evaluable for efficacy and safety. They were a median age of 78 (range, 64 to 92). About half (52%) were male, and 78% had an ECOG performance status of grade 0 or 1.
Forty-four percent had moderate renal function impairment with a creatinine clearance between 30 and 60 mL/min. Thirty percent had B symptoms, 22% had bulky disease, and 52% had extra-nodal involvement.
Patients received 1.8 mg/kg of brentuximab intravenously on day 1 of a 21-day cycle. Response was assessed by CT scan during cycles 2, 4, 8, and 16, and by CT plus PET scan during cycles 2 and 8.
The median follow-up was 8.7 months. Dr Forero-Torres pointed out that, initially, “there were no progressions,” and all patients achieved tumor reduction.
The ORR was 93%, the CR rate was 70%, the partial response rate was 22%, and the rate of stable disease was 7%.
The median duration of response was 9.1 months (range, 0.03 to 13.14), and the median progression-free survival was 10.5 months (range, 2.6 to 14.3). For patients who had a CR, the median progression-free survival was about 12 months, Dr Forero-Torres said.
The median number of treatment cycles administered per patient was 8 (range, 3 to 23). Patients discontinued treatment primarily because of progressive disease (41%) or adverse events (AEs, 37%).
AEs occurring in 20% or more of patients were constipation, decreased appetite, diarrhea, peripheral edema, nausea, fatigue, and peripheral sensory neuropathy. All were grade 1 or 2, except for peripheral sensory neuropathy, which also had about 20% grade 3 events.
Grade 3 or higher treatment-related AEs included peripheral sensory neuropathy (n=7), peripheral motor neuropathy (n=2), rash (n=2), and 1 patient each with anemia, increased aspartate aminotransferase, asthenia, neutropenia, orthostatic hypotension, generalized rash, and maculopapular rash.
Serious AEs (SAEs) were minimal, Dr Forero-Torres said, and included 1 patient each with pyrexia, orthostatic hypotension, asthenia and rash, and deep vein thrombosis.
Seven patients discontinued treatment due to peripheral sensory neuropathy, 2 due to peripheral motor neuropathy, and 1 due to orthostatic hypotension.
Dr Forero-Torres emphasized that there were no grade 4 AEs, no AE-related deaths, and no deaths within 30 days of the last dose of medication.
Brentuximab plus dacarbazine
Fourteen of 18 patients in the combination arm were evaluable for efficacy and safety. Their median age was 72.5 (range, 62 to 87), 72% were male, 67% had an ECOG status of grade 0 or 1, and 56% had normal renal function with a creatinine clearance greater than 80 mL/min.
Forty-four percent exhibited B symptoms, 11% had bulky disease, and 50% had extra-nodal involvement.
They received brentuximab at 1.8 mg/kg plus dacarbazine at 375 mg/m2 for cycles 1-12, followed by monotherapy for cycles 13-16.
At the time of the interim analysis, 83% of patients were still on treatment, “so this is very early preliminary data,” Dr Forero-Torres noted.
All of the patients achieved tumor reduction, and 4 patients achieved a CR.
They had a median treatment duration of 16.7 weeks (range, 3 to 36), received a median of 5.5 cycles (range, 1 to 12), and had a median follow-up time of 19.1 weeks (range, 6.1 to 36.1).
The most common grade 1 or 2 AEs were peripheral sensory neuropathy (33%), nausea (33%), diarrhea (28%), constipation (28%), fatigue (22%), alopecia (22%), arthralgia (22%), and headache (22%).
Grade 3 AEs or SAEs, with 1 patient each, were C difficile colitis (SAE), hypotension (SAE), and hyperglycemia.
Dr Forero-Torres noted that investigators observed “robust antitumor activity” among these older patients receiving front-line brentuximab.
The cohort combining brentuximab with bendamustine is currently enrolling patients.
The study is sponsored by Seattle Genetics, Inc., developer of brentuximab vedotin (Adcetris).![]()
*Information in the abstract differs from that presented at the meeting.
Ibrutinib proves active in high-risk CLL

Credit: Mary Ann Thompson
Single-agent ibrutinib can elicit a high response rate in patients with high-risk chronic lymphocytic leukemia (CLL), results of a phase 2 trial suggest.
The Bruton’s tyrosine kinase inhibitor prompted a 92% objective response rate in patients who had previously untreated or relapsed/refractory CLL with either 17p deletion (del 17p) or tumor protein 53 (TP53) aberrations.
Researchers reported this and other results of the trial in The Lancet Oncology.
“Ibrutinib treatment results observed in CLL patients with del 17p or TP53 aberrations are very encouraging given that these patients have a high relapse rate after chemotherapy and are in need of tolerable, effective, and durable treatment options,” said study author Mohammed Farooqui, DO, of the National Heart, Lung, and Blood Institute in Bethesda, Maryland.
He and his colleagues studied 51 patients in this trial, 35 with previously untreated CLL and 16 with relapsed or refractory CLL. Forty-seven of the patients (92%) had del 17p, and 4 patients carried the TP53 aberration but did not have del 17p.
The study’s primary endpoint was overall response rate after 24 weeks. Secondary endpoints included safety, overall survival, progression-free survival, best response, and nodal response.
The median follow-up for all patients was 24 months (15 months for the previously untreated cohort). At 24 weeks, 48 patients were evaluable for response, assessed according to the modified IWCLL 2008 criteria.
Response rates
At 24 weeks, 92% (n=44) of the 48 evaluable patients achieved an objective response. Fifty percent of all evaluable patients achieved a partial response (n=24)—55% of previously untreated patients (n=18) and 40% of relapsed/refractory patients (n=6).
As for best response, 10% of all patients achieved a complete response (n=5)—12% of previously untreated patients (n=4) and 7% of relapsed/refractory patients (n=1). And 67% of patients had a partial response (n=32)—70% of previously untreated patients (n=23) and 60% of relapsed/refractory patients (n=9).
After 8 weeks on therapy, ibrutinib was associated with a more than 50% mean reduction in tumor burden in the bone marrow (44%), lymph nodes (70%), and spleen (79%). After 24 weeks of therapy, the rates of tumor burden reduction (> 50%) increased to 83%, 93%, and 95%, respectively.
Survival and safety
The estimated progression-free survival at 24 months for all patients on an intention-to-treat basis was 82%. Forty-two of the 51 patients (82%) continued on ibrutinib treatment without disease progression.
The estimated overall survival at 24 months was 80% for all patients—84% for previously untreated patients and 74% for patients with relapsed or refractory disease.
At the final follow-up, 8 (16%) patients had died—5 (10%) from progressive disease, 2 (4%) from infection, and 1 (2%) patient with a sudden, unexplained death that may have been treatment-related.
The most common adverse events (occurring in more than 30% of all patients) potentially related to ibrutinib were arthralgia (59%), diarrhea (51%), rash (47%), nail ridging (43%), bruising (33%), and muscle spasms (31%).
The most frequent grade 3 or 4 hematologic adverse events were neutropenia (24%), anemia (14%), and thrombocytopenia (10%). The most common nonhematologic grade 3 adverse event was pneumonia, which occurred in 3 patients (6%).
Nine patients (18%) discontinued treatment. The reasons for discontinuation included disease progression in 5 patients (10%) and death for 3 patients (6%).
This research was sponsored by the Intramural Research Program of the National Heart, Lung, and Blood Institute and the National Cancer Institute; Danish Cancer Society; Novo Nordisk Foundation; National Institutes of Health Medical Research Scholars Program; and Pharmacyclics Inc.
Ibrutinib is jointly developed and commercialized by Pharmacyclics and Janssen Biotech, Inc. ![]()

Credit: Mary Ann Thompson
Single-agent ibrutinib can elicit a high response rate in patients with high-risk chronic lymphocytic leukemia (CLL), results of a phase 2 trial suggest.
The Bruton’s tyrosine kinase inhibitor prompted a 92% objective response rate in patients who had previously untreated or relapsed/refractory CLL with either 17p deletion (del 17p) or tumor protein 53 (TP53) aberrations.
Researchers reported this and other results of the trial in The Lancet Oncology.
“Ibrutinib treatment results observed in CLL patients with del 17p or TP53 aberrations are very encouraging given that these patients have a high relapse rate after chemotherapy and are in need of tolerable, effective, and durable treatment options,” said study author Mohammed Farooqui, DO, of the National Heart, Lung, and Blood Institute in Bethesda, Maryland.
He and his colleagues studied 51 patients in this trial, 35 with previously untreated CLL and 16 with relapsed or refractory CLL. Forty-seven of the patients (92%) had del 17p, and 4 patients carried the TP53 aberration but did not have del 17p.
The study’s primary endpoint was overall response rate after 24 weeks. Secondary endpoints included safety, overall survival, progression-free survival, best response, and nodal response.
The median follow-up for all patients was 24 months (15 months for the previously untreated cohort). At 24 weeks, 48 patients were evaluable for response, assessed according to the modified IWCLL 2008 criteria.
Response rates
At 24 weeks, 92% (n=44) of the 48 evaluable patients achieved an objective response. Fifty percent of all evaluable patients achieved a partial response (n=24)—55% of previously untreated patients (n=18) and 40% of relapsed/refractory patients (n=6).
As for best response, 10% of all patients achieved a complete response (n=5)—12% of previously untreated patients (n=4) and 7% of relapsed/refractory patients (n=1). And 67% of patients had a partial response (n=32)—70% of previously untreated patients (n=23) and 60% of relapsed/refractory patients (n=9).
After 8 weeks on therapy, ibrutinib was associated with a more than 50% mean reduction in tumor burden in the bone marrow (44%), lymph nodes (70%), and spleen (79%). After 24 weeks of therapy, the rates of tumor burden reduction (> 50%) increased to 83%, 93%, and 95%, respectively.
Survival and safety
The estimated progression-free survival at 24 months for all patients on an intention-to-treat basis was 82%. Forty-two of the 51 patients (82%) continued on ibrutinib treatment without disease progression.
The estimated overall survival at 24 months was 80% for all patients—84% for previously untreated patients and 74% for patients with relapsed or refractory disease.
At the final follow-up, 8 (16%) patients had died—5 (10%) from progressive disease, 2 (4%) from infection, and 1 (2%) patient with a sudden, unexplained death that may have been treatment-related.
The most common adverse events (occurring in more than 30% of all patients) potentially related to ibrutinib were arthralgia (59%), diarrhea (51%), rash (47%), nail ridging (43%), bruising (33%), and muscle spasms (31%).
The most frequent grade 3 or 4 hematologic adverse events were neutropenia (24%), anemia (14%), and thrombocytopenia (10%). The most common nonhematologic grade 3 adverse event was pneumonia, which occurred in 3 patients (6%).
Nine patients (18%) discontinued treatment. The reasons for discontinuation included disease progression in 5 patients (10%) and death for 3 patients (6%).
This research was sponsored by the Intramural Research Program of the National Heart, Lung, and Blood Institute and the National Cancer Institute; Danish Cancer Society; Novo Nordisk Foundation; National Institutes of Health Medical Research Scholars Program; and Pharmacyclics Inc.
Ibrutinib is jointly developed and commercialized by Pharmacyclics and Janssen Biotech, Inc. ![]()

Credit: Mary Ann Thompson
Single-agent ibrutinib can elicit a high response rate in patients with high-risk chronic lymphocytic leukemia (CLL), results of a phase 2 trial suggest.
The Bruton’s tyrosine kinase inhibitor prompted a 92% objective response rate in patients who had previously untreated or relapsed/refractory CLL with either 17p deletion (del 17p) or tumor protein 53 (TP53) aberrations.
Researchers reported this and other results of the trial in The Lancet Oncology.
“Ibrutinib treatment results observed in CLL patients with del 17p or TP53 aberrations are very encouraging given that these patients have a high relapse rate after chemotherapy and are in need of tolerable, effective, and durable treatment options,” said study author Mohammed Farooqui, DO, of the National Heart, Lung, and Blood Institute in Bethesda, Maryland.
He and his colleagues studied 51 patients in this trial, 35 with previously untreated CLL and 16 with relapsed or refractory CLL. Forty-seven of the patients (92%) had del 17p, and 4 patients carried the TP53 aberration but did not have del 17p.
The study’s primary endpoint was overall response rate after 24 weeks. Secondary endpoints included safety, overall survival, progression-free survival, best response, and nodal response.
The median follow-up for all patients was 24 months (15 months for the previously untreated cohort). At 24 weeks, 48 patients were evaluable for response, assessed according to the modified IWCLL 2008 criteria.
Response rates
At 24 weeks, 92% (n=44) of the 48 evaluable patients achieved an objective response. Fifty percent of all evaluable patients achieved a partial response (n=24)—55% of previously untreated patients (n=18) and 40% of relapsed/refractory patients (n=6).
As for best response, 10% of all patients achieved a complete response (n=5)—12% of previously untreated patients (n=4) and 7% of relapsed/refractory patients (n=1). And 67% of patients had a partial response (n=32)—70% of previously untreated patients (n=23) and 60% of relapsed/refractory patients (n=9).
After 8 weeks on therapy, ibrutinib was associated with a more than 50% mean reduction in tumor burden in the bone marrow (44%), lymph nodes (70%), and spleen (79%). After 24 weeks of therapy, the rates of tumor burden reduction (> 50%) increased to 83%, 93%, and 95%, respectively.
Survival and safety
The estimated progression-free survival at 24 months for all patients on an intention-to-treat basis was 82%. Forty-two of the 51 patients (82%) continued on ibrutinib treatment without disease progression.
The estimated overall survival at 24 months was 80% for all patients—84% for previously untreated patients and 74% for patients with relapsed or refractory disease.
At the final follow-up, 8 (16%) patients had died—5 (10%) from progressive disease, 2 (4%) from infection, and 1 (2%) patient with a sudden, unexplained death that may have been treatment-related.
The most common adverse events (occurring in more than 30% of all patients) potentially related to ibrutinib were arthralgia (59%), diarrhea (51%), rash (47%), nail ridging (43%), bruising (33%), and muscle spasms (31%).
The most frequent grade 3 or 4 hematologic adverse events were neutropenia (24%), anemia (14%), and thrombocytopenia (10%). The most common nonhematologic grade 3 adverse event was pneumonia, which occurred in 3 patients (6%).
Nine patients (18%) discontinued treatment. The reasons for discontinuation included disease progression in 5 patients (10%) and death for 3 patients (6%).
This research was sponsored by the Intramural Research Program of the National Heart, Lung, and Blood Institute and the National Cancer Institute; Danish Cancer Society; Novo Nordisk Foundation; National Institutes of Health Medical Research Scholars Program; and Pharmacyclics Inc.
Ibrutinib is jointly developed and commercialized by Pharmacyclics and Janssen Biotech, Inc. ![]()
Drug gets orphan designation for WM

The US Food and Drug Administration (FDA) has granted orphan drug designation for IMO-8400, an antagonist of the endosomal Toll-like receptors (TLRs) 7, 8 and 9, for the treatment of Waldenström’s macroglobulinemia (WM).
The designation provides the drug’s maker, Idera Pharmaceuticals, with certain incentives, including eligibility for federal grants, research and development tax credits, and 7 years of marketing exclusivity if the product is approved.
Preclinical studies have shown that, in WM and other B‐cell lymphomas characterized by the MYD88 L265P oncogenic mutation, TLR signaling is overactivated. And this enables tumor cell survival and proliferation.
About 90% of WM patients are reported to harbor the MYD88 L265P mutation.
In research presented at the 2014 AACR Annual Meeting, investigators showed that IMO-8400 decreased the viability of mutated WM cells and diffuse large B-cell lymphoma (DLBCL) cells in vitro. The drug also decreased tumor growth and prolonged survival in mice with MYD88 L265P-positive DLBCL.
Now, Idera is conducting a phase 1/2 trial (NCT02092909) of IMO-8400 in patients with WM who have a history of relapse or failure to respond to one or more prior therapies. The protocol includes 3 dose-escalation cohorts of IMO-8400 administered subcutaneously.
The trial’s independent data review committee has completed its review of 4-week safety data from the second dose cohort (1.2 mg/kg/week) and has determined that Idera may open enrollment in the third dose cohort (2.4 mg/kg/week).
Final 24-week safety and clinical activity data are anticipated in the second half of 2015.
Aside from WM, Idera is pursuing clinical development of IMO-8400 in DLBCL patients harboring the MYD88 L265P mutation and in rare autoimmune diseases, including dermatomyositis. ![]()

The US Food and Drug Administration (FDA) has granted orphan drug designation for IMO-8400, an antagonist of the endosomal Toll-like receptors (TLRs) 7, 8 and 9, for the treatment of Waldenström’s macroglobulinemia (WM).
The designation provides the drug’s maker, Idera Pharmaceuticals, with certain incentives, including eligibility for federal grants, research and development tax credits, and 7 years of marketing exclusivity if the product is approved.
Preclinical studies have shown that, in WM and other B‐cell lymphomas characterized by the MYD88 L265P oncogenic mutation, TLR signaling is overactivated. And this enables tumor cell survival and proliferation.
About 90% of WM patients are reported to harbor the MYD88 L265P mutation.
In research presented at the 2014 AACR Annual Meeting, investigators showed that IMO-8400 decreased the viability of mutated WM cells and diffuse large B-cell lymphoma (DLBCL) cells in vitro. The drug also decreased tumor growth and prolonged survival in mice with MYD88 L265P-positive DLBCL.
Now, Idera is conducting a phase 1/2 trial (NCT02092909) of IMO-8400 in patients with WM who have a history of relapse or failure to respond to one or more prior therapies. The protocol includes 3 dose-escalation cohorts of IMO-8400 administered subcutaneously.
The trial’s independent data review committee has completed its review of 4-week safety data from the second dose cohort (1.2 mg/kg/week) and has determined that Idera may open enrollment in the third dose cohort (2.4 mg/kg/week).
Final 24-week safety and clinical activity data are anticipated in the second half of 2015.
Aside from WM, Idera is pursuing clinical development of IMO-8400 in DLBCL patients harboring the MYD88 L265P mutation and in rare autoimmune diseases, including dermatomyositis. ![]()

The US Food and Drug Administration (FDA) has granted orphan drug designation for IMO-8400, an antagonist of the endosomal Toll-like receptors (TLRs) 7, 8 and 9, for the treatment of Waldenström’s macroglobulinemia (WM).
The designation provides the drug’s maker, Idera Pharmaceuticals, with certain incentives, including eligibility for federal grants, research and development tax credits, and 7 years of marketing exclusivity if the product is approved.
Preclinical studies have shown that, in WM and other B‐cell lymphomas characterized by the MYD88 L265P oncogenic mutation, TLR signaling is overactivated. And this enables tumor cell survival and proliferation.
About 90% of WM patients are reported to harbor the MYD88 L265P mutation.
In research presented at the 2014 AACR Annual Meeting, investigators showed that IMO-8400 decreased the viability of mutated WM cells and diffuse large B-cell lymphoma (DLBCL) cells in vitro. The drug also decreased tumor growth and prolonged survival in mice with MYD88 L265P-positive DLBCL.
Now, Idera is conducting a phase 1/2 trial (NCT02092909) of IMO-8400 in patients with WM who have a history of relapse or failure to respond to one or more prior therapies. The protocol includes 3 dose-escalation cohorts of IMO-8400 administered subcutaneously.
The trial’s independent data review committee has completed its review of 4-week safety data from the second dose cohort (1.2 mg/kg/week) and has determined that Idera may open enrollment in the third dose cohort (2.4 mg/kg/week).
Final 24-week safety and clinical activity data are anticipated in the second half of 2015.
Aside from WM, Idera is pursuing clinical development of IMO-8400 in DLBCL patients harboring the MYD88 L265P mutation and in rare autoimmune diseases, including dermatomyositis.
Certain cancers primarily result from ‘bad luck’
in the bone marrow
Scientists have created a statistical model that measures the proportion of cancer incidence, across many tissue types, caused mainly by random mutations that occur when stem cells divide.
By their measure, two-thirds of adult cancers—including certain leukemias—can be explained primarily by “bad luck,” when these random mutations occur in genes that can drive cancer growth.
The remaining third are due to environmental factors and inherited genes.
“All cancers are caused by a combination of bad luck, the environment, and heredity, and we’ve created a model that may help quantify how much of these three factors contribute to cancer development,” said Bert Vogelstein, MD, of the Johns Hopkins University School of Medicine.
Dr Vogelstein and Cristian Tomasetti, PhD, also of the Johns Hopkins University School of Medicine, detailed these findings in Science.
The pair came to their conclusions by searching the scientific literature for information on the cumulative number of stem cell divisions in 31 tissue types during an average individual’s lifetime.
The researchers knew that cancer arises when tissue-specific stem cells make random mistakes, or mutations. But the actual contribution of these random mistakes to cancer incidence, in comparison to the contribution of hereditary or environmental factors, was unclear.
To sort out the role of random mutations in cancer risk, the team charted the number of stem cell divisions in 31 tissues and compared these rates with the lifetime risks of cancer in the same tissues among Americans.
From this data scatterplot, Drs Tomasetti and Vogelstein determined the correlation between the total number of stem cell divisions and cancer risk to be 0.804. Mathematically, the closer this value is to 1, the more stem cell divisions and cancer risk are correlated.
“Our study shows, in general, that a change in the number of stem cell divisions in a tissue type is highly correlated with a change in the incidence of cancer in that same tissue,” Dr Vogelstein said.
One example is in colon tissue, which undergoes 4 times more stem cell divisions than small intestine tissue in humans. Likewise, colon cancer is much more prevalent than small intestinal cancer.
“You could argue that the colon is exposed to more environmental factors than the small intestine, which increases the potential rate of acquired mutations,” Dr Tomasetti said.
However, the scientists observed the opposite in mouse colons, which had a lower number of stem cell divisions than in their small intestines. In mice, cancer incidence is lower in the colon than in the small intestine. The researchers believe this supports the role of the total number of stem cell divisions in the development of cancer.
Using statistical theory, the pair calculated how much of the variation in cancer risk can be explained by the number of stem cell divisions, which is 0.804 squared, or, in percentage form, approximately 65%.
Finally, the scientists classified the types of cancers they studied into two groups. They calculated which cancer types had an incidence predicted by the number of stem cell divisions and which had higher incidence.
They found that 22 cancer types—including acute myeloid leukemia and chronic lymphocytic leukemia—could be largely explained by the “bad luck” factor of random DNA mutations during cell division.
The other 9 cancer types had incidences higher than predicted by “bad luck” and were presumably due to a combination of bad luck plus environmental or inherited factors.
“We found that the types of cancer that had higher risk than predicted by the number of stem cell divisions were precisely the ones you’d expect, including lung cancer, which is linked to smoking; skin cancer, linked to sun exposure; and forms of cancers associated with hereditary syndromes,” Dr Vogelstein said.
“This study shows that you can add to your risk of getting cancers by smoking or other poor lifestyle factors. However, many forms of cancer are due largely to the bad luck of acquiring a mutation in a cancer driver gene regardless of lifestyle and heredity factors. The best way to eradicate these cancers will be through early detection, when they are still curable by surgery.”
The researchers noted that some cancers, such as breast and prostate cancer, were not included in the report because the team was unable to find reliable stem cell division rates in the scientific literature.
They hope other scientists will help refine their statistical model by finding more precise stem cell division rates.
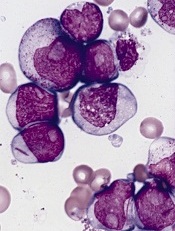
in the bone marrow
Scientists have created a statistical model that measures the proportion of cancer incidence, across many tissue types, caused mainly by random mutations that occur when stem cells divide.
By their measure, two-thirds of adult cancers—including certain leukemias—can be explained primarily by “bad luck,” when these random mutations occur in genes that can drive cancer growth.
The remaining third are due to environmental factors and inherited genes.
“All cancers are caused by a combination of bad luck, the environment, and heredity, and we’ve created a model that may help quantify how much of these three factors contribute to cancer development,” said Bert Vogelstein, MD, of the Johns Hopkins University School of Medicine.
Dr Vogelstein and Cristian Tomasetti, PhD, also of the Johns Hopkins University School of Medicine, detailed these findings in Science.
The pair came to their conclusions by searching the scientific literature for information on the cumulative number of stem cell divisions in 31 tissue types during an average individual’s lifetime.
The researchers knew that cancer arises when tissue-specific stem cells make random mistakes, or mutations. But the actual contribution of these random mistakes to cancer incidence, in comparison to the contribution of hereditary or environmental factors, was unclear.
To sort out the role of random mutations in cancer risk, the team charted the number of stem cell divisions in 31 tissues and compared these rates with the lifetime risks of cancer in the same tissues among Americans.
From this data scatterplot, Drs Tomasetti and Vogelstein determined the correlation between the total number of stem cell divisions and cancer risk to be 0.804. Mathematically, the closer this value is to 1, the more stem cell divisions and cancer risk are correlated.
“Our study shows, in general, that a change in the number of stem cell divisions in a tissue type is highly correlated with a change in the incidence of cancer in that same tissue,” Dr Vogelstein said.
One example is in colon tissue, which undergoes 4 times more stem cell divisions than small intestine tissue in humans. Likewise, colon cancer is much more prevalent than small intestinal cancer.
“You could argue that the colon is exposed to more environmental factors than the small intestine, which increases the potential rate of acquired mutations,” Dr Tomasetti said.
However, the scientists observed the opposite in mouse colons, which had a lower number of stem cell divisions than in their small intestines. In mice, cancer incidence is lower in the colon than in the small intestine. The researchers believe this supports the role of the total number of stem cell divisions in the development of cancer.
Using statistical theory, the pair calculated how much of the variation in cancer risk can be explained by the number of stem cell divisions, which is 0.804 squared, or, in percentage form, approximately 65%.
Finally, the scientists classified the types of cancers they studied into two groups. They calculated which cancer types had an incidence predicted by the number of stem cell divisions and which had higher incidence.
They found that 22 cancer types—including acute myeloid leukemia and chronic lymphocytic leukemia—could be largely explained by the “bad luck” factor of random DNA mutations during cell division.
The other 9 cancer types had incidences higher than predicted by “bad luck” and were presumably due to a combination of bad luck plus environmental or inherited factors.
“We found that the types of cancer that had higher risk than predicted by the number of stem cell divisions were precisely the ones you’d expect, including lung cancer, which is linked to smoking; skin cancer, linked to sun exposure; and forms of cancers associated with hereditary syndromes,” Dr Vogelstein said.
“This study shows that you can add to your risk of getting cancers by smoking or other poor lifestyle factors. However, many forms of cancer are due largely to the bad luck of acquiring a mutation in a cancer driver gene regardless of lifestyle and heredity factors. The best way to eradicate these cancers will be through early detection, when they are still curable by surgery.”
The researchers noted that some cancers, such as breast and prostate cancer, were not included in the report because the team was unable to find reliable stem cell division rates in the scientific literature.
They hope other scientists will help refine their statistical model by finding more precise stem cell division rates.
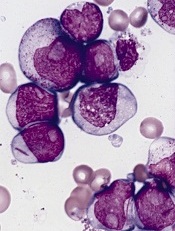
in the bone marrow
Scientists have created a statistical model that measures the proportion of cancer incidence, across many tissue types, caused mainly by random mutations that occur when stem cells divide.
By their measure, two-thirds of adult cancers—including certain leukemias—can be explained primarily by “bad luck,” when these random mutations occur in genes that can drive cancer growth.
The remaining third are due to environmental factors and inherited genes.
“All cancers are caused by a combination of bad luck, the environment, and heredity, and we’ve created a model that may help quantify how much of these three factors contribute to cancer development,” said Bert Vogelstein, MD, of the Johns Hopkins University School of Medicine.
Dr Vogelstein and Cristian Tomasetti, PhD, also of the Johns Hopkins University School of Medicine, detailed these findings in Science.
The pair came to their conclusions by searching the scientific literature for information on the cumulative number of stem cell divisions in 31 tissue types during an average individual’s lifetime.
The researchers knew that cancer arises when tissue-specific stem cells make random mistakes, or mutations. But the actual contribution of these random mistakes to cancer incidence, in comparison to the contribution of hereditary or environmental factors, was unclear.
To sort out the role of random mutations in cancer risk, the team charted the number of stem cell divisions in 31 tissues and compared these rates with the lifetime risks of cancer in the same tissues among Americans.
From this data scatterplot, Drs Tomasetti and Vogelstein determined the correlation between the total number of stem cell divisions and cancer risk to be 0.804. Mathematically, the closer this value is to 1, the more stem cell divisions and cancer risk are correlated.
“Our study shows, in general, that a change in the number of stem cell divisions in a tissue type is highly correlated with a change in the incidence of cancer in that same tissue,” Dr Vogelstein said.
One example is in colon tissue, which undergoes 4 times more stem cell divisions than small intestine tissue in humans. Likewise, colon cancer is much more prevalent than small intestinal cancer.
“You could argue that the colon is exposed to more environmental factors than the small intestine, which increases the potential rate of acquired mutations,” Dr Tomasetti said.
However, the scientists observed the opposite in mouse colons, which had a lower number of stem cell divisions than in their small intestines. In mice, cancer incidence is lower in the colon than in the small intestine. The researchers believe this supports the role of the total number of stem cell divisions in the development of cancer.
Using statistical theory, the pair calculated how much of the variation in cancer risk can be explained by the number of stem cell divisions, which is 0.804 squared, or, in percentage form, approximately 65%.
Finally, the scientists classified the types of cancers they studied into two groups. They calculated which cancer types had an incidence predicted by the number of stem cell divisions and which had higher incidence.
They found that 22 cancer types—including acute myeloid leukemia and chronic lymphocytic leukemia—could be largely explained by the “bad luck” factor of random DNA mutations during cell division.
The other 9 cancer types had incidences higher than predicted by “bad luck” and were presumably due to a combination of bad luck plus environmental or inherited factors.
“We found that the types of cancer that had higher risk than predicted by the number of stem cell divisions were precisely the ones you’d expect, including lung cancer, which is linked to smoking; skin cancer, linked to sun exposure; and forms of cancers associated with hereditary syndromes,” Dr Vogelstein said.
“This study shows that you can add to your risk of getting cancers by smoking or other poor lifestyle factors. However, many forms of cancer are due largely to the bad luck of acquiring a mutation in a cancer driver gene regardless of lifestyle and heredity factors. The best way to eradicate these cancers will be through early detection, when they are still curable by surgery.”
The researchers noted that some cancers, such as breast and prostate cancer, were not included in the report because the team was unable to find reliable stem cell division rates in the scientific literature.
They hope other scientists will help refine their statistical model by finding more precise stem cell division rates.
CARs come in different makes and models

Credit: NIAID
SAN FRANCISCO—CTL019, a chimeric antigen receptor (CAR) T cell targeting CD19, is not the only CAR in the production line.
Investigators at the National Cancer Institute in Bethesda, Maryland, and Memorial Sloan Kettering Cancer Center (MSKCC) in New York City are also pursuing CAR T-cell therapy.
These groups are using a retroviral platform to transduce the T cells rather than a lentiviral one, as is the case with CTL019.
Investigators reported progress to date on these makes of CARs at the 2014 ASH Annual Meeting.
Daniel W. Lee III, MD, of the National Cancer Institute, reported on a phase 1 study of CD19 CAR T cells in children and young adults with CD19+ acute lymphoblastic leukemia or non-Hodgkin lymphoma.
And Jae H. Park, MD, of MSKCC, presented data from a trial of JCAR015—autologous T cells genetically modified to express a 19-28z CAR targeting CD19—in patients with B-cell acute lymphoblastic leukemia.
The study is sponsored by MSKCC, but JCAR015 is a product of Juno Therapeutics.

Credit: NIAID
SAN FRANCISCO—CTL019, a chimeric antigen receptor (CAR) T cell targeting CD19, is not the only CAR in the production line.
Investigators at the National Cancer Institute in Bethesda, Maryland, and Memorial Sloan Kettering Cancer Center (MSKCC) in New York City are also pursuing CAR T-cell therapy.
These groups are using a retroviral platform to transduce the T cells rather than a lentiviral one, as is the case with CTL019.
Investigators reported progress to date on these makes of CARs at the 2014 ASH Annual Meeting.
Daniel W. Lee III, MD, of the National Cancer Institute, reported on a phase 1 study of CD19 CAR T cells in children and young adults with CD19+ acute lymphoblastic leukemia or non-Hodgkin lymphoma.
And Jae H. Park, MD, of MSKCC, presented data from a trial of JCAR015—autologous T cells genetically modified to express a 19-28z CAR targeting CD19—in patients with B-cell acute lymphoblastic leukemia.
The study is sponsored by MSKCC, but JCAR015 is a product of Juno Therapeutics.

Credit: NIAID
SAN FRANCISCO—CTL019, a chimeric antigen receptor (CAR) T cell targeting CD19, is not the only CAR in the production line.
Investigators at the National Cancer Institute in Bethesda, Maryland, and Memorial Sloan Kettering Cancer Center (MSKCC) in New York City are also pursuing CAR T-cell therapy.
These groups are using a retroviral platform to transduce the T cells rather than a lentiviral one, as is the case with CTL019.
Investigators reported progress to date on these makes of CARs at the 2014 ASH Annual Meeting.
Daniel W. Lee III, MD, of the National Cancer Institute, reported on a phase 1 study of CD19 CAR T cells in children and young adults with CD19+ acute lymphoblastic leukemia or non-Hodgkin lymphoma.
And Jae H. Park, MD, of MSKCC, presented data from a trial of JCAR015—autologous T cells genetically modified to express a 19-28z CAR targeting CD19—in patients with B-cell acute lymphoblastic leukemia.
The study is sponsored by MSKCC, but JCAR015 is a product of Juno Therapeutics.
CAR is feasible in majority of ALL patients, team says

Credit: Bill Branson
SAN FRANCISCO—A chimeric antigen receptor (CAR) T-cell therapy is feasible in 90% of heavily pretreated or transplanted patients with acute lymphoblastic leukemia (ALL) and can serve as a bridge to transplant, according to investigators.
Daniel W. Lee III, MD, of the National Cancer Institute in Bethesda, Maryland, reported on a phase 1 study of this CD19 CAR T-cell therapy in children and young adults with CD19+ ALL or non-Hodgkin lymphoma at the 2014 ASH Annual Meeting (abstract 381*).
Twenty-one patients were enrolled on the trial. They had a preparative regimen of fludarabine and cyclophosphamide and were infused with CAR T cells 11 days after the peripheral blood mononuclear cells were collected.
Dose levels were 1 x 106 CAR+ T cells/kg, 3 x 106 CAR+ T cells/kg, or the maximum number of cells generated if below either one of these levels. Two patients received less than the dose assigned and were not evaluated for toxicity.
Patients were a median age of 13 years (range, 5 to 27). Fourteen were male, 20 had ALL, and 1 had diffuse large B-cell lymphoma.
All had detectable disease, and 2 were CNS2 at the time of T-cell infusion. Six had primary refractory disease, 8 had at least 1 prior stem cell transplant, and 4 had prior immunotherapy.
The investigators determined that the maximally tolerated dose was 1 x 106 CAR+ T cells/kg. The dose-limiting toxicities were related to cytokine release syndrome (CRS), which was reversible if managed appropriately with tocilizumab, with or without steroids.
Grade 3 adverse events possibly related to therapy included fever (47%), febrile neutropenia (37%), electrolyte disturbance (29%), CRS (16%), hypotension (11%), transaminitis (16%), and 5% each for hypertension, prolonged QTc, dysphasia, LV systolic dysfunction, multiorgan failure, hypoxia, and pulmonary edema.
Grade 4 events possibly related to treatment included electrolyte disturbance (5%), CRS (16%), hypotension (11%), cardiac arrest (5%), and hypoxia (5%). There was no evidence of graft-vs-host disease.
The complete response (CR) rate was 67% in the intent-to-treat population and 70% in patients with ALL.
“Those patients who responded tended to have some degree of cytokine release syndrome, whereas those patients who did not respond or had stable disease did not have any CRS,” Dr Lee said. “But, also, it’s important to note that you don’t have to have severe grade 3 or grade 4 CRS in order to have significant response.”
Dr Lee also pointed out that in vivo CAR T-cell expansion significantly correlated with response (P=0.0028). And CRS severity correlated with IL-6 (P=0.0002), INF-γ (P=0.0002), C-reactive protein (P=0.0015), and CAR (P=0.0011).
At a median follow-up of 10 months, minimal residual disease-negative patients had a 79% leukemia-free survival. Overall survival was 52% for all patients enrolled. Two patients had CD19-negative relapses.
The investigators also found that CAR T cells can eliminate CNS leukemia, with 11 of 17 patients (65%) having CAR T cells detectable in their cerebrospinal fluid.
The team concluded that this therapy is feasible in 90% of heavily pretreated or transplanted ALL patients and can serve as a bridge to transplant.
*Information in the abstract differs from that presented at the meeting.

Credit: Bill Branson
SAN FRANCISCO—A chimeric antigen receptor (CAR) T-cell therapy is feasible in 90% of heavily pretreated or transplanted patients with acute lymphoblastic leukemia (ALL) and can serve as a bridge to transplant, according to investigators.
Daniel W. Lee III, MD, of the National Cancer Institute in Bethesda, Maryland, reported on a phase 1 study of this CD19 CAR T-cell therapy in children and young adults with CD19+ ALL or non-Hodgkin lymphoma at the 2014 ASH Annual Meeting (abstract 381*).
Twenty-one patients were enrolled on the trial. They had a preparative regimen of fludarabine and cyclophosphamide and were infused with CAR T cells 11 days after the peripheral blood mononuclear cells were collected.
Dose levels were 1 x 106 CAR+ T cells/kg, 3 x 106 CAR+ T cells/kg, or the maximum number of cells generated if below either one of these levels. Two patients received less than the dose assigned and were not evaluated for toxicity.
Patients were a median age of 13 years (range, 5 to 27). Fourteen were male, 20 had ALL, and 1 had diffuse large B-cell lymphoma.
All had detectable disease, and 2 were CNS2 at the time of T-cell infusion. Six had primary refractory disease, 8 had at least 1 prior stem cell transplant, and 4 had prior immunotherapy.
The investigators determined that the maximally tolerated dose was 1 x 106 CAR+ T cells/kg. The dose-limiting toxicities were related to cytokine release syndrome (CRS), which was reversible if managed appropriately with tocilizumab, with or without steroids.
Grade 3 adverse events possibly related to therapy included fever (47%), febrile neutropenia (37%), electrolyte disturbance (29%), CRS (16%), hypotension (11%), transaminitis (16%), and 5% each for hypertension, prolonged QTc, dysphasia, LV systolic dysfunction, multiorgan failure, hypoxia, and pulmonary edema.
Grade 4 events possibly related to treatment included electrolyte disturbance (5%), CRS (16%), hypotension (11%), cardiac arrest (5%), and hypoxia (5%). There was no evidence of graft-vs-host disease.
The complete response (CR) rate was 67% in the intent-to-treat population and 70% in patients with ALL.
“Those patients who responded tended to have some degree of cytokine release syndrome, whereas those patients who did not respond or had stable disease did not have any CRS,” Dr Lee said. “But, also, it’s important to note that you don’t have to have severe grade 3 or grade 4 CRS in order to have significant response.”
Dr Lee also pointed out that in vivo CAR T-cell expansion significantly correlated with response (P=0.0028). And CRS severity correlated with IL-6 (P=0.0002), INF-γ (P=0.0002), C-reactive protein (P=0.0015), and CAR (P=0.0011).
At a median follow-up of 10 months, minimal residual disease-negative patients had a 79% leukemia-free survival. Overall survival was 52% for all patients enrolled. Two patients had CD19-negative relapses.
The investigators also found that CAR T cells can eliminate CNS leukemia, with 11 of 17 patients (65%) having CAR T cells detectable in their cerebrospinal fluid.
The team concluded that this therapy is feasible in 90% of heavily pretreated or transplanted ALL patients and can serve as a bridge to transplant.
*Information in the abstract differs from that presented at the meeting.

Credit: Bill Branson
SAN FRANCISCO—A chimeric antigen receptor (CAR) T-cell therapy is feasible in 90% of heavily pretreated or transplanted patients with acute lymphoblastic leukemia (ALL) and can serve as a bridge to transplant, according to investigators.
Daniel W. Lee III, MD, of the National Cancer Institute in Bethesda, Maryland, reported on a phase 1 study of this CD19 CAR T-cell therapy in children and young adults with CD19+ ALL or non-Hodgkin lymphoma at the 2014 ASH Annual Meeting (abstract 381*).
Twenty-one patients were enrolled on the trial. They had a preparative regimen of fludarabine and cyclophosphamide and were infused with CAR T cells 11 days after the peripheral blood mononuclear cells were collected.
Dose levels were 1 x 106 CAR+ T cells/kg, 3 x 106 CAR+ T cells/kg, or the maximum number of cells generated if below either one of these levels. Two patients received less than the dose assigned and were not evaluated for toxicity.
Patients were a median age of 13 years (range, 5 to 27). Fourteen were male, 20 had ALL, and 1 had diffuse large B-cell lymphoma.
All had detectable disease, and 2 were CNS2 at the time of T-cell infusion. Six had primary refractory disease, 8 had at least 1 prior stem cell transplant, and 4 had prior immunotherapy.
The investigators determined that the maximally tolerated dose was 1 x 106 CAR+ T cells/kg. The dose-limiting toxicities were related to cytokine release syndrome (CRS), which was reversible if managed appropriately with tocilizumab, with or without steroids.
Grade 3 adverse events possibly related to therapy included fever (47%), febrile neutropenia (37%), electrolyte disturbance (29%), CRS (16%), hypotension (11%), transaminitis (16%), and 5% each for hypertension, prolonged QTc, dysphasia, LV systolic dysfunction, multiorgan failure, hypoxia, and pulmonary edema.
Grade 4 events possibly related to treatment included electrolyte disturbance (5%), CRS (16%), hypotension (11%), cardiac arrest (5%), and hypoxia (5%). There was no evidence of graft-vs-host disease.
The complete response (CR) rate was 67% in the intent-to-treat population and 70% in patients with ALL.
“Those patients who responded tended to have some degree of cytokine release syndrome, whereas those patients who did not respond or had stable disease did not have any CRS,” Dr Lee said. “But, also, it’s important to note that you don’t have to have severe grade 3 or grade 4 CRS in order to have significant response.”
Dr Lee also pointed out that in vivo CAR T-cell expansion significantly correlated with response (P=0.0028). And CRS severity correlated with IL-6 (P=0.0002), INF-γ (P=0.0002), C-reactive protein (P=0.0015), and CAR (P=0.0011).
At a median follow-up of 10 months, minimal residual disease-negative patients had a 79% leukemia-free survival. Overall survival was 52% for all patients enrolled. Two patients had CD19-negative relapses.
The investigators also found that CAR T cells can eliminate CNS leukemia, with 11 of 17 patients (65%) having CAR T cells detectable in their cerebrospinal fluid.
The team concluded that this therapy is feasible in 90% of heavily pretreated or transplanted ALL patients and can serve as a bridge to transplant.
*Information in the abstract differs from that presented at the meeting.